Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 17/48/02. The contractual start date was in December 2017. The final report began editorial review in June 2018 and was accepted for publication in October 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Aceves-Martins et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Food insecurity (FI) is a social and economic problem that involves difficulties in accessing sufficient, safe and nutritious food that is necessary to meet individuals’ dietary requirements and preferences for a healthy life. 1 FI is a multifaceted phenomenon, with each stage typified by conditions and experiences of food insufficiency and behavioural responses. 2 FI may be experienced when there is uncertainty about future food availability and access, insufficiency in the amount and kind of food required for an optimal and healthy nutrition status or the need to use socially unacceptable ways to acquire food. 3
Food insecurity can be defined as the inadequate or unreliable availability of safe, nutritionally adequate food, or inadequate or uncertain capability of acquiring adequate foods in socially conventional and safe ways. 4 However, the UK governmental authorities have cautioned against attempting to capture all aspects of FI in one definition: ‘The factors that impact on household food security are complex. There are multiple indicators, such as quality, variety and desirability of diet as well as total intake, not all of which are measured consistently. It is therefore, very difficult and potentially misleading to attempt to develop a single classification of food insecurity’ (contains Parliamentary information licensed under the Open Parliament Licence v3.0). 5
Food has a vital role in the functioning and welfare of the family unit, which places further stress on food-insecure children. FI in children is contingent not only on food but also on related areas of children’s daily lives, such as school, their personal welfare and their responsibilities to other family members. Children’s experiences of FI are evident in three areas of their self: cognitive (the child is aware that food is scarce and that coping strategies are used by the family), emotional (the child experiences feelings associated with FI, such as worry, sadness or anger) and physical (the child experiences feelings such as hunger, pain, tiredness or weakness). In addition, children may take responsibility for their FI by participating in pertinent adults’ strategies to manage their limited resources, initiating their own strategies or generating their own resources to obtain food or money for food. 6,7
There are a number of potential negative developmental consequences for children experiencing FI, for example poor health, poor dietary intake, high consumption of energy-dense foods, inadequate intake of micronutrients, behavioural problems, poor school performance, absenteeism from school, lower levels of physical activity, delayed language development and atypical social interactions. 7–11
A report published in 2017 by the Food and Agriculture Organization of the United Nations and other international organisations such as United Nations International Children’s Emergency Fund (UNICEF) and the World Health Organization (WHO)12 shows that, after a prolonged decline, world FI appears to be on the rise again. The estimated worldwide number of undernourished people increased from 777 million in 2015 to 815 million in 2016. The report further states that it is unclear whether the recent increase in hunger and FI indicates the beginning of an upwards trend or reflects a more transient situation. Nevertheless, the recent increase has caused a growing concern among national and international organisations and governmental authorities around the globe. Food security (FS) is one of the determinants of nutritional outcomes, especially for children. 12
It is therefore important to improve current understanding of the extent and consequences of FI in children, as well as to consider any strategy or programme undertaken to address it. It is worth pointing out that the Food Foundation (a non-governmental organisation – http://foodfoundation.org.uk/) is currently conducting an independent inquiry into FI affecting children in the UK, in association with the Office of the Children’s Commissioner, England, Wales, Northern Ireland and Scotland. This rapid review was undertaken as part of this national inquiry.
General objective
To determine the nature, extent and consequences of FI affecting children (aged ≤ 18 years) in the UK.
Specific objectives
This rapid review will focus on five research questions (RQs):
-
What is the nature and what are the determinants of child FI in high-income countries?
-
What are the incidence, prevalence and costs of child FI in the UK (including recent trends)?
-
What is the impact of FI on children’s health and social well-being in high-income countries?
-
What interventions exist to reduce, eliminate or mitigate the effects of child FI in high-income countries?
-
What is the cost-effectiveness of existing interventions that aim to reduce, eliminate or mitigate the effects of child FI in high-income countries?
Chapter 2 Methods
Inclusion criteria
Type of studies
All study designs were considered in this review. Quantitative or qualitative assessments of FI either from young people themselves (if available) or from any parent, relative, caregiver or professionals who engage with them were included.
Type of participants
Children from birth to 18 years old (at the start of the study or evaluation) of any ethnicity or sex living in specified high-income countries were included. If samples included people aged > 18 years but the mean age was ≤ 18 years, the study was included.
According to a UNICEF report published in 2015,9 children as young as 7 years can respond accurately to questionnaire items sensitive to FI. However, as not all studies in the literature were likely to provide experiences of FI from children, for children aged > 7 years we included both direct (from children) and indirect (from parent/caregiver) experiences or assessments of FI. Furthermore, with the intention of evaluating child FI in depth, we included studies that focused solely on child FI, as well as studies that measured or addressed child FI alongside household FI, as long as they provided outcomes measured in children (using tools that included any question about or measure of FI in children living in the household).
Type of setting
To gain a broad understanding of the nature and consequences of child FI, as well as of the interventions designed to address it, the literature from countries with developed economies, according to the Organisation for Economic Co-operation and Development categorisation,13 were included. However, in recent years, an economic recession has been experienced by several countries in Europe, resulting in diverse responses in the affected countries, for example public budget cuts and health and welfare sector austerity measures. 14,15 There is growing evidence to suggest that the different governmental responses to this economic crisis and its consequences (e.g. unemployment, inflation of food prices, reduction in salaries and growing costs of fuel and housing) may have an impact on a broad set of social, economic and health domains and contribute to the increased prevalence of FI. 14,15 Nevertheless, not all European countries facing such hardship have experienced these problems, and statistics of FI differ among countries. 16 For the purpose of this rapid review, we focused only on those European countries (the UK, France, Germany and Italy) that are part of the G7 (major developed economies worldwide). We also included Ireland because of its regional proximity and similarity to the UK in terms of social and political context, as well as the Nordic countries, which are among the most affluent countries worldwide and where FI has been successfully tackled by well-established social security schemes. 17 Thus, studies or reports from the following industrialised countries were deemed suitable for inclusion: the UK, Ireland, France, Germany, Italy, Sweden, Norway, Denmark, Finland, Iceland, Canada, the USA, Japan, Australia and New Zealand.
Exclusion criteria
Reports were excluded if they were published before 1995, focused solely on household FI, measuring outcomes on adults (with the exception of longitudinal studies where children were followed into adulthood, with suitable measurements of FI), or related to the agricultural or farming aspects of FI. Studies that considered the target population as food insecure for participating in a programme, without a measurement of FI in participants, were also excluded.
Search strategy
Reports from 1995 onwards were included in this rapid review to focus on information conducted under contemporary epidemiological and environmental circumstances of children’s FI, focusing on high-income countries (listed above). All searches were restricted to English-language publications.
Published literature was sought from health-care, nutrition, education and social science databases. The literature searches were designed to address RQs 3–5, but any information identified in the search results that was relevant to RQs 1 and 2 above was also retrieved. The databases searched on 4 December 2017 were MEDLINE (including In-Process & Other Non-Indexed Citations and E-pub ahead of print files), EMBASE, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Commonwealth Agricultural Bureaux (CAB) abstracts, The Cochrane Library, the Education Resources Information Centre (ERIC), PsycINFO, the Social Science Citation Index and the Applied Social Sciences Index and Abstracts (ASSIA). No study design restriction was applied. Appendix 1 provides full details of search strategies.
Other methods of identifying relevant information sources
Reference lists of identified studies were scrutinised for additional publications, and experts in the field were contacted for additional relevant reports. References of included studies were screened. Any references not identified in our search and meeting the inclusion criteria were retrieved and data were extracted. Furthermore, the websites of UK government, public and private institutions, charities and international organisations concerned with child health and poverty were consulted for relevant documents and information (the complete list of relevant websites searched is presented in Appendix 1, Sources of grey literature: websites consulted). From the results of scoping searches, it was anticipated that these sources would provide the majority of the evidence for the overviews to address RQs 1 and 2.
Data screening, selection and synthesis
The review process for the selection and synthesis of the current relevant evidence was based on the following stages.
-
Title/abstract screening (by one reviewer, with 10% checked by a second reviewer).
-
Full-text screening (by one reviewer, with 10% checked by a second reviewer).
-
Categorisation of texts screened according to the RQ of interest.
-
Data extraction (by one reviewer and double checked by a second reviewer).
-
Information recorded included authors, title of the publication, journal or source, publication year, study design, aim of the study, study period, geographical location, inclusion criteria, exclusion criteria, number of participants, age of participants (children or adolescents), tool or survey used to measure child FI, person who provided information on child FI (children themselves, parents, other), main findings (e.g. factors related to FI, young people’s experience of FI, prevalence of FI, nutritional and non-nutritional consequences of FI, results of interventions to reduce or mitigate FI), source of funding, and whether the analysed sample was part of any project/study or evaluation programme.
-
Data synthesis
For all RQs, the information extracted was tabulated and described narratively. If results were available for children, adults or households, only those reported for children or households with children were considered. Alongside the description of the results, we recorded how FI was measured in children. Measurement of FI was categorised as direct (when information on FI was directly retrieved from children) or indirect (when information of FI was retrieved from a parent/caregiver or another person). Furthermore, the health impact was categorised as direct (health and nutritional outcomes measured in children) or indirect (measures of food access including stability in food access, household income or household food production).
Chapter 3 Results
Overall characteristics and results of the included studies
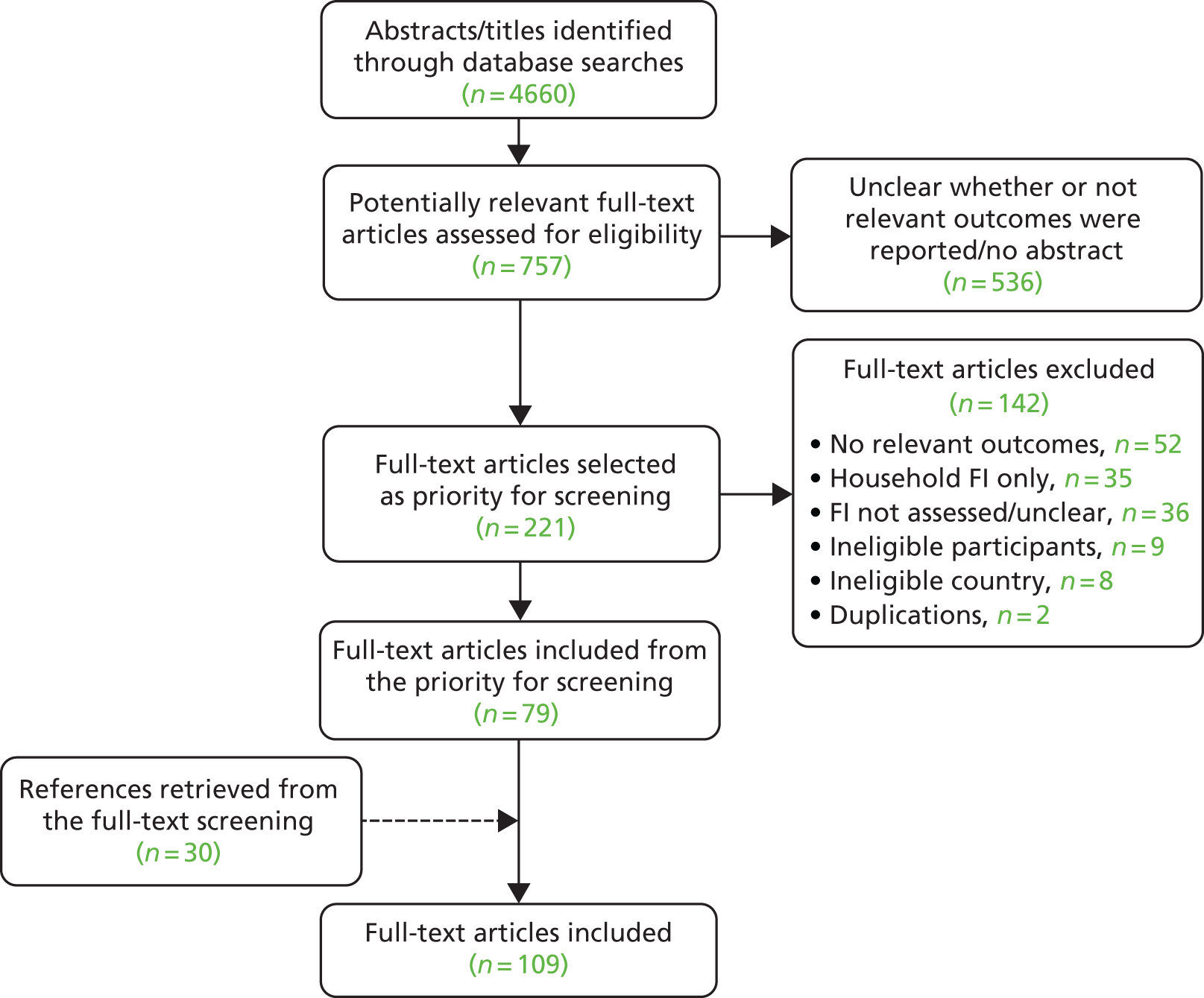
From 4660 initially retrieved references published in the current literature, 757 potentially relevant abstracts were assessed for eligibility. As this was a large number of references for full-text screening in the context of a rapid review, it was decided to select only those abstracts that explicitly mentioned child FI.
Therefore, 221 articles were selected for full-text screening, of which 79 were included for screening. The main reasons for exclusion were the lack of relevant outcomes, household FI measurements (without child-specific measurements), lack of assessment of FI and ineligible participants or countries. During data extraction of the 79 included articles, the references were screened and a further 30 studies were identified as potentially relevant, assessed for eligibility and incorporated. This totalled 109 published references included in this rapid review. It was noticed that a number of the 30 articles included at the reference screening stage had appeared on the original list of 4660 abstracts. For completeness, this list was rescreened and a further 30 potentially relevant articles were identified. However, because of the time and resource constraints that are typical of rapid reviews, we were not able to include these studies. It is worth pointing out that the 30 studies did not mention child FI in their abstracts and had not appeared on the reference lists of any studies included in this rapid review; therefore, it was considered unlikely that any important information would be missed. Figure 1 presents the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of study selection.
FIGURE 1.
The PRISMA flow chart.
The grey literature that had been identified by the initial scoping searches was scrutinised systematically by one reviewer but the process was not documented owing to its more ad hoc nature.
Overall, of the 109 included studies, 57 addressed RQ 1 (nature and determinants of child FI),6,18–73 73 addressed RQ 3 (impact of FI on children’s health and social well-being),9,12,19–21,24,26–29,36,39,41,42,44,45,47,51–54,56–58,60,61,63,66,67,69,72–114 15 addressed RQ 4 (interventions to tackle child FI),26,50,71,74,78,83,98,115–122 and none addressed RQ 2 (incidence, prevalence and costs of child FI in the UK) or RQ 5 (cost-effectiveness of interventions). Thirty-six studies addressed more than one RQ. 19–21,24,26–29,36,39,41,42,44,45,47,50–54,56–58,60,61,63,66,67,69,71–74,78,83,98 Figure 2 shows the studies identified for each RQ.
FIGURE 2.
Overview of included studies.
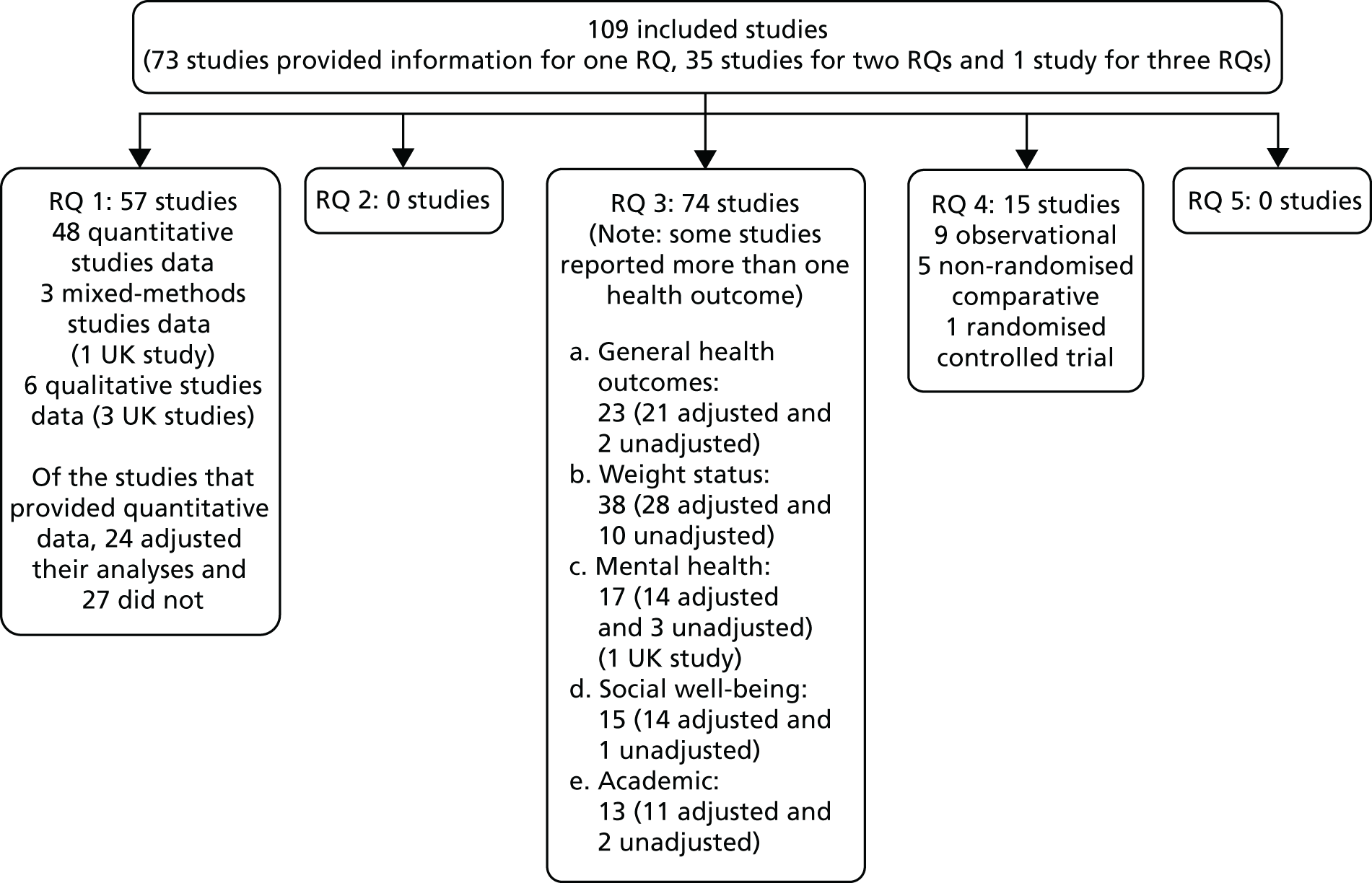
Most of the studies identified were from North America (91 from the USA and 10 from Canada),21,23,27,42,43,45,46,68,75,76 five were from the UK,19,30–32,59 one was from Ireland,106 one was from Australia54 and one was from New Zealand. 122
Of the 109 studies included in the review, 100 were quantitative studies,9,12,18–24,26–29,33,35–54,56–58,60,61,63–82,84–123 six were qualitative studies6,25,30–32,55 and three were mixed-methods studies. 59,62,64 Of the 100 quantitative studies, 73 were cohort or cross-sectional observational studies,9,21,22,24,26–29,33,36–38,41,43–54,57,58,60,61,63–71,73–79,81,82,84–88,97–116 20 were longitudinal cohort studies,12,18–20,23,35,39,40,42,56,72,80,89–96 two were randomised controlled trials (RCTs)122,123 and five were non-randomised comparative studies. 117–121
The age of the target population varied across studies. Twenty-four studies included children aged < 5 years, 22 studies included adolescents (aged > 10 years), 62 studies included both children and adolescents of various ages, one study interviewed parents 48 hours after giving birth and again at 12, 36 and 60 months after giving birth,37 and one study included stakeholders engaging with school-aged children. 31 The characteristics of participants are further detailed in Appendix 2.
Child food insecurity measurements
Studies that focused solely on child FI and those that included measures of child FI alongside household FI were considered suitable for inclusion, as long as they reported outcomes measured in children. From each included study, childhood FI measurements were identified and tabulated (see Appendix 3).
Overall, the most commonly used tool to measure FI in children (or their households) was the 18-item United States Department of Agriculture Household FS Module (referred to hereafter as the 18-item USDA module). Overall, 51 studies used the 18-item USDA module as the main tool for measuring FI,9,12,18,20,21,24,26,28–30,34,35,39–41,43,44,49,51,53,56–58,66,67,71,72,80–83,85,86,88–96,100,103,104,110,113,115,116,120,123 eight used a modified version of it,27,45,46,64,75,97,109,121 six used only the eight child-specific items of the tool,37,38,48,50,63,74 and six used individual items of it (rather than those identified as child-specific items). 47,65,78,102,105,108 The 18-item USDA module was developed in 1995 as a result of a co-operative effort among US federal government agencies and private sector experts, through the Food and Nutrition Service and Economic Research Service of the US Department of Agriculture (USDA) and the Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) of the US Department of Health and Human Services. 2 The original tool has been slightly modified over the years and uses a continuous, linear scale, which measures the degree of severity of FI/hunger experienced by a household in terms of a single numerical value. The tool comprises 10 items that evaluate FI in adults in the household, and eight items that evaluate FI in children of the household. 124 The unit of measure used for the scale is a matter of convention; the USDA guide suggests a classification of households with one or more children based on the following four main categories.
-
Raw score 0: high FS or food secure – household members have no, or minimal, presence of FI.
-
Raw score 1–2: marginal FS or food insecure without hunger – household members report FI, with concerns on the adequacy of the household food supply and in modifications to household food management.
-
Raw score 3–7: low FS or food insecure with hunger (moderate) – adult household members report a reduction in food intake to an extent that indicates that adults have repeatedly experienced a physical sensation of hunger. In food-insecure households with children, such reductions are not yet observed in children.
-
Raw score 8–18: very low FS or food insecure with hunger (severe) – adult household members have reduced the children’s food intake, indicating that the children have experienced hunger.
Apart from the 18-item USDA module, the USDA has provided additional tools that have been used in the literature, for example the 6-item USDA module,22 7-item USDA module19 and 16-item USDA module. 54 The USDA also adopted a tool developed by researchers at the University of Southern Mississippi125 as ‘The Child Food Security Survey Module’, which assesses FI in children aged ≥ 12 years by means of a 9-item module. This module (or some of its items) was used by nine studies included in this rapid review. 50,52,60,62,68,77,98,107,112
With regard to other tools used to measure FI, four studies used the Radimer/Cornell Measures of Hunger and FI: two out of the four studies used the 12-item version36,61 and two studies used the 10-item version. 33,59 One further study used three questions adapted from the Radimer/Cornell tool. 23 Four studies used the Community Childhood Hunger Identification Project (CCHIP) survey. 69,73,99,117
To assess FI, some studies used questionnaires or graphic tools generated or adapted by the investigators, or semistructured interviews. For example, some studies, which reported results from the Health Behaviour in School-Aged Children (HBSC) study, asked participants (adolescents) the following question: ‘Some young people go to school or to bed hungry because there is not enough food at home. How often does this happen to you?’76,84,106 Another study asked participants the following single question: ‘Has [the child] ever expressed being hungry because the family has run out of food or money to buy food?’42 One study assessed FI and hunger through a graphic survey (cartoons) for children118 and another assessed this by using an analogue scale that consisted of a cardboard cut-out doll with an adjustable stomach, which allowed children to dynamically assess hunger and satiety. 122 Seven studies measured FI through interviews (in-depth face to face or semistructured) with children or with parents and stakeholders involved with food-insecure children. 6,25,30–32,55,97
Twenty-one studies measured FI directly from children or adolescents,6,25,52,55,60,62,64,68,70,76,77,79,84,98,106,107,111,112,114,118,122 eight included measurements from both the parent/caregiver and the child/adolescent,22,30,32,47,50,69,73,101 one included measurements from parent(s)/caregiver(s), the child/adolescent and school staff,117 72 included only the parents’/caregivers’ evaluation of child FI or household FI,12,18–21,23,24,26–29,33–41,43–46,48,49,51,53,54,56–59,61,63,65–67,71,72,74,75,78,82,83,85,86,88–96,99,100,102–105,108–110,113,116,119–121,123,126 five reported that measurement of FI was provided by a primary caregiver (adult or older sibling living in the household, not specifically the parents)9,42,80,81,97 and in one study FI was reported by a caseworker in child protection services. 87
Research question 1: what is the nature and what are the determinants of child food insecurity in high-income countries?
Fifty-seven studies investigated the relationship between child FI and various individual, familial, socioeconomic, demographic or cultural factors. 6,18–73 Of these 57 studies, six were qualitative studies6,25,30–32,55 and three were mixed-methods studies. 59,62,64 With regard to the qualitative and mixed-methods studies, one reported the experiences of stakeholders31 whereas the remaining studies reported the experiences of children, adolescents or parents. Owing to the multifactorial nature of FI, there are different variables that could relate (positively or negatively) with FI. From the included studies, 24 considered factors related to child FI and adjusted their analyses for potentially explanatory or confounding variables. 18,20–24,26,27,35,37,38,40,42,48–51,53,54,61,65,70–72 The characteristics most frequently assessed were children’s demographic characteristics (e.g. age, sex or ethnicity), parental factors [e.g. socioeconomic status (SES), employment, immigration status, marital status] and household characteristics (e.g. neighbourhood SES, number of people living in the household, adults in the household). Eight studies reported both adjusted and unadjusted analyses. 26,37,40,48,50,51,53,71 The findings of the main studies that assessed factors related to child FI and adjusted their analyses for potential explanatory or confounding variables are presented in Appendix 4, and the main findings of the studies that assessed factors relating to child FI but did not adjust their analyses for potential explanatory or confounding variables are presented in Appendix 5.
Results from quantitative data
A number of factors that were likely to increase the risk of child FI were identified in the 51 studies that used quantitative or mixed methods. Factors reported in more than one quantitative study with analyses adjusted for appropriate variables are summarised in Table 1.
| Category | Studies reporting outcome [author, date, country (number of participants)] | Summary of factor(s) related to child FI |
|---|---|---|
| Material deprivation |
Carter et al. 2012, Canada23 (n = 1746) Kenney 2008, USA37 (n = 1073) |
One study reported that material deprivation is associated with greater FI for children37 and the other study did not23 |
| Parents’ employment |
Sharkey et al. 2011, USA61 (n = 610) Ramsey et al. 2011, Australia54 (n = 185) |
One or both parents being unemployed was significantly associated with an increased risk of child FI |
| Number of people in household |
Egeland et al. 2011, Canada27 (n = 388) Jacknowitz et al. 2015, USA35 (n = 7850) |
Compared with food-secure households, child food-insecure households showed a greater ratio of children to adults in the home and a greater prevalence of household crowding |
| Neighbourhood social cohesion and disorder |
Carter et al. 2012, Canada23 (n = 1746) Kimbro et al. 2012, USA40 (n = 11,610) |
Low social cohesion, high social deprivation, high disorder and unsafe neighbourhoods were environmental factors related to child FI |
| Emotional status |
Jacknowitz et al. 2015, USA35 (n = 7850) Zaslow et al. 2009, USA72 (n = 10,221) |
Households with higher levels of FI had higher levels of depression. Changes in maternal depression (becoming depressed or recovering from depression) were associated with transitioning into and out of FI, respectively |
| FI in parents |
Bruening et al. 2017, USA22 (n = 55) Morrissey et al. 2016, USA49 (n = 12,550) |
Adolescents were more likely to be food insecure if their mothers were food insecure. Children in high-poverty neighbourhoods were more likely to be food insecure or live with a food-insecure adult |
| Living location |
Carter et al. 2012, Canada23 (n = 1746) Jacknowitz et al. 2015, USA35 (n = 7850) Morrissey et al. 2016, USA49 (n = 12,550) |
Living in rural areas rather than in urban areas was not associated with an increased risk of FI |
| Living property characteristics |
Broughton et al. 2006, Canada21 (n = 142) Egeland et al. 2011, Canada27 (n = 388) Kirkpatrick et al. 2010, Canada42 (n = 9142) Ramsey et al. 2011, Australia54 (n = 185) |
Living in public, rented or assisted housing was significantly associated with an increased risk of child FI |
| Children’s ageing |
Kirkpatrick et al. 2010, Canada42 (n = 5809) Carter et al. 2012, Canada23 (n = 1746) Whitbeck et al. 2006, USA70 (n = 428) Ramsey et al. 2011, Australia54 (n = 185) |
Mixed, inconsistent findings: one study reported a negative association between age and FI,23 two studies reported a positive relationship42,70 and one study reported no relationship54 |
| Number of parents in household |
Arteaga et al. 2017, USA18 (n = 2150) Carter et al. 2012, Canada23 (n = 1746) Kimbro et al. 2012, USA40 (n = 11,610) Ramsey et al. 2011, Australia54 (n = 185) |
Children in single-parent families were more likely to report FI. Household FI risk was higher in two-parent families |
| Maternal age |
Arteaga et al. 2017, USA18 (n = 2150) Carter et al. 2012, Canada23 (n = 1746) Kersey et al. 2007, USA38 (n = 4278) Kimbro et al. 2012, USA40 (n = 11,610) |
Mixed, inconsistent findings: two studies reported a positive association between maternal age and FI,18,40 one study reported a negative association between maternal age of < 21 years and FI38 and one study reported no association23 |
| Ethnicity |
Bhargava et al. 2008, USA20 (n = 7635) Jacknowitz et al. 2015, USA35 (n = 7850) Kimbro et al. 2012, USA40 (n = 11,610) Morrissey et al. 2016, USA49 (n = 12,550) Nalty et al. 2013, USA50 (n = 48) |
Hispanic children reported significantly higher FI levels than children of other ethnicities. Children from African American neighbourhoods were more likely to experience FI than those from white neighbourhoods |
| Number of siblings |
Kirkpatrick et al. 2010, Canada42 (n = 9142) Egeland et al. 2011, Canada27 Bhargava et al. 2008, USA20 (n = 7635) Kimbro et al. 2012, USA40 (n = 11,610) Sharkey et al. 2011, USA61 (n = 610) Ramsey et al. 2011, Australia54 (n = 185) |
Overall, there was a significant association between child FI and the number of siblings/children in the household. One study reported no association54 |
| Parents’ education |
Bhargava et al. 2008, USA20 (n = 7635) Kersey et al. 2007, USA38 (n = 4278) Kimbro et al. 2012, USA40 (n = 11,610) Morrissey et al. 2016, USA49 (n = 12,550) Yu et al. 2010, USA71 (n = 3799) Ramsey et al. 2011, Australia54 (n = 185) |
Higher levels of education reported by parents (or mothers) were associated with lower levels of child FI. One study reported no association54 |
| Parental nativity |
Arteaga et al. 2017, USA18 (n = 2150) Carter et al. 2012, Canada23 (n = 1746) Chilton et al. 2009, USA24 (n = 7216) Kersey et al. 2007, USA38 (n = 4278) Miller 2016, USA48 (n = 36,302) Sharkey et al. 2011, USA61 (n = 610) Ramsey et al. 2011, Australia54 (n = 185) |
In general, children in immigrant families in the USA were more likely to experience FI than those in non-immigrant families. Conversely, an Australian study showed that children with a parent born outside Australia were less likely to be food insecure than those with Australian-born parents |
| SES/household income |
Kirkpatrick et al. 2010, Canada42 (n = 3333) Broughton et al. 2006, USA21 (n = 142) Carter et al. 2012, Canada23 (n = 1746) Dunifon and Kowaleski-Jones 2003, USA26 (n = 1600) Jacknowitz et al. 2015, USA35 (n = 7850) Morrissey et al. 2016, USA49 (n = 12,550) Papas et al. 2016, USA51 (n = 74) Sharkey et al. 2011, USA61 (n = 610) Yu et al. 2010, USA71 (n = 3799) Ramsey et al. 2011, Australia54 (n = 185) |
Low family income or low SES was associated with an increased risk of child FI |
In summary, there are a number of factors that may be pivotal for child FI. FI is a multifactorial problem and the factors described above may increase its likelihood. The majority of factors investigated in the 24 studies that adjusted their findings for relevant explanatory or confounding variables were associated with an increased risk of FI and a more vulnerable environment for children (e.g. material deprivation, parents’ employment, number of people in household, neighbourhood social cohesion and disorder, FI in parents, living property characteristics, number of parents in household, number of siblings, ethnicity, parents’ education, mother’s depression and SES/household income). Three studies showed that living in a rural area did not increase the risk of FI compared with living in an urban area. There were conflicting findings for the relationships between FI and children’s ageing and maternal age.
Most of the reviewed studies were observational and not designed to rigorously assess relevant factors associated with FI. Some studies were small and may have been underpowered. Tools to measure FI varied across studies. Twenty-six studies provided only a crude association between FI and potential factors related to FI without adjusting analyses for explanatory or confounding variables. Jacknowitz et al. 35 pointed out that ascertaining whether some potential triggers of FI are actually predictors or are actually consequences of FI can be quite challenging. Furthermore, some factors may be much more critical than others, especially in children. For instance, Carter et al. 23 observed that the effect sizes for household-level factors (e.g. SES or single-parent family status) were higher than those for other related factors. Despite these limitations, there were consistent patterns across most of the studies reviewed.
Findings from qualitative studies
Six out of the 57 studies that addressed RQ 1 used qualitative methods6,25,30–32,55 and three used mixed methods. 59,62,64 Four studies6,25,30,55 evaluated children’s and adolescents’ experiences of FI, one study evaluated the experiences of stakeholders engaging with food-insecure children31 and two studies evaluated both children’s and stakeholders’ experiences. 32,62 One study64 that was linked to one of the qualitative studies included55 evaluated the perception of FI in a sample of homeless youth living in two shelters. One study conducted in the UK interviewed parents of at-risk food-insecure children and used a mixed methodology;59 however, the findings of the interviews with parents were not clearly reported in the manuscript. The general characteristics of the children and stakeholders populations included in the seven studies that reported qualitative data are presented in Table 2.
| Study authors and year of publication | Country | Population |
|---|---|---|
| Harvey 201630 | UK | 19 children aged 5–11 years recruited from Kids Company (London, UK) (a UK charity providing support for deprived inner-city children) |
| Harvey-Golding et al. 201532 | UK | 15 children, mainly white British (mean age 9 years). Parents/caregivers of participating children were also invited to participate (n = 16, mean age = 41.1 years) as were school staff (n = 16, mean age = 41 years) from three participating free-breakfast schools |
| Harvey-Golding et al. 201631 | UK | 19 stakeholders of schools located in communities within the bottom half of neighbourhoods ranked on indicators of deprivation |
| Connell et al. 200525 | USA | 32 children aged 11–16 years from two after-school programmes for low-income children in a mid-sized city and from a rural middle school with a high rate of eligibility for free and reduced-price school meals |
| Fram et al. 20116 | USA | 26 children aged 9–16 years from families recruited from food pantries, soup kitchens, social services agencies and community centres |
| Richards and Smith 200755 | USA | 56 children (6–13 years) living in homeless shelters |
| Smith and Richards 200864 | USA | 202 youths (6–18 years) living in homeless shelters |
| Shtasel-Gottlieb et al. 201562 | USA | 12 children between sixth and twelfth grade from low-income families in a predominantly minority urban community and stakeholders |
Children’s and adolescents’ experiences of food insecurity
Six studies6,25,30,32,55,62 provided information on children and adolescents’ experiences of FI. Five of these studies used qualitative methods6,25,30,32,55 and one used mixed methods (both qualitative and quantitative). 62 Sample sizes ranged from 12 to 56 participants and the age of participants ranged from 5 to 16 years.
It is worth noting that two studies55,64 were conducted by the same authors in the same homeless shelters in the USA but assessed children of different age groups. The study by Smith and Richards64 assessed the perceptions of FI and coping mechanisms to avoid hunger in a sample of homeless young people (aged 9–18 years), and that of Richards and Smith55 assessed the perceptions of FI among younger children (aged 6–13 years). 55 It is unclear whether or not there was a degree of overlap between the two studies in terms of participants. Furthermore, Smith and Richards64 modified the adult USDA FI assessment tool in order to adapt it for use with adolescents.
Overall, findings of the qualitative studies indicated that children did not normally talk to each other about lack of food at home. However, they could describe or acknowledge when a peer or another family was running out of food. Most were unaware that FI was prevalent in their community. 25,62
Qualitative studies reported children’s perceptions or experiences of FI in terms of cognitive (e.g. children talked about scarcity of food),6,25,30,32,55,62 physical (e.g. hunger, pain and weakness related to lack of sufficient food)6,30 and emotional awareness (e.g. negative feelings associated with FI). 6,25,30,62 They also considered the social interactions and behavioural reactions (e.g. coping strategies) of food-insecure children. Table 3 presents a summary of the relevant qualitative studies according to the main identified themes.
| Themes identified | Subthemes identified | Study authors, year of publication and country | Quotation |
|---|---|---|---|
| Lack of food and causes of FI | Lack of food or money to buy food in the household | Harvey 2016, UK30 | Yeah, ’cos when my mum doesn’t have a lot of money, well, that’s when we don’t have enough [food]Female, 9 years old |
| Connell et al. 2005, USA25 | [. . .] it was the bills. They had so many bills that they had to pay and had to cut back on some stuffAge not reported | ||
| Harvey 2016, UK30 | Researcher: And so, is that when you come here [Kids Company, UK children’s charity] and have your dinner?Participant: I just don’t eatMale, 10 years old | ||
| Harvey 2016, UK;30 Fram et al. 2011, USA;6 Connell et al. 2005, USA25 | In some studies children reported that their parents or caregivers talked to them openly about the lack of money or food and used expressions such as ‘unaffordable’, ‘wait until I get paid’ or ‘go to play’ when they were asking for something to eat | ||
| Hunger | Harvey 2016, UK30 | Researcher: Do you ever go to bed with an empty tummy . . . a hungry tummy?Participant: [nods to indicate agreement]Male, 5 years oldMy tummy’s achingFemale, 7 years oldYour belly hurts, and sometimes you’ll feel like you’ll vomitFemale, 10 years old | |
| Fram et al. 2011, USA6 | Angry, mad, go to sleep basically, [. . .] you feel like you’ve got a bunch of cramps in your stomach and you’ll be light-headedAge not reported | ||
| Coping and eating strategies | Need to eat less or distribute food among siblings | Fram et al. 2011, USA6 | I normally don’t eat it that much.Age not reported |
| Harvey 2016, UK30 | [. . .] my two baby sisters, because they need food, they share with me. They get one each and I get the rest because I’m the littlest that goes to schoolFemale, 7 years old | ||
| Eating really fast | Connell et al. 2005, USA25 | Yeah, ’cause when they get food they try to eat it all up so that it will take a long time before they get hungry againAge not reported | |
| Sleeping to alleviate hunger | Harvey 2016, UK30 | I feel hungry. I just want to sleep ’cos when you sleep [. . .] when I [go] to bed hungry and sleep, I’m not hungryFemale, 9 years old | |
| Social strategies | Social confidence | Fram et al. 2011, USA6 | [. . .] we had to keep going over to my friend’s house back and forth asking if she had butter and milk and eggs [. . .] I really didn’t feel good about it because I’m not comfortable asking people thatAge not reported |
| Connell et al. 2005, USA25 | They send you to borrow some flour. Our neighbour do that all the time. She borrow flour and eggs all the time so that she can finish cooking. We borrow flour all the time. We always run outAge not reported | ||
| Feeling responsible for managing/stretching food resources | Fram et al. 2011, USA6 | [My sister] would sometimes ask me to ask for a fruit snack or a banana and I would say, no, we’re running low, we could use those for tomorrow for lunchAge not reported | |
| Connell et al. 2005, USA25 | . . . I go in my house and I do everything that I can for my little brother, my little sister, and my friends so I just bring them something to eatAge not reported | ||
| Finding ways of generating resources for food or money to buy food | Fram et al. 2011, USA6 | [. . .] we’ll like get together and we’ll find a way to get money up, not, we ain’t got to sell no drugs though, [. . .] We’ll find some way [. . .]Age not reported | |
| Household characteristics | Noticing barriers to accessing food | Harvey 2016, UK30 | [. . .] She was going to take me to the cinema but because she didn’t have enough money she was going to save it on foodFemale, 9 years old |
| Connell et al. 2005, USA25 | His daddy died and his mama didn’t have a jobAge not reported[. . .] the parents might eat once a day and the kids eat regular like they do every dayAge not reported | ||
| Connell et al. 2005, USA25 | One of the included studies reported that 7 out of 32 interviewed children admitted that their parents or caregivers preferred to smoke, drink alcohol, or buy drugs or clothes rather than buying food. No quotations provided | ||
| Limited cooking and storage space or lack of appliances | Richards and Smith 2007, USA55 | We have a small fridge, so nothin’ won’t hardly fit in thereAge not reported | |
| Harvey 2016, UK30 | [. . .] sometimes ’cos of the slow cooker we have to have leftovers and it might just be bread or noodles . . . I don’t want thatFemale, 9 years old | ||
| Poor access to shops in the neighbourhood and lack of transport | Richards and Smith 2007, USA55 | We gotta walk here, ’cause my mom don’t have a car no more. So we got to walk basically we walk a lot, except for, like we don’t walk two days of the weekAge not reported. . . Like we have to walk from here all the way to the [food stamp office] – that’s a long wayAge not reported | |
| Sources of food | Frequent takeaway meals or junk food or eating less desirable, unhealthy food because there was no other choice | Harvey 2016, UK30 | If there’s not enough to eat at home, we buy some chicken and chipsResearcher:OK. So, from the takeaway?Participant:YeahMale, 10 years oldWell every Friday we have chicken and chips but my mum said it’s not healthyFemale, 8 years old |
| Connell et al. 2005, USA25 | [. . .] Change to lower class meals like eating a whole lot of canned food instead of fixing up some proper mealsAge not reported | ||
| School lunches | Connell et al. 2005, USA25 | . . . eat a lot at school and then when you come home you won’t be hungry for another hour or 4 hoursAge not reported | |
| Food banks | Harvey 2016, UK30 | If there’s not school, like sometimes we don’t do lunches. [. . .] On Sundays we do shopping [food banks], so we have to leave it until we do shopping on SundaysFemale, 10 years old |
Stakeholders’ experiences of dealing with children food insecurity
Two of the identified qualitative studies assessed the perspective of senior stakeholders with regard to child FI. 31,62 One of the studies interviewed parents, but no quotations or qualitative information from such interviews were provided in the manuscript. 59
Harvey-Golding et al. 31 explored the perspectives of senior stakeholders using one-on-one semistructured interviews regarding the provision of a school breakfast programme around the UK. The sample comprised 19 participants (eight from local authorities and 11 employed in senior roles within mainstream primary schools or special schools where pupils experienced multiple levels of deprivation) who were involved in the free school breakfast programme.
School staff reported being able to identify children from food-insecure households or those at risk of FI, for example they could identify children who were not going to have quality breakfast at home and observed that were the working parents and those who did not claim benefits who were struggling the most. Concerns were also raised about those in low-paid jobs or multiple jobs and those who were living in private rented and/or multiple occupation accommodation: ‘Lower paid jobs and they’re on the breadline, they’re in rented accommodation and multiple occupation. ‘Cause some do two jobs’. 31
Some school staff reported that they were aware of families experiencing increased FI during weekends and school holidays and expressed concern that some children might not be fed during the holidays. In some cases, school staff took the initiative of organising food provision to families during school holidays via a local food bank and stressed the need for breakfast provision during school holidays: ‘I think for some children, some families there is a definite, definite need, you know we’ve had to give food parcels out and things’ and ‘Individual teachers, individual welfare assistants and learning support assistants, actually paying for some kind of food out of their own money’. 31
Overall, among stakeholders, the school breakfast programme was considered a positive way to alleviate hunger, improve children’s health and nutritional status and start the school day. However, stakeholders noticed that some students may eat breakfast twice (once at home and once at school), raising concerns about the risk of increased calorie intake. 31
With regard to families, the programme was thought to alleviate the rushed morning routines for certain families and was considered particularly beneficial for low-income families, families with multiple children and families with disabilities: ‘I think it’s an amazing scheme if you have got one, two or three kids in particular’. 31 However, some stakeholders raised concerns about the fact that the programme could potentially remove parental responsibility and promote poor parenting practices: ‘They know that they are going to get their breakfast, they get their dinners. Where the parents are not feeding them they know that they are going to be fed’. 31
It was considered that the impact of the programme varied across the different local communities. In more deprived communities, the programme was considered extremely beneficial to families experiencing FI and food poverty. In general, stakeholders felt that the programme alleviated FI in the community, improved health and nutrition and had the potential to reduce stigma and inequality: ‘It doesn’t make anybody feel different. Everybody is the same. It has got a very positive ethos in school’. 31 However, there were concerns that the programme may contribute to increased overweight and obesity levels, as in less deprived areas, children may eat breakfast twice. 31
Shtasel-Gottlieb et al. 62 conducted a two-phase, mixed-methods study. In the first phase, 2350 students from sixth to twelfth grade completed an anonymous survey that included the youth self-report form of the 9-item USDA module and demographic questions. In the second phase, 20 adult key informant interviews and four semistructured student focus groups were performed to explain the findings from phase 1. The adult key informants were members of school staff, parents, government officials, church officials, community organisers and local health providers. Most stakeholders recognised FI as a community concern and were not surprised by the prevalence of FI in the community: ‘I would think it would be higher’. 62
Some stakeholders noted that very low FS motivated youths to reach out to the community, which had the potential to offer a supportive environment for young food-insecure people: ‘Because they don’t have their parents [to support them] maybe they turn to their community and each other more’. Stakeholders felt that community-level initiatives (e.g. food pantries, school breakfast/lunch programmes, and summer food programmes) were useful to address the needs of food-insecure youths: ‘School programs for some families are the foundation of their food [and] their capacity to provide food’. However, they were aware of potential barriers to accessing community resources: ‘For some families it might be a pride issue for them not to go. I think people feel like they’re failing their families if they can’t provide them the basic needs’. Some students pointed out that the stigma and embarrassment surrounding FI and food poverty might prevent young people from reaching out to their peers: ‘People could start talking to each other and . . . people who are too scared to even say that they don’t have food’. 62
Other stakeholders suggested that some families may encounter difficulties in accessing community resources due to language and cultural differences (‘There are a ton of resources out there, but they aren’t in one central place’; ‘there are a lot of immigrant families and [certain ethnic groups] are really isolated a lot of times too’) or to high instability at home (‘domestic violence, drug and alcohol abuse, [or] absentee parents’). 62
Research question 2: what are the incidence, prevalence and costs of child food insecurity in the UK (including recent trends)?
Information on the prevalence of child FI in the UK was sparse. No information regarding the incidence and costs of child FI in the UK, or recent trends, was identified.
The 2017 UNICEF report indicates that 19.5% of children aged < 15 years in the UK live with a respondent who is moderately or severely food insecure and 10.4% live with a respondent who is severely food insecure. 127 FI was assessed using the Food Insecurity Experience Scale (FIES), which was introduced to the Gallup World Poll (an annual large-scale, population-based household survey, covering the majority of the world’s countries) in 2014. The FIES is based on three existing tools used to assess FI in household-based surveys: the US Household FS Scale, the Household FI Access Scale, and the Latin American and Caribbean FS Scale. It is an experience-based metric, which assesses direct responses to questions about access to adequate food. The FIES is considered to complement existing measures of other dimensions of FI. 128
For the high-income countries considered in this rapid review, Table 4 reports the proportion of children aged < 15 years who live with a respondent who is food insecure.
| Country | n | FIES-M+, mean % (95% CI) | FIES-S, mean % (95% CI) |
|---|---|---|---|
| UK | 1992 | 19.5 (15.8 to 23.1) | 10.4 (7.5 to 13.3) |
| Ireland | 601 | 17.9 (15.2 to 20.7) | 7.3 (5.6 to 9.0) |
| France | 486 | 6.0 (4.3 to 7.7) | 1.3 (0.5 to 2.2) |
| Germany | 418 | 4.9 (3.2 to 6.7) | 1.2 (0.4 to 2.0) |
| Italy | 450 | 8.8 (6.5 to 11.1) | 1.1 (0.4 to 1.9) |
| Sweden | 1985 | 4.1 (2.6 to 5.5) | 0.6 (0.1 to 1.0) |
| Norway | 480 | 5.2 (3.4 to 6.9) | 1.7 (0.8 to 2.6) |
| Denmark | 551 | 8.5 (6.5 to 10.5) | 1.2 (0.6 to 1.8) |
| Finland | 274 | 7.8 (5.4 to 10.1) | 0.9 (0.2 to 1.6) |
| Iceland | 225 | 8.4 (5.0 to 11.8) | 3.5 (1.5 to 5.4) |
| Canada | 513 | 11.9 (9.3 to 14.5) | 3.3 (2.1 to 4.4) |
| USA | 508 | 19.6 (16.4 to 22.8) | 6.9 (5.0 to 8.4) |
| Japan | 403 | 1.4 (0.5 to 2.3) | 0.3 (–0.1 to 0.7) |
| Australia | 421 | 16.0 (12.8 to 19.1) | 4.9 (3.2 to 6.6) |
| New Zealand | 484 | 10.9 (8.6 to 13.3) | 3.2 (1.8 to 4.5) |
Table 4 shows that the UK figure for moderate or severe FI is the highest (19.5%) among European countries and only marginally smaller than the US figure (19.6%). Likewise, the UK figure for severe FI is notably higher (10.4%) than that of all other high-income countries, including the USA. The country with the most similar FIES profile to the UK is Ireland, which is not surprising given its regional proximity and comparable social and political environment.
Poverty in the UK
Recently published statistics on poverty in the UK (House of Commons Briefing Paper 2018) show that in 2015/16 in the UK, there were 3.7 million children in absolute low income or absolute poverty and 4.0 million children in relative low income or relative poverty. 129 The proportion of children living in relative poverty (in households with an income < 60% of median household income in that year) is expected to increase sharply from 30% in 2015/16 to 37% in 2021/22 based on incomes after housing costs are deducted, and from 20% to 27% based on incomes before housing costs are deducted. The proportion of children living in absolute poverty (in households with an income < 60% of the 2010/11 median, uprated for inflation) is also expected to rise, from 27% in 2015/16 to 31% in 2021/22 based on incomes after housing costs, and from 17% to 22% based on incomes before housing costs. 129
Research question 3: what is the impact of food insecurity on children’s health and social well-being in high-income countries?
From the results of the search strategies, 74 studies that investigated the relationship between FI status and children’s health and well-being outcomes were identified. The results of these studies are presented, for clarity, according to five main categories: general health outcomes, weight status, mental health outcomes, social well-being outcomes and academic outcomes. The results of the studies that adjusted their analyses for explanatory or confounding variables are summarised below. The results of the studies that did not adjust their analyses for explanatory or confounding variables are reported in Appendix 6. A quantitative synthesis of findings was deemed unfeasible because of the lack of consistency in the definition and measurement of FI across studies, as well as the variation in terms of children’s characteristics, settings and type of outcomes between studies. Further details of the main studies that adjusted their analyses for explanatory or confounding variables are presented in Appendix 7.
General health outcomes
Table 5 summarises the results of the 21 studies (adjusted analyses)21,24,26–29,39,42,44,45,54,60,63,66,69,76,82,83,88,95,106 that assessed the relationship between FI and children’s general health status or health problems (e.g. psychosomatic symptoms, anaemia, asthma, number of hospitalisations). Three studies used self-reported health data from the children or adolescents involved. 60,76,106 Nine studies reported the caregivers’ assessment of the children’s general health. 21,26,39,44,45,54,69,83,95 Nine studies used data from national health surveys or blood samples. 24,27–29,42,63,66,82,88 The results of two studies73,99 that did not adjust their analyses for explanatory or confounding variables are reported in Appendix 6.
| Study authors, year of publication and country | Health outcome(s) measured | Measurement tools | Number of participants | Summary of results | Main explanatory or confounding variables considered |
|---|---|---|---|---|---|
| Molcho et al. 2007, Ireland106 | Psychosomatic symptoms (e.g. headaches, stomach aches, backaches, feeling dizzy) | Self-reported data through the HBSC Survey130 | 3596 children | Children living in food poverty reported physical symptoms more often than those not living in food poverty (p < 0.05) | Age and social class (according to the father’s occupation) |
| Broughton et al. 2006, Canada21 | Iron depletion | Caregiver’s report of child’s overall health status; haematological tests | 142 households with children | Less than 7% in either the FS or the FI group had indications of iron depletion (p-values not presented) | Household income |
| Egeland et al. 2011, Canada27 | Health status and anaemia | Caregiver’s report of child’s overall health status, haematological samples and the Nunavut Inuit Health Survey131 | 388 children | No significant difference in the proportion of children with anaemia between food-secure and food-insecure homes. There was no significant traditional food by FS interaction term noted for iron deficiency (p = 0.84). Children from severely food-insecure homes were significantly less likely to have their health rated as ‘excellent/very good’ by their parents (39%, 34/88) than children (54%, 86/159) from food-secure homes (RR 0.7, 95% CI 0.5 to 1) | Household characteristics |
| Kirkpatrick et al. 2010, Canada42 (longitudinal study) | Health status, asthma prevalence | Caregiver reported through the Canadian National Longitudinal Survey Of Children And Youth132 | 5809 children aged 10–15 years; 3333 youths aged 16–21 years | Higher odds of poor health were observed in children (but not in youths) who had experienced hunger than in those who were never hungry (OR 2.5, 95% CI 1.3 to 4.6). Children and youths who ever experienced hunger were 2.4 times more likely to have asthma (OR 2.4, 95% CI 1.1 to 4.9). Youths (but not children) were more likely to have asthma (OR 6.1, 95% CI 1.4 to 25.9) if their caregiver reported two or more hunger episodes over time | Child and household sociodemographic variables associated with poverty |
| Pickett et al. 2015, Canada76 | Psychosomatic symptoms (e.g. headaches, stomach aches, backaches, feeling dizzy) | Self-reported data through the HBSC Survey | 25,912 adolescents | Children who reported experiencing hunger ‘sometimes’ or ‘often or always’ were 1.9 and 4.4 times more likely to report psychosomatic symptoms (OR 1.9, 95% CI 1.8 to 2.0; OR 4.4, 95% CI 3.7 to 5.2, respectively) | Family’s SES characteristics and practices, school food and nutrition programmes |
| Marjerrison et al. 2011, Canada45 | Hospitalisations | The caregiver completed a telephone-administered questionnaire | 183 children with type 1 or 2 diabetes | Children from food-insecure households were 3.7 times more likely to have been admitted to hospital previously than children from food-secure families (OR 3.7, 95% CI 1.5 to 8.7) | FS status; child, parent and household characteristics |
| Chi et al. 2014, USA82 | Dental caries | NHANES data | 2206 children | Children from low- or very low-FS households had significantly higher untreated caries (prevalence ratio 2.0, 95% CI 1.1 to 3.6; p = 0.03; prevalence ratio 1.7, 95% CI 1.0 to 2.9; p = 0.05, respectively) than children with full FS. There was no difference in untreated caries between children from fully and marginally food-secure households (p = 0.17) | Age; SES |
| Chilton et al. 2009, USA24 | Health status | NHANES data | 19,275 mothers | Children of immigrants to the USA living in food-insecure households were 1.7 times more likely than food-secure households to have their health reported as ‘fair’ or ‘poor’ (OR 1.7; p < 0.001) | Immigrant status and other relevant covariates |
| Cook et al. 2004, USA83 | Health status, hospitalisation | Caregiver’s report of child’s overall health status and number of hospitalisations | 11,539 caregivers of children from the C-SNAP | Children enrolled in the C-SNAP who were living in food-insecure households had significantly greater odds of ‘fair/poor’ health than those in food-secure households (OR 1.9, 95% CI 1.7 to 2.2; p < 0.05). Children in food-insecure households were 1.3 times more likely to have been hospitalised since birth (OR 1.3, 95% CI 1.2 to 1.5) | Child and maternal characteristics, health insurance and day care status, participation in food assistance programmes |
| Dunifon and Kowaleski-Jones 2003, USA26 | Health limitations that affected participation in daily activities | Caregiver’s report of child’s overall health status | 3500 school-aged children from the NSLP | An increase in FI was associated with an 8% increase in the odds of health limitations (β 1.1, SE 2.0; p < 0.01) | Sociodemographic characteristics of children and their families |
| Eicher-Miller et al. 2009, USA28 | Anaemia | NHANES data | 11,247 children | The odds of an iron deficiency anaemia diagnosis were 10.7 (p = 0.01), 8.1 (p = 0.002) and 3.0 (p = 0.02) times more among food-insecure children aged 3–5 years, 6–11 years and 12–15 years, respectively, than among their counterparts | Clustering, stratification, survey cycle year, sex, ethnicity, and poverty-to-income ratio |
| Eicher-Miller et al. 2011, USA29 | Bone health | NHANES data | 5270 children | Bone mineral content was lower in males aged 8–11 years from food-insecure households than in their food-secure counterparts (p ≤ 0.05). Females and males of other age groups did not significantly differ in bone mineral content | Survey year, poverty, ethnicity, BMI, physical activity, meals eaten at school per week and smoking habits from participants |
| Holben and Taylor 2015, USA88 | Blood glucose, total cholesterol, triglycerides, blood pressure | NHANES data | 7435 children and adolescents | No statistically significant differences in levels of blood glucose, total cholesterol, triglycerides and blood pressure across levels of household FS were reported. Participants from high-FS households had significantly higher mean HDL values than those from food-insecure households (p = 0.019) | Age, ethnicity, sex |
| Ryu and Bartfeld 2012, USA95 (longitudinal study) | Health status | Caregiver’s report of child’s overall health status | 6651 children | 88.5% of children with no observed household FI were in ‘very good’ or ‘excellent’ health, compared with 67% to 79% of those with 1, 2, or 3 years of FI and 58.1% of those with household FI in all observed years | Sociodemographic and household characteristics |
| Kimbro et al. 2015, USA39 (longitudinal study) | Health status | Caregiver’s report of child’s overall health status | 6300 children | Child health status was significantly poorer if the child experienced a transition into FI or was food insecure at both measurement periods, than if the child remained food secure over time (p-values not reported) | Child, parent and neighbourhood sociodemographic characteristics |
| Mangini et al. 2015, USA44 | Asthma | Caregiver’s report through the ECLS-K survey133 | 11,099 children | Food-insecure household was associated with a higher incidence of asthma (OR 1.0, 95% CI 1.0 to 1.1). Marginal FI was associated with 34% higher odds of asthma (95% CI 1.3 to 1.4). When marginally food-insecure households were grouped with food-insecure households, the OR for asthma was 1.36 (95% CI 1.3 to 1.4) | Child, parents and household characteristics |
| Shanafelt et al. 2016, USA60 | Health status | Self-reported health | 904 students | Food-insecure adolescents were significantly less likely than food-secure adolescents to report ‘excellent’ or ‘very good’ health (OR 0.4, 95% CI 0.3 to 0.6; p < 0.01) | Grade level, sex, free and reduced-price lunch status, ethnicity, weight |
| Skalicky et al. 2006, USA63 | Anaemia | Haematological data from the C-SNAP | 626 children | Food-insecure children had 2.4 greater odds of having iron deficiency with anaemia than food-secure children (OR 2.4, 95% CI 1.1 to 5.2; p = 0.02). The proportion of children having anaemia and iron deficient-no anaemia did not differ significantly between food-insecure and food-secure households | Caregiver and household characteristics, whether or not the child was ever breastfed |
| Tester et al. 2016, USA66 | Lipid profiles | NHANES data | 1072 adolescents | Those reporting marginal FS were almost twice as likely to have elevated TG (≥ 90 mg/dl) (OR 1.9, 95% CI 1.1 to 3.0), elevated TG-to-HDL-C ratio (OR 1.7, 95% CI 1.1 to 2.8) and Apo B level of ≥ 90 mg/dl (OR 2.0, 95% CI 1.2 to 3.4) as high-FS adolescents | Sociodemographic characteristics |
| Weinreb et al. 2002, USA69 | Health status | Caregivers responses to questions adapted from the National Health Interview Survey134 | 180 preschool children, 228 school children | For preschool-aged children, moderate hunger was a significant predictor of health conditions (p = 0.03). In school-aged children, severe hunger was a significant predictor of chronic conditions (p = 0.05) | Housing status, mother’s distress, low birthweight, and child life events |
| Ramsey et al. 2011, Australia54 | Health status | Caregiver reports of child’s overall health status | 185 children aged 3–17 years | Health status was not associated with child FI (p > 0.05) | Household income |
In summary, food-insecure children were more likely to report poorer health status, poorer health indicators or more symptoms than food-secure children. Findings were largely consistent across studies. Only one study did not find an association between FI and poor health54 and another study found a higher risk of poor health in children (10–15 years), but not in youths (16–21 years). With regard to specific health problems, some, for example asthma or dental caries, were reported more frequently in food-insecure children than in their food-secure counterparts. 42,44,82 For others, such as anaemia or iron depletion, the evidence was mixed and not clear-cut. 63 Compared with food-secure children, food-insecure children were also more likely to report more hospitalisations (as a proxy of health status). 45,83
Weight status
Thirty-eight studies investigated the relationship between weight status and child FI. 12,20,21,27,28,36,45,51,52,54,56,57,60,61,63,67,74–76,78–81,85,86,88,97,98,100,102–105,109,111–113,123 Twenty-eight of these studies adjusted their analyses for explanatory or confounding variables (Table 6)12,20,21,28,36,51,54,56,67,74–76,78–81,85,86,88,97,100,102–105,109,112,113 and 10 did not (see Appendix 6). 27,45,52,57,60,61,63,98,111,123 The majority of studies involved assessment of weight and height by a trained health professional. In some studies, the data were reported by the caregiver54 or self-reported by children or adolescents. 76,79,112 All studies that adjusted their analyses for explanatory or confounding variables used weight measurements to calculate body mass index (BMI) as weight (kg)/height (m2). Most studies (adjusted and unadjusted analyses) used the CDC growth charts, and a few36,54,76 used WHO or International Obesity Task Force (now known as World Obesity/Policy & Prevention) growth charts, or the US NCHS78 growth reference or other categorisation systems. Only one study did not report the tool used for the categorisation of weight status. 79
| Study authors, year of publication and country | Measurement tool | BMI classification used | Number of participants | Summary of results | Main explanatory or confounding variables considered |
|---|---|---|---|---|---|
| Broughton et al. 2006, Canada21 | Height and weight were measured | CDC growth reference | 142 pre-schoolers | Pre-schoolers in food-insecure households were twice as likely to be reported as overweight/obese as those in food-secure households (p-value not reported) | Household income |
| Mark et al. 2012, Canada75 | Height and weight were measured | CDC growth reference | 8938 youths | In the two lowest-income groups (n = 2280), boys from food-insecure households had a higher prevalence of overweight (mean 45.0, 95% CI 31.1 to 58.9) than boys from food-secure households (mean 27.1, 95% CI 21.8 to 32.4; p = 0.03). This difference was not statistically significant for girls | Age |
| Pickett et al. 2015, Canada76 | Self-reported height and weight | WHO growth reference | 25,912 adolescents from the HBSC study | HBSC participants reporting hunger ‘sometimes’ or ‘often or always’ were 1.2 times more likely to self-report an overweight/obese status than those who reported as ‘never’ suffering from hunger | Child, parent and food assistance characteristics |
| Barroso et al. 2016, USA78 | Weight was measured | NCHS growth reference | 240 children | Cutting the size of the child’s meals and visiting a food bank (as indicators of FI) were not statistically related to child weight-for-length (p > 0.05). Children whose mothers reported ever having received SNAP were twice as likely to be overweight as those who had never received SNAP (95% CI 1.04 to 3.90) | Child and maternal characteristics and dietary pattern |
| Bhargava et al. 2008, USA20 (longitudinal study) | Height and weight were measured by ECLS research staff | CDC growth reference | 7635 children from the ECLS | Household FI score was a not a significant predictor of weight (p > 0.05). Households with children who were taller and heavier for their ages reported significantly higher FI levels (p < 0.05) | Child, parent and household characteristics |
| Bruening and Johnson 2015, USA79 | Self-reported height and weight | Not reported | 5869 adolescents | Food-insecure youths were 1.2 times more likely to self-report overweight or obesity (p = 0.047) | Sociodemographic characteristics |
| Burke et al. 2016, USA80 (longitudinal study) | Height and weight were measured by ECLS research staff | CDC growth reference | 15,827 children from the ECLS | No significant differences in BMI growth between food-insecure and food-secure children. Significant differences in BMI growth in females based on household FS. Between kindergarten and eighth grade, females in food-insecure households increased BMI growth by 2.87% (95% CI 1.27 to 4.49) compared with females in food-secure households (p < 0.05). This result was not significant in males | Child characteristics, time-invariant and time-variant variables |
| Casey et al. 2006, USA81 | Height and weight were measured by a NHANES health technician | CDC growth reference | 6995 children from the NHANES | The risk of obesity was 1.3 times (95% CI 1.0 to 1.7) greater in food-insecure children than in food-secure children (p = 0.03) | Child, parent and household characteristics |
| Eicher-Miller et al. 2009, USA28 | Height and weight were measured by a NHANES health technician | CDC growth reference | 11,247 children and adolescents from the NHANES | Differences of BMI status across food-insecure and food-secure groups were significant depending on age group [e.g. the difference in the 6–11 years group was not significant (p = 0.0806), but was significant in the 12–15 years group (p = 0.0021)], with fewer food-insecure adolescents classified as obese or overweight | NHANES clustering and stratification |
| Gundersen et al. 2008, USA86 | Height and weight were measured by a NHANES health technician | CDC growth reference | 841 children and adolescents from the NHANES | Increases in maternal stressors (e.g. family structure, financial, mental and physical health problems) increased the probability of being overweight or obese for children in food-secure households but decreased these odds for children in food-insecure households (p > 0.05). An increase in maternal stressors amplified the probability of being overweight or obese in food-secure 3- to 10-year-olds (p < 0.05) | Child and mother characteristics |
| Gundersen et al. 2009, USA85 | Height and weight were measured by a NHANES health technician | CDC growth reference | 2516 children and adolescents from the NHANES | The association between FI and obesity was not significant. This non-significance persisted when the analysis was performed by ethnicity subgroups (non-Hispanic white, non-Hispanic African American, and Hispanic) and sex | Demographic characteristics |
| Holben and Taylor 2015, USA88 | Height and weight were measured by a NHANES health technician | CDC growth reference | 7435 adolescents from the NHANES | Children living in low- and very low-FS households were 1.2 and 1.4 times, respectively, more likely to have obesity (p = 0.036), and 1.4 and 1.5 times, respectively, more likely to have central obesity as measured by waist circumference (p = 0.002) | Age, ethnicity and sex |
| Jyoti et al. 2005, USA11 (longitudinal study) | Height and weight were measured by ECLS research staff | CDC growth reference | Approximately 21,000 children from the ECLS | Children from persistently food-insecure households had a 0.35 kg/m2 greater gain in BMI (p < 0.028) and a 0.65 kg greater gain in weight (p < 0.026) than children from persistently food-secure households. The association between kindergarten FI, higher BMI and weight was among girls only (p = 0.015). Becoming food insecure was associated significantly with greater weight and BMI gains among boys (p = 0.019) but not among girls (p = 0.10) | Child, parent, household and neighbourhood time-varying and time-invariant characteristics |
| Kaiser et al. 2002, USA36 | Height and weight were measured by research staff | WHO/NCHS growth reference | 211 families | No significant differences (p > 0.05) were found between children weight-for-height z-score or height-for-age z-score and levels of FI | Mother’s acculturation score |
| Kaur et al. 2015, USA97 | Height and weight were measured by a NHANES health technician | CDC growth reference | 9701 children from the NHANES | Significant differences in obesity prevalence between food-insecure and food-secure children at both the child and the household level. However, child-level food insecure was not associated with obesity. On the other hand, at a household level, food insecure was associated to obesity only in 6- to 11-year-old children (OR 1.8, 95% CI 1.3 to 2.5), but not in 2- to 5-year-old children (OR 0.9, 95% CI 0.5 to 1.5) | Child and household characteristics |
| Kohn et al. 2014, USA74 | Height and weight were measured by a NHANES health technician | CDC growth reference | 1321 children and adolescents from the NHANES | In low-income food-insecure youths, food assistance participation was not associated with BMI z-score, high waist circumference or categorical weight status for any specification of food assistance (p > 0.05). Food-secure youth, but not food-insecure youth, participating in food assistance programmes had increased body weight measurements | Child, parent and household characteristics |
| Kuku et al. 2012, USA100 | Height and weight were measured by research staff | CDC growth reference | 959 children from a US data set (Child Development Supplement of the Panel Study Dynamics) | No significant association between food insecure and obesity was found. However, results showed that among boys who were at lower levels of FS, an increase in the number of affirmative FI responses was associated with a higher probability of obesity. This association was not observed among girls | Child characteristics |
| Lohman et al. 2009, USA102 | Height and weight were measured by research staff | CDC and IOTF growth references | 1011 adolescents | FI was not related to weight status. However, there was a significant interaction between maternal stressors (i.e. unemployment, disabilities, low self-esteem, psychological distress, low support network) and FI. Adolescents classified as food insecure whose mothers reported the presence of maternal stressors were 1.7 times more likely to report obesity (p < 0.05). As maternal stressors increased in child food-insecure households, an adolescent’s probability of being overweight or obese increased from approximately 35% to 70%, depending on the stressors experienced | FI, stressor indices (unemployment, disabilities, low self-esteem, psychological distress, low support network), and the interaction of these indices with FI |
| Martin and Ferris 2007, USA103 | Height and weight were measured by research staff | CDC growth reference | 212 children | Children in households with low incomes (< 100% of poverty levels) were half as likely to be overweight as those in households with higher incomes (OR 0.4, 95% CI 0.2 to 0.9; p = 0.03). However, food insecure did not increase the odds of childhood overweight (p = 0.37) | Child, parent and household characteristics |
| Matheson et al. 2002, USA104 | Height and weight were measured by research staff | CDC growth reference | 124 children | Children from food secure households weighed more than those from food-insecure households (p = 0.04). The food-insecure children’s body weights were within the normal range | Age and sex |
| Metallinos-Katsaras et al. 2009, USA105 | Height and weight were measured | CDC growth reference | 8493 children | Girls < 2 years old from food-insecure households were 40% less likely to be overweight (OR 0.6, 95% CI 0.5 to 0.9) than their food-secure counterparts. Girls from 2 to 5 years of age living in food-insecure households with hunger were 1.5 times more likely to report overweight (OR 1.5, 95% CI 1.0 to 2.1) | Maternal education and ethnicity |
| Papas et al. 2016, USA51 | Height and weight were measured by research staff | CDC growth reference | 74 mother–child dyads | Food-insecure children were 10.2 times (OR 10.2, 95% CI 1.2 to 85.5) more likely to be obese than food-secure children. However, maternal overweight/obesity moderated this association. Those living in a low-FS household with an obese mother were 9.5 times (OR 9.5, 95% CI 1.2 to 81) more likely to be obese, and those with very low FS and an obese mother were 32 times (OR 32, 95% CI 2.6 to 391) more likely to report obesity | Parent and household characteristics |
| Rose and Bodor 2006, USA56 (longitudinal study) | Height and weight were measured by ECLS research staff | CDC growth reference | 16,889 children from the ECLS | Children from food-insecure households were 20% less likely to be overweight (p = 0.027). There was a significant interaction between household food-secure status and maternal education (p < 0.05). food insecure was negatively associated with weight gain over time (OR 0.7, 95% CI 0.6 to 0.9) | Child, parent, household and neighbourhood characteristics |
| Speirs et al. 2016, USA109 | Height and weight were measured by research staff | CDC growth reference | 438 pre-school children | Household food insecure and child food insecure were not associated with either overweight/obesity or BMI-for-age z-score (p > 0.05). However, girls from food-insecure households were more likely than girls from food-secure households to have a higher BMI z-score (p < 0.05) | Child, parent and household characteristics |
| Trapp et al. 2015, USA67 | Height and weight were measured by research staff | CDC growth reference | 222 caregivers with young children | No direct association between household FS status and child overweight/obesity. Findings showed an increase in child BMI percentile with increasing age among households reporting high FS (p < 0.02). This effect was not observed in households reporting any degree of FI | Household food-secure status, maternal, demographic and psychosocial characteristics |
| Willis and Fitzpatrick 2016, USA112 | Self-reported height and weight | CDC growth reference | 324 adolescents | Significant direct association between FI and weight status among early adolescents (p < 0.001). The association was no longer significant after adjustment for psychosocial factors (e.g. depression) | Adolescent characteristics |
| Winicki and Jemison 2003, USA113 | Height and weight were measured by ECLS research staff | CDC growth reference | 21,260 children from the ECLS | Overweight rates increased with more severe FI category; however, the difference was not significant (p < 0.05) | Household characteristics |
| Ramsey et al. 2011, Australia54 | Parent-reported height and weight | WHO growth reference | 185 households with children | There was no association between FI and overweight/obesity in children (p > 0.05) | Household income |
In summary, the evidence was mixed. Six studies that adjusted their analyses for explanatory or confounding variables found that food-insecure children were more likely to be categorised as overweight/obese,21,76,78,79,88 but seven other studies (adjusted analyses) did not find an association between child food insecure and weight status. 20,36,54,67,85,103,104 Some studies found the association between child FI and weight status to depend on sex,74,75,80,100,105,109 age,28 psychosocial or parental characteristics51,86,102,112 and the tool used for measuring FI. 97 One longitudinal cohort study found that persistently food-insecure children had a greater weight gain over time than persistently food-secure children. 12 However, other longitudinal studies that assessed the same children cohort [Early Childhood Longitudinal Study (ECLS)] did not report a weight gain in food-insecure children over time. 56,113 Most of the studies that did not adjust their analyses for explanatory or confounding variables found that weight status or BMI was unrelated to food-secure status (see Appendix 6). 27,45,52,57,60,61,63,98 Only one study111 showed that youths who reported no hunger were least likely to have a BMI greater than or equal to the 95th percentile. However, caution is advised when interpreting these results as they could be explained by potential relevant factors that were not accounted for. The studies that used data from National Health and Nutrition Examination Survey (NHANES) or ECLS cohorts conducted secondary analyses of existing data sets and assessed different explanatory or confounding variables (see Table 6). Results were almost equally split between studies that showed a significant association between FI and weight status and those that did not.
Mental health outcomes
In total, 17 studies19,26,39,41,47,53,54,69,73,76,89,92,93,96,99,106,108 investigated the association between FI and children’s mental health outcomes. Fourteen studies adjusted their analyses for explanatory or confounding variables (Table 7)19,26,39,47,53,54,69,76,89,92,93,96,106,108 and three did not (see Appendix 6). 41,73,99 The ‘adjusted’ studies used scales or scores to evaluate mental health outcomes such as externalising or internalising behaviours,19,26,39,69,76,89,92 behavioural problems or difficulties54,93,96,108 and mental health disorders. 47,53,106
| Study authors, year of publication and country | Mental health outcome(s) measured | Measurement tools | Number of participants | Summary of results | Main explanatory or confounding variables considered |
|---|---|---|---|---|---|
| Belsky et al. 2010, UK19 | Children’s cognitive, behavioural, and emotional development | Children’s and teachers’ reports on externalising scale | 2125 school-aged children | Association between FI and children’s emotional problems was significant in adjusted analyses (β 0.2, SE 0.1; p < 0.05) | Income level, maternal personality, and household sensitivity to children’s needs |
| Molcho et al. 2007, Ireland106 | Mental symptoms (i.e. feeling irritable, bad tempered or more nervous or having difficulties sleeping) | Self-reported data through the HBSC Survey | 8424 school-aged children | Boys who reported experiencing food poverty were more likely to feel low (OR 2.6, 95% CI 2.3 to 2.8), afraid (OR 2.2, 95% CI 1.8 to 2.5) or dizzy (OR 2.4, 95% CI 2.1 to 2.7) than those who did not report food poverty. Girls who reported experiencing food poverty were more likely to feel dizzy (OR 2.0, 95% CI 1.7 to 2.2), afraid (OR 2.2, 95% CI 2.0 to 2.5) or tired and exhausted (OR 2.0, 95% CI 1.8 to 2.2) than those who did not report food poverty | Age and social class (according to the father’s occupation) |
| Pickett et al. 2015, Canada76 | Behaviour problems (i.e. internalising/externalising behaviours) | Self-reported data through the HBSC Survey | 25,912 school-aged children | Children who experienced hunger ‘sometimes’ or ‘often or always’ were more likely to report internalising negative emotional problems than those who ‘never’ experienced hunger (OR 2.1, 95% CI 2.0 to 2.2, and OR 3.8, 95% CI 3.2 to 4.4, respectively). They were also more likely to report externalising negative behavioural problems than those ‘never’ experiencing hunger (OR 1.2, 95% CI 1.1 to 1.3 and OR 2.0, 95% CI 1.7 to 2.4, respectively) | Child and parent sociodemographic characteristics |
| Dunifon and Kowaleski-Jones 2003, USA26 | Behavioural problems (i.e. internalising/externalising behaviours) | Reported by mother through Behaviour Problems Index | 3500 school-aged children | Increased FI was associated with decreased levels of positive behaviours (β –0.17, SE 0.06; p < 0.001) | Child and parent sociodemographic characteristics |
| Howard 2011, USA89 (longitudinal study) | Interpersonal relationships, self-control, externalising behaviour | Children’s and teachers’ reports from the ECLS-K study | 4710 children | Children experiencing FI at any time had lower social skills than those who were food secure. FI was also found to negatively affect children’s non-cognitive skill development. Children who experienced an early transition from FI in first grade to FS in third grade showed a large impairment that persisted through to fifth grade (p < 0.05) | Child, parent and household sociodemographic characteristics |
| Huang et al. 2010, USA92 (longitudinal study) | Children behavioural problems (externalising/internalising behaviours) | Caregiver’s report through the Behaviour Problem Index | 416 children | FI was positively associated with both externalising and internalising behavioural problems. In particular, FI indirectly affected externalising (p = 0.05) and internalising problems (p = 0.061) through parenting stress | Child and household head characteristics, household characteristics |
| Huang and Vaughn 2016, USA93 (longitudinal study) | Children’s behavioural problems (externalising/internalising behaviours) | Children’s and teachers’ reports in the ECLS-K study | 7348 children | Overall, FI was not associated with change in children’s behaviour problems (externalising or internalising behaviours). The authors indicated that the impact of FI on children’s behaviour problems could be episodic or interact with specific developmental stages. However, results might differ depending on the sex and the persistency of FI | Child, parent and household sociodemographic characteristics |
| Johnson and Markowitz 2017, USA96 (longitudinal study) | Children’s behaviour in terms of hyperactivity, conduct problems | Children’s and teachers’ reports in the ECLS-K study | 3700 children | As the level of FI increased across early childhood, the negative associations with behavioural outcomes increased accordingly. Specifically, any one episode of FI in early childhood was associated with increased hyperactivity (β 0.3, SE 0.1; p = 0.02) and conduct problems (β 0.3, SE 0.1; p = 0.05) | Demographic and household economic variables theoretically or empirically linked to FI |
| Kimbro et al. 2015, USA39 (longitudinal study) | Behavioural problems (i.e. interpersonal skills, self-control, internalising and externalising behaviours) | Children and children’s teachers reports in the ECLS-K study | 6300 children | Teachers reported poorer scores for interpersonal skills, self-control, and internalising and externalising behaviours for children who experienced FI (no p-values presented). Children who transitioned into FI had significantly inferior ratings on interpersonal skills, self-control and externalising behaviours, compared with children who were food secure | Child, parent and neighbourhood sociodemographic characteristics |
| McLaughlin et al. 2012, USA47 | Mental disorders according to a DSM-IV classification (mood, anxiety behaviour and substance disorders) | Self-reported through modified version of Composite International Diagnostic Interview and caregiver’s report of major symptoms | 6483 adolescent–parent pairs | A higher FI score was associated with greater odds of any past-year mental disorder and past-year mood, anxiety, behaviour, and substance disorders (OR 1.2 for each). The association between FI and mood disorders was stronger for adolescents with a low family income (OR 1.2–1.6 for adolescents in the lowest three quartiles compared with adolescents in the highest quartile) and was stronger for adolescents with higher levels of relative deprivation (OR 1.1) | Family SES, extreme poverty and family income |
| Poole-Di Salvo et al. 2016, USA53 | Mental health problems | Parent-reported Strengths and Difficulties Questionnaire (as a measure of mental health) from the ECLS-K study | 8600 adolescents | Household FI was independently associated with more than a twofold increased risk of parent-reported mental health problems among adolescents (OR 2.3, 95% CI 1.6 to 3.2) | Adolescent, parent and neighbourhood characteristics |
| Slack and Yoo 2005, USA108 | Behavioural problems | Caregiver’s in-person interview in the US Illinois Families Study | 942 families | Food hardship was positively associated with externalising behaviour problems for younger children (p < 0.01) and with internalising behaviour problems for both age groups (3–5 and 6–12 years; p < 0.01). Food hardship was not found to be related to older children’s externalising behaviour problems (p > 0.05) | Parent characteristics (such as parental stress, warmth, and depression) |
| Weinreb et al. 2002, USA69 | Behavioural problems (i.e. internalising/externalising problems) | Caregiver’s report through the Child Behaviour Check List | 180 preschool children and 228 school-aged children | School-aged children with severe hunger had parent-reported anxiety scores that were more than double the scores of children with no hunger (OR 2.2, SE 1.12; p < 0.05) and significantly higher internalising and externalising behaviour problems (p = 0.04). Similarly, for preschool-aged children, severe hunger was associated with internalising behaviour problems compared with children with no hunger (p < 0.05) | Type of housing, mother’s distress level, and stressful life events |
| Ramsey et al. 2011, Australia54 | Emotional symptoms or behavioural difficulties | Caregiver’s report through a strengths and difficulties questionnaire | 185 children | Children living in food-insecure households were more likely to report borderline or atypical emotional symptoms (OR 2.4, 95% CI 1.1 to 5.4; p < 0.05) or behavioural difficulties (OR 2.4, 95% CI 1.0 to 5; p < 0.05) than their counterparts | Household income |
In summary, 7 out of the 14 studies that adjusted their analyses for explanatory or confounding variables found an association between FI and children’s emotional or behavioural problems,19,26,54,69,76,92,108 one found an association between FI and children’s mental health symptoms,106 and two reported an association between FI and children’s mental health disorders. 47,53 In addition, three longitudinal studies showed a detrimental effect of FI on mental health markers, such as social skills, internalising and externalising behaviours and hyperactivity. 39,89,96 By contrast, another longitudinal study did not find an association between FI and the developmental change in children’s behavioural problems. 93 The authors suggested that the impact of FI on children’s behaviour could be episodic or could interact with developmental phases over time.
Social well-being outcomes
Fifteen studies9,12,58,76,77,84,87,90,91,94,106,107,110,114,117 investigated the association between FI and children’s social well-being outcomes [i.e. happiness, life satisfaction, social skills, quality of life (QoL), lifestyles, physical fighting, misconduct, bullying, rereport to social protection services]. Fourteen studies9,12,58,76,77,84,87,90,91,94,106,107,110,114 adjusted their analyses for explanatory or confounding variables (Table 8) and one117 did not (see Appendix 6). The data were self-reported by children,9,76,77,84,91,106,107,114,117 the caregiver,94 the children’s teachers12,90 or caseworkers in child protection services. 87
| Study authors, year of publication and country | Outcome(s) measured | Measurement tools | Number of participants | Summary of results | Main explanatory or confounding variables considered |
|---|---|---|---|---|---|
| Molcho et al. 2007, Ireland106 | Life satisfaction and happiness | Self-reported data through the HBSC Survey | 8424 adolescents | Boys and girls reporting food poverty were 2.1 times and 2.2 times, respectively, more likely to report low life satisfaction (p < 0.05) and 50% and 60%, respectively, less likely to report that they felt happy about their life (p < 0.05) than their food-secure counterparts | Age and social class (according to the father’s occupation) |
| Pickett et al. 2015, Canada76 | Frequency of physical fighting and talking back to teachers (as a measure of social delinquency) | Self-reported data through the HBSC Survey | 25,912 students | Those reporting hunger ‘sometimes’ were 1.3 times more likely to self-report frequent physical fighting (p < 0.05), and those reporting hunger ‘often or always’ were 1.8 times more likely to self-report frequent physical fighting (p < 0.05) than those who ‘never’ experienced hunger. In addition, those reporting hunger ‘sometimes’ or ‘often or always’ were 40% and 60%, respectively, less likely to report internalised-positive feelings than those who ‘never’ experienced hunger (p < 0.05) | Child, parent, household and sociodemographic characteristics and food assistance programmes characteristics |
| Baer et al. 2015, USA77 | Housing problems (e.g. homelessness, utilities shut off) and substance use problems | Self-reported data through ‘The Online Advocate’ survey | 400 adolescents and young adults | Those reporting low FS or very low FS were from 3.1 (95% CI 1.8 to 5.5) to 3.3 (95% CI 1.8 to 6.0) times more likely to report housing issues (p < 0.001). Those reporting very low FS were 4.5 (95% CI 2.3 to 9.2) times more likely to report substance use problems (p < 0.001) | Age, sex and ethnicity |
| Casey et al. 2005, USA8 | QoL | Self-reported through the Paediatric Quality of Life Initiative | 399 children | Children in households reporting FI recorded significantly lower psychosocial function (p = 0.017), physical function (p = 0.006) and total QoL score (p = 0.005) than children in food-secure households. The results differed by age group, with the youngest children (3–8 years) reporting significantly inferior physical functioning (p = 0.001), and teenagers (12–17 years) living in food-insecure households scoring lower in psychosocial functioning (p = 0.007) | Age, sex and ethnicity |
| Edwards and Taub 2017, USA84 | Bullying (victimisation and perpetration) | Self-reported through the HBSC survey | 12,642 adolescents | Significant difference in bullying victimisation (p < 0.001) and bullying perpetration (p < 0.001) in food-insecure children (fifth to tenth grade) compared with their food-secure peers. Older food-insecure children (ninth to tenth grade) reported more bullying victimisation, and also engaged in more bullying perpetration (p < 0.05). Students who reported FI, at least occasionally, experienced greater bullying victimisation than those who did not report FI (p < 0.008). In addition, more boys in the overall sample engaged in bullying perpetration than girls (p < 0.05) | Grade, sex, FI level |
| Fram et al. 2015, USA114 | Lifestyles | Self-reported through dietary recalls and a self-administered physical activity checklist | 3605 children | FI was associated with higher calorie consumption (p = 0.02), more fat (p = 0.04) and sugar (p = 0.05) intake, a diet that was lower in vegetables (p = 0.02) and a variety of perceived barriers (e.g. feeling too tired) to exercising (p < 0.001) | Child characteristics |
| Howard 201190 (longitudinal study) | Social skills | Teachers’ reports on social skills scores | 4710 children | There was a significant (p < 0.05) negative relationship between FI and children’s social skill scores. Children who experienced a transition from FI in first grade to FS in third grade had significantly lower social skill scores (p = 0.019). The association was significant among boys (p < 0.05) but not among girls (p = 0.56) | Child characteristics |
| Howard 201391 (longitudinal study) | Dietary behaviours | Self-reported fruit and vegetables consumption | 5670 children | Food-insecure children reported a lower weekly consumption of fruit (p < 0.05) but a higher amount of carrots and potatoes (p < 0.05) than children with very low FS | Child and ecological factors influencing consumption of fruit and vegetables |
| Jackson and Vaughn 2017, USA94 (longitudinal study) | Misconduct (i.e. fighting, bullying, stealing, cheating, lying, and defying/misbehaving) | Caregiver-reported | 5323 adolescents | Among boys, persistent exposure to FI during childhood was associated with greater involvement in fighting/bullying (OR 1.7, 95% CI 1.4 to 2.1), stealing (OR 1.7, 95% CI 1.3 to 2.2), cheating/lying (OR 1.4, 95% CI 1.2 to 1.6) and defying/misbehaving (OR 1.3, 95% CI 1.1 to 1.5). Participating in multiple forms of misconduct was 168% higher among boys exposed to persistent FI than among those who were raised in consistently food-secure households. These results were not significant in girls | Adolescent, parent, household and neighbourhood characteristics |
| Helton 2016, USA87 | Rereport to child protection services | Caseworker reports | 3580 families with children | 12% of families with food-neglected children were rereported to child protection services, compared with 8% of families without food-neglected children. Food neglect predicted a greater risk of rereport (HR 3.0) than of other forms of maltreatment (p < 0.05) | Maltreatment types, caregiver mental health problems, and covariates |
| Jyoti et al. 2005, USA11 (longitudinal study) | Social skills and behaviours | Children’s and teachers’ reports in the ECLS-K study | Approximately 21,000 children | Children from food-insecure households at kindergarten demonstrated a 0.08-point greater decline in social skills score than children from food-secure households (p < 0.05). Association between kindergarten FI and change in social skills was significant for boys only (p < 0.001). Transitioning from food insecure to food secure was associated with a greater increase in social skills for girls (p < 0.001) and a smaller increase in social skills for boys (p < 0.038). Becoming food insecure was associated with a greater decline in social skills among girls (p < 0.005) but greater improvement in social skills for boys (p < 0.050) | Time varying and time-invariant for child, parent and neighbourhood household characteristics |
| Rossen and Kobernik 2016, USA58 | Dietary behaviours | Caregivers’ complete recalls for < 6-year-olds; 6- to 11-year-olds completed the recalls with assistance; and ≥ 12-year-olds self-reported | 5136 children | Children experiencing very low FS consumed fewer whole grains (p > 0.05), more solid fats (p > 0.05) and more added sugars (p > 0.05) than their food-secure counterparts. However, FI was mostly not associated with dietary intake (p > 0.05) | Child characteristics |
| Sharkey et al. 2012, USA107 | Dietary behaviours | Self-reported 24 hours’ dietary recall | 50 children | Very low FS was associated with greater intakes of total energy (p < 0.05), calcium (p < 0.05) and percentage of calories from added sugar (p < 0.001) | Child characteristics |
| To et al. 2014, USA110 | Physical activity | Self-reported through questionnaire and accelerometer | 2261 children and adolescents | Food-insecure children registered less moderate to vigorous physical activity than food-secure children (coefficient 25.24; p = 0.02). However, FI was not related with adherence to physical activity guidelines or time spent doing sedentary activities (p > 0.05) | Child and household characteristics |
In summary, FI was associated with poor social well-being, poor QoL and unhealthy lifestyles in children and adolescents in all 14 studies. In particular, FI was associated with poorer scores on happiness and life satisfaction,106 poorer social skills scores,90 more frequent housing problems (e.g. homelessness),77 substance abuse,77 frequent bullying engagement,84 frequent physical fighting,76 poorer diet quality91,107,114 and lower QoL scores. 9 One longitudinal study found that persistent household FI during childhood was linked to physical fighting and other misconduct (bullying, stealing, lying and defying behaviour) among boys, but not girls. 94 A sex difference was also reported in another longitudinal study, which observed that changes in social skills scores over time were dependent on the transition from FI to FS (or vice versa) and sex. 12 One study reported differences in QoL scores according to age, with food-insecure children (3–8 years) reporting lower scores in physical functioning and food-insecure adolescents (12–17 years) reporting lower scores in psychosocial functioning. 9 One study showed that families with a history of food neglect had a greater risk of being rereported to the child protection services in a shorter time than families without food neglect. 87
Academic outcomes
Thirteen studies examined the relationship between FI and children’s academic performance. 12,19,26,39,54,60,69,72,73,77,96,99,113 Eleven studies adjusted their analyses for explanatory or confounding variables (Table 9)12,19,26,39,54,60,69,72,77,96,113 and two did not (see Appendix 6). 73,99 The outcomes more often assessed were reading and maths scores, school attendance and cognitive development. Most of the outcomes were self-reported, obtained through tests or teacher reported. One study assessed parent-reported outcomes. 54
| Study authors, year of publication and country | Outcome(s) measured | Measurement tools | Number of participants | Summary of results | Main explanatory or confounding variables considered |
|---|---|---|---|---|---|
| Belsky et al. 2010, UK19 | Cognitive development, IQ score | Self-reported through Wechsler Intelligence Scale for Children | 2125 school-aged children | Children in food-insecure households had significantly lower IQs and higher levels of behavioural and emotional problems than their food-secure counterparts (p < 0.001). FI predicted lower child IQ, but once household income was added to the model, the association was no longer significant | Household income and nonmaterial household characteristics |
| Baer et al. 2015, USA77 | Educational problems | Self-reported data through ‘The Online Advocate’ survey | 400 children and young people | FI was linked to educational problems such as unmet learning disability and dropping out of high school (low FS: OR 2.4, 95% CI 1.1 to 5.3; p = 0.03; very low FS: OR 3.9, 95% CI 1.8 to 8.4; p < 0.01) | Age, sex and ethnicity |
| Dunifon and Kowaleski-Jones, 2003, USA26 | Childhood activities, school attendance, performance of schoolwork | Self-reported through Woodcock–Johnson Psycho-Educational Battery | 3500 school-aged children enrolled in the NSLP | Significant association between FI and children’s academic scores (p > 0.05). Students receiving food aids (NSLP) had lower maths scores than those who did not receive food aids | Household sociodemographic characteristics |
| Johnson and Markowitz 2017, USA96 (longitudinal study) | Children’s kindergarten reading and maths outcomes | Children’s teachers’ reports in the ECLS-K study | Approximately 3700 children | Negative associations between earlier FI (at 9 months and 2 years) and school outcomes. Very low FI at 9 months was linked to reduced reading scores (p = 0.03) while low FS at 9 months was associated with decreased maths scores (p = 0.03); very low FI at 2 years was associated with decreased approaches to learning (p = 0.04) and reduced maths skills (p = 0.03). In general, as the intensity of FI increased across early childhood, so too did negative associations with outcomes | Sociodemographic and household economic variables |
| Jyoti et al. 2005, USA11 (longitudinal study) | Academic achievement (reading and maths scores) | Children’s teachers’ reports in the ECLS-K study | Approximately 13,500 children | Negative association between kindergarten FI and change in maths score was significant only for girls (β –1.8; p < 0.017). Children from households transitioning from FS to FI showed a smaller increase in reading (p = 0.0007) and maths scores (p < 0.005) than children from households who remained food secure. These differences were significant regardless of sex | Child and household characteristics |
| Kimbro et al. 2015, USA39 (longitudinal study) | Academic achievement (reading, maths and science scores) | Children’s teachers’ reports in the ECLS-K study | 6300 children | Children who were food insecure at first grade did had significantly lower academic achievement scores in reading, maths and science than children who were food secure, and those who were food insecure at both kindergarten and first grade scored lowest on all three measures. However, when the analyses were adjusted for relevant covariates, no significant association was found between FI transitions (into and out of FI) and children’s academic achievement outcomes | Child and household characteristics (including family structure, household income, parental employment status, occupational prestige, education and the number of siblings in the household) |
| Shanafelt et al. 2016, USA60 | School attendance | School records from participants of the US BreakFAST Project | 904 children | Food-insecure students were more likely to have a lower cumulative attendance, grade-point average (p < 0.01) and be in a lower grade-point percentile than their food-secure counterparts (p < 0.01). Food-insecure adolescents were more likely to show a lower attendance rate than food-secure adolescents (p < 0.01), but this was no longer statistically significant after adjustment (p = 0.15) | Grade level, sex, free and reduced-price lunch status, ethnicity and weight categories |
| Winicki and Jemison 2003, USA113 | Academic achievement (reading and maths scores) | Children’s teachers’ report in the ECLS-K study | 21,260 children | Negative effect of FI on maths scores and on learning (p < 0.05). However, for children at or below 150% of the federal poverty level, the FI measures did not explain maths scores or learning | Explanatory variables that were indicators of increasingly severe levels of FI |
| Weinreb et al. 2002, USA69 | Academic scores, developmental delay, learning disabilities, repeat of a school year or missing days in school | Self-reported through the Wechsler Individual Achievement Test Screener | 180 preschool-aged children and 228 school-aged children | Compared with preschool and school-aged children who were moderately or not hungry, those who experienced severe hunger showed poorer academic scores, developmental delay and learning disabilities, and were likely to repeat a school year or miss days in school. However, these differences were not statistically significant (p > 0.05) | Housing status |
| Zaslow et al. 2009, USA72 (longitudinal study) | Children’s cognitive development | Children’s teachers’ reports in the ECLS-B | 8944 children | No direct effect of FI on children’s cognitive development (p > 0.05). Higher levels of FI worked indirectly through depression and parenting practices to influence mental proficiency in toddlerhood. High levels of FI were positively associated with depression (β 0.180). In turn, depression was negatively associated with more positive parenting practices (β –0.033), and positive parenting practices were positively associated with mental proficiency at 24 months (β 0.081; p < 0.001) | Child, parent and household sociodemographic characteristics |
| Ramsey et al. 2011, Australia54 | Days away from school due to illness | Caregiver reported | 185 households with children aged 3–17 years | Children who were living in food-insecure households were 3.5 times more likely to have days away from school because of illness (OR 3.5, 95% CI 1.4 to 8.5; p < 0.05) and 5.4 times more likely of having to cut down on activities because of illness (OR 5.4, 95% CI 1.4 to 20.1; p < 0.05) | Household income |
In summary, 5 out of the 11 studies that reported adjusted results showed some detrimental effects of FI on children’s academic outcomes, such as lower intelligence quotient (IQ) scores,19 lower reading or maths scores,96 lower school attendance54,60 and dropping out of high school more frequently. 77 Three studies found no effects of FI on academic outcomes. 26,69,113 One study that used data from the ECLS found that FI worked indirectly through depression and parenting practices to influence mental proficiency in toddlerhood. 72 A longitudinal study found negligible impacts of FI transitions on academic outcomes in first grade once child and family characteristics were taken into account. 39 By contrast, another longitudinal study found that FI was associated with developmental outcomes and that the association differed by sex. 12
Research question 4: what interventions exist to reduce, eliminate or mitigate the effects of child food insecurity in high-income countries?
Fifteen studies assessed the effects of interventions, programmes or food aids designed to eliminate, reduce or mitigate the effects of child FI. 26,50,71,74,78,83,98,115–122 Fourteen studies were conducted in the USA and evaluated federal programmes of food aid,26,50,71,74,78,83,98,115–121 and one study, a 1-year stepped-wedge cluster RCT, was conducted in New Zealand. 122
Of the included studies, six evaluated school-based food provision programmes,26,50,98,117,118,122 six evaluated nutrition assistance federal programmes,74,78,83,115,116,121 two evaluated programmes that provide an extra money during the summer holidays,119,120 and another evaluated a nutrition assistance federal programme and informal/community food support, such as food pantries, Meals on Wheels and soup kitchens. 71 The characteristics of these food aid programmes are summarised in Table 10 and further information is reported in Appendix 8. Among the qualitative studies identified for RQ 1, the study by Harvey-Golding et al. 31 reports qualitative information on the perspective of senior stakeholders involved in the UK Universal School Breakfast Programme and is summarised below.
| Study authors, year of publication and country | Brief summary of programme/intervention | Population | Outcome(s) measured | Summary of results | Main explanatory or confounding variables considered |
|---|---|---|---|---|---|
| Barroso et al. 2016, USA78 | The SNAP offers nutrition assistance to low-income individuals and families and provides economic benefits to communities (previously known as food stamp programme) | Children from Hispanic mothers enrolled in the USA WIC programme. 240 mother–child dyads | Child weight, weight-for-length | After adjusting results for potential confounders, receiving SNAP was positively associated with child weight status. Children whose mothers reported ever having received SNAP were 2.01 times more likely to be overweight than children whose mothers did not report ever having received SNAP (OR 2, 95% CI 1.0 to 3.9; p < 0.05) | Child characteristics and eating behaviours |
| Canter et al. 2017, USA115 | Double-value coupon programme recruited during SNAP transaction at a farmer’s market or during pick-up from child care | 148 caregivers recruited from several agencies serving low-income families | Fruit and vegetable intake, physical activity, sleep, FI | Food-insecure children consumed significantly fewer servings of vegetables (p < 0.05). Physical activity significantly predicted fruit and vegetable intake (p < 0.01). However, double-value coupon programme service usage did not have a significant impact on children’s fruit and vegetable consumption | Child characteristics |
| Cook et al. 2004, USA83 | Three US federal programmes of food aid are considered in this study: food stamps, which help people with low income to buy food; WIC, which provides supplemental foods and nutrition education for low-income pregnant, breastfeeding, and non-breastfeeding postpartum women; and TANF, an emergency fund that provides food assistance | 11,539 caregivers | Parent-reported health status and number of hospitalisations since birth | Receiving food stamps attenuated (but did not eliminate) the association between FI and children’s fair/poor health. For children in households not receiving food stamps, being food insecure increased the odds of fair/poor health by 2.1 times, after controlling for other covariates and adding ‘receiving food stamps’ into the analyses. A similar pattern was seen for TANF benefits; however, the interaction was not significant. In the analysis of hospitalisation since birth, there was no significant interaction between receiving food stamps or TANF benefits and FI. No results for the WIC programme were reported | Child and parent characteristics |
| Cook et al. 2006, USA116 | The food stamps programme is a food-purchasing assistance initiative for low- and no-income people across the USA (later renamed as SNAP) developed by the US Federal Government, which funds a variety of services to help low-income families with children | 17,158 caregivers of children aged ≤ 3 years | Parent-reported health status and number of hospitalisations since birth | Children in food stamps programme participating households that were classified as households with child FI had lower odds of fair/poor health (OR 1.7, 95% CI 1.3 to 2.2) than children in similar households not participating in the food stamps programme (OR 2.1, 95% CI 1.8 to 2.5). Participation in food stamps programme reduced the odds of fair/poor health by 24% and 42% in food-insecure households and households with child FI, respectively | Child and parent characteristics |
| Dunifon and Kowaleski-Jones 2003, USA26 | The NSLP is a federal nutrition programme that provides nutritious foods to school-aged children. Families according to their income are eligible for free or reduced-price NSLP lunches | ≈3500 children | Health limitations, behavioural problems, and academic achievement | Participating in the NSLP was found to be associated with increased externalising behaviour (p < 0.05), an 82% increase in the odds of having a health limitation (p < 0.05), and lower maths scores (p < 0.05). An increase in FI was associated with decreased level of positive behaviours and increased odds of health limitations | Child, parent and household characteristics |
| Ecker and Sifers 2013, USA118 (non-randomised comparative study) | The BackPack Food Program is a weekend food programme that aims to reduce hunger among school-aged children through the distribution of easy-to-prepare food in children’s backpacks every Friday or the last day of school prior to a long weekend | 1380 children from three schools with the highest percentage of students receiving free and reduced lunches in the Midwest of USA | Hunger and children’s behaviours | Direct observations of on-task behaviour were recorded for 52 students. Overall, there was not a significant increase in students’ on-task behaviour (p = 0.19) or a significant decrease in students’ self-reported hunger levels (p = 0.54). Almost all parents (98%) reported that the programme benefited their family, and made a difference to the well-being of their child | Unadjusted |
| Gordon et al. 2017, USA119 (non-randomised comparative study) | The SEBTC was a programme in which low-income households with children eligible for free or reduced-price meals received benefits per school-aged child per summer month (about US$60). Benefits were delivered through an electronic benefit transfers cards that could be used to purchase food via existing programmes such as SNAP or WIC system | Approximately 67,000 children from around 42,000 households were involved in the SEBTC | Parent-reported FS and dietary quality | Average rates of very low FS among children in the no-benefit group were higher than those in the benefit group (p < 0.001). In general, the SEBTC programme significantly improved children’s healthier eating, with increased consumption of fruits and vegetables, whole grains and dairy products and reduced consumption of sugar sweetened beverages (p < 0.001) – with the exception of sugar-sweetened beverages in SNAP households | Differences in populations across sites, parent and demographic characteristics |
| Khan et al. 2011, USA98 | Free school breakfast available to all school children in a school in Vermont | 373 children | Self-reported FS | The majority of surveyed children were classified as food secure (79.6%), 15.8% were classified as food insecure without hunger, and 4.6% were classified as food insecure with hunger. A statistically significant relationship between FS and eating breakfast at home was found. Children who were food insecure (with or without hunger) were less likely to eat breakfast at home than children who were food secure (67.1% vs. 81.4%; p = 0.007) | Unadjusted |
| Kleinman et al. 2002, USA117 (non-randomised comparative study) | A USBP in the Boston Public Schools | 97 children; inner-city students in grades 4 to 6 | Child nutritional risk status, hunger, psychosocial functioning and academic performance | Children whose nutritional status improved recorded significantly larger increases in school breakfast participation than children whose nutritional status stayed the same or worsened (p < 0.001). For those who improved their nutritional intake, significant improvements were recorded in functioning (p < 0.01) and maths grades (p < 0.05), as well as a significant decrease in the number of days away from school (p < 0.001) | Unadjusted |
| Klerman et al. 2017, USA120 (non-randomised comparative study) | SEBTC programme in 16 US sites between 2011 and 2013. Authors performed a random-assignment evaluation where benefit amounts, participating sites, details of the intervention, and households sample size varied across geographical regions. In 2011 and 2012, households were assigned to a SEBTC benefit group (US$60 per school-aged child per month) or to a zero-benefit control group. In 2013, to test the differential impact of benefits – US$60 relative to US$30 – all randomised households were issued the some SEBTC benefits (either US$60 or US$30 per school-aged child per month) with no zero-benefit control group. The benefit amounts were given through SNAP or WIC sites | Summer survey n = 48,449; spring survey n = 41,793 households | Parent-reported FS | SEBTC improved children’s FS in both SNAP and WIC sites. A US$30 SEBTC benefit per child improved FS (p < 0.01) but generally had a smaller impact than the US$60 benefit (p < 0.01). After adjusting the analyses for household characteristics, the authors reported significant variations in the impact of the US$60 monthly benefits compared with no benefits | FI status; adolescent, household and school characteristics |
| Kohn et al. 2014, USA74 | SNAP and WIC benefits. School meal participation was defined as the child eating free or reduced-price school breakfast and/or school lunch at least once a week during the school year | 1321 young people | Weight status | Prevalence of overweight and obesity was not significantly different for children participating in food programmes compared with non-participating children. Among low-income, food-insecure children, food assistance participation was not associated with BMI scores, high waist circumference or weight status for any specification of food assistance (adjusted analyses). However, analyses by sex showed that low-income, food-secure girls participating in food assistance programmes (SNAP or WIC) other than school meals alone had higher BMI score (β 0.4, 95% CI 0.1 to 0.7) and greater risk of high waist circumference (OR 2.2, 95% CI 1.0 to 4.6) | Child and parent characteristics |
| Korenman et al. 2013, USA121 (non-randomised comparative study) | The federal CACFP reimburses child care providers for meals and snacks served at participating preschools, day care homes, afterschool programmes and homeless shelters, according to a child’s family income | 10,700 children from the ECLS Birth Cohort | Children’s nutrition-related outcomes and FI | Low-income children participating in CACFP were 1.4 times more likely to consume two or more cups/day of milk (OR 1.4, 95% CI 1.0 to 1.9; p < 0.05) and 1.6 times more likely to consume two or more servings/day of vegetables (OR 1.6, 95% CI 1.6 to 2.1; p < 0.05). However, there was no change in FI status (p > 0.05) | Household characteristics and food participation programme |
| Nalty et al. 2013, USA50 | School-based nutrition programmes such as SNAP, WIC, NSLP, School Breakfast Programme and SFSP | Residents of rural areas along the Texas–Mexico border (48 mother–child dyads) | Parent- and child-report of FS | Child FI improved significantly from summer to school months with protection during school offered by the school breakfast programme and NSLP. Children who took part in these programmes were 70% less likely to report FI (OR 0.3, 95% CI 0.1 to 0.5; p < 0.001). However, SFSP and SNAP did not reduce the burden of FI during the summer (p > 0.05) | Maternal characteristics |
| Yu et al. 2010, USA71 | Food stamps and informal/community food supports (e.g. food pantries, Meals on Wheels and soup kitchens) | 3799 households (710 African American households and 3089 Caucasian households) | FS | In both ethnic groups child FS was positively related to food stamp programme participation and informal food supports. Although informal food supports positively predicted child FS in both ethnic groups (p < 0.001), participation in the food stamps programme predicted greater child FS (p < 0.001) among Caucasian households but not among African American households | Sociodemographic and household characteristics |
| Mhurchu et al. 2013, New Zealand122 (cluster RCT) | 1-year, stepped-wedge, cluster RCT in low-SES schools to investigate the effects of a free daily SBP | 424 children | School attendance and academic achievement | Significant decrease in children’s self-reported hunger (p < 0.001). No significant effects of the SBP on children’s school attendance (p > 0.05) and academic achievements | Child characteristics |
In summary, studies varied in terms of the characteristics of the interventions/food aid programmes assessed, characteristics of the sample population, setting and range of outcomes assessed. There is some evidence that food assistance programmes, which provide benefits to low-income households with school-aged children, may improve children’s FS;50,120 reduce, but not eliminate, the effects of FI on poor health;83,116 and promote children’s healthier eating patterns with increased consumption of fruit and vegetables and dairy products. 119,121 Nevertheless, one of the studies pointed out that even with food coupons, it may be challenging for families to buy fresh food (e.g. fruit and vegetables). 115 It is worth noting that although food assistance programmes may improve children’s FS, the impact on FI may vary according to the type and level of benefits50,120 and the rate of utilisation of food support and may be different in different ethnic groups. 71 A cluster RCT showed that free school breakfast programmes may have had positive effects in reducing children’s short-term hunger but did not have an impact on children’s school attendance and academic performance. 122
Other findings (qualitative data)
Some of the studies included in this rapid review that evaluated food assistance programmes provided qualitative information on some specific aspects of the programmes. Harvey-Golding et al. ,31 for example, investigated the beliefs, views and attitudes among key stakeholders served by a council-wide universal free school breakfast (UFSB) initiative in the north-west of England. A sample of 19 stakeholders (school staff and local authorities) were recruited from three primary schools participating in the UFSB scheme to take part in semistructured interviews and small focus groups. They reported that the prevalent perception of the participants was that the UFSB programme contributed to the mitigation of FI in the community: ‘I think it just takes the pressure off them and it just gives them the knowledge that the child is gonna come to school, have something to eat to set them up for the day till lunch time’. 31 Similarly, the programme was considered an important feature for those parents experiencing working poverty and who were potentially not eligible for free school meals. Furthermore, senior level stakeholders (local authorities and primary school staff) involved in the implementation of the programme, claimed that the programme could help teachers as well – considering that in many cases teachers ended up to buy food for children who came to school without eating at home. They also maintained that the programme was an opportunity for some children to have a wider and healthier food choice as well as a way to increase their autonomy and independence. In general, the UFSB programme was perceived by senior school staff as a way of alleviating hunger among children in schools. Before the start of the UFSB programme, staff reported that some children consumed high-calorie/low-nutrition snack foods and beverages in school, such as crisps and carbonated drinks. These behaviours changed after the programme started: ‘I have not seen in months, children walking to school eating junk. I did see that before breakfast came along’. In addition, parents were less likely to provide children with money to buy breakfast as they were receiving something of nutritional value at school. 31 Some senior staff felt that the programme had the potential to improve punctuality because children were more likely to arrive on time, owing to the appeal of a free breakfast: ‘I am aware that kids now get to school earlier than what they did’, ‘Where the parents are not feeding them they know that they are going to be fed’. 31 Following the introduction of the UFSB programme, children were more alert and less likely to lose concentration in class. The programme was also assumed to provide children with opportunities to interact with their peers and staff while eating breakfast. In addition, senior school staff considered that the programme was effective in reducing children’s anxieties about being hungry and, therefore, was beneficial for learning. Likewise, school breakfast was considered to have a positive impact on the school environment, providing a calm and positive start to the school day. 31
Local authorities and schools staff were aware of the potential negative impact of the UFSB programme on children’s health, such as encouraging overeating and increasing obesity levels: ‘There is some concern that maybe some children are double eating in the morning’. 31 It was perceived that a small minority of children, perhaps from more affluent areas of the community, were eating breakfast twice, at home and at school: ‘If they are getting an unhealthy breakfast at home in the more affluent families, and then getting a healthy one at school it is still adding calories’. 31 To prevent potentially unwanted impacts of consuming breakfast twice, it was considered that communication with parents needed to be improved as a matter of urgency: ‘We need to get the right message to parents that we will be providing breakfast for those kids’. 31 Moreover, other issues raised by the participants were problems related to high-sugar items at school and concerns about obesity and dental health among children, because providing practical breakfast items that were healthy and balanced in terms of nutrients proved difficult: ‘The handheld one does offer a real challenge in getting a good variety of healthy items in there’ or ‘We used to have fruit juice on. That’s now had to come off. [. . .] It was public health, because it has an impact on dental health’ or ‘I was looking at one of the waffles, I’ve got the pack in front of me here and the, on the traffic light system they have now on the packets, it’s red for fat, saturates and sugars [. . .]’. 31
Although some senior school staff considered that the universal provision of the UFSB programme was necessary to remove barriers, maintain equality and eliminate stigma, others felt that a more targeted approach would have had a greater impact and would save resources: ‘I mean it’s very expensive and I’d like to think it was more targeted, rather than universal’. 31
Research question 5: what is the cost-effectiveness of existing interventions that aim to reduce, eliminate or mitigate the effects of child food insecurity in high-income countries?
None of the studies included in this rapid review evaluated the cost-effectiveness of interventions developed to reduce, eliminate or mitigate the effects of FI in children living in high-income countries. Similarly, there was no evidence from the grey literature to answer this RQ.
Chapter 4 Summary of the grey literature
The main themes identified during scrutiny of the grey literature relating to child FI were breakfast clubs, holiday hunger, food banks, necessity of measurement of household FI, and the relationship between obesity and FI in children.
Breakfast clubs
The 2017 Kellogg’s (Battle Creek, MI, USA) survey of secondary school teachers showed that 82% of teachers witnessed teenagers arriving at school hungry every day and that 62% of school staff described seeing children arriving at school hungry on a weekly basis. 135,136
The proportion of schools, on average, that provide breakfast clubs is 85% in the UK, 72% in Scotland and 96% in Wales. In England, provision ranges from 82% to 91%. In the UK, there are universal free school meals for infant-aged pupils (i.e. reception, years 1 and 2). In Scotland, all children in primary 1 to primary 3 are eligible for free school meals. 135,136
A Department for Education evaluation of breakfast clubs in schools with high levels of deprivation reported that around one-third to two-fifths of pupils attending breakfast clubs were eligible for free school meals. 137 Kellogg’s also reported a correlation between the proportion of pupils eligible for free school meals and the proportion of schools with a breakfast club. 136
A large proportion of secondary schools (79%) reported thinking that their breakfast club would have to close, with school funding being main reason (86%), followed by the extra staff requirement (44%) and breakfast club-specific funding cuts (39%). By contrast, 5% of primary and secondary school teachers think that it is unlikely that their breakfast club will close. Around half of schools (54%) report that their breakfast club is operating below capacity. 135,136
The Kellogg’s audit of school breakfast club provision in the UK reported that teachers believed that breakfast clubs make a substantial difference to pupils’ attendance and concentration in class and have a longer-term effect on examination results. 135 In addition, 45% and 49% of schools said that their club had improved attendance and concentration, respectively. Overall, 15% of schools reported an improvement in examination results, which they linked to their breakfast club.
A report by the Sheffield Political Economy Research Institute of children’s experiences of food and poverty showed that peer-reviewed evidence on outcomes of breakfast club provision surrounding education, health, social inclusion and family life are extremely varied and far from conclusive. 138 Several studies showed improvements in some outcomes but not in others, and some outcomes showed declines. These findings are reinforced (and partly informed) by the published studies of Shemilt et al. 139 and Murphy et al. ,140 which showed improvements in some outcomes (e.g. concentration, nutritional intake at breakfast time, skipping classes) but no effect on others (e.g. skipping breakfast). Furthermore, one study reported ‘disbenefits’ in the form of negative behaviours. 139
The Department for Education137 conducted a ‘semisystematic’ literature review of school breakfast clubs as part of its evaluation of breakfast clubs in schools with high levels of deprivation. Five out of the six studies identified by the Department for Education review were not relevant to the present rapid review because they did not assess child FI specifically. Nevertheless, for completeness and to complement the findings of this rapid review their results are reproduced in Table 11. Full details of the sixth study122 are reported in section RQ 4 of this rapid review.
| Programme name | Study design | Description of programme | What was learnt about what works? |
|---|---|---|---|
| Welsh Government: school breakfast clubs140 | Cluster RCT + process | Universal free breakfast provision in Welsh primary schools. Held in nine local authority areas, covering 111 schools | Better targeting of pupils who are not eating breakfast at home is needed. There was no reduction in breakfast skipping or classroom behaviour after introducing breakfast clubs, generally because those who accessed breakfast at school were those who would otherwise have eaten at home |
| School breakfast clubs, England139 | Cluster RCT and observational analysis | Breakfast clubs in 30 schools with high deprivation in England |
It is hard to conduct RCTs in this setting, given the lack of control evaluators have over recruitment, eligibility checking and implementation Inadequate supervision could lead to clubs becoming boisterous or disruptive The evaluation showed improvements in concentration, attendance and fruit eating |
| New Zealand Free School Breakfast Programme122 | Stepped-wedge cluster RCT | Universal free breakfast to 14 primary schools in deprived areas of New Zealand |
There was no effect on school attendance or academic achievement, but some effect on satiety after introducing breakfast clubs Some positive impact was found on attendance but only among those who attended > 50% of the time |
| New York City, Breakfast in the Classroom141 | Cross-sectional survey comparing Breakfast in the Classroom and non-Breakfast in the Classroom schools | Universal free breakfast, offered in the classroom, in elementary schools in deprived areas of New York City |
Those setting up clubs need to bear in mind that children skip breakfast for a variety of reasons (predominantly a lack of time, lack of hunger and dieting to lose weight); this diversity needs to be taken into account For every student who ate breakfast who otherwise would not have done, three ate breakfast twice |
| Australia: healthy food for all, evaluation of the school breakfast programme142 | Annual online survey to participating schools | Long-running national programme (running since 2001) serving 369 schools in Western Australia | Problems identified in breakfast clubs mainly related to a lack of volunteers or staff to run the clubs, and problems with food products running out, not being available or going off |
| US Department of Agriculture, Food and Nutrition Service: Evaluation of the school breakfast programme pilot project143 | Experimental design including treatment and control schools | Evaluation of a pilot of universal free breakfast provision (as compared with the control provision that pupils pay for, get free or get at a reduced price depending on family income). Pilot covered 79 elementary schools in six districts |
There was a substantial increase in participation in the first year of the pilot, which was maintained in the following 2 years Participation by students from lower-income families doubled across the 2 years of implementation Participation was much higher in schools where breakfast was eaten in the classroom rather than in a cafeteria There was no clear impact on academic test scores or on attendance, tardiness or discipline |
Holiday hunger
An All-Party Parliamentary Group on Hunger, involving UK Members of Parliament and Peers, published a report in April 2017 that focused on hunger among children during the school holidays. 144 The report stated that up to 3 million children in the UK are at risk of hunger during the school holidays, when free school meals received during school term time are not available. It is estimated that there are up to around 1 million children in this group. In London alone, it has been estimated that school holidays involve a struggle for food for over half a million children. Accordingly, there is a notable increase in the pressure on food banks during the school holidays. 144 A further indicator of the issue is highlighted by school staff at the start of the school term; for example, a National Union of Teachers (NUT) survey found that 78% of teachers reported children arriving at school hungry after the holidays. 145 Furthermore, 39% of UK teachers in a Kellogg’s survey reported believing that pupils do not get enough to eat during the holidays. 144
The long summer break has been shown to have a negative effect on the educational levels of low-income children who are not engaged in learning during the holidays. Of note, mathematics and spelling performance are particularly susceptible to adverse effects, and children can take up to 7 weeks to make up this loss of learning. 144,146 The NUT survey reported that 78% of teachers believed that hunger in the holidays has a negative effect on children’s education. 145 In addition, 69% and 57% were concerned about the negative effects of such hunger on children’s social well-being and physical health, respectively. 144
It has been reported that children who attend free meal and activities programmes in the school holidays eat more healthily, participate in more exercise, behave better and return to school in a more positive condition than if they had not attended. 144
A number of schools around the country have responded to the need for year-round nutrition for children. For example, free school holiday meals and activities have recently been approved for families in need in Aberdeen, highlighting a growing recognition of the issue of holiday hunger. 147
A recent report highlighted four challenges that breakfast and holiday clubs face: inaccessibility (availability, capacity, opening hours and cost vary and can be a barrier for some children), unreliability (clubs do not always run continuously over time), unaccountability (provision is often voluntary without formal oversight) and social acceptability (implications of social exclusion, embarrassment and stigma for children using the facilities). 138
Food banks
The information regularly published by the Trussell Trust on food banks is reported to be the most frequently cited in the context of FI. 148–150 In addition to food banks, there is some government ‘food aid’ in the UK; families receiving specific income-related benefits can be eligible for free school meals. People on such benefits with children aged < 4 years can also receive vouchers to purchase fresh and infant formula milk and fresh or frozen fruit and vegetables. 151
Between 2012/13 and 2013/14, provision to children by Trussell Trust food banks rose by 252%. Provision to children has since risen by a further 69%. 138 Latest figures from the Trussell Trust reported that 1,332,952 3-day emergency food parcels were distributed to people in crisis between 1 April 2017 and 31 March 2018, representing a 13% increase on the previous year. Of these, 484,026 went to children. 149 The Trussell Trust further reported that half of children helped by food banks over the summer holiday months are of primary school age. 150
Necessity of measuring household food insecurity
The need to routinely measure household FI in the UK was evident in the grey literature. The UK government does not currently measure household FI and there is no way of knowing the actual extent of the issue. 5,152,153 Approximately 77% of adults in the UK think that the government should routinely measure FI, and Members of Parliament have called for the government to introduce such measures. Steps to measure household FI are being taken in Scotland, Wales and Northern Ireland, but measurement is not consistent across countries and a complete picture of household FI in the UK is not possible. To effectively tackle household FI, robust measurements of its extent are necessary. As there is no single tool able to capture all the dimensions of FI, a combination of different measures is necessary to fully understand the extent, causes and consequences of FI. The Food and Agriculture Organisation of the United Nations launched the Voices of the Hungry project in 2013 in an attempt to broaden the set of existing indicators. This project led to the development of the Food Insecurity Experience Scale (FIES), which provides information about the adequacy of people’s access to food by asking them directly about their experiences. 128 The UK Department of Health has previously stated that, in view of the FAO initiative, it has no plans to independently measure and monitor FI. 5 Nevertheless, the UK Food Foundation has suggested the addition of standardised questions on FI (as used in the UN FAO Food Insecurity Experience Scale) into existing UK surveys such as the Office for National Statistics Living Costs and Food Survey,154 or the Health Survey for England. 155
Overall, the grey literature was silent on the measurement of child FI. 5,128,156,157
Obesity and food insecurity in children
The relationship between obesity and FI in children has been investigated in both the published and the grey literature. The Food Research and Action Centre reported mixed results from studies based in the USA. 158 For example, one study found no association between obesity and household FS status in low-income children aged 8–17 years. 85 By contrast, children aged 12–18 years from low-FS households were more likely to be obese than those from high-FS households. 88 Furthermore, low-income children experiencing persistent household FI during infancy and early childhood were 22% more likely to be obese at 2–5 years than those from food-secure households. The reasons for the link between obesity and FS are reported to be multifactorial. 159 For example, lack of full grocery facilities in low-income areas,160–162 reliance on public transport by people on low incomes,163 relatively high cost (and poorer quality) of healthy foods as compared with less healthy foods in lower-income neighbourhoods,164,165 prevalence of fast-food-type outlets in low-income communities (and, in particular, near schools)166–168 and limited access to health care. 169 In addition, eating behaviours of people with FI, for example overeating when food is available,170–172 and the psychological aspects of being food insecure, such as stress, depression and anxiety, may also be contributing factors. 47,173 Of particular relevance to children in lower-income neighbourhoods may be the lack of opportunities for physical activity. This may present itself in terms of fewer facilities, such as parks and green spaces, unattractive or unsafe facilities, or the inability to afford organised sports expenses or transport costs. 174,175
In the UK, the Obesity Health Alliance has predicted that 60% of 5- to 11-year old boys in the highest category of deprivation will be overweight or obese by 2020, compared with 16% of boys in the least deprived category. An average of 1 in 5 girls in the same age group is predicted to be overweight or obese by 2020, regardless of level of deprivation. 176
Chapter 5 Overall results
Overall, 109 studies published in the literature assessing FI in children in high-income countries were included in this rapid review. The majority (93%) of studies were conducted in North America (the USA and Canada). Only five studies were conducted in the UK. Regarding the specified RQs, 52% of included studies assessed factors linked to FI (RQ 1), 68% assessed the impact of FI on children’s health outcomes (RQ 3), 14% reported findings of food assistance programmes (RQ 4), and 34% of the studies assessed more than one RQ. None of these studies assessed the incidence, the prevalence or the recent trends of child FI in the UK (RQ 2) or the cost-effectiveness of food assistance programmes (RQ 5).
All of the included studies measured FI in children through a variety of methods (e.g. surveys, face-to-face interviews, analogue scales or vignettes and cartoons). However, most of the tools (68%) used to measure child FI involved parental reports (e.g. the 18-item USDA module) that assess FI in the household (including children living in it). Only eight studies (7%) used the version of the USDA module that has been modified to collect answers directly from young people. Even where the same tool was used across studies, some authors used modified scoring systems and categories, which made it challenging to summarise evidence.
Fifty-seven studies provided information on the nature and determinants of child FI (RQ 1); in particular, 51 provided quantitative data and six provided qualitative data. Several factors were identified that might be pivotal for food-insecure children. According to the 24 studies that adjusted their analyses for explanatory or confounding variables, factors associated with FI included material deprivation, parents’ employment, number of people in household, neighbourhood social cohesion and disorder, emotional status, living property characteristics, number of parents in household, ethnicity, number of siblings, parents’ education and SES/household income.
Qualitative data showed that children’s experience of FI (even in children as young as 5 years) includes cognitive, physical and emotional awareness, as well as social and behavioural responsiveness to FI. Children demonstrated awareness of adults or family behaviours towards FI as well as of the household characteristics that contributed to increase FI. Moreover, one study showed that children at risk of FI might also express concerns regarding the lack of food.
None of the included studies identified from the current literature assessed the incidence, prevalence and costs of child FI in the UK. According to the UK House of Commons Poverty in the UK Statistics 2018 report,129 4.0 million children were estimated to live in relative poverty (relative low income) and 3.7 million were estimated to live in absolute poverty (absolute low income) in 2015/16. Similarly, data from the 2017 UNICEF report Prevalence and Correlates of Food Insecurity Among Children Across the Globe127 indicate that 19.5% of children aged < 15 years in the UK are living with a respondent who is moderately or severely food insecure, and 10.4% live with a severely food-insecure respondent. 127 These appear to be the most up-to-date data on the prevalence of child FI in the UK and are widely cited in the FI literature.
Seventy-four studies evaluated the impact of FI on children’s health and social well-being. Child FI was linked to a range of negative outcomes including poor general and mental health, developmental, psychological and behavioural problems, disrupted social interactions and poor academic performance. For some other outcomes, the evidence was mixed, and the association was less clear (e.g. weight status, attachment to parents, mental proficiency).
Fifteen studies reported findings of food assistance programmes. Most of the programmes attenuated, but did not eliminate, FI or any outcome related to it. Most of the published studies lacked a detailed description of the methodology and/or the intervention provided, which made interpreting the results challenging. Furthermore, none of the studies evaluated the cost-effectiveness and sustainability of the programme under consideration.
Chapter 6 Discussion
This rapid review aimed to determine the nature, extent and consequences of FI affecting children aged ≤ 18 years in the UK. FI is a multifactorial phenomenon associated with a number of factors (mainly linked to SES and demographic characteristics) that might result in the limited or uncertain availability of food and in the limited or uncertain ability to access food and, hence, may affect children’s health outcomes.
The main aim of this rapid review was to assess factors more likely to be associated with FI, the impact of FI on children’s health and social well-being and the findings of food programmes designed to tackle FI in both children and adolescents. However, one of the main challenges of the review was to identify studies that explicitly measured FI in children as well as interventions to reduce or mitigate the effects of FI in children. Ultimately, 109 studies that described measurements of child FI were included in this rapid review. Only five studies were conducted in the UK and three of these provided qualitative data. Overall, there was a lack of consistency in how FI was defined and measured across studies. Some studies reported parent-led measurements (i.e. ‘indirect measurement’) and included measurements of household FI along with child-specific measurements. Although information collected from parents/families is important in establishing the extent and consequences of child FI, there is evidence showing that some parents try to ‘shield’ their children from FI,25 and such ‘shielding’ may affect the reliability of data as different effect sizes in outcomes have been shown in sensitivity analyses comparing child-level FI measures with household measurements. 74,177 To date, there is not an established gold standard for the assessment of FI in children or adolescents. According to the 2015 UNICEF report on the measurement of FI among children,9 children as young as 7 years can respond accurately to questionnaire items sensitive to FI. Results from this rapid review showed that 19.2% of the studies measured FI directly from children or adolescents, and 6% included both children’s and parents’/caregivers’ measurements. As indicated by the 2015 UNICEF report, there is a need to develop a tool to assess child FI, to allow for a reliable and valid ‘direct’ measurement. 10
The process should ideally involve children and adolescents as much as possible to ensure that their FI experiences, views and beliefs are taken into account and fully integrated into the development and implementation of any novel instrument. 178
To fully understand the complexity and multifactorial nature of FI and guide efforts that aim to tackle it, it is crucial to identify factors that may cause or increase its risk. According to the results presented in this rapid review, some factors that may lead to a vulnerable environment for children and adolescents appear to increase the risk of FI, for example having a low SES, being homeless or living in public housing, having unemployed parents or living with a large number of siblings. Notably, these associations do not imply causality, as the direction of the relationship with FI is not further explicated.
Evidence regarding some other factors potentially linked to FI was inconsistent across studies. For example, some of the studies based in the USA found a significant association between parental immigration status and FI (i.e. households with foreign parents were more likely to suffer from FI). However, results from other countries were less clear; for example, a Canadian study23 did not find any significant association, while an Australian study showed that households with a parent born outside Australia were 60% less likely to be FI than households with an Australian-born parent. 54 The assessment of factors that may lead to, or increase, FI is complex because of the nature of FI, as well as the political, economic and sociocultural differences in terms of food systems and welfare programmes that exist across communities and across countries. 179 Furthermore, the majority of evidence was reported in observational studies, which were not properly designed to rigorously assess the determinants of FI, and provided only a crude association between FI and factors that may increase the risk of FI without taking into account relevant explanatory or confounding variables. Moreover, it was very challenging to determine whether some potential associated factors of FI were actually predictors or consequences of changes in FI. For instance, it has been shown that FI may work indirectly through parental depression and parenting practices to influence security of attachment among children. 72 Therefore, a certain degree of caution is required when interpreting the results of this rapid review.
Most qualitative studies reported children’s perceptions or experiences in terms of cognitive (e.g. being aware that food is scarce), emotional (e.g. feelings associated with FI, such as sadness) and physical (e.g. experience of hunger, pain, tiredness or weakness) awareness of FI. 6,180 In addition, some qualitative studies reported children’s social (e.g. being pressured to eat with other family, friends or neighbours) and behavioural (e.g. responsibility for managing food resources to shield their loved ones, overeating or eating less desirable foods because there was no other choice) reactions to FI.
Two of the included studies recorded stakeholders’ and parents’ perceptions and points of view regarding child FI. The results showed that school teachers may be able to identify children at risk of FI. The WHO has identified schools as the target setting for health promotion among children and adolescents, as schools are ideal environments for promoting academic achievement as well as safety and mental, physical and emotional health in young people. 181 School-based interventions can play a crucial role in health promotion among young people, as children and adolescents generally attend school 5 days per week, for around 6 hours per day, throughout much of the calendar year. Furthermore, school teachers reported that, despite being expensive and resources driven, food programmes implemented in schools and community centres might reduce stigma and inequality among young people.
However, stakeholders expressed their concerns about the lack of food aid during weekends and school holidays, as well as the need for funding and resources to implement and run such programmes. Similar concerns have been raised by the Food and Agriculture Organization of the United Nations, with the general recommendation that food assistance programmes should offer opportunities for promoting sustainable improvements in FS. 182
The studies included in this rapid review showed a number of possible associations between FI and health outcomes in children. However, there are a number of issues worth considering. The measurement of FI varied across studies. There was variation in how some outcomes were measured: some were measured directly by health professionals or research staff, whereas others were reported by parents or by children or adolescents themselves. Such self-reports may not be accurate and might potentially bias results. 183 The results varied according to the type of data and the statistical analyses used. For instance, five of the included studies used data from the US ECLS cohort to examine the association between FI and children’s weight status. 12,20,56,80,113 Even though the same data set was used, results were not consistent across studies (with a possible overlap of participants between studies): two studies found a significant association between FI and children’s weight status,12,56 one found a trend towards association,113 one found no association20 and the remaining study found differences between boys and girls. 80 Such variations may be explained by the covariates included in the statistical analyses, as well as the type of analyses performed, which could affect the results and their interpretation. The same issue is evident between studies that adjusted results for potential explanatory or confounding variables (usually related to children’s, parents’ or households’ characteristics) and those that did not. The differences in the methods used across studies may significantly alter the results, leading to very different conclusions regarding the magnitude and relevance of observed effects. 184
Overall, and despite the identified methodological issues, several physical, mental, developmental and social well-being outcomes were linked to FI in children and adolescents. In some cases, the association was clear and significant across studies, whereas in others the strength of the association varied across studies. In general, most of the included studied reported a negative association between FI and health and social well-being outcomes in children. However, in some cases it was difficult to determine whether FI was a risk factor for children or an indicator of other types of deprivation.
This rapid review identified 15 studies (most from the USA) that assessed the effects of interventions/programmes designed to eliminate, reduce or mitigate the effects of child FI. Results varied and, in general, showed that effects of FI are attenuated, but not eradicated, by food assistance programmes. It is worth noting that many programmes were designed and implemented to mitigate the effects of FI but not to solve the problem of FI. In addition, many studies did not provide a full description of the intervention (such as frequency, duration, intensity, quality of food aids, personnel involved) and, therefore, it was not possible to determine which aspects and components of the programme were more likely to be effective. Most studies did not include a control intervention and only one of the included studies was a cluster RCT122 (a school breakfast programme in New Zealand reported a significant decrease in children’s self-reported short-term hunger during the intervention phase as compared with the control, but no other school attendance or academic achievement outcomes changed significantly with the programme).
In high-income countries, the assessment of food assistance programmes to tackle child FI is likely to be complex, not only because of the multifactorial nature of FI, but also because of the complexity of country-specific public and private food assistance initiatives, which involve a combinations of roles, actors, practices and resources. 185
Limitations
There are some limitations to consider regarding this rapid review. Owing to time and resource constraints, 30 potentially relevant articles were not included in the review and the quality of the included studies was not evaluated. Few studies conducted in the UK were identified. The lack of consistency with regard to study characteristics, characteristics of children and households, measurements of FI and types of outcomes meant that it was not feasible to perform a quantitative synthesis of results and it was challenging to provide a general overview.
Research needs and future challenges
There is an urgent need to monitor and report FI in children in the UK. No evidence on the prevalence or incidence of FI in children in the UK was identified and it appears that other indices are commonly used as proxy measures of FI. Therefore, better measurement and monitoring is needed to permit an accurate and reliable assessment of the extent of the problem in the UK.
Income and poverty measures do not provide clear information about FS, even though FI and hunger can arise from limited economic resources, especially in young children. 2 No single indicator can completely capture FI or hunger. For this reason, information on a variety of specific conditions, experiences and behaviours that serve as indicators is needed. Several organisations advocate for systems to measure and monitor individual children’s experiences of FI. 10 In addition, there is a need to assess levels of severity of FI. 2 Such efforts need to ensure that children and adolescents are involved as much as possible, so that their FI experiences are understood and taken into account.
No studies evaluating interventions to reduce, mitigate or eliminate child FI in the UK were identified in the literature, and the majority of the studies were from the USA. In general, there was a lack of detail about the characteristics of the interventions and the methodology used, which made it challenging to synthesise evidence and interpret findings. There is a clear need to conduct evaluations of possible interventions/programmes to tackle child FI in the UK and to identify mechanisms and processes through which these interventions/programmes may work and produce benefits. In particular, more information is needed on measurements and targeted interventions for young, more vulnerable populations, for example children who are homeless. Furthermore, future research should report methods, characteristics of the study population and characteristics of the intervention in detail to permit an adequate and accurate interpretation of findings and, particularly, of the impact of the intervention on children’s outcomes.
Future research should also clarify the mediating effects of demographic and social characteristics, family stressors and parenting practices in the relationship between FI and children’s outcomes.
It would also be interesting to explore whether or not health-care systems could be used in the future as support networks for FI young people. Similarly, it would be useful, especially in the UK context, to further engage the role of public health research in addressing child FI.
Chapter 7 Conclusions
Food insecurity is a serious problem, and children may be one of the most vulnerable populations to suffer its consequences. In high-income countries, several factors (personal, socioeconomic, cultural, parental and/or household characteristics) were frequently related to FI in children (aged ≤ 18 years). Furthermore, several health and social well-being outcomes were associated with FI in children and adolescents. However, in some cases, the association was strong and significant across studies, but in others was less clear. Nevertheless, the overall pattern of associations was the same across studies and showed a negative relationship between FI and children’s health and social-well-being. The interventions or food assistance programmes reported in the literature attenuated, but did not eliminate, FI or any outcome related to it. Moreover, there was no information on the cost-effectiveness and sustainability of such programmes.
At present, there are no prevalence or incidence studies assessing FI in children in the UK. However, some national and international reports that used proxy indicators have shown that children’s poverty and FI have increased in recent years. Considering the short- and long-term detrimental effects of FI on child health and well-being, a better measurement and monitoring system is needed to permit a reliable assessment of the extent of the problem, including levels of severity, in the UK.
Food security is a human right, involving social justice, public health, food systems and policies. Viewed in an international context or within a country, state or local community, FS is crucial not only at the society and household levels, but also at an individual level. Adequate assessment of this problem is crucial for better identification of vulnerable populations (such as children and adolescents), and also for better administration of resources, development of programmes and implementation of policies that aim to tackle it.
There is a clear need to conduct evaluations of possible interventions/programmes to tackle child FI in the UK and to identify mechanisms and processes through which these interventions/programmes may be effective and sustainable.
Future research, especially studies assessing the effects and impact of FI on children’s outcomes, should be adequately designed, analysed and reported. Future studies should also consider the mediating effects of demographic and social characteristics, family stressors and parenting practices in the relationship between FI and children’s health and social well-being outcomes.
Acknowledgements
The authors are grateful to Flora Douglas (Robert Gordon University, Aberdeen), Ada Garcia (Human Nutrition, School of Medicine, University of Glasgow), Aixa Aleman-Diaz (WHO-Collaborating Centre for International Child & Adolescent Health Policy, Child and Adolescent Health Research Unit, University of St Andrews), Martin Caraher (Centre for Food Policy, City, University of London) and Stephen Whybrow (Rowett Institute of Nutrition & Health, University of Aberdeen) for providing comments on the research protocol and methodological guidance as members of the advisory group for this rapid review and to Lara Kemp for her secretarial support.
Contributions of authors
Magaly Aceves-Martins acted as systematic reviewer, drafted the original protocol, led the day-to-day running of this review and reviewed the available evidence on child FI.
Moira Cruickshank acted as systematic reviewer and reviewed the available evidence on child FI.
Cynthia Fraser acted as information specialist, and developed and ran the search strategies.
Miriam Brazzelli acted as project lead and supervised and co-ordinated all aspects of this review.
All authors contributed to the writing of this rapid review and approved its final version.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Food and Agricultural Organization of the United Nations . Trade Reforms and Food Security 2003. www.fao.org/docrep/005/y4671e/y4671e00.htm (accessed May 2018).
- Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security 2000. https://fns-prod.azureedge.net/sites/default/files/FSGuide_0.pdf (accessed May 2018).
- Department for Work and Pensions . Households Below Average Income: 1994 95 to 2015 16 2017. www.gov.uk/government/uploads/system/uploads/attachment_data/file/600091/households-below-average-income-1994-1995-2015-2016.pdf (accessed May 2018).
- Mindell J, Erens B, Nelson M, Finglas P. Low Income Diet and Nutrition Survey (LIDNS) 2007.
- McGuiness F, Brown J, Ward M. Household Food Insecurity Measurement in the UK. Debate Pack CDP 2016/0238. London: UK Parliament; 2016.
- Fram MS, Frongillo EA, Jones SJ, Williams RC, Burke MP, DeLoach KP, et al. Children are aware of food insecurity and take responsibility for managing food resources. J Nutr 2011;141:1114-19. https://doi.org/10.3945/jn.110.135988.
- Bernal J, Frongillo EA, Herrera HA, Rivera JA. Food insecurity in children but not in their mothers is associated with altered activities, school absenteeism, and stunting. J Nutr 2014;144:1619-26. https://doi.org/10.3945/jn.113.189985.
- Casey PH, Szeto KL, Robbins JM, Stuff JE, Connell C, Gossett JM, et al. Child health-related quality of life and household food security. Arch Pediatr Adolesc Med 2005;159:51-6. https://doi.org/10.1001/archpedi.159.1.51.
- Fram MS, Bernal J, Frongillo EA. The Measurement of Food Insecurity Among Children: Review of Literature and Concept Note. Office of Research Working Paper WP-2015-08 2015. www.oecd-ilibrary.org/children-and-youth/the-measurement-of-food-insecurity-among-children_30d5a92c-en (accessed May 2018).
- Jaffe K, Bernal J, Herrera HA. Relation between shame, nutrition and happiness in children. Acta Cient Venez 2014;65:29-3.
- Jyoti DF, Frongillo EA, Jones SJ. Food insecurity affects school children’s academic performance, weight gain, and social skills. J Nutr 2005;135:2831-9. https://doi.org/10.1093/jn/135.12.2831.
- The State of Food Security and Nutrition in the World 2017. Building Resilience for Peace and Food Security. Rome: Food and Agriculture Organization of the United Nations; 2017.
- Organization for Economic Co-operation and Development . OECD Members and Partners 2018. www.oecd.org/about/membersandpartners/ (accessed May 2018).
- Carney M. Compounding crises of economic recession and food insecurity: a comparative study of three low-income communities in Santa Barbara County. Agri Human Values 2012;29:185-201.
- Karanikolos M, Mladovsky P, Cylus J, Thomson S, Basu S, Stuckler D, et al. Financial crisis, austerity, and health in Europe. Lancet 2013;381:1323-31. https://doi.org/10.1016/S0140-6736(13)60102-6.
- Loopstra R, Reeves A, Stuckler D. Rising food insecurity in Europe. Lancet 2015;385. https://doi.org/10.1016/S0140-6736(15)60983-7.
- Borch A, Kjaernes U. The prevalence and risk of food insecurity in the Nordic region: preliminary results. J Consumer Policy 2016;39:261-74. https://doi.org/10.1007/s10603-016-9316-x.
- Arteaga I, Potochnick S, Parsons S. Decomposing the household food insecurity gap for children of U.S.-born and foreign-born Hispanics: evidence from 1998 to 2011. J Immigr Minor Health 2017;19:1050-8. https://doi.org/10.1007/s10903-017-0561-0.
- Belsky DW, Moffitt TE, Arseneault L, Melchior M, Caspi A. Context and sequelae of food insecurity in children’s development. Am J Epidemiol 2010;172:809-18. https://doi.org/10.1093/aje/kwq201.
- Bhargava A, Jolliffe D, Howard LL. Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study-Kindergarten. Br J Nutr 2008;100:438-44. https://doi.org/10.1017/S0007114508894366.
- Broughton MA, Janssen PS, Hertzman C, Innis SM, Frankish CJ. Predictors and outcomes of household food insecurity among inner city families with preschool children in Vancouver. Can J Public Health 2006;97:214-16.
- Bruening M, Lucio J, Brennhofer S. Mother and adolescent eating in the context of food insecurity: findings from urban public housing. Matern Child Health J 2017;21:1911-17. https://doi.org/10.1007/s10995-017-2306-z.
- Carter MA, Dubois L, Tremblay MS, Taljaard M. Local social environmental factors are associated with household food insecurity in a longitudinal study of children. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-1038.
- Chilton M, Black MM, Berkowitz C, Casey PH, Cook J, Cutts D, et al. Food insecurity and risk of poor health among US-born children of immigrants. Am J Public Health 2009;99:556-62. https://doi.org/10.2105/AJPH.2008.144394.
- Connell CL, Lofton KL, Yadrick K, Rehner TA. Children’s experiences of food insecurity can assist in understanding its effect on their well-being. J Nutr 2005;135:1683-90. https://doi.org/10.1093/jn/135.7.1683.
- Dunifon R, Kowaleski-Jones L. The influences of participation in the National School Lunch Program and food insecurity on child well-being. Soc Serv Rev 2003;77:72-9. https://doi.org/10.1086/345705.
- Egeland GM, Williamson-Bathory L, Johnson-Down L, Sobol I. Traditional food and monetary access to market-food: correlates of food insecurity among Inuit preschoolers. Int J Circumpolar Health 2011;70:373-83. https://doi.org/10.3402/ijch.v70i4.17836.
- Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. Food insecurity is associated with iron deficiency anemia in US adolescents. Am J Clin Nutr 2009;90:1358-71. https://doi.org/10.3945/ajcn.2009.27886.
- Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. Food insecurity is associated with diet and bone mass disparities in early adolescent males but not females in the United States. J Nutr 2011;141:1738-45. https://doi.org/10.3945/jn.111.142059.
- Harvey K. ‘When I go to bed hungry and sleep, I’m not hungry’: children and parents’ experiences of food insecurity. Appetite 2016;99:235-44. https://doi.org/10.1016/j.appet.2016.01.004.
- Harvey-Golding L, Donkin LM, Defeyter MA. Universal free school breakfast: a qualitative process evaluation according to the perspectives of senior stakeholders. Front Public Health 2016;4. https://doi.org/10.3389/fpubh.2016.00161.
- Harvey-Golding L, Donkin LM, Blackledge J, Defeyter MA. Universal free school breakfast: a qualitative model for breakfast behaviors. Front Public Health 2015;3. https://doi.org/10.3389/fpubh.2015.00154.
- Himmelgreen DA, Perez-Escamilla R, Segura-Millan S, Peng Y, Gonzalez A, Singer M, et al. Food insecurity among low-income Hispanics in Hartford, Connecticut: implications for public health policy. Hum Organ 2000;59:334-42. https://doi.org/10.17730/humo.59.3.76557m317748l414.
- Holben DH, McClincy MC, Holcomb JP, Dean KL, Walker CE. Food security status of households in Appalachian Ohio with children in Head Start. J Am Diet Assoc 2004;104:238-41. https://doi.org/10.1016/j.jada.2003.09.023.
- Jacknowitz A, Morrissey T, Brannegan A. Food insecurity across the first five years: triggers of onset and exit. Children Youth Serv Rev 2015;53:24-33. https://doi.org/10.1016/j.childyouth.2015.03.012.
- Kaiser LL, Melgar-Quiñonez HR, Lamp CL, Johns MC, Sutherlin JM, Harwood JO. Food security and nutritional outcomes of preschool-age Mexican-American children. J Am Diet Assoc 2002;102:924-9. https://doi.org/10.1016/S0002-8223(02)90210-5.
- Kenney CT. Father doesn’t know best? Parents’ control of money and children’s food insecurity. J Marriage Fam 2008;70:654-69. https://doi.org/10.1111/j.1741-3737.2008.00512.x.
- Kersey M, Geppert J, Cutts DB. Hunger in young children of Mexican immigrant families. Public Health Nutr 2007;10:390-5. https://doi.org/10.1017/S1368980007334071.
- Kimbro RT, Denney JT. Transitions into food insecurity associated with behavioral problems and worse overall health among children. Health Aff 2015;34:1949-55. https://doi.org/10.1377/hlthaff.2015.0626.
- Kimbro RT, Denney JT, Panchang S. Individual, family and neighborhood characterisrics abd children’s food insecurity. J Appl Res Children 2012;3.
- King C. Soft drinks consumption and child behaviour problems: the role of food insecurity and sleep patterns. Public Health Nutr 2017;20:266-73. https://doi.org/10.1017/S1368980016002093.
- Kirkpatrick SI, McIntyre L, Potestio ML. Child hunger and long-term adverse consequences for health. Arch Pediatr Adolesc Med 2010;164:754-62. https://doi.org/10.1001/archpediatrics.2010.117.
- Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J Nutr 2008;138:604-12. https://doi.org/10.1093/jn/138.3.604.
- Mangini LD, Hayward MD, Dong YQ, Forman MR. Household food insecurity is associated with childhood asthma. J Nutr 2015;145:2756-64. https://doi.org/10.3945/jn.115.215939.
- Marjerrison S, Cummings EA, Glanville NT, Kirk SF, Ledwell M. Prevalance and associations of food insecurity in children with diabetes mellitus. J Pediatr 2011;158:607-11. https://doi.org/10.1016/j.jpeds.2010.10.003.
- McIsaac KE, Stock DC, Lou W. Household food security and breast-feeding duration among Canadian Inuit. Public Health Nutr 2017;20:64-71. https://doi.org/10.1017/S136898001600166X.
- McLaughlin KA, Green JG, Alegría M, Jane Costello E, Gruber MJ, Sampson NA, et al. Food insecurity and mental disorders in a national sample of U.S. adolescents. J Am Acad Child Adolesc Psychiatry 2012;51:1293-303. https://doi.org/10.1016/j.jaac.2012.09.009.
- Miller DP. Accessibility of summer meals and the food insecurity of low-income households with children. Public Health Nutr 2016;19:2079-89. https://doi.org/10.1017/S1368980016000033.
- Morrissey TW, Oellerich D, Meade E, Simms J, Stock A. Neighborhood poverty and children’s food insecurity. Children Youth Services Rev 2016;66:85-93. https://doi.org/10.1016/j.childyouth.2016.05.006.
- Nalty CC, Sharkey JR, Dean WR. School-based nutrition programs are associated with reduced child food insecurity over time among Mexican-origin mother-child dyads in Texas Border Colonias. J Nutr 2013;143:708-13. https://doi.org/10.3945/jn.112.168757.
- Papas MA, Trabulsi JC, Dahl A, Dominick G. Food Insecurity Increases the odds of obesity among young Hispanic children. J Immigr Minor Health 2016;18:1046-52. https://doi.org/10.1007/s10903-015-0275-0.
- Poole A, Ruiz CS, Shows AR, Chen JJ. Household food security status, food perceptions, dietary behaviors and weight status in Southeast Texas adolescents. insights to action. Academy of Nutrition and Dietetics. Food and Nutrition Conference and Expo, Houston TX, October 19–22, 2013. J Acad Nutr Diet 2013;113.
- Poole-Di Salvo E, Silver EJ, Stein RE. Household food insecurity and mental health problems among adolescents: what do parents report?. Acad Pediatr 2016;16:90-6. https://doi.org/10.1016/j.acap.2015.08.005.
- Ramsey R, Giskes K, Turrell G, Gallegos D. Food insecurity among Australian children: potential determinants, health and developmental consequences. J Child Health Care 2011;15:401-16. https://doi.org/10.1177/1367493511423854.
- Richards R, Smith C. Environmental, parental, and personal influences on food choice, access, and overweight status among homeless children. Soc Sci Med 2007;65:1572-83. https://doi.org/10.1016/j.socscimed.2007.06.013.
- Rose D, Bodor JN. Household food insecurity and overweight status in young school children: results from the Early Childhood Longitudinal Study. Pediatrics 2006;117:464-73. https://doi.org/10.1542/peds.2005-0582.
- Rose-Jacobs R, Black MM, Casey PH, Cook JT, Cutts DB, Chilton M, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics 2008;121:65-72. https://doi.org/10.1542/peds.2006-3717.
- Rossen LM, Kobernik EK. Food insecurity and dietary intake among US youth, 2007–2010. Pediatr Obes 2016;11:187-93. https://doi.org/10.1111/ijpo.12044.
- Sellen DW, Tedstone AE, Frize J. Food insecurity among refugee families in East London: results of a pilot assessment. Public Health Nutr 2002;5:637-44. https://doi.org/10.1079/PHN2002340.
- Shanafelt A, Hearst MO, Wang Q, Nanney MS. Food insecurity and rural adolescent personal health, home, and academic environments. J Sch Health 2016;86:472-80. https://doi.org/10.1111/josh.12397.
- Sharkey JR, Dean WR, Johnson CM. Association of household and community characteristics with adult and child food insecurity among Mexican-origin households in colonias along the Texas-Mexico border. Int J Equity Health 2011;10. https://doi.org/10.1186/1475-9276-10-19.
- Shtasel-Gottlieb Z, Palakshappa D, Yang F, Goodman E. The relationship between developmental assets and food security in adolescents from a low-income community. J Adolesc Health 2015;56:215-22. https://doi.org/10.1016/j.jadohealth.2014.10.001.
- Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J 2006;10:177-85. https://doi.org/10.1007/s10995-005-0036-0.
- Smith C, Richards R. Dietary intake, overweight status, and perceptions of food insecurity among homeless Minnesotan youth. Am J Hum Biol 2008;20:550-63. https://doi.org/10.1002/ajhb.20780.
- Sonik R, Parish SL, Ghosh S, Igdalsky L. Food insecurity in U.S. households that include children with disabilities. Except Child 2016;83:42-57. https://doi.org/10.1177/0014402916651847.
- Tester JM, Laraia BA, Leung CW, Mietus-Snyder ML. Dyslipidemia and food security in low-income US adolescents: National Health and Nutrition Examination Survey, 2003–2010. Prev Chronic Dis 2016;13. https://doi.org/10.5888/pcd13.150441.
- Trapp CM, Burke G, Gorin AA, Wiley JF, Hernandez D, Crowell RE, et al. The relationship between dietary patterns, body mass index percentile, and household food security in young urban children. Child Obes 2015;11:148-55. https://doi.org/10.1089/chi.2014.0105.
- Wadsworth L. Food insecurity in Nova Scotia youths. J Nutr Educ Behav 2012;44. https://doi.org/10.1016/j.jneb.2012.03.128.
- Weinreb L, Wehler C, Perloff J, Scott R, Hosmer D, Sagor L, et al. Hunger: its impact on children’s health and mental health. Pediatrics 2002;110. https://doi.org/10.1542/peds.110.4.e41.
- Whitbeck LB, Chen X, Johnson KD. Food insecurity among homeless and runaway adolescents. Public Health Nutr 2006;9:47-52. https://doi.org/10.1079/PHN2005764.
- Yu M, Lombe M, Nebbitt VE. Food stamp program participation, informal supports, household food security and child food security: a comparison of African American and Caucasian households in poverty. Children Youth Services Rev 2010;32:767-73. https://doi.org/10.1016/j.childyouth.2010.01.015.
- Zaslow M, Bronte-Tinkew J, Capps R, Horowitz A, Moore KA, Weinstein D. Food security during infancy: implications for attachment and mental proficiency in toddlerhood. Matern Child Health J 2009;13:66-80. https://doi.org/10.1007/s10995-008-0329-1.
- Murphy JM, Wehler CA, Pagano ME, Little M, Kleinman RE, Jellinek MS. Relationship between hunger and psychosocial functioning in low-income American children. J Am Acad Child Adolesc Psychiatry 1998;37:163-70. https://doi.org/10.1097/00004583-199802000-00008.
- Kohn MJ, Bell JF, Grow HM, Chan G. Food insecurity, food assistance and weight status in US youth: new evidence from NHANES 2007–08. Pediatr Obes 2014;9:155-66. https://doi.org/10.1111/j.2047-6310.2012.00143.x.
- Mark S, Lambert M, O’Loughlin J, Gray-Donald K. Household income, food insecurity and nutrition in Canadian youth. Can J Public Health 2012;103:94-9.
- Pickett W, Michaelson V, Davison C. Beyond nutrition: hunger and its impact on the health of young Canadians. Int J Public Health 2015;60:527-38. https://doi.org/10.1007/s00038-015-0673-z.
- Baer TE, Scherer EA, Fleegler EW, Hassan A. Food insecurity and the burden of health-related social problems in an urban youth population. J Adolesc Health 2015;57:601-7. https://doi.org/10.1016/j.jadohealth.2015.08.013.
- Barroso CS, Roncancio A, Moramarco MW, Hinojosa MB, Davila YR, Mendias E, et al. Food security, maternal feeding practices and child weight-for-length. Appl Nurs Res 2016;29:31-6. https://doi.org/10.1016/j.apnr.2015.03.009.
- Bruening M, Johnson K. 197. Social support mediates the relationship between food insecurity and weight status among adolescents in New Mexico. J Adolesc Health 2015;56:S101-2. https://doi.org/10.1016/j.jadohealth.2014.10.202.
- Burke MP, Frongillo EA, Jones SJ, Bell BB, Hartline-Grafton H. Household food insecurity is associated with greater growth in body mass index among female children from kindergarten through eighth grade. J Hunger Environment Nutr 2016;11:227-41. https://doi.org/10.1080/19320248.2015.1112756.
- Casey PH, Simpson PM, Gossett JM, Bogle ML, Champagne CM, Connell C, et al. The association of child and household food insecurity with childhood overweight status. Pediatrics 2006;118:e1406-13. https://doi.org/10.1542/peds.2006-0097.
- Chi DL, Masterson EE, Carle AC, Mancl LA, Coldwell SE. Socioeconomic status, food security, and dental caries in US children: mediation analyses of data from the National Health and Nutrition Examination Survey, 2007–2008. Am J Public Health 2014;104:860-4. https://doi.org/10.2105/AJPH.2013.301699.
- Cook JT, Frank DA, Berkowitz C, Black MM, Casey PH, Cutts DB, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr 2004;134:1432-8. https://doi.org/10.1093/jn/134.6.##.
- Edwards OW, Taub GE. Children and youth perceptions of family food insecurity and bullying. School Mental Health 2017;9:263-72. https://doi.org/10.1007/s12310-017-9213-8.
- Gundersen C, Garasky S, Lohman BJ. Food insecurity is not associated with childhood obesity as assessed using multiple measures of obesity. J Nutr 2009;139:1173-8. https://doi.org/10.3945/jn.109.105361.
- Gundersen C, Lohman BJ, Garasky S, Stewart S, Eisenmann J. Food security, maternal stressors, and overweight among low-income US children: results from the National Health and Nutrition Examination Survey (1999–2002). Pediatrics 2008;122:e529-40. https://doi.org/10.1542/peds.2008-0556.
- Helton JJ. Food neglect and maltreatment re-report. Children Youth Services Rev 2016;71:77-83. https://doi.org/10.1016/j.childyouth.2016.10.042.
- Holben DH, Taylor CA. Food insecurity and its association with central obesity and other markers of metabolic syndrome among persons aged 12 to 18 years in the United States. J Am Osteopath Assoc 2015;115:536-43. https://doi.org/10.7556/jaoa.2015.111.
- Howard LL. Does food insecurity at home affect non-cognitive performance at school? A longitudinal analysis of elementary student classroom behavior. Econ Educ Rev 2011;30:157-76. https://doi.org/10.1016/j.econedurev.2010.08.003.
- Howard LL. Transitions between food insecurity and food security predict children’s social skill development during elementary school. Br J Nutr 2011;105:1852-60. https://doi.org/10.1017/S0007114510005623.
- Howard LL. Food insecurity experiences predict children’s fruit and vegetable consumption in the USA. ISRN Nutrition 2013;2013. https://doi.org/10.5402/2013/426029.
- Huang J, Oshima KM, Kim Y. Does food insecurity affect parental characteristics and child behavior? Testing mediation effects. Soc Serv Rev 2010;84:381-40. https://doi.org/10.1086/655821.
- Huang J, Vaughn MG. Household food insecurity and children’s behaviour problems: new evidence from a trajectories-based study. Br J Soc Work 2016;46:993-1008. https://doi.org/10.1093/bjsw/bcv033.
- Jackson DB, Vaughn MG. Household food insecurity during childhood and adolescent misconduct. Prev Med 2017;96:113-17. https://doi.org/10.1016/j.ypmed.2016.12.042.
- Ryu JH, Bartfeld JS. Household food insecurity during childhood and subsequent health status: the early childhood longitudinal study – kindergarten cohort. Am J Public Health 2012;102:e50-5. https://doi.org/10.2105/AJPH.2012.300971.
- Johnson AD, Markowitz AJ. Associations between household food insecurity in early childhood and children’s kindergarten skills. Child Dev 2017;21.
- Kaur J, Lamb MM, Ogden CL. The association between food insecurity and obesity in children-the National Health and Nutrition Examination Survey. J Acad Nutr Diet 2015;115:751-8. https://doi.org/10.1016/j.jand.2015.01.003.
- Khan S, Pinckney RG, Keeney D, Frankowski B, Carney JK. Prevalence of food insecurity and utilization of food assistance program: an exploratory survey of a Vermont middle school. J Sch Health 2011;81:15-20. https://doi.org/10.1111/j.1746-1561.2010.00552.x.
- Kleinman RE, Murphy JM, Little M, Pagano M, Wehler CA, Regal K, et al. Hunger in children in the United States: potential behavioral and emotional correlates. Pediatrics 1998;101. https://doi.org/10.1542/peds.101.1.e3.
- Kuku O, Garasky S, Gundersen C. The relationship between childhood obesity and food insecurity: a nonparametric analysis. Appl Econ 2012;44:2667-77. https://doi.org/10.1080/00036846.2011.566192.
- Larson N, Bruening M, MacLehose R, Story M, Neumark-Sztainer D. Household food insecurity: links to adolescent eating patterns and weight status. J Acad Nutr Diet 2012;112. https://doi.org/10.1016/j.jand.2012.06.326.
- Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann JC. Adolescent overweight and obesity: links to food insecurity and individual, maternal, and family stressors. J Adolesc Health 2009;45:230-7. https://doi.org/10.1016/j.jadohealth.2009.01.003.
- Martin KS, Ferris AM. Food insecurity and gender are risk factors for obesity. J Nutr Educ Behav 2007;39:31-6. https://doi.org/10.1016/j.jneb.2006.08.021.
- Matheson DM, Varady J, Varady A, Killen JD. Household food security and nutritional status of Hispanic children in the fifth grade. Am J Clin Nutr 2002;76:210-17. https://doi.org/10.1093/ajcn/76.1.210.
- Metallinos-Katsaras E, Sherry B, Kallio J. Food insecurity is associated with overweight in children younger than 5 years of age. J Am Diet Assoc 2009;109:1790-4. https://doi.org/10.1016/j.jada.2009.07.007.
- Molcho M, Gabhainn SN, Kelly C, Friel S, Kelleher C. Food poverty and health among schoolchildren in Ireland: findings from the Health Behaviour in School-aged Children (HBSC) study. Public Health Nutr 2007;10:364-70. https://doi.org/10.1017/S1368980007226072.
- Sharkey JR, Nalty C, Johnson CM, Dean WR. Children’s very low food security is associated with increased dietary intakes in energy, fat, and added sugar among Mexican-origin children (6-11 y) in Texas border Colonias. BMC Pediatr 2012;12. https://doi.org/10.1186/1471-2431-12-16.
- Slack KS, Yoo J. Food hardship and child behavior problems among low-income children. Soc Serv Rev 2005;79:511-36. https://doi.org/10.1086/430894.
- Speirs KE, Fiese BH. STRONG Kids Research Team . The relationship between food insecurity and BMI for preschool children. Matern Child Health J 2016;20:925-33. https://doi.org/10.1007/s10995-015-1881-0.
- To QG, Frongillo EA, Gallegos D, Moore JB. Household food insecurity is associated with less physical activity among children and adults in the U.S. population. J Nutr 2014;144:1797-802. https://doi.org/10.3945/jn.114.198184.
- Widome R, Neumark-Sztainer D, Hannan PJ, Haines J, Story M. Eating when there is not enough to eat: eating behavior and perceptions of food among food-insecure youths. Am J Public Health 2009;99:822-8. https://doi.org/10.2105/AJPH.2008.139758.
- Willis DE, Fitzpatrick KM. Psychosocial factors as mediators of food insecurity and weight status among middle school students. Appetite 2016;103:236-43. https://doi.org/10.1016/j.appet.2016.04.022.
- Winicki J, Jemison K. Food insecurity and hunger in the kindergarten classroom: its effect on learning and growth. Contemp Econ Policy 2003;21:145-57. https://doi.org/10.1093/cep/byg001.
- Fram MS, Ritchie LD, Rosen N, Frongillo EA. Child experience of food insecurity is associated with child diet and physical activity. J Nutr 2015;145:499-504. https://doi.org/10.3945/jn.114.194365.
- Canter KS, Roberts MC, Davis AM. The role of health behaviors and food insecurity in predicting fruit and vegetable intake in low-income children. Child Health Care 2017;46:131-50. https://doi.org/10.1080/02739615.2015.1124772.
- Cook JT, Frank DA, Levenson SM, Neault NB, Heeren TC, Black MM, et al. Child food insecurity increases risks posed by household food insecurity to young children’s health. J Nutr 2006;136:1073-6. https://doi.org/10.1093/jn/136.4.1073.
- Kleinman RE, Hall S, Green H, Korzec-Ramirez D, Patton K, Pagano ME, et al. Diet, breakfast, and academic performance in children. Ann Nutr Metab 2002;46:24-30. https://doi.org/10.1159/000066399.
- Ecker ME, Sifers SK. The BackPack Food Program’s effects on U.S. elementary students’ hunger and on-task behavior. J Child Nutr Manage 2013;37.
- Gordon AR, Briefel RR, Collins AM, Rowe GM, Klerman JA. Delivering summer electronic benefit transfers for children through the Supplemental Nutrition Assistance Program or the Special Supplemental Nutrition Program for Women, Infants, and Children: benefit use and impacts on food security and foods consumed. J Acad Nutr Diet 2017;117:367-75.e2. https://doi.org/10.1016/j.jand.2016.11.002.
- Klerman JA, Wolf A, Collins A, Bell S, Briefel R. The effects the summer electronic benefits transfer for children demonstration has on children’s food security. Appl Econ Perspective Policy 2017;39:516-32. https://doi.org/10.1093/aepp/ppw030.
- Korenman S, Abner KS, Kaestner R, Gordon RA. The Child and Adult Care Food Program and the nutrition of preschoolers. Early Child Res Q 2013;28:325-36. https://doi.org/10.1016/j.ecresq.2012.07.007.
- Mhurchu CN, Gorton D, Turley M, Jiang Y, Michie J, Maddison R, et al. Effects of a free school breakfast programme on children’s attendance, academic achievement and short-term hunger: results from a stepped-wedge, cluster randomised controlled trial. J Epidemiol Community Health 2013;67:257-64. https://doi.org/10.1136/jech-2012-201540.
- Jansen EC, Kasper N, Lumeng JC, Brophy Herb HE, Horodynski MA, Miller AL, et al. Changes in household food insecurity are related to changes in BMI and diet quality among Michigan Head Start preschoolers in a sex-specific manner. Soc Sci Med 2017;181:168-76. https://doi.org/10.1016/j.socscimed.2017.04.003.
- Economic Research Service . U.S. Household Food Security Survey Module: Three-Stage Design With Screeners 2012. www.ers.usda.gov/media/8271/hh2012.pdf (accessed May 2018).
- Connell CL, Nord M, Lofton KL, Yadrick K. Food security of older children can be assessed using a standardized survey instrument. J Nutr 2004;134:2566-72. https://doi.org/10.1093/jn/134.10.2566.
- Canter KS. The role of health behaviors and food insecurity in predicting food intake in low-income children. Dissertation Abstracts International: Section B: The Sciences and Engineering 2016;77.
- Pereira AL, Handa S, Holmqvist G. Prevalence and Correlates of Food Insecurity Among Children Across the Globe. Innocenti Working Paper WP-2017-09. Florence: UNICEF Office of Research; 2017.
- Food and Agriculture Organization of the United Nations . Voices of the Hungry 2013. www.fao.org/in-action/voices-of-the-hungry/background/en (accessed May 2018).
- McGuiness F. Poverty in the UK: Statistics. Briefing Paper 7096. London: UK Parliament; 2018.
- Inchley J, Currie D, Vieno A, Torsheim T, Ferreira-Borges C, . Adolescent Alcohol-Related Behaviours: Trends and Inequalities in the WHO European Region, 2002–2014 (2018) 2018. www.euro.who.int/en/publications/abstracts/adolescent-alcohol-related-behaviours-trends-and-inequalities-in-the-who-european-region,-20022014-2018 (accessed 26 October 2018).
- The International Polar Year Nunavut Inuit Child Health Survey 2007–2008. n.d. www.mcgill.ca/cine/files/cine/child_inuit_health_survey_aug_31.pdf (accessed October 2018).
- Statistics Canada . National Longitudinal Survey of Children and Youth (NLSCY). n.d. www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=56797 (accessed October 2018).
- National Center for Education Statistics . Early Childhood Longitudinal Program (ECLS) n.d. https://nces.ed.gov/ecls/ (accessed October 2018).
- Centers for Disease Control and Prevention . National Health Interview Survey n.d. www.cdc.gov/nchs/nhis/quest_doc.htm (accessed October 2018).
- Kellogg Company . An Audit of School Breakfast Club Provision in the UK: A Report by Kellogg’s 2014. www.kelloggs.co.uk/content/dam/europe/kelloggs_gb/pdf/R5_Kelloggs%20Breakfast%20Club%20Audit%20APSE.pdf (accessed May 2018).
- Kellogg Company . The Future of School Breakfast Clubs: A Funding Crisis in the UK 2017. www.kelloggs.co.uk/en_GB/what-we-believe/breakfasts-for-better-days/breakfast-club-network.html (accessed May 2018).
- Graham N, Puts E, Beadle S. Evaluation of Breakfast Clubs in Schools With High Levels Of Deprivation 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/603946/Evaluation_of_Breakfast_Clubs_-_Final_Report.pdf (accessed May 2018).
- Lambie-Mumford H, Sims L. Children’s Experiences of Food And Poverty: The Rise and Implications of Charitable Breakfast Clubs and Holiday Hunger Projects in the UK. Sheffield Political Economy Research Institute; 2017.
- Shemilt I, Harvey I, Shepstone L, Swift L, Reading R, Mugford M, et al. A national evaluation of school breakfast clubs: evidence from a cluster randomized controlled trial and an observational analysis. Child Care Health Dev 2004;30:413-27. https://doi.org/10.1111/j.1365-2214.2004.00453.x.
- Murphy S, Moore GF, Tapper K, Lynch R, Clarke R, Raisanen L, et al. Free healthy breakfasts in primary schools: a cluster randomised controlled trial of a policy intervention in Wales, UK. Public Health Nutr 2011;14:219-26. https://doi.org/10.1017/S1368980010001886.
- Van Wye G, Seoh H, Adjoian T, Dowell D. Evaluation of the New York City Breakfast in the Classroom program. Am J Public Health 2013;103:e59-64. https://doi.org/10.2105/AJPH.2013.301470.
- Davies C. School Breakfast Program 2011 Evaluation Report. Perth, WA: Healthy Food for All; 2012.
- Food and Nutrition Services . Evaluation of the School Breakfast Program Pilot Project. Final Report 2004. https://fns-prod.azureedge.net/sites/default/files/SBPPFinal.pdf (accessed May 2018).
- Forsey A. Hungry Holidays: A Report on Hunger Amongst Children During School Holidays 2017. https://feedingbritain.files.wordpress.com/2015/02/hungry-holidays.pdf (accessed May 2018).
- National Education Union . NUT Survey on Holiday Hunger 2017. www.teachers.org.uk/news-events/conference-2017/nut-survey-holiday-hunger (accessed May 2018).
- Feeding Britain . Ending Hunger in the Holidays 2018. www.feedingbritain.org/Handlers/Download.ashx?IDMF=123ee6f1-631d-48d7-94a5-a801dd2ac89a (accessed May 2018).
- Aberdeen City Council . Councillors Give Backing to School Holiday Meals Initiative [News Item] 2018. https://news.aberdeencity.gov.uk/councillors-give-backing-to-school-holiday-meals-initiative/ (accessed May 2018).
- Scottish Government . Dignity: Ending Hunger Together in Scotland. Report of the Independent Working Group on Food Poverty 2016. https://beta.gov.scot/publications/dignity-ending-hunger-together-scotland-report-independendent-working-group-food/ (accessed May 2018).
- The Trussell Trust . The Trussel Trust: Latest Stats 2018. www.trusselltrust.org/ (accessed May 2018).
- The Trussell Trust . Half of Children Helped by Foodbanks Over Summer Holiday Months Are Primary School Children [News Item] 2017. www.trusselltrust.org/2017/07/25/half-children-helped-foodbanks-summer-holiday-months-primary-school-students/ (accessed May 2018).
- Downing E, Kennedy S, Fell M. Food Banks and Food Poverty. Standard Note SN06657 2014. http://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN06657 (accessed May 2018).
- Forsey A. An Evidence Review for the All-Party Parliamentary Inquiry into Hunger in the United Kingdom 2015. https://feedingbritain.files.wordpress.com/2015/02/food-poverty-appg-evidence-review-final.pdf (accessed May 2018).
- Forsey A. Britain’s Not-so-Hidden Hunger 2016. https://feedingbritain.files.wordpress.com/2017/01/437488_tso_britains-not-so-hidden-hunger.pdf (accessed May 2018).
- Office for National Statistics . Living Costs and Food Survey. User Guidance and Technical Information for the Living Costs and Food Survey n.d. www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/methodologies/livingcostsandfoodsurvey (accessed November 2018).
- Food Foundation . Measuring Household Food Insecurity in the UK and Why We MUST Do It: 4 Facts You Should Know n.d. https://foodfoundation.org.uk/wp-content/uploads/2016/07/MeasuringHouseholdFoodInsecurity.pdf (accessed November 2018).
- Church Action on Poverty . Step up to the Plate: Towards a UK Food and Poverty Strategy 2018. www.church-poverty.org.uk/news/pressroom/resources/reports/stepuptotheplate/view (accessed May 2018).
- Tait C. Hungry for Change 2015. https://fabians.org.uk/publication/hungry-for-change/ (accessed May 2018).
- Food Research and Action Center . Understanding the Connections: Food Insecurity and Obesity 2015. http://frac.org/wp-content/uploads/frac_brief_understanding_the_connections.pdf (accessed May 2018).
- Metallinos-Katsaras E, Must A, Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet 2012;112:1949-58. https://doi.org/10.1016/j.jand.2012.08.031.
- Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966–2007. Preventing Chronic Disease 2009;6.
- Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prevent Med 2009;36:74-81. https://doi.org/10.1016/j.amepre.2008.09.025.
- Bell J, Mora G, Hagan E, Rubin V, Karpyn A. Access to Healthy Food and Why It Matters: A Review of the Research 2013. www.policylink.org/find-resources/library/access-to-healthy-food-and-why-it-matters (accessed 23 October 2018).
- Ver Ploeg M, Mancino L, Todd JE, Clay DM, Scharadin B. Where Do Americans Usually Shop for Food and How Do They Travel To Get There? Initial Findings from the National Household Food Acquisition and Purchase Survey. Washington, DC: U.S. Department of Agriculture, Economic Research Service; 2015.
- Andreyeva T, Blumenthal DM, Schwartz MB, Long MW, Brownell KD. Availability and prices of foods across stores and neighborhoods: the case of New Haven, Connecticut. Health Affairs 2008;27:1381-8. https://doi.org/10.1377/hlthaff.27.5.1381.
- Evans A, Banks K, Jennings R, Nehme E, Nemec C, Sharma S, et al. Increasing access to healthful foods: a qualitative study with residents of low-income communities. Int J Behav Nut Phys Act 2015;12. https://doi.org/10.1186/1479-5868-12-S1-S5.
- Fleischhacker SE, Evenson KR, Rodriguez DA, Ammerman AS. A systematic review of fast food access studies. Obesity Reviews 2011;12:e460-71. https://doi.org/10.1111/j.1467-789X.2010.00715.X.
- Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health 2012;102:1644-54. https://doi.org/10.2105/AJPH.2012.300865.
- Kestens Y, Daniel M. Social inequalities in food exposure around schools in an urban area. Am J Prevent Med 2010;39:33-40. https://doi.org/10.1016/j.amepre.2010.03.014.
- Smith JC, Medalia C. Health Insurance Coverage in the United States: 2014. U.S. Census Bureau, Current Population Reports, P60-253. Washington, DC: U.S. Government Printing Office; 2015.
- Bruening M, MacLehose R, Loth K, Story M, Neumark-Sztainer D. Feeding a family in a recession: food insecurity among Minnesota parents. Am J Public Health 2012;102:520-6. https://doi.org/10.2105/AJPH.2011.300390.
- Dammann K, Smith C. Food-related attitudes and behaviors at home, school, and restaurants: perspectives from racially diverse, urban, low-income 9- to 13-year-old children in Minnesota. J Nutr Educ Behav 2010;42:389-97. https://doi.org/10.1016/j.jneb.2009.09.003.
- Olson CM, Bove CF, Miller EO. Growing up poor: long-term implications for eating patterns and body weight. Appetite 2007;49:198-207. https://doi.org/10.1016/j.appet.2007.01.012.
- Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low-income Supplemental Nutrition Assistance Program participants and income-eligible nonparticipants. J Nutr 2015;145:622-7. https://doi.org/10.3945/jn.114.199414.
- Neckerman KM, Lovasi GS, Davies S, Purciel M, Quinn J, Feder E, et al. Disparities in urban neighborhood conditions: evidence from GIS measures and field observation in New York City. J Public Health Policy 2009;30:264-85. https://doi.org/10.1057/jphp.2008.47.
- Bruton CM, Floyd MF. Disparities in built and natural features of urban parks: comparisons by neighborhood level race/ethnicity and income. J Urban Health 2014;91:894-907. https://doi.org/10.1007/s11524-014-9893-4.
- Obesity Health Alliance . 3 in 5 of England’s Most Deprived Boys Will Be Overweight or Obese by 2020 [News Item] 2016. http://obesityhealthalliance.org.uk/2016/10/11/3-5-englands-deprived-boys-will-overweight-obese-2020/ (accessed May 2018).
- Nord M, Coleman A, Andrews N, Carlson S. Household Food Security in the United States, 2009 2010. www.ers.usda.gov/webdocs/publications/44776/7024_err108_1_.pdf?v=41056 (accessed May 2018).
- Aceves-Martins M, Aleman-Diaz AY, Giralt M, Solà R. Involving young people in health promotion, research and policy-making: practical recommendations [published online ahead of print May 18 2018]. Int J Qual Health Care 2018. https://doi.org/10.1093/intqhc/mzy113.
- International Food Policy Research Institute . 2018 Global Food Policy Report 2018. https://reliefweb.int/sites/reliefweb.int/files/resources/132488.pdf (accessed May 2018).
- Bernal J, Frongillo EA, Herrera H, Rivera J. Children live, feel, and respond to experiences of food insecurity that compromise their development and weight status in peri-urban Venezuela. J Nutr 2012;142:1343-9. https://doi.org/10.3945/jn.112.158063.
- Health Promoting Schools: An Effective Approach to Early Action on Noncommunicable Disease Risk Factors. Geneva: WHO; 2017.
- The State of Food and Agriculture. Rome: Food and Agriculture Organization of the United Nations; 2006.
- Aceves-Martins M, Whitehead R, Inchley J, Giralt M, Currie C, Solà R. Self-reported weight and predictors of missing responses in youth. Nutrition 2018;53:54-8. https://doi.org/10.1016/j.nut.2018.01.003.
- Jean-Jacques M, Persell SD, Hasnain-Wynia R, Thompson JA, Baker DW. The implications of using adjusted versus unadjusted methods to measure health care disparities at the practice level. Am J Med Qual 2011;26:491-50. https://doi.org/10.1177/1062860611403135.
- Arcuri S, Brunori G, Galli F. Insights on the role of private and public actors in food assistance provision: a literature review for high income countries. Economia Agro Alimentare Food Economy 2017;19:119-50. https://doi.org/10.3280/ECAG2017-001006.
- Winston P, Angel R, Burton L, Cherlin A, Moffitt RM, Wilson WJ. Welfare, Children, and Families: A Three-City Study, Overview and Design Report. Balitmore, MD: John Hopkins University; 1999.
- Dolan M, Smith K, Casanueva C, Ringeisen H. NSCAWII Baseline Report: Introduction to NSCAWII. OPRE Report #2011–27a. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2011.
- Dowd K, Dolan M, Wallin J, Miller K, Biemer P, Aragon-Logan E, et al. National Survey of Child and Adolescent Well-being II (NSCAW II) Combined Waves 1–2, Data File User’s Manual, Restricted Release Version. NY: Cornell University, National Data Archive on Child Abuse and Neglect; 2011.
- Casanueva C, Tueller S, Dolan M, Testa M, Smith K, Day O. Examining predictors of re-reports and recurrence of child maltreatment using two national data sources. Child Youth Serv Rev 2015;48:1-13. https://doi.org/10.1016/j.childyouth.2014.10.006.
Appendix 1 Food insecurity search strategies
MEDLINE and EMBASE
Date range searched: EMBASE, 1980 to 2017 week 49; Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R), 1946 to 4 December 2017.
Via Ovid multifile search: http://shibboleth.ovid.com/.
Date of search: 4 December 2017.
Search strategy
-
Food Insecurity/ use emez (1678)
-
Food Security/ use emez (3231)
-
food insecurity.kw. (1038)
-
food security.kw. (1644)
-
Food Supply/ use ppez (10,963)
-
(food adj3 (security or insecurity or poverty or poor or sufficien$ or insufficien$)).tw. (16,718)
-
Hunger/ (15,298)
-
or/1-7 (40,860)
-
adolescent/ or child/ or child, preschool/ use ppez (5,297,230)
-
exp juvenile/ use emez (3,166,098)
-
(child$ or boy? or girl? or household? or famil$).tw. (4,907,551)
-
9 or 10 or 11 (8,592,312)
-
8 and 12 (12,407)
-
exp africa/ or exp caribbean region/ or exp central america/ or exp “gulf of mexico”/ or exp latin america/ or exp south america/ or exp antarctic regions/ or exp arctic regions/ or exp asia/ (2,493,168)
-
13 not 14 (7997)
-
Food Assistance/ (1467)
-
Food Services/ use ppez (5374)
-
(food adj2 (bank? or pantry or pantries or aid or parcel?)).tw. (1255)
-
(voucher? or stamp?).tw. (10,597)
-
(club? adj2 (breakfast or lunch or supper or food)).tw. (104)
-
(meal? adj2 (school or nurser$ or free)).tw. (2216)
-
(holiday adj2 (club? or food or kitchen)).tw. (20)
-
magic breakfast.tw. (0)
-
(trussell or fareshare).tw. (111)
-
((food or meal? or breakfast or lunch or supper or nutrition$) adj3 (program$ or project? or scheme? or support or school)).tw. (51,209)
-
or/16-25 (67,019)
-
15 and 26 (1496)
-
exp Child Behavior/ (64,220)
-
Child Behavior Disorders/ use ppez (21,646)
-
exp Child Development/ (99,622)
-
exp Child Development Disorders, Pervasive/ (87,868)
-
Developmental Disabilities/ use ppez (19,298)
-
Developmental Disorder/ use emez (32,407)
-
exp Neurodevelopmental Disorders/ use ppez (178,860)
-
Child Health/ (22,651)
-
Child growth/ use emez (11,451)
-
Diet/ (341,126)
-
Child Nutrition/ use emez (15,195)
-
Nutritive Value/ (27,150)
-
(child$ adj3 (health or develop$ or disorder$ or well being or social)).tw. (273,004)
-
(child adj3 (mental or psychiat$ or psychologic$ or cognitiv$)).tw. (26,908)
-
(child adj3 (growth or height or weight or diet or nutrit$)).tw. (12,022)
-
(child adj3 (academic or reading or numer$ or verbal or speech or learn$)).tw. (3350)
-
or/28-43 (1,022,534)
-
15 and 44 (2383)
-
exp “costs and cost analysis”/ use ppez (224,968)
-
exp economic evaluation/ use emez (269,065)
-
economics/ (255,203)
-
health economics/ use emez (34,892)
-
exp health care cost/ use emez (257,803)
-
exp economics,hospital/ use ppez (23,588)
-
exp economics,medical/ use ppez (14,400)
-
economics,pharmaceutical/ use ppez (3003)
-
pharmacoeconomics/ use emez (6692)
-
exp models, economic/ use ppez (14,182)
-
exp decision theory/ (13,447)
-
monte carlo method/ (60,837)
-
markov chains/ (15,527)
-
exp technology assessment, biomedical/ (23,358)
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minimis$)).ab. (288,499)
-
economics model$.tw. (127)
-
(economic$ or pharmacoeconomic$).tw. (502,318)
-
(price or prices or pricing).tw. (77,919)
-
budget$.tw. (57,824)
-
(value adj1 money).tw. (61)
-
(expenditure$ not energy).tw. (58,544)
-
markov$.tw. (45,252)
-
monte carlo.tw. (83,728)
-
(decision$ adj2 (tree? or analy$ or model$)).tw. (45,263)
-
or/46-69 (1,687,881)
-
(metabolic adj cost).tw. (2531)
-
((energy or oxygen) adj (cost or expenditure)).tw. (56,771)
-
70 not (71 or 72) (1,686,109)
-
15 and 73 (1490)
-
(food adj1 (security or insecurity)).ti. (4178)
-
75 and child$.tw,kw,hw. (1408)
-
27 or 45 or 74 or 76 (4900)
-
77 not (letter or note or comment or editorial or abstract).pt. (4319)
-
limit 78 to english language (4156)
-
limit 79 to yr=“1995 – 2017” (3866)
CAB abstracts
Date range searched: 1990 to 2017 week 47.
Via Ovid: http://shibboleth.ovid.com/.
Date of search: 4 December 2017.
Search strategy
-
food security/ (18,731)
-
(food adj3 (security or insecurity or poverty or poor or sufficienc$ or insufficienc$)).tw. (29,876)
-
Hunger/ (3642)
-
or/1-3 (32,379)
-
exp children/ or adolescents/ (125,323)
-
(child$ or boy? or girl?).tw. (168,810)
-
5 or 6 (168,810)
-
4 and 7 (2651)
-
exp developing countries/ (1,583,325)
-
8 not 9 (1152)
-
limit 10 to (english language and yr="1996 - 2017”) (1089)
PsycINFO
Date range searched: 1987 to November week 2 2017.
Via Ovid: http://shibboleth.ovid.com/.
Date of search: 4 December 2017.
Search strategy
-
(food adj3 (security or insecurity or poverty or poor or sufficienc$ or insufficienc$)).tw. (1512)
-
Hunger/ (1034)
-
food insecurity.id. (398)
-
food security.id. (211)
-
or/1-4 (2471)
-
(child$ or boy? or girl? or adolescent?).af. (1,324,695)
-
5 and 6 (1347)
-
(africa or asia or “south america” or “central america”).af. (120,026)
-
7 not 8 (1041)
-
limit 9 to (english language and yr=“1996 - 2017”) (977)
CINAHL
Date range searched: 1982 to December 2017.
Via EBSCOhost: http://search.ebscohost.com.
Date of search: 4 December 2017.
Search strategy
-
S1 (MH “Food Security”)
-
S2 TX ( food N3 (security or insecurity) ) OR TX ( food N3 (poverty or poor) ) OR TX ( food N3 (insufficienc* or sufficienc*))
-
S3 S1 OR S2
-
S4 (MH “Child+”) OR (MH “Adolescence+”)
-
S5 TX (child* or boy* or girl* or household or family)
-
S6 S4 OR S5
-
S7 S3 AND S6
-
S8 (MH “Africa+”) OR (MH “Central America+”) OR (MH “South America+”) OR (MH “West Indies+”) OR (MH “Asia+”)
-
S9 S7 NOT S8
-
S10 S7 NOT S8- Published Date: 19960101-20171231 Narrow by Language:- english
ERIC
Date range searched: 1996 to December 2017.
Via EBSCOhost: http://search.ebscohost.com.
Date of search: 4 December 2017.
Search strategy
-
S1 TX ( food N3 (insecurity or security) ) OR TX ( food N3 (poverty or poor) ) TX ( food N3 (insufficienc* or sufficienc*) )
-
Limiters – Date Published: 19960101-20171231 Narrow by Language: - english
ASSIA
Date range searched: 1996–2017.
Via ProQuest: www.proquest.com.
Date of search: 4 December 2017.
Search strategy
(MAINSUBJECT.EXACT(“Food security”) OR ab((food W3 (security OR insecurity OR poverty OR poor OR insufficienc* OR sufficienc*))) OR ti((food W3 (security OR insecurity OR poverty OR poor OR insufficienc* OR sufficienc*)))) AND (la.exact(“ENG”) AND yr(1996-2017))
Social Science Citation Index
Database: =SSCI Timespan=1996–2017.
Via Web of Knowledge: www.webofknowledge.com.
Date of search: 4 December 2017.
Search strategy
-
# 1# 2 6,166 (TS=food security) AND LANGUAGE: (English)
-
#2 2,859 (TS=food insecurity) AND LANGUAGE: (English)
-
# 3 363 (TS=food sufficiency) AND LANGUAGE: (English)
-
# 4 422 (TS=food insufficiency) AND LANGUAGE: (English)
-
# 5 2,911 (TS=food poverty) AND LANGUAGE: (English)
-
# 6 9,308 (#1 OR #2 OR #3 OR #4 OR #5) AND LANGUAGE: (English)
-
# 7 408,518 (TS= (child* or boy* or girl*)) AND LANGUAGE: (English)
-
# 8 1,885 (#6 and #7) AND LANGUAGE: (English)
-
# 9 66,757 (TS=developing countr*) AND LANGUAGE: (English)
-
# 10 185,281 (TS=(Russia* or india* or Pakistan* or china or Chinese)) AND LANGUAGE: (English)
-
# 11 63,416 (TS=(carribean or mexic* or argentin* or brazil* or chile*)) AND LANGUAGE: (English)
-
# 12 145,371 (TS=(africa* or Egypt* or Ethiopia* or Kenya* or tanzania* or Uganda* or niger*)) AND LANGUAGE: (English)
-
# 13 421,820 #12 OR #11 OR #10 OR #9
-
# 14 1,070 (#8 NOT #13) AND LANGUAGE: (English) Refined by: DOCUMENT TYPES: ( ARTICLE )
The Cochrane Library
Cochrane Database of Systematic Reviews: Issue 12 of 12, December 2017.
Cochrane Central Register of Controlled Trials: Issue 11 of 12, November 2017.
Via The Cochrane Library: www.thecochranelibrary.com.
Date of search: 4 December 2017.
Search strategy
-
#1 food next/3 (security or insecurity or poverty or poor or insufficienc* or sufficienc*):ti,ab,kw (Word variations have been searched) (194)
-
#2 MeSH descriptor: [Child] explode all trees (250)
-
#3 MeSH descriptor: [Adolescent] explode all trees (93,070)
-
#4 (child* or boy* or girl* or household or family):ti,ab,kw (Word variations have been searched) (124,680)
-
#5 #2 or #3 or #4 (188,198)
-
#6 #1 and #5 (140)
-
#7 MeSH descriptor: [Africa] explode all trees (6140)
-
#8 MeSH descriptor: [Central America] explode all trees (250)
-
#9 MeSH descriptor: [South America] explode all trees (2131)
-
#10 MeSH descriptor: [Caribbean Region] explode all trees (391)
-
#11 MeSH descriptor: [Asia] explode all trees (16,815)
-
#12 #7 or #8 or #9 or #10 or #11 (25,256)
-
#13 #6 and not #12 (91)
Sources of grey literature: websites consulted
UK national and regional sources
UK Parliament All Parliamentary Party Group on Hunger: www.parliament.uk/
UK Department of Health: www.gov.uk/government/organisations/department-of-health
Scottish Government Working Group: www.gov.scot/
NHS Health Scotland: www.healthscotland.com/
Royal College of Paediatrics & Child Health: www.rcpch.ac.uk/
Scottish Food Coalition: www.foodcoalition.scot/
Food Standards Agency: www.food.gov.uk/
Food Foundation: http://foodfoundation.org.uk/
Food Ethics Council: www.foodethicscouncil.org/
Food Research Collaboration: http://foodresearch.org.uk/
Food Poverty Alliance: www.povertyalliance.org/
Healthy Living UK: http://healthylivinguk.org/
Feeding Britain: https://feeding-britain.org/
Community Food & Health Scotland: www.communityfoodandhealth.org.uk/
Joseph Rowntree Foundation: www.jrf.org.uk/
Church Action on Poverty: www.church-poverty.org.uk/
Child Poverty Action Group: www.cpag.org.uk/
Poverty & Social Exclusion: www.poverty.ac.uk/
Fabian Society: www.fabians.org.uk/
Shake Up Your Wake Up: www.shakeupyourwakeup.com/
Magic Breakfast: www.magicbreakfast.com/
The Trussell Trust: www.trusselltrust.org/
FareShare: http://fareshare.org.uk/
British Red Cross: www.redcross.org.uk/
Sustain: www.sustainweb.org/foodpoverty/
International sources
UNICEF: www.unicef-irc.org/
UN Food & Agriculture Organization: www.fao.org/
United States Department of Agriculture Food and Nutrition Services: www.fns.usda.gov/
Food Insecurity Policy Research: http://proof.utoronto.ca/
Child Trends (US): www.childtrends.org/
Joint Centre for Poverty Research: www.eurofoodbank.org/
United States Department of Agriculture Food Programs [SNAP, Special Supplemental Nutrition Programme for Women, Infants and Children (WIC), School Breakfast, School Lunch, Summer Food, Fresh Fruit and Vegetables, etc.]: www.fns.usda.gov/programs-and-services
European Federation of Food Banks: www.eurofoodbank.org/
Appendix 2 General characteristics of included studies
| Study authors and year of publication | Country | Study design | Children’s age | Population | Number of participants/sample size | RQ addressed | Project/study/programme |
|---|---|---|---|---|---|---|---|
| Belsky et al. 201019 | UK | Longitudinal | 5–12 years | Families with same-sex twins | 2123 children | 1 and 3 | Environmental Risk Longitudinal Twin Study |
| Harvey 201630 | UK | Qualitative | 5–11 years median 9 years) | Participants recruited from Kids Company (UK charity that supports inner-city deprived children) | 19 children | 1 | Kids Company (registered charity in the UK). Data used: spring 2014 |
| Harvey-Golding et al. 201532 | UK | Qualitative | Mean 9 years | Three primary schools located in an area of high socioeconomic deprivation | 15 children | 1 | None reported |
| Harvey-Golding et al. 201631 | UK | Qualitative | Stakeholders | Participating schools located in communities within the bottom half of neighbourhoods ranked on indicators of deprivation | 19 stakeholders | 1 | UFSB |
| Sellen et al. 200259 | UK | Mixed methods | < 5 years | Refugee population living in east London | 30 families | 1 | Refugee Education Team and Community Renewal Programme |
| Molcho et al. 2007106 | Ireland | Observational | 10–17 years | Nationally representative sample of schools | 8424 students | 3 | (Irish) HBSC study. Data used: 2002 |
| Broughton et al. 200621 | Canada | Observational | 2–5 years | Families from low-income neighbourhoods who spoke English, Cantonese or Mandarin | 142 households with children | 1 and 3 | None reported |
| Carter et al. 201223 | Canada | Longitudinal | 4–10 years | Children born and raised in Québec | 1746 children | 1 | Québec Longitudinal Study of Child Development |
| Egeland et al. 201127 | Canada | Observational | 3–5 years | Inuit pre-schoolers in Canada’s Nunavut Territory | 374 children | 1 and 3 | Nunavut Inuit Child Health Survey. Data used: 2007–8 |
| Kirkpatrick and Tarasuk 200843 | Canada | Observational | 1–18 years | Participants living in private residences across Canada | 7353 children and adolescents | 1 | Canadian Community Health Survey. Data used: 2004 (cycle 2.2) |
| Kirkpatrick et al. 201042 | Canada | Longitudinal | 10–21 years | Data from a national longitudinal survey | 9142 (5809 children and 3333 youth) | 1 and 3 | Canadian National Longitudinal Survey of Children and Youth. Data used: 1994–2004/5 |
| Marjerrison et al. 201145 | Canada | Observational | Mean 11.8 years, SD 4 years | Households with a child with insulin-requiring diabetes mellitus | 183 families | 1 and 3 | None reported |
| Mark et al. 201275 | Canada | Observational | 9–18 years | Participants living in private dwellings in Canada | 8938 | 3 | Canadian Community Health Survey. Data used: 2004 (cycle 2.2) |
| McIsaac et al. 201746 | Canada | Observational | 3–5 years | Population based, cross-sectional survey of Inuit children in the Canadian territory of Nunavut | 215 caregivers | 1 | The Nunavut Inuit Child Health Survey. Data used: 2007–8 |
| Pickett et al. 201576 | Canada | Observational | 11–15 years | Nationally representative sample of schools | 25,912 students | 3 | (Canadian) HBSC study. Data used: 2009–10 |
| Wadsworth 201268 | Canada | Observational | 7–11 years | Students in seventh to eleventh grades | 918 students | 1 | Keeping Pace provincial health surveillance project |
| Arteaga et al. 201718 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Hispanic children | 2150 in 1998 and 2800 in 2011 | 1 | ECLS-K. Data used: 1998–9, 2010–11 |
| Baer et al. 201577 | USA | Observational | 15–25 years (mean 18 years) | Youths living in urban Boston |
15–17 years, n = 172 18–25 years, n = 228 |
3 | The Online Advocate study |
| Barroso et al. 201678 | USA | Observational | 12–24 months (mean 17 months, SD 4.2 months) | Hispanic low-income people enrolled in a WIC programme | 240 mother–child dyads | 3 and 4 | The WIC programme in the South-Western USA |
| Bhargava et al. 200820 | USA | Longitudinal | Mean 73 months | Children from kindergarten to fifth grade | 7635 children | 1 and 3 | ECLS-K. Data used: 1999–2003 |
| Bruening and Johnson 201579 | USA | Observational | Mean 15.8 years, SD 1.2 years | Youths part of The New Mexico Youth Risk and Resiliency Survey | 5869 adolescents | 3 | None reported |
| Bruening et al. 201722 | USA | Observational | Mean 14.6 years, SD 2.3 years | Participants from six public housing sites located in low-income neighbourhoods who spoke English or Spanish | 55 adolescents | 1 | None reported (reported as a pilot study) |
| Burke et al. 201680 | USA | Longitudinal | Baseline: males mean 68.8 months (SD 4.5 months); females mean 68.1 months (SD 4.1 months) | Children from kindergarten to eighth grade | Varied according time point: maximum included n = 15,158 (1999) to minimum included n = 5753 (2007) | 3 | ECLS-K. Data used: fall 1998; spring 1999; spring 2002; spring 2004; and spring 2007 |
| Canter et al. 2017115 | USA | Observational | 5–10 years (mean 7.7 years, SD 1.7 years) | English-speaking parents with a child (aged 5–10 years) in their care, who received services through an organisation devoted to serving low-income families in a large metropolitan area in the USA | 148 children | 4 | None reported |
| Casey et al. 20058 | USA | Observational | 3–17 years | Counties selected on population size, % of population who were African American, % of people living below the federal poverty level | 399 children | 3 | None reported |
| Casey et al. 200681 | USA | Observational | 3–17 years | Representative sample of the US population | 6995 children | 3 | NHANES. Data used: 1999–2002 |
| Chi et al. 201482 | USA | Observational | 5–17 years | Representative sample of the US population | 2206 children | 3 | NHANES. Data used: 2007–8 |
| Chilton et al. 200924 | USA | Observational | 0–3 years | Participants recruited at emergency departments and paediatric care clinics being seen for conditions that were not life-threatening, if mothers spoke English or Spanish | 19,275 mothers | 1 and 3 | C-SNAP. Data used: 1998–2005 |
| Connell et al. 200525 | USA | Qualitative | 11–16 years | Children from two after-school programmes for low-income children in a mid-sized central city and from a rural middle school with a high rate of eligibility for free and reduced-price school meals | 32 children | 1 | This study was the first phase of a three-phase research project designed to develop a FS survey module that could be administered directly to children |
| Cook et al. 200483 | USA | Observational | ≤ 36 months | Children whose adult caregivers were interviewed at the six C-SNAP sites | 11,539 caregivers | 3 and 4 | C-SNAP. Data used: 1998–2004 |
| Cook et al. 2006116 | USA | Observational | ≤ 36 months | Participants recruited at emergency departments and paediatric care clinics being seen for conditions that were not life-threatening, if mothers spoke English or Spanish | 17,130 caregivers | 4 | C-SNAP. Data used: 1998–2002 |
| Dunifon and Kowaleski-Jones 200326 | USA | Observational | 6–12 years | US nationally representative sample | 1854 children | 1, 3 and 4 | Study evaluating the NSLP by using data from data from the Child Development Supplement of the Panel Study of Income Dynamics. Data used: 1997 |
| Ecker and Sifers 2013118 | USA | Non-randomised comparative | Kindergarten through sixth grade (ages not specified) | Schools with high % of students receiving free/reduced lunches | 192 students (hunger surveys were evaluated for 82 students) | 4 | BackPack Food Program |
| Edwards and Taub 201784 | USA | Observational | 11–16 years | Nationally representative sample from elementary, middle and high schools across the USA | 12,642 students | 3 | US HBSC study. Data used: 2009–10 |
| Eicher-Miller et al. 200928 | USA | Observational | 3–19 years (mean 14.6 years SD 2.3 years) | Representative children and adolescents from non-institutionalised and civilian US population | 11,247 children and adolescents | 1 and 3 | NHANES. Data used: 1999–2000, 2001–2 and 2003–4 |
| Eicher-Miller et al. 201129 | USA | Observational | 8–19 years | Representative = children and adolescents from non-institutionalised and civilian US population | 5270 children and adolescents | 1 ands 3 | NHANES. Data used: 2001–2 and 2003–4 |
| Fram et al. 20116 | USA | Qualitative | 9–16 years | Families from homes in rural and non-rural areas recruited from food pantries, soup kitchens, social services agencies and community centres | 26 children and adolescents | 1 | None reported |
| Fram et al. 2015114 | USA | Observational | Mean 10.1 years, SD 0.8 years | Ethnically diverse, low-income fourth and fifth grade children and their families | 3605 children | 3 | Secondary analysis of the Network for a Healthy California – Childrens PowerPlay! Campaign. Data collected for 2012 |
| Gordon et al. 2017119 | USA | Non-randomised comparative | School-aged children (ages not specified) | Households with eligible school-aged children certified for reduced or free meals | 27,092 children (with FI measurement) | 4 | The Summer Electronic Benefit Transfer for Children demonstration piloted summer food assistance through electronic benefit transfers, through either the WIC or the SNAP. Data used: evaluation sample in 2012 |
| Gundersen et al. 200886 | USA | Observational | Mean 8.3 years, SD 3.7 years | Households below 200% of the poverty line with a female adult and at least one child from a nationally representative sample | 841 children in 425 households | 3 | NHANES. Data used: 1999–2002 and the current population survey |
| Gundersen et al. 200985 | USA | Observational | 8–17 years (mean 12 years) | Households below 200% of the poverty line from a nationally representative sample | 2516 children | 3 | NHANES. Data used: 2001–4 |
| Helton 201687 | USA | Observational | 0–17 years (mean 7 years) | Children involved in Child Protective Services investigations of allegations of maltreatment | 3580 children | 3 | The National Survey of Child and Adolescent Well-Being and the National Child Abuse and Neglect Data System. Data used: 2010 |
| Himmelgreen et al. 200033 | USA | Observational | 1–6 years | Low-income Hispanic caregivers recruited from churches, shelters and other community centres | 248 caregivers of children | 1 | Maternal/child health programmes delivered by the Hispanic Health Council, Hartford Hospital, Connecticut Children’s Medical Centre and the WIC |
| Holben et al. 200434 | USA | Observational | Households with children (ages not specified) | Households with children currently enrolled in Head Start (which involves provision of supplemental resources, such as meals and snacks) | 297 households | 1 | Head Start |
| Holben and Taylor 201588 | USA | Observational | 12–18 years (mean 14.9 years, SD 0.1 years) | Participants with waist circumference data | 7435 adolescents | 3 | NHANES. Data used: 1999–2006 |
| Howard 201189 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | 4710 children | 3 | ECLS-K. Data used: 1999–2003 |
| Howard 201190 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | 4710 children | 3 | ECLS-K. Data used: 1999–2004 |
| Howard 201391 | USA | Longitudinal | 10–13 years (2004 cohort), 13–16 years (2007 cohort) | Students enrolled in over 1200 kindergartens in the USA | 5670 children | 3 | ECLS-K. Data used: 2004–7 |
| Huang et al. 201092 | USA | Longitudinal | Mean 9.5 years, SD 3.5 years | Households with an income of less than 200% of the poverty threshold and where parents were the primary caregivers; from a nationally representative sample | 416 children from 249 households | 3 | Child Development Supplement to the Panel Study of Income Dynamics. Waves included 1997 and 2002 |
| Huang and Vaughn 201693 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | Sample size ranges from 6032 to 7144 depending on the time point and missing data | 3 | ECLS-K. Data used: 1999–2003 |
| Jacknowitz et al. 201535 | USA | Longitudinal | 9 months (2001–2), 2 years (2003–4), 4 years (2005–6) | Nationally representative sample of children from infancy to the time they entered school | Baseline analysis sample was 7850 | 1 | ECLS-B. Data used: 2001–8 |
| Jackson and Vaughn 201794 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | Sample sizes ranged from 6531 to 7028 children depending on the time point and missing data | 3 | ECLS-K. Data used: 1999–2007 |
| Jansen et al. 2017123 | USA | RCT | Mean 4.4 years, SD 0.6 years | Pre-schoolers in Head Start programme from urban and rural areas | 501 children | 3 | Growing Healthy Study, a cluster-randomised community-based obesity intervention trial from Head Start programme. Data used: 2011–15 |
| Ryu and Bartfeld 201295 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA. Analyses were limited to children with full household FS status measurements at all four time points | 7326 children | 3 | ECLS-K. Data used: 1999–2007 |
| Johnson and Markowitz 201796 | USA | Longitudinal | 9 months (2001–2), 2 years (2003–4), 4 years (2005–6) | Students living in households with incomes at or below 185% of the poverty lines from those enrolled in a nationally representative sample of children from infancy to the time they entered school | 3700 children | 3 | ECLS-B. Data used: 1999–2008 |
| Jyoti et al. 200511 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | Sample sizes ranged from 13,500 to 11,400 children depending on the time point and missing data | 3 | ECLS-K. Data used: 1999–2002 |
| Kaiser et al. 200236 | USA | Observational | 3–6 years | Spanish- and English-speaking Mexican American families | 211 families with preschool children | 1 and 3 | Head Start, Healthy Start, the federal WIC |
| Kaur et al. 201597 | USA | Observational | 2–11 years | Nationally representative sample of the US civilian non-institutionalised population | 9701 children | 3 | NHANES. Data used: 2001–10 |
| Kenney 200837 | USA | Observational | Within 48 hours of the child’s birth, and then at 12, 36 and 60 months | Nationally representative sample of non-marital births in the USA | 1073 couples | 1 | Fragile Families and Child Wellbeing Study data and In-Home Longitudinal Study of Pre-School Children |
| Kersey et al. 200738 | USA | Observational | < 3 years | Participants recruited from a clinic serving a low-income, urban, diverse population | 4278 caregivers | 1 | None reported |
| Khan et al. 201198 | USA | Observational | 10–14 years | Children attending a public middle school | 373 children and adolescents | 3 and 4 | School receiving free lunch |
| Kimbro et al. 201240 | USA | Longitudinal | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | 11,610 children | 1 | ECLS-K. Data used: 1999–2002. Data merged with Census 2000 contextual for analysis purposes |
| Kimbro and Denney 201539 | USA | Longitudinal | First grade (6–9 years), third grade (8–11 years) and fifth grade (10–13 years) | Students living in household incomes below 300% of the federal poverty level from those enrolled in over 1200 kindergartens in the USA | 6300 children | 1 and 3 | ECLS-K. Data used: 2010–12 |
| King 201741 | USA | Observational | 5 years | Predominantly unmarried mothers | 2829 mothers | 1 and 3 | Fragile Families and Child Wellbeing Study. Data used: collected at the fifth year |
| Kleinman et al. 199899 | USA | Observational | < 12 years | Families with at least one child | 328 families | 3 | CCHIP |
| Kleinman et al. 2002117 | USA | Non-randomised comparative | Fourth to sixth grades (ages not specified) | Inner-city students eligible for UFSB programme | 97 children | 4 | Collaborative study of a UFSB in the Boston Public Schools |
| Klerman et al. 2017120 | USA | Non-randomised comparative | School-aged children (ages not specified) | Households with school-aged children who, in the prior school year, were certified for free or reduced-price school meals | Summer survey, n = 48,449; spring survey, n = 41,793 | 4 | Summer Electronic Benefits Transfer for Children |
| Kohn et al. 201474 | USA | Observational | 4–17 years | Children from families below the 200% poverty line | 1321 children and adolescents | 3, 4 | NHANES. Data used: 2007–8 |
| Korenman et al. 2013121 | USA | Non-randomised comparative | 4 years | Nationally representative sample of children from infancy to the time they entered school | 4050 students, of whom 1850 participated in the CACFP | 4 | CACFP from Head Start Centres analysed using data of ECLS-B |
| Kuku et al. 2012100 | USA | Observational | 0–12 years | Children from households below 200% of the poverty line from nationally representative survey | 959 children | 3 | Child Development Supplement of the Panel Study of Income Dynamics. Data used: 2003 |
| Larson et al. 2012101 | USA | Observational | Middle- and high-school students (ages not specified) | Households of middle- and high-school students who participated the population-based EAT study | 1983 households | 3 | Eat Study. Data used: 2009–10 |
| Lohman et al. 2009102 | USA | Observational | 10–15 years (mean 12 years, SD 1.4 years) | Children and their mothers from low-income neighbourhoods with income less than twice the poverty line | 1011 adolescents | 3 | Welfare, Children, and Families: A Three-City Study. Data used: 1999 |
| Mangini et al. 201544 | USA | Observational | 6–9 years, 8–11 years and 10–13 years | Students enrolled in over 1200 kindergartens in the USA | 11,099 children | 1, 3 | ECLS-K. Data used: 2002 |
| Martin and Ferris 2007103 | USA | Observational | 2–12 years (mean 5.7 years) | Community centres that primarily served low-income families in the second poorest medium-sized city in the USA | 200 parents and their 212 children | 3 | None reported |
| Matheson et al. 2002104 | USA | Observational | Mean 10.7 years | Mothers of students enrolled in eight elementary schools | 124 mother–child dyads | 3 | Study conducted as part of a school-based obesity prevention study funded by the National Cancer Institute. No further details provided |
| McLaughlin et al. 201247 | USA | Observational | 13–17 years | Adolescents and parents for whom data were available | 6483 adolescent–parent dyads | 1 and 3 | National Comorbidity Survey Replication Adolescent Supplement |
| Metallinos-Katsaras et al. 2009105 | USA | Observational | 1–5 years | Mothers from low-income families | 8493 mothers | 3 | Data from low-income families participating at one of nine WIC children clinics in Massachusetts |
| Miller 201648 | USA | Observational | 6–9 years, 8–11 years and 10–13 years | Children who lived with their biological mothers and had valid information on child FI and the nativity of parents and children enrolled in over 1200 kindergartens in the USA | 12,934 families | 1 | ECLS-K. Data used: 1999–2007 |
| Morrissey et al. 201649 | USA | Observational | Mean 5.5 years | Sample was limited to non-missing data on FS or household poverty level | 12,550 children | 1 | ECLS-K. Data used: 2010–11. In addition, the US Census Bureau’s 2008–12 American Community Survey. Five-year estimates and USDA’s Food Environment Atlas 2010 data |
| Murphy et al. 199873 | USA | Observational | Elementary grades (third through fifth) and middle-school grades (eighth) (ages not specified) | Participants enrolled in schools with free meals for all children | 204 children | 1 and 3 | Collaborative study of a free breakfast programme in the Philadelphia and Baltimore public schools |
| Nalty et al. 201350 | USA | Observational | 6–11 years (mean 8.5 years, SD 1.4 years) | Residents of rural areas along the USA–Mexico border | 48 mother–child dyads | 1 and 4 | None reported |
| Papas et al. 201651 | USA | Observational | 2–8 years (mean 4.8 years, SD 1.9 years) | Low-income Hispanic families | 74 mothers and children | 1 and 3 | None reported |
| Poole et al. 201352 | USA | Observational | Mean 16.6 years, SD 1.1 years | High-school students | 193 adolescents | 1 and 3 | Unclear |
| Poole-Di Salvo et al. 201653 | USA | Observational | 12–16 years | Eighth-grade students enrolled in over 1200 kindergartens in the USA | Approximately 8600 students | 1 and 3 | ECLS-K. Data used 2007 |
| Richards and Smith 200755 | USA | Qualitative | 6–13 years (mean 9.8 years, SD 1.6 years) | Participants recruited from homeless shelters | 56 children | 1 | None reported |
| Rose and Bodor 200656 | USA | Longitudinal | 6–9 years and 8–11 years | Students enrolled in over 1200 kindergartens in the USA | 12,890 children | 1 and 3 | ECLS-K. Data used: 1999 and 2000 |
| Rose-Jacobs et al. 200857 | USA | Observational | 4–36 months | English-, Spanish-, or Somali-speaking caregivers | 2010 caregiver/child dyads | 1 and 3 | C-SNAP. Data used: 2004–5 |
| Rossen and Kobernik 201658 | USA | Observational | 2–15 years | Nationally representative US data | 5136 children and adolescents | 1 and 3 | NHANES: Data used: 2007–10 |
| Shanafelt et al. 201660 | USA | Observational | Nineth and tenth grade (ages not specified) | Participants of a RCT of a school breakfast intervention among 16 high schools in rural Minnesota, USA | 904 students | 1 and 3 | Project BreakFAST (Fuelling Academics and Strengthening Teens). Baseline data used |
| Sharkey et al. 201161 | USA | Observational | NR | Residents of rural areas along the USA–Mexico border | 484 households with children | 1 and 3 | Colonia Household and Community Food Resource Assessment. Data used: 2009 |
| Sharkey et al. 2012107 | USA | Observational | 6–11 years (mean 9.1 years, SD 1.3 years) | Residents of rural areas along the USA–Mexico border | 50 mother and child dyads | 3 | None reported |
| Shtasel-Gottlieb et al. 201562 | USA | Mixed methods | Middle-school (grades sixth to eighth) and high-school (grades ninth to twelfth) students (ages not specified) | Adolescents from a low-income, urban community | 2350 in the observational study and 12 in the qualitative study | 1 | None reported |
| Skalicky et al. 200663 | USA | Observational | 6–36 months | Low-income children utilising the paediatric emergency department | 626 children | 1 and 3 | Data obtained from the Boston Medical Centre (1996–2001), people interviewed as part of C-SNAP |
| Slack and Yoo 2005108 | USA | Observational | 3–12 years | Families with a primary caregiver transitioning from welfare to work | 942 families | 3 | Illinois Families Study. Data used: waves 1 and 2 |
| Smith and Richards 200864 | USA | Mixed methods | 9–18 years (mean 11.6 years, SD 2.0 years) | Participants recruited from homeless shelters | 202 children and adolescents | 1 | None reported |
| Sonik et al. 201665 | USA | Observational | Households with children (< 18 years) | Nationally representative sample of the non-institutionalised US civilian population | 24,729 households | 1 | Survey of income and programme participation. Data used: 2004 and 2008 (waves 5 and 6) |
| Speirs et al. 2016109 | USA | Observational | Mean 39 months | Families with a preschool-aged child | 438 families | 3 | Synergistic Theory and Research on Obesity and Nutrition Group Kids (STRONG Kids) programme. Data used: 2009–10 (wave 1) |
| Tester et al. 201666 | USA | Observational | 12–18 years | Low-income households (below 200% of the federal poverty line) from a nationally representative sample in the USA | 1072 adolescents | 1 and 3 | NHANES. Data used: 2003–10 |
| To et al. 2014110 | USA | Observational | 6–17 years | Low-income households (below 350% of the federal poverty line) from a nationally representative sample in the USA | 3049 children and adolescents | 3 | NHANES. Data used: 2003–6 |
| Trapp et al. 201567 | USA | Observational | 24–48 months (mean 35 months, SD 8.7 months) | Hispanic or African American caregivers participating in an obesity prevention/reversal study | 222 children | 1 and 3 | Steps to Growing Up Healthy Study |
| Weinreb et al. 200269 | USA | Observational | 2.5–17 years (preschool-aged: mean 4 years; school-aged: mean 10 years) | Participants were part of a larger study consisting of 220 homeless and 216 low-income, never homeless mothers and 627 dependent children | 203 school-aged children and 152 preschool-aged children | 1 and 3 | Unmatched case–control study of family homelessness |
| Whitbeck et al. 200670 | USA | Observational | 16–19 years (mean 17.4 years, SD 1.1 years) | Homeless or runaway youths | 428 adolescents | 1 | Baseline data from a 3-year longitudinal study of homeless and runaway youths in the USA Midwest |
| Widome et al. 2009111 | USA | Observational | Middle- and high-school students (ages not specified) | Young, ethnically diverse middle and high-school student population | 4746 adolescents | 3 | Project EAT (Eating Among Teens) |
| Willis and Fitzpatrick 2016112 | USA | Observational | Mean 11 years | Fifth to seventh grade students in a middle school | 324 students | 3 | None reported |
| Winicki and Jemison 2003113 | USA | Observational | Kindergarten children (ages not specified) | Students enrolled in over 1200 kindergartens in the USA | 18,847 children | 3 | ECLS-K. Data used: 1998–9 |
| Yu et al. 201071 | USA | Observational | Households with children (< 18 years) | Households with children with income below 185% poverty of the federal poverty level | 3799 households | 1 and 4 | Individuals who completed both CPS and the FS Supplement in 2003 |
| Zaslow 200972 | USA | Longitudinal | Infants and toddlers (ages not specified) | Nationally representative sample of children from infancy to the time they entered school | 7894 children | 1 and 3 | ECLS-B. Data used: 2001–4 |
| Ramsey et al. 201154 | Australia | Observational | 3–17 years | 1000 households in the most disadvantaged districts in Brisbane, QLD, Australia | 185 households | 1 and 3 | Data were collected from the most disadvantaged districts in Brisbane, QLD, Australia |
| Mhurchu et al. 2013122 | New Zealand | RCT | 5–13 years (mean 9.4 years, SD 2 years) | Participants recruited from low-income schools that did not have an existing breakfast programme | 424 students | 4 | Some schools received the Red Cross Breakfast in Schools programme, and others received the breakfast programme provided by the private sector |
Appendix 3 Measurement of food insecurity
| Study authors and year of publication | Country | Person(s) reporting child FI | Child FI measurement tool | Term used to present FI in the results |
|---|---|---|---|---|
| Belsky et al. 201019 | UK | Parents/caregivers | 7-item USDA FS Survey Module | Families that were ever FI |
| Harvey 201630 | UK | Parents/caregivers and children/adolescents | Children: one-to-one semistructured interviews; parents/caregivers: 18-item USDA Household FS Survey Module | Family FS |
| Harvey-Golding et al. 201631 | UK | Senior stakeholders involved in the implementation and delivery of a food aid programme | One-on-one semistructured interviews | FI |
| Harvey-Golding et al. 201532 | UK | Parents/caregivers and children/adolescents | Semistructured interviews | FI and hunger |
| Sellen et al. 200259 | UK | Parents/caregivers | 10-item Radimer/Cornell Measure of Hunger and FI | Household, caregiver and index child of FI |
| Molcho et al. 2007106 | Ireland | Adolescents | HBSC survey item: ‘Some young people go to school or to bed hungry because there is not enough food at home. How often does this happen to you?’ | Food poverty |
| Broughton et al. 200621 | Canada | Parents/caregivers | 18-item USDA module | FI, anxiety about a household’s food supply, or reduced quality or quantity of food consumed |
| Carter et al. 201223 | Canada | Parents/caregivers | Three questions adapted from the Radimer/Cornell Measure of Hunger and FI | FI |
| Egeland et al. 201127 | Canada | Parents/caregivers | 18-item USDA module (modified by Indian and Northern Affairs Canada) | Household FI and child FI |
| Kirkpatrick and Tarasuk 200843 | Canada | Parents/caregivers | 18-item USDA module | Household FI |
| Kirkpatrick et al. 201042 | Canada | Primary caregiver (any adult or older sibling living in the household, not specifically the parents) | One question: ‘Has [the child] ever experienced being hungry because the family has run out of food or money to buy food?’ | Hunger |
| Marjerrison et al. 201145 | Canada | Parents/caregivers | 18-item USDA module (adapted for the Canadian population) | Food-insecure families |
| Mark et al. 201275 | Canada | Parents/caregivers | 18-item USDA module (adapted for the Canadian population) | FI |
| McIsaac et al. 201746 | Canada | Parents/caregivers | 18-item USDA module, adapted and modified by authors | Household FS |
| Pickett et al. 201576 | Canada | Adolescents | HBSC survey: ‘Some young people go to school or to bed hungry because there is not enough food at home. How often does this happen to you?’ | Hunger |
| Wadsworth 201268 | Canada | Children | 9-item USDA child module | FI |
| Arteaga et al. 201718 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Baer et al. 201577 | USA | Adolescents | 9-item USDA Self-Administered FS Survey Module for Youths (for 12–17 years) | Personal and household-level FS |
| Barroso et al. 201678 | USA | Parents/caregivers | Questionnaire about Growth and Nutrition (which included three adapted questions form the 18-item USDA module). In addition, demographic information about the amount of food assistance dollars obtained monthly and food bank use | FI |
| Bhargava et al. 200820 | USA | Parents/caregivers | 18-item USDA module | Personal and household-level FS |
| Bruening and Johnson 201579 | USA | Adolescents | The New Mexico Youth Risk and Resiliency Survey | Food-insecure adolescents |
| Bruening et al. 201722 | USA | Parents/caregivers and children/adolescents | 6-item USDA module modified for self-administration | FI |
| Burke et al. 201680 | USA | Primary caregiver (any adult or older sibling living in the household) | 18-item USDA module | Household FI |
| Canter et al. 2017115 | USA | Parents/caregivers | 18-item USDA module | Household FI and child FI |
| Casey et al. 20058 | USA | Primary caregiver (any adult or older sibling living in the household, not specifically the parents) | 18-item USDA module | FI |
| Casey et al. 200681 | USA | Primary caregiver (any adult or older sibling living in the household, not specifically the parents) | 18-item USDA module | Household FI and child FI |
| Chi et al. 201482 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Chilton et al. 200924 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Connell et al. 200525 | USA | Children | Individual semistructured interview | Child FI |
| Cook et al. 200483 | USA | Parents/caregivers | 18-item USDA module | Household FI and hunger |
| Cook et al. 2006116 | USA | Parents/caregivers | 18-item USDA module | FI |
| Dunifon and Kowaleski-Jones 200326 | USA | Parents/caregivers | 18-item USDA module | Household FI and child FI |
| Ecker and Sifers 2013118 | USA | Children | A hunger (graphic) survey | Hunger |
| Edwards and Taub 201784 | USA | Adolescents | HBSC survey: ‘Some young people go to school or to bed hungry because there is not enough food at home. How often does this happen to you?’ | FS |
| Eicher-Miller et al. 200928 | USA | Parents/caregivers | 18-item USDA module | Child FI |
| Eicher-Miller et al. 201129 | USA | Parents/caregivers | 18-item USDA module | FI |
| Fram et al. 20116 | USA | Children | Semistructured interview | Household FI |
| Fram et al. 2015114 | USA | Children | 5 items from the Child FS Assessment (CFSA) | Child FI |
| Gordon et al. 2017119 | USA | Parents/caregivers | VLFS among children during summer (as assessed using the 30-day FS measure. Unclear if it is 18-item USDA module) | Household and child with very low FS |
| Gundersen et al. 200886 | USA | Parents/caregivers | 18-item USDA module | Household and child FI |
| Gundersen et al. 200985 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Helton 201687 | USA | Caseworker | Limited Maltreatment Classification System | Food neglection |
| Himmelgreen et al. 200033 | USA | Parents/caregivers | 10-item Radimer/Cornell Measure of Hunger and FI | Household FI, adult FI and child hunger |
| Holben et al. 200434 | USA | Parents/caregivers | 18-item USDA module | FI and childhood hunger |
| Holben and Taylor 201588 | USA | Parents/caregivers | 18-item USDA module | FS |
| Howard 201189 | USA | Parents/caregivers | 18-item USDA module | Household and child FI. Transition between FI and FS |
| Howard 201190 | USA | Parents/caregivers | 18-item USDA module | Household and child FI. Transition between FI and FS |
| Howard 201391 | USA | Parents/caregivers | 18-item USDA module | FI |
| Huang et al. 201092 | USA | Parents/caregivers | 18-item USDA module | FI |
| Huang and Vaughn 201693 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Jacknowitz et al. 201535 | USA | Parents/caregivers | 18-item USDA module | FI in a household and child level |
| Jackson and Vaughn 201794 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Jansen et al. 2017123 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Ryu and Bartfeld 201295 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Johnson and Markowitz 201796 | USA | Parents/caregivers | 18-item USDA module | Family FS |
| Jyoti et al. 200511 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Kaiser et al. 200236 | USA | Parents/caregivers | 12-item Radimer/Cornell FS scale | Household, adult and child FI |
| Kaur et al. 201597 | USA | Primary caregiver (any adult or older sibling living in the household, not specifically the parents) | 18-item USDA module. In addition, individuals in households with an affirmative response to at least one of the 18-item USDA module were asked the five personal FI questions referenced ‘the last 30 days’ during the personal interview | Child FI |
| Kenney 200837 | USA | Parents/caregivers | Child-specific questions (8 items) from the 18-item USDA module | Child FI and child hunger |
| Kersey et al. 200738 | USA | Parents/caregivers | Child-specific questions (8 items) from the 18-item USDA module | FI and childhood hunger |
| Khan et al. 201198 | USA | Children | 9-item USDA child module | Child FI |
| Kimbro et al. 201240 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Kimbro et al. 201539 | USA | Parents/caregivers | 18-item USDA module | FI |
| King 201741 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Kleinman et al. 199899 | USA | Parents/caregivers | CCHIP survey | Hunger |
| Kleinman et al. 2002117 | USA | Parents/caregivers and child/adolescents and school staff | CCHIP survey (parents) and Child Hunger Index Child Report (children) | Hunger |
| Klerman et al. 2017120 | USA | Parents/caregivers | 18-item USDA module | Child FI and child hunger |
| Kohn et al. 201474 | USA | Parents/caregivers | Child-specific questions (8 items) from the 18-item USDA module | Child FI |
| Korenman et al. 2013121 | USA | Parents/caregivers | 18-item Current Population Survey – FS Scale | FI for the family |
| Kuku et al. 2012100 | USA | Parents/caregivers | 18-item USDA module | FI |
| Larson et al. 2012101 | USA | Parents/caregivers and children/adolescents | Adolescents Eat Survey; parents/caregivers completed the 6-item USDA module | Food insufficiency and household FI |
| Lohman et al. 2009102 | USA | Parents/caregivers | Three questions from the 18-item USDA module | FI |
| Mangini et al. 201544 | USA | Parents/caregivers | 18-item USDA module | Food-insecure household |
| Martin and Ferris 2007103 | USA | Parents/caregivers | 18-item USDA module | Household FS and hunger |
| Matheson et al. 2002104 | USA | Parents/caregivers | 18-item USDA module | Household FS and hunger |
| McLaughlin et al. 201247 | USA | Parents/caregivers and children/adolescents | Four items from the 18-item USDA module (answered by adolescents and parents) | FI and hunger |
| Metallinos-Katsaras et al. 2009105 | USA | Parents/caregivers | Four-question subscale of the 18-item USDA module | Household FS and hunger |
| Miller 201648 | USA | Parents/caregivers | Child-specific questions from the 18-item USDA module | Children FI |
| Morrissey et al. 201649 | USA | Parents/caregivers | 18-item USDA module | Household FS, adult FS and child FS |
| Murphy et al. 199873 | USA | Parents/caregivers and children/adolescents | CCHIP survey | Child hunger |
| Nalty et al. 201350 | USA | Parents/caregivers and children/adolescents | Child-specific questions (8 items) from the 18-item USDA and module 9-item USDA child module | Child FI |
| Papas et al. 201651 | USA | Parents/caregivers | 18-item USDA module | Household FS |
| Poole et al. 201352 | USA | Adolescents | 9-item USDA child module | FI |
| Poole-Di Salvo et al. 201653 | USA | Parents/caregivers | 18-item USDA module | FI |
| Richards and Smith 200755 | USA | Children | In-depth face-to-face interviews | Hunger and food availability |
| Rose and Bodor 200656 | USA | Parents/caregivers | 18-item USDA module | FS |
| Rose-Jacobs et al. 200857 | USA | Parents/caregivers | 18-item USDA module | Household FI and hunger |
| Rossen and Kobernik 201658 | USA | Parents/caregivers | 18-item USDA module | Child FI |
| Shanafelt et al. 201660 | USA | Children | 9-item USDA child module | Food-insecure children |
| Sharkey et al. 201161 | USA | Parents/caregivers | 12-item Radimer/Cornell FS scale | Assessed for household, caregiver and index child FI |
| Sharkey et al. 2012107 | USA | Children | 9-item USDA child module | Child FI |
| Shtasel-Gottlieb et al. 201562 | USA | Adolescents | 9-item USDA child module | Adolescent FI |
| Skalicky et al. 200663 | USA | Parents/caregivers | Child-specific questions (8 items) from the 18-item USDA module | Children FI |
| Slack and Yoo 2005108 | USA | Parents/caregivers | Four-items subscale of the 18-item USDA module | Food hardship |
| Smith and Richards 200864 | USA | Adolescents | 18-item USDA module. Adapted and modified by the authors | FI |
| Sonik et al. 201665 | USA | Parents/caregivers | One question measuring childhood FI (whether children had sufficient food to eat) + five-item subscale of 18-item USDA module | Household and child FI |
| Speirs et al. 2016109 | USA | Parents/caregivers | 18-item USDA module modified by asking participants to consider only the target child | Household and child FI |
| Tester et al. 201666 | USA | Parents/caregivers | 18-item USDA module | Household FS |
| To et al. 2014110 | USA | Parents/caregivers | 18-item USDA module | Household FS |
| Trapp et al. 201567 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Weinreb et al. 200269 | USA | Parents/caregivers and children/adolescents | CCHIP | Hunger–food insufficiency |
| Whitbeck et al. 200670 | USA | Adolescents | Three items adapted from the 16-item USDA module | FI |
| Widome et al. 2009111 | USA | Adolescents | Two items adapted from the 1999 USDA FS/Hunger Core Module: 3-stage design, with screeners | Hunger, FI and household food availability |
| Willis and Fitzpatrick 2016112 | USA | Children | Five items from 9-item USDA child module | FI score |
| Winicki and Jemison 2003113 | USA | Parents/caregivers | 18-item USDA module | FI |
| Yu et al. 201071 | USA | Parents/caregivers | 18-item USDA module | Child FS and household FI |
| Zaslow 200972 | USA | Parents/caregivers | 18-item USDA module | Household FI |
| Ramsey et al. 201154 | Australia | Parents/caregivers | 16-item USDA module | FI |
| Mhurchu et al. 2013122 | New Zealand | Children and parents | Children: modified version of ‘Freddy’ an analogue FI scale; parents: CCHIP Scale | Hunger and FS |
Appendix 4 Results of studies investigating factors related to child food insecurity (adjusted findings)
| Category | Subcategory | Study authors, year of publication and country | n | Main explanatory or confounding variables | Main results |
|---|---|---|---|---|---|
| Children’s characteristics | Sex | Whitbeck et al. 2006, USA70 | 428 | Adolescent’s characteristic variables, history at home (neglect and/or abuse by caretakers) and on the street (ever on street) | Male sex was positively associated with FI (p < 0.001). However, this variable lost significance when more characteristics were added to the analysis |
| Child ageing | Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parental characteristics, number of people in the household, neighbourhood characteristics and transitions of FS status over time | As children aged, household FI became less likely, but this association was not statistically significant (p > 0.05) | |
| Kirkpatrick et al. 2010, Canada42 | 5809 | Child and household sociodemographic characteristics | Higher odds of experiencing hunger were observed with increasing age (OR 1.2, 95% CI 1.0 to 1.4) in children aged 10–15 years | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | Children’s ageing was not statistically associated with FI (p > 0.05) | ||
| Whitbeck et al. 2006, USA70 | 428 | Adolescent’s characteristic variables, history at home (neglect and/abuse by caretakers) and on the street (homeless) | Older adolescents were those most likely to report FI (p < 0.001). This variable remained significant across analyses | ||
| Child health | Jacknowitz et al. 2015, USA35 | 7850 | Child characteristics and transitions of FS status over time | Deterioration of children’s health predicted the transition to low or very low FS at the child (p < 0.05) and household level (p < 0.001) | |
| Children with disabilities | Sonik et al. 2016, USA65 | 24,729 households with children (3948 had disabilities) | Sociodemographic variables including presence of an adult with a disability | Any FI was 55% greater in families including children with disabilities (OR 1.6, 95% CI 1.5 to 1.8). Very low FS was 70% greater (OR 1.7, 95% CI 1.5 to 2.0), and child FI was 38% greater (OR 1.4, 95% CI 1.2 to 1.7) but was significant only in the model for very low FI (OR 0.7, 95% CI 0.5 to 0.9). For families below 185% federal poverty line, results were similar. Having a child with a disability increased odds of any FI by 44% (OR 1.6, 95% CI 1.4 to 1.8), very low FS by 65% (OR 1.7, 95% CI 1.5 to 2.1) and child FI by 31% (OR 1.4, 95% CI 1.1 to 1.6) | |
| Supportiveness | Whitbeck et al. 2006, USA70 | 428 | Adolescent’s characteristic variables, history at home (neglect and/abuse by caretakers) and on the street (homeless) | The size of adolescents’ social network was negatively related to FI. The larger the social network, the less likely the adolescent was to experience FI (p < 0.001) | |
| Substance abuse | Whitbeck et al. 2006, USA70 | 428 | Adolescent’s characteristic variables, history at home (neglect and/abuse by caretakers) and on the street (homeless) | Substance abuse was positively associated with FI (p < 0.001). However, this variable lost significance when food strategies were added into the model | |
| Cultural factors | Ethnicity | Bhargava et al. 2008, USA20 | 7635 | Child characteristics | Hispanic households reported significantly higher FI levels, whereas African American households reported lower FI (p < 0.05) |
| Jacknowitz et al. 2015, USA35 | 7850 | Child characteristics and transitions of FS status over time | Being non-Hispanic African American (p < 0.001) or Hispanic (p < 0.001) may trigger the transition into a low or very low FS at the child and household level | ||
| Morrissey et al. 2016, USA49 | 12,550 | Child, parent and neighbourhood characteristics | Hispanic children were more likely than children of other ethnicities to experience FI at all levels (p < 0.001) | ||
| Nalty et al. 2013, USA50 | 48 | Parent and food assistance characteristics | Mothers of Mexican ethnicity were 4.5 times more likely to report FI than those of white ethnicity (OR 4.5, 95% CI 1.5 to 13.2; p < 0.001) | ||
| Household/family structure | Parent at household | Arteaga et al. 2017, USA18 | 2150 | Child, parent and household variables | Household FI risk was higher in a two biological parent household than in other family structures (p < 0.001) |
| Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics. transitions of FS status over time | Single-parent families were 2.5 times more likely to be FI (p ≤ 0.001) | ||
| Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Children with single mothers were nearly three times more likely to be FI at kindergarten and third grade than children with two parents (p < 0.001) | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | Single parents with children reported more FI (46.8%) than couples with children (29%). Single-parent families were 1.8 times more likely to report FI than FS (p < 0.05) | ||
| Number of siblings | Bhargava et al. 2008, USA20 | 7635 | Child characteristics | Greater number of siblings was associated with higher FI (p < 0.05) | |
| Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Compared with food-secure children, children who experienced FI were more likely to have more siblings in the household (p-value not reported) | ||
| Kirkpatrick et al. 2010, Canada42 | 10–15 years (n = 5809), 16–21 years (n = 3333) | Child and household sociodemographic characteristics | Higher odds of experiencing hunger were observed with increasing number of children in the household (OR 1.4, 95% CI 1.1 to 1.9) in children aged 10–15 years | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | No significant association between number of children in the household and FI (p = 0.65) | ||
| Sharkey et al. 2011, USA61 | 610 | Demographic characteristics, food sources and behaviours also included | Statistically significant positive association between child FI and number of children in the household (p ≤ 0.001) | ||
| Egeland et al. 2011, Canada27 | 388 | Household characteristics | The number of children (aged ≤ 18 years) in the home was positively related to FI (OR 1.2, 95% CI 1.0 to 1.4) | ||
| Number of people in household | Egeland 2011, Canada27 | 388 | Household characteristics | Tendency for a greater ratio of children to adults in the home (p ≤ 0.10), and a greater prevalence of household crowding (more than one person/room) was found in food insecure than in food-secure homes. The number of children (≤ 18 years) in the home was positively related to FI (OR 1.2, 95% CI 1.0 to 1.4) | |
| Jacknowitz et al. 2015, USA35 | 7850 | Child characteristics and transitions of FS status over time | Increasing the number of adults in the household (p < 0.10) may aid in the transition of exiting low or very low FS in children | ||
| Head of household | Yu et al. 2010, USA71 | 3089 Caucasian, 710 African | Household characteristics | In Caucasian and African American households, child FI was positively associated with having a female head of household (p < 0.05) | |
| Neighbourhood/community characteristics | Neighbourhood social cohesion and disorder | Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics and transitions of FS status over time | Low social cohesion (OR 1.4, 95% CI 1.1 to 1.9; p ≤ 0.01) and high disorder (OR 1.8, 95% CI 1.3 to 2.3; p ≤ 0.001) significantly increased the odds of FI |
| Neighbourhood social cohesion and disorder | Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Significant differences in the likelihood of FI existed when parents reported their neighbourhood as not safe or somewhat safe compared with those who reported it very safe to play outside (p < 0.05) | |
| Poole-Di Salvo et al. 2016, USA53 | 8600 | Adolescent and family characteristics | No association between FI and living in an unsafe neighbourhood (OR 1.2, 95% CI 0.9 to 1.7) | ||
| Living location | Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics, transitions of FS status over time | Living in a small or rural town did not significantly increase the odds of FI (OR 0.9, 95% CI 0.6 to 1.3; p > 0.05) compared with those living in a metropolitan area | |
| Jacknowitz et al. 2015, USA35 | 7850 | Child characteristics and transitions of FS status over time | Moving homes may trigger the entry into low- or very low-FS status at a child (p < 0.001) and household level (p < 0.001) | ||
| Morrissey et al. 2016, USA49 | 12,550 | Neighbourhood and household characteristics, food access | Children living in rural areas were 2 and 1 percentage points less likely to live in food-insecure households or with food-insecure adults, respectively, and marginally significantly less likely to experience FI themselves than those in urban areas. Furthermore, children in high-poverty rural tracts were 2 percentage points less likely to be food insecure than those in high-poverty urban tracts (p < 0.05) | ||
| Living location | Egeland et al. 2011, Canada27 | 388 | Household characteristics | Child food-insecure homes were more likely to be public housing and in need of major repairs and to report income support than child food-secure homes (p < 0.05) | |
| Homelessness | Whitbeck et al. 2006, USA70 | 428 | Adolescent’s characteristic history at home (neglect and/abuse by caretakers) and on the street (homeless) | Being homeless was related to FI (p < 0.001). This variable remained significant across models | |
| Ethnic group neighbourhoods | Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Children in neighbourhoods that had fewer white individuals and more African American and Hispanic individuals were more likely to be food insecure (p < 0.001) | |
| Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Food-insecure children live in neighbourhoods with higher proportions of linguistically isolated residents, as well as nearly 16% of residents who are foreign born (p < 0.001) | ||
| Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Relative to living in a white/high-SES neighbourhood, living in an African American/low-SES neighbourhood put children at over twice the odds of FI (p < 0.05) | ||
| Neighbourhood SES | Morrissey et al. 2016, USA49 | 12,550 | Neighbourhood and household characteristics, food access | The likelihood of FI increased as neighbourhood poverty level increases (p < 0.05). However, the associations between neighbourhood poverty and FI largely disappeared with background characteristics added, with the exception of living in a high-poverty tract (≥ 40%), which was associated with a 1 percentage point increase in the likelihood of child FI (p < 0.05) | |
| Parent characteristics | Parental nativity status and mother’s citizenship status | Arteaga et al. 2017, USA18 | 2150 | Child, parent and household characteristics | FI among households with children was significantly higher for foreign-born mothers than for US-born mothers (p < 0.05) |
| Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics, transitions of FS status over time | Mothers’ immigrant status did not significantly increase the odds of FI (OR 1.4, 95% CI 0.8 to 2.3; p > 0.05) | ||
| Chilton et al. 2009, USA24 | 7216 | Child and maternal characteristics, maternal symptoms | Immigrant households were more likely to report FI for mothers who had been in the USA 0–5 years (OR 2.4, 95% CI 2.2 to 2.8; p < 0.001); for those who had been in the USA 6–10 years (OR 2.1, 95% CI 1.8 to 2.4; p < 0.001); and for those who had been in the USA ≥ 11 years (OR 1.4, 95% CI 1.2 to 1.7; p < 0.001). All of these odds increased when the model was controlled by maternal symptoms, and were statistically significant | ||
| Kersey et al. 2007, USA38 | 4278 caregivers | Child, socioeconomic and demographic, maternal and food assistance characteristics | US-born Latino children in Mexican immigrant families had much higher rates of child hunger than non-immigrant, non-Latino children at (p < 0.01). In addition, Latino families had much higher rates of household FI than non-Latinos, at 53.1% vs. 15.6% (p < 0.01). After adjusting, Latino children were more likely to be hungry (OR 13.0, 95% CI 5.9 to 28.7; p < 0.01) and in food-insecure households (OR 6.6, 95% CI 5.2 to 8.3; p < 0.01) than non-Latino children | ||
| Miller 2016, USA48 | 36,302 | Child, family and food assistance programmes covariates | Initial rates of child FI were significantly higher among first- (p < 0.001) and second- (p < 0.001) generation children of immigrants than for children of US-born parents. For low-income families with US-born parents, these rates increased over time, as they did for families with second-generation children, albeit at a slower rate. Families with first-generation immigrant children had the highest initial levels of FI, which subsequently declined over time | ||
| Miller 2016, USA48 | 36,302 | Child, family and food assistance programmes covariates | Additional years of living with children in the USA were associated with increased rates of children FI for US-born children and parents (p < 0.001). However, adjustment for participation in food assistance programmes had little bearing on findings | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | Households with a parent born outside Australia were 60% less likely to be FI than households with an Australian-born parent (p < 0.001) | ||
| Sharkey et al. 2011, USA61 | 610 | Demographic characteristics, parental eating behaviours and food assistance programme participation | There was an independently associated with increasing levels of a child FI for children of mothers born in Mexico (OR 2.13; p < 0.01) | ||
| Emotional status | Jacknowitz et al. 2015, USA35 | 7850 | Child characteristics and transitions of FS status over time | Mothers’ entry into depression was trigger for entrance into to low or very low FS at a child level (p < 0.001) and a household level (p < 0.001). Furthermore, a mother exiting depression could aid, at a child level, exiting low- or very low-FI status (p < 0.001) and a household level (p < 0.001) | |
| Zaslow et al. 2009, USA72 | 10,221 | Parent, household and child characteristics | FI was positively associated with depression (p < 0.001). However, FI works indirectly through depression and parenting practices to influence insecure attachment. Households with higher levels of FI have higher levels of depression, and higher levels of depression reduce positive parenting, and more positive parenting was associated with more positive mental proficiency at 24 months | ||
| Mothers’ age | Arteaga et al. 2017, USA18 | 2150 | Child, parent and household characteristics | Mothers’ age was positively related to FI (p < 0.05) | |
| Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics and transitions of FS status over time | Mothers’ age differences did not significantly increase the odds of FI (p > 0.05) | ||
| Kersey et al. 2007, USA38 | 4278 | Child, socioeconomic and demographic, maternal and food assistance characteristics | Young maternal age (< 21 years) was negatively associated with FI (OR 0.7, 95% CI 0.5 to 0.8; p < 0.01) | ||
| Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | Children with younger mothers were, on average, significantly more likely to be food insecure at both kindergarten and third grade (p < 0.001) | ||
| Education | Bhargava et al. 2008, USA20 | 7635 | Children’s characteristics | Households where parents were more educated and incomes were higher reported significantly lower FI levels (p < 0.05) | |
| Kersey et al. 2007, USA38 | 4278 | Child, socioeconomic and demographic, maternal and food assistance characteristics | Increased maternal education level was negatively associated with FI (OR 0.9, 95% CI 0.8 to 1.0; p < 0.01) | ||
| Kimbro et al. 2012, USA40 | 11,610 | Socioeconomic variables, parent and child characteristics, food aids received | At both kindergarten and third grade, significant differences in the likelihood of FI existed when the mother’s education was reported to be high school to some college or bachelor’s degree or more compared with those reporting less than high school (p < 0.001). The odds of FI for children at kindergarten were reduced 60% in families where mother’s education reached at least a bachelor’s degree | ||
| Morrissey et al. 2016, USA49 | 12,550 | Neighbourhood and household characteristics, as well as food access | Children whose parents lacked a high-school degree were more likely to live in food-insecure households or with food-insecure adults than those with more educated parents (p < 0.05) | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | Parent’s highest level of education was not associated with FI status (p = 0.16). The OR of reporting FI by parents with highest level of education (twelfth grade) was 1.0 (95% CI 0.5 to 1.9) compared with those educated to a level beyond twelfth grade | ||
| Yu et al. 2010, USA71 | 3089 Caucasian, 710 African American | Household characteristics | In Caucasian households, child FS was positively associated with the level of education attained by the head of a household (p < 0.05). In addition, in the African American model analysis the level of education attained by the head of a household predicted child FS (p < 0.05) | ||
| Risk personality profiles | Kenney 2008, USA37 | 1073 | Parental money system and father’s control system characteristics | If the father had a drug or alcohol problem, the odds of child FI were OR 2.1 (p < 0.001) | |
| Supportiveness | Kenney 2008, USA37 | 1073 | Parental money system and father’s control system characteristics | Mother’s report of her partner’s supportiveness was associated with a reduced likelihood (OR 0.5; p < 0.05) of child FI | |
| Skills | Broughton et al. 2006, USA21 | 142 | Household income | Parents with less personal capacity in terms of self-rated cooking skills had eight times the odds of FI compared with households with the greatest resources (p-value not reported) | |
| FI in parents | Bruening et al. 2017, USA22 | 55 | Adolescents’ characteristics, maternal immigration status | Adolescents had 3.5 times higher odds of being food insecure if their mothers were food insecure (OR 3.5, 95% CI 1.0 to 13.0; p < 0.058) | |
| Morrissey et al. 2016, USA49 | 12,550 | Neighbourhood and household characteristics, food access | Children in high-poverty tracts were 11 percentage points more likely to live with food-insecure adult or experience FI themselves (p < 0.05) | ||
| Employment | Ramsey et al. 2011, Australia54 | 185 | Equalised household income | The OR of reporting FI in unemployed or unable to work parents was 3.4 (95% CI 1.1 to 10.7) compared with full-time workers (p < 0.05) | |
| Sharkey et al. 2011, USA61 | 610 | Demographic characteristics, parental eating behaviours and food assistance programme participation | Having a partner unemployed increased the odds of child FI (OR 4.0; p < 0.001), as did having a partner employed part time (OR 2.9; p < 0.001) | ||
| Socioeconomic characteristics | Material deprivation | Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics and transitions of FS status over time | According to adjusted analysis, material deprivation did not significantly increase the odds of FI (OR 1.1, 95% CI 0.9 to 1.5; p > 0.05) |
| Kenney 2008, USA37 | 1073 | Parental money system and father’s control system characteristics | The odds of child FI were about 1.7 times higher (OR 1.7, SE 0.13; p < 0.001) among parents who reported material hardship than among those who did not | ||
| SES/household income | Broughton et al. 2006, USA21 | 142 | Household income | Low income was the primary risk factor for FI (p-value not reported) | |
| Carter et al. 2012, Canada23 | 1746 | Socioeconomic variables, parent characteristics, number of people in the household, neighbourhood characteristics and transitions of FS status over time | Having a medium SES (OR 3.5, 95% CI 2.1 to 5.9; p ≤ 0.001) or low SES (OR 8.4, 95% CI 5.0 to 14.1; p ≤ 0.001) significantly increased the odds of FI, compared with high-SES children | ||
| Dunifon and Kowaleski-Jones 2003, USA26 | 1600 | Child and family characteristics | Family income was significantly and negatively associated with the continuous FI measure (p < 0.01). Family income was the most significant predictor of FI (OR 1.00, z-score 2.0; p < 0.01) | ||
| Jacknowitz et al. 2015, USA35 | 7850 | Child characteristics and transitions of FS status over time | An income decrease triggered the transition to a low- or very low-FS status at a child level (p < 0.001) and at a household level (p < 0.001). An increase in the income could aid, at child level, exit from the low- or very low-FI status (p < 0.001) and at a household level (p < 0.001) | ||
| Kirkpatrick et al. 2010, Canada42 | 3333 | Child and household sociodemographic characteristics | Among youth aged 16–21 years lower odds of ever being hungry were observed with increasing income (OR 1.0, 95% CI 0.9 to 1.0) | ||
| Morrissey et al. 2016, USA49 | 12,550 | Neighbourhood and household characteristics, as well as food access | Children in poor (< 100% federal poverty line) or low-income households (between 100% and 200% federal poverty line) were more likely to live in food-insecure households or with food-insecure adults than those above 200% federal poverty line | ||
| Papas et al. 2016, USA51 | 74 | Household income, number of children in the household, length of time living in the USA, and educational attainment | Household income was associated with FI status. Households at the federal poverty line for a household of four were less likely to be report FI than those who were living on incomes below the federal poverty line (OR 0.2, 95% CI 0.1 to 0.7) | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | Those in the lowest category of equalised household income reported FI more frequently (56.5%) than the middle category (27.6%) and the higher category income (7.4%) (p < 0.001). Those living in the lowest equalised household income were 16.2 times (OR 16.2, 95% CI 3.5 to 74.5) and those in the middle category were 4.8 times (OR 4.8, 95% CI 1.0 to 22.5) times more times more likely to report FI than those in the highest category | ||
| Sharkey et al. 2011, USA61 | 610 | Demographic characteristics, parental eating behaviours and food assistance programme participation | Reporting household income > 100% federal poverty line was associated with less child FI (OR 0.1; p < 0.05) | ||
| Yu et al. 2010, USA71 | 3089 Caucasian, 710 African | Household characteristics | In Caucasian and African American households child FS was negatively associated with household FS and household income (p < 0.05) | ||
| Income management | Kenney 2008, USA37 | 1073 | Parental money system and father’s control system characteristics | The odds of child FI were over 2.5 times higher (p < 0.01) when the father controlled pooled income than when the mother did. The odds of FI were almost 2.3 times higher (p < 0.01) when both parents ‘equally’ controlled pooled income than when the mother alone did | |
| Living property characteristics | Broughton et al. 2006, USA21 | 142 | Household income | Households with less-equipped kitchen facilities had three times (95% CI 1.1 to 11.1) the odds of FI compared with households with the greatest resources (p-value not reported) | |
| Egeland et al. 2011, Canada27 | 388 | Household characteristics | Child food-insecure homes were more likely to be public housing (RR 1.4, 95% CI 1.1 to 1.9; p < 0.05) | ||
| Kirkpatrick et al. 2010, Canada42 | 9142 | Child and household sociodemographic characteristics | Higher odds of experiencing hunger were observed if they reported to ever having lived in a rented dwelling (OR 5.9, 95% CI 2.6 to 13.4) for 10- to 15-year-old participants and (OR 2.3, 95% CI 1.0 to 5.1) for 16- to 21-year-old participants | ||
| Ramsey et al. 2011, Australia54 | 185 | Equalised household income | Those renting a housing tenure (53.7%) or living in assisted housing (49%) reported FI more often than those owning their own homes (27.6%) (p < 0.001). However, OR was not statistically significant (OR 0.9, 95% CI 0.4 to 2.3; p > 0.05) | ||
| Social deprivation | Carter et al. 2012, Canada23 | 1746 | SES variables, parental characteristics, number of people in the household, neighbourhood characteristics and transitions of FS status over time | Social deprivation (the strength of family social ties within an area considering the proportion of persons aged ≥ 15 years who were separated, divorced or widowed, proportion of people aged ≥ 15 years of age who lived alone, and proportion of single-parent families who were living in the enumeration area) significantly increased the odds of food-insecure households (OR 1.6, 95% CI 1.2 to 2.3; p ≤ 0.01) |
Appendix 5 Results of studies investigating factors relating to child food insecurity (unadjusted findings)
| Category | Subcategory | Study author, year and country | n a | Summary of main results |
|---|---|---|---|---|
| Children’s characteristics | Sex | Wadsworth 2012, Canada68 | 918 | Significant differences between sexes in each evaluated grade, with girls reporting deeper experiences at all levels of FI than boys (no p-value provided) |
| Shtasel-Gottlieb et al. 2015, USA62 | 2350 | FI did not differ between sexes (p < 0.001) | ||
| Papas et al. 2016, USA51 | 74 | No statistically significant difference in child FI between sexes (p > 0.05) | ||
| Murphy et al. 1998, USA73 | 204 | Hunger category scores differed by sex, with girls more likely to be at risk of hunger than boys (p < 0.001) | ||
| Age | Nalty et al. 2013, USA50 | 48 | Children living in FI were slightly younger than those living in FS (p = 0.04) | |
| Papas et al. 2016, USA51 | 74 | No statistically significant difference in age (p > 0.05) of FI vs. FS | ||
| Poole-Di Salvo et al. 2016, USA53 | 8600 | Higher percentages of FI (15.5%) in children below eighth grade than in those in eighth grade (9.4%) and ninth grade or above (9.4%) (p < 0.001) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 | Children living in FI were younger than those living in FS (p < 0.001) | ||
| Shtasel-Gottilieb et al. 2015, USA62 | 2350 | Higher prevalence of FI in higher scholar grades (p < 0.001) | ||
| Wadsworth 2012, Canada68 | 918 | Significantly older students living in FI compared with younger students were reported (p-value not reported) | ||
| Birthweight | Kimbro et al. 2012, USA40 | 11,610 | Children low in birthweight were likely to be in FI at kindergarten (p < 0.001). However, this weight disadvantage was overcome by third grade (p > 0.05) | |
| King 2017, USA41 | 2829 | Lower birthweight in food-insecure children than in those living in FS (9.8% vs. 11.8%) (p < 0.001) | ||
| Mangini et al. 2015, USA44 | 11,099 | Higher likelihood of low birthweight in food-insecure households than in food-secure households (p < 0.001) | ||
| Rose and Bodor 2006, USA56 | 12,890 | Birthweight differences were significantly associated with household FS status (p < 0.05) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 | No statistically significant difference between households with FI and households with FS with respect to low birthweight (p = 0.46) | ||
| Weinreb et al. 2002, USA69 | 355 | School-aged children reporting severe hunger were more likely to have had low birthweight than those with no hunger (p < 0.005) | ||
| Insurance | Mangini et al. 2015, USA44 | 11,099 | Children in food-insecure households more likely to be uninsured than children in food-secure households (p < 0.001) | |
| Miller 2016, USA48 | 36,302 | Significantly lower baseline reports of child FI for children reported as health insured than for those not reported as health insured (p < 0.001) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of being uninsured or using public health insurance for food-insecure children than for food-secure children (p < 0.001) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 | Significant difference in child FI with respect to insurance (public insurance FS 83% vs. 92% FI; no insurance FS 2% vs. 4 FI; private insurance FS 15% vs. 4% FI) (p < 0.001) | ||
| Dunifon and Kowaleski-Jones 2003, USA26 | 1600 | If the child was insured, there was a negative association with the continuous FI measure (p < 0.01) | ||
| Smoking | Eicher-Miller et al. 2011, USA29 | 5270 | Compared with food-secure males, a significantly greater proportion of food-insecure males aged 16–19 years were smokers (p = 0.001) | |
| Tester et al. 2016, USA66 | 1072 | Significant differences in FI among low-income adolescents when smoking (p = 0.02) | ||
| Immigrant status | Kirkpatrick and Tarasuk 2008, Canada43 | 7353 | No statistically significant difference in FS and FI between children born in Canada, and children who immigrated to Canada < 10 years ago or > 10 years ago (p > 0.05) | |
| Parental and familial characteristics | Ethnicity | Kenney 2008, USA37 | 1073 | No statistically significant association between mother’s ethnicity and FI across all ethnic groups included (non-Hispanic African descendants, Mexican/Central American, Puerto Rican and other Hispanic) (p > 0.05) |
| King 2017, USA41 | 2829 | Higher likelihood of mother of a child in FI to be African descendant (56.6 vs. 50.2%) or Hispanic (26.0 vs. 24.2%) (p < 0.001) than FS groups | ||
| Eicher-Miller et al. 2011, USA29 | 5270 | Greater proportion of FI reported by Mexican Americans than by non-Hispanic Caucasian population (p < 0.001) | ||
| Kimbro et al. 2012, USA40 | 11,610 | Significant differences in likelihood of FI among non-Hispanic African descendants, Hispanic and Asian compared with non-Hispanic Caucasian children in kindergarten and third grade (p < 0.01) | ||
| Mangini et al. 2015, USA44 | 11,099 | Higher likelihood of children in food-insecure households to be non-Hispanic Caucasian compared with children in FS (p < 0.001) | ||
| Miller 2016, USA48 | 36,302 | Significantly higher baseline rates of child FI if mother reported herself as Hispanic compared with those who did not (p < 0.05) | ||
| Poole et al. 2013, USA52 | 193 | More reported FI by African descendent students than other ethnic groups (p = 0.029) | ||
| Poole-Di Salvo et al. 2016, USA53 | 8600 | Significant difference in the ethnicity of households that reported FI (p < 0.001) among non-Hispanic African descendants (16.8%), Hispanic (13.3%), Caucasian (7.1%) and other (12.1%) (p = 0.001) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 | More Hispanic caregivers reported as food insecure than food secure (p < 0.001) than white participants (p < 0.001) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of children in FI to be non-Hispanic African descendants or Mexican American than those in FS (p < 0.001) | ||
| Shanafelt et al. 2016, USA60 | 791 | Higher likelihood of children in FI to be non-Caucasian than those in FS (p < 0.001) | ||
| Rose and Bodor 2006, USA56 | 16,889 | Fewer reports of FI by Caucasian adolescents than by non-Caucasian adolescents (p < 0.001) | ||
| Tester et al. 2016, USA66 | 1072 | Significant differences among Hispanic and African descendant low-income adolescents in FI and those from other ethnicities (p = 0.004) | ||
| Weinreb et al. 2002, USA69 | 203 | High likelihood of Caucasian and Puerto Rican school-aged children to report severe hunger signs (p < 0.01) | ||
| Yu et al. 2010, USA71 | 3089 Caucasian, 710 African | Higher FS reported for Caucasian households than for African descendant households (p = 0.003). No differences were found in child FI | ||
| Shtasel-Gottilieb et al. 2015, USA62 | 2350 | More reported FI by Hispanic households (p < 0.001) | ||
| Parent characteristics | Caregiver nativity or citizenship status | Kimbro et al. 2012, USA40 | 11,610 | Significant differences in the likelihood of FI for both kindergarten and third grade children whose mothers were born in foreign countries compared with those with mothers born in the USA (p < 0.001) |
| Kimbro et al. 2015, USA39 | 6300 | Higher likelihood of FI for children with a foreign-born parent (p-value not reported) | ||
| Mangini et al. 2015, USA44 | 11,099 | Higher likelihood of FI for children with a mother born outside the USA (p < 0.001) | ||
| Papas et al. 2016, USA51 | 74 | No statistically significant FI differences considering maternal characteristics or number of years living in the USA (p > 0.05) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 | Less frequent reports of FI (55%) than FS (79%) for mothers born in the USA (p < 0.001) | ||
| Sellen et al. 2002, UK59 | 30 | FI present in the entire refugee sample in the UK. Severe FI (with child hunger) for people with shorter lengths of stay (p = 0.021) | ||
| Sellen et al. 2002, UK59 | 30 | No difference in prevalence of child hunger whether or not an immigration decision had been reached. Similar for those families appealing against a negative decision and those granted status to remain (p-value not reported) | ||
| Skalicky et al. 2006, USA63 | 626 | Higher likelihood of reporting FI for caregiver immigrants to the USA (p < 0.001) | ||
| Emotional status | Miller 2016, USA48 | 36,302 | Significantly higher initial rates of children FI among households that reported mother depressive symptoms in cross-sectional and longitudinal data compared with those that did not (p < 0.001) | |
| King 2017, USA41 | 2829 | Greater probability of reporting FI for children with mothers who reported depression (14.0% vs. 29.7%) compared with children in FS (p < 0.001) | ||
| Poole-Di Salvo et al. 2016, USA53 | 8600 | More FI from parents who reported being depressed (28.5%) than from those who did not report being depressed (6.7%) by means of an unadjusted analysis (p-value not reported) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 | More FI from mothers who reported depressive symptoms (48%) than from those who did not report depressive symptoms (29%) (p < 0.001) | ||
| Trapp et al. 2015, USA67 | 222 | Caregivers from food-insecure households were more likely to report depressive symptoms (27%) compared with those from food-secure households (9%) (p < 0.001) | ||
| Weinreb et al. 2002, USA69 | 355 | Higher rates of major depression, post-traumatic stress disorder and anxiety disorders for mothers of preschool-aged children with severe hunger (p-value not reported) | ||
| Mothers’ age | Himmelgreen et al. 2000, USA33 | 248 | Caregivers of food-secure children were younger than those of food-insecure children (p < 0.05). In addition, as the age of the caretakers increased, so did the severity of FI (p < 0.05) | |
| Kimbro et al. 2015, USA39 | 6300 | More likelihood of FI for children with a younger mother compared with children who were food-secure (p-value not reported) | ||
| Papas et al. 2016, USA51 | 74 | No statistically significant differences of FI in maternal characteristics, including age of the mother (p > 0.05) | ||
| Poole-Di Salvo et al. 2016, USA53 | 8600 | No statistical difference among age of mothers reporting FI: < 30 years (10.5%), 30–47 years (10.4%), > 47 years (8.9%) (p = 0.558) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 caregivers | Less likelihood of being ≥ 21 years for caregivers who reported household FI (p = 0.03) | ||
| Education | King 2017, USA41 | 2829 | More children with FI had mothers with high school as the educational level achieved (74.4% vs. 61.8%) (p < 0.001) | |
| Mangini et al. 2015, USA44 | 11,099 | Higher likelihood of children in households with FI having mothers with a low educational level compared with children in households with FS (p < 0.001) | ||
| Marjerisson et al. 2011, Canada45 | 183 | Higher levels of education in parents of households with FS (p < 0.05) | ||
| McLaughlin et al. 2012, USA47 | 6483 | Negative association between FI and parental education | ||
| Poole-Di Salvo et al. 2016, USA53 | 8600 | Statistically significant difference between households that reported FI and highest degree earned by parent: less than high-school diploma (23.7%), high-school diploma/equivalent (12.8%), bachelor’s degree (3.7%), master’s degree/doctorate (2.3%) (p < 0.001) | ||
| Rose and Bodor 2006, USA56 | 16,889 | Significant association between maternal education and household FS status (p < 0.05). Those reporting less than a high-school education level (30.6%) reported FI more often (12.7%). College graduate mothers reported less FI (3.9%) than FS (23.9%) (p-value not reported) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of FI in children having less educated parents than children with FS (p < 0.001) | ||
| Sellen et al. 2002, UK59 | 30 | Non-significant trend of refugee mothers of children with hunger being on average 3 years younger than those of children without hunger (p = 0.086) | ||
| Skalicky et al. 2006, USA63 | 626 | Higher likelihood of FI in caregivers having less than a college education (p < 0.01) | ||
| Tester et al. 2016, USA66 | 1072 | No significant differences among low-income adolescents’ FS in terms of mother’s education (p > 0.05) | ||
| Risk personality profiles | Belsky et al. 2010, UK19 | 2123 | Higher likelihood of mothers in households with FI to have high-risk personality profiles (low conscientiousness, extraversion and agreeableness, and high neuroticism), with their households being less sensitive to children’s needs (p < 0.001) | |
| King 2017, USA41 | 2829 | Children in households with FI with mothers who reported domestic violence (0.6% vs. 1.3%) (p < 0.001) compared with food-secure households | ||
| King 2017, USA41 | 2829 | Children in households with FI had mothers who reported having previous drug or alcohol problems (12.2% vs. 24.8%) compared with food-secure children (p < 0.001) | ||
| Weinreb et al. 2002, USA69 | 203 | More likelihood of school-aged children who reported severe hunger having mothers with a lifetime diagnosis of post-traumatic stress disorder or substance abuse (p-value not reported) | ||
| Supportiveness | King 2017, USA41 | 2829 | Children in households with FI had mothers who reported having lower social support (2.4% vs. 3.2%) compared with food-secure households (p < 0.001) | |
| Sellen et al. 2002, USA59 | 30 | No difference in the indicators of social support from family and friends in families with and without child hunger (p > 0.05) | ||
| FI in parents | Kaiser et al. 2002, USA36 | 211 | Current FI was correlated with having experienced food insufficiency as a child for mothers (p < 0.001) and fathers (p < 0.009) | |
| Employment | Kimbro et al. 2012, USA40 | 11,610 | Significant differences, at both kindergarten and third grade level, in the likelihood of FI when no parent works full time than in those with at least one parent working full time (p < 0.001) | |
| King 2017, USA41 | 2829 | More likelihood of FI in children having a mother unemployed compared with children with FS (61.2% vs. 53.5%) (p < 0.001) | ||
| Papas et al. 2016, USA51 | 74 mother/child dyads | No statistically significant differences in maternal characteristics, including employment and income (p > 0.05), between food-secure and food-insecure participants | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 caregivers | More food-secure caregivers (49%) reported being employed than food-insecure caregivers (36%) (p < 0.001) | ||
| Skalicky et al. 2006, USA63 | 626 | Higher likelihood of FI in unemployed caregivers (p = 0.04) | ||
| Health status | Miller 2016, USA48 | 36,302 | Significantly higher initial rates of FI among children with a mother with poor health than among children with a mother with a fair health reported in adjusted models (p < 0.05) | |
| Poole-Di Salvo et al. 2016, USA53 | 8600 | Higher likelihood of FI reported by parents with fair/poor health (27.2%) than by those with excellent/very good/good health (7.6%) (p < 0.001) | ||
| Marjerisson et al. 2011, Canada45 | 183 | No statistically significant difference between families with FI that reported living with adults with a medical condition (50%) and households with FS (35%) (p = 0.18) | ||
| Household/familiar structure | Parent at household | King 2017, USA41 | 2829 | Higher likelihood of children in FI having separated or non-resident mothers (p < 0.001) |
| Kirkpatrick and Tarasuk 2008, Canada43 | 7353 | Statistically significant difference in FI in terms of household size (i.e. number of adults) (p < 0.001) | ||
| Marjerisson et al. 2011, Canada45 | 183 | Statistically significant difference in reported FI (45%) for parents in single homes with respect to FS (12.1%) (p < 0.001) | ||
| Marjerisson et al. 2011, Canada45 | 183 | Compared with food-secure households, a higher proportion of food-insecure households had only one adult who contributed to the household income. On the contrary, a higher proportion of food-secure households had two adults who contributed to the household income | ||
| Poole-Di Salvo et al. 2016, USA53 | Approximately 8600 | Married couples reported less FI (5.6%) than those unmarried (20.5%) (p < 0.001) | ||
| Rose-Jacobs et al. 2008, USA57 | 2010 caregivers | No difference in FI or FS with respect to marital status (p = 0.61) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of children with FI to have unmarried or cohabiting parents than children who were food-secure (p < 0.001) | ||
| Tester et al. 2016, USA66 | 1072 | Significant differences among low-income adolescents in FS in terms of partnered status of the household (p = 0.01) | ||
| Number of siblings | Kimbro et al. 2012, USA40 | 11,610 | Significantly higher likelihood of children with more siblings to be in FI at both kindergarten and third grade (p < 0.001) | |
| Kirkpatrick and Tarasuk 2008, Canada43 | 7353 | Higher likelihood of FI in households with a larger number of children (from 0–11 years) than with a smaller number of children living in the household (p < 0.05) | ||
| Miller 2016, USA48 | 36,302 | Significantly higher initial rates of FI among households with a larger number of children than among those reporting fewer children | ||
| Papas et al. 2016, USA51 | 74 | No statistically significant differences in food-insecure household characteristics, including the number of residing children (p > 0.05) | ||
| Marjerisson et al. 2011, Canada45 | 183 | No significant difference for FI and FS groups in terms of number of children in the homes (p-value not reported) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | More likelihood of children in FI living in larger households (p < 0.001) | ||
| Number of people in household | Sellen et al. 2002, UK59 | 30 | No difference between families with and without child hunger for refugee population in terms of level of education, self-efficacy score of mothers, size or composition of household, child-to-caregiver ratio, lone care giving, presence of father, or indicators of social support from family and friends (p < 0.05) | |
| Skalicky et al. 2006, USA63 | 626 | Higher likelihood of FI for children living in households with five or more members (p = 0.03) | ||
| Living with a smoker | Eicher-Miller et al. 2009, USA28 | 11,247 | Significantly greater proportion of participants with FI in households with a smoker (p < 0.001) | |
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of FI in children living with a smoker (p < 0.001) | ||
| Head of household | Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of FI in children living in female-headed households (p < 0.001) | |
| Socioeconomic characteristics | Material deprivation | King 2017, USA41 | 2829 | More FI in children with mothers who experienced greater material hardship (1.9% vs. 0.9%) (p < 0.001) |
| SES/household income | Belsky et al. 2010, UK19 | 2123 | Households with FI had lower incomes than households with FS (p < 0.001) | |
| Eicher-Miller et al. 2009, USA28 | 11,247 | Significantly greater proportion of FI in participants of all age groups living in a household with a poverty-to-income ratio of > 1.0 (p < 0.001) | ||
| Eicher-Miller et al. 2011, USA29 | 5270 | Significantly greater proportion of FI in participants of all age groups living in a household with a poverty-to-income ratio of > 1.0 (p < 0.001) | ||
| Kaiser et al. 2002, USA36 | 211 | Significant association between FI and SES (r = –0.44) (p < 0.001) | ||
| Kimbro et al. 2012, USA40 | 11,610 | Significant differences in the likelihood of FI by household income in children living in households with 100–200% federal poverty level, 200–300% federal poverty level and > 300% federal poverty level compared with those living in < 100% federal poverty level at both kindergarten and third grade (p < 0.001) | ||
| Kimbro et al. 2015, USA39 | 6300 | Higher likelihood of children in FI to have low SES than children who were in FS (p-value not reported) | ||
| Kirkpatrick and Tarasuk 2008, Canada43 | 7353 | Statistically significant difference between FI and FS with respect to income adequacy in children population (among all categories: lowest, lower middle, middle, upper middle, upper) and between both sexes (p-value not reported) | ||
| Mangini et al. 2015, USA44 | 11,099 | More likelihood of children in food-insecure households 57% living below the poverty level compared with children in food-secure households 15% above the poverty level (p < 0.001) | ||
| McLaughlin et al. 2012, USA47 | 6483 | Negative association between FI and family income | ||
| Rose and Bodor 2006, USA56 | 16,889 | Significantly more FI reported in those households with lower poverty–index ratio than those with a higher poverty-to-index ratio (p < 0.05) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of children in FI to fall below the federal poverty threshold than food-secure children (p < 0.001) | ||
| Poole-Di Salvo et al. 2016, USA53 | 8600 | More FI (29.8%) reported by children living in households below the poverty threshold than by those at or above poverty threshold (5.0%) (p < 0.001) | ||
| Living property characteristics | Marjerisson et al. 2011, Canada45 | 183 | More frequently reported FS from families reported living in a dwelling owned by a household member than from families not doing so (92.9% vs. 52.5%) (p < 0.01) | |
| McIsaac et al. 2017, Canada46 | 215 | Lower likelihood of caregivers from food-secure households living in public housing (p < 0.001) | ||
| Rossen and Kobernik 2016, USA58 | 5136 | Less likelihood of children in FI living in an owned house (p < 0.001) | ||
| Social deprivation | McLaughlin et al. 2012, USA47 | 6483 | Significantly higher levels of relative deprivation (i.e. lower family income in relation to others in the community) associated with lower FI scores (p-value not reported) | |
| Rossen and Kobernik 2016, USA58 | 5136 | Higher likelihood of food-insecure children living in areas of high deprivation. Higher levels of deprivation were associated with children in FI than with children who were in FS (p < 0.001) | ||
| Neighbourhood/community characteristics | Neighbourhood social cohesion and disorder | McLaughlin et al. 2012, USA47 | 6483 | Greater FI in adolescents living in areas with higher degrees of community-level inequality |
| Poole-Di Salvo et al. 2016, USA53 | Approximately 8600 | Less FI (7.5%) in households that reported living in a safer neighbourhood than in those in unsafe neighbourhood (19.2%) (p < 0.001). When adjusted this association lost statistical significance | ||
| Rossen and Kobernik 2016, USA58 | 5136 | More likelihood of food-insecure children living in places with higher levels of crime than children living in safer areas (p < 0.001) | ||
| Living location | Rose and Bodor 2006, USA56 | 16,889 | No statistically significant difference with respect to level of urbanisation in the area food-insecure participants lived in (central city, urban fringe or rural) (p > 0.05) | |
| Rossen and Kobernik 201658 | 5136 | More FI in children residing in smaller, more urban counties (p < 0.001) | ||
| Holben et al. 2004, USA34 | 152 | 25.6 times more likely for families without reliable transportation to experience hunger compared with those with reliable transportation | ||
| Homelessness | Weinreb et al. 2002, USA69 | 355 | More than half of school-aged children with severe hunger were homeless, compared with 30% with no hunger (p = 0.02) |
Appendix 6 Results of studies that assessed health, social well-being and academic outcomes and did not adjust their analyses for explanatory or confounding variables
| Study author, year of publication and country | Outcome measured | Tool of measurement | Number of participants | Summary of results |
|---|---|---|---|---|
| Kleinman et al. 1998, USA99 | Health status score | PSC | 328 families with a child aged < 12 years | 20% of hungry children (12/56) were classified as dysfunctional by the PSC, compared with 6% of those at risk for hunger (10/161) and 3% of those who were not hungry (3/111) (p < 0.01) |
| Murphy et al. 1998, USA73 | Health status score | PSC | 204 children | Child hunger was significantly associated with parent-reported measures of children’s symptoms (p < 0.001) |
| Study author, year of publication and country | Outcome measured | BMI categorisation tool | Number of participants | Summary of results |
|---|---|---|---|---|
| Egeland et al. 2011, Canada27 | Height and weight measured by nurses | CDC growth reference | 374 children | No difference in the BMI percentile was found between food-insecure children (90 percentile) and food-secure children (90 percentile) (p > 0.05) |
| Marjerrison et al. 2011, Canada45 | Height and weight measured by nurses or dietitian | None. BMI considered as a scale | 183 households with child with insulin-dependent diabetes mellitus | Mean BMI did not differ between children from food-insecure families and those from food-secure families (p-value not reported) |
| Khan et al. 2011, USA98 | Self-reported weight and height | CDC growth reference | 373 adolescents | No statistical significance regarding the BMI classification and FI/FS status (p = 0.549) |
| Rose Jacobs et al. 2008, USA57 | Height and weight measured by project staff or medical staff | CDC growth reference | 2010 families | FI vs. FS groups did not differ significantly (p > 0.05) with respect to child’s mean weight-for-age z-score or in the categorical classification as underweight or overweight |
| Shanafelt et al. 2016, USA60 | Height and weight measured at school | CDC growth reference | 904 children | There was no significant difference across FI and FS categories and weight categories (p = 0.19) |
| Sharkey et al. 2012, USA61 | Weight measured at each visit | CDC growth reference | 50 children | BMI status was not significantly associated with FS status (p-value not presented) |
| Skalicky et al. 2006, USA63 | Unclear | Not reported | 626 children | Food-insecure children were no more likely than food-secure children to be at risk of energy protein undernutrition (p = 0.38) or overweight (p = 0.73) |
| Poole et al. 2013, USA52 | Height and weight was measured | Not reported | 193 adolescents | BMI was unrelated to FS status (p-value not reported) |
| Widome et al. 2009, USA111 | Height and weight measured by trained research staff | CDC growth reference | 4746 young people | Youths who reported no hunger in the past year were least likely to have a BMI greater than or equal to the 95th percentile (p = 0.01) |
| Study author, year of publication and country | Outcome measured | Tool of measurement | Number of participants | Summary of results |
|---|---|---|---|---|
| King 2016, USA41 | Behavioural outcomes | Child Behaviour Checklist | 2829 children | The negative impact of soft drink consumption on behavioural problems was greater for food-insecure children; the risk of aggressive behaviours was significantly higher for children who consumed two (0.9 SD; p < 0.05) and four or more (0.9 SD; p < 0.01) soft drinks daily. In addition, children who consumed one (0.5 SD; p < 0.05) and four or more (0.5 SD; p < 0.01) soft drinks daily showed higher attention problems |
| Kleinman et al. 1998, USA99 | History of mental health counselling | CCHIP survey | 328 families with at least one child | Hungry children were significantly more likely to have a past or current history of mental health counselling than other children in the sample (p < 0.01). 21% of hungry children, 12% of those at risk of hunger, and 5% of not hungry children reported a history of mental health counselling |
| Kleinman et al. 1998, USA99 | Special education services and academic failure (repeating a grade) | CCHIP survey | 328 families | Hungry children were significantly more likely to receive special education services (p < 0.05), with 29% (16/56) of ‘hungry’ children 15% (24/161) of ‘at risk for hunger’ children and 14% (15/111) of ‘not hungry’ children receiving special education services. Furthermore, hunger was also related to a child’s history of academic failure (repeating a grade), although differences were not statistically significant (p < 0.10) |
| Larson et al. 2012, USA101 | Adolescent eating patterns | Food Frequency Questionnaire | 1983 households with adolescents | FS status was associated with energy-adjusted intakes of dairy, calcium and vitamin D as well as family dinner frequency among adolescent females and males. When analysing by sex, among males, FS status was also inversely associated with BMI z-score |
| Murphy et al. 1998, USA73 | Psychosocial functioning | Child Behaviour Checklist and PSC | 204 school-aged children | Children who were hungry, or at risk of hunger, were twice as likely to be classified as having impaired functioning as those classified as not hungry (p < 0.05) |
Appendix 7 Descriptions of studies that investigated the association between child food insecurity and health outcomes and adjusted their analyses for explanatory or confounding variables
General health outcomes
The study by Pickett et al. 76 contributed to the HSBC study, which is a WHO collaborative study of health and health risk behaviours. The authors collected data on food poverty and psychosomatic symptoms from 25,912 children aged 11–15 years from 436 Canadian schools. After adjusting analyses for family’s SES, characteristics and practices, school food and nutrition programmes, they showed that hunger was reported by 25% of participants. Children who reported experiencing hunger ‘sometimes’ or ‘often or always’ were 1.9 and 4.4 times more likely [odds ratio (OR) 1.9, 95% confidence interval (CI) 1.8 to 2.0; OR 4.4, 95% CI 3.7 to 5.2, respectively] to suffer from psychosomatic symptoms (e.g. headaches, stomach aches, backaches, feeling dizzy) than those who reported having ‘never’ experienced hunger.
Molcho et al. 106 used HBSC study (Irish) data and observed similar results to those reported by Pickett et al. 76 Children living in food poverty reported physical symptoms more often (e.g. headaches, stomach aches, backaches) than those who did not suffer from food poverty (p < 0.05).
The survey conducted by Egeland et al. 27 assessed 388 children aged 3–5 years among the Canadian Inuit community. The authors showed that parents reported similar rates of ‘excellent’ or ‘very good’ health from children’s FS (54.0%) and food-insecure homes (47.6%). However, children from severe child food-insecure homes were significantly less likely to have their health rated as ‘excellent/very good’ by their parents (39%, 34/88) than children (54%, 86/159) from child food-secure homes (risk ratio 0.7, 95% CI 0.5 to 1). In addition, there was no significant difference in the proportions of children from child food-insecure and food-secure homes who had anaemia. There was a not a significant traditional food by FS interaction term (p = 0.09). In further analyses, the authors found that 31.6% of food-insecure children who did not consume traditional food were anaemic, compared with 14.9% of those who did consume traditional food in the past day. There was no significant traditional food by FS interaction term noted for iron deficiency (p = 0.84).
Kirkpatrick et al. 42 used longitudinal data from the Canadian National Longitudinal Survey of Children and Youth (NLSCY) on a sample of children aged 10–15 years (n = 5809) and young people aged 16–21 years (n = 3333). They found that more than 1 in 10 children (13.5%) were rated as being in poor health; 32.9% of those who had ever experienced hunger were reported to be in poor health, compared with 12.8% of those who had never experienced hunger. After adjusting for baseline health and other potential confounders, higher odds of poor health were observed in children (but not youths) who had experienced hunger than in those who were never hungry (OR 2.5, 95% CI 1.3 to 4.6). In the combined cohort of children and young people, hunger was associated with higher odds of poor health; in the sex-stratified analyses, this effect persisted for girls (OR 2.4, 95% CI 1.3 to 4.4) but not for boys (OR 1.4, 95% CI 0.7 to 2.9). In the study sample, 32.7% of children (36.9% of ever hungry vs. 32.6% of never hungry) and 30.5% of youths (41.7% of ever hungry vs. 30.1% of never hungry) were reported to have a diagnosed chronic condition. No associations were observed in either children or youths between a diagnosis of chronic health condition and hunger. Diagnosed asthma was reported in 24.8% of ever-hungry children compared with 18.0% of never-hungry children (10–15 years, n = 5809) and 11.7% of youths aged 16–21 years (27.1% of ever hungry vs. 11.1% of never-hungry youths; n = 3333). When both primary caregiver and youth hunger reports were considered, a significant association between ever experiencing hunger and asthma was observed among youths, with those who ever experienced hunger being 2.4 times more likely to have asthma (OR 2.4, 95% CI 1.1 to 4.9). For youths, but not for children, the analysis showed higher odds (OR 6.1, 95% CI 1.4 to 25.9) of asthma among those with two or more caregiver-reported hunger episodes over time.
Broughton et al. 21 reported significantly lower median serum zinc levels in children aged 2–5 years from food-insecure households than in those living in food-secure situations (n = 142). Holben and Taylor88 analysed NHANES data from 7435 young people aged 12–18 years and reported no statistically significant differences in mean levels of blood glucose, total cholesterol, triglycerides and blood pressure across levels of household FI. Participants from high-FS households had significantly higher mean high-density lipoprotein (HDL) (‘good cholesterol’) values then those from food-insecure households (p = 0.019). Overall, 3.1% (n = 246) of all participants presented at least two additional markers indicative of metabolic syndrome. The mean number of metabolic syndrome risk factors increased as FI increased (high FS mean 0.3, 95% CI 0.3 to 0.4; marginal FS mean 0.4, 95% CI 0.3 to 0.5; low FS mean 0.4, 95% CI 0.3 to 0.5; and very low FS mean 0.5, 95% CI 0.4 to 0.6). The difference among categories was statistically significant (p = 0.018).
Chi et al. 82 used NHANES data from 2206 children aged 5–17 years. Children from low- or very low-FS households had significantly higher untreated caries (prevalence ratio 2.0, 95% CI 1.1 to 3.6; p = 0.03 and prevalence ratio 1.7, 95% CI 1.0 to 2.9; p = 0.05) than children with full FS. There was no difference in untreated caries between children from fully and those from marginally food-secure households (p = 0.17).
Chilton et al. 24 observed that children who were immigrants to the USA and were living in food-insecure households were 1.7 times more likely to have their health reported as ‘fair’ or ‘poor’ (OR 1.7, p < 0.001 after adjusting results for immigrant status and other relevant covariates). When considering the length of stay in the USA, these odds decreased to 1.1 for those who had been in the USA for 6–10 years (the relationship was no longer significant; p = 0.15) and decreased even more for those who had been in the USA for more than 11 years (OR 1; p = 0.93). FI was considered a significant mediator of the increased odds of fair/poor child’s health among immigrants who had been in the USA for 0–5 years (p < 0.001) and 6–10 years (p < 0.001).
Cook et al. ,83 after adjusting analyses for study site, child’s ethnicity, health insurance and day care status, mother born in the USA, caregiver’s age, employment, marital and education status, and household receipt food assistance programmes, showed that children enrolled in the Children Sentinel Nutrition Assessment Programme (C-SNAP) who were living in food-insecure households had significantly greater odds of ‘fair/poor’ health than those in food-secure households (OR 1.9, 95% CI 1.7 to 2.2). In particular, compared with children in food-secure households, children in food-insecure households with hunger were 2.3 times more likely to have their health rated as ‘fair/poor’ (OR 2.3, 95% CI 1.9 to 2.8) and those in food-insecure households without hunger were 1.7 times more likely to have their general health rated as ‘fair/poor’ (OR 1.7, 95% CI 1.5 to 2.0).
Dunifon and Kowaleski-Jones26 examined the association between FI and participation in the US National School Lunch Program (NSLP) in a sample of school-aged children (n = 3500). They used the 18-item USDA module to assess FI and measured health limitations with a variable indicating whether or not the child had any health limitations (reported by the parent) that affected participation in childhood activities, school attendance or the performance of schoolwork. A child with a limitation in any area was given a score of one. The rest were given scores of zero. The authors found that 10% of the 6- to 12-year-old children lived in households that would be classified as FI by the USDA and an additional 7% lived in households that would be classified as marginally food-insecure. An increase in FI was associated with an 8% increase in the odds of health limitations [β 1.1, standard error (SE) 2.0; p < 0.01]. 26
Eicher-Miller et al. 28 used NHANES data from 11,247 children aged 3–19 years. They reported that, after adjustment for clustering, stratification, survey cycle year, sex, ethnicity and poverty-to-income ratio, the odds of iron deficiency anaemia were 10.7 (p = 0.01), 8.1 (p = 0.002) and 3.0 (p = 0.02) times more likely among food-insecure children aged 3–5 years, 6–11 years and 12–15 years, respectively, than among their food-secure counterparts. The total dietary iron intake was 1.9 times as likely (p < 0.001) to be below the Estimated Average Requirement among food-insecure children aged 16–19 years than among their food-secure counterparts. Skalicky et al. 63 assessed 626 children aged < 36 months and found that the proportion of children with anaemia and iron deficient without anaemia did not differ significantly between food-secure and food-insecure children. However, when adjusting for US-born caregiver, caregiver education, employment, welfare status, household size and child ever breastfed, food-insecure children were 2.4 times more likely to be iron deficient with anaemia (OR 2.4, 95% CI 1.1 to 5.2; p = 0.02) than food-secure children. There was no association between child FI and anaemia without iron deficiency or iron deficiency without anaemia.
Eicher-Miller et al. 29 used NHANES data from 5270 children aged 8–19 years. After adjusting results for potential confounders (survey year, poverty-to-income ratio, ethnicity, BMI, physical activity, meals eaten at school per week, and personal smoking) they found that bone mineral content was lower in males 8–11 years old from food-insecure households than in their food-insecure counterparts (p ≤ 0.05). Females and males of other age groups did not significantly differ in bone mineral content. Survey-adjusted univariate analysis revealed differences in calcium-related dietary proportions among FS and FI groups. Only males aged 8–11 years from food-insecure households were found to differ from their food-secure counterparts. They were more than twice (OR 2.5, 95% CI 1.1 to 5.8; p = 0.03) as likely to report less than the USDA Food Guide recommendations for servings of dairy and 2.3 times (OR 2.3, 95% CI 1.3 to 4.0; p < 0.001) more likely to have a calcium intake less than the estimated average requirement than males from households with FS.
Ryu et al. 95 examined the exposure to household FI over a period of 9 years among a sample of children (n = 6651) selected when they were in kindergarten and assessed the consequences of FI on children’s parent-reported general health in eighth grade. Among children with no household FI at baseline or subsequent observations, 84.4% had ‘very good’ or ‘excellent’ proxy-reported health at the start of kindergarten, compared with 78.5% of those with 1 year of FI and 65–70% of those with 2, 3 or 4 years of FI. By eighth grade, the health differences according to the children’s FS history were more apparent: 88.5% of children with no observed household FI were in ‘very good’ or ‘excellent’ health compared with 67–79% of those with 1, 2 or 3 years of FI and 58.1% of those with household FI in all observed years. Compared with children who were food-secure at all time points, children with 3 years of reported household FI had an estimated 92% increase in their odds of lower health status and children living in food-insecure households during the 4 years of observations had an estimated 209% increase in their odds of lower health status. Adjusting the models to a higher average income significantly reduced the odds of poor, fair or good health, whereas the number of years in FI had no significant link to health outcomes. Lower health at baseline was also strongly linked to lower health in eighth grade.
Marjerrison et al. 45 found that the mean glycated haemoglobin (HbA1c) concentration was higher in children from food-insecure households than in those from food-insecure households [mean 9.5%, standard deviation (SD) 2.1%, vs. mean 9%, SD 1.5%; p = 0.039] (n = 183). There was no statistically significant difference between the FI and FS groups in the number of diabetes mellitus-related visits to the emergency department. Children living in a food-insecure household were less likely to use an insulin pump (p = 0.002). FI did not predict HbA1c concentrations of > 9.0%. The authors noted that families implemented various strategies to manage the financial load of diabetes mellitus. One of the most common strategies was to buy cheaper food so that the money could be used to purchase supplies (19/40; 47.5%) and having another family member eat less so that the child with diabetes mellitus could have sufficient food (20/40; 50%). Furthermore, some of the interviewed families (n = 5) reported reusing needles and/or testing blood glucose less often than recommended because of the high cost of materials.
In the study by Mangini et al. ,44 the evaluation of asthma in 11,099 third grade children was assessed in the Early Childhood Longitudinal Study – Kindergarten cohort (ECLS-K). The overall results showed that besides ethnicity, asthma prevalence differed by FS, household poverty status, child’s BMI and birthweight. In non-Hispanic white, non-Hispanic African American and Hispanic children, the prevalence of asthma was higher in those from food food-insecure households. In the adjusted (by ethnicity; household poverty status in relation to census thresholds; child sex; maternal nativity and education; child health insurance; height, weight, and birthweight; and household income) analysis for the entire sample (n = 11,099), higher odds of asthma were associated with a food-insecure household (OR 1.0, 95% CI 1.0 to 1.1). In particular, marginal FI was associated with 34% higher odds of asthma (95% CI 1.3 to 1.4). Similarly, when marginally food-insecure households were grouped with food-insecure households, the OR for asthma was 1.36 (95% CI 1.3 to 1.4). In Hispanic children, a 35% higher odds of asthma was associated with FI, whereas poverty increased asthma by 34% (95% CI 1.3 to 1.4), and the odds more than doubled for Hispanic children in food-insecure and poor households (OR 2.3, 95% CI 2.2 to 2.4). In non-Hispanic African American children, FI was negatively associated with asthma (OR 0.6, 95% CI 0.5 to 0.6), whereas FI and poverty together were positively associated with asthma (OR 1.8, 95% CI 1.7 to 1.8). In non-Hispanic white children, FI was positively associated with asthma (OR 1.2, 95% CI 1.2 to 1.2), as was the combination of FI and poverty (OR 1.8, 95% CI 1.7 to 1.8).
Shanafelt et al. 60 used a student survey to assess the personal health of food-insecure adolescents from rural schools in Minnesota, USA (n = 904). They observed that, compared with their food-secure counterparts, food-insecure adolescents reported poorer health (p < 0.01). After adjusting for grade level, sex, free and reduced-price lunch status, ethnicity and weight categories, food-insecure adolescents were significantly less likely to report ‘excellent’ or ‘very good’ health (OR 0.4, 95% CI 0.3 to 0.6; p < 0.01).
Tester et al. 66 used NHANES data from 1072 adolescents aged 12–18 years and reported a trend towards poorer lipid profiles (higher levels triglycerides or low-density lipoprotein) for food-insecure adolescents, but the results were not associated with FS status. Those reporting marginal FS were almost two times more likely (OR 1.9, 95% CI 1.1 to 3.0) to have elevated triglycerides (≥ 90 mg/dl) (OR 1.7, 95% CI 1.1 to 2.8), elevated triglyceride-to-high-density lipoprotein cholesterol (HDL-C) ratio (OR 2.0, 95% CI 1.2 to 3.4) and Apo B level of ≥ 90 mg/dl. However, these results were not significant for those reporting low or very low FS. The interaction between FS and sex was significant for HDL-C (p = 0.014); females were almost three times more likely to have low HDL-C (OR 2.7, 95% CI 1.1 to 6.4) when categorised as marginal FS, although not with low or very low FS. No associations were seen in male adolescents.
Weinreb et al. 69 collected health data from homeless and low-income mothers and their children (180 preschool-aged children and 228 school-aged children) in Massachusetts, USA. They found (unadjusted analyses) that, compared with their food-secure counterparts, school-aged children with severe hunger were more likely to have more chronic health conditions (mean 3.4 vs. 1.8; p = 0.002) and more stressful life events (mean 8.8 vs. 6.0; p = 0.009). Similarly, in the past year preschool-aged children with severe hunger experienced more traumatic life events than children free from hunger (mean 8.5 vs. 6.0; p = 0.02). Preschool-aged children with severe hunger also had more health conditions in the past year (2.8 vs. 1.9 for the no hunger group and vs. 2.6 for the modest hunger group; p = 0.004). For preschool-aged children, moderate hunger was a significant predictor of health conditions after controlling for explanatory variables (p = 0.03). In school-aged children, severe hunger was a significant predictor of chronic conditions after adjusting for housing status, mother’s distress, low birthweight and child life events (p = 0.05).
Ramsey et al. 54 collected data from 185 households with children aged 3–17 years in socioeconomically disadvantaged urban areas in Australia by means of a parent-completed questionnaire. They showed that a greater proportion of children from food-insecure households experienced poorer general health than their food-secure counterparts (p = 0.01). However, after adjusting the analyses for household income, health was no longer associated with children FI (p > 0.05).
Six studies27,45,57,63,83,116 exploring the relationship between FI and number of hospitalisations had mixed results. Cook et al. 83 found (adjusted analyses) that, compared with their food-secure counterparts, children in food-insecure households were 1.3 times more likely to have been hospitalised since birth (OR 1.3, 95% CI 1.2 to 1.5). Marjerrison et al. 45 assessed children with insulin-dependent diabetes and observed that children from food-insecure families had a higher rate of hospitalisation in the previous year (30% vs. 10.5%; p = 0.002) than those from food-secure families. Similarly, Skalicky et al. 63 found that, compared with food-secure children, food-insecure children were more likely to have had one or more hospitalisations (p = 0.02). The remaining three studies did not find any significant relationship between FI and rate of hospitalisation. 27,57,116
Weight status
Barroso et al. 78 performed a cross-sectional secondary data analysis of a sample of 240 low-income Mexican American mother–child dyads. The children were enrolled in the WIC and were free of any major disease. The mean age of the 240 children was 17.0 months (SD 4.2 months) and the mean age of the mothers was 26.2 years (SD 5.8 years). Cutting the size of the child’s meal, running out of money for food, running out of food and visiting a food bank (as indicators of FI) were not significantly associated with child weight-for-length. However, receiving food stamps or Supplemental Nutrition Assistance Program (SNAP) was positively associated with child weight-for-length in that children whose mothers reported ever having received SNAP were twice as likely to be overweight as children whose mothers did not report ever having received SNAP (95% CI 1.0 to 3.9). Children who consumed desserts were 2.9 times more likely to be overweight than children who did not consume desserts (95% CI 1.2 to 6.9). In addition, children’s calorie intake was significantly associated with child weight-for-length.
Bruening and Johnson79 examined potential protective factors that mediated the relationship between FI and overweight/obesity among 5869 adolescents in New Mexico. After adjusting results for sociodemographic characteristics, FI was significantly associated with overweight/obesity (OR 1.2; p = 0.047).
Casey et al. 81 used data from the US NHANES 1999–2002 on 6995 children aged 3–7 years to assess the association between household and child FI with childhood overweight status. Children classified as FI were significantly more likely to be at risk of obesity (38.8% vs. 28.8%; p ≤ 0.01) and to be overweight (21.1% vs. 14.5%; p ≤ 0.01) than children classified as food-secure. However, when stratified by age groups, this difference was statistically significant (p ≤ 0.05) only for the 3- to 5-year-olds (36.9% vs. 21.6%) and the 12- to 17-year-olds (38.3% vs. 30.1%). After adjusting the analyses for child age, ethnicity, sex and household poverty index, the risk of obesity was 1.3 times greater in food-insecure children than in those who were food secure (OR 1.3, 95% CI 1.0 to 1.7; p = 0.03).
Kaiser et al. 36 presented data from a cross-sectional survey of 211 low-income Mexican American families with children of preschool age (aged 3–6 years) conducted in California, USA. Weight-for-height z-scores, height-for-age z-scores and the percentage of overweight (85th percentile weight-for-height z-scores) were calculated. Families who reported household FI showed the highest mean weight-for-height z-scores. Although the prevalence of child overweight and obesity was high (14% were above the 85th percentile weight-for-height z-scores and 23% were above the 95th percentile), no significant differences were found in weight or height status of children by level of FI.
Papas et al. 51 investigated the association between FI and obesity among 74 low-income, Hispanic mother–child dyads. The majority of households were FI (74%) and one-third (30%) of children were obese. After adjusting for marital status, monthly household income and the number of children in the household, FI status was significantly associated with childhood obesity (OR 10.2, 95% CI 1.2 to 85.5; p < 0.05), with stronger associations observed within households where mothers were overweight/obese than in those where mothers were of a normal weight.
Pickett et al. 76 used data collected in Canada for the HBSC study to investigate the association between FI and weight status in a large sample (n = 25912) of adolescents (aged 11–15 years). After adjusting for potentially relevant factors, results showed that those reporting hunger ‘sometimes’ or ‘often or always’ were more likely to self-report an overweight/obese status (OR 1.2, 95% CI 1.1 to 1.4, and OR 1.3, 95% CI 1.0 to 1.6, respectively) than those who reported to have ‘never’ experienced hunger.
Willis and Fitzpatrick112 examined the association between FI and weight status among youth, as well as the potential mediation by psychosocial factors. Cross-sectional data were collected from fifth to seventh grade students (n = 324) in a middle school in Arkansas, USA. The mean age of students was 11 years. FI, depression and perceived social status all showed significant associations with weight status. Overall, this study shows that there was a significant (p < 0.001) association between FI and weight status among early adolescents. This association remained consistent after controlling for sex, poverty and ethnicity (p < 0.05). However, the addition of psychosocial factors, such as perceived social status and depression, were important mediators of the FI–obesity association.
Studies that did not find a significant relationship between FI and weight are described below.
Kuku et al. 100 examined data from 959 children (aged 0–12 years) from a nationally representative US data set (the Child Development Supplement of the Panel Study of Income Dynamics). The results of their parametric analyses showed that there was no significant relationships between childhood obesity and FI. By contrast, non-parametric results (using a continuous measure of FI) showed that the probability of being obese varied according the level of FI experienced by the child (increased for food-secure children and decreased as FI became more extreme). They concluded that the relationship between FI and obesity is complex and non-linear and differs by demographic and economic subgroups.
Lohman et al. 102 examined a sample of adolescents (n = 1011) aged 10–15 years and their low-income families from the Welfare, Children, and Families: A Three-City Study, Overview and Design Report,186 and adjusted the results for FI and relevant maternal stressor indices. They found that there was no direct association between FI, maternal or family stressors and overweight or obesity. However, the interaction of FI and maternal stressors (i.e. unemployed, disability, low self-esteem, high psychological distress, poor health and low social support) was significantly linked to the probability of being overweight or obese (i.e. an increase in maternal stressors increased the adolescents’ probability of being overweight or obese) (p < 0.05).
Martin and Ferris103 examined the relationship between childhood overweight and FI in a sample of 212 children aged 2–12 years. They did not find (unadjusted analyses) a significant association between FI and childhood overweight. After adjusting results for potential confounders [i.e. household income level, child age (2–5 years or 6–12 years), child sex, single parenthood and parents’ educational level], they found that having an obese parent significantly increased the odds of a child being overweight (OR 2.6, 95% CI 1.2 to 5.4; p = 0.02) and that children in households with incomes < 100% of poverty were half as likely to be overweight as those in higher-income households (OR 0.4, 95% CI 0.2 to 0.9; p = 0.03). However, there was no significant association between childhood overweight and FI.
Ramsey et al. 54 investigated the associations between FI and health and developmental outcomes in 185 children aged 3–17 years from socioeconomically disadvantaged suburbs in Australia. After adjustment for household income, weight status was not associated with FI. Children from food-insecure households did not have a greater probability of being underweight/normal weight or overweight/obesity than their food-secure counterparts (OR 0.9, 95% CI 0.4 to 2.1; p > 0.05).
Speirs et al. 109 explored the relationships between household and child FI and child overweight using a sample of 438 preschool-aged children aged 2–5 years in the USA. They found that neither household nor child FI was significantly associated with overweight/obesity or BMI scores. However, after adjusting the results for potential confounders (i.e. maternal ethnicity, maternal age, maternal BMI, household income, parental education, child sex and child age), they observed a significant positive relationship between household FI and BMI scores for girls (OR 2.1, 95% CI 0.6 to 7.5; p = 0.01) but not for boys (OR 0.8, 95% CI 0.2 to 2.7; p > 0.05).
Trapp et al. 67 explored the association between household FI, dietary intake and BMI in 222 low-income, preschool-aged children (aged 2–4 years).They did not find a direct association between household FI and child overweight/obesity. When the analyses were stratified by ethnicity, household FI was not associated with child weight among all ethnic groups. They also reported that the proportion of overweight/obese children in highly food-secure households nearly doubled between 2 and 3 years of age (p < 0.02). This increase in weight among age groups was not observed for households reporting any degree of FI.
One study reported mixed results across age groups. Metallinos-Katsaras et al. 105 examined the relationship between overweight and household FI with/without hunger in low-income children in the USA. Data were collected on 8493 children aged 1 month to 5 years and analysed by sex and age groups using logistic regression. Significant interactions were found between household FI and age groups (p < 0.05) and child sex (p < 0.10). After adjusting results for potential confounders (i.e. ethnicity, age and maternal education), they observed that among children < 2 years, household FI was associated with reduced odds of overweight compared with food-secure households. This association was statistically significant for girls (OR 0.6, 95% CI 0.5 to 0.9; p < 0.05), but not for boys (OR 0.8, 95% CI 0.6 to 1.1; p > 0.05). Among 2- to 5-year-old girls, households reporting FI with hunger were positively associated with greater odds of being overweight compared with food-secure households (OR 1.5, 95% CI 1.1 to 2.1; p < 0.05).
Data from the US National Health and Nutrition Examination Survey
Six of the included studies used data from the NHANES conducted in the USA. 28,74,85,86,88,97 Two studies showed a relationship between FI and children’s weight. Eicher-Miller et al. 28 collected data from 11,247 children and showed that the prevalence of being ‘at risk of overweight’ and ‘overweight’ was significantly higher among children aged 3–19 years who were living in food-insecure households than among children aged 3–5 years (p = 0.0246) and 12–15 years (p = 0.002) in food-secure households. Kaur et al. 97 studied a sample of 9701 children aged 2–11 years and reported a significant difference in the prevalence of obesity between food-secure and food-insecure children at both a child level and a personal level (p < 0.001).
Three studies found no relationship between FI and weight status. The study by Gundersen et al. 86 investigated the associations between FI and the probability of being ‘at risk of overweight’ or ‘overweight’ in 841 children aged 3–17 years. Overall, no direct association between FI and childhood overweight was found.
A further study by Gundersen et al. 85 showed that food-insecure children (n = 2516) aged 8–17 years were no more likely to be obese than their food-secure counterparts. Five different measurements of obesity (i.e. BMI, waist circumference, triceps skinfold thickness, trunk fat mass and percentage of body fat) were used in the study. After adjusting results for potential confounders (i.e. child age, ethnicity, sex and family income), the association between FI and obesity was not significant for five measures of obesity. This non-significant association remained when subgroups analyses were performed according to ethnic groups (non-Hispanic whites, non-Hispanic African Americans, and Hispanics) and sex. Kohn et al. 74 collected data from 1321 low-income, food-insecure children aged 4–17 years. After adjusting results for potential confounders (i.e. child age, sex, ethnicity, family poverty status, health insurance type, sex of primary respondent, primary respondent age and education), they found that food assistance participation was not associated with BMI scores, high waist circumference or categorical weight status.
One study reported mixed results regarding the relationship between FI and childhood weight. Holben and Taylor88 analysed results from 7435 adolescents aged 12–18 years and found no significant differences in mean BMI-for-age percentiles by household FS status (p = 0.087). However, after adjusting the results for potential confounders (i.e. age, ethnicity and sex), they observed that participants classified as marginally food secure (OR 1.4, 95% CI 1.1 to 1.9; p < 0.001) and low food secure (OR 1.4, 95% CI 1.1 to 1.8; p < 0.001) were significantly more likely than their high food-secure counterparts to be overweight. In addition, those from marginally food-secure households (OR 1.3, 95% CI 1.0 to 1.7; p = 0.036) and very low-FS households (OR 1.4, 95% CI 1.0 to 1.8; p = 0.036) were more likely to be obese that their counterparts. In central obesity measurements (waist circumference), significant differences were also found between levels of FS status (p < 0.001). Participants from low- (OR 1.4, 95% CI 1.1 to 1.8; p = 0.002) or very low-FS households (OR 1.5, 95% CI 1.1 to 2.0; p = 0.002) had a significantly higher mean percentage of waist circumference thresholds (see Appendix 8 for more details).
Longitudinal data from the US Early Childhood Longitudinal Study – Kindergarten cohort
Five of the included studies used data from the US ECLS-K12,20,56,80,113 to investigate the association between FI and childhood weight status. The ECLS-K started in 1998 by observing 19,684 children enrolled in 1277 US schools. Children and their households were observed in kindergarten and first, third and fifth grades. One study found a negative association between FI and children’s weight. Rose et al. 56 analysed data from 16,889 children (1480 were classified as food insecure and 15,409 as food secure) and found that children from food-insecure households were 20% less likely to be overweight than those from food-secure households (p = 0.027).
Two studies found no association between FI and weight. Bhargava et al. 20 used an ECLS-K data set covering 11,479 children from kindergarten to fifth grade to assess the relationships between household FI and body weight. Complete data were analysed on 7635 children (mean age 73 months). Results were adjusted for ethnicity, age, parental education, number of siblings, health limitations in respondent, television watching, parental care, physical exercise and family income. Household FI was not a significant predictor of weight and BMI scores (p > 0.05). Winicki and Jemison113 found that children from food-secure households weighed less than other children, but the differences were not statistically significant. Moreover, the BMI of children increased with increasing level of FI but, again, the differences were not statistically significant.
Two studies found mixed results for boys and girls. Burke et al. 80 used ECLS-K data from 15,827 children aged 6–14 years and showed that food insecure girls in kindergarten had an average BMI of 1.1% lower (95% CI –1.9% to –0.3%) than food secure girls. Between kindergarten and eighth grade, food insecure girls’ BMI increased by 2.9% (95% CI 1.3% to 4.5%) compared with that of food secure girls. For boys, based on FI status, significant differences in BMI were observed. Jyoti et al. 11 used a ECLS-K sample of 13,500 children for whom data were available at kindergarten and a sample of 11,400 children for whom data were available at third grade. After adjusting for many individual, parent and household explanatory variables, they found that children from persistently food-insecure households had a 0.4 kg/m2 greater gain in BMI (p < 0.028) and a 0.7 kg greater gain in weight (p < 0.026) than children from persistently food-secure households. These associations were significant among girls (β 0.6 kg/m2, p = 0.0022, and β 1.0 kg, p = 0.0024, respectively) but not among boys. Becoming food insecure was associated significantly with greater weight gains and BMI gains among boys (β 1.2 kg; p = 0.019) but non-significantly with smaller weight and BMI gains among girls (p > 0.05).
Studies that used ECLS-K data showed that the association of FI with weight in children might be complex and several factors or explanatory variables may affect the magnitude and direction of results. Bhargava et al. 20 used data from the 1998–19 and 2010–11 cohorts and included weight and height as explanatory variables in their analyses. They observed that households with children taller and/or heavier for their ages reported significantly higher FI levels. However, household FI was not a significant predictor of weight and BMI scores. Burke et al. 80 used the 1998, 1999, 2002, 2004 and 2007 ECLS-K cohorts and analysed data by sex. They observed significant differences in BMI growth between food secure and food-insecure households with girls but not in households with boys. The association shifted over time; girls in food-insecure households at the start of the study (n = 7808) had a BMI that was 1.1% lower than that of girls in food-secure households (p < 0.01). However, by eighth grade, girls in food-insecure households had a BMI that was 1.7% higher than that of girls in food-secure households (p < 0.01). BMI growth from kindergarten to eighth grade among girls in food-insecure households was 2.9% greater (p < 0.001) than the growth among girls in food-secure households.
Mental health outcomes
Belsky et al. 19 examined the role of FI in the aetiology of children’s cognitive and mental health problems. They used data from a prospective longitudinal study of 2125 school-aged children (sample initiated in 1999–2000) to test the associations between household FI and children’s cognitive, behavioural and emotional development. They reported (unadjusted analyses) that children living in food-insecure households had higher levels of behavioural and emotional problems at 12 age of years than their food-secure counterparts (p < 0.001). The relationship between FI and children’s behavioural problems was largely independent of household income (β 0.2, SE 0.1; p < 0.05), but became weak and non-significant when results were adjusted for income level, maternal personality and household sensitivity to children’s needs (p > 0.05). By contrast, the association between FI and children’s emotional problems remained significant in both unadjusted and adjusted analyses (β 0.2, SE 0.1; p < 0.05).
Huang et al. 92 used longitudinal data from 416 children (mean age 9.5 years) and adjusted results for the household head’s characteristics, household characteristics and child’s characteristics to explore the association between FI and children’s behavioural problems (externalising and internalising behaviours). FI was positively associated with both externalising and internalising behavioural problems. In particular, they found that FI could impact on indirectly externalising and internalising problems through parenting stress.
Johnson and Markowitz96 used data (n = 3700) from the longitudinal US Early Childhood Longitudinal Survey – Birth cohort (ECLS-B) study to examine the association of FI with children’s behaviour in terms of hyperactivity, conduct problems and approaches to learning. They found that as the level of FI increased across early childhood, the negative associations with behavioural outcomes increased accordingly. Specifically, any one episode of FI in early childhood was associated with increased hyperactivity (β 0.3, SE 0.1; p = 0.02) and conduct problems (β 0.3, SE 0.1; p = 0.05).
Molcho et al. 106 used data from the 2002 HBSC study, a cross-sectional survey that administered a self-completion questionnaire to a nationally representative random sample of school-children (n = 8424) aged 10–17 years from 176 schools in the Republic of Ireland. All analyses were adjusted for age and social class (according to the father’s occupation), and were conducted independently for boys and girls. They observed that both boys and girls experiencing FI reported mental symptoms more frequently. Symptoms such as feeling irritable, bad tempered, more nervous or having difficulties sleeping were significantly higher in children who reported food poverty than in those who did not report food poverty (both sexes; p < 0.05). Boys who reported experiencing food poverty were more likely to feel low (OR 2.6, 95% CI 2.3 to 2.8), afraid (OR 2.2, 95% CI 1.8 to 2.5) or dizzy (OR 2.4, 95% CI 2.1 to 2.7) than those who did not report food poverty. Girls who reported experiencing food poverty were more likely to feel dizzy (OR 2.0, 95% CI 1.7 to 2.2), afraid (OR 2.2, 95% CI 2.0 to 2.5) or tired and exhausted (OR 2.0, 95% CI 1.8 to 2.2) than those who did not report food poverty.
Howard89 analysed the ECLS-K data from 4710 children enrolled in first, third and fifth grade (1999–2003) and found that children experiencing FI at any time had lower social skills (assessed in terms of interpersonal relationships, self-control, approaches to learning and externalising behaviour) than children who were food secure. FI was also found to affect negatively children’s non-cognitive skill development. In particular, children who experienced an early transition from FI in first grade to FS in third grade showed a large impairment that persisted through to fifth grade (p < 0.05).
In a further publication based on the same data set, Howard90 showed a significant (p < 0.05) negative relationship between FI and children’s social skill scores. Children who experienced a transition from FI in first grade to FS in third grade had significantly lower social skill scores (p = 0.019). The association was significant among boys (p < 0.05) but not among girls (p = 0.56).
Slack and Yoo108 used data from the US Illinois Families Study, a 6-year panel of families that had a primary caregiver transitioning from welfare to work. Data from 942 families with at least one child were used to explore the relationship between food hardship and behaviour problems in children aged 3–5 years and children aged 6–12 years. Food hardship was positively associated with externalising behaviour problems for younger children (p < 0.01) and with internalising behaviour problems for both age groups (p < 0.01). Food hardship was not found to be related to older children’s externalising behaviour problems (p > 0.05). However, all of these relationships were mediated by parental characteristics (such as parental stress, warmth and depression).
Pickett et al. 76 used HBSC survey data from 25,912 Canadian children aged 11–15 years. After adjusting results for potential confounders, they observed that children who experienced hunger ‘sometimes’ or ‘often or always’ were more likely to report internalising negative emotional problems than those who reported ‘never’ suffering from hunger (OR 2.1, 95% CI 2.0 to 2.2, and OR 3.8, 95% CI 3.2 to 4.4, respectively). Furthermore, those reporting hunger ‘sometimes’ or ‘often or always’ were more likely to report externalising negative behavioural problems than those who reported ‘never’ suffering from hunger (OR 1.2, 95% CI 1.1 to 1.3, and OR 2.0, 95% CI 1.7 to 2.4, respectively).
Weinreb et al. 69 assessed 180 preschool children aged 2.5–6 years and 228 school-children aged 6–17 years who participated in an unmatched case–control study of homeless, low-income families in the USA. For both groups of children, severe hunger was a predictor of internalising problems after controlling for possible explanatory variables (p < 0.001). After adjusting results for type of housing, mother’s distress level and stressful life events, school-aged children with severe hunger had parent-reported anxiety scores that were more than double the scores for children with no hunger and significantly higher internalising behaviour problems than children with no hunger. Similarly, for preschool-aged children, severe hunger was associated with internalising behaviour problems compared with children with no hunger.
McLaughlin et al. 47 examined whether FI was associated with past-year mental disorders using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, in 6483 adolescent–parent pairs who took part into the US National Comorbidity Survey Replication Adolescent Supplement survey. They found that a higher FI score was associated with greater odds of any past-year mental disorder (OR 1.2) and greater odds of past-year mood, anxiety, behaviour and substance disorders (OR 1.2 for each). After controlling for standard indicators of family SES, FI remained significantly associated with greater odds of adolescents’ mental disorders. The magnitude of the associations between FI and mental disorders was unchanged when controlling for extreme poverty and family income and minimally attenuated when controlling for childhood adversities. There was also a positive interaction between FI and either family income (p = 0.008) or relative deprivation (p = 0.005). The association between FI and mood disorders was stronger for adolescents with a low family income (OR 1.2–1.6 for adolescents in the lowest three quartiles compared with adolescents in the highest quartile) and was stronger for adolescents with higher levels of relative deprivation (OR 1.1).
Poole-Di Salvo et al. 53 used cross-sectional data from the 2007 set (eighth grade) of the ECLS-K from 8600 adolescents and found (unadjusted analyses) that adolescents with household FI had significantly higher rates of parent-reported mental health problems than those with household FS. Compared with food-secure adolescents, adolescents who lived in food-insecure households had a significantly increased risk of emotional (OR 2.5, 95% CI 1.6 to 3.7), conduct (OR 1.5, 95% CI 1.0 to 2.3), peer problems (OR 1.6, 95% CI 1.0 to 2.4), less optimal pro-social behaviour (OR 1.5, 95% CI 1.0 to 2.2) and hyperactivity (OR 1.5, 95% CI 1.0 to 2.2). After adjusting the results for appropriate variables, household FI was independently associated with more than a twofold increased risk of parent-reported mental health problems among adolescents (OR 2.3, 95% CI 1.6 to 3.2).
Ramsey et al. 54 assessed 185 children aged 3–17 years from socioeconomically disadvantaged suburbs in Australia. After adjusting results for household income, the authors found that children living in food-insecure households were more likely to report borderline or atypical emotional symptoms (OR 2.4, 95% CI 1.1 to 5.4; p < 0.05) or behavioural difficulties (OR 2.4, 95% CI 1.0 to 5.3; p < 0.05).
Dunifon and Kowalwski-Jones26 evaluated the effects of FI and of participating in the US NSLP in a sample of 3500 school-aged children (6–12 years). They found that participation in the NSLP was associated with increased externalising behaviour. An increase in FI was associated with decreased levels of positive behaviours (β –0.17, SE 0.06; p < 0.001). Boys showed more behaviour problems than girls.
Huang and Vaughn93 used longitudinal data from 7348 children in the ECLS-K. After adjusting results for child characteristics, household characteristics and parental characteristics they found that FI was not associated with developmental change in children’s behaviour problems. They observed that the impact of FI on children’s behaviour problems could be episodic or interact with specific developmental stages.
Kimbro et al. 39 used data from 6300 children in the ECLS-K. They found that, in general, for children who experienced FI, teachers reported poorer scores with regard to interpersonal skills, self-control, and internalising and externalising behaviours. However, they reported two exceptions: (1) internalising behaviours among children who transitioned into FI were not significantly different from those observed among children who were never FI and (2) externalising behaviours among children who transitioned out of FI were not significantly different from those observed in children who were food secure. After adjustment for confounding factors, children who transitioned from FS to FI showed significantly worse ratings on interpersonal skills, self-control, and externalising behaviours than children who were food secure.
Social well-being outcomes
Zaslow et al. 72 used data from 8944 children aged 9–24 months in the ECLS-B to explore the associations between household FI during infancy and attachment and mental proficiency in toddlerhood. They found that FI had no significant direct association with being insecurely attached. Instead, FI worked indirectly through depression and parenting practices to influence security of attachment and mental proficiency in toddlerhood. FI appeared to be positively associated with depression (β 0.2; p < 0.001), which, in turn, was negatively associated with positive parenting (β –0.03; p < 0.05). The likelihood of insecure attachment reduced when more positive parenting practices were put in place (β –0.04; p < 0.05).
Baer et al. 77 assessed 400 participants aged 15–25 years (mean 18 years) living in Boston, USA, who completed a web-based screening tool. The survey aimed at identifying problems in seven health-related social domains. After adjustment for age, sex and ethnicity, FI was significantly associated with cumulative burden of social problems (p < 0.001). In particular, FI was associated with housing problems (OR 2.8, 95% CI 1.8 to 4.4) and substance use (OR 2.5, 95% CI 1.5 to 4.3). More specifically, compared with food-secure participants, those reporting low (n = 70) or very low FS (n = 60) were 3.1 times (OR 3.1, 95% CI 1.8 to 5.5; p < 0.001) and 3.3 times more likely (OR 3.3, 95% CI 1.8 to 6; p < 0.001) to report housing issues. Furthermore, those reporting very low FS were at higher risk of alcohol and drugs abuse and tobacco use (OR 4.5, 95% CI 2.3 to 9.2; p < 0.001).
Pickett et al. 76 used HBSC data from 25,912 children aged 11–15 years from 436 Canadian schools. After adjustment for potential confounding factors, compared with their ‘never’ hungry counterparts, children who experienced hunger ‘sometimes’ or ‘often or always’ were less likely to report emotional well-being feelings (OR 0.6, 95% CI 0.5 to 0.6, and OR 0.5, 95% CI 0.4 to 0.5, respectively) and pro-social behaviours (OR 0.8, 95% CI 0.8 to 0.9, and OR 0.8, 95% CI 0.7 to 1.0, respectively) and more likely to report frequent physical fighting (OR 1.3, 95% CI 1.2 to 1.4, and OR 2.3, 95% CI 2.0 to 2.7, respectively) and to talk back to teachers (OR 1.3, 95% CI 1.2 to 1.4, and OR 1.8, 95% CI 1.5 to 2.1, respectively).
Helton87 used a sample of 3580 children up to 17 years old from the US National Survey of Child and Adolescent Well-Being187,188 and the corresponding administrative data files from the National Child Abuse and Neglect Data System (NCANDS). 189 They examined families with and without an allegation of child food neglect with regard to the time to re-report following the close of a maltreatment investigation. ‘Food neglect’ was described as the inadequate provision of food and a form of FI. The findings showed that around 12% of families with children who were experiencing food neglect were re-reported within 100 days of the index investigation, compared with 8% of families without food neglect. Within 1 year, around one-third (34%) of food-neglected children were re-reported compared with about 24% of families without food neglect. After adjustment for maltreatment types, caregiver mental health problems and other relevant covariates, food neglect predicted a greater risk of re-report [hazard ratio (HR) 3.0, 95% CI 1.2 to 7.9; p < 0.05] than did other forms of maltreatment (e.g. shelter neglect HR 0.3, 95% CI 0.1 to 0.8, and receiving interventions from the Child Protective Services HR 0.7, 95% CI 0.5 to 1.0).
Two studies assessing the relationship between FI and children’s social well-being stratified the results by sex. 11,94 Jyoti et al. 11 used data from ≈13,500 children enrolled in the ECLS-K cohort and found that children from food-insecure households at kindergarten showed a greater decline in social skills assessed by teachers questionnaires than children from food-secure households. Stratification by sex showed that the association between kindergarten FI and change in social skills was significant only for boys (β –0.1; p < 0.001). After controlling for relevant variables, the association between kindergarten FI and social skills was significant only among girls. In the full sample, persistent FI was not associated with differential changes in social skills over time when compared with persistent FS. Transitioning from FI to FS was associated with a greater increase in social skills score for girls (p < 0.001) and a smaller increase for boys (p < 0.038). By contrast, becoming FI was associated with a greater decline in social skills score among girls (β –0.135; p < 0.005) but with a greater improvement in social skills score among boys (β 0.124; p < 0.050).
Jackson and Vaughn94 used data from the ECLS-K cohort (≈7000 children aged 13–14 years). After adjusting results for potential confounders, FI and FI persistence were predictive of most forms of misconduct for boys. Persistent exposure to FI during childhood was associated with greater involvement in fighting/bullying (OR 1.7, 95% CI 1.4 to 2.1), stealing (OR 1.7, 95% CI 1.3 to 2.2), cheating/lying (OR 1.4, 95% CI 1.2 to 1.6), and defying misbehaving (OR 1.3, 95% CI 1.1 to 1.5) for boys. Participating in multiple forms of misconduct was 168% higher among boys exposed to persistent FI than among those who were raised in consistently food-secure households. For girls, however, household FI generally failed to predict adolescent misconduct.
Pickett et al. 76 used data from the HBSC survey conducted in Canada among 25,912 children aged 11–15 years. They found (adjusted analyses) that those reporting hunger ‘sometimes’ or ‘often or always’ were more likely (OR 1.3, 95% CI 1.2 to 1.4, and OR 2.3, 95% CI 1.9 to 2.7, respectively) to self-report frequent engagement in bullying than those who reported ‘never’ suffering from hunger. Furthermore, those reporting hunger ‘sometimes’ or ‘often or always’ were more likely (OR 1.8, 95% CI 1.7 to 2.0, and OR 2.6, 95% CI 2.2 to 3.0, respectively) to self-report frequent victimisation by bullying than those who reported ‘never’ suffering from hunger. Edwards and Taub84 also used data from the HBSC (US version) and found a statistically significant difference in bullying victimisation (p < 0.001) and bullying perpetration (p < 0.001) in fifth to tenth grade children with FI as compared with their food-secure peers. All effect sizes were small, but pairwise comparisons indicated that students who faced FI at least occasionally experienced greater bullying victimisation than those who did not (p < 0.008). Further analyses showed a statistically significant difference in bullying perpetration.
One study assessed life satisfaction among school children (aged 10–17 years). Molcho et al. 106 assessed measures of life satisfaction and performed analyses adjusted for sex, age and paternal social class. They found that children reporting food poverty were significantly more likely to feel dissatisfied with their life while children not experiencing food poverty were less likely to report a low life satisfaction (OR 2.2, 95% CI 1.95 to 2.43, and OR 2.3, 95% CI 2.1 to 2.5, respectively). The same results were observed for happiness indicators. Children reporting food poverty were less likely to report happiness.
Casey et al. 8 performed a cross-sectional survey of 399 children in the USA aged 3–17 years and reported the effects of FI on children’s QoL. Children in food-insecure households scored significantly lower on physical (p = 0.006) and psychosocial function (p = 0.017) and on total child health-related QoL (p = 0.005) than children in food-secure households. The youngest children (3–8 years) in food-insecure households scored significantly lower in physical functioning than their food-secure counterparts (median 6.1, 95% CI 2.5 to 9.7; p = 0.001). By contrast, teenagers (12–17 years) in food-insecure households recorded significantly lower scores in psychosocial functioning (median 7.3, 95% CI 2.1 to 12.5; p = 0.007). The youngest children (median 4.8, 95% CI 0.7 to 8.9; p = 0.002) and teenagers (median 5.0, 95% CI 0.5 to 9.5; p = 0.03) in food-insecure households scored significantly lower in the total health-related QoL. In subgroup analyses by ethnicity, African American males in food-insecure households scored significantly lower on physical function (p < 0.05) and total child health-related QoL (p < 0.05) but there were no differences for white males by level of FI. African American females, but not white females, in food-insecure households scored lower in psychosocial (p = 0.08) and total child health-related QoL (p = 0.06). Further analyses adjusted for child age, ethnicity, sex and family income showed that FI status was significantly associated with total child health-related QoL (median 3.5, 95% CI 0.4 to 6.7; p = 0.03) and physical function (median 3.3, 95% CI 0.1 to 6.4; p ≤ 0.05). The association of FI with psychosocial function was not significant (median 3.6, 95% 0.05 to 7.4; p = 0.06).
Academic performance
Baer et al. 77 assessed 400 children and young people aged 15–25 years (mean 18 years) who lived in Boston, USA, and completed a web-based screening tool. The survey aimed to identify problems in seven health-related social domains including education. After controlling for age, sex and ethnicity, they found that FI was associated with educational problem, such as unmet learning disability and dropping out of high school (low FS OR 2.4, 95% CI 1.1 to 5.3, p = 0.03; very low FS OR 3.9, 95% CI 1.8 to 8.4, p < 0.01).
Belsky et al. 19 used data from a UK prospective longitudinal study of 2125 school-aged children (sample constructed in 1999–2000) to test the association between household FI and children’s cognitive development. After adjusting results for potential confounders, they showed that at age 12 years, children in food-insecure households (n = 278) had significantly lower IQs and higher levels of behavioural and emotional problems than their food-secure counterparts (p < 0.001). FI predicted lower child IQ but once household income was added to the model, the association was no longer significant.
Kimbro et al. 39 used longitudinal data from 6300 children in kindergarten and first grade who were part of the ECLS-K cohort. They found (unadjusted analyses) that children who were food insecure at kindergarten and/or first grade had significantly lower academic achievement scores in reading, maths and science, than with children who were food secure, and that children who were food insecure at both kindergarten and first grade scored lowest on all three measures. However, after adjusting their analyses for children and family characteristics (e.g. child sex, child birthweight, family structure household income, parental employment status, occupational prestige, education level, number of siblings in the household), they found no significant associations between FI transitions (into and out of FI) and children’s academic achievement outcomes.
Ramsey et al. 54 collected data from 185 households with children aged 3–17 years in socioeconomically disadvantaged urban areas in Australia by means of a parent-completed questionnaire. After adjusting for household income, children who were living in food-insecure households were 3.5 times more likely to have days away from school because of illness (OR 3.5, 95% CI 1.4 to 8.5; p < 0.05.) and 5.4 times more likely to cut down on activities because of illness (OR 5.4, 95% CI 1.4 to 20.1; p < 0.05).
Johnson and Markowitz96 used longitudinal data from a recent birth cohort of US-born children in low-income households (n = 2800–3700) to investigate the association between childhood FI and children’s kindergarten reading and maths outcomes. After adjustment for standard demographic and household economic variables, they observed broadly negative associations between earlier FI (at 9 months and 2 years) and school outcomes. Very low FI at 9 months was linked to reduced reading scores (p = 0.03), whereas low FS at 9 months was associated with decreased maths scores (p = 0.03); very low FI at 2 years was associated with decreased approaches to learning (p = 0.04) and reduced maths skills (p = 0.03). In general, as the intensity of FI increased across early childhood, so too did negative associations with outcomes.
Jyoti et al. 11 used data from ≈13,500 children from the ECLS-K cohort and found that children from households experiencing FI at kindergarten demonstrated a smaller increase in maths (β –2.3; p < 0.001) and reading scores (β –4.4; p < 0.001). After controlling for explanatory variables, the association between kindergarten FI and change in mathematics score remained negative, even though this was significant only for girls (β –1.8; p < 0.017). Persistent FI was not associated with differential changes in mathematics and reading scores when compared with persistent FS in the full sample. Children from households transitioning from FS to FI showed a smaller increase in reading score (p = 0.0007) and in mathematics scores (p < 0.005) than children from households who remained food secure. These differences were significant regardless of sex.
Shanafelt et al. 60 used data from 904 children in ninth and tenth grade from the US BreakFAST (Fuelling Academics and Strengthening Teens) project, which enrolled students from 16 high schools in Minnesota, USA. After adjustment for grade level, sex, free and reduced-price lunch status, race, and weight categories, they found that food insecure students were more likely to have a lower cumulative attendance, have a lower grade-point average (p < 0.01) and be in a lower grade-point percentile than their food-secure counterparts (p < 0.01). Food-insecure adolescents were more likely to show a lower attendance rate than food-secure adolescents (p < 0.01), but this was no longer statistically significant after adjustment (p = 0.15).
Winicki and Jemison113 used data from the ECLS-K cohort. Of the 21,260 children entering kindergarten, 18,847 provided valid responses to the FS survey module and 3335 had at least one affirmative response. A negative relationship between maths scores and FI was observed. After adjusting results for explanatory variables, there was a negative effect of FI on maths scores and on learning (p < 0.05). However, for children ≤ 150% of the federal poverty level, FI measures did not explain maths scores or learning.
Three studies found no relationship between FI and children’s academic performance. Dunifon and Kowaleski-Jones,26 who examined the association between FI and participation in the US NSLP in a sample of school-aged children (n = 3500), did not find a significant association between FI and children’s academic scores (p > 0.05). Weinreb et al. 69 collected data from homeless and low-income mothers and their children (180 preschool-aged children and 228 school-aged children in the USA). Unadjusted analyses showed that, compared with preschool and school-aged children who were moderately or not hungry, those who experienced severe hunger showed poorer academic scores, developmental delay and learning disabilities, and were likely to repeat a school year or miss days in school. However, these differences were not statistically significant. Zaslow et al. 72 analysed data from a longitudinal nationally representative sample of infants and toddlers (n = 8944) aged 9–24 months from the ECLS-B. For the analyses, they derived parent and child assessment data from the 9- and 24-month interviews. After adjustment for mother’s/father’s individual characteristics, household-level characteristics, child characteristics and child-care characteristics, there was no direct effect of FI on children cognitive development (p > 0.05). Higher levels of FI worked indirectly through depression and parenting practices to influence mental proficiency in toddlerhood. High levels of FI were positively associated with depression (β 0.180). In turn, depression was negatively associated with more positive parenting practices (β –0.033) and positive parenting practices were positively associated with mental proficiency at 24 months (β 0.081; p < 0.001).
Appendix 8 Descriptions of studies that assessed food assistance programmes
Cook et al. 83 evaluated whether or not receiving food stamps or Temporary Assistance to Needy Families (TANF) benefits modified the associations between FI and health status or hospitalisation records for children aged ≤ 3 years. The food stamps programme was a food-purchasing assistance initiative for low- and no-income people across the USA (later renamed SNAP) developed by the US Federal Government, which funds a variety of services (e.g. child care, education and job training, transportation, aid to children at risk of abuse and neglect) to help low-income families with children. They conducted a multisite retrospective cohort study with cross-sectional surveys at urban medical centres in five US states and Washington DC between August 1998 and December 2001. Caregivers of 11,539 children were interviewed and the results showed that, for risk factors for fair/poor health, there was a significant interaction between receiving food stamps and FI. Receiving food stamps attenuated (but did not eliminate) the association between FI and children’s fair/poor health. For children in households not receiving food stamps, being food insecure increased the odds of fair/poor health by 2.1 times; after controlling for other covariates and adding ‘receiving food stamps’ into the analyses, being food insecure increased the odds of fair/poor health by 1.5 times. A similar pattern was seen for TANF benefits; however, the interaction was not significant. In the analysis of hospitalisation since birth, there was no significant interaction between receiving food stamps or TANF benefits and FI.
A later study from the same authors116 aimed to determine whether child FI increased the risks posed by household FI to child health and whether or not the USA food stamps programme could modify these effects. From August 1998 to June 2004, 17,158 caregivers of children aged ≤ 3 years were interviewed in six urban medical centres. It is unclear if there is overlap with the participants involved in the Cook et al. 83 study. In line with the results of the previous study by Cook et al. ,83 participation in the food stamps programme reduced, but did not eliminate, the positive associations of both household FI and child FI with parents’ ratings of children health as fair/poor. In subgroup analyses stratified by food stamps programme participation, after controlling for potential confounders (i.e. child’s ethnicity, health insurance status, day-care attendance, mother born in the USA, caregiver’s age, employment status, marital status and education level), children in food-insecure households receiving food stamps programme benefits had lower odds of fair/poor health (OR 1.4, 95% CI 1.1 to 1.8) than children in food-insecure households not participating in the food stamps programme (OR 1.6, 95% CI 1.3 to 2.0). Similarly, children in food stamps programme participating households that were classified as households with child FI had lower odds of fair/poor health (OR 1.7, 95% CI 1.3 to 2.2) than children in similar households not participating in the food stamps programme (OR 2.1, 95% CI 1.8 to 2.5). Participation in the food stamps programme reduced the odds of fair/poor health by 24% and 42% in food-insecure households and households with child FI, respectively.
The study by Canter et al. 115 evaluated participation in a state-level double-value coupon programme with the aim of assessing the potential impact of participation on children’s FI, physical activity, sedentary behaviour, sleep, and fruit and vegetables consumption. Participants were recruited from several agencies serving low-income households in a large metropolitan area in the USA. Participants were parents or caregivers of children aged 5–10 years who were English speaking and received services through an organisation supporting low-income families. Potential participants were approached during their usual service usage (i.e. during SNAP transaction at a farmer’s market). Initially, 148 participants were recruited and, of these, 109 were received services through a state-level double-value coupon programme. Thirty-nine participants were recruited while receiving services through other organisations providing services to low-income families. Food-insecure children consumed significantly fewer servings of vegetables (p < 0.05). Physical activity significantly predicted fruit and vegetables intake (p < 0.01). However, double-value coupon programme service usage did not have a significant impact on children’s fruit and vegetables consumption.
The study by Dunifon and Kowaleski-Jones26 examined child- and family-specific factors that could predict FI and participation in the US NSLP, as well as the effects on children of FI and of participating in the NSLP. The NLSP is a federally sponsored nutrition programme that aims to provide nutritious foods to school-aged children at no, or reduced, cost. Families are eligible for free NSLP lunches or reduced-price lunches according to their income. The authors used data from ≈3500 children aged 6–12 years to examine how FI and participation in the NLSP could affect children’s development. Participating in the NSLP was found to be associated with increased externalising behaviour (p < 0.05), an 82% increase in the odds of having a health limitation (p < 0.05) and lower maths scores (β 1.9, SE 0.8; p < 0.05). An increase in FI was associated with decreased level of positive behaviours and increased odds of health limitations. The authors concluded that participation in the NSLP was detrimental to children and explained that omitted variables might have biased the association between NSLP participation and children’s outcomes. In particular, children participating in the NSLP differed in ‘unmeasured’ ways from those not participating, and these unmeasured variables might be associated with the observed negative outcomes. For this reason, the authors conducted analyses comparing the outcomes of siblings within the same family (one of whom participated in the NSLP and one of whom did not). In these analyses, participation in the NSLP was not a significant predictor of any of the child outcomes, suggesting that the initial full sample results were probably due to unmeasured family-specific factors that biased the association between NSLP participation and child outcomes, particularly when predicting children’s test scores and health limitations. Overall, FI was associated with children’s health and behaviour and participation in the NSLP did not predict improved outcomes for children. FI was significantly predicted by family income, number of siblings and food stamps receipts.
Ecker and Sifers118 evaluated the US ‘BackPack Food Program’, which distributes easy-to-prepare food in children’s backpacks every Friday or on the last day of school before a long weekend. The food packs contained child-friendly, single-serving, non-perishable items for breakfast, lunch and a snack each day. Three schools with the highest percentage of students receiving free and reduced-price lunches in the Midwest of the USA were included in the study. The proportion of children eligible for free or reduced-price meals in the three schools were 43%, 47% and 46%, respectively. The evaluation included direct observation of students in the classroom (n = 52), student hunger surveys (n = 82) and satisfaction surveys conducted with students (n = 192), parents (n = 138) and teachers (n = 82). One baseline observation and three follow-up observations were collected. Results indicate that there was not a significant increase in students’ on-task behaviour (p = 0.19) or a significant decrease in students’ self-reported hunger levels (p = 0.54). The satisfaction surveys showed that nearly all (97%) of the children reported looking forward to the food and 60% reported sharing the food with other children in the home. Almost all parents (98%) reported that the programme benefited their family and that the programme had made a difference to the well-being of their child. More than half of the adults (53%) indicated that it was difficult to provide enough food for everyone in the home, and 14% said that they or another adult in the home would have had to skip a meal without the programme. Teachers reported improvements in students’ energy levels, emotional well-being and behaviour.
Gordon et al. 119 piloted the Summer Electronic Benefit Transfer for Children (SEBTC), a programme created by the Food and Nutrition Service of the USDA to provide food benefits during the summer to households with eligible school-aged children. Low-income households with children eligible for free or reduced-price meals received US$60 benefits per school-aged child per summer month. Benefits were delivered through an electronic benefit transfers cards that could be used to purchase food via existing programmes, such as SNAP or WIC. Approximately 67,000 children from around 42,000 households were involved in the SEBTC. Initial household interviews provided a baseline for household SES, demographic characteristics and FS status during the school year. Interviews (which took place 30 days after SEBTC benefits started) allowed the research team to measure effects of SEBTC on FS and children’s food consumption. Around 60% of assessed households received SNAP benefits and 22% received WIC benefits at baseline. The SEBTC programme improved children’s FS substantially for both SNAP and WIC households. Average rates of FI were 46.6% for the no-benefit group and 38.8% for the benefit group in SNAP-households (p < 0.001), and 41.9% for the no-benefit group and 32.8% for the benefit group in WIC-households (p < 0.001). Despite lower levels of SEBTC participation and redemptions in WIC households than in SNAP households, the impact of SEBTC on very low child FS was not significantly different among SNAP and WIC households. In general, the SEBTC programme significantly improved children’s eating behaviours in the direction of healthier eating with increased consumption of fruits and vegetables, whole grains and dairy products and reduced consumption of sugar-sweetened beverages (p < 0.001), with the exception of sugar-sweetened beverages in SNAP households.
Klerman et al. 120 implemented and evaluated the SEBTC programme in 16 US sites between 2011 and 2013. Benefit amounts, participating sites, details of the intervention and household sample size varied across geographical regions. In 2011 and 2012, households were randomised either to an SEBTC benefit group (US$60 per school-aged child per month) or to a zero-benefit control group. In 2013, to test the differential impact of benefits, all randomised households were issued some SEBTC benefits (either US$60 or US$30 per school-aged child per month), with no zero-benefit control group. Overall, across all years, households in the US$60 group redeemed 82% of benefits and those in the US$30 group redeemed 74% of benefits. A random sample of nearly 50,000 households was selected to be part of the impact evaluation. These households were interviewed in the spring before the end of the school year and again in the summer. Results showed that a US$60 SEBTC benefit per eligible child per month cut child very low FS by nearly one-third (p < 0.01) and reduced FI by approximately one-fifth (p < 0.01). Prevalence of child FI in the absence of SEBTC was 43.0% and SEBTC reduced the prevalence to 35.7% (p < 0.01). A US$30 SEBTC benefit per child improved FS (p < 0.01) but generally had a smaller impact than the US$60 benefit (p < 0.01). After adjusting the analyses for household characteristics, the authors reported significant variations in the impact of the US$60 monthly benefits compared with no benefits. For instance, reductions in child very low FS in the summer were larger for those who were less food secure at baseline. Households that were child food insecure in the spring also experienced greater reductions in the summer. In summer, impacts on very low FS and FI were larger for households with three or more children and with an adolescent at home. The authors considered these moderators as proxy measures for need. Reductions of child FI during the summer were also larger for households receiving SNAP in the spring and for households headed by an African American adult.
Khan et al. 98 assessed FI and the relationship between FI and participation in school breakfast and lunch programmes in 373 school children aged 10–14 years in Vermont, USA. Approximately 40% of the children were eligible for free or reduced-price meals and free breakfast was available to all school children. Information on the breakfast provision or numbers partaking was not reported. The majority of children were classified as food secure (79.6%), 15.8% were classified as food insecure without hunger and 4.6% were classified as food insecure with hunger. A statistically significant relationship between FS and eating breakfast at home was found. Children who were food insecure (with or without hunger) were less likely to eat breakfast at home than children who were food secure (67.1% vs. 81.4%; p = 0.007). No difference was found between eating school breakfast or eating school lunch, as the majority of food-secure and food-insecure children ate lunch at school (91.5% vs. 93.4%, respectively). Furthermore, of the food-insecure children, only three did not eat breakfast at school (two of these did eat breakfast at home).
Kleinman et al. 117 assessed whether or not nutrient intake and academic and psychosocial functioning improved after the start of a US UFSB programme in the Boston Public Schools. Information was collected from 97 inner-city students in fourth to sixth grades prior to the start of the programme and again after 6 months. The results indicate that 19% of the students had improved their nutrient intake, 64% were unchanged and 18% were at increased nutritional risk. Children whose nutritional status improved recorded significantly larger increases in school breakfast participation than children whose nutritional status stayed the same or worsened (p < 0.001). Children who improved their nutritional intake reported a significant decrease in symptoms of hunger compared with children whose nutritional status remained the same. Children who reported worsening their nutritional status had an increase in symptoms of hunger (p < 0.001). Furthermore, those who improved their nutritional intake showed significant improvements in functioning according to the Paediatric Symptom Checklist scores, compared with children whose nutritional status remained the same, or children whose nutritional intake category worsened (p < 0.01). Only changes in maths grades were found to be significantly improved (p < 0.05). Children who improved their nutritional intake significantly reduced the number of days on which they were absent from school (mean –4.4 days) compared with children whose nutritional intake did not change (mean –1.7 days) or children whose nutritional intake worsened (mean 3.0 days; p < 0.01). There was no significant decrease in tardiness among children with increased breakfast participation.
Korenman et al. 121 involved a sample of 4-year-old children drawn from the US ECLS-B to obtain estimates of associations between Child and Adult Care Food Program (CACFP) participation and children’s food consumption (e.g. milk, fruit, vegetables, fast food and sweets), children’s overweight/underweight status and family FI. The CACFP reimburses child care providers for meals and snacks served to children in their care through participating preschools, day care homes, after-school programmes and homeless shelters, according to a child’s family income. Results (unadjusted analyses) indicated that CACFP participants (n = 2200) and their families were much more likely than non-participants were (n = 1850) to experience FI. Children were food insecure in 20% of CACFP households versus 4% of non-participant households. In addition, CACFP participants were more likely to report the use of food stamps, TANF, SNAP, WIC or Head Start. CACFP participants were less likely than non-participants to limit consumption of sodas and fast food; nevertheless, they were more likely to consume the recommended number of servings of milk, juice, fruit or vegetables, and more likely to limit consumption of sweet snacks. CACFP participants were also more likely than non-participants to be overweight or at risk of overweight (p < 0.05). After adjusting the results for potential confounders, low-income children participating in CACFP were 1.4 times more likely to consume two or more cups of milk per day (OR 1.4, 95% CI 1.0 to 1.9; p < 0.05) and 1.6 times more likely to consume two or more servings of vegetables per day (OR 1.6, 95% CI 1.6 to 2.1; p < 0.05) than non-participants.
Nalty et al. 50 assessed mothers’ and children’s (aged 6–11 years) perspectives and experiences of child FI, including the effects of school-based and summertime nutrition programmes. Participants (48 mother–child dyads) were residents of rural areas along the Texas–Mexico border, which are communities that may lack sanitary conditions, water/drain systems and paved roads, often consist of self-build housing and are inhabited predominantly by people of Hispanic immigrant population. Data were collected through surveys during two waves between July 2010 and March 2011. Participation in school-based nutrition programmes, such as SNAP, WIC, NSLP, School Breakfast Program and Summer Food Service Program (SFSP), was recorded. Child FI was more prevalent in the summer than during the school year (62.5% vs. 18.8%; p = 0.02). With regard to mothers’ perspectives, there was no change in child FS from summer to school months (58.3% vs. 47.9%; p = 0.46). Children and mothers reported different rates of FI during the summer and school year, but these were not significantly different. After adjustment for the significant effects of school-based nutrition programmes and single parenthood, child FI improved significantly from summer to school months with protection during school offered by the school breakfast programme and NSLP as children who took part in these programmes were 70% less likely to report FI (OR 0.3, 95% CI 0.1 to 0.5; p < 0.001). However, SFSP and SNAP did not reduce the burden of FI during the summer (p > 0.05).
Barroso et al. 78 performed secondary analyses of data collected from 374 children aged 12–24 months as part of a longitudinal study that assessed the effects of a public health nursing intervention on optimal childhood growth for low-income, minority children from Hispanic mothers who were enrolled in the US WIC programme. Participants received nutrition education every 6 months. After adjusting results for potential confounders, receiving SNAP was positively associated with child weight status. Children whose mothers reported ever having received SNAP were 2.01 times more likely to be overweight than children whose mothers did not report ever having received SNAP (OR 2, 95% CI 1.0 to 3.9; p < 0.05).
Kohn et al. 74 used data from the US NHANES 2007–8 to assess whether or not participation in food assistance programmes was a risk factor for overweight and obesity in children aged 4–17 years and whether FI was a moderator of this association. School meal participation was defined as the child eating free or reduced-price school breakfast and/or school lunch at least once a week during the school year. Characteristics differed significantly by food assistance participation including age, non-white ethnicity, poverty levels and FI. Prevalence of overweight and obesity were not significantly different for children participating in food programmes compared with non-participating children. Among children participating in one food programme, school meals had the highest single-programme participation. Among low-income, food-insecure children, food assistance participation was not associated with BMI scores, high waist circumference or weight status for any specification of food assistance (adjusted analyses). However, analyses by sex showed that low-income, food secure girls participating in food assistance programmes (SNAP or WIC) other than school meals alone had higher BMI score (β 0.4, 95% CI 0.1 to 0.7) and greater risk of high waist circumference (OR 2.2, 95% CI 1.0 to 4.6). BMI scores remained elevated (β 0.3, 95% CI 0.1 to 0.6) and risk of high waist circumference approached significance (OR 2.2; p = 0.05) when analyses were corrected for differences in potential selection bias between programmes. Furthermore, among food secure boys, any food assistance participation was positively associated with all measures of weight status in analyses with direct adjustments: BMI scores (β 0.4, 95% CI 0.1 to 0.7), high waist circumference (OR 2.5, 95% CI 1.2 to 5.1) and overweight or obesity (vs. normal weight) (OR 1.7, 95% CI 1.1 to 2.8).
Yu et al. 71 examined how the effects of household characteristics, food stamps programme participation (SNAP), informal food supports (e.g. informal/community food supports, such as food pantries, Meals on Wheels and soup kitchens), household FS and child FS, differ between African American and Caucasian households. They used data from 3799 low-income participants (710 African American households and 3089 Caucasian households) who completed the Current Population Survey and the 2003 FS survey. African American households reported more participation in the food stamps programme (47.0% vs. 28.1%; p < 0.001) and more informal food supports (21.8% vs. 17.7%, respectively; p < 0.05) than Caucasian households. On the other hand, Caucasian households reported higher levels of household FS (p = 0.003). Among Caucasian households, food stamps programme participation was positively associated with female headship of a household and number of children, and negatively associated with age, hours of work and household income. Among African American households, food stamps programme participation was positively associated with female headship of a household, and negatively associated with the age of the head of a household, level of education held by the head of a household, hours of work and household income. In both ethnic groups, child FS was positively related to food stamp programme participation and informal food supports. Informal food supports positively predicted child FS in both ethnic groups (p < 0.001), but participation in the food stamps programme predicted greater child FS (p < 0.001) among Caucasian households but not among African American households.
Mhurchu et al. 122 conducted a 1-year stepped-wedge, cluster RCT in 14 low-SES schools in New Zealand to investigate the effects of a free school breakfast programme on children’s school attendance. Participating schools (clusters) crossed over from control to intervention phase in different terms throughout the school year, according to four specified different sequences. Eligible schools were low-income schools that did not have any ongoing breakfast programme, and eligible participants were children aged 5–13 years who did not have food allergies. The intervention was a free daily school breakfast programme, provided either by the national Red Cross Breakfast in Schools programme or by the private sector. A total of 424 children were enrolled in the trial, with an average of 30 children per school. Compared with the control phase, a significant decrease in children’s self-reported short-term hunger was observed during the intervention phase (p < 0.001). There were no statistically significant effects of the free school breakfast programme on children’s school attendance. The odds of children achieving an attendance rate of < 95% was 0.76 (95% CI 0.6 to 1.0) during the intervention phase and OR 0.9 (95% CI 0.7 to 1.3) during the control phase, giving an overall OR of 0.8 (95% CI 0.6 to 1.1; p = 0.19). There were no significant effects of the school breakfast programme on children’s academic outcomes.
List of abbreviations
- ASSIA
- Applied Social Sciences Index and Abstracts
- BMI
- body mass index
- CAB
- Commonwealth Agricultural Bureaux
- CACFP
- Child and Adult Care Food Program
- CCHIP
- Community Childhood Hunger Identification Project
- CDC
- Centers for Disease Control and Prevention
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- ECLS
- Early Childhood Longitudinal Study
- ECLS-B
- Early Childhood Longitudinal Survey – Birth cohort
- ECLS-K
- Early Childhood Longitudinal Study – Kindergarten cohort
- ERIC
- Education Resources Information Centre
- FI
- food insecurity
- FIES
- Food Insecurity Experience Scale
- FS
- food security
- HbA1c
- glycated haemoglobin
- HBSC
- Health Behaviour in School-Aged Children
- HDL
- high-density lipoprotein
- HDL-C
- high-density lipoprotein cholesterol
- HR
- hazard ratio
- IQ
- intelligence quotient
- NCHS
- National Center for Health Statistics
- NHANES
- National Health and Nutrition Examination Survey
- NSLP
- National School Lunch Program
- NUT
- National Union of Teachers
- OR
- odds ratio
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL
- quality of life
- RCT
- randomised controlled trial
- RQ
- research question
- SD
- standard deviation
- SE
- standard error
- SEBTC
- Summer Electronic Benefit Transfer for Children
- SES
- socioeconomic status
- SFSP
- Summer Food Service Program
- SNAP
- Supplemental Nutrition Assistance Program
- TANF
- Temporary Assistance to Needy Families
- UFSB
- universal free school breakfast
- UNICEF
- United Nations International Children’s Emergency Fund
- USDA
- United States Department of Agriculture
- WHO
- World Health Organization
- WIC
- Special Supplemental Nutrition Programme for Women, Infants and Children
