Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3006/02. The contractual start date was in April 2011. The final report began editorial review in November 2016 and was accepted for publication in June 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Wouter Poortinga, Nikki Jones and Simon Lannon received funding from Carmarthenshire County Council to conduct a health impact survey study from 2009 to 2016. Jonathan Morgan was responsible for delivering the Carmarthenshire Homes Standard improvement programme.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Rodgers et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background and aims
Background to the project
The Welsh Housing Quality Standard (WHQS) was introduced by the Welsh Government in 2002 as a standard to be achieved by all social landlords (local authorities and housing associations/registered social landlords) in Wales by 2012 and to be maintained thereafter. 1 The goal was to ensure that all socially rented homes in Wales were in a good state of repair; safe and secure; adequately heated, fuel efficient and well insulated; provided with up-to-date kitchens and bathrooms; well managed; located in attractive and safe environments; and, as far as possible, suited to the specific needs of the household. Similar standards were introduced in England in 2000 and in Northern Ireland (as per the Decent Homes Standard in England) and Scotland in 2004. 2,3 It has been made clear that the Standard does not apply to housing in the private sector in Wales, although the need for improvement is not dissimilar, and, in parts of the private sector, may be even more pressing. 4
Aims of the project
We investigated the health impact of bringing housing to a national quality standard. Our research questions examined changes in health events for council house residents after their homes received at least one cointervention of a concentrated housing intervention. Changes in routinely collected health event data were used as a proxy for health impact. Our primary research question was:
-
What is the change in emergency hospital admission rates for cardiovascular, respiratory and injury-related conditions (combined) for tenants aged ≥ 60 years?
The secondary research questions investigated emergency admission rate changes separately for each of the three categories of conditions, respiratory, cardiovascular and injuries, for both older tenants and tenants of all ages.
We were also interested in capturing changes in health events managed in the community that may not have resulted in a hospital admission, and asked:
-
What are the changes in emergency department attendances, general practitioner (GP) treatments for mental health and respiratory conditions, and attendances at the GP for respiratory conditions?
We also asked:
-
What is the impact on costs associated with health-care utilisation?
Our main analyses of interest evaluated the direct impact of changes in health-care utilisation as a result of living in a home while it was brought up to standard. We were also interested to see if the effects remained in the longer term. Therefore, we analysed, as a separate group, those people who either were already living in a home that had received the improvements or had moved into a study home in which the improvements had already been made.
This report presents the impact of the housing improvement on emergency admissions to hospital (see Chapter 3), the impact on health-care utilisation in primary care and accident and emergency hospital attendances (see Chapter 4), and the economic impact (see Chapter 5).
Chapter 2 The housing intervention
We have included sufficient details on the intervention to capture the degree of flexibility or tailoring of the intervention that took place. This chapter follows the TIDieR (Template for Intervention Description and Replication) reporting guidelines. 5
Background to housing quality standards: the Welsh Housing Quality Standard
The Welsh Government introduced the WHQS in 2002 to be achieved by all social landlords (local authorities and housing associations/registered social landlords) in Wales by 2012 and to be maintained thereafter. 6 Political devolution after 1999 and the creation of the National Assembly for Wales, with enhanced responsibilities for much of national-level housing policy in Wales, provided the impetus for developing a common standard for all social rented housing in Wales and was prefaced in the Assembly’s first National Housing Strategy, Better Homes for People in Wales. 6
The WHQS sets out a basic set of requirements with the aim of ensuring that all socially rented homes in Wales are in a good state of repair; safe and secure; adequately heated, fuel efficient and well insulated; provided with up-to-date kitchens and bathrooms; well managed; located in attractive and safe environments; and, as far as possible, suited to the specific needs of the household. Similar standards had already been introduced in England in 2000 and subsequently in Northern Ireland and Scotland in 2004. 2,3,7 There are differences between the detailed requirements of the individual housing quality standards, and it is generally accepted that cointerventions of the WHQS are more challenging than those set elsewhere. There are 10 broad components for which social landlords in Wales are expected to report compliance annually: roofs and associated components, windows, external doors, kitchens, bathrooms, energy rating, central heating systems, electrical systems, mains-powered smoke detectors, gardens and external storage.
Social landlords in Wales have adopted different approaches to the delivery of the WHQS, and different time scales have emerged for achieving it. The housing stock options considered by Welsh local authorities, essentially whether to retain their council-owned stock or pursue stock transfer (where supported by tenants), and uncertainties over the availability of sufficient financial resources have delayed progress towards the achievement of the WHQS. The 10-year target of attaining the standard for all social housing in Wales was perhaps overly ambitious, given these uncertainties. However, at the outset there was no consistent baseline against which to measure progress towards meeting the WHQS and, until 2010, no consistent monitoring of landlord compliance. As a result, the Welsh Government agreed extensions to the original 2012 deadline with individual local authorities and housing associations and, subsequently, has set a revised deadline of 2020 for all Welsh social landlords to achieve the WHQS.
Delivery of the housing intervention
In 2003, Carmarthenshire County Council (CCC) consulted a sample of 1000 tenants about their views on the WHQS. Following this, in 2005, the council took the decision to retain its ownership and management of the council housing stock and to set its own housing quality standard, the Carmarthenshire Homes Standard (CHS), which is a standard slightly higher than the WHQS. With the agreement of the Welsh Government, a time scale for full compliance with the WHQS/CHS was set for 2015. This is the intervention this study has considered in seeking to evaluate the health impacts of housing improvements. The council adapted the WHQS for its sheltered housing stock and added the installation of carbon monoxide detectors and feature fireplaces, neither of which is part of the WHQS. Although there is not a perfect match between these compliance categories and those demanded by Welsh Government in relation to the WHQS, there is considerable overlap. Hereafter, the application of housing standards, as carried out by CCC, is referred to as ‘the intervention’. In terms of assessing the intervention, we examined if each of the eight housing work cointerventions met and complied with the CHS quality standard (Box 1). Further details about the intervention are provided in Appendix 1 (see Table 12).
All homes owned by CCC were brought up to standard for each of the following cointerventions:
-
Windows and doors.
-
Kitchens. a
-
Bathrooms. a
-
Loft insulation.
-
Wall insulation (internal or external).
-
Heating systems, including boilers, new radiators and new fireplace surrounds. a
-
Electrical systems, including rewiring, adding power sockets, smoke detectors, carbon monoxide detectors and security lights, and installing extractor fans in bathrooms and kitchens.
-
Garden paths.
Materials chosen by tenants were used for these cointerventions (see Figure 20).
Carmarthenshire County Council also developed an environmental works project to enable local residents to identify and prioritise improvements to their wider environment.
Logic model of housing improvements
The anticipated impacts on health of these cointerventions are described in the literature using logic models. 8 The models can be used to infer longer-term health impacts that could not be detected during the lifespan of previous evaluations. The possible pathways between housing improvement and health are visually mapped according to the best available evidence on the health and socioeconomic impacts. The health impacts of internal housing improvement interventions have not yet been adequately evaluated. 9 A simplified version of this logic model was tailored to the GoWell programme. 10 We have adapted the housing improvements to health pathways for the CHS intervention (Table 1).
| Health condition | Housing risk factors | Associated housing conditions | Relevant housing improvements |
|---|---|---|---|
| Fall and burn injuries | Slip hazard |
Slippery surfaces Ventilation |
Kitchens and bathrooms Electrical systems |
| Trip hazard | Trailing wires | Electrical systems | |
| Fall hazard |
Window open low to ground Uneven steps/no handrails |
Windows and doors Garden paths |
|
| Respiratory health | Damp and mould | Thermal efficiency | Insulation |
| Cold | Weatherproofing | Heating | |
| Overcrowding | Ventilation | Kitchens and bathrooms | |
| Circulatory conditions | Cold | Thermal efficiency | Insulation |
| Thermal efficiency | Windows and doors | ||
| Heating affordability and functioning | Heating | ||
| Concerns about crime and antisocial behaviour | Windows and doors | ||
| Mental health | Stress | External quality and appearance | Insulation |
| Anxiety | Heating | ||
| Depression | Damp and mould | Kitchens and bathrooms | |
| Fuel poverty | |||
| Overcrowding | Windows and doors | ||
| Concerns about crime and antisocial behaviour |
Community engagement
The intervention was delivered by contractors on behalf of a CCC team who reported to an overarching Steering Group and a Tenant Involvement Group made up of a wide range of tenants from across the county. This provided a mechanism for tenant views to be expressed to the team, in addition to newsletters, reports and regular surveys. Carmarthenshire recognised at the start that the involvement of tenants in the development of the programme would be the main factor in its successful delivery.
Carmarthenshire County Council liaised with the tenants network to establish the intervention programme roll-out, and gave households several choices for the type of materials to be used for their new kitchens and bathrooms (see Appendix 2). In 2014, the council also started working with its tenants and other stakeholders to consider what further improvements might be required beyond 2015, a programme known as the Carmarthenshire Homes Standard Plus (CHS+).
It was noted above that the CHS was developed in consultation with the council’s own tenants. CCC has continued to encourage tenant involvement and community engagement in the evolution of the CHS (and now CHS+) and to link the CHS to other council strategies (e.g. its corporate, sustainable development and affordable warmth strategies). As a result of the further engagement with tenants, Carmarthenshire’s business plan for the delivery of CHS+ has been developed around three main themes: supporting tenants and residents, investing in tenants’ homes and providing more homes. Improving standards through the CHS+ is integral to all three.
Carmarthenshire County Council has recognised that both resident involvement and community engagement are essential in the delivery of CHS (and CHS+). The council has also developed a CHS sustainability strategy to help council tenants to live more sustainably by reducing carbon emissions, minimising waste, encouraging recycling, maximising employment and training opportunities, and promoting safe, attractive and sustainable environments. The council took some before-and-after photographs to show tenants the appearance of the externally visible improvements (Figure 1).
FIGURE 1.
Photographs illustrating the (a) before and (b) after picture of housing improvements in Carmarthenshire. Reproduced with permission from Jonathan Morgan, Carmarthenshire Country Council, 2017.


Considerable consultation was undertaken to consider how the different cointerventions might be organised and rolled out across different estates and parts of the county. It was a highly complex process to agree the prioritising of work and achieve an appropriate balance across different localities, and at the same time linking this to available funding and resources. Nevertheless, work programmes were developed to ensure the delivery of the intervention from the end of 2007–8 to the completion of the programme in December 2015.
The council wants to deliver an excellent housing service and it conducts regular satisfaction surveys. In its 2012–15 council housing business plan, it reported 91% overall tenant satisfaction with intervention works and 95% tenant satisfaction with the performance of the council’s contractor partners.
Our study research team had engagement from the council housing tenants from the outset of the project through Study Steering Committee meetings. The housing upgrades were delivered in a pragmatic order, with no prioritisation or selection of tenants who were most in need. Ms Pam Every, a lay representative and the chairperson of the Llanelli Tenants Network, liaised with the council, attended the launch of CHS intervention with the First Minister for Wales, and was involved in interpreting the results and in our ongoing plans for dissemination.
Organising and delivering housing standards
Carmarthenshire County Council is managing the intervention using PRINCE (Projects in a Controlled Environment) II project management procedures. A team of seven council officers reports monthly to a Project Steering Group made up of directors and heads of service who are responsible for the internal monitoring of progress. The project team also reports on a regular basis to a liaison group made up of tenant representatives, meeting with area-based housing staff and members of the project team to discuss project proposals and provide feedback of wider tenant views. Information is also provided to all tenants through newsletters and reports.
Study design considerations
We noted above that CCC took a decision in 2005 to retain its council housing stock and developed a programme to deliver the intervention between 2005 and 2015. However, some other social landlords were not able to achieve the WHQS within the original time scale, and in a small number of cases did not expect to achieve WHQS until 2017 or later. In these cases, progress towards achieving the WHQS has been much slower because of significant shortfalls between investment needs and available resources, ongoing financial uncertainties, rejection of the transfer option by tenants and limitations on organisational and contractor capacities, and much of the work will be done during the period 2015–20. Welsh Government ministers have now indicated a revised target of no later than 2020 for all Welsh social landlords to attain WHQS compliance, although most are expected to do so by the end of 2017.
We originally selected one such local authority as a comparator in the expectation that its compliance levels in relation to the different cointerventions of the WHQS would be significantly lower, during the study period, than those in the main intervention locality. This landlord was not expected to achieve the WHQS until 2020. We received data from our intended comparator area but, following efforts to recategorise data fields to allow a direct intervention comparison between regions, it was apparent that many more properties than expected were recorded as reaching housing quality standards. This is likely to be because of ongoing works of maintenance and improvement. Furthermore, the pressure of reporting compliance with the WHQS in this region is different, resulting in data recording what is essentially a different intervention. Thus, we were unable to use the region as a comparator as intended. Instead, we used an internal comparator comprising people living in homes that had not yet received a cointervention as a reference group, with an adjustment for any trends present within the wider region (rest of Carmarthenshire).
The internal reference groups meant there was a different reference group for each housing cointervention assessed. They included residents of homes that could have undergone any type of housing improvement other than the one being analysed. All homes had at least one intervention.
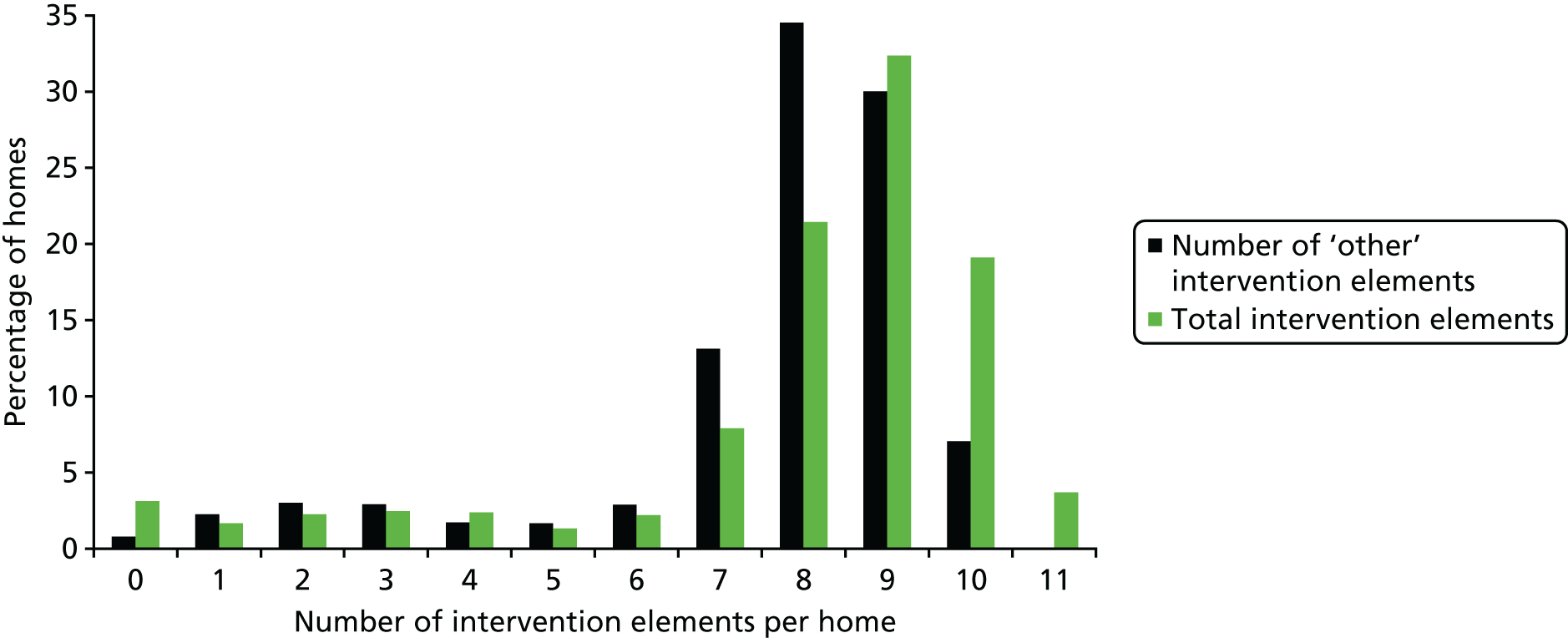
It is challenging to illustrate exhaustively the case mix of properties in terms of intervention. To illustrate the ‘perfect complexity’ of the intervention at the household level, the large number of variations in the intervention order and number received by each home. For the 11 intervention cointerventions, there are 2047 possible combinations of intervention. We consider that the intervention delivery was sufficiently complex to have been effectively delivered in a random pattern. This is illustrated by comparing the overall pattern of the intervention with that of a single cointervention: windows and doors (Figure 2). Overall, there were few homes that had only one cointervention, and also few that required all cointerventions, with 8–10 being the most frequent number of cointerventions received per home (before combining all electrical work into one ‘electrical systems’ cointervention, there were 11 separate categories of work). There were 9159 properties and, of these, 4802 properties had windows and doors fitted during the study period. Of the 4802 homes that had windows and doors fitted (see Table 2), only 38 (< 1%) homes had this single cointervention only during the study period. We estimate that this would be a maximum of 55 older residents, some of whom will have moved or died during the decade-long study period; there is no reason to suggest that there was a disproportionate number of people living in these homes.
FIGURE 2.
Intervention delivery: number of interventions (1–11 cointerventions) overall and number of ‘other’ interventions for homes that received windows and doors (1–10 other cointerventions).
The complex housing intervention proceeded stepwise over a considerable period of time, complicating the evaluation and limiting study design choice. Intervention details are described above, as well as in detail in Appendix 1 (see Table 12). Properties receiving all cointerventions constituting the intervention often had different intervention dates for each and were spread over an 8-year period throughout the study. This is because the programme was designed with a ‘rolling’ design to minimise the amount of disruption due to the works, allowing people to remain in their homes for the duration of the intervention. Additionally, the number of cointerventions needed and the extent of work required was dependent on the condition of the property at the start of the study and a number of other factors such as property type and year of build. Some properties required considerably more work than others to achieve WHQS compliance status. This means that properties received different interventions at different periods throughout the improvement programme. However, the work programme was designed at the start of the intervention, meaning that the timing of different cointerventions was independent of need and the extent of work required.
All homes had at least one intervention, but this is not true of individuals. In addition to the complexity of the intervention being evaluated, the migration of individuals generated by a high churn rate of residents typical of social housing occupancy created additional challenges to effectively capture the effects of the intervention at an individual level. We were assured by CCC that there was no change in the policy for allocating homes and no reason to suggest that the case mix of tenants was different following the intervention programme.
The only criterion of the dynamic cohort was that an individual had to live in a study home (that eventually would experience at least one cointervention during the study period) for a minimum of 60 days. It is a non-trivial task to convert the property-level intervention information into individual-level data. Consider that it is possible for some individuals to be in a reference group for multiple cointerventions. Conversely, an individual could live in multiple properties and could have experienced more than the maximum number interventions received by each home.
It is important to note that (apart from excluding younger people from our primary outcome of older residents) we have not excluded any groups of people from our analyses. There were three groups in each of our analyses, as follows.
-
The ‘never compliant’ reference group were tenants who lived in their home while that particular cointervention did not meet the housing quality standard. They may have moved into another home before the work was completed to make their former home compliant.
-
The main exposure (1) group includes those tenants who were living in their home at the time it had the work completed for a particular cointervention and ‘became compliant’. This group was compared with the reference group. We have focused on presenting these results in the report.
-
The second exposure (2) group, comprising tenants who either were living in the home that already met the housing quality standard for a particular cointervention or moved into a home after the cointervention was complete, are our second ‘always compliant’ group. We have included the results from this group analysed against the reference group for a particular cointervention in our ‘additional analyses’ results sections (see Chapter 3, Results, Additional analyses, and Chapter 4, Results, Additional analyses).
We repeated our analyses, including the three reference and exposure groups, and the eight cointerventions, for each of our primary and secondary health outcomes.
To help illustrate this complex housing intervention and the migration of tenants, we have provided a conceptual diagram to illustrate some of the combinations and challenges we have taken into account in our analyses (Figure 3).
FIGURE 3.
Conceptual diagram of the housing intervention.
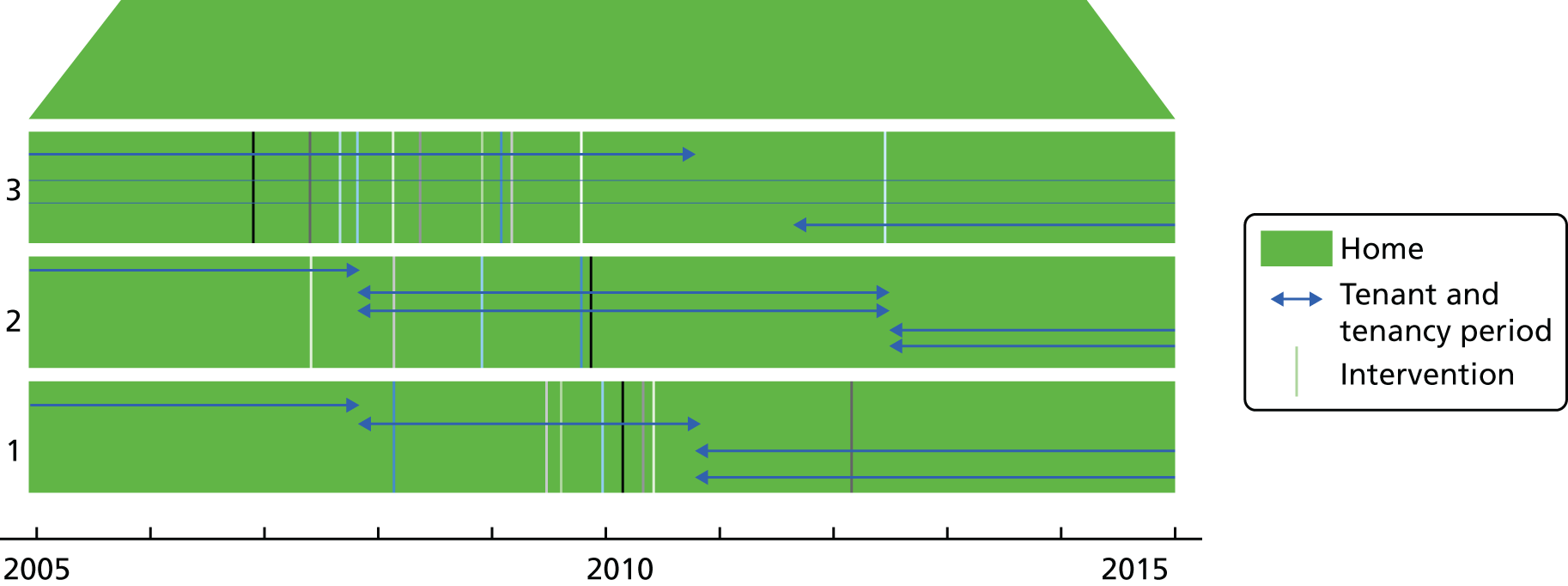
The conceptual diagram (see Figure 3) shows three homes; each large block is a different home. The vertical lines are the cointerventions that are delivered to each home in a different order; a different number is delivered to each home. The horizontal lines represent individual tenants who have different tenancy periods during the study period. In home 1, the first tenant, who lived there before the start of the study period, moved out at the end of 2007 before the first cointervention was delivered in 2008. This tenant would be in the reference group for the ‘blue’ cointervention. The tenant in home 2 is in the exposure (1) group for the ‘pink’ cointervention. The two tenants moving into home 2 at the end of 2007 are in the exposure (2) group for the ‘pink’ cointervention, and in the exposure (1) group for the rest.
Residential environment changes
A housing improvement programme may act as a catalyst for wider neighbourhood regeneration. 11–13 We wanted to assess if wider environmental area changes occurred as a result of investment in the homes. This would help us interpret the results from our statistical models assessing changes in health events as a result of the housing improvements.
An established environmental quality audit tool was updated and validated as part of the research to assess the impacts of the housing intervention on the overall quality of the neighbourhood environment. 14,15 It was expected that the housing intervention would result in measurable improvements in the overall quality of the neighbourhood environment, and that these improvements would be linked to work that contributes to the external appearance of the property and the estate environment in general.
The revised Residential Environment Assessment Tool (REAT 2.0) [www.ncbi.nlm.nih.gov/pubmed/28260806 (accessed 18 October 2017)] study found a medium-sized increase in overall neighbourhood quality, showing the wider changes associated with a concentrated housing improvement programme. As expected, postcodes with the greatest externally visible improvements had the highest increase in neighbourhood quality. However, the effect was not statistically significant. This is most likely due to a scaling back of the gardens and estates part of the programme. The gardens and estates improvement was reduced from more general beautification to a focus only on making garden paths safe. The results regarding changes in residential environmental quality are reported in detail in Appendix 3 and in a working paper. 16
Chapter 3 The effect on emergency hospital admissions of a housing intervention meeting national housing quality standards: a longitudinal study using data linkage
This chapter follows the STROBE (Strengthening of the Reporting of Observational Studies in Epidemiology) reporting guidelines for observational study designs (www.strobe-statement.org). 17
Parts of this chapter have been reproduced from Rodgers et al. 18 This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
Background/rationale
This chapter examines changes in health-care utilisation, as a proxy for health, following housing improvements to bring council homes up to a national quality standard. Poor housing quality has been associated with negative health impacts globally. 19 To reduce health inequalities, distinguished researchers such as Sir Michael Marmot recommend that policies focus on wider determinants of health, including housing. 20–22 However, some housing policy has been implemented despite evidence from housing interventions suggesting small or unclear health effects. 23 Countries in temperate regions with fewer energy-efficient homes, including the UK, Greece, Portugal and Ireland, have more excess winter deaths, indicating that variations in winter mortality are caused by differences in indoor temperatures, health-care spending and socioeconomic circumstances. 24 Direct health impacts of cold housing and fuel poverty are thought to cause 33% and 40% of respiratory and cardiovascular diseases, respectively. 25 Housing quality standards require maintenance through continuing investment in ageing housing stock. 20 Quantifiable evidence of the health impact and associated costs of health-care utilisation as a result of poor housing quality is needed to ensure sufficient investment.
Poor health has been associated with poor housing quality in a number of cross-sectional studies. 23 A systematic review of the effects of improvements to housing found some evidence of health benefits following changes to thermal conditions, particularly when these interventions were targeted towards those with chronic respiratory conditions. 26,27 Evidence of health improvements not specifically targeted at vulnerable groups were less clear; authors noted that impacts measured for everyone in a housing improvement area may conceal health improvements for vulnerable population subgroups. Studies had a relatively limited follow-up and used self-reported health in most cases. 25 The review concluded that precise housing conditions and mechanisms causing poor health need further investigation using robust study designs.
Evidence on whole-home housing-led interventions remains unclear. 27 Multiple cointerventions of a national housing intervention and impact on self-reported physical and mental health was evaluated using a quasi-experimental design. There were positive associations with mental health (kitchens and bathrooms, front doors) and physical health (fabric works) but a negative effect on physical health following the installation of central heating. 23 Three waves of cross-sectional surveys had 1011 participants contributing to all waves to constitute a 5-year longitudinal data set. 23 The authors were unable to randomise the allocation or to a waiting list but used the waiting list as a control. The use of survey data directly from participants introduces bias and restricts follow-up duration. However, the ability to assess changes in well-being directly as a result of the housing intervention rather than waiting for changes in health service utilisation is advantageous for studies with a limited number of participants and short follow-up periods. 27 Consideration has been given to whether or not a whole-house intervention prevents the onset of long-term conditions; follow-up time was up to 5 years for about half of the participants, but there was no evidence of preventing the onset of new conditions in this period. 10
A limited number of studies have used a randomised controlled design with longitudinal data. However, when studies have achieved randomisation, the number of participants is relatively small, limiting subgroup analyses. A larger randomised controlled trial (RCT)28 allocated 436 homes to the treatment group and had a waiting list for 406 control group homes to receive fall-prevention home modifications. After adjusting for age, previous falls, sex and ethnic origin, the intervention resulted in a 26% reduction in the per-year rate of injuries due to falls at home, compared with the control group. The 950 low-income participants were followed up using objective data for just over 3 years, a period suitable for modifications having an immediate impact on health such as falls. However, follow-up times have been equally as short for respiratory and cardiovascular conditions that are likely to result in impacts after a longer time period. 29 The results were limited by the collection of health outcomes for the entire duration of the study without correcting for deaths and migration during the intervention period.
A RCT30 of child participants with asthma allocated 200 to an intervention group and 209 to a control group. Non-polluting heating was installed, with the control group on a waiting list. Child self-report and parental-reported health data were collected at baseline and at 1-year follow-up. At follow-up, only 349 (39%) of 899 eligible households had completed all requirements, with exclusions due to moving home, lack of interest or withdrawal from the trial for unknown reasons. Attempts were made to investigate bias in reporting by the children by including questions about health outcomes not expected to be associated with the heating upgrades (e.g. vomiting or a twisted ankle). Some reporting bias was found. In addition, a direct comparison of self-reported and objective data found a significant reduction in school absences recorded by statutory school records, but not when using parental-reported data. Therefore, it may be possible to randomise allocation of a housing intervention, but the required longer-term follow-up means that a RCT using self-report data only may include various forms of bias. This could reduce the robustness of this study design to render it less than the ‘gold standard’.
In contrast to RCTs, observational studies have their own set of limitations. It is difficult to control for the multiple associations between poverty, poor housing and poor health. 31 Lack of randomisation means that there is doubt about the equivalency of an intervention and a reference group. We propose that data linkage studies may be used to adjust for multiple confounders. These studies allow the use of thousands of people in the wider region to adjust results for trends, and the creation of multiple reference groups for those waiting for different parts of the intervention. To our knowledge there have been no evaluations of housing interventions using data linkage and routinely collected data; however, there have been non-intervention data linkage studies investigating the health and education outcomes for children resident in social housing compared with the rest of the regional population. 32
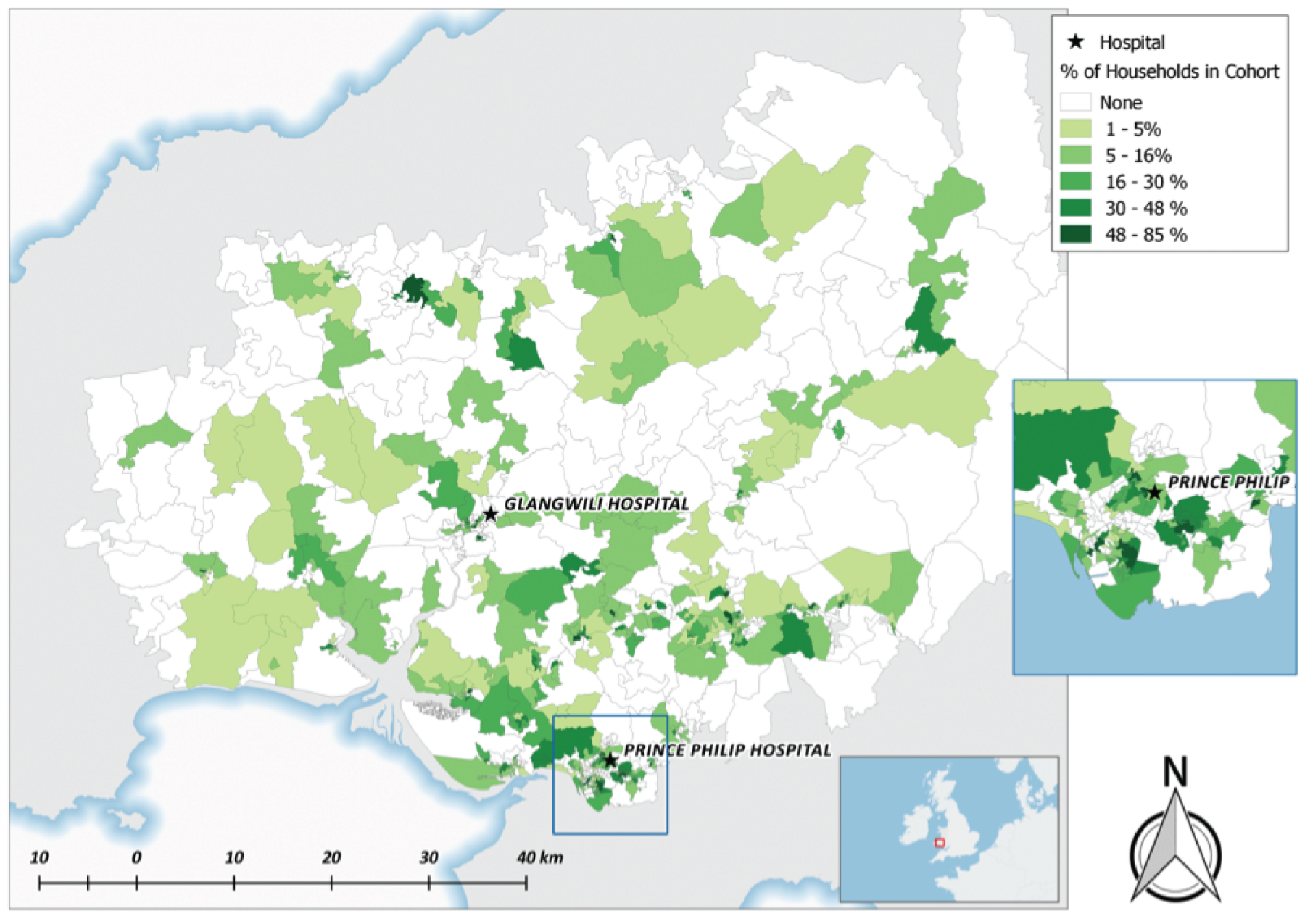
Concentrated investment in national housing standards was used to deliver a comprehensive housing investment programme, which comprised multiple work cointerventions, with potential health impact pathways to improve a wide range of health conditions, including falls and burns, as well as the more commonly studied cardiovascular and respiratory conditions that typically see an impact from warmth or energy efficiency measures. We used a decade of linked health data to examine whether or not each cointervention of a comprehensive housing intervention had an impact on the health of residents living in council homes (social or public housing), in Carmarthenshire, as determined by their emergency admissions to hospital. Data linkage has not previously been used to study the effects of housing improvements, and nor has this wide range of outcomes been evaluated. More than 9000 council homes distributed throughout Carmarthenshire received the intervention (Figure 4).
FIGURE 4.
Percentage of study homes receiving at least one work cointervention by small area geography (Census, 2011 lower super output areas). Contains OS data © Crown copyright and database right (2015).
Objectives
We used more than a decade of unique total-population, linked health data to investigate whether or not emergency hospital admission rates for respiratory conditions, cardiovascular conditions and fall and burn injuries for council tenants aged ≥ 60 years were associated with properties receiving at least one cointervention of a concentrated housing intervention. Several secondary hypotheses were specified to investigate emergency admission rate changes separately for each of the three conditions, respiratory, cardiovascular and injuries, for both older tenants and all ages.
Our main analyses of interest evaluated the direct impact of changes in health-care utilisation for those individuals living in homes that were brought up to standard. We were also interested to see if effects would be detected in the longer term. Therefore, we analysed, as a separate group, those people who either were living in a home that already met the national standard or moved into a home during the study window but after the improvements had already been made.
Methods
Study design
In a longitudinal panel design, we flagged all homes receiving the housing intervention, the residents benefiting from the intervention and their health-care utilisation, as recorded in an anonymised databank, for the period before and throughout the duration of the intervention. 33
Using a longitudinal design we were able to observe outcomes in high temporal resolution monthly intervals for all subjects in this study. This approach maximised the use of individual level health data, which could be aggregated into any desired time interval, before, during and after the intervention, and allowed us to overcome the logistical difficulties identified with the difference in differences method. It also utilises the availability of detailed intervention data to determine which components of the intervention were delivered to each home, and when, along with who lived in those homes during that time.
Our panel design method enabled us to evaluate associations between meeting housing standards and health events over time. It allowed any underlying temporal trends or systematic (or any other) changes affecting the study group to be taken into account, providing more confidence that estimated effects are attributable to the intervention. This is important for our study outcomes for which calendar period could confound the occurrence of admissions for cardiovascular and respiratory admissions, as well as fall-related injuries.
This approach also allowed analyses of the individual cointerventions and made it possible to isolate their effects. A difference in differences analyses comparing outcomes before the start of the intervention with those observed after the entire intervention is completed is not suited to an evaluation of individual cointerventions to quantify which have the strongest effects. Multiple testing using different time periods for each cointervention would violate conditions of independence, and cointerventions may have complex interacting effects on the outcomes that could not be accounted for using just two time periods: before and after a change in quality for each cointervention. Our longitudinal panel design allowed a more general approach to evaluate all of the components of the intervention together.
Our longitudinal approach provided effect estimates for each cointervention of the complex intervention by simultaneously (1) observing changes in health events, as a proxy for health outcomes, in relation to the housing quality status during an individuals’ period of tenancy, and (2) adjusting for trends in the wider population.
Our longitudinal study design used repeated measures of health service utilisation during the study period, and covariates indicating compliance with housing quality standards, generated retrospectively based on the delivery of each housing cointervention. The analysis of health events over time was the most appropriate method to evaluate and account for all the components of the complex intervention while fully utilising the longitudinal routine health data sets.
For each cointervention, we categorised exposure based on whether or not an individual was exposed to completion of the cointervention during their period of tenancy. We also considered the effect of the regeneration work on people who moved into homes that were already at the required standard for a cointervention. Our reference group for each cointervention were residents in homes that that did not have an upgrade for that particular cointervention. Individuals were categorised differently for each cointervention and we did not have static exposure groups. Individuals living in a home that received a cointervention were categorised as such irrespective of the specific time that the intervention was delivered. Intervention roll-out was not associated with residents’ needs or demographic profiles, and so receipt of a cointervention in the first or last month of the study, or in any intervening month, was assumed to be random across the population.
Health records were counted monthly for the entire time during which people were resident in a study home, and rates of health events were compared between exposed individuals and those in the reference group for each cointervention.
Data sources and measurement
The type and date of improvements for each housing cointervention, the dates of assessment for compliance and the outcome from those assessments (including work not required or work declined), along with addresses, were sent to our trusted third party, who anonymised these data into a databank [Secure Anonymised Information Linkage (SAIL)]. 33 The data analyst worked closely with CCC to determine the data preparation rules to identify compliance status from the housing quality standards data. These administrative data were collected for the primary purpose of reporting progress towards government targets.
Dates of intervention work were used to determine when a property became compliant with the national standards for each individual property throughout the study period. The duration of work was not recorded in the data; the date represents when housing standards were assessed, often at the point of completion for each cointervention. If a specific cointervention was recorded as compliant but there was no date of work, then the property was assumed to be compliant for that cointervention throughout the study period. That is, the cointervention was assumed to be compliant from 1 January 2005. Once a property received a housing cointervention improvement it was recorded as compliant, and we assumed that there would be no deterioration of the cointervention during the study.
For properties for which a cointervention of work was not applicable (e.g. a ground-floor flat would not be assessed for loft insulation), we have coded those cointerventions as not required and they were excluded from effect estimates for the specific cointervention. If cointerventions of work were declined by the tenant, these were recorded as an acceptable fail in the data; we coded the cointervention as non-compliant. Tenants of these properties were allocated to a reference group for the relevant cointerventions.
Property-level data were linked to individuals resident in those homes, using the Welsh Demographic Service data set, to determine which individuals lived in each property throughout the study. Individuals who moved between homes were treated as separate observations; that is, the condition of their previous home was not taken into account in analysing observations recorded at subsequent addresses. The start and end dates of periods lived at each address were obtained for all study participants. These provided the periods of follow-up for study participants and allowed us to derive a single exposure per person and per cointervention. Study participants were all tenants registered as living in one of the council homes for at least 60 days, between January 2005 and March 2015. The Welsh Demographic Service data set was also used to select all other properties in the region, and individuals registered during the study period for at least 60 days, to create a regional comparator group used to adjust for background trends.
The housing cointerventions were added as independent variables of interest: (1) windows and doors, (2) kitchens, (3) bathrooms, (4) heating systems, (5) wall insulation, (6) loft insulation, (7) electrical system and (8) garden paths. The intervention variable categories represented, for each person, whether the cointervention was already at the required standard, brought up to standard during their period of tenancy, not up to standard during their period of tenancy or not required. All electrical components of the regeneration programme (i.e. smoke detectors, carbon monoxide detectors, security lights, kitchen and bathroom extractor fans and internal rewiring) were represented by a single variable, ‘electrical system’.
Emergency admissions for the period January 2005 to March 2015 for all participants were extracted from the Patient Episode Dataset for Wales (PEDW), which contains complete admissions for Welsh residents. 34 Monthly counts of emergency admissions for cardiovascular and respiratory conditions, and injuries (falls and burns) were generated for each participant (see Appendix 4), along with indicators of cointervention compliance.
Our analysis compared changes in counts of emergency admissions before, during and after the intervention period, analysing individual-level data as a ‘panel’ study. Rates of emergency admissions were derived for the regional comparator group (rest of Carmarthenshire, for each month and by age, sex, comorbidity and income deprivation) and included as a covariate to adjust for background trends in admissions. The programme of work was not implemented in respect of tenants’ needs and, therefore, there was little potential for confounding by indication.
Our outcome variables consisted of emergency hospital admissions for cardiovascular and respiratory conditions and injuries (falls and burns) extracted from the PEDW. Emergency hospital admissions for these health conditions could reasonably occur as a result of poor housing and be altered as a result of housing improvements.
Potentially confounding variables included age (< 25, 25–39, 40–49, 50–59, 60–69, 70–79 and ≥ 80 years), sex (also extracted from the Welsh Demographic Service data set), comorbidity (0 or ≥ 1), income deprivation (Welsh Index of Multiple Deprivation35 income domain from 1, least deprived, to 3, most deprived), rurality (Office for National Statistics36 classification: 1, village and hamlet; 2, town and fringe; and 3, urban) and year of study (2005, 2006, . . ., 2015). These potentially confounding variables were available in the databank and were included in every model.
Statistical methods
We used a negative binomial model to examine the effects of multiple housing cointervention compliance on the rates of emergency admissions, while adjusting for potential confounders (sex, age, comorbidities, deprivation index and rurality classification).
The study made use of an internal reference group. The properties that received an intervention for the individual cointerventions were compared with a reference group of people living in homes that did not receive the cointervention during their tenancy.
A longitudinal analysis was carried out using a panel design with repeated observations for each participant. A multilevel model structure with monthly observations over time (level 1) nested within individuals (level 2) allowed us to take account of clustering of observations over time using random effects. This structure also enabled the handling of unbalanced data, when the number of observations varied for individuals: an artefact of a dynamic cohort. The outcome, Yjk, is the number of events for individual k, within month j where an event is counted as per the definition of emergency hospital admissions.
Given that µjk is the expectation of outcome Yjk conditional on covariates Xpk, p = 1, 2, . . ., P, and Yjk ∼ Poisson (µjk), thus the marginal model relates E(Yjk|Xk) via the log-link function. We used the negative binomial distribution, which is a two-parameter extension of the one-parameter Poisson distribution.
The explanatory variables X1, X2, . . ., XP included the variables of interest (the cointervention-level indicators of compliance) as well as the potentially confounding variables. Their associated regression coefficients β1, β2, . . ., βP represent the estimated effects on a log-scale of the mean counts of health events.
The number of person-days observed in each month is denoted by mjk. To adjust for the non-constant observation periods among individuals, we included log(mjk) as an offset in the modelling framework.
The final model can be expressed as:
where uk denotes the individual-specific random effect, and the ranges for j and k vary depending on the outcome modelled, as described below. 37
Results
The intervention
Between January 2007 and March 2015, 46,272 housing work cointerventions were carried out to meet the national housing quality standard (Table 2). About 2% of properties did not undergo work owing to tenants declining the work, and 10% did not require the work (e.g. there was no loft to insulate) (see Table 2). By the end of the study period, approximately 7% of homes in the data we received had not met the quality standards between cointerventions. For each home, the complex intervention activity varied considerably: up to 102 months for a home receiving multiple cointerventions, with a median of 54 months.
| Cointervention | Category, n (%) | ||||
|---|---|---|---|---|---|
| Met standard (from start) | Met standard (work completed) | Did not meet standard (other) | Did not meet standard (decline) | Work not required | |
| Windows and doors | 4129 (45.1) | 4802 (52.4) | 227 (2.5) | 1 (0.0) | 0 (0.0) |
| Wall insulation | 2477 (27.0) | 6030 (65.8) | 645 (7.0) | 1 (0.0) | 6 (0.1) |
| Loft insulation | 4065 (44.4) | 2908 (31.8) | 543 (5.9) | 588 (6.4) | 1055 (11.5) |
| Heating systems | 334 (3.6) | 7087 (77.4) | 894 (9.8) | 398 (4.3) | 446 (4.9) |
| Kitchens | 445 (4.9) | 7430 (81.1) | 991 (10.8) | 293 (3.2) | 0 (0.0) |
| Bathrooms | 566 (6.2) | 7504 (81.9) | 839 (9.2) | 250 (2.7) | 0 (0.0) |
| Electrical systems | 263 (2.9) | 8394 (91.6) | 492 (5.4) | 10 (0.1) | 0 (0.0) |
| Garden paths | 3892 (42.5) | 2767 (30.2) | 229 (2.5) | 0 (0.0) | 2270 (24.8) |
| Total (average) | 16,438 (22.4) | 46,272 (63.2) | 5086 (6.9) | 1696 (2.3) | 3777 (10.3) |
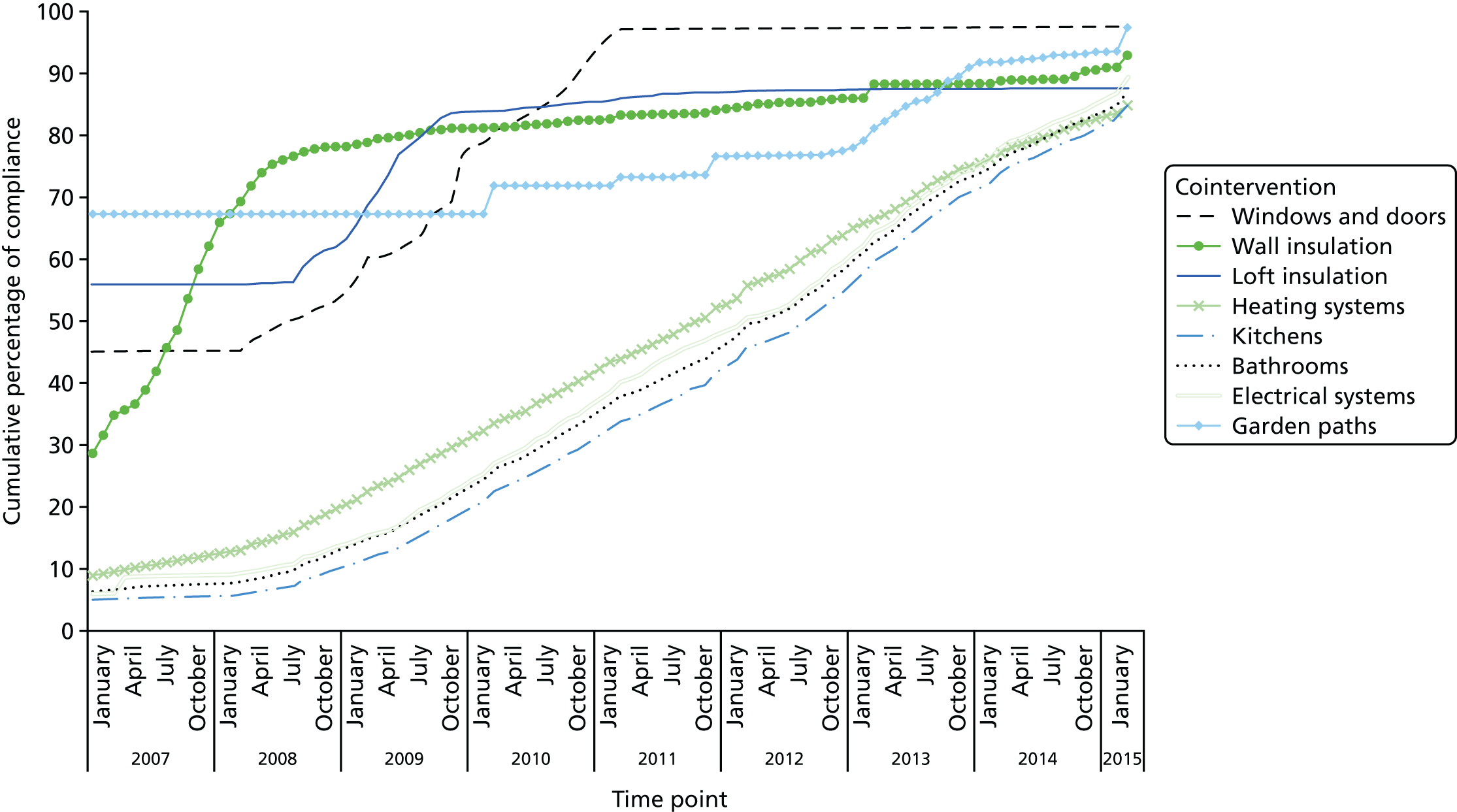
The cumulative proportion of properties meeting housing quality standards for each work cointervention increased steadily throughout the study period (Figure 5). The cointerventions of loft insulation, wall insulation, windows and doors and gardens met the required housing standard more than the other cointerventions at the start of the study period.
FIGURE 5.
Cumulative proportion of properties meeting housing quality standards over the intervention period by cointervention.
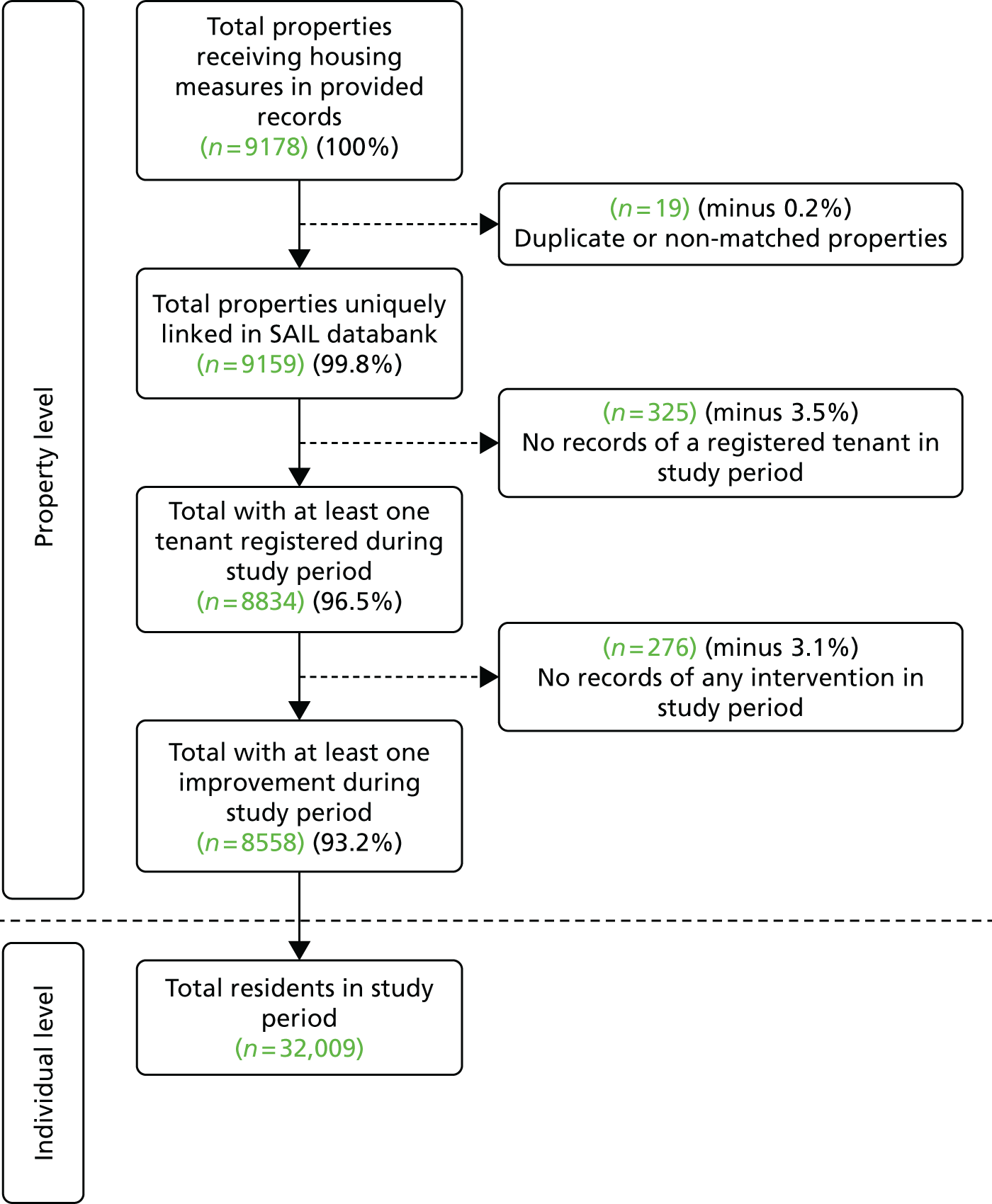
The number of properties reduced at each stage of data preparation processing. The original 9178 addresses provided by CCC were reduced to 8558 addresses retained for analysis after undergoing data anonymisation and linkage to intervention home residents (Figure 6).
FIGURE 6.
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram of study homes from receipt of data from CCC, through anonymised data linkage, to the selection of only those homes with registered tenants.
Cohort profiles
During the entire study period 32,009 participants (of all ages) were registered to a study home. The study population remained stable during the study period, with an average number of 18,031 people observed per year. Over 45% of all participants were registered to a study home for the entire observation window, contributing to 10.25 years or 123 monthly records. Overall, there was a total of 183,553 person-years of follow-up for all residents living in study homes. All homes and people in the region not in our study but within the rest of Carmarthenshire region provided a large number of person-years for follow-up (Table 3). Health-care utilisation was intentionally captured only for the time during which the resident was registered at the property; therefore, there is no loss to follow-up.
| Group | Number of homes | Number of people | Follow-up (person-years) |
|---|---|---|---|
| Study group | 8588 | 32,009 | 183,533 |
| Rest of Carmarthenshire | 70,286 | 231,200 | 1,628,554 |
Residents of council homes had higher proportions of individuals in the younger and older age groups than did the wider population, and the distribution of income deprivation also showed differences between the two groups (Table 4); the majority of individuals within our study group are in the two most deprived income quintiles compared with the rest of Carmarthenshire, where the majority of individuals are in the three middle-income quintiles.
| Characteristic | Group, n (%) | |
|---|---|---|
| Intervention home residents | Rest of Carmarthenshire | |
| Total | 32,009 (100) | 231,200 (100) |
| Age group (years) | ||
| < 25 | 13,943 (43.6) | 81,899 (35.4) |
| 25–39 | 5435 (17.0) | 43,885 (19.0) |
| 40–49 | 2922 (9.1) | 29,393 (12.7) |
| 50–59 | 2655 (8.3) | 28,681 (12.4) |
| 60–69 | 2774 (8.7) | 22,767 (9.8) |
| 70–79 | 2362 (7.4) | 14,895 (6.4) |
| ≥ 80 | 1918 (6.0) | 9680 (4.2) |
| Sex | ||
| Male | 15,173 (47.4) | 114,196 (49.4) |
| Female | 16,836 (52.6) | 117,004 (50.6) |
| Income deprivation quintile | ||
| Most deprived | 10,165 (31.8) | 23,137 (10.0) |
| More | 10,647 (33.3) | 54,856 (23.7) |
| Mid | 7538 (23.5) | 65,050 (28.1) |
| Less | 3273 (10.2) | 63,853 (27.6) |
| Least deprived | 386 (1.2) | 24,304 (10.5) |
| Rurality classification | ||
| Urban | 17,973 (56.1) | 99,952 (43.2) |
| Town | 5276 (16.5) | 32,690 (14.1) |
| Village and hamlet | 8760 (27.4) | 98,558 (42.6) |
| Comorbidity status | ||
| No comorbidities | 29,426 (91.9) | 219,485 (94.9) |
| At least one comorbidity | 2583 (8.1) | 11,715 (5.1) |
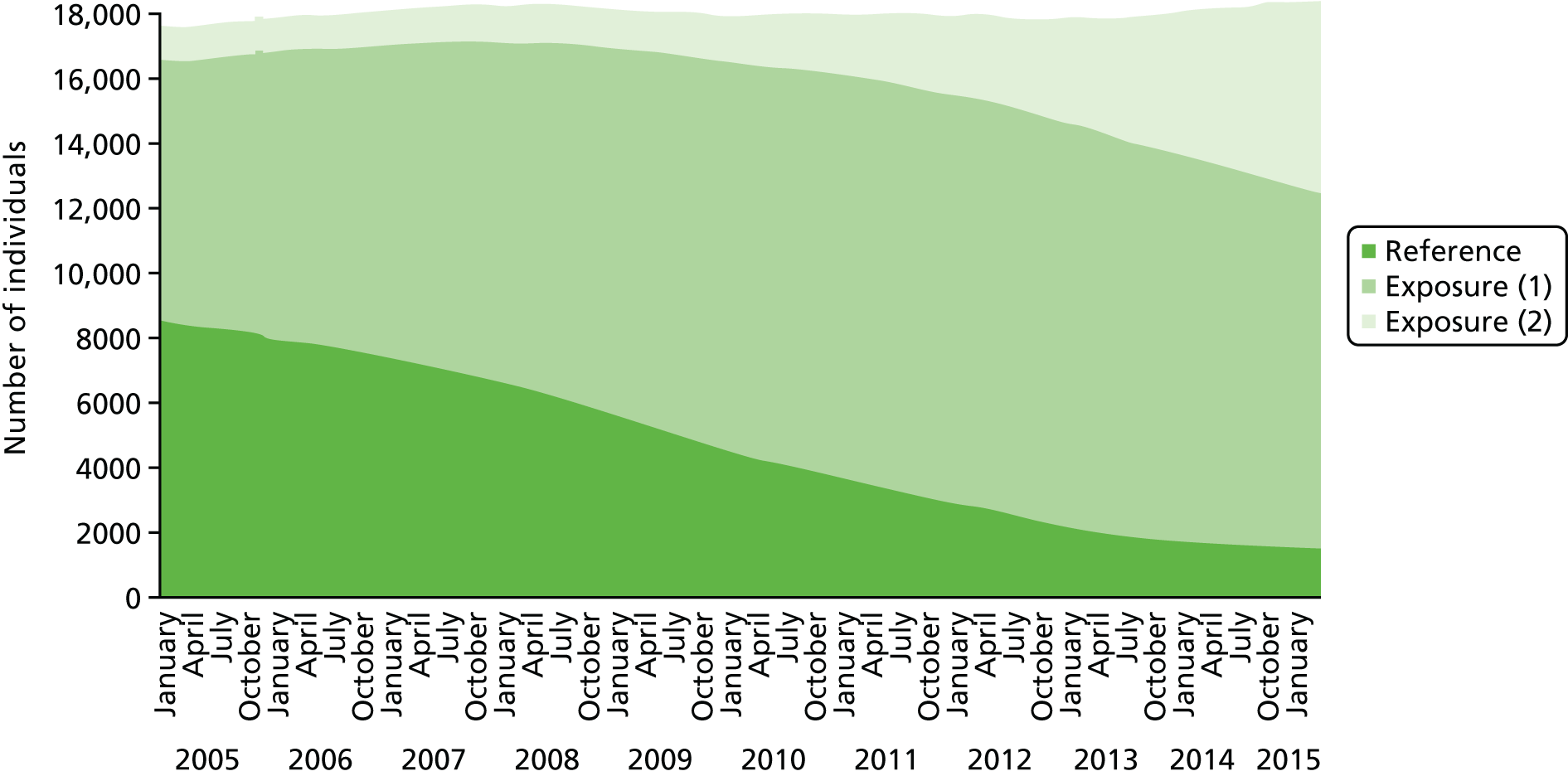
The number of people within each exposure and reference group varied between cointerventions. Generally, as the delivery of the intervention progressed and higher proportions of homes met the national standards, the number of people who lived in a home while work was carried out increased (exposure group 1), along with the number of people moving into properties that were already up to standard (exposure group 2). Conversely, the number of people who lived in homes that did not meet national standards decreased over the study window (reference group, Figure 7).
FIGURE 7.
Number of individuals registered to intervention homes for the electrical system cointervention, for each exposure group, by study month.
At the end of the study period, the vast majority of homes (96.5%) had received at least one cointervention of any type (see Figure 6), and it is worth noting that the properties themselves received the intervention but the individuals whose tenancy ended before this happened were used as the reference group. There could be bias in this group due to changes in people living in the property before and after the work was completed. However, discussions with the council assured us that there was no change in policy for allocating homes and there was no reason to suggest that the case mix of tenants was different following the intervention programme.
The numbers of participants within the exposure and reference groups differed for each work cointervention; for example, for electrics, exposure (1) = 13,358, reference = 12,726. The characteristics of these two groups are shown in Table 5.
| Characteristic | Group, n (%) | |
|---|---|---|
| Reference | Exposure (1) | |
| Total | 13,358 (100.0) | 12,726 (100.0) |
| Age group (years) | ||
| < 25 | 5804 (43.4) | 5021 (39.5) |
| 25–39 | 2271 (17.0) | 2174 (17.1) |
| 40–49 | 1001 (7.5) | 1424 (11.2) |
| 50–59 | 890 (6.7) | 1365 (10.7) |
| 60–69 | 970 (7.3) | 1384 (10.9) |
| 70–79 | 1114 (8.3) | 967 (7.6) |
| ≥ 80 | 1308 (9.8) | 391 (3.1) |
| Sex | ||
| Male | 6278 (47.0) | 6051 (47.5) |
| Female | 7080 (53.0) | 6675 (52.5) |
| Income deprivation quintile | ||
| Most deprived | 4172 (31.2) | 4274 (33.6) |
| More | 4455 (33.4) | 4224 (33.2) |
| Mid | 3240 (24.3) | 2730 (21.5) |
| Less | 1355 (10.1) | 1328 (10.4) |
| Least deprived | 136 (1.0) | 170 (1.3) |
| Rurality classification | ||
| Urban | 7537 (56.4) | 7278 (57.2) |
| Town | 1936 (14.5) | 2027 (15.9) |
| Village and hamlet | 3885 (29.1) | 3421 (26.9) |
| Comorbidity status | ||
| No comorbidities | 12,075 (90.4) | 11,863 (93.2) |
| At least one comorbidity | 1283 (9.6) | 863 (6.8) |
Outcome data
Study group participants (of all ages) had 10,524 emergency admissions relating to cardiovascular conditions, respiratory conditions, falls or burns, which accounted for approximately one-third of all emergency admissions (33.7%) recorded in the PEDW, and 10.4% had at least one admission for any of our conditions of interest (Table 6). Monthly counts fluctuated during the study period (see Table 14).
| Outcome | Group, n (%) | |
|---|---|---|
| All ages | Aged ≥ 60 years | |
| ≥ 1 cardiovascular condition, respiratory condition or injury (falls and burns) | 10,524 (10.4) | 7296 (27.0) |
| ≥ 1 cardiovascular condition | 4661 (5.1) | 3720 (16.9) |
| ≥ 1 respiratory condition | 4907 (5.2) | 2849 (10.9) |
| ≥ 1 injury (falls and burns) | 956 (1.4) | 700 (4.4) |
Main results
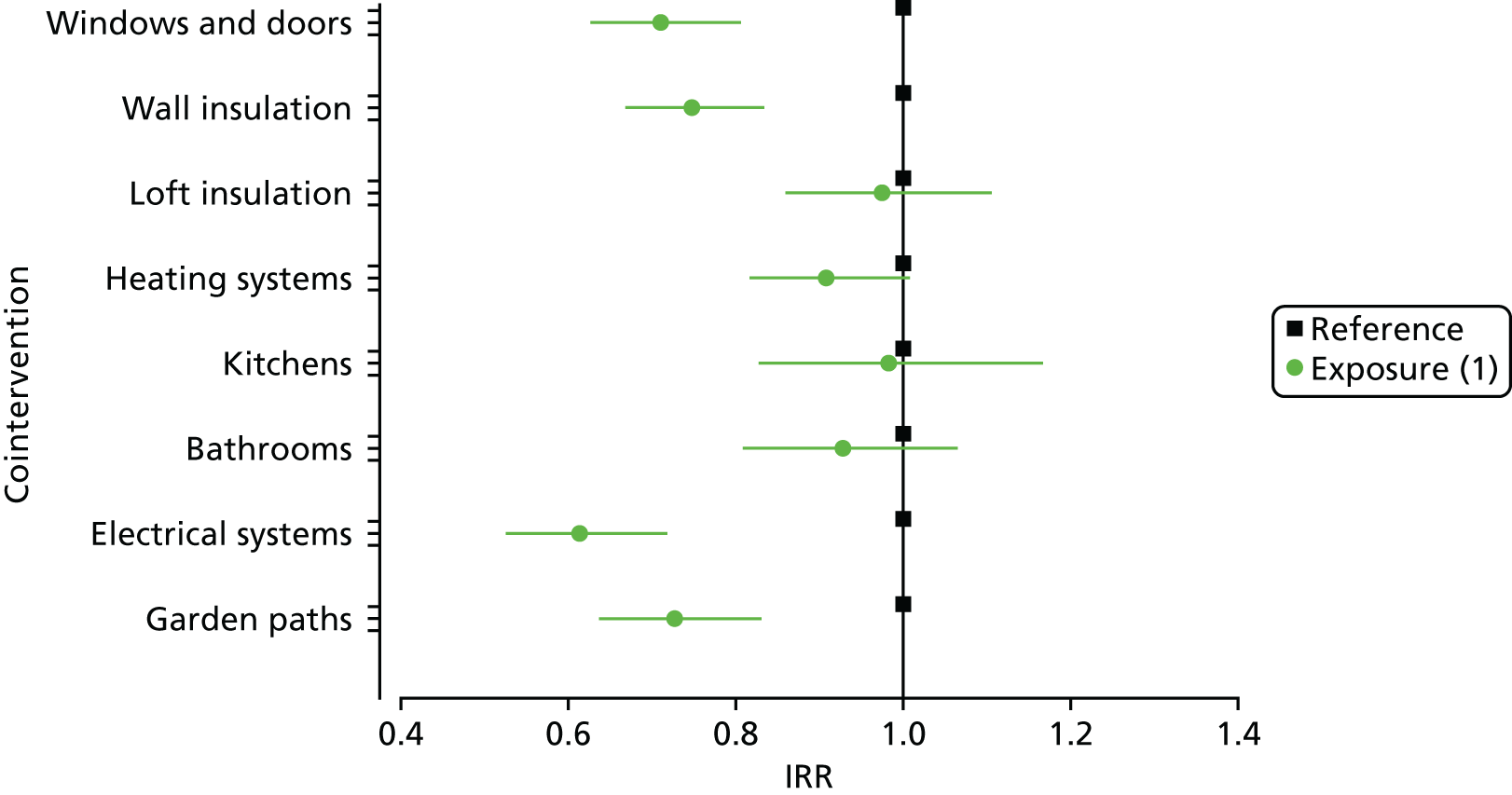
Model coefficients were converted to incidence rate ratios (IRRs) to aid interpretation, representing, for each housing cointervention, the change in outcome rates for participants who were allocated to an exposure group, because they lived in a home while it was upgraded, compared with a reference group of participants living in homes that did not receive improvement work during their tenancy, while holding all other variables in the model constant. An IRR equal to 1 indicated that there was no difference between outcome rates compared with the reference group; an IRR < 1 or > 1 indicated a decrease or an increase, respectively, in events for the exposure group relative to the reference group. We report here on our main exposure group (1) for tenants receiving the work while living in the home, and at the end of this chapter we report on a secondary exposure group (2) for people living in homes that were already compliant when they moved in. We also report p-values; owing to multiple hypothesis testing, we have reduced the local level of significance to a p-value of < 0.01 in our formal tests. This is to ensure that the overall, or global, level of significance was still at the 95% level. 38 Please note that for the purposes of presenting results graphically we used 95% confidence intervals (CIs).
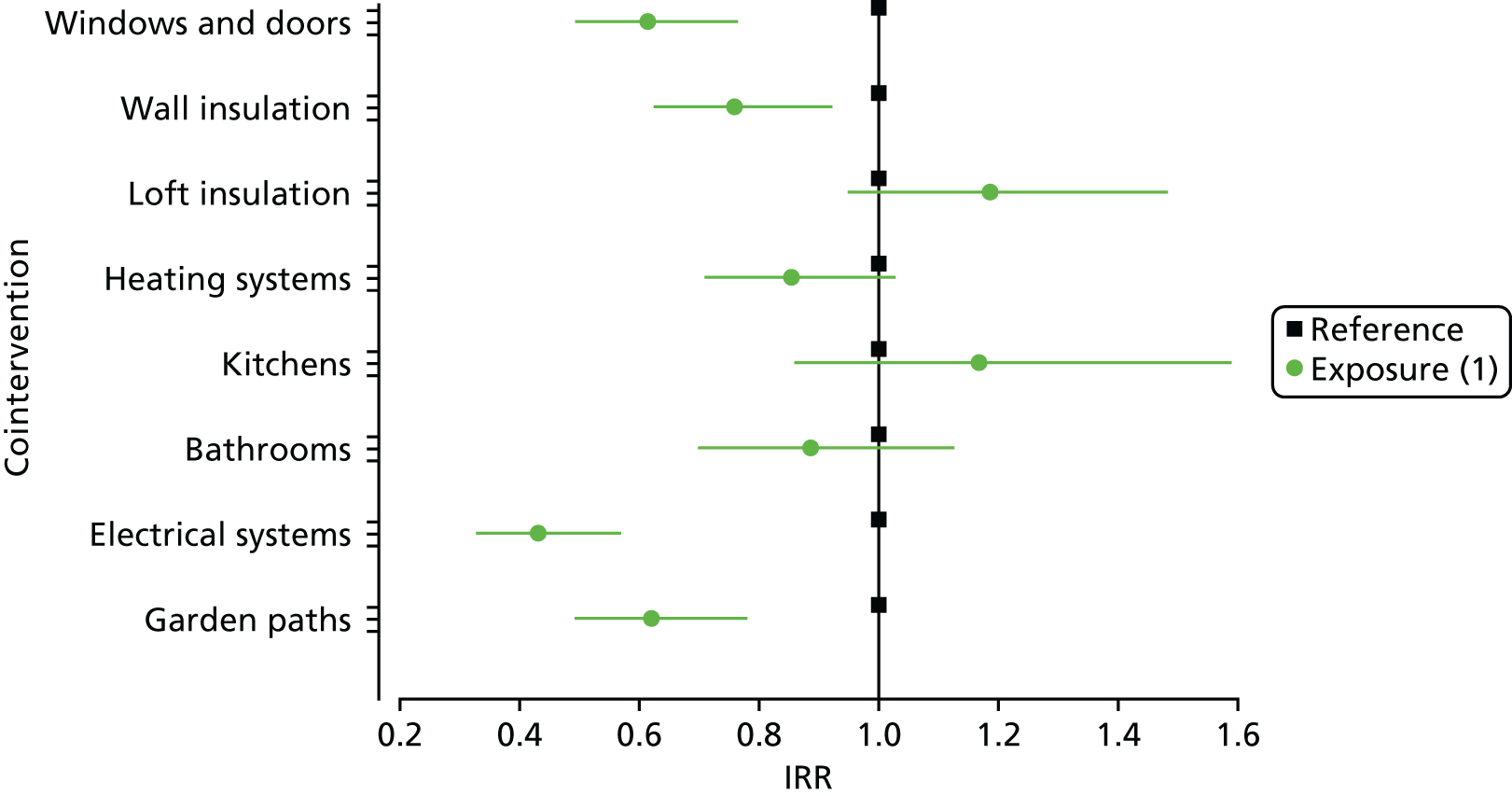
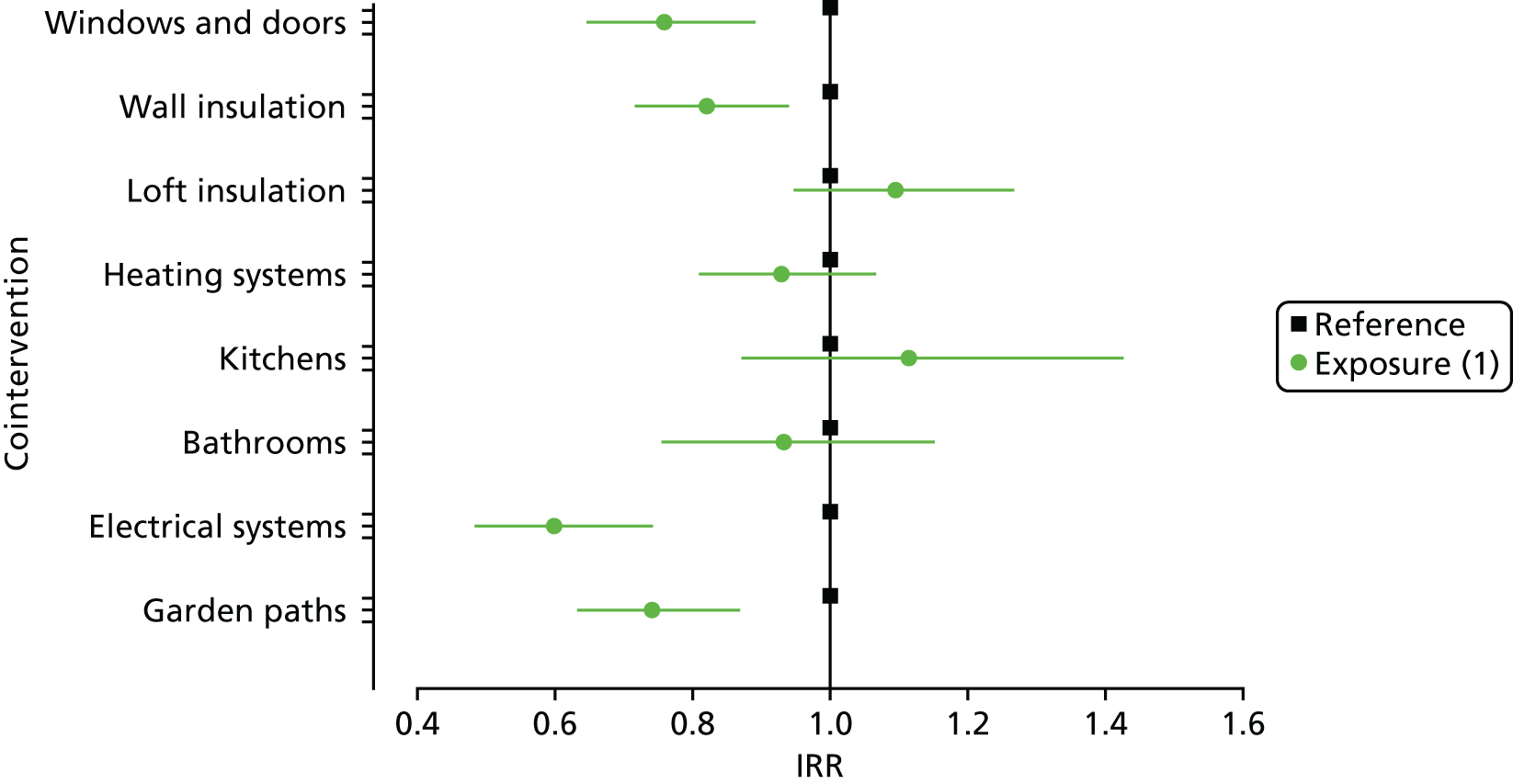
Emergency admissions combined: older residents
Figure 8 shows the IRR for emergency admissions for the combined conditions for participants aged ≥ 60 years by cointervention. Residents aged ≥ 60 years who were living in homes while the electrical systems were upgraded had 39% fewer emergency hospital admissions than those in the reference group (IRR 0.61, 95% CI 0.53 to 0.72; p < 0.01). A reduction in admissions was also found to be associated with windows and doors (IRR 0.71, 95% CI 0.63 to 0.81; p < 0.01), wall insulation (IRR 0.75, 95% CI 0.67 to 0.84; p < 0.01) and garden path improvements (IRR 0.73, 95% CI 0.64 to 0.83; p < 0.01). There were no changes in emergency admissions associated with heating upgrades (IRR 0.91, 95% CI 0.82 to 1.01; p = 0.072), loft insulation (IRR 0.98, 95% CI 0.86 to 1.11; p = 0.695), new kitchens (IRR 0.98, 95% CI 0.83 to 1.17; p = 0.843) or new bathrooms (IRR 0.93, 95% CI 0.81 to 1.06; p = 0.287).
FIGURE 8.
Incidence rate ratios of emergency admissions for combined conditions for participants aged ≥ 60 years by cointervention.
Emergency admissions for cardiovascular conditions: older residents
For older residents living in homes while wall insulation was installed, there were statistically significant associations with lower rates of emergency admissions for cardiovascular conditions (IRR 0.73, 95% CI 0.63 to 0.85; p < 0.01), compared with the reference group (Figure 9). There were no changes in emergency admissions associated with upgrading windows and doors (IRR 0.81, 95% CI 0.69 to 0.96; p = 0.016), new bathrooms (IRR 0.94, 95% CI 0.78 to 1.13; p = 0.532) or new kitchens (IRR 0.91, 95% CI 0.73 to 1.13; p = 0.395), installing loft insulation (IRR 0.86, 95% CI 0.73 to 1.02; p = 0.083), electrical system upgrades (IRR 0.80, 95% CI 0.66 to 0.99; p = 0.036) or heating upgrades (IRR 0.94, 95% CI 0.82 to 1.08; p = 0.389).
FIGURE 9.
Incidence rate ratios of emergency admissions for cardiovascular conditions for participants aged ≥ 60 years by cointervention.
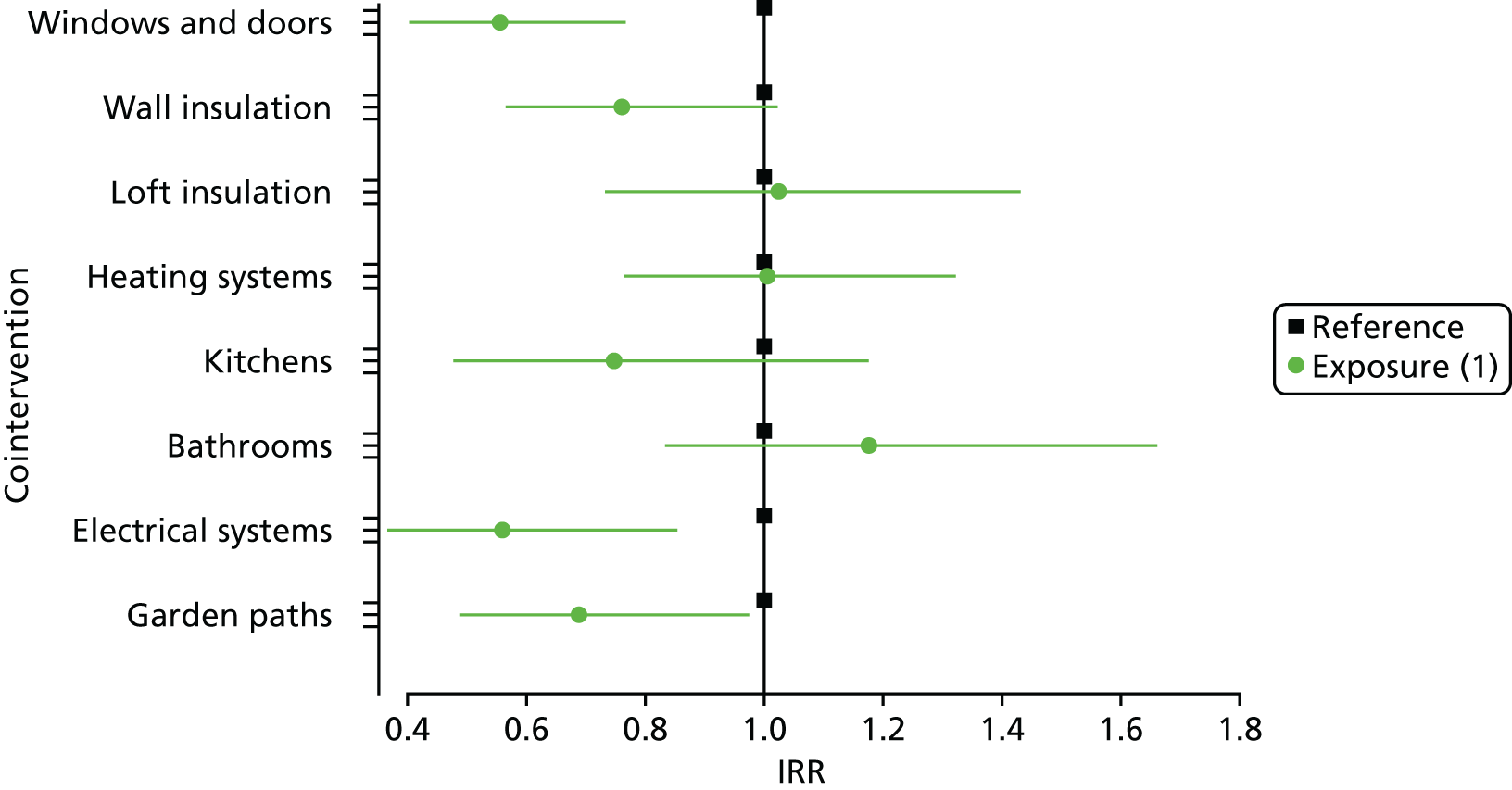
Emergency admissions for respiratory conditions: older residents
We found that there were fewer emergency admissions for respiratory conditions among participants aged ≥ 60 years who were living in homes that were receiving upgrades to windows and doors (IRR 0.61, 95% CI 0.49 to 0.76; p < 0.01), wall insulation (IRR 0.76, 95% CI 0.62 to 0.92; p < 0.01), electrical systems upgrades (IRR 0.43, 95% CI 0.33 to 0.57; p < 0.01) and garden path improvements (IRR 0.62, 95% CI 0.49 to 0.78; p < 0.01) than among those in the reference group (Figure 10). There were no changes in emergency admissions associated with upgrading bathrooms (IRR 0.89, 95% CI 0.70 to 1.13; p = 0.322), kitchens (IRR 1.17, 95% CI 0.86 to 1.59; p = 0.326), loft insulation (IRR 1.18, 95% CI 0.95 to 1.48; p = 0.138) or heating (IRR 0.85, 95% CI 0.71 to 1.03; p = 0.093).
FIGURE 10.
Incidence rate ratios of emergency admissions for respiratory conditions for participants aged ≥ 60 years by cointervention.
Emergency admissions for falls and burns: older residents
We found that there were fewer emergency admissions for injuries among participants aged ≥ 60 years who were living in homes that were receiving upgrades to windows and doors (IRR 0.56, 95% CI 0.40 to 0.77; p < 0.01) and electrical systems (IRR 0.56, 95% CI 0.37 to 0.85; p < 0.01) than among those living in reference group properties that did not receive upgrades during follow-up (Figure 11). There were no changes in emergency admissions associated with upgrading wall insulation (IRR 0.76, 95% CI 0.57 to 1.02; p = 0.070), new bathrooms (IRR 1.18, 95% CI 0.83 to 1.66; p = 0.354), new kitchens (IRR 0.75, 95% CI 0.48 to 1.17; p = 0.209), loft insulation (IRR 1.02, 95% CI 0.73 to 1.43; p = 0.887), garden path improvements (IRR 0.69, 95% CI 0.49 to 0.97; p = 0.035) or heating upgrades (IRR 1.01, 95% CI 0.77 to 1.32; p = 0.966).
FIGURE 11.
Incidence rate ratios of emergency admissions for injuries for participants aged ≥ 60 years by cointervention.
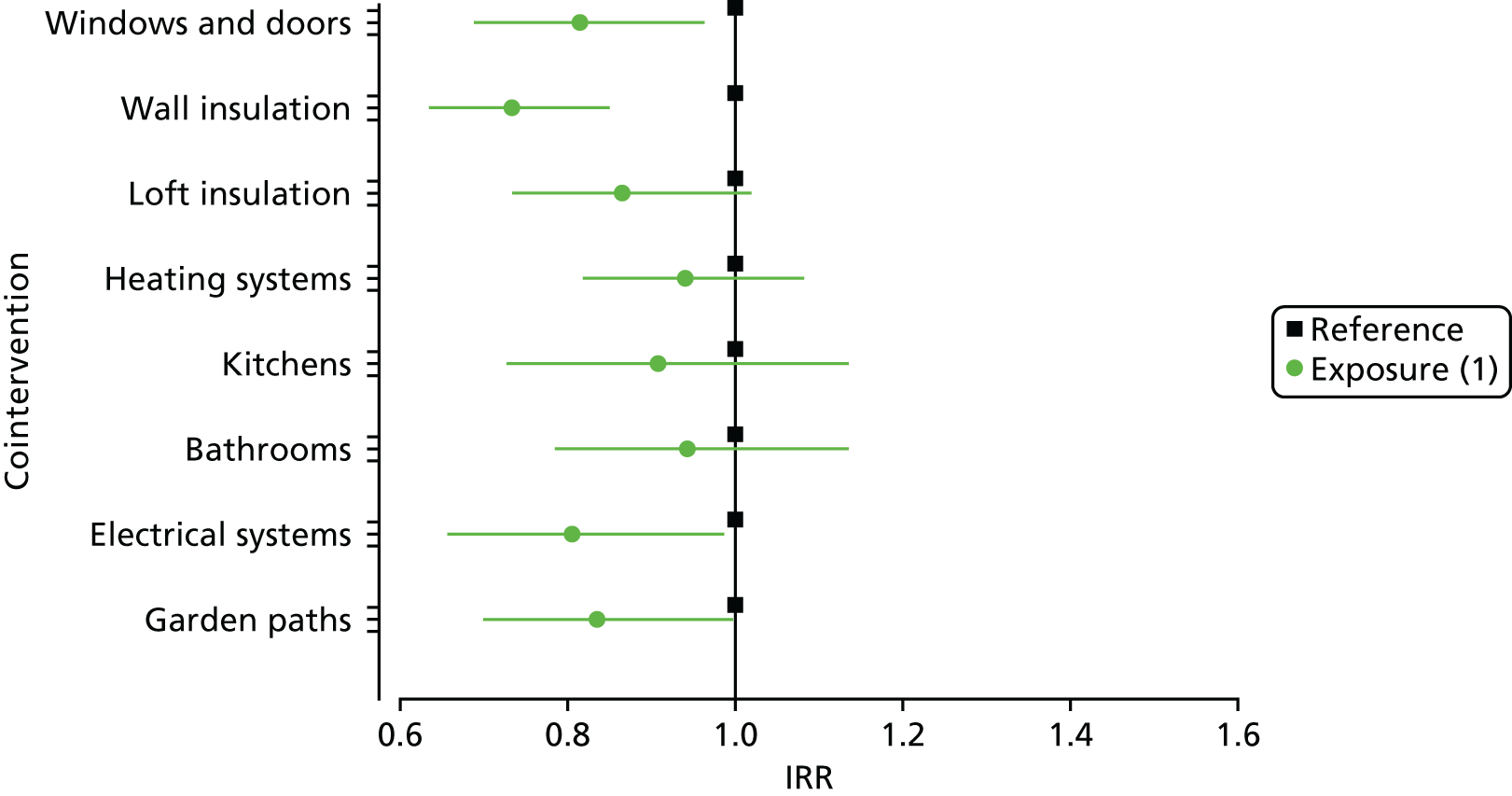
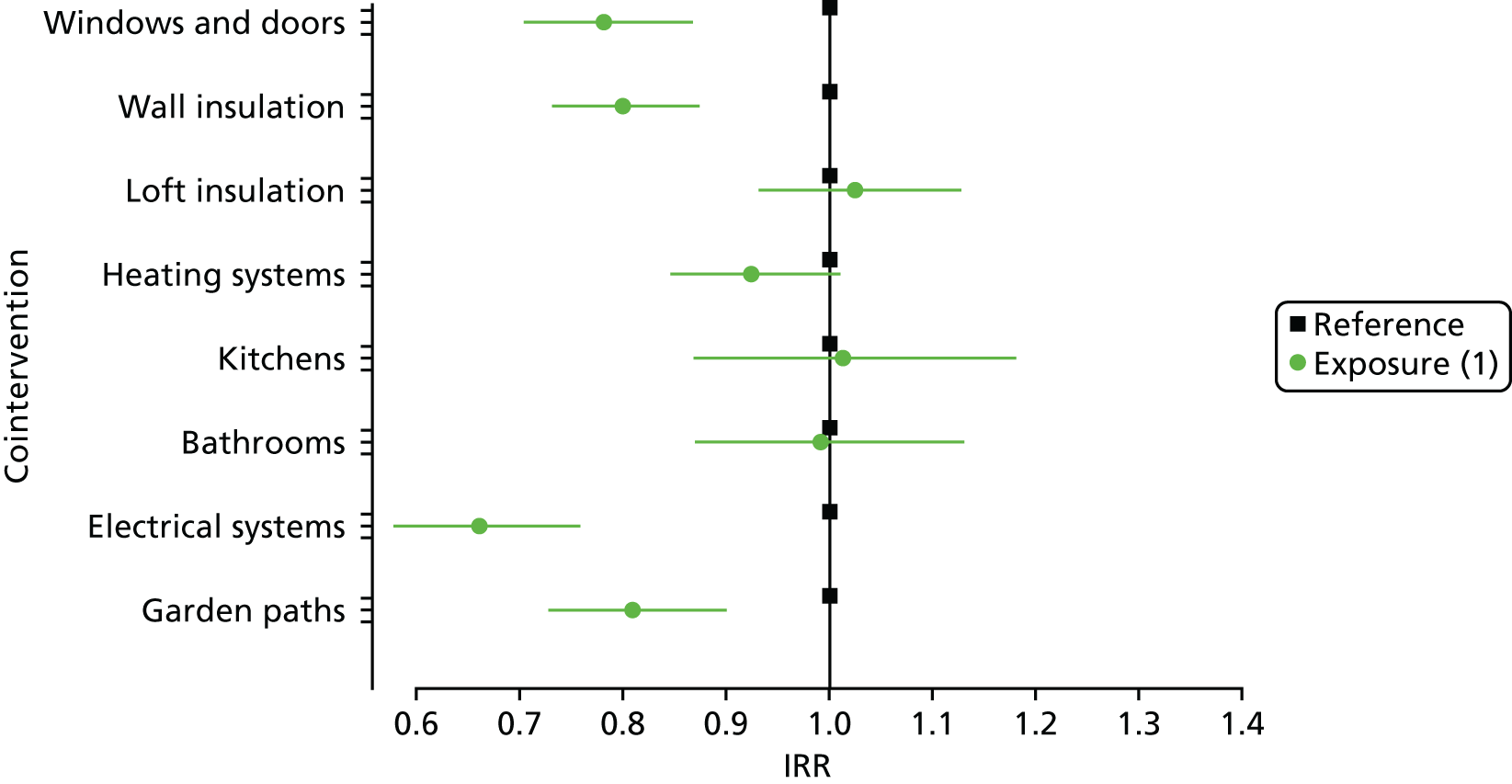
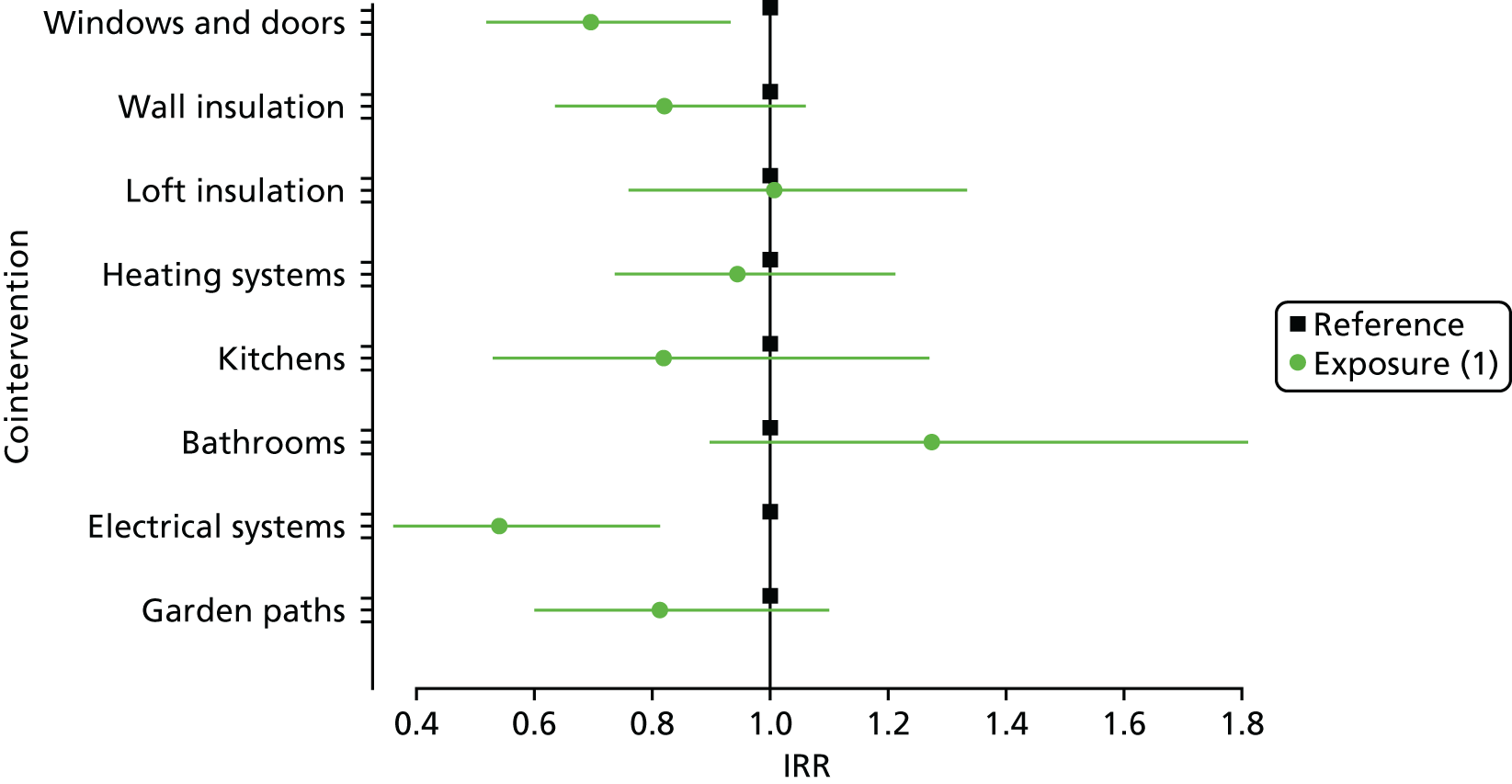
Emergency admissions combined: all ages
The effects found for the older residents remained for all ages (Figure 12). People of all ages had 34% fewer combined admissions if they lived in homes while the electrical systems were upgraded than if they were in the reference group (IRR 0.66, 95% CI 0.58 to 0.76; p < 0.01). A reduction in admissions was also found to be associated with windows and doors upgrades (IRR 0.78, 95% CI 0.70 to 0.87; p < 0.01), wall insulation (IRR 0.80, 95% CI 0.73 to 0.87; p < 0.01) and garden path improvements(IRR 0.81, 95% CI 0.73 to 0.90; p < 0.01). There were no changes in emergency admissions associated with heating upgrades (IRR 0.92, 95% CI 0.85 to 1.01; p = 0.083), loft insulation (IRR 1.02, 95% CI 0.93 to 1.13; p = 0.618), new kitchens (IRR 1.01, 95% CI 0.87 to 1.18; p = 0.867) or new bathrooms (IRR 0.99, 95% CI 0.87 to 1.13; p = 0.900).
FIGURE 12.
Incidence rate ratios of emergency admissions for combined conditions for participants of all ages by cointervention.
Emergency admissions for cardiovascular conditions: all ages
We found that there were fewer emergency admissions for cardiovascular conditions among individuals (of all ages) who were living in homes that were receiving wall insulation during the study window (IRR 0.74, 95% CI 0.65 to 0.85; p < 0.01) (Figure 13). There were no changes in emergency admissions associated with upgrading bathrooms (IRR 0.99, 95% CI 0.82 to 1.19; p = 0.907), kitchens (IRR 0.95, 95% CI 0.77 to 1.17; p = 0.635), loft insulation (IRR 0.93, 95% CI 0.80 to 1.08; p = 0.327), electrical system upgrades (IRR 0.79, 95% CI 0.65 to 0.96; p = 0.016), windows and doors upgrades (IRR 0.82, 95% CI 0.70 to 0.96; p = 0.015) or heating upgrades (IRR 0.93, 95% CI 0.82 to 1.06; p = 0.286).
FIGURE 13.
Incidence rate ratios of emergency admissions for cardiovascular conditions for participants of all ages by cointervention.
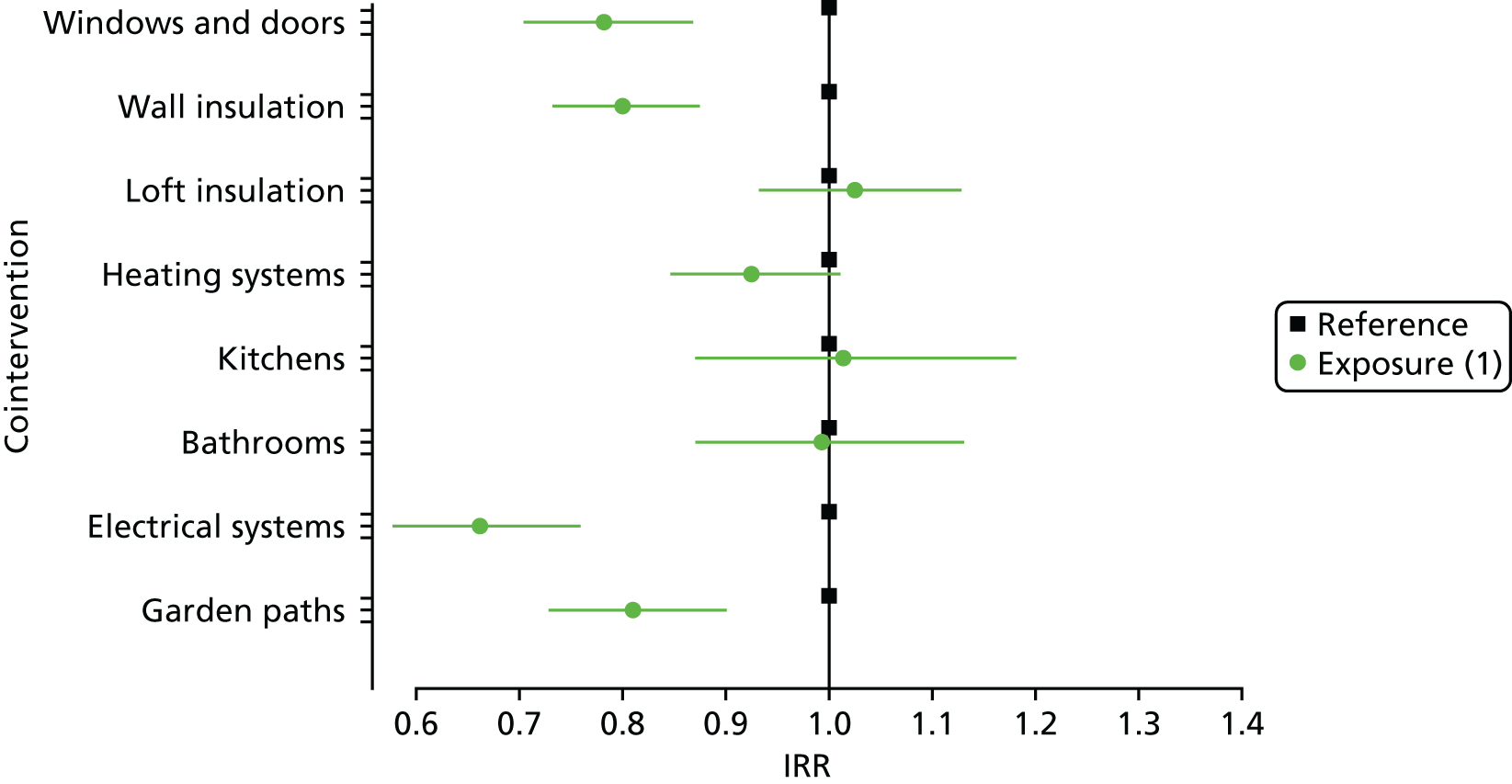
Emergency admissions for respiratory conditions: all ages
The intervention was associated with a statistically significant difference in emergency admissions for respiratory conditions among individuals of all ages; the electrical system cointervention was associated with the largest decrease for those living in homes that reached the required housing quality standard for a cointervention during the observation period (IRR 0.60, 95% CI 0.48 to 0.74; p < 0.01), compared with those in a reference group (Figure 14). Similarly, associations were also found with fewer emergency admissions for individuals living in properties reaching quality standards for windows and doors (IRR 0.76, 95% CI 0.65 to 0.89; p < 0.01), wall insulation (IRR 0.82, 95% CI 0.72 to 0.94; p < 0.01) and garden paths (IRR 0.74, 95% CI 0.63 to 0.87; p < 0.01) than for those in the reference group. There were no changes in emergency admissions associated with upgrading bathrooms (IRR 0.93, 95% CI 0.75 to 1.15; p = 0.510), kitchens (IRR 1.11, 95% CI 0.87 to 1.43; p = 0.393), loft insulation (IRR 1.09, 95% CI 0.95 to 1.27; p = 0.225) or heating (IRR 0.93, 95% CI 0.81 to 1.07; p = 0.293).
FIGURE 14.
Incidence rate ratios of emergency admissions for respiratory conditions for participants of all ages by cointervention.
Emergency admissions for falls and burns: all ages
We found that there were fewer emergency admissions relating to injuries among individuals (of all ages) living in properties that underwent upgrades to electrical systems (IRR 0.54, 95% CI 0.36 to 0.81; p < 0.01) than among those living in properties in the reference group for that cointervention (Figure 15). There were no changes in emergency admissions associated with upgrading wall insulation (IRR 0.82, 95% CI 0.63 to 1.06; p = 0.129), new bathrooms (IRR 1.27, 95% CI 0.90 to 1.81; p = 0.178), new kitchens (IRR 0.82, 95% CI 0.53 to 1.27; p = 0.370), loft insulation (IRR 1.01, 95% CI 0.76 to 1.33; p = 0.969), window and door upgrades (IRR 0.70, 95% CI 0.52 to 0.93; p = 0.015) or heating upgrades (IRR 0.94, 95% CI 0.73 to 1.21; p = 0.648).
FIGURE 15.
Incidence rate ratios of emergency admissions for injury-related conditions for participants of all ages by cointervention.
Additional analyses
We reported on our primary exposure group (1) above, which required people to be resident in the homes while the cointervention was upgraded. We also compared events for those living in homes not meeting national standards with events for those in a second exposure group (2). This group of people either were already living in a home that reached the required standard for the cointervention or during the study had moved into a home that already had the work completed. Many of the results for this second exposure group followed those for the primary exposure group, particularly for our primary outcome for older residents and combined emergency admissions. We report the main differences between exposure (1) and exposure (2) here, and the complete results are in Appendix 4.
We found that tenants of all ages living in homes that already met the housing quality standard for heating had a statistically significant association with more emergency admissions for combined conditions compared with the reference group (IRR 1.23, 95% CI 1.10 to 1.38; p < 0.01). This was somewhat in contrast to tenants who were living in homes while their new boiler was fitted, which demonstrated an (albeit non-significant) association with fewer admissions (IRR 0.91, 95% CI 0.85 to 1.01; p = 0.083). People of all ages whose homes already met housing standards for heating systems also had a significant increase in respiratory conditions for heating systems already in their home (respiratory: IRR 1.31, 95% CI 1.11 to 1.55; p < 0.01). Separately, neither cardiovascular conditions nor injuries were significantly associated with heating upgrades.
Discussion
Our primary health outcome was combined respiratory, cardiovascular and injuries (falls and burns) emergency hospital admissions for council housing tenants aged ≥ 60 years. There was a measurable reduction in emergency admissions associated with several cointerventions. When we examined different categories of emergency admission, the largest reduction was for respiratory conditions, although there were still decreases for admissions relating to cardiovascular conditions and to fall and burn injuries.
Secondary outcomes included the evaluation of residents of all ages who received the cointerventions of a housing intervention. This group also had fewer emergency admissions to hospital for cardiovascular and respiratory conditions and for fall and burn injuries. The ratios of rates between intervention and reference groups varied between cointerventions. The largest reduction for an intervention group was due to the electrical systems upgrade cointervention, which was associated with 57% fewer emergency admissions for respiratory conditions than in the reference group. In addition, fitting new windows and doors, as well as wall insulation, was associated with a reduction in emergency admissions. Several other cointerventions showed an association with fewer emergency admissions, but these were not statistically significant.
We analysed separately those tenants who either lived in a home with cointerventions that already met national housing quality standards or had moved into a home already meeting the standard. The broadly similar findings between our main exposure group, whose homes received the intervention while they were a tenant, and this second exposure group have encouraging implications for the sustainability of effects beyond tenants occupying properties at the time of the intervention.
The strengths of our study included our use of routinely collected data for a complete housing cohort; removal of possible selection, participation or recall biases; a large number of person-years of follow-up; and the adjustment for multiple confounders to ensure that findings may be generalised to similar housing interventions. We had complete data for hospital admissions and death registrations and were able to censor people who moved out of intervention homes, allocating exact exposures to the intervention by the number of days registered to a property. We were able to examine council housing population subgroups using individual-level data, removing the possibility of concealing health improvements within areas for the total council housing population receiving the intervention. We analysed all people living in council intervention homes for whom we had health records within the databank, which was close to 100%. Our study design allowed us to estimate the effects of each work cointervention to evaluate this complex intervention, and the impact on each of our outcomes for older tenants and all ages, making direct comparisons between groups depending on their exposure status.
Housing interventions are a policy intervention, generally funded by local and central government, and often viewed as a natural experiment. Randomisation of the council homes to intervention exposure and reference groups was not possible because the intervention had already begun at the time this study commenced. As with all observational studies, there always remains the potential for residual confounding. We were limited by a lack of knowledge of the precise status of homes before they were brought up to CHS standards. For example, for some cointerventions the dose received was unknown; the home might have had a full rewiring, or simply received a few additional power sockets to achieve compliance. The model assumes independence between work cointerventions, whereas in reality the causal mechanism influencing individual-level health events are likely to arise through a combination of cointerventions that work together to achieve effects, such as thermal conditions being influenced by windows and doors, loft and wall insulation. Therefore, the effect estimates cannot be added together to create combined effect estimates.
The electrical cointervention was associated with the largest difference in emergency admissions (for respiratory-related conditions). The improvements carried out within this remit of work included installing additional power sockets, fitting security lighting outside the property, installing hard-wired smoke detectors and carbon monoxide alarms and installing electrical ventilation in kitchens and bathrooms. These items were installed simultaneously by the same contractor. It is, therefore, challenging to theorise the causal mechanism influencing the reduction in admissions found in this study because there is likely to be a combination of factors contributing to this effect.
Heating system upgrades, including the installation of new boilers and radiators, were associated with increases in admission rates for those tenants who moved into or lived in a home already meeting this housing quality standard. This increase was not found for those who were registered as living in the property at the time the intervention was implemented. The use of a new boiler is an ‘active’ intervention, meaning that residents must use it correctly to gain the greatest benefit. There was no guidance provided to those who moved into a home already fitted with a boiler meeting housing standards. In contrast, people who were living in the property when the boiler was fitted may have received some instruction in the most efficient use of their new boiler from the contractor.
Garden path improvement results should be interpreted with caution because tenants were given the option to pay for improvements that were not simply related to path safety but included beautification work to their gardens. This is a higher standard than the national WHQS. Therefore, the results may represent a biased subset of population who were able to afford the work or were inclined to invest in their garden.
This is the largest and most comprehensive analysis to date of the effect of bringing housing quality to national standards using a concentrated programme of work, and the effect that this has on health-care utilisation. This was made possible using data linkage at household and individual levels, and the findings highlight a substantial potential for multicomponent housing programmes to improve health overall as evaluated using a proxy of health-care utilisation. We analysed subgroups of population and health service utilisation for several conditions expected to change as a result of several housing quality improvements. The results shown here provide evidence for health benefits, indicated by a reduction in emergency admissions to hospital, following improvements in social housing conditions that could be achieved through the implementation of a similar programme of work.
Chapter 4 The effect of the housing intervention on other health outcomes: a longitudinal study using data linkage
This chapter describes the evaluation of the effect of the intervention on health service utilisation other than emergency admissions, which were described in Chapter 3. The focus of this chapter is on capturing the use of primary care physician services for people with respiratory and mental health conditions, and attendances at emergency departments that did not necessarily result in a hospital admission. For the respiratory and mental health outcomes, we created each condition-specific cohort before counting relevant treatments (respiratory and mental health) and GP attendances (respiratory). The emergency department attendance data set captured changes during the ongoing intervention period, beginning in 2011.
What impact has the intervention had on general practitioner health events?
Links between cold and damp housing for respiratory and cardiovascular conditions were discussed in the previous chapter. Links also exist for common mental health disorders (CMDs); these were made in the late 19th century, but only relatively recently has more evidence been published. 39,40 Thermal efficiency has been shown to have an effect on CMDs, with the causal pathways including the financial inability to heat homes, prolonged thermal discomfort, stigmatisation and worries about the consequences of substandard housing. 25,39,41–44
Objectives
Our objective was to create condition-specific cohorts for all ages to answer the following questions.
-
What impact did the intervention have on GP prescriptions for asthma and chronic obstructive pulmonary disease (COPD) treatments (amounts of relievers and preventers, and total prescribed)?
-
What impact did the intervention have on GP attendances for individuals with asthma and COPD conditions?
-
What impact did the intervention have on GP-recorded common mental health events?
Methods
The methodological approach used to analyse the effect of the intervention follows that described in Chapter 3 for emergency admissions. The data sources used to measure the outcome variable and the definition of that variable are detailed here, along with the subcohorts of participants included in these analyses, which distinguish the only differences in the modelling specification.
An analysis of GP events was conducted on residents whose GP was signed up as a data provider for the SAIL databank (i.e. residents whose GP was signed up to the SAIL databank at the time of writing the final results and had GP records available during the study window). Therefore, our 32,009 study participants were restricted to 20,021 people for whom GP data were available. Once our study period was taken into account, there were 18,327 individuals with available data, from which we created condition-specific cohorts.
Participants
We further restricted analyses for GP-based outcomes by creating two subcohorts for individuals with GP records indicating that they had (1) asthma or COPD or (2) a CMD. Residents were selected for inclusion in the asthma and COPD cohort if they had relevant diagnosis, symptom or treatment Read codes at any point (see Table 18). To create the CMD subcohort, we used an algorithm designed to identify cases of patients with CMDs (anxiety and depression), with a sensitivity of 0.32, a specificity of 0.96 and a positive predictive value of 0.74. 45,46
We took the decision to first identify diagnosed individuals because it was necessary to ensure that outcomes were not confounded by treatments prescribed for other reasons. For example, respiratory symptoms related to viral infections are not affected by household conditions. Antidepressant medication may be used to treat other conditions; both selective serotonin reuptake inhibitors and tricyclic antidepressants are used to treat chronic pain. These outcomes were measured only for those individuals whose conditions were ‘active’ and may have feasibly been affected by the intervention. All historical data were used to define the asthma and COPD cohort because GPs treating such patients with a known history of these conditions are not likely to re-enter a diagnosis code with all subsequent activity relating to that condition. Patients are not often cured of these conditions, so any previous diagnosis was assumed to remain valid for all follow-up beyond that date.
Asthma and chronic obstructive pulmonary disease prescriptions outcome variable
General practitioner event records containing Read codes for relevant treatments (see Appendix 4) were extracted for each individual in the asthma and COPD subcohort. The number of unique prescriptions per day was aggregated into monthly counts of GP treatments for asthma and COPD for each individual throughout the study period (and according to the exposure periods as described above).
Asthma and chronic obstructive pulmonary disease general practitioner attendance outcome variable
For the same subcohort we wanted to know if individuals visited their GP more or less often following the intervention. We created a method to estimate the number of visits per month to allow a measurement of proportional change. This was required so that we could utilise the GP data held in the SAIL databank, which do not allow the identification of GP visits. Instead, all GP activity is recorded, such as records for recording symptoms, diagnoses, test results and administrative records. The total number of GP records was counted for each month a person was included in the study, and multiplied by a proportion depending on their age and year of GP record to estimate the number of visits in order to analyse proportional changes.
Common mental health disorder outcome variable
For each individual in the CMD cohort, and for the months identified as a CMD case, unique mental health treatment Read codes (see Appendix 5, Table 15) were counted per day and aggregated into monthly counts.
Results
After selecting residents with the relevant conditions from the GP data, there were 8662 people in the asthma and COPD cohort and 2562 people in the CMD cohort (Tables 7 and 8 show the corresponding cohort profiles). Differences for the CMD cohort were as expected, with about two-thirds of the cohort female.
| Characteristic | Group, n (%) | |
|---|---|---|
| Intervention home residents | Rest of Carmarthenshire | |
| Total | 8662 (100) | 57,523 (100) |
| Age group (years) | ||
| < 25 | 3672 (42.4) | 21,788 (37.9) |
| 25–39 | 1328 (15.3) | 9485 (16.5) |
| 40–49 | 678 (7.8) | 6182 (10.7) |
| 50–59 | 747 (8.6) | 6618 (11.5) |
| 60–69 | 874 (10.1) | 6257 (10.9) |
| 70–79 | 820 (9.5) | 4503 (7.8) |
| ≥ 80 | 543 (6.3) | 2690 (4.7) |
| Sex | ||
| Male | 3916 (45.2) | 26,863 (46.7) |
| Female | 4746 (54.8) | 30,660 (53.3) |
| Income deprivation quintile | ||
| Most deprived | 2547 (29.4) | 5265 (9.2) |
| More | 2428 (28.0) | 11,608 (20.2) |
| Mid | 2416 (27.9) | 17,671 (30.7) |
| Less | 1174 (13.6) | 17,537 (30.5) |
| Least deprived | 97 (1.1) | 5442 (9.5) |
| Rurality classification | ||
| Urban | 4055 (46.8) | 19,932 (34.7) |
| Town | 1333 (15.4) | 8165 (14.2) |
| Village and hamlet | 3274 (37.8) | 29,426 (51.2) |
| Comorbidity status | ||
| No comorbidities | 7636 (88.2) | 52,708 (91.6) |
| At least one comorbidity | 1026 (11.8) | 4815 (8.4) |
| Characteristic | Group, n (%) | |
|---|---|---|
| Intervention home residents | Rest of Carmarthenshire | |
| Total | 2562 (100) | 14,779 (100) |
| Age group (years) | ||
| < 25 | 651 (25.4) | 2635 (17.8) |
| 25–39 | 782 (30.5) | 4140 (28.0) |
| 40–49 | 363 (14.2) | 2844 (19.2) |
| 50–59 | 292 (11.4) | 2290 (15.5) |
| 60–69 | 228 (8.9) | 1471 (10.0) |
| 70–79 | 172 (6.7) | 924 (6.3) |
| ≥ 80 | 74 (2.9) | 475 (3.2) |
| Sex | ||
| Male | 855 (33.4) | 5104 (34.5) |
| Female | 1707 (66.6) | 9675 (65.5) |
| Income deprivation quintile | ||
| Most deprived | 736 (28.7) | 1411 (9.5) |
| More | 681 (26.6) | 2980 (20.2) |
| Mid | 755 (29.5) | 4614 (31.2) |
| Less | 356 (13.9) | 4473 (30.3) |
| Least deprived | 34 (1.3) | 1301 (8.8) |
| Rurality classification | ||
| Urban | 1208 (47.2) | 5174 (35.0) |
| Town | 351 (13.7) | 1825 (12.3) |
| Village and hamlet | 1003 (39.1) | 7780 (52.6) |
| Comorbidity status | ||
| No comorbidities | 2313 (90.3) | 13,762 (93.1) |
| At least one comorbidity | 249 (9.7) | 1017 (6.9) |
Statistically significant associations with lower rates of prescribed medications were found among the exposure group of individuals with a history of asthma or COPD (of all ages) who were living in homes that received new windows and doors during their tenancy (IRR 0.92, 95% CI 0.88 to 0.97; p < 0.01), compared with the reference group (Figure 16).
FIGURE 16.
Incidence rate ratios for prescriptions for participants with a history of asthma or COPD of all ages by cointervention.
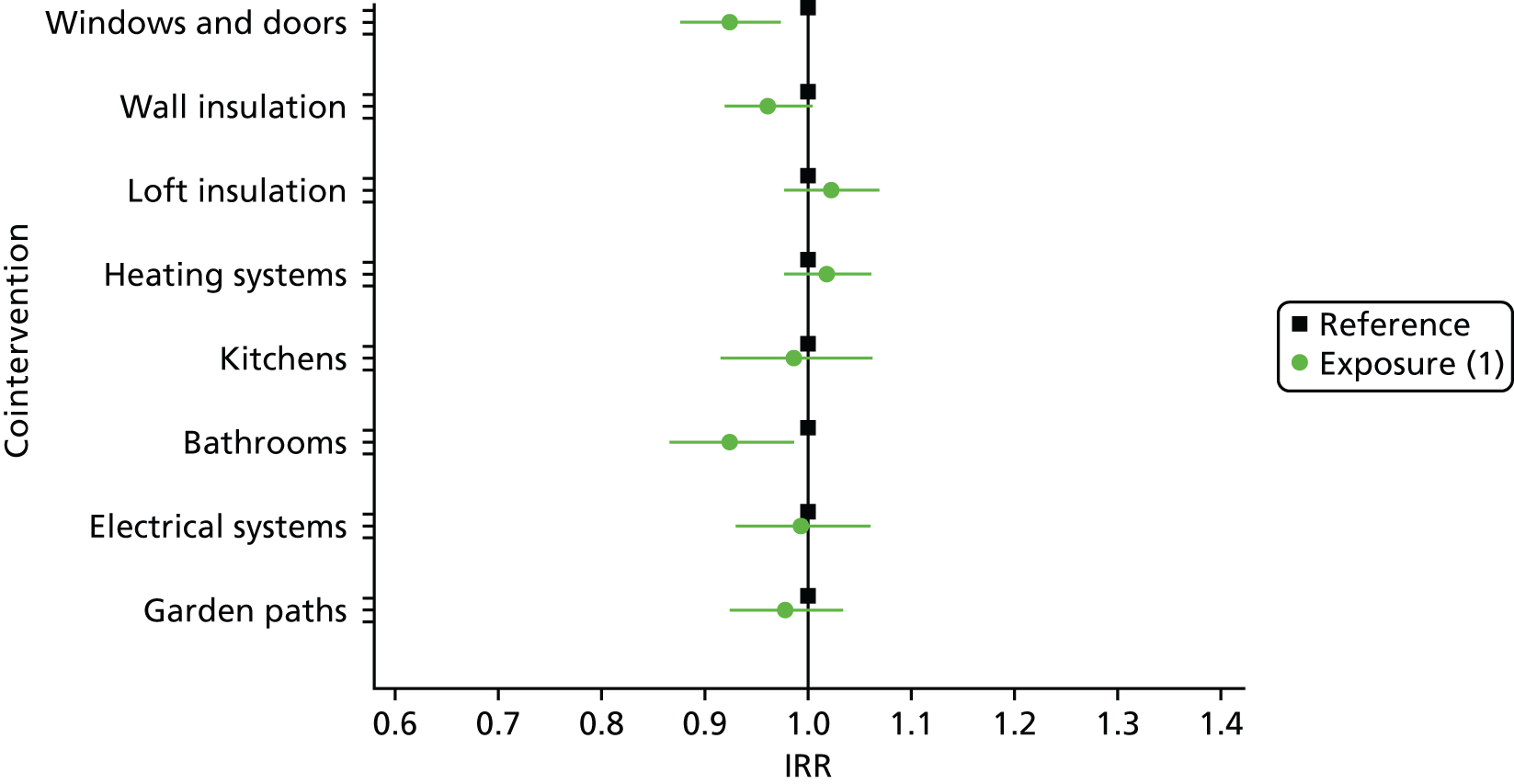
Statistically significant associations with lower rates of GP attendances were found among individuals in the asthma and COPD cohort (of all ages) living in properties while they received upgraded electrical systems, compared with the reference group (IRR 0.91, 95% CI 0.87 to 0.95; p < 0.01) (Figure 17).
FIGURE 17.
Incidence rate ratios for GP attendances for participants with a history of asthma or COPD by cointervention.
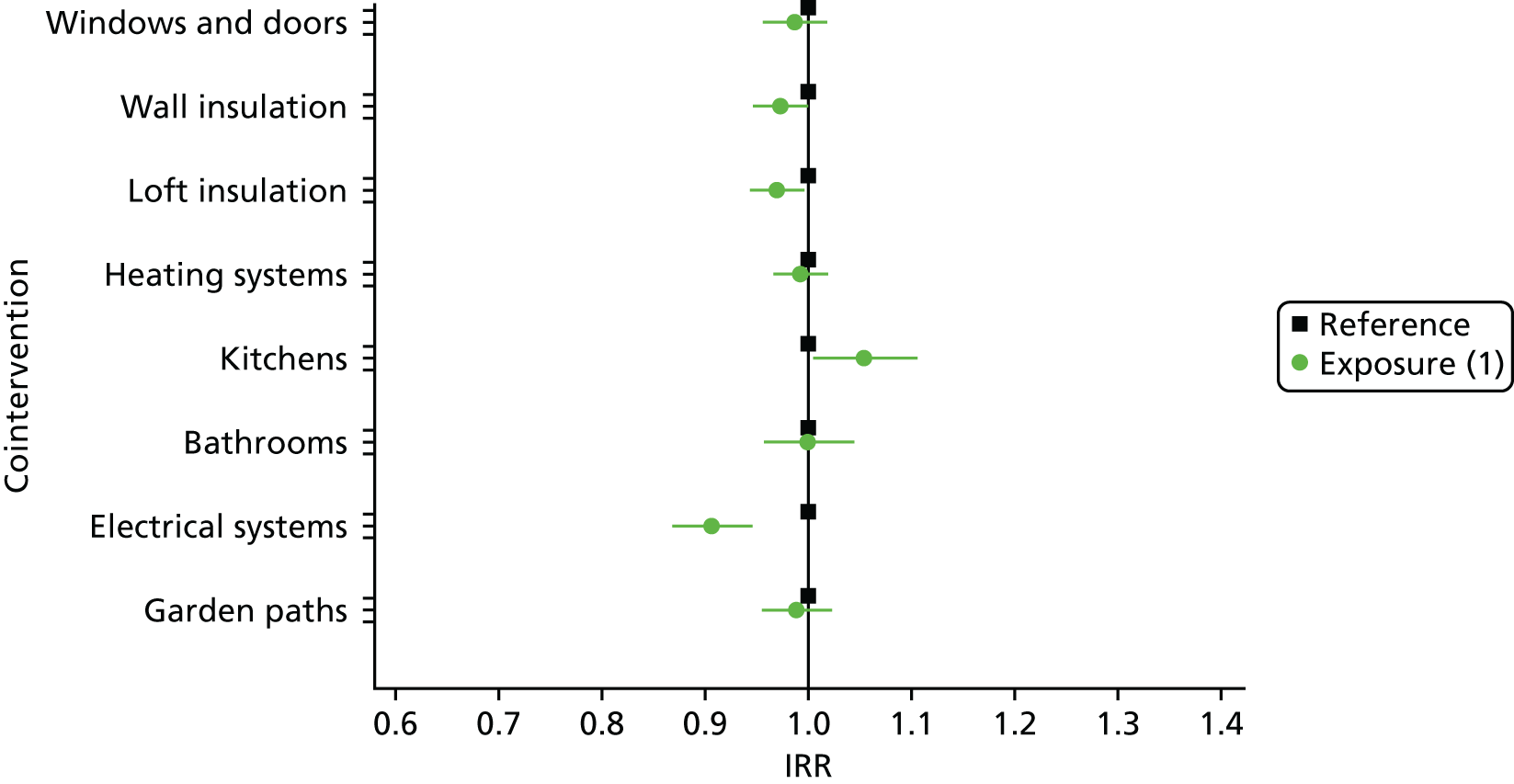
There were no statistically significant associations between any of the cointerventions and prescribed medications among those with a CMD (Figure 18).
FIGURE 18.
Incidence rate ratios for prescribed medications for participants with a CMD by cointervention.
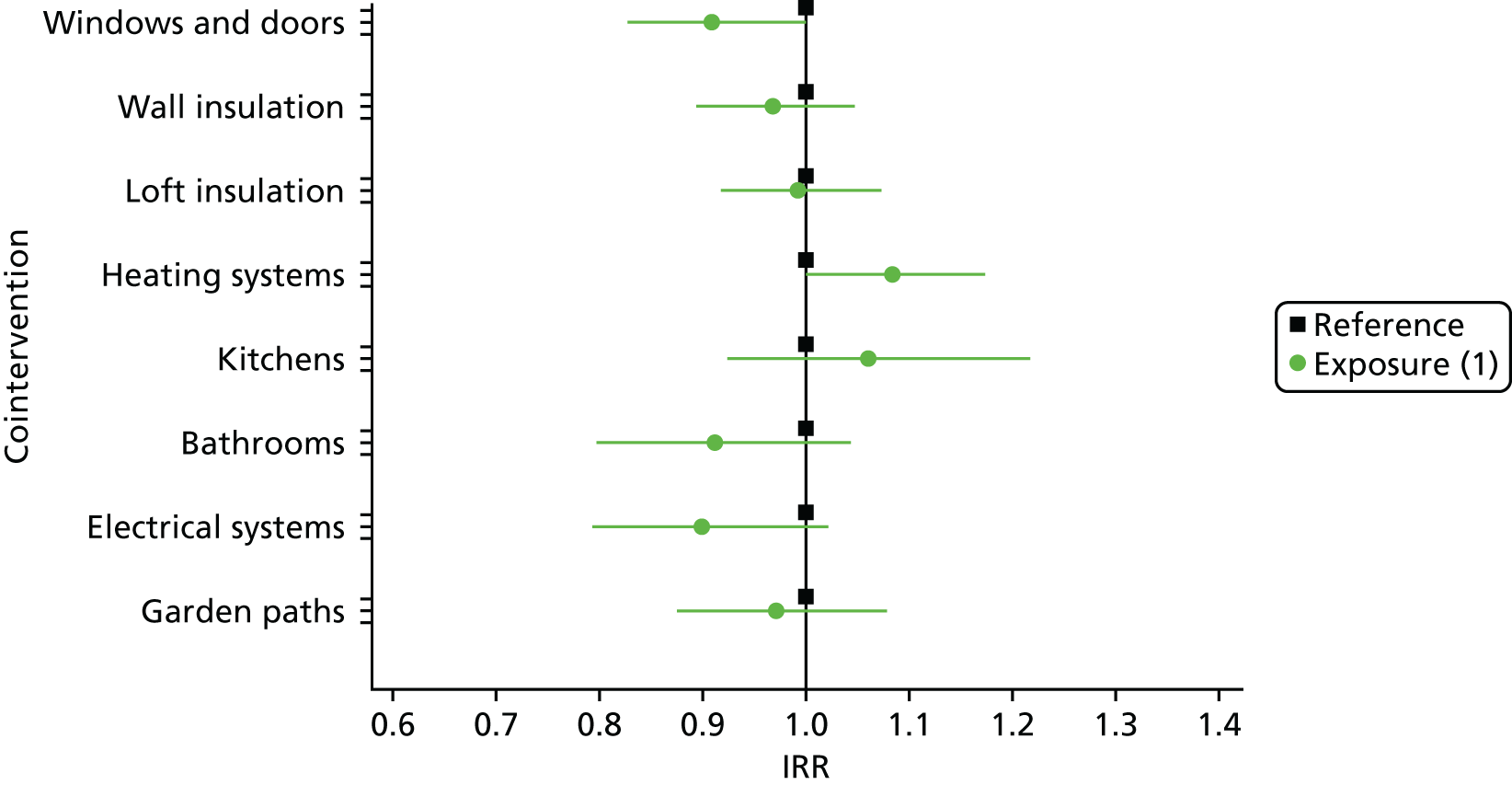
Additional analyses
We also investigated the impact of being exposed to good-quality housing through living in a home that already met the standards for a particular housing cointervention. This may be through longer-term exposure to good-quality housing, or because people moved into a home during the study and that work cointervention was already complete.
There were fewer asthma and COPD prescriptions associated with those people who lived in homes that were already up to the recommended standard for wall insulation (IRR 0.95, 95% CI 0.91 to 0.99; p = 0.016) than with those in the reference group. Although this was not statistically significant at our local level of p-value of < 0.01, as with all tests, it is possible that there was an effect despite the lack of statistical significance. In this case the small sample size may have prevented a statistically significant effect associated being realised with the smaller asthma and COPD cohort (see Figure 29).
Respiratory patients whose homes already met housing standards for boilers had an association with more GP contacts (IRR 1.06, 95% CI 1.02 to 1.09; p < 0.01) than those in the reference group. People with asthma or COPD who lived in properties while they had a new kitchen fitted generally had more GP contacts (IRR 1.05, 95% CI 1.01 to 1.11), although this was not significant at the multiple testing correction level (p = 0.030). In contrast, those already living in homes with a kitchen that met the standard were associated with lower rates of GP contacts for asthma and COPD (IRR 0.92, 95% CI 0.87 to 0.97; p < 0.01) than those in the reference group.
There were (albeit non significant) associations with lower rates of prescribed medications among individuals with a history of CMD living in properties that already met housing quality standards for kitchens compared with the reference group (IRR 0.83, 95% CI 0.70 to 0.97; p = 0.023). As for the COPD/asthma cohort, there may have been an effect but the sample size was too small to show statistical significance.
What impact has the intervention had on emergency department attendances for all injuries occurring at home?
Injuries and the potential pathways relating to housing cointerventions were described in Chapter 2, with further consideration in Chapter 3 for fall and burn injuries. Here we investigate the impact of the housing cointerventions on emergency attendances. These include more minor injuries that did not necessarily result in a hospital admission.
Methods
The methodological approach used to analyse the effect of the housing interventions on emergency department attendances for injuries occurring at home follows that described above for emergency admissions. The data sources used to measure the outcome variable and the definition of that variable are detailed here, along with the subcohort of participants included in this analysis, which distinguish the only differences in the modelling specification.
Participants
The analysis was restricted to individuals registered to an intervention home between 1 January 2011 and 31 March 2015 because Emergency Department Data Set (EDDS) [www.publichealthwalesobservatory.wales.nhs.uk/edds (accessed 1 November 2017)] data collection was not nationally mandated before this period.
Variables
The EDDS was used to define injuries likely to have occurred at home and that could be attributed to a housing intervention. The EDDS contains standardised emergency department diagnostic and treatment codes and International Classification of Diseases, Tenth Edition (ICD-10)47 codes that were used to create the injury outcome definition (see Appendix 6, Table 16) for all new attendances, excluding follow-up or preoperative appointments. Only injuries that occurred in the individual’s own home were selected based on the ‘location type’ (01 at home, 14 other specified or 99 unspecified). Criteria also included ‘mechanism of injury’ (not equal to 98 non-injury) and ‘activity’ code (not equal to 01 work, 2 education, 3 sport, 6 road traffic collision or 98 non-injury).
Counts of identified attendances were aggregated into monthly counts for each individual throughout their follow-up period. Any records indicating a new attendance containing diagnostic or treatment codes relating to an injury occurring at home were selected to define an injury outcome.
Results
After selecting residents with the relevant conditions from EDDS data, there were 24,366 people in the emergency department cohort (Table 9). People living in homes while windows and doors upgrade work was carried out were not associated with a significant reduction in injuries (IRR 0.79, 95% CI 0.65 to 0.96; p = 0.021). This was a result of setting the CI at 99% (p < 0.01) to account for multiple hypothesis testing. It is important to remember that absence of evidence is not evidence of absence. 48 However, there was a significant association with lower rates of emergency department attendance found for individuals who had always lived in a home that met standards for windows and doors, compared with the reference group (IRR 0.76, 95% CI 0.62 to 0.93; p < 0.01).
| Characteristic | Group, n (%) | |
|---|---|---|
| Intervention home residents | Rest of Carmarthenshire | |
| Total | 24,366 (100) | 193,129 (100) |
| Age group (years) | ||
| < 25 | 9699 (39.8) | 60,171 (31.2) |
| 25–39 | 4240 (17.4) | 33,756 (17.5) |
| 40–49 | 2539 (10.4) | 26,138 (13.5) |
| 50–59 | 2211 (9.1) | 24,941 (12.9) |
| 60–69 | 2337 (9.6) | 23,886 (12.4) |
| 70–79 | 1841 (7.6) | 14,753 (7.6) |
| ≥ 80 | 1499 (6.2) | 9484 (4.9) |
| Sex | ||
| Male | 11,533 (47.3) | 95,558 (49.5) |
| Female | 12,833 (52.7) | 97,571 (50.5) |
| Income deprivation quintile | ||
| Most deprived | 7708 (31.6) | 19,132 (9.9) |
| More | 8154 (33.5) | 45,773 (23.7) |
| Mid | 5646 (23.2) | 54,360 (28.1) |
| Less | 2543 (10.4) | 53,708 (27.8) |
| Least deprived | 315 (1.3) | 20,156 (10.4) |
| Rurality classification | ||
| Urban | 13,697 (56.2) | 84,278 (43.6) |
| Town | 4062 (16.7) | 26,889 (13.9) |
| Village and hamlet | 6607 (27.1) | 81,962 (42.4) |
| Comorbidity status | ||
| No comorbidities | 22,363 (91.8) | 182,448 (94.5) |
| At least one comorbidity | 2003 (8.2) | 10,681 (5.5) |
Higher rates of attendance were found for those living in a property while the garden path was made safe (IRR 1.20, 95% CI 1.07 to 1.35; p < 0.01) than for the reference group. A similar result was found for those living in homes already meeting national standards for garden paths (IRR 1.16, 95% CI 1.04 to 1.30; p < 0.01). The remaining cointerventions were not associated with changes in emergency department attendances for either exposure group (Figure 19). The full results are given in Table 17 (see also Figure 32).
FIGURE 19.
Incidence rate ratios for emergency department attendances relating to injuries for participants of all ages by cointervention.
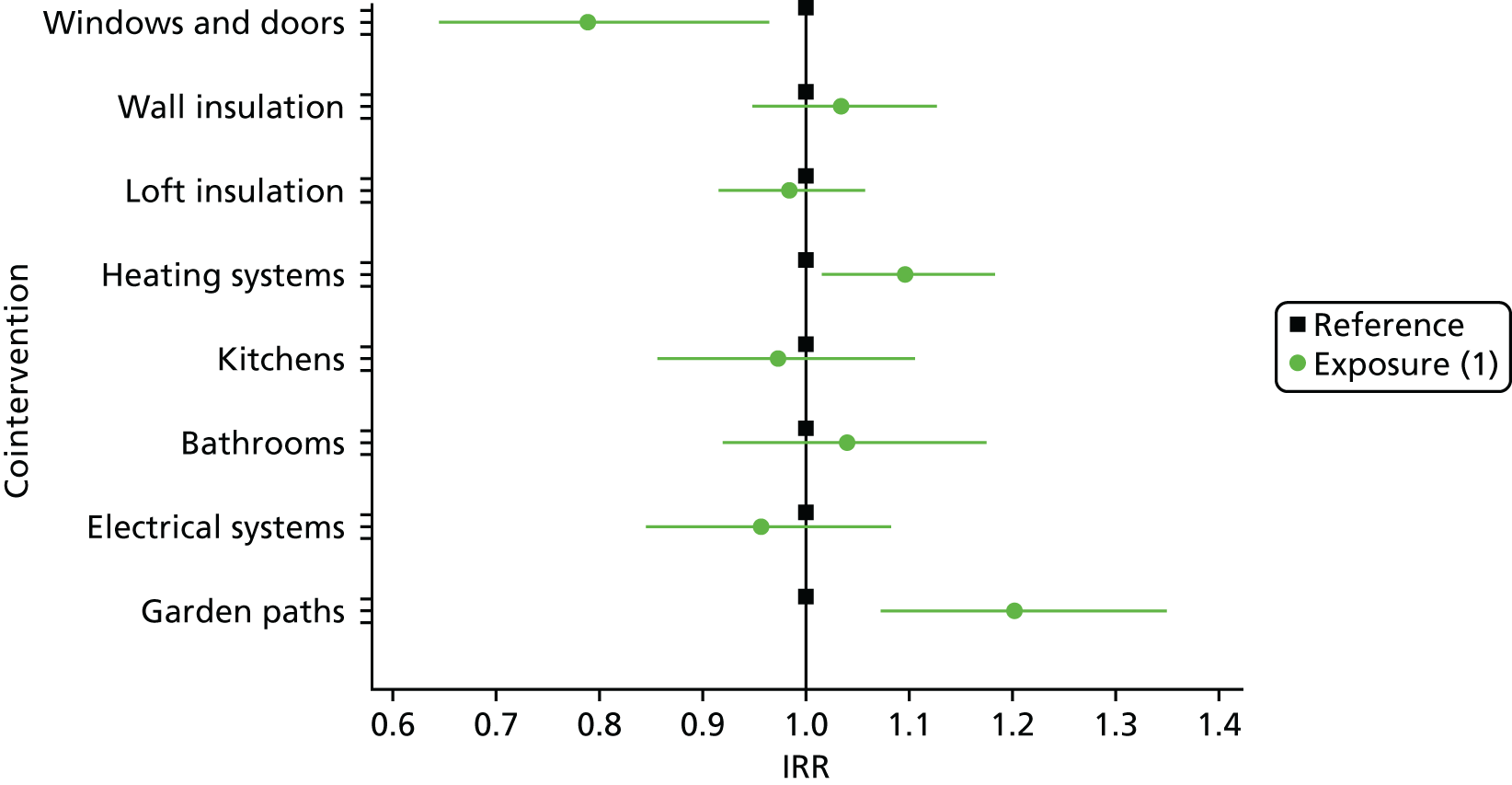
Discussion and conclusion
There were few statistically significant associations of the use of primary care physician services for respiratory and CMDs, and attendances at emergency departments, as a result of this housing intervention.
It may be that a lack of well-being was established for generations and throughout the community. Corresponding ill health and health-care utilisation behaviour for individuals, including GP consultations, may have been set previously. We propose that there was insufficient opportunity to alter established behaviour and ill health to result in significant reductions in health events, despite the potentially long follow-up periods during this decade-long intervention evaluation. 10
Equally, despite a lack of statistical significance, it is possible there was a practical effect. The people with pre-existing respiratory conditions and CMDs may have experienced an effect on their health service utilisation, compared with the reference group, that would have been significant had the sample size been larger.
Our methods targeted people who had at least one chronic condition (COPD/asthma or CMD). They were likely to have regularly visited the GP for a period of time sufficient to have set habits that may be difficult to change. We also know that people who are socially disconnected and feel lonely (particularly older adults) rate their physical health lower. 49,50 As a result, lonely people are more likely to visit their GP and to use other health services often, even if their symptoms are lessening. Studies have demonstrated that loneliness is also a predictor of use of accident and emergency services independent of chronic illness. 51
People with respiratory conditions whose kitchens already met the housing standard had fewer GP contacts, but those with a new kitchen showed a (non-significant) increase in GP contacts (p = 0.030). Similarly, those with a respiratory condition who had always lived in a home with a compliant boiler also had more GP contacts, but those who were living in the home while the boiler was fitted did not. Further in-depth qualitative work is needed to understand these results. Continued investments in housing and very long-term intergenerational data linkage studies may be needed to assess educational and other outcomes that may contribute to changes in health-care utilisation in the longer term. 52
People with injuries attending an accident and emergency room had an increased number of attendances associated with the garden path cointervention. The increase is likely to be for minor injuries because the individuals were not necessarily admitted to hospital, and is opposite to emergency admissions, which reduced (see Chapter 3). There was a significant reduction in fall and burn injuries for those people who always had garden paths meeting the housing standard. This could be from increased mobility due to overconfidence in navigating gardens using outside paths; and could be for those people who moved into a home with recently upgraded paths, rather than those people who have lived in a home that was always compliant for the paths cointervention. Our previous work indicated that ≥ 2 home moves for young children were associated with an increased risk of emergency admissions (IRR 1.33, 95% CI 1.18 to 1.51). 53 Therefore, this may be an indication of moving into an unfamiliar home, as opposed to related to the garden paths themselves.
Chapter 5 Does the intervention represent value for money?
Introduction
Health economic studies are intended to inform policy-makers and health-care decision-makers, enabling them to identify which interventions, policies or services provide the best value for money. The challenge when undertaking evaluation of public health interventions is that their objectives and outcomes are often captured using different methods and measures and not those recommended for use in economic evaluation in the UK. The ‘reference case’ employed by the National Institute for Health and Care Excellence (NICE) for health technology assessment (HTA) specifies which methods are appropriate and consistent with the NHS objective of maximising health gain from limited resources. 54 This includes the use of the quality-adjusted life-year (QALY). Public health interventions and outcomes are complex and not necessarily represented by a single metric such as the QALY; thus, NICE has developed guidance for methods for the economic evaluation of such interventions. 55
Public health interventions have multidimensional (economic, social and environmental) and intertemporal aims that differentiate them from many other types of intervention. 56 Public health initiatives should be regarded as an investment in the health of the nation and not be expected to generate relatively short payback periods. 57 Therefore, they do not fit into narrow definitions and perspectives of cost-effectiveness. Investing in housing regeneration is an example of a public health intervention and involves an integrated set of activities aiming to reverse economic, social, environmental and physical decline to achieve long-lasting improvement to the area.
There is some evidence that improving and regenerating social housing stock by increasing energy efficiency through insulation and other measures to improve heat conservation, such as double glazing, and also that the provision of more efficient heating, improves the health of residents and is potentially a cost-effective investment benefiting national health services. 58 There has been little previous evidence on the health impacts of new kitchens and bathrooms because this type of intervention has not been evaluated previously. Public sector investment in housing regeneration such as the application of the CHS has the potential to generate health economic impacts.
This chapter describes the analyses undertaken to assess the health economic impact of the housing intervention.
Perspective and constraints
Public health interventions such as social housing regeneration schemes are complex, as is measuring their impact. These interventions may deliver health benefits for people living in these areas and also deliver benefits to the NHS through the reduced use of NHS services, thereby releasing resources for other purposes. Regeneration schemes also have diverse stakeholders because they have an impact on the NHS, public sector and social services and owners and landlords of the housing, as well as on the occupants of the housing. An improvement in appearance also has an impact on the neighbourhood. Interventions of this type are generally paid for not by the NHS, but from local authority budgets, although the interests of these two stakeholders have moved closer together.
The principle of (re)organising expenditure across public sector organisations to optimise public health benefits is technically possible but it has political and organisational challenges. However, changes in the UK NHS and local authorities such as the ‘devolution’ in Greater Manchester have created a unified budget, suggesting that ‘joined-up’ spending on one sector (housing) delivering benefits in another (health) is possible and could be undertaken in Wales.
Policy-makers, who have increasingly limited budgets, have to consider the opportunity cost of spending some of their budget on regeneration schemes; money spent on housing regeneration will limit the funds available for other projects. Thus, evidence of value for money from all perspectives, including the NHS, is vital to inform decisions about regeneration policy.
Value for money depends on several factors, including the setting for the intervention and the perspective of the evaluator. Public health recommendations for investment consider equity and value for money, the balance between the estimated cost of each intervention and the expected outcomes for the diverse community of stakeholders and beneficiaries, which would include but not be limited to health benefits. An important consideration for public health interventions may be the time over which return on investment is expected or needed, that is, the duration needed for the benefits of an intervention, policy or service to be realised and for the financial impact, potential savings or reduction in health-care service utilisation to be compared with the initial expenditure on the intervention. Budget and political cycles may constrain investment in projects that deliver benefits a long time in the future and drive preferences to have the benefits of investment within the time period of the budget or political cycle; this is often shorter than the period of time over which the intervention benefits can be seen.
Economic studies for public health
The importance of having robust and meaningful evidence on the cost and consequences of public health interventions and the necessary divergence from the HTA reference case has been accepted by decision-making bodies such as NICE, and there is increasing recognition that an analysis within this area of health economics must take into account the wider context of public health. NICE recognised this distinction by producing specific health economic guidance for public health. 55 This guidance has broadened the approach to take into account stakeholder perspectives additional to the NHS, such as that of local authorities. While the guidance draws on many aspects of the NICE HTA reference case, there are also important differences that NICE recommends taking into account when framing a suitable health economic analysis for a public health intervention such as housing regeneration. NICE public health guidance also presents the pros and cons of the different methods of economic analysis available for the evaluation of public health interventions and the options for their use in differing contexts.
Different types of health economic studies
Health economic analyses take many forms, have different purposes and can be divided into two distinct groups: cost studies and economic evaluation studies. Descriptions of the main types of health economic analysis are given in Box 2.
-
Cost-offset analysis establishes whether or not health-care utilisation decreases as a result of a health intervention. A total offset occurs when general health-care savings exceed the cost of the health-care intervention, effectively resulting in the treatment paying for itself.
-
Cost-minimisation analysis addresses assessment of costs if the health benefits of the competing health-care technologies have been demonstrated to have clinically equivalent outcomes.
-
Cost–consequences analysis considers all of the health and non-health benefits of an intervention across different sectors and reports them in a disaggregated form. It accepts that different types of benefit cannot be captured using the same units. All impacts and costs are considered (even if the impacts cannot be costed) when deciding which interventions represent the best value. This distinguishes it from a cost–benefit analysis.
-
Cost-effectiveness analysis typically involves measuring a specific, one-dimensional health or clinical outcome, for example ‘asthma attacks averted’.
-
Cost–utility analysis is a special type of cost-effectiveness in which multidimensional health outcomes are reduced to a single dimension reflecting individuals’ preferences for the diverse health outcomes. The most commonly used outcome in a cost–utility analysis is the QALY. For both cost-effectiveness and cost–utility studies, value for money is identified using a measure of the additional cost per additional outcome ratio (e.g. an incremental cost per QALY ratio) and comparing that with an external threshold or with the ratio achieved by alternative policies.
-
Cost–benefit analysis involves the measurement and valuation of all outcomes of interest in monetary terms. Here the value for money is identified by positive net economic benefit associated with the interventions (i.e. the monetary value of the outcomes exceeds the net costs of the intervention less any costs savings achieved elsewhere).
Cost studies concentrate on identifying the resources, impacts and costs related to providing interventions and any cost offsets that may arise. There are three main types of cost study: cost-offset study, cost-minimisation analysis and cost–consequences analysis. Economic evaluations differ, as they take account of both costs and benefits, are always comparative analyses and take three main forms: cost-effectiveness analysis, cost–utility analysis and cost–benefit analysis.
Although methods such as cost–utility analysis are identified as the preferred approach, within the NICE reference case for HTA, the NICE public health guidelines recognise that there are some disadvantages associated with cost–utility analysis. These are related to the narrowness of the cost–utility analysis approach, which focuses only on health benefits rather than the broader benefits (i.e. non-health benefits) often associated with public health interventions. 55 NICE more recently took account of the need to ensure that the method of economic analysis chosen is more inclusive and that a corresponding change in perspective not limited to a NHS perspective is considered for public health interventions. 55 Thus, considering appropriate metrics is often a key issue when developing a suitable analytical framework for such health economics studies. However, when differing metrics are used to value different outcomes, as often happens when impacts of public health interventions are assessed, undertaking an economic analysis can be challenging. To accommodate these issues, NICE guidelines place more emphasis on the use of cost–consequences and cost–benefit analyses, compared with cost-effectiveness and cost–utility analyses, when assessing public health interventions. 55 These approaches ensure that relevant impacts or benefits (to health, non-health or community) are considered, to enable local authorities (and other organisations interested in improving people’s health) to review, from their perspective, whether or not a public health intervention represents value for money. It is worth noting that not all of these costs need to be monetised in order to complete deliberations.
Economic analyses in housing studies
Despite their importance, there is a limited number of full health economic evaluations of housing improvement programmes. Health economic studies addressing the impact of housing improvements were reviewed by Fenwick et al. in 2013. 58 Their systematic review of published health economic analyses undertaken as part of studies of the health impacts of housing improvement schemes found 29 studies reporting costs and/or economic analysis. 58 Twenty-five of these were cost studies reporting only cost data and/or benefits to the recipients. Of these, the authors suggest, 11 could have been extended to undertake a full economic evaluation. The review also found three further studies in which the authors stated that they had undertaken a cost–benefit analysis economic evaluation. However, they did not include a monetary valuation of all important outcomes, and therefore none of the studies was a true cost–benefit analysis. Three studies generally reported modest net benefits across some or all of a range of outcomes, and cost savings. A single study, accurately reporting a full economic evaluation (a cost-effectiveness analysis), was undertaken by Barton et al. 59 They captured changes in residents’ health-related quality of life and used changes to generate utilities for the cost-effectiveness analysis. 58 They reported that the intervention (upgrading heating, replacing doors and windows and providing insulation) was more costly and less effective than the status quo, but suggested that the 1-year time horizon of the study was too short to realise these outcomes.
Since the 2012 review, there have been other UK-based housing studies that are cost studies and not full economic evaluations. The Gentoo social housing and sustainability group undertook a pilot study60 of the health impacts of housing improvement in people with COPD living in 12 homes with poor insulation. Information on health status and use of NHS resources was collected (by survey) from residents, who had their home energy efficiency ratings increased through the installation of double glazing, efficient boilers, and loft and cavity wall insulation. Outcomes for intervention home residents were compared with those for people with COPD in the area who did not have their homes improved. The researchers compared health-care utilisation in the winter period pre and post installation and found that residents had fewer attendances post installation. Over an 18-month period, participants self-reported that GP appointments reduced by 60%, accident and emergency attendances reduced by 30%, outpatient appointments reduced by 22% and emergency admissions reduced by 25%. 60
The second, and larger, recent cost study by Warm Homes for Health was cofunded by Gentoo and Nottingham City Homes and was based on a similar Gentoo programme of improvements focused on heating and insulation. A cost analysis has been reported so far, with the intention to also undertake a cost-effective analysis. 61 There were 228 participating households, most with two tenants. Baseline survey data recorded that participants were generally socioeconomically deprived and in poor health: 77% of households had an income of < £15,000 per year, about half of the average household income for the UK. After installation of housing improvements, health service use reduced and NHS cost savings were estimated at > £50,000. The authors suggest that this can be extrapolated to potential savings of £1B per year in health service use costs if the 4.8 million ‘unhealthy’ UK homes were to receive similar housing improvements. 61
We found a good-quality intervention study evaluating home modifications for the prevention of falls in the general population. 28 This New Zealand-based study provided the basis for a cost–benefit analysis of home modifications, enabling the monetisation and extrapolation of the benefits of these interventions. Even using conservative assumptions, estimates suggested that this programme was beneficial, reducing fall injury costs by 33%. 62
Aims and objectives of the economic analysis of meeting housing quality standards
Our research contributes to the evidence discussed in the previous studies. Instead of using self-report survey data, our study utilises objective routinely collected health and housing data available in the SAIL databank. 33,63,64 The use of routinely collected health data and data linkage to households undergoing the improvement work allowed the evaluation team to retrospectively extract health-care utilisation from the databank despite the work having begun at the start of the study. 65 The study reported here focuses on the impact on the utilisation of secondary health-care services, including emergency admissions of people living in homes that received the housing intervention compared with people living in homes before interventions were implemented. 66
The aim of the health economic analysis is to consider the costs and consequences of the application of the intervention in the form of a cost–consequences analysis.
Methods
The methods for defining and analysing emergency hospital admissions were described in Chapter 3 (see Methods). These outcomes were used for the cost–consequences analysis, the most appropriate methodological approach for considering value for money and economic analysis in this study. NICE recommends cost–consequences analysis as an acceptable approach for public health interventions such as housing improvements because the analysis accepts that different types of benefit cannot be expressed using the same units. This cost–consequences analysis considers resource use and cost impacts of the intervention and all the benefits of the intervention across different NHS sectors and reports them separately in a disaggregated form. NHS impacts and costs are considered to enable decision-makers to determine if the intervention represents good value.
The ideal comparator for an economic evaluation would be ‘business as usual’ in the same area. However, because all of the council housing stock was improved as part of the intervention to bring houses up to the housing quality standard, there was no remaining council housing in Carmarthenshire that would have enabled a contemporaneous comparison with the application of CHS. Instead, the comparison was completed at the level of the cointervention; tenants in homes that did not have one of the eight cointerventions completed were the reference group. There were, therefore, different intervention exposure and reference groups for each cointervention. Adjustments were made for several potentially confounding variables, including the differing age structure of the population over the programme time horizon, and for background trends in health-care utilisation for the remainder of the population living in the same region: the ‘rest of Carmarthenshire’ (see Chapter 3, Methods).
The perspectives of the cost–consequences analysis reported here are those of the Welsh local authority (costs) and the Welsh NHS (consequences).
The time horizon for the analysis is 10 years and 3 months, the study period; the housing improvement investments were made during that time. The lifespan of the cointerventions of the CHS intervention can range from 10 years for a smoke alarm to 12 years for a new central heating boiler to 15 years for a new bathroom or 60 years for work on paths and gardens, and will benefit a series of residents moving in and out of the property. To estimate the appropriate time horizon for the study, we considered the length of time a resident lived in the property, and thus was exposed to the new cointerventions, and may have been expected to accumulate potential health benefits. Given that the shortest lifespan of a cointervention was 10 years, we are confident that a 10-year time horizon for the economic analysis was appropriate and generalisable to other settings. Extrapolating beyond the 10-year time horizon of the study is inappropriate given the level of migration into, out of and between study properties, and the uncertainty about how much health benefit remains with the individual after they have left the property.
Health outcomes
Our primary health outcome was emergency hospital admissions for cardiovascular conditions, respiratory conditions and fall and burn injuries. Outcome data were obtained from routinely collected data, as described in Chapter 3.
Resource use and costs
Health service-related costs were identified for the primary outcome and estimated to facilitate the cost–consequences analysis. The resource use is the outcome itself, comprising contact with the health services, and the corresponding costs were derived from NHS Healthcare Resource Groups. Our approach enabled the resources and costs relating to hospital admissions to be estimated using routine data. This includes potential benefits to the NHS, in terms of reduced contacts with the NHS, and consequent potential capacity or cost impact on the NHS.
Results
Outcomes
The results for all health outcomes can be found in Appendix 7, Table 17.
Intervention costs
The cost for each cointervention was obtained from the local authority. These are shown in Table 10. All costs are presented in British pounds at 2015 prices and tariffs. One cointervention, loft insulation, had no budgetary impact or cost to the local authority at the time because funding for this cointervention was available through Welsh Government grant funding. There was, however, a real cost to obtaining and fitting the loft insulation, and so we obtained this cost from the local authority and included it in the overall estimate of the costs of the intervention in order to make our results generalisable. The most expensive cointerventions in terms of cost per unit were external wall insulation at £9000 per unit delivered (the least frequently delivered cointervention) and double-glazed windows and doors at £3500 per unit delivered. Central heating boilers, new bathrooms and electrical system-related cointerventions were the most frequently delivered cointerventions.
| Cointervention | Average cost (£)b | Estimated lifetime yearsb | Average property cost per year (£) | Average cost per persona per year (£) | Number of properties | Total cost (£) |
|---|---|---|---|---|---|---|
| Double glazed windows and doors | 3500 | 20 | 175 | 76 | 4802 | 16,807,000 |
| External wall insulationc | 9000 | 30 | 300 | 130 | 663 | 5,968,955 |
| Cavity wall insulationc | 1000 | 25 | 40 | 17 | 5367 | 5,366,783 |
| Loft insulation | 225 | 10 | 23 | 10 | 2908 | 654,300 |
| Heating | 5752 | 15 | 383 | 167 | 7087 | 40,764,424 |
| Bathroom | 2349 | 25 | 94 | 41 | 7504 | 17,626,896 |
| Kitchens | 3298 | 15 | 220 | 96 | 7430 | 24,504,140 |
| Electrics | 3159 | 20 | 158 | 69 | 7744 | 24,463,296 |
| CO detectord | NA | 10 | 7701 | |||
| Smoke alarmd | NA | 10 | 8394 | |||
| Security lightsd | NA | 10 | 7667 | |||
| Paths | 700 | 60 | 12 | 5 | 2767 | 1,936,900 |
| Total spend | 138,092,694 |
The budget that CCC spent on meeting the intervention that we evaluate in this study was £144,807,000. Our bottom-up costing of the intervention was £138,092,694. This results in a difference of £6.7M. This was probably due to additional costs for major works and associated costs to work packages in order for the homes to comply with the housing standard. Not all properties are uniform and several would have had various issues requiring rectification before the component was replaced, for example meter relocation, gas connection or pantry removal for kitchen size compliance.
Health outcome costs
Individual-level data were used to calculate the costs of each emergency admission and each condition category based on Healthcare Resource Group cost codes attached to each person’s admission data. We averaged the costs for each year and then inflated these to present data (2015) costs for our study population and their specific emergency admission health-care utilisation.
Costs and consequences
Table 11 shows the effect of the intervention on the percentage reduction in hospital admissions for people aged ≥ 60 years, who received at least some of the cointerventions, compared with those who did not receive any of the cointerventions of the CHS. The estimated number of admissions saved is based on a rate of 147 admissions per 1000 person-years observed in those residents aged ≥ 60 years. The average cost of an admission (for the combined conditions) was £2952. After adjusting for inflation, the average cost was £3462. The installation of electrical upgrades delivered the greatest number of admissions saved per 1000 persons per year (57 admissions) and the greatest estimated savings per 1000 persons per year (£198,455). Taking the conservative effect size of only a 28% reduction and 41 admissions saved would result in savings of £142,480, as indicated by the lower bound of the CI. Below, we have calculated the admission reduction in real terms for CCC social housing, and for another, larger, fictitious region.
| Cointervention | Decrease (%) (95% CI) | Estimated number of admissions saved | Minimum, maximum | Estimated savings (£) (95% CI) |
|---|---|---|---|---|
| Windows and doors | 29 (19 to 37) | 43 | 28, 54 | 147,569 (96,683 to 188,278) |
| Wall insulation | 25 (16 to 33) | 37 | 24, 49 | 127,215 (81,417 to 167,923) |
| Loft insulation | 2 (–11 to 24) | 3 | –16, 35 | 10,178 (–55,981 to 122,139) |
| Heating systems | 9 (–1 to 28) | 13 | –2, 35 | 45,802 (–5089 to 142,496) |
| Kitchens | 2 (–17 to 27) | 3 | –1, 41 | 10,178 (–86,515 to 137,407) |
| Bathrooms | 7 (–6 to 29) | 10 | –9, 43 | 35,624 (–30,535 to 147,585) |
| Electrical systems | 39 (28 to 47) | 57 | 41, 69 | 198,455 (142,480 to 239,163) |
| Garden paths | 27 (17 to 36) | 40 | 25, 53 | 137,392 (86,506 to 183,189) |
Carmarthenshire social housing older residents
In a population of 7054 older residents who have not received the intervention, the expected number of admissions per annum would be 1037 using the baseline admission rate of 147 per 1000 persons. With a reduction of 28%, it is estimated that the number of admissions per annum could be reduced to 741 for older residents who have received the intervention. This is based on the intervention effect reducing the admission rate to 106 emergency admissions per 1000 persons.
Therefore, we invite policy-makers to use these per 1000 population estimates to calculate the potential cost of admissions saved for older housing residents in their region(s) of interest.
Another region social housing older residents
The same baseline rate of 147 per 1000 person years for those aged ≥ 60 years in a larger region with 28,000 older people in social housing would have estimates of 28,000 147/1000 = 4116 admissions, reduced to 2964 each year, assuming a similar demographic composition of older people. For the electrical systems cointervention, this is an admission reduction of 28,000 57/1000 = 1596. This translates into a potential cost saving of £5,556,740 per year [£198,455 cost saving per 1000 people per year 28 (thousand)]. Taking the lower estimate of admissions saved provides estimated cost savings of £142,480 28 (thousand) = £3,989,440, again assuming a similar demographic composition of older people.
Discussion and conclusions
The application of the intervention to meet housing quality standards was an intensive programme with a number of separate cointerventions, all of which have been evaluated individually for their health and economic impact. Housing intervention evaluations reported in the literature have generally been less extensive but have many of the cointerventions in common: new boilers, loft insulation and double-glazed windows and doors. These core cointerventions are typical of housing regeneration schemes and have been commented on elsewhere in this report (see Chapter 2, The housing intervention, Delivery of the housing intervention).
The study population for the entire study was 32,009 individuals (of all ages) registered to an intervention address. The total number of individuals within the rest of Carmarthenshire group was 231,200.
Overall, the study population had the highest percentage of individuals aged ≥ 60 years (22%), compared with the rest of Carmarthenshire (20.5%), and also had a slightly higher proportion of females than males (52.6% vs. 47.4%). A fuller description of the populations is provided in Chapter 3 within the ‘cohort profiles’ section. Generalising from this study to other regeneration schemes and locations is not unreasonable, but the characteristics of populations and other settings will need to be considered when interpreting these results.
The investment made by CCC resulted in a reduction in emergency admissions for those people aged ≥ 60 years and thus created cost offsets for the NHS, which we have estimated. Our results show that several of the separate cointerventions contributed to a reduction in emergency admissions in the population aged ≥ 60 years. The cointerventions that were not associated with statistically significant changes in outcomes simply incurred the costs. There may well have been benefits of these cointerventions but this study did not capture them. The value of a reduction in admissions to hospital and the estimated impact of these reductions observed in this study may be over and above the estimated savings. Potentially of more value to a health-care provider than savings is the opportunity to reorganise capacity and resources to optimise care provision. In the UK, emergency admissions to hospital are a major concern for the NHS, costing £12.5B and representing 67% of hospital bed-days in England in 2013. 68 A hospital admission for any of the reasons reported here can have far-reaching consequences. This is especially true for an older individual with comorbidities who may experience in life changes as a result of the underlying cause of emergency admission and not return to live independently following their discharge from hospital. 69
The estimated economic impact arising from the reduction in emergency admissions for the NHS reported here is likely to be a considerable underestimate; discharge from hospital often incurs follow-up contacts in primary, community, acute social and specialist ambulatory care, none of which have been captured in this study. The ‘cost offset’ from investing in one or more of the cointerventions not only reduces the consumption of health-care resources, but may release capacity in the community and ambulatory care. This resource could be deployed elsewhere, for example into further housing improvements and modifications.
The strengths relating to the use of routine data are clear in this study. Data on resource use and health events are available before, during and after the intervention and do not rely on self-report and recall bias, and the health-care events can be related to specific health problems. The use of routine data also facilitates an analysis of subgroups of the populations to identify the populations for whom the CHS delivers the greatest benefit, enabling targeting of housing improvements in the future. The costs we applied to the NHS contacts were not based on aggregated standard tariffs, as is usual; instead, we devised a method to calculate the costs of each of our condition categories based on the Healthcare Resource Group cost codes attached to each person’s emergency admission data. Therefore, the tariffs were not aggregated for all secondary care delivered in Wales, but instead have been tailored to our study population and primary outcome, representing more realistic costs to the hospitals in our study region. Although these costs may be different from the actual costs to the hospitals, they are more accurately defined than costs generally used within health economic studies. 70
The retrospective collection of hospital admissions limited the data to recording only part of the picture, the receipt of the intervention (costs) and health events before, during and after the intervention (consequences to the NHS). We did not undertake a cost–benefit analysis, one approach recommended by NICE for evaluating public health interventions. 71 NICE accepts that this approach poses challenges in terms of obtaining all of the necessary data to undertake analysis. 55 This study was not suitable for cost–benefit analysis because data were not available on the impacts of the housing intervention on society as a whole. Neither was it possible, using routine data alone, which generally do not include quality of life data, to undertake a cost–utility analysis to estimate the value of the CHS in terms of cost per QALY. This would have enabled a comparison of the value of investing in housing improvements with that of other public health investments. Ideally, data on the impact on health-related quality of life, relating to either the process of installing cointerventions (which may have caused stress) or an emergency hospital admission, would be captured routinely in future to allow a complete economic evaluation from the perspective of society as a whole.
This analysis shows a positive impact – a reduction – in the use of NHS resources and considerable cost savings per person year, which can be offset against the cost of implementing the intervention. In an integrated housing and health budget, the cost offsets would be tangible and potentially allow funds to be vired between budgets.
Chapter 6 Discussion and conclusions
This complex interdisciplinary study required substantial consideration of the study design to most effectively capture the rolling programme of multiple cointerventions improving the quality of social housing over a period of > 8 years, together with objectively recorded health events for the dynamic study population for our study decade.
Housing intervention and public health outcomes
Evaluating the health impact of large-scale housing interventions is challenging because of a number of factors, including the additional complexities of house moves and the long time taken to complete multicomponent interventions. There have been attempts to use RCTs to evaluate housing interventions, but follow-up for longer interventions is likely to have introduced bias. 28 We have used a privacy-protecting data linkage system to track individuals across time and residences. Data linkage systems enable previously intractable evaluations of large-scale interventions and natural experiments to be conducted using routinely collected data. 72
A managed programme meeting modern home standards resulted in improvements to social housing residents’ health, as measured by emergency hospital admissions. However, it is beyond the scope of this study to say if a cointervention on its own would deliver these health improvements. CCC recognised that its tenants should be involved in the development of the programme of housing improvement work. The control given to tenants, and the faith in their council to make changes considered important to local residents, is likely to have contributed to the successful delivery and improved health outcomes, measured using health-care events. 73
Fit with previous research
A systematic review by Thomson et al. 27 summarised housing investment and associated health effects. There were health improvements from housing investments targeted to those who were most vulnerable, authors concluded, but programmes that delivered improvements across areas may have concealed associated health improvements for those with the greatest potential to benefit. There is also a need for follow-up to assess people’s longer-term outcomes. 26,27 Routine data utilised in our evaluation reduced loss to follow-up, and data linkage at household and individual levels allowed us to follow up people for up to 10 years (183,553 person-years of follow-up).
Since then there have been a number of additional papers published on evaluating health outcomes as a result of housing interventions. The GoWell study used self-report survey data to directly assess changes in health and well-being and, unlike our data linkage study, did not have to wait for changes in health service utilisation. Although limited to a 5-year follow-up for 1011 participants, the authors found positive associations with mental health (kitchens and bathrooms, and front doors) and physical health (fabric works), and a negative effect on physical health following the installation of central heating. 23 Our study did not rely on self-report survey data and we have captured health service utilisation (as a proxy of health outcomes) for everyone who lived in an intervention home, even if it was for as little as 60 days, thereby limiting the possibility of a sampling bias.
Despite the limitations of the routine data (capturing only the GP-reported CMDs) we were able to see a trend of reduced prescriptions for the small CMD cohort who lived in a home while it was fitted with new windows and doors (IRR 0.91, 95% CI 0.83 to 1.00; p = 0.046). This suggests that there may be the potential for significant associations in a larger cohort and agreement with the GoWell results.
We found a negative effect on our asthma/COPD cohort in terms of a significant increase in GP contacts for those who were living in a home that already had a boiler (heating system) meeting the national standard, similar to the negative effect on physical health found by GoWell. However, this was not sustained by the asthma/COPD cohort who lived in a home while the heating system work was completed; there was no association with either visits or prescriptions.
The GoWell study and the current evaluation both modelled separate cointerventions within one statistical model. The GoWell study had four cointerventions, whereas we had eight, the rolling programme making it more complex to disentangle other interventions occurring in the same home. The GoWell study modelled time since intervention, which we recommend for future research. Increasingly complex models are possible despite the dynamic cohort censoring those who migrated or died. A New Zealand-based study achieved randomisation for a more limited programme of fall prevention home improvements; their relatively short follow-up period effectively captured falls but did not censor people. 28 To lengthen the period of follow-up, to capture changes in cardiovascular outcomes for example, it would be necessary to add censoring to reduce bias. The New Zealand Home Injury Prevention Intervention study found a 39% reduction in home injury rate,28 which is in line with the 44% reductions we found for older resident emergency admissions for injuries (associated with both the windows and doors and the electrical system upgrades).
Our results, using objective rather than self-reported outcomes, provide new evidence to support the theory that bringing homes to a national housing quality standard has a beneficial impact on residents. We showed that there are fewer resulting emergency hospital admissions for older people and for those of all ages. The objective data from primary care, including GP contacts and prescriptions, contained more mixed results, but largely showed statistically significant reductions in health-care utilisation, supporting the conclusions of other studies that have used self-reported health data. It is important to note that an absence of statistical significance does not equate to no effect. Overall, we found evidence to support the theory that housing interventions are beneficial for health and have the potential to save money.
Context and methodological implications
Routine data have strengths including objective, historical data collection. Data are generally collected routinely and consistently for everyone. However, the detail in these data is sometimes lacking; for example, quality-of-life and patient-recorded outcome measures are often not recorded. They often omit details researchers are interested in, such as the precise geographic location of an injury occurrence. For example, using the emergency department attendance data, we inferred that injuries occurred in the home by excluding all mention of other locations. This may have led us to include more injuries than necessary, although we know from the literature that, for older people in particular, most injuries do occur in the home.
Routine data are collected for reasons other than research, which can make their use challenging. Hospital admissions data have an ICD-10 coding structure that has been in place for several decades, and qualified clinical coders have their ICD-10 codes audited regularly for the purpose of service evaluation. 47 These data record the most severe conditions that require a stay in hospital and yet the reason for admission often changes during the course of an admission episode, requiring researchers to create selection rules from multiple codes. In illustration, we chose the primary diagnosis code from the admission record for each hospital stay because underlying conditions and clinical complications may develop, and so subsequent records may not fully reflect the underlying reason for the admission.
In contrast, Read codes recorded in general practice do not have an equivalent structure. Relatively recent audit requirements (Quality and Outcomes Framework) are now in place for some conditions, for example mental health. Read code recording has changed through time as the Quality and Outcomes Framework rules have been updated, making longitudinal research more complex. Additionally, we know that it is incorrect to assume that all conditions present for the population are reported to a GP. Community surveys for mental health and well-being found that the majority of mental illness was not reported to a GP. 45 Therefore, there may be an increase in well-being that is not captured using routine data.
Although routine data have allowed us to evaluate this intervention using retrospective links from individuals living in intervention homes during the relevant periods, we acknowledge the data limitations. We do not have quality-of-life data, which would be central to most survey-based studies. Although we used a long follow-up period, routinely collected data do not allow us to understand how people’s lives have changed in their home. Research using mixed methods is necessary to examine the wider health and well-being impacts of the improvements. Members of the research team were involved in a separate survey-based longitudinal investigation of the social and health impacts of the intervention. There were five waves of survey data collected in 2009–16, focused on subjective health outcomes (e.g. self-reported respiratory symptoms and mental well-being) and non-health outcomes (e.g. self-reported housing quality, thermal satisfaction and fuel poverty). Alongside the current project, the research team were further engaged in a mixed-methods evaluation to determine the wider health and psychosocial impacts of an energy-performance programme that took place in Wales between 2010 and 2015. 74 These studies have shown that routine data, in combination with field studies, can provide a comprehensive evaluation of the impacts of housing improvement programmes.
There were several additional confounders that we would have liked to include had they been available in the databank. These include employment status, individual-level deprivation, lifetime health status at baseline and smoking status. These data exist in routinely collected data sets and may become available for further analyses of outcomes associated with this intervention. Additionally, it is likely that we have not taken all confounding into account. For example, residual confounding could exist because older occupants of remediated homes were able to remain in the community for longer as a result of their improved homes. It is possible that rates of age-related conditions in those aged ≥ 80 years would then be higher among those in the improved homes.
The study did not examine changes in educational outcomes, which are likely to have a large impact on life chances and health. For older people with established ill health, improved housing will not provide a cure, but we have shown that resulting emergency hospital admissions were reduced. The provision of suitable space, through heating more rooms or the provision of a kitchen table, may result in long-term educational attainment improvements and health improvements for future generations. 8
Furthermore, we did not have information on the size of the intervention. Improvements from a poor state of repair to a compliant condition could well have a greater impact on health and well-being than improvements in a house that was already in a reasonable state. This can be assessed only if data on the initial state of repair and the size of intervention are collected, which, unfortunately, was not possible in this study.
Although we isolated each cointervention within our statistical analyses and reported on the impact of each on our health outcomes, we acknowledge that there is potentially a cumulative impact for a number of housing improvements on the housing tenants and their health service utilisation. This is due to the rolling nature of the intervention and the potential for tenants to receive from one to eight cointerventions, in any order, over an 8-year period. We suggest that our approach is useful in estimating the association of health service utilisation with a particular cointervention. However, in practice, implementing one housing cointervention on its own is unlikely to cause the reduction as seen in our results. The benefits of being part of a community-wide intervention with a strong community engagement component should not be understated.
We believe that our comparison groups were random in terms of the delivery of the intervention, and there was no reason that different groups of people would have lived in the homes before and after the cointerventions were completed. Although we cannot definitively say that our analyses have resolved potential confounding because the study was not randomly allocated, we have shown as clearly as possible that the random delivery of the intervention and unbiased allocation of people to homes means that there was as little confounding as is humanly possible without a RCT being completed. Not all policy questions suit a trial design, but this one does,75 assuming that future projects can have timely input from an evaluation team. This was a real-world trial without random allocation. Policy-makers often prefer making decisions on the basis of efficacy trials run under ideal circumstances and frequently exclude patients with protocol deviations;76 if we had excluded people who moved home during the decade study period, or who lived in a home receiving all of the interventions, we would have had very few individuals remaining. On the trial continuum of efficacy to effectiveness, this is towards the effectiveness end. We hope that, along with other topical research studies, this (costed) effectiveness trial will help policy-makers to make necessary policy decisions.
Implications of key findings
In Chapter 5, we outlined the complexities of assessing the costs and benefits of housing interventions. We followed this with cost and consequence estimates for the housing cointerventions that resulted in a statistically significant reduction in emergency admissions. Emergency admissions have substantial costs compared with community preventative measures. We estimate that there are considerable cost savings directly to the NHS from emergency admission reductions.
Furthermore, reduction in admissions to hospital and their impact, as observed in this study, have value in addition to the estimated savings. Avoiding a hospital admission often has far-reaching consequences for individuals and for a health-care system. Providing a health-care provider with the ability to release capacity, and the opportunity to reorganise resources to optimise care provision, is valuable.
Housing professionals will have to make decisions about housing improvement investments in the light of the needs of their own communities; evidence presented in this report may help to inform these decisions. We have provided a quantified estimate of the impact on several public health outcomes. Consideration of the health-care utilisation impacts is needed because they may offset the costs of the housing improvements. Housing improvements may result in positive health and wider societal impacts for future generations that this decade-long study has not been able to quantify.
Conclusions
The results demonstrated a reduction in health service utilisation and, by proxy, an improvement in health outcomes, as a consequence of housing improvements. These results are relevant to developed countries in temperate regions implementing national housing standards for residents of social housing. There will be differences in the expected benefits depending on the baseline condition of the properties and the extent of work carried out under each cointervention to meet housing quality standards. The heterogeneity of work carried out in housing interventions was noted in a systematic literature review as the main obstacle to generalising evidence from different programmes of work. 77 Some cointerventions that are more clearly defined, such as boiler standards or loft insulation, are not likely to differ much between improvement programmes. The extent and type of work carried out to improve bathrooms or kitchens has a broader scope and, therefore, potentially poses more difficulty in completing this intervention elsewhere. However, the use of standard reporting guidelines has maximised the potential for implementation elsewhere using similar evaluation methods.
A decade ago we understood that the public health interventions most likely to reduce health inequalities were those that operate at a higher societal level than one-to-one clinical interventions. 78 The more deprived the individuals, the more events conspire to prevent them from obtaining excellent preventative services and faithfully following the advice required to achieve full health benefits. 52 Universally legislated measures, such as water fluoridation, reach everyone. A national housing standard applied to all homes, not just social housing, may be considered a universally legislated measure and could reduce health inequalities.
The following are recommendations for future work to underpin the operation and management of future projects.
-
A system should be implemented to promote early communication between government and academics, allowing more effective health and economic evaluations of large-scale non-health-care interventions.
-
A standard system using a comment data specification for recording data on housing interventions is required for research purposes. A minimum data set should be defined and then used by each housing/local authority, including validated and reliable complete data on geographical location, and compliance with national standards. This includes the geographical location with complete address data and the National Land and Property Gazetteer-generated Unique Property Reference Number to facilitate data linkage.
-
A vast number of data are held in local authorities that, if held in a research-ready format, could be used in a system-wide natural experiment evaluation to benefit the effective planning and delivery of a variety of services. To allow the evaluation of system-wide changes, data should be held in a person-home (Unique Property Reference Number) based ‘data spine’ common across all departments. A data research contact person should be identified to update an online catalogue of all ‘research-ready’ data and to be the first point of contact for researchers.
-
Future housing interventions should include information for residents moving into homes that have boilers and other active systems, so that they have knowledge of the most effective and beneficial use of their systems.
We make the following recommendations for further research.
-
Randomised controlled trials should still be pursued and built into large-scale housing improvement projects from conception, if possible. Shortening the total intervention period for each home would reduce the complexity of the evaluation challenges. The utilisation of routinely collected data augmented with survey data would provide an ideal study design.
-
Improved reporting standards for measuring, recording and reporting housing quality standards are needed to ensure that regions may be used as meaningful comparators. Specifically, we recommend:
-
more detail to be collected on the start and finish dates for each cointervention
-
more data on the scale of the intervention (how much change has occurred) for each intervention cointervention
-
detailed expenditure data for each intervention cointervention at the household level.
-
-
Standards should be extended to the private sector and evaluations completed for people living in homes that are believed to be at a lower standard than that for social housing.
-
More complex analysis should be completed including multivariate mixed models of outcomes. We modelled each outcome in a separate model in our study, which assumed independence between outcomes. More statistical resource would be required to complete this. Modelling of time-dependent interaction effects and seasonally adjusted lags with longer periods of follow-up could also be undertaken with additional resource, as could an exploration of any interactions between cointerventions; for example, did boilers and windows have a greater combined effect?
-
Qualitative studies should be undertaken to attempt to understand the causal mechanisms underlying the changes in health service utilisation and include a quality-of-life measure. Utilising these data with other routinely collected data from other sectors could make possible an evaluation of the costs and benefits of housing improvements across health, education, social care and other services such as charitable organisations.
Acknowledgements
Funding acknowledgement
The work was undertaken at Swansea University Medical School, made possible by the following grant: Centre for the Improvement of Population Health through E-records Research (CIPHER) and Farr Institute capital enhancement. CIPHER and the Farr Institute are funded by Arthritis Research UK, the British Heart Foundation, Cancer Research UK, the Chief Scientist Office (Scottish Government Health Directorates), the Economic and Social Research Council, the Engineering and Physical Sciences Research Council, the Medical Research Council, the National Institute for Health Research, the National Institute for Social Care and Health Research (Welsh Government) and the Wellcome Trust (grant reference MR/K006525/1).
The work had the support of the Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council (RES-590-28-0005), the Medical Research Council, the Welsh Government and the Wellcome Trust (WT087640MA), under the auspices of the UKCRC, is gratefully acknowledged.
We are grateful to the members of the study steering committee for their contribution and guidance. We are also grateful to Dr Gwyneth Davies for reviewing the primary care Read codes for respiratory outcomes.
We acknowledge the contribution of CCC to this project in allowing us to use its investment programme to consider health impact on tenants. Specific thanks go to its leader, the executive board member for housing, the chief executive, the director for communities and the head of housing and public protection for fully supporting the project throughout.
We would like to thank CCC employees who assisted with the project, Mr Kevin Evans and Mr Andy Griffiths, for assistance with housing data queries.
The study made use of anonymised data held in the SAIL system, which is part of the national e-health records research infrastructure for Wales. The authors would like to acknowledge all of the data providers who made anonymised data available for research.
The authors would like to acknowledge Mr Gareth Peters of Cardiff University for developing the REAT 2.0 application and website, and Mrs Tatiana Calve, formerly of Cardiff University, for her work on the REAT 2.0.
Contributions of authors
Dr Sarah E Rodgers (Associate Professor in Epidemiology) is project scientific manager of this project and has led and been involved in every aspect of the research. She carried out the baseline cohort analysis and led the writing of the report.
Ms Rowena Bailey (Statistician) contributed to the preparation of the data, produced the descriptive summaries of the data, carried out the negative binomial regression analyses and contributed to the cost–consequences analysis.
Mr Rhodri Johnson (Data Analyst) liaised with CCC to obtain and interpret intervention data, carried out coding and analysis on the PEDW, GP, accident and emergency, Office for National Statistics and Welsh Demographic Service data sets and managed the daily study tasks.
Professor Wouter Poortinga (Professor of Environmental Psychology) conceived the research, led the evaluation of the housing intervention on the neighbourhood environment, and contributed to the statistical analysis and to the writing of the report. He was part of the project management team.
Dr Robert Smith (Senior Lecturer in Housing) conceived the research, advised on housing standards and relevance to the research, and led the writing of housing quality standards for the report.
Professor Damon Berridge (Chairperson in Applied Statistics) took over as senior statistician on Frank Dunstan’s retirement, advising on the optimal model specification to maximise utility of the complex longitudinal data. He contributed to the interpretation of model results and the writing of the final report.
Ms Pippa Anderson (Head of Swansea Centre for Health Economics) advised on health economics and led the writing of Chapter 5.
Professor Ceri Phillips (Professor in Health Economics) advised on health economics.
Dr Simon Lannon (Research Fellow in Energy and Environmental Modelling) conceived the research and contributed to the evaluation of the housing intervention on the neighbourhood environment, the development of the REAT application and the remote REAT 2.0 feasibility study. He led the digital map analysis and provided background information for the housing interventions.
Ms Nikki Jones (Researcher in Neighbourhood Quality) contributed to the evaluation of the housing intervention on the neighbourhood environment, conducted statistical analyses and led the remote REAT 2.0 feasibility study. She further contributed to the writing of the report and provided background information for the housing interventions.
Professor Frank D Dunstan (Professor of Medical Statistics) advised on the technical aspects of the statistical analyses.
Mr Jonathan Morgan (Housing Services Manager – Investment and Support) contributed to improving the research team’s understanding of details of the housing improvements programme, advised on the interpretation of results and contributed to report writing.
Mrs Sandra Y Evans (Stock Analyst) collated and provided property address and intervention data, liaised with the research team to interpret intervention data, and provided cost data and a narrative to explain the difference in costs between the council figures and research data.
Mrs Pam Every (Lay Person) provided important context to the research team as a tenant of the housing undergoing improvements, including confirmation of unbiased work delivery. She was involved in result interpretation and dissemination.
Professor Ronan A Lyons (Professor of Public Health) is the principal investigator and was involved in all aspects of the research, including the conception, design and compilation of clinical coding sets for use in the record-linked data sets, and contributed to report writing.
Publications
Lyons RA, Hutchings H, Rodgers SE, Hyatt MA, Demmler J, Gabbe BJ, et al. Development and use of a privacy-protecting total population record linkage system to support observational, interventional, and policy relevant research. Lancet 2012;380:S6.
Rodgers SE, Bailey R, Johnson R, Berridge D, Poortinga W, Lannon S, et al. Emergency hospital admissions associated with a non randomised housing intervention meeting national housing quality standards: a longitudinal data linkage study [published online ahead of print June 20 2018]. J Epidemiol Community Health 2018.
Rodgers SE, Heaven M, Lacey A, Macey S, Poortinga W, Dunstan FD, et al. Cohort profile: the housing regeneration and health study. Int J Epidemiol 2012;43:52–60.
Lyons R, Ford D, Moore L, Rodgers S. Use of data linkage to measure the population health effect of non-health-care interventions. Lancet 2013;383:1517–19.
Rodgers SE, Bailey R, Johnson R, Berridge D, Poortinga W, Dunstan F, Lyons RA. Effects of national housing quality standards on hospital emergency admissions: a quasi-experiment using data-linkage. Lancet 2016;388:S3.
Poortinga W, Lannon S, Jones N, Rodgers SE, Johnson RD, Calve T, et al. Neighborhood quality and attachment: validation of the Revised Residential Environment Assessment Tool (REAT 2.0). Environ Behav 2017;49:255–82.
Data sharing statement
Access to data held within the SAIL databank is governed by the SAIL Information Governance Review Process. Data access requests should be made to saildatabank@swansea.ac.uk, referencing ‘Carmarthenshire Housing 0160’.
Requests for access to intervention data should be made to the data custodian (CCC).
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- The Welsh Housing Quality Standard: Guidance for Social Landlords on Interpretation and Achievement of the WHQS. Cardiff: Welsh Assembly Government; 2002.
- A Decent Home: Definition and Guidance for Implementation. London: Department for Communities and Local Government; 2006.
- Neilson M. Scottish Housing Quality Standard. Edinburgh: Scottish Government; 2004.
- Improving Lives and Communities: Homes in Wales. Cardiff: Welsh Assembly Government; 2010.
- Hoffmann TC, Glasziou P, Boultron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- The Welsh Housing Quality Standard Revised Guidance for Social Landlords on Interpretation and Achievement of the Welsh Housing Quality Standard. Cardiff: Welsh Government; 2008.
- Interim House Condition Survey. Belfast: Northern Ireland Housing-Executive; 2004.
- Thomson H, Thomas S. Developing empirically supported theories of change for housing investment and health. Soc Sci Med 2015;124:205-14. https://doi.org/10.1016/j.socscimed.2014.11.043.
- Gibson M, Petticrew M, Bambra C, Sowden AJ, Wright KE, Whitehead M. Housing and health inequalities: a synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health Place 2011;17:175-84. https://doi.org/10.1016/j.healthplace.2010.09.011.
- Curl A, Kearns A. Can housing improvements cure or prevent the onset of health conditions over time in deprived areas?. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2524-5.
- Carley M. Housing and Neighbourhood Renewal: Britain’s New Urban Challenge. London: Policy Studies Institute, University of Westminster; 1990.
- Carter T, Smith S. Neighbourhood Improvement: The Role of Housing and Housing Institutions. Elsevier Publishing; 2012.
- Cole I, Foden M, Robinson D, Wilson I. Interventions in Housing and the Physical Environment in Deprived Neighbourhoods. Evidence from the New Deal for Communities Programme. London: Department for Communities and Local Government; 2010.
- Dunstan F, Weaver N, Araya R, Bell T, Lannon S, Lewis G, et al. An observation tool to assist with the assessment of urban residential environments. J Environ Psychol 2005;25:293-305. https://doi.org/10.1016/j.jenvp.2005.07.004.
- Poortinga W, Calve T, Jones N, Lannon S, Rees T, Rodgers SE, et al. Neighborhood quality and attachment: validation of the Revised Residential Environment Assessment Tool. Environ Behav 2016. http://dx.doi.org/10.1177/0013916516634403.
- Jones N, Poortinga W, Lannon S, Calve T. The Effect of a Housing Intervention on the Quality of the Neighbourhood Environment. Cardiff: Welsh School of Architecture; 2016.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;12:453-7. https://doi.org/10.1136/bmj.39335.541782.AD.
- Rodgers SE, Bailey R, Johnson R, Berridge D, Poortinga W, Lannon S. Emergency hospital admissions associated with a non randomised housing intervention meeting national housing quality standards: a longitudinal data linkage study [published online ahead of print June 20 2018]. J Epidemiol Community Health 2018. https://doi.org/10.1136/jech-2017-210370.
- Developing Guidance for Health Protection in the Built Environment – Mitigation and Adaptation Responses. Geneva: World Health Organization; 2010.
- Marmot M. Fair Society, Healthy Lives. London: The Marmot Review; 2010.
- Health Equity Through Action on the Social Determinants of Health. Geneva: World Health Organization; 2008.
- McAuley A, Denny C, Taulbut M, Mitchell R, Fischbacher C, Graham B, et al. Informing investment to reduce inequalities: a modelling approach. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0159256.
- Curl A, Kearns A, Mason P, Egan M, Tannahill C, Ellaway A. Physical and mental health outcomes following housing improvements: evidence from the GoWell study. J Epidemiol Community Health 2015;69:12-9. https://doi.org/10.1136/jech-2014-204064.
- Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health 2003;57:784-9. https://doi.org/10.1136/jech.57.10.784.
- The Health Impacts of Cold Homes and Fuel Poverty The Health Impacts of Cold Homes and Fuel Poverty. London: The Baring Foundation; 2011.
- Osman L, Douglas G, Ayres J, Ludbrook A, Kyle G, Milne K, et al. Energy Efficiency Improvement and Health Status of COPD Patients: A Report to the Eaga Partnership Charitable Trust. Kendal: Eaga Partnership Charitable Trust; 2007.
- Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socio-economic outcomes: a systematic review. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.4073/csr.2013.2.
- Keall MD, Pierse N, Howden-Chapman P, Cunningham C, Cunningham M, Guria J, et al. Home modifications to reduce injuries from falls in the Home Injury Prevention Intervention (HIPI) study: a cluster-randomised controlled trial. Lancet 2015;385:231-8. https://doi.org/10.1016/S0140-6736(14)61006-0.
- Osman LM, Ayres JG, Garden C, Reglitz K, Lyon J, Douglas JG. A randomised trial of home energy efficiency improvement in the homes of elderly COPD patients. Eur Respir J 2010;35:303-9. https://doi.org/10.1183/09031936.00187708.
- Howden-Chapman P, Pierse N, Nicholls S, Gillespie-Bennett J, Viggers H, Cunningham M, et al. Effects of improved home heating on asthma in community dwelling children: randomised controlled trial. BMJ 2008;337. https://doi.org/10.1136/bmj.a1411.
- Wilkinson P, Pattenden S, Armstrong B, Fletcher A, Kovats RS, Mangtani P, et al. Vulnerability to winter mortality in elderly people in Britain: population based study. BMJ 2004;329. https://doi.org/10.1136/bmj.38167.589907.55.
- Martens PJ, Chateau DG, Burland EM, Finlayson GS, Smith MJ, Taylor CR, et al. The effect of neighborhood socioeconomic status on education and health outcomes for children living in social housing. Am J Public Health 2014;104:2103-13. https://doi.org/10.2105/AJPH.2014.302133.
- Ford DV, Jones KH, Verplancke JP, Lyons RA, John G, Brown G, et al. The SAIL Databank: building a national architecture for e-health research and evaluation. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-157.
- Public Health Wales Observatory . Patient Episode Database for Wales (PEDW) n.d. www.publichealthwalesobservatory.wales.nhs.uk/PEDW (accessed 18 October 2017).
- Welsh Government . Welsh Index of Multiple Deprivation n.d. http://gov.wales/statistics-and-research/welsh-index-multiple-deprivation/?lang=en (accessed 18 October 2017).
- Office for National Statistics . Rural/Urban/Local/Authority/(LA)/Classification/(England) n.d. www.ons.gov.uk//methodology/geography/geographicalproducts/ruralurbanclassifications/2001ruralurbanclassification/ruralurbanlocalauthoritylaclassificationengland (accessed 1 November 2017).
- Berridge D, Crouchley R. Multivariate Generalized Linear Mixed Models Using R. Boca Raton, FL: CRC Press; 2011.
- Sedgwick P. Multiple hypothesis testing and Bonferroni’s correction. BMJ 2014;349. https://doi.org/10.1136/bmj.g6284.
- Liddell C, Guiney C. Living in a cold and damp home: frameworks for understanding impacts on mental well-being. Public Health 2015;129:191-9. https://doi.org/10.1016/j.puhe.2014.11.007.
- Weber GA. Improved tenement homes for American cities. Munic Aff 1897;1:745-62.
- Evans J, Hyndman S, Stewart-Brown S, Smith D, Petersen S. An epidemiological study of the relative importance of damp housing in relation to adult health. J Epidemiol Community Health 2000;54:677-86. https://doi.org/10.1136/jech.54.9.677.
- Ormandy D, Ezratty V. Thermal discomfort and health: protecting the susceptible from excess cold and excess heat in housing. Adv Build Energy Res 2015;10:84-98. https://doi.org/10.1080/17512549.2015.1014845.
- Evans GW. The built environment and mental health. J Urban Health 2003;80:536-55. https://doi.org/10.1093/jurban/jtg063.
- Shenassa ED, Daskalakis C, Liebhaber A, Braubach M, Brown M. Dampness and mold in the home and depression: an examination of mold-related illness and perceived control of one’s home as possible depression pathways. Am J Public Health 2007;97:1893-9. https://doi.org/10.2105/AJPH.2006.093773.
- John A, McGregor J, Fone D, Dunstan F, Cornish R, Lyons RA, et al. Case-finding for common mental disorders of anxiety and depression in primary care: an external validation of routinely collected data. BMC Med Inform Decis Mak 2016;16. https://doi.org/10.1186/s12911-016-0274-7.
- McGregor J, Brooks C, Chalasani P, Chukwuma J, Hutchings H, Lyons RA, et al. The Health Informatics Trial Enhancement Project HITE: Using routinely collected primary care data to identify potential participants for a depression trial. Trials 2012;11. https://doi.org/10.1186/1745-6215-11-39.
- International Classification of Diseases Version 2016. Geneva: World Health Organization; 2016.
- Altman DG, Bland JM. Statistics notes: absence of evidence is not evidence of absence. BMJ 1995;311. https://doi.org/10.1136/bmj.311.7003.485.
- Cornwell EY, Waite LJ. Social disconnectedness perceived isolation and health among older adults. J Health Soc Behav 2009;50:31-48. https://doi.org/10.1177/002214650905000103.
- Bolton M. Loneliness – The State We’re In. Abingdon: Age UK Oxfordshire; 2012.
- Geller J, Janson P, McGovern E, Valdini A. Loneliness as a predictor of hospital emergency department use. J Fam Pract 1999;48:801-4.
- Frank J. Public health interventions to reduce inequalities: what do we know works?. Can J Public Health 2012;103:5-7.
- Hutchings HA, Evans A, Barnes P, Demmler JC, Heaven M, Healy MA, et al. Pediatrics 2016;138. https://doi.org/10.1542/peds.2015-2836.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Methods for the Development of NICE Public Health Guidance (Third Edition): Introduction. London: NICE; 2012.
- Roberto CA, Kawachi I. Behavioral Economics and Public Health. Oxford: Oxford University Press; 2015.
- Phillips CJ, Fordham R, Marsh K, Bertranou E, Davies S, Hale J, et al. Exploring the role of economics in prioritization in public health: what do stakeholders think?. Eur J Public Health 2011;21:578-84. https://doi.org/10.1093/eurpub/ckq121.
- Fenwick E, Macdonald C, Thomson H. Economic analysis of the health impacts of housing improvement studies: a systematic review. J Epidemiol Community Health 2013;67:835-45. https://doi.org/10.1136/jech-2012-202124.
- Barton A, Basham M, Foy C, Buckingham K, Somerville M. Torbay Healthy Housing Group . The Watcombe Housing Study: the short term effect of improving housing conditions on the health of residents. J Epidemiol Community Health 2007;61:771-7. https://doi.org/10.1136/jech.2006.048462.
- Burns P, Coxon J. Boiler on Prescription Trial Closing Report. Sunderland: Gentoo Group; 2016.
- Edwards RT, Bray N. The Warm Homes for Health project: exploring the cost-effectiveness of improving population health through better housing. Lancet 2014;384. https://doi.org/10.1016/S0140-6736(14)62206-6.
- Keall MD, Pierse N, Howden-Chapman P, Guria J, Cunningham CW, Baker MG. Cost-benefit analysis of fall injuries prevented by a programme of home modifications: a cluster randomised controlled trial. Inj Prev 2017;23:22-6. http://dx.doi.org/10.1136/injuryprev-2015-041947.
- Jones KH, Ford DV, Jones C, Dsilva R, Thompson S, Brooks CJ, et al. A case study of the Secure Anonymous Information Linkage SAIL Gateway: A privacy-protecting remote access system for health-related research and evaluation. J Biomed Inform 2013;50:196-204. https://doi.org/10.1016/j.jbi.2014.01.003.
- Lyons RA, Jones KH, John G, Brooks CJ, Verplancke JP, Ford DV, et al. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak 2009;9. https://doi.org/10.1186/1472-6947-9-3.
- Rodgers SE, Demmler JC, Dsilva R, Lyons RA. Protecting health data privacy while using residence-based environment and demographic data. Health Place 2012;18:209-17. https://doi.org/10.1016/j.healthplace.2011.09.006.
- Rodgers SE, Heaven M, Lacey A, Poortinga W, Dunstan FD, Jones KH, et al. Cohort profile: the housing regeneration and health study. Int J Epidemiol 2014;43:52-60. https://doi.org/10.1093/ije/dys200.
- Office for National Statistics . Average Household Size 2013. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/populationandhouseholdestimatesfortheunitedkingdom/2011-03-21#average-household-size (accessed 8 December 2017).
- Emergency Admissions to Hospital: Managing the Demand. London: Department of Health; 2013.
- Cornwell J, Levenson R, Sonola L, Poteliakhoff E. Continuity of Care for Older Hospital Patients: A Call for Action. London: The King’s Fund; 2012.
- 2016/17 National Tariff Payment System. Leeds: NHS England; 2016.
- Judging Whether Public Health Interventions Offer Value for Money. London: NICE; 2013.
- Fone D, Morgan J, Fry R, Rodgers S, Orford S, Farewell D, et al. Change in alcohol outlet density and alcohol-related harm to population health (CHALICE): a comprehensive record-linked database study in Wales. Public Health Res 2016;4.
- Rogers A, Huxley P, Evans S, Gately C. More than jobs and houses: mental health quality of life and the perceptions of locality in an area undergoing urban regeneration. Soc Psychiatry Psychiatr Epidemiol 2008;43:364-72. https://doi.org/10.1007/s00127-008-0316-2.
- Grey CNB, Jiang S, Nascimento C, Rodgers S, Johnson R, Lyons RA, et al. The short-term health and psychosocial impacts of domestic energy efficiency investments in low-income areas: a controlled before and after study. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4075-4.
- Whitty CJ. What makes an academic paper useful for health policy?. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0544-8.
- Gartlehner G, Hansen RA, Nissman D, Lohr KN, Carey TS. Criteria for Distinguishing Effectiveness from Efficacy Trials in Systematic Reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2006.
- Thomson H, Petticrew M, Douglas M. Health impact assessment of housing improvements: incorporating research evidence. J Epidemiol Community Health 2003;57:11-6. https://doi.org/10.1136/jech.57.1.11.
- Macintyre S. Inequalities in Health in Scotland: What are They and What Can We Do About Them?. Glasgow: Medical Research Council Social & Public Health Sciences Unit; 2007.
- Taylor RB, Gottfredson SD, Brower S. Block crime and fear: defensible space local social ties and territorial functioning. J Res Crime Delinquency 1984;21:303-31. https://doi.org/10.1177/0022427884021004003.
- Perkins DD, Wandersman A, Rich RC, Taylor RB. The physical environment of street crime: defensible space territoriality and incivilities. J Environ Psychol 1993;13:29-4. https://doi.org/10.1016/S0272-4944(05)80213-0.
- Newman O. Defensible Space. New York, NY: Macmillan; 1972.
- Cozens PM, Saville G, Hillier D. Crime prevention through environmental design (CPTED): a review and modern bibliography. Prop Manag 2005;23:328-56. https://doi.org/10.1108/02637470510631483.
- Lee AC, Maheswaran R. The health benefits of urban green spaces: a review of the evidence. J Public Health 2011;33:212-22. https://doi.org/10.1093/pubmed/fdq068.
- Badland HM, Opit S, Witten K, Kearns RA, Mavoa S. Can virtual streetscape audits reliably replace physical streetscape audits?. J Urban Health 2010;87:1007-16. https://doi.org/10.1007/s11524-010-9505-x.
- Clarke P, Ailshire J, Melendez R, Bader M, Morenoff J. Using Google Earth to conduct a neighborhood audit: reliability of a virtual audit instrument. Health Place 2010;16:1224-9. https://doi.org/10.1016/j.healthplace.2010.08.007.
- Rundle AG, Bader MD, Richards CA, Neckerman KM, Teitler JO. Using Google Street View to audit neighborhood environments. Am J Prev Med 2011;40:94-100. https://doi.org/10.1016/j.amepre.2010.09.034.
- THIN Database. London: University College London; 2015.
- THIN Data: Strengths and Limitations. London: University College London; 2013.
Appendix 1 The intervention
We have included sufficient detail here to enable the housing intervention to be repeated. We have followed the TIDieR guidelines.
| Item | Description | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brief name (1) | The CHS: improvements to council housing to the CHS. The CHS was determined by Carmarthenshire tenants to ensure that we complied with the WHQS. Tenants were consulted to define the standard, which is a higher than the WHQS | ||||||||||||||||||||||
| Why (2) | Poor housing is recognised as a determinant of poor health; the WHQS sets out a basic set of requirements aiming to ensure that all social rented homes in Wales are:
|
||||||||||||||||||||||
There are 10 component headings within the WHQS. These are:
|
|||||||||||||||||||||||
CCC grouped improvements into four work packages:
|
|||||||||||||||||||||||
This research concentrates on eight specific cointerventions of work:
|
|||||||||||||||||||||||
| What: materials (3) | There was a large amount of variation in materials used owing to the variation in housing type and condition, the specific needs of tenants and the number of types of works or interventions that were carried out | ||||||||||||||||||||||
| A full list of materials is available on request from CCC | |||||||||||||||||||||||
| Interventions were carried out to meet minimum standards of the WHQS, plus CHS has extras including the installation of CO detectors and feature fireplaces and the adaptation of the WHQS in relation to sheltered housing and environmental improvements | |||||||||||||||||||||||
| What: procedures (4) | A general process was followed whereby CCC employees held discussions with residents before work was allocated to building contractors | ||||||||||||||||||||||
| The overall programme of works was agreed with tenants before any of the works started. It was agreed that:works should be spread out across the county as far as possiblethey would be carried out on an estate-by-estate basis | |||||||||||||||||||||||
Annual work programmes were set to deliver improvements to all council homes. Tenants were informed, through a work programme booklet, of when the work was planned to be carried out. This was updated periodically as the programme evolved. The length of time for the works to be carried out varied depending on the needs of the household but was generally a maximum of 3 weeks for internal works. All works were carried out with the tenants in situ, unless there were exceptional circumstances. The points below describe the general process from initial communication with tenants through to work completion
|
|||||||||||||||||||||||
Owing to the variation in property type, existing standard and state of repair of each housing cointervention, the instructions and decisions on whether to renew or upgrade each cointervention varied considerably. The following aims to describe the key components used in this decision:
|
|||||||||||||||||||||||
| Who provided (5) | Work was carried out through a CHS contractor framework, made up of up to eight contractors. Work was allocated to individual contractors following the tendering process. All contractors were Wales based; a number were local (Carmarthenshire) contractors and one was an internal CCC contractor (in-house property services division) | ||||||||||||||||||||||
| How (6) | Work carried out by contractors according to annual work programmes that were periodically updated and communicated to tenants | ||||||||||||||||||||||
| Where (7) | All socially rented properties owned by CCC requiring upgrades to meet national housing standards (WHQS/CHS) located in Carmarthenshire, UK | ||||||||||||||||||||||
| When and how much (8) | Properties received between 1 and 11 improvements depending on state of repair compared with the WHQS/CHS. The total investment, across all work, was in excess of £200M | ||||||||||||||||||||||
| Tailoring (9) | Adaptions were made for a number of reasons, depending on property characteristics and tenant need (e.g. when a tenant had a disability, the bathroom requirements were adapted to suit the tenant) | ||||||||||||||||||||||
| Modifications (10) | Initially the gardens and estates works were intended to beautify the areas; however, owing to budget constraints this was reined back to cover health and safety aspects only. Around 50 properties received the enhanced works before modification of the works | ||||||||||||||||||||||
| How well: planned (11) | The original aim was to upgrade every property for every aspect of the WHQS/CHS by 2013; however, this was extended to December 2015, making the evaluation more complex | ||||||||||||||||||||||
| How well: actual (12) |
Compliance at 31 March 2016 is detailed below for 8930 properties according to CCC data, which differ from the final data set used in the main analysis owing to data linkage and slight time period differences CointerventionProperties completed, n (%)Windows8929 (99.99)Wall insulation8355 (93.56)Loft insulation8111 (90.83)Boilers7990 (89.47)Kitchens8084 (90.53)Bathroom8226 (92.12)Electrics8430 (94.40)Smoke alarms8766 (98.16)CO detectors8400 (94.06)Security lights8281 (92.73) |
Cointervention | Properties completed, n (%) | Windows | 8929 (99.99) | Wall insulation | 8355 (93.56) | Loft insulation | 8111 (90.83) | Boilers | 7990 (89.47) | Kitchens | 8084 (90.53) | Bathroom | 8226 (92.12) | Electrics | 8430 (94.40) | Smoke alarms | 8766 (98.16) | CO detectors | 8400 (94.06) | Security lights | 8281 (92.73) |
| Cointervention | Properties completed, n (%) | ||||||||||||||||||||||
| Windows | 8929 (99.99) | ||||||||||||||||||||||
| Wall insulation | 8355 (93.56) | ||||||||||||||||||||||
| Loft insulation | 8111 (90.83) | ||||||||||||||||||||||
| Boilers | 7990 (89.47) | ||||||||||||||||||||||
| Kitchens | 8084 (90.53) | ||||||||||||||||||||||
| Bathroom | 8226 (92.12) | ||||||||||||||||||||||
| Electrics | 8430 (94.40) | ||||||||||||||||||||||
| Smoke alarms | 8766 (98.16) | ||||||||||||||||||||||
| CO detectors | 8400 (94.06) | ||||||||||||||||||||||
| Security lights | 8281 (92.73) |
Appendix 2 Tenant choice forms
The information tenants received as part of CCC’s engagement strategy allowed them to choose the materials used in making improvements to their bathrooms, kitchens and fireplaces (Figure 20).
FIGURE 20.
First page (of 12) from tenant engagement leaflet describing material choices for improvements to kitchens, bathrooms and fireplaces. Reproduced with permission from Jonathan Morgan, Carmarthenshire Country Council, 2017.
Appendix 3 The revised Residential Environment Assessment Tool
The results reported in this appendix are described in more detail elsewhere. 16
Objective: An established environmental quality audit tool14,15 was updated and validated, as part of the research, to assess the impacts of the housing intervention on the overall quality of the neighbourhood environment. It was expected that the housing intervention would result in measurable improvements in the overall quality of the neighbourhood environment, and that these improvements would be linked to work that contributes to the external appearance of the property and the estate environment in general.
The instrument: The REAT 2.0 was developed from the original REAT neighbourhood assessment tool created in 2001. It is an instrument designed for auditors to assess the quality of the neighbourhood environment. 14 The original tool was amended to facilitate data collection and include a more explicit theoretical structure, resulting in a shorter instrument. 15
The REAT 2.0 instrument includes several dimensions that contribute to a summary score of neighbourhood quality (Table 13). The neighbourhood condition dimension is intended to capture the quality or condition of public and private spaces. 79,80 The natural surveillance dimension is designed to capture the cointerventions of street and property surveillance. 81,82 The natural cointerventions dimension records green cointerventions in both public (e.g. a park or tree-lined road) and private (e.g. a front garden) spaces. 83
| Street level | Property level | |
|---|---|---|
| Neighbourhood condition | Litter in public space | Property maintenance |
| Condition of public space | Garden maintenance | |
| Vandalism/graffiti in public space | External beautification | |
| Natural surveillance | View of the street | View of windows and doors |
| Natural cointerventions | Natural cointerventions in public space | Trees in front gardens |
| Purposively planted vegetation in front gardens |
REAT 2.0 has high levels of inter-rater reliability, with kappa coefficients (κ) of ≥ 0.77 for individual categorical items and Spearman’s rank correlation coefficients (ϱ) of ≥ 0.97 for the overall and constituent component scores. REAT 2.0 was also validated against residents’ own perceptions of the neighbourhood through a neighbourhood quality perceptions survey. This showed that the instrument has sound construct and predictive validity. 15
The development of the tool included the creation of a mobile application to facilitate field observations and data entry (http://reat.cardiff.ac.uk). Its development and validity are reported in detail elsewhere. 16
Method: The research took place in the three major urban areas in Carmarthenshire (Llanelli, Carmarthen and Ammanford). All postcode areas in which one or more homes were scheduled to receive at least one external intervention were selected for the study. REAT 2.0 was used for baseline assessments of 282 postcodes in 2012. Because the intervention programme had started before the evaluation study, a large number of homes had already received a number of improvements before baseline REAT 2.0 data could be collected. Follow-up assessments of the same 282 postcodes were carried out in 2014. The neighbourhood quality scores arising from both rounds of assessment were subsequently weighted using importance judgements derived from the neighbourhood perception survey. 16
Information regarding the timing, nature and volume of intervention work that was conducted within the postcodes was provided by the council. In total, 58% of the postcodes contained houses that received some sort of work between the two assessments; 48% of the postcodes contained houses that received internal work (e.g. upgrading of kitchens and bathrooms, electrical systems); and 48% of the postcodes contained houses that received external work, most of which (41%) only involved security lighting.
Analysis: A repeated measures analysis of variance was conducted to determine whether or not there was an overall improvement in neighbourhood quality between the assessments. A mixed-design analysis of variance was conducted to determine whether or not the observed increases in neighbourhood quality were greater in postcodes that had received more work under the housing intervention programme.
Results: A statistically significant medium-sized increase was found in overall neighbourhood quality [F(1,257) = 48.758; p = 0.000; η2 = 0.159]. Postcodes were categorised according to the amount of externally visible intervention that had taken place (interventions in < 25% of properties within the postcode, n = 189; 25 to < 50%, n = 39; 50 to < 75%, n = 15; and ≥ 75%, n = 15). The mean increase in the overall REAT 2.0 score was the highest for the group with the largest intervention dose (0.73) as compared with other groups, the largest of which had a mean increase in the overall REAT 2.0 score of 0.34. However, the differences between these groups were non-significant [F(3,254) = 0.936; p = 0.424; η2 = 0.011].
Other results: The mobile REAT 2.0 application was developed and tested in the field. Although the application did not speed up data collection itself, it saved time needed for data entry and also proved reliable in adverse weather conditions. 16
An additional study was conducted to examine the feasibility of conducting REAT 2.0 assessments remotely with Google Street View™ (Google Inc., Mountain View, CA, USA). 84–86 A subsample (n = 102) of the study postcodes were selected for remote assessments using a newly developed online REAT 2.0 facility (REAT view; see http://reat.cardiff.ac.uk). The study found moderate correlations between the remote and on-site REAT assessments, with discrepancies likely to be due to the different viewpoint afforded by the Street View camera and temporal differences in streetscape photography. Furthermore, remote assessments took nearly twice as long as on-site assessments, suggesting that, unless an area is difficult to access or travel costs are a particular issue, remote assessments should be used with caution.
Discussion: There was a statistically significant, medium-sized increase in the overall neighbourhood quality during the 2 years from baseline to follow-up. Those with the greatest number of externally visible improvements had the highest increase in neighbourhood quality. Although the latter effect was not statistically significant, it is suggestive of a dose effect but with insufficient statistical power to confirm.
The external ‘gardens and estates’ improvements were scaled back from beautification to safety considerations only. The scale-back, combined with scheduling changes, meant that only 164 of the 282 (58%) postcodes contained homes that had received any external improvement, and only 48 of the 282 (17%) contained properties that received garden improvements at the time of the 2014 post-test assessment. Furthermore, postcodes included in the study may have had only one or two council owned homes with planned or completed interventions. The ecological nature of this part of the study meant that 61% of homes were not council housing in various stages of (dis)repair, undergoing an unknown amount of improvement. This will have diluted the intervention dose and the potential for REAT 2.0 to detect improvements at the level of the postcode.
Conclusion: The study has shown that investments in existing housing stock have the potential to improve the outlook of neighbourhoods. Despite a number of shortcomings relating to difficulties conducting evaluations of existing practical interventions, this is, to our knowledge, the first study that has conducted detailed neighbourhood quality assessments at multiple time points to examine the wider neighbourhood impacts of a programme to improve housing standards in social housing. The REAT 2.0 tool is suitable for assessing areas undergoing housing improvements, with or without planned regeneration, and would be useful to evidence the wider area level economic and social benefits of housing improvement work.
Appendix 4 Counts of health events, by month
| Period | Emergency hospital admission outcomes | ED outcome | GP outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admission: combined (≥ 60 years) | Admission: cardiovascular (≥ 60 years) | Admission: respiratory (≥ 60 years) | Admission: injuries (≥ 60 years) | Admission: combined (all ages) | Admission: cardiovascular (all ages) | Admission: respiratory (all ages) | Admission: injuries (all ages) | ED attendances: injuries (all ages) | GP visits: respiratory (all ages) | GP prescriptions: respiratory (all ages) | GP prescriptions: CMD (all ages) | |
| January 2005 | 63 | 32 | 24 | 7 | 95 | 37 | 43 | 15 | NA | 7825 | 1468 | 597 |
| February 2005 | 75 | 38 | 30 | 7 | 97 | 43 | 45 | 9 | NA | 7789 | 1328 | 614 |
| March 2005 | 69 | 30 | 34 | 5 | 98 | 37 | 51 | 10 | NA | 8142 | 1448 | 733 |
| April 2005 | 43 | 20 | 19 | * | 74 | 34 | 35 | 5 | NA | 7721 | 1400 | 748 |
| May 2005 | 60 | 31 | 24 | 5 | 86 | 42 | 37 | 7 | NA | 7831 | 1441 | 772 |
| June 2005 | 62 | 39 | 17 | 6 | 82 | 43 | 30 | 9 | NA | 8282 | 1503 | 820 |
| July 2005 | 50 | 25 | 23 | * | 68 | 34 | 32 | * | NA | 7748 | 1437 | 804 |
| August 2005 | 64 | 40 | 18 | 6 | 87 | 50 | 28 | 9 | NA | 7897 | 1543 | 838 |
| September 2005 | 59 | 37 | 17 | 5 | 89 | 49 | 34 | 6 | NA | 8533 | 1487 | 774 |
| October 2005 | 72 | 43 | 18 | 11 | 102 | 51 | 37 | 14 | NA | 8647 | 1436 | 832 |
| November 2005 | 65 | 31 | 27 | 7 | 92 | 40 | 43 | 9 | NA | 8845 | 1556 | 824 |
| December 2005 | 72 | 35 | 30 | 7 | 112 | 40 | 59 | 13 | NA | 7758 | 1544 | 754 |
| January 2006 | 65 | 38 | 21 | 6 | 104 | 46 | 50 | 8 | NA | 8295 | 1591 | 809 |
| February 2006 | 56 | 30 | 19 | 7 | 86 | 36 | 43 | 7 | NA | 7560 | 1439 | 769 |
| March 2006 | 54 | 28 | 19 | 7 | 89 | 34 | 47 | 8 | NA | 8390 | 1516 | 874 |
| April 2006 | 59 | 24 | 27 | 8 | 91 | 33 | 49 | 9 | NA | 7220 | 1327 | 775 |
| May 2006 | 55 | 33 | 15 | 7 | 83 | 40 | 34 | 9 | NA | 8108 | 1580 | 825 |
| June 2006 | 63 | 33 | 25 | 5 | 90 | 44 | 39 | 7 | NA | 8069 | 1593 | 829 |
| July 2006 | 63 | 36 | 25 | * | 90 | 45 | 40 | 5 | NA | 7518 | 1536 | 860 |
| August 2006 | 58 | 33 | 19 | 6 | 89 | 42 | 39 | 8 | NA | 7561 | 1491 | 878 |
| September 2006 | 60 | 35 | 21 | * | 85 | 42 | 35 | 8 | NA | 8066 | 1532 | 790 |
| October 2006 | 73 | 44 | 16 | 13 | 100 | 50 | 34 | 16 | NA | 8515 | 1543 | 817 |
| November 2006 | 58 | 38 | 17 | * | 76 | 45 | 27 | * | NA | 8634 | 1607 | 742 |
| December 2006 | 64 | 41 | 20 | * | 96 | 46 | 46 | * | NA | 7486 | 1531 | 710 |
| January 2007 | 61 | 27 | 28 | 6 | 94 | 32 | 52 | 10 | NA | 8552 | 1680 | 733 |
| February 2007 | 61 | 32 | 22 | 7 | 79 | 34 | 35 | 10 | NA | 7532 | 1509 | 712 |
| March 2007 | 53 | 33 | 11 | 9 | 74 | 41 | 24 | 9 | NA | 8144 | 1623 | 755 |
| April 2007 | 70 | 40 | 24 | 6 | 86 | 46 | 34 | 6 | NA | 7513 | 1606 | 679 |
| May 2007 | 50 | 28 | 17 | 5 | 79 | 38 | 33 | 8 | NA | 7883 | 1633 | 719 |
| June 2007 | 45 | 29 | 11 | 5 | 64 | 37 | 21 | 6 | NA | 7431 | 1465 | 694 |
| July 2007 | 41 | 22 | 14 | 5 | 75 | 32 | 33 | 10 | NA | 7678 | 1621 | 725 |
| August 2007 | 56 | 25 | 27 | * | 78 | 31 | 40 | 7 | NA | 7509 | 1562 | 701 |
| September 2007 | 54 | 29 | 20 | 5 | 86 | 39 | 37 | 10 | NA | 7505 | 1454 | 656 |
| October 2007 | 81 | 44 | 28 | 9 | 108 | 55 | 42 | 11 | NA | 8728 | 1752 | 726 |
| November 2007 | 76 | 32 | 35 | 9 | 100 | 36 | 55 | 9 | NA | 7986 | 1622 | 648 |
| December 2007 | 54 | 30 | 21 | * | 80 | 35 | 40 | 5 | NA | 6879 | 1641 | 598 |
| January 2008 | 66 | 26 | 37 | * | 96 | 33 | 57 | 6 | NA | 7514 | 1625 | 681 |
| February 2008 | 45 | 26 | 12 | 7 | 74 | 31 | 31 | 12 | NA | 7480 | 1564 | 622 |
| March 2008 | 67 | 34 | 24 | 9 | 94 | 44 | 39 | 11 | NA | 6842 | 1504 | 631 |
| April 2008 | 57 | 28 | 22 | 7 | 79 | 35 | 36 | 8 | NA | 7198 | 1591 | 667 |
| May 2008 | 61 | 36 | 20 | 5 | 84 | 45 | 30 | 9 | NA | 7043 | 1593 | 642 |
| June 2008 | 50 | 27 | 18 | 5 | 69 | 32 | 30 | 7 | NA | 7347 | 1624 | 672 |
| July 2008 | 59 | 31 | 22 | 6 | 78 | 38 | 33 | 7 | NA | 7576 | 1620 | 664 |
| August 2008 | 62 | 37 | 19 | 6 | 83 | 45 | 28 | 10 | NA | 6584 | 1464 | 559 |
| September 2008 | 47 | 27 | 17 | * | 77 | 35 | 35 | 7 | NA | 7652 | 1789 | 610 |
| October 2008 | 56 | 28 | 23 | 5 | 80 | 37 | 34 | 9 | NA | 7748 | 1732 | 606 |
| November 2008 | 75 | 39 | 30 | 6 | 102 | 45 | 49 | 8 | NA | 7149 | 1590 | 544 |
| December 2008 | 71 | 32 | 34 | 5 | 109 | 36 | 65 | 8 | NA | 7256 | 1970 | 591 |
| January 2009 | 68 | 31 | 30 | 7 | 90 | 39 | 42 | 9 | NA | 7432 | 1710 | 605 |
| February 2009 | 46 | 21 | 20 | 5 | 72 | 31 | 34 | 7 | NA | 6594 | 1547 | 581 |
| March 2009 | 48 | 23 | 19 | 6 | 75 | 27 | 40 | 8 | NA | 7715 | 1739 | 627 |
| April 2009 | 49 | 25 | 20 | * | 72 | 31 | 34 | 7 | NA | 7043 | 1704 | 545 |
| May 2009 | 57 | 33 | 22 | * | 78 | 42 | 34 | * | NA | 6883 | 1547 | 487 |
| June 2009 | 51 | 22 | 25 | * | 79 | 30 | 43 | 6 | NA | 7471 | 1840 | 580 |
| July 2009 | 64 | 27 | 27 | 10 | 96 | 34 | 51 | 11 | NA | 7370 | 1721 | 604 |
| August 2009 | 42 | 21 | 16 | 5 | 67 | 29 | 29 | 9 | NA | 6627 | 1583 | 499 |
| September 2009 | 47 | 25 | 15 | 7 | 70 | 30 | 31 | 9 | NA | 7535 | 1880 | 554 |
| October 2009 | 45 | 17 | 20 | 8 | 77 | 25 | 38 | 14 | NA | 7891 | 1838 | 525 |
| November 2009 | 57 | 27 | 22 | 8 | 93 | 37 | 46 | 10 | NA | 6940 | 1663 | 458 |
| December 2009 | 68 | 38 | 25 | 5 | 106 | 43 | 53 | 10 | NA | 7518 | 1774 | 468 |
| January 2010 | 47 | 27 | 15 | 5 | 77 | 36 | 33 | 8 | NA | 6326 | 1569 | 377 |
| February 2010 | 63 | 33 | 25 | 5 | 91 | 41 | 43 | 7 | NA | 6625 | 1470 | 392 |
| March 2010 | 45 | 21 | 17 | 7 | 70 | 26 | 35 | 9 | NA | 7223 | 1743 | 539 |
| April 200 | 52 | 31 | 20 | * | 80 | 36 | 43 | * | NA | 6415 | 1453 | 422 |
| May 2010 | 62 | 30 | 24 | 8 | 86 | 38 | 38 | 10 | NA | 6103 | 1499 | 394 |
| June 2010 | 49 | 29 | 19 | * | 70 | 37 | 31 | * | NA | 6851 | 1658 | 432 |
| July 2010 | 49 | 30 | 17 | * | 69 | 38 | 27 | * | NA | 6500 | 1549 | 402 |
| August 2010 | 46 | 28 | 14 | * | 61 | 38 | 18 | 5 | NA | 6139 | 1542 | 431 |
| September 2010 | 56 | 27 | 20 | 9 | 73 | 35 | 28 | 10 | NA | 6955 | 1683 | 421 |
| October 2010 | 49 | 28 | 19 | * | 69 | 35 | 31 | * | NA | 6751 | 1541 | 402 |
| November 2010 | 54 | 20 | 30 | * | 84 | 27 | 52 | 5 | NA | 7104 | 1823 | 395 |
| December 2010 | 69 | 29 | 35 | 5 | 106 | 36 | 63 | 7 | NA | 6291 | 1806 | 366 |
| January 2011 | 68 | 25 | 37 | 6 | 97 | 33 | 55 | 9 | 276 | 6485 | 1679 | 335 |
| February 2011 | 47 | 23 | 22 | * | 79 | 30 | 46 | * | 240 | 6648 | 1612 | 388 |
| March 2011 | 54 | 32 | 22 | * | 88 | 43 | 43 | * | 335 | 7002 | 1763 | 414 |
| April 2011 | 49 | 29 | 18 | * | 69 | 35 | 29 | 5 | 346 | 6209 | 1625 | 416 |
| May 2011 | 51 | 24 | 23 | * | 69 | 31 | 32 | 6 | 352 | 6503 | 1744 | 443 |
| June 2011 | 52 | 35 | 15 | * | 70 | 39 | 28 | * | 330 | 6692 | 1706 | 410 |
| July 2011 | 46 | 28 | 15 | * | 65 | 34 | 27 | * | 373 | 6282 | 1604 | 389 |
| August 2011 | 56 | 31 | 20 | 5 | 73 | 38 | 29 | 6 | 359 | 6490 | 1801 | 425 |
| September 2011 | 64 | 32 | 24 | 8 | 91 | 42 | 39 | 10 | 338 | 6540 | 1663 | 370 |
| October 2011 | 55 | 27 | 24 | * | 78 | 35 | 38 | 5 | 346 | 6869 | 1765 | 399 |
| November 2011 | 60 | 31 | 18 | 11 | 77 | 36 | 30 | 11 | 295 | 6802 | 1804 | 384 |
| December 2011 | 78 | 39 | 34 | 5 | 103 | 44 | 52 | 7 | 304 | 6252 | 1744 | 358 |
| January 2012 | 60 | 23 | 29 | 8 | 81 | 31 | 40 | 10 | 308 | 6662 | 1790 | 364 |
| February 2012 | 60 | 26 | 27 | 7 | 83 | 34 | 42 | 7 | 256 | 6477 | 1718 | 355 |
| March 2012 | 67 | 37 | 27 | * | 99 | 45 | 47 | 7 | 311 | 6631 | 1793 | 402 |
| April 2012 | 68 | 34 | 25 | 9 | 95 | 45 | 41 | 9 | 328 | 6054 | 1652 | 347 |
| May 2012 | 64 | 28 | 29 | 7 | 98 | 38 | 51 | 9 | 399 | 6616 | 1861 | 382 |
| June 2012 | 50 | 25 | 20 | 5 | 82 | 39 | 36 | 7 | 337 | 5713 | 1629 | 331 |
| July 2012 | 58 | 27 | 24 | 7 | 87 | 33 | 44 | 10 | 350 | 6536 | 1811 | 350 |
| August 2012 | 47 | 25 | 18 | * | 76 | 36 | 34 | 6 | 332 | 6240 | 1832 | 357 |
| September 2012 | 63 | 35 | 21 | 7 | 79 | 43 | 29 | 7 | 354 | 5327 | 1454 | 299 |
| October 2012 | 58 | 27 | 23 | 8 | 86 | 38 | 40 | 8 | 315 | 6173 | 1767 | 346 |
| November 2012 | 58 | 27 | 25 | 6 | 85 | 36 | 41 | 8 | 292 | 5682 | 1680 | 309 |
| December 2012 | 58 | 21 | 34 | * | 87 | 28 | 56 | * | 229 | 5091 | 1751 | 303 |
| January 2013 | 65 | 29 | 28 | 8 | 91 | 41 | 41 | 9 | 277 | 6141 | 1741 | 387 |
| February 2013 | 53 | 30 | 22 | * | 85 | 41 | 41 | * | 249 | 5876 | 1514 | 324 |
| March 2013 | 77 | 31 | 36 | 10 | 99 | 37 | 52 | 10 | 283 | 5923 | 1666 | 312 |
| April 2013 | 64 | 28 | 29 | 7 | 79 | 31 | 41 | 7 | 267 | 6027 | 1730 | 328 |
| May 2013 | 56 | 21 | 30 | 5 | 82 | 30 | 47 | 5 | 360 | 6055 | 1747 | 320 |
| June 2013 | 61 | 31 | 27 | * | 83 | 36 | 42 | 5 | 334 | 5781 | 1580 | 339 |
| July 2013 | 54 | 36 | 15 | * | 74 | 45 | 25 | * | 392 | 6229 | 1839 | 317 |
| August 2013 | 57 | 33 | 20 | * | 75 | 42 | 29 | * | 336 | 5760 | 1655 | 274 |
| September 2013 | 67 | 36 | 26 | 5 | 91 | 42 | 40 | 9 | 357 | 5561 | 1594 | 286 |
| October 2013 | 48 | 27 | 17 | * | 82 | 37 | 39 | 6 | 268 | 5639 | 1670 | 258 |
| November 2013 | 62 | 30 | 28 | * | 91 | 32 | 53 | 6 | 255 | 5158 | 1511 | 234 |
| December 2013 | 65 | 26 | 34 | 5 | 93 | 34 | 53 | 6 | 258 | 4177 | 1333 | 207 |
| January 2014 | 60 | 28 | 22 | 10 | 85 | 40 | 35 | 10 | 276 | 4696 | 1390 | 212 |
| February 2014 | 62 | 36 | 22 | * | 89 | 43 | 42 | * | 266 | 4430 | 1202 | 199 |
| March 2014 | 65 | 35 | 22 | 8 | 91 | 42 | 38 | 11 | 360 | 4880 | 1179 | 202 |
| April 2014 | 59 | 25 | 25 | 9 | 86 | 30 | 45 | 11 | 306 | 2695 | 741 | 110 |
| May 2014 | 73 | 29 | 30 | 14 | 109 | 40 | 52 | 17 | 355 | 2721 | 710 | 114 |
| June 2014 | 63 | 36 | 22 | 5 | 89 | 44 | 37 | 8 | 393 | 2834 | 773 | 110 |
| July 2014 | 76 | 33 | 35 | 8 | 99 | 36 | 50 | 13 | 359 | 2686 | 761 | 105 |
| August 2014 | 55 | 34 | 16 | 5 | 78 | 43 | 27 | 8 | 311 | 2347 | 704 | 82 |
| September 2014 | 61 | 29 | 28 | * | 83 | 38 | 39 | 6 | 361 | 2788 | 806 | 97 |
| October 2014 | 62 | 32 | 25 | 5 | 84 | 39 | 37 | 8 | 335 | 2914 | 797 | 90 |
| November 2014 | 41 | 14 | 19 | 8 | 72 | 23 | 41 | 8 | 277 | 2609 | 681 | 96 |
| December 2014 | 69 | 35 | 30 | * | 120 | 41 | 71 | 8 | 245 | 2773 | 923 | 98 |
| January 2015 | 87 | 34 | 41 | 12 | 118 | 43 | 59 | 16 | 229 | 2844 | 763 | 89 |
| February 2015 | 62 | 34 | 22 | 6 | 95 | 43 | 45 | 7 | 272 | 2696 | 688 | 80 |
| March 2015 | 71 | 38 | 27 | 6 | 104 | 46 | 50 | 8 | 294 | 2221 | 567 | 49 |
Appendix 5 Read codes for common mental health disorder treatments and diagnoses
Treatment and symptom or diagnosis Read codes used in the algorithm to identify CMD cases, and to count treatments when classified as a case (Table 15). 45
| Drug treatment Read codes |
|---|
| Antidepressants |
| d71.. |
| d72.. |
| d73.. |
| d74.. |
| d75.. |
| d76.. |
| d77.. |
| d78.. |
| d79.. |
| d7a.. |
| d7b.. |
| d7c.. |
| d7d.. |
| d7e.. |
| d7f.. |
| d7g.. |
| d7h.. |
| d81.. |
| d83.. |
| d84.. |
| d85.. |
| d91.. |
| da1.. |
| da2.. |
| da3.. |
| da4.. |
| da5.. |
| da6.. |
| da7.. |
| da9.. |
| daA.. |
| daB.. |
| daC.. |
| daD.. |
| gde.. |
| Hypnotics |
| d11.. |
| d12.. |
| d13.. |
| d14.. |
| d15.. |
| d16.. |
| d17.. |
| d18.. |
| d1a.. |
| d1b.. |
| d1c.. |
| d1d.. |
| d1f.. |
| d1g.. |
| d1h.. |
| d1i.. |
| Anxiolytics |
| d21.. |
| d22.. |
| d23.. |
| d24.. |
| d25.. |
| d26.. |
| d27.. |
| d28.. |
| d29.. |
| d2a.. |
| d2b.. |
| d2c.. |
| d2d.. |
| d2f.. |
| d2g.. |
| Depression and anxiety Read codes |
| Depression diagnoses |
| Eu32. |
| Eu320 |
| Eu321 |
| Eu322 |
| Eu324 |
| Eu32y |
| Eu32z |
| Eu33. |
| Eu330 |
| Eu331 |
| Eu332 |
| Eu334 |
| Eu33y |
| Eu33z |
| Eu341 |
| E118. |
| E135. |
| E2B.. |
| E2B1. |
| E291. |
| E204. |
| E2B0. |
| E112. |
| E1120 |
| E1121 |
| E1122 |
| E1123 |
| E1125 |
| E1126 |
| E112z |
| E113. |
| E1130 |
| E1131 |
| E1132 |
| E1133 |
| E1135 |
| E1136 |
| E1137 |
| E113z |
| Anxiety diagnoses |
| Eu41. |
| Eu410 |
| Eu411 |
| Eu413 |
| Eu41y |
| Eu41z |
| E200. |
| E2000 |
| E2001 |
| E2002 |
| E2004 |
| E2005 |
| E200z |
| Mixed depression/anxiety diagnoses |
| E2003 |
| Eu412 |
| Depression symptoms |
| 1B17. |
| 1B1U. |
| 1BQ.. |
| 1BT.. |
| 1BU.. |
| 2257 |
| Anxiety symptoms |
| 1B13. |
| 2258 |
| 1B12. |
| R2y2. |
| 2259 |
Appendix 6 Emergency Department Data Set definitions of injuries occurring at home
We used the EDDS to define injuries occurring at home. We searched for new attendances only (attendance group = 01), with other criteria applied to identify injuries occurring in the home: ‘location type’ equal to 01 (at home), 14 (other specified), or 99 (unspecified), ‘mechanism of injury’ not equal to 98 (non-injury) and ‘activity’ code not equal to 01 (work), 2 (education), 3 (sport), 6 (road traffic collision) or 98 (non-injury). We included records with emergency diagnostic codes listed in Table 16, or ICD-10 codes S00–99, T00–65 or T71 in diagnostic positions 1 to 6, or emergency treatment codes 3Z (‘dressing’), 4Z (‘wound closure’) or 6Z (‘manipulation’) in treatment positions 1 to 6.
| Diagnostic code | Description |
|---|---|
| 01A | Laceration |
| 01B | Contusion |
| 01C | Abrasion |
| 01D | Soft-tissue inflammation |
| 01Z | Wound, other or unspecified |
| 02A | Glasgow Coma Score of 15 |
| 02B | Glasgow Coma Score of < 15 |
| 02C | Dental injury |
| 02Z | Head injury, other or unspecified |
| 03A | Open fracture |
| 03B | Closed fracture |
| 03C | Fracture dislocation |
| 03Z | Fracture, other or unspecified |
| 04A | Sprain |
| 04B | Dislocation |
| 04C | Subluxation |
| 04Z | Joint injury, other or unspecified |
| 05Z | Amputation, other or unspecified |
| 06A | Muscle injury |
| 06B | Tendon injury |
| 06C | Nerve injury |
| 06D | Visceral injury |
| 06E | Vascular injury |
| 06Z | Soft-tissue injury, other or unspecified |
| 07A | Electric |
| 07D | Scald |
| 07G | Hypothermia |
| 07Z | B, S and T conditions, other/unspecified |
Appendix 7 Results for all outcomes and both exposure groups
All results for both primary and secondary outcomes, including emergency hospital admissions, GP outcomes and emergency attendances, are given in Table 17. The results are for our main exposure group (1). These are people who were living in the home when the cointervention was installed. This is the direct health impact for people living in homes that were directly brought up to the housing quality standard. We also provide results for our second exposure group (2). These are for people who were either already living in a home that met housing quality standards at the start of the evaluation period, or moved into an intervention home during the evaluation where the relevant cointervention had been installed as part of the intervention.
| Cointervention | Unadjusted IRR (95% CI) | Adjusted IRR (95% CI) | ||
|---|---|---|---|---|
| Exposure (1) | Exposure (2) | Exposure (1) | Exposure (2) | |
| Emergency admissions for combined conditions for participants of all ages | ||||
| Windows and doors | 0.79 (0.70 to 0.89) | 0.87 (0.78 to 0.97) | 0.78 (0.70 to 0.87) | 0.91 (0.82 to 1.00) |
| Wall insulation | 0.89 (0.80 to 0.99) | 0.94 (0.85 to 1.04) | 0.80 (0.73 to 0.87) | 0.90 (0.82 to 0.98) |
| Loft insulation | 1.27 (1.13 to 1.42) | 1.30 (1.18 to 1.42) | 1.02 (0.93 to 1.13) | 1.01 (0.93 to 1.09) |
| Heating systems | 0.65 (0.58 to 0.72) | 0.77 (0.68 to 0.88) | 0.92 (0.85 to 1.01) | 1.23 (1.10 to 1.38) |
| Kitchens | 0.84 (0.69 to 1.02) | 0.80 (0.65 to 0.97) | 1.01 (0.87 to 1.18) | 1.02 (0.86 to 1.20) |
| Bathrooms | 1.16 (0.98 to 1.37) | 1.35 (1.13 to 1.63) | 0.99 (0.87 to 1.13) | 0.93 (0.80 to 1.07) |
| Electrical systems | 0.68 (0.58 to 0.80) | 0.65 (0.55 to 0.76) | 0.66 (0.58 to 0.76) | 0.79 (0.69 to 0.90) |
| Garden paths | 0.85 (0.75 to 0.96) | 0.98 (0.88 to 1.08) | 0.81 (0.73 to 0.90) | 0.86 (0.79 to 0.94) |
| Emergency admissions for cardiovascular conditions for participants of all ages | ||||
| Windows and doors | 0.88 (0.74 to 1.04) | 0.90 (0.77 to 1.05) | 0.82 (0.70 to 0.96) | 0.95 (0.82 to 1.10) |
| Wall insulation | 0.89 (0.77 to 1.03) | 0.86 (0.74 to 0.99) | 0.74 (0.65 to 0.85) | 0.80 (0.70 to 0.92) |
| Loft insulation | 1.25 (1.07 to 1.47) | 1.32 (1.16 to 1.50) | 0.93 (0.80 to 1.08) | 0.91 (0.81 to 1.03) |
| Heating systems | 0.56 (0.49 to 0.65) | 0.60 (0.50 to 0.72) | 0.93 (0.82 to 1.06) | 1.21 (1.01 to 1.44) |
| Kitchens | 0.72 (0.56 to 0.93) | 0.69 (0.53 to 0.91) | 0.95 (0.77 to 1.17) | 1.05 (0.83 to 1.32) |
| Bathrooms | 1.21 (0.96 to 1.52) | 1.57 (1.22 to 2.01) | 0.99 (0.82 to 1.19) | 0.89 (0.72 to 1.09) |
| Electrical systems | 0.89 (0.71 to 1.12) | 0.68 (0.55 to 0.85) | 0.79 (0.65 to 0.96) | 0.83 (0.68 to 1.01) |
| Garden paths | 0.95 (0.79 to 1.13) | 1.09 (0.94 to 1.26) | 0.92 (0.78 to 1.09) | 0.99 (0.86 to 1.14) |
| Emergency admissions for respiratory conditions for participants of all ages | ||||
| Windows and doors | 0.75 (0.63 to 0.89) | 0.86 (0.74 to 1.01) | 0.76 (0.65 to 0.89) | 0.88 (0.76 to 1.02) |
| Wall insulation | 0.87 (0.75 to 1.01) | 1.01 (0.87 to 1.17) | 0.82 (0.72 to 0.94) | 0.95 (0.83 to 1.09) |
| Loft insulation | 1.30 (1.11 to 1.52) | 1.30 (1.14 to 1.48) | 1.09 (0.95 to 1.27) | 1.11 (0.98 to 1.25) |
| Heating systems | 0.74 (0.63 to 0.86) | 1.01 (0.84 to 1.20) | 0.93 (0.81 to 1.07) | 1.31 (1.11 to 1.55) |
| Kitchens | 1.00 (0.76 to 1.32) | 0.87 (0.65 to 1.15) | 1.11 (0.87 to 1.43) | 0.98 (0.75 to1.27) |
| Bathrooms | 1.09 (0.85 to 1.38) | 1.25 (0.96 to 1.63) | 0.93 (0.75 to 1.15) | 0.95 (0.75 to 1.20) |
| Electrical systems | 0.56 (0.44 to 0.71) | 0.63 (0.50 to 0.79) | 0.60 (0.48 to 0.74) | 0.79 (0.64 to 0.98) |
| Garden paths | 0.78 (0.65 to 0.93) | 0.92 (0.80 to 1.06) | 0.74 (0.63 to 0.87) | 0.80 (0.71 to 0.92) |
| Emergency admissions for injuries for participants of all ages | ||||
| Windows and doors | 0.70 (0.55 to 0.91) | 0.78 (0.62 to 0.99) | 0.70 (0.52 to 0.93) | 0.83 (0.63 to 1.09) |
| Wall insulation | 1.11 (0.89 to 1.39) | 1.12 (0.89 to 1.41) | 0.82 (0.63 to 1.06) | 0.87 (0.67 to 1.13) |
| Loft insulation | 1.34 (1.05 to 1.72) | 1.38 (1.11 to 1.70) | 1.01 (0.76 to 1.33) | 1.00 (0.79 to 1.28) |
| Heating systems | 0.66 (0.53 to 0.82) | 0.56 (0.40 to 0.77) | 0.94 (0.73 to 1.21) | 0.92 (0.64 to 1.34) |
| Kitchens | 0.54 (0.36 to 0.81) | 0.68 (0.43 to 1.10) | 0.82 (0.53 to 1.27) | 1.05 (0.63 to 1.75) |
| Bathrooms | 1.57 (1.11 to 2.21) | 1.15 (0.76 to 1.75) | 1.27 (0.90 to 1.81) | 0.80 (0.51 to 1.25) |
| Electrical systems | 0.59 (0.41 to 0.85) | 0.71 (0.49 to 1.01) | 0.54 (0.36 to 0.81) | 0.69 (0.46 to 1.03) |
| Garden paths | 0.92 (0.70 to 1.20) | 0.82 (0.66 to 1.03) | 0.81 (0.60 to 1.10) | 0.72 (0.56 to 0.92) |
| Emergency admissions for combined conditions for participants aged ≥ 60 years | ||||
| Windows and doors | 0.70 (0.61 to 0.81) | 0.80 (0.70 to 0.92) | 0.71 (0.63 to 0.81) | 0.80 (0.71 to 0.90) |
| Wall insulation | 0.70 (0.61 to 0.79) | 0.73 (0.64 to 0.83) | 0.75 (0.67 to 0.84) | 0.73 (0.65 to 0.82) |
| Loft insulation | 0.93 (0.80 to 1.08) | 1.00 (0.88 to 1.13) | 0.98 (0.86 to 1.11) | 0.93 (0.84 to 1.04) |
| Heating systems | 0.82 (0.72 to 0.93) | 0.97 (0.82 to 1.16) | 0.91 (0.82 to 1.01) | 1.03 (0.88 to 1.20) |
| Kitchens | 1.00 (0.81 to 1.23) | 1.12 (0.90 to 1.40) | 0.98 (0.83 to 1.17) | 1.09 (0.90 to 1.32) |
| Bathrooms | 0.97 (0.82 to 1.14) | 1.08 (0.89 to 1.30) | 0.93 (0.81 to 1.06) | 0.93 (0.79 to 1.09) |
| Electrical systems | 0.60 (0.50 to 0.72) | 0.66 (0.54 to 0.79) | 0.61 (0.53 to 0.72) | 0.66 (0.56 to 0.78) |
| Garden paths | 0.70 (0.60 to 0.82) | 0.82 (0.72 to 0.93) | 0.73 (0.64 to 0.83) | 0.83 (0.74 to 0.92) |
| Emergency admissions for cardiovascular conditions for participants aged ≥ 60 years | ||||
| Windows and doors | 0.75 (0.62 to 0.89) | 0.84 (0.71 to 1.00) | 0.81 (0.69 to 0.96) | 0.91 (0.78 to 1.07) |
| Wall insulation | 0.67 (0.57 to 0.79) | 0.67 (0.57 to 0.79) | 0.73 (0.63 to 0.85) | 0.72 (0.62 to 0.84) |
| Loft insulation | 0.80 (0.67 to 0.97) | 0.92 (0.79 to 1.07) | 0.86 (0.73 to 1.02) | 0.87 (0.76 to 1.00) |
| Heating systems | 0.80 (0.69 to 0.93) | 0.99 (0.80 to 1.24) | 0.94 (0.82 to 1.08) | 1.12 (0.91 to 1.37) |
| Kitchens | 0.92 (0.72 to 1.18) | 1.16 (0.89 to 1.52) | 0.91 (0.73 to 1.13) | 1.18 (0.92 to 1.51) |
| Bathrooms | 0.94 (0.77 to 1.16) | 1.10 (0.87 to 1.38) | 0.94 (0.78 to 1.13) | 0.91 (0.74 to 1.12) |
| Electrical systems | 0.77 (0.61 to 0.97) | 0.75 (0.60 to 0.94) | 0.80 (0.66 to 0.99) | 0.79 (0.64 to 0.98) |
| Garden paths | 0.74 (0.61 to 0.90) | 0.87 (0.74 to 1.02) | 0.84 (0.70 to 1.00) | 0.94 (0.81 to 1.10) |
| Emergency admissions for respiratory conditions for participants aged ≥ 60 years | ||||
| Windows and doors | 0.66 (0.52 to 0.85) | 0.76 (0.60 to 0.95) | 0.61 (0.49 to 0.76) | 0.69 (0.57 to 0.85) |
| Wall insulation | 0.71 (0.57 to 0.89) | 0.76 (0.61 to 0.95) | 0.76 (0.62 to 0.92) | 0.71 (0.58 to 0.86) |
| Loft insulation | 1.18 (0.92 to 1.51) | 1.16 (0.93 to 1.43) | 1.18 (0.95 to 1.48) | 1.08 (0.89 to 1.31) |
| Heating systems | 0.84 (0.68 to 1.04) | 0.99 (0.73 to 1.32) | 0.85 (0.71 to 1.03) | 0.92 (0.70 to 1.20) |
| Kitchens | 1.21 (0.85 to 1.73) | 1.05 (0.73 to 1.51) | 1.17 (0.86 to 1.59) | 0.97 (0.70 to 1.34) |
| Bathrooms | 0.99 (0.75 to 1.31) | 1.14 (0.83 to 1.57) | 0.89 (0.70 to 1.13) | 1.01 (0.77 to 1.33) |
| Electrical systems | 0.43 (0.31 to 0.58) | 0.54 (0.39 to 0.74) | 0.43 (0.33 to 0.57) | 0.51 (0.39 to 0.67) |
| Garden paths | 0.68 (0.52 to 0.88) | 0.81 (0.66 to 1.01) | 0.62 (0.49 to 0.78) | 0.76 (0.62 to 0.91) |
| Emergency admissions for injuries for participants aged ≥ 60 years | ||||
| Windows and doors | 0.58 (0.44 to 0.77) | 0.66 (0.51 to 0.86) | 0.56 (0.40 to 0.77) | 0.64 (0.47 to 0.86) |
| Wall insulation | 0.88 (0.67 to 1.14) | 0.94 (0.72 to 1.24) | 0.76 (0.57 to 1.02) | 0.86 (0.63 to 1.16) |
| Loft insulation | 1.06 (0.78 to 1.43) | 1.02 (0.79 to 1.32) | 1.02 (0.73 to 1.43) | 0.91 (0.68 to 1.22) |
| Heating systems | 0.87 (0.68 to 1.12) | 0.91 (0.60 to 1.37) | 1.01 (0.77 to 1.32) | 1.11 (0.71 to 1.75) |
| Kitchens | 0.62 (0.42 to 0.94) | 0.88 (0.55 to 1.42) | 0.75 (0.48 to 1.17) | 1.04 (0.61 to 1.76) |
| Bathrooms | 1.16 (0.85 to 1.60) | 0.79 (0.52 to 1.19) | 1.18 (0.83 to 1.66) | 0.66 (0.42 to 1.04) |
| Electrical systems | 0.61 (0.42 to 0.89) | 0.86 (0.59 to 1.25) | 0.56 (0.37 to 0.85) | 0.76 (0.50 to 1.15) |
| Garden paths | 0.69 (0.51 to 0.95) | 0.64 (0.50 to 0.83) | 0.69 (0.49 to 0.97) | 0.62 (0.46 to 0.82) |
| Prescribed medications for participants with a CMD | ||||
| Windows and doors | 0.87 (0.79 to 0.96) | 0.93 (0.85 to 1.01) | 0.91 (0.83 to 1.00) | 0.94 (0.86 to 1.02) |
| Wall insulation | 0.97 (0.89 to 1.05) | 1.01 (0.93 to 1.09) | 0.97 (0.89 to 1.05) | 1.00 (0.92 to 1.08) |
| Loft insulation | 0.96 (0.89 to 1.04) | 0.96 (0.89 to 1.02) | 0.99 (0.92 to 1.07) | 0.94 (0.88 to 1.01) |
| Heating systems | 1.01 (0.93 to 1.09) | 0.96 (0.87 to 1.06) | 1.08 (1.00 to 1.17) | 0.98 (0.89 to 1.08) |
| Kitchens | 1.05 (0.91 to 1.20) | 0.81 (0.69 to 0.95) | 1.06 (0.92 to 1.22) | 0.83 (0.70 to 0.97) |
| Bathrooms | 0.96 (0.84 to 1.10) | 1.12 (0.97 to 1.30) | 0.91 (0.80 to 1.04) | 1.08 (0.93 to 1.25) |
| Electrical systems | 0.93 (0.82 to 1.06) | 1.08 (0.96 to 1.22) | 0.90 (0.79 to 1.02) | 1.06 (0.94 to 1.20) |
| Garden paths | 0.98 (0.88 to 1.09) | 0.98 (0.90 to 1.07) | 0.97 (0.87 to 1.08) | 0.98 (0.90 to 1.07) |
| Respiratory prescriptions for participants with a history of asthma and COPD of all ages | ||||
| Windows and doors | 0.93 (0.88 to 0.98) | 0.97 (0.92 to 1.02) | 0.92 (0.88 to 0.97) | 0.96 (0.91 to 1.00) |
| Wall insulation | 0.97 (0.93 to 1.01) | 0.95 (0.91 to 1.00) | 0.96 (0.92 to 1.00) | 0.95 (0.91 to 0.99) |
| Loft insulation | 1.06 (1.01 to 1.11) | 1.07 (1.03 to 1.12) | 1.02 (0.98 to 1.07) | 1.04 (1.00 to 1.08) |
| Heating systems | 1.00 (0.96 to 1.05) | 1.04 (0.99 to 1.10) | 1.02 (0.98 to 1.06) | 1.04 (0.99 to 1.10) |
| Kitchens | 0.98 (0.91 to 1.06) | 0.96 (0.88 to 1.04) | 0.99 (0.92 to 1.06) | 0.98 (0.90 to 1.06) |
| Bathrooms | 0.95 (0.88 to 1.01) | 1.02 (0.94 to 1.09) | 0.92 (0.87 to 0.99) | 0.99 (0.93 to 1.07) |
| Electrical systems | 1.00 (0.94 to 1.07) | 0.99 (0.92 to 1.06) | 0.99 (0.93 to 1.06) | 0.95 (0.89 to 1.02) |
| Garden paths | 1.01 (0.96 to 1.07) | 1.01 (0.96 to 1.06) | 0.98 (0.92 to 1.03) | 0.98 (0.94 to 1.03) |
| GP contacts for participants with a history of asthma and COPD | ||||
| Windows and doors | 0.96 (0.93 to 0.99) | 0.97 (0.94 to 1.00) | 0.99 (0.96 to 1.02) | 1.00 (0.97 to 1.03) |
| Wall insulation | 0.99 (0.96 to 1.02) | 1.01 (0.98 to 1.04) | 0.97 (0.95 to 1.00) | 1.01 (0.99 to 1.04) |
| Loft insulation | 1.00 (0.97 to 1.03) | 1.03 (1.01 to 1.06) | 0.97 (0.94 to 1.00) | 1.01 (0.99 to 1.04) |
| Heating systems | 0.93 (0.91 to 0.96) | 0.98 (0.94 to 1.01) | 0.99 (0.97 to 1.02) | 1.06 (1.02 to 1.09) |
| Kitchens | 1.02 (0.97 to 1.08) | 0.92 (0.87 to 0.97) | 1.05 (1.01 to 1.11) | 0.92 (0.87 to 0.97) |
| Bathrooms | 0.98 (0.94 to 1.03) | 1.02 (0.97 to 1.07) | 1.00 (0.96 to 1.05) | 1.04 (0.99 to 1.09) |
| Electrical systems | 0.95 (0.91 to 0.99) | 0.99 (0.95 to 1.03) | 0.91 (0.87 to 0.95) | 0.99 (0.95 to 1.03) |
| Garden paths | 1.01 (0.97 to 1.05) | 1.01 (0.98 to 1.04) | 0.99 (0.96 to 1.02) | 0.99 (0.96 to 1.01) |
| Emergency department attendances relating to injuries for participants of all ages | ||||
| Windows and doors | 0.77 (0.63 to 0.94) | 0.75 (0.62 to 0.91) | 0.79 (0.65 to 0.96) | 0.76 (0.62 to 0.93) |
| Wall insulation | 0.96 (0.88 to 1.04) | 0.93 (0.86 to 1.01) | 1.03 (0.95 to 1.13) | 0.99 (0.91 to 1.08) |
| Loft insulation | 0.93 (0.87 to 1.00) | 0.97 (0.91 to 1.03) | 0.98 (0.92 to 1.06) | 0.98 (0.92 to 1.05) |
| Heating systems | 1.18 (1.10 to 1.27) | 1.16 (1.07 to 1.26) | 1.10 (1.02 to 1.18) | 1.06 (0.97 to 1.15) |
| Kitchens | 0.98 (0.87 to 1.11) | 0.98 (0.86 to 1.13) | 0.97 (0.86 to 1.11) | 0.96 (0.83 to 1.10) |
| Bathrooms | 1.02 (0.91 to 1.14) | 0.94 (0.83 to 1.07) | 1.04 (0.92 to 1.18) | 1.03 (0.90 to 1.18) |
| Electrical systems | 1.00 (0.89 to 1.12) | 1.11 (0.99 to 1.25) | 0.96 (0.85 to 1.08) | 1.03 (0.91 to 1.16) |
| Garden paths | 1.14 (1.02 to 1.28) | 1.10 (0.99 to 1.23) | 1.20 (1.07 to 1.35) | 1.16 (1.04 to 1.30) |
The reference and exposure groups are different for each cointervention.
FIGURE 21.
Incidence rate ratios of emergency admissions for combined conditions for participants aged ≥ 60 years, by cointervention.
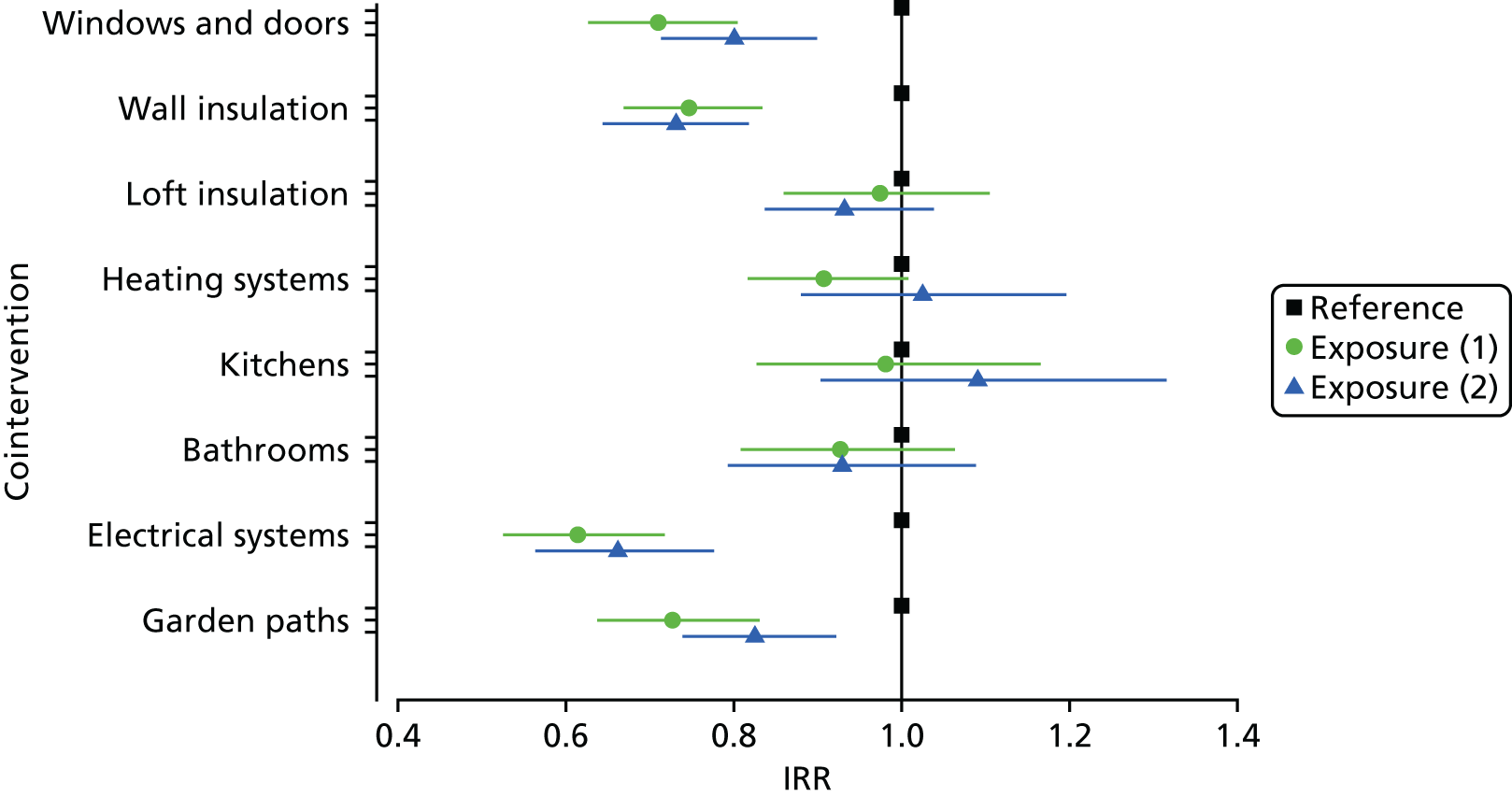
FIGURE 22.
Incidence rate ratios of emergency admissions for cardiovascular conditions for participants aged ≥ 60 years, by cointervention.
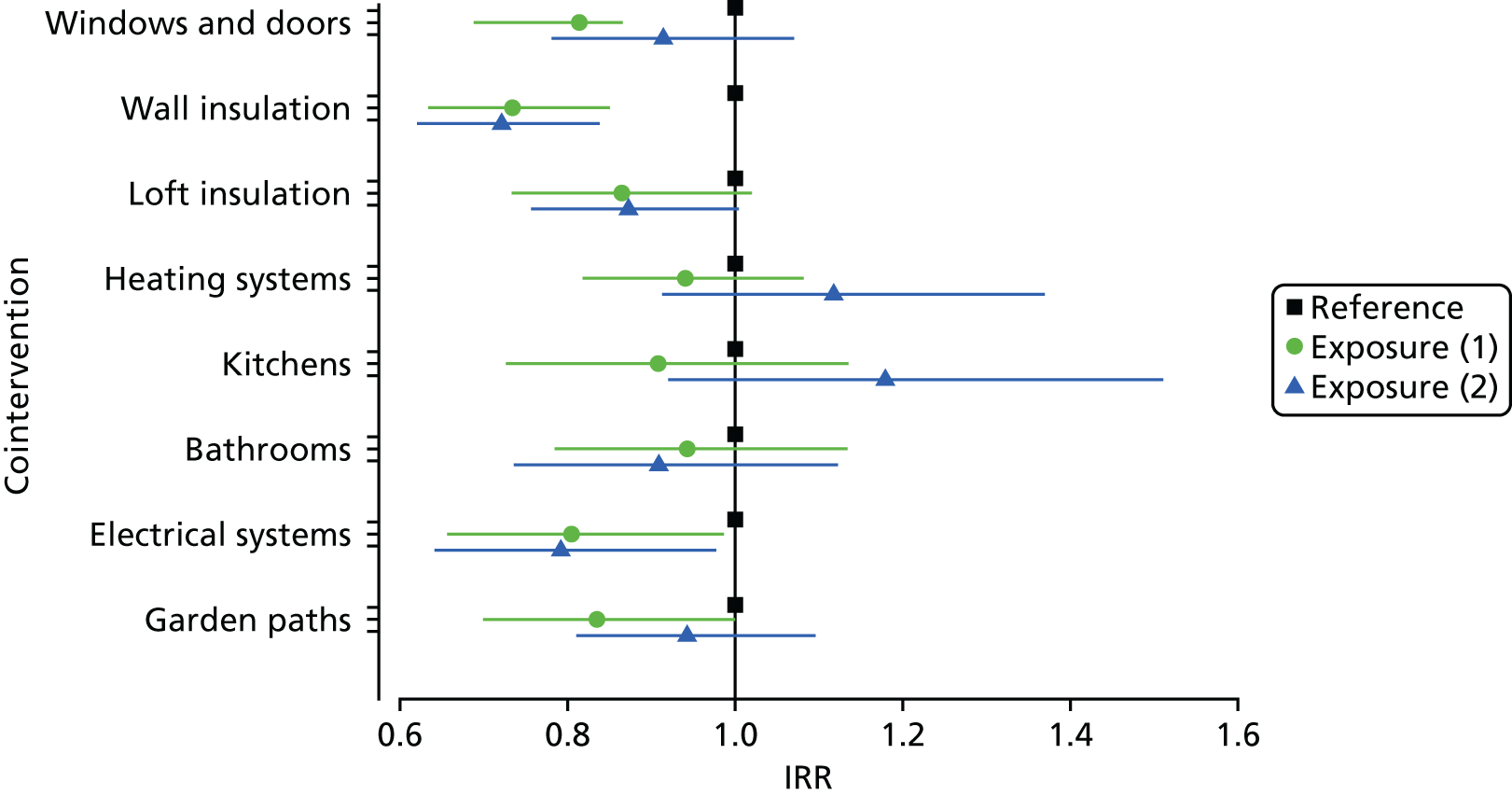
FIGURE 23.
Incidence rate ratios of emergency admissions for respiratory conditions for participants aged ≥ 60 years, by cointervention.
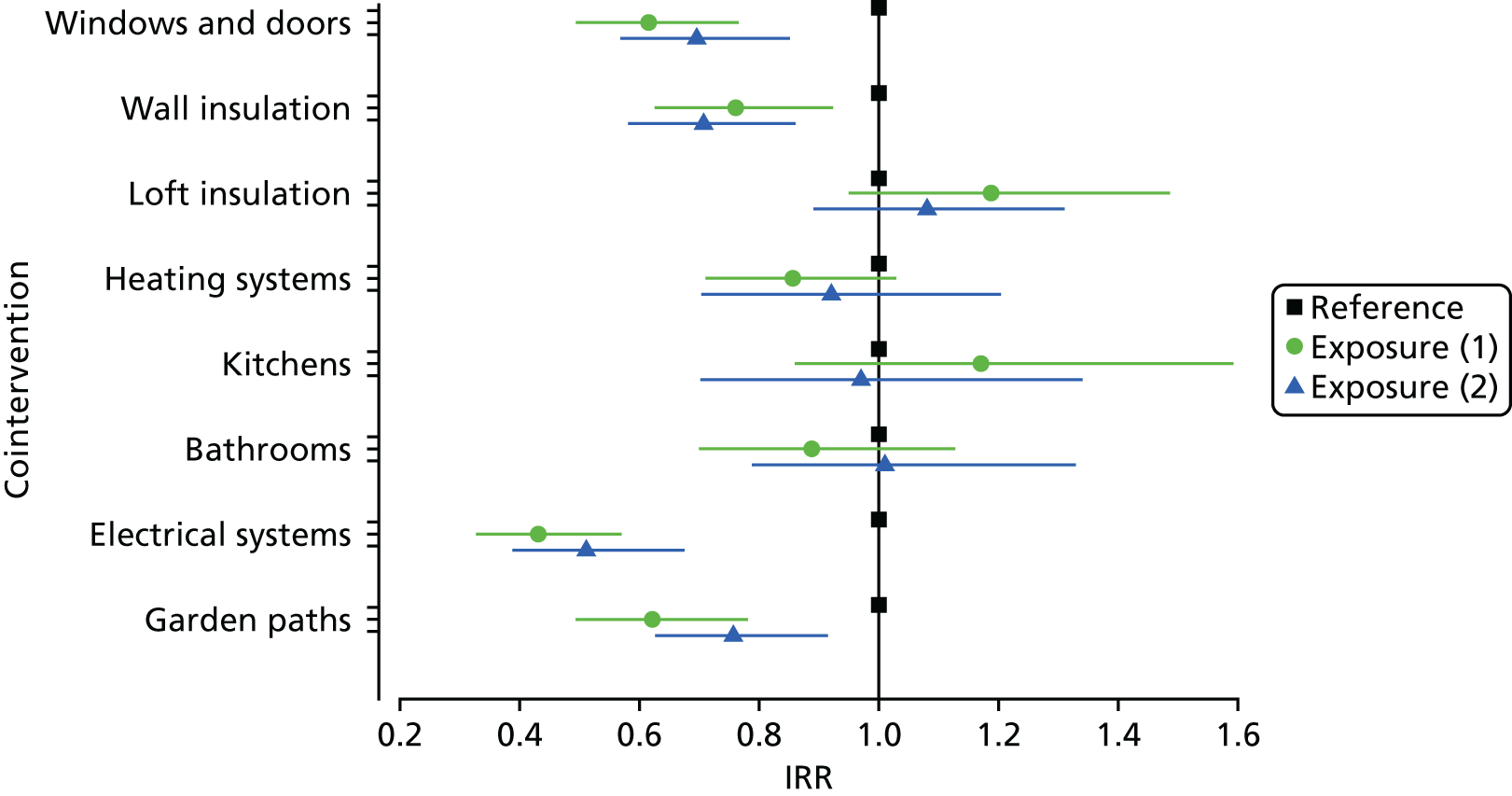
FIGURE 24.
Incidence rate ratios of emergency admissions for injuries for participants aged ≥ 60 years, by cointervention.
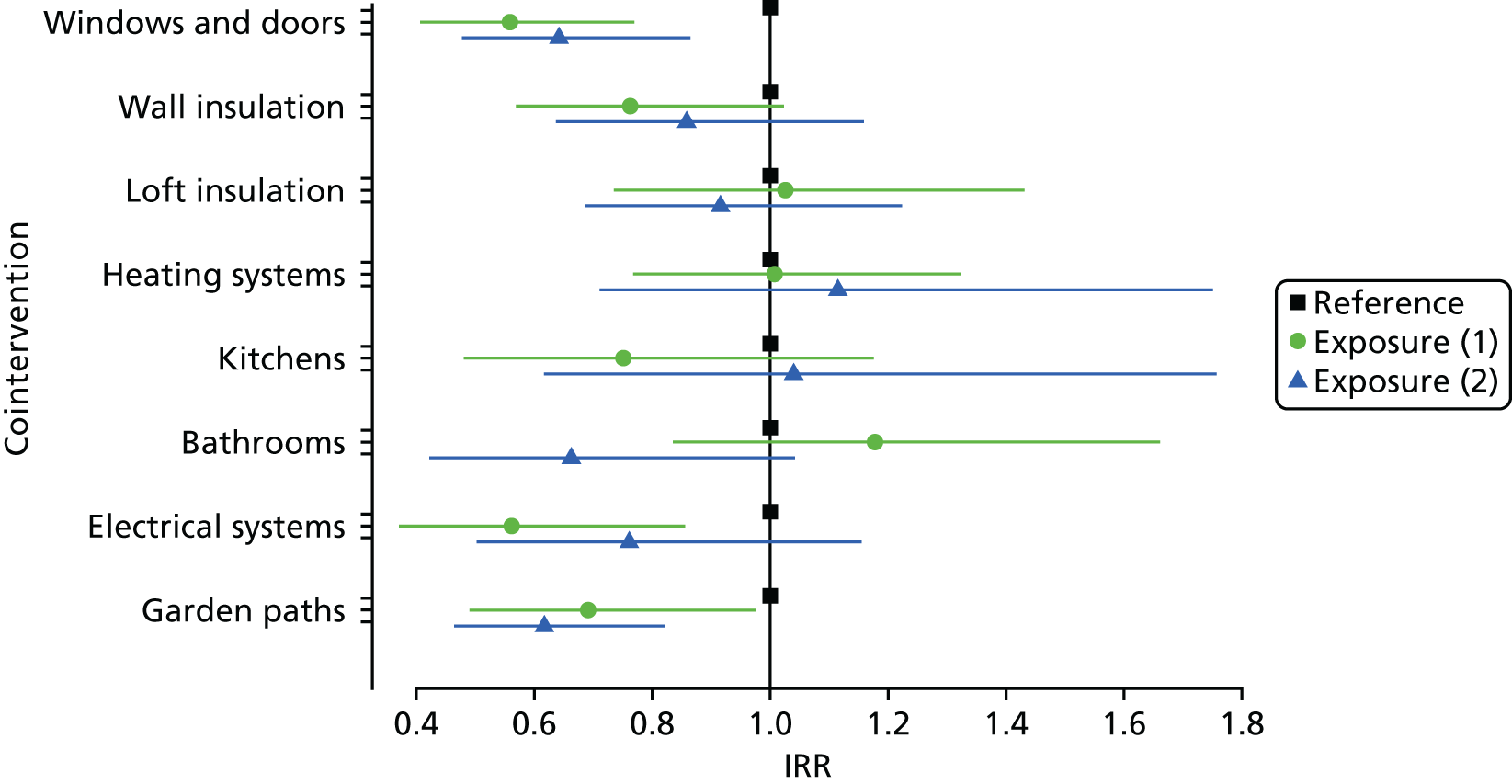
FIGURE 25.
Incidence rate ratios of emergency admissions for combined conditions for participants of all ages, by cointervention.
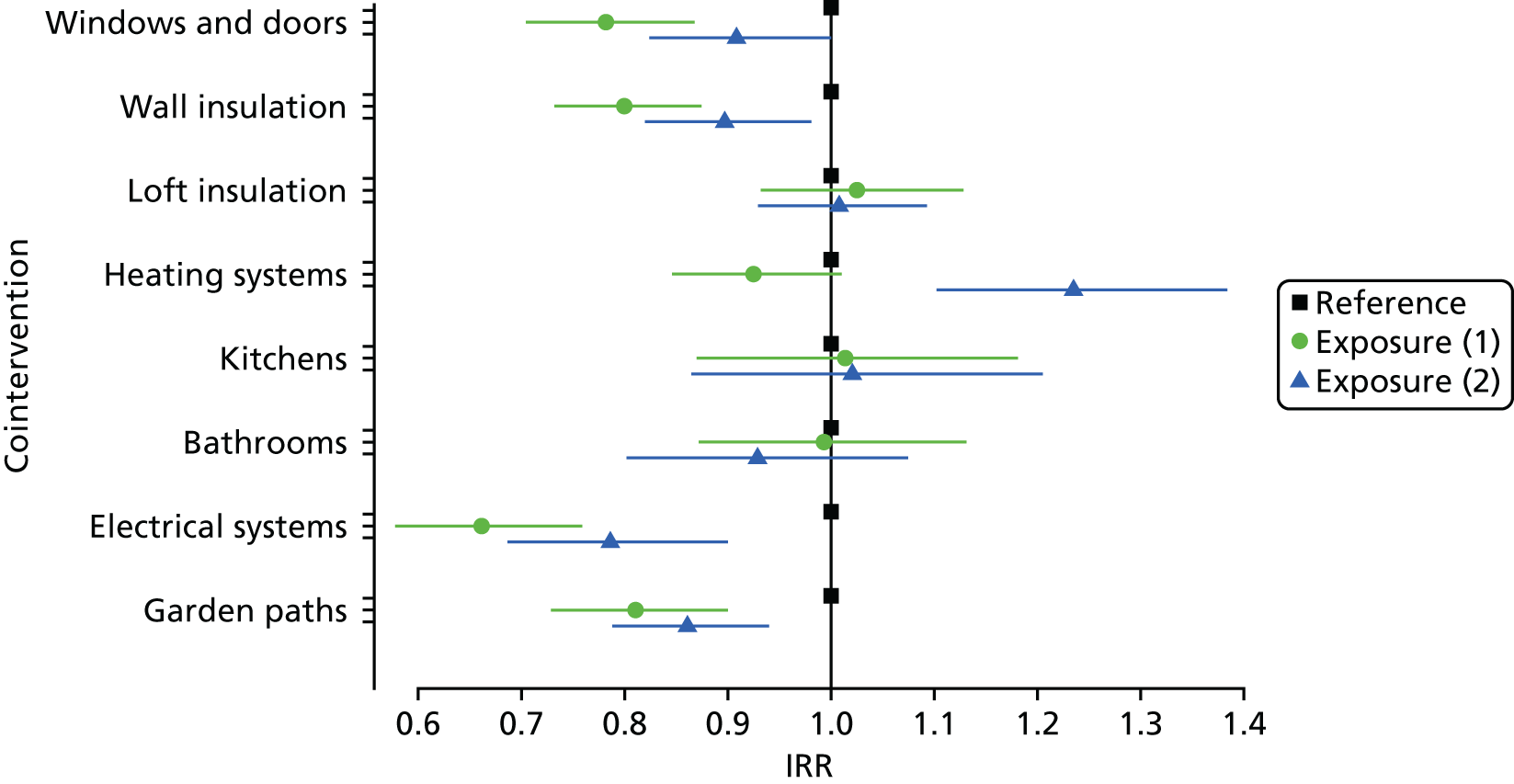
FIGURE 26.
Incidence rate ratios of emergency admissions for cardiovascular conditions for participants of all ages, by cointervention.
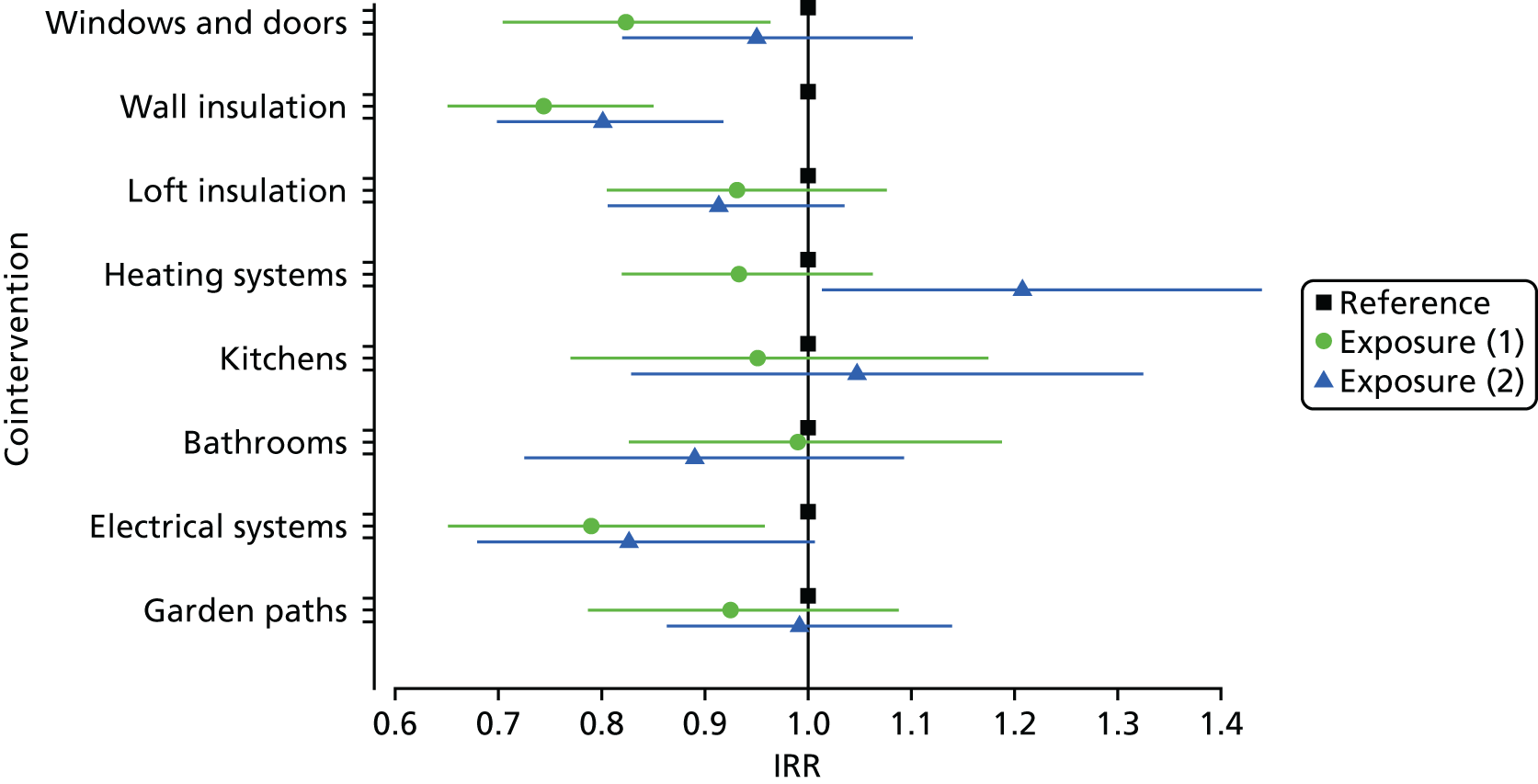
FIGURE 27.
Incidence rate ratios of emergency admissions for respiratory conditions for participants of all ages, by cointervention.
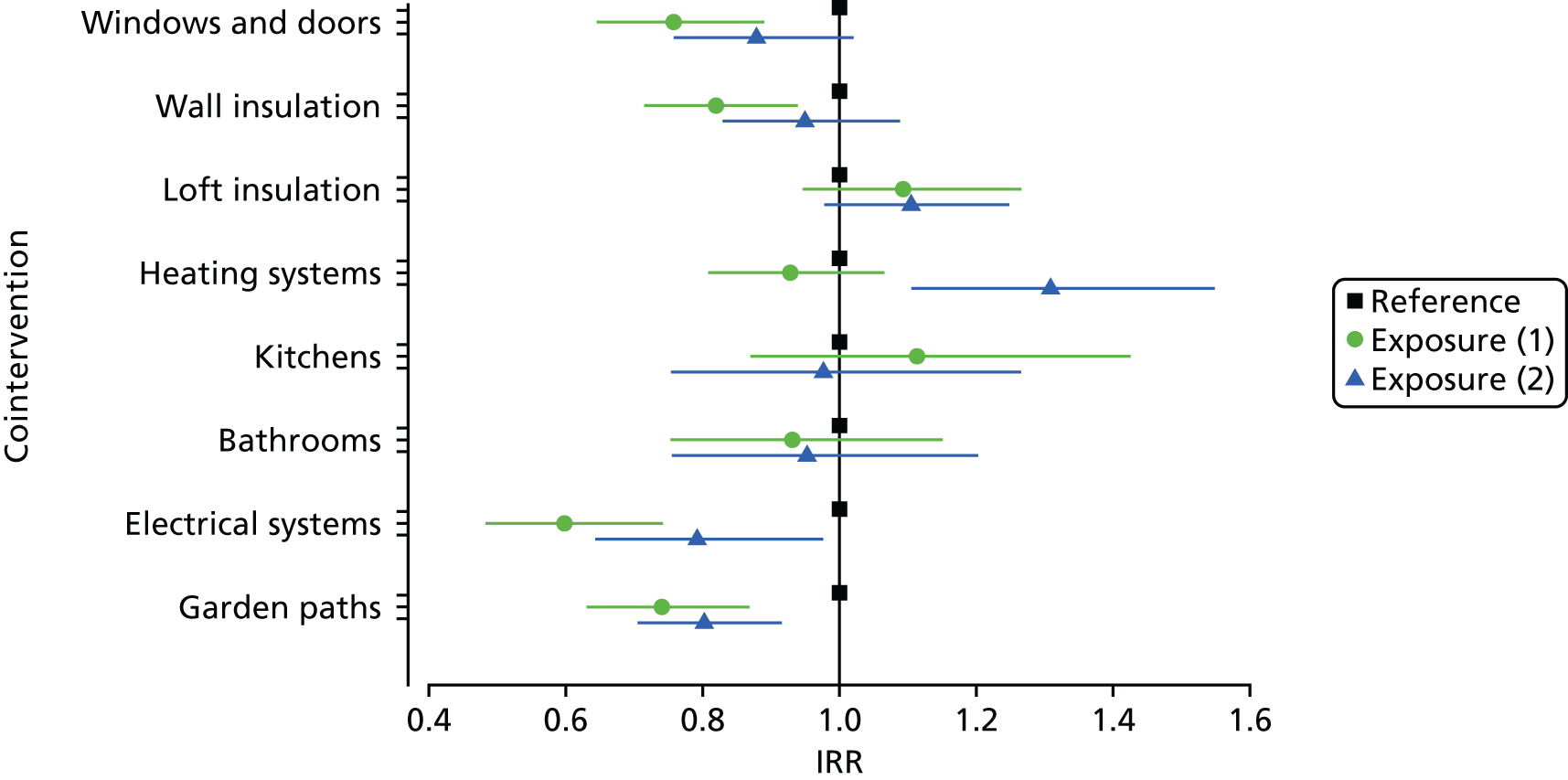
FIGURE 28.
Incidence rate ratios of emergency admissions for injury-related conditions for participants of all ages, by cointervention.
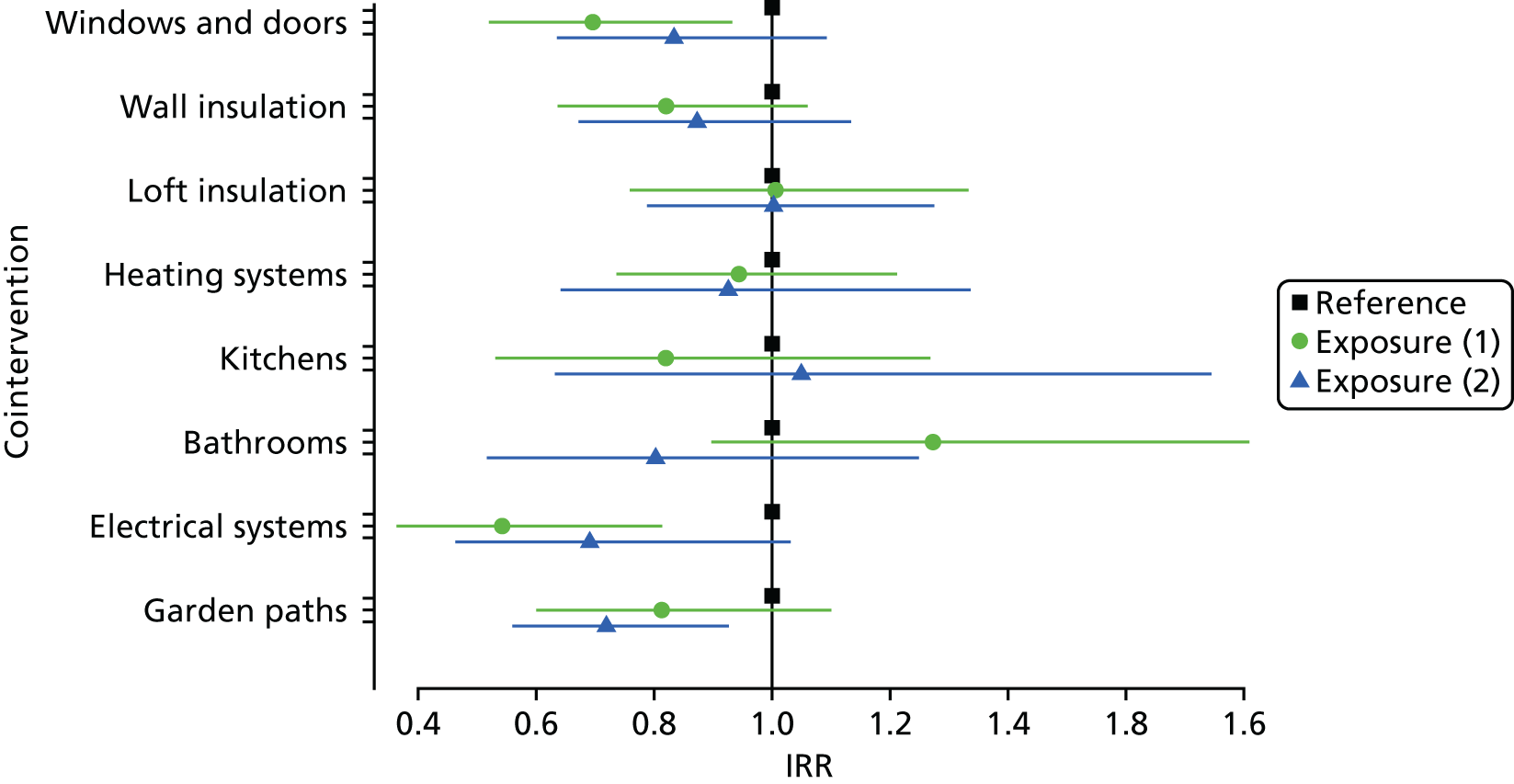
FIGURE 29.
Incidence rate ratios for respiratory prescriptions for participants with a history of asthma and COPD of all ages, by cointervention.
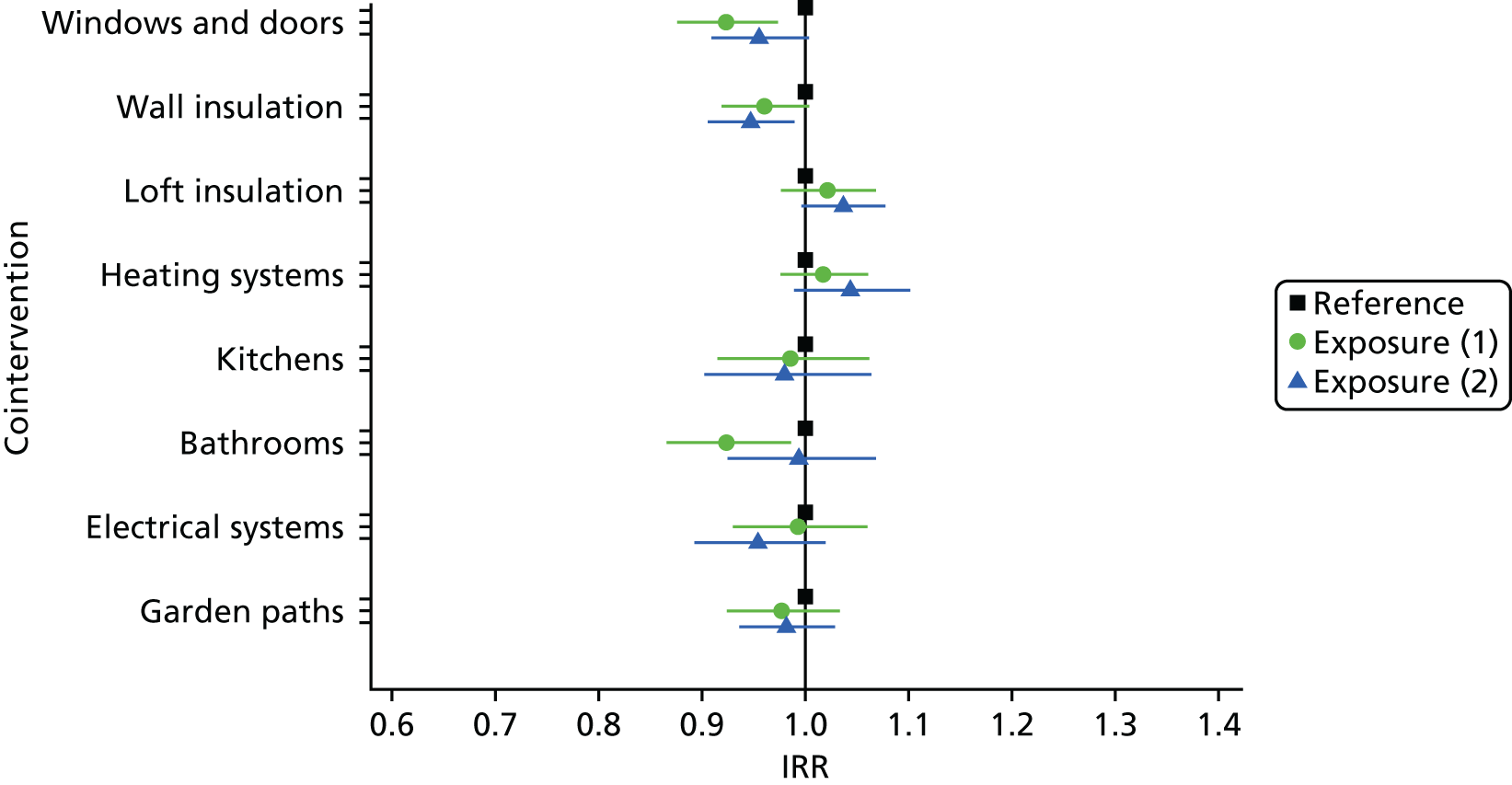
FIGURE 30.
Incidence rate ratios for GP contacts for participants with a history of asthma and COPD, by cointervention.
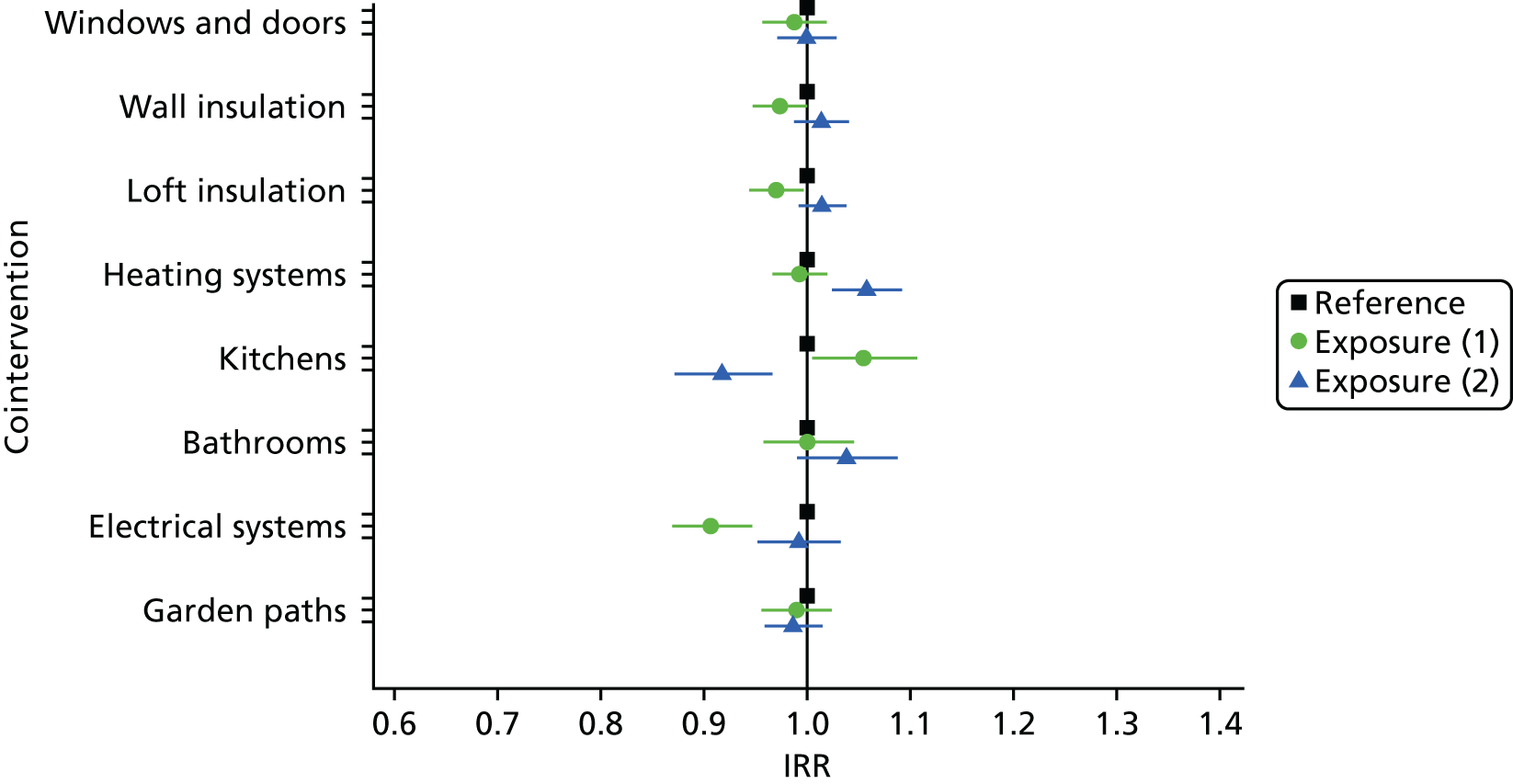
FIGURE 31.
Incidence rate ratios for prescribed medications for participants with a CMD, by cointervention.
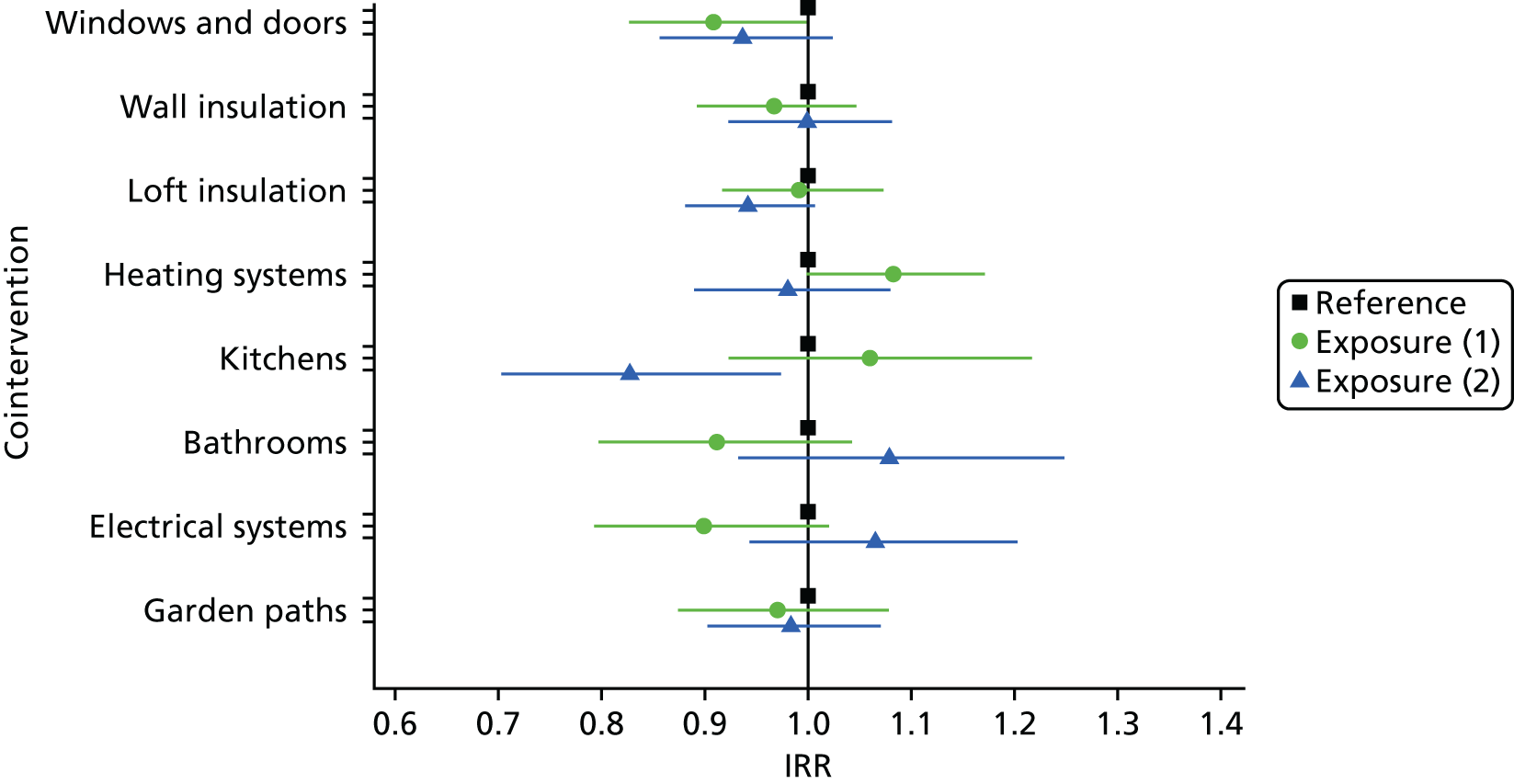
FIGURE 32.
Incidence rate ratios for emergency department attendances, by cointervention.
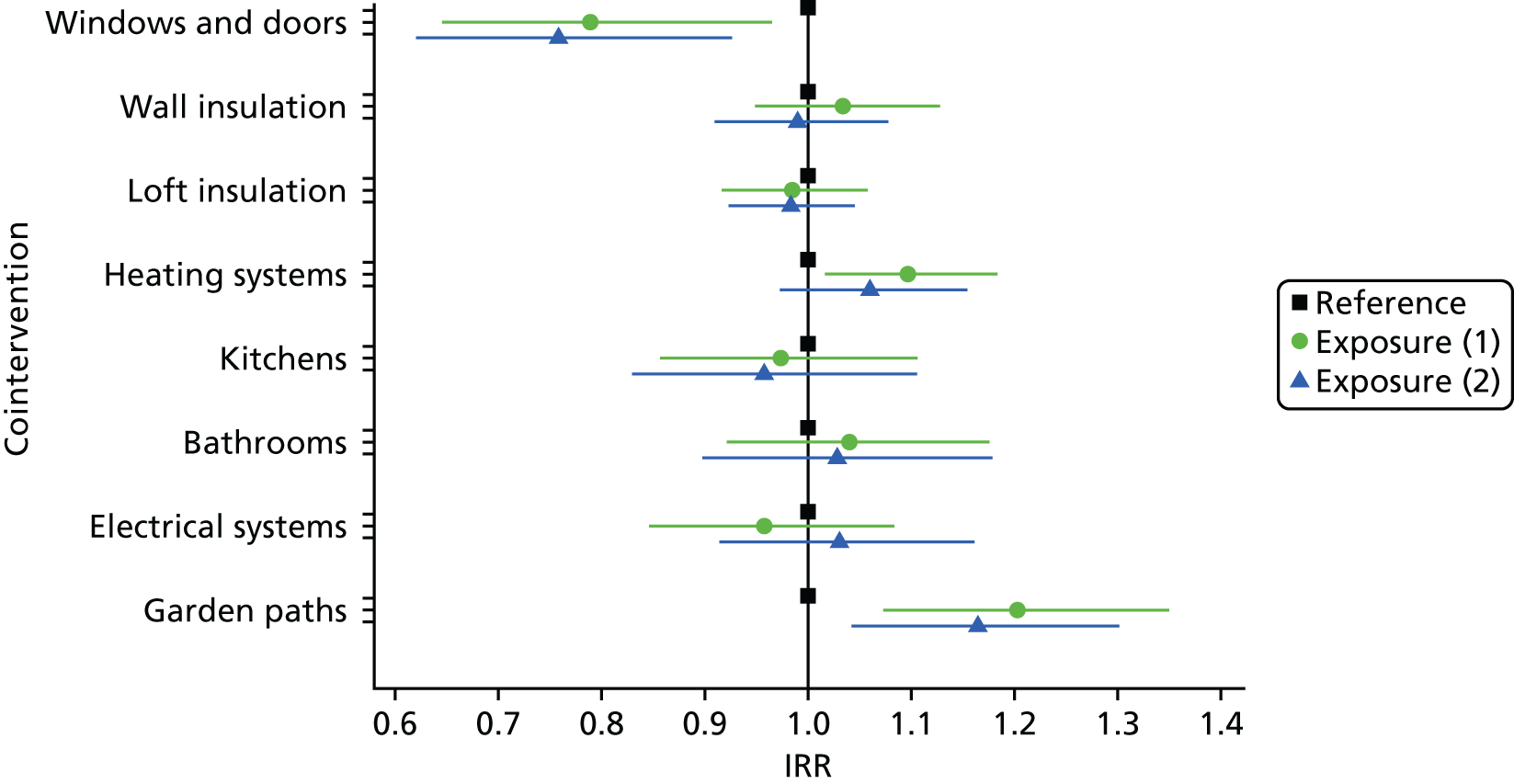
Appendix 8 Primary outcome and hospital admission codes
Hospital admission outcomes were defined using PEDW data within the SAIL databank, which contains anonymised hospital admission data for all Wales-based NHS hospital residents. The specific outcomes are described as emergency admissions to hospital for combined cardiovascular and respiratory conditions, and combined falls and burns. Secondary outcomes are emergency admissions for each of the four listed conditions. We describe our approach of extracting and classifying admissions.
We selected first episodes within a continuous inpatient stay for emergency admissions that were hypothesised as more likely to indicate the main reason of admission.
The primary diagnosis position was used to determine the reason for admission using ICD-10 codes. In cases when the primary diagnosis code recorded was a symptom or other factor influencing health rather than a clinically defined condition, we searched subsequent diagnosis code positions within the episode for the first clinically defining diagnosis code to classify the admission reason. An exception to this rule was created when no clinically defined conditions were present but the first diagnosis code indicated symptoms involving cardiovascular or respiratory systems.
Cardiovascular conditions were identified when the primary diagnosis code was in the ICD-10 ’diseases of the circulatory system’ chapter and respiratory conditions were selected when a primary diagnosis was in the ICD-10 ‘diseases of the respiratory system’ chapter.
Falls were identified when the primary diagnosis code was a traumatic injury, combined with a fall code in any subsequent diagnosis position that occurred in the home. Fall codes determined to be reasonably likely to have an association with the home environment were included, and the fourth character of the fall code was used to select falls occurring in the home.
Records with primary diagnosis burn codes, paired with a cause of burn code in any subsequent diagnosis position that occurred in the home, were selected as burn admissions. Cause of burn codes determined to be reasonably likely to have an association with the home environment were included, and the fourth character of the cause code was used to select burns occurring in the home.
Emergency admission episodes were aggregated into episode counts for monthly time periods from baseline through to follow-up.
Appendix 9 Read codes for asthma and chronic obstructive pulmonary disease cohort creation
For residents with GP data, we created a register of people who had a treatment, symptom or diagnosis suggesting that they had asthma or COPD at any point within their GP data record present in the SAIL databank. The Read codes are listed in Table 18; any mention of any code resulted in the person entering the register. All prescription codes used were counted for each month that the person was in the study.
| c11% | c6A% | 6630 | 663r. | H33z0 | R060F | |
| c12% | c6B% | 6635 | 663s. | H33z1 | R060G | |
| c13% | c71% | 8793 | 663t. | H33z2 | R060H | |
| c14% | c72% | 8794 | 663u. | H33zz | 14B3. | |
| c15% | c74% | 8795 | 663U. | H35y7 | 663K. | |
| c16% | cA1% | 8796 | 663v. | H47y0 | 66YL. | |
| c17% | cA2% | 8797 | 663V. | 1737 | 66YL. | |
| c18% | cd1% | 8798 | 663V0 | 2326 | H31.. | |
| c19% | cd2% | 173A. | 663V1 | 173B. | H36.. | |
| c1A% | ce1% | 178.. | 663V2 | 173e. | H37.. | |
| c1B% | ce3% | 178A. | 663V3 | 23D2. | H38.. | |
| c1C% | ce4% | 178B. | 663w. | 663a. | H39.. | |
| c1D% | ce5% | 1J70. | 663W. | 663b. | H3A.. | |
| c1a% | cf1% | 1O2.. | 663x. | 663c. | H3y.. | |
| c1E% | cg1% | 663.. | 663y. | 663F. | H3z.. | |
| c1c% | cg2% | 663d. | 66Y9. | 663G. | ||
| c22% | cg3% | 663e. | 66YC. | 663g1 | ||
| c23% | cg4% | 663e0 | 66YK. | 663g2 | ||
| c25% | cg5% | 663e1 | 66YP. | 663g3 | ||
| c31% | cg7% | 663f. | 66Yq. | 663g4 | ||
| c32% | ch1% | 663j. | 66Yr. | 663L. | ||
| c33% | ch2% | 663 J. | 8H2P. | 663l. | ||
| c34% | ch3% | 663m. | H3120 | 663M. | ||
| c41% | ci1% | 663n. | H33.. | 663S. | ||
| c42% | cj1% | 663N. | H330. | 663T. | ||
| c43% | ck1% | 663N0 | H3300 | 663Y. | ||
| c51% | cl1% | 663N1 | H3301 | 663z. | ||
| c53% | 1780 | 663N2 | H330z | 663Z0 | ||
| c61% | 1781 | 663O. | H331. | 663Z1 | ||
| c62% | 1782 | 663O0 | H3310 | H302. | ||
| c63% | 1783 | 663p. | H3311 | H3121 | ||
| c64% | 1784 | 663P. | H331z | H32.. | ||
| c65% | 1785 | 663P0 | H332. | H4640 | ||
| c66% | 1786 | 663P1 | H333. | H581. | ||
| c67% | 1787 | 663P2 | H334. | H5y16 | ||
| c68% | 1788 | 663q. | H335. | R0609 | ||
| c69% | 1789 | 663Q. | H33z. | R060E | ||
| 1825 | H06.. | H060F | H06z1 | H23z. | H270z | H5105 |
| 1827 | H060. | H060v | H07.. | H24.. | H28.. | H5109 |
| 23D5. | H0600 | H060w | H2. . . | H240. | H2y.. | H510z |
| 4JU9. | H0601 | H060x | H20.. | H241. | H2z.. | H511. |
| 4JUA. | H0602 | H060z | H200. | H243. | H30.. | H5110 |
| 4JUB. | H0603 | H061. | H201. | H24y. | H300. | H511z |
| 4JUK. | H0604 | H0610 | H202. | H24y7 | H301. | H51y. |
| A0222 | H0605 | H0611 | H203. | H24yz | H302. | H5303 |
| A521. | H0606 | H0612 | H20y. | H24z. | H30z. | H564. |
| A54x4 | H0607 | H0613 | H20y0 | H25.. | H357. | H56y1 |
| A551. | H0608 | H0614 | H20z. | H26.. | H5010 | Hyu08 |
| A730. | H0609 | H0615 | H21.. | H260. | H5012 | Hyu0A |
| A741. | H060A | H0616 | H22.. | H261. | H5014 | Hyu0B |
| A7850 | H060B | H0617 | H23.. | H263. | H51.. | Hyu0D |
| A79A. | H060C | H061z | H231. | H270. | H510. | Hyu0H |
| A7y02 | H060D | H062. | H232. | H2700 | H5103 | Hyu1. |
| AyuKN | H060E | H06z. | H233. | H2701 | H5104 | Hyu10 |
For the GP visits outcome, we also included Read codes indicating lower respiratory conditions; we also only searched for records for the study period for this outcome.
Appendix 10 General practice attendances
General practitioner data held in the SAIL databank do not allow the identification of GP visits; we therefore created a method to estimate the number of visits per month to allow proportional change to be measured. Total GP records were counted for each month that a person was included in the study and then multiplied by a proportion, depending on the age and year of GP record, to arrive at the dependant variable.
We used data obtained from The Health Improvement Network (THIN) database87 to calculate what proportion of records related to a GP visit. We hypothesised that proportions would change over time, by sex and by age, and, therefore, the approach required a review of proportion trends stratified by these variables. Following the analysis, sex was excluded, as there was minimal difference in proportions of events as visits. The final algorithm to derive attendances from proportions of events was based on year of event and age band (Table 19).
| Year of GP record | Age band (years), % | |||||
|---|---|---|---|---|---|---|
| 0–5 | 6–20 | 21–40 | 41–60 | 61–80 | > 80 | |
| 2005 | 40 | 40 | 27 | 21 | 17 | 13 |
| 2006 | 40 | 23 | 27 | 19 | 15 | 12 |
| 2007 | 40 | 21 | 23 | 17 | 14 | 13 |
| 2008 | 40 | 17 | 20 | 14 | 13 | 12 |
| 2009 | 40 | 19 | 20 | 14 | 11 | 12 |
| 2010 | 40 | 21 | 19 | 14 | 11 | 12 |
| 2011 | 40 | 18 | 17 | 13 | 11 | 11 |
| 2012 | 40 | 14 | 15 | 12 | 11 | 10 |
| 2013 | 40 | 9 | 16 | 13 | 11 | 11 |
| 2014 | 40 | 9 | 16 | 13 | 11 | 11 |
| 2015 | 40 | 9 | 16 | 13 | 11 | 11 |
There are a number of strengths and limitations of THIN data88 that may limit the accuracy of the derived GP visit outcome.
List of abbreviations
- CCC
- Carmarthenshire County Council
- CHS
- Carmarthenshire Homes Standard
- CHS+
- Carmarthenshire Homes Standard Plus
- CI
- confidence interval
- CMD
- common mental health disorder
- COPD
- chronic obstructive pulmonary disease
- EDDS
- Emergency Department Data Set
- GP
- general practitioner
- HTA
- health technology assessment
- ICD-10
- International Classification of Diseases, Tenth Edition
- IRR
- incidence rate ratio
- NICE
- National Institute for Health and Care Excellence
- PEDW
- Patient Episode Dataset for Wales
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REAT 2.0
- revised Residential Environment Assessment Tool
- SAIL
- Secure Anonymised Information Linkage
- TIDieR
- Template for Intervention Description and Replication
- WHQS
- Welsh Housing Quality Standard
