Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 14/67/20. The contractual start date was in January 2016. The final report began editorial review in February 2019 and was accepted for publication in August 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Emma McIntosh is a member of the National Institute for Health Research (NIHR) Public Health Research (PHR) Research Funding Board. Ian S Young is a member of the Health Technology Assessment (HTA) National Stakeholder Advisory Group (2015 to present). Frank Kee was a member of the NIHR PHR Research Funding Board and PHR Prioritisation Group (2009–19). Dunla Gallagher received funding from Slimming World (Miles-Bramwell Executive Services Ltd, Alfreton, UK) for work conducted prior to her involvement in this study.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by McGirr et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background to the research
The aim of this chapter is to provide a review of the literature related to overweight and obesity in the postpartum period that informed the development of the intervention and the design of the pilot randomised controlled trial (RCT).
Specifically, this chapter describes weight-related trends during and after pregnancy, evidence-based interventions aimed at improving weight and related health outcomes in postpartum women and highlights some gaps in this evidence. The rationale for utilising mobile phone technology as a method of delivering a postpartum weight management intervention is also described. The present study aimed to address the identified gaps in the evidence.
Although no limitations were placed on the country of origin when searching the literature, owing to the nature of the fields of interest (postpartum weight management interventions and using modern technologies to change weight-related behaviour), the majority of the evidence discussed below originates from developed countries including the USA, Australia, countries within Europe and the UK.
Maternal overweight and obesity and the associated risks
Overweight and obesity are one of the major public health challenges of the 21st century, owing to their widespread prevalence and recognised impact on morbidity and mortality. 1 Adult obesity has nearly doubled worldwide since 1980,2 with commensurate trends among women of reproductive age. 3 In the UK, first-trimester obesity increased more than two-fold between 1989 and 2007 from 7.6% to 15.6%. 4
Being overweight or obese at the start of pregnancy is associated with increased risks of adverse health outcomes for mothers and babies. In comparison with women of a healthy weight, women who are overweight or obese and their offspring may be at a significantly increased risk of experiencing gestational diabetes, pre-eclampsia, hypertension, depression, caesarean section, postpartum haemorrhage, induction of labour, preterm birth, stillbirth, foetal defects, congenital abnormalities and infant death,5–8 and there is an increased risk of offspring adiposity continuing into childhood. 9,10 Weight gain between successive pregnancies is associated with increased risk of gestational diabetes, hypertension, caesarean section, large for gestational age birth weight (birth weight above the 90th percentile) and perinatal mortality. 11,12
Weight gain trends during and after pregnancy
Women are at an increased risk for weight gain during the reproductive years, and this weight gain can set women on an upwards weight trajectory for the decades ahead. 13 It has been estimated that between 40% and 65% of women in the UK gain too much weight during pregnancy. 14 This trend is particularly evident in women who start their pregnancy overweight or obese,15 as well as among those of a lower socioeconomic status. 16
Excessive gestational weight gain and a high pre-pregnancy body mass index (BMI) are both predictors of postpartum weight retention17–21 and are influenced by many other maternal factors, including diet and physical activity behaviours, breastfeeding, sleep, ethnicity, maternity leave, income and mental health. 13,21 Failure to lose pregnancy-related weight by 6 months post partum is considered an important predictor of obesity and associated conditions in mid-life;22,23 many women with obesity attribute the onset of the condition to weight gained in pregnancy. 24 Between 40% and 50% of women who are overweight pre pregnancy move into the obese BMI category by 12 months postpartum. 25 For women who start pregnancy obese, 97% will remain obese after 1 year26 and 40% may gain two or more BMI units between their first and second pregnancies. 27 Although many women will return to their pre-pregnancy weight within 1 year of delivery, it has been estimated that between 15% and 27% of women have major postpartum weight retention (> 4 kg) at 1 year. 20,25,28 Furthermore, two studies20,29 have identified a risk of additional weight gain between 1 and 2 years postpartum, particularly in women who were overweight or obese at the 1-year postpartum time point.
The postpartum period can also be viewed as the ‘interpregnancy’ period for many women, as they will go on to have more children and will experience subsequent pregnancies. 13 Given that the times during and after pregnancy are periods of significant risk for the onset and maintenance of long-term weight-related issues,21,30 not only will this pose risks to women’s health,15 but it may also increase the risk of adverse outcomes during subsequent pregnancies. 11,12,31,32
The postpartum period represents a unique and challenging period in a woman’s life, both emotionally and physically. Women often struggle with weight management at this stage in life and face many barriers to taking positive action, such as lack of time, tiredness and prioritising their children’s needs. 33–36 Pregnancy and motherhood are major life events, and changes in lifestyle and maternal priorities may help explain postpartum weight retention and further weight gain trends. 19,37
Financial costs associated with pregnancy and postpartum overweight and obesity
The increased prevalence of obesity, in general, is currently estimated to cost the NHS > £6B per year and, by 2050, if we include indirect costs to the wider economy (such as those to social care and education), these costs are forecast to rise to nearly £50B. 38 A UK-based study39 found that a pregnant woman with a BMI of ≥ 25 kg/m2 led to NHS costs of up to 37% more than their those of their counterparts with a healthy weight (BMI of between 18.5 kg/m2 and 24.9 kg/m2). The increased costs were as a result of greater health service utilisation by both mothers and their babies as a consequence of adverse outcomes associated with maternal overweight and obesity. 40–42 Weight reduction prior to women becoming pregnant through pre-conception or interpregnancy/postpartum interventions would be a positive step in reducing these costs. Although it is not possible to fully quantify the direct costs and total savings of interventions seeking to tackle postnatal overweight and obesity, the need for additional health care to treat weight-related conditions is commonly accepted. 43–45 The need to identify cost-effective interventions for reducing weight and to evaluate the associated health-care costs is pressing.
Evidence-based strategies to support postpartum weight management
Current health-care guidance suggests that health professionals should advise women who have had a baby in the previous 2 years to eat healthily and keep active to encourage postpartum weight reduction. 45,46 The postpartum period could be an ideal time to intervene to shape new health behaviours as women have shown motivation for weight loss during this time,47,48 and they may have a heightened awareness of their own and their families’ health, and so may be receptive to information about lifestyle. 13 It is also a time when many women start to prepare for the next pregnancy, so there is the potential to set women on a positive course for subsequent pregnancies. 13 However, women have highlighted a need for additional weight management support during the postpartum period as little is currently provided. 17,49,50
Systematic review evidence49,51–54 and the National Institute for Health and Care Excellence (NICE) public health guidance45 both highlight gaps in knowledge about effective and appropriate weight management interventions for women during the postpartum period. There is systematic review evidence to suggest that diet and physical activity interventions delivered post partum have a moderate but positive influence on maternal weight,51–54 and that interventions combining diet and activity behaviour change may be more successful,49,52,53 as well as interventions that included self-regulatory behaviour change techniques (BCTs), such as self-monitoring of weight. 49 van der Pligt et al. 53 conducted a systematic review of intervention studies in which postpartum weight was a main outcome and any combination of diet, physical activity and weight monitoring were intervention components. Study populations included women with singleton pregnancies who were recruited either during or after pregnancy, provided that the intervention was delivered into the postpartum period. There were 11 studies53 included in the review (n = 1227), 10 of which were RCTs and one was a non-randomised trial. Interventions were delivered by a range of health professionals (nurses, fitness instructors, dietitians, trained counsellors and study assistants). The comparison groups received ‘usual care’, which often involved the provision of some general advice on healthy eating and physical activity, for example a leaflet. Seven of the included studies reported a decrease in postpartum weight retention (i.e. a decrease in the number of participants who did not return to their pre-pregnancy weight) in the intervention group. Six of these seven interventions employed both diet and physical activity components, and five of these seven studies recruited overweight and obese populations only. However, there were shortcomings in the quality of included studies, such as lack of descriptions of the randomisation and blinding processes. The heterogeneity of intervention settings and health professionals responsible for delivering the interventions makes it difficult to determine the important aspects of intervention delivery. Only two studies out of 11 were underpinned by theoretical frameworks, so this evidence limits our understanding of the usefulness of particular theories and BCTs, or how they interact with context, in improving outcomes in overweight or obese postpartum women. In addition, no study examined cost-effectiveness. 53 A later systematic review by Lim et al. 49 included 46 studies using either combined diet and activity, or diet or activity only interventions, to reduce weight in postpartum women within 1 year following birth, compared with usual care control conditions or a comparison of two different interventions. Thirty-three of the studies included were RCTs and were included in a meta-analysis (n = 1892); the other 13 studies that were included were single-arm interventions (n = 6) or non-randomised trials (n = 7). The meta-analysis results indicated that combining diet and physical activity advice may be most effective, resulting in a pooled weight loss of 2.3 kg, with subgroup differences showing greater weight loss as a result of interventions that included self-monitoring. 49 However, this review continued to experience similar methodological shortcomings in the included studies in terms of studies being rated as having high to medium risks of bias as a result of inadequacies in the reporting of randomisation and blinding processes, and heterogeneity in the analyses due to differing intervention approaches, with a lack of detail provided on the active ingredients of interventions.
A notable methodological limitation of the included trials in the presented systematic reviews51–53 is that they have experienced high levels of participant attrition and poor engagement, highlighting the difficulty in engaging and maintaining contact with women in the postpartum period. 13 This period of major physiological, psychological and social change poses many challenges for women’s weight management and their ability to engage in behaviour change interventions; what works at other life stages may not necessarily work at this time. 13 The intervention setting and mode of delivery are key considerations when developing appropriate postpartum weight management interventions. 13 Interventions for overweight or obese postpartum women delivered in community settings, using group approaches, have presented difficulties for new mothers at this challenging time, and have raised concerns about reach and retention, particularly for disadvantaged groups,53,55–58 creating a potential to increase health inequalities. 59,60 For example, despite high initial motivation to enrol in the active mothers postpartum study,55 and the provision of group sessions multiple times per week, at various times of day, women found it difficult to attend owing to the competing needs of their baby and home- and work-life. Thus, despite considerable evidence that group approaches are associated with significant weight loss in the general population,61 they may not be feasible for the postpartum period. Furthermore, given the significant variability in postpartum weight gain trajectories,62 the optimal time to engage women in postpartum weight management during this challenging period is still unknown. 53 It is probable that flexibility regarding time to opt in is needed to engage women in postpartum interventions when they are ready, rather than dictating a narrow opt-in window. 13
The challenges of engaging and retaining women in postpartum weight management interventions has led to the suggestion that a highly flexible and individualised approach to weight loss interventions is needed in the postpartum period, shifting away from structured community-based programmes, to home-based or more adaptable ‘anytime, anyplace’ approaches, such as those enabled by mobile technologies. 53,55–58 However, in the described systematic reviews by van der Pligt et al. 53 and Lim et al. ,49 no study had used modern technologies, such as mobile phones, as an alternative to traditional face-to-face support. One study63 used modern technology (an online diet planner) as an adjunct to traditional face-to-face support. Employing mobile technologies to change diet, weight and physical activity presents a promising and expanding area of behavioural research, but, at the time that our research was conceived, was one that had not been exploited extensively, or trialled in new mothers carrying excess weight. 64–66 Systematic reviews and RCTs published since our funding application for the Supporting MumS are discussed later (see Chapter 5).
Weight management intervention delivery by short message service
The availability, adaptability and low cost of mobile technologies provide a promising format for delivering lifestyle intervention programmes on a sustained basis,67 and the NHS aims to embrace the potential of digital strategies for improving the health of people in the UK. 68 Short message service- (SMS-) delivered interventions have the advantage of wide reach, flexible scheduling and individual tailoring of content, thus making them an attractive proposition to support women in the busy postpartum period and represent an approach that may help address health inequalities. Use of mobile phones and other technical devices has become integral to how individuals communicate and plan their daily lives. Mobile phone ownership is widespread among all sectors of society, irrespective of socioeconomic status, and SMS is available on every type of mobile phone and across all phone companies. Such widespread usage serves to reinforce the image of mobile health (mHealth) becoming an important component of future health-care practice. 69,70 Unlike web-based interventions or applications (hereafter referred to as ‘apps’), which require ownership of a smartphone or tablet, and individuals taking the initiative to use them, SMS is a relatively simple mode of communication that uses basic mobile technology. An intervention using SMS can be reactive as well as proactive, instant, more direct, delivered in a timely manner and does not necessarily rely on initiation by the participant. 66 SMS is an ideal vehicle for reach, engagement and ‘proportionate universalism’, that is SMS can be universally delivered at a scale and intensity that is proportionate to the degree of need to reduce health inequalities, as recommended by Marmot71 and NICE. 72 Exploiting the real-time advantages offered by mobile technologies to deliver weight management support in the postpartum period has the potential to empower women and encourage behaviours that may improve maternal health in both the short and the long term. 67
Early evidence has shown that SMS is an acceptable and feasible mode of intervention delivery and has positive effects on weight management and weight-related behaviours. 64–66,73 Napolitano et al. 73 demonstrated the feasibility and acceptability of SMS as a method for promoting healthy behaviours for weight loss in a group of 52 (mostly female) college students. A systematic review74 of behaviour change interventions using SMS as the main method of intervention delivery (14 studies; n = 3512 participants) highlighted a positive impact on short-term behavioural outcomes, including diet, physical activity, smoking and clinical care, such as diabetes management, in 13 of the included studies. 74 However, study quality was low, with only six of the 14 studies using a RCT design. One study was a clustered randomised comparative trial, one was a randomised crossover trial and the other six were single, pre–post design studies. The ability to compare studies was limited as the interventions were aimed at changing different behaviours. The authors of this review highlighted a need to improve trial methodology to allow the full potential of SMS-delivered interventions to be explored. Another systematic review, by Aguilar-Martínez et al. ,75 specifically examined studies that had used mobile phone technologies as a tool for weight loss in adults with overweight or obesity. Of 10 included studies, two used SMS or multimedia messaging service (MMS) to demonstrate the potential of these methods for supporting weight loss. One of these two studies used a pre–post intervention design (n = 927 participants);76 the intervention involved a 12-week programme of diet, exercise and behaviour modification advice delivered once a week via SMS and was shown to reduce the mean weight, waist circumference and BMI measurements. The other study77 used a RCT design (n = 75 participants) and compared an intervention group which received a 16-week SMS- and MMS-delivered intervention alongside paper-based nutritional advice with a control group which received the paper-based nutritional advice only. The intervention group showed a greater weight loss, on average, than the control group. The remaining studies in the review by Aguilar-Martínez et al. 75 used apps or web-based programmes. However, their review highlighted that frequent self-recording of weight seemed to be important, as was the personalisation of the intervention (counselling and individualised feedback), and that a social support system could act as a motivational tool.
Weight management research has been dominated by trials of interventions mainly focusing on weight loss. Such evidence has illustrated that clinically relevant weight loss is attainable in the short-term, but longer-term (≥ 6 months’) follow-up highlights the challenge of weight loss maintenance,78–80 which is key to maintaining clinical benefits. 81 There is increasing recognition of the need to focus attention on weight loss maintenance and, specifically, the need to design interventions for this purpose. 79 Often, the behaviour change theories that inform intervention research assume that the processes used to initiate behaviour change (such as changes in diet and physical activity to achieve weight loss) also facilitate maintenance of the behaviour. 82 However, accumulating evidence shows that some strategies involved in supporting initial change are qualitatively different from those involved in maintenance of change. 83–85 This suggests that adapted and new BCTs may be crucial to sustain behavioural and weight changes in the long term.
In terms of the evidence for using SMS as a method to encourage behaviours associated with weight loss maintenance, the work of Gerber et al. 86 and Shaw et al. 82 has indicated early feasibility and acceptability of using SMS in this way. Gerber et al. 86 investigated the feasibility of mobile phone SMS to enable ongoing communication with African American women participating in a weight management programme. Ninety-five African American women participated in this pilot study and received regularly scheduled messages; > 4500 messages were transmitted during the first 4 months, with only 114 returned as undeliverable. The participants reported positive attitudes towards incoming messages, with only one participant declining to continue after enrolment. Shaw et al. 82 developed a theoretically driven automated SMS app to deliver weight loss-sustaining messages following a structured weight loss programme, which was found to be acceptable and feasible in a small (n = 16 participants) uncontrolled pilot study. Using technology-based weight management approaches appeared to be well accepted, with up to 74% of participants accessing and reviewing the weight management materials immediately after receipt. 82
Cost-effectiveness of SMS interventions for postpartum weight management and loss
Current guidance from NICE on weight management before, during and after pregnancy45 and its associated review of the cost-effectiveness of weight management interventions following childbirth,87 both outline the potential of postpartum interventions to reduce the long-term risks of heart disease, cancer, obesity and diabetes. In their review, Duenas et al. 87 concluded that weight management interventions following childbirth are shown to be effective in the short term. However, long-term effects were highly dependent on the modelling of key assumptions, and economic results were reliant on the long-term impact of the short-term effects. Thus, although the authors were able to extract data from observational studies that suggested a 15-year impact on weight change and a lifelong impact on survival, definitive causal effects could not be attributed. Therefore, these long-term economic estimates using standard probabilistic sensitivity analysis are likely to have high levels of structural uncertainty. 87 The guidance stipulates that more observational studies are required to aid future clarification of the long-term impact of interventions in this area.
Two studies in postpartum women have examined cost-effectiveness: a cost–utility analysis conducted in Sweden alongside a RCT of a 12-week dietary treatment (involving an initial counselling session, one home visit and SMS support every 2 weeks)88 and a cost-effectiveness review of existing postpartum weight loss RCTs. 89 Both studies found the interventions to be cost-effective. Hagberg et al. 88 calculated (with no remaining effect assumption after the follow-up year) the cost per quality-adjusted life-year (QALY) to be US$8643 (≈£6720.57). With an assumption of 1 year of effect beyond the 1-year follow-up, the cost-effectiveness ratio was US$3477 (≈£2703.62). Rawdin et al. 89 undertook their analysis from the perspectives of the UK NHS and Personal Social Services, and estimated an incremental cost-effectiveness ratio of £7355, which is below the NICE guidance90 willingness-to-pay threshold of £20,000.
Searching the existing literature base, no cost-effectiveness studies of a mHealth SMS postpartum weight management intervention were identified. As outlined earlier, postpartum weight management interventions show promise of being cost-effective. However, reviews of digital health interventions have demonstrated that few evaluations have captured data that sufficiently allow for the full consideration of economic outcomes and overall effectiveness and cost-effectiveness of the interventions. 91–95 As Graybill et al. 96 emphasise, currently, alternative technologies such as mHealth are in their infancy as they are commonly outside many health-care systems remit and normal practice. The delivery of digital health programmes is currently not standardised and this heterogeneity and uncertainty around the broader societal benefits make it difficult for decision-makers to make fully informed decisions when comparing different programmes. 97
Rationale for the current study
The rationale for this study was to develop and conduct a pilot RCT of a new individually tailored, SMS-delivered weight management intervention for postpartum women, and to include a specifically designed weight loss maintenance intervention component to help women transition from weight loss to weight loss maintenance by encouraging successful and sustainable self-regulation and habit formation. Future research should address the shortcomings noted in previous trials and carefully consider how to make weight management interventions an attractive and attainable proposition for women who are juggling multiple, competing demands in the postpartum period. The use of SMS could offer a flexible approach to weight management for women during this demanding period of their lives, allowing sustained contact over a longer period of time to help support women in changing behaviours for weight loss and weight loss maintenance while allowing for flexible scheduling, individual tailoring and the embedding of evidence-based BCTs. 98–100 Specifically, in our study we aimed to adapt an existing, successful smoking cessation SMS intervention (txt2stop). 98
Txt2stop
The txt2stop intervention is an evidence- and theory-based automated smoking cessation programme comprising theory-based individually tailored messages and behaviour change support, delivered via SMS, that aims to motivate and support adults to continuously abstain from smoking. 98,100 It was shown to be effective in significantly increasing biochemically verified continuous abstinence at 6 months in the intervention group (10.7%) compared with the control group (4.9%), corresponding to a relative risk of 2.20 [95% confidence interval (CI) 1.80 to 2.68; p < 0.0001]. This effect was evidenced in all socioeconomic groups and in younger and older smokers. 98 The success of the txt2stop intervention has resulted in the establishment of new services providing smoking cessation support delivered by SMS in the UK,101 evidencing the scalability and implementation of this intervention design. We chose to adapt this successful pre-existing SMS platform.
Generalisability and sustainability
The economic burden of treating obesity is projected to increase by £1.9B–2B per year in the UK by 2030. 102 Hence, there is a pressing need to identify cost-effective ways of promoting weight loss and, importantly, weight loss maintenance, in different population groups. Some weight loss interventions are very resource intensive and expensive, which can limit their potential for scale-up and implementation,103 and concerns have been raised that other interventions could increase health inequalities. 59,60 From the perspective of health professionals, who have reported multiple barriers to support weight management (such as lack of time and lack of knowledge),61 use of mobile technologies to facilitate the delivery of evidence-based weight management interventions might free up resources to deal with other health needs.
A SMS approach can be delivered flexibly for sustained contact with women over the medium to long term, with the ability to easily re-engage individuals after life events that disrupt weight management progress (e.g. illness, stress), at a low cost that is not attainable with other intervention approaches, such as group-based and in-person interventions. Extended contact following weight loss interventions is considered best practice for weight loss maintenance;80 without it, most individuals will regain weight in the longer term. The present study will inform the available evidence on developing interventions targeting weight loss maintenance. 79 It will also pilot methods for establishing the cost-effectiveness of delivering such an intervention.
Aim of this study
The aim of the present study was to adapt and pilot-test an evidence- and theory-based tailored SMS-delivered intervention supporting behaviour change for weight loss and weight loss maintenance in postpartum women with overweight or obesity.
Study design
The study was conducted in two stages. Stage 1 involved the adaptation of the txt2stop intervention98 for the development of a theory-based tailored SMS-delivered intervention supporting overweight and obese women’s behaviour change for weight loss and weight loss maintenance in the postpartum period, along with the development of a SMS-delivered active control focusing on child development (see Chapter 2). Personal and public involvement (PPI) is recommended in the development of new digital interventions;104 this recommendation was considered throughout the design of the study and will be discussed at different stages throughout the present report, where relevant. Stage 2 was a two-arm pilot RCT with an embedded process evaluation (see Chapters 3 and 4). The rationale for conducting a pilot RCT was to examine the feasibility and acceptability of delivering all aspects of a full RCT of the intervention, including a cost-effectiveness evaluation, as recommended by the Medical Research Council (MRC) framework for complex interventions. 105 A process evaluation was conducted to address specific research questions related to the delivery of the intervention and the contextual factors influential in the trial outcomes, as well as to pilot-test measures to be used for assessing mechanisms of impact. 106
Overall objectives
-
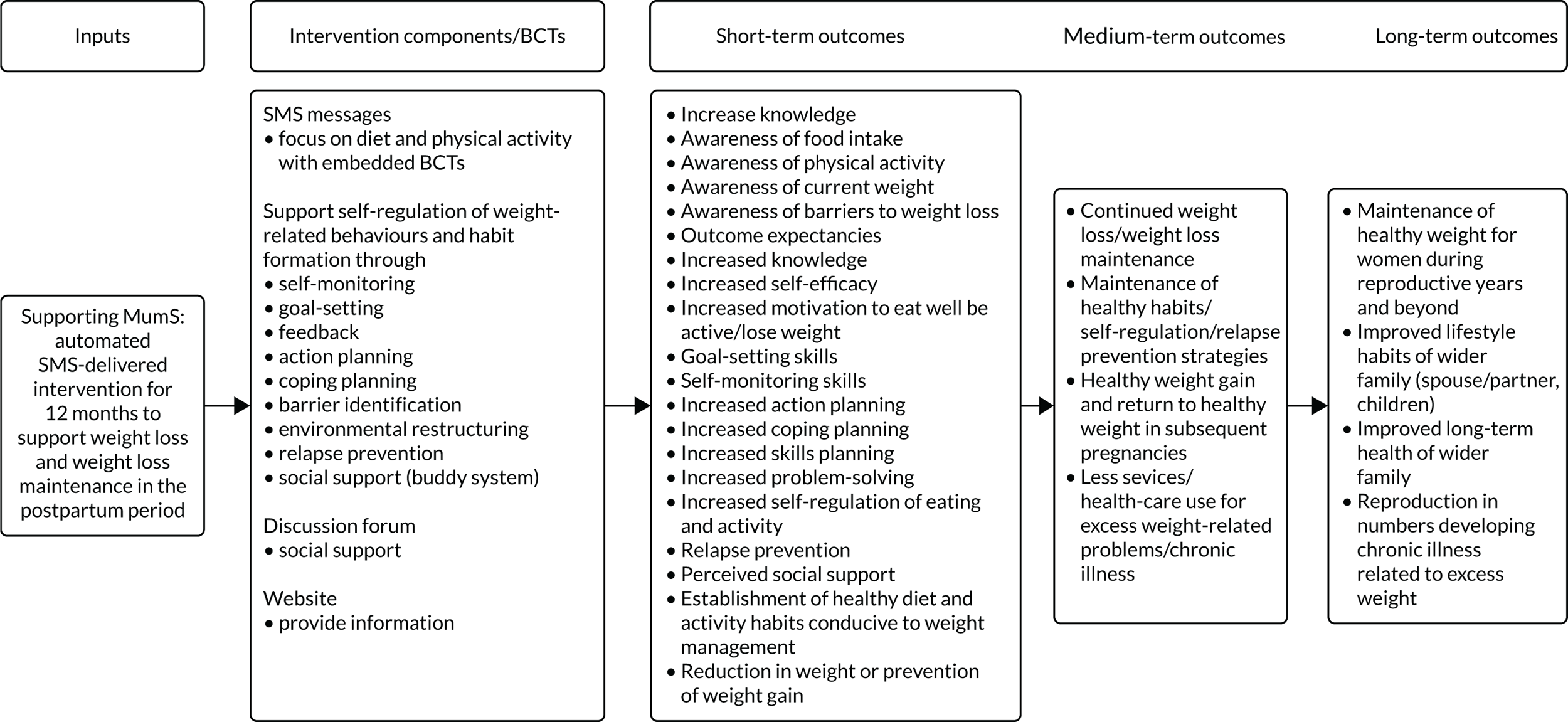
To review BCTs used in the txt2stop intervention and, through assimilation of relevant systematic review evidence, behaviour change theories and the NICE guidance,45 build a logic model for a SMS-delivered weight management intervention in postpartum women who are overweight or obese.
-
To create a library of SMS messages, with PPI, to support weight loss and weight loss maintenance in postpartum women with overweight or obesity.
-
To develop an intervention manual, including a library of messages and recruitment materials and a protocol for a pilot RCT of the SMS-delivered intervention.
-
To conduct a pilot RCT to test recruitment and randomisation strategies (including willingness to be randomised to an active control and retention and attrition rates between groups), examine fidelity of implementation and acceptability of the intervention and active control treatments, identify valid and acceptable (to the PPI members) research instruments to be used in a full RCT, provide variability data on weight loss and weight loss maintenance on which to base a formal power calculation for a full RCT, and to assess outcome data collection processes.
-
To assess pilot data in relation to predefined stop/go progression criteria for a full RCT (see Chapter 3) to inform the decision of whether or not to proceed to a full RCT.
Chapter 2 The development and personal and public involvement testing of the Supporting MumS intervention and active control content
The MRC guidance on developing and evaluating complex interventions105 was used to guide the development and pilot testing of the Supporting MumS intervention. This guidance105 highlights that best practice in intervention development is to adopt a systematic approach that uses the best available evidence, has an appropriate theoretical basis and tests the intervention in a phased approach, starting with a pilot, or series of pilots, to address key uncertainties, followed by more definitive evaluation studies.
The present National Institute for Health Research (NIHR) report describes the development and pilot testing of the Supporting MumS intervention, reported in line with the MRC guidance105 (Table 1).
| MRC guidance stage | Activity | Report section |
|---|---|---|
| 1. Developing complex intervention | ||
| Identifying the evidence base | Review of evidence on postpartum weight management – reviewing published literature and existing systematic reviews | Chapter 1: background |
| Identifying and developing appropriate theory | Identifying relevant behaviour change theory for weight management | Chapter 2: intervention development |
| Modelling process and outcomes | Using chosen theory and literature to inform intervention content; testing intervention content with target group; refining intervention according to feedback | Chapter 2: intervention development |
| 2. Feasibility/piloting: pilot RCT | ||
| Pilot RCT | Pilot RCT with specific progression criteria (see Table 5) | Chapter 3: methods; Chapter 4: results |
This chapter reports the development of the Supporting MumS intervention (stage 1 of the MRC guidance). PPI was an integral part of the intervention development process (see Personal and public involvement in intervention and active control development).
Identifying the evidence base
A review of the evidence on postpartum weight management, including consideration of findings from previous RCTs, systematic reviews and qualitative research, was used to inform the key features of the intervention and the pilot RCT (see Chapter 1).
Identifying/developing appropriate theory
The intention from the outset was to develop an intervention that supported weight loss and weight loss maintenance. No single behavioural theory that fully explains the behaviour change process currently exists. The current intervention was based on two complementary theoretical accounts to target specific behaviour change phases: (1) the motivational and volitional phases to support the initiation of change, followed by (2) the maintenance phase to support sustaining change. Modelling of the initiation of change was guided by the health action process approach (HAPA),107 which outlines a motivational and an action-oriented volitional phase in the initiation of behaviour change. The theoretical approach chosen to guide the intervention development for weight loss was the HAPA. 107 HAPA is a comprehensive sociocognitive model that has been successfully used to predict and change lifestyle behaviours, including weight-related behaviours. 108 Moreover, HAPA has successfully informed the content of previous NIHR-funded SMS-delivered interventions. 108–110 The weight loss aspect of the intervention was shaped by the specific behaviour change phases encompassed by HAPA, including the motivational and volitional phases. The specific psychological processes to increase motivation include outcome and risk perceptions, as well as task self-efficacy (i.e. the belief a person has in their ability to perform a behaviour). In the volitional phase, action-focused processes are specified such as action planning (i.e. specifying the necessary steps needed to change behaviour), coping planning (i.e. specifying how to overcome possible barriers) and maintenance self-efficacy (i.e. the belief in one’s ability to continue change in the long-term).
The selection of maintenance processes was based on a systematic review of > 100 behavioural theories that synthesised theoretical explanations for maintenance of behaviour change. 84 Maintenance specific processes include (1) maintenance motives such as appreciation of the behavioural outcomes, enjoyment of the new behaviour and congruence of the new behaviour with one’s identity and values; (2) habits that enable automatic performance of behaviour; (3) resources to uphold behaviour change, both psychological and physical; (4) self-regulation to monitor whether or not the new behaviour is maintained; and (5) social/environmental support for maintenance. These processes are in line with several leading theories of behaviour change maintenance. 84,111–113
Thus, the intervention targeted specific behaviour change phases, including: (1) the motivational and volitional phases to support the initiation of change; followed by (2) the maintenance phase to support sustaining change (Table 2).
| Change phase | |||
|---|---|---|---|
| Motivation | Volition | Maintenance | |
| Psychological processesa | |||
| BCTsa (phase specific) |
|
|
|
| BCTsa (universal for diet and activity behaviour change and weight management) |
|
|
|
Modelling process and outcomes
The work conducted in this phase is summarised in the following sections:
-
SMS messages: key considerations (length, frequency, timing, tone, key messages on diet and activity, links).
-
Operationalising the key behaviour change techniques in the weight loss and weight loss maintenance phases [bidirectional messages, targeted messages (breastfeeding, smoking, weight loss, weight loss maintenance), self-monitoring weight, self-monitoring diet and activity, goal setting and feedback, slip-ups and relapse prevention, social support, action planning, coping planning].
-
Additional intervention components: discussion forum and study website.
-
Personal and public involvement in intervention and active control development.
Deciding on relevant behaviour change techniques
The BCTs to be incorporated into the intervention were chosen based on a number of different evidence sources, namely the theoretical basis for the intervention described above, published qualitative research with postpartum women,34,114–118 the NICE guidelines on weight management,119,120 systematic reviews of techniques and components used in successful diet and physical activity interventions,121,122 systematic reviews of weight loss maintenance lifestyle interventions123,124 and mHealth interventions,64,65 and a systematic review of systematic reviews examining the BCTs associated with effectiveness in weight management RCTs [McGirr, Dombrowski, Holmes & McKinley, 2018, Queen’s University Belfast (QUB), manuscript under review]. Based on this literature, a number of BCTs were consistently associated with successful weight loss, notably goal-setting, self-monitoring and feedback. A full list of the BCTs employed, along with examples of SMS messages, are shown in Table 3.
| BCT | Example message |
|---|---|
| Goal-setting (outcome) | We’ve talked the talk, now it’s time to walk the walk :). Set your weight loss target today – text us the weight you hope to be in 6 months’ time. For help with setting a weight target that is realistic for you, check out this link: www.nhs.uk/Livewell/weight-loss-guide/Pages/set-your-target-weight.aspx |
| Provide information on consequences of behaviour to the individual | WEEK 10! Need some extra motivation this week? Make a list of how you’ll feel when you reach your weight loss target, e.g. healthier, more confident. Keep this in mind for the week ahead |
| Goal-setting (behaviour) | WEEK 14. Have you set your activity goal for the week ahead? Text Y11 for yes or N11 for no |
| Prompt self-monitoring of behaviour | Monitoring food intake helps with successful weight loss! Are you still recording what you eat? Let us know – text Y7 for yes or N7 for no |
| Prompt self-monitoring of behaviour outcome | What are the scales saying this week? Text us e.g. 11 st 5, or 73.3 kg |
| Action planning | Check your kitchen – if you have healthy foods in there you are much more likely to eat healthily! Do you have fruit and vegetables in the house this week to snack on? Text Y28 for yes or N28 for no |
| Provide instruction on how to perform the behaviour | When to weigh yourself? Pick a time that suits you each week and stick to it. First thing in the morning, after you go to the loo and before you get dressed is best |
| Barrier identification/problem-solving | Looking after a baby and finding the time to exercise can be hard. One solution is to exercise with your baby. Check this link for fun activities you can try out – www.parenting.com/gallery/exercises-to-do-with-your-baby?page=0 |
| Provide feedback on performance |
What about the goal you set last week, did you reach it? Text Y2 for yes and N2 for no (yes/no reply triggers a feedback message) Want some feedback on your weight? Look no further than your scales! Text us your weight followed by UP, DOWN, SAME (reply triggers a feedback message depending on progress) |
| Stress management/emotional control training | Does your mind often win in the battle against your stomach? It’s easy to eat without hunger. Next time, ask yourself these two Q’s first: ‘Am I really hungry?’, ‘Do I really need it?’ Self-talk helps prevent mindless eating (or, in other words, eating without thinking):) |
| Environmental restructuring | Tempted to buy fizzy drinks? Wait! . . . if it’s not in the house you can’t drink it! Sparkling/soda water with a wedge of lemon/lime (or any fruit you like) is a good swap – gives the zing without calories! |
| Plan social support/social change | If you’re a lone wolf, it’s time to join a pack! Support increases weight loss success, so team up with friends/family, or chat to other mums online. The Supporting MumS forum is a great place to start – http://supportingmums.boards.net |
| Provide information on where and when to perform the behaviour | Info overload? No need to make all changes at once! Small steps go a long way in shifting the lbs! Pick two changes to focus on the next time you are out shopping and then try to repeat each week – it will become a habit before you know it! |
| Set graded tasks | Tummy-toning tip: baby amused on the floor? Set the timer on your phone and try a 30-second plank beside them. Challenge yourself to a longer plank each day |
| Prompt practice | Fill up on fuel, not on calories! Outdo the marketer’s trick of placing unhealthy snacks beside the till at the petrol station. Reach for our good old fruit friends or nuts if you fancy something to munch on |
| Time management | Tired and time-tied? Dinner plans can sometimes go out the window! But who says you have to make a fancy meal? Pasta and pesto, oven chips and fish fingers (with some frozen or tinned peas/beans) make quick and handy dinners |
| Prompting generalisation of a target behaviour | Are you able to manage those tempting food situations any better now than before Supporting MumS? Text Y35 for yes and N35 for no |
| Prompt self-talk | There will be times in your weight loss journey when things won’t be perfect. That’s life! Supporting MumS is about aiming for progression not perfection :) Use this mantra – ‘I’m doing the best I can’ – to keep any negative thoughts away |
| Relapse prevention/coping planning | Mmmm smell it, feel it . . . WANT IT! What do you do next . . . eat it? Next time you are faced with this situation, have a plan of action. Could you walk outside, or do something to distract yourself (e.g. call someone, go online)? Text us what you’ll do next time. E.g. ‘step outside’ |
| Prompt rewards contingent on effort or progress towards behaviour | It’s normal for weight loss to slow down or even stay the same for a while, so don’t let it effect your motivation if this happens – congratulate yourself on your success so far! |
| Prompt focus on past success | Love yourself slim in WEEK 19. Think of a time you achieved something you were proud of and how it made you feel. Keep this is mind :) |
| Teach to use prompts/cues | Are you in an ‘I can do this’ kind of mood? Now is a great time to plan your meals for the week. It will mean you’ll be more likely to make healthy food choices on days when you need that extra little bit of motivation! Here’s a sample meal plan to get you started – www.bhf.org.uk/heart-matters-magazine/nutrition/eat-well-on-a-budget/sample-menus |
| Model/demonstrate the behaviour | Strengthening that all-important core will help your pelvic floor muscles recover. Especially after all it’s been through! Some Pilates moves like the plank are a good place to start. Check out this site to see what you might manage – www.nhs.uk/conditions/nhs-fitness-studio/pages/pilates-for-beginners.aspx |
SMS messages: key considerations
Overall, the intervention was designed to encourage a self-guided approach to lifestyle behaviour change and weight management as supported by the literature. 125–127 In line with existing evidence, the intervention focused on dietary intake as well as physical activity to address energy balance alongside appropriate BCTs to support lifestyle change and weight management. The messages aimed to:
-
contain information for weight loss, including advice, practical tips and external resources
-
provide encouragement and motivation, discourage guilt and encourage self-reflection
-
provide information in layers to avoid overwhelming women with too much at once, with reinforcement of key messages at regular intervals
-
include selected BCTs
-
include real-life situations relevant to postpartum women that they could relate to/address key barriers to weight management for this population, for example family environment triggers such as finishing the kids’ left-overs
-
adopt a friendly accessible tone, including humour, to encourage engagement.
The SMS messages were drafted by three members of the study team and commented on and refined by other members of the multidisciplinary study team, with PPI input (see Personal and public involvement in intervention and active control development).
Key considerations when developing the SMS message library were: (1) message length, (2) message frequency, (3) message timing, (4) tone, (5) key messages on diet and activity to be conveyed and (6) using links to signpost to other information sources and tools.
Message length
One of the challenges in writing the SMS messages was to consider message length. Smartphones can accept messages that are > 160 characters, but, for participants with older models, the messages may come through twice. It was not possible to keep all messages to < 160 characters as some concepts needed some explanation, but message length was kept as tight as possible and was tested with PPI members.
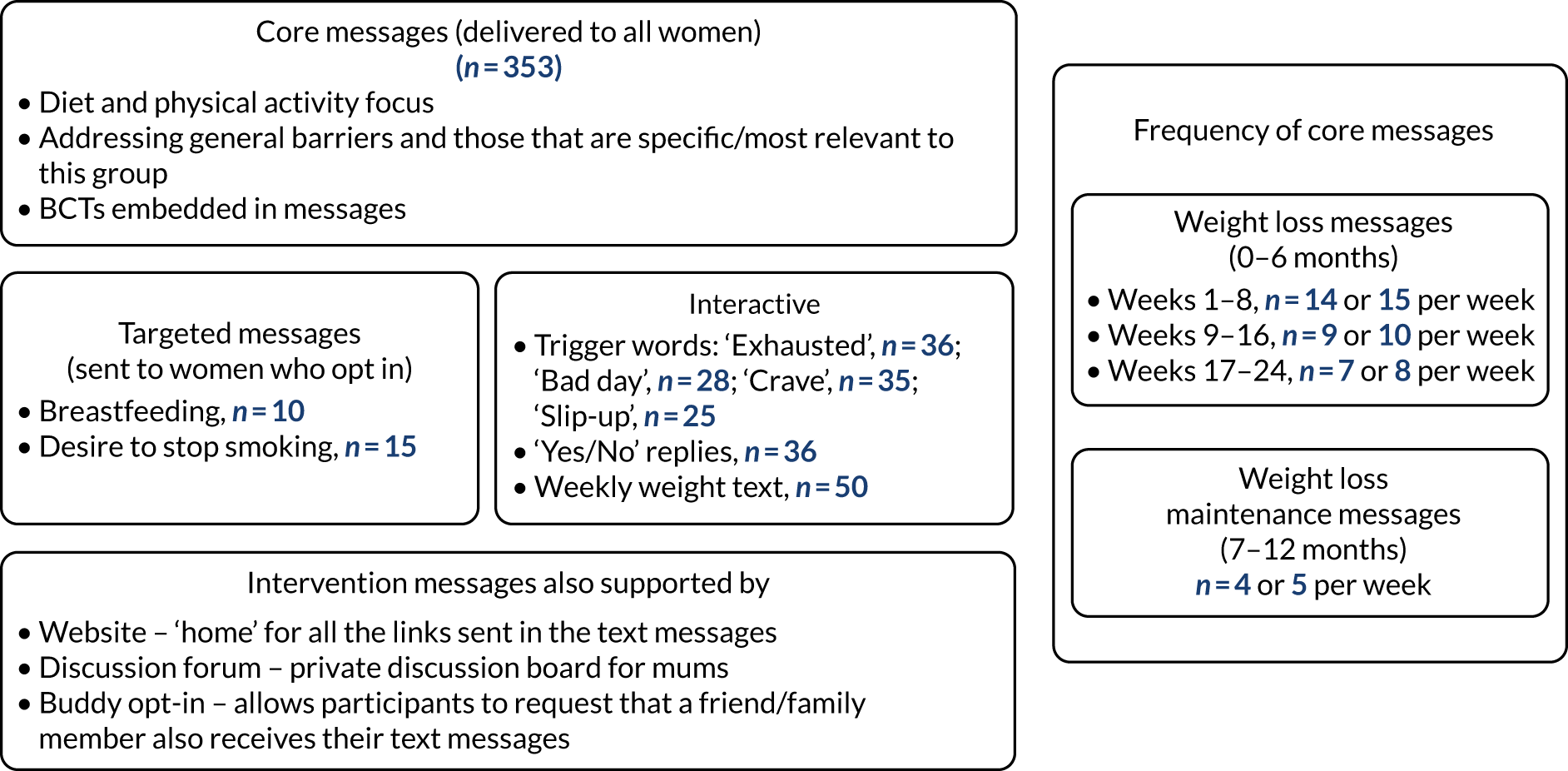
Frequency of messages
For the intervention group, the number of messages was dictated by the nature of the content that needed to be delivered alongside an awareness that too many messages would probably mean messages were ignored. PPI participants were asked for their opinion on the frequency of SMS messages (see Personal and public involvement in intervention and active control development). The intervention consisted of 353 core messages, that is messages that were delivered by the system to all participants: 217 in the weight loss phase and 136 in the weight loss maintenance phase. Given the amount of content to be delivered in the weight loss phase in terms of providing information on diet and physical activity and addressing barriers and embedding BCTs in an engaging and motivational way, a greater number of messages were provided in the weight loss phase (n = 217, months 0–6) relative to the weight loss maintenance phase (n = 136, months 7–12). The number of SMS messages sent during the first 6 months started at a rate of 15 per week and was tapered to eight per week. Fewer messages were sent in the weight loss maintenance phase as the emphasis in this phase was on reinforcing self-regulation techniques, instilled during the first 6 months of the intervention, and focusing more on maintenance-relevant strategies such as relapse prevention and dealing with slip-ups. However, it was also important to maintain enough contact with the participants during months 7–12 to ensure that they still felt supported at this crucial stage in the weight management process, when the potential to return to old ways and regain weight is high. For this reason, the number of messages was kept at four or five per week.
Timing of SMS messages
When participants signed up to the study, they were asked the time of day they preferred to get the message and also what times of day they wanted to be kept message-free, for example 19.00–07.00. The first message was sent to participants on the day they were randomised. Two messages were sent each day between weeks 1 and 8 and they were programmed to arrive at different times to avoid predictability, for example day 1: 11.00 and 20.00, day two: 09.00 and 20.00, day 3: 10.00 and 17.00, day 4: 09.00 and 16.00. As message frequency decreased, SMS messages were sent at various times on different days to avoid predictability; however, the message asking participants to weigh themselves (see Operationalising the key behaviour change techniques in the weight loss and weight loss maintenance phases) was always sent on the same day of the week.
Tone of messages
The messages were written in an informal, friendly style using humour and emojis to engage participants, as evidence indicates that how a message is portrayed can affect how a person responds to that message in relation to changing behaviour. 128 Information on who created the SMS messages (‘nutritionists at QUB alongside other mums’) was provided in the initial messages. To prevent SMS messages from becoming repetitive, some were written as if they came from another mother. These ‘mum’s tips’ were placed sporadically across weeks 1–52, and were included to offer mothers a chance to relate to and learn from another person’s weight management journey and so help to increase self-efficacy.
Key messages on diet and physical activity
The intervention content focused on diet and physical activity, as the effectiveness of targeting dietary change on improving weight outcomes is supported by the literature, see Chapter 1. The key dietary advice incorporated in the intervention focused on creating a calorie deficit, eating regularly (not skipping meals), portion size, healthy snacking, food swaps, social eating, emotional eating, recognising and avoiding food triggers both inside and outside the home environment, shopping for food, cooking, takeaways, drinks, mindful eating, hungry days, weekends and coping/planning for special occasions or other temptations. Barriers to changing diet and activity behaviours were also addressed, including lack of time and tiredness, which are particularly pertinent for this population.
The key messages on physical activity focused on the importance of activity for overall health, guidance on the specific recommendations for physical activity in relation to weight loss and weight loss maintenance, its important role in maintenance of weight loss and a wide range of practical ways for increasing activity, as scheduling activity can be a struggle for women at this stage of life. Walking was introduced first as a form of activity that is accessible to the majority of mothers: they can easily take their baby along with no special equipment required and it is a low-risk activity with recognised health benefits. In line with the self-directed ethos of the intervention, messages also suggested other types of activity throughout the intervention period, encouraging women to find something they might enjoy.
The messages initially focused on dietary change, with messages relating to physical activity being introduced at week 8, in order to focus on one behaviour change before introducing the next activity. Evidence suggests that physical activity on its own is not an effective approach for weight loss, but does become more important in terms of maintaining weight loss. 53,129
Self-monitoring and goal-setting for diet and physical activity were actively encouraged throughout the intervention (see Operationalising the key behaviour change techniques in the weight loss and weight loss maintenance phases).
Using links
Web links were inserted into messages for several purposes, for example to provide more information or guidance on a particular topic such as exercise videos; to signpost to tools to help self-monitor diet and activity; and to give practical advice such as recipe ideas or freezer-friendly meals.
Operationalising the key behaviour change techniques in the weight loss and weight loss maintenance phases
A cluster of BCTs, supported by an evidence base, was selected to be embedded within the Supporting MumS intervention messages and specifically linked to the relevant phases and psychological processes of behaviour change (see Table 3). Intervention BCTs were employed in two ways: (1) phase-specific BCT use and (2) universal BCT use. BCTs specific to a particular phase were operationalised for that phase only. For example, information about the health consequences of obesity (i.e. outcome expectancies) is relevant to motivate people to change, but, once behaviour change has been initiated, this becomes less relevant. Likewise, prompting participants to review their achievements resulting from their weight loss efforts (i.e. satisfaction with outcomes) is only relevant following engagement in behaviour change for some time. Universal BCTs were used throughout the intervention and adapted for the relevant phases of behaviour change. For instance, the setting of weight goals was used throughout the intervention. However, the content of the goals was adjusted depending on whether weight loss was being promoted, or whether participants were being asked to engage in weight loss maintenance.
The BCTs that were considered to be key components based on evidence and theory were operationalised in a number of ways: through the use of bidirectional messages – targeted messages according to weight management progress, eating triggers and other weight-related behaviours (smoking and breastfeeding); self-monitoring weight; self-monitoring diet and activity; and providing social support and messages on action planning and coping planning.
Interactive components: bidirectional messages
Interactive components were included in the core messages that were sent to all participants to encourage engagement and allow provision of feedback. Feedback is important for intervention effectiveness and can serve a number of functions, such as encouraging self-reflection, prompting goal-setting and even preventing a relapse in a trigger situation. One of the interactive features employed questions to emphasise key aspects of the intervention or encourage particular behaviours or self-reflection, for example ‘Did you set a goal this week? Did you achieve your goal? Text us yes or no’.
In total there were 36 ‘yes/no’ messages sent during the 12-month intervention period. When participants replied ‘yes’ or ‘no’, an automated message that was specific for that response was sent to the participant.
Other interactive features included being able to text trigger words and receive an automated reply, and transmission of a weekly weight text, see below.
Targeted messages
Women received targeted messages that were based on data collected at baseline and/or weight loss progress. A bank of text messages was created specifically for women who were breastfeeding and also for women who were interested in smoking cessation. Women opted in to receive these additional messages at baseline, and this was configured on the SMS platform at the time of randomisation.
Breastfeeding
Women who are breastfeeding may be concerned that losing weight will have a negative effect on milk quality and quantity. Evidence to date130 indicates that, once lactation is established, overweight women can restrict their energy intake and exercise aerobically to promote a weight loss of 1 lb/0.5 kg per week, without affecting infant growth. Therefore, a set of SMS messages was created to alleviate participant fears or concerns in relation to weight management while breastfeeding. In total, 10 breastfeeding messages were provided and programmed for delivery in the weight loss phase only, in weeks 1–5, 7–9, 13 and 16. One breastfeeding message was sent each week (except in week 2 when two messages tailored for breastfeeding were sent) so that participants were not overburdened with messages.
Smoking cessation
Smoking cessation is associated with some weight gain and is a barrier to quitting. 131 Therefore, messages were created to provide additional support and encouragement in this regard for women who wanted to stop smoking. Smoking cessation messages were delivered in weeks 1, 14 and 16–24 of the weight loss phase and in weeks 26–28 of the weight loss maintenance phase to encourage and provide sustained support and information to those trying to quit (15 messages in total). One message was sent in each of these weeks so as not to overburden participants. Apart from week 1, messages were not sent about smoking cessation until week 14 in order to avoid overwhelming participants with too many behaviour changes at once; therefore, the intervention conveyed key messages and BCTs related to diet, activity and weight management before addressing smoking cessation.
Weight loss maintenance progress
Weight loss tends to plateau at 6 months and at this stage the focus of the SMS intervention shifted to weight loss maintenance. From month seven onwards, women may have been losing weight or gaining weight or trying to maintain their weight and so they received feedback according to whether their weight had gone up or down or stayed the same (see Self-monitoring of weight). This allowed the provision of real-time feedback, which has been found to be important in effective interventions. 132 The contingent reinforcement highlights achievements or prompts women to take appropriate action. 133
Self-monitoring of weight
Monitoring of weight has been shown to be associated with successful weight loss and weight loss maintenance. 129 Weight self-monitoring was incorporated into the intervention via a weekly message asking women to weigh themselves and send back their weight (e.g. ‘Just a reminder to step on the scales and text us your weight when you do e.g. 11 st 5 or 73.3 kg. All of your texts to SMS will be kept strictly confidential!’) Weekly weight-reporting via SMS has been shown to support self-monitoring and has been found to be feasible in previous trials. 77,133 Reporting weight via SMS was used only for self-monitoring, as weight was measured objectively at study visits (see Chapter 3). In addition to asking women to weigh themselves weekly and respond with their weight, the messages also reminded women why stepping on the scales was important and gave instructions on how to weigh themselves (i.e. preferably the same day of the week, same time and wearing similar clothing), and also reminded women that they could call in to their local pharmacy or shopping centre to weigh themselves.
In the weight loss phase, months 0–6, if women replied with their weight, there was no further message from the system. In the weight loss maintenance phase, the messages reminding women to weigh themselves and report their weight continued, but a feedback feature was added depending on whether women were continuing to lose weight, trying to maintain their weight loss or regaining weight. Hence, in months 7–12, the weekly weight SMS message asked women to send their weight and also add ‘up’ or ‘down’ or ‘same’ in relation to how they did last week (e.g. ‘Weekly weighing = your very own early warning system! Step on the scales today and text us your weight followed by UP, DOWN, SAME. e.g. “10 st 7 SAME” or “66.7 kg SAME”.’). The ‘up’ or ‘down’ or ‘same’ triggered an automated response providing positive encouragement to keep up the good work if their weight went down or stayed the same, or one that offered ideas and information on what to do if their weight went up, as well as messages discouraging feelings of guilt and encouraging them not to dwell on weight gain and to get back on track as soon as possible.
Self-monitoring of diet and activity
Keeping track of diet and activity is known to be positively associated with weight management. 134 Participants were encouraged to monitor their food intake and physical activity to raise awareness of their usual eating and activity patterns and identify where they would like to make changes. The SMS messages suggested a range of options for self-monitoring, such as keeping diaries of food intake and/or activity, using a step counter, using self-monitoring apps or simply recording on paper, for example ‘Keep tabs on your fitness as well as your food. Recording what activities you do, and for how long, will increase your chances of weight loss success. As with food, anything goes- pen & paper, a pedometer, a fitness tracker App on your phone.’. Messages such as this were sent regularly throughout the study to encourage this practice.
Goal-setting and feedback
Participants received guidance on goal-setting for weight loss, dietary change and physical activity via the SMS messages, including examples of how to set specific, measurable, achievable, realistic and timely (SMART) goals, along with guidance on recommended rates of weight loss to help with setting realistic goals. Participants were prompted to set and review goals via prompts, for example ‘Heaps of food for thought this week. Have you thought about what one of your food goals could be? Here’s some inspiration: “I will have a portion of fruit with my breakfast 5 days this week”.’. Messages also asked them to reflect on their progress in relation to the goals they set, for example ‘What about the goal you set last week? Did you reach it? Text Y2 for yes or N2 for no.’. The ‘yes/no’ response triggered an appropriate feedback message, providing support, reinforcement and encouragement; see Interactive components: bidirectional messages.
Slip-ups and relapse prevention
Lapses in good intentions are common in weight loss programmes and can make people feel disempowered, with small slip-ups risking a prolonged return to old and unhelpful behaviours. To support women in such situations, a number of potential trigger points were selected, in conjunction with PPI input (see Personal and public involvement in intervention and active control development). These were ‘slip-up’, ‘crave’, ‘bad day’ and ‘exhausted’. Women could send these trigger words at any time and would receive a reply from a bank of messages specific for that trigger. The real-time responses were designed to provide practical suggestions and support to prevent relapses. This trigger word function has been included in other SMS interventions, such as the txt2stop trial. 98
For messages sent with the word ‘crave’, replies focused on resisting temptation when it was experienced, for example through the use of urge-surfing (allowing cravings to pass without acting on them),135 as well as messages to encourage moderation if they gave in and to ‘get back on track’ again. For ‘slip up’, replies emphasised that it was normal to have slip-ups and encouraged women not to feel guilty. Replies for ‘exhausted’ included suggestions, other than caffeine and sugar, to help combat tiredness, ways of coping with lack of sleep and advice on visiting their general practitioner (GP) if prolonged tiredness persists. ‘Bad-day’ replies included ideas to lift their mood. Women were informed about the trigger words on day 17 of the intervention and were also reminded about them on 8–13 occasions throughout the 12 months of the intervention delivery. From weeks 3–52, participants could send the words ‘crave’ or ‘bad day’; from week 24 they could send the word ‘exhausted’; and in weeks 26–52 they could also send the word ‘slip-up’. Messages were sent out sequentially from a list of available messages. The following numbers of messages for each trigger word were developed: ‘exhausted’, n = 36; ‘crave’, n = 35; ‘bad day’, n = 28; ‘slip-up’, n = 25. Women were not limited in the number of times they could utilise this function.
Social support
Social support was facilitated throughout the SMS intervention using a buddy system (as used previously in txt2stop)98 whereby a participant could nominate a friend or family member to receive the same SMS messages that they were receiving and so be in a better position to provide support to them. Participants were sent the instructions on how to do this in the SMS messages, for example ‘Having support increases weight loss success! Why not have a friend/partner/family member receive the same SMS text messages as you? To do this, reply to this message with Support followed by the person’s mobile number. e.g. Support 07800000000.’. Participants could request a friend/family buddy at any stage and reminders of this facility were sent throughout the intervention period. Messages were also sent to participants to tell them about the value that support can play in weight loss success.
Action planning
Messages were developed to provide participants with knowledge on how they could make plans that would be readily actioned and so would be more likely to lead to achievement of diet and activity goals, for example, ‘Were you able to plan your meals this week? Text Y4 for yes and N4’; ‘Have you made any food swaps recently? Text Y17 for yes and N17 for no’; ‘Keep it, see it, eat it! Check your kitchen– if you have healthy foods in there you are much more likely to eat healthily! Do you have fruit and vegetables in the house this week to snack on? Text Y28 for yes or N28 for no’.
Coping planning
Holiday seasons, special events, social occasions and weekends can all act to undo weight management efforts. 136,137 In line with the theoretical basis of the intervention, support for coping planning was particularly important for maintenance of behaviour to help develop self-efficacy to deal with such situations, and so SMS messages were written to support women in this regard, for example ‘Birthdays? Holidays? Weddings? Do any situations throw your healthy eating plans off track? You’re not alone! Sometimes the best tactic is to accept it, and then plan ahead. If you know you will eat more on a family weekend away, make a plan (e.g. what activity you will do and what you will eat) to get back to your healthy new lifestyle on the Monday’; ‘How have you been coping with tempting situations? Have you been able to resist? Text Y16 for yes and N16 for no’.
Additional intervention components: discussion forum and study website
All the BCTs selected for inclusion in the intervention were embedded in the SMS messages. Two additional components were added to complement the SMS messages with a view to assess how useful these additional elements would be in the pilot RCT.
The first component was a discussion forum, which acted as an additional means of social support. Given the importance of social support for lifestyle behaviour change and weight management, this element was added to allow an opportunity for mothers to talk to other mothers in the intervention, and was complementary to the friends/family social support facilitated via the SMS platform, as previously described. Participants were sent a message informing them of the study forum, along with log-in details. Messages were also sent to remind participants about the forum throughout the duration of the intervention and about the value that support can play in weight loss success.
The other additional component of the intervention was a web page that was established to act as a ‘home’ for all of the web links included in the SMS messages. The web page provided access to the links for participants who might not have been able to access websites from their mobile phone or for those who preferred looking at the internet on larger screens. The web links on the web page were ordered by topic, for easy navigation.
Developing the active control group messages
An active control, as used successfully in the txt2stop trial,98 was developed for the present study. Many similar interventions employ a ‘usual care’ control group; however, the WeighWell feasibility study58 demonstrated the potential for differential attrition rates between the intervention and control groups when a ‘usual care’ control group was used in a postpartum weight loss intervention with women from areas of social disadvantage. Because women volunteering to participate are likely to want to lose weight, being randomised to a usual care or ‘do-nothing’ arm is likely to generate strong patient preferences; employing an active control in these situations might offer an opportunity to create equipoise and enhance satisfaction with randomisation.
As for the intervention messages, the active control SMS messages were drafted by three members of the study team and commented on and refined by other members of the multidisciplinary study team and PPI group (see Personal and public involvement in intervention and active control development). The messages that were developed related to general child care and development, and the content was consistent with evidence-based information provided by the NHS Start4life information service for parents. 138 The active control, therefore, did not mention the target behaviours and did not contain the active ingredients of the intervention (diet and physical activity content and embedded BCTs related to weight loss).
The active control messages were developed for mothers with babies aged ≥ 6 weeks (women had to be at least 6 weeks postpartum to enrol in the study). Relevant messages were created for mothers with a child aged up to 36 months, as women could opt in at any stage up to 24 months postpartum. Women received messages that coincided with the age of their baby, that is if their baby was 6 months old when they were enrolled, they started receiving messages corresponding to this age.
The active control messages were designed to include:
-
A play idea/activity each week.
-
Information on specific milestones, for example developmental steps (crawling, rolling, walking, talking, potty training). Such information was always communicated to mothers with a note of reassurance to assuage concern if their child was not at that stage just yet, as all babies develop differently. Mothers were also advised to speak to their GP or health visitor if they were concerned in any way.
Other messages involved information on home safety, or separation anxiety or information relevant at a particular stage of development. In the Text4baby study139 (the first free, national, health service delivered via SMS in the USA providing information to pregnant women and new mothers to help them improve their health and the health of their babies), three messages per week seemed acceptable to mothers so it was decided to send three messages each week to the active control group in the present study.
There was no bidirectional functionality for the active control messages.
Setting up the SMS platform
The study used the SMS platform used for the txt2stop trial,98 but added to its functionality to allow provision of feedback. The platform enabled messages to be sent to participants at a specified date and time and in a specified order. Other features of the existing SMS platform that were utilised were the trigger-word function described previously; the facility for the participant to text the word STOP at any time if they no longer wanted to receive the messages (in that event, they would still continue in the study unless they also formally withdrew from the study assessments); and the facility to text the word PAUSE if they wanted to pause the messages for a period of time because of planned or unplanned life events, for example holidays or bereavement. If a participant paused the intervention, when they wanted to restart the messages, they contacted the study team who then informed the SMS database programme manager. Messages were restarted from where they left off and the rest of the messages were delivered as for the other participants.
The SMS platform also sent messages on breastfeeding and smoking to women who indicated a desire to receive such messages at their baseline assessments. This was configured on the SMS system at the point of randomisation and the relevant messages were then sent out in addition to the core messages.
Additional programming was carried out to include the participant’s name in the welcome message, as suggested from the PPI work. Feedback from the PPI members indicated that they welcomed the use of some emojis; this was facilitated through the SMS platform using simple symbols, for example a smiley face :), to ensure compatibility across different mobile phones.
Additional programming was also carried out to allow the system to send feedback messages to participants when they responded to the ‘yes/no’ questions or the weight reply messages ‘UP, DOWN or SAME’ in the weight loss maintenance phase. The system was programmed to automatically detect the words ‘UP’, ‘DOWN’ or ‘SAME’ and a message was sent from the appropriate weight reply message library.
Some programming was also required to send the active control messages. This was necessary to adjust message delivery according to the age of the baby at the study outset. Women could opt in to the study any time up to 24 months postpartum, with the study lasting 12 months; therefore, messages were created for babies and toddlers aged from 6 weeks to 36 months. When participants were randomised to the active control, an online calculator selected the appropriate starting point for their messages to ensure that they coincided with the age of their child.
Once set up, the study team tested the delivery of the core messages and interactive features over a period of a few weeks. Issues that were picked up were then resolved before the system went live and the first participant was recruited.
A summary of all the intervention components described is shown in Figure 1.
FIGURE 1.
The supporting MumS study: summary of the intervention components.
Personal and public involvement in intervention and active control development
The PPI is described in this section according to the GRIPP2-SF (Guidance for Reporting Involvement of Patients and the Public 2-Short Form) subheadings. 140
Aim
The aim of PPI was to help develop a SMS-delivered intervention for weight loss and weight loss maintenance in the postpartum period. To achieve this, the intervention development involved close consultation with postpartum women with respect to the following elements:
-
choosing the name
-
developing initial test SMS messages
-
reviewing the full library of SMS messages.
Personal and public involvement consultations were conducted via a mother and toddler group and a Sure Start group in the Belfast area (Sure Start is a programme that supports parents with children aged < 4 years living in disadvantaged areas in Northern Ireland); in addition, three women who had recently had a baby were recruited, two of whom struggled with their weight. These three women were recruited through word of mouth via QUB researchers and asked to join the study writing team. PPI representatives were paid for their time and input, according to the principles of INVOLVE. 141 Because the PPI representatives had each recently had a baby, they provided input and feedback via telephone or e-mail, as this was the easiest way for them to fit in PPI with their busy lives as new mothers.
Methods and results for the personal and public involvement elements
Choosing the name
The study team created a list of 13 potential study names. The names did not mention weight loss because the study had an active control group. This list was shared with the rest of the project management team, which ranked the names, and a reduced shortlist of eight study names was then tested with PPI representatives. This consisted of one mother and toddler group in Belfast visited by a QUB researcher, together with feedback from other new mothers who were friends or relatives of the QUB study team; in total, 18 women were asked to indicate their preferred study name. The most popular name, based on feedback from postpartum women, was ‘SNAP’. However, subsequent searching showed that various SNAP studies already existed, including a NIHR-funded project examining nicotine replacement therapy in pregnancy. SMS was the second most popular choice, standing for ‘Supporting MumS’.
Reviewing the initial test SMS messages
An initial collection of 30 SMS messages was written by members of the study team; 14 intervention messages and six active control messages were then selected for PPI testing. The aim of this testing was to get initial thoughts from PPI representatives on the tone, length, style and content of messages; the inclusion of links; the use of ‘emojis’; and, importantly, to get an instant reaction from women if they felt that any messages were unsuitable.
To carry out this work, a Sure Start group in the Belfast area was contacted to seek permission to attend the group and collect feedback on the drafted messages. Two researchers went along to the group and asked mothers to view the messages and provide any comments beside each message (see Appendix 1). Ten mothers took part. Alongside this, the 20 draft messages were posted or e-mailed to the three women who had recently had a baby who were recruited as PPI representatives for the duration of the study.
Overall feedback on the initial draft messages indicated that women thought that the messages were catchy and encouraging, with an appropriate tone. They felt that the content would provide them with determination not to give up on weight loss goals. They liked the practical cooking tips and they preferred shorter messages. Active control messages were well received and no major refinements were needed based on the initial feedback.
Taking into account this feedback on the most appropriate terminology to be used in messages, as well as the feedback on the length and tone of messages, the intervention messages were drafted for weeks 1–12 and the rest of the active control messages were also drafted.
Reviewing the full library of SMS messages
The PPI representatives reviewed the first 12 weeks of the weight loss messages (n = 146) for tone, length, clarity and acceptability. The messages were presented in a table with four columns after each message: ‘like it’, ‘it’s OK’, ‘don’t like it’ and ‘other comments/suggestions’. These were sent for feedback by post/e-mail according to each woman’s preference. The feedback was collated by study researchers and examples of how messages were then refined have been tabulated (see Appendix 2). After receiving feedback on the messages designed for the first 12 weeks, the intervention messages for weeks 13–24 were drafted (n = 94) and the PPI process above was repeated. Examples of how messages were refined as a result of this feedback are shown in Appendix 3. The feedback received on the SMS messages that were designed for the first 6 months of the intervention was used to develop those relevant to the next 6 months; these had a greater focus on weight loss maintenance. Following a similar process, banks of messages for the trigger words and tailored messages for breastfeeding, smoking cessation and weight ‘up/down/same’ replies were drafted.
A health psychologist in the study team contributed to drafting the weight loss maintenance messages to ensure that habit formation and initiation was embedded in the messages. The SMS messages for months 7–12, as well as trigger word replies and tailored messages, were sent to the PPI group for comment. Examples of message refinement after feedback from the PPI group on weight loss maintenance, trigger words, weight replies and tailored messages are shown in Appendix 4. Based on the initial PPI group comments on the active control messages, the full library (consisting of messages related to child health and development for infants aged 6 weeks to 36 months) was generated by the study team and sent for PPI feedback. For examples of refinements made to the messages after PPI feedback on the active control library, see Appendix 5.
Personal and public involvement discussion and conclusion
Patient and public involvement was essential for the development of this SMS-delivered intervention to guide the tone and content of the individual messages and to ensure that the messages were sensitive to the needs of women at this unique stage in life. This process is likely to have made a major contribution to creating an intervention that is acceptable to the target group.
Personal and public involvement reflections
To fit in with the busy lives of women who have recently had a baby, the team were guided by women when it came to how best to get their input and feedback on the intervention development; post, e-mail and telephone were primarily used. Using this approach allowed us to gather detailed feedback but in a way that was convenient for the women involved.
Three women formed the core PPI group for this study. Given the nature of the PPI work, that is feedback on the individual SMS messages for the intervention and active control, this was felt to be sufficient to gain a range of views and resulted in an intervention that was highly acceptable to the target group (see Chapter 4). Further PPI work would be necessary to tailor this intervention for different cultural groups, as the PPI representatives in this instance were all of white ethnicity.
Chapter 3 Methods
Setting
The trial took place at one site in Belfast (Northern Ireland, UK).
Ethics approval and study sponsor
The trial was conducted in compliance with the requirements outlined in the Economic and Social Research Council Framework for Research Ethics, and was granted ethics approval by the QUB School of Medicine, Dentistry and Biomedical Sciences Research Ethics Committee (reference number 16.49). QUB acted as the sponsor for the study, and local standard operating procedures for the approval and monitoring of research were followed.
Design
The study schema describes the two stages of the study (Figure 3). Stage 1, the intervention development, was described previously (see Chapter 2). Stage 2 was a parallel, two-arm pilot RCT to examine the feasibility and acceptability of the intervention, active control and trial methods to inform the decision on whether or not to proceed to a multicentre full RCT to test the effectiveness of the Supporting MumS intervention.
FIGURE 3.
Schematic representation of the Supporting MumS study.
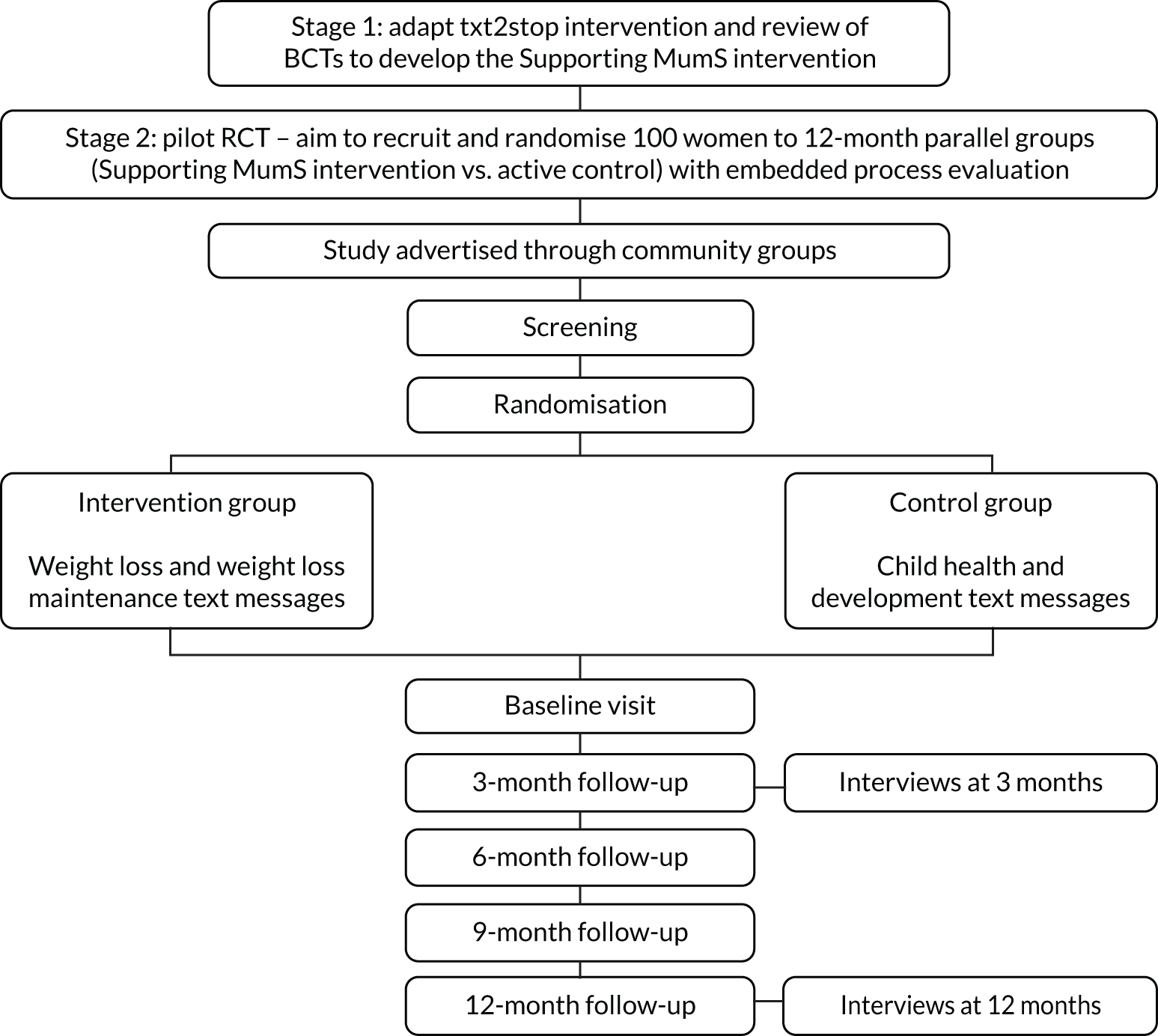
Recruitment
Community groups located in urban areas (in Belfast) and rural areas (in Co. Tyrone) and aimed at mothers of young children were identified through internet searches, social media advertising and community posters, and used to access the target population. A database was used to collate the contact details of the identified groups; these included mother and toddler groups in churches, breastfeeding support groups, ‘rhythm-and-rhyme’ groups in community libraries and Sure Start centres. Facilitators in these settings were contacted initially via telephone or e-mail and asked for permission for a researcher to visit the group to promote the study. If permission was granted, a researcher conducted a group visit, which involved speaking to mothers and disseminating leaflets. Study posters were left for display. Copies of the study leaflet and poster are available on the project web page (www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). When it was not feasible for the researcher to conduct a face-to-face group visit, posters and leaflets were posted directly to the group facilitators.
Several attempts were made to engage with health visitors involved in the childhood immunisation programme, as a potential avenue for recruiting participants. Other general community settings, including libraries, pharmacies and GP surgeries, were contacted and asked to display posters and leaflets in public spaces. The study poster was also advertised through the QUB staff newsletter.
During the recruitment period, owing to a slower than expected rate of recruitment through the targeted community groups, a decision was made to use social media to further promote the study. An advertisement was disseminated through a study Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) page (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020), and a Facebook newsfeed was used to disseminate the study poster that targeted women aged between 18 and 45 years who lived within a 40-km radius of Belfast. Relevant parenting websites (e.g. www.parentingni.org; accessed 27 January 2020) and Facebook groups (e.g. WaterTots NI) were contacted to ask if an advert could appear on their online locations, and organisations in Belfast aimed at families (e.g. NI4Kids: a newsletter targeting parents/guardians of young children aged < 11 years)142 were e-mailed to ask if a short paragraph summarising the research could be included in their quarterly newsletters. The contact details of child-care centres around Belfast and Co. Tyrone were also collated as an option for accessing the target population for recruitment.
The posters, advertisements and leaflets provided information about the study along with contact details of the research team. Women interested in taking part could contact the study administrator via e-mail, SMS, telephone call or Facebook messenger. As the study employed an active control to encourage retention, the purpose of the study was advertised as testing two new SMS interventions: messages about child, health and development or messages about weight management. This aimed to minimise women’s preference for one group over another. Although this approach could be criticised for not being transparent about the purpose of the study, the information sheet clearly described that women had a 50 : 50 chance of being assigned to receive messages about child health and development or messages about weight management, thus preserving participant autonomy. The acceptability of the active control was explored in interviews (see Chapter 4, Research question three: was the retention rate acceptable?).
Screening and eligibility criteria
At the initial point of contact with the study administrator, any woman who was interested in taking part was asked to provide her name, e-mail address or home address and a telephone number, as well as a suitable time for a researcher to make contact. Following this, a participant information sheet was e-mailed or posted to the woman, according to her preferred method (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). After 48 hours had passed, one of the researchers telephoned the woman to check if she had received and read the information sheet and to answer any queries she had. If the woman wished to proceed with study participation, she was then screened according to the inclusion and exclusion criteria using the study screening form (Table 4). A full copy of the study screening form is available at www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/ (accessed 27 January 2020). If the woman was not initially contactable, one more attempt was made to contact the woman for screening.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
During the screening process, women were asked to provide their measured/estimated weight and height, which were used to calculate their BMI. Women meeting the eligibility criteria were invited to take part and an appointment to complete consent and baseline measures was arranged. Owing to the potential inaccuracy of self-reported anthropometric measures, women’s eligibility, in terms of having a BMI of ≥ 25 kg/m2, was confirmed during the baseline visit by the researcher, prior to the collection of baseline data. All other inclusion and exclusion criteria were based on self-reported information. Women screened as ineligible were informed and thanked for their interest and time.
Sample size
There is no consensus on the optimal sample size for pilot RCTs; however, the literature143,144 suggests that, when the objective is to estimate the standard deviation (SD) with sufficient precision (to minimise the number of trial patients included in both the pilot and the main study), a sample size of at least 50 participants per group is advisable. Therefore, the target sample size for the present study was 100 participants. A sample of this size would allow a sufficiently precise estimate of the recruitment rate with 95% CIs for the true recruitment rate within ±10%. The sample size of 50 participants in each group would allow a sufficiently precise estimate of the retention rate with 95% CIs for the true proportion retained, likely, at least, to be within ±15%. The pilot RCT would, thus, provide data on both attrition and primary end point variability to inform the sample size for the full RCT, which will be based on weight-related outcomes (weight loss and weight loss maintenance).
Informed consent
Written informed consent was obtained from all women, prior to randomisation, during home visits at baseline. A copy of the participant consent form is included on the project web page (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). Women were made aware of what the study involved and that they could withdraw from the research at any time without having to give a reason for doing so. They were also given the opportunity to ask questions before providing their written consent. A letter was sent to each participant’s GP, with the participant’s permission, to inform the GP of their patient’s involvement in the study and what the study entailed (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020).
Randomisation
Baseline assessments were conducted prior to randomisation. Eligible women were randomised to one of two groups using a block randomisation approach. Randomisation was carried out independently via a secure remote web-based system that was linked directly with the SMS delivery platform hosted by the London School of Hygiene & Tropical Medicine (LSHTM). Participants became aware of their group allocation at the point when they started to receive the SMS messages.
Blinding
The researchers collecting outcome data had no access to the randomisation system and were blinded to treatment group. Participants were requested not to talk to the researcher about the study or their group allocation. It was intended that different researchers would conduct the face-to-face quantitative data collections and the qualitative interviews, as the latter would involve discussion of the SMS messages that the participant had received.
Study outcomes
The main study outcome was to assess the pilot RCT performance in relation to the predefined stop/go progression criteria for a full RCT. Stop/go criteria for proceeding to a full RCT were based on the following acceptability and feasibility outcomes:
-
acceptability of the intervention and active control (satisfaction rating, qualitative views, willingness to be randomised)
-
feasibility of recruitment – successful recruitment: at least 80% of pilot RCT target (i.e. at least n = 80) and participants recruited from across the socioeconomic spectrum
-
retention rate consistent with, or superior to, other weight loss interventions in overweight and obese postpartum women (at least 65% in the intervention group and 60% in the control group56,123,124)
-
no evidence of substantial, differential attrition between the intervention and active control groups; this was defined as a difference in attrition rate between groups of > 20%
-
evidence of positive indicative effects of the intervention – change in anthropometric measures over time.
Quantitative and qualitative data were used to assess outcomes. The pilot RCT research questions and associated progression criteria, and details of the data that were used to address these research questions, are summarised in Table 5.
| Research questions | Progression criteria | Data source | Data examined | Process evaluation component |
|---|---|---|---|---|
| 1. Was it feasible to recruit participants to the study? | Feasibility of recruitment: successful recruitment – at least 80% of pilot RCT target (i.e. at least n = 80) across the socioeconomic spectrum |
|
|
|
| 2. Was the recruitment strategy appropriate? | ||||
| 3. Was the retention rate acceptable? | Retention rate consistent with, or superior to, other weight loss interventions in overweight or obese postpartum women (i.e. at least 65% in the intervention group and 60% in the control group56,123,124) |
|
|
|
| 4. What sample size would be required in a full RCT? |
|
|
|
|
What are the views of women regarding the acceptability and perceived benefits of the:
|
Acceptability of the intervention and active control |
|
|
|
| 7. What are the indicative effects of the intervention on weight loss and weight loss maintenance? | Evidence of positive indicative effects: change in anthropometric measures over time |
|
|
|
| 8. Can data for the proposed end points be successfully collected? |
|
Data examined for:
|
|
|
| 9. Can all components of the trial be successfully delivered? |
|
|
|
|
| 10. What fine-tuning of the intervention content or delivery is required for a full RCT? |
|
|
Quantitative data collection process
Quantitative data collection during delivery of the 12-month intervention took place at baseline and at 3, 6, 9 and 12 months. A database was used to manage the timetable of visit due dates. Women were contacted by the research team via SMS between 1 and 2 weeks in advance of their follow-up due date to arrange a suitable time to complete the data collection visit. Three attempts were made to contact women by SMS to arrange the follow-up appointments. If no response was received, a letter was posted to the participant’s home address to let her know that the research team were trying to contact her to arrange her next appointment and if she no longer wished to take part to let the research team know, otherwise she would be contacted again when her next follow-up was due (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020).
Women were offered a preferred choice of location for the baseline and outcome data collection visits, including home visits by a member of the research team, or meeting in the QUB research centre or the woman’s place of work. This choice was offered in recognition of the difficulties postpartum women may face in attending data collection appointments. A reminder SMS message was sent out 1 day before the arranged appointment that offered women the chance to rearrange the appointment if it no longer suited them. When a home visit was made at the arranged time and the woman was not available, an attempt was made to rearrange this appointment. Steps were taken to ensure the safety of the researchers while they were conducting visits to participants’ homes. The clerical assistant working on the study was made aware of the arrangements for study visits. The researcher conducting the visit would send a text message to the clerical assistant (or principal investigator if the clerical assistant was absent) when she had arrived at the participant’s home. The researcher would send another message to confirm when she had safely left. If no confirmation message had been received 1 hour after the scheduled appointment time, the clerical assistant was to ring the researcher and follow local standard operating procedures for lone working and reporting safety concerns, if required.
An overview of the data collected by the researcher at each time point is shown in Table 6. Researcher-administered anthropometric measurements, blood pressure (BP) and information on demographics and characteristics of the participants were recorded on case report forms (CRFs) (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). Height (shoes removed) was measured to the nearest 0.1 cm using a portable stadiometer. Weight (shoes and heavy clothing removed) was measured to the nearest 0.1 kg using calibrated digital scales. These measurements were used to calculate BMI [weight (kg) ÷ height2 (m2)] at each time point. Waist circumference (excess clothing removed) was measured to the nearest 0.5 cm using the Seca 201 ergonomic circumference measuring tape (Seca GmbH & Co. KG, Hamburg, Germany). BP was measured three times in the right arm using an automated Omron M3 Sphygmomanometer (Omron Corporation, Kyoto, Japan). Participants were asked to sit quietly for 5 minutes before the measurements were started, and were given an additional 2 minutes of rest between each measurement. The mean values of the second and third systolic and diastolic BP measurements were recorded. If a woman’s BP measurements were high (systolic BP of > 140 mmHg or diastolic BP of > 90 mmHg), she was informed that a letter would be sent to her GP (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020).
| Measure collected | Time point | ||||
|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 9 months | 12 months | |
| Height (m) | ✓ | ||||
| Weight (kg) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Waist circumference (cm) | ✓ | ✓ | ✓ | ✓ | ✓ |
| BP (mmHg) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Demographic and participant characteristics, including date of birth, ethnicity, employment, education, income, marital status, parity, infant feeding, weight history, smoking status, alcohol intake, medical information and technology usage | ✓ | ||||
Self-report questionnaires were used to collect data on other study outcomes (Table 7). After initial development of this questionnaire, completion of it was pilot-tested by three women who had recently had a baby (two women from the PPI group and one woman who was a friend of a member of the research team). Feedback from this process suggested that the questionnaire was easy to understand and complete; however, all three women felt that it was too long. Therefore, several of the scales that had been included were removed (measures of perceived stress, weight self-efficacy and behaviour change satisfaction), shortened (social support for diet and physical activity, and body image satisfaction) or replaced (shorter measure of physical activity). It was also noticed that one of the health economics outcome measures, ICEpop CAPability measure for Adults (ICECAP-A) (see Table 7), had been omitted by mistake, so it was added to the final versions of the questionnaires. Full copies of the study questionnaire booklets can be found at www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/ (accessed 27 January 2020).
| Study end point | Measure used | Time point (months) |
|---|---|---|
| Feasibility and acceptability outcomes | ||
| Satisfaction with SMS messages | Study-specific questions | 0, 3, 6, 9, 12 |
| Acceptability of intervention, active control and study methods | Study-specific questions | 12 |
| Economic evaluation | ||
| Within trial health and social care cost data | ||
| Health service resources use | Questions on health resource usage (e.g. GP, hospitalisations and prescription medicines) | 0, 3, 6, 9, 12 |
| Medication usage | Questions on over-the-counter medications | 0, 3, 6, 9, 12 |
| Healthy lifestyle-related costs | Questions on personal expenditure on healthy lifestyle | |
| Exercise-related costs | Questions on costs of exercise (e.g. gym, fitness/health applications and average time spent exercising/walking daily) | 0, 3, 6, 9, 12 |
| Food and drink costs | Questions on weekly cost of groceries (i.e. healthy eating may cost more), alcohol and smoking products | 0, 3, 6, 9, 12 |
| Outcome measures | ||
| Health-related quality of life | EQ-5D-5L (including visual analogue scale)145 | 0, 3, 6, 9, 12 |
| Capability well-being | ICECAP-A146,147 | 0, 3, 6, 9, 12 |
| Effectiveness evaluation | ||
| Outcome measures | ||
| Dietary intake | Fat and fibre barometer148 | 0, 3, 6, 9, 12 |
| Physical activity | IPAQ-SF,149 pedometer step count and diary | 0, 3, 6, 9, 12 |
| Sugar intake | Study-specific questions | 0, 3, 6, 9, 12 |
| Alcohol consumption | Study-specific questions | 0, 3, 6, 9, 12 |
| Infant feeding | Infant feeding survey150 | 0, 3, 6, 9, 12 |
| Mental health | EPDS151 | 0, 3, 6, 9, 12 |
| Body image satisfaction | Body areas satisfaction and self-classified weight scales of the MBSRQ152 | 0, 3, 6, 9, 12 |
| Confidence/importance/desire for weight loss and weight loss maintenance | Study-specific questions | 0, 3, 6, 9, 12 |
| Mediators of intervention effect | ||
| Habit formation and automaticity of behaviours | Self-report habit index (four items)153 | 0, 3, 6, 9, 12 |
| Intention and self-efficacy for diet and physical activity | HAPA154 and action and coping self-efficacy155 | 0, 3, 6, 9, 12 |
| Self-regulation | Self-regulation of eating behaviour questionnaire156 | 0, 3, 6, 9, 12 |
| Social support | Social support for eating and social support for exercise scales (three items)157 | 0, 3, 6, 9, 12 |
| Goal-setting for diet and exercise | Study-specific questions | 0, 3, 6, 9, 12 |
| Weight self-monitoring | Study-specific questions | 0, 3, 6, 9, 12 |
| Weight loss motivation | Motivation for weight loss scale158 | 0, 3, 6, 9, 12 |
| Dietary and exercise monitoring | Study-specific questions | 0, 3, 6, 9, 12 |
| Self-esteem | Rosenberg Self-Esteem Scale159 | 0, 3, 6, 9, 12 |
| Sleep | Pittsburgh Sleep Quality Index160 | 0, 3, 6, 9, 12 |
| Weight loss programme engagement | Study-specific questions | 0, 3, 6, 9, 12 |
At each study visit, the questionnaire booklet was given to the participant and they were asked to complete it within 1 week and post it back to the research team in the self-addressed prepaid envelope provided to them. Participants also received a sealed pedometer [Digi-walker™ CW-701 series (Yamax Ltd, Bridgnorth, UK) with the screen taped so participants could not view their step count] and a pedometer diary at each study visit. Women were asked to wear the pedometer for 7 days and to use the pedometer diary (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020) to record the times it was worn along with any issues of note in relation to wearing the pedometer, for example forgot to wear or forgot to put on after having a shower. Participants were sent a reminder SMS message on their last day of wearing the pedometer to ask them to post it back in the addressed prepaid envelope that they were provided with and also a reminder to return the questionnaire booklet if it had not yet been received.
To maximise completion of study assessments at each study time point, participants in both groups were offered a £20 One4All shopping voucher (GVS Gift Voucher Shop Ltd, Hemel Hempstead, UK; www.one4all.com/) for each study visit completed as a thank-you for their time and effort. This was posted to the participant once the completed questionnaire and pedometer were received.
Data on proposed study end points
The pilot RCT tested the data collection methods that would be used in a full RCT that could allow an effectiveness and cost-effectiveness evaluation (if stop/go criteria were met) of the Supporting MumS intervention, including measuring mediators and moderators of the intervention effect. The proposed study end points and how and when these were measured are detailed in Table 7. Validated scales were used when possible.
To capture data related to mental health, the Edinburgh Postnatal Depression Scale (EPDS)151 was used. The maximum score on this measure is 30; referral to a health professional is recommended if a respondent scores ≥ 9, and a score of ≥ 13 is indicative of postnatal depression. When participants provided consent, they were informed that the information would be passed to their GP should this happen. Scores were calculated by the research team after the follow-up visit and a letter was sent to the participant and their GP to inform them of scores of ≥ 9 (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020).
Data entry and cleaning
Case report forms and baseline questionnaire data were entered into a Microsoft Access® (Microsoft Corporation, Redmond, WA, USA) database by the study administrator, then exported to Microsoft Excel® (Microsoft Corporation) spreadsheets. An online data entry platform (Qualtrics; Qualtrics International Ltd, Provo, UT and Seattle, WA, USA; www.qualtrics.com/uk/) was used to enter the questionnaire data for all other time points. Data entry into Qualtrics was completed by the study administrator, research project students and the study postdoctoral researcher. The data were exported from the Qualtrics system into Microsoft Excel spreadsheets. A quality control check of 10% of all data entries was conducted and queries resolved when necessary.
Economic evaluation
In line with the UK’s NICE guidance for public health economic evaluations,161 the economic evaluation was conducted from a NHS and Personal Social Services perspective, but with an additional societal perspective applied to capture the broader impact. These health and personal perspectives can help to investigate the broader impact of the intervention, including the direct cost to participants and indirect costs. As recommended by the NICE public health methods guidelines,161 both costs and health outcomes are to be discounted at the same annual rate of 1.5%. The assessment of within-trial health care, social care and personal resource use data and outcomes measures in economic evaluation were previously detailed (see Table 7).
Process evaluation
In line with MRC guidance,105,106 and the aim of the pilot RCT, a process evaluation was performed to examine fidelity, acceptability, dose, reach, recruitment, retention, contamination and context and test methods that would be used to assess mechanisms of impact in a full RCT.
The process evaluation was informed by both qualitative and quantitative data. The process evaluation framework summarises the issues examined as part of the process evaluation, along with the methods used (Table 8).
| Process evaluation component | Issues examined | Method |
|---|---|---|
| Fidelity | Fidelity of delivery |
|
| Fidelity of blinding | Researcher observations | |
| Acceptability | Acceptability and perceived benefits of intervention and active control |
|
| Acceptability and willingness to be randomised |
|
|
| Acceptability of study measures and trial procedures |
|
|
| Dose | Dose of intervention received |
|
| Reach | Who received the intervention | Baseline characteristics of the sample population |
| What intervention was received |
|
|
| Recruitment | Recruitment rates |
|
| Success of recruitment strategies | Study records | |
| Retention | Retention and attrition rates including pregnancy exclusion | Study records |
| Explanations of retention rates |
|
|
| Contamination | Awareness of intervention content by active control group participants | Participant interviews |
| Weight management services usage | Questionnaires | |
| Mechanisms of impact | Ability to measure theorised mediators of effect | Questionnaires |
| Context | Variability in indicative effects |
|
| Contextual factors impacting intervention delivery, receipt or effectiveness |
|
Qualitative data collection process
Qualitative data collection adopted a phenomenological approach whereby semistructured telephone interviews were used to explore participants’ experiences of taking part, including those randomised to the intervention and active control groups. The study progression criteria and process evaluation framework (see Tables 5 and 8) guided the research questions and the topics that the interviews were intended to explore. The semistructured nature of the interviews allowed participants to expand on subjects as they wished.
At baseline, all participants were asked for their consent to take part in telephone interviews with a researcher at months 3 and 12 (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). Women were advised that the interview was optional and that they could decide not to take part at any stage. During completion of the quantitative data collection visits at 3 and 12 months, those women who had provided their consent at baseline were asked by the researcher if they wanted to proceed with an interview. If willing, a preferred date and time to conduct the interview was arranged. Only women who participated in the quantitative data collection visits were approached for interview. When an interview had been arranged but the participant was unable to be contacted at the arranged time, one more attempt was made to contact the woman to rearrange the interview.
Telephone interviews were conducted by study researchers (CM, CR, AW, RON; for details on the credentials of these researchers, see Contributions of authors). Caroline McGirr and Ciara Rooney were known to some of the women as they had been involved in study recruitment and home visits for quantitative data collection. This may have allowed a rapport to be developed easily, but may also have led participants to give more positive responses when evaluating the intervention and active control.
Researchers were based in quiet and private rooms in the Centre for Public Health, QUB. Participants were contacted at the arranged time and a verbal introduction to the interview was provided that detailed the purpose of the interviews, how the data would be collected and transcribed and how confidentiality would be maintained. Women were advised that they were free to skip any questions that they preferred not to answer and that the interview could be stopped at any time. They were then asked to provide verbal consent to proceed with the interview.
Semistructured interview schedules appropriate for each time point and each group were developed and agreed on by the research team. Full copies of the interview schedules are included on the project web page (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). Interviews conducted at 3 months focused on women’s initial acceptability of taking part, including their views about the content, clarity, relevance and personalisation of the SMS messages, their motivations for taking part and their satisfaction with the randomisation process and group allocation, their opinions on the recruitment and study methods and research instruments, any unintended consequences of the intervention such as adverse effects on health or well-being, and any perceived benefits or shortcomings of the intervention and active control messages. Following the 3-month interviews, and based on experience, some additional questions were added to the 12-month interview schedule to address topics of interest that had not yet been explored. However, the 12-month interview schedule was not changed once the interviews commenced. Interviews at 12-months explored the same topics as those examined at 3 months to determine any changes in attitudes over time.
The first two interviews completed were used to pilot the interview schedule with the potential to disregard data if major issues were identified. However, no major difficulties were found in using the question schedule; therefore, the data from these interviews were retained. The researchers used the relevant topic guide to direct the interview towards discussion of topics of interest, but allowed participants to expand on issues relevant to the intervention or active control as they wished. Probes were used to encourage women to elaborate short responses and the researchers provided clarification for any questions that were unclear. Furthermore, prior to bringing the discussion to a close, women were asked if there was anything else of importance to discuss that had not yet been captured during the interview. No repeat interviews were conducted.
Interviews were audio-recorded using a portable recording device. Audio files were transferred to secure password-protected computer servers, then deleted from the recording device. Audio files were transcribed verbatim by external transcription services.
As the population of women eligible for interview was limited to those who had taken part in the trial and were still enrolled, qualitative data collection did not aim to achieve data saturation. Rather, all eligible and willing women were interviewed to capture all available views in relation to evaluating the intervention, active control and study methods. In total, 70 women (intervention: n = 35; active control: n = 35) were interviewed at 3 months and 37 women (intervention: n = 16; active control: n = 21) were interviewed at 12 months (see Chapter 4).
Assessing intervention engagement
A description of the interactive components of the intervention and the methods by which engagement with the intervention was assessed are shown in Table 9. Engagement data were obtained from the LSHTM SMS delivery platform, which recorded all of the replies received from each participant for the duration of the intervention, including date, time and message content. Raw data, stored by randomisation identifier, were transferred from the LSHTM-based platform to a study database in QUB and matched to a three-digit participant identifier. Data were organised according to the relevant intervention component. If women withdrew or had to stop because they became pregnant, their engagement data were used until the time they withdrew/stopped.
| Interactive component | Description of interactive component | How engagement was assessed |
|---|---|---|
| Weekly weight prompt |
|
|
| ‘Yes/no’ questions | Participants received a SMS asking them a question and asking them to reply ‘yes’ or ‘no’. Twenty ‘yes/no’ messages were sent between months 0 and 6, and 16 ‘yes/no’ messages were sent between months 7 and 12. Participants were instructed to reply in a specific format according to the question sequence, e.g. ‘Y1’ or ‘N1’, then, for the next message, ‘Y2’, ‘N2’ etc. |
|
| Trigger words | Participants could text trigger words and receive a supportive message in return. The four trigger words were: ‘Bad day’, ‘Crave’, ‘Exhausted’ and ‘Slip-up’ |
|
| Additional SMS/response to core messages | A number of other messages were received by the server. Some were spontaneous, others were in response to core messages that asked rhetorical questions or to ‘text us’ a reply |
|
| Discussion forum | An online discussion forum where participants could post anonymously and engage with other participants |
|
| Buddy system | Participants could nominate a family member or friend to receive the same core messages as them, for support and engagement, by texting ‘SUPPORT’ followed by a mobile number |
|
Weight SMS messages and ‘yes/no’ questions
These features have been previously described in Chapter 2.
The raw data obtained from the SMS delivery platform were manipulated to assess a number of parameters:
-
To count the number of replies to the initial message, sent on day 7 of the intervention, asking participants to text their goal weight, that is the weigh that they would like to be in 6 months.
-
To allow checks on the fidelity of sending the weekly weight SMS message and the ‘yes/no’ questions using date of randomisation and Excel formulae to calculate scheduled delivery date and check this against messages actually sent. Across the core messages, 36 SMS messages asked the participant a question and requested a response to be sent in the form of ‘Y1’ or ‘N1’ (with the number corresponding to an automated response specific to that question), for example ‘Have you tried to lose weight before? Text Y1 for “Yes” or N1 for “No”.’ In total, women were due to receive a SMS message prompting them to weigh themselves 50 times over the course of the 12 months of intervention delivery.
-
To examine engagement with the weight SMS message, raw data on weight replies received from each participant were extracted, including if they replied, what they replied, if they replied in the correct format (this was important because for weeks 25–52, participants were instructed to reply with their weight and UP’, ‘DOWN’, or ‘SAME’ according to how their weight had changed since the previous week, which triggered an automated reply), and if they included additional information in their message. Total weight-prompting SMS messages sent and total weight replies received were calculated for each participant for weeks 1–24 (weight loss phase) and 25–51 (weight loss maintenance phase), and weight SMS messages were expressed as a percentage of the total number of SMS messages that were sent.
-
To examine engagement with the ‘yes/no’ questions – the same process as for the weight SMS messages, as described in the previous point, was followed.
-
For women who withdrew or had to stop because they became pregnant, their engagement data were used until the time they withdrew/stopped, and engagement with weight and ‘yes/no’ responding was expressed as a percentage of the total number of SMS messages they were sent.
-
Fidelity of automated replies to the weight ‘UP’/‘DOWN’/‘SAME’ and ‘yes/no’ questions was examined by viewing messages sent by women and system replies.
Trigger words
The total number of trigger words used by each participant along with the date they were sent was recorded, and the fidelity of automated replies to the trigger words was checked.
Spontaneous texts
The total number of spontaneous messages received for each participant was recorded. These were checked to identify if they were truly spontaneous or were in response to a rhetorical question in the core message sent, for example ‘Out with the old and in with the new! Think back to the start of SMS. What new habits have you formed? Text us! E.g. “more fruit”, “eat breakfast” etc.’.
Buddy system
Details of any participant using the buddy system were recorded, along with the date the participant requested this support.
Discussion forum
The number of participants using the forum and the number of posts to the discussion forum were recorded.
Statistical analysis
Quantitative data analysis
Statistical analyses were largely descriptive. The eligibility, recruitment, retention and pregnancy exclusion rates for the sample were described using a Consolidated Standards of Reporting Trials (CONSORT)162 flow chart. Binomial exact 95% CIs were calculated for retention proportions. Baseline characteristics of the recruited samples (total study sample and interview samples) were summarised and tabulated by trial arm, as well as for responders and non-responders at final follow-up. To examine the success of collecting data on proposed study end points, the percentage of completeness for returned questionnaires and missing values for each outcome measure at baseline and at 12 months’ follow-up were reported. Summaries of anthropometric measures (weight and waist circumference) by trial arm were presented. Continuous variables were summarised using the mean and SD or median and interquartile range (IQR) for skewed distribution. Categorical variables were summarised using the percentage in each category. Exploratory effectiveness analyses using analysis of covariance and logistic regression models were conducted to examine the indicative effects of the intervention on anthropometric outcomes (including weight change between baseline and 3 months, between baseline and 6 months, between baseline and 9 months, between baseline and 12 months, between 3 and 6 months, between 6 and 9 months and between 9 and 12 months, adjusted for baseline weight; the proportion of women losing ≥ 5 kg or 5% of body weight; the proportion of women gaining ≥ 5 kg or 5% of body weight; and waist circumference change between baseline and 3 months, between baseline and 6 months, between baseline and 9 months, between baseline and 12 months, between 3 and 6 months, between 6 and 9 months and between 9 and 12 months, adjusted for baseline measurements). The analysis of these anthropometric outcomes excluded missing cases. Intention-to-treat analyses of weight change between baseline and 12 months imputed weight data for non-responders at 12 months’ follow-up using the last observation carried forward (LOCF) and baseline observation carried forward (BOCF) methods. Hypothesis testing was not included as the study was not powered to provide definitive results on effectiveness, but indicative intervention effects with 95% CIs were reported. Statistical Product and Service Solutions (SPSS) software version 22.0 (IBM Corporation, Armonk, NY, USA) was used to support statistical analysis.
The analysis of engagement data was completed using SPSS version 25.0. Data were analysed descriptively as for the other quantitative variables above. The percentage engagement with the weight prompts and ‘yes/no’ SMS messages at 3, 6 and 12 months were calculated for each participant. Participants were classified as ‘high’ or ‘low’ engagers using the median cut-off point: participants with replies to weight prompts or ‘yes/no’ messages less than or equal to the median at each time point were considered to be ‘low’ engagers, participants with replies greater than the median were considered to be ‘high’ engagers. This is similar to the method used in the Motivated Mums programme,163 and a more simplified method than that adopted in the Growing Healthy study. 164 Baseline sociodemographic characteristics and changes in weight, BMI and waist circumference from baseline to month 12 for high and low engagers were analysed using independent samples t-tests (exploratory analysis of indicative effects only). Proportions of high/low engagers losing ≥ 5 kg or gaining ≥ 5 kg were also assessed. Examining weight gain or loss relative to the threshold of 5 kg was of interest to understand what proportion of participants experienced substantial loss or gain in weight of a magnitude that could affect health risks and was relevant to the thresholds for substantial postpartum weight retention examined in other studies. 20,25,28
Economic data analysis
For the purpose of the pilot study, a full cost-effectiveness analysis (CEA) was not conducted. However, one will be conducted if taken forward to a full RCT. To examine the success of collecting data that would be used in a CEA in a full RCT, the percentage of completeness for returned questionnaires was calculated and the missing values for resource use, personal costs and economic outcome measures were recorded at baseline and at all follow-up time points.
Qualitative data analysis
Thematic analysis was used to analyse the qualitative data. Caroline McGirr and Dunla Gallagher started by reading transcripts to check the accuracy and anonymisation of the transcription and to familiarise themselves with the data. Interviewees were not asked to check the transcripts. Caroline McGirr, Dunla Gallagher and Michelle C McKinley met as a working group and, together, coded four interviews. An early visual thematic map was developed to organise the generated codes. For the purposes of this report, to examine feasibility and acceptability outcomes, a deductive coding framework was developed to allow mapping of the qualitative data against the study research questions and progression criteria (see Tables 5 and 8). Interviews were coded and categorised according to predetermined themes based on the study objectives (e.g. perceived benefits of the intervention), while allowing flexibility for unexpected findings to be added to the coding framework (e.g. unintended consequences).
Caroline McGirr and Dunla Gallagher independently coded 50% of the remaining transcripts and carried out extensive discussion throughout the analysis process to achieve agreement and reliability of the findings. Each researcher coded six transcripts; then they met to discuss their interpretations of concepts and to achieve consensus on how to code content. Suggested changes to the coding framework were agreed on and any disagreements discussed with Michelle C McKinley until a decision was reached. Detailed notes of analytic discussions were documented so that decisions remained transparent. This process was repeated until all of the data had been analysed and a final coding framework was produced. Interviewees were not asked to check the study findings. Thematic analysis was supported by NVivo software version 12.0 (QSR International, Warrington, UK).
The data were presented using quotations from participants to reflect themes and subthemes. Where quotes are presented (see Chapter 4), the respondent’s name has been omitted, but their three-digit participant identifier, along with their allocated group and the time point of the interview, have been included to describe the sources of quotations.
Changes to the protocol
There were no changes to the study protocol. A 4-month, no-cost extension was requested towards the end of the study owing to staffing changes in the research team.
Chapter 4 Results
This chapter presents the results of the study, which are organised according to the research questions for the pilot RCT (see Table 5). The relevant stop/go progression criteria are highlighted throughout this chapter.
Research question 1: was it feasible to recruit participants to the study?
The CONSORT flow diagram, Figure 4, details the recruitment, randomisation and follow-up of participants in the pilot RCT. In total, 100 women were recruited and randomised (intervention, n = 51; active control, n = 49) to the pilot RCT between February and June 2017. The recruitment progression criterion, and how it was met, is outlined in Box 1.
FIGURE 4.
The CONSORT flow diagram of the Supporting MumS pilot RCT.
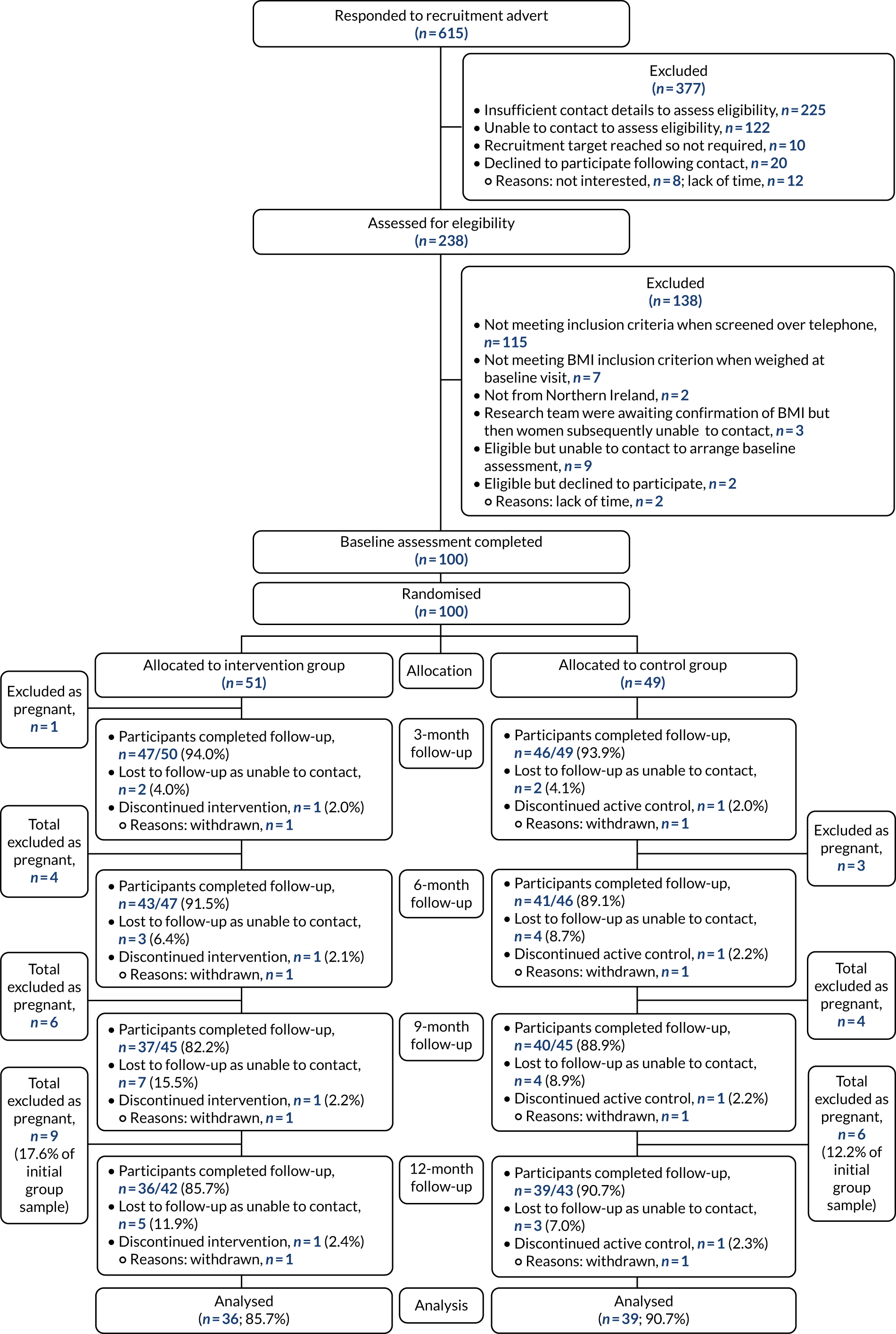
The study successfully recruited 100% of the target sample, thus meeting the progression criterion for a full RCT. Recruitment took 1 month longer than anticipated (5 months rather than 4 months).
Criterion met: yes.
The completion of the telephone screening procedure, used to determine a woman’s eligibility to take part in the study, led to the exclusion of 117 women. Of these, 115 women were excluded as, based on self-reported information, they did not meet the inclusion criteria. The remaining two women were excluded as they did not reside in the study area. Based on self-reported weight, a further seven women went ahead with a baseline visit, but subsequently had to be excluded when their weight (and calculated BMI), as measured by the researcher, were found to be below the inclusion threshold.
Research question 2: was the recruitment strategy appropriate?
Details of the recruitment strategies employed, the number of women recruited and the time taken to recruit using each strategy are shown in Table 10. Recruitment focused on community settings, such as in-person visits to mother and toddler groups and breastfeeding support groups, alongside displaying information about the study in places such as libraries and health centres and using social media to promote the study. Other planned recruitment strategies were not used extensively as the target sample size had been reached. These other strategies included disseminating information through the QUB staff newsletter, placing an advert in the NI4Kids newsletter and local shopping centres or targeting a greater number of health centres. The research team were unable to engage health visitors to use child immunisation appointments as a recruitment strategy.
| Recruitment strategies | Number of venues willing to be recruited (number of venues contacted) | Women recruited (n) | Effort and estimated total time required | Estimated time (hours) to recruit one participant |
|---|---|---|---|---|
| Social mediaa | 10 (19) | 67 |
|
0.25 |
| Word of mouth | N/A | 14 | N/A | N/A |
| Mother and toddler groups | 51 (121)b | 12 |
|
8.25 |
| Library | 21 (21)c | 5 |
|
8 |
| Breastfeeding group | 5 (8) | 2 |
|
5 |
| Health centres | 2 (2) | 0 | Create list of contact details then send e-mail and post materials: 16 hours | N/A |
| Pharmacies | 6 (6) | 0 | Travel and deliver materials to pharmacy: 0.5 hours | N/A |
| Nurseries | 11 (11) | 0 |
|
N/A |
| Soft play areas | 1 (3) | 0 | Visit to see managers: 2 hours | N/A |
| Health fair | 1 (1) | 0 | Attend health fair and organise contact: 8 hours | N/A |
The largest proportion of women were recruited through social media (67%), followed by word of mouth (14%), mother and toddler groups (12%), libraries (5%) and breastfeeding groups (2%).
There were some challenges in recruiting via community groups. The numbers of women attending community groups varied widely, from approximately 4 to 24, depending on the area, and some women attended multiple groups in an area, thereby reducing the overall number of women reached. In addition, many of the adults attending groups with children were grandparents or childminders, rather than the target population. These caregivers were still informed about the study and were asked to pass on the leaflet to the child’s mother. However, given the weight-related criterion required for study entry, it may have been difficult for a third-party person to pass on the information or leaflet to the child’s mother, if that person was afraid of causing offence.
Alongside face-to-face recruitment, social media was employed, using Facebook advertising for 1 month, in tandem with one Sure Start group leader posting on their Sure Start Facebook group page. Two-thirds of participants were recruited by these means. In particular, after a researcher attended a Sure Start group that no one came to, the Sure Start leader shared the study poster on their Sure Start Facebook group page along with a comment to highlight the opportunity to receive £100 vouchers for taking part. The Facebook post was ‘liked’ 104 times, ‘shared’ 233 times and there were 365 comments in which recipients had ‘tagged’ others so that they would see the post. The text comments provided by recipients indicated that offering this monetary incentive motivated some of them to contact the research team to enquire further about the study and, potentially, sign up.
Time taken to recruit participants
The time taken to recruit one participant was calculated for each recruitment strategy (see Table 10). Each woman who responded to the study adverts (n = 615) was e-mailed the information leaflet or sent a text requesting further contact details. A total of 238 women were subsequently contacted by telephone to screen for eligibility and, if appropriate, a baseline visit was arranged; each telephone call lasted approximately 15 minutes. Further contact with a woman may have been required where the researcher had to delay recruitment in order to discuss queries regarding a woman’s eligibility with the wider research team, then make further contact. Therefore, it was estimated that it took 70 hours to complete all screening assessments, including leaving voicemail messages and re-contacting participants who were not available.
Characteristics of the populations recruited according to recruitment strategy
The summary characteristics of the populations recruited via each method are presented in Table 11. Overall, there were no notable differences in the characteristics of women recruited using different approaches, with the exception of women recruited from breastfeeding groups. Two women were recruited this way and both were married, employed and in the highest education and income bracket.
| Characteristic | Social media (N = 67) | Word of mouth (N = 14) | Mother and toddler groups (N = 12) | Library (N = 5) | Breastfeeding groups (N = 2) |
|---|---|---|---|---|---|
| Age at baseline (years) | |||||
| Mean (SD) | 32.7 (45) | 29.6 (3.7) | 34.7 (2.6) | 32.8 (3.0) | 33 (2.8) |
| Employment status, n (%) | |||||
| Full time | 36 (53.7) | 9 (64.3) | 4 (33.3) | 4 (80.0) | 2 (100) |
| Part time | 16 (23.9) | 3 (21.4) | 7 (58.3) | 1 (20) | 0 (0) |
| Self-employed | 4 (6) | 1 (7.1) | 0 (0) | 0 (0) | 0 (0) |
| Unemployed | 11 (16.4) | 1 (7.1) | 1 (8.3) | 0 (0) | 0 (0) |
| Household income (£), n (%) | |||||
| < 14,999 | 5 (7.5) | 1 (7.1) | 0 (0) | 0 (0) | 0 (0) |
| 15,000–29,999 | 13 (19.4) | 4 (28.6) | 4 (33.3) | 1 (20) | 0 (0) |
| 30,000–49,999 | 27 (40.3) | 6 (42.9) | 3 (25.0) | 2 (40) | 0 (0) |
| ≥ 50,000 | 22 (32.8) | 3 (21.4) | 5 (41.7) | 2 (40) | 2 (100) |
| Average household income (%) | |||||
| Income < £29,000 | 26.9 | 35.7 | 33.3 | 20 | 0 |
| Education, n (%) | |||||
| University level | 44 (65.7) | 9 (64.3) | 7 (58.3) | 3 (60.0) | 2 (100) |
| A levels/further education | 20 (29.9) | 4 (28.6) | 4 (33.3) | 2 (40.0) | 0 (0) |
| GCSE level or below | 3 (4.5) | 1 (7.1) | 1 (8.3) | 0 (0) | 0 (0) |
| Marital status, n (%) | |||||
| Single | 8 (11.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Married/civil partnership | 52 (77.6) | 9 (64.3) | 12 (100) | 5 (100) | 2 (100) |
| Living with partner | 7 (10.4) | 5 (35.7) | 0 (0) | 0 (0) | 0 (0) |
| Weeks postpartum | |||||
| Mean (SD) | 44 (32.1) | 31.1 (23.1) | 32.9 (24.6) | 45.5 (26.8) | 14 (7.5) |
Characteristics of the recruited population at baseline
Descriptive statistics summarising the baseline characteristics of the recruited population according to randomised group were tabulated (Table 12). Although the recruitment strategies targeted venues based in Belfast and Co. Tyrone, the women recruited were located across all six counties in Northern Ireland. The majority of those recruited were located in Co. Antrim (56%) and Co. Down (19%), but another 11% of participants lived in Co. Tyrone, 8% in Co. Armagh, 5% in Co. Derry/Londonderry and 1% in Co. Fermanagh. The sample ranged in age between 22 and 44 years, with an average age of 32.5 years, and 99% were of white ethnicity. Nearly half (48%) of the women recruited were < 6 months postpartum, a further 22% were 6–12 months postpartum and 30% were between 12 and 24 months postpartum. The majority of the sample were married or living with a partner (92%) and 42% were first-time mothers. Most participants were employed (87%), 65% were educated to degree level and 28% of the sample had a household income of < £30,000. The intervention and active control groups were comparable in terms of these characteristics.
| Characteristic | Intervention (N = 51) | Active control (N = 49) | Overall (N = 100) |
|---|---|---|---|
| Age at baseline (years) | |||
| Mean (SD) | 32.8 (3.8) | 32.2 (4.7) | 32.5 (4.3) |
| Range | 24–40 | 22–44 | 22–44 |
| Ethnicity, n (%) | |||
| White | 51 (100) | 48 (98.0) | 99 (99.0) |
| Other | 0 (0) | 1 (2) | 1 (1) |
| Employment status, n (%) | |||
| Full time | 33 (64.7) | 22 (44.9) | 55 (55.0) |
| Part time | 12 (23.5) | 15 (30.6) | 28 (28.0) |
| Self-employed | 0 (0) | 5 (10.2) | 5 (5.0) |
| Unemployed | 6 (11.8) | 7 (14.3) | 13 (13.0) |
| Household income (£), n (%) | |||
| < 14,999 | 4 (7.8) | 2 (4.1) | 6 (6.0) |
| 15,000–29,999 | 9 (17.6) | 13 (26.5) | 22 (22.0) |
| 30,000–49,999 | 20 (39.2) | 18 (36.7) | 38 (38.0) |
| ≥ 50,000 | 18 (35.3) | 16 (32.7) | 34 (34.0) |
| Education, n (%) | |||
| Postgraduate degree | 17 (33.3) | 11 (22.4) | 28 (28.0) |
| Undergraduate degree | 17 (33.3) | 20 (40.8) | 37 (37.0) |
| Further education | 13 (25.5) | 9 (18.4) | 22 (22.0) |
| A levels | 2 (3.9) | 6 (12.2) | 8 (8.0) |
| O levels/GCSEs | 2 (3.9) | 2 (4.1) | 4 (4.0) |
| Primary school | 0 (0) | 1 (2.0) | 1 (1.0) |
| Marital status, n (%) | |||
| Single | 3 (5.9) | 5 (10.2) | 8 (8.0) |
| Married/civil partnership | 45 (88.2) | 35 (71.4) | 80 (80.0) |
| Living with partner | 3 (5.9) | 9 (18.4) | 12 (12.0) |
| Body composition | |||
| BMI (kg/m2) | |||
| Median (IQR) | 30.7 (27.6–33.2) | 31.3 (27.6–34.7) | 31.2 (27.6–33.3) |
| Range | 25.4–42.6 | 25.4–50.4 | 25.4–50.4 |
| 25.0–29.9 kg/m2 (overweight), n (%) | 23 (45.1) | 23 (46.9) | 46 (46.0) |
| > 30.0 kg/m2 (obese), n (%) | 28 (54.9) | 26 (53.1) | 54 (54.0) |
| Weight (kg) | |||
| Median (IQR) | 82.0 (76.8–92.6) | 81.6 (73.7–91.0) | 81.8 (75.2–91.1) |
| Range | 60.8–115.4 | 61.6–141.5 | 60.8–141.5 |
| Waist circumference (cm), median (IQR) | 102.6 (98–108.8) | 102 (95.8–111.8) | 102.3 (97–110) |
| Self-reported pre-pregnancy weight (kg), median (IQR) | 73.0 (68.9–85.0) | 76.2 (68.3–86.8) | 76.2 (68.9–86.4) |
| Current smoker, n (%) | 0 (0) | 7 (14.3) | 7 (7) |
| Consumes alcohol, n (%) | 45 (88.2) | 39 (79.6) | 84 (84.0) |
| Parity, n (%) | |||
| One child | 19 (37.3) | 23 (46.9) | 42 (42.0) |
| Two children | 16 (31.4) | 16 (32.7) | 32 (32.0) |
| Three children | 14 (27.5) | 9 (18.4) | 23 (23.0) |
| Four children | 2 (3.9) | 1 (2.0) | 3 (3.0) |
| Postpartum opt-in time point at baseline (months postpartum), n (%) | |||
| < 6 | 22 (43.1) | 26 (53.1) | 48 (48.0) |
| 6–12 | 11 (21.6) | 11 (22.4) | 22 (22.0) |
| 12–18 | 6 (11.8) | 5 (10.2) | 11 (11.0) |
| 18–24 | 12 (23.5) | 7 (14.3) | 19 (19.0) |
| Health problems limiting physical activity, n (%) | 7 (13.7) | 8 (16.3) | 15 (15.0) |
| Currently part of a weight loss programme, n (%) | 15 (29.4) | 11 (22.4) | 26 (26.0) |
| Using a step counter at baseline, n (%) | 16 (32.0) | 17 (37.0) | 33 (34.0) |
| Self-weighing frequency, n (%) | |||
| Daily | 4 (8.0) | 6 (13.3) | 10 (11.1) |
| Weekly | 19 (38.0) | 18 (40.0) | 37 (38.0) |
| Never/rarely | 22 (44.0) | 11 (24.4) | 33 (36.7) |
| Frequency of consuming two portions of fruit daily, n (%) | |||
| Less than one day per week/never | 7 (14.0) | 8 (18.0) | 15 (16.0) |
| 1 or 2 days per week | 10 (20.0) | 14 (32.0) | 24 (25.5) |
| ≥ 3 days per week | 33 (65.6) | 22 (50.0) | 55 (58.5) |
| Daily portions of vegetables, n (%) | |||
| < 1 portion | 5 (10.0) | 8 (18.2) | 13 (13.8) |
| > 1.00 to < 2.99 portions | 30 (60.0) | 17 (38.6) | 47 (50.0) |
| > 3 portions | 15 (30.0) | 19 (43.2) | 34 (36.2) |
| Women who are very confident in their ability to lose weight at baseline, n (%) | 34 (68.0) | 32 (72.7) | 66 (70.2) |
| Women who are very confident in keeping weight off in the long term, n (%) | 22 (44.0) | 18 (41.0) | 40 (42.0) |
| Women getting < 5 hours of sleep per night, n (%) | 7 (14.0) | 2 (4.0) | 10 (10.5) |
| Letter sent to woman’s GP regarding EPDS score, n (%)a | 77 (34.0) | 19 (43.0) | 36 (38.0) |
Box 2 discusses the progression criterion related to recruiting across the socioeconomic spectrum.
The recruited sample included women from across the socioeconomic spectrum; however, the proportion of women in the lowest two income groups versus the highest two income groups was 28% versus 72%.
Criterion met: yes.
Research question 3: was the retention rate acceptable?
Of the 100 women who were recruited to the pilot RCT, 15 women became pregnant during the follow-up period and had to withdraw from the study, leaving a sample of 85 women (see Figure 4). Of the remaining 85 women, 75 (88.2%, 95% CI 79% to 94%) remained in the trial by the 12-month follow-up, with group-specific retention rates of 36 out of 42 (85.7%, 95% CI 71% to 95%) women in the intervention group and 39 out of 43 (90.7%, 95% CI 78% to 97%) women in the active control group. When pregnancies (n = 15), withdrawals (n = 2) and loss to follow-up (n = 8) are considered together, 75% of the 100 women who were randomised completed the 12-month follow-up.
Two women withdrew from the study, one from each group, and both withdrew before the 3-month follow-up. One of these women withdrew because of dissatisfaction with the study procedures being followed, as her GP was informed she had scored > 9 on the EPDS. In line with our duty of care to participants, the participant information sheet informed participants that the information they provided would remain confidential ‘unless there is a serious risk of harm to you or others’ (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). Therefore, if a woman scored > 9 on the EPDS, we informed her GP of the result, making it clear in the letter that the EPDS was a screening questionnaire and was not diagnostic of postnatal depression. Women gave consent for their GP to be informed of any medical issues detected during study visits; elevated BP was given as an example (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020). The trial procedures were reviewed when this participant withdrew from the study and, although the information sheet and consent form could not be amended as all women had been recruited, the procedure for informing a GP was amended to include sending a copy of the letter that was being sent to the GP (see www.journalslibrary.nihr.ac.uk/programmes/phr/146720/#/; accessed 27 January 2020) to the woman for her information, along with a copy of her consent form. No other complaints about this trial procedure were received; in fact, several women commented that they were grateful that the letter had been sent to their GP as it created an opportunity to have a conversation with their GP that they would not have initiated themselves. For a full RCT, the information sheet and consent form should be amended to make it clear to participants that their GP may be informed if there are concerns about physical or mental well-being.
The second woman withdrew from the study as she reported having limited time to participate. Eight women were unable to be contacted for follow-up at 12 months. The attrition rates between the randomised groups were comparable [intervention: n = 6 (14.3% withdrew/lost to follow-up); active control: n = 4 (9.3% withdrew/lost to follow-up)]. A comparison was made of the summary demographic and baseline characteristics for women who completed the 12-month follow-up and those who did not (Table 13).
| Characteristic | Completed the 12-month follow-up | |
|---|---|---|
| Yes (N = 75) | No (N = 10a) | |
| Age at baseline (years) | ||
| Mean (SD) | 32.6 (4.2) | 32.6 (5.3) |
| Range | 22–42 | 26–44 |
| Ethnicity, n (%) | ||
| White | 74 (98.7) | 10 (100) |
| Other | 1 (1.3) | 0 (0) |
| Employment status, n (%) | ||
| Full time | 41 (54.7) | 6 (60.0) |
| Part time | 22 (29.3) | 1 (10.0) |
| Self-employed | 4 (5.3) | 1 (10.0) |
| Unemployed | 8 (10.7) | 2 (20.0) |
| Household income (£), n (%) | ||
| < 14,999 | 3 (4.0) | 1 (10.0) |
| 15,000–29,999 | 17 (22.7) | 3 (30.0) |
| 30,000–49,999 | 29 (38.7) | 4 (40.0) |
| ≥ 50,000 | 26 (34.7) | 2 (20.0) |
| Education, n (%) | ||
| Postgraduate degree | 21 (28.0) | 3 (30.0) |
| Undergraduate degree | 28 (37.3) | 3 (30.0) |
| Further education | 18 (24.0) | 3 (30.0) |
| A levels | 5 (6.7) | 1 (10.0) |
| O levels/GCSEs | 2 (2.7) | 0 (0) |
| Primary school | 1 (1.3) | 0 (0) |
| Marital status, n (%) | ||
| Single | 6 (8.0) | 2 (20.0) |
| Married/civil partnership | 62 (82.6) | 7 (70.0) |
| Living with partner | 7 (9.3) | 1 (10.0) |
| Body composition | ||
| BMI (kg/m2) | ||
| Median (IQR) | 30.3 (27.6–33.1) | 33.3 (30.0–35.7) |
| Range | 25.4–50.4 | 25.4–42.1 |
| 25.0–29.9 kg/m2 (overweight), n (%) | 37 (49.3) | 2 (20.0) |
| > 30.0 kg/m2 (obese), n (%) | 38 (50.7) | 8 (80.0) |
| Weight (kg) | ||
| Median (IQR) | 80.6 (74.8–90.4) | 89.5 (71.8–93.4) |
| Range | 60.8–141.5 | 62.6–115.4 |
| Waist circumference (cm), median (IQR) | 102.6 (97.0–110.0) | 107.7 (97.3–114.8) |
| Self-reported pre-pregnancy weight (kg), median (IQR) | 76.2 (68.9–86.4) | 76.2 (60.3–90.0) |
| Current smoker, n (%) | 4 (5.3) | 1 (10.0) |
| Consumes alcohol, n (%) | 63 (84.0) | 9 (90.0) |
| Parity, n (%) | ||
| One child | 28 (37.3) | 7 (70.0) |
| Two children | 25 (33.3) | 1 (10.0) |
| Three children | 21 (28.0) | 1 (10.0) |
| Four children | 1 (1.3) | 1 (10.0) |
| Postpartum opt-in time point at baseline (months postpartum), n (%) | ||
| < 6 | 39 (52.0) | 3 (30.0) |
| 6–12 | 17 (22.7) | 1 (10.0) |
| 12–18 | 8 (10.7) | 2 (20.0) |
| 18–24 | 11 (14.7) | 4 (40.0) |
Women who completed the 12-month follow-up were broadly similar to non-completers in terms of sociodemographic characteristics. Women educated to below degree level were as likely to be retained as those educated to above degree level. However, a higher proportion of those who did not complete the 12-month follow-up were obese, first-time mothers and at a later stage postpartum at baseline than completers (80% vs. 51% obese, 70% vs. 37% first-time mothers and 60% vs. 35.4% between 12 and 24 months postpartum for completers and non-completers, respectively). One variable at baseline, self-reported weight before pregnancy, was missing for three participants who completed the 12-month follow-up; all other baseline variables had a 100% completion rate for completers and non-completers.
Box 3 highlights the progression criteria related to retention and attrition rates.
The retention rates of participants in both groups exceeded 80% at each follow-up time point, leading to a retention rate of 85.7% of women in the intervention group and 90.7% of women in the active control group at final follow-up.
Less than 20% differential attrition between the intervention and active control groupsThe attrition rates between the randomised groups were comparable (intervention: 14.3% withdrew/lost to follow-up; active control: 9.3% withdrew/lost to follow-up).
Criteria met: yes.
Qualitative telephone interviews
Of the 100 women providing consent at baseline to take part in the pilot RCT, four declined to take part in the qualitative interviews. All women who had a 3-month visit and had consented to interviews were asked at their visit if they would still like to take part in a telephone interview. In total, 70 women (intervention: n = 35; active control: n = 35) out of 87 (80.5%) were interviewed at this time point. Seventeen women were not interviewed: 15 were unable to be contacted and two women declined when approached; one said she did not have sufficient telephone reception to take part and the other declined for an unknown reason. At 12 months, 37 women (intervention: n = 16; active control: n = 21), out of 75 (49.3%) completing the follow-up, were interviewed. An interview time had been arranged for a further 31 women, but contact at the arranged time was unsuccessful and remained unsuccessful after one more attempt was made to contact these women. In addition to the four women who were not approached as they had declined to take part at baseline, a further three women declined to take part when approached at 12 months. Two of these women declined because of the length of the previous interview and the third woman felt that she had no new information to add.
The baseline demographics and characteristics of the women who took part in the interviews at 3 and 12 months have been summarised (see Appendix 6, Table 26, and Appendix 7, Table 27). At both interview time points, the participants who were interviewed provided a good representation across all demographics and anthropometric categories relative to the characteristics of the overall sample. The women who were interviewed included both high engagers and low engagers with the weight reply messages and the ‘yes/no’ reply messages. Self-reported weight before pregnancy was missing for four women interviewed at 3 months; there were no other missing baseline variables for this study sample.
At 3 months, the duration of most interviews was between 10 and 20 minutes for control participants and between 15 and 30 minutes for intervention participants. At 12 months, interview duration ranged from 8 to 15 minutes for control participants and from 10 to 30 minutes for intervention participants.
Research question 4: what sample size would be required in a definitive trial?
An indicative sample size calculation for a full RCT was conducted based on an independent samples t-test comparing the mean weight change from baseline to 12 months and assuming a SD of 7.5 kg for the weight change from baseline to 12 months, based on the active control group in the pilot RCT. Therefore, with 594 completing participants (297 participants in each group), the study would have > 90% power to detect a statistically significant difference, at the 5% level, in the mean weight change from baseline of 2 kg between the intervention and active control groups. This mean difference of 2 kg is accepted as being associated with metabolic health benefits and is frequently used to power weight loss studies in this field. 165 A similar sample size calculation was also conducted based on a chi-squared test comparing the proportion gaining > 5 kg in the intervention and active control groups and assuming that approximately 21% of the active control group would gain 5 kg, as seen in the pilot RCT. Therefore, with 594 participants completing the trial, the trial would have > 90% power to detect a reduction in the proportion of women gaining 5 kg of approximately 11% in the intervention group compared with the active control group (i.e. 21% of the active control group gaining 5 kg compared with 10% of the intervention group gaining 5 kg). This is a smaller difference than seen in the pilot RCT. Allowing for a pregnancy rate of 15% (as observed in the pilot RCT) and a loss to follow-up rate of 15% (12% loss to follow-up was experienced in the pilot RCT), the proposed sample size for a multicentre full RCT would be 425 participants in each of the intervention and active control groups, with a total sample size of 850 women.
Research questions 5 and 6: what are the views of women regarding the acceptability and perceived benefits of the (5) SMS-delivered intervention and (6) active control?
Participant-reported satisfaction with the intervention
At each data collection point, participants were asked to rate how satisfied they were with the SMS messages that they received on a five-point Likert scale ranging from ‘very satisfied’ to ‘very dissatisfied’. Approximately 80–90% of participants reported being ‘mostly satisfied’ or ‘very satisfied’ at all data collection time points (Table 14). Between 2.2% and 6.1% of participants were ‘mostly dissatisfied’ at any time point and no participants were ‘very dissatisfied’ with the intervention SMS at any time point.
| Time point (months) | Participants responding (n) | Response, n (%) | ||||
|---|---|---|---|---|---|---|
| Very satisfied | Mostly satisfied | Neither | Mostly dissatisfied | Very dissatisfied | ||
| 3 | 46 | 10 (21.7) | 29 (63.0) | 6 (13.0) | 1 (2.2) | 0 (0) |
| 6 | 39 | 17 (43.6) | 16 (41.0) | 5 (12.8) | 1 (2.6) | 0 (0) |
| 9 | 35 | 8 (22.9) | 20 (57.1) | 6 (17.1) | 1 (2.9) | 0 (0) |
| 12 | 33 | 9 (27.3) | 20 (60.6) | 2 (6.1) | 2 (6.1) | 0 (0) |
Women who reported, in the questionnaires, that they were dissatisfied with the SMS messages that they received were asked to provide additional written comments to explain their reasons for dissatisfaction. Issues with timing, frequency and impact of the messages were indicated:
Timing – I don’t have time to read during the day with baby. Have asked times to be changed at interview. Content – don’t find extremely helpful. Engagement – confused with requests for info or text when craving, etc.
226, intervention, 3-month questionnaire
Too many. Have totally lost effect and come at same time so very predictable. Barely read them now.
226, intervention group, 6-month questionnaire
They didn’t really catch my attention. After I read them, I quickly forgot about them.
009, intervention group, 12-month questionnaire
Sometimes they make me feel guilty and bad about my eating habits.
348, intervention group, 12-month questionnaire
At the final follow-up, participants were asked to rate their agreement with positive statements related to specific aspects of the SMS message content, including ease of understanding, helpfulness, interest, timing and frequency. Between 82% and 97% of participants in the intervention group either agreed or strongly agreed with all of the statements (Table 15).
| Statement | Participants responding (n) | Rating, n (%) | ||
|---|---|---|---|---|
| Agree/strongly agree | Neither agree or disagree | Disagree/strongly disagree | ||
| Supporting MumS study texts were easy to understand | 33 | 32 (97.0) | 0 (0) | 1 (3.0) |
| Supporting MumS study texts were helpful | 33 | 27 (81.8) | 2 (6.1) | 4 (12.1) |
| Supporting MumS study texts were interesting | 33 | 27 (81.8) | 2 (6.1) | 4 (12.1) |
| An appropriate number of Supporting MumS study texts were received during the study | 33 | 28 (84.4) | 3 (9.1) | 2 (6.1) |
| Supporting MumS study texts were delivered at appropriate times | 32 | 30 (90.9) | 0 (0) | 2 (6.1) |
Views gathered in the qualitative interviews provided further detail in relation to participants’ satisfaction with the intervention SMS. In general, receiving the intervention was perceived very positively and women did not consider there to be any negative aspects of being involved. The length, tone and clarity of the messages were all considered to be acceptable. Women were able to read and understand the advice easily and there was a manageable amount of information in each SMS message, supported by the inclusion of links to relevant websites that allowed participants to access additional information if they wanted to:
There’s enough in it that is actually worth reading, you know, there’s content in it that’s valid but it’s just perfect ‘cos it’s not too long and wordy but it’s not too short and missing the point, you know, you’ve sort of struck the balance between giving as much information and advice as you can without it being too much you think ‘aww I’ll have to read that later’.
010, intervention group, 3 months
Women commented on the importance of the variety of SMS messages received. Continuously changing the focus of the messages to provide advice on different aspects of weight management or a healthy lifestyle helped to maintain women’s interest in the information that they were receiving. In addition, participants differed in their preferences for types of SMS message: some commented on liking the more practical advice, for example meal plans and recipes; others preferred the emotional support provided by the coping and relapse prevention SMS messages; and others appreciated acknowledgement of barriers and set-backs in weight management, which encouraged them to try to reset their goals. Using these different approaches meant that individuals could relate to the messages that used their preferred approach, even if they disliked some of the other messages:
They’ve been varied enough but I’ve not looked at my phone and went ‘aww I know this already’, it’s all been interesting enough, you know, and the variety has been very good, it’s not like I’m getting too much of one, there’s a good amount of thinking about like your shopping, thinking about your meal sizes, thinking about exercise and stuff like that.
181, intervention group, 3 months
The majority of women felt that the number and frequency of SMS messages that they were receiving were acceptable. The daily frequency acted as a constant reminder to think about their weight-related behaviours and women looked forward to receiving the advice. A small number of women felt that they received too many SMS messages and so they tended to ignore them. A few women commented on the importance of the SMS messages continuing to be delivered at the weekends, which tended to be when they were more likely to adopt less healthy behaviours:
There can be quite a lot of texts when actually it’s quite nice to keep you on track and keep your head in it, you know . . . I think I’m getting really one or two every day, which is quite full on, but yeah not in a bad way or anything.
246, intervention group, 3 months
Once or twice a day I would receive them generally . . . also over the weekend; I think it’s good that you get them over the weekend too, that’s pretty important. So yeah, the frequency’s fine.
009, intervention group, 3 months
At the start of the study, women were asked their preferred time to receive messages. The default window for delivery was any time between 10.00 and 23.00; unless another time was specified, SMS messages were sent routinely between these times. In the interviews, some women spoke about liking the routine timing of SMS message delivery and how they looked forward to receiving an anticipated message. However, quite a few women discussed how the timing of receipt of the SMS message could be an issue that could affect their chance of being read. For those on maternity leave, quite often the receipt of SMS messages clashed with other organised activities with their child, which tended to be in the morning or when they were busy with child-care responsibilities throughout the day, meaning they may not have had time to read the messages. For those who had returned to work, often their busy working days meant that they were unable to read SMS messages in real time. A few women suggested that receiving SMS messages in the evening instead may be better, as they would have more time to absorb the information and this was also the time when they were more likely to engage in unhealthy eating behaviours. However, SMS message timing was an issue for only a minority of women, given that most of the women agreed that the SMS messages were delivered at appropriate times (see Table 15):
My only issue or suggestion with it was around the timing of the text messages that I get because generally they always come through at 10.00 in the morning and then sometimes at 12.00 noon . . . but really over the last few months when I’ve been off we’ve been going out to, you know, either baby or toddler activities in the morning like Mums and tots or maybe a baby class or whatever . . . 90% of them are 10 o’clock in the morning . . . so the text message, the text message always comes through at 10 o’clock is like the worst possible time of the day to get my attention.
009, intervention group, 3 months
I think if you would get a one-off in the morning, you might disregard it when you’re busy but to get a couple throughout the day then keeps you in mind . . . Just thinking really, the evenings . . . for me, around sort of 9, when I– 9, then by the time you sit down, you know, a wee reminder at that sort of time in the night might be helpful so as I don’t reach for the nibble, when you finally get sitting down.
016, intervention group, 3 months
There was also a specific issue with the timing of weight self-monitoring messages (whereby women were sent a weekly SMS message to prompt them to weigh themselves and then respond with their weight). A few women commented that they already had a habit of weighing themselves on a specific day, so the weight SMS message did not serve as a reminder to do this. Other women said that they would prefer to weigh themselves on certain days. For example, many did not want to weigh themselves on a Monday morning if they had engaged in weight-promoting behaviours over the weekend:
I don’t really like the ones asking for the weight . . . it’s always the one that makes me thing ‘ah no, not on a Monday’. I think the time that I am most likely to maybe fall off the wagon a wee bit of the weekend, whenever I get that on the Monday I think ‘ah, no’.
028, intervention group, 3 months
Participant-reported satisfaction with the active control
As for the intervention group, participants in the active control group rated how satisfied they were with the SMS messages they received on a five-point Likert scale ranging from ‘very satisfied’ to ‘very dissatisfied’. Levels of satisfaction with the active control SMS messages were similar to those reported for the intervention group (Table 16): 80–90% of participants were either ‘very satisfied’ or ‘mostly satisfied’ at each time point, and < 3% reported being ‘mostly dissatisfied’ or ‘very dissatisfied’ with the received messages.
| Time point (months) | Participants responding (n) | Response, n (%) | ||||
|---|---|---|---|---|---|---|
| Very satisfied | Mostly satisfied | Neither | Mostly dissatisfied | Very dissatisfied | ||
| 3 | 41 | 20 (48.7) | 17 (41.5) | 4 (9.8) | 0 (0) | 0 (0) |
| 6 | 34 | 22 (64.7) | 9 (26.5) | 1 (2.9) | 1 (2.9) | 1 (2.9) |
| 9 | 38 | 21 (55.3) | 16 (42.1) | 1 (2.6) | 0 (0) | 0 (0) |
| 12 | 33 | 18 (50.0) | 10 (27.8) | 3 (8.3) | 1 (2.8) | 0 (0) |
One woman provided a free-text response on the 6-month questionnaire to explain why she was mostly dissatisfied with the active control SMS messages:
Information about toddler groups or education projects would be useful.
183, active control group, 6-month questionnaire
Active control group participants were also asked in the final follow-up questionnaire to rate the extent to which they agreed with positive statements about specific aspects of the active control SMS messages, including ease of understanding, helpfulness, interest, timing and frequency (Table 17). Between 85% and 97% of participants agreed or strongly agreed with the statements about the active control SMS messages.
| Statement | Participants responding (n) | Rating, n (%) | ||
|---|---|---|---|---|
| Agree/strongly agree | Neither agree or disagree | Disagree/strongly disagree | ||
| Supporting MumS study texts were easy to understand | 33 | 32 (97.0) | 0 (0) | 0 (0) |
| Supporting MumS study texts were helpful | 32 | 28 (84.8) | 2 (9.1) | 2 (6.1) |
| Supporting MumS study texts were interesting | 32 | 30 (90.9) | 2 (6.2) | 0 (0) |
| An appropriate number of Supporting MumS study texts were received during the study | 32 | 32 (97.0) | 0 (0) | 0 (0) |
| Supporting MumS study texts were delivered at appropriate times | 31 | 28 (84.8) | 1 (3.0) | 2 (6.1) |
The interview data supported these findings: women spoke very positively about the active control SMS messages received. The length, tone and clarity of the SMS messages were all considered to be acceptable and the information was easy to understand. There was enough information in the SMS messages to be considered useful without being unmanageable. The inclusion of links was perceived positively as it meant that, should women want more information, they could access it, and not including all detailed information in the main body of the text avoided women ignoring the text completely. Participants were satisfied with the frequency with which they were receiving SMS messages, with a few commenting on how they were expecting, or would not mind receiving, more messages. Women in the active control group did not express any difficulties with the time of day that they received the SMS messages:
They’re easy to read, they’re short and the information you’re getting is enough, you know, it’s the snippet of information that makes you sit down and think about it . . . I kind of thought there would’ve been more but no, I think three is just enough, you know, you’re not getting, getting them all the time, you’re not getting tortured but you’re getting enough information, that’s nice, you know, you’re kind of waiting and thinking ‘oh, I wonder when I’ll get my next one!’.
012, active control group, 3 months
They were a good length and there was enough information in them, but still you could sort of scan over them quickly because, you know, you’re running about doing this that and whatever during the day and it didn’t take up a lot of time.
007, active control group, 12 months
Women felt that the SMS message content was good as it provided information in relation to a variety of aspects of child development, which made mothers consciously think about how they could better support their child’s development. As with the intervention group, women in the active control group had individual preferences for the types of SMS messages that they received and the inclusion of advice on a variety of topics meant that women could engage with their preferred information. Even when women considered the received information as something they already knew, they still felt that the SMS messages acted as useful reminders. However, one woman suggested that there could have been some tailoring of the advice specifically for multiparous women, for example to include ideas of how to support sibling interactions or how to balance the demands of multiple children:
I thought it was great, it was nice, some of the wee messages were great and there were lots of nice play ideas and different wee things that were quite useful, like, information wise, I just thought it was lovely.
039, active control group, 12 months
All the stuff I’ve probably read somewhere, not all the stuff but a few of the things I’ve maybe read somewhere before, but it’s good to jog your memory, you know, after a couple of years ‘oh right OK, that again’ so . . . even if it’s somebody’s third or fourth child or something, it’s surprising how easy you forget things so it is, it’s really beneficial either way.
006, active control group, 3 months
I have an older child so I have some of an idea but still they are very different girls so some of the text messages may be more apt than others, because they’re very different babies.
023, active control group, 3 months
The majority of women in the active control group felt that there was no need to change the SMS messages in any way. However, a few women felt that the SMS message content did not match up to their child’s stage of development, for example sometimes they were receiving advice related to developmental milestones that their child had already reached, making the information obsolete. Some of these women recommended that, if it was not possible to exactly align the messages to their child’s developmental stage, then it would be preferable to receive it earlier, which would allow them to prepare for reaching milestones. It was also noted by these participants that this issue was more salient when their child was younger, as many changes happened over a short period of time, whereas it became less of an issue in the later stages of the active control delivery period, when their child was older and major developmental milestones were less frequent:
There’s nothing that’s obviously stuck out for me to question, do you know what I mean? I’ve taken it and I’ve identified or it’s made best treatment or it’s prepared me for, maybe, what’s coming in the future type of thing, so there’s nothing really that I would feel like I would challenge.
076, active control group, 3 months
I think some of the messages I found, I don’t know, obviously, like, all children are different . . . I found that they’ve either, some of them, have come a bit late in terms of it being stuff that we’ve already had to deal with . . .. I think certainly stuff like that the messages could be . . . whatever the subject– the message is about, it could be sort of pre-emptive, so if it was sent earlier then it would get the parents thinking about ‘this was going to be happening and’ or ‘this was going to be– need to start thinking about this’.
007, active control group, 3 months
It would just be helpful if they were more tailored to the particular age development.
021, active control group, 3 months
The evidence supporting women’s satisfaction with the active control was strengthened from the data gathered during the interviews, when all those interviewed said that they would recommend taking part in the study to other mothers and friends and that they would be happy to sign up for the study again:
I definitely would recommend taking part in these kind of things; I think it’s good to, to be able to help mums and, you know, to be there and support ‘cause it’s not an easy, an easy job, but sometimes it’s exhausting and thankless and monotonous and other times it’s very exciting and rewarding and stuff, it’s just a very strange . . . anyway, we can support mums to, kind of, to do anything to help them and improve where they’re at, I think that’s good.
023, active control group, 12 months
I would recommend it and I would be happy to take part as well.
467, active control group. 3 months
Women’s views regarding group allocation and willingness to be randomised
Women were not interviewed directly following randomisation, but during the telephone interviews conducted at 3 months. Participants in both groups were asked about their reasons for taking part in the study and whether or not they had a preference at the outset in relation to which group they were assigned to. Women seemed to have a good understanding of the randomisation process, in that they knew that they had an equal chance of being allocated to either group.
For women who went on to be assigned to the intervention group (n = 36), some indicated that struggles with their weight and a desire for support to lose weight had encouraged them to take part in the study. Half of this group (18/36, 50%) said that they were happy that they had been randomised to receive the weight management advice. However, many of these women also discussed initial perceptions of how the active control messages pertaining to child health and development would have been of benefit to them as well, with one participant saying she would have preferred to have been randomised to receive the active control messages as her family lived far away and, as such, she felt that she lacked support or advice in terms of her child’s development:
I found, you know, after having my daughter I put on quite a lot of weight, so I have. So yes, I did want to go onto it [intervention] particularly, but the other one obviously I, would’ve been very helpful as well, you know, the development.
015, intervention group, 3 months
I probably would’ve wanted to be in the weight loss group a bit more but I would’ve been interested in the child development ones as well.
009, intervention group, 3 months
Although many of the women in the active control group indicated an initial preference for the intervention group owing to weight concerns (13/35, 37%), the majority of these women still reported a high level of satisfaction with the SMS messages that they were receiving (see Tables 21 and 22). This indicated that, despite initial preferences for group allocation, randomisation did not affect their willingness to engage with the active control. Receiving SMS messages related to child health and development was perceived as beneficial and participants said that they would recommend the active control to other mothers. A few women commented that they would still be interested in receiving the weight management SMS messages at the end of the study, which would allow them the benefit of having received both sets of messages:
I wanted to be on the weight loss one just because it’s something I’ve struggled with for a long, long time and, I suppose, for selfish reasons, I was sort of hopin’ that I would, it would help me in that aspect . . . as I say, I wasn’t taking part in the study for my own personal reasons, I was wanting to do it to be of help, but whenever [researcher] told me what the two groups were I was sort of going ‘oh, I’ll keep my fingers crossed’, yeah, I mean it doesn’t, it’s, I’m not disappointed.
007, active control group, 3 months
My whole time at the moment is spent on weight loss, so I was kind of hoping I was going to be in it, but the child development is excellent so I don’t mind.
467, active control group, 3 months
I’d definitely recommend it. And I’d love to get the second part, you know, the kind of healthy ones, I’d love to get them.
012, active control group, 12 months
There were women in each of the randomised groups [intervention: 13/36 (36%); active control: 9/35 (26%)] who said that they had not had a specific preference in terms of group allocation and that they were happy to take part in the study to receive either intervention. Their motivation for taking part in the study was to help with research in general, or they had expected benefits from receiving either the intervention or active control SMS messages. Therefore, including the active control component was an important part of the study design and meant that some women (11/31, 35%) actually had a preference for receiving the SMS messages related to child health and development, particularly those who were first time mothers, those who already engaged in behaviours to support positive weight management or those who were not concerned about their weight:
I’m not disappointed that I’ve ended up in the development group because I’m getting text messages and I find that useful, so it wasn’t that I would’ve not wanted to take part if I had’ve ended up in this group, so it [my interest] was sort of equal for both [groups].
024, active control group, 3 months
I attend a weight loss group anyway, I go to Weight Watchers [WW International, Inc., New York, NY, USA] at the minute, so I kind of thought it would be nice to get the child development.
012, active control group, 3 months
A few participants in both groups indicated that their preference had changed during the course of the study. One of the participants who was receiving the intervention felt that a lack of sleep was negatively affecting her motivation to engage with the weight management advice and, as such, she now would have preferred the active control SMS messages. A few participants in the active control group, who initially signed up to the study with an interest in receiving weight management advice, had a change in attitude as a result of how beneficial they were finding the receipt of SMS messages related to child health and development.
Perceived benefits of the intervention
All of the women in the intervention group who were interviewed at 12 months said that they would recommend the SMS-delivered intervention to other mothers and that they would take part in the study again if given the choice. Some of the women emphasised that there was a lack of support in the postpartum period, recognising the many barriers to weight management after having a baby, a time when balancing work and family commitments, changing routines and other people’s needs could take priority:
I think it is a brilliant type thing and definitely something, not only for a study, but would be brilliant if it was offered to people just after they had babies because you really do struggle with weight loss after you’ve had kids and that’s really, really, I know it sounds like it’s a lie or whatever for people to say, like you don’t have time, it really is very hard to fit it in with working and with small kids and it is definitely good to have some extra support there and something you can read back on and something you can get tips on.
001, intervention group, 12 months
There is literally nothing like after the midwife comes out and helps you with your baby the first couple of days . . . that’s you left to go; there really isn’t, even for mental health and weight loss and all them type of things, there’s really nothing.
001, intervention group, 3 months
Of note in the interviews was women’s ability to accurately recall the content of many of the SMS messages, indicating that they had engaged and taken on board the included advice. The majority of women emphasised how the SMS messages made the consideration of weight management salient in their everyday lives. Providing continuous advice served as constant reminders for women to be conscious of their weight-related behaviours and encouraged and motivated them to think about their behaviours more, as well as providing them with ideas on how they could adopt healthier behaviours. Furthermore, having to reply to messages made them feel accountable to someone else, in that they had to be truthful about how well they were doing in terms of their weight management:
I think the most important thing for me being back to work is just to have, kind of, the words of encouragement and those wee reminders about, you know . . . ‘don’t reach for the biscuit, reach for the fruit’. I think there were wee reminders to just stay on track because it’s very easy to let these things go by the wayside. I do re-read them and I haven’t deleted any messages because I like to be able to scroll back and look at the link and just look at the advice that you’re sending. To be honest, it’s not new but I think just having it in one central area and being able to go in and re-read it if you get the time or the opportunity to do it, it’s really beneficial.
028, intervention group, 3 months
It’s like a daily reminder . . . just keeps you mindful, you know, when you get the wee text message it’s like ‘oh yeah’, you know, you might be thinking about skipping the gym and then a wee text message comes through and it motivates you.
016, intervention group, 3 months
Delivering the intervention by SMS had several benefits. It meant that women could retain the information and access it at their convenience, as well as having a library of weight management advice at hand should they require it. The majority of women said that they briefly read the SMS message at the time of receipt, but would often go back over the messages at a later stage, although a few had deleted them owing to a lack of mobile phone memory space. In comparison with face-to-face advice, receiving SMS messages was less burdensome for participants, especially during this busy period of their lives. At the same time, some women felt that they could easily ignore the SMS messages if they were not motivated to engage with them or if they did not have time to read them. A few women perceived the intervention as non-judgemental and non-stigmatising, as the SMS delivery allowed them an element of anonymity that would not be there if they had to meet someone face to face:
You couldn’t get face-to-face support to the same per cent that you get the text support . . . like, I’ve done Slimming World [Alfreton, UK] and that sort of weekly weigh-in is good, you know, seeing someone face to face for advice and support but in terms . . . that’s the beauty of this, the likes of Slimming World, you don’t get to make your consistent text messages and that is a big support ‘cause it just a constant reminder, you know, when you’re having your breakfast or when you’re going to work or in the middle of the day.
016, intervention group, 3 months
Sometimes if you’re having a particularly bad week, you know, you’re just sort of thinking ‘oh my goodness, more pressure about losing weight’, but at the end of the day you can ignore them if you wish or you can stop at any time, so I don’t think that’s a negative.
009, intervention group, 3 months
It’s a stranger who’s not judging me if, you know, it’s a text message, it’s not someone going ‘oh I can see that you’ve been eating such and such’, it’s just like a nice gentle ‘hey remember to look after yourself’, you know.
181, intervention group, 3 months
A few women reported feeling isolated during the postpartum period, especially if on maternity leave from work. Receiving the intervention SMS messages made them feel as though they were being supported and that they were not alone, especially when SMS message content empathised with women by acknowledging the many struggles they may experience in relation to weight management after having a baby. Many women found the messages related to relapse prevention to be motivating. The length of intervention delivery was particularly beneficial: women may have experienced dips in their motivation to lose weight, but the continuation of SMS messages during this time helped them to refocus. However, one woman said that she felt that, when she had sent information to say her weight had gone up, the response SMS message, to what she perceived as a ‘failure’, could actually have used harsher language:
They are supportive in their tone in that, you know, you’re kind of championing us on saying ‘you’re doing a great job and don’t forget you’re a tired Mum’, you know, it’s very empathetic in terms of the needs of parents that some of it’s almost like you guys understand that we are tired! And there’s not always time for exercise . . . just to get a text message to say, you know, ‘everybody falls off the wagon and that’s OK, just reset your goals’, it helps me get focused again rather than just giving up.
010, intervention group, 3 months
This sort of notion that you’re not the only person that struggles with this, you know, that everybody that has children, they don’t automatically get back into their stick insect shape, that it is a battle . . . and everybody maybe falls off the wagon, but it’s about getting back up again, you know, that does help you feel, you know, you’re not a ‘Supermum’ but there’s a whole lot of mums out there that aren’t ‘Supermums’ either and that’s OK . . . the text messages and the fact that you are hearing what some Mums said through the text message.
158, intervention group, 3 months
At the start it was kind of like ‘right’, you know, ‘get stuck in, let’s do this’ and really motivated. I did lose a wee bit of motivation, but there were some links you sent about great foods ideas and things like that, everything you do you get a wee bit deflated, but I have to say, the ideas were brilliant. I did take a wee dip, but I got back up there, you know. So, it was really, really good for motivation, definitely.
061, intervention group, 12 months
The length of time postpartum women had reached when they were recruited to the study may have influenced the extent to which they benefited from the SMS messages in terms of behaviour changes. One woman, who was recruited during the early postpartum period, felt that this had not been a good time for her to utilise the advice she was being given as she was breastfeeding and felt restricted in how much activity she could do as a result, but yet was receiving advice to engage in more physical activity.
Perceived benefits of the active control
Participants’ views in relation to the perceived benefits of the active control indicated that the SMS messages helped make women better understand their child’s developmental stages and made them more aware of how they were interacting with their child. The SMS messages provided women with some useful ideas on how they could help encourage their child’s development, for example by utilising play ideas, which, in turn, led them to engage more with their child:
Reminding you to do the wee different play things and different sort of things . . . I do like the wee play ones ‘cause it’s sort of like to have wee ideas, different wee things you can do and, sort of, looked into wee things like sensory stuff and things for that . . . helping them with their development really, so anything that can sort of help bring them along . . . but, at the same time, like, I did like the wee one about the immunisation ‘cause then I could just click on it and I was able to read up about it ‘cause I knew they were coming up and know what to expect so it’s all been great.
039, active control group, 3 months
There would have been maybe areas where I was maybe getting frustrated with [child] and then a wee message would come through and sort of remind me that she is only a 2-year-old, this is normal and lots of other mums are going through the same sort of stages and sort of helped ground me a wee bit in those cases.
007, active control group, 12 months
I definitely think I have learned things from it and hopefully put some of it into practice so, yeah.
019, active control, 12 months
Some of the women also perceived there to be emotional benefits from receiving the active control, in that they felt supported and part of a wider network of people. A few commented on how receiving the SMS message provided them with a feeling of self-worth and reassurance that they were doing a good job as a mother because they were supporting their child’s development:
It just makes me feel like I’ve a tiny bit of significance, if you know what I mean? Being a stay-at-home mum, you don’t really get much significance; it makes me feel like I’m part of something.
076, active control group, 3 months
You’re always comparing to other people’s babies because they’re able to do this and your baby’s not, so it’s great to get the development text that kind of reassures you that you are doing a good job and that everything is OK . . . I think a lot of new mums sort of feel a bit isolated, you know, the way you have the new baby and you’re at home and you don’t really tend to go out for the first while, so it’s lovely just getting that wee text message to, even just to reassure you’re not on your own, sort of thing . . . and then just getting the information that’s relevant to you and knowing you are doing a good job, that you’re doing everything to the best that you can do.
012, active control group, 3 months
The mode of delivery was seen as beneficial, as the SMS messages provided a sufficient amount of information without being too time-consuming. The SMS messages, and included links, could be retained and accessed as and when mothers felt was convenient or when the information would be of most use to them. Receiving the active control SMS messages was considered a handy adjunct to mothers’ own efforts, as they would have been likely to have sought out this information themselves. Instead, the information arrived from a trustworthy source, and was perceived to be of great benefit. One woman said she would forward some of the SMS messages on to her husband to share the information:
You’re always sort of looking and reading different things and having those apps that tell you what to expect or what to do or give ideas, whereas this one actually just delivers it right to you so you don’t even have to go looking for it . . . it means, even if you are busy or whatever, that it’s there whenever you can and you don’t have to look for it yourself it just comes to you and it’s nice.
039, active control group, 3 months
They’re helpful, just because I thought that maybe, it’s not just an opinion and it’s probably linked to the NHS website where you’re given details of government position on weaning or play or to make your home safe and all of those things.
278, active control group, 3 months
I never delete a text so there has been a couple of times where I’ve gone back thinking ‘did I miss one of those today?’ . . . so, they are there if I ever chose to go back and look at them.
024, active control group, 3 months
This benefit may have been heightened for second-time mothers as a few acknowledged that they were less likely to have sought out information in relation to their child’s health and development when they had older children. In addition, the advice could have changed since their last child and the SMS message provided them with the updated information:
I think I took for granted that, because I’d done it before, that I knew loads of things anyway, and didn’t necessarily need to know any different ideas for play and stuff like that, but it was wee things that I hadn’t tried before, so it was great. I used to read books with [older child] constantly and be ‘right OK she should be doing this, this and this’ . . . second time around I wasn’t paying as much attention to it then the odd text message was good to be ‘right, that’s where she’s at or where she should be at’. I just feel it’s [the study] quite nice, like I think it’s one of those things it would be nice, like, as a new mum sort of got them because there were so many different wee tips and ideas and the thing about immunisation around that time, it’s just reassurance about things as well. So yeah, it was just really lovely. It would be really nice if everybody could have them.
039, active control group, 12 months
There may have been some unintended benefits in relation to weight management associated with taking part in the active control. One woman commented on how the importance placed on child engagement in the active control messages had motivated her to focus on weight management, as it reminded her about her desire to be physically fit and healthy enough to be able to actively engage with her children:
[It was a] real motivation for me, even though I’m not in the fitness group, but just knowing, I suppose, and with child development, the reason for me losing weight has been about being there for my children and being able to run after them and play with them and stuff, because I had put on such weight that it was hard for me to kind of have the energy to do stuff, so I think that was the driving force, just even knowing that was part of the study, just to help to reassure me to keep going with that.
023, active control group, 12 months
Box 4 highlights the progression criteria related to acceptability of the intervention and active control.
Both groups indicated a high level of satisfaction with the SMS messages that they were receiving, and perceived there to be benefits to both the intervention and the active control conditions. The interview data provided some suggestions from participants about improvements that could be made to the SMS messages or their delivery, which will be discussed later in this chapter. Overall, the intervention and active control were acceptable to women.
Criteria met: yes.
Research question 7: what are the indicative effects of the intervention on weight loss and weight loss maintenance?
Weight outcomes are reported as continuous variables of mean weight change between follow-up time points (Table 18) and as proportional data in terms of percentage of women meeting weight change milestones (Table 19).
| Time point (months) | Participants (n) | Weight change (kg) in intervention group, mean (SD) | Participants (n) | Weight change (kg) in active control group, mean (SD) | Adjustedb mean difference in weight (kg) (95% CI) |
|---|---|---|---|---|---|
| 0–12 | 36 | –1.75 (6.7) | 39 | 0.19 (7.5) | –1.67 (–4.88 to 1.55) |
| 0–3 | 39 | –0.89 (2.7) | 41 | –0.19 (3.1) | –0.61 (–1.90 to 0.67) |
| 0–6 | 38 | –1.44 (4.0) | 39 | –0.27 (5.7) | –1.10 (–3.34 to 1.15) |
| 0–9 | 34 | –1.90 (6.0) | 39 | –0.49 (6.8) | –1.28 (–4.26 to 1.70) |
| 3–6 | 38 | –0.50 (2.6) | 39 | –0.15 (4.1) | –0.35 (–1.93 to 1.24) |
| 6–9 | 34 | –0.47 (2.7) | 39 | –0.22 (2.9) | –0.18 (–1.47 to 1.11) |
| 9–12 | 34 | 0.14 (3.4) | 38 | 0.65 (2.6) | –0.48 (–1.90 to 0.94) |
| Weight loss or gain | Intervention (N = 36), n (%) | Active control (N = 39), n (%) | OR (95% CI) |
|---|---|---|---|
| Weight loss | |||
| ≥ 5-kg loss | 8 (22.2) | 9 (23.1) | 0.95 (0.32 to 2.81) |
| Lost ≥ 5% body weight | 11 (30.6) | 10 (25.6) | 1.28 (0.47 to 3.50)a |
| Weight gain | |||
| ≥ 5-kg gain | 3 (8.3) | 8 (20.5) | 0.35 (0.09 to 1.45) |
| Gained ≥ 5% body weight | 3 (5.9) | 10 (20.4) | 0.26 (0.07 to 1.05)b |
Analysis of weight change for completers at 12 months
Based on the analysis of weight data for the population completing the follow-up at 12 months (n = 75), between baseline and 12 months the intervention group lost, on average, 1.75 kg, whereas the active control group gained 0.19 kg, corresponding to a mean difference in weight change, between the intervention and active control groups, at 12 months of –1.67 kg (95% CI –4.88 kg to 1.55 kg), adjusting for baseline (see Table 18).
Intention-to-treat analysis
A LOCF analysis was performed by using the last recorded weight measurements for those lost to follow-up at 12 months (intervention: n = 6; active control: n = 4). Weight measurements were carried forward from measurements at baseline (n = 5), 3 months (n = 2), 6 months (n = 2) and 9 months (n = 1). The LOCF analysis found an average weight loss of 1.60 kg in the intervention group (n = 42), compared with an average weight gain of 0.17 kg in the active control group (n = 43), corresponding to a mean difference in weight change between groups, adjusting for baseline, of –1.59 kg (95% CI –4.43 kg to 1.26 kg), which was 0.08 kg less than that found in the analysis of complete cases. A BOCF analysis, which imputed baseline weight measurements for non-completers at 12 months into the analysis of weight change, found that the intervention group lost, on average, 1.50 kg, whereas the active control group gained 0.17 kg, corresponding to a mean difference in weight change between groups of –1.48 kg (95% CI –4.32 kg to 1.36 kg), adjusting for baseline, which was 0.19 kg less of a difference than that found in the completers’ analysis.
Proportional weight outcomes
The proportion of women gaining ≥ 5 kg in weight between baseline and 12 months was 8.3% in the intervention group and 20.5% in the active control group; women in the intervention group were less likely to have gained ≥ 5% of their baseline weight by the 12-month follow-up than women in the active control group (see Table 19). The proportions of women losing ≥ 5 kg of weight between baseline and 12 months were similar in the randomised groups, but women in the intervention group were more likely to have lost ≥ 5% of their body weight across the course of the 12-month SMS messages delivery period than those in the active control group (see Table 19).
Waist circumference
Waist circumference outcomes are reported as continuous variables of mean change in waist circumference measurements between follow-up time points (Table 20). Between baseline and 12 months, mean waist circumference in the intervention and active control groups was reduced by 4.27 cm and 5.97 cm, respectively, corresponding to a mean difference at 12 months, adjusting for baseline, of 0.92 cm (95% CI 0.70 cm to 1.14 cm). Reductions in mean waist circumference between each time point were observed in both groups, with the exception of the intervention group between months 9 and 12 in which there was an increase in waist circumference of 0.27 cm.
| Time point (months) | Participants (n) | Waist circumference change (cm) in the intervention group, mean (SD) | Participants (n) | Waist circumference change (cm) in the active control group, mean (SD) | Adjusteda mean difference in waist circumference (cm) (95% CI) |
|---|---|---|---|---|---|
| 0–12 | 34 | –4.27 (8.1) | 36 | –5.97 (9.6) | 0.92 (0.70 to 1.14) |
| 0–3 | 39 | –0.94 (5.8) | 41 | –1.28 (7.2) | 0.19 (–2.77 to 3.15) |
| 0–6 | 38 | –2.62 (6.0) | 39 | –3.18 (7.5) | 0.27 (–2.85 to 3.40) |
| 0–9 | 34 | –4.30 (8.1) | 38 | –3.19 (8.1) | –1.41 (–5.22 to 2.40) |
| 3–6 | 38 | –1.61 (5.5) | 39 | –1.77 (5.1) | –0.03 (–2.46 to 2.39) |
| 6–9 | 34 | –1.66 (4.9) | 38 | –0.26 (4.9) | –1.50 (–3.85 to 0.85) |
| 9–12 | 32 | 0.14 (6.4) | 34 | –2.14 (7.0) | 2.42 (–0.91 to 5.75) |
A further analysis was performed to examine if engagement with the interactive features was associated with intervention effectiveness. Women who completed follow-up assessments at each of the study time points were classified as low or high engagement with the weight SMS messages and ‘yes/no’ questions based on the number of times that they replied. The median number of responses, for each type of message, was used as the threshold for classifying women as high or low engagers (i.e. above or below the median, respectively) (see Chapter 3). Across the course of the intervention, high engagers with the weight SMS message replies lost more weight than low engagers, with a mean difference between low and high engagers at 3, 6 and 12 months of –2.8 kg, –3.65 kg and 1.82 kg, respectively (see Appendix 8, Table 28). High engagers with the ‘yes/no’ replies lost more weight than low engagers, with a mean difference between low and high engagers at 3, 6 and 12 months of –2.03 kg, –3.27 kg and –2.01 kg, respectively (see Appendix 9, Table 29).
The baseline characteristics of the low and high engagers were summarised (see Appendix 10, Table 30). There were no significant differences in the baseline characteristics of high- and low-weight text engagers at 3, 6 and 12 months, with one exception: participants who were low engagers across the time points stated that they received enough help from family/friends (95–100%), compared with around 70% of high engagers who stated that they received enough help from family/friends. This perceived social support was significantly different between low and high engagers at 3, 6 and 12 months (p < 0.05).
Participant engagement
Participant engagement with the interactive SMS components for those completing the first 6 months and those completing the full 12 months of the intervention has been summarised (see Appendix 11, Table 31). In week 2, all participants were asked to send the weight that they would like to achieve in 6 months’ time; 24 (48%) participants replied with a goal weight. One participant did not receive this SMS message as there were complications in SMS message delivery at the beginning of the study for this participant.
Weight engagement
Engagement with weight SMS messages was lower between months 0 and 6 than between months 7 and 12, with 47.4% and 77.8% of participants responding to the weekly prompt to step on the scales and text the research team their weight at each time point, respectively (see Appendix 11, Table 31). Two participants replied to all of the weight SMS messages in the first 6 months and two participants replied to all of the weight SMS messages in months 7–12, one of whom was the same participant; therefore, this participant had 100% engagement. Engagement with the weight replies was sustained over the 12-month intervention.
‘Yes/no’ engagement
There was a high level of engagement with the ‘yes/no’ SMS messages, with 95% of participants sending a reply between months 0 and 6 and 86% of participants sending a reply between months 7 and 12 (see Appendix 11, Table 31). Between 0 and 6 months, 17 participants texted between one and 10 times, whereas 24 participants replied between 20 and 26 times. Between 7 and 12 months, 10 participants replied between one and eight times, whereas 21 participants replied between nine and 16 times.
Trigger word engagement
In terms of participant engagement with the trigger words feature (see Appendix 12, Table 32), 19 participants texted a trigger word between one and three times in the first 6 months and seven participants texted a trigger word between one and three times between months 7 and 12. Engagement with the trigger words ‘crave’, ‘bad day’, ‘exhausted’, ‘slip-up’ was greater in the first 6 months of intervention delivery (31 trigger words texted) than in months 7–12 of intervention delivery (13 trigger words texted). Thirty-eight per cent of the trigger words sent in the first 6 months and 46% of the trigger words sent between months 7 and 12 were sent by the participant on the same day that they received a text informing them or reminding them about the trigger words.
When asked about the trigger words in the interviews, many of the participants felt that this option could be useful as it would allow them to ask for support at a time when they required it. Some women indicated that they were unable to recall what the words were or were unsure what would happen if they did text a trigger word. One participant suggested including some information to say:
If you tell us how you are feeling, we might have some more advice.
016, intervention group, 3 months
I mean, you ask now about what is probably the most useful text– that is probably I think is the best things that you can actually because that’s at a time when it’s convenient to you and it’s relevant to you rather than when the text messages are coming through, you’re maybe not necessarily thinking about weight loss or exercising or something, but it is good that you can text when you’re feeling you have a problem.
001, intervention group, 3 months
I haven’t used any of those yet; I’ve actually forgot about them until you’d mentioned it there.
020, intervention group, 3 months
A few other women said that it was during their busiest times when they were most likely to need to use the trigger words, when there were many barriers to being able to make healthy choices, but it was during these times that they were also too busy to send a message including a trigger word. For those who had used the trigger words, the responses received were viewed as positive and useful.
There were a few explanations provided from the interviews that shed light on women’s levels of engagement with the two-way message aspects of the intervention. A lack of response to SMS messages did not necessarily mean that women were not engaging with the advice. One woman explained how she was unable to respond because she had no credit on her mobile phone. Another woman did not send responses as she was unsure about whether or not she would be charged for the automated response that she would receive from the study, whereas others said that they were too busy to respond but still found the SMS messages useful:
The only problem I’m having with them is, you see the way you can text back to things? My only issue is I can’t text back a lot of the time because I only have credit to O2 [Telefónica UK Limited, Slough, UK] numbers. So, if it’s not an O2 number, then if I don’t have credit on my phone, then I can’t respond to it.
001, intervention group, 3 months
The only negative I can say about myself was just sometimes when I was so busy I would have looked at it, glanced at it and maybe looked back on it, and then forget, that was the only thing, to maybe reply or, you know, or look at the links or, that would be the only thing, but I really found it beneficial.
061, intervention group, 12 months
Some women spoke about how they avoided responding to the requests for their weight when they had gained weight as they were disappointed in themselves, but they may still have been engaging with the advice to self-weigh:
I don’t [respond to weight texts] to be quite honest but that’s my issue because I’m not losing any and it it’s come up, I’m like ‘no, frig off’ . . . I would be weighing myself but I’ve just been disappointed in my progress.
010, intervention group, 3 months
Responses to self-reflection SMS message asking an open question
During the 12 months of intervention delivery, SMS messages were sent to participants asking open questions to promote self-reflection, for example ‘Out with the old and in with the new! Think back to the start of SMS. What new habits have you formed? Text us! E.g. “more fruit”, “eat breakfast”, etc.’. Seven of these SMS messages were included in the first 6 months and one in months 7–12. There were 15 responses to these questions in the first 6 months and six responses during months 7–12.
Additional spontaneous SMS messages
There were a small number of spontaneous responses to SMS messages (see Appendix 12, Table 32).
Interview data on indicative effects
The indicative effects of the intervention were further evidenced by participants’ accounts provided in the interviews. Some women spoke about experiencing weight loss as a result of the study, and others highlighted positive impacts on confidence, self-esteem, perceived support, feeling energised and eating and activity behaviours, which contributed to their weight loss success:
Your text messages helped me to lose a bit of weight, then I was more confident about going to the gym but if I hadn’t’ve lost that weight, no way. Now I’ve went to the gym . . . I’ve lost weight and I know one of the reasons why I’m losing it is because of these text messages. And I definitely know that I’ve grown in confidence and even my self-esteem has improved. So, it is nice to be part of, even though I don’t engage in the discussion forums, it’s still nice to be part of a network that, you know, if I do need support it’s literally at the touch of a text, you know . . . I’m definitely benefitting from it.
158, intervention group, 3 months
I think I’m, like, a stone lighter now than I was 12 weeks ago . . . And that’s something that I would’ve been a stone heavier if I hadn’t done something about it.
181, intervention group, 3 months
Women spoke about how the advice provided in the study had given them useful ideas for how they could implement small but long-term changes into their daily routines and set realistic goals for themselves, for example healthy food swaps, monitoring portion sizes, planning meals and fitting short periods of exercise into their daily lives. They emphasised how the SMS messages had made them think about adopting healthier habits that they had not thought of before, and which were feasible to do in the face of barriers posed by their current lifestyles, such as child-care responsibilities:
It was fantastic, getting you into a new way of thinking and a new healthier way of thinking and ways that you could, you know, actually keep up your exercise and everything because with me, personally, I’ve three wee ones, and sometimes it is hard getting them out, but if I can maybe get them sitting with their toys and then even get a YouTube [YouTube, LLC, San Bruno, CA, USA] workout on that’s fantastic, and I would never have thought of that before starting this study.
568, intervention group, 12 months
I work on the fifth floor, so my goal was ‘right [name] you’re working 5 days this week . . . I’m going to walk them five sets of stairs . . . because I’m up and down the stairs like a yoyo all day but it is faster to kind of just jump in the lift and away you go, you know, but I made that point, that’s my target . . . so it’s things like that where I would never have thought about, my routine, go straight to the lift.
061, intervention group, 12 months
For those who felt that they had not been successful in losing weight, the intervention was still perceived as beneficial in that it provided them with motivation and continued reminders to think about their weight management, and it could successfully encourage them to adopt some healthier behaviours:
I sort of feel a bit of a hypocrite having not lost any weight at the minute but, you know, it’s kept my motivation up for exercise, you know, I’ve not given up on it, and hopefully I can get back on track with the weight . . . I think it’s brilliant, you know, a wee daily reminder is exactly what you need, stops you putting that biscuit into your mouth sometimes.
016, intervention group, 3 months
Box 5 highlights the progression criterion related to the positive indicative effects of the intervention.
There is supporting evidence to suggest that the intervention may have a positive effect on weight loss and prevention of weight gain during the postpartum period.
Criterion met: yes.
Research question 8: can data for the proposed end points be successfully collected?
Data for the proposed study end points were collected in two ways. First, anthropometric and physical outcomes were collected by the researchers at the follow-up visits and recorded on CRFs. A CRF capturing these outcomes was successfully returned for each participant that completed the follow-up at each time point (0 months, n = 100; 3 months, n = 93; 6 months, n = 84; 9 months, n = 77; and 12 months, n = 75). The percentages of complete and missing data for these researcher-measured outcomes at the baseline and 12-month follow-up time points are summarised in Table 21. There were very few missing responses for data collected by the researcher. In terms of the methods used to ensure accuracy in these measurements, there were some difficulties encountered in attempting to leave a rest period of 5 minutes between BP readings owing to mothers having to attend to young children.
| Variable | Intervention, n (%) | Active control, n (%) | Overall, n (%) | |||
|---|---|---|---|---|---|---|
| Baseline (N = 51) | 12 months (N = 36) | Baseline (N = 49) | 12 months (N = 39) | Baseline (N = 100) | 12 months (N = 75) | |
| Height | ||||||
| Complete | 51 (100) | a | 49 (100) | a | 100 (100) | a |
| Missing | 0 (0) | 0 (0) | 0 (0) | |||
| Weight | ||||||
| Complete | 51 (100) | 36 (100) | 49 (100) | 39 (100) | 100 (100) | 75 (100) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Waist circumference | ||||||
| Complete | 51 (100) | 34 (94.4) | 49 (100) | 36 (92.3) | 100 (100) | 70 (93.3) |
| Missing | 0 (0) | 2 (5.6) | 0 (0) | 3 (7.7) | 0 (0) | 5 (6.7) |
| Blood pressure | ||||||
| Complete | 51 (100) | 35 (97.2) | 49 (100) | 39 (100) | 100 (100) | 74 (98.7) |
| Missing | 0 (0) | 1 (2.8) | 0 (0) | 0 (0) | 0 (0) | 1 (1.3) |
The second way in which proposed study end points were measured was by the use of a participant self-report questionnaire that was left with participants at the follow-up visits for them to return by post after completion. The rate of returned questionnaires for each follow-up time point is described in Table 22. At all follow-up time points, a lower percentage of women in the active control group than in the intervention group returned their questionnaires.
| Time point (months) | Intervention | Active control | Overall | |||
|---|---|---|---|---|---|---|
| Completed follow-up (N) | Questionnaire received, n (%) | Completed follow-up (N) | Questionnaire received, n (%) | Completed follow-up (N) | Questionnaire received, n (%) | |
| 0 | 51 | 50 (98.0) | 49 | 45 (91.8) | 100 | 95 (95.0) |
| 3 | 47 | 46 (97.9) | 46 | 41 (89.1) | 93 | 87 (93.5) |
| 6 | 43 | 39 (90.7) | 41 | 34 (82.9) | 84 | 73 (86.9) |
| 9 | 37 | 35 (95.6) | 40 | 38 (95.0) | 77 | 73 (94.8) |
| 12 | 36 | 33 (91.7) | 39 | 33 (84.6) | 75 | 66 (88.0) |
Missing data for proposed health outcomes and mediators
Based on only those questionnaires that were returned at the baseline and 12-month time points, levels of missing data for the outcomes measured using these questionnaires were examined (Tables 23 and 24). Missing data were determined by the complete cases available for the proposed study end point, that is the ability to score validated scales as per the authors’ instructions or the completeness of individual items for study-specific questions. The percentage of missing data for health outcomes and mediators ranged from 1.1% to 15.8% at baseline and from 0% to 15.2% at 12 months, with the majority of outcome measures showing < 4% of missing responses (see Table 23). The level of missing scores for the physical activity outcome, measured using the International Physical Activity Questionnaire-Short Form, was noticeably higher.
| Variable | Intervention, n (%) | Active control, n (%) | Overall, n (%) | |||
|---|---|---|---|---|---|---|
| Baseline (N = 50) | 12 months (N = 33) | Baseline (N = 45) | 12 months (N = 33) | Baseline (N = 95) | 12 months (N = 66) | |
| Dietary intake (20 items) | 0 (0) | 0 (0) | 3 (6.7) | 2 (6.1) | 3 (3.2) | 2 (3.0) |
| Physical activity (10 items) | 7 (14.0) | 4 (12.1) | 8 (17.8) | 6 (18.2) | 15 (15.8) | 10 (15.2) |
| Sugar intake (4 items) | 1 (2.0) | 0 (0) | 2 (6.7) | 1 (3.0) | 4 (4.2) | 1 (1.5) |
| Alcohol consumption (1 item) | 0 (0) | 0 (0) | 2 (4.4) | 1 (3.0) | 2 (2.1) | 1 (1.5) |
| Infant feeding (5 items) | 0 (0) | 0 (0) | 1 (2.2) | 0 (0) | 1 (1.1) | 0 (0) |
| Mental health (10 items) | 0 (0) | 0 (0) | 2 (4.4) | 0 (0) | 2 (2.1) | 0 (0) |
| Body image satisfaction (9 items) | 0 (0) | 1 (3.0) | 2 (4.4) | 1 (3.0) | 2 (2.1) | 2 (3.0) |
| Self-classified weight (2 items) | 1 (2.0) | 1 (3.0) | 3 (6.7) | 0 (0) | 4 (4.2) | 1 (1.5) |
| Desire to lose weight (1 item) | 0 (0) | 0 (0) | 1 (2.2) | 0 (0) | 1 (1.1) | 0 (0) |
| Importance of weight loss/weight loss maintenance (1 item) | 0 (0) | 0 (0) | 1 (2.2) | 2 (6.1) | 1 (1.1) | 2 (3.0) |
| Confidence for weight loss/weight loss maintenance (2 items) | 0 (0) | 1 (3.0) | 2 (4.4) | 2 (6.1) | 2 (2.1) | 3 (4.5) |
| Habit formation (8 items) | 0 (0) | 3 (9.1) | 1 (2.2) | 0 (0) | 1 (1.1) | 3 (4.5) |
| Intention and self-efficacy for diet and physical activity (47 items) | 0 (0) | 1 (3.0) | 2 (4.4) | 1 (3.0) | 2 (2.1) | 2 (3.0) |
| Self-regulation of eating behaviour (5 items) | 1 (2.0) | 0 (0) | 1 (2.2) | 1 (3.0) | 2 (2.1) | 1 (1.5) |
| Social support (3 items) | 0 (0) | 0 (0) | 1 (2.2) | 0 (0) | 1 (1.1) | 0 (0) |
| Goal-setting for diet (1 item) | 0 (0) | 0 (0) | 2 (4.4) | 1 (3.0) | 2 (2.1) | 1 (1.5) |
| Goal-setting for physical activity (1 item) | 0 (0) | 0 (0) | 1 (2.2) | 1 (3.0) | 1 (1.1) | 1 (1.5) |
| Weight self-monitoring (1 item) | 0 (0) | 0 (0) | 1 (2.2) | 0 (0) | 1 (1.1) | 0 (0) |
| Weight loss motivation (24 items) | ||||||
| Health reasons | 2 (4.0) | 1 (3.0) | 1 (2.2) | 4 (12.1) | 3 (3.2) | 5 (7.6) |
| For others | 2 (4.0) | 1 (3.0) | 2 (4.4) | 2 (6.1) | 4 (4.2) | 3 (4.5) |
| For oneself | 1 (2.0) | 3 (9.1) | 1 (2.2) | 2 (6.1) | 2 (2.1) | 5 (7.6) |
| Dietary self-monitoring (1 item) | 0 (0) | 0 (0) | 2 (4.4) | 1 (3.0) | 2 (2.1) | 1 (1.5) |
| Physical activity self-monitoring (1 item) | 0 (0) | 0 (0) | 1 (2.2) | 1 (3.0) | 1 (1.1) | 1 (1.5) |
| Self-esteem (10 items) | 0 (0) | 1 (3.0) | 2 (4.4) | 1 (3.0) | 2 (2.1) | 2 (3.0) |
| Sleep (19 items) | 3 (6.0) | 4 (12.1) | 3 (6.7) | 2 (6.1) | 6 (6.3) | 6 (9.1) |
| Weight loss programme engagement (2 items) | 0 (0) | 0 (0) | 1 (2.2) | 0 (0) | 1 (1.1) | 0 (0) |
| Economic costs and outcomes | Time point, n (%) | ||||
|---|---|---|---|---|---|
| Baseline (N = 95) | 3 months (N = 87) | 6 months (N = 73) | 9 months (N = 73) | 12 months (N = 66) | |
| GP surgery attendance | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Nurse | 1 (1.1) | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) |
| Other | 1 (1.1) | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) |
| A&E attendance | 1 (1.1) | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) |
| Outpatient clinic | 1 (1.1) | 2 (2.3) | 0 (0) | 2 (2.7) | 0 (0) |
| Inpatient treatment | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hospitalisation | 2 (2.1) | 2 (2.3) | 2 (2.7) | 0 (0) | 0 (0) |
| Prescriptions | 1 (1.1) | 0 (0) | 0 (0) | 1 (1.4) | 3 (4.5) |
| Over-the-counter medications | 1 (1.1) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) |
| Medicine costs | 1 (1.1) | 3 (3.4) | 1 (1.4) | 3 (4.1) | 2 (3.0) |
| Use of lifestyle services and clubs | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Food and non-alcoholic costs | 1 (1.1) | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) |
| Alcoholic drink costs | 1 (1.1) | 3 (3.4) | 0 (0) | 0 (0) | 0 (0) |
| Takeaway meals and snacks | 1 (1.1) | 2 (2.3) | 0 (0) | 0 (0) | 0 (0) |
| Meals, snacks and drinks away from home | 1 (1.1) | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) |
| Smoking or vaping | 1 (1.1) | 4 (4.6) | 0 (0) | 0 (0) | 0 (0) |
| Health and fitness apps purchased | 1 (1.1) | 1 (1.1) | 1 (1.4) | 0 (0) | 0 (0) |
| Time spent exercising | 4 (4.2) | 2 (2.3) | 2 (2.7) | 0 (0) | 1 (1.5) |
| ICECAP-A (5 items) | 1 (1.1) | 1 (1.1) | 1 (1.4) | 0 (0) | 0 (0) |
| EQ-5D-5L (5 items) | 0 (0) | 0 (0) | 1 (1.4) | 1 (1.4) | 0 (0) |
| EQ-5D VAS | 2 (2.1) | 0 (0) | 1 (1.4) | 0 (0) | 1 (1.5) |
During data analysis, a printing error was identified in the 12-month intervention questionnaires. One of the items used to measure motivation for weight loss, which asked participants to rate how much they agreed with the statement ‘I want to lose weight to have better success with others’, was missing from the paper questionnaires at this time point. This item was removed from the calculation of the score for the subscale ‘for others’, for the intervention group only, at 12 months. The levels of missing data are based on the questions that the participant could respond to.
During the scoring of the Pittsburgh Sleep Quality Index,160 it was identified that there were five additional items (partner-reported responses in relation to participant’s sleep) that had been included in the questionnaire at each time point, but which did not contribute to the scoring of this scale. Rather, they are used for clinical assessments of sleep conditions.
Pedometer data
A summary of participants’ adherence to wearing and returning the pedometers is shown in Appendix 13, Table 33. The percentage of pedometers returned that contained data decreased across the time points from 88% at baseline to 62.3% at month 12. At months 9 and 12, 4% and 12% of women were not given a pedometer, respectively; this was either because the participant said they did not want to wear the pedometer as they kept forgetting to wear it, or because the participant had not returned their pedometer on more than one previous occasion. At month 6, there was a peak in the number of pedometers returned, but data were wiped for 21.4% of those returned. Pedometers had a memory of 14 days; the month 6 assessments took place around Christmas and, although some measures were in place to take account of this seasonal disruption (e.g. rather than arranging to give a pedometer at the visit, it was posted out later to the participant), there was still an increase in wiped data. The number of pedometer diaries returned after each data collection time point is shown in Appendix 14, Table 34. Returned pedometer diaries decreased from 93% at baseline to 72% at month 12. The highest percentage of diaries not returned was at month 9 (22%).
Economic data
Based on the returned questionnaires at each data collection time point, the levels of missing data for the costs, health resource use and economic outcomes measured using these questionnaires have been summarised (see Table 24). There was a low level of missing data, which remained consistent across all of the follow-up time points. It was noted that, although data were captured on prevalence of the use of prescription medicines, the questionnaire did not allow participants to provide details of what medications were prescribed. Therefore, it could not be established whether these were as a result of postpartum or weight-related conditions. More detailed descriptive summaries of the economic costs and outcome data are provided elsewhere (see Appendix 15, Tables 35–40).
Research question 9: can all components of the pilot randomised controlled trial be successfully delivered?
Fidelity of SMS message delivery
System-maintained records of planned SMS message delivery were compared with records of sent SMS messages to assess the fidelity of SMS message delivery. Overall, 100% of participants received all of the intervention SMS messages (excluding those that were pregnant/withdrawn and one participant who paused her SMS messages 1 week before the intervention finished, as she was going on holiday and did not want the messages to be restarted).
For participants receiving the active control SMS messages for the entire 12 months (excluding those that were pregnant or withdrawn), participants received all of the messages except for the introductory message (welcome and website login details) in many cases. The welcome message should have been delivered to all participants regardless of the age of their baby when they signed up, but was delivered only to women who had a very young baby (aged 7 weeks).
Some fidelity issues were noted when system message logs, retained by the automated SMS delivery platform, were examined. One intervention participant did not receive SMS messages for 11 days after week 6. The participant sent a message to the SMS delivery system to notify the research team that she had not received messages for > 1 week. One of the system administrators responded 6 days later and the SMS messages were re-started and receipt acknowledged by the participant later that day. For participants receiving the intervention SMS messages for the entire 12 months (excluding those that were pregnant/withdrawn/paused), 85% (34/40) received their messages as scheduled. Six participants (15%) experienced a 1-week gap in receiving their SMS messages because of an issue with the server; no women complained about this and for these women the intervention was delivered over 53 weeks rather than 52 weeks, but all SMS messages were still delivered.
In summary, the fidelity of SMS message delivery was satisfactory in that, despite some delay in sending some of the SMS messages to the intervention group, all SMS messages were sent to participants as planned. Messages were stopped for those wishing to no longer receive them once they notified the researcher and were restarted appropriately as requested. The system was unable to provide information on when or whether or not the participant actually opened the SMS message, for example if their phone was off, their battery was low or they were out of signal.
Fidelity of SMS message responses
Fidelity of automated replies to weight SMS messages from system
Weight SMS messages: participants were asked to text ‘up’ or ‘down’ or ‘same’ along with their weight during months 7–12; this triggered an automated response, as described previously (see Chapter 2). Engagement with these components and replying in the correct format varied. In total, 123 out of 400 replies were in the format as instructed (see Appendix 11, Table 31). When the replies were examined, it became clear that the system was not sending automated replies to these 123 women. Instead, it was sending automated replies if the women had just texted the word ‘up’ or ‘down’ or ‘same’ without any additional information such as weight, which they were instructed to reply. Hence, this aspect of the intervention was not delivered as planned.
Fidelity of automated replies to ‘yes/no’ questions
The majority of replies were in the correct format; therefore, most participants received the appropriate response (see Appendix 11, Table 31). Participants not responding in the correct format, for example if additional information was included as well as the Y12/N12, did not receive a response.
Fidelity of automated replies to the trigger words
Responses to trigger words were not sent if the software system did not recognise the trigger word that was texted in. This meant that 91% of trigger word messages sent by participants received an automated reply in the first 6 months versus 77% of trigger words receiving an automated reply between months 7 and 12 (see Appendix 12, Table 32).
Fidelity of blinding
It was intended that researchers collecting outcome data would be blinded to group allocation. To achieve this, ideally, different researchers would have conducted the qualitative interviews and participants would not have divulged their group allocation during the outcome assessment visits. In practice, neither of these were possible; several participants did make reference to their group allocation during the follow-up visits and, with only two researchers conducting outcome assessments, it was not possible to have the interviews conducted by different researchers.
Acceptability of the study methods
The questionnaire at 12 months and the qualitative interviews at both 3 and 12 months gathered data on participants’ views in relation to different aspects of the study methods (Table 25). Most women reported that the study methods were ‘easy’ or ‘very easy’, but there were women who experienced difficulties in wearing the pedometer.
| Study method | Group, n (%) | |
|---|---|---|
| Intervention (N = 33) | Active control (N = 33) | |
| Location of visits | ||
| Response | ||
| Easy/very easy | 33 (100) | 32 (94.0) |
| No strong opinion | 0 (0) | 0 (0) |
| Difficult/very difficult | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.0) |
| Duration of visits | ||
| Response | ||
| Easy/very easy | 33 (100) | 31 (94.0) |
| No strong opinion | 0 (0) | 0 (0) |
| Difficult/very difficult | 0 (0) | 0 (0) |
| Missing | 0 (0) | 2 (6.0) |
| Blood pressure measurement | ||
| Response | ||
| Easy/very easy | 33 (100) | 32 (97.0) |
| No strong opinion | 0 (0) | 0 (0) |
| Difficult/very difficult | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.0) |
| Height measurement | ||
| Response | ||
| Easy/very easy | 32 (96.9) | 31 (93.9) |
| No strong opinion | 1 (3.0) | 1 (3.0) |
| Difficult/very difficult | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.0) |
| Weight measurement | ||
| Response | ||
| Easy/very easy | 31 (94.0) | 33 (100) |
| No strong opinion | 1 (3.0) | 0 (0) |
| Difficult/very difficult | 1 (3.0) | 0 (0) |
| Missing | 0 (0) | 0 (0) |
| Waist measurement | ||
| Response | ||
| Easy/very easy | 32 (97.0) | 31 (93.9) |
| No strong opinion | 0 (0) | 1 (3.0) |
| Difficult/very difficult | 1 (3.0) | 0 (0) |
| Missing | 0 (0) | 1 (3.0) |
| Completing questionnaire | ||
| Response | ||
| Easy/very easy | 29 (87.8) | 28 (84.8) |
| No strong opinion | 3 (9.1) | 3 (9.1) |
| Difficult/very difficult | 1 (3.0) | 1 (3.0) |
| Missing | 0 (0) | 1 (3.0) |
| Wearing pedometer | ||
| Response | ||
| Easy/very easy | 23 (69.7) | 17 (51.5) |
| No strong opinion | 3 (9.1) | 8 (24.2) |
| Difficult/very difficult | 7 (21.2) | 6 (18.2) |
| Missing | 0 (0) | 2 (6.0) |
The interview data provided further detail regarding women’s opinions of the study methods used, as described below.
Home visits
Over 90% of visits at each time point were completed at the participant’s own home as the preferred method. Offering women the choice to complete data collection visits at home was considered to be extremely helpful, especially if women had returned to work, in that the appointment was quick, easy and convenient and it could be flexibly arranged to fit in with their other responsibilities. Furthermore, women felt that cancelling and re-organising appointments when needed was easy to do. Being able to complete data collection visits in this way was often a deciding factor on whether or not women were willing to sign up to the study:
‘Come and talk to me on my territory’, gives you that edge definitely. Maybe that’s one of the reasons why I chose to sign up.
158, intervention group, 3 months
I think, had I not had the option for a home visit, I may have thought differently about the study.
023, active control group, 3 months
Some women discussed barriers that would have stood in the way of them completing data collection visits elsewhere; for example, some of the women were unable to drive and, even for those who did, the inconvenience of arranging child care or the hassle of bringing their children with them to complete study tasks meant that home visits were appreciated:
. . . ‘cause I don’t need to worry about getting me or the baby ready.
134, active control group 3 months
The friendliness and professionalism of the researchers who conducted the home visits was emphasised by many participants. Women felt that the visiting researchers were non-judgemental when measuring their weight, as well as being punctual for the arranged visits:
Not being judged when stepping on the scale . . . arrived when they said they would arrive.
158, intervention group, 3 months
Awk lovely, they were both lovely, the girls that had been out.
076, active control group, 3 months
Vouchers
The majority of women believed that the purpose of giving vouchers to participants was to compensate them for the time they spent accurately completing the study assessments and returning them. One woman perceived the vouchers as a reward for losing weight. Others thought that the vouchers were offered as an incentive to get women to sign up to the study and a few said that it had influenced their decision to take part:
I suppose just as a thank-you for our time and commitment to it, but em, and it also just, I imagine it was an incentive to get people to sign up for it . . . I think the One4All is fantastic . . . I mean it’s brilliant, you know, nearly every conceivable shop is on it.
016, intervention group, 3 months
I thought that was excellent for somebody that’s on maternity leave and is coming to the end of pay towards the end of maternity leave as well, I think, it’s been good to have that, that little treat for yourself as well, you know, where you don’t feel guilty about spending a little bit of money on you ‘cause you’ve, like, worn a pedometer for a week.
023, active control group, 3 months
The type of voucher was well accepted as it could be spent in many shops and women could choose to either spend them on their babies or on themselves. Receiving the vouchers was seen as a positive and generous bonus to taking part; quite a few women commented that they would still have been interested in the study regardless of whether the vouchers were included:
I don’t think it was necessary; that’s not the reason I signed up . . . but it was a nice touch.
158, intervention group, 3 months
Questionnaire booklet
Women felt that the questionnaire booklet was mainly clear and easy to complete, and many participants thought that it was good that it was left with them to complete in their own time, that it could be completed in chunks and that it included mostly multiple-choice questions. However, some participants felt that the questions could be repetitive and a few women expressed difficulties with the limited response options provided for questions:
They were quite long, but you had a good period of time to fill them out and send them back, so it kind of made it OK. You know, if you had to have it done, say, at the visit, it would have been a bit harder.
012, active control group, 12 months
It’s not like you’ve to sit and write a big paragraph or anything; they’re fine.
014, intervention group, 3 months
Sometimes I just felt the scale of responses on some of them were maybe not quite obvious to the question.
009, intervention group, 3 months
In terms of the length of the questionnaire, the majority of women found this acceptable and reported that it generally took them between 20 and 30 minutes to complete, but there were a few women who felt that the questionnaire was slightly too long:
. . . the questions themselves are not terribly long.
181, intervention group, 3 months
. . . long but not too much bother.
570, intervention group, 12 months
Some participants noted how providing responses to some questions really made them think about their behaviours or health and well-being, such as what they were feeding their children or how they were feeling:
Oh I thought they were good and I found as mine went on, mine started to change you know, just my overall health and well-being.
061, intervention group, 12 months
Pedometer
Participants were initially happy to wear the pedometer for 7 days, but many found it problematic as it came off their clothing easily, so they had to choose clothing that would allow them to wear it, and others had difficulties in remembering to put it on:
It was grand, again remembering just to put it on.
024, active control group, 3 months
It happened to fall off the first day and I actually forgot to wear it for 3 days.
061, intervention group, 12 months
. . . like, you don’t even need to wear tights because it’s a long dress, so I’m having to wear tights just so I can put the pedometer on.
174, intervention group, 12 months
Participants did not perceive any issues with completing or returning the step diaries, but remembering to fill it in was difficult for some participants.
Unintended impacts of the study methods
A few women who were interviewed in the active control group discussed how aspects of the study methods, including taking part in the study visits that involved weight checks and using the pedometer, despite the screen not being visible, may have been beneficial for helping them to track their health and weight, or to encourage them to try to lose weight or adopt healthier behaviours:
I’ve kind of just enjoyed being part of it . . . the fact of someone coming out and taking my weight and stuff like that, I suppose it made me kind of think about that a bit more you know.
071, active control group, 3 months
It’s quite good actually wearing the pedometer as well ‘cause it makes me go out and walk.
006, active control group, 3 months
Because, you know, maybe 2 or 3 months down the line someone is going to be coming out to your house and you sort of feel, not pressure in a way, but you’re conscious of that and that’s helped me in a way . . . it’s been good in that sense because I’m part of the study and I’m conscious that there’s a weight loss element to it or that there’s a weigh-in element to it, which is helping me, sort of, stay motivated.
024, active control group, 3 months
Participants’ experiences of receiving and accessing additional intervention and active control components
Breastfeeding SMS messages
A total of 32 women opted to receive breastfeeding SMS messages when asked at the baseline visit (before randomisation they were asked if they wished to receive additional SMS messages in relation to breastfeeding). Of these, 14 women went on to be randomised to the intervention group and the other 18 women were randomised to the active control group. The qualitative interviews explored women’s reasons for opting not to receive breastfeeding SMS messages, as well as women’s experiences of receiving the messages. Those women who did not opt to receive the breastfeeding SMS messages mainly did so either because they were no longer breastfeeding at recruitment stage or because they were not breastfeeding their babies. Among those women who received the breastfeeding SMS messages and who took part in the interviews, there was poor recall of the content of the SMS messages that were related to breastfeeding and, overall, women did not report finding these SMS messages particularly useful. The main reasons given for this were because women who were breastfeeding tended to access other breastfeeding support services for advice, or had previous experiences of breastfeeding:
I suppose I’ve been breastfeeding quite a while, you know, my wee boy’s 1 and I’ve breastfed my other wee boy, so I kind of feel my breastfeeding, I’m in a few breastfeeding support groups, and I kind of feel I know everything.
010, intervention group, 3 months
Smoking SMS messages
None of the women within the sample randomised to the intervention group chose to receive SMS messages related to smoking behaviours. Three women who went on to be randomised to the active control group had asked to receive these SMS messages if they were allocated to the intervention group.
Buddy system
Throughout the intervention delivery, participants were reminded that they could utilise the buddy system, whereby a nominated person received the weight management SMS messages for the purposes of being able to support them in their behaviour change (see Chapter 2). Three participants opted into the buddy system. Reasons for low engagement with this component were investigated in the interviews. Some participants taking part in the interviews were unable to recall the details of this optional intervention component, in that they had not paid much attention to the SMS message received that related to the buddy system or they felt that the information provided on this option was unclear. Of those who were aware of the buddy system option, the main reasons given for not utilising this component were lack of interest, that adequate support was already being received from other people in their lives or women being unable to identify a suitable person to receive the messages. Some women felt that they could not approach the subject of receiving weight-related SMS messages with another person or ask them to sign up for receiving SMS messages, whereas others could not identify someone who would want to, or need to, receive the SMS messages:
No that’s not something I did; it must’ve been one of the messages that I flicked past through because I wasn’t aware of it . . . to be honest, it’s not something I’d be interested in.
010, intervention group, 3 months
I probably would’ve opted for my husband, but he kind of knows that I want to lose weight and he’s supportive of it without being pushy so I didn’t really feel there was any need for him to be receiving them as well. Plus, he also, like, I didn’t think it was useful to him personally as he’s quite good and runs marathons so I didn’t see the benefit, really, of him receiving more information.
009, intervention group, 3 months
Supporting MumS study website
Participants from both groups had access to the study website, which provided details about the study, what it involved and why it was being conducted (see Appendix 16). They were also able to log in, which would bring them to a group-specific section of the website, providing information relevant to the randomised group, such as a list of the links that were provided in the SMS messages. Throughout the study, intervention participants were reminded that they could access the study website for more ideas and links to other sources of information. Women were asked about their use of the study website during the interviews at 3 and 12 months.
Some women were unable to recall details of the website, or said that they did not access it owing to time constraints or because they felt that the information provided in the SMS messages was adequate. Of those who did report accessing the website, the majority said that they did so at the start of the study to find further information on the study purpose and what it involved. This information had been useful, but they had not perceived any further need to engage with the website in the long term:
I went on it just initially when I was looking to find out information about the study, just on top of what’s been on the leaflet, that’s all that I used them for . . . it was fine, gave you all the information that I needed.
009, intervention group, 3 months
It’s more the time, probably, that prevents you from getting to look at things, isn’t it?
599, active control group, 12 months
The women who did actively use the website felt that it was useful having all of the links in one place. They also reported that the layout and visual appearance of the website was acceptable. A few participants said that they had experienced difficulties in signing in to the website:
I went on a few times to look at some of the video links . . . I quite liked it, I thought it was easy enough to navigate through and there were good wee pointers throughout it.
028, intervention group, 3 months
Links
The SMS messages sent to the intervention and active control groups included links to websites where participants could access further information. Participants’ experiences of receiving and using these links were examined in the qualitative interviews. Many women reported using the links to seek additional information to what was provided in the SMS message, especially if they thought that it was something that was particularly relevant to them. Most of the women in the active control group had accessed some of the received links and had found them useful, and a few women said that it was good to have the links to allow them to easily access the included information when needed:
I clicked on some of the links because that one yesterday was like a, it was Parents.com [www.parents.com]. And I definitely read a link to NHS and stuff like that.
039, active control group, 12 months
It’s always good to get more information and they are always there then, so even if [child] wasn’t at that stage, you got the message, you know, and you can always go back through it again and find the link so yeah, it was useful that way.
019, active control group, 12 months
However, one participant commented on how the links were not beneficial to her as she received the SMS message including links at an inconvenient time of day, and receiving them later on in the day may have made her more likely to access the additional information.
The ones with the links, I’m not getting the benefit of because . . . it’s more to do, I think, with the times because if they were coming through later and I had time at maybe 8 o’clock at night I would be more likely to click on the links and so on.
009, intervention group, 3 months
Participants in the intervention group also welcomed messages that contained links and most women were able to recall accessing particular links and had found them useful:
I do like the ones with the links so I do, I find them very helpful so I do . . . I would click on them and then sort of write things down in the wee notebook . . . I’ve clicked on the NHS one as well a few times and then I think there’s been one for the Department of Health as well.
015, intervention group, 3 months
Discussion forum
One participant accessed the study forum during the study. The interview data provided a number of explanations for the lack of engagement with this component. Some women said that they were not interested in engaging with this type of platform or would not feel comfortable discussing their weight management in a forum with other women, or that they preferred to read discussion boards but not post on them. Others said that they already used pre-existing forums, such as NetMums (www.netmums.com), and so they did not have a need for this option. One woman, who went on to access the forum, said she initially experienced difficulties with access, which may have prevented others from engaging. Time limitations also stopped some mothers from using this option, even though they felt that it could have been beneficial. A few women said they would talk to their friends rather than engaging in a forum, and one woman said that just taking part in the study made her feel as though she was part of a support network:
I’d just find it really uncomfortable talking to other Mummies on it and stuff . . . it’s also time as well, just didn’t really have the time . . . I would be alright talking to people I would know, or anything like that, but not others.
001, intervention group, 12 months
I’m on a couple of online forums already so – so I just hadn’t much interest in joining another one, you know?
010, intervention group, 3 months
If I had time I would, you know I suppose that’s just, as such, another commitment that I wouldn’t take on at the minute, but I know whenever I was in maternity leave I really enjoyed parenting forums, you know, and that was something that really did work for me when I had more time . . . I found those kinds of forums really supportive.
016, intervention group, 3 months
Although I would look online at the discussion forums, I’m just not there yet where I’d maybe post something up.
158, intervention group, 3 months
Contamination
To assess the extent to which there could have been contamination between the intervention and active control groups, women in the active control group who participated in the interviews at 12 months were asked if they knew anyone else taking part in the study. If they did, they were subsequently asked for details on any study-related discussions that they had had with those persons. The majority of women (15 of 21 interviewed) reported that they were not aware of anyone else taking part in the study. The other six women said that they each knew one other person who was taking part. Four of these women said that they had never discussed the study with that person and were not aware of that person’s group allocation. The other two women said that they were aware of the other person’s group allocation, one of whom was in the active control group, but, beyond this, they had not discussed the study. For the one woman who knew a person allocated to the intervention group, that person had withdrawn from the study after 1 month’s participation owing to pregnancy. The only other evidence that indicated that there could have been some contamination between the group was during one of the 3-month interviews, when a participant in the active control group mentioned specific details about the ‘trigger words’ interactive component of the intervention. However, she spoke about this in the context of perceiving the active control SMS messages as beneficial for supporting women and reducing social isolation in the postpartum period. Furthermore, there was no indication that having this knowledge about the intervention component could have had any influence on the active control participant in terms of her weight management or health behaviours:
I know when the, the sort of physical, healthy-eating sort of ones come in, [name] was saying you could text, I think it was a trigger, and then get like information on that so, you know, it’s really good that you’re, you know, that you’re not on your own.
012, active control group, 3 months
Overall satisfaction with taking part in the study
In the final follow-up questionnaire, participants were asked to rate their satisfaction with the overall experience of taking part in the study (see Appendix 17, Table 41). The majority of women in both groups were ‘very satisfied’ or ‘mostly satisfied’ in terms of their overall experience as a participant in the study (97% and 87.1% for the active control and intervention groups, respectively), with 93.9% of the intervention group and 90.9% of the active control group saying they would recommend the study to other mothers. However, it is noted that this summary is based on only those women who took part at final follow-up and does not include the views of those who were lost to follow-up. The response for one participant in the active control group was recorded as missing, but she had included a text comment stating ‘I found the whole process quite easy. It didn’t put any extra responsibility on me, it was straight forward to participate in’.
For the minority of women who reported that they were dissatisfied with the study, the reasons given included a lack of perceived benefit of the intervention or active control, or the reiteration of some of the earlier issues noted with receiving the SMS messages, including timing. In the intervention group, a few women felt pressured by the SMS messages when they were struggling to manage their weight:
It was fine, staff were lovely but the text messages were of little to no benefit. I’m not sure it was an effective use of resources and university time.
004, active control group, 12-month questionnaire
I don’t think it had much impact or influence on my weight loss. Often, I didn’t find the texts memorable or motivating.
009, intervention group, 12-month questionnaire
Weigh-in day changes from Thursday – Tuesday without notification. Kept forgetting about the change.
310, intervention group, 12-month questionnaire
I felt like I was constantly being reminded about being overweight.
348, intervention group, 12-month questionnaire
For me the frequency of messages. I felt more pressure to lose weight and as an emotional eater, this did not help. The messages with a question got my attention more – a lot of the others weren’t fully read as I was too busy.
590, intervention group, 12-month questionnaire
Research question 10: what fine-tuning of the intervention content or delivery is required for a full randomised controlled trial?
Based on the results from the previous sections, a number of areas for fine-tuning were identified for the intervention or study assessments that should be considered for a full RCT.
Recruitment
-
Aim to increase recruitment of women from lower socioeconomic groups for a full RCT.
-
Aim to increase the ethnic diversity of the sample for a full RCT.
SMS messages
-
Ensure that the active control group receive an initial welcome message regardless of whether they sign up at 6 weeks or a later time point.
-
Ensure that the weight SMS message is delivered to participants on the same day throughout the intervention, for example not on a Sunday, and, preferably, on a day that women choose if they have a preference or an already established weigh-in day.
-
Add a facility for participants to change the time they receive the SMS message during the intervention if their circumstances or preferences change, for example returning to work.
-
Incorporate further reminders of trigger words.
-
Enhance quality assurance: more checks on SMS message delivery to ensure that they are going out as planned.
-
Check on the programming of weight replies in the maintenance phase with refinement of programming and further testing.
-
Add a facility for women to alter active control SMS messages if they find they do not coincide well with their child’s stage of development.
-
Carry out further PPI regarding the buddy system SMS messages to ensure that such messages are clear and understandable.
-
Make it free to reply to SMS messages.
Other intervention components
-
Remove the discussion forum as it was not used by participants.
Study assessments
-
The pedometer was not acceptable to the target group: consider other wearable devices or rely on self-reported questionnaire data.
-
Put in place a system whereby participants can report if they are pregnant prior to the study visits so that researcher time is not wasted making a journey and then finding out that the participant is pregnant.
-
Questionnaire amendments: resolve the error in the printing of the ‘motivation for weight loss’ scale in the 12-month intervention group questionnaire. Remove the five partner-reported items from the Pittsburgh Sleep Quality Index160 used in the questionnaires, as these questions are not required to establish sleep quality using this measure. The resource use questionnaire would need to be refined for use in a full economic evaluation of the Supporting MumS intervention to include a question to capture details of prescribed medications.
Chapter 5 Discussion
This project was funded under the NIHR Public Health Research programme funding call 14/67 ‘Weight management after pregnancy’, which aimed to address the research question: what are the effective and cost-effective interventions for weight management after pregnancy?
The first 12 months of the project developed the SMS message library and interactive features of the intervention in conjunction with PPI. In the following 24 months, a pilot RCT with pre-defined progression criteria relating to feasibility, acceptability and indicative effects was conducted. The pilot RCT met all of its progression criteria: 100 postpartum women were recruited and randomised to receive messages about weight management or an active control (messages about child health and development) for 12 months. Retention of women at the follow-up visits at 3, 6, 9 and 12 months was high. The intervention was rated highly by women and there was evidence of a positive effect on weight loss or prevention of weight gain, particularly among those that engaged with weight self-monitoring and interactive SMS messaging. The intervention was fully automated. This chapter presents a discussion of the main elements of the intervention and pilot RCT.
Feasibility of recruitment
We have demonstrated that it was feasible to recruit participants to a randomised SMS evaluation study. The recruitment target of 100 postpartum women who were overweight or obese and had a baby in the previous 24 months was achieved. Recruitment took 1 month longer than anticipated (5 months instead of 4 months) and this (pro rata) would need to be factored into the timeline for a full RCT.
The use of multiple recruitment strategies is prudent with this population, which can be hard to recruit. One recent study of postpartum women recruited women from general practices only and was unable to meet the recruitment target of 60 women: 16 were recruited. 166 In the Supporting MumS pilot RCT, multiple community-based approaches were used to reach postpartum women. The majority of participants were recruited via social media, which included paid advertisements and also a post from a mother and toddler group leader, with the latter being the biggest contributor to the sample recruitment. The salience of this post on social media, coming directly from a trusted source, and the fact that the leader highlighted that vouchers were offered as a thank-you for participation in the research, probably contributed to the success of recruitment. A potential ‘trusted source’ recruitment route that did not prove successful in this pilot RCT was the promotion of the study via the childhood immunisation programme. Efforts were made to engage with health visitors involved with the childhood immunisation programme in Northern Ireland but, beyond initial e-mail exchanges, further discussions were not possible within the recruitment time frame of the study. Reasons for this are unclear, but are possibly owing to the timeline for the pilot RCT or competing demands on the staff’s time. This avenue of recruitment should be explored again in a full RCT, as health visitors will come into contact with women of all sociodemographic and ethnic groups on several occasions throughout the postpartum period. Promotion of this intervention in that context would be consistent with the health-care ethos of ‘making every contact count’167 and could represent one route to implementation, should a full RCT demonstrate effectiveness.
Based on the interviews with women at 3 months, offering vouchers as a thank-you for participation and completion of the study assessments is likely to have had a positive influence on the decision to participate for some women, although others indicated that they would have participated regardless of the vouchers being offered. Women also mentioned in the interviews that the home visits influenced their decision to participate because of the convenience factor.
The sample that was recruited included women with different levels of education and household income; however, 65% of the sample were educated to degree level or above and 72% had a household income in the highest two categories (> £30,000). Increasing representation of women across the education and income spectrum should be a key aim for a full RCT. Likewise, 99% of the sample were of white ethnic origin (98% of the population of Northern Ireland is of white ethnic origin168) and a full RCT should include sites that will allow recruitment of a more ethnically diverse sample of women, with cultural adaptation of the language, links and suggestions used in messages as indicated through PPI consultation.
Retention
The retention in the pilot RCT was high in both the intervention (86%) and the active control (91%) groups. Previous trials with this target group have been compromised by high levels of attrition in general, and by differential attrition49,58,169 between the intervention and the active control groups. In a systematic review by Dodd et al. 170 of postpartum weight management interventions, 10 of the 27 studies included reported an attrition rate of > 20%.
A number of strategies were included in this pilot RCT to encourage retention, namely the use of an active control to avoid disappointment after randomisation, home visits to overcome logistical barriers to participation in outcome assessments and vouchers that were given to women on completion of each data collection visit (five visits at £20 per visit) in recognition of the time women were giving up to participate. The study was presented to women as being a trial of two interventions with a 50 : 50 chance of receiving either the weight management messages or the child health and development messages. Women reported a high level of satisfaction with the active control and described several benefits of it in the interviews, with several women seeing it as something that would be useful to all women after they have had a baby.
The home visits and vouchers were presented to women as being related to the ‘research’ part of the study, that is the collection of outcomes. These methods are likely to have helped retention, but they may also have been considered by women to be part of the intervention, even though the intervention was fully automated. Although women seemed to link the vouchers to returning their questionnaires, one woman did comment that she felt uneasy accepting the vouchers if she had not lost weight, so it is possible that some women considered them to be part of the intervention. Likewise, the home visits may have acted as a motivator to engage with the intervention, even though they were very brief and the researchers did not engage in any discussion about behaviour change. The vouchers for completion of study assessments and home visits to collect outcome data were implemented for both the intervention and the control groups; thus, between-group differences in outcomes relate to the SMS intervention. It is important, however, to consider if the vouchers and SMS might interact with the effectiveness of the SMS in the design of a full RCT. Furthermore, the home visits made it as convenient as possible to take part in the study but they did add significantly to the workload for the researchers, and appropriate safety protocols had to be in place to protect the researchers.
At the end of the pilot RCT, several women who received the active control said they would also like to have received the other messages as well at the end of the study. This is something that should be factored into the cost of a full RCT, especially as one of the entry criteria was a BMI of ≥ 25 kg/m2. Funding was not available for this, but a booklet based on the intervention content was developed and given to the active control group at the end of the study.
There were some differences in the characteristics of women who completed the 12-month follow-up compared with those who did not: a higher proportion of non-completers were first time mothers, were between 12 and 24 months postpartum and had a BMI of > 40 kg/m2. This may indicate that women with these characteristics found it more difficult to stay in the study; however, the number of non-completers was low (n = 10), and interviews did not provide any particular indication that these factors were related to engagement with the intervention. This is something that could be explored further in a full RCT. Encouragingly, women educated to below degree level were as likely to be retained as those educated to above degree level.
The interactive features in the Supporting MumS intervention means that, in a future full RCT, it will be possible to explore non-usage attrition and so help to distinguish between reasons for stopping use of the intervention versus reasons for dropping out of the RCT. 171
Acceptability and perceived benefits of the intervention and active control
Data on acceptability were captured via questionnaire responses and in interviews with women at 3 and 12 months. Women who took part in the interviews reflected a range of sociodemographic backgrounds and included a mixture of ‘low’ and ‘high’ engagers.
Satisfaction ratings with the intervention and active control were high, one participant was mostly dissatisfied with the intervention messages, two participants were mostly dissatisfied with the control messages indicating that they felt mostly dissatisfied with the SMS messages they received. No participants indicated they were very dissatisfied. Between 82% and 97% of participants indicated that they found the SMS messages to be easy to understand, helpful, interesting and appropriate in terms of number and timing. In addition, women also commented favourably on the different types of messages and liked the fact that the messages also came at the weekend, when routines change and compliance with weight management efforts can be put to the test. A few women indicated that they would like to have modified the times that they received the SMS messages to better fit with usual routines or to accommodate changing routines. Some women in the active control group felt that the messages did not coincide well with the developmental stage of their child; the facility to adjust this would enhance the acceptability of the active control further.
The high acceptability of the SMS messages is likely to have been influenced by the PPI in the creation and refinement of the message library. Although PPI can extend the time it takes to create the intervention, this investment is worthwhile when the result is a highly acceptable intervention that is valued by the target group.
Even though delivery of the intervention and active control was fully automated, many women discussed feeling supported as a key benefit of taking part that was particularly welcomed at a time when they can feel isolated. After pregnancy, appointments covering maternal health and well-being become very limited; the focus of most interactions with health professionals after pregnancy is the baby’s health. Women have reported receiving much less, if any, physical activity and weight loss advice after pregnancy than during pregnancy. 172,173
The SMS messages were described as encouraging, non-judgemental, non-stigmatising, reassuring and empathetic. They acted as reminders to stay on track or to get back on track after a dip in motivation and prompted positive decisions. Importantly, women could engage with them at a time that suited them and also look back over previous messages they had received. In the interviews, women were able to readily recall specific details about the SMS message content and the different styles of messages. Some women also appreciated the anonymity of the delivery via SMS message but, at the same time, they discussed a feeling of accountability.
The active control SMS messages also elicited many positive responses from women including feeling supported, reassured and encouraged. Others appreciated increasing feelings of self-worth as a mother, indicating a potential benefit of these messages in their own right for postpartum women.
Engagement with the intervention components
Two-way messages
Participants engaged well with the weight replies and the ‘yes/no’ SMS messages, with a few participants replying to every message and the majority replying to over half of the messages. This engagement was sustained across the 12 months of the intervention.
In the first 6 months, nearly half of the participants texted at least one trigger word and, in the last 6 months, about 20% of participants texted a trigger word. Thus, use of the trigger words was lower in the second half of the intervention. ‘Bad day’ and ‘crave’ were the most frequently sent words in months 0–6, and ‘slip-up’ and ‘bad day’ were the most frequently texted words in months 7–12. More reminders about the trigger words are likely to encourage more use of this support system, as over one-third of the trigger words sent by participants were sent on the same day that participants were informed or reminded about them. It is possible that the trigger words were needed more in the earlier stages of the intervention, when self-regulatory skills and habits were being developed.
Two elements of the intervention were added to provide social support, but both were rarely used. The buddy system option was rarely used for a variety of reasons, including not paying attention to the SMS message informing them about the buddy system, a lack of interest in this option or feeling that they were already well supported. Women did discuss feeling well supported by the SMS messages, so it is possible that this element was not required.
Similar to the buddy system, participants did not use the discussion forum and, in interviews, they indicated that they did not feel that they needed this form of support. Even though the discussion forum was a closed group that was available only to intervention group participants, women indicated that they had no desire to post any discussions.
Based on these observations, it is likely that the buddy system and discussion forum would not be valuable to include in a full RCT.
Evidence of positive indicative effects
The change in anthropometric measures demonstrated an overall loss of 1.75 kg in the intervention group and a gain of 0.19 kg in the active control group at 12 months. Eight per cent (n = 3) of women in the intervention group gained ≥ 5 kg, compared with 20% (n = 8) of women in the active control group, hence indicating that the intervention may have helped to attenuate postpartum weight gain. Several studies174–177 have also demonstrated that the postpartum period is a vulnerable time for weight gain, namely weight gain that originates during the postpartum period.
An exploratory analysis was conducted to examine if engaging with the interactive SMS messages was associated with weight change. Thus, based on the number of replies to the weekly weight SMS message and the ‘yes/no’ SMS message, participants were classified as ‘low’ or ‘high’ engagers (below and above median number of responses). Analysis of the weight change in ‘high’ versus ‘low’ engagers for the weight replies and the ‘yes/no’ SMS message revealed notable differences: weight change for those who sent weight replies was –2.66 kg for ‘high’ engagers and –0.84 kg for ‘low’ engagers; weight change for those who sent ‘yes/no’ replies was –3.9 kg for ‘high’ engagers and –0.4 kg for ‘low’ engagers. This underlines the value of adding the two-way messages to the intervention and encouraging self-monitoring and reporting of weight: those that engaged most with these messages were more successful in their weight loss efforts.
Pilot randomised controlled trial methodology
Presenting the study to women
The study was presented to women as an offer of one of two interventions, with a 50 : 50 chance of being assigned to receive SMS messages about either child health and development or weight management. Recruitment materials stated that weight at time of recruitment was an inclusion criterion. The study was presented in this way to offset the randomisation disappointment that may have contributed to differential attrition in other postpartum studies. Feedback from participants and study retention rates support the use of this approach in a full RCT.
Screening participants
Women who were interested in taking part in the study were screened for inclusion over the telephone. This included asking for self-reported weight to assess if they were potentially eligible. If they were, a researcher visited the woman to obtain consent and conduct baseline assessments, but, before doing so, weight was measured by the researcher to confirm eligibility. This resulted in seven women being excluded, as their measured weight was lower than their self-reported weight and they did not meet the weight criterion. This needs to be factored into the workload for researchers when recruiting for a full RCT.
Home visits
Women were offered the choice of the researcher visiting them in their own home to collect the study data or attending the Centre for Public Health at QUB. Overall, the vast majority of follow-up appointments were home visits, and, although this is more demanding on the researcher’s time, feedback from women supports the decision to offer home visits to facilitate participation and retention of postpartum women who are already juggling multiple demands on their time.
Data quality and acceptability of questionnaires
Data completion in returned questionnaires was high; there were very few missing responses, indicating good acceptability and comprehension of the measures used. The questionnaires were pilot-tested and refined before using them in the pilot RCT, which probably improved acceptability. Questionnaire return was slightly higher for the intervention group than for the active control group; this would need to be monitored in a full RCT.
For the cost-effectiveness questionnaires, the costs collected in the pilot RCT were appropriate. The well-being and health-related quality of life (HRQoL) instruments and the resource use data collection instrument would be appropriate for an economic evaluation in a full RCT. The evidence of personal costs linked to weight loss endeavours underline the importance of including a societal perspective for the Supporting MumS economic evaluation alongside the UK NHS and Personal Social Services perspectives. 161 Some minor amendments to the questionnaires would be desirable for a full RCT, such as the addition of categories to the resource use form based on those that are common to postpartum treatment (identified via the pilot RCT), and refinements to capture details of medications prescribed. Only prescription use was collected in the pilot RCT, with no information on medication prescribed and its relevance to postpartum health or a participant’s weight.
Pedometer
A sealed pedometer (the screen was covered so a participant could not view the steps) and pedometer diary were used to collect data on steps per day as an objective indicator of physical activity at each follow-up assessment. Participants were asked to wear the pedometer for 7 days and then post it back to the team in a pre-paid envelope; pedometers with a long memory life were chosen to allow for delays in wearing/returning. Overall, compliance with wearing the pedometer and completing the pedometer diary decreased over the course of the study. When women did wear the pedometer, the quality of data obtained was good. However, women struggled to wear the pedometer for a number of reasons and several pedometers were not returned. When rating the different aspects of the study assessments, women rated pedometers as the least acceptable assessment. A wrist-worn accelerometer with data not visible to participants might be a more acceptable alternative.
Contamination
The majority of participants were recruited via mother and baby groups, social media and word of mouth, and so contamination between study groups was a possibility. At the 12-month interview, participants were asked if they knew anyone else who was taking part in the study; there was no evidence that participants had shared information or discussed their group allocation. This is something that should be considered further in preparations for a full RCT.
Blinding of the outcome assessment
Blinding of the outcome assessment was not possible in the pilot RCT, as some participants made reference to their group allocation during the follow-up visits. Furthermore, with only two researchers conducting outcome assessments, it was not possible to have the 3- and 12-month interviews conducted by different researchers. Reminding participants not to discuss the messages at the start of each visit would help minimise the disclosure of group allocation. With more staff, it would be possible to ensure that the follow-up interviews are not conducted by researcher(s) responsible for conducting other outcome assessments.
Fidelity of delivery of intervention and active control messages
Examination of SMS message delivery data indicated that all participants received all of the intervention or active control messages according to their group allocation. There were a few, temporary, issues with timing of delivery when some intervention SMS messages were stalled in the system owing to a technical difficulty with the server. However, this was resolved fairly quickly and all messages were delivered. In some instances, the automated feedback SMS message programming did not always work as intended. These elements would need to be revisited and resolved, and enhanced quality assurance procedures put in place, before a full RCT examining effectiveness of the intervention was conducted.
Refinements to study protocol or intervention for a full randomised controlled trial
A number of amendments that would be worth making to the study protocol were identified, including minor edits to questionnaire items and minor changes to the intervention elements, such as additional options for tailoring message timing. If targeting a broader range of ethnicities for a full RCT, which would be desirable, cultural adaptation of the messages in terms of language, links and suggestions would be necessary to ensure relevance and acceptability. This should involve a similar PPI approach to that used to develop the SMS message library for the pilot RCT.
Strengths and limitations of the Supporting MumS intervention pilot study
Strengths
A major strength of this study was the production of a library of SMS messages, informed by PPI and explicitly based on behaviour change maintenance theory and incorporating BCTs that are known to be positively associated with weight management. Michie et al. 104 highlight the importance of engaging with the target group in the development of technology interventions. The PPI in this study helped to ensure that the intervention was well accepted by the target group. A further strength was the successful recruitment of postpartum women and high retention in the pilot RCT, both of which have been challenges encountered in previous postpartum RCTs. Furthermore, engagement with the weight replies and with ‘yes/no’ two-way messages was sustained over the 12 months of the intervention, providing further evidence of acceptability and demonstrating the potential for sustained long-term contact with participants, which is conducive to the maintenance of behaviour change. The intervention itself remains novel in the literature, being one of the few UK-based studies in this field, and one of very few interventions that are delivered by fully automated SMS messages, with two-way messages and feedback provided through interactive features. Systematic reviews discussed previously (see Chapter 1) and in Findings in context,49,53,74,75,170,178–181 indicate gaps in the evidence on SMS interventions and interventions addressing postpartum weight loss, many of which have been addressed through the development and pilot testing in the feasibility RCT, or would be addressed in a full RCT.
Limitations
The pilot study participants were predominantly of white ethnicity (99%), which is reflective of the Northern Irish population (98.2% white ethnicity, according to the 2011 census). 168 An aspiration for a full RCT would be to adapt the intervention for a wider range of ethnic groups and to choose recruitment sites that would allow effectiveness testing in a broad range of ethnicities. Similarly, a desire for a full RCT would be to increase the proportion of women from lower socioeconomic groups, as 65% of the sample were educated to degree level or above, 55% were in full-time employment and 72% were in the highest income category.
Staff numbers meant that it was not possible for the 3- and 12-month interviews to be conducted by a researcher who was not involved in outcome assessments, but this may be something that could be factored into the staffing arrangements for a full RCT. Reasons for loss to follow-up were not recorded and it would be useful to try to gather some feedback on this in a full RCT. As discussed in Retention, it is possible, for some women, that the home visits and vouchers for participation were viewed as part of the intervention and interacted with the SMS messages. This possibility needs to be considered when developing the protocol for a full RCT.
It is possible that participants in the control group may have modified their behaviour as a result of taking part in the study, as one control group participant commented that she had been motivated to become more active. The likely impact of this ‘Hawthorne effect’182 on the study findings is difficult to quantify, but it probably reduced between-group differences in outcomes. As for the intervention group, the active control was fully automated and the only contact participants had with study personnel was for outcome data collection, which was standardised for both groups. As part of outcome data collection, participants were asked to wear a sealed pedometer (i.e. they could not read the steps it recorded). This could have contributed to the Hawthorne effect; the pilot RCT results found that the pedometer was the least preferred data collection method and was often lost, damaged or not returned, so it is unlikely that it would be used in a full RCT.
Findings in context
Systematic reviews of SMS interventions for weight management
Since 2015, there have been several systematic reviews178–181 examining the effectiveness of using SMS messages in weight management interventions, all of which provide evidence that supports the use of this mode of delivery.
Siopsis et al. 181 investigated the efficacy of weight management interventions (RCTs or before-and-after studies) using SMS messages. Their search up until October 2013 identified 14 studies, nine of which were conducted in adults. A meta-analysis of six of the adult studies indicated a weighted mean change in body weight among intervention participants of –2.56 kg, compared with –0.37 kg in control participants.
A systematic review and meta-analysis by Schippers et al. 180 examined RCTs testing the effect of interventions delivered via mobile phones on weight loss. Of the 12 studies included, five compared a group receiving a SMS intervention with a control group that received no intervention; all noted a higher weight loss in the intervention groups (weight change ranging from –0.53 kg to –6.76 kg) than in the control groups (weight change ranging from –4.49 kg to 1.14 kg).
The most recent systematic review in this area was published by Job et al. 178 It examined the effectiveness of extended-contact interventions for weight management for adults, delivered via SMS message. Extended-contact interventions were considered to be interventions delivered for ≥ 1 month(s) following an initial weight loss intervention; SMS messages had to provide > 50% of the contacts during the extended-contact intervention period. Seven studies were included, but only three of these were RCTs. This small number of studies provided some evidence that extended-contact, SMS-delivered interventions can be effective. A number of recommendations for future research were made, such as the need for fully powered trials with longer durations and to include interactive components via SMS (two-way messages); clear consideration and better reporting of BCTs; the need to conduct mediation analysis; measurements of diet and physical activity outcomes and examination of their effect on weight maintenance; and consideration of external validity including implementation indicators, economic evaluation and maintenance of outcomes. The Supporting MumS study has already addressed some of these suggestions in its intervention design and pilot RCT and would address the others (e.g. mediation analysis, economic evaluation, implementation indicators) in a full RCT.
A further systematic review by Holmes et al. 179 examined the impact of digital technologies for communicating messages on weight loss maintenance. Seven RCTs were included, three of which used SMS for intervention delivery: one among children aged 10–14 years183 and two among adults. 184,185 Both of the studies with adults focused on weight loss maintenance and found that the interventions showed benefits for weight loss maintenance and maintenance of positive lifestyle changes. The authors of the systematic review179 discussed the potential value of exploring ways of automating feedback to participants, while maintaining the sense of human contact and a personal touch, to overcome reliance on a human operator, which limits potential for scale-up and implementation. The Supporting MumS study adopted a fully automated approach to intervention delivery while still delivering feedback to participants, and PPI engagement when developing the SMS library helped ensure that the tone and style of the SMS messages maintained a sense of human contact.
Based on the most recent systematic reviews described in the previous paragraph, the Supporting MumS study remains unique in the literature in several ways. Notably, few RCTs of text messaging interventions to support weight management have used SMS as the sole or predominant mode of delivery, few have used automated delivery and two-way messages, few incorporate weight loss and weight loss maintenance evidence and few have lasted ≥ 12 months.
Randomised controlled trials of SMS interventions for weight management
Since the above systematic reviews were published, a number of RCTs have examined the effect of SMS interventions on weight loss186–191 or weight loss maintenance192,193 or the prevention of weight gain. 194
Four RCTs186,189–191 used one-way SMS messages in a weight loss intervention. Newton et al. 186 examined the efficacy of a church-based weight loss intervention incorporating mHealth technology on weight loss in a cluster RCT. Eight churches were randomly assigned to either intervention or delayed intervention for 6 months. The intervention group attended group sessions (n = 10) and received SMS messages (five messages per week, one-way). There was a significant difference in weight change between the intervention and control group: intervention group, –1.5 kg; control group, 0.11 kg. Stephens et al. 190 conducted a mHealth weight loss intervention among 62 young adults with overweight or obesity. In this 3-month intervention, the control group received a lifestyle counselling session whereas the intervention group received a multicomponent intervention consisting of two lifestyle counselling sessions, a smartphone diet and activity self-monitoring app and individualised SMS messages from a health coach (the frequency was variable, according to participant preference, from once a week to up to three messages per day; one-way). There was a significant difference in weight change between the intervention and control groups: intervention group, –1.8 kg; control group, 0.3 kg. Ahn and Choi189 tested a one-way SMS intervention in 80 participants with obesity and observed a modest but statistically significant difference in weight change in the intervention group (three messages per week for 12 weeks), compared with the control group (no messages); BMI was significantly lower in the intervention group than in the control group after 12 weeks (27.9 kg/m2 vs. 28.2 kg/m2, adjusted for baseline BMI; weight change in kg was not reported in paper). Silina et al. 191 recruited 123 participants with overweight or obesity and randomised them to one of two groups: a control group (advice on lifestyle) or an intervention group that received advice on lifestyle plus a SMS message (one-way) once every 2 weeks for 1 year. There was a significant difference in weight change between the intervention and control groups: intervention group, 2.40 kg; control group, 1.02 kg.
Two weight loss SMS RCTs have used a combination of one-way and two-way text messages. Zwickert et al. 188 compared the effect of a low-intensity, SMS-only intervention with a high-intensity SMS plus e-mail intervention on weight loss in 60 obese adults in Australia. Both groups received a 12-session cognitive–behavioural therapy intervention. The low-intensity intervention consisted of a one-way daily SMS message for months 0–6, with no intervention after this time point. The high-intensity intervention also received a one-way daily SMS message during months 0–6, but, in addition, they were sent a weekly SMS message requiring a response during months 0–6, a weekly SMS message requiring a response and self-reported weight from months 6–9 and e-mail support from a therapist (maximum three e-mail responses per week). The intervention ceased at month 9 and participants were followed up at 3, 6, 9 and 15 months. Weight loss rates at 15 months were 7.5% for the high-intensity group and 5.1% for the low-intensity group. There was no significant difference between groups in weight change at any of the follow-up points. As both groups lost > 5% body weight, the authors concluded that the study supports SMS messages as a way to support weight loss alongside a group-based cognitive–behavioural therapy intervention. Axley et al. 187 conducted a small (n = 30 participants) RCT in patients with non-alcoholic fatty liver disease. The control group received lifestyle counselling; the intervention group received lifestyle counselling plus three SMS messages (one-way and two-way) weekly for 22 weeks. There was a significant difference in weight change between the intervention and control groups: intervention group, –3.14 kg; control group, 0.82 kg).
Lombard et al. 194 set out to prevent weight gain with a 1-year cluster RCT conducted in 41 towns in Australia among women aged 18–50 years; 301 women were allocated to the control and 348 were allocated to the intervention. The 1-year self-management intervention consisted of one group session at the start, a SMS message each month starting at week 4, a telephone coaching session at week 12 and a programme manual. SMS messages were one-way only. The control group received one general women’s health education session. There was a significant difference in mean weight change between the groups at 1 year (control, 0.44 kg; intervention, –0.48 kg), with authors concluding that a low-intensity lifestyle programme can prevent weight gain over time in women.
Two RCTs have examined text messaging and weight loss maintenance. Kulendran et al. 193 examined the effect of two different styles of SMS messages on weight loss maintenance in obese adolescents in a small, 12-week pilot study with 27 participants. After randomisation, one group received SMS messages giving information and advice on weight loss (one-way messages) and the other group received the same advice but were asked to commit to following the advice (two-way messages). The BMI of adolescents in the commitment group did not change, but the BMI of adolescents in the information group increased. This pilot study indicated that the two-way messages that asked participants to commit to suggested changes were helpful for weight loss maintenance. Lauti et al. 192 designed a SMS intervention to support weight loss maintenance after sleeve gastrectomy surgery. Ninety-five patients were recruited 18 months after surgery and were randomly assigned to receive standard care or SMS support (daily text message each morning, one-way) for 1 year. There was no significant difference in weight regain between groups.
With one exception,192 all of these studies observed significant between-group differences in weight loss or prevention of weight gain or weight loss maintenance in the SMS groups compared with controls, across a range of population groups and in men and women. SMS messages formed a substantial component of the interventions in these studies and was used as the sole delivery mode in three189,191,192 out of nine studies. Most of the studies used one-way SMS messages (seven out of nine studies186,189–194), thus limiting the interactivity of the intervention; two studies187,188 used two-way messaging and none of the studies incorporated replies to the two-way messaging. Three studies were ≤ 3 months in duration.
The number of weight management interventions using SMS continues to grow and these studies will help to address current uncertainties about this mode of delivery, including optimal frequency/intensity, importance of interactivity, value of automation, effect of tailoring and whether SMS should be sole intervention or is most effective when combined with other forms of support. The Supporting MumS study makes a novel and important contribution to this field as there is currently a lack of fully automated SMS interventions, especially in which SMS is the main mode of delivery, and also a lack of interventions incorporating two-way messaging and replies to two-way messaging to encourage engagement and deliver specific BCTs.
Systematic reviews of interventions for weight management in the postpartum period
A review of systematic reviews and meta-analyses by Farpour-Lambert et al. 195 examined evidence for an effect of postpartum interventions on postpartum weight retention. Fifteen systematic reviews were included: nine focused on pregnancy, three focused on postpartum and three covered both during and after pregnancy (the systematic review by Dodd et al. 170 was not included). Overall, combined diet and activity interventions reduced postpartum weight retention in women of any BMI (weighted mean difference –2.57 kg to –2.30 kg), but this was based on evidence judged to be of very low quality according to the Revised Assessment of Multiple Systematic Reviews (R-AMSTAR)196 quality assessment tool. The data for participants with overweight or obesity was judged to be of moderate to very low quality, and the reduction in postpartum weight retention in these participants was –3.60 kg to –1.22 kg.
Since this application was submitted, a number of systematic reviews examining the effectiveness of weight loss interventions in the postpartum period have been published. Sherifali et al. 67 examined the effectiveness of electronic health (eHealth) technologies on weight management in pregnant and postpartum women and also reviewed the efficacy of eHealth technologies on nutrition and physical activity. They included RCTs, non-RCTs, before-and-after studies and pilot studies, with a minimum intervention period of 3 months. Ten studies that were included were published between 1990 and 2016. EHealth technologies included mobile phone text messaging, mobile phone or tablet apps, web-based, e-mails, personal digital assistant, handheld computer and home computer. Four of the 10 studies focused on the postpartum period. 63,197–199 The interventions mainly used web-based interventions, with one study using SMS messages alongside the web-based component. 199 The pooled analysis for eHealth interventions showed a statistically significant mean difference in weight loss of –2.55 kg (95% CI –3.81 kg to –1.28 kg) and mean difference in BMI of –0.87 kg/m2 (95% CI –1.56 kg/m2 to 0.18 kg/m2), relative to the control conditions. None of the studies examined the separate effect of contact with a health professional from the effects of the eHealth intervention alone. The systematic review concluded that there was evidence of benefits of eHealth technologies on weight management in pregnant women; however, they noted that many interventions combined eHealth with other intervention components, and so further research is needed to examine the independent effects of the different eHealth technologies on weight management.
Dodd et al. 170 examined weight loss in postpartum dietary and/or physical activity interventions in a systematic review that included studies published up to November 2017. A total of 27 trials met the inclusion criteria: two used diet intervention alone, five used physical activity alone and 20 combined diet and physical activity; weight outcome data were available for 75% of these. Meta-analysis indicated that combined diet and physical activity interventions (n = 12 studies) resulted in a mean difference in weight loss of –2.49 kg, compared with no intervention. This systematic review noted an overall participant withdrawal rate of 25% and, as for previous reviews in this area, indicated a need to develop appropriate ways of recruiting and engaging with this population to achieve sustained behaviour change.
Interventions for weight management in the postpartum period
Since the most recent systematic review (Dodd et al. 170), which searched literature up to September 2017, a number of weight management trials in postpartum women have been published, the majority of which have been feasibility or pilot studies. These studies highlight interventions that show promise in postpartum women, and, in particular, the use of technology seems to be well received. However, issues of poor recruitment and retention still affect some studies in this area. 166,175,200 The five feasibility and pilot RCTs described in the following paragraphs, all from the USA, have used different intervention approaches ranging from group based to the use of technology to deliver postpartum weight management interventions.
Gilmore et al. 201 conducted a 4-month pilot RCT of the E-Moms mHealth intervention delivered by a smartphone app. As well as the app, participants, who were at an early postpartum stage (< 8 weeks), were provided with a Bluetooth (Bluetooth Special Interest Group, Kirkland, WA, USA) scale and accelerometer that fed data to the app. A registered dietitian provided individualised advice if a participant’s weight deviated for about 3 consecutive days from their ideal weight zone; this support was provided by telephone, e-mail or SMS message. The control group received the usual Women, Infants and Children (WIC) service consisting of standard advice for postpartum nutrition and weight management through their WIC clinic (WIC Moms). The overall attrition rate was 12.5% (WIC Moms, 20%; E-Moms, 5%) and there was some evidence that high adherence (n = 5/19, based on compliance with daily weighing and logging step counts) to the intervention resulted in weight loss, but the pilot nature of the study meant that it was not powered for hypothesis testing. There was also some evidence that, overall, E-Moms prevented weight gain during the 16-week follow-up: WIC Moms gained 2.1% of body fat, compared with the 0.03% gain in the E-Moms group. The team concluded that further development of the intervention to improve adherence is needed.
Wright et al. 200 examined the feasibility of implementing a postpartum weight retention intervention trial in partnership with a community-based organisation serving low-income families with social service support. The intervention was multicomponent: an initial 90-minute class in a local neighbourhood venue followed by another class 6 weeks later, as well as 45-minute home visits at 6 and 12 months post delivery. Between the initial and follow-up class, women were encouraged to wear a pedometer, to use a baby carrier (provided) and to participate in an associated 20-minute exercise programme. They received daily motivational SMS messages and were asked to reply to 42 days of SMS messages, reporting footsteps and baby carrier time. There was no control group; 17 participants who were between 6 and 12 weeks postpartum were recruited over 3 months by community health workers. Attrition was 30% at 6 weeks, 35% at 6 months and 47% at 1 year. There was good engagement with the self-monitoring reporting via SMS in the 6-week intensive intervention: 82% of women texted at least three times per week. There was evidence of weight loss in 58% of the completers at 6 weeks (mean weight loss 0.45 kg; IQR –4.1 kg to 1.8 kg) and 78% of completers at 1 year (mean weight loss 2.3 kg; IQR –14.5 kg to 0.3 kg). However, the observed high attrition rate indicates that there may be issues with acceptability of this intervention.
Another RCT by Joshi et al. 175 used a group-based approach to deliver a behavioural weight management intervention in postpartum African American women in the USA. The intervention was an eight-session, in-person, group-based, weekly weight-loss programme that focused on supervised exercise (resistance training or dancing) and nutrition education, and was based on the Diabetes Prevention Program. 202 Women were randomised to the intervention (n = 32) or usual care (n = 30); 16 women from the intervention group and 19 from the usual care group completed the 8-week follow-up. Mean attendance at group sessions was 40% and about one-third of women (11/32) attended no sessions. Both groups gained weight (2.4-kg gain in the intervention group; 2.2-kg gain in the usual care group). The attrition and lack of engagement observed indicates that this was not a viable intervention.
Two studies testing the use of technology to deliver the intervention to postpartum women show promise. Waring et al. 203 examined the feasibility and acceptability of delivering a postpartum intervention via Facebook in a non-controlled pilot study in the USA. A total of 19 participants who were between 6 weeks and 12 months postpartum and had BMIs of between 25 kg/m2 and 45 kg/m2 were recruited to the 12-week intervention. The intervention was delivered by a private Facebook group and was based on the Diabetes Prevention Program,202 but adapted for postpartum and Facebook delivery. It consisted of Facebook posts, links to online articles, support and encouragement, and a topic of the day provided by two coaches, with an obstetrician and physical therapist available to answer questions. Retention was high (95%) and average 12-week weight loss was 4.8% (SD 4.2%). Thus, this intervention approach appeared to be feasible and acceptable to women and supports the need for further research to assess effectiveness.
Herring et al. 177 conducted a pilot RCT of a pregnancy and postpartum intervention in socioeconomically deprived African American women (n = 66; 36% overweight, 64% obese). The intervention was implemented in early pregnancy through to 6 months postpartum and included several components: weekly to monthly health coach calls, behaviour change goals, interactive self-monitoring text messages, skills training and support through Facebook. Outcomes were assessed at 6 months postpartum and also at 12 months postpartum (6 months after the intervention ceased). Relative to the usual care control group, postpartum weight retention was lower in the intervention group at 6 months postpartum: the proportion at or below early pregnancy weight at 6 months was 56% versus 29% for the intervention and control groups, respectively, but this finding was not maintained at 12 months postpartum. Overall retention was 76%; 68% of participants responded to > 50% of the self-monitoring SMS messages in the postpartum period. The intervention was acceptable and feasible and supports a larger definitive study.
Therefore, some postpartum weight management interventions show potential for effectiveness to date, with those employing technology perhaps being more acceptable for this group because they fit better within the lives of women at this stage of life. Less intensive, self-directed approaches that can be delivered remotely lend themselves to delivering the sustained contact that is needed for long-term behaviour change. Even though recruitment rates may suggest that postpartum women have similar interest in remotely delivered versus in-person weight management interventions,204 the reality of engaging with in-person protocols remains a challenge, as observed in some of the studies described in the previous paragraphs. Furthermore, depending on the level of automation and human interaction, options for scale-up and implementation are expanded for technology-based or technology-assisted interventions. 205 The full potential of using technology in this way in postpartum weight management has not been realised, particularly with regard to SMS support as a primary mode of delivery.
A further gap in this field is the lack of CEAs in postpartum weight management studies, as well as studies examining the effect of such interventions on HRQoL or psychological health; currently, few studies have included longer-term follow-up to examine weight loss maintenance and other maternal and infant health outcomes. It is also becoming more apparent that weight gain originating in the postpartum period is not uncommon in postpartum women and so prevention of weight gain is a viable goal for postpartum studies. 37,206
Based on the evidence from systematic reviews and RCTs described in this chapter, the novelty of the Supporting MumS intervention is apparent in terms of the strong trial design that has been developed, with specific consideration of the needs of postpartum women, and the novel intervention that has been developed in consultation with postpartum women and is delivered in a way that is acceptable to women and has the potential for scale-up and implementation at low cost.
Research recommendations
This work has advanced our understanding of how to carry out research with postpartum women. Feedback from women indicated that the home visits for data collection were a good way to facilitate participation in the research and it is likely that these will have contributed to good retention and data completion:
-
The use of multiple recruitment strategies is prudent with this population, which can be hard to recruit. Social media was the most successful recruitment approach used in this pilot study.
-
Allowing a wider window postpartum to opt in to weight management studies takes into consideration the significant variation in women’s lived experience of the postpartum period and allows them to opt in at a time of their choosing.
-
The active control employed in this study worked well; the messages about child health and development were well received by women and may be worth exploring as an intervention in its own right for mums, dads, grandparents and other caregivers.
Based on this study and evidence from the literature in this field, some considerations and priorities for future research in this area are as follows:
-
There is a need for longer-term interventions in this field that specifically address weight loss maintenance as well as weight loss.
-
Follow-up of participants in the longer term is needed to explore maintenance of any changes in weight and health behaviours after interventions cease.
-
Studies should seek to examine spill-over effects on the wider family from interventions targeted at mothers.
-
Trials should explore cost-effectiveness, potential for scale-up and routes to implementation.
-
Studies employing technology show promise for postpartum women, but robust trials are needed; many interventions to date combine eHealth with other intervention components and so further research is needed to examine the independent effects of the different eHealth technologies on weight management. Studies examining the separate effect of contact with a health professional from the effects of the eHealth intervention alone are lacking.
-
With regard to SMS interventions, more studies are needed to address gaps in the evidence regarding the optimal frequency/intensity, importance of interactivity, value of automation, effect of tailoring and whether SMS should be sole intervention or is most effective when combined with other forms of support.
Conclusion
An evidence- and theory-based SMS-delivered intervention was successfully developed in conjunction with postpartum women with overweight and obesity. The intervention was acceptable to women and was feasible to implement in 12-month pilot RCT. Progression criteria for a full RCT were met and a full RCT should examine the effectiveness and cost-effectiveness of the intervention. Some minor refinements need to be made to the intervention and trial procedures based on the findings of the pilot study before conducting a multicentre full RCT.
Acknowledgements
The intervention costs were provided by the Public Health Agency, Northern Ireland.
We would like to acknowledge the following people who have contributed to this study:
-
The women who contributed to the PPI work and those who participated in the study.
-
Miss Kerrie-Ann Forsythe, clerical officer for the Supporting MumS study, QUB.
-
Dr Roisin O’Neill, Dr Amy Wotherspoon and Dr Amy McGowan, post-doctoral research fellows, QUB, who assisted with study visits.
-
Miss Lauren Edge, second-year medical student, QUB, who assisted with data entry.
-
Miss Eimer McGuickian, third-year medical student, QUB, who assisted with data entry and study administration.
-
Mr Irrfan Ahamed, software engineer, London School of Hygiene & Tropical Medicine, who provided technical support for the automated SMS system throughout the study.
Study Steering Committee
-
Ms Caroline Bloomfield (chairperson), Public Health Agency, Northern Ireland.
-
Ms Janet Calvert, Public Health Agency, Northern Ireland.
-
Dr Nicola Heslehurst, Institute of Health and Society, Newcastle University.
-
Dr Emma Frew, Institute of Applied Health Research, Birmingham University.
-
Professor Chris Patterson, Centre for Public Health, QUB.
-
Ms Sabrina Lynn, Southern Health and Social Care Trust.
Contributions of authors
Caroline McGirr (https://orcid.org/0000-0002-6474-7037) (PhD Student, Nutrition) co-wrote the text messages and was involved in all aspects of the study set-up, recruitment, data collection, data analysis and interpretation. She wrote substantial sections of the intervention development (see Chapter 2), methods (see Chapter 3) and results (see Chapter 4) for the final report.
Ciara Rooney (https://orcid.org/0000-0001-9307-7768) (Post-Doctoral Research Fellow, Public Health Nutrition) co-wrote the text messages and was involved in all aspects of the study set-up, recruitment and data collection and entry.
Dunla Gallagher (https://orcid.org/0000-0002-6037-1351) (Post-Doctoral Research Fellow, Health Psychology) was involved in all aspects of the data analysis and interpretation and wrote substantial sections of the background (see Chapter 1), methods (see Chapter 3) and results (see Chapter 4) for the final report.
Stephan U Dombrowski (https://orcid.org/0000-0001-9832-2777) (Assistant Professor, Health Psychology) was a co-investigator, contributed to the writing of the text messages, the study design and interpretation of findings.
Annie S Anderson (https://orcid.org/0000-0002-0047-4500) (Professor, Public Health Nutrition) was a co-investigator and contributed to the study design and the interpretation of findings.
Christopher R Cardwell (https://orcid.org/0000-0002-2689-4335) (Senior Lecturer, Medical Statistics) was a co-investigator, contributed to the study design and the interpretation of findings, and oversaw the statistical analysis.
Caroline Free (https://orcid.org/0000-0003-1711-0006) (Professor, Primary Care and Epidemiology) was a co-investigator, contributed to the study design and the interpretation of findings, and oversaw the set-up of the automated SMS platform.
Pat Hoddinott (https://orcid.org/0000-0002-4372-9681) (Professor, Primary Care) was a co-investigator and contributed to the writing of the text messages, the study design and the interpretation of findings.
Valerie A Holmes (https://orcid.org/0000-0001-6229-5703) (Senior Lecturer, Diabetes) was a co-investigator and contributed to the study design and interpretation of the findings.
Emma McIntosh (https://orcid.org/0000-0001-6340-3083) (Professor, Health Economics) was a co-investigator, contributed to the study design and interpretation of the findings, and oversaw the collection and analysis of the health economics data.
Camilla Somers (https://orcid.org/0000-0001-6227-8508) (Post-Doctoral Research Fellow, Health Economics) analysed the cost-effectiveness data, contributed to the interpretation of the findings and wrote relevant sections of the methods (see Chapter 3) and results (see Chapter 4) sections for the final report.
Jayne V Woodside (https://orcid.org/0000-0002-5691-4659) (Professor, Human Nutrition) was a co-investigator and contributed to the study design and the interpretation of findings.
Ian S Young (https://orcid.org/0000-0003-3890-3152) (Professor, Medicine) was a co-investigator and contributed to the study design and the interpretation of findings.
Frank Kee (https://orcid.org/0000-0002-0606-8167) (Professor, Public Health) was a co-investigator and contributed to the study design and the interpretation of findings.
Michelle C McKinley (https://orcid.org/0000-0003-3386-1504) (Reader, Nutrition) co-wrote the text messages and led the design and overall conduct of the study and writing of the report.
Publications
McKinley MC, Rooney C, McGirr C, on behalf of the Supporting MumS research team. Supporting MumS pilot RCT Study Design. Poster presentation at the Association for the Study of Obesity on the Island of Ireland (ASOI) conference ‘Implementing Obesity Policy into Practice’, Dublin, 27 April 2016.
McKinley MC, Rooney C, McGirr C, on behalf of the Supporting MumS research team. When do Women Opt In to Postpartum Weight Management? Findings from the Supporting Mums (SMS) Pilot Intervention. Poster presentation at the World Obesity Hot Topic conference ‘Obesity and Reproduction – the cradle of the epidemic’. Leuven, 9 November 2017.
McKinley MC, McGirr C, Rooney C, on behalf of the Supporting MumS research team. Postpartum and Inter-pregnancy Weight Management: Challenges and Opportunities. Oral presentation at the Association for Study of Obesity Northern Ireland symposium on Weight Management before, during and after pregnancy, Belfast, 24 January 2018.
McKinley MC, McGirr C, Rooney C, on behalf of the Supporting MumS research team. Weight Management After Pregnancy: Challenges and Opportunities. Oral presentation at the 5th UK Congress on Obesity, Symposium on ‘Weight management and diet quality before and after pregnancy: public perception, priority areas and what interventions work?’ Newcastle upon Tyne, 6–7 September 2018.
McGirr C, Rooney C, Gallagher D, McKinley MC, on behalf of the Supporting MumS research team. Making Use of Opportunities to Detect Postnatal Depression in Postpartum Research – Evidence from the Supporting MumS (SMS) Study. Poster presentation at the 14th UK Society of Behavioural Medicine Annual Scientific Meeting. Birmingham, 12–13 December 2018.
McGirr C, Gallagher D, Rooney C, McKinley MC, on behalf of the Supporting MumS research team. Use of an Active Control in Weight Management Research – The Supporting MumS Study. Oral presentation at the 28th Nutrition Society Irish Section Postgraduate conference, Portrush, 13–15 February 2019.
McGirr C, Gallagher D, Rooney C, McKinley MC, on behalf of the Supporting MumS research team. A Lifestyle Intervention for Weight Loss and Maintenance of Weight Loss in the Postpartum Period. Oral presentation at the Northern Ireland (NI) British Psychological Society annual conference (Association for the Study of Obesity NI and Division of Health Psychology NI joint event on weight management), Belfast, 11 April 2019.
Gallagher D, McGirr C, Rooney C, McKinley MC, on behalf of the Supporting MumS research team. Acceptability of a Novel Text Message-delivered Intervention for Weight Loss and Maintenance of Weight Loss in the Postpartum Period: the Supporting Mums Study. Poster presentation at the 26th European Congress on Obesity, Glasgow, 28 April–1 May 2019.
McGirr C, Gallagher D, Rooney C, McKinley MC, on behalf of the Supporting MumS research team. Use of an Active Control in Weight Management Research – the Supporting MumS Study. Oral presentation at the 26th European Congress on Obesity, Glasgow, 28 April–1 May 2019.
Gallagher D, McGirr C, Rooney C, McKinley MC, on behalf of the Supporting MumS research team. The Supporting MumS study: A Pilot Randomised Controlled Trial of an SMS-delivered Intervention for Weight Loss and Maintenance of Weight Loss in the Postpartum Period. Oral presentation at the International Society of Behavioural Nutrition and Physical Activity scientific conference, Prague, 4–7 June 2019.
McGirr C, Gallagher D, Rooney C, McKinley MC, on behalf of the Supporting MumS research team. The Supporting MumS study: Development of a Text-Message Library to Support Weight Loss and Maintenance of Weight Loss in the Postpartum Period. Poster presentation at the International Society of Behavioural Nutrition and Physical Activity scientific conference, Prague, 4–7 June 2019.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Haslam DW, James WP. Obesity. Lancet 2005;366:1197-209. https://doi.org/10.1016/S0140-6736(05)67483-1.
- NCD Risk Factor Collaboration . Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016;387:1377-96. https://doi.org/10.1016/S0140-6736(16)30054-X.
- Public Health England . UK Prevalence of Maternal Obesity 2015 n.d. http://webarchive.nationalarchives.gov.uk/20170110171101/https://www.noo.org.uk/NOO_about_obesity/maternal_obesity_2015/prevalence (accessed January 2017).
- Heslehurst N, Rankin J, Wilkinson JR, Summerbell CD. A nationally representative study of maternal obesity in England, UK: trends in incidence and demographic inequalities in 619 323 births, 1989–2007. Int J Obes 2010;34:420-8. https://doi.org/10.1038/ijo.2009.250.
- Scott-Pillai R, Spence D, Cardwell CR, Hunter A, Holmes VA. The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004–2011. BJOG 2013;120:932-9. https://doi.org/10.1111/1471-0528.12193.
- Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev 2015;16:621-38. https://doi.org/10.1111/obr.12288.
- Bhattacharya S, Campbell DM, Liston WA, Bhattacharya S. Effect of body mass index on pregnancy outcomes in nulliparous women delivering singleton babies. BMC Public Health 2007;7. https://doi.org/10.1186/1471-2458-7-168.
- Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA 2014;311:1536-46. https://doi.org/10.1001/jama.2014.2269.
- Schellong K, Schulz S, Harder T, Plagemann A. Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0047776.
- Godfrey KM, Inskip HM, Hanson MA. The long-term effects of prenatal development on growth and metabolism. Semin Reprod Med 2011;29:257-65. https://doi.org/10.1055/s-0031-1275518.
- Cnattingius S, Villamor E. Weight change between successive pregnancies and risks of stillbirth and infant mortality: a nationwide cohort study. Lancet 2016;387:558-65. https://doi.org/10.1016/S0140-6736(15)00990-3.
- Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet 2006;368:1164-70. https://doi.org/10.1016/S0140-6736(06)69473-7.
- McKinley MC, Allen-Walker V, McGirr C, Rooney C, Woodside JV. Weight loss after pregnancy: challenges and opportunities. Nutr Res Rev 2018;31:225-38. https://doi.org/10.1017/S0954422418000070.
- Crozier SR, Inskip HM, Godfrey KM, Cooper C, Harvey NC, Cole ZA, et al. Southampton Women’s Survey Study Group . Weight gain in pregnancy and childhood body composition: findings from the Southampton Women’s Survey. Am J Clin Nutr 2010;91:1745-51. https://doi.org/10.3945/ajcn.2009.29128.
- Catalano PM, Shankar K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ 2017;356. https://doi.org/10.1136/bmj.j1.
- Cheney K, Berkemeier S, Sim KA, Gordon A, Black K. Prevalence and predictors of early gestational weight gain associated with obesity risk in a diverse Australian antenatal population: a cross-sectional study. BMC Pregnancy Childbirth 2017;17. https://doi.org/10.1186/s12884-017-1482-6.
- Christenson A, Johansson E, Reynisdottir S, Torgerson J, Hemmingsson E. Women’s perceived reasons for their excessive postpartum weight retention: a qualitative interview study. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0167731.
- Linné Y, Dye L, Barkeling B, Rössner S. Long-term weight development in women: a 15-year follow-up of the effects of pregnancy. Obes Res 2004;12:1166-78. https://doi.org/10.1038/oby.2004.146.
- Linné Y, Dye L, Barkeling B, Rössner S. Weight development over time in parous women – the SPAWN study – 15 years follow-up. Int J Obes Relat Metab Disord 2003;27:1516-22. https://doi.org/10.1038/sj.ijo.0802441.
- Lipsky LM, Strawderman MS, Olson CM. Maternal weight change between 1 and 2 years postpartum: the importance of 1 year weight retention. Obesity 2012;20:1496-502. https://doi.org/10.1038/oby.2012.41.
- Gore SA, Brown DM, West DS. The role of postpartum weight retention in obesity among women: a review of the evidence. Ann Behav Med 2003;26:149-59. https://doi.org/10.1207/S15324796ABM2602_07.
- Rooney BL, Schauberger CW, Mathiason MA. Impact of perinatal weight change on long-term obesity and obesity-related illnesses. Obstet Gynecol 2005;106:1349-56. https://doi.org/10.1097/01.AOG.0000185480.09068.4a.
- Kirkegaard H, Stovring H, Rasmussen KM, Abrams B, Sorensen TI, Nohr EA. How do pregnancy-related weight changes and breastfeeding relate to maternal weight and BMI-adjusted waist circumference 7y after delivery? Results from a path analysis. Am J Clin Nutr 2014;99:312-9. https://doi.org/10.3945/ajcn.113.067405.
- Leslie WS, Gibson A, Hankey CR. Prevention and management of excessive gestational weight gain: a survey of overweight and obese pregnant women. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-10.
- Siega-Riz AM, Herring AH, Carrier K, Evenson KR, Dole N, Deierlein A. Sociodemographic, perinatal, behavioral, and psychosocial predictors of weight retention at 3 and 12 months postpartum. Obesity 2010;18:1996-2003. https://doi.org/10.1038/oby.2009.458.
- McBain RD, Dekker GA, Clifton VL, Mol BW, Grzeskowiak LE. Impact of inter-pregnancy BMI change on perinatal outcomes: a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 2016;205:98-104. https://doi.org/10.1016/j.ejogrb.2016.07.487.
- Jain AP, Gavard JA, Rice JJ, Catanzaro RB, Artal R, Hopkins SA. The impact of interpregnancy weight change on birthweight in obese women. Am J Obstet Gynecol 2013;208:205-7. https://doi.org/10.1016/j.ajog.2012.12.018.
- Gunderson EP, Abrams B, Selvin S. Does the pattern of postpartum weight change differ according to pregravid body size?. Int J Obes Relat Metab Disord 2001;25:853-62. https://doi.org/10.1038/sj.ijo.0801631.
- Østbye T, Peterson BL, Krause KM, Swamy GK, Lovelady CA. Predictors of postpartum weight change among overweight and obese women: results from the Active Mothers Postpartum study. J Womens Health 2012;21:215-22. https://doi.org/10.1089/jwh.2011.2947.
- Nehring I, Schmoll S, Beyerlein A, Hauner H, von Kries R. Gestational weight gain and long-term postpartum weight retention: a meta-analysis. Am J Clin Nutr 2011;94:1225-31. https://doi.org/10.3945/ajcn.111.015289.
- Bogaerts A, Van den Bergh BR, Ameye L, Witters I, Martens E, Timmerman D, et al. Interpregnancy weight change and risk for adverse perinatal outcome. Obstet Gynecol 2013;122:999-1009. https://doi.org/10.1097/AOG.0b013e3182a7f63e.
- Gunderson EP, Abrams B, Selvin S. The relative importance of gestational gain and maternal characteristics associated with the risk of becoming overweight after pregnancy. Int J Obes Relat Metab Disord 2000;24:1660-8. https://doi.org/10.1038/sj.ijo.0801456.
- Siega-Riz AM, Evenson KR, Dole N. Pregnancy-related weight gain—a link to obesity?. Nutr Rev 2004;62:S105-11. https://doi.org/10.1111/j.1753-4887.2004.tb00079.x.
- Montgomery KS, Bushee TD, Phillips JD, Kirkpatrick T, Catledge C, Braveboy K, et al. Women’s challenges with postpartum weight loss. Matern Child Health J 2011;15:1176-84. https://doi.org/10.1007/s10995-010-0681-9.
- Montgomery KS, Best M, Aniello TB, Phillips JD, Hatmaker-Flanigan E. Postpartum weight loss: weight struggles, eating, exercise, and breast-feeding. J Holist Nurs 2013;31:129-38. https://doi.org/10.1177/0898010112464120.
- Graham M, Uesugi K, Olson C. Barriers to weight-related health behaviours: a qualitative comparison of the socioecological conditions between pregnant and post-partum low-income women. Matern Child Nutr 2014;12:349-61. https://doi.org/10.1111/mcn.12135.
- Olson CM, Strawderman MS, Hinton PS, Pearson TA. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int J Obes Relat Metab Disord 2003;27:117-27. https://doi.org/10.1038/sj.ijo.0802156.
- Public Health England . The Impact of Obesity London: Public Health England 2016. www.noo.org.uk/LA/impact/economic (accessed January 2017).
- Morgan KL, Rahman MA, Macey S, Atkinson MD, Hill RA, Khanom A, et al. Obesity in pregnancy: a retrospective prevalence-based study on health service utilisation and costs on the NHS. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-003983.
- Hinkle SN, Schieve LA, Stein AD, Swan DW, Ramakrishnan U, Sharma AJ. Associations between maternal prepregnancy body mass index and child neurodevelopment at 2 years of age. Int J Obes 2012;36:1312-19. https://doi.org/10.1038/ijo.2012.143.
- Whitaker RC. Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics 2004;114:e29-36. https://doi.org/10.1542/peds.114.1.e29.
- Athukorala C, Rumbold AR, Willson KJ, Crowther CA. The risk of adverse pregnancy outcomes in women who are overweight or obese. BMC Pregnancy Childbirth 2010;10. https://doi.org/10.1186/1471-2393-10-56.
- Kitzmiller JL, Elixhauser A, Carr S, Major CA, de Veciana M, Dang-Kilduff L, et al. Assessment of costs and benefits of management of gestational diabetes mellitus. Diabetes Care 1998;21:B123-30.
- Simon J, Gray A, Duley L. Magpie Trial Collaborative Group . Cost-effectiveness of prophylactic magnesium sulphate for 9996 women with pre-eclampsia from 33 countries: economic evaluation of the Magpie Trial. BJOG 2006;113:144-51. https://doi.org/10.1111/j.1471-0528.2005.00785.x.
- National Institute for Health and Care Excellence . Weight Management Before, During and After Pregnancy 2010.
- Centre for Maternal and Child Enquiries, Royal College of Obstetricians and Gynaecologists . CMACE/RCOG/Joint/Guideline:/Management/of/Women/With/Obesity/in/Pregnancy 2010.
- Heslehurst N, Dinsdale S, Sedgewick G, Simpson H, Sen S, Summerbell CD, et al. An evaluation of the implementation of maternal obesity pathways of care: a mixed methods study with data integration. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0127122.
- Johnson M, Campbell F, Messina J, Preston L, Buckley Woods H, Goyder E. Weight management during pregnancy: a systematic review of qualitative evidence. Midwifery 2013;29:1287-96. https://doi.org/10.1016/j.midw.2012.11.016.
- Lim S, O’Reilly S, Behrens H, Skinner T, Ellis I, Dunbar JA. Effective strategies for weight loss in post-partum women: a systematic review and meta-analysis. Obes Rev 2015;16:972-87. https://doi.org/10.1111/obr.12312.
- Dinsdale S, Branch K, Cook L, Shucksmith J. ‘As soon as you’ve had the baby that’s it . . .’ a qualitative study of 24 postnatal women on their experience of maternal obesity care pathways. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3289-1.
- Nascimento SL, Pudwell J, Surita FG, Adamo KB, Smith GN. The effect of physical exercise strategies on weight loss in postpartum women: a systematic review and meta-analysis. Int J Obes 2014;38:626-35. https://doi.org/10.1038/ijo.2013.183.
- Amorim Adegboye AR, Linne YM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev 2013;7. https://doi.org/10.1002/14651858.CD005627.pub3.
- van der Pligt P, Willcox J, Hesketh KD, Ball K, Wilkinson S, Crawford D, et al. Systematic review of lifestyle interventions to limit postpartum weight retention: implications for future opportunities to prevent maternal overweight and obesity following childbirth. Obes Rev 2013;14:792-805. https://doi.org/10.1111/obr.12053.
- Choi J, Fukuoka Y, Lee JH. The effects of physical activity and physical activity plus diet interventions on body weight in overweight or obese women who are pregnant or in postpartum: a systematic review and meta-analysis of randomized controlled trials. Prev Med 2013;56:351-64. https://doi.org/10.1016/j.ypmed.2013.02.021.
- Østbye T, Krause KM, Lovelady CA, Morey MC, Bastian LA, Peterson BL, et al. Active Mothers Postpartum: a randomized controlled weight-loss intervention trial. Am J Prev Med 2009;37:173-80. https://doi.org/10.1016/j.amepre.2009.05.016.
- Craigie AM, Macleod M, Barton KL, Treweek S, Anderson AS. WeighWell team . Supporting postpartum weight loss in women living in deprived communities: design implications for a randomised control trial. Eur J Clin Nutr 2011;65:952-8. https://doi.org/10.1038/ejcn.2011.56.
- O’Toole ML, Sawicki MA, Artal R. Structured diet and physical activity prevent postpartum weight retention. J Womens Health 2003;12:991-8. https://doi.org/10.1089/154099903322643910.
- Macleod M, Craigie AM, Barton KL, Treweek S, Anderson AS. WeighWell team . Recruiting and retaining postpartum women from areas of social disadvantage in a weight-loss trial – an assessment of strategies employed in the WeighWell feasibility study. Matern Child Nutr 2013;9:322-31. https://doi.org/10.1111/j.1740-8709.2011.00393.x.
- Hoddinott P, Allan K, Avenell A, Britten J. Group interventions to improve health outcomes: a framework for their design and delivery. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-800.
- White M, Adams J, Heywood P, Babones SJ. Social Inequality and Public Health. Bristol: Policy Press; 2009.
- Madigan CD, Daley AJ, Lewis AL, Jolly K, Aveyard P. Which weight-loss programmes are as effective as Weight Watchers®?: non-inferiority analysis. Br J Gen Pract 2014;64:e128-36. https://doi.org/10.3399/bjgp14X677491.
- Devine CM, Bove CF, Olson CM. Continuity and change in women’s weight orientations and lifestyle practices through pregnancy and the postpartum period: the influence of life course trajectories and transitional events. Soc Sci Med 2000;50:567-82. https://doi.org/10.1016/S0277-9536(99)00314-7.
- Colleran HL, Lovelady CA. Use of MyPyramid menu planner for moms in a weight-loss intervention during lactation. J Acad Nutr Diet 2012;112:553-8. https://doi.org/10.1016/j.jand.2011.12.004.
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLOS Med 2013;10. https://doi.org/10.1371/journal.pmed.1001362.
- Lyzwinski LN. A systematic review and meta-analysis of mobile devices and weight loss with an intervention content analysis. J Pers Med 2014;4:311-85. https://doi.org/10.3390/jpm4030311.
- Shaw R, Bosworth H. Short message service (SMS) text messaging as an intervention medium for weight loss: a literature review. Health Informatics J 2012;18:235-50. https://doi.org/10.1177/1460458212442422.
- Sherifali D, Nerenberg KA, Wilson S, Semeniuk K, Ali MU, Redman LM, et al. The effectiveness of eHealth technologies on weight management in pregnant and postpartum women: systematic review and meta-analysis. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8006.
- Scottish Government . Scotland’s Digital Future. A Strategy for Scotland 2011.
- Bert F, Giacometti M, Gualano MR, Siliquini R. Smartphones and health promotion: a review of the evidence. J Med Syst 2014;38. https://doi.org/10.1007/s10916-013-9995-7.
- European Observatory on Health Systems and Policies . Building resilient and innovative health systems. EuroHealth 2013;19:1-52.
- Marmot M. Fair Society, Healthy Lives: The Marmot Review. Strategic Review of Health Inequalities in England Post-2010. London: The Marmot Review; 2010.
- National Institute for Health and Care Excellence . Behaviour Change: Individual Approaches 2014.
- Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity 2013;21:25-31. https://doi.org/10.1002/oby.20232.
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 2009;36:165-73. https://doi.org/10.1016/j.amepre.2008.09.040.
- Aguilar-Martínez A, Solé-Sedeño JM, Mancebo-Moreno G, Medina FX, Carreras-Collado R, Saigí-Rubió F. Use of mobile phones as a tool for weight loss: a systematic review. J Telemed Telecare 2014;20:339-49. https://doi.org/10.1177/1357633X14537777.
- Joo NS, Kim BT. Mobile phone short message service messaging for behaviour modification in a community-based weight control programme in Korea. J Telemed Telecare 2007;13:416-20. https://doi.org/10.1258/135763307783064331.
- Patrick K, Raab F, Adams MA, Dillon L, Zabinski M, Rock CL, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res 2009;11. https://doi.org/10.2196/jmir.1100.
- Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technol Assess 2004;8. https://doi.org/10.3310/hta8210.
- Sniehotta FF, Simpson SA, Greaves CJ. Weight loss maintenance: an agenda for health psychology. Br J Health Psychol 2014;19:459-64. https://doi.org/10.1111/bjhp.12107.
- Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev 2012;13:509-17. https://doi.org/10.1111/j.1467-789X.2011.00972.x.
- Penn L, White M, Lindström J, den Boer AT, Blaak E, Eriksson JG, et al. Importance of weight loss maintenance and risk prediction in the prevention of type 2 diabetes: analysis of European Diabetes Prevention Study RCT. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0057143.
- Shaw RJ, Bosworth HB, Hess JC, Silva SG, Lipkus IM, Davis LL, et al. Development of a theoretically driven mHealth text messaging application for sustaining recent weight loss. JMIR Mhealth Uhealth 2013;1. https://doi.org/10.2196/mhealth.2343.
- Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol 2000;19:64-9. https://doi.org/10.1037/0278-6133.19.Suppl1.64.
- Kwasnicka D, Dombrowski SU, Sniehotta F, White M. What does theory tell us about behaviour change maintenance? A structured review. Psychol Health 2013;28:247-8.
- Sciamanna CN, Kiernan M, Rolls BJ, Boan J, Stuckey H, Kephart D, et al. Practices associated with weight loss versus weight-loss maintenance results of a national survey. Am J Prev Med 2011;41:159-66. https://doi.org/10.1016/j.amepre.2011.04.009.
- Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics J 2009;15:17-25. https://doi.org/10.1177/1460458208099865.
- Duenas A, Rawdin A, Chilcott J, Messina J, Johnson M, Campbell F, et al. The cost-effectiveness of weight management interventions following childbirth. Sheffield: School of Health and Related Research (ScHARR); 2010.
- Hagberg LA, Brekke HK, Bertz F, Winkvist A. Cost-utility analysis of a randomized controlled weight loss trial among lactating overweight/obese women. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-38.
- Rawdin AC, Duenas A, Chilcott JB. The cost-effectiveness of weight management programmes in a postnatal population. Public Health 2014;128:804-10. https://doi.org/10.1016/j.puhe.2014.07.005.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2004.
- Bergmo TS. Can economic evaluation in telemedicine be trusted? A systematic review of the literature. Cost Eff Resour Alloc 2009;7. https://doi.org/10.1186/1478-7547-7-18.
- Bensink M, Hailey D, Wootton R. A systematic review of successes and failures in home telehealth: preliminary results. J Telemed Telecare 2006;12:8-16. https://doi.org/10.1258/135763306779380174.
- Darkins A, Ryan P, Kobb R, Foster L, Edmonson E, Wakefield B, et al. Care Coordination/Home Telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health 2008;14:1118-26. https://doi.org/10.1089/tmj.2008.0021.
- Polisena J, Coyle D, Coyle K, McGill S. Home telehealth for chronic disease management: a systematic review and an analysis of economic evaluations. Int J Technol Assess Health Care 2009;25:339-49. https://doi.org/10.1017/S0266462309990201.
- Rojas SV, Gagnon MP. A systematic review of the key indicators for assessing telehomecare cost-effectiveness. Telemed J E Health 2008;14:896-904. https://doi.org/10.1089/tmj.2008.0009.
- Graybill EM, McMeekin P, Wildman J. Can aging in place be cost effective? A systematic review. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0102705.
- Dávalos ME, French MT, Burdick AE, Simmons SC. Economic evaluation of telemedicine: review of the literature and research guidelines for benefit-cost analysis. Telemed J E Health 2009;15:933-48. https://doi.org/10.1089/tmj.2009.0067.
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 2011;378:49-55. https://doi.org/10.1016/S0140-6736(11)60701-0.
- Jepson RG, Harris FM, Platt S, Tannahill C. The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-538.
- Michie S, Free C, West R. Characterising the ‘Txt2Stop’ smoking cessation text messaging intervention in terms of behaviour change techniques. J Smok Cessat 2012;7:55-60. https://doi.org/10.1017/jsc.2012.12.
- NHS . Smokefree: Support Services n.d. www.nhs.uk/smokefree/help-and-advice/support (accessed December 2018).
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815-25. https://doi.org/10.1016/S0140-6736(11)60814-3.
- Cobiac L, Vos T, Veerman L. Cost-effectiveness of Weight Watchers and the Lighten Up to a Healthy Lifestyle program. Aust N Z J Public Health 2010;34:240-7. https://doi.org/10.1111/j.1753-6405.2010.00520.x.
- Michie S, Yardley L, West R, Patrick K, Greaves F. Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7126.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008;57:1-29. https://doi.org/10.1111/j.1464-0597.2007.00325.x.
- Irvine L, Crombie IK, Cunningham KB, Williams B, Sniehotta FF, Norrie J, et al. Modifying alcohol consumption to reduce obesity: a randomized controlled feasibility study of a complex community-based intervention for men. Alcohol Alcohol 2017;52:677-84. https://doi.org/10.1093/alcalc/agx067.
- Crombie IK, Irvine L, Falconer DW, Williams B, Ricketts IW, Jones C, et al. Alcohol and disadvantaged men: a feasibility trial of an intervention delivered by mobile phone. Drug Alcohol Rev 2017;36:468-76. https://doi.org/10.1111/dar.12455.
- Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie D, Jones C, et al. Texting to Reduce Alcohol Misuse (TRAM): main findings from a randomized controlled trial of a text message intervention to reduce binge drinking among disadvantaged men [published online ahead of print June 1 2018]. Addiction 2018. https://doi.org/10.1111/add.14229.
- Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Ann Behav Med 2009;38:4-17. https://doi.org/10.1007/s12160-009-9118-3.
- Nigg CR, Borrelli B, Maddock J, Dishman RK. A theory of physical activity maintenance. Appl Psychol 2008;57:544-60. https://doi.org/10.1111/j.1464-0597.2008.00343.x.
- Kanfer FH, Goldstein AP. Helping People Change: A Textbook of Methods. Oxford: Pergamon Press; 1975.
- Evenson KR, Aytur SA, Borodulin K. Physical activity beliefs, barriers, and enablers among postpartum women. J Womens Health 2009;18:1925-34. https://doi.org/10.1089/jwh.2008.1309.
- Saligheh M, McNamara B, Rooney R. Perceived barriers and enablers of physical activity in postpartum women: a qualitative approach. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0908-x.
- Groth SW, David T. New mothers’ views of weight and exercise. MCN Am J Matern Child Nurs 2008;33:364-70. https://doi.org/10.1097/01.NMC.0000341257.26169.30.
- Neiterman E, Fox B. Controlling the unruly maternal body: losing and gaining control over the body during pregnancy and the postpartum period. Soc Sci Med 2017;174:142-8. https://doi.org/10.1016/j.socscimed.2016.12.029.
- Fox B, Neiterman E. Embodied motherhood:women’s feelings about their postpartum bodies. Gender Soc 2015;29:670-93. https://doi.org/10.1177/0891243215591598.
- National Institute for Health and Care Excellence . Obesity: Identification, Assessment and Management 2014. www.nice.org.uk/guidance/cg189 (accessed February 2015).
- National Institute for Health and Care Excellence . Weight Management: Lifestyle Services for Overweight or Obese Adults 2014. www.nice.org.uk/guidance/ph53 (accessed February 2015).
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. https://doi.org/10.1037/a0016136.
- Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, et al. IMAGE Study Group . Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-119.
- Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 2014;348. https://doi.org/10.1136/bmj.g2646.
- Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 2007;107:1755-67. https://doi.org/10.1016/j.jada.2007.07.017.
- Catenacci VA, Odgen L, Phelan S, Thomas JG, Hill J, Wing RR, et al. Dietary habits and weight maintenance success in high versus low exercisers in the National Weight Control Registry. J Phys Act Health 2014;11:1540-8. https://doi.org/10.1123/jpah.2012-0250.
- Marinilli Pinto A, Gorin AA, Raynor HA, Tate DF, Fava JL, Wing RR. Successful weight-loss maintenance in relation to method of weight loss. Obesity 2008;16:2456-61. https://doi.org/10.1038/oby.2008.364.
- Tang J, Abraham C, Greaves C, Yates T. Self-directed interventions to promote weight loss: a systematic review of reviews. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.2857.
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56-69. https://doi.org/10.1093/epirev/mxq004.
- Madigan CD, Daley AJ, Lewis AL, Aveyard P, Jolly K. Is self-weighing an effective tool for weight loss: a systematic literature review and meta-analysis. Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0267-4.
- Lovelady C. Balancing exercise and food intake with lactation to promote post-partum weight loss. Proc Nutr Soc 2011;70:181-4. https://doi.org/10.1017/S002966511100005X.
- Tian J, Venn A, Otahal P, Gall S. The association between quitting smoking and weight gain: a systematic review and meta-analysis of prospective cohort studies. Obes Rev 2015;16:883-901. https://doi.org/10.1111/obr.12304.
- Allen JK, Stephens J, Patel A. Technology-assisted weight management interventions: systematic review of clinical trials. Telemed J E Health 2014;20:1103-20. https://doi.org/10.1089/tmj.2014.0030.
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med 2006;355:1563-71. https://doi.org/10.1056/NEJMoa061883.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011;111:92-102. https://doi.org/10.1016/j.jada.2010.10.008.
- Appelhans BM, French SA, Pagoto SL, Sherwood NE. Managing temptation in obesity treatment: a neurobehavioral model of intervention strategies. Appetite 2016;96:268-79. https://doi.org/10.1016/j.appet.2015.09.035.
- Racette SB, Weiss EP, Schechtman KB, Steger-May K, Villareal DT, Obert KA, et al. Influence of weekend lifestyle patterns on body weight. Obesity 2008;16:1826-30. https://doi.org/10.1038/oby.2008.320.
- Díaz-Zavala RG, Castro-Cantú MF, Valencia ME, Álvarez-Hernández G, Haby MM, Esparza-Romero J. Effect of the holiday season on weight gain: a narrative review. J Obes 2017;2017. https://doi.org/10.1155/2017/2085136.
- NHS . Start 4 Life: Baby n.d. www.nhs.uk/start4life/baby/ (accessed January 2017).
- Whittaker R, Matoff-Stepp S, Meehan J, Kendrick J, Jordan E, Stange P, et al. Text4baby: development and implementation of a national text messaging health information service. Am J Public Health 2012;102:2207-13. https://doi.org/10.2105/AJPH.2012.300736.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
- National Institute for Health Research . INVOLVE n.d. www.invo.org.uk/ (accessed January 2017).
- NI4Kids . NI4kids Family Life n.d. https://ni4kids.com/ (accessed December 2017).
- Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-264.
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res 2011;45:626-9. https://doi.org/10.1016/j.jpsychires.2010.10.008.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Al-Janabi H, Peters TJ, Brazier J, Bryan S, Flynn TN, Clemens S, et al. An investigation of the construct validity of the ICECAP-A capability measure. Qual Life Res 2013;22:1831-40. https://doi.org/10.1007/s11136-012-0293-5.
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167-76. https://doi.org/10.1007/s11136-011-9927-2.
- Wright JL, Scott JA. The Fat and Fibre Barometer, a short food behaviour questionnaire: reliability, relative validity and utility. Australian J Nutr Dietet 2000;57:33-9.
- Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport 2000;71:114-20. https://doi.org/10.1080/02701367.2000.11082794.
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010. Leeds: NHS Digital; 2012.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. https://doi.org/10.1192/bjp.150.6.782.
- Cash TF. The Multidimensional Body-Self Relations Questionnaire: MBSRQ Users’ Manual. Norfolk: VA; 2000.
- Gardner B, Abraham C, Lally P, de Bruijn GJ. Towards parsimony in habit measurement: testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-102.
- Sniehotta F, Schwarzer R, Scholz U, Schuz B. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol 2005;35:565-76. https://doi.org/10.1002/ejsp.258.
- Schwarzer R, Renner B. Social-cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Health Psychol 2000;19:487-95. https://doi.org/10.1037/0278-6133.19.5.487.
- Kliemann N, Beeken RJ, Wardle J, Johnson F. Development and validation of the Self-Regulation of Eating Behaviour Questionnaire for adults. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0414-6.
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med 1987;16:825-36. https://doi.org/10.1016/0091-7435(87)90022-3.
- Meyer AH, Weissen-Schelling S, Munsch S, Margraf J. Initial development and reliability of a motivation for weight loss scale. Obes Facts 2010;3:205-11. https://doi.org/10.1159/000315048.
- Rosenberg M. Conceiving the Self. New York, NY: Basic Books; 1979.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-21. https://doi.org/10.1016/0165-1781(89)90047-4.
- National Institute for Health and Care Excellence . Methods for the Development of NICE Public Health Guidance (Third Edition) 2012.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c332.
- Polheber A, Feutz K. Implementing an evidence-based outpatient program to reduce postpartum weight retention. Nurs Womens Health 2017;21:284-95. https://doi.org/10.1016/j.nwh.2017.06.008.
- Denney-Wilson E, Laws R, Russell CG, Ong KL, Taki S, Elliot R, et al. Preventing obesity in infants: the growing healthy feasibility trial protocol. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009258.
- Phelan S, Hagobian T, Brannen A, Hatley KE, Schaffner A, Muñoz-Christian K, et al. Effect of an internet-based program on weight loss for low-income postpartum women: a randomized clinical trial. JAMA 2017;317:2381-91. https://doi.org/10.1001/jama.2017.7119.
- Haste A, Adamson AJ, McColl E, Araujo-Soares V, Bell R. Problems recruiting and retaining postnatal women to a pilot randomised controlled trial of a web-delivered weight loss intervention. BMC Res Notes 2018;11. https://doi.org/10.1186/s13104-018-3305-x.
- NHS Health Education England . Making Every Contact Count n.d. www.makingeverycontactcount.co.uk/ (accessed February 2019).
- Northern Ireland Statistics and Research Agency . Census 2011: Key Statistics for Northern Ireland n.d. www.nisra.gov.uk/sites/nisra.gov.uk/files/publications/2011-census-results-key-statistics-northern-ireland-report-11-december-2012.pdf (accessed June 2019).
- Wilkinson SA, van der Pligt P, Gibbons KS, McIntyre HD. Trial for reducing weight retention in new mums: a randomised controlled trial evaluating a low intensity, postpartum weight management programme. J Hum Nutr Diet 2015;28:15-28. https://doi.org/10.1111/jhn.12193.
- Dodd JM, Deussen AR, O’Brien CM, Schoenaker DAJM, Poprzeczny A, Gordon A, et al. Targeting the postpartum period to promote weight loss: a systematic review and meta-analysis. Nutr Rev 2018;76:639-54. https://doi.org/10.1093/nutrit/nuy024.
- Eysenbach G, Jadad AR. Evidence-based patient choice and consumer health informatics in the internet age. J Med Internet Res 2001;3. https://doi.org/10.2196/jmir.3.2.e19.
- van der Pligt P, Olander EK, Ball K, Crawford D, Hesketh KD, Teychenne M, et al. Maternal dietary intake and physical activity habits during the postpartum period: associations with clinician advice in a sample of Australian first time mothers. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0812-4.
- Ferrari RM, Siega-Riz AM, Evenson KR, Moos MK, Melvin CL, Herring AH. Provider advice about weight loss and physical activity in the postpartum period. J Womens Health 2010;19:397-406. https://doi.org/10.1089/jwh.2008.1332.
- Abebe DS, Von Soest T, Von Holle A, Zerwas SC, Torgersen L, Bulik CM. Developmental trajectories of postpartum weight 3 years after birth: Norwegian Mother And Child Cohort study. Matern Child Health J 2015;19:917-25. https://doi.org/10.1007/s10995-014-1593-x.
- Joshi PP, Quintiliani LM, McCarthy AC, Gilmore A, Mahesri M, Sullivan LM, et al. A randomized controlled feasibility trial in behavioral weight management for underserved postpartum African American women: the RENEW study. Prev Chronic Dis 2018;15. https://doi.org/10.5888/pcd15.170400.
- Huseinovic E, Bertz F, Brekke HK, Winkvist A. Two-year follow-up of a postpartum weight loss intervention: results from a randomized controlled trial. Matern Child Nutr 2018;14. https://doi.org/10.1111/mcn.12539.
- Herring SJ, Cruice JF, Bennett GG, Darden N, Wallen JJ, Rose MZ, et al. Intervening during and after pregnancy to prevent weight retention among African American women. Prev Med Rep 2017;7:119-23. https://doi.org/10.1016/j.pmedr.2017.05.015.
- Job JR, Fjeldsoe BS, Eakin EG, Reeves MM. Effectiveness of extended contact interventions for weight management delivered via text messaging: a systematic review and meta-analysis. Obes Rev 2018;19:538-49. https://doi.org/10.1111/obr.12648.
- Holmes WS, Moorhead SA, Coates VE, Bond RR, Zheng H. Impact of digital technologies for communicating messages on weight loss maintenance: a systematic literature review. Eur J Public Health 2019;29:320-8. https://doi.org/10.1093/eurpub/cky171.
- Schippers M, Adam PC, Smolenski DJ, Wong HT, de Wit JB. A meta-analysis of overall effects of weight loss interventions delivered via mobile phones and effect size differences according to delivery mode, personal contact, and intervention intensity and duration. Obes Rev 2017;18:450-9. https://doi.org/10.1111/obr.12492.
- Siopis G, Chey T, Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. J Hum Nutr Diet 2015;28:1-15. https://doi.org/10.1111/jhn.12207.
- McCambridge J, Wilton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 2014;67:267-77. https://doi.org/10.1016/j.jclinepi.2013.08.015.
- de Niet J, Timman R, Bauer S, van den Akker E, Buijks H, de Klerk C, et al. The effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: a randomized controlled trial. Pediatr Obes 2012;7:205-19. https://doi.org/10.1111/j.2047-6310.2012.00048.x.
- Donaldson EL, Fallows S, Morris M. A text message based weight management intervention for overweight adults. J Hum Nutr Diet 2014;27:90-7. https://doi.org/10.1111/jhn.12096.
- Fjeldsoe BS, Goode AD, Phongsavan P, Bauman A, Maher G, Winkler E, et al. Evaluating the maintenance of lifestyle changes in a randomized controlled trial of the ‘Get Healthy, Stay Healthy’ program. JMIR Mhealth Uhealth 2016;4. https://doi.org/10.2196/mhealth.5280.
- Newton RL, Carter LA, Johnson W, Zhang D, Larrivee S, Kennedy BM, et al. A church-based weight loss intervention in African American adults using text messages (LEAN Study): cluster randomized controlled trial. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.9816.
- Axley P, Kodali S, Kuo YF, Ravi S, Seay T, Parikh NM, et al. Text messaging approach improves weight loss in patients with nonalcoholic fatty liver disease: a randomized study. Liver Int 2018;38:924-31. https://doi.org/10.1111/liv.13622.
- Zwickert K, Rieger E, Swinbourne J, Manns C, McAulay C, Gibson AA, et al. High or low intensity text-messaging combined with group treatment equally promote weight loss maintenance in obese adults. Obes Res Clin Pract 2016;10:680-91. https://doi.org/10.1016/j.orcp.2016.01.001.
- Ahn A, Choi J. A one-way text messaging intervention for obesity. J Telemed Telecare 2016;22:148-52. https://doi.org/10.1177/1357633X15591129.
- Stephens JD, Yager AM, Allen J. Smartphone technology and text messaging for weight loss in young adults: a randomized controlled trial. J Cardiovasc Nurs 2017;32:39-46. https://doi.org/10.1097/JCN.0000000000000307.
- Silina V, Tessma MK, Senkane S, Krievina G, Bahs G. Text messaging (SMS) as a tool to facilitate weight loss and prevent metabolic deterioration in clinically healthy overweight and obese subjects: a randomised controlled trial. Scand J Prim Health Care 2017;35:262-70. https://doi.org/10.1080/02813432.2017.1358435.
- Lauti M, Kularatna M, Pillai A, Hill AG, MacCormick AD. A randomised trial of text message support for reducing weight regain following sleeve gastrectomy. Obes Surg 2018;28:2178-86. https://doi.org/10.1007/s11695-018-3176-1.
- Kulendran M, King D, Schmidtke KA, Curtis C, Gately P, Darzi A, et al. The use of commitment techniques to support weight loss maintenance in obese adolescents. Psychol Health 2016;31:1332-41. https://doi.org/10.1080/08870446.2016.1204452.
- Lombard C, Harrison C, Kozica S, Zoungas S, Ranasinha S, Teede H. Preventing weight gain in women in rural communities: a cluster randomised controlled trial. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1001941.
- Farpour-Lambert NJ, Ells LJ, Martinez de Tejada B, Scott C. Obesity and weight gain in pregnancy and postpartum: an evidence review of lifestyle interventions to inform maternal and child health policies. Front Endocrinol 2018;9. https://doi.org/10.3389/fendo.2018.00546.
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358. https://doi.org/10.1136/bmj.j4008.
- Kim C, Draska M, Hess ML, Wilson EJ, Richardson CR. A web-based pedometer programme in women with a recent history of gestational diabetes. Diabet Med 2012;29:278-83. https://doi.org/10.1111/j.1464-5491.2011.03415.x.
- Nicklas JM, Zera CA, Seely EW, Abdul-Rahim ZS, Rudloff ND, Levkoff SE. Identifying postpartum intervention approaches to prevent type 2 diabetes in women with a history of gestational diabetes. BMC Pregnancy Childbirth 2011;11. https://doi.org/10.1186/1471-2393-11-23.
- Herring SJ, Cruice JF, Bennett GG, Davey A, Foster GD. Using technology to promote postpartum weight loss in urban, low-income mothers: a pilot randomized controlled trial. J Nutr Educ Behav 2014;46:610-15. https://doi.org/10.1016/j.jneb.2014.06.002.
- Wright C, Mogul M, Acevedo G, Aysola J, Momplaisir F, Schwartz S, et al. Preparing for a trial to test a postpartum weight retention intervention among low income women: feasibility of a protocol in a community-based organization. BMC Womens Health 2018;18. https://doi.org/10.1186/s12905-018-0517-0.
- Gilmore LA, Klempel MC, Martin CK, Myers CA, Burton JH, Sutton EF, et al. Personalized mobile health intervention for health and weight loss in postpartum women receiving women, infants, and children benefit: a randomized controlled pilot study. J Womens Health 2017;26:719-27. https://doi.org/10.1089/jwh.2016.5947.
- Diabetes Prevention Program Research Group . The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002;25:2165-71. https://doi.org/10.2337/diacare.25.12.2165.
- Waring ME, Moore Simas TA, Oleski J, Xiao RS, Mulcahy JA, May CN, et al. Feasibility and acceptability of delivering a postpartum weight loss intervention via Facebook: a pilot study. J Nutr Educ Behav 2018;50:70-4. https://doi.org/10.1016/j.jneb.2017.09.025.
- Silfee VJ, Lopez-Cepero A, Lemon SC, Estabrook B, Nguyen O, Rosal MC. Recruiting low-income postpartum women into two weight loss interventions: in-person versus Facebook delivery. Transl Behav Med 2019;9:129-34. https://doi.org/10.1093/tbm/iby013.
- Tsai AG, Nicholson WK. Losing weight during the postpartum period. JAMA 2017;317:2375-6. https://doi.org/10.1001/jama.2017.7036.
- Walker LO, Sterling BS, Kim M, Arheart KL, Timmerman GM. Trajectory of weight changes in the first 6 weeks postpartum. J Obstet Gynecol Neonatal Nurs 2006;35:472-81. https://doi.org/10.1111/j.1552-6909.2006.00062.x.
Appendix 1 Examples of the refinement of the initial 14 draft intervention SMS messages, based on personal and public involvement feedback
| Initial message | PPI comments | Refined message |
|---|---|---|
| Did you know that people who skip breakfast are more likely to snack on high calorie foods mid-morning, and consume more calories during the day than breakfast eaters? Next time you think about skipping breakfast, think again! Try to even eat something small like a slice of toast until you get into a better routine |
Language patronising, ‘did you know?’ . . . Start the message off catchy |
Cook yourself thin! Meals you prepare at home can have up to 50% less calories than meals you eat when dining out. Next time you feel like you don’t have time, think of your waistline. It’s amazing what you can make up in just 20 minutes! E.g. tuna pasta bake, with frozen peas. Click here for recipes |
| Lost the inspiration to keep going? Losing weight can help you to feel more confident . . . no more worrying about camouflaging those wobbly bits! Why not find your favourite jeans, the ones you couldn’t wear when you were pregnant, and imagine yourself wearing them again? This could help you to stick to your plan | ‘Wobbly bits’ OK to use now at 6 months, but much more sensitive earlier | If you ever feel like stalling have these 2 things in mind: (1) The rewards you will enjoy when you reach your target weight (maybe it’s fitting into your favourite jeans?). (2) Success takes time, so keep calm and carry on :) |
Appendix 2 Examples of message refinement after personal and public involvement feedback focusing on weight loss SMS messages during weeks 1–12
| Text message | Feedback | Refined message |
|---|---|---|
| Congratulations on the birth of your baby and welcome to the Supporting MumS (SMS) study :) The SMS team are nutritionists who have joined up with mums in the same boat as you, to come up with weight loss and healthy lifestyle tips to keep you feeling at your best. We look forward to having you on board! Read more here – http://go.qub.ac.uk/supportingmums | Perhaps personalise to include mothers’ name/gender of baby | Congratulations [insert mother’s forename] on the birth of your baby and welcome to the Supporting MumS (SMS) study :) The SMS team are nutritionists who have joined up with mums in the same boat as you, to come up with weight loss and healthy lifestyle tips to keep you feeling at your best. We look forward to having you on board! Read more here – http://go.qub.ac.uk/supportingmums |
| Rome wasn’t built in a day, and neither are new habits. By making small changes and repeating them often they will soon become second nature | Give examples | Rome wasn’t built in a day, and neither are new habits. By making small changes and repeating them often they will soon become second nature. Text us one small change you could try to turn into a habit over the next couple of weeks. E.g. ‘drink a glass of water first thing in the morning’ |
| It might not come around often, but next time you have a bit of extra time (and energy!) to make a meal, make more and freeze it. You can grab it quickly when you’ve run out of steam someday. You don’t need to spend more to add more, an extra can of veg can go a long way | Give examples | It might not come around often, but next time you have a bit of extra time (and energy!) to make a meal, make more and freeze it. You can grab it quickly when you’ve run out of steam someday. You don’t need to spend more to add more, an extra can of veg can go a long way. E.g. spaghetti bolognaise, chilli con carne, chicken curry, veg soup. Click here for more ideas – www.jamieoliver.com/family/freezer-friendly-recipes/ |
| Reminder – set your weekly goal | Give more tips | Reminder – set your weekly goal. All out of ideas? Here’s some inspiration – ‘I am going to swap my white bread, pasta and cereal for wholegrain options when I do my shop this weekend’ |
| Visiting family or they’re coming over to you? Sweet or savoury snacks (or both!) are likely to be out in force. It’s not about ‘all or nothing’ though. It’s when you feel your hand reaching out for another that it’s time to step away;) | Healthy alternatives to entertaining guests | Visiting family or they’re coming over to you? Sweet or savoury snacks (or both!) are likely to be out in force. It’s not about ‘all or nothing’ though. It’s when you feel your hand reaching out for another that it’s time to step away;) If you’re hosting, here are some quick and healthy nibble ideas: veg sticks and hummus, fruit salad, unsalted nuts |
| Find yourself with a quiet half hour sitting watching T.V.? Why not try to be proactive when the advertisements come on . . . use this time to prepare some meals. You could wash the vegetables, peel, chop, or cook. By the end of your T.V. programme you could have a meal almost prepared, if not cooked for another day! |
Not sure I’ve had too many quiet half hours in front of the T.V. unless I’m wrecked, in which case no cooking is going to get done! I’m a great fan of the slow cooker and made ‘dump bags’ that I could just put in in the morning and it would be prepared in the evening. You can freeze the dump bags |
Message replaced The demands of motherhood can make even showering seem like a luxury, never mind cooking! Mum’s tip: ‘My slow cooker was a lifesaver – I’d throw the ingredients in and stick it on – it did all the cooking for me and made enough for a few dinners!’ |
Appendix 3 Examples of message refinement after personal and public involvement feedback focusing on weight loss SMS messages during weeks 13–24
| Initial message | Feedback | Refined message |
|---|---|---|
| Busy week ahead? Set a realistic plan of when you can add in some activity. To save time, try making more meals to freeze – these should see you through the week! | Give examples | Busy week ahead? Set a realistic plan of when you can add in some activity. To save time, try making more meals to freeze – these should see you through the week! For ideas click on the link, or why not look for/share ideas on the SMS forum? www.goodtoknow.co.uk/recipes/pictures/34832/things-you-can-make-in-bulk-and-freeze/1 |
| Stock up on snacks! Healthy snacks in your drawer at work, or in a carry bag for when you are leaving the house, can make you less tempted to reach for less healthy nibbles. Try grapes, unsalted nuts or popcorn or pumpkin/sunflower seeds | Links to healthy snack ideas | Stock up on snacks! Healthy snacks in your drawer at work, or in a carry bag for when you are leaving the house, can make you less tempted to reach for less healthy nibbles. Try grapes, unsalted nuts or popcorn or pumpkin/sunflower seeds. For more ideas click on this link – www.bbcgoodfood.com/recipes/collection/healthy-snack |
| Thirsty or hungry?! It’s really easy to mistake hunger for thirst. Tip: next time you are getting something to eat, have a glass of water first to make sure it’s not just fluids your body wants;) | Might be good to have this one earlier than week 19 | Moved message to week 13 |
| Great! You are really getting in control of your new healthy lifestyle – keep going! Why not get ahead of the game and prepare for possible future slip ups | This is demoralising | Great! You are really getting in control of your new healthy lifestyle – keep going! |
Appendix 4 Examples of message refinement after personal and public involvement feedback focusing on weight loss maintenance messages (months 7–12), trigger words, weight replies and tailored SMS messages
| Text message | Feedback | Refinement |
|---|---|---|
| Crazy day . . . just in the door an hour later than planned . . . and dinner to sort out. If this was you, would you have a plan of attack in action? | Give example of how to overcome this, quick meal ideas | Crazy day . . . just in the door an hour later than planned . . . and dinner to sort out. If this was you, what would your plan of action be? Here are some ideas to help – www.bhf.org.uk/heart-matters-magazine/nutrition/cooking-skills/quick-healthy-meals |
| Fantastic you have the determination and willpower needed to maintain your new weight. Hope you feel chuffed :) | Unsure about using chuffed | Fantastic you have the determination and willpower needed to maintain your new weight. Hope you feel proud :) |
| Reminder about support service |
Most people that have lost weight and kept it off have done so with support from family and friends! Visit our SMS forum (http://supportingmums.boards.net) to chat with other mums, or get your friend/partner/family member to receive SMS texts for extra support – text ‘Support’ followed by the person’s mobile number to sign up. E.g. Support 0780000000. (messages like this have been added in more frequently to the weight loss maintenance phase) |
|
| If they text ‘crave’, congratulate them for asking for support before giving in | Congratulations on texting crave before giving in to your craving. You have the willpower to keep up your new healthy lifestyle. Be proud of yourself! | |
| Weigh-in day! Text us your weight this week and whether it has gone UP, DOWN or stayed the SAME from last week. E.g. 10 st 7 SAME or 66.7 kg SAME | Remind women all weights are confidential | Weigh-in day! Text us your weight this week and whether it has gone UP, DOWN or stayed the SAME from last week. E.g. 10 st 7 SAME or 66.7 kg SAME. Reminder, all texts are completely confidential! |
Appendix 5 Examples of message refinement after personal and public involvement feedback focusing on active control SMS messages
| Initial message | Feedback | Refined message |
|---|---|---|
| Travelling in the car? It’s important that your little one is buckled securely into their seat. They might be curious to try and undo it. Having books, toys and sing-songs can help keep them occupied | Check safety recommendations for car seat with government guidelines | Travelling in the car? It’s important that your little one is buckled securely into their seat. They might be curious to try and undo it – if this happens pull over and re-do it. Check your baby seat meets government safety guidelines. Read more here – www.gov.uk/child-car-seats-the-rules/using-a-child-car-seat-or-booster-seat |
| Might seem daft, but it’s a good idea to chat to your baby early on. Even though they won’t understand you, they will find your voice soothing and it will help their language development | This is negative | Babies recognise their parents’ voices from early on! Keep chatting to them to help encourage their language development |
| Cries and coos? You may have noticed your little one has started making other noises like cooing/chuckling. Show you’re listening by cooing/talking back | Tell mum why to talk back | Cries and coos? You may have noticed your little one has started making other noises like cooing/chuckling. Show you’re listening and encourage language development by cooing/talking back |
| Good toys for a 12-week-old baby? Anything goes, but bright, colourful, noisy toys are likely to be a hit | Explain why | Good toys for a 12-week-old baby? Anything goes, but bright, colourful, noisy toys (sorry!) are likely to be a hit. These are the easiest for your baby to see and will help with his/her sensory development |
Appendix 6 Data table of demographics and baseline characteristics of those who took part in the qualitative interviews at 3 months
| Characteristic | Intervention (N = 35) | Active control (N = 35) | Overall (N = 70) |
|---|---|---|---|
| Age at baseline (years) | |||
| Mean (SD) | 33.8 (3.7) | 32.2 (7.9) | 33 (4.4) |
| Employment status, n (%) | |||
| Full time | 22 (62.9) | 17 (48.6) | 39 (55.7) |
| Part time | 9 (25.7) | 11 (31.4) | 20 (28.6) |
| Self-employed | 0 (0) | 3 (8.6) | 3 (4.3) |
| Unemployed | 4 (11.4) | 4 (11.4) | 8 (11.4) |
| Household income (£), n (%) | |||
| < 14,999 | 2 (5.7) | 0 (0) | 2 (2.9) |
| 15,000–29,999 | 6 (17.1) | 8 (22.9) | 14 (20.0) |
| 30,000–49,999 | 14 (40.0) | 14 (40.0) | 28 (40.0) |
| ≥ 50,000 | 13 (37.1) | 13 (37.1) | 26 (37.1) |
| Education, N (%) | |||
| Postgraduate degree | 14 (40.0) | 7 (20.0) | 21 (30.0) |
| Undergraduate degree | 11 (31.4) | 16 (45.7) | 27 (38.6) |
| Further education | 8 (22.9) | 5 (14.3) | 13 (18.6) |
| A levels | 2 (5.7) | 4 (11.4) | 6 (8.6) |
| O levels/GCSEs or below | 0 (0) | 3 (8.6) | 3 (4.3) |
| Marital status, n (%) | |||
| Single | 2 (5.7) | 3 (8.6) | 5 (7.1) |
| Married/civil partnership | 31 (88.6) | 26 (74.3) | 58 (82.8) |
| Living with partner | 2 (5.7) | 6 (17.2) | 7 (10.0) |
| Body composition | |||
| BMI (kg/m2) | |||
| Median (IQR) | 30.4 (28.4–32.3) | 29.1 (26.8–33.9) | 31.0 (27.5–32.8) |
| 25.0–29.9 kg/m2 (overweight), n (%) | 16 (45.7) | 18 (51.4) | 34 (48.6) |
| > 30.0 kg/m2 (obese), n (%) | 19 (54.3) | 17 (48.6) | 36 (51.4) |
| Weight (kg), median (IQR) | 81.4 (76.8–87.4) | 83.6 (72.2–90.2) | 80.2 (74.5–89.1) |
| Waist circumference (cm), median (IQR) | 103.0 (99.0–106.0) | 98.5 (94.5–114.0) | 101.9 (97–108.9) |
| Self-reported pre-pregnancy weight (kg), median (IQR) | 73.0 (69.9–88.9) | 76.2 (67.0–86.4) | 74.4 (68.9–86.6) |
| Parity, n (%) | |||
| One child | 13 (37.1) | 17 (48.6) | 30 (42.9) |
| Two or more children | 22 (62.9) | 18 (51.4) | 40 (57.1) |
| Postpartum opt-in time point at baseline (months postpartum), n (%) | |||
| < 6 | 13 (37.1) | 20 (57.1) | 33 (47.1) |
| 6–12 | 10 (28.6) | 8 (22.9) | 18 (25.7) |
| 12–18 | 4 (11.4) | 5 (14.3) | 9 (12.9) |
| 18–24 | 8 (22.9) | 2 (5.7) | 10 (14.3) |
| Recruitment source, n (%) | |||
| Social media | 24 (68.6) | 23 (65.7) | 47 (67.1) |
| Mother and toddler group | 4 (11.4) | 8 (22.9) | 12 (17.1) |
| Word of mouth | 4 (11.4) | 4 (11.4) | 8 (11.4) |
| Library | 3 (8.6) | 0 (0) | 3 (4.3) |
| Weight status at 3 months, n (%) | |||
| Stayed the same/lost weight | 19 (54.3) | 15 (42.9) | 34 (48.6) |
| Gained weight | 16 (45.7) | 20 (57.1) | 36 (51.4) |
| Engagement at 3 months with weight texts, n (%) | |||
| High engagera | 17 (48.6) | – | |
| Low engagera | 18 (51.4) | – | |
| Engagement at 3 months with ‘yes/no’ texts, n (%) | |||
| High engagera | 11 (21.4) | – | |
| Low engagera | 24 (68.6) | – | |
Appendix 7 Data table of demographics and baseline characteristics of those who took part in the qualitative interviews at 12 months
| Characteristic | Intervention (N = 16) | Active control (N = 21) | Overall (N = 37) |
|---|---|---|---|
| Age at baseline (years) | |||
| Mean (SD) | 32.4 (3.5) | 32.0 (3.5) | 32.2 (3.5) |
| Employment status, n (%) | |||
| Full time | 11 (68.8) | 9 (42.9) | 20 (54.1) |
| Part time | 3 (18.8) | 8 (381) | 11 (29.7) |
| Self-employed | 0 (0) | 2 (9.5) | 2 (5.4) |
| Unemployed | 2 (12.5) | 2 (9.5) | 4 (10.8) |
| Household income (£), n (%) | |||
| < 14,999 | 1 (6.3) | 0 (0) | 1 (2.7) |
| 15,000–29,999 | 3 (18.8) | 7 (33.3) | 10 (27.0) |
| 30,000–49,999 | 6 (37.5) | 7 (33.3) | 13 (35.1) |
| ≥ 50,000 | 6 (37.5) | 7 (33.3) | 13 (35.1) |
| Education N (%) | |||
| Postgraduate degree | 6 (37.5) | 5 (25.0) | 11 (29.7) |
| Undergraduate degree | 3 (18.8) | 10 (47.6) | 13 (35.1) |
| Further education | 7 (43.8) | 2 (9.5) | 9 (24.3) |
| A levels | 0 (0) | 2 (9.5) | 2 (5.4) |
| O levels/GCSEs or below | 0 (0) | 2 (9.5) | 2 (5.4) |
| Marital status, n (%) | |||
| Single | 2 (12.5) | 1 (4.8) | 3 (8.1) |
| Married/civil partnership | 13 (81.3) | 17 (81.0) | 30 (81.1) |
| Living with partner | 1 (6.3) | 3 (14.3) | 4 (10.8) |
| Body composition | |||
| BMI (kg/m2) | |||
| Median (IQR) | 29.6 (26.7–32.6) | 31.3 (27.4–34.0) | 30.0 (27.3–33.0) |
| 25.0–29.9 kg/m2 (overweight), n (%) | 9 (56.3) | 10 (47.6) | 19 (51.4) |
| > 30.0 kg/m2 (obese), n (%) | 7 (43.7) | 11 (52.4) | 18 (48.6) |
| Weight (kg), median (IQR) | 79.8 (76.2–82.4) | 79.2 (72.4–95.6) | 79.6 (74.7–89.6) |
| Waist circumference (cm), median (IQR) | 103.0 (98.0–105.9) | 103.0 (94.3–117.5) | 103.0 (96.0–110.5) |
| Self-reported pre-pregnancy weight (kg), median (IQR) | 69.9 (65.0–85.7) | 80.0 (69.6–89.2) | 73.0 (68.0–87.5) |
| Parity, n (%) | |||
| One child | 3 (18.8) | 7 (33.3) | 10 (27.0) |
| Two or more children | 13 (81.2) | 14 (66.7) | 27 (72.9) |
| Postpartum opt-in time point at baseline (months postpartum), n (%) | |||
| < 6 | 4 (25.0) | 14 (66.7) | 18 (48.6) |
| 6–12 | 4 (25.0) | 3 (14.3) | 7 (18.9) |
| 12–18 | 1 (6.3) | 3 (14.3) | 4 (10.8) |
| 18–24 | 7 (43.8) | 1 (4.8) | 8 (21.6) |
| Recruitment source, n (%) | |||
| Social media | 10 (62.5) | 12 (57.1) | 22 (59.5) |
| Mother and toddler group | 1 (6.3) | 6 (28.6) | 7 (18.9) |
| Word of mouth | 4 (25.0) | 3 (14.3) | 7 (18.9) |
| Library | 1 (6.3) | 0 (0) | 1 (2.7) |
| Weight status at 3 months, n (%) | |||
| Stayed the same/lost weight | 11 (68.8) | 10 (47.6) | 21 (56.8) |
| Gained weight | 5 (31.3) | 11 (52.4) | 16 (43.2) |
| Engagement at 3 months with weight texts, n (%) | |||
| High engagera | 8 (50) | – | |
| Low engagera | 8 (50) | – | |
| Engagement at 3 months with ‘yes/no’ texts, n (%) | |||
| High engagera | 7 (43.8) | – | |
| Low engagera | 9 (56.3) | – | |
Appendix 8 Data table showing changes in anthropometry according to engagement with weight SMS message replies
| Changes in anthropometric measures | 3 months | 6 months | 12 months | |||
|---|---|---|---|---|---|---|
| High engagera | Low engagerb | High engagera | Low engagerb | High engagera | Low engagerb | |
| n | 21 | 26 | 21 | 22 | 18 | 18 |
| Change in weight from baseline (kg), mean (SD) | –2.2 (2.46) | 0.6 (2.27) | –3.15 (4.4) | 0.5 (2.83) | –2.66 (6.77) | –0.84 (6.65) |
| Change in waist circumference from baseline (cm), mean (SD) | –3.1 (6.13) | 0.6 (4.47) | –5.0 (6.52) | –0.83 (4.53) | –8.9 (20.6) | –3.6 (7.54)c |
| Change in BMI from baseline (kg/m2), mean (SD) | –0.8 (0.88) | 0.4 (0.82) | –1.12 (1.64) | 0.15 (1.03) | –0.99 (2.49) | –0.31 (2.39) |
Appendix 9 Data table showing changes in anthropometry according to engagement with ‘yes/no’ SMS message replies
| Changes in anthropometric measures | 3 months | 6 months | 12 months | |||
|---|---|---|---|---|---|---|
| High engagera | Low engagerb | High engagera | Low engagerb | High engagera | Low engagerb | |
| n | 17 | 30 | 19 | 24 | 16 | 20 |
| Change in weight from baseline (kg), mean (SD) | –1.18 (0.39) | 1.57 (0.50) | –1.21 (0.42) | 1.38 (0.49) | –3.9 (7.95) | 0.4 (4.33) |
| Change in waist circumference from baseline (cm), mean (SD) | –1.3 (0.45) | 0.26 (0.99) | –4.6 (6.74) | –1.5 (4.86) | –9.4 (21.19) | –3.5 (7.35)c |
| Change in BMI from baseline (kg/m2), mean (SD) | –0.67 (0.80) | 0.26 (0.99) | –1.10 (1.71) | 0.03 (–0.19) | –1.1 (2.62) | –0.32(2.29) |
Appendix 10 Data table showing baseline anthropometric and socioeconomic characteristics of participants with high and low engagement with weight SMS message replies
| Baseline anthropometric and socioeconomic characteristics | 3 monthsa | p-value | 6 monthsa | p-value | 12 monthsa | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| High engager | Low engager | High engager | Low engager | High engager | Low engager | ||||
| Baseline visit (n) | 21 | 26 | 21 | 22 | 18 | 18 | |||
| Characteristic, median (IQR) | |||||||||
| Weight (kg) | 79.6 (7.3) | 82.7 (17.9) | 0.199 | 79.6 (7.3) | 82.0 (21.4) | 0.198 | 79.8 (8.7) | 82.2 (20.4) | 0.743 |
| BMI (kg/m2) | 29.6 (5.2) | 30.8 (4.4) | 0.152 | 29.6 (6.01) | 31.3 (4.0) | 0.166 | 29.9 (5.27) | 30.2 (4.3) | 0.239 |
| Waist circumference (cm) | 101.0 (6.5) | 102.8 (10.5) | 0.716 | 101.0 (6.5) | 103.0 (10.5) | 0.559 | 102.0 (8.7) | 102.8 (10.9) | 0.988 |
| Gestational weight gainb | 12.7 (6.4) | 9.5 (7.0) | 0.898 | 12.7 (6.4) | 9.5 (6.9) | 0.884 | 12.7 (8.6) | 9.5 (6.2) | 0.293 |
| Age (years) | 34.0 (7) | 33 (6) | 0.700 | 34 (6) | 34 (7) | 0.695 | 33.5 (6) | 33.5 (6) | 0.899 |
| Weeks postpartum (weeks) | 28.7 (57.9) | 32.0 (46.1) | 0.700 | 26.9 (58.7) | 37.8 (44) | 0.409 | 24.2 (69.6) | 40.2 (44.8) | 0.389 |
| BMI (kg/m2), n (%) | |||||||||
| 25–29.99 | 11 (52.4) | 12 (46.2) | 0.448 | 11 (52.4) | 9 (40.9) | 0.327 | 9 (50.0) | 9 (50.0) | 1.00 |
| ≥ 30 | 10 (47.6) | 14 (53.8) | 10 (47.6) | 13 (59.1) | 9 (50.0) | 9 (50.0) | |||
| Education, n (%) | |||||||||
| < Degree level | 7 (33.3) | 8 (30.8) | 0.549 | 7 (33.3) | 7 (31.8) | 0.586 | 7 (38.9) | 6 (33.3) | 1.00 |
| ≥ Undergraduate degree | 14 (66.7) | 18 (69.2) | 14 (66.7) | 15 (68.2) | 11 (61.1) | 12 (66.7) | |||
| Household income (£ per year), n (%) | |||||||||
| < 30,000 | 5 (23.8) | 6 (23.1) | 0.610 | 5 (23.8) | 4 (18.2) | 0.468 | 6 (33.3) | 3 (16.7) | 0.443 |
| ≥ 30,000 | 16 (76.2) | 20 (76.9) | 16 (76.2) | 18 (81.8) | 12 (66.7) | 15 (83.3) | |||
| Help from family/friends, n (%) | |||||||||
| Enough help | 14 (66.7) | 0.002c | 15 (71.4) | 21 (95.5) | 0.041c | 12 (66.7) | 18 (100) | 0.019c | |
| Not enough help | 7 (33.3) | 6 (28.6) | 1 (4.5) | 6 (33.3) | 0 (0) | ||||
Appendix 11 Data table summarising intervention participant engagement with the interactive SMS intervention features
| Interactive component | 0–6 months | 7–12 months |
|---|---|---|
| Weekly weight SMS messages | ||
| Weight SMS messages sent to each participant (n) | 23 | 27 |
| Participants replying to weight SMS messages/total number of participants, n/N (%) | 39/43 (47.4)a | 28/36 (77.8)b |
| Participants replying to weight SMS messages by responses (n) | ||
|
22 | 15 |
|
21 | 13 |
|
989 | 972 |
| Total weight replies received | 469 | 400 |
| Weight replies in correct formatc,d (n) | 269 | 123 |
| Weight replies in incorrect format (n) | 200 | 277 |
|
79 | 1 |
|
0 | 56 |
|
0 | 18 |
|
0 | 202 |
| Total weight replies that received a system automated response, n (%) | N/A | 50 (12.5) |
| ‘Yes/no’ SMS messages | ||
| ‘Yes/no’ SMS messages sent to each participant (n) | 20 | 16 |
| Participants replying to any ‘yes/no’ SMS messages/total number of participants, n/N (%) | 41/43 (95.3)a | 31/36 (86.1)b |
| Participants replying to ‘yes/no’ SMS messages by responses (n) | ||
|
17 | 10 |
| Replied to > 50% of SMS messages | 24 | 21 |
| ‘Yes/no’ replies in instructed formatf (n) | 460 | 272 |
| ‘Yes/no’ replies with extra information added (n) | 12 | 2 |
| Total ‘yes/no’ replies that received a system automated response, n/N (%) | 460/460 (100%) | 272/272 (100%) |
Appendix 12 Data table summarising intervention participant engagement with the trigger words and core and spontaneous SMS intervention functions
| Engagement component | 0–6 monthsa | 7–12 monthsb |
|---|---|---|
| Trigger words | ||
| Number of participants texting a trigger word | 19 | 7 |
| Total number of trigger words texted | 34 | 13 |
|
12 | 4 |
|
12 | 1 |
|
7 | 3 |
|
3 | 5 |
| Trigger word SMS messages that received a system automated response, n/N (%) | 31/34 (91) | 10/13 (77) |
| Core SMS messages | ||
| Total core SMS messages asking open questions (n) | 7 | 1 |
| Responses to core SMS messages asking open questions (n) | 15 | 6 |
| Responses to goal weight SMS message sent at the start of the intervention (n) | 24 | 0 |
| Spontaneous SMS messages | ||
| Total number of additional spontaneous texts | 3 | 15 |
| Replies to the automated ‘yes/no’ replies | 1 | 3 |
| Gift card/pedometer queries | 2 | 3 |
| Pause | 0 | 2c |
| Replies to final SMS message | 0 | 2 |
| Other additional texts | 0 | 4 |
Appendix 13 Data table summarising the status of pedometers
| Pedometer status | Month, n (%) | ||||
|---|---|---|---|---|---|
| 0 (N = 100) | 3 (N = 93) | 6 (N = 84) | 9 (N = 77) | 12 (N = 75) | |
| Returned and contained data | 88 (88.0) | 80 (86.0) | 64 (76.2) | 55 (71.4) | 47 (62.3) |
| Returned but damaged | 1 (1.0) | 1 (1.1) | 0 (0) | 0 (0) | 0 (0) |
| Returned but data wiped | 5 (5.0) | 4 (4.3) | 18 (21.4) | 6 (7.8) | 4 (5.3) |
| Lost in post | 2 (2.0) | 2 (2.2) | 0 (0) | 1 (1.3) | 2 (2.7) |
| Not returned; unknown reason | 3 (3.0) | 5 (5.4) | 2 (2.4) | 7 (9.1) | 7 (9.3) |
| Participant lost pedometer | 1 (1.0) | 0 (0) | 0 (0) | 3 (3.9) | 2 (2.7) |
| Returned but battery dead | 0 (0) | 1 (1.0) | 0 (0) | 2 (2.3) | 2 (2.7) |
| No pedometer given | 0 (0) | 0 (0) | 0 (0) | 3 (3.9) | 9 (12.0) |
Appendix 14 Data table summarising the return of pedometer diaries
| Pedometer diary | Month, n (%) | ||||
|---|---|---|---|---|---|
| 0 (N = 100) | 3 (N = 93) | 6 (N = 84) | 9 (N = 77) | 12 (N = 75) | |
| Returned | 93 (93.0) | 84 (90.3) | 69 (82.1) | 57 (74.0) | 54 (72.0) |
| Not returned | 7 (7.0) | 9 (9.7) | 15 (17.9) | 17 (22.0) | 12 (16.0) |
| Not given | 0 (0) | 0 (0) | 0 (0) | 3 (4.0) | 9 (12.0) |
Appendix 15 Economic costs and outcomes data
Resource use
Table 35 shows the NHS resource use quantities (mean number of visits, SD, median, minimum and maximum) that were accumulated over the 12-month intervention period for the active control and intervention groups. Each analysis includes only those cases that had complete resource use data at all five data collection time points. The pilot RCT results illustrate that, for the intervention group, nurse and GP visits were the most frequent NHS resource use. The active control group reported using GP, nurse and inpatient treatment resources most. Table 35 also illustrates that, aside from outpatient clinic visits, the intervention recipient group reported higher resource use; however, there was only a marginal difference between the active control and the intervention groups.
| NHS resource use (visits) | Intervention | Active control | Mean difference | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | ||
| GP | 31 | 3.87 | 4.15 | 3 | 0 | 17 | 29 | 3.31 | 2.65 | 2 | 0 | 11 | –0.56 |
| Nurse | 31 | 1.13 | 1.50 | 1 | 0 | 5 | 29 | 1.24 | 1.50 | 1 | 0 | 5 | 0.11 |
| A&E | 30 | 0.2 | 0.48 | 0 | 0 | 2 | 27 | 0.18 | 0.47 | 0 | 0 | 2 | –0.05 |
| Outpatient clinic | 26 | 0.62 | 1.20 | 0 | 0 | 4 | 27 | 0.63 | 1.04 | 0 | 0 | 4 | 0.01 |
| Inpatient treatment | 30 | 0.20 | 0.48 | 0 | 0 | 2 | 29 | 0.21 | 0.41 | 0 | 0 | 1 | 0.01 |
| Hospital stay | 30 | 0.30 | 0.95 | 0 | 0 | 5 | 28 | 0.50 | 1.20 | 0 | 0 | 4 | 0.20 |
The results also provided information on non-categorised resource use items, shown in Table 36 (complete-case analysis). The results show that the active control group recorded a larger number of midwife visits. Free-text comments revealed that the intervention group reported using the services of both a counsellor and a physiotherapist. The active control group reported no further NHS resource use.
| Resource use | Intervention | Active control | ||
|---|---|---|---|---|
| Visits (n) | Patients (n) | Visits (n) | Patients (n) | |
| Midwife | 1 | 1 | 30 | 1 |
| Physiotherapist | 2 | 2 | 0 | 0 |
| Breastfeeding specialist | 0 | 0 | 1 | 1 |
| Counsellor | 2 | 2 | 0 | 0 |
In both the active control and the intervention groups, there was a prevalent use of prescription medication, as shown in Table 37. The intervention group reported higher prescription medication use across the 12-month period than the active control group, in which only 29.0% (9/31) of participants reported using prescription medication at 12 months, compared with 65.6% (21/32) of the intervention participants.
| Time point | Intervention, n (%) | Active control, n (%) | ||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Baseline | 32 (64.0) | 18 (36.0) | 28 (63.6) | 16 (36.4) |
| 3 months | 22 (47.8) | 24 (52.2) | 22 (53.7) | 19 (46.3) |
| 6 months | 7 (17.9) | 32 (82.1) | 6 (17.6) | 28 (82.4) |
| 9 months | 19 (54.3) | 16 (45.7) | 18 (48.6) | 19 (51.4) |
| 12 months | 21 (65.6) | 11 (34.4) | 9 (29.0) | 22 (71.0) |
Personal costs
Details of participants’ personal food, health and medication costs (mean number of visits, SD, median, minimum and maximum) across both the intervention and active control groups over the 12-month intervention period (complete-case analysis) are presented in Table 38. The results illustrate that the mean participant costs were higher for all items except health and fitness apps among the active control group than the intervention group. The study shows that, across the intervention, the personal cost to participants was £70.60 higher in the active control group than in the intervention group. These pilot RCT results indicate that the proportion of personal costs were positively affected by the intervention.
| Personal costs collected | Intervention | Active control | Mean difference (£) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (£) | SD (£) | Median (£) | Minimum (£) | Maximum (£) | n | Mean (£) | SD (£) | Median (£) | Minimum (£) | Maximum (£) | ||
| Over-the-counter medication cost | 27 | 8.85 | 12.70 | 2.00 | 0.00 | 40.00 | 27 | 26.16 | 48.26 | 9.00 | 0.00 | 210.00 | 17.31 |
| Cost of lifestyle services and clubs | 31 | 178.75 | 188.22 | 120.00 | 0.00 | 695.00 | 28 | 179.27 | 218.65 | 127.50 | 0.00 | 1080.00 | 0.51 |
| Food and non-alcoholic costs | 31 | 401.81 | 150.71 | 360.00 | 160.00 | 820.00 | 29 | 408.52 | 139.44 | 390.00 | 205.00 | 685.00 | 6.71 |
| Alcoholic drink costs | 30 | 32.95 | 36.31 | 25.00 | 0.00 | 160.00 | 28 | 33.71 | 36.28 | 20.5.00 | 0.00 | 106.00 | 0.76 |
| Takeaway meals and snacks | 31 | 55.87 | 36.62 | 50.00 | 0.00 | 150.00 | 28 | 69.43 | 46.36 | 77.00 | 7.00 | 165.00 | 13.56 |
| Meals, snacks and drinks away from home | 31 | 76.10 | 50.51 | 75.00 | 0.00 | 190.00 | 29 | 112.38 | 76.95 | 95.00 | 10.00 | 335.00 | 36.28 |
| Smoking or vaping | 29 | 1.52 | 6.39 | 0.00 | 0.00 | 33.00 | 28 | 11.61 | 35.88 | 0.00 | 0.00 | 150.00 | 10.10 |
| Health and fitness apps purchased | 23 | 20.67 | 76.92 | 0.00 | 0.00 | 370.00 | 19 | 5.99 | 13.40 | 0.00 | 0.00 | 55.00 | –14.68 |
| Total cost | £776.52 | £847.07 | |||||||||||
Outcome measures for economic evaluation
ICECAP-A
The results shown in Table 39 illustrate that, across the active control and intervention groups, there was marginal difference. The completeness of the ICECAP-A questionnaire at 12 months was 100% (33/33) for both groups, including the participants who completed and returned the follow-up questionnaire at 12 months, as reported in Chapter 4. The results show that there was a small improvement in the intervention group ICECAP-A scores over the 12 months (relative to baseline) whereas the active control group revealed no improvement and had a lower mean tariff score at the end of the intervention period of 0.91, compared with 0.95 for the intervention group. The results demonstrate that it is possible to measure and value a longitudinal change (or lack of change) in participant well-being over the course of the intervention using this measure; therefore, it will be taken forward in the full RCT.
| Time point | Intervention | Active control | Mean difference | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | ||
| Tariff score | |||||||||||||
| Baseline | 50 | 0.89 | 0.12 | 0.93 | 0.51 | 1 | 44 | 0.89 | 0.10 | 0.91 | 0.51 | 1 | –0.002 |
| 3 months | 46 | 0.89 | 0.11 | 0.93 | 0.49 | 1 | 41 | 0.92 | 0.08 | 0.94 | 0.62 | 1 | 0.03 |
| 6 months | 38 | 0.91 | 0.11 | 0.93 | 0.51 | 1 | 33 | 0.91 | 0.08 | 0.92 | 0.70 | 1 | –0.0005 |
| 9 months | 35 | 0.92 | 0.07 | 0.93 | 0.65 | 1 | 38 | 0.90 | 0.11 | 0.92 | 0.44 | 1 | –0.02 |
| 12 months | 33 | 0.95 | 0.06 | 0.95 | 0.79 | 1 | 33 | 0.91 | 0.08 | 0.91 | 0.69 | 1 | –0.04 |
| ICECAP-A score change | |||||||||||||
| 3 months – baseline | 45 | 0.01 | 0.11 | 0 | –0.24 | 0.35 | 41 | 0.04 | 0.09 | 0.01 | –0.13 | 0.34 | 0.03 |
| 6 months – baseline | 38 | 0.03 | 0.07 | 0.02 | –0.19 | 0.16 | 33 | 0.01 | 0.07 | 0 | –0.21 | 0.14 | –0.01 |
| 9 months – baseline | 35 | 0.05 | 0.11 | 0.02 | –0.12 | 0.39 | 38 | 0.02 | 0.09 | 0.01 | –0.26 | 0.22 | –0.03 |
| 12 months – baseline | 33 | 0.06 | 0.08 | 0.03 | –0.05 | 0.26 | 33 | 0.01 | 0.08 | 0 | –0.19 | 0.25 | –0.05 |
EuroQol-5 Dimensions, five-level version
The results shown in Table 40 summarise the EuroQol-5 Dimensions, five-level version (EQ-5D-5L), questionnaire data at baseline and at 3, 6, 9 and 12 months (complete-case analysis). Similar to the ICECAP-A, the completeness of the EQ-5D-5L questionnaire at 12 months was 100% (33/33) for both groups. The results show that, in both the intervention and the active control groups, there was a slight improvement in the visual analogue scale scores over the 12-month period, with a larger improvement seen in the active control group (3.74) than in the intervention group (2.15). However, in tariff scores and overall utility change from baseline, the intervention group showed an overall positive improvement in reported utility whereas the active control group reported the same score at 12 months as at baseline. It is clear to see that the largest difference in tariff scores was reported at 9 months, with the intervention group reporting a mean score of 0.96 and the active control group reporting a mean score of 0.86. Only the intervention group reported a positive utility change over the 12-month complete-case analysis, and the results also indicate that the intervention produced a larger QALY gain than that produced by the active control. Similarly to the ICECAP-A results, a longitudinal change over time could be identified from the EQ-5D-5L results, and this change could be measured and valued.
| Time point | Intervention | Active control | Mean difference | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | ||
| VAS | |||||||||||||
| Baseline | 50 | 77.94 | 17.39 | 80 | 20 | 100 | 43 | 75.35 | 14.39 | 75 | 40 | 100 | –2.59 |
| 3 months | 46 | 77.30 | 15.25 | 80 | 30 | 100 | 41 | 77.54 | 13.28 | 80 | 35 | 100 | 0.23 |
| 6 months | 39 | 79.79 | 13.52 | 80 | 45 | 100 | 33 | 74.54 | 14.11 | 75 | 35 | 95 | –5.25 |
| 9 months | 35 | 79.94 | 11.35 | 80 | 60 | 100 | 38 | 76.66 | 14.71 | 80 | 22 | 95 | –3.28 |
| 12 months | 32 | 80.09 | 16.19 | 85 | 20 | 95 | 33 | 79.09 | 12.51 | 80 | 36 | 96 | –1.00 |
| Tariff score | |||||||||||||
| Baseline | 48 | 0.90 | 0.09 | 0.88 | 0.7 | 1 | 47 | 0.9 | 0.13 | 0.88 | 0.35 | 1 | –0.02 |
| 3 months | 44 | 0.87 | 0.15 | 0.88 | 0.44 | 1 | 44 | 0.88 | 0.12 | 0.88 | 0.54 | 1 | 0.01 |
| 6 months | 36 | 0.91 | 0.10 | 0.94 | 0.65 | 1 | 36 | 0.89 | 0.13 | 0.88 | 0.53 | 1 | –0.02 |
| 9 months | 33 | 0.96 | 0.07 | 1 | 0.8 | 1 | 39 | 0.86 | 0.13 | 0.88 | 0.58 | 1 | –0.1 |
| 12 months | 33 | 0.93 | 0.1 | 1 | 0.69 | 1 | 33 | 0.9 | 0.12 | 0.88 | 0.58 | 1 | –0.03 |
| Utility change | |||||||||||||
| 3 months – baseline | 43 | –0.05 | 0.14 | 0 | –0.48 | 0.16 | 44 | –0.03 | 0.09 | 0 | –0.23 | 0.23 | 0.02 |
| 6 months – baseline | 36 | –0.00 | 0.11 | 0 | –0.35 | 0.16 | 36 | –0.02 | 0.13 | 0 | –0.37 | 0.23 | –0.02 |
| 9 months – baseline | 33 | 0.05 | 0.1 | 0 | –0.15 | 0.26 | 39 | –0.02 | 0.12 | 0 | –0.23 | 0.39 | –0.07 |
| 12 months – baseline | 33 | 0.01 | 0.09 | 0 | –0.16 | 0.23 | 33 | –0.00 | 0.09 | 0 | –0.20 | 0.23 | –0.02 |
| QALY | |||||||||||||
| 12 months – baseline | 29 | 0.92 | 0.07 | 0.92 | 0.75 | 1 | 31 | 0.89 | 0.09 | 0.90 | 0.62 | 1 | –0.03 |
Appendix 16 Screenshot of study website

Appendix 17 Data table of participant-reported overall satisfaction with taking part
| Group | Responses (n) | Response, n (%) | ||||
|---|---|---|---|---|---|---|
| Very satisfied | Mostly satisfied | Neither | Mostly dissatisfied | Very dissatisfied | ||
| Intervention | 33 | 18 (54.5) | 11 (33.3) | 2 (6.1) | 1 (3.0) | 1 (3.0) |
| Active control | 33 | 21 (63.6) | 11 (33.3) | 1 (3.0) | 0 (0) | 0 (0) |
List of abbreviations
- BCT
- behaviour change technique
- BMI
- body mass index
- BOCF
- baseline observation carried forward
- BP
- blood pressure
- CEA
- cost-effectiveness analysis
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CRF
- case report form
- eHealth
- electronic health
- EPDS
- Edinburgh Postnatal Depression Scale
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- HAPA
- health action process approach
- HRQoL
- health-related quality of life
- ICECAP-A
- ICEpop CAPability measure for Adults
- IQR
- interquartile range
- LOCF
- last observation carried forward
- LSHTM
- London School of Hygiene & Tropical Medicine
- mHealth
- mobile health
- MMS
- multimedia messaging service
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PPI
- personal and public involvement
- QALY
- quality-adjusted life-year
- QUB
- Queen’s University Belfast
- RCT
- randomised controlled trial
- SD
- standard deviation
- SMS
- short message service
- SPSS
- Statistical Product and Service Solutions
- WIC
- Women, Infants and Children