Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 11/3050/30. The contractual start date was in September 2016. The final report began editorial review in October 2016 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
John Norrie reports that he was a member of the National Institute for Health Research (NIHR)/Health Technology Assessment (HTA) Commissioning Board 2010–16, is a member of the NIHR Journals Editorial Board (2015–present) and is deputy chairperson of the NIHR/HTA General Board (2016–present). Carol Emslie reports grants and non-financial support from the Scottish Health Action on Alcohol Problems, grants from the NIHR HTA programme and non-financial support from the British Sociological Association Alcohol Study Group outside the submitted work. She is also a member of the Alcohol Research UK Grants Advisory Panel (unpaid position). Peter T Donnan reports grants from Novo Nordisk Ltd, GlaxoSmithKline plc and AstraZeneca plc outside the submitted work. He is also is a member of the New Drugs Committee of the Scottish Medicines Consortium.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Crombie et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Alcohol and disadvantaged groups
Alcohol-related morbidity and mortality represent a major public health challenge. The cost of alcohol to society has been estimated at > £55B per year in England1 and > £3.5B per year in Scotland. 2 These costs occur through lost productivity, increased health-care and other public sector costs, and social disruption.
Brief interventions, based on psychological theories of behaviour change, have been developed to tackle alcohol-related problems. There is extensive evidence that they are effective,3–6 although some recent large studies have found them to be ineffective7–9 or possibly harmful. 10 To date, most studies have been conducted in health-care settings, often with individuals who are seeking help.
The risk of alcohol-related harm is substantially higher in disadvantaged groups. 11,12 Alcohol is a major cause of inequalities in health. 11,13,14 Part of the explanation for this may lie in the patterns of drinking; although socioeconomically disadvantaged individuals may not drink more on average, they are more likely to binge drink. 15–17 Binge drinking used to refer to an extended period of several days’ drinking, but is now defined as drinking more than a specified amount, such as eight UK units of alcohol, in a single session. 18
The group who binge drink most frequently in the UK is young to middle-aged disadvantaged men. 16 They may not be reached by current initiatives to tackle excessive drinking as the uptake of public health interventions among socially disadvantaged men is low. 19 There is a need for an intervention that accesses and effectively reduces binge drinking in this hard-to-reach population.
Interventions to reduce inequalities
Behaviour change interventions are less effective, and often ineffective, with disadvantaged/low income groups. 20–23 Indeed, there is concern that interventions may widen inequalities in health. 24–27 A systematic review of smoking cessation found that there were more barriers to change for disadvantaged groups, particularly pro-smoking norms, additional cues to smoking and increased stress. 23 Evaluations of smoking cessation interventions suggest that the lower effectiveness is due not to lower initial uptake, but to lower sustained compliance with the intervention. 28,29 This could be because disadvantaged individuals are less likely to translate intentions to change into action to modify behaviour. 30 Qualitative research suggests that disadvantaged individuals who live in poorly resourced and stressful environments are isolated from wider social norms and have limited opportunities for respite and recreation. 31 Fear of being judged and fear of failure have also been identified as barriers to change. 32 These findings suggest that interventions should be tailored to disadvantaged groups. 33,34 There is a paucity of evidence on interventions to reduce alcohol consumption or binge drinking in disadvantaged individuals.
Recruitment and retention
Recruitment to randomised controlled trials (RCTs) is a major problem. 35 Only a minority of trials reach their intended sample size on time and many require extensions and additional resources to boost recruitment. 35–37 As a consequence, poor recruitment is the major cause of discontinued trials. 38,39 Several systematic reviews40–43 have sought to identify strategies for increasing recruitment to trials. Recommended strategies include using financial incentives, using opt-out, making trial materials culturally sensitive, and making multiple attempts at contact. Direct personal contact, by telephone or face to face, has been found to be substantially more effective than passive approaches, such as mass media or mail. 44
The recruitment of individuals of lower socioeconomic status to trials is particularly difficult because they are less willing to participate in research studies. 45–49 Barriers to research participation include distrust of research, concern about confidentiality, fear of authority, lack of knowledge, lack of time and perceived lack of benefit from participation. 50–54 Strategies to address the reluctance of disadvantaged groups include those mentioned for trials in the general population, but also stress personal contact, the use of sensitive and culturally relevant communication, and attention to the benefits of participation.
The retention of disadvantaged groups is also challenging. 23,55,56 Several systematic reviews55,57,58 and a survey of clinical trials units in the UK59 have identified strategies to improve retention in general population studies. In addition, strategies for retention of disadvantaged groups have been identified. 52,55,56,60–62 These include maintaining contact during follow-up, several contact strategies, the use of a financial incentive, multiple attempts at contact, sending reminders and making the interview convenient for participants. 52,55,57,58,60,61,63–65
Text message interventions
Text messaging provides a method for delivering brief alcohol interventions that has the potential to reach large numbers of individuals at low cost. Recent systematic reviews have shown that there is good evidence that text messages can promote smoking cessation66–68 and increase adherence to antiretroviral therapy. 69,70 The quality of the primary studies in many other areas is a cause for concern. 66,68 No studies have tackled binge drinking among disadvantaged men, although text messaging interventions are particularly well suited to young to middle-aged men because their ownership of mobile phones is high.
Background to the study
We recently completed a National Institute for Health Research (NIHR)-funded feasibility study that demonstrated that all stages of a trial of a brief intervention delivered by mobile phone could be completed successfully. 71 It identified a high frequency of hazardous drinking among disadvantaged men, creating a pressing need for effective interventions to tackle their binge drinking. The success of the feasibility study led to the recommendation that a full trial to assess the effectiveness and cost-effectiveness of the text message intervention should be conducted.
Overview of full trial
This study tested the effectiveness of a novel text message intervention designed to reduce binge drinking among disadvantaged men. It was a four-centre, parallel group, pragmatic, individually randomised controlled trial. The four centres covered major regions of Scotland: Tayside, Glasgow, Forth Valley and Fife. Men aged 25–44 years from areas of high deprivation were recruited. Deprivation was measured using the Scottish Index of Multiple Deprivation (SIMD),72 which is similar to the English Index of Multiple Deprivation. Men were recruited from areas classified as being in the most disadvantaged quintile. The required sample size was 798 men.
The text message intervention was a series of 112 interactive text messages delivered by mobile phone over a 12-week period. The intervention drew on literature from alcohol brief interventions, communication theory, and behaviour change theories and techniques. The control group received an attentional control comprising 89 text messages on general health topics.
The primary outcome was the proportion of men binge drinking (consuming > 8 units of alcohol) on ≥ 3 occasions in the previous 28 days. It was assessed at 12 months post intervention. Secondary outcomes covered heavy binge drinking (> 16 units of alcohol), total mean consumption and frequency of hazardous or harmful drinking [Alcohol Use Disorders Identification Test (AUDIT)] at 12 months post intervention, and binge drinking and heavy binge drinking at 3 months post intervention.
The economic evaluation took a societal perspective and modelled the potential cost-effectiveness of the intervention assuming a nationwide implementation. Data were collected on the resources required for recruitment and the implementation of the intervention. These were used to predict the costs relating to national rollout where resources will be costed according to their opportunity cost.
Research questions
Three research questions were specified in the protocol.
-
Can a brief intervention delivered by mobile phone reduce the frequency of binge drinking among disadvantaged men?
-
Is the intervention cost-effective?
-
Which components of the behaviour change strategy (intentions to avoid becoming drunk, self-efficacy for refusing drinks, goal-setting and action-planning for reducing binge drinking frequency) are associated with changes in drinking behaviour?
Chapter 2 Development of the text message intervention
Introduction
The behaviour change intervention was designed to promote a sustained reduction in the frequency of binge drinking. The challenge was to develop an empirically and theoretically based complex intervention to engage socially disadvantaged men long enough to guide them through the steps to behaviour change. The tailoring of interventions to the needs and circumstances of disadvantaged groups is strongly recommended. 33,34,73 The intervention was developed from the one used in the feasibility study, which was designed in collaboration with the user group. 71 The method of delivery, text messages with no face-to-face contact, proved to be highly acceptable to the target group, so it was used again.
Systematic reviews have shown that text message interventions can successfully modify adverse health behaviours. 66,74 Several recent studies have reported that mobile phone interventions have the potential to modify drinking in people attending emergency departments,75–77 students,78,79 young people,80 adults81 and dependent drinkers. 82 Mobile phone ownership in the target age group in the UK is > 95%,83 and phone users frequently check their phones,84 so study participants would be likely to open and read the messages. Previous studies report that text messages are usually read soon after delivery. 85 Text messaging is particularly suited to the target group because little effort is required to receive the intervention and texts can be accessed at times that suit the participants. In addition, each text message can be read quickly and reread if desired. Men who may not want to commit time to reading leaflets or large sections of text may prefer to receive concise text messages.
Overview
Evidence from several areas was used to create the intervention. Initially, the psychological theory that would underpin the intervention was decided. Evidence from alcohol brief interventions was reviewed and effective behavioural change techniques were included. A narrative was used to structure the text messages and to ensure that the participants’ interest could be maintained over the intervention period. The storyline was designed to increase engagement, provide coherence to the text messages and illustrate the process of behaviour change. Communication theory was reviewed to ensure that the overall ethos of the intervention was engaging for and acceptable to the recipients. Finally, successful techniques used in the design of the text messages for the feasibility study were also incorporated. In particular, focus groups with disadvantaged men, which were conducted in the feasibility study, identified levers for behaviour change, as well as approaches to be avoided.
Key findings from the feasibility study
Focus groups investigated men’s attitudes about taking part in a text message intervention and their beliefs about cutting down. 71 They gave insight into the target group’s patterns of drinking, and their knowledge about alcohol-related harms and the benefits of reduced drinking. The common pattern of drinking was periods of abstinence interspersed with infrequent heavy-drinking days. Many men believed that their drinking behaviours, motives and desire to change were significantly different from when they were younger. They had adopted the role of the ‘mature drinker’, which came with social roles and responsibilities (employee, husband/partner, parent). Most men were aware of the harms associated with alcohol misuse, but had low perceived personal risk. They made it clear that in an intervention they would not want to be preached at or told what to do.
The feasibility study also found that the text message brief intervention could engage participants86 and had the potential to reduce binge drinking. 71 Participants enjoyed the interactive nature of the intervention and gave carefully considered personal responses to the questions asked in the text messages. They engaged with the cognitive antecedents to reducing drinking as they were discussed in the text messages. Although the intervention addressed intention to change, it did not provide sufficient assistance on methods to achieve behaviour change and maintain the new behaviour. The intervention would need to be modified to incorporate a psychological theory that addresses volition as well as motivation to change behaviour. In addition, a period of 1 month would not be sufficient to address all of the steps required to change behaviour, so it should be extended to 3 months.
Psychological theory underpinning the intervention
The behaviour change strategy was based on the Health Action Process Approach (HAPA). 87 The HAPA model suggests that behaviour change occurs through two distinct phases: a pre-intentional or motivational phase and a volitional phase. The volitional phase is made up of separate components: a planning and action phase, and a maintenance phase. HAPA was chosen as it addresses the intention–behaviour gap,88 identified as a weakness in some behavioural change theories. Although HAPA was used as the overarching structure around which the intervention was developed, it drew on other social cognition models, such as subjective norms from the theory of planned behaviour,89 self-monitoring from social cognitive theory90 and control theory. 91 It also used empirical data from the feasibility study. Finally, behaviour change techniques suitable for use in alcohol interventions were incorporated. 92
Alcohol brief interventions
The first trial of a brief intervention for heavy alcohol use was conducted in 1962. 93 Since then, over 50 trials have been conducted in primary care and their results have been synthesised in 26 systematic reviews. 94 The consistent finding is that the interventions were effective for hazardous and harmful drinking in middle-aged men. However, there is insufficient evidence of effectiveness in women and in older and younger drinkers. Evidence from other settings is less persuasive. For example, in patients from emergency departments, trauma care centres, hospitals and community pharmacies, the evidence is mixed. 95,96
Despite the evidence on effectiveness, the mechanism of action of brief interventions is not known,97–99 in part because alcohol brief interventions are very heterogeneous. The time for the delivery of the interventions varies between 5 and 60 minutes, with a median of 25 minutes. 5 The content of the interventions also varies substantially. 5,94 They can contain motivational interviewing, feedback and advice, self-monitoring of alcohol consumption, self-help manuals, counselling and cognitive–behavioural therapy. 5,94,100 It is unclear whether or not interventions based on the principles of motivational interviewing may be more effective than other approaches. 97,99 One review of reviews has suggested that effective interventions contain at least two of three elements: feedback on drinking, advice and goal-setting. 101 A more recent review found that promoting self-monitoring was the only technique that appeared effective. 92 Bien et al. ,100 in their very widely cited paper, summarised the common components of effective brief interventions with the acronym FRAMES: Feedback on current consumption; Responsibility of the individual for his drinking; Advice to change; Menu of change strategies; Empathy in the delivery; and Self-efficacy for action.
Narratives in interventions
A narrative was used to engage the participants and to illustrate the key steps in the behaviour change process. Braddock and Price Dillard102 describe a narrative as ‘a cohesive, causally linked sequence of events that takes place in a dynamic world subject to conflict, transformation, and resolution through non-habitual, purposeful actions performed by character’. Narrative is increasingly being used as a tool for behaviour change. 103 Instead of presenting facts and arguments for changing behaviour, a narrative intervention translates these into actions and experiences of characters within a chronological series of events. 104 Narratives have been used in a range of health behaviour change studies (e.g. risks associated with sunbeds, vaccination for human papillomavirus, smoking cessation and alcohol use104), although none delivered through text messaging has been reported. In the present study, the narrative follows a central character, Dave, as he gradually realises that he drinks too much and decides to reduce his consumption. It charts his efforts, successes and relapses, and concludes with Dave enjoying the financial and social benefits of moderated drinking.
There are several advantages of using narrative. Information presented in a narrative has a stronger effect on knowledge, attitudes and intentions than the same information in a non-narrative format. 105 Narrative is particularly useful for changing perceived social norms and behavioural intentions. 106 It can ‘strengthen existing prosocial beliefs and behaviours as well as counteract unhealthy ones’. 107 Resistance to behaviour change is overcome because individuals are engaged in the narrative. 103
To be effective for behaviour change, the narrative and the characters in it have to engage the reader, a process aided if the protagonists are culturally similar to the target audience. 108,109 The narrative also has to be plausible and internally consistent. 110 The depiction of a character who succeeds against the odds can boost motivation for personal goals. 111
Logic model
A logic model was used to aid the development of the intervention (Table 1). Logic models help to clarify how the intervention will lead to behaviour change and, in the longer term, to improved health and social well-being. 112 A review of a problem (behaviour to be changed and the target group) clarifies what is to be achieved. It can also identify challenges, such as resistance of disadvantaged groups to conventional health-promotion interventions. The intervention strategy, the intervention goals and the outputs specify how the aim will be achieved. In this study, the initial requirements for behaviour change were an increased awareness and personal relevance of the harms of alcohol and the benefits of moderated drinking. Altering risk perception and alcohol expectancies are prerequisites for increased motivation to change. Setting goals and making action plans would lead to reduced drinking, but only if self-efficacy for action was also increased. Furthermore, to prevent relapse, reduced drinking would have to be maintained. This could be achieved by increasing the salience of the benefits of reduced drinking. Thus, the short-term benefits of moderated drinking can be used to encourage longer-term reductions. This will lead to improved health and social well-being for the individual and a reduction in the costs of alcohol-related harms for society.
| Problem | ➡ | Intervention/strategy | ➡ | Intervention goals | ➡ | Output | ➡ | Outcomes | ➡ | Impact | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Short term | Long term | ||||||||||
| Binge drinking is common among young to middle-aged disadvantaged men | Design a cost-effective alcohol intervention that will appeal to the target group | Recruit socially disadvantaged men who regularly binge drink | Increased personal relevance of alcohol-related harms | Decrease the number of episodes of binge drinking | Maintenance of healthy drinking patterns | Reduction in inequalities through improved health and fewer social problems and family disruption | |||||
| Disadvantaged men may be reluctant to engage with health-promoting interventions | Incorporate a narrative to engage the men in the steps involved in changing behaviour | Increase awareness of alcohol-related harms | Intentions to drink at safe levels | Reduce/prevent:
|
Prevention of physical, mental and social problems:
|
Reduced costs to:
|
|||||
| Conventional alcohol brief interventions may not reach this group |
The intervention is based on the HAPA and uses behaviour change techniques The causal model: |
Deliver the intervention by text message to make it acceptable to the target group Change alcohol expectancies by encouraging men to consider the benefits of reduced drinking Change drinking behaviour through goal-setting and action-planning Maintain moderate/safe drinking levels |
Goals/action plans to drink at safe levels Strategies to maintain safe drinking levels Moderated drinking by individuals |
Increase salience of benefits of reduced drinking Increase self-efficacy to change |
Increased productivity due to the reduction in sick time taken Shift in attitudes towards alcohol Change in drinking culture |
||||||
Stages in the development of the intervention
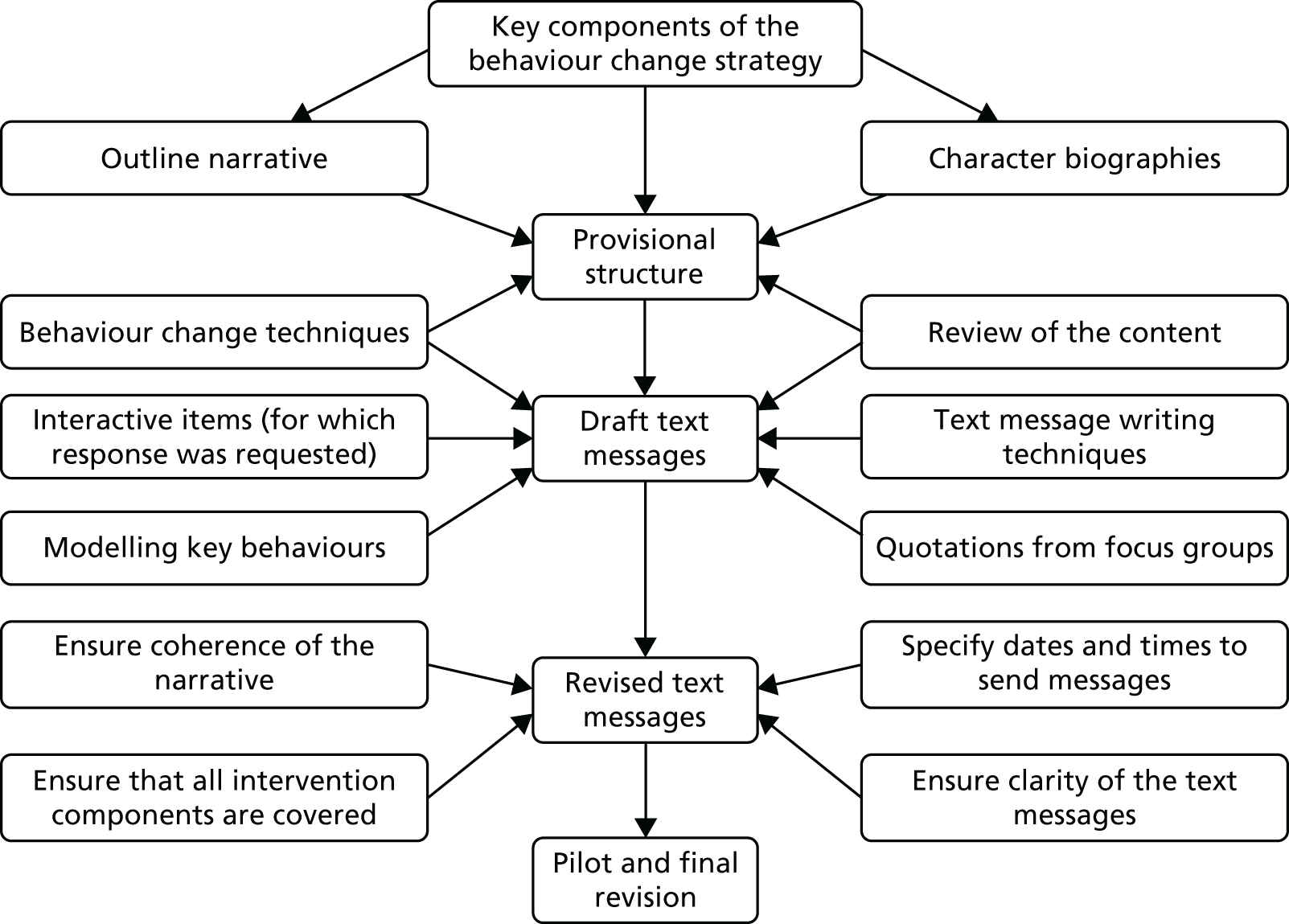
The intervention was developed in four stages (Figure 1): (1) establishing the provisional structure of the intervention, (2) drafting the text messages, (3) revising the content of the text messages and (4) piloting and final revisions. In practice, there was much iteration in the writing process, with modifications made to the narrative and to the text messages as the structure and content of individual text messages were developed. An extended piloting process was required to ensure that the narrative was coherent when rendered into text messages and that all components of the behaviour change strategy were adequately addressed.
FIGURE 1.
Stages in writing the text messages.
Stage 1: establishing the provisional structure
Building on the logic model, key elements of the intervention were reviewed to create a provisional structure. These were the behaviour change model (HAPA)87 and relevant behaviour change techniques. 92 This provided a framework to establish how the narrative would depict the process of behaviour change, who the characters in the narrative would be and how the intervention could be delivered within the time frame of 3 months.
Key components of the behaviour change strategy
To establish a framework and timetable for the delivery of the intervention, the components of HAPA to be incorporated at each stage were addressed in three parts (Box 1). In the motivational phase, the pre-intentional motivational processes that lead to behavioural intentions include changing alcohol expectancies and perceptions of personal risk from alcohol-related harm. Increasing self-efficacy and gaining social support are also essential at this and all subsequent stages of the intervention.
-
Alcohol expectancies.
-
Perception of risk.
-
Action self-efficacy.
-
Social support.
-
Action self-efficacy.
-
Coping self-efficacy.
-
Action control (how to cope in a high-risk situation).
-
Goal-setting.
-
Action-planning.
-
Social support.
-
Recovery self-efficacy.
-
Coping self-efficacy.
-
Action control (how to cope in a high-risk situation).
-
Social support.
The volitional phase of HAPA was divided into two parts. Initially, action-planning and coping-planning were tackled. This included the setting of goals and drawing up of action plans and coping plans. Subsequently, maintenance of the new behaviour, including lapse and relapse, was addressed (see Box 1). A recent review of behavioural theory113 has identified four factors that are important in maintenance. These were incorporated into the intervention: (1) satisfaction with behavioural outcome (e.g. financial gain or weight loss from reduced drinking); (2) self-regulatory processes (e.g. self-monitoring and planning); (3) identity (i.e. ensuring that processes and outcomes of behaviour change are consistent with the attitudes and values of the participants); and (4) social and environmental factors (e.g. making plans for how to deal with high-risk drinking situations).
Character biographies
To enable the detailed storyline to be developed, the number and the nature of the characters were decided. The number of characters was limited to ensure that the study participants could follow their individual stories. Constraints imposed by embedding the narrative in text messages meant that background information on each character was limited.
The feasibility study71 identified distinct drinking behaviours within the target group: men who regularly drank over the binge-drinking threshold (> 8 units of alcohol in a session) and those who engaged in very heavy binge drinking (> 16 units of alcohol in a session). A common pattern of drinking was periods of abstinence interspersed with infrequent heavy-drinking days. Another common feature was that many men believed that their drinking behaviours, motives and desire to change were significantly different from when they were younger. They perceived this as a shift towards the role of a ‘mature drinker’, which came with social roles and responsibilities (employee, husband/partner, parent). This ‘mature drinker’ identity was desirable and important for being able to fulfil responsibilities and commitments to family or work.
The first task was to ensure that the characters in the narrative embodied these characteristics. Participants would be more likely to feel a personal connection if the characters were similar to them. The narrative was portrayed through a lead character, Dave, his wife (Christine) and several minor characters who were friends (Box 2). Dave was presented as someone who believed he was a mature drinker (a family man with responsibilities), but who had been a heavy binge drinker in the past. He was designed to be likeable and someone who would succeed in changing his behaviour. However, so that the participants would empathise with his experiences, he also faced disappointment and failure before finally achieving his goals. Dave was resilient and reflective, allowing him to learn from his failures and disappointments. He modelled the process of reflection on his drinking to encourage participants to review their own behaviour, motivations and circumstances.
Dave is a family man who is married to Christine. He initially believes that he is a mature drinker. He subsequently realises that he is a regular binge drinker and becomes aware of the potential risks from his drinking. He models behaviour change techniques that are likely to work, but also experiences lapses along the way. In the end he achieves his goal to cut down on his drinking and is satisfied with the outcome of the changes he has made.
Peripheral characters (Dave’s friends)Stevie is the unmarried ‘antagonist’ character. He has few responsibilities, is unemployed and lives with his mother. Stevie often encourages everyone around him to drink.
Dougie has had serious alcohol-related problems in the past. He lives with a long-suffering partner (Sadie) but has a troubled relationship. He also tries to change his drinking, but gets it wrong more often than Dave.
Alec is a reformed, now mature, sensible drinker. He is respected by the others and is a role model for Dave.
The minor characters, like the protagonist, were also people with whom the participants could identify (either currently, or as someone who would represent their younger self or an older role model). These characters were more likely to fail in achieving their goals, but they were also designed to elicit empathy and sympathy from participants. Different drinking patterns (e.g. reformed heavy drinker, regular heavy binge drinker) were allocated to the characters, and then other demographic characteristics were introduced (i.e. employed/unemployed; single/in a relationship/family man).
Outline narrative
A narrative, based on the lives of these characters, was written out in full before it was considered how this could be rendered into text messages. Dave set out on a journey to moderated drinking, modelling the key steps in the process to behaviour change (Box 3). For example, action planning to reduce alcohol consumption should specify when a new behaviour will be adopted, where it will be carried out and how it will be achieved. This process of action planning was described in a text message, and then illustrated in a subsequent message by Dave going through the process of identifying the where, when and how he would cut down. Similarly, when relapse prevention was addressed, Dave explained how it had happened to him and why he was determined to keep to his original plan to reduce his drinking. Dave’s fallibility encourages ‘buy-in’, as men identify with him and his determination could inspire them to emulate him. In general, if participants empathise with the character, the texts (e.g. perceived risk, benefits of moderated drinking) become more relevant and concrete and are more likely to lead to behaviour change.
Self-monitoring of drinking.
Risk perception.
Modifying outcome expectancies.
Intention to reduce drinking.
Subjective norms.
Goal-setting.
Action-planning.
Action self-efficacy.
Success at sticking to the plan.
Lapse.
Coping-planning.
Coping self-efficacy.
Satisfaction with changed drinking pattern.
Rewards for achieving goals.
Narratives frequently evoke emotional responses and these can have strong effects over and above more rational cognitive approaches. Thus, emotive topics were used to increase motivation to change; for example, one of the character’s partner and child leave home because of problems caused by alcohol. The character’s setbacks were subsequently resolved after drinking problems had been tackled. The impact of these fraught situations, and their subsequent resolution, will be greater if the participants identify with the character.
Self-efficacy is essential in achieving behaviour change. The intervention aimed to increase self-efficacy throughout the intervention period (task self-efficacy, coping self-efficacy and maintenance self-efficacy). Using characters to model behaviours allowed the intervention to focus on self-efficacy for specific concrete behaviours rather than general self-efficacy beliefs. Furthermore, it can engender self-efficacy through vicarious experience, particularly if the men identify with the characters in the narrative.
Inclusion of behaviour change techniques
Several taxonomies of behaviour change techniques to aid the design of interventions have been published,114,115 including one for alcohol interventions. 92 A list of the relevant techniques that have been suggested for alcohol interventions92 was incorporated into the narrative (e.g. providing normative information about others’ behaviour and experiences and facilitating goal-setting and action-planning).
Review of content
To assess the completeness of the provisional intervention, the sections of the narrative were laid out in a matrix that specified the intended impact of each section, the behavioural construct that was being addressed, the behaviour change techniques employed and the proposed mechanism of change. This ensured that the key components of the behaviour change strategy and the relevant behaviour change techniques were covered in the intervention.
Stage 2: drafting text messages
The complete narrative was rendered in a series of 112 text messages, each with one or more of the following purposes:
-
delivering the narrative (to engage participants)
-
increasing the salience of the harms of heavy drinking and the benefits of moderated drinking
-
modelling steps in the behaviour change process
-
giving information or facts (to augment the behaviour change strategy portrayed in the narrative)
-
asking questions (to monitor, in real time, participants’ reactions to the components of the intervention)
-
comments from other characters (anonymised quotations from the feasibility study participants to reinforce the part of the intervention being delivered)
-
adding humour (to increase engagement).
The salience of harms was increased by asking participants if they or their friends had experienced harms. This avoided the possibly patronising approach of telling experienced drinkers about harms with which they were already familiar. The feasibility study showed that most men were well aware of these harms. 71 It also increased the personal relevance of the harms. A similar approach was used with benefits, in which participants were asked to identify how their lives might be improved if they drank less.
The major constraint in writing the text messages was the permitted length of a text message (160 characters). Thus, the storyline had to be fairly simple and straightforward enough to be delivered in a few words. Although smartphones can send messages that are more than 160 characters (i.e. combining two or more messages at once), there is a danger that the participants will be deterred by large blocks of text.
The text messages were constructed so that the main character, Dave, appeared to be a recipient of the intervention. Thus, he commented on the text messages, answered questions and modelled behaviours that were expected from the behaviour change strategy. To simplify the narrative, Dave was the only character who sent messages, although he discussed at length what was happening in the lives of the other characters. The narrative had to be sufficiently engaging so that participants could remember what was happening from day to day. Achieving this with one or two text messages per day was challenging. Messages containing narrative were identified either by Dave introducing himself or signing off at the end of the message. When possible, messages about changing behaviour and advice about reducing drinking were modelled by the characters. This avoided didactic delivery of the intervention, which preliminary work in the feasibility study had found to be unwelcome.
Interactive items for key components of the intervention
The use of interactive text messages was central to the intervention. Mobile phone etiquette requires reciprocation, so messages that ask questions are likely to be answered. 116 Those in the target group were frequent mobile phone users and, therefore, were likely to engage in text message conversations. The feasibility study showed that participants engaged with the cognitive antecedents to reducing drinking, and with important steps on the causal chain to behaviour change. 86 This feature was capitalised on by asking questions on the key components of HAPA and the behaviour change strategy. For example, participants were asked ‘If you made a goal to cut down a bit on your drinking, what would it be? Text me your answer’ or ‘What would you do if you got into a situation where you were expected to drink far more than you intended? Text me your answer’. The responses to these questions provided an indication of engagement with the intervention in real time.
The feasibility study found that many of the participants gave carefully considered personal responses to the questions set. 86 Participants are likely to spend more time thinking about the content of the message if a response is sought. In addition, committing thoughts to a written response may reinforce the intention or action specified.
Quotations from the feasibility study
The feasibility study produced a wealth of data ‘in the participants’ own words’ both from focus groups and from text message responses from those who received the intervention. 71 Anonymised quotations from the feasibility study delivered information in language appropriate for the target group. Texts that showed other people sharing personal experiences could also give participants confidence to give their own replies. This technique was used to illustrate harms from alcohol misuse, to model new behaviours and to report achievements and benefits from changing behaviour. The quotations were presented as coming from men other than the characters in the narrative. For example, to illustrate risk perception, one message said ‘John from Dundee says “I’ve woke up in the cells a few times because of drink. If i was sober it would never have happened” ’. To reinforce their authenticity, the quotations were not corrected for spelling or grammar.
Specifying dates and times to send messages
The first text message was sent on the Monday evening following randomisation. This enabled messages to be tailored to the day of the week. The feasibility study revealed that a common pattern is heavy drinking at the weekend followed by sobriety during the week. Text messages sent on Friday and Saturday were therefore delivered in the afternoon or early evening before the men went out drinking. Messages sent on Sunday were generally delivered later in the evening to give the participants a little more time to recover from a hangover. Midweek text messages were sent at variable times, often after the working day. Messages were sent at different times and on different days of the week to avoid predictability.
Participants received 112 messages in total. They received at least one message on every day for the first 5 weeks. The maximum number of messages sent in a day was four. From week 6 onwards, occasional days were missed. It is essential to strike a balance between maintaining engagement with the participants, passing on the information necessary, and not overburdening them with the number of messages. Previous research offers differing views on message frequency. One systematic review suggests that retention is higher if the number of messages is varied over time,117 while another reported that interventions when message frequency decreased were more effective than those with constant frequencies. 74 All of the messages in the intervention were unique, although some topics (e.g. self-efficacy and maintenance of a new behaviour) were revisited at different stages of the intervention.
Use of linked messages
On days when more than one text message was sent to participants, the messages were often sent in pairs or groups of three or four. This device has several purposes. Linked messages enabled more complex messages to be sent, as some of the psychological constructs could not be explained in a single message. They were also used to extend the time the participants thought about a topic. The first message was often used to seed an idea, while the follow-up text messages encouraged reflection on the topic. Combinations of messages were also used to add suspense and build a storyline. Paired messages could also pose a question, with the answer provided later in the day. The time delay between linked messages varied from 3 minutes to 4 hours.
Making the intervention acceptable
Communication theory was used to guide the design of the text messages. It proposes that, to be effective, a message must be attended to, comprehended, processed, accepted and acted on. 118 Four features of a message affect the likelihood of behaviour change: the source (i.e. credibility) of the message, its style and content, the nature of the recipient and the context (the circumstances in which the message is received). 67,119 The name of the university was used to give credibility to the study and the intervention, and it was also mentioned on all written material given to the men during recruitment. To establish a relationship, participants were sent a welcoming text message that included their first name. Text messages did not include messaging slang as this could be construed as unprofessional coming from a credible source (i.e. a university). Communication theory suggests that interesting and unexpected statements can be used to maintain interest. Thus, humour was used throughout the intervention period.
Stage 3: revision of the text messages
Ensuring coherence of the narrative and the behaviour change strategy
When the intervention had been rendered into text messages, it was reviewed to ensure that all of the components of the intervention had been preserved (i.e. the key components of HAPA and the behaviour change techniques). The storyline was also checked to ensure the narrative was coherent. The messages were read by colleagues who knew the storyline of the narrative and the behaviour change techniques and processes that should be incorporated into the intervention. They were asked to establish whether or not the behaviour change strategy was intact and addressed in sufficient detail and also whether or not the reader could follow the narrative when it was reduced to a series of text messages. This process was then repeated with colleagues unfamiliar with the narrative and the intervention. Text messages were read and reread to identify any ambiguous statements and to ensure that the unedited direct quotations from the feasibility study were easily understood.
Stage 4: piloting and final revisions
The final piloting used 24 volunteers who were given background information on the study and were told about the fictional characters in the narrative. They were given all of the text messages on paper and asked to provide written comments, both on the overall approach and on individual text messages. The volunteers commonly engaged with the characters and the narrative as if they were real by responding to the text messages rather than commenting on their content. The volunteers’ comments gave reassurance that the texts were clear and readily understood. They also showed that the use of characters made the intervention appear more realistic and less daunting. The volunteers also found the overall approach supportive. Finally, they suggested how the narrative could be amended: for example, one of the minor characters, Stevie, had been left with an unresolved drink problem. The narrative was amended to show that Stevie successfully tackled his drinking and also found a girlfriend.
A second round of piloting involved volunteers who received the text messages on their mobile phones. This was primarily used to test the delivery system, but also helped determine whether or not the frequency and timing of the messages were acceptable.
The control package
The control group also received a series of text messages over the 3-month intervention period. This was designed to be an attentional control, which did not mention alcohol or include any messages on changing health behaviour. Every week a different health topic was covered, for example physical activity, sexual health, diet, mental health, sleep quality, hearing and foot health. The text messages provided facts, trivia and jokes on the topics. Although the control messages did not include a narrative, the characters did play a minor role. For example, to increase engagement and introduce humour, some messages appeared to come from Dave in the form of ‘useless information’, such as ‘Dave’s useless information for today: The average person has at least seven dreams a night’ or ‘Dave’s useless information for today: A sneeze can reach 100 mph, a cough only 60 mph’.
To promote engagement, men were asked one question per week. This was usually a multiple-choice question on the topic of the week, for example ’What is the biggest organ in the body? (a) liver (b) lungs (c) skin (d) brain. Text me your answer please‘ and ‘What is bromodosis? (a) painful toes (b) smelly feet (c) ingrown toenails (d) dropped arches. Text me your answer please’. These questions encouraged interaction without asking participants to give the considered personal responses required from the intervention group.
Summary
This structured approach has led to the design of a text message intervention with a strong theoretical basis. The process was highly iterative to enable a theory of behaviour change and a set of behaviour change techniques to be embedded in a coherent narrative. These were successfully rendered in a series of short text messages (maximum length 160 characters). The use of characters helped make the intervention realistic and allowed key behavioural activities to be modelled. Pilot testing revealed strong support for the intervention.
Chapter 3 Study methods
The study was a four-centre, parallel-group, pragmatic, individually randomised controlled trial that sought to reduce the frequency of binge drinking in disadvantaged men. The study protocol is available on the NIHR website120 and was published in the journal Trials. 121 The study was approved by the East of Scotland Research Ethics Service REC1 (REC reference 13/ES/0058).
Recruitment
Study group
Men aged 25–44 years from areas of high deprivation were recruited. Recruitment was conducted in four centres that cover major regions of Scotland: Tayside, Glasgow, Forth Valley and Fife. Level of deprivation was measured using the SIMD,72 which is similar to the English Index of Multiple Deprivation. Men were recruited from areas classified as being in the most disadvantaged quintile. Recruitment was conducted from March 2014 to December 2014.
Inclusion/exclusion criteria
Men were included in the study if they had ≥ 2 episodes of binge drinking (> 8 units of alcohol in a single session) in the preceding 28 days. Exclusion criteria were as follows: men who were currently attending care at an alcohol problem service and men who would not be contactable by mobile phone for any part of the intervention period.
Techniques to promote recruitment
Recruitment employed several evidence-based techniques. 40–43 It involved direct personal contact (face to face or by telephone), involved multiple attempts at contact and used an approach based on respectful treatment. 122,123 An opt-out strategy was used. A financial incentive was offered for participating in the study. High-street vouchers to the total of £50 were offered, although this was divided across the whole study: £10 at completion of the baseline questionnaire, £20 during the delivery of the text messages and a further £10 for completion of the questionnaires at 3 months and 12 months post intervention. The incentive was given for continued participation and was not linked to drinking behaviour.
To ensure good coverage of disadvantaged men, two recruitment strategies were employed, each to recruit half of the target of 798 men. One used primary care registers and the other used a community outreach method, time–space sampling (TSS).
Strategy 1: recruitment through general practice registers
Potential participants were identified from the practice lists of 20 general practices by staff from the Scottish Primary Care Research Network (SPCRN). These lists contain data on age, sex and postcode. Postcodes were used to derive the SIMD score. 124 Men who lived in the highest deprivation quintile were randomly selected by SPCRN staff to give a maximum of 200 potential participants from each practice list. General practitioners (GPs) screened the list and sent potential participants a letter inviting them to take part (see Appendix 1). The letter was personally addressed, mentioned the appropriate local university (Dundee, Stirling or Glasgow Caledonian) and stated that a financial incentive would be given. The accompanying participant information sheet (see Appendix 2) carried the university’s logo and stressed the confidentiality of the study. An opt-out strategy was used for recruitment. The name, address and telephone number of those who did not decline to take part were provided to the researchers by the SPCRN. The researchers contacted these individuals by telephone approximately 2 weeks after the GP letter was sent. Attempts at contact by telephone were made at different times of the day and on different days of the week.
Strategy 2: time–space sampling
Time–space sampling125 is a community outreach strategy that recruits participants from a number of venues and involves sampling at different times of the day and on different days of the week. The specific features of the strategy were based on findings from the feasibility study,71 augmented by fieldwork, to identify appropriate venues and suitable times for recruitment. A variety of venues were explored for their potential for recruitment, including town centres, workplaces, community groups, football grounds, charities that support long-term unemployed people, supermarkets, housing associations and main shopping streets in disadvantaged areas.
Fieldwork
Areas classified by the SIMD as being in the most deprived quintile were identified from a government website. 126 Maps of high-deprivation areas within towns were produced using an online mapping resource (Google MapsTM, Google, Inc., Mountain View, CA, USA). The maps were printed with sufficient detail to show street names and reference points to provide a detailed guide for fieldwork. Sources of potential participants were public houses, job centres, community centres, pharmacies, sports facilities, bookmakers and supermarkets. These were identified by using Google Street ViewTM (Google, Inc., Mountain View, CA, USA) and from local authority websites. Google Street View was also employed to identify routes of access and car parking.
The initial fieldwork established that few people were encountered in housing estates in areas of high deprivation. Instead, they tended to congregate in high streets in, or adjacent to, areas of high deprivation, where facilities such as public houses, bookmakers, convenience stores and supermarkets are common. The fieldwork showed that recruiting from the streets around these venues was more productive than recruiting inside the venues. It also established that distributing leaflets and using gatekeepers were largely unproductive.
Initial screening
A researcher approached men in the selected areas who appeared to be in the age range (25–44 years). Potential participants were asked about their age and their current drinking levels. The study was described to those who reported binge drinking (> 8 units of alcohol in a single session) at least twice in the previous 4 weeks. All participants were told that the study was about alcohol and health. They were given a participant information sheet (see Appendix 2) and a consent form (see Appendix 3) to read, and their mobile phone number was obtained. About 24 hours after the potential participants received the participant information sheet and consent form, the researcher telephoned them to discuss the study and ascertain their eligibility by administering the screening questionnaire (see Appendix 4).
Informed consent
Informed consent was obtained by text message. This method was successfully used in the feasibility study. 71 Individuals who verbally agreed to take part were sent a text message asking if they understood what was involved and if they were willing to take part. Consent was obtained when the participant positively responded to the text message. These messages were stored electronically. In addition, the research assistant completed the consent form while interviewing the participant and signed and dated the form, including the time at which the text message giving consent was received.
Randomisation
The randomisation was carried out using the secure remote web-based system provided by the Tayside Clinical Trials Unit. Randomisation was stratified by participating centre and the recruitment method and restricted using block sizes of randomly varying lengths. The allocation ratio was 1 : 1, intervention to control.
Allocation concealment
The researchers appointed to carry out the recruitment enrolled the participants. The researchers entered key data items (mobile phone number, study identification number and preferred first name) into the web-based randomisation system. This system automatically assigned men to one of the treatment arms and subsequently delivered the appropriate set of text messages. The researchers who conducted the baseline and follow-up interviews had no access to this system and were unaware to which treatment group the men had been assigned.
Training
The importance of staff training was recently emphasised in a survey of UK clinical trials units. 59 The research assistants who carried out the recruitment and baseline data collection received a formal training programme, comprising three 2-hour sessions of didactic lectures, tutorial sessions and role play. These sessions covered the background to the study and the details of the recruitment strategies and data collection techniques. The need for a sensitive approach to recruitment, based on ‘respectful treatment’,122,123 was described. Researchers were encouraged to value potential participants and to thank them for listening to the outline of the study. In addition to the formal training, two further sessions were held at which progress towards recruitment targets and experience with recruitment techniques were reviewed. Ongoing mentoring formed an important part of training, during which researchers’ recruitment experiences, successes and failures were discussed.
The training on data collection covered the purposes of all of the data items, but focused on the measurement of alcohol consumption. The diversity of alcoholic beverages was described, highlighting how bottled and canned drinks with a specific brand name could vary in volume and strength. The training enabled the researchers to explore this diversity. Role play gave practice in eliciting accurate details of specific drinks consumed, from which detailed drinking histories were prepared. At initial sessions, those playing the role of the drinker were forthcoming with the details of their drinking, but became progressively more reticent in subsequent sessions. This provided those playing the role of the researcher with experience of the careful probing needed to elicit full details of alcohol consumption. Finally, researchers practised calculating the frequency of binge drinking, heavy binge drinking and total alcohol consumption from detailed drinking histories. After each episode of training, supportive feedback was given as part of a group discussion.
Measuring binge drinking
In this study, binge drinking is defined as > 8 UK units of alcohol in a single session. This criterion is widely used in national surveys in the UK. 127 It corresponds to > 64 g of ethanol. The measure used in the USA is ≥ 5 drinks in a single session, which amounts to ≥ 70 g of ethanol. 128 Thus, the definitions are similar but not identical. The study recorded the number of binge-drinking episodes over the 28 days before the interview. Other approaches, such as recording the amount consumed on the heaviest drinking day in the past week, have been criticised. 127
This study also uses > 16 units of alcohol as the threshold for heavy binge drinking to identify those who are consuming very large amounts of alcohol in a single session. There is increasing concern about those who consume sufficient alcohol to be at risk of serious acute adverse effects (e.g. blackout or poisoning). 129 This measure was obtained by doubling the level for binge drinking. The same approach has been proposed for the USA, giving a threshold of ≥ 10 drinks. 129
Data collection methods
All baseline (see Appendix 5) and outcome data (see Appendices 6 and 7) were collected by telephone interview by research assistants blinded to treatment arm. The timeline follow back130 methodology was followed, using the modification for telephone use. 131 Because recent studies have emphasised the importance of measuring the strength and volume of drinks,132,133 the approach was adapted to obtain detailed information on the alcohol consumed on every drinking occasion over the previous 28 days. The initial questions identified how many days in the last 4 weeks participants had consumed alcohol and what they had consumed on each day. Attention was given to eliciting details of the type of drink, for example lager or cider, the brand, the size of servings and the number of servings. Further questions were asked to establish these details. If participants had difficulty describing their drinking, the researcher would ask them to consider the most recent week and then work backwards from there. Once the participant had provided this information, they were asked again about any special occasions not accounted for (e.g. social or sporting events, weddings and drinks with meals out).
When a drink had been poured at home, particularly spirits and wine, participants were asked how their measure compared with a standard pub measure. If consumption was stated as a range of drinks (e.g. ‘2–3 single vodkas’), the mid-point of the range was taken (i.e. 2.5 single vodkas). Similarly, if the number of drinking days was stated as a range (e.g. 2–3 days in a week), this was taken as 2.5 days in a week or 10 days in the last 4 weeks. If the participant could not remember specific drinks (e.g. ‘4 pints of lager, I don’t know which brand’), researchers referred to a ‘standard drinks list’ to ensure consistency.
This detailed questioning provided a list of the type and volume of every drink consumed with sufficient detail for the alcoholic strength to be determined from a look-up table of drinks. The look-up table was compiled from the websites of two major supermarket chains, which provide the volumes and strengths of most common drinks. This was supplemented, when necessary, by the alcohol manufacturer’s own website. The total units of alcohol were calculated for each drinking day. From these data, the number of moderate drinking days (≤ 8 units of alcohol), the number of binge-drinking days (> 8 units of alcohol) and the number of heavy binge-drinking days (> 16 units of alcohol) were established. The data also enabled the total number of units of alcohol consumed over 28 days to be calculated. The process of aggregating drinking and calculating the different measures of consumption was conducted independently by two members of the research team. Differences were resolved by discussion.
Baseline data collection
Alcohol consumption was measured by the methods described above. To minimise research participation effects, which could influence the impact of the intervention, the number of data collected at baseline was kept to a minimum. Recent systematic reviews134,135 indicate that baseline questions can lead participants to re-evaluate drinking behaviour. Thus, questions on topics such as knowledge of the harms of alcohol, or intentions to reduce consumption, were not asked.
Individual-level sociodemographic status was assessed using marital status, employment status and educational attainment. The participants’ postcodes were used to derive the SIMD score. In addition, a single question from the Fast Alcohol Screening Test (FAST)136 was used to determine whether or not participants suffered episodes of memory loss following drinking sessions.
Follow-up methods
Several evidence-based techniques were used in this study to promote retention: financial incentives; credibility of source (the use of the university logo on letterhead); personalised contacts (the use of the participant’s preferred first name); regular contact (through keeping-in-touch text messages); multiple attempts at contact; and the use of multiple methods of contact (letters, texts, telephone calls and, when the information was available, e-mails and partner’s mobile phone). 52,55,57,58,60,61,63–65
The follow-up interviews were conducted by telephone from August 2014 to February 2016. Each week a computer-generated list identified men due to be followed up in the next week. These men were sent a letter 1 week in advance reminding them that they were due to be contacted, and that they would receive a £10 voucher for completing the follow-up interview. An automated text message reminder was also sent 3 days before follow-up was due. Multiple attempts at contact were made at various times of day and on various days of the week. After several unsuccessful attempts, a voicemail message was left and a reminder text message was sent by the researcher. When the information was available, other contact methods were also tried: landlines, mobile phone numbers of partners and e-mail addresses. Subsequently, up to three letters were sent, with reply-paid envelopes, requesting updated contact details and convenient times for contact. Finally, for men recruited through general practice registers, the practice was contacted to request updated contact information.
Data collection at the first follow-up
The first follow-up was carried out 3 months post intervention (see Appendix 6). Data on alcohol consumption were collected, using the method described above. Two secondary outcomes were measured: the proportion of men consuming > 8 units of alcohol, and the proportion consuming > 16 units of alcohol, on ≥ 3 occasions in the previous 28 days. No other data were collected at this follow-up to minimise question behaviour effects. 134,135 Participants were also asked for any change of address to ensure that their gift vouchers would be correctly delivered. The researchers collecting the data were blind to treatment allocation.
Data collection at final follow-up
The final follow-up was carried out 12 months post intervention (see Appendix 7). The primary outcome and three secondary outcomes were measured at this follow-up. The primary outcome was the proportion of men consuming > 8 units of alcohol on ≥ 3 occasions in the previous 28 days. Two secondary outcomes of alcohol consumption were also measured at final follow-up: the proportion of men with ≥ 3 occasions of heavy binge drinking (> 16 units of alcohol in a session) and the mean alcohol consumption over 28 days. The method of collecting the data on alcohol consumption was described above. Finally, the AUDIT137 was used to determine the frequency of hazardous and harmful drinking. Questions were also asked about attempts to reduce drinking and the success of these attempts. Questions on self-efficacy for refusing drinks were taken from a validated questionnaire. 138 Health status was measured by the EuroQol-5 Dimensions, five-level version (EQ-5D-5L),139 a validated quality-of-life questionnaire designed to be simple to administer. Contacts with police/criminal justice, plus accident and emergency and other health-care usage, were measured by the widely used short Service Use Questionnaire (S Parrot, Department of Health Sciences, University of York, 2012 personal communication). Well-being was measured using the four Office for National Statistics Personal Well-being questions. 140 Finally, questions were asked about the acceptability of the study methods and recall of the text messages.
The sequence of questions in the follow-up questionnaire was arranged to obtain data on the primary and secondary outcomes first, followed by perceived changes in drinking over 12 months and the data for the economic evaluation, and, finally, participants’ views on the study methods (see Appendix 7). This ensured that questions on alcohol consumption were not influenced by responses to questions on other topics. It also meant that the most important data would be obtained if the interview was terminated early.
Sample size calculation
The sample size calculation is based on the hypothesised difference in the proportion of frequent binge drinking between intervention and control groups at the 12-month post-intervention assessment. It uses the finding from the feasibility study that 57% of men consumed > 8 units of alcohol on ≥ 3 occasions in the previous 28 days. 71 The proposed effect size was that the intervention would reduce the frequency of binge drinking from 57% to 46%, a net reduction of 11%. A recent systematic review of conventional brief interventions5 found an 11% difference in frequency of binge drinking between intervention and control groups. To detect a reduction in the frequency of binge drinking in this way from 57% to 46% (at the 5% significance level with a power of 80%) would require a sample size of 319 per group, or 638 in total. The required sample size was then increased by 20% to allow for losses to follow-up, making the total sample size 798. We expected that the loss to follow-up would be less than this, as the loss in our 3-month feasibility study was only 4%. However, as most alcohol brief intervention trials have a loss to follow-up of > 20%,5 it was prudent to make suitable allowance.
Statistical methods
The analysis of treatment effects was conducted by intention to treat.
Methods for descriptive statistics
Binary variables (including primary and secondary outcomes as well as baseline binary variables) were summarised as number of observations, number of missing values, and number and percentage overall and per treatment group. Continuous variables (total alcohol consumption at 12 months post intervention and total alcohol consumption at baseline) were summarised as number of observations, number of missing values, mean, standard deviation (SD), standard error of the mean, median, and range overall and per treatment group.
Analysis of primary outcome
Logistic regression141 was used to investigate the effect of the intervention on the primary outcome, that is, whether or not the participant had consumed > 8 units of alcohol on ≥ 3 occasions in the previous 28 days at 12 months post intervention (proportion drinking > 8 units of alcohol on ≥ 3 occasions at 12 months). Three models were fitted to the primary outcome:
-
the unadjusted model (only treatment group as a fixed factor in the model)
-
the model adjusted for one baseline drinking variable (whether or not the participant had consumed > 8 units of alcohol on ≥ 3 occasions in the 28 days before the beginning of the study)
-
a full model adjusted for baseline drinking as for model 2 and the baseline covariates of method of recruitment (general practice registers/TSS), recruitment centre, age group, living with a partner (yes/no), employed (yes/no), further education (yes/no), SIMD score (1–10) and question 2 from the FAST. 136
Model 3 is considered the primary analysis and models 1 and 2 are presented for information. The treatment effect of the intervention on the primary outcome was the difference in proportions, or odds ratios (ORs), between the two groups with the 95% confidence interval (CI). Unadjusted treatment effect estimates were compared with corresponding estimates adjusted for baseline and other model covariates.
Analysis of secondary outcomes
The binary secondary outcomes (> 8 units of alcohol on ≥ 3 occasions at 3 months post intervention, > 16 units of alcohol on ≥ 3 occasions at 3 months and > 16 units of alcohol on ≥ 3 occasions at 12 months, and an AUDIT score of > 7 at 12 months post intervention) were analysed using the same analysis plan as for the primary outcome based on the logistic regression model. The adjustment for baseline drinking used the alcohol measure that was the equivalent of the secondary outcome (e.g. for the proportion drinking > 16 units of alcohol on ≥ 3 occasions at 12 months, the adjustment used the proportion drinking > 16 units of alcohol on ≥ 3 occasions at baseline). However, as the AUDIT was not administered at baseline, the adjusted models for the proportion with an AUDIT score of > 7 at 12 months used whether or not the participant had consumed > 8 units of alcohol on ≥ 3 occasions in the 28 days before the beginning of the study (> 8 units of alcohol on ≥ 3 occasions at baseline).
For total alcohol consumption at 12 months post intervention, owing to the skewness of the data, a generalised linear model assuming a gamma distribution and log-link function141 was used in the analysis. Again, three models were fitted as described above to this secondary outcome: the unadjusted model (only treatment group as a fixed factor in the model), the model adjusted for baseline (total alcohol consumption at baseline) and the full model adjusted for baseline and the other covariates listed above for the analysis of the primary outcome. The treatment effect of the intervention on this outcome was measured as the mean difference in consumption between treatment groups with the 95% CI.
Sensitivity analysis for missing data
Multiple imputation methods were used to assess the sensitivity of primary outcome results to missing data. Generalised linear models were used for multiple imputations, assuming that data were missing at random. 142 Multiple imputation included the explanatory variables used in the fully adjusted model above plus the primary and secondary outcomes. All primary and secondary outcome variables at baseline and at the 3-month and 12-month follow-ups were used, as was additional information collected at the 12-month follow-up interviews. This included demographic data at the 12-month follow-up, several questions on participant experiences in the study, and items from the Service Use Questionnaire, the EQ-5D-5L and the Office for National Statistics Personal Well-being questionnaire.
Economic evaluation
The methods for the economic evaluation are presented in Chapter 9.
Patient and public involvement
The trial design was informed by findings from the feasibility study, particularly from the focus groups with disadvantaged men. In addition, the pilot trial with disadvantaged men explored their views of the study design and conduct to identify ways in which these could be improved. Two user group representatives were involved throughout the development and conduct of the full RCT. They attended project meetings and assisted in developing the recruitment methods, reviewing the use of incentives, commenting on the data collection questionnaires and assessing the overall acceptability of the study methods. Volunteers also reviewed the text message intervention and the narrative on which it was based.
Changes to the protocol
The Readiness Ruler143 was not used in the final follow-up questionnaire. This question asks participants to choose one option, from four, that best describes their current drinking status: (1) I never think about my drinking, (2) sometimes I think about drinking less, (3) I have decided to drink less, and (4) I am already trying to cut back on my drinking. This question was not used because it was anticipated that some participants would have made changes to their alcohol consumption, either by cutting down or by stopping completely. Those who had done so might find that none of the options were applicable. Thus, participants in this study were instead asked:
-
Have you tried to reduce your drinking in the past year?
-
Did you set a goal to cut down on your drinking?
-
If yes, how did you try to achieve your goal?
-
If you managed to cut down, have you continued to drink less?
The FAST136 was not used in the final follow-up questionnaire; the AUDIT137 was used instead. The AUDIT comprises 10 questions, all of which are included in the FAST. Many published studies have used the AUDIT, and so, to allow comparison with these, the AUDIT was used in this study. However, the wording of one question common to the FAST and the AUDIT differs slightly. In the AUDIT, the final questions asks ‘Has a relative or friend, doctor or other health worker been concerned about your drinking and suggested that you cut down?’ The three possible responses are no; yes, but not in the last year; and yes, during the last year. In the FAST, the question asks ‘In the last year, has a relative or friend, doctor or other health worker been concerned about your drinking and suggested that you cut down?’ Here the possible responses are: no; yes, on one occasion; and yes, on more than one occasion. This modification was made for the FAST to ensure that the result focused on the last year. 144 This minor difference between the questionnaires means that we cannot report a total FAST score. Thus, the AUDIT is reported instead of the FAST.
The goal-setting and action-planning scales developed by Renner et al. 145 were not used. Initial piloting showed that the burden of answering the many questions on each scale was too great for telephone interviews. Instead, a few specific questions were asked about goal-setting, action-planning and coping-planning.
Chapter 4 Recruitment and baseline assessment
Introduction
This chapter presents the data on recruitment and describes the drinking patterns and demographic characteristics of the study participants. It also explores the implications of the findings for the recruitment of a group usually considered hard to reach.
Results
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Figure 2) shows the passage of individuals through the study. A total of 3603 men were assessed for inclusion in the study, of whom 704 were not eligible (e.g. they had not consumed > 8 units of alcohol on ≥ 2 occasions in the previous 28 days or were not within the target age range). A further 1485 men were not contactable by telephone, and 589 declined. It should be noted that the distinction between not eligible and not interested could be blurred, as some men may have said that they were not interested to avoid discussing their alcohol consumption and others may have said that they did not drink enough as a convenient way of refusing to participate.
FIGURE 2.
The CONSORT flow diagram. Reproduced from Crombie et al. 146 © 2018 The Authors. Addiction published by John Wiley & Sons Ltd on behalf of Society for the Study of Addiction. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
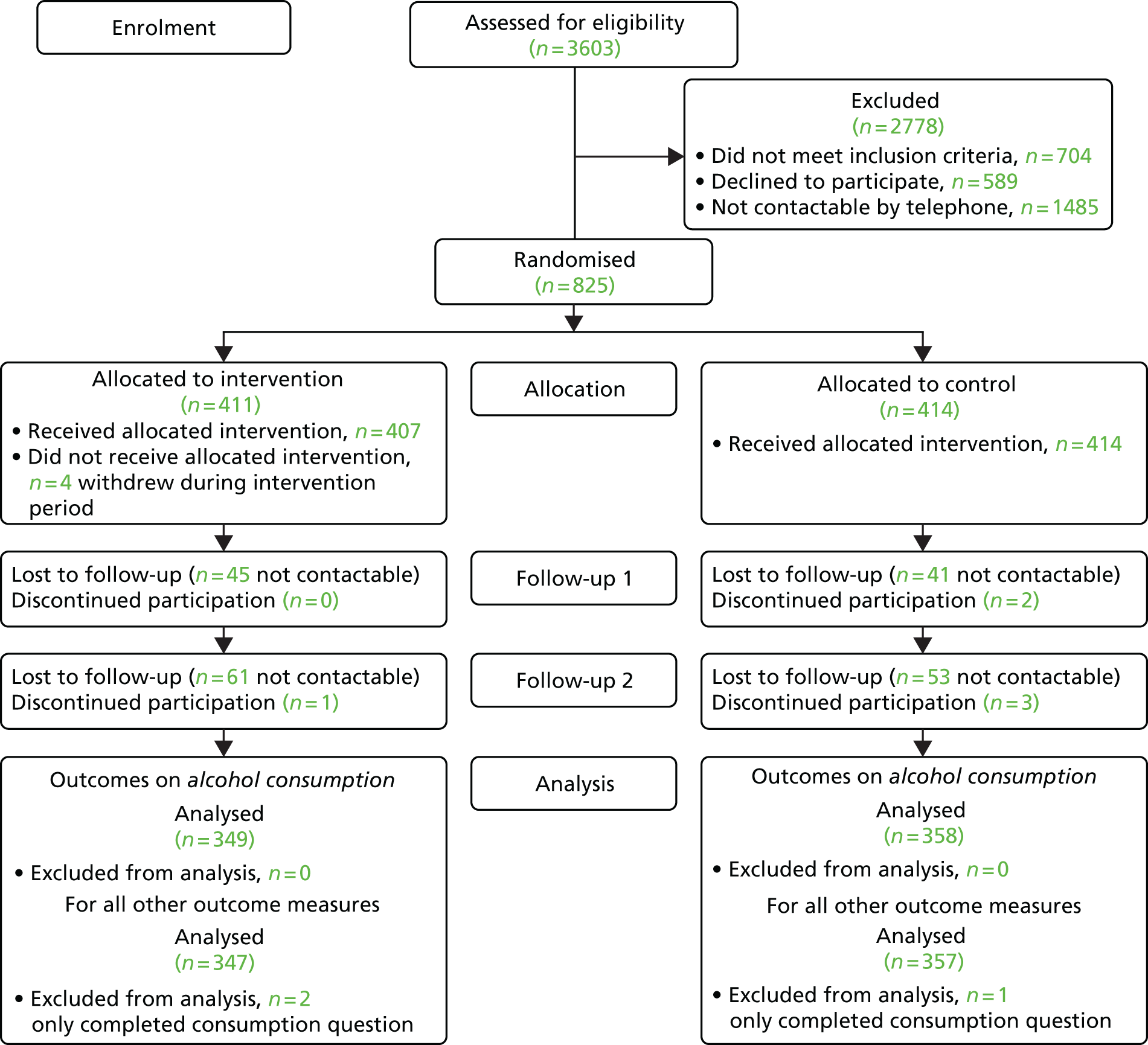
The target of 798 men was exceeded, with 825 men recruited in total. Both recruitment strategies were successful (Table 2), although slightly more men were recruited from general practice registers than by community outreach (TSS). Recruitment targets were met in three of the four centres. There was a small shortfall in numbers of men recruited from general practice registers in Forth Valley, but this was compensated by additional men recruited from Fife.
| Centre | Recruitment method, n (%) | Total, n (%) | |
|---|---|---|---|
| General practice registers | TSS | ||
| Tayside | 102 (23.9) | 100 (25.1) | 202 (24.5) |
| Fife | 132 (30.9) | 99 (24.9) | 231 (28.0) |
| Forth Valley | 88 (20.6) | 98 (24.6) | 186 (22.5) |
| Glasgow | 105 (24.6) | 101 (25.4) | 206 (25.0) |
| Total | 427 | 398 | 825 |
Most men (84%) had ≥ 3 binge-drinking sessions (> 8 units of alcohol) in the previous 28 days, and almost half had ≥ 3 heavy binge-drinking sessions (> 16 units of alcohol) (Table 3). Participants had almost 20 alcohol-free days over the 28-day period. On average, the participants had 6.6 binge-drinking sessions in 28 days, or 1.65 per week.
| Drinking pattern | Method of recruitment | Total (N = 825), n (%) | p-value | |
|---|---|---|---|---|
| General practice registers (N = 427) | TSS (N = 398) | |||
| Number (%) of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) in previous 28 days | 350 (82.0) | 346 (86.9) | 696 (84.4) | 0.050a |
| Number (%) of men with ≥ 3 occasions of heavy binge drinkingb (> 16 units of alcohol) in previous 28 days | 171 (40.0) | 221 (55.5) | 392 (47.5) | < 0.001a |
| Mean consumption in past 28 days (units) (SD) | 105.6 (89.0) | 164.4 (162.2) | 134.0 (132.8) | < 0.001c |
| Mean number of binge-drinking sessions (> 8 units of alcohol) (SD) | 5.87 (4.6) | 7.34 (5.8) | 6.58 (5.2) | < 0.001c |
| Mean number of heavy binge-drinking sessionsb (> 16 units of alcohol) (SD) | 2.66 (3.7) | 4.55 (5.7) | 3.57 (4.8) | < 0.001c |
| Mean number of alcohol-free days (SD) | 20.60 (5.4) | 19.10 (6.3) | 19.88 (5.9) | < 0.001c |
| Frequency of being unable to remember what happened the night before because of drinking, n (%) | ||||
| Never | 296 (69.3) | 206 (51.8) | 502 (60.8) | < 0.001a |
| Less than monthly | 99 (23.2) | 136 (34.2) | 235 (28.5) | |
| Monthly | 28 (6.6) | 38 (9.5) | 66 (8.0) | |
| Weekly or more | 4 (0.9) | 18 (4.5) | 22 (2.7) | |
There were marked and statistically significant differences in the drinking patterns of the men recruited by the two methods (see Table 3). Those recruited by TSS had slightly more binge-drinking sessions (> 8 units of alcohol in a session) and more heavy binge-drinking sessions (> 16 units of alcohol in a session). Mean consumption was 56% higher in the men recruited by TSS than in those recruited from general practice registers. This occurred partly because of the increased frequency of binge- and heavy binge-drinking sessions, but also because more alcohol was consumed during these heavy-drinking sessions. The higher frequency of episodes of forgetting what happened the night before, among the men recruited by TSS, is consistent with their higher frequency of heavy binge drinking.
The men had a mean age of 35 years; just over half were living with a partner and over one-third were unemployed (Table 4). Over 60% of men had only high school education and over three-quarters lived in the most disadvantaged quintile. There were also differences in the demographic characteristics between men recruited through general practices and those recruited by TSS (see Table 4). Thus, in comparison with men recruited from general practice registers, significantly more of the men recruited by TSS were single and unemployed. Some TSS men lived in slightly more affluent areas, although all of these men were recruited from areas of social disadvantage. At the baseline assessment, a few men recruited from general practice registers gave an address that had a SIMD score of ≥ 3. Although these men had been selected from the registers because their recorded address corresponded to a SIMD score of ≤ 2, they had moved since their records were last updated. Their address at the time of recruitment was used.
| Characteristic | Recruitment method, n (%) | Total (N = 825), n (%) | p-valuea | |
|---|---|---|---|---|
| General practice registers (N = 427) | TSS (N = 398) | |||
| Age group (years) | ||||
| 25–34 | 210 (49.2) | 226 (56.8) | 436 (52.8) | 0.029 |
| 35–44 | 217 (50.8) | 172 (43.2) | 389 (47.2) | |
| Marital statusb | ||||
| Married/lives with a partner | 256 (60.1) | 192 (48.2) | 448 (54.4) | 0.001 |
| Single | 170 (39.9) | 206 (51.8) | 376 (45.6) | |
| Employment status | ||||
| Employed | 332 (77.8) | 196 (49.2) | 528 (64.0) | < 0.001 |
| Unemployed | 95 (22.2) | 202 (50.8) | 297 (36.0) | |
| Highest educational attainment | ||||
| High school | 264 (61.8) | 246 (61.8) | 510 (61.8) | 0.240 |
| Vocational qualification/further training | 120 (28.1) | 124 (31.2) | 244 (29.6) | |
| University degree | 43 (10.1) | 28 (7.0) | 71 (8.6) | |
| SIMD decile | ||||
| 1–2 (most deprived) | 410 (96.0) | 226 (56.8) | 636 (77.1) | < 0.001 |
| ≥ 3 | 17 (4.0) | 172 (43.2) | 189 (22.9) | |
Table 3 showed that men recruited by TSS had a higher mean consumption than those recruited from general practice registers. Table 5 extends this analysis by exploring the independent effects of recruitment method and demographic factors on mean consumption. It shows that, overall, those who were single had higher mean consumption than men with a partner. Similarly, those who were unemployed had higher consumption than those who were employed. However, within each level of the demographic factors, men recruited by TSS had higher mean consumption than those recruited from general practice registers. Table 5 also shows that, for each recruitment method, the demographic factors have independent effects on alcohol consumption.
| Characteristic | Recruitment method, mean consumption (SD) | Total, mean (SD) | |
|---|---|---|---|
| General practice registers | TSS | ||
| Marital status | |||
| Married/lives with partner | 99.3 (69.3) | 137.9 (120.5) | 115.8 (96.5) |
| Single | 115.4 (111.9) | 189.2 (190.1) | 155.8 (163.5) |
| Employment status | |||
| Employed | 100.6 (74.6) | 136.9 (118.4) | 114.1 (94.9) |
| Unemployed | 123.1 (125.9) | 191.1 (192.1) | 169.3 (176.3) |
There is also clear evidence of an interaction between the demographic factors and recruitment method. The influence of community outreach (TSS) was much larger for single men than for men with a partner. Similarly, community outreach has a larger effect for unemployed men than for men in employment. Thus, not only do recruitment method and socioeconomic factors exert independent effects on alcohol consumption, there is also an interaction effect.
The treatment groups were similar in all demographic characteristics (Table 6). The groups were also similar in all of the measures of alcohol consumption (Table 7). It is notable that binge-drinking sessions accounted for most of the alcohol consumed (93%).
| Characteristic | Group, n (%) | Total (N = 825), n (%) | |
|---|---|---|---|
| Intervention (N = 411) | Control (N = 414) | ||
| Age group (years) | |||
| 25–34 | 221 (53.8) | 215 (51.9) | 436 (52.8) |
| 35–44 | 190 (46.2) | 199 (48.1) | 389 (47.2) |
| Marital statusa | |||
| Married/lives with a partner | 224 (54.6) | 224 (54.1) | 448 (54.4) |
| Single | 186 (45.4) | 190 (45.9) | 376 (45.6) |
| Employment status | |||
| Employed | 276 (67.2) | 252 (60.9) | 528 (64.0) |
| Unemployed | 135 (32.8) | 162 (39.1) | 297 (36.0) |
| Highest educational attainment | |||
| High school | 250 (60.8) | 260 (62.8) | 510 (61.8) |
| Vocational qualification/further training | 132 (32.1) | 112 (27.1) | 244 (29.6) |
| University degree | 29 (7.1) | 42 (10.1) | 71 (8.6) |
| SIMD decile | |||
| 1–2 (most deprived) | 314 (76.4) | 322 (77.8) | 636 (77.1) |
| ≥ 3 | 97 (23.6) | 92 (22.2) | 189 (22.9) |
| Drinking pattern | Group | Total (N = 825) | |
|---|---|---|---|
| Intervention (N = 411) | Control (N = 414) | ||
| Number (%) of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) in previous 28 days | 342 (83.2) | 354 (85.5) | 696 (84.4) |
| Number (%) of men with ≥ 3 occasions of heavy binge drinkinga (> 16 units of alcohol) in previous 28 days | 191 (46.5) | 201 (48.6) | 392 (47.5) |
| Mean consumption in past 28 days (units) (SD) | 133.0 (132.7) | 134.9 (133.0) | 134.0 (132.8) |
| Proportion of total units consumed during binge-drinking sessions (> 8 units of alcohol) (%) | 92.4 | 92.6 | 92.5 |
| Mean number of binge-drinking sessions (> 8 units of alcohol) (SD) | 6.51 (5.2) | 6.65 (5.2) | 6.58 (5.2) |
| Mean number of heavy binge-drinking sessionsa (> 16 units of alcohol) (SD) | 3.55 (5.0) | 3.59 (4.7) | 3.57 (4.8) |
| Mean number of alcohol-free days (SD) | 19.90 (5.9) | 19.86 (5.8) | 19.88 (5.9) |
| Frequency of being unable to remember what happened the night before because of drinking, n (%) | |||
| Never | 257 (62.5) | 245 (59.2) | 502 (60.8) |
| Less than monthly | 113 (27.5) | 122 (29.5) | 235 (28.5) |
| Monthly | 27 (6.6) | 39 (9.4) | 66 (8.0) |
| Weekly or more | 14 (3.4) | 8 (1.9) | 22 (2.7) |
Discussion
This study succeeded in recruiting a substantial number of disadvantaged men to an intervention aimed at reducing binge drinking. The participants engaged frequently in binge drinking and heavy binge drinking, but they also had a high proportion of alcohol-free days. Two recruitment strategies were used and both achieved their targets, a major achievement with a social group often considered to be hard to reach. However, there was a marked difference in the men according to recruitment strategy. The community outreach approach (TSS) produced a sample who were much more likely to have a higher mean consumption and to binge drink more frequently.
Interpretation of baseline drinking
The pattern of drinking was one dominated by binge-drinking sessions interspersed with periods of sobriety. Overall, the mean consumption of alcohol was lower than in many other studies of alcohol brief interventions. In this study, the average consumption over 28 days was 134 units, corresponding to 268 g of alcohol per week. A systematic review5 found that in studies among men, the average consumption was much higher, at 377 g per week. However, in the present study, the frequency of binge drinking, 1.65 times per week, was much higher than in the systematic review5 (0.9 times per week). Our findings support previous studies that have shown that although socioeconomically disadvantaged groups may not drink more on average, they are more likely to binge drink. 15–17
A striking finding is that 93% of the alcohol that the participants drank was consumed in binge-drinking sessions. This could partly explain why disadvantaged men, who do not drink more heavily than more affluent men, experience much higher rates of alcohol-related harm. 14,147,148 It also emphasises the need for interventions directed at binge drinking.
Assessment of the recruitment process
The recruitment target for this study, 798 men,121 was exceeded in a social group considered to be hard to reach. 45–49 Several factors may have contributed to the success of recruitment. These include the use of evidence-based strategies to improve recruitment: financial incentives, direct contact (face to face or telephone) and, for those on general practice registers, an opt-out approach and multiple attempts at contact. 40–43,149 In addition, the study was designed to require little effort from the participants, and common barriers, such as the requirement to travel or to attend a clinic, were avoided.
The study also used a sensitive approach based on ‘respectful treatment’122,123 in which the needs and views of potential participants take priority. This was encouraged through formal training sessions and informal, but regular, mentoring of the researchers who recruited participants. The recruiters recognised that potential participants could have a distrust of the research or concerns about the effort involved in participation. 50–53 Thus, men who were willing to listen to a description of the study were viewed as helping us, and the men who agreed to participate have done us a great favour. This perspective may have aided recruitment and helped researchers deal more easily with the disappointment of refusal.
The opening remarks may also have been important for recruitment. For community outreach, some phrases would often initiate a conversation: ‘Excuse me, would you happen to be in the age range 25–44?’ or ‘Excuse me, could you help me out?’ Other phrases were found to prompt immediate refusal: ‘Have you got a minute?’ and ‘Can I have a moment of your time?’ When contacting men recruited from general practice registers, it was helpful to mention the letter that had been sent out by their GP. This established credibility and may have eased concern that the call might be from a sales person. Once a relationship was established, a fuller description of the study was given, resolving any doubts or concerns that the men may have had.
Previous studies have found that recruitment by community outreach is often less successful than that using other strategies. 50 A recent study150 reported that community outreach was ineffective in recruiting socially disadvantaged smokers. The question then is why the method succeeded in the present study. A possible reason is the method and manner of the approach. Preliminary fieldwork was used to establish promising venues. The approach involved direct personal contact with potential participants. Methods such as using gatekeepers to identify potential participants and distributing leaflets proved ineffective. Direct face-to-face contact has been found to be more successful149 because it enables potential participants to receive an explanation about what to expect and can clarify misapprehensions.
Comparisons of the groups identified by the two recruitment strategies
A key finding from this study was the difference between the men according to recruitment strategy. Those recruited by community outreach had a higher mean consumption and a higher frequency of binge drinking. The difference in alcohol consumption patterns between the two recruitment strategies can be partly explained by sociodemographic factors such as marital and employment status. However, within each level of the demographic factors, there are marked differences in alcohol consumption between the men recruited by TSS and those recruited from general practice registers. Those recruited by community outreach had consistently higher alcohol consumption. Furthermore, there is a multiplicative effect on consumption of community outreach with being single or being unemployed.
The explanation for the relationship between recruitment method, sociodemographic factors and alcohol consumption is complex. It would be expected that unemployed men would be more likely to be recruited by community outreach, as this was mainly carried out during working hours, when men in employment would be working. However, this explanation does not easily explain why fewer single men, and fewer heavy drinkers, were recruited from general practice registers. Possibly a form of self-selection bias was in operation. Those who drink heavily are less likely to participate in surveys. 151–153 Non-responders to surveys are also more likely to suffer alcohol-related morbidity and mortality. 49,154 This bias could operate when men on general practice registers are contacted by telephone. In contrast, the face-to-face contact of community outreach could provide a more sympathetic and supportive approach, which could also emphasise the non-demanding nature of the study. This may help overcome reluctance of heavy drinkers to participate. It could also reduce the barriers that are experienced by disadvantaged groups, such as distrust of research, concern about confidentiality, fear of authority and lack of benefit from participation. 50–54
In summary, the recruitment strategies were successful for recruiting disadvantaged men. Those recruited frequently engaged in binge drinking but had few moderate drinking sessions. Thus, most of the alcohol consumed was drunk in binge-drinking sessions, which may place those men at high risk of alcohol-related harm. The community outreach approach may be a better method of recruiting hard-to-reach groups with adverse social circumstances. The methods used in this study could be usefully employed in future studies wanting to test interventions to reduce inequalities in health by tackling adverse health behaviours in disadvantaged groups.
Chapter 5 Evaluation of the text message intervention
Introduction
The intervention group and the control group both received a series of Short Message Service (SMS) messages which were delivered over 12 weeks by a computer programme. The novel intervention was based on the HAPA87 and incorporated evidence-based behaviour change techniques. 92 The intervention group received 112 messages, which addressed the components of HAPA. The intervention was presented as a narrative in which fictional characters modelled the key steps in the behaviour change process. This was interspersed with text messages giving information about alcohol, questions on the behaviour change process, and humour.
The control group were sent 89 text messages on a variety of health topics unrelated to alcohol. The control messages provided only facts and trivia on these topics or were humorous. The messages did not incorporate a psychological model or use any behaviour change techniques. They were designed to engage the participants without raising awareness of issues around alcohol misuse and they were not designed to influence health behaviours. Although the control package did not include a narrative, characters were used to pass on information.
This chapter reports on the fidelity of delivery of the intervention and engagement with the study. The feasibility study on which the full trial was based71 showed that men responded enthusiastically to a text message intervention and that the content of their responses gave insight into men’s reactions to the components of the behaviour change strategy. 86 The chapter also explores whether or not the text messages elicited the intended reaction from participants.
Methods
Fidelity of delivery of the text messages
Short Message Service messages can be tracked to determine whether or not they have been delivered to the recipient’s mobile phone. The computer system that sent the text messages recorded and stored information on delivery status. Delivery status was recorded as delivered (the phone had reception and was switched on) or undelivered (the phone was switched off or it had no signal for 24 hours). The programme could not record whether or not messages delivered to the phones were opened by the recipients. The proportion of text messages recorded as delivered to the participants’ mobile phone was monitored as a measure of fidelity of delivery of the intervention.
Responses to the text messages
The computer package that delivered the messages also electronically stored text message responses received from participants. Participants were told that responding to the questions was voluntary, but also that they could send a response at any time to any of the messages received. All of the responses received were anonymised and collated by the Health Informatics Centre at the University of Dundee.
Although both treatment groups received messages that prompted a response, the purpose of the questions posed differed between the groups. For the intervention group, questions were designed to reinforce key components of the intervention and to monitor engagement with the psychological constructs of the intervention in real time. Twenty-one of the 112 messages sent to the intervention group sought a response. The purpose of questions in the control arm was simply to maintain interest in the study. Thus, 12 multiple-choice questions were posed, one per week on health topics. These questions did not require the participants to reflect on their own health behaviour in any way or to give a personalised response.
Engagement with the study and the behaviour change intervention was measured in seven ways.
-
Intervention and control groups
-
counts of responses to the text messages
-
counts of the use of key words that demonstrate satisfaction with the text messages
-
counts of words that indicate reflection on drinking
-
-
Intervention group only
-
counts of responses to the multiple-choice questions
-
the nature of responses to the multiple-choice questions
-
counts of responses to the open-ended questions
-
the nature of responses to the open-ended questions.
-
Characteristics of the participants who responded to the text messages
To investigate the factors that influenced engagement with the study, the demographic characteristics of the participants and their baseline drinking were compared with the frequency of responding to text message questions. Participants were divided into three groups (low, medium and high responders), according to the number of questions they answered. For the intervention arm, who were asked 21 questions, the groups were 0–5 questions answered (low responders), 6–14 questions answered (medium responders) and 15–21 questions answered (high responders). Control participants were asked 12 questions, so the groups were 0–4 questions answered (low responders), 5–8 questions answered (medium responders) and 9–12 questions answered (high responders).
Results
Fidelity of delivery of the text messages
The intervention package comprised 112 SMS text messages. Thus, a total of 46,032 messages were sent to the 411 participants during the intervention period. The control group participants received 89 text messages each, amounting to 36,846 messages sent out. Of the total of 82,878 messages sent to all of the participants, 79,218 messages (95.6%) were delivered to the participants’ phones. Fidelity of delivery was similar in both treatment groups. Participants in the intervention group received 95.5% of messages sent, while those in the control group received 95.7%.
A few (4.4%) of the 82,878 messages were recorded as undelivered (the phone was switched off or it had no signal for 24 hours). Two hundred and seventy-six men (33%) failed to receive one or more messages. Of those who missed messages, the number of undelivered messages per participant in the intervention group ranged from 1 to 112, with a median of 6 messages missed. For the control group, the range was 1–74 (median 3.5).
Participants who missed more than six messages were more likely to be single and unemployed (Table 8). They were also heavier drinkers at baseline than those who received all of the messages, and were more likely to have been recruited by TSS.
| Factor | Number of missed messages, n (%) | Total (N = 825), n (%) | ||
|---|---|---|---|---|
| 0 (N = 549) | 1–5 (N = 154) | ≥ 6 (N = 122) | ||
| Age group (years) | ||||
| 25–34 | 289 (66.3) | 87 (20.0) | 60 (13.8) | 436 |
| 35–44 | 260 (66.8) | 67 (17.2) | 62 (15.9) | 389 |
| Marital statusa | ||||
| Married/lives with a partner | 325 (72.5) | 70 (15.6) | 53 (11.8) | 448 |
| Single | 224 (59.6) | 83 (22.1) | 69 (18.4) | 376 |
| Employment status | ||||
| Employed | 390 (73.9) | 90 (17.0) | 48 (9.1) | 528 |
| Unemployed | 159 (53.5) | 64 (21.5) | 74 (24.9) | 297 |
| Highest educational attainment | ||||
| High school | 327 (64.1) | 93 (18.2) | 90 (17.6) | 510 |
| Vocational qualification/further training | 167 (68.4) | 46 (18.9) | 31 (12.7) | 244 |
| University degree | 55 (77.5) | 15 (21.1) | 1 (1.4) | 71 |
| SIMD decile | ||||
| 1–2 (most deprived) | 437 (68.7) | 106 (16.7) | 93 (14.6) | 636 |
| ≥ 3 | 112 (59.3) | 48 (25.4) | 29 (15.3) | 189 |
| Recruitment method | ||||
| General practice registers | 318 (74.5) | 69 (16.2) | 40 (9.4) | 427 |
| TSS | 231 (58.0) | 85 (21.4) | 82 (20.6) | 398 |
| Group | ||||
| Intervention | 275 (66.9) | 67 (16.3) | 69 (16.8) | 411 |
| Control | 274 (66.2) | 87 (21.0) | 53 (12.8) | 414 |
| Mean units consumed in previous 28 days (SD) | 121.6 (113.2) | 144.4 (135.0) | 176.4 (190.5) | 134.0 (132.8) |
Responses to the text messages
Frequency of responses received to the text messages
Participants in both groups responded enthusiastically to the text messages. Responses were received from 92% of participants in the intervention group (380 men) and from 94% of participants in the control group (388 men). The total number of responses received from participants in the two arms of the study are not comparable because of the differences in the nature of the text messages. The intervention group received many more text messages that asked questions, the majority of which required free-text responses. In contrast, almost all of the questions sent to the control group were multiple choice and required only a single-letter response.
Intervention group
A total of 7481 responses were received to the 112 messages from the men in the intervention group. The number of responses per participant ranged from 0 to 81 (mean 18.2, median 17). Although 35% of the participants (142 men) responded > 20 times, another 33% responded ≤ 10 times (Figure 3).
FIGURE 3.
Intervention group: frequency of responses to text messages.
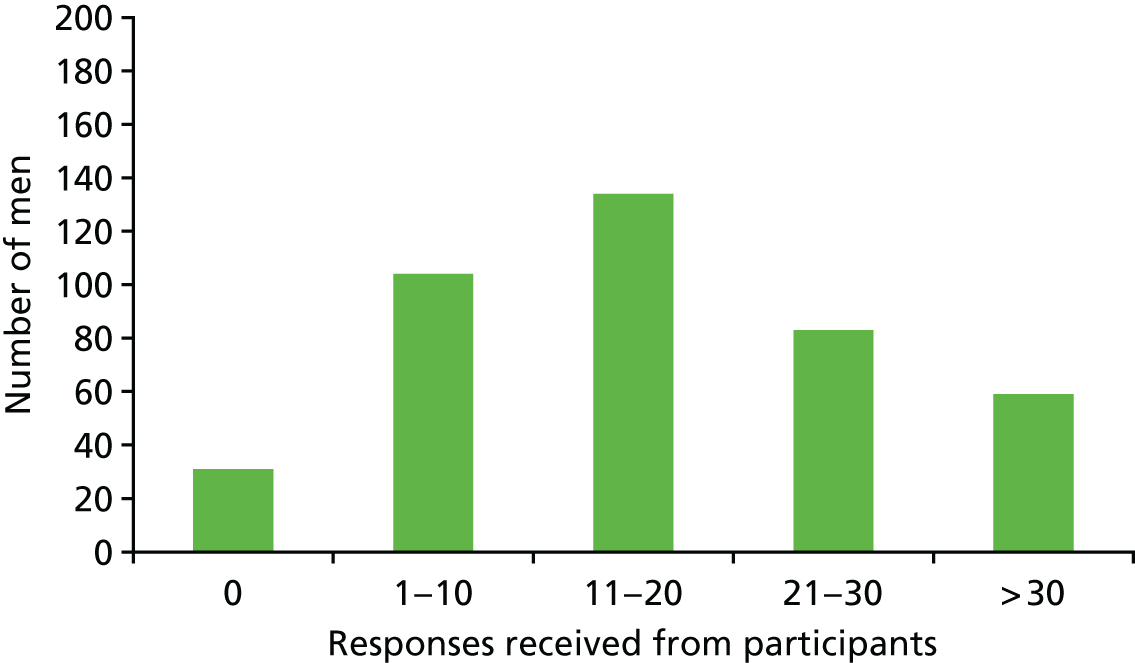
Control group
The control group received fewer text messages than the intervention group, and also received fewer messages that prompted a response. Thus, 5605 responses were received to the 89 messages sent out to each man (Figure 4). Although the range of responses received was similar to the intervention group, 0–77, the mean and median number of responses received was lower (mean 13.5, median 10.5 per man). Only 19% responded > 20 times.
FIGURE 4.
Control group: frequency of responses to text messages.
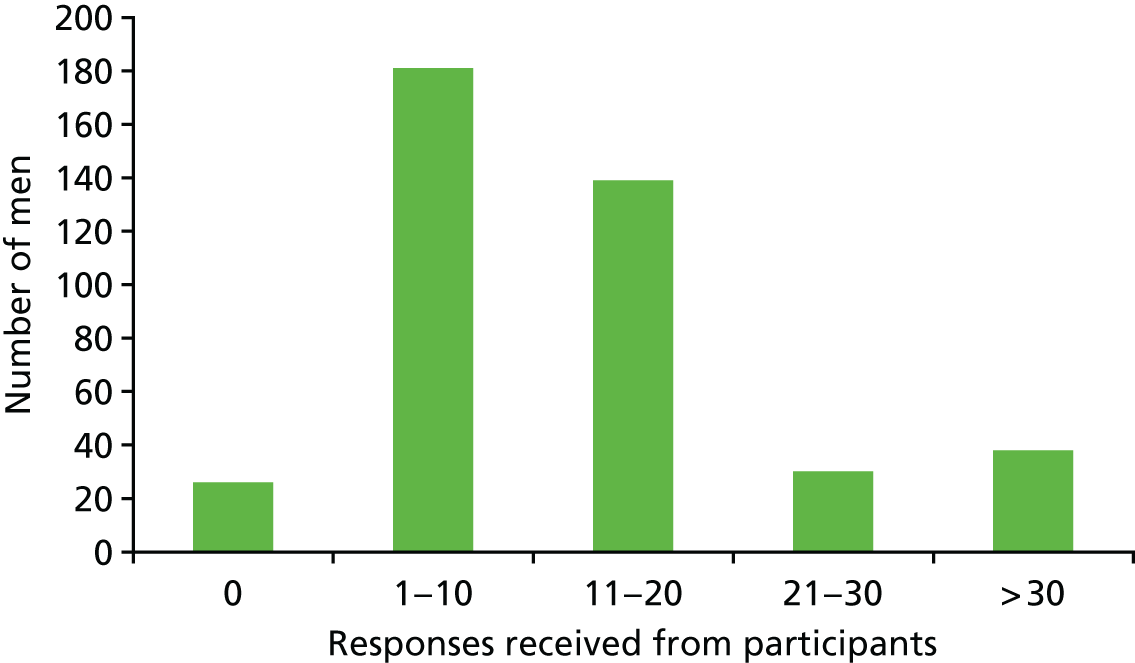
Responses to individual text messages
Intervention group
The intervention group messages were divided into four types (Figure 5). The blue bars represent responses to text messages that presented the narrative; the black bars represent responses to facts, supporting information or humour; the dark green bars represent the responses to messages that sought a response from participants; and the light green bars represent responses to messages that asked a question, but also provided an answer, such that a response was not expected.
FIGURE 5.
Intervention group: frequency of responses by type of text message.
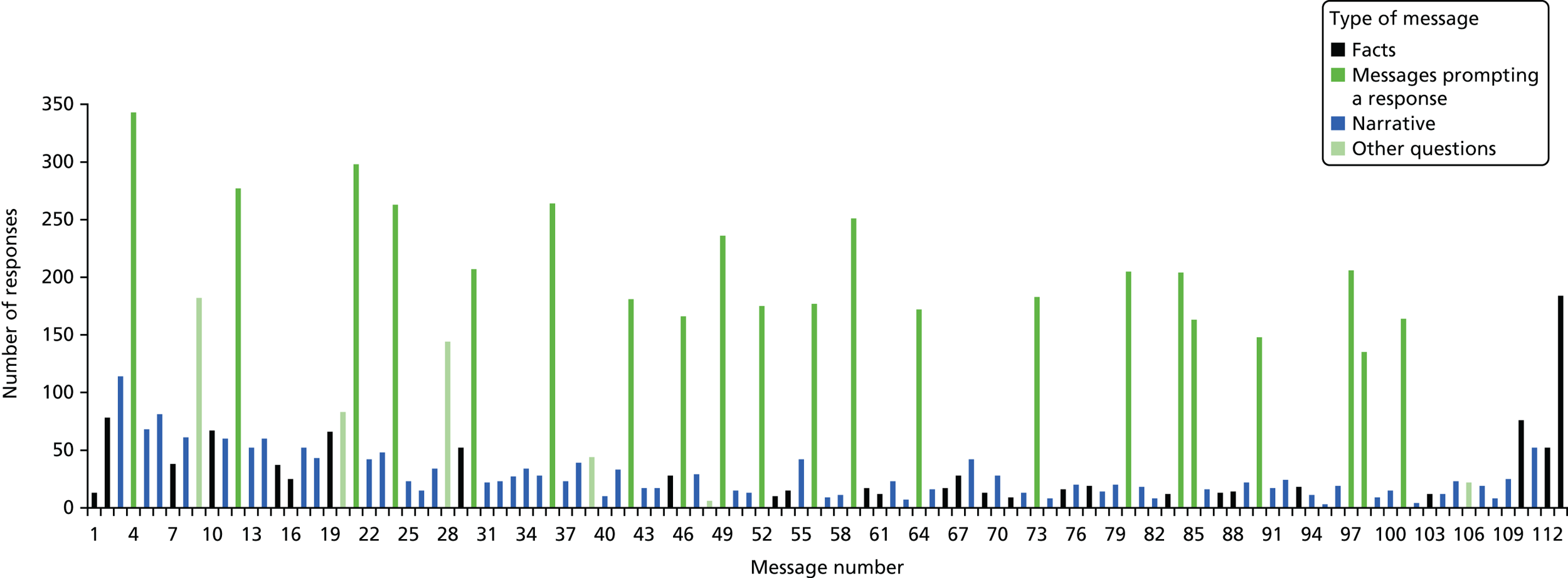
The mean number of responses per man to messages that asked a question was 10.7 (median 11). The number of replies to the 91 messages that did not seek a response was slightly less (mean of 7.5 messages per man, median 3), but each of these messages received some responses. Many of these were responses to events occurring within the narrative, such as offering support and sympathy to characters when they were struggling to reduce their alcohol consumption.
There was some attenuation in the number of men answering questions over the 12-week period. This could be partly due to the nature of the questions. For example, some questions asked the men about specific actions such as setting a goal to reduce drinking (message number 56) or making a plan (message number 64). Participants who had not considered doing this may not have responded because they felt that the questions were not relevant.
The final bar on the histogram represents the 184 responses that were not related to any particular message. These included queries about gift vouchers, details on change of addresses or telephone numbers and general comments about the study or how the participant was feeling.
Control group
Two types of messages were sent to the control group (Figure 6): facts and trivia on health topics (black bars) and multiple-choice questions (green bars). The control group participants also demonstrated high levels of engagement with the study. The frequency of responding to the questions was lower than in the intervention group (mean 6.7, median 7). For the 77 text messages that did not ask a question, the number of responses was also lower than in the intervention group (mean of 6.9 messages per man, median 2). Apart from answering the questions, men commented on the health topics or responded to the humorous messages, often coming up with jokes of their own. The multiple-choice questions, one per week, did not seek the personalised responses required by the intervention group. Nevertheless, the questions were sufficient to sustain the men’s interest over the 3-month period. As in the intervention arm, the first question received more responses than any other question (283 responses from the 414 men). There was less variation in the number of responses received to the control text messages. Some attenuation was observed over the period, particularly over the last 3 weeks of the intervention. The topics being discussed during these 3 weeks [e.g. foot health (206 responses), tiredness (189 responses) and hearing (175 responses)] may have had less appeal than topics covered earlier [e.g. physical activity (260 responses), sexual health (253 responses) or oral health (263 responses)].
FIGURE 6.
Control group: frequency of responses by type of text message.
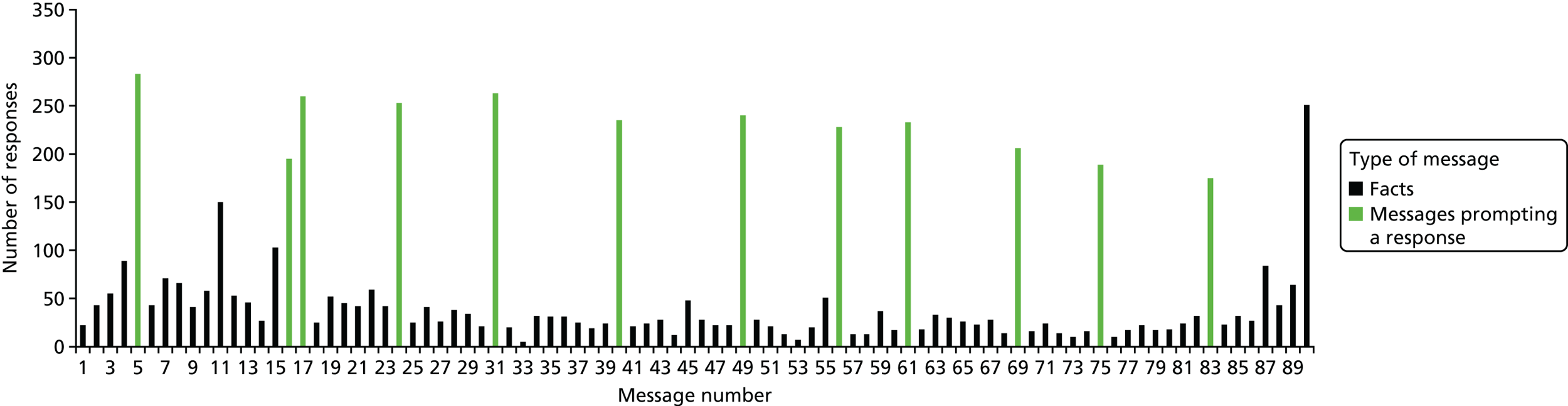
The final bar on the histogram shows the 251 responses from the control participants that were not related to any particular message. In addition to the queries about gift vouchers and details of change of addresses and telephone numbers, many men came up with more trivia and jokes on the health topics.
Engagement with the text messages
To investigate further the level of engagement with the text messages, a count of key words was performed on the database of responses received from the participants. The first group of words addresses general engagement with the study (Table 9). Phrases such as ‘lol’ or ‘haha’ are consistent with enjoyment and pleasure, while ‘thanks’ and ‘no problem’ suggest that the participants appreciated the study. The number of responses were similar in both groups. The role of the character Dave differed depending on the arm of the study. In the intervention group text messages, Dave was portrayed as a peer, who demonstrated changing his behaviour through a narrative. In the control text messages, Dave was much less prominent and did not have a storyline to support his role. He simply passed on interesting or humorous information to the participants, and many replied to him.
| Key word | Responses (n) | |
|---|---|---|
| Intervention | Control | |
| Lol | 264 | 313 |
| Thank [s] | 116 | 213 |
| Haha | 73 | 75 |
| No problem | 48 | 32 |
| Dave [ie] | 119 | 100 |
| Voucher | 34 | 47 |
| Sorry | 50 | 27 |
| Advice [se] | 7 | 9 |
The second set of key words relate to alcohol and behaviour change (Table 10). Whereas hundreds of the responses from the intervention group mentioned alcohol and drinking, few from the control group did so. This is because the control group received no messages about alcohol or about changing health behaviours. The number of references to different types of alcohol reflected the drinks most commonly consumed by the men (i.e. beer, vodka and lager).
| Key word | Occurrences in replies (n) | |
|---|---|---|
| Intervention | Control | |
| Drink | 1305 | 28 |
| Beer | 236 | 4 |
| Health | 210 | 18 |
| Alcohol | 186 | 11 |
| Stop[ped] | 173 | 19 |
| Pub | 125 | 6 |
| Drunk | 107 | 6 |
| Vodka | 103 | 2 |
| Lager | 85 | 3 |
| Change | 76 | 14 |
| Binge | 64 | 1 |
| Sober | 36 | 0 |
Intervention group responses to text messages that sought a response
Text messages that sought a response were an integral part of the behaviour change intervention. These questions were designed to reinforce key components of the intervention by getting the men to reflect on their drinking and think carefully about the antecedents to changing their behaviour. Reviewing the content of these responses gave an assessment of engagement with the psychological constructs of the intervention and key steps in the behaviour change process in real time.
The questions were distributed over the first 10 weeks of the intervention period, with a maximum of four questions being asked during 1 week. Table 11 presents the questions asked of the participants, the psychological constructs being addressed and the number of responses received from the participants. Questions during the first few weeks were designed to address the motivational phase of the HAPA. Thus, early text messages asked the men to self-monitor, record and report how much they usually drank. Questions in this phase also encouraged men to think about the pros and cons of their current level of drinking and to consider the potential benefits of cutting down. Text messages in the volitional phase helped the men to set goals and make action plans by first demonstrating how to do it and then gently asking the men what their own goal and plans would be. Maintenance of a new behaviour, which presents many challenges, is a key component of the HAPA. The second half of the intervention period encouraged maintenance by asking questions about doing alternative activities and making plans on how to cope in situations in which drinking would be expected. Self-efficacy, which is essential throughout the behaviour change process, was addressed in both phases of the intervention. Study participants demonstrated engagement with the messages from the beginning of the intervention period, with the first question receiving the greatest number of responses.
| Text number | Question | Psychological construct | Number of responsesa |
|---|---|---|---|
| 4 | We all drink for different reasons. What’s the main reason you drink? (a) it’s a habit (b) to feel better (c) to have fun (d) to cope. Text me your answer | Self-perception of motives for drinking | 343 |
| 12 | Do you try to keep track of what you drink on a night out? It can be hard. What’s your usual amount? Text me your answer | Self-monitoring of drinking behaviour | 277 |
| 21 | Did you manage to count how much you drank over the weekend? Text me your answer | Self-monitoring of drinking behaviour | 298 |
| 24 | Can you think of any reasons why it might be a good idea for you to cut down a bit on your drinking? Please text me your answer | Outcome expectancies | 263 |
| 30 | Have you or your mates had any problems caused by alcohol? Please let me know. We’ve all been there | Risk perception | 207 |
| 36 | In the past week have you thought about cutting back a bit on your drinking? Text me (a) yes (b) no (c) maybe | Ideation/reflection/consideration of reducing drinking | 264 |
| 42 | Can you think of someone who’d be happy if you made a change? What would you hear them say? Please text me your answer | Subjective norms (normative beliefs) | 181 |
| 46 | Many people want to cut back a bit. Can you tell me what would be good about that for you? | Outcome expectancies | 166 |
| 49 | How much would you save each month if you drank half as much? Count up your savings and text me the sum | Outcome expectancies | 242 |
| 52 | By saving your cash you could treat yourself to something special too. Picture what you would like and text me back your answer |
Outcome expectancies Positive reinforcement |
175 |
| 56 | If you made a goal to cut down a bit on your drinking, what would it be? Text me your answer | Goal setting to reduce drinking | 177 |
| 59 | How confident are you that you could cut back a bit? (a) absolutely certain (b) pretty sure (c) maybe (d) no chance. Text me back please | Action self-efficacy | 252 |
| 64 | If you made a plan, what would it be? Text me your answer | Action plan to reduce drinking | 172 |
| 73 | What would you do if you got into a situation where you were expected to drink far more than you intended? Text me your answer |
Coping-planning/maintenance self-efficacy Existence, content and quality of coping plans |
183 |
| 80 | Would you feel comfortable about refusing a drink when you’re out with your mates and drinking in rounds? Text me back please | Coping/maintenance self-efficacy | 205 |
| 84 | If you had an unplanned binge, how confident are you that you could get back on track next time? (a) absolutely certain (b) pretty sure (c) maybe (d) no chance | Coping self-efficacy | 204 |
| 85 | Have you thought about doing something different with your time? What could you do to avoid a drinking session? Text me your answer |
Ideation/reflection/consideration of behaviour change Existence, content and quality of plans |
163 |
| 90 | Getting a result from changing things makes the effort involved worthwhile. What would make it worthwhile if you cut back a bit? Text me your answer | Outcome expectancies | 148 |
| 97 | In the past 3 months have you (a) thought about changing your drinking (b) set a goal to change it (c) made a plan of how to do it (d) never thought about it? | Measures whether or not participants had thought about goal-setting and planning and whether or not it actually took place | 206 |
| 98 | If you have cut down on the drinking a bit, have you noticed any differences to you or your family? Let me know please | Reported benefits of reducing drinking | 135 |
| 101 | Think about times when you are tempted to drink far too much. What could you do to stop it happening? Text me your answer |
Coping/maintenance self-efficacy Existence, content and quality of plans |
164 |
Five of the questions were multiple choice and these attracted the most responses from the men (Table 12). The first question was designed to identify the type of drinkers in the study, and it was based on the Drinking Motives Questionnaire,155 which categorises reasons for drinking as social, coping or enhancement. Some men gave several reasons for drinking, but the majority of men who selected a single option (220 men out of the 327 who responded) reported that they drank ‘to have fun’.
| Question and possible answers | Number of responsesa |
|---|---|
| We all drink for different reasons. What’s the main reason you drink? (Message 4) | |
| A – It’s a habit | 33 |
| B – To feel better | 18 |
| C – To have fun | 220 |
| D – To cope | 17 |
| Multiple answers, other reasons, duplicate response, additional comments | 55 |
| In the past week have you thought about cutting back a bit on your drinking? (Message 36) | |
| A – Yes | 115 |
| B – No | 90 |
| C – Maybe | 55 |
| Additional comments | 5 |
| How confident are you that you could cut back a bit? (Message 59) | |
| A – Absolutely certain | 124 |
| B – Pretty sure | 66 |
| C – Maybe | 39 |
| D – No chance | 10 |
| Multiple answers, other response, additional comments | 13 |
| If you had an unplanned binge, how confident are you that you could get back on track next time? (Message 84) | |
| A – Absolutely certain | 114 |
| B – Pretty sure | 56 |
| C – Maybe | 27 |
| D – No chance | 2 |
| Other response | 5 |
| In the past 3 months have you . . . (Message 97) | |
| A – Thought about changing your drinking | 80 |
| B – Set a goal to change it | 41 |
| C – Made a plan of how to do it | 42 |
| D – Never thought about it | 42 |
| Additional comments | 1 |
Message 36, sent out at the end of the third week of the intervention, was used to evaluate whether the participants had reflected on their own drinking patterns in response to the intervention or had thought about cutting down. Forty-four per cent of the 260 men who responded said that they had thought about cutting down, while 35% of respondents said that they had not.
Two questions [at the end of week 5 (message 59) and at the beginning of week 10 (message 84)] assessed action self-efficacy and recovery/coping self-efficacy, respectively. More than half of the men who responded to the message on action self-efficacy (51%) expressed very high confidence levels, while 20% said that they lacked confidence. The number of men who responded to the question on recovery self-efficacy was smaller, but 56% of those who did respond had very high confidence levels.
Message 97 asked men to report on actual changes to their drinking during the intervention period. Of the 205 men who responded, 20% had set a goal to reduce drinking and 20% had made a plan of how to achieve their goal. Twenty per cent of the respondents revealed that they had never thought about changing their drinking, while 39% stated that they had at least thought about changing.
The remaining 16 messages that sought responses were open-ended questions that required the participants to reflect on the part of the behaviour change strategy being addressed (see Table 11). Many of the responses gave carefully considered answers and contained personal details. Very often these responses were longer than the 160 characters that are permitted in one text message. To illustrate the nature of engagement with components of the behaviour change process, verbatim responses to selected questions are presented.
Outcome expectancies/risk perception
Text number 24, ‘Can you think of any reasons why it may be a good idea for you to cut down a bit on your drinking? Please text me your answer’, was designed to encourage re-evaluation of current drinking behaviour. Posing it as a question encouraged the participants to reflect on the pros and cons of their drinking and the potential risks. By giving a response, the participant was required to present an argument for change and commit it to text. Fifty-six per cent of the participants (230 men) identified a range of potential benefits. These fell into four categories:
-
Short-term/immediate benefits:
-
Feel much fresher and more active without it!
-
Be healthier and no more satardays with a sorehead.
-
To remember ur night reduce cost and hangover.
-
-
Health:
-
To be in a better mental and physical shape.
-
My liver function test came bck very high,and the drink is obviously a major reason.
-
Cut down on my drinking help save my liver any other alcohol related diseases no hangovers.
-
-
Family:
-
To try for a baby again with the missus.
-
I feel guilty when i am hungover around the kids.
-
I want to cut down so I don’t become to ill with the alcohol and want to c my wee boy grow up big and healthy.
-
So your kids dont see that as the norm, and drink because they see me doin it.
-
-
Financial:
-
Money, it can be expensive.
-
Saving Money!
-
Bank balance, productivity on sundays.
-
Many men listed several reasons for cutting down:
A few good reasons for cutting down on drinking for me is better mental and physical health and the ability to enjoy my kids more as a heavy drinking session drains your body.
My answer for cutting down drinking,save money,better health,u wont get a beer belly, better relationships. <name>
The reasons a [I] would cut down is for my children my health plus a [I] find my weekends more enjoyable without a hangover.
Save money. Stop wasting days lying in bed/on couch with hangovers. Stops the wife falling out with me. Remember more of my life instead of forgetting what I’ve been up to when had to much to drink.
A few men felt that they did not need to cut down:
I like when I drink. I dont drink to much :-).
No when I drink it is in moderation.
No I don’t think I need to cut down.
No not at this point in time.
Perception of harms
Text number 30, sent during the third week – ‘Have you or your mates had any problems caused by alcohol? Please let me know. We’ve all been there’ – was designed to address outcome expectancies and risk perception. Almost half (195) of the participants replied to this question. A few men (n = 31) said that they had never experienced alcohol-related harm, but 97 men reported personal problems, 39 reported harms experiences by friends and family members, while another 22 reported both personal problems and harms experienced by friends and family members. Some men gave very personal responses of problems that had occurred from their own drinking and how they had been affected by other people’s drinking:
The odd assault charge but nothing realy note worthy.
I tried to sleep with my sister in law. <name>
Problems caused by drinking? Oh yes . . . Prison, Hospitalisation (illness/injurys), Breakups, Job losses, Evictions, STI’s, Money troubles . . . I could go on and on.
Apart from a day of work,and a bad hangover not really?
Iv spent more than my fair share of nites in police custody, lost the love of my life and a few friends too and been in alot of scraps n all because the drink and boy do i regret it n hope i will learn one day.
Yeah my step dad was an boozer and would slap me and my mum around. <name>
Not me or friends as such but I’ve suffered it first hand as my Mum has a drink problem.
Others reported problems that their friends had experienced. These included:
I’ve had a friend that’s died because of drink. Fell off a balcony in a block of flats.
Yes a few pals have lost there marriage because of alcohol.
Not me, but my pals have had Broken marriage, injured when getting home, lost jobs, & died from alcohol poisoning.
My mate lost everything his family and business all because he decided to drive after a few, he killed a woman and seriously injured a her husband in a crash.
Lost a good friend and a couple of other guys i knew,and it hits home the long term damage it can cause.
Subjective norm
Text number 42 asked ‘Can you think of someone who’d be happy if you made a change? What would you hear them say? Please text me your answer?’ This text message used the psychological concept of ‘subjective norm’ (an individual’s perception of social normative pressures, or relevant others’ beliefs that he or she should or should not perform certain behaviours). It sought to encourage participants to identify people who would approve of their decision to reduce their drinking in order to increase their motivation to change. This question elicited responses from 176 participants (43%), many of which were deeply personal. Parents, partners, family members and friends were all identified as people who would be pleased to see a reduction in drinking. Some men gave detailed responses about what their family and friends would say:
My kids they would say well done dad.
My wife. She would say at least she wouldn’t have to worry where I was and what I was up to?
My girlfriend would be happy.less chance i’d be ending up dead like her father.
My gran.youll lose that horrible beer belly.
My wife, she’s get more money for shoes!!
My wife <name>. Maybe take her out more she would probably say got my husband back.
A few men could not think of anyone who would be pleased:
I’ve racked my brain for this question and i can’t think of anyone. Sorry.
No. Dont know anyone. Im single one.
Some men simply felt that they did not drink enough to cause concern to family and friends:
Nobody i don’t drink excessively.
I dont have anyone that would say i drink too much and need to cut back . . .
Nobody thinks I drink much . . . so I don’t have an answer to this question.
Goal-setting and action-planning
Setting goals and making action plans are essential steps in changing a health behaviour. Text number 56 in week 5 of the intervention asked ‘If you made a goal to cut down a bit on your drinking, what would it be? Text me your answer.’ More than 40% of participants (172 men) responded to this question, 158 of whom suggested goals to reduce consumption, either by reducing the frequency of drinking occasions or by reducing the amount consumed on drinking occasions:
Stop Drinking during the week!
Restrict it to weekends.
Cut down one day a week.
Stop earlier in the evening or at very least slow down compared to others.
Buy a 12pack fortnightly instead of weekly.
To just have a tin of juice back at the pub after football on a Saturday instead of a pint which leads onto more pints.
Home before clubs open.
When drinking, take note of how much I’m actually consuming and stay away from binge drinking!
To cut out drinkin into early hours of mornin. And avoid awful hangovers.
Action plans should provide the details on how personal goals will be achieved. One text message therefore explained: ‘When you make a plan it always works better if you make sure you say: WHEN; WHERE; and HOW you will do it.’ This message was followed by ‘If you made a plan, what would it be? Text me your answer.’ One hundred and sixty-seven men responded to this question. Of these, 29 men had no plan. The remainder presented plans that varied greatly in content. Some men took a cue from the message and gave a very structured plan:
Plan- WHEN: tonight. WHERE: watching the footie. PLAN: No more than 3 drinks.
When: Saturday night. Where: the golf club. How: go home for tea rather than stay all afternoon and evening.
WHEN: Monday, WHERE: at home, HOW: not having a can of beer with the nfl game.
Others presented less structured, basic plans that could be interpreted as intentions:
Only drink one night this weekend.
A plan I would make would be not to have a couple of cans before going to the pub.
Im going to not buy beer for at home after the pub so i dont drink when i get in from pub.
For others, plans appeared to be aspirations rather than a concrete plan to be followed:
Avoid social situations.
Try and save money.
Go out later and come home sooner. Simple.
Actual benefits of reduced drinking
During week 10, towards the end of the intervention period, participants were asked ‘If you have cut down on the drinking a bit, have you noticed any differences to you or your family? Let me know please.’ This question asked about actual benefits that the men had experienced as a result of reducing their drinking, rather than being a hypothetical question.
Those who reported benefits identified a range of health, personal, family and financial benefits:
Felt more energetic n good about myself. Family have noticed this too. <name>
Yes cut down, mrs moans less.
Little things like not having memory blanks from a night out the morning after.
More money,doing more family things and my temper is not so short.
We are closer than we have been recently.
The main difference I have noticed is I feel a lot better the next day, so rather than lying in the feotal position on the couch the whole day, I can get up and do stuff with the mrs.
Better sleep . . . better at work . . . more motivated . . .
I’ve managed to buy some new clothes in a smaller size with the money I’ve saved and the kids see a bit more of me.
A few men reported no benefits, but thought that they needed more time to feel these:
<name> here No differences yet suppose it will take time
Not really maybe in more time.
Finally, some men reported that they had not cut down, although some of these appeared to be more aware of their drinking:
I don’t think I’ve cut down any although I have been more aware of what I’m drinking.
Not cut down on my drinking yet.
Had a set back so not cut down.
Haven’t cut down no difference.
Characteristics of the participants who responded to the text messages
The demographic characteristics of the high, medium and low responders were explored for the intervention group and control group separately, before the treatment groups were compared. Men in the intervention group who were high responders (compared with medium and low responders) were more likely to be in the older age group (35–44 years); be living with a partner; be employed; have attended further education; be living in the most disadvantaged areas; and have been recruited through general practice registers (Table 13). The characteristics of the high responders in the control group were very similar, although the differences between the high and low responders were less marked than in the intervention group (Table 14).
| Factor | Level of response, n (%) | Total (N = 411), n | ||
|---|---|---|---|---|
| High (N = 158) | Medium (N = 129) | Low (N = 124) | ||
| Age group (years) | ||||
| 25–34 | 69 (31.2) | 75 (33.9) | 77 (34.8) | 221 |
| 35–44 | 89 (46.8) | 54 (28.4) | 47 (24.7) | 190 |
| Marital statusa | ||||
| Married/lives with a partner | 106 (47.3) | 61 (27.2) | 57 (25.4) | 224 |
| Single | 52 (28.0) | 67 (36.0) | 67 (36.0) | 186 |
| Employment status | ||||
| Employed | 131 (47.5) | 80 (29.0) | 65 (23.6) | 276 |
| Unemployed | 27 (20.0) | 49 (36.3) | 59 (43.7) | 135 |
| Highest educational attainment | ||||
| High school | 84 (33.6) | 76 (30.4) | 90 (36.0) | 250 |
| Vocational qualification/further training | 56 (42.4) | 44 (33.3) | 32 (24.2) | 132 |
| University degree | 18 (62.1) | 9 (31.0) | 2 (6.9) | 29 |
| SIMD decile | ||||
| 1–2 (most deprived) | 128 (40.8) | 94 (29.9) | 92 (29.3) | 314 |
| ≥ 3 | 30 (30.9) | 35 (36.1) | 32 (33.0) | 97 |
| Recruitment method | ||||
| General practice registers | 91 (42.7) | 65 (30.5) | 57 (26.8) | 213 |
| TSS | 67 (33.8) | 64 (32.3) | 67 (33.8) | 198 |
| Factor | Level of responses, n (%) | Total (N = 414), n | ||
|---|---|---|---|---|
| High (N = 167) | Medium (N = 132) | Low (N = 115) | ||
| Age group (years) | ||||
| 25–34 | 82 (38.1) | 69 (32.1) | 64 (29.8) | 215 |
| 35–44 | 85 (42.7) | 63 (31.7) | 51 (25.6) | 199 |
| Marital status | ||||
| Married/lives with a partner | 94 (42.0) | 69 (30.8) | 61 (27.2) | 224 |
| Single | 73 (38.4) | 63 (33.2) | 54 (28.4) | 190 |
| Employment status | ||||
| Employed | 119 (47.2) | 81 (32.1) | 52 (20.6) | 252 |
| Unemployed | 48 (29.6) | 51 (31.5) | 63 (38.9) | 162 |
| Highest educational attainment | ||||
| High school | 98 (37.7) | 87 (33.5) | 75 (28.8) | 260 |
| Vocational qualification/further training | 45 (40.2) | 31 (27.7) | 36 (32.1) | 112 |
| University degree | 24 (57.1) | 14 (33.3) | 4 (9.5) | 42 |
| SIMD decile | ||||
| 1–2 (most deprived) | 137 (42.5) | 105 (32.6) | 80 (24.8) | 322 |
| ≥ 3 | 30 (32.6) | 27 (29.3) | 35 (38.0) | 92 |
| Recruitment method | ||||
| General practice registers | 112 (52.3) | 66 (30.8) | 36 (16.8) | 214 |
| TSS | 55 (27.5) | 66 (33.0) | 79 (39.5) | 200 |
Responses requiring attention
In addition to responding to the content of the intervention, participants sent messages if they needed to get in touch with the research team. They had been asked to tell the study team if they had a change of address or telephone number, or if they wanted to withdraw from the study. Most importantly, they could report adverse events or any distress they were experiencing. Thus, anonymised responses from the participants were screened daily by the trial manager. A member of the research team responded to 80 text messages received from participants. The most frequent queries were about gift vouchers (27 messages). A few men, particularly at the beginning of the intervention period, had some misperceptions or misunderstandings about the nature of the intervention and the content of the text messages. Thus, 15 men were contacted to provide further explanation of what was involved and to reassure them. Nine men sent messages indicating that they no longer wanted to receive the messages. All of these men were called and, following a discussion with the researcher, two were withdrawn from the study. The other seven were happy to remain in the study. Messages from six men suggested that they were distressed in some way. Two men indicated that they wanted to die and two reported having other psychiatric problems. Some also reported drug-related problems. All of these men responded to, and appreciated, telephone calls from the researchers. They were given information on where to seek help and all of them remained in the study. A further six men, by answering questions posed in the intervention, reported drinking very large amounts of alcohol. These men were advised to contact their GP to seek help for their alcohol problems. Finally, 17 men were contacted for a variety of other reasons. For example, some asked if their friends or partners could take part, others reported a change of address, problems with their mobile phones or that they were going on holiday.
Discussion
This study has shown that a theoretically based behaviour change intervention can be rendered into a series of SMS messages and delivered with high fidelity to young to middle-aged disadvantaged men who regularly binge drink. The methods used to monitor the delivery and evaluate the impact of the messages showed that the interactive text messages maintained the interest of the participants over the 3-month intervention period. It also showed that men in the intervention group engaged with key components of the behaviour change process. Nineteen of the 21 questions attracted responses from at least 40% of the participants. At the end of the intervention period, almost one-quarter of men reported a range of health, personal, family and financial benefits that had resulted from reducing their alcohol consumption. To put this into context, the sample size calculation was based on the estimate that only 11% of men would reduce their frequency of binge drinking to detect a statistically significant effect of the intervention.
Fidelity of delivery is essential for the success of a behaviour change intervention. 156 More than 95% of the text messages were delivered to the participants’ mobile phones. Of those who failed to receive some of the messages, the majority missed very few. Two-thirds of the participants received all of the messages and < 10% missed more than six.
Another important aspect of fidelity of delivery is ensuring that the recipients have understood the intervention and are able to perform the new skills that have been taught. 157 The text messages sent to the intervention group were designed to explore both of these requirements. A careful evaluation of the responses to the questions that tapped into key components of the behaviour change mechanism showed a high degree of engagement with the cognitive antecedents to reducing drinking. For example, participants gave details on self-monitoring of their alcohol consumption, their reasons for cutting down, setting goals and making action plans, and the benefits of reducing drinking. Participants gave deeply personal details of their experiences and none of the responses received rejected the suggestion that reducing alcohol consumption would be beneficial. Many comments on drinking behaviour suggested that the participants were reducing consumption or at least thinking about doing so. Some were able to report real health and social benefits. These benefits translated into positivity and some men indicated that they were looking towards a better future for themselves and their families (e.g. ‘I want to be around to see my son growing up’).
An added advantage of the text message intervention was that the participants could open the messages at a time that suited them. They were not committed to participating in intervention sessions at specific times. They could also read and reread the messages, which gave them the opportunity to revisit salient parts of the intervention, so that the intervention was received and the responses were sent in ‘real time’ and in the ‘real world’. 158 This is described as ecological momentary assessment,159 whereby the impact of the intervention is monitored as participants go about their daily business.
An analysis of the responses confirmed that the impact of the text messages differed greatly between the two study groups. Responses from participants in the intervention group demonstrated engagement with components of the behaviour change process. The control messages enlisted much less emotional involvement than the intervention group messages, although the responses conveyed levels of engagement and enjoyment that were comparable with the intervention group. Overall, very few men in the control group mentioned alcohol in their responses.
Interest was maintained in the study throughout the intervention period, although some attenuation was observed in the number of men responding to the later questions. For intervention group participants, this was partly because of the nature of the questions posed during the last few weeks of the intervention. Some of the later questions were relevant only to those men who had already made changes (i.e. questions asked about coping-planning, strategies to maintain reduced drinking and the benefits of reduced consumption). For men who had not changed their drinking, some of the questions asked would have appeared less relevant.
A key issue is the interpretation of the lack of responses to questions. This does not necessarily show a lack of engagement with the intervention. There may be many reasons why participants did not respond to the messages. Participants may not have had time to compose the response or may not have had credit on their phones. Some men may have reacted as intended but thought that it was not necessary to respond. It is likely that the total number of responses underestimates the true level of engagement with the study.
Socially disadvantaged people are less likely to participate in research48,49 and less likely to engage with health promotion. However, most study participants engaged with the text messages from the outset. The approach taken to deliver the intervention without face-to-face contact may have been attractive to this group. Ownership of mobile phones is very high83 and text messaging is often the preferred means of communication. 160 Such a familiar method of communication may have encouraged engagement with the study from people who would be reluctant to engage in direct contact.
The monitoring of responses to the text messages identified several instances when men expressed concerns about the study, and a few men who appeared to be in some distress. When investigated further, all of the concerns raised were resolved. This highlights the need to address issues arising in intervention studies that do not involve direct contact with participants. Research studies have a duty of care to participants and, given that the process is technically simple, it would seem essential that in all text message studies the responses received should be monitored.
Conclusions
This empirically and theoretically based complex intervention, delivered by text message, engaged socially disadvantaged men. Most of the participants received the complete set of text messages and almost all responded to the messages. The men expressed enjoyment and satisfaction with the study and very few voiced any dislike of the messages. Content analysis has shown that the text messages were understood and that the participants were able to use the cognitive and behavioural skills demonstrated in the narrative (e.g. self-monitoring of alcohol consumption, goal-setting and action-planning). By the end of the intervention period, almost one-quarter of men in the intervention group reported that they had experienced a range of health, personal, family and financial benefits from reducing their alcohol consumption.
Chapter 6 First follow-up
Introduction
The first follow-up was scheduled at 3 months after the end of the intervention, which was 6 months after the baseline assessment, as the text messages were sent over a 12-week period. The aim was to detect whether or not there were short-term changes in alcohol consumption. This was intended to aid the interpretation of any changes in the frequency of binge drinking at 12 months post intervention, which is the primary outcome measure for the trial. This chapter presents a descriptive analysis of two prespecified secondary outcomes: the proportion of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) and the proportion of men with ≥ 3 occasions of heavy binge drinking (> 16 units of alcohol) in the preceding 28 days. It also explores whether or not loss to follow-up could have introduced bias into the observed results.
Results
In total, 737 of the 825 men (89.3%) were followed up. Retention rates were almost identical for the two treatment groups: 89.1% (366/411) for the intervention group and 89.6% (371/414) for the control group. There was a marked, and similar, fall in the two treatment groups of the proportion of men with ≥ 3 occasions of binge drinking: the intervention group fell by 37.4% and the control group fell by 40.5% (Table 15). The proportion of men with ≥ 3 occasions of heavy binge drinking followed a similar pattern, with large falls in both groups. The falls in the proportions of men with binge and heavy binge-drinking sessions are accompanied by falls in the mean number of these drinking sessions. For example, in the intervention group, the mean number of binge-drinking sessions fell from 6.49 to 3.82 (i.e. by 2.67 sessions) and the mean number of heavy binge-drinking sessions fell by 1.65 sessions. As a result of these falls, the mean number of non-drinking days increased by 2.2 days. The same pattern of changes is seen in the control group.
| Alcohol consumption in the previous 28 days | Group | |||
|---|---|---|---|---|
| Intervention | Control | |||
| Baseline (N = 366) | 3-month follow-up (N = 366) | Baseline (N = 371) | 3-month follow-up (N = 371) | |
| Percentage of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) | 82.2 | 44.8 | 85.2 | 44.7 |
| Percentage of men with ≥ 3 occasions of heavy binge drinking (> 16 units of alcohol)a | 46.2 | 22.1 | 48.3 | 20.2 |
| Mean number of binge-drinking sessions (> 8 units of alcohol) (SD) | 6.49 (5.3) | 3.82 (5.4) | 6.57 (5.2) | 3.85 (5.4) |
| Mean number of heavy binge-drinking sessions (> 16 units of alcohol) (SD) | 3.58 (5.1) | 1.93 (4.4) | 3.55 (4.6) | 1.74 (4.2) |
| Mean number of alcohol-free days (SD) | 19.9 (5.9) | 22.1 (6.0) | 19.9 (5.8) | 21.8 (6.3) |
| Mean consumption in previous 28 days (units) (SD) | 131.6 (132.0) | 77.6 (113.3) | 133.0 (134.3) | 78.7 (115.7) |
| Proportion of total units consumed during binge-drinking sessions (> 8 units of alcohol) (%) | 92.3 | 61.8 | 92.5 | 64.2 |
The mean consumption of alcohol in the previous 28 days also fell substantially and by similar amounts in the two groups: 54.0 units in the intervention group and 54.3 units in the control group (see Table 15). The fall in mean consumption occurred through falls in the frequency of binge drinking and reductions in the amount consumed in binge-drinking sessions. Individuals differed in the way in which their consumption changed (Table 16). Thus, two-thirds of the 192 men who drank > 150 units of alcohol at baseline reduced their consumption at follow-up, and 60 of these men reduced to ≤ 50 units of alcohol. Among the men who drank between 50 and 100 units, a few (n = 38), increased their consumption, but most (n = 164), reduced their consumption. Overall, at every category of baseline alcohol consumption, most men had reduced their consumption at follow-up. Approximately 10% of the men in each category reduced their consumption to zero.
| Baseline: participants’ consumption in previous 28 days (units) | First follow-up: participants’ consumption in previous 28 days (units) | Total (units) | ||||
|---|---|---|---|---|---|---|
| 0 | ≤ 50 | > 50–100 | > 100–150 | > 150 | ||
| ≤ 50 | 19 | 85 | 18 | 7 | 5 | 134 |
| > 50–100 | 25 | 139 | 67 | 23 | 15 | 269 |
| > 100–150 | 12 | 61 | 38 | 16 | 15 | 142 |
| > 150 | 17 | 43 | 42 | 29 | 61 | 192 |
| Total | 73 | 328 | 165 | 75 | 96 | 737 |
Loss to follow-up
The drinking patterns at baseline among those lost to follow-up was explored to identify whether or not bias could have been introduced. Table 17 shows that those lost to follow-up in the two groups had very similar drinking patterns at baseline and none of the differences approached statistical significance. Although there are small differences between the treatment groups, these sometimes favour one group and sometimes favour the other.
| Factor | Group | Total (N = 88), mean (SD) | p-value | |
|---|---|---|---|---|
| Intervention (N = 45) | Control (N = 43) | |||
| Percentage of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) | 91.1 | 88.4 | 89.8 | 0.672a |
| Percentage of men with ≥ 3 occasions of binge drinking (> 16 units of alcohol) | 48.9 | 51.2 | 50.0 | 0.831a |
| Mean consumption in previous 28 days (units) (SD) | 145.0 (138.6) | 150.8 (122.0) | 147.8 (130.0) | 0.835b |
| Proportion of total units that are consumed during binge-drinking sessions (> 8 units of alcohol), % (SD) | 93.1 (14.4) | 93.2 (18.0) | 93.1 (16.2) | 0.977b |
| Mean number of binge-drinking sessions (> 8 units of alcohol) (SD) | 6.71 (5.1) | 7.28 (5.3) | 6.99 (5.2) | 0.611b |
| Mean number of heavy binge-drinking sessions (> 16 units of alcohol) (SD) | 3.33 (4.4) | 3.98 (4.9) | 3.65 (4.6) | 0.517b |
| Mean number of alcohol-free days (SD) | 19.64 (5.9) | 19.40 (5.8) | 19.52 (5.8) | 0.843b |
| Frequency of being unable to remember what happened the night before because of drinking, n (%) | ||||
| Never | 25 (55.6) | 26 (60.5) | 51 (58.0) | 0.283a |
| Less than monthly | 15 (33.3) | 9 (20.9) | 24 (27.3) | |
| Monthly | 4 (8.9) | 8 (18.6) | 12 (13.6) | |
| Weekly or more | 1 (2.2) | 0 (0.0) | 1 (1.1) | |
The men who were not followed up differed slightly in their drinking patterns from those who were followed up (Table 18). Those not followed up were more likely to have ≥ 3 binge, and heavy binge, drinking sessions. Their mean alcohol consumption was also higher. However, although the direction of effect is consistent, all of these differences were small and none was statistically significant.
| Factor | Followed up | p-value | |
|---|---|---|---|
| No (N = 88) | Yes (N = 737) | ||
| Percentage of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) | 89.8 | 83.7 | 0.139a |
| Percentage of men with ≥ 3 occasions of binge drinking (> 16 units of alcohol) | 50.0 | 47.2 | 0.621a |
| Mean consumption in previous 28 days (units) (SD) | 147.8 (130.0) | 132.3 (133.1) | 0.301b |
| Proportion of total units consumed during binge-drinking sessions (> 8 units of alcohol), % (SD) | 93.1 (16.2) | 92.4 (15.8) | 0.702b |
| Mean number of binge-drinking sessions (> 8 units of alcohol) (SD) | 6.99 (5.2) | 6.53 (5.2) | 0.439b |
| Mean number of heavy binge-drinking sessions (> 16 units of alcohol) (SD) | 3.65 (4.6) | 3.56 (8.4) | 0.878b |
| Mean number of alcohol-free days (SD) | 19.52 (5.8) | 19.92 (5.9) | 0.546b |
| Frequency of being unable to remember what happened the night before because of drinking, n (%) | |||
| Never | 51 (58.0) | 451 (61.2) | 0.175a |
| Less than monthly | 24 (27.3) | 211 (28.6) | |
| Monthly | 12 (13.6) | 54 (7.3) | |
| Weekly or more | 1 (1.1) | 21 (2.8) | |
The men who were not followed up differed markedly from those followed up in terms of their demographic characteristics (Table 19). Thus, a substantially larger proportion of those lost to follow-up were single, were unemployed or had lower educational attainment. They were also, on average, younger and were much more likely to have been recruited by TSS. All of these differences were statistically significant.
| Characteristic | Followed up, n (%) | p-value | |
|---|---|---|---|
| No (N = 88) | Yes (N = 737) | ||
| Age (years), mean (SD) | 32.3 (5.1) | 34.9 (5.4) | < 0.001a |
| Recruitment method | |||
| General practice registers | 24 (27.3) | 403 (54.7) | < 0.001b |
| TSS | 64 (72.7) | 334 (45.3) | |
| Marital statusc | |||
| Married/lives with a partner | 32 (36.4) | 416 (56.5) | < 0.001b |
| Single | 56 (63.6) | 320 (43.5) | |
| SIMD decile | |||
| 1–2 (most deprived) | 59 (67.0) | 577 (78.3) | 0.018b |
| ≥ 3 | 29 (33.0) | 160 (21.7) | |
| Employment status | |||
| Employed | 29 (33.0) | 499 (67.7) | < 0.001b |
| Unemployed | 59 (67.0) | 238 (32.3) | |
| Highest educational attainment | |||
| High school | 57 (64.8) | 453 (61.5) | 0.027b |
| Vocational qualification/further training | 30 (34.1) | 214 (29.0) | |
| University degree | 1 (1.1) | 70 (9.5) | |
Discussion
This chapter has presented the results of the interim follow-up. Only two secondary outcome measures were prespecified in the protocol to be assessed at this follow-up. As such, it would be inappropriate to draw conclusions about effectiveness at this stage. However, these analyses found that, at the interim follow-up, the differences between treatment groups on all measures of alcohol consumption (amounts consumed and frequency of binge drinking) were small. Conventional alcohol brief interventions in primary care show a difference in the frequency of binge drinking of 11% and a difference in mean consumption of 10%. 5 In contrast, the differences seen in this interim analysis are much smaller.
The most striking finding from these analyses was the large fall in all measures of alcohol consumption seen in both groups. Large falls are often seen in the control groups of trials of alcohol brief interventions. 135,161 Possible explanations for these falls will not be explored here. Instead, a thorough review of possible explanations for the findings from the interim and final follow-up analyses will be presented in Chapter 8.
The retention rate was high at 3 months post intervention. This could be a consequence of the use of several evidence-based techniques such as financial incentives, maintaining regular contact, and multiple methods of and attempts at contact. It is notable that during the process of getting in touch only two men requested not to be contacted again, suggesting that the multiple attempts caused little or no inconvenience to the participants.
The possibility of bias due to loss to follow-up in the interim analyses is low. Loss to follow-up in this study was low in comparison with that found in conventional brief interventions in which outcomes were measured 6 months after baseline. 5 Retention rates were high and almost identical in the two treatment arms. Furthermore, those lost to follow-up in the two treatment arms were almost identical in their levels of baseline alcohol consumption. Finally, those who completed this follow-up had broadly similar levels of alcohol consumption at baseline to those who were not followed up. These findings suggest that loss-to-follow-up bias is unlikely to be an explanation for the similarity in groups at the interim follow-up.
The men who were lost to follow-up were markedly different in terms of demographic characteristics from those retained in the study. This suggests that mechanisms other than heavy alcohol consumption may be responsible for the loss of these men. One possibility is that two related factors, life stresses and low income, explain the loss to follow-up.
Chapter 7 Final follow-up
Introduction
The final follow-up took place 12 months after the end of the intervention, which was 15 months after the baseline assessment. This chapter presents the analysis of all of the primary and secondary outcomes. This includes those measured at 12 months post intervention: ≥ 3 occasions of binge drinking (> 8 units of alcohol in a session), mean consumption of alcohol (units over 28 days), ≥ 3 occasions of heavy binge drinking (> 16 units of alcohol in a session) and a score of > 7 on the AUDIT. 137 It also covers those measured at 3 months post intervention: ≥ 3 occasions of binge drinking (> 8 units of alcohol in a session) and ≥ 3 occasions of heavy binge drinking. Only the fitted regression models and treatment effects are presented for the outcomes measured at 3 months post intervention. The chapter also investigates whether or not loss to follow-up bias could have affected the estimates of treatment effect. Exploratory analyses are also conducted to determine whether factors such as recall of the text messages or perceived benefits of study participation could help explain the findings on effectiveness. The results for the economic analysis are presented in Chapter 9.
Results
Of the 825 men who were randomised, 707 were followed up at 12 months post intervention. Complete data were obtained for all men, except for three on whom only data on alcohol consumption were collected (note that these three men did not complete the AUDIT). The retention rate at 12 months was 85.6%, only slightly lower than the retention rate of 89.3% at the first follow-up. The retention rates at 12 months were similar in the two treatment arms: 84.9% in the intervention group and 86.5% in the control group. There was considerable overlap in follow-up status at 3 and 12 months (Table 20), with 687 (83%) men being followed up on both occasions. However, of the 737 men who were followed up at 3 months, 50 (6.8%) were not followed up at 12 months, and of the 88 men not followed up at 3 months, 20 (22.7%) were followed up at 12 months.
| Followed up at 3 months | Followed up at 12 months | ||
|---|---|---|---|
| Yes | No | Total | |
| Yes | 687 | 50 | 737 |
| No | 20 | 68 | 88 |
| Total | 707 | 118 | 825 |
Substantial falls were seen on all measures of alcohol consumption. For all participants, the proportion of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol in a session) fell from 83.7% to 44.7%. The mean consumption of alcohol (units over 28 days) also fell substantially, from 128.8 to 78.3 units.
Descriptive analysis of the primary and secondary outcomes measured at 12 months post intervention
Simple tabulations
Table 21 presents the baseline and final follow-up data for the intervention and control groups. The primary outcome for the trial was the proportion of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol in a session). At final follow-up, the difference in the proportion of men meeting this criterion was higher, by 6.3%, in the control group than in the intervention group. The absolute fall from baseline in the proportion of men meeting this criterion was 40.7% in the intervention group and 37.4% in the control group (see Table 21).
| Factor | Group | |||
|---|---|---|---|---|
| Intervention | Control | |||
| Baseline (N = 349) | 12-month follow-up (N = 349) | Baseline (N = 358) | 12-month follow-up (N = 358) | |
| Percentage of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) | 82.2 | 41.5 | 85.2 | 47.8 |
| Percentage of men with ≥ 3 occasions of heavy binge drinking (> 16 units of alcohol)a | 45.8 | 17.5 | 46.9 | 18.7 |
| Mean number of binge-drinking sessions (> 8 units of alcohol) (SD) | 6.25 (4.9) | 3.62 (5.1) | 6.66 (5.4) | 4.07 (5.7) |
| Mean number of heavy binge-drinking sessions (> 16 units of alcohol) (SD) | 3.40 (4.7) | 1.84 (4.4) | 3.51 (4.7) | 1.70 (4.0) |
| Mean number of alcohol-free days (SD) | 20.2 (5.6) | 21.8 (6.2) | 19.8 (5.9) | 21.5 (7.0) |
| Mean consumption in previous 28 days (units) (SD) | 125.1 (120.4) | 77.2 (119.8) | 132.4 (135.4) | 79.4 (120.0) |
| Proportion of total units consumed during binge-drinking sessions (> 8 units of alcohol) (%) | 92.4 | 60.2 | 92.3 | 63.3 |
The secondary outcomes for alcohol consumption were the proportion of men with ≥ 3 heavy binge-drinking sessions (> 16 units of alcohol in a session) and total alcohol consumption over 28 days. The falls from baseline in the frequencies of heavy binge drinking were almost identical: the intervention group showed a fall of 28.3% and the control group showed a fall of 28.2%.
The fall in mean consumption of alcohol over 28 days in the intervention group was 47.9 units, which was slightly smaller than the fall of 53 units seen in the control group. The mean fall in consumption conceals considerable variation between individuals (Table 22). The majority of men (57.6%) moved to a lower consumption group, many (30.7%) stayed in the same consumption group and a few (11.7%) moved to a higher consumption group.
| Distribution of baseline consumption (units)a | Men in consumption categories at final follow-upa (n) | ||||
|---|---|---|---|---|---|
| 0 units | ≤ 50 units | > 50–100 units | > 100–150 units | > 150 units | |
| ≤ 50 | 20 | 82 | 22 | 3 | 5 |
| > 50–100 | 31 | 116 | 70 | 21 | 21 |
| > 100–150 | 15 | 47 | 53 | 13 | 11 |
| > 150 | 17 | 52 | 31 | 25 | 52 |
The final secondary outcome measured at 12 months post intervention was the proportion of men with a score of > 7 on the AUDIT. Scores of > 7 are indicative of hazardous or harmful drinking; 72.6% were AUDIT positive in the intervention group and 68.3% were positive in the control group. For completeness, the distribution of AUDIT scores in the two treatment arms is shown in Table 23. The mean AUDIT scores in the two treatment arms were also similar: 10.96 in the intervention group and 10.97 in the control group.
| Total AUDIT score at final follow-up | Group, n (%) | Total (N = 704),a n (%) | |
|---|---|---|---|
| Intervention (N = 347) | Control (N = 357) | ||
| 0–7 | 95 (27.4) | 113 (31.7) | 208 (29.5) |
| 8–15 | 190 (54.8) | 177 (49.6) | 367 (52.1) |
| 16–19 | 33 (9.5) | 36 (10.1) | 69 (9.8) |
| 20–40 | 29 (8.4) | 31 (8.7) | 60 (8.5) |
The potential bias from loss to follow-up
Three sets of analyses were conducted to assess whether or not loss to follow-up could have influenced the observed outcomes at 12 months post intervention. The first compared the baseline drinking of the men in each treatment group who were subsequently lost to follow-up (Table 24). The two treatment groups were similar on all measures of alcohol consumption, with none of the differences approaching statistical significance.
| Factor | Group | Total (N = 118), % | p-value | |
|---|---|---|---|---|
| Intervention (N = 62) | Control (N = 56) | |||
| Percentage of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol) | 88.7 | 87.5 | 88.1 | 0.839a |
| Percentage of men with ≥ 3 occasions of heavy binge drinking (> 16 units of alcohol) | 50.0 | 58.9 | 54.2 | 0.331a |
| Mean consumption in previous 28 days (units) (SD) | 177.6 (182.2) | 151.0 (116.5) | 165.0 (154.4) | 0.351b |
| Proportion of total units consumed during binge-drinking sessions (> 8 units of alcohol) (%) | 92.4 | 94.0 | 93.1 | 0.569a |
| Frequency of being unable to remember what happened the night before because of drinking, n (%) | ||||
| Never | 39 (62.9) | 38 (67.9) | 77 (65.3) | 0.371a |
| Less than monthly | 16 (25.8) | 13 (23.2) | 29 (24.6) | |
| Monthly | 4 (6.5) | 5 (8.9) | 9 (7.6) | |
| Weekly or more | 3 (4.8) | 0 (0.0) | 3 (2.5) | |
The second analysis of the impact of loss to follow-up compared the baseline consumption of the men who were followed up at 12 months with that of those who were not followed up at 12 months (Table 25). This shows that those not followed up had slightly higher frequencies of binge drinking, had a higher mean consumption and had fewer alcohol-free days. Although only the mean consumption showed a significant difference, it seems likely that more heavier drinkers were lost to follow-up.
| Factor | Followed up | p-value | |
|---|---|---|---|
| No (N = 118) | Yes (N = 707) | ||
| Percentage of men with ≥ 3 occasions of binge drinking (> 8 units) | 88.1 | 83.7 | 0.223a |
| Percentage of men with ≥ 3 of heavy binge drinking (> 16 units) | 54.2 | 46.4 | 0.114a |
| Mean number of alcohol-free days | 19.1 (6.5) | 20.0 (5.7) | 0.108b |
| Mean consumption in previous 28 days (units) (SD) | 165.0 (154.4) | 128.8 (128.2) | 0.017b |
| Proportion of total units consumed during binge-drinking sessions (> 8 units) (%) | 93.1 | 92.4 | 0.632a |
| Frequency of being unable to remember what happened the night before because of drinking, n (%) | |||
| Never | 77 (65.3) | 425 (60.1) | 0.751a |
| Less than monthly | 29 (24.6) | 206 (29.1) | |
| Monthly | 9 (7.6) | 57 (8.1) | |
| Weekly or more | 3 (2.5) | 19 (2.7) | |
The final assessment of the impact of loss to follow-up compared the demographic characteristics at baseline of men who were followed up with those of men who were not followed up (Table 26). This showed that over three-quarters of those not followed up had been recruited by TSS. Furthermore, those not followed up were more likely to be single, to be unemployed and to have had only high school education. All of the differences, except for age, were highly statistically significant.
| Factor | Followed up, n (%) | p-valuea | |
|---|---|---|---|
| No (N = 118) | Yes (N = 707) | ||
| Recruitment method | |||
| General practice registers | 28 (23.7) | 399 (56.4) | < 0.001 |
| TSS | 90 (76.3) | 308 (43.6) | |
| Age group (years) | |||
| 25–29 | 34 (28.8) | 167 (23.6) | 0.549 |
| 30–34 | 35 (29.7) | 200 (28.3) | |
| 35–39 | 27 (22.9) | 189 (26.7) | |
| 40–44 | 22 (18.6) | 151 (21.4) | |
| Marital statusb | |||
| Married/lives with a partner | 48 (40.7) | 400 (56.7) | 0.001 |
| Single | 70 (59.3) | 306 (43.3) | |
| SIMD decile | |||
| 1–2 (most deprived) | 79 (66.9) | 557 (78.8) | 0.005 |
| ≥ 3 | 39 (33.1) | 150 (21.2) | |
| Employment status | |||
| Employed | 44 (37.3) | 484 (68.5) | < 0.001 |
| Unemployed | 74 (62.7) | 223 (31.5) | |
| Highest educational attainment | |||
| High school | 89 (75.4) | 421 (59.5) | < 0.001 |
| Vocational qualification/further training | 29 (24.6) | 215 (30.4) | |
| University degree | 0 (0.0) | 71 (10.0) | |
Model fitting and treatment effects
Primary outcome
Logistic regression was used to estimate the treatment effect. Three models were fitted: (1) no adjustment, (2) adjustment for baseline binge drinking only and (3) full adjustment for baseline covariates (Table 27). All produced similar estimates of treatment effect. The primary outcome measure showed a modest, statistically non-significant reduction in the frequency of binge drinking in the intervention group compared with the control group. For the fully adjusted model, which was the one prespecified in the statistical analysis plan, the estimate was 0.79 (95% CI 0.57 to 1.08; p = 0.14). This corresponds to a net reduction of 5.7% in the proportion of men who binge drink on ≥ 3 occasions (95% CI –13.3% to 1.9%). The CIs indicate that there is considerable uncertainty in the estimate of the treatment effect. Multiple imputation was conducted to take account of men lost to follow-up. The treatment effect was very similar to that for the fully adjusted model, giving an OR of 0.77 (95% CI 0.55 to 1.09; p = 0.143).
| Model, OR (95% CI) | p-valueb | |||
|---|---|---|---|---|
| Unadjusted | Adjusted for baseline drinking | Fully adjusted | ||
| Primary outcome | ||||
| % > 8 units on ≥ 3 occasions at 12 months (n = 347, 358)c | 0.78 (0.58 to 1.05) | 0.79 (0.59 to 1.07) | 0.79 (0.57 to 1.08) | 0.140 |
| Secondary outcomes | ||||
| % > 8 units on ≥ 3 occasions at 3 months (n = 364, 371)c | 1.00 (0.75 to 1.34) | 1.04 (0.77 to 1.40) | 1.05 (0.77 to 1.44) | 0.751 |
| % > 16 units on ≥ 3 occasions at 3 months (n = 364, 371)c | 1.12 (0.79 to 1.60) | 1.17 (0.81 to 1.70) | 1.22 (0.83 to 1.81) | 0.314 |
| % > 16 units on ≥ 3 occasions at 12 months (n = 347, 358)c | 0.92 (0.63 to 1.35) | 0.93 (0.62 to 1.38) | 0.97 (0.64 to 1.46) | 0.871 |
| % AUDIT positived (n = 345, 357)c | 1.23 (0.89 to 1.70) | 1.28 (0.92 to 1.78) | 1.34 (0.95 to 1.89) | 0.095 |
| Mean difference (95% CI) in consumption at 12 months (n = 347, 358)c | –2.18 (–19.49 to 15.13) | 4.66 (–10.10 to 19.42) | 4.46 (–11.1 to 20.03) | 0.573 |
A prespecified subgroup analysis examined the effect of recruitment method on the primary outcome. The baseline data (see Chapter 4) showed large differences in demographic characteristics and alcohol consumption between men recruited from general practice registers and those recruited by TSS. For the group recruited from general practice registers, the net reduction in the proportion of men who binge drink on ≥ 3 occasions was 8.6% (95% CI –18.7% to 1.5%), whereas the reduction was much lower for the TSS group: 2.1% (95% CI –13.5% to 9.4%).
All secondary outcomes (at 3 months and 12 months post intervention)
Logistic regression models were also fitted for the four binary secondary outcomes (see Table 27). The intervention group showed small relative increases in the frequencies of binge drinking (> 8 units on ≥ 3 occasions) and heavy binge drinking (> 16 units on ≥ 3 occasions) at the 3-month follow-up. At the 12-month follow-up there was a small relative reduction in the frequency of heavy binge drinking. The frequency of hazardous or harmful drinking, as measured by the AUDIT, was slightly higher in the intervention group. The CIs for all binary variables were wide and none of the p-values approached statistical significance.
An analysis of total alcohol consumption over 28 days (at 12 months post intervention) using the generalised linear gamma model showed that, in the absence of any baseline adjustments, the intervention group had a lower level of consumption. However, this was reversed when adjustment was made for baseline consumption and for the other baseline covariates. The effect of intervention on this secondary outcome was not significant and the small fluctuations in treatment effects across the three models were most likely due to chance.
Summary of the treatment effects
The primary outcome showed a modest, statistically non-significant benefit of the intervention, which translates to a 5.7% reduction in the frequency of binge drinking. This is approximately half of the hypothesised value (11%) that was used as the basis for the sample size calculation. A prespecified analysis showed that the net reduction was larger in men recruited from general practice registers (8.6%) than in those recruited by TSS (2.1%). One secondary outcome shows a small benefit of the intervention but others suggest a small benefit for the control. None of these effects is statistically significant. The treatment effects are clustered around the value for no effect of the intervention and all have wide CIs.
Other measures of the impact of the intervention
Four questions from a drinking refusal self-efficacy questionnaire162 were used to assess the participants’ perceived ability to resist drinking. These revealed high or moderately high perceived self-efficacy, but with small, non-significant and consistent differences in favour of the intervention group (Table 28).
| Self-efficacy statement | Group, n (%) | p-valuea | |
|---|---|---|---|
| Intervention (N = 349) | Control (N = 357) | ||
| Able to resist alcohol | |||
| When you are watching TV | 336 (96.8) | 340 (95.2) | 0.119 |
| When someone offers you a drink | 302 (87.0) | 295 (82.6) | 0.401 |
| When your friends are drinking | 252 (72.6) | 255 (71.4) | 0.927 |
| When you are bored | 304 (87.6) | 311 (87.1) | 0.334 |
In response to a further question about whether or not they had tried to reduce their drinking, significantly more men in the intervention group said that they had tried to reduce their alcohol consumption (63.7% vs. 55.5%; p = 0.027). Table 29 shows that men who reported trying to drink less had reduced their alcohol consumption much more than men who said that they had not tried. The effects are similar in the two groups, although the fall in the frequency of binge drinking is greater in the intervention group and the fall in mean consumption is greater in the control group.
| Intervention group: reported attempting to reduce | Control group: reported attempting to reduce | |||
|---|---|---|---|---|
| Yes (n = 221) | No (n = 126) | Yes (n = 197) | No (n = 158) | |
| Change in binge drinking (%)a | –46.2 | –30.2 | –41.1 | –32.3 |
| Change in mean consumption (units) | –61.4 | –24.1 | –74.0 | –27.5 |
Participant recall of the content of the intervention (or control) text messages was assessed by a series of open questions. No prompting of specific issues was given and participants could give no answer, one answer or more than one answer. In response to a general question about what they remembered, substantially more men in the intervention group remembered the characters in the text messages (Table 30). The control group were more likely to give no answer, to remember the texts that asked questions or to say simply that they liked the messages.
| Question | Group (n) | Total (N) | |
|---|---|---|---|
| Intervention | Control | ||
| Thinking back to the text messages you received, what do you remember about them? | |||
| Remember nothing about the messages | 43 | 70 | 113 |
| Remember the characters’ experiences | 225 | 76 | 301 |
| Liked the messages | 51 | 142 | 193 |
| They made me think | 24 | 6 | 30 |
| The questions asked | 55 | 83 | 138 |
| Other | 18 | 43 | 61 |
Participants were also asked whether or not they found the comments from the characters helpful. Slightly more men in the intervention group (231, 67%) than in the control group (211, 59%) responded ‘yes’. Among those making a positive response, more men in the intervention group cited engagement with the narrative or increased awareness of alcohol consumption as their reason (Table 31). In contrast, those in the control group were more likely to say that they enjoyed the study or that it made them think in general.
| Comment | Group (n) | Total (N) | |
|---|---|---|---|
| Intervention | Control | ||
| Made them aware of, or think about, their alcohol consumption | 63 | 22 | 85 |
| Raised awareness, or made them think in general | 36 | 52 | 88 |
| Engaged with the narrative or other people’s views | 86 | 12 | 98 |
| Enjoyment or appreciation of the study | 18 | 53 | 71 |
| Other/nothing specific | 49 | 74 | 123 |
About three-quarters of the participants said that they had benefited from participating in the study, with almost exactly the same number in the intervention (275, 79.3%) and control (273, 76.5%) groups. However, more men in the intervention group reported as benefits an increased awareness of drinking or of having reduced or stopped drinking (Table 32).
| Reported benefit | Group (n) | Total (N) | |
|---|---|---|---|
| Intervention | Control | ||
| Raised awareness of, or made them think about, their alcohol intake | 134 | 102 | 236 |
| Stopped or reduced drinking | 43 | 30 | 73 |
| Raised awareness, or made them think in general | 37 | 58 | 95 |
| Financial benefits (gift vouchers) | 19 | 17 | 36 |
| Enjoyment or appreciation of the study | 18 | 49 | 67 |
| Engaged with the narrative | 24 | 7 | 31 |
| Other/nothing specific | 31 | 36 | 67 |
The acceptability of the study methods was assessed by four indirect questions that assessed the participants’ experiences of the study (Table 33). Almost all participants enjoyed taking part and would recommend the study to other people, and about four-fifths discussed the study with friends or family. Fewer participants, about half, showed the text messages to others, possibly because text messages are considered personal. The intervention and control groups gave similar levels of response.
| Question | Group, n (%) | Total, n (%) | |
|---|---|---|---|
| Intervention | Control | ||
| Discussed the study with others | 290 (83.8) | 278 (77.9) | 568 (80.8) |
| Showed the text messages to others | 172 (49.7) | 201 (56.8) | 373 (53.3) |
| Enjoyed taking part in the study | 336 (99.1) | 349 (99.7) | 685 (99.4) |
| Would recommend the study to others | 328 (95.3) | 344 (97.5) | 672 (96.4) |
Adverse events
Three serious adverse events (deaths) occurred during the study. Two of the deaths occurred while the participants were in the intervention phase of the study and one occurred after the first follow-up interview had been completed. No information on the circumstances of the deaths were received. However, there was no reason to suspect that participation in the study could have contributed to the participants’ deaths in any way. All serious adverse events were reported to the ethics committee.
Discussion
The five main findings from this chapter are that (1) the retention rate was high; (2) the intervention had a modest, statistically non-significant effect on the primary outcome; (3) the treatment effect was much larger in men recruited from general practice registers than in those recruited by TSS; (4) the secondary outcomes on consumption at final follow-up showed inconsistent results, one with a small (non-significant) advantage to the intervention group, the other four with small (non-significant) advantages to the control group; and (5) there were large falls in alcohol consumption in both groups. Other key findings from the analyses are as follows: the acceptability of the study methods was high; the large differences found in the recall of the text messages reflected the differences in the content of the text messages received; and differences were seen between treatment groups in the perceived benefits of study participation.
The discussion of the findings on the effectiveness of the intervention needs to take into account the findings from other chapters, particularly the chapters on the interim follow-up and the evaluation of the text message responses. Thus, it is covered in a subsequent chapter (see Chapter 8), which reviews all relevant findings, and the wider literature, to explore the interpretation of the treatment effects and their implications.
The only statistically significant difference between the intervention and control groups was in the proportion of men who reported having attempted to reduce their drinking. This finding has to be treated with caution because it was not a prespecified outcome measure and could simply be a consequence of multiple statistical significance testing. It also presents a numerical challenge. More men in the intervention group said that they had tried to reduce their consumption. Furthermore, men who said that they had tried to reduce their consumption had reduced their drinking more than men who said they had not tried. This would imply that the intervention group should have lower alcohol consumption. The explanation is that in the control group the men who said that they had tried to reduce their consumption did so to a greater extent than the equivalent men in the intervention group. Their greater reduction in consumption compensates for their smaller number.
Retention
The retention rate of 86% was high, particularly for a study of disadvantaged men. It is much higher than that seen in most previous brief interventions. The Cochrane review of brief interventions in primary care by Kaner et al. 5 found that the average retention rate was 73%. Furthermore, in the present study, retention was almost identical in the two treatment arms, suggesting that loss to follow-up bias would be low. In contrast, conventional alcohol brief intervention trials show, on average, a significantly higher loss to follow-up in the intervention group. 5 Possibly the use of a financial incentive, £10 each for the two follow-up interviews, aided retention.
Acceptability of study methods
The high acceptability of the study methods is consistent with an overt aim of the study design: to make participation as easy and enjoyable as possible. The use of financial incentives may also have contributed to the acceptability. It seems likely that the high retention rate is due to this level of acceptability. This finding has obvious implications for other studies targeting socioeconomically disadvantaged groups: use incentives and make participation as simple, enjoyable and worthwhile as possible.
Recall of the text messages
Similar numbers of men in the intervention and control groups recalled the content of the text messages. However, the details of what was recalled differed greatly between the treatment arms: the intervention group remembered specifics about the content and characters in the text messages, and being made to think about their drinking. In contrast, the control group’s recollections tended to be phrased in general terms, most often saying that they liked the messages. The important point about the differences in recollection is that they were sustained at 12 months after the messages stopped, indicating the strength of the impact of the text messages.
Impact of participating in the study
There was some evidence that the intervention group had thought more about their drinking and were more likely to have attempted to reduce their consumption. These reports did not translate into lower consumption than in the control group.
An unexpected finding was that many men in the control group reported that participating in the study made them think about their alcohol intake. Although more men in the intervention group gave this response, the reports from the control group need an explanation, particularly because alcohol was not mentioned in the control text messages. Possibly the detailed questions on alcohol, which were asked at the beginning of the interview, influenced replies to later questions. The men may have been attempting to please the researchers conducting a study on alcohol. This is the phenomenon of demand characteristics,163 which holds that participants in studies often try to please researchers. If this did occur in the control group, then an effect of similar size might be expected in the intervention.
In summary, the intervention had a modest statistically non-significant effect on the primary outcome and small inconsistent and non-significant effects on the secondary outcomes. There was considerable uncertainty in the estimates of the treatment effect. Interventions with disadvantaged individuals commonly have much smaller treatment effects than studies in the general population. Further research is needed to reduce the uncertainty around the treatment effect.
Chapter 8 Explanations for the major findings at follow-up
Introduction
Two main findings emerged from the analysis of the primary and secondary outcomes: that large falls occurred in alcohol consumption in both intervention and control groups; and that the intervention had a modest and statistically non-significant effect on the primary outcome and inconsistent and small non-significant effects on the secondary outcomes. This chapter explores these findings in depth, drawing on results from across the study and the wider literature. It explores possible methodological weaknesses and sources of bias to clarify whether or not these could help to explain the observed results.
Possible explanations for the fall in alcohol consumption
Large falls in consumption are commonly seen in control groups in trials of alcohol brief interventions. 135,161 The fall in consumption seen in the control group in this study is large, at the upper end of the magnitude of falls identified in reviews of control group effects. 135,161 It is, thus, unusually but not exceptionally large.
The sustained nature of the fall
Any explanation(s) for the fall would need to account for the sustained nature of the fall: the mean falls from baseline at the 3-month and the 12-month follow-ups were almost identical. Furthermore, at these two follow-ups the overall levels of consumption were similar. Three trials of alcohol brief interventions have included two follow-up assessments at times comparable with those in this study. Curry et al. 164 and Reiff-Hekking et al. 165 showed large sustained falls in the frequency of binge drinking and in the mean consumption in both intervention and control groups; Richmond et al. 166 did not report on binge drinking but showed large sustained falls in mean consumption.
Several possible explanations for the sustained fall in this study were considered. These include regression to the mean,167 social desirability bias,168 research participation effects,169 demand characteristics,163 contemporaneous change in alcohol consumption and self-selection bias.
Regression to the mean
Individuals who are selected for a study because they have a high value on a measure (such as alcohol consumption) will, on average, have a lower value when measured on a subsequent occasion. 170–173 This phenomenon, regression to the mean, will affect all trials that use a high value of a measure (e.g. alcohol consumption) as an entry criterion. An empirical demonstration of this in a cohort study showed that the size of the fall in AUDIT score increased progressively as the threshold for entry was increased. 174
The present study selected men who had a least two binge-drinking sessions in the previous 28 days, so some fall in alcohol consumption would be expected. Furthermore, it would result in a sustained fall. Thus, at least some of the observed fall in alcohol consumption in the intervention and control groups will be due to this phenomenon. The question is how much of the reduction is due to it, and whether or not an additional explanation needs to be sought for the full size of the fall.
We replicated the empirical study of McCambridge et al. ,174 who investigated the potential effects of regression to the mean by setting different entry criteria. The replication used data from the first follow-up and the final follow-up and included only those men who completed both follow-ups (n = 687). Three types of entry criteria were applied to the participants at the first follow-up: no criterion, a minimum of two binge-drinking sessions in the previous 28 days (criterion 1) and a minimum of three binge-drinking sessions in the previous 28 days (criterion 2). This was carried out separately for two measures of alcohol consumption: the percentage of men with ≥ 3 occasions of binge drinking (> 8 units of alcohol in a session) and mean consumption over 28 days. With no entry requirement, there was little change in alcohol consumption between the first and second follow-ups (Table 34). The application of criterion 1 resulted in a fall in both measures of alcohol consumption. Criterion 2 produced much larger falls in the alcohol consumption measures. However, even these larger falls were not as great as those seen in this study between baseline and final follow-up: the actuals falls were –33.6% (proportion of men with ≥ 3 occasions of binge drinking) and –50.5 units of alcohol. To put this into context, criterion 1 was the one used for selecting men for entry into this trial. To the extent that this analysis reflects what happened at recruitment, it suggests that regression to the mean can explain only a part of the observed fall between baseline and final follow-up. This is consistent with the empirical study of McCambridge et al. ,174 which showed that regression to the mean has only modest effects unless a very high bar to entry is imposed.
| Eligibility criteria (must have been followed up at both 3 and 12 months) | Absolute change in alcohol consumption | |
|---|---|---|
| Men with ≥ 3 binge-drinking sessions (%) | Mean consumption over 28 days (units of alcohol) | |
| No entry criterion (n = 687) | +0.7 | +2.1 |
| Entry criterion 1 (n = 386) | –16.3 | –12.2 |
| Entry criterion 2 (n = 303) | –31.7 | –18.3 |
Social desirability bias
Social desirability bias is the extent to which individuals report their behaviour, for example alcohol consumption, in a way that they think is socially desirable. 168 Participants report what they think is appropriate, acceptable or desired by others. Substantial under-reporting of alcohol consumption in surveys is widely recognised. Much of this is likely to be due to social desirability bias, although part could be due to the incomplete recall of consumption. Self-reported alcohol consumption provides estimates which are only 40–60% of those from data on alcohol sales. Recent data from four English speaking countries show that the survey data account for only between 31% and 57.5% of the alcohol sold. 175 The figure for Scotland is 54%. 176 However, it is unclear how under-reporting would produce the large fall seen from baseline to follow-up. Social desirability bias, or incomplete recall, might be expected to operate to a similar extent at baseline and at the follow-up assessments, and thus might not produce the consistent large falls over time. A more nuanced argument would be that social desirability bias could increase because of participation in the research. This possibility is explored in the next section.
Research participation effects
Concerns about the effects of research participation on the behaviour of study subjects are longstanding. 169,177 In this trial, several study factors could influence participant behaviour: screening and recruitment,178,179 the process of gaining informed consent180 and the administration of the baseline questionnaire. 134,181 In particular, the detailed alcohol history that was taken at baseline interview in this study could have had such an effect. Moos182 has outlined a mechanism by which this could occur: assessment could raise awareness of risky drinking, leading to self-monitoring and to the recognition that consumption is higher than would be wanted. This could increase motivation to change and, thus, lead to reduced drinking. However, a recent overview of reviews134 and a commentary paper183 concluded that the effects of research participation are small and inconsistent, suggesting that they are unlikely to explain the size of falls in consumption seen in this study. Furthermore, Moos182 has suggested that an effect of research participation is likely to be short term and, if so, could not explain the large sustained fall in consumption observed at the 12-month follow-up.
Demand characteristics
Demand characteristics could be viewed as a type of research participation effect or a special type of social desirability bias. It holds that participants in research studies may act in ways that they think will please the researchers. 163 If participants guess the purpose of a study, in this case to reduce alcohol consumption, they may under-report their alcohol consumption to please the researcher. 184 Possibly the magnitude of under-reporting may depend on the amount of benefit participants believe they gained from the research. In this study, where the aim was to reduce alcohol consumption, participant satisfaction was high. This may have encouraged participants to under-report their consumption to a greater extent at follow-up than at baseline. Under this argument, it might expected that the intervention group, who received many text messages about reducing consumption, would have a stronger motivation to under-report their consumption. As the intervention and control groups reported similar large falls in alcohol consumption, demand characteristics may not account for the observed results. McCambridge et al. 184 have also pointed out the paucity of research on this topic outside laboratory settings. Although demand characteristics may have a role, their contribution at present is purely theoretical. In addition, the magnitude of the effect might be expected to attenuate over time, as occurs with most behaviour change interventions. 113 No attenuation of effect was seen between the 3-month and the 12-month follow-ups, suggesting that demand characteristics might not explain the observed falls in consumption.
Contemporaneous changes in alcohol consumption
The baseline data were collected from March to December 2014 and the follow-up interviews were conducted during the period August 2014–February 2016. If national alcohol consumption had fallen from 2014, then part of the fall observed in this study could have been due to contemporaneous change. In fact, alcohol consumption in Scotland (measured by alcohol sales data and self-reports in surveys) fell from 2008 to 2013, rose slightly in 2014176 and rose again in 2015 to the level seen in 2011. 185
Self-selection bias
A very large, high-quality trial (Project MATCH)186 of three treatments for alcoholics found that all three produced very similar outcomes: approximately 30% of participants were abstinent at the 1-year follow-up, and this was sustained at 3 years. A more recent reanalysis of the original data raised the possibility of a different explanation for the abstinence rates. 187 It showed that almost all of the treatment effect had occurred by the first week of the planned 12-week treatment programme. Furthermore, a group of participants who dropped out before receiving any treatment experienced two-thirds to three-quarters of the improvement seen in those who completed the treatment plan. A possible explanation for these findings is that those who ‘decide to enter treatment are likely to reduce their drinking’. 187 In other words, those who are highly motivated to reduce their drinking are more likely to participate in trials. Although Project MATCH was conducted with people with alcoholism, a similar phenomenon could occur among hazardous drinkers. This would explain the large falls in consumption frequently observed in control groups of alcohol brief intervention trials. 135,161 Self-selection would also explain the sustained fall in consumption. At present, selection bias remains a hypothesis that needs to be tested in further research.
In summary, only regression to the mean is capable of explaining a sustained fall in alcohol consumption, but most probably it can only explain part of the observed fall. At present, there is insufficient evidence to conclude whether social desirability, research participation effects or self-selection bias played a role.
Why the intervention had a modest, statistically non-significant effect on the primary outcome
There are several possible explanations for the modest, statistically non-significant effect of the intervention, which can be conveniently grouped as study-specific factors and the nature of the target group. Before exploring these explanations, the results of the present study need to be put into the context of existing and recent research findings, particularly the recent studies on alcohol brief interventions and text message studies to reduce alcohol consumption.
Recent studies on alcohol brief interventions
Evidence from two systematic reviews5,6 shows that alcohol brief interventions are effective, although the effects are small. The reviews found that the proportion of men who engaged in binge drinking (heavy drinking) was reduced by 11%5 and 12%. 6 In contrast, this study found that the net reduction in binge drinking was 5.7%. It also found that the reduction in binge drinking in men recruited through general practice registers was higher (8.6%, 95% CI –18.7% to 1.5%) than in those recruited by TSS (2.1%, 95% CI –13.5% to 9.4%). Both of the reviews5,6 concluded that there was no evidence that brief interventions are effective with dependent drinkers.
Since the publication of these reviews, five large trials7–10,188 of alcohol brief interventions, which found that the intervention was ineffective or possibly harmful, have been published. Three of these trials formed the SIPS (Screening and Intervention Programme for Sensible Drinking) research programme in which the intervention was evaluated in primary care,7 accident and emergency departments8 and criminal justice. 9 All three studies found that the brief intervention was not effective, as the primary outcome was similar in the active treatment and control groups. A separate study10 in primary care found that, at follow-up, the intervention group had a statistically significantly higher alcohol consumption than the control group. Finally, a complex study188 that addressed four risk behaviours (smoking, alcohol use, exercise and healthy eating) found no significant effect on alcohol use. The last of these did report that the intervention increased intentions to change, the number of attempts at change and perceived success in achieving change, but these did not result in measured behaviour change.
Text message studies to reduce alcohol consumption
Several recent studies have explored the use of text messages to tackle hazardous or harmful drinking. Two studies, one with vocational school students81 and the other with mandated college students,189 used an uncontrolled before-and-after design, making it difficult to draw conclusions about effectiveness. Four studies78,190–192 on text messaging were conducted with college students and none showed a significant effect on alcohol consumption. One study190 stated that there was no significant effect of the intervention; another study,192 which intended only to assess feasibility and acceptability, also reported no significant effect on alcohol. The third study191 reported a significant effect in a subgroup, and, finally, a very small study78 reported a significant effect on a secondary outcome measure (readiness to change drinking). A further, large study193 of university students, which compared two smartphone apps with a control group, found that one of the apps significantly increased alcohol consumption.
Text message studies have also been conducted outside the educational environment. One study76 of emergency department attendees claimed that a text message intervention can lead to small reductions in the self-reported number of heavy drinking days and in the number of drinks consumed per drinking day. However, the authors reported that there was differential loss of heavy drinkers at follow-up (more heavy drinkers were lost in the intervention group). After adjustment for the losses by multiple imputation, the intervention effect became non-significant. Finally, a pilot study82 on dependent drinkers found a statistically non-significant difference in favour of the intervention. In summary, although the technology appears to work well, there is a lack of convincing evidence that text messages are effective in reducing alcohol consumption.
Potential limitations of the study
Randomised controlled trials can suffer from problems of design and conduct, which impair their ability to detect the effect of interventions. The following section places particular attention on the biases identified in the Cochrane risk-of-bias tool194 and those for which there is strong evidence of bias. 195 It also follows the recommendation of the Cochrane group and considers those design features of a trial that could have contributed to the inconclusive findings.
Insufficient statistical power
This study was large, much larger than most published trials on alcohol brief interventions. 5,6 The sample size calculation assumed that 20% of men would be lost to follow-up, but in the event only 14% did not complete the final follow-up. Thus, the study had a higher power than was stated in the original protocol. However, the power to detect an effect could have been reduced by the large fall in alcohol consumption seen in the control group (and, by implication, the intervention group), which could increase the variance of the outcome measure.
Lack of blinding of participants to the purpose of the study
If study participants are aware that the purpose of a study is to reduce alcohol consumption, they may under-report their consumption to please the researcher. In this study, participants were told that the research was investigating alcohol and health and that the aim was to identify ways to reduce alcohol consumption. Thus, demand characteristics, or social desirability (described above), could have encouraged them to report a lower alcohol consumption than was the case. This could result in non-differential misclassification of the outcome with the most likely effect of biasing the estimate of treatment effect to the null. 196,197 It is unclear whether this form of bias to the null could explain the study findings. All trials of alcohol brief interventions would have suffered from the same bias, but many detected significant effects of treatment. 5,6
Poor allocation concealment
The nature of the treatment group should be concealed from study participants and from the observers making the baseline and follow-up measurements. In drug trials, blinding of participants can cover the look, taste and smell of the medication. In this study, an attempt was made to conceal treatment status (intervention or control) by providing the two groups with a similar number of text messages. However, the content of the text messages received by the intervention group would have revealed that they were being encouraged to reduce their drinking. This might have resulted in a greatly increased social desirability effect in the intervention group, leading to a greater reduction in their consumption. This was not the case.
Another possibility is that awareness of the purpose of the messages induced psychological reactance,198 reducing social desirability or even encouraging participants to exaggerate their consumption. Neither possibility seems likely because of the similar high level of satisfaction with the study methods found in both groups. Furthermore, the effect would need to be sustained to the 12-month follow-up. This seems unlikely, as the effects of most behavioural interventions attenuate over time. 113
A further feature of allocation concealment is that the researchers making the baseline and outcome measurements should be blind to the participants’ treatment status. Randomisation in this study was by a remote web-based system to which none of the researchers had access, and so they remained unaware of treatment allocation while the outcomes were being measured.
Data collection methods
One limitation of this study is that it used self-reported alcohol consumption, which could be influenced by social desirability bias. 168 The validity of self-reports of alcohol consumption is a longstanding concern of researchers. There was a consensus that self-report methods provide a reliable and valid way of measuring alcohol consumption. 199 However, more recent studies have drawn attention to the importance of measuring the strength and volume of drinks132,133 and episodes of binge drinking. 200 Thus, we modified the data collection method, timeline follow back,130 to collect detailed information in order to increase the accuracy of the estimates of alcohol consumption.
A change in data collection methods between baseline and follow-up might have influenced the results. Efforts were made to minimise this through staff training and ensuring regular contact between research staff to ensure a consistent approach. The data on alcohol consumption were collected using the same questions at the baseline and follow-up interviews.
Loss to follow-up
Alcohol brief intervention studies commonly have average loss to follow-up rates of 27%, with a significantly higher loss to follow-up in the intervention group. 5 It is suggested that a loss to follow-up of > 20% gives rise to concern. 201,202 In this study, loss to follow-up was 14% and almost identical in the intervention and control groups. Furthermore, the finding that, among those lost to follow-up, alcohol consumption was similar in those in the intervention and control groups suggests that bias due to loss to follow-up is unlikely. Finally, the multiple imputation to take account of missing data produced an almost identical treatment effect to that from the main analysis. Thus, loss to follow-up bias cannot explain the study findings.
Poorly designed intervention
The intervention had a strong theoretical and empirical basis. The intervention was designed around the HAPA,87 a behaviour change model that describes the adoption, initiation and maintenance of a new behaviour as a process that involves a motivational and a volitional phase. It also incorporated behaviour change techniques from the taxonomy developed by Michie et al. 92 The intervention drew heavily on the components of alcohol brief interventions, which have been shown to have a modest but significant effect on mean consumption and binge drinking. 5,6
A possible weakness of the intervention is that it may have been too subtle. It used the technique from motivational interviewing, raising the participants’ awareness of the discrepancy between the impact of their current drinking and their social roles and responsibilities. Possibly a more direct approach, emphasising the harms of drinking and accompanied by advice to cut down, would have been more effective. However, it is also possible that such an approach could cause some irritation to participants, as text messages from someone they do not know telling them that they drink too much might not be welcomed. Such an approach is commonly used in health-care settings, where a doctor may give such advice, but could be less acceptable in a community-based study.
Inappropriate delivery method
As alcohol brief interventions delivered face to face are effective, it is possible that the weakness lies in the use of text messages for delivery. A cardinal feature of text message interventions is that they are delivered in small packages over an extended period. In contrast, conventional alcohol brief interventions are commonly delivered in a single session or a few linked sessions. Possibly the separation of the components of text message intervention over a 12-week period reduced the overall effectiveness. If, for example, texts increasing risk awareness were distant from those encouraging goal-setting and action-planning, then the motivation for action would be reduced. However, in this study that was not the case. Texts aimed at motivation were spread throughout the intervention: indeed, there was regular reinforcement of key steps in the behaviour change sequence. Furthermore, behaviour change interventions delivered by mobile phone have been shown to be effective in some circumstances, particularly smoking cessation and adherence to treatment in patients with human immunodeficiency virus infection. 66
Poor fidelity of delivery of the intervention
A major advantage of text message interventions is that they are sent automatically to a participant’s phone. Electronic monitoring of this revealed that almost all of the text messages had been received by the participants’ phones. Furthermore, the frequency of responses to the messages confirmed that participants had opened and read the texts.
Poor engagement with the intervention
The study was designed to encourage engagement of the men with the intervention. Several approaches were adopted: using language tailored to the target group, sending welcoming text messages and using participants’ first names in text messages. The intervention was also designed to be interactive by prompting men to send responses to some of the text messages they received. These responses showed high levels of engagement with key components of the intervention.
Limited duration of intervention delivery
The intervention was delivered over a period of 3 months. Possibly an intervention delivered over a longer period would be more effective. Disadvantaged individuals are less likely to translate intentions to change into action to modify behaviour. 30 Thus, a longer-term intervention could place more emphasis on the volitional components of behaviour change and reinforce commitment to reducing alcohol consumption.
Attentional control
The study used an active or attentional control which could have influenced drinking behaviour. The control group received almost as many texts as the intervention group and the texts were focused on health, which may have made men think about their health and their drinking. The control group were as likely to engage with their text messages. However the questions in their texts were mainly of a type found in trivia quizzes and had a multiple choice format. Responses to these questions only required a single letter answer. In contrast the questions in the intervention were more challenging, which required review and disclosure of drinking behaviour. Participants gave considered responses to the questions which indicated engagement with the key steps of the behaviour change process.
Research participation effects
McCambridge et al. 177 have suggested a novel mechanism by which research participation could bias the estimate of treatment effect. Suppose only a small number of individuals are susceptible to behaviour change, and that most of them respond to the research participation effects by reducing their drinking. This will occur to an equal extent in the intervention and control groups, but it will leave a reduced number of participants who would respond to the effects of the intervention, biasing the observed treatment effect to the null. At present this is just a hypothesis, but if true it suggests that brief alcohol intervention studies underestimate the real effect of the intervention. Under this hypothesis, the null effect in the present study could have occurred if research participation effects were larger than in previous studies, or if the intervention were much weaker than in other studies. Again, however, the effects of this mechanism might be expected to attenuate over time, and it is unlikely to be able to explain the sustained fall.
The nature of the target group
Behaviour change interventions are less effective, or ineffective, in disadvantaged/low-income groups, although they can still have modest statistically significant effects. 20–22 Evaluations of smoking cessation interventions suggest that the lower effectiveness is due not to lower initial uptake, but to lower sustained compliance with the intervention. 28,29 Fear of being judged and fear of failure have also been identified as barriers for disadvantaged groups. 32
Possibly the social and physical environment in which the men lived could have overwhelmed their intentions to drink more moderately. There is convincing evidence that area characteristics influence health outcomes. 203–205 A review of interventions to promote smoking cessation found that there were more barriers to change for disadvantaged groups, particularly pro-smoking norms, additional cues to smoking and increased stress. 23 Qualitative research suggests that disadvantaged individuals who live in poorly resourced and stressful environments are isolated from wider social norms and have limited opportunities for respite and recreation. 31
Living in a disadvantaged neighbourhood could also lead to heavier alcohol consumption. 206 Poverty and poor neighbourhoods can increase stress,207 which in turn increases the frequency of binge drinking. 208 Low-income groups encounter a higher frequency of daily hassles209 and alcohol outlets are more common in disadvantaged neighbourhoods. 210 Stress and alcohol cues (such as the ready availability of alcohol) could increase motivation to drink. 211 More research is needed into the impact of these barriers on intervention effectiveness, and on strategies to overcome their effects. 34
An interesting finding from a prespecified analysis was that the intervention had a much larger effect in men recruited from general practice registers than in those recruited through TSS. The latter group were more likely to be unemployed and single and to have lower educational attainment. They were also more likely to be heavier drinkers. Thus, the finding of lower effectiveness in the TSS group is consistent with the explanation that stress and the hassles of daily living reduced the effectiveness of the intervention. If true, it raises the question of whether it would be better to intervene on men recruited from general practice registers, because effectiveness is higher, or whether the TSS group, whose need may be greater, should receive higher priority. As all of the men in the study are at high risk of alcohol-related harm, this a challenging ethical issue.
Summary and implications
This chapter has reviewed many possible explanations for the main study findings, but unanswered questions remain. It has been shown that a fall in alcohol consumption following entry to a study is a common event in intervention studies. The large falls in alcohol consumption seen in both the intervention and the control groups in this study can be partly explained by regression to the mean, but it seems likely that other factors are also involved. This could be important. If some unknown factor contributed to the observed fall, it could be exploited in national efforts to reduce the frequency of heavy drinking.
A careful review of the study found that there were no major weaknesses in study design. The finding of a modest, statistically non-significant effect of the intervention could reflect the difficulty of changing health behaviours in disadvantaged groups. The intervention could have been weakened by not stating explicitly to participants that they were drinking too much and that this was causing harm to themselves and their families and friends. This approach was not adopted in case the men felt that they were being preached at and, thus, disengaged from the study. It remains possible that the more frank approach would have been successful.
The additional challenges to behaviour change in disadvantaged groups suggest that intervention studies may need to have greater power to detect effects than in studies in the general population. 23 In particular, the hypothesised treatment effect should be much smaller. This would reduce the cost-effectiveness of the intervention so that policy-makers will need to decide how much they are willing to pay to reduce inequalities in health. This discussion should include the non-health benefits of the intervention; for example, the costs of alcohol misuse are much greater for criminal justice and social services than they are for health. 2,212
Bias to the null could have occurred in the study. Research participation and social desirability could lead to non-differential misclassification of the outcome, biasing the intervention effect to the null. This seems a less likely explanation, because it cannot easily account for the sustained fall over the 12-month follow-up period. The effect of behaviourally based explanations would be expected to attenuate over time.
It could be argued that, even if differential misclassification had only a small effect, efforts should be made to design studies to minimise research participation effects. However, doing so could be problematic. In this study, considerable effort was made to promote engagement with the intervention, and several evidence-based techniques were used to increase retention. These could have increased the impact of research participation effects and social desirability. However, failing to foster engagement, or having a high loss to follow-up, could have more deleterious effects. The evidence suggests that research participation effects are small,135,177 whereas there is strong evidence that loss to follow-up can cause substantial bias. 195 The tension between the efforts to maximise retention and those to minimise the research participation effect is not widely recognised.
One implication of the finding on effectiveness is that a different approach may be required to tackle binge drinking in disadvantaged men. Possibly the intervention would need to be sustained over several months to combat the attenuating effect of adverse social circumstances. Measures to increase the price of alcohol could be helpful, as several studies have shown that the drinking of those in the lowest socioeconomic group is most affected by price increases. 213–215
In summary, alcohol is a major cause of inequalities in health, and there is a pressing need for an intervention to tackle hazardous and harmful drinking in disadvantaged groups. The study found that the intervention had a modest, statistically non-significant effect on alcohol consumption in disadvantaged men. The intervention had a strong theoretical and empirical basis, and participants engaged as intended with key components of the behaviour change strategy. The most likely reason for the modest treatment effect is the difficulty of changing adverse health behaviours in disadvantaged men, although part of the lack of effect could be an inherent limitation in the ability of text message interventions to change behaviour. Given the magnitude of the problem of health inequalities, and the political priority attached to reducing them, further research into the issues raised in this study would appear urgent.
Chapter 9 Economic evaluation
Introduction
Text message interventions have been widely used in health care and in disease prevention,66–70 often on the assumption that they provide a low-cost method of improving health outcomes. However, formal cost-effectiveness evaluations have seldom been conducted. 216,217 This large community-based study provides an opportunity to explore more fully the costs of text message interventions. Because disadvantaged men are less likely to volunteer for behaviour change interventions, an active recruitment strategy was needed. Thus, the findings are directly applicable to hard-to-reach groups. The recruitment costs were estimated in detail because this information would be essential for making decisions about a national or local rollout of the text message intervention. These costs could be omitted to enable comparisons to be made with studies that have used passive or opportunistic recruitment. Furthermore, the recruitment costs are those extra costs that are needed to reach this population group and need to be considered when considering rolling out this text message intervention in practice. There is a need to know about both the costs and the cost-effectiveness of this approach such that policy-makers can decide on whether this intervention provides good value for money compared with competing alternatives for the available resources. Opportunistic screening and brief intervention have been reported to be effective and cost-effective218 but there is no evidence about the cost-effectiveness of text message interventions that tackle harmful drinking.
The collection of evidence to inform the economic evaluation of the brief intervention delivered by text messages was conducted alongside the trial. First, this evidence is used in the economic evaluation that considered the ‘within trial’ short-term cost-effectiveness adopting the perspective of the government [costs of running the programme plus the 12-month follow-up cost of health care, social care and criminal justice services vs. the reduction in binge drinking at the 12-month follow-up and the short-term quality-adjusted life-years (QALYs)]. Second, the cost-effectiveness included a long-term perspective including the modelled impact on government costs (health care and social care), as well as wider societal impacts on crime and workplace harms. It also considered the predicted impact on QALYs up to 30 years post intervention.
Two recruitment methods were used in the trial: TSS and recruitment from general practice registers. The method used has implications for the cost of recruitment and may also have implications for the effectiveness of the intervention given the differences in the characteristics of the men recruited by each method. Thus, the cost-effectiveness analysis was performed for the two strategies combined, taking into account the number likely to be recruited using each method and then for each recruitment method separately.
The incremental cost, incremental effectiveness and cost-effectiveness ratios were estimated for two possible populations. These populations were designed to help to inform future decisions about a local implementation of the intervention and a larger national rollout. Considering the implications of both the size and the structure of the intervention on value for money is particularly important because some of the intervention costs are fixed and there are likely to be economies of scale when the intervention is rolled out to a larger population. The first population considered was ‘an equivalent trial population’ (a population of the same size and structure as the recruited trial population) and the second population was for a nationwide rollout. Intervention rollout in both populations was compared with a ‘do-nothing’ scenario, which represents standard practice. Naturally the programme cost (recruitment and implementation) of the ‘do-nothing’ scenario was assumed to be zero, and the service costs and the effectiveness outcomes of the ‘do-nothing’ scenario were assumed to be equivalent to those of the control arm of the trial.
Methods
Below we outline the methods used to estimate the programme costs, including the costs of recruitment and intervention implementation. The programme costs form part of the short-term cost to government and are also relevant for other interventions that aim to target hard-to-reach groups such as disadvantaged men. Then we describe how we used the trial evidence to estimate the impact of the brief intervention on other short-term costs to the government, taking into consideration health, social and criminal justice services use costs. We then describe the effectiveness measures, the frequency of binge drinking (≥ 3 occasions of > 8 units of alcohol) at 12 months post intervention and QALYs in the 12 months post intervention. Then we explain the methods used to capture the uncertainty in both costs and outcome. The longer-term impact of the intervention on costs and QALYs (from the 12-month follow-up to 30-year follow-up) was estimated with modelling based on the Sheffield Alcohol Policy Model. 219–221 For the short-term analysis, both costs and outcomes are not discounted as the time frame between the major cost expenditure and effectiveness outcomes is short, and discounting will play a very limited role. However, for the longer-term modelling, both costs and QALYs are discounted at 3.5% per annum as per National Institute for Health and Care Excellence (NICE) guidance. 222 The analysis was conducted using the Stata® statistical software package (version 14.0; StataCorp LP, College Station, TX, USA), IBM SPSS Statistics version 22 (2013; IBM Corporation, Armonk, NY, USA) and SAS 9.4 (2013; SAS Institute Inc., Cary, NC, USA).
Costs
Programme costs
Data collection
A log book was used during the trial as the primary source for collecting information relevant for estimating the programme costs, the cost of recruitment and the cost of implementing the text message intervention if it was decided to rollout the intervention in practice. The log book recorded the times taken for tasks of the trial and was kept by staff involved in various stages of the trial, including one trial manager, one trial administrator, four research assistants and three SPCRN representatives. Detailed in the log book was the amount of time staff members spent on training, recruiting, making telephone calls to participants for the baseline interview and preparing materials to be sent to the participants. Some examples of log book items for the general practice register recruitment method include e-mailing invitations and reminders to practices, making telephone calls to recruit practices and searching practice databases for potential participants. For the TSS recruitment method, some examples of log book items are time spent locating recruitment venues, travelling between venues and identifying potential participants on site. It was noted which tasks were solely for research purposes and, therefore, would not be required in a standard rollout of the intervention.
In addition to the log book, the costs of the message delivery system within the trial and estimates on the likely cost implications if rolled out on a larger scale were obtained from the Health Informatics Centre at the University of Dundee. The unit costs of items such as stationery and postage were obtained from the University of Dundee purchasing department and the Royal Mail. The pay scales of the appropriate staff levels for each task were sourced from the NHS and the University of Dundee. Costs recorded before 2016 were updated to 2016 prices using the 2016 quotes as obtained from the service providers. All costs are presented in 2016 Great British pounds.
Costing methods
The programme costs, including those of recruitment and text message intervention implementation, were estimated for the following three steps of the intervention: (1) identify potential participants from targeted venues (the TSS method) or from general practice registers (the general practice method), (2) contact potential participants to conduct screening questionnaires and recruit those who were eligible and (3) deliver the intervention via text messages. To estimate the programme costs per participant, and particularly to allocate fixed costs, such as renting servers to send text messages to individuals, costs were first estimated as if the programme was rolled out to a population of the same size and structure as that recruited in the trial. This was labelled as the ‘equivalent trial population’. In the trial, although both the intervention and control groups were actively recruited and received messages, only the intervention group received messages designed to change their drinking behaviour. However, when estimating the cost of rolling out the intervention in practice compared with doing nothing, all participants were assumed to have received the ‘active’ messages from the intervention. To estimate the recruitment costs, the costs for both the general practice and TSS groups, regardless of whether they ended up in the intervention or control group, were utilised because they all provided a valid estimate of the cost of recruiting such a population group if the intervention were rolled out in practice. The costs of adopting TSS and general practice recruitment strategies were presented jointly and then independently.
Staff costs were estimated as the staff time recorded in the log book for the tasks multiplied by the wage rate of the proposed staff levels, and then inflated by 45%223 to reflect the overhead costs of the organisation running the programme. This included costs for utilities, general management and support services. On-costs were also included and assumed to be 31%224 of the wage rate. 223 The assumed unit costs for inputs can be found in Table 35. For men who refused to take part in the trial, were not reachable by telephone or were not eligible, we assumed that the incurred staff and material costs were borne evenly by actual participants receiving the intervention in each centre. As the costs incurred for unsuccessful recruitment are likely to be a major component of the recruitment cost in practice, they were split evenly for actual participants in each centre and varied only at the centre level. Furthermore, because costs for successful recruitment are similar within centres by construction, the uncertainty in costs is estimated using the centre-level variation adjusted for centre recruitment size. This is instead of examining the individual-level variation in costs, which would underestimate the true uncertainty involved. A normal distribution for the average recruitment costs per recruited participant in each centre was assumed in the absence of knowledge about the likely distribution of centre average costs per participant.
Multiple gift vouchers were used in the trial to encourage programme enrolment, engagement and retention, and to compensate for participants’ time completing follow-up surveys for research purposes. In the costing of the intervention, a £10 gift voucher after enrolment and another £10 gift voucher during the intervention were included, as this was considered critical to obtain recruitment and engagement rates if the programme was rolled out in practice. Although in the trial an additional £20 in gift vouchers was sent to participants during the intervention, this was not included in the costing of the intervention rollout, as this was considered to be more for improving participant retention for research purposes rather than for encouraging engagement. Vouchers used to improve the follow-up rate for research purposes were also excluded, as these were not considered to be required at rollout. Costs for other research purposes, such as staff time conducting 3- and 12-month post-intervention questionnaires and maintaining the research database at follow-up points, were recorded separately and not included in the estimated programme costs. Costs for using the text messages application software were incurred as a one-off cost for both the equivalent trial population and the nationwide rollout.
For rollout to the equivalent trial population, the costs related to the text delivery system, the time for the programmer to monitor delivery and the time for the trial manager to oversee the programme were assumed to be needed for 1 year. The manager’s time overseeing the programme refers to the time for miscellaneous management matters not related to specific programme tasks (e.g. supervision of staff). For rollout of the programme in England and Scotland, the text delivery system was assumed to be needed for 5 years, as was the trial manager’s time overseeing the programme. The costs for the text message delivery system, the trial manager’s time and the programme’s website are split evenly across participants. The uncertainty of the mean cost at nationwide rollout was assumed to be the same as the variation of the mean estimated from the equivalent trial population. The mean cost and the variation of the mean was the weighted average based on the expected numbers recruited.
For the nationwide rollout in England and Scotland, the programme reach was projected using the male population at the appropriate age range multiplied by the proportion likely to be disadvantaged, approached and recruited. We took the population of men aged 25–44 years from the 2011 UK Census,225 assuming that 20% of this population were from areas classified as being in the most disadvantaged quintile. This is the target population of the programme. The proportions of the targeted population who could be reached by TSS by and general practice recruitment methods were assumed to be 20% and 97%, respectively. 226 The likelihood of successful recruitment for TSS and general practice recruitment was estimated based on the observed success rates from the trial. The uncertainty of the programme reach and its impact on cost and cost-effectiveness outcomes were demonstrated in a one-way sensitivity analysis.
In the nationwide rollout scenario, where both recruitment methods were employed together, we assume that the general practice method would be implemented first, with the TSS method thereafter given the much wider reach of the general practice recruitment method. As some participants recruited by general practice registers could also be approached during TSS recruitment, we assume an additional cost of 25% per potential participant for TSS method to account for the additional time spent identifying those who were already captured by the general practice method. Similarly, it was assumed that, for the nationwide rollout, the number recruited by the TSS method would be 50% less than if the TSS recruitment was employed alone, given the potential overlap in general practice and TSS populations.
Short-term costs to government
Data collection
Besides the costs of implementing the programme, the overall short-term costs of the intervention to government, including the use of health care, social and criminal justice services, were collected at the 12-month post-intervention follow-up by the short Service Use Questionnaire (courtesy of S Parrot at the Department of Health Sciences, University of York, UK). The questionnaire asked about service use in the previous 6 months and this was used to extrapolate the cost of service use for the 12-month period post intervention. No service use questions were asked at baseline or during the intervention owing to concerns that this could cause contamination to the trial result by triggering reflection and improvement in alcohol consumption. 134 Thus, it was assumed conservatively that there were no differences in service use during the text message intervention period.
Costing methods
To estimate the costs of health-care, social and criminal justice services, the collected service uses were multiplied by the average unit prices of the services obtained from various sources. 2,223,227,228 Health-care and social costs recorded before 2015 were updated to 2015 prices according to the hospital and community health services pay and prices index. 223 The costs were then updated to 2016 prices assuming a 1% inflation rate as estimated for 2014–15 by the hospital and community health services pay and prices index. 223 The costs for criminal justice services before 2016 were inflated to 2016 prices using the general inflation rate estimated by the Bank of England. All costs are presented in 2016 Great British pounds (£). The cost implications of health-care, social and criminal justice services use were then inferred using the estimated cost difference between intervention and control groups, namely the incremental cost after adjusting for participants’ baseline characteristics using the same set of variables as reported in Chapter 3. Table 35 summarises the unit cost inputs that were used in estimating the costs of service use during 12 months’ follow-up.
| Type of cost | Cost details | Source | |
|---|---|---|---|
| Programme costs | |||
| Staff salary | Hourly wage (£)a | Nominal annual salary (£)b | |
| Project manager (local government) | 37 | 30,000–35,000 | NHS pay scales 2016–17229 |
| Grade 6, spine point 4 recruiter | 28 | 26,274 | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| NHS grade 4–5 administrative post | 23 | 20,000–22,000 | NHS pay scales 2016–17229 |
| NHS grade 3 administrative post | 19 | 16,000–18,000 | NHS pay scales 2016–17229 |
| Text system programmer | 40 | 35,600–37,800 | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| Reimbursement per participating general practice | 240 | NHS Primary Care Network cost231 | |
| Stationery, voucher and phone costs | Unit price | ||
| PIS pack (three sheets, one postcard and one envelope) | 0.308 | University of Dundee purchasing department 2016232 | |
| Letter | 0.055 | University of Dundee purchasing department 2016232 | |
| Postcard | 0.098 | University of Dundee Design and Print services 2016 | |
| Postage | 0.550 | Royal Mail costs for second class postage stamps 2016233 | |
| Envelope | 0.045 | University of Dundee purchasing department 2016232 | |
| Gift voucher | 10 | Gift voucher cost for initial recruitment and intervention engagement 2016 | |
| Phone cost (handset and contract) for 1 year | 240 | Textlocal 2016 (Chester, UK; www.textlocal.com) | |
| Costs related to text system | Costs (£) | Cost type | |
| Text messages application software | 5000 | One-off for the trial; no cost for rollout | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| Set-up of the message delivery system | 2500 | One-off | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| Testing and amendment of the message delivery system | 1000 | One-off for a 1-year programme, twice in a 5-year period | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| Dedicated telephone number for enquiries | 180 | Per year | Textlocal 2016 |
| Server hosting charge (back-up, recovery and services) | 2000 | Per year | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| Project management for IT | 500 | Per year | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| Text system programmer’s time (monitoring and maintenance) | 4385 | Per year | University of Dundee Academic and HE Support Staff pay scales 2016230 |
| SMS at £0.036 per message for bundles of 50,000 messages (112 messages per participant) | 4032 | Per participant | Textlocal 2016 |
| SMS at £0.029 per message for bundles of 100,000 messages (112 messages per participant) | 3.248 | Per participant | Textlocal 2016 |
| SMS at £0.026 per message for bundles of 250,000 messages (112 messages per participant) | 2.912 | Per participant | Textlocal 2016 |
| Programme’s information web page | 1000 | One-off | Assumptionc |
| Project manager’s time overseeing the programme | 6160 | Per year | Trial estimation |
| Costs of service use | Cost per use (£) | Reference unit cost | |
| Health-care services | |||
| Accident and emergency | 133 | Accident and emergency attendance | NHS reference average costs 2014–15227 |
| Night in hospital | 1581 | Non-elective inpatient (excluding excess bed-days) | NHS reference average costs 2014–15227 |
| 306 | Excess bed-days | NHS reference average costs 2014–15227 | |
| Admitted to hospital but not overnight | 728 | Day case | NHS reference average costs 2014–15227 |
| Outpatient appointment | 115 | Outpatient attendance | NHS reference average costs 2014–15227 |
| Visited doctor | 66 | GP per patient contact | Curtis and Burns223 |
| Doctor visited you | 72 | GP home visit | Curtis and Burns223 |
| Visited nurse | 38 | Face-to-face contact in district nursing services | Curtis and Burns223 |
| Nurse visited you | 46 | Face-to-face contact in health visiting services | Curtis and Burns223 |
| Prescriptions | 24 | GP prescription costs per consultation | Curtis and Burns223 |
| Social care services | |||
| Visited by social worker | 74 | Social worker plus travel | Curtis and Burns223 |
| Went to see social worker | 56 | Social worker | Curtis and Burns223 |
| Visited by care worker/advisor | 86 | Senior social worker plus travel | Curtis and Burns223 |
| Went to see care worker/advisor | 72 | Senior social worker | Curtis and Burns223 |
| Criminal justice services | |||
| Arrested/cautioned/fined | 88 | Average cost of probation, supervised attendance order, restriction of liberty order and fine | Costs of the Criminal Justice System in Scotland 2014–15228 |
| Appeared peace/sheriff court | 267 | Sheriff Court and Justice of the Peace Court | Costs of the Criminal Justice System in Scotland 2014–15228 |
| Appeared high court | 82,546 | High Court of Justiciary | Costs of the Criminal Justice System in Scotland 2014–15228 |
| Day in prison | 89 | Cost per prisoner per year | Ministry of Justice234 |
Effectiveness
Two effectiveness outcomes were considered separately in the cost-effectiveness analyses in the short term: (1) frequency of binge drinking at the 12-month follow-up and (2) QALYs within the 12 months post intervention. The impact of the intervention on these outcomes and the uncertainty around these were estimated using the same methodology as described in Chapter 3, adjusting for participants’ baseline characteristics. QALYs were estimated using the EQ-5D-5L235 utility scores reported at 12 months post intervention and applied to the whole 12-month period post intervention. EQ-5D-5L data at baseline and during the intervention were not collected to minimise potential contamination through changed behaviour if too many questions on health were asked. 134 QALYs for participants who died before the 12-month post-intervention follow-up were assumed to be zero for the whole 12-month period post intervention. The impact of the intervention on QALYs was estimated using a generalised linear model framework with an identity link function and Gaussian distribution, controlling for the same baseline characteristics as the primary analysis. The distribution family of Gaussian was chosen to accommodate the negative EQ-5D-5L utility states, as these negative states are believed to be valid and no other standard distribution reflected the distribution. As changes in drinking frequencies are unlikely to fully translate into health changes in the first year after the intervention, it was expected that any change in QALYs due to the intervention was likely to be small at the 12-month post-intervention follow-up. The trial was not powered to detect small QALY differences and thus it was expected that there would be large uncertainties around the 12-month post-intervention follow-up QALY results.
At nationwide rollout, the effectiveness outcomes for the programme were assumed to be the same as the equivalent trial population for the TSS and general practice recruitment methods. For the combined recruitment strategy, we assume that the effectiveness outcome at nationwide rollout is the weighted average of the effectiveness of the two recruitment methods estimated from the trial.
Incremental cost-effectiveness ratios
The incremental cost-effectiveness ratios, defined as the incremental cost divided by the incremental effectiveness, were estimated to present the additional cost that is required to achieve one additional unit of effectiveness (cost per one less person with ≥ 3 occasions of binge drinking and cost per QALY). The cost-effectiveness of adopting TSS and general practice registers recruitment strategies were presented jointly and then individually as subgroup analysis had shown that the cost-effectiveness results of the combined strategies at nationwide rollout are essentially driven by the cost-effectiveness of the different recruitment strategies and their projected coverage.
Uncertainty
To account for uncertainty at nationwide rollout, a probabilistic sensitivity analysis was undertaken in which 10,000 random draws from the distribution of costs and effectiveness were taken. The distribution of the (incremental) programme cost was constructed based on the mean and standard error of the programme costs as estimated from the equivalent trial population. The distribution of the incremental short-term costs to government, defined as the sum of the programme and services use costs, was estimated in the same manner and was adjusted for participants’ baseline characteristics using the same set of variables as reported in Chapter 3. The treatment effect of the intervention as estimated in Chapter 3 was used to estimate the incremental effectiveness. From 10,000 random draws, the incremental cost-effectiveness ratios were estimated. The cost-effectiveness acceptability curves were plotted and then interpreted against a set of assumed willingness-to-pay thresholds.
One-way sensitivity analysis
In addition to the probabilistic sensitivity analysis, uncertainty in cost and effectiveness outcomes at nationwide rollout was explored using a one-way sensitivity analysis for key modelling assumptions in which the distributions of the uncertainty were unknown. More specifically, we considered scenarios when (1) the trial manager’s time overseeing the project rose by 10-fold (varying costs); (2) only a percentage of the projected population was reached (varying costs); (3) the intervention effect for participants who received the intervention but were lost to follow-up was included using multiple imputation (varying effectiveness) described in Chapter 3; and (4) the presence of control intervention effect, whereby 10% of the control group’s reduction in binge drinking was assumed to be due to the control intervention itself. This includes factors such as being recruited to a study on alcohol, being asked about current alcohol consumption and receiving text messages on general health topics instead of a true ‘do-nothing’ scenario (varying effectiveness). The incremental cost-effectiveness ratios for the alternative scenarios were estimated and the uncertainties around the incremental cost-effectiveness ratios were presented using cost-effectiveness acceptability curves where the probabilities of the intervention being cost-effective at various assumed willingness-to-pay thresholds were summarised.
Modelling long-term costs and outcomes post 12-month follow-up
The long-term impact of the intervention on costs and QALYs was estimated with economic modelling based on the alcohol consumption observed at the 12-month follow-up. We adapted the model structure of an existing alcohol policy appraisal model, the Sheffield Alcohol Policy Model,219–221 to estimate the impact of alcohol consumption on population health. The Sheffield model utilises potential impact fractions and alcohol-attributable fractions to estimate the harm resulting from both the mean (total weekly units of alcohol) and the peak (units of alcohol consumed on the heaviest drinking day in the previous 7 days) alcohol consumption of individuals. 219 A range of acute and chronic health conditions and social harms (crime and workplace harms) attributable to alcohol were considered in the Sheffield model, and impacts on costs were quantified in monetary terms and for health in QALYs.
Based on the Sheffield model, the impact of the intervention was modelled from the 12-month follow-up for another 29 years to allow the full impact of the consumption change on outcomes to be assessed. Health risks were estimated in age subgroups (defined as 25–34, 35–44, 45–54, 55–64 and ≥ 75 years) based on the mean and peak alcohol consumption. The perspective of the model is that of the government (costs to NHS and social services) and the drinkers (quality of life), counting the costs of morbidity, mortality, social harms and health-related quality of life. All costs and QALYs were discounted at a rate of 3.5% based on NICE convention222 and costs were presented in 2016 prices.
Model parameters
Consumption
The consumption change due to the brief intervention in the first year of the modelling period was estimated based on the observed difference in the consumption at the 12-month post-intervention follow-up between the intervention and control groups.
To obtain participant-level mean and peak consumption predictions if they were in the control and intervention groups, we used the method of recycled predictions. 236 Here we predicted the alcohol consumption at 12 months post intervention as if all participants were in the control group, and then as if all participates were in the intervention group controlling for the same baseline characteristics as in the primary analysis. Quantile regressions (0.1, 0.2, 0.3, 0.4, 0.5, 0.6, 0.7, 0.8, 0.9) were employed to conduct the recycled predictions, to allow the distribution of mean and peak to be estimated. This allows the impact of the intervention to vary across the population. For instance, the impact of the intervention might be different for those who were otherwise expected to become light drinkers versus heavy drinkers. Each individual was randomly allocated one consumption quantile from the nine consumption quantiles (0.1 to 0.9) to predict the mean and peak weekly consumption. Consumption predictions were made for the TSS and general practice recruitment methods respectively to allow for the projected population each recruitment method could reach if rolled out nationwide to vary. The combined recruitment strategy for the nationwide impact was presented as the main result of the model.
Beyond the first year of the modelling period, consumption of individuals in the intervention group was assumed to rebound linearly towards their predicted consumption had they been in the control group over a period of 7 years. The choice of 7 years was based on the findings of Fleming et al. 237
Consumption risk and outcome
Following the Sheffield model,220,221 the effect of consumption on health and social harm was estimated using the mean and peak weekly consumption. Risk functions relating alcohol consumption to health and social risk and the relevant alcohol-attributable fractions were sourced from the Sheffield model, versions 2.0220 and 3.0. 221
More specifically, consideration was given to morbidity and mortality for 39 health conditions, social harm in terms of 20 crimes, employment and work absence. When morbidity and mortality events occurred in the same year, one event was chosen randomly. Similarly for competing mortality events, one was randomly chosen.
The impacts of health and social harms on quality of life were derived from the Sheffield model. 220 Utilities for individuals who were estimated to have multiple morbidity conditions were estimated as the product of the utility for each health condition. A utility for an individual who died was estimated as the half of the individual’s utility in the previous year. For those with no harm estimated, the utility for the general population of the age range was applied. The cost of each morbidity, mortality and social harm event was sourced from the Sheffield model, version 2.0,220 unless otherwise noted.
Data sources for model parameters are summarised in Table 36, along with the key modelling assumptions.
| Parameter/assumption | Source |
|---|---|
| Cost | |
| Diabetes mellitus (type 2) | Kanavos et al., 2012238 |
| Pneumonia | Delgleize et al., 2016239 |
| Absenteeism | CIPD, 2015240 |
| Unemployment | Office for National Statistics, 2016241 |
| Other causes of death | Chitnis et al., 2012242 |
| All other costs | Sheffield model 2.0220 |
| Outcome | |
| Risk functions (consumption to health and social harms) | Purshouse et al., 2009;220 Angus et al., 2016221 (Sheffield model) |
| Impact of harm on quality of life | Purshouse et al., 2009220 |
| All other cause of death | Office for National Statistics, 2005243 |
| Key modelling assumptions | |
| Time horizon | 30 years |
| Intervention effect | Consumption of the intervention group was assumed to rebound linearly towards that of the control group over a period of 7 years in accordance with Fleming et al.237 |
Results
A summary of the short-term cost to government, including programme costs and short-term service use costs estimated for the equivalent trial population and the programme rolled out in England and Scotland, is presented in Table 37. The detailed programme costs estimated for the equivalent trial population and services use are documented in Appendix 8 (see Tables 41–46). Participants (n = 3) who did not provide information on service use at the final follow-up were dropped when service use cost was estimated.
| Type of cost | Recruitment method, £ (95% CI) | |||||
|---|---|---|---|---|---|---|
| Equivalent trial population (number of participants recruited/projected)a | Projected population, England and Scotland (number of participants recruited/projected) | |||||
| Combined strategy (n = 825) | TSS only (n = 398) | General practice registers only (n = 427) | Combined strategy (n = 248,417) | TSS only (n = 61,556) | General practice registers only (n = 217,639) | |
| Short-term incremental cost to government (intervention – ‘do nothing’) per participantb | 511 (–32 to 1112) | 925 (–624 to 2472) | 341 (–35 to 717) | 357 (–156 to 869) | 865 (–680 to 2409) | 285 (–82 to 651) |
| Incremental programme cost (intervention – ‘do nothing’) per participant | 133.40 (143.37 to 180.78) | 177.81 (163.47 to 192.14) | 147.42 (124.28 to 170.55) | 96.85 (83.25 to 110.43) | 118.55 (109.71 to 127.39) | 91.26 (76.99 to 105.51) |
| Step 1: identifying potential participants (£) | 58.24 | 76.67 | 41.07 | 47.86 | 76.67 | 41.07 |
| Step 2: recruiting participants (£) | ||||||
| Staff making calls | 16.42 | 11.60 | 20.92 | 19.77 | 11.60 | 20.92 |
| Stationery and vouchers | 12.08 | 12.04 | 12.12 | 12.11 | 12.04 | 12.12 |
| Step 3: intervention (£) | ||||||
| IT system and staff related | 24.03 | 45.49 | 42.68 | 3.11 | 3.72 | 3.14 |
| Voucher related | 13.93 | 14.01 | 13.85 | 13.87 | 14.01 | 13.85 |
| Other programme costs (£) | ||||||
| Project manager overseeing the programme | 7.47 | 15.48 | 14.43 | 0.12 | 0.50 | 0.14 |
| Web page development | 1.21 | 2.51 | 2.34 | 0.00 | 0.02 | 0.00 |
| Incremental service use cost [intervention – control(‘do nothing’)], adjusted | 378 (–175 to 931) | 747 (–787 to 2280) | 194 (–159 to 546) | 262 (–237 to 761) | Same as the equivalent trial population | |
| Service use cost unadjusted meansc | ||||||
| Intervention | 1672 (1093 to 2253) | 2656 (1375 to 3937) | 914 (654 to 1175) | |||
| Control | 1432 (1000 to 1863) | 2169 (1232 to 3106) | 853 (643 to 1063) | |||
| Intervention – control | 241 (–478 to 960) | 487 (–1084 to 2059) | 62 (–271 to 394) | 114 (–372 to 601) | Same as the equivalent trial population | |
| Health care (£) | 437 | 929 | 61 | 169 | ||
| Social care (£) | –152 | –400 | 44 | –11 | ||
| Criminal justice (£) | –45 | –42 | –44 | –44 | ||
| Total incremental cost to government (programme and services use) | 391,571 (–76,491 to 859,164) | 344,315 (–270,650 to 958,663) | 121,603 (–35,105 to 278,154) | 88,606,610 (–38,824,172 to 215,907,152) | 53,252,466 (–41,859,336 to 148,268,891) | 61,980,377 (–17,892,865 to 141,773,550) |
| Total incremental effect (95% CI) (number of participants with drinking frequency reduced)d | 47 (–16 to 110) | 8 (–37 to 54) | 37 (–6 to 80) | 19,363 (–6470 to 45,197) | 1293 (–5786 to 8310) | 18,717 (–3265 to 40,698) |
For the equivalent trial population rollout, it was estimated that the short-term incremental cost to government for an average participant was £511 with the combined recruitment strategy. The average programme costs per participant were £133, £178, and £147, respectively, when the combined recruitment strategy, the TSS method and the general practice method, respectively, were employed. The cost per participant at the ‘identifying potential participants’ stage was estimated to be approximately £77 when only the TSS method was used, which was almost twice that of £41 when only the general practice method was used. However, the TSS method was estimated to be almost 50% cheaper at the ‘recruiting participants’ stage when potential participants were called for screening and consent for enrolment in the programme. At the intervention stage, the intervention costs, including costs related to the information technology (IT) system, system monitoring and maintenance, were estimated. The average cost at this step was largely driven by the number of participants involved and their share of the fixed IT system cost, namely ‘economies of scale’.
For nationwide rollout, the target population the programme could reach for a nationwide rollout in England and Scotland was estimated to be 248,417 when a combined recruitment method was adopted, 61,556 when the TSS recruitment method only was employed, and 217,639 when the general practice recruitment method only was employed (the population projection is detailed in Appendix 8, Tables 46–48). The short-term incremental cost to government for an average participant was estimated to be £375, lower than that of the equivalent trial population driven by the lower programme and service use cost with the general practice recruitment strategy. The average programme cost per participant for nationwide rollout was estimated to be £87, £102, and £83, respectively, for the combined recruitment strategy, the TSS method and the general practice method. This was lower than the costs incurred for the trial population as participants were estimated to have a smaller cost share for renting the IT system and for the trial manager’s time overseeing the project. If both recruitment methods were employed at rollout of the programme in England and Scotland, the estimated cost would be £24M (95% CI £21M to £27M). This could result in approximately 20,000 (95% CI –6500 to 45,000) fewer disadvantaged men with ≥ 3 occasions of binge drinking.
The incremental cost and effectiveness outcomes used in the cost-effectiveness analysis for nationwide rollout are summarised in Table 37, followed by the estimated incremental cost-effectiveness ratios. From a short-term government cost perspective where costs of services use were included, the mean cost to government to obtain one fewer person with ≥ 3 occasions of binge drinking is estimated to be £4576 with a combined recruitment strategy. As expected, changes in QALYs were minimal in the first year despite the drinking frequencies being reduced, and large uncertainties were found around these minimal changes (Table 38). Based on the point estimates, the intervention group was dominated, with the intervention estimated to be less effective and more costly on average than the ‘do-nothing’ approach.
| Components | Recruitment method | ||
|---|---|---|---|
| Combined strategy | TSS | General practice registers | |
| Incremental short-term government cost (intervention – control), £ (95% CI) | 357 (–156 to 869) | 865 (–680 to 2409) | 285 (–82 to 651) |
| Incremental effectiveness (intervention – control) | |||
| People with ≥ 3 occasions of binge drinking (> 8 units of alcohol) reduced, % (95% CI) | 0.078a (–0.012 to 0.168) | 0.021 (–0.094 to 0.135) | 0.086 (–0.015 to 0.187) |
| QALY gained (95% CI) | –0.006 (–0.037 to 0.025) | –0.003 (–0.038 to 0.031) | –0.007 (–0.037 to 0.024) |
| Incremental cost-effectiveness ratios (cost/effectiveness)b | |||
| Additional cost per one fewer person with ≥ 3 occasions of binge drinking (£) | 4576 | 41,196 | 3311 |
| Cost per QALY gained | Dominatedc | ||
The uncertainties around the incremental cost-effectiveness ratios for the nationwide rollout were demonstrated using cost-effectiveness planes as presented in Figure 7. There were large uncertainties around the short-term government costs and large uncertainty in relative terms for the QALY results given that the estimated QALY change itself was very small.
FIGURE 7.
Cost-effectiveness planes for nationwide rollout. (a) Proportion of people with ≥ 3 occasions of binge drinking, with short-term cost to government; and (b) short-term QALYs, with short-term costs to government. Note: to enhance the clarity of the graphs, the cost-effectiveness planes plotted only 1000 points for each recruitment strategy from a random draw of the 10,000 bootstrapped replications. Acceptability curves were plotted using all 10,000 replications.
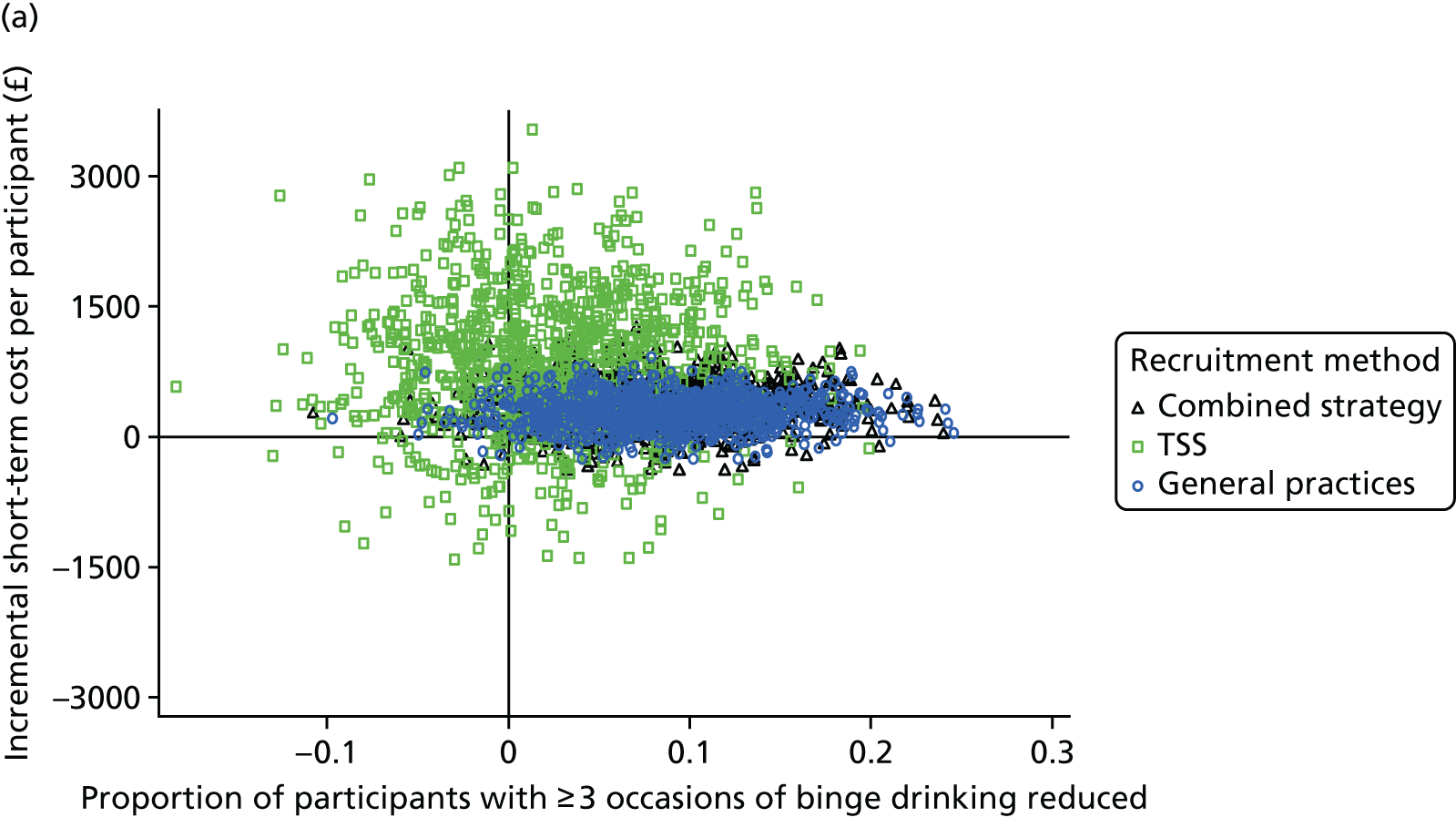
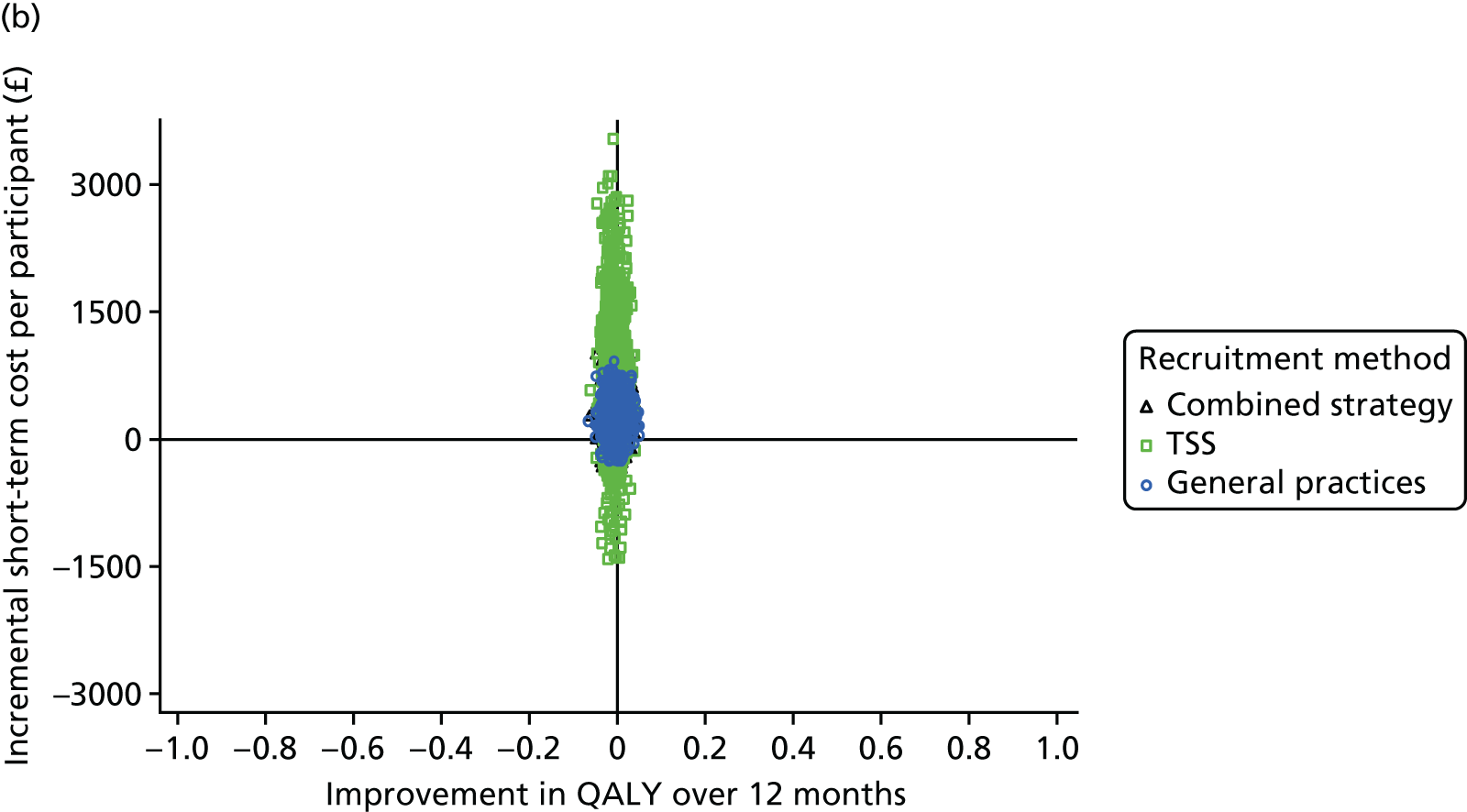
Sensitivity analysis
One-way sensitivity analyses were conducted for four alternative scenarios at nationwide rollout for the two effectiveness outcomes.
Cost per one fewer person with ≥ 3 occasions of binge drinking
For the cost per one fewer person with ≥ 3 occasions of binge drinking, the sensitivity analysis results were compared with the base-case results at nationwide rollout (Table 39). The uncertainties of these results for each alternative scenario were highlighted using acceptability curves as presented in Figure 8.
| Scenarios | Recruitment method (£) | ||
|---|---|---|---|
| Combined strategy | TSS | General practice registers | |
| Base-case scenario at nationwide rollout | 4576 | 41,196 | 3311 |
| Sensitivity analysis | |||
| AS1: when the programme manager’s time overseeing the project rises 10-fold | 5833 | 41,410 | 3326 |
| AS2: when only a percentage of the projected population were reached |
10% reached: 5856 90% reached: 5819 |
10% reached: 41,762 90% reached: 41,203 |
10% reached: 3351 90% reached: 3312 |
| AS3: lost to follow-up included using multiple imputation | 4148 | 39,323a | 2998a |
| AS4: 10% of control group reduction in binge drinking was due to the control intervention itself (rather than what would have happened with no intervention) | 3148 | 13,864 | 2363 |
FIGURE 8.
Acceptability curves for the primary outcome for combined strategy at nationwide rollout, base case and AS 1, 2, 3 and 4: short-term cost to government. AS, alternative scenario.
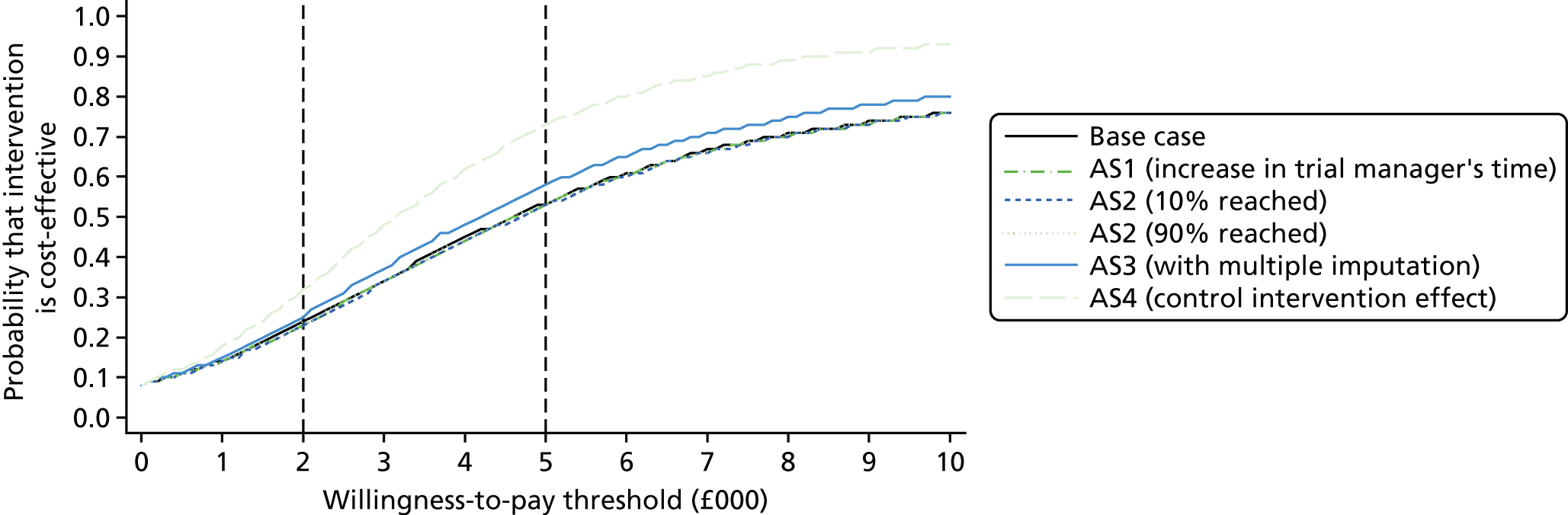
In alternative scenarios 1 (costs were varied by increasing the programme manager’s time overseeing the project) and 2 (reducing the projected population the programme could reach), there were minimal changes in the estimated incremental cost-effectiveness ratios. In alternative scenario 3 (effectiveness outcomes were varied by including the multiple imputation results for people who were in the trial during the intervention period but not available for the 12-month follow-up), the incremental cost-effectiveness ratios were estimated to be lower. For the combined strategy, confidence that the programme is cost-effective in the short-term was estimated to be approximately 58% for a government willingness-to-pay threshold of £5000.
In alternative scenario 4 [a control intervention effect (compared with a true ‘do-nothing’ approach) of 10% was assumed for the decrease in the primary outcome between baseline and 12 months post intervention], the cost-effectiveness ratios were estimated to be lower at £3148 for the combined recruitment strategy than for the base case. Confidence that the programme is cost-effective at a £5000 government willingness-to-pay threshold would be 70% for the combined recruitment strategy in this case.
Short-term cost per quality-adjusted life-year gained
For alternative scenarios 1–3, the point estimates for the QALY analysis suggest that the intervention was dominated (more costly and less effective). Thus, it is redundant to estimate the incremental cost-effectiveness ratios. Alternative scenario 4, with a possible control intervention effect, cannot be estimated, as EQ-5D-5L data were not collected at baseline.
The acceptability curves for the alternative scenarios on short-term cost per QALY gained are presented in Figure 9. As £20,000–30,000 per QALY gained is typically considered cost-effective under the NICE technology assessment framework,244 the willingness-to-pay thresholds of £20,000 and £30,000 were plotted.
FIGURE 9.
Acceptability curves for QALYs for AS 1, 2 and 3: short-term cost to government. AS, alternative scenario.
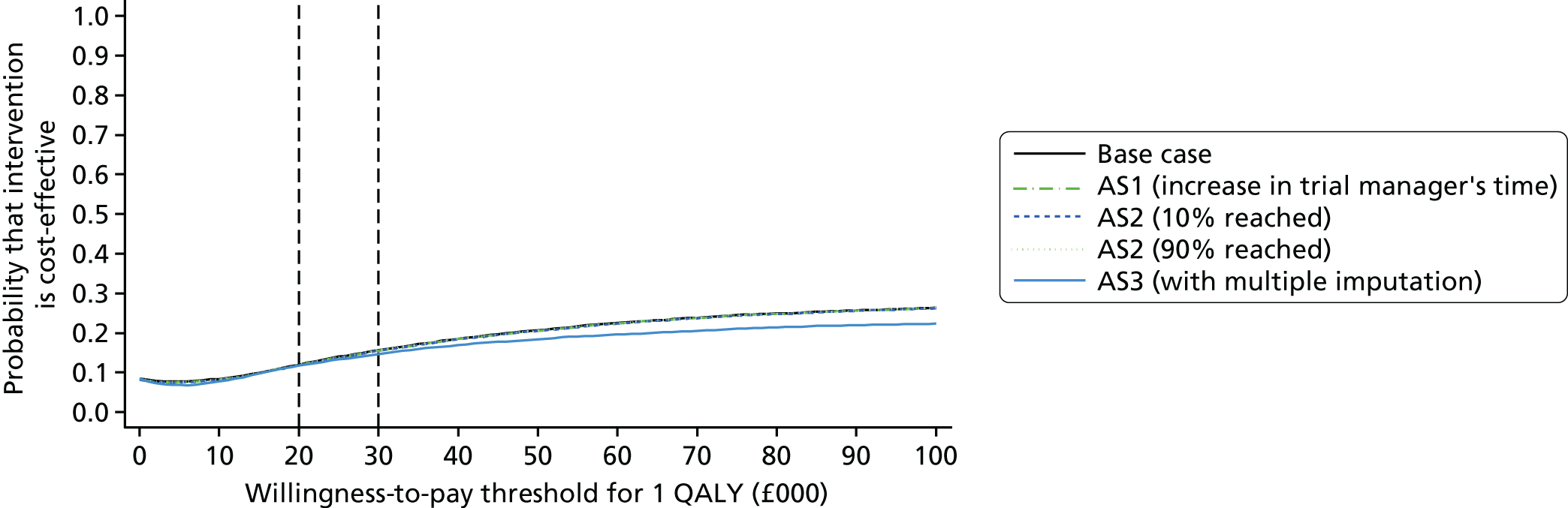
As shown in Figure 10, when considering only the QALY gains to 12 months post intervention we are only 15% confident that the intervention would be cost-effective at a government willingness-to-pay threshold of £30,000 per QALY.
FIGURE 10.
Estimated distribution of consumption at the 12-month follow-up for control and intervention groups (by combined recruitment strategy and by each recruitment method individually). Mean weekly consumption for (a) combined strategy; (c) general practice registers; (e) TSS; and peak weekly consumption for (b) combined strategy; (d) general practice registers; and (f) TSS.
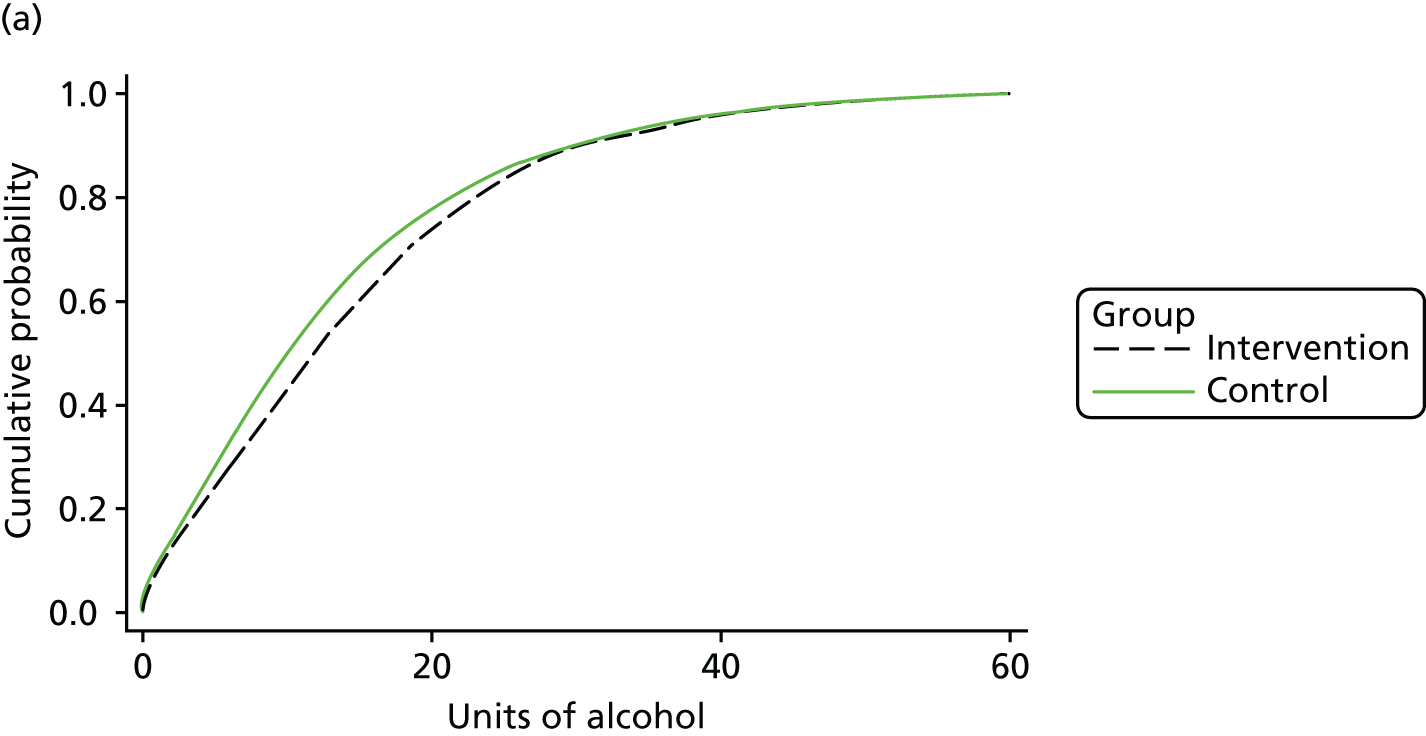
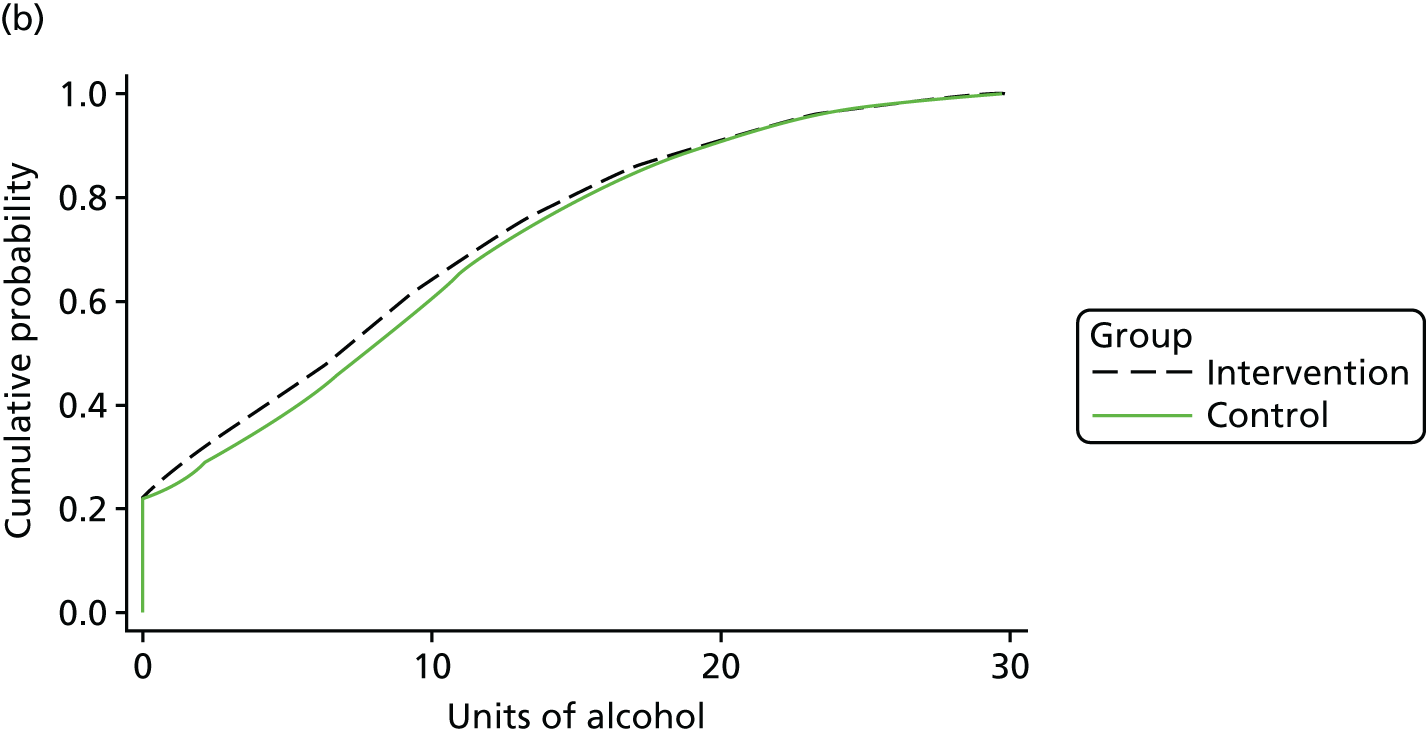
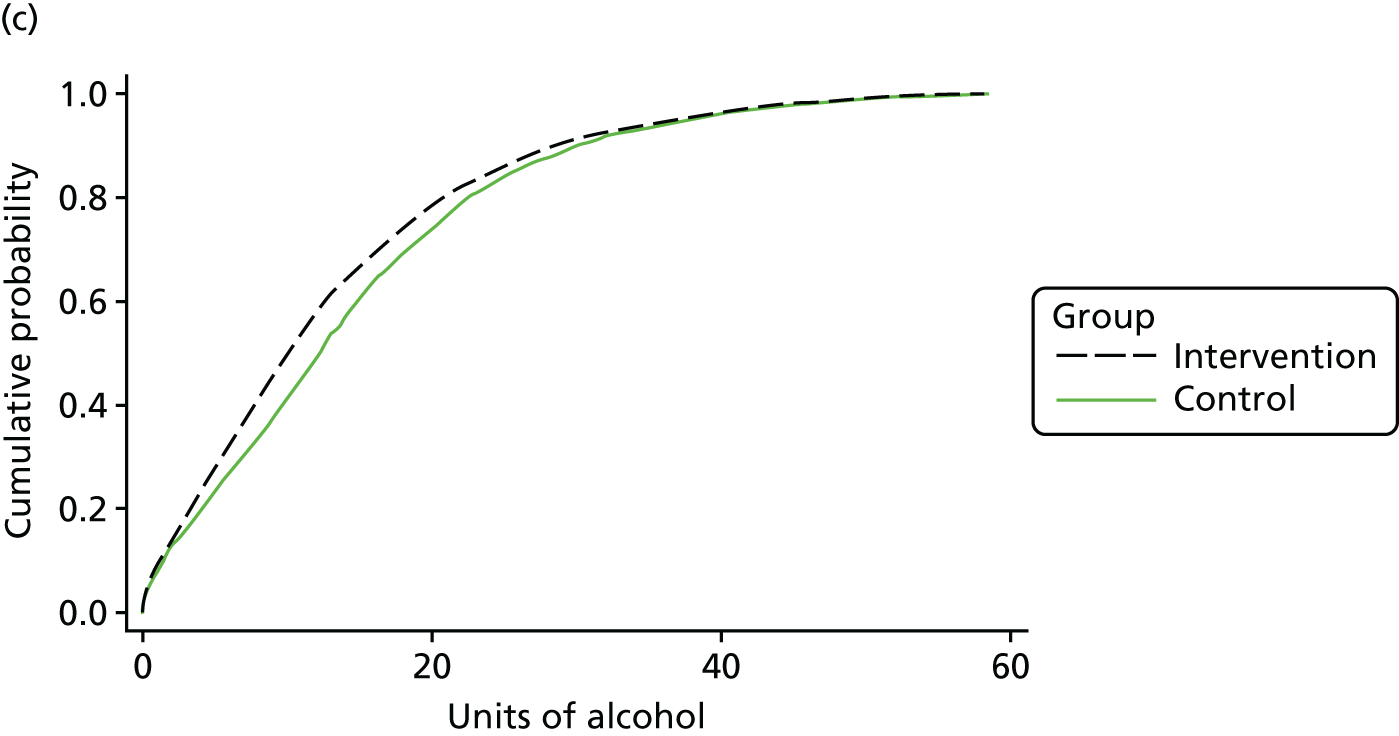
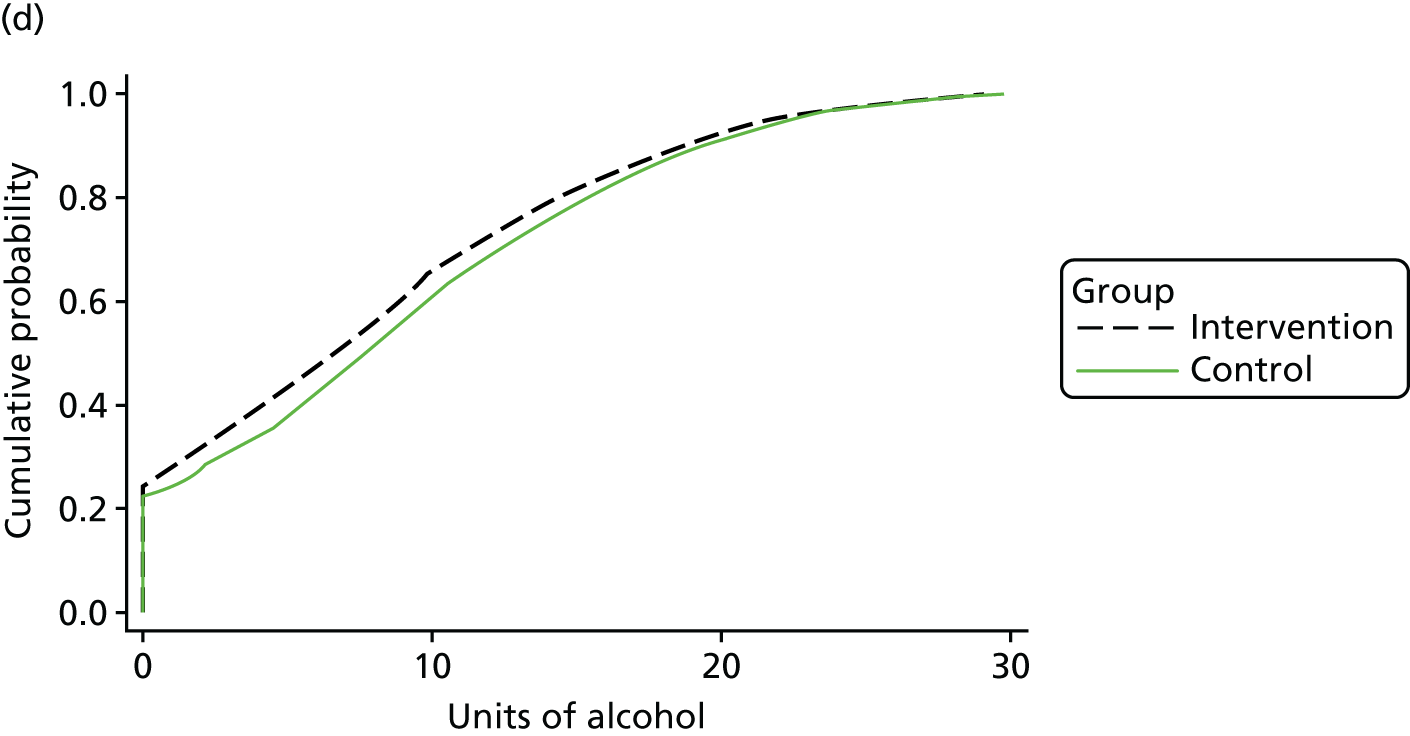
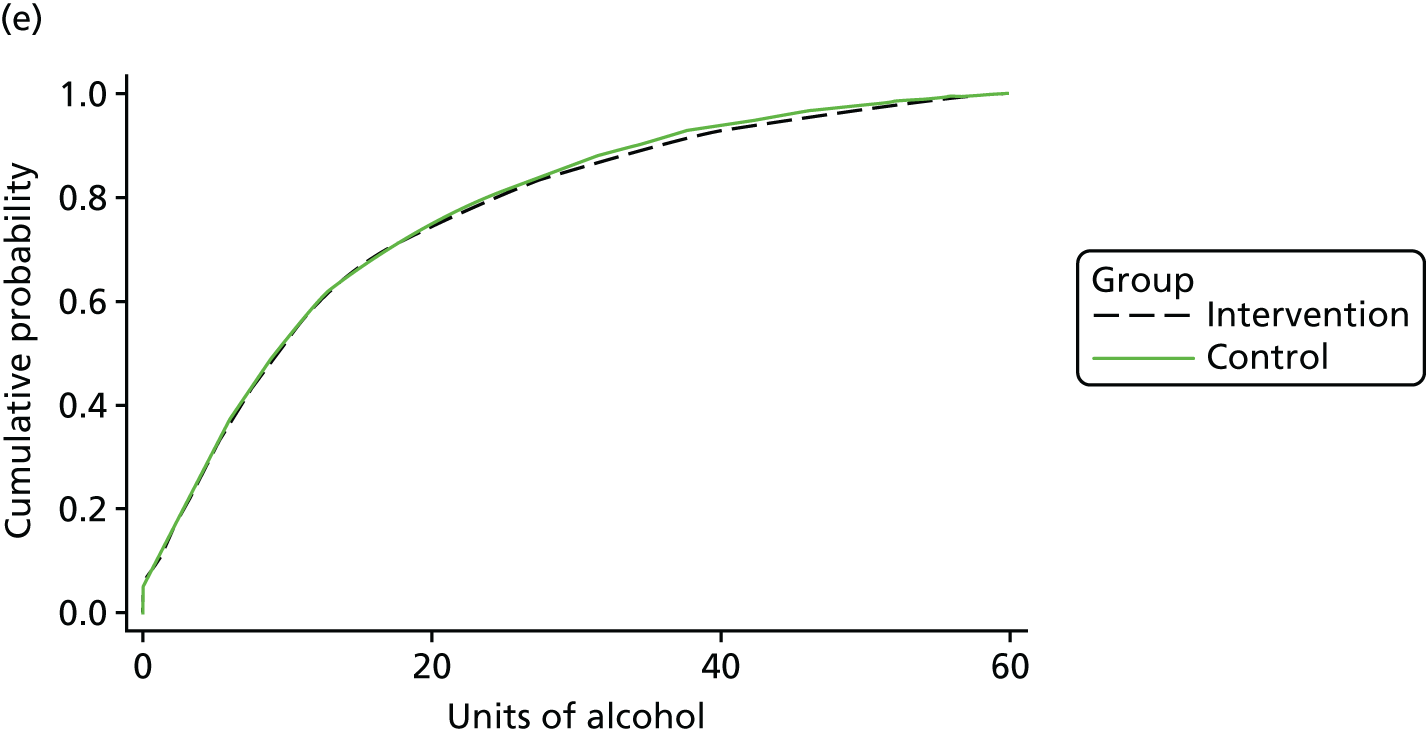
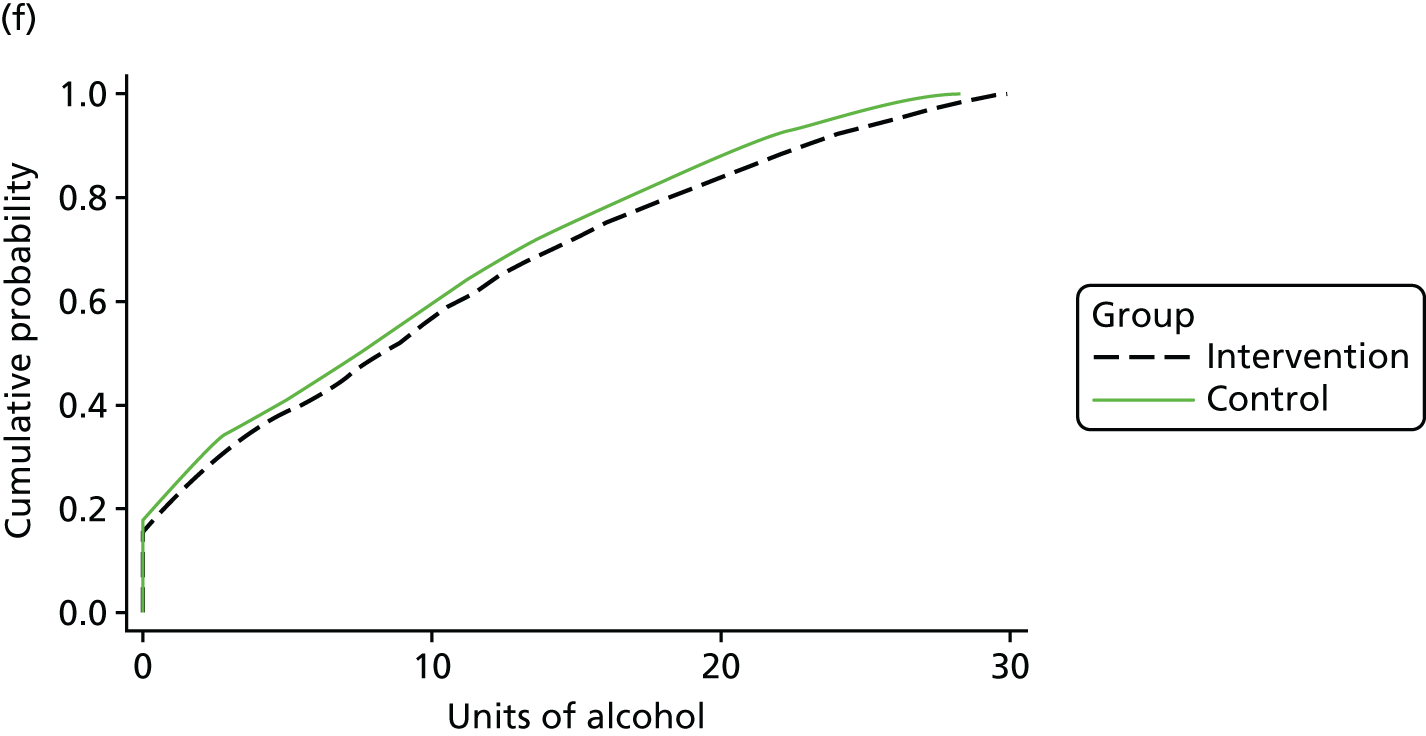
Modelling the long-term cost-effectiveness using the Sheffield model
Based on the 12-month follow-up trial data, the projected distribution of alcohol consumption for participants in the control and the intervention groups are presented in Figure 10. Individuals are ranked from the lightest drinkers to the heaviest drinkers on each consumption measure. The predictions for participants recruited by TSS and general practice recruitment methods are also presented separately below. As shown in Figure 10, with combined recruitment for more moderate drinkers at the 12-month follow-up, it was estimated that the intervention group would drink approximately 2 units fewer each week and 1 unit less in their peak session than if they were in the control group. But at the heavier drinking end of the population at 12-month follow-up it was estimated that there would be very little impact of the intervention on peak drinking levels. The combined recruitment results are heavily driven by the large number of participants projected to be recruited via general practices and we can see the similar consumption patterns in the general practice subgroup in Figure 10. For the TSS subgroup, the intervention mostly appeared to have very little impact on mean weekly consumption (although in the upper tail of heavy drinkers, the intervention group were estimated to have higher mean weekly drinking levels than the control group) and the intervention was also estimated to have increased peak consumption especially for the heaviest drinkers at 12 month follow-up. Given that there seems to be little change in mean weekly consumption but higher peak consumption, it could be that men are having fewer drinking sessions (fewer binge sessions) but more intense drinking sessions when they do drink.
These predicted drinking levels at 12 months were then combined with the assumption that any differences observed between the intervention and control groups at the 12-month follow-up would linearly decline over the next 7 years, such that after 7 years the intervention group would again be drinking at the same levels as the control group. The modelling assumption that the impact of the brief intervention on both mean and peak alcohol consumption declines in a linear fashion over a period of 7 years is demonstrated in Figure 11. In particular for the intervention group, it is assumed that the mean weekly consumption across the whole population increases from 13 units per week at the 12-month follow-up to the control group level of 15 units per week after 7 more years. Similarly, peak consumption for the intervention group increases from an estimated average of 8.5 units of alcohol in their heaviest drinking session in the previous week at the 12-month follow-up to the control group level of an average of 9 units after 7 more years.
FIGURE 11.
Linear decline of the intervention effect on average projected (a) mean weekly consumption and (b) peak weekly consumption in the previous week.
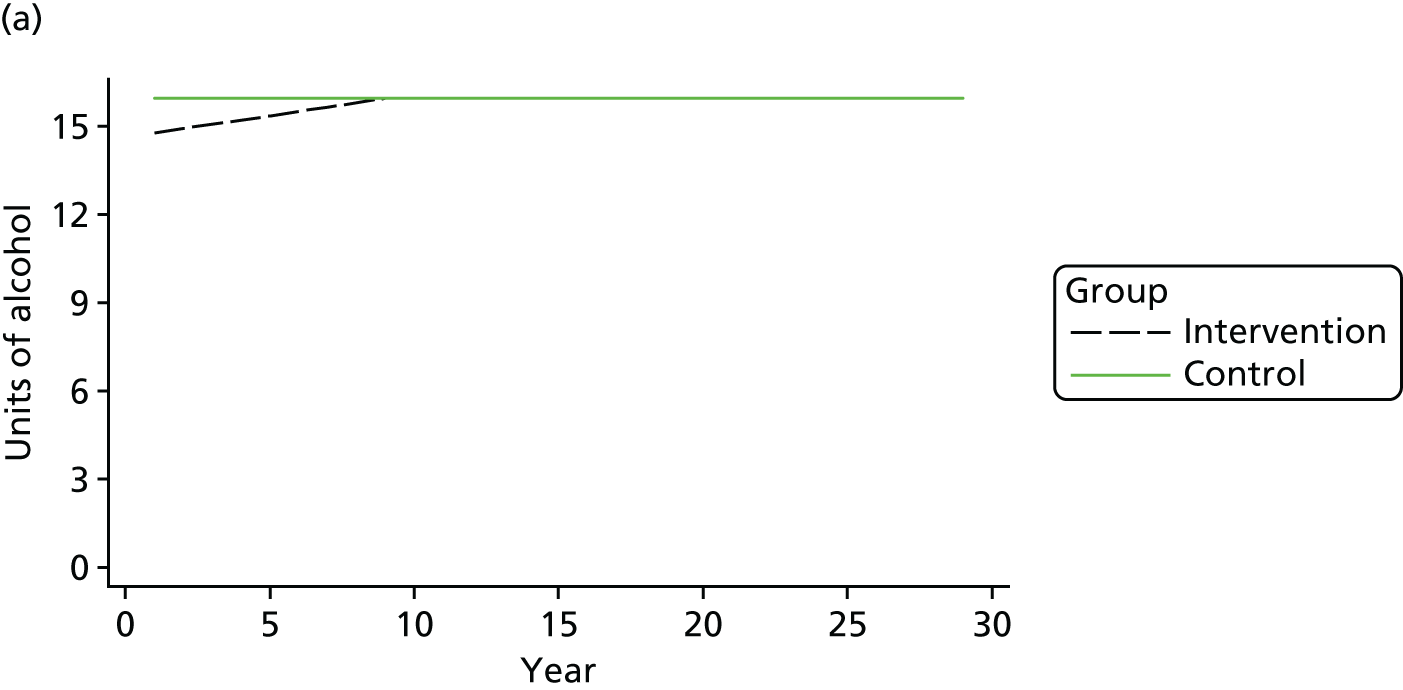
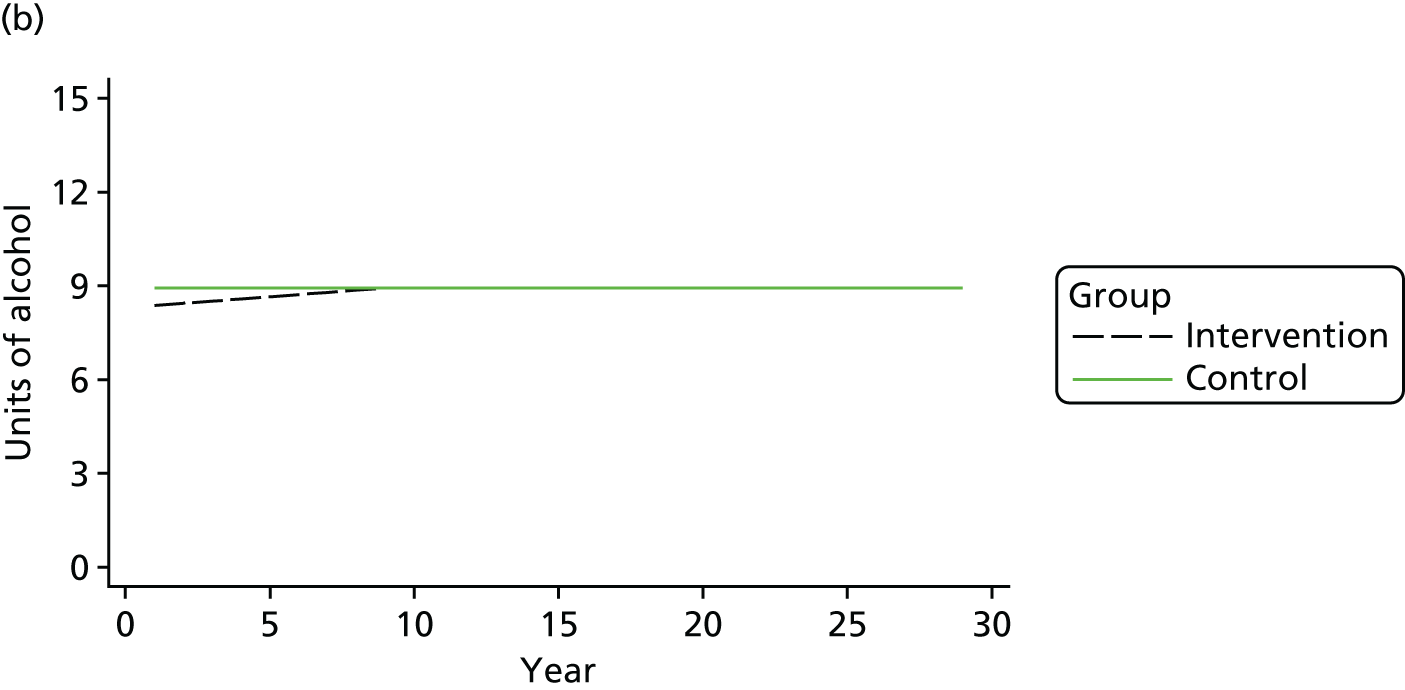
Next, these estimated mean and peak drinking distributions for both the intervention and the control groups were used as inputs in the model to project the likely differences in alcohol-related harm over the next 29 years. The model results combined with the short-term follow-up results are summarised in Table 40, and the incidences for the specific health and social harms from the model are detailed in Appendix 8 (see Table 50). Overall, the intervention was estimated to be dominated when the short-term follow-up and the model results were combined. Owing to the small difference in both mean and peak consumption at final 12-month follow-up between the intervention and control groups, only a small cost difference and utility benefit was estimated from year 1 to year 30 and the utility benefit was smaller than the estimated utility loss within the initial 12-month follow-up period.
| Intervention – control | Total effect over 30 years post intervention | Model results over the time horizon (1–30 years) | Intervention and short-term follow-up (0–1 year) |
|---|---|---|---|
| Base case | |||
| Incremental cost (discounted 3.5%) (£) | 300 | –57 | 357 |
| QALYs gained (discounted 3.5%) | –0.0034 | 0.0029 | –0.0063 |
| Incremental cost-effectiveness ratio | Dominated | Dominated | |
| One-way sensitivity analysis | |||
| No discounting | |||
| Incremental cost (£) | 246 | –111 | 357 |
| QALYs gained | –0.0030 | 0.0033 | –0.0063 |
| Incremental cost-effectiveness ratio | Dominated | Dominated | |
| Cost and utility discounted by 1.5% | |||
| Incremental cost (£) | 274 | –83 | 357 |
| QALYs gained | –0.0031 | 0.0032 | –0.0063 |
| Incremental cost-effectiveness ratio | Dominated | Dominated | |
| Model time horizon 19 years | |||
| Incremental cost (£) | 325 | –32 | 357 |
| QALYs gained | –0.0021 | 0.0042 | –0.0063 |
| Incremental cost-effectiveness ratio | Dominated | Dominated | |
Table 41 shows the modelling results and long-term cost-effectiveness by the general practice and TSS recruitment strategies separately. For the general practice recruitment method alone, the projected benefits in QALYs gained within the modelled period were still outweighed by the loss observed within the 12-month follow-up. Because the intervention was estimated to increase mean weekly consumption in the TSS group for the heaviest drinkers and to have increased peak consumption, the model showed further substantial losses in QALYs over the year 1 to year 30 horizon. Thus, the estimated cost-effectiveness of the intervention for the TSS group becomes even less favourable once we consider the potential long-term impact of the intervention.
| Intervention – control | Total effect over 30 years post intervention | Model results over the time horizon (1–30 years) | Intervention and short-term follow-up (0–1 year) |
|---|---|---|---|
| General practice registers | |||
| Incremental cost (discounted 3.5%) (£) | 203 | –82 | 285 |
| QALYs gained (discounted 3.5%) | –0.0015 | 0.0055 | –0.0070 |
| Incremental cost-effectiveness ratio | Dominated | Dominated | |
| TSS | |||
| Incremental cost (discounted 3.5%) (£) | 874 | 9 | 865 |
| QALYs gained (discounted 3.5%) | –0.0180 | –0.0150 | –0.0030 |
| Incremental cost-effectiveness ratio | Dominated | Dominated | |
Discussion
This is the first text message intervention study tackling harmful drinking that has incorporated an economic evaluation. The programme cost per participant was estimated to be £97 (95% CI £83 to £110), and was mostly driven by the costs at the active recruiting stage: over 80% of the cost per participant, £80 with a £10 gift voucher included, was incurred at recruitment, when men from disadvantaged areas were approached, screened and recruited. The delivery of the intervention itself, on the other hand, was estimated to cost less than £20 on average per participant, inclusive of another £10 gift voucher. Compared with the literature on alcohol screening and brief intervention, in which the median costs per screened participant were estimated to be between £9 and £21 and median costs per brief intervention £26 to £81245 (see Appendix 8, Table 51, for conversion to 2016 £), the cost of the text message programme seems only slightly more expensive. The main difference in costs is the large recruitment costs of the current text message programme compared with the cheaper ‘opportunistic’ recruitment for alcohol brief interventions delivered in primary care.
Although the estimated cost per participant to recruit and implement the intervention was modest, there was a lack of evidence that the intervention would be cost effective. The estimated impacts on patterns of alcohol consumption, downstream cost implications and QALYs were modest, inconsistent and uncertain. The short term incremental government costs, including both the costs of the programme and the costs of health and social care and criminal justice services 12 months post intervention, were estimated to be £357 (95% CI –£156 to £869) per participant for nationwide rollout. If the programme was rolled out in England and Scotland, it was estimated that there could be approximately 20,000 (95% CI –6500 to 45,000) fewer disadvantaged men who had ≥ 3 occasions of binge drinking at a programme cost of £24M (95% CI £21M to £27M) with TSS and general practice recruitment methods combined. This would result in an average government cost of £4576 per one fewer person with ≥ 3 occasions of binge drinking at the first year post-intervention.
The QALY difference between intervention and control groups was minimal in the first year after the programme was delivered, with the intervention group having slightly worse QALYs on average. With a higher cost and a QALY loss, this meant that, in the short term, it was estimated that the intervention was dominated by a ‘do-nothing’ approach in terms of costs per QALYs. However, there is large uncertainty around the QALY results, as the current trial was not powered to detect the expected small impacts on QALYs within the 12 months post intervention. In addition, the estimated QALY loss at the 12-month follow-up may be inconsistent with the reduced binge drinking frequency in the intervention group compared with the control group, as indicated by the primary outcome, although there is a chance that reduced binge drinking resulted in lower quality of life in the short term.
The major health implications are likely to be experienced after the 12-month post-intervention follow-up. To allow the longer-term impact of the brief intervention to be considered, a modelling approach was employed based on the observed mean and peak consumption at the 12-month follow-up. Adapting the structure of the Sheffield model, the current gold standard for modelling future implications for changes in drinking behaviour,219 a small discounted QALY gain in favour of the intervention and a very small discounted cost saving compared with the control group was estimated from years 1 to 30. However, when the model results were combined with the short-term follow-up using the QALY results, the intervention was still dominated by the ‘do-nothing’ option.
We also estimated the subgroup cost-effectiveness by recruitment method. We found that, overall, the evidence suggested that the general practice method compared with a ‘do-nothing’ approach appeared more cost effective than recruitment by TSS compared with a ‘do-nothing’ approach, with both a lower cost per participant of recruitment and implementation and a larger estimated effectiveness in reducing the level of binge drinking to < 3 sessions in the previous 28 days. However, there is considerable uncertainty around the impact of the intervention on the cost to government of health, social and criminal justice service use, as well as uncertainty around the effectiveness of the intervention and, therefore, considerable uncertainty about the impact on the long-term costs and QALYs. The long-term modelling results for the general practice subgroup suggest that even small changes in alcohol consumption patterns for this high-risk group may result in worthwhile long-term QALY gains relative to the cost of the intervention.
Although the intervention appeared more cost-effective in the general practice subgroup, the TSS recruitment method was able to reach a distinctly more disadvantaged group who had higher levels of drinking and were more likely to be single and unemployed (see Chapter 4). These men also had much higher levels of health, social and criminal justice service use than the men recruited through the general practice method (see Appendix 8, Table 52). This implies that if only the general practice recruitment method is used, some of these men may not be reached.
Given that disadvantaged men may not volunteer for interventions that are offered through the primary health-care sector, there may also be an equity or equal access argument for spending additional funds to be able to reach these men. 246 This will be especially important for men who would be recruited through the TSS method. Although the cost of active recruitment is higher, society may prefer to pay more to improve the health of the most disadvantaged in our society and thus reduce health inequalities. 247
As an alternative to active recruitment at a local or national level, it may be possible to reduce recruitment costs by using mass media campaigns, manned helplines and websites. This could improve the cost-effectiveness of the intervention, but, at the same time, it may recruit different types of drinkers from those engaged in the current study. The cost-effectiveness of the text message intervention may also depend on the general motivation among the disadvantaged male population at the time of implementation. For example, the text message intervention may be more cost-effective if it is implemented simultaneously with policies that increase the general motivation to reduce alcohol consumption, such as minimum pricing for alcohol.
Several limitations of the current economic evaluation are worth noting. Information on service use (health-care, social and criminal justice services) and EQ-5D-5L scores were not collected at baseline or at the 3-month follow-up to limit the number of questions that could themselves act to reduce subsequent alcohol consumption. Consequently, owing to the lack of data collection at the baseline and early follow-up periods, we conservatively assume that there would be no difference in service use or in EQ-5D-5L scores over the 3-month intervention period, which could lead to a potential underestimation of the intervention’s impact. In addition, we assume that the differences in QALYs observed at the 12-month follow-up were the differences for the whole preceding 12-month period. The cost to government in terms of service use 12 months post intervention was estimated using the self-reported service use and applying the average cost for each service, both of which may lead to bias. We used an adapted version of the Sheffield Alcohol Policy Model to consider the long-term impact of the brief intervention using the model’s two critical inputs: the peak consumption in the previous week and the mean weekly consumption of alcohol over the previous month. This may underestimate the impact on harms of the current trial, because, rather than reducing the peak consumption, the intervention aimed to reduce the number of binge-drinking sessions. The observed reduction in mean alcohol consumption could be due to a reduction in binge-drinking sessions rather than a reduction in the amount of alcohol consumed in one session or low-intensity sessions. This may have implications for the projected benefits, as a reduction in alcohol consumption from binge-drinking sessions may be more beneficial than a reduction in the number of low-intensity drinking sessions. 248,249
Future economic evaluations of interventions targeted at reducing binge drinking would benefit from larger sample sizes in trials to improve statistical power to allow more robust economic conclusions to be made, including about the impact on QALYs and service use costs. This is especially important for low-cost interventions, in which even a small improvement in the patterns of alcohol consumption may mean that the intervention provides good value for money. In addition, the economic evaluation of alcohol interventions, in general, would benefit from longer-term follow-up, potentially through linkage with administrative data sources to minimise the cost of follow-up, to better capture the potential downstream reduction in service use and improvements in health, which is where many of the expected benefits from improvement in drinking behaviour are likely to occur.
Chapter 10 Conclusions
Alcohol misuse is a major contributor to inequalities in health. After several years of decline, alcohol consumption has recently started to increase. There is a pressing need for an effective, low-cost intervention to tackle binge drinking in disadvantaged groups.
The study successfully recruited a large number of disadvantaged men to a trial of an alcohol intervention. This makes it one of the largest trials of an alcohol brief intervention, a major achievement with a hard-to-reach group. The retention rate was high, much higher than most previous trials on alcohol interventions. Loss to follow-up is unlikely to have been a cause of significant bias.
The intervention had a strong empirical and theoretical basis, and it incorporated the elements of brief alcohol interventions. A narrative structure was used to deliver an intervention based on a behaviour change model (the HAPA)87 that included a range of specific behaviour change techniques. Characters in the narrative were used to convey information on alcohol and its harms and the benefits of reduced consumption. They also modelled the processes involved in changing behaviour. These features were successfully rendered in a series of short text messages that were delivered over a 3-month period.
The text message intervention was delivered with high fidelity. The responses to the text messages showed that many participants engaged enthusiastically with the intervention and that the texts were fully understood. The honest, and indeed candid, nature of many responses suggests that participants had sufficient trust in the research study to share their experiences, feelings and intentions. Possibly the anonymity provided by the medium of text messages made participants feel more confident about disclosing personal details.
Many participants identified personal reasons to reduce binge drinking and reported setting goals and making action plans. About one-quarter described the benefits that they had enjoyed after reducing their drinking. This highlights the potential of responses to text messages to monitor participant reactions to intervention components in real time.
The main finding was that the intervention had a modest statistically non-significant effect on the primary outcome and small inconsistent and non-significant effects on the secondary outcomes. The observed modest and non-significant effect of the intervention could have several explanations. It could reflect the difficulty of changing health behaviours commonly encountered in disadvantaged groups. It is also possible that non-differential misclassification biased the treatment effect to the null.
Disadvantaged individuals are less likely to respond to behaviour change interventions and there is a widespread concern that, without adequate tailoring to disadvantaged groups, interventions could widen inequalities. Several studies have investigated barriers to changing health behaviours in disadvantaged groups, particularly for smoking cessation, but evidence on barriers to reducing alcohol consumption and binge drinking is sparse. Future research should urgently address this issue.
The differences in the characteristics of the men identified by the two recruitment strategies raises an important issue. Men recruited by TSS had a higher mean consumption and a higher frequency of binge drinking than those recruited from general practice registers at the baseline interviews; they were also more likely to be single and to be unemployed. These findings suggest that men recruited by TSS may have more stressful lives with less social support, making it more difficult to change their drinking behaviour. This could explain why the treatment effect of the intervention on the primary outcome was much lower in the TSS group. The combination of heavier drinking and more stressful lives could also explain why the economic analysis found much higher costs for health, social care and criminal justice services in the men recruited by TSS. These findings confirm the need to tackle binge drinking in this group.
The additional challenges to behaviour change suggest that intervention studies with disadvantaged groups may need to have greater power to detect effects than studies in the general population. In particular, the hypothesised treatment effect should be smaller. This would reduce the cost-effectiveness of the intervention. Society will need to decide how much it is willing to pay to reduce inequalities in health. This discussion should include the non-health benefits of the intervention; for example, the costs of alcohol misuse are much greater for criminal justice and social services than they are for health.
Another important finding was that alcohol consumption fell substantially from baseline to outcome assessment in both intervention and control groups. The falls in both groups were similar on several measures of alcohol consumption. They could partly be the result of regression to the mean. As alcohol consumption is self-reported, the falls could also be due to social desirability bias, research participation effects or self-selection by motivated individuals. However, there is no evidence to support these possible explanations.
Further research is needed to identify the mechanisms that explain the large falls in alcohol consumption commonly seen in trials of alcohol brief interventions. These could be sources of bias that could be controlled for in further studies. Alternatively, they could be mechanisms of behaviour change that could be exploited in future interventions. Those conducting future trials should recognise that large falls in alcohol consumption in control groups are common and take account of this in their sample size calculations.
The economic evaluation showed that the assessment of cost-effectiveness was inconclusive. Although the cost per man of recruiting to and implementing the intervention was modest, the intervention’s impacts on patterns of alcohol consumption, QALYs and downstream costs were inconsistent and uncertain.
Over 80% of the intervention cost was incurred in recruiting the participants. Disadvantaged men are reluctant to engage in health promotion interventions and this cost may need to be met if society is to reduce inequalities in health caused by harmful drinking.
Overall, this study suggests that text message interventions have promise for tackling adverse health behaviours in disadvantaged men. The methods for recruitment, retention and engagement could be used in future research studies. The facility to monitor, in real time, participant responses to individual text messages can identify whether or not the intervention components are achieving their intended effects. The outstanding challenge is to develop effective interventions for individuals who live in areas of disadvantage. The methods developed for this study provide a platform for the design and testing of interventions to reduce inequalities in health.
Limitations of the study
The study used an active control that, combined with the recruitment procedures and baseline assessments, could have biased the treatment effect towards the null.
Although the loss to follow-up was smaller than in most alcohol brief intervention studies, it is still possible that this could have introduced bias. This seems unlikely because the retention rates are similar in the intervention and control groups and multiple imputation to adjust for missingness had no effect on the estimated treatment effect.
Awareness that they were involved in an alcohol study could have caused participants to under-report their consumption levels, biasing treatment effects towards the null.
It is possible that the period of 3 months of text messages was insufficient to provide a lasting change in drinking behaviour. In addition, the text messages may have been phrased too gently, following the principles of motivational interviewing, such that a more blunt approach could have been more successful. However, this approach runs the risk of antagonising participants so that they disengage from the intervention.
Recommendations for further research
-
Conduct a future trial to reduce the uncertainty around the treatment effect of the intervention. It could also test whether or not the intervention is significantly less effective in men recruited by the TSS method, and explore possible explanations for this.
-
Assess the impact of the use of an attentional control (general health text messages) by including a second minimal control (no text messages).
-
Test whether or not a more direct and frank approach, stressing the harm of their current drinking, would be acceptable to disadvantaged men.
-
Explore the barriers to reducing binge drinking in disadvantaged men to enable strategies to overcome them to be developed.
-
Identify the mechanism(s) responsible for falls in alcohol consumption in the control group.
-
Explore the impact of regression to the mean by recruiting participants to an alcohol study without setting an entry criterion. After follow-up the participants could be divided into four groups based on baseline alcohol consumption: no alcohol, low consumption, moderate consumption and high consumption.
-
Explore the impact of research participation effects by using a factorial design with the factors baseline assessment (screening only vs. full drinking history) and techniques to promote recruitment and retention (no techniques vs. evidence-based techniques).
-
Conduct a feasibility study to assess the utility and acceptability of biomarkers to measure alcohol consumption in disadvantaged men.
-
Investigate the impact of an extended intervention (i.e. at least 12 months) for reducing alcohol consumption in disadvantaged men.
-
Use the methods of recruitment, retention and text message delivery to test the effectiveness of interventions designed to tackle other adverse health behaviours in disadvantaged groups.
Acknowledgements
We are indebted to the men who participated so willingly in the study.
We are grateful to Dr S Parrot for use of the Short Service Use questionnaire.
We would like to thank the 20 general practices for helping to recruit participants. Recruitment through general practice was co-ordinated through the SPCRN, and we are grateful to Marie Pitkethley, Kim Stringer and Tracy Ibbotson for the efforts they made to make this a success.
We are grateful to Amy Howie, who provided administration support for the trial. She was also responsible for ensuring that the participants received their gift vouchers on time.
We thank Jillian Hart and Judith Connell for recruiting participants from the Forth Valley and Glasgow sites.
We would like to thank Sean and Lee (User Group Representatives) who attended steering group meetings and contributed to the study design and interpretation of the findings.
Finally, we would like to thank the members of the Trial Steering Committee, Professor John Frank (chairperson), Professor Jonathan Chick, Mr Philip McLoone and Mr Mike Alcock, for their support, guidance and encouragement.
Contributions of authors
Professor Iain K Crombie (Professor of Public Health) was the chief investigator for the study and the principal investigator for the Tayside site. He designed the study and supervised its conduct. He contributed to the intervention development, the training and supervision of the research assistants and the analysis of the data, and he wrote the final report.
Dr Linda Irvine (Senior Research Fellow, Public Health) was the trial manager and the principal investigator for the Fife site. She also contributed to the study design, the intervention development, the training and supervision of the research assistants, the follow-up interviews, the analysis of the data and the writing of the final report. She led on the writing of the text messages and wrote the chapters on intervention development (see Chapter 2) and the evaluation of the text message intervention (see Chapter 5).
Professor Brian Williams (Professor of Health Services Research and Director of Health & Wellbeing Research) contributed to the study design and the text message intervention. He suggested the inclusion of a narrative in the intervention. He also provided critical comment on the final report.
Professor Falko F Sniehotta (Professor of Behavioural Medicine and Health Psychology) contributed to the study design and the text message intervention.
Dr Dennis J Petrie (Associate Professor, Health Economics) designed the economic evaluation. He undertook the analysis with Dr Li Huang, co-wrote the chapter on the economic evaluation (see Chapter 9) and provided critical comment on the final report.
Dr Claire Jones (Senior Software Engineer) was responsible for the web-based randomisation system. She created, ran and monitored the message delivery system, the system for recording receipt of SMS text messages and the mechanism for storing text message responses from participants.
Professor John Norrie [Professor of Clinical Trials and Biostatistics, Director, Centre for Healthcare Randomised Trials (CHaRT)] contributed to the study design, advised on sample size and data analysis, and provided critical comment on the final report.
Dr Josie MM Evans (Reader in Public Health) was the principal investigator at the Forth Valley site. She supervised the recruitment of participants and also provided critical comment on the final report.
Carol Emslie (Reader, Substance Use and Misuse) was the principal investigator at the Glasgow site. She supervised the recruitment of participants.
Dr Peter M Rice (Addictions Psychiatrist) advised on alcohol questionnaires and alcohol-related problems.
Dr Peter W Slane (GP) advised on recruitment methods and contributed to the study design.
Professor Gerry Humphris (Professor of Health Psychology) contributed to the study design and the text message intervention.
Professor Ian W Ricketts [Professor (Emeritus) in Computer Science] contributed to the design of the text message delivery system.
Dr Ambrose J Melson (Research Associate, Mental Health and Wellbeing) contributed to the text message intervention and provided critical comment on the final report.
Professor Peter T Donnan (Professor of Epidemiology and Biostatistics, Director of Dundee Epidemiology and Biostatistics Unit and Co-Director of Tayside Clinical Trials Unit) undertook the statistical analysis and contributed to the writing of the chapters on quantitative analysis.
Mr Andrew McKenzie (Research Assistant, Public Health) recruited participants from general practices and by community outreach in Tayside, Glasgow and Forth Valley. He conducted follow-up interviews, assisted with the analysis of the trial data and contributed to the writing of the final report.
Dr Li Huang (Research Fellow, Health Economics) undertook the economic evaluation with Dr Dennis J Petrie and co-wrote the economic evaluation chapter (see Chapter 9).
Dr Marcus Achison (Research Assistant, Public Health) recruited participants from general practices and by community outreach in Fife, Glasgow and Forth Valley, conducted follow-up interviews and provided critical comment on the final report.
All authors contributed to the final report.
Publications
Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie D, Jones C, et al. Texting to Reduce Alcohol Misuse (TRAM): main findings from a randomized controlled trial of a text message intervention to reduce binge drinking among disadvantaged men [published online ahead of print June 1 2018]. Addiction 2018.
Data sharing statement
For research purposes, data can be obtained from the corresponding author: Professor Iain K Crombie, University of Dundee, Division of Population Health Sciences, School of Medicine, The Mackenzie Building, Kirsty Semple Way, Dundee, DD2 4BF. E-mail: i.k.crombie@dundee.ac.uk.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Lister G, Fordham R, Mugford M, Olukoga A, Wilson E, McVey D. Evaluating Social Marketing for Health: The Need for Consensus. The Societal Cost of Potentially Preventable Illness n.d.
- The Societal Cost of Alcohol Misuse in Scotland for 2007. Edinburgh: Scottish Government; 2010.
- Raistrick D, Heather N, Godfrey C. Review of the Effectiveness of Treatment for Alcohol Problems. London: The National Treatment Agency for Substance Misuse; 2006.
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med 2005;165:986-95. https://doi.org/10.1001/archinte.165.9.986.
- Kaner EF, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;2. https://doi.org/10.1002/14651858.CD004148.pub3.
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 2012;157:645-54. https://doi.org/10.7326/0003-4819-157-9-201211060-00544.
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.e8501.
- Drummond C, Deluca P, Coulton S, Bland M, Cassidy P, Crawford M, et al. The effectiveness of alcohol screening and brief intervention in emergency departments: a multicentre pragmatic cluster randomized controlled trial. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0099463.
- Newbury-Birch D, Coulton S, Bland M, Cassidy P, Dale V, Deluca P, et al. Alcohol screening and brief interventions for offenders in the probation setting (SIPS Trial): a pragmatic multicentre cluster randomized controlled trial. Alcohol Alcohol 2014;49:540-8. https://doi.org/10.1093/alcalc/agu046.
- Hilbink M, Voerman G, van Beurden I, Penninx B, Laurant M. A randomized controlled trial of a tailored primary care program to reverse excessive alcohol consumption. J Am Board Fam Med 2012;25:712-22. https://doi.org/10.3122/jabfm.2012.05.120070.
- Mackenbach JP, Kulhánová I, Bopp M, Borrell C, Deboosere P, Kovács K, et al. Inequalities in alcohol-related mortality in 17 European countries: a retrospective analysis of mortality registers. PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001909.
- Probst C, Roerecke M, Behrendt S, Rehm J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol 2014;43:1314-27. https://doi.org/10.1093/ije/dyu043.
- Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, et al. European Union Working Group on Socioeconomic Inequalities in Health . Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008;358:2468-81. https://doi.org/10.1056/NEJMsa0707519.
- Schmidt LA, Mäkelä P, Rehm J, Room R, Blas E, Kurup AS. Equity, Social Determinants and Public Health Programmes. Geneva: World Health Organization; 2010.
- Grittner U, Kuntsche S, Gmel G, Bloomfield K. Alcohol consumption and social inequality at the individual and country levels – results from an international study. Eur J Public Health 2013;23:332-9. https://doi.org/10.1093/eurpub/cks044.
- Fone DL, Farewell DM, White J, Lyons RA, Dunstan FD. Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-002337.
- Päljarvi T, Suominen S, Car J, Koskenvuo M. Socioeconomic disadvantage and indicators of risky alcohol-drinking patterns. Alcohol Alcohol 2013;48:207-14. https://doi.org/10.1093/alcalc/ags129.
- Berridge V, Herring R, Thom B. Binge drinking: a confused concept and its contemporary history. Soc Hist Med 2009;22:597-60. https://doi.org/10.1093/shm/hkp053.
- Blaxter M. Evidence for the Effect on Inequalities in Health of Interventions Designed to Change Behaviour. Bristol: Department of Social Medicine, University of Bristol; 2007.
- Niederdeppe J, Fiore MC, Baker TB, Smith SS. Smoking-cessation media campaigns and their effectiveness among socioeconomically advantaged and disadvantaged populations. Am J Public Health 2008;98:916-24. https://doi.org/10.2105/AJPH.2007.117499.
- Michie S, Jochelson K, Markham WA, Bridle C. Low-income groups and behaviour change interventions: a review of intervention content, effectiveness and theoretical frameworks. J Epidemiol Community Health 2009;63:610-22. https://doi.org/10.1136/jech.2008.078725.
- Bull ER, Dombrowski SU, McCleary N, Johnston M. Are interventions for low-income groups effective in changing healthy eating, physical activity and smoking behaviours? A systematic review and meta-analysis. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006046.
- Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction 2011;106:1568-85. https://doi.org/10.1111/j.1360-0443.2011.03467.x.
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013;67:190-3. https://doi.org/10.1136/jech-2012-201257.
- Brown T, Platt S, Amos A. Equity impact of interventions and policies to reduce smoking in youth: systematic review. Tob Control 2014;23:e98-105.
- Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities?. PLOS Med 2010;7. https://doi.org/10.1371/journal.pmed.1000320.
- Vander Ploeg KA, Maximova K, McGavock J, Davis W, Veugelers P. Do school-based physical activity interventions increase or reduce inequalities in health?. Soc Sci Med 2014;112:80-7. https://doi.org/10.1016/j.socscimed.2014.04.032.
- Kotz D, West R. Explaining the social gradient in smoking cessation: it’s not in the trying, but in the succeeding. Tob Control 2009;18:43-6. https://doi.org/10.1136/tc.2008.025981.
- Hiscock R, Judge K, Bauld L. Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation?. J Public Health 2011;33:39-47. https://doi.org/10.1093/pubmed/fdq097.
- Conner M, McEachan R, Jackson C, McMillan B, Woolridge M, Lawton R. Moderating effect of socioeconomic status on the relationship between health cognitions and behaviors. Ann Behav Med 2013;46:19-30. https://doi.org/10.1007/s12160-013-9481-y.
- Stead M, MacAskill S, MacKintosh AM, Reece J, Eadie D. ‘It’s as if you’re locked in’: qualitative explanations for area effects on smoking in disadvantaged communities. Health Place 2001;7:333-43. https://doi.org/10.1016/S1353-8292(01)00025-9.
- Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health 2009;31:258-77. https://doi.org/10.1093/pubmed/fdp008.
- Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health 2008;98:216-21. https://doi.org/10.2105/AJPH.2007.114777.
- Passey M, Bonevski B. The importance of tobacco research focusing on marginalized groups. Addiction 2014;109:1049-51. https://doi.org/10.1111/add.12548.
- Sully BG, Julious SA, Nicholl J. A reinvestigation of recruitment to randomised, controlled, multicenter trials: a review of trials funded by two UK funding agencies. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-166.
- McDonald AM, Knight RC, Campbell MK, Entwistle VA, Grant AM, Cook JA, et al. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials 2006;7. https://doi.org/10.1186/1745-6215-7-9.
- Fletcher B, Gheorghe A, Moore D, Wilson S, Damery S. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2011-000496.
- Kasenda B, von Elm E, You J, Blümle A, Tomonaga Y, Saccilotto R, et al. Prevalence, characteristics, and publication of discontinued randomized trials. JAMA 2014;311:1045-51. https://doi.org/10.1001/jama.2014.1361.
- Williams RJ, Tse T, DiPiazza K, Zarin DA. Terminated trials in the ClinicalTrials.gov results database: evaluation of availability of primary outcome data and reasons for termination. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0127242.
- Watson JM, Torgerson DJ. Increasing recruitment to randomised trials: a review of randomised controlled trials. BMC Med Res Methodol 2006;6. https://doi.org/10.1186/1471-2288-6-34.
- Mapstone J, Elbourne D, Roberts I. Strategies to improve recruitment to research studies. Cochrane Database Syst Rev 2007;2. https://doi.org/10.1002/14651858.MR000013.pub3.
- Caldwell PH, Hamilton S, Tan A, Craig JC. Strategies for increasing recruitment to randomised controlled trials: systematic review. PLOS Med 2010;7. https://doi.org/10.1371/journal.pmed.1000368.
- Treweek S, Lockhart P, Pitkethly M, Cook JA, Kjeldstrøm M, Johansen M, et al. Methods to improve recruitment to randomised controlled trials: Cochrane systematic review and meta-analysis. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-002360.
- McDonald PW. Population-based recruitment for quit-smoking programs: an analytic review of communication variables. Prev Med 1999;28:545-57. https://doi.org/10.1006/pmed.1998.0479.
- Turrell G, Patterson C, Oldenburg B, Gould T, Roy MA. The socio-economic patterning of survey participation and non-response error in a multilevel study of food purchasing behaviour: area- and individual-level characteristics. Public Health Nutr 2003;6:181-9. https://doi.org/10.1079/PHN2002415.
- Lorant V, Demarest S, Miermans PJ, Van Oyen H. Survey error in measuring socio-economic risk factors of health status: a comparison of a survey and a census. Int J Epidemiol 2007;36:1292-9. https://doi.org/10.1093/ije/dym191.
- Goodman A, Gatward R. Who are we missing? Area deprivation and survey participation. Eur J Epidemiol 2008;23:379-87. https://doi.org/10.1007/s10654-008-9248-0.
- Demarest S, Van der Heyden J, Charafeddine R, Tafforeau J, Van Oyen H, Van Hal G. Socio-economic differences in participation of households in a Belgian national health survey. Eur J Public Health 2013;23:981-5. https://doi.org/10.1093/eurpub/cks158.
- Gorman E, Leyland AH, McCartney G, White IR, Katikireddi SV, Rutherford L, et al. Assessing the representativeness of population-sampled health surveys through linkage to administrative data on alcohol-related outcomes. Am J Epidemiol 2014;180:941-8. https://doi.org/10.1093/aje/kwu207.
- UyBico SJ, Pavel S, Gross CP. Recruiting vulnerable populations into research: a systematic review of recruitment interventions. J Gen Intern Med 2007;22:852-63. https://doi.org/10.1007/s11606-007-0126-3.
- Ejiogu N, Norbeck JH, Mason MA, Cromwell BC, Zonderman AB, Evans MK. Recruitment and retention strategies for minority or poor clinical research participants: lessons from the Healthy Aging in Neighborhoods of Diversity Across the Life Span Study. Gerontologist 2011;51:S33-45. https://doi.org/10.1093/geront/gnr027.
- Nagler RH, Ramanadhan S, Minsky S, Viswanath K. Recruitment and retention for community-based eHealth interventions with populations of low socioeconomic position: strategies and challenges. J Commun 2013;63:201-20. https://doi.org/10.1111/jcom.12008.
- Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-42.
- Ellard-Gray A, Jeffrey NK, Choubak M, Crann SE. Finding the hidden participant: solutions for recruiting hidden, hard-to-reach, and vulnerable populations. Int J Qual Methods 2015;14. https://doi.org/10.1177/1609406915621420.
- Nicholson LM, Schwirian PM, Groner JA. Recruitment and retention strategies in clinical studies with low-income and minority populations: progress from 2004–2014. Contemp Clin Trials 2015;45:34-40. https://doi.org/10.1016/j.cct.2015.07.008.
- Pescud M, Pettigrew S, Wood L, Henley N. Insights and recommendations for recruitment and retention of low socio-economic parents with overweight children. Int J Soc Res Methodol 2015;18:617-33. https://doi.org/10.1080/13645579.2014.931201.
- Robinson KA, Dinglas VD, Sukrithan V, Yalamanchilli R, Mendez-Tellez PA, Dennison-Himmelfarb C, et al. Updated systematic review identifies substantial number of retention strategies: using more strategies retains more study participants. J Clin Epidemiol 2015;68:1481-7. https://doi.org/10.1016/j.jclinepi.2015.04.013.
- Brueton VC, Tierney JF, Stenning S, Meredith S, Harding S, Nazareth I, et al. Strategies to improve retention in randomised trials: a Cochrane systematic review and meta-analysis. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-003821.
- Bower P, Brueton V, Gamble C, Treweek S, Smith CT, Young B, et al. Interventions to improve recruitment and retention in clinical trials: a survey and workshop to assess current practice and future priorities. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-399.
- David MC, Alati R, Ware RS, Kinner SA. Attrition in a longitudinal study with hard-to-reach participants was reduced by ongoing contact. J Clin Epidemiol 2013;66:575-81. https://doi.org/10.1016/j.jclinepi.2012.12.002.
- Kleschinsky JH, Bosworth LB, Nelson SE, Walsh EK, Shaffer HJ. Persistence pays off: follow-up methods for difficult-to-track longitudinal samples. J Stud Alcohol Drugs 2009;70:751-61. https://doi.org/10.15288/jsad.2009.70.751.
- Cotter RB, Burke JD, Stouthamer-Loeber M, Loeber R. Contacting participants for follow-up: how much effort is required to retain participants in longitudinal studies?. Eval Program Plann 2005;28:15-21. https://doi.org/10.1016/j.evalprogplan.2004.10.002.
- Robinson KA, Dennison CR, Wayman DM, Pronovost PJ, Needham DM. Systematic review identifies number of strategies important for retaining study participants. J Clin Epidemiol 2007;60:757-65. https://doi.org/10.1016/j.jclinepi.2006.11.023.
- Booker CL, Harding S, Benzeval M. A systematic review of the effect of retention methods in population-based cohort studies. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-249.
- Davis LL, Broome ME, Cox RP. Maximizing retention in community-based clinical trials. J Nurs Scholarsh 2002;34:47-53. https://doi.org/10.1111/j.1547-5069.2002.00047.x.
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLOS Med 2013;10. https://doi.org/10.1371/journal.pmed.1001362.
- Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.CD006611.pub2.
- Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD007457.pub2.
- Mbuagbaw L, van der Kop ML, Lester RT, Thirumurthy H, Pop-Eleches C, Ye CL, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): an individual patient data meta-analysis of randomised trials. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003950.
- Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0088166.
- Crombie IK, Falconer DW, Irvine L, Williams B, Ricketts IW, Humphris G, et al. Reducing alcohol-related harm in disadvantaged men: development and feasibility assessment of a brief intervention delivered by mobile phone. Public Health Res 2013;1.
- Scottish Indices of Deprivation 2003. Oxford: University of Oxford; 2003.
- Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci 2012;1248:107-23. https://doi.org/10.1111/j.1749-6632.2011.06202.x.
- Head KJ, Noar SM, Iannarino NT, Grant Harrington N. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc Sci Med 2013;97:41-8. https://doi.org/10.1016/j.socscimed.2013.08.003.
- Suffoletto B, Callaway C, Kristan J, Kraemer K, Clark DB. Text-message-based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcohol Clin Exp Res 2012;36:552-60. https://doi.org/10.1111/j.1530-0277.2011.01646.x.
- Suffoletto B, Kristan J, Callaway C, Kim KH, Chung T, Monti PM, et al. A text message alcohol intervention for young adult emergency department patients: a randomized clinical trial. Ann Emerg Med 2014;64:664-72. https://doi.org/10.1016/j.annemergmed.2014.06.010.
- Suffoletto B, Kristan J, Chung T, Jeong K, Fabio A, Monti P, et al. An interactive text message intervention to reduce binge drinking in young adults: a randomized controlled trial with 9-month outcomes. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0142877.
- Mason M, Benotsch EG, Way T, Kim H, Snipes D. Text messaging to increase readiness to change alcohol use in college students. J Prim Prev 2014;35:47-52. https://doi.org/10.1007/s10935-013-0329-9.
- Berman AH, Gajecki M, Sinadinovic K, Andersson C. Mobile interventions targeting risky drinking among university students: a review. Curr Addict Rep 2016;3:166-74. https://doi.org/10.1007/s40429-016-0099-6.
- Wright CJ, Dietze PM, Crockett B, Lim MS. Participatory development of MIDY (Mobile Intervention for Drinking in Young people). BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-2876-5.
- Haug S, Schaub MP, Venzin V, Meyer C, John U, Gmel G. A pre-post study on the appropriateness and effectiveness of a Web- and text messaging-based intervention to reduce problem drinking in emerging adults. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2755.
- Lucht MJ, Hoffman L, Haug S, Meyer C, Pussehl D, Quellmalz A, et al. A surveillance tool using mobile phone short message service to reduce alcohol consumption among alcohol-dependent patients. Alcohol Clin Exp Res 2014;38:1728-36. https://doi.org/10.1111/acer.12403.
- Office for National Statistics . Mobile or Smartphone Users By Age Group, GB, 2012. FOI Request: Mobile and Smartphone Usage. Ref Number: 001478 2012. www.ons.gov.uk/ons/about-ons/business-transparency/freedom-of-information/what-can-i-request/previous-foi-requests/people-and-places/mobile-and-smartphone-usage/index.html (accessed 31 March 2017).
- Andrews S, Ellis DA, Shaw H, Piwek L. Beyond self-report: tools to compare estimated and real-world smartphone use. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0139004.
- Douglas N, Free C. ‘Someone batting in my corner’: experiences of smoking-cessation support via text message. Br J Gen Pract 2013;63:e768-76. https://doi.org/10.3399/bjgp13X674459.
- Irvine L, Falconer DW, Jones C, Ricketts IW, Williams B, Crombie IK. Can text messages reach the parts other process measures cannot reach: an evaluation of a behavior change intervention delivered by mobile phone?. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0052621.
- Schwarzer R. Modeling health behaviour change: how to predict and modify the adoption and maintenance of health behaviours. Appl Psychol 2008;57:1-29.
- Sutton S. How does the health action process approach (HAPA) bridge the intention-behavior gap? An examination of the model’s causal structure. Appl Psychol 2008;57:66-74. https://doi.org/10.1111/j.1464-0597.2007.00326.x.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-221. https://doi.org/10.1016/0749-5978(91)90020-T.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull 1982;92:111-35. https://doi.org/10.1037/0033-2909.92.1.111.
- Michie S, Whittington C, Hamoudi Z, Zarnani F, Tober G, West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction 2012;107:1431-40. https://doi.org/10.1111/j.1360-0443.2012.03845.x.
- McCambridge J. Fifty years of brief intervention effectiveness trials for heavy drinkers. Drug Alcohol Rev 2011;30:567-8. https://doi.org/10.1111/j.1465-3362.2011.00379.x.
- O’Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol 2014;49:66-78. https://doi.org/10.1093/alcalc/agt170.
- Field CA, Baird J, Saitz R, Caetano R, Monti PM. The mixed evidence for brief intervention in emergency departments, trauma care centers, and inpatient hospital settings: what should we do?. Alcohol Clin Exp Res 2010;34:2004-10. https://doi.org/10.1111/j.1530-0277.2010.01297.x.
- Brown TJ, Todd A, O’Malley C, Moore HJ, Husband AK, Bambra C, et al. Community pharmacy-delivered interventions for public health priorities: a systematic review of interventions for alcohol reduction, smoking cessation and weight management, including meta-analysis for smoking cessation. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009828.
- Gaume J, McCambridge J, Bertholet N, Daeppen JB. Mechanisms of action of brief alcohol interventions remain largely unknown – a narrative review. Front Psychiatry 2014;5. https://doi.org/10.3389/fpsyt.2014.00108.
- Heather N. Toward an understanding of the effective mechanisms of alcohol brief interventions. Alcohol Clin Exp Res 2014;38:626-8. https://doi.org/10.1111/acer.12336.
- Bertholet N, Palfai T, Gaume J, Daeppen JB, Saitz R. Do brief alcohol motivational interventions work like we think they do?. Alcohol Clin Exp Res 2014;38:853-9. https://doi.org/10.1111/acer.12274.
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction 1993;88:315-35. https://doi.org/10.1111/j.1360-0443.1993.tb00820.x.
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. U.S. Preventive Services Task Force . Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2004;140:557-68. https://doi.org/10.7326/0003-4819-140-7-200404060-00017.
- Braddock K, Dillard JP. Meta-analytic evidence for the persuasive effect of narratives on beliefs, attitudes, intentions, and behaviors. Commun Monogr 2016;83:1-24. https://doi.org/10.1080/03637751.2015.1128555.
- Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ Behav 2007;34:777-92. https://doi.org/10.1177/1090198106291963.
- Shen FY, Sheer VC, Li RB. Impact of narratives on persuasion in health communication: a meta-analysis. J Advert 2015;44:105-13. https://doi.org/10.1080/00913367.2015.1018467.
- Murphy ST, Frank LB, Chatterjee JS, Baezconde-Garbanati L. Narrative versus nonnarrative: the role of identification, transportation, and emotion in reducing health disparities. J Commun 2013;63:116-37. https://doi.org/10.1111/jcom.12007.
- Moran MB, Murphy ST, Frank L, Baezconde-Garbanati L. The ability of narrative communication to address health-related social norms. Int Rev Soc Res 2013;3:131-49. https://doi.org/10.1515/irsr-2013-0014.
- Miller-Day M, Hecht ML. Narrative means to preventative ends: a narrative engagement framework for designing prevention interventions. Health Commun 2013;28:657-70. https://doi.org/10.1080/10410236.2012.762861.
- Larkey LK, Hecht M. A model of effects of narrative as culture-centric health promotion. J Health Commun 2010;15:114-35. https://doi.org/10.1080/10810730903528017.
- de Graaf A. The effectiveness of adaptation of the protagonist in narrative impact: similarity influences health beliefs through self-referencing. Hum Commun Res 2014;40:73-90. https://doi.org/10.1111/hcre.12015.
- Cho H, Shen L, Wilson K. Perceived realism: dimensions and roles in narrative. Communic Res 2012;20:1-24.
- Prestin A. The pursuit of hopefulness: operationalizing hope in entertainment media narratives. Media Psychol 2013;16:318-46. https://doi.org/10.1080/15213269.2013.773494.
- Abroms LC, Whittaker R, Free C, Mendel Van Alstyne J, Schindler-Ruwisch JM. Developing and pretesting a text messaging program for health behavior change: recommended steps. JMIR Mhealth Uhealth 2015;3. https://doi.org/10.2196/mhealth.4917.
- Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev 2016;10:277-96. https://doi.org/10.1080/17437199.2016.1151372.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. https://doi.org/10.1037/0278-6133.27.3.379.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Spagnolli A, Gamberini L. Interacting via SMS: practices of social closeness and reciprocation. Br J Soc Psychol 2007;46:343-64. https://doi.org/10.1348/014466606X120482.
- Poorman E, Gazmararian J, Parker RM, Yang B, Elon L. Use of text messaging for maternal and infant health: a systematic review of the literature. Matern Child Health J 2015;19:969-89. https://doi.org/10.1007/s10995-014-1595-8.
- Fishbein M, Cappella JN. The role of theory in developing effective health communications. J Commun 2006;56:S1-S17. https://doi.org/10.1111/j.1460-2466.2006.00280.x.
- Briñol P, Petty RE. Fundamental processes leading to attitude change: implications for cancer prevention communications. J Commun 2006;56:S81-104. https://doi.org/10.1111/j.1460-2466.2006.00284.x.
- Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie DJ, Jones C, et al. Reducing Binge Drinking Among Disadvantaged Men Through an Intervention Delivered by Mobile Phone: A Multi-Centre Randomised Controlled Trial n.d. www.nets.nihr.ac.uk/projects/phr/11305030 (accessed 6 March 2018).
- Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie D, Evans JM, et al. A mobile phone intervention to reduce binge drinking among disadvantaged men: study protocol for a randomised controlled cost-effectiveness trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-494.
- Sixsmith J, Boneham M, Goldring JE. Accessing the community: gaining insider perspectives from the outside. Qual Health Res 2003;13:578-89. https://doi.org/10.1177/1049732302250759.
- Flanagan SM, Hancock B. ‘Reaching the hard to reach’ – lessons learned from the VCS (voluntary and community sector). A qualitative study. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-92.
- Scottish Index of Multiple Deprivation 2004 Technical Report. Scottish Executive; 2004.
- Semaan S. Time-space sampling and respondent-driven sampling with hard-to-reach populations. Methodol Innov 2010;5:60-75. https://doi.org/10.4256/mio.2010.0019.
- Scottish Government . The Scottish Index of Multiple Deprivation n.d. www.scotland.gov.uk/Topics/Statistics/SIMD (accessed 6 March 2018).
- McAlaney J, McMahon J. Establishing rates of binge drinking in the UK: anomalies in the data. Alcohol Alcohol 2006;41:355-7. https://doi.org/10.1093/alcalc/agl025.
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA 2003;289:70-5. https://doi.org/10.1001/jama.289.1.70.
- Patrick ME. A call for research on high-intensity alcohol use. Alcohol Clin Exp Res 2016;40:256-9. https://doi.org/10.1111/acer.12945.
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students’ recent drinking history: utility for alcohol research. Addict Behav 1986;11:149-61. https://doi.org/10.1016/0306-4603(86)90040-7.
- Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend 1996;42:49-54. https://doi.org/10.1016/0376-8716(96)01263-X.
- Greenfield TK, Kerr WC. Alcohol measurement methodology in epidemiology: recent advances and opportunities. Addiction 2008;103:1082-99. https://doi.org/10.1111/j.1360-0443.2008.02197.x.
- Bond JC, Greenfield TK, Patterson D, Kerr WC. Adjustments for drink size and ethanol content: new results from a self-report diary and transdermal sensor validation study. Alcohol Clin Exp Res 2014;38:3060-7. https://doi.org/10.1111/acer.12589.
- McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0023748.
- Bernstein JA, Bernstein E, Heeren TC. Mechanisms of change in control group drinking in clinical trials of brief alcohol intervention: implications for bias toward the null. Drug Alcohol Rev 2010;29:498-507. https://doi.org/10.1111/j.1465-3362.2010.00174.x.
- Manual for the Fast Alcohol Screening Test (FAST). London: Health Development Agency; 2002.
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care . Second Edition. Geneva: World Health Organization, Department of Mental Health and Substance Dependence; 2001.
- Oei TP, Young RS, Allen JP, Wilson VB. Assessing Alcohol Problems. A Guide for Clinicians and Researchers. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003.
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337-43. https://doi.org/10.3109/07853890109002087.
- Dolan P, Layard R, Metcalfe R. Measuring Subjective Wellbeing for Public Policy: Recommendations on Measures. Special paper No. 23. London: Centre for Economic Performance; 2011.
- Fox J. Applied Regression Analysis and Generalized Linear Models. Sage Publications, Inc.; 2008.
- Little R, Rubin D. Statistical Analysis with Missing Data. New York, NY: Wiley; 2002.
- Heather N, Smailes D, Cassidy P. Development of a Readiness Ruler for use with alcohol brief interventions. Drug Alcohol Depend 2008;98:235-40. https://doi.org/10.1016/j.drugalcdep.2008.06.005.
- Hodgson R, Alwyn T, John B, Thom B, Smith A. The FAST Alcohol Screening Test. Alcohol Alcohol 2002;37:61-6. https://doi.org/10.1093/alcalc/37.1.61.
- Renner B, Schwarzer R, Kwon S, Spivak Y, Panzer M. Risk and Health Behaviors. Documentation of the Scales of the Research Project: ‘Risk Appraisal Consequences in Korea’ (RACK). Second Edition. Berlin: International University Bremen & Freie Universität Berlin; 2007.
- Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie D, Jones C, et al. Texting to Reduce Alcohol Misuse (TRAM): main findings from a randomized controlled trial of a text message intervention to reduce binge drinking among disadvantaged men [published online ahead of print June 1 2018]. Addiction 2018. https://doi.org/10.1111/add.14229.
- Grittner U, Kuntsche S, Graham K, Bloomfield K. Social inequalities and gender differences in the experience of alcohol-related problems. Alcohol Alcohol 2012;47:597-605. https://doi.org/10.1093/alcalc/ags040.
- Loring B. Alcohol and Inequities: Guidance for Addressing Inequities in Alcohol-related Harm. Copenhagen: World Health Organization Regional Office for Europe; 2014.
- Harkins C, Shaw R, Gillies M, Sloan H, MacIntyre K, Scoular A, et al. Overcoming barriers to engaging socio-economically disadvantaged populations in CHD primary prevention: a qualitative study. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-391.
- Thompson TP, Greaves CJ, Ayres R, Aveyard P, Warren FC, Byng R, et al. Lessons learned from recruiting socioeconomically disadvantaged smokers into a pilot randomized controlled trial to explore the role of Exercise Assisted Reduction then Stop (EARS) smoking. Trials 2015;16. https://doi.org/10.1186/1745-6215-16-1.
- Zhao J, Stockwell T, Macdonald S. Non-response bias in alcohol and drug population surveys. Drug Alcohol Rev 2009;28:648-57. https://doi.org/10.1111/j.1465-3362.2009.00077.x.
- Maclennan B, Kypri K, Langley J, Room R. Non-response bias in a community survey of drinking, alcohol-related experiences and public opinion on alcohol policy. Drug Alcohol Depend 2012;126:189-94. https://doi.org/10.1016/j.drugalcdep.2012.05.014.
- Meiklejohn J, Connor J, Kypri K. The effect of low survey response rates on estimates of alcohol consumption in a general population survey. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0035527.
- Christensen AI, Ekholm O, Gray L, Glümer C, Juel K. What is wrong with non-respondents? Alcohol-, drug- and smoking-related mortality and morbidity in a 12-year follow-up study of respondents and non-respondents in the Danish Health and Morbidity Survey. Addiction 2015;110:1505-12. https://doi.org/10.1111/add.12939.
- Cooper ML, Russell M, Skinner JB, Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychol Assess 1992;4:123-32. https://doi.org/10.1037/1040-3590.4.2.123.
- Steckler A, Linnan L. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey Bass; 2002.
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Health Psychol 2004;23:443-51. https://doi.org/10.1037/0278-6133.23.5.443.
- Cohn AM, Hunter-Reel D, Hagman BT, Mitchell J. Promoting behavior change from alcohol use through mobile technology: the Future of Ecological Momentary Assessment. Alcohol Clin Exp Res 2011;35:2209-15. https://doi.org/10.1111/j.1530-0277.2011.01571.x.
- Schüz N, Cianchi J, Shiffman S, Ferguson SG. Novel technologies to study smoking behavior: current developments in ecological momentary assessment. Curr Addict Rep 2015;2:8-14. https://doi.org/10.1007/s40429-015-0039-x.
- Faulkner X, Culwin F. When fingers do the talking: a study of text messaging. Interact Comput 2005;17:167-85. https://doi.org/10.1016/j.intcom.2004.11.002.
- Jenkins RJ, McAlaney J, McCambridge J. Change over time in alcohol consumption in control groups in brief intervention studies: systematic review and meta-regression study. Drug Alcohol Depend 2009;100:107-14. https://doi.org/10.1016/j.drugalcdep.2008.09.016.
- Oei TP, Hasking PA, Young RM. Drinking refusal self-efficacy questionnaire-revised (DRSEQ-R): a new factor structure with confirmatory factor analysis. Drug Alcohol Depend 2005;78:297-30. https://doi.org/10.1016/j.drugalcdep.2004.11.010.
- Orne MT. On the social psychology of the psychological experiment: with particular reference to demand characteristics and their implications. Am Psychol 1962;17. https://doi.org/10.1037/h0043424.
- Curry SJ, Ludman EJ, Grothaus LC, Donovan D, Kim E. A randomized trial of a brief primary-care-based intervention for reducing at-risk drinking practices. Health Psychol 2003;22:156-65. https://doi.org/10.1037/0278-6133.22.2.156.
- Reiff-Hekking S, Ockene JK, Hurley TG, Reed GW. Brief physician and nurse practitioner-delivered counseling for high-risk drinking. Results at 12-month follow-up. J Gen Intern Med 2005;20:7-13. https://doi.org/10.1111/j.1525-1497.2005.21240.x.
- Richmond R, Heather N, Wodak A, Kehoe L, Webster I. Controlled evaluation of a general practice-based brief intervention for excessive drinking. Addiction 1995;90:119-32. https://doi.org/10.1111/j.1360-0443.1995.tb01016.x.
- Heather N. Interpreting null findings from trials of alcohol brief interventions. Front Psychiatry 2014;5. https://doi.org/10.3389/fpsyt.2014.00085.
- Davis CG, Thake J, Vilhena N. Social desirability biases in self-reported alcohol consumption and harms. Addict Behav 2010;35:302-11. https://doi.org/10.1016/j.addbeh.2009.11.001.
- McCambridge J, Kypri K, Elbourne D. Research participation effects: a skeleton in the methodological cupboard. J Clin Epidemiol 2014;67:845-9. https://doi.org/10.1016/j.jclinepi.2014.03.002.
- Gill JS, Zezulka AV, Beevers DG, Davies P. Relation between initial blood pressure and its fall with treatment. Lancet 1985;1:567-9. https://doi.org/10.1016/S0140-6736(85)91219-X.
- Morton V, Torgerson DJ. Regression to the mean: treatment effect without the intervention. J Eval Clin Pract 2005;11:59-65. https://doi.org/10.1111/j.1365-2753.2004.00505.x.
- Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol 2005;34:215-20. https://doi.org/10.1093/ije/dyh299.
- Finney JW. Regression to the mean in substance use disorder treatment research. Addiction 2008;103:42-5. https://doi.org/10.1111/j.1360-0443.2007.02032.x.
- McCambridge J, Kypri K, McElduff P. Regression to the mean and alcohol consumption: a cohort study exploring implications for the interpretation of change in control groups in brief intervention trials. Drug Alcohol Depend 2014;135:156-9. https://doi.org/10.1016/j.drugalcdep.2013.11.017.
- Stockwell T, Zhao J, Greenfield T, Li J, Livingston M, Meng Y. Estimating under- and over-reporting of drinking in national surveys of alcohol consumption: identification of consistent biases across four English-speaking countries. Addiction 2016;111:1203-13. https://doi.org/10.1111/add.13373.
- Beeston C, Reid G, Robinson M, Craig N, McCartney G, Graham L, et al. Monitoring and Evaluating Scotland’s Alcohol Strategy. Third Annual Report. Edinburgh: NHS Health Scotland; 2013.
- McCambridge J, Kypri K, Elbourne D. In randomization we trust? There are overlooked problems in experimenting with people in behavioral intervention trials. J Clin Epidemiol 2014;67:247-53. https://doi.org/10.1016/j.jclinepi.2013.09.004.
- Quirk A, MacNeil V, Dhital R, Whittlesea C, Norman I, McCambridge J. Qualitative process study of community pharmacist brief alcohol intervention effectiveness trial: can research participation effects explain a null finding?. Drug Alcohol Depend 2016;161:36-41. https://doi.org/10.1016/j.drugalcdep.2016.01.023.
- McCambridge J. From question-behaviour effects in trials to the social psychology of research participation. Psychol Health 2015;30:72-84. https://doi.org/10.1080/08870446.2014.953527.
- Felix L, Keating P, McCambridge J. Can obtaining informed consent alter self-reported drinking behaviour? A methodological experiment. BMC Med Res Methodol 2015;15. https://doi.org/10.1186/s12874-015-0032-z.
- Clifford PR, Davis CM. Alcohol treatment research assessment exposure: a critical review of the literature. Psychol Addict Behav 2012;26:773-81. https://doi.org/10.1037/a0029747.
- Moos RH. Context and mechanisms of reactivity to assessment and treatment. Addiction 2008;103:249-50. https://doi.org/10.1111/j.1360-0443.2007.02123.x.
- McCambridge J. [Commentary] Research assessments: instruments of bias and brief interventions of the future?. Addiction 2009;104:1311-2. https://doi.org/10.1111/j.1360-0443.2009.02684.x.
- McCambridge J, de Bruin M, Witton J. The effects of demand characteristics on research participant behaviours in non-laboratory settings: a systematic review. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0039116.
- Brown L, Campbell-Jack D, Gray L, Hovald P, Kirkpatrick G, Knudsen L, et al. The Scottish Health Survey. 2015 edition, Volume 1, Main Report. Edinburgh: Scottish Government; 2016.
- Project MATCH Research Group . Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcohol Clin Exp Res 1998;22:1300-11. https://doi.org/10.1111/j.1530-0277.1998.tb03912.x.
- Cutler RB, Fishbain DA. Are alcoholism treatments effective? The Project MATCH data. BMC Public Health 2005;5. https://doi.org/10.1186/1471-2458-5-75.
- Butler CC, Simpson SA, Hood K, Cohen D, Pickles T, Spanou C, et al. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: a cluster randomised trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f1191.
- Suffoletto B, Merrill JE, Chung T, Kristan J, Vanek M, Clark DB. A text message program as a booster to in-person brief interventions for mandated college students to prevent weekend binge drinking. J Am Coll Health 2016;64:481-9. https://doi.org/10.1080/07448481.2016.1185107.
- Moore SC, Crompton K, van Goozen S, van den Bree M, Bunney J, Lydall E. A feasibility study of short message service text messaging as a surveillance tool for alcohol consumption and vehicle for interventions in university students. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-1011.
- Riordan BC, Conner TS, Flett JAM, Scarf D. A brief orientation week ecological momentary intervention to reduce university student alcohol consumption. J Stud Alcohol Drugs 2015;76:525-9. https://doi.org/10.15288/jsad.2015.76.525.
- Bendtsen M, Bendtsen P. Feasibility and user perception of a fully automated push-based multiple-session alcohol intervention for university students: randomized controlled trial. JMIR Mhealth Uhealth 2014;2. https://doi.org/10.2196/mhealth.3233.
- Gajecki M, Berman AH, Sinadinovic K, Rosendahl I, Andersson C. Mobile phone brief intervention applications for risky alcohol use among university students: a randomized controlled study. Addict Sci Clin Pract 2014;9. https://doi.org/10.1186/1940-0640-9-11.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Savovic J, Jones HE, Altman DG, Harris RJ, Juni P, Pildal J, et al. Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Ann Intern Med 2012;157:429-38. https://doi.org/10.7326/0003-4819-157-6-201209180-00537.
- Copeland KT, Checkoway H, McMichael AJ, Holbrook RH. Bias due to misclassification in the estimation of relative risk. Am J Epidemiol 1977;105:488-95. https://doi.org/10.1093/oxfordjournals.aje.a112408.
- Delgado-Rodríguez M, Llorca J. Bias. J Epidemiol Community Health 2004;58:635-41. https://doi.org/10.1136/jech.2003.008466.
- Miller CH, Lane LT, Deatrick LM, Young AM, Potts KA. Psychological reactance and promotional health messages: the effects of controlling language, lexical concreteness, and the restoration of freedom. Hum Commun Res 2007;33:219-40. https://doi.org/10.1111/j.1468-2958.2007.00297.x.
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction 2003;98:1-12. https://doi.org/10.1046/j.1359-6357.2003.00586.x.
- Stahre M, Naimi T, Brewer R, Holt J. Measuring average alcohol consumption: the impact of including binge drinks in quantity-frequency calculations. Addiction 2006;101:1711-8. https://doi.org/10.1111/j.1360-0443.2006.01615.x.
- Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet 2002;359:781-5. https://doi.org/10.1016/S0140-6736(02)07882-0.
- Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders-Algra M, et al. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies?. Arch Dis Child 2008;93:458-61. https://doi.org/10.1136/adc.2007.127316.
- Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci 2010;1186:125-45. https://doi.org/10.1111/j.1749-6632.2009.05333.x.
- Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally?. Int J Epidemiol 2003;32:357-66. https://doi.org/10.1093/ije/dyg084.
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health 2001;55:111-22. https://doi.org/10.1136/jech.55.2.111.
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Soc Sci Med 2005;61:965-75. https://doi.org/10.1016/j.socscimed.2004.12.027.
- Santiago CD, Wadsworth ME, Stump J. Socioeconomic status, neighborhood disadvantage, and poverty-related stress: prospective effects on psychological syndromes among diverse low-income families. J Econ Psychol 2011;32:218-30. https://doi.org/10.1016/j.joep.2009.10.008.
- Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol Alcohol 2005;40:453-60. https://doi.org/10.1093/alcalc/agh176.
- Jacob R, Arnold LD, Hunleth J, Greiner KA, James AS. Daily hassles’ role in health seeking behavior among low-income populations. Am J Health Behav 2014;38:297-306. https://doi.org/10.5993/AJHB.38.2.15.
- Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: does the availability of alcohol play a role?. Int J Epidemiol 2005;34:772-80. https://doi.org/10.1093/ije/dyi026.
- Amlung M, MacKillop J. Understanding the effects of stress and alcohol cues on motivation for alcohol via behavioral economics. Alcohol Clin Exp Res 2014;38:1780-9. https://doi.org/10.1111/acer.12423.
- Jarl J, Johansson P, Eriksson A, Eriksson M, Gerdtham UG, Hemström O, et al. The societal cost of alcohol consumption: an estimation of the economic and human cost including health effects in Sweden, 2002. Eur J Health Econ 2008;9:351-60. https://doi.org/10.1007/s10198-007-0082-1.
- Mäkelä P, Herttua K, Martikainen P. The socioeconomic differences in alcohol-related harm and the effects of alcohol prices on them: a summary of evidence from Finland. Alcohol Alcohol 2015;50:661-9. https://doi.org/10.1093/alcalc/agv068.
- Vandenberg B, Sharma A. Are alcohol taxation and pricing policies regressive? Product-level effects of a specific tax and a minimum unit price for alcohol. Alcohol Alcohol 2016;51:493-502. https://doi.org/10.1093/alcalc/agv133.
- Holmes J, Meng Y, Meier PS, Brennan A, Angus C, Campbell-Burton A, et al. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. Lancet 2014;383:1655-64. https://doi.org/10.1016/S0140-6736(13)62417-4.
- Thirumurthy H, Lester RT. M-health for health behaviour change in resource-limited settings: applications to HIV care and beyond. Bull World Health Organ 2012;90:390-2. https://doi.org/10.2471/BLT.11.099317.
- Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J Telemed Telecare 2011;17:41-8. https://doi.org/10.1258/jtt.2010.100322.
- Babor T, Cactano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No Ordinary Commodity. New York, NY: Oxford University Press; 2003.
- Brennan A, Meier P, Purshouse R, Rafia R, Meng Y, Hill-Macmanus D, et al. The Sheffield Alcohol Policy Model – a mathematical description. Health Econ 2015;24:1368-88. https://doi.org/10.1002/hec.3105.
- Purshouse R, Brennan A, Latimer N, Meng Y, Rafia R, Jackson R, et al. Modelling to Assess The Effectiveness and Cost-Effectiveness of Public Health Related Strategies and Interventions to Reduce Alcohol Attributable Harm in England Using the Sheffield Alcohol Policy Model Version 2.0. Report to the NICE Public Health Programme Development Group. Sheffield: University of Sheffield; 2009.
- Angus C, Holmes J, Robert P, Meier P, Brennan A. Model-based Appraisal of the Comparative Impact of Minimum Unit Pricing and Taxation Policies in Scotland. An Adaptation of the Sheffield Alcohol Policy Model Version 3. Sheffield: School of Health and Related Research (ScHARR), University of Sheffield; 2016.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit (PSSRU), University of Kent; 2015.
- Curtis LA. Unit Costs of Health and Social Care. Canterbury: Personal Social Services Research Unit (PSSRU), University of Kent; 2014.
- Office for National Statistics . 2011 Census n.d. www.ons.gov.uk/census/2011census (accessed 14 February 2018).
- NHS Digital . 2010 PCO Data – Attribution Data Set GP Registered Populations 2010. https://data.gov.uk/dataset/attribution-dataset-gp-registered-populations (accessed 31 March 2017).
- Reference Costs 2014–15. London: Department of Health and Social Care; 2015.
- Scottish Crime Statistic 2014–15. Edinburgh: Scottish Government; 2016.
- Royal College of Nursing . NHS Pay Scales 2016–17 n.d. www.rcn.org.uk/employment-and-pay/nhs-pay-scales-2016-17 (accessed 16 Febraury 2018).
- University of Dundee . Single Pay Spine for Academic and HE Support Staff n.d. www.dundee.ac.uk/finance/our-services/payroll/salary-scales/single-pay-spine/ (accessed 16 February 2018).
- NHS Research Scotland . Primary Care Network n.d. www.nhsresearchscotland.org.uk/research-areas/primary-care (accessed 16 February 2018).
- University of Dundee . Procurement 2016. www.dundee.ac.uk/procurement/ (accessed 16 February 2018).
- Royal Mail . Our Prices n.d. www.royalmail.com/current-postage-prices/ (accessed 16 February 2018).
- Costs Per Place and Costs Per Prisoner by Individual Prison. National Offender Management Service Annual Report and Accounts 2015–16. Management Information Addendum. London: Ministry of Justice; 2016.
- Devlin N, Shah K, Feng Y, Mulhern B, van Hout B. Valuing Health-Related Quality of Life: An EQ-5D-5L Value Set for England. Research Paper 16/01. London: Office of Health Economics; 2016.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. New York, NY: Oxford University Press; 2014.
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res 2002;26:36-43. https://doi.org/10.1111/j.1530-0277.2002.tb02429.x.
- Kanavos P, van den Aardweg S, Schurer W. Diabetes Expenditure Burden of Disease and Management in 5 EU Countries. London: LSE Health, London School of Economics; 2012.
- Delgleize E, Leeuwenkamp O, Theodorou E, Van de Velde N. Cost-effectiveness analysis of routine pneumococcal vaccination in the UK: a comparison of the PHiD-CV vaccine and the PCV-13 vaccine using a Markov model. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010776.
- Absence Management Annual Survey Report 2015. London: CIPD; 2015.
- Annual Survey of Hours and Earnings: 2016 Provisional Results. London: Office for National Statistics; 2016.
- Chitnis X, Georghiou T, Steventon A, Bardsley M. The Impact of the Marie Curie Nursing Service on Place of Death and Hospital Use at the End of Life. London: The Nuffield Trust; 2012.
- Mortality Statistics. Review of the Registrar General on Deaths by Cause, Sex and Age, in England and Wales, 2005. London: Office for National Statistics; 2006.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013 2013. www.nice.org.uk/process/pmg9/chapter/the-appraisal-of-the-evidence-and-structured-decision-making (accessed 31 March 2017).
- Bray JW, Zarkin GA, Hinde JM, Mills MJ. Costs of alcohol screening and brief intervention in medical settings: a review of the literature. J Stud Alcohol Drugs 2012;73:911-9. https://doi.org/10.15288/jsad.2012.73.911.
- Crombie IK, Falconer DW, Irvine L, Norrie J, Williams B, Slane PW. Risky single-occasion drinking and disadvantaged men: will recruitment through primary care miss hazardous drinkers?. Alcohol Clin Exp Res 2013;37:1577-81. https://doi.org/10.1111/acer.12123.
- Robson M, Asaria M, Cookson R, Tsuchiya A, Ali S. Eliciting the level of health inequality aversion in England. Health Econ 2017;26:1328-34. https://doi.org/10.1002/hec.3430.
- Heckley G, Jarl J, Gerdtham UG. Frequency and intensity of alcohol consumption: new evidence from Sweden. Eur J Health Econ 2017;18:495-517. https://doi.org/10.1007/s10198-016-0805-2.
- Byrnes J, Shakeshaft A, Petrie D, Doran C. Can harms associated with high-intensity drinking be reduced by increasing the price of alcohol?. Drug Alcohol Rev 2013;32:27-30. https://doi.org/10.1111/j.1465-3362.2012.00482.x.
Appendix 1 General practitioner letter of invitation
Appendix 2 Participant information sheet
Appendix 3 Participant consent form
Appendix 4 Screening questionnaire
Appendix 5 Baseline questionnaire
Appendix 6 First follow-up questionnaire
Appendix 7 Final follow-up questionnaire
Appendix 8 Economic evaluation: supplementary tables
| Type of cost | Centre | Staff level appropriate at rollout | |||
|---|---|---|---|---|---|
| Tayside | Fife | Forth Valley | Glasgow | ||
| Step 1: identifying potential participants | |||||
| Training | |||||
| Manager training recruiters | 256.31 | 256.31 | 256.31 | 256.31 | Project manager |
| Recruiters’ time for training | 577.23 | 577.23 | 577.23 | 577.23 | Grade 6, spine point 4 |
| Locating venue and identifying potential participants | Grade 6, spine point 4 | ||||
| At venue | 5087.34 | 2907.32 | 3997.33 | 3082.42 | |
| Travelling | 432.92 | 2039.55 | 1236.24 | 981.29 | |
| Number of potential participants identified | 233 | 123 | 168 | 171 | |
| PIS packs for potential participants | |||||
| Preparation time | 614.27 | 324.27 | 442.9 | 450.82 | Grade 3 administrative post |
| Stationery cost | 84.58 | 44.65 | 60.98 | 62.07 | |
| Total cost (step 1) | 7052.66 | 6149.34 | 6571.01 | 5410.15 | |
| Staff | 6968.08 | 6104.69 | 6510.02 | 5348.08 | |
| Stationery | 84.58 | 44.65 | 60.98 | 62.07 | |
| Step 2: recruiting participants from potential participants | |||||
| Call to screen and give message consent | |||||
| Staff time | 744.82 | 614.56 | 611.10 | 737.89 | Grade 6, spine point 4 |
| Phone cost for 1 year | 120 | 120 | 120 | 120 | |
| Extra PIS packs and consent form | Grade 3 administrative post | ||||
| Number of extra sent | 2.25 | 2.25 | 2.25 | 2.25 | |
| Preparation time | 5.93 | 5.93 | 5.93 | 5.93 | |
| Material cost | 2.05 | 2.05 | 2.05 | 2.05 | |
| Number of participants recruited | 100 | 99 | 98 | 101 | |
| Sent vouchers by post | Grade 3 administrative post | ||||
| Staff time (10 minutes for each voucher) | 263.64 | 261.00 | 258.36 | 266.27 | |
| Vouchers, printing and postage | 1060.50 | 1049.90 | 1039.29 | 1071.11 | |
| Lost vouchers | |||||
| Staff time (10 minutes for each voucher) | 5.27 | 5.27 | 5.27 | 5.27 | Grade 3 administrative post |
| Vouchers, printing and postage | 21.21 | 21.21 | 21.21 | 21.21 | |
| Total cost (step 2) | 2223.43 | 2079.92 | 2063.22 | 2229.74 | |
| Staff | 1019.66 | 886.76 | 880.66 | 1015.37 | |
| Stationery, vouchers and phone | 1203.76 | 1193.16 | 1182.55 | 1214.37 | |
| Cost per participant (steps 1 and 2) | 92.76 | 83.12 | 88.10 | 75.64 | |
| Step 3: intervention (all participants treated as in the intervention group) | |||||
| Vouchers | |||||
| Sent vouchers by post | |||||
| Staff time (10 minutes for each voucher) | 1049.27 | Grade 3 administrative post | |||
| Vouchers, printing and postage | 4220.79 | ||||
| Lost vouchers | |||||
| Staff time (10 minutes for each voucher) | 15.82 | Grade 3 administrative post | |||
| Vouchers, printing and postage | 63.63 | ||||
| Total voucher-related cost | 5349.51 | ||||
| One-year system cost | |||||
| Text messages application software | 5000 | ||||
| Set-up of the message delivery system | 2500 | ||||
| Testing and amendment of the message delivery system | 1000 | ||||
| Dedicated phone number for enquiries | 180 | ||||
| Server hosting charge | 2000 | ||||
| Project management for IT | 500 | ||||
| Text system programmer’s time for monitoring and maintenance | 4385 | ||||
| Bundles of SMS (112 messages per participant) | 1605 | ||||
| Total system cost | 17,170 | ||||
| Total cost (step 3) | 22,519 | ||||
| Cost per participant (step 3) | 56.80 | ||||
| Vouchers | 13.44 | ||||
| System | 43.14 | ||||
| Type of cost | Centre | Staff level appropriate at rollout | |||
|---|---|---|---|---|---|
| Tayside | Fife | Forth Valley | Glasgow | ||
| Step 1: identifying potential participants | |||||
| Send initial e-mails to general practices | 55.58 | 55.58 | 55.58 | 55.58 | Grade 4–5 administrative post |
| Phone non-responders | – | 101.50 | 368.58 | – | Project manager |
| Number of practices recruited | 5 | 5 | 6 | 4 | |
| Visit practices and complie lists of potential participants | 670.16 | 618.67 | 538.05 | 244.89 | Grade 4–5 administrative post |
| At venue or calling | 509.05 | 457.56 | 376.94 | 83.78 | |
| Travel | 161.11 | 161.11 | 161.11 | 161.11 | |
| GP screening (£162 each practice) | 1200 | 1200 | 1440 | 960 | |
| Collect list, prepare and send PIS packs | |||||
| Packs sent to each centre | 431.78 | 637.19 | 714.53 | 309.33 | |
| Collect list and prepare letters | 375.39 | 381.03 | 405.19 | 251.33 | Grade 4–5 administrative post |
| At venue or calling | 56.39 | 256.17 | 309.33 | 58.00 | |
| Travel | 717.62 | 818.96 | 739.53 | 494.85 | |
| Material cost | 245.79 | 280.51 | 253.30 | 169.49 | |
| Time to prepare packs | 206.13 | 206.13 | 247.35 | 164.90 | Grade 3 administrative post |
| General practices sending out packs | 13.15 | 16.07 | 12.86 | 9.48 | |
| Receiving postcards, editing and transferring lists | 431.78 | 637.19 | 714.53 | 309.33 | Grade 4–5 administrative post |
| Number of potential participants identified | 724 | 885 | 708 | 522 | |
| Compile list of potential participants to be contacted | 6.72 | 0.52 | 0.42 | 0.31 | Grade 3 administrative post |
| Manager training recruiters | 128.16 | 128.16 | 128.16 | 128.16 | Project manager |
| Recruiters’ time for training | 288.62 | 288.62 | 288.62 | 288.62 | Grade 6, spine point 4 |
| Total cost (step 1) | 3963.70 | 4351.90 | 4786.96 | 2825.60 | |
| Staff | 3246.08 | 3532.94 | 4047.43 | 2330.76 | |
| Stationery | 717.62 | 818.96 | 739.53 | 494.85 | |
| Step 2: recruiting participants from potential participants | |||||
| Call to screen and give message consent | |||||
| Staff time | 1621.44 | 1492.34 | 1089.62 | 1574.88 | Grade 6, spine point 4 |
| Phone cost for 1 year | 120 | 120 | 120 | 120 | |
| Extra PIS packs and consent form | |||||
| Number of extra sent | 43 | 43 | 43 | 43 | |
| Preparation time for each pack | 113.36 | 113.36 | 113.36 | 113.36 | Grade 3 administrative post |
| Material cost | 39.26 | 39.26 | 39.26 | 39.26 | |
| Number of participants recruited | 102 | 132 | 88 | 105 | |
| Sent vouchers by post | |||||
| Staff time (10 minutes for each voucher) | 268.91 | 348.00 | 232.00 | 276.82 | Grade 3 administrative post |
| Vouchers, printing and postage | 1081.71 | 1399.86 | 933.24 | 1113.53 | |
| Lost vouchers | |||||
| Staff time (10 minutes for each voucher) | 0.66 | 0.66 | 0.66 | 0.66 | Grade 3 administrative post |
| Vouchers, printing and postage | 2.65 | 2.65 | 2.65 | 2.65 | |
| Total cost (step 2) | 3248.00 | 3516.13 | 2530.79 | 3241.16 | |
| Staff | 2004.38 | 1954.36 | 1435.64 | 1965.72 | |
| Stationery, vouchers and phone | 1243.62 | 1561.77 | 1095.15 | 1275.44 | |
| Total cost per participant (steps 1 and 2) | 70.70 | 59.61 | 83.16 | 57.78 | |
| Step 3: intervention (all participants treated as in the intervention group) | |||||
| Vouchers | |||||
| Sent vouchers by post | |||||
| Staff time (10 minutes for each voucher) | 1125.73 | Grade 3 administrative post | |||
| Vouchers and printing and postage | 4528.34 | ||||
| Lost vouchers | |||||
| Staff time (10 minutes for each voucher) | 3.95 | Grade 3 administrative post | |||
| Vouchers and printing and postage | 15.91 | ||||
| Total voucher-related cost | 5673.92 | ||||
| One-year system cost | |||||
| Text messages application software | 5000 | ||||
| Set-up of the message delivery system | 2500 | ||||
| Testing of and amendments to the message delivery system | 1000 | ||||
| Dedicated phone number for enquiries | 180 | ||||
| Server hosting charge | 2000 | ||||
| Project management for IT | 500 | ||||
| Text system programmer’s time for monitoring and maintenance | 4385 | ||||
| Bundles of SMS (112 messages per participant) | 1721 | ||||
| Total system cost | 17,286 | ||||
| Total cost (step 3) | 23,960 | ||||
| Cost per participant (step 3) | 53.77 | ||||
| Voucher related | 13.29 | ||||
| System related | 40.48 | ||||
| Type of cost | Recruitment method | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TSS only | General practice registers only | Combined methods | ||||||||||
| Tayside | Fife | Forth Valley | Glasgow | Tayside | Fife | Forth Valley | Glasgow | Tayside | Fife | Forth Valley | Glasgow | |
| Step 1: identifying potential participants | ||||||||||||
| Staff on site or in office | 65.35 | 41.06 | 53.81 | 43.24 | 29.69 | 23.60 | 40.65 | 20.11 | 47.35 | 31.09 | 47.58 | 31.45 |
| Staff travelling | 4.33 | 20.60 | 12.61 | 9.72 | 2.13 | 3.16 | 5.35 | 2.09 | 3.22 | 10.64 | 9.18 | 5.83 |
| Stationery | 0.85 | 0.45 | 0.62 | 0.61 | 7.04 | 6.20 | 8.40 | 4.71 | 3.97 | 3.74 | 4.30 | 2.70 |
| Step 2: recruiting participants from potential participants | ||||||||||||
| Staff making calls | 10.20 | 8.96 | 8.99 | 10.05 | 19.65 | 14.81 | 16.31 | 18.72 | 14.97 | 12.30 | 12.45 | 14.47 |
| Stationery and vouchers | 12.04 | 12.05 | 12.07 | 12.02 | 12.19 | 11.83 | 12.44 | 12.15 | 12.12 | 11.93 | 12.25 | 12.09 |
| Step 3: intervention | ||||||||||||
| Voucher related | 13.44 | 13.44 | 13.44 | 13.44 | 13.29 | 13.29 | 13.29 | 13.29 | 13.36 | 13.35 | 13.37 | 13.36 |
| IT system and staff related | 43.14 | 43.14 | 43.14 | 43.14 | 40.48 | 40.48 | 40.48 | 40.48 | 22.90 | 22.90 | 22.90 | 22.90 |
| Project manager overseeing the programme | 12.69 | 12.82 | 12.95 | 12.56 | 12.44 | 9.61 | 14.42 | 12.08 | 6.28 | 5.49 | 6.82 | 6.16 |
| Web page | 2.51 | 2.51 | 2.51 | 2.51 | 2.34 | 2.34 | 2.34 | 2.34 | 1.21 | 1.21 | 1.21 | 1.21 |
| Total cost per participant | 164.54 | 155.03 | 160.14 | 147.30 | 139.25 | 125.33 | 153.69 | 125.98 | 125.38 | 112.64 | 130.06 | 110.17 |
| Service use | Group, mean (SD) | |
|---|---|---|
| Intervention (n = 347) | Control (n = 357) | |
| Health-care services use | ||
| Accident and emergency department | 0.46 (1.28) | 0.37 (1.14) |
| Night in hospital | 1.28 (11.31) | 0.21 (0.95) |
| Admitted to hospital but not overnight | 0.10 (0.56) | 0.16 (0.87) |
| Outpatient appointment | 1.89 (19.45) | 0.91 (2.97) |
| Visited doctor | 3.38 (5.91) | 3.36 (4.81) |
| Doctor visited you | 0.04 (0.58) | 0.03 (0.24) |
| Visited nurse | 0.60 (1.70) | 0.69 (5.26) |
| Nurse visited you | 0.02 (0.26) | 0 (0) |
| Prescriptions | 7.59 (27.88) | 7.50 (26.34) |
| Social care services | ||
| Visited by social worker | 0.36 (2.69) | 0.37 (3.15) |
| Went to see social worker | 0.98 (9.54) | 0.89 (9.42) |
| Visited by care worker/advisor | 0.60 (6.37) | 2.17 (27.02) |
| Went to see care worker/advisor | 0.35 (3.11) | 0.65 (6.35) |
| Criminal justice services | ||
| Arrested/cautioned/fined | 0.25 (1.05) | 0.24 (0.91) |
| Appeared peace/sheriff court | 0.17 (0.91) | 0.18 (1.50) |
| Appeared high court | 0 (0) | 0 (0) |
| Day in prison | 1.18 (14.04) | 1.67 (16.28) |
| Type of cost | Recruitment method | Staff level | |
|---|---|---|---|
| TSS | General practice registers | ||
| Step 1 | NA | NA | |
| Step 2 reminder letters, more vouchers sent | |||
| Pre first follow-up | |||
| RA time (10 minutes per letter) | 1531.59 | 1643.19 | |
| Stationery (£0.60 per letter) | 240.79 | 258.34 | |
| Post first follow-up and lost vouchers | |||
| RA time | 1289.15 | 1554.68 | |
| Stationery and vouchers (£10.60 per pack) | 3552.7 | 4284.4 | |
| Pre second follow-up | |||
| RA time (10 minutes per letter) | 1531.59 | 1643.19 | |
| Stationery (£0.60 per letter) | 240.79 | 258.34 | |
| Post second follow-up and lost vouchers | |||
| RA time | 1189.10 | 1543.13 | |
| Stationery and vouchers (£10.60 per pack) | 2553.58 | 2739.64 | |
| Step 2 research total | 12,129.26 | 13,924.92 | |
| Step 3 intervention | |||
| Monitor for undelivered messages and take action | 504.68 | 135.85 | Project manager |
| Read responses and take action | 320.39 | 108.68 | Project manager |
| Maintain and update database (1 minute per entry) | 24,637.43 | 26,432.62 | Grade 3 administrative post |
| Data extracts | 500 | 500 | |
| Step 3 research total | 25,962.50 | 27,177.14 | |
| Research total | 38,091.76 | 41,102.06 | |
| Number of participants | 398 | 427 | |
| Research cost per participant | 95.71 | 96.26 | |
| Projection | Population (%) | Source | ||
|---|---|---|---|---|
| Scotland | England | Total | ||
| Population that could be recruited, n | 5311 | 56,244 | 61,556 | |
| Population in 2011, n | 5,295,000 | 53,012,456 | 58,307,456 | |
| Could be targeted and recruited | 0.10 | 0.11 | ||
| Men aged 25–44 years | 13 | 14 | 2011 Census225 | |
| Disadvantaged | 20 | 20 | Assumption | |
| Reached | 20 | 20 | Assumption | |
| Agreed as potential participants | 34 | 34 | From this trial | |
| Participated | 57 | 57 | From this trial | |
| Projection | Population (%) | Source | ||
|---|---|---|---|---|
| Scotland | England | Total | ||
| Population could be recruited, n | 18,779 | 198,860 | 217,639 | |
| Population in 2011, n | 5,295,000 | 53,012,456 | 58,307,456 | |
| Could be targeted and recruited | 0.35 | 0.38 | ||
| Men aged 25–44 years | 13 | 14 | 2011 Census225 | |
| With general practice registration | 97a | 97a | PCO226 and 2011 Census225 | |
| Disadvantaged | 20 | 20 | Assumption | |
| Reached and recruited | 14 | 14 | From this trial | |
| Projection | Population (n) | ||
|---|---|---|---|
| Scotland | England | Total | |
| Population that could be recruited | 21,434 | 226,983 | 248,417 |
| From general practice registers | 18,779 | 198,860 | 217,639 |
| From TSS | 2656 | 28,122 | 30,778 |
| Health and social harm | Rate (%) | ||
|---|---|---|---|
| Difference (intervention – control) | Intervention | Control | |
| Acute conditions | |||
| Mental and behavioural disorders due to use of alcohol | 0.0000 | 0.0007 | 0.0007 |
| Ethanol poisoning | 0.0000 | 0.0000 | 0.0000 |
| Methanol poisoning | 0.0000 | 0.0000 | 0.0000 |
| Toxic effect of alcohol, unspecified | 0.0000 | 0.0000 | 0.0000 |
| Accidental poisoning by exposure to alcohol | 0.0004 | 0.0004 | 0.0000 |
| Chronic conditions | |||
| Alcohol-induced pseudo-Cushing’s syndrome | 0.0000 | 0.0000 | 0.0000 |
| Degeneration of the nervous system | 0.0000 | 0.0000 | 0.0000 |
| Alcoholic polyneuropathy | 0.0000 | 0.0000 | 0.0000 |
| Alcoholic myopathy | –0.0007 | 0.0000 | 0.0007 |
| Alcoholic cardiomyopathy | 0.0004 | 0.0004 | 0.0000 |
| Alcoholic gastritis | 0.0000 | 0.0051 | 0.0051 |
| Alcoholic liver disease | –0.0018 | 0.0073 | 0.0092 |
| Chronic pancreatitis (alcohol induced) | 0.0007 | 0.0007 | 0.0000 |
| Malignant neoplasm of lip, oral cavity and pharynx | 0.0055 | 0.4472 | 0.4417 |
| Malignant neoplasm of oesophagus | –0.0187 | 1.2059 | 1.2246 |
| Malignant neoplasm of colon and rectum | 0.0194 | 0.9675 | 0.9480 |
| Malignant neoplasm of liver and intrahepatic bile ducts | 0.0051 | 0.1343 | 0.1291 |
| Malignant neoplasm of larynx | –0.0015 | 0.2341 | 0.2355 |
| Malignant neoplasm of breast | 0.0000 | 0.0000 | 0.0000 |
| Diabetes mellitus (type 2) | –0.0936 | 5.8480 | 5.9416 |
| Epilepsy and status epilepticus | –0.0095 | 1.8061 | 1.8157 |
| Cardiac arrhythmias | 0.0095 | 6.2747 | 6.2652 |
| Haemorrhagic stroke | –0.0037 | 0.5536 | 0.5573 |
| Lower respiratory infections: pneumonia | 0.0000 | 0.0000 | 0.0000 |
| Cirrhosis of the liver (excluding alcoholic liver disease) | –0.0484 | 1.4594 | 1.5079 |
| Hypertensive diseases | 0.0143 | 0.1915 | 0.1772 |
| Acute and chronic pancreatitis | –0.0059 | 0.8955 | 0.9014 |
| Social harms | |||
| Road traffic accidents: non-pedestrian | –0.0029 | 0.0029 | 0.0059 |
| Pedestrian traffic accidents | 0.0004 | 0.0004 | 0.0000 |
| Water transport accidents | 0.0000 | 0.0000 | 0.0000 |
| Air/space transport accidents | 0.0000 | 0.0000 | 0.0000 |
| Fall injuries | 0.0004 | 0.0238 | 0.0235 |
| Work/machine injuries | 0.0000 | 0.0015 | 0.0015 |
| Firearm injuries | 0.0000 | 0.0000 | 0.0000 |
| Drowning | –0.0004 | 0.0000 | 0.0004 |
| Inhalation of gastric contents | 0.0007 | 0.0007 | 0.0000 |
| Fire injuries | –0.0011 | 0.0007 | 0.0018 |
| Accidental excessive cold | 0.0000 | 0.0000 | 0.0000 |
| Intentional self-harm | –0.0055 | 0.0048 | 0.0103 |
| Assault | –0.0004 | 0.0051 | 0.0055 |
| More serious wounding | –0.0022 | 0.0114 | 0.0136 |
| Less serious wounding | 0.0327 | 1.4323 | 1.3996 |
| Assault on a constable | 0.0077 | 0.1185 | 0.1108 |
| Assault without injury | –0.0081 | 1.1509 | 1.1590 |
| Criminal damage | –0.0789 | 5.7420 | 5.8209 |
| Theft from the person | –0.0018 | 0.0150 | 0.0169 |
| Robbery | 0.0011 | 0.0183 | 0.0172 |
| Robbery (business) | –0.0004 | 0.0007 | 0.0011 |
| Burglary in a dwelling | –0.0007 | 0.0316 | 0.0323 |
| Burglary not in a dwelling | 0.0004 | 0.0268 | 0.0264 |
| Theft of a pedal cycle | 0.0011 | 0.0114 | 0.0103 |
| Theft from vehicle | –0.0070 | 0.1519 | 0.1589 |
| Aggravated vehicle taking | –0.0007 | 0.0007 | 0.0015 |
| Theft of vehicle | –0.0018 | 0.0260 | 0.0279 |
| Other theft | 0.0000 | 0.0418 | 0.0418 |
| Theft from shops | –0.0161 | 1.1582 | 1.1744 |
| Violent disorder | 0.0018 | 0.0026 | 0.0007 |
| Total sexual offence | –0.0154 | 0.1244 | 0.1398 |
| Homicide | 0.0000 | 0.0007 | 0.0007 |
| Unemployment | –0.1721 | 11.0071 | 11.1791 |
| Absenteeism | –0.0220 | 0.3933 | 0.4153 |
| Mortality | |||
| Death due to alcohol | 0.0668 | 11.3824 | 11.3156 |
| All causes of death | 0.0994 | 38.1018 | 38.0023 |
| 2016 GBP (£) | 2009 USD ($) | Source | |
|---|---|---|---|
| Median costs per screening | 9–21 | 10–25 | Bray et al., 2012245 |
| Median costs per brief intervention | 26–81 | 30–95 | Bray et al., 2012245 |
| Type of costs | Recruitment method | Difference; p-value | |
|---|---|---|---|
| TSS (n = 396) | General practice (n = 308) | ||
| Health-care services | 1552 | 784 | 768; 0.006 |
| Social-care services | 473 | 49 | 424; 0.003 |
| Criminal justice services | 383 | 50 | 333; 0.006 |
List of abbreviations
- AUDIT
- Alcohol Use Disorders Identification Test
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FAST
- Fast Alcohol Screening Test
- GP
- general practitioner
- HAPA
- Health Action Process Approach
- IT
- information technology
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SIMD
- Scottish Index of Multiple Deprivation
- SMS
- Short Message Service
- SPCRN
- Scottish Primary Care Research Network
- TSS
- time–space sampling
