Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 12/153/39. The contractual start date was in April 2017. The final report began editorial review in February 2018 and was accepted for publication in September 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Ruth Kipping received grants from North Somerset Council and Gloucestershire Council. Ruth Kipping and Rona Campbell received grants from Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer). Laura Johnson received grants from the Elizabeth Blackwell Institute (University of Bristol) and the Wellcome Trust. Laurence Moore received grants from the Medical Research Council (MRC) and from the Scottish Government Chief Scientist Office. Rona Campbell (2015–current), Laurence Moore (2009–15) and Russell Jago (2014–current) were members of the National Institute for Health Research (NIHR) Public Health Research (PHR) Research Funding Board. William Hollingworth was a member of the NIHR Health Technology Assessment Clinical Evaluation and Trials Board. Rona Campbell was a member of the MRC Public Health Intervention Development (PHIND) Scheme Funding Board and the Board of DECIPHer Impact.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Kipping et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Parts of this chapter have been reproduced from Kipping et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Preschool children’s physical activity, nutrition and weight: a national priority
In England, 22.6% of children starting primary school are overweight or obese. 2 Obesity rates increase with deprivation; 12.7% in the most deprived areas are obese, compared with 5.8% in the least deprived decile. It is predicted that 17% of children aged 2–11 years in England will be overweight in 2020 and a further 13% will be obese. 3 Therefore, it is a priority that interventions are developed, tested and implemented with preschool-aged children to reduce their risk of developing obesity and chronic diseases.
Among children, physical activity (PA) is associated with lower levels of cardiometabolic risk factors, including blood lipids, blood pressure and improved psychological well-being. 4 Patterns of PA track moderately from childhood to adulthood, suggesting that it is linked to both short- and long-term health among children. 5 Furthermore, review evidence has identified that preschool children (aged 3 to 4.9 years) who had higher levels or increased amounts of PA were associated with improved measures of adiposity, motor skill development, psychosocial health and cardiometabolic health. 6
The English Chief Medical Officer’s recommendations are that children < 5 years of age who are capable of walking should be physically active for at least 3 hours per day and sedentary time should be minimised. 7 There is no guidance about screen time in the UK. In 2012, only 10% of 2- to 4-year-olds in England were classified as meeting the current guidelines for children < 5 years7 of at least 3 hours of PA per day. In addition, 3- to 4-year-olds in the UK are sedentary for an average of 10–11 hours per day. 7,8
A diet that is high in fruit and vegetables and low in saturated fat has been associated with reduced risk of many forms of cancer, adult heart disease and all-cause mortality. 9 Dietary patterns are often set during childhood. Children aged 1.5–10 years in the UK do not eat sufficient amounts of fruit and vegetables, and 32% of boys and 18% of girls are reported as having eaten no fruit during a 4-day period. 10 The latest national recommendation is that intake of free sugars should provide no more than 5% of total energy intake for adults and children aged > 2 years. 11 Intake of non-milk extrinsic sugars (NMES) is 12% of total daily energy intake for 1- to 3-year-olds and 13% for 4- to 10-year-olds. 12 Soft drinks contribute 10% to the intake of NMES in 1- to 3-year-olds and 13% to the intake of NMES in 4- to 10-year-olds. Saturated fat intake is also higher than the recommended 11% of total daily energy intake, at 14.6% for 1- to 3-year-olds and 13.3% for 4- to 10-year-olds. Preschool-aged children in low-income populations are more likely to consume table sugar and soft drinks than those in more affluent groups. 13
A study of the prevalence of dental caries among a sample of 5-year-old children in state-funded schools in England found that 24.7% of children had some obvious tooth decay in 2014/15. 14 The average number of teeth that were decayed, missing or filled in the whole sample was 0.8, and among those with decay it was 3.4. There is a clear correlation between higher deprivation and dental decay (R2 = 0.47) at local authority level. Poor oral health can have a negative impact on sleeping, eating, speaking, playing and socialising for children. 15 Furthermore, it is the most common reason for admission for hospital in children aged 5–9 years in England. 16 A Public Health England commissioning toolkit for oral health reviewed the evidence for a wide range of oral health interventions and found that there was some evidence for the effectiveness of healthy food and drink policies in early childhood settings and recommended this approach. 17 Furthermore, the review found that oral health training for the wider professional workforce appeared promising although there was a lack of randomised controlled trials (RCTs).
Three systematic reviews of obesity prevention, PA and nutrition in young children each identified a lack of studies in young children and a clear need for more research with robust study designs. 18–20 The 2011 Cochrane review of obesity prevention in children identified research gaps for effective interventions for children aged 0–5 years. 20 In addition, this review recommended that studies must better report the impacts on the environment, setting and sustainability. Studies should also test interventions that are guided by theory-based frameworks such as the socioecological model.
Rationale for a feasibility study on physical activity and improved nutrition in child-care settings
Child-care settings provide opportunities to deliver interventions at the population level. 21 Ninety-seven per cent of children aged 3–4 years in England attend some form of government-funded early years education, of whom 39% attend day-care providers outside school settings. 22 In England, government-funded child care for 3- and 4-year-olds increased from 15 to 30 hours/week in September 201723 (with certain conditions on parental employment), which has the potential to increase the amount of time children spend in child-care settings. However, not all child-care settings are health-promoting environments. Child-care settings provide scalable opportunities to deliver interventions at the population level. 21 The 2012 Early Years Foundation Stage (EYFS) statutory framework sets the standards to ensure that children learn, develop and are kept healthy and safe. 24 The EYFS includes somewhat limited standards for PA and healthy diet and requires nurseries to maintain a high staff to child ratio (1 : 4 for 2-year-olds, and 1 : 13 for 3- to 5-year-olds). 24 This provides nursery staff with contact during mealtimes to apply the techniques of taste exposure, encouragement, praise, and modelling of healthy eating. Furthermore, the settings can constrain or enable PA. A systematic review of the role of peers in eating behaviours and PA found that there was some evidence to support the role of peers. 25 Four out of the six PA studies reported that children were more active when peers were present. However, large peer group size was negatively associated with PA in two cross-sectional studies. 26,27 All nutrition interventions in the review reported that children’s eating behaviours may be influenced by their peers.
The Children’s Food Trust published voluntary guidelines for food in early years settings in 2012. 28 In addition, PA guidelines for young children in England were published in 2011. 7 The English 2016 Childhood Obesity strategy is very limited with respect to preschool children,29 but local authorities in England and Wales are increasingly developing and implementing their own programmes to support healthy interventions in early years settings. We have reviewed the local authority websites for the Core Cities in England and found all (except one) have some form of healthy early years programme. In Wales, the Healthy and Sustainable Pre-School Scheme was started in 2011 on seven health topics: Nutrition and Oral Health; Physical Activity/Active Play; Mental and Emotional Health, Wellbeing and Relationships; Environment; Safety; Hygiene; and Workplace Health and Wellbeing. 30 These programmes all include nutrition and some have additional health topics. However, none of these programmes has been evaluated for effectiveness through a RCT. Therefore, new approaches are required to prevent obesity and reduce inequalities in early years settings.
Assessment of PA in 3- to 5-year-old children at preschool has shown that they are physically inactive during most of their time in preschool, with only 3% of time engaged in moderate to vigorous physical activity (MVPA). MVPA is closely associated with cardiorespiratory fitness and body mass index (BMI) in adolescence; therefore, it is of concern that such a small proportion of time in preschool is spent in MVPA. Furthermore, about 80% of time is spent in sedentary activities. 31 However, studies have found different levels; one study found that children aged 3–4 years in the UK (in particular boys) spent more time in MVPA and were less sedentary when in child care than when at home. 32 The particular preschool that a child attends is a strong predictor of PA levels, and being outdoors is one of the most powerful correlates of PA in children. 31 The lack of MVPA in preschool settings may be influenced by space constraints, a lack of equipment, a lack of policies and a lack of scheduled times for free play and outdoor play and a lack of staff training in PA promotion. 19 A systematic review of interventions to increase PA in child-care settings concluded that regularly provided, structured PA programmes can increase the amount and intensity of PA undertaken. 33
Larson et al. 18 reviewed the regulations, practices, policies and interventions for promoting healthy eating and PA and for preventing obesity in children attending child care. The review identified a lack of strong regulation in child-care settings in relation to health behaviours, such as PA and diet. A 2016 Cochrane review of strategies to improve healthy eating, PA and obesity prevention in child-care services found that:
Weak and inconsistent evidence of the effectiveness of such strategies in improving the implementation of policies and practices, childcare service staff knowledge or attitudes, or child diet, physical activity or weight status. Further research in the field is required.
Wolfenden et al. 33
There is ample opportunity within child-care settings to improve nutritional quality, oral health, time engaged in PA and promotion of health behaviours by caregivers. Other than Nutrition And Physical Activity Self Assessment for Child Care (NAP SACC) (see NAP SACC), a small number of RCTs based in child-care settings that aim to improve nutrition and/or PA or sedentary time with 2- to 4-year-olds have been published (Table 1). The studies focused on education, staff development, and addressing child-care policies or opportunities for increasing PA. Many, but not all, of the studies reported small changes in children’s PA, sedentary time or nutrition in the short term. Only one intervention showed an effect on weight. 40 There was a lack of long-term follow-up or demonstration of effect across a wide range of anthropometric and behavioural changes. Only four of the studies were in the UK and none of these targeted both diet and PA within child-care settings.
| Name of study/first author | Type of intervention | Setting; country (age range) | Results for the intervention arm compared with the control arm |
|---|---|---|---|
| Family Focused Active Play34 | Family-focused intervention to decrease sedentary time and increase PA for 10 weeks | Surestart Centres; England (3–4.9 years) | 1.5% and 4.3% less sedentary time during week and weekend days, respectively, and 4.5% and 13.1% more PA during week and weekend days, respectively |
| Active Play35 | 6-week local authority staff-led training (active play) to help preschool staff deliver 60-minute weekly sessions compared with a resource pack | Preschools attached to Surestart Centres; England (3–4.9 years) | Assessment of 162 children found no evidence for differences in total fundamental movement skill, object control skill or locomotor skills scores |
| Alhassan36 | An increase of 60 minutes per day in time spent outdoors for 2 days | Head Start Centers; USA (3–5 years) | No difference in total daily PA |
| Specker37 | Children assigned to gross motor or fine motor group for 1 year | Nursery; USA (3–5 years) | Time spent in vigorous activity was higher in the gross motor group at 18 months but not 24 months |
| Brocodile the Crocodile38 | Seven educational sessions encouraged to reduce time spent watching TV | Nursery; USA (2.6–5.5 years) | –4.7 hours per week television/video viewing (95% confidence interval –8.4 to –1.0 hours per week; p = 0.02) |
| CHERRY39 | An exploratory trial, focused on family-centred nutrition | Children’s Centres; England (1.5–5 years) | Positive, but non-significant, changes in fruit and vegetables, decreasing sugary drinks and snacks |
| Healthy Caregivers/Children40 | Curricula for teachers/parents, menu modifications and policies for nutrition, PA and screen time | Children’s Centres; USA (2–5 years) | Mean child BMI increased in control centres from 0.43 to 0.55 kg/m2 and smaller increases were seen in intervention centres (0.46 to 0.49 kg/m2). The environmental assessment (EPAO) total nutrition score improved in the intervention centres (12.4 to 13.5) with no change in control schools (12.5 to 12.6). Little changes in the EPAO PA scores |
| Hip-Hop to Health41 | Healthy eating and PA lessons for 14 weeks | Preschools; USA; (3–5 years) | More MVPA (difference between adjusted group means = 7.46 minutes per day, p = 0.02) and less total screen time (−27.8 minutes per day, p = 0.05). No differences in BMI, zBMI, or dietary intake |
| Move and Learn42 | Integration of PA into preschool half-day over 8 weeks | Preschools; USA; (3–5 years) | In 2 out of the 8 weeks, the levels of PA were higher than in the other weeks |
| Munch and Move43 | Professional development to promote healthy eating and PA among children | Preschools; Australia; (mean age 4.4 years) | FMS improved (p < 0.001) and the number of FMS sessions increased by 1.5 per week (p = 0.05). Sweetened drinks reduced by 0.13 servings (46 ml) (p = 0.05) |
| PAKT44,45 | 30-minute/day PA intervention delivered by preschool teachers, with homework over 1 year | Preschools; Germany; (mean age 4.7 years) | The intervention found no evidence for improvement in PA measured by accelerometers between groups |
| Preschool nutritional intervention46 | Sessions by nutritionists with some parent involvement. Activities covered different foods, preparing food and eating behaviour | Preschools; Germany; (3–6 years) | Fruit and vegetable intakes increased by 0.23 and 0.15 portions per day (p < 0.001 and p < 0.05, respectively). No changes in water or sugary drinks consumed |
| MAGIC47 | Nursery and home elements with enhanced PA programme and materials for home | Nursery; Scotland; (mean age 4.2 years) | No differences in BMI, PA or sedentary behaviour |
| SHAPES48 | Ecological PA intervention in preschools: preschool teachers trained to engage children in PA during (1) structured, teacher-led PA opportunities in the classroom; (2) structured and unstructured PA opportunities at recess; and (3) PA integrated into preacademic lessons | Preschools; USA; (4 years) | Children in intervention schools engaged in more MVPA than children in control schools (7.4 and 6.6 minutes per hour, respectively; p = 0.01). In the analysis by gender there was evidence of a difference for girls (6.8 vs. 6.1 minutes per hour of MVPA, respectively; p = 0.04) but not for boys (7.9 vs. 7.2 minutes per hour, respectively; p = 0.1) |
| Tigerkids49 | Modules on PA, fruit and vegetables and waste | Preschools; Germany; (3–5 years) | Higher consumption of fruit and vegetables at 6 months, which was sustained at 18 months |
| Toy box50,51 | Preschool-based, family-involved intervention to influence obesity-related behaviours in 4- to 6-year-olds in Europe | Preschools; six European countries; (4–6 years) | Evaluation of the effectiveness of the study of 472 preschool children (mean age 4.43 years) from 27 kindergartens in Flanders found small increases in PA in the whole sample. The greatest effects were found in boys and in preschoolers from high-SES kindergartens |
Ongoing randomised controlled trials
Internationally, several trials in early years settings or with families of preschool children are currently being conducted with the aim of improving nutrition and/or PA, which further demonstrates the importance of improving health for this age group:
-
Jump Start is a multicomponent PA intervention for children aged 3–5 years in Australia. The intervention uses lessons in preschool and a home-based component with the primary outcome of total activity (accelerometer measured) during centre hours. 52
-
The Healthy Start-Départ Santé intervention is being tested in preschools with children aged 3–5 years in Canada. The intervention aims to enable parents and preschool staff to integrate PA and health eating into the day. 53
-
The DAGIS study (increased health and wellbeing in preschool) is a preschool intervention that is being developed with the aim of reducing inequalities in energy balance-related behaviours in preschoolers aged 3–5 years in Finland. 54,55
-
In Norway, a web-based programme to reduce food-related fears and promote healthy dietary habits in 1-year-olds is being studied through a trial design with two different interventions. 56
-
The physical Literacy in the Early Years (PLEY) Project in Nova Scotia (Canada) is aiming to determine if 3- to 5-year-old children who participate in active outdoor play in Childcare Centres, facilitated by educators trained in embedding loose parts into outdoor play spaces, develop greater physical literacy. 57
-
Smart Moms is a 6-month smartphone intervention in North Carolina (USA) that aims to reduce sugar-sweetened beverage and juice consumption among children aged 3–5 years with overweight or obese mothers. 58
-
The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) is a trial in Australia testing a 33-month intervention using web-based materials and Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) with parents of infants, alongside the pre-existing six 2-hour sessions given quarterly to first-time parents. 59
NAP SACC
The NAP SACC intervention was chosen to be adapted and piloted in the UK in this study. 60 NAP SACC, which was developed in the USA, is focused on improving nutrition and PA environment, policies and practices in child-care centres through self-assessment and targeted technical assistance. It addresses PA, sedentary behaviours and nutrition by allowing providers to choose where they focus change. The NAP SACC approach, which uses data, evidence-based action-planning, choice, support, engagement and ownership, tailoring and sustained change, has been used in other UK public health interventions. RCTs of NAP SACC in the USA have demonstrated the feasibility and acceptability of the intervention, the effectiveness of improving the environmental audit nutrition score [11% improvement from a baseline Environment and Policy Assessment and Observation (EPAO) score of 8.6],60 increase in nursery staff’s knowledge of childhood obesity, healthy eating, personal health and working with families (all at a p < 0.05 level), decrease in children’s body mass index z-scores (zBMI) (p = 0.02)61 (a measure of relative weight adjusted for child age and sex) and an increase in accelerometer-measured PA by 17% (p < 0.05) and a 46.2% increase in vigorous activity (p < 0.05). 62 NAP SACC was updated in 2014 and the revised online version, called ‘Go NAP SACC’, includes expanded best practices and is the version which NAP SACC UK is based on, excluding the materials for breastfeeding. 63
NAP SACC is one of the few interventions that works with child-care providers to produce sustainable changes in the child-care environment and promote improvements in children’s activity levels and nutritional intake. NAP SACC has been widely adopted throughout the USA, which demonstrates that it is a model that, if shown to be effective, could easily be disseminated in the UK. NAP SACC has not previously been assessed for feasibility or acceptability of use in the UK or with direct measures of nutrition or BMI. In addition, some issues of fidelity to the intervention were encountered in the US trial, which were addressed through this feasibility study.
NAP SACC UK
The development and final version of NAP SACC UK (Nutrition And Physical Activity Self Assessment for Child Care UK version), following the phase 1 study, is outlined in detail in Chapter 2. To orientate the reader, the NAP SACC UK intervention, as used in the feasibility study, involved health visitors (called NAP SACC UK partners) supporting nursery staff to (1) review the nutrition, oral health, PA and screen time environment, policies and practices against best practice and national guidelines, (2) support staff to set goals and (3) provide targeted assistance over 5 months. Two workshops were delivered to nursery staff by local experts. A home intervention [website, short message service (SMS) and e-mails] was developed to support parents to set goals.
The subsequent chapters outline the methods and results for the two phases of the feasibility RCT and the two substudies. This is followed by the lessons learnt and discussion.
Chapter 2 The NAP SACC UK feasibility study overview
Parts of this chapter have been reproduced from Kipping et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
In this chapter the feasibility study aims and objectives, study design, progression criteria, trial registration, governance, ethics, safety and public involvement are outlined.
Study aim and objectives
The aim of the feasibility study was to evaluate the feasibility and acceptability of implementing and trialling an adaptation of the NAP SACC intervention, with a home component in nursery settings. The study had one primary objective and three secondary objectives.
Primary objective
-
To assess whether or not prespecified criteria relating to the feasibility and acceptability of the intervention and trial design are met sufficiently for progression to a full-scale RCT.
Secondary objectives
-
To explore the experiences of nursery staff, the intervention delivery team and parents/carers, in terms of acceptability, barriers, fidelity to and facilitators of the intervention, data collection methods and participant burden, and the feasibility of long-term follow-up with the aim of informing refinement of the intervention and study design prior to a potential full-scale RCT.
-
To pilot primary and secondary outcome measures and economic evaluation methods, and determine the practicality of data linkage for BMI through the Child Measurement Programme in England66 and Wales,67 in advance of a potential full-scale RCT.
-
To calculate the sample size required for a full-scale RCT and to estimate likely recruitment, attendance, adherence and retention rates.
Feasibility study design
The feasibility study had two phases:
-
Phase 1: intervention adaptation and development, in which the NAP SACC materials were adapted for use in the UK and the NAP SACC UK home component to involve parents/carers was created.
-
Phase 2: feasibility cluster RCT with embedded process evaluation and health economic methods (Figures 1 and 2). The logic model for the NAP SACC UK intervention is shown in Figure 3.
FIGURE 1.
Phase 1 flow diagram.
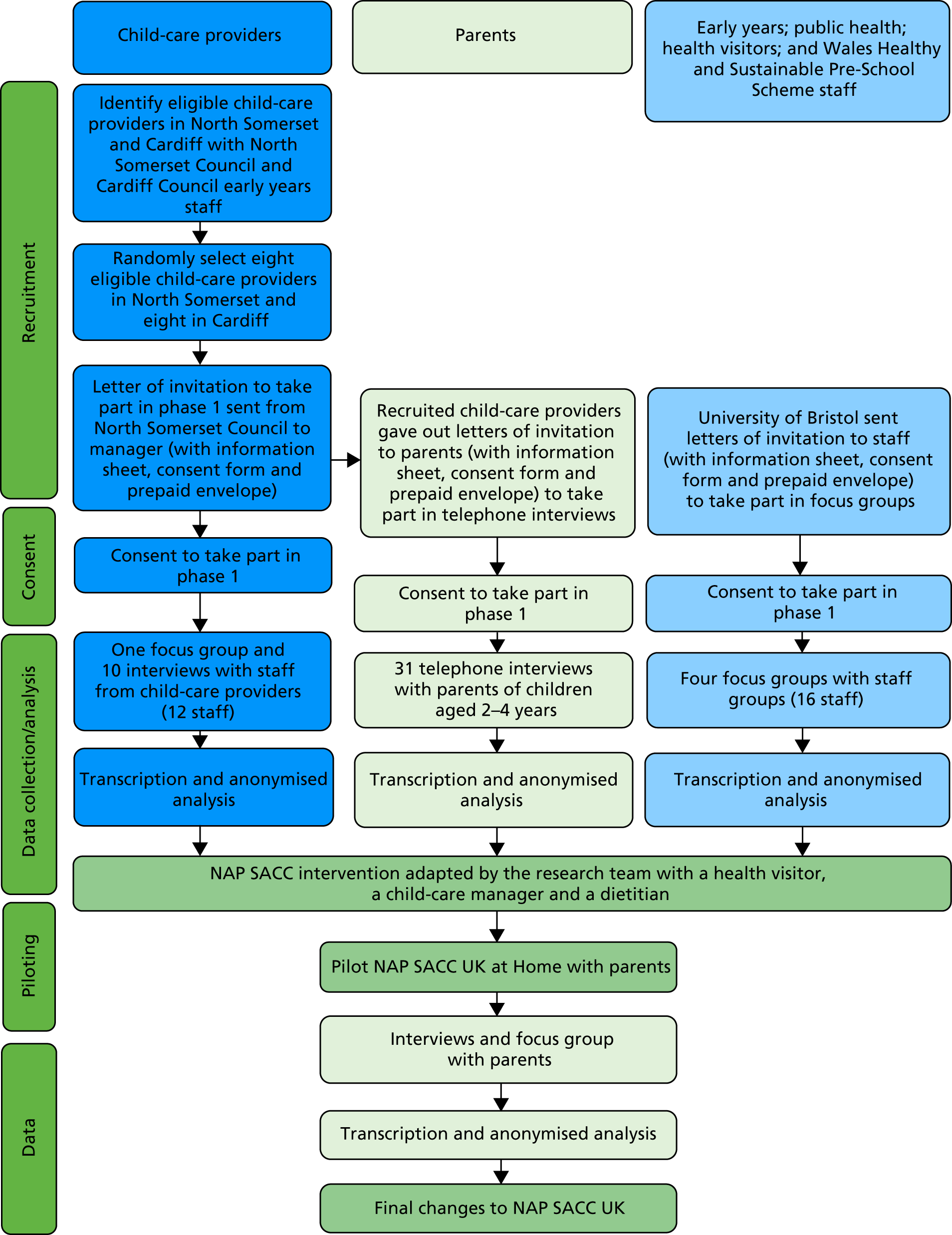
FIGURE 2.
Phase 2 flow diagram.
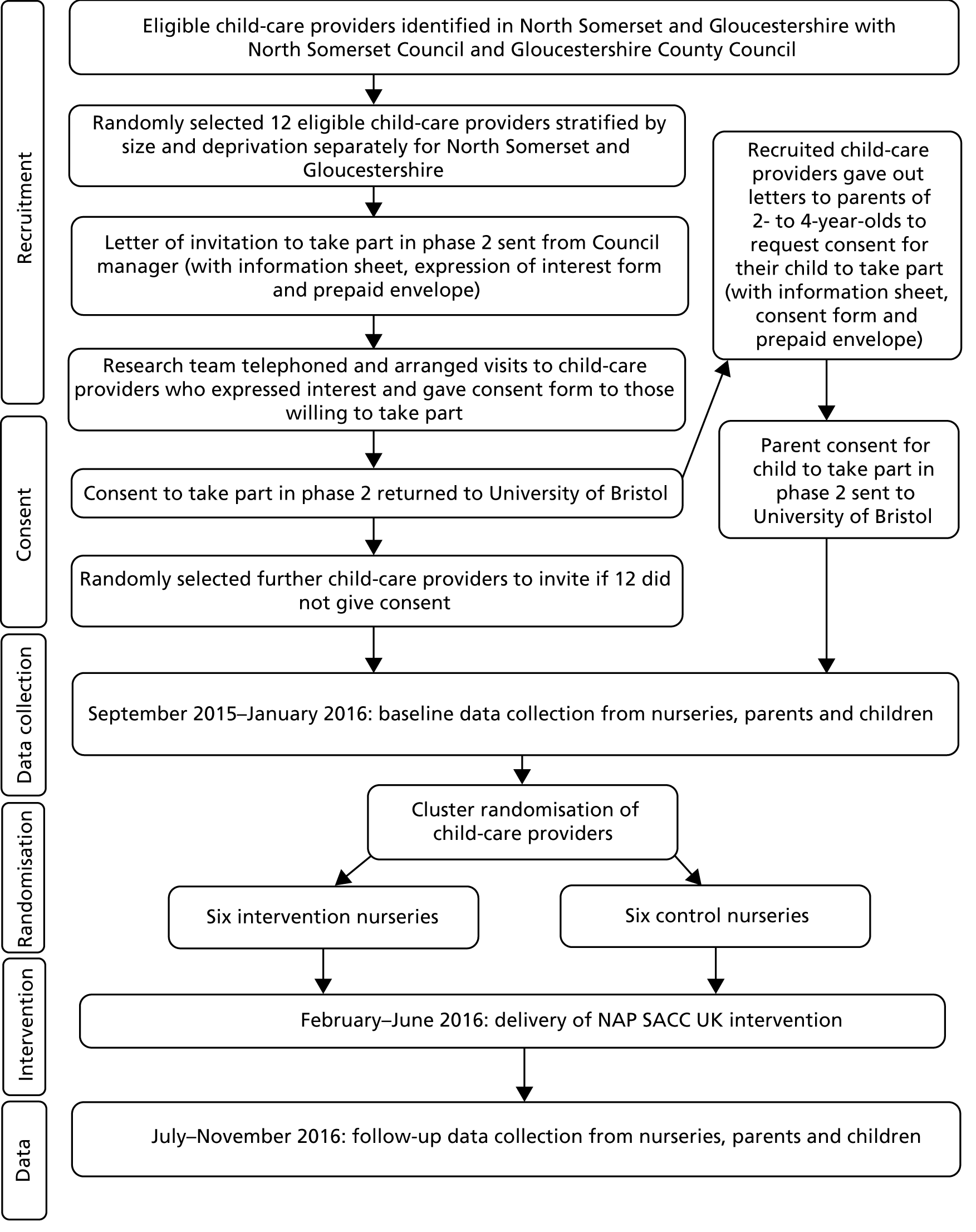
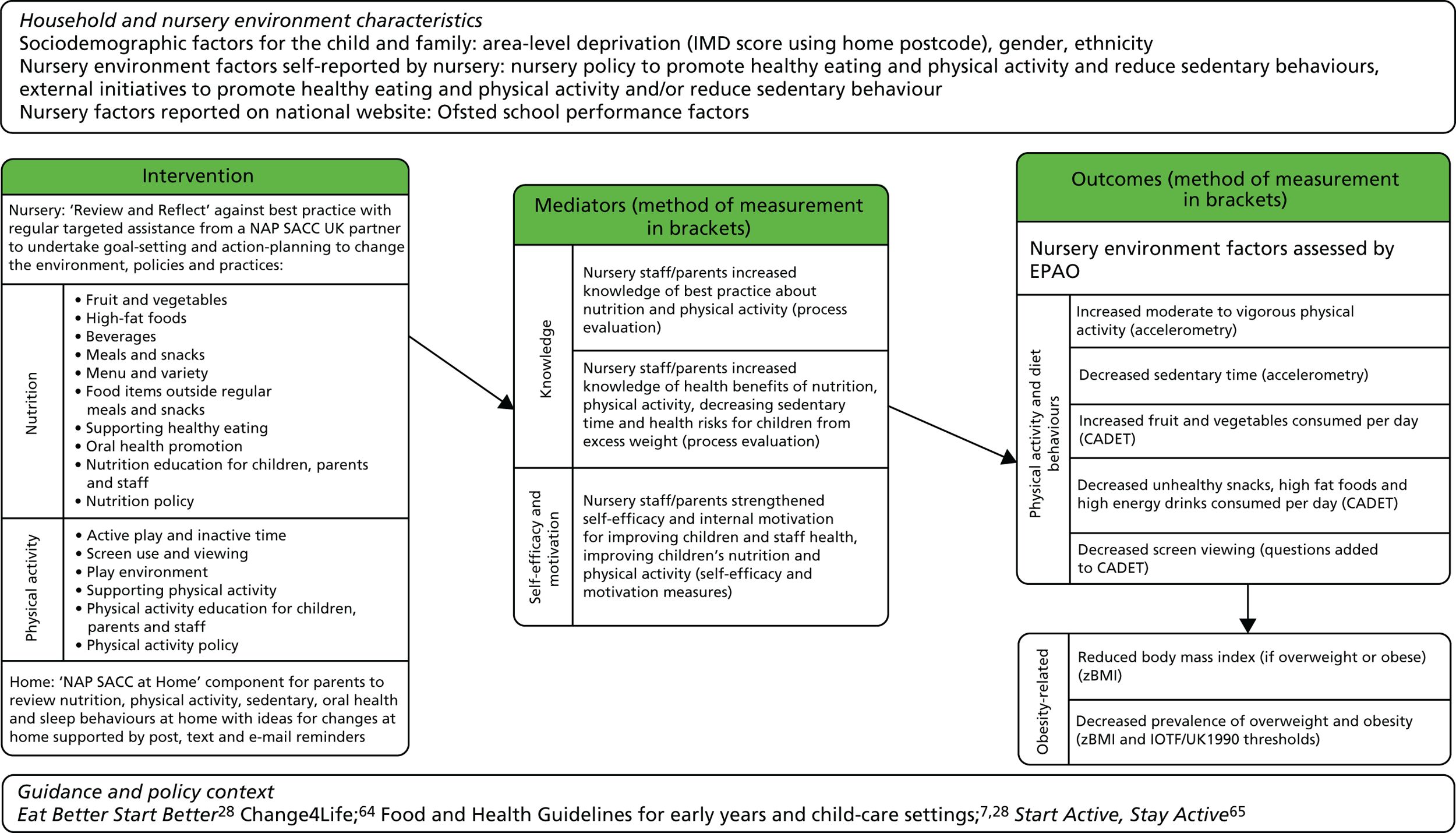
FIGURE 3.
Logic model of NAP SACC UK. IOTF, International Obesity Task Force.
The protocol for the study has been published. 1
Progression criteria
The predefined progression criteria for the trial, as agreed with the external Trial Steering Committee (TSC) and the funder [National Institute for Health Research (NIHR)], were the following.
Criterion 1: feasibility
-
Was it feasible to implement the NAP SACC UK intervention in child-care providers? This was assessed according to (1) at least 40% of contacted eligible child-care providers expressing a willingness in principle to take part in the feasibility trial in response to an invitation to take part; and (2) a synthesis from the different aspects of the process evaluation [observation, interviews and analysis of meeting logs between NAP SACC UK partners (health visitors) and child-care providers].
Criterion 2: acceptability of intervention
-
Was the intervention acceptable to NAP SACC UK partners? This was assessed via interviews with partners and analysis of meeting logs between NAP SACC UK partners and child-care providers.
-
Was the intervention acceptable to the majority of child-care managers, staff and parents/carers? This was assessed via interviews with managers, staff and parents/carers.
Criterion 3: acceptability of the trial design
-
Were the trial design and methods acceptable? This was assessed according to (1) expressions of interest from eligible child-care settings; (2) interviews with child-care providers about randomisation and data collection; (3) at least a 40% parental opt-in consent rate for measurements with eligible 2- to 4-year-old children; (4) a maximum loss to follow-up of three providers (or no more than two in any arm) or 40% of children; (5) a synthesis of interviews with parents/carers about data collection.
Trial registration, governance and ethics
The study was approved by Wales Research Ethics Committee 3 prior to recruitment and data collection commencing (formative work 14/WA/1134; pilot RCT 15/WA/0043; process evaluation 15/WA/035). The trial protocol was registered with Current Controlled Trials (ISRCTN16287377: www.isrctn.com/ISRCTN16287377). Ethics approval for the mediator questionnaire substudy was obtained from the Faculty of Health Sciences Research Ethics Committee at the University of Bristol (reference 41585). Ethics approval for the nursery food photography feasibility substudy was obtained from the University of Bristol School for Policy Studies Research Ethics Committee in November 2017. The feasibility RCT was overseen by a TSC, comprising an independent chairperson and four independent members. The TSC met approximately 6-monthly throughout the study (with one 12-month gap), meeting five times in total, to examine trial progress, conduct and scientific credibility. This was a pilot trial with no interim analysis and, therefore, the TSC and funder agreed that a separate Data Monitoring and Safety Committee was not necessary.
Safety
Child-care providers were given contact details for the trial manager and were able to contact the study team if they had any concerns or parents/carers report concerns. Nursery managers and those delivering the intervention (health visitors and trainers) were asked to contact the study team within 5 working days if any untoward incident or adverse event (AE) occurred to a member of staff or child, as a direct result of taking part in NAP SACC UK, or because of changes that have occurred in the nursery environment as a result of participation in NAP SACC UK. Study-specific AE/incident report forms were available to be used to record information on the event. No AEs or serious AEs were reported associated with the intervention or trial.
Public involvement
A patient and public involvement group was set up early in the project to provide advice and guidance. Parents, child-care staff, health visitors, local authority early years staff, public health specialists, health improvement staff and a dietitian were invited to participate. The first meeting was held in March 2015, during phase 1 of the project, as phase 2 (a feasibility RCT) was being planned. The topics discussed included the wording of parent questionnaires, wording of the questionnaire around future use of anonymised data, the content and delivery of the nursery staff workshops that made up a key component of the intervention, the home component, ‘NAP SACC at Home’, and suitable thank you gifts for the children involved. This first meeting was well attended (nine lay members). The next meeting, held in February 2016 with the same group invited, was very poorly attended (one lay member). This meeting was held after baseline data collection, prior to the intervention. The main topic for discussion was the home component, ‘NAP SACC at Home’, particularly how to engage parents and children, the suitability of sending tips by text and e-mail, how to encourage parents to set goals, and the use of a NAP SACC UK Facebook group.
The final meeting was held in July 2017 at the end of the study. This time only nursery managers were invited (five attended) and the meeting was used to discuss improvements that could be made to the NAP SACC intervention and data collection methods following issues identified during the feasibility study. Topics discussed included how to approach nurseries and parents to improve recruitment, incentives for nurseries to participate, dietary measures and the possibility of weighing or photographing food consumed by children, intervention delivery and the impact of the government-funded 30 hours of child care due to start in September 2017. This was a very useful meeting with good engagement from nursery managers, who provided useful insights.
Changes made to the protocol and intervention following phase 1
Change of phase 2 study site
During the funding process, NIHR suggested that an urban area with greater ethnic diversity be included in addition to North Somerset to ensure greater generalisability. The plan was to keep Bristol available for a full trial and, therefore, we proposed that Cardiff be involved. There was subsequently a change of site from Cardiff to Gloucestershire, which required a protocol amendment. Full details of this decision are shown in Table 30, Appendix 1. This was agreed with the sponsor, TSC and NIHR. The collaborators’ agreement was signed by the two new organisations. This created a delay in recruitment of nurseries in Gloucestershire, but the change improved our understanding of the feasibility of undertaking this study by involving another local authority area in England given the complexity of interventions and different nursery provision encountered in Wales.
Shortening the intervention
As recruitment of nurseries was delayed by the change to include Gloucestershire, we agreed with the TSC to shorten the intervention to 5 months. Therefore, baseline data collection was carried out from September 2015 to January 2016. Randomisation took place in February 2016. The intervention period was 1 February 2016 to 30 June 2016. The NAP SACC UK at Home element was launched to parents in April and May 2016. Follow-up data collection was completed at 8 out of the 12 nurseries in July 2016. The remaining four nurseries were left until September 2016 to assess the feasibility of following up those children who had left nursery to start school.
Chapter 3 Feasibility study phase 1: methods
This chapter provides an overview of the study aims and objectives, study design, methods and results of phase 1 of the study where we adapted NAP SACC to the UK setting and developed a home component.
Phase 1 eligibility and recruitment
A purposive sample of eight child-care providers in North Somerset and eight child-care providers in Cardiff were sent a letter inviting the child-care provider staff to take part in a focus group or telephone interview to inform the development of the NAP SACC UK trial. A letter, project information sheet, reply envelope and form indicating if they wish to participate in a focus group or telephone interview were sent. The sample of child-care providers included private day nurseries as well as community preschools and Children’s Centre nurseries but did not include parent-and-child playgroups or crèches. North Somerset and Cardiff were selected because these are the areas where the RCT was originally intended to take place, Gloucestershire was substituted for Cardiff for phase 2. The two areas provided diverse localities within England and Wales, including urban and rural settings, with a range of deprivation and ethnicity indices.
Health visitors in North Somerset, Wales Healthy and Sustainable Pre-School Scheme (WHASPS) staff in Cardiff and early years staff working at local authorities in North Somerset and Cardiff were sent the same information inviting them to take part in separate focus groups. Written informed consent was taken before the focus groups and telephone interviews commenced.
Phase 1 data collection procedures
Twelve (75%) nurseries were recruited, eight in North Somerset and four in Cardiff. The recruited child-care settings were asked to send parents with children aged 2–4 years a letter, project information sheet, reply envelope and form indicating if they wish to participate in a telephone interview to discuss the NAP SACC UK intervention and trial.
Interviews were conducted with parents in sufficient numbers until saturation was reached and followed a semistructured format with follow-up probes on key topics of interest. Questions focused on ways in which the NAP SACC intervention could be adapted to involve parents and methods of maximising participation in the trial. Each telephone interview lasted 30–45 minutes, was conducted by a trained researcher and was recorded using an Olympus DS-2200 Digital recorder (Olympus DS-2200 Digital recorder, 2 Corporate Center Drive, Melville, NY, USA).
Focus groups were initially chosen as the method of data collection for nursery, early years and public health staff. Focus groups are an effective method of collecting qualitative data as the thoughts and ideas of some members of the group can often encourage others to verbalise their responses in a comfortable, safe and supportive environment. 68 Each focus group lasted 45–60 minutes, was conducted by a trained moderator and was recorded using an Olympus DS-2200 digital recorder.
The focus groups had a semistructured design with follow-up probes on key topics of interest. Questions focused on which aspects of NAP SACC needed to be adapted to incorporate UK guidance, recommendations and terminology; how NAP SACC could be adapted to include parents; what additional training could be provided to child-care staff to increase structured active play; how the intervention could be promoted to child-care providers; what factors might influence low participation and adherence to the programme and study; and what strategies should be used to maximise participation.
Owing to the logistical difficulties of arranging focus groups with nursery staff, it was later decided to hold telephone interviews for most nursery staff. The same topic guides were used for the nursery staff interviews as they were for the focus groups and ethics approval was given for the change.
In addition to discussing how NAP SACC could be adapted to the UK during focus groups and interviews, potential changes to NAP SACC were discussed during meetings with a group of local experts, including a community dietitian, oral health and PA specialists, as well as with the study Trial Management Group, the TSC and the founder of NAP SACC (and co-applicant), Dianne Ward.
Phase 1 data analysis
The interview and focus group recordings were transcribed verbatim and anonymised. Tapes were erased and destroyed after transcription. All identifying data were removed from the transcripts. The qualitative software analysis package NVivo (Version 10, QSR International, Warrington, UK) was used to support analysis and data management. As the data were exploratory, a thematic analytical approach was used. A member of the research team indexed a subset of transcript data to construct a coding framework. Codes were then applied to the remaining transcript data. Codes were assembled to construct emergent themes, which were refined and agreed through discussions between the research team. All participant narratives were equally privileged in the generation of new theoretical and empirical insights. Anonymised data were presented in the form of quotes.
Feasibility study phase 1: results
This chapter presents the results from phase 1 of the feasibility study, which aimed to inform the adaptation of the NAP SACC intervention for use in the UK and the creation of a home component and to refine the RCT methods.
Recruitment
Participant characteristics are shown in Table 2. A total of 12 nursery managers, 31 parents and 15 public health and early years staff participated in the study. More than 90% of the participants were female. Four focus groups were conducted with public health and early years staff, along with one focus group for nursery staff. All 31 parents were interviewed by telephone.
| Place | Group | Number | Total | |
|---|---|---|---|---|
| In focus groups | Of interviews | |||
| North Somerset | Parents (all) | N/A | 21 | 21 |
| Low-SES parents | N/A | 1 | 1 | |
| Middle-SES parents | N/A | 12 | 12 | |
| High-SES parents | N/A | 8 | 8 | |
| Nursery managers | 2 | 6 | 8 | |
| Public health/early years staffa | 6 | N/A | 6 | |
| Cardiff | Parents | N/A | 10 | 10 |
| Low-SES parents | N/A | 0 | 0 | |
| Middle-SES parents | N/A | 5 | 5 | |
| High-SES parents | N/A | 5 | 5 | |
| Nursery managers | N/A | 4 | 4 | |
| Public health/early years staffb | 9 | N/A | 9 | |
| Total | Parents (all) | N/A | 31 | 31 |
| Nursery managers | 2 | 10 | 12 | |
| Public health/early years staffb | 15 | N/A | 15 | |
Child-care context
Table 3 shows the breakdown of nurseries by location, socioeconomic status (SES), type of nursery, number of 2- to 4-year-old children registered at the nursery, and meal and/or snack provision. The SES of the nursery was based on the Index of Multiple Deprivation (IMD)69 in England and the Welsh Index of Multiple Deprivation (WIMD)70 in Wales. The IMD is an English Government-produced measure of deprivation that includes assessments of income, employment, health and education. 69 WIMD is the official measure of relative deprivation for small areas in Wales, which includes assessments of income, employment, health, education, access to services, community safety, physical environment and housing. 70 The IMD/WIMD was obtained for the postcode of each nursery and thus represented a measure of deprivation for the nursery and not the individual participant. The nurseries were then stratified into low-, middle- and high-SES tertiles.
| Child-care setting number | Location of child-care setting | SES of child-care setting | Type of child-care setting | Number of 2- to 4-year-old children at child-care setting | Food provided |
|---|---|---|---|---|---|
| 1 | North Somerset | High | Community preschool | 40 | Meals and snacks |
| 2 | North Somerset | High | Community preschool | 16 | Snack only |
| 3 | North Somerset | Middle | Private day nursery | 48 | Meals and snacks |
| 4 | North Somerset | Middle | Children’s centre nursery | 105 | Meals and snacks |
| 5 | North Somerset | High | Community preschool | 45 | Snack only |
| 6 | North Somerset | Low | Private day nursery | 35 | Meals and snacks |
| 7 | North Somerset | Middle | Private day nursery | 60 | Meals and snacks |
| 8 | North Somerset | Middle | Private day nursery | 42 | Meals and snacks |
| 9 | Cardiff | High | Private day nursery | 50 | Meals and snacks |
| 10 | Cardiff | Low | Private day nursery | 30 | Meals and snacks |
| 11 | Cardiff | Middle | Private day nursery | 63 | Meals and snacks |
| 12 | Cardiff | High | Community preschool | 55 | Snack only |
Eight nurseries were based in North Somerset, of which four were registered as private day nurseries, three as community preschools and one as a children’s centre nursery. Four nurseries were based in Cardiff, of which three were registered as private day nurseries and one as a community preschool. Across both sites, two nurseries were classified as low SES, five were middle SES and five were high SES. The number of 2- to 4-year-old children registered at the nurseries ranged from 16 to 105. A total of 75% of the sample of nurseries provided meals and snacks for children, which were prepared in-house. The remainder, all of which were community preschools offering sessional care, provided snacks only. Information regarding the ethnic diversity of the child-care settings was unavailable but one-third of the nurseries were based in Cardiff, which is ethnically diverse (17.2% from a non-white background). 70
Nursery environment
Healthy nursery environment: nutrition (parents and nursery managers)
Parents and nursery staff generally reported a good standard of nutrition in nurseries:
We take fruit in, in the morning. So that’s part of the routine, is putting the fruit together in a bowl. And . . . if you bring in something more unusual than just an apple or a banana then they . . . sort of talk about it with the children.
Parent_Mid_SES_Nursery_1
With us the majority of the time we have fruit and natural yoghurt for dessert, there’s always veg either in with the meal or as part of the meal.
Manager_High_SES_Nursery_9
However, knowledge of and use of nutritional guidance varied between settings, ranging from specific food safety guidance for caterers, to recipes from early years magazines, to no guidance at all:
. . . the owner and the management team and the cook . . . we all throw ideas about what we are going to provide.
Nursery Manager_High SES_Nurser_9
We usually follow the Safer Food Better Business for Caterers guidance and also the schools’ guidance as well, the local authority guidance as well . . . and of course anything else that comes out via research . . .
Manager_Mid_SES_Nursery_4
. . . that’s between me, as the owner, and my cook as what we can cook and what we can afford . . .
Manager_Mid_SES_Nursery_3
. . . Um at the moment we just get it from, you know, early years magazines, etc.
Manager_Mid_SES_Nurser_4
Interestingly, none of the North Somerset settings had used, or even heard of, the Children’s Food Trust’s 2012 report, Eat Better, Start Better: Voluntary Food and Drink Guidelines for Early Years Settings in England. 28
Healthy nursery environment: physical activity (parents and nursery managers)
Parents and staff of most nurseries reported that there was space and equipment for children to be physically active:
It’s a new building and they’ve got a very large central play area, as well as a separate outdoor play area.
Parent_Mid_SES_Nursery_4
They’ve got an outdoor area at the front and back . . . they are always out on bikes or they have a couple of little plastic cars, so they are always charging around out there.
Parent_Mid_SES_Nursery_7
. . . we’ve got . . . the Sticky Kids’ CDs [compact discs] which we do, and we’re outside nearly all day.
Manager_Low_SES_Nursery_6
However, one setting had only indoor space available to children:
This playgroup doesn’t have a garden . . . so they are very much confined to indoors . . . with regards to physical activity as far as I know there’s not massive of stuff organised.
Parent_High_SES_Nursery_12
The majority of parents also reported that their children spent time outdoors at their nursery, but there was variation in whether this was ‘all weather’ or only on fine days:
My son especially loves the outside and I think that’s why he really enjoys it there. He has in the past got upset because he couldn’t go outside because it’s raining.
Parent_High_SES_Nursery_5
We have to make sure they have wellies and waterproofs so yes they can go out anytime.
Parent_Mid_SES_Nursery_7
Some parents reported that their child’s nursery never took children off premises for PA or outdoor play, which they had mixed reactions to:
Because they’ve got quite good outdoor facilities, the garden is big enough, they don’t really need to. They are in the city centre so I don’t think it’s very practical to be honest.
Parent_Mid_SES_Nursery_11
I don’t think they take them outside. It is a shame . . . there is park land within 2 minutes of where they are, so they definitely could take them outside.
Parent_High_SES_Nursery_12
Screen time mainly consisted of children taking turns on a computer, and was reasonably limited across settings:
We’ve only literally got one computer, and to be fair that’s not on every day.
Manager_ Mid_SES_Nursery_8
However, one nursery reported that they relied on the television to keep children occupied while cleaning the nursery:
This week’s been particularly bad weather, so while I need to clear up my dining room, which is also our playroom, I use the television because it’s been wet and windy and they haven’t wanted to go outside.
Manager_Mid_SES_Nursery_3
NAP SACC intervention
Nursery staff were asked to look at the questions on the self-assessment form and provide feedback on their clarity, appropriateness and fit with UK standards. They were also asked to comment on the length of the draft document. Overall, nursery staff were positive about the NAP SACC approach of self-assessment:
. . . I thought they were quite . . . reflective and . . . not too off-putting either . . . and you just literally tick boxes, which is what we always like.
Manager_Mid_SES_Nursery_3
You know, when you said 70 questions I thought, ‘Ooh’. But actually they’re quite straightforward.
Manager_High_SES_Nursery_2
However, the absence of a section on oral health in the self-assessment form was noted to be a growing concern in nurseries:
. . . one thing that has come to our attention in nurseries . . . is children’s teeth . . . more so than obesity, I feel. We have three children at the nursery . . . one . . . is 2 years old and her teeth are rotten . . . another little boy . . . has a hole in his tooth . . . another little girl . . . has got holes in her teeth . . . to the point where she needs them out. And I think . . . we need to put . . . oral health in there somewhere.
Manager_Mid_SES_Nursery_3
Regarding the action-planning document, nursery staff suggested reducing the number of goals required to be set over a 6-month period:
I don’t know whether 10 would be manageable in 6 months, besides everything else that people have to do as well. 10 just seems quite a lot. I’ve got action plans that I might have 10 on but I’m going to spend a whole year covering those. 6 months to do 10 is quite a lot I think.
Manager_Low_SES_Nursery_10
We usually have, when we do anything in child care, we usually use three or four goals, targets.
Manager_Mid_SES_Nursery_3
They also welcomed improved links with health visitors:
We never ever see a health visitor, so I think that’s amazing.
Manager_Mid_SES_ Nursery_2
However, health visitors and WHASPS expressed concern over their capacity to deliver training workshops for nursery staff:
My area, there’s lots of health visitors, so we’d probably be able to achieve it. But in other places, like here, [town name], they may not be able to because there’s quite a few nurseries and not many health visitors, so they might struggle to get round each one, with getting their work done as well.
Health_Visitor_North_Somerset
I think having to give presentations maybe takes us into a different level of time commitment.
WHASP_Cardiff
When asked if the proposed workshop topics of ‘childhood overweight’, ‘nutrition for children, ‘physical activity for children’ and ‘personal health and wellness for staff’ would be of interest to child-care staff, nursery managers expressed a particular need for more staff training in children’s PA:
. . . although physical development is now a prime area for us to promote, a lot of us have not had any training about how to promote that, you know, the types of activities, and it’s not easily available.
Manager_High_SES_Nursery_5
However, concerns were raised about the sensitivity of the topic ‘personal health and wellness for staff’:
. . . that could be quite a tricky area, couldn’t it? Um especially if you’re modelling the obesity one, because you could have some staff that could be slightly overweight that could take offence at that . . . it would have to be handled very carefully, wouldn’t it?’
Manager_ Mid_SES_Nursery_4
Developing a home component
In general, parents welcomed the idea of including a home learning component in the NAP SACC UK intervention:
If I was given something like that . . . um I’d have just welcomed the advice and I wouldn’t think you were trying to tell me what to do; you’re just trying to help me in the right direction. If there are a few things that I can improve upon, then brilliant.
Parent_High_SES_Nursery_2
However, many parents were concerned that this part of the intervention could be deemed to be invasive or ‘preachy’:
There’s a fine line with becoming too involved with how a parent is raising their child, so I would be cautious.
Parent_High_SES_Nursery_12
I think sometimes some people might think it’s a bit patronising. It’s quite obvious that children shouldn’t just sit around and watch TV [television], they need exercise.
Parent_Mid_SES_Nursery_3
Some parents cautioned that the home component may be received differently depending on social background:
I think there are some types of parents that will be hard to reach, so if you approach it in a non-judgemental way and you make it easily accessible for everyone no matter what background, I imagine there are some people who don’t have much money . . . they will feel different and I think it’s making those people feel welcome because it’s help for everyone.
Parent_Mid_SES_Nursery_11
Healthy/low-cost recipe and PA ideas were reported to be most attractive to parents as part of the home component:
Sometimes it’s cheaper or easier to buy junk food. So I think recipes is a good one, giving ideas.
Parent_Mid_SES_Nursery_11
I think a lot more should be available for children, I’ve been looking at gymnastics and dance classes for my daughter and they are just so expensive . . . you would love to send your children to all these classes, but you need ideas of things that don’t cost, or don’t cost a lot of money.
Parent_Midd_SES_Nursery_4
Many parents welcomed the idea of sharing healthy eating and PA ideas with others, and tip-sharing forums were suggested, either online (e.g. using social media) or at a physical meet-up:
You could probably maybe do workshops for parents, ways of getting vegetables into foods, things like that. It would give you a boost to do the right thing, wouldn’t it?
Parent_Low_SES_Nursery_6
It would be really handy to have a Facebook page with ideas of what you could cook for dinner tonight. A healthy meal that you could do, or something that you could do with the children.
Parent_Mid_SES_Nursery_4
Others suggested that the home component would be most successful if linked in with the nursery’s activities:
You could do something coming from the nurseries, like a welcome pack, or once a quarter maybe linked to the seasons, something like that. Different vegetables and things . . . In that you could have a couple of recipe ideas, or activities you can do at this time of year, or even go for a long walk and collect autumn leaves, pine cones to make Christmas decorations, all that sort of stuff. Seasonal fruit and veg and a couple of nice recipes to do with it. A little fun activity pack.
Parent_Mid_SES_Nursery_7
Parent–child cookery sessions and demonstrations at the nursery were also appealing:
I wonder whether if you had some kind of demo maybe, I don’t know whether the preschool would be involved with that. You could have a kind of demo, someone come along and cook something, and the children and the parents all stay together and have like a buffet or party, that maybe encourages the children to try something they haven’t and maybe the parents as well.
Parent_High_SES_Nursery_1
Finally, parents highlighted the importance of involving children in the home component as much as possible, as they were regarded by parents as ‘key’ to change in the home:
So anything that involves the parent going IN, I think they would be keen on and involving the children as well will mean once you’ve left this event, you take it home and if the children’s imagination has been captured and you’ve been there together, then I think that would be a very good way of getting the information home.
Parent_Mid_SES_Nursery_4
Development of NAP SACC UK and NAP SACC UK at Home
NAP SACC UK
Following discussions with nursery managers, it was decided to change the name of the NAP SACC UK self-assessment form to the Review and Reflect form as the research team felt that the word self-assessment evoked a sense that the nursery was being examined in a manner similar to Ofsted (England) or Estyn (Wales), which was potentially off-putting for staff. The form itself was also revised using the English guidelines Eat Better, Start Better – Voluntary Food and Drink Guidelines for Early Years Settings in England,28 as these are seen as current best practice for nurseries in the UK. This meant including questions on salt, breakfast, types of protein and dairy served, puddings and snacks, as well as adapting foods originating in the USA to UK alternatives. Given the concerns raised by the nursery manager and NHS oral health specialist about oral health in nursery-aged children, three questions on oral health were added to the child nutrition section of the form, including how staff promote oral health to children, capacity for professional development and training in oral health, information and support for families and existence of a policy on oral health. Furthermore, after discussion with Welsh Healthy and Sustainable Pre-School Scheme staff, a question was also added about whether or not the nursery had a PA policy that included active travel. After making these amendments and adaptations, the original Go NAP SACC form (excluding the breastfeeding section) was reduced to 80 items.
Following feedback from nursery staff about the manageable number of goals to be achieved in 6 months, the action-planning document was reduced from 10 goals to 8. Owing to the concerns of some nursery managers about their ability to release staff for training, and also the potential sensitivity of some of the workshop topics, the number of training workshops available to nursery staff was condensed from five workshops on ‘obesity’, ‘healthy eating’, ‘physical activity’, ‘personal health and wellness’ and ‘working with families’, to two workshops, each lasting 3 hours, on ‘nutrition and oral health’ and ‘physical activity’. Instead of being delivered by a ‘nurse partner’, as in the USA, these workshops were delivered by a local expert. This differed to the original plan for workshops to be delivered by health visitors and Welsh Healthy and Sustainable Preschool staff, as feedback suggested that this would be burdensome for staff who already had large caseloads. However, because of the interest from nurseries in improving links with health visitors, these workshops were attended by a health visitor, who then became the NAP SACC UK partner for that nursery, maintaining regular contact with the facility to provide support and guidance in making their improvements over a 6-month period. Table 4 summarises the changes made from NAP SACC US to NAP SACC UK.
| Step | NAP SACC | |
|---|---|---|
| USA | UK | |
| 1 | 99-item self-assessment (excluding breastfeeding section), ‘Go NAP SACC’63 | 80-item Review and Reflect based on ‘Go NAP SACC’63 and revised with UK guidance |
| 2 | Action-planning (10 goals) | Two workshops (3 hours) delivered by local experts with participating health visitors |
| 3 | Five workshops delivered by nurse consultant | Action-planning (8 goals) |
| 4 | Targeted technical assistance from nurse consultant | Targeted technical assistance from NAP SACC UK partner (health visitor) |
| 5 | Evaluate, revise and repeat | Evaluate, revise and repeat |
Development of NAP SACC UK at Home
Drawing on feedback from parents about the proposed home component of NAP SACC UK, a digital media intervention was developed (NAP SACC UK at Home). The steps of NAP SACC UK at Home are outlined below:
-
Sign up: parents are invited to sign up to take part in NAP SACC UK at Home. This involved logging on to the NAP SACC UK at Home website and registering an e-mail address and mobile phone number for correspondence or returning the information on paper to the NAP SACC UK office.
-
Tailoring support: parents were asked to complete a questionnaire about their family habits at home with respect to the areas covered by the home component to allow tailoring of support. An e-mail or text was sent in response, suggesting areas of focus for the goals. The first 50 parents who completed the questionnaire received a free family swimming voucher, redeemable at local swimming pools.
-
Goal-setting and action-planning: parents were asked to set goals for change and plan actions to meet the goals in the areas of eating, drinking, oral health, sleeping, indoor play, outdoor play, television (TV) and screen-viewing behaviours.
-
Tailored suggestions: parents received fortnightly tips and suggestions to prompt behaviour changes in the areas where support was requested. These were sent via Facebook, text and e-mails or by post for those not online.
-
Review: parents were encouraged to review their goals and actions, to consider what worked and what could be approached differently, to set new goals and actions and consider other areas for change.
Summary
The phase 1 study found that nurseries reported a generally good standard of nutrition, but the extent to which nutrition guidance was used varied between settings, with some using no nutritional guidance at all. Most nurseries had space for the children to be physically active, which was usually outdoors. There was variation in the extent to which the outdoor space was used ‘all weather’ or on fine days only. Screen time was limited across settings, with few including television time in their daily routines. Children’s oral health was highlighted to be a growing concern in nurseries, and this concern was reinforced by an NHS oral health specialist, who was a member of our group of expert advisors to NAP SACC UK. Adaptations to NAP SACC were made in the light of the phase 1 study and NAP SACC UK at Home was created.
Chapter 4 Feasibility cluster randomised controlled trial phase 2: methods
Parts of this chapter have been reproduced from Kipping et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
This chapter describes the methods used in the feasibility cluster RCT.
Sample size, eligibility, recruitment and randomisation
The sample size for this feasibility study was not informed by a power calculation. The sample size of 12 nurseries was chosen to provide information on variability within and between nurseries at baseline and follow-up, response rates and intracluster correlation coefficients (ICCs) in anticipation of a larger trial. A larger sample would not have been appropriate for a feasibility study and 12 participants was deemed a sufficient sample for the process evaluation, which was the most important part of this feasibility study.
The study took place in nurseries in two areas of England (North Somerset and Gloucestershire) and in the homes of children recruited to the study. North Somerset is a rural area adjacent to Bristol, with 14.1% of children living in poverty (per cent of children aged < 16 years in families receiving means-tested benefits and low income in 2012). 71 Gloucestershire is a large rural county to the north of Bristol. The health of people in Gloucestershire is generally better than the England average; however, 13.8% of children live in poverty. 72
The inclusion criteria for child-care providers were that they must be a day nursery, private nursery school, maintained nursery school, children’s centre with nursery, or preschool, in North Somerset or Gloucestershire. Excluded child-care settings were child minders, crèches, playgroups, primary school reception classes (where schools operate an early-admission policy to admit children aged 4 years) and au pairs. Settings were eligible if they had a minimum of 20 children aged 2–4 years who attend the child-care providers for at least 12 hours per week over 50 weeks of the year, or 15 hours per week in term time.
The NAP SACC UK study was discussed with North Somerset child-care provider managers at meetings convened by North Somerset Council and advertised in the Council’s early years newsletter. These opportunities were not available in Gloucestershire because of timing of recruitment. Child-care providers were sent a letter from the Council, project information sheet, reply envelope and form indicating if they wish to participate and reason for their response. Non-responders were followed up with a reminder and then a telephone call. All interested child-care providers were contacted by telephone to discuss the study following which, if the provider was still interested, they were offered a visit to discuss the intervention and study in more detail. A £200 incentive was provided to all participating nurseries at the end of the study.
Randomisation involved allocation to two arms: NAP SACC UK or usual practice. Twelve child-care providers (six in each area) were recruited to the trial, of which six were randomised to the control group and six to the intervention (three in each area). Allocation was conducted by an independent statistician at the Bristol Randomised Trials Collaboration, blind to the identity of the child-care providers. Stratified randomisation was used to ensure balance for (1) deprivation (using IMDs for the local super output area for 2010, where the provider is located), (2) size of child-care provider [small (≤ 48 children) or large (> 48 children)] depending on number of children attending, details obtained from the Council, Ofsted website or the nurseries own website] and (3) location (North Somerset and Gloucestershire). To achieve reasonably equally sized groups for randomisation, 12 groups were created across each of the two areas, with six lists created for each of low, medium and high IMD score. Each of the six lists by IMD category combinations was divided into two equal groups according to size.
Parents/carers were given a letter, project information sheet, reply envelope and form indicating if they wish to give consent for their child to take part in the study (sent at the end of August 2015). Research staff attended all nurseries late afternoon on between 1 and 3 days (depending on staff availability) to talk to parents about recruitment and answer any questions. All children received a small thank you gift [packet of stickers or a Mr Men™ (Mister Men Limited, London, UK) book] after each of the two data collections to encourage the prompt return of accelerometers.
The NAP SACC UK intervention
The NAP SACC UK intervention is based on the online Go NAP SACC intervention73 (but delivered in person) and was adapted for use in the UK during phase 1 of the feasibility study. It is based on social cognitive theory and the socioeconomic framework. In the feasibility study, the intervention was delivered by health visitors (NAP SACC UK partners) and local experts delivered the workshops for nursery staff. The intervention used in the NAP SACC UK feasibility trial is summarised using the Template for Intervention Description and Replication (TIDieR)74 12-item checklist in Table 5. The intervention also contained a home-based component, informed by other studies of behaviour change with parents/carers of young children use of digital media, and interviews and focus groups with parents/carers, nursery managers and health visitors. The intended behaviour change techniques used in the different elements of the NAP SACC UK intervention are outlined in Appendix 5, Table 32.
| Item | Description |
|---|---|
| Name | NAP SACC UK |
| Why |
NAP SACC UK is an intervention delivered in child-care settings with the aim of improving the nutrition, oral health and PA environment, through a process of self-assessment and targeted assistance. NAP SACC UK is a theory-based programme that employs components of social cognitive theory and socioecological framework. The objectives of the programme are to improve the nutritional quality, variety and quantity of food served, increase the amount and quality of PA, and to improve oral health education, staff–child interactions and staff behaviours around nutrition and PA and child-care provider policies on nutrition and PA NAP SACC at Home Phase 1 work included interviews with parents, which indicated an interest in a digital media intervention for parents, where tips and ideas could be given without being invasive or ‘preachy’ |
| What: materials |
The NAP SACC UK intervention is based around a self-assessment tool completed by nursery managers. This document, called the Review and Reflect, is an 80-item multiple-choice questionnaire, completed by the nursery manager, covering areas in nutrition, oral health, PA and play, outdoor play and learning, and screen time Following completion of the Review and Reflect, the nursery manager along with the NAP SACC UK partner agree on eight goals: three nutrition, three PA and a further two of the nursery’s choice. These are recorded on the ‘NAP SACC UK Action-planning’ document Intervention materials are not yet available for access because of the possibility of undertaking a full-scale trial NAP SACC at Home The NAP SACC at Home intervention is based around a website called ‘NAP SACC at Home’. This contains a page where parents can register their details, an initial questionnaire, goal-setting area and information pages. Additional materials included a NAP SACC at Home Facebook page, and paper copies of resources for those without internet access |
| What: procedures |
The NAP SACC UK intervention is a five stage process:NAP SACC at Home The NAP SACC at Home part of the intervention has the following stages: |
| Who provided |
The main part of the intervention was delivered by NAP SACC UK partners, who in this study were health visitors. Health visitors are qualified nurses or midwives who have undertaken further training and qualifications in child health, health promotion, public health and education. Additionally, to undertake the role of NAP SACC partner, health visitors were given further training consisting of a 0.5-day session led by a senior early years nutrition health improvement specialist, a PA specialist and an oral health specialist, and a further 2-hour ‘top-up’ training session mid-way through the intervention Workshops were delivered by specialists. The nutrition workshop was delivered by a senior early years health improvement specialist with a background in paediatric dietetics. The PA workshop was delivered by a PA expert NAP SACC at Home The NAP SACC at Home part of the intervention was delivered remotely via a website (or paper copies) and via Facebook. The content of the website and Facebook page was developed by the study team, and the website was designed and built by a specialist digital media company |
| How |
The main part of the intervention was delivered face to face; this included going through the Review and Reflect and action-planning, and the workshops. Other parts of the intervention, such as on-going support and advice from the NAP SACC UK partner, could be provided over the telephone, or by e-mail All parts of the intervention were delivered to participating nurseries individually. Some parts may have been delivered on a one-to-one basis (e.g. nursery manager and NAP SACC UK partner setting goals), whereas other parts, such as the workshop, would have been delivered to a whole group of staff from one nursery NAP SACC at Home The NAP SACC at Home part of the intervention was delivered remotely via a website (or paper copies) and via Facebook. Parents were able log on at a time convenient to them, on laptops, PCs or mobile devices |
| Where |
The NAP SACC UK intervention is delivered in the nursery itself. The NAP SACC UK partner offers visits to the nursery as necessary, and the workshops take place at the nursery, unless the nursery request otherwise NAP SACC at Home Parents were able access materials via the internet from their own home, or wherever was convenient |
| When and how much |
The NAP SACC UK intervention took place over 5 months. The initial face-to-face meetings between health visitors and nursery managers lasted ≥ 2 hours. The average number of advice/support opportunities given was 2.2 face-to-face meetings, 1.8 telephone calls and 2.8 e-mails The nutrition workshops were 3 hours and the PA workshops were 2.5 hours NAP SACC at Home Parents were able to access the website as often as they liked during the intervention period. Individually tailored texts/e-mails were sent to parents on a fortnightly basis |
| Tailoring |
The technical assistance offered by the NAP SACC UK partner would depend on the goals that the nursery had set NAP SACC at Home The NAP SACC at Home component was specifically tailored to suit the parents’ needs. Parents answered a questionnaire when they registered and this enabled appropriate information, hints and tips to be sent to them, depending on which areas they set goals in |
| Modifications | The intervention was originally intended to be 6 months long. This was reduced to 5 months part-way through the study to allow time for data collection |
| How well: planned | A process evaluation was conducted alongside the RCT, which looked at both adherence and fidelity. This involved the use of observations, logs, semistructured interviews and document analysis |
| How well: actual | The NAP SACC UK intervention was implemented as planned, with two exceptions: (1) the parent website was used by only 14% of parents and (2) one intervention nursery did not fully implement the intervention |
Outcome measures
Primary outcomes
The primary outcome of this feasibility RCT was the acceptability of the intervention and the trial methods, assessed against pre-set progression criteria (see Progression criteria). Progression criteria were agreed with the NIHR Public Health Research funding board and an independent TSC and were assessed using a range of methods.
Secondary outcomes
The secondary outcomes were measured at baseline (T0) prior to the intervention and 8–10 months after the baseline measurements (T1) (follow-up was deliberately staggered to assess the feasibility of following up children aged 4 years as they moved to school). These assessments were to inform the choice of primary outcomes for a full-scale trial and particularly whether or not the outcomes require data collection from parents/carers and children, or if the outcomes could be the environmental audit and zBMI using data linkage from the National Child Measurement Programme (NCMP). The outcomes included:
-
child accelerometer-measured activity
-
children’s height and weight
-
child food and drink intake, specifically of fruit and vegetables, snacks and sugar-sweetened drinks
-
child screen time
-
EPAO instrument score
-
parental and nursery staff mediators
-
family costs
-
health-related quality of life (HRQoL).
Data collection
As this feasibility study was not designed to assess efficacy, effectiveness or cost-effectiveness, data collection was designed primarily to assess feasibility and acceptability. All measurements were completed at baseline and again at follow-up, except for the baseline nursery audits and demographic information provided on consent forms. Data collection methods comprised the following.
Accelerometry measured activity
We used ActiGraph GT1M accelerometers (Actigraph, Pensacola, FL, USA), which have been extensively validated for assessment of PA among children. Accelerometers were fitted by NAP SACC UK researchers on the day of data collection, and instructions for their use were given to parents/carers on the same day.
Anthropometric measures of children
All anthropometric measurements were completed by DBS-checked trained fieldworkers with a member of nursery staff present. Weight was measured without shoes in light clothing to the nearest 0.1 kg using a Seca digital scale (Seca, Birmingham, UK). Height was measured to the nearest 0.1 cm without shoes using a portable Harpenden stadiometer (Holtain Ltd, Pembrokeshire, UK). Fieldworkers were trained to ensure correct position for height assessment. The ethics committee requested that the research team wrote to nursery managers alerting them to any children who were on or above the 99th zBMI centile for their age and sex, with context regarding the concerns about obesity in children, and advising them to follow their usual child protection procedures.
Children’s food and drink intake specifically fruit and vegetables, snacks and sugar-sweetened drinks
Dietary assessment was performed using the Child and Diet Evaluation Tool (CADET) prospective ticklist record for all foods consumed in a 24-hour period, an instrument validated for use in intervention studies with young children. 75,76 The CADET assesses the intake of 15 food groups, and CADET data were recorded by researchers undertaking observation of the children at all snacktimes and mealtimes at the nurseries and by parents/carers completing the CADET form at home for the child’s food and drink consumption before and after nursery. At baseline, the data were collected on paper forms with four children observed by one researcher. At follow-up, the data were recorded on paper and transferred to Google Nexus (Google Inc., Mountain View, CA, USA) tablets in the nursery. In a sample of four nurseries, CADET data collection at home was piloted over a weekend in addition to the weekday of nursery data collection; for two of these nurseries, the data were returned by parents on paper and in two nurseries they were collected from the parents by a researcher over the telephone. For the two nurseries where CADET was provided over the telephone, a NAP SACC UK researcher made up to four attempts to contact the parents/carers by telephone.
Sedentary time
Sedentary time was assessed by gathering details of screen time and quiet play time on a weekend day; the questions were based on those used in the Toybox study. 77 Sedentary time was assessed via questions at the end of the CADET tool completed by parents/carers.
Environment and Policy Assessment and Observation instrument score
The EPAO instrument was developed for the NAP SACC programme and assesses child-care nutrition and PA environments, policies, and practices. It was developed using the standards, recommendations and research literature on which the NAP SACC intervention itself was based. It has been tested for validity and reliability in nursery settings in the USA. 78 The EPAO, modified to accommodate the expanded best practices in 2014, consists of a 1-day observation and review of pertinent centre documents using 189-item questions and 16 free-text sections, with the average of all subscale scores representing total nutrition, indoor play, outdoor play and sedentary time scores. The EPAO from the USA was adapted to ensure consistency with the NAP SACC UK intervention and consistency with English descriptions of food. The EPAO instrument was administered at each of the nurseries by researchers who received specific training. This task was usually shared between two fieldworkers (morning and afternoon) as the form was long and required constant attention.
Parental and nursery staff mediators
Parental and nursery staff knowledge (e.g. nutrition, oral health, PA and sedentary behaviours), self-efficacy and motivation were assessed using tools created for this study. The reliability and validity of the tools are being explored in a separate study to inform whether or not they need further refinement for use in a full-scale trial. A paper questionnaire covering parent/carer mediators was completed by parents/carers.
Data linkage
The feasibility of zBMI data linkage with the NCMP data held by Local Authorities in England66 in the first year of primary school at age 4–5 years was examined in principle. All parents/carers of consented children were sent a further consent form in the post at the end of the study to request consent to link their child’s height and weight data measured through the NCMP (the data linkage did not take place because the study finished before the data were collected in schools).
Intervention data collection procedures comprised the following.
The home component
This was evaluated with respect to data from the record of parental use of the website, goal-setting, sent text messages, sent e-mails and Facebook group activity.
The Review and Reflect tool
Nursery staff completed a Review and Reflect tool at the beginning and end of the intervention. This provided an indication of the staff’s assessment of any changes in the nursery environment, policy and practice relating to nutrition, PA, sedentary behaviours and oral health. This tool is based on the original and revised NAP SACC self-assessment tool.
Goal-setting forms
Nursery staff completed a form to outline their eight intended goals at the beginning of the intervention and this was sent to the research team.
Data were collected by the research team and casual fieldworkers. Training for all staff took place prior to data collection, which covered background of the trial, the structure of nursery visits and role of the fieldworkers, practice measurements in pairs, an explanation of the study protocols and standard operating procedures including the call-in protocol, the policy on working hours, the lone working policy, and the protocol for concern about a child observed during fieldwork. Fieldworkers for follow-up data collection were trained prior to data collection. Google Nexus tablets were trialled for collecting nursery CADET data at all nurseries during follow-up data collection. The tablets were encrypted and made secure with a passcode. Data were entered offline and uploaded later when the tablet was connected to the internet.
Data storage and management
The secure, web-based electronic data capture system REDCap was used to store study data. This tool was created specifically for clinical research. The study team built and modified electronic forms in the database with support from a university clinical data systems manager.
Data from questionnaires were stored in anonymised form using participant identification (ID) numbers. REDCap contains functionality that allowed the team to e-mail survey links directly to participants. It was used in this way to collect follow-up parent/carer questionnaire data, for those parents/carers who provided an e-mail address on their child’s consent form (the majority). NVivo data analysis software was used to store, code and undertake thematic analysis of anonymised transcripts of the process evaluation data. All data collected will be made freely and openly available for other researchers to use via the data.bris Research Data Repository (where consent was given for data to be shared); this will take place at an appropriate time with respect to a possible full trial.
Data analysis
The statistical analyses were primarily descriptive, providing estimates of eligibility, recruitment, intervention delivery and retention rates among this study population, with 95% confidence intervals (CIs) calculated to incorporate between-provider variation where appropriate. Summary statistics were calculated for the outcome measures using means and standard deviations (SDs) by allocation arm and key demographic variables to inform the sample size and recruitment plan for the main trial, if warranted. Differences were explored for what was identified to be the primary outcome for a future trial by study location (North Somerset/Gloucestershire) and deprivation (high vs. low). Comparisons were made between those who completed the study and those who dropped out to investigate if this is a potential source of bias. Missing data were not imputed for the purposes of the feasibility study. However, the extent of missing data was examined and described to inform the full trial. Stata® v14 (StataCorp LP, College Station, TX, USA) statistical software was used for all analyses.
As this was a feasibility study, the sample size was not based on a power calculation, so the sample cannot provide a usefully precise estimate of the intervention effect. However, we were able to determine likely recruitment rate of nurseries and children, adherence to the intervention, and intracluster correlations in anticipation of a larger trial.
For qualitative data we aimed for a maximum variation sample of interviewees to achieve a broad perspective on the salient issues. Emergent issues from earlier interviews and focus groups were explored in subsequent interviews and the number of interviews undertaken was determined by data saturation (no new issues or themes emerging from within/across participants). All interviews and focus groups were audio-taped and transcribed verbatim. All the transcripts were read and reread in order to gain an overall understanding of participants’ views and experiences. Data were coded in NVivo software, and analysed thematically, allowing comparisons to be made within and across the interviews. Quotations which best represented the nature of each theme were extracted. In the process evaluation of the feasibility trial a total of 40 interviews were carried out and transcribed. One transcriber working within the University of Bristol was paid to transcribe 11 interviews; an outside transcriber with previous experience of working with the University transcribed 24 interviews, and the remaining five interviews were transcribed by one of the NAP SACC UK team members.
Physical activity
Children wore accelerometers for 5 days including week and weekend days. Periods of 60 minutes with zero values were interpreted as time that the monitor was not worn. 79 A day was considered valid if 8 hours of data were recorded. 80 Mean minutes of sedentary time (using two thresholds of 0–25 and 0–199 counts per 15 seconds using the criteria proposed by Evenson and Puyau81,82 were used to inform choice in a full trial). Mean minutes of light, moderate to vigorous intensity PA were then processed (thresholds of 200–799, and ≥ 800 counts per 15 seconds). Mean accelerometer counts per minute (which provide an indication of the overall volume of PA in which the children engage) were also calculated as this approach facilitates comparison with studies that may have applied a different cut-point. The accelerometer data were checked for outliers; informed by previous studies with children we excluded implausibly high values, such as might occur when a participant uses a trampoline, using a cap of 11,714 counts per minute. 83 Any values above this were capped at this maximum number. Consequently, the activity was still recorded as vigorous activity, but any biologically implausible peaks of activity were removed.
Anthropometric measures of children
Analysis consisted of height, weight, zBMI and proportion of overweight and obese (as determined by the UK1990 age and gender reference charts84 at 85% and 95% centiles, respectively), with further sensitivity analysis conducted using the International Obesity Task Force thresholds. 85
Children’s food and drink intake specifically fruit and vegetables, snacks and sugar-sweetened drinks
Colleagues at the University of Leeds, who designed the CADET tool, coded and analysed the CADET tick list food diary in DANTE, a Microsoft Access® (Microsoft Corporation, Redmond, WA, USA)-based food diary analysis programme designed by the Nutrition Epidemiology Group at the University of Leeds. 75 Frequency was assumed to be equal to one portion. Portion sizes were based on average food intakes of children from the National Diet and Nutrition Survey86 and were age and gender specific. Nutrient values were obtained from the food composition tables of McCance and Widdowson and their supplements. 87
We assessed children’s diet quality based on their adherence to the nationally recognised Children’s Food Trust voluntary food and drink guidelines for early years settings. 28 This is in line with NAP SACC UK aiming to increase nursery staff’s knowledge of nutrition and improve dietary provision consistent with the Children’s Food Trust. Furthermore, examining diet by way of adherence to dietary guidelines instead of total intake means that the results can be interpreted against these guidelines and, therefore, have practical implications for public health policy. The Children’s Food Trust guidelines are underpinned by a nutrient framework88 and encompass four food groups on which to base meals and snacks: starchy foods; fruit and vegetables; non-dairy protein sources (meat, fish, and alternatives); and milk and dairy foods, with additional guidance on desserts, pudding and cakes, drinks, fat, salt and sugar. Appendix 6, Table 33, contains a list of food items included in each food group as defined by the Children’s Food Trust. Consequently, some food items were included in more than one food groups (e.g. baked beans were included in both the fruit and vegetables and the non-dairy protein sources food groups).
We operationalised these guidelines (hereon known as NAP SACC UK Nutrition Best Practice Standards) when possible, based on the number of main meals and snacks children consumed on the day of observation separately. Main meals included breakfast, lunch or tea (dinner), and snacks included morning and afternoon snack. We assigned children a score of 1 for each respective standard they met and 0 if they did not meet a standard. The scores were summed to derive an overall NAP SACC UK Nutrition Best Practice Standards score (range 0–9 for two meals, 0–8 for one meal, 0–5 for two snacks and 0–3 for one snack).
Individual dietary intakes of fruit and vegetables, snacks and sugar-sweetened drinks during nursery attendance were assessed, but we were not able to accurately calculate intake of these foods while children were at home. Although parents were asked to report their children’s food intake using a home food diary, the response rate of this assessment was low, and many parents filled in the diary on a different date from the nursery observation. As a result, we were not able to estimate the daily dietary intake of the aforementioned foods in order to compare it by setting (nursery vs. home), in line with the presented results on PA. Therefore, and also taking into account that the intervention involved training nursery staff to follow the CFT’s guidelines, the NAP SACC UK Nutrition Best Practice Standards score was considered as the dietary outcome of the study. We computed descriptive statistics for adherence with the NAP SACC UK Nutrition Best Practice Standards by intervention arm.
Screen time
Screen time and time spent in quiet play were separately categorised into < 1 hour, 1–2 hours and > 2 hours. In the absence of UK guidelines for screen time this categorisation was informed by the American and Australian guidelines that children aged 2–5 years should have screen time or television time limited to 1 hour89 or < 1 hour90 per day.
EPAO
Analysis consisted of total EPAO score, EPAO subscores and scores for the components identified for change by the nursery.
Parent-completed questionnaire about child and family
Details were summarised on parent socioeconomic status, family variables (siblings), hours child spends at nursery per day and per week, age of child, parent ethnicity and child ethnicity.
Health economics
Our aim was to pilot measures of resource use and estimate more precisely the cost of the intervention to inform a full-scale trial. We measured key cost components for the public sector, child-care providers and parents. We delineated resource use (e.g. hours), unit costs (e.g. cost per hour) and calculated mean provider and parental costs in the intervention and control groups. We estimated incremental costs and 95% CIs for descriptive purposes. We anticipated that the NAP SACC UK intervention would be unlikely to affect HRQoL in the short term, and any effect on HRQoL is more likely in the long term through changes in dietary habits, PA and BMI. However, we piloted a measure of HRQoL in order to explore any changes over the course of the trial and examine associations between PA and HRQoL.
The HRQoL was measured using the Paediatric Quality of Life Inventory (PedsQL) 4.0 for children aged 2–4 years91 at baseline and 8–10 months later. The instrument has been tested for reliability and validity in community settings91 including comparing HRQoL between preschool children with or without obesity. 92 The inventory has 21 items rating HRQoL in four domains: physical function, emotional function, social function and nursery function. Parents rated their child’s functioning related to each item on a scale of 0 to 4 (0 = never a problem, 1 = almost never a problem, 2 = sometimes a problem, 3 = often a problem, 4 = almost always a problem). The PedsQL items were reverse scored and linearly transformed onto a scale of 0–100, for ease of interpretation, so that higher PedsQL scores indicated better HRQoL. Missing observations were imputed, as per the PedsQL scoring instructions. 93
Family expenditure on PA of the 2- to 4-year-old child was collected from the parent questionnaire at baseline and 8–10 months later. Parents were asked to list all the physical activities their 2- to 4-year-old child had participated in over the past week and the associated cost, if any, of each activity (entry fees, membership, etc.). A subsequent question asked how many miles in the car were travelled to get to the activity. Expenditure on transport was calculated using the HM Revenue and Customs tax rates per business mile, costed at 45p per mile. 94 The cost of transport to the activities was added to the expenditure on physical activities to generate the total weekly expenditure on PA of the 2- to 4-year-old. Parents were also asked to estimate the time spent on their child being physically active including travel and waiting time. This time was converted into hours per week.
Data on food expenditure were collected through the parent questionnaire, where parents were asked to estimate how much they spent on food in either the last week or the last month. Data were converted to weekly expenditure. Food expenditure was separated into five domains: supermarket shop, convenience shop, takeaway food, café/restaurant food and other (e.g. school dinner money). Parents were also asked if the spending on food in that period had been typical.
Health-care use was collected through the parent questionnaire in which parents were asked to detail visits to health-care providers in the last month. These data were collected at baseline and at the 8- to 10-month follow-up. This included, general practitioner (GP)/family doctor, therapist (e.g. physiotherapist, dietitian) and hospital inpatient and outpatient visits. The costs of health-care use of the 2- to 4-year-old children were calculated by multiplying the mean number of visits by the associated Department for Health and Social Care NHS Reference Costs 2015–201695 and the Personal Social Services Research Unit Health and Social Care Unit Costs 2016. 96 At follow-up, a subsample of 35 parents were randomly selected (by the trials unit) to recall health-care use over the past 5 months (rather than the last month) to compare parent recall. These data were divided by five to give a monthly average.
Data were collected on parent time taken off work and the associated costs. Parents were asked how many days they had taken off work in the past month associated with the health of their 2- to 4-year-old child. Time taken off work was separated into three domains: paid time off work, unpaid time off work and annual leave days off work. The cost of paid time off was calculated by taking the average weekly salary from the Average Salary of Hours and Earnings Survey 2016. 97 The national median weekly salary of £539.00 was divided by five to provide a day rate of £107.80. This number was then multiplied by the number of paid days’ work parents took off because of their 2- to 4-year-old child’s health.
The costs to nurseries of preparing for and delivering the intervention were estimated using the reported time that nursery staff attended the workshop, recorded time with the health visitors and additional information from the nursery logs. The cost of the intervention to the nurseries was estimated using the average hourly rate for nursery workers and managers. 98 However, it was at the discretion of the nursery how they pay staff to attend the workshop. Not all nurseries paid their staff to attend the workshop.
All data relating to cost and HRQoL were combined with the parental mediator questionnaire and given to parents by nursery staff to return by post to the research team. At follow-up, all parents/carers who had provided an e-mail address on their child consent forms were e-mailed a link to complete the parent/carer questionnaire online, using the study’s database. Non-responders were sent a paper copy. Data were analysed using Stata MP 14.2 statistics and data analysis package. Mean differences at follow-up were tested using paired t-tests for food expenditure, PA expenditure, PedsQL score and child health-care costs. Costs and outcomes are presented in a cost–consequence table.
Process evaluation
Qualitative data collection and analysis
The aim of the process evaluation was to examine the feasibility and acceptability of the NAP SACC intervention and study design according to three prespecified progression criteria (see Chapter 2, Progression criteria). The design of the process evaluation used three relevant parts of the RE-AIM framework (Reach, Adoption and Implementation). 99 The key process evaluation questions (progression criteria) and the data collection methods used are outlined in Table 6. Data were collected through (1) semistructured interviews with key stakeholders (i.e. NAP SACC partners, nursery managers and staff, and parents), (2) non-participant observations (of nursery workshops and meetings between NAP SACC partners and nursery managers) and (3) document analysis of NAP SACC partner logs, Review and Reflect forms and goal-setting forms.
| Progression criteria | Methods | Details |
|---|---|---|
| 1. Was it feasible to implement the NAP SACC intervention with child-care providers? |
Non-participant observations Semistructured interviews Document analysis |
Observation of NAP SACC UK partner training (n = 1) Observations of nursery workshops (n = 10) Observations of NAP SACC UK partner/nursery manager meetings (n = 5) Interviews with NAP SACC UK partners (n = 4) Interviews with nursery managers (n = 12) Interviews with nursery staff (n = 4) Analysis of completed logs (n = 5), Review and Reflect forms (n = 5) and goal-setting forms (n = 5) |
| 2. Was the intervention acceptable to NAP SACC Partners and the majority of child-care managers, staff and parents? |
Non-participant observations Semistructured interviews Document analysis |
Observations of nursery workshops (n = 10) Observations of NAP SACC UK partner/nursery manager meetings (n = 5) Interviews with NAP SACC UK partners (n = 4) Interviews with nursery managers (n = 12) Interviews with nursery staff (n = 4) Analysis of completed logs (n = 5), Review and Reflect forms (n = 5) and goal-setting forms (n = 5) |
| 3. Were the trial design and methods acceptable? | Semistructured interviews |
Interviews with NAP SACC UK partners (n = 4) Interviews with nursery managers (n = 12) Interviews with nursery staff (n = 4) |
Non-participant observation
All observations were conducted by Jane Collingwood (trial co-ordinator, maternity cover), with the exception of the NAP SACC UK partner training and one nutrition workshop (in nursery 3), both conducted by Rowan Brockman (research associate). The purpose of the nursery workshop observations was to assess the fidelity, feasibility and acceptability of the workshops by documenting its delivery and its receipt by nursery staff. Observations focused on who and how many staff attended, the workshop format, elements that worked well/less well, and the behaviour, interest and engagement demonstrated by the workshop facilitators and participants. Observations were recorded using a semistructured observation schedule in order to document prespecified information while also allowing for unstructured qualitative observations to be included.
The purpose of NAP SACC partner/nursery manager meeting observations was to assess the fidelity, feasibility and acceptability of these meetings and focused on the style of interaction (e.g. mutual decision-making or led by participant, supportive or critical, etc.), aspects that worked well/less well, and the behaviour, interest and enthusiasm displayed by the NAP SACC partner and manager. Observations were recorded using a semistructured observation schedule.
Semistructured interviews
Semistructured interviews were conducted with key stakeholders (NAP SACC UK partners, nursery managers and staff, and parents) to assess the fidelity, feasibility and acceptability of both the intervention and the research design. We aimed to interview all NAP SACC UK partners and all nursery managers, as well as one member of nursery staff from each intervention nursery. We also sought to interview 20 parents from both intervention and control nurseries.
Interviews with NAP SACC UK partners, nursery managers and nursery staff were conducted face to face or over the telephone, according to the participants’ preferences. All parent interviews were conducted over the telephone. Semistructured interview guides specific to each stakeholder group (Table 7) were used for all interviews to ensure that key topics were covered while allowing participants to discuss other issues they felt were important. Interviews were audio-recorded on an encryptable device and transcribed verbatim. All interviews were conducted by Rebecca Langford, with the exception of four parent interviews conducted by Ruth Kipping.
| Stakeholder group | Number | Method | Key topic areas |
|---|---|---|---|
| NAP SACC UK partners | 4 |
In person (n = 3) Telephone (n = 1) |
|
| Nursery managers | 12 |
In person (n = 9) Telephone (n = 3) |
|
| Nursery staff | 4 | In person (n = 4) |
|
| Parents | 20 | Telephone (n = 20) |
|
Document analysis
Three sets of documents were collected and analysed as part of the process evaluation: NAP SACC UK partner logs, Review and Reflect forms and goal-setting forms. NAP SACC UK partners were asked to log costs incurred in their participation in the NAP SACC UK study. Partners logged the date, type (e-mail, telephone, face-to-face meeting) and duration of contacts with each nursery. They also recorded travelling distance and time for the economic evaluation. These logs were analysed alongside other process evaluation data in relation to the key progression criteria.
Review and Reflect forms were either completed individually by the nursery manager and then discussed with the NAP SACC UK partner or completed alongside discussion with the partner during one of their meetings. These forms were reviewed and updated at a follow-up meeting between the manager and partner. Data from these forms were used to document changes made within the nurseries and to triangulated with other forms of data (e.g. interviews).
Forms documenting the goals set by the nurseries were also collected and compared against data from the follow-up Review and Reflect forms and interview data to assess progress made.
Data analysis
Interview transcripts were entered into NVivo software to aid data management and analysis. Qualitative interview data were analysed using techniques associated with thematic context analysis and grounded theory. Initially, Rebecca Langford read through all transcripts to familiarise herself with the data. Rebecca Langford then coded four transcripts line by line to identify themes and develop an initial coding framework. Rebecca Langford and Ruth Kipping independently applied this coding framework to two further transcripts. The results from this independent coding were compared, any discrepancies discussed and revisions were made to the framework. Rebecca Langford applied the revised framework to all subsequent transcripts, making revisions where necessary in discussion with Ruth Kipping as appropriate. Observation data were entered into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet for analysis, with these data being compared and contrasted with interview data, where relevant, to support cross-checking and triangulation. Data from NAP SACC UK partner logs, Review and Reflect forms and goal-setting forms were entered into the REDCap data management system. Data from interviews, observations and document analysis were triangulated to identify confirmatory or contradictory data.
All analysis was conducted by Rebecca Langford, in discussion with other members of the research team. Rebecca Langford is an experienced qualitative researcher who started work on the study to conduct the process evaluation after the intervention had been delivered and the majority of follow-up data had been collected. Rebecca Langford had no other role in the design or management of the trial or in collecting (quantitative) outcome data. This distance from the wider NAP SACC study allowed her to take a critical and objective view of the intervention and research process.
Chapter 5 Feasibility cluster randomised controlled trial phase 2: results
In this section of the report, we describe the nursery and child recruitment rates at baseline and retention (which relate to progression criteria 1a, 3a, 3c, 3d; see Chapter 4, Progression criteria, for the full criteria) and the characteristics of the nurseries and children participating in the study. The findings related to the other progression criteria are presented in Chapter 7, Process evaluation, where the process evaluation is presented. We report the quantitative data analyses examining the secondary outcomes and mediators, followed by the pilot health economic and quality-of-life outcome measures.
Recruitment, retention and participant characteristics
Figure 4 summarises participation in the feasibility trial, with reasons for withdrawal from the study following the Consolidated Standards of Reporting Trials (CONSORT) guidance. Of the 14 nurseries approached in North Somerset, six (42.9%) gave consent to take part in the study. In Gloucestershire, of the 24 approached, six (25.0%) consented to participate, giving an overall consent rate of 31.6%. No large nurseries in the highest deprivation group were recruited in Gloucestershire. At least one nursery was recruited in each of the other five groups. Reasons for declining to take part included being too busy, staffing issues, financial issues and feeling that they did not need the intervention. No nurseries were lost to follow-up.
FIGURE 4.
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
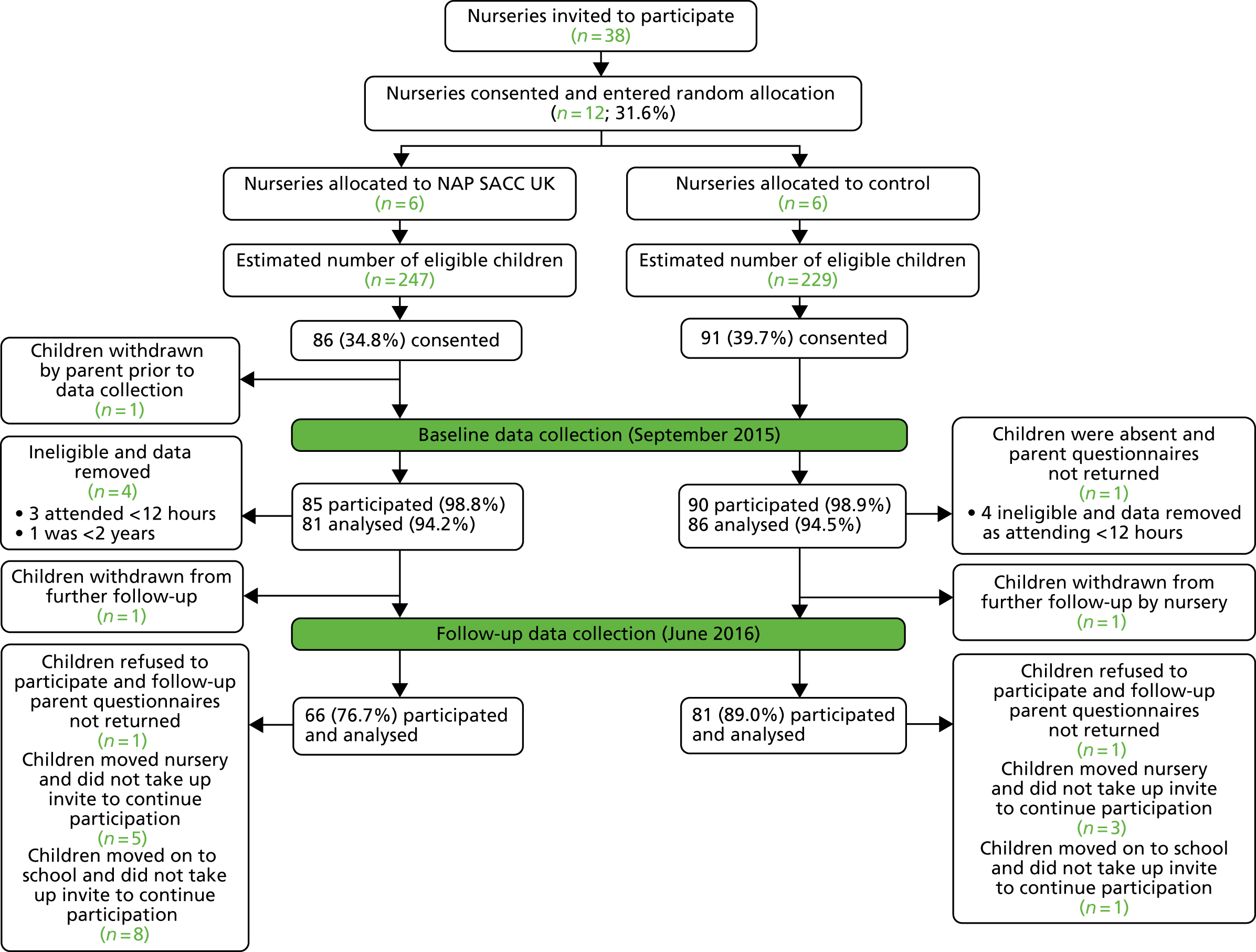
There were estimated to be 476 children potentially eligible to take part in the study. Of the 221 potentially eligible children in North Somerset, 97 (43.9%) parents provided consent for their child to take part in the measurements and 80 (31.4%) out of 255 potentially eligible children in Gloucestershire were given consent. The parental consent for all children was 37.2%. The 177 consented children were invited to take part in baseline data collection; one (0.6%) child’s consent was withdrawn by the parents prior to data collection commencing. A total of 175 out of the 176 remaining children provided some baseline data (99.4%) (one child was absent from nursery and parents did not complete baseline parental questionnaire). A further eight (4.5%) children were removed because they were ineligible, leaving 167 out of 168 children with data in the baseline analysis.
At the follow-up data collection, 147 (87.5%) out of 168 children at baseline participated in data collection. Two (1.2%) children had consent withdrawn, two (1.2%) refused to participate in measurements and their parents did not return follow-up questionnaires, eight (4.8%) moved nursery and nine (5.4%) moved to primary school and did not take up the offer to continue participation. Out of the 476 potentially eligible children at baseline, 147 (30.9%) children provided data at baseline and follow-up. This comprised 66 children in the intervention arm and 81 children in the control arm. Sending a link to the parental questionnaire by e-mail to a subgroup of parents at follow-up yielded a completion rate of 28% with 87% for those parents sent the questionnaire by post at follow-up. In the pilot of collecting weekend food and drink consumption CADET data from parents in two nurseries, 51.6% of parents returned the paper copy. For the parents in the two nurseries where data were collected over the telephone, the research staff had difficulty reaching the parents/carers even after four attempts at phoning.
The completeness of data by item for nurseries, children and parents is shown in Table 8 and the characteristics of nurseries, children and parents by study arm at baseline are shown in Table 9.
| Data item | Baseline, n (%) | Follow-up, n (%) |
|---|---|---|
| Nursery | ||
| Nursery mediator questionnaire | 31 (12 nurseries, 2.6 per nursery) | 23 (8 nurseries, 1.9 per nursery, 2.9 per nursery that replied) |
| Nursery EPAO | 6 (100) | 6 (100) |
| Nursery completed Review and Reflect form | 3 (50) | 3 (50) |
| Childrena | ||
| Height | 162 (96.4) | 138 (83.1) |
| Weight | 161 (95.6) | 139 (83.7) |
| Accelerometer worn and returnedb | 140 (83.3) | 122 (73.5) |
| Accelerometer with valid wear time for 1 day | 124 (73.8) | 94 (56.6) |
| CADET nurseryc | 153 (91.1) | 130 (78.3) |
| CADET home | 139 (82.7) | 79 (47.6) |
| Parent | ||
| Parent HRQoL and cost questionnaire | 125 (74.4) | 86 (51.8) |
| Parent mediator questionnaire | 125 | 79d |
| Characteristic | Intervention | Control | ||
|---|---|---|---|---|
| N | Mean (SD) or n (%) | N | Mean (SD) or n (%) | |
| Nursery | ||||
| Size of nursery, mean (SD) number of eligible children | 6 | 65 (17.4) | 6 | 53 (21.3) |
| Nursery size | ||||
| n (%) small | 6 | 2 (33.3%) | 6 | 4 (66%) |
| n (%) large | 6 | 4 (66%) | 6 | 2 (33.3%) |
| Nursery IMD,a mean (SD) | 6 | 17.2 (14.3) | 6 | 10.5 (5.7) |
| Nursery IMDa | ||||
| n (%) low IMD | 6 | 2 (33.3%) | 6 | 2 (33.3%) |
| n (%) medium IMD | 6 | 2 (33.3%) | 6 | 2 (33.3%) |
| n (%) high IMD | 6 | 2 (33.3%) | 6 | 2 (33.3%) |
| Nursery mediator questionnaire PA, mean (SD) | ||||
| Knowledge | 16 | 4.19 (1.64) | 15 | 4.07 (1.28) |
| Motivation | 15 | 4.54 (0.45) | 15 | 4.45 (0.84) |
| Self-efficacy | 16 | 4.43 (0.47) | 15 | 4.46 (0.57) |
| Nursery mediator questionnaire nutrition, mean (SD) | ||||
| Knowledge | 16 | 10.88 (3.30) | 15 | 11.00 (1.13) |
| Motivation | 15 | 4.47 (0.50) | 15 | 4.58 (0.51) |
| Self-efficacy | 16 | 4.36 (0.36) | 15 | 4.58 (0.29) |
| EPAO total score, mean (SD) | 6 | 1.76 (1.24) | 6 | 1.92 (1.22) |
| EPAO total nutrition score, mean (SD) | 6 | 1.92 (1.23) | 6 | 1.97 (1.23) |
| EPAO total physical score, mean (SD) | 6 | 1.59 (1.23) | 6 | 1.86 (1.22) |
| Children | ||||
| Height, mean (SD) (cm) | 59 | 95.25 (5.81) | 75 | 97.24 (6.13) |
| Weight, mean (SD) (kg) | 58 | 15.14 (2.23) | 76 | 15.86 (2.24) |
| zBMI, mean (SD) [zBMI unit (UK1990)] | 62 | 0.45 (1.03) | 69 | 0.51 (0.86) |
| Accelerometer valid wear time for nursery day | ||||
| MVPA (minutes) | 61 | 23.13 (12.32) | 60 | 21.90 (12.42) |
| LVPA (minutes) | 61 | 122.30 (30.75) | 60 | 124.64 (35.49) |
| Sedentary time (minutes) | 61 | 509.20 (74.34) | 60 | 493.65 (58.07) |
| Proportion of children who consumed ≥ 2 main meals and adhered to best practice standards, number of children (%) | 48 | 4 (8.3%) | 23 | 4 (17.4%) |
| Proportion of children who consumed 1 main meal and adhered to best practice standards, number of children (%) | 21 | 6 (28.6%) | 46 | 4 (8.7%) |
| Proportion of children who consumed 2 snacks and adhered to best practice standards, number of children (%) | 23 | 3 (13.0%) | 26 | 14 (53.9%) |
| Proportion of children who consumed 1 snack and adhered to best practice standards, number of children (%) | 37 | 28 (75.7%) | 43 | 28 (65.1%) |
| Child HRQoL, PedsQL mean (SD) | 32 | 85.9 (8.2) | 45 | 87.7(10.4) |
| Parent | ||||
| Parent cost questionnaire | ||||
| Mean (SD) £ family weekly food expenditure | 28 | 93.2 (34.3) | 42 | 109.3 (40.4) |
| Mean (SD) £ child weekly PA expenditure | 26 | 8.9 (10.5) | 40 | 10.7 (8.0) |
| Parent mediator questionnaire PA, mean (SD) | ||||
| Knowledge | 56 | 4.11 (1.64) | 68 | 4.35 (1.29) |
| Motivation | 56 | 4.17 (0.55) | 68 | 4.24 (0.62) |
| Self-efficacy | 56 | 4.23 (0.53) | 69 | 4.37 (0.49) |
| Parent mediator questionnaire nutrition, mean (SD) | ||||
| Knowledge | 56 | 9.71 (2.40) | 68 | 10.13 (2.12) |
| Motivation | 56 | 4.26 (0.67) | 69 | 4.36 (0.56) |
| Self-efficacy | 56 | 4.45 (0.47) | 68 | 4.48 (0.60) |
| Parent highest educational attainment, number of parents with first degree or higher (%) | 50 | 31 (61.7%) | 85 | 63 (78.8%) |
Outcomes
Physical activity and sedentary time
The number of children who met the criteria of ≥ 480 minutes per day of accelerometer wear time is shown in Appendix 4, Table 31. The results of complete-case PA and sedentary time are presented in Table 10. The mean minutes of activity per day was 152 and 148 minutes in the intervention and control arms, respectively. This highlighted that, on average, children did not meet the Chief Medical Officer’s recommended 180-minute daily activity guideline. 7 The data show suggestion of promise for the intervention increasing MVPA on nursery days in the intervention arm (24.0–32.5 minutes) compared with the control arm (21.6–24.4 minutes) and total activity (151.6–172.1 minutes in the intervention arm vs. 148.1–154.2 minutes in the control arm); differences between arms were not seen on non-nursery days. Some caution is required in interpreting these data because not all children had valid wear-time data.
| Accelerometer measurement | Intervention, mean (SD) | Control, mean (SD) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Nursery day | n = 22 | n = 37 | ||
| Mean MVPA minutes per day | 24.00 (14.3) | 32.50 (14.8) | 21.57 (12.3) | 24.41 (12.9) |
| Mean total activity minutes per day | 151.63 (77.02) | 172.05 (38.98) | 148.05 (44.25) | 154.19 (43.33) |
| Mean light minutes per day | 127.63 (30.8) | 139.55 (28.1) | 126.48 (34.9) | 129.78 (32.8) |
| Mean sedentary minutes per day | 518.42 (77.0) | 480.15 (68.7) | 493.65 (55.1) | 472.84 (56.8) |
| Mean counts per minute | 573.88 (186.6) | 698.94 (190.1) | 571.08 (162.3) | 625.21 (175.3) |
| Non-nursery day | n = 14 | n = 29 | ||
| Mean MVPA minutes per day | 23.02 (12.9) | 28.03 (11.2) | 21.60 (9.9) | 25.90 (13.1) |
| Mean total activity minutes per day | 143.48 (45.84) | 164.06 (37.50) | 133.56 (33.86) | 156.75 (38.35) |
| Mean light minutes per day | 120.46 (33.8) | 136.03 (31.4) | 111.97 (30.1) | 130.84 (30.0) |
| Mean sedentary minutes per day | 496.15 (74.7) | 509.03 (62.8) | 506.88 (63.4) | 500.27 (75.3) |
| Mean counts per minute | 569.83 (207.4) | 623.32 (145.54) | 544.78 (136.1) | 622.87 (161.9) |
Anthropometric
Results of complete-case zBMI are presented in Table 11. The proportions of children in each arm of the study at baseline and follow-up who were overweight and obese are given, as determined by the UK1990 age and gender reference charts84 at 85% and 95% centiles and International Obesity Task Force (IOTF) reference points. 85 There were some differences at baseline, with children in the control arm being taller (97.2 cm in the control arm; 95.3 cm in the intervention arm) being heavier (15.9 kg in the control arm; 15.1 kg in the intervention arm) and having a greater zBMI (0.46 in the control arm; 0.39 in the intervention arm). There was also a lower proportion of overweight and obese children in the control arm by both measures (23.2% UK1990 and 19.6% IOTF in the control arm; 31.7% UK1990 and 26.8% IOTF in the intervention arm) and there were more obese children by the UK1990 measure (10.7% in the control arm; 7.3% in the intervention arm). At follow-up, the mean height and weight increased in both arms, with a greater increase in zBMI in the intervention arm (0.46 to 0.29 in the control arm; 0.39 to 0.49 in the intervention arm). The proportion overweight or obese decreased in both arms by both measures (23.2% to 19.6% UK1990 in the control arm and 31.7% to 24.4% UK1990 in the intervention arm; 19.6% to 12.5% IOTF in the control arm and 26.8% to 17.1% IOTF in the intervention arm) except IOTF obesity, which increased in the control arm (1.8% to 3.6%). However, because the numbers are small, these differences in proportion should be considered with caution.
| Anthropometric measure | Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Height (cm) | 59 | 95.25 (5.81) | 59 | 100.42 (6.00) | 75 | 97.24 (6.13) | 75 | 102.5 (5.93) |
| Weight (kg) | 58 | 15.14 (2.23) | 58 | 16.71 (2.35) | 76 | 15.86 (2.24) | 76 | 17.2 (2.41) |
| zBMI | 41 | 0.39 (1.09) | 41 | 0.49 (0.85) | 56 | 0.46 (0.88) | 56 | 0.29 (0.92) |
| Overweight or obese (UK1990), n (%)a | 13 | 31.7 | 10 | 24.4 | 13 | 23.2 | 11 | 19.6 |
| Obese (UK1990), n (%)a | 3 | 7.3 | 2 | 4.9 | 6 | 10.7 | 4 | 7.1 |
| Overweight or obese (IOTF), n (%) | 11 | 26.8 | 7 | 17.1 | 11 | 19.6 | 10 | 12.5 |
| Obese (IOTF), n (%) | 2 | 4.9 | 1 | 2.4 | 1 | 1.8 | 2 | 3.6 |
Diet
The proportions of children who consumed two or more main meals at nursery (control, n = 18; intervention, n = 30) and adhered to the NAP SACC UK Nutrition Best Practice Standards are shown in Table 12. Overall, there was good adherence to the standards, where the average scores at follow-up were 6.9 and 6.4 out of 9.0 in the control and intervention arms, respectively. There was little difference between the two arms post intervention. However, the proportion of children who met the recommendation for starchy foods (three per day) was higher in the intervention arm than in the control arm. Conversely, a smaller proportion of children in the intervention arm consumed a portion of fruit and a portion of vegetables at each meal. Nevertheless, children in the intervention arm appeared more likely to consume a variety (four types) of fruit and vegetables over the course of the day. In both arms, the proportion of children who did not eat processed meat or fish products was relatively low (≤ 60%).
| Best practice standard | Intervention (N = 30), n (%) | Control (N = 18), n (%) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Starchy food | ||||
| A portion as part of each meal | 30 (100.0) | 30 (100.0) | 17 (94.4) | 18 (100.0) |
| Three types over the course of the day | 19 (63.3) | 21 (70.0) | 7 (38.9) | 4 (22.2) |
| Processed potatoes never consumed | 27 (94.4) | 22 (73.3) | 18 (100.0) | 17 (95.7) |
| Fruit and vegetables | ||||
| A portion of fruit and a portion of vegetables at each meal | 16 (53.3) | 13 (43.3) | 15 (83.3) | 16 (88.9) |
| Four types of fruit and vegetables over the course of the day | 23 (76.7) | 22 (73.3) | 15 (83.3) | 11 (61.1) |
| Meat, fish, eggs, beans and other non-dairy sources of protein | ||||
| A portion as part of each meal | 15 (50.0) | 16 (53.3) | 11 (61.1) | 13 (72.2) |
| Processed meat and fish products never consumed | 18 (60.0) | 12 (40.0) | 10 (55.6) | 10 (55.6) |
| Desserts, puddings and cakes | ||||
| Milk-based or fruit-based desserts | 27 (90.0) | 26 (86.7) | 16 (88.9) | 18 (100.0) |
| Beverages | ||||
| Did not consume sugary drinkb | 30 (100.00) | 30 (100.0) | 18 (100.0) | 17 (94.4) |
| NAP SACC UK best practice standards score, mean (SD) | 6.8 (1.3) | 6.4 (1.4) | 7.1 (1.8) | 6.9 (1.3) |
The diet quality of children who consumed one main meal (control, n = 27; intervention, n = 14) was generally good (Table 13). There were differences between the arms for the average NAP SACC UK Nutrition Best Practice Standard scores at follow-up (6.6 vs. 5.1 out of 8.0 in the control and intervention arms, respectively). In both arms, < 40% of the children met the standard regarding one portion of fruit and one portion of vegetables.
| Best practice standard | Intervention (N = 14), n (%) | Control (N = 27), n (%) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Starchy food | ||||
| A portion as part of each meal | 14 (100.0) | 13 (92.9) | 25 (92.6) | 27 (100.0) |
| Processed potatoes never consumed | 14 (100.0) | 12 (85.7) | 26 (96.3) | 27 (100.0) |
| Fruit and vegetables | ||||
| A portion of fruit and a portion of vegetables at each meal | 5 (35.7) | 3 (21.4) | 8 (29.6) | 10 (37.0) |
| Two types of fruit and vegetables over the course of the day | 12 (85.7) | 8 (57.1) | 24 (88.9) | 21 (77.8) |
| Meat, fish, eggs, beans and other non-dairy sources of protein | ||||
| A portion as part of each meal | 8 (57.1) | 3 (21.4) | 14 (51.9) | 20 (74.1) |
| Processed meat and fish products never consumed | 12 (85.7) | 6 (42.9) | 21 (77.8) | 23 (85.2) |
| Desserts, puddings and cakes | ||||
| Milk-based or fruit-based desserts | 12 (85.7) | 13 (92.9) | 23 (85.2) | 24 (88.9) |
| Beverages | ||||
| Did not consume sugary drinkb | 13 (92.9) | 14 (100.0) | 27 (100.0) | 27 (100.0) |
| NAP SACC UK best practice standard score, mean (SD) | 6.4 (1.3) | 5.1 (1.0) | 6.2 (1.2) | 6.6 (1.2) |
Tables 14 and 15 show the proportion of children who met the NAP SACC UK Nutrition Best Practice Standards for snacks. There was high adherence to the standards for children who had one or two snacks at nursery. Among children who had two snacks, the average NAP SACC UK Nutrition Best Practice Standard scores at follow-up were 3.7 and 4.4 out of 5.0 in the control and intervention arms, respectively. There was suggestion of promise that the mean score in the intervention arm was higher than in the control arm. A higher proportion of children in the intervention arm met the standards regarding starchy food, fruit and vegetables, and high-sugar or high-fat snacks than did those the control arm. Among children who had one snack only, the average NAP SACC UK Nutrition Best Practice Standards score was also higher in the intervention arm.
| Best practice standard | Intervention (N = 13), n (%) | Control (N = 12), n (%) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Starchy food | ||||
| As part of at least one snack per day | 8 (61.5) | 8 (61.5) | 11 (91.7) | 1 (8.3) |
| Fruit and vegetables | ||||
| A portion of fruit or vegetables with some snacks | 13 (100.0) | 12 (92.3) | 9 (75.0) | 10 (83.3) |
| Did not consume dried fruit as a snack | 13 (100.0) | 13 (100.0) | 11 (91.7) | 12 (100.0) |
| High-sugar or high-fat snacks | ||||
| Did not consume as a snack | 7 (53.9) | 11 (84.6) | 7 (58.3) | 9 (75.0) |
| Beverages | ||||
| Did not consume sugary drinkb | 12 (92.3) | 13 (100.0) | 12 (100.0) | 12 (100.0) |
| NAP SACC UK best practice standard score, mean (SD) | 4.1 (0.5) | 4.4 (0.7) | 4.2 (0.9) | 3.7 (0.5) |
| Best practice standard | Intervention (N = 13), n (%) | Control (N = 20), n (%) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Fruit and vegetables | ||||
| Did not consume dried fruit as a snack | 12 (92.3) | 13 (100.0) | 19 (95.0) | 12 (60.0) |
| High-sugar or high-fat snacks | ||||
| Did not consume as a snack | 11 (84.6) | 11 (84.6) | 19 (95.0) | 15 (75.0) |
| Beverages | ||||
| Did not consume sugary drinka | 13 (100.0) | 13 (100.0) | 20 (100.0) | 20 (100.0) |
| NAP SACC UK best practice standard score, mean (SD) | 2.8 (0.6) | 2.8 (0.4) | 2.9 (0.3) | 2.4 (0.6) |
Screen-viewing and sedentary activities
Parents reported their child’s time spent screen-viewing across a range of screen devices and in quiet play before and after nursery and on Saturdays. Table 16 shows that in the intervention arm from baseline to follow-up, fewer children watched TV or took part in sedentary activities for between 1 and 2 or ≥ 2 hours on nursery days, in contrast with the control arm where more children did. Fewer children in the intervention arm watched TV or engaged with sedentary activities for > 2 hours on a Saturday and there was no change or an increase in the control arm for each.
| Time spent screen-viewing or in quiet play | Intervention (N = 17), n (%) | Control (N = 38), n (%) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Time spent screen-viewinga in child’s free time before and after nursery | ||||
| ≤ 1 hour | 11 (64.7) | 15 (88.2) | 32 (84.2) | 27 (71.1) |
| > 1 hour and < 2 hours | 3 (17.7) | 2 (11.8) | 5 (13.2) | 8 (21.1) |
| ≥ 2 hours | 3 (17.7) | 0 (0.0) | 1 (2.6) | 3 (7.9) |
| Time spent screen-viewinga on Saturday | ||||
| ≤ 1 hour | 5 (29.4) | 5 (29.4) | 12 (31.6) | 16 (42.1) |
| > 1 hour and < 2 hours | 5 (29.4) | 8 (47.1) | 19 (50.0) | 15 (39.5) |
| ≥ 2 hours | 7 (41.2) | 4 (23.5) | 7 (18.4) | 7 (18.4) |
| Time spent in quiet playb in child’s free time before and after nursery | ||||
| ≤ 1 hour | 6 (35.3) | 6 (35.3) | 25 (65.8) | 15 (39.5) |
| > 1 hour and < 2 hours | 3 (17.7) | 4 (23.5) | 10 (26.3) | 17 (44.7) |
| ≥ 2 hours | 8 (47.1) | 7 (41.2) | 3 (7.9) | 6 (15.8) |
| Time spent in quiet playb on Saturday | ||||
| ≤ 1 hour | 1 (5.9) | 2 (11.8) | 7 (18.9) | 4 (10.5) |
| > 1 hour and < 2 hours | 3 (17.7) | 2 (11.8) | 8 (21.6) | 10 (26.3) |
| ≥ 2 hours | 13 (76.5) | 13 (76.5) | 22 (59.5) | 24 (63.2) |
Environment and Policy Assessment and Observation
The EPAO total score and subscale scores were scored from zero to three. The mean EPAO scores for the total, subscores of nutrition and PA and subheadings are shown in Table 17. At baseline the total score and all subscores (with the exception of beverages provided and feeding environment) were scored slightly higher in the control nurseries. The lowest recorded subscore was in nutrition education and professionalism in intervention and control nurseries and the highest subscores were beverages, oral health and screen time. At follow-up, there were overall small decreases in subscores in the control arm and a combination of increases and some decreases in the intervention arm. The greatest change was recorded to be in oral health in the intervention arm.
| EPAO score | Intervention (n = 12) | Control (n = 12) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Total score | 1.76 (1.24) | 1.76 (1.30) | 1.92 (1.22) | 1.74 (1.28) |
| Total nutrition | 1.92 (1.23) | 1.93 (1.25) | 1.97 (1.23) | 1.83 (1.23) |
| Total PA | 1.59 (1.23) | 1.58 (1.58) | 1.86 (1.22) | 1.65 (1.32) |
| Nutrition | ||||
| Foods provided | 2.25 (1.24) | 2.40 (1.01) | 2.42 (0.97) | 2.17 (1.12) |
| Beverages provided | 3.00 (0.00) | 2.72 (0.75) | 2.94 (0.23) | 2.94 (0.23) |
| Oral health | 2.50 (1.22) | 2.83 (0.41) | 3.00 (0.00) | 2.83 (0.37) |
| Feeding environment | 1.56 (1.24) | 1.43 (1.27) | 1.32 (1.19) | 1.43 (1.15) |
| Nutrition education and professionalism | 0.56 (0.86) | 0.72 (1.02) | 1.00 (1.20) | 0.33 (0.58) |
| PA | ||||
| PA and play | 1.41 (1.12) | 1.23 (1.36) | 1.53 (1.31) | 1.35 (1.36) |
| Outdoor play | 1.30 (1.15) | 1.42 (1.23) | 1.81 (1.11) | 1.50 (1.22) |
| Screen time | 2.83 (0.56) | 2.92 (1.30) | 2.83 (0.55) | 2.88 (0.60) |
Review and Reflect
The six intervention nursery managers completed the Review and Reflect 80 questions, where they self-rated themselves on a scale from one to four, with one being the lowest level of acceptable practice and four being best practice. Table 18 shows the self-reported data for the three nurseries whose managers returned the completed Review and Reflect forms at baseline and follow-up. The reported nutrition summary score was higher than any of the PA, outdoor play or screen scores. The oral health and policies were the lowest scored sections of the Review and Reflect. The self-reported scores increased from baseline to follow-up in all four summary scores with an overall improvement of 9% and mean difference of 0.26 (95% CI –0.15 to 0.67).
| Summary scores | Baseline scores (n = 3) | Follow-up scores (n = 3) |
|---|---|---|
| Child nutrition and oral health summary score | 3.07 (0.20) | 3.24 (0.18) |
| Food provided | 3.07 (0.20) | 3.38 (0.21) |
| Beverages provided | 3.44 (0.51) | 3.56 (0.51) |
| Oral health | 2.00 (0.33) | 2.11 (0.51) |
| Feeding environment | 3.24 (0.29) | 3.51 (0.16) |
| Menus and variety | 3.00 (1.00) | 3.00 (0.00) |
| Nutrition education and professional development | 2.29 (0.38) | 2.95 (0.08) |
| Nutrition policy | 2.00 (1.00) | 2.33 (1.15) |
| PA and play summary score | 2.67 (0.29) | 2.98 (0.15) |
| Time provided | 2.78 (0.12) | 3.22 (0.19) |
| Indoor play environment | 3.33 (0.76) | 3.50 (0.50) |
| PA staff practices | 3.08 (0.14) | 3.25 (0.25) |
| PA education and professional development | 2.33 (0.31) | 2.80 (0.35) |
| PA policy | 1.00 (0.00) | 1.00 (0.00) |
| Outdoor play and learning summary score | 2.57 (0.90) | 2.71 (0.10) |
| Outdoor play | 3.25 (0.75) | 3.42 (0.52) |
| Outdoor physical environment | 2.63 (0.45) | 2.74 (0.53) |
| Outdoor play education and professional development | 2.00 (0.88) | 2.22 (0.51) |
| Outdoor play policy | 1.00 (0.00) | 1.00 (0.00) |
| Screen time summary score | 2.48 (0.33) | 2.6 (0.23) |
| Screen time availability and staff practices | 3.25 (0.50) | 3.58 (0.52) |
| Screen time education | 1.33 (0.58) | 1.66 (0.58) |
| Screen time policy | 1.00 (0.00) | 1.00 (0.00) |
Mediators
The mediators identified in the logic model were assessed by parents and nursery staff completing questionnaires that assessed motivation, self-efficacy and knowledge across the domains of nutrition and PA, with each question having a five point rating of agreement. Table 19 shows the parental mediators and Table 20 shows the nursery staff mediators at baseline and follow-up by study arm. In the intervention arm, there were small increases from baseline to follow-up in all parental mediator measures except PA knowledge. In the control arm, there were small increases in all parental PA mediators and decreases or no meaningful change in any of the parental nutrition mediators. In the intervention arm, there were small increases from baseline to follow-up in all nursery staff mediator measures, except no change in nutrition self-efficacy. In the control arm, there were decreases in all nursery mediators, except for a small increase in PA self-efficacy.
| Parental reported mediator | Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| PA, play and sedentary time | ||||||||
| Knowledge | 32 | 4.00 (1.30) | 32 | 3.78 (1.41) | 41 | 4.15 (1.15) | 41 | 4.56 (1.23) |
| Motivation | 32 | 4.12 (0.52) | 32 | 4.33 (0.53) | 40 | 4.24 (0.60) | 40 | 4.29 (0.49) |
| Self-efficacy | 32 | 4.20 (0.51) | 32 | 4.28 (0.58) | 41 | 4.39 (0.52) | 41 | 4.43 (0.47) |
| Nutrition and oral health | ||||||||
| Knowledge | 32 | 9.97 (2.24) | 32 | 10.69 (1.84) | 41 | 10.34 (2.16) | 41 | 10.22 (2.12) |
| Motivation | 32 | 4.25 (0.66) | 32 | 4.39 (0.55) | 41 | 4.32 (0.55) | 41 | 4.34 (0.51) |
| Self-efficacy | 32 | 4.37 (0.49) | 32 | 4.49 (0.54) | 40 | 4.52 (0.45) | 40 | 4.49 (0.47) |
| Nursery staff reported mediator | Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| PA, play and sedentary time | ||||||||
| Knowledge | 16 | 4.19 (1.64) | 12 | 5.08 (0.90) | 15 | 4.07 (1.28) | 11 | 4.64 (1.69) |
| Motivation | 15 | 4.54 (0.45) | 11 | 4.76 (0.32) | 15 | 4.45 (0.84) | 11 | 4.36 (0.76) |
| Self-efficacy | 16 | 4.43 (0.47) | 12 | 4.58 (0.39) | 15 | 4.46 (0.57) | 10 | 4.54 (0.43) |
| Nutrition and oral health | ||||||||
| Knowledge | 16 | 10.88 (3.30) | 12 | 12.09 (2.02) | 15 | 11.00 (1.13) | 11 | 10.20 (2.66) |
| Motivation | 15 | 4.47 (0.50) | 11 | 4.66 (0.38) | 15 | 4.58 (0.51) | 10 | 4.28 (0.89) |
| Self-efficacy | 16 | 4.36 (0.36) | 10 | 4.35 (0.54) | 15 | 4.58 (0.29) | 10 | 4.38 (0.49) |
Data linkage
Parents (n = 138) were asked at the end of data collection to give consent (in principle) for data linkage to the NCMP66 height and weight data (which is collected in primary schools in Reception and Year 6). Fifty-six (41%) parents returned the consent form and 51 (91%) of these gave consent for data linkage and four (7%) declined; therefore, 37% of all invited parents gave consent. This study did not intend to undertake data linkage because of the timescales.
Health economics
Intervention costs
The costs associated with the health visitors’ training were £1355.71 (see Appendix 7, Table 34). Health visitors travelled from North Somerset and Gloucestershire to Bristol for this training. The total cost of the workshop delivery in nurseries, including trainers’ time, refreshments, equipment and administration was £4372.83. Workshop costs only varied in terms of travel expenses, but nursery 12 participated in part of the intervention only, so the costs for this nursery were less (see Appendix 7, Table 35). The reported time of the health visitors’ attendance at each of the nurseries, attendance at the workshops, their preparation time and travel costs for each nursery are shown in Appendix 7, Table 36. Again, nursery 12 did not undertake the whole intervention, so the health visitor only attended this nursery for 2.5 hours. The total cost of the health visitors delivering the intervention and workshop attendance was £2181.13.
The mean (SD) cost incurred by each nursery of the intervention delivery was £717.22 (£260.05) (Table 21). The mean (SD) cost of health visitor intervention delivery, including workshop delivery, per nursery was £1092.32 (£197.90). The NAP SACC UK at Home element cost £11,946.95 (see Appendix 7, Table 37), but this was not included in the cost–consequence table as this was a one-off cost and NAP SACC UK at Home will not be continued.
| Costs and consequences | Intervention | Control |
|---|---|---|
| Cost of health visitor intervention delivery per nursery including workshop,a mean | 1092.32 (197.90) | N/A |
| Cost of intervention to nursery, mean | 717.22 (260.05) | N/A |
| Parental weekly food spend, mean difference between baseline and follow-up | 16.64 (51.56) | 2.52 (46.23) |
| Parental weekly PA spend, mean difference between baseline and follow-up | 4.47 (12.91) | 4.73 (28.00) |
| Child health-care costs, mean difference between baseline and follow-up | 6.59 (112.91) | –5.40 (32.72) |
| PedsQL score, mean difference between baseline and follow-up | 0.41 (7.39) | –1.67 (8.58) |
Health-related quality of life
A total of 124 parents (72.1%) completed the questionnaire about the child’s quality of life, expenditure on food and PA and child health-care use at baseline. A total of 86 parents (50%) completed the questionnaire at follow-up. The complete case for HRQoL analysis was 77 (44.8%). Parents reported few problems with their child’s HRQoL, the median score for the physical health, social health and nursery health domains being between 90 and 100. There were minimal changes in domain scores between baseline and follow-up for children in both the intervention and the control nurseries (Table 22). There was no change in the total score for intervention nurseries. The mean difference (SD) for the total score at follow-up was 0.41 (7.39) for the intervention arms and –1.67 (8.58) for the control arms (see Table 21).
| PedsQL score | Intervention (n = 32) | Control (n = 45) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Total PedsQL | ||||
| Mean (SD) | 85.93 (7.53) | 86.34 (8.58) | 87.65 (8.74) | 85.98 (10.45) |
| Median | 86.90 | 86.90 | 89.88 | 89.88 |
| Range | 64.29–96.43 | 64.29–100 | 57.14–100 | 60.71–100 |
| Physical health | ||||
| Mean (SD) | 86.79 (9.74) | 88.91 (9.02) | 91.59 (9.65) | 90.77 (10.31) |
| Median | 90.62 | 90.63 | 93.75 | 93.75 |
| Range | 65.63–100 | 71.88–100 | 65.63–100 | 62.50–100 |
| Emotional function | ||||
| Mean (SD) | 74.84 (11.29) | 74.03 (16.75) | 75.00 (15.73) | 74.64 (14.71) |
| Median | 75 | 75 | 75 | 75 |
| Range | 50–100 | 25–100 | 45–100 | 40–100 |
| Social function | ||||
| Mean (SD) | 92.10 (9.81) | 89.68 (11.47) | 92.14 (12.40) | 88.57 (14.70) |
| Median | 95 | 95 | 100 | 95 |
| Range | 60–100 | 55–100 | 45–100 | 50–100 |
| Nursery function | ||||
| Mean (SD) | 91.94 (12.26) | 91.67 (11.18) | 95.83 (7.64) | 90.67 (11.52) |
| Median | 100 | 100 | 100 | 95.83 |
| Range | 41.67–100 | 58.33–100 | 75–100 | 66.67–100 |
Food and physical activity costs
There was a small increase in self-reported family food expenditure between baseline and follow-up in both the intervention and the control arms (Table 23). This increase may be the result of inflation. Total weekly expenditure in both arms at follow-up was approximately £110 with large variances in expenditure between families. Some of the variance may be attributed to household size. Most expenditure was spent on supermarket food. More than 90% of parents stated that their reported spending on food and drink in the last week/month was typical at baseline and follow-up.
| Weekly spend | Intervention (n = 28) | Control (n = 42) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Total spend (£) | 93.26 (34.28) | 109.90 (51.63) | 109.33 (40.42) | 111.85 (46.29) |
| Supermarket shop/delivery | 76.25 (30.01) | 77.10 (33.36) | 83.54 (35.08) | 83.72 (34.68) |
| Convenience shop | 5.98 (7.36) | 11.78 (14.86) | 8.84 (9.53) | 10.60 (9.17) |
| Takeaway | 3.41 (5.24) | 8.10 13.00) | 4.11 (6.76) | 6.07 (10.54) |
| Café/restaurant | 6.07 (13.63) | 10.08 (14.01) | 10.77 (15.13) | 9.04 (13.18) |
| Other (e.g. school dinner money) | 1.54 (4.42) | 2.10 (9.47) | 2.06 (3.78) | 2.54 (6.05) |
There was a small increase in weekly PA expenditure for parents in both the intervention and the control nurseries (Table 24). The mean (SD) increase at follow-up was £4.47 (£12.91) for the intervention arm and £4.73 (£28.00) for the control arm. Total time spent by parents on their child’s weekly PA including travel and waiting time also increased for both the intervention and the control nurseries. Baseline data collection occurred in autumn/winter and follow-up data collection in July, which may have had an impact on these results.
| Weekly spend and time | Intervention (n = 26) | Control (n = 40) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Total cost including fees and travel costs (£) | 8.87 (10.50) | 13.34 (13.04) | 10.70 (8.04) | 15.43 (28.73) |
| Total time spent, including travelling and waiting (hours) | 3.91 (2.63) | 4.78 (3.49) | 4.74 (3.69) | 6.30 (5.46) |
Child health-care use
Parents reported infrequent health-care use at baseline and follow-up (Table 25). There were small changes in total (SD) monthly child health-care costs from baseline to follow-up in intervention nursery children [£6.59 (£112.91)] and control nursery children [–£8.13 (£41.22)] (see Table 25). Parents in intervention and control arms reported < 1 day of time off work due to illness of their child at follow-up (see Appendix 7, Table 38).
| Baseline | Intervention (N = 31) | Control (N = 43) | ||
|---|---|---|---|---|
| n | Cost (£) | n | Cost (£) | |
| At GP practice/community health centre | ||||
| GP/family doctor | 0.33 (0.61) | 12.77 (21.89) | 0.28 (0.70) | 10.05 (25.24) |
| Therapist (e.g. physiotherapist, osteopath, dietitian) | 0 | 0 | 0 | 0 |
| Other | 0.07 (0.25) | 9.58 (37.97) | 0.11 (0.32) | 8.40 (24.66) |
| Hospital care | ||||
| Ambulatory | 0.02 (0.15) | 2.72 (17.84) | 0.12 (0.32) | 2.70 (17.84) |
| Inpatient | 0 | 0 | 0 | 0 |
| Total | 0.42 (0.76) | 25.07 (53.03) | 0.51 (0.90) | 21.16 (55.30) |
| Follow-up | ||||
| At GP practice/community health centre | ||||
| GP/family doctor | 0.25 (0.54) | 8.83 (19.38) | 0.16 (0.63) | 5.86 (22.51) |
| Therapist (e.g. physiotherapist, osteopath, dietitian) | 0.03 (0.18) | 2.81 (15.63) | 0 | 0 |
| Other | 0 | 0 | 0.005 (0.03) | 1.14 (5.27) |
| Hospital care | ||||
| Ambulatory | 0.06 (0.21) | 6.93 (24.42) | 0.10 (0.37) | 6.28 (25.26) |
| Inpatient | 0.006 (0.04) | 10.38 (57.80) | 0 | 0 |
| Total | 0.34 (0.76) | 28.94 (94.79) | 0.27 (0.93) | 13.27 (32.88) |
Process evaluation
Data collected
Non-participant observations of both PA and nutrition nursery workshops were conducted in five out of the six intervention nurseries. Nursery 12 did not fully implement the intervention and, therefore, did not hold any workshops. Observations of NAP SACC UK partner/nursery manager meetings were conducted in the five intervention nurseries implementing the intervention. One observation (nursery 3) was of an initial meeting between the NAP SACC UK partner and the nursery manager and focused on discussing the Review and Reflect form. The remaining four meetings were of subsequent meetings between the NAP SACC UK partner and the nursery manager, and focused on reviewing progress made, changes implemented and outstanding actions.
Interviews were conducted with all NAP SACC UK partners and all managers in both intervention and control nurseries. Interviews with nursery staff members were conducted in four of the six intervention nurseries: nursery 12 did not implement the intervention and, therefore, no interview was carried out; one staff member (from nursery five) declined to be interviewed. We did not interview staff members in control nurseries. We aimed to interview 20 parents with invitations sent out by post. In total, 97 invitations were sent and 20 parents [intervention, n = 10; control, n = 10 (all mothers)] agreed to be interviewed (21% response rate). Interviews with NAP SACC UK partners and nursery managers lasted approximately 1 hour. Interviews with nursery staff were shorter (between 30 minutes and 1 hour) and interviews with parents were between 15 and 30 minutes.
Three NAP SACC UK partners returned completed logs documenting the interactions with nurseries. One partner did not return a log as her assigned nursery (12) did not fully implement the intervention. Baseline Review and Reflect forms were completed for four intervention nurseries: two nurseries (9 and 12) did not return their forms. Follow-up Review and Reflect forms were available for four nurseries: one form was not returned (nursery three) and one did not fully implement the intervention (nursery 12) and, therefore, did not complete the follow-up form.
Documents outlining the agreed goals set for each intervention nursery were available for the five nurseries implementing the intervention.
Progression criteria 1: feasibility
This section of the process evaluation aims to answer the following question: was it feasible to implement the NAP SACC UK intervention in child-care providers? Overall, the NAP SACC UK intervention was implemented with good fidelity (Table 26), with two exceptions. First, the parent website was not well used. Second, one intervention nursery (nursery 12) did not fully implement the intervention (but participated in data collection).
| NAP SACC UK intervention element | Implementation |
|---|---|
| NAP SACC UK partner training |
Training session held December 2015 (2.5 hours) for three partners. Fourth partner received one-to-one training in January 2016 ‘Top-up’ session held May 2016 (2 hours) |
| Nursery staff workshops | Workshops held in fivea/six nurseries, March–April 2016 |
| Review and Reflect | Form completed in all six intervention nurseries |
| Nursery goal-setting | Fivea/six nurseries set goals |
| On-going support | NAP SACC UK partner support provided to fivea/six nurseries via face-to-face meetings, e-mails and telephone calls |
| Parent website |
Parent website launched (April 2016) 12 parents (14%) logged onto site, of whom:29 e-mails/texts were sent out |
NAP SACC UK partner training
The training session for three NAP SACC UK partners was held in December 2015. This half-day session included an overview of the NAP SACC UK research study and training on how to support nurseries to improve nutrition, PA and oral health. Training was provided by local topic experts: a senior early years nutrition specialist, an independent PA trainer and an oral health promotion specialist. NAP SACC UK partners were provided with a resource pack containing relevant national guidance on nutrition, PA and oral health and copies of relevant study documents (e.g. Review and Reflect tool and resource log). One NAP SACC UK partner (Partner_Int_21) was unable to attend this training session and received a one-to-one session with Ruth Kipping in January 2016, providing her with the same information and documentation.
A second ‘top-up’ training session for NAP SACC UK partners was held in May 2016 to assess the nurseries’ progress and identify any problems or need for additional support. It was attended by three of the four NAP SACC UK partners, as well as the trial principal investigator, the trial manager and the nutrition, PA and oral health trainers.
Nursery staff workshops
Two workshops for nursery staff (focusing on PA and nutrition) were held in five out of the six intervention nurseries between March and April 2016. Nursery 12 did not fully implement the intervention and, therefore, did not implement any workshops. However, a 20-minute one-to-one session was conducted between the nutrition facilitator and the nursery’s cook on 14 April 2016.
The workshops were held either on a Saturday morning (n = 3) or on a workday evening (after the nursery had closed, n = 8), according to nursery preference. Workshops lasted between 2 and 3 hours (mean = 2 hours and 35 minutes) and refreshments were provided.
The PA workshops were all facilitated by the same person, an independent PA partner. The nutrition workshops were delivered by two different facilitators: a senior early years nutrition specialist (two workshops) and an early years health improvement specialist (three workshops). Both nutrition facilitators work in local authority public health teams, but were employed directly by NAP SACC UK to deliver the workshops.
The workshop facilitators used a variety of activities to engage nursery staff, including Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) presentations, group discussions, quizzes, food props and games. Observations of workshops described all three facilitators as highly enthusiastic and engaging. Information was delivered in a straightforward and uncomplicated way and was pitched at the right level to keep the staff engaged. As one partner described:
[the workshop] was very hands on . . . a really good way to tap into people’s skill levels really. People had a laugh, they were relaxed.
Partner_Int_21
The workshop observers noted facilitators adapted the content of the workshop to the needs and interests of the nurseries, for example by considering how the physical spaces available to the nurseries could be best used to promote PA.
Review and Reflect
Review and Reflect forms were completed in all six intervention nurseries. It was intended that the nursery manager would fill in the Review and Reflect form in advance (in collaboration with other staff, when necessary) and then discuss it with the NAP SACC UK partner during their initial meeting; however, it is only clear that this happened in two nurseries (nurseries 1 and 3). The NAP SACC UK partner assigned to nurseries 8 and 9 said that neither manager had filled in the Review and Reflect form before their initial meeting because ‘they just didn’t have time’ (Partner_Int_14), although this contradicts interview data from the manager of nursery 8. It is unclear what happened in the two remaining nurseries (5 and 12). Most interviewees did not comment on the benefits of filling in the form independently or with the NAP SACC UK partner. However, one partner (Partner_Int_14) noted that although it ‘slowed us down’, completing the form together generated more conversation and ‘made it easier for me to work with them to set the goals’.
Nursery goal-setting
Goals were set in five out of the six nurseries. Nurseries were asked to set three nutrition and three PA goals, and two additional goals that could relate to nutrition, PA or oral health, according to their own priorities. As described in the phase 1 results, oral health was a novel element of the UK NAP SACC UK study added because of formative research in stage 1 of the study. However, to ensure comparability with the US version of the NAP SACC UK study, the research team specified that only a maximum of two goals could focus on oral health. Three nurseries set eight goals and two nurseries set seven goals.
There was some confusion as to when goals were meant to be set (either before or after the workshops). Although it was intended that nurseries would set specific goals during the workshops, this did not happen in any nursery. This did not appear to be because they ran out of time, and several workshops ran for less than the scheduled 3 hours. In four nurseries (1, 5, 8 and 9), goals were set during manager–partner meetings, with the workshops happening afterwards. In the fifth nursery (3) the Review and Reflect form and goal-setting were completed after the workshops because of scheduling problems.
Two partners (Partner_Int_14 and Partner_Int_25) felt that the nurseries should have completed the workshops first and then set their goals. This would have meant that they were ‘a bit more equipped with the knowledge’ to be able to identify suitable goals (Partner_Int_14), with the other partner adding ‘it’s difficult for them to know what they want to change when they’ve not done the workshops’ (Partner_Int_25). However, one partner noted that it was important to ensure that the Review and Reflect form (if not the goal-setting) was complete before the workshops to prevent managers providing biased answers. This view was confirmed by the manager at nursery 3 (where the Review and Reflect form was completed after the workshops):
I feel my judgement was hindered slightly because I already had the knowledge of the [workshops] in my brain when I done the Review and Reflect score . . . so I was maybe slightly semi-biased when I done it . . . Saying I was maybe slightly better than what we were.
Manager_Int_1
Examples of the types of nutrition goals set included staff role modelling positive eating behaviours, asking children ‘are you still hungry?’ rather than ‘do you want some more?’, changes to menus (e.g. providing more varied breakfast foods, removing biscuits as snacks or increasing oily fish portions), increasing heathy eating activities offered and providing information on healthy eating to parents. PA goals included developing a nursery PA policy, providing more active stories and games, staff role modelling of PA and providing information to parents on PA. Three nurseries (1, 5 and 8) also included specific goals on promoting oral health through nursery activities and dental visits.
Specific goals set by each nursery and progress made, are set out in Appendix 8, Table 42. Progress was made on most goals, in part because many were relatively simple to implement. For example, many menu changes (e.g. offering fruit at breakfast or removing biscuits as snacks) were quick and easy to achieve. Interview data also suggested that goals requiring behavioural change (e.g. adult’s role modelling more PA or asking children if they were still hungry) had also been implemented.
Although some managers noted some initial resistance or scepticism from staff about behavioural changes, all explained that this resistance had been overcome. For example, staff in one nursery did not believe that the portion sizes (which had been revised in light of the NAP SACC UK nutrition workshop) were correct. However, the manager discussed the guidance with the staff and explained that ‘the fact that obesity is so high, this is the reason why, because it’s down to us overfeeding them’. She continued, ‘it took a little while for some staff to come round but we’re kind of getting there now which is good’ (Manager_Int_1). Similarly, the manager and deputy manager at one nursery noted how staff seemed daunted by the idea of ensuring three hours of PA every day, but worked with the staff to find ways to achieve this:
So it was, you know, ‘Go and research it,’ or, ‘We’ll try and give you ideas’ . . . Or they might come back and say, ‘Well, I can’t do this for this.’ We’ll have a look at it, ‘Well actually you can,’ or, ‘Actually, no, you’re right. You can’t. Let’s have a look at doing it a different way’.
Manager_Int_4
Some goals had not yet been achieved; these tended to be those which required more time and effort, particularly on the part of the nursery manager (e.g. writing new nursery policies). For example, managers at nurseries 1 and 5 had not yet written their nutrition and/or PA policies.
On-going support
Intervention nurseries were offered support from NAP SACC UK partners in order to discuss their Review and Reflect forms, set goals and support the nursery manager and staff in making the specified changes. Support was provided via e-mails, telephone calls or further face-to-face meetings. The details of this support were collated from the NAP SACC UK partner logs and are summarised in Appendix 8, Table 39.
Initial partner–manager meetings took place face to face on nursery premises and all lasted > 2 hours. Of the five nurseries implementing the intervention, all had at least one further face-to-face meeting with their NAP SACC UK partner to review progress made. Additional support was offered via e-mails and telephone calls, although some of these telephone calls were to set up subsequent face-to-face meetings rather than offering substantive support. NAP SACC UK partners described using e-mails and telephone calls to pass on relevant information to nurseries (e.g. about National Smiles Month, Partner_Int_21) or to check on progress and offer general support and encouragement.
Parent website
A summary of the use of the NAP SACC UK website is shown in Appendix 8, Table 40. The website was promoted to parents at the six intervention nurseries with a free child’s mug featuring the website address, a flyer and a parent information sheet. All intervention parents with an e-mail address were e-mailed with a link to the website and a parent newsletter including a link to the website was sent out 1 month later. Parents were offered a free family swimming voucher at the local authority’s swimming pools as an incentive, if they completed the ‘Healthy Habits’ section and set a goal on the website. The parent website was not well used, with only 12 parents (14%) logging on to the website. All 12 parents completed the ‘Healthy Habits’ survey and seven set a goal (see Appendix 8). Goals focused on sleep (n = 3), increasing outdoor play (n = 2), eating (n = 1) and screens and seated time (n = 1) (see Appendix 8, Table 41). All 12 parents were sent e-mails to encourage the setting of a (further) goal, but none did so.
As part of the website registration process, parents provided a mobile phone number. Targeted text messages based on the parents’ answers to the ‘Healthy Habits’ survey were sent to the 12 parents. Parents received between one and three text messages, depending on how early they signed-up to the website. No parent received more than one text message per week to avoid overload, and no parent unsubscribed from these messages.
A NAP SACC UK closed Facebook group was set up for intervention parents to complement the website. The plan was for the research team to send suggestions for goals, information about health changes and recipes, with the aim of generating discussion and support between parents. No parents at any intervention nursery joined the Facebook group.
Withdrawal from the intervention: nursery 12
One intervention nursery (12) did not fully implement the NAP SACC UK intervention (but participated in follow-up data collection). The nursery manager completed the Review and Reflect form with the NAP SACC UK partner, but no goals were set and no staff workshops were held. The primary reason for the nursery withdrawing was staff found the requirement to attend after-hours training workshops unacceptable. The letter of agreement between the nursery and the university stated that participation in the study would involve two out-of-hours training workshops. However, the letter of agreement was signed by the nursery’s deputy manager and it became clear in the manager interview that she was unaware of this requirement.
It is important to note, however, that the out-of-hours training was unacceptable because nursery staff had very recently completed several weeks of mandatory (out-of-hours) first aid training. Out-of-hours training was therefore not inherently unacceptable to staff, rather the specific timing of the NAP SACC UK workshops (following shortly after other mandatory training in this nursery) made it so. Indeed much training in nursery settings is conducted out of hours and the five other intervention nurseries all rated the NAP SACC UK workshops extremely highly.
Although NAP SACC UK staff offered alternative solutions to this problem (including conducting workshops during the nursery day), none was acceptable to the manager. A series of communication problems between the nursery manager, the NAP SACC UK partner and NAP SACC UK study staff led to the point when the manager discussed withdrawing her nursery from the study. As a result, the study principal investigator (RK) was unblinded in order to discuss the situation with the manager, resulting in the nursery agreeing to remain within the study for data collection purposes, but not fully implementing the intervention. Therefore, nursery 12 did not set any goals nor did it hold any staff workshops. However, a 20-minute one-to-one session was held between the nursery cook and the nutrition workshop facilitator where key points from the nutrition training workshop were summarised.
Progression criteria 2: intervention acceptability
This section of the process evaluation aims to answer the following question: was the intervention acceptable to NAP SACC UK partners and the majority of child-care managers, staff and parents?
Overall, levels of acceptability of the NAP SACC UK intervention to NAP SACC UK partners and nursery managers and staff was high. One manager explained that: ‘It’s been thoroughly enjoyable to take part in it . . . it’s been an absolute benefit . . . I would recommend it to any other nursery’ (Manager_Int_1). A staff member from a different nursery described the intervention as ‘eye-opening’, explaining that for ‘us who have been in for a long [time] . . . you sort of get stuck in your ways and it’s just shown us different ways of doing things’ (Staff_Int_6). NAP SACC UK partners were also generally positive about the intervention, describing it as ‘a practical, useful intervention’ (Partner_Int_25) and ‘a fantastic idea’ (HV_ Int_14), although this partner explained that it worked well because the ‘nurseries are really buying in to it’, noting that ‘it would be very difficult, I think, to be with a nursery that aren’t quite so keen’.
In general, parents were unaware of specific changes occurring in the nursery because of NAP SACC, but were supportive of the nurseries’ participation in research and their child’s involvement in it. For example, one parent noted: ‘I just think it’s a very useful thing to be doing to be honest. I’m glad to be part of it’ (Parent_Int_38). However, the very low uptake of the website suggests this intervention element was unacceptable to parents.
NAP SACC UK partner training
The partners appreciated the NAP SACC UK training describing it as ‘useful’ (Partner_Int_16) and ‘well done’ (Partner_Int_25) and that it ‘ironed out any questions, made it clear what we had to do’ Two partners had not expected to learn much from the nutrition session as this topic was well-covered in their health visiting role. However, both reported finding it useful, for example in making them aware of the Children’s Food Trust Voluntary Guidance for Early Years settings28 or in demonstrating the amount of sugar present in certain drinks. The PA session particularly appreciated because, as one partner explained, ‘that wasn’t something I’d had . . . formal training on’, adding ‘[health visitors] focus a lot on what people are eating but you forget about the other side which is very important’ (Partner_Int_25). The training lasted 2.5 hours; two partners felt it should have been longer, describing how each of the three trainers (for nutrition, PA and oral health) were ‘tied for time’ (Partner_Int_25) and that one session (oral health) had run out of time.
A second ‘top-up’ training session was held for NAP SACC UK partners in May 2016. This aimed to provide study staff with a sense of how the intervention was progressing and to assess whether partners required additional information or resources in order to support the nurseries. One partner (Partner_Int_16) found it helpful to hear about other partners’ experiences working with their nurseries. Another (Partner_Int_25) felt it was useful ‘because we all came in with specific things, challenges that we’d had’ and were able to share learning and ideas. However, she added ‘it was all a bit late, we’d nearly finished by then. So we probably could have done with that one a bit sooner’. Additional resources, particularly on oral health, were requested by the partners and were e-mailed out shortly after this meeting. Although the partners perceived this top-up training to be useful, for a group of experienced staff such as these health visitors, it does not appear to be an essential part of the NAP SACC UK intervention. In terms of this feasibility study, it was however useful in checking progress and allowing an opportunity for any specific problems to be identified and resolved.
Although not a specific requirement of the intervention, all four partners described how they did some additional preparation outside the two training workshops to prepare for working with the nurseries. This involved familiarising themselves with the literature and resources provided by NAP SACC UK and ensuring that they understood what they needed to do with the nurseries. As one partner explained:
I wanted to prepare myself. I think I couldn’t have walked out of that room at that training session and gone straight to a nursery. I wanted to be able to read through the Review and Reflect tool and also I was cross-referencing with the . . . guidance that the nursery would adhere to.
Partner_Int_14
How long each partner spent preparing was not specifically logged but one partner said she spent ‘about a day in total’ (Partner_Int_14) and all partners were reimbursed for one day of preparation time.
Nursery staff workshops
Nursery managers, nursery staff and the NAP SACC UK partners were all highly enthusiastic about the two NAP SACC UK training workshops. Indeed, the enthusiasm and inspiration created by the workshops appears to have been the most important part of the whole NAP SACC UK intervention for many of the nursery staff. The workshops were variously described as ‘invaluable’ (Manager_Int_10), ‘absolutely brilliant’ (Staff_Int_6) and ‘inspiring’ (Partner_Int_21). One manager explained:
The [staff] that did the workshops thoroughly enjoyed them, and they were really good, and you know I would recommend them to anybody. They were definitely worth doing.
Manager_Int_7
One manager admitted to feeling nervous beforehand about having external staff come in to run the training, explaining:
It’s always a bit hard when you have a professional coming into your setting, you feel as though you’re being sort of criticised.
Manager_Int_1
However, these fears were not realised and her staff found the workshops to be extremely positive: ‘Luckily none of that came into play or anything. Yeah, they were absolutely brilliant both of them.’
Workshop style and facilitation
The interactive nature of the workshops and the lively and engaging manner of the facilitators were important in engaging the staff, particularly at the end of a long working day. As one manager explained:
We had the physical activity training after a long day at work for most of us, and we were kind of all like, ‘Oh it’s training.’ And actually we all kind of came away like, ‘My gosh, I’ve got so much energy. I just want to do this and I want to do this . . . and it kind of re-inspired us’.
Manager_Int_11
Both workshops were reported as being pitched at the right level for staff. As one manager noted, her staff had a range of academic abilities and backgrounds from apprentices to staff with degrees, but the workshops were ‘very tailored to absolutely everybody’ (Manager_Int_1). This was echoed by another manager who said ‘everybody got something out of it’ (Manager_Int_7).
The skill and personality of the facilitators appeared crucial in creating the right atmosphere for the workshops and in inspiring staff. One staff member described how during a quiz activity in the nutrition session some friendly competition emerged between groups and the nutrition facilitator ‘sort of went with that’ and ‘she really got us engaged’ (Staff_Int_12). The PA facilitator, in particular, was highly praised for his ability to engage staff. The NAP SACC UK partner attended one nursery workshop explained:
I think they were a little shy to begin with some of them, and then he got them really going . . . He was really good and really engaged them and people started to relax.
Partner_Int_21
This was corroborated by the manager of this nursery who explained:
[The facilitator] had like a funny character to him . . . So it was kind of like we felt like we knew him, and that was funny . . . I guess you just kind of felt at home or felt at ease. So you took on a lot more and you had a laugh and a joke, but you didn’t lose sight of where you were going.
Manager_Int_11
Physical activity workshops
Several participants explained how the PA workshops made them think more creatively about ways to help children be physical active and reflect on their own practice:
It wasn’t until we actually had the training days that we realised actually that we could have done more, and had specific activities outside. It tended to just be free flow, so children were spending most of the time sat on the floor not participating in the activity. And we kind of just thought ‘oh it’s ok, they’re outside, they’re running in and out, that’s fine, that’s all the activity that they need.
Manager_Int_1
Several participants described how the PA facilitator had given them many creative ideas for incorporating PA into the everyday activities of the nursery. One staff member described with enthusiasm being shown different ways to use ordinary objects for PA:
For example, with tennis racquets, you don’t need just for playing tennis. You can do various activities with them. I think it’s just opened our eyes to think, ‘Actually, there are new ways of doing it’.
Staff_Int_6
The NAP SACC UK partner attending this same workshop also noted how the facilitator:
. . . got them thinking about story time, how can you have story time just not where they’re sat on their bottoms watching you with your book, how can you bring that story to life and have the children going on a bear hunt round the room?
Partner_Int_14
A NAP SACC UK partner (Partner_Int_21) described how, for a different nursery (3), some staff felt ‘out of their comfort zone’ being asked to act ‘as if they were on CBeebies [BBC, London, UK]’ to encourage PA during story time. She explained that this was ‘gently talked about [in the workshop] . . . and that’s something they’ve worked on’, adding that one member of staff had subsequently received funding from the local authority to attend storytelling workshops.
The PA workshop in particular received high praise from the participants. One manager, for example, said ‘We absolutely loved the physical activity [workshop]. Absolutely loved it’ (Manager_Int_11), while another felt that they got more from this workshop than the nutrition session (Manager_Int_4). One exception to this came from nursery 9 where the manager and staff member interviewed, despite describing the workshop as ‘very good’ (Staff_Int_6), felt that the session could have been more interactive:
The physical activity one was less interactive . . . it was more sort of PowerPoint based, so it was more talk . . . I think because it was physical activity we expected it to be active.
Manager_Int_7
Observation of this workshop did not suggest the delivery of this particular session was different from any of the other PA workshops delivered.
Nutrition workshops
Some of the enthusiasm for the PA sessions appears to be because this was often a novel training topic for them; nurseries were much more likely to have received other training on nutrition and healthy eating. Nonetheless, the nutrition workshops were also praised and several participants commented on how much they had learnt. One staff member commented that ‘we came out [of the nutrition workshop] and actually we wanted to know more . . . we could have stayed there another hour’ (Staff_Int_6), while another was reminded that nutrition is ‘not something to be sort of shoved on a shelf somewhere and forgotten about’ (Manager_Int_10). Participants seemed to particularly appreciate advice on portion sizes. One manager explained that they had been looking for information on portion control prior to NAP SACC UK but:
. . . everywhere we looked everyone was saying something completely different with regards to how much children should be eating . . . So it was great to have [the nutrition workshop facilitator] to come in and for us to actually share this is what we’re doing, is this all correct? That was absolutely perfect for us.
Manager_Int_1
One manager noted a discrepancy between the advice they received from NAP SACC UK and that from an oral health programme (Smiles Better) which they had recently been involved in. The NAP SACC UK training recommended including oily fish on their menu once every week, while the Smiles Better training suggested including it three out of four weeks. The staff member at this same nursery also noted the NAP SACC UK nutrition training ‘did overlap quite a lot’ with the training they had received from the Smiles Better programme (Staff_Int_3).
Timing and attendance
Workshops were held either on a workday evening (n = 8) or on a Saturday morning (n = 3), according to nursery staff preference. Attendance at the workshops ranged from four to eight staff, with a mean of six.
The timing of these session elicited mixed views from participants, with some nurseries reporting good attendance while others reported poorer participation. The manager of nursery 3 explained that despite the voluntary nature of the workshops, staff attendance has been ‘absolutely great’ (Manager_Int_1), although she did acknowledge that having both workshops as part of a scheduled nursery inset day would have been easier for them. Other participants described their lack of enthusiasm at the thought of training after a long day, but reported coming away from the workshops feeling inspired and enthused (Manager_Int_11_and_12).
Nonetheless, asking staff to attend training out of hours did pose difficulties for some nurseries and consequently limited attendance. One staff member at nursery 9 noted that only five people attended the Saturday morning session, explaining that ‘some of the staff work 40 plus hours a week and they’ve obviously got stuff that they do on a weekend and they just couldn’t make it’ (Staff_Int_3). The nursery manager also commented on this, saying that ‘it would have been nice if more had attended but . . ., we do a long day and then having to do a couple of hours in an evening, I can understand why’ (Manager_Int_4).
A similar problem was reported at nursery 8 where only 4 out of 13 staff attended the evening nutrition workshop. The staff member noted that ‘that’s not unusual for staff meetings’ (Staff_Int_6), with the manager acknowledging that ‘a lot of [staff] have got children of their own, and their children are doing things, or they’ve got partners who work away and all those sort of complications.’ (Manager_Int_7). However, attendance at this particular nursery was complicated by the fact it had recently been taken over by a nursery chain. New staff were contractually obliged to attend out-of-hours staff training, while staff on the old contracts were not. The manager noted this issue (although not confined to NAP SACC UK training) had created ‘a little bit of . . . tension’ (Manager_Int_7).
Because of the voluntary nature of the out-of-hours NAP SACC UK training, it was not always possible to ensure that the ‘right’ staff were attending. The priority for the study was to ensure that early years practitioners with responsibility for NAP SACC UK’s target age range (2- to 4-year-olds) attended the training. However, one manager noted that ‘it tended to be more the baby practitioners that attended the physical workshop’ than those working with 2- to 4-year-olds (Manager_Int_4). We did not record how many staff working with 2- to 4-year-olds attended the training in each nursery.
Participants reported the length of the sessions (ranging from 2–3 hours) as being appropriate, although one manager commented that they ‘could have been a little bit longer and certain things more in depth’ (Manager_Int_1). Another manager commented it had been difficult to ask staff to attend a 3-hour session as their after-work team meetings only usually lasted 1–1.5 hours. However, splitting the two 3-hour workshops over four 1.5-hour sessions would have been equally difficult to expect staff to attend. Having the training as part of an inset day would have improved attendance but as they had recently been taken over by a chain no inset days were being scheduled at that time (Manager_Int_7).
NAP SACC UK partner attendance and delivery
Three NAP SACC UK partners attended at least one workshop in each nursery that they were working with (no workshops were held at nursery 12 so the partner could not attend). Partners did not report any problems in attending these out-of-hours workshops. One noted that attending the evening workshop meant a very long day (08.00 to 20.00) but that ‘it wasn’t a problem because . . . the trainers were so engaging, it was actually fine’ (Partner_Int_25).
All three partners found it beneficial to attend the workshops. One explained that it was ‘really helpful to do those workshops with the nurseries, just so you can kind of see the staff and what their attitudes are’ (HV_Int_25). Another suggested it had been important in establishing a good rapport with the nursery staff:
It gave me a chance to meet the staff, and also hopefully it gave them a chance to see, as the Health Visitor, I was also saying ‘Oh wow, this has got a lot of sugar in hasn’t it?’ That kind of showed we’ve all got something to learn.
Partner_Int_21
However, one partner suggested that the role of the partner at these workshops should be made clearer:
I suppose it’s helpful to know, if you’re going along, are you going along to support delivery of the workshops or are you a participant?
Partner_Int_25
One partner admitted that ‘how much [attending the workshop] actually altered my meetings with the managers and our goals and things like that [is] hard to say’ (Partner_Int_14); however, another partner felt that it had been very useful in helping her with the rest of her NAP SACC UK role in the nursery. She explained that it had been useful to see:
. . . which bits [the staff] were enthusiastic about because then it really helped when you were then doing the goal-setting. You’ve got an idea in your head of – because they’re not going to make changes about things they aren’t in the least bit interested in . . . And then when you’re doing the goal-setting with them you can kind of say, ‘Oh, well, you know, people seemed to be quite enthusiastic about this’.
Partner_Int_25
Partners were asked how they would feel about delivering these workshops in any future roll-out of NAP SACC UK. All three agreed that with further training they would be happy to take on this role, noting that they have a lot of experience in delivering this type of training within their health visiting roles, albeit to parents rather than nursery staff (note, this is in contrast to the findings from the formative focus groups discussed in phase 1). However, one partner noted that ‘I don’t think I’d be ever quite as enthusiastic as [the PA facilitator], because he’s so passionate about it’ (Partner_Int_14). Given the success of these workshops appeared largely related to the enthusiasm and personality of the facilitators, the skills and attributes of the workshop facilitators in any subsequent roll-out would require careful consideration.
Staff training budgets
Although NAP SACC UK workshops were provided free of charge, they did potentially incur a cost to nurseries in terms of paid overtime or time off in lieu; the acceptability of this was explored in nursery manager interviews. In addition, we asked about nursery staff training budgets and their views on paying for the NAP SACC UK workshops.
Of the five nurseries implementing the workshops, all but one (nursery 9) paid staff for attending the training or gave them time off in lieu. The manager at nursery 9 explained that staff were not usually paid to attend training, but were expected to attend voluntarily as part of their personal development. The staff member interviewed (Staff_Int_3) at this nursery felt that this accounted for the poorer attendance at the workshops. The costs incurred by the nurseries for these workshops were estimated to range from £478 to £691 (mean £610) and are discussed in greater detail in Chapter 6, Health economics.
Of the 12 nurseries participating in this study, four had dedicated staff training budgets. Exact figures were only given for two nurseries: a total of £100 and £150 per term for the whole nursery. In the remaining nurseries, training requests were considered on a case-by-case basis according to the needs of the nursery and interests of staff, with mandatory training (e.g. child first aid) taking priority. In at least two nurseries it appeared staff were sometimes expected to pay the course costs for any non-mandatory training they wished to attend (although they may have been paid or given time off in lieu for attending). Unsurprisingly, free training was more likely to be approved by nursery management than courses with registration fees. Often only one or two staff would be sent on a training course, with the expectation they would cascade the information back to other staff.
Most staff were not in favour of charging for NAP SACC UK workshops, with one manager noting that the free training was a major incentive to take part in the study (Manager_Int_10). One staff member felt that her nursery would not have paid for the nutrition workshops ‘because there was nothing [new]. We were hot on that anyway’ (Staff_Int_3). However, her manager was more equivocal saying they ‘possibly’ would have considered the training if there had been a charge but would only have allowed one person to attend (Manager_Int_4). This was echoed by managers at nurseries 1 and 5, who would also have limited the number of staff attending to limit costs. The manager at nursery 8 noted that any training charge would require approval from their chain head office, making participation in the study more problematic. Interestingly, one manager explained that now she knew how good the workshops were she would have paid for them, but that ‘at the time, most probably not’ (Manager_Int_1).
Review and Reflect
Both the NAP SACC UK partners and the nursery managers reported finding the process of completing and discussing the Review and Reflect form very useful. One manager explained that ‘it showed us what we are doing good and just the tweaks we needed to change that improved it’ (Manager_Int_4). It was, however, also described as ‘extremely time-consuming’ (Manager_Int_1), often taking about 2 hours to complete, which led one partner to quip ‘by the end of it I needed a lie down!’ (HV_Int_14). Finding time to complete the lengthy form within a busy nursery day was problematic, meaning that it was sometimes put ‘on the backburner slightly’ (Manager_Int_1) or even compromised the quality of the data provided:
[It] was really longwinded . . . By the end of it we were just like, ‘Oh, we’ll just tick that one, and we’re not really too sure’.
Manager_Int_11
Another staff member felt that it was too repetitive, explaining that ‘we just felt that we were just ticking the same thing over and over again’ (Staff_Int_11). Revising the form to be simpler, shorter, and less ‘wordy’ was suggested by one partner (Partner_Int_25).
None the less, the benefits of completing the process were reported, with one manager noting that ‘once you actually got into doing it, it was absolutely fine’ (Manager_Int_7). One partner felt that it was a useful way to get the managers really thinking about their practice:
Certainly with them all pulling their menus out and it’s like, ‘Oh gosh, no, I didn’t think about that’, and, ‘Oh yeah, look at that pattern, look at that. We’re offering too many biscuits there’. Just gets them really thinking about it.
Partner_Int_14
Some managers had filled in the form before meeting with the NAP SACC UK partner, while others completed it with the partner during their first meeting. Some of those who did the latter commented on the benefits of completing it in this way (the former group did not mention this in interviews). One partner explained that ‘because I’d been involved in actually the completion of the questionnaire . . . that made it easier for me to work with them to set the goals’ (Partner_Int_14). This was backed up by the nursery manager who said ‘you could do it on your own, but it was nicer to have somebody to sort of bounce things off’ (Manager_Int_4). Equally, another partner felt that completing the form with the manager ‘gave me an oversight really, and also what restrictions they have from a financial point of view’ (Partner_Int_21).
Nursery goal-setting
Both nursery staff and NAP SACC UK partners appreciated the fact that many of the goals set were simple and easy to implement – little ‘tweaks’ to menus or practice, rather than more daunting changes. Examples of these changes included cutting up fruit rather than offering whole pieces, adding details of local dentists to registration packs, taking chairs away to encourage children to stand, creating an ‘open door’ policy that allowed children to choose to play inside or out, and using resources that they already had but in new ways. As one staff member explained that the changes ‘were easy things to do. They weren’t major things’ (Staff_Int_3). One partner felt that these easily achievable goals were key to getting the nurseries on-board:
They’re just small goal-setting . . . they’re inexpensive goal-setting . . . and I liked that because I thought that was practical, not too big a jump for the nurseries.
Partner_Int_16
Some nursery staff talked about how the process of being involved in NAP SACC UK and setting goals had provided a welcome opportunity to reflect on their usual practice and be more mindful about their interactions with the children:
Quite a lot of us we found were dug down in routine, more so thinking, ‘We need to do this now, we need to do this, we need to do this in our routine’, rather than thinking, ‘Actually what are we doing as adults that promote what children are doing, and like physically wise and activity wise?’.
Manager_Int_11
Another manager talked about how the changes implemented as a result of NAP SACC UK had become ingrained in their nursery practice:
I think because it has become so ingrained in what we do. For example, our chef, she devised all of our menus for the summer taking some of the learning that we’ve gained through NAP SACC, and so therefore every time she puts the menus together that’s how she will write them, informed with that as well. So, it now has become part of our make-up and it’s quite early on . . . but at the moment it’s quite ingrained in what we do.
Manager_Int_10
Nutrition goals
All nurseries who had set goals to modify their menus had achieved them (although see Barriers to setting or implementing goals for barriers to changing the menu in nursery 1). Staff at one nursery commented on their improved understanding of portion control as a result of the NAP SACC UK nutrition workshop, with the manager explaining that ‘we’re not overfeeding them any more’ (Manager_Int_1). However, one of the changes most frequently commented on, and implemented by several nurseries, was simply changing the language staff used when offering second helpings of food:
I think the thing that was actually the most useful was this thing about asking children whether they’re still hungry or not [rather than ‘do you want some more’] . . . I’d never thought about it . . . And actually that whole concept of just changing one phrase that you use when you interact with a child, but actually that makes a massive difference, because they’re making a decision based on their own body and their own needs, not on what the child next to them is doing.
Manager_Int_7
Another positive change was that one (nursery 3) now allowed staff to eat for free to encourage them to eat with the children and role modelling positive eating behaviours. As this nursery was part of a local chain, this new practice had been rolled out to three other nurseries (not involved in the NAP SACC UK trial). The NAP SACC UK partner for this nursery felt that this was a hugely positive change because ‘socialisation and eating, that’s the key element to children’s healthy attitude to food’ (HV_Int_21). The staff member interviewed at this nursery also felt that this change had resulted in considerable benefits:
I can see personally with some children who are not too sure about food, and it’s kind of ‘I don’t want to try that’, I’ve noticed if I sit with them . . . they have watched me and they have eaten what I’m eating, and they will try it with me. And I think that’s such a benefit to those children and for all children as well to see I am eating my vegetables, and they can copy me and copy that behaviour as well.
Staff_Int_2
Changes were also made with regard to providing parents with extra information on nutrition. One nursery held a parents evening including nutritional information, displaying a noticeboard signposting parents to relevant resources and provided information on their website (nursery 5). The manager of this nursery noted that staff were now more willing to speak to parents about nutritional issues (e.g. suggesting healthier alternatives to chocolate bars in lunchboxes). The manager explained that they can now ‘provide some background information as to why we’re actually saying it, as opposed to it’s just a personal opinion, it’s got some more clout behind it now [because of NAP SACC UK]’ (Manager_Int_10).
Another manager (Manager_Int_11) set a goal to provide parents with information on healthy packed lunches and explained it had made a ‘massive difference’ with the children now coming ‘in with healthier lunches, or I should say a balanced lunch.’ This nursery now included the packed lunch guidance in their welcome packs for all new families, explaining that:
As soon as they say, ‘Oh, we’re thinking of bringing a packed lunch’, rather than kind of feeling like we’re targeting them, it’s just, ‘Oh, this is standard that we give out’, just so that the information is there for them ready.
Manager_Int_11
Physical activity goals
Physical activity goals tended to fall into three categories: devising policies, engaging with parents, and changes to staff practices and/or use of equipment and space. Of the three nurseries planning to write and implement a new PA policy, only one (nursery 9) had done so; progress had been hampered in the other two nurseries because of managers’ lack of time. Four nurseries (1, 3, 8 and 9) set goals to provide parents with information about PA. All four nurseries had done this, although in one case (nursery 1) it was not clear whether or not the changes made (e.g. moving parent information display to a more accessible area) were specifically attributable to NAP SACC UK.
Interviews tended to focus on the changes to staff practices and the use of their space and equipment in creating more opportunities for PA. For example, one nursery (1) had ‘revamped’ their garden to make better use of it by introducing wooden boxes at different heights to encourage jumping, as well as creating a ‘mud kitchen’. A manager at nursery 3 explained how they had changed their approach to using their outdoor space:
We did have set garden times before, but during our [NAP SACC UK PA workshop] he said it was best for children to choose whether they want to play inside or outside which is what we now do, down to his advice.
Manager_Int_1
Other examples of changes to practice included buying a compact disc (CD) player to encourage children (and staff) to be physically active to music even when it was very wet outside, using different games or equipment while outside to get the children to be more active or staff discussing their own hobbies and interests (e.g. hockey or gymnastics) with children.
An important consequence of the intervention was the space it gave to staff to concentrate on the importance of children’s PA. One staff member commented that their involvement in NAP SACC UK had ‘opened their eyes’ to new ways of promoting PA and that ‘it just made us reflect on our practice’ (Staff_Int_6). Another manager felt that the NAP SACC UK training had given staff permission to focus on encouraging and enjoying PA with the children:
It was just quite nice to like see the staff actually relaxing a bit more and not worried about, ‘Oh, we need to go to do that next because actually so and so is already in there doing it and we’re out here enjoying our time’. And obviously for the children it was, ‘Oh, the adults do it too, they have fun, they play the spot game, they chase us round’.
Manager_Int_11
Barriers to setting or implementing goals
As noted above, most goals set by the nurseries had been achieved. The exceptions to this were where policies had not been written or specific activities (e.g. a Fitness Fun week or dental visit) had not yet been arranged (see Appendix 8, Table 42). However, it became apparent from the interviews that some nurseries had chosen not to set certain goals because they were aware that they were not achievable. For example, one NAP SACC UK partner explained that she did not broach creating a PA policy with one of her nurseries as it was part of a large, national chain and it ‘would have been far more challenging for them to actually try and implement policies without a huge delay . . . it would have gone through a lot of red tape and wouldn’t have been achieved within the timeframe that we had.’ (HV_Int_14, referring to nursery 8). By way of contrast, one manager wondered if being part of a chain would have helped him achieve his goal of creating a new PA policy because ‘because you’ll have other departments that put that sort of thing together and it’s not down to one individual’ (Manager_Int_10).
A lack of space was also noted as a barrier in some nurseries. Toothbrushing was not set as a goal in one nursery because they did not have space to accommodate the extra movement of children and staff needed to facilitate this. Another manager commented on their limited outdoor space as a barrier to increasing PA, but went on to add that this meant that they just had ‘to use that [space] wisely’ (Manager_Int_1).
One NAP SACC UK partner raised the issue of a potential conflict of interest between running the nursery as a profitable business and introducing healthy changes that might prove unpopular with parents. She felt that one of her nurseries would not have been keen to introduce a ‘water only’ policy for fear of this reason:
[Nursery 1] wouldn’t have gone for a water only [policy] . . . because that might alienate some of the parents. . . So I suppose, as a private nursery, there is a balance between wanting to put these healthy things in place . . . it’s difficult, because you’re wanting people to carry on sending them and paying. And they can equally go to another nursery down the road if they don’t like the food.
Partner_Int_25
However, it was not clear from this interview whether or not this was a goal that had been discussed and subsequently rejected or an assumption on the part of the partner; neither the manager nor staff member interviewed at this nursery mentioned this issue.
Two partners raised some concerns about having the right nursery staff involved in the planning and goal-setting process to ensure that actions were followed through. The partner working with nursery 3 was disappointed that NAP SACC UK activities were delegated to the nursery’s ‘graduate leader’ and that the nursery’s cook did not attend the nutrition workshop or any meetings between the partner and the deputy. She noted that although the planned changes to the menu (e.g. including oily fish) appeared to have been implemented, she ‘couldn’t actually pin [the graduate leader] down to how the cook had integrated that’, and had not seen the new menus to verify this change (Partner_Int_21).
The partner for nursery 1 similarly noted problems with ensuring the right people were involved. As she noted, ‘the person I was dealing with didn’t have any say on budget. And they did try to make changes that they couldn’t, couldn’t do really, because the owners wouldn’t agree to it’ (HV_Int_25). This frustration was echoed by the nursery manager who described the difficulties of trying to implement without having the authority to purchase the necessary resources:
So we are still waiting for the resources to come through. [The owners] did say, ‘Yes, go and buy them’, but they haven’t given me a budget. So I’m a bit reluctant to just go out and buy things and then them tell me, you have spent too much, or not enough.
Manager_Int_11
Budgetary constraints were a significant barrier for this nursery and prevented the manager from making changes to the nursery menu. This nursery operated on a very tight budget that the owners (who were not involved in the NAP SACC UK goal-setting process) were unable or unwilling to increase. The manager felt that the children were currently served too much bread at teatime (both toast and sandwiches) and wanted to offer alternatives, such as hummus and vegetable wraps. However, this had not been possible:
[The owners] know it’s too much bread, but it works in the budget . . . So when you can’t exceed like 40p for a loaf of bread, how could you possibly buy a thing of wraps and something to fill the wraps?
Manager_Int_11
The owners had tried to be flexible on this issue by allowing the manager to use any underspend on new items like hummus, but as the manager explained that ‘we are so tight on budget, it’s very rare that we would have enough to buy hummus and wraps’ (Manager_Int_11).
Because of these constraints, changing the teatime menu was not set as specific NAP SACC UK goal. However, the staff were continuing to push for changes with the owners, for example by feeding back the fact the children were not eating the food provided at teatime, which led to a lot of food wastage (something that was confirmed by the whole-day EPAO observation for this nursery). The manager also used their participation in NAP SACC UK study as leverage:
I don’t think it will ever be at a point where it’s changed fully. But I do think [the owners] are being more flexible. And I think that has come from the study, and that we’ve come back and said, ‘We’re learning this. We want to try it, please let us’.
Manager_Int_11
Nonetheless, their inability to implement the changes that they wanted had affected the staff’s enjoyment and engagement with NAP SACC UK. As the manager explained, staff struggled with the nutrition workshops because they knew they would be unable to make the changes suggested:
Obviously we took everything on-board, but I think deep down a lot of us kind of thought, maybe we were a little bit more deflated because we kind of thought, ‘Actually we know we can’t do that’.
Manager_Int_11
Length of intervention
Managers and nursery staff felt that the amount of time they had to set goals, attend workshops and implement changes (approximately 5 months) was appropriate. One manager explained that ‘it’s not something that can be done in a few weeks and it has to be allowed to embed, not only in the minds of staff, but also to see the differences in children as well’ (Manager_Int_10). Another manager acknowledged if they had had to make lots of substantial changes they may have needed longer, but ‘because we were quite good with it all already I suppose it was fine. We didn’t need that much [time]’ (Manager_Int_7). However, one manager commented that although they had achieved their goals, ‘I feel we need more time to ensure everything is completely embedded’ (Manager_Int_1). She felt that being followed up after an additional 6 months would be an incentive to continue working on their goals. One NAP SACC UK partner felt that because it had taken time to arrange dates for the staff workshops, it had felt a bit rushed towards the end, although her two nurseries had still managed to achieve most of their goals: ‘By the time we’d done the workshops and the goal-setting, it was nearly time to finish’ (Partner_Int_25).
On-going support
On-going support was provided in the form of e-mails or telephone calls, and was used as an informal means of checking progress towards the nurseries’ goals. The level of support appeared to be quite light touch, with one partner explaining that she had not needed to provide ‘a lot of support really, more guidance to what their goals were and signposting them to what resources there were and how they could achieve the goals’ (Partner_Int_25). Another partner felt that neither nursery she was assigned to required much support as they were already highly motivated and had quickly met their goals:
When I e-mailed [both nurseries] a month afterwards . . . both of them came back with, ‘We’re pretty much there’ . . . They didn’t need any help because, like I said, they were great to start with, there wasn’t a huge amount to work with.
Partner_Int_14
Nonetheless, managers reported finding this on-going support useful. For example, the manager from nursery 1 appreciated the outside perspective offered by the partner and found the positive feedback received very motivating: ‘to actually have somebody outside that actually picked up on [the changes made] . . . that was quite positive and just kind of kept you going really’ (Manager_Int_11). Other managers appreciated the opportunity to build relationships with the partners as child health professionals. One manager (nursery 5) described the contact with the partner as ‘an important link’ and ‘invaluable’ (Manager_Int_10), and another described the benefits of their growing relationship:
[It’s] been useful to know that someone who knows what we are doing, we could just give a [tele]phone call to or drop an e-mail to and say, ‘Oh, we’re looking for this. Do you have anything?’ Or, vice versa, she might see something and think, ‘Oh yeah, [nursery 1] might want that’.
Manager_Int_11
One partner appeared to be unclear as to what was expected of her in this support role and, at times, uncomfortable in pursuing it. She noted that both nursery managers were very busy and she had struggled to arrange meetings to offer support admitting that ‘I do feel like I’m harassing them’ (Partner_Int_25). She did not feel she that offered the nurseries a lot of support, but ‘more guidance to what their goals were and signposting them to what resources there were and how they could achieve the goals’ and went on to add:
I don’t think I really got to that point where . . . they were ringing me up saying, ‘Oh, how can we do this?’ I didn’t really have that relationship with them. I don’t know quite why that was.
Partner_Int_25
Parent website
Only 12 parents (14%) used the website, indicating low acceptability for this intervention element. Of the 10 intervention parents interviewed, five had used the website and five had not. Three parents were unaware of its existence, while the remaining two parents knew about it but did not ‘get around to looking at it’ (Parent_Int_32). As one explained: ‘it was just one of those things that I just, it hasn’t been a priority really’ (Parent_Int_19).
Of the parents who did use the website, two explicitly mentioned they had been motivated by the free swimming voucher offered. Another parent accessed the website briefly but did not set any goals, explaining that: ‘I think probably if I wanted advice or anything I would turn to the internet anyway and good old Google for ideas’ (Parent_Int_22) rather than consulting a site like NAP SACC UK. Other comments included that the website was ‘bright and colourful’ (Parent_Int_23) and that logging on, completing the Healthy Habits form and setting goals ‘wasn’t difficult’ (Parent_Int_17) and was ‘pretty self-explanatory’ (Parent_Int_29).
Two parents discussed whether or not setting goals had made any difference to their interactions with their child. One parent said, ‘I wouldn’t say it made any difference to what I was doing’ (Parent_Int_29). She did try to find new ways of making fruit and vegetable more appealing to her daughter; for example, by arranging fruit in the shape of a butterfly, but that ‘the novelty wore off after about a minute’. Another felt she did ‘try to be much more conscious of what I was giving her [to eat]’ (Parent_Int_34) but noted progress on this goal had tailed off over the summer holidays when they were out of their normal routine.
One parent appreciated the e-mails she received from NAP SACC UK, but two parents who received text messages found these less helpful. One explained that the messages were ‘nothing that I didn’t know’ (Parent_Int_29), while another felt the texts (on screen time) were irrelevant to her:
I thought it was quite silly because we don’t give her really screen time anyway. They were clearly sort of generic texts, which I expected from the study that I’d set this goal and then I’d kind of have text encouragement re the goal [that I’d set on healthy eating].
Parent_Int_34
Future delivery of NAP SACC UK: the NAP SACC UK partner role
Within the NAP SACC UK trial, the partner role was taken on by health visitors. This group of professionals was deemed to be most similar in terms of skills and professional background to the child-care health partners used in the US NAP SACC study. Health visitors are qualified nurses with specific training and responsibility for children aged 0–5 years and their families. Four health visitors were employed within the NAP SACC UK trial, two from each local authority area, with this work taking place and being remunerated outside their normal contracted hours.
The health promotion work that NAP SACC UK enabled them to do with the nurseries was seen by all four health visitors as a ‘fundamental part’ of their role because they were commissioned to ‘work with children under the age of 5 [years] and their families within the community setting’ (Partner_Int_25). One health visitor felt that they were the ‘best partners to work with nurseries’ because they were the ‘only consistent professionals that are seeing that age group, outside of the nurseries’ (Partner_Int_21).
Although other staff were suggested as being able to take on parts of the NAP SACC UK partner role, there was a feeling that the health visitors’ training and experience brought something to the role that others could not. For example, one health visitor described their approach as more ‘in-depth’ and ‘holistic’ and felt strongly that the NAP SACC UK partner needed to have a specific background in health.
The professional status of the health visitors was highly valued by the nursery staff. One manager explained that: ‘So she, being a health visitor . . . that is her profession so I think it is a good thing doing [the Review and Reflect form] with her’ (Manager_Int_4). Another staff member focused specifically on the benefit of establishing a ‘professional relationship’ with their health visitor:
It’s nice that I’ve got that professional relationship now with our health visitor. So I know that I can call her any time and she’ll come down even after the study has finished and come and see us, which I’m sure she would have done anyway but I know now that I’ve got that professional relationship . . . Probably it would be nice for all settings to have that one named health visitor that you’ve really got that professional relationship with, that you can just contact at any time, I think is really beneficial to every nursery.
Staff_Int_2, emphasis added
However, one health visitor queried if the partner role was making the best use of their skills as health visitors. As she explained, ‘I think what we did, you didn’t need to be a health visitor to do that’ (Partner_Int_25). She would have preferred to have more interaction with the parents and children (rather than just nursery staff), which fitted better with her skills and experience as a health visitor:
Ideally I would have been more involved with the nursery and seeing the kids eating, but that didn’t really happen . . . I didn’t have any contact with the children at all . . . I think it would be nice to have some sort of face-to-face input with the parents, rather than just being a separate person that helps the nursery. So being a bit more involved with the whole thing.
Partner_Int_25
In her view, her skills were in these areas and her time would have been better spent on this, rather than filling in the time-consuming Review and Reflect form:
It probably wasn’t the best use of time . . . we deal with public and groups and things on a daily basis – it would be better to not be doing form filling so much.
Partner_Int_25
Although the health visitors all enjoyed their NAP SACC UK role and felt strongly that it was (or at least should be) an important part of their role, they were also very clear they did not have the capacity to deliver it at present. Their existing workload was so great that even their commissioned services were not always being fulfilled. As one explained: ‘We can’t even do our basic, provide the basic service . . . we’re missing out bits because we haven’t got the capacity to do it’ (Partner_Int_6). While another commented:
We are commissioned to do certain things . . . [and] although part of it is building community capacity and that kind of health promotion thing . . . that’s what disappears by the wayside when we are swamped with child protection, high levels of need . . . We just don’t have the time unfortunately.
Partner_Int_14
In light of this pressure, any additional workload (such as NAP SACC UK) would simply not be delivered: ‘I mean if you put this on health visitors to do routinely, I think it just wouldn’t get done.’ (Partner_Int_16).
One solution to this capacity issue would be to create a specialist health visiting role, exempt from other health visitor duties, to deliver NAP SACC UK to a series of nurseries:
You could employ health visitors, just health visitors to do that . . . but I think, you’d have to be dedicated to do that work. You couldn’t be doing [other health visiting work] because unfortunately, when it comes up against child protection work, you end up having to prioritise the child protection work.
Partner_Int_16
One health visitor felt that this ‘would be a really good health visiting role’ and would ensure that you had ‘somebody doing it that’s really enthusiastic and passionate about it’, which she felt was important to its success (Partner_Int_25). Importantly, this model of ‘specialist’ roles already exists within the health visiting service (e.g. with specialist mental health positions).
Another issue with asking health visitors to take on this role routinely was identified by one participant who pointed out the lack of overlap between the geographical area in which health visitors work and nursery catchment areas:
The difficulty is that we work within a geographical post coded area, so all our families would be in a particular area. As we know, if there was a nursery sitting in the middle they could be coming from anywhere . . . sounds a bit jobs worth, but . . . that nursery wouldn’t necessarily be totally our patch.
Partner_Int_4
Both family support workers (FSWs) and nursery nurses were suggested by health visitors as potentially being able to act as NAP SACC UK partners. FSWs are employed by local children’s centres, providing outreach to families identified as being in need, and running parent training and support programmes. Nursery nurses work as part of the health visiting team undertaking a variety of tasks, such as child development reviews and weaning classes.
Although both groups of staff potentially had skills and experience relevant to the NAP SACC UK partner role, neither routinely work with nursery settings, and one partner raised concerns about their lower levels of training (particularly the FSWs) and the impact that this might on the integrity of the intervention:
Sometimes we’ve found that [the FSWs have] said something different to what we’ve said. And then some families pick up on that and then there’s a big issue about, ‘Oh she told us that and she said that,’ and it’s a bit disjointed . . . So there was a bit of conflict going on there.
Partner_Int_16
She also expressed reservations about whether or not FSWs could be adequately trained up to the on the NAP SACC role:
It depends how well you want to deliver it. And that sounds awful, doesn’t it? I don’t mean it like that. I mean how much in-depth, how holistic you want it to be?
Partner_Int_16
Nursery nurses were felt to be a more obvious choice for the NAP SACC UK partner role because of their specific background in health. However, it was also noted they are unlikely to have spare capacity to take on this role and one participant noted that some health visiting teams no longer employed nursery nurses.
Progression criteria 3: trial design acceptability
This section of the process evaluation aims to answer the following question: were the trial design and methods acceptable? We also explored any potential harms or additional benefits arising from the study and any changes occurring within control settings as a result of their involvement with the study.
Nursery participation
Nursery and child recruitment rates in Gloucestershire were lower than in North Somerset. There are a number of possible reasons for this. First, the recruitment period was longer in North Somerset. Gloucestershire was chosen later in the study to replace Cardiff, resulting in a shorter period in which to recruit nurseries, coinciding with the busy Christmas/New Year period. Second, because of the longer recruitment period, promotion of the NAP SACC UK study at local authority meetings for early years providers took place in North Somerset prior to recruiting nurseries, but not in Gloucestershire. Third, there were fewer on-going initiatives (e.g. the Bristol Standard or ‘Smiles Better’ oral health programme) in early years settings in North Somerset, suggesting that NAP SACC UK faced less ‘competition’ for participation.
In interviews, nursery staff were asked their reasons for participating in the study. These are discussed below with no discernible differences in responses identified between nursery staff in the two different areas.
Several managers took part in the study because they had a particular interest in child nutrition and had previously undertaken study in this area (e.g. on a foundation child-care degree). Others described a general interest in seeing what they could learn as a nursery from participating: “We just kind of thought, ‘Why not? We haven’t got anything to lose, and probably stuff to gain, things to learn” (Manager_Int_11). Another was keen to support research in general, explaining ‘as a company we love new research and we love being part of new ideas’ (Manager_Int_1).
The intervention happening at the just right time was an incentive for two nurseries. One manager explained that ‘every year we look for a focus for the nursery, and [NAP SACC UK] came around at the right time’ (Manager_Int_10), while the other nursery was in the process of updating their menus and the manager felt that ‘it would be a positive to look at the guidelines and see what we’re expected to do’ (Staff_Int_3). For both of these nurseries, the fact that the intervention seemed manageable and ‘quite an easy process to deliver’ (Manager_Int_10) was another incentive. As one described: ‘It was something that I felt, you know, that as a nursery we could do this’ (Manager_Int_4).
For some managers, the opportunity to reflect on their own practice was a particular incentive. One manager wanted to take part ‘just to sort of reassure that we’re doing everything that we should be doing and just picking up anything that we were not doing correctly’ (Manager_Int_4). Another explained that she had worked in child care for 20 years and ‘I don’t want to get to the stage when you get complacent. So I’m always looking at things, how we can improve things, or ways that we can do things better’ (Manager_Int_9).
Other managers were keen to take part in something that could improve their children’s health. It was a way ‘to get the best for our children . . . one way of actually helping these children, the adults of the future, to actually learn more about their diet and what choices they can make’ (Manager_Int_8). For one manager working with a more deprived nursery intake, it was particularly appealing because she had already identified these health issues in her children:
We do have children here that have significant issues like with the dental care, and the children that are overweight. And we also have a significant number of children who live in flats, who obviously that physical exercise issue is more of an issue for them . . . I thought it was something that would be good to reflect on and good to think about, and maybe sort of prioritise.
Manager_Int_7
Recruiting children
For children to take part in the NAP SACC UK study, parents had to provide written consent. Parent information sheets and consent forms were sent to parents of eligible children in sealed envelopes via nurseries. Participation rates ranged from 18.9% to 81.3% of eligible children.
Most nursery staff acknowledged the difficulty of engaging parents in new initiatives, such as NAP SACC UK. As one manager explained that:
[The parents] just didn’t seem very involved at all. And I don’t think that’s down to NAP SACC, I just think that is down to the parents really. When we tried new things and provide open evenings . . . they don’t really seem interested either.
Manager_Int_1
A number of staff acknowledged that ‘parents don’t read the correspondence’ (Staff_Int_3) and it was often a challenge to get required forms and signatures back to the nursery. As a result, two nurseries said they now ask parents to complete important forms at the nursery rather than send them home.
Because initial child recruitment to the study was slow, a NAP SACC UK member of staff attended all 12 nurseries on 29 occasions in total at pick-up times to speak with parents about the study. Several managers felt that this had helped with recruitment:
Because we weren’t getting many consent forms back, the suggestion was maybe [NAP SACC staff] actually came in physically in person to the nursery and actually sat, and during our busiest period when we knew parents were going to be in and out. And that worked because it just gave the parents a bit more reassurance of what it was . . . I think that definitely helped with them actually coming out in person.
Manager_Int_5
However, a couple of managers expressed some reservations about this method suggesting that ‘parents felt a bit put upon’ (Manager_Int_9) or even might have found this ‘a little bit intimidating’ (Manager_Int_7).
Some nursery staff suggested that they should be more involved in the recruitment process to increase participation. To reduce burden on nurseries, staff were not asked to get involved in recruitment but were simply handed sealed information packs to parents. However, some staff found this frustrating as parents would ask them about the study but they were unable to help:
Where the parents were getting envelopes with information and I think it would have been handy for the [staff] to have had some information. Because obviously the parents were then asking the [staff] questions and they didn’t necessarily know the answer.
Manager_Int_5
Two managers also felt it would have been useful to have a list of who had signed up so they knew who needed to be chased up:
Because we had a list of the parents who had taken the information . . . and we didn’t know [if they had signed up]. Some [forms] was coming back to us and some didn’t. And so we were chasing them and we didn’t know because they might have sent [the form] back [to NAP SACC].
Manager_Int_15
Randomisation
Although some managers of control nurseries expressed disappointment at not receiving the intervention, all accepted and understood the importance of the randomisation process. However, it became apparent in interviews that two nurseries did not fully understand their allocation to the control arm. One manager was unaware that her nursery was in the control arm; she thought that the intervention consisted solely of the children’s height, weight and accelerometry assessments. Another control manager thought that her nursery had been allocated to the control arm because they had been assessed as already doing everything they needed to do with regard to nutrition and PA:
So how did you feel about being put in the control group?
It was good. It just means we know we’re doing everything right really, so it’s good to know that we’re doing what we can.
OK, so is it your understanding that you were put in the control because you’re already doing everything that you need to do?
As far as I’m aware [laughs].
Height and weight measures
Nursery staff reported few problems with regard to weighing and measuring children in the nursery setting. Several staff said the children were to take part ‘because [they] love doing that sort of thing’ (Manager_Int_10). Another explained that:
One or two had little meltdown . . . but that’s to be expected with 2-, 3-year-olds, but generally it went absolutely fine. It was absolutely brilliant.
Manager_Int_1
Taking the measurements created some disruption to the nursery day because each child had to be accompanied by a member of nursery staff. One manager provided an extra member of staff on these days to ensure that the correct adult–child ratio was maintained while one staff member left the room. Another manager explained that they used a quiet area of the room to take the measurements rather than taking the children outside. She admitted ‘if we’d have had to take them out of the room it could have been a bit more of a problem’ (Manager_Int_5).
Staff in one nursery prepared children for the measurements, explaining the day before exactly what would happen and reassuring them about the process. The way in which the NAP SACC UK research staff handled the measurements was praised by several nurseries, both in terms of their interactions with the children and in being flexible to fit in with the usual nursery schedule and practices as far as possible. No parent reported any reservations about allowing their child to be measured.
Accelerometry measures
The majority of nursery staff and parents reported the children enjoyed wearing the accelerometry belts, particularly because NAP SACC UK staff presented them as ‘superhero’ belts:
The children absolutely loved them. A couple of children didn’t want to take them off after the end of the week . . . they thought it gave them superpowers.
Manager_Int_1
In most cases, nursery staff reported few problems with getting the children to wear the belts, in part because the children could see their peers wearing them too. Some parents reported finding it more difficult to get their child to wear the belt at home. Both nursery staff and parents found it harder to persuade the children to wear the belts for the follow-up measurements because the novelty had worn off.
Although the majority of children wore the belts (87.5% at baseline and 73.5% at follow-up), a number of minor problems were reported by nursery staff and parents. Some children found the belts uncomfortable to wear (e.g. straps were too tight or too long, or rubbed against their skin, especially in hot weather). There were also some issues with ensuring that the children were wearing the belts at the right time. One manager, for example, explained that ‘most of them will take them off before they go out in the garden, which is probably the time when they’re moving around,’ adding that the children got too hot when they were running around or were frustrated with staff constantly moving the belts back into the right position on the hip (Manager_Int_11). Some parents reported forgetting to put the belt on, especially after swimming or having a bath. In addition, some nurseries reported issues with belts getting mixed up or misplaced. Although most accelerometers were returned, one manager felt awkward having to ‘nag’ parents to bring them back in, but went on to add that ‘we’re used to doing that!’ (Manager_Int_24). There was only one comment about the safety of the belts, where a manager reported a parent was reluctant to let her child wear the belt because she might put it round her neck.
Observations
In general, nursery staff did not report many problems with either the mealtime observations or the whole-day EPAO observation: ‘That was fine . . . They just sort of melted to the background and didn’t really cause any issues or anything. You just hardly know they’re there’ (Manager_Int_10). However, some practical issues were raised regarding the logistics of having extra people in the nursery setting conducting the observations. One staff member noted that their nursery is very small and having two extra observers in their small kitchen was difficult (Staff_Int_12). Another manager spoke about the inconvenience of letting the observers in and out of the nursery between the mealtimes:
We have five mealtimes a day including the snacks. So you’ve got breaks in-between them, and like where are they going to go and what are they going to do? It kind of takes up space in the nursery. I think most of them did go out off site. And then it’s letting them back in and signing them back in again.
Staff_Int_3
There were mixed comments regarding how staff felt about being observed. In several cases, nursery staff reported being used to being observed, for example by visiting parents, Ofsted and other professionals: ‘We are quite used to that, we have staff being observed . . . so they are used to that and it doesn’t faze them’ (Manager_Int_9). Some participants also reported the friendly and unobtrusive manner of the NAP SACC UK researchers meant that it was easy to carry on as normal. As one staff member (Staff_Int_2) commented that ‘They just kind of tucked themselves out the way and were quietly watching and observing’. However, others reported finding it ‘a little bit strange’ (Manager_Int_7) or even ‘scary’ (Staff_Int_12) being watched so closely. One manager described how her staff found the whole-day EPAO observation a bit intrusive:
Staff did find that quite evasive [sic] and obviously rifling through the books . . . it’s like someone coming into your home and start looking through your cupboards . . . That was the only bit they’ve obviously said they found uncomfortable.
Manager_Int_8
There were mixed responses regarding the impact that the observations had on staff behaviour. Several participants felt that staff had not significantly changed their interactions as a result: ‘[The staff] just carried on as normal and you actually end up forgetting they’re there really’ (Staff_Int_6). However, two managers believed that their staff may have changed their behaviour. In one case this was because staff were feeling uncomfortable:
I think that some of them were maybe a little bit more sort of nervous, in the same way that they would be when Ofsted are here and you kind of like become a little bit edgy . . . So I wouldn’t say it changed what they did, but it may have changed the way they did it a little bit.
Manager_Int_7
In the other, the manager felt the staff may have been trying to give a good impression:
Because they knew what NAP SACC were there for I think they made sure our targets were being achieved and that you can clearly see that they were.
Manager_Int_1
By contrast, the children appeared to be unaffected by and often unaware of the observations, again partly because they are used to having visitors to the nursery. Most participants therefore felt that ‘it didn’t really change the children’s behaviour at all’ (Staff_Int_2), with only one participant stating that ‘the children sort of played up a tiny little bit, because I think obviously there was new people in the room’ (Staff_Int_12).
The only negative comments about the observations came from staff at nursery 12, and appeared to relate to a misunderstanding about the purpose of the two different observations: the mealtime observations of children’s food consumption for completion of the CADET food diary and the EPAO. During her interview, the manager described the difference between the two sets of observers who came to her nursery:
So we had two different lots of people that came out to observe, and they were just so different. The one group that came, they came in the room with the children, saw what they were eating, came outside to play with them, observed them, really good. And the other lot, oh, they just sat in the office the WHOLE DAY!
Manager_Int_9
Although we cannot verify this, we believe that the first pair of observers were completing the EPAO assessment, which comprises an extremely detailed observation of all aspects of the nursery environment and staff practices. These observers would therefore have been present at the nursery all day, interacting with staff and children in order to check details to complete the EPAO form. The second pair of observers were probably there to record only what the children ate at mealtimes and, in order to stay out of the way, would return to the office in between meals.
The difference between these pair of observers clearly frustrated the manager, who felt that the second observers simply were not getting an accurate reflection of what their nursery was like.
Parent questionnaires
Parents were sent a questionnaire to complete at baseline and follow-up, comprising questions on the child’s quality of life (PedsQL), spending on food and physical activities, health-care use and mediators such as knowledge, self-efficacy and motivation.
In most cases, parents reported no problems with the questionnaire, describing it as ‘straightforward’ and ‘self-explanatory’. Some parents noted that it was ‘quite thorough’ and took some time to fill out, but no-one described this as a particular problem. As one parent commented that ‘it did take quite a bit of time, but you could see the relevance in it so I didn’t mind doing it’ (Parent_Int_18).
Part of the questionnaire asked about their child’s use of GP, health visitor or A&E health-care services. At follow-up this questionnaire was modified so that parents were randomly selected to receive a questionnaire asking about this health-care use either over the past month or since February 2016 (last 5 months). Parents who were asked about use in the past month reported no problems recalling these details. Those asked to think about the previous 5 months also generally reported no problems because their children were generally very healthy and, therefore, had not used any/many of these services: ‘It was quite easy, because he hadn’t been [ill]. . . so there wasn’t anything to remember’ (Parent_Int_18).
However, some parents did find this question difficult to answer:
. . . I was thinking, ‘Gosh, how am I going to remember from February?’ So I don’t think I do remember very well. So I think I kind of [laughs] guessed.
Parent_Int_26
This was particularly the case if the child had accessed health-care services on more than one occasion:
[my son] has been to the Doctor a few times but I wouldn’t be able to remember if it was in the last 5 months or not. Hospital would be a bit more significant, so I would remember that I think.
Parent_Int_35
Most parents agreed that being asked to recall only the previous month would have been much easier.
The questionnaire also assessed potential mediators including knowledge, self-efficacy and motivation. A minority of parents reported some problems with the phrasing of these questions and they may need to be modified for use in any further trial. For example, one parent was unable to distinguish between questions that asked ‘I feel able to [e.g. provide my children with fruit at all main meals]’ and ‘I am motivated to . . .’. For her, ‘they weren’t any different to me. You kind of completed them the same.’ (Parent_Int_29). Another parent felt that the answers from these questions could be ‘misleading’ with people ticking the same response for very different reasons. As she explained:
You know the questions ‘Do you feel able to reduce the amount of fizzy drinks . . .?’ [My daughter’s] never had fizzy drinks in her life, ever. So do I feel able to reduce it? ‘No’ because she never has it. What do I put? She never has it . . . But you could also answer, if you have a child that really loves Coke [Coca-Cola®; The Coca-Cola Company, Atlanta, GA, USA] and you were really struggling with their behaviour and you were pulling your hair out, then you may feel that I’ve got trapped into this behaviour, which I don’t feel happy with, but I can’t reduce the Coke because it would be even worse. So you could end up with two people on the far ends of the spectrum answering the same thing.
Parent_Int_19
One parent admitted that it was hard to answer these questions completely honestly ‘because obviously every parent likes to think they would feed their child lots of fruit and veg’, while another admitted some questions ‘ended up making me feel a bit guilty’ because ‘I know what the right answer is, and am I, you know, am I giving an answer that makes me a bad parent?’ (Parent_Int_30).
Food diary
Many parents reported no difficulties in completing the food diary. It was variously described as ‘fine’, ‘straightforward’ and ‘easy’. However, other parents admitted finding some elements of the form confusing. Several parents reported being unclear as to which days and which meals they were supposed to complete. For example, one parent commented:
I didn’t understand whether you wanted, the day she goes to nursery, do I then check up the menu and put that in, or do the nursery fill that out? . . . So like today, do I then go and ask what she’s had for lunch and put that down?
Parent_Int_40
Another parent found it difficult to decide which category to put certain foods under.
[My son] likes brioche but it’s not listed. Is it bread? Is it a cake? I don’t know . . . And so I was like it’s not toast, it’s not pastry, it’s just brioche. So I was struggling a bit, like should I just write it down, I don’t know what to do.
Parent_Int_17
Another parent felt that because the form was so detailed with different options, it was difficult to complete. She felt that it would have been easier to simply write down what her child ate at each meal rather than having to flick through pages of different options (Parent_Int_22). Another suggestion was to reorder the listed food items to make it easier to complete (e.g. including ‘milk’ next to the breakfast cereals category).
Nursery staff interviews confirmed some parents were confused over how to complete the food diary. One manager explained that some parents ‘found the food diary quite difficult to understand’ (Manager_Int_7) with other staff confirming parents were often confused about which days/meals they were meant to complete. As one manager explained:
Some parents just did that day that they had that [accelerometer] belt on, so they just did the food for that day. Some parents did the food for the whole week, or however long the booklet was for. Some people just did for the nursery day and just put ‘Not applicable, at nursery’. So it was a bit of a mixture of things.
Manager_Int_9
Although nursery staff were generally willing to explain the diary to the parents, one staff member noted that they had not actually seen the instructions given to parents (sent out in sealed packs), which made it difficult for them to help:
Because obviously they’re sealed so we don’t – we can’t like explain it to them. So obviously we just gave them the packs. So maybe it might be nice if we had a copy of the pack so we know what’s in them . . . so we could say like, ‘You’ve got to do this’ when we’re doing our handover.
Staff_Int_12
Involvement in research study
In general, nursery managers did not report finding participation in the NAP SACC UK study burdensome. One manager commented that the NAP SACC UK staff had taken on much of the administration of the study and ‘that was probably one of the best things about the study’. As she explained:
When we first got involved I was a little bit apprehensive about how much extra work it would mean for us. But no they have actually been great, they’ve been the ones taking on the admin role and then everything, so really good.
Manager_Int_1
Another manager added:
A lot of it has been managed really well, almost to kind of take the pressure off us a little bit . . . It’s not been a burden on us at all.
Manager_Int_5
However, one manager did admit that there had been ‘more to [the study] than I perhaps initially perceived’ and that his lack of time to dedicate to the study was why some goals (e.g. writing policies) had not been met (Manager_Int_10). A couple of managers mentioned the height and weight measurements had created some disruption in the nursery because each child needed to be accompanied by a member of nursery staff, but as one explained, ‘we knew in advance when it was coming, so as long as we were able to prepare for that and accommodate for it, that was fine’ (Manager_Int_11). Another manager said their staff had had to help some parents filling in their food diaries, but they had been happy to do this (Manager_Int_7).
The NAP SACC UK staff were praised by many nursery staff for their ability to interact positively with the children and to undertake their role with the minimum disruption to the nursery. One manager, for example, described the NAP SACC UK researchers as ‘fantastic’ and said ‘your team were great in adapting to us’ and fitting in with the nursery schedule and practices (Manager_Int_24).
The majority of nursery managers felt communication between the NAP SACC UK team and themselves had been good. As one commented: ‘I think the communication has been fine all the way through. I don’t think it’s been too much and I don’t think it’s been too little. I think it’s been just right.’ (Manager_Int_5). Most communication had been with the trial manager via e-mails and telephone calls. Managers felt that e-mails were generally the most appropriate method of communication as they were able to respond at a convenient time and provided with written confirmation of arrangements. However, one manager felt that personal telephone calls had been useful at the start of the project to build rapport with the NAP SACC UK staff and another explained that they appreciated being telephoned as a prompt to act on e-mails that they may have forgotten about.
Some minor issues were raised regarding communication. One manager felt that ‘things were very done sort of last-minutey, which doesn’t work quite well with us as a setting’ (Manager_Int_1). She explained that they needed at least 2 weeks’ notice for data collection to arrange enough staff cover. Two other managers suggested that being given a timetable at the start of the study explaining when things would be happening (e.g. data collection, staff workshops, observations) would have been helpful. There were also comments about the number of different NAP SACC UK staff who came into the nursery for different reasons. For example, one manager said:
[It] would have been nice if we had the same people come in. Because each time it was someone different and each day it was someone different as well, that just the consistency of the same person, just because from our point of view we’re quite strict on who we let in and everything and who can just wander.
Manager_Int_13
Communication appeared to have been more difficult with nursery 12 and lack of full understanding of what the intervention entailed contributed to their decision to not take part in the intervention. As described in Withdrawal from the intervention: nursery 12, staff at nursery 12 were unwilling to attend the out-of-hours NAP SACC UK workshops and the nursery manager interview revealed she had been unaware of the requirement for this training:
So when you signed up . . . was it outlined there that [the training] was going to be in the evenings?
No.
So you weren’t aware of that at all?
No. We didn’t even know to be fair, I don’t think we did, that there was staff training.
The letter of agreement between the nursery and NAP SACC UK stated that nurseries allocated to the intervention arm would need to ‘ensure as many nursery staff as possible attend two workshop sessions’ and that these workshops ‘will take place during an evening and on a Saturday morning’. In this nursery, the letter of agreement was signed by the deputy manager and thus the manager was not fully aware of the requirements of the study.
The nursery manager also added the fact that both she and the trial manager worked part time had not helped matters:
When you rang the office [the trial manager] works part time, I work part time, that’s the nature of the job, you know, it was someone else you were speaking to and like I say, it was different people organising different appointments, and things like that.
Manager_Int_9
Harms and wider benefits
No significant harms were reported by nursery staff, partners or parents regarding the NAP SACC UK trial. However, some wider benefits from participation in the study were noted by partners and nursery staff.
One partner provided her nursery with health advice for children outside the NAP SACC UK age range by providing them with updated guidance on baby weaning best practice. She also explained:
It’s highlighted things for me that now going into other nurseries I would probably take some leaflets with me if I was just going to observe a child, and say ‘Oh actually I’ve brought this for you, maybe you might like to look it up on the website and tap into that?’.
Partner_Int_21
Another partner described how, as a result of her involvement with NAP SACC UK, her health visiting team were now asking other nurseries and children’s centres to include questions about dental registration on their registration forms (Partner_Int_25).
As noted earlier, one nursery now allowed staff to eat a free meal with the children and this practice had since been rolled out to other nurseries in their local chain. This same nursery had also rolled out their new menus, revised in light of NAP SACC UK Best Practice Standards, to their other nurseries.
Changes in control settings
Managers of control nurseries were asked whether or not they had made any changes around PA, nutrition and oral health during the intervention period and, if so, if these changes were related to their participation in the NAP SACC UK trial.
In most cases, managers indicated that they had continued with their normal practice, which may have included providing activities for the children around, for example, healthy eating. However, in two nurseries there appeared to have been some more direct changes resulting from their involvement with the NAP SACC UK study. The manager of nursery 7, for example, explained that her staff may have changed what they were eating in front of the children because the nursery was involved in the study:
I think it’s probably made the [staff] a bit more aware about what they’re doing when they’re bringing in their own snacks and stuff. Rather than bringing in a fizzy drink to have, they’re bringing their water or at snacktimes they make sure they’re having fruit, the same as what the children are having, and that kind of thing.
Manager_Int_5
Another manager explained that her nursery had started raising awareness of the sugar content of foods with parents by promoting sugar apps and putting up displays in nursery corridors. When asked if this had happened as a result of their involvement with NAP SACC UK, she answered:
I guess . . . I think it’s just because we’re now part of the programme we’ve actually been able to sort of, it gives us a bit more clout. We’ve said we’ve been part of this research programme and we want to address it, so in the newsletter we’ve been giving information to parents about taking part in the research. We’ve got the display up in the corridor for them to look at. We’ve been sending out leaflets with their packs.
Manager_Int_8
However, it should be noted that this nursery was also participating in the ‘Smiles Better’ programme at the same time and this campaign had provided the information and leaflets that the nursery were giving out. This activity was therefore likely to have happened anyway, regardless of their participation in the NAP SACC UK study.
Summary
Progress against the progression criteria is summarised in Table 27. Recruitment of nurseries (31.6%) and children (35.3%) was lower than the progression criteria of 40%, but both were exceeded in one of the two study areas. No nurseries withdrew from the study. The intervention was delivered as planned in five out of the six intervention nurseries with high levels of feasibility and acceptability (there were particular circumstances in the sixth nursery), with the exception of the home component. It was feasible to recruit and train health visitors to deliver the intervention, but health visitors reported that they may not have capacity to deliver the intervention in the future alongside their usual workload.
| Progression criteria | Summary of progress |
|---|---|
|
Feasibility 1a. At least 40% nurseries willing to participate |
31.6% overall (42.9% in North Somerset; 25.0% in Gloucestershire) |
| 1b. Synthesis of process evaluation elements regarding feasibility of intervention |
Overall NAP SACC UK proved feasible to implement, with the majority of intervention elements delivered with fidelity Two exceptions: (1) one recruited nursery decided not to take part in intervention and (2) NAP SACC UK at Home (website) not well used |
|
Acceptability: intervention 2a. Was the intervention acceptable to NAP SACC UK partners? |
NAP SACC UK was highly acceptable to NAP SACC UK partners, but concerns were raised about their capacity. Alternative models of delivery were suggested including specialised health visitors dedicated to deliver NAP SACC UK, nursery nurses or health improvement staff |
| 2b. Was the intervention acceptable to the majority of nursery managers, staff and parents? | NAP SACC UK was highly acceptable to most nursery managers and staff. They particularly valued the workshops and contact with a named NAP SACC partner. Parents were often unaware of the specific changes made within the nurseries |
|
Acceptability: trial design 3a. Expressions of interest from eligible nurseries |
31.6% overall (42.9% in North Somerset; 25.0% in Gloucestershire) |
| 3b. Acceptability of randomisation and data collection | Randomisation was acceptable to nursery staff, although some did not fully understand how they were allocated. Data collection measures (height/weight, accelerometery, observations, and questionnaires) were acceptable to staff and did not cause disruption. Parents were highly supportive of the research process |
| 3c. At least 40% parental opt-in consent rate | 35.3% overall (43.5% in North Somerset; 30.8% in Gloucestershire) |
| 3d. Maximum loss to follow-up of (1) three providers and (2) 40% of children | (1) No losses and (2) 14.2% children (3 children withdrawn, 2 refused, 8 nursery movers, 11 children moved to school) |
| 3e. Synthesis of parents’ views of data collection | Overall parents reported data collection measures to be acceptable |
The trial methods and design were acceptable and feasible. The number of children lost to follow-up was 24 (14.2%), and this was due to withdrawing consent (1.8%), child refusal to participate on the day (1.2%), children moving to primary school (6.5%) or children moving nursery (4.7%). The response rate was 145 (85.8%) at follow-up. Although the study was not powered to measure effectiveness, accelerometer measured total PA and MVPA were higher in the intervention arm than in the control arm after the intervention. The ICC for total activity was estimated at 0.02 (95% CI < 0.0001 to 0.95). Assuming a coefficient of variation in participating children per nursery of 0.4, 30% incomplete data and an ICC of 0.05, 720 children at 52 nurseries will give 90% power at the 5% significance level to detect a 17-minute increase. The average cost of delivering the intervention was estimated at £1184 per nursery, and nurseries incurred, on average, an additional £717 for staff to attend the two workshops.
Chapter 6 Mediators questionnaire test–retest substudy: methods
This chapter provides the study aims, methods and results of the mediator questionnaire test–retest substudy.
Mediator questionnaire test–retest reliability study overview
The aims of the current study were to test the NAP SACC UK parent and nursery staff questionnaire mediators for (1) acceptability by examining response rates and missing data, (2) maximising the internal consistency of the scales using Cronbach’s α coefficients and (3) reliability by conducting test–retest analyses using weighted kappa coefficients and paired t-tests.
Development of the mediator questions
The mediator questions for parents and nursery staff (see Appendices 2 and 3) were based on the questionnaire items used in the Active for Life Year 5101 study and were adapted using the NAP SACC UK self-assessment form. The self-efficacy, motivation and knowledge questions were split into two sections: children’s nutrition/oral health and children’s PA. All the self-efficacy questions started with the same stem, ‘I feel able to’, and were followed by dietary, PA or oral health-related behaviours where the response options were: 1 – ‘Disagree a lot’, 2 – ‘Disagree a little’, 3 – ‘Not sure’, 4 – ‘Agree a little’ and 5 – ‘Agree a lot’. The same health-related behaviours were included in the motivation questions but used the stem, ‘I am motivated to’. The motivation response options were: 1 – ‘Never’, 2 – ‘Sometimes’, 3 – ‘I don’t know’, 4 – ‘Most of the time’ and 5 – ‘Always’. Multiple-choice questions were set for the knowledge items and varied in terms of having one or multiple correct response options.
Sample and recruitment
Nurseries from Bristol, UK, were recruited through postal invitations followed by an e-mail invitation 10 days later. Participating nursery managers recruited nursery staff and parents via e-mail. Parents were also recruited via an online advert on the survey forum of the UK-based parenting website (www.netmums.com). Inclusion criteria were nursery staff and parents or guardians who worked with or had 2- to 4-year-old children. Written informed consent was obtained from the nursery managers and online consent was gained from each participant prior to data collection commencing.
Data collection
Nursery managers were instructed to send a link to the online nursery staff questionnaire via e-mail to all nursery staff who worked with 2- to 4-year-olds. This was repeated for the parent questionnaire to parents who had 2- to 4-year-old children. Participants were asked to provide their e-mail address at the end of the questionnaire and those who did were automatically sent the questionnaire again 1 week later. They were sent a reminder e-mail a further 3 days later. Participants’ questionnaires were included if the second administration of the questionnaire was completed between 7 and 11 days after the first administration. Each participant was reimbursed with a £10 voucher on completion of the first and second administrations of the questionnaire.
Data analysis
Descriptive statistics were used to summarise the participant characteristics, response rates and missing data. Using the data from the first administration of the questionnaire, Cronbach’s α coefficients were calculated to determine the internal consistency of the four scales: nutrition self-efficacy, PA self-efficacy, nutrition motivation and PA motivation. Values of at least 0.7 were considered acceptable. 102 To assess test–retest reliability of the items, weighted kappa coefficients for ordinal variables103 were calculated. To interpret the kappa coefficient results, the cut-off points detailed by Landis and Koch104 were used: 0.00–0.20 = ‘slight’; 0.21–0.40 = ‘fair’; 0.41–0.60 = ‘moderate’; 0.61–0.80 = ‘substantial’; and 0.81–1.00 = ‘almost perfect’ agreement. For the knowledge questions, the percentage of correct answers was derived for each participant and paired t-tests were carried out on these continuous test and retest summed scores.
Chapter 7 Mediator questionnaire test–retest substudy: results
Participants
Demographic characteristics for the 82 parents and 69 nursery staff are shown in Appendix 9, Table 43. Most parents were in the 31–35 years age group (43.9%) whereas nursery staff were mainly in the 25–30 years age category (31.9%). The highest level of education was a university degree for both parents (41.5%) and nursery staff (37.7%).
Acceptability and missing data
The number of times that individuals gave consent on the questionnaire link was 130 and 103 for parents and nursery staff respectively; it was not possible to distinguish whether or not the same individuals clicked consent multiple times, as they did not have to provide any identifying information (e.g. e-mail addresses). A total of 102 parents completed the first administration of the questionnaire and 88 parents (86.3%) completed it for the second administration. For the nursery staff questionnaire, 86 and 74 (86.0%) participants completed the first and second administrations, respectively. A total of 73 (89.0%) and 70 (85.4%) parents completed all the self-efficacy and motivation questions in the first and second questionnaire, respectively. The number of nursery staff participants completing all the questions was 58 (84.1%) for the first and 61 (88.4%) for the second administration.
Cronbach’s α coefficients
The Cronbach α coefficients of the items within the four scales from the parent questionnaire are presented in Appendix 9, Tables 44 and 45. The final column represents the α coefficients for the test scale if the item is removed. The overall Cronbach’s α for the scale is also presented in the final column. The nutrition self-efficacy scale shows an acceptable level of internal consistency (α = 0.80). The PA self-efficacy scale has the weakest internal consistency in the parent questionnaire but is still at an acceptable level (α = 0.73). The removal of the item 17 relating to the provision of opportunities to walk to/from nursery would noticeably improve the internal consistency of the scale (α = 0.81). The nutrition motivation scale shows a high level of internal consistency (α = 0.86). The PA motivation scale demonstrates the highest overall Cronbach’s α (α = 0.89). Unlike the equivalent item in the PA self-efficacy scale, the removal of the item 37 has less of an effect on the internal consistency (α = 0.92).
Appendix 9, Table 45, shows the Cronbach α coefficients for the nursery staff questionnaire. The nutrition self-efficacy and the nutrition motivation scales both had α coefficients of 0.89, which shows a high level of internal consistency. Both the PA self-efficacy and the PA motivation scales also demonstrated high levels of internal consistency as the Cronbach’s α coefficients were 0.91.
Test–retest analyses
Test–retest analyses found that most of the weighted kappa coefficients for individual items fell under the ‘moderate’ category for the parent (75.0%) questionnaire and for the nursery staff (55.8%) questionnaire (see Appendix 9, Table 46). Paired t-tests found that knowledge scores for parents were higher in the questionnaire’s second administration [t = –3.23, degrees of freedom (df) = 81; p = 0.002] but there was no strong evidence for a substantial increase in the nursery staff’s score in the second administration (t = –0.67, df = 68; p = 0.503).
Summary
Participating nursery managers recruited nursery staff and parents via e-mail, and the respective questionnaires were sent out as a weblink and completed twice, 1 week apart. A small number of parents were recruited online (via www.netmums.com; London, UK). The acceptability of the questionnaires was explored by looking at response rates and missing data. Cronbach’s α coefficients were used to look at the internal consistency of the four scales (i.e. nutrition self-efficacy, PA self-efficacy, nutrition motivation and PA motivation). Test–retest analyses (weighted kappa coefficients and paired t-tests) were used to determine whether or not the items/scales are reliable. We have produced a novel tool that can be used to measure parental and nursery staff’s self-efficacy, motivation and knowledge towards diet, oral health and PA. Overall, these analyses have demonstrated that the scales show good internal consistency and test–retest reliability.
Chapter 8 Nursery food photography feasibility substudy: methods
This chapter provides the study aims and objectives, study design and methods of the nursery food photography feasibility substudy.
Overview
An additional feasibility study was undertaken after the end of the feasibility trial with the aim to ascertain the feasibility and acceptability of taking photographs of the foods and drinks served to 2- to 4-year-olds in nurseries to estimate portion size served and caloric intake of individual children (to replace CADET in a full trial as a method of collecting nutrition data in nurseries). This study also aimed to determine the number of children from whom one researcher could feasibly collect complete food and drink data to inform a future trial.
Sample and recruitment
A purposeful sample of nurseries within Bristol, to allow for variation in deprivation and meal provision (nursery-provided food and family-provided food), were invited to take part, with the aim of recruiting four nurseries. Nurseries were approached by e-mail and provided with an invitation letter, nursery information sheet, consent form and camera policy. Nursery managers were given 2 weeks to respond with a reminder e-mail sent after 1 week. The camera policy included details regarding storage of the camera during non-eating times and a requirement that the nursery manager check the photographs at the end of the data collection day to ensure that there were no concerns about inappropriate use of the camera. It was requested that the policy was signed along with the consent form.
Once a nursery manager had consented to taking part in the study, a date for data collection was arranged and nursery managers were asked to briefly explain mealtimes, locations and serving arrangements. Following this, information packs for all parents/carers of 2- to 4-year-olds that were going to be present on the day of data collection were posted to the nursery managers. The packs included a letter, an information sheet, an opt-out consent form and a stamped addressed envelope. Nursery managers were asked to hand these to parents/carers. Parents/carers were given 2 weeks to provide opt-out consent if they did not want their child to take part in the study.
Data collection
Two researchers visited each nursery for 1 full day of data collection. Photographs were taken of as many consented children’s food and drink as possible. Researchers followed the Fieldworkers’ Standard Operating Procedures that were developed for this study.
A set of laminated cards were prepared to be placed next to the children’s plates for each photograph. A standard credit-card-sized marker was printed on the laminated card to aid perspective adjustment and later portion size estimation. Dry-wipe marker pens were used to indicate on the laminated card the type of meal, whether the photograph was taken before or after eating and whether the photograph was of the first or second helping. The researcher ID and participant ID were written on the front of the laminated card, with the child’s name written on the back so that all meals throughout the day could be matched to that child. The laminated cards were left at the nurseries after data collection.
The type and number of drinks were recorded in one-quarter cup increments on a fieldworker data collection sheet to save time having to take ‘before’ and ‘after’ photographs of each refill of drink. A full cup of water was also weighed to determine the volume of water being drunk based on the one-quarter cup increments recorded on the data collection sheet. A researcher took one photograph before the meal and one after, at a 45-degree angle and approximately at arm’s-length distance to include all the food on the plate. The aim was for no part of the child to be in the photograph, however, it was anticipated that occasionally part of a child’s hand, arm or body would be shown in the photograph. If a child received additional portions, a photograph was taken of the ‘empty’ plate before and after an additional serving to capture a photograph of the new portion and then a final photo when the child had finished eating to capture any leftovers or confirm that the entire serving was consumed.
To optimise portion size estimation for each food in a mixed meal, foods should be separated on the plate and not layered on top of one another (e.g. pasta on one side and sauce on the other side of the plate, or sandwiches opened up to reveal the contents). To overcome the time demands of separating foods on each individual child’s plate, a portion was provided to the researchers with foods separated. For composite meals (e.g. cottage pie, curry) the researchers asked the nursery staff for a detailed description of the ingredients and quantities and for a portion. When a meal could not be weighed, standard recipes were used based on the National Diet and Nutrition Survey nutrient data bank.
In nurseries that allowed packed lunches, each consenting child’s packed lunch was photographed and each element weighed and recorded. A new pair of latex gloves was used for each packed lunch to avoid cross-contamination of allergens.
At the end of the data collection day, nursery staff who were present on the day were asked to complete a short questionnaire about their views and acceptability of the data collection method. The nursery manager was asked to check all the photograph thumbnails to confirm they had no concern about the content of the photographs.
Data analysis
The photographs were annotated as relevant and submitted for analysis to Pennington Biomedical Research Center (PBRC), an organisation based in the USA that specialises in estimating food portion and nutrient data using food photography. 105–107 No information that could identify a child or nursery was sent to PBRC. Processing of photographs involved trained members of the PBRC team using the photographs and annotations to match foods pictured to food in a UK food composition database. Once a matching food was chosen, the portion size of the food was estimated by comparing the photograph to standard photographs of that food where portion size (grams) was known. The standard marker included within photographs was used to rescale photographs to the same size as the standard photographs, which aided accurate estimation of portion sizes. Portion size and food composition information was then combined to generate nutrient contents of the meal eaten. Questionnaire data from nursery staff were entered into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet and summarised using descriptive statistics. Fieldworkers were asked to complete detailed observation notes and these were analysed thematically.
Chapter 9 Nursery food photography feasibility substudy: results
Recruitment
Of the seven nurseries invited, four (57%) gave consent to take part in the nursery food photography feasibility substudy. Reasons for non-participation by nurseries were staff shortages, tight workloads and changes, for example, in management structures. One nursery mentioned not wishing to take part because of a small dining area that would have been a struggle to accommodate any extra adults or equipment. The nurseries were all located in Bristol and differed in their size, IMD and types of meals provided. One nursery permitted packed lunches. One nursery had a chef and three nurseries received their meals from external catering companies. In addition to lunch and snacks, two nurseries provided breakfast and two provided an afternoon meal.
Nursery managers estimated a total of 153 eligible children to be present on the days of data collection. A total of 180 letters were given to parents by nursery staff giving information about the study and the opportunity to opt their child out of the study; seven opt-out consent forms (4%) were received.
On each day of data collection, the two fieldworkers collected data from one group of children throughout the day. In two nurseries, researchers followed children aged 3–4 years, and in two other nurseries researchers followed children aged 2 years. Across the nurseries, data from a total of 51 children were collected on at least one eating occasion. Of these 51 children, 26 (51%) had data for all eating occasions at nursery on the day of data collection.
Staff present at mealtimes and throughout the day of data collection were asked to complete the staff questionnaire (see Appendix 10) at the end of the day. All 19 staff who were approached completed and returned the questionnaire.
A total of 307 photographs were taken across the days of data collection. When staff looked through photographs at the end of the day, one photograph was deleted as the photograph included the participant’s name on the nursery place mat. Figure 5 gives an example of before-and-after photographs.
FIGURE 5.
(a) Before and (b) after photographs of a meal in a nursery.
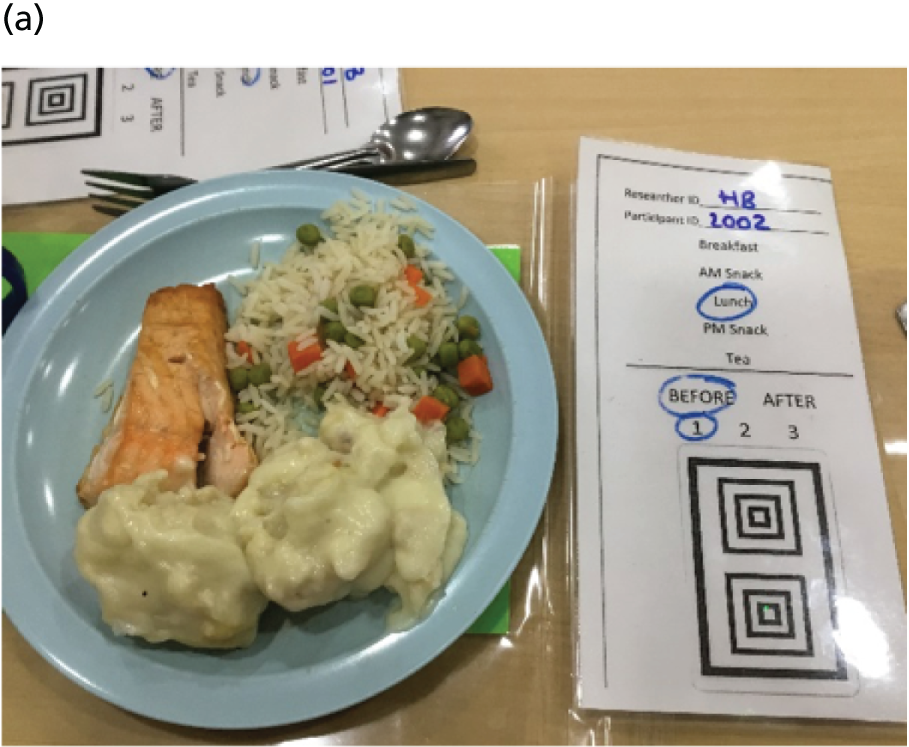
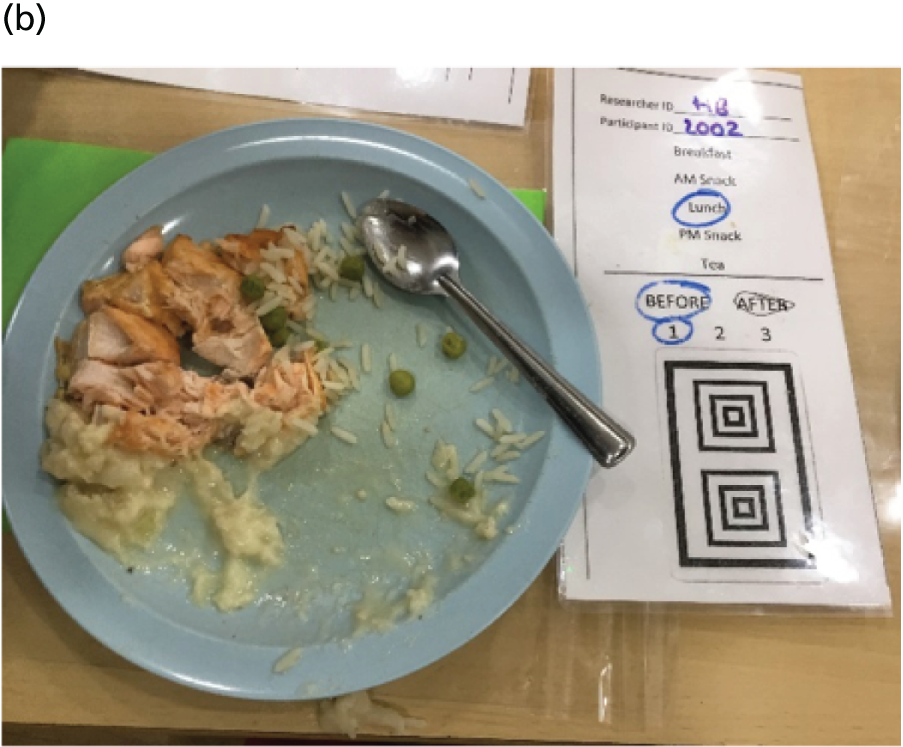
Feasibility of data collection
It is feasible to use a tablet in nurseries for photographic data collection. In combination with a written observation sheet to capture anything not photographed, a good estimate of what children aged 2–4 years at nurseries eat and drink throughout the day can be made. The wide screen of the tablet made it easy to capture all food items and the laminated ID card in one photograph. It was often not feasible to take photographs at a 45-degree angle and an arm’s length away, given the small space provided for each plate at the table, but this did not have an impact on the estimation of portion size.
Acceptability to children
The field notes and comments by nursery staff demonstrated the study was acceptable to the children at the nurseries. Children were happy and comfortable with the presence of researchers and taking a photograph before and after of their plate. Some children showed interest in the laminated ID card and played with it. At times, children would look at researchers, speak or wave to researchers and try to look at the photographs that were being taken of their food. However, in general, taking the photographs did not disrupt their eating experience. One child asked us not to take photographs of their plate; this did not discourage or influence the other children at the table and the child was not distressed and was happy for us to continue with the other children.
Acceptability for nursery staff
The questionnaire responses, field notes and comments made by staff throughout the day of data collection demonstrated that nursery staff generally found the study and the process of taking photographs of food acceptable. Staff were happy with the tablet being stored in the room and with researchers taking the tablet from this location prior to each eating occasion. All nursery managers checked the photographs on the tablet at the end of the day and this did not take longer than a couple of minutes. They all stated that they were happy with the process of checking the photographs.
A total of 89% of all staff indicated that they felt well informed about the data collection process. Fourteen out of 18 staff (77.7%) agreed or strongly agreed that the process of taking photographs did not disrupt the staff, and 12 out of 17 staff (70.5%) indicated the process did not disrupt the children. Overall, 17 out of 19 staff (89%) agreed or strongly agreed that they found the process of taking photographs before and after each snack and meal acceptable. Only one member of staff indicated concern about the content of the photographs taken and this member of staff strongly disagreed or disagreed with all other statements that were provided in the nursery staff questionnaire. No other information was provided on the questionnaire to allow these strong views to be interpreted. Thirteen out of 16 staff (81.3%) said that they were aware that a member of staff checked all the photographs at the end of the day. All but one staff member (94.7%) agreed or strongly agreed that they found it acceptable for researchers to be given details of the food eaten. One staff member commented that the use of video could be considered for capturing what children eat.
There were some challenges in working with the staff, such as staff assuming that they were being observed in how they co-operated and dealt with children at mealtimes, and staff being unaware of the study taking place or what was required of them and the children. These challenges were often addressed through speaking with the staff during the break times and developing a rapport with them so that they would ensure that the children waited for us to take the photograph and identified the correct children. All of the staff we worked with were happy to do this and were committed to helping the researchers; however, all staff needed to be briefed on how they should help the researchers.
It transpired that tablets and photographic equipment are commonly used within nurseries to take pictures of the children’s learning and progress. One nursery communicated that they had recently started using tablets to record in written format approximately how much and what children ate at the different mealtimes (not using photographs).
Weighing of sample portions and food ingredients
It was acceptable for nursery staff to weigh a sample portion of each composite meal that was served. When asked, nursery staff were happy to provide a sample portion and answer any questions about the food content. In the staff questionnaire, 14 out of the 16 staff members (85.5%) who answered the question indicated that they found it acceptable for researchers to weigh a sample plate of food served to the children.
Three nurseries used external catering companies to provide the food to children. The information provided to nursery about the exact ingredients at times covered only the allergens present in the meals, not the specific ingredients. Therefore, it is not necessarily possible to obtain this information about every single item of food served to children.
Photographing drinks
It was not feasible to capture what children drank in photographs because drinks were often served following the food being served, or throughout the meal, and children were often able to help themselves. The type of drink and quantity drank can be captured through the observation sheet. In three nurseries, the cups used for children were identical, whereas the cup sizes in one nursery varied. When cup sizes are the same, it is possible to measure the volume of the cup and estimate when a child drinks one-quarter or a half or the volume. At some nurseries, children had access to either individual water bottles or cups of water throughout the day.
Packed lunches
It is uncommon for all children to have packed lunches. Only a small proportion of children registered at the nursery that permitted packed lunches brought packed lunches. The initial estimate by the nursery manager was that seven children (9%) would bring in packed lunches on the day of data collection.
It was feasible to ask nursery staff to collect the packed lunches prior to lunch being served and for fieldworkers to take photographs of the food in a different room. It was acceptable for the fieldworkers to take apart the lunch and for the other fieldworker to take the photograph and to note what the packed lunch contained. In some circumstances, the individual items, particularly homemade unidentified composite foods, could not be identified. It was difficult to take the ‘after’ photograph following lunch as there were usually multiple wrapped items of the packed lunch that took a large space on the table.
Coding by Pennington Biomedical Research Center
It was feasible to upload all photographs from the tablet and to annotate these in accordance with the file requirements of the PBRC. The photographs and the observation sheet, both containing the participant IDs, were submitted for the portion size to be estimated.
Lessons learnt
Taking photographs of meals
The feasibility of taking the before-and-after photographs of the child’s meals is dependent on the way that the meal is served, and a different approach is needed for different meal types. We encountered several types and the methods required for each are outlined in Appendix 10.
Estimates of researchers needed for data collection
Two fieldworkers are needed for data collection. The number of children whom fieldworkers can follow throughout the day is dependent on the style in which the meals are served. As drink consumption needs to be recorded observationally, and some food items (e.g. fruit that children could help themselves to) needs to be recorded on an observation sheet, it is not feasible for one researcher to do both tasks at the same time as this would result in missing data. Thus, we found that two researchers working together, one taking photographs with the tablet and watching for the children to be served and to finish their meal, while the other records all observational data, would optimise the number of children who could be followed.
The serving style and also the number of children per table is still important to estimate how many children could be followed throughout the day by two researchers. Two researchers can usually follow one table of children in order to accurately record the number of additional food portions and drinks of water the children take. We found that we could follow up to 10 children if they were all seated at the same table. If the meal was served in a rolling fashion, as was most common for snacktime, it was possible to follow all the children present at the meal as approximately four children at a time would be given their portion and, only once they had finished, would more children be called up to get theirs.
The co-operation of the staff is essential in identifying which children we are following and asking children to wait for the photograph to be taken. Letting the nursery know which children were going to be followed can help the staff prepare for the arrival of researchers.
Summary
It is feasible to collect diet data in a nursery setting by taking photographs. A combination of photographic and observational data collection using two fieldworkers together means that up to 10 children can be followed in 1 day, providing that the children are seated at the same table for all meals and that children are served sequentially.
Chapter 10 Lessons learnt from the NAP SACC UK feasibility trial
In this chapter, the practical lessons relating to recruitment, data collection and intervention delivery are examined with a view to informing a full-scale trial. These lessons will also be relevant to the design of other trials within nursery settings. The lessons draw from the process evaluation, experiences of the research team, and discussions with co-applicants, the TSC, the founder of NAP SACC (Professor Dianne Ward), and the lay advisory group. Specific quotes and issues raised in the process evaluation are not repeated here but presented in the form of practical recommendations.
Recruitment
Recruitment of a local authority to participate in a trial should include a thorough check of other early years/preschool health initiatives (including non-health initiatives), which could make recruitment difficult or affect the control groups. This learning particularly draws on the phase 1 findings and decision to change the second local authority from Wales to Gloucestershire, but also the experience within Gloucestershire of other initiatives. The impact of this for recruitment to a full trial could be that it will be more difficult to recruit cities in particular, because many have developed healthy preschool programmes or have other city-wide early years initiatives. It may also mean that recruitment of early years settings may be more difficult in local authorities that are part of the ‘Bristol Standard’ family, where many early years settings are undertaking the Bristol Standard quality improvement programme. These considerations will be taken into account in choice of local authorities for a future full trial.
It was helpful attending the local authority’s regular meeting with child-care providers to inform nursery managers of the trial and, if the study progressed to a full-scale trial, this level of local engagement would be important. Nursery recruitment may be aided by creating a short online film, with interviews from managers, NAP SACC UK partners and parents from the feasibility study highlighting what it involved, as well as the nursery staff and NAP SACC UK partners’ enthusiasm for the intervention and the acceptability of the feasibility study. This approach has been used by GoActive108 (www.cedar.iph.cam.ac.uk/research/directory/goactivestudy/). The film should feature nurseries from deprived areas to highlight potential benefits of reducing health inequalities to attract large nurseries in deprived areas. A future trial should ensure that the memorandum of understanding is signed by the manager (not deputy, to avoid the problem encountered at one nursery, which did not fully take part in the intervention) after a briefing meeting with staff and the manager.
To increase child recruitment rates, the acceptability of using parental opt-out consent for some or all data should be discussed with the ethics committee (of note, opt-out consent was used in the nursery food photography substudy and is used routinely by NCMP for national data collection). Recruitment of children could be increased by involving nursery staff in communicating with parents about the study. This would require a member of the research team to discuss the study and child eligibility with staff (not only the manager) and show staff the recruitment packs. This process could also reduce the number of ineligible children included in the denominator. Attendance by research staff when parents are collecting their children on at least three afternoons per nursery may increase recruitment, allowing parents to consider the study and ask questions. Nursery staff should be provided with a list of children for whom no response has been received so that they can remind parents to return the consent form.
Professor Dianne Ward, the founder of NAP SACC in the USA, has identified lessons for conducting environmental interventions in early years settings. These include:
-
Ensure that the intervention is based on a behaviour change theory.
-
An advisory group should inform the intervention and delivery.
-
Realistic recruitment targets should consider the economic nature of child care.
-
Data collection needs to be flexible with realistic sample size calculations because of high rates of child (and sometimes provider) turnover.
-
Interventions that are relatively easy to implement are more likely to appeal to a wide variety of providers. 109
Of particular note for the NAP SACC UK study is the reality that recruitment, particularly dual recruitment of nurseries and children/parents, is challenging and requires resources and time. Such realism is required with consideration for the sample size and resource requirement for a future trial, particularly if meaningful dietary measures are to be included.
Data collection
Although the acceptability of children wearing accelerometers was good, the number of children meeting the wear-time criteria of ≥ 480 minutes per day was not large. A number of studies that used accelerometers with preschool children have a used less strict wear-time criteria for valid days of accelerometer data. For example, Pate et al. ’s study in US preschools included children in the analysis if they provided accelerometer data for ≥ 50% of the school day for 3 days, with a full day being > 6 hours (e.g. 180 minutes per day minimum wear time). 48 Stanley et al. 52 considered > 3 hours per day on ≥ 1 day as valid wear time for a study in a preschool setting.
Given the turnover of children between early years settings and progression to primary school, consideration should be given to a repeat cross-sectional study design within the RCT to maximise assessment of environmental changes on the children within the nursery at each time point.
The use of laptop computers for CADET data collection was not trialled as it would have been cumbersome to use a laptop in the nursery environment. The use of tablets should be explored further for data collection if adequate battery power and speed of data entry is possible with different devices or models; however, paper data collection was acceptable and practical.
In a full-scale trial, parents should not be asked to report costs of food and PA, health-care use or time off work, because there were too many missing data, these data were highly variable and these costs were unlikely to be affected to a great extent by the intervention.
The methods used in the food photography substudy should be adopted for a phase 3 trial to give more detailed information about portion size and food/drink consumption. Among the parents who responded, a high percentage gave consent for data linkage to NCMP height and weight data collected in schools. Therefore, requesting opt-out consent for data linkage to NCMP should be included in a full trial.
The EPAO data were collected on 1 day for each nursery at baseline and follow-up. With the variability of activities, weather and food provided between days we were concerned that one day of observation was not reliable. The EPAO provides useful contextual information about the nurseries, but it is questionable whether or not it is a reliable enough measure to be included as an outcome measure in a full trial. The original development of the instrument concluded the tool is a ‘stable and reasonably accurate instrument . . . However, a more robust, less subjective measure would be more appropriate for researchers seeking an outcome measure to assess intervention impact.’110
A phase 3 trial should measure how the intervention is sustained over time with respect to staff turnover and whether changes are embedded as ‘the way things are done’ or diluted. Furthermore, an objective measure of oral health should be included as a secondary outcome.
Intervention delivery
To ensure timely completion of the Review and Reflect form and maximise the number of nursery staff attending the two workshops (to coincide with inset days, or avoid planned annual leave and nursery closures), the NAP SACC UK partner and nursery manager meetings and two workshops should be booked with all nurseries at an early stage and prior to randomisation (cancelling the dates in control nurseries after randomisation). This would have the additional advantage of nursery managers being fully aware of the time commitment required for the intervention prior to randomisation as a further check, in addition to the signed memorandum of understanding.
The timing of the elements of the intervention should be:
-
NAP SACC UK partner and nursery manager meet to jointly complete the Review and Reflect tool.
-
Workshop includes the manager highlighting areas for potential improvement identified in the Review and Reflect tool.
-
Staff suggest goals at end of workshop and confirm action plan with NAP SACC UK partner in subsequent meeting.
The intervention should be extended to 1 year to include two cycles of the Review and Reflect and goal-setting process, with a supplementary workshop after 6 months. Process data suggest partners and managers focused initially on easy-to-achieve goals. Allowing for a second cycle of goal-setting would encourage them to extend their goals beyond the ‘easy wins.’ As the workshops appeared important in motivating staff, an additional workshop at this point is recommended to encourage commitment from staff. The intervention could be improved by providing template copies of relevant policies (e.g. nutrition, PA, screen time, oral health, dental registration questions for registration pack).
Communication with nurseries at the beginning and throughout the intervention should make clear when the support from the NAP SACC UK partner will end. In addition, for the control nurseries, there should be ongoing communication so there is not a long period between annual data collection periods. Consideration of provision of an alternative health intervention could be considered for control groups (e.g. sun protection or hand hygiene).
During baseline data collection, it was observed that a small number of children in approximately half of the nurseries were bringing in packed lunches from home. An information sheet111 is available from the Children’s Food Trust on healthy packed lunches for early years and the national Change4Life website112 has a page with ideas for packed lunches. This information could be included in the information provided to the NAP SACC UK partners in a phase 3 trial, as an additional resource. Staff from Public Health England and the Children’s Food Trust anticipated government policy to increase free early years education from 15 to 30 hours for 3- to 4-year-olds (for parents working a minimum number of hours) and in September 2017 may increase lunchbox provision (Alison Burton, Public Health England, 2017, personal communication, and Patricia Mucavele, Children’s Food Trust, 2017, personal communication). 23 The five nursery managers attending the lay advisory group thought that increases in lunchboxes would be minimal but would increase in some settings. Therefore, the Review and Reflect tool should also incorporate best practice standards for lunchbox provision. The design of this could further be supported by work on lunchbox quality in the UK,113 Australia43 and USA. 114
The pressure of health visitors’ capacity to deliver the intervention necessitates flexibility to consider different models of delivery. If NAP SACC UK is delivered by a less experienced group of staff in a future trial, additional training will be necessary to ensure that these individuals are adequately supported. This should be provided at an earlier stage of the intervention, with additional top-up training to allow staff to discuss emerging issues.
Summary
The feasibility study has identified a number of modifications to improve recruitment, data collection and intervention delivery. These are summarised in Table 28.
| Theme | Recommendation |
|---|---|
| Recruitment | Create an online film with participants from the feasibility study to aid recruitment |
| Use local authority meetings with nurseries to promote the trial | |
| Face-to-face meetings to be held with all the nursery managers to ensure that they fully understood what participation and randomisation would involve | |
| Research staff to meet nursery staff prior to child recruitment (at team meeting or visiting staff in each room) to explain the study, eligibility of children and child recruitment process | |
| Managers (not deputies) to sign a ‘memorandum of understanding’ outlining the intervention, research process and commitment to take part | |
| Research staff to be present in every recruited nursery late afternoon on 3 days, during each child recruitment period, in order to meet parents and answer any questions face to face to facilitate child recruitment | |
| Discuss with ethics committee the acceptability of parental opt-out consent for some or all child data collection | |
| Data | Repeated cross-sectional study design within the RCT to maximise assessment of environmental changes on the children within the nursery at each time point |
| At the point of requesting consent for child data collection, parental opt-out consent for data linkage to NCMP data should be requested | |
| Collection of portion size and calorie intake for snacks and meals using remote food photography methodology | |
| An objective measure of oral health should be included as a secondary outcome | |
| Consider removing EPAO as an outcome measure or using a summary measure | |
| Health economic data should be reduced and focused on intervention costs and PedsQL | |
| Intervention | Intervention period to include two cycles of the Review and Reflect and goal-setting process (one cycle in the pilot), over 1 full year, with a supplementary workshop after 6 months |
| Nursery owners (as well as managers and staff) to be invited to attend the workshops to engage the decision-makers | |
| Intervention to be delivered by either a health visitor or other public health/health improvement/health professional with appropriate skills | |
| Lunchbox best practice elements should be added to the intervention | |
| Consider use of alternative intervention for control nurseries |
Chapter 11 Discussion
Summary of findings
The phase 1 study found that nurseries reported a generally good standard of nutrition, but the extent to which nutrition guidance was used varied between settings, with some using no guidance. Most nurseries had space for children to be physically active, which was usually outdoors. There was variation in the extent to which the outdoor space was used regardless of weather, or only on dry days. Screen time was limited across settings, with few including television time in their daily routines. Children’s oral health was highlighted as a growing concern in nurseries, and this concern was reinforced by an NHS oral health specialist who was a member of our group of expert advisors to NAP SACC UK. Adaptations to NAP SACC were made in the light of the phase 1 study and NAP SACC UK at Home was created.
In the phase 2 feasibility RCT, recruitment of nurseries (31.6%) and children (35.3%) was lower than the progression criteria of 40%, but both were exceeded in one of the two study areas. No nurseries withdrew from the study. The intervention was delivered as planned in five out of the six intervention nurseries with high levels of feasibility and acceptability (there were particular circumstances in the sixth nursery), with the exception of the home component. It was feasible to recruit and train health visitors to deliver the intervention, but health visitors reported they may not have capacity to deliver the intervention alongside their usual workload.
The trial methods and design were acceptable and feasible. The number of children lost to follow-up was 24 (14.2%), because of withdrawing consent (1.8%), child refusal to participate on the day (1.2%), children moving to primary school (6.5%) or children moving nursery (4.7%). Eighty-five per cent (n = 145) of children were followed up for data collection, but not all children provided all data at baseline and follow-up. Although the study was not powered to measure effectiveness, accelerometer-measured total PA and MVPA were higher in the intervention arm than in the control arm after the intervention. The ICC for total activity was 0.02 (95% CI < 0.0001 to 0.95). The average cost of delivering the intervention was estimated at £1184 per nursery; nurseries incurred on average an additional £717 for staff attendance at two workshops.
The two substudies found the mediator questionnaire to be reliable and the methods of collecting diet data using photography to estimate portion size to be feasible.
Progression criteria
Chapter 5, Table 27, outlines the trial outcomes for each of the progression criteria. These criteria were met in full except for the recruitment of nurseries and children and the feasibility of the NAP SACC UK at Home component. Although the overall recruitment rates for nurseries and children were below the target 40%, both were exceeded in North Somerset, where the length of recruitment was longer, and the independent TSC agreed that these data showed recruitment is feasible.
Intervention acceptability
The intervention was implemented with high fidelity except that (1) one nursery did not implement the intervention because of staff workload (we concluded that the issues for this nursery were not generalisable and would add visits to all nursery managers and staff at recruitment to avoid this in a future trial) and (2) the digital home component was used by only 14% of parents. The process evaluation showed that the NAP SACC UK intervention was feasible to implement in a UK nursery. The mean number of staff per nursery attending workshops was seven. The workshops and contact with health visitors were highly valued. The mean number of goals set was eight. Reported changes included menu modifications, reducing portion sizes and sugary snacks, role modelling PA and eating, and active story telling. The intervention was highly acceptable to the NAP SACC UK partners and they reported that they enjoyed delivering the intervention. Concerns were raised by NAP SACC UK partners as to how, if rolled out, this would fit into their (health visitor) current workload as they are already overstretched. Suggestions included having dedicated NAP SACC UK health visitors (separate to normal health visitors duties), using other staff groups (e.g. health improvement staff) or having a generic job description for a set of key skills.
The intervention was found to be highly acceptable to nursery managers and staff. Workshops were frequently mentioned as the part of the intervention most valued by these groups, along with the contact with a named health visitor. Parents who were interviewed were supportive of the research process taking place in the nursery, but were usually unaware of the changes that had taken place because of the intervention.
Research feasibility and acceptability
The trial design and methods were highly acceptable. Some nursery staff did not fully understand the randomisation process, but the majority of staff found it an acceptable process. Staff reported that the data collection process was acceptable and caused little disruption; similarly, parents reported the data collection to be acceptable. No nurseries left the trial, and only 14.2% (24/169) of children were lost to follow-up, primarily because they left the nursery (either to a different nursery or to school).
Indication of affordability
The study included piloting cost-effectiveness measures through the use of logs and questionnaires to estimate intervention costs. The mean cost of the intervention was £1184.39 (SD £209.48) per nursery or £27 per 2- to 4-year-old child. The majority of this cost was attributed to the staff time required to deliver the intervention. Depending on who delivers the workshop training and the support to nurseries, local authorities could potentially absorb most of the costs of delivering the intervention within currently commissioned services (e.g. health visiting) or provision by local authority staff. Alternatively, the intervention could be funded by public health or early years local authority departments and commissioned as an externally provided service.
Suggestion of promise
The accelerometer data showed suggestion of promise for the intervention increasing MVPA and total activity on nursery days in the intervention arm compared with the control arm, which was not seen to the same extent on non-nursery days. We would aim to increase the number of children with valid wear time of the accelerometers by using methods adopted in a study by Pate et al. 48 in nurseries in the USA. In Pate et al. ’s study,48 research staff returned to the nursery each morning to give replacement accelerometers to children who did not arrive wearing the accelerometer given the previous day. Furthermore, families were given a $25 gift card at the end of each data collection period.
There was further suggestion of promise for the knowledge and motivation of parents and nursery staff, reduction in screen time and sedentary activities at home, increase in the quality of snack provision, and decrease in the proportion of children who are overweight or obese.
Implications for future research
Phase 3 trial
The NAP SACC UK intervention and trial methods were feasible and acceptable and we found suggestion of promise in the feasibility trial. Therefore, only minimal refinements to intervention content are required. The feasibility trial supports the case for a phase 3 effectiveness trial. The feasibility work has informed the design of a full-scale trial and a multicentre trial has been funded by NIHR (PHR NIHR 127551) which will start in July 2019, informed by a range of sample size calculations (see Appendix 11, Table 47) to detect a 17-minute increase in total activity on nursery days immediately post intervention.
The PICO (Participants, Intervention, Control, Outcomes) for a full trial is shown in Box 1, and Table 29 outlines the key steps of the NAP SACC UK interventions as they will be used in the full trial over 12 months. Steps 1–4 will take place over 6 months and steps 5–7 over the following 6 months.
-
Nurseries with children aged 2–4 years eating at least one main meal per day.
-
Nursery staff.
-
Children aged 2–4 years attending a participating nursery for at least 12 hours per week.
-
NAP SACC UK intervention delivered by health or health improvement staff over 12 months.
-
Usual practice.
To investigate the effect of the NAP SACC UK intervention immediately post intervention compared with usual practice for children aged 2–4 years who attend nursery for at least 12 hours per week on:
-
accelerometer-assessed mean total activity time on nursery days.
-
average calories consumed across all eating occasions on nursery days.
-
Accelerometer-assessed mean daily moderate to vigorous physical activity time per nursery day.
-
Accelerometer-assessed mean daily sedentary time per nursery day.
-
Average size (calories) of food served across all eating occasions in nursery per day.
-
Average grams of core food consumed across all eating occasions in nursery per day.
-
Average grams of non-core food consumed across all eating occasions in nursery per day.
-
The ratio of average grams of core food to average grams of non-core food consumed across all eating occasions in nursery per day.
-
zBMI determined from weight and height measured in nurseries by two fieldworkers.
-
Proportion of children who are overweight/obese, determined by the UK age and gender reference charts at 85% and 95% centiles.
-
Environmental and Policy Assessment and Observation (EPAO) UK Instrument score.
-
Child quality of life measured using PedsQL.
-
Cost-effectiveness.
| Time period | NAP SACC UK intervention components |
|---|---|
| First 6 months | 1. Self-Assessment: 80 multiple-choice questions to assess 19 key areas in nutrition and PA with response options ranging from minimal to best practice |
| 2. Action-planning: eight areas selected for improvement with an action plan | |
| 3. Workshop delivery: nursery staff receive two workshops (each 3 hours) led by nutrition and PA specialists | |
| 4. Targeted technical assistance: NAP SACC UK partner maintains regular contact with the child-care setting to provide support and guidance in making their improvements | |
| Second 6 months | 5. Evaluate: the self-assessment is repeated |
| 6. Workshop delivery: 2-hour workshop for staff with NAP SACC UK partner and experts to remind staff of the intervention aims, review progress and set eight goals and actions | |
| 7. Targeted technical assistance: NAP SACC partner maintains regular contact with the nursery to provide support and guidance in making their improvements |
Strengths and limitations
This is a study in the UK that has tested the feasibility of a combined nutrition and PA environmental intervention in nurseries, with the additional component of oral health. The adaptation of the intervention from the USA was well informed by communication with parents, nursery managers and providers of services in early years settings.
For a feasibility study, it was a strength that two local authorities were involved, which included a range of city, small town and rural areas and neither area was adjacent to the university (where settings are more likely to be exposed to opportunities to take part in research), therefore giving a good indication of recruitment in other areas of the country. The intervention and trial methods were tested in a good number of nurseries and with a large number of children. Rates of nursery and child recruitment were reasonable. The retention of nurseries was excellent and retention of children was good where the children stayed within the nurseries; we deliberately tested the feasibility of following children beyond their time in nursery with the progression to school.
Objective measures of PA, diet, zBMI and the nursery environment were collected from participants at two time points. The study incorporated a detailed process evaluation that has allowed us to address the progression criteria from the perspectives of parents, nursery staff and NAP SACC UK partners. The study further benefited from a detailed test of measures of HRQoL and cost to inform a future assessment of cost-effectiveness.
The intervention was provided free to nurseries. Although the nurseries incurred the cost of staff time to take part, none of the six intervention nurseries raised this as a concern and only one nursery decided not to take part prior to recruitment because of this particular concern. All children in nurseries were potentially able to benefit from improvements made by the nurseries.
We have reported the intervention in accordance with the TIDieR framework and CONSORT reporting guidelines (with the CONSORT flow diagram; see Figure 4).
The data collection using CADET allowed us to assess food consumption by food group but not by portion size, because some nurseries reported making changes in portion size and this was not measured objectively. The number of children with complete accelerometer data at baseline and follow-up for the required wear time was low. Response rates from parents to complete the parent questionnaire were lower at follow-up. Both could be addressed through use of incentives and different protocols for data collection in a full trial;48 we would not intend to measure parental costs of diet and PA, health-care use or time off work (because there were too many missing data, these data were highly variable and these costs were unlikely to be affected much by the intervention).
We were not aware that there were two other quality improvement programmes available to nurseries in Gloucestershire prior to recruitment and, therefore, these were not part of the exclusion criteria for recruiting nurseries. Many nurseries in Gloucestershire were taking part in the ‘Bristol Standard’ and the pilot ‘Smiles Better award’. The Bristol Standard addresses 10 dimensions of educational quality (including health dimensions) across the nursery environment through a process of self-reflection, evaluation and goal-setting by nursery staff. Two out of the six recruited nurseries in Gloucestershire were also involved with the Bristol Standard. The Smiles Better award addresses oral health. The recruitment rate may have been higher had we excluded nurseries participating in other non-health quality improvement programmes in Gloucestershire. This was discussed after recruitment with the TSC; the TSC advised it would have been reasonable for nursery participation in quality improvement programmes, other than NAP SACC UK, to have been included in the exclusion criteria. If this had been an exclusion criterion the nursery recruitment rate would probably have been higher. The eligibility criteria for a future trial will need to consider whether or not nurseries should be excluded if they are already committed to other quality improvement programmes because of the capacity of nurseries to take part in multiple programmes.
We did not recruit any large nurseries in the highest deprivation group. Nurseries did not need to give a reason for not taking part and, therefore, we have limited information as to why these nurseries chose not take part. It is possible that the large nurseries in more deprived areas have more children who do not have English as a first language and have more children aged 2 years accessing the free child care that is means-tested for 2-year-olds. Therefore, these nurseries may have a greater workload and taking part in a research study may be regarded to be an additional burden. For a full trial, as part of the recruitment, we will include large and deprived nurseries in a recruitment video and ensure that issues regarding the benefits of reducing health inequalities are highlighted, to help large nurseries in deprived areas to identify with other nurseries that took part and to make the study feel manageable, attractive and of importance to their children.
In this study, zBMI was used as the measure of adiposity for children. We recognise that this cannot provide data on fat mass and fat-free mass, which may be important and could be detected by other approaches, such as dual-energy X-ray absorptiometry (DEXA) scans. 115 However, these methods are not applicable for use within a large field study and it would not be feasible to use such an approach in a definitive trial without substantial increases in participant burden and research cost. Thus, despite the potential limitations zBMI is the most appropriate measure for this study.
Conclusions and recommendations
The NAP SACC UK intervention (without the home component) and trial design have been found to be acceptable to nursery staff, parents and NAP SACC UK partners. The delivery of a cluster RCT, with process and economic evaluations, was feasible. The data indicate that NAP SACC UK has promise to increase PA levels of children aged 2–4 years during their time at nursery. Collectively, the findings from this study support the progression to a phase 3 trial of NAP SACC UK. A multicentre cluster randomised controlled trial to evaluate the effectiveness and cost-effectiveness of NAP SACC UK has been funded by NIHR (and will start in July 2019).
Acknowledgements
We thank all the children, parents/carers, nursery staff, health visitors and trainers (specifically Jessica Williams, Mike Squire, Hayley Burton and Auriol Barker) who took part in NAP SACC UK. We thank all the NAP SACC UK staff including fieldworkers (with particular thanks to Sarah Harding, Tom Reid and Manmita Rai and Jane Collingwood), administrative staff, computing and data management staff (with particular thanks to Xabier Baquedano, Mai Baquedano and Sam Story), research governance staff (Anna Brooke) and finance staff (Alex Mikulski and Kathryn Mellor). We thank Becky Pollard and Jon Roberts (North Somerset Council), Julie Bishop (Public Health Wales), Janine Newbury (North Somerset Community Partnership), Sarah Scott and Ruth Lewis (Gloucestershire County Council) and Jane Hayhurst (Gloucestershire Care Services NHS Trust) and their staff for their support for the study. We also thank the chairperson and members of the TSC for their advice and support: Professor Russell Viner, University College London and London NHS Foundation Trust; Professor Sian Robinson, University of Southampton; Justine Britton, University of Bristol; Dr Brad Metcalf, University of Exeter; Claire Wilson, Health Visitor.
This study was designed and delivered in collaboration with the Bristol Randomised Trials Collaboration, a UK Clinical Research Collaboration (UKCRC) Registered Clinical Trials Unit in receipt of NIHR CTU support funding. The work was undertaken with the support of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research Centre of Excellence. Joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. Funding from the Elizabeth Blackwell Institute at the University of Bristol paid for work in collaboration with PBRC for the remote food photography substudy.
Contributions of authors
Dr Ruth Kipping (Senior Research Fellow, Public Health) was the principal investigator, obtained the funds for the study and wrote the first draft of the monograph.
Dr Rebecca Langford (Research Associate, Public Health) undertook the process evaluation, collected and analysed the data wrote the results for publication and wrote the process evaluation methods and results sections of the monograph.
Dr Rowan Brockman (Research Associate, Public Health) collected and analysed data from the phase 1, wrote the phase 1 methods and results sections of the monograph and contributed to adapting the NAP SACC intervention and writing the mediator questionnaires.
Ms Sian Wells (Trial Manager, Public Health) managed the study and the ethics applications, collected phase 1 data, was involved with adapting the NAP SACC intervention, adapting the self-assessment tool and the EPAO and contributed to writing the monograph.
Professor Chris Metcalfe (Professor, Medical Statistics) was co-applicant, co-designed the study, oversaw the data analysis and interpretation and contributed to writing the monograph.
Dr Angeliki Papadaki (Senior Lecturer, Nutrition) was co-applicant, co-designed the study, advised on the diet data analysis and interpretation and contributed to writing the monograph.
Dr James White (Senior Lecturer, Public Health) was co-applicant, co-designed the study, advised on the data analysis and interpretation and contributed to writing the monograph.
Professor William Hollingworth (Professor, Health Economics) was co-applicant, co-designed the study, oversaw the data analysis and interpretation of the economic and health-related quality-of-life interpretation and contributed to writing the monograph.
Professor Laurence Moore (Professor, Public Health) was co-applicant, co-designed the study, advised on the management of the study, data analysis and interpretation and contributed to writing the monograph.
Professor Dianne Ward (Professor, Nutrition and Physical Activity) was co-applicant, co-designed the study, advised on the management of the study, data analysis and interpretation and contributed to writing the monograph.
Professor Rona Campbell (Professor, Public Health) was co-applicant, co-designed the study, advised on the management of the study, data analysis and interpretation and contributed to writing the monograph.
Mr Bryar Kadir (Research Associate, Medical Statistics) conducted the analysis of the data.
Ms Laura Tinner (PhD student, Public Health) conducted the analysis of the health economic and health-related quality-of-life data, EPAO as well as the cost of intervention delivery data. She undertook the design, data collection and analysis of the nursery food photography feasibility substudy.
Dr Vanessa Er (Research Associate, Public Health) conducted the analysis and interpretation of the diet data, and contributed to writing the diet section of the monograph.
Ms Kaiseree Dias (PhD student, Public Health) conducted the design, data collection and analysis of the mediators’ questionnaire test retest substudy.
Ms Heide Busse (PhD student, Public Health) undertook the design, data collection and analysis of the nursery food photography feasibility substudy.
Ms Jane Collingwood (Trial Co-ordinator, Public Health) co-ordinated the study, undertook data collection and contributed to writing the monograph.
Dr Alexandra Nicholson (Trial Co-ordinator, Public Health) managed the study and contributed to writing the monograph.
Dr Laura Johnson (Senior Lecturer, Nutrition) co-designed the nursery food photography feasibility substudy and contributed to the data analysis, interpretation and contributed to writing the monograph.
Professor Russell Jago (Professor, Physical Activity) was co-applicant, co-designed the study, advised on the management of the study, data analysis and interpretation and contributed to writing the monograph.
All authors reviewed various sections of the monograph and made critical revisions to relevant sections. All approved the final submission.
Publications
Brockman R, Jago R, White J, Campbell R, Hollingworth W, Metcalfe C, et al. NAP SACC UK: Adapting a US Environmental Intervention in UK Nurseries to Increase Physical Activity and Healthy Eating in 2–4 Year Olds. Oral Presentation. Bristol: South West Public Health Scientific Conference 2016; 2016.
Langford R, Jago R, White J, Moore L, Papadaki A, Hollingworth W, et al. A physical activity, nutrition and oral health intervention in nursery settings: process evaluation of the NAP SACC UK feasibility cluster RCT. BMC Public Health 2019;19:865.
Brockman R, Jago R, White J, Campbell R, Hollingworth W, Metcalfe C, et al. NAP SACC UK: Adapting a US Environmental Intervention in UK Nurseries to Increase Physical Activity and Healthy Eating in 2–4 Year Olds. Oral Presentation. Norwich: UKCRC 2016 Conference; 2016.
Brockman R, Jago R, White J, Campbell R, Hollingworth W, Metcalfe C, et al. Parents’ and staff’s views of adapting the Nutrition and Physical Activity Self-Assessment for Childcare in UK nurseries to improve physical activity and healthy eating. Lancet 2016;388:S22.
Kipping R, Jago R, Metcalfe C, White J, Papadaki A, Campbell R, et al. NAP SACC UK: protocol for a feasibility cluster randomised controlled trial in nurseries and at home to increase physical activity and healthy eating in children aged 2–4 years. BMJ Open 2016;6:e010622.
Kipping R, Langford R, White J, Metcalfe C, Papadaki A, Hollingworth W, et al. NAP SACC UK: Feasibility Cluster Randomised Controlled Trial and Process Evaluation of an Environmental Intervention in Nurseries and a Web-Based Home Intervention to Increase Physical Activity, Oral Health and Healthy Eating in Children Aged 2–4 years. Oral Presentation. Bristol: South West Public Health Scientific Conference 2017; 2017.
Kipping R, Langford R, White J, Metcalfe C, Papadaki A, Hollingworth W, et al. NAP SACC UK: Feasibility Cluster Randomised Controlled Trial and Process Evaluation of an Environmental Intervention in Nurseries and a Web-Based Home Intervention to Increase Physical Activity, Oral Health and Healthy Eating in Children Aged 2–4 years. Oral Presentation. Victoria, BC: ISBNPA conference 2017; 2017.
Kipping R, Langford R, White J, Metcalfe C, Papadaki A, Hollingworth W, et al. NAP SACC UK: Feasibility Cluster Randomised Controlled Trial and Process Evaluation of an Environmental Intervention in Nurseries and a Web-Based Home Intervention to Increase Physical Activity, Oral Health and Healthy Eating in Children Aged 2–4 years. Poster Presentation. Manchester: Society of Social Medicine conference 2017; 2017.
Er V, Dias K, Papadaki A, White J, Metcalfe C, Jago R, et al. Are Diet and Physical Activity Associated with zBMI in 2–4-year olds in North Somerset and Gloucestershire: A Cross-Sectional Study. Oral Presentation. Bristol: South West Public Health Scientific Conference 2018; 2018.
Tinner L, Kipping R, White J, Jago R, Metcalfe C, Hollingworth W, et al. Are Quality of Life and Family Expenditure on Physical Activity Associated with Physical Activity in 2–4-year-olds in North Somerset and Gloucestershire? Oral Presentation. Bristol: South West Public Health Scientific Conference 2018; 2018.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Kipping R, Jago R, Metcalfe C, White J, Papadaki A, Campbell R, et al. NAP SACC UK: protocol for a feasibility cluster randomised controlled trial in nurseries and at home to increase physical activity and healthy eating in children aged 2–4 years. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010622.
- NHS Digital . National Child Measurement Programme England, 2016 17 School Year 2017. https://digital.nhs.uk/catalogue/PUB30113 (accessed 12 December 2017).
- National Heart Forum . Obesity Trends for Children Aged 2–11: Analysis from the Health Survey for England, London: National Heart Forum; 1993–2007 2009.
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr 2005;146:732-7. https://doi.org/10.1016/j.jpeds.2005.01.055.
- Malina RM. Physical activity and fitness: pathways from childhood to adulthood. Am J Hum Biol 2001;13:162-72. https://doi.org/10.1002/1520-6300(200102/03)13:2<162::AID-AJHB1025>3.0.CO;2-T.
- Timmons BW, Leblanc AG, Carson V, Connor Gorber S, Dillman C, Janssen I, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl Physiol Nutr Metab 2012;37:773-92. https://doi.org/10.1139/h2012-070.
- Department of Health and Social Care . UK Physical Activity Guidelines 2011.
- Hesketh KR, McMinn AM, Ekelund U, Sharp SJ, Collings PJ, Harvey NC, et al. Objectively measured physical activity in four-year-old British children: a cross-sectional analysis of activity patterns segmented across the day. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/1479-5868-11-1.
- Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao E, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 2014;349. https://doi.org/10.1136/bmj.g4490.
- Department of Health and Social Care . National Diet and Nutrition Survey Headline Results from Year 1 of the Rolling Programme (2008 2009) 2010.
- Scientific Advisory Committee on Nutrition . Carbohydates and Health 2015.
- Public Health England . National Diet and Nutrition Survey Results from Years 5 and 6 (combined) of the Rolling Programme (2012 2013–2013 2014) 2016.
- Nelson M, Erens R, Bates B, Church S, Boshier T. Low Income Diet and Nutrition Survey: Summary of Key Findings. Norwich: The Stationery Office; 2007.
- Public Health England . National Dental Epidemiology Programme for England: Oral Health Survey of Five-Year-Old Children 2015 2016. www.nwph.net/dentalhealth/14_15_5yearold/Protocol_2014_15_5%20yr%20olds%20v2.pdf (accessed 1 February 2018).
- Nuttall N, Harker R. Impact of Oral Health: Children’s Dental Health in the United Kingdom, 2003. London: The Stationery Office; 2004.
- Health and Social Care Information Centre . Monthly Topic of Interest: Children in Hospital Episode Statistics – July 2012 to June 2013 2013.
- Public Health England . Local Authorities Improving Oral Health: Commissioning Better Oral Health for Children and Young People 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/321503/CBOHMaindocumentJUNE2014.pdf (accessed 1 February 2018).
- Larson N, Ward DS, Neelon SB, Story M. What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. J Am Diet Assoc 2011;111:1343-62. https://doi.org/10.1016/j.jada.2011.06.007.
- Ward D, Vaughn A, McWilliams C, Hales D. Interventions for increasing physical activity at childcare. Med Sci Sports Exerc 2010;42:526-34. https://doi.org/10.1249/MSS.0b013e3181cea406.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. https://doi.org/10.1002/14651858.CD001871.pub3.
- National Institute for Health and Care Excellence (NICE) . Review 6: The Effectiveness of Public Health Interventions to Improve the Nutrition of 2 to 5 Year Old Children 2008.
- Department for Education . Statistical First Release 20 2014: Provision for Children Under Five Years of Age in England: January 2014 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/324065/SFR20-2014_Text1.pdf (accessed 25 January 2016).
- English Government . Help Paying For Childcare n.d. www.gov.uk/help-with-childcare-costs/free-childcare-and-education-for-2-to-4-year-olds (accessed 3 August 2017).
- Department of Education . Statutory Framework for the Early Years Foundation Stage 2012.
- Ward SA, Bélanger MF, Donovan D, Carrier N. Relationship between eating behaviors and physical activity of preschoolers and their peers: a systematic review. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0374-x.
- Brown WH, Pfeiffer KA, Mciver K, . Social and environmental factors associated with preschoolers’ non-sedentary physical activity. Child Dev 2009;80:45-58. https://doi.org/10.1111/j.1467-8624.2008.01245.x.
- Gubbels JS, Kremers SP, van Kann DH, . Interaction between physical environment, social environment, and child characteristics in determining physical activity at child care. Health Psychol 2011;30:84-90. https://doi.org/10.1037/a0021586.
- Children’s Food Trust . Eat Better Start Better: Voluntary Food and Drink Guidelines for Early Years Settings in England – A Practical Guide 2012.
- HM Government . Child Obesity: A Plan for Action 2016. www.gov.uk/government/uploads/system/uploads/attachment_data/file/546588/Childhood_obesity_2016__2__acc.pdf (accessed 17 August 2017).
- NHS Wales . Welsh Network of Healthy School Schemes n.d. www.wales.nhs.uk/sitesplus/888/page/82249#pre (accessed 15 January 2018).
- Pate RR, McIver K, Dowda M, Brown WH, Addy C. Directly observed physical activity levels in preschool children. J Sch Health 2008;78:438-44. https://doi.org/10.1111/j.1746-1561.2008.00327.x.
- Hesketh KR, Griffin SJ, Van Sluijs EM. UK Preschool-aged children’s physical activity levels in childcare and at home: a cross-sectional exploration. Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0286-1.
- Wolfenden L, Jones J, Williams CM, Finch M, Wyse RJ, Kingsland M, et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev 2016;10. https://doi.org/10.1002/14651858.CD011779.pub2.
- O’Dwyer MV, Fairclough SJ, Knowles Z, Stratton G. Effect of a family focused active play intervention on sedentary time and physical activity in preschool children. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-117.
- Foulkes JD, Knowles Z, Fairclough SJ, Stratton G, O’Dwyer M, Ridgers ND, et al. Effect of a 6-week active play intervention on fundamental movement skill competence of preschool children. Percept Mot Skills 2017;124:393-412. https://doi.org/10.1177/0031512516685200.
- Alhassan S, Sirard JR, Robinson TN. The effects of increasing outdoor play time on physical activity in Latino preschool children. Int J Pediatr Obes 2007;2:153-8. https://doi.org/10.1080/17477160701520108.
- Specker B, Binkley T, Fahrenwald N. Increased periosteal circumference remains present 12 months after an exercise intervention in preschool children. Bone 2004;35:1383-8. https://doi.org/10.1016/j.bone.2004.08.012.
- Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med 2004;158:170-6. https://doi.org/10.1001/archpedi.158.2.170.
- Watt RL. Exploratory and Developmental Trial of a Family Centred Nutrition Intervention Delivered in Children’s Centres. London: University College London; 2012.
- Natale R, Ludwig D, Sardinas K, Change Martinez C, Palenzuela J, Sunil M, et al. NIFA poster abstract healthy caregivers Healthy Children Phase 2 (HC2): relationship between childcare center nutrition and physical activity environment and child body mass index over one school year. J Nut Edu Behav 2017;49:S119-20. https://doi.org/10.1016/j.jneb.2017.05.107.
- Fitzgibbon ML, Stolley MR, Schiffer LA, Braunschweig CL, Gomez SL, Van Horn L, et al. Hip-hop to health Jr. obesity prevention effectiveness trial: postintervention results. Obesity 2011;19:994-1003. https://doi.org/10.1038/oby.2010.314.
- Trost SG, Fees B, Dzewaltowski D. Feasibility and efficacy of a ‘move and learn’ physical activity curriculum in preschool children. J Phys Act Health 2008;5:88-103. https://doi.org/10.1123/jpah.5.1.88.
- Hardy LL, King L, Kelly B, Farrell L, Howlett S. Munch and move: evaluation of a preschool healthy eating and movement skill program. Int J Behav Nutr Phys Act 2010;7. https://doi.org/10.1186/1479-5868-7-80.
- Roth K, Mauer S, Obinger M, Ruf KC, Graf C, Kriemler S, et al. Prevention through Activity in Kindergarten Trial (PAKT): a cluster randomised controlled trial to assess the effects of an activity intervention in preschool children. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-410.
- Roth K, Kriemler S, Lehmacher W, Ruf KC, Graf C, Hebestreit H. Effects of a physical activity intervention in preschool children. Med Sci Sports Exerc 2015;47:2542-51. https://doi.org/10.1249/MSS.0000000000000703.
- Breitenstein L, Fischer JE. De Bock . Positive impact of a pre-school-based nutritional intervention on children’s fruit and vegetable intake: results of a cluster-randomized trial. Pub Health Nutr 2012;15:466-75. https://doi.org/10.1017/S136898001100200X.
- Reilly JJ, Kelly L, Montgomery C, Williamson A, Fisher A, McColl JH, et al. Physical activity to prevent obesity in young children: cluster randomised controlled trial. BMJ 2006;333. https://doi.org/10.1136/bmj.38979.623773.55.
- Pate RR, Brown WH, Pfeiffer KA, Howie EK, Saunders RP, Addy CL, et al. An intervention to increase physical activity in children: a randomized controlled trial with 4-year-olds in preschools. Am J Prev Med 2016;51:12-2. https://doi.org/10.1016/j.amepre.2015.12.003.
- Bayer O, von Kries R, Strauss A, Mitschek C, Toschke AM, Hose A, et al. Short- and mid-term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster-randomized trial. Clin Nutr 2009;28:122-8. https://doi.org/10.1016/j.clnu.2009.01.001.
- Manios Y, Grammatikaki E, Androutsos O, Chinapaw MJ, Gibson EL, Buijs G, et al. A systematic approach for the development of a kindergarten-based intervention for the prevention of obesity in preschool age children: the ToyBox-study. Obes Rev 2012;13:3-12. https://doi.org/10.1111/j.1467-789X.2011.00974.x.
- De Craemer M, De Decker E, Verloigne M, De Bourdeaudhuij I, Manios Y, Cardon G. ToyBox-study group . The effect of a kindergarten-based, family-involved intervention on objectively measured physical activity in Belgian preschool boys and girls of high and low SES: the ToyBox-study. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/1479-5868-11-38.
- Stanley RM, Jones RA, Cliff DP, Trost SG, Berthelsen D, Salmon J, et al. Increasing physical activity among young children from disadvantaged communities: study protocol of a group randomised controlled effectiveness trial. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3743-0.
- Bélanger M, Humbert L, Vatanparast H, Ward S, Muhajarine N, Chow AF, et al. A multilevel intervention to increase physical activity and improve healthy eating and physical literacy among young children (ages 3–5) attending early childcare centres: the Healthy Start-Départ Santé cluster randomised controlled trial study protocol. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-2973-5.
- ISRCTN Registry . Increased Health and Wellbeing in Preschools n.d. www.isrctn.com/ISRCTN57165350 (accessed 1 February 2018).
- Määttä S, Lehto R, Nislin M, Ray C, Erkkola M, Sajaniemi N, et al. DAGIS research group . Increased health and well-being in preschools (DAGIS): rationale and design for a randomized controlled trial. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1744-z.
- ISRCTN Registry . A Web-Based Program to Reduce Food-Related Fears and Promote Healthy Dietary Habits in Toddlers n.d. www.isrctn.com/ISRCTN98064772 (accessed 1 February 2018).
- ISRCTN Registry . Physical Literacy in the Early Years (PLEY) Project : A Loose Parts Intervention to Promote Active Outdoor Play in Preschool Aged Children n.d. www.isrctn.com/ISRCTN14058106 (accessed 1 February 2018).
- Nezami BT, Lytle LA, Tate DF. A randomized trial to reduce sugar-sweetened beverage and juice intake in preschool-aged children: description of the Smart Moms intervention trial. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3533-8.
- Campbell KJ, Hesketh KD, McNaughton SA, Ball K, McCallum Z, Lynch J, et al. The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) Program: a cluster-randomized controlled trial of an early intervention to prevent childhood obesity. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-2836-0.
- Ward DS, Benjamin SE, Ammerman AS, Ball SC, Neelon BH, Bangdiwala SI. Nutrition and physical activity in child care: results from an environmental intervention. Am J Prev Med 2008;35:352-6. https://doi.org/10.1016/j.amepre.2008.06.030.
- Alkon A, Crowley AA, Neelon SE, Hill S, Pan Y, Nguyen V, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-215.
- Bonis M, Loftin M, Ward D, Tseng TS, Clesi A, Sothern M. Improving physical activity in daycare interventions. Child Obes 2014;10:334-41. https://doi.org/10.1089/chi.2014.0040.
- The University of North Carolina at Chapel Hil . Go NAPSACC n.d. https://gonapsacc.org/ (accessed 15 January 2018).
- Change4Life . Change4Life n.d. www.nhs.uk/change4life.
- Stay Active: A Report on Physical Activity from the Four Home Countries’ Chief Medical Officers . Department of Health, Physical Activity, Health Improvement and Protection 2011. www.gov.uk/government/publications/start-active-stay-active-a-report-on-physical-activity-from-the-four-home-countries-chief-medical-officers.
- NHS Digital . National Child Measurement Programme n.d. http://content.digital.nhs.uk/ncmp (accessed 29 August 2017).
- NHS Wales . Child Measurement Programme for Wales n.d. www.wales.nhs.uk/siteplus/888/page/67762 (accessed 12 February 2019).
- Krueger R, Casey M. Focus Groups. A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications; 2000.
- Ministry of Housing, Communities and Local Government . National Statistics English Indices of Deprivation 2015 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 12 February 2019).
- Welsh Government . Stats Wales. Ethnicity by Area and Ethnic Group n.d. https://statswales.gov.wales/Catalogue/Equality-and-Diversity/Ethnicity/ethnicity-by-area-ethnicgroup (accessed 1 February 2018).
- Public Health England . North Somerset Unitary Authority Health Profile 2015 n.d. https://fingertips.phe.org.uk/profile/health-profiles (accessed 27 January 2016).
- Public Health England . Gloucestershire County Health Profile 2015 n.d. https://fingertips.phe.org.uk/profile/health-profiles (accessed 27 January 2016).
- NAP SACC . Go NAP SACC n.d. https://gonapsacc.org/ (accessed 15 Janaury 2018).
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Cade JE, Frear L, Greenwood DC. Assessment of diet in young children with an emphasis on fruit and vegetable intake: using CADET – Child and Diet Evaluation Tool. Public Health Nutr 2006;9:501-8. https://doi.org/10.1079/PHN2005871.
- Christian MS, Evans CE, Nykjaer C, Hancock N, Cade JE. Measuring diet in primary school children aged 8–11 years: validation of the Child and Diet Evaluation Tool (CADET) with an emphasis on fruit and vegetable intake. Eur J Clin Nutr 2015;69:234-41. https://doi.org/10.1038/ejcn.2014.160.
- Latomme J, Cardon G, De Bourdeaudhuij I, Iotova V, Koletzko B, Socha P, et al. Effect and process evaluation of a kindergarten-based, family-involved intervention with a randomized cluster design on sedentary behaviour in 4- to 6- year old European preschool children: The ToyBox-study. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0172730.
- Ward DS, Mazzucca S, McWilliams C, Hales D. Use of the Environment and Policy Evaluation and Observation as a Self-Report Instrument (EPAO-SR) to measure nutrition and physical activity environments in childcare settings: validity and reliability evidence. Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0287-0.
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181-8. https://doi.org/10.1249/mss.0b013e31815a51b3.
- Konstabel K, Veidebaum T, Verbestel V, Moreno LA, Bammann K, Tornaritis M, et al. Objectively measured physical activity in European children: the IDEFICS study. Int J Obes 2014;38:135-43. https://doi.org/10.1038/ijo.2014.144.
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557-65. https://doi.org/10.1080/02640410802334196.
- Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res 2002;10:150-7. https://doi.org/10.1038/oby.2002.24.
- Rich C, Geraci M, Griffiths L, Sera F, Dezateux C, Cortina-Borja M. Quality control methods in accelerometer data processing: identifying extreme counts. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0085134.
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9. https://doi.org/10.1136/adc.73.1.25.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320:1240-3. https://doi.org/10.1136/bmj.320.7244.1240.
- Gregory J, Lowe S, Bates, CJ, Prentice A, Jackson LV, Smithers G, et al. National Diet and Nutrition Survey: Young People Aged 4 to 18 Years. Volume I: Report of the Diet and Nutrition Survey 2000.
- Finglas PM, Roe MA, Pinchen HM, Berry R, Church SM, Dodhia SK, et al. McCance and Widdowson’s The Composition of Foods, Seventh Summary Edition. Cambridge: Royal Society of Chemistry; 2015.
- Wall C, Mucavele P, Sharp L. Development and implementation of voluntary food and drink guidelines for early years settings in England. Nutr Bull 2012;37:251-6. https://doi.org/10.1111/j.1467-3010.2012.01981.x.
- American Academy of Pediatrics . American Academy of Pediatrics Announces New Recommendations for Children’s Media Use 2016. www.aap.org/en-us/about-the-aap/aap-press-room/pages/american-academy-of-pediatrics-announces-new-recommendations-for-childrens-media-use.aspx (accessed 15 January 2018).
- Australian Department of Health . Get Up and Grow – Caring for Our Kids – Staff Hand Book – Healthy Eating and Physical Activity 2012. www.health.gov.au/internet/publications/publishing.nsf/Content/gug-indig-hb∼inactivitiy (accessed 15 January 2018).
- Varni JW, Seid M, Kurtin PS. PedsQL™ 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Med Care 2001;39:800-12. https://doi.org/10.1097/00005650-200108000-00006.
- Kuhl ES, Rausch JR, Varni JW, Stark LJ. Impaired health-related quality of life in preschoolers with obesity. J Pediatr Psychol 2012;37:1148-56. https://doi.org/10.1093/jpepsy/jss090.
- Varni J.W. Scaling and Scoring of the Pediatric Quality of Life Inventory™ PedsQL 2017. www.pedsql.org/PedsQL-Scoring.pdf (accessed 15 August 2017).
- HM Revenue and Customs . Expenses and Benefits Business Mileage n.d. www.gov.uk/expenses-and-benefits-business-travel-mileage/rules-for-tax (accessed 15 August 2017).
- Department for Health and Social Care NHS Reference Costs . NHS Reference Costs 2015–2016 n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/577083/Reference_Costs_2015-16.pdf (accessed 15 August 2017).
- Personal Social Services Research Unit . Health and Social Care Unit Costs 2016 n.d. www.pssru.ac.uk/project-pages/unit-costs/2016/ (accessed 15 August 2017).
- Office of National Statistics . Average Salary of Hours and Earnings Survey 2016 n.d. www.ons.gov.uk (accessed 15 August 2017).
- Payscale . Nursery Worker Salary n.d. www.payscale.com/research/UK/Job=Nursery_Worker/Hourly_Rate (accessed 15 August 2017).
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Langford R, Jago R, White J, Moore L, Papadaki A, Hollingworth W, et al. A physical activity, nutrition and oral health intervention in nursery settings: process evaluation of the NAP SACC UK feasibility cluster RCT. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-7102-9.
- Lawlor DA, Howe LD, Anderson EL, Kipping RR, Campbell R, Wells S, et al. The Active for Life Year 5 (AFLY5) school-based cluster randomised controlled trial: effect on potential mediators. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-2734-5.
- Bland JM, Altman DG. Cronbach’s alpha. BMJ 1997;314. https://doi.org/10.1136/bmj.314.7080.572.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Abingdon-on-Themes: Taylor & Francis; 2013.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Nicklas T, Saab R, Islam NG, Wong W, Butte N, Schulin R, et al. Validity of the remote food photography method against doubly labeled water among minority preschoolers. Obesity 2017;25:1633-8. https://doi.org/10.1002/oby.21931.
- Nicklas T, Saab R, Islam NG, Wong W, Butte N, Schulin R, et al. Validity of a digital diet estimation method for use with preschool children. J Acad Nutr Diet 2018;118:252-60.
- Nicklas TA, O’Neil CE, Stuff J, Goodell LS, Liu Y, Martin CK. Validity and feasibility of a digital diet estimation method for use with preschool children: a pilot study. J Nutr Educ Behav 2012;44:618-23. https://doi.org/10.1016/j.jneb.2011.12.001.
- Brown HE, Whittle F, Jong ST, Croxson C, Sharp SJ, Wilkinson P, et al. A cluster randomised controlled trial to evaluate the effectiveness and cost-effectiveness of the GoActive intervention to increase physical activity among adolescents aged 13–14 years. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014419.
- Benjamin Neelon SE, Østbye T, Hales D, Vaughn A, Ward DS. Preventing childhood obesity in early care and education settings: lessons from two intervention studies. Child Care Health Dev 2016;42:351-8. https://doi.org/10.1111/cch.12329.
- Benjamin SE, Neelon B, Ball SC, Bangdiwala SI, Ammerman AS, Ward DS. Reliability and validity of a nutrition and physical activity environmental self-assessment for child care. Int J Behav Nutr Phys Act 2007;4. https://doi.org/10.1186/1479-5868-4-29.
- Children’s Food Trust . Healthy Packed Lunches for Early Years n.d. http://media.childrensfoodtrust.org.uk/2015/05/CFT-Packed-Lunch-Guidance.pdf (accessed 4 January 2018).
- Change4Life . Healthier Lunchboxes n.d. www.nhs.uk/change4life/recipes/healthier-lunchboxes#lmM05E27QghKqM5O.97 (accessed 4 January 2018).
- Evans CEL, Greenwood DC, Thomas JD, Cleghorn CL, Kitchen MS, Cade JE. SMART lunch box intervention to improve the food and nutrient content of children’s packed lunches: UK wide cluster randomised controlled trial. J Epidemiol Community Health 2010;64:970-6. https://doi.org/10.1136/jech.2008.085837.
- Roberts-Gray C, Briley ME, Ranjit N, Byrd-Williams CE, Sweitzer SJ, Sharma SV, et al. Efficacy of the Lunch is in the Bag intervention to increase parents’ packing of healthy bag lunches for young children: a cluster-randomized trial in early care and education centers. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-015-0326-x.
- Jensen NS, Camargo TF, Bergamaschi DP. Comparison of methods to measure body fat in 7-to-10-year-old children: a systematic review. Public Health 2016;133:3-13. https://doi.org/10.1016/j.puhe.2015.11.025.
- Abraham C, Michie S. A taxonomy of behaviour change techniques used in interventions. Health Psy 2008;27:379-87. https://doi.org/10.1037/0278-6133.27.3.379.
- Office for National Statistics . Annual Survey of Hours and Earnings: 2016 Provisional Results n.d. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2016provisionalresults (accessed 31 January 2018).
- Change4Life . Food Facts n.d. www.nhs.uk/change4life/food-facts (accessed 31 January 2018).
- Henry. Healthy Start, Brighter Future . Healthy Recipes n.d. www.henry.org.uk/recipes (accessed 31 January 2018).
Appendix 1 Changes to protocol
| Challenge encountered during phase 1 | Specifics | Implications |
|---|---|---|
| Four other public health preschool initiatives were taking place in Wales or Cardiff and, therefore, a general feeling that NAP SACC UK was not needed |
Wales Healthy and Sustainable Preschool Scheme Cardiff Gold Standard Healthy Snack Award Scheme Flying Start dietitians working with preschool settings in Cardiff Wales Designed to Smile (toothbrushing) |
We needed to exclude the most deprived settings where these initiatives were targeted and it would have created duplication or confusion introducing NAP SACC UK Potential implication for recruiting nurseries because of availability of other initiatives and, therefore, a general view that NAP SACC UK was not a priority |
| Engaging partners in Cardiff with the intervention |
Some Wales Healthy and Sustainable Pre-School Scheme staff felt that the study was duplicating their existing programme Cardiff Council did not want to send the letter to recruit nurseries to phase 1 or provide contact details for the nurseries; a combination of time constraints and concern about being associated with the research |
Lack of local support and endorsement for the work |
| Different provision of government funding of free nursery education at age 3 in Wales and England |
Funding in Wales provides five free sessions per week of 2.5 hours each at specific providers Funding in England provides up to 15 hours free each week which can be used at any registered child-care provider |
Children who receive the free sessions in Wales are unlikely to stay for lunch or tea and, therefore, will be excluded from the trial because we require that they receive a meal, whereas in England the funding is used more flexibly at any registered child-care provider towards the total cost of child care |
| Poorer response from Cardiff nurseries to invitations to take part in the phase 1 interviews | In North Somerset all nurseries (n = 8) responded positively to taking part in the interviews, whereas in Cardiff only four out of seven contacted responded positively | Potential implication for recruiting because of availability of other initiatives |
| Experience suggests that we would be unlikely to include other areas of Wales in a full trial because of these issues | Unlikely to continue with a full trial in Wales and, therefore, more appropriate to undertake feasibility work in another area in England |
Appendix 2 Parent mediator questionnaire
Appendix 3 Nursery staff mediator questionnaire
Appendix 4 Supplementary outcome data
| Days | Intervention, n (%) | Control, n (%) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| 0 | 5 (7.5) | 9 (17.6) | 11 (15.1) | 19 (26.8) |
| 1 | 6 (9.0) | 9 (17.6) | 3 (4.1) | 4 (5.6) |
| 2 | 4 (6.0) | 6 (11.8) | 2 (2.7) | 4 (5.6) |
| 3 | 10 (14.9) | 5 (9.8) | 11 (15.1) | 11 (15.5) |
| 4 | 14 (20.9) | 7 (13.7) | 14 (19.2) | 10 (14.1) |
| 5 | 16 (23.9) | 7 (13.7) | 17 (23.3) | 12 (16.9) |
| 6 | 6 (9.0) | 2 (3.9) | 12 (16.4) | 9 (12.7) |
| 7 | 6 (9.0) | 6 (11.8) | 3 (4.1) | 2 (2.8) |
Appendix 5 The NAP SACC UK intervention elements and related behaviour change techniques employed
Using the taxonomy developed by Abraham and Michie,116 Table 32 describes the intended behaviour change techniques used in the different elements of the NAP SACC UK intervention. However, it is important to note that NAP SACC UK does not solely aim to change behaviours, but also targets the nursery environment.
| Intervention element | Associated behaviour change technique(s) |
|---|---|
| NAP SACC UK partner training |
Provide information about behaviour–health link Provide information on consequences Provide instruction |
| Review and Reflect self-assessment |
Prompt review of behavioural goals Prompt intention formation Prompt self-monitoring of behaviour |
| Goal-setting |
Prompt specific goal-setting Prompt intention formation Prompt barrier ID |
| Staff workshops |
Provide information about behaviour–health link Provide information on consequences Prompt intention formation Provide instruction Model or demonstrate the behaviour Prompt self-monitoring of behaviour Prompt ID as a role model |
| On-going support |
Provide general encouragement Provide feedback on performance Use follow-up prompts Time management |
| NAP SACC at Home website |
Provide information about behaviour–health link Provide information on consequences Prompt intention formation Provide general encouragement |
Appendix 6 CADET definition for food groups/items
| Food item (in CADET) | Description |
|---|---|
| Starchy foodsa | |
| C1 | Sandwich (tick filling separately). Bread, roll, toast crumpet |
| C3 | Garlic bread, naan, paratha |
| C4 | Chapati, pitta bread, wrap, roti, etc. |
| C5 | Cracker, crispbread, etc. (note: also included if consumed as snacks) |
| J1 | Pizza |
| J2 | Boiled rice |
| J3 | Fried rice |
| J4 | Noodles |
| J5 | Pasta – plain, couscous |
| J6 | Pasta with tomato sauce (no meat) |
| J7 | Pasta with cheese sauce |
| J8 | Pasta with meat, fish (and sauce) |
| J9 | Yorkshire pudding, pancake |
| L1 | Boiled, mashed, jacket (potato) |
| P2 | High-fibre [e.g. Bran flakes® (Kellogg’s, Battle Creek, MI, USA), Weetabix® (Weetabix, Kensington Blvd Lakeville, MN, USA), Shreddies® (Nestlé UK, Welwyn Garden City, UK), muesli] |
| P3 | Other [e.g. Cornflakes® (Kellogg’s, Battle Creek, MI, USA), Rice Krispies® (Kellogg’s, Battle Creek, MI, USA), etc.] |
| P4 | Porridge, Ready Brek® (Weetabix, Kensington Blvd Lakeville, MN, USA) |
| Processed potatoes | |
| L2 | Chips, roast, potato faces, etc. |
| Fruit and vegetables | |
| K1 | Mixed vegetables |
| K2 | Tomatoes |
| K3 | Cucumber |
| K4 | Coleslaw |
| K5 | Other salad vegetables (e.g. lettuces) |
| K6 | Stir-fried vegetables |
| K7 | Broccoli, Brussels sprouts, cabbage |
| K8 | Courgettes |
| K9 | Spinach |
| K10 | Parsnips |
| K11 | Radish |
| K12 | Leeks |
| K13 | Carrots |
| K14 | Cauliflower |
| K15 | Peas, sweetcorn |
| K16 | Celery |
| K17 | Peppers, red, green, yellow, etc. |
| K18 | Other vegetable |
| K19 | Baked beans – only counted as one portion |
| K20 | Lentils, dahl – only counted as one portion |
| K21 | Other beans – only counted as one portion |
| M1 | Fruit salad (tinned or fresh) |
| M2 | Apple |
| M3 | Pear |
| M4 | Banana |
| M5 | Orange, satsuma, etc. |
| M6 | Grapes |
| M7 | Melon, watermelon |
| M8 | Pineapple |
| M9 | Strawberry, raspberry, etc. |
| M10 | Peach, nectarine, plum, apricot, mango |
| M11 | Kiwi |
| M12 | Other fresh fruit |
| M13 | Dried fruit |
| A6 | Fruit juice (pure)/smoothies – only counted as one portion |
| Meat, fish, eggs, beans and other non-dairy sources of protein | |
| E4 | Quiche – meat, fish or vegetable |
| E5 | Scrambled egg, omelette, fried egg |
| E6 | Poached, boiled egg |
| F1 | Chicken, turkey – sliced or plain |
| F3 | Chicken, turkey – in a creamy sauce, curry (e.g. korma or tikka masala) |
| G1 | Other meats – sliced roast, steak, chops |
| G2 | Other meats – stew casserole, mince, curry or keema |
| G9 | Offal (e.g. liver, kidney) |
| H3 | White fish (not fried) (e.g. cod, haddock, plaice) |
| H4 | Tuna or other oily fish (including can or fresh) |
| H5 | Shellfish (e.g. prawns, mussels) |
| K19 | Baked beans |
| K20 | Lentils, dahl |
| K21 | Other beans |
| I3 | Quorn, veggie mince, sausages, etc. |
| Processed meat and fish products | |
| F2 | Chicken, turkey – nuggets, dippers, Kiev, etc. |
| G3 | Other meats – beef burger, hamburger, doner, kebab |
| G4 | Bacon |
| G5 | Ham |
| G6 | Sausages |
| G7 | Sausage roll, meat pie, pasty, fried dumplings |
| G8 | Corned beef, luncheon meats, salami, pepperoni |
| H1 | Fish fingers |
| H2 | Fried fish in batter (as in fish and chips) |
| Dairy | |
| A1 | Milk, milky drink, lassi |
| B7 | Yoghurt, fromage frais |
| E1 | Hard cheese (e.g. Cheddar, red Leicester) |
| E2 | Cheese spread, triangle, string |
| E3 | Cottage cheese |
| N3 | Cream, custard |
| N4 | Mousse, milk puddings (e.g. rice pudding) |
| P5 | Milk on cereal |
| Desserts | |
| B7 | Yogurt or fromage frais |
| M1 | Fruit salad (tinned or fresh) |
| N4 | Mousse, milk puddings (e.g. rice pudding) |
| N2–3 and N5–6b | Ice cream, frozen dessert [e.g. Vienetta® (Unilever, Surrey, UK)]; cream, custard; cakes, buns, sponge pudding; sweet pies, tarts, crumbles |
| High-sugar or high-fat snacks | |
| B1 | Crisps, savoury snacks [Cheddars (Jacob’s, Dublin, Republic of Ireland)] |
| B3 | Cereal bar, muesli bar, flapjack |
| B4 | Chocolate biscuit |
| B5 | Other biscuit |
| B6 | Croissant, waffles, Pop-Tarts (Kellogg’s, Battle Creek, MI, USA) |
| N1 | Jelly, ice lolly |
| N2 | Ice cream, frozen dessert (e.g. Vienetta) |
| N3 | Cream, custard |
| N4 | Mousse, milk puddings (e.g. rice pudding) |
| N5 | Cakes, buns, sponge pudding |
| N6 | Sweet pies, tarts, crumbles |
| O1 | Sweets, toffees, mints |
| O2 | Chocolate bars [e.g. Mars® (Mars Food UK Limited, Melton Mowbray, UK), Galaxy® (Mars Food UK Limited, Melton Mowbray, UK)] |
| cN2–6 should only be consumed during mealtimes as milk- or fruit-based desserts | |
| Sugary drink | |
| A3 | Drinking chocolate, etc. |
| A4 | Fizzy drink (pop/cola), squash, fruit drink [e.g. Ribena® (Lucozade Ribena Suntory, The Royal Forest Factory, Coleford, UK)] |
| A5 | Diet, low-calorie drink (including fizzy low calorie) |
Appendix 7 Supplementary health economic tables
| Cost item | Total | Total cost (£) |
|---|---|---|
| Health visitor time | 4 days | 520.00 |
| Health visitor travel | 258 miles | 88.75 |
| Trainer cost | N/A | 700.00 |
| Other | N/A | 19.96 |
| Refreshments | N/A | 27.00 |
| Total | N/A | 1355.71 |
| Trainers time per nursery | Travel costs (£) | Cost of time (£) | Total cost (£) |
|---|---|---|---|
| Nursery 001 | 11.25 | 574.64 | 585.89 |
| Nursery 003 | 10.80 | 574.64 | 585.44 |
| Nursery 005 | 5.13 | 574.64 | 579.77 |
| Nursery 008 | 30.69 | 574.64 | 605.33 |
| Nursery 009 | 18.00 | 574.64 | 592.64 |
| Nursery 012 | 34.70 | 350.00 | 384.75 |
| Total trainer costs | 110.57 | 3223.20 | 3333.82 |
| Equipment costs | N/A | N/A | 369.06 |
| Refreshments | N/A | N/A | 220.00 |
| Administration | N/A | N/A | 450.00 |
| Total | 110.57 | 3223.20 | 4372.88 |
| Time or cost | Total time | Cost of time (£)a | Travel costs (£) | Total costs (£) |
|---|---|---|---|---|
| Health visitor preparation time | 4 days | 524.32 | N/A | 524.32 |
| Health visitor total contact time per nursery including attending workshop | ||||
| Nursery 001 | 2.5 days | 325.00 | 33.75 | 358.75 |
| Nursery 003 | 3.5 days | 463.64 | 10.80 | 474.44 |
| Nursery 005 | 2.5 days | 325.00 | 39.15 | 364.15 |
| Nursery 008 | 1.5 days | 195.00 | 9.36 | 204.36 |
| Nursery 009 | 1.5 days | 195.00 | 7.83 | 202.83 |
| Nursery 012 | 2.5 hours | 46.43 | 5.85 | 52.28 |
| Total health visitor costs (£) | 2074.39 | 106.74 | 2181.13 | |
| Element | Total cost (£) |
|---|---|
| Website domain | 8.38 |
| Photo credits for study website | 61.00 |
| Website development from circle interactive | 7920.00 |
| Casual web developers | 2718.39 |
| Promotional flyers, swimming vouchers and information sheets | 404.10 |
| Promotional mugs | 835.08 |
| Total | 11,946.95 |
| Days or cost | Intervention (n = 33) | Control (n = 45) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Total time off (days) | 0.36 (1.03) | 0.73 (1.68) | 0.18 (0.91) | 0.33 (0.85) |
| Paid time off (not using paid annual leave) | 0.33 (0.30) | 0.36 (1.14) | 0.09 (0.47) | 0.22 (0.64) |
| Using paid annual leave (days) | 0 | 0.21 (0.93) | 0.04 (0.21) | 0.04 (0.30) |
| Unpaid time off work (days) | 0.06 (0.35) | 0.15 (0.87) | 0.04 (2.98) | 0.07 (0.33) |
| Cost of paid time off work (£)a | 32.67 (106.05) | 39.20 (122.96) | 9.58 (16.63) | 23.96 (68.52) |
Appendix 8 Supplementary process evaluation data
| Nursery | NAP SACC UK partner | Start/end date of support period | Details of contacts |
|---|---|---|---|
| 1 | ID 902 | 9 March 2016 to 28 June 2016 |
E-mail contacts: 1 Telephone contacts: 1 (15 minutes) Meetings: 2 (150 minutes, 150 minutes) |
| 3 | ID 903 | 4 February 2016 to 20 June 2016 |
E-mail contacts: 1 Telephone contacts: 3 (10 minutes, 5 minutes, 10 minutes) Meetings: 3 (135 minutes, 90 minutes, 90 minutes) |
| 5 | ID 902 | 9 March 2016 to 6 July 2016 |
E-mail contacts: 2 Telephone contacts: 3 (30 minutes, 5 minutes, 20 minutes) Meetings: 2 (150 minutes, 150 minutes) |
| 8 | ID 901 | 4 March 2016 to 14 June 2016 |
E-mail contacts: 5 Telephone contacts: 1 (10 minutes) Meetings: 2 (180 minutes, 60 minutes) |
| 9 | ID 901 | 22 February 2016 to 13 June 2016 |
E-mail contacts: 5 Telephone contacts: 1 (15 minutes) Meetings: 2 (180 minutes, 60 minutes) |
| 12 | ID 904 | March 2016 | Nursery did not fully implement intervention. However, one meeting with NAP SACC UK partner ID 904 took place to complete Review and Reflect form |
| Logged on to website (n) | Completed Healthy Habits (n) | Set ≥ 1 goal (n) | Text/e-mails sent (n) |
|---|---|---|---|
| 12 | 12 | 7 | 29 |
| Area | Goal |
|---|---|
| Sleep | I will encourage my child to do more calming activities in the hour before bedtime |
| I will create a calm sleep environment at bedtime | |
| Outdoor play | I will get outside with my child more |
| I will plan more outdoor activities to do with my child | |
| Eating | I will increase my child’s fruit and veg intake |
| Screens and seated time | I will reduce the amount of time that my child spends watching TV |
| Nursery | Area | Goal | Progress made assessed by Review and Reflect form and qualitative data | |
|---|---|---|---|---|
| 1 | Nutrition | Staff to ask children if still hungry before offering second portions | Review and Reflect | Q27. When children request seconds, staff ask them if they are still hungry before serving more food. Score went from ‘rarely or never’ to ‘often’. Comment: ‘Children are using the language more – about whether they’re hungry’ |
| Qualitative | The staff are a bit more, ‘Are you still hungry?’ rather than just, ‘Oh yeah, I’ll just feed you because you’ve asked for it.’ Actually checking and having those conversations with the children . . . And just generally I think the staff are just having it more at the front of their minds rather than at the backManager_Int_11We started saying, ‘Are you hungry? Like do you want more food?’ Like we’ve been asking them the questionStaff_Int_12 | |||
| Introduce activities focused on healthy eating | Review and Reflect | Q33. Staff incorporate healthy eating learning into their children’s formal daily activities, play and learning experiences. Score went from ‘Once per month or less’ to ‘2–3 times per month’. Comment: ‘More putting foods into groups and thinking about why we need foods’ | ||
| Qualitative | I think it’s just like we’ve become a lot more active in promoting that. Before we would kind of do cooking activities alongside [the cook], but it would be more like cakes, biscuits, like yummy treats that we’d send home with them. Whereas now it has become a lot more involved with getting them to make their own tea and things and, yeah, cutting up the vegetables and things like thatStaff_Int_12 | |||
| Provide information on guidance on children’s lunchboxes | Review and Reflect | Not covered in Review and Reflect | ||
| Qualitative | One of the goals we had was just to have more information for us as well as the parents on packed lunches . . . We did have it on display for the parents to look at and take photos of, like the poster and things, where they wanted to . . . Children are coming in with healthier lunches, or more so I should say a balanced lunchStaff_Int_11 | |||
| PA | Create a policy on PA with an attached appendix about screen time | Review and Reflect | Q54. Our written policya on PA includes the following topics. Score remained ‘No written policy’. Comment: ‘Planning to write garden and activity policy’ | |
| Qualitative | I think the policies didn’t really happenPartner_Int_25 | |||
| Create and provide parents with some guidance on PA, outdoor play and screen time | Review and Reflect | Q53. Information or education for families on children’s PA includes the following topics. Score remained at ‘none’. Comment: ‘Need to write policy – action plan for NAP SACC UK’ | ||
| Qualitative | Manager talked about moving the parent information display to a different location to make it more accessible to parents and the ways in which they tried to engage parents. Unclear, however, whether this had changed as a result of this NAP SACC UK goal | |||
| Adults actively involve themselves in and role model PA | Review and Reflect | Q47. Staff role-model good PA habits. Score remained at ‘often’. Comment: ‘More often – staff now more involved and children’s attention held more’ | ||
| Qualitative | And obviously for the children it was, ‘Oh, the adults do it too, you know, they have fun, they play the spot game, they chase us round the rivet.’ Whatever it is that we were doing, we will actually be more involved, and for a longer periodManager_Int_11 | |||
| Additional areas | Promote oral hygiene and health | Review and Reflect | Q18. We promote oral health in the following ways. Score remained at 0–1 ticks. Comment: ‘Action plan for NAP SACC UK – no change at present but owner has agreed to fund equipment’ | |
| Qualitative | So we are still waiting for the resources to come through. [The owners] did say, ‘Yes, go and buy them,’ but they haven’t given me a budgetManager_Int_11 | |||
| Collect more information on portion sizes and share these with staff | Review and Reflect | Not covered in Review and Reflect | ||
| Qualitative | We had to like sort out foods from like different categories and then we had to say what portion sizes it was for a child of a certain age. And that was just to actually have a visual, was actually really usefulManager_Int_11 | |||
| Nursery 3 | Nutrition | Role modelling positive meal behaviours | Review and Reflect | No follow-up Review and Reflect form available |
| Qualitative | Staff can now eat for free now to encourage positive eating behaviours (Partner_Int_2121)Our employer has given us free meals to eat with the children so we don’t have to pay. So we eat a child’s portion with the children, I think that’s helped as well so our employer is very much on boardStaff_Int_2 | |||
| Re-visit menu choices to include oily fish | Review and Reflect | No follow-up Review and Reflect form available | ||
| Qualitative | Our menus have changed as well recently as well, so we’re looking at what we’ve got in our menus, and made sure it is balanced as well, making sure we’ve got that fish in there and everythingStaff_Int_2Partner added that the new menu had been rolled out to the other two nurseries in their local chain (not participating in NAP SACC UK) (Partner_Int_21) | |||
| Education of parents – sharing information | Review and Reflect | No follow-up Review and Reflect form available | ||
| Qualitative | We’ve spoken about obviously the NAP SACC study with [parents], we asked them for menu ideas and we’re doing our menusStaff_Int_2 | |||
| PA | Adult led role modelling activities | Review and Reflect | No follow-up Review and Reflect form available | |
| Qualitative | Both manager and staff indicated there were implementing more activities to encourage PA, but unclear if these included adult-led role modellingI think physical activity wise we do a lot more things like parachutes, so a lot more physical activities outside and insideStaff_Int_2 | |||
| Use storytelling as a delivery mechanism/changing passive to activities. | Review and Reflect | No follow-up Review and Reflect form available | ||
| Qualitative | We had the storytelling within the physical activity training . . . over time it’ll develop even more . . . We can come up with a story ourselves, and then we encourage children to move around. So if was the Hungry Caterpillar [by Eric Carle, Penguin Books Ltd, London, UK] they could wriggle on the floor or they could jump up into a butterflyStaff_Int_2 | |||
| Use more varied resources for being active | Review and Reflect | No follow-up Review and Reflect form available | ||
| Qualitative | We spend a lot more time outside, not only down to do with the weather but down to do with NAP SACC too . . . We did have set garden times before, but during our physical play discussion that we had when somebody came in he said it was best for children to choose whether they want to play inside or outside which is what we now do down to his advice and everything . . . And we monitor children on a daily basis, so those ones that we know haven’t had much time on scooters, or bikes or running around or anything like that. So do set games with the children, especially our preschoolers, of ‘What’s the time Mr Wolf?’ and ‘duck, duck, goose,’ and things like that, to really get them up and activeManager_Int_1 | |||
| Additional. areas | Sharing information with our other settings (looking up what information is out there) | Review and Reflect | No follow-up Review and Reflect form available | |
| Qualitative | No qualitative data on this | |||
| Nursery 5 | Nutrition | Regulate portion sizes | Review and Reflect |
Q20. Meals and snacks are served to preschool children in the following way Comment: some children putting lots on plate, others being very fussy and only putting a little on; needing staff intervention |
| Qualitative | No qualitative data on this | |||
| Provide a template for packed lunches | Review and Reflect | Q37. Families are offered information and support on child nutrition. Score increased from less than once per year to two times per year or more | ||
| Qualitative | Since we started NAP SACC we have provided parents with information via our website and also information on parents’ evenings that we’ve held and general discussions during the day . . . For example, some children come here with lunchboxes and if staff now see something in there that they think, well, they shouldn’t really have that, you know, it’s either a chocolate treat or something like that, then we will talk to parents about it and suggest other alternativesManager_Int_10 | |||
| Devise a policy on child nutrition | Review and Reflect |
Q39. Our written policy on child nutrition includes the following topics. No policy yet Comment: planning to write as part of action plan |
||
| Qualitative | Manager had not written any policies yet due to lack of time (Manager_Int_10) | |||
| PA | Staff to provide active stories and games | Review and Reflect |
Q41. The amount of adult-led PA our nursery provides for 2–4 year old children each day is. Score went from ‘less than 30 minutes’ to ‘45–59 minutes’ Comment: ‘Summer – outside more. More active learning’ |
|
| Qualitative | No qualitative data on this | |||
| To provide information on PA to parents | Review and Reflect | No data provided in the Review and Reflect form | ||
| Qualitative | But since we started NAP SACC we have provided parents with information via our website and also information on parents’ evenings that we’ve held and general discussions during the day. So it’s become something which is more pushed up in terms of importance that we will talk to parents aboutManager_Int_10 | |||
| Devise policy on physical development | Review and Reflect |
Q54. Our written policya on PA includes the following topics. Score stayed at ‘No written policy or policy does not include these topics’ Comment: ‘Planning to do. NAP SACC UK policy’ |
||
| Qualitative | Manager had not written any policies yet due to lack of time (Manager_Int_10) | |||
| Additional areas | Implement a program on oral hygiene | Review and Reflect | Score remained at 0–1 ticks. Comment ‘Planning to put in toothbrushing’ | |
| Qualitative | Manager had not written any policies yet due to lack of time (Manager_Int_10) | |||
| Nursery 8 | Nutrition | Offer three different starchy foods at breakfast (e.g. to include crackers/breadsticks) | Review and Reflect |
Q2. Breakfast is an important meal for young children. Score went from 2–3 ticks to 4 ticks. Addition tick(s) not indicated on paper form Comment: ‘Introduced toast as well as cereal’ |
| Qualitative | . . . one of the things that we needed to do was add, we just had cereal for breakfast, three types of cereal, and we needed to add another starch-based product into our breakfast. So now we provide bread as well, so they have that choice, they have toast as a choice as wellManager_Int_7 | |||
| Nursery to offer oral health as a topic – dentist visit | Review and Reflect |
Q18. We promote oral health in the following ways. Score went from 2 ticks to 3 ticks. Addition tick for ‘Staff give children a practical demonstration of how to brush their teeth and maintain good oral hygiene’ Comment: ‘Dental role play – health promotions equipment and dental nurse visit to talk to the children’ |
||
| Qualitative | We had the dentist in that spoke to the children about dental hygiene, and then we’d include the parents in thatManager_Int_7We do it all through play, through role play. We hired some dental stuff from the NHS. So we had a proper like role play areaStaff_Int_6 | |||
| Families to be offered information on Change4life118 and Henry Portion Sizes119 | Review and Reflect |
Q37. Families are offered information and support on child nutrition. Score went from ‘less than once per year’ to ‘2 times per year or more’ Comment: ‘Change 4 life sugar swaps’ |
||
| Qualitative | We’ve used things like the food smart brochures and given those to parents. And the bonds for babies about weaning and breastfeeding and all those sorts so that parents have got information there that is. For our parents a lot of them are not really well educated, we have a lot that English is a second language so they need information that’s quite visual, which the sugar smart is. It is, it’s good because it’s colourful isn’t it, and it’s visualManager_Int_7 | |||
| PA | PA board in multipurpose room. To be discussed at activity workshop | Review and Reflect | Q46. Staff incorporate PA into daily routines, transitions between activities, and other planned activities. Score went from ‘Sometimes’ to ‘Each time they see an opportunity’ Comments: ‘Physical activity board in room. College to start physical activity workshop for children as part of their workshop. Doing Barnardo’s Toddle Waddle walk by canal’ | |
| Qualitative | And also the physical development workshop I think has opened our eyes to different ways we can do things. For example, with tennis racquets, you don’t need just for playing tennis. You can do various activities with them. I think it’s just opened our eyes to think, ‘Actually, there are new ways of doing it,’ or, ‘Actually, we do do that, but we need to do it more.’ It’s just made us reflect on our practise, you know, more than what we didStaff_Int_6 | |||
| Fitness fun week | Review and Reflect |
Q50. Staff talk with children informally & formally about the importance of PA. Score went from ‘Sometimes’ to ‘Each time they see an opportunity’ Comments: ‘Fitness for week goals set. Staff went to discuss with college’ |
||
| Qualitative | No qualitative data on this | |||
| Information sharing with parents about PA | Review and Reflect | Q53. Information or education for families on children’s PA includes the following topics. Score went from ‘Sometimes’ to ‘Each time they see an opportunity’ | ||
| Qualitative | No qualitative data on this | |||
| Additional areas | Asking the children ‘Are you still hungry?’ | Review and Reflect |
Q27. When children request seconds, staff ask them if they are still hungry before serving more food. Score went from ‘rarely or never’ to ‘always’ Comment: ‘Now asking routinely’ |
|
| Qualitative | I think the thing that was actually the most useful was this thing about asking children whether they’re still hungry or not, because it was something that we had never, I’d never thought about itManager_Int_7 | |||
| Introduce toast/rice cakes/breadsticks at breakfast and offer both cereal and toast, etc. | Review and Reflect |
Q9. The starchy foods we serve. Score went from ‘Include at least 3 types over the course of the week’ to ‘Include at least 3 types over the course of the day incorporating both white and wholegrain products’ Comment: ‘Toast at breakfast’ |
||
| Qualitative | . . . one of the things that we needed to do was add, we just had cereal for breakfast, three types of cereal, and we needed to add another starch-based product into our breakfast. So now we provide bread as well, so they have that choice, they have toast as a choice as wellManager_Int_7 | |||
| Nursery 9 | Nutrition | Review of menu to ensure oily fish included each week | Review and Reflect | No baseline Review and Reflect form available |
| Qualitative | We added an extra fish on. Because we’ve got a four week menu, so we made sure there’s fish in each of the weeksInt. 3So we have actually changed our menu and put oily fish on once a week. We’ve done it as a best practiceManager_Int_4 | |||
| Week 1 include fruit with an ice-cream served | Review and Reflect | No baseline Review and Reflect form available | ||
| Qualitative | Include fruit with all ice cream. I think we had some ice cream cornets that were served with fruit for that oneStaff_Int_3 | |||
| Remove rich tea biscuits and reduce snacks to once a week | Review and Reflect | No baseline Review and Reflect form available | ||
| Qualitative | We had Rich Tea biscuits on the menu for snacks and things like that, well that’s come offStaff_Int_3 | |||
| PA | Information to parents on PA and Change4life website, etc. | Review and Reflect | No baseline Review and Reflect form available | |
| Qualitative | Also information to parents on child nutrition, which I’ve got leaflets and things like that forStaff_Int_3 | |||
| Introduction of PA policy | Review and Reflect | No baseline Review and Reflect form available | ||
| Qualitative | Policy written and awaiting sign off by managing director of chain (Staff_Int_3)We’ve done a lot of staff meetings about the NAP SACC and what we’re expected to do about the physical development policy and just encouraged the staff to do lots of things throughout the dayStaff_Int_3 | |||
| Incorporating more activity into at least one circle time/story time per day | Review and Reflect | No baseline Review and Reflect form available | ||
| Qualitative | We’ve just encouraged them to be a bit more different in what they do, so instead of walking they’ll do a bit of jogging and things like that . . . And stories, when they’re telling stories they can get up and walk around and things like that, rather than just sitting down. And there’s not so much sitting now. There’s a lot of movement involvedStaff_Int_3But a lot of information we gathered from the internet on how to fit in physical development into children’s every day, things like that, which is what I spoke about, trying to do circle times and story times and being a lot more active in those times, not expecting them to sit for so long and doing much more activities outside as wellStaff_Int_3 | |||
| Additional areas | Information to parent on child nutrition | Review and Reflect | No baseline Review and Reflect form available | |
| Qualitative | Also information to parents on child nutrition, which I’ve got leaflets and things like that forStaff_Int_3 | |||
| Offer fruit bowl at breakfast | Review and Reflect | No baseline Review and Reflect form available | ||
| Qualitative | And also offer a fruit bowl at breakfast. Because we weren’t, unless the children asked for it, we weren’t really offering it. But now that we’ve got a fruit bowl out on show, they’re showing a lot more interest in it. So they are eating a lot more fruit at breakfastStaff_Int_3 | |||
| 12 | N/A – nursery did not set any goals | |||
Appendix 9 Supplementary mediator questionnaire test–retest data
| Characteristics | Number |
|---|---|
| Parent | n = 82 |
| Age (years), n (%) | |
| < 25 | 3 (3.66) |
| 25–30 | 12 (14.6) |
| 31–35 | 36 (43.9) |
| 36–40 | 25 (30.5) |
| ≥ 41 | 6 (7.32) |
| Highest level of education, n (%) | |
| Did not complete secondary school | 1 (1.22) |
| GCSE or GNVQ level or equivalent | 7 (8.54) |
| A levels or advanced GNVQ or equivalent | 9 (11.0) |
| University degree | 34 (41.5) |
| Postgraduate degree or higher | 31 (37.8) |
| Employment status, n (%) | |
| Student | 6 (7.32) |
| Housewife/househusband | 12 (14.6) |
| Full time | 21 (25.6) |
| Part time | 41 (50.0) |
| Unemployed | 2 (2.44) |
| Number of children, mean (SD) | 1.68 (0.735) |
| Number of children, n (%) | |
| 1 | 36 (43.9) |
| 2 | 39 (47.6) |
| 3 | 4 (4.88) |
| 4 | 3 (3.66) |
| Nursery staff | n = 69 |
| Age (years), n (%) | |
| < 25 | 17 (24.6) |
| 25–30 | 22 (31.9) |
| 31–35 | 11 (15.9) |
| 36–40 | 5 (7.25) |
| ≥ 41 | 14 (20.3) |
| Highest level of education, n (%) | |
| GCSE or GNVQ level or equivalent | 16 (23.2) |
| A levels or advanced GNVQ or equivalent | 21 (30.4) |
| University degree | 26 (37.7) |
| Postgraduate degree or higher | 6 (8.70) |
| Scale | Cronbach’s α |
|---|---|
| Nutrition self-efficacy scale | |
| 1. I feel able to provide my children with fruit at all main meals | 0.77 |
| 2. I feel able to provide my children with vegetables at all main meals | 0.78 |
| 3. I feel able to reduce the amount of processed meat, fish or potato products served to my children at all main meals | 0.78 |
| 4. I feel able to provide my children with home-cooked meals each week | 0.78 |
| 5. I feel able to reduce the number of high-sugar or high-fat snacks served to my children each week | 0.76 |
| 6. I feel able to reduce the amount of sugary breakfast cereals served to my children each week | 0.78 |
| 7. I feel able to reduce the number of fizzy drinks and cordials served to my children each week | 0.78 |
| 8. I feel able to increase the amount of water served to my children each week | 0.80 |
| 9. I feel able to make changes to the portion sizes served to my children each week | 0.79 |
| 10. I feel able to increase how often my children brush their teeth with fluoride toothpaste | 0.78 |
| Alpha for overall scale | 0.80 |
| PA self-efficacy scale | |
| 11. I feel able to provide my children with time for indoor activities and games each week | 0.70 |
| 12. I feel able to provide my children with space for indoor activities and games each week | 0.68 |
| 13. I feel able to provide my children with toys/equipment for indoor activities and games each week | 0.71 |
| 14. I feel able to provide my children with time for outdoor play and games each week | 0.67 |
| 15. I feel able to provide my children with space for outdoor play and games each week | 0.66 |
| 16. I feel able to provide my children with toys/equipment for outdoor play and games each week | 0.69 |
| 17. I feel able to provide my children with opportunities for walking to/from nursery each week | 0.81 |
| 18. I feel able to provide my children with opportunities for outdoor play regardless of the weather | 0.71 |
| 19. I feel able to reduce the amount of time the adults in my household spend using screens across the week | 0.73 |
| 20. I feel able to reduce the amount of time the children in my household spend using screens across the week | 0.72 |
| Alpha for overall scale | 0.73 |
| Nutrition motivation scale | |
| 21. I am motivated to provide my child with fruit at all main meals | 0.85 |
| 22. I am motivated to provide my child with vegetables at all main meals | 0.85 |
| 23. I am motivated to reduce the amount of processed meat, fish or potato products served to my child at all main meals | 0.84 |
| 24. I am motivated to provide my child with home-cooked meals | 0.86 |
| 25. I am motivated to reduce the number of high-sugar or high-fat snacks served to my child | 0.84 |
| 26. I am motivated to reduce the amount of sugary breakfast cereals served to my child | 0.84 |
| 27. I am motivated to reduce the number of fizzy drinks and cordials served to my child | 0.85 |
| 28. I am motivated to increase the amount of water served to my child | 0.85 |
| 29. I am motivated to make changes to the portion sizes served to my child | 0.87 |
| 30. I am motivated to increase how often my child brushes their teeth with fluoride toothpaste | 0.85 |
| Alpha for overall scale | 0.86 |
| PA motivation scale | |
| 31. I am motivated to provide my child with time for indoor activities and games | 0.88 |
| 32. I am motivated to provide my child with space for indoor activities and games | 0.87 |
| 33. I am motivated to provide my child with toys/equipment for indoor activities and games | 0.88 |
| 34. I am motivated to provide my child with time for outdoor play and games | 0.87 |
| 35. I am motivated to provide my child with space for outdoor play and games | 0.86 |
| 36. I am motivated to provide my child with toys/equipment for outdoor play and games | 0.87 |
| 37. I am motivated to provide my child with opportunities for walking to/from nursery | 0.92 |
| 38. I am motivated to provide my child with opportunities for outdoor play regardless of the weather | 0.87 |
| 39. I am motivated to reduce the amount of time the adults in my household spend using screens | 0.89 |
| 40. I am motivated to reduce the amount of time the children in my household spend using screens | 0.88 |
| Alpha for overall scale | 0.89 |
| Scale | Cronbach’s α |
|---|---|
| Nutrition self-efficacy scale | |
| 1. I feel able to serve fruit and vegetables to children at all main meals | 0.89 |
| 2. I feel able to limit the amount of processed meat, fish or potato products served to children | 0.87 |
| 3. I feel able to limit the amount of salt used in food for children | 0.87 |
| 4. I feel able to limit the number of high-sugar or high-fat snacks served to children | 0.88 |
| 5. I feel able to limit the use of cakes and/or other sweet or high fat foods to celebrate event | 0.88 |
| 6. I feel able to make changes to the types of beverage provided to children | 0.87 |
| 7. I feel able to make changes to how we promote oral health at nursery | 0.88 |
| 8. I feel able to make changes to how staff role-model healthy eating foods served at meal and snacktimes | 0.87 |
| 9. I feel able to make changes to how staff incorporate healthy eating learning into children’s daily activities | 0.87 |
| 10. I feel able to increase staff access to professional development in child nutrition | 0.88 |
| 11. I feel able to increase communication with parents about child nutrition | 0.88 |
| 12. I feel able to make changes to our written policy on child nutrition | 0.87 |
| Alpha for overall scale | 0.89 |
| Physical activity self-efficacy scale | |
| 13. I feel able to provide an appropriately sized indoor space for children’s physical activity and play | 0.90 |
| 14. I feel able to provide appropriate indoor toys and equipment for children’s physical activity and play | 0.90 |
| 15. I feel able to increase the amount of time provided for indoor physical activity and play for children | 0.90 |
| 16. I feel able to increase the amount of adult-led indoor physical activity and play for children | 0.90 |
| 17. I feel able to provide an appropriately sized outdoor space for children’s physical activity and play | 0.90 |
| 18. I feel able to provide appropriate outdoor toys and equipment for children’s physical activity and play | 0.90 |
| 19. I feel able to increase the amount of time provided for outdoor physical activity and play for children | 0.90 |
| 20. I feel able to increase the amount of adult-led outdoor physical activity and play for children | 0.91 |
| 21. I feel able to make changes to the amount of screen time allowed in our nursery per child | 0.91 |
| 22. I feel able to make changes to how staff role-model good physical activity habits | 0.90 |
| 23. I feel able to make changes to how staff incorporate physical activity learning into children’s daily activities | 0.90 |
| 24. I feel able to increase staff access to professional development in children’s physical activity | 0.90 |
| 25. I feel able to increase communication with parents about children’s physical activity | 0.90 |
| 26. I feel able to make changes to our written policy on children’s physical activity | 0.90 |
| Alpha for overall scale | 0.91 |
| Nutrition motivation scale | |
| 27. I am motivated to serve fruit and vegetables to children at all main meals | 0.90 |
| 28. I am motivated to limit the amount of processed meat, fish or potato products served to children | 0.89 |
| 29. I am motivated to limit the amount of salt used in food for children | 0.89 |
| 30. I am motivated to limit the number of high-sugar or high-fat snacks served to children | 0.88 |
| 31. I am motivated to limit the use of cakes and/or other sweet or high fat foods to celebrate events | 0.88 |
| 32. I am motivated to make changes to the types of beverage provided to children | 0.88 |
| 33. I am motivated to make changes to how we promote oral health at nursery | 0.88 |
| 34. I am motivated to make changes to how staff role-model healthy eating foods served at meal and snacktimes | 0.89 |
| 35. I am motivated to make changes to how staff incorporate healthy eating learning into children’s daily activities | 0.88 |
| 36. I am motivated to increase staff access to professional development in child nutrition | 0.88 |
| 37. I am motivated to increase communication with parents about child nutrition | 0.89 |
| 38. I am motivated to make changes to our written policy on child nutrition | 0.89 |
| Alpha for overall scale | 0.89 |
| Physical activity motivation scale | |
| 39. I am motivated to provide an appropriately sized indoor space for children’s physical activity and play | 0.90 |
| 40. I am motivated to provide appropriate indoor toys and equipment for children’s physical activity and play | 0.90 |
| 41. I am motivated to increase the amount of time provided for indoor physical activity and play for children | 0.90 |
| 42. I am motivated to increase the amount of adult-led indoor physical activity and play for children | 0.90 |
| 43. I am motivated to provide an appropriately sized outdoor space for children’s physical activity and play | 0.90 |
| 44. I am motivated to provide appropriate outdoor toys and equipment for children’s physical activity and play | 0.90 |
| 45. I am motivated to increase the amount of time provided for outdoor physical activity and play for children | 0.89 |
| 46. I am motivated to increase the amount of adult-led outdoor physical activity and play for children | 0.90 |
| 47. I am motivated to make changes to the amount of screen time allowed in our nursery per child | 0.90 |
| 48. I am motivated to make changes to how staff role-model good physical activity habits | 0.90 |
| 49. I am motivated to make changes to how staff incorporate physical activity learning into children’s daily activities | 0.89 |
| 50. I am motivated to increase staff access to professional development in children’s physical activity | 0.90 |
| 51. I am motivated to increase communication with parents about children’s physical activity | 0.90 |
| 52. I am motivated to make changes to our written policy on children’s physical activity | 0.91 |
| Alpha for overall scale | 0.91 |
| Parent questionnaire scales | ||||||
|---|---|---|---|---|---|---|
| n (%) | ||||||
| Number of items | 0 < 0.2 | 0.2 < 0.4 | 0.4 < 0.6 | 0.6 < 0.8 | 0.8 < 1.0 | |
| Slight | Fair | Moderate | Substantial | Almost perfect | ||
| Nutrition self-efficacy | 10 | 0 | 1 (10.0) | 7 (70.0) | 2 (20.0) | 0 |
| Physical activity self-efficacy | 10 | 0 | 0 | 8 (80.0) | 1 (10.0) | 1 (10.0) |
| Nutrition motivation | 10 | 0 | 2 (20.0) | 7 (70.0) | 1 (10.0) | 0 |
| Physical activity motivation | 10 | 0 | 0 | 8 (80.0) | 2 (20.0) | 0 |
| Total | 40 | 0 | 3 (7.50) | 30 (75.0) | 6 (15.0) | 1 (2.50) |
| Nursery staff questionnaire scales | ||||||
| Number of items | 0 < 0.2 | 0.2 < 0.4 | 0.4 < 0.6 | 0.6 < 0.8 | 0.8 < 1.0 | |
| Slight | Fair | Moderate | Substantial | Almost perfect | ||
| Nutrition self-efficacy | 12 | 0 | 3 (25.0) | 7 (58.3) | 2 (16.7) | 0 |
| Physical activity self-efficacy | 14 | 0 | 2 (14.3) | 10 (71.4) | 2 (14.3) | 0 |
| Nutrition motivation | 12 | 1 (8.33) | 5 (41.7) | 6 (50.0) | 0 | 0 |
| Physical activity motivation | 14 | 0 | 7 (50.0) | 6 (42.8) | 1 (7.14) | 0 |
| Total | 52 | 1 (1.92) | 17 (32.7) | 29 (55.8) | 5 (9.62) | 0 |
Appendix 10 Supplementary nursery food photography data
The feasibility of taking before-and-after photographs of the child’s meals is dependent on the way the meal is served and a different approach is needed for different meal types. We encountered several types and the methods required for each are outlined here.
Food served on a plate by staff and distributed to children
This approach is most common with younger children, in nurseries where meals are delivered by an external company and for hot meals. With this style it is possible to take the before-and-after photograph as children are unable to help themselves and photographs can often be taken before children start to eat the food. If any additional items are served throughout the meal, this can be captured in the observation sheet. For this approach, approximately 10 children from the same table can be followed by two researchers; one researcher takes the photographs and the other researcher makes notes about drinks and any additional items served on the observation sheet.
Food served on serving plates and bowls in the centre of the table for children to help themselves (to put onto their own plate)
This approach is more common with older children, although most are still assisted in serving themselves. It is usual with more substantial hot meals, such as lunch. For example, there might be a central plate with meat slices, another with potatoes and another with vegetables and the children use a spoon to serve themselves. In this case it is possible to take the before-and-after photograph as well as photographs for additional portions as it is rare that a child will be allowed more than two additional portions. Staff assistance is required to tell fieldworkers when a child is having an additional portion. The laminated card needs to be altered between portions, which can make the wait longer for the child. For this approach, up to eight children from one table can be followed by two researchers.
Food served at the table with platters in the centre for children to help themselves (either with or without their own plate)
This approach is most common with snacktimes and teatime (Figure 6). Nursery staff will have access to a fruit bowl or a trolley with the food on and will sit at the table with the children, chop up the food into portions and then put it in the middle of the table. In this case, it is possible only to take an ‘after’ photograph of the food to capture what is left over, the data must be captured through an observation sheet. Children may take several small portions and often they take from the central plate and eat straight away, without putting the food onto their own plate. It is therefore not feasible to take all before photographs for this type of serving.
FIGURE 6.
Photograph of food served on a platter at snacktime.

Food served in a rolling fashion
For some meals, some nurseries serve the children a few at a time. For example, four children may come to a small table and be served. Only once these children have finished and left the table are other children called to be served. If the food served is on a plate, it is possible to take photographs of all the children’s food as they are being served a few at a time. However, the style of the meal may still be ‘grazing’ with platters of different food in the middle, with the difference that children are called at different times. In this case the observation sheet can be used to record all items that were taken by the child and only the after photograph can be taken. This indicates how much food was not eaten. Rolling fashion serving takes longer than meals at which all children are served at the same time, but the researchers can capture a larger number of children.
Single identical item of food served to all children
In some meal occasions, one single identical item of food is served to all children (i.e. sealed yoghurt pot). On these occasions, the researchers can record an example photograph of the item and then record on the observation sheet who has been given this item. An after photograph can be taken to record how much of the item has been eaten and is left over.
Appendix 11 Full-trial sample size calculations
| Power | Total activity difference | ICC | Number of children per arm | Number of nurseries per arm | Number of children | Total nurseries | Number of children per arm if child attrition at 20% | Number of nurseries per arm if child attrition at 20% | Number of children per arm if child attrition at 30% | Number of nurseries per arm if child attrition at 30% |
|---|---|---|---|---|---|---|---|---|---|---|
| 80 | 17 | 0.01 | 126 | 9 | 252 | 18 | 158 | 12 | 180 | 13 |
| 80 | 17 | 0.02 | 140 | 10 | 280 | 20 | 175 | 13 | 200 | 15 |
| 80 | 17 | 0.05 | 196 | 14 | 392 | 24 | 245 | 18 | 280 | 20 |
| 80 | 17 | 0.1 | 266 | 19 | 532 | 38 | 333 | 24 | 380 | 28 |
| 90 | 17 | 0.01 | 168 | 12 | 336 | 24 | 210 | 15 | 240 | 18 |
| 90 | 17 | 0.02 | 182 | 13 | 364 | 26 | 228 | 17 | 260 | 19 |
| 90 | 17 | 0.05 | 252 | 18 | 504 | 36 | 315 | 23 | 360 | 26 |
| 90 | 17 | 0.1 | 350 | 25 | 700 | 50 | 438 | 32 | 500 | 36 |
Glossary
- Civi CRM
- Web-based customer relationship management software.
- PedsQL
- Measurement model for the paediatric quality-of-life inventory.
- UK1990
- The age and gender reference charts for body mass index z-scores established from the cohort in the UK in 1990.
List of abbreviations
- AE
- adverse event
- BMI
- body mass index
- CADET
- Child and Diet Evaluation Tool
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DECIPHer
- Development and Evaluation of Complex Interventions for Public Health Improvement
- df
- degrees of freedom
- EPAO
- Environment and Policy Assessment and Observation
- EYFS
- Early Years Foundation Stage
- FSW
- family support worker
- GP
- general practitioner
- HRQoL
- health-related quality of life
- ICC
- intracluster correlation coefficient
- ID
- identification
- IMD
- Index of Multiple Deprivation
- IOTF
- International Obesity Task Force
- MVPA
- moderate to vigorous physical activity
- NAP SACC
- Nutrition And Physical Activity Self Assessment for Child Care
- NAP SACC UK
- Nutrition And Physical Activity Self Assessment for Child Care UK version
- NCMP
- National Child Measurement Programme
- NIHR
- National Institute for Health Research
- NMES
- non-milk extrinsic sugars
- PA
- physical activity
- PBRC
- Pennington Biomedical Research Center
- PedsQL
- Paediatric Quality of Life Inventory
- PICO
- Participants, Intervention, Control, Outcomes
- RCT
- randomised controlled trial
- SD
- standard deviation
- SES
- socioeconomic status
- TIDieR
- Template for Intervention Description and replication
- TSC
- Trial Steering Committee
- TV
- television
- UKCRC
- UK Clinical Research Collaboration
- WHASPS
- Wales Healthy and Sustainable Pre-School Scheme
- WIMD
- Welsh Index of Multiple Deprivation
- zBMI
- body mass index z-scores
