Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 15/49/08. The contractual start date was in October 2016. The final report began editorial review in January 2020 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Caldwell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Parts of this chapter are reproduced or adapted from Caldwell et al. 1 © 2019 The Author(s). Published by Elsevier Ltd. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Description of the problem
Common mental disorders are a key cause of morbidity in children and young people (CYP). Globally, depressive disorders are the third largest cause of adolescent disability-adjusted life-years (DALYs) lost, and anxiety disorders are the fifth cause of DALYs lost for adolescent girls. 2 In the UK, the most common mental disorders among CYP are anxiety, depressive and conduct disorders. NHS Digital figures from 2017 suggest that 7.2% of 5- to 19-year-olds have an anxiety disorder, 2.1% a depressive disorder and 4.6% a conduct disorder. 3 In this report, we will refer to anxiety, depressive and conduct disorders as ‘common mental disorders’ (CMDs), as these are the disorders with the highest prevalence among CYP in the UK. Although the prevalence of CMDs tends to increase with age, it is noted that rates of anxiety and depressive disorders have increased among CYP in the UK over the last 20 years, in contrast to the stability of diagnoses for conduct and hyperactivity disorders. 3–5 However, as many CYP or their guardians do not seek help,6,7 these figures may represent an underestimate. 8,9
Children and young people with a mental health disorder are more likely to engage in risky behaviours, such as smoking and substance use; are more likely to self-harm; and are more likely to be excluded from school. 10–16 Although the causes are multifactorial, with genetic and environmental factors contributing to susceptibility, the distribution of CMDs is socially and economically patterned. 17 For example, young people with a common mental disorder are nearly twice as likely as those without a disorder to be living with a lone parent, more than twice as likely to have unemployed parents and more likely to have parents with low incomes and fewer qualifications and living in social housing. 11 Evidence from the UK Millennium Cohort18 suggests that children from low-income families are four times more likely to have a mental health problem than those from higher-income families. Longitudinal evidence suggests a linear relationship between the frequency of disorder episodes and the likelihood of adverse social outcomes. In a cohort of CYP aged 16–21 years from New Zealand,19 the odds of later welfare dependence were 1.34 [95% confidence interval (CI) 1.09 to 1.64] times higher among those reporting 1–4 episodes of depression than among those reporting no episodes of major depression. The odds among those reporting ≥ 10 episodes were 2.42 (95% CI 1.31 to 4.45) times higher than among those reporting none.
Although there is ongoing debate about the drivers of increased prevalence,20 there is robust evidence to suggest that lifetime trajectories of CMDs are established by mid-adolescence,21 with half of all disorders recognisable by age 14 years and three-quarters by age 25 years. 22 The Royal College of Psychiatrists has stated that greater personal, social and economic benefits can be generated by intervening early in the life course than by intervening at any other time. 22 However, Child and Adolescent Mental Health Services (CAMHS) worldwide are under-resourced. 23 In the UK, the Local Government Association estimates that > 338,000 children were referred to CAMHS in 2017, but fewer than one-third had received treatment within the year. 24 Even in the advent of optimal access and treatment, one economic modelling study has suggested that < 30% of the burden of CMDs could be alleviated by treatment alone. 25
Description of the intervention
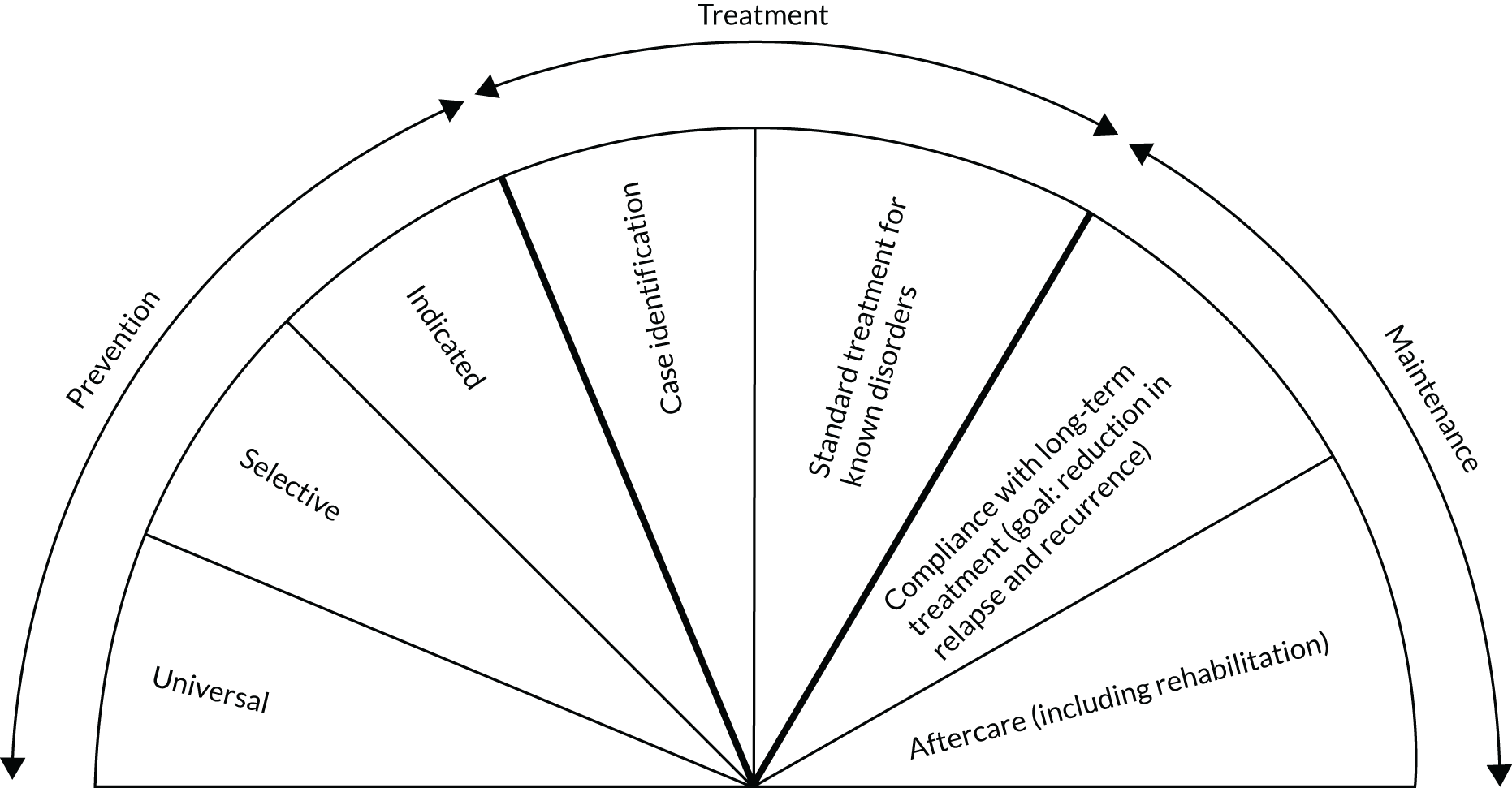
Against this background, there has been a growing focus on the primary prevention of CMDs among CYP. Primary prevention aims to prevent the onset of disease before clinically relevant symptoms are detectable and, therefore, targets a seemingly ‘healthy’ population. According to the National Academy of Medicine (NAM) (formerly known as the Institute of Medicine), primary prevention encompasses the prevention of disorder-specific symptoms, reduction of preclinical symptoms and prevention (or delay) of disorder onset. 26 The NAM definition of primary prevention also refers to universal, selective and indicated prevention26,27 and is distinguished from mental health promotion (Figure 1). Universal prevention addresses whole populations regardless of their risk status or susceptibility to a CMD. Selective prevention targets subgroups with higher than average risk of developing a mental disorder; risk can be defined as biological, psychological or social factors. Indicated prevention focuses on individuals with detectable, but subclinical, symptoms of a CMD. Increasingly, the boundary between indicated prevention and ‘early intervention’ is being blurred by clinicians. 28 The NAM framework views mental health promotion as a focus on encouraging mental health and the enhancement of well-being, rather than the prevention of illness.
FIGURE 1.
The mental health intervention spectrum for mental disorders. Reproduced with permission from Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. 26 Copyright © National Academy of Sciences. All rights reserved.
In the UK, schools are at the forefront of the prevention agenda. For example, the green paper Transforming Children and Young People’s Mental Health Provision29 calls for mental health leads to be embedded in schools and a greater role for schools in cross-sectoral support teams. The 2019 green paper Advancing our Health: Prevention in the 2020s30 takes this further, with subsequent policy announcements giving schools statutory responsibility for children’s mental health and well-being. Across the UK, school-based education is compulsory between the ages of 5 and 16 years,31 with further statutory provision for 16- to 18-year-olds in England. In 2019, 8.82 million pupils were enrolled in England,32 698,000 in Scotland,33 234,550 in Wales34 and 330,000 in Northern Ireland. 35
Multiple systematic reviews examining school-based preventative interventions for CMDs have been published in recent years, and taken together the results suggest a small but positive effect of psychological and educational interventions. For example, for the prevention of anxiety and depression, Werner-Seidler et al. 36 evaluated both universal and targeted (selective and indicated) interventions in school settings and found a small beneficial effect on both depression (Hedges’ g 0.23, 95% CI 0.19 to 0.28) and anxiety (Hedges’ g 0.20, 95% CI 0.14 to 0.25). Johnstone et al. 37 focused on universal interventions in school settings and observed a positive effect on symptoms of depression (Hedges’ g 0.17, 95% CI 0.06 to 0.28), but not on anxiety (Hedges’ g 0.09, 95% CI –0.07 to 0.26). Stockings et al. 38 included multiple settings in their review, and included both universal and targeted populations. They concluded that universal (Cohen’s d –0.11, 95% CI –0.16 to –0.05) and targeted interventions (Cohen’s d –0.33, 95% CI –0.46 to –0.20) to prevent depression are effective in the short term. They observed that universal prevention had a positive effect on anxiety (Cohen’s d –0.16, 95% CI –0.27 to –0.06), but that indicated prevention did not (Cohen’s d –0.01, 95% CI –0.27 to 0.26). Rasing et al. 39 focused on targeted interventions only, in any setting, and concluded that depression symptoms were reduced [standardised mean difference (SMD) –0.25, 95% CI –0.38 to –0.12], but not anxiety (SMD –0.19, 95% CI –0.36 to 0.03).
Much research into the prevention of conduct disorder has focused on indicated parenting programmes to prevent antisocial/disruptive behaviour in young children. Meta-analyses of indicated parenting programmes suggest that they have a positive effect. For example, Piquero et al. 40 report a medium effect size for preventing antisocial behaviour (Hedges’ g 0.37; p < 0.001). Meta-analyses of school-based universal interventions have focused on reducing broader ‘externalising’ or general behaviour problems, rather than on the prevention of conduct disorder. For example, Lipsey and Wilson41 found that both universal school-based interventions (Hedges’ g 0.21; p < 0.05; Q76 212; p < 0.05) and indicated interventions (Hedges’ g 0.29; p < 0.05; Q108 300; p < 0.05) had a small beneficial effect in terms of preventing outcomes of disruptive behaviour.
Rationale for the current study
It can be argued that no two preventative interventions are exactly alike, as they are made up of combinations of components, each delivered with differing degrees of fidelity and intensity, to slightly different populations and settings. However, in a standard meta-analysis, intervention complexity and variation are overlooked when studies are combined to form a single comparator for analysis (e.g. ‘CMD intervention’ compared with control). This ‘lumping’, or conflating, of potentially disparate interventions can induce statistical heterogeneity. Estimates of statistical heterogeneity (variability across intervention effects) in meta-analyses of preventative CMD interventions can be substantial. Although heterogeneity may be inevitable in public health meta-analyses,42 it should nevertheless be minimised because of the consequences for policy recommendations and decision-making. 43 For example, in a random-effects meta-analysis, the precision (certainty) with which the average intervention effect is estimated decreases as heterogeneity increases, that is CIs are wider.
The need to ‘lump’ interventions, and control conditions, can be avoided by using a network meta-analysis (NMA). 44 A NMA combines direct and indirect estimates of intervention effect to allow the simultaneous comparison of multiple interventions in a single evidence synthesis. Crucially, a NMA retains the distinct identity of each intervention analysed. 45 It also enables the ranking of interventions according to the probability that each is the best, or worst, for a given outcome. The effect of intervention components (individually or in combination) can be modelled in a meta-analysis using metaregression methods. 46 Work since 201447–49 has highlighted the importance and feasibility of NMAs in public health, and how they can be used to explore and minimise heterogeneity in evidence syntheses. A component-level NMA is ideally suited to synthesising preventative CMD interventions, as the complexity of interventions can be incorporated, while providing the coherent and quantitative assessment of effectiveness necessary for decision-making.
Aims and objectives
The overall aim of this project was to identify the most effective and cost-effective intervention component(s), or combination of components, for the universal and targeted prevention of common mental health problems among CYP. For the purposes of this project, CMDs were defined as anxiety, depressive and conduct disorders. This focus was clarified in a protocol update (see the following section and Table 1 for details).
This aim was addressed by the following objectives:
-
consult with CYP and their parents/guardians to inform the outcomes of interest for the systematic review
-
conduct a systematic review of educational setting-based (1) universal and (2) targeted interventions for the primary prevention of anxiety, depression and conduct disorder that have been evaluated in randomised controlled trials (RCTs)
-
develop a classification scheme, or taxonomy, of components used in preventative mental health interventions
-
conduct intervention-level and component-level NMAs to identify effective interventions and components of interventions
-
conduct an economic evaluation to determine the most cost-effective component, or combinations of components, of targeted and universal interventions by condition and setting.
Changes to protocol, clarifications and additional analyses
The protocol was updated in October 2018, to reflect decisions made at the searching and screening stages of the review. These are listed in Searching and screening, with full details and accompanying rationale reported in Table 1 Further changes and clarifications were made at the analysis stage and are listed in Analysis for transparency.
| Deviation or clarification | Proposal or original protocol | Date | Review stage and change | Rationale |
|---|---|---|---|---|
| Project began: October 2016 | ||||
| Deviation | Proposal and protocol | November 2016 | Searching: reduced number of databases searched | The proposal stated that 12 databases would be searched. In consultation with an information specialist, we derived a more efficient approach involving three stages:
|
| Deviation | Proposal and protocol | December 2016 | Screening: change to inclusion criteria | In the original proposal, we stated that the relevant age range would be 5–25 years. To increase relevance to school settings in the UK, the lower age limit was changed to age 4 years. Studies were included if the majority of children were aged ≥ 5 years, or if the mean age was approximately 5 years with a ‘small’ standard deviation. Studies in which the majority of children were < 4 years of age were excluded |
| Deviation | Proposal and protocol | December 2016 | Screening: change to inclusion criteria | In the original proposal, we stated that the relevant age range would be 5–25 years. The original upper age limit was selected to allow sufficient time for multiple follow-ups in tertiary settings, and was not intended to reflect age at baseline (entry to trial). This approach was difficult to operationalise during pilot data extraction, as studies had a wide age range at baseline, spanning the upper age limit (e.g. ages 18–28 years at baseline). Therefore, this was modified to include studies in which the majority of participants were aged ≤ 19 years at baseline |
| Clarification | Proposal and protocol | December 2016 | Screening: clarification of inclusion criteria | ‘Community’ was defined in the protocol inclusion criteria as ‘school affiliated’ and the examples ‘after-school and holiday clubs, church groups, youth clubs and student unions’ given as an illustration. During screening, ‘school affiliated’ was operationalised as ‘attached or linked to a specific school setting’. Studies that used schools as the source of recruitment but that were conducted ‘off-site’ at home or in other community settings were not eligible for inclusion. Multisetting studies that were primarily based in schools were included. This was to ensure that the school was not simply be the point of recruitment for an intervention that was then (entirely) carried out elsewhere |
| Project paused: April 2017 to February 2018 | ||||
| Clarification | Protocol | April 2018 | Data extraction: clarification to conditions included | The original proposal listed CMDs as obsessive–compulsive disorder, phobia, post-traumatic stress, panic disorder, anxiety, depression and conduct disorder. We stated in the proposal that we anticipated focusing on the most common: anxiety, depression and conduct disorder. However, the original protocol did not reflect this anticipated focus clearly enough, and a clarification was needed. After staff absence, to ensure efficiency and expedite the review, a modification was made to the protocol to ensure that the explicit focus was on anxiety, depression and conduct disorder. At the stage this decision was made, data extraction for depression and conduct disorder studies had not started, but was under way for anxiety |
| Clarification | Protocol | January 2019 | Analysis: clarification of analysis plans | Educational settings were divided into UK-specific primary, secondary and tertiary groupings for the purposes of analysis, and studies were grouped on the basis of the mean age (or range) and mapped to a primary, secondary or tertiary setting for analysis. This was not made explicit in the original protocol, which implied that the intervention should be delivered in one of these settings. This would not have been practical from an international perspective, owing to differences in educational systems (e.g. middle and junior-high schools). Studies were grouped on the basis of the mean age (or range) and mapped to a UK-equivalent primary, secondary or tertiary setting for analysis |
| Deviation | Protocol | January 2019 | Analysis: change to analysis plan | We planned to analyse ‘inequality’ as a main outcome. However, few studies reported inequality as a primary outcome; instead, we carried out post hoc subgroup analyses by SES, sex and ethnicity. These characteristics were selected post hoc, on the basis of the most commonly reported study characteristics |
| Deviation | Protocol | January 2019 | Analysis: change to analysis plan | In the protocol, we stated that we would conduct metaregression by intervention intensity, defined as total session time (number of sessions × duration in minutes). However, we determined that this would not be meaningful in a NMA with differing classes of intervention. It would have been possible to conduct the metaregression in a subgroup analysis of psychological therapies only |
| Deviation | Protocol | May 2019 | Analysis: change to outcome measure | In response to reviewer comments on Caldwell et al.,1 we added a post hoc composite ‘internalising’ outcome for inclusion in the NMA. We defined internalising outcomes as combined, or total, scores from depression and anxiety symptom scales. For example, the ‘internalising’ subscale of the SDQ or the total score from the DASS |
| Deviation | Protocol | June 2019 | Analysis: change to analysis plan | Parental reporting of child symptoms was a secondary outcome and, as such, it was not anticipated that we would conduct a NMA. However, based on external evidence of a discrepancy between CYP and parent reports, and that some included studies reported only a parent outcome, we conducted a post hoc analysis of parent-reported outcomes |
| Clarification | Protocol | October 2019 | Analysis: change to analysis plan | In the protocol, we stated that a cost-effectiveness analysis would be conducted if there was sufficient evidence to build and populate a model. If this were not the case, then a cost–consequence analysis would be conducted. We did not identify sufficient evidence to build and populate a model; therefore, we did not conduct a cost-effectiveness analysis. We did, however, conduct a cost–consequence analysis. This, therefore, does not constitute a change from protocol, but we report it here for transparency |
Searching and screening
-
The number of databases searched was reduced from the original proposal. Instead, we followed Cochrane Methodological Expectations of Cochrane Intervention Reviews (MECIR) conduct guidelines50,51 on the selection of primary databases and applied approaches for optimising search strategies. 52–54
-
The protocol stated that the relevant age range for inclusion was 5–25 years. This was difficult to operationalise in practice, and changes were made to the age limits so that the report covers the age range 4–18 years.
-
We clarified the intended intervention setting as ‘educational-setting based’. In the original proposal, we stated that the review would be conducted for ‘school and community based . . . prevention interventions’, and defined ‘community’ as ‘school affiliated’ settings. The clarification here pertains to the definition of ‘school affiliated’, which was operationalised as ‘formally attached or linked to a specific school setting’.
-
A further clarification relates to the definition of CMDs. In this review, CMDs were defined in reference to their prevalence. The updated protocol clarified that the clinical conditions of interest were anxiety, depressive and conduct disorders, as these are the most common across the included age groups.
Analysis
-
The educational setting for each study was categorised as UK-specific primary, secondary and tertiary groupings for the purposes of analysis only. This was not made explicit in the original protocol, which implied that the intervention should be delivered in one of these settings.
-
We planned to analyse ‘inequality’ as a main outcome. However, owing to a lack of data, this was not possible; instead, we considered subgroup analyses by socioeconomic status (SES), sex and ethnicity. These characteristics were selected post hoc, based on participant characteristic data that had been extracted.
-
We planned to conduct a metaregression of intervention intensity, in which intensity was defined as total session time (number of sessions × duration in minutes). However, we determined that this would not be meaningful in a NMA with differing classes of intervention, and so the analysis was not conducted.
-
In response to reviewer comments on Caldwell et al. ,1 we added a post hoc analysis for a composite internalising symptoms outcome (which combined depression and anxiety symptom scores).
-
A post hoc NMA of parent-reported child symptoms was conducted.
-
In the protocol, we stated that a cost-effectiveness analysis would be done if there was sufficient evidence to build and populate a model. As an alternative, we planned a cost–consequence analysis. We found that there was insufficient evidence for a cost-effectiveness analysis, and so a cost–consequence analysis is reported.
Chapter 2 Methods for assessing effectiveness
In this chapter, we describe the methods and process applied for the systematic review and NMA. The protocol for the study was registered with PROSPERO (CRD42016048184). Changes from the protocol and clarifications relating to inclusion criteria are listed in Chapter 1 and are described in detail in Table 1. They are also briefly noted throughout this chapter.
Patient and public involvement
As part of the systematic review process, we consulted with the Advice Leading to Public Health Advancement (ALPHA) research advisory group of young people aged 14–21 years, facilitated by the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer) Centre at Cardiff University. 55 The aim was to identify health and social outcomes of importance to young people that could be considered in the systematic review. On the basis of this focus group, we included a post hoc outcome looking at the impact of prevention interventions on the stigma associated with mental disorders. We also met with members of The Caerphilly County Borough Parent Network to explore their views on young people’s mental health and the role of schools in preventing and identifying problems. 56 There were no outcomes from that focus group that fed directly into this report.
Methods for the systematic review of effectiveness studies
Criteria for considering studies for this review
In the absence of direct head-to-head evidence comparing interventions, indirect comparisons can be made across a connected network of interventions. For example, the effect of intervention C against intervention B (BC) can be obtained indirectly from the effect of C against intervention A (AC), minus the effect of B against A (AB). The combination of indirect and direct evidence across a network of intervention comparisons is known as a NMA.
The following eligibility criteria were specified to address the key consistency assumption required for a valid NMA. In a three-intervention network, the consistency assumption requires the true BC intervention effect estimated in the B versus C trials to be the same as the BC intervention effect estimated by the A versus C and A versus B trials (had they also included the B and C arms). 57 For this to hold, one should check that the populations included across all trials in the analysis are comparable to each other, with respect to any potential effect-modifying characteristics. 58 This requirement has been conceptualised as ‘joint randomisability’ of the interventions for the target population. 59 ‘Joint randomisability’ implies that a hypothetical, multiarm trial of every included intervention would be reasonable, in principle, and that all participants would be randomisable to any of the interventions included. 60 This requires clearly and specifically defined inclusion criteria, to ensure the included studies, populations and interventions are sufficiently comparable. Further details on NMA are provided in Methods for the evidence synthesis of effectiveness studies.
Study design
Parallel-group RCTs and quasi-randomised controlled trials were eligible for inclusion. We defined quasi-randomised trials as those for which allocation was based on a pseudo-random sequence, such as the order in which participants were recruited or their date of birth. Both individually randomised and cluster randomised trials were eligible for inclusion. We did not plan to exclude crossover trials, but only the first period was considered eligible for inclusion.
Population
We followed the NAM’s definition of primary prevention, which refers to universal, selective and indicated populations (see Figure 1). 27 Briefly, universal prevention addresses whole populations not defined on the basis of risk; selective prevention is targeted at subgroups with a higher than average risk of developing a mental disorder; and indicated prevention is targeted at high-risk subgroups and/or individuals with detectable, but subclinical, symptoms of a mental disorder. In the first instance, we used author-reported classifications of the intended prevention level. However, when interventions were delivered to a whole class or school with the same at-risk characteristic (such as schools in low-income areas), they were combined with universal prevention. Studies were excluded if the intervention was described by the author as indicated prevention, but baseline symptoms scores were suggestive of clinically meaningful symptom levels (see Definition of disorder).
Age
As noted in Chapter 1, the eligible age range was modified during the screening stage of the review. Further details of this change to protocol are provided in Table 1.
Studies including participants between the ages of 4 and 18 years (age at study recruitment), in full- or part-time education, were eligible for inclusion. The lower age limit was set in accordance with the de facto school starting age in England and Wales. However, owing to global differences in school starting age, we determined that studies implemented in preschool settings would be eligible for inclusion if (1) the mean age of participants was 5 years or (2) the majority of enrolled children were aged 5 years at the time of the baseline assessment. The upper age limit reflects the minimum age of entry to higher (tertiary) education in England and Wales. However, studies were eligible for inclusion if the mean age of participants at baseline was ≤ 19 years. Studies targeted at young people not in education or training were excluded.
Definition of disorder
The original proposal listed CMDs among CYP as obsessive–compulsive disorder, phobia, post-traumatic stress, panic disorder, anxiety, depression and conduct disorder. However, we anticipated focusing on anxiety, depression and conduct disorder, as they are the most common, and we expected the greatest number of studies for these conditions. The structure and connectivity of a network are important considerations in a NMA, as estimates can be obtained only for connected networks, and sparsely populated networks with few participants can lead to imprecise estimates. 57 Further details of this clarification to the original protocol are provided in Table 1.
Studies were included if they were explicitly aimed at the primary prevention of anxiety, depression and/or conduct disorder as operationalised according to categorical or clinically referenced definitions of disorder [e.g. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)]. 61 This was to differentiate studies addressing related mental health constructs, such as emotional health or well-being, which were excluded (see Interventions and comparators). Studies were eligible if they focused on either prevention of disorder onset or prevention of symptoms.
However, studies that addressed individual symptoms, or combinations of symptoms, associated with anxiety, depression and conduct disorder, but without explicitly linking these to a clinically identifiable disorder, were excluded. For example, interventions to prevent insomnia, rumination or low self-esteem were excluded, even though these symptoms are associated with depressive and/or anxiety disorders, and interventions to prevent truancy, bullying or aggressive behaviour were excluded, even though these behaviours are associated symptoms of conduct disorder. Studies were included only if they addressed the whole condition, not individual symptoms or combinations of associated symptoms. We consulted trial registrations and protocols, when available, for further information.
Studies in indicated populations were eligible if participants had subclinical mental disorder symptoms as identified by a screening instrument, an interview or a teacher referral. Subclinical symptoms could be defined in reference to diagnostic criteria such as the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10)- or DSM-5-categorised disorders, or ‘in research’ via use of a disorder-specific screening instrument, for example the Children’s Depression Inventory or Revised Children’s Manifest Anxiety Scale. The boundary between indicated prevention and early intervention (treatment) is debated,26,27 with no definitive diagnostic threshold. Studies were excluded if baseline measures were suggestive of clinically meaningful symptoms in > 40% of participants, even if the study had been defined as indicated prevention by the author. Young people at risk of comorbid mental health disorders were eligible for inclusion. However, we excluded studies for which > 40% of participants had an identifiable or pre-existing mental disorder. To ensure a clinically homogeneous population for analysis, studies in which the whole population had a diagnosis of attention deficit hyperactivity disorder (ADHD) or an autism spectrum disorder were excluded, as these form distinct diagnostic categories.
Setting
As noted in Chapter 1, the operationalisation of setting was clarified from the original proposal. Full details are provided in Table 1.
Interventions implemented in an educational setting were eligible for inclusion. For the purposes of analysis, this was operationalised as being primary, secondary or tertiary educational settings. However, to accommodate global differences in educational systems, we did not restrict to interventions implemented in these settings if the age eligibility criteria were met. For example, an intervention delivered in a kindergarten setting would be eligible for inclusion if the mean age of participants was 5 years, or the majority of enrolled children were aged 5 years at the time of the baseline assessment. Interventions implemented in school-affiliated settings (e.g. after-school and holiday clubs) were eligible for inclusion if they were implemented on school grounds. This clarification from the original protocol is explained in Table 1. Studies that used schools as the source of recruitment but for which the intervention was not school based were excluded.
Health service settings, such as primary care and outpatient and inpatient settings, were excluded. Interventions implemented in young offender institutions and for looked-after children in residential care were also excluded. Interventions implemented in low-income countries (LICs), middle-income countries (MICs) or high-income countries (HICs) were eligible, as defined by 2017 World Bank classifications. 62
Interventions and comparators
Inclusion criteria
Interventions were eligible for inclusion if they addressed a universal, selective or indicated population, and the primary study aim was to prevent anxiety, depression or conduct disorder.
Eligible intervention types included psychological and psychosocial, educational or physical interventions that were implemented in educational settings, either individually or in groups. Inclusion was not restricted by mode of delivery. Interventions were included if delivered by peer educators, teachers, youth workers, clinicians, health visitors, school nurses or counsellors. However, digital and online interventions were eligible for inclusion only if they were primarily delivered in the education setting or were a clear adjunct to a wider programme delivered in the school/educational setting (e.g. as homework).
All relevant non-pharmacological control interventions were considered eligible for inclusion, for example standard provision/usual curriculum, waiting list, no intervention, attention control or ‘placebo’ interventions, and other active psychological and psychosocial, educational or physical interventions. Further details on active and control interventions are provided in Chapter 3.
Exclusion criteria
The following intervention exclusion criteria were informed by the need to ensure the validity of the NMA. The key assumption underpinning a NMA is described in the Cochrane handbook59 as ‘transitivity’, but is also known as the consistency assumption. Regarding the interventions included in the network, transitivity requires ‘all competing interventions of a systematic review to be jointly randomizable’59 and that intervention A is ‘similar’ when it appears in the A versus B and A versus C studies.
Assessment of transitivity for public health interventions is not straightforward. To ensure the validity of the NMA, we included only interventions for which the primary aim in a given study was to prevent anxiety, depression or conduct disorder. Unless the study was explicitly focused on disorder-specific prevention, then mental health promotion, awareness, literacy or information interventions were not eligible for inclusion. Social and emotional well-being and positive psychology interventions to improve mental well-being were also excluded, as research suggests that well-being is a separate construct to mental ill health. 63,64 When possible, we consulted trial protocols or registrations if this was ambiguous in the publication. Interventions designed to target prevention of behaviours or social problems that might be on the causal pathway to a mental disorder (e.g. prevention of stress, anti-bullying interventions, substance abuse prevention) were also excluded. Similarly, classroom management and school readiness interventions were not eligible. ‘Parenting’ interventions such as parent management training or parenting skills interventions were not eligible for inclusion. However, interventions that took place in schools, with a parenting component, were eligible if the parenting component was not > 50% of the whole intervention.
Outcomes
According to the NAM classification of primary prevention, the overall, longer-term aim of preventative interventions ‘is the reduction of the occurrence of new cases’26 of mental disorders. However, it also recognises the importance of shorter-term prevention in terms of reducing symptoms, which, in turn, may delay or reduce the risk of the onset of the disorder. All are considered beneficial at a population level and are ‘worthwhile goals of prevention’. 26 In this report, we focus on the effect of prevention interventions on symptoms of anxiety, depression and conduct disorder. The main outcome was prevention or reduction of disorder-specific symptoms for self-reported anxiety, depression and conduct disorder.
All validated disease-specific measurement scales for CYP were eligible for inclusion. When studies reported multiple outcome measures, we applied a prespecified hierarchy to select the most appropriate outcome for analysis from each study (see Appendix 1). We did not exclude studies reporting a composite mental health scale from the systematic review [e.g. the Strengths and Difficulties Questionnaire (SDQ)]; however, they were not combined with disorder-specific scales in the main NMA. In a change from protocol (see Table 1), a post hoc analysis for composite ‘internalising’ symptom scales was conducted. For example, measurement scales reporting a total or combined score across depression and anxiety symptoms, such as a total Revised Children’s Anxiety and Depression Scale (RCADS) score, or a composite outcome such as the SDQ ‘emotional symptoms’ subscale, were included in this post hoc outcome.
The following additional primary and secondary outcomes were also specified a priori. However, in the absence of a core outcome set65 or guidelines for the selection of measurement scales for school-based mental health interventions,66 we determined that an inclusive approach to additional primary and secondary outcomes was appropriate. Therefore, we did not specify how these outcomes should be measured in advance, or which scales should be used. Instead, we extracted outcomes as reported by the study authors.
Additional primary outcomes were as follows:
-
self-reported well-being, as defined by study author(s)
-
self-reported suicidal ideation, behaviour and self-harm, as reported by study author(s)
-
intervention impact on inequalities in health, as defined by study author(s).
The primary time point of interest was immediately post intervention. However, as sustainability of intervention effect is an important question for public mental health,67 we also report results for mid-term (6–12 months) and longer-term (13–24 months) follow-ups. If studies had a follow-up of ≥ 25 months, these results were also extracted.
Secondary outcomes of interest were as follows:
-
Mental health-related stigma, as defined by study author(s). During our initial patient and public involvement (PPI) focus groups, reducing the stigma associated with mental health problems was identified as an important outcome for young people.
-
Acceptability of an intervention to young people, as reported by the study author(s).
-
Parent-reported prevention or reduction of disorder-specific symptoms, as reported by the study author(s).
-
Self-reported problem behaviour, such as substance use or involvement in violence.
-
Academic attainment, as defined by the study author(s).
Study identification, inclusion and data extraction
Identification of studies
As noted in Chapter 1, the approach to searching was modified from that of the original proposal. Full details and explanation are reported in Table 1.
The revised search strategy involved three stages, which might be considered to combine the ‘known items’ and ‘law of diminishing returns’ approaches described by Booth,52 to optimise searching. First, working with an information specialist (SDa) and following the Cochrane MECIR guidance on conducting searches,50,51 we searched MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials (CENTRAL) and PsycInfo electronic databases. The search strategies for each electronic database are described in Appendix 1. The final searches were carried out on 4 April 2018. Searches were not restricted by language, country or date of publication.
Second, in addition to the database searches, we conducted searches of Epistemonikos (www.epistemonikos.org; Epistemonikos Foundation, Santiago, Chile) to identify published systematic reviews of interventions for the prevention of CMDs among CYP. Epistemonikos was searched on 16 November 2016. The reference lists from these reviews were added to the results of the database searches, ready for screening.
Finally, after screening, we conducted an informal scoping search of the Education Resources Information Center (ERIC) database. This was to check whether further relevant studies could be located, cross-referencing with those already identified from the previously mentioned approaches. If scoping revealed further relevant studies, a formal search was planned. In response to reviewer comments on the draft version of this report, the ERIC scoping searches were formalised and extended to the British Education Index (BEI). Further details are reported in Appendix 1.
Screening for study inclusion/exclusion was independently assessed by two reviewers (SRD, JCP, DMC, PC); disagreement was resolved by a third reviewer if necessary (SRD, JCP, DMC, PC, SEH). Owing to the volume of potentially relevant studies retrieved, reasons for study exclusion were recorded at full-text screening only.
We used a standardised data extraction form in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) to extract information from included studies. Data were extracted by one reviewer and checked by a second (SRD, CF, PC, JCP, DMC). Discrepancies were discussed and a consensus reached. Disagreements were resolved by a third reviewer if necessary. The following information was extracted from the papers:
-
Study design and the target CMD of intervention (i.e. anxiety, depression or conduct disorder); whether the intervention was universal or targeted (indicated or selected); and number of participants recruited, randomised and assessed (or clusters, if a cluster RCT).
-
Details of participants (country, intervention setting, age, sex, ethnicity).
-
Details of intervention as reported by trial author. Narrative description of components and delivery process for experimental and control interventions. This included number of sessions; intervention dose (calculated as intensity of intervention: total session time × duration in minutes); whether the intervention was group or individual, face to face or digital; who facilitated the intervention; and intervention fidelity measures.
-
Outcome(s) assessed and all follow-up time points.
-
Risk-of-bias assessment, including additional assessment for cluster trials.
-
Mean total symptom score and standard deviation (SD) at baseline and follow-up time points for primary measurement scale, change from baseline or mean difference between arms; details on whether results were for completers only or use of methods for handling missing data such as last observation carried forward; and intracluster correlation coefficient (ICC), the statistical model used to account for clustering (if any).
Study authors were contacted for additional data, if necessary.
Classification of interventions and components
Eligible interventions were psychological and psychosocial, educational, or physical interventions. Following previous studies,68–72 and based on author-reported descriptions, the content of psychological and psychosocial interventions was classified into four broad intervention types: cognitive–behavioural, behavioural, third wave and interpersonal. Physical interventions were further classified as exercise or biofeedback. Further categories identified were a combined mindfulness/relaxation intervention, psychoeducational and psychosupportive interventions, and occupational therapy. Control interventions were classified into four categories: no intervention, waiting list, usual curriculum and attention controls. 72–74 A full description of all interventions is given in Chapter 3.
We also conducted an intervention component analysis (ICA)75 to identify features of intervention content and process, influenced by the why, what, who, how, when and how much domains of the Template for Intervention Description and Replication (TIDieR). 76 We applied the constant comparative method,77 whereby the intervention descriptions reported by authors were used to develop a coding scheme to classify the components of each intervention and control. If necessary, descriptions were supplemented by intervention manuals and/or correspondence with the study author. ICA is an iterative and inductive process. One reviewer (SRD) developed and piloted a list of provisional component codes based on published studies. 46,68,72,78 The components were discussed with a second reviewer and a preliminary coding exercise was then undertaken on a sample of interventions by a wider group (SRD, DMC, JK and SEH), and the coding scheme was further refined based on discussion. The refined coding scheme was then applied inductively by one researcher (SDa) and audited by another (DMC). Iterative coding refinements were made until application failed to reveal any new information and the component categories could be described as ‘saturated’.
The working definitions of each intervention and control classification and the classifications of intervention components are provided in Chapter 3.
Assessment of risk of bias in included studies
Two reviewers independently used the Cochrane Risk of Bias tool79 to assess whether there was a high, low or unclear risk of bias in the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessor, incomplete outcome data, selective outcome reporting and other sources of bias (including cluster-specific issues such as contamination, recruitment bias and unit-of-analysis errors). All eligible studies were included in the NMA regardless of their risk-of-bias classification, and sensitivity analyses examined the impact of excluding studies deemed to be at high and unclear risks of bias for random sequence generation and allocation concealment.
Methods for the evidence synthesis of effectiveness studies
Data preparation
For continuous outcomes, data were extracted for number randomised to each intervention arm at baseline, and baseline mean and SD, and number assessed at follow-up, and follow-up mean and SD (for each time point listed previously). If the mean change from baseline was reported, then this was extracted, together with the standard error (SE) for the mean change from baseline (if reported). Data were extracted for complete cases. However, if authors reported means and SEs from an appropriate model accounting for participant dropout or non-response, this was preferred.
For analysis, we used the standardised mean change from baseline, as a variety of outcome measurement scales were used across the studies. An adjustment for small sample size was applied, following the formula for Hedges’ g. 80 For studies that did not report mean change from baseline, we derived this from reported baseline and follow-up means and SDs. 81 Here we assumed a correlation coefficient of 0.7, based on previous analyses. 82 This value was explored in sensitivity analyses. Results are summarised using SMDs and 95% credible intervals (CrIs).
For dichotomous outcomes, data were extracted for available cases unless authors clearly reported events and number of participants following the intention-to-treat principle. Dichotomous outcomes were summarised using odds ratios (ORs) and 95% CrIs.
If key statistics (e.g. SDs) were not available in the published report, we contacted trial authors for further information. In cases of non-response, or if missing data were not available, we did not impute the data and these studies were excluded from the NMA (but not the systematic review).
For cluster randomised trials that did not account for the effect of clustering, we followed the advice in the Cochrane handbook (section 16.3.4)81 for calculating an approximate sample size. We reviewed reported ICCs from all included papers and used an ICC estimate of 0.03, which is the mean of the values reported and is similar to ICCs used in previous public health systematic reviews. 68,83–85 This value was also explored in sensitivity analyses.
Pairwise and network meta-analyses
Both standard pairwise meta-analyses and NMAs were conducted. A NMA was planned for each primary outcome and for the primary time point only.
A NMA allows data on multiple interventions to be pooled in a single analysis. 86 It is considered a ‘core method’ by Cochrane59 and is routinely used in National Institute for Health and Care Excellence (NICE) technology appraisals and guidelines. 87,88 For the novice, the Cochrane handbook81 provides an accessible introduction; for further depth, we recommend consulting tutorials and introductory papers on NMA. 44,45,60,89–92 However, we describe the fundamentals in the following paragraphs.
A NMA requires that the intervention comparisons made in RCTs can be displayed pictorially as a network of comparisons that are ‘connected’ (i.e. there is a path from any one intervention to another formed by RCT evidence). 59,93 In the absence of direct head-to-head evidence comparing interventions, indirect comparisons can be made via common comparator(s) across the network. For example, the effect of intervention C against intervention B can be obtained from the effect of C against A, minus the effect of B against A. The combination of indirect and direct evidence across a network of intervention comparisons is known as a NMA.
The validity of a NMA assumes that there are no differences between studies in factors that might interact with the intervention effect (effect modification). This is the same assumption made in a pairwise meta-analysis,57 but in a NMA applies across intervention comparisons. It is therefore important to consider separate analyses according to factors that may be potential effect modifiers. In the first instance, separate analyses were conducted by population (universal or targeted) and setting (primary, secondary or tertiary education). Separate analyses were run for the main outcomes of self-reported anxiety, self-reported depression and self-reported conduct disorder symptoms. Following research suggesting common mechanisms and pathways within internalising and externalising disorders (transdiagnostic factors),94–97 we ran analyses across (1) all studies aiming to prevent depression and/or anxiety and (2) studies aiming to prevent conduct disorder. That is, studies contributing to either the depression or anxiety outcome analyses could be studies that aimed to prevent (1) anxiety (2) depression or (3) anxiety and depression. Studies contributing to the analysis of the conduct disorder outcome were only those aiming to prevent conduct disorder. We explore this decision further in a subgroup analysis (see Subgroup, metaregression and sensitivity analyses). A visual check of the inclusion/exclusion characteristics of trials in each network was conducted, to ensure that potential effect modifiers were evenly distributed across studies.
Network plots were drawn in Stata® version 15 (StataCorp LP, College Station, TX, USA) to allow visual inspection of network connectedness. 98
For the primary time point of post intervention only, we considered three NMA models, each allowing for increasing specificity of intervention detail:46,82
-
Intervention-level model – interventions were analysed as ‘clinically meaningful units’. 48 For example, cognitive–behavioural therapy (CBT) was analysed as a distinct intervention to psychoeducation or third wave-based interventions.
-
Additive model – components nested within intervention. A main intervention effect was estimated (as per the intervention-level model), plus additional effects for specific components within each intervention. For example, we estimated an overall CBT effect, which represents the effect for CBT interventions with components that were common across all the included CBT interventions, and also estimated the additional effect of CBT interventions containing a psychoeducation component, a mindfulness component and so on.
-
Full interaction model – components nested within intervention: under this model, each unique combination of intervention and components was considered as a separate intervention. For example, CBT with cognitive + behavioural + psychoeducation components was considered a distinct intervention to CBT with cognitive + behavioural + psychoeducation + relaxation components.
For follow-up time points, where we anticipated finding fewer studies, we ran the intervention-level model only as prespecified in the protocol. Intervention-level analyses were implemented in a Bayesian framework using OpenBUGS software (version 3.2.3). Component analyses were implemented in WinBUGS99 (version 1.4.3; MRC Biostatistics Unit, Cambridge, UK). Statistical details are reported in Appendix 1. Data and WinBUGS code can be obtained by contacting the corresponding author. Vague prior distributions were specified for intervention effect and heterogeneity parameters (see Appendices 1 and 3). We assessed convergence for the intervention-level NMA based on three chains using the Brooks–Gelman–Rubin diagnostic tool and history plots in OpenBUGS. Specific convergence details for each model and population/setting analysis are reported in the model fit tables in Appendix 3, Table 29–46.
Random-effects models were run for the main outcomes, assuming a common between-study SD (known as ‘homogeneous variance’). 100 However, we assessed both fixed- and random-effects models on the basis of model fit. Heterogeneity was evaluated by examining the posterior median between-study SD (τ) and 95% CrIs from the random-effects model, and by comparing model fit of the fixed- and random-effects models. Model fit was measured by the posterior mean of residual deviance. In addition, we examined the deviance information criterion (DIC), which penalises model fit with model complexity. Differences of ≥ 5 points in posterior mean residual deviance and the DIC were considered meaningful, with lower values preferred. 101 Model fit statistics are reported in Appendix 3.
As described previously, a key assumption for a valid NMA is that of consistency between the direct and indirect evidence. If the effect estimates from the direct and indirect evidence in a network do not agree, this is known as inconsistency. The strict inclusion/exclusion criteria described previously were specified to avoid inconsistency, but they do not guarantee consistency. For this reason, the statistical agreement of the evidence was formally checked. Consistency was assessed by comparing the goodness of fit of a model assuming consistency with that of one allowing for inconsistency (i.e. a model that provides effect estimates based on direct evidence only). A common between-study SD was also assumed for these inconsistency models. 57
Pairwise meta-analyses were also conducted when head-to-head evidence was available. The method of estimation is similar to the NMA, except that the consistency assumption is removed such that intervention effects for separate comparisons are unrelated and separate intervention effects can be estimated. 57 Estimates are reported for the post-intervention time point only and are from a random-effects model that assumes that the heterogeneity parameter is common across intervention comparisons. This better reflects the assumption made in the NMA and, therefore, allows a fair comparison of the intervention effect estimates obtained from both approaches.
Subgroup, metaregression and sensitivity analyses
Metaregression and subgroup analyses were performed in OpenBUGS following the Evidence Synthesis Technical Support Unit code available from the NICE Decision Support Unit’s website and described in Dias et al. 102,103 Subgroup analyses were conducted to assess whether or not intervention effects differed by intended focus of the intervention, for example if interventions addressing anxiety had a larger effect on anxiety outcomes than interventions intended to focus on depression but which also recorded anxiety outcomes.
Metaregression was planned for the intervention-level NMA and main outcomes only, to examine if intervention effects differed by mode of intervention delivery and who facilitated intervention delivery:
-
Mode of intervention delivery – interventions were categorised as being delivered face to face or via a computer/internet. To explore whether or not intervention effects were modified by mode of delivery, we fitted a metaregression model for face-to-face (covariate value = 0) and computer/internet (covariate = 1) interventions. A random-effects NMA model was fitted. However, the regression coefficient for the covariate was assumed to be a fixed effect across studies. The between-study SD was assumed to be common for face-to-face and computer/internet interventions. Vague priors were specified.
-
Who facilitated intervention delivery – interventions were categorised as being facilitated by a teacher or a mental health professional (MHP). There was considerable variation within the category of ‘MHP’ and it should be regarded as a simplification. Here, MHP included school counsellors, qualified psychotherapists and graduate and post-doctoral psychology students. Graduate and post-doctoral students included those studying general psychology, educational psychology or counselling psychology, when specified. We fitted a metaregression model that enabled us to estimate the intervention effect at each value of the covariate (0 or 1), for each intervention, comparing the effect of each facilitator (e.g. CBT-teacher vs. CBT-MHP vs. usual care). To allow for networks containing multiarm studies with more than two interventions facilitated by a teacher or MHP, a hierarchical model was fitted. In this hierarchical model, a regression coefficient for each intervention was assumed to come from a normal distribution with a common mean and between-intervention SD. The between-intervention SD was assumed to be common for each value of the covariate. Vague priors were specified.
We explored the potential for small-study effects using comparison-adjusted funnel plots. 98
Sensitivity analyses were conducted for the intervention-level NMA, main outcomes and primary time point only. Analyses explored the robustness of results to the following:
-
Excluding studies deemed to have a high/unclear risk of bias on the domains of random sequence generation and allocation concealment.
-
The ICC value of 0.03 for cluster randomised trials. Sensitivity analyses were conducted assuming an ICC of 0.01 and 0.06.
-
The correlation value of 0.7 assumed for calculating change from baseline SD. Sensitivity analyses were conducted assuming a correlation of 0.6 and 0.8.
Interpreting the results and evaluating evidence of effect
As described previously, summary effect estimates and their 95% CrIs from the NMA are reported. In interpreting these statistical findings, we followed the guidance from the Cochrane handbook (section 15.3) that interpretation of results from a meta-analysis should not rely on statements of ‘statistical significance’ or thresholds implying ‘significance’. 104 Instead, we interpret the strength of statistical evidence on a graduated scale from weaker to stronger evidence of an intervention effect. 105,106
In Chapter 9, we also provide a summary of these statistical findings for the primary outcomes of anxiety, depression and conduct disorder symptoms at the primary time point of post intervention. This interpretation forms the basis of the conclusions for the report. The criteria used are based on the considerations outlined in Chapters 14107 and 15104 of the Cochrane handbook. These considerations are informed by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) domains of imprecision, inconsistency (heterogeneity), risk of bias and publication bias. It is not a formal application of the GRADE rating system, which necessitates up- or downgrading of the evidence on the basis of the assessments to form an overall assessment of ‘quality’. 107
Specifically, our interpretation of the evidence is not solely based on the magnitude and direction of the summary point estimate, but also incorporates an evaluation of all of the following:
-
the precision of the effect estimate, as described by the 95% CrI
-
the extent of the between-study heterogeneity observed in each analysis, as described by τ and its 95% CrI
-
the risk-of-bias assessment
-
the possibility of non-reporting biases or evidence of small-study effects.
Chapter 3 Intervention and component categorisation
In this chapter, we describe the intervention classifications and the components used in the NMAs reported in Chapters 4 and 5.
Main ‘intervention-level’ classification
The main ‘intervention-level’ classifications were assigned based on the trial authors’ descriptions and classifications used in previous systematic reviews. 36–39,68,108–113 Many interventions to prevent anxiety and depression have been adapted from existing clinical interventions for treatment which, in turn, are grounded in identifiable therapeutic traditions. In adapting therapeutic interventions for a prevention context, some developers have retained the reference to the underlying therapy on which they are based, for example cognitive–behavioural therapy. Although these preventative interventions focus on the same techniques, exercises and skills that underpin the clinical ‘therapeutic’ intervention, the term ‘therapy’ may be considered a misnomer in a preventative context. As such, it may be preferable and more accurate to consider these preventative interventions as ‘interventions based on the principles of CBT’. However, for conciseness and consistency with the trial literature we retain the use of ‘therapy’ when using intervention abbreviations throughout the report (e.g. CBT).
Behavioural therapy
Behavioural therapy is a group of allied techniques that focus on behavioural models of psychology and seek to modify overt maladaptive behaviours. In the current review, we categorised interventions based on behavioural activation, self-monitoring, role-playing, exposure to feared stimuli or scheduling pleasant activities as being behavioural in nature.
Cognitive–behavioural therapy
Cognitive–behavioural therapy can be considered a family of allied techniques, based in both behavioural and cognitive models of psychology, that utilise a set of overlapping cognitive and behavioural techniques. CBT is based on the proposition that a person’s behaviour is influenced by their cognitive activity (and vice versa), and that cognitions can be monitored and altered (cognitive restructuring). In turn, emotions and behaviour can be modified via this cognitive change. CBT interventions for treatment of CMDs typically include a psychoeducation component; however, in preventative interventions, this may not always be present.
Third-wave interventions
This was a composite category. Third-wave psychotherapies emphasise mindfulness, acceptance and flexibility. They tend to focus on a person’s relationship to their cognitions and emotions, encouraging an acceptance of thoughts, rather than modifying their content. Interventions that described themselves as mindfulness-based CBT, acceptance and commitment therapy or dialectical behavioural therapy were included in this classification. Third-wave preventative interventions were distinguished from mindfulness meditation or relaxation interventions that did not explicitly address cognitions or behaviours.
Interpersonal therapy
From a treatment perspective, interpersonal therapy (IPT) is based on the relationship between mood symptoms and interpersonal relationships. It seeks to relieve symptoms via resolving interpersonal conflict and difficulties. In the preventative context, IPT addresses the relationship between young people significant adults (e.g. teachers, parents), with regard to avoiding/resolving conflict via improved coping communication skills. The techniques used attempt to improve interpersonal skills may include role play, problem-solving exercises and practising effective communication.
Mindfulness meditation and relaxation-based interventions
In the present review, mindfulness/relaxation is a composite category and is distinct from third-wave interventions. Relaxation includes breathing exercises, muscle relaxation and yoga from the Iyengar or Hatha traditions (as opposed to more vigorous traditions). Mindfulness meditation interventions were included in this category if they focused solely on meditation or relaxation without incorporating aspects of traditional ‘talking’ psychotherapeutic approaches.
Biofeedback
Biofeedback is a mind–body intervention that uses physiological monitoring devices or equipment to learn to control physiological responses, such as heart rate. Users may monitor their heart rate variability using pulse oximetry, for example while completing a standard deep-breathing exercise. The feedback received helps the participant learn how to influence the negative, or undesired, response (e.g. a stress response). Smartphone applications and ‘consumer wearables’ have been developed for monitoring stress, anxiety and sleep problems.
Exercise
In this review, we classified an exercise intervention as a cardiovascular intervention designed to raise heart rate and breathing to (at least) a moderate intensity level, for example dancing, running and team sports.
Cognitive bias modification
Cognitive bias modification (CBM) relates to a group of approaches, including attention and interpretation bias training, that aim to retrain cognitive distortions. CBM evolved from a visual attention task (a dot-probe task), in which a participant is exposed to a series of threatening and neutral stimuli via computer, such as angry and neutral faces, and the speed of their response to a ‘probe’ is measured (e.g. where on the screen the angry or neutral face was displayed). In individuals with a CMD, attention tends to be selectively directed towards the negative image and response times to the probe are slower. CBM for the treatment of anxiety disorders seeks to ‘retrain’ this selective attention bias towards the positive stimulus. In preventative interventions for CYP, CBM tasks may be embedded in engaging and user-friendly formats such as interactive video games (‘CBM gamification’).
Occupational therapy
Occupational therapy interventions are based on engaging CYP in meaningful daily activities or ‘occupations’. Interventions are skill based and aim to enable CYP to successfully engage with, and participate in, developmentally appropriate everyday events. For example, an intervention might focus on a favourite activity to increase self-esteem, or schoolwork may be modified to create a positive learning environment and reduce stress.
Control groups
On the basis of previous research,68,72–74 we distinguished the following separate control groups. We note that, in the included trials, psychoeducation and psychosupport were sometimes considered as active interventions in their own right. Their inclusion under a ‘control group’ heading does not affect the findings.
Psychoeducation
Often a component of CBT-based interventions, psychoeducation can also be used as a distinct intervention. It typically involves a systematic approach to providing background information, for example what the cause or symptoms of a mental disorder are and advice regarding the mental disorder and/or explaining the approaches that can help to mitigate symptoms. Written materials or presentations may be provided.
Psychosupport and counselling
Often a component of other interventions, psychosupportive interventions are also used in a stand-alone format. In the current report, we combined psychosupportive and counselling-based interventions into one category. Here it refers to a non-specific, possibly therapeutic, intervention that could include listening, signposting to further services, or forming an attachment or therapeutic alliance.
Usual curriculum
If an active intervention took place during a regular timetabled class and participants in the control group continued to receive the regular class curriculum, the control intervention was classified as standard provision or ‘usual curriculum’. This included a variety of different classes and could have included a ‘well-being’ or health lesson or a standard timetabled academic lesson (such as history or mathematics).
Waiting list
If participants in the control group were explicitly told (e.g. via informed consent processes) that they would receive the active intervention at a later date, the control condition was categorised as a waiting list. Although participants were also likely to be receiving usual curriculum or a no-intervention control, the use of an explicit waiting list design takes precedence in our categorisation.
No intervention
A no-intervention control categorisation was used to differentiate between a control condition in which participants received something and a control condition in which participants were not involved in any structured activity. This classification was applied when the active intervention was held outside regular timetabled classes (e.g. after school) and the participants were not described as being in a waiting list control.
Attention control
A control was classified as attention control if it was a de novo intervention provided to the participants for the purpose of the research study.
Component classifications
As described in Chapter 2, ICA is a subjective process. We defined an intervention component as a potentially active ingredient or constituent part of a main ‘therapy-level’ intervention. In a NMA, components can be included as indicator variables in a network metaregression; as such, they are pragmatic classifications related to the techniques used, and may not pertain to psychotherapeutic schools or traditions. We did not assume the presence of a component based on the therapy-based intervention-level classification assigned by study authors, but on the details provided about what was done. For example, if an author stated that the intervention was CBT based, we did not assume that it contained a psychoeducation, cognitive or behavioural component unless it was clearly stated in the paper (or intervention manual if applicable). We coded only what was clearly reported, and discuss this further in the limitations section of the discussion (see Chapter 10).
Component classifications should also be read independently from the similar-sounding main intervention-level classifications mentioned previously. For example, an intervention-level CBT classification may be defined by the following illustrative combinations of components, depending on what was reported:
-
CBT intervention 1 – psychoeducation + cognitive + behavioural + relaxation + exercise
-
CBT intervention 2 – cognitive + behavioural
-
CBT intervention 3 – psychoeducation + cognitive.
Behavioural
A behavioural component was one in which techniques included helping participants to practise and acquire new skills to cope or manage difficult emotions, moods or behaviours. This component includes strategies used in behavioural activation, social skills exercises (including how to make friends, be a good friend and support your friends), role play, assertiveness training, interpersonal work and activity scheduling and contingency management including goal-setting, planning and decision-making activities, problem-solving and exposure. Following Hetrick et al. ,68 this component was initially subdivided into four further subcomponents: (1) social skills training, (2) problem-solving, (3) exposure and (4) ‘other’ behavioural categories. However, this resulted in unconnected networks, so results are reported for a ‘lumped’ behavioural component only.
Cognitive
This component label was applied when an intervention included strategies or techniques designed to identify and replace cognitive distortions with more accurate and adaptive ones, for example recognising and understanding thoughts and feelings, using positive self-talk and challenging negative self-talk and thoughts.
Third wave
During the ICA, we observed that standard CBT, third wave interventions and mindfulness/relaxation interventions were often based on combinations of the same components. We included a third wave component category to ensure differentiation between these ‘therapy-level’ interventions. The component definition is the same as described previously for the intervention level analysis.
Mindfulness
Mindfulness techniques included guided meditation, colouring and drawing, and exercises to practise being in the moment and being free from judgemental thoughts and distractions. On completion of the component coding, we observed that a mindfulness component was always present in conjunction with a relaxation component.
Relaxation
Separate mindfulness and relaxation components were specified to allow for relaxation techniques that were not defined as meditation or mindfulness. This included strategies such as progressive muscle relaxation, abdominal breathing exercises, cue-controlled relaxation, and identification of physiological arousal (‘body clues’) approaches.
Physiological
A component was coded as physiological if it involved the process of displaying involuntary or subthreshold physiological processes, usually by electronic instrumentation, and learning to voluntarily influence those processes by making changes in cognition.
Bias modification
This component was present only in the main therapy-level intervention, CBM, as described previously. However, on completion of coding, it was retained as a separate component, as the four studies that could be described as evaluating a CBM intervention were assessed as containing different combinations of components:
Psychoeducation
Psychoeducation was also included as a component of broader interventions. The definition applied at the component level is the same as described previously for the intervention-level analysis.
Additional process and implementation classifications
We also extracted information on the following implementation and process components of interventions: number of sessions, duration of intervention (minutes), mode of delivery (face to face or digital), group or individual delivery, who the facilitator was and whether or not training was provided, and whether or not intervention fidelity was monitored. The characteristics of interventions, the components and process details are provided in Chapters 4 and 5 and in Appendix 2. We did not include the process components in the NMA owing to concerns regarding a lack of power and network connectedness. 82
Chapter 4 Effectiveness of educational setting-based interventions for preventing anxiety
Parts of this chapter are reproduced or adapted from Caldwell et al. 1 © 2019 The Author(s). Published by Elsevier Ltd. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes substantial additions and formatting changes to the original text, as well as changes to the reporting approach.
In this chapter, we report the systematic review and NMA results for studies reporting an anxiety outcome only. Studies reporting a depression outcome are reported in Chapter 5 and additional and secondary outcomes are reported in Chapter 6.
Systematic review results
Studies included in the review
The overall Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for the whole review is reported in Figure 2. A total of 11,990 citations were screened, and 1512 full-text articles were retrieved for further screening. Of these, 142 studies were identified as eligible for inclusion in either the anxiety, depression or conduct disorder reviews. Fifty-four studies reported both an anxiety and a depression outcome. The full list of included studies can be found in Appendix 2.
FIGURE 2.
Study selection process: PRISMA flow diagram for whole systematic review. a, Not mutually exclusive. Some studies reported both anxiety and depression outcomes. Of 142 studies, 54 reported both anxiety and depression outcomes. Seven did not report either. Forty-eight of 109 studies contributing to the NMA reported both an anxiety and a depression outcome. b, Study was included in the NMA at any of the follow-up time points. Note that references to the main study publication and articles awaiting classification are listed in Appendix 2.
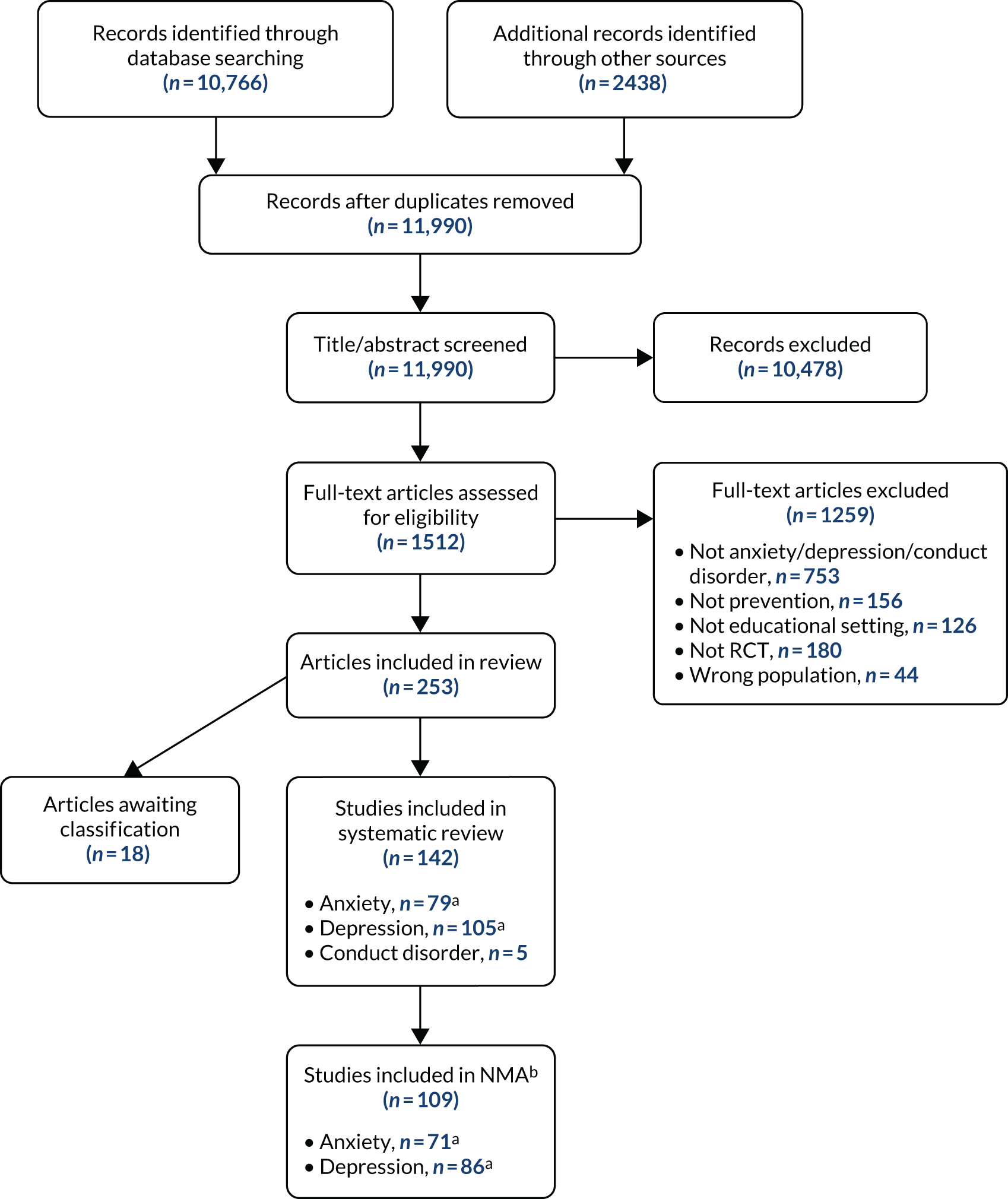
Of the 142 studies eligible for the review, 79 included a self-reported anxiety outcome; the details are reported in this chapter. Studies reporting a depression or conduct disorder outcome are reported separately in Chapters 5 and 7. Among the studies reporting an anxiety outcome, the primary focus of 38 studies was the prevention of anxiety whereas 13 were focused on the prevention of depression and 28 addressed both anxiety and depression. Subgroup analyses examining whether or not intervention effects differed by intended focus of the intervention are reported in Exploring heterogeneity and small-study effects.
Study characteristics are reported in Appendix 2. Included studies were published between 1982 and 2018, and randomised between 22 and 5030 participants (median 184 participants). There were 43 cluster randomised studies, of which four reported cluster-adjusted means and SDs and 35 reported model-based estimates. Thirty-six were individually randomised trials. Seventy-three studies reported a post-intervention end point, 38 reported a follow-up of between 6 and 12 months and seven reported a follow-up of between 13 and 24 months. Studies could report more than one follow-up time point; details of studies reporting multiple time points are in Appendix 2.
Forty-four studies were classified as universal and 35 were classified as targeted (27 indicated, eight selective). Twenty-seven studies were implemented in primary schools, 45 in secondary schools, five in tertiary education and two across multiple settings (i.e. two or more settings). Seventy studies were conducted in HICs, with eight conducted in MICs and one in a LIC. Of the studies conducted in HICs, five were conducted in lower-income settings, as specified by the trial authors. Categorisation of LICs and MICs was based on 2017 World Bank classifications. 62
Risk-of-bias assessment
Study-level risk-of-bias assessments are reported in Appendix 2. Thirteen of the 79 studies reporting an anxiety outcome were assessed as being at low risk of bias for both random sequence generation and allocation concealment. A further 13 studies reported a suitable randomisation approach, but did not report sufficient details of allocation concealment to allow assessment (i.e. unclear). Fifty studies were judged as having unclear risk of bias for both random sequence generation and allocation concealment. Two studies were judged to have an unclear risk of bias for randomisation and a low risk of bias for allocation concealment. One study was judged to have a low risk of bias for randomisation and a high risk of bias for allocation concealment.
Seventy-three studies were judged to be at high or unclear risk of bias for participant blinding. The six studies judged to have a low risk of bias for participant blinding used active controls or alternative interventions. Study protocols and/or trial registrations were available for 23 studies, of which 20 were considered to have a low risk of bias, and three an unclear risk of bias, for selective outcome reporting. For cluster randomised trials, we also considered how recruitment, randomisation and analysis were conducted under the Cochrane Risk of Bias tool heading of ‘other bias’. Of 43 cluster RCTs, 19 were judged to be at high risk for ‘other bias’.
Interventions and components identified in the review
Table 2 reports the interventions and components identified for studies reporting a self-reported anxiety outcome. Seventeen studies compared three or more interventions. Sixty-two studies included an intervention based on CBT, eight included a relaxation/mindfulness-based intervention, one included an intervention based on CBT + IPT, three included a ‘third-wave’ intervention, four used methods of biofeedback, two included an exercise intervention and two used CBM approaches. One study used an occupational therapy-based intervention. With regard to non-active comparators, 27 studies were waiting list controlled, 17 were ‘usual curriculum’ controlled, 16 had a no-intervention control and 14 used an attention control.
| Study | Focusa | Classification | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention level | Component level, for active intervention only | |||||||||||||
| Armb 1 | Armb 2 | Armb 3 | Armb 4 | Psychoeducation | Cognitive | Behavioural | Mindfulness | Third wave | Relaxation | Physiological | Exercise | BM | ||
| Universal secondary setting | ||||||||||||||
| Araya et al.118 2013 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Aune and Stiles119 2009 | Anxiety | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Baker and Butler120 1984 | Anxiety | CBT | CBT | – | + | + | – | – | + | – | – | – | ||
| – | + | + | – | – | + | – | – | – | ||||||
| Barrett et al.121 2005 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Bonhauser et al.122 2005 | Anxiety + depression | Exercise | Exercise | – | – | – | – | – | – | – | + | – | ||
| Bonhauser et al.122 2005 | – | – | – | – | – | – | – | + | – | |||||
| Britton et al.123 2014 | Anxiety + depression | (Attention control) | Mindfulness/relaxation | – | – | – | + | – | + | – | – | – | ||
| Burckhardt et al.124 2015 | Anxiety + depression | (Attention control) | Mindfulness/relaxation | – | – | – | – | – | + | – | – | – | ||
| Calear et al.125 2009 | Anxiety + depression | (Waiting list) | CBT | – | + | + | – | – | + | – | – | – | ||
| Calear et al.126 2016 | Anxiety | (Waiting list) | CBT | CBT | + | + | + | + | – | + | – | – | – | |
| + | + | + | + | – | + | – | – | – | ||||||
| Calear et al.127 2016 | Anxiety | (Waiting list) | CBT | + | + | + | + | – | + | – | – | – | ||
| Gillham et al.128 2006 | Anxiety + depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Gucht et al.129 2017 | Anxiety + depression | (Usual curriculum) | Third wave | + | – | – | – | + | – | – | – | – | ||
| Hiebert et al.130 1989 | Anxiety | (Attention control) | Mindfulness/relaxation | + | – | – | – | – | + | + | – | – | ||
| Hodas131 2016 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Johnson et al.132 2016 | Anxiety + depression | (Usual curriculum) | Third wave | – | – | – | + | + | + | – | – | – | ||
| Johnson et al.133 2017 | Anxiety + depression | (Usual curriculum) | Third wave | Third wave | – | – | – | + | + | + | – | – | – | |
| Johnson et al.133 2017 | – | – | – | + | + | + | – | – | – | |||||
| Lock and Barrett134 2003 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Lowry-Webster et al.135 2001 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Perry et al.136 2017 | Depression | (Attention control) | CBT | + | + | + | – | – | + | – | – | – | ||
| Potek137 2012 | Anxiety | (Waiting list) | Mindfulness/relaxation | + | – | – | + | – | + | – | – | – | ||
| Roberts et al.138 2003 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Roberts et al.139 2010 | Anxiety + depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Rodgers and Dunsmuir140 2015 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Sheffield et al.141 2006 | Depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Stallard et al.142 2013 | Depression | (Usual curriculum) | (Attention control) | CBT + IPT | + | + | + | – | – | + | – | – | – | |
| Tomba et al.143 2010 | Anxiety + depression | CBT | CBT | + | + | + | – | – | + | – | – | – | ||
| Tomba et al.143 2010 | + | + | + | – | – | + | – | – | – | |||||
| Wong et al.144 2014 | Anxiety + depression | (Usual curriculum) | CBT | CBT | + | + | + | – | – | – | – | – | – | |
| Wong et al.144 2014 | + | + | + | – | – | – | – | – | – | |||||
| Universal primary setting | ||||||||||||||
| Ahlen et al.145 2018 | Anxiety + depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Attwood et al.146 2012 | Anxiety | (Attention control) | CBT | + | + | + | – | – | – | – | – | – | ||
| Barrett and Turner147 2001 | Anxiety | (Usual curriculum) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Barrett and Turner147 2001 | + | + | + | – | – | + | – | – | – | |||||
| Bouchard et al.148 2013 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Collins et al.149 2014 | Anxiety | (Usual curriculum) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Collins et al.149 2014 | + | + | + | – | – | + | – | – | – | |||||
| Essau et al.150 2012 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Gallegos151 2008 | Anxiety + depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Johnstone et al.152 2014 | Anxiety + depression | (Usual curriculum) | CBT | – | + | + | – | – | + | – | – | – | ||
| Miller et al.153 2010 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Miller et al.154 2011 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Miller et al.154 2011 | Anxiety | (Attention control) | CBT | + | + | + | – | – | + | – | – | – | ||
| Pattison and Lynd-Stevenson155 2001 | Depression | (No intervention) | (Attention control) | CBT | CBT | – | + | + | – | – | – | – | – | – |
| Pattison and Lynd-Stevenson155 2001 | – | + | + | – | – | – | – | – | – | |||||
| Pophillat et al.156 2016 | Anxiety + depression | (Usual curriculum) | CBT | + | + | – | – | – | – | – | – | – | ||
| Rooney et al.157 2006 | Depression | (No intervention) | CBT | – | + | + | – | – | + | – | – | – | ||
| Ruttledge et al.158 2016 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Stallard et al.159 2014 | Anxiety | (Usual curriculum) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Stallard et al.159 2014 | + | + | + | – | – | + | – | – | – | |||||
| Targeted secondary setting | ||||||||||||||
| Balle and Tortella-Feliu160 2010 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Berry and Hunt161 2009 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Cova et al.162 2011 | Depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Dobson et al.163 2010 | Anxiety + depression | (Attention control) | CBT | – | + | + | – | – | – | – | – | – | ||
| Fitzgerald et al.114 2016 | Anxiety | (Attention control) | CBM | – | – | – | – | – | – | – | – | + | ||
| Gaete et al.164 2016 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Gillham et al.165 2012 | Depression | (No intervention) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Gillham et al.165 2012 | + | + | + | – | – | + | – | – | – | |||||
| Hiebert et al.130 1989 | Anxiety | (Waiting list) | Mindfulness/relaxation | Biofeedback | + | – | – | – | – | + | + | – | – | |
| Hiebert et al.130 1989 | – | – | – | – | – | – | + | – | – | |||||
| Hunt et al.166 2009 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Jordans et al.167 2010 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Kiselica et al.168 1994 | Anxiety | Psychosupport | CBT | + | + | + | – | – | + | – | – | – | ||
| Owen and Lanning169 1982 | Anxiety | (Waiting list) | Mindfulness/relaxation | CBT | CBT | – | – | – | – | – | + | – | – | – |
| Owen and Lanning169 1982 | + | + | – | – | – | – | – | – | – | |||||
| Owen and Lanning169 1982 | + | + | – | – | – | + | – | – | – | |||||
| Peng et al.170 2015 | Anxiety + depression | (No intervention) | Exercise | – | – | – | – | – | + | – | + | – | ||
| Rice171 2009 | Anxiety | (Attention control) | CBT | Mindfulness/relaxation | + | + | + | – | – | + | – | – | – | |
| Rice171 2009 | – | – | – | – | – | + | – | + | – | |||||
| Scholten et al.172 2016 | Anxiety | (Attention control) | Biofeedback | – | – | – | – | – | + | + | – | – | ||
| Sheffield et al.141 2006 | Depression | (No intervention) | CBT | CBT | CBT | + | + | + | – | – | – | – | – | – |
| Sheffield et al.141 2006 | + | + | + | – | – | – | – | – | – | |||||
| Sheffield et al.141 2006 | + | + | + | – | – | – | – | – | – | |||||
| Sportel et al.117 2013 | Anxiety | (No intervention) | CBM | CBT | – | + | – | – | – | – | – | – | + | |
| Sportel et al.117 2013 | – | + | + | – | – | – | – | – | – | |||||
| Topper et al.173 2017 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Targeted primary setting | ||||||||||||||
| Cooley-Strickland et al.174 2011 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Manassis et al.175 2010 | Anxiety + depression | (Attention control) | CBT | + | + | – | – | – | – | – | – | – | ||
| McLoone et al.176 2012 | Anxiety | (Waiting list) | CBT | CBT | + | + | + | – | – | – | – | – | – | |
| McLoone et al.176 2012 | + | + | + | – | – | – | – | – | – | |||||
| Mifsud and Rapee177 2005 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Miller et al.178 2011 | Anxiety | (Attention control) | CBT | + | + | + | – | – | + | – | – | – | ||
| Schoneveld et al.115 2016 | Anxiety | (Attention control) | Biofeedback | – | – | + | – | – | + | + | – | + | ||
| Schoneveld et al.116 2018 | Anxiety | CBT | Biofeedback | – | + | + | – | – | + | – | – | – | ||
| Schoneveld et al.116 2018 | – | – | + | – | – | – | + | – | + | |||||
| Simpson179 2008 | Anxiety + depression | (Attention control) | CBT | + | + | + | – | – | – | – | – | – | ||
| Siu180 2007 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Tokolahi et al.181 2018 | Anxiety + depression | (Waiting list) | Occupational therapy | – | – | – | – | – | – | – | – | – | ||
| van Starrenburg et al.182 2017 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Targeted tertiary/university setting | ||||||||||||||
| Cui et al.183 2016 | Depression | (Waiting list) | Psychosupport | CBT | + | + | + | – | – | + | – | – | – | |
| Ellis et al.184 2011 | Depression | (No intervention) | Psychosupport | CBT | + | + | + | – | – | + | – | – | – | |
| Higgins185 2007 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Seligman et al.186 1999 | Anxiety + depression | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Seligman et al.187 2007 | Anxiety + depression | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Multiple/mixed settings | ||||||||||||||
| Liddle and Macmillan188 2010 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Velásquez et al.189 2015 | Anxiety + depression | (Waiting list) | Mindfulness/relaxation | – | – | – | – | – | + | – | – | – | ||
Table 2 also reports the combinations of components identified across all studies reporting an anxiety outcome (at any time point) by population and setting. Components are reported by intervention arm level, and not at the trial level. When there are multiarm trials (i.e. three or more arms) with multiple ‘active’ interventions, intervention components are reported on separate lines. There were 99 active intervention arms, of which 67 had a psychoeducation component. Seventy-eight interventions had a cognitive component, 75 had a behavioural component, eight had a mindful component, four had third-wave components, 60 had a relaxation component, six had a physiological component, four arms had an exercise component and four had a bias modification component.
Further intervention process and delivery characteristics are reported in Appendix 2. The number of sessions implemented ranged from 2 to 120 [mean 11.13 (SD 13.44) sessions]. As a proxy for intervention dose, we calculated the intervention intensity as total session time (number of sessions × duration in minutes). This ranged from 135 to 10,800 minutes [mean 740.15 (SD 1295.60) minutes]. A total of 90% of interventions were delivered to whole classrooms or small groups. Forty-three per cent of interventions were delivered by a MHP, school counsellor or student psychologist, and 10% were delivered by miscellaneous external professionals. Twenty-two per cent of studies used interventions delivered by teachers. Fifteen per cent of studies involved a combination of both teaching and a MHP/psychology professional. Four studies implemented interventions via computer. Two studies could not be classified.
Network meta-analysis results
Of the 79 studies reporting an anxiety outcome, 71 (n = 33,377 participants) contributed data to the NMA for anxiety (across all settings and time points). Forty-eight of these studies also reported a depression outcome and contributed to the depression NMA reported in Chapter 5. The network plot for all studies reporting an anxiety outcome across all populations and settings is reported in Figure 3.
FIGURE 3.
Network plot of all eligible studies reporting an anxiety outcome. OT, occupational therapy; third wave, third-wave CBT-based therapies. The plot edges (lines) connecting each pair of interventions represent a direct comparison and are proportional to the number of trials making that direct comparison. Intervention ‘nodes’ are proportional to the number of participants randomised to each intervention.
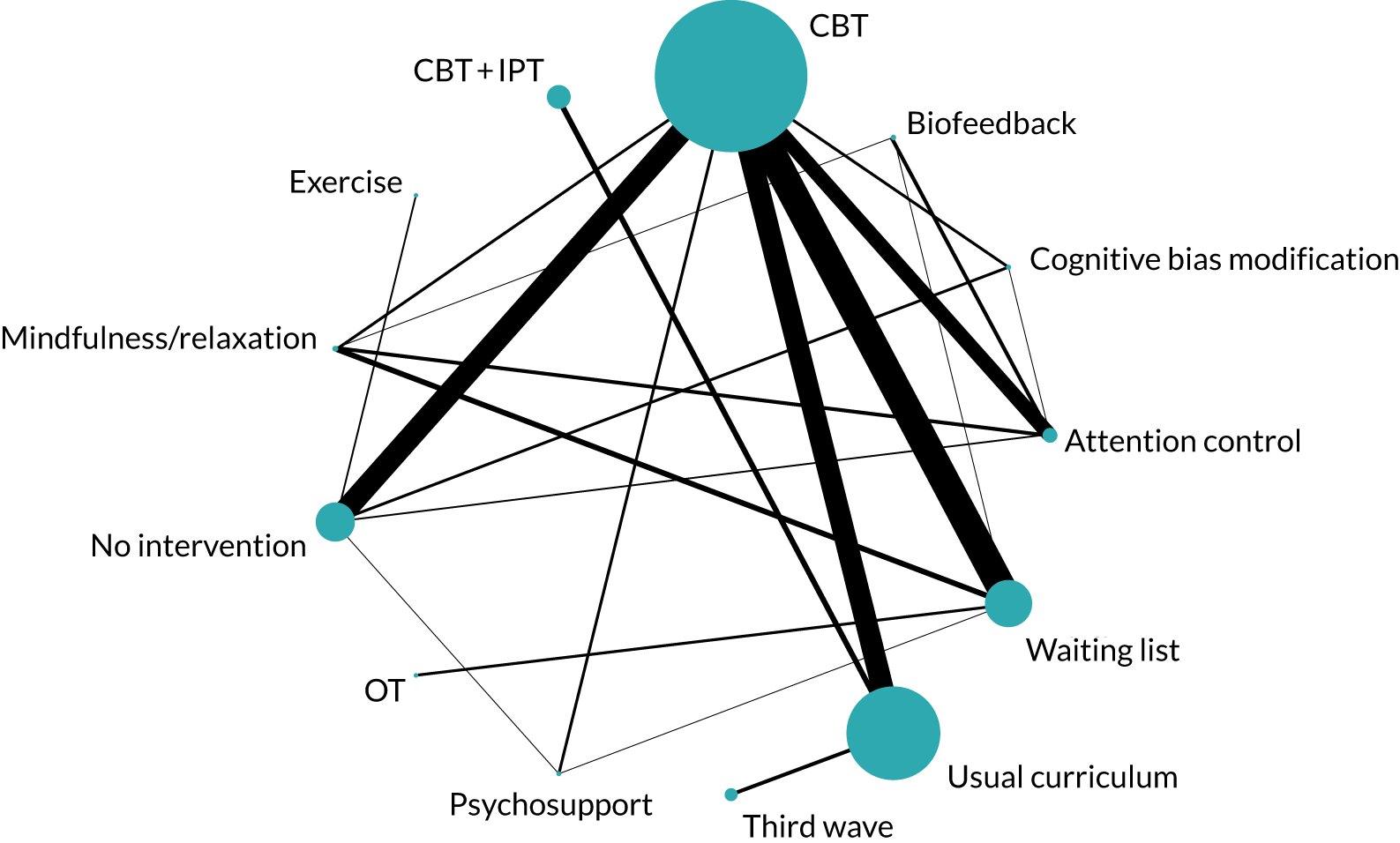
Analyses were conducted separately by population, setting and follow-up time point. Three models were compared for each analysis: a main effects (intervention-level) model, an additive component model and a full interaction component model for the primary time point of immediately post intervention. The longer-term follow-ups of 6–12, 13–24 and ≥ 25 months are reported for the standard intervention-level NMAs only. When data were available from head-to-head trials, we conducted pairwise meta-analyses. The results are reported alongside NMA results in Table 3. Full NMA and pairwise results are reported in Appendix 4.
| Setting | Intervention | Reference intervention | NMA | Direct meta-analysis | Number of direct trials | ||
|---|---|---|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | ||||
| Universal secondary | CBT | Usual curriculum | –0.15 | –0.34 to 0.04 | –0.15 | –0.33 to 0.02 | 3 |
| Third wave | Usual curriculum | 0.03 | –0.14 to 0.20 | 0.04 | –0.10 to 0.19 | 3 | |
| Mindfulness/relaxation | Usual curriculum | –0.65 | –1.14 to –0.19 | NA | NA | 0 | |
| Universal primary | CBT | Usual curriculum | –0.07 | –0.23 to 0.05 | –0.08 | –0.24 to 0.04 | 6 |
| Targeted secondary | CBT | No intervention | 0.03 | –0.11 to 0.16 | 0.03 | –0.10 to 0.16 | 4 |
| CBM | No intervention | –0.17 | –0.45 to 0.11 | –0.21 | –0.54 to 0.15 | 1 | |
| Exercise | No intervention | –0.47 | –0.86 to –0.09 | –0.47 | –0.86 to –0.08 | 1 | |
| Biofeedback | No intervention | –0.18 | –0.55 to 0.21 | NA | NA | 0 | |
| Mindfulness/relaxation | No intervention | 0.03 | –0.42 to 0.48 | NA | NA | 0 | |
| Targeted primary | CBT | Waiting list | –0.38 | –0.84 to 0.07 | –0.35 | –0.79 to 0.09 | 5 |
| Occupational therapy | Waiting list | 0.11 | –0.91 to 1.14 | 0.11 | –0.93 to 1.16 | 1 | |
| Biofeedback | Waiting list | –0.38 | –1.50 to 0.72 | NA | NA | 0 | |
Universal population, secondary setting
Post intervention
The analysis-specific network diagram is reported in Figure 4. Twenty-one studies (n = 10,208 participants) contributed to the analysis for the main time point of immediately post intervention. 119,120,125–141,143,144 Most studies in this network were judged to be at unclear risk of bias. The risk of bias was judged to be unclear for 13 studies and low for three studies in both the randomised sequence generation and allocation concealment domains. In four studies, the risk of bias was judged to be low for randomisation but unclear for allocation concealment. In one study, the risk of bias was judged to be unclear for randomisation but low for allocation concealment. Sixteen studies included an intervention based on CBT, three were based on third-wave interventions, and two were mindfulness/relaxation-based interventions; the reference intervention was usual curriculum (see Appendix 2 for details). All reported results are from a random-effects NMA model unless otherwise stated. Model fit and selection statistics suggested that a consistency model was appropriate. Of the three models fitted (intervention, additive and full interaction), the additive model was preferred, suggesting evidence for effect modification by components. All model fit statistics are reported in Appendix 3. Results reported in the following sections are SMDs and 95% CrIs.
FIGURE 4.
Network plot for universal population, secondary setting: post-intervention anxiety outcome.
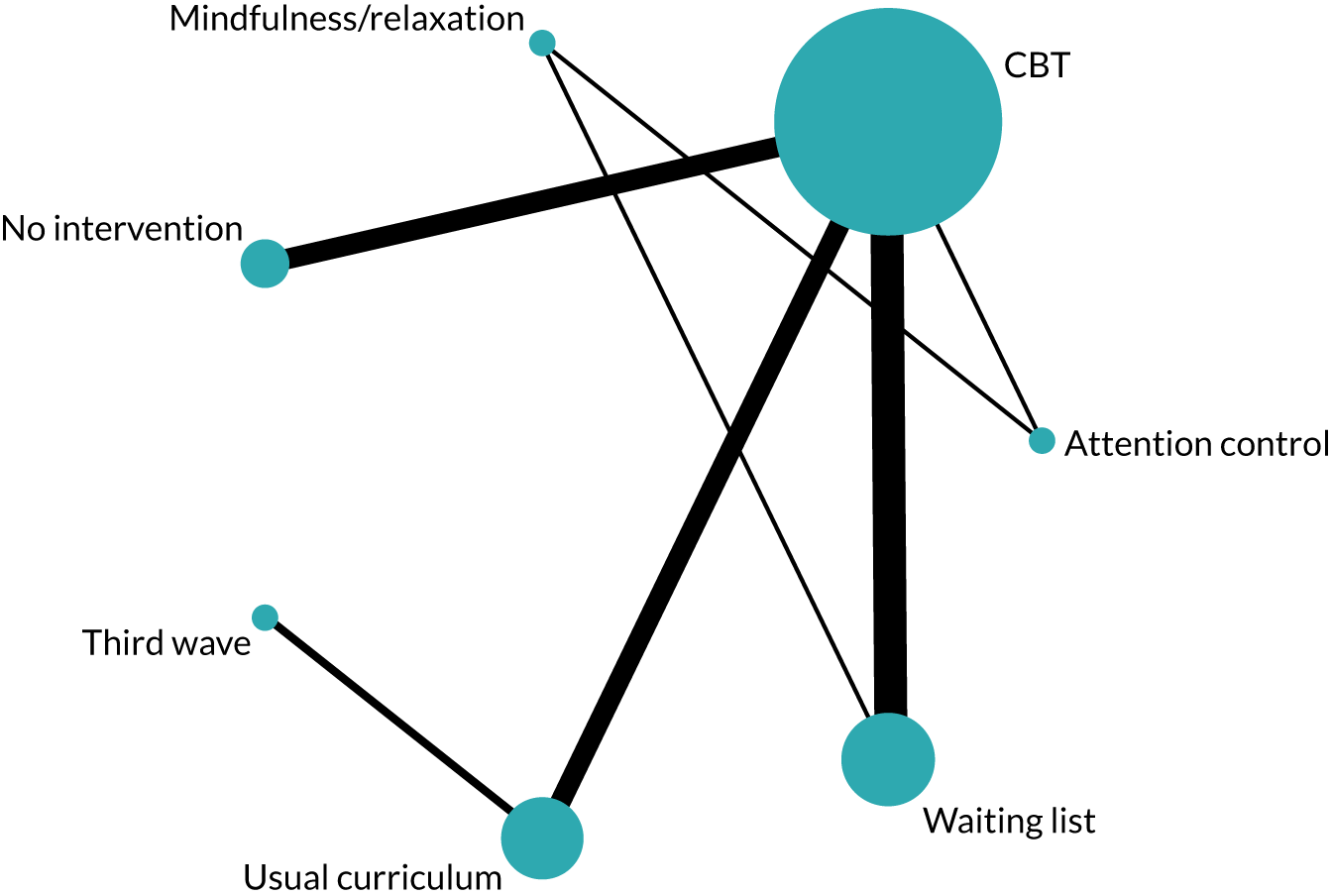
Intervention-level model
Between-study posterior median SDs (τ) were indicative of moderate heterogeneity (τ 0.11, 95% CrI 0.02 to 0.22). Table 3 reports SMDs (and 95% CrIs) for each active intervention relative to usual curriculum. There was weak evidence of a modest effect of CBT in preventing symptoms of anxiety post intervention (SMD –0.15, 95% CrI –0.34 to 0.04). Mindfulness/relaxation interventions (SMD –0.65, 95% CrI –1.14 to –0.19) reduced symptoms relative to usual curriculum. However, this finding must be interpreted in the context of the possible small-study effects observed in the funnel plot reported in Appendix 6, Figure 17, and the ratings of unclear risk of bias. Only two small mindfulness/relaxation studies (n = 30,130 and n = 79137 participants) contributed to the network, and both were rated as having an unclear risk of bias for random sequence generation and allocation concealment. There was a lack of evidence for the effect of third-wave interventions (SMD 0.03, 95% CrI –0.14 to 0.20).
Additive model: components nested within intervention
Component-level models were fitted to evaluate whether or not the observed between-study heterogeneity in the intervention model could be explained by differences in intervention components.
We fitted an additive model with components nested within interventions, such that a main intervention effect was estimated, plus an additional effect for the inclusion of a specific component. Results are reported as regression coefficients (β-values and 95% CrIs) describing the increase or decrease in SMD via the addition of each component to each intervention. The coefficients can be interpreted as the additional effect of each specific component over and above the ‘common’ intervention-level effect.
All CBT interventions in the universal secondary network included a cognitive and a behavioural component. We estimated the additional effect of including a psychoeducational, mindfulness or relaxation component to cognitive and behavioural components. The between-study heterogeneity was reduced compared with that of the intervention-level analysis (τ 0.06, 95% CrI 0.00 to 0.21) (see Appendix 3). The effect of any CBT intervention including a psychoeducation component was to reduce the SMD (β –0.39, 95% CrI –0.78 to 0.01). The effect of including a mindfulness component in a CBT intervention was to increase the SMD (β 0.57, 95% CrI 0.08 to 1.03) (i.e. less effective at reducing anxiety). There was no evidence to suggest an effect of adding a relaxation component to CBT (β 0.07, 95% CrI –0.21 to 0.38).
Table 4 reports the SMDs for all specific additive combinations of intervention components. Under the additive component model, it is possible to estimate an effect for all combinations, even in the absence of directly observable trials. Relative to a usual curriculum control, there is some evidence that the combination of cognitive + behavioural + psychoeducation components is effective at reducing anxiety post intervention in universal secondary settings (SMD –0.30, 95% CrI –0.59 to –0.01). There is a lack of evidence for all other combinations.
| Population/setting | Main intervention | Components (within main intervention) | Study arms (n) | Model, SMD (95% CrI) | |
|---|---|---|---|---|---|
| Additive | Full interaction | ||||
| Universal secondary, anxiety | CBT | (Cognitive + behavioural) | 2 | 0.09 (–0.17 to 0.36) | 0.09 (–0.22 to 0.40) |
| (Cognitive + behavioural) + psychoeducation | 6 | –0.30 (–0.59 to –0.01) | –0.30 (–0.62 to 0.02) | ||
| (Cognitive + behavioural) + relaxation | 2 | 0.16 (–0.22 to 0.57) | –31.49 (–144.2 to 90.84) | ||
| (Cognitive + behavioural) + psychoeducation + relaxation | 6 | –0.23 (–0.62 to 0.19) | –0.21 (–0.66 to 0.26) | ||
| (Cognitive + behavioural) + psychoeducation + mindfulness + relaxation | 3 | 0.34 (–0.12 to 0.82) | –31.32 (–144 to 91.01) | ||
| (Cognitive + behavioural) + mindfulness | 0 | 0.66 (–0.02 to 1.31) | – | ||
| (Cognitive + behavioural) + mindfulness + relaxation | 0 | 0.73 (0.03 to 1.45) | – | ||
| (Cognitive + behavioural) + psychoeducation + mindfulness | 0 | 0.27 (–0.10 to 0.64) | – | ||
Full interaction model: components nested within intervention
Under a full interaction model, each different combination of intervention and components is considered as a separate intervention. For example, a CBT intervention with cognitive + behavioural + psychoeducation components is considered to be distinct from CBT with cognitive + behavioural + psychoeducation + relaxation components. However, the power to estimate and detect evidence of interactions is limited by the data available for each distinct combination. For the universal secondary anxiety analysis, there were sufficient data to estimate the effects for CBT-based interventions only, although we note that power was low and convergence was problematic. Model fit statistics suggested that the full interaction model was slightly preferred over the intervention-level model, but that the additive effect model is preferred overall (see Appendix 3). However, for completeness, we also report the full interaction results in Table 4. There was weak evidence that CBT with cognitive + behavioural + psychoeducation components is effective relative to usual curriculum (SMD –0.30, 95% CrI –0.62 to 0.02). The between-study posterior median SD was suggestive of low to moderate heterogeneity (τ 0.09, 95% CrI 0.01 to 0.24). Regression coefficients are reported in Appendix 3, but yielded very imprecise estimates of change in SMD.
Universal, secondary, further time points: intervention-level effects
Full results for the following time points are reported in Appendix 6. Details for studies contributing to each time point are reported in Appendix 2.
Fifteen studies (n = 13,150 participants), comparing seven interventions, were included in the analysis for 6–12 months post intervention. 118,125,126,128,129,131,133–136,138,139,141–143 Twelve studies included an intervention based on CBT, one study included a CBT + IPT intervention and two studies included a third-wave intervention. There was no evidence to suggest that any intervention reduced symptoms of anxiety between 6 and 12 months, relative to usual curriculum (CBT: SMD –0.11, 95% CrI –0.34 to 0.11; third wave: SMD –0.05, 95% CrI –0.32 to 0.22; and CBT + IPT: SMD –0.02, 95% CrI –0.42 to 0.36). Between-study heterogeneity was moderate (τ 0.15, 95% CrI 0.06 to 0.37).
Three studies (n = 1077 participants) contributed to the analysis for 13–24 months post intervention, all of which included an intervention based on CBT. 136,138,139 There was no evidence to suggest that CBT-based interventions prevented symptoms of anxiety between 13 and 24 months, relative to usual curriculum (SMD –0.01, 95% CrI –2.84 to 2.81).
One study (n = 92 participants) reported a follow-up time point of 30 months. 139 The SMD for the effect of CBT relative to usual curriculum was –0.23 (95% CrI –0.55 to 0.08). The study was rated as having an unclear risk of bias for random sequence generation and allocation concealment.
Universal population, primary setting
Post intervention
The analysis-specific network diagram for universal primary settings is reported in Figure 5. Fifteen studies from 14 publications (n = 5605 participants) contributed to the analysis for the main time point of immediately post intervention. 145–158 Thirteen studies were deemed to have an unclear risk of bias and one study was deemed to have a low risk of bias for both randomised sequence generation and allocation concealment domains. One study was judged to be at unclear risk of bias for randomisation but at low risk of bias for allocation concealment. All studies included an intervention based on CBT. Model fit and selection statistics suggested that a random-effects consistency model was appropriate. Fit was similar across all three models (intervention, additive and full interaction) but indicated that the intervention-level model was preferred (see Appendix 3). Therefore, we report effect estimates from the intervention-level analysis only. Regression coefficients from the additive and full interaction models are reported in Appendix 3.
FIGURE 5.
Network plot for universal population, primary setting: post-intervention anxiety outcome.
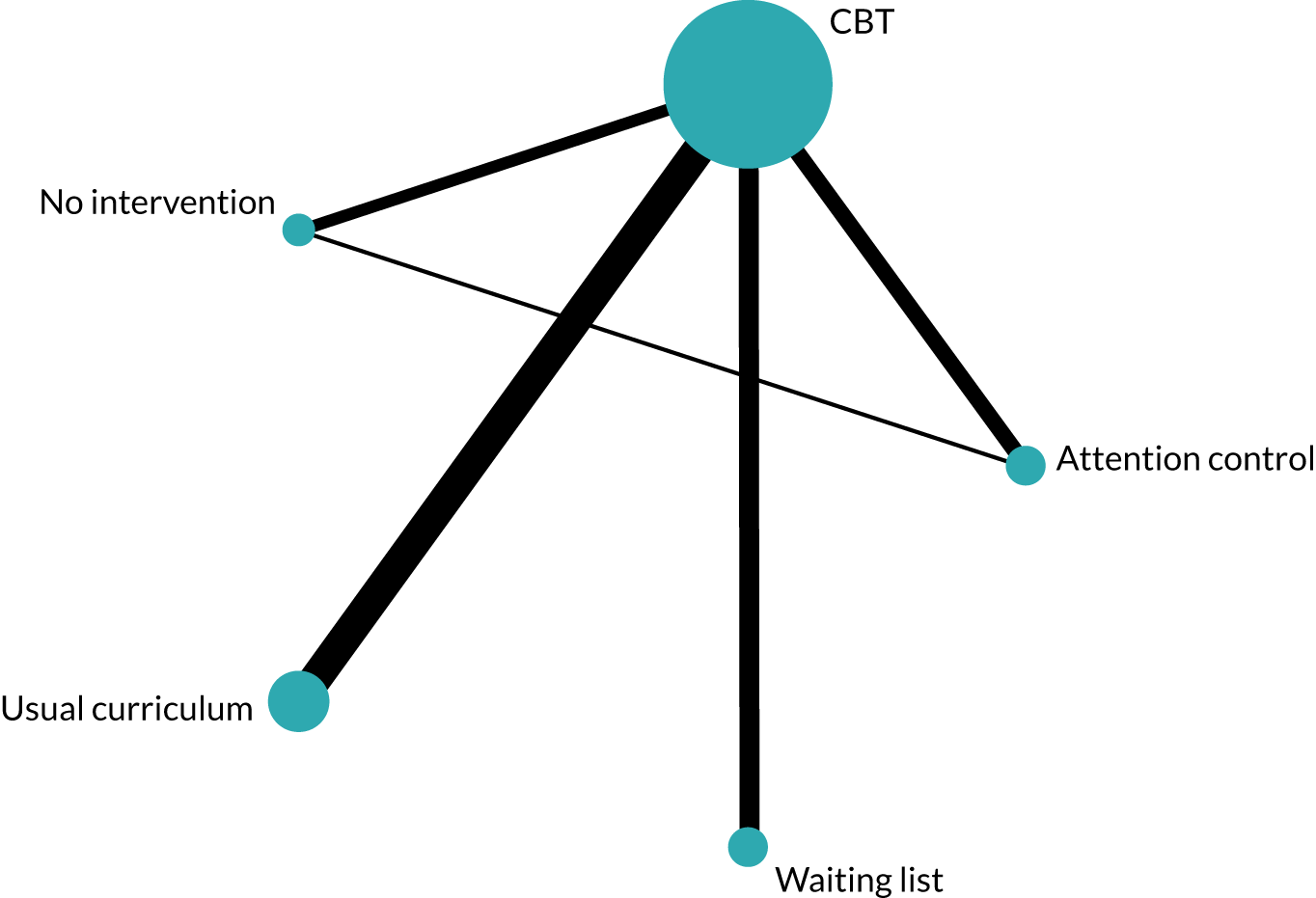
Intervention-level model
Between-study posterior median SDs were indicative of moderate heterogeneity (τ 0.10, 95% CrI 0.01 to 0.26). There was weak evidence of a very small effect of CBT relative to usual curriculum (SMD –0.07, 95% CrI –0.23 to 0.05) (see Table 3).
Universal, primary, further time points: intervention-level effects
Ten studies (n = 4794 participants) contributed to the analysis for 6–12 months post intervention, all of which evaluated a CBT-based intervention. 145,149–152,154,155,157,159 Between-study posterior median SDs were indicative of substantial heterogeneity (τ 0.22, 95% CrI 0.08 to 0.45). There was no evidence that CBT reduced symptoms of anxiety at between 6 and 12 months, relative to usual curriculum (SMD –0.11, 95% CrI –0.35 to 0.11) (see Appendix 5).
Three studies (n = 1603 participants) contributed to the analysis for 13–24 months post intervention, all of which included an intervention based on CBT. 152,157,159 There was no evidence to suggest that CBT-based interventions prevented symptoms of anxiety at between 13 and 24 months, relative to usual curriculum (SMD 0.00, 95% CrI –0.68 to 0.71; τ 0.13).
One study (n = 910 participants) reported a follow-up time point of 30 months. 152 This study provided weak evidence of a small effect of CBT relative to usual curriculum (SMD –0.12, 95% CrI –0.26 to 0.02). The study was deemed to be at unclear risk of bias for random sequence generation and allocation concealment.
Targeted population, secondary setting
Post intervention
The analysis-specific network diagram for targeted secondary settings is reported in Figure 6. Fifteen studies (n = 2383 participants) contributed to the analysis for the main time point of immediately post intervention. 114,117,130,141,160–163,165,167,168,170–173 Three studies were deemed to be at low risk of bias and seven were deemed to be at unclear risk of bias for randomised sequence generation and allocation concealment. Four studies were deemed to be at low risk of bias for randomised sequence generation and at unclear risk for allocation concealment. Five studies were multiarm and compared multiple active interventions. Twelve studies included an intervention based on CBT, two studies examined biofeedback interventions, two studies included a CBM intervention, two studies included a mindfulness/relaxation intervention and one study evaluated study an exercise intervention. Model fit and selection statistics suggested that a random-effects consistency model was appropriate. Model fit was similar across all three intervention models (main intervention, additive and full interaction) (see Appendix 3). There was no evidence of effect modification by intervention components in targeted secondary settings. The intervention-level model is preferred, and regression coefficients from the additive and full interaction models are reported in Appendix 3.
FIGURE 6.
Network plot for targeted population, secondary setting: post-intervention anxiety outcome.
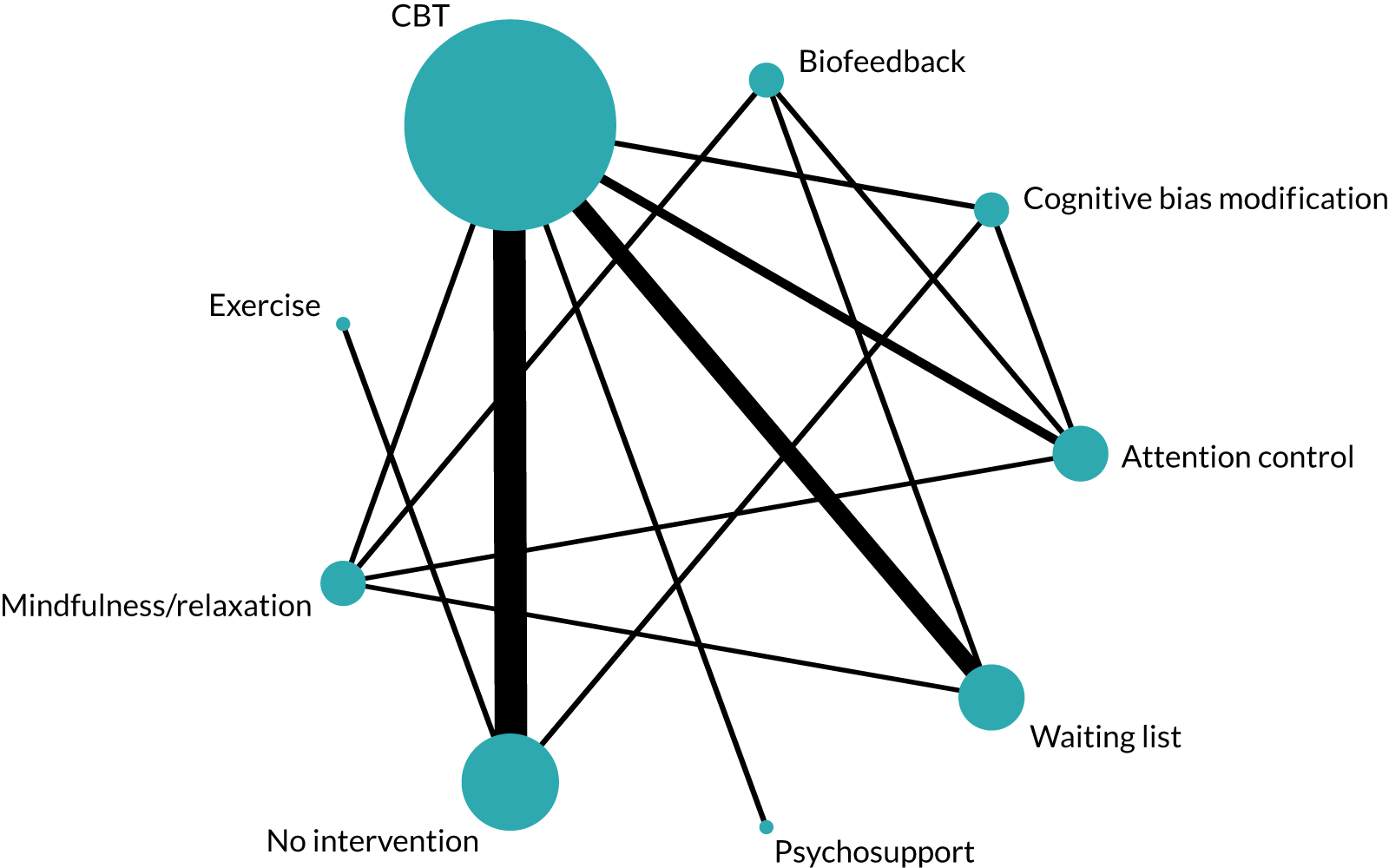
Intervention-level effects
There was mild to moderate between-study heterogeneity (τ 0.06, 95% CrI 0.00 to 0.21). Table 3 reports SMDs (and 95% CrIs) for each active intervention, relative to no intervention. There was no evidence of an effect for CBT (SMD 0.03, 95% CrI –0.11 to 0.16), biofeedback (SMD –0.18, 95% CrI –0.55 to 0.21), CBM (SMD –0.17, 95% CrI –0.45 to 0.11) or mindfulness/relaxation (SMD 0.03, 95% CrI –0.42 to 0.48). There was evidence that exercise reduced post-intervention anxiety symptoms, relative to no intervention (SMD –0.47, 95% CrI –0.86 to –0.09). However, exercise was evaluated in only one study, which was judged to be at unclear risk of bias for random sequence generation and allocation concealment.
Targeted, secondary, further time points: intervention-level effects only
Six studies (n = 1284 participants) contributed to the analysis for 6–12 months post intervention, of which all included a CBT-based intervention and one included a CBM intervention (three-arm study). 117,141,160,163,165,173 There was evidence of mild to moderate between-study heterogeneity (τ 0.06, 95% CrI 0.00 to 0.25). There was no evidence that either CBT (SMD 0.05, 95% CrI –0.12 to 0.20) or CBM (SMD –0.14, 95% CrI –0.53 to 0.24) reduced anxiety at between 6 and 12 months, relative to no intervention.
One study (n = 260 participants),166 deemed to be at unclear risk of bias, provided evidence for a small effect of CBT, relative to no intervention, for the prevention of anxiety between 13 and 24 months’ follow-up (SMD –0.26, 95% CrI –0.52 to –0.01) and at 48 months’ follow-up (SMD –0.39, 95% CrI –0.65 to –0.14).
Targeted population, primary setting
Post intervention
The analysis-specific network diagram for targeted primary settings is reported in Figure 7. Eleven studies (n = 1314) contributed to the analysis for the post-intervention time point. 115,116,174–182 Three studies were deemed to be at low risk of bias and six studies were deemed to be at unclear risk of bias for both the randomisation and allocation concealment domains. A further two studies were rated as having an unclear risk of bias for allocation concealment, but a low risk of bias for random sequence generation. One study compared two active interventions. Ten studies included an intervention based on CBT, one examined a biofeedback intervention and one included an occupational therapy intervention. Model fit and selection statistics indicated that a random-effects consistency model was appropriate. Model fit was similar across all three intervention models (main intervention, additive and full interaction), but suggested that the intervention-level model was preferred (see Appendix 3). Regression coefficients from the additive and full interaction models are reported in Appendix 3.
FIGURE 7.
Network plot for targeted population, primary setting: post-intervention anxiety outcome. OT, occupational therapy.
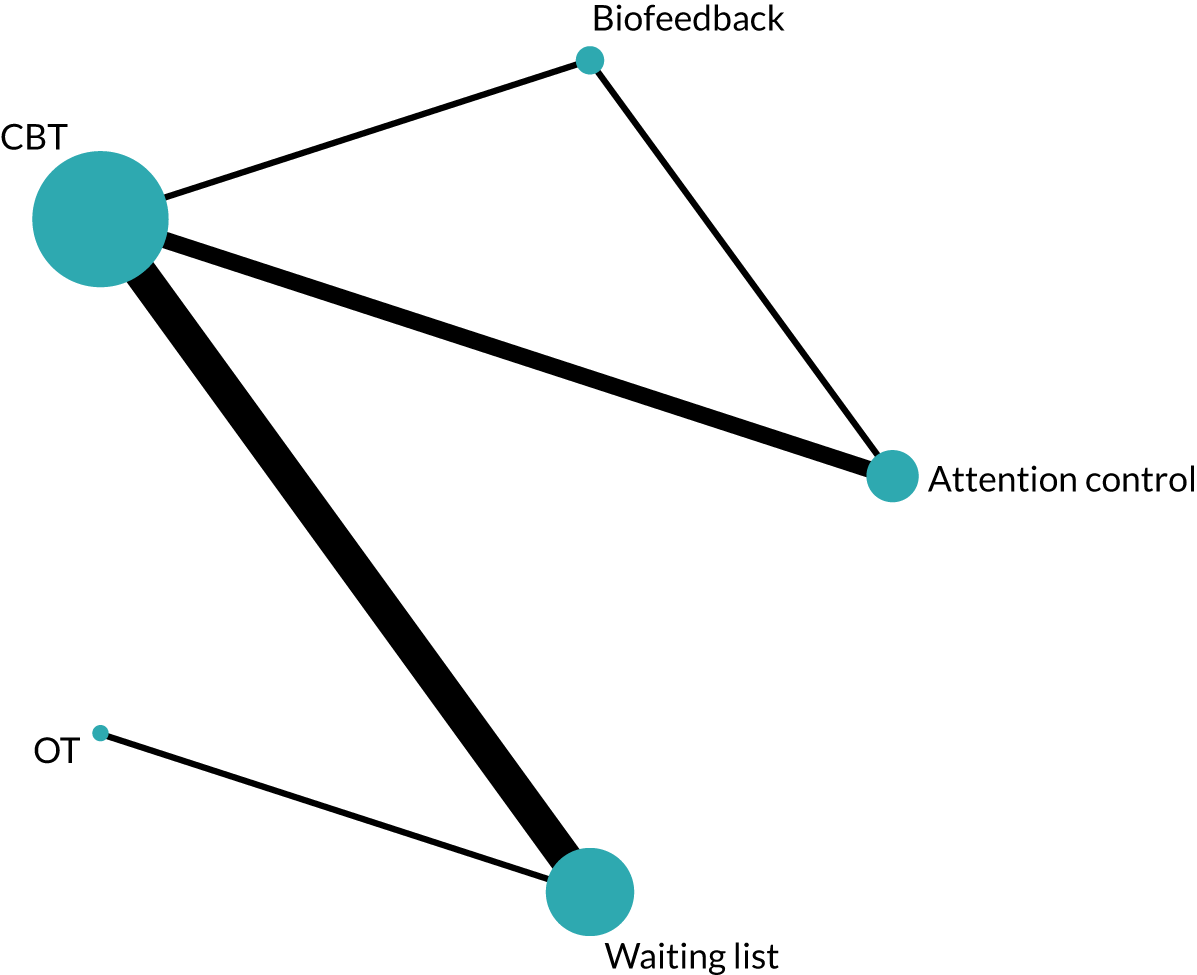
Intervention-level effects
There was evidence of substantial between-study heterogeneity (τ 0.42, 95% CrI 0.21 to 0.89). Table 3 reports SMDs (95% CrIs) for each intervention relative to a waiting list. There was weak evidence of an effect for CBT (SMD –0.38, 95% CrI –0.84 to 0.07), but a lack of evidence for biofeedback (SMD –0.38, 95% CrI –1.50 to 0.72) or occupational therapy (SMD 0.11, 95% CrI –0.91 to 1.14).
Targeted, primary, further time points: intervention-level effects only
Five studies (n = 713 participants) contributed to the analysis for 6–12 months post intervention, of which five included a CBT-based intervention and one included a biofeedback intervention (one study compared two active interventions). 116,175–178 The between-study posterior median SD was indicative of substantial heterogeneity (τ 0.52, 95% CrI 0.15 to 2.51). There was no evidence that either CBT (SMD –0.17, 95% CrI –1.37 to 1.06) or biofeedback (SMD –0.28, 95% CrI –2.49 to 1.93) reduced anxiety symptoms at between 6 and 12 months, relative to a waiting list. No studies reported a follow-up of > 12 months post intervention.
Targeted population, tertiary/university setting
The analysis-specific network diagram is reported in Figure 8. Four studies (n = 743 participants) contributed to the analysis for the main post-intervention time point, of which all included an intervention based on CBT. 183,184,186,187 Owing to insufficient data in this network, the component models were not fitted.
FIGURE 8.
Network plot for targeted population, tertiary/university setting: post-intervention anxiety outcome.
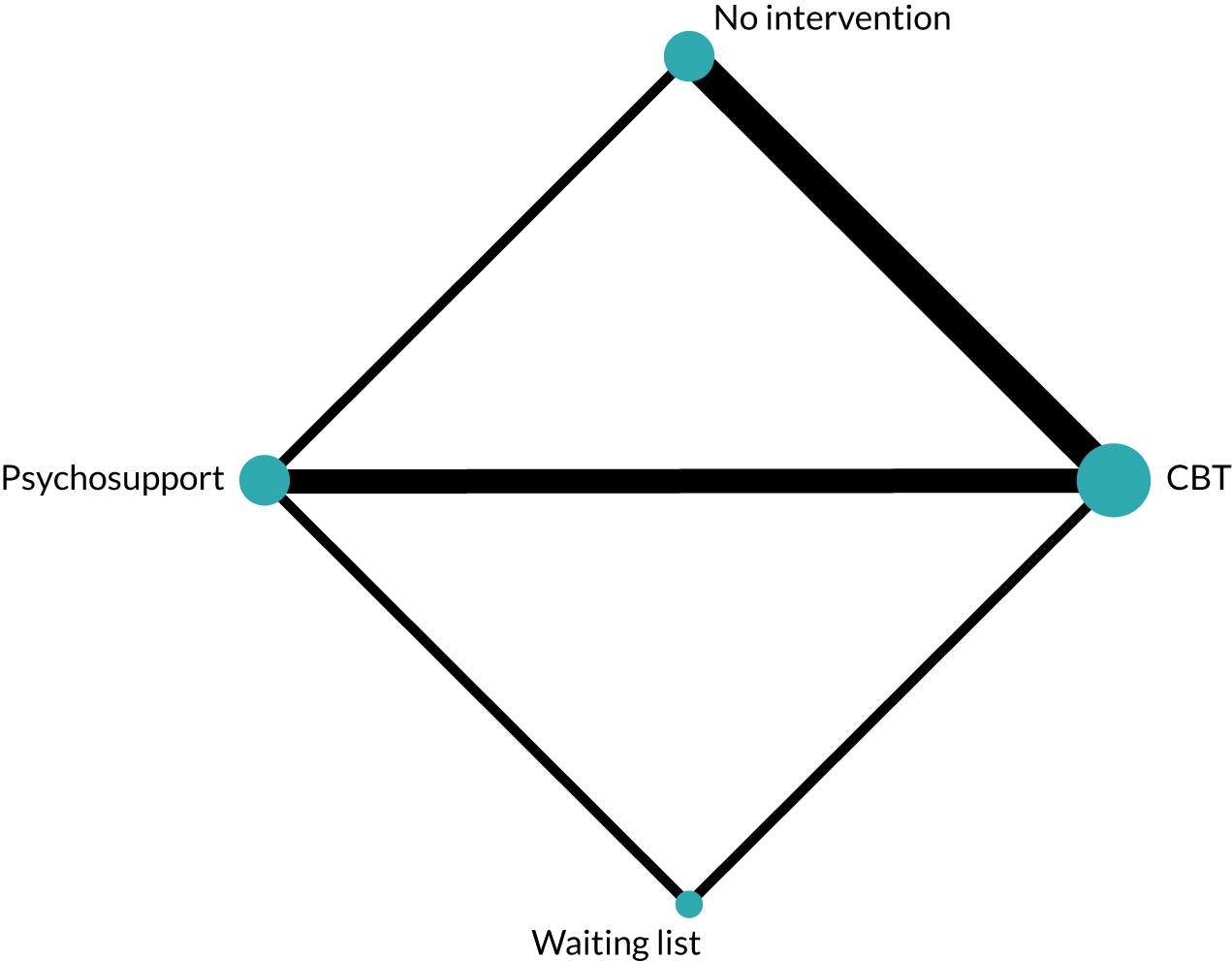
Intervention-level model
Post intervention, and 6–12 and 13–24 months post intervention
Model fit and selection statistics suggested that a random-effects consistency model was reasonable (see Appendix 3). However, the between-study posterior median SDs were indicative of substantial heterogeneity (τ 0.43, 95% CrI 0.05 to 2.24). This was considerably reduced in the unrelated intervention effects model (τ 0.21, 95% CrI 0.01 to 2.68), and may indicate the presence of inconsistency. For this reason, results are not reported. However, this potential inconsistency should be interpreted in the light of the inclusion criteria that interventions needed to be delivered in the educational institution, and the unanticipated limitations this caused for the tertiary/university setting analyses. We consider the limitations in Chapter 10, Limitations relating to inclusion criteria.
Exploring heterogeneity and small-study effects
Subgroup analyses, metaregression and sensitivity analyses were conducted for the intervention-level NMA, for the main outcome and for the primary end point of post intervention only. The comparison-adjusted funnel plots suggest that small study effects are possible in the universal primary and secondary settings analyses. That is, smaller studies may be reporting more beneficial results than larger studies among non-active controlled trials reporting an anxiety outcome (see Appendix 6). This is a potentially important finding. Of all the populations and settings considered in this chapter, the universal analyses provided the strongest evidence for a reduction in anxiety post intervention. There was no evidence to suggest the presence of small-study effects for the analyses of targeted populations in either setting.
A metaregression was conducted for intervention mode of delivery (face to face or via computer), and for intervention facilitator (teacher or a MHP). There was no evidence of effect modification by facilitator or mode of delivery for any population or setting combination (see Appendix 6). However, for the universal primary analysis, there was weak evidence that teacher-delivered CBT interventions (SMD –0.05, 95% CrI –0.21 to 0.08) may be slightly less effective than MHP-delivered CBT interventions (SMD –0.18, 95% CrI –0.42 to 0.00).
Subgroup analyses were conducted to evaluate if intervention effects differed by intended focus of the intervention. For each population and setting combination, intervention estimates were compared across three subgroups: (1) interventions that aimed to prevent anxiety (2) interventions that aimed to prevent only depressive symptoms and (3) interventions that aimed to prevent both anxiety and depression.
For the universal secondary and universal primary anxiety networks, there was very weak evidence that intervention focus was important. Interventions focused on preventing anxiety appeared to have a larger effect on anxiety symptoms than those focusing on depression or combined depression and anxiety. However, CrIs overlapped, and we did not conduct a statistical test to examine subgroup differences. For targeted populations, there was some evidence to suggest that interventions focusing on both anxiety and depression were slightly more effective than interventions focused on anxiety alone. However, we emphasise that these results are to be considered descriptive only. Full results are reported in Appendix 6.
Sensitivity analyses: risk of bias
Sensitivity analyses were conducted for the intervention-level NMA, for the main outcome and primary end point of post intervention only. We explored the robustness of the findings to excluding studies judged to be at high/unclear risk of bias for the domains of random sequence generation and allocation concealment.
Having removed studies judged to be at high/unclear risk of bias, few studies were eligible for inclusion. In the universal secondary network, only three studies125,126,141 of three interventions (waiting list, no intervention and CBT) remained after excluding studies judged to be at high risk of bias, and there was no evidence of an effect for CBT (SMD –0.07, 95% CrI –0.77 to 0.58), relative to a waiting list control (Table 5). For targeted secondary interventions, there were three studies judged to be at low risk of bias comparing four interventions (waiting list, no intervention, CBT and CBM). 117,141,167 There was no evidence of a beneficial effect for either CBT (SMD 0.07, 95% CrI –0.25 to 0.41) or CBM (SMD –0.20, 95% CrI –0.69 to 0.30), relative to no intervention. One study was judged to be at low risk of bias in the universal primary network. 145 A sensitivity analysis was not possible for the targeted primary network.
| Population/setting | Intervention | Reference intervention | Trials (n) | SMD (95% CrI) | |
|---|---|---|---|---|---|
| Low risk of bias | All | ||||
| Universal secondary | CBT | Waiting list | 3 | –0.07 (–0.77 to 0.58) | –0.09 (–0.24 to 0.03) |
| Universal primary | CBT | Usual curriculum | 1 | –0.01 (–0.18 to 0.17)a | –0.07 (–0.23 to 0.05) |
| Targeted secondary | CBT | No intervention | 3 | 0.07 (–0.25 to 0.41) | 0.03 (–0.11 to 0.16) |
| CBM | No intervention | –0.20 (–0.69 to 0.30) | –0.17 (–0.45 to 0.11) | ||
Sensitivity analyses: intracluster correlation coefficient and change from baseline scores
When cluster randomised trials did not explicitly account for clustering in their analyses, we followed the advice in the Cochrane handbook (section 16.3.4)81 for calculating an approximate sample size, using an ICC of 0.03. We explored the robustness of this decision in a best-case/worst-case sensitivity analysis using ICCs of 0.01 and 0.06, respectively. All results were robust to alternative ICC values. To calculate the standardised mean change from baseline, we assumed a correlation of 0.7, which was based on previous analyses (see Chapter 2, Data preparation). Sensitivity analyses were robust to using correlation values of 0.6 and 0.8 (see Appendix 6).
Summary of main results
Seventy-nine studies met the inclusion criteria for the anxiety prevention review, most of which (n = 66) were deemed to be at high or unclear risk of bias for random sequence generation and/or allocation concealment. In addition, there was evidence of possible small-study effects in the universal primary and universal secondary networks. Moderate levels of heterogeneity were observed in all analyses.
A more detailed interpretation of the results, applying the criteria outlined in Chapter 3, is considered in Chapter 9. Seventy-one studies contributed data to the NMA. In the universal secondary network, there was evidence that mindfulness/relaxation interventions (SMD –0.65, 95% CrI –1.14 to –0.19) reduced symptoms of anxiety, relative to usual curriculum. There was weak evidence for a small effect of CBT in reducing self-reported anxiety symptoms (SMD –0.15, 95% CrI –0.34 to 0.04). However, the two mindfulness/relaxation studies were connected to the network only via single small studies. 130,137 Both studies were rated as having an unclear risk of bias for random sequence generation and allocation concealment. The CBT estimate is based on 16 studies (n = 8851 participants),119,120,125–128,131,134–136,138–141,143,144 of which three (n = 4001 participants) were judged to be at low risk of bias for random sequence generation and allocation concealment. 125,126,141 This could, therefore, be considered a more robust finding (because of the lower risk of bias).
There was evidence of effect modification by intervention components for the CBT interventions in the universal secondary network. The additive components analysis suggests that a CBT intervention with a psychoeducation component was more effective than other CBT combinations. There was a reduction in the SMD of –0.39 (95% CrI –0.78 to 0.01) for CBT interventions with a psychoeducation component.
Studies included in the universal primary network were mostly judged to be at unclear risk of bias. There was weak evidence of a very small effect that CBT prevented symptoms of anxiety, relative to usual curriculum, at post intervention.
For the targeted secondary analysis there was evidence that exercise was effective, relative to no intervention (SMD –0.47, 95% CrI –0.86 to –0.09). However, this was based on a single study, connected to the network via no intervention (n = 121 participants) and judged to be at unclear risk of selection bias. 170 There was no evidence of an effect for any other type of intervention in this network.
There was weak evidence to suggest that CBT was effective, relative to waiting list, in the targeted primary analysis at post intervention.
There was evidence of inconsistency in the targeted tertiary/university network. We consider this, and the limitations imposed by the inclusion criteria on the validity of the university network, in Chapter 10, Limitations relating to inclusion criteria.
Chapter 5 Effectiveness of educational setting-based interventions for preventing depression
The main findings for the intervention-level NMA reported in this chapter are reproduced or adapted from Caldwell et al. 1 © 2019 The Author(s). Published by Elsevier Ltd. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes substantial additions and formatting changes to the original text, as well as changes to the reporting approach.
In this chapter, we report the systematic review and NMA results for studies reporting a depression outcome only.
Systematic review
Studies included in the review
The overall PRISMA flow diagram for the project can be seen in Figure 2. There were 105 studies reporting a self-reported depression outcome. The full list of included studies can be found in Appendix 2. Of these 105 studies, the primary focus of 62 studies was the prevention of depression, 29 focused on the prevention of anxiety and depression, and 14 focused on the prevention of anxiety alone. A subgroup analysis to explore whether or not intervention effects varied depending on intended intervention focus is reported subsequently in Exploring heterogeneity and small-study effects.
Study characteristics are reported in Appendix 2. Included studies were published between 1993 and 2018, and randomised between 16 and 8873 participants (median 198). Fifty-three studies were cluster randomised, of which seven reported cluster-adjusted means (SEs) and 29 reported results from appropriate models. The median number of clusters was 13 [interquartile range (IQR) 8–22 clusters]. Fifty-two were individually randomised trials. Ninety-seven studies reported a post-intervention end point, 64 reported a follow-up of between 6 and 12 months, and 18 reported a follow-up of between 13 and 24 months. Six reported a follow-up of ≥ 25 months.
Fifty-seven studies were classified as universal and 48 as targeted (38 indicated, 10 selective). Twenty studies were implemented in a primary school setting, 72 in secondary school, eight in tertiary education and five across multiple settings. A total of 94 studies were conducted in HICs, with 10 conducted in MICs and one in a LIC. Of the studies conducted in HICs, seven were conducted in lower-income settings, as specified by the trial authors.
Risk-of-bias assessment
Study-level risk-of-bias assessments are reported in Appendix 2. Seventeen of the 105 studies reporting a depression outcome were assessed as being at low risk of bias for both random sequence generation and allocation concealment. A further 21 studies reported a suitable randomisation approach, but did not report sufficient details of allocation concealment to allow assessment. Seven studies were judged as being at low risk of bias for participant blinding; all were active, or attention controlled. Study protocols and/or trial registrations were available for 27 studies, of which 25 were judged to be at low risk of bias for selective outcome reporting. Two studies were judged as being at unclear risk of bias. One reported a trial registration number that we could not locate, and the primary outcome was not clear for the other. For cluster randomised trials, we also considered how recruitment, randomisation and analysis were conducted under the Cochrane Risk of Bias tool heading of ‘other bias’. Of 53 cluster RCTs, 18 were judged to be at high risk and 16 at unclear risk of ‘other bias’.
Interventions and components identified in the review
Table 6 reports the interventions and components identified for studies reporting a self-reported depression outcome. Twenty-three studies were multiarm, comparing three or more interventions. Seventy-six studies included an intervention based on CBT, five studies included an intervention based on a combination of CBT + IPT and four were based on IPT alone. Four studies included a relaxation/mindfulness-based intervention, six included a third-wave intervention, four included a behavioural intervention, two included an exercise intervention and one used a CBM approach. One study used an occupational therapy-based intervention. With regard to non-active comparators, 26 studies were waiting list controlled, 33 were usual curriculum controlled, 27 had a no-intervention control and nine used an attention control. Two studies were classified as having a psychoeducation control group and six were classified as having a psychosupport control.
| Study | Focusa | Classification | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention level | Component level for active intervention only | |||||||||||||
| Armb 1 | Armb 2 | Armb 3 | Armb 4 | Psychoeducation | Cognitive | Behavioural | Mindfulness | Third wave | Relaxation | Physiological | Exercise | Bias modification | ||
| Universal secondary | ||||||||||||||
| Araya et al.118 2013 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Aune and Stiles119 2009 | Anxiety | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Barrett et al.121 2005 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Barry et al.190 2017 | Depression | (Usual curriculum) | CBT | + | + | – | – | – | – | – | – | – | ||
| Bonhauser et al.122 2005 | Anxiety + depression | Exercise | Exercise | – | – | – | – | – | – | – | + | – | ||
| Bonhauser et al.122 2005 | – | – | – | – | – | – | – | + | – | |||||
| Burckhardt et al.124 2015 | Anxiety + depression | (Attention control) | Mindfulness/relaxation | – | – | – | + | – | + | – | – | – | ||
| Burckhardt et al.191 2016 | Anxiety + depression | (Usual curriculum) | Third wave | + | – | + | + | + | + | – | – | – | ||
| Calear et al.125 2009 | Anxiety + depression | (Waiting list) | CBT | – | + | + | – | – | + | – | – | – | ||
| Calear et al.126 2016 | Anxiety | (Waiting list) | CBT | CBT | + | + | + | + | – | + | – | – | – | |
| Calear et al.126 2016 | Anxiety | + | + | + | + | – | + | – | – | – | ||||
| Calear et al.127 2016 | Anxiety | (Waiting list) | CBT | + | + | + | + | – | + | – | – | – | ||
| Chaplin et al.192 2006 | Depression | (No intervention) | CBT | CBT | – | + | + | – | – | + | – | – | – | |
| Chaplin et al.192 2006 | Depression | – | + | + | – | – | + | – | – | – | ||||
| Clarke et al.193 1993 | Depression | (Usual curriculum) | Psychoeducation | + | – | – | – | – | – | – | – | – | ||
| Clarke et al.193 1993 | Depression | (Usual curriculum) | Behavioural therapy | + | – | + | – | – | – | – | – | – | ||
| Gillham et al.128 2006 | Anxiety + depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Gillham et al.194 2007 | Depression | (No intervention) | (Attention control) | CBT | – | + | + | – | – | + | – | – | – | |
| Gucht et al.129 2017 | Anxiety + depression | (Usual curriculum) | Third wave | + | – | – | – | + | – | – | – | – | ||
| Hodas131 2016 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Horowitz et al.195 2007 | Depression | (Usual curriculum) | CBT | IPT | + | + | + | – | – | – | – | – | – | |
| Horowitz et al.195 2007 | Depression | + | – | + | – | – | – | – | – | – | ||||
| Johnson et al.132 2016 | Anxiety + depression | (Usual curriculum) | Third wave | – | – | – | + | + | + | – | – | – | ||
| Johnson et al.133 2017 | Anxiety + depression | (Usual curriculum) | Third wave | Third wave | – | – | – | + | + | + | – | – | – | |
| Johnson et al.133 2017 | Anxiety + depression | – | – | – | + | + | + | – | – | – | ||||
| Kindt et al.196 2014 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Lock and Barrett134 2003 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Lowry-Webster et al.135 2001 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Merry et al.197 2004 | Depression | (Attention control) | CBT + IPT | – | + | + | – | – | + | – | – | – | ||
| Perry et al.136 2017 | Depression | (Attention control) | CBT | + | + | + | – | – | + | – | – | – | ||
| Pössel et al.198 2004 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | – | – | – | – | ||
| Pössel et al.199 2011 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | – | – | – | – | ||
| Pössel et al.200 2013 | Depression | (Usual curriculum) | (Attention control) | CBT | + | + | + | – | – | – | – | – | – | |
| Raes et al.201 2014 | Depression | (Usual curriculum) | Third wave | + | – | – | + | + | + | – | – | – | ||
| Rivet-Duval et al.202 2011 | Depression | (Waiting list) | CBT + IPT | – | + | + | – | – | + | – | – | – | ||
| Roberts et al.138 2003 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Roberts et al.139 2010 | Anxiety + depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Rose et al.203 2014 | Depression | (Attention control) | CBT + IPT | CBT + IPT | – | + | + | – | – | + | – | – | – | |
| Rose et al.203 2014 | Depression | – | + | + | – | – | + | – | – | – | ||||
| Sawyer et al.204 2010 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Shatté205 1997 | Depression | (No intervention) | (Attention control) | CBT | – | + | + | – | – | – | – | – | – | |
| Sheffield et al.141 2006 | Depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Spence et al.206 2003 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Stallard et al.142 2013 | Depression | (Usual curriculum) | (Attention control) | CBT + IPT | + | + | + | – | – | + | – | – | – | |
| Tak et al.207 2016 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | – | – | – | – | ||
| Tomba et al.143 2010 | Anxiety + depression | CBT | CBT | + | + | + | – | – | + | – | – | – | ||
| Tomba et al.143 2010 | + | + | + | – | – | + | – | – | – | |||||
| Wong et al.144 2014 | Anxiety + depression | (Usual curriculum) | CBT | CBT | + | + | + | – | – | – | – | – | – | |
| Wong et al.144 2014 | Anxiety + depression | + | + | + | – | – | – | – | – | – | ||||
| Universal primary | ||||||||||||||
| Ahlen et al.145 2018 | Anxiety + depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Barrett and Turner147 2001 | Anxiety | (Usual curriculum) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Barrett and Turner147 2001 | Anxiety | + | + | + | – | – | + | – | – | – | ||||
| Cardemil et al.208 2007 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | – | – | – | – | ||
| Essau et al.150 2012 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Gallegos151 2008 | Anxiety + depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Gillham209 1994 | Depression | (No intervention) | CBT | CBT | – | + | + | – | – | + | – | – | – | |
| Gillham209 1994 | – | + | + | – | – | + | – | – | – | |||||
| Johnstone et al.152 2014 | Anxiety + depression | (Usual curriculum) | CBT | – | + | + | – | – | + | – | – | – | ||
| Mendelson et al.210 2010 | Depression | (Waiting list) | Mindfulness/relaxation | – | – | – | + | – | + | – | – | – | ||
| Pattison and Lynd-Stevenson155 2001 | Depression | (No intervention) | (Attention control) | CBT | CBT | – | + | + | – | – | – | – | – | – |
| Pattison and Lynd-Stevenson155 2001 | Depression | – | + | + | – | – | – | – | – | – | ||||
| Pophillat et al.156 2016 | Anxiety + depression | (Usual curriculum) | CBT | + | + | + | – | – | + | – | – | – | ||
| Quayle et al.211 2001 | Depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Rooney et al.157 2006 | Depression | (No intervention) | CBT | – | + | + | – | – | + | – | – | – | ||
| Soffer212 2003 | Depression | (No intervention) | (Attention control) | Behavioural therapy | – | – | + | – | – | – | – | – | – | |
| Stallard et al.159 2014 | Anxiety | (Usual curriculum) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Stallard et al.159 2014 | Anxiety | + | + | + | – | – | + | – | – | – | ||||
| Targeted secondary | ||||||||||||||
| Arnarson and Craighead213 2009 | Depression | (Waiting list) | CBT + IPT | – | + | + | – | – | + | – | – | – | ||
| Balle and Tortella-Feliu160 2010 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Berry and Hunt161 2009 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Clarke et al.214 1995 | Depression | (No intervention) | CBT | – | + | – | – | – | – | – | – | – | ||
| Congleton215 1995 | Depression | (Waiting list) | CBT | + | + | – | – | – | – | – | – | – | ||
| Cova et al.162 2011 | Depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
| Dobson et al.163 2010 | Anxiety + depression | (Attention control) | CBT | – | + | + | – | – | – | – | – | – | ||
| Fitzgerald et al.114 2016 | Anxiety | (Attention control) | CBM | – | – | – | – | – | – | – | – | + | ||
| Fung et al.216 2016 | Anxiety + depression | (Waiting list) | Mindfulness/relaxation | – | – | – | + | – | + | – | – | – | ||
| Gaete et al.164 2016 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | – | – | – | – | ||
| Gillham et al.165 2012 | Depression | (No intervention) | CBT | CBT | + | + | + | – | – | + | – | – | – | |
| Gillham et al.165 2012 | Depression | + | + | + | – | – | + | – | – | – | ||||
| Hunt et al.166 2009 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Jordans et al.167 2010 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Livheim et al.217 2015 | Depression | Psychosupport | Third wave | – | – | – | – | + | – | – | – | – | ||
| McCarty et al.218 2011 | Depression | (Usual curriculum) | CBT | – | + | + | – | – | + | – | – | – | ||
| McCarty et al.219 2013 | Depression | Psychosupport | CBT | – | + | + | – | – | + | – | – | – | ||
| Noël et al.220 2013 | Depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Peng et al.170 2015 | Anxiety + depression | (No intervention) | Exercise | – | – | – | – | – | + | – | + | – | ||
| Poppelaars et al.221 2016 | Depression | (Waiting list) | CBT | CBT | CBT | + | + | – | – | – | – | – | – | – |
| Poppelaars et al.221 2016 | Depression | – | + | + | – | – | – | – | – | – | ||||
| Poppelaars et al.221 2016 | Depression | + | + | + | – | – | – | – | – | – | ||||
| Puskar et al.222 2003 | Depression | (No intervention) | CBT | – | + | + | – | – | + | – | – | – | ||
| Rohde et al.223 2014 | Depression | Psychoeducation | CBT | CBT | – | + | + | – | – | – | – | – | – | |
| Rohde et al.223 2014 | Depression | – | + | + | – | – | – | – | – | – | ||||
| Sheffield et al.141 2006 | Depression | (No intervention) | CBT | CBT | CBT | + | + | + | – | – | – | – | – | – |
| Sheffield et al.141 2006 | Depression | + | + | + | – | – | – | – | – | – | ||||
| Sheffield et al.141 2006 | Depression | + | + | + | – | – | – | – | – | – | ||||
| Stallard et al.142 2013 | Depression | (Usual curriculum) | (Attention control) | CBT + IPT | + | + | + | – | – | + | – | – | – | |
| Stice et al.224 2008 | Depression | Psychoeducation | Psychosupport | CBT | CBT | – | + | + | – | – | – | – | – | – |
| Stice et al.224 2008 | Depression | + | – | + | – | – | – | – | – | – | ||||
| Stoppelbein225 2003 | Depression | (Attention control) | CBT | + | + | + | – | – | + | – | – | – | ||
| Topper et al.173 2017 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Wijnhoven et al.226 2014 | Depression | (Waiting list) | CBT | – | + | – | – | – | – | – | – | – | ||
| Woods and Jose227 2011 | Depression | (Usual curriculum) | CBT | + | + | + | – | – | – | – | – | – | ||
| Young et al.228 2006 | Depression | Psychosupport | IPT | + | – | + | – | – | – | – | – | – | ||
| Young et al.229 2010 | Depression | Psychosupport | IPT | + | – | + | – | – | – | – | – | – | ||
| Young et al.230 2016 | Depression | Psychosupport | IPT | + | – | + | – | – | – | – | – | – | ||
| Targeted primary | ||||||||||||||
| Cowell et al.231 2009 | Depression | (No intervention) | Psychosupport | – | – | – | – | – | – | – | – | – | ||
| Jaycox et al.232 1994 | Depression | (Waiting list) | CBT | – | + | + | – | – | + | – | – | – | ||
| Manassis et al.175 2010 | Anxiety + depression | (Attention control) | CBT | + | + | – | – | – | – | – | – | – | ||
| Simpson179 2008 | Anxiety + depression | (Attention control) | CBT | + | + | + | – | – | – | – | – | – | ||
| Siu180 2007 | Anxiety + depression | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| Tokolahi et al.181 2018 | Anxiety + depression | (Waiting list) | Occupational therapy | – | – | – | – | – | – | – | – | – | ||
| Universal tertiary/university setting | ||||||||||||||
| Reynolds et al.233 2011 | Depression | (Usual curriculum) | Behavioural therapy | – | – | + | – | – | – | – | – | – | ||
| Targeted tertiary/university setting | ||||||||||||||
| Cui et al.183 2016 | Depression | (Waiting list) | Psychosupport | CBT | + | + | + | – | – | + | – | – | – | |
| Ellis et al.184 2011 | Depression | (No intervention) | Psychosupport | CBT | + | + | + | – | – | + | – | – | – | |
| Higgins185 2007 | Anxiety | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Peden et al.234 2000 | Depression | (No intervention) | CBT | – | + | – | – | – | – | – | – | – | ||
| Seligman et al.186 1999 | Anxiety + depression | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Seligman et al.187 2007 | Anxiety + depression | (No intervention) | CBT | + | + | + | – | – | + | – | – | – | ||
| Takagaki et al.235 2016 | Depression | (No intervention) | Behavioural therapy | + | – | + | – | – | – | – | – | – | ||
| Multiple/mixed settings | ||||||||||||||
| Liddle and Macmillan188 2010 | Anxiety | (Waiting list) | CBT | + | + | + | – | – | + | – | – | – | ||
| McLaughlin236 2011 | Depression | Psychosupport | CBT | – | + | + | – | – | + | – | – | – | ||
| Stice et al.237 2007 | Depression | (Waiting list) | CBT | + | + | + | – | – | – | – | – | – | ||
| Velásquez et al.189 2015 | Anxiety + depression | (Waiting list) | Mindfulness/relaxation | – | – | – | – | – | + | – | – | – | ||
| Yu238 2002 | Depression | (No intervention) | CBT | + | + | + | – | – | – | – | – | – | ||
Table 6 also reports the combinations of components identified across all studies reporting a depression outcome (at any time point) by population and setting. Components identified were psychoeducation, cognitive, behavioural, mindful, third wave, relaxation, physiological, exercise and CBM. There were 123 active intervention arms from the 105 studies reporting a self-reported depression outcome. Of these active intervention arms, 72 had a psychoeducation component, 96 had a cognitive component, 100 had a behavioural component, 11 had mindful components, seven had third-wave components, 61 had a relaxation component, two had an exercise component and one had a CBM component. The most frequently identified combinations were psychoeducation + cognitive + behavioural (26 study arms), psychoeducation + cognitive + behavioural + relaxation (28 arms) and cognitive + behavioural + relaxation (17 arms).
Further intervention process and delivery characteristics are reported in Appendix 2. The number of intervention sessions implemented ranged from 2 to 120 [median 10 (IQR 8–12) sessions]. As a proxy for intervention dose, we calculated the intervention intensity as total session time (number of sessions × duration in minutes); this ranged from 135 to 10,800 minutes [median 600 (IQR 450–900) minutes]. Ninety per cent of interventions were delivered to whole classrooms or small groups. In 52 studies, interventions were delivered by a MHP, school counsellor or student psychologist. In 10 studies, interventions were delivered by miscellaneous external professionals. Twenty studies used interventions delivered solely by teachers. Fifteen studies involved a combination of teaching, psychology and other professionals. Three studies implemented interventions via computer. Five studies could not be classified.
Network meta-analysis results
Of the 105 studies in the depression review, 86 studies (50,159 participants) contributed to the NMA for depression. Studies not contributing to the NMA are listed in Appendix 2. The network plot for all studies reporting a depression outcome across all populations and settings is reported in Figure 9. The plot edges (lines) connecting each pair of interventions represent a direct comparison and are proportional to the number of trials making that direct comparison. Intervention ‘nodes’ are proportional to the number of participants randomised to each intervention.
FIGURE 9.
Network plot for all eligible studies reporting a depression outcome. OT, occupational therapy; SH, self-help; third wave, third-wave CBT-based therapies.
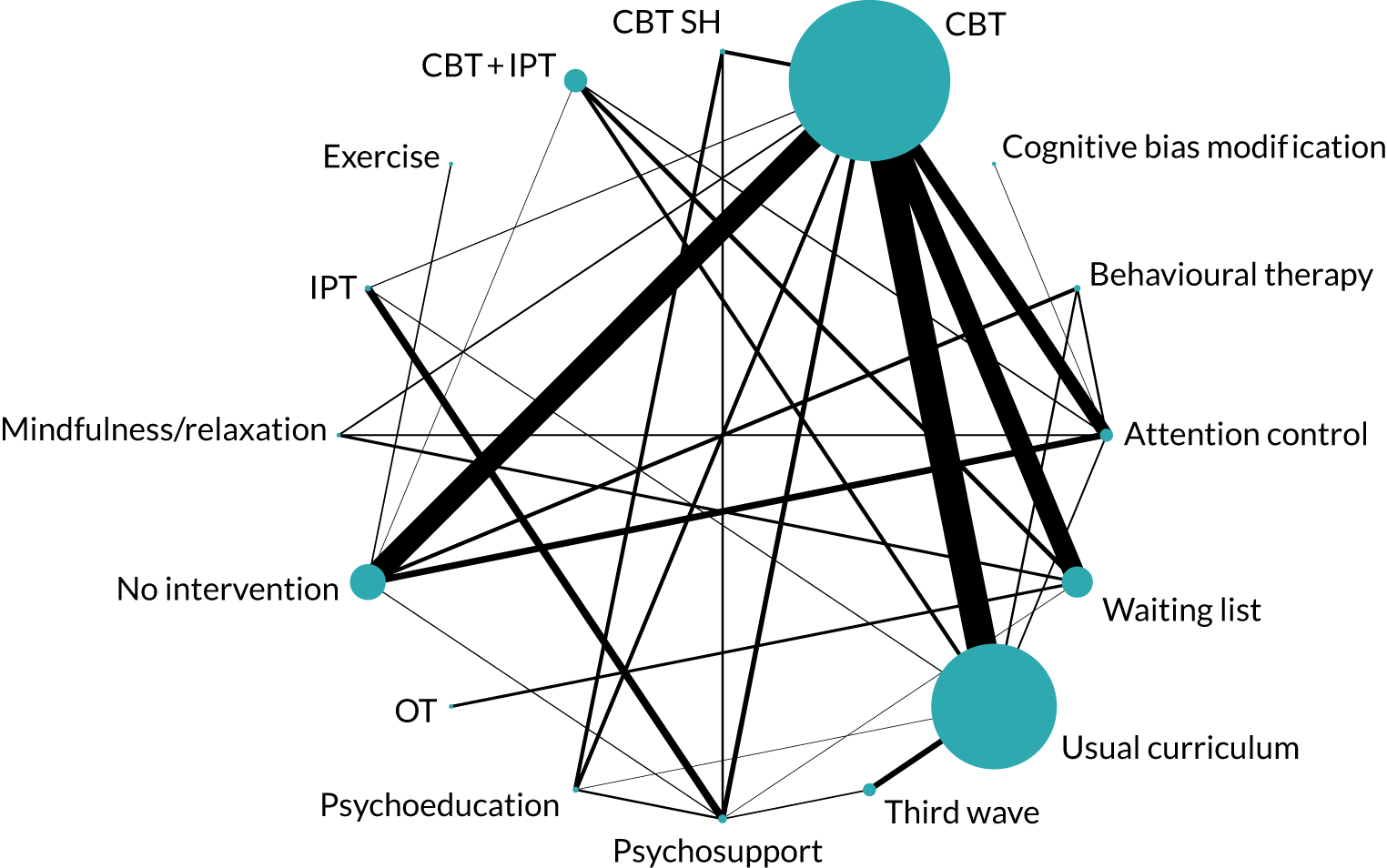
Model details are described in Chapter 2 and Appendix 1. Three models were compared for each analysis. We report the results from an intervention-level main effect, a nested additive component and a full interaction component model. Results are reported by population, setting and follow-up time point. The longer-term follow-ups of 6–12, 13–24 and ≥ 25 months are reported for the main intervention-level model only. When data were available from head-to-head trials, we conducted pairwise meta-analyses. The results are reported alongside NMA results in Table 7. Full NMA and pairwise results are reported in Appendix 4.
| Setting | Intervention | Reference intervention | NMA | Direct meta-analysis | Number of trials | ||
|---|---|---|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | ||||
| Universal secondary | CBT | Usual curriculum | –0.04 | –0.16 to 0.07 | –0.05 | –0.17 to 0.06 | 11 |
| CBT + IPT | Usual curriculum | –0.18 | –0.46 to 0.08 | NA | NA | 0 | |
| Behavioural therapy | Usual curriculum | –0.02 | –0.40 to 0.37 | –0.02 | –0.40 to 0.37 | 1 | |
| IPT | Usual curriculum | –0.03 | –0.36 to 0.29 | –0.10 | –0.47 to 0.26 | 1 | |
| Third wave | Usual curriculum | –0.03 | –0.21 to 0.14 | –0.02 | –0.19 to 0.14 | 4 | |
| Universal primary | CBT | Usual curriculum | –0.13 | –0.44 to 0.17 | –0.11 | –0.37 to 0.16 | 6 |
| Behavioural therapy | Usual curriculum | –0.10 | –1.04 to 0.80 | NA | NA | 0 | |
| Targeted secondary | CBT | No intervention | –0.22 | –0.58 to 0.13 | –0.16 | –0.47 to 0.15 | 5 |
| IPT | No intervention | –0.65 | –1.50 to 0.16 | NA | NA | 0 | |
| Third wave | No intervention | –0.68 | –1.83 to 0.47 | NA | NA | 0 | |
| CBM | No intervention | –0.90 | –2.20 to 0.40 | NA | NA | 0 | |
| Exercise | No intervention | –0.28 | –1.13 to 0.58 | –0.28 | –1.12 to 0.57 | 1 | |
| Targeted primary | CBT | Waiting list | –0.48 | –2.49 to 1.50 | –0.48 | –2.48 to 1.47 | 2 |
| Occupational therapy | Waiting list | –0.10 | –2.94 to 2.71 | –0.10 | –2.87 to 2.69 | 1 | |
Universal population, secondary setting
Post intervention
The analysis-specific network diagram is reported in Figure 10. Thirty-four studies (18,094 participants) contributed to the analysis for the main time point of immediately post intervention, of which nine were multiarm trials. 119,125–129,131–136,138,139,141,143,144,190,192–203,205–207 Six studies were deemed to be at low risk of bias, and 18 studies were deemed to be at unclear risk of bias, for both random sequence generation and allocation concealment. Five studies were rated as having an unclear risk of bias for randomisation and a low risk of bias for allocation concealment. Three studies were rated as having a low risk of bias for randomisation and an unclear risk of bias for allocation concealment. Two studies were rated as having an unclear risk of bias for randomised sequence generation and a high risk of bias for allocation concealment. Twenty-five studies included an intervention based on CBT, one included an intervention based on IPT and three included an intervention based on a combination of CBT and IPT. Four interventions were based on third wave and one was based on behavioural therapy. All reported results are from a random-effects NMA model unless otherwise stated. Model fit and selection statistics suggested that a consistency model was appropriate. Of the three component models fitted (intervention, additive and full interaction), the additive model was preferred, suggesting evidence for effect modification by components. All model fit statistics are reported in Appendix 3. Results are reported as SMDs and 95% CrIs.
FIGURE 10.
Network plot for universal population, secondary setting: post-intervention depression outcome.
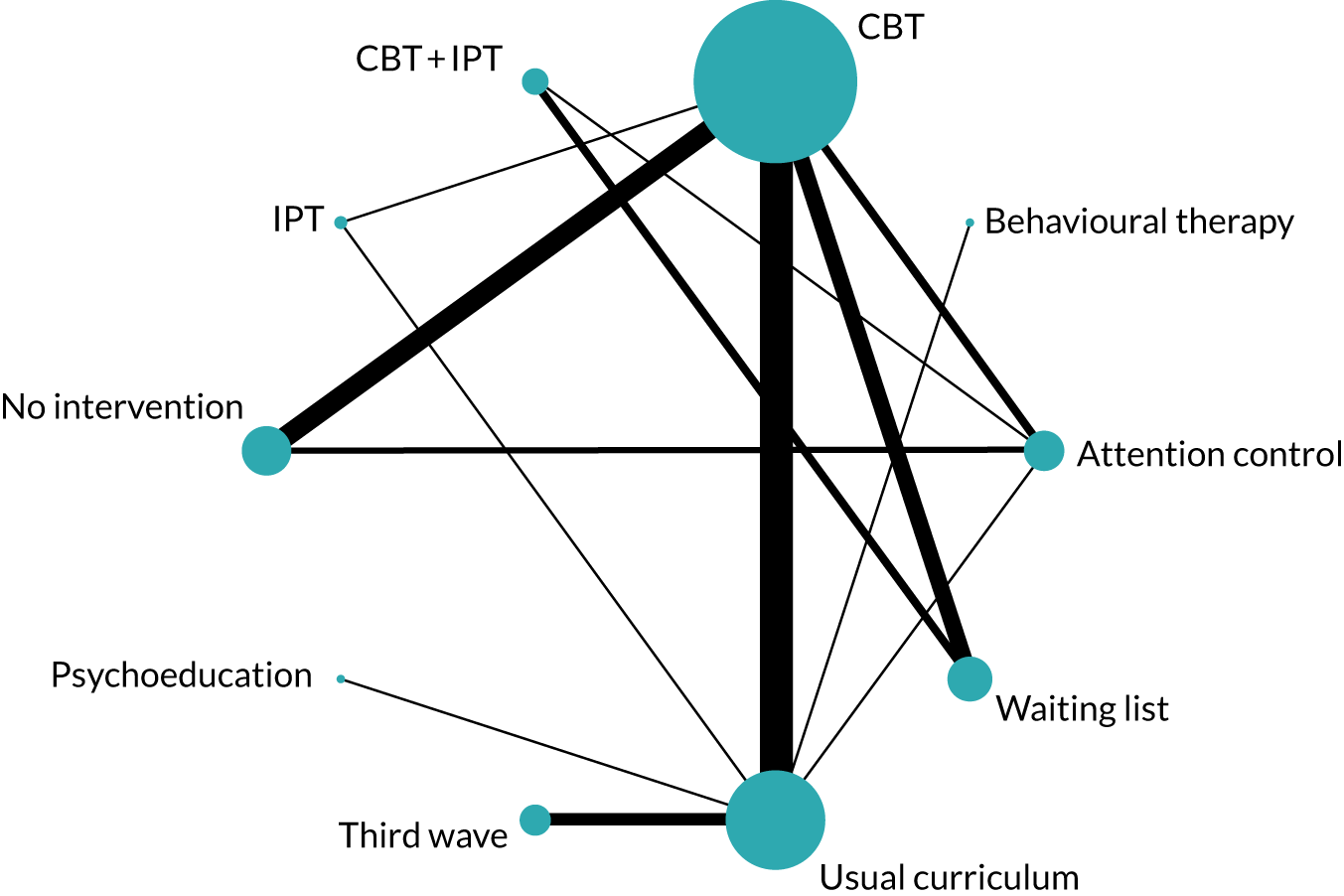
Intervention-level effects
The between-study posterior median SD (τ) was indicative of moderate heterogeneity (τ 0.15, 95% CrI 0.10 to 0.22). Table 7 reports SMDs (95% CrIs) for each intervention relative to usual curriculum. There was weak evidence of a very small effect of CBT (SMD –0.04, 95% CrI –0.16 to 0.07) in preventing symptoms of depression post intervention. There was weak evidence of a small effect of CBT + IPT (SMD –0.18, 95% CrI –0.46 to 0.08) in preventing symptoms at the post-intervention time point. There was no evidence to suggest that IPT (SMD –0.03, 95% CrI –0.36 to 0.29), third-wave therapies (SMD –0.03, 95% CrI –0.21 to 0.14) or behavioural therapy (SMD –0.02, 95% CrI –0.40 to 0.37) are effective.
Additive model: components nested within intervention
Component-level models were fitted to evaluate whether or not the observed between-study heterogeneity in the intervention model could be explained by differences in intervention components. It was possible to estimate additive component effects in CBT and third-wave interventions.
The between-study posterior median SD was indicative of moderate heterogeneity (τ 0.14, 95% CrI 0.08 to 0.22). All CBT interventions included a cognitive component, and additive effects were estimated for psychoeducation, behavioural, mindful and relaxation components. The regression coefficients are reported in Appendix 3 and suggest that there was no evidence of effect modification by components for CBT interventions. Table 8 reports the SMDs for all specific additive combinations of intervention components. Relative to a usual curriculum control, there was weak evidence that a cognitive plus a behavioural component may be effective at reducing symptoms of depression post intervention in universal secondary settings (SMD –0.11, 95% CrI –0.28 to 0.05). There was a lack of evidence for all other combinations.
| Population/setting/outcome | Main intervention | Components (within main intervention) | Study arms (n) | SMD (95% CrI) | |
|---|---|---|---|---|---|
| Additive model | Full interaction model | ||||
| Universal/secondary/depression | CBT | Cognitive + psychoeducational + behavioural | 11 | 0.01 (–0.12 to 0.13) | –0.03 (–0.15 to 0.09) |
| Cognitive + psychoeducational | 1 | –0.55 (–1.33 to 0.20) | –0.57 (–1.33 to 0.21) | ||
| Cognitive + behavioural + relaxation | 4 | –0.10 (–0.31 to 0.11) | –0.11 (–0.4 to 0.17) | ||
| Cognitive + behavioural | 4 | –0.11 (–0.28 to 0.05) | –0.03 (–0.15 to 0.09) | ||
| Cognitive + psychoeducational + behavioural + relaxation | 6 | 0.02 (–0.18 to 0.22) | 0.02 (–0.20 to 0.24) | ||
| Cognitive + psychoeducational + behavioural + mindfulness + relaxation | 3 | –0.01 (–0.4 to 0.38) | –0.02 (–0.46 to 0.41) | ||
| Cognitive + mindfulness | 0 | –0.70 (–1.6 to 0.18) | – | ||
| Cognitive + relaxation | 0 | –0.66 (–1.47 to 0.13) | – | ||
| Cognitive + psychoeducational + mindfulness | 0 | –0.59 (–1.44 to 0.26) | – | ||
| Cognitive + behavioural + relaxation | 0 | –0.54 (–1.33 to 0.24) | – | ||
| Cognitive + psychoeducational + mindfulness +relaxation | 0 | –0.57 (–1.44 to 0.29) | – | ||
| Cognitive + psychoeducational + behavioural + mindfulness | 0 | –0.03 (–0.4 to 0.35) | – | ||
| Cognitive + behavioural + mindfulness | 0 | –0.14 (–0.59 to 0.30) | – | ||
| Cognitive + behavioural + mindfulness + relaxation | 0 | –0.13 (–0.58 to 0.32) | – | ||
| Cognitive + mindfulness + relaxation | 0 | –0.69 (–1.6 to 0.21) | – | ||
| Third wave | Third wave + psychoeducational | 1 | –0.05 (–0.38 to 0.27) | –0.05 (–0.40 to 0.30) | |
| Third wave + mindfulness + relaxation | 3 | 0.10 (–0.12 to 0.33) | 0.11 (–0.13 to 0.35) | ||
| Third wave + psychoeducational + mindfulness + relaxation | 1 | –0.35 (–0.70 to 0.00) | –0.35 (–0.72 to 0.02) | ||
All third-wave interventions contained a third-wave component, and additive effects were estimated for psychoeducation and a combined mindfulness + relaxation component. Owing to the data structure, it was not possible to estimate the effects for mindfulness and relaxation components separately. The impact of including a psychoeducation component in third-wave interventions was to reduce the SMD by –0.45 (β –0.45, 95% CrI –0.87 to –0.04). Although this regression coefficient indicates the presence of effect modification, Table 8 shows that there was still only weak evidence that a third-wave intervention (when made up of third wave + mindfulness + relaxation components) is effective at reducing symptoms of depression relative to a usual curriculum (SMD –0.35, 95% CrI –0.70 to 0.00). We note that this is based on evidence from a single study.
Full interaction model: components nested within intervention
Table 8 also reports the number of studies comparing each unique combination of components for CBT and third-wave interventions for the full interaction component model. Model fit and regression coefficients are reported in Appendix 3. The between-study posterior median SD for the full interaction model was suggestive of moderate heterogeneity (τ 0.15, 95% CrI 0.10 to 0.23). There was no evidence of a differential effect of CBT or third wave by intervention components in universal secondary settings.
Universal, secondary, further time points: intervention-level effects
Twenty-eight studies (19,817 participants) contributed to the analysis for 6–12 months post intervention, eight of which were multiarm trials. 118,125,126,128,129,131,133–136,138,139,141–143,194–203,205–207 Twenty-one studies included an intervention based on CBT, four studies included a CBT + IPT intervention and one study evaluated an IPT-based intervention. Three studies included a third-wave-based intervention. The between-study posterior median SD was indicative of low heterogeneity (τ 0.08, 95% CrI 0.02 to 0.15). There was weak evidence, of small effects, to suggest that CBT (SMD –0.02, 95% CrI –0.10 to 0.06), CBT + IPT (SMD –0.10, 95% CrI –0.26 to 0.05) and third-wave interventions (SMD –0.13, 95% CrI –0.27 to 0.01) could prevent symptoms of depression, compared with a usual curriculum comparator. The third-wave studies were judged to be at low risk of bias. The CBT and CBT + IPT studies were judged to be at mostly unclear risk of selection bias (see Appendix 2). There was no evidence to support IPT (SMD 0.11, 95% CrI –0.13 to 0.35) reducing symptoms at 6–12 months, relative to usual curriculum.
Eight studies (7584 participants) contributed to the analysis for 13–24 months post intervention, seven of which included an intervention based on CBT and one that included an intervention based on CBT + IPT. 136,138,139,194,197,204,206,207 There was no evidence to suggest that CBT-based (SMD –0.04, 95% CrI –0.20 to 0.14) or CBT + IPT (SMD –0.10, 95% CrI –0.57 to 0.39) interventions prevented symptoms of depression at 13–24 months, relative to usual curriculum. The between-study posterior median SD was indicative of low heterogeneity (τ 0.07, 95% CrI 0.00 to 0.35).
We combined studies reporting time points closest to 36 months post intervention. Three studies (1303 participants) reported time points between 30 and 36 months post intervention. 138,194,206 All evaluated a CBT intervention. There was no evidence of an effect for preventing symptoms (SMD –0.14, 95% CrI –2.89 to 2.63), compared with usual curriculum.
Universal population, primary setting
Post intervention
The analysis-specific network diagram is reported in Figure 11. Twelve studies (4116 participants) contributed to the analysis for the main time point of immediately post intervention. 145,147,150–152,155–157,208,209,211,212 Eleven included an intervention based on CBT and one study evaluated a behavioural intervention. Model fit and selection statistics were suggestive of slight lack of fit, but a consistency model was preferred. Model fit was similar across all three component models fitted (intervention, additive and full interaction), but suggests that the intervention-level model was appropriate (see Appendix 3). Therefore, we report effect estimates from the random-effects intervention-level NMA only. Regression coefficients from the additive and full interaction models are reported in Appendix 3.
FIGURE 11.
Network plot for universal population, primary setting: post-intervention depression outcome.
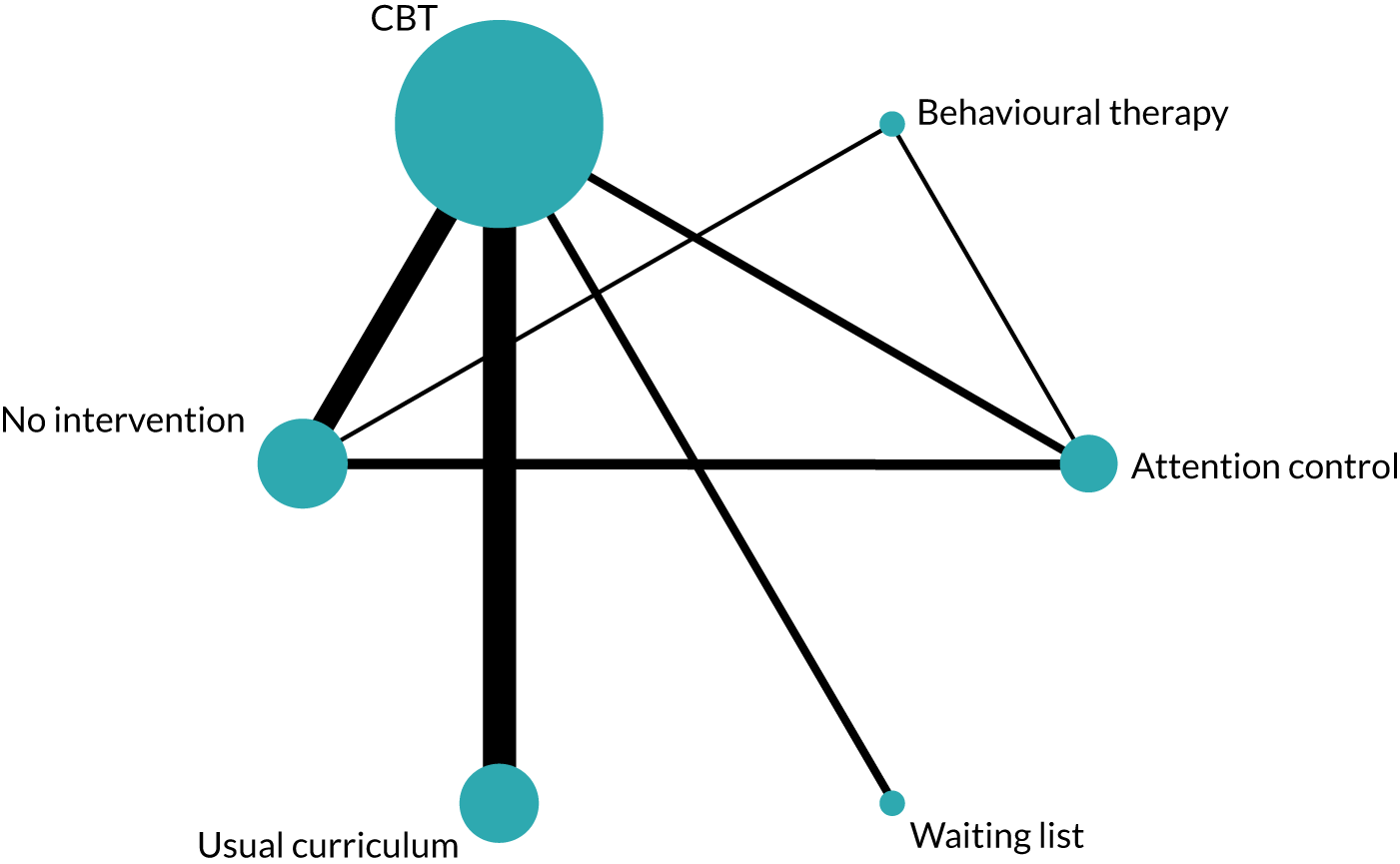
Intervention-level effects
The between-study posterior median SD was indicative of moderate to substantial heterogeneity (τ 0.32, 95% CrI 0.18 to 0.59). Table 7 reports SMDs (95% CrIs) for each intervention, relative to usual curriculum. There was a lack of evidence that CBT (SMD –0.13, 95% CrI –0.44 to 0.17) or behavioural therapy (SMD –0.10, 95% CrI –1.04 to 0.80) reduced self-reported symptoms of depression post intervention.
Additive model: components nested within intervention
The between-study posterior median SD was indicative of high heterogeneity (τ 0.37, 95% CrI 0.20 to 0.70). All CBT interventions included a cognitive and a behavioural component, and additive effects could be estimated for psychoeducation and relaxation components only. However, there was no evidence for effect modification; regression coefficients are reported in Appendix 3, Table 40.
Full interaction model: components nested within intervention
The between-study posterior median SD was suggestive of high heterogeneity (τ 0.39, 95% CrI 0.21 to 0.78). There was no evidence of effect modification by intervention components for CBT in universal primary settings; regression coefficients are reported in Appendix 3, Table 40.
Universal, primary, further time points: intervention-level effects
Nine studies (4134 participants) contributed to the analysis for 6–12 months post intervention, all of which evaluated a CBT-based intervention. 145,150–152,155,157,159,208,211 The between-study posterior median SDs were indicative of moderate to substantial heterogeneity (τ 0.21, 95% CrI 0.06 to 0.56). There was weak evidence, of a small effect, that CBT prevents symptoms of depression at 6–12 months, relative to usual curriculum (SMD –0.15, 95% CrI –0.43 to 0.09).
Three studies (1602 participants) contributed to the analysis for 13–24 months post intervention, all of which included an intervention based on CBT. 152,157,159 There was no evidence to suggest that CBT-based interventions prevented symptoms of depression at 13–24 months, relative to usual curriculum (SMD –0.03, 95% CrI –0.62 to 0.55).
One study (910 participants) reported a follow-up time point of 30 months post intervention. 152 There was evidence that CBT prevented symptoms of depression at 30 months’ follow-up (SMD –0.27, 95% CrI –0.42 to –0.13).
Targeted population, secondary setting
Post intervention
The analysis-specific network diagram for targeted secondary settings is reported in Figure 12. Twenty-four studies (3669 participants) contributed to the analysis for the main time point of immediately post intervention. 114,141,160–163,165,167,170,173,214,215,217–219,221–224,226–230 Four studies were deemed to be at low risk of bias and seven studies were deemed to be at unclear risk of bias for both random sequence generation and allocation concealment. Eleven studies were judged to be at low risk of bias for random sequence generation but at unclear risk of bias for allocation concealment, and two studies were judged to be at unclear risk of bias for random sequence generation but at low risk of bias for allocation concealment. Eighteen studies included an intervention based on CBT, three studies included IPT-based interventions, one study evaluated a third-wave intervention, one included a CBM intervention and one evaluated an exercise intervention. Model fit and selection statistics were suggestive of slight lack of fit, but a consistency model was considered reasonable. Model fit was similar across all three component models (intervention, additive and full interaction). Reported results are from a random-effects, consistency intervention-level NMA. Full model fit details are provided in Appendix 3.
FIGURE 12.
Network plot for targeted population, secondary setting: post-intervention depression outcome.
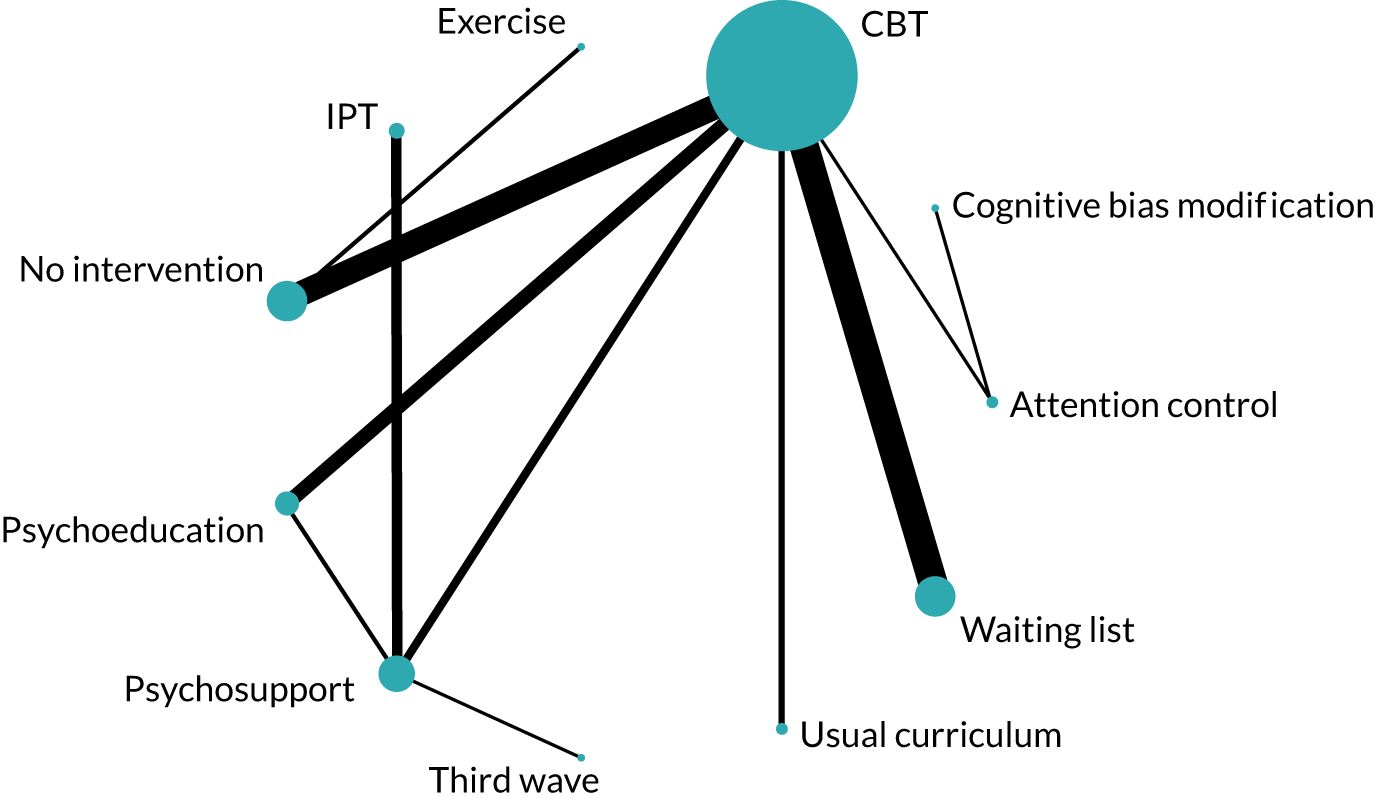
Intervention-level effects
There was evidence of moderate to substantial between-study heterogeneity (τ 0.38, 95% CrI 0.25 to 0.58). Table 7 reports SMDs (95% CrIs) for each intervention relative to no intervention. There was no evidence of an effect for any intervention: CBT (SMD –0.22, 95% CrI –0.58 to 0.13); CBM (SMD –0.90, 95% CrI –2.20 to 0.40); IPT (SMD –0.65, 95% CrI –1.50 to 0.16); exercise (SMD –0.28, 95% CrI –1.13. to 0.58); and third wave (SMD –0.68, 95% CrI –1.83 to 0.47).
Component models: additive and full interaction
Regression coefficients are reported for both the additive and full interaction models in Appendix 3, Table 42. There was no evidence of effect modification according to components for CBT interventions in a targeted secondary setting.
Targeted, secondary, further time points: intervention-level effects only
Seventeen studies (2728 participants) contributed to the analysis for 6–12 months post intervention, of which 14 included a CBT-based intervention and three included an IPT intervention. 141,160,163,165,173,214,218,219,221–224,226–230 There was evidence of high levels of between-study heterogeneity (τ 0.44, 95% CrI 0.27 to 0.71). There was no evidence that either CBT (SMD –0.04, 95% CrI –0.51 to 0.41) or IPT (SMD –0.49, 95% CrI –1.49 to 0.48) prevented symptoms of depression at 6–12 months, relative to no intervention.
Five studies (1089 participants) provided data for the NMA of 13–24 months’ follow-up. 166,218,223,224,229 Four evaluated a CBT intervention and one evaluated an IPT-based intervention. Between-study heterogeneity was high (τ 0.58, 95% CrI 0.12 to 3.08). There was no evidence that CBT (SMD –0.18, 95% CrI –2.56 to 2.16) or IPT (SMD 0.09, 95% CrI 3.81 to 3.93) reduced symptoms of depression at 13–24 months post intervention.
One study (260 participants), judged to be at unclear risk of bias, provided no evidence to suggest that CBT prevented symptoms at 48 months’ follow-up (SMD –0.27, 95% CrI –1.05 to 0.50). 166
Targeted population, primary setting
Post intervention
The analysis-specific network diagram for targeted primary settings is reported in Figure 13. Five studies (497 participants) contributed to the analysis for the post-intervention time point, of which four included an intervention based on CBT, and one examined an occupational therapy-based intervention. 175,179–181,232 One study was deemed to be at low risk of bias for both random sequence generation and allocation concealment, and three studies were deemed to be at unclear risk of bias. One study was deemed to be at low risk of bias for random sequence generation but at unclear risk of bias for allocation concealment. Model fit statistics are reported in Appendix 3. There were limited data available for the component-level models; however, model fit was similar across the three models. The between-study posterior median SD was lowest for the intervention-level model; it is on this basis that the intervention-level model is preferred here (see Appendix 3). All reported results are from a consistency random-effects NMA model unless otherwise stated.
FIGURE 13.
Network plot for targeted population, primary setting: post-intervention depression outcome. OT, occupational therapy.
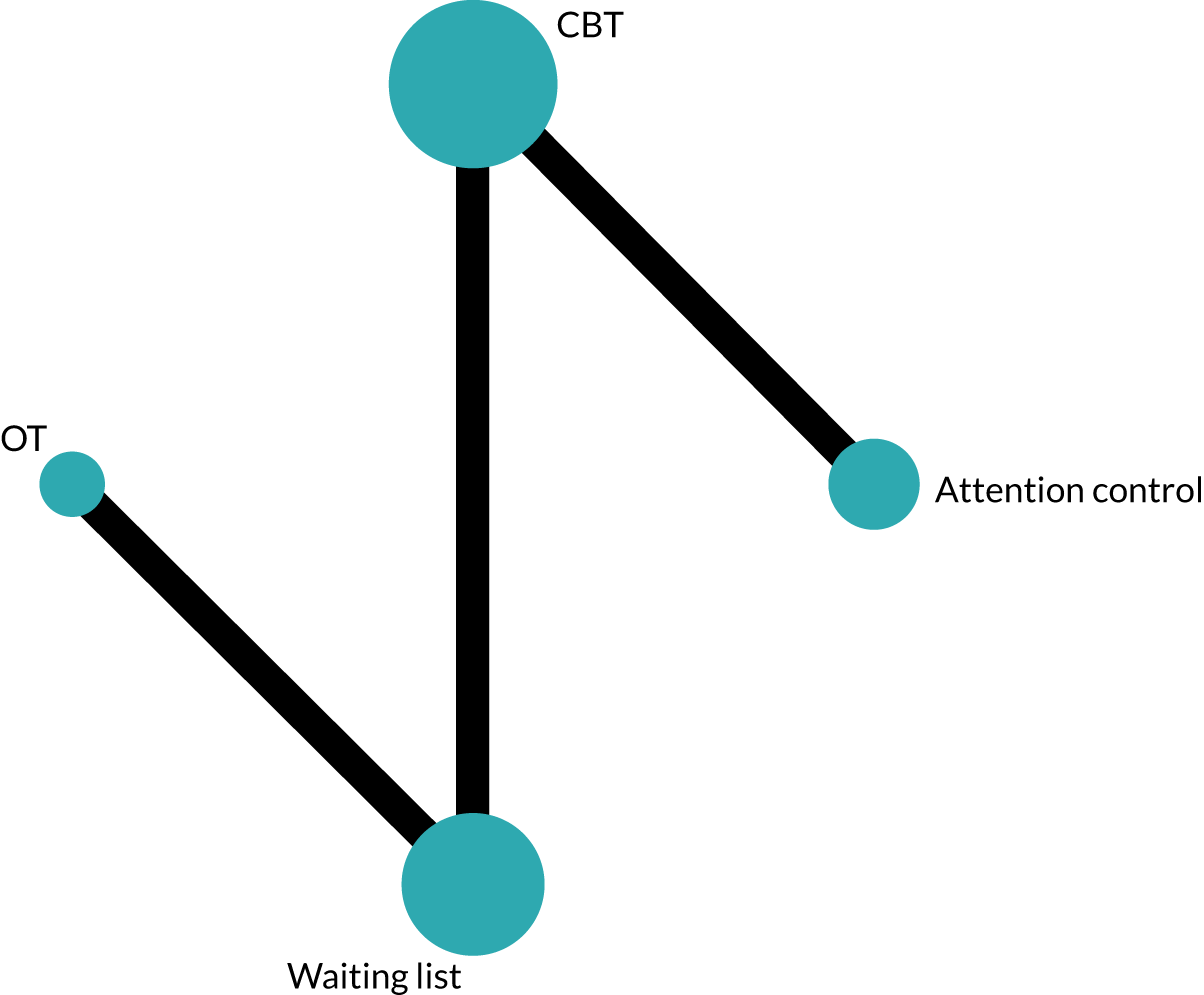
Intervention-level effects
There was evidence of substantial between-study heterogeneity (τ 0.60, 95% CrI 0.08 to 3.80). Table 7 reports SMDs (95% CrIs) for each intervention relative to a waiting list. There was no evidence of an effect for CBT (SMD –0.48, 95% CrI –2.49 to 1.50) or occupational therapy (SMD –0.10, 95% CrI –2.94 to 2.71) at the immediate post-intervention time point.
Component models: additive and full interaction
For the additive component model, the between-study posterior median SD tended to the prior (τ 2.48, 95% CrI 0.12 to 4.87), as did the regression coefficient for occupational therapy (β –8.97, 95% CrI –144.7 to 144.5). As a result, we conclude that data were insufficient to estimate additive or full interaction effects for targeted primary settings.
Targeted, primary, further time points: intervention-level effects only
Two studies (230 participants) reported follow-up at 6–12 months, both of which included a CBT-based intervention. 175,232 A fixed-effects NMA was conducted. There was weak evidence that CBT (SMD –0.34, 95% CrI –0.72 to 0.05) prevented symptoms of depression at 6–12 months, relative to a waiting list. There was weak evidence from one study (83 participants), judged to be at unclear risk of bias, that CBT prevented symptoms of depression at 24 months’ follow-up, compared with a waiting list (SMD –0.50, 95% CrI –0.96 to 0.05). 232
Targeted population, tertiary/university setting
The analysis-specific network diagram is reported in Figure 14. Five studies (789 participants) contributed to the analysis for the main time point of post intervention, four of which included an intervention based on CBT and one of which included an intervention based on behavioural therapy. 183,184,186,187,235 Model fit and selection statistics suggested that a random-effects consistency model was reasonable (see Appendix 3); however, the between-study posterior median SD was indicative of substantial heterogeneity (τ 0.51, 95% CrI 0.12 to 2.50). This was considerably reduced in the unrelated intervention effects model (τ 0.26, 95% CrI 0.02 to 2.48), and may indicate the presence of inconsistency. Therefore, results for the tertiary setting are not reported. This possible inconsistency should also be interpreted in the light of the inclusion criteria adopted in this review, that interventions needed to be delivered in the educational institution itself, and the unanticipated limitations it caused for the tertiary/university setting analyses. We consider the limitations in Chapter 10.
FIGURE 14.
Network plot for targeted population, tertiary/university setting: post-intervention depression outcome.
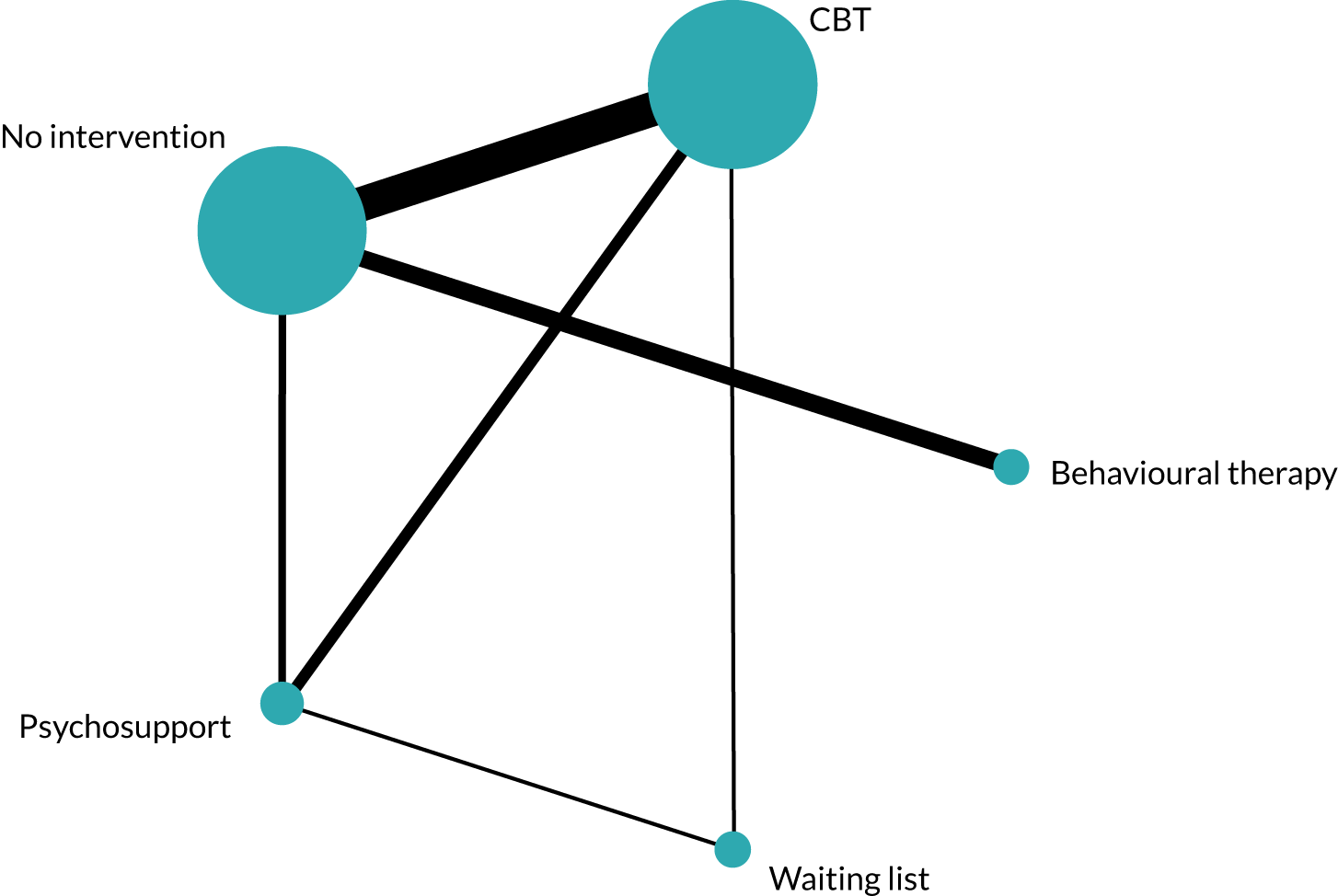
Exploring heterogeneity and small-study effects
Subgroup analyses, metaregression and sensitivity analyses were conducted for the intervention-level NMA, for the main outcome and primary end point of post intervention only. Comparison-adjusted funnel plots did not provide evidence of small-study effects (see Appendix 6). However, the small number of studies available for the primary settings makes interpretation difficult.
Metaregression was conducted for intervention mode of delivery (face to face or via computer) and for intervention facilitator (teacher or a MHP). There was no evidence of effect modification by facilitator or mode of delivery for any population or setting combination (see Appendix 6).
Subgroup analyses were conducted to assess whether or not intervention effects differed by intended focus of the intervention, for example whether or not interventions addressing depression had a larger effect on anxiety outcomes than interventions intended to focus on anxiety but which also recorded depression outcomes. For each population and setting combination, intervention estimates were compared across three subgroups: (1) interventions that aimed to prevent anxiety (2) interventions that aimed to prevent depression only and (3) interventions that aimed to prevent both anxiety and depression. The results are reported in Appendix 6 but should be considered descriptive only. For the universal secondary network, there was some evidence that intervention focus was important. Interventions focused on preventing depression appear to have a larger effect on self-reported symptoms of depression than those focusing on anxiety or combined depression and anxiety. However, CrIs overlap, and we did not conduct a statistical test to examine subgroup differences.
Sensitivity analyses: risk of bias
Sensitivity analyses were conducted for the intervention-level NMA, for the main outcome and primary end point of post intervention only. We explored the robustness of the findings to excluding studies judged to be at high/unclear risk of bias for the randomised sequence generation and allocation concealment domains.
Having removed studies judged to be at high/unclear risk of bias for randomisation and allocation concealment, only six studies of six interventions remained in the universal secondary depression network. 125,126,141,196,197,201 However, only five studies formed a connected network. 125,126,141,196,201 Restricting to studies judged to have a low risk of bias, there was no evidence that CBT (SMD 0.02, 95% CrI –0.77 to 0.80) or third-wave (SMD –0.35, 95% CrI –1.15 to 0.45) interventions are effective to prevent symptoms of depression in universal secondary settings (Table 9). For targeted secondary interventions, only four studies of four interventions could be included in the analysis of studies judged to have a low risk of bias, and there was no evidence that CBT was effective. 141,167,219,226 One study was judged to be at low risk of bias in the universal primary network. 145 A sensitivity analysis was not possible for the targeted primary network.
| Population/setting | Reference intervention | Intervention | Number of studies | SMD (95% CrI) | |
|---|---|---|---|---|---|
| Low risk of bias studies | All studies | ||||
| Universal secondary | Usual curriculum | CBT | 5 | 0.02 (–0.77 to 0.80) | –0.04 (–0.16 to 0.07) |
| Usual curriculum | Third wave | –0.35 (–1.15 to 0.45) | –0.03 (–0.21 to 0.14) | ||
| Universal primary | Usual curriculum | CBT | 1 | –0.10 (–0.29 to 0.09)a | –0.13 (–0.44 to 0.17) |
| Targeted secondary | No intervention | CBT | 4 | 0.07 (–1.33 to 1.49) | –0.22 (–0.58 to 0.13) |
Sensitivity analyses: intracluster correlation coefficient and change from baseline scores
When cluster-randomised trials did not explicitly account for clustering in their analyses, we followed the advice in the Cochrane handbook (section 16.3.4)81 for calculating an approximate sample size, using an ICC of 0.03. We explored the robustness of this decision in a best-case/worst-case sensitivity analysis using ICCs of 0.01 and 0.06, respectively. Results were robust to alternative ICC values.
When necessary, we derived mean change from baseline from reported baseline and follow-up means and SDs. To do so, we assumed a correlation coefficient of 0.7, which was based on previous analyses. 82 We conducted sensitivity analyses using correlation values of 0.6 and 0.8. Results were robust to alternative correlation values (see Appendix 6).
Summary of main results
A total of 105 studies met the inclusion criteria for the depression prevention review, of which 88 were judged to be at high or unclear risk of bias for random sequence generation and/or allocation concealment. Eighty-six studies contributed data to the NMA across all settings and time points. Moderate levels of heterogeneity were observed in all analyses, and high levels of heterogeneity were observed in some analyses. There was no suggestion of small-study effects in the depression networks.
At the primary time point of post intervention, there was weak evidence from 34 studies to suggest that CBT (SMD –0.04, 95% CrI –0.16 to 0.07) and CBT + IPT (SMD –0.18, 95% CrI –0.46 to 0.08) may be effective in universal secondary settings. In all other populations and settings, there was no evidence to suggest that any type of intervention was effective for preventing depression at the post-intervention time point. The interpretation of these results and the implications for conclusions are presented in Chapter 9.
At 6–12 months’ follow-up, there was weak evidence to suggest that CBT (SMD –0.02, 95% CrI –0.10 to 0.06), CBT + IPT (SMD –0.10, 95% CrI –0.26 to 0.05) and third-wave interventions (SMD –0.13, 95% CrI –0.27 to 0.01) may reduce depression, compared with usual curriculum, in universal secondary settings. There was also weak evidence that CBT reduced self-reported depression at 6–12 months, relative to usual curriculum, in universal primary settings (SMD –0.15, 95% CrI –0.43 to 0.09), and relative to a waiting list in targeted primary settings (SMD –0.34, 95% CrI –0.72 to 0.05). In targeted primary settings, there was weak evidence, from a single study judged to be at unclear risk of bias, for the beneficial effect of CBT-based interventions (relative to a waiting list) at 13–24 months’ follow-up (SMD –0.50, 95% CrI –0.96 to 0.05).
In all other populations and settings, at all remaining time points, there was an absence of evidence that any type of intervention was effective.
Owing to possible statistical inconsistency, we do not report the results for tertiary education settings. As noted in Chapter 4, we consider this, and the limitations imposed by the inclusion criteria on the validity of the tertiary/university network, in Chapter 10.
Chapter 6 Additional primary outcomes and secondary outcomes from studies focusing on prevention of depression and/or anxiety
In the preceding chapters, we reported the effectiveness results for the main outcomes of self-reported anxiety and depression. In this chapter, we report the additional outcomes from all studies focusing on anxiety, depression or anxiety and depression.
Additional primary outcomes
Self-reported psychological well-being
Of the 137 studies focused on preventing anxiety, depression, or both depression and anxiety, 15 reported an outcome of self-reported psychological well-being, life satisfaction or quality of life. Five studies reported measuring well-being using the Warwick–Edinburgh Mental Wellbeing Scale,124,126,127,132,133 seven studies reported a measure of life satisfaction124,131,159,181,187,203,239 and two studies reported a quality-of-life measure. 129,235 One study reported a measure of social functioning206 and one used the Ryff Scales of Psychological Well-being. 143 Planned NMAs by population and setting were not possible; data are reported by outcome measure and study in Table 10. From their model-based analysis, Calear et al. 16 reported that there were no differences between interventions for school-led CBT and a waiting list (Cohen’s d –0.08, 95% CI –0.29 to 0.13) or between health service-led CBT and a waiting list (Cohen’s d –0.06, 95% CI –0.21 to 0.09). Using the data reported in the paper, we calculated the difference in mean change from baseline at post intervention, which suggested a small drop in well-being at post intervention. For each of the remaining 12 studies, summary intervention effects were compatible with both an increase and a decrease in well-being/life satisfaction.
| Study | Population | Setting | Comparisona | Results, mean difference (95% CI) |
|---|---|---|---|---|
| Warwick–Edinburgh Mental Wellbeing Scale | ||||
| Calear et al.126 2016 | Universal | Secondary | CBT vs. CBT vs. waiting list | Post intervention: –2.07 (–3.56 to –0.58) |
| Post intervention: –1.09 (–2.32 to –0.14) | ||||
| Calear et al.127 2016 | Universal | Secondary | CBT vs. waiting list | Post intervention: 1.85 (–0.35 to 4.05) |
| Johnson et al.132 2016 | Universal | Secondary | Third wave vs. usual curriculum | Post intervention: 0.01 (–0.12 to 0.14) |
| Johnson et al.133 2017 | Universal | Secondary | Third wave vs. third wave vs. usual curriculum | Post intervention: 0.02 (–0.10 to 0.14) |
| Post intervention: –0.06 (–0.18 to 0.06) | ||||
| Burckhardt et al.124 2015 | Universal | Secondary | Mindfulness/relaxation vs. attention control | Post intervention data not reported |
| Life satisfaction scales | ||||
| Hodas131 2016 | Universal | Secondary | CBT vs. waiting list | Post intervention: 1.74 (–1.28 to 4.76) |
| Khalsa et al.239 2012 | Universal | Secondary | Mindfulness/relaxation vs. usual curriculum | Post intervention: 0.03 (–0.29 to 0.35) |
| Rose et al.203 2014 | Universal | Secondary | CBT + IPT vs. CBT + IPT vs. waiting list | Post intervention: 0.13 (–0.12 to 0.38) |
| Post intervention –0.13 (–0.37 to 0.11) | ||||
| Burckhardt et al.124 2015 | Universal | Secondary | Mindfulness/relaxation vs. attention control | Post intervention data not reported |
| Stallard et al.159 2014 | Universal | Primary | CBT vs. CBT vs. usual curriculum | 12-month follow-up: –0.58 (–1.26 to 0.10) |
| 12-month follow-up: 0.03 (–0.66 to 0.72) | ||||
| Tokolahi et al.181 2018 | Targeted | Primary | Occupational therapy vs. waiting list | Post intervention: –0.45 (–3.39 to 2.49) |
| Seligman et al.187 2007 | Targeted | Tertiary | CBT vs. no intervention | Post intervention: 0.10 (–1.06 to 1.26) |
| Quality of life, social functioning and Ryff Scales of Psychological Well-being | ||||
| Quality of life | ||||
| Gucht et al.129 2017 | Universal | Secondary | Third wave vs. usual curriculum | Post intervention: 0.09 (–0.26 to 0.44) |
| Takagaki et al.235 2016 | Targeted | University | Behavioural therapy vs. no intervention | Post intervention: 0.05 (0.02 to 0.08) |
| Social functioning | ||||
| Spence et al.206 2003 | Universal | Secondary | CBT vs. usual curriculum | Post intervention: 0.22 (–0.70 to 1.14) |
| Ryff Scales of Psychological Well-being | ||||
| Tomba et al.143 2010 | Universal | Secondary | CBT vs. CBT | Multiple subscales reported: autonomy, environmental mastery, personal growth, positive relations, purpose in life and self-acceptance |
Self-reported suicidal ideation, behaviour and self-harm
Author-defined suicidal ideation, behaviour or self-harm was referenced in 34 studies narratively or quantitatively. However, of these, the majority (n = 21) excluded participants reporting suicidal thoughts or behaviours and/or removed questions asking about suicide and self-harm from the baseline questionnaires. Some studies reported that the removal of questions was requested by participating schools or education authorities. Eleven studies reported that suicidal thoughts and behaviours were measured at baseline and that participants were referred to further services when necessary. However, nine did not then provide details on whether or not these students continued in the study, nor did they provide follow-up measures. The full details of these studies are reported in Appendix 7.
Seven studies reported participants experiencing suicidal thoughts or self-harm at post intervention. 123,136,142,162,221,235,240 Details are reported in Table 11. Three studies were conducted in a universal secondary setting and formed a connected network via attention control. However, NMA model fit was suggestive of inconsistency, and combined results are not reported. Two studies were conducted in a targeted secondary setting, one in an indicated tertiary setting and one in a universal primary setting. There was no evidence to suggest that educational setting-based interventions to prevent anxiety and/or depression had an impact on suicidal ideation or thoughts of self-harm for CYP.
| Study | Analysis (population, setting) | Comparison | Outcome | Results |
|---|---|---|---|---|
| Perry et al.136 2017 | Universal, secondary | Attention control vs. CBT | Suicidal ideation | OR 0.83 (95% CrI 0.28 to 2.40) |
| aStallard et al.142 2013 | Universal, secondary | Attention control vs. usual curriculum | Self-harm thoughts | OR 0.87 (95% CrI 0.72 to 1.04) |
| Attention control vs. CBT + IPT | OR 0.83 (95% CrI 0.70 to 1.00) | |||
| Britton et al.123 2014 | Universal, secondary | Attention control vs. mindfulness/relaxation | Suicidal ideation or self-harm | Not estimable |
| Poppelaars et al.221 2016 | Indicated, secondary | Waiting list vs. CBT | Suicidal ideation | OR 2.20 (95% CrI 0.29 to 65.56) |
| Cova et al.162 2011 | Indicated, secondary | No intervention vs. CBT | Self-harm | Results not presented because of missing SDs |
| Roberts et al.240 2018 | Universal, primary | Usual curriculum vs. CBT vs. CBT | Suicidal ideation | For suicidal ideation, there was no significant group time interaction [F(2,198) = 2.84, p = 0.061]. There were, however, significant main effects for group [F(2,198) = 3.41, p = 0.035] and time [F(1,198) = 6.14, p = 0.014] |
| Takagaki et al.235 2016 | Indicated, tertiary/university | No intervention vs. behavioural activation | Suicidal ideation | OR 0.39 (95% CrI 0.05 to 2.28) |
Inequalities in health
None of the included studies reported the impact of the intervention on inequalities in health;241 therefore, we conducted post hoc subgroup analyses on the basis of available data. Data had been extracted on participant characteristics, including SES, sex and ethnicity (see Chapter 2). Descriptions of SES, sex and ethnicity, as defined by study authors, are reported in Appendix 7. Owing to insufficient data, subgroup analyses could not be conducted by sex or ethnicity for any population or setting. Subgroup analyses for studies conducted in lower socioeconomic settings (as described by the author) are reported.
Eleven studies reported being conducted in lower SES settings, of which three were conducted in MICs118,122,189 and eight in HICs. 139,140,152,156,157,196,208,210 Interventions evaluated in lower SES settings were CBT relative to usual curriculum, no intervention or a waiting list. Unfortunately, for the primary time point of post intervention, data were available for only seven studies conducted in HICs. 139,140,152,156,157,196,208 The results suggest that, in the case of interventions in secondary school settings, those delivered in lower SES settings may be less effective than those delivered in higher/mixed SES settings in reducing self-reported symptoms of anxiety. However, owing to the number of studies available, it was necessary to conduct fixed-effects analyses for the lower SES subgroup. This was not observed for self-reported depression, although it is of interest that the SMD for CBT compared with usual curriculum in higher/mixed SES settings was –0.07 (95% CrI –0.20 to 0.06); in lower SES settings, the SMD was 0.04 (95% CrI –0.06 to 0.15).
Table 12 reports the subgroup analysis findings. There was no evidence of a difference by SES for either self-reported depression or anxiety in primary educational settings. However, for self-reported anxiety, the SMD of CBT compared with usual curriculum in higher/mixed SES settings was 0.15 (95% CrI –0.37 to 0.02); in lower SES settings, the SMD was 0.05 (95% CrI –0.08 to 0.18).
| Population/setting | Outcome | Comparison | SES, SMD (95% CrI) | |
|---|---|---|---|---|
| Low | High/mixed | |||
| Universal secondary | Depression | CBT vs. usual curriculum | 0.04 (–0.06 to 0.15)a | –0.07 (–0.20 to 0.06) |
| Anxiety | CBT vs. usual curriculum | 0.09 (–0.11 to 0.29)a | –0.29 (–0.50 to –0.07) | |
| Universal primary | Depression | CBT vs. usual curriculum | –0.23 (–0.60 to 1.13) | –0.05 (–0.55 to 0.45) |
| Anxiety | CBT vs. usual curriculum | 0.05 (–0.08 to 0.18)a | –0.15 (–0.37 to 0.02) | |
Combined depression and anxiety scores and other ‘internalising’ outcomes
As described in Chapter 1, Changes to protocol, clarifications and additional analyses, and Table 1, a post hoc decision was made to assess composite ‘internalising’ outcomes, for example outcome scales that reported combined anxiety and depression scores (such as total Depression, Anxiety and Stress Scale or RCADS scores) or ‘internalising’ subscales of broader psychological functioning measures such as the SDQ. Six studies reported an internalising outcome, with useable data at post intervention, and are reported in Table 13 by population and setting. 119,123,163,171,216,219 Four studies in targeted secondary settings provided sufficient data for inclusion in a random-effects NMA. 163,171,216,219 Model fit statistics suggested that a consistency model was reasonable; however, the posterior median between-study SD was indicative of substantial heterogeneity (τ 0.97, 95% CrI 0.03 to 9.03) and tended to the prior distribution [uniform(0,10)]. Consequently, we report only study-specific SMDs in Table 13.
| Study | Population | Setting | Time | Comparison | Results, SMD (95% CrI) |
|---|---|---|---|---|---|
| Britton et al.123 2014 | Universal | Secondary | Post intervention | Attention control vs. mindfulness/relaxation | 0.12 (–0.32 to 0.54) |
| Aune and Stiles119 2009 | Universal | Secondary | Post intervention | No intervention vs. CBT | –0.02 (–0.10 to 0.06) |
| Fung et al.216 2016 | Targeted | Secondary | Post intervention | Waiting list vs. mindfulness/relaxation | –0.19 (–0.83 to 0.44) |
| McCarty et al.219 2013 | Targeted | Secondary | Post intervention | Psychosupport vs. CBT | –0.33 (–0.62 to –0.05) |
| Rice171 2009 | Targeted | Secondary | Post intervention | Attention control vs. CBT | 0.08 (–0.89 to 1.04) |
| Rice171 2009 | Targeted | Secondary | Post intervention | Attention control vs. mindfulness/relaxation | 0.41 (–0.31 to 1.13) |
| Dobson et al.163 2010 | Targeted | Secondary | Post intervention | Attention control vs. CBT | 0.19 (–0.26 to 0.64) |
A fixed-effects NMA was possible for a further two studies142,206 reporting a 12-month follow-up in a universal secondary setting, as they formed a connected network via usual curriculum.. However, there was no evidence that interventions based on CBT (SMD 0.03, 95% CrI –0.14 to 0.20) or CBT + IPT (SMD 0.01, 95% CrI –0.16 to 0.17) were more effective than usual curriculum for improving composite internalising outcomes at a 12-month follow-up.
Secondary outcomes
Acceptability and attendance
Intervention acceptability was defined by study authors. We anticipated considerable variability in the reporting of acceptability outcomes, but have combined them here under loose categories relating to (1) attitudes towards and satisfaction with intervention, (2) enjoyment and utility, and (3) attendance. Thirty-three studies reported a summary of acceptability of the intervention to study participants in terms of satisfaction or enjoyment and are summarised in Tables 14 and 15 by population and setting. Attendance data, as reported by authors, are reported in Appendix 7, Table 72.
| Study | Satisfaction |
|---|---|
| Baker and Butler120 1984 | This was measured using the Attitudes Toward Treatment Scale, a 14-item Likert-type scale, with possible scores ranging from 14 to 98. Higher scores indicate a higher degree of satisfaction. Treatment group: mean score 75.47 (SD 12.93); control group: mean score 63.69 (SD 10.02) |
| Potek137 2012 | On a 10-point Likert scale, the intervention group gave an average rating of 8.05 (SD 0.99, minimum 5.93, maximum 9.57). Higher scores indicate a higher degree of satisfaction |
| Fung et al.216 2016 | On a scale of 1–10, the author reports ‘moderate levels of satisfaction’ among participants (mean score 7.21, SD 0.67) |
| Kiselica et al.168 1994 | . . . female participants had a more favourable attitude toward training experience than did male participants, regardless of the treatment condition they were assigned to |
| McCarty et al.218 2011 | Participants were asked how satisfied they were with group membership: ‘very much’, 48%; ‘pretty much’, 36%; and ‘all right’, 13%. One student disliked the group ‘a little’ and felt ‘embarrassed’ (3%) |
| McCarty et al.219 2013 | Satisfaction: 83% liked their intervention group ‘very much’ or ‘pretty much’. Comfort: 84% of students were comfortable in their intervention group |
| Stice et al.224 2008 | In the two group-based interventions, 76% and 71% of respondents were ‘pleased’ or ‘very pleased’ with their assigned group. In the bibliotherapy group, 29% reported being ‘pleased’ or ‘very pleased’ |
| Higgins185 2007 | On a scale of 1–5, the mean satisfaction score was 4.0 (SD 0.47). The author describes this as showing that most participants were ‘somewhat satisfied’ with the workshop |
| Study | Enjoyment and usefulness of intervention |
|---|---|
| Stallard et al.142 2013 | Usual PSHE was preferred over both classroom-based CBT and attention control PSHE: liking (F 7.11, df 2970; p < 0.01), usefulness (F 6.46, df 2966; p < 0.01), relevance (F 8.84, df 2963; p < 0.01) |
| Merry et al.197 2004 | Enjoyment and usefulness were assessed using five-point Likert scales. Enjoyment: both the RAP-Kiwi intervention (mean score 3.0, SD 1.1) and attention control (mean score 3.7, SD 1.0) were rated ‘reasonably enjoyable’. Usefulness: RAP-Kiwi mean score 2.9 (SD 1.1); attention control mean score 3.1 (SD 1.1). Higher values indicate greater enjoyment and usefulness |
| Johnson et al.133 2017 | On a 10-point Likert scale, enjoyment and interest were rated as follows: mean score 6.92 (median 7.0, range 0–10). Higher values indicate greater enjoyment |
| Tak et al.207 2016 | Rated on a four-point Likert-scale. Authors report that participants did not like the intervention (mean score 1.58, SD 0.69) and did not find it useful (mean score 1.96, SD 0.85). Higher values indicate greater enjoyment and usefulness |
| Roberts et al.139 2010 | SLS: the ‘Learning to negotiate’ lessons were rated most enjoyable by students and ‘Networks’ the least enjoyable. Role plays were the most popular activities. A total of 68.7% to 79.0% rated the utility of SLS as average or higher |
| OTS: the most enjoyable activities were games and quizzes. A total of 67.3% rated the utility of OTS as average or higher | |
| Lowry-Webster et al.135 2001 | Participants were asked ‘How much did you enjoy the FRIENDS program?’; 31.1% enjoyed it ‘a lot’, 53.7% enjoyed it ‘some’, 14.2% ‘a little’ and 1% ‘not at all’ |
| Johnson et al.132 2016 | On a 10-point Likert scale, student enjoyment and interest was rated as follows: mean score 6.67 (median 7.0, range 0–10). Higher values indicate greater enjoyment and interest |
| Spence et al.206 2003 | A total of 42% would recommend the course to other students, 31% would maybe recommend it and 27% would not recommend the course. A total of 34% expected to use the skills learnt, 49% thought that they would maybe use the skills, and 17% did not think that they would use the skills in their everyday life |
| Rivet-Duval et al.202 2011 | Intervention participants rated the usefulness and acceptability of the programme as high (mean score 4.57, SD 0.78). (No detail provided on scale) |
| Britton et al.123 2014 | A total of 82% of students felt more focused, more able to concentrate or less distracted, and 88% reported feeling more relaxed and calmer |
| Calear et al.127 2016 | Over 60% of participants found the website to be useful or very useful . . . over 50% . . . reported they would use the website again and a further 10% had already recommended the website to a friend |
| Poppelaars et al.221 2016 | On a five-point scale, the mean response for liking OVK was 3.13 (SD 1.09); for SPARX, it was 3.16 (SD 1.35). The mean response for programme usefulness in daily life was 3.07 (SD 1.19) for OVK and 2.72 (SD 1.26) for SPARX |
| Cova et al.162 2011 | A total of 71.6% strongly agreed or agreed that participation was enjoyable, and 8.7% strongly disagreed or disagreed. A total of 79.0% strongly agreed or agreed that the intervention was useful, and 13.5% strongly disagreed or disagreed |
| Livheim et al.217 2015 | A total of 91% of participants ‘gave exclusively positive feedback’ about the intervention. Half stated that it was ‘very valuable’ and the remainder that it was ‘quite valuable’. All would recommend the course to a friend |
| Woods and Jose227 2011 | Participants reported the following positive aspects of the intervention: confectionery rewards, missing lessons and playing games. Negative aspects: amount of reading and writing required and ‘out-of-date’ scenarios |
| Ahlen et al.145 2018 | A total of 80% of participants in the high level of supervision group, compared with 68% in the low level of supervision group, enjoyed Friends for Life ‘much or some’ |
| Mendelson et al.210 2010 | The authors conducted focus groups:. . . students generally had a positive experience in the program and felt they learned skills that helped them in their day-to-day lives |
| Pophillat et al.156 2016 | The proportion of children who enjoyed the intervention was 92% |
| Soffer212 2003 | A total of 100% of participants in the behavioural intervention and 79% in the attention control group responded that they ‘would like to be in a program like this again’ |
| Attwood et al.146 2012 |
Most reported applying the skills learnt in their daily life. However, the authors note that content was challenging for some younger participants |
| Stallard et al.159 2014 | A total of 934 participants in the active arm responded that the intervention was fun, 742 thought that it had helped them and 787 would recommend the intervention to a friend |
| Essau et al.150 2012 | The authors state that children were asked whether or not they enjoyed the programme and if they used the skills taught. However, no results are reported |
| Ruttledge et al.158 2016 | A total of 68% of respondents found FRIENDS for Life ‘very useful’ or ‘somewhat useful’ |
| Schoneveld et al.116 2018 | On a five-point scale, participants were asked to rate (1) ‘I found it fun to participate in the intervention’ [CBT: mean score 2.35 (SD 1.39); biofeedback: mean score 2.77 (SD 1.18)] and (2) ‘I can use what I learned in my daily life well’ [CBT: mean score 2.96 (SD 0.95); biofeedback: mean score 2.13 (SD 1.38)] |
| Schoneveld et al.115 2016 | On a five-point scale, participants were asked to rate (1) ‘I liked to play the game’ [control: mean score 2.74 (SD 1.24); biofeedback: mean score 1.90 (SD 1.38); p ≤ 0.001) and (2) ‘I can use what I learned in my daily life well’ [control: mean score 1.72 (SD 1.28); biofeedback: mean score 1.68 (SD 1.29)] |
Attitudes and satisfaction with intervention
Eight studies reported satisfaction with the intervention (see Table 14). Two studies120,137 reported an overall satisfaction outcome in a universal secondary setting. Both used Likert-type scales and suggested that students were highly satisfied with the interventions. In targeted secondary settings, five studies reported a satisfaction or attitude to ‘treatment’ measure. 168,216,218,219,224 However, results were reported for the experimental/active intervention arms only, and not for controls. All reported that participants were satisfied with their intervention assignment. One study185 in a targeted tertiary setting reported satisfaction with intervention assignment, with a mean score of 4.0 (SD 0.47) on a five-point scale, suggesting that the majority of participants were satisfied with the intervention.
Intervention enjoyment and utility
Twenty-five studies reported enjoyment or utility of intervention. In universal secondary settings, 11 studies reported an acceptability outcome assessing enjoyment or usefulness of the intervention. 123,127,132,133,135,139,142,197,202,206,207 However, only two studies reported comparative data for all arms of the study. Stallard et al. 142 note that the control group intervention: ‘Usual PSHE [personal, social and health education] was rated more positively than both classroom-based CBT and attention control PSHE for liking [F 7.11, df (degrees of freedom) 2970; p < 0.01], usefulness (F 6.46, df 2966; p < 0.01) and relevance for their age (F 8.84, df 2963; p < 0.01).’ Merry et al. 197 compared intervention arms on a five-point Likert scale, where five was the most positive score and one the most negative. The programmes were rated by the students as reasonably enjoyable. The control group intervention received slightly higher ratings than the experimental intervention for both enjoyment and utility (see Table 15). The majority of studies reported that participants enjoyed the intervention and found it useful. Only one study reported negative enjoyment and utility feedback from students207 (see Table 15).
In universal primary settings, eight studies reported some detail for enjoyment or usefulness of the intervention. 145,146,150,156,158,159,210,212 Two studies evaluating the FRIENDS anxiety programme reported an acceptability outcome assessing enjoyment or usefulness. 158,159 In Ruttledge et al. ,158 68% of the children found the FRIENDS for Life programme ‘very useful’ or ‘somewhat useful’. Stallard et al. 159 reported that 74% of participants enjoyed the intervention, 59% thought that it had been helpful and 62% would recommend it to a friend. Across all studies, results suggest that participants generally found the interventions enjoyable and useful (see Table 15).
Four studies reported enjoyment/utility in targeted secondary settings. 162,217,221,227 Poppelaars et al. 221 provided comparative data for two CBT-based interventions and concluded that acceptability was similar across the programmes. Woods and Jose227 conducted semistructured focus groups at the end of a CBT intervention, Adolescents Coping with Emotions. The focus groups were conducted in New Zealand, with the majority of participants being Maori and Pacific Islander students and identifying trust in the group as an important benefit of the intervention. In addition, some participants noted that the insight gained about thinking processes was useful. Participants liked the use of confectionery as a reward, and identified the games played and missing class as good aspects of the programme. However, they also felt that the intervention used out-of-date scenarios and that there was too much reading and writing involved in the sessions. Livheim et al. 217 reported that most participants (91%) gave exclusively positive feedback on the evaluation of the acceptance and commitment therapy-based intervention and all reported that they would recommend it to a friend. The majority of students included in Cova et al. ’s162 study enjoyed (71.6%) and found the CBT intervention useful (79%).
Two studies provided information on enjoyment in a targeted primary setting. 115,116 Schoneveld et al. 116 noted that children enjoyed both the experimental and control interventions equally (CBT vs. biofeedback). However, in an earlier trial, in which the control intervention was a commercially available computer game, children clearly preferred the control intervention. 115
Attendance and dropouts from intervention
Only one study explicitly mentioned attendance as a proxy for acceptability of the intervention to participants. Congleton215 noted that attendance was excellent and that this reflected how much the students enjoyed the course and the importance of convenient timetabling.
Across all other studies, attendance was reported descriptively. Study-specific attendance details, as reported by trial author, are reported in Appendix 7.
Parent-reported child anxiety, depression or internalising outcomes
A post hoc decision was made to analyse parent-reported child anxiety, depression or internalising symptoms. For some of the studies, participants were considered too young for self-reported measures and parents were the primary respondents. In universal primary settings, five studies145,146,156,158,242 provided baseline and follow-up data on parent-reported child anxiety outcomes. From a random-effects NMA, there was no evidence that CBT-based interventions reduced parent-reported child anxiety symptoms relative to usual curriculum (SMD –0.10, 95% CrI –2.13 to 1.83).
Six studies115,116,176,177,181,182 provided both baseline and follow-up data to enable a NMA for targeted primary settings. There was no evidence that CBT-based interventions (SMD –0.43, 95% CrI –1.08 to 0.14), biofeedback (SMD –0.48, 95% CrI –1.76 to 0.72) or occupational therapy (SMD 0.05, 95% CrI –1.07 to 1.19) reduced parent-reported child anxiety symptoms relative to a waiting list.
Academic attainment
Seven studies reported academic attainment data. 131,136,137,145,159,168,174 Various measures of attainment were used; we report study-specific results in Table 16. Across all studies, there was no evidence of an effect of intervention on academic outcomes.
| Study | Measure | Results, mean difference (95% CI) |
|---|---|---|
| Ahlen et al.145 2018 | Teacher-rated five-point scale | 0.01 (–0.10 to 0.12) |
| Cooley-Strickland et al.174 2011 | WIAT-reading (age equivalent) | 0.30 (–0.24 to 0.83) |
| Cooley-Strickland et al.174 2011 | WIAT-mathematics (age equivalent) | 0.30 (–0.20 to 0.80) |
| Hodas131 2016 | Mathematics computation (age equivalent) | Results reflect an older age of students in a waiting list group |
| Hodas131 2016 | Reading comprehension | Results reflect an older age of students in a waiting list group |
| Kiselica et al.168 1994 | Quarterly GPA | Univariate F tests revealed [no] significant differences between the treatment and control participants for GPA |
| Perry et al.136 2017 | Final exam results (standardised) | Notably, academic outcomes did not differ between the 2 groups p = 0.41 |
| Potek137 2012 | SAT language assessment | –0.10 (–1.60 to 1.40) |
| aStallard et al.159 2014 | SAT reading | 0.10b (–0.56 to 0.76) |
| aStallard et al.159 2014 | SAT mathematics | 1.83b (1.13 to 2.53) |
| aStallard et al.159 2014 | SAT writing | 0.68b (0.02 to 1.34) |
| aStallard et al.159 2014 | SAT reading | 0.93b (0.30 to 1.57) |
| aStallard et al.159 2014 | SAT mathematics | 1.15b (0.45 to 1.85) |
| aStallard et al.159 2014 | SAT writing | 1.48b (0.84 to 2.12) |
Problem behaviours
Few studies reported problem behaviours, and those that did reported substance use. The following results are reported as per the original publications. In a universal secondary setting, Stallard et al. 142 reported that there was evidence of a beneficial effect of CBT + IPT on cannabis use at 6 months (OR 0.56, 95% CI 0.38 to 0.82) and at 12 months (OR 0.70, 95% CI 0.48 to 0.93), but not on alcohol or ‘street drug’ use. In targeted secondary settings, Stice et al. 224 reported that CBT reduced ‘substance use’ (F[6,674] 3.60; p = 0.002) relative to control and Topper et al. 173 reported that there was ‘no significant difference’ between the intervention and control groups for binge drinking (Cohen’s d 0.22). In a tertiary/university setting, Reynolds et al. 233 reported results from the Alcohol Use Disorders Identification Test (AUDIT) and concluded that there was ‘no significant difference’ observed between the intervention and control groups for alcohol consumption or alcohol problems, although they also report that:
. . . a significant interaction of the orientation group effect with the linear effect of time was found, suggesting differential change for the [intervention] and [control] groups across the three time points. The overall percentage of youth above the clinical cut off for the BATD [behavioural activation treatment for depression] group generally decreased over time.
Mental health-related stigma
During our initial PPI work, reducing the stigma associated with mental health problems was identified as an important outcome for young people. Only one study reported a mental health-related stigma outcome. In Perry et al. ,136 stigma was measured using a nine-item subscale of the Depression Stigma Scale, an 18-item scale that assesses personal and perceived stigma towards depression, on which higher scores indicate greater stigma. At the immediate post-intervention time point, there was no evidence of a reduction in personal or perceived stigma in the SPARX (smart, positive, active, realistic, X-factor thoughts) computerised CBT group, compared with the attention control intervention (mean difference –0.50, 95% CI –2.90 to 1.90).
Chapter 7 Effectiveness of educational setting-based interventions for preventing conduct disorder
Systematic review results
Studies included in the review
The overall PRISMA flow diagram for the project is reported in Figure 2. Twenty-seven papers relating to five studies met our eligibility criteria for inclusion in the conduct disorder review. Included studies were published between 1999 and 2018, and randomised between 225 and 891 participants (median 245 participants). All studies were cluster randomised, of which four reported results from appropriate models incorporating the multilevel nature of the data.
One study was classified as universal243 and four were classified as targeted244–247 (all indicated). All studies were conducted in primary school settings, with age at baseline ranging from 4.2 to 7.91 years. The majority of study participants were boys. In the four indicated studies, the proportion of boys ranged from 69% to 74% of participants. Four studies were conducted in HICs,243,244,246,247 and one was conducted in a MIC. 245 Of the studies conducted in HICs, all were conducted in lower-income settings, as specified by the trial authors.
Owing to intervention complexity and the flexible nature of the intervention implementation, we were not able to calculate an average ‘dose’, as was done for anxiety and depression outcomes.
Risk-of-bias assessments are reported in Figure 15 by individual study. Three studies were judged as having unclear risk of bias for random sequence generation and allocation concealment. 243,244,247 All studies were judged to be at high risk of bias for participant and outcome assessor blinding. Prospective trial registrations were available for one study. 245 For cluster randomised trials we also considered how recruitment, randomisation and analysis were conducted under the Cochrane Risk of Bias tool heading of ‘other bias’. Four studies were judged to be at high or unclear risk for ‘other bias’.
FIGURE 15.
Conduct disorder risk-of-bias assessments by domain and study. +, Low risk of bias; –, high risk of bias; ?, unclear risk of bias.
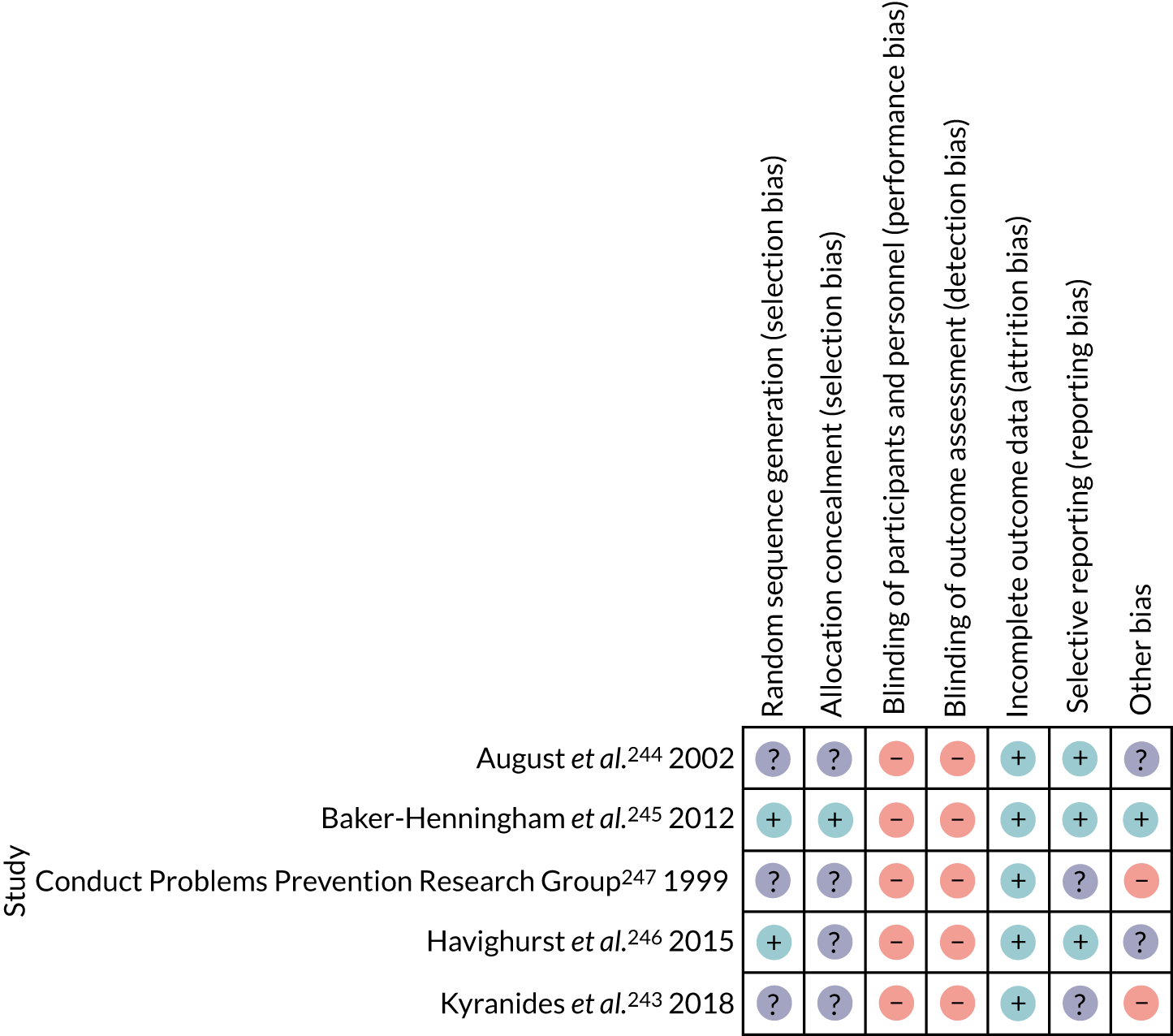
Owing to the diversity of interventions, outcome measures and time points reported by the studies, results are reported narratively by trial, and by date of publication. Owing to this diversity, intervention components are also described narratively, by study, where these could be identified from trial reports. Unless otherwise stated, statistical summaries are reported as described in the original publications.
Fast Track: the Conduct Problems Prevention Research Group247
The Fast Track trial247 was a cluster randomised trial of 54 primary schools in the USA. Beginning in 1991, the trial followed participants for > 20 years. The indicated prevention intervention was delivered over 10 years, targeting children in primary school settings with early-starting disruptive behaviour. The aim of the intervention was to prevent long-term severe and chronic conduct problems, including psychological disorder. The study compared a multicomponent intervention (n = 445) with a no-intervention control (n = 446). Children who were within the top 10% of a combined parent–teacher screen for externalising behaviour problems were invited to take part. The mean age of child participants was 6.5 years (SD 0.48 years); 69% were boys, 51% were African American and 47% were European American. The schools were in areas of high crime and poverty.
Seven intervention components were implemented, the content of which changed each year to be developmentally appropriate for the children and based on the families’ needs. There was insufficient detail provided in the reports to describe the exact nature of these changes. The intervention described subsequently is from the primary school phase of the project (i.e. grades 1–3, ages 6–9 years).
The school-based component was delivered to whole classrooms, and not just to the students enrolled in the Fast Track trial. The PATHS® (Promoting Alternative THinking Strategies) intervention was delivered by classroom teachers across two or three lessons per week across the whole school year. PATHS is a social and emotional learning intervention that focuses on children managing and understanding their behaviour and emotions and includes social and problem-solving skills training. Fidelity was checked by Fast Track educational co-ordinators via weekly classroom and teacher visits. Educational co-ordinators were usually ex-teachers.
There were five parent and/or child components: parent groups, child social skills training groups, parent–child sharing time, child–peer pairing and academic tutoring. Parent groups, child social skills training groups and parent–child sharing time ran during a weekly 2-hour enrichment programme held at school but outside school hours. A total of 22 sessions was offered. Average attendance was 78% for the child group and 71% for the parent group. The child groups focused on reviewing and practising skills in emotional understanding and communication, friendship-building, self-control and social problem-solving. The parent groups focused on parenting skills, self-control and building positive family–school relationships.
Individual support was provided to children and parents by family co-ordinators; this formed the home visiting component. Visits focused on problem-solving and encouraging parental empowerment and self-efficacy. Family co-ordinators typically had advanced degrees in counselling or social work. Home visits were typically every other week across the first year of the intervention. Children were also provided with academic tutoring three times each week for 30-minute sessions during school hours, delivered by ‘paraprofessional tutors’.
Seventy-two per cent of participants received > 50% of each of the following intervention components: parent group, child social skills group, peer pairing and tutoring. Overall, 81% of participants received at least 50% of the recommended number of home visits (i.e. at least six visits). All programme staff attended a 3-day cross-site workshop. Fidelity was monitored using intervention manuals, weekly supervisory telephone calls and weekly staff meetings.
Multiple assessment scales were administered; primary outcomes were not specified. Appropriate multilevel models were conducted for the end of year 1 analyses, but not for later time points. At the end of grade 1 (i.e. 1 year into the intervention), the following effect sizes (Cohen’s d) were reported by the Conduct Problems Prevention Research Group,247 as computed from the F-value and degrees of freedom. Parent ratings of child behaviour change (Cohen’s d 0.50, 95% CI 0.25 to 0.76) and teacher ratings of child behaviour change (Cohen’s d 0.53, 95% CI 0.28 to 0.79) suggested a beneficial effect of the intervention, compared with the control. However for externalising behaviours, parent ratings on the Child Behaviour Checklist (CBCL) (Cohen’s d 0.04, 95% CI –0.15 to 0.26) and teacher ratings on the Teacher Report Form (Cohen’s d 0.02, 95% CI –0.19 to 0.24) suggested no evidence of a difference between intervention and control groups at the end of grade 1. At the end of grade 3, parent ratings of child behaviour change (β 0.18, 95% CI 0.04 to 0.32) and teacher ratings of child behaviour change (β 0.24, 95% CI 0.12 to 0.35) also suggested a beneficial effect for the intervention, compared with the control. However, the parent-rated CBCL was not reported and the teacher-rated Teacher Report Form (β –0.05, 95% CI –1.42 to 1.32) externalising problems scales suggested no evidence of a difference between the intervention and control groups at the end of grade 3.
Three further measures were reported at the end of grade 3. Academic progress in reading (β 0.06, 95% CI –0.06 to 0.17) and mathematics (β 0.08, 95% CI –1.42 to 1.32), and clinical diagnosis of oppositional defiant disorder (ODD) or conduct disorder (β 0.02, 95% CI –0.04 to 0.08). There was no evidence to suggest an intervention effect on these outcomes. Note that the 95% CIs for these effect sizes and regression coefficients are an approximation248 based on data reported by the Conduct Problems Prevention Research Group across two papers. 247,249
In grades 7 and 8, there was no evidence of a difference between intervention and control groups for the parent-rated CBCL (β 1.50, 95% CI –0.15 to 3.15) or the teacher-rated Teacher Report Form (β –0.33, 95% CI –2.45 to 1.79) externalising problems scales. Hyperactivity was also reported and was reduced in the intervention group, compared with the control group.
An independent analysis of the data suggests that there was also little evidence of an effect on mental health outcomes during ‘the high school years’ (i.e. between 9 and 13 years of follow-up). 250 However, the Fast Track trial team conducted a further follow-up, 20 years from baseline (when participants were aged 25 years). On the basis of self-reported outcomes, there was strong evidence for a beneficial effect of the intervention for a composite outcome of any externalising, internalising or substance use problem (OR 0.59, 95% CI 0.43 to 0.81). The authors of the paper state that this is equivalent to a number needed to treat of 8. For diagnosis of antisocial personality disorder, there was a benefit of the intervention, relative to the control (OR 0.60, 95% CI 0.39 to 0.93), but not for attention deficit hyperactivity disorder (OR 0.65, 95% CI 0.39 to 1.08). There was no evidence to suggest that the intervention prevented diagnoses of anxiety (OR 0.79, 95% CI 0.47 to 1.33) or depression (OR 0.68, 95% CI 0.42 to 1.08). Analyses were based on the intention-to-treat principle and appropriately accounted for clustering.
Substance use outcomes included alcohol abuse (OR 0.69, 95% CI 0.48 to 0.99), binge drinking (OR 0.75, 95% CI 0.55 to 1.01), heavy marijuana use (OR 0.76, 95% CI 0.45 to 1.30) and serious substance use (OR 0.58, 95% CI 0.36 to 0.92). There was no evidence of a difference between intervention and control groups for having graduated from high school (OR 0.93, 95% CI 0.68 to 1.27) or currently being in full-time education or employment (OR 0.84, 95% CI 0.60 to 1.18).
Early Risers Skills for Success: August et al.244
The Early Risers ‘Skills for Success’ study244 was a cluster randomised trial for the prevention of serious behaviour problems, as indicated by aggressive–disruptive behaviour. Ten schools were randomised to a multicomponent intervention and 10 were randomised to no intervention. Participants were screened prior to trial entry, to ensure that they were at high risk of a serious conduct problem, as assessed by a T-score of ≥ 58 on the CBCL aggression subscale (which was teacher rated). A total of 245 children were included in the trial: 124 in intervention schools and 121 in control schools. The mean age of participants at baseline was 6.6 years (SD 0.6 years) and 69% were male. Schools were in semirural midwestern USA, in low to low–middle socioeconomic areas. There have been multiple follow-ups of the participants, the latest being 10 years from the start of intervention (i.e. 5 years post intervention).
The intervention was multicomponent and multiphase. Beginning in the summer preceding grade 1 (i.e. year 1 of the intervention) and continuing over the next 2 years (i.e. 3 years in total), students attended a 6-week summer school, equivalent to 432 hours of programme content. Participants received academic content, enrichment activities and small-group social skills training. Peer mentoring was also used. It is not clear who delivered the summer school component of the intervention. In years 4 and 5, ‘booster’ summer camps were offered, each of 6 days’ duration.
The second intervention component was a monitoring and mentoring programme overseen by ‘family advocates’, who provided weekly support to the participants and teachers in their regular school setting. Support provided was flexible, depending on student needs. The third component was a biweekly family programme, based on the Incredible Years intervention, delivered concurrently, but separately, to parents and children. The Incredible Years programme is described elsewhere as being based on CBT principles, but was not described as such here. 251 Twenty-nine sessions, over 3 years, were offered, and were equivalent to 58 hours in total. However, attendance was low [mean 39% (SD 29%)]. In years 4 and 5, six family sessions were offered. In addition to the previously mentioned core intervention components, a personalised home visitation component was available on the basis of individual need.
Approximately 60% participated across all three intervention components in the first 3 years, and 67% participated in three or more components offered during the booster phase. The intervention was manualised, and training was provided to all staff. Intervention fidelity was measured via log books and checked during unannounced visits by ‘fidelity technicians’.
At the end of the main intervention (year 3), externalising outcomes were reported as a composite across a maximum of four measurement scales for outcomes of (1) aggression, (2) hyperactivity and (3) impulsivity. The scales were the Teacher Observation of Classroom Adaptation, the Parent Observation of Classroom Adaptation, the Behavior Assessment System for Children (BASC) – Teacher Rating Scale (BASC-TRS) and the BASC – Parent Rating Scale (BASC-PRS). Teacher-reported academic achievement was also a composite outcome combined across four separate scales (the broad reading and applied problems composite scores from the Woodcock–Johnson Tests of Achievement-Revised, the Learning Problems scale of the BASC-TRS, and the Cognitive Competence scale of the Teacher’s Scale of Child’s Actual Competence and Social Acceptance). An intention-to-treat, three-level model was appropriately conducted, given the clustered nature of the data; however, the school level was retained for the aggression analysis only.
At the end of year 3, intervention participants (n = 199) showed a greater improvement in academic achievement than control participants. However, there was no evidence of an effect for aggression, hyperactivity or impulsivity, and quantitative results were not reported. At the end of year 6 (n = 151), outcomes included self-reported conduct disorder symptoms and diagnosis, ODD symptoms and diagnosis, and self-reported drug use. Based on the means and SDs reported by the authors, we calculated that there was no evidence that the intervention prevented self-reported conduct disorder symptoms (mean difference –0.20, 95% CI –0.91 to 0.51). However, there was evidence to suggest that, for ODD symptoms, the intervention was beneficial (mean difference –1.53, 95% CI –2.58 to –0.48). The authors reported that the ODD effect size was 0.47 (p ≤ 0.01). The effect size for conduct disorder symptoms was not reported. There was no evidence that conduct disorder or ODD diagnoses differed across the intervention and control groups. There was no evidence of an effect for tobacco or alcohol use.
At 10 years from baseline (n = 129), self-reported conduct disorder and ODD were reported. The authors report that the Early Risers intervention was associated with fewer conduct disorder and ODD symptoms in late high school. The estimated mean number of conduct disorder symptoms per participant was 1.81 lower (95% CI 0.34 to 3.30) in the programme group than in the control group and the mean number of ODD symptoms was 1.56 lower (95% CI 0.47 to 2.63).
Incredible Years teacher programme: Baker-Henningham et al.245
Baker-Henningham et al. 245 reported a cluster randomised trial for the indicated prevention of disruptive and aggressive/destructive behaviours. Twenty-four preschools were included and were randomised to either the Incredible Years intervention group (n = 12) or a control group (n = 12). It was not clear from the paper what intervention the control group received, although the trial registration (ISRCTN 35476268) suggests that it was information only. Children were selected for inclusion by a teacher-rated scale based on the ICD-10 criteria for conduct disorder. Three children with the highest scores in each class were enrolled in the study. A total of 225 children aged 3–6 years were included (113 in the intervention group and 112 in the control group). The mean age of participants was 4.2 years (SD 0.9 years), and 69% of participants were boys. Schools were in Kingston, Jamaica, and in ‘disadvantaged’ inner-city areas with high levels of community violence.
The intervention evaluated was the Incredible Years Teacher Training programme, tailored to a Jamaican context. Few details on the intervention were provided in the paper, but it included collaborative and experiential learning; individual goal-setting and self-monitoring; building teachers’ self-efficacy; a focus on teachers’ cognitions, behaviour and emotions; and emphasis on teachers’ ability to generalise the skills learnt. The Incredible Years programme has been described elsewhere as being based on CBT principles, but we note that it was not described as such here. 251 The intervention lasted for 6 months. To ensure fidelity, intervention teachers attended eight full-day training workshops over the period of the intervention and received in-class support from a psychology graduate with previous experience in Incredible Years. The authors reported that teachers attended a median of eight workshops (range 2–8 workshops), with 95% attending at least six workshops; 89% of teachers received all four in-class consultations.
The primary outcome was directly observed in-class child behaviour and reported as frequency of aggressive/destructive behaviours (as defined by a study manual). Secondary outcomes of interest were teacher and parent reports of child behaviour. Teacher-reported child conduct problems were measured using the Sutter–Eyberg Student Behavior Inventory™ (SESBI), and the SDQ was used to measure behaviour difficulties and prosocial skills. Parent-reported child conduct problems were measured using the Eyberg Child Behavior Inventory™ (ECBI), and the SDQ was used to measure behaviour difficulties and prosocial skills. Hyperactivity and attention difficulties were also measured using Conners Global Index. These scales formed a composite outcome of ‘behavioural difficulties’. Child school attendance was taken from school records.
Statistical analyses appropriately accounted for the clustered nature of the data. For the author-reported primary outcome, the intervention reduced the number of directly observed conduct problems (effect size 0.42, 95% CI 0.12 to 0.71). For author-reported secondary outcomes, the intervention reduced the number of teacher-reported behavioural difficulties (effect size 0.47, 95% CI 0.18 to 0.76) and parent-reported behavioural difficulties (effect size 0.22, 95% CI 0.03 to 0.42), relative to the control group. School attendance was also higher in the intervention group than in the control group (effect size 0.30, 95% CI 0.05 to 0.55). Children in the intervention group were less likely to be rated in the clinical range for conduct disorder by teachers (OR 0.31, 95% CI 0.11 to 0.92) than by parents (OR 0.56, 95% CI 0.27 to 1.16).
Multisystemic early intervention: Havighurst et al.246
Havighurst et al. 246 reported a cluster RCT of a multisystemic indicated intervention for primary school-aged children at risk of presenting with conduct disorder. Thirty-three schools in lower socioeconomic areas of Victoria, Australia, were included and were randomised to either the intervention (n = 14) or to a waiting list group (n = 19). Children between the ages of 5 and 9 years were eligible, and those scoring in the top 8% on a joint parent–teacher screen for behaviour problems (using the Conduct Problems Risk Screen) were invited to participate in the study. A total of 113 child participants were randomised to the intervention, and 118 were randomised to the waiting list control group. The mean age was 7.05 years (SD 1.06 years) and 74% of participants were boys.
The intervention contained separate parent, child and school components. The parent component was delivered across eight 2-hour sessions and focused on emotion socialisation coaching, whereby parents learn to respond positively to their children’s emotions. Average parent attendance was six sessions, with 78% of parents attending five or more. The intervention was delivered by clinical or educational psychologists, social workers, speech and language therapists, or occupational therapists. To ensure fidelity, intervention facilitators attended 2-day training, followed an intervention manual and completed weekly checklists. Intervention fidelity was rated as consistently high, with 100% of the foundation skills delivered and 78% of the optional skills delivered.
The child component focused on skills in emotional competence, de-escalation of anger and social problem-solving. Eight sessions were delivered to small groups during school time. Groups were facilitated by two professionals: an intervention clinician and a member of school staff (often a school psychologist or teacher). Average attendance was 7.3 sessions, with 84 children (92.3%) attending at least six sessions. To ensure fidelity, intervention facilitators attended a half-day training, followed a structured intervention manual and completed weekly checklists. One hundred per cent of the child programme content was covered in all groups.
In addition to the parent and child components, schools were also offered the choice between two universal interventions. Seven schools (32 children) received the PATHS intervention, and an additional seven schools received a Professional Learning Package (59 children). Fidelity was not measured.
Follow-up assessments were conducted 10 months post baseline. The following effect estimates are based on adjusted means as reported by the authors. Primary outcomes of interest included parent-reported child behaviour, as measured by the Eyberg Child Behavior Inventory (ODD, conduct disorder and hyperactivity subscales), and teacher-reported child behaviour, as measured by the total SDQ score. Statistical analyses appropriately accounted for the clustered nature of the data and were based on the intention-to-treat principle. For parent-reported child behaviour, there was a beneficial effect of the intervention for conduct disorder (mean difference –2.94, 95% CI –3.43 to –2.45), ODD (mean difference –4.75, 95% CI –5.51 to –3.99) and hyperactivity (mean difference –3.47, 95% CI –3.89 to –3.05), relative to a waiting list control. For teacher-reported child behaviour, the intervention reduced the total SDQ score, relative to the control group (mean difference –1.56, 95% CI –1.80 to –1.32).
Kyranides et al.243
Kyranides et al. 243 reported a small (three schools) cluster RCT of a universal intervention for preventing conduct disorder and callous unemotional traits among children between the ages of 7 and 9 years. Three schools in areas of low SES were randomised to either a skills-building intervention (n = 1) or usual curriculum control (n = 2). Ninety-four children were allocated to the intervention and 210 to the control. The mean age was 7.9 years (SD 0.74 years) and 51% of participants were female.
The (unnamed) intervention was 8 weeks long, with one 45-minute session delivered each week during school hours. The intervention was based on CBT with an added emotional component and aimed to increase children’s awareness of their own and others’ emotions, teach self-control and emotion regulation, promote a positive self-concept, improve social skills and peer relations, and develop problem-solving and communication skills. The intervention was delivered to whole classes by PhD (Doctor of Philosophy) students with master’s degrees in school psychology. An intervention manual was provided, and fidelity was monitored by the research supervisor.
Primary outcomes of interest to this review are the parent-reported Checkmate Child Symptom Inventory-4 to assess symptoms of conduct disorder and the Antisocial Process Screening Device to assess impulsivity. Analyses did not consider clustering. Immediately post intervention (mean difference –0.67, 95% CI –1.30 to –0.04) and at 9 months post intervention (mean difference –0.93, 95% CI –1.32 to –0.55), there was evidence to suggest that conduct disorder symptoms were reduced in the intervention group, relative to the control group. Impulsivity was reported for the post-intervention time point only: the result suggested that there was a beneficial effect of the intervention, relative to the usual curriculum control (mean difference –1.03, 95% CI –1.72 to –0.34).
Summary
Only two studies clearly specified a post-intervention time point. 243,245 Results for all studies at the time point most closely approximating post intervention are summarised in Table 17. All studies reported parent- or teacher-reported outcomes. Only one study reported the primary review outcome of conduct disorder symptoms;243 the remainder reported externalising behaviours or behaviour difficulties.
| Study | Time point | Outcome | Scale | Results |
|---|---|---|---|---|
| aConduct Problems Prevention Research Group247 | 3 years from baselinea | Child behaviour change | Not clear |
|
| 3 years from baseline | Externalising behaviours | CBCL |
|
|
| August et al.244 2002 | 3 years from baselinea | Externalising behaviours | Multiscale composite | . . . no overall Intervention X Time interaction for aggression, hyperactivity or impulsivity |
| Baker-Henningham et al.245 2012 | Post intervention | Observations of child behaviour | DPICS and MOOSES | Effect size 0.42 (95% CI 0.12 to 0.71) |
| Post intervention | Behaviour difficulties | Multiscale composite |
|
|
| Havighurst et al.246 2015 | 10 months from baselineb | Child behaviour | Eyberg Child Behavior Inventory (subscales) | Parent:
|
| 10 months from baseline | Child behaviour | SDQ | Teacher: MD –1.56 (95% CI –1.80 to –1.32) | |
| Kyranides et al.243 2018 | Post intervention | Conduct disorder symptoms | Checkmate Child Symptom Inventory-4 | Parent: MD –0.67 (95% CI –1.30 to –0.04) |
Two studies243,245 implemented school-only interventions, one of which described the intervention as based on CBT principles. 243 For the primary time point of post intervention, both studies reported evidence of a beneficial effect of intervention. One study245 was judged to be at low risk of bias for allocation concealment and randomised sequence generation; the other243 was judged to be at unclear risk of bias for both domains.
Three studies implemented multisystemic, multicomponent and multiphase ‘packages’ of interventions. 244,246,247 Based on the components reported, it is possible that the child-focused school-based components of these interventions were informed by cognitive–behavioural principles. However, none of the authors identified them as CBT-based interventions and their results were reported at the combined ‘package’ level. The studies also reported different follow-up time points. At the (presumed) post-intervention time point, Havighurst et al. 246 reported strong evidence of a beneficial effect of the intervention for parent-reported child behaviour, relative to a waiting list control. This study was rated as having a low risk of bias for randomised sequence generation, but an unclear risk of bias for allocation concealment. No further follow-up time points were reported.
Two studies244,247 reported interventions that, in addition to being multisystemic, were implemented in stages over several years, so it is difficult to discern a ‘post-intervention’ time point. The Fast Track247 study did not clearly specify a primary outcome, and the outcome measures reported vary at each time point. At 1 year and 3 years from baseline, the authors reported a beneficial effect of intervention for child behaviour change, but not for externalising behaviours. At 7 years’ follow-up, the authors reported no evidence of an effect of the intervention for reducing externalising behaviours. Finally, at 20 years’ follow-up, the authors reported a composite internalising, externalising and substance use self-reported outcome and concluded that there was strong evidence of an effect of the intervention. The Fast Track247 study rated as having an unclear risk of bias for both randomised sequence generation and allocation concealment.
At 3 years from baseline, August et al. 244 reported that there was no evidence that the Early Risers intervention reduced teacher-/parent-reported externalising behaviours. At 6 years from baseline, there was no evidence that the intervention prevented self-reported conduct disorder symptoms, although there was a beneficial effect for self-reported ODD symptoms. At 10 years from baseline, the authors reported that there was evidence that the intervention was associated with fewer self-reported conduct disorder symptoms, relative to no intervention. The study was rated as having an unclear risk of bias for both randomised sequence generation and allocation concealment.
Chapter 8 Economic evaluation
As described in Chapter 1, the aim of the economic study was to assess the costs and consequences for intervention components, or combinations of components, that were found to be effective, compared with usual curriculum, in the NMA. Costs and consequences were considered separately for:
-
targeted interventions to prevent anxiety, depression or conduct disorders among (1) primary school-aged children, (2) secondary school-aged children/young people and (3) university-aged young people
-
universal interventions for (1) primary school-aged children, (2) secondary school-aged children and (3) university-aged young people.
For the economic evaluation, we included interventions for which there was robust evidence of an intervention effect in one of the populations considered in the NMA. The intervention-level NMA results (see Chapters 4 and 5) found that CBT interventions (including those combined with IPT) were effective, compared with usual curriculum, at the post-intervention follow-up time point for universal secondary populations. There was also evidence that mindfulness/relaxation interventions reduced symptoms of anxiety. However, the findings were not considered robust because of small study size and unclear risk of bias for the key domains of randomisation and allocation concealment. Similarly, there was evidence that exercise reduced symptoms of anxiety in the targeted secondary analysis. However, this was based on a single study on a network ‘spur’, which was judged to be at unclear risk of bias. There was potential inconsistency in the tertiary/university setting analyses and NMA findings were not reported. We therefore analysed costs and consequences for CBT and CBT + IPT in a universal secondary population. For completeness, we extrapolate the costs for CBT interventions to primary and targeted secondary settings (as CBT was included in the NMA for these settings).
Results from the component NMA suggested that the only intervention component for which there was robust evidence of effectiveness, compared with usual curriculum, was the inclusion of a psychoeducation component in CBT interventions in a universal secondary school setting. We therefore only present costs and consequences for the inclusion of a psychoeducation component in a CBT intervention in the universal secondary population.
If sufficient evidence was available, we planned to conduct full model-based cost-effectiveness analyses for all identified groups. However, there was no robust evidence that any of the interventions were effective at ≥ 6 months post intervention, based on the NMAs. We therefore did not consider that a full model-based cost-effectiveness analysis would be of value, as it was unlikely to demonstrate cost-effectiveness of any of the interventions, compared with usual curriculum, in any of the populations, based on the evidence identified in our review.
The economic study also aimed to review previous economic evaluations of school-based interventions to provide up-to-date and rigorously collated information on costs and cost-effectiveness to inform both future intervention development and implementation decisions. We aimed to complement the effectiveness results by reviewing current literature describing the costs and cost-effectiveness of educational setting-based interventions for preventing anxiety, depression or conduct disorder among CYP. We also aimed to undertake a microcosting study for effective interventions, assigning appropriate costs to the constituent components of the interventions when feasible, for use in the cost–consequence analysis.
Methods
We first describe the methods for the narrative review of previous economic evaluations of educational setting-based interventions that aimed to prevent anxiety, depression or conduct disorder among CYP. We then describe the methods for the microcosting study of the inclusion of a psychoeducation component in universal secondary CBT interventions described in a cost–consequence analysis.
Narrative review
Search strategy
We searched for relevant studies describing economic evaluations of educational setting-based preventative interventions in several ways:
-
The body of abstracts identified in the detailed systematic review described in Chapter 2 was restricted by terms to identify costing studies (e.g. ‘economic evaluation’, ‘cost’).
-
The search strategy used for the systematic review (described in Chapter 2 and Appendix 1, and carried out on 4 April 2018) was reproduced and applied to the full extent of the NHS Economic Evaluation Database (NHS EED; date range searched: 1968 to 2014) on 22 May 2019 (see Appendix 8).
-
Potentially relevant articles were sought by searching for economic evaluations of interventions described in the clinical effectiveness studies included in the NMA (see Chapters 4 and 5). The 142 included articles were inspected for details of trial registration and, when present, the registration record was searched for ‘cost’ or ‘economic’, which might have indicated an intention to conduct an economic analysis. References to the words ‘cost’ or ‘economic’ in the text of the included articles themselves were followed up when appropriate. Authors were contacted to request details of publications if we believed that an economic study may have been carried out but were unable to locate the report.
-
As a supplemental search, economic evaluations associated with the interventions tested in the 142 included effectiveness articles were sought using the Google Scholar (Google Inc., Mountain View, CA, USA) forward citation search functionality. 252,253
The original searches described in Chapter 2 were based on RCTs and may have missed relevant decision models. Therefore, a scoping search was carried out in MEDLINE to assess the likelihood of modelling articles having been missed (see Appendix 8), with the intention of reproducing and repeating the initial searches without the RCT restriction if it appeared that a substantial body of modelling articles had been missed.
Inclusion criteria
The following inclusion criteria were agreed by Joanna C Thorn, Deborah M Caldwell and Nicky J Welton prior to screening articles:
-
educational setting-based intervention
-
intervention designed explicitly to prevent anxiety, depression or conduct disorder
-
intervention aimed at CYP aged 4–18 years
-
original study based on a RCT with an embedded economic evaluation or an economic decision model.
All population, intervention, comparator and outcome inclusion criteria for the effectiveness review were reflected in the economic search. We did not include papers that were written in languages other than English, conference abstracts or review papers. Titles and abstracts were screened for inclusion, and full texts were obtained for all articles that either clearly met the inclusion criteria or for which inclusion was unclear. Screening of both abstracts and full texts was carried out by one author (JT), with a second opinion (DMC) sought when necessary. Reasons for exclusion were recorded for articles rejected after full-text screening.
Data extraction and quality control
Data covering study characteristics (publication date, unit of randomisation, location, setting, study design, type of model, model time horizon or empirical follow-up period, size of study, comparator), intervention details (description of intervention, intervention cost, condition targeted, population, type of intervention) and economic details (type of economic analysis, outcomes measured, sources of outcomes, discount rate, resources included and source of resources, cost year, currency, perspective) were extracted from included studies using a bespoke form in Microsoft Access® (Microsoft Corporation, Redmond, WA, USA). Verbatim descriptions of the study conclusions were also extracted. The quality of the included studies was qualitatively assessed against the Drummond et al. 254 10-point checklist for RCTs and the Philips et al. 255 checklist for decision models. Costs were converted to Great British pounds using purchasing power parity figures256 and inflated to 2018 equivalents257 for comparison purposes.
Data synthesis
Included interventions were categorised as targeted (indicated or selective) or universal, and the cost-effectiveness analyses were described in a narrative review.
Intervention costing
The NMA results (see Tables 3, 4, 7 and 8) suggested that CBT-based interventions were the most likely to produce positive outcomes, with CBT + IPT-based interventions also showing some indication of effect for preventing depression in a universal secondary-age population. Results from the component NMA indicated that the only component for which there was evidence of a beneficial effect in universal secondary CBT interventions was a psychoeducation component, with CBT interventions with psychoeducational components reducing the standardised anxiety score by –0.39 (95% CrI –0.78 to 0.01). Therefore, our intervention costing analysis (and subsequent component breakdown) focused on CBT interventions that incorporated identifiable psychoeducation components and CBT + IPT interventions. As there are considerable similarities between interventions designed to prevent depression and those focusing on anxiety (with some interventions explicitly targeting both), we included both depression and anxiety interventions in the costing estimate without distinguishing between them.
Studies describing universal secondary CBT interventions with a psychoeducation component were identified from the systematic review described in Chapter 2. Details of the interventions were extracted (i.e. year of publication, number of sessions offered, average session duration, size of group, number of group leaders, professional background of leaders, provision of a manual, training, materials, provision of parent sessions and other costs). Further details of the interventions were sought from intervention websites and from linked papers describing the branded interventions in more detail. Through scrutinising the extracted data, an ‘indicative’ intervention was developed. Unit costs for the individual elements for a universal intervention in a secondary population were identified in the UK context, and cost estimates were calculated for the ‘indicative’ intervention. The CBT cost estimates were extrapolated to primary populations and targeted interventions. A similar extraction process was carried out for CBT + IPT interventions.
Component costing
When the CBT intervention was described in sufficient detail (either in the paper itself or by consulting the intervention manual), the approximate proportion of each intervention devoted to psychoeducation elements was estimated. Psychoeducation was defined to include the provision of information, the explanation of symptoms, advice on managing the condition and the provision of written materials,258 while excluding practical experiences (such as role play) and activities based on the individual’s own life experience. Intervention descriptions and manuals were scrutinised carefully, and elements of psychoeducation were identified. The approximate time commitment to each psychoeducation element was estimated, summed for each intervention and expressed as a proportion of the whole intervention. An approximate estimate of the cost that could be ascribed to psychoeducation components was derived based on the overall cost of the indicative intervention.
Cost–consequence analysis
The intervention costs and consequences (SMD relative to usual curriculum post intervention) that could be ascribed to the ‘indicative’ interventions and psychoeducation components are presented as a cost–consequence table (Table 19). If no effectiveness estimates are available relative to usual curriculum, the results relative to a waiting list are reported; if these are also not available, then the results relative to no intervention are presented.
Results
Narrative review of previous economic evaluations
Article selection
A flow diagram summarising the identification and selection of articles is given in Figure 16. A total of 434 titles and abstracts were screened for inclusion; full texts were obtained for 36 articles. Eight articles, reporting on six study time points, were deemed to meet the inclusion criteria.
FIGURE 16.
Study selection process: flow diagram for review of economic evaluations.
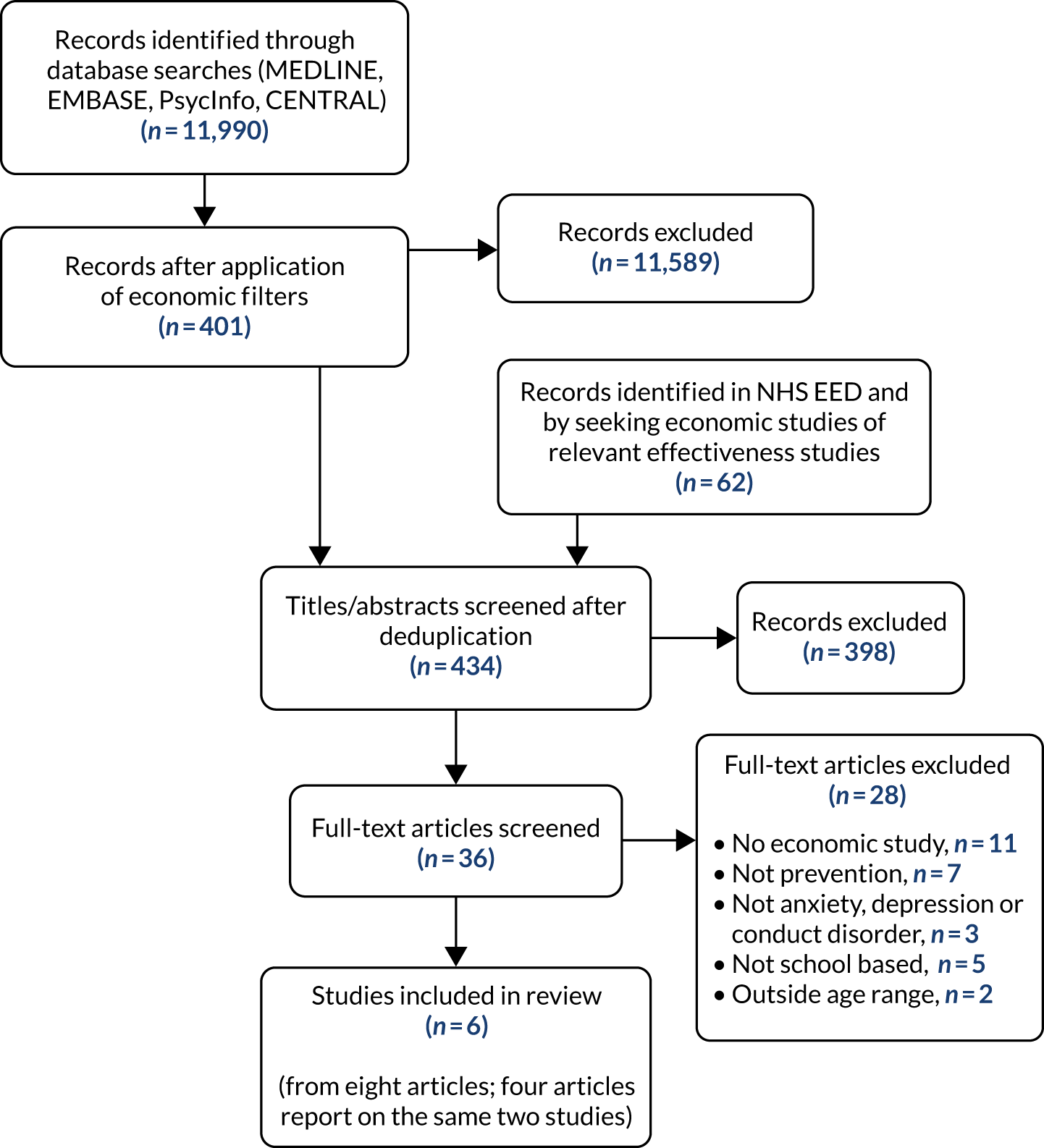
Only 3 of the 137 depression and anxiety effectiveness articles (2.2%) included in Chapters 4 and 5 were found to have published economic evaluations. Three further authors of effectiveness papers were contacted to request details of potential economic evaluations. All three authors confirmed that no economic study had been published, although one is still planning to complete and publish the study in future. Of the five included conduct disorder studies (see Chapter 7), only one (i.e. Fast Track247) had undergone economic evaluation. The additional scoping search carried out in MEDLINE to identify economic decision model papers returned 186 potentially relevant articles. The search identified both of the modelling papers that had already been identified in the original review,259,260 but did not identify any additional articles. Based on this finding, we did not conduct further searches for economic decision model papers in the other databases searched in the systematic review. Although there is a possibility that we may have missed some decision model papers, we think that this is unlikely.
Included studies characteristics
The six included studies were published between 2006 and 2017, with costs reported in currency years from 2003 to 2014. The numbers of participants in the studies describing RCTs ranged from 308 to 3357. Two studies described universal interventions, three studies reported on an indicated intervention (of which two included a universal component) and the final study considered both universal and indicated interventions. Two analyses were based on economic decision models (both Markov models) and four analyses were based on data from RCTs. The follow-up period ranged from 6 months to 14 years for the trial-based analysis, and the model horizons were 5 or 10 years. Interventions were compared with usual provision (n = 4) or no intervention (n = 2). Additional characteristics are summarised in Table 18, and the extracted data are provided in Appendix 8.
| Characteristic | n |
|---|---|
| Condition | |
| Anxiety | 1 |
| Depression | 3 |
| Conduct disorder | 2 |
| Economic evaluation type | |
| Cost-effectiveness analysis | 3 |
| Cost–utility analysis | 4 |
| Cost–consequence analysis | 1 |
| Setting | |
| Primary school | 4 |
| Secondary school | 5 |
| Study design | |
| RCT | 4 |
| Decision model | 2 |
| Jurisdiction | |
| USA | 2 |
| UK | 2 |
| Australia | 2 |
Quality of articles
The study by Mihalopoulos et al. 260 met the majority of the Philips checklist criteria. 255 However, the intervention was not described in adequate detail, half-cycle corrections were neither incorporated nor discussed and there were weaknesses in both the assessment of uncertainty and description of data incorporation. Lee et al. 259 published a very detailed supplementary document alongside the article, thereby meeting most of the reporting requirements, although the cycle length was not explicitly stated and parameter distribution choices were stated but not justified. Structural uncertainty and heterogeneity did not appear to have been explored in either article.
The analysis reported by Anderson et al. 261 lacked sensitivity analyses for exploring uncertainty and did not discuss generalisability, but was otherwise well reported. Although there was no discussion of generalisability or comparison with other studies and no subgroups were considered, the study by Stallard et al. 262 generally conformed to the requirements of the Drummond checklist. 254 The 2006/7 articles by Foster and Jones263,264 did not adequately report the effectiveness of the intervention, and did not include all costs that might have been relevant. Discounting was neither described fully nor justified, and results were not compared with those of other studies. As no incremental analysis was conducted in the 2010 study,250 the study quality was not assessed.
Costs and cost-effectiveness
A range of economic analysis perspectives was studied, including the health, social services, education and criminal justice sectors, leading to a wide range of resources being included in the analyses. Interventions were typically complex and ranged in cost from approximately £45 per participant to > £60,000. The intervention for conduct disorder involved multisystemic, multicomponent and sequentially delivered individual and group interventions over a 10-year period, whereas the interventions for depression and anxiety were all based on CBT methods. Outcomes considered in the economic analyses included utilities [either quality-adjusted life-years (QALYs) or DALYs averted], as well as other clinical outcomes. The studies are described in more detail below.
Prevention of anxiety
Stallard et al. 159,262 studied a universal intervention for anxiety prevention in primary schools in the UK. The FRIENDS intervention is a CBT-based programme that teaches children to recognise anxiety and develop strategies to address anxious feelings. The intervention was delivered by either a teacher or an external health educator, and both were compared against usual curriculum provision in a three-arm trial. The cost-effectiveness of the programme was assessed at 6 months in terms of the cost per unit reduction in primary outcome (RCADS score), and a cost–utility analysis was conducted using the Child Health Utility-9 Dimensions (CHU-9D) instrument to measure health-related quality-of-life data from which QALYs were derived. The economic analyses were carried out from the joint health, social services and education sectors perspective. Therefore, resources considered in the study (measured using an adapted Client Service Receipt Inventory instrument administered by parental interview) included hospital stays, accident and emergency visits, outpatient appointments, general practitioner (GP) visits and visits to psychology practitioners or social workers, and medications. The scope of the study appeared to be condition-specific resource use, except for hospital events, which encompassed all-cause resource use. It was unclear whether use of social services was condition specific or all cause. A very detailed breakdown of the intervention costs was provided, leading to a total of £62.96 per child if the intervention was delivered by school staff and £59.16 per child if delivered by external health staff (inflated to 2018 costs). Point estimates suggested that the intervention was more costly, but less effective (by 0.004 QALYs), than the control, that is the intervention was dominated. The economic analysis provided further evidence that the intervention was unlikely to be cost-effective, with a probability of cost-effectiveness of < 35% at all societal willingness-to-pay values for the intervention delivered by health staff. Furthermore, the analysis was based on complete cases for CHU-9D measurements. This may have led to bias, as it is possible that those individuals without complete data were less likely to have benefited from the programme. The cost of teacher time for delivering the intervention was treated as zero. This strategy implies that there was no opportunity cost associated with alternative learning activities from the teachers’ point of view.
Prevention of depression
Three studies (one RCT and two decision models) addressed interventions aiming to prevent depression. The RCT evaluated the CBT-based Resourceful Adolescent Program (RAP) from the perspective of the NHS and social care in the UK. 261 We note that, in the present review, the RAP was classified as CBT + IPT, a combined intervention type, in line with the description of the intervention in Merry et al. 197 and Hetrick et al. 68 The study was described in both a report to the funder and a journal article. The more recently published paper has been treated here as the primary account, with the funder report consulted for further detail when necessary. The RAP is a universal intervention that was delivered in secondary schools, recruiting young people aged 12–16 years. Cost-effectiveness was assessed after 12 months of follow-up in relation to both QALYs (measured using the EuroQoL-5 Dimensions questionnaire) and clinical symptoms of low mood (measured using the Mood and Feelings Questionnaire-Short Version). Resources considered in the study included hospital stays, accident and emergency visits, outpatient appointments, GP visits and visits to psychology practitioners. Details of medications were collected but not reported, as the data were considered unreliable. The cost associated with delivering the intervention (£46.15 per child in 2018 equivalent) was relatively small, and a detailed breakdown was reported. For both the cost-effectiveness and cost–utility analyses, the point estimates suggested that the intervention was both more costly and less effective than the control (usual class provision within school), albeit with considerable uncertainty around the results. The intervention was deemed ‘highly unlikely’ to be cost-effective.
The two model-based analyses were conducted in the Australian context following the Assessing Cost-Effectiveness in Prevention framework. 259,260 The studies shared a common author, and both were based on ‘hypothetical’ interventions developed by the project team following a literature review and meta-analysis. In both cases, the intervention was compared with no intervention, focused on children aged 11–17 years, considered DALYs averted as the economic outcome measure and used Markov models. The earlier (2012) study260 involved a model time horizon of 5 years and a health sector perspective. The more recent (2017) model259 was extended to 10 years and included both health and education sectors in the perspective. Intervention costs were estimated by Lee et al. 259 at £12.90 per child for the universal intervention and £259.25 per child for the indicated intervention (2018 prices). The incremental cost-effectiveness ratios (ICERs) were found to be AU$7350 per DALY averted for a universal intervention and AU$19,550 per DALY averted for the indicated intervention in Lee et al. ,259 and AU$5400 per DALY averted for an indicated intervention in Mihalopoulos et al. 260 Assessed against a standard societal willingness-to-pay threshold of $50,000 per DALY averted, both studies concluded that school-based preventative interventions represent good value for money. However, as the studies focused on the prevention of major depression with three health states only (healthy, diseased and dead), the lack of granularity in terms of addressing the spectrum of disease severity limits the usefulness of the analyses in informing implementation decisions.
Prevention of conduct disorder
Three articles, all by the same author group and relating to the same study, described the Fast Track intervention, designed to prevent conduct disorder in the USA. The intervention was assessed at two time points (10 years263,264 and 13 years250 post randomisation). Two articles described the same study at the same time point, with one reporting an ICER and the other reporting the net monetary benefit statistic. As these cost-effectiveness statistics would usually be reported together, and the articles are identical in many aspects, the two articles have been treated as one for the purposes of this review. The Fast Track intervention took a long-term approach to the prevention of conduct disorder. Children were identified as ‘at risk’ at age 6–7 years and were given intensive support through multiple activities over a 10-year period, including parent training, group meetings, friendship development and promotion of reading skills (see Chapter 7). The multifaceted intervention was very costly, at US$58,283 (cost year: 2014) (£60,478 in 2018 Great British pounds) per child.
The stated perspective of the economic analysis was that of a third-party payer, but the intervention cost was the only resource included. Cost-effectiveness at 10 years was found to be US$3,481,433 per case of conduct disorder averted, with only a 1% probability of cost-effectiveness at an assumed societal willingness-to-pay value of US$1M. However, the authors explicitly note that the intervention was designed for effectiveness, not cost-effectiveness. Possible future effects were addressed approximately by estimating the costs associated with an enduring criminal lifestyle, and incorporating this estimate into the societal willingness-to-pay value, but no other potential offsets (such as the effect on health or social care, or directly on the education system) were included in the analysis. Only the intervention was costed. A subgroup analysis suggested that the intervention may be cost-effective for children at the highest risk of developing conduct disorder; however, it was unclear whether this analysis was prespecified or conducted post hoc.
By the 13-year follow-up, evidence for cost-effectiveness had dissipated, and the study concluded that ‘[t]he most intensive psychosocial intervention ever fielded did not produce meaningful and consistent effects on costly outcomes’. 250 This study took a much broader perspective than previously, but, citing the lack of intervention effect as a justification, the authors presented marginal effects for group differences for a number of resources, instead of deriving any formal cost-effectiveness statistics combining costs and outcomes. Relevant resources included health-care use, criminal justice interactions, substance use and educational service use. Full data sets were not available for all variables. For example, medication use was available for years 4–13 only, and health-care use was available for years 7–13 only. Costs associated with health-care use and delinquency were investigated, although no unit costs were reported for the resources used. Both outpatient mental health-care use and general any-cause health service use costs were higher in the control group, these costs being, respectively, US$1344 and US$1106 lower per participant in the intervention group. Costs associated with the criminal justice system showed no difference between the groups. Weaknesses in the trial development and conduct were identified, and tension arising from the differing background perspectives of the study team was apparent. For example, the author was critical of developmental psychology as a discipline, of the lack of data-sharing in the project and of the lack of prespecified analysis plans, leading to concerns over chance findings.
Intervention costs
Extracted elements of the interventions described in 20 papers evaluating universal CBT interventions with a psychoeducation component identified via the ICA (see Chapters 4 and 5) are given in Appendix 8. The number of sessions for children ranged from 3 to 30, with a median of 10 sessions. Session duration ranged from 35 to 120 minutes (median 50 minutes). Group sizes ranged from 4 to 30 participants, with a median of 25. Parent sessions formed part of the intervention in only five studies, with low attendance cited as an issue in two of these studies. The group leaders included teachers (n = 8), psychologists (n = 11) and students (n = 5) (sometimes in combination). Groups were led by either one (n = 12) or two (n = 7) individuals (the exact leadership was unclear in one study). Of the 12 groups led by one individual, four were led by psychologists and eight by teachers. Training for delivering the intervention (when described) took a number of forms, including self-participation in the intervention, workshops varying from 90 minutes to 5 days (n = 9, median 1 day) and co-leading a cohort. A facilitator manual was provided in 16 out of 20 interventions, and workbooks or worksheets were supplied in 13 out of 20 interventions.
A ‘typical’ universal secondary CBT intervention might, therefore, comprise 10 sessions of 50 minutes, each session each delivered to 25 children at a time by one teacher who had received 1 day of specific intervention training. Typically a manual would be provided for facilitators, and workbooks for the participants. Unit costs associated with these elements in the UK context are given in Appendix 8. This leads to an estimated overall intervention cost of £43 per student from the school budget perspective. At the school level, this would represent approximately £1825 per (small) two-form entry school, or £7300 per larger eight-form entry school in the first year. A two-form entry school is one that has an annual intake of two classes of approximately 30 students each, who then progress through the school as a stable cohort. An eight-form entry school is approximately four times as large. If this universal intervention were delivered in a primary school, the teacher costs would be slightly lower, leading to an approximate cost of £42 per student. Assuming that a targeted (indicated or selective) intervention would be delivered to a smaller group of students (e.g. 10), the cost per student would be £95 in a secondary setting or £91 in a primary setting. Similarly, based on three articles describing universal secondary CBT + IPT interventions, a typical CBT + IPT intervention might have both workbooks and a manual, and consist of 11 sessions of 60 minutes each, delivered by one teacher to 10 students after 2 days’ training. This leads to an estimated cost of £157 per student.
Component analysis
Seven CBT interventions were described in sufficient detail to attempt to assign a very approximate proportion of the intervention devoted to psychoeducation: e-couch (33%), ThisWayUp (40%), Penn Resilience Program (30%), LARS&LISA (20%), Op Volle Kracht (50%) and two unnamed interventions (12% and 100%). Overall, approximately one-third of the ‘typical’ intervention could be assigned as psychoeducation. The potential cost of incorporating a psychoeducation component might, therefore, represent approximately £14 per student (i.e. approximately £600 per two-form entry school or £2400 per eight-form entry school).
Cost–consequence analysis
Intervention costs and consequences in SMDs that could be ascribed to the ‘indicative’ CBT interventions for a universal secondary population are presented in Table 19, alongside extrapolated intervention costs for similar interventions in primary and targeted populations. Adding IPT to CBT in a universal secondary population is more costly than CBT alone, driven mainly by additional teacher training and delivery to smaller groups of students. Although the estimated SMD shows a bigger reduction in depression score, compared with usual curriculum, than for CBT alone, the estimate is very uncertain. There is no evidence for the effect of CBT + IPT on anxiety in the universal secondary population. Further evidence on the relative efficacy of CBT and CBT + IPT would be required to justify the additional intervention cost. No studies used a usual curriculum control in either secondary or primary targeted populations. There is some evidence that CBT is effective compared with a waiting list for reducing anxiety in a targeted primary population, but this difference may not extend to comparisons with usual curriculum.
| Setting/intervention | Intervention cost per student (£) | CBT for, SMD (95% CrI) | |
|---|---|---|---|
| Anxiety | Depression | ||
| Secondary | |||
| Universal | |||
| CBT | 43 | –0.145 (–0.342 to 0.042) vs. usual curriculum | –0.040 (–0.156 to 0.074) vs. usual curriculum |
| CBT + IPT | 157 | N/A | –0.184 (–0.454 to 0.085) vs. usual curriculum |
| Targeted | |||
| CBT | 95 | 0.028 (–0.108 to 0.164) vs. no intervention | –0.217 (–0.579 to 0.1307) vs. no intervention |
| Primary | |||
| Universal | |||
| CBT | 42 | –0.072 (–0.234 to 0.051) vs. usual curriculum | –0.131 (0.441 to 0.174) vs. usual curriculum |
| Targeted | |||
| CBT | 91 | –0.384 (–0.846 to 0.067) vs. waiting list | –0.477 (–2.486 to 1.50) vs. waiting list |
In Table 20, we report the intervention costs and consequences (SMD) for CBT with or without a psychoeducation component in a universal secondary population. Because all of the CBT interventions in the NMA for this population contained cognitive and behavioural components, the comparison is between CBT with just cognitive and behavioural components and CBT with cognitive, behavioural and psychoeducation components. We give results for both anxiety and depression outcomes, although the NMA results only show evidence of a difference for the anxiety outcome. We also report estimated intervention costs, based on our microcosting of typical interventions with these components as described in the RCTs. Adding a psychoeducation component increases intervention costs, but there is evidence that anxiety symptom scores improve post intervention.
| Population/setting/intervention | Intervention cost per student (£) | Intervention vs. usual curriculum, SMD (95% CrI) | |
|---|---|---|---|
| Anxiety | Depression | ||
| Secondary | |||
| Universal | |||
| CBT (cognitive + behavioural) | 29 | 0.092 (–0.171 to 0.357) | –0.112 (–0.278 to 0.052) |
| CBT (cognitive + behavioural + psychoeducation) | 43 | –0.301 (–0.593 to –0.014) | 0.005 (–0.118 to 0.132) |
Discussion
Review of previous economic studies
The body of evidence described in this review is both small and heterogeneous. Conditions being targeted, interventions and cost-effectiveness analyses were all variable. It was, therefore, not possible to synthesise the results numerically. Multiple perspectives for the analyses were taken, leading to the resources included in the analyses varying widely. The potential long-term costs associated with missing school15,16 (such as lifetime earning capacity) were not estimated in any of the studies. All included studies appropriately compared the intervention with usual provision, or with no intervention (i.e. the model-based studies). Although an active control comparator is appropriate (and necessary) for investigating effectiveness mechanisms, economic analyses are most informative for decision-makers when compared with usual care/curriculum. The two model-based analyses suggested that hypothetical interventions could be cost-effective in the Australian context. However, the trial-based analyses suggested that the interventions were unlikely to be cost-effective in the UK or the USA. For the one intervention that was considered potentially cost-effective in a high-risk subgroup at an interim point of the study, the effect disappeared with longer-term follow-up. There was little empirical costing evidence to inform decisions on the implementation of preventative interventions.
Cost–consequences analysis
The figures used to obtain intervention costs were based on a highly stylised, ‘indicative’ universal intervention that was assumed to be delivered as specified, and there are many ways in which differences might occur in the real world. Although it was assumed that there would be no room hire costs if the intervention were delivered on school premises, there could be heating, lighting or security overheads if the intervention were delivered outside school hours. It is possible that a project manager or administrator would be required to oversee the intervention if it were rolled out across the country. The salary of the teacher delivering the intervention could vary according to experience. Delivery by a psychologist instead of a teacher would affect the salary costs, and psychologists additionally undergo supervision meetings as part of their professional conduct. The intervention would be more costly if two individuals led it instead of one. The detailed intervention cost breakdown by Stallard et al. 262 illustrated the variability in individual components that go into making up an intervention, with small changes in delivery method (e.g. the requirement for travel) leading to big differences in costs between methods. Stallard et al. ’s262 work suggested that it is a fallacy to assume that delivery by schoolteachers is less costly than delivery by health-care specialists. None of the interventions described here explicitly mentioned a licence fee, and potential administration costs have not been considered. Deriving a value for the opportunity cost of time diverted from other learning activities in school is currently considered problematic and has not been taken into account here. Despite these caveats, this simplistic model serves to give an idea of the costs that might accrue to a school budget in the first year of implementation. Subsequent years would incur lower training outlay, assuming that the same teachers deliver the course. The limited details of interventions described in the published reports meant that it was challenging to assign accurate proportions to psychoeducation components.
Implementation might be more attractive if it could be demonstrated that the intervention has a positive effect on educational outcomes or reduces the need to pay for educational psychologists in the future. However, the systematic review found that few studies of effectiveness had considered educational attainment outcomes (see Chapter 6). Future work should consider developing methodologies for evaluating both effectiveness and cost-effectiveness in terms of school outcomes, as well as the outcomes more typically encountered in health-care studies.
The cost–consequence analysis was based only on the intervention costs (i.e. the effect on health-care use was not addressed). It is worth noting that the beneficial effects of an intervention that aims to prevent or reduce symptoms of anxiety may also extend to reducing depression, and vice versa, which would increase the value of such an intervention. A comparison of costs and standardised outcomes in a cost–consequence analysis is difficult to interpret; ideally, a full cost-effectiveness analysis based on a recognised clinical outcome would be conducted. However, we did not find sufficient evidence for the efficacy of these interventions at 6 months’ post-intervention (and longer) follow-up for the development of a cost-effectiveness model to be useful at the present time. An economic model needs to capture long-term costs and benefits, which may be substantial, as issues with mental health and conduct disorder during school years have been shown to be associated with a range of health and behavioural problems as adults,4 which are costly to society. 265 However, further research is needed to develop and evaluate effective interventions for the prevention of mental health and conduct disorders in school-age children before the longer-term consequences of such interventions can be fully assessed.
To ensure high-quality information for decision-makers, it is imperative that future reports of school-based interventions to prevent anxiety, depression or conduct disorder are described in some detail and that the cost implications of interventions are adequately measured.
Chapter 9 Summary and interpretation of key findings
In this chapter, we draw together the findings from the systematic review, NMA and economic evaluation. Based on the criteria for interpretation described in Chapter 2, we summarise our overall interpretation of the evidence from the NMA for the primary time point of immediately post intervention. This summary forms the basis for the implications for practice, implications for research and the conclusions reported in Chapter 10.
Systematic review
The full results of the systematic review are reported in Chapters 4–7 and are summarised briefly here. The effectiveness results are based on searches conducted in April 2018. A total of 11,990 citations were screened, and 1512 full-text articles were retrieved for screening. The review included 142 studies of > 63,500 randomised participants. Of the 142 studies, 92 were judged to be at unclear risk of bias for random sequence generation, 115 were judged to be at high or unclear risk of bias for allocation concealment and 133 were judged to be at high or unclear risk of bias for blinding of participants. We identified a protocol or trial registration for only 32 studies. This represents 23% of included studies published post 2000.
Of the 142 eligible studies, 71 contributed data to the NMA for the prevention of anxiety, 86 were included for the NMA for depression and five contributed to the narrative summary for the prevention of conduct disorder. Note that there was an overlap of studies contributing to the anxiety and depression NMA, with 47 studies reporting both an anxiety and a depression outcome.
Network meta-analyses by population and setting
This is a large and complex review, with 32 possible intervention-level NMAs conducted (condition × setting × population × time point), from which we reported 57 intervention effect estimates of the primary outcomes of self-reported symptoms of anxiety or depression. This number of analyses does not include the component NMAs or subgroup or sensitivity analyses, and does not include the additional and secondary outcomes. Below we report the findings for our primary outcomes at the primary time point of post intervention, for the intervention-level and component-level NMA. Note that, to ensure conciseness in this chapter, we concentrate on interpreting findings for which the relevant results chapter has indicated that there may be statistical evidence of an effect, as described in Chapter 2. However, for full reporting of all results and intervention effect estimates, see Chapters 4 and 5.
Anxiety: universal population, secondary setting
This was a well-populated network of 21 studies and 10,208 participants. The between-study heterogeneity was moderate across the network. The risk of bias for random sequence generation and allocation concealment was deemed to be mostly unclear. At the post-intervention time point, we found weak evidence of a small beneficial effect of CBT-based interventions (SMD –0.15, 95% CrI –0.34 to 0.04), relative to usual curriculum. There was statistical evidence that mindfulness/relaxation interventions (SMD –0.65, 95% CrI –1.14 to –0.19) were effective in preventing symptoms of anxiety. However, the CrIs for the mindfulness/relaxation effect estimate were relatively imprecise, and the effect estimate is based on two small studies, which were judged to be at unclear risk of bias for the domains of random sequence generation and allocation concealment. We also note that there was variation between the study-level effect estimates of the two mindfulness/relaxation studies. One study130 (with 30 participants) reports a large effect estimate of mindfulness/relaxation relative to a waiting list (SMD –1.01, 95% CrI –1.67 to –0.35). The second study137 compared mindfulness/relaxation with an attention control and reports a smaller effect (79 participants, SMD –0.32, 95% CrI –0.72 to 0.08). Finally, the statistical findings for both CBT and mindfulness/relaxation should be interpreted considering the possible evidence of asymmetry from the comparison-adjusted funnel plots, which suggests the presence of small-study effects or other non-reporting bias.
Anxiety: universal population, primary setting
This was a small network of 15 studies, but with a reasonable number of participants (n = 5605). There was moderate between-study heterogeneity across the network. Thirteen studies were judged to be at unclear risk of bias for random sequence generation and allocation concealment, one was judged to be at low risk of bias for both domains and one was judged to be at low risk of bias for random sequence generation only. There was weak evidence for a very small beneficial effect of CBT (SMD –0.07, 95% CrI –0.23 to 0.05), relative to usual curriculum. The comparison-adjusted funnel plot was suggestive of small-study effects or other non-reporting bias.
Anxiety: targeted population, secondary setting
This was a small network of 15 studies (2383 participants). There was mild to moderate between-study heterogeneity across the network. Three studies were judged to be at low risk of bias and seven were judged to be at unclear risk of bias for randomised sequence generation and allocation concealment. Four studies were judged to be at low risk of bias for randomised sequence generation and at unclear risk of bias for allocation concealment. There was evidence that exercise was effective in reducing self-reported anxiety in targeted secondary settings, relative to no intervention (SMD –0.47, 95% CrI –0.86 to –0.09). However, the width of the CrI indicates a relatively imprecise estimate, and exercise was evaluated in only one small study170 (with 121 participants) that was judged to be at unclear risk of bias for random sequence generation and allocation concealment. We caution against overinterpreting the finding for exercise-based interventions in this network. There was no evidence of effectiveness for the other interventions. The comparison-adjusted funnel plot did not suggest the presence of small-study effects or other non-reporting bias.
Anxiety: targeted population, primary setting
The targeted primary network was the smallest of all those considered for the prevention of anxiety with only 11 studies (1314 participants). There was substantial between-study heterogeneity (τ 0.42, 95% CrI 0.21 to 0.89) across the network. Three studies were judged to be at low risk of bias and six studies at unclear risk of bias for both the randomisation and allocation concealment domains. A further two studies were judged to be at unclear risk of bias for allocation concealment, but at low risk of bias for random sequence generation. Although there was weak evidence of a beneficial effect for CBT relative to a waiting list (SMD –0.38, 95% CrI –0.84 to 0.07), the CrI for the estimate is relatively wide. There was no evidence of small-study effects or other non-reporting biases for this network; however, the number of studies is at the lower end required for this analysis to be meaningful. 266
Anxiety: tertiary/university setting
There was evidence of (statistical) inconsistency in the NMA for the prevention of anxiety in tertiary settings; therefore, we do not report effectiveness findings. The inclusion criterion that interventions needed to be implemented in the educational setting may have limited the number of eligible studies, which, in turn, may have contributed to the lack of model fit observed. The limitations are discussed further in Chapter 10.
Depression: universal population, secondary setting
At the post-intervention time point, this was the most connected network, including the greatest number of studies (34 studies; 18,094 participants), of which 25 included an intervention based on CBT. Most studies were rated as having an unclear risk of bias for at least one domain. The between-study heterogeneity was moderate across the entire network. There was weak evidence of a very small beneficial effect for CBT, compared with usual curriculum (SMD –0.04, 95% CrI –0.16 to 0.07). There was also some evidence that CBT + IPT (SMD –0.18, 95% CrI –0.46 to 0.08) was effective at reducing depressive symptoms. The comparison-adjusted funnel plots did not indicate small-study effects or other non-reporting biases.
Depression: universal population, primary setting
This was a small network of 12 studies (4116 participants) of six interventions. Only one study did not include a CBT comparator, yet the between-study heterogeneity was considered to be moderate to substantial. One study was rated as having a low risk of bias and 11 studies were rated as having an unclear risk of bias for both random sequence generation and allocation concealment. There was no evidence of an effect for any intervention relative to usual curriculum. The comparison-adjusted funnel plots did not indicate small-study effects or other non-reporting biases.
Depression: targeted population, secondary setting
Twenty-four studies contributed to this NMA. However, it was small in terms of participants (n = 3669). There was evidence of moderate to substantial between-study heterogeneity across the network. Most studies were rated as having a low risk of bias on at least one of the domains; however, allocation concealment was rated as having an unclear risk of bias in 18 studies. There was no evidence of an effect for any intervention relative to no intervention. The comparison-adjusted funnel plot did not indicate small-study effects or other non-reporting biases.
Depression: targeted population, primary setting
There were five studies (497 participants) in this NMA. Between-study heterogeneity was substantial. One study was judged to be at low risk of bias for both random sequence generation and allocation concealment, and three studies were judged to be at unclear risk of bias. One study was rated as having a low risk of bias for random sequence generation, but an unclear risk of bias for allocation concealment. There was no evidence of an effect for either CBT or occupational therapy, relative to a waiting list. A funnel plot was reported but not interpreted because of the small number of studies included.
Depression: tertiary/university setting
We observed evidence of inconsistency in the NMA for the prevention of anxiety in tertiary settings; therefore, it was not appropriate to report effectiveness findings. As a consequence of the inclusion criteria, few studies were included, which may have contributed to the lack of model fit. The limitations of the inclusion criteria are discussed in Chapter 10.
Anxiety and depression: component network meta-analysis
The taxonomy of intervention components was reported in Chapter 3. We report the anxiety and depression component NMA findings in Chapters 4 and 5. There was little robust evidence that specific combinations of components were more effective than others. The exception was a psychoeducation component: it appears that the addition of a psychoeducation component to CBT may result in a more effective preventative intervention. The mechanism for this finding is not clear. In the psychotherapeutic literature, Pompoli et al. 72 found that the addition of a psychoeducation component to CBT decreased the odds of remission from adult panic disorder symptoms (i.e. made remission less likely), whereas López-López et al. 82 found no evidence that adding psychoeducation to CBT changed the effectiveness for treatment of depression in adults (SMD 0.04, 95% CrI –0.66 to 0.75). Both the Pompoli et al. 72 and López-López et al. 82 studies were conducted in clinical adult populations, and the present study is in non-clinical child and adolescent populations, and mechanisms of psychoeducation may vary. To aid future intervention development, investigation of the potential mechanism(s) of psychoeducation should be conducted and could also explore the possibility that the mechanism of effect is likely to vary across adult and CYP populations.
Anxiety and depression: subgroup analyses
For the primary time point of post intervention, we explored whether or not effects observed in the NMA varied by mode of delivery, facilitator and focus of the intervention. On balance, there was a lack of evidence of effect modification by facilitator or mode of delivery for any population or setting combination. There was weak evidence that interventions facilitated by MHPs may be more effective. There was some evidence to suggest that interventions focused on preventing anxiety had a larger effect on reducing self-reported symptoms of anxiety than those focused on both depression and anxiety, or depression alone, and that interventions focused on preventing depression had a larger effect on reducing symptoms of depression than those focused on both depression and anxiety, or anxiety alone. However, this was not a formal statistical comparison, and, owing to the absence of participant blinding, we cannot rule out possible Hawthorne effects. Therefore, we do not consider this as providing evidence for, or against, the transdiagnostic hypothesis.
Anxiety and depression: additional primary and secondary outcomes
Additional primary and secondary outcomes were also analysed for the primary time point. There was no evidence to suggest that primary or secondary educational setting-based interventions to prevent anxiety or depression improved well-being, reduced suicidal ideation or self-harm, improved academic attainment or improved parent reports of child mental disorder symptoms. Subgroup analyses to examine whether or not intervention effects varied according to SES suggested that interventions delivered in lower SES settings may be slightly less effective than those delivered in higher/mixed SES settings. However, this is based on low SES subgroups with a maximum of four studies, and these findings may not be considered reliable. We did not test for subgroup differences. As regards intervention acceptability, most studies reported that participants were satisfied with their intervention assignment and interventions were rated by the students as reasonably enjoyable. It is of note that only two studies reported the comparative or relative enjoyment across all intervention arms. In both studies, participants preferred the control interventions.
Conduct disorder
Owing to the diversity of interventions, outcome measures and time points reported by the conduct disorder studies, results were reported narratively. Five studies were included, of which three were judged as having an unclear risk of bias for random sequence generation and allocation concealment. One study was judged as having a low risk of bias for both domains, and one was judged to be at low risk of bias for randomisation and unclear risk for allocation concealment. No study reported the primary outcome of self-reported conduct disorder symptoms at post intervention. Instead, results from parent and teacher reports and secondary measures of externalising behaviours at post intervention were summarised. There was evidence from two studies of classroom-based interventions and one study of a multisystemic intervention that externalising behaviours were reduced post intervention. Evidence of a beneficial effect was mixed from two studies of multisystemic, multicomponent and multiphase interventions. In the short term (between 1 and 3 years), there was no evidence to support intervention effectiveness. However, both studies reported evidence over the longer term (5–20 years) of a beneficial effect of the interventions for preventing self-reported conduct disorder symptoms.
Interpretation of network meta-analysis results across all networks: post intervention
With regard to comparative effectiveness at the primary post-intervention time point, we conclude that there is weak statistical evidence to support the effectiveness of school-based anxiety and depression prevention interventions, that effect sizes are modest and the evidence is not robust. CBT-based interventions were the most commonly used across the networks analysed. Despite this, across most networks, there was only weak statistical evidence to suggest that CBT-based interventions may be effective. There was evidence from the universal secondary analyses that mindfulness/relaxation interventions are effective in preventing symptoms of anxiety, and evidence from the targeted secondary anxiety analyses that exercise is effective. However, we are cautious about the overinterpretation of these results because they are based on few studies (two and one, respectively), which were judged to be at unclear risk of bias. We note that there was also weak evidence from the universal secondary depression NMA that CBT + IPT is effective at preventing depressive symptoms. However, the three studies including a CBT + IPT intervention were also rated as having mostly unclear risk of bias.
The evidence base is not robust and further weakens the statistical findings. We note that the risk of bias for random sequence generation and allocation concealment was rated as unclear across most of the networks. Meta-epidemiological evidence suggests that, for subjective outcomes (such as self-rated anxiety or depression), inadequate or unclear allocation concealment exaggerates intervention effect estimates. 267 In the context of this review, the observed intervention-level effects are beneficial relative to control, but they are ‘small’. 268 The potential impact of selection bias on these effect estimates should be considered in their interpretation. Future work using bias-adjusted NMA could explore the likely impact further. 269
The possibility of non-reporting bias in the universal anxiety analyses, in particular, must be considered in the interpretation of the statistical findings. There was some evidence that small negative studies were absent from the anxiety analyses. Adjusting for these studies would probably further attenuate the modest effects observed.
The between-study heterogeneity was at least moderate in 9 of the 10 primary analyses, and mild to moderate in one. It is broadly accepted that statistical heterogeneity is inevitable in meta-analysis. 270 However, steps should be taken to minimise potential sources of heterogeneity in advance of analysis, for example by defining coherent review inclusion and exclusion criteria. This is because the extent of between-study heterogeneity has implications for the interpretation and generalisability of results. 43,103 To illustrate the difficulties heterogeneity causes for the decision-maker, we can consider a predictive interval. 271,272 A 95% prediction interval estimates where the true intervention effects are expected to lie in a new study, or if the intervention were to be rolled out to similar populations (as those included in the analysis). In the presence of heterogeneity, the prediction interval fully encapsulates the uncertainty in intervention effect and will be wider than the CI or CrI. For example, in the universal secondary anxiety analysis (see Chapter 4), the ‘best-bet’ intervention for preventing anxiety is CBT [SMD –0.15 (95% CrI –0.34 to 0.04) vs. usual curriculum]. However, the corresponding 95% prediction interval is–0.47 to 0.16. We can interpret this interval as the 95% range of true SMDs to be expected if we were to implement CBT in secondary schools. That is, having considered the heterogeneity in the existing evidence for a narrowly defined set of interventions, we cannot rule out the possibility that a real-world implementation of CBT to school children might be harmful. We note that the observed heterogeneity was not explained by the subgroup analyses or metaregression, adding to the uncertainty for decision-makers seeking to implement a disorder-specific preventative intervention.
Key findings of the economic evaluation
The body of evidence described in the review of economic evidence was small (six studies) and heterogeneous. The CMD addressed, intervention type and cost-effectiveness analyses differed across the studies identified in the review. It was, therefore, not possible to quantitatively synthesise the findings. Across the studies reviewed, multiple perspectives for the analyses were taken, leading to the resources included in the analyses also varying widely. The potential long-term costs associated with missing school (such as lifetime earning capacity) were not estimated in any of the studies. The two model-based analyses reviewed suggested that hypothetical interventions could be cost-effective in the Australian context. However, the trial-based analyses suggested that the interventions were unlikely to be cost-effective in the UK or the USA. For the one intervention that was potentially cost-effective in a high-risk subgroup at an interim point of the study, the effect had disappeared with longer-term follow-up. There was very little empirical costing evidence to inform decisions on the implementation of preventative interventions.
We developed a highly stylised, ‘indicative’ CBT intervention for a microcosting study based on a universal secondary school setting. Taking the perspective of a single secondary school budget, an estimated intervention cost of £43 per student was derived. Although there are several ways in which a ‘real-world’ CBT intervention may differ, the simplistic model provides an indication of the costs that might accrue to a school budget in the first year of implementation. We also considered the costs of including a psychoeducation component within a CBT intervention, on the basis of the component NMA effectiveness results. We estimated that the potential cost of incorporating a psychoeducation component in the indicative CBT intervention might represent approximately £14 per student. Adding a psychoeducation component increases intervention costs, but this may be offset by the slightly greater improvement in anxiety scores post intervention. However, there was only weak evidence for an improvement in symptoms of depression post intervention in universal secondary settings.
Chapter 10 Discussion
In this chapter, we place the findings summarised in the Chapter 9 in context, with reference to the existing literature, and we discuss the limitations of the study. The implications for practice and research are discussed and conclusions presented.
Comparison with other studies
Depression and anxiety
In placing the findings reported here in context, it may be informative to compare the effect sizes from the present analysis with those observed in psychotherapeutic meta-analyses for the treatment of childhood depression and anxiety. The most robust evidence observed in our primary analyses was in universal secondary settings, in which there was weak evidence of a small benefit for CBT-based interventions (anxiety: SMD –0.15, 95% CrI –0.34 to 0.04; depression: SMD –0.04, 95% CrI –0.16 to 0.07). This can be contrasted with the evidence for group CBT relative to treatment as usual, observed by Zhou et al. 273,274 from a NMA of psychotherapies for treatment of anxiety274 (SMD –0.84, 95% CI –1.47 to –0.21) and depression273 (SMD –0.32, 95% CI –0.60 to –0.08).
Our results are largely consistent with the findings from large-scale RCTs of school-based prevention of anxiety and depression. Twelve RCTs included in our NMA had sample sizes of > 1000 at baseline. 118,119,125,126,141,142,151,159,196,204,206,207 All were passive-controlled RCTs (in two studies the control was a waiting list, in two it was no intervention and in eight it was the usual curriculum). Eight of the 12 RCTs concluded that there was no evidence of an effect of the intervention on self-reported symptoms of anxiety and/or depression, of which five were at low risk of bias for both random sequence generation and allocation concealment (Table 21). We also compared our findings with those of 20 systematic reviews of RCTs published since 2005. A summary of the review characteristics is provided in Appendix 9. Reviews were identified via a combination of non-systematic scoping searches in MEDLINE, PsycInfo, EMBASE and Google Scholar. Nineteen concluded that there were beneficial effects of anxiety and depression prevention programmes for CYP. Most noted that effect sizes were small; however, some were interpreted as showing ‘significant reductions’,113 as ‘consequential’,275 of ‘practical relevance’276 or providing ‘strong support’111 for the effect of interventions. Only one review reported that ‘Results of the various programs . . . are not particularly positive . . . the effects (if there are any) are not sustained over time’. 277 Two reviews were more cautious in their interpretation of the small positive effects, noting that when preventative interventions were compared with an attention control, they ‘showed a sobering lack of effect’. 68,278 We consider possible reasons for the difference in our findings and those of some systematic reviews below.
| Study | Randomiseda (n) | Consent/baseline (n) | Risk of bias | Author reported that intervention was effective | |
|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | ||||
| Araya et al.118 2013 | 2512 | 2508 | Low | Unclear | ✗ |
| Calear et al.127 2016 | Not clear | 1767 | Low | Low | ✗ |
| Kindt et al.196 2014 | 1440 | 1343 | Low | Low | ✗ |
| Sawyer et al.204 2010 | 8873 | 5633 | Unclear | Low | ✗ |
| Sheffield et al.141 2006 | 2479 | 1226 | Low | Low | ✗ |
| Stallard et al.142 2013 | 5761 | 5030 | Low | Low | ✗ |
| Stallard et al.159 2014 | 1448 | 1362 | Low | Unclear | ✗ |
| Tak et al.207 2016 | 1390 | 1341 | Unclear | Low | ✗ |
| Aune and Stiles119 2009 | 2148 | 1748 | Unclear | Unclear | ✓ |
| Calear et al.125 2009 | NR | 1477 | Low | Low | ✓ |
| Gallegos126 2008 | 1070 | 1030 | Unclear | Unclear | ✓ |
| Spence et al.206 2003 | Not clear | 1500 | Unclear | Unclear | ✓ |
Confirmation and developer bias
Confirmation bias may explain the differing interpretations between the present study and previously published reviews. 279 There has been debate about whether systematic reviews should be carried out by those with no conflicts of interest or by subject experts, who are best placed to understand the nuances of study inclusion/exclusion and interpretation of findings. 280 In an empirical study in which subject experts and methodologists were shown the same meta-analysis, Panagiotou and Ioannidis281 observed that subject experts were more likely than methodologists to over-interpret the pooled effect from a meta-analysis. Furthermore, subject experts who had also published a ‘statistically significant’ study showing a positive intervention effect were even more likely to over-interpret findings and to overlook the importance of the between-study heterogeneity on the overall interpretation.
There was some evidence to suggest that preventative RCTs involving the original intervention developer(s) observed stronger intervention effects, although the mechanism was not clear. 282,283 For example, it is possible that implementation and fidelity to intervention are superior in developer-led trials. The impact of so-called ‘developer bias’ on systematic reviews is unknown; however, in the case of 14 of the 20 reviews we identified, the first or senior author was a researcher who subsequently developed/published a school-based RCT to prevent anxiety or depression. Owing to an increased emphasis on reducing research waste,284 it is increasingly common for intervention developers or triallists to first conduct a systematic review. Further research could consider the role of developer bias in systematic reviews.
Inclusion criteria and meta-analytic method
Differences in inclusion criteria should also be considered. We investigate whether or not there was a discrepancy between the studies included in the present review and the 20 reviews described above (see Appendix 9). Reviews for which there was a > 40% discrepancy were Horowitz and Garber285 (57%), Neil and Christensen111 (42%), Neil and Christensen112 (48%), Stice et al. 113 (46%) and Teubert276 (58%). For example, of the 30 studies included in Horowitz and Garber,285 only 13 were included in the present review. The main inclusion differences related to the earlier reviews having broader inclusion criteria, for example severity of symptoms;113,276 inclusion of interventions for children of divorce or alcoholics;113,285 and interventions to address situational (state) anxiety, such as test and public speaking276 or stress reduction. 111,112,276
The choice of meta-analytic method could be a further explanation for findings differing across reviews. Of the 14 reviews conducting a meta-analysis, 10 used a random-effects model, two used a fixed-effects model and two used an undefined model to estimate a pooled effect. Nine summarised intervention effects using Cohen’s d and nine using Hedges’ g. In the present review, we fitted both fixed- and random-effects models, but presented results from the random-effects models based on statistical evidence of heterogeneity. We summarised effects using Hedges’ g, which is observed to be less biased in the presence of small studies (i.e. < 20 participants). Durlak286 states that the Hedges’ g correction typically amounts to a 4% reduction in effect when the total sample size is 20 participants, and around 2% when the sample size is 50. In the present analysis, four studies had sample sizes of ≤ 20 participants, and 19 had sample sizes of ≤ 50. Therefore, the impact of the adjustments made by Hedges’ g is likely to be small.
There are several ways to estimate the SMD; here we used the (standardised) difference in mean change from baseline (also known as change score) and we standardised using the pooled baseline SD. A common alternative is to use the final values (also known as post-intervention score, or follow-up score). It is not clear which approach was taken in the previous meta-analyses. However, using final values may not be appropriate when randomisation is questionable or when there is baseline imbalance in factors that may interact with the outcome. For example, if participants randomised to the control arm have higher depression symptom scores at baseline than those in the active arm, one cannot confidently conclude that the final values reflect the effect of the intervention, rather than severity of initial illness. In such cases, using final values may overestimate the effect of an intervention. In addition, our analyses were conducted in a Bayesian framework, in contrast to all 20 previous reviews, which took a frequentist approach. In a Bayesian analysis, the uncertainty in all parameters is fully represented. In particular, it takes full account of uncertainty in the between-studies SD in a random-effects model. Frequentist methods typically assume that the between-studies SD is known with certainty; as a result, Bayesian CrIs tend to be wider than frequentist CIs for random-effects models. 287
Standard pairwise meta-analysis and network meta-analysis
A further difference between the present review and those described previously is that we separated intervention and control groups into their distinct types. We a priori identified four distinct control conditions: attention control, waiting list, no intervention and usual curriculum. This was based on the psychotherapeutic literature, in which it was established that control group choice contributes to differences in effect size estimate. 73,74 To explore the possible impact of this decision, we ran a simple analysis ‘lumping’ these control conditions to form a single comparator. To emulate previous analyses more closely, we also included psychoeducation and psychosupport conditions in the conflated ‘control’ condition. Primary and secondary settings were also combined, but we kept universal and targeted populations separate. We also ran a second analysis combining psychological interventions, to form a ‘psychological intervention versus control’-type analysis.
When control conditions were conflated, our results were consistent with previous reviews, that is intervention effects for CBT versus ‘control’ now indicated a beneficial effect of CBT in every network at post intervention (see Appendix 9). This suggests that previously observed beneficial effects may have been a consequence of differential control group effects being obscured by ‘lumping’. However, the impact of lumping control groups in meta-analyses of public mental health interventions should be explored further. Certainly, in the psychotherapeutic literature, the use of a waiting list has been called a ‘nocebo’73 and a technique ‘to prove your therapy is effective, even when it is not’. 74 Future preventative and public health trials should also consider the importance of control groups at the feasibility or pilot stages of development.
Conduct disorder
The preliminary signs of conduct problems often emerge during early childhood. As a result, school-based interventions specifically aimed at the prevention of conduct disorder have been implemented in primary school settings. In recent years, however, interventions for preventing conduct disorders have largely focused on parenting skills, in community or home settings (e.g. Family Check-up, Nurse Family Partnership, Triple P). 288 The 2013 NICE guidelines on recognition of, intervention for and management of conduct disorders among CYP289 included a review of classroom-based interventions for selective and indicated prevention of conduct disorders. Noting that only 53% of the eligible studies included sufficient data for inclusion in a meta-analysis, the NICE guidelines concluded that, for selective interventions, the mean teacher-rated antisocial behaviour in the intervention groups was SMD –0.43 (95% CI –0.96 to –0.09). However, it is unlikely that teachers could have been blinded to intervention allocation. Conversely, there was no evidence of an effect when rated by an external observer (SMD –0.43, 95% CI –0.96 to 0.09) or for parent-reported antisocial behaviour (SMD –0.13, 95% CI –0.39 to 0.13).
We found few reviews explicitly referring to the prevention of conduct disorder, and most were conducted in the 1990s. 290–294 Instead, authors have focused on the prevention of collections of behaviours associated with conduct disorder, for example interventions that aim to prevent multiple risk behaviours such as substance misuse, aggression and stealing. 295 For example, in an early review of the prevention of ODD and conduct disorder, Tremblay et al. 293 state:
To our surprise, we found no preventative interventions that met our selection criteria . . . We thus broadened the scope and selected studies with outcome measures related to CD [conduct disorder]/ODD symptoms including court recorded or self-report delinquency, self-, parent- or teacher-rated measures of aggressive externalising behaviour and observer measures of aversive behaviour in the classroom. We generally refer to these outcomes using the term Disruptive Behaviour Disorders.
Tremblay et al. 293
More recent reviews taking this broader approach for school settings, such as Park-Higgerson et al. ,296 suggest that there is no evidence of an effect for interventions reducing aggression and violence, compared with the control (effect size –0.09, 95% CI –0.23 to 0.05). 296 de Vries et al. 297 examined prevention programmes for adolescents showing early signs of antisocial and disruptive behaviour problems. For interventions in a school setting, there was no evidence of an effect relative to usual curriculum [β –0.19 (SE 0.33)]. However, in a 2018 Cochrane review84 of interventions to prevent multiple risk behaviours, a positive effect of universal school-based interventions to prevent a composite outcome of ‘anti-social behaviour and offending’ was observed (OR 0.81, 95% CI 0.66 to 0.98). 84 We note that studies contributing to such reviews may not even reference conduct or disruptive behaviour disorders in their aims or backgrounds. We return to the issue of defining conduct disorder subsequently, in the limitations section.
Strengths and limitations of the study
To the best of our knowledge, this is the first NMA of preventative mental health interventions and the first to review the comparative effectiveness of distinct psychological, educational and physical interventions in a single analysis for CYP.
Limitations relating to search strategy
There is growing interest in improving the efficiency of study identification in systematic reviews. 54,298–302 However, there is no consensus on the number of databases to search or for defining appropriate ‘stopping rules’ or abbreviated search strategies. 52,53 A limitation of the present study is, therefore, that we searched only four electronic health-related and psychology databases. The selection of databases was consistent with the Cochrane MECIR conduct standards for searching, and included reference list searching of published systematic reviews and scoping searches to inform the ‘stopping’ strategy. The electronic database searches retrieved all but two eligible studies previously included in published systematic reviews; neither of these contributed to the NMA. 188,303 The scoping searches of two educational databases (ERIC and BEI) did not identify any further eligible studies. However, the possibility that potentially eligible studies have been missed cannot be ruled out emphatically.
Limitations relating to inclusion criteria
The inclusion and exclusion criteria were specified to minimise the potential for between-study heterogeneity and to address the assumption of consistency for the NMA. This condition was satisfied in 8 of the 10 networks, with inconsistency being noted in the two tertiary/university-level analyses. Nevertheless, we consider the implications of the narrow inclusion criteria below.
Definition of disorder
To be eligible for inclusion in the present review, the explicit aim of a study had to be the prevention of anxiety, depression or conduct disorder. These might be considered as ‘disorder-specific’ prevention interventions, although, in practice, some sought to prevent both anxiety and depression. The focus of the present review was the prevention of anxiety, depression and conduct disorder, and not specific diagnostic subtypes of disorders. Although we did not exclude studies focusing on specific disorders (e.g. social anxiety), our preferred outcome was a total symptom score. This approach is consistent with a population health perspective,304 the existing trial literature and previous systematic reviews. Only one study119 focused on the prevention of a specific anxiety disorder (social anxiety), and none addressed the prevention of subtypes of depression or conduct disorder.
To reduce the risk of selective outcome reporting, studies were not selected on the basis of reported outcomes. That is, studies were not selected on the basis of whether or not they reported anxiety, depression or conduct disorder outcomes. Selective outcome reporting can occur when studies measure multiple outcomes but select only those that are ‘statistically significant’ for publication. In turn, this can cause bias in a body of evidence and overestimate the effect of interventions. Prospective trial registration and protocols reduce the likelihood of selective reporting; however, this was not made a mandatory requirement in medicine until 2008. We are not aware of a current similar requirement within psychological science. As noted in Chapter 9, only 32 of the 142 studies included in this review had protocols or trial registrations readily available. We therefore chose a conservative approach of including studies based on the stated intent of the trial, as written in the publication.
The decision to restrict inclusion to disorder-specific prevention interventions is likely to have had the biggest impact for the review of conduct disorder. Fairchild et al. 305 note that conduct disorder is a highly heterogeneous disorder and they state there are > 32,000 different symptom profiles that could lead to a diagnosis. Such clinical variation is likely to pose an even bigger problem for primary preventative studies with regard to defining a target population. Over the preceding 25 years (since the publication of the DSM-IV), clinical language has evolved and, in the present review, it was not easy to judge whether or not study authors were using the terms ‘problems’ and ‘disorders’ interchangeably. Again, in the absence of trial registrations and protocols, we chose a conservative approach and restricted to ‘disorders’. A related concern refers to our reliance on DSM-5 criteria and the decision to exclude neurodevelopmental and neurobiological conditions. In DSM-III, -IV and -IV Text Revision (spanning 1980–2012), conduct disorders were categorised together with ADHD under ‘Attention-deficit and disruptive behavior disorders’. In DSM-5,61 they were separated. Conduct disorders are now grouped under ‘Disruptive, Impulse-Control, and Conduct Disorders’ and ADHD is separately considered under the ‘Neurodevelopmental Disorders’ heading. It is not clear whether or not older studies considered ‘conduct disorder’ as a catch-all for ‘disruptive behaviour disorders’, which historically included ADHD. In a NMA of psychosocial interventions for the treatment of childhood disruptive behaviour disorders, Epstein et al. 306 conclude that future studies must more clearly identify the target population for intervention. We echo their conclusion here, for preventative interventions.
Intervention focus
To minimise potential between-study heterogeneity and to address the assumption of consistency for the NMA, we included a narrowly defined set of interventions. Unless it was clear that the aim of the intervention was to prevent anxiety, depression or conduct disorder, we excluded interventions focused on mental health promotion. Similarly, we excluded studies addressing the related constructs of social and emotional well-being and positive mental health. Here we followed the NAM’s definition of mental health promotion as interventions that ‘aim to enhance an individual’s ability to achieve developmentally appropriate tasks and a positive sense of self-esteem, mastery, well-being and social inclusion, and strengthen their ability to cope with adversity’. 27 Recent evidence has suggested that well-being is only weakly correlated (r = 0.2) with mental illness in children,64 raising doubts that interventions targeting one will necessarily affect the other. 63 However, some interventions may aim to address both prevention and promotion, for example the Aussie Optimism Program. 152 In such instances, we referred to trial registrations and protocols to inform our inclusion decision. However, given the absence of trial registrations or protocols, it was difficult to operationalise this distinction, and this is a limitation of the review.
In common with previously published systematic reviews that focused on disorder-specific prevention of anxiety, depression or conduct disorder,36–39,68 we did not include interventions that primarily addressed the prevention of substance use, bullying or stress, although these factors have been shown to be associated with later mental ill health. We also excluded classroom management and social and emotional learning interventions. Classroom management interventions use conditioning and reinforcement to encourage prosocial behaviours and reduce challenging behaviours in their classrooms (e.g. providing clear expectations and routines, stating clear rules and consequences, and consistently using praise and other rewards). Consequently, interventions such as the Good Behaviour Game were not included in our review. However, there is recent evidence that these interventions do affect general conduct outcomes for children and are cost-effective in a UK context. 307 This could be considered a limitation of the findings for conduct disorder.
Mental health is multifaceted, with biological and environmental factors contributing to the development of a disorder. A further limitation of this review is that the interventions included are largely ‘downstream’. That is, they are focused on changing an individual’s cognitions, emotions or mood, without addressing the wider ‘upstream’ social determinants of mental health or the complex adaptive systems in which interventions are implemented. 308 It is, therefore, important to situate our findings in the context that there are calls to reframe preventative mental health towards a broader dimensional approach309,310 and incorporate other perspectives, such as a developmental psychopathological perspective to prevention. 311 In psychology and psychiatry, this has manifested in calls for a ‘paradigm shift’ away from the categorical approach to diagnosing mental disorders (e.g. ICD and DSM). 312–314 In public health, the focus has shifted to whole-school, systemic interventions as a wider, structural approach to tackle the increasing prevalence of CYP with mental health problems. Whole-school interventions have shown promise for physical health outcomes83 and emotional well-being;315 however, there is limited evidence, to date, that they are effective in the prevention of CMDs. 83,316 The present review is limited by the absence of these perspectives; future work should be considered to evaluate the comparative effectiveness of such interventions.
Defining population
We followed the NAM’s intervention spectrum for mental disorders, which defines three populations: universal, selective and indicated. By definition, participants in universal interventions are included irrespective of diagnostic status; consequently, studies included in the universal analyses will have included CYP with diagnosed mental health conditions at baseline. As noted in Chapter 1, a definitive boundary between indicated prevention and early intervention (i.e. treatment) is difficult to draw. Our eligibility criteria sought to minimise the inclusion of CYP with clinical conditions in the ‘targeted’ analyses, but, in the absence of clearly defined scale cut-off points or diagnostic tests for anxiety, depression or conduct disorder, we relied on author descriptions of participants. As a result, we cannot rule out the possibility that some of the participants in the ‘targeted’ analyses may also have had clinically diagnosable conditions. Here we reflect that the distinction between indicated prevention and early intervention is a qualitative one and is likely to rest with the intent of the triallist. If the intent of a study is to decrease the likelihood of the onset of a mental disorder or decrease detectable, but subclinical, symptoms, it can be considered prevention. If the aim of the study is to reduce existing, clinically meaningful or diagnosed symptoms, it can be considered treatment.
The inclusion criteria meant that there were few studies of eligible university-based interventions. In the original protocol, we stated that the upper age limit for eligible studies was 25 years, which was intended to allow for follow-up time points. As described in Table 1, this was difficult to operationalise, and was modified to be ≤ 19 years at baseline. In turn, this limited the eligible university population and is likely to have excluded interventions specifically aimed at older undergraduate and postgraduate students. The inclusion criterion that the intervention should be educational setting based was also restrictive. In tertiary education institutions, many interventions were delivered in health-care settings (e.g. primary care, psychology clinics) or remotely, without supervision (e.g. via mobile phone, internet). As a comparison, a 2019 review with broader inclusion criteria included 62 studies of preventing anxiety and depression in university students. 317 This larger review concluded that the overall effect size was moderate (Hedges’ g 0.65, 95% CIs 0.57 to 0.73). In combination with the potential for inconsistency observed in the tertiary NMAs, the small number of included tertiary/university studies is a further limitation of the present review; therefore, we do not make inferences about the effect of interventions in that setting.
Limitations relating to outcomes
Although agreement between parent- and child-reported symptoms is typically low, multi-informant measures of mental disorder symptoms among CYP are often considered preferable to single report. 318–320 Therefore, it may be considered a limitation that our primary outcomes were only symptoms self-reported by CYP. Parent-reported child symptoms were included as a secondary outcome; however, only 12% of the anxiety and depression studies included a parent report. All studies included for the prevention of conduct disorder included a parent and/or teacher report. Self-reported outcomes may be at higher risk of performance bias than observer-rated outcomes owing to lack of blinding to intervention allocation. In trials of school-based interventions, however, it is also questionable whether or not parents and teachers can be successfully blinded. Furthermore, the outcome of interest for decision-makers wanting to reduce the burden of common mental disorders is likely to be clinical diagnosis or service use, not symptoms. Clinical diagnosis was infrequently reported for the anxiety and depression studies, but was reported for the longer-term follow-ups in the conduct disorder studies.
Other limitations
The typology of interventions was based on previous literature, piloting and discussion among our team. However, the use of the constant comparative method was time-consuming and, inevitably, subjective. We sought greater objectivity by one reviewer initially drawing up a list of components, which was refined by a second reviewer through discussion. The list was further reviewed by two additional members of the team. Their suggested modifications were piloted and a final classification scheme constructed. This scheme was then applied and further refined during data extraction, until no further components were identified (saturation). Relying on published papers also generated problems for classifying components. To ensure a consistent approach across all studies, we did not assume the presence of a component unless it was explicitly stated in the paper or confirmed via correspondence with the authors. Inevitably, the taxonomy reflects the narrow set of interventions on which it is based, and it may not generalise to other preventative mental health interventions, as a result of the inclusion and exclusion criteria adopted here. Owing to the subjectivity of classification and lack of a consistent format for reporting of intervention details, there is potential for component misclassification. 321 It is also of note that the classification scheme that we developed for anxiety and depression did not generalise to conduct disorder interventions. As a result, we do not claim this as a definitive taxonomy, but a contribution to the growing literature.
Few studies reported sufficient detail to judge how randomisation or allocation concealment had been conducted; consequently, the risk of bias for these domains are mostly judged to be unclear. Many studies also had short follow-up periods, and it was not always clear whether reported follow-up periods referred to post intervention or from baseline. Only 13% of studies of anxiety and depression prevention studies reported a follow-up of > 1 year, and 5% reported a follow-up of > 2 years. For conduct disorder, two studies reported longer-term follow-ups and both indicated strong evidence of an effect (although they were not cost-effective; see Chapter 8).
Implications for practice
In this review, we conclude that there is weak evidence to support the effectiveness of school-based anxiety, depression or conduct disorder prevention interventions, but that it is not robust evidence. The available economic evidence for a UK context suggests that school-based anxiety and depression prevention interventions are ‘highly unlikely’ to be cost-effective, compared with usual curriculum, especially when the usual curriculum already contains a personal, social and health education aspect. 261,322 For conduct disorder, the US-based Fast Track cost-effectiveness evaluation suggests that it is unlikely that such a comprehensive, multisystemic approach would be implemented in practice. 250,263,264
However, the policy environment in the UK has recently placed schools front and centre in the prevention, early detection and support of students with mental health needs. Therefore, schools and local authorities may need access to comprehensive and independent sources of information to ensure that they are not susceptible to exaggerated claims or ‘trends’ about what works for the mental health of CYP. 323,324 Examples of freely accessible, evidence-based repositories and services include Evidence for Impact325 and the Early Intervention Foundation. 326 However, bespoke evidence-based services could also be useful to support schools that have identified specific mental health needs, and could emulate those run by AskFuse327 for Public Health and the Avon and Wiltshire Mental Health Partnership NHS Trust’s BEST in Mental Health328 evidence service for treatment of mental disorders.
Local government, education authorities, schools and universities should be made aware that few studies have measured potential harms or side effects of the interventions. This may include explicit harms, social harms or equity harms. 329 For example, in our study, we observed weak evidence that depression and anxiety prevention interventions may be more beneficial in higher-income settings than in low-income settings. The opportunity cost of implementing a potentially harmful intervention (one that has the potential to increase symptoms) should be considered by those commissioning interventions. Lorenc and Oliver329 describe this as ‘the potential benefits which may be forgone as a result of committing resources to ineffective or less effective interventions’.
Implications for research
The following implications for research are described in priority order.
Although overall evidence was weak, and risk of bias was judged to be unclear, the component NMA provided evidence that CBT interventions including a psychoeducation component may be effective for the prevention of anxiety and depression in universal secondary settings. There was also evidence that exercise and mindfulness/relaxation interventions were effective for symptoms of anxiety in universal secondary settings, although this was not robust. In the light of these findings, a future RCT in a secondary school setting might consider a multiarm design comparing CBT with mindfulness/relaxation with an attention control. It may also be of interest to explore the impact of including an active exercise component. However, before progression to a RCT, further work is undoubtedly necessary to optimise the content of such an intervention,330 including exploring the mechanisms of action for psychoeducation components for CYP. Such work should be conducted in consultation with CYP. What is clear is that any future RCTs of preventative mental health interventions must be well designed and include an economic evaluation.
Further research on the importance of control conditions for all public health interventions should also be a priority. Until then, we echo Merry and Hetrick’s331 conclusions and suggest that RCTs of interventions to prevent CMDs should use an active control (attention control or alternative intervention) and that waiting list controls should be discouraged.
It has been suggested that intervention effects can emerge over a longer time period in public health. 332,333 However, the majority of studies included in this report reported a post-intervention time point only, and we are not able to confirm or refute this observation. For anxiety and depression, only 18 trials from the 137 included had outcomes available at > 12 months post intervention and only seven trials reported time points at > 24 months. Follow-up periods were longer for the conduct disorder studies, and the positive study-level findings from the 20-year follow-up of Fast Track247 suggest that school-based RCTs should plan for longer follow-up periods. The possibility of using data linkage could be considered as an adjunct or substitute for primary data collection where resources are a concern.
Future preventative intervention studies should also include measurements of potential harms and/or side effects. However, it is not clear from our review what harms or side effects should be measured, and further research on core outcome sets should consider this issue. 334 Consideration of prevention of common mental health disorders from a systems perspective335 may also help to identify such unintended consequences.
Finally, the reporting of basic methodological aspects of the included studies was inadequate and scientific journals should ensure that the Consolidated Standards of Reporting Trials (CONSORT) guidance,336 and its extension to Social and Psychological interventions,337 is fully adhered to. To improve reporting of intervention components, authors should be encouraged to complete TIDieR reporting guideline for complex interventions and comparator conditions. The work reported in this monograph contributes to the growing literature around components of mental health interventions. However, the field lacks consensus and future work should focus on agreeing a taxonomy for preventative mental health interventions and control conditions.
Conclusions
With regard to the comparative effectiveness of school-based anxiety, depression and conduct disorder prevention interventions, there is a lack of robust evidence that any one type of intervention can be preferred across all populations and settings. However, in making this statement, we reiterate that the present review specifically addressed prevention of clinically referenced disorders. These conclusions, therefore, relate to a narrowly defined set of largely ‘downstream’ interventions, which focus on changing an individual’s cognitions, emotions or behaviours, without addressing wider ‘upstream’ social determinants of mental health (e.g. SES) or the complex, adaptive systems in which interventions are implemented. 288
Acknowledgements
This work was undertaken with the support of DECIPHer, one of the UK Clinical Research Collaboration Public Health Centres of Excellence. We thank the ALPHA young people’s public input advisory group based in DECIPHer and the parents who attended the parenting PPI session in Bargoed, Wales.
Contributions of authors
Deborah M Caldwell (https://orcid.org/0000-0001-8014-7480) (Senior Lecturer in Public Health) co-conceived the project, co-led and contributed to the systematic review and components analysis, conducted intervention-level NMAs and drafted the report.
Sarah R Davies (https://orcid.org/0000-0003-1321-7826) (Deputy Managing Editor, Cochrane Developmental, Psychosocial and Learning Problems group) co-led and contributed to the systematic review and component analysis and commented on the draft report.
Joanna C Thorn (https://orcid.org/0000-0001-8962-2428) (Research Fellow) led the economic evaluation, drafted Chapter 8 and commented on report drafts.
Jennifer C Palmer (Senior Research Associate) and Paola Caro (PhD student) contributed to the systematic review and commented on report drafts.
Sarah E Hetrick (https://orcid.org/0000-0003-2532-0142) (Associate Professor of Youth Mental Health) co-conceived the project, contributed to the systematic review and components analysis, and commented on report drafts.
David Gunnell (https://orcid.org/0000-0002-0829-6470) (Professor of Epidemiology) co-conceived the project and commented on report drafts.
Sumayya Anwer (https://orcid.org/0000-0002-1740-0399) (Research Fellow) contributed to component-level NMAs.
José A López-López (https://orcid.org/0000-0002-9655-3616) (Lecturer in Psychological Methods) contributed to intervention-level NMAs and commented on the report.
Clare French (https://orcid.org/0000-0002-6943-7353) (Senior Research Associate) contributed to the systematic review and commented on the report.
Judi Kidger (https://orcid.org/0000-0002-1054-6758) (Senior Lecturer in Public Health) co-conceived the project, contributed to the components analysis and commented on the draft report.
Sarah Dawson (https://orcid.org/0000-0002-6682-063X) (Information Specialist) provided guidance on and executed the electronic database searches.
Rachel Churchill (https://orcid.org/0000-0002-1751-0512) (Professor in Evidence Synthesis) co-conceived the project and provided guidance and advice on project direction and the component analysis.
James Thomas (https://orcid.org/0000-0003-4805-4190) (Professor of Social Research and Policy) co-conceived the project and commented on the report.
Rona Campbell (https://orcid.org/0000-0002-1099-9319) (Professor of Public Health Research) co-conceived the project and commented on the report.
Nicky J Welton (Professor in Statistical and Health Economic Modelling) co-conceived the project, contributed to intervention-level NMAs, led component-level NMAs, supervised the economic evaluation, drafted sections of the report and provided comments on the report.
Publication
Caldwell DM, Davies SR, Hetrick SE, Palmer JC, Caro P, López-López JA, et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry 2019;6:1011–20.
Data-sharing statement
Requests for access to extracted study data should be addressed to the corresponding author. Intervention and component-level NMA WinBUGS code is available from https://research-information.bris.ac.uk/en/persons/deborah-m-caldwell/projects/ or by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Caldwell DM, Davies SR, Hetrick SE, Palmer JC, Caro P, López-López JA, et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry 2019;6:1011-20. https://doi.org/10.1016/S2215-0366(19)30403-1.
- World Health Organization . Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation 2017.
- NHS Digital . Mental Health of Children and Young People in England, 2017 [PAS] n.d. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2017/2017 (accessed 31 December 2019).
- Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet 2014;383:1404-11. https://doi.org/10.1016/S0140-6736(13)62116-9.
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet 2011;377:2093-102. https://doi.org/10.1016/S0140-6736(11)60512-6.
- Perkins A, Ridler J, Browes D, Peryer G, Notley C, Hackmann C. Experiencing mental health diagnosis: a systematic review of service user, clinician, and carer perspectives across clinical settings. Lancet Psychiatry 2018;5:747-64. https://doi.org/10.1016/S2215-0366(18)30095-6.
- Martínez-Hernáez A, DiGiacomo SM, Carceller-Maicas N, Correa-Urquiza M, Martorell-Poveda MA. Non-professional-help-seeking among young people with depression: a qualitative study. BMC Psychiatry 2014;14. https://doi.org/10.1186/1471-244X-14-124.
- Carrellas NW, Biederman J, Uchida M. How prevalent and morbid are subthreshold manifestations of major depression in adolescents? A literature review. J Affect Disord 2017;210:166-73. https://doi.org/10.1016/j.jad.2016.12.037.
- Cameron IM, Lawton K, Reid IC. Recognition and subsequent treatment of patients with sub-threshold symptoms of depression in primary care. J Affect Disord 2011;130:99-105. https://doi.org/10.1016/j.jad.2010.10.010.
- Kidger J, Heron J, Lewis G, Evans J, Gunnell D. Adolescent self-harm and suicidal thoughts in the ALSPAC cohort: a self-report survey in England. BMC Psychiatry 2012;12. https://doi.org/10.1186/1471-244X-12-69.
- National Collaborating Centre for Mental Health . Depression in Children and Young People: Identification and Management in Primary, Community and Secondary Care 2005.
- Champion KE, Mather M, Spring B, Kay-Lambkin F, Teesson M, Newton NC. Clustering of multiple risk behaviors among a sample of 18-year-old Australians and associations with mental health outcomes: a latent class analysis. Front Public Health 2018;6. https://doi.org/10.3389/fpubh.2018.00135.
- Pailing AN, Reniers RLEP. Depressive and socially anxious symptoms, psychosocial maturity, and risk perception: associations with risk-taking behaviour. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0202423.
- Bannink R, Broeren S, Heydelberg J, van’t Klooster E, Raat H. Depressive symptoms and clustering of risk behaviours among adolescents and young adults attending vocational education: a cross-sectional study. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1692-7.
- Finning K, Ford T, Moore DA, Ukoumunne OC. Emotional disorder and absence from school: findings from the 2004 British Child and Adolescent Mental Health Survey. Eur Child Adolesc Psychiatry 2020;29:187-98. https://doi.org/10.1007/s00787-019-01342-4.
- Finning K, Moore D, Ukoumunne OC, Danielsson-Waters E, Ford T. The association between child and adolescent emotional disorder and poor attendance at school: a systematic review protocol. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0523-6.
- Hagell A, Shah R, Viner R, Hargreaves D, Varnes L, Heys M. The Social Determinants of Young People’s Health: Identifying the Key Issues and Assessing How Young People Are Doing in the 2010s n.d. www.health.org.uk/publications/the-social-determinants-of-young-people%E2%80%99s-health (accessed 31 December 2019).
- Gutman LM, Joshi H, Parsonage M, Schoon I. Children of the New Century: Mental Health Findings from the Millennium Cohort Study n.d. www.centreformentalhealth.org.uk/sites/default/files/2018-09/newcentury.pdf (accessed 31 December 2019).
- Fergusson DM, Boden JM, Horwood LJ. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. Br J Psychiatry 2007;191:335-42. https://doi.org/10.1192/bjp.bp.107.036079.
- Bor W, Dean AJ, Najman J, Hayatbakhsh R. Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Aust N Z J Psychiatry 2014;48:606-16. https://doi.org/10.1177/0004867414533834.
- Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry 2015;56:370-93. https://doi.org/10.1111/jcpp.12372.
- Royal College of Psychiatrists . No Health Without Public Mental Health: The Case for Action. Position Statement PS4 2010 n.d. www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/position-statements/ps04_2010.pdf?sfvrsn=b7316b7_4 (accessed 31 December 2019).
- Rocha TB, Graeff-Martins AS, Kieling C, Rohde LA. Provision of mental healthcare for children and adolescents: a worldwide view. Curr Opin Psychiatry 2015;28:330-5. https://doi.org/10.1097/YCO.0000000000000169.
- Local Government Association . CAMHS – Facts and Figures n.d. www.local.gov.uk/about/campaigns/bright-futures/bright-futures-camhs/child-and-adolescent-mental-health-and (accessed 31 December 2019).
- Andrews G, Issakidis C, Sanderson K, Corry J, Lapsley H. Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry 2004;184:526-33. https://doi.org/10.1192/bjp.184.6.526.
- Mrazek PJ, Haggerty RJ. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academies Press; 1994.
- National Research Council and Institute of Medicine . Preventing Mental, Emotional, and Behavioral Disorders Among Young People Progress and Possibilities 2009.
- Arango C, Díaz-Caneja CM, McGorry PD, Rapoport J, Sommer IE, Vorstman JA, et al. Preventive strategies for mental health. Lancet Psychiatry 2018;5:591-604. https://doi.org/10.1016/S2215-0366(18)30057-9.
- Department of Health and Social Care, Department for Education . Transforming Children and Young People’s Mental Health Provision: A Green Paper n.d. www.gov.uk/government/consultations/transforming-children-and-young-peoples-mental-health-provision-a-green-paper (accessed 31 December 2019).
- Cabinet Office, Department of Health and Social Care . Advancing Our Health: Prevention in the 2020s n.d. www.gov.uk/government/consultations/advancing-our-health-prevention-in-the-2020s (accessed 31 December 2019).
- UK Government . School Leaving Age n.d. www.gov.uk/know-when-you-can-leave-school (accessed 31 December 2019).
- Department for Education . Schools, Pupils and Their Characteristics: January 2019 n.d. www.gov.uk/government/statistics/schools-pupils-and-their-characteristics-january-2019 (accessed 31 December 2019).
- Scottish Government Learning Directorate . Summary Statistics for Schools in Scotland No. 10: 2019 Edition n.d. www.gov.scot/publications/summary-statistics-schools-scotland-no-10-2019-edition/ (accessed 31 December 2019).
- Welsh Government StatsWales . Pupils Present on Census Day by Local Authority and Sector n.d. https://statswales.gov.wales/Catalogue/Education-and-Skills/Schools-and-Teachers/Schools-Census/Pupil-Level-Annual-School-Census/Pupils/pupilspresentcensusday-by-localauthorityregion-sector (accessed 31 December 2019).
- Department for Education Northern Ireland . School Enrolments – Northern Ireland Summary Data n.d. www.education-ni.gov.uk/publications/school-enrolments-northern-ireland-summary-data (accessed 31 December 2019).
- Werner-Seidler A, Perry Y, Calear AL, Newby JM, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev 2017;51:30-47. https://doi.org/10.1016/j.cpr.2016.10.005.
- Johnstone KM, Kemps E, Chen J. A meta-analysis of universal school-based prevention programs for anxiety and depression in children. Clin Child Fam Psychol Rev 2018;21:466-81. https://doi.org/10.1007/s10567-018-0266-5.
- Stockings EA, Degenhardt L, Dobbins T, Lee YY, Erskine HE, Whiteford HA, et al. Preventing depression and anxiety in young people: a review of the joint efficacy of universal, selective and indicated prevention. Psychol Med 2016;46:11-26. https://doi.org/10.1017/S0033291715001725.
- Rasing SPA, Creemers DHM, Janssens JMAM, Scholte RHJ. Depression and anxiety prevention based on cognitive behavioral therapy for at-risk adolescents: a meta-analytic review. Front Psychol 2017;8. https://doi.org/10.3389/fpsyg.2017.01066.
- Piquero AR, Jennings WG, Diamond B, Farrington DP, Tremblay RE, Welsh BC, et al. A meta-analysis update on the effects of early family/parent training programs on antisocial behavior and delinquency. J Exp Criminol 2016;12:229-48. https://doi.org/10.1007/s11292-016-9256-0.
- Wilson SJ, Lipsey MW. School-based interventions for aggressive and disruptive behavior: update of a meta-analysis. Am J Prev Med 2007;33:130-43. https://doi.org/10.1016/j.amepre.2007.04.011.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. https://doi.org/10.1136/bmj.327.7414.557.
- Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 2005;25:646-54. https://doi.org/10.1177/0272989X05282643.
- Caldwell DM, Welton NJ. Approaches for synthesising complex mental health interventions in meta-analysis. Evid Based Ment Health 2016;19:16-21. https://doi.org/10.1136/eb-2015-102275.
- Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005;331:897-900. https://doi.org/10.1136/bmj.331.7521.897.
- Welton NJ, Caldwell DM, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol 2009;169:1158-65. https://doi.org/10.1093/aje/kwp014.
- Higgins JPT, López-López JA, Becker BJ, Davies SR, Dawson S, Grimshaw JM, et al. Synthesising quantitative evidence in systematic reviews of complex health interventions. BMJ Global Health 2019;4. https://doi.org/10.1136/bmjgh-2018-000858.
- Melendez-Torres GJ, Bonell C, Thomas J. Emergent approaches to the meta-analysis of multiple heterogeneous complex interventions. BMC Med Res Methodol 2015;15. https://doi.org/10.1186/s12874-015-0040-z.
- Achana F, Hubbard S, Sutton A, Kendrick D, Cooper N. An exploration of synthesis methods in public health evaluations of interventions concludes that the use of modern statistical methods would be beneficial. J Clin Epidemiol 2014;67:376-90. https://doi.org/10.1016/j.jclinepi.2013.09.018.
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf MI, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019). n.d.
- Higgins JPT, Lasserson T, Chandler J, Tovey D, Thomas J, Flemyng E, et al. Methodological Expectations of Cochrane Intervention Reviews (MECIR) n.d. https://community.cochrane.org/mecir-manual (accessed 20 August 2020).
- Booth A. How much searching is enough? Comprehensive versus optimal retrieval for technology assessments. Int J Technol Assess Health Care 2010;26:431-5. https://doi.org/10.1017/S0266462310000966.
- Nussbaumer-Streit B, Klerings I, Wagner G, Heise TL, Dobrescu AI, Armijo-Olivo S, et al. Abbreviated literature searches were viable alternatives to comprehensive searches: a meta-epidemiological study. J Clin Epidemiol 2018;102:1-11. https://doi.org/10.1016/j.jclinepi.2018.05.022.
- Halladay CW, Trikalinos TA, Schmid IT, Schmid CH, Dahabreh IJ. Using data sources beyond PubMed has a modest impact on the results of systematic reviews of therapeutic interventions. J Clin Epidemiol 2015;68:1076-84. https://doi.org/10.1016/j.jclinepi.2014.12.017.
- DECIPHer . Advice Leading to Public Health Advancement: ALPHA – DECIPHer’s Research Advisory Group of Young People n.d. https://decipher.uk.net/public-health-improvement-research-networks-phirns/public-involvement-alpha/ (accessed 20 August 2020).
- The Parent Network Caerphilly County Borough . Why We Got Together n.d. www.parentcaer.org.uk/ (accessed 20 August 2020).
- Dias S, Ades AE, Welton NJ, Jansen JP, Sutton AJ. Network Meta Analysis for Decision-Making. Hoboken, NJ: John Wiley & Sons, Inc.; 2018.
- Jansen JP, Naci H. Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-159.
- Chaimani A, Caldwell DM, Li T, Higgins JPT, Salanti G, Higgins JPT, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019). n.d.
- Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods 2012;3:80-97. https://doi.org/10.1002/jrsm.1037.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition 2013. https://doi.org/10.1176/appi.books.9780890425596.
- The World Bank Group . World Bank Country and Lending Group n.d. https://datahelpdesk.worldbank.org/ (accessed 20 August 2020).
- Haworth CM, Carter K, Eley TC, Plomin R. Understanding the genetic and environmental specificity and overlap between well-being and internalizing symptoms in adolescence. Dev Sci 2017;20. https://doi.org/10.1111/desc.12376.
- Patalay P, Fitzsimons E. Correlates of mental illness and wellbeing in children: are they the same? Results from the UK Millennium Cohort Study. J Am Acad Child Adolesc Psychiatry 2016;55:771-83. https://doi.org/10.1016/j.jaac.2016.05.019.
- Clarke M, Williamson PR. Core outcome sets and systematic reviews. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0188-6.
- Farber G, Wolpert M, Kemmer D. Common Measures for Mental Health Science: Laying the Foundations. June 2020 n.d. https://wellcome.ac.uk/sites/default/files/CMB-and-CMA-July-2020-pdf.pdf (accessed 19 August 2020).
- Whelan J, Love P, Pettman T, Doyle J, Booth S, Smith E, et al. Cochrane update: predicting sustainability of intervention effects in public health evidence: identifying key elements to provide guidance. J Public Health 2014;36:347-51. https://doi.org/10.1093/pubmed/fdu027.
- Hetrick SE, Cox GR, Witt KG, Bir JJ, Merry SN. Cognitive behavioural therapy (CBT), third-wave CBT and interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. Cochrane Database Syst Rev 2016;8. https://doi.org/10.1002/14651858.CD003380.pub4.
- Barth J, Munder T, Gerger H, Nüesch E, Trelle S, Znoj H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLOS Med 2013;10. https://doi.org/10.1371/journal.pmed.1001454.
- Hunot V, Moore TH, Caldwell DM, Furukawa TA, Davies P, Jones H, et al. ‘Third wave’ cognitive and behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.CD008704.pub2.
- Shinohara K, Honyashiki M, Imai H, Hunot V, Caldwell DM, Davies P, et al. Behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.CD008696.pub2.
- Pompoli A, Furukawa TA, Efthimiou O, Imai H, Tajika A, Salanti G. Dismantling cognitive–behaviour therapy for panic disorder: a systematic review and component network meta-analysis. Psychol Med 2018;48:1945-53. https://doi.org/10.1017/S0033291717003919.
- Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H, et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatr Scand 2014;130:181-92. https://doi.org/10.1111/acps.12275.
- Cuijpers P, Cristea IA. How to prove that your therapy is effective, even when it is not: a guideline. Epidemiol Psychiatr Sci 2016;25:428-35. https://doi.org/10.1017/S2045796015000864.
- Sutcliffe K, Thomas J, Stokes G, Hinds K, Bangpan M. Intervention Component Analysis (ICA): a pragmatic approach for identifying the critical features of complex interventions. Syst Rev 2015;4. https://doi.org/10.1186/s13643-015-0126-z.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Hetrick SE, Bailey A, Rice SM, Simmons MB, McKenzie JE, Montague AE, et al. A qualitative analysis of the descriptions of cognitive behavioural therapy (CBT) tested in clinical trials of depressed young people. J Depress Anxiety 2015;4. https://doi.org/10.4172/2167-1044.1000172.
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive-behavioral treatment for depression. J Consult Clin Psychol 1996;64:295-304. https://doi.org/10.1037//0022-006x.64.2.295.
- Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Borenstein M, Hedges LV, Higgins JPT, Rothstein H. Introduction to Meta Analysis. Hoboken, NJ: John Wiley & Sons, Inc.; 2009.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]. The Cochrane Collaboration; 2011.
- López-López JA, Davies SR, Caldwell DM, Churchill R, Peters TJ, Tallon D, et al. The process and delivery of CBT for depression in adults: a systematic review and network meta-analysis. Psychol Med 2019;49:1937-47. https://doi.org/10.1017/S003329171900120X.
- Langford R, Bonell C, Jones H, Pouliou T, Murphy S, Waters E, et al. The World Health Organization’s Health Promoting Schools framework: a Cochrane systematic review and meta-analysis. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1360-y.
- MacArthur G, Caldwell DM, Redmore J, Watkins SH, Kipping R, White J, et al. Individual-, family-, and school-level interventions targeting multiple risk behaviours in young people. Cochrane Database Syst Rev 2018;10. https://doi.org/10.1002/14651858.CD009927.pub2.
- Arikpo D, Edet ES, Chibuzor MT, Odey F, Caldwell DM. Educational interventions for improving primary caregiver complementary feeding practices for children aged 24 months and under. Cochrane Database Syst Rev 2018;5. https://doi.org/10.1002/14651858.CD011768.pub2.
- Higgins JP, Whitehead A. Borrowing strength from external trials in a meta-analysis. Stat Med 1996;15:2733-49. https://doi.org/10.1002/(SICI)1097-0258(19961230)15:24<2733::AID-SIM562>3.0.CO;2-0.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013. Process and Methods [PMG9] n.d. www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 (accessed 20 August 2020).
- National Institute for Health and Care Excellence . Developing NICE Guidelines: The Manual. Process and Methods [PMG20] n.d. www.nice.org.uk/process/pmg20/chapter/introduction (accessed 20 August 2020).
- Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med 2013;159:130-7. https://doi.org/10.7326/0003-4819-159-2-201307160-00008.
- Mavridis D, Giannatsi M, Cipriani A, Salanti G. A primer on network meta-analysis with emphasis on mental health. Evid Based Ment Health 2015;18:40-6. https://doi.org/10.1136/eb-2015-102088.
- Leucht S, Chaimani A, Cipriani AS, Davis JM, Furukawa TA, Salanti G. Network meta-analyses should be the highest level of evidence in treatment guidelines. Eur Arch Psychiatry Clin Neurosci 2016;266:477-80. https://doi.org/10.1007/s00406-016-0715-4.
- Molloy GJ, Noone C, Caldwell D, Welton NJ, Newell J. Network meta-analysis in health psychology and behavioural medicine: a primer. Health Psychol Rev 2018;12:254-70. https://doi.org/10.1080/17437199.2018.1457449.
- Salanti G, Kavvoura FK, Ioannidis JP. Exploring the geometry of treatment networks. Ann Intern Med 2008;148:544-53. https://doi.org/10.7326/0003-4819-148-7-200804010-00011.
- Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, et al. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. J Abnorm Child Psychol 2008;36:187-206. https://doi.org/10.1007/s10802-007-9169-5.
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol 1998;107:216-27. https://doi.org/10.1037//0021-843x.107.2.216.
- Eaton NR, Rodriguez-Seijas C, Carragher N, Krueger RF. Transdiagnostic factors of psychopathology and substance use disorders: a review. Soc Psychiatry Psychiatr Epidemiol 2015;50:171-82. https://doi.org/10.1007/s00127-014-1001-2.
- Forbes MK, Tackett JL, Markon KE, Krueger RF. Beyond comorbidity: toward a dimensional and hierarchical approach to understanding psychopathology across the life span. Dev Psychopathol 2016;28:971-86. https://doi.org/10.1017/S0954579416000651.
- Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0076654.
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS – a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 2000;10:325-37. https://doi.org/10.1023/A:1008929526011.
- Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 2004;23:3105-24. https://doi.org/10.1002/sim.1875.
- Spiegelhalter DJ, Best NG, Carlin BP, van der Linde A. Bayesian measures of model complexity and fit. J R Statist Soc 2002;64:583-639. https://doi.org/10.1111/1467-9868.00353.
- Dias S, Sutton AJ, Welton NJ, Ades AE. Heterogeneity: Subgroups, Meta-Regression, Bias and Bias-Adjustment [Internet]. NICE DSU Technical Support Document No. 3. London: National Institute for Health and Care Excellence; 2012.
- Dias S, Sutton AJ, Welton NJ, Ades AE. Evidence synthesis for decision making 3: heterogeneity – subgroups, meta-regression, bias, and bias-adjustment. Med Decis Making 2013;33:618-40. https://doi.org/10.1177/0272989X13485157.
- Schünemann HJ, Vist GE, Higgins JPT, Santesso N, Deeks JJ, Glasziou P, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019) n.d. www.training.cochrane.org/handbook (accessed 31 December 2019).
- Sterne JA, Davey Smith G. Sifting the evidence – what’s wrong with significance tests?. BMJ 2001;322. https://doi.org/10.1136/bmj.322.7280.226.
- Kirkwood BR, Sterne JAC. Essential Medical Statistics. Hoboken, NJ: John Wiley & Sons, Inc.; 2003.
- Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019). n.d.
- Corrieri S, Heider D, Conrad I, Blume A, König HH, Riedel-Heller SG. School-based prevention programs for depression and anxiety in adolescence: a systematic review. Health Promot Int 2014;29:427-41. https://doi.org/10.1093/heapro/dat001.
- Calear AL, Christensen H. Systematic review of school-based prevention and early intervention programs for depression. J Adolesc 2010;33:429-38. https://doi.org/10.1016/j.adolescence.2009.07.004.
- Moreno-Peral P, Conejo-Cerón S, Rubio-Valera M, Fernández A, Navas-Campaña D, Rodríguez-Morejón A, et al. Effectiveness of psychological and/or educational interventions in the prevention of anxiety: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 2017;74:1021-9. https://doi.org/10.1001/jamapsychiatry.2017.2509.
- Neil AL, Christensen H. Australian school-based prevention and early intervention programs for anxiety and depression: a systematic review. Med J Aust 2007;186:305-8. https://doi.org/10.5694/j.1326-5377.2007.tb00906.x.
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin Psychol Rev 2009;29:208-15. https://doi.org/10.1016/j.cpr.2009.01.002.
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol 2009;77:486-503. https://doi.org/10.1037/a0015168.
- Fitzgerald A, Rawdon C, Dooley B. A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behav Res Ther 2016;84:1-8. https://doi.org/10.1016/j.brat.2016.06.003.
- Schoneveld EA, Malmberg M, Lichtwarck-Aschoff A, Verheijen GP, Engels RC, Granic I. A neurofeedback video game (MindLight) to prevent anxiety in children: a randomized controlled trial. Comput Hum Behav 2016;63:321-33. https://doi.org/10.1016/j.chb.2016.05.005.
- Schoneveld EA, Lichtwarck-Aschoff A, Granic I. Preventing childhood anxiety disorders: is an applied game as effective as a cognitive behavioral therapy-based program?. Prev Sci 2018;19:220-32. https://doi.org/10.1007/s11121-017-0843-8.
- Sportel BE, de Hullu E, de Jong PJ, Nauta MH. Cognitive bias modification versus CBT in reducing adolescent social anxiety: a randomized controlled trial. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0064355.
- Araya R, Fritsch R, Spears M, Rojas G, Martinez V, Barroilhet S, et al. School intervention to improve mental health of students in Santiago, Chile: a randomized clinical trial. JAMA Pediatr 2013;167:1004-10. https://doi.org/10.1001/jamapediatrics.2013.2361.
- Aune T, Stiles TC. Universal-based prevention of syndromal and subsyndromal social anxiety: a randomized controlled study. J Consult Clin Psychol 2009;77:867-79. https://doi.org/10.1037/a0015813.
- Baker SB, Butler JN. Effects of preventive cognitive self-instruction training on adolescent attitudes, experiences, and state anxiety. J Prim Prev 1984;5:17-26. https://doi.org/10.1007/BF01332030.
- Barrett P, Lock S, Farrell L. Developmental differences in universal preventive intervention for child anxiety. Clin Child Psychol Psychiatry 2005;10:539-55. https://doi.org/10.1177/1359104505056317.
- Bonhauser M, Fernandez G, Püschel K, Yañez F, Montero J, Thompson B, et al. Improving physical fitness and emotional well-being in adolescents of low socioeconomic status in Chile: results of a school-based controlled trial. Health Promot Int 2005;20:113-22. https://doi.org/10.1093/heapro/dah603.
- Britton WB, Lepp NE, Niles HF, Rocha T, Fisher NE, Gold JS. A randomized controlled pilot trial of classroom-based mindfulness meditation compared to an active control condition in sixth-grade children. J Sch Psychol 2014;52:263-78. https://doi.org/10.1016/j.jsp.2014.03.002.
- Burckhardt R, Manicavasagar V, Batterham PJ, Miller LM, Talbot E, Lum A. A web-based adolescent positive psychology program in schools: randomized controlled trial. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4329.
- Calear AL, Christensen H, Mackinnon A, Griffiths KM, O’Kearney R. The YouthMood Project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J Consult Clin Psychol 2009;77:1021-32. https://doi.org/10.1037/a0017391.
- Calear AL, Batterham PJ, Poyser CT, Mackinnon AJ, Griffiths KM, Christensen H. Cluster randomised controlled trial of the e-couch Anxiety and Worry program in schools. J Affect Disord 2016;196:210-17. https://doi.org/10.1016/j.jad.2016.02.049.
- Calear AL, Christensen H, Brewer J, Mackinnon A, Griffiths KM. A pilot randomized controlled trial of the e-couch anxiety and worry program in schools. Internet Interv 2016;6:1-5. https://doi.org/10.1016/j.invent.2016.08.003.
- Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, et al. School-based prevention of depression and anxiety symptoms in early adolescence: a pilot of a parent intervention component. School Psychol Q 2006;21:323-48. https://doi.org/10.1521/scpq.2006.21.3.323.
- Gucht K, Griffith JW, Hellemans R, Bockstaele M, Pascal-Claes F, Raes F. Acceptance and Commitment Therapy (ACT) for adolescents: outcomes of a large-sample, school-based, cluster-randomized controlled trial. Mindfulness 2017;8:408-16. https://doi.org/10.1007/s12671-016-0612-y.
- Hiebert BA, Kirby B, Jaknavorian A. School-based relaxation: attempting primary prevention. Can J Couns 1989;23:273-87.
- Hodas R. An investigation of the relationship between positive and negative mental health factors and academic performance among early adolescent girls. Diss Ab Int B Sci Eng 2016;76.
- Johnson C, Burke C, Brinkman S, Wade T. Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav Res Ther 2016;81:1-11. https://doi.org/10.1016/j.brat.2016.03.002.
- Johnson C, Burke C, Brinkman S, Wade T. A randomized controlled evaluation of a secondary school mindfulness program for early adolescents: do we have the recipe right yet?. Behav Res Ther 2017;99:37-46. https://doi.org/10.1016/j.brat.2017.09.001.
- Lock S, Barrett PM. A longitudinal study of developmental differences in universal preventive intervention for child anxiety. Behav Change 2003;20:183-99. https://doi.org/10.1375/bech.20.4.183.29383.
- Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study. Behav Change 2001;18:36-50. https://doi.org/10.1375/bech.18.1.36.
- Perry Y, Werner-Seidler A, Calear A, Mackinnon A, King C, Scott J, et al. Preventing depression in final year secondary students: school-based randomized controlled trial. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8241.
- Potek R. Mindfulness as a school-based prevention program and its effect on adolescent stress, anxiety and emotion regulation. Diss Abs Int B Sci Eng 2012;73.
- Roberts C, Kane R, Thomson H, Bishop B, Hart B. The prevention of depressive symptoms in rural school children: a randomized controlled trial. J Consult Clin Psychol 2003;71:622-8. https://doi.org/10.1037/0022-006x.71.3.622.
- Roberts CM, Kane R, Bishop B, Cross D, Fenton J, Hart B. The prevention of anxiety and depression in children from disadvantaged schools. Behav Res Ther 2010;48:68-73. https://doi.org/10.1016/j.brat.2009.09.002.
- Rodgers A, Dunsmuir S. A controlled evaluation of the ‘FRIENDS for Life’ emotional resiliency programme on overall anxiety levels, anxiety subtype levels and school adjustment. Child Adolesc Ment Health 2015;20:13-9. https://doi.org/10.1111/camh.12030.
- Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, et al. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol 2006;74:66-79. https://doi.org/10.1037/0022-006X.74.1.66.
- Stallard P, Phillips R, Montgomery AA, Spears M, Anderson R, Taylor J, et al. A cluster randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of classroom-based cognitive-behavioural therapy (CBT) in reducing symptoms of depression in high-risk adolescents. Health Technol Assess 2013;17. https://doi.org/10.3310/hta17470.
- Tomba E, Belaise C, Ottolini F, Ruini C, Bravi A, Albieri E, et al. Differential effects of well-being promoting and anxiety-management strategies in a non-clinical school setting. J Anxiety Disord 2010;24:326-33. https://doi.org/10.1016/j.janxdis.2010.01.005.
- Wong N, Kady L, Mewton L, Sunderland M, Andrews G. Preventing anxiety and depression in adolescents: a randomised controlled trial of two school-based internet-delivered cognitive behavioural therapy programmes. Internet Interv 2014;1:90-4. https://doi.org/10.1016/j.invent.2014.05.004.
- Ahlen J, Hursti T, Tanner L, Tokay Z, Ghaderi A. Prevention of anxiety and depression in Swedish school children: a cluster-randomized effectiveness study. Prev Sci 2018;19:147-58. https://doi.org/10.1007/s11121-017-0821-1.
- Attwood M, Meadows S, Stallard P, Richardson T. Universal and targeted computerised cognitive behavioural therapy (Think, Feel, Do) for emotional health in schools: results from two exploratory studies. Child Adolesc Ment Health 2012;17:173-8. https://doi.org/10.1111/j.1475-3588.2011.00627.x.
- Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: preliminary results from a universal school-based trial. Br J Clin Psychol 2001;40:399-410. https://doi.org/10.1348/014466501163887.
- Bouchard S, Gervais J, Gagnier N, Loranger C. Evaluation of a primary prevention program for anxiety disorders using story books with children aged 9–12 years. J Prim Prev 2013;34:345-58. https://doi.org/10.1007/s10935-013-0317-0.
- Collins S, Marks Woolfson L, Durkin K. Effects on coping skills and anxiety of a universal school-based mental health intervention delivered in Scottish primary schools. School Psychol Int 2014;35:85-100. https://doi.org/10.1177/0143034312469157.
- Essau CA, Conradt J, Sasagawa S, Ollendick TH. Prevention of anxiety symptoms in children: results from a universal school-based trial. Behav Ther 2012;43:450-64. https://doi.org/10.1016/j.beth.2011.08.003.
- Gallegos J. Preventing Childhood Anxiety and Depression: Testing the Effectiveness of a School-Based Program in Mexico 2008.
- Johnstone J, Rooney RM, Hassan S, Kane RT. Prevention of depression and anxiety symptoms in adolescents: 42 and 54 months follow-up of the Aussie Optimism Program-Positive Thinking Skills. Front Psychol 2014;5. https://doi.org/10.3389/fpsyg.2014.00364.
- Miller LD, Short C, Garland EJ, Clark S. The ABCs of CBT (cognitive behavior therapy): evidence-based approaches to child anxiety in public school settings. J Couns Dev 2010;88:432-9. https://doi.org/10.1002/j.1556-6678.2010.tb00043.x.
- Miller LD, Laye-Gindhu A, Liu Y, March JS, Thordarson DS, Garland EJ. Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behav Res Ther 2011;49:315-23. https://doi.org/10.1016/j.brat.2011.02.006.
- Pattison C, Lynd-Stevenson R. The prevention of depressive symptoms in children: the immediate and long-term outcomes of a school-based program. Behav Change 2001;18:92-102. https://doi.org/10.1375/bech.18.2.92.
- Pophillat E, Rooney RM, Nesa M, Davis MC, Baughman N, Hassan S, et al. Preventing internalizing problems in 6–8 year old children: a universal school-based program. Front Psychol 2016;7. https://doi.org/10.3389/fpsyg.2016.01928.
- Rooney R, Roberts C, Kane R, Pike L, Winsor A, White J, et al. The prevention of depression in 8- to 9-year-old children: a pilot study. Aust J Guidance Couns 2006;16:76-90. https://doi.org/10.1375/ajgc.16.1.76.
- Ruttledge R, Devitt E, Greene G, Mullany M, Charles E, Frehill J, et al. A randomised controlled trial of the FRIENDS for Life emotional resilience programme delivered by teachers in Irish primary schools. Educ Child Psychol 2016;33:69-8.
- Stallard P, Skryabina E, Taylor G, Phillips R, Daniels H, Anderson R, et al. Classroom-based cognitive behaviour therapy (FRIENDS): a cluster randomised controlled trial to Prevent Anxiety in Children through Education in Schools (PACES). Lancet Psychiatry 2014;1:185-92. https://doi.org/10.1016/S2215-0366(14)70244-5.
- Balle M, Tortella-Feliu M. Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety Stress Coping 2010;23:71-85. https://doi.org/10.1080/10615800802590652.
- Berry K, Hunt CJ. Evaluation of an intervention program for anxious adolescent boys who are bullied at school. J Adolesc Health 2009;45:376-82. https://doi.org/10.1016/j.jadohealth.2009.04.023.
- Cova F, Rincon P, Melipillan R. Evaluation of the efficacy of a prevention program for depression in female adolescents. Ter Psicol 2011;29:245-50. https://doi.org/10.4067/S0718-48082011000200011.
- Dobson KS, Hopkins JA, Fata L, Scherrer M, Allan LC. The prevention of depression and anxiety in a sample of high-risk adolescents: a randomized controlled trial. Can J Sch Psychol 2010;25:291-310. https://doi.org/10.1177/0829573510386449.
- Gaete J, Martinez V, Fritsch R, Rojas G, Montgomery AA, Araya R. Indicated school-based intervention to improve depressive symptoms among at risk Chilean adolescents: a randomized controlled trial. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0985-4.
- Gillham JE, Reivich KJ, Brunwasser SM, Freres DR, Chajon ND, Kash-Macdonald VM, et al. Evaluation of a group cognitive-behavioral depression prevention program for young adolescents: a randomized effectiveness trial. J Clin Child Adolesc Psychol 2012;41:621-39. https://doi.org/10.1080/15374416.2012.706517.
- Hunt C, Andrews G, Crino R, Erskine A, Sakashita C. Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Aust N Z J Psychiatry 2009;43:300-4. https://doi.org/10.1080/00048670902721152.
- Jordans MJ, Komproe IH, Tol WA, Kohrt BA, Luitel NP, Macy RD, et al. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial. J Child Psychol Psychiatry 2010;51:818-26. https://doi.org/10.1111/j.1469-7610.2010.02209.x.
- Kiselica MS, Baker SB, Thomas RN, Reedy S. Effects of stress inoculation training on anxiety, stress, and academic performance among adolescents. J Couns Psychol 1994;41:335-42. https://doi.org/10.1037/0022-0167.41.3.335.
- Owen H, Lanning W. The effects of three treatment methods upon anxiety and inappropriate attentional style among high school athletes. Int J Sport Psychol 1982;13:154-62.
- Peng S, Qi A, Yuan F. Experimental study on the effects of exercise prescription on the mental health of left-behind school children in rural areas. Rev Argent Clin Psicol 2015;24:267-76.
- Rice CL. Reducing anxiety in middle school and high school students: a comparison of cognitive–behavioral therapy and relaxation training approaches. Diss Ab Int A Humanit Soc Sci 2009;69.
- Scholten H, Malmberg M, Lobel A, Engels RC, Granic I. A randomized controlled trial to test the effectiveness of an immersive 3D video game for anxiety prevention among adolescents. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0147763.
- Topper M, Emmelkamp PM, Watkins E, Ehring T. Prevention of anxiety disorders and depression by targeting excessive worry and rumination in adolescents and young adults: a randomized controlled trial. Behav Res Ther 2017;90:123-36. https://doi.org/10.1016/j.brat.2016.12.015.
- Cooley-Strickland MR, Griffin RS, Darney D, Otte K, Ko J. Urban African American youth exposed to community violence: a school-based anxiety preventive intervention efficacy study. J Prev Interv Community 2011;39:149-66. https://doi.org/10.1080/10852352.2011.556573.
- Manassis K, Wilansky-Traynor P, Farzan N, Kleiman V, Parker K, Sanford M. The feelings club: randomized controlled evaluation of school-based CBT for anxious or depressive symptoms. Depress Anxiety 2010;27:945-52. https://doi.org/10.1002/da.20724.
- McLoone JK, Rapee RM. Comparison of an anxiety management program for children implemented at home and school: lessons learned. Sch Ment Health 2012;4:231-42. https://doi.org/10.1007/s12310-012-9088-7.
- Mifsud C, Rapee RM. Early intervention for childhood anxiety in a school setting: outcomes for an economically disadvantaged population. J Am Acad Child Adolesc Psychiatry 2005;44:996-1004. https://doi.org/10.1097/01.chi.0000173294.13441.87.
- Miller LD, Laye-Gindhu A, Bennett JL, Liu Y, Gold S, March JS, et al. An effectiveness study of a culturally enriched school-based CBT anxiety prevention program. J Clin Child Adolesc Psychol 2011;40:618-29. https://doi.org/10.1080/15374416.2011.581619.
- Simpson AT. The roles of self-regulation and coping in a preventative cognitive–behavioural intervention for school-age children at-risk for internalizing disorders. Diss Ab Int B Sci Eng 2008;69.
- Siu FYA. Internalizing problems among primary school children in Hong Kong: Prevalence and treatment. Diss Ab Int A Humanit Soc Sci 2008;69.
- Tokolahi E, Vandal AC, Kersten P, Pearson J, Hocking C. Cluster-randomised controlled trial of an occupational therapy intervention for children aged 11–13 years, designed to increase participation to prevent symptoms of mental illness. Child Adolesc Ment Health 2018;23:313-27. https://doi.org/10.1111/camh.12270.
- van Starrenburg ML, Kuijpers RC, Kleinjan M, Hutschemaekers GJ, Engels RC. Effectiveness of a cognitive behavioral therapy-based indicated prevention program for children with elevated anxiety levels: a randomized controlled trial. Prev Sci 2017;18:31-9. https://doi.org/10.1007/s11121-016-0725-5.
- Cui L, He F, Han Z, Yang R, Xiao J, Oei TP. A brief group cognitive–behavioral program for the prevention of depressive symptoms in Chinese college students. Int J Group Psychother 2016;66:291-307. https://doi.org/10.1080/00207284.2015.1111098.
- Ellis L, Campbell A, Sethi S, O’Dea B. Comparative randomized trial of an online cognitive–behavioral therapy program and an online support group for depression and anxiety. J Cyber Ther Rehabil 2011;4:461-7.
- Higgins DM. Preventing generalized anxiety disorder in an at-risk sample of college students: a brief cognitive–behavioral approach. Diss Ab Int B Sci Eng 2007;67.
- Seligman MEP, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prev Treat 1999;2. https://doi.org/10.1037//1522-3736.2.0008a.
- Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behav Res Ther 2007;45:1111-26. https://doi.org/10.1016/j.brat.2006.09.010.
- Liddle I, Macmillan S. Evaluating the FRIENDS programme in a Scottish setting. Educ Psychol Pract 2010;26:53-67. https://doi.org/10.1080/02667360903522785.
- Velásquez AM, López MA, Quiñonez N, Paba DP. Yoga for the prevention of depression, anxiety, and aggression and the promotion of socio-emotional competencies in school-aged children. Educ Res Eval 2015;21:407-21. https://doi.org/10.1080/13803611.2015.1111804.
- Barry M, Murphy M, O’Donovan H. Assessing the effectiveness of a cognitive behavioural group coaching intervention in reducing symptoms of depression among adolescent males in a school setting. Int Coach Psychol Rev 2017;12:101-9.
- Burckhardt R, Manicavasagar V, Batterham PJ, Hadzi-Pavlovic D. A randomized controlled trial of strong minds: a school-based mental health program combining acceptance and commitment therapy and positive psychology. J Sch Psychol 2016;57:41-52. https://doi.org/10.1016/j.jsp.2016.05.008.
- Chaplin TM, Gillham JE, Reivich K, Elkon AG, Samuels B, Freres DR, et al. Depression prevention for early adolescent girls: a pilot study of all girls versus co-ed groups. J Early Adolesc 2006;26:110-26. https://doi.org/10.1177/0272431605282655.
- Clarke GN, Hawkins W, Murphy M, Sheeber L. School-based primary prevention of depressive symptomatology in adolescents: findings from two studies. J Adolesc Res 1993;8:183-204. https://doi.org/10.1177/074355489382004.
- Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, et al. School-based prevention of depressive symptoms: a randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. J Consult Clin Psychol 2007;75:9-19. https://doi.org/10.1037/0022-006X.75.1.9.
- Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. J Consult Clin Psychol 2007;75:693-706. https://doi.org/10.1037/0022-006X.75.5.693.
- Kindt KC, Kleinjan M, Janssens JM, Scholte RH. Evaluation of a school-based depression prevention program among adolescents from low-income areas: a randomized controlled effectiveness trial. Int J Environ Res Public Health 2014;11:5273-93. https://doi.org/10.3390/ijerph110505273.
- Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. J Am Acad Child Adolesc Psychiatry 2004;43:538-47. https://doi.org/10.1097/00004583-200405000-00007.
- Pössel P, Horn AB, Groen G, Hautzinger M. School-based prevention of depressive symptoms in adolescents: a 6-month follow-up. J Am Acad Child Adolesc Psychiatry 2004;43:1003-10. https://doi.org/10.1097/01.chi.0000126975.56955.98.
- Pössel P, Adelson JL, Hautzinger M. A randomized trial to evaluate the course of effects of a program to prevent adolescent depressive symptoms over 12 months. Behav Res Ther 2011;49:838-51. https://doi.org/10.1016/j.brat.2011.09.010.
- Pössel P, Martin NC, Garber J, Hautzinger M. A randomized controlled trial of a cognitive–behavioral program for the prevention of depression in adolescents compared with nonspecific and no-intervention control conditions. J Couns Psychol 2013;60:432-8. https://doi.org/10.1037/a0032308.
- Raes F, Griffith JW, Van der Gucht K, Williams JMG. School-based prevention and reduction of depression in adolescents: a cluster-randomized controlled trial of a mindfulness group program. Mindfulness 2014;5:477-86. https://doi.org/10.1007/s12671-013-0202-1.
- Rivet-Duval E, Heriot S, Hunt C. Preventing adolescent depression in Mauritius: a universal school-based program. Child Adolesc Ment Health 2011;16:86-91. https://doi.org/10.1111/j.1475-3588.2010.00584.x.
- Rose K, Hawes DJ, Hunt CJ. Randomized controlled trial of a friendship skills intervention on adolescent depressive symptoms. J Consult Clin Psychol 2014;82:510-20. https://doi.org/10.1037/a0035827.
- Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: a randomised controlled study of the beyond blue schools research initiative. J Child Psychol Psychiatry 2010;51:199-20. https://doi.org/10.1111/j.1469-7610.2009.02136.x.
- Shatté AJ. Prevention of depressive symptoms in adolescents: issues of dissemination and mechanisms of change. Diss Ab Int B Sci Eng 1997;57.
- Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: an evaluation of the problem solving for life program. J Consult Clin Psychol 2003;71:3-13. https://doi.org/10.1037//0022-006x.71.1.3.
- Tak YR, Lichtwarck-Aschoff A, Gillham JE, Van Zundert RM, Engels RC. Universal school-based depression prevention ‘Op Volle Kracht’: a longitudinal cluster randomized controlled trial. J Abnorm Child Psychol 2016;44:949-61. https://doi.org/10.1007/s10802-015-0080-1.
- Cardemil EV, Reivich KJ, Beevers CG, Seligman ME, James J. The prevention of depressive symptoms in low-income, minority children: two-year follow-up. Behav Res Ther 2007;45:313-27. https://doi.org/10.1016/j.brat.2006.03.010.
- Gillham JE. Preventing depressive symptoms in school children. Diss Ab Int B Sci Eng 1995;55.
- Mendelson T, Greenberg MT, Dariotis JK, Gould LF, Rhoades BL, Leaf PJ. Feasibility and preliminary outcomes of a school-based mindfulness intervention for urban youth. J Abnorm Child Psychol 2010;38:985-94. https://doi.org/10.1007/s10802-010-9418-x.
- Quayle D, Dziurawiec S, Roberts C, Kane R, Ebsworthy G. The effect of an optimism and lifeskills program on depressive symptoms in preadolescence. Behav Change 2001;18:194-203. https://doi.org/10.1375/bech.18.4.194.
- Soffer AG. School-Based Social Skills Training to Reduce Children’s Depressive Symptomatology 2003.
- Arnarson EO, Craighead WE. Prevention of depression among Icelandic adolescents. Behav Res Ther 2009;47:577-85. https://doi.org/10.1016/j.brat.2009.03.011.
- Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry 1995;34:312-21. https://doi.org/10.1097/00004583-199503000-00016.
- Congleton AB. The Effect of a Cognitive–Behavioral Group Intervention on the Locus of Control, Attributional Style, and Depressive Symptoms of Middle School Students 1995.
- Fung J, Guo S, Jin J, Bear L, Lau A. A pilot randomized trial evaluating a school-based mindfulness intervention for ethnic minority youth. Mindfulness 2016;7:819-28. https://doi.org/10.1007/s12671-016-0519-7.
- Livheim F, Hayes L, Ghaderi A, Magnusdottir T, Högfeldt A, Rowse J, et al. The effectiveness of acceptance and commitment therapy for adolescent mental health: Swedish and Australian pilot outcomes. J Child Fam Stud 2015;24:1016-30. https://doi.org/10.1007/s10826-014-9912-9.
- McCarty CA, Violette HD, McCauley E. Feasibility of the positive thoughts and actions prevention program for middle schoolers at risk for depression. Depress Res Treat 2011;2011. https://doi.org/10.1155/2011/241386.
- McCarty CA, Violette HD, Duong MT, Cruz RA, McCauley E. A randomized trial of the Positive Thoughts and Action program for depression among early adolescents. J Clin Child Adolesc Psychol 2013;42:554-63. https://doi.org/10.1080/15374416.2013.782817.
- Noël LT, Rost K, Gromer J. Depression prevention among rural preadolescent girls: a randomized controlled trial. Sch Soc Work J 2013;38:1-18.
- Poppelaars M, Tak YR, Lichtwarck-Aschoff A, Engels RC, Lobel A, Merry SN, et al. A randomized controlled trial comparing two cognitive–behavioral programs for adolescent girls with subclinical depression: a school-based program (Op Volle Kracht) and a computerized program (SPARX). Behav Res Ther 2016;80:33-42. https://doi.org/10.1016/j.brat.2016.03.005.
- Puskar K, Sereika S, Tusaie-Mumford K. Effect of the Teaching Kids to Cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs 2003;16:71-80. https://doi.org/10.1111/j.1744-6171.2003.tb00350.x.
- Rohde P, Stice E, Shaw H, Brière FN. Indicated cognitive behavioral group depression prevention compared to bibliotherapy and brochure control: acute effects of an effectiveness trial with adolescents. J Consult Clin Psychol 2014;82:65-74. https://doi.org/10.1037/a0034640.
- Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive–behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: a randomized efficacy trial. J Consult Clin Psychol 2008;76:595-606. https://doi.org/10.1037/a0012645.
- Stoppelbein LA. Primary prevention: an evaluation of a high-school based cognitive–behavioral program. Diss Ab Int B Sci Eng 2004;64.
- Wijnhoven LA, Creemers DH, Vermulst AA, Scholte RH, Engels RC. Randomized controlled trial testing the effectiveness of a depression prevention program (‘Op Volle Kracht’) among adolescent girls with elevated depressive symptoms. J Abnorm Child Psychol 2014;42:217-28. https://doi.org/10.1007/s10802-013-9773-5.
- Woods B, Jose P. Effectiveness of a school-based indicated early intervention program for Maori and Pacific adolescents. J Pac Rim Psychol 2011;5:40-5. https://doi.org/10.1375/prp.5.1.40.
- Young JF, Mufson L, Davies M. Efficacy of Interpersonal Psychotherapy-Adolescent Skills Training: an indicated preventive intervention for depression. J Child Psychol Psychiatry 2006;47:1254-62. https://doi.org/10.1111/j.1469-7610.2006.01667.x.
- Young JF, Mufson L, Gallop R. Preventing depression: a randomized trial of interpersonal psychotherapy-adolescent skills training. Depress Anxiety 2010;27:426-33. https://doi.org/10.1002/da.20664.
- Young JF, Benas JS, Schueler CM, Gallop R, Gillham JE, Mufson L. A randomized depression prevention trial comparing interpersonal psychotherapy – adolescent skills training to group counseling in schools. Prev Sci 2016;17:314-24. https://doi.org/10.1007/s11121-015-0620-5.
- Cowell JM, McNaughton D, Ailey S, Gross D, Fogg L. Clinical trial outcomes of the Mexican American Problem Solving program (MAPS). Hisp Health Care Int 2009;7:179-89. https://doi.org/10.1891/1540-4153.7.4.178.
- Jaycox LH, Reivich KJ, Gillham J, Seligman ME. Prevention of depressive symptoms in school children. Behav Res Ther 1994;32:801-16. https://doi.org/10.1016/0005-7967(94)90160-0.
- Reynolds EK, Macpherson L, Tull MT, Baruch DE, Lejuez CW. Integration of the brief behavioral activation treatment for depression (BATD) into a college orientation program: depression and alcohol outcomes. J Couns Psychol 2011;58:555-64. https://doi.org/10.1037/a0024634.
- Peden AR, Hall LA, Rayens MK, Beebe LL. Reducing negative thinking and depressive symptoms in college women. J Nurs Scholarsh 2000;32:145-51. https://doi.org/10.1111/j.1547-5069.2000.00145.x.
- Takagaki K, Okamoto Y, Jinnin R, Mori A, Nishiyama Y, Yamamura T, et al. Behavioral activation for late adolescents with subthreshold depression: a randomized controlled trial. Eur Child Adolesc Psychiatry 2016;25:1171-82. https://doi.org/10.1007/s00787-016-0842-5.
- McLaughlin C. Evaluating the effect of an empirically-supported group intervention for students at-risk for depression in a rural school district. Diss Ab Int B Sci Eng 2011;71.
- Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: an elusive search for a psychosocial placebo control condition. Behav Res Ther 2007;45:863-76. https://doi.org/10.1016/j.brat.2006.08.008.
- Yu L. Preventing depressive symptoms in Chinese children. Diss Abs Int B Sci Eng 2000;60.
- Khalsa SB, Hickey-Schultz L, Cohen D, Steiner N, Cope S. Evaluation of the mental health benefits of yoga in a secondary school: a preliminary randomized controlled trial. J Behav Health Serv Res 2012;39:80-9. https://doi.org/10.1007/s11414-011-9249-8.
- Roberts CM, Kane RT, Rooney RM, Pintabona Y, Baughman N, Hassan S, et al. Efficacy of the Aussie Optimism Program: promoting pro-social behavior and preventing suicidality in primary school students. A randomised-controlled trial. Front Psychol 2018;8. https://doi.org/10.3389/fpsyg.2017.01392.
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013;67:190-3. https://doi.org/10.1136/jech-2012-201257.
- Pahl KM, Barrett PM. Preventing anxiety and promoting social and emotional strength in preschool children: a universal evaluation of the Fun FRIENDS Program. Adv Sch Ment Health Promot 2010;3:14-25. https://doi.org/10.1080/1754730X.2010.9715683.
- Kyranides MN, Fanti KA, Katsimicha E, Georgiou G. Preventing conduct disorder and callous unemotional traits: preliminary results of a school based pilot training program. J Abnorm Child Psychol 2018;46:291-303. https://doi.org/10.1007/s10802-017-0273-x.
- August GJ, Hektner JM, Egan EA, Realmuto GM, Bloomquist ML. The early risers longitudinal prevention trial: examination of 3-year outcomes in aggressive children with intent-to-treat and as-intended analyses. Psychol Addict Behav 2002;16:S27-39. https://doi.org/10.1037/0893-164x.16.4s.s27.
- Baker-Henningham H, Scott S, Jones K, Walker S. Reducing child conduct problems and promoting social skills in a middle-income country: cluster randomised controlled trial. Br J Psychiatry 2012;201:101-8. https://doi.org/10.1192/bjp.bp.111.096834.
- Havighurst SS, Duncombe M, Frankling E, Holland K, Kehoe C, Stargatt R. An emotion-focused early intervention for children with emerging conduct problems. J Abnorm Child Psychol 2015;43:749-60. https://doi.org/10.1007/s10802-014-9944-z.
- The Conduct Problems Prevention Research Group . Initial impact of the Fast Track prevention trial for conduct problems: I. The high-risk sample. J Consult Clin Psychol 1999;67:631-47. https://doi.org/10.1037/0022-006X.67.5.631.
- Wilson DB. Practical Meta-Analysis Effect Size Calculator [Online Calculator] n.d. https://campbellcollaboration.org/research-resources/effect-size-calculator.html (accessed 1 December 2019).
- Conduct Problems Prevention Research Group . Using the Fast-Track randomized prevention trial to test the early-starter model of the development of serious conduct problems. Dev Psychopathol 2002;14:925-43. https://doi.org/10.1017/S0954579402004133.
- Foster EM. Costs and effectiveness of the fast track intervention for antisocial behavior. J Ment Health Policy Econ 2010;13:101-19.
- Battagliese G, Caccetta M, Luppino OI, Baglioni C, Cardi V, Mancini F, et al. Cognitive–behavioral therapy for externalizing disorders: a meta-analysis of treatment effectiveness. Behav Res Ther 2015;75:60-71. https://doi.org/10.1016/j.brat.2015.10.008.
- Atkinson LZ, Cipriani A. How to carry out a literature search for a systematic review: a practical guide. BJPsych Adv 2018;24:74-82. https://doi.org/10.1192/bja.2017.3.
- Martín-Martín A, Orduna-Malea E, Thelwall M, Delgado López-Cózar E. Google Scholar, Web of Science, and Scopus: a systematic comparison of citations in 252 subject categories. J Informetr 2018;12:1160-77. https://doi.org/10.1016/j.joi.2018.09.002.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8. https://doi.org/10.3310/hta8360.
- Organisation for Economic Co-operation and Development (OECD) . Purchasing Power Parities (PPP) n.d. https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm#indicator-chart (accessed 20 November 2019).
- Bank of England . Inflation Calculator n.d. www.bankofengland.co.uk/monetary-policy/inflation/inflation-calculator (accessed 20 November 2019).
- National Institute for Health and Care Excellence (NICE) . Common Mental Health Problems: Identification and Pathways to Care. Clinical Guideline [CG123] 2011.
- Lee YY, Barendregt JJ, Stockings EA, Ferrari AJ, Whiteford HA, Patton GA, et al. The population cost-effectiveness of delivering universal and indicated school-based interventions to prevent the onset of major depression among youth in Australia. Epidemiol Psychiatr Sci 2017;26:545-64. https://doi.org/10.1017/S2045796016000469.
- Mihalopoulos C, Vos T, Pirkis J, Carter R. The population cost-effectiveness of interventions designed to prevent childhood depression. Pediatrics 2012;129:e723-30. https://doi.org/10.1542/peds.2011-1823.
- Anderson R, Ukoumunne OC, Sayal K, Phillips R, Taylor JA, Spears M, et al. Cost-effectiveness of classroom-based cognitive behaviour therapy in reducing symptoms of depression in adolescents: a trial-based analysis. J Child Psychol Psychiatry 2014;55:1390-7. https://doi.org/10.1111/jcpp.12248.
- Stallard P, Skryabina E, Taylor G, Anderson R, Ukoumunne OC, Daniels H, et al. A cluster randomised controlled trial comparing the effectiveness and cost-effectiveness of a school-based cognitive-behavioural therapy programme (FRIENDS) in the reduction of anxiety and improvement in mood in children aged 9/10 years. Public Health Res 2015;3. https://doi.org/10.3310/phr03140.
- Foster EM, Jones D. Conduct Problems Prevention Research Group . Can a costly intervention be cost-effective?: an analysis of violence prevention. Arch Gen Psychiatry 2006;63:1284-91. https://doi.org/10.1001/archpsyc.63.11.1284.
- Foster EM, Jones DE. The economic analysis of prevention: an illustration involving children’s behavior problems. J Ment Health Policy Econ 2007;10:165-75.
- Suhrcke M, Pillas D, Selai C. Social Cohesion for Mental Wellbeing Among Adolescents. Copenhagen: WHO Regional Office for Europe; 2008.
- Page MJ, Higgins JPT, Sterne JAC, Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019). n.d.
- Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 2008;336:601-5. https://doi.org/10.1136/bmj.39465.451748.AD.
- Schäfer T, Schwarz MA. The meaningfulness of effect sizes in psychological research: differences between sub-disciplines and the impact of potential biases. Front Psychol 2019;10. https://doi.org/10.3389/fpsyg.2019.00813.
- Dias S, Welton NJ, Marinho VCC, Salanti G, Higgins JPT, Ades AE. Estimation and adjustment of bias in randomized evidence by using mixed treatment comparison meta-analysis. J R 2010;173:613-29. https://doi.org/10.1111/j.1467-985X.2010.00639.x.
- Higgins JP. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 2008;37:1158-60. https://doi.org/10.1093/ije/dyn204.
- Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc 2009;172:137-59. https://doi.org/10.1111/j.1467-985X.2008.00552.x.
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342. https://doi.org/10.1136/bmj.d549.
- Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, et al. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: a systematic review and network meta-analysis. World Psychiatry 2015;14:207-22. https://doi.org/10.1002/wps.20217.
- Zhou X, Zhang Y, Furukawa TA, Cuijpers P, Pu J, Weisz JR, et al. Different types and acceptability of psychotherapies for acute anxiety disorders in children and adolescents: a network meta-analysis. JAMA Psychiatry 2019;76:41-50. https://doi.org/10.1001/jamapsychiatry.2018.3070.
- Waddell C, Hua JM, Garland OM, Peters RD, McEwan K. Preventing mental disorders in children: a systematic review to inform policy-making. Can J Public Health 2007;98:166-73. https://doi.org/10.1007/BF03403706.
- Teubert D. A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. J Anxiety Disord 2011;25:1046-59. https://doi.org/10.1016/j.janxdis.2011.07.001.
- Bernaras E, Jaureguizar J, Garaigordobil M. Child and adolescent depression: a review of theories, evaluation instruments, prevention programs, and treatments. Front Psychol 2019;10. https://doi.org/10.3389/fpsyg.2019.00543.
- Lawrence PJ, Rooke SM, Creswell C. Review: Prevention of anxiety among at-risk children and adolescents – a systematic review and meta-analysis. Child Adolesc Ment Health 2017;22:118-30. https://doi.org/10.1111/camh.12226.
- Gorman DM. ‘Everything works’: the need to address confirmation bias in evaluations of drug misuse prevention interventions for adolescents. Addiction 2015;110:1539-40. https://doi.org/10.1111/add.12954.
- Gøtzsche PC, Ioannidis JPA. Content area experts as authors: helpful or harmful for systematic reviews and meta-analyses?. BMJ 2012;345. https://doi.org/10.1136/bmj.e7031.
- Panagiotou OA, Ioannidis JP. Primary study authors of significant studies are more likely to believe that a strong association exists in a heterogeneous meta-analysis compared with methodologists. J Clin Epidemiol 2012;65:740-7. https://doi.org/10.1016/j.jclinepi.2012.01.008.
- Gorman DM, Conde E. Conflict of interest in the evaluation and dissemination of ‘model’ school-based drug and violence prevention programs. Eval Program Plann 2007;30:422-9. https://doi.org/10.1016/j.evalprogplan.2007.06.004.
- Holder H. Prevention programs in the 21st century: what we do not discuss in public. Addiction 2010;105:578-81. https://doi.org/10.1111/j.1360-0443.2009.02752.x.
- Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet 2009;374:86-9. https://doi.org/10.1016/S0140-6736(09)60329-9.
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol 2006;74:401-15. https://doi.org/10.1037/0022-006X.74.3.401.
- Durlak JA. How to select, calculate, and interpret effect sizes. J Pediatr Psychol 2009;34:917-28. https://doi.org/10.1093/jpepsy/jsp004.
- Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR. Bayesian methods in health technology assessment: a review. Health Technol Assess 2000;4. https://doi.org/10.3310/hta4380.
- Petitclerc A, Tremblay RE. Childhood disruptive behaviour disorders: review of their origin, development, and prevention. Can J Psychiatry 2009;54:222-31. https://doi.org/10.1177/070674370905400403.
- National Collaborating Centre for Mental Health . Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition, Intervention and Management. National Clinical Guideline Number 158 2013.
- Miller LS. Preventive interventions for conduct disorders: a review. Child Adolesc Psychiatr Clin N Am 1994;3:405-20. https://doi.org/10.1016/S1056-4993(18)30507-8.
- Boyle MH, Offord DR. Primary prevention of conduct disorder: issues and prospects. J Am Acad Child Adolesc Psychiatry 1990;29:227-33. https://doi.org/10.1097/00004583-199003000-00011.
- Kamps DM, Tankersley M. Prevention of behavioral and conduct disorders: trends and research issues. Behav Disord 1996;22:41-8. https://doi.org/10.1177/019874299602200103.
- Tremblay RE, LeMarquand D, Vitaro F, Quay HC, Hogan AE. Handbook of Disruptive Behavior Disorders. New York, NY: Springer Science+Business Media; 1999.
- Reid JB. Prevention of conduct disorder before and after school entry: relating interventions to developmental findings. Dev Psychopathol 1993;5:243-62. https://doi.org/10.1017/S0954579400004375.
- Wilson DB, Gottfredson DC, Najaka SS. School-based prevention of problem behaviors: a meta-analysis. J Quant Criminol 2001;17:247-72. https://doi.org/10.1023/A:1011050217296.
- Park-Higgerson HK, Perumean-Chaney SE, Bartolucci AA, Grimley DM, Singh KP. The evaluation of school-based violence prevention programs: a meta-analysis. J Sch Health 2008;78:465-79. https://doi.org/10.1111/j.1746-1561.2008.00332.x.
- de Vries SL, Hoeve M, Assink M, Stams GJ, Asscher JJ. Practitioner review: Effective ingredients of prevention programs for youth at risk of persistent juvenile delinquency – recommendations for clinical practice. J Child Psychol Psychiatry 2015;56:108-21. https://doi.org/10.1111/jcpp.12320.
- Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0644-y.
- Ross-White A, Godfrey C. Is there an optimum number needed to retrieve to justify inclusion of a database in a systematic review search?. Health Info Libr J 2017;34:217-24. https://doi.org/10.1111/hir.12185.
- Lorenzetti DL, Topfer LA, Dennett L, Clement F. Value of databases other than medline for rapid health technology assessments. Int J Technol Assess Health Care 2014;30:173-8. https://doi.org/10.1017/S0266462314000166.
- Shemilt I, Khan N, Park S, Thomas J. Use of cost-effectiveness analysis to compare the efficiency of study identification methods in systematic reviews. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0315-4.
- O’Mara-Eves A, Thomas J, McNaught J, Miwa M, Ananiadou S. Using text mining for study identification in systematic reviews: a systematic review of current approaches. Syst Rev 2015;4. https://doi.org/10.1186/2046-4053-4-5.
- Dadds MR, Roth JH. Prevention of anxiety disorders: results of a universal trial with young children. J Child Fam Stud 2008;17:320-35. https://doi.org/10.1007/s10826-007-9144-3.
- Rose G. Sick individuals and sick populations. Int J Epidemiol 1985;14:32-8. https://doi.org/10.1093/ije/14.1.32.
- Fairchild G, Hawes DJ, Frick PJ, Copeland WE, Odgers CL, Franke B, et al. Conduct disorder. Nat Rev Dis Primers 2019;5. https://doi.org/10.1038/s41572-019-0095-y.
- Epstein RA, Fonnesbeck C, Potter S, Rizzone KH, McPheeters M. Psychosocial interventions for child disruptive behaviors: a meta-analysis. Pediatrics 2015;136:947-60. https://doi.org/10.1542/peds.2015-2577.
- Ford T, Hayes R, Byford S, Edwards V, Fletcher M, Logan S, et al. Training teachers in classroom management to improve mental health in primary school children: the STARS cluster RCT. Public Health Res 2019;7. https://doi.org/10.3310/phr07060.
- Keshavarz N, Nutbeam D, Rowling L, Khavarpour F. Schools as social complex adaptive systems: a new way to understand the challenges of introducing the health promoting schools concept. Soc Sci Med 2010;70:1467-74. https://doi.org/10.1016/j.socscimed.2010.01.034.
- Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018;392:1553-98. https://doi.org/10.1016/S0140-6736(18)31612-X.
- Shah JL, Scott J, McGorry PD, Cross SPM, Keshavan MS, Nelson B, et al. Transdiagnostic clinical staging in youth mental health: a first international consensus statement. World Psychiatry 2020;19:233-42. https://doi.org/10.1002/wps.20745.
- Ialongo NS, Rogosch FA, Cicchetti D, Toth SL, Buckley J, Petras H, et al. Developmental Psychopathology: Theory and Method, Volume 1. Hoboken, NJ: John Wiley & Sons, Inc.; 2006.
- Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, et al. A hierarchical taxonomy of psychopathology can transform mental health research. Perspect Psychol Sci 2019;14:419-36. https://doi.org/10.1177/1745691618810696.
- Kotov R, Krueger RF, Watson D. A paradigm shift in psychiatric classification: the Hierarchical Taxonomy Of Psychopathology (HiTOP). World Psychiatry 2018;17:24-5. https://doi.org/10.1002/wps.20478.
- Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry 2014;13:28-35. https://doi.org/10.1002/wps.20087.
- Goldberg JM, Sklad M, Elfrink TR, Schreurs KMG, Bohlmeijer ET, Clarke AM. Effectiveness of interventions adopting a whole school approach to enhancing social and emotional development: a meta-analysis. Eur J Psychol Educ 2019;34:755-82. https://doi.org/10.1007/s10212-018-0406-9.
- Kidger J, Araya R, Donovan J, Gunnell D. The effect of the school environment on the emotional health of adolescents: a systematic review. Pediatrics 2012;129:925-49. https://doi.org/10.1542/peds.2011-2248.
- Rith-Najarian LR, Boustani MM, Chorpita BF. A systematic review of prevention programs targeting depression, anxiety, and stress in university students. J Affect Disord 2019;257:568-84. https://doi.org/10.1016/j.jad.2019.06.035.
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull 1987;101:213-32. https://doi.org/10.1037/0033-2909.101.2.213.
- Sourander A, Helstelä L, Helenius H. Parent-adolescent agreement on emotional and behavioral problems. Soc Psychiatry Psychiatr Epidemiol 1999;34:657-63. https://doi.org/10.1007/s001270050189.
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull 2005;131:483-509. https://doi.org/10.1037/0033-2909.131.4.483.
- James A, Yavchitz A, Ravaud P, Boutron I. Node-making process in network meta-analysis of nonpharmacological treatment are poorly reported. J Clin Epidemiol 2018;97:95-102. https://doi.org/10.1016/j.jclinepi.2017.11.018.
- Stallard P, Sayal K, Phillips R, Taylor JA, Spears M, Anderson R, et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: pragmatic cluster randomised controlled trial. BMJ 2012;345. https://doi.org/10.1136/bmj.e6058.
- Sense about Science . Brain Gym n.d. https://archive.senseaboutscience.org/data/files/resources/55/braingym_final.pdf (accessed 31 December 2019).
- Macnamara B. Schools Are Buying ‘Growth Mindset’ Interventions Despite Scant Evidence That They Work Well n.d. https://theconversation.com/schools-are-buying-growth-mindset-interventions-despite-scant-evidence-that-they-work-well-96001 (accessed 31 December 2019).
- Evidence 4 Impact (E4I) . What Is Evidence 4 Impact? n.d. www.evidence4impact.org.uk/ (accessed 31 December 2019).
- Early Intervention Foundation . Early Intervention Foundation n.d. www.eif.org.uk/ (accessed 31 December 2019).
- Fuse: The Centre for Translational Research in Public Health . AskFuse n.d. www.fuse.ac.uk/askfuse/ (accessed 31 December 2019).
- Avon and Wiltshire Mental Health Partnership NHS Trust . About BEST n.d. http://best.awp.nhs.uk/about-best/ (accessed 31 December 2019).
- Lorenc T, Oliver K. Adverse effects of public health interventions: a conceptual framework. J Epidemiol Community Health 2014;68:288-90. https://doi.org/10.1136/jech-2013-203118.
- Collins LM, Baker TB, Mermelstein RJ, Piper ME, Jorenby DE, Smith SS, et al. The multiphase optimization strategy for engineering effective tobacco use interventions. Ann Behav Med 2011;41:208-26. https://doi.org/10.1007/s12160-010-9253-x.
- Merry S, Hetrick S. Prevention of depression and anxiety: is the whole better than the sum of the parts?. Evid Based Ment Health 2017;20. https://doi.org/10.1136/eb-2016-102425.
- Waters E, Doyle J, Jackson N, Howes F, Brunton G, Oakley A. Cochrane Collaboration . Evaluating the effectiveness of public health interventions: the role and activities of the Cochrane Collaboration. J Epidemiol Community Health 2006;60:285-9. https://doi.org/10.1136/jech.2003.015354.
- Walugembe DR, Sibbald S, Le Ber MJ, Kothari A. Sustainability of public health interventions: where are the gaps?. Health Res Policy Syst 2019;17. https://doi.org/10.1186/s12961-018-0405-y.
- National Institute for Health Research School for Public Health Research . Identifying and Validating a Core Public Mental Health Outcome Set n.d. https://sphr.nihr.ac.uk/research/public-mental-health/identifying-and-validating-a-core-public-mental-health-outcome-set-pmh-wp2/ (accessed 19 August 2020).
- Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, et al. The need for a complex systems model of evidence for public health. Lancet 2017;390:2602-4. https://doi.org/10.1016/S0140-6736(17)31267-9.
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c869.
- Grant S, Mayo-Wilson E, Montgomery P, Macdonald G, Michie S, Hopewell S, et al. CONSORT-SPI 2018 Explanation and Elaboration: Guidance for reporting social and psychological intervention trials. Trials 2018;19. https://doi.org/10.1186/s13063-018-2735-z.
- Dias S, Welton NJ, Sutton AJ, Ades AE. NICE DSU . Technical Support Document 2: A Generalised Linear Modelling Framework for Pairwise and Network Meta-Analysis of Randomised Controlled Trials. Report by the Decision Support Unit n.d. http://nicedsu.org.uk/wp-content/uploads/2017/05/TSD2-General-meta-analysis-corrected-2Sep2016v2.pdf (accessed 22 March 2021).
- Anticich SAJ, Barrett PM, Silverman W, Lacherez P, Gillies R. The prevention of childhood anxiety and promotion of resilience among preschool-aged children: a universal school-based trial. Adv Sch Ment Health Promot 2013;6:93-121. https://doi.org/10.1080/1754730X.2013.784616.
- Eather N, Morgan PJ, Lubans DR. Effects of exercise on mental health outcomes in adolescents: findings from the CrossFit™ teens randomized controlled trial. Psychol Sport Exerc 2016;26:14-23. https://doi.org/10.1016/j.psychsport.2016.05.008.
- Haden SC, Daly L, Hagins M. A randomised controlled trial comparing the impact of yoga and physical education on the emotional and behavioural functioning of middle school children. Focus Altern Complement Ther 2014;19:148-55. https://doi.org/10.1111/fct.12130.
- Department for Education . School Workforce in England: November 2018 n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/811622/SWFC_MainText.pdf (accessed 6 April 2021).
- HM Revenue and Customs . Rates and Thresholds for Employers 2018 to 2019 n.d. www.gov.uk/guidance/rates-and-thresholds-for-employers-2018-to-2019 (accessed 6 April 2021).
- Department for Education . Pension Grants for Schools, Local Authorities and Music Education Hubs n.d. www.gov.uk/government/publications/teachers-pension-employer-contribution-grant-tpecg/pension-grant-methodology (accessed 6 April 2021).
- Department for Education . School Teachers’ Pay and Conditions Document 2019 and Guidance on School Teachers’ Pay and Conditions n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832634/School_teachers_pay_and_conditions_2019.pdf (accessed 6 April 2021).
- Willis Palmer . Government Announces Mental Health Training for Teachers n.d. www.willispalmer.com/government-announces-mental-health-training-for-teachers/ (accessed 6 April 2021).
- Department for Education . Schools, Pupils and Their Characteristics: January 2018 n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/719226/Schools_Pupils_and_their_Characteristics_2018_Main_Text.pdf (accessed 6 April 2021).
- Fisak BJ, Richard D, Mann A. The prevention of child and adolescent anxiety: a meta-analytic review. Prev Sci 2011;12:255-68. https://doi.org/10.1007/s11121-011-0210-0.
- Ahlen J, Lenhard F, Ghaderi A. Universal prevention for anxiety and depressive symptoms in children: a meta-analysis of randomized and cluster-randomized trials. J Prim Prev 2015;36:387-403. https://doi.org/10.1007/s10935-015-0405-4.
- Brunwasser SM, Garber J. Programs for the prevention of youth depression: evaluation of efficacy, effectiveness, and readiness for dissemination. J Clin Child Adolesc Psychol 2016;45:763-83. https://doi.org/10.1080/15374416.2015.1020541.
- Waldron SM, Stallard P, Grist R, Hamilton-Giachritsis C. The ‘long-term’ effects of universal school-based anxiety prevention trials: a systematic review. Mental Health Prevent 2018;11:8-15. https://doi.org/10.1016/j.mhp.2018.04.003.
Appendix 1 Methods for systematic review and network meta-analysis
Decision rule for choosing between multiple-report scales
Decision rule for depression scales
-
Scores that combine depression and other symptoms will be excluded (e.g. scales that measure ‘internalising symptoms’ or combined anxiety and depression scores).
-
Choice between multiple scales:
-
use self-reports in preference to clinician-rated scales
-
use instruments with well-studied psychometric properties
-
use inventories aimed at paediatric populations in preference to inventories aimed at the general population
-
use instruments specifically targeted to measure depressive symptoms in preference to instruments with a broader scope
-
use most commonly reported scale across studies.
-
Decision rule for anxiety scales
-
Scores that combine anxiety and other symptoms will be excluded (e.g. total RCADS score would be excluded as it is a combined depression and anxiety score, whereas the RCADS total anxiety subscale score would be included in preference).
-
Use total anxiety scores when available:
-
If total anxiety score is not available but a generalised anxiety subscale score is available, we will use the subscale score. (For universal populations, we think that most interventions are likely to be targeting non-specific anxiety and are not sure what the importance of separation and social anxiety are. Furthermore, some other subscales, e.g. post-traumatic stress disorder, obsessive–compulsive disorder, are no longer considered anxiety disorders in the DSM-5.)
-
-
Choice between multiple scales:
-
use inventories of general symptoms in preference to instruments targeting specific anxiety domains.
-
if several inventories of general symptoms are available, use those aimed at the general population in preference to instruments aimed at identifying patients with anxiety disorders.
-
use most commonly reported scale across studies.
-
Search strategies used for each database
MEDLINE
Date range searched: inception to 4 April 2018.
Date searched: 4 April 2018.
Search strategy
-
CHILD, PRESCHOOL/or CHILD/or ADOLESCENT/or YOUNG ADULT/
-
(child* or boy* or girl* or kids or juvenil* or minors or paediatric* or pediatric* or adolesc* or preadolesc* or preadolesc* or pubert* or pubescen* or prepube* or prepube* or teen* or (young adj (adult* or people or patient* or men* or women* or male or female or survivor* or offender* or minorit*)) or youth* or student* or undergrad*).ti,ab,kf.
-
(child* or adolesc* or paediatr* or pediatr*).jn.
-
or/13
-
EDUCATION/
-
SCHOOLS/or SCHOOLS, NURSERY/
-
SCHOOL HEALTH SERVICES/or SCHOOL NURSING/
-
STUDENTS/or UNIVERSITIES/
-
(preschool or kindergarten or school* or college* or campus* or classroom* or curricul* or teacher or gatekeeper or pupil*).ti,ab,kf.
-
PEER GROUP/
-
((peer or peers) adj (education or group or relation* or support* or intervention* or leader*)).ti,ab,kf.
-
student* union.ti,ab,kf.
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) adj2 (camp or club or group)).ti,ab,kf.
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) adj based).ti,ab,kf.
-
or/5-14
-
ADAPTATION, PSYCHOLOGICAL/
-
EMOTIONS/
-
MENTAL HEALTH/
-
SOCIAL ADJUSTMENT/
-
exp STRESS, PSYCHOLOGICAL/
-
(mental health or mental* ill* or psychiatric).ti,ab,kf.
-
(wellbeing or well being).ti,ab,kf.
-
(stress* or distress*).ti,ab,kf.
-
or/16-23
-
DEPRESSION/
-
DEPRESSIVE DISORDER
-
MOOD DISORDERS
-
(depress* or dysthymi* or affective disorder* or affective symptom* or mood* or mental).ti.
-
(depress* adj2 (adolescent* or child* or anaclitic* or episode* or disorder or scale* or score* or symptom* or unipolar)).ti,ab,kf.
-
((depress*or mood* or mental or psychological or wellbeing or well being or emotion*) adj2 (improve* or onset or prevent* or reduc*)).ti,ab,kf.
-
((Axis 1 or Axis I) adj disorder*).ab.
-
or/25-31
-
exp ANXIETY DISORDERS/
-
ANXIETY/
-
anxi*.ti.
-
(anxi* adj3 (adolescent* or child* or disorder* or general* or interpersonal or separation or social*)).ti,ab,kf.
-
(phobi* or agoraphobi* or PTSD or post trauma* or posttrauma or panic* or OCD or obsess* or compulsi* or GAD or stress disorder* or stress reaction* or acute stress or neurosis or neuroses or neurotic or psychoneuro* or (school adj2 (refusal or avoid*)) or social avoidance or mutism).ti,ab,kf.
-
(((anxi* or fear or fright) adj3 (perform* or athlet* or music* or act* or test* or exam*)) or math* anxiety).ti,ab,kf.
-
(public adj3 (speak* or speech)).ti,ab,kf.
-
or/33-39
-
CONDUCT DISORDER/
-
CHILD BEHAVIOR DISORDERS/
-
JUVENILE DELINQUENCY/
-
SOCIAL BEHAVIOR/
-
SOCIAL BEHAVIOR DISORDERS/
-
((behavi* or conduct or personalit*) adj2 (agressi* or nonagressi* or antisocial or anti social or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internali#ing or externali#ing or problem*)).ti,ab,kf.
-
((conduct or behavi* or antisocial or anti social or dyssocial or emotional* or internali#ing or externali#ing) adj3 (problem* of difficult* or psychopathol*)).ti,ab,kf.
-
(oppositional adj3 (defiant* or disorder*)).ti,ab,kf.
-
or/41-48
-
PREVENTIVE HEALTH SERVICES/or “EARLY INTERVENTION (education)”/or HEALTH LITERACY/or PATIENT EDUCATION AS TOPIC/or HEALTH PROMOTION/or PRIMARY PREVENTION/or SECONDARY PREVENTION/
-
prevention & control.fs.
-
prevent*.ti,kf.
-
prevention of.ab,kf.
-
(prevent* adj2 (intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial)).ti,ab,kf.
-
((early or brief) adj intervention*).ti,ab,kf. 56 ((universal or targeted) adj2 (program* or intervention*)).ti,ab,kf.
-
(vulnerabl* or at risk or (risk adj2 reduc*)).ti,ab,kf.
-
RISK/or RISK FACTORS/
-
exp ACCIDENTS/
-
BEREAVEMENT/or GRIEF/
-
SOCIAL PROBLEMS/
-
BULLYING/
-
CHILD OF IMPAIRED PARENTS/
-
CHILD, ORPHANED/
-
CRIME VICTIMS/
-
exp DISASTERS/
-
DIVORCE/
-
LIFE CHANGE EVENTS/
-
RUNAWAY BEHAVIOR/
-
URBAN POPULATION/
-
RURAL POPULATION/
-
SURVIVORS/
-
VIOLENCE/
-
WARFARE/
-
social problems/or exp civil disorders/or exp crime/or exp human rights abuses/or exp parental death/or poverty/or exp social behavior disorders/or domestic violence/or exp child abuse/or exp ethnic violence/or physical abuse/or exp terrorism/or torture/or exposure to violence/or exp “warfare and armed conflicts”/
-
“dissent and disputes”/or family conflict/or psychosocial deprivation/
-
or/50-76
-
RANDOMIZED CONTROLLED TRIAL/or PRAGMATIC CLINICAL TRIAL/
-
Randomized Controlled Trial.pt.
-
(randomi#ed or randomi#ation).ab,ti,kf.
-
(RCT or (random* adj3 (administ* or allocat* or assign* or class* or cluster* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*))).ab.
-
at random.ab.
-
placebo.ab.
-
trial.ti,kf.
-
or/78-84
-
(treatmentasusual or (treatment* adj2 usual) or (standard adj2 care) or (standard adj2 treatment) or (routine adj2 care) or (usual adj2 medication*) or (usual adj2 care) or TAU).ti,ab,kf.
-
(waitlist* or waitlist* or waitinglist* or wait* list* or (waiting adj (condition or control)) or WLC).ti,ab,kf.
-
(((delay* adj3 (start or treatment*)) or no intervention or no treatment* or notreatment or non treatment* or nontreatment* or nontreatment or minim* treatment* or untreated group* or untreated control* or without any treatment) and (control* or group*)).ti,ab,kf.
-
((no intervention* or non intervention* or nonintervention* or without any intervention*) and (control* or group*)).ti,ab,kf.
-
or/86-89
-
85 or 90
-
4 and 15 and (24 or 32 or 40 or 49) and 77 and 91
-
((universal or indicated or targeted or at risk) and prevent* and (anxiety or depress* or conduct) and (child* or adolesc* or school*)).mp.
-
((prevent* adj (program* or intervention)) and (anxiety or depress* or conduct) and (child* or adolesc* or school*)).mp.
-
93 or 94.
PsycInfo
Date range searched: inception to 4 April 2018.
Date searched: 4 April 2018.
Search strategy
-
“3580”.cc. [= Classification Code: Educational/Vocational Counseling & Student Services]
-
exp school based intervention/
-
school*.ti.
-
or/1-3
-
(child* or boy* or girl* or kids or juvenil* or minors or paediatric* or pediatric* or adolesc* or preadolesc* or pre-adolesc* or pubert* or pubescen* or prepube* or pre-pube* or teen* or (young adj (adult* or people or patient* or men* or women* or male or female or survivor* or offender* or minorit*)) or youth* or student* or undergrad*).ti,ab,id.
-
pediatrics/
-
child psychiatry/or child psychopathology/or child psychology/
-
adolescent psychiatry/or adolescent psychopathology/or adolescent psychology/
-
child psychotherapy/or adolescent psychotherapy/
-
childhood development/or early childhood development/or adolescent development/
-
students.hw.
-
(“160” or “180” or “200” or “320”).ag. [= Age Group Field/Codes: preschool 2–5; school age 6–12; adolescence 13–17; young adulthood 18–29]
-
or/5-12
-
education/
-
education/or elementary education/or high school education/or higher education/or middle school education/or multicultural education/or nontraditional education/or preschool education/or private school education/or public school education/or secondary education/or special education/
-
schools/or academic settings/or boarding schools/or charter schools/or exp colleges/or elementary schools/or graduate schools/or high schools/or institutional schools/or junior high schools/or kindergartens/or middle schools/or nongraded schools/or nursery schools/
-
school environment/or college environment/
-
school facilities/or campuses/or classrooms/or “learning centers (educational)”/or school libraries/
-
community facilities/or community mental health centers/or exp libraries/
-
“summer camps (recreation)”/
-
curriculum/
-
exp extracurricular activities/or exp after school programs/
-
(preschool or nursery or kindergarten or school* or college* or university or universities or campus* or classroom* or curricul* or gatekeeper or pupil*).ti,ab,id.
-
peers/or peer counseling/or peer tutoring/
-
((peer or peers) adj (education or group or relation* or support* or intervention* or leader*)).ti,ab,id.
-
student* union.ti,ab,id.
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) adj3 (camp* or club*1 or group*1)).ti,ab,id.
-
((primary or secondary or tertiary) adj educat*).ti,ab,id.
-
((detention or refugee*) adj (camp*1 or centre*1 or center*1)).ti,ab,id.
-
or/14-29
-
“3300”.cc. [ = Classification Code: Health & Mental Health Treatment & Prevention]
-
primary mental health prevention/
-
mental health/or well being/
-
Stress/or Distress/
-
emotional adjustment/
-
“resilience (psychological)”/or coping behavior/or psychological stress/
-
*affective disorders/
-
major depression/or dysthymic disorder/or reactive depression/or “depression (emotion)”/
-
(depress* adj3 (adolescent* or infant* or child* or student* or anaclitic* or episode* or disorder or scale* or score* or symptom* or unipolar)).ti,ab,id.
-
((depress* or mood* or mental or psychological or wellbeing or well being or emotion*) adj3 (improve* or onset or prevent* or reduc*)).ti,ab,id.
-
(depress* or dysthymi* or affective disorder* or affective symptom* or mood* or mental).ti,id.
-
((axis 1 or axis I) adj disorder*).ti,ab,id.
-
exp anxiety/
-
anxiety disorders/or acute stress disorder/or death anxiety/or generalized anxiety disorder/or exp obsessive compulsive disorder/or panic disorder/or post-traumatic stress/or exp posttraumatic stress disorder/or separation anxiety disorder/
-
phobias/or acrophobia/or agoraphobia/or claustrophobia/or ophidiophobia/or school phobia/or social phobia/
-
fear/or panic/or panic attack/
-
(anxi* adj3 (adolescent* or child* or disorder* or general* or interpersonal or separation or social*)).ti,ab,id.
-
(phobi* or agoraphobi* or PTSD or post trauma* or posttrauma* or panic* or OCD or obsess* or compulsi* or GAD or stress disorder* or stress reaction* or acute stress or neurosis or neuroses or neurotic or psychoneuro* or (school adj3 (refusal or avoid*)) or social avoidance or mutism).ti,ab,id.
-
(((anxi* or fear or fright) adj3 (perform* or athlet* or music* or act* or test* or exam*)) or math* anxiety).ti,ab,id.
-
(public adj3 (speak* or speech)).ti,ab,id.
-
conduct disorder/or explosive disorder/or oppositional defiant disorder/
-
*behavior disorders/
-
exp juvenile delinquency/
-
exp antisocial behavior/
-
((behavi* or conduct or personalit*) adj3 (agressi* or nonagressi* or antisocial or anti social or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internalizing or externalizing or internalising or externalising or problem*)).ti,ab,id.
-
((conduct or behavi* or antisocial or anti social or dyssocial or emotional* or internalizing or externalizing or internalising or externalising) adj3 (problem* of difficult* or psychopathol*)).ti,ab,id.
-
(oppositional adj3 (defiant* or disorder*)).ti,ab,id.
-
or/33-57
-
early intervention/
-
“onset (disorders)”/
-
health promotion/or exp health education/or health knowledge/or health literacy/
-
mental health programs/
-
public health/
-
prevention/or preventive medicine/
-
“3365”.cc.
-
prevent*.ti,id.
-
prevention of.ab.
-
(prevent* adj3 (intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial)).ti,ab,id.
-
((early or brief) adj3 intervention*).ti,ab,id.
-
((universal or targeted) adj3 (program* or intervention*)).ti,ab,id.
-
(vulnerabl* or at risk or (risk adj3 reduc*)).ti,ab,id.
-
at risk populations/or predisposition/or risk factors/or “susceptibility (disorders)”/
-
orphans/or orphanages/
-
bullying/or conflict/or emotional abuse/or school violence/or teasing/or threat/or victimization/
-
school dropouts/
-
runaway behavior/
-
exp Crime Victims/
-
exp violent crime/
-
exp violence/
-
trauma/
-
rural environments/
-
urban environments/
-
exp neighborhoods/
-
exp social issues/
-
war/or conflict/
-
accidents/or exp disasters/
-
exp transportation accidents/
-
survivors/
-
bereavement/or grief/
-
divorce/or child custody/
-
parental death/or exp parental absence/
-
life changes/
-
child abuse/or abandonment/or child neglect/
-
family conflict/or domestic violence/or emotional abuse/
-
(bereave* or bullying or divorce or foster care or grief or humanitarian or orphan* or RTA or refugee* or survivor* or victim* or war).ti,ab,id.
-
(stigma or help seeking).ti,ab,id,hw.
-
or/59-96
-
treatment effectiveness evaluation.sh.
-
clinical trials.sh.
-
mental health program evaluation.sh.
-
placebo.sh.
-
randomi#ed.ti,ab.
-
(random* adj3 (administ* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab.
-
RCT.ab,id.
-
(waitlist* or wait-list* or waiting-list* or wait* list* or (waiting adj (condition or control)) or WLC).ti,ab,id.
-
placebo.ti,ab,id.
-
at random.ab.
-
((no intervention* or non intervention* or non-intervention* or without any intervention*) adj3 (control* or group*)).ti,ab,id.
-
(reference group or observation group or control group).ti,ab,id.
-
trial.ti.
-
or/98-110
-
(4 or (13 and 30)) and (31 or 58) and 97 and 111
-
(4 or (13 and 30)) and 32 and 111
-
4 and 58 and 111
-
or/112-114.
EMBASE
Date range searched: inception to 4 April 2018.
Date searched: 4 April 2018.
Search strategy
-
juvenile/or exp child/or exp adolescent/or young adult/
-
(child* or boy* or girl* or kids or juvenil* or minors or paediatric* or pediatric* or adolesc* or preadolesc* or preadolesc* or pubert* or pubescen* or prepube* or prepube* or teen* or (young adj (adult* or people or patient* or men* or women* or male or female or survivor* or offender* or minorit*)) or youth* or student* or undergrad*).ti,ab,kw.
-
(child* or adolesc* or paediatr* or pediatr*).jn.
-
or/1-3
-
school/or college/or community college/or high school/or kindergarten/or middle school/or nursery school/or primary school/or university/
-
education/or curriculum/or education program/or learning environment/or exp special education/
-
school health service/
-
exp student/
-
(preschool or kindergarten or school* or college* or campus* or classroom* or curricul* or teacher or gatekeeper or pupil*).ti,ab,kw.
-
peer group/
-
((peer or peers) adj (education or group or relation* or support* or intervention* or leader*)).ti,ab,kw.
-
student* union.ti,ab,kw.
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) adj2 (camp or club or group)).ti,ab,kw.
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) adj based).ti,ab,kw.
-
or/5-14
-
mental health/or community mental health/or psychological well being/
-
mental stress/or *stress/
-
(mental health or mental* ill* or psychiatric).ti,kw.
-
(wellbeing or well being).ti,kw.
-
(stress* or distress*).ti,kw.
-
*wellbeing/
-
or/16-21
-
depression/or dysthymia/or *major depression/or “mixed anxiety and depression”/
-
mood disorder/
-
mood/or *emotion/
-
(depress* or dysthymi* or affective disorder* or affective symptom* or mood* or mental).ti.
-
(depress* adj2 (adolescent* or child* or anaclitic* or episode* or disorder or scale* or score* or symptom* or unipolar)).ti,ab,kw.
-
((depress* or mood* or mental or psychological or wellbeing or well being or emotion*) adj2 (improve* or onset or prevent* or reduc*)).ti,ab,kw.
-
((Axis 1 or Axis I) adj disorder*).ab.
-
or/23-29
-
*anxiety/
-
exp anxiety disorder/
-
anxi*.ti.
-
(anxi* adj3 (adolescent* or child* or disorder* or general* or interpersonal or separation or social*)).ti,ab,kw.
-
(phobi* or agoraphobi* or PTSD or post trauma* or posttrauma or panic* or OCD or obsess* or compulsi* or GAD or stress disorder* or stress reaction* or acute stress or neurosis or neuroses or neurotic or psychoneuro* or (school adj2 (refusal or avoid*)) or social avoidance or mutism).ti,ab,kw.
-
(((anxi* or fear or fright) adj3 (perform* or athlet* or music* or act* or test* or exam*)) or math* anxiety).ti,ab,kw.
-
(public adj3 (speak* or speech)).ti,ab,kw.
-
or/31-37
-
conduct disorder/
-
*behavior disorder/
-
psychosocial disorder/
-
juvenile delinquency/or delinquency/
-
problem behavior/
-
*social adaptation/
-
((behavi* or conduct or personalit*) adj2 (agressi* or nonagressi* or antisocial or anti social or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internali#ing or externali#ing or problem*)).ti,ab,kw.
-
((conduct or behavi* or antisocial or anti social or dyssocial or emotional* or internali#ing or externali#ing) adj3 (problem* of difficult* or psychopathol*)).ti,ab,kw.
-
(oppositional adj3 (defiant* or disorder*)).ti,ab,kw.
-
oppositional defiant disorder/
-
or/39-48
-
Prevention/or Preventive Medicine/
-
Prophylaxis/
-
primary prevention/or secondary prevention/
-
health promotion/or health education/or health literacy/
-
pc.fs.
-
prevent*.ti,kw.
-
prevention of.ab.
-
(prevent* adj2 (intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial)).ti,ab,kw.
-
((early or brief) adj intervention*).ti,ab,kw.
-
((universal or targeted) adj2 (program* or intervention*)).ti,ab,kw.
-
(vulnerabl* or at risk or (risk adj2 reduc*)).ti,ab,kw.
-
risk/or risk factor/
-
risk of developing.ab.
-
exp “accidents and accident related phenomena”/
-
exp emotional deprivation/
-
exp grief/
-
social problem/or exp abuse/or bullying/or exp crime/or divorce/or exp human rights abuse/or exp social discrimination/or exp social exclusion/or exp violence/
-
orphaned child/
-
exp victim/
-
exp disaster/
-
life event/
-
coping behavior/or runaway behavior/
-
“population and population related phenomena”/or high risk population/or minority group/or rural population/or urban population/or vulnerable population/
-
exp survivor/
-
exp warfare/
-
conflict/or family conflict/
-
early intervention/
-
or/50-76
-
randomized controlled trial/
-
(randomi#ed or randomi#ation).ab,ti,kw.
-
(RCT or (random* adj3 (administ* or allocat* or assign* or class* or cluster* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*))).ab.
-
at random.ab.
-
trial.ti,kw.
-
or/78-82
-
4 and 15 and (22 or 30 or 38 or 49) and 77 and 83.
Cochrane Central Register of Controlled Trials
Date range searched: inception to 4 April 2018.
Date searched: 4 April 2018.
Search strategy
#1 MeSH descriptor: [Child] explode all trees
#2 MeSH descriptor: [Adolescent] this term only
#3 MeSH descriptor: [Young Adult] this term only
#4 (child* or boy* or girl* or kids or juvenil* or minors or paediatric* or pediatric* or adolesc* or preadolesc* or pre-adolesc* or pubert* or pubescen* or prepube* or pre-pube* or teen* or (young next (adult* or people or patient* or men* or women* or male or female or survivor* or offender* or minorit*)) or youth* or student* or undergrad*):ti,ab,kw (Word variations have been searched)
#5 child* or adolesc* or paediatr* or pediatr*:so
#6 (#1 or #2 or #3 or #4 or #5)
#7 MeSH descriptor: [Education] this term only
#8 MeSH descriptor: [Schools] this term only
#9 MeSH descriptor: [Schools, Nursery] this term only
#10 MeSH descriptor: [Students] this term only
#11 MeSH descriptor: [Universities] this term only
#12 (preschool or kindergarten or school* or college* or campus* or classroom* or curricul* or teacher or gatekeeper or pupil*):ti,ab,kw (Word variations have been searched)
#13 MeSH descriptor: [Peer Group] this term only
#14 ((peer or peers) next (education or group or relation* or support* or intervention* or leader*)):ti,ab,kw (Word variations have been searched)
#15 “student* union”:ti,ab,kw (Word variations have been searched)
#16 ((church or communit* or holiday* or religi* or spiritual* or youth or vacation) near/3 (camp or club or group)):ti,ab,kw (Word variations have been searched)
#17 ((church or communit* or holiday* or religi* or spiritual* or youth or vacation) near/3 based):ti,ab,kw (Word variations have been searched)
#18 university or universities:ti,ab,kw (Word variations have been searched)
#19 (primary or secondary or tertiary) next educat*:ti,ab,kw (Word variations have been searched)
#20 (#7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19)
#21 MeSH descriptor: [Depression] this term only
#22 MeSH descriptor: [Depressive Disorder] this term only
#23 MeSH descriptor: [Mood Disorders] this term only
#24 depress* or dysthymi* or affective disorder* or affective symptom* or mood* or mental:ti (Word variations have been searched)
#25 depress* near/3 (adolescent* or child* or anaclitic* or episode* or disorder or scale* or score* or symptom* or unipolar):ti,ab,kw (Word variations have been searched)
#26 ((depress* or mood* or mental or psychological or wellbeing or well being or emotion*) near/3 (improve* or onset or prevent* or reduc*)):ti,ab,kw
#27 (axis 1 or axis I) next disorder*
#28 MeSH descriptor: [Anxiety Disorders] explode all trees
#29 MeSH descriptor: [Anxiety] this term only
#30 MeSH descriptor: [Performance Anxiety] this term only
#31 (anxi* near/3 (adolescent* or child* or disorder* or general* or interpersonal or separation or social*))
#32 (phobi* or agoraphobi* or PTSD or post trauma* or posttrauma or panic* or OCD or obsess* or compulsi* or GAD or stress disorder* or stress reaction* or acute stress or neurosis or neuroses or neurotic or psychoneuro* or (school near/3 (refusal or avoid*)) or social avoidance or mutism)
#33 (((anxi* or fear or fright) near/3 (perform* or athlet* or music* or act* or test* or exam*)) or math* anxiety)
#34 (public near/3 (speak* or speech))
#35 MeSH descriptor: [Conduct Disorder] this term only
#36 MeSH descriptor: [Child Behavior Disorders] this term only
#37 MeSH descriptor: [Juvenile Delinquency] this term only
#38 MeSH descriptor: [Social Behavior] this term only
#39 MeSH descriptor: [Social Behavior Disorders] explode all trees
#40 ((behavi* or conduct or personalit*) near/3 (agressi* or nonagressi* or antisocial or anti social or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internalizing or externalizing or internalising or externalising or problem*))
#41 ((conduct or behavi* or antisocial or anti social or dyssocial or emotional* or internalizing or externalizing or internalising or externalising) adj3 (problem* of difficult* or psychopathol*))
#42 (oppositional near/3 (defiant* or disorder*))
#43 ((conduct disorder*) near/3 (onset or prevent*))
#44 MeSH descriptor: [Adaptation, Physiological] this term only
#45 MeSH descriptor: [Emotions] this term only
#46 MeSH descriptor: [Mental Health] this term only
#47 MeSH descriptor: [Social Adjustment] this term only
#48 MeSH descriptor: [Stress, Psychological] this term only
#49 (mental health or mental* ill* or psychiatric)
#50 (wellbeing or well-being or “well being”)
#51 stress* or distress*
#52 (#21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51)
#53 (#6 and #20 and #52) [Population + Setting + Condition] (n = 10686 Trials)
[Prevention/Risk Factors]
#54 MeSH descriptor: [Preventive Health Services] this term only
#55 MeSH descriptor: [Early Intervention (Education)] this term only
#56 MeSH descriptor: [Health Literacy] this term only
#57 MeSH descriptor: [Patient Education as Topic] this term only
#58 MeSH descriptor: [Health Promotion] this term only
#59 MeSH descriptor: [Primary Prevention] this term only
#60 MeSH descriptor: [Secondary Prevention] this term only
#61 prevent*:ti (Word variations have been searched)
#62 prevent*:kw (Word variations have been searched)
#63 “prevention of”
#64 (prevent* near/3 (intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial))
#65 ((early or brief) next intervention*)
#66 ((universal or targeted) near/3 (program* or intervention*))
#67 (vulnerabl* or “at risk” or (risk near/3 reduc*))
#68 MeSH descriptor: [Risk] explode all trees
#69 MeSH descriptor: [Accidents] explode all trees
#70 MeSH descriptor: [Bereavement] explode all trees
#71 MeSH descriptor: [Bullying] this term only
#72 MeSH descriptor: [Child of Impaired Parents] this term only
#73 MeSH descriptor: [Child, Orphaned] this term only
#74 MeSH descriptor: [Crime Victims] this term only
#75 MeSH descriptor: [Disasters] explode all trees
#76 MeSH descriptor: [Divorce] explode all trees
#77 MeSH descriptor: [Life Change Events] this term only
#78 MeSH descriptor: [Runaway Behavior] this term only
#79 MeSH descriptor: [Urban Population] this term only
#80 MeSH descriptor: [Rural Population] this term only
#81 MeSH descriptor: [Survivors] this term only
#82 MeSH descriptor: [Violence] explode all trees
#83 MeSH descriptor: [Warfare] explode all trees
#84 MeSH descriptor: [Family Conflict] this term only
#85 MeSH descriptor: [Psychosocial Deprivation] this term only
#86 MeSH descriptor: [Poverty] this term only
#87 (bereave* or bullying or divorce or foster care or grief or humanitarian or orphan* or RTA or refugee* or survivor* or victim* or war)
#88 (#54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 or #66 or #67 or #68 or #69 or #70 or #71 or #72 or #73 or #74 or #75 or #76 or #77 or #78 or #79 or #80 or #81 or #82 or #83 or #84 or #85 or #86 or #87 or #87)
#89 #53 and #88 [Population + Setting + Condition + Prevention/Risk Factors] (n = 3575)
#90 (#26 or #43) and #6 and #20 [(MH or Conduct Disorder Prevention) + Population + Setting] (n = 1273)
#91 #89 or #90.
Scoping searches of educational databases
Following our updated protocol, a scoping search of the ERIC was conducted. A simple search was conducted on 29 March 2018 and no further relevant studies were identified. On this basis, we considered the likely ‘law of diminishing returns’52 and determined that further formal literature searches would be increasingly unlikely to return further eligible citations. However, in response to reviewers’ comments on the draft version of this report, we conducted formal scoping searches on 11 April 2020 using the ERIC and BEI. The full search strategy is described subsequently. The total citations returned were 2570. One reviewer screened the titles and abstracts of a random 10% of the citations returned and 18 full texts were retrieved. Of these, eight studies were identified as eligible for inclusion in the review. However, all had been identified via the original search strategy and were previously included.
We used EBSCOhost databases to search the ERIC and BEI. The following search terms were used:
S26 S19 AND S25 (n = 2570)
S25 (S20 OR S21 OR S22 OR S23 OR S24) [Prevention/Promotion or Risk Factors]
S24 TI (orphan* or “school dropout*” or runaway* or “run away*” or bullying or conflict or abuse or abused or abandonment or “abandoned child*” or (child* N2 neglect*) or “foster care” or (parent* N2 absen*) or violence or teasing or threatened or victim* or crime or criminal or trauma or rural or urban or environment* or neighborhood* or neighbourhood* or “social issues” or poverty or war or accidents or RTA or humanitarian or refugee* or disaster* or survivor* or death or bereavement or grief or grieving or divorce or custody or stigma or “help seeking”) OR AB (orphan* or “school dropout*” or runaway* or “run away*” or bullying or conflict or abuse or abused or abandonment or “abandoned child*” or “child neglect” or “edge of care” or “foster care” or (parent* N2 absen*) or violence or teasing or threatened or victim* or crime or criminal or trauma or rural or urban or environment* or neighborhood* or neighbourhood* or “social issues” or poverty or war or accidents or RTA or humanitarian or refugee* or disaster* or survivor* or death or bereavement or grief or grieving or divorce or custody or stigma or “help seeking”)
S23 TI (vulnerabl* or “at risk” or (risk N3 reduc*)) or “risk population*” or predisposition or pre-disposition or “risk factor” or “susceptibility) OR AB (vulnerabl* or “at risk” or (risk N3 reduc*)) or “risk population*” or predisposition or pre-disposition or “risk factor” or “susceptibility)
S22 TI (intervention or ((universal or targeted) W3 (program* or intervention*))) OR AB ((universal or targeted) W3 (program* or intervention*)) OR SU Intervention
S21 TI (promot* or prevent*) OR AB (prevention OR (prevent* N3 (intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial)))
S20 TI (onset or ((early or brief) N3 intervention*) or “health promotion” or “health education” or “health knowledge” or “health literacy” or “mental health program*” or “public health”) OR AB (((early or brief) N3 (onset or intervention*)) or “health promotion” or “health education” or “health knowledge” or “health literacy” or “mental health program*” or “public health”)
S19 (S10 AND S18)
S18 (S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17) [RCT Filter]
S17 TI (trial) OR AB (trial)
S16 TI (placebo) OR AB (placebo)
S15 TI (“reference group” or “observation group” or “control group”) OR AB (“reference group” or “observation group” or “control group”)
S14 TI ((“no intervention*” or “non intervention*” or “without any intervention*”) and (control* or group*)) OR AB ((“no intervention*” or “non intervention*” or “without any intervention*”) and (control* or group*))
S13 TI (WLC or waitlist* or (wait* W2 (list or condition or control))) OR AB (WLC or waitlist* or (wait* W2 (list or condition or control)))
S12 TI (randomized or randomised or “at random” or RCT or (random* N3 (administ* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*))) OR AB (randomized or randomised or “at random” or RCT or (random* N3 (administ* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)))
S11 TI ((program* N3 (evaluat* or effectiveness))
S10 (S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9) [Depression/Anxiety/Conduct]
S9 TI ((behavi* or dyssocial or emotional* or internalizing or externalizing or internalising or externalising) N3 (problem* of difficult* or psychopathol*)) OR AB ((conduct or behavi* or antisocial or “anti social” or dyssocial or emotional* or internalizing or externalizing or internalising or externalising) N3 (problem* of difficult* or psychopathol*))
S8 TI ((behavi* or conduct or personalit*) N3 (agressi* or nonagressi* or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internalizing or externalizing or internalising or externalising or problem*)) OR AB ((behavi* or conduct or personalit*) N3 (agressi* or nonagressi* or antisocial or “anti social” or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internalizing or externalizing or internalising or externalising or problem*))
S7 TI (conduct or delinquen* or defiant or antisocial* or anti-social* or “explosive disorder*” or (behavio* W2 disorder*) OR AB (“conduct disorder*” or “explosive disorder*” or (oppositional W3 (defiant or disorder*)) or (behavio* W2 disorder*) or “juvenile delinquency” or “antisocial behavior”)
S6 TI (PTSD or “post-trauma*” or posttrauma* or “stress disorder*” or “stress reaction*” or “acute stress”) OR AB (PTSD or “post-trauma*” or posttrauma* or “stress disorder*” or “stress reaction*” or “acute stress”)
S5 TI (neurosis or neuroses or neurotic or psychoneuro* or (school N3 (refusal or avoid*)) or “social avoidance” or mutism) OR AB (neurosis or neuroses or neurotic or psychoneuro* or (school N3 (refusal or avoid*)) or “social avoidance” or mutism)
S4 TI (anxiety or GAD or fear or panic or phobi* or acrophobi* or agoraphobi* or claustrophobi* or ophidiophobi* or obsess* or compulsi or OCD) OR AB (anxiety or GAD or fear or panic or phobi* or acrophobi* or agoraphobi* or claustrophobi* or ophidiophobi* or obsess* or compulsi or OCD)
S3 TI ((affective W2 disorder*) or depressi* or depressed or dysthymi* or mood* or ((“axis 1” or “axis I”) W2 disorder*)) OR AB ((affective W2 disorder*) or depressi* or depressed or dysthymi* or mood* or ((“axis 1” or “axis I”) W2 disorder*))
S2 TI (distress or “psychological stress” or “psychological adjustment” or “emotional adjustment” or resilience or (coping N2 behavio*)) OR AB (“psychological distress” or “psychological stress” or “psychological adjustment” or “emotional adjustment” or (coping N2 behavio*))
S1 TI (mental* or psychological or wellbeing or “well being”) OR AB ((mental* or psychological) W2 (health* or wellbeing or “well being”).
Further statistical details for intervention-level and component-level network meta-analysis models
For each study i and arm k, the mean outcome is denoted by yi,k with SE sei,k. The baseline SD pooled across arms is sdi and Hedges’ g adjustment factor:
where ni,k is the number assessed in study i and arm k (i.e. complete cases).
The likelihood for the observed data is assumed to be normally distributed:
where θi,k is the standardised mean outcome for the intervention in arm k. The NMA model is put on the standardised mean scale so that intervention effects are SMDs.
We fitted three different NMA models that differed in the level of detail with which the intervention effects were modelled: (1) an intervention-level model, (2) an additive component model and (3) a full interaction component model. These three models are described subsequently. The models are fitted using a Bayesian Monte Carlo Markov chain approach evaluated in WinBUGS. WinBUGS code differed slightly for each population and outcome because of the evidence available for each of the possible intervention/component combinations.
Intervention-level network meta-analysis model
The intervention-level model is the standard NMA model,338 whereby the effect of each intervention is estimated as a ‘clinically meaningful’ unit. For example, here we estimate a CBT effect that is assumed to be the same regardless of the components comprising the CBT interventions. We describe a random-effects model because, although fixed-effects models were fitted, there was substantial heterogeneity, and so only results from random-effects models are presented. The standardised mean outcome for study i, arm k, is the sum of a standardised mean outcome on arm 1, µi, and a SMD, δi,k, for the intervention on arm k relative to the intervention on arm 1:
The random-effects NMA model assumes that the SMDs, δi,k, come from a common normal distribution with a mean that represents the appropriate SMD for the intervention comparison made, and a between-study SD, τ:
where Inti,k indicates the intervention on arm k of study i, and dk is the pooled estimate of intervention k. Flat normal priors are given to the µi and dk parameters, and a uniform(0,5) prior is given to τ. A standard correction is applied to incorporate correlations in the estimates from trials with three or more arms.
Additive component level (nested within interventions)
For a given intervention, the SMD comprises a sum of SMDs for the components that it includes (see Welton et al. 46). Equation 4 then becomes:
where Ci,k,j is an indicator for whether the intervention on arm k of study i contains component j (Ci,k,j = 1) or not (Ci,k,j = 0), and βk,j is the additional SMD for intervention k when component j is included. Flat normal priors are given to the βk,j parameters, and all other priors are as for the intervention-level model.
Note that, for the model to be identifiable, a reference combination of components is defined for each intervention, with SMD dk, and the regression coefficients βk,j are only estimated for additional components over and above the reference combination of components. For example, for universal interventions in the secondary population with anxiety as an outcome, all CBT interventions contain a cognitive and a behavioural component, and so this (cognitive + behavioural) forms the reference CBT intervention. Additional effects of psychoeducation, mindfulness and relaxation are estimated.
For some interventions, sets of components always co-occur, and so only a single regression coefficient can be estimated for the joint inclusion of components in that set. For example, for universal interventions in the secondary population with anxiety as an outcome, third-wave interventions were either with or without both mindfulness and relaxation components. Third-wave without any additional components, therefore, forms the reference intervention, and an additional effect is estimated for the addition of both mindfulness and relaxation components.
Full interaction component model (nested within interventions)
Equation 5 assumes that the inclusion of additional components has an additive effect, so that, for example, adding a psychoeducation component to a CBT intervention with cognitive and behavioural components has the same change in SMD as addition of a psychoeducation component to a CBT with cognitive, behavioural and relaxation components. The full interaction model46 relaxes this assumption and estimates a separate effect for each combination of components. Equation 5 then becomes:
where βk,c1,c2 is the additional SMD for intervention k when components are included as indicated by c1,c2. Flat normal priors are given to the βk,c1,c2 parameters, and all other priors are as for the intervention-level model.
Note that, as for the additive model, a reference combination of components is defined for each intervention, with SMD dk, and the regression coefficients βk,c1,c2 are estimated only for combinations of components that are different from the reference combination.
Code for the network meta-analysis components models
The code on which the component level models are based is available in Dias et al. 338 The adaptation to component-level NMA is based on WinBUGS code reported in Welton et al. 46
The WinBUGS code for all three models implemented in this report and an example dataset are available from https://research-information.bris.ac.uk/en/persons/deborah-m-caldwell/projects or by contacting the corresponding author.
Appendix 2 Results from systematic review
Primary reference for studies included in the review
This list of references provides the primary reference only for the studies included in the review.
Ahlen J, Hursti T, Tanner L, Tokay Z, Ghaderi A. Prevention of anxiety and depression in Swedish school children: a cluster-randomized effectiveness study. Prev Sci 2018;19:147–58. 145
Anticich SAJ, Barrett PM, Silverman W, Lacherez P, Gillies R. The prevention of childhood anxiety and promotion of resilience among preschool-aged children: a universal school-based trial. Adv Sch Ment Health Promot 2013;6:93–121. 339
Araya R, Fritsch R, Spears M, Rojas G, Martinez V, Barroilhet S, et al. School intervention to improve mental health of students in Santiago, Chile: a randomized clinical trial. JAMA Pediatr 2013;167:1004–10. 118
Attwood M, Meadows S, Stallard P, Richardson T. Universal and targeted computerised cognitive behavioural therapy (Think, Feel, Do) for emotional health in schools: results from two exploratory studies. Child Adolesc Ment Health 2012;17:173–8. 146
Aune T, Stiles TC. Universal-based prevention of syndromal and subsyndromal social anxiety: a randomized controlled study. J Consult Clin Psychol 2009;77:867–79. 119
Baker SB, Butler JN. Effects of preventive cognitive self-instruction training on adolescent attitudes, experiences, and state anxiety. J Prim Prev 1984;5:17–26. 120
Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: preliminary results from a universal school-based trial. Br J Clin Psychol 2001;40:399–410. 147
Barrett P, Lock S, Farrell L. Developmental differences in universal preventive intervention for child anxiety. Clin Child Psychol Psychiatry 2005;10:539–55. 121
Barry M, Murphy M, O’Donovan H. Assessing the effectiveness of a cognitive behavioural group coaching intervention in reducing symptoms of depression among adolescent males in a school setting. Int Coach Psychol Rev 2017;12:101–9. 190
Bonhauser M, Fernandez G, Püschel K, Yañez F, Montero J, Thompson B, Coronado G. Improving physical fitness and emotional well-being in adolescents of low socioeconomic status in Chile: results of a school-based controlled trial. Health Promot Int 2005;20:113–22. 122
Bouchard S, Gervais J, Gagnier N, Loranger C. Evaluation of a primary prevention program for anxiety disorders using story books with children aged 9–12 years. J Prim Prev 2013;34:345–58. 148
Britton WB, Lepp NE, Niles HF, Rocha T, Fisher NE, Gold JS. A randomized controlled pilot trial of classroom-based mindfulness meditation compared to an active control condition in sixth-grade children. J Sch Psychol 2014;52:263–78. 123
Burckhardt R, Manicavasagar V, Batterham PJ, Miller LM, Talbot E, Lum A. A web-based adolescent positive psychology program in schools: randomized controlled trial. J Med Internet Res 2015;17:e187. 124
Burckhardt R, Manicavasagar V, Batterham PJ, Hadzi-Pavlovic D. A randomized controlled trial of strong minds: a school-based mental health program combining acceptance and commitment therapy and positive psychology. J Sch Psychol 2016;57:41–52. 191
Calear AL, Christensen H, Mackinnon A, Griffiths KM, O’Kearney R. The YouthMood Project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J Consult Clin Psychol 2009;77:1021–32. 125
Calear AL, Batterham PJ, Poyser CT, Mackinnon AJ, Griffiths KM, Christensen H. Cluster randomised controlled trial of the e-couch Anxiety and Worry program in schools. J Affect Disord 2016;196:210–17. 126
Calear AL, Christensen H, Brewer J, Mackinnon A, Griffiths KM. A pilot randomized controlled trial of the e-couch anxiety and worry program in schools. Internet Interv 2016;6:1–5. 127
Cardemil EV, Reivich KJ, Beevers CG, Seligman ME, James J. The prevention of depressive symptoms in low-income, minority children: two-year follow-up. Behav Res Ther 2007;45:313–27. 208
Chaplin TM, Gillham JE, Reivich K, Elkon AG, Samuels B, Freres DR, et al. Depression prevention for early adolescent girls: a pilot study of all girls versus co-ed groups. J Early Adolesc 2006;26:110–26. 192
Clarke GN, Hawkins W, Murphy M, Sheeber L. School-based primary prevention of depressive symptomatology in adolescents: findings from two studies. J Adolesc Res 1993;8:183–204. 193
Collins S, Marks Woolfson L, Durkin K. Effects on coping skills and anxiety of a universal school-based mental health intervention delivered in Scottish primary schools. School Psychol Int 2014;35:85–100. 149
Dadds MR, Roth JH. Prevention of anxiety disorders: results of a universal trial with young children. J Child Fam Stud 2008;17:320–35. 303
Eather N, Morgan PJ, Lubans DR. Effects of exercise on mental health outcomes in adolescents: findings from the CrossFit™ teens randomized controlled trial. Psychol Sport Exerc 2016;26:14–23. 340
Essau CA, Conradt J, Sasagawa S, Ollendick TH. Prevention of anxiety symptoms in children: results from a universal school-based trial. Behav Ther 2012;43:450–64. 150
Gallegos J. Preventing Childhood Anxiety and Depression: Testing the Effectiveness of a School-based Program in Mexico. PhD thesis. Austin, TX: The University of Texas at Austin; 2008. 151
Gillham JE. Preventing depressive symptoms in school children. Diss Ab Int B Sci Eng 1995;55:4119. 209
Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, Seligman MEP. School-based prevention of depression and anxiety symptoms in early adolescence: a pilot of a parent intervention component. School Psychol Q 2006;21:323–48. 128
Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, et al. School-based prevention of depressive symptoms: a randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. J Consult Clin Psychol 2007;75:9–19. 194
Gucht K, Griffith JW, Hellemans R, Bockstaele M, Pascal-Claes F, Raes F. Acceptance and Commitment Therapy (ACT) for adolescents: outcomes of a large-sample, school-based, cluster-randomized controlled trial. Mindfulness 2017;8:408–16. 129
Haden SC, Daly L, Hagins M. A randomised controlled trial comparing the impact of yoga and physical education on the emotional and behavioural functioning of middle school children. Focus Altern Complement Ther 2014;19:148–55. 341
Hiebert BA, Kirby B, Jaknavorian A. School-based relaxation: attempting primary prevention. Can J Couns 1989;23:273–87. 130
Hodas R. An investigation of the relationship between positive and negative mental health factors and academic performance among early adolescent girls. Diss Ab Int B Sci Eng 2016;76(12-B(E)). 131
Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. J Consult Clin Psychol 2007;75:693–706. 195
Johnson C, Burke C, Brinkman S, Wade T. Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav Res Ther 2016;81:1–11. 132
Johnson C, Burke C, Brinkman S, Wade T. A randomized controlled evaluation of a secondary school mindfulness program for early adolescents: do we have the recipe right yet? Behav Res Ther 2017;99:37–46. 133
Johnstone J, Rooney RM, Hassan S, Kane RT. Prevention of depression and anxiety symptoms in adolescents: 42 and 54 months follow-up of the Aussie Optimism Program-Positive Thinking Skills. Front Psychol 2014;5:364. 152
Khalsa SB, Hickey-Schultz L, Cohen D, Steiner N, Cope S. Evaluation of the mental health benefits of yoga in a secondary school: a preliminary randomized controlled trial. J Behav Health Serv Res 2012;39:80–90. 239
Kindt KC, Kleinjan M, Janssens JM, Scholte RH. Evaluation of a school-based depression prevention program among adolescents from low-income areas: a randomized controlled effectiveness trial. Int J Environ Res Public Health 2014;11:5273–93. 196
Lock S, Barrett PM. A longitudinal study of developmental differences in universal preventive intervention for child anxiety. Behav Change 2003;20:183–99. 134
Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study. Behav Change 2001;18:36–50. 135
Mendelson T, Greenberg MT, Dariotis JK, Gould LF, Rhoades BL, Leaf PJ. Feasibility and preliminary outcomes of a school-based mindfulness intervention for urban youth. J Abnorm Child Psychol 2010;38:985–94. 210
Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. J Am Acad Child Adolesc Psychiatry 2004;43:538–47. 197
Miller LD, Short C, Garland EJ, Clark S. The ABCs of CBT (cognitive behavior therapy): evidence-based approaches to child anxiety in public school settings. J Couns Dev 2010;88:432–9. 153
Miller LD, Laye-Gindhu A, Liu Y, March JS, Thordarson DS, Garland EJ. Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behav Res Ther 2011;49:315–23. 154
Pahl KM, Barrett PM. Preventing anxiety and promoting social and emotional strength in preschool children: a universal evaluation of the Fun FRIENDS Program. Adv Sch Ment Health Promot 2010;3:14–25. 242
Pattison C, Lynd-Stevenson R. The prevention of depressive symptoms in children: the immediate and long-term outcomes of a school-based program. Behav Change 2001;18:92–102. 155
Perry Y, Werner-Seidler A, Calear A, Mackinnon A, King C, Scott J, et al. Preventing depression in final year secondary students: school-based randomized controlled trial. J Med Internet Res 2017;19:e369. 136
Pophillat E, Rooney RM, Nesa M, Davis MC, Baughman N, Hassan S, Kane RT. Preventing internalizing problems in 6–8 year old children: a universal school-based program. Front Psychol 2016;7:1928. 156
Pössel P, Horn AB, Groen G, Hautzinger M. School-based prevention of depressive symptoms in adolescents: a 6-month follow-up. J Am Acad Child Adolesc Psychiatry 2004;43:1003–10. 198
Pössel P, Adelson JL, Hautzinger M. A randomized trial to evaluate the course of effects of a program to prevent adolescent depressive symptoms over 12 months. Behav Res Ther 2011;49:838–51. 199
Pössel P, Martin NC, Garber J, Hautzinger M. A randomized controlled trial of a cognitive–behavioral program for the prevention of depression in adolescents compared with nonspecific and no-intervention control conditions. J Couns Psychol 2013;60:432–8. 200
Potek R. Mindfulness as a school-based prevention program and its effect on adolescent stress, anxiety and emotion regulation. Diss Abs Int B Sci Eng 2012;73:3272. 137
Quayle D, Dziurawiec S, Roberts C, Kane R, Ebsworthy G. The effect of an optimism and lifeskills program on depressive symptoms in preadolescence. Behav Change 2001;18:194–203. 211
Raes F, Griffith JW, Van der Gucht K, Williams JMG. School-based prevention and reduction of depression in adolescents: a cluster-randomized controlled trial of a mindfulness group program. Mindfulness 2014;5:477–86. 201
Reynolds EK, Macpherson L, Tull MT, Baruch DE, Lejuez CW. Integration of the brief behavioral activation treatment for depression (BATD) into a college orientation program: depression and alcohol outcomes. J Couns Psychol 2011;58:555–64. 233
Rivet-Duval E, Heriot S, Hunt C. Preventing adolescent depression in Mauritius: a universal school-based program. Child Adolesc Ment Health 2011;16:86–91. 202
Roberts C, Kane R, Thomson H, Bishop B, Hart B. The prevention of depressive symptoms in rural school children: a randomized controlled trial. J Consult Clin Psychol 2003;71:622–8. 138
Roberts CM, Kane R, Bishop B, Cross D, Fenton J, Hart B. The prevention of anxiety and depression in children from disadvantaged schools. Behav Res Ther 2010;48:68–73. 139
Roberts CM, Kane RT, Rooney RM, Pintabona Y, Baughman N, Hassan S, et al. Efficacy of the Aussie Optimism Program: promoting pro-social behavior and preventing suicidality in primary school students. A randomised-controlled trial. Front Psychol 2018;8:1392. 240
Rodgers A, Dunsmuir S. A controlled evaluation of the ‘FRIENDS for Life’ emotional resiliency programme on overall anxiety levels, anxiety subtype levels and school adjustment. Child Adolesc Ment Health 2015;20:13–19. 140
Rooney R, Roberts C, Kane R, Pike L, Winsor A, White J, Brown A. The prevention of depression in 8- to 9-year-old children: a pilot study. Aust J Guidance Couns 2006;16:76–90. 157
Rose K, Hawes DJ, Hunt CJ. Randomized controlled trial of a friendship skills intervention on adolescent depressive symptoms. J Consult Clin Psychol 2014;82:510–20. 203
Ruttledge R, Devitt E, Greene G, Mullany M, Charles E, Frehill J, Moriarty M. A randomised controlled trial of the FRIENDS for Life emotional resilience programme delivered by teachers in Irish primary schools. Educ Child Psychol 2016;33:69–89. 158
Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: a randomised controlled study of the beyond blue schools research initiative. J Child Psychol Psychiatry 2010;51:199–209. 204
Shatté AJ. Prevention of depressive symptoms in adolescents: issues of dissemination and mechanisms of change. Diss Ab Int B Sci Eng 1997;57:7236. 205
Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, McLoone J. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol 2006;74:66–79. 141
Soffer AG. School-based Social Skills Training to Reduce Children's Depressive Symptomatology. PhD thesis. New York, NY: City University New York; 2003. 212
Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: an evaluation of the problem solving for life program. J Consult Clin Psychol 2003;71:3–13. 206
Stallard P, Phillips R, Montgomery AA, Spears M, Anderson R, Taylor J, et al. A cluster randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of classroom-based cognitive-behavioural therapy (CBT) in reducing symptoms of depression in high-risk adolescents. Health Technol Assess 2013;17(47). 142
Stallard P, Skryabina E, Taylor G, Phillips R, Daniels H, Anderson R, Simpson N. Classroom-based cognitive behaviour therapy (FRIENDS): a cluster randomised controlled trial to Prevent Anxiety in Children through Education in Schools (PACES). Lancet Psychiatry 2014;1:185–92. 159
Tak YR, Lichtwarck-Aschoff A, Gillham JE, Van Zundert RM, Engels RC. Universal school-based depression prevention ‘Op Volle Kracht’: a longitudinal cluster randomized controlled trial. J Abnorm Child Psychol 2016;44:949–61. 207
Tomba E, Belaise C, Ottolini F, Ruini C, Bravi A, Albieri E, et al. Differential effects of well-being promoting and anxiety-management strategies in a non-clinical school setting. J Anxiety Disord 2010;24:326–33. 143
Velásquez AM, López MA, Quiñonez N, Paba DP. Yoga for the prevention of depression, anxiety, and aggression and the promotion of socio-emotional competencies in school-aged children. Educ Res Eval 2015;21:407–21. 189
Wong N, Kady L, Mewton L, Sunderland M, Andrews G. Preventing anxiety and depression in adolescents: a randomised controlled trial of two school-based internet-delivered cognitive behavioural therapy programmes. Internet Interv 2014;1:90–4. 144
Arnarson EO, Craighead WE. Prevention of depression among Icelandic adolescents. Behav Res Ther 2009;47:577–85. 213
Balle M, Tortella-Feliu M. Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety Stress Coping 2010;23:71–85. 160
Berry K, Hunt CJ. Evaluation of an intervention program for anxious adolescent boys who are bullied at school. J Adolesc Health 2009;45:376–82. 161
Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry 1995;34:312–21. 214
Congleton AB. The Effect of a Cognitive–Behavioral Group Intervention on the Locus of Control, Attributional Style, and Depressive Symptoms of Middle School Students. PhD thesis. Lexington, KY: University of Kentucky; 1995. 215
Cooley-Strickland MR, Griffin RS, Darney D, Otte K, Ko J. Urban African American youth exposed to community violence: a school-based anxiety preventive intervention efficacy study. J Prev Interv Community 2011;39:149–66. 174
Cova F, Rincon P, Melipillan R. Evaluation of the efficacy of a prevention program for depression in female adolescents. Ter Psicol 2011;29:245–50. 162
Cowell JM, McNaughton D, Ailey S, Gross D, Fogg L. Clinical trial outcomes of the Mexican American Problem Solving program (MAPS). Hisp Health Care Int 2009;7:179–89. 231
Cui L, He F, Han Z, Yang R, Xiao J, Oei TP. A brief group cognitive–behavioral program for the prevention of depressive symptoms in Chinese college students. Int J Group Psychother 2016;66:291–307. 183
Dobson KS, Hopkins JA, Fata L, Scherrer M, Allan LC. The prevention of depression and anxiety in a sample of high-risk adolescents: a randomized controlled trial. Can J Sch Psychol 2010;25:291–310. 163
Ellis L, Campbell A, Sethi S, O’Dea B. Comparative randomized trial of an online cognitive–behavioral therapy program and an online support group for depression and anxiety. J Cyber Ther Rehabil 2011;4:461–7. 184
Fitzgerald A, Rawdon C, Dooley B. A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behav Res Ther 2016;84:1–8. 114
Fung J, Guo S, Jin J, Bear L, Lau A. A pilot randomized trial evaluating a school-based mindfulness intervention for ethnic minority youth. Mindfulness 2016;7:819–28. 216
Gaete J, Martinez V, Fritsch R, Rojas G, Montgomery AA, Araya R. Indicated school-based intervention to improve depressive symptoms among at risk Chilean adolescents: a randomized controlled trial. BMC Psychiatry 2016;16:276. 164
Gillham JE, Reivich KJ, Brunwasser SM, Freres DR, Chajon ND, Kash-Macdonald VM, et al. Evaluation of a group cognitive-behavioral depression prevention program for young adolescents: a randomized effectiveness trial. J Clin Child Adolesc Psychol 2012;41:621–39. 165
Higgins DM. Preventing generalized anxiety disorder in an at-risk sample of college students: a brief cognitive–behavioral approach. Diss Ab Int B Sci Eng 2007;67:5406. 185
Hunt C, Andrews G, Crino R, Erskine A, Sakashita C. Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Aust N Z J Psychiatry 2009;43:300–4. 166
Jaycox LH, Reivich KJ, Gillham J, Seligman ME. Prevention of depressive symptoms in school children. Behav Res Ther 1994;32:801–16. 232
Jordans MJ, Komproe IH, Tol WA, Kohrt BA, Luitel NP, Macy RD, de Jong JT. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial. J Child Psychol Psychiatry 2010;51:818–26. 167
Kiselica MS, Baker SB, Thomas RN, Reedy S. Effects of stress inoculation training on anxiety, stress, and academic performance among adolescents. J Couns Psychol 1994;41:335–42. 168
Liddle I, Macmillan S. Evaluating the FRIENDS programme in a Scottish setting. Educ Psychol Pract 2010;26:53–67. 188
Livheim F, Hayes L, Ghaderi A, Magnusdottir T, Högfeldt A, Rowse J, et al. The effectiveness of acceptance and commitment therapy for adolescent mental health: Swedish and Australian pilot outcomes. J Child Fam Stud 2015;24:1016–30. 217
Manassis K, Wilansky-Traynor P, Farzan N, Kleiman V, Parker K, Sanford M. The feelings club: randomized controlled evaluation of school-based CBT for anxious or depressive symptoms. Depress Anxiety 2010;27:945–52. 175
McCarty CA, Violette HD, McCauley E. Feasibility of the positive thoughts and actions prevention program for middle schoolers at risk for depression. Depress Res Treat 2011;2011:241386. 218
McCarty CA, Violette HD, Duong MT, Cruz RA, McCauley E. A randomized trial of the Positive Thoughts and Action program for depression among early adolescents. J Clin Child Adolesc Psychol 2013;42:554–63. 219
McLaughlin C. Evaluating the effect of an empirically-supported group intervention for students at-risk for depression in a rural school district. Diss Ab Int B Sci Eng 2011;71:5820. 236
McLoone JK, Rapee RM. Comparison of an anxiety management program for children implemented at home and school: lessons learned. Sch Ment Health 2012;4:231–42. 176
Mifsud C, Rapee RM. Early intervention for childhood anxiety in a school setting: outcomes for an economically disadvantaged population. J Am Acad Child Adolesc Psychiatry 2005;44:996–1004. 177
Miller LD, Laye-Gindhu A, Bennett JL, Liu Y, Gold S, March JS, et al. An effectiveness study of a culturally enriched school-based CBT anxiety prevention program. J Clin Child Adolesc Psychol 2011;40:618–29. 178
Noël LT, Rost K, Gromer J. Depression prevention among rural preadolescent girls: a randomized controlled trial. Sch Soc Work J 2013;38:1–18. 220
Owen H, Lanning W. The effects of three treatment methods upon anxiety and inappropriate attentional style among high school athletes. Int J Sport Psychol 1982;13:154–62. 169
Peden AR, Hall LA, Rayens MK, Beebe LL. Reducing negative thinking and depressive symptoms in college women. J Nurs Scholarsh 2000;32:145–51. 234
Peng S, Qi A, Yuan F. Experimental study on the effects of exercise prescription on the mental health of left-behind school children in rural areas. Rev Argent Clin Psicol 2015;24:267–76. 170
Poppelaars M, Tak YR, Lichtwarck-Aschoff A, Engels RC, Lobel A, Merry SN, et al. A randomized controlled trial comparing two cognitive–behavioral programs for adolescent girls with subclinical depression: a school-based program (Op Volle Kracht) and a computerized program (SPARX). Behav Res Ther 2016;80:33–42. 221
Puskar K, Sereika S, Tusaie-Mumford K. Effect of the Teaching Kids to Cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs 2003;16:71–80. 222
Rice CL. Reducing anxiety in middle school and high school students: a comparison of cognitive–behavioral therapy and relaxation training approaches. Diss Ab Int A Humanit Soc Sci 2009;69:2607. 171
Rohde P, Stice E, Shaw H, Brière FN. Indicated cognitive behavioral group depression prevention compared to bibliotherapy and brochure control: acute effects of an effectiveness trial with adolescents. J Consult Clin Psychol 2014;82:65–74. 223
Scholten H, Malmberg M, Lobel A, Engels RC, Granic I. A randomized controlled trial to test the effectiveness of an immersive 3D video game for anxiety prevention among adolescents. PLOS ONE 2016;11:e0147763. 172
Schoneveld EA, Malmberg M, Lichtwarck-Aschoff A, Verheijen GP, Engels RC, Granic I. A neurofeedback video game (MindLight) to prevent anxiety in children: a randomized controlled trial. Comput Hum Behav 2016;63:321–33. 115
Schoneveld EA, Lichtwarck-Aschoff A, Granic I. Preventing childhood anxiety disorders: is an applied game as effective as a cognitive behavioral therapy-based program? Prev Sci 2018;19:220–32. 116
Seligman MEP, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prev Treat 1999;2. 186
Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behav Res Ther 2007;45:1111–26. 187
Simpson AT. The roles of self-regulation and coping in a preventative cognitive–behavioural intervention for school-age children at-risk for internalizing disorders. Diss Ab Int B Sci Eng 2008;69:3862. 179
Siu FYA. Internalizing problems among primary school children in Hong Kong: prevalence and treatment. Diss Ab Int A Humanit Soc Sci 2008;69:115. 180
Sportel BE, de Hullu E, de Jong PJ, Nauta MH. Cognitive bias modification versus CBT in reducing adolescent social anxiety: a randomized controlled trial. PLOS ONE 2013;8:e64355. 117
Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: an elusive search for a psychosocial placebo control condition. Behav Res Ther 2007;45:863–76. 237
Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: a randomized efficacy trial. J Consult Clin Psychol 2008;76:595–606. 224
Stoppelbein LA. Primary prevention: an evaluation of a high-school based cognitive–behavioral program. Diss Abs Int B Sci Eng 2004;64:4066. 225
Takagaki K, Okamoto Y, Jinnin R, Mori A, Nishiyama Y, Yamamura T, et al. Behavioral activation for late adolescents with subthreshold depression: a randomized controlled trial. Eur Child Adolesc Psychiatry 2016;25:1171–82. 235
Tokolahi E, Vandal AC, Kersten P, Pearson J, Hocking C. Cluster-randomised controlled trial of an occupational therapy intervention for children aged 11–13 years, designed to increase participation to prevent symptoms of mental illness. Child Adolesc Ment Health 2018;23:313–27. 181
Topper M, Emmelkamp PM, Watkins E, Ehring T. Prevention of anxiety disorders and depression by targeting excessive worry and rumination in adolescents and young adults: a randomized controlled trial. Behav Res Ther 2017;90:123–36. 173
van Starrenburg ML, Kuijpers RC, Kleinjan M, Hutschemaekers GJ, Engels RC. Effectiveness of a cognitive behavioral therapy-based indicated prevention program for children with elevated anxiety levels: a randomized controlled trial. Prev Sci 2017;18:31–9. 182
Wijnhoven LA, Creemers DH, Vermulst AA, Scholte RH, Engels RC. Randomized controlled trial testing the effectiveness of a depression prevention program (‘Op Volle Kracht’) among adolescent girls with elevated depressive symptoms. J Abnorm Child Psychol 2014;42:217–28. 226
Woods B, Jose P. Effectiveness of a school-based indicated early intervention program for Maori and Pacific adolescents. J Pac Rim Psychol 2011;5:40–50. 227
Young JF, Mufson L, Davies M. Efficacy of Interpersonal Psychotherapy-Adolescent Skills Training: an indicated preventive intervention for depression. J Child Psychol Psychiatry 2006;47:1254–62. 228
Young JF, Mufson L, Gallop R. Preventing depression: a randomized trial of interpersonal psychotherapy-adolescent skills training. Depress Anxiety 2010;27:426–33. 229
Young JF, Benas JS, Schueler CM, Gallop R, Gillham JE, Mufson L. A randomized depression prevention trial comparing interpersonal psychotherapy – adolescent skills training to group counseling in schools. Prev Sci 2016;17:314–24. 230
Yu L. Preventing depressive symptoms in Chinese children. Diss Abs Int B Sci Eng 2000;60:6389. 238
August GJ, Hektner JM, Egan EA, Realmuto GM, Bloomquist ML. The early risers longitudinal prevention trial: examination of 3-year outcomes in aggressive children with intent-to-treat and as-intended analyses. Psychol Addict Behav 2002;16:S27–39. 244
Baker-Henningham H, Scott S, Jones K, Walker S. Reducing child conduct problems and promoting social skills in a middle-income country: cluster randomised controlled trial. Br J Psychiatry 2012;201:101–8. 245
Havighurst SS, Duncombe M, Frankling E, Holland K, Kehoe C, Stargatt R. An emotion-focused early intervention for children with emerging conduct problems. J Abnorm Child Psychol 2015;43:749–60. 246
Kyranides MN, Fanti KA, Katsimicha E, Georgiou G. Preventing conduct disorder and callous unemotional traits: preliminary results of a school based pilot training program. J Abnorm Child Psychol 2018;46:291–303. 243
The Conduct Problems Prevention Research Group. Initial impact of the Fast Track prevention trial for conduct problems: I. The high-risk sample. J Consult Clin Psychol 1999;67:631–47. 247
References to studies awaiting classification
Unable to locate full text
Boogar IR. [Effectiveness of the Teasdale Cognitive Therapy on depression reduction in guidance and high school students.] Psychol Res 2012;14:25–40.
Dadsetan P, Anari A, Sedghpour BS. Social anxiety disorders and drama-therapy. J Iran Psychol 2008;4:115–123.
Diner MD. The differential effects of meditation and systematic desensitization on specific and general anxiety. Diss Abs Int B Sci Eng 1978;39:1950.
Kahn RHC. The Effect of a Group Support Intervention Program on Depression, Social Adjustment, and Self-esteem of Adolescents in an Overseas American International School. PhD thesis. Washington, DC: The Catholic University of America; 1989.
Ma HX, Liu MT, Zhang FY. Improving the academic emotions of high-school students by rational-emotive educational mode. Chin J Clin Psychol 2012;20:116–119.
Mirzamani SM, Azvar F, Dolatshahi B, Askari A. [Efficacy of life skills training on reduce depressive symptoms in student population.] J Res Behav Sci 2012;10:124–32.
Moharreri F, Yazdi A. Evaluation of the effectiveness of the Friends for Life Program on children’s anxiety and depression. Iran J Psychiatry 2017;12:272–280.
Short C. Universal Prevention Program for Anxiety Symptoms in School Aged Children: Taming Worry Dragons. Master’s thesis. Vancouver, BC: University of British Columbia; 2005.
Zou M, Han RS. Attributive training in junior school students with high-level anxiety. Chin Ment Health J 2008;3:358–371. Abstract available from http://en.cnki.com.cn/Article_en/CJFDTOTAL-ZXWS200805016.html (accessed 18 May 2021).
No author details. Effectiveness of group cognitive–emotional skills training on improvement of anxiety management in primary school children. Iran J Psychiatry 2012;7 (CENTRAL database).
Conference abstracts
Rezaei Ghalechi E, Sadeghi Movahhed F. Teaching Coping Skills Affects on Decreasing Mental Disorders Symptoms of Students. EPA 2013 – 21st European Congress of Psychiatry, Nice, 6–9 April 2013.
Tze-Chun T, Shih-Yin H. Efficacy of school-based interpersonal psychotherapy to adolescents of early detected depressive and suicide ideations: randomized control study. Early Interv Psychiatry 2010;4(Suppl. 1):1–200.
Davis H. Youth Clubs: Outcome of a Community-based Intervention for Prevention of Mental Health Disorders in Adolescence. European Child Psychiatry Research Group – invitational meeting, Oslo, 5–7 September 1996 (found on the CENTRAL database).
Other
Eimecke S, Pauschardt J, Mattejat F. [Prevention of childhood anxiety and depression: efficacy of an additional parent training program.] Verhaltenstherapie 2010;20:193–200.
Tsutsumi A. Effects of a psycho-educational program for preventing depression in junior high and high school students. Jpn J Educ Psychol 2015;63:323–37.
St Onge J, Stephenson R, Kumar BS. Validation of the FRIENDS anxiety prevention program for children in Canada. Can J Community Ment Health 2016;35:25–40.
Silvestri L, Dantonio M, Eason S. The effects of a self-development program and relaxation/imagery training on the anxiety levels of at-risk fourth grade students. J Instr Psychol 1996;23:167–73.
Petersen A, Leffert A, Graham B, Alwin J, Ding S. Promoting Mental Health During the Transition into Adolescence. In Schulenberg J, Maggs JL, Hierrelmann AK, editors. Health Risks and Developmental Transitions During Adolescence. New York, NY: Cambridge University Press; 1997. pp. 471–97.
Details of studies included in systematic review of anxiety and depression prevention
Tables 22 and 23 report the focus of the intervention, study design, population, setting and age range (if reported) for 137 studies included in the review for depression and anxiety prevention. A total of 79 studies reported an anxiety outcome and 105 reported a depression outcome.
| Study | Target | Study design | Population | Setting | Age (SD) (years) | Anxiety scale | In NMA?a | Follow-up time point(s) (months) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post intervention | 1–5 | 6–12 | 13–24 | ≥ 25 | ||||||||
| Aune and Stiles119 2009 | Anxiety | Cluster randomised | Universal | Secondary | 10–15 | SCARED | Yes | 0 | ||||
| Baker and Butler120 1984 | Anxiety | Cluster randomised | Universal | Secondary | 16–18 | STAI | Yes | 0 | ||||
| Calear et al.126 2016 | Anxiety | Cluster randomised | Universal | Secondary | 12–18 | SCAS, GAD-7 | Yes | 0 | 6, 12 | |||
| Calear et al.127 2016 | Anxiety | Cluster randomised | Universal | Secondary | 13–17 | SCAS, GAD-7 | Yes | 0 | 3 | |||
| Hiebert et al.130 1989 | Anxiety | Individually randomised | Universal | Secondary | 13–14 | STAI | Yes | 0 | ||||
| Lock and Barrett134 2003 | Anxiety | Cluster randomised | Universal | Secondary | Not clear | RCMAS, SCAS | Yes | 0 | 12 | |||
| Potek137 2012 | Anxiety | Individually randomised | Universal | Secondary | 14–17 | MASC | Yes | 0 | ||||
| Rodgers and Dunsmuir140 2015 | Anxiety | Individually randomised | Universal | Secondary | 12–13 | SCAS | Yes | 0 | 4 | |||
| Calear et al.125 2009 | Anxiety and depression | Cluster randomised | Universal | Secondary | 12–17 | RCMAS | Yes | 0 | 6 | |||
| Gillham et al.128 2006 | Anxiety and depression | Individually randomised | Universal | Secondary | 11–13 | RCMAS | Yes | 0 | 6, 12 | |||
| Gucht et al.129 2017 | Anxiety and depression | Cluster randomised | Universal | Secondary | 14–21 | YSR-anxiety | Yes | 0 | 12 | |||
| Hodas131 2016 | Anxiety and depression | Individually randomised | Universal | Secondary | 12–14 | RCMAS | Yes | 0 | 6 | |||
| Johnson et al.132 2016 | Anxiety and depression | Cluster randomised | Universal | Secondary | 13.63 (0.43) | DASS-anxiety | Yes | 0 | 3 | |||
| Johnson et al.133 2017 | Anxiety and depression | Cluster randomised | Universal | Secondary | 13.44 (0.33) | DASS-anxiety | Yes | 0 | 6,12 | |||
| Lowry-Webster et al.135 2001 | Anxiety and depression | Cluster randomised | Universal | Secondary | 10–13 | RCMAS, SCAS | Yes | 0 | 12 | |||
| Roberts et al.139 2010 | Anxiety and depression | Cluster randomised | Universal | Secondary | 11–13 | RCMAS | Yes | 0 | 6 | 18 | ||
| Tomba et al.143 2010 | Anxiety and depression | Cluster randomised | Universal | Secondary | 11.41 | RCMAS | Yes | 0 | 6 | |||
| Wong et al.144 2014 | Anxiety and depression | Cluster randomised | Universal | Secondary | 14–16 | GAD-7 | Yes | 0 | ||||
| Araya et al.118 2013 | Depression | Cluster randomised | Universal | Secondary | 14.5 (0.90) | RCADS-anxiety | Y-12 | 3 | 12 | |||
| Perry et al.136 2017 | Depression | Cluster randomised | Universal | Secondary | 16–17 | SCAS | Yes | 0 | 6 | 18 | ||
| Roberts et al.138 2003 | Depression | Cluster randomised | Universal | Secondary | 11–13 | RCMAS | Yes | 0 | 6 | 18 | 30 | |
| Sheffield et al.141 2006 | Depression | Cluster randomised | Universal | Secondary | 13–15 | SCAS | Yes | 0 | 6, 12 | |||
| Stallard et al.142 2013 | Depression | Cluster randomised | Universal | Secondary | 12–16 | RCADS-GA | Y-12 | 6, 12 | ||||
| Barrett et al.121 2005 | Anxiety | Cluster randomised | Universal | Secondary | 9–16 | SCAS | No | |||||
| Bonhauser et al.122 2005 | Anxiety and depression | Cluster randomised | Universal | Secondary | 15.3 (0.92) | HADS | No | 0 | ||||
| Britton et al.123 2014 | Anxiety and depression | Individually randomised | Universal | Secondary | 11.79 (0.41) | STAI | No | 0 | ||||
| Burckhardt et al.124 2015 | Anxiety and depression | Cluster randomised | Universal | Secondary | 14–16 | DASS-anxiety | No | 0 | 5 | |||
| Attwood et al.146 2012 | Anxiety | Individually randomised | Universal | Primary | 10–12 | SCAS | Yes | 0 | ||||
| Barrett and Turner147 2001 | Anxiety | Cluster randomised | Universal | Primary | 10–12 | RCMAS, SCAS | Yes | 0 | ||||
| Bouchard et al.148 2013 | Anxiety | Individually randomised | Universal | Primary | 9–12 | MASC | Yes | 0 | ||||
| Collins et al.149 2014 | Anxiety | Cluster randomised | Universal | Primary | 9–10 | SCAS | Yes | 0 | 6 | |||
| Essau et al.150 2012 | Anxiety | Cluster randomised | Universal | Primary | 9–12 | SCAS | Yes | 0 | 6, 12 | |||
| Miller et al.153 2010 | Anxiety | Cluster randomised | Universal | Primary | 7–12 | MASC | Yes | 0 | ||||
| Miller et al.154 2011 | Anxiety | Cluster randomised | Universal | Primary | 7–13 | MASC | Yes | 0 | 6 | |||
| Miller et al.154 2011 | Anxiety | Cluster randomised | Universal | Primary | 7–13 | SCAS | Yes | 0 | 12 | |||
| Ruttledge et al.158 2016 | Anxiety | Cluster randomised | Universal | Primary | 9–13 | SCAS | Yes | 0 | 3 | |||
| Stallard et al.159 2014 | Anxiety | Cluster randomised | Universal | Primary | 9–10 | RCADS-GA | Y-12 | 12 | 24 | |||
| Ahlen et al.145 2018 | Anxiety and depression | Cluster randomised | Universal | Primary | 8–11 | SCAS | Yes | 0 | 12 | |||
| Gallegos151 2008 | Anxiety and depression | Cluster randomised | Universal | Primary | 9–11 | SCAS | Yes | 0 | 6 | |||
| Johnstone et al.152 2014 | Anxiety and depression | Cluster randomised | Universal | Primary | 9–10 | SCAS | Yes | 0 | 6 | 18 | 30, 42, 54 | |
| Pophillat et al.156 2016 | Anxiety and depression | Cluster randomised | Universal | Primary | 6–8 | SCAS | Yes | 0 | ||||
| Pattison and Lynd-Stevenson155 2001 | Depression | Individually randomised | Universal | Primary | 9–12 | STAI | Yes | 0 | 8 | |||
| Rooney et al.157 2006 | Depression | Cluster randomised | Universal | Primary | 8–9 | RCMAS | Yes | 0 | 9 | 18 | ||
| Velásquez et al.189 2015 | Anxiety and depression | Individually randomised | Universal | M | NR | Modified SDQ-anxiety | No | 0 | ||||
| Balle and Tortella-Feliu160 2010 | Anxiety | Individually randomised | Targeted | Secondary | 11–17 | SCAS | Yes | 0 | 6 | |||
| Berry and Hunt161 2009 | Anxiety | Cluster randomised | Targeted | Secondary | 12–15 | SCARED | Yes | 0 | ||||
| Fitzgerald et al.114 2016 | Anxiety | Individually randomised | Targeted | Secondary | 15–18 | SCARED | Yes | 0 | 3 | |||
| Hiebert et al.130 1989 | Anxiety | Individually randomised | Targeted | Secondary | 15–17 | STAI | Yes | 0 | ||||
| Hunt et al.166 2009 | Anxiety | Cluster randomised | Targeted | Secondary | 11–13 | RCMAS, SCAS | Y-24 | 0 | 24 | 48 | ||
| Kiselica et al.168 1994 | Anxiety | Individually randomised | Targeted | Secondary | 14–15 | STAI | Yes | 0 | 3 | |||
| Rice171 2009 | Anxiety | Individually randomised | Targeted | Secondary | 10–18 | MASC | Yes | 0 | 2 | |||
| Scholten et al.172 2016 | Anxiety | Individually randomised | Targeted | Secondary | 11–15 | SCAS | Yes | 0 | 3 | |||
| Sportel et al.117 2013 | Anxiety | Cluster randomised | Targeted | Secondary | 12–15 | RCADS-social anxiety | Yes | 0 | 6, 12 | |||
| Owen and Lanning169 1982 | Anxiety | Individually randomised | Targeted | Secondary | 15–16 | STAI | No | 0 | ||||
| Dobson et al.163 2010 | Anxiety and depression | Individually randomised | Targeted | Secondary | 13–18 | BAI | Yes | 0 | 3 | 6 | ||
| Jordans et al.167 2010 | Anxiety and depression | Cluster randomised | Targeted | Secondary | 11–14 | SCARED | Yes | 0 | ||||
| Peng et al.170 2015 | Anxiety and depression | Cluster randomised | Targeted | Secondary | 14.2 (2.34) | Mental Health Test-anxiety | Yes | 0 | ||||
| Topper et al.173 2017 | Anxiety and depression | Individually randomised | Targeted | Secondary | 15–22 | MASQ | Yes | 0 | 3 | 12 | ||
| Cova et al.162 2011 | Depression | Individually randomised | Targeted | Secondary | 14–15 | BAI | Yes | 0 | ||||
| Gaete et al.164 2016 | Depression | Individually randomised | Targeted | Secondary | 13–18 | RCADS | No | 3 | ||||
| Gillham et al.165 2012 | Depression | Individually randomised | Targeted | Secondary | 10–15 | RCMAS | Yes | 0 | 6 | |||
| Sheffield et al.141 2006 | Depression | Cluster randomised | Targeted | Secondary | 13–15 | SCAS | Yes | 0 | 6, 12 | |||
| Cooley-Strickland et al.174 2011 | Anxiety | Individually randomised | Targeted | Primary | 9–10 | RCMAS | Yes | 0 | ||||
| McLoone et al.176 2012 | Anxiety | Individually randomised | Targeted | Primary | 7–10 | SCAS | Yes | 0 | 12 | |||
| Mifsud and Rapee177 2005 | Anxiety | Cluster randomised | Targeted | Primary | 8–11 | SCAS | Yes | 0 | 6 | |||
| Miller et al.178 2011 | Anxiety | Cluster randomised | Targeted | Primary | 7–12 | SCAS | Yes | 0 | 3 | 12 | ||
| Schoneveld et al.115 2016 | Anxiety | Individually randomised | Targeted | Primary | 8–13 | SCAS | Yes | 0 | 3 | |||
| Schoneveld et al.116 2018 | Anxiety | Individually randomised | Targeted | Primary | 7–12 | SCAS | Yes | 0 | 3 | 6 | ||
| van Starrenburg et al.182 2017 | Anxiety | Individually randomised | Targeted | Primary | 7–13 | SCAS | Yes | 0 | 3 | |||
| Manassis et al.175 2010 | Anxiety and depression | Individually randomised | Targeted | Primary | 8–11 | MASC | Yes | 0 | 12 | |||
| Simpson179 2008 | Anxiety and depression | Individually randomised | Targeted | Primary | 7–11 | MASC | Yes | 0 | ||||
| Siu180 2007 | Anxiety and depression | Individually randomised | Targeted | Primary | 7–10 | SCARED | Yes | 0 | ||||
| Tokolahi et al.181 2018 | Anxiety and depression | Cluster randomised | Targeted | Primary | 7–12 | MASC | Yes | 0 | ||||
| Cui et al.183 2016 | Depression | Individually randomised | Targeted | University | 19.42 (1.66) | Zung | Yes | 0 | 6 | |||
| Ellis et al.184 2011 | Depression | Individually randomised | Targeted | University | 18–25 | DASS-anxiety | Yes | 0 | ||||
| Higgins185 2007 | Anxiety | Individually randomised | Targeted | University | 17–19 | BAI, GAD | Yes | 0 | 1 | 6, 12 | ||
| Seligman et al.186 1999 | Anxiety and depression | Individually randomised | Targeted | University | 19 (NR) | BAI | Yes | 0 | 3 | 36 | ||
| Seligman et al.187 2007 | Anxiety and depression | Individually randomised | Targeted | University | 19 (NR) | BAI | Yes | 0 | 1,3 | |||
| Liddle and Macmillan188 2010 | Anxiety | Individually randomised | Targeted | M | 8–14 | SCAS | No | 0 | ||||
| Study | Target | Study design | Population | Setting | Age (SD) (years) | Depression scale | In NMA? | Follow-up time point(s) (months) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post intervention | 1–5 | 6–12 | 13–24 | ≥ 25 | ||||||||
| Ahlen et al.145 2018 | Anxiety and depression | Cluster randomised | Universal | Primary | 8–11 | CDI | Yes | 0 | 12 | |||
| Araya et al.118 2013 | Depression | Cluster randomised | Universal | Secondary | 14.5 (0.90) | BDI | Y-12 | 3 | 12 | |||
| Arnarson and Craighead213 2009 | Depression | Individually randomised | Targeted | Secondary | 14–15 | CDI | No | |||||
| Aune and Stiles119 2009 | Anxiety | Cluster randomised | Universal | Secondary | 10–15 | SMFQ | Yes | 0 | ||||
| Balle and Tortella-Feliu160 2010 | Anxiety | Individually randomised | Targeted | Secondary | 11–17 | CDI | Yes | 0 | 6 | |||
| Barrett and Turner147 2001 | Anxiety | Cluster randomised | Universal | Primary | 10–12 | CDI | Yes | 0 | ||||
| Barrett et al.121 2005 | Anxiety | Cluster randomised | Universal | Secondary | 9–16 | CDI | No | |||||
| Barry et al.190 2017 | Depression | Individually randomised | Universal | Secondary | 15–16 | CES-D | Yes | 0 | ||||
| Berry and Hunt161 2009 | Anxiety | Cluster randomised | Targeted | Secondary | 12–15 | CES-D | Yes | 0 | ||||
| Bonhauser et al.122 2005 | Anxiety and depression | Cluster randomised | Universal | Secondary | 15.3 (0.92) | HADS | No | 0 | ||||
| Burckhardt et al.124 2015 | Anxiety and depression | Cluster randomised | Universal | Secondary | 14–16 | DASS-depression | No | 0 | 5 | |||
| Burckhardt et al.191 2016 | Anxiety and depression | Cluster randomised | Universal | Secondary | 15–18 | DASS-depression | No | 0 | ||||
| Calear et al.125 2009 | Anxiety and depression | Cluster randomised | Universal | Secondary | 12–17 | CES-D | Yes | 0 | 6 | |||
| Calear et al.126 2016 | Anxiety | Cluster randomised | Universal | Secondary | 12–18 | CES-D | Yes | 0 | 6, 12 | |||
| Calear et al.127 2016 | Anxiety | Cluster randomised | Universal | Secondary | 13–17 | CES-D | Yes | 0 | 3 | |||
| Cardemil et al.208 2007 | Depression | Individually randomised | Universal | Primary | 10–12 | CDI | Yes | 0 | 3 | 6 | ||
| Chaplin et al.192 2006 | Depression | Individually randomised | Universal | Secondary | 11–14 | CDI | Yes | 0 | ||||
| Clarke et al.193 1993 | Depression | Cluster randomised | Universal | Secondary | 14–16 | CES-D | Yes | 0 | 3 | |||
| Clarke et al.193 1993 | Depression | Cluster randomised | Universal | Secondary | 14–16 | CES-D | Yes | 0 | 3 | |||
| Clarke et al.214 1995 | Depression | Individually randomised | Targeted | Secondary | 14–16 | CES-D | Yes | 0 | 6, 12 | |||
| Congleton215 1995 | Depression | Individually randomised | Targeted | Secondary | 12–14 | CDI | Yes | 0 | ||||
| Cova et al.162 2011 | Depression | Individually randomised | Targeted | Secondary | 14–15 | BDI | Yes | 0 | ||||
| Cowell et al.231 2009 | Depression | Cluster randomised | Targeted | Primary | 10.4 (0.78) | CDI | No | 0 | 95 | |||
| Cui et al.183 2016 | Depression | Individually randomised | Targeted | University | 19.42 (2.43) | Zung | Yes | 0 | 6 | |||
| Dobson et al.163 2010 | Anxiety and depression | Individually randomised | Targeted | Secondary | 13–18 | CDI, CES-D | Yes | 0 | 3 | 6 | ||
| Ellis et al.184 2011 | Depression | Individually randomised | Targeted | University | 18–25 | DASS-depression | Yes | 0 | ||||
| Essau et al.150 2012 | Anxiety | Cluster randomised | Universal | Primary | 9–12 | RCADS-depression | Yes | 0 | 6, 12 | |||
| Fitzgerald et al.114 2016 | Anxiety | Individually randomised | Targeted | Secondary | 15–18 | RCADS-depression | Yes | 0 | 3 | |||
| Fung et al.216 2016 | Anxiety and depression | Individually randomised | Targeted | Secondary | 12–14 | PHQ-9 | No | 0 | ||||
| Gaete et al.164 2016 | Depression | Individually randomised | Targeted | Secondary | 13–18 | BDI | No | 3 | ||||
| Gallegos151 2008 | Anxiety and depression | Cluster randomised | Universal | Primary | 9–11 | CDI | Yes | 0 | 6 | |||
| Gillham209 1994 | Depression | Individually randomised | Universal | Primary | 10–12 | CDI | Yes | 0 | ||||
| Gillham et al.128 2006 | Anxiety and depression | Individually randomised | Universal | Secondary | 11–13 | CDI, CDRS | Yes | 0 | 6, 12 | |||
| Gillham et al.194 2007 | Depression | Individually randomised | Universal | Secondary | 11–14 | CDI, CDRS | Yes | 0 | 6, 12 | 18, 24 | 36 | |
| Gillham et al.165 2012 | Depression | Individually randomised | Targeted | Secondary | 10–15 | CDI, RADS | Yes | 0 | 6 | |||
| Gucht et al.129 2017 | Anxiety and depression | Cluster randomised | Universal | Secondary | 14–21 | YSR-affect | Yes | 0 | 12 | |||
| Higgins185 2007 | Anxiety | Individually randomised | Targeted | University | 17–19 | BDI | Yes | 0 | 1 | 6, 12 | ||
| Hodas131 2016 | Anxiety and depression | Individually randomised | Universal | Secondary | 12–14 | CDI | Yes | 0 | 6 | |||
| Horowitz et al.195 2007 | Depression | Individually randomised | Universal | Secondary | 14–15 | CDI, CES-D | Yes | 0 | 6 | |||
| Hunt et al.166 2009 | Anxiety | Cluster randomised | Targeted | Secondary | 11–13 | CDI | Y-24 | 0 | 24 | 48 | ||
| Jaycox et al.232 1994 | Depression | Cluster randomised | Targeted | Primary | 10–13 | CDI, RCDS | Yes | 0 | 6, 12 | 18, 24 | ||
| Johnson et al.132 2016 | Anxiety and depression | Cluster randomised | Universal | Secondary | 13.63 (0.43) | DASS-depression | Yes | 0 | 3 | |||
| Johnson et al.133 2017 | Anxiety and depression | Cluster randomised | Universal | Secondary | 13.44 (0.33) | DASS-depression | Yes | 0 | 6, 12 | |||
| Johnstone et al.152 2014 | Anxiety and depression | Cluster randomised | Universal | Primary | 9–10 | CDI | Yes | 0 | 6 | 18 | 30, 42, 54 | |
| Jordans et al.167 2010 | Anxiety and depression | Cluster randomised | Targeted | Secondary | 11–14 | DSRS | Yes | 0 | ||||
| Kindt et al.196 2014 | Depression | Cluster randomised | Universal | Secondary | 11–16 | CDI | Yes | 0 | 6, 12 | |||
| Liddle and Macmillan188 2010 | Anxiety | Individually randomised | Targeted | M | 8–14 | CDI | No | 0 | ||||
| Livheim et al.217 2015 | Depression | Individually randomised | Targeted | Secondary | 12–17 | RADS | Yes | 0 | ||||
| Lock and Barrett134 2003 | Anxiety | Cluster randomised | Universal | Secondary | NR | CDI | Yes | 0 | 12 | |||
| Lowry-Webster et al.135 2001 | Anxiety and depression | Cluster randomised | Universal | Secondary | 10–13 | CDI | Yes | 0 | 12 | |||
| Manassis et al.175 2010 | Anxiety and depression | Individually randomised | Targeted | Primary | 8–11 | CDI | Yes | 0 | 12 | |||
| McCarty et al.218 2011 | Depression | Individually randomised | Targeted | Secondary | 13 (0.38) | MFQ, CDRS | Yes | 0 | 6, 12 | 18 | ||
| McCarty et al.219 2013 | Depression | Individually randomised | Targeted | Secondary | 11–15 | MFQ | Yes | 0 | 6, 12 | |||
| McLaughlin236 2011 | Depression | Individually randomised | Targeted | M | 10–15 | CES-D, BDI | No | 0 | ||||
| Mendelson et al.210 2010 | Depression | Cluster randomised | Universal | Primary | 9–11 | SMFQ | No | 0 | ||||
| Merry et al.197 2004 | Depression | Individually randomised | Universal | Secondary | 13–15 | RADS, BDI | Yes | 0 | 6, 12 | 18 | ||
| Noël et al.220 2013 | Depression | Individually randomised | Targeted | Secondary | 13–15 | CES-D | No | 0 | ||||
| Pattison and Lynd-Stevenson155 2001 | Depression | Individually randomised | Universal | Primary | 9–12 | CDI | Yes | 0 | 8 | |||
| Peden et al.234 2000 | Depression | Individually randomised | Targeted | University | 18–24 | CES-D, BDI | No | 0 | 6 | 18 | ||
| Peng et al.170 2015 | Anxiety and depression | Cluster randomised | Targeted | Secondary | 14.2 (2.34) | Mental Health Test-depression | Yes | 0 | ||||
| Perry et al.136 2017 | Depression | Cluster randomised | Universal | Secondary | 16–17 | MDI | Yes | 0 | 6 | 18 | ||
| Pophillat et al.156 2016 | Anxiety and depression | Cluster randomised | Universal | Primary | 6–8 | CDI | Yes | 0 | ||||
| Poppelaars et al.221 2016 | Depression | Cluster randomised | Targeted | Secondary | 11–16 | RADS | Yes | 0 | 3 | 6, 12 | ||
| Pössel et al.198 2004 | Depression | Cluster randomised | Universal | Secondary | 13–14 | CES-D | Yes | 0 | 3 | 6 | ||
| Pössel et al.200 2013 | Depression | Cluster randomised | Universal | Secondary | 14–16 | CDI | Yes | 0 | 4 | 8, 12 | ||
| Pössel et al.199 2011 | Depression | Cluster randomised | Universal | Secondary | 12–13 | Self-reported questionnaire – depression | Yes | 0 | 6, 12 | |||
| Puskar et al.222 2003 | Depression | Individually randomised | Targeted | Secondary | 14–18 | RADS | Yes | 0 | 6, 12 | |||
| Quayle et al.211 2001 | Depression | Individually randomised | Universal | Primary | 11–12 | CDI | Yes | 0 | 6 | |||
| Raes et al.201 2014 | Depression | Cluster randomised | Universal | Secondary | 13–20 | DASS-depression | Yes | 0 | 6 | |||
| Reynolds et al.233 2011 | Depression | Cluster randomised | Universal | University | 17.9 (0.53) | DASS-depression | No | 0 | 6 | |||
| Rivet-Duval et al.202 2011 | Depression | Individually randomised | Universal | Secondary | 12–16 | RADS | Yes | 0 | 6 | |||
| Roberts et al.138 2003 | Depression | Cluster randomised | Universal | Secondary | 11–13 | CDI | Yes | 0 | 6 | 18 | 30 | |
| Roberts et al.139 2010 | Anxiety and depression | Cluster randomised | Universal | Secondary | 11–13 | CDI | Yes | 0 | 6 | 18 | ||
| Rohde et al.223 2014 | Depression | Individually randomised | Targeted | Secondary | 13–19 | CES-D | Yes | 0 | 6, 12 | 18, 24 | ||
| Rooney et al.157 2006 | Depression | Cluster randomised | Universal | Primary | 8–9 | CDI | Yes | 0 | 9 | 18 | ||
| Rose et al.203 2014 | Depression | Cluster randomised | Universal | Secondary | 9–14 | CDI, RADS | Yes | 0 | 6, 12 | |||
| Sawyer et al.204 2010 | Depression | Cluster randomised | Universal | Secondary | 13.1 (0.50) | CES-D | Yes | 24 | ||||
| Seligman et al.186 1999 | Anxiety and depression | Individually randomised | Targeted | University | 19 (NR) | BDI | Yes | 0 | 3 | 36 | ||
| Seligman et al.187 2007 | Anxiety and depression | Individually randomised | Targeted | University | 19 (NR) | BDI | Yes | 0 | 1, 3 | |||
| Shatté205 1997 | Depression | Individually randomised | Universal | Secondary | 12–14 | CDI | Yes | 0 | 4 | 8, 12 | ||
| Sheffield et al.141 2006 | Depression | Cluster randomised | Universal | Secondary | 13–15 | CDI, CES-D | Yes | 0 | 6, 12 | |||
| Sheffield et al.141 2006 | Depression | Cluster randomised | Targeted | Secondary | 13–15 | CDI, CES-D | Yes | 0 | 6, 12 | |||
| Simpson179 2008 | Anxiety and depression | Individually randomised | Targeted | Primary | 7–11 | CDI | Yes | 0 | ||||
| Siu180 2007 | Anxiety and depression | Individually randomised | Targeted | Primary | 7–10 | RCDS | Yes | 0 | ||||
| Soffer212 2003 | Depression | Individually randomised | Universal | Primary | 10–11 | RCDS | Yes | 0 | 1 | |||
| Spence et al.206 2003 | Depression | Cluster randomised | Universal | Secondary | 12–14 | BDI | Yes | 0 | 12 | 24 | 36, 48 | |
| Stallard et al.142 2013 | Depression | Cluster randomised | Universal | Secondary | 12–16 | RCADS-depression | Y-12 | 6, 12 | ||||
| Stallard et al.142 2013 | Depression | Cluster randomised | Targeted | Secondary | 12–16 | RCADS-depression | No | 6, 12 | ||||
| Stallard et al.159 2014 | Anxiety | Cluster randomised | Universal | Primary | 9–10 | RCADS-depression | Y-12 | 12 | 24 | |||
| Stice et al.237 2006 | Depression | Individually randomised | Targeted | M | 15–22 | BDI | No | 0 | 1 | 6 | ||
| Stice et al.224 2008 | Depression | Individually randomised | Targeted | Secondary | 14–19 | BDI | Yes | 0 | 6, 12 | 24 | ||
| Stoppelbein225 2003 | Depression | Cluster randomised | Targeted | Secondary | 15 (NR) | CDI | No | 0 | 6 | |||
| Tak et al.207 2016 | Depression | Cluster randomised | Universal | Secondary | 12–14 | CDI | Yes | 0 | 6, 12 | 18, 24 | ||
| Takagaki et al.235 2016 | Depression | Individually randomised | Targeted | University | 18–19 | BDI | Yes | 0 | ||||
| Tokolahi et al.181 2018 | Anxiety and depression | Cluster randomised | Targeted | Primary | 7–12 | CDI | Yes | 0 | ||||
| Tomba et al.143 2010 | Anxiety and depression | Cluster randomised | Universal | Secondary | 11.41 (0.56) | Kellner’s | Yes | 0 | 6 | |||
| Topper et al.173 2017 | Anxiety and depression | Individually randomised | Targeted | Secondary | 15–22 | CDI | Yes | 0 | 3 | 12 | ||
| Velásquez et al.189 2015 | Anxiety and depression | Individually randomised | Universal | M | NR | Modified SDQ-depression | No | 0 | ||||
| Wijnhoven et al.226 2014 | Depression | Individually randomised | Targeted | Secondary | 11–15 | CDI, CES-D | Yes | 0 | 1 | 6 | ||
| Wong et al.144 2014 | Anxiety and depression | Cluster randomised | Universal | Secondary | 14–16 | PHQ-9 | Yes | 0 | ||||
| Woods and Jose227 2011 | Depression | Individually randomised | Targeted | Secondary | 14 (NR) | CDI | Yes | 0 | 2 | 12 | ||
| Young et al.228 2006 | Depression | Individually randomised | Targeted | Secondary | 11–16 | CES-D | Yes | 0 | 3 | 6 | ||
| Young et al.229 2010 | Depression | Individually randomised | Targeted | Secondary | 13–17 | CES-D, CDRS | Yes | 0 | 6, 12 | 18 | ||
| Young et al.230 2016 | Depression | Individually randomised | Targeted | Secondary | 13.42 (1.23) | CES-D | Yes | 0 | 6 | |||
| Yu238 2002 | Depression | Individually randomised | Targeted | M | 8–15 | CDI | No | 0 | 3 | 6 | ||
| Study | Reason | Not included in anxiety NMA | Not included in depression NMA |
|---|---|---|---|
| Arnarson and Craighead213 2009 | Data not available | – | ✗ |
| Barrett et al.121 2005 | Data not useable | ✗ | ✗ |
| Bonhauser et al.122 2005 | Not connected to network | ✗ | ✗ |
| Britton et al.123 2014 | Data not available | ✗ | – |
| aBurckhardt et al.124 2015 | Data not available | ✗ | ✗ |
| aBurckhardt et al.191 2016 | Data not available | – | ✗ |
| Cowell et al.231 2009 | Not connected to network | – | ✗ |
| Fung et al.216 2016 | Data not available | – | ✗ |
| Gaete et al.164 2016 | Post-intervention time point not reported | ✗ | ✗ |
| Liddle and Macmillan188 2010 | Mixed age group (8–14 years) | ✗ | ✗ |
| McLaughlin236 2011 | Mixed age group (10–15 years) | – | ✗ |
| Mendelson et al.210 2010 | Data not available | – | ✗ |
| Noël et al.220 2013 | Data not available | – | ✗ |
| Owen and Lanning169 1982 | Baseline measures not reported | ✗ | – |
| Peden et al.234 2000 | Data not available | – | ✗ |
| Reynolds et al.233 2011 | Not connected to network | – | ✗ |
| Stallard et al.142 2013 | Study used in universal analysis only | – | ✗ |
| Stice et al.237 2006 | Mixed age group (15–22 years) | – | ✗ |
| Stoppelbein225 2004 | Data not available | – | ✗ |
| Velásquez et al.189 2015 | Mixed age group (ages not reported) | ✗ | ✗ |
| Yu238 2000 | Mixed age group (8–15 years) | – | ✗ |
| Study | Target | Study design | Population | Setting | Age (years) | Outcome |
|---|---|---|---|---|---|---|
| Anticich et al.339 2013 | Anxiety | Cluster randomised | Universal | Primary | 4–7 | Preschool Anxiety Scale |
| Dadds and Roth303 2008 | Anxiety | Cluster randomised | Universal | Primary | 3–7 | Anxiety Disorders Interview Schedule-Parent Version |
| Eather et al.340 2016 | Anxiety and depression | Cluster randomised | Universal | Secondary | 15–16 | SDQ-total |
| Haden et al.341 2014 | Anxiety and depression | Individually randomised | Universal | Primary | 10–11 | CBCL-parent rated |
| Khalsa et al.239 2012 | Anxiety and depression | Cluster randomised | Universal | Secondary | 15–19 | Behaviour Assessment System for Children |
| Pahl and Barrett242 2010 | Anxiety | Cluster randomised | Universal | Primary | 4–6 | Preschool Anxiety scale |
| Roberts et al.240 2018 | Anxiety and depression | Cluster randomised | Universal | Primary | 9–12 | SDQ-total |
| Study | Type | Setting | Age (years) | Country | Control | Intervention | Sessions (n) | Intensity (minutes) | Delivered by | Format | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | |||||||||
| Ahlen et al.145 2018 | Universal | Primary | 8–11 | HIC | Usual curriculum | CBT | 10 | 600 | Teacher | Face to face | Group | ||
| Anticich et al.339 2013 | Universal | Primary | 4–7 | HIC | Waiting list | Psychosupport | CBT | 10 | NR | Teacher | Face to face | Group | |
| Araya et al.118 2013 | Universal | Secondary | 14.5 | MIC | Usual curriculum | CBT | 11 | 660 | Psychologist | Face to face | Group | ||
| Attwood et al.146 2012 | Universal | Primary | 10–12 | HIC | Attention control | CBT | 6 | 270 | Researcher | Multimedia/computer based | Group/individual | ||
| Aune and Stiles119 2009 | Universal | Secondary | 10–15 | HIC | No intervention | CBT | 3 | 135 | Psychologist | Face to face | Group | ||
| Baker and Butler120 1984 | Universal | Secondary | 16–18 | HIC | CBT self-help | CBT | 8 | 360 | Teacher | Face to face | Group | ||
| Barrett and Turner147 2001 | Universal | Primary | 10–12 | HIC | Usual curriculum | CBT | CBT | 10 | 750 | Teachers or Psychologist | Face to face | Group | |
| Barrett et al.121 2005 | Universal | Secondary | 9–16 | HIC | No intervention | CBT | 10 | 525 | Psychologist | Face to face | Group | ||
| Barry et al.190 2017 | Universal | Secondary | 15–16 | HIC | Usual curriculum | CBT | 4 | Not clear | ‘Coach’ | Face to face | Group | ||
| Bonhauser et al.122 2005 | Universal | Secondary | 15.3 | MIC | Exercise | Exercise | 120 | 10,800 | Teacher | Face to face | Group | ||
| Bouchard et al.148 2013 | Universal | Primary | 9–12 | HIC | Waiting list | CBT | 10 | 750 | Psychologist | Face to face | Group | ||
| Britton et al.123 2014 | Universal | Secondary | 11.79 | HIC | Attention control | Mindfulness/relaxation | 30 | 225 | Teacher | Face to face | Group | ||
| Burckhardt et al.124 2015 | Universal | Secondary | 14–16 | HIC | Attention control | Mindfulness/relaxation | 6 | 360 | NA | Multimedia/computer based | Group | ||
| Burckhardt et al.191 2016 | Universal | Secondary | 15–18 | HIC | Usual curriculum | Third wave | 16 | 480 | Psychologist | Face to face | Group | ||
| Calear et al.125 2009 | Universal | Secondary | 12–17 | HIC | Waiting list | CBT | 5 | 150 | Teacher | Multimedia/computer based | Group | ||
| Calear et al.126 2016 | Universal | Secondary | 12–18 | HIC | Waiting list | CBT | CBT | 6 | 210 | Teacher or MHP supported | Multimedia/computer based | Group | |
| Calear et al.127 2016 | Universal | Secondary | 13–17 | HIC | Waiting list | CBT | 6 | 210 | Teacher | Multimedia/computer based | Group | ||
| Cardemil et al.208 2007 | Universal | Primary | 10–12 | HIC | Usual curriculum | CBT | 12 | 1080 | Psychologist | Face to face | Group | ||
| Chaplin et al.192 2006 | Universal | Secondary | 11–14 | HIC | No intervention | CBT | CBT | 12 | 1080 | Teacher and researchers | Face to face | Group | |
| Clarke et al.193 1993 | Universal | Secondary | 14–16 | HIC | Usual curriculum | Psychoeducation | 3 | 150 | Teacher | Face to face | NA | ||
| Clarke et al.193 1993 | Universal | Secondary | 14–16 | HIC | Usual curriculum | Behavioural therapy | 5 | 250 | Teacher | Face to face | NA | ||
| Collins et al.149 2014 | Universal | Primary | 9–10 | HIC | Usual curriculum | CBT | 10 | NR | Teacher or school counsellor | Face to face | Group | ||
| Dadds and Roth303 2008 | Universal | Primary | 3–7 | HIC | No intervention | CBT | 6 | NR | Psychologist | Face to face | Group | ||
| Eather et al.340 2016 | Universal | Secondary | 15–16 | HIC | Waiting list | Exercise | 16 | 960 | Fitness instructor | Face to face | Group | ||
| Essau et al.150 2012 | Universal | Primary | 9–12 | HIC | Waiting list | CBT | 10 | 600 | Psychologist | Face to face | Group | ||
| Gallegos151 2008 | Universal | Primary | 9–11 | MIC | Usual curriculum | CBT | 10 | 600 | Teacher | Face to face | Group | ||
| Gillham209 1995 | Universal | Primary | 10–12 | HIC | No intervention | CBT | 12 | 1440 | Psychologist | Face to face | Group | ||
| Gillham et al.128 2006 | Universal | Secondary | 11–13 | HIC | No intervention | CBT | 8 | 720 | Researchers and psychologist | Face to face | Group | ||
| Gillham et al.194 2007 | Universal | Secondary | 11–14 | HIC | No intervention | Attention control + psychosupport | CBT | 12 | 1080 | Teachers, school counsellors and psychologists | Face to face | Group | |
| Gucht et al.129 2017 | Universal | Secondary | 14–21 | HIC | Usual curriculum | Third wave | 4 | 480 | Teacher | Face to face | Group | ||
| Haden et al.341 2014 | Universal | Primary | 10–11 | HIC | Usual curriculum | Mindfulness/relaxation | 36 | 3240 | Teacher | Face to face | Group | ||
| Hiebert et al.130 1989 | Universal | Secondary | 13–14 | HIC | Attention control | Mindfulness/relaxation | 11 | 660 | Teacher and school counsellor | Face to face | Group | ||
| Hodas131 2016 | Universal | Secondary | 12–14 | HIC | Waiting list | CBT | 7 | 455 | Psychologist | Face to face | Group | ||
| Horowitz et al.195 2007 | Universal | Secondary | 14–15 | HIC | Usual curriculum | IPT | CBT | 8 | 720 | Psychologist | Face to face | Group | |
| Johnson et al.132 2016 | Universal | Secondary | 13.63 | HIC | Usual curriculum | Third wave | 9 | 495 | Psychologist | Face to face | Group | ||
| Johnson et al.133 2017 | Universal | Secondary | 13.44 | HIC | Usual curriculum | Third wave | Third wave | 9 | 450 | Psychologist | Face to face | Group | |
| Johnstone et al.152 2014 | Universal | Primary | 9–10 | HIC | Usual curriculum | CBT | 10 | 600 | Teacher | Face to face | Group | ||
| Khalsa et al.239 2012 | Universal | Secondary | 15–19 | HIC | Usual curriculum | Mindfulness/relaxation | 27.5 | 825 | Yoga trainer | Face to face | Group | ||
| Kindt et al.196 2014 | Universal | Secondary | 11–16 | HIC | Usual curriculum | CBT | 16 | NR | Teacher | Face to face | Group | ||
| Lock and Barrett134 2003 | Universal | Secondary | NR | HIC | No intervention | CBT | 10 | 750 | Teacher | Face to face | Group | ||
| Lowry-Webster et al.135 2001 | Universal | Secondary | 10–13 | HIC | Waiting list | CBT | 10 | 600 | Teacher | Face to face | Group | ||
| Mendelson et al.210 2010 | Universal | Primary | 9–11 | HIC | Waiting list | Mindfulness/relaxation | 48 | 2160 | Yoga trainer | Face to face | Group | ||
| Merry et al.197 2004 | Universal | Secondary | 13–15 | HIC | Attention control | CBT + IPT | 11 | NR | Teacher | Face to face | Group | ||
| Miller et al.153 2010 | Universal | Primary | 7–12 | HIC | Waiting list | CBT | NR | NR | Teacher | Face to face | Group | ||
| Miller et al.154 2011 | Universal | Primary | 7–13 | HIC | Waiting list | CBT | 9 | NR | Teacher and school counsellor | Face to face | Group | ||
| Miller et al.154 2011 | Universal | Primary | 7–13 | HIC | Attention control | CBT | 9 | 540 | Teacher and school counsellor | Face to face | Group | ||
| Pahl and Barrett242 2010 | Universal | Primary | 4–6 | HIC | Waiting list | CBT | 9 | 270 | Psychologist | Face to face | Group | ||
| Pattison and Lynd-Stevenson155 2001 | Universal | Primary | 9–12 | HIC | No intervention | Attention control | CBT | CBT | 10 | 1200 | Child MHPs | Face to face | Group |
| Perry et al.136 2017 | Universal | Secondary | 16–17 | HIC | Attention control | CBT | 7 | 175 | NA | Multimedia/computer based | Group | ||
| Pophillat et al.156 2016 | Universal | Primary | 6–8 | HIC | Usual curriculum | CBT | 10 | NR | Teacher | Face to face | Group | ||
| Pössel et al.198 2004 | Universal | Secondary | 13–14 | HIC | Usual curriculum | CBT | 10 | 900 | Psychologist or graduate students | Face to face | Group | ||
| Pössel et al.199 2011 | Universal | Secondary | 12–13 | HIC | Usual curriculum | CBT | 10 | 900 | Psychologist or graduate students | Face to face | Group | ||
| Pössel et al.200 2013 | Universal | Secondary | 14–16 | HIC | Usual curriculum | Attention control | CBT | 10 | 900 | Psychologist or graduate students | Face to face | Group | |
| Potek137 2012 | Universal | Secondary | 14–17 | HIC | Waiting list | Mindfulness/relaxation | 6 | 270 | Psychologist | Face to face | Group | ||
| Quayle et al.211 2001 | Universal | Primary | 11–12 | HIC | Waiting list | CBT | 8 | 640 | Psychologist | Face to face | Group | ||
| Raes et al.201 2014 | Universal | Secondary | 13–20 | HIC | Usual curriculum | Third wave | 8 | 800 | Psychologist | Face to face | Group | ||
| Reynolds et al.233 2011 | Universal | University | 17.9 | HIC | Usual curriculum | Behavioural therapy | 14 | 1680 | Psychologist | Face to face | Group | ||
| Rivet-Duval et al.202 2011 | Universal | Secondary | 12–16 | MIC | Waiting list | CBT + IPT | 11 | 660 | Teacher | Face to face | Group | ||
| Roberts et al.138 2003 | Universal | Secondary | 11–13 | HIC | Usual curriculum | CBT | 12 | NR | Psychologist | Face to face | Group | ||
| Roberts et al.139 2010 | Universal | Secondary | 11–13 | HIC | Usual curriculum | CBT | 20 | 1200 | Teacher | Face to face | Group | ||
| Roberts et al.240 2018 | Universal | Primary | 9–12 | HIC | Usual curriculum | CBT | CBT | 20 | 1200 | Teacher | Face to face | Group | |
| Rodgers et al.140 2015 | Universal | Secondary | 12–13 | HIC | Waiting list | CBT | 10 | 600 | Psychologist | Face to face | Group | ||
| Rooney et al.157 2006 | Universal | Primary | 8–9 | HIC | No intervention | CBT | 8 | 480 | Psychologist | Face to face | Group | ||
| Rose et al.203 2014 | Universal | Secondary | 9–14 | HIC | Waiting list | CBT + IPT | CBT + IPT | 11 | 495 | Psychologist | Face to face | Group | |
| Ruttledge et al.158 2016 | Universal | Primary | 9–13 | HIC | Waiting list | CBT | 10 | NR | Teacher | Face to face | Group | ||
| Sawyer et al.204 2010 | Universal | Secondary | 13.1 | HIC | Usual curriculum | CBT | 30 | 900 | Teacher | Face to face | Group | ||
| Shatté205 1997 | Universal | Secondary | 12–14 | HIC | No intervention | Attention control | CBT | 12 | 1440 | Teachers and psychologist | Face to face | Group | |
| Sheffield et al.141 2006 | Universal | Secondary | 13–15 | HIC | No intervention | CBT | 8 | 380 | Teachers and psychologist | Face to face | Group | ||
| Soffer212 2003 | Universal | Primary | 10–11 | HIC | No intervention | Attention control | Behavioural therapy | 8 | 320 | Psychologist | Face to face | Group | |
| Spence et al.206 2003 | Universal | Secondary | 12–14 | HIC | Usual curriculum | CBT | 8 | 380 | Teacher | Face to face | Group | ||
| Stallard et al.142 2013 | Universal | Secondary | 12–16 | HIC | Usual curriculum | Attention control | CBT + IPT | 9 | 495 | Facilitator | Face to face | Group | |
| Stallard et al.159 2014 | Universal | Primary | 9–10 | HIC | Usual curriculum | CBT | CBT | 9 | 540 | Teacher and facilitator | Face to face | Group | |
| Tak et al.207 2016 | Universal | Secondary | 12–14 | HIC | Usual curriculum | CBT | 16 | 800 | Teacher and psychologist | Face to face | Group | ||
| Tomba et al.143 2010 | Universal | Secondary | 11.41 | HIC | CBT | CBT | 6 | 720 | Psychologist | Face to face | Group | ||
| Velásquez et al.189 2015 | Universal | Primary/secondary | NR | MIC | Waiting list | Mindfulness/relaxation | 24 | 2880 | Yoga trainer | Face to face | Group | ||
| Wong et al.144 2014 | Universal | Secondary | 14–16 | HIC | Usual curriculum | CBT | CBT | 6 | 240 | Teacher | Multimedia/computer based | Group | |
| Arnarson and Craighead213 2009 | Indicated | Secondary | 14–15 | HIC | No intervention | CBT + IPT | 14 | NR | Psychologist | Face to face | Group | ||
| Balle and Tortella-Feliu160 2010 | Selective | Secondary | 11–17 | HIC | Waiting list | CBT | 6 | 270 | Psychologist | Face to face | Group | ||
| Berry and Hunt161 2009 | Indicated | Secondary | 12–15 | HIC | Waiting list | CBT | 8 | 480 | Psychologist | Face to face | Group | ||
| Clarke et al.214 1995 | Indicated | Secondary | 14–16 | HIC | No intervention | CBT | 15 | 675 | School psychologist | Face to face | Group | ||
| Congleton215 1995 | Selective | Secondary | 12–14 | HIC | Waiting list | CBT | 8 | 480 | Psychologist | Face to face | Group | ||
| Cooley-Strickland et al.174 2011 | Indicated | Primary | 9–10 | HIC | Waiting list | CBT | 13 | 780 | Psychologist | Face to face | Group | ||
| Cova et al.162 2011 | Indicated | Secondary | 14–15 | MIC | No intervention | CBT | 11 | 990 | Psychologist | Face to face | Group | ||
| Cowell et al.231 2009 | Selective | Primary | 10.4 | HIC | No intervention | Psychosupport | 6 | NR | Nurse | Face to face | Group | ||
| Cui et al.183 2016 | Indicated | University | 19.42 | MIC | Waiting list | CBT | Psychosupport | 8 | 960 | Psychologist | Face to face | Group | |
| Dobson et al.163 2010 | Indicated | Secondary | 13–18 | HIC | Attention control | CBT | 15 | 675 | Psychologist | Face to face | Group | ||
| Ellis et al.184 2011 | Indicated | University | 18–25 | HIC | No intervention | CBT | Psychosupport | 3 | 300 | NA | Multimedia/computer based | Individual | |
| Fitzgerald et al.114 2016 | Indicated | Secondary | 15–18 | HIC | Attention control | BM | 4 | NR | Researcher | Multimedia/computer based | Group | ||
| Fung et al.216 2016 | Indicated | Secondary | 12–14 | HIC | Waiting list | Third wave | 12 | 720 | Psychologist | Face to face | Group | ||
| Gaete et al.164 2016 | Indicated | Secondary | 13–18 | MIC | Usual curriculum | CBT | 8 | 360 | Psychologist | Face to face | Group | ||
| Gillham et al.165 2012 | Indicated | Secondary | 10–15 | HIC | No intervention | CBT | CBT | 10 | 900 | Teacher and school counsellor | Face to face | Group | |
| Hiebert et al.130 1989 | Indicated | Secondary | 15–17 | HIC | Waiting list | Mindfulness/relaxation | BIO | 8 | 320 | Psychologist | Face to face | Individual | |
| Higgins185 2007 | Indicated | University | 17–19 | HIC | No intervention | CBT | 2 | 240 | Psychologist | Face to face | Group | ||
| Hunt et al.166 2009 | Indicated | Secondary | 11–13 | HIC | No intervention | CBT | 10 | 500 | Teacher and school counsellor | Face to face | Group | ||
| Jaycox et al.232 1994 | Indicated | Primary | 10–13 | HIC | Waiting list | CBT | 12 | 1080 | Psychologist | Face to face | Group | ||
| Jordans et al.167 2010 | Selective | Secondary | 11–14 | LIC | Waiting list | Mixed | 15 | 900 | Researcher | Face to face | Group | ||
| Kiselica et al.168 1994 | Indicated | Secondary | 14–15 | HIC | Psychoeducation | CBT | 8 | 480 | Counsellors | Face to face | Group | ||
| Liddle and Macmillan188 2010 | Selective | Primary/secondary | 8–14 | HIC | Waiting list | CBT | 10 | NR | Psychologist | Face to face | Group | ||
| Livheim et al.217 2015 | Indicated | Secondary | 12–17 | HIC | Psychosupport | Third wave | 8 | NR | Psychologist | Face to face | Group | ||
| Manassis et al.175 2010 | Indicated | Primary | 8–11 | HIC | Attention control | CBT | 12 | 720 | Psychologist | Face to face | Group | ||
| McCarty et al.218 2011 | Indicated | Secondary | 13 | HIC | Usual curriculum | CBT | 12 | NR | Not clear | Face to face | Group | ||
| McCarty et al.219 2013 | Indicated | Secondary | 11–15 | HIC | Psychosupport | CBT | 12 | 600 | Therapists | Face to face | Group | ||
| McLaughlin236 2011 | Indicated | Primary/secondary | 10–15 | HIC | Psychosupport | CBT | 10 | 500 | Psychologist | Face to face | Group | ||
| McLoone et al.176 2012 | Indicated | Primary | 7–10 | HIC | Waiting list | CBT | CBT | 10 | 600 | School counsellors | Face to face | Group | |
| Mifsud and Rapee177 2005 | Indicated | Primary | 8–11 | HIC | Waiting list | CBT | 8 | 480 | School counsellors | Face to face | Group | ||
| Miller et al.178 2011 | Indicated | Primary | 7–12 | HIC | Attention control | CBT | 9 | 540 | Teacher and school counsellor | Face to face | Group | ||
| Noël et al.220 2013 | Indicated | Secondary | 13–15 | HIC | Waiting list | CBT | 12 | Students | Face to face | Group | |||
| Owen and Lanning169 1982 | Indicated | Secondary | 15–16 | HIC | Waiting list | Mindfulness/relaxation | CBT | CBT | 6 | 180 | Counsellors | Face to face | Group |
| Peden et al.234 2000 | Indicated | University | 18–24 | HIC | No intervention | CBT | NR | NR | NA | Face to face | Group | ||
| Peng et al.170 2015 | Selective | Secondary | 14.2 | MIC | No intervention | Exercise | 24 | NR | NR | Face to face | Group | ||
| Poppelaars et al.221 2016 | Indicated | Secondary | 11–16 | HIC | Waiting list | CBT | CBT | CBT | 8 | 480 | Psychologist | Face to face | Individual |
| Puskar et al.222 2003 | Indicated | Secondary | 14–18 | HIC | No intervention | CBT | 10 | 450 | Nurse | Face to face | Group | ||
| Rice171 2009 | Indicated | Secondary | 10–18 | HIC | Attention control | CBT | Mindfulness/relaxation | 16 | 560 | Psychologist | Face to face | Group | |
| Rohde et al.223 2014 | Indicated | Secondary | 13–19 | HIC | Psychoeducation | CBT | CBT | 6 | 360 | Psychologist or self-help | Face to face | Group | |
| Scholten et al.172 2016 | Indicated | Secondary | 11–15 | HIC | Attention control | Biofeedback | 6 | 360 | Researcher | Multimedia/computer based | Individual | ||
| Schoneveld et al.115 2016 | Indicated | Primary | 8–13 | HIC | Attention control | Biofeedback | 5 | 300 | Researcher | Multimedia/computer based | Group | ||
| Schoneveld et al.116 2018 | Indicated | Primary | 7–12 | HIC | CBT | Biofeedback | 6 | 360 | Master’s students and psychologist | Multimedia/computer based | Group | ||
| Seligman et al.186 1999 | Selective | University | 19 | HIC | No intervention | CBT | 8 | 960 | Psychologist | Face to face | Group/individual | ||
| Seligman et al.187 2007 | Selective | University | 19 | HIC | No intervention | CBT | 8 | 960 | Psychologist | Face to face/multimedia | Group | ||
| Sheffield et al.141 2006 | Indicated | Secondary | 13–15 | HIC | No intervention | CBT | CBT | CBT | 8 | 380 | Teachers or school counsellor or both | Face to face | Group |
| Simpson179 2008 | Indicated | Primary | 7–11 | HIC | Attention control | CBT | 12 | 1080 | NR | Face to face | Group | ||
| Siu180 2007 | Indicated | Primary | 7–10 | HIC | Waiting list | CBT | 8 | NR | Counsellors | Face to face | Group | ||
| Sportel et al.117 2013 | Indicated | Secondary | 12–15 | HIC | No intervention | BM | CBT | 20 | 900 | NA | Multimedia/computer based | Individual | |
| Stallard et al.142 2013 | Indicated | Secondary | 12–16 | HIC | Usual curriculum | Usual curriculum | CBT + IPT | 9 | 495 | Facilitator | Face to face | Group | |
| Stice et al.237 2006 | Indicated | Secondary/university | 15–22 | HIC | Waiting list | CBT | 4 | 240 | Psychologist | Face to face | Group | ||
| Stice et al.224 2008 | Indicated | Secondary | 14–19 | HIC | No intervention | CBT self-help | Psychosupport | CBT | 6 | 360 | Self-help or psychologist | Face to face | Group |
| Stoppelbein225 2003 | Indicated | Secondary | 15 | HIC | Attention control | CBT | 10 | 500 | Psychologist | Face to face | Group | ||
| Takagaki et al.235 2016 | Indicated | University | 18–19 | HIC | No intervention | Behavioural therapy | 5 | 300 | Psychologist | Face to face | Group | ||
| Tokolahi et al.181 2018 | Selective | Primary | 7–12 | HIC | Waiting list | Occupational therapy | 8 | 480 | Occupational therapist | Face to face | Group | ||
| Topper et al.173 2017 | Selective | Secondary | 15–22 | HIC | Waiting list | CBT | 6 | 540 | Psychologist | Face to face | Group | ||
| van Starrenburg et al.182 2017 | Indicated | Primary | 7–13 | HIC | Waiting list | CBT | 12 | 720 | Psychologist | Face to face | Group | ||
| Wijnhoven et al.226 2014 | Indicated | Secondary | 11–15 | HIC | Waiting list | CBT | 8 | 400 | Therapist | Face to face | Group | ||
| Woods and Jose227 2011 | Indicated | Secondary | 14 | HIC | Usual curriculum | CBT | 8 | 720 | School counsellors | Face to face | Group | ||
| Young et al.228 2006 | Indicated | Secondary | 11–16 | HIC | Psychosupport | CBT | 10 | 900 | Psychologist/social worker | Face to face | Group/individual | ||
| Young et al.229 2010 | Indicated | Secondary | 13–17 | HIC | Psychosupport | IPT | 10 | 900 | Psychologist | Face to face | Group/individual | ||
| Young et al.230 2016 | Indicated | Secondary | 13.42 | HIC | Psychosupport | IPT | 11 | 450 | Psychologist | Face to face | Group/individual | ||
| Yu238 2002 | Indicated | Primary/secondary | 8–15 | MIC | No intervention | CBT | 10 | 1200 | Teacher | Face to face | Group | ||
Risk-of-bias assessments for studies reporting anxiety or depression outcome
Risk-of-bias judgements were made for 137 studies included in the review of studies to prevent anxiety and/or depression. Each study was assessed using the Cochrane Risk of Bias tool, version 1.0,79 which rates the risk of bias as low, unclear or high. For ‘other bias’, we considered cluster trials only, and examined bias arising from the timing of identification and recruitment of participants (recruitment bias). We also considered unit-of-analysis errors (not accounting for clustering) and possibility of contamination across clusters.
| Study | Population | Setting | Risk of bias | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Selective reporting | Incomplete outcome data | Other bias (cluster RCTs) | |||
| Ahlen et al.145 2018 | Universal | Primary | Low | Low | High | High | Lowa | High | High |
| Anticich et al.339 2013 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | Unclear |
| Araya et al.118 2013 | Universal | Secondary | Low | Unclear | High | High | Lowb | Low | Unclear |
| Arnarson and Craighead213 2009 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | High | NA |
| Attwood et al.146 2012 | Universal | Primary | Unclear | Unclear | Unclear | Unclear | Unclear | High | NA |
| Aune and Stiles119 2009 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | High |
| Baker and Butler120 1984 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | High |
| Balle and Tortella-Feliu160 2010 | Selective | Secondary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Barrett and Turner147 2001 | Universal | Primary | Unclear | Unclear | High | High | High | High | High |
| Barrett et al.121 2005 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | Unclear |
| Barry et al.190 2017 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Berry and Hunt161 2009 | Indicated | Secondary | Low | Unclear | High | High | Unclear | Low | Low |
| Bonhauser et al.122 2005 | Universal | Secondary | Unclear | Unclear | High | High | High | Low | High |
| Bouchard et al.148 2013 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | Unclear |
| Britton et al.123 2014 | Universal | Secondary | Low | High | High | High | Unclear | Low | NA |
| Burckhardt et al.124 2015 | Universal | Secondary | Low | Unclear | Unclear | Unclear | Unclearb | High | Low |
| Burckhardt et al.191 2016 | Universal | Secondary | Unclear | Unclear | High | High | High | High | High |
| Calear et al.125 2009 | Universal | Secondary | Low | Low | High | High | Lowb | Low | Low |
| Calear et al.126 2016 | Universal | Secondary | Low | Low | High | High | Unclearb | Low | Low |
| Calear et al.127 2016 | Universal | Secondary | Unclear | Unclear | High | High | Lowb | Low | Unclear |
| Cardemil et al.208 2007 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | NA |
| Chaplin et al.192 2006 | Universal | Secondary | Low | Unclear | High | High | Unclear | High | NA |
| Clarke et al.193 1993 | Universal | Secondary | Unclear | Unclear | High | High | High | Low | High |
| Clarke et al.193 1993 | Universal | Secondary | Unclear | Unclear | High | High | High | High | High |
| Clarke et al.214 1995 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | High | NA |
| Collins et al.149 2014 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | High |
| Congleton215 1995 | Selective | Secondary | Unclear | Unclear | High | High | Lowa | High | NA |
| Cooley-Strickland et al.174 2011 | Indicated | Primary | Unclear | Unclear | High | High | High | Unclear | High |
| Cova et al.162 2011 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Cowell et al.231 2009 | Selective | Primary | Unclear | Unclear | High | High | Unclear | Unclear | High |
| Cui et al.183 2016 | Indicated | University | Unclear | Unclear | High | High | Unclear | Low | High |
| Dadds and Roth303 2008 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | High |
| Dobson et al.163 2010 | Indicated | Secondary | Low | Unclear | Low | Low | Lowb | Unclear | NA |
| Eather et al.340 2016 | Universal | Secondary | Low | Low | High | High | Unclearb | Unclear | High |
| Ellis et al.184 2011 | Indicated | University | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Essau et al.150 2012 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | Unclear |
| Fitzgerald et al.114 2016 | Indicated | Secondary | Unclear | Unclear | Low | Low | Lowb | Unclear | NA |
| Fung et al.216 2016 | Indicated | Secondary | Unclear | High | High | High | Unclear | Low | NA |
| Gaete et al.164 2016b | Indicated | Secondary | Low | Low | High | High | Lowb | Unclear | NA |
| Gallegos151 2008 | Universal | Primary | Unclear | Unclear | High | High | Lowa | Unclear | High |
| Gillham209 1995 | Universal | Primary | Unclear | Unclear | High | High | Lowa | Unclear | NA |
| Gillham et al.128 2006 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Gillham et al.194 2007 | Universal | Secondary | Low | Unclear | High | High | Unclear | Unclear | NA |
| Gillham et al.165 2012 | Indicated | Secondary | Low | Unclear | High | High | Lowb | Unclear | NA |
| Gucht et al.129 2017 | Universal | Secondary | Low | Unclear | High | High | Unclear | High | High |
| Haden et al.341 2014 | Universal | Primary | Unclear | High | High | High | Unclear | Low | NA |
| Hiebert et al.130 1989 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Hiebert et al.130 1989 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Higgins185 2007 | Indicated | University | Unclear | Unclear | High | High | Unclear | High | NA |
| Hodas131 2016 | Universal | Secondary | Unclear | Unclear | High | High | Lowa | High | NA |
| Horowitz et al.195 2007 | Universal | Secondary | Low | High | High | High | Unclear | Low | NA |
| Hunt et al.166 2009 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Jaycox et al.232 1994 | Indicated | Primary | Unclear | Unclear | High | High | Unclear | High | NA |
| Johnson et al.132 2016 | Universal | Secondary | Low | Unclear | High | High | Unclear | Low | NA |
| Johnson et al.133 2017 | Universal | Secondary | Low | Unclear | High | High | Lowb | Low | NA |
| Johnstone et al.152 2014 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | Low |
| Jordans et al.167 2010 | Selective | Secondary | Low | Low | High | High | Lowb | Low | Low |
| Khalsa et al.239 2012 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | High |
| Kindt et al.196 2014 | Universal | Secondary | Low | Low | High | High | Lowb | High | Low |
| Kiselica et al.168 1994 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Liddle and Macmillan188 2010 | Selective | Primary/secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Livheim et al.217 2015 | Indicated | Secondary | Low | Unclear | High | High | High | Unclear | NA |
| Lock and Barrett134 2003 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | High |
| Lowry-Webster et al.135 2001 | Universal | Secondary | Unclear | Unclear | High | High | High | High | High |
| Manassis et al.175 2010 | Indicated | Primary | Low | Unclear | Low | Low | Lowb | Low | NA |
| McCarty et al.218 2011 | Indicated | Secondary | Unclear | Unclear | High | High | Lowb | Unclear | NA |
| McCarty et al.219 2013 | Indicated | Secondary | Low | Low | Unclear | Unclear | Unclear | Unclear | NA |
| McLaughlin236 2011 | Indicated | Primary/secondary | Low | High | Low | Low | Lowa | Unclear | NA |
| McLoone et al.176 2012 | Indicated | Primary | Low | Unclear | High | High | High | Unclear | High |
| Mendelson et al.210 2010 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | High |
| Merry et al.197 2004 | Universal | Secondary | Low | Low | Low | Low | Unclear | High | NA |
| Mifsud and Rapee177 2005 | Indicated | Primary | Unclear | Unclear | High | High | High | High | High |
| Miller et al.153 2010 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | High |
| Miller et al.154 2011 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Unclear | High |
| Miller et al.178 2011 | Indicated | Primary | Unclear | Unclear | High | High | Unclear | Low | High |
| Miller et al.154 2011 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | Low |
| Noël et al.220 2013 | Indicated | Secondary | Low | Unclear | High | High | Unclear | Low | NA |
| Owen and Lanning169 1982 | Indicated | Secondary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Pahl and Barrett242 2010 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | High |
| Pattison and Lynd-Stevenson155 2001 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Peden et al.234 2000 | Indicated | University | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Peng et al.170 2015 | Selective | Secondary | Unclear | Unclear | High | High | Unclear | Low | Unclear |
| Perry et al.136 2017 | Universal | Secondary | Unclear | Low | Low | Low | Lowb | Low | Low |
| Pophillat et al.156 2016 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | Low |
| Poppelaars et al.221 2016 | Indicated | Secondary | Unclear | Low | High | High | Lowb | Low | Low |
| Pössel et al.198 2004 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | Unclear |
| Pössel et al.199 2011 | Universal | Secondary | Unclear | Unclear | High | High | High | High | Unclear |
| Pössel et al.200 2013 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | Unclear |
| Potek137 2012 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Puskar et al.222 2003 | Indicated | Secondary | Low | Unclear | High | High | Unclear | High | NA |
| Quayle et al.211 2001 | Universal | Primary | Unclear | Unclear | High | High | Unclear | High | NA |
| Raes et al.201 2014 | Universal | Secondary | Low | Low | High | High | Unclear | Low | Unclear |
| Reynolds et al.233 2011 | Universal | University | Unclear | Unclear | Unclear | Unclear | Unclear | Low | Low |
| Rice171 2009 | Indicated | Secondary | Unclear | Unclear | Unclear | Unclear | Lowa | High | NA |
| Rivet-Duval et al.202 2011 | Universal | Secondary | Unclear | High | High | High | Unclear | Low | NA |
| Roberts et al.138 2003 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Low | Unclear |
| Roberts et al.139 2010 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | Unclear |
| Roberts et al.240 2018 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Low | Unclear |
| Rodgers et al.140 2015 | Universal | Secondary | Unclear | Unclear | High | High | High | Unclear | NA |
| Rohde et al.223 2014 | Indicated | Secondary | Low | Unclear | High | High | Unclear | Low | NA |
| Rooney et al.157 2006 | Universal | Primary | Unclear | Unclear | High | High | Unclear | Unclear | Unclear |
| Rose et al.203 2014 | Universal | Secondary | Unclear | Unclear | Unclear | Unclear | Unclear | Low | Unclear |
| Ruttledge et al.158 2016 | Universal | Primary | Low | Unclear | High | High | Unclear | Low | Unclear |
| Sawyer et al.204 2010 | Universal | Secondary | Unclear | Low | High | High | Unclear | Unclear | Low |
| Scholten et al.172 2016 | Indicated | Secondary | Low | Unclear | Unclear | Unclear | Lowb | Low | NA |
| Schoneveld et al.115 2016 | Indicated | Primary | Low | Low | Unclear | Unclear | Lowb | Low | NA |
| Schoneveld et al.116 2018 | Indicated | Primary | Low | Low | Low | Low | Lowb | Low | NA |
| Seligman et al.186 1999 | Selective | University | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Seligman et al.187 2007 | Selective | University | Unclear | Unclear | High | High | Unclear | Unclear | NA |
| Shatté205 1997 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Sheffield et al.141 2006 | Universal | Secondary | Low | Low | High | High | Unclear | Low | High |
| Sheffield et al.141 2006 | Indicated | Secondary | Low | Low | High | High | Unclear | Low | High |
| Simpson179 2008 | Indicated | Primary | Unclear | Unclear | Low | Low | Unclear | Low | NA |
| Siu180 2007 | Indicated | Primary | Unclear | Unclear | High | High | Unclear | Low | NA |
| Soffer212 2003 | Universal | Primary | Unclear | Unclear | High | High | Lowa | Unclear | NA |
| Spence et al.206 2003 | Universal | Secondary | Unclear | Unclear | High | High | Unclear | High | Unclear |
| Sportel et al.117 2013 | Indicated | Secondary | Low | Low | High | High | Lowb | High | Unclear |
| Stallard et al.142 2013b | Universal | Secondary | Low | Low | High | High | Lowb | High | Low |
| Stallard et al.142 2013b | Indicated | Secondary | Low | Low | High | High | Lowb | High | Low |
| Stallard et al.159 2014b | Universal | Primary | Low | Low | High | High | Lowb | Low | Low |
| Stice et al.237 2006 | Indicated | Secondary/university | Unclear | Unclear | High | High | Unclear | Low | NA |
| Stice et al.224 2008 | Indicated | Secondary | Low | Unclear | High | High | Lowb | Low | NA |
| Stoppelbein225 2003 | Indicated | Secondary | Unclear | Unclear | Unclear | Unclear | Lowa | High | Low |
| Tak et al.207 2016 | Universal | Secondary | Unclear | Low | High | High | Lowb | Unclear | Low |
| Takagaki et al.235 2016 | Indicated | University | Low | Low | High | High | Lowb | Low | NA |
| Tokolahi et al.181 2018 | Selective | Primary | Low | Low | High | High | Lowb | Low | Low |
| Tomba et al.143 2010 | Universal | Secondary | Unclear | Unclear | Unclear | Unclear | Unclear | Low | High |
| Topper et al.173 2017 | Selective | Secondary | Unclear | Low | High | High | Lowb | Low | NA |
| van Starrenburg et al.182 2017 | Indicated | Primary | Unclear | Unclear | High | High | Unclearb | Low | NA |
| Velásquez et al.189 2015 | Universal | Primary/secondary | Unclear | Unclear | High | High | Unclear | Low | Unclear |
| Wijnhoven et al.226 2014 | Indicated | Secondary | Low | Low | High | High | Unclear | Low | NA |
| Wong et al.144 2014 | Universal | Secondary | Low | Unclear | High | High | Lowb | High | Unclear |
| Woods and Jose227 2011 | Indicated | Secondary | Low | Unclear | High | High | Unclear | High | NA |
| Young et al.228 2006 | Indicated | Secondary | Low | Unclear | Unclear | Unclear | Unclear | Low | NA |
| Young et al.229 2010 | Indicated | Secondary | Low | Unclear | Unclear | Unclear | Lowb | Low | NA |
| Young et al.230 2016 | Indicated | Secondary | Low | Unclear | Unclear | Unclear | Unclear | Low | NA |
| Yu238 2002 | Indicated | Primary/secondary | Unclear | Unclear | High | High | Unclear | Unclear | NA |
Studies reporting facilitator fidelity and integrity measures
| Study | Facilitator fidelity/integrity |
|---|---|
| Ahlen et al.145 2018 | Teachers received regular e-mails and visits to check schedule adherence. Most teachers (n = 17) completed all 10 sessions, two completed eight sessions and one completed six of the 10 scheduled sessions. Sessions were not recorded satisfactorily |
| Aune and Stiles119 2009 | Adherence and competence were rated as very good to excellent (adherence: mean = 5.33, competence: mean = 5.67) |
| Barrett and Turner147 2001 | 88–92% concordance reported |
| Barrett et al.121 2005 | 88.8–95.6% concordance between session and manual content was reported |
| Burckhardt et al.191 2016 | Sessions were audio-recorded. Adherence to acceptance and commitment therapy was scored on a four-point Likert scale where 1 = minimal and 4 = very high adherence. The mean across all session components was 3.0 |
| Clarke et al.193 1993 | Mean compliance for evaluated sessions was 86.2% (range 61–100%) compliance |
| Clarke et al.214 1995 | Sessions were audio-recorded. Adherence averaged 93.9% compliance (SD 5.2%, range 77.8–100% protocol compliance) |
| Collins et al.149 2014 | Authors reported a high level of fidelity to intervention content by lesson and facilitator groups. Mean fidelity rating across all sessions: 6.31 (on a seven-point scale) |
| Dadds and Roth303 2008 | Across all sessions, mean adherence to the manual/ intended intervention was 96% (range 83–100%) |
| Dobson et al.163 2010 | Adherence to intervention protocol was assessed by audio-tape. The first author listened to randomly selected tapes and tried to identify the intervention. Identification was 100% accurate. The authors stated that this suggests ‘strong adherence to treatment protocols’ |
| Essau et al.150 2012 | Adherence to the intervention content ranged from 78[%] to 97% |
| Gallegos151 2008 | Compliance with the programme manual was reported by classroom. The mean compliance across all classrooms was 2.07 (four-point scale, 1 = extremely well and 4 = not at all) |
| Gillham et al.194 2007 | Sessions were audio-taped and integrity scores rated on a seven-point scale (7 = excellent coverage). Integrity score for degree of items covered: PRP mean 4.9 (SD 0.48); PEP mean 4.4 (SD 0.36). Integrity score for percentage of items covered satisfactorily: PRP 80% (SD 7.5%); PEP 68% (SD 5.7%) |
| Gillham et al.165 2012 | PRP sessions were audio-taped:On average, group leaders covered 68% of the integrity items to some degree (rated ≥ 2) and 47% of the items satisfactorily (rated ≥ 4) |
| Hunt et al.166 2009 | Facilitators were asked to rate their compliance to intervention content and aims. A total of 49.0% complied ‘extremely well’ and 44.8% ‘moderately well’. Sessions were also audio-recorded; however, only 40% of schools provided usable audio-tapes. Of these, only half (55%) were rated as complying moderately or extremely well to the intervention content and activities |
| Johnson et al.133 2017 | An average proficiency score of 5 out of 6 was given for facilitator adherence and competence |
| Johnstone et al.152 2014 | Implementation integrity was recorded by 88.46% of teachers in a logbook. The average content covered was mean 95.6% (SD 5.31%) |
| Kindt et al.196 2014 | A total of 16 out of 28 teachers filled out adherence reports for OVK. On average, 80.5% of lessons were taught (95.3% of the first eight and 65.5% of the last eight lessons) |
| McCarty et al.219 2013 | For the Positive Thoughts and Actions intervention, video-recordings were reviewed; the mean facilitator adherence to core concepts of the intervention was 92%, (range 73–100%). For the control intervention, audio-recorded interviews were reviewed; the mean facilitator adherence was 92% (range 80–96%) |
| Miller et al.154 2011 | Two sessions were audio-recorded. Adherence to intervention content and objectives ranged from 96.4% (session 3) to 83.3% (session 6) |
| Miller et al.178 2011 | Sessions were audio-recorded and rated by graduate students using a Likert scale. Adherence to programme objectives ranged from 76.85% to 79.51% |
| Miller et al.154 2011 | Sessions were audio-recorded and rated by graduate students using a Likert scale. Adherence to programme objectives ranged from 76.85% to 79.51% |
| Pahl and Barrett242 2010 | Facilitators completed logbooks. Mean adherence to the manual was 94% (range 90–98%) |
| Pössel et al.200 2013 | Facilitators recorded their adherence to the intervention manual after each session. Adherence was 91.6% in the CBT intervention and 92.4% in the control intervention |
| Roberts et al.138 2003 | Facilitators completed integrity checklists. The mean percentage of content covered was 74.11%. Sessions were also audio-recorded. No difference between facilitator-rated adherence and independent assessment of session recordings was reported |
| Roberts et al.139 2010 | The mean percentage of teacher-reported intervention adherence in the SLS lessons was 95.3% (range 87.3–98.3%). The mean percentage of teacher-reported content adherence in the OTS lessons was 98.04% (range 97.5–100%). Independent assessment agreed with teachers’ reporting (100% agreement) |
| Roberts et al.240 2018 | Intervention content comprised 10 modules. Average module implementation for SLS: teacher training-only arm, 9.16 (SD 2.02); teacher training + coaching, 9.24 (SD 1.74). Average module implementation for OTS: teacher training-only arm, 7.92 (SD 3.25); teacher training + coaching arm, 8.06 (SD 3.56) |
| Rodgers and Dunsmuir140 2015 | Random sessions were video-recorded. Protocol fidelity and integrity checks ‘showed concordance between session and manual content (89%)’ |
| Rohde et al.223 2014 | Sessions were recorded. Adherence and competence were rated on 10-point scales, on which higher scores indicated higher adherence/competence. The mean adherence was 7.0 (SD 0.7) and mean competence was 7.1 (SD 0.7) |
| Rose et al.203 2014 | No deviations from the manualized programs were observed |
| Ruttledge et al.158 2016 | All teachers returned the fidelity checklist confirming that they had delivered all 10 sessions of the programme in sequence and covered the key components |
| Sawyer et al.204 2010 | Session materials were manualised, and teachers completed checklists on session content completion. Checklists were returned by 36–44% of teachers across the 3 years. Teachers covered a mean of 70% of content and activities in Year 8 (range 17–100%), a mean of 70% in Year 9 (range 21–100%) and a mean of 74% in Year 10 (range 20–100%) |
| Sheffield et al.141 2006 (universal) | The mean number of program elements completed each session was 85% |
| Sheffield et al.141 2006 (indicated) | The mean number of program elements completed each session was > 92% |
| Soffer212 2003 | Sessions were audio-taped and were evaluated by independent assessors, who concluded that ‘All sessions met 100% adherence to the treatment manuals’ |
| Spence et al.206 2003 | All teachers reported 100% of the materials were completed in five sessions (sessions 1, 2, 6, 7 and 8). Half of the teachers did not complete the remaining sessions or only partially completed the content (sessions 3–5) |
| Stallard et al.142 2013 | Of the 36 classroom-based CBT sessions observed to assess intervention fidelity, 31 covered all the core tasks, with at least 75% of core tasks being covered in the remaining five sessions |
| Stallard et al.159 2014 | One session from each school was audio-taped and evaluated independently. In the health-led intervention, 100% of sessions delivered the core intervention tasks and home activities. In the school-led intervention, 60% of the sessions implemented all the core tasks and home activities and 32% delivered all core tasks, but not home activities |
| Stice et al.224 2008 | Adherence to intervention components and facilitator competence were evaluated. Cognitive behavioural intervention: 96% of intervention components were delivered and 94% of items were delivered with good competence. Supportive–expressive intervention: 100% of components were fully adhered to and 94% of items were delivered with good competence |
| Tak et al.207 2016 | Facilitators completed a self-reported questionnaire for assessing fidelity:Program fidelity was 80% |
| Takagaki et al.235 2016 | Sessions were audio-recorded. A checklist was used to evaluate the facilitators’ adherence to intervention content and protocol:. . . the therapist’s adherence to the protocol was 100% |
| Topper et al.173 2017 | Sessions were audio-taped:On average, 93% of the essential and required elements of the protocol were completed per session |
| Young et al.230 2016 | Sessions were audio-recorded and followed a manual. Sessions were rated by an ‘experienced clinician’; 98.5 % of techniques were delivered with fidelity. A total of 49% of techniques were satisfactorily delivered and 49.5% were rated superior for delivery |
Appendix 3 Network meta-analysis results
Model fit tables: by population, setting and outcome
Tables 29–46 report model fit statistics for each population, setting and time point analysis. Model fit for depression (Tables 38–46) and anxiety outcomes (Tables 29–37) are reported in separate tables. We assessed both fixed- and random-effects models on the basis of model fit. Component-level models were fitted assuming consistency and random-effects only. Heterogeneity was evaluated by examining the posterior median between-study SD (τ) and 95% CrIs from the random-effects model, and by comparing model fit of the fixed- and random-effects models. Model fit was measured by the posterior mean of residual deviance. In addition, we examined the DIC, which penalises model fit with model complexity. Differences of ≥ 5 points for posterior mean residual deviance and DIC were considered meaningful, with lower values preferred. 101 Inconsistency was assessed by comparing the goodness of fit of a model, assuming consistency with one allowing for inconsistency (i.e. a model that provides effect estimates based on direct evidence only). A common between-study variance was also assumed for both the consistency and inconsistency models.
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Convergenced | Chains |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Universal | Secondary | Post intervention | Fixed effect, consistency | 45 | 92.9 | 112.8 | 27 | – | 40,000 | 3 |
| Post intervention | Random effects, consistency | 49.5 | 102.0 | 35.4 | 0.11 (0.02 to 0.22) | 100,000 | 3 | |||
| Post intervention | Random effects, inconsistency | 49.9 | 102.2 | 35.2 | 0.15 (0.01 to 0.20) | 30,000 | 3 | |||
| Component-level NMA (random effects, consistency) | ||||||||||
| Universal | Secondary | Post intervention | Interventione | 45 | 49.3 | 101.7 | 35.3 | 0.11 (0.02 to 0.22) | 20,000 | 2 |
| Post intervention | Additive component levelf | 47.6 | 100.5 | 35.8 | 0.06 (0.00 to 0.21) | 40,000 | 2 | |||
| Post intervention | Full interaction component level | 48.2 | 102.6 | 37.7 | 0.09 (0.01 to 0.24) | 200,000 | 2 | |||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + psychoeducation | –0.39 | –0.78 to 0.01 |
| CBT + mindfulness | 0.57 | 0.08 to 1.03 | |
| CBT + relaxation | 0.07 | –0.21 to 0.38 | |
| Full interaction | CBT + relaxation | –31.58 | –144.30 to 90.75 |
| CBT + psychoeducation | –0.39 | –0.83 to 0.06 | |
| CBT + psychoeducation + relaxation | –0.30 | –0.84 to 0.27 | |
| CBT + psychoeducation + mindfulness + relaxation | –31.41 | –144.10 to 90.93 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Convergenced | Chains |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Universal | Primary | Post intervention | Fixed effect, consistency | 34 | 43.0 | 145.7 | 19 | – | 20,000 | 3 |
| Random effects, consistency | 37.4 | 145.8 | 24.6 | 0.10 (0.01 to 0.26) | 100,000 | 3 | ||||
| Random effects, inconsistency | 39.7 | 148.4 | 25.0 | 0.08 (0.00 to 0.26) | 200,000 | 3 | ||||
| Component-level NMA (random effects, consistency) | ||||||||||
| Universal | Primary | Post intervention | Interventione | 34 | 37.6 | 145.7 | 24.6 | 0.09 (0.00 to 0.26) | 20,000 | 2 |
| Additive component levelf | 36.0 | 147.5 | 27.8 | 0.13 (0.01 to 0.34) | 20,000 | 2 | ||||
| Full interaction component level | 36.0 | 148.6 | 28.9 | 0.15 (0.01 to 0.36) | 20,000 | 2 | ||||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + psychoeducation | –0.13 | –0.51 to 0.22 |
| CBT + relaxation | 0.20 | –0.17 to 0.55 | |
| Full interaction | CBT + psychoeducation | 0.11 | –0.53 to 0.74 |
| CBT + relaxation | –0.24 | –0.97 to 0.49 | |
| CBT + psychoeducation + relaxation | –0.01 | –0.63 to 0.62 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Convergenced | Chains |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Targeted | Secondary | Post intervention | Fixed effect, consistency | 36 | 38.0 | 104.4 | 23 | – | 50,000 | 3 |
| Random effects, consistency | 36.3 | 105.8 | 26.1 | 0.06 (0.00 to 0.21) | 100,000 | 3 | ||||
| Random effects, inconsistency | 37.7 | 110.1 | 28.9 | 0.06 (0.00 to 0.23) | 150,000 | 3 | ||||
| Component-level NMA (random effects, consistency) | ||||||||||
| Targeted | Secondary | Post intervention | Interventione | 36 | 36.01 | 105.4 | 26 | 0.06 (0.00 to 0.22) | 20,000 | 2 |
| Additive component levelf | 37.6 | 109.5 | 28.6 | 0.08 (0.00 to 0.26) | 30,000 | 2 | ||||
| Full interaction component level | 37.4 | 109.1 | 28.3 | 0.08 (0.00 to 0.26) | 20,000 | 2 | ||||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + psychoeducation | 0.12 | –0.53 to 0.74 |
| CBT + relaxation | –0.04 | –0.29 to 0.23 | |
| Full interaction | CBT + psychoeducation | 0.88 | –193.90 to 196.50 |
| CBT + relaxation | 0.12 | –0.50 to 0.72 | |
| CBT + psychoeducation + relaxation | 0.08 | –0.57 to 0.69 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Convergenced | Chains |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Targeted | Primary | Post intervention | Fixed effects, consistency | 25 | 53.3 | 83.8 | 15 | – | 100,000 | 3 |
| Random effects, consistency | 23.9 | 61.5 | 22.2 | 0.42 (0.21 to 0.89) | 60,000 | 3 | ||||
| Random effects, inconsistency | 24.0 | 61.8 | 22.2 | 0.43 (0.21 to 0.91) | 50,000 | 3 | ||||
| Component-level NMA (random effects, consistency) | ||||||||||
| Targeted | Primary | Post intervention | Interventione | 25 | 23.9 | 62.3 | 22.2 | 0.42 (0.21 to 0.89) | 20,000 | 2 |
| Additive component levelf | 23.2 | 62.3 | 22.9 | 0.70 (0.31 to 2.28) | 20,000 | 2 | ||||
| Full interaction component level | 23.3 | 62.6 | 23.0 | 0.69 (0.30 to 2.29) | 20,000 | 2 | ||||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + psychoeducation | 0.08 | –3.11 to 3.33 |
| CBT + behavioural | 0.06 | –2.54 to 2.63 | |
| CBT + relaxation | –0.31 | –1.84 to 1.16 | |
| Full interaction | CBT + behavioural + relaxation | –0.32 | –3.75 to 3.24 |
| CBT + psychoeducation + behavioural | 0.05 | –2.46 to 2.64 | |
| CBT + psychoeducation + relaxation | –0.26 | –2.82 to 2.29 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Chains | Convergenced |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Targeted | Tertiary/university | Post intervention | Fixed effect, consistency | 10 | 16.9 | 39.9 | 7.0 | – | 2 | 10,000 |
| Post intervention | Random effects, consistency | 10.7 | 36.6 | 9.9 | 0.43 (0.05 to 2.24) | 2 | 100,000 | |||
| Post intervention | Random effects, inconsistency | 9.8 | 35.1 | 9.4 | 0.21 (0.01 to 2.68) | 2 | 50,000 | |||
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Chains | Convergenced |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Universal | Secondary | Post intervention | Fixed effect, consistency | 76 | 139.7 | 212.4 | 43.0 | – | 3 | 30,000 |
| Post intervention | Random effects, consistency | 78.3 | 172.3 | 64.3 | 0.15 (0.10 to 0.22) | 3 | 100,000 | |||
| Post intervention | Random effects, inconsistency | 80.0 | 175.1 | 65.5 | 0.15 (0.09 to 0.23) | 3 | 100,000 | |||
| Component-level NMA (random effects, consistency) | ||||||||||
| Universal | Secondary | Post intervention | Interventione | 76 | 78.3 | 172.3 | 64.3 | 0.15 (0.10 to 0.22) | 2 | 20,000 |
| Post intervention | Additive component levelf | 77.2 | 173.9 | 67 | 0.14 (0.08 to 0.22) | 2 | 20,000 | |||
| Post intervention | Full interaction component level | 77.6 | 176.5 | 69.2 | 0.15 (0.10 to 0.23) | 2 | 20,000 | |||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | Cognitive + psychoeducation | 0.12 | –0.05 to 0.29 |
| Cognitive + behavioural | 0.56 | –0.21 to 1.34 | |
| Cognitive + mindfulness | –0.03 | –0.40 to 0.34 | |
| Cognitive + relaxation | 0.01 | –0.17 to 0.20 | |
| Third wave + psychoeducation | –0.45 | –0.87 to –0.04 | |
| Third wave + (mindfulness + relaxation) | –0.30 | –0.77 to 0.17 | |
| Full interaction | Cognitive + behavioural | 0.00 | 0.00 to 0.00 |
| Cognitive + behavioural + relaxation | –0.08 | –0.36 to 0.19 | |
| Cognitive + psychoeducation | –0.53 | –1.31 to 0.25 | |
| Cognitive + psychoeducation + behavioural + relaxation | 0.05 | –0.17 to 0.28 | |
| Cognitive + psychoeducation + behavioural + mindfulness + relaxation | 0.01 | –0.42 to 0.44 | |
| Third wave + psychoeducation | 0.16 | –0.26 to 0.58 | |
| Third wave + mindfulness + relaxation | –0.30 | –0.81 to 0.21 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Chains | Convergenced |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Universal | Primary | Post intervention | Fixed effect, consistency | 29 | 66.4 | 127.3 | 17.0 | – | 3 | 30,000 |
| Post intervention | Random effects, consistency | 28.9 | 98.7 | 26 | 0.32 (0.18 to 0.59) | 3 | 100,000 | |||
| Post intervention | Random effects, inconsistency | 28.8 | 98.4 | 25.7 | 0.28 (0.15 to 0.52) | 3 | 200,000 | |||
| Component-level NMA (random effects, consistency) | ||||||||||
| Universal | Primary | Post intervention | Interventione | 29 | 28.8 | 98.6 | 26 | 0.33 (0.18 to 0.60) | 2 | 20,000 |
| Post intervention | Additive component levelf | 28.8 | 99.5 | 26.9 | 0.37 (0.20 to 0.70) | 2 | 20,000 | |||
| Post intervention | Full interaction component level | 28.9 | 100.1 | 27.3 | 0.39 (0.21 to 0.78) | 2 | 20,000 | |||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + psychoeducation | 0.02 | –0.91 to 0.96 |
| CBT + relaxation | –0.09 | –0.73 to 0.52 | |
| Full interaction | CBT + psychoeducation | –0.35 | –1.40 to 0.69 |
| CBT + relaxation | –0.36 | –1.94 to 1.25 | |
| CBT + psychoeducation + relaxation | –0.29 | –1.72 to 1.16 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Chains | Convergenced |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Targeted | Secondary | Post intervention | Fixed effect, consistency | 55 | 144.1 | 252.4 | 34.0 | – | 3 | 30,000 |
| Post intervention | Random effects, consistency | 57.6 | 183.2 | 51.4 | 0.38 (0.25 to 0.58) | 3 | 100,000 | |||
| Post intervention | Random effects, inconsistency | 58.7 | 184.7 | 51.7 | 0.37 (0.24 to 0.58) | 3 | 150,000 | |||
| Component-level NMA (random effects, consistency) | ||||||||||
| Targeted | Secondary | Post intervention | Interventione | 55 | 57.5 | 183.1 | 51.4 | 0.38 (0.25 to 0.58) | 2 | 20,000 |
| Post intervention | Additive component levelf | 58.0 | 184.3 | 52.0 | 0.35 (0.21 to 0.58) | 2 | 20,000 | |||
| Post intervention | Full interaction component level | 58.1 | 185.8 | 53.5 | 0.38 (0.24 to 0.62) | 2 | 20,000 | |||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + cognitive | –0.20 | –1.02 to 0.62 |
| CBT + psychoeducation | 0.37 | –0.09 to 0.84 | |
| CBT+ behavioural | –0.10 | –0.61 to 0.40 | |
| CBT + relaxation | 0.22 | –0.24 to 0.71 | |
| Full interaction | Cognitive + behavioural | –0.11 | –0.71 to 0.53 |
| Cognitive + behavioural + relaxation | –0.16 | –0.95 to 0.64 | |
| Cognitive + psychoeducation | 0.55 | –0.28 to 1.38 | |
| Cognitive + psychoeducation + behavioural | 0.11 | –0.51 to 0.73 | |
| Cognitive + psychoeducation + behavioural + relaxation | 0.50 | –0.27 to 1.29 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Convergenced | Chains |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | ||||||||||
| Targeted | Primary | Post intervention | Fixed effect, consistency | 10 | 15.5 | 41.2 | 8.0 | – | 10,000 | 3 |
| Post intervention | Random effects, consistency | 10.3 | 38.1 | 10.5 | 0.60 (0.08 to 3.80) | 60,000 | 3 | |||
| Post intervention | Random effects, inconsistency | 10.3 | 38 | 10 | 0.60 (0.07 to 3.79) | 100,000 | 3 | |||
| Component-level NMA (random effects, consistency) | ||||||||||
| Targeted | Primary | Post intervention | Interventione | 10 | 10.3 | 38.1 | 10.1 | 0.62 (0.07 to 3.74) | 20,000 | 2 |
| Post intervention | Additive component levelf | 10.0 | 37.8 | 10.4 | 2.48 (0.12 to 4.87) | 50,000 | 2 | |||
| Post intervention | Full interaction component level | 9.9 | 37.7 | 9.9 | 2.43 (0.12 to 4.87) | 40,000 | 2 | |||
| Component model | Intervention | Regression coefficient | 95% CrI |
|---|---|---|---|
| Additive | CBT + psychoeducation | –0.73 | –9.65 to 8.19 |
| CBT + behavioural | –0.21 | –9.10 to 8.59 | |
| CBT + relaxation | –5.62 | –144.70 to 144.50 | |
| Full interaction | Cognitive + behavioural + relaxation | –16.39 | –99.72 to 96.58 |
| Cognitive + psychoeducation + behavioural | –0.28 | –9.10 to 8.41 | |
| Cognitive + psychoeducation + behavioural + relaxation | –17.12 | –100.40 to 95.73 |
| Population | Setting | Time point | Model | Data pointsa | Residual devianceb | DIC | P D c | SD (τ) (95% CrI) | Convergenced |
|---|---|---|---|---|---|---|---|---|---|
| Intervention-level NMA | |||||||||
| Targeted | Tertiary/university | Post intervention | Fixed effect, consistency | 12 | 22.4 | 51.0 | 9.0 | – | 30,000 |
| Post intervention | Random effects, consistency | 12.5 | 44.0 | 12.0 | 0.51 (0.12 to 2.50) | 70,000 | |||
| Post intervention | Random effects, inconsistency | 11.8 | 43.0 | 11.6 | 0.26 (0.02 to 2.48) | 150,000 | |||
Appendix 4 Full network meta-analysis and standard pairwise meta-analyses
The following tables report the random-effects consistency results for all populations and settings and are presented alongside the pairwise meta-analyses, if data were available.
Pairwise meta-analyses were conducted for all intervention and control comparisons for which direct head-to-head evidence was available. The method of estimation is similar to the NMA, except that the consistency assumption is removed, such that intervention effects for separate comparisons are unrelated and separate intervention effects can be estimated. Estimates are reported for the immediate post-intervention main time point only and are from a random-effects model that assumes that the heterogeneity parameter is common across intervention comparisons. This better reflects the assumption made in the NMA and, therefore, allows a fair comparison of the intervention effect estimates obtained from both approaches. Vague prior distributions were used for all parameters, and convergence is reported in the model fit tables above (Tables 29–46).
Intervention effect estimates are reported as standardised mean differences and interventions labelled numerically. Intervention comparisons are interpreted as the ‘higher’ number relative to the ‘lower’ number, that is smd[1,5] is the relative intervention effect of 5 over 1. For example, smd[1,5] –0.15, (95% CrI –0.34 to 0.04) would be interpreted as intervention 5 is reducing anxiety, compared with intervention 1.
Analysis-specific intervention numbers are provided as footnotes to each table and differ across analyses.
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | –0.05 | –0.28 to 0.18 | NA | |
| smd[1,3] | –0.07 | –0.34 to 0.19 | NA | |
| smd[1,4] | –0.15 | –0.51 to 0.15 | NA | |
| smd[1,5] | –0.15 | –0.34 to 0.04 | –0.15 | –0.33 to 0.02 |
| smd[1,6] | 0.03 | –0.14 to 0.20 | 0.04 | –0.10 to 0.19 |
| smd[1,7] | –0.65 | –1.14 to –0.19 | NA | |
| smd[2,3] | –0.02 | –0.25 to 0.21 | NA | |
| smd[2,4] | –0.10 | –0.43 to 0.17 | NA | |
| smd[2,5] | –0.09 | –0.24 to 0.03 | –0.07 | –0.19 to 0.04 |
| smd[2,6] | 0.08 | –0.20 to 0.37 | NA | |
| smd[2,7] | –0.60 | –1.05 to –0.17 | –1.08 | –1.76 to –0.39 |
| smd[3,4] | –0.08 | –0.44 to 0.23 | NA | |
| smd[3,5] | –0.07 | –0.27 to 0.11 | –0.07 | –0.25 to 0.10 |
| smd[3,6] | 0.10 | –0.21 to 0.42 | NA | |
| smd[3,7] | –0.58 | –1.07 to –0.12 | NA | |
| smd[4,5] | 0.01 | –0.24 to 0.30 | –0.06 | –0.32 to 0.19 |
| smd[4,6] | 0.18 | –0.17 to 0.59 | NA | |
| smd[4,7] | –0.50 | –0.90 to –0.10 | –0.29 | –0.75 to 0.16 |
| smd[5,6] | 0.18 | –0.07 to 0.44 | NA | |
| smd[5,7] | –0.51 | –0.94 to –0.08 | NA | |
| smd[6,7] | –0.68 | –1.20 to –0.19 | NA | |
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | 0.02 | –0.20 to 0.22 | NA | |
| smd[1,3] | 0.23 | –0.15 to 0.60 | NA | |
| smd[1,4] | –0.17 | –0.51 to 0.17 | NA | |
| smd[1,5] | –0.07 | –0.23 to 0.05 | –0.08 | –0.24 to 0.04 |
| smd[2,3] | 0.20 | –0.18 to 0.58 | NA | |
| smd[2,4] | –0.19 | –0.54 to 0.16 | NA | |
| smd[2,5] | –0.10 | –0.26 to 0.06 | –0.09 | –0.25 to 0.05 |
| smd[3,4] | –0.39 | –0.83 to 0.04 | –0.38 | –0.97 to 0.22 |
| smd[3,5] | –0.30 | –0.65 to 0.05 | –0.31 | –0.65 to 0.03 |
| smd[4,5] | 0.09 | –0.22 to 0.40 | 0.11 | –0.27 to 0.47 |
| Intervention comparisona | NMA | Pairwise | |||
|---|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | ||
| smd[1,2] | 0.30 | 0.09 to 0.53 | NA | ||
| smd[1,3] | –0.09 | –0.39 to 0.22 | NA | ||
| smd[1,4] | 1.08 | 0.52 to 1.64 | NA | ||
| smd[1,5] | 0.03 | –0.11 to 0.16 | 0.03 | –0.10 to 0.16 | |
| smd[1,6] | –0.18 | –0.55 to 0.21 | NA | ||
| smd[1,7] | 0.03 | –0.42 to 0.48 | NA | ||
| smd[1,8] | –0.17 | –0.45 to 0.11 | –0.21 | –0.54 to 0.15 | |
| smd[1,9] | –0.47 | –0.86 to –0.09 | –0.47 | –0.87 to –0.08 | |
| smd[2,3] | –0.40 | –0.71 to –0.09 | NA | ||
| smd[2,4] | 0.77 | 0.20 to 1.34 | NA | ||
| smd[2,5] | –0.28 | –0.45 to –0.11 | –0.27 | –0.46 to –0.10 | |
| smd[2,6] | –0.48 | –0.86 to –0.11 | –0.58 | –1.17 to 0.01 | |
| smd[2,7] | –0.28 | –0.71 to 0.15 | –0.24 | –0.82 to 0.33 | |
| smd[2,8] | –0.48 | –0.79 to –0.17 | NA | ||
| smd[2,9] | –0.77 | –1.22 to –0.34 | NA | ||
| smd[3,4] | 1.17 | 0.56 to 1.78 | NA | ||
| smd[3,5] | 0.12 | –0.17 to 0.40 | –0.03 | –0.43 to 0.38 | |
| smd[3,6] | –0.08 | –0.38 to 0.20 | –0.03 | –0.36 to 0.30 | |
| smd[3,7] | 0.12 | –0.31 to 0.55 | –0.10 | –0.75 to 0.58 | |
| smd[3,8] | –0.08 | –0.36 to 0.20 | –0.01 | –0.36 to 0.34 | |
| smd[3,9] | –0.38 | –0.87 to 0.11 | NA | ||
| smd[4,5] | –1.05 | –1.60 to –0.50 | –1.05 | –1.59 to –0.52 | |
| smd[4,6] | –1.25 | –1.91 to –0.60 | NA | ||
| smd[4,7] | –1.05 | –1.75 to –0.36 | NA | ||
| smd[4,8] | –1.25 | –1.86 to –0.64 | NA | ||
| smd[4,9] | –1.55 | –2.23 to –0.87 | NA | ||
| smd[5,6] | –0.20 | –0.56 to 0.16 | NA | ||
| smd[5,7] | 0.00 | –0.43 to 0.43 | NA | ||
| smd[5,8] | –0.20 | –0.46 to 0.07 | NA | ||
| smd[5,9] | –0.50 | –0.91 to –0.09 | NA | ||
| smd[6,7] | 0.20 | –0.24 to 0.65 | NA | ||
| smd[6,8] | 0.00 | –0.37 to 0.38 | NA | ||
| smd[6,9] | –0.30 | –0.84 to 0.25 | NA | ||
| smd[7,8] | –0.20 | –0.67 to 0.27 | NA | ||
| smd[7,9] | –0.50 | –1.09 to 0.09 | NA | ||
| smd[8,9] | –0.30 | –0.78 to 0.17 | NA | ||
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | –0.35 | –1.05 to 0.33 | NA | |
| smd[1,3] | –0.38 | –0.84 to 0.07 | –0.35 | –0.79 to 0.09 |
| smd[1,4] | 0.11 | –0.91 to 1.14 | 0.11 | –0.93 to 1.16 |
| smd[1,5] | –0.38 | –1.50 to 0.72 | NA | |
| smd[2,3] | –0.03 | –0.54 to 0.49 | –0.03 | –0.55 to 0.50 |
| smd[2,4] | 0.47 | –0.77 to 1.71 | NA | |
| smd[2,5] | –0.03 | –1.16 to 1.11 | NA | |
| smd[3,4] | 0.50 | –0.62 to 1.62 | NA | |
| smd[3,5] | 0.00 | –1.01 to 1.01 | 0.00 | –1.04 to 1.03 |
| smd[4,5] | –0.50 | –2.01 to 1.01 | NA | |
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | 0.00 | –0.19 to 0.19 | NA | |
| smd[1,3] | 0.02 | –0.16 to 0.20 | NA | |
| smd[1,4] | 0.07 | –0.12 to 0.26 | 0.31 | –0.05 to 0.69 |
| smd[1,5] | –0.04 | –0.16 to 0.07 | –0.05 | –0.17 to 0.06 |
| smd[1,6] | –0.03 | –0.21 to 0.14 | –0.02 | –0.19 to 0.14 |
| smd[1,7] | –0.19 | –0.46 to 0.08 | NA | |
| smd[1,8] | –0.03 | –0.36 to 0.29 | –0.10 | –0.47 to 0.26 |
| smd[1,9] | –0.13 | –0.49 to 0.22 | –0.13 | –0.49 to 0.22 |
| smd[1,10] | –0.02 | –0.40 to 0.37 | –0.02 | –0.40 to 0.37 |
| smd[2,3] | 0.02 | –0.18 to 0.23 | NA | |
| smd[2,4] | 0.07 | –0.14 to 0.28 | NA | |
| smd[2,5] | –0.04 | –0.20 to 0.11 | –0.02 | –0.18 to 0.13 |
| smd[2,6] | –0.04 | –0.30 to 0.22 | NA | |
| smd[2,7] | –0.19 | –0.41 to 0.04 | –0.21 | –0.46 to 0.05 |
| smd[2,8] | –0.03 | –0.39 to 0.33 | NA | |
| smd[2,9] | –0.14 | –0.54 to 0.26 | NA | |
| smd[2,10] | –0.02 | –0.45 to 0.41 | NA | |
| smd[3,4] | 0.05 | –0.15 to 0.24 | –0.03 | –0.30 to 0.23 |
| smd[3,5] | –0.06 | –0.21 to 0.08 | –0.05 | –0.20 to 0.10 |
| smd[3,6] | –0.06 | –0.31 to 0.19 | NA | |
| smd[3,7] | –0.21 | –0.49 to 0.07 | NA | |
| smd[3,8] | –0.05 | –0.41 to 0.30 | NA | |
| smd[3,9] | –0.16 | –0.55 to 0.24 | NA | |
| smd[3,10] | –0.04 | –0.47 to 0.38 | NA | |
| smd[4,5] | –0.11 | –0.27 to 0.05 | –0.22 | –0.56 to 0.12 |
| smd[4,6] | –0.11 | –0.36 to 0.15 | NA | |
| smd[4,7] | –0.25 | –0.51 to 0.00 | –0.18 | –0.55 to 0.18 |
| smd[4,8] | –0.10 | –0.46 to 0.26 | NA | |
| smd[4,9] | –0.20 | –0.60 to 0.19 | NA | |
| smd[4,10] | –0.09 | –0.51 to 0.34 | NA | |
| smd[5,6] | 0.00 | –0.20 to 0.21 | NA | |
| smd[5,7] | –0.14 | –0.39 to 0.10 | NA | |
| smd[5,8] | 0.01 | –0.32 to 0.33 | NA | |
| smd[5,9] | –0.09 | –0.46 to 0.28 | NA | |
| smd[5,10] | 0.02 | –0.38 to 0.43 | NA | |
| smd[6,7] | –0.15 | –0.47 to 0.17 | NA | |
| smd[6,8] | 0.00 | –0.37 to 0.37 | NA | |
| smd[6,9] | –0.10 | –0.49 to 0.29 | NA | |
| smd[6,10] | 0.02 | –0.40 to 0.44 | NA | |
| smd[7,8] | 0.15 | –0.25 to 0.56 | NA | |
| smd[7,9] | 0.05 | –0.39 to 0.49 | NA | |
| smd[7,10] | 0.17 | –0.30 to 0.64 | NA | |
| smd[8,9] | –0.10 | –0.58 to 0.37 | NA | |
| smd[8,10] | 0.02 | –0.49 to 0.52 | NA | |
| smd[9,10] | 0.12 | –0.40 to 0.64 | NA | |
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | –0.09 | –0.77 to 0.54 | NA | |
| smd[1,3] | 0.13 | –0.40 to 0.65 | NA | |
| smd[1,4] | –0.07 | –0.79 to 0.62 | NA | |
| smd[1,5] | –0.13 | –0.44 to 0.17 | –0.11 | –0.37 to 0.16 |
| smd[1,6] | –0.10 | –1.04 to 0.80 | NA | |
| smd[2,3] | 0.22 | –0.48 to 0.96 | NA | |
| smd[2,4] | 0.02 | –0.83 to 0.88 | NA | |
| smd[2,5] | –0.04 | –0.60 to 0.56 | –0.06 | –0.56 to 0.49 |
| smd[2,6] | –0.01 | –1.05 to 1.04 | NA | |
| smd[3,4] | –0.20 | –0.79 to 0.37 | –0.15 | –0.71 to 0.39 |
| smd[3,5] | –0.26 | –0.69 to 0.17 | –0.29 | –0.66 to 0.08 |
| smd[3,6] | –0.23 | –1.03 to 0.55 | –0.12 | –0.88 to 0.64 |
| smd[4,5] | –0.06 | –0.68 to 0.59 | NA | |
| smd[4,6] | –0.03 | –0.84 to 0.78 | NA | |
| smd[5,6] | 0.03 | –0.85 to 0.88 | NA | |
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | 0.22 | –0.27 to 0.70 | NA | |
| smd[1,3] | 0.04 | –0.72 to 0.82 | NA | |
| smd[1,4] | –0.81 | –1.81 to 0.18 | NA | |
| smd[1,5] | 0.02 | –0.62 to 0.66 | NA | |
| smd[1,6] | –0.22 | –0.58 to 0.13 | –0.16 | –0.47 to 0.15 |
| smd[1,7] | –0.68 | –1.83 to 0.47 | NA | |
| smd[1,8] | –0.65 | –1.50 to 0.16 | NA | |
| smd[1,9] | –0.90 | –2.20 to 0.40 | NA | |
| smd[1,10] | –0.28 | –1.13 to 0.58 | –0.28 | –1.12 to 0.57 |
| smd[1,11] | 0.12 | –0.50 to 0.72 | NA | |
| smd[2,3] | –0.18 | –0.92 to 0.59 | NA | |
| smd[2,4] | –1.03 | –2.01 to –0.04 | NA | |
| smd[2,5] | –0.20 | –0.82 to 0.43 | NA | |
| smd[2,6] | –0.44 | –0.77 to –0.11 | –0.40 | –0.71 to –0.08 |
| smd[2,7] | –0.90 | –2.03 to 0.25 | NA | |
| smd[2,8] | –0.87 | –1.70 to –0.06 | NA | |
| smd[2,9] | –1.12 | –2.40 to 0.17 | NA | |
| smd[2,10] | –0.50 | –1.48 to 0.49 | NA | |
| smd[2,11] | –0.10 | –0.70 to 0.49 | NA | |
| smd[3,4] | –0.85 | –2.02 to 0.28 | NA | |
| smd[3,5] | –0.02 | –0.90 to 0.83 | NA | |
| smd[3,6] | –0.26 | –0.95 to 0.41 | –0.25 | –0.94 to 0.40 |
| smd[3,7] | –0.72 | –2.01 to 0.56 | NA | |
| smd[3,8] | –0.69 | –1.73 to 0.30 | NA | |
| smd[3,9] | –0.94 | –2.37 to 0.46 | NA | |
| smd[3,10] | –0.32 | –1.47 to 0.81 | NA | |
| smd[3,11] | 0.08 | –0.78 to 0.90 | NA | |
| smd[4,5] | 0.83 | –0.24 to 1.91 | NA | |
| smd[4,6] | 0.59 | –0.34 to 1.52 | 0.59 | –0.34 to 1.52 |
| smd[4,7] | 0.14 | –1.30 to 1.57 | NA | |
| smd[4,8] | 0.16 | –1.05 to 1.35 | NA | |
| smd[4,9] | –0.09 | –0.92 to 0.75 | –0.09 | –0.91 to 0.74 |
| smd[4,10] | 0.53 | –0.77 to 1.85 | NA | |
| smd[4,11] | 0.93 | –0.13 to 1.98 | NA | |
| smd[5,6] | –0.24 | –0.78 to 0.30 | –0.22 | –0.71 to 0.26 |
| smd[5,7] | –0.70 | –1.65 to 0.26 | –0.70 | –1.65 to 0.25 |
| smd[5,8] | –0.67 | –1.21 to –0.16 | –0.67 | –1.20 to –0.16 |
| smd[5,9] | –0.92 | –2.28 to 0.43 | NA | |
| smd[5,10] | –0.30 | –1.36 to 0.76 | NA | |
| smd[5,11] | 0.09 | –0.56 to 0.75 | 0.26 | –0.55 to 1.08 |
| smd[6,7] | –0.46 | –1.55 to 0.64 | NA | |
| smd[6,8] | –0.43 | –1.19 to 0.31 | NA | |
| smd[6,9] | –0.68 | –1.93 to 0.57 | NA | |
| smd[6,10] | –0.06 | –0.98 to 0.86 | NA | |
| smd[6,11] | 0.33 | –0.16 to 0.83 | 0.22 | –0.59 to 1.02 |
| smd[7,8] | 0.02 | –1.08 to 1.11 | NA | |
| smd[7,9] | –0.22 | –1.88 to 1.43 | NA | |
| smd[7,10] | 0.40 | –1.03 to 1.83 | NA | |
| smd[7,11] | 0.79 | –0.37 to 1.95 | NA | |
| smd[8,9] | –0.25 | –1.70 to 1.22 | NA | |
| smd[8,10] | 0.37 | –0.80 to 1.57 | NA | |
| smd[8,11] | 0.77 | –0.06 to 1.62 | NA | |
| smd[9,10] | 0.62 | –0.92 to 2.18 | NA | |
| smd[9,11] | 1.02 | –0.33 to 2.36 | NA | |
| smd[10,11] | 0.40 | –0.65 to 1.44 | NA | |
| Intervention comparisona | NMA | Pairwise | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| smd[1,2] | –0.72 | –3.56 to 2.10 | NA | |
| smd[1,3] | –0.48 | –2.49 to 1.50 | –0.48 | –2.48 to 1.47 |
| smd[1,4] | –0.10 | –2.94 to 2.71 | –0.10 | –2.87 to 2.69 |
| smd[2,3] | 0.25 | –1.76 to 2.21 | 0.25 | –1.73 to 2.21 |
| smd[2,4] | 0.62 | –3.39 to 4.60 | NA | |
| smd[3,4] | 0.38 | –3.06 to 3.84 | NA | |
Appendix 5 Further time points: results from the intervention-level network meta-analysis
| Population and setting | Intervention | Reference | Follow-up (months) | |||||
|---|---|---|---|---|---|---|---|---|
| 6–12 | 13–24 | ≥ 25 | ||||||
| SMD | 95% CrI | SMD | 95% CrI | SMD | 95% CrI | |||
| Universal, secondary | CBT | Usual curriculum | –0.11 | –0.34 to 0.11 | –0.01 | –2.84 to 2.81 | –0.23 | –0.55 to 0.08 |
| Third wave | Usual curriculum | –0.05 | –0.32 to 0.22 | – | – | – | – | |
| CBT + IPT | Usual curriculum | –0.02 | –0.42 to 0.36 | – | – | – | – | |
| Universal, primary | CBT | Usual curriculum | –0.11 | –0.35 to 0.11 | 0.00 | –0.68 to 0.71 | –0.12 | –0.26 to 0.02 |
| Targeted, secondary | CBT | No intervention | 0.05 | –0.12 to 0.20 | –0.26 | –0.52 to –0.01a | –0.39 | –0.65 to –0.14a |
| CBM | No intervention | –0.14 | –0.53 to 0.24 | – | – | – | – | |
| Targeted, primary | CBT | Waiting list | –0.17 | –1.37 to 1.06 | – | – | – | – |
| Biofeedback | Waiting list | –0.28 | –2.49 to 1.93 | – | – | – | – | |
| Population and setting | Intervention | Reference | Follow-up (months) | |||||
|---|---|---|---|---|---|---|---|---|
| 6–12 | 13–24 | ≥ 25 | ||||||
| SMD | 95% CrI | SMD | 95% CrI | SMD | 95% CrI | |||
| Universal, secondary | CBT | Usual curriculum | –0.02 | –0.10 to 0.06 | –0.04 | –0.20 to 0.14 | –0.14 | –2.89 to 2.63 |
| Third wave | Usual curriculum | –0.13 | –0.27 to 0.01 | – | – | – | – | |
| CBT + IPT | Usual curriculum | –0.10 | –0.26 to 0.05 | –0.10 | –0.57 to 0.39 | – | – | |
| IPT | Usual curriculum | 0.11 | –0.13 to 0.35 | – | – | – | – | |
| Universal, primary | CBT | Usual curriculum | –0.15 | –0.43 to 0.09 | –0.03 | –0.62 to 0.55 | –0.27 | –0.42 to –0.13a |
| Targeted, secondary | CBT | No intervention | –0.04 | –0.51 to 0.41 | –0.18 | –2.56 to 2.16 | –0.27 | –1.05 to 0.50a |
| IPT | No intervention | –0.49 | –1.49 to 0.48 | 0.09 | –3.81 to 3.93 | – | – | |
| Targeted, primary | CBT | Waiting list | –0.34 | –0.72 to 0.05b | –0.50 | –0.96 to 0.05a | – | – |
Appendix 6 Exploring heterogeneity and publication bias
Comparison-adjusted funnel plots to explore potential small study effects
A funnel plot is a graph of the study-level treatment effect estimates plotted against their SE. In a standard funnel plot, the vertical axis (SE) is reported in reverse, so that studies with smaller SEs are seen at the top of the plot (typically larger studies). Comparison-adjusted funnel plots follow this convention, but are modified to allow for multiple treatments and multiple comparisons from NMA. In the following graphs, we plot active treatments versus inactive control only. The x-axis reports the difference of each study’s estimate (yiXY) from the direct summary effect for each comparison (yiXY − µXY), and the y-axis reports the SE of yiXY. The red line represents the null hypothesis that the comparison-specific pooled effect estimates do not differ from the study-specific effect sizes. In the absence of small-study effects, all points should be symmetrical around the null.
Following Chaimani et al. ,98 the comparisons included in these funnel plots are for a control compared with an active intervention. Specific interventions are listed after each graph.
FIGURE 17.
Comparison-adjusted funnel plot: universal population, secondary setting – anxiety. 1 = usual curriculum, 2 = waiting list, 3 = no intervention, 4 = attention control, 5 = CBT, 6 = third wave and 7 = mindfulness/relaxation.
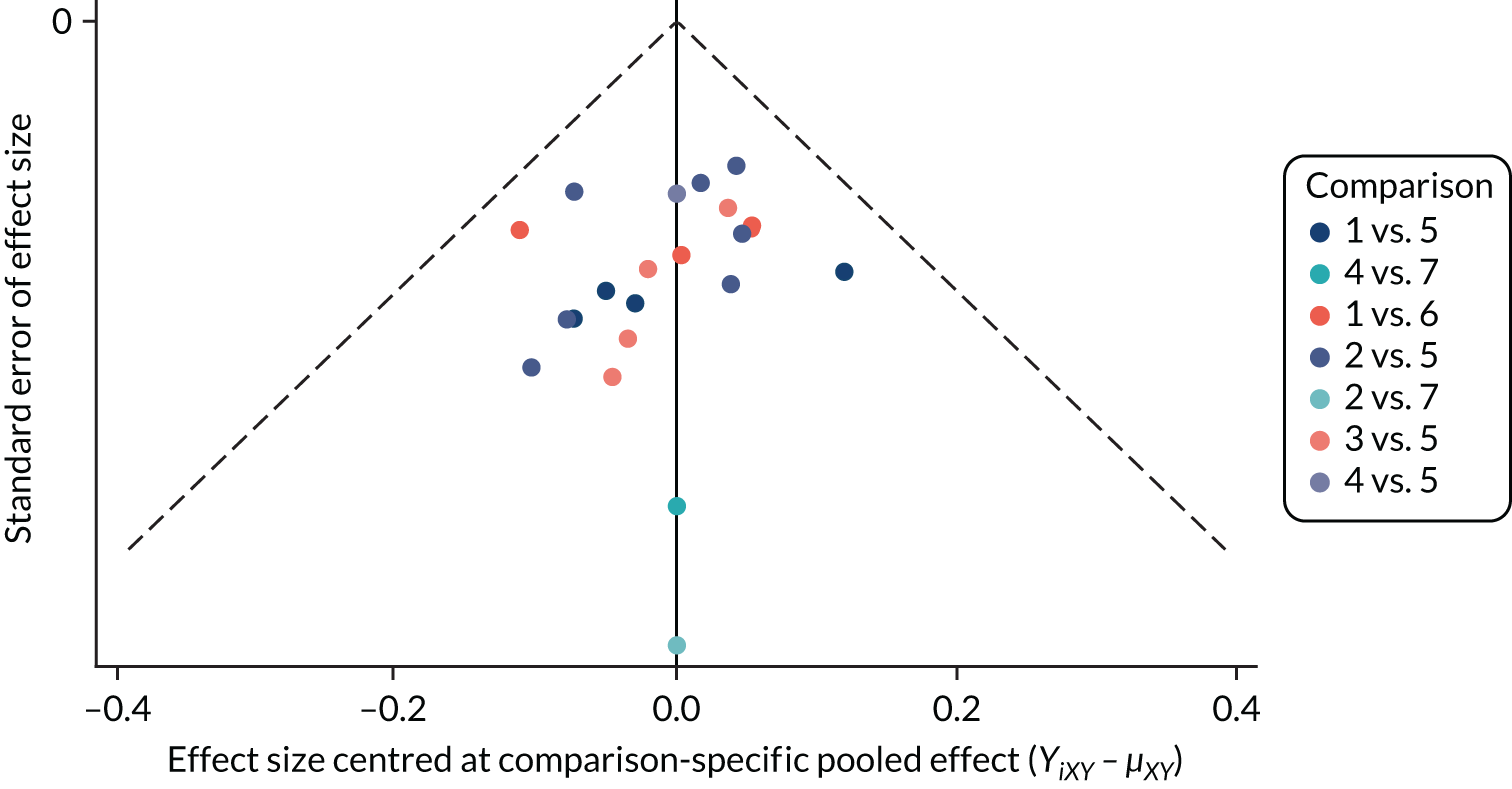
FIGURE 18.
Comparison-adjusted funnel plot: universal population, primary setting – anxiety. 1 = usual curriculum, 2 = waiting list, 3 = no intervention, 4 = attention control and 5 = CBT.
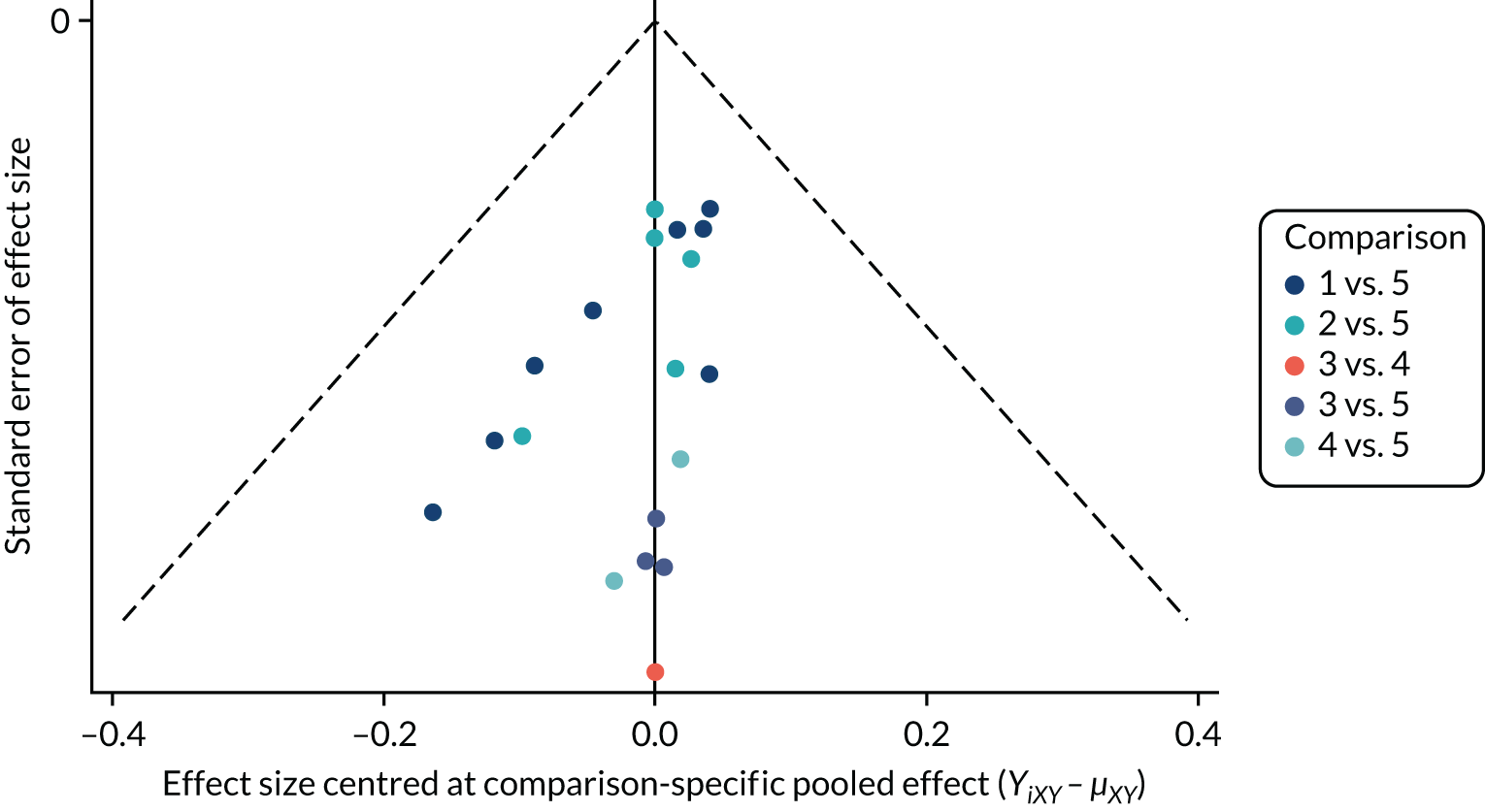
FIGURE 19.
Comparison-adjusted funnel plot: targeted population, secondary setting – anxiety. 1 = no intervention, 2 = waiting list, 3 = attention control, 4 = CBT, 5 = mindfulness/relaxation, 6 = bias modification, 7 = biofeedback and 8 = exercise.
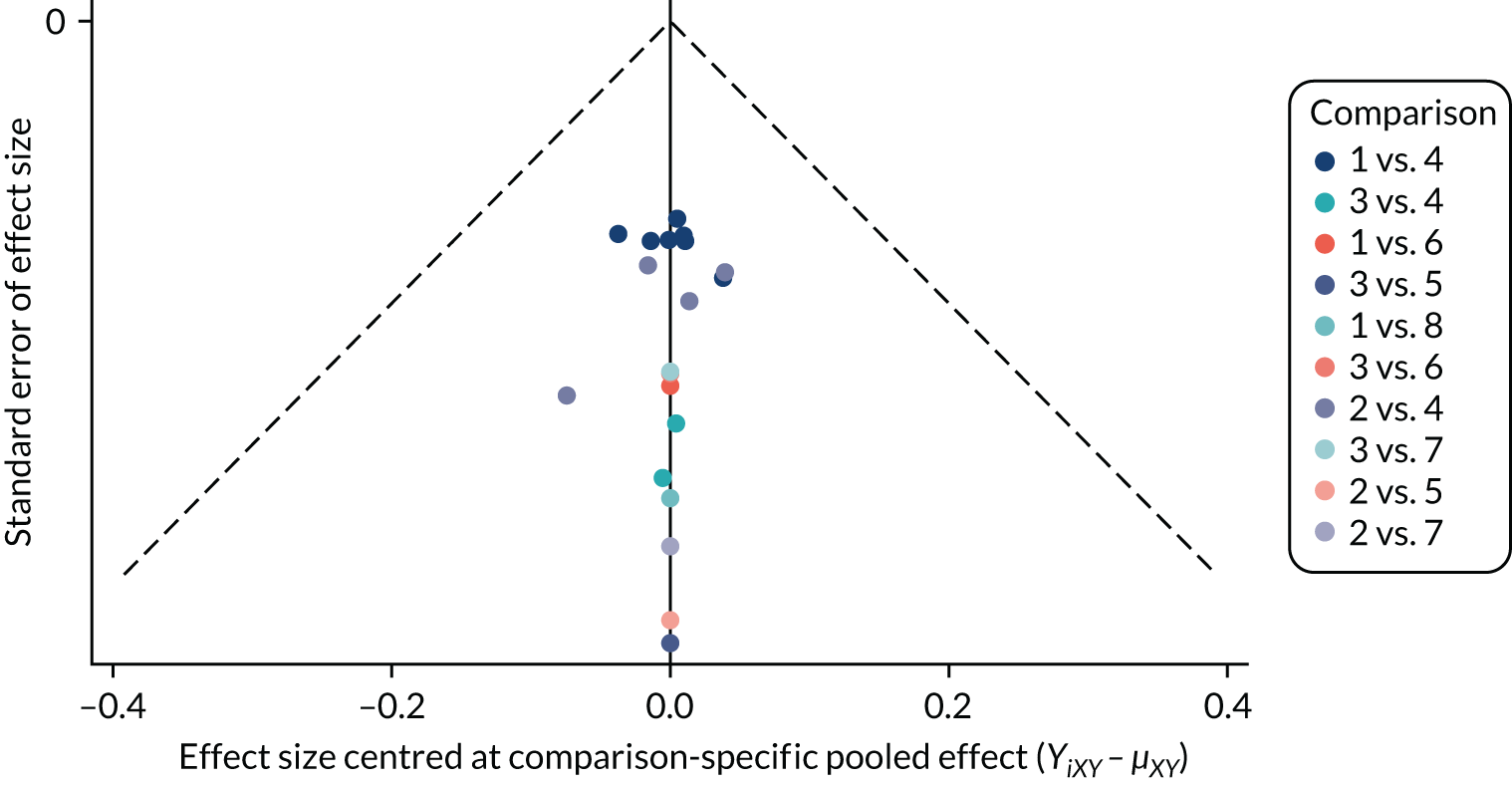
FIGURE 20.
Comparison-adjusted funnel plot: targeted population, primary setting – anxiety. 1 = waiting list, 2 = attention control, 3 = CBT and 4 = occupational therapy.
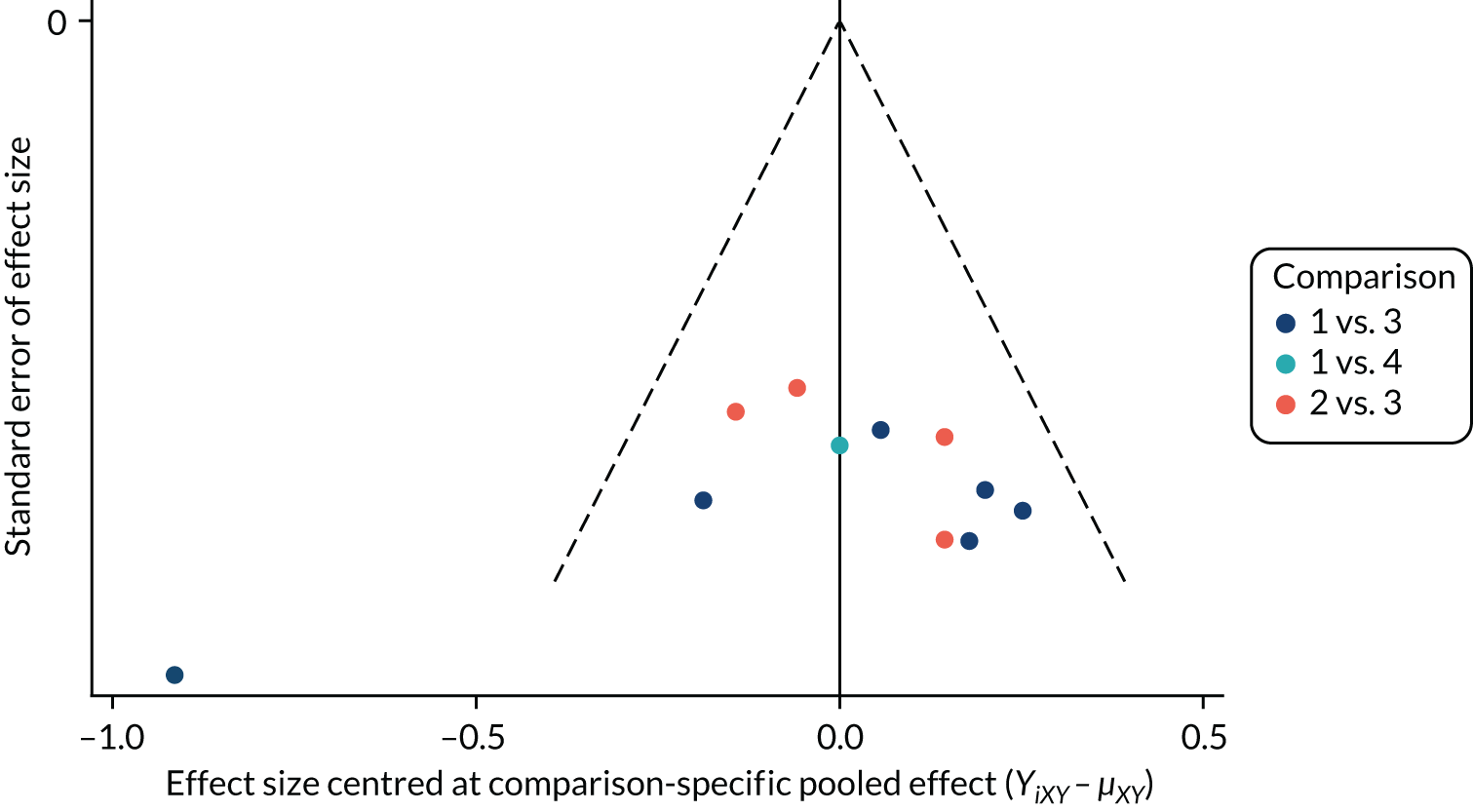
FIGURE 21.
Comparison-adjusted funnel plot: universal population, secondary setting – depression. 1 = usual curriculum, 2 = waiting list, 3 = no intervention, 4 = attention control, 5 = CBT, 6 = third wave, 7 = IPT, 8 = IPT + CBT and 9 = behavioural therapy.
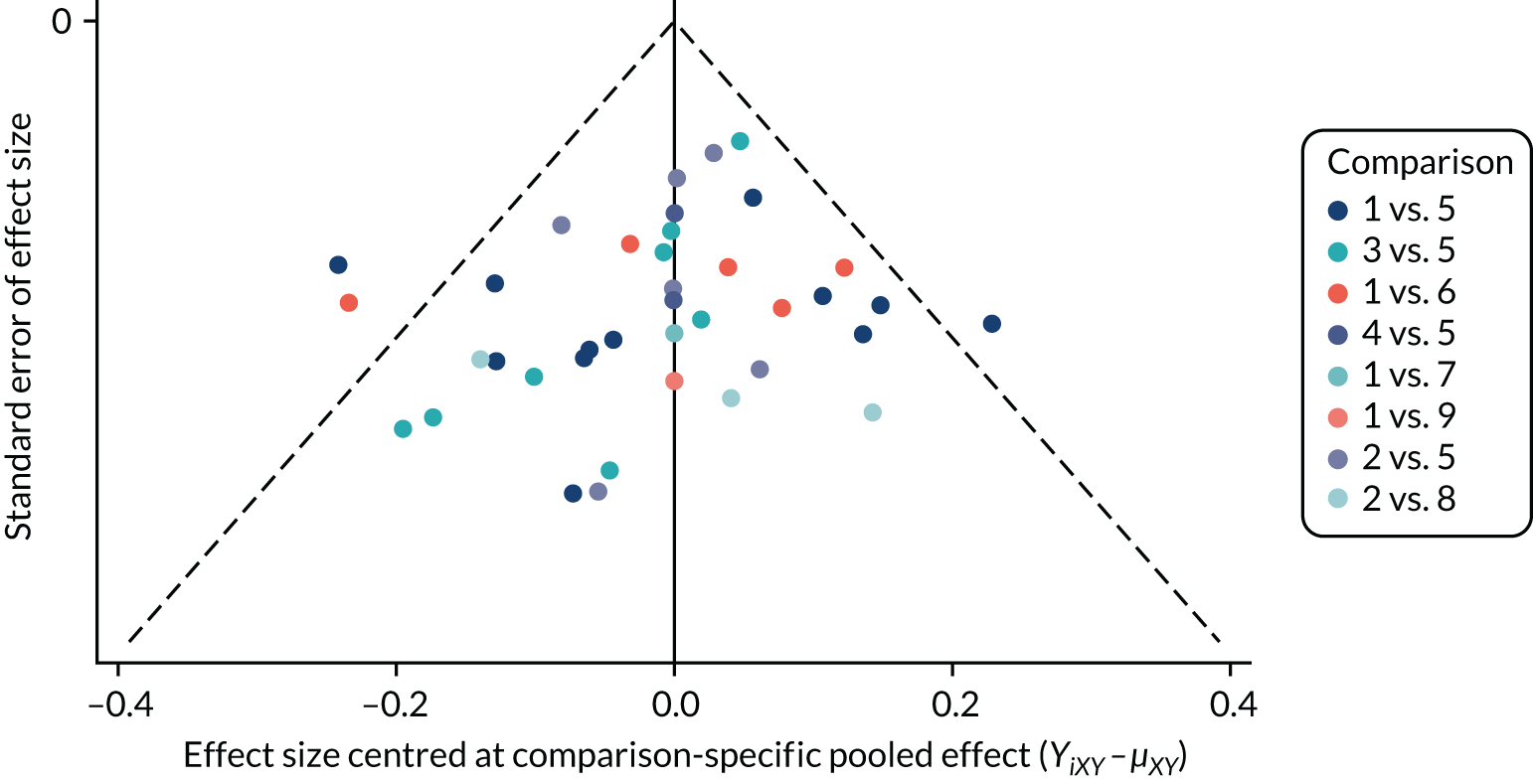
FIGURE 22.
Comparison-adjusted funnel plot: universal population, primary setting – depression. 1 = usual curriculum, 2 = waiting list, 3 = no intervention, 4 = attention control, 5 = CBT and 6 = behavioural therapy.
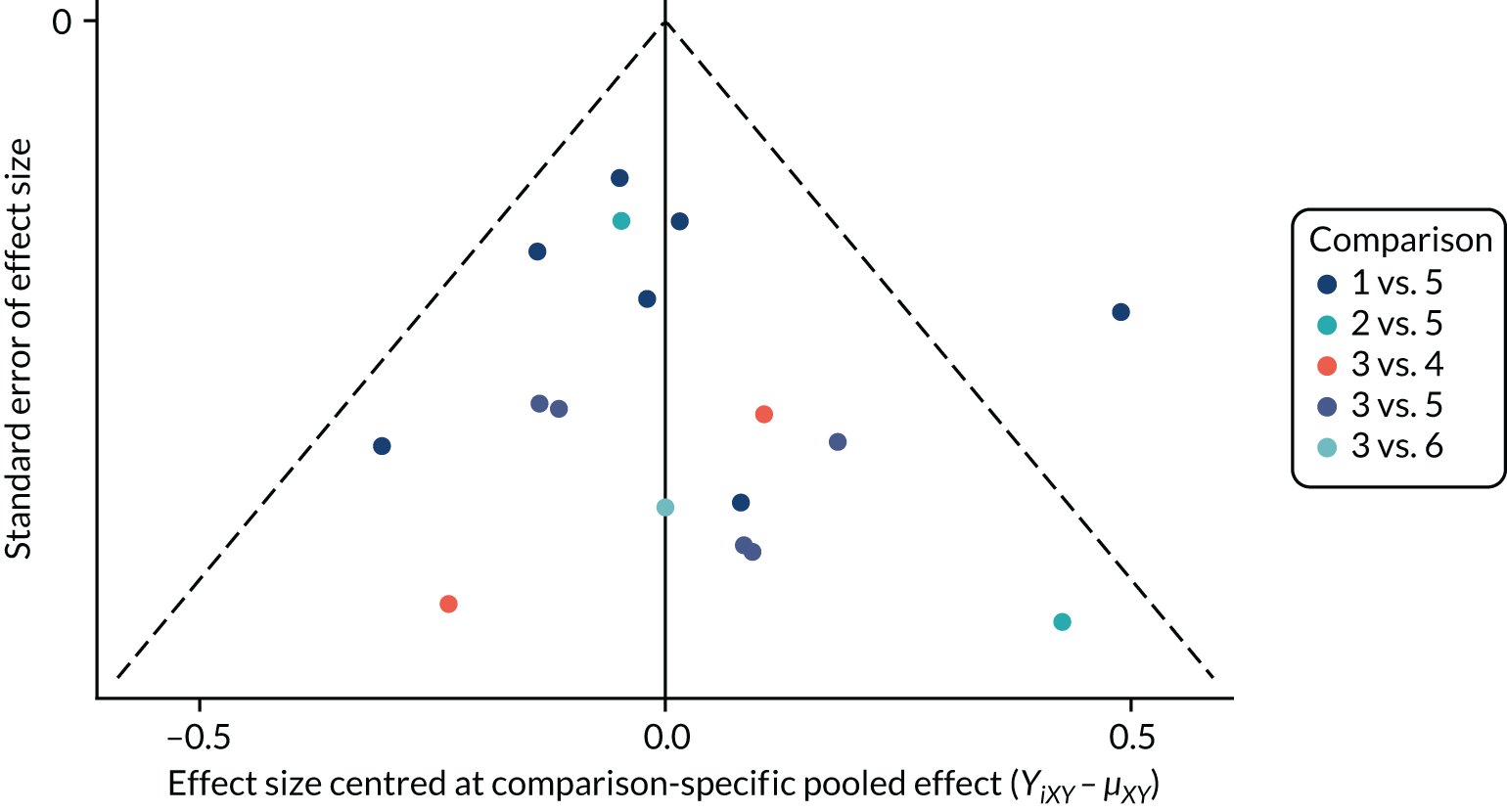
FIGURE 23.
Comparison-adjusted funnel plot: targeted population, secondary setting – depression. 1 = no intervention, 2 = waiting list, 3 = usual curriculum, 4 = attention control, 6 = CBT, 9 = exercise and 10 = cognitive bias modification.
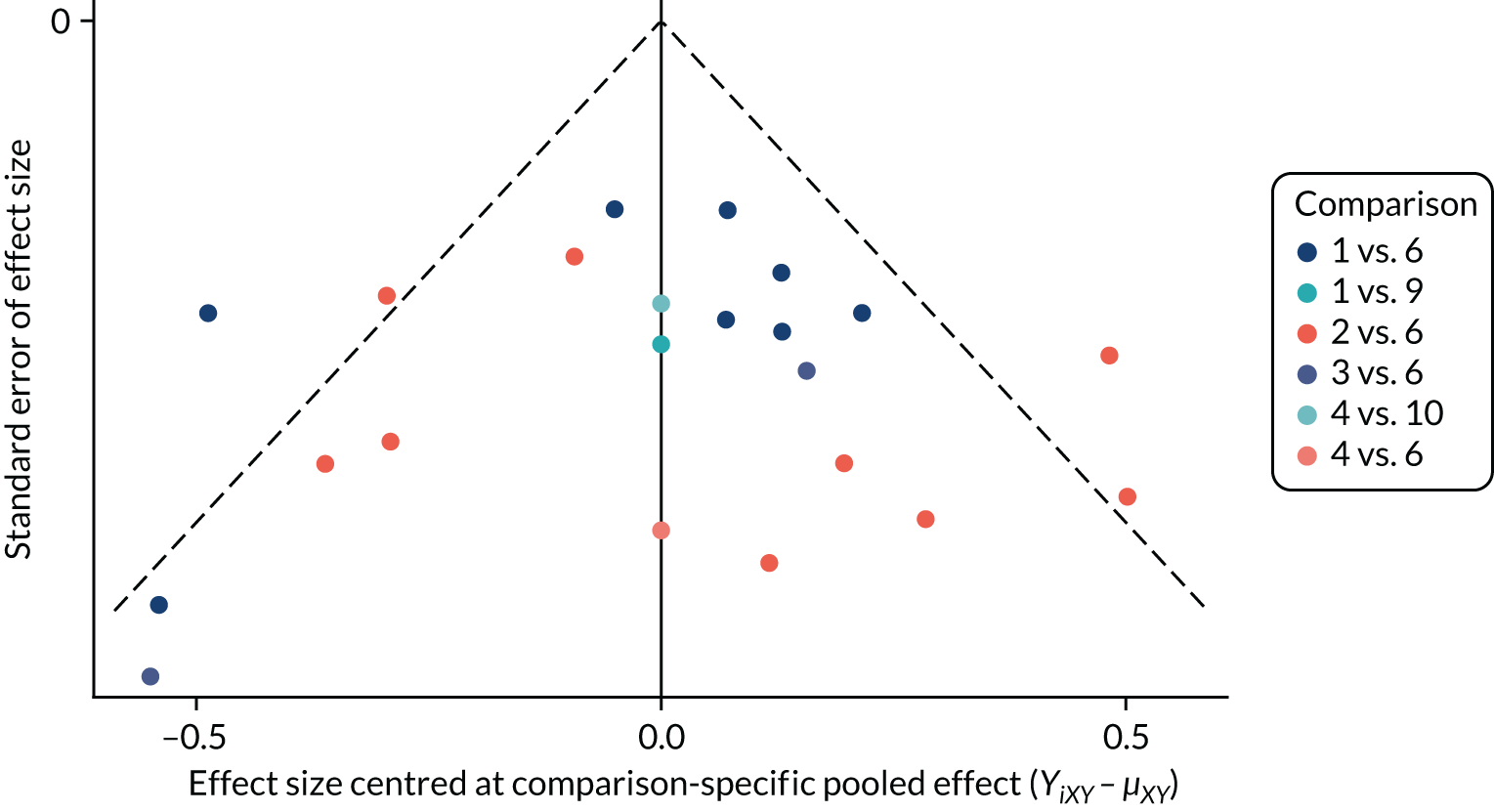
FIGURE 24.
Comparison-adjusted funnel plot: targeted population, primary setting – depression. 1 = waiting list, 2 = attention control, 3 = CBT and 4 = occupational therapy.
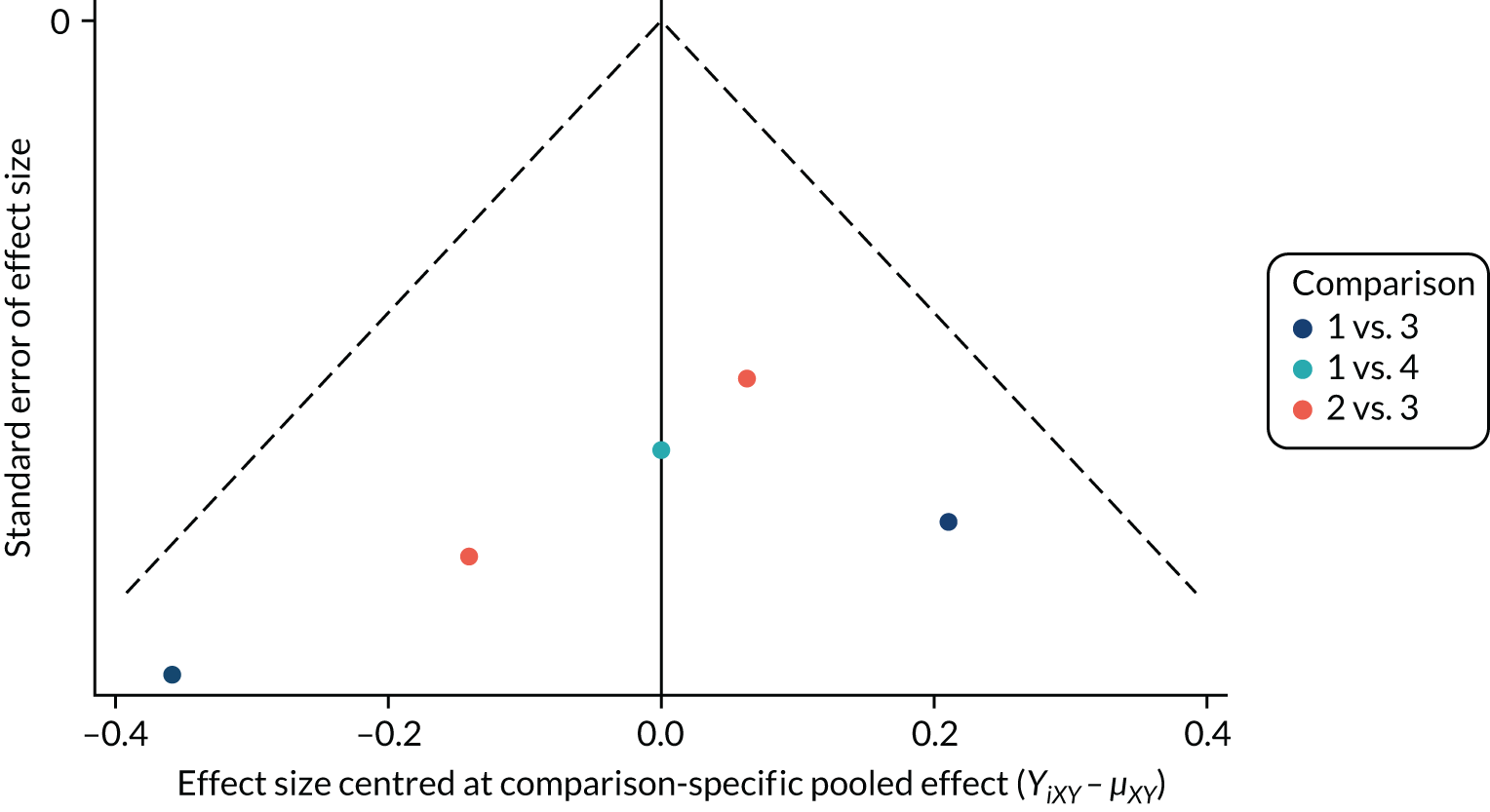
Meta regression, subgroup analysis and risk-of-bias sensitivity analysis
Facilitator delivering intervention: metaregression
Interventions were categorised as being delivered by a teacher or a MHP. There was considerable variation in the classification of ‘MHP’ and it should therefore be regarded as a simplification. Here, MHP includes school counsellors, qualified psychotherapists, and graduate and post-doctoral psychology students (which included general psychology, educational psychology or counselling psychology, if specified). In most studies, MHPs were external to the educational setting; however, this was not always the case.
Metaregression analyses
Facilitator metaregression
Meta-regression and subgroup analyses were performed in OpenBUGS following the Evidence Synthesis Technical Support Unit code available from the NICE Decision Support Unit website and described in Dias et al. 102,103 Interventions that varied by person of delivery were CBT, third-wave and mindfulness/relaxation interventions. To explore whether or not intervention effects were modified by person delivering the intervention (teacher or MHP), we fitted a metaregression model for intervention–teacher (0) and intervention–MHP (1). This enables us to estimate the intervention effect at each value of the covariate, for each intervention, including multiarm trials that compared the effect of both facilitators. When there were two or more interventions that were delivered by a teacher or MHP, a random-effects NMA model was fitted and we assumed a hierarchical model for the regression coefficient across interventions (CBT, third wave and mindfulness/relaxation), whereby the regression coefficients were assumed to come from a normal distribution with mean (m.beta) and precision (tau.beta). The between-studies SD was assumed to be common for each value of the covariate. We estimated a between-intervention SD (sd.beta) for the covariate regression coefficients. Vague priors were specified.
When only a single intervention varied by person delivering it, a fixed covariate effect (as for mode of delivery) was fitted.
| Intervention-facilitator | SMD | 95% CrI | Number of studies |
|---|---|---|---|
| CBT – teacher | –0.13 | –0.32 to 0.06 | 9 |
| CBT – MHP | –0.17 | –0.42 to 0.03 | 6 |
| Third wave – teacher | –0.10 | –0.38 to 0.19 | 1 |
| Third wave – MHP | 0.10 | –0.10 to 0.29 | 2 |
| Mindfulness/relaxation – teacher | –0.48 | –1.02 to 0.08 | 1 |
| Mindfulness/relaxation – MHP | –0.95 | –1.68 to –0.27 | 1 |
| Intervention | Regression coefficient | 95% CrI | |
| CBT | –0.4 | –0.23 to 0.10 | |
| Third wave | 0.20 | –0.15 to 0.53 | |
| Mindfulness/relaxation | –0.48 | –1.39 to 0.22 | |
| Parameter | Posterior mean | 95% CrI | |
| m.beta | –0.11 | –1.29 to 0.94 | |
| sd.beta | 0.58 | 0.04 to 1.83 | |
| Posterior median between-study SD | 0.10 (95% CrI 0.01 to 0.22) | ||
| Intervention-facilitator | SMD | 95% CrI | Number of studies |
|---|---|---|---|
| CBT – teacher | –0.05 | –0.21 to 0.08 | 6 |
| CBT – MHP | –0.18 | –0.42 to 0.00 | 4 |
| Intervention | Regression coefficient | 95% CrI | |
| CBT | –0.14 | –0.33 to 0.03 | |
| Posterior median between-study SD | 0.10 (95% CrI 0.01 to 0.26) | ||
| Intervention-facilitator | SMD | 95% CrI | Number of studies |
|---|---|---|---|
| CBT – other | 0.01 | –0.18 to 0.20 | 2 |
| CBT – MHP | 0.00 | –0.22 to 0.22 | 7 |
| Biofeedback – other | –0.04 | –0.59 to 0.53 | 1 |
| Biofeedback – MHP | –0.27 | –0.88 to 0.32 | 1 |
| Intervention | Regression coefficient | 95% CrI | |
| CBT | –0.01 | –0.23 to 0.20 | |
| Biofeedback | –0.20 | –0.96 to 0.39 | |
| Parameter | Posterior mean | 95% CrI | |
| m.beta | –0.08 | –1.62 to 1.29 | |
| sd.beta | 0.57 | 0.00 to 1.89 | |
| Posterior median between-study SD | 0.08 (95% CrI 0.00 to 0.29) | ||
| Intervention-facilitator | SMD | 95% CrI | Number of studies |
|---|---|---|---|
| CBT – teacher | –0.07 | –0.21 to 0.08 | 10 |
| CBT – MHP | –0.01 | –0.15 to 0.14 | 8 |
| Third wave – teacher | –0.07 | –0.37 to 0.23 | 1 |
| Third wave – MHP | –0.02 | –0.22 to 0.17 | 3 |
| CBT + IPT – teacher | –0.21 | –0.53 to 0.11 | 2 |
| CBT + IPT – MHP | –0.07 | –0.43 to 0.31 | 1 |
| Intervention | Regression coefficient | 95% CrI | |
| CBT | 0.06 | –0.10 to 0.22 | |
| Third wave | 0.05 | –0.29 to 0.36 | |
| CBT + IPT | 0.13 | –0.20 to 0.55 | |
| Parameter | Posterior mean | 95% CrI | |
| m.beta | 0.08 | –0.53 to 0.72 | |
| sd.beta | 0.18 | 0.01 to 1.48 | |
| Posterior median between-study SD | 0.14 (95% CrI 0.08 to 0.22) | ||
| Intervention-facilitator | SMD | 95% CrI | Number of studies |
|---|---|---|---|
| CBT – teacher | –0.19 | –0.52 to 0.14 | 4 |
| CBT – MHP | 0.08 | –0.46 to 0.57 | 5 |
| Intervention | Regression coefficient | 95% CrI | |
| CBT | 0.27 | –0.30 to 0.80 | |
| Posterior median between-study SD | 0.30 (95% CrI 0.12 to 0.60) | ||
| Intervention-faciliator | SMD | 95% CrI | Number of studies |
|---|---|---|---|
| CBT – other | –0.10 | –0.49 to 0.27 | 14 |
| CBT – MHP | –0.30 | –0.67 to 0.06 | 2 |
| Intervention | Regression coefficient | 95% CrI | |
| CBT | –0.20 | –0.52 to 0.13 | |
| Posterior median between-study SD | 0.35 (95% CrI 0.22 to 0.55) | ||
Mode of delivery metaregression
Interventions were categorised as being delivered face to face or via computer/internet (multimedia). Across all networks, the only intervention that varied by mode of delivery was CBT. To explore whether or not intervention effects were modified by mode of delivery, we fitted a metaregression model for CBT-face to face (covariate = 0) and CBT-multimedia (covariate = 1). This enabled us to estimate the intervention effect for both CBT-face to face and CBT-multimedia. A random-effects NMA model was fitted, but the regression coefficient for the covariate was assumed a fixed effect across studies. The between-studies SD was assumed to be common for CBT-face to face and CBT-multimedia.
Results are reported for universal secondary settings only, as there were insufficient data available for meaningful analysis in other populations/settings.
| Intervention-facilitator | SMD | 95% CrI |
|---|---|---|
| CBT – face to face | –0.03 | –0.14 to 0.09 |
| CBT – multimedia | –0.15 | –0.38 to 0.07 |
| Intervention | Regression coefficient | 95% CrI |
| CBT | –0.12 | –0.34 to 0.10 |
| Posterior median between-study SD | 0.15 (95% CrI 0.09 to 0.22) | |
| Intervention-facilitator | SMD | 95% CrI |
|---|---|---|
| CBT – face to face | –0.14 | –0.36 to 0.07 |
| CBT – multimedia | –0.16 | –0.42 to 0.10 |
| Intervention | Regression coefficient | 95% CrI |
| CBT | –0.02 | –0.27 to 0.23 |
| Posterior median between-study SD | 0.12 (95% CrI 0.02 to 0.24) | |
Subgroup analysis: examining whether or not intervention effect is modified by the intended focus of the intervention
For each population, setting and outcome combination, intervention estimates are compared across three subgroups: (1) interventions that aimed to prevent symptoms of anxiety (2) interventions that aimed to prevent only symptoms of depression and (3) interventions that aimed to prevent both symptoms of anxiety and symptoms of depression. The interest here is whether or not interventions designed specifically to prevent one clinical disorder might still affect the other. An intervention on the prevention of anxiety may also report the effect on depressive symptoms, for example.
| Focusa | Comparisonb | Studiesc (n) | SMDd | 95% CrI | SDe | 95% CrI |
|---|---|---|---|---|---|---|
| Universal, secondary: self-reported depression | ||||||
| Anxiety | CBT vs. no intervention | 4 | 0.05 | –0.13 to 0.22 | 0.04 | 0.00 to 0.33 |
| Depression | CBT vs. no intervention | 18 | –0.14 | –0.36 to 0.06 | 0.18 | 0.10 to 0.30 |
| Anxiety + depression | CBT vs. no intervention | 10 | 0.05 | –0.33 to 0.47 | 0.13 | 0.01 to 0.32 |
| Universal, secondary: self-reported anxiety | ||||||
| Anxiety | CBT vs. no intervention | 7 | –0.12 | –0.96 to 0.72 | 0.35 | 0.02 to 1.43 |
| Depression | CBT vs. no intervention | 4 | 0.00 | –5.26 to 5.25 | 1.66 | 0.12 to 4.74 |
| Anxiety + depression | CBT vs. no intervention | 10 | –0.05 | –0.91 to 0.38 | 0.16 | 0.03 to 0.37 |
| Universal, primary: self-reported depression | ||||||
| Anxiety | CBT vs. usual curriculum | 2 | 0.18 | –0.06 to 0.41 | Fixed-effects analysis | |
| Depression | CBT vs. usual curriculum | 6 | –0.57 | –1.51 to 0.37 | 0.34 | 0.03 to 0.96 |
| Anxiety + depression | CBT vs. usual curriculum | 4 | –0.16 | –0.42 to 0.13 | 0.17 | 0 to 0.78 |
| Universal, primary: self-reported anxiety | ||||||
| Anxiety | CBT vs. usual curriculum | 9 | –0.37 | –0.64 to –0.12 | 0.08 | 0.00 to 0.32 |
| Depression | CBT vs. no intervention | 2 | –0.31 | –0.61 to 0.00 | Fixed-effects analysis | |
| Anxiety + depression | CBT vs. usual curriculum | 4 | 0.04 | –0.16 to 0.27 | 0.07 | 0.00 to 0.61 |
| Targeted, secondary: self-reported depression | ||||||
| Anxiety | CBT vs. waiting list | 2 | –0.21 | –0.49 to 0.08 | Fixed-effects analysis | |
| Depression | CBT vs. waiting list | 17 | –0.33 | –0.86 to 0.20 | 0.38 | 0.24 to 0.62 |
| Anxiety + depression | CBT vs. waiting list | 3 | –0.67 | –3.65 to 2.33 | 0.78 | 0.00 to 4.56 |
| Targeted, secondary: self-reported anxiety | ||||||
| Anxiety | CBT vs. no intervention | 8 | 0.13 | –0.95 to 1.18 | 0.33 | 0.03 to 1.34 |
| Depression | CBT vs. no intervention | 3 | 0.00 | –0.15 to 0.16 | 0.08 | 0.00 to 0.26 |
| Anxiety + depression | CBT vs. waiting list | 3 | –0.21 | –1.27 to 0.84 | 0.45 | 0.01 to 2.66 |
| Targeted, primary: self-reported anxiety | ||||||
| Anxiety | CBT vs. waiting list | 7 | –0.16 | –0.41 to 0.09 | 0.14 | 0.00 to 0.48 |
| Anxiety + depression | CBT vs. waiting list | 4 | –1.43 | –5.47 to 2.60 | 1.19 | 0.02 to 4.52 |
Sensitivity analyses
| Intervention | ICC = 0.01 | ICC = 0.06 | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| Universal, secondary, depression (19/34 trials) | ||||
| CBT | –0.04 | –0.16 to 0.07 | –0.04 | –0.16 to 0.08 |
| Third wave | –0.04 | –0.21 to 0.14 | –0.03 | –0.20 to 0.14 |
| IPT + CBT | –0.18 | –0.46 to 0.09 | –0.18 | –0.45 to 0.08 |
| IPT | –0.03 | –0.37 to 0.30 | –0.03 | –0.34 to 0.29 |
| Behavioural therapy | –0.02 | –0.40 to 0.37 | –0.02 | –0.41 to 0.38 |
| Universal, primary, depression (7/12 trials) | ||||
| CBT | –0.13 | –0.44 to 0.18 | –0.13 | –0.44 to 0.17 |
| Behavioural therapy | –0.09 | –1.04 to 0.82 | –0.1 | –1.03 to 0.79 |
| Targeted, secondary, depression (5/24 trials) | ||||
| CBT | –0.21 | –0.58 to 0.14 | –0.21 | –0.58 to 0.14 |
| Third wave | –0.68 | –1.83 to 0.47 | –0.68 | –1.84 to 0.48 |
| IPT | –0.65 | –1.50 to 0.16 | –0.65 | –1.50 to 0.17 |
| CBM | –0.89 | –2.20 to 0.41 | –0.89 | –2.21 to 0.41 |
| Exercise | –0.28 | –1.11 to 0.55 | –0.28 | –1.11 to 0.55 |
| Targeted, primary, depression (1/5 trials) | ||||
| CBT | –0.47 | –2.46 to 1.54 | –0.48 | –2.48 to 1.50 |
| Occupational therapy | –0.1 | –2.92 to 2.76 | –0.1 | –2.90 to 2.72 |
| Universal, secondary, anxiety (12/21 trials) | ||||
| CBT | –0.15 | –0.34 to 0.04 | –0.15 | –0.34 to 0.04 |
| Third wave | 0.03 | –0.15 to 0.21 | 0.04 | –0.13 to 0.20 |
| Mindfulness/relaxation | –0.66 | –1.16 to –0.19 | –0.64 | –1.12 to –0.19 |
| Universal, primary, anxiety (11/15 trials) | ||||
| CBT | –0.08 | –0.24 to 0.04 | –0.07 | –0.23 to 0.06 |
| Targeted, secondary, anxiety (5/15 trials) | ||||
| CBT | 0.03 | –0.10 to 0.16 | 0.03 | –0.11 to 0.17 |
| Biofeedback | –0.17 | –0.55 to 0.21 | –0.17 | –0.55 to 0.21 |
| Mindfulness/relaxation | 0.04 | –0.41 to 0.49 | 0.03 | –0.41 to 0.48 |
| CBM | –0.17 | –0.44 to 0.10 | –0.17 | –0.45 to 0.13 |
| Exercise | –0.47 | –0.83 to –0.12 | –0.47 | –0.89 to –0.04 |
| Targeted, primary, anxiety (2/11 trials) | ||||
| CBT | –0.39 | –0.85 to 1.14 | –0.38 | –0.85 to 0.07 |
| Occupational therapy | 0.11 | –0.93 to 0.72 | 0.11 | –0.93 to 1.15 |
| Biofeedback | –0.39 | –1.50 to 0.72 | –0.38 | –1.51 to 0.73 |
| Intervention | C = 0.6 | C = 0.8 | ||
|---|---|---|---|---|
| SMD | 95% CrI | SMD | 95% CrI | |
| Universal, secondary, depression (34 trials) | ||||
| CBT | –0.04 | –0.15 to 0.07 | –0.04 | –0.16 to 0.07 |
| Third wave | –0.03 | –0.2 to 0.13 | –0.03 | –0.21 to 0.14 |
| IPT + CBT | –0.18 | –0.44 to 0.08 | –0.18 | –0.45 to 0.08 |
| IPT | –0.03 | –0.34 to 0.28 | –0.03 | –0.36 to 0.29 |
| Behavioural therapy | –0.02 | –0.39 to 0.35 | –0.02 | –0.39 to 0.36 |
| Universal, primary, depression (12 trials) | ||||
| CBT | –0.13 | –0.44 to 0.17 | 0.13 | –0.44 to 0.18 |
| Behavioural therapy | –0.08 | –1.04 to 0.84 | 0.12 | –1.03 to 0.77 |
| Targeted, secondary, depression (24 trials) | ||||
| CBT | –0.21 | –0.57 to 0.13 | –0.22 | –0.59 to 0.13 |
| Third wave | –0.67 | –1.83 to 0.48 | –0.68 | –1.83 to 0.45 |
| IPT | –0.63 | –1.47 to 0.18 | –0.71 | –1.56 to 0.13 |
| CBM | –0.89 | –2.2 to 0.40 | –0.91 | –2.22 to 0.39 |
| Exercise | –0.28 | 1.12 to 0.56 | –0.28 | –1.13 to 0.58 |
| Targeted, primary, depression (5 trials) | ||||
| CBT | –0.47 | –2.46 to 1.45 | –0.48 | –2.55 to 1.57 |
| Occupational therapy | –0.10 | –2.85 to 2.64 | –0.10 | –3.00 to 2.77 |
| Universal, secondary, anxiety (21 trials) | ||||
| CBT | –0.19 | –0.41 to 0.01 | –0.21 | –0.45 to 0.00 |
| Third wave | 0.03 | –0.15 to 0.21 | 0.03 | –0.18 to 0.25 |
| Mindfulness/relaxation | –0.69 | –1.22 to –0.18 | –0.77 | –1.29 to –0.28 |
| Universal, primary, anxiety (15 trials) | ||||
| CBT | –0.06 | –0.21 to 0.06 | –0.08 | –0.24 to 0.04 |
| Targeted, secondary, anxiety (15 trials) | ||||
| CBT | 0.03 | –0.11 to 0.17 | 0.03 | –0.10 to 0.17 |
| Biofeedback | –0.18 | –0.59 to 0.17 | –0.16 | –0.52 to 0.17 |
| Mindfulness/relaxation | 0.02 | –0.48 to 0.12 | 0.04 | –0.36 to 0.44 |
| CBM | –0.17 | –0.42 to 0.11 | –0.17 | –0.42 to 0.11 |
| Exercise | –0.47 | –0.89 to –0.05 | –0.47 | –0.83 to –0.11 |
| Targeted, primary, anxiety (11 trials) | ||||
| CBT | –0.38 | –0.83 to 0.06 | –0.39 | –0.86 to 0.07 |
| Occupational therapy | 0.11 | –0.88 to 1.10 | 0.11 | –0.95 to 1.17 |
| Biofeedback | –0.38 | –1.45 to 0.68 | –0.39 | –1.53 to 0.75 |
Appendix 7 Additional outcomes
Suicidal ideation, behaviour and self-harm outcomes
| Study | Population | Setting | Quotation/details |
|---|---|---|---|
| McCarty et al.218 2011 | Indicated | Secondary | Suicidal ideation was an exclusion criterion |
| Tokolahi et al.181 2018 | Selective | Primary | Reporting parasuicidal and/or suicidal thoughts or behaviours was an exclusion criterion |
| Young et al.230 2016 | Indicated | Secondary | Reporting significant suicidal ideation or non-suicidal self-injury (n = 11) was an exclusion criterion |
| Kindt et al.196 2014 | Universal | Secondary | The question on suicide was removed from the Child Depression Inventory. The authors reported that this was ‘to optimize collaboration with school officials and parents’ |
| McCarty et al.219 2013 | Indicated | Secondary | Current suicidal ideation was an exclusion criterion |
| Peden et al.234 2000 | Indicated | University | Current suicidal ideation was an exclusion criterion |
| Rohde et al.223 2014 | Indicated | Secondary | Current/acute suicidal ideation was an exclusion criterion |
| Young et al.229 2010 | Indicated | Secondary | Suicidal ideation or self-harm behaviours were exclusion criteria |
| Livheim et al.217 2015 | Indicated | Secondary | Suicidality was an exclusion criterion |
| Cowell et al.231 2009 | Selective | Primary | Suicidal ideation was an exclusion criterion |
| Wijnhoven et al.226 2014 | Indicated | Secondary | Suicidal ideation was an exclusion criterion |
| Seligman et al.186 1999 | Selective | University | Students who were considered at current suicide risk were excluded |
| Study | Population | Setting | Quotation/details |
|---|---|---|---|
| Hodas et al.131 2016 | Universal | Secondary | The question on suicidal ideation was removed from the Child Depression Inventory |
| Johnstone et al.152 2014 | Universal | Primary | The question on suicidal ideation was removed from the Child Depression Inventory. The authors note this was because school officials expressed concern about its appropriateness for primary-aged children |
| Pophillat et al.156 2016 | Universal | Primary | The question on suicidal ideation was removed from the Child Depression Inventory. The authors note this was removed ‘in accordance with the Western Australia Department of Education’s standards’ |
| Soffer et al.212 2003 | Universal | Primary | The author reported not using the Children’s Depression Inventory at all, as the Board of Education ‘did not approve . . . due to its explicit assessment of suicidality’ |
| Tak et al.207 2016 | Universal | Secondary | The question on suicidal ideation was removed ‘due to ethical considerations’ (scale used: Child Depression Inventory) |
| Chaplin et al.192 2006 | Universal | Secondary | The question on suicidal ideation was removed ‘at the request of school administrators’ (scale used: Child Depression Inventory) |
| Gillham et al.165 2012 | Indicated | Secondary | Questions on suicidal ideation were removed ‘at the request of school administrators’ (scales used: Child Depression Inventory and Reynolds Adolescent Depression Scale) |
| Horowitz et al.195 2007 | Universal | Secondary | Question on suicidal ideation was removed ‘because of concerns of the participating schools’ (scale used: Child Depression Inventory) |
| Pössel et al.200 2013 | Universal | Secondary | Question on suicidal ideation was removed ‘at the request of the school, as is common in school-based research’ (scale used: Child Depression Inventory) |
Socioeconomic status, biological sex and ethnicity
| Trial | Setting | Sex | Ethnicity | Socioeconomic Status |
|---|---|---|---|---|
| Ahlen et al.145 2018 | Primary | Mixed | NC | Median of household income US$6000–7000/month |
| Anticich et al.339 2013 | Primary | Mixed | Study conducted in Australia. Catholic preschools and primary schools in the greater metropolitan area of Brisbane. Participants described as ‘white’ | . . . working to middle class |
| Araya et al.118 2013 | Secondary | Mixed | NC | ‘Socially deprived’. Author reported School Social Deprivation Index, mean (SD) 0.85 (0.1) 0.85 (0.1) |
| Attwood et al.146 2012 | Primary | Boys | NC | NC |
| Aune and Stiles119 2009 | Secondary | Mixed | Study conducted in Norway:. . . less than 3% non-Caucasian | NC |
| Baker and Butler120 1984 | Secondary | Mixed | Caucasian | NC |
| Barrett and Turner147 2001 | Primary | Mixed | . . . predominantly from Anglo-Saxon families with English as their primary language | 75.35% dual-parent and 11.55% single-parent families. . . varying levels of socio-economic advantage . . . |
| Barrett et al.121 2005 | Secondary | Mixed | The majority of children . . . were white, Anglo-Saxon, Catholic or Protestant Christian | diverse levels of socio-economic status . . . working to middle class |
| Barry et al.190 2017 | Secondary | Boys | The majority of participants stated that they were ‘white, white Irish or any other white background’ | NR |
| Bonhauser et al.122 2005 | Secondary | Mixed | No information provided. Study was conducted in Santiago, Chile | . . . a low socioeconomic area . . . The percentage of the population living below the poverty level . . . is 15% |
| Bouchard et al.148 2013 | Primary | Mixed | NC | Schools were representative of ‘low-, average-, high-, and very high-income neighbourhoods’ |
| Britton et al.123 2014 | Secondary | Mixed | NC | an independent Quaker school |
| Burckhardt et al.124 2015 | Secondary | Mixed | NC | . . . schools were among the highest . . . socioeconomic status compared to other schools in Australia |
| Burckhardt et al.191 2016 | Secondary | Mixed | NC | 76% of the students were in the top quartile of socio-economic advantage |
| Calear et al.125 2009 | Secondary | Mixed | 94% of participants stated that English was their first language. Other languages were Chinese, Hindi, Arabic and Indonesian | . . . a mix of public, private, coeducational, single-sex, metropolitan, and rural schools from six Australian states |
| Calear et al.126 2016 | Secondary | Mixed | 88% reported that English was their first language. Other languages reported were Chinese, Vietnamese, Indian and Arabic | NC |
| Calear et al.127 2016 | Secondary | Mixed | 97% of participants reported English as their first language | NC |
| Cardemil et al.208 2007 | Primary | Mixed |
School 1: 77.2% Latino, 11.7% African American, 7.8% Caucasian and 2.8% Asian School 2: 98.9% African American, 0.6% Asian, 0.2% Latino and 0.2% Caucasian |
School 1: 95.3% of students from low-income households School 2: 89.8% of students from low-income families |
| Chaplin et al.192 2006 | Secondary | Girls | Mostly white (88.7%), with 4.1% African American, 1.5% Latino, 1% Asian American and 4.6% more than one race or ethnicity | Median family annual income was ≥ US$100,000 |
| Clarke et al.193 1993a | Secondary | Mixed | 90% of enrolled students identified as White | . . . schools were located in predominantly middle-class neighborhoods |
| Clarke et al.193 1993b | Secondary | Mixed | 90% of enrolled students identified as White | . . . schools were located in predominantly middle-class neighborhoods |
| Collins et al.149 2014 | Primary | Mixed | Participants were described as 98% British white | 6.9% of students were eligible for free school meals. . . schools were located in relatively affluent suburbs |
| Dadds and Roth303 2008 | Primary | Mixed | 86.8% of participants were described as white, Anglo-Saxon | The majority of participants are described as ‘working to middle class’ |
| Eather et al.340 2016 | Secondary | Mixed | NC | NC |
| Essau et al.150 2012 | Primary | Mixed | The majority were of German origin (95%). Others identified Southern and Eastern European backgrounds. A total of 63% identified as catholic and 10.9% as protestant | 72% of parents reported having a high school or equivalent educational level |
| Gallegos151 2008 | Primary | Mixed | The study was conducted in the metropolitan area of Monterrey, Northern Mexico. No further information is given | The author described most people living in the local area as being of a medium SES, ‘ranked as number 6’ [Instituto Nacional de Estadística Geografía e Informática (INEGI; National Institute of Statistics, Geography, and Information)] |
| Gillham209 1995 | Primary | Mixed | NC | NC |
| Gillham et al.128 2006 | Secondary | Mixed | Most students stated that they were from Caucasian backgrounds. Two students were of African American descent, one of Asian descent, and one student defined their ethnicity as ‘other’ |
Suburban Philadelphia A total of 47% had household incomes of > US$100,000, 34% of US$60,000–99,999. 19% of < US$60,000 |
| Gillham et al.194 2007 | Secondary | Mixed | The majority of students were of Caucasian descent, < 10% African American descent, < 2% Latino descent and < 3% Asian descent | School 1: 39% reported income of > US$100,000; 72% of > US$60,000. In schools 2 and 3, 84% and 66%, respectively, reported family income of < US$60,000 |
| Gucht et al.129 2017 | Secondary | Mixed | The study was conducted in a Dutch-speaking region of Belgium | NC |
| Haden et al.341 2014 | Primary | Mixed | Study was conducted in New YorkMost participants were . . . White | Most participants had a household income in the US$10,000–75,000 or > US$125,000 range |
| Hiebert et al.130 1989 | Secondary | Mixed | The study was conducted in a large suburban area in Western Canada | NC |
| Hodas131 2016 | Secondary | Girls |
School 1: 72% of students were Caucasian School 2: 45% of students were African American and 43% were Caucasian |
School 1: affluent households ‘. . . who are able to afford the nearly US$27,000 annual tuition’ School 2: economically diverse |
| Horowitz et al.195 2007 | Secondary | Mixed | 79% Caucasian, 13% African American, 2% Latino, 1% Asian American, 1% Native American, 3% mixed heritage | Students came from working to middle class communities |
| Johnson et al.132 2016 | Secondary | Mixed | NC | 16.2% low SES, 39% medium SES, 44.8% high SES |
| Johnson et al.133 2017 | Secondary | Mixed | NC | . . . a broad range of socioeconomic (SES) demographics |
| Johnstone et al.152 2014 | Primary | Mixed | NC | Schools were in the ‘poorest (bottom 30%) in the Western Australian Department of Education and Training School Database’ |
| Khalsa et al.239 2012 | Secondary | Mixed | Students attending the school were described as ‘90% white’ | A total of 17% of students were described as from a low-income population |
| Kindt et al.196 2014 | Secondary | Mixed | The authors report that approximately 50% of participants were classed as being an ‘ethnic minority’ | Schools were eligible for the study if ≥ 30% of their students came from low-income areas |
| Lock and Barrett134 2003 | Secondary | Mixed | NC | The schools were described as being ‘socio-economically diverse’ |
| Lowry-Webster et al.135 2001 | Secondary | Mixed | NC | No details on SES were given. The study was conducted in catholic schools in the Brisbane metropolitan area |
| Mendelson et al.210 2010 | Primary | Mixed | A total of 83.5% of students self-identified as African American, 4.1% as Latino, 4.1% as white, and 7.2% as ‘mixed race’ | No details on SES were given. Study was conducted in Baltimore City public schools |
| Merry et al.197 2004 | Secondary | Mixed | Children attending the school were predominantly from Maori and Pakeha backgrounds | School 1 was in a lower socioeconomic urban area; school 2 was in a middle-class rural district |
| Miller et al.153 2010 | Primary | Mixed | . . . a population that spoke English in 88% of homes . . . | . . . an unemployment rate of 5.5% . . . |
| Miller et al.154 2011 | Primary | Mixed | 36% Canadian aboriginal – First Nations, Native American, Metis, and Inuit | NC |
| Miller et al.154 2011 | Primary | Mixed | 18% spoke a language other than English in the home | NC |
| Pahl and Barrett242 2010 | Primary | Mixed | NC | A total of 19% of families had an annual income of < US$40,000, 38.7% between US$40,001 and $80,000, and 28% between US$80,001 and US$100,000 |
| Pattison and Lynd-Stevenson155 2001 | Primary | Mixed | NC | The study is described as being based in ‘a rural town south of Adelaide’ |
| Perry et al.136 2017 | Secondary | Mixed | Roughly 43% spoke a language other than English at home | Participants were from selective and partially selective state/public funded schools in metropolitan Sydney, Australia |
| Pophillat et al.156 2016 | Primary | Mixed | NC | ‘. . . a very low socioeconomic status area in Perth,’ Western Australia |
| Pössel et al.198 2004 | Secondary | Mixed | NC | NC |
| Pössel et al.199 2011 | Secondary | Mixed | NC | . . . a wide range of social classes is likely to be represented . . . economically different regions of the area are represented |
| Pössel et al.200 2013 | Secondary | Mixed | The sample was 72.8% Caucasian, 14.7% African American, 5.4% Latino, 1.4% Asian/Pacific Islander, 0.8% Native American, 4.4% mixed heritage, and 0.6% ‘other’ | Participants were working to middle class. A total of 29% of the students were eligible for free or subsidised school meals |
| Potek et al.137 2012 | Secondary | Mixed | Total sample was 77.4% white; 16.1% black; 3.2% Latino and 3.2% East Asian | NC |
| Quayle et al.211 2001 | Primary | Girls | NC | The study was conducted in a private girls’ school in a high socioeconomic suburb of Perth, Western Australia |
| Raes et al.201 2014 | Secondary | Mixed | NC | NC |
| Reynolds et al.233 2011 | University | Mixed | Participants were 57.7% white, 12.7% African American, 11.3% Hispanic, 8.5% Asian or Pacific Islander, 5.6% Asian Indian and 4.2% self-identified as ‘other’ | NC |
| Rivet-Duval et al.202 2011 | Secondary | Mixed | A total of 97.5% of participants were Mauritian and were ‘. . . representative of the ethnic (primarily Creole, Hindu and Muslim) and religious (primarily Christian, Hindu and Muslim) backgrounds of the Mauritian population’ | Household income: 10% < Rs5000, 19% between Rs5000 and Rs15,000, 33% between Rs15,000 and Rs25,000 and 38% > Rs25,000 |
| Roberts et al.138 2003 | Secondary | Mixed | Participants were 74% Australian, 3% Australian Aboriginal, 5% UK and Ireland, 3% European, 0.5% other non-English speaking and 15% not stated | Mothers’ and fathers’ level of education, respectively:
|
| Roberts et al.139 2010 | Secondary | Mixed | Participants were 44% Australian, 4% other English speaking, 7% other non-English speaking and 44% not stated |
Annual family income (Aus$): 14% < $20,000, 30% $20,000–50,000; 13% > $50,000 and 43% not stated |
| Roberts et al.240 2018 | Primary | Mixed | Participants were 80.7% Australian, 1.7% Australian Aboriginal, 9.2% other English-speaking countries, 5% Asian, 1.9% European, and 1.5% other non-English speaking countries | NC |
| Rodgers and Dunsmuir140 2015 | Secondary | Mixed |
School 1: 68% white Irish, 18% Irish travelling community and 14% foreign nationals School 2: 92% white Irish, 0% Irish travelling community and 8% foreign nationals School 3: 88% white Irish, 0% Irish travelling community and 12% foreign nationals |
. . . a socially disadvantaged catchment area in a major city in Ireland |
| Rooney et al.157 2006 | Primary | Mixed | NC | The study was conducted in schools in ‘low socioeconomic areas’ |
| Rose et al.203 2014 | Secondary | Mixed | Mixed | Mixed |
| Ruttledge et al.158 2016 | Primary | Mixed | NC | Mixed |
| Sawyer et al.204 2010 | Secondary | Mixed | NC | 81% of participants had at least one parent in full-time employment |
| Shatté205 1997 | Secondary | Mixed | NC | NC |
| Sheffield et al.141 2006 | Secondary | Mixed | . . . a broad range of social and cultural backgrounds, consistent with the Australian population . . . | NC |
| Soffer212 2003 | Primary | Mixed | Participants were 60% Caucasian, 14% African American, 8% Hispanic American, 8% Asian American, 4% mixed ethnicity and 6% other ethnicity | Average Hollingshead Index: 35.37 (SD 11.67). Most parents reported occupations in the middle-income range |
| Spence et al.206 2003 | Secondary | Mixed |
Other students reported a ‘variety of ethnic backgrounds typical of the Australian population’ |
Average SES score was 4.55 (SD 2.66). The authors describe this as ‘typical of the SES distribution of Australia’ and ‘. . . indicative of lower middle SES’ |
| Stallard et al.142 2013 | Secondary | Mixed | . . . were representative of schools in the United Kingdom for ethnicity | . . . schools were representative of schools in the United Kingdom for deprivation (eligibility for free school meals), pupil absence rates, and academic ability (examination results and proportion of children with identified special educational needs) |
| Stallard et al.159 2014 | Primary | Mixed | Participants were 94% white British, 6% ‘non-white’ | ‘Family affluence’: 2% low; 29% medium; 69% high. Eligibility for free school meals was lower than the national average (12.4% vs. 18.2%) |
| Tak et al.207 2016 | Secondary | Mixed | A total of 79% described as Dutch, 21% ‘other’ and 16.9% were from ethnic minorities. The authors note this is lower than the general population (20.3 %) | NC |
| Tomba et al.143 2010 | Secondary | Mixed | NC | NC |
| Velásquez et al.189 2015 | Mixed (primary/secondary) | Mixed | Study was conducted in Bogotá, Colombia | . . . a disadvantaged area |
| Wong et al.144 2014 | Secondary | Mixed | NC | NC |
| Study | Setting | Sex | Ethnicity | SES |
|---|---|---|---|---|
| Arnarson and Craighead213 2009 | Secondary | Mixed | NC | NC |
| Balle and Tortella-Feliu160 2010 | Secondary | Mixed | NC | NC |
| Berry and Hunt161 2009 | Secondary | Boys | 74% of families were of an Anglo-Saxon, 17% were of Middle Eastern and 9% were from an Asian ethnic background | 54% of parents had not completed tertiary education; 76% were from lower to middle-class backgrounds as classified by annual income |
| Clarke et al.214 1995 | Secondary | Mixed | 92.5% of participants were ‘non-Hispanic white’ | Median parent education was 1 to 2 years of college |
| Congleton215 1995 | Secondary | Mixed | 92% of participants were described as ‘Caucasian’ | 25% of participants received subsidised or free school meals |
| Cooley-Strickland et al.174 2011 | Primary | Mixed | 92% African American, 8% ‘biracial’ | The schools in this study were in disadvantaged areas. 90% of the students in the schools received subsidised or free school meals |
| Cova et al.162 2011 | Secondary | Girls | NC | NC |
| Cowell et al.231 2009 | Primary | Mixed | Not specifically referenced. However, schools were selected if the student body was ≥ 30% from Latino ethnic backgrounds | 80% of families reported annual incomes of < US$26,000 |
| Cui et al.183 2016 | University | Mixed | NC | NC |
| Dobson et al.163 2010 | Secondary | Mixed | NC | NC |
| Ellis et al.184 2011 | University | Mixed | NC | NC (participants were university students) |
| Fitzgerald et al.114 2016 | Secondary | Mixed | 93% white; 2% black; 2% Asian; 0% Irish Traveller; 1% other and 2% unknown | Classified using ‘School disadvantage status’ (DEIS): non-DEIS 82%; DEIS 18% |
| Fung et al.216 2016 | Secondary | Mixed | 52.6% of students described themselves as self-identified Latino and 47.4% as Asian American | No details on participants but school district in an ethnically diverse, low-income area |
| Gaete et al.164 2016 | Secondary | Mixed | NC | The majority of participants were from ‘low socio-economic families’ |
| Gillham et al.165 2012 | Secondary | Mixed | Less than 1% Native American, 4% Asian, < 1% Pacific Islander/Native Hawaiian, 12% African American, 77% European American, 3% Latino/a, 4% other | Reported mothers’ and fathers’ education level. The majority had 'some college' education and above (respectively): 79% and 69% |
| Hiebert et al.130 1989 | Secondary | Mixed | NC | NC |
| Higgins185 2007 | University | Mixed | 95% of participants described themselves as Caucasian, 2.6% as Asian, 1.3% as African American and 1.3% as other | NC |
| Hunt et al.166 2009 | Secondary | Mixed | No information given. Schools were Catholic secondary schools in Sydney | NC |
| Jaycox et al.232 1994 | Primary | Mixed | Details provided for the intervention group: 80% Caucasian, 17% African American, 3% other | Total family income (intervention group):
|
| Jordans et al.167 2010 | Secondary | Mixed |
|
Details of family income not provided. Nepal is classified as a LIC |
| Kiselica et al.168 1994 | Secondary | Mixed | White | Participants lived in an area described as ‘middle-class and lower middle-class’ |
| Liddle and Macmillan188 2010 | Mixed (primary/secondary) | Mixed | NC (Scottish setting) | NC |
| Livheim et al.217 2015 | Secondary | Girls | NC | NC |
| Manassis et al.175 2010 | Primary | Mixed | Ethnicity as reported by families was 56.8% Caucasian, 12.8% Asian, 8.1% East Indian, 6.8% Hispanic, 5.4% Filipino, 3.3% black, and 6.8% mixed/other | Our sample was [. . . ] economically diverse |
| McCarty et al.218 2011 | Secondary | Mixed | Details provided for intervention group:
|
Parental education was reported for the intervention group: 64% had a bachelor’s degree or higher |
| McCarty et al.219 2013 | Secondary | Mixed | Details provided for in intervention group:
|
|
| McLaughlin236 2011 | Mixed (primary/secondary) | Mixed | 94% Caucasian, 2% Hispanic, 2% African American, 2% Asian and/or Pacific Islander, and < 1% American Indian | Information not provided for sample. 11% of students in the school district were eligible for subsidised or free school meals |
| McLoone et al.176 2012 | Primary | Mixed | NC | Reported for school-based intervention group, mothers' and fathers' occupational status (respectively): 25% and 2% unemployed, 32% and 15% trade/clerical, 44% and 84% professional |
| Mifsud and Rapee177 2005 | Primary | Mixed | Reported for the intervention group: 78% Australian, 17% other country, 5% Aboriginal | Sample details not reported. Intervention was run in areas with high levels of socioeconomic disadvantage |
| Miller et al.178 2011 | Primary | Mixed | Ethnicity not reported. However, 48% of the sample did not speak English as their first language with their families (18% spoke Chinese, proportion of other languages not reported) | NC |
| Noël et al.220 2013 | Secondary | Girls | Reported for intervention group only: 80% African American, 15% non-Hispanic white and 5% Hispanic | NC |
| Owen and Lanning169 1982 | Secondary | Boys | NR | NR |
| Peden et al.234 2000 | University | Girls | NC | NC |
| Peng et al.170 2015 | Secondary | Mixed | NC | NC |
| Poppelaars et al.221 2016 | Secondary | Girls | Detail not reported. Authors state that 94.7% of participants had been born in the Netherlands | NC |
| Puskar et al.222 2003 | Secondary | Mixed | NC | NC |
| Rice171 2009 | Secondary | Mixed | NC | NC |
| Rohde et al.223 2014 | Secondary | Mixed | The participants are described as 6% Hispanic, 2% Asian Americans, 1% African Americans, 72% Caucasian, 1% Native American and 18% other or mixed ethnic background | Parental education 39% high school graduate or less, 26% some college, 22% college graduate and 13% graduate degree |
| Scholten et al.172 2016 | Secondary | Mixed | Authors state that 97.8% of participants had been born in the Netherlands | ‘The majority’ of students in the sample were academically high achievers (‘high streamed education tracks’) |
| Schoneveld et al.115 2016 | Primary | Mixed | 89.7% of participants were 'of Dutch descent' | NC |
| Schoneveld et al.116 2018 | Primary | Mixed | 91.4% of participants had been born in the Netherlands | NC |
| Seligman et al.186 1999 | University | Mixed | NC | NC |
| Seligman et al.187 2007 | University | Mixed | NC | NC |
| Sheffield et al.141 2006 | Secondary | Mixed | Sample specific details not provided. Authors state that sample reflected the Australian population for social and cultural background | NC |
| Simpson179 2008 | Primary | Mixed | 56% ‘Caucasian’, 38% Asian/South Asian descent and 6% were from other or mixed ethnic backgrounds | Household annual income: 35.2% > CAN$80,000 and 24.6% < CAN$35,000. Mothers’ education: 68.5% some post-secondary education, 14% did not complete high school and 8.8% completed high school. Fathers’ education: 40% some post-secondary education, 19.3% did not finish high school and 7% finished high school |
| Siu180 2008 | Primary | Mixed | NC | NC |
| Sportel et al.117 2013 | Secondary | Mixed | NC | NC |
| Stallard et al.142 2013 | Secondary | Mixed | Information not explicitly provided. However, the schools are described as ‘representative of schools in the United Kingdom for ethnicity' | Specific details not reported. However, schools are described as 'representative of schools in the United Kingdom for deprivation pupil attendance and academic ability’ |
| Stice et al.237 2007 | Mixed (secondary/university) | Mixed | 17% Asians, 6% blacks, 55% ‘Caucasian’, 15% Hispanics, 7% other/mixed ethnic background | Parental education level: 20% high school graduate or less, 20% some college, 34% college graduate, 26% graduate degree |
| Stice et al.224 2008 | Secondary | Mixed | 2% Asian, 9% African American, 46% ‘Caucasian’, 33% Hispanic and 10% other/mixed ethnic heritage | Parental education level: 26% high school graduate or less, 17% some college, 35% college graduate, 18% graduate degree |
| Stoppelbein225 2003 | Secondary | Mixed | 88% ‘Caucasian’, 10% African American, 2% Asian American | SES: 18% lower, 22% lower middle, 51% middle, 9% upper middle |
| Takagaki et al.235 2016 | University | Mixed | NC | NC |
| Tokolahi et al.181 2018 | Primary | Mixed | 35% New Zealand English, 16% Maori, 18% Pacific, 10% Asian, 20% other | NC |
| Topper et al.173 2017 | Secondary | Mixed | NC | NC |
| van Starrenburg et al.182 2017 | Primary | Mixed | 92.9% of participants and 90.8% of their mothers were born in the Netherlands | Mothers’ education level: 55% completed a vocational education, 25% had college or higher education. 40% of the families had a household income considered ‘low to average’ |
| Wijnhoven et al.226 2014 | Secondary | Girls | 98% of the participants were ‘of Dutch origin’ | NC |
| Woods and Jose227 2011 | Secondary | Mixed | 45% of participants identified themselves as Maori and 55% as Pacific | Schools were representative of a range of SESs |
| Young et al.228 2006 | Secondary | Mixed | 92.7% of participants identified as Hispanic | [H]alf reported a gross household income of $25,000 or less |
| Young et al.229 2010 | Secondary | Mixed | 73.7% Hispanic, 39% African American | NC |
| Young et al.230 2016 | Secondary | Mixed | 19.9% African American, 4.3% Asian and 8.1% other/mixed race. 38.2% Hispanic and 38.2% white ‘non-minority, non-Hispanic’ | Participants reported a wide range of annual household incomes: 17.3% < US$25,000, 38.4% US$25,000–90,000, and 44.3% > US$90,000 |
| Yu238 2002 | Mixed (primary/secondary) | Mixed | NC | Intervention group parental education level: (father and mother, respectively) 5% and 4% primary school, 9% and 6% junior school, 29% and 34% senior school, 28% and 45% college, 28% and 11% more than college. Intervention group parental income level: 17% < 1000 yuan; 25% 1001–2000 yuan; 24% 2001–3000 yuan; 17% 3001–4000 yuan; 17% > 4001 yuan |
Intervention attendance and engagement
Table 72 reports student attendance figures, as reported by trial author.
| Study | Attendance |
|---|---|
| Ahlen et al.145 2018 | Non-attendance ranged between 4.2% and 6.1% (at class level) |
| Araya et al.118 2013 | 80.5% of intervention group participants attended ≥ 6 sessions |
| Bonhauser et al.122 2005 | Authors report that 87% of the sessions were completed |
| Burckhardt et al.124 2015 | 8.0% of intervention group participants did not return any of their workbooks from any of the sessions, 15.5% returned 1–2 workbooks, 20.8% returned 3–4 workbooks and 55.6% returned 5–6 session workbooks |
| Calear et al.125 2009 | 62% of the intervention group completed three or more sections (‘modules’) of the intervention. 32.7% completed all sections. [mean number of sections completed, 3.16 (SD 1.68)] |
| Calear et al.126 2016 | School-based intervention: 78% completed 2 weeks, 43% completed at least 4 weeks and 36% completed all 6 weeks of the intervention. Health service intervention: 87% completed 2 weeks, 65% completed at least 4 weeks and 50% completed all 6 weeks of the intervention |
| Calear et al.127 2016 | 45% completed all 6 weeks of the intervention |
| Chaplin et al.192 2006 | Single-sex PRP intervention: attendance mean = 7.03 sessions (SD 4.15). Co-educational PRP intervention: attendance = mean 5.04 sessions (SD 3.56) |
| Clarke et al.214 1995 | Average intervention group attendance = 72% (range 13% to 100%) |
| Congleton215 1995 | Except for one participant, all attended at least six of the eight sessions; 69% attended all eight sessions |
| Cooley-Strickland et al.174 2011 | All participants attended at least 12 of the 13 sessions |
| Cova et al.162 2011 | Universal intervention: 76.5% of the participants attended eight or more sessions; 3.4% attended six or fewer sessions (mean = 8.86 sessions). Indicated intervention: in the indicated modality of the programme, 43% attended six or fewer sessions and 8.9% did not attend any session (mean = 6 sessions) |
| Cowell et al.231 2009 | Participants in the north side intervention groups attended an average of eight classes. Participants in the south side intervention group received an average of 4.72 classes (t = −2.47, df = 109, p = 0.02) |
| Cui et al.183 2016 | Cognitive behavioural intervention: 56% of participants attended all eight sessions and 85% attended at least six sessions. Supportive group intervention: 53% of participants attended all sessions and 82% attended at least six sessions |
| Eather et al.340 2016 | Across all sessions the attendance was 94% for the intervention group |
| Essau et al.150 2012 | 21 children missed one session, 14 missed two sessions, and 6 missed three sessions. All children missing as session had a 1 : 1 catch-up session before their next group session. All these children received an individual session before joining the next group session |
| Fung et al.216 2016 | The average number of sessions attended was 10.28 out of 12 sessions (85.63%) |
| Gaete et al.164 2016 | An average of 55.5% participants attended each session (SD = 5.9; range, 45.0–66.4%) |
| Gillham et al.128 2006 | Average number of sessions attended was 5.5 out of eight; 14% of participants attended two or fewer sessions; 45% of participants attended seven or more sessions |
| Gillham et al.194 2007 | PRP intervention: average number of sessions attended was 6.71 (SD = 4.22); 16% did not attend any sessions. PEP intervention: average number of sessions attended was 7.11 (SD = 4.43); 15% of participants did not attend any sessions |
| Gillham et al.165 2012 | 84% of students attended at least one session of the main intervention and 44% attended the booster session at 5 months |
| Johnson et al.132 2016 | 87% of participants attended six or more out of the eight sessions |
| Johnson et al.133 2017 | For the first two sessions, attendance was 40%. By the end of the intervention, involvement was 9% |
| Johnstone et al.152 2014 | The average number of sessions attended was 9.03 (SD 2.143) |
| Khalsa et al.239 2012 | 73.4% of sessions were attended (SD 0.2%) |
| Livheim et al.217 2015 | Acceptance and commitment intervention: attended an average of 5.8 out of eight sessions |
| McCarty et al.218 2011 | 94% of parents received three or more sessions (out of four) |
| McCarty et al.219 2013 | 85% of parents participated in both home visit sessions, 38% attended both parent workshop sessions, 22% attended one workshop and 40% did not attend either workshop |
| Mendelson et al.210 2010 | Intervention attendance varied by school. School 1: 73.5% completed at least 75% of sessions and school 2: 40% of students attended 75% of sessions |
| Mifsud and Rapee177 2005 | A mean of 7.38 of eight sessions were attended (SD 0.58) by students |
| Perry et al.136 2017 | 88% of participants completed at least four sessions |
| Poppelaars et al.221 2016 | Participants completed an average of 6.77 (SD 1.17) out of eight lessons. All participants received at least four sessions |
| Pössel et al.200 2013 | Cognitive–behavioural prevention programme: participants attended a mean of 8.5 (SD 2.3) sessions. Non-specific control: mean of 8.6 (SD 2.0) sessions were attended |
| Puskar et al.222 2003 | Students attended an average of nine sessions |
| Quayle et al.211 2001 | Most participants attended ‘three or four sessions.’ 8.3% of participants attended seven sessions and 21% attended five or more sessions |
| Roberts et al.138 2003 | Attendance ranged from 87% to 99% over the 12 sessions |
| Roberts et al.139 2010 | SLS intervention: 5.2% of students missed at least 25% of the sessions. OTS intervention: 9% of students missed at least 25% of the sessions |
| Rohde et al.223 2014 | Cognitive behavioural intervention: participants attended an average of 5.3 sessions (SD 0.9); 48% attended all six sessions. All students received at least three sessions |
| Schoneveld et al.115 2016 | 80.9% of participants completed all game sessions. Mean = 4.71 sessions (SD 0.69) |
| Seligman et al.186 1999 | 85% of participant attended the workshop |
| Seligman et al.187 2007 | 84% of participant attended the workshop |
| Sheffield et al.141 2006 (universal) | Mean number of sessions attended was > 90% |
| Sheffield et al.141 2006 (indicated) | Mean attendance rate was 75% of the sessions |
| Siu180 2008 | Only eight students missed one session |
| Sportel et al.117 2013 | A small proportion of participants (n = 16) did not complete the intervention |
| Stallard et al.142 2013 | Classroom-based CBT intervention: median sessions attended was 89% (quartiles 67–100%); 80% of students attended at least 60% of planned sessions. Attention control group: median sessions attended was 100% (quartiles 88–100); 95% of students attended at least 60% of sessions |
| Stallard et al.159 2014 | Classroom CBT intervention: 80% of participants attended at least 60% of the sessions. Attention control group: 93% of participants attended at least 60% of the sessions |
| Stice et al.224 2008 | Cognitive–behavioural intervention: 44% of participants attended all sessions; 86% attended at least three of the six sessions. Supportive group intervention: 45% attended all sessions; 89% attended at least three of the six sessions |
| Tak et al.207 2016 | Attendance data for main intervention not reported. However, 67.8% of participants completed the booster session |
| Takagaki et al.235 2016 | 98.4% of participants completed all sessions |
| Topper et al.173 2017 | Group intervention: mean number of sessions attended was 4.59 (SD 1.43). Internet intervention: mean number of sessions attended was 3.96 (SD 1.65) |
| Velásquez et al.189 2015 | 21 participants were classified as low attenders and 47 were classified as high attenders |
| Young et al.228 2006 | Intervention participants attended a mean of 6.9 sessions (SD 1.0) |
| Young et al.229 2010 | IPT-AST intervention: participants attended an average of 5.22 group sessions (SD 2.55). School counselling intervention: students attended an average of 3.76 sessions (SD 2.53) |
| Young et al.230 2016 | IPT-AST intervention: mean number of sessions attended by participants was 6.80 (SD 1.85). Group counselling intervention mean sessions attended was 6.18 (SD 1.85) |
Appendix 8 Economic evaluation
Search carried out in the NHS Economic Evaluation Database
NHS Economic Evaluation Database (1968 to 2014) was searched on 22 May 2019.
Search strategy
-
MeSH DESCRIPTOR child, preschool
-
MeSH DESCRIPTOR child
-
MeSH DESCRIPTOR adolescent
-
MeSH DESCRIPTOR young adult
-
(child* or boy* or girl* or kids or juvenil* or minors or paediatric* or pediatric* or adolesc* or preadolesc* or pre-adolesc* or pubert* or pubescen* or prepube* or pre-pube* or teen* or (young NEAR0 (adult* or people or patient* or men or women or man or woman or male* or female* or survivor* or offender* or minorit*)) or youth* or student* or undergrad*)
-
(child* or adolesc* or paediatr* or pediatr*):so
-
#1 OR #2 OR #3 OR #4 OR #5 OR #6
-
MeSH DESCRIPTOR education
-
MeSH DESCRIPTOR schools
-
MeSH DESCRIPTOR schools, nursery
-
MeSH DESCRIPTOR school health services
-
MeSH DESCRIPTOR school nursing
-
MeSH DESCRIPTOR students
-
MeSH DESCRIPTOR universities
-
preschool or kindergarten or school* or college* or campus* or classroom* or curricul* or teacher* or gatekeeper* or pupil*
-
MeSH DESCRIPTOR peer group
-
((peer or peers) NEAR0 (education or group or relation* or support* or intervention* or leader*))
-
student* union
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) NEAR1 (camp or club or group))
-
((camp or club or group) NEAR1 (church or communit* or holiday* or religi* or spiritual* or youth or vacation))
-
((church or communit* or holiday* or religi* or spiritual* or youth or vacation) NEAR0 based)
-
#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21
-
MeSH DESCRIPTOR adaptation, psychological
-
MeSH DESCRIPTOR emotions
-
MeSH DESCRIPTOR mental health
-
MeSH DESCRIPTOR social adjustment
-
MeSH DESCRIPTOR stress, psychological EXPLODE ALL TREES
-
mental health or mental* ill* or psychiatric
-
wellbeing or well being
-
stress* or distress*
-
#23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30
-
MeSH DESCRIPTOR depression
-
MeSH DESCRIPTOR depressive disorder
-
MeSH DESCRIPTOR mood disorders
-
(depress* or dysthymi* or affective disorder* or affective symptom* or mood* or mental):ti
-
(depress* NEAR1 (adolescent* or child* or anaclitic* or episode* or disorder or scale* or score* or symptom* or unipolar)) or ((adolescent* or child* or anaclitic* or episode* or disorder or scale* or score* or symptom* or unipolar) NEAR1 depress*)
-
((depress* or mood* or mental or psychological or wellbeing or well being or emotion*) NEAR1 (improve* or onset or prevent* or reduc*)) or ((improve* or onset or prevent* or reduc*) NEAR1 (depress* or mood* or mental or psychological or wellbeing or well being or emotion*)) 780
-
(Axis 1 or Axis I) NEAR0 disorder*
-
#32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38
-
MeSH DESCRIPTOR anxiety disorders EXPLODE ALL TREES
-
MeSH DESCRIPTOR anxiety
-
anxi*:ti
-
(anxi* NEAR2 (adolescent* or child* or disorder* or general* or interpersonal or separation or social*)) or ((adolescent* or child* or disorder* or general* or interpersonal or separation or social*) NEAR2 anxi*)
-
(phobi* or agoraphobi* or PTSD or post trauma* or posttrauma or panic* or OCD or obsess* or compulsi* or GAD or stress disorder* or stress reaction* or acute stress or neurosis or neuroses or neurotic or psychoneuro* or (school NEAR1 (refusal or avoid*)) or ((refusal or avoid*) NEAR1 school) or social avoidance or mutism)
-
(((anxi* or fear or fright) NEAR2 (perform* or athlet* or music* or act* or test* or exam*)) or math* anxiety or ((perform* or athlet* or music* or act* or test* or exam*) NEAR2 (anxi* or fear or fright)))
-
(public NEAR2 (speak* or speech)) or ((speak* or speech) NEAR2 public)
-
#40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46
-
MeSH DESCRIPTOR conduct disorder
-
MeSH DESCRIPTOR child behavior disorders
-
MeSH DESCRIPTOR juvenile delinqency
-
MeSH DESCRIPTOR social behavior
-
MeSH DESCRIPTOR social behavior disorders
-
((behavi* or conduct or personalit*) NEAR1 (agressi* or nonagressi* or antisocial or anti social or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internalising or internalizing or externalising or externalizing or problem*)) or ((agressi* or nonagressi* or antisocial or anti social or dyssocial or defiant or delinquen* or disturb* or disrupt* or disorder* or internalising or internalizing or externalising or externalizing or problem*) NEAR1 (behavi* or conduct or personalit*))
-
((conduct or behavi* or antisocial or anti social or dyssocial or emotional* or internalising or internalizing or externalising or externalizing) NEAR2 (problem* or difficult* or psychopathol*)) or ((problem* or difficult* or psychopathol*) NEAR2 (conduct or behavi* or antisocial or anti social or dyssocial or emotional* or internalising or internalizing or externalising or externalizing))
-
oppositional NEAR2 (defiant* or disorder*)
-
#48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55
-
MeSH DESCRIPTOR preventive health services
-
MeSH DESCRIPTOR early intervention (education)
-
MeSH DESCRIPTOR health literacy
-
MeSH DESCRIPTOR patient education as topic
-
MeSH DESCRIPTOR health promotion
-
MeSH DESCRIPTOR primary prevention
-
MeSH DESCRIPTOR secondary prevention
-
prevent*:ti
-
prevention of
-
(prevent* NEAR1 (intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial)) or ((intervention or educat* or pilot or program* or project or protocol* or training or universal or targeted or primary or secondary or selective or indicated or study or trial) NEAR1 prevent*)
-
(early or brief) NEAR0 intervention*
-
((universal or targeted) NEAR1 (program* or intervention*))
-
vulnerabl* or at risk or (risk NEAR1 reduc*) or (reduc* NEAR1 risk)
-
MeSH DESCRIPTOR risk
-
MeSH DESCRIPTOR risk factors
-
MeSH DESCRIPTOR accidents EXPLODE ALL TREES
-
MeSH DESCRIPTOR bereavement
-
MeSH DESCRIPTOR grief
-
MeSH DESCRIPTOR social problems
-
MeSH DESCRIPTOR bullying
-
MeSH DESCRIPTOR child of impaired parents
-
MeSH DESCRIPTOR child, orphaned
-
MeSH DESCRIPTOR crime victims
-
MeSH DESCRIPTOR disasters EXPLODE ALL TREES
-
MeSH DESCRIPTOR divorce
-
MeSH DESCRIPTOR life change events
-
MeSH DESCRIPTOR runaway behavior
-
MeSH DESCRIPTOR urban population
-
MeSH DESCRIPTOR rural population
-
MeSH DESCRIPTOR survivors
-
MeSH DESCRIPTOR violence
-
MeSH DESCRIPTOR warfare
-
MeSH DESCRIPTOR civil disorders EXPLODE ALL TREES
-
MeSH DESCRIPTOR crime EXPLODE ALL TREES
-
MeSH DESCRIPTOR human rights abuses EXPLODE ALL TREES
-
MeSH DESCRIPTOR parental death EXPLODE ALL TREES
-
MeSH DESCRIPTOR poverty
-
MeSH DESCRIPTOR social behavior disorders EXPLODE ALL TREES
-
MeSH DESCRIPTOR domestic violence
-
MeSH DESCRIPTOR child abuse EXPLODE ALL TREES
-
MeSH DESCRIPTOR ethnic violence EXPLODE ALL TREES
-
MeSH DESCRIPTOR physical abuse
-
MeSH DESCRIPTOR terrorism EXPLODE ALL TREES
-
MeSH DESCRIPTOR torture
-
MeSH DESCRIPTOR exposure to violence
-
MeSH DESCRIPTOR warfare and armed conflicts EXPLODE ALL TREES
-
MeSH DESCRIPTOR dissent and disputes
-
MeSH DESCRIPTOR family conflict
-
MeSH DESCRIPTOR psychosocial deprivation
-
#57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74 OR #75 OR #76 OR #77 OR #78 OR #79 OR #80 OR #81 OR #82 OR #83 OR #84 OR #85 OR #86 OR #87 OR #88 OR #89 OR #90 OR #91 OR #92 OR #93 OR #94 OR #95 OR #96 OR #97 OR #98 OR #99 OR #100 OR #101 OR #102 OR #103 OR #104 OR #105
-
MeSH DESCRIPTOR randomized controlled trial
-
MeSH DESCRIPTOR pragmatic clinical trial
-
randomised or randomized or randomisation or randomization
-
(RCT or (random* NEAR2 (administ* or allocat* or assign* or class* or cluster* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or substitut* or treat*)) or ((administ* or allocat* or assign* or class* or cluster* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or substitut* or treat*) NEAR2 random*))
-
at random
-
placebo
-
trial
-
#107 OR #108 OR #109 OR #110 OR #111 OR #112 OR #113
-
treatment-as-usual or (treatment* NEAR1 usual) or (usual NEAR1 treatment*) or (standard NEAR1 care) or (standard NEAR1 treatment) or (routine NEAR1 care) or (usual NEAR1 medication*) or (usual NEAR1 care) or TAU
-
waitlist* or wait-list* or waiting-list* or wait* list* or (waiting NEAR0 (condition or control)) or WLC
-
((delay* NEAR2 (start or treatment*)) or ((start or treatment) NEAR2 delay*) or no intervention or no treatment* or no-treatment or non treatment* or nontreatment* or non-treatment* or minim* treatment* or untreated group* or untreated control* or without any treatment) and (control* or group*)
-
(no intervention* or non intervention* or non-intervention* or without any intervention*) and (control* or group*)
-
#115 OR #116 OR #117 OR #118
-
#114 OR #119
-
#7 AND #22 AND (#31 OR #39 OR #47 OR #56) AND #106 AND #120
-
(universal or indicated or targeted or at risk) and prevent* and (anxiety or depress* or conduct) and (child* or adolesc* or school*)
-
(prevent* NEAR0 (program* or intervention)) and (anxiety or depress* or conduct) and (child* or adolesc* or school*)
-
#122 OR #123
-
#120 AND #124
-
#121 OR #125
-
#126 IN NHSEED
Scoping search carried out in MEDLINE for economic decision models
As the original literature searches for the effectiveness analyses were conducted for RCTs only, we conducted an additional scoping search to ascertain if we were likely to have missed publications of model-based economic analyses. The following search strategy was implemented in MEDLINE. No additional citations were located, and a full search was not conducted. The scoping search of MEDLINE was 1946 to present, and the search was carried out on 17 June 2019.
Search strategy
-
decision model*.mp.
-
markov.mp.
-
Decision Trees/or decision tree*.mp.
-
economic model*.mp. or Models, Economic/
-
cohort model*.mp.
-
simulation model*.mp.
-
1 or 2 or 3 or 4 or 5 or 6
-
depression.mp. or Depression/
-
Anxiety/or anxiety.mp. or Anxiety Disorders/
-
conduct disorder.mp. or Conduct Disorder/
-
8 or 9 or 10
-
Child Psychiatry/or child*.mp. or Psychology, Child/or Child/
-
adolescent*.mp. or Adolescent Psychiatry/or Adolescent/
-
Young Adult/or young*.mp.
-
12 or 13 or 14
-
7 and 11 and 15
Characteristics of studies contributing to the economic evaluation
| Study | ||||||
|---|---|---|---|---|---|---|
| Mihalopoulos et al.260 2012 | Anderson et al.261 2014 | Foster250 2010 | Foster and Jones263,264 2006 and 2007 | Lee et al.259 2017 | Stallard et al.262 2015 | |
| Condition | Depression | Depression | Conduct disorder | Conduct disorder | Depression | Anxiety |
| Intervention type | Indicated | Universal | Indicated with a universal component | Indicated with a universal component | Universal and indicated | Universal |
| Intervention | ‘Representative’ intervention, CBT based | RAP (CBT) | Fast Track (multicomponent) | Fast Track (multicomponent) | ‘Hypothetical’ intervention (group psychological) | FRIENDS (CBT) |
| Comparator | No intervention | Usual PSHE | Usual provision | Usual provision | No intervention | Usual school provision |
| Setting (school) | Secondary | Secondary | Primary and secondary | Primary and secondary | Primary and secondary | Primary |
| Age range (years) | 11–17 | 12–16 | 6–16 | 6–17 | 11–17 | 9–10 |
| Type of economic analysis | CUA | CEA, CUA | CCA | CEA | CUA | CUA, CEA |
| Study type | Model | Trial | Trial | Trial | Model | Trial |
| Model type | Markov | N/A | N/A | N/A | Markov | N/A |
| Model time horizon | 5 years | N/A | N/A | N/A | 10 years | N/A |
| Follow-up period | N/A | 12 months | 12–14 years | 10 years | N/A | 6 months |
| Participants (n) | N/A | 3357 | 891 | 891 | N/A | 308 |
| Cost of intervention | AU$47M total | £41.96 per child | US$58,000 per child | US$58,283 per child | £55.92 per child for school led, £52.55 for health led | |
| Perspective | Health sector | NHS and social care | Payer for intervention, criminal justice, education | Third-party payer | Health and education sector | Health sector (NHS) and the education/social services sector |
| Location | Australia | UK | USA | USA | Australia | UK |
| Resources included | Intervention, cost ‘offsets’ defined as average annual cost of treating depression, parental time and travel | Inpatient stays, A&E attendances, outpatient visits, GP for any reason, GP for psychological problems, GP nurse, school nurse, counsellor, community mental health service, child psychologist, social worker, other professional | Outpatient visits, nights as an inpatient, number of admissions (for emotional/behavioural or any other reason), medication, repeating a grade, special education, arrests, court appearances, police contacts, detention centre stays, jail stays | Intervention only | Intervention, ‘cost offsets’ (health care) | Overnight hospital stays, A&E visits, outpatient appointments, GP for any reason, GP for worry/anxiety/happiness, GP nurse, school nurse, counsellor, child mental health service, child psychologist, social worker, other professional, medication |
| Unit of randomisation | N/A | Year group | School | School | N/A | School |
| Currency | Australian dollars | GBP | US dollars | US dollars | Australian dollars | GBP |
| Publication year | 2012 | 2014 | 2010 | 2006/7 | 2017 | 2015 |
| Trial registration | N/A | ISRCTN19083628 | NCT01653535 (follow-up) | NCT01653535 (follow-up) | N/A | ISRCTN23563048 |
| Outcomes | DALYs averted | SMFQ, QALYs | Range of antisocial behaviour measures | Conduct disorder diagnosis averted | DALY | QALYs |
| Source of outcomes | N/A | EQ-5D | Self-reported, parent reported, agency records | Diagnostic Interview Schedule of Children | N/A | CHU-9D |
| Discount rate (%) | 3 | N/A | N/A | 5 | 3 | N/A |
| Cost year | 2003 | 2014 | Not stated | 2004 | 2013 | 2013 |
| Source of resource use | Literature | CSRI | Parent-completed Service Assessment for Children and Adolescents, adolescent self-reported, review of agency records, Life Changes assessment | Study records | N/A | CSRI parent interview |
| Conclusions | After school screening, screening and the psychological intervention represent good value-for-money. Such an intervention needs to be seriously considered in any national package of preventive health services | . . . the universal provision of classroom-based CBT is unlikely to be either more effective or less costly than usual school provision | . . . the intervention lacked both the breadth and depth of effects on costly outcomes to demonstrate cost-effectiveness or even effectiveness | Results indicate the intervention is cost-effective for the children at highest risk | School-based psychological interventions appear to be cost-effective | . . . find limited evidence to support the universal provision of specific anxiety prevention programmes in UK primary schools. Although we found no evidence that the universal provision of the FRIENDS programme was cost-effective over a 6-month period, this conclusion needs to be treated with caution |
| Study | Number of sessions | Average session time (minutes) | Group size (n) | Parent sessions | Facilitator (number) | Manual | Training | Materials | Other costs |
|---|---|---|---|---|---|---|---|---|---|
| Calear et al.126 2016 | 6 | 35 | 30 | Teacher or specialist (1) | Yes | No training | Unclear | ||
| Calear et al.127 2016 | 6 | 35 | 30 | Teacher (1) | Yes | No training | Unclear | ||
| Hodas131 2016 | 10 | 50 | 4 | 2 Doctoral students/1 psychologist and 2 undergraduates (2) | No | Unclear | Worksheets | ||
| Rodgers and Dunsmuir140 2015 | 10 | 60 | 11 | Psychologist (1) | Yes | 1 day | Workbooks | ||
| Lowry-Webster et al.135 2001 | 10 | 75 | 30 | 3 (low turnout) | Teacher (1) | Yes | 1 day | Workbooks | 2 booster sessions |
| Wong et al.144 2014 | 6.5 | 40 | 30 | Teacher (1) | Yes | No training | Worksheets | ||
| Gillham et al.128 2006 | 8 | 90 | 11 | 6 × 90 minutes | Psychologist (2) | Yes | Developer, junior staff were trained (no details) | Unclear | |
| Lock and Barrett134 2003 | 12 | 75 | 30 | 3 (low turnout) | Psychologist (1) | Yes | 1 day | Workbooks | |
| Tomba et al.143 2010 | 6 | 120 | 20 | Psychologist (2) | Yes | Training on recruitment | Handouts | ||
| Horowitz et al.195 2007 | 8 | 90 | 11 | Psychologist and student (2) | Yes | Training workshops (no details) | Workbooks | ||
| Kindt et al.196 2014 | 16 | 50 | 25 | Teacher (1) | Yes | 4 days | Workbooks | Remote advice | |
| Pössel et al.198 2004 | 10 | 90 | 16 | Psychologist or postgraduates (2) | Yes | Participation | Unclear | ||
| Pössel et al.199 2011 | 10 | 90 | 27 | Psychologist or postgrads (2) | Yes | Participation, co-presenting | Unclear | ||
| Tak et al.207 2016 | 16 | 50 | 13 | Psychologist (1) | No | 5 days | Workbook | 2-hour booster | |
| Aune and Stiles119 2009 | 3 | 45 | 30 | 1 day, nurses; 60 minutes, parents; 90 minutes, carers | Teacher (1) | No | 90 minutes, teachers | Booklet, website, handouts | Newspaper advertisement |
| Barrett et al.121 2005 | 10 | 50 | 25 | 4 × 2-hour sessions (10 participants) | Psychologist (1) | Yes | Training (unspecified amount) | Workbook, booklet | 2 booster sessions |
| Barry et al.190 2017 | 4 | 40 | 13 | Unclear (0) | No | Unclear | |||
| Pössel et al.200 2013 | 10 | 90 | 8 | Psychologist and postgraduate (2) | Yes | Participation | |||
| Sawyer et al.204 2010 | 30 | 42 | 30 | Teacher (1) | Yes | 1 day | Workbook, poster, homework sheet, CD, DVD | ||
| Sheffield et al.141 2006 | 8 | 47 | 30 | Teacher (1) | Yes | 1 day (6 hours) | Workbook, notes, poster, handouts |
| Study | Number of sessions | Average session time (minutes) | Size of group (n) | Parent sessions | Facilitator (number) | Manual | Training | Materials | Other costs |
|---|---|---|---|---|---|---|---|---|---|
| Merry et al.197 2004 | 11 | 70 | 23 | NA | Teacher (1) | Yes | 2.5 days | Workbook | NA |
| Rivet-Duval et al.202 2011 | 11 | 60 | 10 | NA | Teacher (1) | Yes | 2 days (16 hours) plus 0.5-day booster | Unclear | NA |
| Rose et al.203 2014 | 20 | 45 | 9 | NA | Psychologist students (1) | Yes | 2 days (1 for each intervention) | Workbook | NA |
Cost data, assumptions and sources
| Cost type | Unit cost (2018) | Assumptions and sources |
|---|---|---|
| Average hourly rate for teachers in the UK |
|
Average salary342 for secondary school classroom teacher (2018) = £37,700 Average salary342 for primary school classroom teacher (2018) = £34,700 |
Employer National Insurance contribution343 @ 13.8% over £8424
|
||
Superannuation contribution = 16.4% (note that the rate rose to 23.6% in 2019, but is covered by a grant)344
|
||
|
||
| Workbook (per student) | £9 | Costs for the workbooks varied between approximately £4 and £12 |
| Manual (per teacher) | £25 | Costs for the intervention manuals varied between approximately £5 and £40 |
| Cost of training one teacher |
|
|
| Average number of students per school347 |
|
|
| Average class size347 |
|
Appendix 9 Comparison of findings with previous systematic reviews
| Study | Conditiona | Populationb | Settingc | Interventiond | Comparatore | Designf | Summary effectg | Meta-analysish | Adjusted cluster?i | Studies included in review (n) | Percentage of studies includedj | Summaryk |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wadell275 2007 | Anxiety, depression and conduct disorder | Universal and targeted | All | Psychological | Not clear | RCT | NAl | No | NAl | 6 | 83 | Results presented by specific programme and p-value |
| Horowitz and Garber285 2006 | Depression | Universal and targeted | Not clear | Not clear | Control | RCT | Hedges’ g | Not clear | Not clear | 30 | 43 | Overall mean effect was 0.16 |
| Neil and Christensen111 2007 | Anxiety and depression | Universal targeted and early intervention | School | Psychological, educational | Not clear | RCT | Cohen’s d | No | Not clear | 24 | 58 | The effect sizes for controlled trials varied from small (0.18) to moderate (0.83) |
| Neil and Christensen112 2009 | Anxiety | Universal targeted and early intervention | School | Psychological, educational, physical | Not clear | RCT | Cohen’s d | NAl | Not clear | 27 | 52 |
|
| Calear and Christensen109 2010 | Depression | Universal targeted and early intervention | School | Psychological, educational | Waiting list, no intervention, usual curriculum, attention control | RCT | Cohen’s d | NAl | Not clear | 42 | 71 | Out of 42 trials, 23 (55%) significantly reduced participants’ depressive symptoms at post test or follow-up, with effect sizes ranging from 0.21 to 1.40. The effect sizes of the 19 trials that did not obtain significant results ranged from –0.54 to 0.73 |
| Stice et al.113 2009 | Depression | Universal and targeted | All | Not clear | Attention control, no intervention, waiting list | RCT, quasi-RCT | r | Random effects | Not clear | 46 | 54 | r = 0.15 (z = 4.96; p < 0.001) |
| Fisak348 2011 | Anxiety | Universal and targeted | All | Psychological | Not clear | RCT, pre–postm | Hedges’ g | Fixed effects | Not clear | 31 | 65 | Anxiety: 0.18 (95% CI 0.13 to 0.23):
|
| Teubert276 2011 | Anxiety | Universal and targeted | Not clear | Not clear | Waiting list, attention control, placebo | RCT | Hedges’ g | Random effects | Not clear | 59 | 42 |
|
| Corrieri108 2014 | Anxiety and depression | Universal and targeted | School | Psychological | RCT (> 100) | Cohen’s d | Not clear | Not clear | 24 | 71 |
|
|
| Ahlen et al.349 2015 | Anxiety and depression | Universal | Not clear | Psychological, educational | Not clear | RCT | Hedges’ g | Random effects | Yes | 30 | 83 |
|
| Brunwasser350 2016 | Depression | Universal and targeted | Not clear | Psychological | No intervention, usual curriculum | RCT | Hedges’ g | Fixed effects | Not clear | 35 | 89 | A review of each specific programme: only pools within each programme for which there were three or more RCTs |
| Stockings et al.38 2016 | Anxiety and depression | Universal and targeted | All | Psychological, educational, physical | No intervention, usual curriculum, waiting list, attention control | RCT | Cohen’s d | Random effects | Not clear | 146 | 60 |
|
| Hetrick68 2016 | Depression | Universal and targeted | All | Psychological | Usual curriculum, no intervention, waiting list, attention control, other | RCT | SMD | Random effects | Yes | 83 | 73 |
|
| Lawrence et al.278 2017 | Anxiety | Targeted | All | Not clear | Waiting list, active | RCT | Hedges’ g | Random effects | Not clear | 16 | 63 |
|
| Waldron351 2018 | Anxiety | Universal | School | Psychological | Waiting list, no intervention, attention control | RCT | Hedges’ g | NAl | NAl | 8 | 100 | NAl |
| Werner-Seidler et al.36 2017 | Anxiety and depression | Universal and targeted | School | Psychological, educational | No intervention, usual curriculum, waiting list, attention control | RCT | Hedges’ g | Random effects | Not clear | 81 | 81 |
|
| Rasing et al.39 2017 | Anxiety and depression | Targeted | All | CBT | No intervention, usual curriculum, waiting list, attention control | RCT | Cohen’s d | Random effects | Not clear | 36 | 81 |
|
| Moreno-Peral et al.110 2017 | Anxiety | Universal and targeted | All | Psychological, educational | RCT | SMD | Random effects | Not clear | 9 | 77 | Anxiety: –0.29 (95% CI –0.47 to –0.10) | |
| Bernaras et al.277 2019 | Depression | Universal and targeted | School | Psychological | Not clear | RCT | NAl | NAl | NAl | 9 | 89 | NAl |
| Johnstone et al.37 2018 | Anxiety and depression | Universal | School | Psychological | Waiting list, usual curriculum, placebo | RCT | Hedges’ g | Random effects | Not clear | 14 | 100 |
|
| Comparison | Depression | Anxiety | ||||||
|---|---|---|---|---|---|---|---|---|
| Universal | Targeted | Universal | Targeted | |||||
| SMD | 95% CrI | SMD | 95% CrI | SMD | 95% CrI | SMD | 95% CrI | |
| CBT vs. controla | –0.08 | –0.16 to –0.01 | –0.25 | –0.43 to –0.08 | –0.07 | –0.13 to –0.03 | –0.19 | –0.34 to –0.05 |
| SDb | 0.17 | 0.12 to 0.23 | 0.38 | 0.28 to 0.54 | 0.06 | 0.01 to 0.14 | 0.29 | 0.18 to 0.43 |
| Psychological interventionc vs. control | –0.09 | –0.15 to –0.02 | –0.31 | –0.48 to –0.14 | –0.06 | –0.12 to –0.02 | NAd | |
| SDb | 0.17 | 0.12 to 0.23 | 0.39 | 0.28 to 0.55 | 0.06 | 0.00 to 0.15 | ||
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- ALPHA
- Advice Leading to Public Health Advancement
- BASC
- Behavior Assessment System for Children
- BASC-TRS
- Behavior Assessment System for Children – Teacher Rating Scale
- BEI
- British Education Index
- CAMHS
- Child and Adolescent Mental Health Services
- CBCL
- Child Behaviour Checklist
- CBM
- cognitive bias modification
- CBT
- cognitive–behavioural therapy
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CHU-9D
- Child Health Utility-9 Dimensions
- CI
- confidence interval
- CMD
- common mental disorder
- CrI
- credible interval
- CYP
- children and young people
- DALY
- disability-adjusted life-year
- DECIPHer
- Development and Evaluation of Complex Interventions for Public Health Improvement
- df
- degrees of freedom
- DIC
- deviance information criterion
- DSM
- Diagnostic and Statistical Manual of Mental Disorders
- ERIC
- Education Resources Information Center
- GP
- general practitioner
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HIC
- high-income country
- ICA
- intervention component analysis
- ICC
- intracluster correlation coefficient
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- ICER
- incremental cost-effectiveness ratio
- IPT
- interpersonal therapy
- IQR
- interquartile range
- LIC
- low-income country
- MECIR
- Methodological Expectations of Cochrane Intervention Reviews
- MesH
- medical subject heading
- MHP
- mental health professional
- MIC
- middle-income country
- NAM
- National Academy of Medicine
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NMA
- network meta-analysis
- ODD
- oppositional defiant disorder
- OR
- odds ratio
- PATHS
- Promoting Alternative THinking Strategies
- PhD
- Doctor of Philosophy
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSHE
- personal, social and health education
- QALY
- quality-adjusted life-year
- RAP
- Resourceful Adolescent Program
- RCADS
- Revised Children’s Anxiety and Depression Scale
- RCT
- randomised controlled trial
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SE
- standard error
- SES
- socioeconomic status
- SMD
- standardised mean difference
- SPARX
- smart, positive, active, realistic, X-factor thoughts
- TIDieR
- Template for Intervention Description and Replication
