Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as award number 15/192/13. The contractual start date was in November 2017. The draft manuscript began editorial review in November 2022 and was accepted for publication in May 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Gong et al. This work was produced by Gong et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Gong et al.
Chapter 1 Background
In areas affected by aircraft noise near major airports, relief periods of lower or absent aircraft noise are valued by residents. These periods may occur in relation to deliberate flight path changes to provide respite or because of changes due to weather variations, especially wind direction. However, it is unclear whether this respite might result in benefits to health endpoints. There is certainly good evidence that long-term exposure to aircraft noise can affect quality of life, cause annoyance and disturb sleep. 1 In recent years, evidence has accumulated which suggests that long-term exposure to transport noise may result in high blood pressure and may also impact cardiovascular health. A meta-analysis of 24 studies of road traffic noise2 published in 2012 and two meta-analyses each of five studies of aircraft noise3,4 published in 2009 and 2015 (comprising seven studies in total) found associations between long-term aircraft noise exposure and hypertension in adults. A meta-analysis from Vienneau et al. in 2015 included 10 studies on transport noise5 (3 of which included aircraft noise) and found associations between long-term noise exposure and ischaemic heart disease (IHD). Vienneau et al.’s updated meta-analysis of 13 studies (13 estimates for road traffic, 5 for aircraft and 3 for railway noise exposure) in 2019 found a 2%, 3% and 1% increase in relative risk of IHD per 10 dB increment in day–evening–night noise levels (Lden) for road, aircraft and railway noise exposure, respectively (although only risk for road traffic noise was statistically significant). 6 A meta-analysis conducted by some of the applicants and authors of this report, which included relevant studies from two meta-analyses6,7 and one literature review,8 as well as new studies published until February 2022, found a 3% and 2% increased risk for IHD incidence and mortality per 10 dB Lden for aircraft noise, respectively, but the risk for mortality was not statistically significant. 9 The applicants’ own BMJ study published in 201310 found that higher long-term average aircraft noise exposures in areas near London Heathrow airport were associated with higher average risks of hospital admission and mortality for heart disease and stroke.
The mechanisms for such effects may include impacts on the autonomic nervous system, either directly or indirectly via psychological annoyance that results in a stress reaction, and/or lack of restorative sleep, both of which will impact on cardiovascular health. 11 Although exposure to aircraft noise could induce adaptation in humans, there is evidence that adaptation to loud noise is typically incomplete,12 in part due to diminished coping resources, as aviation noise sources are typically outside the control of the individual. 13
Extremely few studies have examined the impact of short-term changes in transport noise on health. Recent experimental studies in humans have documented short-term rises in blood pressure and cardiovascular risk markers in the blood following aircraft noise exposure during sleep14 and a small panel study has shown changes in heart rate variability can be induced with daytime noise exposures (not specifically transport noise). 15,16 A case-crossover study of cardiovascular mortality in relation to road traffic noise in Madrid over a 3-year period,15,16 recently updated to 7 years of follow-up,17 found short-term (lag 0 and lag 1) increases in IHD and myocardial infarction mortality that were independent of air pollution exposures. This road noise study may not be directly applicable to aircraft noise, which is a qualitatively different type of sound. Also, aircraft noise may vary around airports due to changes in flight paths because of wind direction and operational conditions, which is not the case for roads, which have fixed geographical positions.
We are aware of only one previous study on short-term impacts of aircraft noise on cardiovascular outcomes. This is a case-crossover study by Saucy (2021) examining around 25,000 cardiovascular deaths near Zürich airport, Switzerland, taking data from the Swiss national cohort. Using the fact that the Swiss mortality records have precise time of death, the authors found that aircraft noise exposure levels in the 2 hours preceding death for night-time deaths were significantly associated with cardiovascular disease (CVD) mortality [odds ratio (OR) 1.44, 95% confidence interval (CI) 1.03 to 2.04] for the highest exposure group [equivalent continuous sound pressure level (LAeq) > 50 dB vs. < 20 dB)]. Aircraft noise was assigned to place of residence; one limitation of the study is that it was not clear whether this was also place of death.
To our knowledge, there is only one study that has examined short-term flight changes in aircraft noise on hospital admissions – the closure of Heathrow airport in 2010 for 6 days following eruption of Iceland’s Eyjafjallajökull volcano. 18 The authors used an interrupted time series design but were unable to detect changes in CVD hospital admissions in areas within the 55 dB(A) noise contour of Heathrow (0.7 million population) over this 6-day period. The authors comment that this may be related to lack of statistical power. To give confidence that analyses can actually detect what might be small increases in risk, such studies would need to include large numbers of people and detailed long-running information on daily aircraft noise levels. Daily variability in population noise exposure is not available from standard sources such as the Civil Aviation Authority (CAA), which is addressed in the proposed research.
Chapter 2 Objectives
The aim of this study was to evaluate the potential short-term impact of aircraft noise exposure on cardiovascular morbidity and mortality in a general population. This is one of the first studies to examine short-term associations of aircraft noise with cardiovascular outcomes and, additionally, to consider impacts of changes in noise levels. The results have potential inference for interventions that reduce aircraft noise levels reduce CVD outcomes in the short term.
This study used variability in night and daytime aircraft noise related to operational and weather-related (e.g. easterly/westerly wind) changes in flight paths in the area around London Heathrow airport, which is one of the top 10 busiest airports in the world, sited in close proximity to a densely population urban area. Our previous study10 found that around 3.6 million people live around London Heathrow airport, who are potentially affected by aircraft noise. There is intense policy interest in studies around London Heathrow, given the potential expansion and addition of a third runway currently under consideration. Given the number of local residents affected and high public interest within London in aircraft noise, Heathrow has one of the most stringent approaches to noise control of major world airports and has conducted a number of trials of flight paths to try to improve noise exposures of local residents. Results from this study should be transferable to other countries.
The specific research questions that we attempted to answer are:
-
Is there a significant short-term impact of aircraft noise on cardiovascular morbidity and mortality?
-
Are there interactions with factors such as age, gender, ethnicity and deprivation that may function as effect modifiers?
-
Is there variability in risk estimates between areas with consistent patterns of noise exposure compared with those with changing patterns of noise exposure?
-
How do risk estimates differ when using different noise metrics?
The objectives were:
-
To obtain daily estimates of day and night-time noise average exposure and the number of noisy events for 2011–15 for the population living around London Heathrow airport.
-
To link the noise estimates to cardiovascular hospital admission and mortality data via postcode of residence.
-
To conduct a case-crossover analysis relating daily changes in aircraft noise to CVD morbidity and mortality, accounting for relevant confounders that also change on a day-to-day basis, such as temperature and air pollution.
-
To identify relevant interactions for areas with consistent patterns of noise exposure versus those with changing patterns of noise exposure, and to further explore interactions with age, gender, ethnicity and deprivation.
Chapter 3 Methods – generating highly time–space resolved aircraft noise exposure data
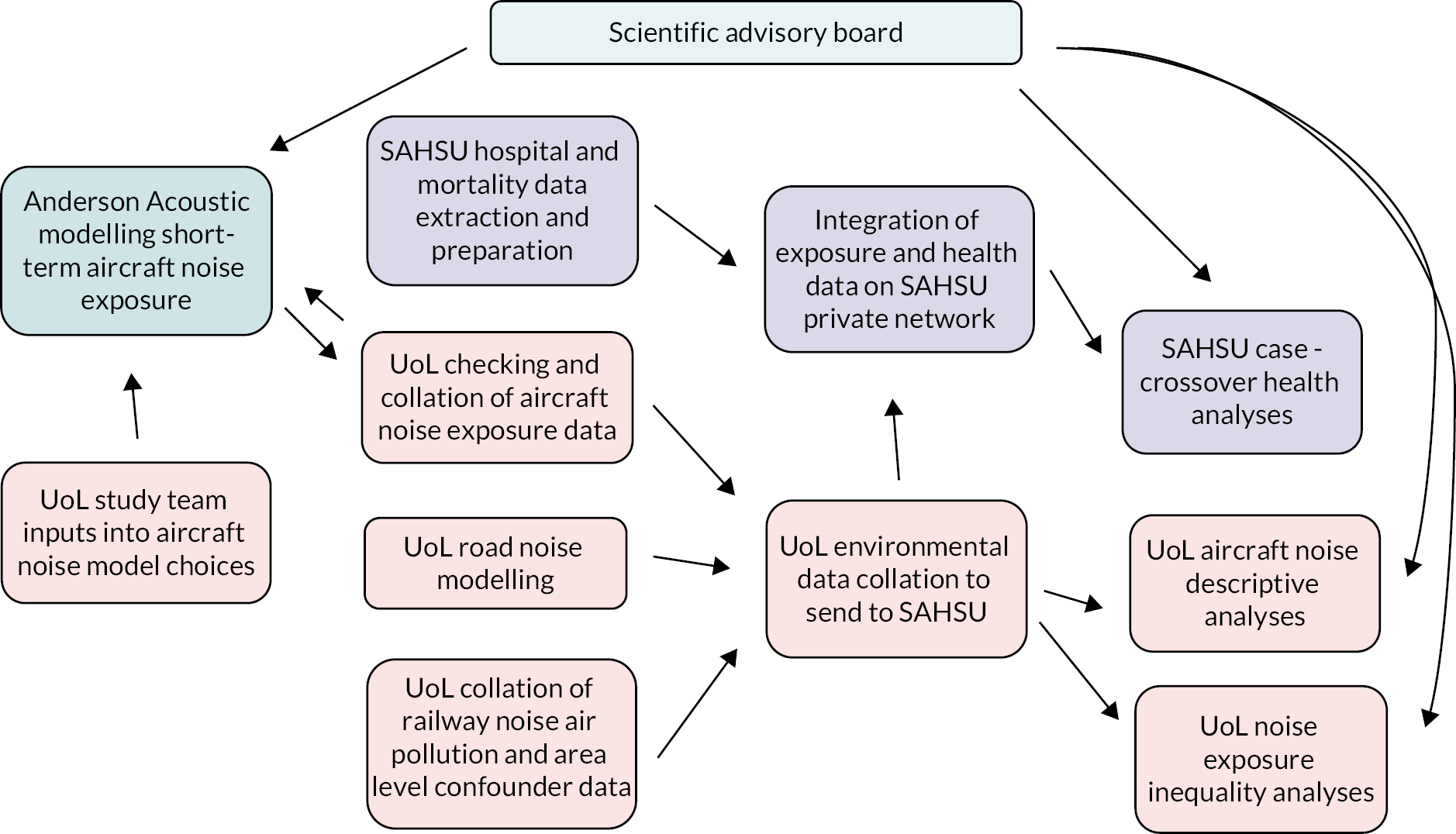
Figure 1 presents the details of the research pathway, indicating which institutions did which tasks.
FIGURE 1.
Research pathway diagram. Key: orange boxes – work conducted at University of Leicester (UoL); purple boxes – work conducted at Small Area Health Statistics Unit (SAHSU), Imperial College, London; cyan box – work conducted by noise consultancy.
We began by introducing the study area, population and period. The model and input data used to generate daily aircraft noise exposure data were then discussed.
Study area, unit and population
The study area’s centroid was at Heathrow airport, covering a bounding box with longitudes extending from −0.901° to −0.031° west, and latitudes from 51.345° to 15.609° north. It covered an approximate distance of 97 km east to west, and 47 km north to south. The study area was designed to capture the outer bounds of the CAA annual average aircraft noise contours in 2011 (Figure 2) that were available when the study was being designed and could be aligned with the population data from the UK 2011 Census (the UK Census takes place every 10 years).
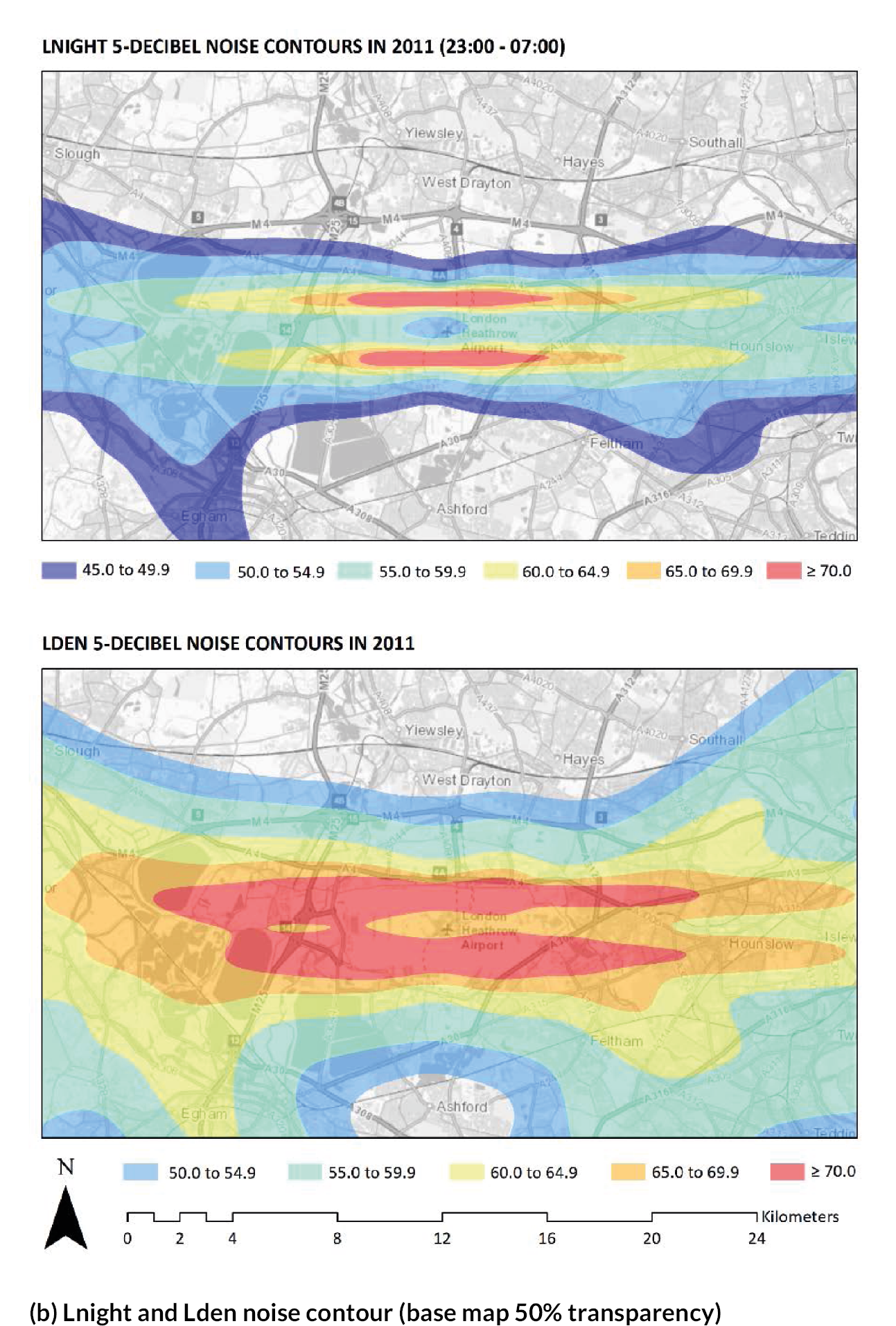
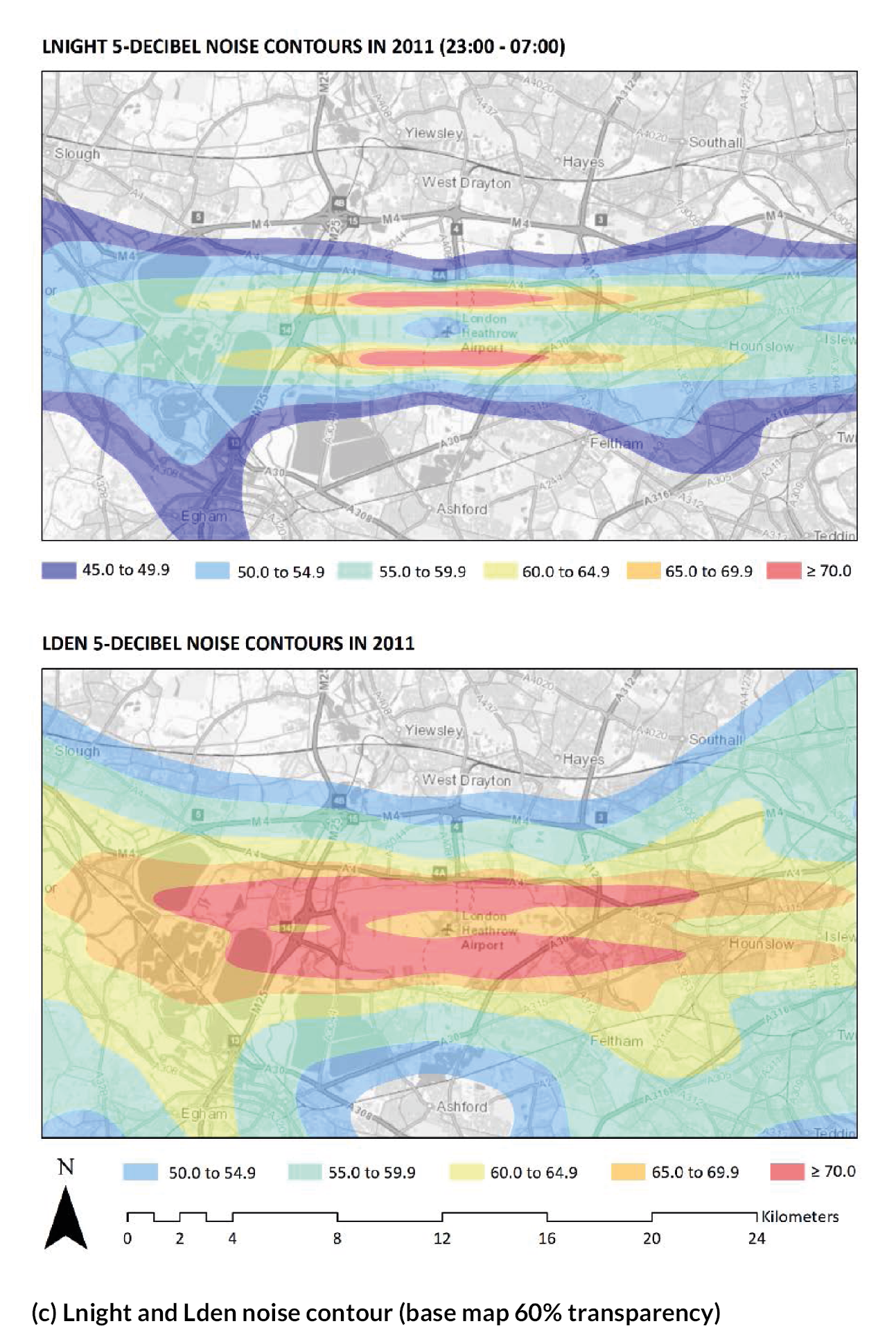
FIGURE 2.
The spatial extent of the Aviation Environmental Design Tool modelling exercise (black bounding box) in relation to the CAA annual average aircraft noise contours for 2011 for Lnight (top) and Lden (bottom). (a) Lnight and Lden noise contour. (b) Lnight and Lden noise contour (base map 50% transparency). (c) Lnight and Lden noise contour (base map 60% transparency). Note: (a) Full Lnight and Lden noise contour, (b) and (c) are the same contour maps but magnified while maintaining a background map with a 50% and 60% transparency level, respectively. (continued)
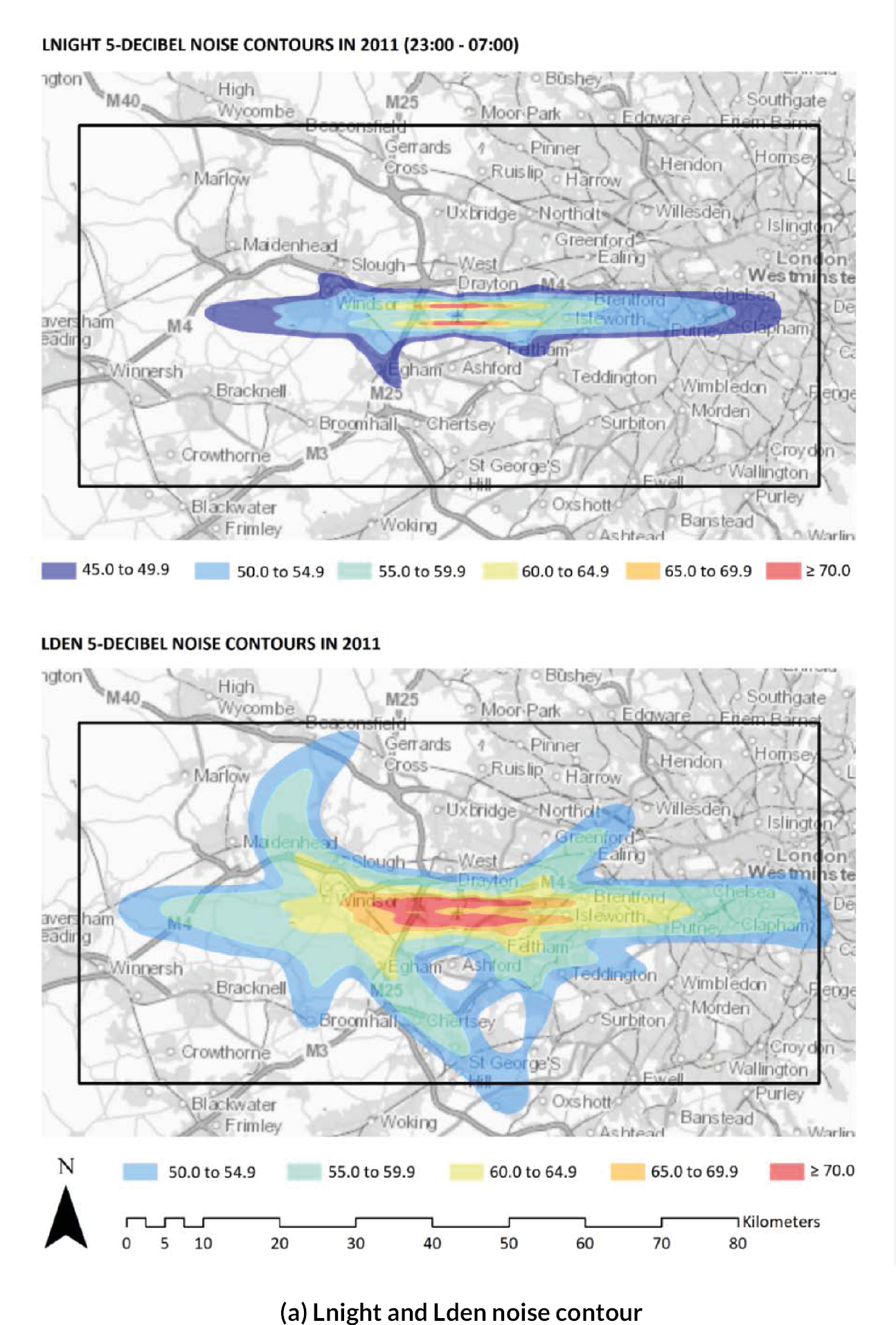
To reduce the computational demands of modelling, a grid resolution of 100 × 100 m was specified near to Heathrow, with a 200 × 200-m resolution then used to the extent of the study area. The inner grid, with a 100-m resolution, covered the area from Datchet to Osterley Park (approximately 25 km east to west) and West Drayton to Ashford (approximately 15 km north to south).
We used postcodes as the unit of analysis because they represented the smallest geographical area in the UK, allowing us to model noise levels with the highest possible spatial resolution (approximately 1.75 million live postcodes across the country in 201619). Postcodes are designed to support postal mail deliveries and small numbers of postcodes in the study area change every year, as new postcodes are created, and old postcodes become redundant from increases in and redistributions of the population over time. The total numbers of postcodes in each year are listed in Table 1.
| Year | Postcodes |
|---|---|
| 2014 | 156,324 |
| 2015 | 155,960 |
| 2016 | 155,558 |
| 2017 | 155,448 |
| 2018 | 155,671 |
Typically, each postcode within the study area consists of 53 residents [standard deviation (SD) 44)] and 22 occupied households (SD 17), based on headcount data from Nomis). 20 The combined population of this boundary box in 2011 was approximately 6.3 million.
Model
Version 3b of the Aviation Environmental Design Tool (AEDT), developed by the US Federal Aviation Administration, was used to assess aircraft noise levels at each of the postcodes within the study area. The AEDT was developed to model aircraft performance in space and time to estimate noise, fuel consumption, emissions and air quality consequences. 21 This tool is actively used by the US government for regulatory studies, research and domestic aviation system planning, as well as domestic and international aviation environmental policy analysis.
Local parameters
Operational procedures and fleet profiles for Heathrow were extracted from the AEDT database. This includes the geographical content for activity around the surface structures (i.e. runways, taxiways and terminals) and airspace (i.e. ground tracks, altitude controls, etc.). Fleet profiles are also provided by (the European Organisation for the Safety of Air Navigation) EUROCONTROL family and International Civil Aviation Organization engine performance.
Heathrow airport’s radar system provided records of flight activity, which included the position, height and speed of all aircraft for 2014–18. The headwind direction was determined by the actual direction of operation. The headwind speed was maintained at the AEDT default of 8 knots during the entire period of each operation. That is, wind direction changes such that it is always directed against aircraft course.
Wind measurements are often used to approximate the headwind direction and aircraft performance parameters such climb (therefore height) and speed; however, such information was comprehensively captured by the radar data system at Heathrow. Wind speed or direction is not used by the AEDT sound propagation calculations, which may be viewed as a limitation of current modelling practices.
Several meteorological parameters were included in the AEDT noise calculations:
-
We evaluated the dry air temperature data measured at Heathrow airport, to reduce the number of required models run. Fluctuations in average temperature were evaluated for 2014–18 by month and time of day (Tables 2–4). The hourly mean dry air temperature measurements were summarised into 32 groups, based on season (n = 4) and time of day (n = 8).
-
Annual mean temperatures are relatively stable for the period 2014–18, ranging from 1.6 to 12.4°C.
-
Seasonal variations in temperature exist. Mean winter months temperatures at Heathrow are 5.8–9.0°C (November–March) and mean summer month temperatures are 14.0–19.5°C (June–August). Summer month temperatures are generally more stable, with lower levels of relative dispersion around the mean. For each model run, the AEDT model used one of the 32 unique temperature values from the 5-year profiles shown in Table 4, which corresponds to the specified ‘day’ and ‘time of day’. In total, 1826 days across the 5 years of 2014–18 were considered, with each day comprising eight irregularly grouped periods (i.e. 14,608 flight-activity noise model surfaces were created).
-
| Time period | Count (N) | Mean (°C) | SD (°C) | CoV (%) | |
|---|---|---|---|---|---|
| All observations | 1 January 2014 to 31 December 2018 | 43,080 | 12 | 6 | 49.9 |
| Month | January | 3720 | 5.9 | 3.5 | 58.9 |
| February | 3378 | 5.8 | 3.5 | 59.1 | |
| March | 3716 | 7.9 | 3.7 | 46.6 | |
| April | 3095 | 10.5 | 3.8 | 36 | |
| May | 3715 | 14 | 4.1 | 29.4 | |
| June | 3600 | 17.3 | 4.1 | 23.6 | |
| July | 3710 | 19.5 | 4.2 | 21.4 | |
| August | 3715 | 17.9 | 3.8 | 21.2 | |
| September | 3542 | 15.6 | 3.7 | 24 | |
| October | 3718 | 12.6 | 3.4 | 26.7 | |
| November | 3451 | 9 | 3.6 | 40.4 | |
| December | 3720 | 7.7 | 3.9 | 51.3 | |
| Year | 2014 | 8752 | 12.4 | 5.5 | 44.5 |
| 2015 | 8256 | 11.9 | 5.4 | 45.5 | |
| 2016 | 8773 | 11.6 | 6.1 | 52.3 | |
| 2017 | 8758 | 12 | 6.1 | 50.6 | |
| 2018 | 8541 | 12.3 | 6.8 | 55.5 | |
| 00.00 | 01.00 | 02.00 | 03.00 | 04.00 | 05.00 | 06.00 | 07.00 | 08.00 | 09.00 | 10.00 | 11.00 | 12.00 | 13.00 | 14.00 | 15.00 | 16.00 | 17.00 | 18.00 | 19.00 | 20.00 | 21.00 | 22.00 | 23.00 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| January | 5.1 | 5 | 4.9 | 4.8 | 4.7 | 4.6 | 4.7 | 4.8 | 4.9 | 5.5 | 6.3 | 7 | 7.5 | 7.8 | 7.8 | 7.6 | 7 | 6.6 | 6.3 | 6.1 | 5.9 | 5.8 | 5.6 | 5.4 |
| February | 4.9 | 4.7 | 4.5 | 4.4 | 4.3 | 4.3 | 4.3 | 4.4 | 4.8 | 5.7 | 6.5 | 7.2 | 7.6 | 7.8 | 8 | 7.8 | 7.5 | 7 | 6.5 | 6.2 | 5.8 | 5.6 | 5.3 | 5.1 |
| March | 6.3 | 6 | 5.8 | 5.6 | 5.5 | 5.4 | 5.4 | 5.9 | 6.8 | 7.9 | 8.8 | 9.7 | 10.4 | 10.7 | 11 | 10.9 | 10.5 | 9.9 | 9.1 | 8.5 | 8 | 7.5 | 7.1 | 6.7 |
| April | 8.3 | 7.9 | 7.6 | 7.4 | 7.2 | 7.2 | 7.7 | 8.8 | 10 | 11.2 | 12.1 | 12.9 | 13.4 | 13.8 | 14 | 13.9 | 13.6 | 13.1 | 12.3 | 11.4 | 10.7 | 10 | 9.3 | 8.7 |
| May | 11.3 | 10.9 | 10.6 | 10.3 | 10.2 | 10.5 | 11.5 | 12.7 | 13.8 | 14.9 | 15.8 | 16.5 | 17.1 | 17.4 | 17.6 | 17.5 | 17.3 | 16.8 | 16.1 | 15.1 | 14.2 | 13.4 | 12.6 | 12 |
| June | 14.5 | 14 | 13.6 | 13.3 | 13.2 | 13.7 | 14.6 | 15.7 | 16.9 | 17.9 | 18.9 | 19.7 | 20.4 | 20.9 | 21.2 | 21.2 | 20.9 | 20.5 | 19.8 | 18.8 | 17.7 | 16.8 | 15.9 | 15.1 |
| July | 16.9 | 16.3 | 15.9 | 15.5 | 15.4 | 15.7 | 16.7 | 17.8 | 19 | 20.2 | 21.2 | 22 | 22.6 | 23.1 | 23.4 | 23.4 | 23.1 | 22.7 | 22.1 | 21.2 | 20.1 | 19.1 | 18.2 | 17.5 |
| August | 15.6 | 15.2 | 14.8 | 14.6 | 14.3 | 14.4 | 15.2 | 16.3 | 17.5 | 18.7 | 19.7 | 20.4 | 20.9 | 21.3 | 21.5 | 21.5 | 21.2 | 20.7 | 19.9 | 18.8 | 18 | 17.3 | 16.6 | 16 |
| September | 13.4 | 13.1 | 12.8 | 12.6 | 12.4 | 12.4 | 12.8 | 13.6 | 14.9 | 16.3 | 17.4 | 18.2 | 18.8 | 19.2 | 19.3 | 19.1 | 18.7 | 18 | 17 | 16.2 | 15.5 | 14.9 | 14.3 | 13.8 |
| October | 11.1 | 10.8 | 10.7 | 10.6 | 10.6 | 10.6 | 10.7 | 11.1 | 11.9 | 13 | 13.9 | 14.7 | 15.3 | 15.5 | 15.6 | 15.3 | 14.7 | 13.9 | 13.3 | 12.8 | 12.5 | 12.1 | 11.7 | 11.3 |
| November | 8 | 7.9 | 7.7 | 7.6 | 7.5 | 7.6 | 7.7 | 7.8 | 8.2 | 9 | 9.8 | 10.4 | 10.9 | 11.1 | 11.1 | 10.7 | 10.2 | 9.8 | 9.5 | 9.2 | 8.9 | 8.7 | 8.4 | 8.1 |
| December | 6.9 | 6.7 | 6.6 | 6.6 | 6.6 | 6.7 | 6.7 | 6.8 | 6.9 | 7.4 | 8.1 | 8.7 | 9.2 | 9.4 | 9.4 | 9.1 | 8.6 | 8.3 | 8 | 7.9 | 7.7 | 7.6 | 7.4 | 7.2 |
| Group | Months | 07.00–15.00 | 15.00–19.00 | 19.00–22.00 | 22.00–23.00 | 23.00–24.00 | 24.00–04.30 | 04.30–06.00 | 06.00–07.00 |
|---|---|---|---|---|---|---|---|---|---|
| Winter | November to March | 8.0 | 8.5 | 7.3 | 6.8 | 6.5 | 5.9 | 5.7 | 5.8 |
| Winter transition | April and October | 13.0 | 13.8 | 11.6 | 10.5 | 10.0 | 9.2 | 8.9 | 9.2 |
| Summer transition | May and September | 16.5 | 17.6 | 14.9 | 13.5 | 12.9 | 11.7 | 11.4 | 12.2 |
| Summer | June to August | 19.9 | 21.4 | 18.6 | 16.9 | 16.2 | 14.8 | 14.5 | 15.5 |
The Ordnance Survey digital terrain model of Great Britain, which has a 50-m horizontal resolution, was passed into the AEDT model to create terrain features. It is an open-height dataset of contours with spot heights, break lines, coastline, lakes, ridges and form lines cross Great Britain with a typical accuracy level greater than 2 m root mean square deviation. With terrain elevation processing, it is possible to adjust sound propagation from the attenuation due to line of sight blockage. It is based on the difference in propagation path length between the direct path and propagation path over the top of terrain features, known as path length difference. The terrain model used only accounts for the elevation of natural landscapes and not manmade features (i.e. buildings).
Model output
A comprehensive set of average ‘A’ frequency weighted noise estimates were provided for eight time bands (see Table 3) over the course of each day (LAeq) for the study period of 1 January 2014 to 31 December 2018. These periods were chosen in discussion with the study advisory board, including industry representatives, to capture conventional periods (i.e. 07.00–19.00 hours – day, 19.00–23.00 hours – evening, 23.00–07.00 hours – night), together with timings that are aligned with Heathrow operations (e.g. 23.30–04.30 hours scheduled night flight ban, 07.00–15.00 hours and 15.00–22.00 hours respite periods). The ‘A’ weighting is the standard weighting of the audible frequencies designed to reflect the response of the human ear to noise (between 500 Hz and 6 kHz).
We used daily noise levels during eight period bands, as mentioned above, to further calculate daily mean aircraft noise levels in four metrics: Lday (07.00–19.00 hours), Leve (19.00–23.00 hours), Lnight (23.00–07.00 hours) and LAeq24 (24-hour average).
In addition, the daily number of flight events exceeding a maximum sound level of 65 A-weighted decibels [dB(A)] in the daytime and 60 dB(A) at night, were estimated at each modelled location (N-Above) from 1 January 2018 to 31 December 2018. For further context, if any of the one-eighth-second periods from an aircraft noise event (generated by a single aircraft operation) exceeds the specified threshold, then that event is counted as one. The N-Above measure cannot exceed the number of operations that occur in the specified period. These event counts are based on the maximum sound level with ‘A’ frequency weighting and fast time weighting.
Limitations identified in the Aviation Environmental Design Tool model
We identified several limitations in the use of the AEDT model, particularly as we extended its use to look at short periods within a single day (it is usually used to provide long-term average noise exposures).
-
Atmospheric pressure, relative humidity and wind speed are set as meteorological constants that reflect the 30-year average at the airport. These simplifications are a limit of current modelling practices, when estimating sub-annual average aircraft noise exposures.
-
The headwind speed is maintained at 8 knots during the entire period of each operation. This may result in inaccurate aircraft performance parameters, such as climb and speed, which are related to the location and intensity of noise.
-
Wind speed or direction is not used by the AEDT sound propagation calculations (i.e. a uniform dispersion in all directions is assumed at all times).
-
The terrain model only accounts for elevation of natural landscapes and not manmade features. Therefore, containment and sheltering effects in urban locations are ignored.
-
The computational demands for creating sub-daily exposure surfaces:
-
Limited the spatial resolution of the model outputs, returning a coarser exposure gradient, although we think that this still gave good exposure contrast for our epidemiological study.
-
Dryer air temperatures were summarised into profiles that accounted for season and time of day across the 5-year study period. Therefore, the influence of unusual temperature events on sound propagation is not accounted for.
-
These factors are likely to lead to exposure misclassification bias. However, annual average aircraft noise surfaces are currently only routinely modelled by the CAA. This study has used several approaches to develop and enhance the existing approach to create sub-annual exposure surfaces:
-
Radar tracks of individual flights were provided by Heathrow airport, with a unique set of aircraft footprints constructed for each modelled period.
-
The created AEDT surfaces cover 1826 days across the 5 years of 2014–18 (i.e. 14,608 flight activity-informed noise surfaces were created vs. 5 annual average surfaces for each noise metric).
-
Actual flight paths were used rather than these being estimated by operational movements being estimated by headwind direction and performance parameters.
-
-
Unique temperature profiles were used, which correspond to the specified ‘season’ and ‘time of day’. Annual average AEDT models only use long-term averages.
We also had a very large dataset to work with, which may offset some of the lack of precision as a result of random bias.
Methods and results: descriptive analysis of daily aircraft noise data
We first examined the descriptive summary of the noise data. The study area annually had between 155,448 and 156,324 postcodes for the period 2014–18. We calculated log-10 logarithmic means, SDs and the 90th percentile for noise levels during the eight time bands (04.30–06.00, 06.00–07.00, 07.00–15.00, 15.00–19.00, 19.00–22.00, 22.00–23.00, 23.00–24.00, 24.00–04.30 hours), as well as four metrics, including LAeq24, Lday (07.00–19.00), Leve (19.00–23.00) and Lnight (23.00–07.00). These statistics were then anti-log transformed and are presented in Table 5. We also presented arithmetic means, SDs and the 90th percentile of number of flight events per time band in the same table.
| Noise metrics | N | Mean | SD | Min | Max | P90 |
|---|---|---|---|---|---|---|
| LAeq 04.30–06.00 hours | 283,706,122 | 43.75 | 53.22 | 0 | 77.69 | 44.72 |
| LAeq 06.00–07.00 hours | 284,476,323 | 50.92 | 58.44 | 7.04 | 80.33 | 52.93 |
| LAeq 07.00–15.00 hours | 284,476,323 | 49.87 | 58.06 | 22.96 | 78.83 | 51.5 |
| LAeq 15.00–19.00 hours | 284,165,204 | 49.44 | 57.67 | 19.84 | 78.9 | 51.09 |
| LAeq 19.00–22.00 hours | 271,590,174 | 49.12 | 57.3 | 17.04 | 78.84 | 50.95 |
| LAeq 22.00–23.00 hours | 284,476,323 | 47.48 | 56.69 | 9.19 | 81.07 | 49.24 |
| LAeq 23.00–24.00 hours | 279,444,325 | 41.06 | 51.54 | 0 | 79.52 | 42.15 |
| LAeq 24.00–04.30 hours | 87,705,638 | 29.81 | 42.3 | 0 | 76.34 | 30.04 |
| Lday | 284,165,204 | 49.73 | 57.17 | 22.79 | 78.29 | 51.76 |
| Leve | 271,590,174 | 48.8 | 56.97 | 16.33 | 78.86 | 51.2 |
| Lnight | 86,618,974 | 44.19 | 51.39 | 4.23 | 74.13 | 46.49 |
| LAeq24 | 83,220,954 | 48.92 | 55.98 | 22.87 | 76.88 | 50.72 |
| N60 04.30–06.00 hours | 56,819,915 | 1 | 2.62 | 0 | 33 | 1 |
| N60 06.00–07.00 hours | 56,819,915 | 3 | 7.39 | 0 | 58 | 9 |
| N65 07.00–15.00 hours | 56,664,244 | 8 | 32.91 | 0 | 388 | 10 |
| N65 15.00–19.00 hours | 56,819,915 | 4 | 16.47 | 0 | 199 | 5 |
| N65 19.00–22.00 hours | 56,819,915 | 3 | 11.87 | 0 | 146 | 3 |
| N65 22.00–23.00 hours | 56,819,915 | 1 | 2.83 | 0 | 47 | 1 |
| N60 23.00–24.00 hours | 56,352,902 | 0 | 1.34 | 0 | 43 | 1 |
| N60 24.00–04.30 hours | 21,171,256 | 0 | 0.67 | 0 | 23 | 1 |
The number of noise observations per period varied throughout the day, with missing values due to the absence of air traffic above the corresponding postcodes. Four periods (06.00–07.00 hours, 07.00–15.00 hours, 15.00–19.00 hours and 22.00–22.00 hours) of the eight specified periods in this study had full numbers of observations (N = 284,476,323). Early morning (04.30–06.00 hours: N = 283,706,122) and night between 19.00 and 24.00 hours (19.00–23.00 hours: N = 271,590,174; 23.00–24.00 hours: N = 279,444,325) had slightly fewer number of observations, whereas night quota period (24.00–04.30 hours) had less than 31% of the total number of observations (N = 87,705,638). For standard noise metrics, Lday and Leve had 284,165,204 and 271,590,174 observations, respectively, which is close to the total number of postcodes. Comparatively, Lnight and LAeq24 had 86,618,974 and 83,220,954 observations, respectively, or approximately 29–30% of total number of postcodes.
The use of multiple periods throughout the day allowed us to explore which periods were the quietest and noisiest, looking at descriptive statistics for postcodes with values assigned (see Table 5). The morning shoulder period (06.00–07.00 hours) was the noisiest, with the highest mean (50.92 dB) and 90th percentile (52.93 dB) noise levels. Daytime (07.00–15.00 hours) aircraft noise levels had a mean noise level of 49.87 dB and the 90th percentile was 51.50 dB, the second highest of all periods. As the noise levels in each postcode in the study area exceeded 22.96 dB, aircraft noise affects nearly every postcode in the area. The quietest periods on average were night shoulder and night quota periods – the mean noise levels across postcodes during 23.00–24.00 hours and 24.00–04.30 hours were 41.06 and 29.81 dB, respectively. The 90th percentiles were 42.15 and 30.04 between 23.00 and 24.00 hours and 24.00 and 04.00 hours. The descriptive summary of noise levels by season is presented in Appendix 1.
The average Lday, Leve, Lnight and LAeq24 levels were 49.73, 48.80, 44.19 and 48.95 dB, respectively. Their 90th percentiles were 51.76, 51.20, 44.19 and 50.57 dB.
For noisy flight event numbers (N65: number of flights > 65 dB day; N60: number of flights > 60 dB night), the means, minima, maxima and 90th percentiles were rounded to the nearest integer to aid the interpretation of the results. The highest number of events occurred during 07.00–15.00 hours (see Table 5), with an average of 8 noisy flight events and with the top 10% of postcodes experiencing 10 events. Morning shoulder (06.00–07.00 hours) had the second highest 90th percentile, with a value of nine noisy flights, but the third highest mean, with a value of 3. During the night quota period (04.30–06.00 hours), the average number of flight events per postcode was one. Comparatively, 23.00–24.00 hours and 24.00–04.30 hours had an average of zero events.
For health analysis purposes, negative noise values as produced by models were ignored.
Correlations
In Table 6, we present the pairwise Pearson correlation coefficients (r) between daily aircraft noise levels at eight specified time bands and standard four noise metrics (LAeq24, Lday, Lnight and Leve), and the daily number of flight events at eight time bands.
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | (15) | (16) | (17) | (18) | (19) | (20) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) LAeq 04.30–06.00 hours | 1.000 | |||||||||||||||||||
| (2) LAeq 06.00–07.00 hours | 0.680 | 1.000 | ||||||||||||||||||
| (3) LAeq 07.00–15.00 hours | 0.425 | 0.725 | 1.000 | |||||||||||||||||
| (4) LAeq 15.00–19.00 hours | 0.343 | 0.632 | 0.845 | 1.000 | ||||||||||||||||
| (5) LAeq 19.00–22.00 hours | 0.309 | 0.574 | 0.764 | 0.868 | 1.000 | |||||||||||||||
| (6) LAeq 22.00–23.00 hours | 0.090 | 0.299 | 0.520 | 0.562 | 0.664 | 1.000 | ||||||||||||||
| (7) LAeq 23.00–24.00 hours | –0.062 | 0.109 | 0.269 | 0.279 | 0.353 | 0.600 | 1.000 | |||||||||||||
| (8) LAeq 24.00–04.30 hours | 0.075 | 0.157 | 0.276 | 0.262 | 0.283 | 0.373 | 0.357 | 1.000 | ||||||||||||
| (9) Lday | 0.415 | 0.723 | 0.974 | 0.928 | 0.831 | 0.555 | 0.286 | 0.284 | 1.000 | |||||||||||
| (10) Leve | 0.275 | 0.546 | 0.755 | 0.855 | 0.977 | 0.771 | 0.417 | 0.315 | 0.820 | 1.000 | ||||||||||
| (11) LAeq24 | 0.445 | 0.744 | 0.950 | 0.924 | 0.901 | 0.665 | 0.366 | 0.306 | 0.980 | 0.901 | 1.000 | |||||||||
| (12) Lnight | 0.682 | 0.912 | 0.769 | 0.698 | 0.682 | 0.495 | 0.310 | 0.289 | 0.778 | 0.680 | 0.818 | 1.000 | ||||||||
| (13) N60 04.30–06.00 hours | 0.296 | 0.440 | 0.421 | 0.377 | 0.385 | 0.229 | 0.066 | 0.114 | 0.431 | 0.369 | 0.465 | 0.497 | 1.000 | |||||||
| (14) N60 06.00–07.00 hours | 0.339 | 0.620 | 0.596 | 0.519 | 0.513 | 0.309 | 0.113 | 0.163 | 0.601 | 0.496 | 0.631 | 0.661 | 0.733 | 1.000 | ||||||
| (15) N65 07.00–15.00 hours | 0.190 | 0.344 | 0.519 | 0.390 | 0.370 | 0.328 | 0.206 | 0.209 | 0.503 | 0.393 | 0.500 | 0.413 | 0.331 | 0.497 | 1.000 | |||||
| (16) N65 15.00–1900 hours | 0.176 | 0.308 | 0.390 | 0.484 | 0.400 | 0.410 | 0.229 | 0.201 | 0.449 | 0.433 | 0.477 | 0.394 | 0.293 | 0.400 | 0.433 | 1.000 | ||||
| (17) N65 19.00–22.00 hours | 0.169 | 0.295 | 0.373 | 0.462 | 0.403 | 0.431 | 0.243 | 0.211 | 0.430 | 0.445 | 0.465 | 0.385 | 0.273 | 0.378 | 0.410 | 0.959 | 1.000 | |||
| (18) N65 22.00–23.00 hours | 0.124 | 0.233 | 0.379 | 0.400 | 0.336 | 0.452 | 0.283 | 0.225 | 0.407 | 0.410 | 0.423 | 0.325 | 0.139 | 0.242 | 0.448 | 0.708 | 0.737 | 1.000 | ||
| (19) N60 23.00–24.00 hours | 0.096 | 0.185 | 0.333 | 0.335 | 0.304 | 0.394 | 0.374 | 0.236 | 0.348 | 0.349 | 0.384 | 0.323 | 0.130 | 0.219 | 0.333 | 0.372 | 0.385 | 0.550 | 1.000 | |
| (20) N60 24.00–04.30 hours | 0.117 | 0.161 | 0.238 | 0.238 | 0.204 | 0.281 | 0.239 | 0.317 | 0.250 | 0.244 | 0.256 | 0.239 | 0.088 | 0.147 | 0.264 | 0.295 | 0.306 | 0.318 | 0.335 | 1.000 |
We found high to very high correlations (coefficient 0.68–0.90) between each pair of the four standard noise metrics (Lday, Lnight, Leve and LAeq24).
In comparison, daily aircraft noise during early morning (04.30–06.00 hours) and late night (24.00–04.30 hours), had a much weaker correlation (coefficient < 0.4) with noise levels during any other time bands. There were moderate to high correlations (coefficient 0.52–0.87) between each pair of daily aircraft noise levels during the day (07.00–15.00 hours), the afternoon (15.00–19.00 hours) and the early evening (19.00–22.00 and 22.00–23.00 hours).
There were weak to moderate correlations (coefficient 0.07–0.48) between the number of flight events and the actual noise levels during the eight time bands, with the exception of N60 06.00–07.00 hours, which had a moderate correlation with noise levels during 06.00–07.00, 07.00–15.00, 15.00–19.00 and 19.00–22.00 hours. Moreover, there were relatively weak correlations between each pair of noisy flight events except for N60 06.00–07.00 hours and N60 04.30–06.00 hours (coefficient 0.73), N65 19.00–22.00 hours and N65 15.00–19.00 hours (coefficient 0.96), N65 22.00–23.00 hours and N65 15.00–19.00 hours (coefficient 0.71), N65 22.00–23.00 hours and N65 22.00–23.00 hours (coefficient 0.55). This may show that the distribution of noisy flight events may differ from that of daily noise levels in dB.
The lower correlations of non-standard and noisy event metrics with the standard noise metrics of Lday, Lnight, Leve and LAeq24 (compared with high correlations between the standard metrics) raises the possibility that standard metrics may miss important characteristics of noise exposure, with potential relevance for impacts on biological systems.
Methods and results: approaches to identifying respite and/or relief period
An important question that we sought to answer was whether there was variability in cardiovascular health risk estimates between areas with consistent noise exposure patterns and those with changing noise exposure patterns. Changing noise exposure can be either a relief, defined as a break from or a reduction in aircraft noise, or respite, defined as a scheduled relief from aircraft noise for a period of time. 22 While the minimum noticeable difference in sound level for humans is often regarded as 3 dB, one report suggests that a relief period should provide at least 5–6 dB reduction for people to notice a difference in sound level, and 7–8 dB to provide a significant break from aircraft noise. 23
We considered three ways to identify these reliefs and/or respite periods:
-
Using areas affected by documented flight changes, especially those designed to provide respite.
-
Defining an arbitrary high and low noise level and number of days experienced for each of these:
-
For morning periods;
-
For afternoon periods;
-
Comparing morning and afternoon periods on the same day.
-
-
Statistically, using CoV of noise for each postcode.
Previous studies on relief/respite
We identified one study by Beghelli et al. that examined the effect of respite on medical costs. 24 This study used a natural experiment of the Early Morning Arrival Trial, which was implemented from 5 November 2012 to 31 March 2013 to provide noise respite to certain communities living near Heathrow airport. The trial identified four exclusion zones (two to the east and two to the west of Heathrow). This trial designated four exclusion zones (two to the east and two to the west of Heathrow). During the trial, each week, night and early morning (23.30–06.00 hours) aircraft movement was rerouted from one set of air traffic exclusion zones to non-exclusion areas. This reroute alternated weekly between two sets of air traffic exclusion zones. Beghelli et al. showed that the trial was associated with a 5.8% decrease in spending on central nervous system treatment, which included the treatment of sleep loss, concentration deficits and other stress-related illnesses in quiet set of zones, compared with control zones, which saw no change in flight movement during the period. 24 However, there was a non-statistically significant increase in medication for CVD during the trial. 24
We did not have information on flight trials to include in our study. However, the trial exclusion zones considered in Beghelli et al. were relatively small, with each zone measuring only 1 nautical mile (1.15 miles) in width25 (our study area was 97 × 47 km) and the period was relatively short (5 months – we had 5 years of data). Linking these trial areas is likely to provide an insufficient sample size for health analyses, especially when using binary outcomes indicating more severe disease (hospital admissions and mortality data).
A priori identification of aircraft noise variability based on respite criteria
Using our daily aircraft noise data, we experimented with using arbitrarily defined cut-off noise levels and numbers of days affected to define areas with detectable noise level changes compared with control areas with much more constant levels of noise, with the aim of seeing whether we could identify sufficient postcodes for health analyses.
We attempted to establish criteria for selecting postcodes (relief group) that were exposed to loud aircraft noise on a significant number of days per year but also had a significant number of relatively quiet days. The difference between loud and quiet noise levels was chosen to be 5 dB in order for people to be able to detect the change in sound level according to a previous report on respite and relief periods. 23 We then modified the selection criteria to identify two control groups of postcodes with varying numbers of days exposed to loud aircraft noise. The number of postcodes belonging to each group and their average noise levels were computed and presented in Tables 7–9.
Since our data split a day into eight time bands, we first focused on the morning shoulder period (06.00–07.00 hours), which was typically the noisiest period of the day, as shown in the preceding section. We arbitrarily identified a relief group that consisted of postcodes with over 100 days of exposure to noise levels above 55 dB and 100 days of exposure to noise levels below 50 dB per year. We chose 55 and 50 dB as our thresholds because a difference of at least 5 dB in sound level is required for people to consciously notice it and also because these are moderate levels of noise at or above mean levels for each time period (Table 7). The first control group consisted of postcodes that were exposed to aircraft noise during morning shoulder period for at least 100 days below 50 dB but between 100 and 200 days above 55 dB during the same period. The second control group includes postcodes that have at least 200 days that were exposed to above 55 dB during morning shoulder period. Table 7 displays the number of postcodes in each group per year, together with their average decibel levels. Between 23,439 and 25,679 postcodes meet the relief group criteria. However, these numbers represent only about 17% of the total number of postcodes. There were between 2084 and 5065 and 18,374 and 22,235 postcodes that met the criteria for control groups I and II. These numbers nevertheless remain small.
| Difference in dB | Year | Relief area criteria | Postcodes (n) | Mean noise levels (dB) | Control area I criteria | Postcodes (n) | Mean noise levels (dB) | Control area II criteria | Postcodes (n) | Mean noise levels (dB) |
|---|---|---|---|---|---|---|---|---|---|---|
| Panel 1: 5 dB difference |
2014 | 100+ days > 55 dB AND 100+ < 50 dB days in a year | 23,439 | 51.27 | 100–200 days > 55 dB AND 100+ days ≤ 50 dB | 5065 | 48.17 | 200+ days > 55 dB | 18,374 | 52.74 |
| 2015 | 24,346 | 52.12 | 3783 | 48.94 | 20,563 | 53.09 | ||||
| 2016 | 25,264 | 51.65 | 3997 | 50.32 | 21,267 | 52.49 | ||||
| 2017 | 24,103 | 54.06 | 2084 | 48.74 | 22,019 | 54.64 | ||||
| 2018 | 25,679 | 51.9 | 3444 | 48.17 | 22,235 | 52.68 | ||||
| Panel 2: 5 dB difference |
2014 | 50+ days > 55 dB AND 50+ days | 25,142 | 50.81 | 100–200 days > 55 dB AND 100+ days ≤ 50 dB | 5065 | 48.9 | 100+ days > 55 dB | 23,439 | 51.27 |
| 2015 | 26,047 | 51.72 | 3783 | 48.94 | 24,346 | 52.12 | ||||
| 2016 | 26,857 | 51.21 | 3997 | 50.32 | 25,264 | 51.65 | ||||
| 2017 | 26,722 | 53.35 | 2084 | 48.74 | 24,103 | 54.06 | ||||
| 2018 | 27,287 | 51.46 | 3444 | 49.82 | 25,679 | 51.9 | ||||
| Panel 2: 7 dB difference |
2014 | 100+ days > 57 dB AND 100+ days | 23,439 | 53.01 | 100–200 days > 57 dB AND 100+ days ≤ 50 dB | 3783 | 50.39 | 200+ days > 57 dB | 18,374 | 54.49 |
| 2015 | 24,346 | 53.82 | 3997 | 50.27 | 20,563 | 55.13 | ||||
| 2016 | 25,264 | 53.33 | 2084 | 52.29 | 21,267 | 54.6 | ||||
| 2017 | 24,103 | 55.89 | 3444 | 50.36 | 22,019 | 56.59 | ||||
| 2018 | 25,679 | 53.52 | 5065 | 48.90 | 22,235 | 54.5 |
W experimented with various noise thresholds and days to identify postcodes with significant variations in aircraft noise levels. In panel 2 of Table 7, instead of 100 days as the relief group identification criterion, we used 50 days. Similarly, we used 100 days as the cut-off for control group II, as opposed to 200 days. In panel 3 of the same table, we adopted a 7 dB noise difference as opposed to the 5 dB difference used in panel 1. Results indicate that the number of postcodes that meet the criteria in panel 2 and 3 is comparable to that in panel 1.
We used the same method to identify the relief group and the two control groups, but with afternoon noise levels (15.00–19.00 hours). Table 8 shows the results, which demonstrate that similarly small number of postcodes met the criteria.
| Difference in dB | Year | Relief area criteria | Postcodes (n) | Mean noise levels (dB) | Control area I criteria | Postcodes (n) | Mean noise levels (dB) | Control area II criteria | Postcodes (n) | Mean noise levels (dB) |
|---|---|---|---|---|---|---|---|---|---|---|
| Panel 1: 5 dB difference |
2014 | 100+ days > 55 dB AND 100+ days in a year | 19,743 | 52.92 | 100–200 days > 55 dB AND 100+ days ≤ 50 dB | 8424 | 51.00 | 200+ days > 55 dB | 11,319 | 57.39 |
| 2015 | 18,769 | 53.62 | 7141 | 51.65 | 11,628 | 57.56 | ||||
| 2016 | 19,872 | 53.28 | 7960 | 51.34 | 11,912 | 57.76 | ||||
| 2017 | 20,712 | 52.65 | 8818 | 50.71 | 11,894 | 57.80 | ||||
| 2018 | 17,861 | 53.25 | 6133 | 50.89 | 11,728 | 57.52 | ||||
| Panel 2: 5 dB difference |
2014 | 50+ days > 55 dB AND 50+ days | 23,668 | 51.42 | 100–200 days > 55 dB AND 100+ days ≤ 50 dB | 8424 | 51.00 | 100+ days > 55 dB | 19,743 | 52.92 |
| 2015 | 23,589 | 51.48 | 7141 | 51.65 | 18,769 | 53.62 | ||||
| 2016 | 23,742 | 51.51 | 7960 | 51.34 | 19,872 | 53.28 | ||||
| 2017 | 24,915 | 51.19 | 8818 | 50.71 | 20,712 | 52.65 | ||||
| 2018 | 22,774 | 51.41 | 6133 | 50.89 | 17,861 | 53.25 | ||||
| Panel 2: 7 dB difference |
2014 | 100+ days > 57 dB AND 100+ days | 15,265 | 55.01 | 100–200 days > 57 dB AND 100+ days ≤ 50 dB | 5608 | 53.29 | 200+ days > 57 dB | 9696 | 59.68 |
| 2015 | 14,641 | 55.57 | 4833 | 53.76 | 9981 | 59.78 | ||||
| 2016 | 15,465 | 55.33 | 5055 | 53.44 | 10,515 | 59.68 | ||||
| 2017 | 15,888 | 54.94 | 5263 | 53.1 | 10,649 | 59.52 | ||||
| 2018 | 13,836 | 55.57 | 3557 | 53.34 | 10,333 | 59.46 |
Finally, we linked morning shoulder (06.00–07.00 hours) noise levels with afternoon (15.00–19.00 hours) noise levels to identify a relief group with a relatively noisy morning shoulder period but a quieter afternoon relative to a control group with significantly noisier morning shoulder and afternoon periods. We identified relief postcodes as those exposed to noise levels above 55 dB during the morning shoulder period but below 50 dB in the afternoon on the same day for at least 100 days per year. The control group consisted of postcodes where morning shoulder period and afternoon noise levels exceeded 55 dB on the same day for at least 200 days per year. Table 9 (top half of panel 1) shows that between 2014 and 2018 there are between 3029 and 5647 postcodes in the relief group, but only between 1655 and 1896 in the control group. We then relaxed the criteria by selecting postcodes that were exposed to noise levels above 55 dB during the morning shoulder period and below 50 dB in the afternoon on the same day but for at least 50 days in a year. The control group comprised all postcodes that were exposed to noise levels above 55 dB during the morning shoulder period and afternoon of the same day for at least 100 days. The results shown in the bottom half of panel 1 of Table 9 display that the number of postcodes in the relief and control groups increased significantly compared with the previous analysis, but the total number remained relatively small. We reapplied the same strategy but increased the noise level difference from 5 to 7 dB to identify relief and control postcodes. The results were presented in panel 2 of Table 9.
| Difference in dB | Year | Relief area criteria | Postcodes (n) | Period (hours) Mean noise level (dB) |
Control area criteria | Postcodes (n) | Period (hours) Mean noise level (dB) |
|---|---|---|---|---|---|---|---|
| Panel 1: 5 dB difference | 2014 | 100+ days > 55 dB morning 07.00–15.00 hours AND 100+ days ≤ 50 dB afternoon on same day | 3029 | 06.00–0.700: 50.34 15.00–19.00: 48.77 |
200+ days > 55 dB in morning and afternoon on same day | 1655 | 06.00–07.00: 57.71 15.00–19.00: 58.28 |
| 2015 | 4009 | 06.00–07.00: 51.19 15.00–19.00: 48.87 |
1689 | 06.00–07.00: 58.55 15.00–19.00: 58.28 |
|||
| 2016 | 4454 | 06.00–07.00: 50.60 15.00–19.00: 48.9 |
1670 | 06.00–07.00: 58.7 15.00–19.00: 58.51 |
|||
| 2017 | 5647 | 06.00–07.00: 50.68 15.00–19.00: 48.7 |
1896 | 06.00–07.00: 60.86 15.00–19.00: 58.74 |
|||
| 2018 | 4090 | 06.00–07.00: 50.68 15.00–19.00: 47.62 |
1483 | 06.00–07.00: 59.18 15.00–19.00: 58.28 |
|||
| 2014 | 50+ days > 55 dB morning 07.00–15.00 hours AND 50+ days ≤ 50 dB afternoon on same day | 6122 | 06.00–07.00: 50.30 15.00–19.00: 48.96 |
100+ days > 55 dB morning and afternoon on same day | 7375 | 06.00–07.00: 54.65 15.00–19.00: 53.96 |
|
| 2015 | 6884 | 06.00–07.00: 51.28 15.00–19.00: 49.1 |
7598 | 06.00–07.00: 55.39 15.00–19.00: 53.86 |
|||
| 2016 | 7312 | 06.00–07.00: 50.69 15.00–19.00: 49.18 |
7742 | 06.00–07.00: 54.97 15.00–19.00: 53.91 |
|||
| 2017 | 12,967 | 06.00–07.00: 53.15 15.00–19.00: 49.25 |
7440 | 06.00–07.00: 57.1 15.00–19.00: 53.64 |
|||
| 2018 | 8011 | 06.00–07.00: 51.08 15.00–19.00: 48.59 |
5811 | 06.00–07.00: 55.64 15.00–19.00: 54.35 |
|||
| Panel 2: 7 dB difference | 2014 | 100+ days > 57 dB morning 07.00–15.00 hours AND 100+ days ≤ 50 dB afternoon on same day | 1235 | 06.00–07.00: 51.96 15.00–19.00: 50.16 |
200+ days > 57 dB morning AND afternoon on same day | 778 | 06.00–07.00: 59.08 15.00–19.00: 60.19 |
| 2015 | 1508 | 06.00–07.00: 52.89 15.00–19.00: 50.39 |
769 | 06.00–07.00: 59.75 15.00–19.00: 60.10 |
|||
| 2016 | 1748 | 06.00–07.00: 52.33 15.00–19.00: 50.39 |
806 | 06.00–07.00: 60.2 15.00–19.00: 60.28 |
|||
| 2017 | 2493 | 06.00–07.00: 54.33 15.00–19.00: 50.11 |
798 | 06.00–07.00: 61.54 15.00–19.00: 60.17 |
|||
| 2018 | 1733 | 06.00–07.00: 52.07 15.00–19.00: 48.59 |
658 | 06.00–07.00: 60.21 15.00–19.00: 59.62 |
|||
| 2014 | 50+ days > 57 dB morning 07.00–15.00 hours AND 50+ days ≤ 50 dB afternoon on same day | 3095 | 06.00–07.00: 52.31 15.00–19.00: 50.7 |
100+ days > 57 dB morning AND afternoon on same day | 4955 | 06.00–07.00: 56.56 15.00–19.00: 55.79 |
|
| 2015 | 3673 | 06.00–07.00: 53.01 15.00–19.00: 50.63 |
4888 | 06.00–07.00: 57.42 15.00–19.00: 55.78 |
|||
| 2016 | 4078 | 06.00–07.00: 52.32 15.00–19.00: 50.55 |
4905 | 06.00–07.00: 57.15 15.00–19.00: 55.95 |
|||
| 2017 | 7481 | 06.00–07.00: 54.76 15.00–19.00: 50.73 |
4693 | 06.00–07.00: 59.14 15.00–19.00: 55.68 |
|||
| 2018 | 4487 | 06.00–07.00: 52.83 15.00–19.00: 50.08 |
3323 | 06.00–07.00: 58.06 15.00–19.00: 56.87 |
In conclusion, using different selection criteria for relief and control postcodes and predefined noise cut-off points to identify areas with large changes in noise levels, we only identified a small proportion of postcodes in the study area (~5000–25,000 postcodes compared with 150,000 overall). Further, some of the predefined control areas had similar or lower noise levels to the areas presumed to have relief periods. We therefore did not conduct health analyses because the small sample size was likely to have been insufficient to detect effects.
Coefficient of variation
The CoV (SD/mean × 100) is a measure of variability that can be used to quantify the day-to-day variability per postcode between 2014 and 2018. A high CoV suggests that daily noise levels within a postcode vary more in a given period.
The 2014–18 descriptive summary of the CoV for daily noise levels by postcode level is presented in Table 10. In this table, for each time band, we calculated the CoV for all seasons (winter, winter transition, summer and summer transition) and additionally by pooled seasonal data across 2014–18 (summer, summer transition, winter and winter transition). Our findings showed that daily noise levels by postcodes varied more during the night. Particularly, 24.00– 04.30 hours had the highest mean CoV (67.33–74.16) of all time bands, followed by 04.30–06.00 and 23.00–24.00 hours. The morning shoulder period (06.00–07.00 hours) had the highest mean daily levels, but its mean CoV (15.98–16.83) was the fifth highest among all time bands. Daytime aircraft noise tended to be less variable.
| Time band | Season | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|---|
| N | Mean | SD | Min | Max | ||
| 04.30–06.00 hours | Four seasons | 164,012 | 44.80 | 16.85 | 3.301 | 112.9 |
| Winter | 164,012 | 44.04 | 16.91 | 2.962 | 109.2 | |
| Winter transition | 164,012 | 46.52 | 18.07 | 3.420 | 126.5 | |
| Summer | 164,012 | 45.92 | 18.91 | 3.424 | 128.0 | |
| Summer transition | 164,012 | 43.91 | 19.66 | 3.339 | 142.0 | |
| 06.00–07.00 hours | Four seasons | 164,012 | 16.59 | 7.980 | 1.655 | 53.11 |
| Winter | 164,012 | 16.51 | 7.952 | 1.641 | 52.79 | |
| Winter transition | 164,012 | 16.49 | 8.004 | 1.314 | 53.56 | |
| Summer | 164,012 | 16.83 | 8.168 | 1.239 | 54.25 | |
| Summer transition | 164,012 | 15.98 | 7.502 | 1.238 | 54.28 | |
| 07.00–15.00 hours | Four seasons | 164,012 | 10.43 | 4.798 | 1.194 | 22.31 |
| Winter | 164,012 | 10.35 | 4.731 | 1.202 | 22.00 | |
| Winter transition | 164,012 | 10.46 | 4.901 | 1.119 | 22.95 | |
| Summer | 164,012 | 10.59 | 5.018 | 1.119 | 23.47 | |
| Summer transition | 164,012 | 9.728 | 4.352 | 1.088 | 22.71 | |
| 15.00–19.00 hours | Four seasons | 164,012 | 10.62 | 4.849 | 1.315 | 23.44 |
| Winter | 164,012 | 10.62 | 4.825 | 1.324 | 23.27 | |
| Winter transition | 164,012 | 10.54 | 4.913 | 1.271 | 23.82 | |
| Summer | 164,012 | 10.60 | 4.968 | 1.252 | 24.15 | |
| Summer transition | 164,012 | 9.892 | 4.364 | 1.269 | 22.54 | |
| 19.00–22.00 hours | Four seasons | 155,951 | 10.29 | 4.155 | 1.388 | 23.56 |
| Winter | 155,951 | 10.13 | 4.074 | 1.366 | 23.11 | |
| Winter transition | 155,951 | 10.42 | 4.349 | 1.387 | 24.24 | |
| Summer | 155,951 | 10.61 | 4.487 | 1.443 | 25.08 | |
| Summer transition | 155,951 | 10.05 | 4.077 | 1.387 | 24.22 | |
| 22.00–23.00 hours | Four seasons | 164,012 | 24.07 | 37.24 | 2.126 | 210.9 |
| Winter | 164,012 | 24.20 | 37.23 | 2.167 | 210.8 | |
| Winter transition | 164,012 | 23.81 | 37.26 | 1.929 | 210.8 | |
| Summer | 164,012 | 23.62 | 37.30 | 1.858 | 210.7 | |
| Summer transition | 164,012 | 23.47 | 37.32 | 1.839 | 210.6 | |
| 23.00–24.00 hours | Four seasons | 164,012 | 45.64 | 35.95 | 8.104 | 255.4 |
| Winter | 164,012 | 48.20 | 36.03 | 8.769 | 263.0 | |
| Winter transition | 164,012 | 41.10 | 35.86 | 6.454 | 241.3 | |
| Summer | 164,012 | 39.12 | 35.97 | 5.863 | 241.2 | |
| Summer transition | 164,012 | 38.08 | 35.99 | 5.730 | 239.3 | |
| 24.00–04.30 hours | Four seasons | 164,012 | 72.13 | 17.84 | 20.16 | 238.4 |
| Winter | 164,012 | 74.16 | 18.89 | 19.26 | 290.6 | |
| Winter transition | 164,012 | 69.09 | 16.76 | 20.46 | 185.2 | |
| Summer | 164,012 | 68.75 | 16.79 | 20.03 | 169.7 | |
| Summer transition | 164,012 | 67.33 | 17.02 | 7.514 | 299.5 |
Methods and results: investigating daily aircraft noise and material and health inequality
The hedonic pricing model suggests that aircraft noise is a negative externality that could have a negative impact on housing prices, resulting in noise inequality where the poor are more likely to reside in noisier areas. 26 A study relating to London Heathrow airport found no evidence that deprived populations were more likely to be exposed to high aircraft noise levels. 27 In fact, the study found that individuals with the highest household income, white ethnicity, and with the lowest area-level income deprivation were more likely to live within a 50 dB contour of aircraft noise. A review examining social inequalities in noise exposure from all sources also found a mixed relationship between deprivation and noise exposure. 28 The question of whether aircraft noise may be associated with deprivation is therefore unclear and is likely to vary between airports and countries.
One issue to consider is that deprivation is a potentially multidimensional concept, encompassing numerous facets of an individual’s life throughout their lifetime. 29 There is limited evidence on the relationship between aircraft noise and non-material deprivation, particularly health inequality, which may be directly linked to health outcomes.
In light of this finding, the purpose of this section of the study was to investigate the relationship between aircraft noise and material and health deprivation.
Deprivation
Given that deprivation has many different aspects, we focused on two: material and health deprivation. We measured material and health deprivation using three variables: Carstairs index of multiple deprivation [census output areas level (COA), 2011 only], fuel poverty rate [lower-layer super output areas level (LSOA), 2014–18] and avoidable death rate per 100,000 [local authority district level (LAD), 2014–18].
-
Carstairs index is a commonly used area-level measure of material deprivation in health studies. 30 It was calculated using four variables from the 2011 Census, including male unemployment, low social class, non-car ownership and overcrowding. This variable has the highest spatial resolution among the three deprivation indicators chosen for this study, due to its geography being COA (the highest spatial resolution of English Census geography of average population of 310 individuals). This indicator is time invariant as only 2011 values were available. Data were obtained via the UK Data Archive (link: www.data-archive.ac.uk, accessed 23 November 2022).
-
Annual fuel poverty rate is used to measure the percentage of households that were unable to maintain standard thermal comfort and safety. 31 Fuel poverty has been increasingly recognised as a distinct form of social and health inequality. 32 It has been hypothesised that cold may be associated with excess winter deaths. 33 A cold home due to fuel poverty has been linked to respiratory problems, arthritis and rheumatism in people of all ages, as well as mental health problems in adolescents. 34 This indicator is annual, covering the period 2014–18. The geographic level is LSOA level (Census geography category with average population of 1500 individuals) and covers the period 2014–18. We extracted fuel poverty from UK annual fuel poverty statistics. 35
-
We used yearly avoidable death rate per 100,000 to measure health inequality. Mortality is an outcome that can be clinically quantified; avoidable mortality is amenable to policy intervention. 36 Avoidable death rate could therefore be used to capture the geographical disparity in health. 36 The definition of avoidable death rate is available from the Office for National Statistics. 37 The data were at LAD level (mean population of approximately 179,361.6 per LAD), covering each year 2014–18. We downloaded the data from the Office for National Statistics. 38
Confounders
We adjusted for the quintiles of percentage of non-white population per LAD, considering that ethnic concentration may be related to both deprivation and aircraft noise levels. These data were obtained from Nomis (www.nomisweb.co.uk, accessed 13 February 2023).
Statistical analyses
Since noise exposure levels were calculated daily, serial correlation is a concern. We specified a random effects model with autoregressive first-order autoregression model disturbance to estimate the association between daily noise levels and quintiles of deprivation.
The equations are specified as:
where i represents individual postcode, j represents individual output areas, k represents individual LSOA, l represents individual LAD, t represents year; noiseit, carstairsj and ethniclt represents daily noise levels (continuous), quintiles of Carstairs index and quantiles of percentage ethnic minority population; yeart is the year fixed effect; ui is the random heterogeneity and eit is error term.
where i represents individual postcode, j represents individual output areas, k represents individual LSOA, l represents individual LAD and t represents year; noiseit, avoidlt and ethniclt represent daily noise levels (continuous), quintiles of avoidable death rate and quantiles of percentage ethnic minority population; yeart is the year fixed effect; ui is the random heterogeneity and eit is error term.
where i represents individual postcode, j represents individual output areas, k represents individual LSOA, l represents individual LAD and t represents year; noiseit, carstairsj, avoidlt, fuelpovkt and ethniclt represent daily noise levels (continuous), quintiles of fuel poverty rate and quantiles of percentage ethnic minority population; yeart is the year fixed effect; ui is the random heterogeneity and eit is error term.
where i represents individual postcode, j represents individual output areas, k represents individual LSOA, l represents individual LAD and t represents year; noiseit, fuelpovkt and ethniclt represent daily noise levels (continuous), quintiles of Carstairs index, quintiles of avoidable death rate, quintiles of fuel poverty rate and quantiles of percentage ethnic minority population; yeart is the year fixed effect; ui is the random heterogeneity and eit is error term.
Each postcode uniquely belongs to an output area, a lower LSOA and a LAD, which enables us to link data.
Our dependent variables included the four noise metrics: LAeq24, Lnight, Leve and Lday.
We conducted four regressions per noise metric. The first regression of each metric included quintiles of Carstairs index and percentage non-white ethnicity. Models 2 and 3 replaced Carstairs index with avoidable death rate and fuel poverty rate, respectively. Model 4 included quintiles for all three measures of deprivation and percentage non-white ethnicity.
All analyses were conducted in Stata using module xtregar. 39
Results
Table 11 shows the descriptive summary of measures of deprivation and percentage non-white ethnicity in the analysis.
| Variables | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|
| N | Mean | SD | Min | Max | |
| Avoidable death rate per 10,000 persons | 284,476,323 | 133.26 | 25.1 | 78 | 209.9 |
| Carstairs index | 284,476,323 | 0.94 | 3.1 | −4.88 | 28.31 |
| Fuel poverty (%) | 284,476,323 | 10.18 | 3.63 | 1.8 | 29.6 |
| Non-white (%) | 284,476,323 | 36.26 | 14.51 | 4.4 | 68.9 |
Table 12 illustrates the pairwise correlations between variables involved in analysis. The noise correlation coefficients between LAeq24, Lday, Leve and Lnight ranged between r = 0.68 and 0.98. The correlation between Lnight and Leve (r = 0.68) was the lowest among all pairs, whereas the correlation between Lday and LAeq24 (r = 0.98) was the highest. For deprivation variables, we used raw values rather than quintiles. The correlation between Carstairs index and both of avoidable death rate and fuel poverty was moderate (r ~ 0.4), while that between fuel poverty rate and avoidable death rate was particularly weak (r = 0.08). There was a fairly weak relationship between each pair of the three deprivation variables and area percentage non-white ethnicity in our data (r 0.08–0.49), with the correlation between the Carstairs index and the percentage non-white ethnicity being the strongest (r = 0.49).
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) |
|---|---|---|---|---|---|---|---|---|
| (1) Lday | 1 | |||||||
| (2) Leve | 0.82 | 1 | ||||||
| (3) LAeq24 | 0.98 | 0.9 | 1 | |||||
| (4) Lnight | 0.78 | 0.68 | 0.82 | 1 | ||||
| (5) Carstairs index | −0.02 | −0.03 | −0.02 | 0.04 | 1 | |||
| (6) Avoidable death rate | 0.15 | 0.15 | 0.19 | 0.23 | 0.42 | 1 | ||
| (7) Fuel poverty rate | −0.07 | −0.09 | −0.08 | −0.03 | 0.36 | 0.08 | 1 | |
| (8) Non-white (%) | −0.13 | −0.14 | −0.15 | −0.07 | 0.49 | 0.41 | 0.36 | 1 |
Tables 13 and 14 demonstrate the main results from regressions. The dependent variables were Lday (07.00–19.00 hours) and Leve (19.00–23.00 hours) in Table 13, and Lnight (23.00–07.00 hours) and LAeq24 (24-hour average) in Table 14. In models 1–3, we separately regressed the association between one measure of deprivation and aircraft noise levels while adjusting for quintiles of percentage non-white ethnicity. The results of these models consistently demonstrated that almost all quintiles of the Carstairs index, avoidable death rate and fuel poverty rate (except for Q5 of the fuel poverty rate) had significant and positive coefficients, regardless of the noise metrics being examined. This evidenced that postcodes near Heathrow airport with the least material or health deprivation experienced the lowest daily noise levels between 2014 and 2018.
| Dependent variables | Lday | Leve | ||||||
|---|---|---|---|---|---|---|---|---|
| Models | Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 |
| Carstairs index Q1 – least deprived (base) | ||||||||
| Q2 | 1.02*** | 0.90*** | 1.02*** | 0.90*** | ||||
| (0.05) | (0.05) | (0.05) | (0.04) | |||||
| Q3 | 0.58*** | 0.35*** | 0.68*** | 0.45*** | ||||
| (0.04) | (0.04) | (0.04) | (0.04) | |||||
| Q4 | 0.09** | −0.21*** | 0.22*** | −0.08** | ||||
| (0.04) | (0.04) | (0.04) | (0.04) | |||||
| Q5 | 0.40*** | −0.01 | 0.48*** | 0.11*** | ||||
| (0.04) | (0.04) | (0.04) | (0.04) | |||||
| Avoidable death rate Q1 – least deprived (base) | ||||||||
| Q2 | 0.08*** | 0.08*** | 0.12*** | 0.13*** | ||||
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Q3 | 0.48*** | 0.49*** | 0.38*** | 0.38*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q4 | 0.76*** | 0.76*** | 0.71*** | 0.71*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q5 | 0.69*** | 0.70*** | 0.69*** | 0.69*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Fuel poverty rate Q1 – least deprived (base) | ||||||||
| Q2 | 0.02*** | 0.02*** | 0.15*** | 0.15*** | ||||
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Q3 | 0.03*** | 0.03*** | 0.12*** | 0.12*** | ||||
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Q4 | 0.04*** | 0.04*** | 0.12*** | 0.12*** | ||||
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Q5 | −0.02*** | −0.01*** | 0.00 | 0.01*** | ||||
| (0.00) | (0.00) | (0.00) | (0.00) | |||||
| Non-white ethnicity (%) Q1 (base) | ||||||||
| Q2 | 0.15*** | 0.17*** | 0.16*** | 0.18*** | −0.48*** | −0.45*** | −0.46*** | −0.43*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.00) | (0.00) | (0.00) | (0.00) | |
| Q3 | −0.12*** | −0.14*** | −0.12*** | −0.14*** | −0.63*** | −0.65*** | −0.62*** | −0.64*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Q4 | −0.57*** | −0.56*** | −0.57*** | −0.55*** | −1.13*** | −1.11*** | −1.12*** | −1.10*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Q5 | −0.78*** | −0.85*** | −0.78*** | −0.84*** | −1.49*** | −1.57*** | −1.47*** | −1.55*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Constant | 43.93*** | 43.92*** | 44.29*** | 43.78*** | 42.78*** | 42.87*** | 43.14*** | 42.57*** |
| (0.03) | (0.01) | (0.01) | (0.03) | (0.03) | (0.01) | (0.01) | (0.03) | |
| Observations (n) | 280,458,080 | 280,458,080 | 280,458,080 | 280,458,080 | 268,178,754 | 268,178,754 | 268,178,754 | 268,178,754 |
| Postcodes (n) | 162,004 | 162,004 | 162,004 | 162,004 | 154,173 | 154,173 | 154,173 | 154,173 |
| Autocorrelation | AR1 | AR1 | AR1 | AR1 | AR1 | AR1 | AR1 | AR1 |
| Dependent variables | Lnight | LAeq24 | ||||||
|---|---|---|---|---|---|---|---|---|
| Models | Model 1 | Model 2 | Model 3 | Model 4 | Model 1 | Model 2 | Model 3 | Model 4 |
| Carstairs index Q1 – least deprived (base) | ||||||||
| Q2 | 2.66*** | 2.42*** | 1.12*** | 0.95*** | ||||
| (0.06) | (0.05) | (0.05) | (0.05) | |||||
| Q3 | 3.13*** | 2.68*** | 0.99*** | 0.66*** | ||||
| (0.05) | (0.05) | (0.05) | (0.04) | |||||
| Q4 | 2.79*** | 2.23*** | 0.57*** | 0.15*** | ||||
| (0.05) | (0.04) | (0.05) | (0.04) | |||||
| Q5 | 3.18*** | 2.45*** | 0.81*** | 0.26*** | ||||
| (0.05) | (0.04) | (0.04) | (0.04) | |||||
| Avoidable death rate Q1 – least deprived (base) | ||||||||
| Q2 | 0.41*** | 0.41*** | 0.17*** | 0.18*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q3 | 1.22*** | 1.13*** | 0.62*** | 0.63*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q4 | 1.59*** | 1.47*** | 1.20*** | 1.20*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q5 | 1.66*** | 1.54*** | 1.11*** | 1.12*** | ||||
| (0.02) | (0.02) | (0.02) | (0.02) | |||||
| Fuel poverty rate Q1 – least deprived (base) | ||||||||
| Q2 | 0.16*** | 0.14*** | 0.07*** | 0.06*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q3 | 0.23*** | 0.22*** | 0.08*** | 0.07*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q4 | 0.13*** | 0.10*** | 0.08*** | 0.07*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Q5 | −0.08*** | −0.11*** | −0.04*** | −0.03*** | ||||
| (0.01) | (0.01) | (0.01) | (0.01) | |||||
| Non-white ethnicity (%) Q1 (base) | ||||||||
| Q2 | −0.51*** | −0.43*** | −0.35*** | −0.52*** | −0.37*** | −0.38*** | −0.34*** | −0.37*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Q3 | −0.42*** | −0.40*** | −0.25*** | −0.53*** | −0.53*** | −0.62*** | −0.50*** | −0.61*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Q4 | −0.95*** | −0.89*** | −0.78*** | −1.04*** | −1.02*** | −1.05*** | −0.99*** | −1.04*** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Q5 | −1.10*** | −1.15*** | −0.88*** | −1.28*** | −1.24*** | −1.43*** | −1.18*** | −1.42*** |
| (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | |
| Constant | 33.33*** | 34.94*** | 35.69*** | 32.91*** | 42.31*** | 42.48*** | 42.95*** | 42.07*** |
| (0.04) | (0.02) | (0.02) | (0.04) | (0.04) | (0.02) | (0.02) | (0.03) | |
| Observations (n) | 85,847,742 | 85,847,742 | 85,847,742 | 85,847,742 | 82,265,795 | 82,265,795 | 82,265,795 | 82,265,795 |
| Postcodes (n) | 162,003 | 162,003 | 162,003 | 162,003 | 154,173 | 154,173 | 154,173 | 154,173 |
| Autocorrelation | AR1 | AR1 | AR1 | AR1 | AR1 | AR1 | AR1 | AR1 |
However, which quintile of deprivation (Q1 least deprived, Q5 least deprived) was the noisiest depended on the deprivation measures and noise metrics used. During the day (07.00–19.00 hours), Q2 of Carstairs index, Q4 of avoidable death rate and Q4 of fuel poverty rate had the highest levels of noise. In the evening (19.00–23.00 hours), Q2 of the Carstairs index, Q4 of the avoidable death rate and Q2 of fuel poverty rate had the highest levels of noise pollution. It is interesting to note, the quintile with the highest levels of aircraft noise exposure at night (23.00–07.00 hours) was Q5, for both the Carstairs index and the avoidable death rate, as well as Q3 for the fuel poverty rate.
There were two interesting exposure–response patterns in relation to this. First, among the three indicators of deprivation, avoidable death rate had the most noticeable gradient. Column (2) of Table 13 demonstrates Q2 and Q3 postcodes were exposed to slightly higher noise levels, whereas Q4 and Q5 postcodes were exposed to significantly higher noise levels during daytime (coefficients: Q2 – 0.08, Q3 – 0.48, Q4 – 0.76 and Q5 – 0.69). The second is that the exposure–response relationship between night-time aircraft noise levels and deprivation was more pronounced than during the day and evening. This gradient was particularly clear when we paired night-time noise with avoidable death rate (coefficients: Q2 – 0.41, Q3 – 1.22, Q4 – 1.59 and Q5 – 1.66). While the relationship did not appear to be linear, it supported an observation that postcodes in local authorities with higher avoidable death rates were more likely to be exposed to a higher level of aircraft noise at night.
We found a stronger association between deprivation and daily aircraft noise at night than during the day or evening in postcodes near Heathrow airport. In comparison with postcodes in Q1, those in Q2–Q5 of the Carstairs index were exposed to noise levels that were 2.66, 3.13, 2.79 and 3.18 dB higher at night, but only 1.02, 0.58, 0.09 and 0.40 dB higher during daytime, and 1.02, 0.68, 0.22 and 0.48 dB higher during evening. The same conclusion is supported by the results that LAeq24 (mean sound levels over the 24 hours) had very similar number of observations as Lnight (N observations: Lnight – 85,847,742 vs. LAeq24 – 82,265,795) but its relationship with deprivation was significantly smaller in size than that of Lnight. The evidence suggests that night-time aircraft noise exposure inequality is of particular concern in postcodes near Heathrow.
Lastly, we found that the fuel poverty rate had a weaker relationship with daily aircraft noise than the Carstairs index and avoidable death rate. There was a negative relationship between the fifth and fourth quintiles of fuel poverty and aircraft noise during some periods.
The above interpretation of the results was based on models that included only one measure of deprivation, but our conclusions held when all deprivation measures were included (model 4).
Methods and results: short-term impact of aircraft noise on cardiovascular morbidity and mortality
One of the main aims of our study was to evaluate short-term impact of aircraft noise on cardiovascular morbidity and mortality. We used a time-stratified case-crossover study design, in which the days when an event of interest occurred are matched with control days within the same month and on the same day of the week. 40,41 This individual-level design naturally adjusts for all time-invariant or slowly time-varying confounders, including sex, smoking behaviour and genetic factors. It uses all cases in the population without the need to recruit additional controls. The case-crossover design is useful in assessing the acute impact of a transient risk factor with minimal bias and has been used widely in environmental epidemiology, predominantly in temperature and air pollution studies as well as aircraft noise. 42,43
Health outcomes data
All hospital episodes and deaths due to primary CVD in the study area from 1 January 2014 to 31 December 2018 were included. We extracted postcode data on all hospital episodes and deaths from the Hospital Episode Statistics from NHS Digital and the mortality data from the Office for National Statistics held by the UK Small Area Health Statistics Unit at Imperial College London. Data were obtained for all events with primary cause of admission or death due to stroke [International Classification of Diseases version 10 (ICD-10) codes I61, I63–I64], coronary heart disease (CHD; ICD-10 I20–I25) and CVD (ICD-10 Chapter I) and linked to postcode-level noise estimates. Time of hospital episode and death were not available. The study was covered by national research ethics approval from the London – South East Research Ethics Committee (reference 17/LO/0846; date of opinion 29 June 2017). Data access to confidential patient information without consent was covered by the Health Research Authority Confidentiality Advisory Group under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (section 251); reference: 20/CAG/0028 (outcome date 24 March 2020, section 251 Register Index Sheet application number A02476).
Confounder data
The environmental confounders included in the models were mean temperature and particulate matter less than 2.5 µm in diameter (PM2.5) concentration. Hourly dry air temperature measurements were captured at three National Oceanic and Atmospheric Administration Integrated Surface Database weather stations within 25 km of the study area. Hourly background measurements of fine PM2.5 were captured by the six UK Automatic Urban and Rural Network sites within 25 km of the study area. Dry air temperature and background PM2.5 concentrations were estimated at each residential postcode using a spatial interpolation technique known as inverse distance-squared weighting.
Individual-level ethnicity data were available for all hospital admissions in the Hospital Episode Statistics data and COA-level Carstairs Index quintile from the 2011 Census was linked to admissions and deaths data. The Carstairs index is a commonly used indicator of material deprivation in health studies. 30,44 All estimates were also adjusted for the effect of holidays.
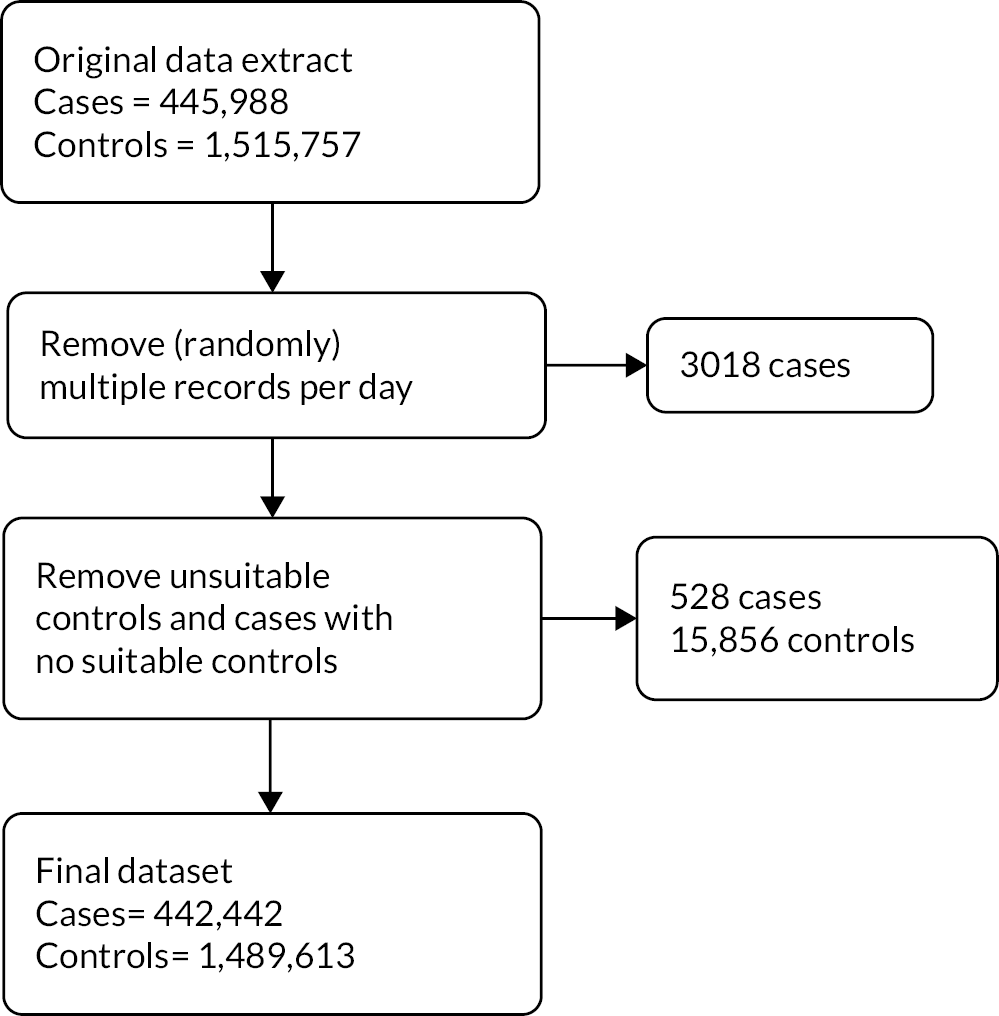
Statistical analyses
Patients with multiple cardiovascular episodes (records) per day (n = 3,018; 0.07% of cases) had one record on the day randomly selected for inclusion. Each episode record represents a patient being seen by a new clinician, so these may relate to the same spell in hospital. Control periods were matched to case periods within the same year and month on the same day of the week, excluding control days on which an additional cardiovascular episode occurred (n = 15,856 controls); 528 cases with no suitable control days were also excluded from analyses. A flowchart of the exclusion criteria and how they affected the numbers of cases and controls is presented in Figure 3.
FIGURE 3.
Hospital episodes exclusion criteria.
Conditional logistic regression was used to estimate the OR and 95% CI per 5-dB increase for the metrics Lday, Leve, Lnight, Lden and LAeq24, as well as for eight distinct periods throughout the 24-hour period relating to aircraft flows. We considered all CVD, CHD only and stroke only for both hospital episode and deaths. Estimates were adjusted for mean temperature, PM2.5 concentration and the effect of holidays, as these are variables that change rapidly in time, while long-term confounders were accounted for by the case-crossover study design. Analyses were also stratified by age, sex, ethnicity, deprivation and season to assess effect modification. All analyses were run in R statistical software45 using the Epi package. 46
Descriptive results
The descriptive summary of our sample is presented in Table 15 (note that the noise estimates relate to postcodes of cases only. This is a subset of all postcodes and descriptive statistics of noise levels differ from estimates in Table 5 relating to all postcodes; in fact, averages are lower than for all postcodes, likely reflecting spatial variability in characteristics of populations by postcode, such as age of individuals who become cases).
| Hospital episodes 2014–18 (n = 442,442) | Deaths 2014–18 (n = 49,443) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All CVD | CHD | Stroke | All CVD | CHD | Stroke | |||||||
| (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | (n) | (%) | |
| Sexa | ||||||||||||
| Male | 256,674 | 58.0 | 81,278 | 69.9 | 21,367 | 52.7 | 26,011 | 52.6 | 12,984 | 61.9 | 4014 | 45.7 |
| Female | 185,749 | 42.0 | 34,941 | 30.1 | 19,199 | 47.3 | 23,432 | 47.4 | 7984 | 38.1 | 4771 | 54.3 |
| Age (years)a | ||||||||||||
| < 65 | 190,732 | 43.1 | 49,936 | 43.0 | 11,420 | 28.2 | 7267 | 14.7 | 3640 | 17.4 | 834 | 9.5 |
| 65+ | 250,705 | 56.7 | 66,260 | 57.0 | 29,106 | 71.7 | 42,176 | 85.3 | 17,328 | 82.6 | 7951 | 90.5 |
| Deprivation | ||||||||||||
| 1 (least) | 57,060 | 12.9 | 15,061 | 13.0 | 5080 | 12.5 | 7239 | 14.6 | 2843 | 13.6 | 1349 | 15.4 |
| 2 | 55,076 | 12.4 | 14,307 | 12.3 | 5104 | 12.6 | 6561 | 13.3 | 2630 | 12.5 | 1275 | 14.5 |
| 3 | 72,775 | 16.4 | 18,735 | 16.1 | 6666 | 16.4 | 8582 | 17.4 | 3541 | 16.9 | 1529 | 17.4 |
| 4 | 106,033 | 24.0 | 27,356 | 23.5 | 9454 | 23.3 | 11,606 | 23.5 | 4984 | 23.8 | 2012 | 22.9 |
| 5 | 151,498 | 34.2 | 40,763 | 35.1 | 14,263 | 35.2 | 15,455 | 31.3 | 6970 | 33.2 | 2620 | 29.8 |
| Season | ||||||||||||
| Summer | 110,255 | 24.9 | 29,215 | 25.1 | 10,095 | 24.9 | 11,260 | 22.8 | 4728 | 22.5 | 2060 | 23.4 |
| Summer transition | 73,835 | 16.7 | 19,730 | 17.0 | 6731 | 16.6 | 7702 | 15.6 | 3231 | 15.4 | 1333 | 15.2 |
| Winter | 184,625 | 41.7 | 47,807 | 41.1 | 16,838 | 41.5 | 22,365 | 45.2 | 9589 | 45.7 | 3933 | 44.8 |
| Winter transition | 73,727 | 16.7 | 19,470 | 16.8 | 6903 | 17.0 | 8116 | 16.4 | 3420 | 16.3 | 1459 | 16.6 |
| Ethnicityb | ||||||||||||
| South Asian | 42,994 | 9.7 | 18,049 | 15.5 | 2711 | 6.7 | ||||||
| Black | 35,245 | 8.0 | 5704 | 4.9 | 4197 | 10.3 | ||||||
| Otherc | 297,390 | 67.2 | 73,658 | 63.4 | 27,582 | 68.0 | ||||||
| Missing | 66,813 | 15.1 | 18,811 | 16.2 | 6077 | 15.0 | ||||||
| Case | Control | Case | Control | |||||||||
| Noise estimates (dB) | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| 24.00–04.30 | 2.01 | 5.99 | 2.04 | 6.03 | 2.07 | 6.08 | 2.06 | 6.06 | ||||
| 04.30–06.00 | 25.80 | 12.53 | 25.81 | 12.52 | 25.72 | 12.38 | 25.71 | 12.41 | ||||
| 06.00–07.00 | 40.77 | 8.80 | 40.79 | 8.79 | 40.59 | 8.62 | 40.60 | 8.62 | ||||
| 07.00–15.00 | 42.43 | 6.97 | 42.42 | 6.96 | 42.43 | 6.83 | 42.43 | 6.85 | ||||
| 15.00–19.00 | 41.93 | 6.94 | 41.92 | 6.94 | 41.94 | 6.82 | 41.92 | 6.84 | ||||
| 19.00–22.00 | 41.85 | 6.87 | 41.84 | 6.87 | 41.79 | 6.77 | 41.77 | 6.78 | ||||
| 22.00–23.00 | 39.51 | 7.41 | 39.49 | 7.41 | 39.48 | 7.41 | 39.49 | 7.40 | ||||
| 23.00–24.00 | 27.92 | 10.89 | 27.94 | 10.90 | 27.59 | 10.91 | 27.64 | 10.93 | ||||
Results for short-term aircraft noise associations with hospital admissions
There was evidence of a small increase in risk for a 5-dB increment in noise during the evening (Leve OR = 1.005, 95% CI 1.000 to 1.010), particularly from 22.00 to 23.00 hours (OR = 1.006, 95% CI 1.002 to 1.010) for all CVD admissions (Table 16). A similar but not statistically significant pattern was estimated for admissions due to CHD. There was no evidence of an increased risk for hospitalisations due to stroke (Figure 4).
| All CVD | CHD | Stroke | |
|---|---|---|---|
| Hosp. episodes | |||
| LAeq24 | 1.003 (0.998 to 1.008) | 1.002 (0.992 to 1.012) | 1.003 (0.986 to 1.020) |
| Lday | 1.002 (0.997 to 1.007) | 1.002 (0.993 to 1.011) | 1.001 (0.986 to 1.017) |
| Leve | 1.005 (1.000 to 1.010) | 1.005 (0.996 to 1.014) | 0.999 (0.984 to 1.015) |
| Lnight | 0.999 (0.995 to 1.003) | 0.997 (0.989 to 1.004) | 1.001 (0.989 to 1.014) |
| Lden | 1.001 (0.997 to 1.006) | 0.999 (0.989 to 1.009) | 1.002 (0.986 to 1.017) |
| Deaths | |||
| LAeq24 | 1.002 (0.987 to 1.017) | 0.993 (0.970 to 1.017) | 0.980 (0.945 to 1.016) |
| Lday | 1.000 (0.986 to 1.014) | 0.994 (0.972 to 1.016) | 0.984 (0.952 to 1.018) |
| Leve | 1.003 (0.988 to 1.017) | 0.990 (0.968 to 1.012) | 0.983 (0.950 to 1.017) |
| Lnight | 0.999 (0.988 to 1.011) | 1.007 (0.989 to 1.025) | 0.981 (0.955 to 1.008) |
| Lden | 1.001 (0.987 to 1.016) | 0.997 (0.975 to 1.020) | 0.969 (0.936 to 1.003) |
FIGURE 4.
Odds ratios and 95% CIs for hospitalisations due to all CVD, CHD and stroke per 5-dB increase LAeq at defined time points throughout the day, evening and night. Estimates adjusted for PM2.5 concentration, mean temperature and holiday effect.
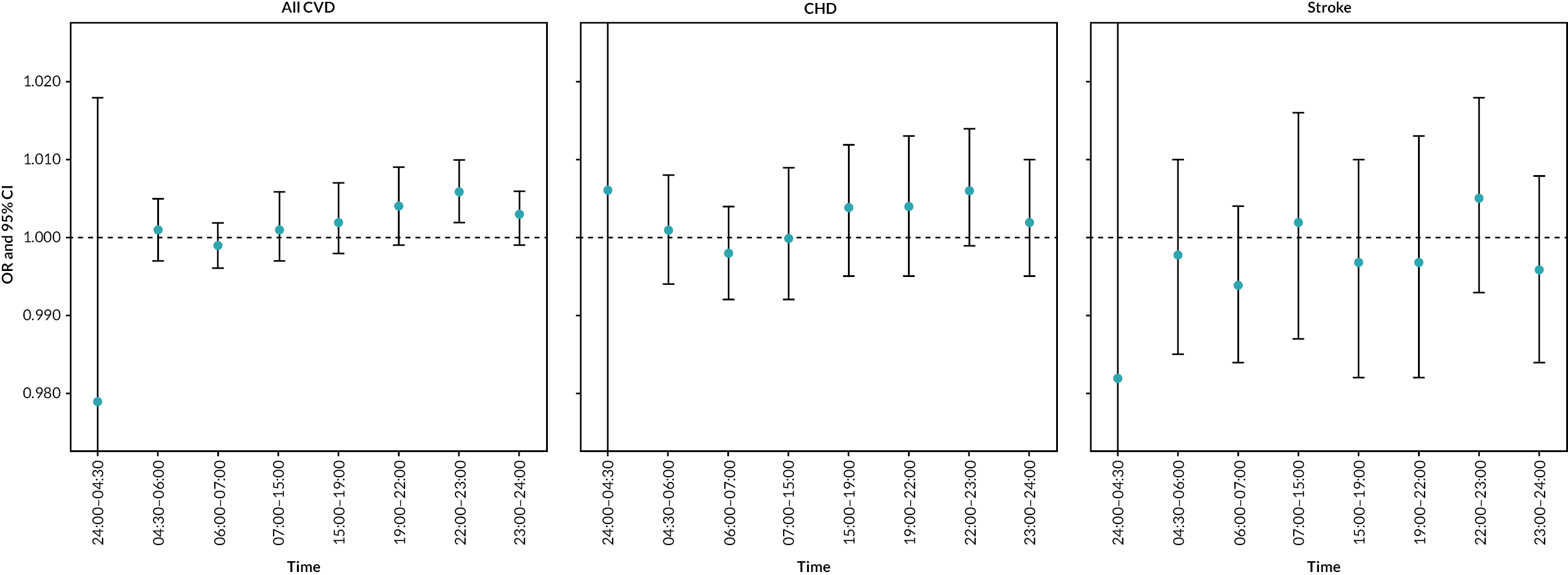
Stratified analyses for cardiovascular admissions can be seen in Figure 5. After stratifying by age and sex, the effect of aircraft noise on cardiovascular admissions was statistically significant in men over the age of 65 years during the daytime (Lday OR = 1.009, 95% CI 1.001 to 1.019) evening (Leve OR = 1.014, 95% CI 1.005 to 1.019) and, to a lesser extent, in women under the age of 65 years during the evening (Leve OR = 1.012, 95% CI 1.000 to 1.023; Figure 5). Similarly, the same figure shows, after stratifying by ethnicity, that an effect for hospitalisations due to all CVD was seen in patients who identified as South Asian during the evening hours 22.00–23.00 hours (OR = 1.004, 95% CI 1.002 to 1.028) and as other ethnicity (not South Asian or black) during the evening (Leve OR = 1.007, 95% CI 1.001 to 1.013). There was no significant effect modification by age, sex or ethnicity evident for CHD or stroke. There was also an increase in risk during late night hours among individuals residing in the third and fourth quintiles of deprivation (Figure 5).
FIGURE 5.
Odds ratios and 95% CIs for hospitalisations due to all CVD per 5-dB increase LAeq, stratified by (a) age-sex, (b) ethnicity, (c) deprivation and (d) season. Estimates adjusted for PM2.5 concentration, mean temperature and holiday effect.
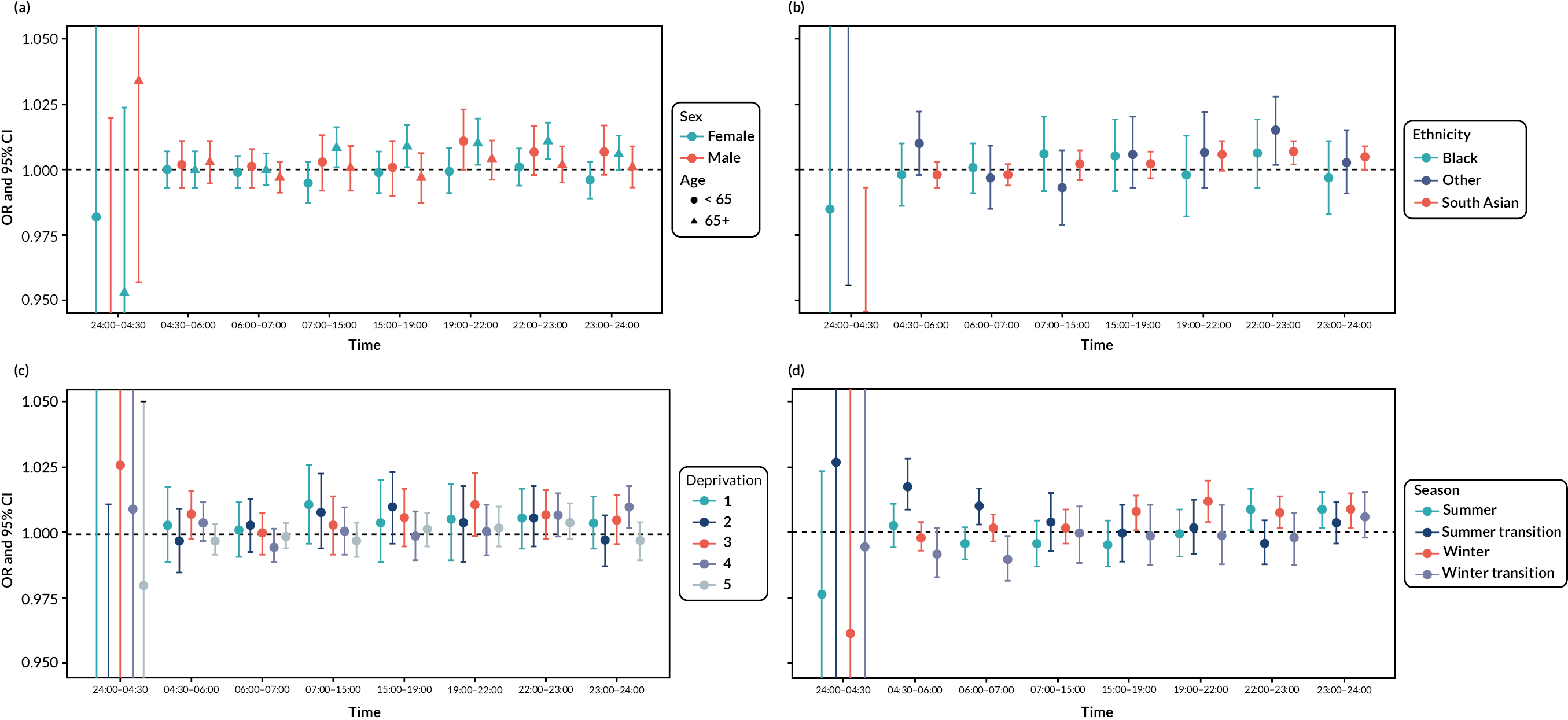
There was also evidence of effect modification by season for all CVD and for CHD. The effect of night-time aircraft noise on all CVD was strongest in the summer (22.00–23.00 hours OR = 1.009, 95% CI 1.001 to 1.017; 23.00–24.00 hours OR = 1.009, 95% CI 1.002 to 1.016) and winter months (22.00–23.00 hours OR = 1.008, 95% CI 1.002 to 1.014; 23.00–24.00 hours OR = 1.009, 95% CI 1.002 to 1.015), and the effect of late afternoon and early evening aircraft noise was only evident in the winter (15.00–19.00 hours OR = 1.008, 95% CI 1.001 to 1.014; 19.00–22.00 hours OR = 1.012, 95% CI 1.004 to 1.020). The effect of early morning aircraft noise was strongest in the summer transition months (04.30–06.00 hours OR = 1.018, 95% CI 1.009 to 1.028; 06.00–07.00 hours OR = 1.010, 95% CI 1.003 to 1.017; Figure 6).
FIGURE 6.
Odds ratio and 95% CIs for hospitalisations CHD (right) per 5-dB increase LAeq, stratified by season. Estimates adjusted for PM2.5 concentration, mean temperature and holiday effect.
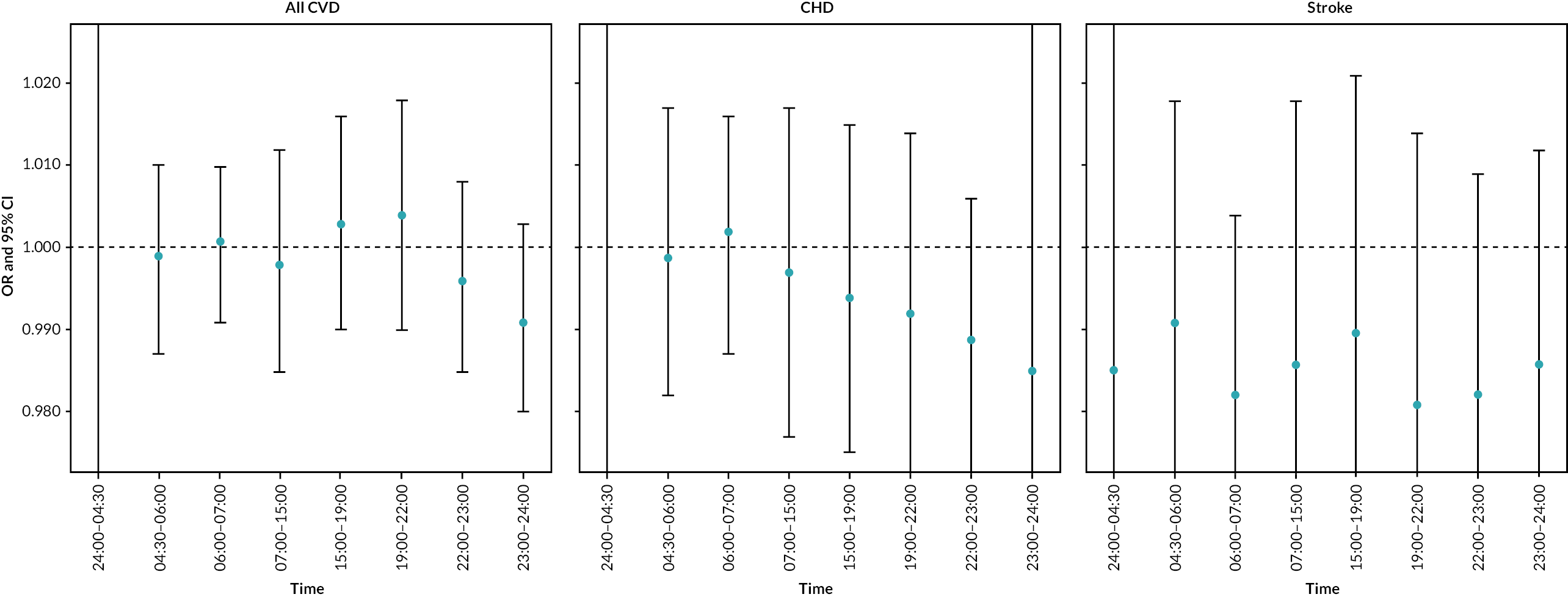
In a sensitivity analysis including only the first hospital episode for the 60.8% of patients with more than one episode (Figure 7), similar patterns were seen as for the main analyses (see Figure 4 and Table 16).
FIGURE 7.
Sensitivity analyses: ORs and 95% CIs for hospital episodes due to all CVD, CHD and stroke per 5-dB increase LAeq at defined time points throughout the day, evening and night, including only the first hospital episode for the 60.8% of patients with more than one episode (n = 269,915). Estimates adjusted for PM2.5 concentration, mean temperature and holiday effect.
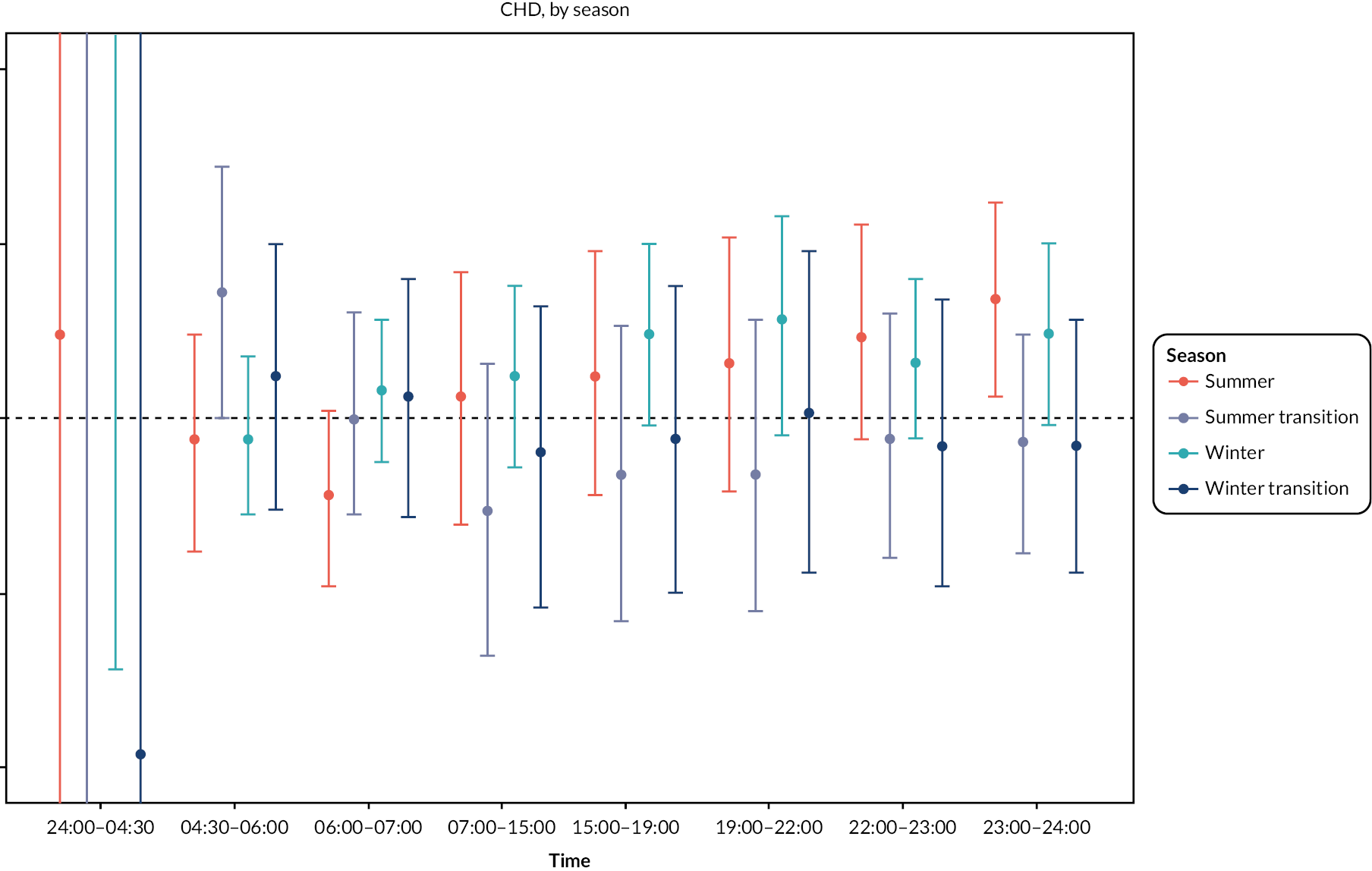
Associations of aircraft noise with mortality
There was no evidence of an association between short-term aircraft noise and deaths due to CVD, CHD or stroke, with wide confidence intervals (Figure 8).
FIGURE 8.
Odds ratios and 95% CIs for deaths due to all CVD, CHD and stroke per 5-dB increase LAeq at defined time points throughout the day, evening and night. Estimates adjusted for PM2.5 concentration, mean temperature and holiday effect.
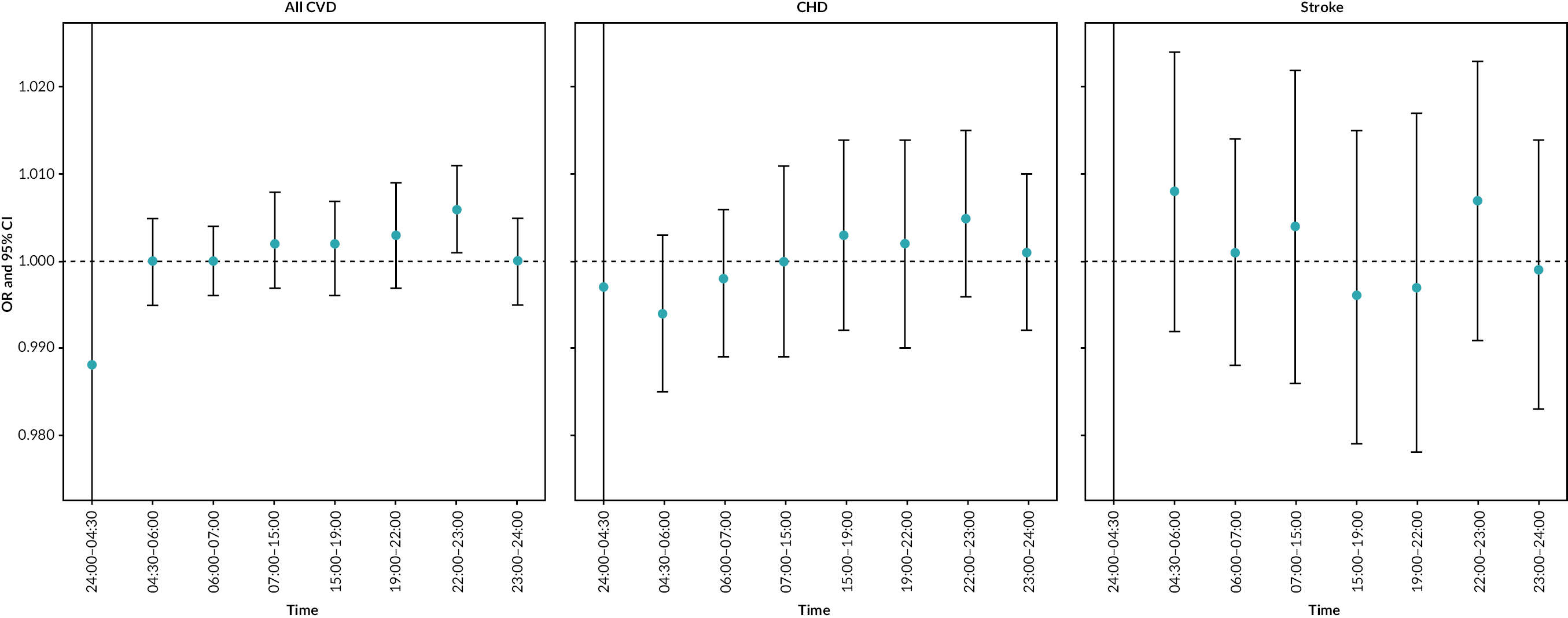
Variability in risk estimates between areas with consistent patterns of noise exposure compared with those with changing patterns of noise exposure
As detailed previously, we used CoV to measure the variability of daily noise levels per postcode between 2014 and 2018. We reran regression analyses stratifying our samples by low (≤ mean) compared with high (> mean) CoV (daily noise levels between 2014 and 2018), to assess the difference in risks of hospitalisation for CVD across regions with low and high availability in noise. The mean CoV for each noise metrics can be found in Table 10. As seen in Table 17, there were increased risks of hospitalisation for CVD throughout the evening hours (19.00–22.00, 22.00–23.00 and 23.00–24.00 hours) in the low CoV group. However, there was a non-significant risk at any time of day in high CoV group.
| Group | Time band (hour) | OR | Lower limit | Upper limit |
|---|---|---|---|---|
| Low CoV (< mean) | 24.00–04.30 | 0.998 | 0.995 | 1.002 |
| 04.30–06.00 | 1.001 | 0.997 | 1.006 | |
| 06.00–07.00 | 1.004 | 0.996 | 1.011 | |
| 07.00–15.00 | 1 | 0.99 | 1.011 | |
| 1.500–19.00 | 1.008 | 0.998 | 1.028 | |
| 19.00–22.00 | 1.012 | 1.002 | 1.023 | |
| 22.00–23.00 | 1.011 | 1.004 | 1.018 | |
| 23.00–24.00 | 1.005 | 1.001 | 1.008 | |
| High CoV (> mean) | 24.00–04.30 | 0.999 | 0.994 | 1.004 |
| 04.30–06.00 | 0.997 | 0.995 | 0.999 | |
| 06.00–07.00 | 0.998 | 0.995 | 1.002 | |
| 07.00–15.00 | 1.002 | 0.997 | 1.006 | |
| 15.00–19.00 | 1.002 | 0.997 | 1.006 | |
| 19.00–22.00 | 1.002 | 0.996 | 1.007 | |
| 22.00–23.00 | 1.004 | 0.999 | 1.009 | |
| 23.00–24.00 | 1.002 | 0.998 | 1.005 |
To explore whether low CoV areas were those with higher noise levels (potentially suggesting high noise and less relief periods), we examined mean noise levels (Table 18). For the latter two periods, mean noise levels were higher in the low CoV postcodes (41 vs. 37 dB for 22.00–23.00 hours; 31 vs. 24 dB for 23.00–24.00 hours), However, for the period 19.00–22.00 hours, the mean noise levels were 41 dB in low CoV areas compared with 43 dB in high CoV areas. We therefore could not readily infer that a lack of relief periods (or at least some periods of lower noise exposure) was related to the association with hospitalisation.
| Period (hours) | Hospital admission | SD | CoV | |
|---|---|---|---|---|
| Mean | Median | |||
| 19.00–22.00 | 41.2 | 40.73 | 5.98 | low |
| 42.59 | 42.21 | 7.72 | high | |
| 22.00–23.00 | 41.02 | 40.32 | 6.61 | low |
| 37.44 | 36.61 | 7.93 | high | |
| 23.00–24.00 | 31.47 | 31.5 | 10.19 | low |
| 24.02 | 23.68 | 10.31 | high | |
Chapter 4 Discussion
Summary of results
Descriptive summary of daily aircraft noise data
We found that the morning shoulder period (06.00–07.00 hours) was the noisiest among all periods (mean 50.92 dB; 90th percentile 52.93 dB). Daytime (07.00–15.00 hours) aircraft noise levels were typically only slightly lower than the morning shoulder period (mean 49.87 dB; 90th percentile 51.50 dB). Night quota periods (23.30–04.30 hours) are typically times when people are sleeping, but we found that the average noise levels across postcodes from 23.00 to 24.00 hours and 24.00 to 04.30 hours were 41.06 and 29.81 dB, respectively.
We found that during 07.00–15.00 hours, postcodes within the study area experienced an average of eight flight events. Morning shoulder (06.00–07.00 hours) had an average of three events, while night-time (04.30–06.00 hours) had an average of one flight event.
Approaches to identifying respite and/or relief period
We did not have information on flight trials so attempted to identify relief periods (caused by e.g. wind direction changes as well as trials) in other ways. A priori definition of appreciable changes in noise did not identify enough postcodes. We therefore examined CoV of daily noise levels at postcodes. Highest variability was seen in night-time periods, with 24.00–04.30 hours having the highest mean CoV, followed by 04.30–06.00 and 23.00–24.00 hours.
Daily aircraft noise and material and health inequality
We examined the relationship between aircraft noise Lday, Leve and LAeq24 and three different deprivation/inequality measures. While postcodes near Heathrow with the least material or health deprivation experienced the lowest daily noise levels between 2014 and 2018, the relationship with deprivation measures, including the Carstairs index and fuel poverty, was complex and did not appear to have a clear gradient. A gradient was more evident between Lnight and avoidable death rate. The fuel poverty rate had a weaker relationship with daily aircraft noise than Carstairs index and avoidable death rate.
Short-term impact of aircraft noise on cardiovascular morbidity and mortality
We included all recorded hospitalisations (n = 442,442) and deaths (n = 49,443) in 2014–18 due to CVD. We used conditional logistic regression to estimate the OR and adjusted for PM2.5 concentration, temperature and holidays. We estimated an increase in risk for a 5-dB increment in noise during the evening (Leve OR = 1.005, 95% CI 1.000 to 1.010), particularly from 22.00 to 23.00 hours (OR = 1.006, 95% CI 1.002 to 1.010) for all CVD admissions. We found some evidence for effect modification by age, ethnicity, deprivation and season, but patterns were not consistent. The findings provide support for a potential mechanism through which aircraft noise may disturb sleep and elevate blood pressure, contributing to increased risk of cardiovascular hospitalisation.
Additionally, we found that an increased risk of CVD hospitalisation for increases in noise during the night-time hours (19.00–22.00, 22.00–23.00 and 23.00–24.00 hours) was only seen in postcodes with lower CoV. The average noise levels in the lower CoV postcodes were higher than other postcodes in two of the three periods – only giving partial support to the hypothesis that areas with higher noise levels and fewer relief periods have higher CVD admission risks. The impact of relief periods needs further research, ideally looking at other relevant outcomes (e.g. sleep disturbance, blood pressure, heart rate variability).
Reflections on what was and what was not successful in the programme
Delays
The dissemination of results was originally scheduled for 31 August 2020. The delays were caused by (1) relocation of the project from Imperial College to the University of Leicester, (2) complexities in the modelling process, which had not been anticipated by the noise consultancy conducting the modelling and (3) the COVID-19 pandemic, which among other impacts, slowed the recruitment of a researcher to conduct the analyses. The NIHR was supportive and responsive to communications about the delays throughout the project and a no-cost extension was agreed.
Strengths
We created and analysed a large dataset, which included daily average noise levels for approximately 155,000 postcodes near Heathrow airport. The AEDT version 3b was used to assess aircraft noise levels at each of the 155,000 postcodes in the vicinity of Heathrow airport from 1 January 2014 to 31 December 2018. These data are probably those with the highest resolution regarding Heathrow airport’s daily aircraft noise levels. Our analysis of noise data concludes that exposure to daily aircraft noise remains an environmental problem for some communities near Heathrow airport.
The study area encompassed around 6.3 million people who resided near Heathrow airport in 2011. The high temporal resolution of our daily aircraft noise exposure data was an additional strength. Thirdly, our noise data were estimated for eight time bands, allowing us to distinguish between different daytime and night-time periods.
In the subsection where we examined the association between daily aircraft noise exposure and deprivation, we used a range of deprivation domains, including not only poverty but also health disparities.
Our study focused on the impact of short-term aircraft noise on cardiovascular morbidity and mortality and, to our knowledge, is one of only three such studies to date. In our analysis of population health, we included nearly all hospitalisations and deaths attributable to CVD, providing sufficient statistical power to detect an effect. By design, the case-crossover design controlled for significant measured and unmeasured confounders, such as lifestyle factors, ethnicity and age. Differentiating the effects of noise during specific times of the day, evening and night provided evidence for certain biological mechanisms observed in previous research.
Patient and public involvement
The methods and results were discussed at meetings of the study scientific advisory board, which includes representatives from the non-governmental Aviation Environment Federation and the Heathrow Association for the Control of Aircraft Noise, a community group set up over 50 years ago to represent people living under the Heathrow flight path.
Equality, diversity and inclusion issues
Our study included 442,442 naturally occurring hospital admissions and 49,443 fatalities from CVD, after removing some duplicate reports and records with no control variables. Males made up 58.0% of hospital admissions, with 56.7% being above the age of 65 years. Among those who stated their ethnicity, 9.4% were black and 11.4% were South Asian.
Limitations
Among the limitations are that the study area was designed to capture outer bounds of the CAA annual average aircraft noise contours in 2011. Some postcodes outside the study area could still be affected by aircraft noise but were not included in the analysis. However, given the spatial and temporal resolution and size of the data, this was a reasonable compromise.
In our analysis of deprivation, we used area-level not individual-level noise and deprivation estimates therefore the ecological fallacy may apply. Heathrow airport is situated close to highly populated areas, some of which are very wealthy, so may not be representative of other airports.
We were only able to examine outdoor noise levels and were not able to take account of housing characteristics, including double glazing, which may have affected indoor noise exposures.
Misclassification bias may also have been introduced because we used noise exposure at small geographical level rather than individual level. Another source of potential misclassification is that individuals may move outside of the postcode to which their exposure has been assigned at different periods throughout the day. We expect less exposure misclassification in the evening and night-time hours because individuals are more likely to be at their postcode of residence during these times. We also expect less misclassification among older individuals throughout the day and night, as they are less likely to travel away from home for work or school during the day. This may partially explain why effect estimates were highest during evening and night-time hours, and among individuals over the age of 65 years. Lastly, exposure misclassification may have been introduced because data on exact time of admission and death were not available, and we were therefore unable to define the precise window of exposure before an event occurs. To compensate for this, we used the average of lag 0 and lag 1 before the event day to ensure the defined exposure window captures the true exposure. Lastly, misclassification bias may be introduced due to moving home; according to English Housing Survey, between 9% and 11.3% of households in England moved home per year between 2011 and 2018. 47
Chapter 5 Conclusion
We have produced one of the most detailed datasets available on aircraft noise exposure at one of the world’s busiest airports, covering a 5-year period at different times of day and night corresponding to airline operation periods. We conducted one of extremely few studies on short-term aircraft noise exposure and CVD hospitalisation and mortality. Our findings suggested that short-term noise exposure during the evening and night-time may be linked to an increased risk of all CVD hospital admissions, which would fit with a role for sleep disturbance. Numbers of deaths were small relative to hospital admissions, and we lacked statistical power to detect associations. Our results also suggest that sustained (low variability) noise exposure may be an important characteristic in relation to the health associations. This is partly supported by evidence that showed a significant association between aircraft noise during night-time and evening and hospital admissions in regions with low noise variability, but this was not consistent as to whether absolute noise levels were higher or lower.
In further analyses, we found some degree of correlation between different measures of deprivation and exposure to aircraft noise. While these were not straightforwardly linear, they did suggest that deprived areas were more exposed, particularly to night-time noise. In health analyses, there were interactions seen with deprivation (Carstairs index) with increase in risk of CVD hospitalisation in relation to acute aircraft noise exposure during late night hours among individuals residing in the third and fourth quintiles of deprivation (but not the most deprived quintile). This analysis is one of very few to investigate the relationship between aircraft noise and heath inequality.
This information can be informative for national health policy, local residents and for airports and help inform future health and exposure studies. As air transport increases post-pandemic, information on noise exposures as well as views from community groups can inform future airport policies.
Recommendations for future research
We recommend the following future studies to further advance the knowledge:
-
Make use of natural experiments to assess the impact of intervention on short-term aircraft noise exposure on CVD.
-
Studies looking at interventions such as double glazing, other noise insulation or flight changes, linking indoor and outdoor noise measurements with objective measures of CVD risk; for example, blood pressure, heart rate variability, sleep and blood biomarkers.
-
Further investigation of the relationship between noise variation and the risk of CVD, using novel noise metrics.
-
Consideration of deprivation and ethnicity in all studies examining associations between aircraft noise and health outcomes as these had effect-modifying impacts in the current study related to cardiovascular health.
Implications for future studies
-
We discovered that the period 24.00–04.30 hours had the greatest daily noise variation. Future studies on the health effects of aircraft noise pollution focused on Heathrow airport are advised to take the variation of night-time noise levels into account. Further work on noisy events is important (we only calculated these for N60 and N65 for 1 year and exploration of lower cut-points and other years would be helpful).
-
We found that the morning quota period (06.00–07.00 hours) had the highest mean daily aircraft noise level per postcode, which contrasts sharply with the mean noise levels during the night quota period (23.30–06.00 hours). This implies that future epidemiological studies focusing on Heathrow airport are recommended to distinguish this period from the regular night-time period (23.00–06.00 hours).
-
We identified a positive link between avoidable death rate and daily aircraft noise exposure, particularly at night. This suggests a link between health deprivation and aircraft noise levels. Future epidemiological studies focusing on Heathrow airport are recommended to consider health deprivation as a potential confounder.
Additional information
Contributions of authors
Xiangpu Gong (https://orcid.org/0000-0002-8985-9756) (Research Associate, Epidemiology) helped to design noise exposure inequalities analyses, conducted the descriptive and exposure inequalities analyses and prepared results for publication.
Nicole Itzkowitz (https://orcid.org/0000-0001-5076-3522) (Research Assistant, Statistics) conducted the health analyses and prepared results for publication.
Calvin Jephcote (https://orcid.org/0000-0003-0464-8448) (Lecturer in Practice and Research Fellow in Geographical Information Science, Exposure Science) developed and collated environmental exposure assessment data, interpreted and prepared results for publication.
Kathryn Adams (https://orcid.org/0000-0002-5305-709X) (Research Assistant, Exposure Science) developed and collated environmental exposure assessment data.
Glory O Atilola (https://orcid.org/0000-0002-4678-2015) (Research Associate, Biostatistics) conducted the health analyses and prepared results for publication.
John Gulliver (https://orcid.org/0000-0003-3423-2013) (Professor of Environmental and Exposure Sciences) designed the study environmental exposure assessments, set up the contract with environmental consultants to provide the aircraft noise data, interpreted and prepared results for publication.
Marta Blangiardo (https://orcid.org/0000-0002-1621-704X) (Professor of Biostatistics) designed the study, designed the statistical analyses, conducted the health analyses, interpreted and prepared results for publication.
Anna Hansell (https://orcid.org/0000-0001-9904-7447) (Professor of Environmental Epidemiology, University of Leicester), initiated the study, conceived and designed the analyses, helped arrange ethics and governance permissions for health data access, set up contract specification with environmental consultants to provide the aircraft noise data, set up the study scientific advisory board, interpreted and prepared the results for publication.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/UTCE9104.
Primary conflicts of interest: Conflicts of interest were reported by Nicole Itzkowitz (NIHR award), John Gulliver (NIHR awards), Anna Hansell (NIHR awards, chair of the Committee on the Medical Effects of Air Pollution, payment for role as PhD examiner in Finland 2022, Travel and subsistence costs for international 2-day meeting in Milan on air pollution).
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data is used (#datasaveslives). You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
The aircraft noise exposure data are available to other academic researchers on request to the corresponding author.
Ethics statement
The study was covered by national research ethics approval from the London – South East Research Ethics Committee, reference 17/LO/0846 (date of opinion, 29 June 2017). Data access to confidential patient information without consent was covered by the Health Research Authority Confidentiality Advisory Group under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (section 251 support), reference: 20/CAG/0028 (outcome date 24 March 2020, section 251 Register Index Sheet application number A02476).
Carstairs index of deprivation (England and Wales, 2011)
The Carstairs index is an indicator of relative deprivation that is commonly used in spatial epidemiology to identify socioeconomic confounding. 48,49 This deprivation index is constructed from four unweighted UK Census variables, which describe the level of male unemployment, overcrowding, private vehicle ownership and social composition in each community.
A revised form of the Carstairs index was constructed for census output area and lower layer super output areas in England and Wales, using the 2001 classification of low social classes devised by Norman. 48,49 The revised low social class variable approximates its counterpart from the 1991 Census, developed to account for Office for National Statistics methodology and classification changes in later censuses.
Datasets from the 2011 Census were obtained from Nomis (www.nomisweb.co.uk), the official online delivery service of labour market statistics provided by the Office for National Statistics. Tables KS602EW, QS409EW, KS404EW and QS607EW contained the necessary information to create the Carstairs index for 2011 across England and Wales.
Table 19 lists the variable names, descriptions and formulas.
| Variable name | Description | Calculation |
|---|---|---|
| Proportion of ‘male unemployment’ (KS602EW) | ‘Unemployed males age 16–74 years’ ÷ ‘economically active males age 16–74 years’ | KS602EW0005 ÷ (KS602EW0002 + KS602EW0003 + KS602EW0004 + KS602EW0005 + KS602EW0006) |
| Proportion of ‘overcrowded households’ (QS409EW) | (‘Over 1 and up to 1.5 persons per room’ + ‘over 1.5 persons per room’) ÷ ‘all households’ | (QS409EW0004 + QS409EW0005) ÷ QS409EW0001 |
| Proportion of ‘households without vehicle ownership’ (KS404EW) | ‘No cars or vans in household’ ÷ ‘all households’ | KS404EW0002 ÷ KS404EW0001 |
| Proportion of ‘persons from a low social class’ (QS607EW) | (L11.2 + L12.2 + L12.4 + L12.5 + L12.7 + L13.1 + L13.2 + L13.4 + L13.5) ÷ ‘all persons’ | (QS607EW0035 + QS607EW0038 + QS607EW0040 + QS607EW0041 + QS607EW0043 + QS607EW0045 + QS607EW0046 + QS607EW0048 + QS607EW0049) ÷ QS607EW0001 |
Each of these variables were z scored (mean-centred and divided by their SD) and all four z scores were summed to return an index value measuring the relative level of deprivation in each community. A value of 0 identifies communities that follow the national average of England and Wales, with negative values identifying increased affluence, and positive values identifying increased levels of deprivation.
Carstairs index values for the 181,408 COA communities in England and Wales were then categorised in quintile groups, to control for any outliers within the data. This procedure was repeated for the 34,753 LSOA communities in England and Wales.
Nitrogen Dioxide Concentration
Nitrogen dioxide (NO2) concentrations from all sources of pollution in µg/m3 were obtained from a land use regression-modelled raster surface with a 50-m grid resolution, developed by Gulliver et al. 50 This pollution model is based on a multivariate regression equation that describes the relationship between sample locations and environmental variables (i.e. rural–urban land cover classifications and road network data within several proximity buffer zones).
Postcode centroids (i.e. points representing the population-weighted centre of each postcode unit) were intersected with the continuous NO2 raster surface, to extract an exposure value at each location.
Road transport noise (annual, 2013)
Modelled road-transport noise estimates were calculated in accordance with the CNOSSOS-EU common framework for noise assessment methods developed by the European Commission (2002/49/EC). For the purposes of this study, the CNOSSOS-EU model algorithms were implemented in PostgreSQL via the PostGIS v2.1 extension, following the protocol described by Morley et al. 51
Annual average daily traffic counts and traffic speeds across the UK road network in 2013 enter the model, together with information relating to the surface roughness of land cover, building heights, wind profiles and average temperatures in 2013.
The CNOSSOS-EU model ran on the ALICE high-performance computing facility at the University of Leicester. Figure 9 (adapted from Gulliver et al. 52), describes the workflow of the CNOSSOS-EU model.
FIGURE 9.
Workflow of the CNOSSOS-EU model.
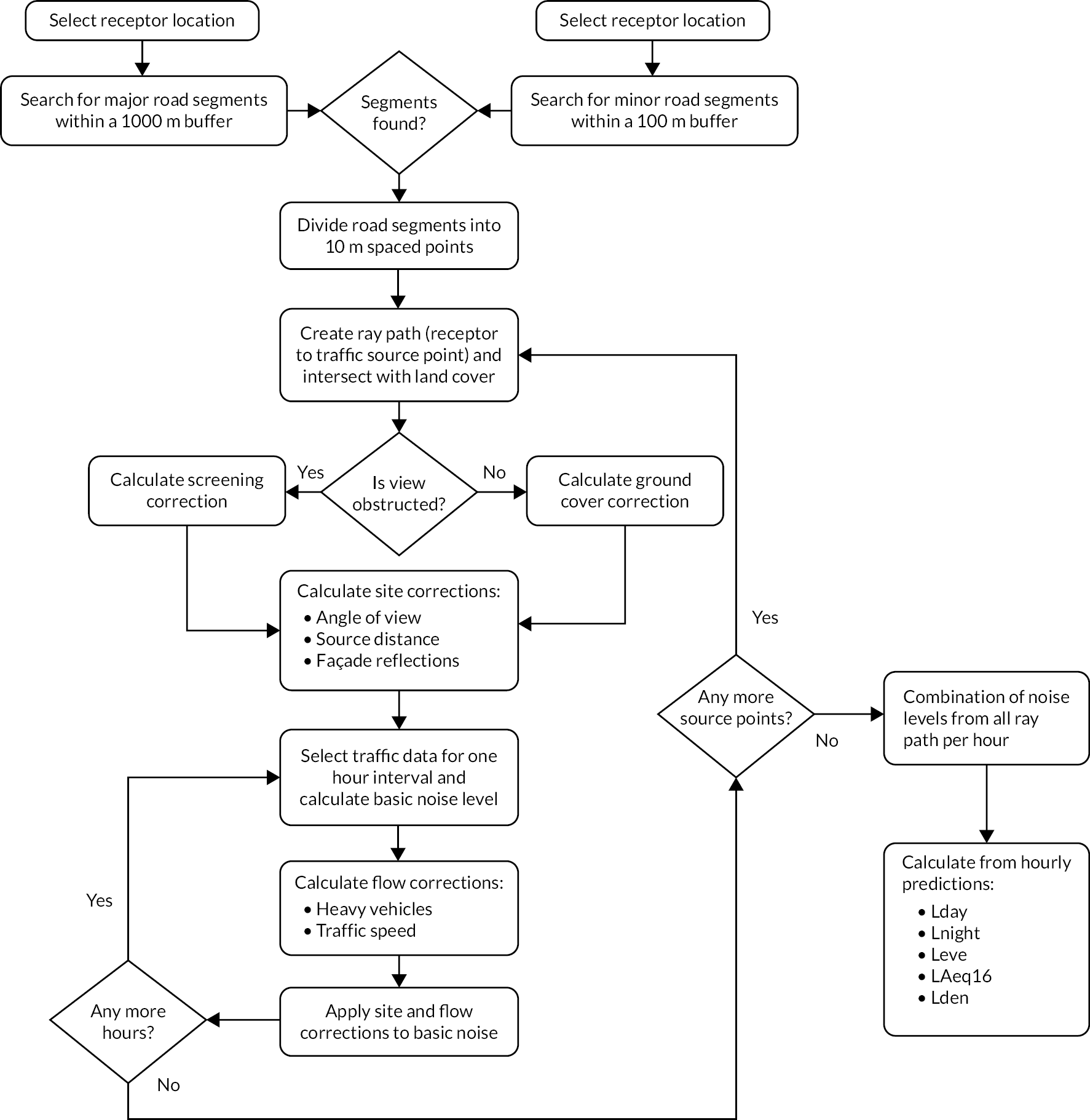
In brief, the coordinates of each receptor (residential postcode centroid) are assigned to the closest building. The building façade that is likely to experience the most noise levels is identified (i.e. traffic count on a nearby road/road distance), and a receptor (point) is placed 1 m away from the building. A geographical information systems operation locates all major roads within a 1000-m radius and all minor roads within a 100-m radius of each receptor.
Noise exposure from road transport was reported in accordance with five noise metrics that are ‘A’ frequency weighted. The ‘A’ weighting is a standard weighting of the audible frequencies designed to reflect the response of the human ear to noise (between 500 Hz and 6 kHz):
-
Lday is the A-weighted equivalent noise level (Leq) over the 12-hour day period (07.00–19.00 hours), also known as the day noise indicator.
-
Levening is the A-weighted equivalent noise level (Leq) over the 4-hour evening period (19.00–23.00 hours), also known as evening noise indicator.
-
Lnight is the A-weighted equivalent noise level (Leq) over the 8-hour night period (23:00–07:00 hours), also known as the night noise indicator.
-
LAeq16 is the A-weighted equivalent noise level (Leq) over the 16-hour day period (07.00–23:00 hours).
-
Lden is the A-weighted equivalent noise level (Leq) over a whole day, but with a penalty of +10 dB(A) for night-time noise (22.00–07.00 hours) and +5 dB(A) for evening noise (19.00–23.00 hours), also known as the day-evening-night noise indicator.
Hospitalisation and death registration data are held by and available through NHS Digital to researchers meeting relevant governance standards (https://digital.nhs.uk/services/data-access-request-service-dars).
All other data are available online. The avoidable death rate can be obtained from government statistics (gov.uk). The Carstairs index is accessible via the UK Data Archive. The Office for National Statistics provides the fuel poverty rate and percentage of non-white population per local authority district.
Information governance statement
The study was covered by national research ethics approval from the London – South East Research Ethics Committee, reference 17/LO/0846 (date of opinion, 29 June 2017). Data access to confidential patient information without consent was covered by the Health Research Authority Confidentiality Advisory Group under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (section 251 support) – HRA CAG reference: 20/CAG/0028 (CAG outcome date 24 March 2020, section 251 Register Index Sheet Application number A02476).
The University of Leicester is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation 2016/679. The University of Leicester acted as data controller and both University of Leicester and Imperial College London acted as data processors (the University of Leicester held the exposure data and made decisions on the analyses). Imperial College London held the health data and we supplied them with the exposure data, which was integrated into the health data, and joint decisions were taken on the health analyses).
For organisations where the sponsoring body is also the data controller under the data protection legislation, the University of Leicester is the data controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our data protection officer here: https://le.ac.uk/policies/insurance/gdpr-notice.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Public Health Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Gong X, Itzkowitz N, Atilola G, Adams K, Jephcote C, Blangiardo M, et al. The association between aircraft noise levels and material and health deprivation. Proceedings of the Inter-Noise conferences, 2022.
Gong X, Adams K, Jephcote C, Itzkowitz N, Atilola G, Blangiardo M, et al. Characteristics of daily aircraft noise near Heathrow Airport. Proceedings of the 2022 UK and Ireland Exposure Science Meeting, 2022.
Itzkowitz N, Gong X, Adams K, Jephcote C, Gulliver J, Hansell A, Blangiardo M. Aircraft noise and cardiovascular morbidity and mortality near Heathrow Airport: a case-crossover study. Proceedings of the 34th Annual Conference of the International Society for Environmental Epidemiology, 2022.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- World Health Organization . Burden of Disease from Environmental Noise: Quantification of Healthy Life Years Lost in Europe 2011. www.who.int/publications/i/item/9789289002295 (accessed 23 November 2022).
- van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens 2012;30:1075-86.
- Babisch W, Kamp I. Exposure-response relationship of the association between aircraft noise and the risk of hypertension. Noise Health 2009;11:161-8.
- Huang D, Song X, Cui Q, Tian J, Wang Q, Yang K. Is there an association between aircraft noise exposure and the incidence of hypertension? A meta-analysis of 16784 participants. Noise Health 2015;17:93-7.
- Vienneau D, Schindler C, Perez L, Probst-Hensch N, Roosli M. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res 2015;138:372-80.
- Vienneau D, Eze IC, Probst-Hensch N, Röösli M. Association between transportation noise and cardio-metabolic diseases: an update of the WHO meta-analysis n.d. https://edoc.unibas.ch/70857/1/ICA_2019_manuscript%20Vienneau%20final.pdf (accessed 23 November 2023).
- Van Kempen E, Casas M, Pershagen G, Foraster M. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health 2018;15.
- Waye KP, van Kempen E. Non-auditory Effects of Noise: An Overview of the State of the Science of the 2017–2020 Period n.d. www.icben.org/2021/ICBEN%202021%20Papers/full_paper_29017.pdf (accessed 23 November 2023).
- Hamilton S, Fenech B, Hansell A, Gong X, Vienneau D. Systematic Review and Meta-analyses of Association between Transportation Noise and Ischaemic Heart Disease Based on Studies Published between 1994–2022 n.d. https://doi.org/10.3397/IN_2022_0393 (accessed 23 November 2023).
- Hansell AL, Blangiardo M, Fortunato L, Floud S, de Hoogh K, Fecht D, et al. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ 2013;347.
- Munzel T, Sorensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J 2016;38:557-64.
- Easterlin RA. Explaining happiness. Proc Natl Acad Sci U S A 2003;100:11176-83.
- Kroesen M, Molin EJ, Van Wee B. Testing a theory of aircraft noise annoyance: a structural equation analysis. J Acoust Soc Am 2008;123:4250-60.
- Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol Off J German Cardiac Soc 2015;104:23-30.
- Walker ED, Brammer A, Cherniack MG, Laden F, Cavallari JM. Cardiovascular and stress responses to short-term noise exposures-a panel study in healthy males. Environ Res 2016;150:391-7.
- Tobias A, Recio A, Diaz J, Linares C. Noise levels and cardiovascular mortality: a case-crossover analysis. Eur J Prev Cardiol 2015;22:496-502.
- Recio A, Linares C, Banegas JR, Diaz J. The short-term association of road traffic noise with cardiovascular, respiratory, and diabetes-related mortality. Environ Res 2016;150:383-90.
- Pearson T, Campbell MJ, Maheswaran R. Acute effects of aircraft noise on cardiovascular admissions: an interrupted time-series analysis of a six-day closure of London Heathrow Airport caused by volcanic ash. Spat Spatio-Temporal Epidemiol 2016;18:38-43.
- Office for National Statistics . Postal Geography n.d. www.ons.gov.uk/methodology/geography/ukgeographies/postalgeography (accessed 23 November 2022).
- Nomis . Postcode Headcounts and Household Estimates – 2011 Census 2013. www.nomisweb.co.uk/census/2011/postcode_headcounts_and_household_estimates (accessed 22 November 2023).
- Federal Aviation Administration . Aviation Environmental Design Tool (AEDT) Version 3b Technical Manual 2019. https://rosap.ntl.bts.gov/view/dot/49814 (accessed 23 November 2023).
- Porter N, Sanchez D, Holgate C. A Review on the State of the Art on Respite. Brighton: Anderson Acoustics; 2016.
- Heathrow Airport Limited . Respite Research 2022. www.heathrow.com/company/local-community/noise/making-heathrow-quieter/respite-research (accessed 23 November 2022).
- Beghelli S, De Coulon A, O’Mahony M. Health benefits of reducing aircraft pollution: evidence from changes in flight paths. J Popul Econ 2023;36:2581-607. https://doi.org/10.1007/s00148-023-00964-y.
- Tucker K, Williams R, Leighton S. Heathrow Airport: Early Morning Arrival Trial, Final Report 2013. https://hacan.org.uk/wp-content/uploads/2022/03/EMAT_final-_report.pdf (accessed 23 November 2022).
- Nelson JP. Hedonic Methods in Housing Markets. New York, NY: Springer; 2008.
- Tonne C, Milà C, Fecht D, Alvarez M, Gulliver J, Smith J, et al. Socioeconomic and ethnic inequalities in exposure to air and noise pollution in London. Environ Int 2018;115:170-9.
- Dreger S, Schüle SA, Hilz LK, Bolte G. Social inequalities in environmental noise exposure: a review of evidence in the WHO European Region. Int J Environ Res Public Health 2019;16.
- Hajat A, MacLehose RF, Rosofsky A, Walker KD, Clougherty JE. Confounding by socioeconomic status in epidemiological studies of air pollution and health: challenges and opportunities. Environ Health Perspect 2021;129.
- Allik M, Brown D, Dundas R, Leyland AH. Developing a new small-area measure of deprivation using 2001 and 2011 census data from Scotland. Health Place 2016;39:122-30.
- Liddell C, Morris C. Fuel poverty and human health: a review of recent evidence. Energy Policy 2010;38:2987-97.
- Simcock N, Walker G, Day R. Fuel poverty in the UK: beyond heating. People Place Policy 2016;10:25-41.
- Mercer JB. Cold: an underrated risk factor for health. Environ Res 2003;92:8-13.
- Dear KB, McMichael AJ. The Health Impacts of Cold Homes and Fuel Poverty. British Medical Journal Publishing Group; 2011.
- Department for Business, Energy and Industrial Strategy . Annual Fuel Poverty Statistics Report: 2022 (2020 Data) 2022. www.gov.uk/government/collections/fuel-poverty-statistics (accessed 23 November 2022).
- Tang KK, Petrie D, Rao DSP. Measuring health inequality with realization of potential life years (RePLY). Health Econ 2009;18:S55-75.
- Office for National Statistics . Avoidable Mortality in the UK QMI 2022. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/methodologies/avoidablemortalityinenglandandwalesqmi (accessed 23 November 2022).
- Office for National Statistics . Avoidable Mortality in Great Britain Statistical Bulletins 2021. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/avoidablemortalityinenglandandwales/previousReleases (accessed 23 November 2022).
- StataCorp . Stata Statistical Software: Release 17 2021.
- Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 1991;133:144-53.
- Mittleman MA, Maclure M, Robins JM. Control sampling strategies for case-crossover studies: an assessment of relative efficiency. Am J Epidemiol 1995;142:91-8.
- Saucy A, Schäffer B, Tangermann L, Vienneau D, Wunderli J-M, Röösli M. Does night-time aircraft noise trigger mortality? A case-crossover study on 24 886 cardiovascular deaths. Eur Heart J 2021;42:835-43.
- Konstantinoudis G, Minelli C, Vicedo-Cabrera AM, Ballester J, Gasparrini A, Blangiardo M. Ambient heat exposure and COPD hospitalisations in England: a nationwide case-crossover study during 2007–2018. Thorax 2022;77:1098-104.
- Carstairs V, Morris R. Deprivation and health in Scotland. Health Bull (Edinb) 1990;48:162-75.
- R Core Team . R: A Language and Environment for Statistical Computing 2018.
- Carstensen B, Plummer M, Laara E, Hills M. Epi: A Package for Statistical Analysis in Epidemiology 2022. https://CRAN.R-project.org/package=Epi (accessed 23 November 2022).
- Department for Levelling Up, Housing and Communities and Ministry of Housing, Communities and Local Government . English Housing Survey Data on New Households and Recent Movers n.d. www.gov.uk/government/statistical-data-sets/new-households-and-recent-movers (accessed 23 November 2022).
- Carstairs V, Morris R. Deprivation and health in Scotland. Aberdeen: Aberdeen University Press; 2002.
- Norman P. Identifying change over time in small area socio-economic deprivation. Appl Spatial Analysis Policy 2010;3:107-38.
- Gulliver J, De Hoogh K, Hansell A, Vienneau D. Development and back-extrapolation of NO2 land use regression models for historic exposure assessment in Great Britain. Environ Sci Technol 2013;47:7804-11.
- Morley D, De Hoogh K, Fecht D, Fabbri F, Bell M, Goodman P, et al. International scale implementation of the CNOSSOS-EU road traffic noise prediction model for epidemiological studies. Environ Pollut 2015;206:332-41.
- Gulliver J, Morley D, Vienneau D, Fabbri F, Bell M, Goodman P, et al. Development of an open-source road traffic noise model for exposure assessment. Environ Model Softw 2015;74:183-93.
Appendix 1 Descriptive summary of daily aircraft noise levels by season
| Season | Variables | Aircraft (N) | Mean | SD | Min | Max | 90th percentile |
|---|---|---|---|---|---|---|---|
| Summer | LAeq 04.30–06.00 | 740,333 | 24.92 | 7.821 | 7.123 | 58.21 | 36.3 |
| LAeq 06.00–07.00 | 740,333 | 40.68 | 6.43 | 16.39 | 76.09 | 48.84 | |
| LAeq 07.00–15.00 | 740,333 | 42.03 | 5.312 | 27.25 | 72.1 | 48.84 | |
| LAeq 15.00–19.00 | 740,333 | 41.69 | 5.238 | 27.7 | 69.67 | 48.4 | |
| LAeq 19.00–22.00 | 740,333 | 41.25 | 5.326 | 22.86 | 68.79 | 48.23 | |
| LAeq 22.00–23.00 | 740,333 | 36.96 | 7.186 | 12.65 | 70.29 | 45.63 | |
| LAeq 23.00–24.00 | 740,333 | 30.64 | 6.505 | 12.65 | 67.17 | 39.68 | |
| LAeq 24.00–04.30 | 696,831 | 14.98 | 6.392 | 0.00 | 55.89 | 22.99 | |
| N60 04.30–06.00 | 155,671 | 0.64 | 1.444 | 0 | 7.196 | 3.09 | |
| N60 06.00–07.00 | 155,671 | 3.194 | 6.206 | 0 | 38.64 | 11.82 | |
| N65 07.00–15.00 | 155,671 | 6.848 | 23.95 | 0 | 323.8 | 12.68 | |
| N65 15.00–19.00 | 155,671 | 3.158 | 11.25 | 0 | 170.4 | 5.95 | |
| N65 19.00–22.00 | 155,671 | 2.331 | 8.247 | 0 | 117.3 | 4.1 | |
| N65 22.00–23.00 | 155,671 | 0.554 | 2.869 | 0 | 33.39 | 0.22 | |
| N60 23.00–24.00 | 155,671 | 0.722 | 1.65 | 0 | 21.24 | 2.67 | |
| N60 24.00–04.30 | 155,671 | 0.338 | 0.856 | 0 | 8 | 1 | |
| Summer transition | LAeq 04.30–06.00 | 740,333 | 23.71 | 6.262 | 10.03 | 54.02 | 32.49 |
| LAeq 06.00–07.00 | 740,333 | 39.88 | 5.662 | 19.47 | 74 | 46.7 | |
| LAeq 07.00–15.00 | 740,333 | 41.65 | 5.658 | 26.46 | 75.11 | 48.41 | |
| LAeq 15.00–19.00 | 740,333 | 41.63 | 5.388 | 27.44 | 74.51 | 48.1 | |
| LAeq 19.00–22.00 | 740,333 | 41.65 | 5.239 | 24.9 | 75.17 | 48.04 | |
| LAeq 22.00–23.00 | 740,333 | 39.94 | 5.111 | 20.97 | 69.87 | 46.54 | |
| LAeq 23.00–24.00 | 740,333 | 30.2 | 6.079 | 12.17 | 63.72 | 38.42 | |
| LAeq 24.00–04.30 | 740,333 | 14.22 | 5.147 | 1.344 | 44.01 | 20.9 | |
| N60 04.30 –.600 | 115,206 | 0.579 | 1.263 | 0 | 5.951 | 2.49 | |
| N60 06.00–07.00 | 115,206 | 2.912 | 5.503 | 0 | 32.62 | 11.44 | |
| N65 07.00–15.00 | 115,206 | 7.738 | 24.23 | 0 | 320.9 | 16.47 | |
| N65 15.00–19.00 | 115,206 | 3.549 | 11.57 | 0 | 163.5 | 7.01 | |
| N65 19.00–22.00 | 115,206 | 2.599 | 8.395 | 0 | 115.5 | 5.03 | |
| N65 22.00–23.00 | 115,206 | 0.796 | 2.306 | 0 | 32.57 | 2.19 | |
| N60 23.00–24.00 | 115,206 | 0.411 | 0.78 | 0 | 8.897 | 1.21 | |
| N60 24.00–04.30 | 115,206 | 0.0768 | 0.132 | 0 | 1.194 | 0.2 | |
| Winter | LAeq 04.30–06.00 | 740,333 | 28.98 | 7.055 | 9.872 | 61.08 | 38.79 |
| LAeq 06.00–07.00 | 740,333 | 41.51 | 5.989 | 18.39 | 74.98 | 49.08 | |
| LAeq 07.00–15.00 | 740,333 | 43.17 | 5.11 | 28.61 | 72.32 | 49.82 | |
| LAeq 15.00–19.00 | 740,333 | 42.6 | 5.111 | 27.97 | 69.86 | 49.13 | |
| LAeq 19.00–22.00 | 740,333 | 42.34 | 5.385 | 24.76 | 74.94 | 49.53 | |
| LAeq 22.00–23.00 | 740,333 | 38.44 | 5.764 | 19.54 | 67.61 | 46.09 | |
| LAeq 23.00–24.00 | 740,333 | 23.72 | 6.442 | 8.987 | 58.05 | 33.31 | |
| LAeq 24.00–04.30 | 727,635 | 12.5 | 5.937 | 0.000267 | 51.31 | 19.93 | |
| N60 04.30–06.00 | 115,206 | 0.911 | 1.943 | 0 | 8.742 | 3.97 | |
| N60 06.00–07.00 | 115,206 | 2.833 | 5.324 | 0 | 30.74 | 11.18 | |
| N65 07.00–15.00 | 115,206 | 8.216 | 23.46 | 0 | 300.4 | 18.89 | |
| N65 15.00–19.00 | 115,206 | 3.873 | 11.67 | 0 | 158.8 | 7.88 | |
| N65 19.00–2.200 | 115,206 | 2.675 | 7.985 | 0 | 108.4 | 5.55 | |
| N65 22.00–23.00 | 115,206 | 0.629 | 1.676 | 0 | 23.24 | 1.77 | |
| N60 23.00–2.400 | 115,206 | 0.21 | 0.379 | 0 | 4.384 | 0.58 | |
| N60 24.00–04.30 | 115,206 | 0.107 | 0.192 | 0 | 2.065 | 0.29 | |
| Winter transition | LAeq 04.30–06.00 | 740,333 | 24.15 | 8.307 | 5.009 | 64.36 | 35.13 |
| LAeq 06.00–07.00 | 740,333 | 41.35 | 6.626 | 13.86 | 78.37 | 49.66 | |
| LAeq 07.00–15.00 | 740,333 | 42.64 | 5.445 | 27.37 | 78.34 | 49.32 | |
| LAeq 15.00–19.00 | 740,333 | 42.33 | 5.466 | 26.41 | 75.24 | 49.3 | |
| LAeq 19.00–22.00 | 740,333 | 42.03 | 5.548 | 21.68 | 75.46 | 48.9 | |
| LAeq 22.00–23.00 | 740,333 | 40.43 | 5.805 | 20.43 | 75.46 | 48.15 | |
| LAeq 23.00–24.00 | 740,333 | 31.11 | 7.531 | 11.91 | 72.29 | 41.34 | |
| LAeq 24.00–04.30 | 702,071 | 14.12 | 5.69 | 7.16E−05 | 53.42 | 21.51 |
List of abbreviations
- AEDT
- Aviation Environmental Design Tool
- CAA
- Civil Aviation Authority
- CHD
- coronary heart disease
- CI
- confidence interval
- COA
- census output areas
- CoV
- coefficients of variation
- CVD
- cardiovascular disease
- dB
- decibel
- EMAT
- Early Morning Arrival Trial
- ICD-10
- International Classification of Diseases Version 10
- IHD
- ischaemic heart disease
- LAD
- local authority district
- LAeq24
- equivalent continuous sound pressure level during 24 h
- Lday
- equivalent continuous sound pressure level during 07.00–19.00 hours
- Leve
- equivalent continuous sound pressure level during 19.00–23.00 hours
- Lnight
- equivalent continuous sound pressure level during 23.00–07.00 hours
- LSOA
- lower layer super output areas
- N60
- number of flights > 60 dB in night-time
- N65
- number of flights > 65 dB in daytime
- NHS
- National Health Service
- NIHR
- National Institute for Health and Care Research
- OR
- odds ratio
- PM2.5
- particulate matter less than 2.5 µm in diameter
- SD
- standard deviation
