Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 14/231/20. The contractual start date was in October 2016. The final report began editorial review in September 2018 and was accepted for publication in June 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Stacy A Clemes, Daniel D Bingham, Natalie Pearson, Yu-Ling Chen, Charlotte Edwardson, Keith Tolfrey, Lorraine Cale, Mike Fray and Sally E Barber report non-financial support from Ergotron, Inc. (Saint Paul, MN, USA), during the conduct of the study. Keith Tolfrey reports non-financial support from Iwantastandingdesk.com (Clitheroe, UK) for EIGER™ student standing desks for other independent sedentary behaviour research in secondary schools.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Clemes et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background and rationale
Sedentary behaviour, physical activity and health in children
Childhood is a critical period for the establishment of healthy lifestyle behaviours, including physical activity. Continual advances in modern technology, economic progress and changes to our environments have resulted in reductions in physical activities associated with daily living, and in sedentary behaviour becoming ubiquitous within all settings of daily life. Sedentary behaviour is a behaviour distinct from physical (in)activity and is currently defined as ‘any waking behaviour characterised by an energy expenditure of ≤ 1.5 metabolic equivalents (METs) while in a sitting, reclining or lying posture’. 1 Although reclining and lying postures are included in the definition, most of the time an individual (young people and adults) spends sedentary will be in a sitting position during waking hours. Participation in regular physical activity has numerous short- and longer-term physiological, psychological and social benefits for young people. 2–4 For example, reviews have shown that physical activity can improve blood pressure, weight status and bone mineral density, and lead to improvements in self-esteem and depression, and, in the longer term, can prevent chronic disease. 2,4 It is acknowledged that physical activity is beneficial to health, and sedentary behaviour has been shown to adversely affect health.
Sedentary time is associated with an increased risk of metabolic syndrome,5 cardiovascular disease,6–8 type 2 diabetes mellitus,7,8 all-cause mortality9 and depression10 in adults. Although the evidence for associations between objectively assessed sedentary time and health outcomes in young people is less consistent,11–13 the proxy sedentary behaviours of television viewing and screen time (the most prolific area of sedentary behaviour research) are unfavourably associated with body composition, fitness, self-esteem, cognitive development, pro-social behaviour, academic achievement in children13,14 and cholesterol in adulthood. 15 Sedentary behaviours in children have, furthermore, been shown to coexist with lower levels of physical activity16 and other ‘unhealthy’ behaviours, such as increased consumption of energy-dense foods, lower intakes of fruits and vegetables,17 and inadequate sleep. 18 Furthermore, recent evidence suggests an association between sedentary behaviour and several markers of inflammation and endothelial dysfunction,19 signalling potential mechanistic links with poor cardiovascular health in children. In addition, the emergence of an increased cardiometabolic health risk profile in some population groups is evident during the first decade of life. 20 For example, British South Asian children have demonstrated higher levels of glycated haemoglobin, fasting insulin and triglycerides, and lower high-density lipoprotein cholesterol than white British children, as well as having a higher sum of all skinfolds and fat mass percentage. 21,22 Therefore, these populations may be more vulnerable to the adverse affects of excessive sedentary time. Indeed, evidence of the influence of sedentary behaviour on the health of young people has prompted many countries to establish public health recommendations for sedentary behaviour. The UK, USA, Canada, Australia and the Netherlands, for example, now recommend that young people should reduce sitting time and break up long periods of sitting as frequently as possible. 23–27
Prevalence of sedentary behaviour in children
In the UK, sitting is the most prevalent behaviour exhibited during waking hours in children, accounting for > 65% of their waking time (or 7.5 hours),28 with some children reportedly sitting for > 10 hours per day (> 70% of waking hours). 29 Accelerometer data from the Health Survey for England have shown that young people (aged 5–15 years) spend, on average, 7 hours per day sedentary. 30 International research shows similar prevalence rates, with data from the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE)31 showing that children across 12 geographically and culturally diverse countries spend an average of 8.6 hours per day sedentary. 31 Similar proportions of waking hours spent sedentary have also been reported in children and adolescents from Canada and the USA. 32,33
Objective (accelerometry) sedentary behaviour data further suggest that children spend the majority of their school time sedentary. 34,35 For example, in children aged 10–12 years, across five European countries, 65% of the time spent at school was sedentary. 35 More recently, research has turned to inclinometer devices to more accurately measure total sedentary time (or sitting specifically), with data from these devices from British, Australian and Malaysian children (aged 8–12 years) further confirming that the majority of their time at school (70–71%), on weekdays (53–69%) and weekend days (60–73%) is spent sitting. 29,36–38
The rising prevalence of sedentary behaviour (and sitting) is of further public health concern because this behaviour in childhood has been shown to increase across key transitions in children’s lives (i.e. from primary to secondary school),39 and has been shown to track into adolescence40 and adulthood. 15 Given the physiological and psychosocial risks related to sedentary behaviour, and the evidence that sedentary behaviour increases as children get older, there is a need for interventions to reduce sedentary behaviour and increase movement in children.
Interventions to reduce sedentary behaviour in young people
The environments and social norms that children are exposed to have dominant influences on their activity behaviour. Given that children spend half of their waking hours at school, it is plausible that the school environment may be a critical influence on their health behaviour patterns41–43 and be a most appropriate target environment for interventions. A plethora of physical activity interventions aimed at young people have been conducted over the past two decades. 44,45 School-based interventions promoting physical activity have been successfully implemented during physical education classes, break times and before and after school hours, and have revealed positive effects on physical activity. 44 Furthermore, there is now growing evidence supporting the use of physical activity as a teaching tool (e.g. physically active learning) and classroom movement breaks, as a means of facilitating classroom management, student attention and focus on task. 46 However, teachers, education departments and organisations frequently cite a crowded curriculum, alongside other barriers, such as lack of knowledge or confidence, as reasons for not implementing physical activity programmes. Thus, alternative methods that do not add to teachers’ workload and require minimal specialist knowledge are required.
With an increasing interest in sedentary behaviour, a number of systematic reviews and meta-analyses have been published, synthesising the interventions that focus on young people. 47,48 Although most interventions specifically targeting sedentary behaviour have been home or school based, sedentary behaviour has typically been targeted as screen time and via behaviour change strategies within non-school settings (i.e. screen time at home),48 the effects of which have been inconclusive. 47 Most interventions specifically targeting sedentary behaviour have not been based on a behaviour change framework or theory. 48 In a recent review of interventions targeting sedentary behaviour, only 10 out of 21 interventions included studies that were theory based. 48 Theoretical frameworks provide a scaffold for intervention development from being an evidence-based source for understanding the behaviour of interest and possible levers of change,49 allowing a systematic evaluation of the intervention outcomes. Theories and frameworks typically utilised in sedentary behaviour interventions to date, again which have largely targeted screen time, include social cognitive theory, behavioural choice theory, the social ecological model and the chronic care model. 48
Although there is an abundance of behaviour change theories, models and frameworks for researchers to use (indeed 83 were identified in a recent systematic review49), the behaviour change wheel (BCW)50 has increasingly received attention within the sedentary behaviour literature. 51,52 The BCW synthesises 19 pre-existing frameworks of behaviour change into a single interface, incorporating a theory of behaviour, intervention functions and associated policy categories, and can be applied to any behaviour in any setting. 50 As policy can only influence behaviour through interventions, which in turn act through capability, opportunity and motivation, the framework is represented as a wheel with an outer layer (policy categories) influencing the next layer (intervention functions), until behaviour is changed at the very centre of the wheel. 50
The capability, opportunity, motivation – behaviour model (COM-B) (sources of behaviour) hypothesises that for specific behaviours to occur, the individual must have both the physical and psychological capability to perform the given behaviour, along with the social and physical opportunity to perform the behaviour, and be motivated to perform the specific behaviour more so than any other behaviours within that moment in time. Within the context of sedentary behaviour, the only interventions that have consistently demonstrated a reduction in sedentary time in younger populations are those utilising a standing desks design within the classroom (i.e. environmental restructuring),53 thus providing a physical opportunity for children to stand and/or break up their sitting time. As children spend up to 6 hours per day in the school environment and owing to the potential reach of school-based interventions to tackle inequalities (i.e. demographic and social/cultural), changing the traditional classroom environment to an activity-permissive one by reducing sitting in this environment (rather than the traditional focus on leisure time screen use) is a promising area of research. Indeed, environmental restructuring to provide a physical opportunity to stand rather than sit would certainly be essential within the classroom environment, as traditional furniture dictates that children spend most of their class time sitting. However, implementing new practices and/or changing existing practices in organisations, such as schools, require changes in individual behaviour (i.e. pupil) and collective behaviour (i.e. teachers/school staff and pupils), and changing behaviour requires an understanding of the influences on behaviour in the context in which they occur. Our understanding of these factors can be enhanced through the theoretical domains framework,54 which provides a theoretical lens through which to view the cognitive, affective, social and environmental influences on behaviour. 55
Interventions to reduce sitting within the classroom environment
There are now a growing number of environmental interventions that aim to reduce classroom sitting time and increase standing and movement, which have been implemented in schools and evaluated for effectiveness through systematic reviews. 56,57 Feasibility studies, including our own,29,58,59 have demonstrated the effectiveness of incorporating sit–stand desks in primary school classrooms over the short term (< 12 weeks). For example, sit–stand desks have been shown to enable pupils to alternate between sitting and standing without disruption to teaching, learning or behaviour. 56 Furthermore, sit–stand desks in classrooms have been shown to be effective in increasing energy expenditure60,61 and standing and movement62 during the school day. In addition, studies have shown that sit–stand desks in classrooms lead to improvements in children’s posture and musculoskeletal comfort,63,64 levels of academic engagement65 and achievement,64 and improved cognitive function. 66 Sitting time has been shown to be reduced by between 44 and 60 minutes per day and standing time increased by between 18 and 55 minutes per day during classroom time at school, over 4 and 9 weeks’ follow-up. 29,59,67 More recently, the impact of standing desks on sitting time in the classroom has been assessed over 16 weeks’ follow-up, with results suggesting a 13% reduction in sitting and a 31% increase in standing at school, relative to baseline. 68 Clearly, incorporating standing desks in classrooms shows great promise for reducing children’s sitting time. However, systematic reviews have concluded that the majority of studies conducted to date have included relatively small samples, have been short in duration, have not included a randomised controlled design and have not assessed the impact of standing desks on academic performance. 56,57,69 Further exploration in this area of research is thus warranted.
Development of the Stand Out in Class study
The feasibility of incorporating sit–stand desks in the classroom environment over a 9-week period was demonstrated in an earlier intervention study we conducted with Year 5 Bradford primary school children. 29 In this feasibility study, we verified a number of our outcome measures (objectively determined sitting time and physical activity, body composition, blood pressure and teacher-reported pupil behaviour). In a novel approach, we replaced three standard desks (sitting six children) with six sit–stand desks. The teacher rotated the children assigned to the intervention group around the classroom in groups of six, according to the lesson being taught, using naturally occurring breaks between lessons to do so, ensuring that each child was exposed to the sit–stand desks once a day for at least 1 hour. Children in the control group continued with their usual practice, with no environmental changes to their classroom. Reductions in classroom sitting of 52 minutes per day were observed within the intervention group and reductions in total daily sitting of 81 minutes per day on school days after 9 weeks were seen. Teachers reported improvements in behaviour and no perceived negative effects on teaching or learning were observed. As part of this feasibility work, we also compared the changes in classroom sitting observed in our sample with data from a related feasibility study conducted in a primary school in Melbourne, Australia. 29 In the Melbourne study,29 every child in the intervention classroom had a sit–stand desk. Despite differences in desk provision, no significant differences in reductions in sitting time were observed between the two studies. Reductions in classroom sitting of 44 minutes per day and reductions in total daily sitting of 68 minutes per day were observed in the Melbourne intervention class. This early work demonstrates the potential of sit–stand desks in the classroom as a way of reducing sitting in children over the short term, irrespective of the type of sit–stand desk provision.
Following this successful feasibility work, the next logical step required was the development of the Stand Out in Class intervention. With the aim of informing a future definitive trial, the Stand Out in Class pilot study was developed to establish procedures for school and participant recruitment, and the acceptability of the intervention and outcome measures, and attrition rates. This intervention was informed by our feasibility work and public and patient involvement (PPI) with teachers and children through informal interviews and workshops (children only), in which our earlier work was described and their feedback on the intervention and proposed measures was obtained. This present study therefore comprises a pilot evaluation of the implementation of standing desks in the classroom through a cluster randomised controlled trial (RCT), with objective measures of sitting and activity, and a range of health- and education-related outcome measures. Rapid increases in sedentary time have been observed in children aged ≥ 11 years, relative to younger age groups. 70 This study targets Year 5 classrooms, comprising children just below this age (9- to 10-year-olds), with the goal of reducing the typical rise in sedentary time seen during the transition into adolescence,39 given also that sedentary behaviours track from childhood into adolescence and adulthood. 40 Furthermore, evidence suggests that children in Year 5 upwards are active participants in their own learning, making them an optimal target for classroom interventions that may facilitate learning. 71 A cluster design is considered appropriate because the intervention is delivered at the classroom level, rather than at an individual level.
Aims and objectives
The aim of this study is to undertake a pilot cluster RCT of the introduction of sit–stand desks in primary school classrooms to inform a future definitive trial.
Pilot trial study objectives
-
Establish and refine a recruitment strategy for schools and pupils.
-
Determine attrition in the trial (schools and children).
-
Determine completion rates for outcome measures (and whether or not these are sufficiently high to provide accurate data in a full trial).
-
Assess whether or not there are any differences in trial recruitment, retention and acceptability between ethnic groups.
-
Assess the acceptability of randomisation to schools.
-
Assess the acceptability of measurement instruments to teachers, children and parents, including the activPAL™ (PAL Technologies Ltd, Glasgow, UK) inclinometer, as the tool for the measurement of the primary outcome.
-
Assess the acceptability of the intervention to teachers, children and parents.
-
Monitor any adverse effects, such as musculoskeletal discomfort and/or disruption to the classroom/learning, to inform the design of a full trial and minimise or eliminate any such effects.
-
Assess intervention fidelity.
-
Derive preliminary estimates of the effect of the intervention on children’s total daily sitting time, physical activity, indicators of health (markers of adiposity and blood pressure), cognitive function, and academic performance, engagement and behaviour.
-
Estimate the standard deviation (SD) of the primary outcome to inform a sample size calculation for a full RCT.
-
Determine the availability and completeness of economic data, and conduct a preliminary assessment of potential cost-effectiveness.
Chapter 2 Study design and methods
This chapter summarises the study protocol for this pilot RCT as originally funded. Some of the material has already appeared in a published format72 and is reproduced here. Reproduced from Clemes et al. 72 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Study design
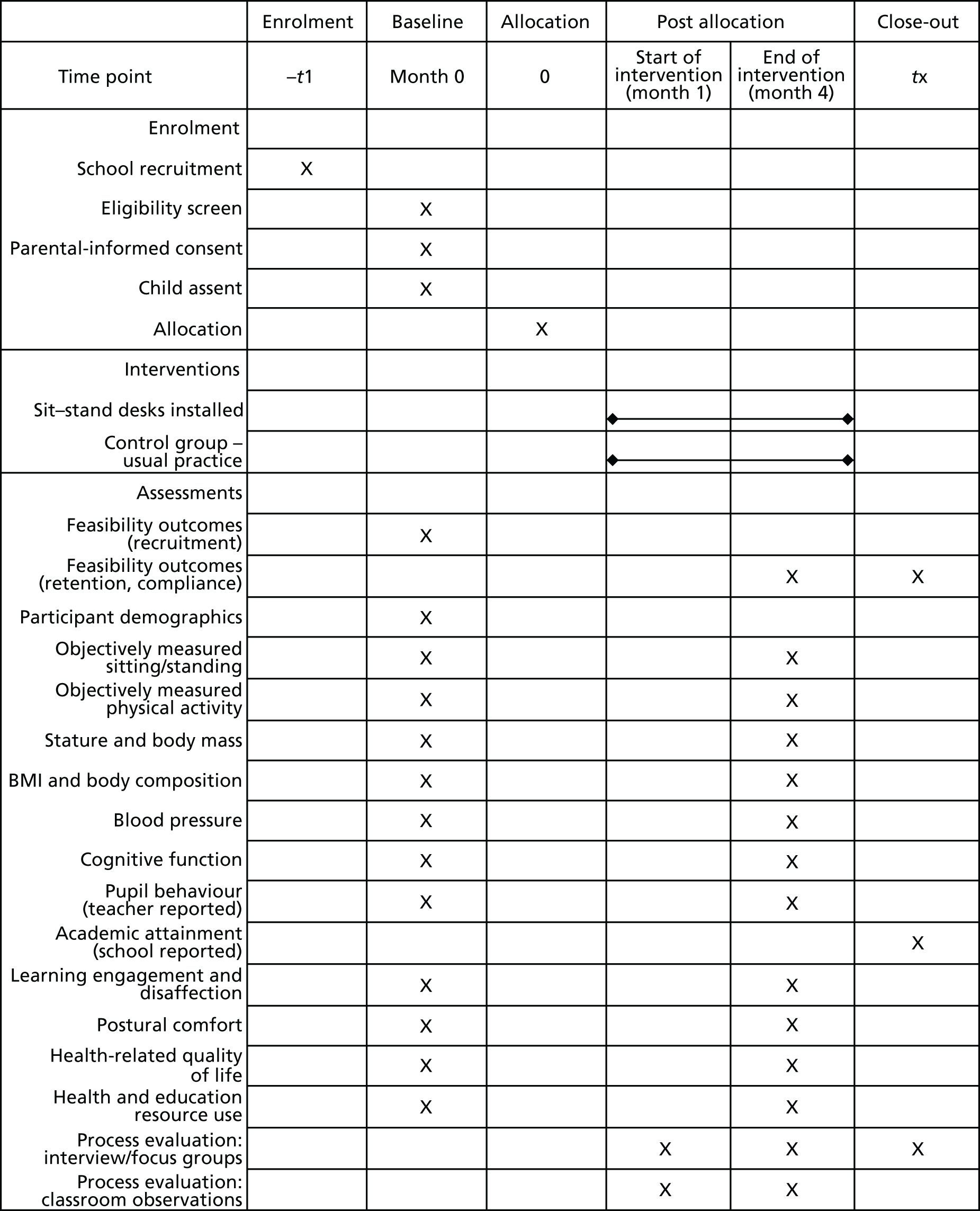
This was a school-based, pilot, two-armed, cluster RCT with economic and process evaluations. Individuals (Year 5 children, aged 9–10 years) were the unit of analysis and schools (clusters) were randomly assigned to one of two conditions: (1) six manually adjustable sit–stand desks incorporated into the classroom environment (intervention condition) or (2) current practice (control condition). Baseline measurements preceded randomisation and the sit–stand desks were installed into the intervention classrooms following this. An identical set of outcome measurements were taken from all participants approximately 7 months after the baseline measures, at the end of Year 5. Figure 1 shows the schedule of enrolment, intervention and outcome measurements.
FIGURE 1.
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) diagram illustrating the design and time scales of the pilot Stand Out in Class RCT. BMI, body mass index. Arrows indicate start and end points of intervention and control period. Reproduced from Clemes et al. 72 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. Includes minor additions and formatting changes to the original.
Ethics approval
Ethics approval for this study was obtained from Loughborough University’s Ethical Advisory Committee (reference R16-P027). All members of the measurement team were required to have a current enhanced disclosure and barring service check and all employees of the Bradford Teaching Hospitals NHS Foundation Trust who undertook data collection completed online training in safeguarding children and information governance.
Study setting
The study was conducted in primary schools in Bradford, UK. Bradford was chosen as the study location given its ethnic composition (predominantly South Asian and white British) and high levels of deprivation, health inequalities and childhood morbidity. 73 Half of all babies born in Bradford are of South Asian origin and 60% of babies are born into the poorest 20% of the population,73 with elevated risk factors for chronic diseases seen in South Asian children in comparison with white children. 20,22 Furthermore, in 2016–17, 38% of Year 6 children in Bradford were overweight or obese according to the National Child Measurement Programme. 74 The setting of this study, therefore, is fundamental in addressing the important issue of health inequalities, in that the intervention will be accessible to all children. In addition, the location enables us to pilot the intervention under challenging circumstances, meaning that, if it proves acceptable, it is likely to be transferable to most schools. At the planning stages of the trial, PPI with local teachers, parents and children demonstrated widespread support for the study, with all of those informally interviewed stating that they would be keen to try sit–stand desks in their classrooms (teachers and children).
Sample size
A recruitment target of eight primary schools, each with at least 15 child participants (approximately 50% of a typical class), was set, giving a minimum total sample of 120 participants. This matches the minimum of four clusters per arm recommended for a definitive cluster RCT75 and exceeds the target minimum sample size recommended for pilot trials. 76 Consequently, the sample should be sufficient to provide clear estimates of recruitment and follow-up for a definitive trial.
School and participant recruitment and eligibility criteria
Government-funded primary schools located in the city of Bradford were invited to take part in the trial. Private and designated special schools and schools with < 25 pupils in Year 5 were not eligible to participate. Schools running a sitting time reduction programme, or with a unique characteristic that precluded comparisons with another school, were also not eligible for participation. The study was publicised to primary schools through existing local networks (e.g. Bradford Primary Improvement Partnership and Bradford’s Public Forum for Education). We aimed to recruit four schools with predominantly South Asian pupils (> 50%) and four with predominantly white British pupils (> 50%). The ethnic composition of the pupils was determined using local school census data.
The following three-stage process was adopted, informed by our earlier feasibility work and PPI with teachers and head teachers, for contacting schools about the study: (1) head teachers/senior teachers were sent an e-mail detailing the study, with the e-mail including a copy of the information sheet for schools; (2) 2 days after sending the e-mail, the school was telephoned and the reception team was asked whether or not the e-mail had been received by the head teacher/senior teachers; and (3) a follow-up telephone call was made to the school to arrange a time for the research team to meet either with the head teacher or with a senior teacher, either over the telephone or in person, to discuss the study in more detail, or to confirm that the school was not interested in participating in the study. Schools interested in participating were sent/given further information about the study, including an information sheet for teachers, and during the follow-up conversations the head teacher, or a nominated senior teacher, was requested to provide written informed consent to participate on behalf of the school. During recruitment, schools were requested to identify a designated lead teacher and were informed that they may be randomised to a current practice control condition in which they would be asked to maintain their usual classroom practice.
Following school recruitment, a member of the research team contacted the designated lead teacher directly via e-mail. The school was then provided with an invitation pack for the parents or guardians of eligible children (9- to 10-year-olds within the nominated Year 5 class of participating schools). The invitation pack contained a detailed information sheet for parents/guardians about the study, an opt-in consent form for the parent or guardian to complete and return if they were happy for their child to participate in the evaluation and an information sheet for children. The packs were given to eligible Year 5 children, who were asked to give them to their parents or guardians. In consultation with the participating Year 5 teachers within the schools, it was agreed that members of the research team, and the teacher, would be present at the school gates during school drop-off and collection times over a 4-day period (after children were given their packs to take home) to speak to parents and guardians about the study, should they have any questions. Completed consent forms were returned by pupils to their teacher, who informed the research team of the children who were to be involved in the evaluation measures.
At the beginning of the baseline measurement session, all methods were fully explained to the participants by a team member who was suitably qualified and experienced, and who was authorised to do so by the principal investigator (PI). Children were then asked to provide verbal and written assent that they were happy to participate, and this was requested again at the start of the follow-up measurement sessions. Children without parental consent or those who did not give their assent to participate in the evaluation were excluded from the evaluation measures, described in Outcome measurements, although they were still able to use the sit–stand desks in their classrooms. Any children in the intervention schools with known contraindications (e.g. those with a musculoskeletal injury, wheelchair users) that would preclude periods of standing were invited to participate in the evaluation measures and encouraged to use the sit–stand desks in a seated posture for inclusivity. These individuals were, however, excluded from the analyses.
Changes from the original protocol/grant application
The original grant application proposed that the intervention would run throughout the entire academic year (≈10 months) while the participants were in Year 5. The intended start date of the grant was originally 1 April 2016 and the desk installation was planned for September 2016. However, owing to delays at the project approval stage, the study did not officially commence until 1 November 2016 and the sit–stand desks were installed in the intervention schools between 27 February 2017 and 3 March 2017 (due to further delays caused by desk availability from the manufacturer). The intervention was therefore shorter (4.5 months) than originally proposed. As one of the project goals was to build on the previous evidence and assess the longer-term acceptability of using sit–stand desks in primary school classrooms, the study team discussed with the Trial Steering Committee (TSC) the possibility of extending the duration of the intervention until December 2017, with the desks remaining with the children as they entered Year 6. The TSC, however, recommended that the intervention be completed as originally planned in July 2017, and this recommendation was supported by expert advisors within the National Institute for Health Research (NIHR). It was felt that extending the trial into Year 6, particularly in terms of the scheduling of a further set of follow-up measures, would place added pressure on the new Year 6 teachers and schools at a critical time when the children would be preparing for and taking their Standard Assessment Tests (SATs). It was also felt that, as a pilot study, the team would still have an adequate number of data to assess the acceptability of the trial following 4.5 months.
The Stand Out in Class intervention
Six sit–stand desks were placed in one Year 5 classroom (replacing three standard desks sitting six children) in each intervention school for two school terms. The research team supported teachers in the development of a classroom rotation plan to ensure that all children in their class were exposed to the sit–stand desks for at least 1 hour per day, on average, across the week. Stools or chairs remained in the classroom and children were free to choose whether they sat or stood when using the sit–stand desks.
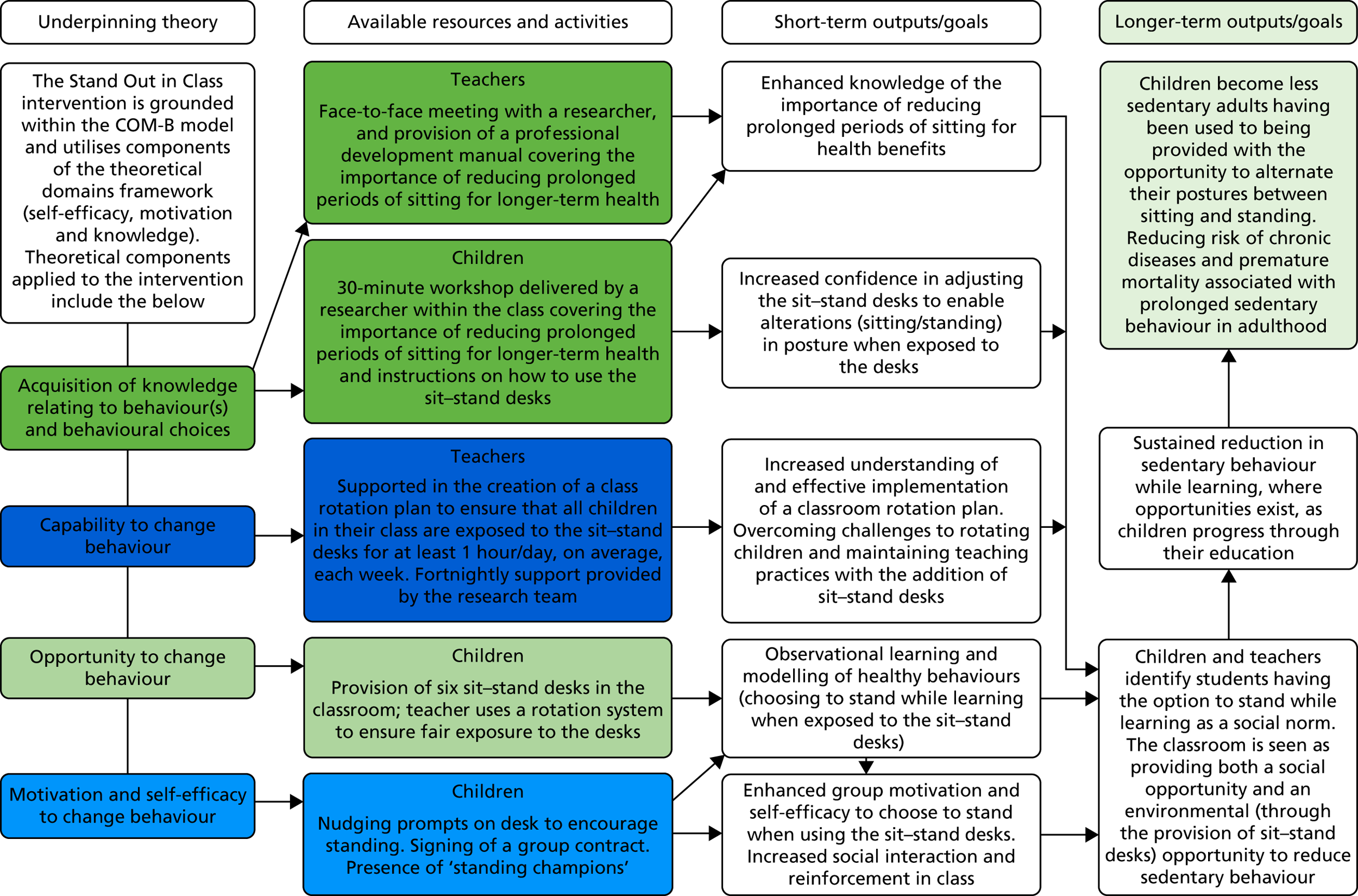
Teachers and pupils in the intervention classrooms received training on sit–stand desk use by the research team and teachers also received a professional development manual (see Report Supplementary Material 1) containing information on the health benefits of reducing prolonged sitting and on correct posture when standing at the desks. The manual and training focused on encouraging correct adoption of the intervention, targeting key barriers to and facilitators of sit–stand desk use. These were identified from our previous work,29,77 from the COM-B, within the BCW,78 and from the theoretical domains framework79 (e.g. self-efficacy, motivation and knowledge). Standardised behaviour change techniques (e.g. goal-setting, instruction)80 were also used during the training with teachers and pupils. A summary of the intervention components is shown in Table 1 and a logic model for the Stand Out in Class intervention, applicable for a definitive trial, is presented in Figure 2. Appendix 1, Table 23, details potential intervention barriers, solutions and hypothesised mediating processes informed by the above theoretical frameworks.
| Intervention component | Target domain | Mediating variable | Description |
|---|---|---|---|
| Adjustable sit–stand desks | Environment | Six adjustable sit–stand desks introduced into the classroom | |
| Nudging prompts | Environment | Children choose to stand rather than sit when using desks |
Stickers placed on each of the sit–stand desks Examples: |
| 2-hour one-to-one meeting | Teacher | Exposure to desks | 2-hour meeting with teacher covering:
|
| Professional development manual | Teacher | Exposure to desks | Covering topics such as:
|
| Planned weekly rotation plan | Teacher | Exposure to desks | Teacher creates a predetermined rotation plan and keeps a record of whether this was adhered to or not (simple tick sheet) |
| Fortnightly support with practitioners | Teacher | Exposure to desks | Telephone or face-to-face meeting with researchers/practitioners to discuss any issues around implementation of rotation plans |
| 30-minute workshop | Children |
Exposure to desks Children choose to stand rather than sit when using desks |
Covering topics such as:
|
| Standing champion/leader | Children |
Exposure to desks Children choose to stand rather than sit when using desks |
One child in a group is chosen as a standing champion, with responsibility of reminding the teacher of the rotation plan |
| Group contract | Children |
Exposure to desks Children choose to stand rather than sit when using desks |
Children asked to sign a class contract that states that I will try my best to:
|
FIGURE 2.
A logic model for the Stand Out in Class intervention, which is applicable for a definitive trial. Adapted with permission from Clemes et al. 81 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
The usual practice control arm
To compare the effects of the intervention against usual practice (i.e. the provision of standard classroom desks), schools assigned to the control arm were requested to continue with their usual practice and lesson delivery, and no environmental changes were made to their classrooms. The Year 5 participants in the control schools were asked to complete the same study measurements as those in the intervention schools, at the same time points. On completion of the study, control schools were offered a report summarising the collected data of their pupils.
Allocation to treatment groups
To assess the acceptability of the intervention and proposed outcome measures for use in a definitive trial across an ethnically diverse sample, recruited schools were stratified based on the ethnic composition of their pupils (see School and participant recruitment and eligibility criteria). Following the completion of baseline measurements, schools within each stratum were randomised by an independent statistician at the Leicester Clinical Trials Unit into the two trial arms [intervention and control, with an allocation ratio of 1 : 1 using a randomisation list in SAS® software (SAS Institute Inc., Cary, NC, USA). [SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries. ® indicates USA registration.] Two schools with predominantly South Asian pupils and two schools with predominantly white British pupils were randomised into the intervention and control arms (four schools in each trial arm). This stratification enabled the examination of whether or not there were differences between South Asian and white British pupils in terms of recruitment and retention, adherence to the outcome measures and preliminary effects of the intervention on outcome measures (objective 4). The statistician performing the analyses was blinded to the schools’ allocation to the study arms, as were the community researchers undertaking the outcome measurements.
Outcome measurements
Trial feasibility-related outcomes
The primary aim of this pilot study was to establish school and participant recruitment and retention rates, the acceptability of the intervention and proposed outcome measures, intervention and measurement fidelity, and the availability and completeness of economic data for an estimation of potential cost-effectiveness, to inform the development of a definitive trial. Study uptake was monitored by recording the number of schools and pupils approached, and the number agreeing to participate (objective 1). Withdrawal rates of schools and children (objective 2) and completion rates for outcome measures were recorded (objective 3), and these feasibility outcomes were compared between ethnic groups (objective 4).
Process evaluation
A series of interviews and focus groups with teachers, children and parents were conducted following the completion of the baseline measures and randomisation to explore the acceptability of the trial procedures, including randomisation (objective 5), and the acceptability of the measurement instruments (objective 6). The acceptability of the intervention (objective 7) and children’s, teachers’ and parents’ perceptions and experiences of the intervention and outcome measures were determined during the intervention through a further set of interviews (n = 4 with teachers from the intervention schools) and focus groups (n = 4 with children from the intervention schools) (objective 8). Potential differences in the trial and intervention acceptability between ethnic groups were explored as part of the analyses from the focus groups (objective 4). Towards the end of the intervention, four one-to-one interviews were also conducted (one per intervention school) with senior staff (head teachers/deputy head teachers) to further examine the acceptability of the intervention (objective 7).
To assess intervention fidelity, intervention classrooms were observed by a member of the research team for the duration of at least half a school day during the spring and summer terms. Field notes were taken to document the occurrence of any intervention components (i.e. use of prompt cards, engagement with a standing champion; see Table 1) during the observation period. In addition, children’s postures during sit–stand desk use were recorded using a postural analysis recording system based on the portable ergonomic observation63 to assess any potential future risk of musculoskeletal injury (objectives 8 and 9). Full details of the process evaluation methods, analyses and results are described in Chapter 5.
Health- and education-related outcome measures
All health-related outcome measurements were taken twice: at baseline prior to randomisation and approximately 7 months after baseline when pupils were at the end of Year 5 (the sit–stand desks remained in the intervention classes until the end of Year 5, while the follow-up measures were taking place).
Proposed primary outcome in a full trial: activPAL-determined sitting time
The likely primary outcome in a definitive trial would be change in average daily school day sitting time. Sitting was measured objectively for 7 consecutive days during each measurement period using the activPAL3 micro accelerometer (PAL Technologies Ltd, Glasgow, UK). All activPALs were initialised and downloaded using manufacturer proprietary software (activPAL Professional v.7.2.32, PAL Technologies Ltd, Glasgow, UK) and data were processed using the freely available ProcessingPAL software (version 1.1, University of Leicester, Leicester, UK; https://github.com/UOL-COLS/ProcessingPAL). The activPAL3 was waterproofed [using a nitrile sleeve and hypoallergenic Hypafix® (BSN medical, Hull, UK) dressing] and participants were requested to wear the device continuously (24 hours/day) on the anterior aspect of their right thigh during each measurement period. Participants were provided with a brief diary during each monitoring period, in which they were requested to document time in bed and any periods of non-wear.
The use of the activPAL to objectively measure sitting has increased in recent years82 and the device is recommended for use in interventions when the primary outcome measure is sitting. 83 It is regarded as the most accurate method of assessing sitting behaviour in free-living settings,84 and has been shown to be almost 100% accurate in measuring sitting, standing, walking and postural transitions in children. 85,86 The device has also been successfully used as a primary outcome measure in previous school-based sedentary behaviour interventions. 29,59,67
Although total daily school day sitting time is likely to be the primary outcome for a future trial, we also extracted classroom and leisure time sitting, standing and stepping times from the activPAL data. This allowed us to specifically examine the impact of the intervention on these behaviours during class time (the environment in which the intervention was administered). Furthermore, any positive (i.e. reductions in sitting) or compensatory effects (increases in sitting) of the intervention on children’s sitting, standing or stepping time out of school hours were examined by extracting activPAL data collected during leisure time.
Periods of non-wear and sleep time were excluded from the analyses using an automated algorithm,87 (applied within the ProcessingPAL software) and supplemented with cross-checking against participants’ diary entries. Owing to the exploratory nature of this study, children were included in the analyses if they had worn the activPAL for at least 8 hours on at least 1 weekday at baseline and follow-up, as applied elsewhere. 29 To assess whether or not the number of valid days of activPAL wear had an effect on the primary outcome (to inform wear time criteria in a definitive trial), sensitivity analyses were undertaken to examine the impact of the number of included days (see Statistical analysis). The variability (SD) of the data from the proposed primary outcome was used to inform a sample size calculation for a definitive trial (objective 11).
Proposed secondary outcomes in a full trial
ActiGraph-determined physical activity
Proposed secondary outcomes for a definitive trial include objectively measured physical activity. Although the activPAL provides a valid measure of posture, it has not been well validated for assessment of various physical activity intensities among children. Therefore, participants were requested to wear the ActiGraph GT3X+ accelerometer (ActiGraph, Pensacola, FL, USA) on the waist continuously (24 hours/day) for 7 consecutive days, concurrently with the activPAL, during each measurement period. The feasibility of collecting ActiGraph data, in addition to activPAL data, was examined in the present study to inform a definitive trial, in which this device could be used as a secondary outcome to examine any positive or negative (i.e. compensatory) effects of the intervention on physical activity, either during or after school hours. ActiGraphs were initialised to record data at 15-second epochs, the devices were initialised and downloaded using ActiLife version 6.13.3 (ActiGraph) and the data were processed using specifically developed and commercially available software (KineSoft version 3.3.20, Loughborough, UK). Periods of non-wear were documented in a brief diary provided with the activPAL and ActiGraph.
Waist-worn accelerometers have traditionally been considered the criterion measure of children’s physical activity. 88 The ActiGraph is the most commonly used accelerometer in field-based research and has been shown to have acceptable reliability and validity in paediatric populations. 89 Times spent in light (26–573 counts/15-second epoch) and moderate- to vigorous-intensity (≥ 574 counts/15-second epoch) activity throughout the day, and during and out of school hours, were extracted from the ActiGraph data using the Evenson cut-off points. 90 ActiGraph-determined sedentary time (≤ 25 counts/15-second epoch) was also extracted for descriptive purposes. In a comparative study examining the classification accuracy of five different ActiGraph cut-off points for determining children’s and adolescents’ physical activity intensity, against indirect calorimetry, the Evenson cut-off points were found to be the most accurate across all intensity levels and are therefore recommended for use in this age group. 91 Periods of non-wear and sleep time were excluded from the analyses during the processing of the ActiGraph data, and supplemented with cross-checking against participants’ diary entries. Owing to the 24-hour wear protocol of the ActiGraphs, a blanket removal of sleep time between 23.00 and 05.59 was undertaken when processing these data. However, to identify periods of sleep occurring outside this time period (i.e. after 06.00 and before 23.00), the three-axis acceleration data from the ActiGraph were used to detect periods of no movement. If these periods exceeded 20 minutes of zero counts, then this additional period was excluded as non-wear/sleep time. The same wear time criteria as applied to the activPAL data (a minimum of 8 hours of wear on at least 1 weekday) was also applied to the ActiGraph data.
Anthropometry
At each measurement point, children’s stature and body mass (both assessed without shoes) were measured directly using standard procedures by trained research staff. Body mass index (BMI) (kg/m2) was calculated and converted to a BMI percentile based on UK reference data. 92 Body composition (percentage body fat and fat mass) was assessed via bioelectrical impedance analysis using Tanita DC-360S body composition scales (Tanita, Tokyo, Japan) which contain specific algorithms for children.
Blood pressure
Blood pressure was measured from the left arm after at least a 5-minute period of quiet sitting using a semi-automated recorder (Omron HEM-907; Omron Corporation, Kyoto, Japan) with a paediatric cuff, in accordance with current recommendations. 93 Three measurements of blood pressure were taken with each measurement, separated by a 2-minute rest period. The mean systolic and diastolic blood pressures recorded from the second and third assessments were calculated and used in the analyses.
Cognitive function
A set of objective cognitive function tests were administered via a validated software package. The software was installed on school computers, enabling study participants to undertake these assessments collectively in the classroom, under the supervision of two researchers. Participants undertook a practice run-through of the cognitive function test battery a day before the test day. The test battery took children approximately 15 minutes to complete and included the Corsi block-tapping test,94 the Stroop test95 and the rapid visual information processing (RVIP) task. 96
The Corsi block-tapping test measures visuospatial working memory capacity. 94 Performance on the Corsi block-tapping test is linearly associated with age in typically developing children97 and the original version has exhibited a test–retest reliability coefficient of 0.7 (Pearson’s correlation coefficient) in 11-year-olds. 98 The test involves participants repeating a sequence of blocks, displayed on a 3 × 3 grid, which individually change colour. The test begins with a sequence of three blocks and proceeds to a maximum of 12. The sequence length increases or decreases by one with every correctly or incorrectly reproduced sequence, respectively. The outcome measure was the mean correctly recalled sequence length, assessed across 12 attempts.
The Stroop test measures sensitivity to interference and the ability to suppress an automated response (by reading colour names in favour of naming the font colour), and is a commonly used measure of selective attention and executive function. 99 The current test comprised two levels: a simple level and a complex level. The simple level involved reading a name of a colour in black font and identifying the colour using the right or left arrow keys on the keyboard. In the complex level, participants were presented with a colour name (i.e. red, green or blue) in a different font colour (e.g. the word ‘red’ in blue font) and were required to identify the colour name (i.e. red in the example given above). The average reaction time of all correct responses for the simple and complex levels were calculated. The complex reaction time measure within this computerised test has been shown to exhibit a test–retest reliability of 0.55 (Pearson’s correlation coefficient) in a combined sample of children and adults. 100
The RVIP task measures sustained attention and has been shown to exhibit an internal reliability coefficient (assessed using Cronbach’s alpha) of 0.49 in school-aged children. 101 The test involves detecting sequences of three consecutive even or odd numbers presented on the screen. Each number is presented individually and changes every 600 milliseconds. Outcomes from this test include the true-positive rate (i.e. the number of correctly identified sequences out of all identifiable sequences) and the miss rate (i.e. the number of missed sequences out of all identifiable sequences), with scores for both measures ranging between 0 and 1. The true-positive rate is considered a measure of accuracy, whereas the miss rate is considered a measure of alertness, with higher and lower values indicating better performance, respectively. Mean reaction times for each correctly identified sequence were also recorded.
Academic progress and attainment
Measures of participants’ academic progress across maths, reading and writing were collected using routine assessment data recorded by the schools. As collecting data relating to pupils’ progress across these key subject areas is not a requirement of the national curriculum, the participating schools did not have a standardised method of collecting these data. Through consultation with participating teachers, attainment data were dichotomised for the purposes of this study into binary classifications of whether or not each participating pupil was meeting expectations in these three key subject areas at a particular time of development and education. With teachers’ guidance, we transformed the attainment data collected by each school, for each participating pupil, into the following variables: ‘yes – pupil is meeting expectations (for maths/writing/reading) of children of that age’ or ‘no – pupil is not meeting expectations (for maths/writing/reading) of children of that age’. Each school’s attainment data collected at the start of the spring term (2016/17 academic year), coinciding with before the intervention commenced, and at the end of the school year (July 2017), were collected and transformed in this way, to ensure standardised data across the eight participating schools. The binary scores calculated for baseline were subtracted from the follow-up scores for maths, reading and writing separately, leading to a nominal variable of ‘change of subject expectation’, which led to three categorical levels: (1) decreased level of expectation (pupil was meeting expected level for the subject, but is no longer meeting expectations); (2) no change in expected level; and (3) increased level of expectation (pupil was not meeting level of expectation, but is now).
Questionnaire measures
The impact of the intervention on participants’ behaviour was assessed using the Strengths and Difficulties Questionnaire, completed by teachers at baseline and follow-up. This questionnaire, when completed by teachers, has been shown to provide a valid indicator of children’s behaviour (convergent validity: Pearson’s correlation coefficient with the Rutter Children Behaviour Questionnaire = 0.92102). In addition, children self-reported their engagement and disaffection with their own learning via the Engagement Versus Disaffection with Learning Questionnaire103 (correlation coefficients between pupil and teacher reports of the components of engagement using this measure range from 0.26 to 0.44104). Postural comfort was reported by participants using a further brief questionnaire. 63
Children completed the Paediatric Quality of Life Inventory (PEDS-QL)105 and EuroQol-5 Dimensions Youth (EQ-5D-Y)106 at each measurement point, to provide a measure of self-reported quality of life. The construct validity of the PEDS-QL has been previously demonstrated, with healthy children displaying significantly higher scores on this measure than acutely or chronically ill children. 105 Responses on the EQ-5D-Y have also been shown to correlate with other measures of children’s health-related quality of life (convergent validity correlation coefficients up to 0.56107). To inform the economic analysis described in more detail in Economic Analysis (objective 12), teachers and parents completed a questionnaire72 created for the purpose of this study, which assessed participants’ health- and education-related resource use at baseline and follow-up.
Basic demographic information (sex, age, ethnicity and postcode, to determine Index of Multiple Deprivation as an indicator of socioeconomic status) was collected at baseline.
School and participant appreciation
As a thank you for participating in this pilot trial, all schools (intervention and control) received a donation of £200 at the end of the study period. A £5 gift voucher was also given to each child following the completion of both the baseline and follow-up measures to encourage a timely return of the accelerometers.
Economic analysis
The availability and completeness of economic data were established as part of this pilot study (objective 12). Resource use information was collected, which included the cost of the sit–stand desks, along with participants’ health-related [e.g. general practitioner (GP) visits] and education-related resource use (e.g. requirements for additional tutoring). Proposed outcomes within a definitive trial were based on two sectors: health and education. For the former, as described in Questionnaire measures, the PEDS-QL105 and EQ-5D-Y106 were collected at baseline and follow-up to assess children’s health-related quality of life. For the latter, the Strengths and Difficulties Questionnaire completed by school teachers for each pupil was used. A preliminary cost-effectiveness analysis was conducted (see Chapter 4) to inform the value of, and to make recommendations for, the design of a full trial. All outcomes collected were presented as a within-trial analysis at baseline and follow-up; however, no formal comparison of the cost and benefit of providing sit–stand desks was conducted for within-trial outcomes. A brief scoping review was conducted to identify existing model(s) that link short-term health outcomes to long-term health effects with this model, informing a preliminary assessment of the long-term health costs and benefits associated with the intervention.
Statistical analysis
The analysis and reporting of this pilot RCT was in line with the Consolidated Standards of Reporting Trials (CONSORT) statement for cluster RCTs. 108 Data were analysed on a complete-case basis. The purpose of the primary analysis was to assess the feasibility of recruitment and adherence/retention of primary schools and pupils to the sit–stand desk intervention. As this was a pilot trial, the primary analyses mainly utilised descriptive statistics. The number of schools approached, the number agreeing to participate, the proportion of children within each school with parental consent to participate in the study evaluation, the number of children completing the study protocol, retention rates and the number providing valid outcome measurement data at baseline and follow-up are described in Chapter 3. Study acceptability data are presented for the sample as a whole and stratified according to study arm (intervention and control) and ethnicity (South Asian and white British).
Although the main aim of this study was to establish acceptability, feasibility, recruitment rates and sample size to inform a definitive trial, and although effectiveness was unlikely to be established with the small sample size, we examined the proposed primary and secondary outcomes for a definitive trial to mimic practice in such a trial. The results from this analysis should, however, be treated as preliminary and interpreted with caution. 109,110 As the number of clusters is low, cluster summary statistics were used rather than multilevel modelling. 111,112 The analyses were conducted using children as the unit of analysis, with change in average total school day sitting time as the primary outcome. A weighted linear regression model was used to compare the intervention arms weighted by the number of participants followed up in each cluster, and adjusted for baseline total daily sitting time on school days and average weekday wear time when awake across the two time points (baseline and 7 months). To examine preliminary effects of the intervention on the secondary outcomes, the same analytical approach was adopted as for the proposed primary outcome (objective 10). These analyses were intended to provide preliminary evidence of the effectiveness of the intervention to, in part, inform the decision of whether or not a definitive trial should be undertaken.
Sensitivity analyses were performed on the proposed primary outcome for a full trial of average weekday sitting time. This was achieved by including pupils who wore the activPAL (with a minimum valid wear time of 8 hours/day) for at least 2, 3 and 4 weekdays, at baseline and follow-up.
An objective of this pilot study was to estimate the SD of the primary outcome to inform a full trial. The intraclass correlation coefficient (ICC) to inform the sample size calculation of a definitive trial was estimated from published literature. The ICC was not estimated from this pilot study because multilevel modelling was considered to be an unsuitable analysis method for the present study, due to the small number of clusters, and an ICC estimate from such a model would not be sufficiently robust to inform a sample size calculation for a definitive trial.
Data management and research governance
Anonymised data were entered into a secure and validated clinical data management system provided by the Leicester Clinical Trials Unit; this database (InferMed Macro v4; Elsevier Ltd, Oxford, UK) included a series of quality control mechanisms to ensure that the data collected were complete and accurate. The study was sponsored by Loughborough University and two groups were created to oversee the research: an independent TSC and a Project Committee. As the study was regarded as low risk, the TSC took on the role of a Data Monitoring Committee, with the intention of reviewing any serious adverse events, should they have arisen, and monitored progress with data collection. The TSC met every 6 months and included the PIs (Stacy A Clemes and Sally E Barber), an independent chairperson, two independent external members (including a statistician) and two school representatives (public members who were teachers from schools separate to those participating in the trial). The Project Committee comprised the PIs, all co-investigators and those concerned with the day-to-day running of the study, and provided update reports for the TSC.
Chapter 3 Results
This chapter presents the quantitative findings from the Stand Out in Class pilot study. This study was primarily designed to address issues surrounding school and participant recruitment, acceptability of the measurement tools and intervention, and school and participant attrition rates and compliance with the measurement tools to inform a future definitive trial. Although the study was not powered to provide information on a treatment effect, preliminary estimates of the effect of the intervention are reported herein to further aid the design of a definitive trial. This chapter reports on the following study objectives:
-
Objective 1 – establish and refine a recruitment strategy for schools and pupils.
-
Objective 2 – determine attrition in the trial (schools and children).
-
Objective 3 – determine completion rates for outcome measures (and whether or not these are sufficiently high to provide accurate data in a full trial).
-
Objective 4 – assess whether or not there are any differences in trial recruitment, retention and acceptability between ethnic groups.
-
Objective 8 – monitor any adverse effects, such as musculoskeletal discomfort and/or disruption to the classroom/learning, to inform the design of a full trial and minimise or eliminate any such effects.
-
Objective 10 – derive preliminary estimates of the effect of the intervention on children’s total daily sitting time, physical activity, indicators of health (markers of adiposity and blood pressure), cognitive function, and academic performance, engagement and behaviour.
-
Objective 11 – estimate the SD of the primary outcome to inform a sample size calculation for a full RCT.
Objective 1: school and participant recruitment
A total of 24 eligible schools were approached for recruitment into this pilot study. Of these 24 schools, the study target number of eight schools consented to take part in the study, with the overall recruitment rate being 33% [95% confidence interval (CI) 0.16% to 0.55%]. Twelve out of the 24 schools did not consent to enter the study (50%) and four out of the 24 schools approached did not respond to the initial e-mail (17%). The characteristics of the participating schools are described in Table 2.
| Trial arm (school number) | Location | Percentage of pupils | |||
|---|---|---|---|---|---|
| Eligible for free school meals | Classified as white British ethnic origin | Classified as South Asian ethnic origin | Whose first language is not English | ||
| Control (1) | Bradford South | 16.9 | 63.2 | 17.5 | 16.3 |
| Control (2) | Bradford West | 21.2 | 10.8 | 76.3 | 69.5 |
| Control (3) | Bradford East | 23.8 | 30.8 | 54.9 | 57.1 |
| Control (4) | Bradford East | 13.1 | 1.1 | 88.3 | 88.6 |
| Intervention (1) | Bradford East | 26.4 | 11.1 | 51 | 74.3 |
| Intervention (2) | Bradford East | 18.2 | 0.6 | 91.8 | 92 |
| Intervention (3) | Bradford South | 14.9 | 89 | 2.8 | 3.9 |
| Intervention (4) | Shipley | 2.3 | 83.5 | 5.6 | 9.1 |
Data from the 2016–17 school census113 show that the proportion of children eligible for free school meals was similar across the recruited schools and declined schools [mean 17.1% (range 2.3–26.4%) vs. mean 17.4% (range 9.6–28.5%), respectively] for the 2016/17 academic year and across the previous 6 years [mean 31.1% (range 6.4–52.4%) vs. mean 29.6% (range 17.4–48.2%), respectively]. There was, however, a difference between the proportion of children whose first language was not English between the recruited and declined schools [mean 51.4% (range 3.9–92%) vs. mean 38.4% (range 0–93.5%), respectively], with eight of the 12 declined schools predominantly containing white British children.
Overall, the proportion of pupils at the eight schools with parental consent to participate in the trial evaluation was 75% (176/234), exceeding the target minimum sample size of 120 participants (see Chapter 2, Sample size).
Objective 2: determine attrition in the trial (schools and children)
All eight participating schools completed the trial; the overall school retention rate was therefore 100%.
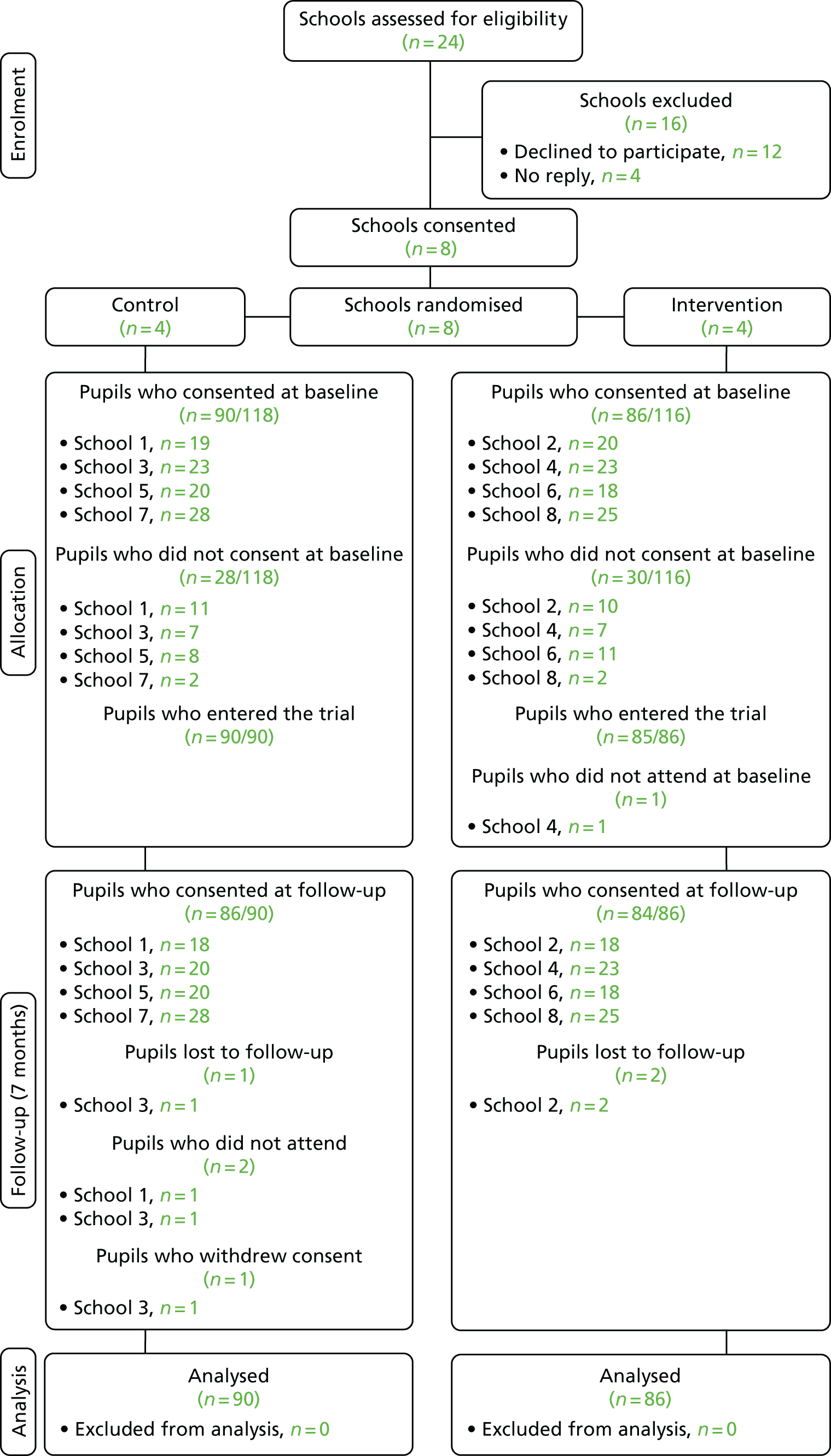
At 7 months’ follow-up, the overall retention of participating children was 97% (170/176). The retention rate of children in the control group was 96% (86/90) and the retention rate of the intervention group was 98% (84/86). A CONSORT flow diagram for the study is shown in Figure 3. Two participants in the control group (2.2%) did not attend the follow-up measures because they were absent from school during the days in which these measures took place. Three participants [one control (1.1%), two intervention (2.3%)] moved away from the area during the study and hence changed schools. One participant in the control group (1.1%) withdrew their assent prior to the follow-up measures. The demographic characteristics of the participating children are shown in Table 3.
FIGURE 3.
A CONSORT flow diagram for the Stand Out in Class pilot RCT. Reproduced with permission from Clemes et al. 81 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
| Demographic characteristic | Trial arm | Overall (N = 176) | |
|---|---|---|---|
| Control (N = 90) | Intervention (N = 86) | ||
| Sex, n (%) | |||
| Male | 50 (55.6) | 48 (55.8) | 98 (55.7) |
| Female | 44 (44.4) | 38 (44.2) | 78 (44.3) |
| Ethnicity, n (%) | |||
| White British | 18 (20.0) | 45 (52.3) | 63 (35.8) |
| South Asian | 59 (65.6) | 26 (30.2) | 85 (48.3) |
| Other | 13 (14.4) | 15 (17.4) | 28 (15.9) |
| Age (years), mean (SD) | 9.3 (0.5) | 9.3 (0.4) | 9.3 (0.5) |
Objective 3: determine completion rates for outcome measures
Overall completion rates for the outcome measures at 7 months’ follow-up (including participants who provided valid data at both baseline and follow-up) were as follows:
-
≥ 63% for activPAL data (proposed primary outcome in a definitive trial)
-
≥ 83% for ActiGraph data
-
≥ 94% for anthropometric measures
-
≥ 69% for blood pressure
-
≥ 89% for cognitive function
-
≥ 97% for the child-reported Body Comfort Survey
-
≥ 97% for the Engagement Versus Disaffection with Learning Questionnaire
-
≥ 91% for teacher-reported Strengths and Difficulties Questionnaire data.
Objective 4: assess whether or not there are any differences in trial recruitment, retention and acceptability between ethnic groups
Table 24 in Appendix 2 displays the recruitment and retention rates for the whole sample and according to ethnic group. Ninety-eight per cent of both white British children and South Asian children provided parental consent and written assent to participate within the trial evaluation. Similarly, 98% of white British children and South Asian children completed the trial. The impact of ethnic group on acceptability of the trial overall is discussed in Chapter 5 as part of the full process evaluation, alongside discussion of objectives 5–7.
Objective 8: monitor any adverse effects, such as musculoskeletal discomfort and/or disruption to the classroom/learning, to inform the design of a full trial and minimise or eliminate any such effects
There were no serious adverse events or adverse events reported throughout the duration of the trial. Specifically, there were no reported adverse effects associated with the intervention that related to musculoskeletal discomfort and/or disruption to the classroom or to learning. Teachers’ and children’s perceptions and experiences of the intervention are discussed in detail in the process evaluation described in Chapter 5. Descriptive statistics summarising preliminary evidence of the impact of the intervention on musculoskeletal comfort, classroom behaviour, engagement with learning and markers of attainment are presented under objective 10 (objective 9, the assessment of intervention fidelity, is also covered in Chapter 5).
Objective 10: derive preliminary estimates of the effect of the intervention on children’s total daily sitting time, physical activity, indicators of health (markers of adiposity and blood pressure), cognitive function, and academic performance, engagement and behaviour
Primary outcome for a subsequent definitive trial
The proposed primary outcome for a future definitive trial is change in mean daily sitting time on weekdays (school days). Mean daily sitting time on weekdays was chosen, given that the intervention was school based. Sitting time measured across the whole school day/weekday was proposed, as this measure encompasses school hours and out-of-school hours and factors in any compensatory effects of the intervention, should any beneficial effects of the intervention experienced during school hours be cancelled out by an increase in sitting after school, for example. Table 4 displays the descriptive statistics for all activPAL variables recorded throughout waking hours on weekdays for the control and intervention groups.
| Waking hours on weekdays | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 57) | Intervention (n = 52) | Control (n = 58) | Intervention (n = 52) | Control (n = 57) | Intervention (n = 52) | |
| Wear time (minutes/day) | 836.3 (88.5) | 843.8 (47.8) | 830.9 (78.6) | 835.4 (64.2) | –3.7 (121.6) | –8.4 (62.3) |
| Time spent sitting (minutes/day) | 520.1 (83.6) | 514 (61.5) | 504.4 (94.0) | 472.0 (73.5) | –15.2 (107.5) | –42.0 (76.6) |
| Time spent standing (minutes/day) | 179.9 (58.6) | 195.4 (38.7) | 176.5 (45.7) | 197.1 (49.4) | –3.0 (50.2) | 1.6 (52.0) |
| Time spent stepping (minutes/day) | 136.3 (44.9) | 134.4 (30.4) | 150.0 (42.1) | 166.4 (41.9) | 14.4 (44.8) | 32.0 (41.1) |
| Percentage of wear time spent sitting | 62.4 (8.8) | 60.9 (5.9) | 60.5 (8.6) | 56.5 (8.2) | –2.0 (8.7) | –4.3 (8.6) |
| Percentage of wear time spent standing | 21.4 (6.3) | 23.2 (4.5) | 21.5 (6.1) | 23.6 (5.7) | 0.1 (5.9) | 0.4 (5.8) |
| Percentage of wear time spent stepping | 16.2 (4.7) | 15.9 (3.5) | 18.1 (4.8) | 19.9 (4.6) | 1.9 (4.6) | 3.9 (4.6) |
| Number of sit to stand transitions | 102.5 (28.7) | 106.4 (23.6) | 104.1 (26.5) | 106.2 (21.4) | 1.6 (25.0) | 0.2 (20.5) |
| Number of days worn | 3.7 (1.3) | 3.5 (0.9) | 3.2 (1.2) | 3.5 (1.4) | –0.5 (1.4) | 0.0 (1.8) |
A weighted linear regression model was calculated to compare the primary outcome for the subsequent definitive trial (change in average weekday sitting time between baseline and 7 months’ follow-up) between pupils in the control group and those in the intervention group. The model was weighted by the number of participants followed up in each cluster (sum of weight = 110 observations). The model was adjusted for baseline average weekday sitting time for each cluster and for average weekday wear time when awake across the two time points (baseline and 7 months). Owing to the exploratory nature of the trial, the results are presented as weighted mean differences with 95% CIs. As the variables in the regression model reflect cluster means rather than individual observations, analytically weighted least squares was the method of estimation used, in which cluster sizes were the weights.
The model revealed that children in the intervention group spent less time sitting than children in the control group. The mean difference (weighted by school size) in change in sitting time (in minutes) adjusted as described above was –30.6 minutes per day (95% CI –56.42 to –4.83 minutes per day).
The addition of baseline season of activPAL data collection to the weighted linear regression model did not affect the difference in sitting time between groups. When follow-up season was included in the model, the adjusted difference in sitting time between groups was –26.64 minutes per day (95% CI –73.08 to 19.79 minutes per day).
Sensitivity analyses of the proposed primary outcome in a definitive trial
Owing to the exploratory nature of this pilot study, participants were included in the preliminary analyses presented in Primary outcome for a subsequent definitive trial if they wore the activPAL for a minimum of 8 hours on at least 1 weekday. To assess whether or not the number of valid days of activPAL wear had an effect on the estimates (to inform wear time criteria in a definitive trial), the preliminary primary outcome analysis described in Primary outcome for a subsequent definitive trial was rerun to include only those participants with specific days of valid activPAL data. These results are presented in Table 5. Similar differences to those described in Primary outcome for a subsequent definitive trial between groups were observed for participants providing at least 2 and 3 valid days of wear; however, these differences appear to be attenuated when considering only participants with at least 4 valid days of activPAL data.
| Days of valid data | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control | Intervention | Control | Intervention | Control | Intervention | |
| At least 1 weekday (control, n = 58; intervention, n = 52) | 520.1 (83.6) | 514 (61.5) | 504.4 (94.0) | 472.0 (73.5) | –15.2 (107.5) | –42.0 (76.6) |
| Intervention vs. control weighted mean difference –30.6 minutes/day (95% CI –56.42 to –4.83 minutes/day) | ||||||
| At least 2 weekdays (control, n = 47; intervention, n = 41) | 522.8 (79.3) | 513.3 (57.5) | 507.1 (92.6) | 471.7 (76.9) | –15.7 (98.1) | –41.6 (71.2) |
| Intervention vs. control weighted mean difference –23.96 minutes/day (95% CI –67.47 to 19.54 minutes/day) | ||||||
| At least 3 weekdays (control, n = 34; intervention, n = 34) | 508.6 (78.9) | 513.9 (58.9) | 511.2 (74.3) | 480.2 (77.7) | 2.5 (80.2) | –33.6 (70.5) |
| Intervention vs. control weighted mean difference –29.17 minutes/day (95% CI –85.57 to 27.24 minutes/day) | ||||||
| At least 4 weekdays (control, n = 26; intervention, n = 19) | 493.0 (73.8) | 525.5 (52.1) | 508.8 (73.3) | 509.4 (63.5) | 15.8 (82.2) | –16.0 (70.7) |
| Intervention vs. control weighted mean difference –6.71 minutes/day (95% CI –77.48 to 64.06 minutes/day) | ||||||
Secondary outcomes for a subsequent definitive trial
activPAL accelerometer secondary outcomes
Table 6 displays the descriptive statistics for activPAL-determined time spent sitting, standing and stepping during school class time for the control and intervention groups. The change in time spent sitting during class time was the main secondary activPAL outcome of interest. On average, control participants experienced an increase in class time sitting at 7 months’ follow-up, whereas a reduction in class time sitting was observed in the intervention group (see Table 6).
| Class time | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 57) | Intervention (n = 52) | Control (n = 58) | Intervention (n = 52) | Control (n = 57) | Intervention (n = 52) | |
| Wear time (minutes/day) | 278.7 (58.1) | 274.5 (48.3) | 291.8 (42.0) | 290.0 (19.0) | 13.4 (67.0) | 11.8 (61.3) |
| Time spent sitting (minutes/day) | 180.2 (47.7) | 188.3 (40.4) | 206.4 (48.3) | 176.4 (41.2) | 25.7 (59.0) | –14.5 (56.6) |
| Time spent standing (minutes/day) | 64.5 (34.0) | 59.2 (21.5) | 56.3 (22.1) | 72.3 (28.6) | –7.8 (28.9) | 12.5 (31.5) |
| Time spent stepping (minutes/day) | 34.0 (15.5) | 27.0 (10.1) | 29.1 (10.7) | 41.4 (17.0) | –4.5 (13.8) | 13.8 (17.2) |
| Percentage of wear time spent sitting | 65.5 (13.2) | 68.8 (9.0) | 70.1 (11.4) | 60.8 (13.5) | 4.4 (12.4) | –7.7 (13.2) |
| Percentage of wear time spent standing | 22.5 (10.4) | 21.4 (6.8) | 19.7 (8.8) | 25.0 (10.0) | –2.7 (9.5) | 3.3 (9.9) |
| Percentage of wear time spent stepping | 12.0 (4.7) | 9.7 (3.2) | 10.1 (4.5) | 14.3 (5.9) | –1.7 (5.3) | 4.4 (5.9) |
In addition, participants in the intervention group experienced an increase in standing and stepping time during class time at follow-up, whereas reductions in these behaviours were observed at follow-up in the control group (see Table 6).
Table 7 displays the descriptive statistics for activPAL-determined time spent sitting, standing and stepping measured after school for the control and intervention groups. On average, both groups experienced reductions in sitting and increases in standing and stepping after school at the 7-month follow-up, suggesting no compensatory effects of the intervention (such as increases in sitting outside of school) in the intervention group.
| After school | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 56) | Intervention (n = 52) | Control (n = 57) | Intervention (n = 52) | Control (n = 56) | Intervention (n = 52) | |
| Wear time (minutes/day) | 381.6 (63.2) | 363.0 (60.4) | 376.0 (84.7) | 367.6 (72.8) | –0.3 (88.0) | 6.8 (59.6) |
| Time spent sedentary (minutes/day) | 258.9 (49.9) | 239.9 (49.9) | 221.8 (76.0) | 217.2 (56.2) | –33.9 (75.2) | –19.6 (59.2) |
| Time spent standing (minutes/day) | 68.6 (25.5) | 72.6 (22.1) | 77.1 (30.6) | 76.0 (28.4) | 9.5 (32.0) | 3.6 (29.6) |
| Time spent stepping (minutes/day) | 54.1 (28.8) | 50.6 (18.5) | 77.1 (37.2) | 74.4 (32.6) | 24.1 (39.7) | 22.8 (31.2) |
| Percentage of wear time spent sedentary | 68.2 (9.3) | 66.0 (7.0) | 58.5 (13.8) | 59.3 (10.7) | –9.6 (14.0) | –6.4 (12.5) |
| Percentage of wear time spent standing | 17.8 (5.6) | 20.0 (5.4) | 20.9 (7.4) | 20.6 (5.8) | 2.9 (7.4) | 0.5 (6.8) |
| Percentage of wear time spent stepping | 14.0 (5.9) | 13.9 (4.5) | 20.7 (8.8) | 20.1 (6.9) | 6.7 (8.6) | 5.9 (7.2) |
Table 25 in Appendix 2 summarises the descriptive statistics for all activPAL variables recorded throughout waking hours across all monitoring days, including both weekdays and weekend days. The trends observed in this table match those reported in Table 4, which summarise the mean daily activPAL variables calculated across weekdays only.
ActiGraph accelerometer secondary outcomes
Table 8 displays the descriptive statistics for all ActiGraph variables recorded throughout waking hours on weekdays for the control and intervention groups. Both groups demonstrated similar reductions in ActiGraph-determined sedentary time and small changes in light-intensity physical activity and moderate- to vigorous-intensity physical activity (MVPA) over the follow-up period.
| Waking hours on weekdays | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 74) | Intervention (n = 72) | Control (n = 74) | Intervention (n = 72) | Control (n = 74) | Intervention (n = 72) | |
| Wear time (minutes/day) | 885.1 (90.5) | 882.6 (84.5) | 827.7 (134.1) | 852.9 (106.8) | –57.4 (125.9) | –29.7 (118.0) |
| Time spent sedentary (minutes/day) | 466.9 (87.3) | 461.8 (75.6) | 422.7 (97.3) | 414.5 (77.9) | –44.2 (74.6) | –47.3 (74.7) |
| Time spent in light physical activity (minutes/day) | 378.2 (61.9) | 383.5 (68.6) | 364.3 (81.2) | 392.7 (70.8) | –13.9 (74.4) | 9.3 (78.3) |
| Time spent in MVPA (minutes/day) | 40.0 (20.5) | 37.4 (17.9) | 40.7 (30.9) | 45.7 (24.7) | 0.7 (24.5) | 8.3 (20.0) |
| Percentage of wear time spent sedentary | 52.6 (7.4) | 52.4 (7.1) | 51.0 (8.6) | 48.6 (7.0) | –1.6 (6.1) | –3.7 (6.2) |
| Percentage of wear time spent in light physical activity | 43 (6.4) | 43.4 (6.2) | 44.0 (6.9) | 46.0 (6.0) | 1.1 (5.5) | 2.6 (5.6) |
| Percentage of wear time spent in MVPA (%) | 4.6 (2.3) | 4.3 (2.1) | 5.0 (3.8) | 5.4 (2.7) | 0.5 (2.8) | 1.1 (2.2) |
| Number of days worn | 3.8 (1.4) | 3.6 (1.3) | 2.8 (1.5) | 3.2 (1.6) | –1.0 (1.3) | –0.4 (1.3) |
Table 9 displays the descriptive statistics for the ActiGraph variables measured during class time and Table 10 displays the same variables measured after school. Children in the control group reduced their ActiGraph-determined sedentary time during the after-school period, whereas the intervention group children reduced their sedentary time both during class time and after school. Children in the intervention group exhibited increases in time in light-intensity physical activity and MVPA during class time and small increases in these behaviours after school, whereas participants from the control group exhibited increases in these behaviours after school only at follow-up.
| Class time | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 74) | Intervention (n = 72) | Control (n = 74) | Intervention (n = 72) | Control (n = 74) | Intervention (n= 72) | |
| Wear time (minutes/day) | 307.0 (8.6) | 288.3 (13.8) | 308.4 (12.2) | 283.0 (27.2) | 1.4 (15.3) | –5.4 (26.9) |
| Time spent sedentary (minutes/day) | 181.5 (32.4) | 170.8 (33.6) | 183.9 (31.6) | 153.2 (33.3) | 2.4 (29.6) | –17.6 (28.3) |
| Time spent in light physical activity (minutes/day) | 116.9 (27.9) | 112.6 (29.7) | 118.3 (29.7) | 123.8 (32.0) | 1.4 (23.7) | 10.3 (37.5) |
| Time spent in MVPA (minutes/day) | 8.6 (6.0) | 4.9 (3.8) | 6.2 (7.4) | 6.9 (5.0) | –2.4 (8.7) | 2.0 (4.7) |
| Percentage of wear time spent sedentary | 59.0 (10.0) | 59.2 (10.9) | 59.7 (10.4) | 54.5 (13.1) | 0.7 (8.7) | –4.7 (12.7) |
| Percentage of wear time spent in light physical activity | 38.1 (9.3) | 39.1 (10.5) | 38.3 (9.2) | 43.6 (10.9) | 0.1 (7.9) | 3.8 (12.4) |
| Percentage of wear time spent in MVPA | 2.8 (2.0) | 1.7 (1.3) | 2.0 (2.3) | 2.5 (1.8) | –0.8 (2.8) | 0.8 (1.7) |
| After school | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 74) | Intervention (n = 72) | Control (n = 74) | Intervention (n = 72) | Control (n = 74) | Intervention (n = 72) | |
| Wear time (minutes/day) | 389.6 (67.3) | 379.1 (57.9) | 358.8 (107.1) | 362.7 (92.0) | –30.8 (105.8) | –16.4 (99.7) |
| Time spent sedentary (minutes/day) | 195.6 (51.4) | 194.1 (44.9) | 155.9 (65.9) | 169.8 (54.2) | –39.8 (60.9) | –24.3 (57.9) |
| Time spent in light physical activity (minutes/day) | 178.6 (41.9) | 169.8 (39.4) | 179.4 (65.7) | 169.0 (52.5) | 0.8 (66.9) | –0.7 (57.8) |
| Time spent in MVPA (minutes/day) | 15.3 (10.4) | 15.2 (8.8) | 23.5 (22.2) | 23.8 (17.5) | 8.2 (19.5) | 8.6 (17.1) |
| Percentage of wear time spent sedentary | 50.0 (9.5) | 51.2 (8.6) | 43.3 (12.7) | 46.2 (10.9) | –6.6 (11.5) | –5.0 (11.2) |
| Percentage of wear time spent in light physical activity | 46.0 (8.4) | 44.8 (7.6) | 49.8 (10.3) | 46.5 (7.4) | 3.8 (10.2) | 1.7 (8.0) |
| Percentage of wear time spent in MVPA | 4.0 (2.8) | 4.1 (2.4) | 6.9 (5.8) | 7.3 (6.9) | 2.8 (4.7) | 3.2 (6.9) |
Health markers (adiposity and blood pressure)
Table 11 displays the descriptive statistics for the anthropometric and blood pressure measurements taken from participants at baseline and follow-up. The changes seen in the anthropometric measurements over the follow-up period are reflective of typical growth-related changes in children of this age.
| Measure | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 90) | Intervention (n = 84) | Control (n = 85) | Intervention (n = 83) | Control(n = 85) | Intervention (n = 81) | |
| Height (cm) | 140.5 (6.6) | 138.3 (6.2) | 144.0 (6.8) | 141.3 (6.4) | 3.3 (1.7) | 2.9 (1.0) |
| Body mass (kg) | 36.3 (9.5) | 35.0 (7.8) | 39.2 (10.6) | 37.7 (8.7) | 3.0 (1.7) | 2.7 (1.7) |
| Per cent body fat: girls (control, n = 40; intervention, n = 35) | 24.4 (8.4) | 23.6 (8.1) | 23.7 (9.1) | 25.0 (8.3) | –0.7 (2.1) | 0.5 (2.8) |
| Per cent body fat: boys (control, n = 50; intervention, n = 49) | 20.6 (8.9) | 19.9 (6.9) | 20.7 (8.9) | 19.0 (6.6) | 0.4 (2.6) | –0.9 (2.4) |
| Fat mass (kg) | 8.8 (5.6) | 8.0 (4.5) | 9.4 (6.2) | 8.9 (5.4) | 0.7 (1.8) | 0.7 (2.1) |
| BMI (kg/m2) | 18.2 (4.0) | 18.2 (3.3) | 18.7 (4.1) | 18.8 (3.5) | 0.6 (0.8) | 0.6 (0.7) |
| Systolic blood pressure (mmHg)a | 102.5 (11.8) | 102.8 (15.2) | 107.3 (11.7) | 110.5 (11.2) | 5.1 (15.8) | 10.2 (17.8) |
| Diastolic blood pressure (mmHg)a | 66.1 (10.2) | 67.3 (14.1) | 66.3 (9.5) | 68.4 (9.7) | 0.2 (12.1) | 2.4 (16.2) |
Cognitive function
Cognitive function was assessed using three separate tests: the Stroop test, the Corsi block-tapping test and the RVIP test. The outcomes derived from these measures are summarised in Table 12. Overall improvements in the performance on most test components were observed in both groups over the follow-up period, probably due to a learning effect of these tests.
| Measure | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control | Intervention | Control | Intervention | Control | Intervention | |
| Stroop test: reaction times – basic level (milliseconds) | 1275.4 (404.6) | 1315.5 (533.4) | 1202.6 (320.0) | 1175.1 (259.5) | –56.1 (408.6) | –126.7 (519.1) |
| Stroop test: reaction times – complex level (milliseconds) | 1733.2 (520.9) | 1733.1 (448.6) | 1586.9 (726.8) | 1612.2 (387.2) | –207.2 (540.5) | –115.5 (384.0) |
| Corsi block-tapping test: mean sequence length (n) | 4.2 (1.1) | 4.1 (1.0) | 4.5 (1.0) | 4.5 (1.1) | 0.3 (1.1) | 0.3 (1.0) |
| RVIP: reaction time (milliseconds) | 648.7 (139.7) | 652.1 (123.1) | 652.2 (121.6) | 650.5 (96.8) | 5.7 (170.9) | –6.2 (148.2) |
| RVIP: accuracy (range 0–1) | 0.20 (0.15) | 0.25 (0.17) | 0.30 (0.20) | 0.31 (0.19) | 0.1 (0.2) | 0.1 (0.2) |
| RVIP: alertness (range 0–1) | 0.53 (0.22) | 0.56 (0.17) | 0.59 (0.17) | 0.59 (0.15) | 0.1 (0.2) | 0.0 (0.2) |
Musculoskeletal comfort
Table 13 presents results from the child-reported Body Comfort Survey (summarised scales), which shows the proportion of pupils who feel good at their desks. At the 7-month follow-up, there was an increase in the proportion of pupils from both groups who reported that they felt better at their desk.
| Body area | Time point, n (%) | |||
|---|---|---|---|---|
| Baseline | Follow-up | |||
| Control (N = 88) | Intervention (N = 83) | Control (N = 86) | Intervention (N = 83) | |
| Neck | 65 (73.9) | 59 (71.1) | 68 (79.1) | 72 (86.8) |
| Arm | 69 (79.3)a | 60 (72.3) | 76 (88.4) | 79 (95.2) |
| Back | 59 (67.8)a | 54 (65.1) | 63 (73.3) | 63 (75.9) |
| Wrists | 70 (79.6) | 57 (69.5)b | 78 (90.7) | 74 (89.2) |
| Hip | 72 (82.8)a | 63 (77.8)b | 78 (90.7) | 72 (86.8) |
| Leg | 67 (77.0)a | 59 (72.0)b | 72 (83.7) | 69 (83.1) |
| Ankle | 74 (84.1) | 63 (75.9) | 74 (86.1) | 72 (86.8) |
Classroom disruption and pupil behaviour
Pupil behaviour, conduct in the classroom and interactions with fellow pupils were examined using the teacher-reported Strengths and Difficulties Questionnaire. Descriptive statistics for this measure for the control and intervention groups at baseline and follow-up, along with the changes in ratings, are summarised in Table 14. The lower the score in each subscale, and the lower the total score, the better the behaviour. The intervention group generally had reduced antisocial and hyperactive behaviours and increased self-control compared with the control group at follow-up.
| Strengths and Difficulties Questionnaire subscale item and total scores | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 83) | Intervention (n = 78) | Control (n = 83) | Intervention (n = 84) | Control (n = 81) | Intervention (n = 78) | |
| Emotional symptoms | 0.9 (1.7) | 2.1 (2.5) | 1.4 (2.2) | 1.9 (2.3) | 0.4 (1.9) | –0.1 (1.9) |
| Conduct problems | 0.7 (1.3) | 1.3 (2.0) | 1.0 (1.8) | 0.8 (1.5) | 0.3 (1.6) | –0.5 (1.5) |
| Hyperactivity | 3.3 (3.2) | 4.2 (3.2) | 3.0 (3.0) | 3.5 (3.1) | –0.3 (2.3) | –0.6 (2.0) |
| Peer relationships problem | 1.3 (1.5) | 1.7 (2.0) | 1.5 (1.6) | 1.6 (1.9) | 0.1 (1.4) | –0.1 (1.6) |
| Prosocial behaviours | 7.4 (2.8) | 7.6 (2.6) | 7.1 (2.6) | 7.9 (2.0) | –0.2 (2.2) | 0.4 (1.9) |
| Internalising factors (emotional + peer) | 2.2 (2.8) | 3.8 (4.0) | 2.8 (3.3) | 3.5 (3.6) | 0.5 (2.6) | –0.2 (2.8) |
| Externalising factors (conduct + hyperactivity) | 4.0 (4.1) | 5.4 (4.8) | 4.1 (4.4) | 4.3 (4.2) | 0.0 (3.2) | –1.1 (2.6) |
| Total difficulties score | 6.2 (5.7) | 9.2 (7.6) | 6.9 (6.0) | 7.8 (6.6) | 0.6 (4.6) | –1.3 (4.5) |
Engagement and disaffection with learning
Participants self-reported their engagement and disaffection with their own learning using the Engagement Versus Disaffection with Learning Questionnaire. Table 15 summarises the scores for each subscale of this measurement tool at baseline and at follow-up, along with the changes in scores calculated over the follow-up period. There were no noticeable between-group differences in the mean change in any subscale score over the trial period.
| Scale | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control (n = 90) | Intervention (n = 82) | Control (n = 86) | Intervention (n = 83) | Control (n = 86) | Intervention (n = 80) | |
| Behavioural engagement | 3.4 (0.6) | 3.4 (0.5) | 3.3 (0.6) | 3.3 (0.5) | 0.0 (0.7) | –0.1 (0.5) |
| Emotional engagement | 3.4 (0.6) | 3.4 (0.6) | 3.3 (0.6) | 3.3 (0.6) | –0.1 (0.6) | –0.1 (0.6) |
| Overall engagement | 3.4 (0.5) | 3.4 (0.5) | 3.3 (0.6) | 3.3 (0.5) | –0.1 (0.6) | –0.1 (0.5) |
| Behavioural disaffection | 3.0 (0.8) | 3.1 (0.7) | 3.2 (0.8) | 3.1 (0.7) | 0.2 (0.9) | 0.0 (0.8) |
| Emotional disaffection | 3.3 (0.7) | 3.2 (0.8) | 3.2 (0.7) | 3.2 (0.7) | 0.0 (0.8) | 0.0 (0.6) |
| Overall disaffection | 3.1 (0.7) | 3.1 (0.7) | 3.2 (0.7) | 3.1 (0.6) | 0.1 (0.7) | 0.0 (0.6) |
Academic progress and attainment
An overview of the results for school performance per class is shown in Appendix 2, Table 26. Table 16 shows the combined data from which the comparisons were made. There were no differences between change in expectation level for maths and writing between the control and intervention groups. However, fewer participants in the intervention group (n = 4) than in the control group (n = 16) experienced a decrease in reading expectation.
| Change | Class, n (%) | |||||
|---|---|---|---|---|---|---|
| Maths | Reading | Writing | ||||
| Control (N = 90) | Intervention (N = 84) | Control (N = 90) | Intervention (N = 84) | Control (N = 90) | Intervention (N = 84) | |
| Decreased | 4 (4.4) | 3 (3.6) | 16 (17.7) | 4 (4.8) | 10 (11.1) | 4 (4.8) |
| No change | 80 (88.9) | 70 (83.3) | 66 (73.3) | 66 (78.6) | 73 (81.1) | 73 (86.9) |
| Increased | 6 (6.7) | 11 (13.1) | 8 (8.9) | 14 (16.7) | 7 (7.8) | 7 (8.3) |
Objective 11: estimate the standard deviation of the primary outcome to inform a sample size calculation for a full randomised controlled trial
Optimum reductions in daily sitting time that lead to health benefits have not yet been established in children. Current UK guidelines for children simply state that ‘all children and young people should minimise the amount of time spent being sedentary (sitting) for extended periods’. 23 Recent data in adults have shown that reallocating 30 minutes of sedentary time per day to light movement is associated with a 2–4% improvement in cardiometabolic biomarkers. 114 In the absence of current information on optimum reductions of sedentary time for health benefits in children, we are guided by the evidence above from adult studies.
The likely primary outcome in a definitive trial would be change in average daily (school day) sitting time, measured by the activPAL (or ActiGraph worn on the thigh, following feasibility testing), after 10 months. The study would be powered to detect a difference of 30 minutes per day between the intervention arm and the control arm. The primary analysis would be performed using linear multilevel models. 115
Under the following assumptions, a sample size of 924 participants (462 participants/arm) from 42 clusters (21 clusters/arm) would be needed for this definitive trial to have 90% power to detect a change in mean total daily (school day) sitting time of 30 minutes per day at the 5% significance level (two tailed):
-
SD of 95 (observed in our pilot study), which equates to a standardised difference of 0.316 (postulated true difference ÷ SD)116
-
average cluster size of 22 (observed in this pilot study)
-
conservative ICC of 0.05 (owing to the lack of previous data to inform this, we have followed recommendations by Campbell et al. 117)
-
coefficient of variation to allow for variation in cluster sizes of 0.11 (based on cluster sizes in this pilot, average of 22 and a range of 18–28).
Inflating the sample size by 25% to allow for potential individual loss to follow-up and non-compliance with the primary outcome (informed by the present study and recent school-based cluster RCTs118,119), and inflating the number of clusters per arm by 1 to allow for whole-cluster dropout, the study would require a sample size of 1276 participants from 58 clusters in total (638 participants and 29 clusters/arm).
Summary
The following chapters present the results relating to other aspects of this pilot trial. The preliminary economic evaluation is presented in Chapter 4 and the process evaluation is described in Chapter 5. A discussion of the overall findings, lessons learnt from this pilot trial and recommendations for further research are presented in Chapter 6.
Chapter 4 Economic evaluation
Introduction
This chapter presents an exploratory economic assessment of the cluster-randomised Stand Out in Class pilot study, addressing objective 12. The health economic evaluation of the Stand Out in Class study represents a particularly valuable contribution to sedentary behaviour research. During a scoping review, we found few intervention studies that explicitly considered the magnitude of the potential health effect of observed changes in sedentary behaviour. Fewer still examined any potential resulting change in cost of health-care resource use.
Given interest in this area as a potential public health intervention, and tightly constrained budgets across the health and education sectors, it is important to maintain an explicit consideration of cost-effectiveness in future work of this nature. Health economic models in this area are underdeveloped and would benefit from refinement to closer reflect the current evidence base of health effects of physical (in)activity. This would enable better representation of the potential health opportunity cost of investments to reduce sedentary behaviour rather than other possible public health investments. 120
Introduction to methods
The economic analysis is split into two main sections:
-
A within-trial analysis of health and education resource use, and summary measures of health and education effects, collected at baseline and at the end of the trial follow-up period. This is presented as a cost–consequence analysis.
-
An extrapolated trial analysis modelling the cost and quality-of-life impact over the long term. This is presented as an indicative cost–utility analysis. An expected value of perfect information (EVPI) analysis is also presented.
Value of information analysis presents an upper estimate of the monetary value of further research into resolving all decision uncertainty of the cost-effectiveness of the current ‘Stand Out in Class’ intervention at varying thresholds, given the changes in physical activity and sedentary behaviour observed in the pilot study. EVPI estimates capture the value of both further research into the effectiveness of this intervention at reducing sedentary time, and the associated health effect of any change in physical activity and/or reduction in sedentary time.
All analyses are presented from a health system and Personal Social Services perspective. A limited range of education outcomes are, however, included in the within-trial analysis. Within-trial analysis presents a cost–consequence analysis of reported health and education outcomes over the trial time horizon (4 months). It was not possible to conduct a cost–utility analysis for within-trial health outcomes. Although the EQ-5D-Y106 and PEDS-QL105 were both collected at baseline and at follow-up, to date these outcome measures have no valuation tariff for valuing surveyed health states into quality-adjusted life-years (QALYs). All self-report measures used to inform these analyses are described in detail in Chapter 2. The education outcomes collected are also limited, as ‘education resource use’ and ‘strengths and difficulties’ questionnaires lack external validity in predicting relevant educational attainment outcomes, such as the outcome of national curriculum assessments.
Extrapolated trial analysis aims to identify the magnitude of potential causal links between changes in sedentary time and/or physical activity observed, and long-term health outcomes. Public health interest in this trial area is driven by the expectation that reducing the level of sedentary behaviour in a cohort of children is important for ongoing health outcomes, including consideration of a residual health effect beyond the scope of the intervention itself.
General methods
Data sources
Impact of intervention
Within-trial analysis utilised three key data sources: (1) health-care resource use was measured by parent-reported survey, which detailed use of a range of common health services over the previous 3 months; (2) health-related quality of life was measured by the EQ-5D-Y (including visual analogue score) and PEDS-QL; and (3) an educational resource use and educational outcome questionnaire relating to pupils’ behaviour (Strengths and Difficulties Questionnaire102) was completed for each pupil by teacher-reported survey. Baseline measurements were taken in January/February 2017 and post-intervention assessments were completed in July 2017.
Parent reports of health-care contacts were combined with closest matching unit costs. Reference costs for non-hospital care were obtained from the latest Personal Social Services Research Unit (PSSRU) report121 in which resource costs for identical or most similar items were available. Hospital-related incidents were costed using the 2016 NHS schedule of reference costs. 122 Data sources for each health-care resource use item are presented online in Report Supplementary Material 2. When relevant, costs were inflated to 2016 pounds using the health and social care factor (Hospital and Community Health Service) reported in PSSRU 2016.
Extrapolated trial analysis utilised the results of surveyed levels of physical activity in the intervention and control groups, measured by the ActiGraph accelerometer. Although the Stand Out in Class study primarily targeted classroom sitting time, there is currently very limited evidence available for the effect of classroom sitting time and other sedentary behaviours on health costs and health-related quality of life, both of which are necessary for health economic modelling (see Scoping review). Physical activity levels (referred to as ‘activity’ throughout this chapter) were therefore measured in METs,123 when health economic evidence was available. The difference in measured activity between the intervention and control groups was calculated and used in long-term disease incidence modelling. Changes in disease incidence resulted in changes in projected health-related costs and quality of life, which informed long-term cost-effectiveness estimates.
Education outcomes are also presented in the economic within-trial analysis. There was insufficient trial reporting on relevant standardised education outcomes to inform detailed evaluation. Although 9- to 10-year-olds in England follow a standardised curriculum, progress tests are not uniform between schools, or even necessarily valid for time point comparisons within schools. The main education outcome considered was therefore the change in reported behavioural difficulties on a teacher-reported Strengths and Difficulties Questionnaire. A cognitive function test was performed; however, individual results were not recorded in the case report form.
Intervention costs
The trial protocol allowed for six desks in each intervention school, allocated between a total class size of 30 children. In each intervention school, access to standing desks was granted to the full class, whether children were enrolled in the trial or not. As class sizes were at full capacity of 30 pupils in all but one school (n = 27), exposure to the intervention was approximately equal if the trial protocol was followed in each school.
In the intervention arm, standing desks were assumed to be an upfront cost split between the current full cohort of 30 pupils and nine future full cohorts of 30 pupils. These future cohorts represent future beneficiaries of the capital assets over an expected 10-year lifespan. Manufacturer correspondence (Carrie Schmitz, Ergotron Inc., 2018, personal communication) advised the best available price for the desks provided in-kind to the trial (Ergotron LearnFit) was £379 per unit, with no discount available on the trial cohort of 24 desks.
The intervention cost, per school, of six standing desks used in the trial was therefore costed as £2274. No financing arrangements were assumed, nor any setup, future service or maintenance costs to the intervention schools, with the manufacturer-supplied 10-year warranty assumed to be comprehensive and costless at point of claim. These assumptions were deemed appropriate for the relatively small number of desks provided to each school; however, any financing cost and opportunity cost of time and labour, for example, to set up standing desks on a greater scale, such as across a full school, would need to be accounted for in a larger intervention.
The intervention cost per pupil over 10 years for a full class size of 30 pupils was calculated to be £7.58. This assumes no opportunity cost of upfront capital investment (e.g. lost bank interest on cash over the 9 additional cohort years). The assumption of no opportunity cost of capital over 10 years would require re-examination for a larger-scale intervention. In the control arm, no environmental changes were made and, thus, no desk-related costs were assumed to be accrued over the course of the trial.
Missing data
Missing data are a concern in cost-effectiveness analysis because costs or health outcomes in individuals with missing data may be systematically different from those with fully observed information. Inappropriate missing data strategies have the potential to bias resource allocation decisions. 124 We followed a recent presentation framework in setting out our missing data strategy below (see Missing data strategy). 125
Description of missing data
Patterns of missingness in data sources used in economic within-trial analysis are detailed online in Report Supplementary Material 2. Participant responses were regarded as ‘complete’ if all items were completed unambiguously. ‘Incomplete’ responses included both partially complete and fully incomplete responses. When responses indicated a range of values, the mean was used. Remaining ambiguous entries were removed and treated as null entries.
The missing data mechanism was primarily participant non-response, meaning that all resource items were incomplete (e.g. due to failure to return a completed survey). Only six respondents were completely lost to follow-up, with no response to any outcome measure (four in the control arm and two in the intervention arm). There was also a small amount of item non-response for individual questions within otherwise complete outcome measures, particularly for the parent-reported health-care resource use. Missing data are non-monotone, with only 33 of 176 (18.8%) respondents having complete data in outcomes of interest in all six survey categories (four outcome measurements, two resource use measurements) at baseline and at follow-up. Thirty-three per cent of respondents had missing data in only one outcome at one of the two collection time points.
Missing data patterns indicated some variation in missingness by trial group, with 23.3% of respondents having no missing data for all main outcome variables in the intervention arm, compared with 14.4% of respondents in the control arm. There was also some indication of variation in missingness patterns by ethnicity, with 54.46% of non-white respondents having missing data in main outcomes for up to only one time point, compared with 48% of white respondents. Missing data were most frequent in the parent-reported health-care resource use survey (44.3%, aggregated across time points) and least frequent in education resource use (0%) and EQ-5D-Y profiles (5.4%, aggregated time points).
For health-care resource use, missingness at baseline appeared a strong predictor of missingness at follow-up (p = 0.01); however, there was strong clustering of missingness at the school level. Accounting for clustering reduced the significance of the null hypothesis of no association between time points (p = 0.11). There was also quite strong evidence for association of missingness between time points in the activity data (p = 0.04) (measured using the ActiGraph), although there was also clustering of completeness at the school level. Accounting for clustering, there was some evidence for rejecting the null hypothesis of no association in missingness in activity levels between time points (p = 0.12). In other outcome categories, there was no evidence of association in missingness between time points.
There was no evidence of association of missingness between outcome types. In the outcome categories with the most missing data, health-care resource use and accelerometer-measured activity, there was only very weak evidence to reject the null hypothesis of no association (p = 0.81 and p = 0.79 adjusted for clustering).
Missing data strategy
Our missing data strategy consisted of two analyses:
-
a multiply imputed analysis, using multiply imputed data sets generated by predictive mean matching from nearest neighbours
-
a complete-case analysis, including only participants with complete responses in each survey type at baseline and follow-up.
Missing data were multiply imputed assuming missingness at random in the base case, with results compared with the complete-case analysis (reported online in Report Supplementary Material 2). Sensitivity to the assumption of missingness at random was not otherwise investigated and testing robustness of conclusions to plausible departures from the ‘missingness at random’ assumption should form a part of future work. Conditional on the observed data, the probability of cost-effectiveness data being missing may still depend on the underlying unobserved values (i.e. data may be ‘missing not at random’). 126 The missing data strategy makes no distinction between within-trial and extrapolated trial outcomes. All relevant outcomes were combined into one data set, allowing utilisation of complete outcomes to inform other, incomplete outcomes.
Multiple imputation methods
Missing data were multiply imputed by chained equations using the mi impute command in Stata® 15 (StataCorp LP, College Station, TX, USA). Nearest neighbour matching with replacement using the 10 nearest neighbours was used to help protect against misspecification of regression equations. 127 Fifty multiply imputed data sets were generated to minimise Monte Carlo error, approximately matching the percentage of missing data in the outcome with the most missing data (health-care resource use). 128 Each imputation had a burn-in of 50 estimates to help the imputation model achieve stable estimates.
In estimating health-care resource use, it was not possible to multiply impute health-care items individually, due to non-convergence. For this reason, resource use was categorised into four broad types: (1) primary care, (2) hospital, (3) mental health and (4) community care. Categorisation of individual resource use items into broad categories is presented in Table 17. Resource use was imputed on a cost scale, after prior calculation of costs from individual items, as there was large variation between costs of individual types of resource use within item categories. Imputing directly on the cost of resource use was therefore more likely to reflect uncertainty in resource cost in each category, rather than trying to later recreate cost outcomes from the predicted number of appointments in each category.
| Costs | |||
|---|---|---|---|
| Primary care | Hospital | Psychological | Community care |
| GP surgery visit: £27.00 | Accident and emergency visit: £137.74 | Psychiatrist appointment: £236.44 | Health visitor home visit: £40.91 |
| GP home visit: £103.94 | Hospital outpatient appointment: £116.92 | Psychologist appointment: £144.70 | District nurse home visit: £26.54 |
| GP telephone call: £14.40 | Inpatient stays:a £389.10/day | Other counsellor/therapist appointment: £59.96 | Social worker office visit: £49.50 |
| GP nurse surgery visit: £12.58 | Mental health nurse appointment: £62.24 | Social worker home visit: £59.40 | |
| GP nurse home visit: £14.37 | |||
| GP nurse telephone call: £6.10 | |||
| Other doctor’s appointment: £39.18 | |||
Multiple imputation estimates were conducted simultaneously by chained equations and included intervention group, school number, as well as participants’ age, sex and ethnicity (16 possible categories) as covariates. A random seed was specified to aid replicability of analysis, with the imputation trace saved to perform post-imputation diagnostics to establish convergence performance. Anthropometric measurements regarded as potential predictors of outcome variables were included in chained equations. These included BMI, fat mass and average blood pressure measurements at baseline and at follow-up.
Multiple imputation used a single-level linear model with no interactions, accounting for clustering at the school level only, using an indicator variable, rather than using multilevel modelling as advised best practice. 129 Single-level (fixed-effect) modelling accounts for some between-cluster variation, explained by cluster-level predictors; however, it is unlikely to explain all between-cluster heterogeneity. Multilevel (random-effects) imputation was not conducted owing to perceived difficulty in implementation, given the small numbers of individuals in each cluster, particularly within the time constraints of the research. Small numbers within each cluster also prevented model fitting of a single-level sensitivity analysis – in imputing data separately for each cluster, which would allow the distributions of imputed values to differ among clusters. Comparable single-level imputation models would not converge using the standard maximum likelihood approach. 130 Future work that investigates the sensitivity of our conclusions to a multilevel imputation strategy would be a valuable contribution to understanding the intervention effect studied in this trial.
The total cost of health-care resource use across all categories and activity values aggregated to a simulated year (accounting for school holidays) were registered as passive outcomes and reconstructed post imputation from imputation estimates of non-aggregated values. EuroQol-5 Dimensions (EQ-5D) responses were imputed, as other variables using predictive mean matching, at the index level. It was not possible to conduct imputation on individual dimensions using ordered logit or probit regression, nor EQ-5D tariff-valued scores, as per best practice. 131 As a result, individual dimensions were reconstructed from the imputed index for each imputation.
Post-imputation estimation
Post-imputation estimation was performed using the Stata command mi estimate to implement Rubin’s rules, adjusting for clustering at the school level. 132 This method was used for all outcome variables, apart from the EQ-5D. The clustering method ‘vce (cluster)’ assumes that observations are independent across groups (in this case, at the school level), but not necessarily within groups. Observations were not clustered by observations across time points within individuals. The mi estimate command also accounts for between-imputation uncertainty in estimation of standard errors and, thus, presents wider Cls than standard analysis, which assumes that the value for each observation is certain.
However, reconstructed EQ-5D dimension scores across 50 imputations were combined using their mode value for each individual. This approach therefore does not fully represent the degree of uncertainty introduced by variation between imputations. However, this method was judged the best approach to ensure eradication of nonsense non-integer values introduced by post-imputation estimation commands and also judged most appropriate for the recommended method of presentation of non-tariff-valued EQ-5D profiles. 133
Within-trial analysis
Methods
Cost–consequence analysis
Costs and consequences across health and education sectors are presented in the intervention and control groups at follow-up. It was not possible to conduct a full cost–utility analysis on data collected in health, as youth tariffs to convert health profiles to QALY weightings are not currently available. 133 Best practice indicates not to use adult weightings to value children’s health state measures. 134 In education, there is currently no known available cost-effectiveness framework outside cost–consequence analysis.
Base-case analysis
All base-case analysis was performed on multiply imputed data sets. A complete-case analysis is presented in scenario analysis, reported online in Report Supplementary Material 2. We compiled simple unadjusted aggregate outcomes for health-related costs and consequences in health and education. We utilised an intervention cost, as set out in Data sources, Intervention costs, of £7.58 per child. A comparison of outcomes at baseline and follow-up is presented. As previously mentioned, no valuation tariffs were available for calculation of QALYs in the trial groups and, for this reason, no incremental cost-effectiveness ratios (ICERs) could be calculated. We did not conduct any regression analysis of within-trial outcomes, nor attempt to stratify results by predefined subgroups, such as ethnicity.
Health-care resource use
The number of health-care contacts by type are presented from the results of complete-case analysis. This is inconsistent with presentation of other within-trial results. Imputation methods used did not directly estimate the number of health-care contacts in patients with missing data. The number of patients with complete data in all categories are presented in each group. Each inpatient day was classified as a separate health-care event. Estimated health-care costs during the survey period were calculated for all patients from reported usage. Mean patient costs in four health categories are presented at baseline and at follow-up for the intervention and control groups.
Education resource use
Education resource use by teacher-reported survey is reported at each time point. Education outcomes are not monetised.
Health outcomes
The EQ-5D-Y and PEDS-QL health profiles are presented at baseline and at follow-up. The percentage of pupils in each EQ-5D health state is reported. PEDS-QL mean scores in each dimension are reported. Presentation of PEDS-QL scoring follows the survey provider’s guidance. 135 PEDS-QL scores are scaled 0–100, with 0 being worst and 100 being best (therefore higher scores represent better health-related quality of life). Valuation of health outcomes into QALYs from EQ-5D-Y profiles was not possible as there were no valid available preference-based tariffs. 134 Use of a mapping algorithm for PEDS-QL was considered; however, mapping methodology relied on stable population preference-based valuation of EQ-5D-Y tariff. 136
Education outcomes
Strengths and Difficulties Questionnaire scores were categorised into four bands, as recommended by the survey developer. 137 The percentage of pupils in each category is reported at baseline and at follow-up, with ‘normal’ representing the best categorisation and ‘very high’ representing children with the most difficulties.
Results
Table 17 summarises resource use categorisation and corresponding reference costs, per resource use, collected from PSSRU121 and NHS Reference Costs 2015–16. 122 For survey items for which a recent reference cost had not been calculated, a close comparator was used for costing. This was applicable for only one resource item, where the survey item ‘other counsellor/therapist’ was assumed to be comparable to the cost of a GP counsellor. Estimating the cost of some other resource items required further assumptions, such as resource items requiring home visits, which involved assumption of the amount and cost of travel time. Assumptions, when made, were kept consistent between closely comparable resource items. Full details of the assumptions for each item are presented in Report Supplementary Material 2 alongside their source.
Recent reference costs were readily available for survey items with the highest reported use, such as GP surgery visits. In less frequently utilised services, costs were less readily available in the literature. For this reason, given relatively low reported use, the impact of assumptions to approximate health-care resource costs in categories where these costs were not directly available is expected to be minimal. Inpatient stays were costed as an average of hospital costs per day, rather than by individual Healthcare Resource Group coding for any procedure named in complete cases. This was expected to limit unexplainable variation in imputed hospital costs due to different Healthcare Resource Group costs of conditions treated in each arm by inpatient stay recorded in complete cases.
Costs are presented in 2016 Great British pounds. When cost estimates were gathered from historical sources, they were inflated to 2016 prices using the Hospital and Community Health Service Index reported by the PSSRU. 121 Total resource costs and outcomes in health and education are presented in Table 18.
| Resource use | Time point | |||
|---|---|---|---|---|
| Baseline | Follow-up | |||
| Control | Intervention | Control | Intervention | |
| Health resource use | ||||
| Total health-care resource use, n | N = 46 | N = 54 | N = 43 | N = 53 |
| Primary care | 20.5 | 47 | 18.5 | 21 |
| Hospital care | 8 | 9 | 9 | 17 |
| Psychological care | 2 | 2 | 15 | 0 |
| Community care | 0 | 1 | 3 | 0 |
| Health-care resource use (mean cost) (£) | N = 90 | N = 86 | N = 90 | N = 86 |
| Primary care | 15.17 | 20.51 | 9.91 | 9.53 |
| Hospital care | 34.73 | 17.79 | 31.39 | 88.57 |
| Psychological care | 6.95 | 5.02 | 11.29 | 16.73 |
| Community care | 1.56 | 0.55 | 2.02 | 1.46 |
| Mean cost (all categories) | 58.42 | 43.88 | 54.62 | 116.29 |
| Intervention cost | 7.58 | |||
| Mean cost (per patient) | 58.42 | 43.88 | 54.62 | 123.87 |
| Education resource use | N = 90 | N = 86 | N = 90 | N = 86 |
| Total education resource use, % | ||||
| Pupils receiving additional tutoring | 1 | 12 | 9 | 12 |
| Disciplinary events | 3 | 13 | 8 | 13 |
| Pupils receiving learning support | 8 | 13 | 7 | 13 |
| Health outcome | N = 90 | N = 86 | N = 90 | N = 86 |
| EQ-5D-Y dimension, % | ||||
| Mobility | ||||
| No problems | 89 | 91 | 83 | 83 |
| Some problems | 9 | 9 | 16 | 16 |
| A lot of problems | 2 | 0 | 1 | 1 |
| Looking after myself | ||||
| No problems | 97 | 9 | 96 | 92 |
| Some problems | 2 | 6 | 4 | 8 |
| A lot of problems | 1 | 0 | 0 | 0 |
| Doing usual activities | ||||
| No problems | 80 | 90 | 84 | 84 |
| Some problems | 19 | 9 | 14 | 16 |
| A lot of problems | 1 | 1 | 1 | 0 |
| Having pain or discomfort | ||||
| No problems | 64 | 60 | 53 | 59 |
| Some problems | 30 | 36 | 44 | 38 |
| A lot of problems | 6 | 3 | 2 | 2 |
| Feeling worried, sad or unhappy | ||||
| Not worried, sad . . . | 78 | 70 | 77 | 73 |
| A bit worried, sad . . . | 22 | 28 | 23 | 27 |
| Very worried, sad . . . | 0 | 2 | 0 | 0 |
| PEDS-QL mean scores (higher score = better health-related quality of life) | ||||
| Physical function | 71.30 | 69.52 | 67.78 | 68.27 |
| Emotional function | 81.34 | 73.79 | 78.52 | 76.19 |
| Social function | 82.37 | 79.33 | 80.92 | 79.75 |
| School function | 79.51 | 72.01 | 72.53 | 69.93 |
| Education outcomes | N = 90 | N = 86 | N = 90 | N = 86 |
| SDQ profiles (‘very high’ = most measured difficulties), % | ||||
| Normal | 81 | 69 | 81 | 76 |
| Slightly raised | 9 | 16 | 12 | 1 |
| High | 7 | 6 | 3 | 6 |
| Very high | 3 | 9 | 3 | 7 |
The number of health-care contacts in complete cases in each trial arm appears to vary. This is largely driven by a small number of high-use patients. In the control arm at follow-up, 11 of 15 instances of ‘psychological care’ are for one pupil who reported weekly counselling appointments. Similarly, in the intervention arm at follow-up, 15 of 17 ‘hospital care’ contacts were for a pupil who received surgery for a burst appendix and therefore required an extended inpatient stay.
In the full base-case cohort, mean costs of hospital care in the intervention arm appear large; however, this was, in part, driven by the previously described surgery for one pupil, costed at £5836.50. Overall, there appears to be little interpretable difference in estimated health-care costs in the prior 3 months between trial arms. The mean cost of the intervention per pupil was comparatively small, and if costed over the same 3-month time horizon, rather than a full year, the mean cost of the intervention during the trial period reduces from £7.58 to £1.90 per pupil.
Education resource use across all categories appears slightly higher in the intervention group than in the control group at follow-up. However, when baseline patterns of resource use are considered, the level of education resource use in the intervention arm appears stable between the two time points, whereas resource use increases in the control arm between summer and winter. Education outcomes collected are, however, difficult to interpret. For example, interpretation of an increase in pupils receiving additional tutoring in the control arm between time points is highly context dependent. This could be due to a change in teaching style within the school, or by revision of expectations by parents. Again, there appears to be little interpretable evidence of divergence in resource use between the intervention and control arms during the trial period that could be attributed to the intervention.
Comparing EQ-5D-Y profiles at follow-up suggests that health outcomes also diverge little between groups. The largest difference was a 6% difference in report of pupils experiencing some pain and discomfort, with a higher number reporting ‘no problems’ in the intervention arm. This corresponds roughly to a difference of five pupils. There were, however, 4% more pupils reporting some anxiety in the intervention arm than in the control arm and a similar 4% increase in reported problems in self-care in the same group.
When assessing EQ-5D-Y profiles between the two time points, a more significant trend emerges of changes in the characteristics of reported health profiles between baseline and follow-up. In both trial arms, the percentage of pupils reporting ‘no difficulties’ in mobility, self-care and pain/discomfort decreases between baseline and follow-up, meaning a higher number of pupils report at least some difficulties in these dimensions. Both trial arms report an increase in mobility problems between baseline and follow-up, a change of 6% in the control arm and 8% in the intervention arm.
The EQ-5D-Y profiles reveal some further divergence between trial arms. Although in the control arm there is an 11% increase in the number of pupils reporting at least some pain, in the intervention arm there is an increase in reported pain of only 1% between time points. In the ‘usual activities’ dimension, there is a 4% increase in reported problems in the intervention group between time points, whereas there is a simultaneous 4% decline in reported problems in the control arm. Reported anxiety simultaneously increases by 3% in the intervention arm, but declines by 1% in the control arm.
The PEDS-QL dimensions follow a similar pattern to EQ-5D-Y outcomes. Health profiles are comparable at follow-up; however, observed differences between groups in health profiles at baseline mean that pupils in the two trial groups have experienced some difference in trends between time points. Both groups report a decline in ‘school function’ between time points, with a 6.98-point decline in the control arm and a 2.08-point decline in the intervention arm. ‘Emotional function’ decreases by 2.82 points in the control arm, but improves by 2.4 points in the intervention arm. There is greater similarity in trends in other dimensions, with both trial arms reporting a decline in physical function between time points (slightly larger in the control group), and small changes in social function showing a slight decrease in the control arm compared with a slight improvement in the intervention arm.
Comparing education outcomes at follow-up, teacher-reported Strengths and Difficulties Questionnaires reveal a greater number of more severe reported difficulties in the intervention arm than in the control arm. There is a 5% difference in reported difficulties, which are distributed among the two highest categorisations of pupil difficulties. When accounting for baseline values, however, an improvement in strengths and difficulties profiles is apparent in both arms, with a much stronger difference observed in the intervention arm. In the intervention group, there is a 7% improvement in the number of pupils categorised within normal ranges by teachers. There is an apparent improvement in reducing reports of both higher- and lower-severity difficulties. In the control arm, there is a 3% improvement in aggregated difficulties profiles. This is due to fewer pupils being classified as ‘high’ difficulty; however, there is a corresponding increase in the number of pupils with difficulties profiles still classified outside a ‘normal’ range. The results of complete-case analysis are presented in scenario analysis (see Report Supplementary Material 2).
Discussion
Main findings
Within-trial analysis reveals no substantial difference in outcomes between trial arms. Suggestive patterns in some outcomes do not appear to sum to a coherent picture across all outcomes describing any clear distinction between trial groups. Overinterpretation of small numbers is a significant risk, with this study underpowered to detect differences in outcomes with a high level of sampling variability.
There is some evidence of differences between the trial arms in health and education outcomes, but less evidence of differences in estimated resource use. Difference in trend was most apparent in PEDS-QL scores and in ‘strengths and difficulties’ profiles, in which there was some evidence to suggest a slight improvement in measured outcomes between time points in the intervention arm compared with the control arm. However, little is known about the sensitivity or external validity of these measures to influence a judgement of the relative importance of sample-measured improvement on these outcomes.
There was no clear difference in EQ-5D-Y profiles between groups. There were changes in reported anxiety and levels of pain and discomfort between time points, which could be interpreted to favour the trend in the intervention arm; however, the balance of other outcomes appears to either favour the control arm or show no difference in the aggregated health profile. It is especially difficult to interpret the relevance of any change in the population-aggregated EQ-5D-Y profile without a valuation tariff to provide generalisation to a measure of average health-related quality of life in each group by an aggregate quality-of-life measure, such as the QALY. Without valuation, it is not easy to establish the relative weight to attribute to any improvement in one domain compared with relative declines in another area. Changes in an individual’s measured health-related quality of life depend on reported values for that individual across all dimensions, rather than one dimension alone; thus, it is particularly difficult to interpret any obvious trend in individual health outcomes from a population-aggregated EQ-5D-Y health profile.
In health-care resource use, although survey-reported estimates suggest a higher cost of total resource use in the intervention arm than in the control arm, this is largely attributable to a single high-cost participant for an apparently unrelated inpatient stay. All cost categories show a high degree of variation, with a potential problem in attribution to the intervention. Any change in health-care resource use resulting from the Stand Out in Class intervention is likely to follow a meandering causal pathway, probably over a long period, and therefore will require a much larger sample size to measure and attribute any difference between trial arms at an appropriate degree of accuracy.
No obvious pattern emerges from the within-trial pilot survey outcomes. Sampling variability was heightened by differential patterns of outcome completeness in health-care resource use between clustered sites. In education resource use, it is similarly difficult to interpret changes in resource use not only due to previously mentioned difficulty in interpretation of the outcomes collected, but also due to little understanding of the sensitivity, stability across time points and external validity of outcomes collected. A larger trial powered to detect significant difference may resolve parameter uncertainty; however, thought should also be given to ensure that outcomes collected in any future trial have a ready, intuitive interpretation.
Impact of scenario analysis
Complete-case analysis reveals a similar picture to the base case, with the largest divergence from the multiply imputed base case in outcomes with highest levels of incompleteness. This meant that although health and education outcomes and education resource use were broadly similar, there was some observed difference in the estimated mean cost of health-care resource use in the complete-case analysis. Complete-case analysis suggested a higher mean cost of health-care resource use in both arms, suggesting some difference in patterns of missing resource information accounted for in regression adjustment on observable characteristics in multiple imputation.
The difference in mean health-care resource use between scenarios was greatest at follow-up. Mean resource use was 9% higher, on average, in complete-case analysis than the multiply imputed base case. The difference was particularly large for the control arm at follow-up (complete-case health-care resource use mean costs were 14% higher) and for the intervention arm at baseline (complete-case health-care resource use mean costs were 11% higher than base-case estimates). For this reason, based on multiply imputed estimates, it appears that high-cost patient subgroups are over-represented in complete-case survey responses of health-care resource use, which is probably only partially corrected by imputation on observed characteristics in base-case analysis. Patterns of resource use in each arm hold roughly consistent proportions between scenarios, but with similarly little distinctive pattern in resource use in complete-case analysis across health cost categories.
Comparison with other studies
Limited randomised research has examined the impact of sedentary behaviour interventions aiming to create an active classroom in primary schools. 56,69 This study adds to existing literature by examining resource use outcomes, as well as a limited range of health and education outcomes. In particular, information regarding health-care resource use during observation periods has not been found in previous known studies of active learning interventions. The study shows that it is feasible to collect outcomes of interest for an economic evaluation. However, evidence gathered remains small scale and over a short time period. Our study does not demonstrate significant new information than previous studies, which have already demonstrated the feasibility of incorporating sit–stand desks into the primary school environment in the short term. 29,58,59
Our study conclusion of no measured difference in education resource use in the trial arm concurs with previous study results of no disruption caused by a sit–stand desk intervention to teaching, learning or behaviour. 29 Education outcomes collected could not, however, be used to corroborate previously gathered evidence of improved levels of academic engagement or achievement. 64,65 Economic analysis of surveyed health outcomes did show a slight improvement in trend in reported pain on EQ-5D-Y profiles, which could be interpreted to corroborate with previous study evidence demonstrating that sit–stand desks lead to improvements in posture and musculoskeletal comfort in children63,64 and adults. 138 However, the origins of reported changes in pain profiles were not analysed in economic analysis. Observed changes in aggregate health profiles were difficult to interpret, with little convincing evidence of differences between arms on EQ-5D-Y profiles; however, some limited evidence of improvement on PEDS-QL-measured quality-of-life scores were seen. Poor balance on baseline characteristics between arms is likely to have impaired our ability to estimate the treatment effect accurately for all outcomes collected in this pilot study.
Strengths and limitations
Health-care resource use surveys were incomplete for a significant proportion of trial participants. Efforts should be made in any future trial analysis to make parental surveys easier to complete, and incentives to encourage responses should be considered. In any future trial, reporting of health-care resource use could be streamlined to minimise reporting and recall bias (e.g. allowing parents to record health-care incidents in real time using a trial-specific application or website). This would also allow closer analysis of the effect of clustering of health-care resource use by school, recording the exact timing of resource use.
It was not possible to calculate QALYs based on the quality-of-life surveys used. Although it is perhaps unlikely that quality-of-life difference would be observed during the short period of within-trial analysis, it is hoped that future work may be able to utilise forthcoming valuations of EQ-5D-Y measures to collate individual health profiles. Difference in average health-related quality of life may be observed over a longer time period, if possible, to calculate individual-level standardised quality-of-life values.
Educational outcomes utilisable as intermediate outcomes for extrapolation to final end points, such as national examination attainment, were absent from trial data collection. Education resource use and Strengths and Difficulties Questionnaires lack significant external validity for measures of interest to policy-makers in education. In consultation with head teachers and teachers/assessment co-ordinators via PPI, further consideration should be given to measuring academic progress to identify appropriate national curriculum-related or standard assessments used by schools, which will enable direct comparison between participating schools in a future trial. In the absence of consensus over such measures, proxies of academic progress, such as attendance and/or in-class behaviour data, which can be measured consistently across schools, should be identified in collaboration with head teachers and teachers. Future analysis should also consider how best to cost limited education resource use items collected.
Some residual imbalance between intervention and control groups, despite randomisation, may have biased the trial results presented, as there is some evidence of differences in key observable characteristics between trial arms at baseline. Outside imbalances mentioned directly in economic analysis, we draw attention to differences between trial arms described in previous chapters. There is an observed difference in school-level averages of English as first language (44.85% intervention arm, 52.9% control arm), reflecting differential ethnic composition, and also a difference in number of pupils in receipt of free school meals (27.1% intervention arm, 35.1% control arm). Both differences are likely to reflect an underlying difference between arms in socioethnic strata and reflect differential barriers to children’s participation in society. Perhaps more crucially, there were also variations in intervention implementation as described in Chapter 5, with only one of four schools implementing the Stand Out in Class intervention as per trial protocol.
The effect of these differences was not investigated formally, nor accounted for in the economic analysis presented. Results presented should therefore be viewed in the context of heterogeneity in baseline characteristics, and type and magnitude of intervention exposure.
Scoping review
Aims and objectives
A scoping review was carried out to identify candidate economic models or comprehensive meta-analyses evaluating the effect of childhood sedentary behaviour on a range of long-term health outcomes. Sedentary behaviour can be defined as time spent sitting, lying or reclining accompanied by low levels of energy expenditure (1.0–1.5 METs). 1 Sedentary behaviours exist across various daily domains: in work, leisure and commuting. 33,139,140 Some distinctions between types of sedentary behaviour go further, categorising sedentary behaviours as discretionary (such as watching television or reading) and non-discretionary (such as sitting at school or during a commute). 141
Our primary research question was:
Are there existing economic or epidemiologic models that could be adapted for economic evaluation, which link childhood sedentary behaviour to expected short- and long-term health outcomes?
A secondary aim of our scoping review was to give an oversight of existing research into the link between sedentary behaviour and health outcomes to guide our methods of evaluation and highlight key issues in the field.
Our secondary research question was therefore:
What is known from the existing literature about the causal association between childhood sedentary behaviour and health outcomes?
In consultation with an information strategist, preliminary MEDLINE searches were carried out (see Search strategy). Only English-language publications were searched.
Search strategy
A comparison of initial search strategies is presented online in Report Supplementary Material 2. Search strategy 1 required article titles to contain ‘sedentary’ in the main title, whereas search strategy 2 allowed ‘sedentary lifestyle’ or variants to be contained in the main text of articles. Search strategy 1 identified 78 records, whereas strategy 2 identified 1540 records.
Abstracts from strategy 1 and a sample of 20 abstracts from strategy 2 were examined for relevance. Given the greater sample size of papers judged potentially relevant, search strategy 2 was selected, with the phrase ‘[review OR economic evaluation]’ added to the search terms to refine the search to more closely identify potential modelling studies. This search identified 208 papers, 182 of which were not duplicates.
All 182 abstracts were examined for relevance to the research question. Papers were examined in more detail if they were determined from the abstract to:
-
examine associations with a quantified health effect (e.g. BMI, cognitive development, depression)
-
consider a relevant population (i.e. aged < 16 years)
-
use an objective measure of physical activity and/or sedentary behaviour
-
include a study design that could indicate evidence of a causal association
-
be a meta-analysis or systematic review, containing evidence regarding more than one health effect, or outcomes relevant for an economic evaluation (e.g. quality of life).
Articles were ranked according to these criteria to prioritise articles for review. There were 12 articles fulfilling four criteria and seven articles fulfilling all five criteria (one was at protocol stage). Results of the scoping review are shown in Report Supplementary Material 2.
Our scoping search revealed studies of varying quality, mostly in high-income countries; however, it also found some evidence gathered in a variety of low- and middle-income settings. The 33 papers examined highlighted some key themes within the field and identified further relevant references. It was apparent that many studies have been undertaken to ascertain population trends and general correlates of sedentary behaviour, as well as testing the effectiveness of interventions aimed to reduce sedentary behaviour. In this field, there was a good range of evidence type, including studies with defined control groups, some with randomised components. Health effects of sedentary interventions were, however, less often studied.
When examining sedentary time, proxies were often used, such as reported television viewing time, rather than objective measurement. The lack of objective measurement and uniform scale, and method of assessment, of sedentary behaviour made comparisons between studies difficult due to levels of heterogeneity in exposure, often hindering the usefulness of reviews or meta-analyses. The type of sedentary behaviour studied is important, with the possibility of health effects from television viewing, for example, to be mediated by unhealthy dietary patterns less common in people who spend more time in other sedentary behaviours (such as reading or studying). 17,142 Comparatively few studies aimed to specifically track sedentary behaviours to short- or long-term health effects in children. In gathering evidence for short-term health effects, comparatively few analyses convincingly account for residual confounding of physical activity levels. Our search highlighted a wider range of evidence for the health effects of sedentary behaviours in adults; however, our assessment of this evidence was limited by our choice of search terms, which explicitly attempted to focus on a paediatric and adolescent population.
Studies that examined health effects of sedentary behaviours in children most often focused on a limited range of outcomes, most commonly around cardiometabolic or adiposity outcomes. Most frequently, short-term outcomes were observed, such as high-density lipoprotein cholesterol or BMI. The six reviews ranked most relevant (i.e. those scoring 5/5) focus primarily on these outcomes; however, they also report other major outcomes. 12,14,142–145 The reviews present a mixed evidence base, with the most relevant reviews suggesting a negative impact of higher sedentary behaviour on paediatric health outcomes, particularly from observational studies not controlling for physical activity levels. The evidence base is, however, inconclusive or shows no health effect of sedentary behaviour in a paediatric population for prospective study designs or when physical activity levels or diet are controlled for. 12,144,145 A full summary of evidence presented in the reviews considered is presented in Report Supplementary Material 2.
Narrative summary of studies considered
Carson et al. ,14 de Rezende et al. 142 and Tremblay et al. 13 focus on non-prospective sources, as well as intervention studies. Perhaps due to the greater number of non-prospective sources considered, the direction of evidence presented suggests an association between lower sedentary time, lower BMI and improved psychosocial outcomes. Tremblay et al. 13 provide a meta-analysis for adiposity outcomes; however, all above papers use a narrative review as their main vehicle of evidence synthesis. No review attempts to control for levels of physical activity, neither do they readily differentiate the conclusions of evidence gathered from objective measures of sedentary behaviour from other sources. Authors cite heterogeneity in exposure and methods of outcome measurement in underlying studies as a limitation to further quantitative synthesis. Nevertheless, Tremblay et al. 13 conclude that the limited RCT evidence examined, ‘coupled with the qualitative syntheses of data from the other study designs, provides consistent evidence of the inverse relationship between sedentary behaviour and health outcomes’.
Biddle et al. ,144 Cliff et al. 12 and van Ekris et al. 145 take a more sceptical view of the evidence available. These reviews focus primarily on prospective studies or those using objective measurement of sedentary behaviours. Cliff et al. 12 provide an estimate of the health impact of sedentary behaviours controlling for moderate to vigorous physical activity levels. Although Carson et al. 14 argue against this approach, due to potential for collinearity in physical activity levels and sedentary behaviour patterns in a regression framework, Cliff et al. 12 nevertheless utilise this approach. As Cliff et al.’s12 focus was on evidence gathered from experimental sources (often based on multicomponent physical activity interventions), Carson et al. ’s14 criticism is less applicable. Carson et al.’s14 criticism is most pertinent for evidence gathered from observational sources, where causality is more difficult to attribute; thus, adjusted regression approaches may eliminate the intervention effect.
Cliff et al. 12 conclude that ‘there is limited available evidence that volume or patterns of sedentary behaviour are associated with health and development in children and young people, particularly from studies with low [risk of bias] that adjust for MVPA’. 12 van Ekris et al. 145 give an evidence synthesis stratified by sedentary behaviour type to help account for heterogeneity in exposure type. This analysis presents a small, non-significant increase in adiposity (BMI) for each additional reported hour of television viewing or computer use. There was no evidence of effect on adiposity in studies using objective measurement of sedentary behaviour. Biddle et al. 144 also conclude that studies using objective accelerometer measurement yield null association between sedentary behaviour (measured by screen time) and adiposity, despite a small dose–response relationship observed from cross-sectional evidence. Biddle et al. 144 conclude that there is no evidence of a causal association between sedentary behaviour and adiposity in youth using Bradford Hill criteria.
Results
The summary of the evidence base of the health effects of sedentary behaviour in children was surprising to us. The evidence base for adverse effects of childhood sedentary behaviour on common health outcomes was expected to be stronger. All authors acknowledge limitations in the evidence base, citing the need for more long-term studies in this area, particularly with robust study designs. Nevertheless, the observed divergence from evidence gathered in adults, for whom there is currently stronger indication of adverse health effects of sedentary behaviours, may have plausible explanation. Some authors suggest that children accumulate their sedentary behaviour in a different way to adults. 146 Altenburg et al. 146 found the children studied to spend ‘most of their sedentary time in bouts of ≥ 5 minutes’ and ‘bouts of ≥ 20 minutes were rare’. Meanwhile, adult studies indicate that prolonged uninterrupted sitting is especially detrimental for cardiometabolic health. 147–149 van Ekris et al. 145 therefore hypothesise ‘that frequent interruptions in children’s sedentary time may prevent them from negative health consequences’. The underlying biology may be the same, but the behaviour was sufficiently different to prevent this being observed.
An alternative explanation may be borne out in the inadequacy of measurement methods to detect sedentary behaviours accurately. Much research uses non-objective measures, such as self- or proxy-reported questionnaires, with serious risk of bias. However, Carson et al. 14 equally note that ‘accelerometers may not be sensitive enough to capture patterns in sedentary time’, and propose future research using inclinometers, ‘which can more accurately capture postures . . . to better understand the health impacts of patterns of sedentary behaviour’. 14,150 The authors therefore believe that the use of accelerometers as the primary instrument of measuring sedentary behaviour objectively limits the potential to find evidence of a health effect. Nevertheless, evidence of the paediatric health effect of sedentary behaviours from inclinometer measures is currently unavailable and therefore cannot be considered in economic model building. Perhaps more notably, evidence of the health effects of sedentary behaviours gathered using any means from screen time studies are likely to be largely incomparable with the in-school evidence generated in this study, if the possible mediating effects of increased snacking while sedentary during screen time is considered a plausible confounding effect. It is not expected that this mediating pathway would be observed to a similar degree within the school environment.
Candidate models
The scoping search found no candidate economic models to assess the health impact of sedentary behaviour in children. This is not surprising, given the limited literature providing robust evidence of an association between sedentary behaviour and adverse health outcomes in children, independent of physical activity levels. Meta-analysis data gathered from the literature was too diverse to attempt to incorporate into a new economic model, given budget and time constraints imposed by the project. Outcomes, exposure types and dosing reported by meta-analysis were considered difficult to translate to a modelling approach that examined health outcomes suitable for economic evaluation. Meta-analyses that did report relevant information on exposure type and dosing generally reported intermediate biological end points as main outcomes, which also lacks sufficient linking evidence for a paediatric population to long-term health outcomes that could be used to understand potential health-related costs and quality of life. A project with greater research resources could undoubtedly make better use of existing evidence in attempting to create a simple economic model synthesising all existing evidence and aiding decision-makers’ understanding of key remaining research uncertainties.
The research team therefore decided to focus on evaluations conducted in the wider sport science literature. Communication with other health economists working in sport science evaluation revealed three candidate economic models, focusing on physical activity rather than sedentary behaviours. 151–154 This approach would provide indicative evidence of the potential health effects and economic value of the trial intervention in a related area in which more robust evidence was available and was, therefore, considered the best use of the quantitative evidence collected. This approach would also aid comparability with existing public health interventions valued with these tools, with the relative comparability of modelling assumptions. Similarly, this would best aid decision-makers by producing generalised outcomes measured in health-related costs and QALYs, which can be used for comparison between different programmes. 155 Nevertheless, patterns of sedentary behaviour are hypothesised to have a health effect independent from overall levels of physical activity, rather than being defined simply by the absence of physical activity. 9,156,157 These papers raise evidence in health outcomes of sedentary behaviours in adults (except Treuth et al. 156), from cardiometabolic disease and all-cause mortality, to a variety of physiological and psychological problems. The limitations of our approach in focusing solely on health effects arising from ‘physical activity’ are therefore recognised and could bias the results against the cost-effectiveness of the intervention, if the true health effects arising from sedentary behaviour are clinically significant.
All three models were Markov-type structured, with each model’s key features summarised in Report Supplementary Material 2. MOVES v.2 model was chosen primarily for its ability to be adapted to model individual-level health effects from person-specific activity values collected during the trial at baseline and at follow-up. Assumptions were more transparent and adaptable than other models considered, and therefore despite evidence being tailored to an adult population (aged > 16 years), this model was deemed most appropriate to make best use of the granularity of continuous individual-level activity data collected during the trial, without aggregation to a binary activity variable. Further detail of the mechanism of the MOVES model is provided in Introduction to MOVES model and also in the updated MOVES v.2 user guide. 151
Extrapolated trial analysis
Introduction
This section presents long-term modelling estimating changes in health-related quality of life and health costs arising from changes in physical activity levels observed in the Stand Out in Class trial over a 30-year time horizon.
Methods
Introduction to MOVES model
The MOVES model is designed to estimate the health-related quality-of-life and cost impact of a change in physical activity induced by a specific intervention. The tool uses epidemiological evidence to estimate the health impact of a change in physical activity on projected incidence of eight common health conditions over a chosen time horizon up to 30 years. The model focuses on the studied health effects of physical activity in adults aged ≥ 16 years, for whom the evidence base of a health effect is greatest.
The tool estimates the incidence of eight health conditions with and without a physical activity intervention to estimate the incremental cost and health-related quality-of-life effect of the intervention over a chosen time horizon. Increased physical activity is modelled to reduce the projected incidence of eight common health conditions for which a dose–response relationship has been rigorously studied. The projected number of incident and prevalent cases over the chosen time horizon are combined with disease-specific cost and quality-of-life sources gathered from the literature. This information is used to estimate the impact of projected changes in disease incidence due to physical activity on health service costs associated with treating and managing the considered health conditions.
Quality-of-life impact is similarly modelled, comparing quality-of-life outcomes in the two projections of disease prevalence with and without the physical activity intervention with age-adjusted general population values. Quality-of-life changes in the model arise directly from changes in the projected prevalence of health conditions and each condition’s associated severity. 158 Quality-of-life changes from incident conditions are modelled as absolute values rather than decrements to age-adjusted values. This means that it is possible that an incident health condition may increase health-related quality of life in the model. It was not possible to rectify this modelling issue in the scope of this work; however, this model deficit is most important for elderly populations who have a lower health-related quality of life, on average, than the young population considered in our analysis.
The magnitude of change in physical activity is modelled using METs, a physiological measure expressing the energy cost of the physical activity undertaken. This is a standard measure of physical activity used regularly in the sport science literature. 159,160 A reference value of 1 MET, for example, is considered the resting metabolic rate. 20 The measure has ratio properties, meaning that an activity of 2 METs can be considered double the energy expenditure than that of an average person at rest.
The MOVES tool models a diminishing health benefit of additional exercise for already active individuals. Similarly, the health decrement from decreasing activity levels from a high baseline activity will result in a smaller change in modelled health than for a less active individual. Thus, the model is less sensitive to changes in activity for highly active individuals than for relatively inactive individuals. This decrement was modelled with an adult population in mind; any change in this inflection for a child population was not considered in the scope of this research.
The model is parameterised using a value of ‘METs per week’, with and without intervention. In the base case, the baseline value was assumed to be the average activity level observed in the control arm at follow-up. The intervention effect was assumed to be the difference between the average activity level observed in the intervention arm and control arm at follow-up. This is reported as the ‘unadjusted’ analysis. We investigate the sensitivity of conclusions to an intervention effect controlling for difference in the activity levels observed in intervention and control arms at baseline. This is reported as the ‘adjusted’ analysis.
Activity levels were measured by the ActiGraph accelerometer in both trial arms (see Chapter 2). MET values were obtained directly from internal ActiGraph processing software (ActiLife) and averaged over a standardised waking wear time period (06.00 to 23.00, as determined by diary entries). Non-wear time was detected during the processing of the ActiGraph data and automatically removed.
Although METs are a standard tool in physical activity research, there is some limitation to their applicability in analysing interventions targeted at reducing sedentary behaviours. 154,161 A growing evidence base suggests an independent association between sedentary behaviours, such as prolonged sitting, and health outcomes, regardless of the levels of physical activity undertaken. Some evidence is suggestive of this health effect in conditions such as obesity, cardiovascular/metabolic markers and some cancers,162,163 leading to characterisations such as the ‘physically active couch potato’ or the ‘active non-couch potato’. 13,164
This highlights a weakness in our modelling approach. By focusing only on the average levels of activity at the two time periods, we do not analyse how that level of activity was achieved, the intensity of bursts of vigorous activity and the length of unbroken sedentary periods. For example, subject A and subject B may achieve the same average level of activity, with one engaging in short periods of high-intensity activity and another achieving a longer dose of lower-intensity activity. Evidence suggests that the distribution of activity may be important, with a hypothesised change in health risk if activity is regularly interspersed throughout the day, rather than achieving the same dose of physical activity in a single burst. 165 However, as above, our scoping review failed to discover any existing models suitable or adaptable for health economic evaluation that assessed the independent health effects of sedentary behaviour from physical activity (see Scoping review).
Model mechanism
MOVES models the projected change in disease incidence resulting from a change in physical activity for type 2 diabetes mellitus, breast cancer, colorectal cancer, coronary heart disease, cerebrovascular disease, dementia, depression and hip fracture. Modelled conditions were based on the UK Chief Medical Officers’ 2011 Department of Health and Social Care report Start Active, Stay Active, summarising the health conditions judged to have strong evidence of an association between physical activity and health, which could be modelled with a dose–response relationship. 23 Evidence has been presented of the impact of physical activity on up to 20 long-term conditions; however, evidence of a health impact on other conditions was not judged sufficiently robust by the Chief Medical Officers’ 2011 report. 23,166
Annual population incidence and treatment effect of physical activity were estimated by the model authors for the eight health conditions. Physical activity interventions are not assumed in the model to affect the number of already prevalent cases, only the incidence of future cases. Population incidence of disease rates are calculated for the general population (which therefore includes active and non-active participants), with incidence rates divided into five age categories, with categories split into 15-year periods until 60 years of age. The modelling approach assumes average population incidence of each disease condition to occur at population average rates of physical activity (adjusted for age group). The model gathers evidence for age-specific incidence from a global source, so performs a direct standardisation based on UK 2011 census data of UK population size in each age category for each sex. 167,168
Evidence for the treatment effect attributed by the model is based on two meta-analyses. 169,170 The source for each health condition is reported in the model user manual, alongside the model authors’ quality assessment of underlying studies. 151 Costs and quality-of-life effects from hip fracture were not considered relevant outcomes for our trial population, with no estimated change in outcomes. Dose–response relationships were not reported stratified by age group in either meta-analysis, so the treatment effect of exercise is assumed to be uniform across age groups. This is likely to bias the direction of modelled association if the true effect of physical activity on health is greater in a population subgroup, such as the very young or very old.
Model authors have added smoothing to treatment effects reported in the meta-analyses to extrapolate over a wider range of potential activity values (0–70 METs/week). Although meta-analyses considered the effect of a fixed dose of physical activity on health, the model aims to estimate the health response of physical activity across a range of values. A comparison of raw and smoothed curves is presented in Report Supplementary Material 2. Smoothing appears generally reasonable for study outcomes derived from the Kyu et al. 169 meta-analysis, with some divergence in modelled patterns of type 2 diabetes mellitus from meta-analysis evidence, with meta-analysis suggesting a stronger health effect of activity than that modelled. It was not possible to compare raw and modelled outcomes for dementia or depression outcomes gathered from the Woodcock et al. 170 study. Insufficient detail was provided in the model handbook to understand the model authors’ choice of smoothing effect for all conditions and this prevented further investigation. Default model assumptions of the shape of the dose–response relationship were therefore not altered in our study.
Further detail of model mechanism is available in the model manual. 151 A full list of adjustments to the standard model specification are presented in Report Supplementary Material 2. Parameters used in the model were not updated to aid comparability and replicability with the standard model.
Model parameterisation
Our analysis uses each participant’s daily average of total measured activity to estimate the average level of wake-time activity at baseline and follow-up in each trial arm. There was no minimum valid observation period of accelerometer wear, as data sparsity meant that the trial protocol of a minimum of 3 days of accelerometer wear time was dropped. This was judged the most pragmatic approach with data available. Activity levels during school hours and out of school time were estimated separately from trial data to understand the independent effect of the intervention on activity during and after school hours. This separation was important owing to potential for a compensation effect in total measured activity levels (i.e. a compensating reduction in magnitude/intensity of out-of-school activity due to any increase in activity during the school day). 171
Activity values measured in METs per week within and outside school during the trial period were therefore scaled up to create a simulated year. This simulated year attempts to describe any variation in activity between the academic year and school holidays. Children were assumed to be in school for 190 days per year (government-mandated minimum). 172 Data collected during weekends were assumed to be representative of activity during holiday periods and therefore multiplied by 175.25 days. This created an estimate of activity over a full year, which was used to simulate the ‘average’ MET per week in each trial arm at baseline and at follow-up.
Metabolic equivalents per week were estimated in the control and the intervention arm by linear regression, adjusting standard errors in mean values for clustering at the school level. In the base case, estimated activity measured in METs per week over the simulated year were compared at follow-up (unadjusted analysis). In a corresponding scenario, the observed difference between groups at follow-up was adjusted for baseline activity values (adjusted analysis). Regression modelling did not investigate the effect of any clustering of activity within individuals between time points.
Estimated values were fed into the model, with probabilistic modelling choosing a random value around the mean value from Student’s t distribution around the modelled standard error, with degrees of freedom specified by regression output. In multiply imputed data sets, the average degrees of freedom from regression estimates were used (4.97–5.46 degrees of freedom). In complete-case analysis, 7 degrees of freedom were used, with t distribution sample size adjusted to match the appropriate complete-case sample. Monte Carlo simulation modelling was used to generate 10,000 simulations for each scenario to represent the effect of parameter uncertainty on cost-effectiveness results.
The MOVES model allows specification of a parameter determining how long the health effect from any change in an individual’s activity is expected to be maintained. Previously reported modelling studies for interventions aiming to reduce sedentary behaviour assume that intervention effects are fully sustained for the first year and then decay at a rate of 50–55% per annum thereafter. 173–176 A 50% decay rate per annum in the health effect of the intervention was therefore assumed in the base case, and sensitivity analysis investigated the effect on cost-effectiveness conclusions when decay rates of 0% and 100% were assumed. These scenarios represent, respectively, a full ongoing health effect across 30 years or an exponential decay to the health effect after the year of the trial intervention.
Estimated costs and health-related quality of life over time horizons considered were discounted at 3.5% per annum, with intervention costs assumed as a one-off event at the beginning of the modelled time horizon. As in within-trial analysis, desks used in the intervention and control arm were modelled to have an expected lifespan of 10 years, meaning that the intervention cost was assumed to be £7.58 per child. Scenario analysis investigated the impact of using a public health discount rate of 1.5% per annum. Probabilistic modelling is presented for all scenarios.
Expected value of perfect information was computed for the base-case model and relevant scenarios. This is computed as the difference between the (1) average of maximum net monetary benefit of either Stand Out in Class or a ‘do nothing’ strategy and (2) average net monetary benefit from the Stand Out in Class intervention. 177 This is calculated over 10,000 scenarios and calculated at maximum and minimum stated willingness-to-pay thresholds set by the National Institute for Health and Care Excellence’s (NICE’s) technology assessments. 178 A 10-year discounted population of all children in the UK aged 9.5 years was chosen to represent the target population of the intervention over its expected time horizon, representing the expected size of the Year 5 school cohort in the UK. Values for the UK population size by age were taken from mid-2017 population estimates. 179
Results
Physical activity
Activity values at baseline and follow-up in each arm are presented in Table 19, with multiply imputed and complete-case values presented alongside for comparison. Multiply imputed values were used for base-case analysis. ‘Simulated average’ values represent the mean METs per day expected over the simulated year described above. These values were used to create the expected METs over the course of the simulated week used as a model parameter.
| Activity modelling | Baseline | Follow-up | ||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| Multiply imputed | n = 90 | n = 86 | n = 90 | n = 86 |
| Mean METs/day | ||||
| Weekday | 1.7982 | 1.8199 | 1.8839 | 1.9050 |
| Weekend | 1.7076 | 1.7933 | 1.9153 | 1.9453 |
| Simulated average | 1.7547 | 1.8071 | 1.8989 | 1.9243 |
| Model parameters | ||||
| Simulated METs/week | 12.2831 | 12.6500 | 13.2926 | 13.4704 |
| Standard error (clustered) | 0.1667 | 0.1592 | 0.2570 | 0.3012 |
| Simulated mean difference between groups (95% CI) | 0.3669 (–0.1537 to 0.8874) | 0.1779 (–0.6880 to 1.0437) | ||
| Complete case | n = 74 | n = 70 | n = 59 | n = 62 |
| Mean METs/day | ||||
| Weekday | 1.7833 | 1.8232 | 1.8857 | 1.8898 |
| Weekend | 1.7115 | 1.7921 | 1.8848 | 1.9404 |
| Simulated average | 1.7488 | 1.8083 | 1.8853 | 1.9141 |
| Model parameters | ||||
| Simulated METs/week | 12.2418 | 12.6579 | 13.1968 | 13.3985 |
| Standard error (clustered) | 0.1845 | 0.2058 | 0.2420 | 0.3566 |
| Simulated mean difference between groups (95% CI) | 0.4161 (–0.2376 to 1.0697) | 0.2017 (–0.8174 to 1.2208) | ||
As is apparent from the complete-case analysis, presented in Table 19 for comparison, there was a higher level of completeness in accelerometer measurement at baseline than at follow-up, which is reflected in the increased standard error around the sample means at follow-up. The increased standard error in the intervention arm at follow-up may also highlight heterogeneity between subgroups within the intervention group, some of whom may have responded particularly strongly to the standing desk intervention in their activity patterns. This possibility was not investigated further in this analysis owing to potential for overinterpretation of small numbers.
Activity levels are higher, on average, across all measures at follow-up than at baseline. As highlighted previously, follow-up data collection was undertaken during the summer months, with longer daytime hours than for the baseline data collection in winter. For this reason, average activity values were collected over a longer period, with an applied wake-time filter of 06.00 to 23.00 at both time periods (based on sleep and wake-time diary entries), thus potentially capturing an increase in daily activity during the summer period.
Comparing trial arms in the multiply imputed data set at follow-up, there is a slightly higher average daily activity level measured in the intervention arm than in the control arm during weekday and weekend monitoring. The difference between outcomes is highest at weekend measurement, in which average daily activity is 1.54% higher in the intervention arm than in the control arm. The difference between arms narrows to 1.12% in weekday activity at follow-up. This translates into an activity difference of 1.34% between arms at follow-up in the simulated year.
In complete-case analysis, the difference between arms in activity levels at follow-up suggests a slightly different pattern. The difference in activity levels between arms during weekday measurement is only 0.22%, with a higher pattern of activity in the control arm. The difference in activity levels widens during weekend observation to 2.95%, translating to a difference in activity over the simulated year to 1.53%. Missing data in complete-case analysis therefore appear to follow a pattern captured by baseline characteristics included in regression adjustment in multiple imputation equations, with imputation estimates rebalancing average activity values by differential adjustment in some of the imputation subgroups considered. The sensitivity of conclusions to alternative specification of multiple imputation equations was not investigated in this analysis; however, this could plausibly form a part of future work.
When also considering the pattern of baseline values, evidence of a difference between groups is starker. If considering the trend between baseline and follow-up time periods, the intervention arm shows a 0.60% lower increase in measured activity between summer and winter time points than in the control arm. The difference between arms is strongest during weekend measurement, for which the difference in trend between time points is 26.83%, with the intervention arm demonstrating considerably less increase in activity from winter to summer. This corresponds to an overall difference in trend between trial arms over the simulated year of 18.73%, showing a larger increase in activity in the control arm than the intervention arm during the trial period.
To describe the potential importance of imbalance in baseline values to study conclusions, mean differences between the intervention and control group at baseline are presented. In both the multiply imputed base case and complete-case analysis, there is some evidence of difference between the levels of activity observed in the intervention and control groups at baseline. In the multiply imputed base case, the difference in activity levels over a simulated average week shows already higher activity in the intervention arm than in the control arm (0.3669 METs/week, 95% CI –0.1537 to 0.8874 METs/week). At follow-up, there is less mean difference between treatment and control groups, albeit with wider CIs, particularly in the complete-case analysis. The reader’s judgement regarding the relevance of slight evidence of true difference between the control and intervention arms’ baseline activity in this small sample should be used to inform the reader’s view of the appropriateness of adjusting estimates of the difference between intervention and control arms at follow-up for any existing difference in baseline activity levels in long-term cost-effectiveness modelling.
Long-term cost-effectiveness
Table 20 shows the main results of long-term probabilistic cost-effectiveness modelling over a 30-year time horizon. In the base case, in which there was no adjustment for baseline activity levels, ‘unadjusted’ modelling of the incremental cost-effectiveness of the Stand Out in Class intervention produced an ICER of £78,986 per QALY. For unadjusted activity levels, probabilistic modelling estimated a 26.67% probability of the Stand Out in Class intervention being cost-effective at the current maximum national willingness to pay for a unit of health (£30,000/QALY gained).
| Model result (scenario) | Base case (3.5% discount, 50% health effect per annum) | 1.5% discount rate | 100% health effect ongoing | 0% health effect ongoing | ||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Predicted change in health-related quality of life (30-years) | 0.00009 | –0.00003 | 0.00012 | –0.00005 | 0.00056 | –0.00023 | 0.00006 | –0.00003 |
| Predicted change in health cost (£) | –0.19 | 0.06 | –0.21 | 0.08 | –1.64 | 0.66 | –0.13 | 0.06 |
| Predicted change in total cost (£) | 7.39 | 7.64 | 7.37 | 7.66 | 5.94 | 8.24 | 7.45 | 7.64 |
| Mean cost-effectiveness ratio | £78,986/QALY | Dominated | £60,430/QALY | Dominated | £10,564/QALY | Dominated | £116,278/QALY | Dominated |
| Probability (%) cost-effective at £20,000/QALY | 15.58 | 5.61 | 22.38 | 9.41 | 57.29 | 31.67 | 5.74 | 2.25 |
| Probability (%) cost-effective at £30,000/QALY | 26.67 | 10.56 | 34.33 | 15.33 | 60.32 | 34.84 | 14.22 | 5.13 |
| EVPI (£) | ||||||||
| EVPI (per person), WTP £20,000 | 0.66 | 0.43 | 1.28 | 0.55 | 11.82 | 7.57 | 0.17 | 0.07 |
| EVPI (per person), WTP £30,000 | 1.69 | 0.90 | 2.84 | 1.23 | 15.61 | 11.97 | 0.57 | 0.22 |
| EVPI (discounted 10-years population), WTP £20,000 | 4,572,088 | 2,982,372 | 8,778,105 | 3,817,901 | 81,370,602 | 52,145,982 | 1,177,843 | 454,909 |
| EVPI (discounted 10-years population), WTP £30,000 | 11,620,021 | 6,224,846 | 19,574,686 | 8,497,135 | 107,464,367 | 82,401,571 | 3,940,340 | 1,488,710 |
When differences between groups in baseline activity levels were accounted for, the Stand Out in Class intervention was dominated by a strategy of ‘do nothing’. In this case, the intervention was, on average, more costly and less effective in improving population health than making no changes to the classroom environment. This is due to a smaller observed change in physical activity levels between time points in the intervention arm than the control arm. At a maximum value of the current NICE threshold, adjusting for differences in baseline levels of physical activity, the estimated probability of the Stand Out in Class intervention being cost-effective was 10.56%. This means that, accounting for uncertainty in the change in physical activity observed, there is only a small chance of the intervention being cost-effective under these assumptions.
Our long-term cost-effectiveness conclusions were moderately sensitive to choice of health services or public health discount rate, with the probabilistic ICER reducing in the unadjusted case by £18,556 when using the public health discount rate of 1.5%. However, it remained unlikely that the intervention was cost-effective, with an estimated 34.33% chance that the intervention was cost-effective at the maximum NICE threshold at the new unadjusted ICER of £60,430 per QALY.
Our conclusions were, however, highly sensitive to assumptions surrounding the ongoing health effect of physical activity beyond the intervention itself. When the health effect of past exercise was assumed to be maintained for the whole modelled time horizon of 30 years, the intervention was highly cost-effective in the unadjusted case at £10,546 per QALY, with a 60.32% chance of being cost-effective at the maximum threshold value. Conversely, in the adjusted case, due to the observed reduction in physical activity being maintained over the whole trial period, there was a corresponding increase in modelled costs and decrease in modelled QALYs. Owing to the increased importance of uncertainty around the health effect when modelled over a longer period, in the adjusted case there was still a moderate chance of the intervention being cost-effective (34.84% at a threshold of £30,000/QALY).
As expected, when the health effect was assumed to decay exponentially after the period of the intervention, the modelled probabilistic ICER increased to £116,278 per QALY in the unadjusted case (14.22% chance cost-effective at £30,000/QALY). The adjusted case remained dominant, with a 5.13% chance of being cost-effective at £30,000 per QALY. Cost-effectiveness results for complete-case analysis are presented in Report Supplementary Material 2. Cost-effectiveness acceptability curves for base-case scenarios are also available in Report Supplementary Material 2.
Expected value of perfect information
Table 20 presents the EVPI to resolve all parameter uncertainty considered in the model. EVPI is calculated for each scenario at the lower and upper NICE cost-effectiveness thresholds, per person and at the population level.
The EVPI results are more sensitive to the scenario modelled than whether or not post-intervention measures of activity levels adjust for baseline activity. At the upper bound of the NICE threshold (i.e. a higher willingness to pay per population QALY generated), there is increased value placed on resolving decision uncertainty regarding the proposed intervention’s cost-effectiveness. For this reason, in the base case, EVPI in the baseline-adjusted analysis was modelled at £0.43–0.90 per person at national thresholds of between £20,000 and £30,000 per QALY. In unadjusted analysis, EVPI per person is modelled at £0.66–1.69 (threshold £20,000–30,000/QALY). At the higher threshold, the EVPI is 11.9% of the modelled cost of the Stand Out in Class intervention per person in the adjusted case and 22.3% of the desk cost in the unadjusted case.
There was only one scenario in which EVPI to resolve all modelled parameter uncertainty was at or higher than the value of the cost of the intervention per person. When the health effect of the standing desk intervention was assumed to be maintained for the full time horizon of 30 years, the EVPI per person in the baseline-adjusted analysis was £7.57–11.97 (threshold £20,000–30,000/QALY). In the unadjusted analysis, the EVPI per person was £11.82–15.61 (threshold £20,000–30,000/QALY). At the upper threshold value, this puts the EVPI in this scenario at 157.9% of the cost of the Stand Out in Class intervention in the adjusted case and 205.9% of the intervention cost in the unadjusted analysis.
The EVPI was calculated at a population level, considering the expected discounted UK population of Year 5 pupils over the intervention lifetime of 10 years. In the base case, the population value of resolving all modelled parameter uncertainty in the health effect of the Stand Out in Class intervention is between £3.0M and £6.2M when differences in baseline activity levels are considered, or £4.6M and £11.6M when not adjusting for difference in baseline activity (threshold £20,000–30,000/QALY). Again, the assumed ‘ongoing health effect’ parameter, determining the proportion of ongoing health effect beyond the intervention period, produced considerable variation between scenarios in population EVPI for the discounted population. Population EVPI values for the discounted population of 10 ‘Year 5’ cohorts across all scenarios considered are presented in Table 20. Across all scenarios considered, the maximum expected value of research to resolve all decision uncertainty was £107M at a threshold of £30,000 per QALY. A comparison plot of the EVPI at different willingness-to-pay thresholds for unadjusted base-case scenarios is presented in Report Supplementary Material 2.
Discussion: long-term cost-effectiveness modelling
Key findings
Based on long-term cost-effectiveness modelling over a 30-year time horizon, the Stand Out in Class intervention is not cost-effective at a threshold of £30,000 per QALY, with a low probability of the intervention being cost-effective based on modelled uncertainty in existing evidence. ICERs show large variation between scenarios; however, in all but one of eight modelled scenarios, this variation does not result in a predicted mean ICER below the upper bound of the UK cost-effectiveness threshold for new health technologies. In base-case analysis, we estimated an ICER of £78,986 per QALY in ‘unadjusted’ analysis, with the treatment being dominated by a strategy of ‘do nothing’ in ‘adjusted’ analysis, which controlled for differences between groups in levels of baseline activity.
The Stand Out in Class intervention is only cost-effective when the ‘unadjusted’ health effect of a standing desk is assumed to be maintained for the whole 30-year period. At face value, this appears to be an unreasonable assumption. However, this is equivalent to assuming that the intervention would produce a long-term behaviour change in the treated population, which meant that their activity levels were consistently above the untreated (at the current magnitude) population over the 30-year period. When phrased as such, this assumption may appear plausible, given recent dialogue of the potential for early intervention to deliver long-term maintenance of intervention-induced behaviour change. 180 However, when incorporating this assumption into a model that adjusts the treatment effect in activity levels for observed differences in activity between trial groups at baseline, the Stand Out in Class intervention is still shown to be more costly and less effective than a ‘do nothing’ strategy, as in all other scenarios that control for differences between groups in baseline activity levels.
Estimates of EVPI present the maximum possible value of future research to resolve all remaining decision uncertainty regarding the cost-effectiveness of the Stand Out in Class intervention, based on the modelling approach used. ‘Perfect information’ can eliminate the possibility of making the wrong decision. For this reason, to maximise population health gain, a health system should be willing to pay for additional evidence to inform a decision, up to a maximum budget constraint, after which the cost of research will exceed the population health benefit from further research. 181 In this case, a proportion of this expected research value is in resolving parameter uncertainty in the health effect of physical activity. A further proportion of this research value is in determining the true value of expected health costs and quality of life for a population with a known disease burden. The remaining value of research uncertainty is in parameter uncertainty regarding the activity inputs (i.e. knowing the true levels of activity in each intervention group at baseline and follow-up).
The expected population value of perfect information for all parameters in base-case analysis is £6.2M in the ‘adjusted’ case and £11.6M in the ‘unadjusted’ case. This assumes the higher value of the national threshold value to produce one ‘unit’ of health (£30,000/QALY). In this case, the value of research that resolved all parameter uncertainty involved in this funding decision would be worth between £6.2M and £11.6M to a national decision-maker.
In the scenario in which we assume an ongoing health effect throughout the intervention period, the EVPI increases to £107.4M in the ‘unadjusted’ case and £82.4M in the ‘adjusted’ case. When the health effect of the intervention is maintained for this longer period, knowing the true change in activity induced by the intervention matters proportionately more.
Neither the expected value of perfect parameter information nor the expected value of sample information were calculated as part of this work. For this reason, we do not have a clear indication of the upper bound of the expected value of further research into activity levels alone, as collected in this trial. We also do not have a clear indication of the expected value of an additional trial, which without incurring unfeasibly large costs to obtain an unlimited sample size, would resolve only a proportion of the total research uncertainty. 182 For this reason, we can conclude only that the further value of research into determining the true health effect of the Stand Out in Class trial is bounded by EVPI estimates, with the value of resolving uncertainty in true levels of activity pre and post intervention being only a proportion of the total EVPI over all parameters presented above.
Comparability with other studies
To the best of our knowledge, this chapter represents the first examination of the long-term cost-effectiveness of active classroom interventions, such as sit–stand desks. Despite public health interest in targeting childhood sedentary behaviours, with the intention of changing these behaviours over the longer term, the cost-effectiveness of such interventions has been less frequently considered. 183 Such interventions are an obvious candidate for public health cost-effectiveness modelling, given that trial outcomes collected are typically short term and expected payoffs occur over a much longer time horizon, with potential overspill between sectors, such as improved education outcomes leading to better health outcomes in later life. 184
Although one systematic review185 found school-based physical activity interventions to be among the most cost-effective in increasing energy expenditure, a separate review186 linking activity gains to changes in health using a generalised cost–utility framework measured in QALYs, revealed all school-based interventions considered to be cost-ineffective at a threshold of US$50,000 per QALY. 185,186 Current work, including this report chapter, has, however, not yet explicitly integrated consideration of potential intersectoral impacts of active classroom interventions into cost-effectiveness analysis. 187 Explicit consideration of intersectoral effects could provide a new perspective on the estimated long-term cost-effectiveness of interventions, such as the Stand Out in Class intervention.
In contextualising the changes in activity levels measured in the trial, in a recent systematic review57 of eight studies of classroom standing desks and sedentary behaviour (three RCTs), all studies reported an increase in standing time and a decrease in sitting time. This review57 did not report activity outcomes in terms of change in METs per hour. Using an average of point estimates of energy expenditure in sitting-type activities, we could expect an approximate activity increase of 0.193 METs per hour for each additional hour spent standing rather than sitting. 188 For this reason, the additional metabolic expenditure of an estimated 40-minute increase in standing time in children, reported by the single study59 reporting outcomes in minutes over waking hours, is likely to have a limited impact on daily average activity. This translates to an estimated increase of 0.0107 METs over a 12-hour waking day. The small impact of the Stand Out in Class intervention on metabolic expenditure levels therefore does not appear inconsistent with wider literature.
Strengths and limitations
In this trial, intervention cost-effectiveness was undermined by study results that demonstrated only small changes in activity, measured by METs. METs are sometimes sidelined in newer research studies of sedentary behaviour. Newer studies often measure the impact of sedentary behaviour interventions on specific related outcomes, such as changes in sitting time, rather than providing a generalised measure. This is due to the perceived insensitivity of METs to detect changes in patterns of sedentary behaviour and the hypothesis of a health effect of sedentary behaviour independent of physical activity. 157,189 However, although there is some evidence of sedentary behaviour patterns influencing a limited range of intermediate health outcomes, such as short-term measures of blood pressure, cholesterol or blood lipids, these outcomes are not currently utilisable in health economic evaluations as their impact on meaningful generalisable measures of population health (such as the QALY) is highly variable. 190 For example, the relevance of changes in blood composition will depend on the cardiac risk profile of the population considered and how long any change in blood composition is maintained. There is currently insufficient evidence not only in the effect of measured sedentary behaviour on surrogate health outcomes, but also of the link between the measured intermediate health outcomes to robust measures of final end points, such as health-related quality of life. This absence is particularly apparent in children.
Our study conclusions utilise a health mechanism mediated by physical activity levels, in which causal links are more readily established. 23 Future work could investigate the plausibility of updating our modelling strategy with current best evidence on the independent health effect of sedentary behaviour; however, such work will require a significant increase in research resources. Given current limitations in available evidence, such research is also unlikely to resolve a meaningful proportion of decision uncertainty in relation to the cost of any such research undertaking.
Even in using METs, significant uncertainty remains in estimating the health impact of changes to activity levels. Questions of the nature of dose–response between activity and health outcomes remain unresolved. 191 Estimation of the dose–response relationships of hypothesised health effects, given different levels of baseline activity, require very large sample sizes. 192 For example, the current model assumption of an attenuating dose–response relationship at higher levels of physical activity is likely to require further examination. There is also particular scepticism regarding current modelled health costs and outcomes in depression, with the evidence base currently heavily relying on use of inconsistent self-report measures of physical activity, with varying use of subjective and direct measures of defining depression criteria. 193,194 This presents a barrier to understanding the nature of a dose–response relationship with an adequate degree of precision.
In this study, we have assumed that health effects of changes in activity in children are equivalent to the modelled risk in young adults (aged ≥ 16 years). This is despite difference in national population guidelines of the recommended level of physical activity per week in the two populations, with recommended levels of activity in children being significantly higher. 23 Any difference in risk profile from additional activity in children compared with an adult population was not addressed as part of this research and may be an important consideration in future analysis. There was also no account in modelling for changes in the trajectory of physical activity with ageing of the modelled cohort (i.e. the population becoming more sedentary with age); additional economic modelling could be used to address this deficiency. 139,195
Chapter 5 Process evaluation
Introduction
This chapter presents the qualitative findings from a detailed process evaluation conducted throughout the Stand Out in Class pilot study. The process evaluation explored key feasibility- and acceptability-related outcomes of the trial surrounding school and participant recruitment, acceptability of randomisation, acceptability of the measurement instruments and the intervention, along with the examination of any negative consequences of the intervention (such as classroom disruption). A detailed assessment of intervention fidelity was also undertaken. This chapter reports on the following study objectives:
-
Objective 1 – establish and refine a recruitment strategy for schools and pupils.
-
Objective 5 – assess the acceptability of randomisation to schools.
-
Objective 6 – assess the acceptability of measurement instruments to teachers, children, parents and guardians, including the activPAL inclinometer as the tool for the measurement of the primary outcome.
-
Objective 7 – assess the acceptability of the intervention to teachers, children, parents and guardians.
-
Objective 8 – monitor any adverse effects, such as musculoskeletal discomfort and/or disruption to the classroom/learning to inform the design of a full trial and minimise or eliminate any such effects.
-
Objective 9 – assess intervention fidelity over the intervention period.
Methods
Process evaluation overview
A series of interviews and focus groups with teachers, children and parents or guardians were conducted following the completion of the baseline measures and randomisation (phase 1), to explore the acceptability of the trial procedures, including randomisation (objective 5) and the acceptability of the measurement instruments (objective 6). Interviews/focus groups with teachers (n = 12 interviews), children (n = 12 focus groups) and parents/guardians (n = 7 interviews/focus groups) were conducted at each of the eight participating schools.
To help refine a recruitment strategy for a future trial, parents or guardians who did not consent their child to participate (identified by teachers who would know which parents had not consented) were asked briefly and informally by researchers visiting the schools at drop-off times or by teachers themselves if they would be willing to share their reasons for not consenting (objective 1). The acceptability of the intervention (objective 7) and children’s, teachers’, and parents and guardians’ perceptions and experiences of the intervention and outcome measures were determined at phase 1 and further explored towards the end of the intervention period (phase 2), through a further set of interviews (n = 4 with teachers from the intervention schools) and focus groups (n = 4 with children from the intervention schools) (objective 8). This included exploring any negative effects, such as discomfort from the monitoring equipment, reasons for non-compliance with the outcome measures or class disruption. Potential differences in the trial and intervention acceptability between ethnic groups were also explored as part of the analyses from the focus groups (objective 4). Towards the end of the intervention period, four interviews were conducted (with senior staff, head teachers/deputy head teachers) at each intervention school to further examine the acceptability of the intervention (objective 7). To assess intervention fidelity, intervention classrooms were observed by a member of the research team on two occasions and children’s posture during sit–stand desk use was recorded to assess any potential future risk of musculoskeletal injury.
Throughout the process evaluation, we used the conceptual framework of Hasson196 to guide the analysis of intervention fidelity and to explore adherence to the intervention (content, coverage, frequency and duration), and potential moderators of adherence to the intervention (including participant responsiveness, strategies used to facilitate implementation, quality of delivery and contextual factors).
Interview and focus group participants: acceptability and fidelity
For the interviews with participating teachers, the study co-ordinator contacted each teacher by e-mail or telephone to invite them to participate. Interviews took place at the school at a time of the teachers’ choosing. For the focus groups with children, teachers were requested by researchers to nominate three boys and three girls within their class who were confident and would want to participate in a focus group. Selected children were asked to take an information sheet and parental consent form home for their parents or guardians to read and to provide written consent for their child to participate in this phase of the research.
For the focus groups with parents and guardians, we aimed to conduct eight focus groups (one for each school) with parents and guardians who had given their consent for their child to participate in the trial. We aimed to have approximately four to six parents or guardians taking part in each focus group. The strategies employed to recruit parents/guardians to focus groups were (1) via a letter sent home from the school to parents and guardians with children who had consented to take part in the trial, detailing an exact time and date of when the focus group was going to take place (all focus groups took place in each of the schools); and (2) schools with a text message system (n = 3) sent out a reminder text on the morning of the focus group. Each of the eight teachers were asked whether or not a translator would be required before the day of the parent and guardian focus group. Only one focus group required a translator. The translator was a member of the Born in Bradford research team who had prior knowledge on the topic guides and the purpose of the focus group. All other focus groups were conducted in English.
Prior to the start of the parent and guardian focus groups, the purpose of the session was described and participants were requested to provide written informed consent. Finally, for the interviews with head teachers and senior members of staff, the study co-ordinator contacted each of the school’s head teachers and senior members of staff by e-mail or telephone to invite them to participate in an interview at the end of the study, to inform the context part of intervention fidelity.
Interview and focus group procedures: acceptability and fidelity
All of the interviews and focus groups, across both phases, used semistructured topic guides (see Report Supplementary Material 3) to ensure consistency. Questions were open ended to enable participants to raise issues important to them. Topic guides for focus groups with children were written in a language suitable for children aged 9–10 years. All interviews and focus groups were audio-recorded digitally.
Informal conversations with non-consenting parents, guardians and children: acceptability
For the informal conversations with non-consenting parents, guardians and children, teachers or researchers spoke to parents and/or children and simply asked ‘what were the reasons for not signing up to be part of the study?’. Researchers and/or school staff recorded the answer given to the question, along with the child’s sex and what relation the parent or guardian was (e.g. mother, father, grandparent, carer). This approach was taken as teachers felt that asking parents and children to a formal focus group or interview to speak about the trial in which they did not want to participate would possibly make them feel uncomfortable and less likely to speak openly.
Classroom observations: assessment of intervention fidelity and musculoskeletal discomfort
As part of the pilot assessment of intervention fidelity, intervention classrooms were observed by a trained researcher for the duration of at least half a school day (3 hours) during the spring (March, April and May) and summer (June, July and August) terms. Therefore, a total of eight observation periods, two per intervention school, took place. During the observation periods, the researcher used an adapted version of the postural observation technique developed by Benden et al. 63 to observe individual children’s postures while working at a height-adjustable desk (either sitting on a stool or standing), during class time. This was to assess potential future risks of musculoskeletal injury (objectives 8 and 9). The observation of individual children lasted for 10 minutes, with the researcher first positioning themselves such that they were able to see the sagittal plane of the individual child. The researcher then started a stopwatch and used the Benden et al. 63 postural observation sheet (see Report Supplementary Material 3) to identify the posture that most closely resembled the position of the child at the start of every minute for 10 minutes. During the 10 minutes, whether the child’s neck was in extension or flexion, or whether or not the child was resting their elbows and/or forearms on the workstation was also recorded.
The sex of each child was also documented by the researcher, along with the time, lesson/subject and month of the year. If a child was absent from their desk at the beginning of a minute during the 10-minute observation, the researcher marked an ‘X’ and treated it as a missing data point for analysis. Similarly, if the observed child moved during a minute of data collection, the researcher noted it in the ‘comments’ section of the data collection sheet.
The fidelity observations occurred at the same time on the same day as the posture observations. While present in the classroom, researchers had informal conversations with children during natural breaks of the day about each of the intervention components. Researchers also observed and tallied the number of boys and girls either sitting or standing while using the sit–stand desks every minute during the posture observations; this measure provided minute-by-minute data of how the sit–stand desks were being used during class time.
Two researchers conducted both posture and group (fidelity) observations. The interobserver agreement, using interval-by-interval agreement was ≥ 85% for each component of the observation tools.
Qualitative data
Audio-recordings were transcribed verbatim with anonymisation of all personal data. Interview data were then analysed using thematic analysis. 197 The process involved the following steps.
Familiarisation
The researcher became immersed in the raw data by ‘repeated reading’ of the transcripts and listed key ideas for coding.
Generating initial codes
Initial codes and a coding framework were developed, informed predominantly by the objectives of this qualitative component (a deductive approach), although novel views expressed by the participants were also captured (an inductive approach).
Searching for themes
The codes were then organised into potential themes and subthemes. At this point, similarities and differences in views ‘within’ and ‘across’ participant groups (teachers, children, parents/guardians, head teachers) were explored. Owing to the similarities between the sound of boys’ and girls’ voices and all the children in general, transcribers could not distinguish between individual children. Therefore, comparisons were made between the different focus groups rather than individual children.
Reviewing themes
Coded data within each potential theme were reviewed and the themes were modified so that they formed a logical order. Each theme was then further reviewed to ensure that it fit within the entire data set.
Defining and naming themes
A short paragraph was produced for each theme and subtheme to define the ‘essence’ of the theme and subtheme and allocate a name.
Classroom observations: musculoskeletal discomfort
For both group and posture data, descriptive statistics are reported. As this is a pilot study, not powered for statistical significance, statistical tests were not performed.
Results
Some quotations in this section are reproduced with permission from Clemes et al. 81 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Interview and focus group participants
Teachers
We recruited four male (n = 3 control, n = 1 intervention) and four female (n = 1 control, n = 3 intervention) teachers. Four teachers were of South Asian ethnicity and four were of white British ethnicity.
Children
A total of 43 children, 22 boys and 21 girls, participated in the phase 1 focus groups; and 24 children, 10 boys and 14 girls, participated in the phase 2 focus groups (intervention schools only).
Parents/guardians
A total of 18 parents and guardians (13 mothers and five fathers) from seven of the eight schools took part in the focus groups and interviews during phase 1. We were unable to recruit any participants from one school after two attempts. The teacher at this school expressed that parents and guardians struggle to find time to attend any event the school organises, including the annual parents’ evening. This was a common theme for all schools.
The findings of the focus groups and interviews from teachers, children, parents and guardians are presented, according to the key study objectives that this chapter set out to address. We include illustrative quotations to highlight key themes and indicate whether quotations came from control (C1–C4) or intervention (I1–I4) schools, and the predominant ethnicity of the school [white British (WB) or South Asian (SA)].
Objective 1: to support the refinement of a recruitment strategy for schools and pupils
The recruitment processes
Teachers
All eight teachers expressed high satisfaction with the recruitment protocol, with the study being clearly explained:
Yeah, it was very well explained and the ideas and the concept behind what you were doing, so I had no hesitation accepting really.
Teacher, C1, WB
Teachers across both control and intervention schools also commented that the recruitment approach was appropriate and suitable for children, especially the way in which the researchers explained to the children that this was a real-life science experiment:
It worked well. I think you got quite a good uptake . . . as a class, so obviously what you were sending out and the conversations you were having with the children got them quite enthused. I think with them, with the children they’re doing something scientific because they all sort of really love science, the idea of doing something scientific with scientists is like ‘yay!’. So jumped in on that.
Teacher, C2, WB
Children
Children across all focus groups reported that recruitment was positive for them, the study was made clear and that everyone had a choice to participate:
It was good because once I got the letter I didn’t understand what it was or not. [Researchers] told us about the letter and our teachers told us about it and told our, told us to tell our mum if we want to go or not because you first need permission off your mum, and that’s why it was a good process because you got told three times.
Child, I1, SA
. . . it’s more like you get to choose to take part and if you don’t want to then it doesn’t matter.
Child, I3, WB
Parent/guardians
Parents’ views on recruitment were also generally very positive:
Um, the impression I got was all the class were asked about it but the children decided whether they wanted to take part in it or not but we had to give consent, so she brought form home and I think give consent by a certain date and then I had to sign it and then she was given full instruction as to what to do with it.
Mother, C1, WB
A small number of parents mentioned that having a parents’ meeting after school to discuss the project would have been useful, as some parents did not understand what it was and that it involved sit–stand desks:
I think if the school have had had a bit of a meeting just to explain that this is what you’re doing because then you just get a sense . . . because we get loads of letters obviously . . . and like sometimes you think ah, another letter.
Father, I3, WB
Equally, parents stated that this might have been difficult to attend:
I think it’s always hard because you’ve got parents that are working and things as well to invite, you know. The school do a really good job of trying to invite you to these things but always people can’t participate.
Mother, I4, WB
Why did parents/children choose not to participate?
Seven out of the eight schools had a minority of children whose parents did not give consent for them to take part in the trial. Reasons for non-consent were collected from children (n = 17), parents (n = 9, eight female and one male) and one grandparent via brief informal interviews conducted by either a researcher or the class teacher. Reasons given for non-consent by children included being away at the time of the study (n = 1), their parents were not happy with their child being monitored (n = 3), their parents or other caregivers were not happy to give consent (n = 3), they were not comfortable with being monitored or being part of the research (n = 5), that they, or their parents, did not receive any information about the study (n = 3) or they forgot to return the consent form (n = 2). For parents and caregivers, key reasons for non-consent were not being aware of receiving information about the study (n = 6), being away at the time of the study (n = 1), their child being ill at the time of the research (n = 2) or that their child reported not wanting to take part in the study (n = 1). Across both parents and children, the most frequent reason for not consenting to the trial was because children either lost or forgot consent forms, or information about the study was never brought home or made clear to parents. This was reported by 11 out of 27 respondents.
Objective 5: assess the acceptability of randomisation to schools
When asking teachers and children about the acceptability of randomisation, both groups expressed that there was a clear understanding of why the randomisation had occurred:
Well yeah because it makes it fair doesn’t it, it keeps everything on a level playing field and you wouldn’t necessarily want to choose your school because you are hand picking, whereas if you randomise it you make it really clear that you have got an equal chance of having desks in and going through doing those, so it just keeps everything fair doesn’t it really.
Teacher, I2, SA
Because then you can look at the schools that have the tables and the schools that didn’t and look at the difference in health.
Child, I3, WB
This was true even with teachers and children from the control schools, who were understandably disappointed not to be receiving the sit–stand desks. However, they still considered their participation in the trial to be positive and clearly understood why it was required:
Well, I completely understand why you need to have a control. You know, we teach the children, that certain investigations need a control, you need something to compare it against . . .
Teacher, C3, SA
Well a bit sad but I felt happy at the same time because at least we’re taking part in something.
Teacher, C4, SA
As for parents and guardians, most thought that it was a fair process:
I think it’s fair, it’s a fair process because it doesn’t . . . it’s a neutral process as well so there’s no bias towards anything and pick and choose, schools that could be biased there so this was like totally random, I think it was fair.
Mother, I2, SA
Objective 6: assess the acceptability of measurement instruments to teachers, children, parents and guardians, including the activPAL inclinometer as the tool for the measurement of the primary outcome
Thoughts on the activPAL
Teachers
When asked questions regarding the acceptability of the activPAL (as a primary outcome measure), the most common theme identified was the sometimes problematic issue of using the medical dressing [Hypafix® Transparent (BSN medical, Hull, UK), also referred to as ‘stickers’ or ‘sticky pads’ by the teachers/children/parents] to attach the monitor. In some cases, this reportedly caused a minority of children to suffer from itchiness, soreness and discomfort, along with some class disruption:
Yeah, it was a bit faffy. Some of the children did complain about getting a bit of a rash, but they like to complain anyway, so it was a bit . . . I don’t want to use the word chaotic, but that was more to do with the fact that the kids were constantly, interested by them so they were focused on them . . .
Teacher, I1, SA
However, teachers did not feel the issues associated with the medical dressing to be significant, as only a few children complained [e.g. ‘there were only a few complaints . . . ’ (Teacher, C2, WB); ‘Only a couple of them had a little reaction to it’ (Teacher, I4, WB)]. Researchers provided plenty of medical dressing so children could always replace it if required {e.g. ‘It wasn’t a big issue [monitor coming off] We had plenty of supplies . . . ’ (Teacher, C1, WB)}, and children also knew how to correctly replace the dressing, which did not cause extra burden for teachers [e.g. ‘Yeah it was absolutely fine, they, you know, they were shown how to put it on correctly, I didn’t have to do anything for them’ (Teacher, I4, WB)]. Teachers also spoke about how children had the resilience to get on with wearing the monitor and do their best to wear it for as long as possible. Teachers also noted that the activPAL monitor was not noticed by the children once they got used to wearing it, with the position of wearing it on the thigh aiding this:
I think once the children got used to wearing that it was OK for them. I think the fact that it stuck to the leg and once they had got their clothes on during the day it is something that they don’t need to worry about, they don’t fuss about, whereas sometimes if it’s out, if it’s on your arm or on your wrist then they start to play with it. So I think the positioning of where it is on the body is good.
Teacher, I2, SA
Children
During the focus groups, 10 out of 43 children reported feeling some discomfort related to the activPAL:
When you tried to take it off it really hurt.
Child, C3, SA
When I took it off I had a bit of like a little rash or a few spots, from the underneath because my leg got quite sweaty.
Child, C1, WB
As with the teachers, children concluded that using medical dressing to wear the activPAL was problematic. The children explained they had to constantly replace the dressing as it became loose, mostly because of bathing or swimming:
Yeah and the stickiness was bad, it kept coming off, so then when I got a new one [sticker] I couldn’t put it on properly.
Child, C4, SA
Parents
The key themes emerging from the parent interviews and focus groups regarding the activPAL were very similar to those of the children and teachers. Four out of 18 (three mothers and one father) reported a mixture of discomfort and itchiness experienced by children when wearing the activPAL, and feelings of confusion and frustration at times around the use of the medical dressing to attach the device, particularly when bathing:
My son found it quite itchy and irritating and he couldn’t put jeans on because it was a bit annoying but otherwise.
Mother, I2, SA
‘The little thing when they were getting a shower, the sticky thing were coming looser and I can remember one night he couldn’t wear it because it literally wouldn’t stick.
Mother, I3, WB
However, the majority of parents and guardians from both control and intervention schools reported no problems regarding their children wearing the activPAL, and some reported that their children liked wearing the monitors:
It’s all right, it doesn’t hurt anyone, you know what I mean, it’s not in no-one’s way or not.
Father, C1, WB
Well, my daughter, she loved it, she’s like ‘mum, I’ve got this on me thigh, I can’t get it wet, I’ve got to change it and it counts me steps’! So she were quite happy with it, I didn’t find ought wrong with it, it weren’t in way for any sort of reasons.
Mother, I1, WB
Thoughts on the ActiGraph
In response to questions regarding the ActiGraph, a clear theme was that the ActiGraph was much easier and more feasible for children to wear than the activPAL; this was true for all teachers (8/8), most children (38/43) and most parents (15/18):
Again, I think that was nice and, nice and easy to wear that one, wasn’t it, so it was comfortable . . . So, no problems with that one.
Teacher, C3, SA
It didn’t really annoy me at all and it felt like nothing was even there.
yes’s to being happy for children to wear this.
However, some children (n = 15) reported that wearing the ActiGraph was uncomfortable during sleep:
It was OK but when I went to sleep it annoyed be a little bit, but I just moved it somewhere else, to my other side of my hip, and it was actually a little comforting because of the elastic band.
Child, C4, SA
Some children reported that it could be improved by being waterproof:
All right. This one it’s good that it goes around your waist because I had the problem for about the other one, and I think it doesn’t really hurt like the other one. But I think like everyone will say if it was waterproof it would be better because we don’t have to take it off.
Child, I3, WB
A small number of parents (n = 3) mentioned that they were not sure how the ActiGraph should have been worn and what it was meant to do:
It slipped down quite a lot. There was a lot of, you know, it seems to be down here rather than up here and then there was a concern as to did it have to be in a certain place? Was it [laughs] monitoring heartbeats or anything that are less likely, you know, it was more a bit of ‘oh well it’s wobbled down and I don’t know where to put my skirt versus where that should lay’, just that kind of uncomfortable. Nothing particularly went wrong with it.
Mother, I4, WB
Other measures
During the focus groups, teachers, children and parents were also asked about the acceptability of the other measures (e.g. physiological, questionnaires) that were taken as part of the trial. For most teachers, there were no issues with any of the measurements taken, but one teacher commented that the Strengths and Difficulties Questionnaire added more time to an already heavy workload:
. . . the only negative would be the questionnaires that take a while to fill in [Strengths and Difficulties Questionnaire]. It’s time-consuming, that’s all it is and for a teacher who already has sort of 60 books to mark with this time of year we’re looking at reports to write, like you name it, we’ve got a massive list of things to do.
Teacher, I2, SA
As for the children, they deemed all but one of the measures to be fun and enjoyable. The one measure a number of the children did not like was the RVIP test, which they reported to find boring and difficult.
Finally, parents felt that the health resource use questionnaire was quite burdensome:
. . . we get so many letters and stuff to read and forms to sign, I forgot about this form . . . I would off put it to one side to finish later but forgot, you know having more than one child is a full time job and they all bring, you know, so many forms to complete [from school].
Mother, I2, SA
Objective 7: assess the acceptability of the intervention to teachers, children and parents
Randomisation into the trial conditions occurred following baseline data collection (January 2017). The sit–stand desks (Ergotron LearnFits) were installed into the intervention classrooms at the very beginning of March 2017; the delay in desk installation was caused by shipping delays experienced by the desk manufacturer. Before the desks were installed, the researchers met with the teachers to provide them with training on the various intervention components. The teachers were provided with the Stand Out in Class training manual (see Report Supplementary Material 1) and a member of the research team met with each intervention teacher individually for approximately 1 hour, when they explained the various intervention components. During this meeting, the researcher encouraged the teacher to consider how they could rotate children in their class across the week, to ensure equal exposure to the desks. The teachers were also asked to consider how they could implement other intervention components.
Once the sit–stand desks were installed and on the first day of exposure to the desks, the researchers led a children’s workshop within each intervention class (including all children in the classroom), in which the various intervention components were described. This workshop concluded with all children, and their teacher and any teaching assistants, signing the social contract. During this visit, the researcher also discussed with the teacher their thoughts on a rotation plan for exposing children to the sit–stand desks and answered any remaining questions about the intervention.
The first phase of the qualitative work to examine the acceptability of the intervention centred around participants’ initial thoughts and experiences of using the sit–stand desks. This information was gathered from focus groups with the children and parents, and through interviews with the teachers conducted a few weeks after the installation of the sit–stand desks (phase 1). Further insights into all intervention components (the desks, training provision, nudging prompts, the social contract, researcher/practitioner support) were gathered towards the end of the intervention (phase 2) through a second set of interviews (with teachers) and focus groups (with children).
Sit–stand desks: initial thoughts before installation
Teachers
All of the teachers initially thought that the sit–stand desks, and the intervention in general, were positive:
They sounded really good, yeah, I thought they sounded like they’d suit my class really well.
Teacher, I4, WB
However, there was some apprehension regarding the size of the desks, not knowing how large the desks would be and the issues this would have in terms of safety in the classroom:
First thought was possibly about safety and how they would work within the classroom, thinking obviously about the size of them, would they be bigger than our normal size desk, would they be smaller . . .
Teacher, I2, SA
One teacher also had concerns regarding how the rotation system would work, but these soon subsided following the training and after a short period of time of using the desks:
I thought it would be good, I also was a bit worried that it would be a pain with the whole, when we were doing that timetable like, ooh, but actually I was wrong, they’ve been fine and the way that we can use them and stuff. Like I said, now, but also as a school in the future it will be really good.
Teacher, I1, SA
Children
One of the common themes stemming from the children’s focus groups was around what others from outside the classroom would think about the desks:
. . . I thought it was sick [having the desks] because if you came into your class and visitors come into your class, they might look at the stand-up tables and they might be thinking that this school likes to do lots of science experiments and do lots of different projects.
Child, I1, SA
Other themes included the perceived positive health benefits of using a standing desk:
I thought it would be good because, like, it’ll help us to sit straight and not always limp down.
Child, I3, WB
I was a bit confused because I didn’t know how sitting down was bad for you but then when you explained I was more ready.
Child, I4, WB
Finally, the benefit of changing behaviour was recognised, in particular that of boys fidgeting in the class:
When I first heard about them I was like, whoa, if we have these in our class it will like really change boys’ behaviours because some boys, not me, are fidgety so it would be good for them to stand up.
Child, I4, WB
Parents
The initial thoughts of parents about the sit–stand desks were mostly positive:
See I think it’s good because . . . you get up don’t you and walk about and want to walk about, kids can do this?
Parent, I3, WB
In addition, parents were pleasantly surprised by the size and quality of the sit–stand desks:
They’re perhaps a little bit bigger actually, you know, as in sturdier than what I imagined them to be.
Parent, I4, WB
Sit–stand desks: initial thoughts after installation and during the first weeks of use
Teachers
Having had the desks in the classrooms for a few weeks, teachers’ views on the desks remained positive and some of their initial anxieties about them did not materialise. One teacher was unsure whether or not the sit–stand desks would hinder their goal of improving handwriting and presentation; however, this was not found to be the case:
No, they’re better . . . the pessimistic side of me was . . . I was a bit, you know, as much as I thought ah brilliant, it will be a different way to explore teaching styles a different way to deal with these different things, the kids will enjoy it, I was thinking our big push is presentation and handwriting in school and I thought if they stood up, will that change, I thought it wouldn’t and actually I would say it certainly has not harmed handwriting and presentation?
Teacher, I1, SA
Another teacher first thought that the children would misbehave with the sit–stand desks, but found that this generally did not happen in practice:
You know, I thought if we’re doing something and they’re . . . will they be constantly putting it up and down? But they’ve been so good with them and, you know, a few teething problems at the beginning but barely anything and they were with the kids that I thought would be fussy and they were fine. You know, no, they were fine, so better.
Teacher, I1, SA
One teacher (I2, SA) reported many positive features of the desks, including the utility of the wheels and the design of the desks (‘Then we have got the wheels and we’ve got the locks on the wheels so we can move the children around. They can take their table and go and join another table if they need to for that work, so they are really useful to move around’); the height adjustment element (‘I also like the fact that they can stand up and they can raise the desk to the appropriate height which is a really nice thing.’); and the accessories with the desks (‘You have got pots so you’ve got places to put your pens, your paper, you’ve got places to put your whiteboards in . . . ’).
Children
Children provided much positive, as well as useful, feedback about the desks and how to improve them. Themes derived from the four focus groups were as follows.
I think they were very helpful because whenever I’m doing my work I’m always like leaning over and it’s always hurting my back. And also whenever I’m sitting down the screen is like upwards so I’m always like this [slouching] and it’s always hurting my body and I don’t like it. But with the stand-up desks I could rather stand up so I don’t crouch like this or I can stand or I can put it up so I don’t have to like sit down on my table like this but look up to the screen like that.
Child, I1, SA
I mean, because I’m quite a fiddler and with the tables you have your own space and I like this.
Child, I3, WB
I liked it because it was only for one person to sit on, for each table. Because normally, when we have to share a table, there’s not enough space.
Child, I2, SA
This is quite random, like it needs to be more stylish, like . . . diamonds and fur and then purpleness.
Child, I3, WB
I think that I really like the design of the top, we have like these little holes where we can put our rulers, our pencils, our whiteboard pens and our water bottles, our purple pen, we could put anything inside and we don’t have to go to the box where we keep our stuff and get it out, where it can just be in front of us.
Child, I1, SA
I dislike about it is that there’s chairs there, there’s stools there and that the brakes, because the brake sometimes can be hard to reach and they’re all at different angles, so I think if they’re both at the same place opposite each other it would be much more better.
Child, I1, SA
. . . they help improve your body posture and each person gets like a fair chance to go on them once a week.
Child, I4, WB
I prefer the like standing up on the tables because I like know that I’m doing the same amount of work and it’s like the same quality but I’m being more healthy whilst doing it.
Child, I4, WB
Yeah. And it also helped me in my presentation because you already know about Penny the Pencil. I think this might, if I get used to the curriculum I might even get up to gold and get about a hundred every single time because you don’t crouch and make your handwriting worse.
Child, I4, WB
I like it because, like, every time you don’t feel comfortable while sitting down, you could just stand up and then you might feel more comfortable.
Child, I3, WB
It’s like it’s a lot better than our tables because when we do our work, sometimes Miss says, sit down to do our work but then now with the stand-up-sit-down tables we can stand up more because I like working when I stand up especially when it’s stuff like art and stuff like that where you have to draw.
Child, I4, WB
Parents
Parents generally considered the sit–stand desks as positive additions to the classrooms, particularly in terms of their ability to promote movement in class:
So I think that’s, I mean the break time that they get is quite limited as well. When they go home they want to have a rest and so sit down a bit more. And then, you know, my son goes to mosque for an hour so he’s sitting down again, so I think it is good for them to be standing up for a while as well.
Parent, I3, WB
Keep themselves active and motivated and, you know, moving about slightly more.
Parent, I4, WB
Sit–stand desks: thoughts and reflections towards the end of the intervention (phase 2 data collection)
Teachers
Towards the end of the intervention, all the teachers expressed that the desks had become part of the classroom. They had thus overcome some of their original worries, which included whether or not the desks would cause a distraction:
Yeah, it, well for me I’m now used to them so before, I think for the first month or so, I was kind of looking at them as to how would they work, how well would they work with the children, would it just be a distraction for them, but now it’s, it’s kind of just the norm for the children, and we’re kind of, we’re used to them and every week when we rotate round we, we just do it steadily.
Teacher, I2, SA
Children
The children felt that having the desks in their classroom had been very positive, with key themes including changing behaviour for the better, having the option to stand and increases in personal space available:
I think of it as really good, because it changes your behaviour as well, so if you stand up and having a test, then you can move them around, rather than three people sitting on each table. It’s good that they have wheels and you can move around with them, and also it helps because when you’re standing up it makes less noise than pulling chairs, or then I go grab things, so it’s much more better than a normal table and chairs.
Child, I1, SA
When I first saw the desks, I thought it was all plain and boring, but now, 5 months later, now it’s really helpful because people who don’t like sitting down, the desk is really useful for them.
Child, I3, WB
Teachers’ training
The teachers reported that they were very pleased with the intervention training that they had received prior to the start of the study. One teacher reflected that having examples of desk use from previous schools had been really informative and that if it was not for the teachers’ training they would not have thought thoroughly about the groups and the fair rotation of the children:
Yeah, I think the fact that the things that you and [other researcher] already had in place from maybe previous schools or already set up was really good [examples of how other schools in previous studies have rotated children]. It gave us time to thrash out how we would do it fairly, how we would get all the children to have a go on the desks because that is something perhaps if you hadn’t of spoken to me about, I may have kept the same children on the desks for 4, 5 or 6 weeks without rotating round. It just meant that we were really structured in the way that we were using the desks and who was on them and everybody getting a turn.
Teacher, I1, SA
Professional development/project manual
The teachers reported that they generally found the professional development manual (intervention guide) helpful and informative. However, three of the four teachers thought that the document was lengthy and that they struggled to have the time to read it thoroughly. It was also generally felt that the training provided alone was sufficient for them to understand the intervention:
Yeah, it’s quite, ah, lengthy . . . I think that was literally on that thing, I did skim it but I did think it was quite lengthy, I think it’s just because those types of things, you can get quite a lot of those throughout the day for different things and it’s always this, you just don’t have time to read it all so I skimmed it.
Teacher, I1, SA
Nudging prompts
Teachers
Reactions to the nudge prompts were mixed. Three of the teachers reported not using the prompts, one teacher felt that the cards were not needed because the children were very engaged with the sit–stand desks and waited to use the cards should children’s interest and engagement decline:
I’ve not had to use them because I am saving them for when they need to get a bit motivated by it all.
Teacher, I1, SA
Another teacher reported that the cards were not used because they were seen as not necessary and a possible distraction:
No we haven’t . . . I felt they haven’t been needed and that they might have been a bit of a distraction. I feel like the children have a lot to remember in the day anyway. I just thought it would be another thing to be checking on and another thing that might get kind of lost, so we didn’t.
Teacher, I3, WB
Other reasons for not using the nudge cards included the perception that they were too childish and not suitable for children this age. However, one teacher felt that the cards were a good addition and gave ownership of the use of these to the standing leader/captain to encourage children to take ownership of the intervention:
We use those cards [nudge cards] and rotate those everyday which means that the children who are on the desk [standing desk], who have standing leader every day they can take ownership rather of it all rather than myself because it’s there for their desk really, it’s there for them.
Teacher, I2, SA
Children
None of the children initially knew what the nudging prompts were until reminded by the researcher. Children from two schools stated that they remembered the nudge prompts, but that these were used only for the first few weeks of having the desks:
. . . oh yeah! We had them at first it was right at the beginning, no one really liked them though [chorus of agreement] . . .
Child, I1, SA
The desk rotation plan
Teachers
The rotation system adopted by each teacher is discussed in detail Objective 9: assess intervention fidelity over the intervention period. Regarding acceptability of the rotation plan, all teachers ensured that their pupils were rotated around the class and that desk exposure was fair across all pupils. The teachers commented that sitting down with a researcher and gaining their help in devising a rotation plan was extremely useful, given their busy workload:
We did it about five or six times [rotation plan during training] in the different groups and then we got the groups that are the main groups but like I say then there’s that ability to then edit it in terms of what I’m teaching but still making sure that everyone gets what they’ve got. But I thought the actual sat down, because it’s one of those things that if I didn’t do it then, I just . . . not that I wouldn’t have done it, because I would have had to, but it’s just one of those things that if you do it there and then and sat down with researchers and just actually working out and making sure I’ve got it in there and then on Monday it was stuck up and they knew straightaway and it could start straightaway, it’s just one of those things that would have got further and further down the list. So, I found that really useful, just sat down talking with you guys and working out the school timetable and just getting that done, so that was probably the most use for me and the most use for the kids as well because they know where they are then.
Teacher, I2, SA
Children
In all schools, the children confirmed that rotation took place consistently throughout the duration of the study. The issues raised by the children centred around how teachers rotated children differently and how two teachers changed the rotation plan during the study. This theme will be discussed in more detail in Objective 9: assess intervention fidelity over the intervention period.
Fortnightly support with researchers/practitioners
Although fortnightly support from the researchers via either telephone or e-mail was planned, this rarely happened in practice. The teachers reported busy workloads, that they seldom checked their e-mails and/or did not have access to a telephone in their classrooms, making contact difficult. Importantly, though, the teachers did not consider that they needed regular contact during the intervention because they felt confident delivering it following the training received:
. . . its really tough to do, it would be like really hard for teachers to do. We are so busy I never really check my e-mails and a telephone conversation is tough because its teaching or its marking or its reports, but if you are getting in touch to come into school I and most teachers will follow up any messages left with reception.
Teacher, I1, SA
The 30-minute workshop with children
Both teachers and children felt that the workshops were useful and acceptable:
Yeah, I thought the talk with the children was fantastic, like honestly, because I said that. ‘I think you [researcher] should be a teacher’, like I thought they were all really engaged, I thought they understood well, I thought all the questions they asked were answered, it was pitched right at their level . . . I loved the examples of how they should use it and the examples given of good posture, bad posture, how the desks should be.
Teacher, I1, SA
I thought it helped, because if we just had them without anyone talking to us we’d be like, how do you get them up?
Child, I3, WB
A small number of children commented that they wanted an actual desk to practise with during the workshop. This applied to one class in which, due to timetabling restrictions, the workshop took place just before the desks were installed:
You could bring in one of them tables to show them how it works so it makes it a lot easier to understand for little children.
Child, I1, SA
Standing champion/leader
Teachers
The standing champion was employed in each of the schools differently, with one teacher forgetting that there should have been a standing champion to motivate children to stand while using the sit–stand desks:
. . . completely forgot about the standing captain!
Teacher, I1, SA
Another teacher rarely used this strategy because it was felt that it was not needed and would have been a distraction:
No we haven’t . . . I felt they haven’t been needed and that they might have been a bit of a distraction. I feel like the children have a lot to remember in the day anyway. I just thought it would be another thing to be checking on and another thing that might get kind or lost, so we didn’t.
Teacher, I3, WB
One teacher drew on the standing champion to encourage children to take ownership and lead the group’s use of the sit–stand desks:
I wanted the children to think I am in charge today everyone using the desks should be using them to stand not to sit down all day, and also to ensure that everyone’s behaviour is good while on the desks. Like I have said I wanted the children to have ownership of this and the standing champion was part of this.
Teacher, I2, SA
The fourth teacher incorporated the standing champion role at the beginning, but expressed that the incentive award proposed for this role was against the school policy:
You know and it just kind of fell a little bit and we’re not really supposed to like offer prizes and things at school . . . That’s sort of the school policy so there was no prize for it so they weren’t as bothered by it.
Teacher, I4, WB
Children
Children’s perspectives of the standing champion element of the intervention differed across schools and, interestingly, differed from the perspectives of the teachers. Children from one school explained that the standing champion would be someone who would inform the teacher about the behaviour of the other children and the use of the sit–stand desks, which was deemed to be positive, as the champion/leader would receive a prize. However, this occurred only during the first few weeks:
A standing champion was actually so good, it was tempting for you to keep your behaviour good because when it was the end of the day and Miss makes a decision who was the champion leader, she gives a prize out to them, so I think it’s really good . . . little gifts, we have a box which she buys toys and then you go and then pick whichever you want . . . It kind of stopped like a couple of months ago.
Child, I1, SA
As for the other class, one child again explained how the teacher implemented the standing champion role, which was awarded daily, instead of weekly, and how it was documented on the class display who had used the desks that day or not. However, as in the other class, this was not sustained:
No, he was like told that he was like in charge of it. There was a different captain every day . . . We had like this sheet of paper next to the window where at the end of the day we have to take it to say who has been on it and if a person hasn’t been on it we just write their name down . . . it stopped a long time probably near the beginning.
Child, I2, SA
Group contract
The group social contract applied by the researchers at the end of the children’s workshop was an aspect that all four teachers praised, enjoyed and used. The teachers reported laminating the contract and displaying it in the classroom as a reminder to the children that they had agreed to use the desks appropriately:
. . . simple and yet great idea, laminated and put it up on the wall. Children this age like these kind of things, and it was great that those who did not take part in the measurement aspects had the chance to have a go at this and they themselves felt they were part of the study even though they did not participate in the measurements.
Teacher, I2, SA
Overview of the trial: positives, negatives and things to change for the future
At the end of the phase 2 interviews and focus groups, the teachers and children were asked for their thoughts about the positive and negative features of the trial and what they would like to change in the future. Themes and example quotations are reported online in Report Supplementary Material 3. Reported in Table 21 are the ratings of acceptability for the trial’s procedures, measures and intervention components. There were no overall differences in the acceptability of the trial or intervention between different ethnic groups.
| Trial procedures, measures and intervention components | Key findings from process evaluation | Acceptability rating | Suggested improvements/changes |
|---|---|---|---|
| Recruitment |
|
A |
|
| Randomisation |
|
A |
|
| activPAL |
|
A/R |
|
| ActiGraph |
|
A |
|
| RVIP |
|
N | |
| Strengths and Difficulties Questionnaire completed by teachers |
|
R |
|
| Health-related resource use questionnaire completed by parents |
|
R |
|
| Sit–stand desks |
|
A | |
| Teacher training |
|
A | |
| Professional development manual |
|
R |
|
| Nudging prompts |
|
N |
|
| Desk rotation |
|
A |
|
| Fortnightly support from researchers/practitioners |
|
N | |
| Children’s workshops |
|
A | |
| Standing champion |
|
N | |
| Group contract |
|
A |
Objective 8: monitor any adverse effects, such as musculoskeletal discomfort and/or disruption to the classroom or learning, to inform the design of a full trial and minimise or eliminate any such effects
Musculoskeletal discomfort
There were no reports of any musculoskeletal discomfort when using the sit–stand desks in the focus groups with the children. Similarly, the results from the child-reported Body Comfort Survey (see Table 13) revealed an increase in the proportion of pupils (from both groups) reporting that they felt better at their desks at follow-up.
Posture
The researchers observed each of the four intervention classes twice, once in the spring term and once in the summer term. A total of 76 10-miunte observations occurred during the observation periods and posture was recorded every minute during each 10-minute observation. Of the 76 observations, 46 (60.5%) were of boys and 30 (39.5%) were of girls. A total of 56 observations (73.7%) took place in the spring and 20 (26.3%) took place in the summer. A complete set of observation data was not achieved for 28 (36.8%) children, due to their movement away from their desk during the observation period. Participants’ postures at 1-minute intervals were therefore examined; this led to 661 data points [boys n = 390 (59%); girls n = 231 (41%)].
Thirty-six per cent of the classroom observations recorded children standing and 64% recorded children sitting at the sit–stand desks. Children were more likely to exhibit unfavourable postures of neck flexion (> 20°) and neck extension (> 20°) when seated at the desks than when standing. A high proportion of children rested their elbows on the desks while working (48%) and there were no apparent differences in this posture between those seated and those standing.
Classroom disruption and pupil behaviour
The teachers reported minimal disruption to classroom and pupil behaviour resulting from the introduction of the desks. Any disruptions that did occur happened during the first few days of using the desks, but quickly settled down. One teacher explained:
Only really the first group for the first day or so and then once they had realised obviously to not to just play with them, I think more often than not it wasn’t necessarily the standing up, it was more lifting of the desk, putting it down, lifting it up.
Teacher, I2, SA
Objective 9: assess intervention fidelity over the intervention period
We report intervention fidelity against the framework of Hasson,196 and fidelity (whether or not the intervention was implemented as planned), dose (frequency and duration of the intervention), reach and contextual factors are reported below. Participant responsiveness to the intervention (e.g. acceptability) is discussed in detail above (see Objective 7: assess the acceptability of the intervention to teachers, children and parents).
Fidelity: whether or not the intervention was implemented as planned
During the observation visits, the researchers documented whether or not the different intervention components (sit–stand desks being used, rotation plan in place, grouping of children as planned, standing champion, social contract, nudge cards) were taking place. A summary of the fidelity results are reported in Table 22.
| School (season) | Sit–stand desks being useda | Rotation plan in placeb | Grouping of children as plannedc | Standing championd | Social contracte | Nudge cardsf |
|---|---|---|---|---|---|---|
| I01 (spring) | Yes | Yes: per protocol, one group of six per half day – displayed in classroom | Yes | Yes: for being well behaved and for using the sit–stand desk regularly to stand, champion also received a physical prize (toy) | Displayed in the classroom: not referred to | Yes: per protocol |
| I02 (spring) | Yes | Yes: one group of six weekly – displayed in classroom | Yes | Yes: as per protocol one child a week to ensure that the rotation plan and groups are correct and make sure people are using desks correctly and safely | Displayed in the classroom: not referred to | Yes: not by protocol – standing champion given a card each day |
| I03 (spring) | Yes | Yes: one group of six daily – displayed in classroom (teacher changed to weekly after 5 weeks) | Yes | No | Not displayed in classroom | No |
| I04 (spring) | Yes | Yes: one group of six daily – displayed in classroom | Yes | Yes: as per protocol one child a week to ensure that the rotation plan and groups are correct and make sure people are using desks correctly and safely | Displayed in the classroom: not referred to | No |
| I01 (summer) | Yes: stools have now been removed, located in the corner of the classroom where children can access them | Yes: no change from protocol | Yes | No | Displayed in the classroom: not referred to | No |
| I02 (summer) | Yes | Yes: no change from spring | Yes | Yes: same as spring | Displayed in the classroom: not referred to | No |
| I03 (summer) | Partially: location of desks moved from spring assessment and stools have been removed completely | Yes: different from summer – first come first served and teacher preference of no rotation | No: it is first come first served | No | Not displayed in classroom | No |
| I04 (summer) | Yes | Yes: one group of six weekly – displayed in classroom | Yes | No | Displayed in the classroom: not referred to | No |
Sit–stand desk use in the classroom
During the spring and summer terms, it was clear from the classroom observations, conversations with children, and from the phase 1 interviews and focus groups that all sit–stand desks were being used across all intervention classes. However, the use of the desks did change during the trial for intervention schools 1 and 3. In intervention school 1, the teacher decided to remove the stools from the sit–stand desks, and did so before the start of every school day and again before lessons began after lunch. Stools were stacked up in the corner of the classroom. The children had the option of using the stools should they so choose, but they were required to collect them. The teacher removed the stools to encourage children to stand:
I noticed they were sitting more and more, you know, I just moved um, put them in the corner, because after all it’s easy it’s just take them away [remove stools, place in the corner] because if there’s a chair there, you’re going to sit down. If there’s not, then you don’t so.
The children viewed this to be acceptable, with one explaining:
I think it’s better if the chairs are in the corner, because when we got them at first we stood up a lot but after a while everyone just sat down, now Miss has moved them we forget to even sit down spend all lesson standing and no one cares . . . well I don’t care!
Child, I1, SA
In intervention school 3, the teacher who was originally recruited to the trial was absent for the first 3 months of the intervention and was absent for the original training. On their return from leave, this teacher observed how the stools were being used and decided to remove them completely:
When I first arrived in the class I noticed that they were using the desks, but mostly sitting, they were on a rota basis, and some children wanted to use a desk to stand but would have to wait a week to have a go, so I removed the stools and reminded the children that if they wanted to sit down, they already had a place in class to sit, the standing desks were there to stand-up on.
Teacher, I3, WB
Rotation plan and grouping of children (intervention dose)
Only one school implemented the rotation system recommended during the initial training and outlined in the intervention protocol (i.e. of two groups of six children using the sit–stand desks every day). Despite this, all schools devised a rotation plan and had it clearly displayed. The two predominantly white British schools had one group of six children use the sit–stand desks daily. The final school opted to have one group of six children use the sit–stand desks per week. Reasons given for not following the protocol included that the twice-a-day rotation was not suited to the dynamics of the particular classroom and a preference for children to manage the rotation themselves:
I don’t think rotating them twice in a day is really feasible within my class the way we run things, with different sets for different classes.
Teacher, I4, WB
. . . they knew where the rota was, they knew when to check it, they knew when they were changing and it’s been absolutely fine for my class to do that themselves and independently, it’s what I promote.
Teacher, I3, SA
One teacher who did follow the twice-daily rotation protocol reported that she had no issues in doing this, but was thankful for the intervention training:
Yeah, it’s not a problem at all, it’s really easy, quick, simple to do rotate . . . But I thought the actual sat down [training], because it’s one of those things that if I didn’t do it then, I just . . . not that I wouldn’t have done it, because I would have had to, but it’s just one of those things that if you do it there and then and sat down with researchers and just actually working out and making sure I’ve got it in there and then on Monday it was stuck up and they knew straightaway and it could start straightaway.
Teacher, I2, SA
Standing champion
Three schools reported to implement a standing champion in the first term, but during the final term only one school had maintained this role. The standing champion role was sometimes used as a reward for children who had been using desks well and/or who had been well behaved. Standing champions were employed to ensure that the rotation plan and groups were correct and that children were using the sit–stand desks correctly and safely.
Social contract
Three of the four classes clearly displayed the social contract signed by all children, with this tending to be displayed alongside the rotation plan and groups. However, during the focus groups, four children expressed that they had no memory of the teachers referring to the social contract:
I thought that it never existed [response to discussion of social contracts], I think we all forgot that it did exist, though.
Child, I1, SA
Nudge cards
Nudge cards were inconsistently used in the intervention. All schools tried using the cards but reports from both the teachers and children indicated that they were of limited value and were thus discontinued. None of the schools used the nudge cards on the days of the observations, in either the spring or summer terms.
Reach
It was clear from the classroom observations and qualitative research that all children had access to the sit–stand desks throughout the trial and that teachers tried to fairly expose children to the desks.
Contextual influences
From the interviews with the teachers and senior members of staff towards the end of the intervention, it was evident that the political, organisational and economic context of the school had no impact on the fidelity of the intervention. The participating teachers were not negatively affected by an increased workload relating to the trial and from the head teachers’ perspectives; two of the head teachers had deliberately selected teachers to participate who were efficient in managing their workloads:
. . . [teacher] is super at managing her time and hence why I agreed it would work with [teacher], other members of staff I would have said no it wouldn’t have been and I think then it would have been a problem.
Head teacher, I1, SA
All schools were fully committed to the study and had no internal organisational or political constraints or issues that had an impact on the fidelity of the intervention. One potential barrier to the use of the desks was seen to be cost had schools had to purchase them themselves:
No there’s been no economical consequences, obviously because we’ve not paid for anything. If we did, then looking at the budget, that wouldn’t be a possibility.
Head teacher, I2, SA
In conclusion, the four intervention schools and head teachers welcomed their involvement in the trial and ensured that the teachers and pupils had full support to participate fully in the intervention.
Chapter 6 Discussion
The need for effective interventions in the UK targeting the primary prevention of chronic diseases by encouraging healthy lifestyles in children has been highlighted in a number of recent reports. For example, the Chief Medical Officer for England’s 2012 annual report, Our Children Deserve Better: Prevention Pays198 and the UK’s Childhood Obesity: A Plan for Action199 highlight the importance of the school environment in promoting healthy behaviours. Sedentary behaviour is highly prevalent in children28 and is adversely associated with adiposity and weight gain, and clustered metabolic risk. 13,200 As sedentary behaviours track from childhood into adulthood,15,40 reducing children’s sitting time could reduce the risk of numerous chronic conditions associated with prolonged sitting in adulthood. 163 In the present study, at baseline our combined sample (intervention and control participants) spent, on average, 8.75 hours per day sitting, accounting for 63% of their waking hours. Over two-thirds (67%) of class time was spent sitting, confirming this environment as a suitable setting for behaviour change.
The purpose of this study was to undertake a pilot cluster RCT to test the feasibility of conducting and evaluating a school-based sit–stand desk intervention to reduce children’s sedentary behaviour. As a consequence, the implications of this study do not, at this stage, relate to practice, but to the feasibility and design of a follow-on full-scale cluster RCT. Study findings are discussed below in relation to the research objectives. When appropriate, the findings are compared with other studies and the lessons learnt from this study inform suggestions for a future trial.
Trial feasibility-related outcomes (objectives 1–4)
Objective 1: establish and refine a recruitment strategy for schools and pupils
A total of 24 eligible schools were approached for recruitment into this pilot study and the target number of eight schools consented to take part (recruitment rate = 33%). This recruitment rate is similar to recruitment rates seen in other primary school-based interventions located in this region201 and elsewhere in England. 202 The eight recruited schools were located predominantly in urban areas throughout the Bradford metropolitan district. Across the eight schools, an average of 17.1% of pupils were eligible for free school meals; this figure matches the 17.2% of children across all schools in Bradford eligible for free school meals, suggesting that the recruited schools were largely representative of schools within this area. Similarly, the proportion of children eligible for free school meals from the 12 schools that declined to participate was 17.4%. In England, in 2017 (the time of the intervention), 14.8% of children were eligible for free school meals,113 demonstrating the slightly higher levels of deprivation within this study setting.
The recruited schools tended to have a higher proportion of children whose first language was not English (51.4%) than schools that declined to participate (38.4%), and schools in Bradford overall (42.3%). 113 In England, in 2017, 20.6% of primary school children were registered as having English not as their first language, highlighting a greater ethnic diversity in the study sample and Bradford population than in national-level data. 113 Of interest, the schools opting into the study were more likely to contain a higher proportion of South Asian children, with schools declining to participate being more likely to contain white British children (8 out of the 12 declined schools). This finding highlights that the present study was effective in recruiting a diverse range of schools into the study, in terms of the ethnic distribution of their pupils; however, additional strategies to recruit schools containing a higher proportion of white British children may need to be incorporated into a full trial.
Within the participating schools, 75% (n = 176) of eligible pupils provided parental consent and written assent to participate in the evaluation measures, which exceeded our target minimum sample size of 120 participants. This recruitment rate is higher than that seen in a recent RCT (59%) examining the effectiveness of a healthy lifestyle programme [the West Midlands ActiVe lifestyle and healthy Eating in School (WAVES) children study] conducted in primary schools from the West Midlands,202 and similar to that reported (79%) in a primary school-based sit–stand desk intervention in the USA. 203 Overall, this pilot RCT has demonstrated the feasibility of our recruitment strategy for both schools and children into the Stand Out in Class study.
Objective 2: determine attrition in the trial (schools and children)
All eight participating schools completed the trial, leading to a 100% school retention rate. At 7 months’ follow-up, the overall retention rate of participating children was 97% (96% from the control group and 98% from the intervention group). Fifty per cent of children not returning for the follow-up measures had moved away from the area during the study and, hence, changed schools.
Objective 3: determine completion rates for outcome measures (and whether or not these are sufficiently high to provide accurate data in a full trial)
Completion rates for the outcome measures ranged from 63% to 97%. The highest completion rates were seen for the anthropometric (94%) and questionnaire-based measures (97%), with the completion rates for these measures being comparable to those reported in the Active for Life Year 5 cluster RCT, a school-based intervention targeting physical activity, sedentary behaviour and fruit and vegetable consumption in children. 119 The lowest completion rate (63%) was observed for the activPAL, with a number of children not providing valid data from this device across the two measurement periods. The proportion of children providing valid activPAL data in the present study is higher than that observed previously in a similar group of children29 and identical to that observed in a recent sit–stand desk RCT in Belgian children. 204 These numbers are lower, however, than those observed (> 90% compliance) in other (non-RCT) classroom-based sit–stand desk interventions in which the activPAL was the primary outcome. 68,205
In comparison with the activPAL, rates of compliance with the wear time criteria for the ActiGraph were higher (83%) when the same wear time criteria were applied (≥ 8 hours on at least 1 weekday). In the Active for Life Year 5 study, 60% of participants complied with their ActiGraph wear time criteria (≥ 8 hours of wear on at least 3 days206). 119 Applying the same criteria to the ActiGraph data in the present study would have resulted in 68% of our sample providing valid data at baseline and follow-up, confirming the feasibility of this device. The acceptability of the activPAL as the proposed primary outcome measure for a definitive trial is discussed further in Objective 6: assess the acceptability of measurement instruments to teachers, children, parents and guardians, including the activPAL inclinometer as the tool for the measurement of the primary outcome. This pilot RCT has highlighted the need for further research to examine how wear protocols can be improved for the activPAL to increase compliance. Aside from this measure, however, completion rates for the remaining measures examined herein were sufficiently high to provide accurate data in a full trial.
Objective 4: assess whether or not there are any differences in trial recruitment, retention and acceptability between ethnic groups
There were no observed differences in trial recruitment, retention or compliance rates between South Asian and white British children. Ninety-eight per cent of white British and South Asian children provided parental consent and written assent to participate in the trial evaluation, and retention rates of 98% were observed in both ethnic groups. Sixty-five per cent of white British children and 68% of South Asian children provided valid activPAL data, whereas 87% and 84% of children within these ethnic groups provided valid ActiGraph data, respectively. No themes emerged during the process evaluation to indicate differences in the acceptability of the trial or intervention between different ethnic groups.
Lessons learnt from the process evaluation (addressing objectives 1 and 5–9)
Table 21 summarises the key lessons learnt regarding the acceptability of the procedures adopted, the measurement tools and the Stand Out in Class intervention, from our detailed process evaluation. Overall, the process evaluation offered a number of positive insights from teachers, children and parents about the recruitment strategy, the acceptability of randomisation, measurement tools and intervention, along with the fidelity of the intervention and its impact on day-to-day classroom management.
Objective 1: establish and refine a recruitment strategy for schools and pupils
Teachers, children and parents all considered the recruitment approach adopted to be appropriate and teachers liked how the study was explained to children by the research team during classroom visits. As highlighted in Trial feasibility-related outcomes (objectives 1–4), Objective 1: establish and refine a recruitment strategy for schools and pupils, 75% of eligible pupils from the participating schools provided parental consent to participate in the trial evaluation. Informal conversations with parents who did not provide informed consent for their child to participate revealed that the most common reason for this was that parents were unaware of the study, through not receiving or not reading the study information sheet sent home with their children. A future trial should explore with schools additional options to inform parents and guardians about the study, such as inclusion of a brief mention of an up and coming study in electronic school newsletters, for example, or via schools’ social media platforms.
Objective 5: assess the acceptability of randomisation to schools
The process of randomisation was regarded as acceptable and fair by teachers, children and parents, and although participants from the control schools expressed disappointment at being randomised into the control arm, participants understood why a control condition was needed. Control arm teachers stated that participating in the study was still a positive experience for their class.
Objective 6: assess the acceptability of measurement instruments to teachers, children, parents and guardians, including the activPAL inclinometer as the tool for the measurement of the primary outcome
The majority of the measurement instruments used within this pilot trial were deemed to be acceptable by teachers, children and parents. Teachers reported that some children experienced irritation on their legs caused by the medical dressing used to attach the activPAL; however, they reported that this occurred in a small minority of children and did not feel that it was a big issue. However, some children also reported that the medical dressing was ‘problematic’ and this was echoed by some parents. Concerns regarding the attachment of the activPALs are reflected in the compliance data reported in Trial feasibility related outcomes (objectives 1–4), Objective 3: determine completion rates for outcome measures (and whether or not those are sufficiently high to provide accurate data in a full trial. Children reported generally preferring the ActiGraph and this was reflected by the higher compliance data seen for this device.
Further research should examine different attachment options for the activPAL in children. In the present study, we adopted a 24-hour wear protocol, with the anticipation that the hypoallergenic Hypafix dressing would stay on the skin for a number of days, and not require children to frequently take the device (and dressing) on and off. This approach has been used successfully in a recent sit–stand desk intervention with 11-year-olds. 68 Other researchers, however, have enclosed the activPAL in a small pocket in an adjustable elasticised belt that is worn at the mid-anterior position of the thigh throughout waking hours only and removed for any water-based activities. 38 This attachment option resulted in high compliance rates (> 90%) in a recent sit–stand desk intervention in 10- to 11-year-olds and has been used successfully in a cross-sectional study with > 200 8- to 11-year-olds. 150,205
Other researchers have recently used the ActiGraph placed on the anterior aspect of the thigh attached using an elasticised belt as the primary outcome measure in recent sit–stand desk interventions in schools. 66,207 When mounted on the thigh, the ActiGraph inclinometer algorithm has been found to be a valid and reliable method of measuring sitting and standing postures. 208,209 The utility of the ActiGraph worn on the thigh and the activPAL placed within an elasticised belt should be explored in a sample of primary school children within the UK, to inform a definitive trial.
Children reported that the RVIP task was difficult and this is reflected by the relatively low levels of accuracy recorded on this test. This test has previously been used in slightly older samples of school children (12- to 13-year-olds),101 and may, therefore, not be appropriate for younger age groups. Some parents reported the health-related resource use questionnaire burdensome to complete and this is reflected in the low completion rate for this measure. Future studies should investigate more appropriate methods of obtaining this information from parents to inform economic evaluations.
Objective 7: assess the acceptability of the intervention to teachers, children, parents and guardians
Initial thoughts about sit–stand desks being installed within classrooms were generally very positive by teachers, children and parents. After a few weeks of the desks being installed, teachers’ views of the intervention remained positive and any initial apprehensions about the desks (including any potential negative impact on handwriting and general behaviour) were not experienced. Towards the end of the intervention, teachers commented on how the desks were now regarded as part of the norm within their classrooms. The overall design and features of the desks, including their wheels, which enabled them to be moved easily, were highlighted as positives by teachers. These comments about the desks fitting in within the classroom and their portability are in agreement with interview data collected from a high school teacher in the USA following installation of six LearnFit desks in their classroom over a 9-week period. 210
Similar to the teachers, children were very positive about the desks throughout the intervention. A number highlighted that their comfort levels when working at the desks improved and some reported feeling healthier by standing up. A number of the children reported that they liked having their own space and they liked having the option to sit or stand when using the desks. These comments about space and having the option to sit or stand mirror those from a sample of 11- to 14-year-olds from a US middle school exposed to six LearnFit desks over 9 weeks. 210 Some children in the present study reported that they felt that the desks improved behaviour within the classroom. This is something that has been reported previously by parents interviewed following a pilot sit–stand desk intervention in a primary school in Texas. 58 In the Texas study, 61% of parents interviewed reported that they felt that the sit–stand desk had a positive impact on their child’s behaviour at school. In the present study, parents were also positive about the intervention, commenting that they liked how the desks promoted movement in class.
Teachers found the training component of the intervention very helpful and found the examples of how they could rotate children around in their class to ensure equal exposure to the desks useful. The project manual provided to teachers after the training, and the use of the nudge cards, were not deemed necessary, however, by the majority of teachers, as they felt confident to deliver the intervention after the training session. Overall, findings from the process evaluation suggest that the Stand Out in Class intervention is acceptable to teachers, children and parents.
Objective 8: monitor any adverse effects, such as musculoskeletal discomfort and/or disruption to the classroom and learning, to inform the design of a full trial and minimise or eliminate any such effects
There were no reports of any adverse effects associated with the intervention in terms of musculoskeletal discomfort reported by children, or disruption to the classroom reported by teachers or children. These findings agree with others who have concluded that sit–stand desks can be introduced into the classroom environment without having a negative impact on student learning, behaviour or musculoskeletal comfort, and without causing classroom disruption. 65,67,205,207,210 Indeed, some evidence suggests that sit–stand desks can have a positive impact on musculoskeletal comfort, with improvements in comfort ratings being observed in children following sit–stand desk use. 63,207
Objective 9: assess intervention fidelity over the intervention period
Limited evidence currently exists on the fidelity of sit–stand desk interventions within the classroom environment. 210 We undertook two classroom observations in each intervention school, one in the spring term and one in the summer term, to examine the fidelity of the Stand Out in Class intervention. It was clear from all observations that all sit–stand desks were being used across all intervention classes. However, the intervention differed slightly across intervention schools as the trial progressed. Two teachers decided to move the provided stools away from the desks to encourage children to stand at the desks, whereas in the remaining intervention schools, the stools were kept with the desks. Throughout the study the intervention teachers also modified how they rotated children around the class to be exposed to the desks. Only one teacher used the per-protocol rotation plan recommended during the training, which involved rotating groups of children at half-daily intervals; two teachers rotated children on a daily basis, so each group of children was exposed to the desks for 1 day per week; and one teacher rotated children on a weekly basis. Following contact with the research team about this rotation plan, this teacher modified it and agreed to rotate the children more frequently. Despite differences in how children were exposed to the desks, it was clear from the classroom observations and qualitative research with teachers and children that all children had access to the sit–stand desks throughout the trial, and all teachers tried to ensure that desk exposure was fair across their class. Although we observed some deviations from the intervention protocol, the observation that teachers started to utilise the desks in their own way suggests that the intervention may have real-world applicability and feasibility.
The addition of more sit–stand desks in classrooms, such as making up 50% of classroom furniture, as suggested elsewhere,210 could be a feasible solution for a future trial. This would probably make it easier for teachers to rotate children around for desk exposure and also, importantly, increase the dose of the intervention. Overall, in the present study, all intervention schools were fully committed to the trial, and participating teachers had the full support of head teachers and senior staff.
Preliminary estimates of intervention effectiveness and sample size calculation for a full trial
Although the main aim of this pilot RCT was to establish key information around recruitment, acceptability and feasibility of the Stand Out in Class intervention, along with the acceptability and feasibility of a range of outcome measures, preliminary estimates of the effectiveness of the intervention on the proposed primary outcome were examined to determine whether or not the intervention shows a positive direction of effect. As the study was not powered to determine effectiveness, these finding should be treated as preliminary.
Objective 10: derive preliminary estimates of the effect of the intervention on children’s total daily sitting time, physical activity, indicators of health (markers of adiposity and blood pressure), cognitive function, and academic performance, engagement and behaviour
A weighted linear regression model, after adjustment for mean baseline weekday sitting time and mean wear time across the measurement time points, revealed that children in the intervention group spent less time sitting than children in the control group did at follow-up. The mean difference (weighted by school size) in change in sitting time over the intervention period was –30.6 minutes per day (95% CI –56.42 to –4.84 minutes per day) between groups. This is a greater reduction in daily sitting time than that observed in a recent sit–stand desk RCT conducted in primary school children in Belgium, in which, relative to the control group, the intervention group experienced a reduction in daily sitting of –13.5 minutes per day at 8–12 weeks’ follow-up. 204 In this study, however, only three sit–stand desks were placed in the classrooms of the intervention schools, which probably explains the reduced effect of the intervention on total daily sitting time. Based on the current findings, and those of Verloigne et al. ,204 it would be logical to suggest that adding more sit–stand desks to the classroom environment, and thus increasing the exposure and ‘dose’ of the intervention, would probably result in even greater reductions in daily sitting time. If examined over a longer time period, with sufficient power, such a study would fill an important gap in the literature by investigating the impact of this intervention on markers of health in children, as discussed in further detail below.
To date, most sit–stand desk interventions in primary schools have reported within-group differences in sitting time over the intervention period, with reductions in mean weekday sitting times ranging from 12 minutes per day to 80 minutes per day in intervention groups. 29,67,68,205,207 Of the few studies that have drawn comparisons between changes in weekday sitting times between intervention and control participants, changes between groups have ranged from +19 to –66 minutes per day. 68,204,205 Although preliminary, this study adds to the very limited evidence base204 from a cluster RCT on the potential impact of a classroom sit–stand desk intervention on changes in weekday sitting time.
No data currently exist in children to inform the magnitude of a reduction in sitting time needed to bring about changes in health markers. Although such optimum reductions in sedentary time in children need to be established to inform public health messaging, data from adults have demonstrated that reallocating just 30 minutes of sedentary time per day to light movement is associated with a 2–4% improvement in cardiometabolic biomarkers. 114 An earlier meta-analysis of RCTs and non-RCTs, examining sedentary behaviour interventions delivered in the school or home environment, reported an overall decrease in children’s sedentary behaviour of 18 minutes per day. 211 The preliminary findings from this study hold promise, therefore, and support the need for further RCTs examining the impact of sit–stand desks in the classroom environment.
Preliminary findings from this study revealed that reductions in sitting and increases in physical activity occurred in both groups after school, suggesting no evidence of compensatory behaviours occurring within the intervention group outside school hours, as reported elsewhere. 67,68 However, these findings should be treated with caution due to the confounding variable of measurement season (see Strengths and limitations).
There were no observed changes in measures of body composition or blood pressure within this study. However, significant reductions in BMI percentile have been observed in a sample of 7- to 9-year-olds exposed to sit–stand desks over a 2-year period in three US primary schools. 203 In the same study, non-significant reductions in BMI percentile were also observed in children exposed to the sit–stand desks for 1 year. In this US study, all standard (seated) desks were replaced with sit–stand desks, suggesting that the intervention ‘dose’ was greater than that observed in the present study. However, as in the present study, stools were provided with the sit–stand desks and children could choose whether to sit or stand throughout their lessons. Sitting time was not directly measured in this study, therefore it is unclear by how much sitting time was reduced over the 1- and 2-year periods. This evidence, however, suggests that such a treatment effect of this simple intervention (i.e. providing children with more opportunities to stand while learning) may be seen over a longer exposure period, with a greater intervention dose, and this should be examined in a definitive trial.
Improvements in cognitive function were seen in both groups, suggestive of a potential learning effect of the cognitive test battery. To date, findings of the impact of sit–stand desks on cognitive function are inconclusive, with preliminary (non-RCT) evidence suggesting that sit–stand desks have a positive impact on some measures of cognitive function, whereas other evidence suggests no effect. 66,212 No evidence currently exists, however, that suggests that sit–stand desks have a negative impact on cognitive function.
Pupil behaviour conduct in the classroom and interactions with fellow pupils were examined using the teacher-reported Strengths and Difficulties Questionnaire. Preliminary observations from this measure indicated that the intervention group generally had reduced antisocial and hyperactive behaviours and increased self-control than the control group at follow-up. Interview data from teachers from US primary and high schools have highlighted observed improvements in behaviour when children use sit–stand desks,58,210 with teachers reporting that student attention and engagement increased during standing.
In this study, we demonstrated the feasibility of collecting academic progress data for maths, reading and writing from schools. However, as data relating to pupils’ progress across these key subject areas are not a requirement of the national curriculum for schools to collect, the lack of standardisation of this measure across participating schools made the interpretation of these data difficult, as we used routine data collected by each school to avoid placing additional burden on schools. When planning further research in this area, consideration in partnership with head teachers and teachers/assessment co-ordinators via PPI should be given to identify appropriate national curriculum-related/standard assessments routinely used by schools, which will enable direct comparisons between participating schools. In the absence of consensus over such measures, proxies of academic progress, such as attendance and/or in-class behaviour data, which can be measured consistently across schools, should be identified in collaboration with head teachers/teachers. Improvements in these measures would also be beneficial to inform an economic evaluation from an education perspective.
Objective 11: estimate the standard deviation of the primary outcome to inform a sample size calculation for a full randomised controlled trial
In this pilot study, a pooled SD of 95 minutes per day was observed in change in school day (weekday) sitting time, the proposed primary outcome in a definitive trial. Using this value, the sample size for a full trial was calculated to be 1276 participants from 58 clusters in total (638 participants and 29 clusters per arm). The sample size incorporates a 25% inflation to allow for losses to follow-up and missing data, along with the addition of one extra school in each arm to allow for whole-cluster dropout.
Lessons learnt from the preliminary economic evaluation
Objective 12: determine availability and completeness of economic data and conduct a preliminary assessment of potential cost-effectiveness
This study has demonstrated that it is feasible to conduct an economic evaluation alongside a cluster RCT of a sit–stand desk intervention within the classroom environment. Our preliminary analysis suggested little evidence of an effect in within-trial or extrapolated economic analyses. Based on current evidence using the most plausible scenarios, the intervention is unlikely to be cost-effective over a 30-year time horizon at a threshold of £30,000 per QALY. However, the Stand Out in Class intervention is typical of broader public health interventions, in that its comparatively small cost and QALY gain result in an ICER that is very sensitive to small changes in intervention cost and effectiveness. 213
Comments on trial design and implementation: suggestions for improvements for a definitive trial
Cluster randomisation appears to have been ineffective in balancing ethnic characteristics between trial arms despite stratification of schools on ethnic characteristics with the intention to achieve ethnic balance. Methods to improve ethnic balance and, therefore, improve precision in estimation of any hypothesised variation in treatment effect across ethnic groups should be considered in any future trial. Incorporation of a range of schools with different deprivation profiles would also add to understanding of which groups benefit most from any such intervention and could be used to inform a distributional cost-effectiveness analysis. No attempt was made to control for ethnic imbalance in all analysis of treatment effect, with multiple imputation only rebalancing missing data within known ethnic categories.
The trial treatment ‘dose’ should also be considered in the light of comments regarding low compliance with the trial protocol rotation plan. If possible, more than six sit–stand desks should be incorporated into the classroom environment to ascertain whether or not the observed treatment effect follows a dose–response relationship.
Areas for future work
We did not investigate the sensitivity of our conclusions to variation in the cost of sit–stand desks and whether or not this was viewed as an incremental cost over replacement of existing worn-out school furniture like for like. There is considerable variation in the cost of standing desks between different model designs and uncertainty in how best to incorporate any costs into economic modelling over their expected time horizon. A recent research briefing suggested that the unit price of a classroom standing desk varies from £25 for a basic model to > £600 for a sophisticated model. 214 How accounting costs are considered is likely to have an impact on cost-effectiveness judgements. There is a valid query of the viability of individual schools being able to cover the high upfront cost of a standing desk intervention, without additional cost of financing over several years. The same research briefing indicates an approximate cost of £270,000 to equip a whole school with standing desks costing £300 each, equipping 30 classrooms, each capable of holding 30 students per class. 214
As costing was conducted as a static classroom in this analysis, with no account of periods of non-use, costing assumptions at the school level would require change, given the current structure of UK primary school teaching, with asset usage being somewhat dynamic, unlike, for example, Italy, where teachers rather than children rotate between classrooms. If an intervention was extended to the whole school, incremental cost-effectiveness estimates may require consideration of children having access to standing desks in more than one classroom for lessons in different subjects. This would mean a higher cost per child, calculated as the total cost of desks in all classrooms divided by the expected population of the whole school over the expected lifespan of the desks.
At the increment, as in this study, the cost of setting up and maintaining these desks was not an important consideration; however, on a whole-school scale, consideration of these costs is likely to be relevant, with the benefit of an ‘active classroom’ environment needing to be compared with the opportunity cost of other potential investments forgone because of expenditure.
The main barrier to the current research agenda is an absence of evidence of an independent health effect of sedentary behaviours on generalised health measures, such as the QALY. Current evidence of health effects reported in intermediate health outcomes have inconclusive effect on measures that have meaningful impact on health-related quality of life. It is acknowledged that further research is needed to explore the impact of low-intensity activity on child and adolescent health, with interest in not only the volume of activity but also the distribution of activity throughout the day and school week. 4,23
Within the existing modelling approach, future work to assess a range of plausible values for the decay parameter in health effect would be particularly valuable, given extreme modelled sensitivity to this parameter. The rate of decay in activity levels, or corresponding health effect, is likely to interact with other environmental factors, including the spread of active workstations and other active living interventions across regions and throughout the life course. Models linking non-health outcomes of physical activity changes to desirable general outcomes (such as improved attendance, classroom behaviour, progress/attainment) would similarly be a valuable addition to analysis, in helping understand the importance of the possible non-health benefits of the Stand Out in Class intervention and similar interventions. A lack of available evidence has prevented further examination of outcomes outside health at this time.
Strengths and limitations
The Stand Out in Class pilot cluster RCT adopted a mixed-methods approach, including quantitative, qualitative and health economic analyses, enabling a thorough evaluation of all trial procedures providing valuable information to inform the design, evaluation and value of conducting a definitive trial. The intervention was based on a theoretical framework and its development was informed by the literature,56,57,69 our early work29 and PPI (including focus groups with children and interviews with teachers and head teachers during the planning stages, along with ongoing consultations with teachers throughout the trial). The study setting is a further strength of this trial. Bradford was chosen as the study location given its ethnic composition (predominantly South Asian and white British) and high levels of deprivation, health inequalities and childhood morbidity. 73 The characteristics of the participating schools suggest that they were largely representative of schools within the Bradford metropolitan district, enabling us to pilot this intervention under challenging circumstances. The acceptability and feasibility findings of this study therefore suggest that this trial would probably be feasible within other settings. Forty-eight per cent of the present sample of children were of South Asian ethnic origin. With the emergence of an increased cardiometabolic health risk profile observed in British South Asian children, in comparison with white British children,22 early health promotion interventions in such higher-risk groups could be an important strategy for reducing ethnicity-related health inequalities later in life. The classroom-based setting of the present intervention is important for addressing health inequalities, in that this environment is accessible to all children.
Delays experienced with the start date of this study (see Chapter 2, Changes from the original protocol/grant application) meant that our intervention duration was shorter than that originally proposed. Originally, baseline measurements were due to take place when children were at the end of Year 4 (in June/July), with the desks being installed into their new Year 5 classroom at the start of term. This would have enabled us to pilot the intervention over 1 school year, with the follow-up measurements planned in the subsequent June/July when participants were at the end of Year 5. With the baseline measurements not taking place until November/December, the differences in the season of the measurements are probably a confounding factor in the present study. This should be mitigated in a further trial, if such a trial begins the baseline measurements earlier and examines the impact of this intervention over an entire academic year. Although not an aim of this present pilot study, based on evidence from a longer-term sit–stand desk intervention in the USA,203 which incorporated both a 1- and 2-year intervention period, a longer-term intervention (≥ 1 year) will be more likely to detect potential health impacts (e.g. favourable changes in markers of adiposity) of the intervention.
Conclusions and suggestions for further research
This pilot study has provided evidence of the acceptability and feasibility of the Stand Out in Class intervention and evaluation measures. Participant recruitment rates exceeded expectations and retention rates at follow-up were high (97%). The majority of evaluation measures were deemed acceptable and important lessons have been learnt on improvements that should be made in the planning of a definitive trial. All participating schools were committed to the trial, and we received widespread engagement and enthusiasm for the intervention from teachers, head teachers, children and parents.
Preliminary quantitative evidence suggests that the intervention may have a positive direction of effect on weekday sitting time, which warrants testing in a definitive cluster RCT. Importantly, quantitative and qualitative data from this study suggest that the introduction of sit–stand desks into the classroom environment did not negatively impact classroom behaviour and children’s learning. These outcomes are likely to be of key interest to schools considering participating in such interventions and/or adopting these desks in the future. Although the amount of change in sedentary time required in children to bring about positive changes in health markers is yet to be established, a longer-term US sit–stand desk intervention revealed favourable reductions in BMI percentile in primary school children. 203 Furthermore, other evidence suggests that sit–stand desks can have a positive impact on musculoskeletal comfort in children, potentially reducing the risk of future musculoskeletal ill health. 63,207 The feasibility findings of the present study, and emerging evidence on the potential health benefits of sit–stand desks, support the need for a definitive trial. Such a trial could provide novel and robust evidence of the longer-term (≥ 12 months) health and education impacts of this intervention and may have the potential to enhance the classroom environment. Based on the findings of the present study, the following recommendations for the planning of a definitive trial are made:
-
As standing provides a potentially important but small increase in metabolism compared with sitting, this stimulus needs to be applied regularly and over a longer time period than the 4.5 months experienced by the children in the current pilot study. A definitive trial should be conducted over a minimum of 1 academic year, and more sit–stand desks should be incorporated into the classroom to (1) make it easier for teachers to rotate children around to be exposed to the desks and (2) increase the overall dose of the intervention. Such a trial could provide novel and robust evidence on the impact of this intervention on sitting time, markers of health and academic progress.
-
Different methods to attach the activPAL accelerometer to children should be examined to improve comfort and compliance with this measure, or alternative measures of objectively classifying children’s posture should be examined (e.g. use of the ActiGraph on the thigh could be investigated).
-
Efforts should be made to make parental surveys easier to complete; reporting of health-care resource use could be streamlined to minimise reporting and recall bias, for example allowing parents to record health-care incidents in real time using a trial-specific application or website.
-
In consultation with head teachers and teachers or assessment co-ordinators via PPI, further consideration should be given to measuring academic progress to identify appropriate national curriculum-related and standard assessments used by schools, which will enable direct comparison between participating schools. In the absence of consensus over such measures, proxies of academic progress, such as attendance and/or in-class behaviour data, which can be measured consistently across schools, should be identified in collaboration with head teachers and teachers.
-
Based on teachers’ feedback in the current study, an infographic detailing the benefits of reducing sitting time should be produced in collaboration with teachers for use in a full trial, instead of the teachers’ handbook, which was deemed to be too long. The nudge prompts should also not be included in a future intervention.
-
The cognitive assessment test battery should not be included in a full trial, given the limited evidence surrounding the links between sedentary behaviour and cognitive function in children and due to the inappropriateness of some of the tests used (e.g. the RVIP) for this age group.
Acknowledgements
We would especially like to thank all schools, head teachers, senior teachers, Year 5 teachers, children and parents who participated in the study. We are very grateful to our international study collaborators: Professor David Dunstan (Baker Heart and Diabetes Institute, Melbourne, Australia), Professor Jo Salmon (Deakin University, Melbourne, Australia) and Dr Jérôme Gijselaers (Welten Institute, the Netherlands) for their continued support and advice throughout the study. We are also very grateful to the independent members of the TSC: Dr Emma Frew (chairperson, Institute of Applied Health Research, University of Birmingham), Dr Kirsten Corder (Medical Research Centre Epidemiology Unit, University of Cambridge), Dr Marco Cattaneo (School of Mathematics and Physical Sciences, University of Hull), Ms Anita Selby (Grove House Primary School, Bradford) and Ms Caron Stone (Haworth Primary School, Keighley). We would also like to thank Ergotron, Inc.; the sit–stand desks used in this study were supplied via an in-kind donation from Ergotron. Ergotron played no role in the study design, data collection or data analyses, or in the preparation of this report. Ergotron have no relevant interests/rights in terms of project outcomes and uses.
This study was funded by the NIHR Public Health Research programme (project number 14/231/20) and supported by the NIHR Leicester Biomedical Research Centre – Lifestyle theme.
Contributions of authors
Stacy A Clemes (https://orcid.org/0000-0001-5612-5898) (Reader in Active Living and Public Health) was the PI and had overall responsibility for the study. She drafted Chapters 2, 3 and 6 and provided a detailed review and edit of Chapters 1, 4 and 5.
Daniel D Bingham (https://orcid.org/0000-0002-5809-7357) (Senior Research Fellow) was the local study co-ordinator in Bradford and was responsible for school and participant recruitment, and overseeing data collection. He was also responsible for the process evaluation and drafted Chapter 5.
Natalie Pearson (https://orcid.org/0000-0003-2060-5966) (Research Associate) was a Loughborough-based study co-ordinator and was responsible for data management and the processing and scoring of the Strengths and Difficulties Questionnaire and the ActiGraph data. She drafted Chapter 1 and contributed to the writing of the results presented in Chapter 3.
Yu-Ling Chen (https://orcid.org/0000-0002-6976-4055) (Research Associate) was a Loughborough-based study co-ordinator (maternity cover for Natalie Pearson for part of the project) and was responsible for data collection and management, and the processing and scoring of the cognitive function and activPAL data. She contributed to the writing of the results presented in Chapter 3.
Charlotte Edwardson (https://orcid.org/0000-0001-6485-9330) (Associate Professor in Physical Activity, Sedentary Behaviour and Health) was responsible for the objective measurement of sedentary behaviour (activPAL) and physical activity (ActiGraph) and oversaw data collection, processing and interpretation of these data.
Rosemary McEachan (https://orcid.org/0000-0003-1302-6675) (Born in Bradford Programme Director) was responsible for qualitative data collection, analysis, preparation and presentation of the qualitative results presented in Chapter 5.
Keith Tolfrey (https://orcid.org/0000-0001-6269-1538) (Reader in Paediatric Exercise Physiology) was responsible for the physiological health assessments and oversaw data collection, processing and interpretation of these data.
Lorraine Cale (https://orcid.org/0000-0003-1485-4499) (Professor in Physical Education and Sport Pedagogy) was responsible for the measurements of academic progress and in-class behaviour, and oversaw data collection, processing and interpretation of these data.
Gerry Richardson (https://orcid.org/0000-0002-2360-4566) (Professor of Health Economics) was responsible for the analysis of the health economic data, and the preparation and presentation of the health economic results in Chapter 4.
Mike Fray (https://orcid.org/0000-0002-6889-128X) (Senior Lecturer in Human Factors Design) was responsible for the assessment of postural comfort and for the in-class observations of intervention participants using their sit–stand desks. He oversaw data collection, processing and interpretation of these data.
James Altunkaya (https://orcid.org/0000-0002-8293-3466) (NIHR Research Methods Fellow) undertook the analysis of the health economic data and drafted the health economic results presented in Chapter 4.
Stephan Bandelow (https://orcid.org/0000-0002-8484-4707) (Senior Lecturer in Psychology) was responsible for the measurements of cognitive function and oversaw data collection, processing and interpretation of these data.
Nishal Bhupendra Jaicim (https://orcid.org/0000-0002-8584-0388) (Medical Statistician) was responsible for the statistical analysis, and the preparation and presentation of the quantitative results.
Sally E Barber (https://orcid.org/0000-0001-9872-6106) (Principal Research Fellow) assisted the PI with the day-to-day management of the trial, provided expertise in children’s health behaviour interventions and health inequalities within the Bradford setting, and oversaw the Bradford-based research staff.
All authors were members of the internal Project Committee for the trial, read drafts and provided revisions on the content of the report and gave final approval for submission.
Publications
Clemes SA, Bingham DD, Pearson N, Chen YL, Edwardson C, McEachan R, et al. Stand Out in Class: restructuring the classroom environment to reduce sedentary behaviour in 9- to 10-year-olds – study protocol for a pilot cluster randomised controlled trial. Pilot Feasibility Stud 2018;4:103.
Clemes SA, Bingham DD, Pearson N, Chen YL, Edwardson CL, McEachan RRC, et al. Stand Out in Class: restructuring the classroom environment to reduce sitting time – findings from a pilot cluster randomised controlled trial. Int J Behav Nutr Phys Act 2020;17:55.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN) – terminology consensus project process and outcome. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0525-8.
- Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Lancet Physical Activity Series Working Group . Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247-57. https://doi.org/10.1016/S0140-6736(12)60646-1.
- Hallal PC, Victora CG, Azevedo MR, Wells JC. Adolescent physical activity and health: a systematic review. Sports Med 2006;36:1019-30. https://doi.org/10.2165/00007256-200636120-00003.
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7. https://doi.org/10.1186/1479-5868-7-40.
- Edwardson CL, Gorely T, Davies MJ, Gray LJ, Khunti K, Wilmot EG, et al. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0034916.
- Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol 2012;41:1338-53. https://doi.org/10.1093/ije/dys078.
- Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia 2012;55:2895-905. https://doi.org/10.1007/s00125-012-2677-z.
- Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med 2011;41:207-15. https://doi.org/10.1016/j.amepre.2011.05.004.
- Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc 2009;41:998-1005. https://doi.org/10.1249/MSS.0b013e3181930355.
- Teychenne M, Ball K, Salmon J. Physical activity, sedentary behavior and depression among disadvantaged women. Health Educ Res 2010;25:632-44. https://doi.org/10.1093/her/cyq008.
- Chinapaw MJ, Proper KI, Brug J, van Mechelen W, Singh AS. Relationship between young peoples’ sedentary behaviour and biomedical health indicators: a systematic review of prospective studies. Obes Rev 2011;12:e621-32. https://doi.org/10.1111/j.1467-789X.2011.00865.x.
- Cliff DP, Hesketh KD, Vella SA, Hinkley T, Tsiros MD, Ridgers ND, et al. Objectively measured sedentary behaviour and health and development in children and adolescents: systematic review and meta-analysis. Obes Rev 2016;17:330-44. https://doi.org/10.1111/obr.12371.
- Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act 2011;8. https://doi.org/10.1186/1479-5868-8-98.
- Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput JP, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab 2016;41:240-65. https://doi.org/10.1139/apnm-2015-0630.
- Hancox RJ, Milne BJ, Poulton R. Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. Lancet 2004;364:257-62. https://doi.org/10.1016/S0140-6736(04)16675-0.
- Pearson N, Braithwaite RE, Biddle SJ, van Sluijs EM, Atkin AJ. Associations between sedentary behaviour and physical activity in children and adolescents: a meta-analysis. Obes Rev 2014;15:666-75. https://doi.org/10.1111/obr.12188.
- Pearson N, Biddle SJ. Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med 2011;41:178-88. https://doi.org/10.1016/j.amepre.2011.05.002.
- Chaput JP, Saunders TJ, Carson V. Interactions between sleep, movement and other non-movement behaviours in the pathogenesis of childhood obesity. Obes Rev 2017;18:7-14. https://doi.org/10.1111/obr.12508.
- Gabel L, Ridgers ND, Della Gatta PA, Arundell L, Cerin E, Robinson S, et al. Associations of sedentary time patterns and TV viewing time with inflammatory and endothelial function biomarkers in children. Pediatr Obes 2016;11:194-201. https://doi.org/10.1111/ijpo.12045.
- Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GJ, Alberti KG, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 2002;324. https://doi.org/10.1136/bmj.324.7338.635.
- Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup PH. Patterns of body size and adiposity among UK children of South Asian, black African-Caribbean and white European origin: Child Heart And health Study in England (CHASE Study). Int J Epidemiol 2011;40:33-44. https://doi.org/10.1093/ije/dyq180.
- Whincup PH, Nightingale CM, Owen CG, Rudnicka AR, Gibb I, McKay CM, et al. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the Child Heart and Health Study in England (CHASE Study). PLOS Med 2010;7. https://doi.org/10.1371/journal.pmed.1000263.
- Chief Medical Officers . Start Active, Stay Active: A Report on Physical Activity from the Four Home Countries’ Chief Medical Officers 2011. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf (accessed 3 September 2018).
- Physical Activity Guidelines Advisory Committee . 2018 Physical Activity Guidelines Advisory Committee Scientific Report 2018. https://health.gov/paguidelines/second-edition/report/ (accessed 3 September 2018).
- Canadian Society for Exercise Physiology . Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep 2016. https://csepguidelines.ca/ (accessed 3 September 2018).
- Australian Government . Australia’s Physical Activity and Sedentary Behaviour Guidelines 2017. www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-phys-act-guidelines (accessed 3 September 2018).
- Physical Activity Guidelines 2017 2017. www.healthcouncil.nl/documents/advisory-reports/2017/08/22/physical-activity-guidelines-2017 (accessed 3 September 2018).
- Steele RM, van Sluijs EM, Cassidy A, Griffin SJ, Ekelund U. Targeting sedentary time or moderate- and vigorous-intensity activity: independent relations with adiposity in a population-based sample of 10-y-old British children. Am J Clin Nutr 2009;90:1185-92. https://doi.org/10.3945/ajcn.2009.28153.
- Clemes SA, Barber SE, Bingham DD, Ridgers ND, Fletcher E, Pearson N, et al. Reducing children’s classroom sitting time using sit-to-stand desks: findings from pilot studies in UK and Australian primary schools. J Public Health 2016;38:526-33. https://doi.org/10.1093/pubmed/fdv084.
- Craig R, Mindell JHV. Health Survey for England 2008. London: Department of Health and Social Care; 2008.
- LeBlanc AG, Katzmarzyk PT, Barreira TV, Broyles ST, Chaput JP, Church TS, et al. Correlates of total sedentary time and screen time in 9–11 year-old children around the world: the international study of childhood obesity, lifestyle and the environment. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0129622.
- Colley RC, Wong SL, Garriguet D, Janssen I, Connor Gorber S, Tremblay MS. Physical activity, sedentary behaviour and sleep in Canadian children: parent-report versus direct measures and relative associations with health risk. Health Rep 2012;23:45-52.
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 2008;167:875-81. https://doi.org/10.1093/aje/kwm390.
- Abbott RA, Straker LM, Mathiassen SE. Patterning of children’s sedentary time at and away from school. Obesity 2013;21:E131-3. https://doi.org/10.1002/oby.20127.
- van Stralen MM, Yildirim M, Wulp A, te Velde SJ, Verloigne M, Doessegger A, et al. Measured sedentary time and physical activity during the school day of European 10- to 12-year-old children: the ENERGY project. J Sci Med Sport 2014;17. https://doi.org/10.1016/j.jsams.2014.05.011.
- Hughes AR, Muggeridge DJ, Gibson AM, Johnstone A, Kirk A. Objectively measured sedentary time in children and their parents. AIMS Public Health 2016;3:823-36. https://doi.org/10.3934/publichealth.2016.4.823.
- Wafa SW, Aziz NN, Shahril MR, Halib H, Rahim M, Janssen X. Measuring the daily activity of lying down, sitting, standing and stepping of obese children using the ActivPAL (TM) activity monitor. J Trop Pediatrics 2017;63:98-103. https://doi.org/10.1093/tropej/fmw052.
- Ridgers ND, Timperio A, Cerin E, Salmon J. Within- and between-day associations between children’s sitting and physical activity time. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2291-3.
- Pearson N, Haycraft E, P Johnston J, Atkin AJ. Sedentary behaviour across the primary-secondary school transition: a systematic review. Prev Med 2017;94:40-7. https://doi.org/10.1016/j.ypmed.2016.11.010.
- Biddle SJ, Pearson N, Ross GM, Braithwaite R. Tracking of sedentary behaviours of young people: a systematic review. Prev Med 2010;51:345-51. https://doi.org/10.1016/j.ypmed.2010.07.018.
- van Sluijs EM, Jones NR, Jones AP, Sharp SJ, Harrison F, Griffin SJ. School-level correlates of physical activity intensity in 10-year-old children. Int J Pediatr Obes 2011;6:e574-81. https://doi.org/10.3109/17477166.2010.518239.
- Morton KL, Atkin AJ, Corder K, Suhrcke M, van Sluijs EM. The school environment and adolescent physical activity and sedentary behaviour: a mixed-studies systematic review. Obes Rev 2016;17:142-58. https://doi.org/10.1111/obr.12352.
- Bonell C, Humphrey N, Fletcher A, Moore L, Anderson R, Campbell R. Why schools should promote students’ health and wellbeing. BMJ 2014;348. https://doi.org/10.1136/bmj.g3078.
- Kriemler S, Meyer U, Martin E, van Sluijs EM, Andersen LB, Martin BW. Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Br J Sports Med 2011;45:923-30. https://doi.org/10.1136/bjsports-2011-090186.
- Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD007651.pub2.
- Daly-Smith AJ, Zwolinsky S, McKenna J, Tomporowski PD, Defeyter MA, Manley A. Systematic review of acute physically active learning and classroom movement breaks on children’s physical activity, cognition, academic performance and classroom behaviour: understanding critical design features. BMJ Open Sport Exerc Med 2018;4. https://doi.org/10.1136/bmjsem-2018-000341.
- Biddle SJ, Petrolini I, Pearson N. Interventions designed to reduce sedentary behaviours in young people: a review of reviews. Br J Sports Med 2014;48:182-6. https://doi.org/10.1136/bjsports-2013-093078.
- Altenburg TM, Kist-van Holthe J, Chinapaw MJ. Effectiveness of intervention strategies exclusively targeting reductions in children’s sedentary time: a systematic review of the literature. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0387-5.
- Michie S, West R, Campbell R, Brown J, Gainforth HL. ABC of Behaviour Change Theories. London: Silverback Publishing; 2014.
- Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. London: Silverback Publishing; 2014.
- Spence JC, Rhodes RE, Carson V. Challenging the dual-hinge approach to intervening on sedentary behavior. Am J Prev Med 2017;52:403-6. https://doi.org/10.1016/j.amepre.2016.10.019.
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev 2016;10:89-112. https://doi.org/10.1080/17437199.2015.1082146.
- Hegarty LM, Mair JL, Kirby K, Murtagh E, Murphy MH. School-based interventions to reduce sedentary behaviour in children: a systematic review. AIMS Public Health 2016;3:520-41. https://doi.org/10.3934/publichealth.2016.3.520.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-37.
- Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0605-9.
- Sherry AP, Pearson N, Clemes SA. The effects of standing desks within the school classroom: a systematic review. Prev Med Rep 2016;3:338-47. https://doi.org/10.1016/j.pmedr.2016.03.016.
- Minges KE, Chao AM, Irwin ML, Owen N, Park C, Whittemore R, et al. Classroom standing desks and sedentary behavior: a systematic review. Pediatrics 2016;137. https://doi.org/10.1542/peds.2015-3087.
- Blake JJ, Benden ME, Wendel ML. Using stand/sit workstations in classrooms: lessons learned from a pilot study in Texas. J Public Health Manag Pract 2012;18:412-15. https://doi.org/10.1097/PHH.0b013e3182215048.
- Hinckson EA, Aminian S, Ikeda E, Stewart T, Oliver M, Duncan S, et al. Acceptability of standing workstations in elementary schools: a pilot study. Prev Med 2013;56:82-5. https://doi.org/10.1016/j.ypmed.2012.10.014.
- Benden ME, Blake JJ, Wendel ML, Huber JC. The impact of stand-biased desks in classrooms on calorie expenditure in children. Am J Public Health 2011;101:1433-6. https://doi.org/10.2105/AJPH.2010.300072.
- Benden ME, Zhao H, Jeffrey CE, Wendel ML, Blake JJ. The evaluation of the impact of a stand-biased desk on energy expenditure and physical activity for elementary school students. Int J Environ Res Public Health 2014;11:9361-75. https://doi.org/10.3390/ijerph110909361.
- Lanningham-Foster L, Foster RC, McCrady SK, Manohar CU, Jensen TB, Mitre NG, et al. Changing the school environment to increase physical activity in children. Obesity 2008;16:1849-53. https://doi.org/10.1038/oby.2008.282.
- Benden ME, Pickens A, Shipp E, Perry J, Schneider D. Evaluating a school based childhood obesity intervention for posture and comfort. Health 2013;5:54-60. https://doi.org/10.4236/health.2013.58A3008.
- Koskelo R, Vuorikari K, Hänninen O. Sitting and standing postures are corrected by adjustable furniture with lowered muscle tension in high-school students. Ergonomics 2007;50:1643-56. https://doi.org/10.1080/00140130701587236.
- Dornhecker M, Blake J, Benden M, Zhao H, Wendel M. The effect of stand-biased desks on academic engagement: an exploratory study. Int J Health Promot Educ 2015;53:271-80. https://doi.org/10.1080/14635240.2015.1029641.
- Wick K, Faude O, Manes S, Zahner L, Donath L. I can stand learning: a controlled pilot intervention study on the effects of increased standing time on cognitive function in primary school children. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15020356.
- Aminian S, Hinckson EA, Stewart T. Modifying the classroom environment to increase standing and reduce sitting. Build Res Inf 2015;43:631-45. https://doi.org/10.1080/09613218.2015.1058093.
- Silva DR, Minderico CS, Pinto F, Collings PJ, Cyrino ES, Sardinha LB. Impact of a classroom standing desk intervention on daily objectively measured sedentary behavior and physical activity in youth. J Sci Med Sport 2018;21:919-24. https://doi.org/10.1016/j.jsams.2018.01.007.
- Hinckson E, Salmon J, Benden M, Clemes SA, Sudholz B, Barber SE, et al. Standing classrooms: research and lessons learned from around the world. Sports Med 2016;46:977-87. https://doi.org/10.1007/s40279-015-0436-2.
- The Health and Social Care Information Centre . Health Survey for England 2008: Volume 1, Physical Activity and Fitness 2009. https://files.digital.nhs.uk/publicationimport/pub00xxx/pub00430/heal-surv-phys-acti-fitn-eng-2008-rep-v1.pdf (accessed 3 September 2018).
- Ginsburg H, Opper S. Piaget’s Theory of Intellectual Development. Englewood Cliffs, NJ: Prentice-Hall Inc.; 1988.
- Clemes SA, Bingham DD, Pearson N, Chen YL, Edwardson C, McEachan R, et al. Stand Out in Class: restructuring the classroom environment to reduce sedentary behaviour in 9-10-year-olds - study protocol for a pilot cluster randomised controlled trial. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0295-3.
- Wright J, Small N, Raynor P, Tuffnell D, Bhopal R, Cameron N, et al. Cohort profile: the born in Bradford multi-ethnic family cohort study. Int J Epidemiol 2013;42:978-91. https://doi.org/10.1093/ije/dys112.
- NHS Digital . National Child Measurement Programme, England, 2016 17 School Year 2017. https://files.digital.nhs.uk/publication/j/n/nati-chil-meas-prog-eng-2016-2017-rep.pdf (accessed 3 September 2018).
- Murray D. Design and Analysis of Group-Randomized Trials. Oxford: Oxford University Press; 1998.
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Statistics 2005;4:287-91. https://onlinelibrary.wiley.com/doi/pdf/10.1002/pst.185.
- Sherry AP, Pearson N, Ridgers ND, Barber SE, Bingham DD, Nagy LC, et al. The Effectiveness of Sit-to-Stand Desks to Reduce Sitting Time Within a Primary School Classroom: An 8 Month Controlled Trial n.d.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. ‘Psychological Theory’ Group . Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. https://doi.org/10.1136/qshc.2004.011155.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Clemes SA, Bingham DD, Pearson N, Chen YL, Edwardson CL, McEachan RRC, et al. Stand Out in Class: restructuring the classroom environment to reduce sitting time – findings from a pilot cluster randomised controlled trial. Int J Behav Nutr Phys Act 2020;17. https://doi.org/10.1186/s12966-020-00958-z.
- Edwardson CL, Winkler EAH, Bodicoat DH, Yates T, Davies MJ, Dunstan DW, et al. Considerations when using the activPAL monitor in field-based research with adult populations. J Sport Health Sci 2017;6:162-78. https://doi.org/10.1016/j.jshs.2016.02.002.
- Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc 2011;43:1561-7. https://doi.org/10.1249/MSS.0b013e31820ce174.
- Atkin AJ, Gorely T, Clemes SA, Yates T, Edwardson C, Brage S, et al. Methods of measurement in epidemiology: sedentary behaviour. Int J Epidemiol 2012;41:1460-71. https://doi.org/10.1093/ije/dys118.
- Aminian S, Hinckson EA. Examining the validity of the ActivPAL monitor in measuring posture and ambulatory movement in children. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-119.
- Davies G, Reilly JJ, McGowan AJ, Dall PM, Granat MH, Paton JY. Validity, practical utility, and reliability of the activPAL in preschool children. Med Sci Sports Exerc 2012;44:761-8. https://doi.org/10.1249/MSS.0b013e31823b1dc7.
- Winkler EA, Bodicoat DH, Healy GN, Bakrania K, Yates T, Owen N, et al. Identifying adults’ valid waking wear time by automated estimation in activPAL data collected with a 24 h wear protocol. Physiol Meas 2016;37:1653-68. https://doi.org/10.1088/0967-3334/37/10/1653.
- Dollman J, Okely AD, Hardy L, Timperio A, Salmon J, Hills AP. A hitchhiker’s guide to assessing young people’s physical activity: deciding what method to use. J Sci Med Sport 2009;12:518-25. https://doi.org/10.1016/j.jsams.2008.09.007.
- Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the computer science and applications (CSA) activity monitor in children. Med Sci Sports Exerc 1998;30:629-33. https://doi.org/10.1097/00005768-199804000-00023.
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557-65. https://doi.org/10.1080/02640410802334196.
- Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011;43:1360-8. https://doi.org/10.1249/MSS.0b013e318206476e.
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9. https://doi.org/10.1136/adc.73.1.25.
- O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 2003;21:821-48. https://doi.org/10.1097/01.hjh.0000059016.82022.ca.
- Corsi PM. Human memory and the medial temporal region of the brain. Diss Abstr Int 1972;34.
- MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychol Bull 1991;109:163-20. https://doi.org/10.1037/0033-2909.109.2.163.
- Bakan P. Extraversion-introversion and improvement in an auditory vigilance task. Br J Psychol 1959;50:325-32. https://doi.org/10.1111/j.2044-8295.1959.tb00711.x.
- Farrell Pagulayan K, Busch RM, Medina KL, Bartok JA, Krikorian R. Developmental normative data for the Corsi block-tapping task. J Clin Exp Neuropsychol 2006;28:1043-52. https://doi.org/10.1080/13803390500350977.
- Orsini A. Corsi’s block-tapping test: standardization and concurrent validity with WISC-R for children aged 11 to 16. Percept Mot Skills 1994;79:1547-54. https://doi.org/10.2466/pms.1994.79.3f.1547.
- Cooper SB, Bandelow S, Nute ML, Dring KJ, Stannard RL, Morris JG, et al. Sprint-based exercise and cognitive function in adolescents. Prev Med Rep 2016;4:155-61. https://doi.org/10.1016/j.pmedr.2016.06.004.
- Gualtieri CT, Johnson LG. Reliability and validity of a computerized neurocognitive test battery, CNS Vital Signs. Arch Clin Neuropsychol 2006;21:623-43. https://doi.org/10.1016/j.acn.2006.05.007.
- Syväoja HJ, Tammelin TH, Ahonen T, Kankaanpää A, Kantomaa MT. The associations of objectively measured physical activity and sedentary time with cognitive functions in school-aged children. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0103559.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Skinner EA, Marchand G, Furrer C, Kindermann T. Engagement and disaffection in the classroom: part of a larger motivational dynamic. J Educ Psychol 2008;100:765-81. https://doi.org/10.1037/a0012840.
- Skinner EA, Kindermann T, Furrer C. A Motivational perspective on engagement and disaffection. Educ Psychol Meas 2009;69:493-525. https://doi.org/10.1177/0013164408323233.
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39. https://doi.org/10.1097/00005650-200108000-00006.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. https://doi.org/10.1007/s11136-010-9648-y.
- Ravens-Sieberer U, Wille N, Badia X, Bonsel G, Burström K, Cavrini G, et al. Feasibility, reliability, and validity of the EQ-5D-Y: results from a multinational study. Qual Life Res 2010;19:887-97. https://doi.org/10.1007/s11136-010-9649-x.
- Campbell MK, Piaggio G, Elbourne DR, Altman DG. CONSORT Group . Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345. https://doi.org/10.1136/bmj.e5661.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10. https://doi.org/10.1186/1471-2288-10-67.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. https://doi.org/10.1111/j.2002.384.doc.x.
- Bland JM, Kerry SM. Statistics notes. Trials randomised in clusters. BMJ 1997;315. https://doi.org/10.1136/bmj.315.7108.600.
- Kerry SM, Bland JM. Analysis of a trial randomised in clusters. BMJ 1998;316. https://doi.org/10.1136/bmj.316.7124.54.
- GOV.UK . Schools, Pupils and Their Characteristics: January 2017 2018. www.gov.uk/government/statistics/schools-pupils-and-their-characteristics-january-2017 (accessed 3 September 2018).
- Buman MP, Winkler EA, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005-2006. Am J Epidemiol 2014;179:323-34. https://doi.org/10.1093/aje/kwt292.
- Snijders T, Boskers R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Thousand Oaks, CA: Sage; 1999.
- Altman DG. Statistics and ethics in medical research: III how large a sample?. Br Med J 1980;281:1336-8. https://doi.org/10.1136/bmj.281.6251.1336.
- Campbell MK, Fayers PM, Grimshaw JM. Determinants of the intracluster correlation coefficient in cluster randomized trials: the case of implementation research. Clin Trials 2005;2:99-107. https://doi.org/10.1191/1740774505cn071oa.
- Harrington DM, Davies MJ, Bodicoat DH, Charles JM, Chudasama YV, Gorely T, et al. Effectiveness of the ‘Girls Active’ school-based physical activity programme: a cluster randomised controlled trial. Int J Behav Nutr Phys Act 2018;15. https://doi.org/10.1186/s12966-018-0664-6.
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348. https://doi.org/10.1136/bmj.g3256.
- Palmer S, Raftery J. Opportunity cost. BMJ 1999;318:1551-2. https://doi.org/10.1136/bmj.318.7197.1551.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: PSSRU, University of Kent; 2017.
- Department of Health and Social Care . NHS Reference Costs 2015–16 2017. www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016 (accessed 7 September 2018).
- Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol 1990;13:555-65. https://doi.org/10.1002/clc.4960130809.
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/10.1007/s40273-014-0193-3.
- Gabrio A, Mason AJ, Baio G. Handling missing data in within-trial cost-effectiveness analysis: a review with future recommendations. Pharmacoecon Open 2017;1:79-97. https://doi.org/10.1007/s41669-017-0015-6.
- Leurent B, Gomes M, Faria R, Morris S, Grieve R, Carpenter JR. Sensitivity analysis for not-at-random missing data in trial-based cost-effectiveness analysis: a tutorial. PharmacoEconomics 2018;36:889-901. https://doi.org/10.1007/s40273-018-0650-5.
- Morris TP, White IR, Royston P. Tuning multiple imputation by predictive mean matching and local residual draws. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-75.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377-99. https://doi.org/10.1002/sim.4067.
- DiazOrdaz K, Kenward MG, Gomes M, Grieve R. Multiple imputation methods for bivariate outcomes in cluster randomised trials. Stat Med 2016;35:3482-96. https://doi.org/10.1002/sim.6935.
- Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol 2009;60:549-76. https://doi.org/10.1146/annurev.psych.58.110405.085530.
- Simons CL, Rivero-Arias O, Yu LM, Simon J. Multiple imputation to deal with missing EQ-5D-3L data: should we impute individual domains or the actual index?. Qual Life Res 2015;24:805-15. https://doi.org/10.1007/s11136-014-0837-y.
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987.
- van Reenen M, Janssen B, Oppe M, Kreimeier S, Greiner W. EQ-5D-Y User Guide – Basic Information on How to Use The EQ-5D-Y Instrument 2018. https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-Y_User_Guide_v1.0_2014.pdf (accessed 7 September 2018).
- Kind P, Klose K, Gusi N, Olivares PR, Greiner W. Can adult weights be used to value child health states? Testing the influence of perspective in valuing EQ-5D-Y. Qual Life Res 2015;24:2519-39. https://doi.org/10.1007/s11136-015-0971-1.
- Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126-39. https://doi.org/10.1097/00005650-199902000-00003.
- Khan KA, Petrou S, Rivero-Arias O, Walters SJ, Boyle SE. Mapping EQ-5D utility scores from the PedsQL™ generic core scales. PharmacoEconomics 2014;32:693-706. https://doi.org/10.1007/s40273-014-0153-y.
- Youth in Mind . Scoring the Strengths &Amp; Difficulties Questionnaire for Age 4–17 or 18+ 2016. www.sdqinfo.org/py/sdqinfo/b3.py?language=Englishqz(UK) (accessed 24 August 2018).
- Agarwal S, Steinmaus C, Harris-Adamson C. Sit-stand workstations and impact on low back discomfort: a systematic review and meta-analysis. Ergonomics 2018;61:538-52. https://doi.org/10.1080/00140139.2017.1402960.
- Davis MG, Fox KR, Hillsdon M, Sharp DJ, Coulson JC, Thompson JL. Objectively measured physical activity in a diverse sample of older urban UK adults. Med Sci Sports Exerc 2011;43:647-54. https://doi.org/10.1249/MSS.0b013e3181f36196.
- Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior determinants and interventions. Am J Prev Med 2011;41:189-96. https://doi.org/10.1016/j.amepre.2011.05.013.
- Pettee Gabriel KK, Morrow JR, Woolsey AL. Framework for physical activity as a complex and multidimensional behavior. J Phys Act Health 2012;9:11-8. https://doi.org/10.1123/jpah.9.s1.s11.
- de Rezende LF, Rodrigues Lopes M, Rey-López JP, Matsudo VK, Luiz Odo C. Sedentary behavior and health outcomes: an overview of systematic reviews. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0105620.
- Tremblay MS, Leblanc AG, Janssen I, Kho ME, Hicks A, Murumets K, et al. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab 2011;36:59-64. https://doi.org/10.1139/H11-012.
- Biddle SJ, García Bengoechea E, Wiesner G. Sedentary behaviour and adiposity in youth: a systematic review of reviews and analysis of causality. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0497-8.
- van Ekris E, Altenburg TM, Singh AS, Proper KI, Heymans MW, Chinapaw MJ. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: a systematic review and meta-analysis. Obes Rev 2016;17:833-49. https://doi.org/10.1111/obr.12426.
- Altenburg TM, de Niet M, Verloigne M, De Bourdeaudhuij I, Androutsos O, Manios Y, et al. Occurrence and duration of various operational definitions of sedentary bouts and cross-sectional associations with cardiometabolic health indicators: the ENERGY-project. Prev Med 2015;71:101-6. https://doi.org/10.1016/j.ypmed.2014.12.015.
- Altenburg TM, Rotteveel J, Dunstan DW, Salmon J, Chinapaw MJ. The effect of interrupting prolonged sitting time with short, hourly, moderate-intensity cycling bouts on cardiometabolic risk factors in healthy, young adults. J Appl Physiol 2013;115:1751-6. https://doi.org/10.1152/japplphysiol.00662.2013.
- Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 2012;35:976-83. https://doi.org/10.2337/dc11-1931.
- Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. Breaks in sedentary time. Diabetes Care 2008;31. https://doi.org/10.2337/dc07-2046.
- Ridgers ND, Salmon J, Ridley K, O’Connell E, Arundell L, Timperio A. Agreement between activPAL and ActiGraph for assessing children’s sedentary time. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-15.
- SportEngland . What Is MOVES? 2018. www.sportengland.org/our-work/health-and-inactivity/what-is-moves/ (accessed 7 September 2018).
- Economics of Chronic Diseases (EConDA) . EConDA Policy Tool (Beta Version 6) 2018. www.econdaproject.com/tools.php (accessed 7 September 2018).
- National Institute for Health and Care Excellence (NICE) . Estimating Return on Investment for Interventions and Strategies to Increase Physical Activity 2014.
- van der Ploeg HP, Hillsdon M. Is sedentary behaviour just physical inactivity by another name?. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0601-0.
- Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull 2010;96:5-21. https://doi.org/10.1093/bmb/ldq033.
- Treuth MS, Catellier DJ, Schmitz KH, Pate RR, Elder JP, McMurray RG, et al. Weekend and weekday patterns of physical activity in overweight and normal-weight adolescent girls. Obesity 2007;15:1782-8. https://doi.org/10.1038/oby.2007.212.
- Owen N, Bauman A, Brown W. Too much sitting: a novel and important predictor of chronic disease risk?. Br J Sports Med 2009;43:81-3. https://doi.org/10.1136/bjsm.2008.055269.
- Sullivan PW, Slejko JF, Sculpher MJ, Ghushchyan V. Catalogue of EQ-5D scores for the United Kingdom. Med Decis Making 2011;31:800-4. https://doi.org/10.1177/0272989X11401031.
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000;32:498-504. https://doi.org/10.1097/00005768-200009001-00009.
- Butte NF, Watson KB, Ridley K, Zakeri IF, McMurray RG, Pfeiffer KA, et al. A youth compendium of physical activities: activity codes and metabolic intensities. Med Sci Sports Exerc 2018;50:246-56. https://doi.org/10.1249/MSS.0000000000001430.
- Thijssen DH. Do not ignore the opposite end of the physical activity spectrum. BMJ 2017;357. https://doi.org/10.1136/bmj.j2709.
- Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 2015;162:123-32. https://doi.org/10.7326/M14-1651.
- Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol 2018;33:811-29. https://doi.org/10.1007/s10654-018-0380-1.
- Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab 2010;35:725-40. https://doi.org/10.1139/H10-079.
- Murphy MH, Blair SN, Murtagh EM. Accumulated versus continuous exercise for health benefit: a review of empirical studies. Sports Med 2009;39:29-43. https://doi.org/10.2165/00007256-200939010-00003.
- World Health Organization . Global Recommendations on Physical Activity for Health 2010. whqlibdoc.who.int/publications/2010/9789241599979_eng.pdf (accessed 3 September 2018).
- Murray CJL, Lopez AD. Harvard School of Public Health . Global Health Statistics: A Compendium of Incidence, Prevalence and Mortality Estimates for Over 200 Conditions 1996. https://apps.who.int/iris/handle/10665/41848 (accessed 7 September 2018).
- Office for National Statistics . 2011 Census: Usual Resident Population by Five-Year Age Group and Sex, United Kingdom and Constituent Countries 2012. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/2011censuspopulationestimatesbyfiveyearagebandsandhouseholdestimatesforlocalauthoritiesintheunitedkingdom (accessed 10 September 2018).
- Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 2016;354. https://doi.org/10.1136/bmj.i3857.
- Woodcock J, Edwards P, Tonne C, Armstrong BG, Ashiru O, Banister D, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: urban land transport. Lancet 2009;374:1930-43. https://doi.org/10.1016/S0140-6736(09)61714-1.
- Mansoubi M, Pearson N, Biddle SJ, Clemes SA. Using sit-to-stand workstations in offices: is there a compensation effect?. Med Sci Sports Exerc 2016;48:720-5. https://doi.org/10.1249/MSS.0000000000000802.
- Long R. The School Day and Year (England). House of Commons Library; 2016.
- Singh V, Suhrcke M, Hardeman W, Sutton S, Wilson ECF. Very Brief Interventions Programme Team . Cost-effectiveness and value of information analysis of brief interventions to promote physical activity in primary care. Value Health 2018;21:18-26. https://doi.org/10.1016/j.jval.2017.07.005.
- Over EA, Wendel-Vos GW, van den Berg M, Reenen HH, Tariq L, Hoogenveen RT, et al. Cost-effectiveness of counseling and pedometer use to increase physical activity in the Netherlands: a modeling study. Cost Eff Resour Alloc 2012;10. https://doi.org/10.1186/1478-7547-10-13.
- Cobiac LJ, Vos T, Barendregt JJ. Cost-effectiveness of interventions to promote physical activity: a modelling study. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000110.
- Jacobs-van der Bruggen MA, Bos G, Bemelmans WJ, Hoogenveen RT, Vijgen SM, Baan CA. Lifestyle interventions are cost-effective in people with different levels of diabetes risk: results from a modeling study. Diabetes Care 2007;30:128-34. https://doi.org/10.2337/dc06-0690.
- Briggs A, Claxton K, Sculpher M. Decision Modelling for Health Economic Evaluation. Oxford: Oxford University Press; 2006.
- McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. PharmacoEconomics 2008;26:733-44. https://doi.org/10.2165/00019053-200826090-00004.
- Office for National Statistics . Estimates of the Population for the UK, England and Wales, Scotland and Northern Ireland – Mid-2017 2018. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed 17 August 2018).
- Bate A. Early Intervention. House of Commons Library; 2017.
- Claxton K, Eggington S, Ginnelly L, Griffin S, McCabe C, Philips Z, et al. A Pilot Study of Value of Information Analysis to Support Research Recommendations for NICE 2005. www.ncbi.nlm.nih.gov/books/NBK425823/pdf/Bookshelf_NBK425823.pdf (accessed 10 September 2018).
- Ades AE, Lu G, Claxton K. Expected value of sample information calculations in medical decision modeling. Med Decis Making 2004;24:207-27. https://doi.org/10.1177/0272989X04263162.
- Wu S, Cohen D, Shi Y, Pearson M, Sturm R. Economic analysis of physical activity interventions. Am J Prev Med 2011;40:149-58. https://doi.org/10.1016/j.amepre.2010.10.029.
- Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy 2009;93:85-92. https://doi.org/10.1016/j.healthpol.2009.07.012.
- Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, König HH. The long-term cost-effectiveness of obesity prevention interventions: systematic literature review. Obes Rev 2012;13:537-53. https://doi.org/10.1111/j.1467-789X.2011.00980.x.
- Laine J, Kuvaja-Köllner V, Pietilä E, Koivuneva M, Valtonen H, Kankaanpää E. Cost-effectiveness of population-level physical activity interventions: a systematic review. Am J Health Promot 2014;29:71-80. https://doi.org/10.4278/ajhp.131210-LIT-622.
- Drost RM, Paulus AT, Ruwaard D, Evers SM. Valuing inter-sectoral costs and benefits of interventions in the healthcare sector: methods for obtaining unit prices. Expert Rev Pharmacoecon Outcomes Res 2017;17:77-84. https://doi.org/10.1586/14737167.2016.1141679.
- Mansoubi M, Pearson N, Clemes SA, Biddle SJ, Bodicoat DH, Tolfrey K, et al. Energy expenditure during common sitting and standing tasks: examining the 1.5 MET definition of sedentary behaviour. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1851-x.
- Pate RR, O’Neill JR, Lobelo F. The evolving definition of ‘sedentary’. Exerc Sport Sci Rev 2008;36:173-8. https://doi.org/10.1097/JES.0b013e3181877d1a.
- Ciani O, Buyse M, Drummond M, Rasi G, Saad ED, Taylor RS. Time to review the role of surrogate end points in health policy: state of the art and the way forward. Value Health 2017;20:487-95. https://doi.org/10.1016/j.jval.2016.10.011.
- LeBlanc AG, Janssen I. Dose-response relationship between physical activity and dyslipidemia in youth. Can J Cardiol 2010;26:201-5. https://doi.org/10.1016/S0828-282X(10)70400-1.
- Kesäniemi A, Riddoch CJ, Reeder B, Blair SN, Sørensen TIa. Advancing the future of physical activity guidelines in Canada: an independent expert panel interpretation of the evidence. Int J Behav Nutr Phys Act 2010;7. https://doi.org/10.1186/1479-5868-7-41.
- Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med 2008;46:397-411. https://doi.org/10.1016/j.ypmed.2008.01.009.
- Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med 2013;45:649-57. https://doi.org/10.1016/j.amepre.2013.08.001.
- Hamer M, Kivimaki M, Steptoe A. Longitudinal patterns in physical activity and sedentary behaviour from mid-life to early old age: a substudy of the Whitehall II cohort. J Epidemiol Community Health 2012;66:1110-15. https://doi.org/10.1136/jech-2011-200505.
- Hasson H. Systematic evaluation of implementation fidelity of complex interventions in health and social care. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-67.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Chief Medical Officer’s Report . Our Children Deserve Better: Prevention Pays 2013. www.gov.uk/government/publications/chief-medical-officers-annual-report-2012-our-children-deserve-better-prevention-pays (accessed 3 September 2018).
- Department of Health and Social Care . Childhood Obesity: A Plan for Action 2018. www.gov.uk/government/publications/childhood-obesity-a-plan-for-action (accessed 3 September 2018).
- Saunders TJ, Chaput JP, Tremblay MS. Sedentary behaviour as an emerging risk factor for cardiometabolic diseases in children and youth. Can J Diabetes 2014;38:53-61. https://doi.org/10.1016/j.jcjd.2013.08.266.
- Barber SE, Akhtar S, Jackson C, Bingham DD, Hewitt C, Routen A, et al. Preschoolers in the playground: a pilot cluster randomised controlled trial of a physical activity intervention for children aged 18 months to 4 years. Public Health Res 2015;3. https://doi.org/10.3310/phr03050.
- Adab P, Pallan MJ, Lancashire ER, Hemming K, Frew E, Barrett T, et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6 and 7 year olds: cluster randomised controlled trial (WAVES study). BMJ 2018;360. https://doi.org/10.1136/bmj.k211.
- Wendel ML, Benden ME, Zhao H, Jeffrey C. Stand-biased versus seated classrooms and childhood obesity: a randomized experiment in Texas. Am J Public Health 2016;106:1849-54. https://doi.org/10.2105/AJPH.2016.303323.
- Verloigne M, Ridgers ND, De Bourdeaudhuij I, Cardon G. Effect and process evaluation of implementing standing desks in primary and secondary schools in Belgium: a cluster-randomised controlled trial. Int J Behav Nutr Phys Act 2018;15. https://doi.org/10.1186/s12966-018-0726-9.
- Contardo Ayala AM, Salmon J, Timperio A, Sudholz B, Ridgers ND, Sethi P, et al. Impact of an 8-month trial using height-adjustable desks on children’s classroom sitting patterns and markers of cardio-metabolic and musculoskeletal health. Int J Environ Res Public Health 2016;13. https://doi.org/10.3390/ijerph13121227.
- Lawlor DA, Peters TJ, Howe LD, Noble SM, Kipping RR, Jago R. The Active for Life Year 5 (AFLY5) school-based cluster randomised controlled trial protocol: detailed statistical analysis plan. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-234.
- Ee J, Parry S, Oliveira BI, McVeigh JA, Howie E, Straker L. Does a classroom standing desk intervention modify standing and sitting behaviour and musculoskeletal symptoms during school time and physical activity during waking time?. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15081668.
- Steeves JA, Bowles HR, McClain JJ, Dodd KW, Brychta RJ, Wang J, et al. Ability of thigh-worn ActiGraph and activPAL monitors to classify posture and motion. Med Sci Sports Exerc 2015;47:952-9. https://doi.org/10.1249/MSS.0000000000000497.
- Edwardson CL, Rowlands AV, Bunnewell S, Sanders J, Esliger DW, Gorely T, et al. Accuracy of posture allocation algorithms for thigh- and waist-worn accelerometers. Med Sci Sports Exerc 2016;48:1085-90. https://doi.org/10.1249/MSS.0000000000000865.
- Erwin H, Beighle A, Routen A, Montemayor B. Perceptions of using sit-to-stand desks in a middle school classroom. Health Promot Pract 2018;19:68-74. https://doi.org/10.1177/1524839917730046.
- van Grieken A, Ezendam NP, Paulis WD, van der Wouden JC, Raat H. Primary prevention of overweight in children and adolescents: a meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-61.
- Mehta RK, Shortz AE, Benden ME. Standing up for learning: a pilot investigation on the neurocognitive benefits of stand-biased school desks. Int J Environ Res Public Health 2015;13. https://doi.org/10.3390/ijerph13010059.
- Owen L, Pennington B, Fischer A, Jeong K. The cost-effectiveness of public health interventions examined by NICE from 2011 to 2016. J Public Health 2018;40:557-66. https://doi.org/10.1093/pubmed/fdx119.
- Case . Stand-Biased Desks 2018. www.cedar.iph.cam.ac.uk/wp-content/uploads/2016/05/Stand-biased-desks.pdf (accessed 24 August 2018).
Appendix 1 The Stand Out in Class intervention
| Barrier | Affected mediating variable | COM-B | Theoretical domains framework | Solution (what, who, how, where) | Behaviour change techniques |
|---|---|---|---|---|---|
| Environmental barriers | |||||
| Lesson activities may require a large amount of space (e.g. A3 poster) and for children to work in groups (cluster of tables, e.g. six children), which may be difficult using the sit–stand desks that seat individual children, not the standard pair of children. Some children may stand, some may sit, therefore sit–stand desks may be seen as impractical for the teacher, and the teacher could tell the children using the six sit–stand desks to sit, not stand | M2: children choosing to stand when using sit–stand desks | Opportunity – physical | Environmental contexts and resources |
What: (1) training manual; (2) one-to-one training; (3) frequent support conversations Who: researchers/practitioners for all three components Where/how: 1 and 2 – school; 3 – school or via telephone When: 1 and 2 – before the desks are introduced into the classroom; 3 – every 2 weeks throughout the intervention |
4.1. Instruction on how to perform the behaviour 5.1. Provide information about health consequences 12.1. Restructuring the physical environment 3.1. Social support (unspecified) |
| Limited classroom size with six sit–stand desks in place | M1: time children are exposed to sit–stand desks | Opportunity – physical | Environmental contexts and resources |
What: (1) training manual; (2) one-to-one training; (3) frequent support conversations Who: researchers/practitioners for all three components Where/how: 1 and 2 – school; 3 – school or via telephone When: 1 and 2 – before the desks are introduced into the classroom; 3 – every 2 weeks throughout the intervention |
4.1. Instruction on how to perform the behaviour 5.1. Provide information about health consequences 12.1. Restructuring the physical environment 3.1. Social support (unspecified) |
| Limited flexibility of the sit–stand desks for the teacher to ask the children to work in groups (traditionally would be around their cluster of tables) | M1: time children are exposed to sit–stand desks | Opportunity – physical | Environmental contexts and resources |
What: (1) training manual; (2) one-to-one training; (3) frequent support conversations/consultation Who: researchers/practitioners for all three components Where/how: 1 and 2 – school; 3 – school or via telephone When: 1 and 2 – before the desks are introduced into the classroom; 3 – every 2 weeks throughout the intervention |
3.1. Social support (unspecified) |
| Teacher might want to place the children with special needs (e.g. eyesight problem or misbehaviour) closer to the front or a specific place in the classroom | M1: time children are exposed to sit–stand desks | Opportunity – physical | Environmental contexts and resources |
What: (1) training manual; (2) one-to-one training; (3) frequent support conversations/consultation Who: researchers/practitioners for all three components Where/how: 1 and 2 – school; 3 – school or via telephone When: 1 and 2 – before the desks are introduced into the classroom; 3 – every 2 weeks throughout the intervention |
3.1. Social support (unspecified) |
| Teacher’s barriers | |||||
| Not understanding the importance of reducing children’s sitting/sedentary time, therefore not rotating children and discouraging standing during lessons | M1: time children are exposed to sit–stand desks |
Capability – psychological Motivation – reflective |
Knowledge |
What: (1) training manual; (2) one-to-one training Who: researchers/practitioners for all three components Where/how: school When: before the desks are introduced into the classroom throughout the intervention |
5.1. Information about health consequences |
| Find it difficult to rotate the children in groups because of some of the needs of the children or because of challenging behaviour of children | M1: time children are exposed to sit–stand desks | Capability – psychological | Cognitive skills |
What: (1) training manual; (2) one-to-one training Who: researchers/practitioners for all three components Where/how: school – face to face When: before the desks are introduced into the classroom throughout the intervention Notes: during training researchers will aid the teachers in identifying possible challenging children, and then one of the activities will be a practice and rehearsal in how to deal with challenging behaviour |
8.1. Behavioural practice/rehearsal |
| After a period of time the teacher does not have belief in the sit–stand desks and ceases to rotate the groups | M1: time children are exposed to sit–stand desks | Motivation – reflective | Belief about capabilities |
What: frequent support conversations Who: researchers/practitioners Where/how: school or via telephone When: every 2 weeks throughout the intervention Notes: researcher will reassure the teacher they can successfully do this, and describe the occasions when they did rotate the children successfully |
15.1. Verbal persuasion about capability 15.3. Focus on past success |
| Rotating the children is difficult and teacher stops rotating because of the added stress and consideration of how to rotate children | M1: time children are exposed to sit–stand desks |
Motivation – automatic Capability – psychological |
Emotion |
What: frequent support conversations Who: researchers/practitioners Where/how: school or via telephone When: every 2 weeks throughout the intervention Notes: researcher will advise on ways to reduce negative emotions to facilitate the rotating of children to the desks; and also advise on/arrange/provide emotional support – e.g. ask for classroom assistant to attend support conversation – this will be a face-to-face meeting |
11.2. Reduce negative emotions 3.2. Social support (practical) |
| The extra time burden during times of stress and time pressure | M1: time children are exposed to sit–stand desks |
Motivation – automatic Capability – psychological |
Emotion |
What: frequent support conversations Who: researchers/practitioners Where/how: school or via telephone When: every 2 weeks throughout the intervention Notes: researcher will advise on ways to reduce negative emotions to facilitate the rotating of children to the desks; and also advise on/arrange/provide emotional support – e.g. ask for classroom assistant to attend support conversation – this will be a face-to-face meeting |
11.2. Reduce negative emotions 3.2. Social support (practical) |
| If the rotation system goes against other grouping systems used in class (e.g. ability or split class system) | M1: time children are exposed to sit–stand desks | Capacity – psychological/physical | Memory, attention and decision processes |
What: (1) training manual; (2) one-to-one training; (3) frequent support conversations Who: researchers/practitioners for all three components Where/how: 1 and 2 – school; 3 – school or via telephone When: 1 and 2 – before the desks are introduced into the classroom; 3 – every 2 weeks throughout the intervention |
4.1. Instruction on how to perform the behaviour 12.1. Restructuring the physical environment 3.1. Social support (unspecified) |
| Teacher forgets to rotate children | M1: time children are exposed to sit–stand desks | Capacity – psychological | Memory, attention and decision processes |
What: children’s workshop. In the children’s workshop, children will be informed of the rotation plan, which will be printed and placed on display in the classroom. ‘Remind teacher’ or something similar will be written in large letters next to the rotation plan display Who: researchers/practitioners ensure the timetable has been printed off, and ensure children and staff (teacher, assistant) know where the plan is kept and why Where/how: school When: during the children’s workshop |
7.1. Prompts/cues |
| Find it difficult to change the standard sitting dynamics during lessons | M1: time children are exposed to sit–stand desks | Motivation – reflective | Belief about capabilities |
What: frequent support conversations Who: Researchers/practitioners Where/how: school or via telephone When: every 2 weeks throughout the intervention Notes: researcher will reassure the teacher they can successfully do this, change the groupings and rotation plan, or position of desks if required. Also, describe to the teacher the occasions when they did rotate the children successfully |
15.1. Verbal persuasion about capability 15.3. Focus on past success 4.1. Instruction on how to perform the behaviour |
| Teachers will often have children in ability tables and this may disrupt the workings of that, therefore will not rotate children, or rotate children equally | M1: time children are exposed to sit–stand desks | Motivation – reflective | Belief about capabilities |
What: frequent support conversations Who: researchers/practitioners Where/how: school or via telephone When: every 2 weeks throughout the intervention Notes: researcher will reassure the teacher they can successfully do this, change the groupings and rotation plan, or position of desks if required. Also, describe to the teacher the occasions when they did rotate the children successfully |
15.1. Verbal persuasion about capability 15.3. Focus on past success 4.1. Instruction on how to perform the behaviour |
| Teacher is absent, so rotation plan is not followed. Or if there is a change in personnel (e.g. part-time teacher, trainee teacher, supply teacher or different teacher for certain classes), there may be inconsistent delivery of the intervention and rotation policy | M1: time children are exposed to sit–stand desks | Capacity – physical | Social support |
What: children’s workshop. Children will be informed of the rotation plan, which will be printed and placed on display in the classroom. ‘Remind teacher’ or something similar will be written in large letters next to the rotation plan display Who: researchers/practitioners ensure the timetable has been printed off, and ensure children and staff (teacher, assistant) know where the plan is kept and why Where/how: school When: during the children’s workshop |
7.1. Prompts/cues |
| Teacher does not have the confidence to manage the group with a proportion of the students standing | M1: time children are exposed to sit–stand desks | Capacity – physical/psychological | Skills; beliefs about capabilities |
What: (1) teacher would be supported by the researchers/practitioners planning the rotation; (2) children will be asked to agree on the rules of using sit–stand desks Who: researchers/practitioners Where/how: school When: 1 – teacher’s training; 2 – before the desks are introduced into the classroom (children’s workshop) |
4.1. Instruction on how to perform the behaviour |
| After a period of time the novelty of the intervention has worn off, leading to reduced compliance or reduced enthusiasm by the teacher to encourage standing | M1: time children are exposed to sit–stand desks | Motivation – reflective | Optimism; belief about capabilities |
What: consulting Who: researchers/practitioners Where/how: frequent (fortnightly) contact with the teacher via telephone/e-mail and visit in person (at school) When: during the period of intervention |
15.1. Verbal persuasion about capability 15.3. Focus on past success 4.1. Instruction on how to perform the behaviour |
| Teacher does not have a clear goal for the time each of the children’s groups should be exposed to the desks | M1: time children are exposed to sit–stand desks | Capability | Skills |
What: (1) teacher’s manual; (2) one-to-one teacher’s training; (3) consulting Who: researchers/practitioners and teachers Where/how: 1 and 2 – school; 3 – telephone/e-mail/in-person meeting When: 1 and 3 – during the period of intervention; 2 – at teacher’s training |
8.1. Behavioural practice/rehearsal |
| Resistant to change: may require a change in teaching practice | M1: time children are exposed to sit–stand desks | Motivation | Skills |
What: (1) one-to-one teacher’s training; (2) consulting Who: researchers/practitioners and teachers Where/how: 1 – school; 2 – telephone/e-mail and visit in person (at school) When: 1 – at teacher’s training; 2 – during the period of intervention |
8.1. Behavioural practice/rehearsal 8.7. Graded tasks |
| Children’s barriers | |||||
| Children do not understand the importance of standing while working, therefore will conform to the usual behaviour of sitting to work when using the sit–stand desks | M2: children choosing to stand when using sit–stand desks | Capability – psychological | Knowledge |
What: workshop for children Who: researchers/practitioners Where/how: school for 30–40 minutes When: before the desks are introduced into the classroom (children’s workshop) |
4.1. Instruction on how to perform the behaviour 5.1. Provide information about health consequences |
| As standing is optional, some children might just choose to sit down from the start. This may affect the attitude of other children in the classroom and cause fewer children to opt to stand | M2: children choosing to stand when using sit–stand desks | Motivation – reflective | Beliefs about consequences |
What: workshop for children Who: researchers/practitioners Where/how: school for 30–40 minutes When: before the desks are introduced into the classroom (children’s workshop) Notes: ask children to list pros and cons of standing up more during workshop. Put the list up in the classroom |
9.2. Pros and cons 7.1. Prompts/cues |
| Children may not relate the health benefits of standing to their own health | M2: children choosing to stand when using sit–stand desks | Motivation – reflective | Beliefs about consequences |
What: workshop for children Who: researchers/practitioners Where/how: school for 30–40 minutes When: before the desks are introduced into the classroom (children’s workshop) Notes: make it clear that sitting down is fine, but try to stand if possible as this is great for your health |
5.1. Provide information about health consequences 9.2. Pros and cons 7.1. Prompts/cues |
| Children may not ‘take to it’ first time. This may take children out of their comfort zone and could make some children physically uncomfortable. Some children may require time to get used to standing in class | M2: children choosing to stand when using sit–stand desks | Capability – physical | Physical skills |
What: workshop for children Who: researchers/practitioners Where/how: school for 30–40 minutes When: before the desks are introduced into the classroom (children’s workshop) Notes: make it clear that sitting down is fine, but try to stand if possible as this is great for your health. Set the goal of standing for the first 10 minutes each time they work at the table. Include a prompt sticker for children to stand at least for the first 10 minutes |
5.1. Provide information about health consequences 8.3. Habit formation 7.1. Prompts/cues |
| Some children may feel self-conscious if they are the only ones who choose to stand. Once other children sit down, they may feel obliged to do the same due to social constraints | M2: children choosing to stand when using sit–stand desks | Opportunity – social | Social influences |
What: (1) workshop for children; (2) teacher awards a standing champion weekly; (3) update of teacher capacity to do this via frequent support conversations Who: 1 and 3 – researchers/practitioners; 2 – teachers Where/how: 1 – school for 30–40 minutes; 2 – school; 3 – school or telephone call When: 1 – before the desks are introduced into the classroom; 2 – weekly; 3 – every 2 weeks Note: Make it clear that even if the child is the only one standing, they are a role model of someone who is working, but also being healthy by reducing the time they are sitting. The teacher rewards a standing champion for each week. The child is given a badge and can wear it for a week. Clear criteria for standing champion are (1) using the desks to stand up safely and sensibly; (2) length of time is not the most important thing, it’s having an attempt |
13.1. Identification of self as role model 10.3. Non-specific reward |
| After a period of time the novelty of standing while working has worn off and children go back to sitting when using the desks | M2: children choosing to stand when using sit–stand desks | Motivation – automatic | Reinforcement |
What: teacher informs researcher (researcher asks) Who: researchers/practitioners and teachers Where/how: school face-to-face meeting or telephone call When: during the intervention Note: during the teacher fortnightly meetings researchers asks about novelty wearing off. If this is the case ask teachers to (1) change stickers on desks; (2) move the desks to a different physical position; (3) change the groupings of children; or (4) change the rotation plan – this is all done with the support of the researcher |
7.1. Prompts/cues 12.1. Restructuring the physical environment 12.2. Restructuring the social environment |
| Children might have very short period of time or no time to move their belongings (stationary/workbooks, etc.) for the rotation | M1: time children are exposed to sit–stand desks | Capability – physical | Environmental context and resources |
What: (1) children will be asked to rotate during the lunch time, which will give them more time to move their belongings; (2) storage basket of personal belongings can be provided if required Who: researchers/practitioners Where/how: school When: before the desks are introduced into the classroom (children’s workshop) |
12.2. Restructuring the social environment 12.1. Restructuring the physical environment |
| Children find standing is tiring | M2: children choosing to stand when using sit–stand desks | Capability – physical | Knowledge |
What: children will be taught how to stand in a good posture. They will also be told they could ‘break up their standing time by sitting down’ Who: researchers/practitioners with children Where/how: school When: before the desks are introduced into the classroom (children’s workshop) |
4.1. Instruction on how to perform the behaviour 5.1. Provide information about health consequences |
Appendix 2 Quantitative analyses
| Schools/pupils | Retention rates (7-month follow-up), n/N [proportion] (95% CI) | ||
|---|---|---|---|
| Control | Intervention | Overall | |
| Schools retained | 4/4 [1.0] (0.40 to 1.0) | 4/4 [1.0] (0.40 to 1.0) | 8/8 [1.0] (0.63 to 1.0) |
| Schools not retained/withdrew consent | 0/4 [0.0] | 0/4 [0.0] | 0/8 [0.0] |
| Pupils who consented | |||
| Overall | 86/90 [0.96] (0.89 to 0.99) | 84/86 [0.98] (0.92 to 1.0)a | 170/176 [0.97] (0.93 to 0.99) |
| White ethnicity | 17/18 [0.94] (0.73 to 0.99) | 45/45 [1.0] (0.92 to 1.0)a | 62/63 [0.98] (0.91 to 1.0)a |
| Asian ethnicity | 57/59 [0.97] (0.88 to 1.0)a | 26/26 [1.0] (0.87 to 1.0)a | 83/85 [0. 98] (0.92 to 1.0)a |
| Other ethnicity | 12/13 [0.92] (0.64 to 1.0)a | 13/15 [0.87] (0.60 to 0.98) | 25/28 [0.89] (0.72 to 0.98) |
| Pupils who completed trial | |||
| Overall | 86/90 [0.96] (0.89 to 0.99) | 84/86 [0.98] (0.91 to 1.0)a | 170/176 [0.97] (0.93 to 0.99) |
| White ethnicity | 17/18 [0.94] (0.73 to 1.0)a | 45/45 [1.0] (0.92 to 1.0)a | 63/62 [0.98] (0.91 to 1.0)a |
| Asian ethnicity | 57/59 [0.97] (0.88 to 1.0)a | 26/26 [1.0] (0.87 to 1.0)a | 83/85 [0.98] (0.92 to 1.0)a |
| Other ethnicity | 12/13 [0.92] (0.64 to 1.0)a | 13/15 [0.87] (0.60 to 0.98) | 25/28 [0.89] (0.72 to 0.98) |
| Pupils who did not attend: overall | 2/90 [0.02] (0.02 to 0.08) | 0/86 [0.0] (0.0 to 0.04)a | 2/176 [0.01] (0.001 to 0.04) |
| Pupils lost to follow-up: overall | 1/90 [0.01] (0.0003 to 0.06) | 2/86 [0.02] (0.003 to 0.08) | 3/176 [0.02] (0.004 to 0.05) |
| Pupils not retained/withdrew consent: overall | 1/90 [0.01] (0.0003 to 0.06) | 0/86 [0.0] (0.0 to 0.04)a | 1/176 [0.006] (0.0001 to 0.03) |
| Mean daily values calculated across weekdays and weekend days | Time point, mean (SD) | Change, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||
| Control(N = 58) | Intervention (N = 52) | Control (N = 58) | Intervention (N = 52) | Control (N = 58) | Intervention (N = 52) | |
| Wear time (minutes/day) | 819.7 (73.4) | 830.7 (51.3) | 826.7 (64.2) | 826.1 (56.1) | 7.0 (136.0) | –4.6 (70.8) |
| Time spent sitting (minutes/day) | 527.8 (81.3) | 518.0 (63.0) | 504.9 (83.6) | 467.0 (71.7) | –22.8 (102.9) | –51.0 (77.3) |
| Time spent standing (minutes/day) | 168.1 (51.3) | 184.1 (36.7) | 171.1 (46.4) | 191.6 (41.5) | 3.0 (42.8) | 7.6 (41.9) |
| Time spent stepping (minutes/day) | 123.8 (31.9) | 128.6 (32.0) | 150.7 (38.6) | 167.5 (41.9) | 26.8 (35.6) | 38.9 (42.0) |
| Percentage of wear time spent sitting | 64.4 (7.9) | 62.3 (6.2) | 61.0 (8.0) | 56.5 (7.5) | –3.4 (8.1) | –5.9 (8.2) |
| Percentage of wear time spent standing | 20.5 (6.1) | 22.2 (4.3) | 20.8 (5.7) | 23.3 (5.3) | 0.3 (5.5) | 1.1 (4.7) |
| Percentage of wear time spent stepping | 15.1 (3.6) | 15.5 (3.6) | 18.3 (4.6) | 20.3 (4.7) | 3.2 (4.1) | 4.8 (4.8) |
| Number of sit to stand transitions | 98.6 (24.7) | 103.5 (21.1) | 102.3 (25.3) | 105.2 (21.2) | 3.7 (20.5) | 1.7 (18.4) |
| Number of days worn | 5.4 (1.7) | 5.0 (1.5) | 4.6 (1.9) | 5.0 (1.9) | –0.8 (2.0) | 0.0 (2.5) |
| School | Time point, n (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | |||||||||||
| Maths | Reading | Writing | Maths | Reading | Writing | |||||||
| Not met | Met | Not met | Met | Not met | Met | Not met | Met | Not met | Met | Not met | Met | |
| Control classes | ||||||||||||
| C01 | 11 (55) | 9 (45) | 7 (35) | 13 (65) | 12 (60) | 8 (40) | 15 (75) | 5 (25) | 15 (75) | 5 (25) | 16 (80) | 4 (20) |
| C02 | 5 (18) | 23 (82) | 10 (36) | 18 (64) | 10 (36) | 19 (64) | 0 (0) | 28 (100) | 4 (14.3) | 24 (85.7) | 6 (21.4) | 22 (78.6) |
| C03 | 6 (27) | 16 (73) | 5 (23) | 17 (77) | 8 (36) | 14 (64) | 6 (27) | 16 (73) | 6 (27) | 16 (73) | 12 (55) | 10 (45) |
| C04 | 9 (45) | 11 (55) | 12 (60) | 8 (40) | 10 (50) | 10 (50) | 8 (40) | 12 (60) | 17 (85) | 3 (15) | 9 (45) | 11 (55) |
| Total | 31 (34) | 59 (66) | 34 (38) | 56 (62) | 40 (44) | 50 (56) | 29 (32) | 61 (68) | 42 (47) | 48 (53) | 43 (48) | 47 (52) |
| Intervention classes | ||||||||||||
| I01 | 5 (21.7) | 18 (78.3) | 6 (26.1) | 17 (73.9) | 8 (34.8) | 15 (65.2) | 7 (30.4) | 16 (69.6) | 7 (30.4) | 16 (69.6) | 10 (43.5) | 13 (56.5) |
| I02 | 1(4) | 24 (96) | 0 (0) | 100 (100) | 1 (4) | 24 (96) | 1 (4) | 24 (96) | 0 (0) | 25 (100) | 2 (8) | 23 (92) |
| I03 | 8 (44.4) | 11 (55.6) | 10 (55.6) | 8 (44.4) | 9 (50) | 9 (50) | 6 (33.3) | 12 (66.7) | 4 (22.2) | 14 (77.8) | 8 (44.4) | 10 (55.6) |
| I04 | 11 (61) | 7 (39) | 12 (67) | 6 (33) | 12 (67) | 6 (33) | 3 (17) | 15 (73) | 7 (39) | 11 (61) | 7 (39) | 11 (61) |
| Total | 25 (30) | 59 (70) | 28 (33) | 56 (67) | 30 (36) | 54 (64) | 17 (20) | 67 (80) | 18 (21) | 66 (79) | 27 (32) | 57 (68) |
List of abbreviations
- BCW
- behaviour change wheel
- BMI
- body mass index
- CI
- confidence interval
- COM-B
- capability, opportunity, motivation – behaviour model
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-Y
- EuroQol-5 Dimensions Youth
- EVPI
- expected value of perfect information
- GP
- general practitioner
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- MET
- metabolic equivalent
- MVPA
- moderate- to vigorous-intensity physical activity
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PEDS-QL
- Paediatric Quality of Life Inventory
- PI
- principal investigator
- PPI
- public and patient involvement
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RVIP
- rapid visual information processing
- SD
- standard deviation
- TSC
- Trial Steering Committee
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/phr08080).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
