Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/112/16. The contractual start date was in October 2019. The draft manuscript began editorial review in November 2022 and was accepted for publication in June 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Wilson et al. This work was produced by Wilson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Wilson et al.
Chapter 1 Introduction
This chapter is adapted from Abotsie et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Background
There is extensive and growing demand for services to meet the needs of young people with poor mental health. 2 Depression is a common health problem during adolescence. Adolescent lifetime prevalence of major depressive disorder (MDD) is 11–20%. 3,4 However, mild/subthreshold depression is much more common in adolescents than full MDD. 5 Such mild depression is associated with significant personal and public health consequences6 and is a strong predictor for future onset of full MDD. 7 Depression in adolescence predicts a range of adverse outcomes in adulthood, including ongoing mental health problems,8 poorer physical health9 and social, legal and financial problems,10 and it is the most prevalent psychiatric disorder in young people who die by suicide. 11 The total annual cost of depression in England has been estimated to be at least £20.2B. 12 However, there is evidence that prompt psychological intervention can prevent relapse and recurrence,13 and therefore intervening early, before depression symptoms become severe, could generate substantial savings.
The majority of adolescents seeking treatment for depression have mild disorders. 14 In the UK, such cases of mild depression are not likely to meet treatment thresholds for specialist (tier 3) Child and Adolescent Mental Health Services (CAMHS). Instead, young people with mild depression are seen by staff working in local authority child and family services or tier 2 NHS-funded mental health services often delivered by third-sector/voluntary agencies. Most of those working with depressed young people within these non-specialist services are not qualified mental health professionals and have no formal training in delivering evidence-based treatments for people with depression.
At present, there is not a standard treatment as usual (TAU) in these non-specialist sectors. There is great variation between and within services about what is offered to young people with low mood, for example, psychoeducation, non-directive counselling and/or behavioural activation. There is usually little specific training and supervision for these interventions. There is no evidence as to whether these interventions are effective, nor whether a systematic intervention with manualised training, delivery and supervision would be more effective and cost-effective than the current approach of non-systematic and varied interventions.
Current guidelines for the treatment of mild depression in children and young people (CYP)15 recommend simple, non-specific psychosocial strategies, such as non-directive supportive therapy. A recent, large network meta-analysis has shown that while non-directive supportive therapy is better than a waiting list (i.e. no treatment) for adolescent depression, it is not significantly better than placebo. 16 It is important to note that the primary studies included in this meta-analysis took place in a range of services for a range of severities of depression. No randomised controlled trials (RCTs) have taken place in the services described above, where most cases of mild depression are treated in the UK. Thus, there is a clear lack of evidence as to how to treat young people accessing these services. 17–19
Study rationale
Interpersonal psychotherapy (IPT) is a National Institute for Health and Care Excellence (NICE)-recommended first-line treatment for adolescents with moderate to severe depression. IPT helps patients to understand the two-way links between their depressive symptoms and current interpersonal relationships. It also helps patients to improve their interpersonal relationships. In doing so, it aims to reduce depressive symptoms. Whereas non-directive supportive therapy aims ‘to help patients accommodate to existing reality rather than try to help them change it’,20 IPT focuses on helping patients to take active steps to improve their relationships in order to decrease their depressive symptoms. Theoretical influences on IPT included Adolf Meyer’s ‘psychobiological’ approach, which emphasised patients’ current interpersonal and psychosocial experiences, and21 Harry Stack Sullivan’s ‘interpersonal’ approach, which conceptualised psychiatry as the scientific study of people and interpersonal processes. 22 Both approaches contrasted with the dominant psychoanalytic approach at that time, which emphasised intrapsychic processes over interpersonal relationships.
Meta-analyses have demonstrated IPT to be superior to control treatments for depression in both adults23 and adolescents16 and to lead to similar outcomes as cognitive–behaviour therapy in both age groups. Crucially, IPT has been shown to be significantly more effective than supportive counselling for depressed adolescents. 24 Given the importance of interpersonal relationships in the causation of adolescent depression,17 and the developmental priority given to interpersonal relationships during adolescence, this approach has high face validity for this age group.
However, in common with other evidence-based treatments for adolescent depression, IPT must be delivered by a qualified mental health professional. As such, it is unlikely to be a feasible treatment option outside of specialist CAMHS. Interpersonal counselling (IPC) is an adaptation of IPT with three main differences: the treatment duration is shorter (three to six sessions); it is designed for clients with mild depression; and it can be delivered by non-mental health professionals after participation in a brief (2-day) training course.
Interpersonal counselling has been found to be an effective treatment for adults with mild to moderate depression. 25,26 A recent trial in Brazil found that staff without prior psychotherapy training were able to successfully deliver IPC to adults with depression. 27 These staff were similarly effective at providing TAU as qualified psychologists. There has yet to be a published trial of the effectiveness or cost effectiveness of this approach in adolescents. An adapted form of IPC designed to meet the needs of young people (IPC-A) has been developed and piloted in a single-arm study by members of the research team. IPC-A was delivered by staff without prior psychotherapy training and was found to be well accepted by staff and young people,28 but its effectiveness as a treatment for adolescent depression has yet to be tested. Although there are many similarities between adult and adolescent depression, there are also important differences, particularly in treatment response. 17 Adult and young people’s services also differ in their organisation, ethos and staff training. 29 Therefore, it cannot be assumed that an effective treatment for adult depression can be transferred to adolescents without evaluation.
There is currently not any evidence to support decision-making regarding which interventions staff members from services providing young people with non-specialist mental health support should be trained to deliver.
Developing skills of staff members by training them to deliver evidence-based interventions will be important to meeting workforce requirements. This study aimed to contribute to this evidence base and is in line with the Department of Health’s Framework for Mental Health Research, which recommends that research should focus on early intervention and involve organisations beyond traditional health services, including local authorities and the voluntary sector. We believed that IPC-A may be effective for young people with mild depression presenting to non-specialist services and may be more effective than current ‘treatment as usual’ (which is not a specific treatment – it is an approach of trying to help young people with one or several strategies that a therapist has learnt about).
It is important to state that while there is a good evidence base for IPT for adolescent depression and evidence that IPC is effective for mild depression in adults, there is minimal evidence that IPT or IPC is more effective than control treatments for anxiety disorders in either age group. 30 This is because depressive and anxiety disorders are different disorders. Although there is increased risk of the second disorder if one is present, they are best conceptualised as different disorders with different core symptoms (low mood vs. anxiety). (For a full discussion of commonalities and differences between depressive and anxiety disorders, please see Wilkinson31) IPT was specifically designed to focus on the link between low mood (and other depressive symptoms) and interpersonal relationships; hence, it should not be assumed that it works for other disorders. Given it is more likely that IPC is effective for depression than anxiety, this initial pilot study focused on young people with mild depression. Given there is no evidence that IPC is effective for depression or anxiety in this clinical setting, we believed it to be ethically acceptable for young people with depression to be randomised to IPC-A or TAU, and for young people with anxiety but not depression to continue to receive TAU, as they would have done before the trial.
This study was intended to provide the information needed to progress to a national full-scale clinical trial of IPC-A delivered by staff without core professional training (referred to in this report as ‘youth mental health workers’). The training (including subsequent supervised casework) required to deliver IPC-A can be completed by staff without prior mental health qualifications in < 12 weeks. Therefore, if found to be an effective treatment, training existing workers as IPC-A therapists could facilitate a rapid and relatively low-cost expansion of the therapy workforce in line with NHS England and government commitments.
Aim and objectives
The research was designed to inform a future trial of the effectiveness and cost effectiveness of the intervention (IPC for adolescents with mild depression). The aim of the research was to answer the following feasibility questions which arose partly from the variability in service models across providers of non-specialist mental health support for young people:
Feasibility question 1
Are trial procedures, including recruitment (of participants and therapists), randomisation, research assessments and follow-up, feasible and acceptable?
Feasibility question 2
How are IPC-A and TAU delivered, and how and why does intervention delivery vary across differing service contexts?
Feasibility question 3
To what extent does contamination of the control arm occur, and should it be mitigated against in a future trial?
Feasibility question 4
Does the interval estimate of benefit of IPC over TAU in depression scores post treatment include a clinically significant effect?
Chapter 2 Feasibility randomised controlled trial – methods
This chapter is adapted from Abotsie et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Design
The study was designed to answer the research question: Is a full-scale RCT of IPC for young people with mild depression delivered in non-specialist community services feasible? In this feasibility RCT, we planned to randomise 60 eligible young people in a 1 : 1 ratio to receive IPC-A or TAU. Participants were invited to take part in an assessment at baseline (pre randomisation) (see Supplementary Material 1) and followed up at 10 and 23 weeks. The feasibility trial aimed to recruit young people presenting with low mood who were receiving support from participating services in Norfolk and Suffolk, UK. A health economics component was included to inform the design of the economic evaluation in a future study. A process evaluation was incorporated to explore how the intervention is implemented across the counties. Qualitative data were collected through site profile questionnaires (SPQs) (see Supplementary Material 2), observations of IPC-A training workshops and supervision, video-/audio-recordings of treatment sessions (both IPC-A and TAU), interviews with participants (and parents) from the IPC-A and TAU arms and focus groups with youth mental health workers (YMHWs) and wider stakeholders.
Setting
The trial aimed to be conducted in two counties in England. While the sites are in the area served by one NHS mental health trust, tier 1/2 services or services for mild depression are not delivered by this mental health trust, as the severity of illness of young people is generally below the thresholds for NHS specialist CAMHS. Treatment at this level is delivered by a range of services locally. Within the two counties, some non-specialist mental health support services for CYP are provided by the County Councils. Teams delivering these services include Early Help teams, Young People’s teams, Family Support services, school nurses and NEET (not in education, employment or training) teams. In addition, non-specialist mental health support is provided by publicly commissioned independent counselling organisations. Such tier 1 or 2 services provide early interventions to CYPs with mild mental health problems and/or difficult family circumstances such as parental drug and alcohol dependency, parental poor mental health and domestic abuse. Most practitioners working in these services are not qualified mental health practitioners but may have some training in counselling, family work and social care. Staff delivering the IPC and TAU interventions would be employees of these organisations who support young people with mild depression as part of their usual job role. We believed having a variety of services involved across two counties would give a good balance of increasing the transferability of findings while keeping the scale of the study manageable within the available resources.
Eligibility criteria and recruitment procedure
Participant eligibility criteria
Inclusion criteria
-
Age 12–18 years.
-
Seeking help for low mood (as the primary presenting difficulty).
-
Able to provide written informed consent or, for under-16s, written informed assent and parent/guardian consent.
-
Of a level of illness where they would normally receive treatment from the service.
Exclusion criteria
-
Learning disability necessitating non-mainstream schooling.
-
Current psychotic disorder.
-
Current substance dependence.
-
Current significant suicidal ideation (Kiddie Schedule for Affective Disorders and Schizophrenia – Present and Lifetime version – ‘suicidal ideation’ threshold – ‘often thinks of suicide and has thought of a specific method’).
In line with the approach used successfully in the pilot, eligibility criteria were kept to a minimum to increase the external validity of the trial in the context of non-specialist services.
Excluded young people would be signposted to appropriate services. Young people would not be excluded based on insufficient English language skills. Interpreting/translation services and foreign language Revised Children’s Anxiety and Depression Scale (RCADS) were available.
There was not a numerical upper severity threshold for depression symptoms or suicidal ideation. However, we anticipated that the criterion ‘of a level of illness where they would normally receive treatment from the service’ would exclude young people presenting with significant suicidal ideation. Participants expressing significant suicidal ideation or planning at the time of screening remained ineligible for the study.
The planned recruitment period for the feasibility RCT was January–December 2020 (12 months). In order to recruit the target 60 participants, it would have been necessary to recruit an average of 5 participants per month across all sites; this was predicted to be lower in early stages of the study and higher in later stages, as more therapists completed training. The aim was to have six IPC therapists trained in each of the two counties who would each treat two to three young people with IPC. With IPC taking around 10 weeks (taking into account holidays), this means that, on average, each participating therapist would have one ongoing IPC case per half of the recruitment year.
Participants would be young people accessing participating services via the service’s standard referral pathways. Young people were triaged and assessed according to each service’s standard procedures. If the assessment identified low mood as a presenting difficulty, the case would be discussed with a clinical member of the research team (without identifying the young person) to ascertain likely suitability for the trial. The service was given the option of using the RCADS depression scale to help determine suitability, with a cut-off of 11 or over suggesting suitability (this cut-off was not an absolute).
Potential suitable young people were invited to participate, and those who expressed an interest met with the trial’s research practitioner, who carried out informed consent procedures and screened the young person to ensure they met the above criteria.
Consent
The Chief Investigator retained overall responsibility for obtaining informed consent but delegated this duty to the study research practitioner who was trained in obtaining valid informed consent according to the ethically approved protocol, principles of Good Clinical Practice and Declaration of Helsinki. The informed consent process included a discussion with the potential participant (and his or her parent/carer if under 16) about the objectives of the study, what he or she would be asked to do if they chose to participate and the possible risks and benefits of participation. Potential participants (and their parent/carer if applicable) were provided with written information and given at least 48 hours to read and consider the information before being asked for consent. Young people and their parents/carers were given the opportunity to ask questions and have these answered in full.
If the young person wished to participate following this process, they were asked to complete a consent form (if 16 or over) or assent form (if under 16) to document the informed consent/assent process and their willingness to participate. For young people under 16, in addition to the child’s assent to participation, the consent of a parent or carer (adult with parental responsibility) was required for the young person to be included in the study. Consent to participate in an interview as part of the process evaluation was sought during the main consent procedures. However, it was not a requirement that a young person consented to a process evaluation interview in order to be included in the study.
We did not include individuals who did not have capacity to give their consent/assent to participation. During the consent process, it was made completely and unambiguously clear that the participant was free to refuse to participate in all or any aspect of the study, at any time, without giving a reason and without incurring any penalty. The participant’s continued willingness to participate was confirmed at each study contact before commencing any research procedures. Participants were free to withdraw from the study at any time up until the time of data analysis without giving a reason and without prejudicing his or her further treatment. Data collected up to the point of withdrawal would be used if the participant (and their parent/carer in the case of participants under 16) consented to this. Every effort was made to ensure that vulnerable young people were protected and participated voluntarily in a safe environment free from coercion or undue influence.
As the reading ages and levels of understanding of potential participants varied and did not necessarily mirror chronological age, and in line with patient and public involvement (PPI) feedback, instead of preparing separate information sheets for children aged 13–15 years and young people aged 16–18 years, we created an ‘easier to read’ version of the information sheet and a ‘detailed’ version. All young people were provided with both versions of the participant information sheet and could choose to read the version they found more accessible or to read both. Members of the Study’s Youth Advisory Panel reviewed the information sheets to ensure the format and language used were appropriate for the target age group.
In addition, informed consent for staff participation was sought prior to the training workshops. All staff members trained in the intervention were given a verbal explanation of the objectives of the study, what he or she would be asked to do if they chose to participate and the possible risks and benefits of participation. Staff were provided with a written information sheet and had the opportunity to ask questions and have these answered in full before deciding whether to participate. If the staff member decided to participate following this process, they were asked to complete a consent form to document this process.
Staff involved in delivering TAU were invited to consent to participation on an individual basis when they were assigned to work with a young participant allocated to the TAU arm. This consenting process was completed by an unblinded member of the research team.
Sample size
We planned to randomise 60 eligible young people in total. The target sample size was not based upon estimation of efficacy but was in keeping with published suggestions32 and was believed to be practically possible within the limits of the project. Further, it was anticipated that a sample of this size would enable the assessment of the rates of recruitment and retention to a reasonable degree of precision. Assuming an attrition rate of around 20%, a sample of 60 would provide a 95% confidence interval (CI) of width 20% (i.e. ± 10%). For a recruitment rate of around 50%, the interval width would be around 25% (i.e. ± 12.5%).
Intervention and control arms
Intervention
Interpersonal counselling for adolescents is a brief, manualised psychological intervention derived from IPT. IPC helps clients to identify the reciprocal interaction between their current depressive symptoms and interpersonal relationships, with a focus on one of four domains: grief, relationship disputes, big changes and loneliness and isolation. The therapist works with the client to identify effective strategies to deal with their interpersonal problems, which should improve depressive symptoms.
Interpersonal counselling for adolescents (IPC-A) is an adapted form of IPC designed to suit the needs of adolescents. The intervention is delivered over three to six (30- to 60-minute) sessions, depending on participant needs. IPC-A is based on the manual developed by Weissman et al.,33 with minor modifications to make it suitable for young people. IPC-A arm participants would also have access to standard health and care provision throughout their participation; the extent to which provision of IPC-A altered use of these services would be monitored using the modified Client Service Receipt Inventory (CSRI).
Staff trained as IPC-A therapists received two full days of initial training. Prior to delivering IPC-A to trial participants, trainees needed to achieve adequate scores on audiotaped ratings of two therapy sessions for each of two cases, write an adequate reflective log of the two cases and attend supervision regularly.
Following successful completion of the training, therapists received clinical supervision weekly, with a maximum of three therapists per group. We intended that supervision would be provided in a group format to allow therapists to explore the theory and practice of IPC through engaging in shared discussions of real-world cases. Each supervision session lasted up to 1.5 hours. There were a number of trained IPC supervisors in the local area who expressed an interest in supervising the delivery of the intervention within the trial. A further two supervisors were trained to supervise IPC: an IPC therapist and IPT practitioner who were trained as IPC leads to supervise trainees in accordance with the treatment manual,28 who would have overall responsibility for co-ordinating the provision of clinical supervision.
Control
The control arm received TAU, the standard support provided by services. At present, there is not a standard TAU in these non-specialist sectors. There is great variation between and within services about what is offered to young people with low mood, for example, psychoeducation, non-directive counselling and/or behavioural activation. There is usually little specific training and supervision for these interventions. Staff received the normal management and supervision that they normally receive for their casework. Hence, treatment was not at a lower standard than before the trial. As therapeutic approach between and within services varies, supervision also varies (as there is not a standard systematic TAU, there is not a standard systematic supervision as usual). Standard supervision for TAU is less frequent and less intense than the systematic supervision for IPC-A. This may affect quality of therapy but may also increase cost (which would be captured in the health economics analysis). Crucially, the trial compared the whole IPC-A package (including training and supervision) against the whole TAU package.
Participants were not denied access to any treatment option available as part of current provision. However, staff providing individual support to TAU participants did not attend any IPC-A training and did not receive any IPC-A supervision to minimise contamination. Staff trained as IPC-A therapists were required to agree not to discuss any aspect of their training or supervision with colleagues not trained in IPC-A. The interventions that constitute TAU for this group were monitored via the modified CSRI and process evaluation.
Although the practitioners who delivered TAU were not qualified mental health professionals (as in the IPC-A arm), they were able to consult with or offer a joint appointment with a mental health professional [e.g. primary mental health worker (PMHW) or clinical psychologist] or signpost/refer the young person to other local services.
Further note on contamination: The relationship between RCT study design in mental health, ethics and contamination is complex. In this case, TAU is the treatment (varied within and across teams) that is currently given as standard to young people with mental health problems. Given the fact that there is no evidence that IPC-A is better than TAU, it is acceptable for this TAU to be given in the study. Contamination would mean that the presence of the trial would mean that young people receiving care in the TAU arm would be receiving IPC-A interventions, which they would not have received if the trial did not exist. This could happen through TAU therapists attending IPC-A training and/or IPC-A therapists in the team talking about IPC-A practice. Such contamination may improve outcomes in the TAU arm, causing a type 2 error. It is ethical to try to avoid contamination because there is no evidence that IPC-A is better than TAU, and we are doing this study to investigate if there could be a difference – we, therefore, need to ensure that TAU really is TAU.
Randomisation and blinding
Randomisation was co-ordinated remotely by the Norwich Clinical Trials Unit (CTU). Participants were randomised in a 1 : 1 allocation ratio, using a stochastic minimisation algorithm to minimise imbalance between groups in baseline symptom severity, gender and study site. Allocation was managed by the Data Management Team at Norwich CTU via a web-based system; it was not accessible by anyone outside of the team, including the research team, trial therapists and participants; thus, allocation concealment was maintained.
Blinding
Research practitioners collecting follow-up data were blind to the participant’s treatment allocation. A second unblinded member of the research team received the outcome of the randomisation via an automated notification from the system set-up and managed by the CTU and passed details of allocation to the clinical service. Given the nature of the intervention, it was not possible for participants and those involved in delivering the intervention to remain blind. Following allocation, all participants in the study and therapists were asked not to reveal the group to which the participants were randomised to the research practitioner. Participants were reminded at the beginning of each contact with the research practitioner post randomisation not to disclose their allocation. Any potentially unblinding data were stored separately in a secured database to which the research practitioner did not have access. As the study’s Chief Investigator and participants’ responsible clinicians were unblind to treatment allocations, no emergency unblinding procedures were required for this study.
Data collection
Participants were young people accessing participating services via the service’s standard referral pathways, as detailed above. Young people were triaged and assessed according to each service’s standard procedures. If this assessment identified low mood as a presenting difficulty, the case would be discussed with a clinical member of the research team (without identifying the young person) to ascertain likely suitability for the trial. Potentially suitable young people (and/or parents/carers) were invited to participate. If they expressed an interest, consent was given to the service to pass on their details to the research team.
Those who expressed an interest met with the trial’s research practitioner who carried out informed consent procedures and screened the young person to ensure they met the eligibility criteria.
Face-to-face, telephone, video call and/or internet-delivered quantitative assessment took place at baseline, 5, 10 and 23 weeks; questionnaires were completed online by the participant with support from the research practitioner. Young people were invited to take part in qualitative interviews at the end of treatment; up to 20 were planned to take part in these. Staff and stakeholders were invited to take part in focus groups.
The following participant data were collected at baseline (face-to-face, telephone and/or video call interview, internet-delivered questionnaires):
-
demographic characteristics of the young person
-
Kiddie Schedule for Affective Disorders and Schizophrenia, depression section34,35
-
RCADS36
-
Family Assessment Device37
-
Cambridge Friendships Questionnaire38
-
Employment, Education or Training in previous 4 weeks (NEET status)
-
Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS)32
-
modified CSRI39
-
Child Health Utility Index 9D (CHU-9D). 40
Follow-up assessments
The following participant data were collected at 5-week follow-up (online with telephone support):
The following participant data were collected at 10- and 23-week follow-up (face-to-face, telephone and/or video call interviews, ± internet-delivered questionnaires):
-
RCADS36
-
Family Assessment Device37
-
Cambridge Friendships Questionnaire38
-
Employment, Education or Training in previous 4 weeks (NEET status)
-
SWEMWBS32
-
modified CSRI39
-
CHU-9D40
The proposed primary outcome measure for a future effectiveness trial was the RCADS, which is a continuous self-rated questionnaire of depressive and anxiety symptoms, with six subscales, including depression. The RCADS is used as the primary outcome measure for emotional disorders in CAMHS in England, as recommended in the Department of Health Children and Young People’s Improved Access to Psychological Therapies (CYP-IAPT) programme. The results from this feasibility study could potentially be benchmarked against results from countrywide CAMHS services. The RCADS is also used as the primary measure in routine English IPT for adolescent practice – the depression scale is used at each session as part of routine IPT-A. We extended this to IPC-A in the pilot36 and weekly RCADS depression was a useful part of therapy and certainly acceptable to young people and therapists; and it was a highly useful primary outcome scale in the research evaluation. The original Chief Investigator was part of a review of adolescent depression measures published in 2015 and found the RCADS to have good psychometric properties. 36
We used the observer-administered K-SADS at baseline to test for presence of Diagnostic and Statistical Manual of Mental Disorders depressive disorders. While not an outcome measure, we used this to help us to describe the sample, in particular what proportion of participants have MDD. The K-SADS is the gold-standard diagnostic interview schedule in adolescents, with excellent validity and reliability. 34
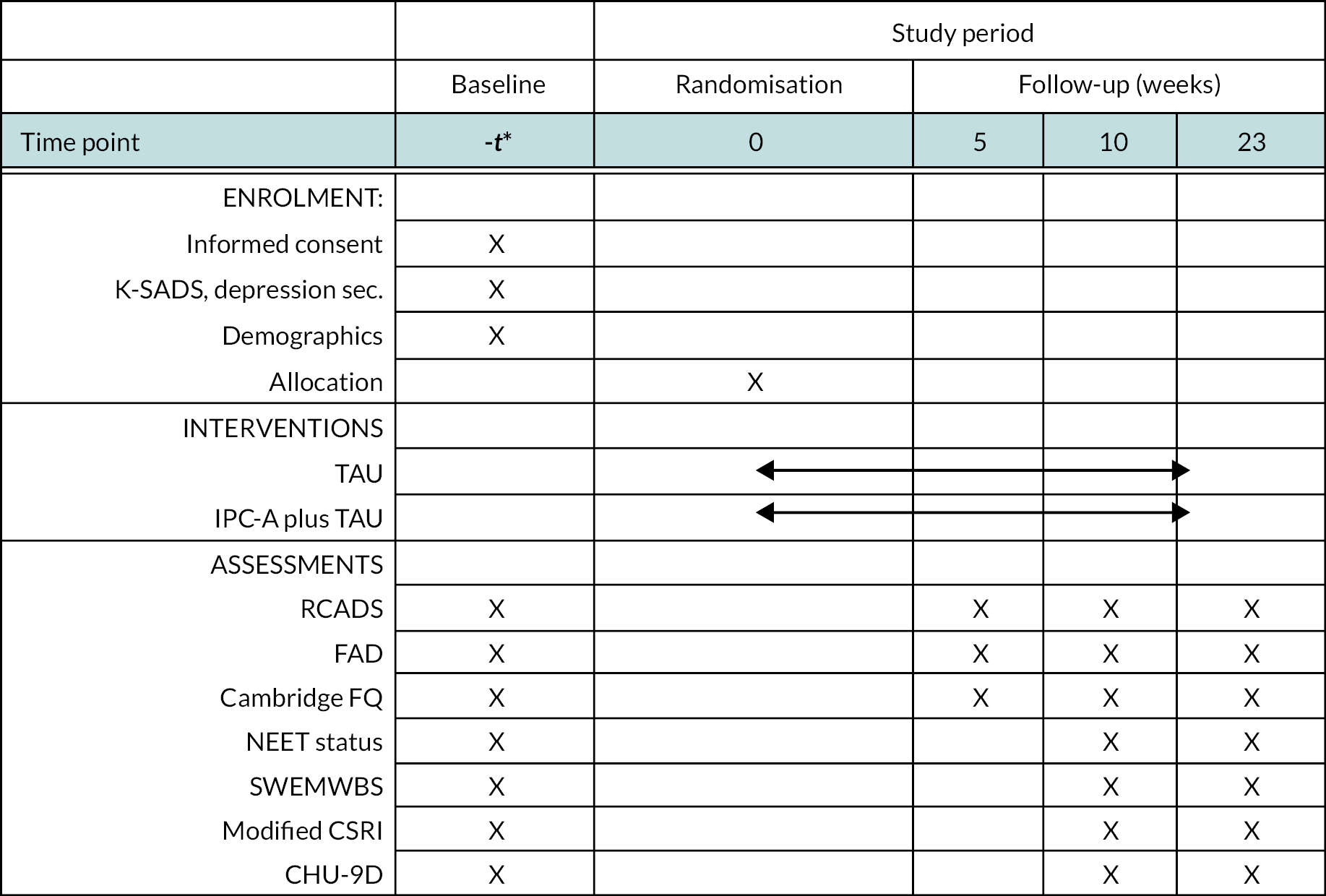
The schedule of enrolment, interventions and assessments in accordance with Standard Protocol Items: Recommendations for Interventional Trials guidelines is shown in Figure 1.
FIGURE 1.
Standard Protocol Items: Recommendations for Interventional Trials figure. FAD, family assessment device; Cambridge FQ, Cambridge Friendship and Relationship Quotient.
Analysis
Statistical analysis plan
Recruitment and retention rates were estimated with 95% CIs. Assuming sufficient information, time until drop-out was analysed using ‘time-to-event’ methods to identify baseline factors likely to be related to drop-out. The proposed primary outcome measure for the definitive RCT was the RCADS depression score at 10 weeks. Although the proposed study was not designed to assess efficacy, the mean between-group difference was estimated using a general linear model including baseline RCADS depression score and treating therapist as a random effect. A 95% CI was constructed to assess whether the treatment benefit was feasibly greater than the minimal clinically significant difference, that is, whether or not it was included within the CI. A similar approach was undertaken for the secondary outcome measures. The rate of completion of each outcome measure was reported. If appropriate, depending on the proportion of missing values, multiple imputation will be undertaken and between-group differences re-estimated as a sensitivity analysis. Further parameters, such as within-group variation, needed for the design of a subsequent full-scale trial, will also be estimated.
A statistical analysis plan (SAP) was written in accordance with Norwich CTU guidance and approved by the independent Data Monitoring Committee (DMC) prior to the formal statistical analysis (see Supplementary Material 3).
Health economic analysis
As this was a feasibility study, it was not considered possible to demonstrate the cost effectiveness of the intervention because the study was not powered to demonstrate effectiveness. However, we collected information to inform the design of an economic evaluation alongside a future definitive trial. The intention was to generate information to inform any future study. Examples would include: the likely cost of the intervention and key components of resource use. It also evaluated the use of the CHU-9D instrument as a potential instrument to use in the future study. 40
The resources required to provide the interventions (IPC and TAU) were recorded. These included training; ongoing clinical supervision; and staff time required to provide the intervention. Each session offered (and its location) in both arms was recorded. Recording of these events was included in the study design in the form of a record sheet. These were combined with appropriate unit cost data to provide an estimate of the cost of providing IPC-A. It is also important to measure any resources related to participants’ mental health in both the intervention and control groups. This was conducted by means of a modified CSRI conducted at baseline, 10 and 23 weeks. Modifications included adjustments to the following aspects of the CSRI. The time frame for recall was adjusted. This was for the last 3 months at baseline and ‘since we last met’ at the 10- and 23-week follow-up. This effectively gave a time frame of the last 10 weeks for the 10-week follow-up and the last 13 weeks for the 23-week follow-up. To reduce burden on participants, the a priori aim was to make the modified CSRI as simple as possible but to still capture relevant and important service use. For this reason, questions were omitted on the following categories: usual living situation; and contacts with criminal justice system. Questions were limited to the following: contacts with specified types of care providers in the school setting; use of inpatient services; use of other secondary care services; contacts with primary care and community health and social services, residential social care services; and use of services by the participants' family. For drugs, named relevant drugs were specified that may have been prescribed for mental health reasons. We also asked about use of other prescribed medicines. For simplicity, no details were recorded of time and travel costs to access services. All demographic data were also deleted from the CSRI, as relevant data were requested elsewhere in the study. Any modifications made were done so in consultation with other ICALM investigators. The CSRI was collected by means of a face-to-face interview, by telephone/teleconference or videocall/video conference, depending on wishes of participants and safety issues arising from COVID-19 infection risk or wider pandemic measures.
The original intention was to analyse resource use data by study arm to highlight any potential areas of differences between trial arms in use of NHS and social care services, including emergency department attendances. However, due to very low numbers, this was not considered to be informative. For this reason, analysis focused on the whole sample, looking at occurrences of missing data, types of resource use reported, patterns over the three time periods and overall performance of the instrument. The measure of health-related quality of life used in the study was the CHU-9D. 40 One important outcome of the feasibility study was an assessment of the suitability of this instrument for use in a future full-scale trial. This was assessed by means of descriptive analysis of the pattern of responses at different time points.
Process evaluation
Please refer to Chapter 4, Data analysis, for details of the analysis for process evaluation.
Progression criteria
The primary intended output of the research was the design of a subsequent trial. The Trial Steering Committee (TSC) planned to assess the trial against the following criteria and make recommendations regarding the suitability of the proposed design for the full-scale trial.
-
Recruitment rate is at least 80% of target.
-
At least 70% of those randomised to receive the intervention attended at least three therapy sessions within the 10-week treatment window.
-
Follow-up assessments are completed by at least 80% of participants at 10 weeks and 70% of participants at 23 weeks.
-
At least 80% of IPC treatment sessions reviewed meet treatment fidelity criteria.
-
Contamination of the control arm can be sufficiently limited for individual randomisation to be justified.
-
The mean RCADS depression scores of the IPC-A and TAU groups at 10 weeks are indicative of a clinically significant difference in depression (3 points).
Governance
Throughout the duration of the study, research processes have been conducted according to the UK Policy Framework for Health and Social Care. A Trial Management Group met on a monthly basis where all aspects of the study were discussed and any issues were identified and resolved. The TSC and DMC were provided with progress reports throughout the duration of the study. Both the committees provided statements of support for the study to be extended beyond the original 2-year timeline due to the suspension of the study during COVID-19.
A provisional SAP was completed at the beginning of the study. Due to the number of changes throughout the study, the SAP was amended following suggestions by the DMC and was approved prior to the analysis being conducted.
Chapter 3 Feasibility randomised controlled trial – results
The project was planned to be conducted over 24 months, beginning on 1 October 2019. Training of identified staff members to deliver IPC-A was planned to commence before the project began and be completed during months 1–3. Recruitment was planned to take place in months 4–15. Follow-up assessments were planned to be completed in month 21. Months 22–24 were to be dedicated to data cleaning, analysis and dissemination.
Although recruitment started as planned in January 2020, the study was suspended in March 2020 due to the first lockdown of the COVID-19 pandemic, which temporarily suspended National Institute for Health and Care Research (NIHR) research activities. The study recommenced in July 2020, with refresher training being offered for therapists. Recruitment then recommenced in September 2020, creating a 7-month delay. By February 2021, however, due to reported impacts on services from continued lockdowns and other COVID-19-related complications, the number of referrals was significantly impacted. Sites had to prioritise urgent cases only or focus only on safeguarding issues. Teams also experienced a change in types of referrals received, reducing the number of trial-eligible young people and lowering the capacity of staff to take on ICALM cases. IPC-A-trained staff also withdrew, citing new pressures resulting from the increased demand and reduced capacity, reducing the number of staff able to carry out the intervention. This difficulty in recruitment prompted changes such as the addition of new delivery sites, offering additional training sessions to train more staff and creating alternative referral pathways (see Recruitment and retention).
In July 2021, due to the ongoing difficulties resulting from the COVID-19 pandemic, and the delay caused by the suspension of the study at the start of the pandemic, an extension was requested and granted by NIHR. According to the revised timeline, recruitment and follow-ups were due to end between December 2021 and February 2022, with March 2022–October 2022 being dedicated to data cleaning, analysis and dissemination. Recruiting sites felt they had begun to normalise and were more positive about their ability to recruit, although the ongoing pressures on the health system limited their ability to prioritise the research trial.
Recruitment and retention
Recruitment of delivery sites
In September 2019, eight teams across Norfolk and Suffolk were approached about taking part in the study. Seven teams (Site-01_Early Help and NEET Team, Site-02_Early Help and NEET Team, Site-03_Early Help and NEET Team, Site-05_Charity, Site-07_Charity, Site-11_Early Help and NEET Team, Site-14_School Nursing) gave their agreement to take part. Six teams were based in Suffolk, and one team was based in Norfolk. The team that declined to take part had previously participated in the single-arm study of IPC-A and stated the reason for declining was that they felt IPC-A did not fit well due to the complexity of their clients.
Site-05_Charity suspended their involvement in December 2020, citing competing pressures and planned to restart their involvement once they had greater capacity; however, this did not happen, and they withdrew from the study in April 2021.
In response to COVID-19, changing team responsibilities and no longer having any teams referring to the study based in Norfolk, it became necessary to recruit further teams to support the study. In May 2021, six additional teams gave their agreement to take part (Site-04_Wellbeing Service, Site-06_Charity, Site-08_Community NHS Trust, Site-09_Family Support Team, Site-12_Family Support Team, Site-13_Family Support Team).
The Family Support Teams provide support through the Family Support Process and child-in-need (CIN) care plans. They work with children and families where there are concerns about the children’s well-being. It is unusual for these teams to get referrals where the only concern is adolescent mental health; there is a much more complex picture, often including a level of relational dysfunction. However, mental health concerns are the norm within their service users. Unlike mental health services, assessments will nearly always include all family members and will most likely be carried out using a Signs of Safety framework.
Site-04_Wellbeing Service offer Tier 2 mental health services to young people aged 4–18. The team consists of children’s wellbeing practitioners (CWPs) (without a core professional mental health qualification) and PMHWs (with a core professional mental health qualification) and provides brief interventions to young people with mild/moderate difficulties. Referrals are via the Site-10_Central referral point, the same referral point as Suffolk Early Help teams. As per trial protocol, staff without a core professional mental health qualification delivered IPC-A as part of the trial.
Site-06_Charity sees young people with mild to moderate mental health difficulties aged between 0 and 21 and works closely with Site-05_Charity. The service has a variety of staff without core mental health qualifications, including CWPs and educational mental health practitioners. Referrals to Site-06_Charity come via either professional or self-referral. Site-06_Charity have a track record of actively participating in research and have a keen awareness of what this involves. Site-06_Charity withdrew in September 2021, citing staff turnover and lack of capacity to train more staff as the reasons for withdrawing.
Site-08_Community NHS Trust provide health advice and support for young people at a universal services level. Part of this role involves delivering time-limited interventions to young people aged 12 and above with new and emerging mental health difficulties. Such interventions are offered by resilience and emotional health practitioners (REHPs), who do not have a core mental health qualification. Most referrals to this service are either from the young person themselves, a parent or a school representative.
A diagram of the sites can be seen in Figure 5.
Of the 13 teams who were sites for the feasibility trial, 7 made referrals to the study, 3 (Site-02_Early Help and NEET Team, Site-06_Charity and Site-08_Community NHS Trust) delivered IPC-A/TAU of which 2 teams provided recordings (Site-08_Community NHS Trust and Site-02_Early Help and NEET Team).
Changes to referral pathways
Although the majority of teams had agreed to offer both IPC-A and TAU, due to difficulties with retention of trained IPC-A staff, clinical capacity, lack of suitable cases and stagnant waiting lists, there were a number of changes to referral pathways as well as the type of intervention teams were able to offer.
Site-04_Wellbeing Service/Site-14_School Nursing
With difficulties due to many young people being ‘stuck’ on the Site-10_Central referral point waiting list, preventing possible eligible referrals, new pathways were sought. There were difficulties with Site-14_School Nursing having limited capacity to deliver the trial, but having eligible young people, and Site-04_Wellbeing Service who had IPC-A trainees but few eligible young people. It was suggested and agreed with locality managers and commissioners to set up a new pathway to allow referrals to the Site-04_Wellbeing Service from the Site-14_School Nursing. Site-14_School Nursing team checked for eligibility and willingness to take part in the study and then referred to the research team for consent and eligibility checks. Site-14_School Nursing would then transfer the case from Site-14_School Nursing to Site-04_Wellbeing Service. If ineligible, the case remained with Site-14_School Nursing. Only at the point of assessment at the Site-04_Wellbeing Service, if a case withdraws from the study or is no longer suitable, would the case stay with Site-04_Wellbeing Service to finish any treatment, as the case would unlikely be suitable for Site-14_School Nursing. If suitable, the research team would be informed, and the case randomised to Site-04_Wellbeing Service for the intervention and informed if the case is TAU or IPC-A. The intervention and the follow-ups would continue as normal.
Site-04_Wellbeing Service and Site-07_Charity
Similar to the Site-14_School Nursing and Site-04_Wellbeing Service pathways, an agreement was set up for Site-04_Wellbeing Service and Site-07_Charity. Site-07_Charity is a charity that offers brief, ‘light touch’ early interventions to young people experiencing mental health difficulties. In terms of the severity of mental health difficulties they offer treatment for, they sit below Site-04_Wellbeing Service, and young people can self-refer. This service is largely made up of counsellors who, due to their training and qualifications, were deemed ineligible to provide IPC-A as part of this study. However, Site-07_Charity offered to provide additional TAU capacity to Site-04_Wellbeing Service, thereby minimising contamination and offering a clear alternative TAU. Site-04_Wellbeing Service would go through their usual process of checking if appropriate for ICALM and then checking if they were interested. The referral form was then sent to the research team to provide an information sheet and consent form, as well as confirming eligibility. If eligible, the young person was then randomised. If the young person was randomised to the TAU arm of the study, Site-07_Charity and Site-04_Wellbeing Service discussed who would deliver the TAU. The staff member of the respective team then completed the participant consent form, and the intervention and the follow-up continued as normal.
Site-04_Wellbeing Service and Site-07_Charity have a contract, which means that any referrals from Wellbeing will be seen within 4 weeks.
Site-10_Central referral point
In a meeting held with team leaders in August 2021, managers highlighted challenges in getting appropriate referrals from the central referral point as a key barrier to recruitment. Managers fed back that due to pressures at the central referral point, the Early Help teams were being allocated more complex cases, instead of the mild cases they are commissioned to take on.
As a result of this feedback, in November 2021, the ICALM study team initiated discussions with representatives from Site-10_Central referral point, Site-02_Early Help and NEET Team and Site-04_Wellbeing Service to set up a fast-tracked referral pathway for suitable ‘green’-rated (low-risk) cases from Site-10_Central referral point to ICALM. The process also received support from a representative from the commissioning group as it was in line with government agenda. Site-10_Central referral point was not a full site for the study; this site supported referrals to the study only.
Delivery site characteristics
An overview of the characteristics of the 13 sites that agreed to take part in the feasibility study is provided in Table 1. Site-10 has not been included as it was a referring site only. Detailed site characteristics can be found in Table 1.
| Site ID | Service type |
|---|---|
| Site-01 | Early Help and NEET |
| Site-02 a | Early Help and NEET |
| Site-03 | Early Help and NEET |
| Site-04 | Wellbeing Service |
| Site-05 | Charity |
| Site-06 a | Charity |
| Site-07 | Charity |
| Site-08 a | Community NHS Trust |
| Site-09 | Family Support |
| Site-11 | Early Help and NEET |
| Site-12 | Family Support |
| Site-13 | Family Support |
| Site-14 | School Nursing |
Staff participants
In May 2021, the format of IPC-A training was significantly altered by being undertaken online due to COVID-19 restrictions and included several sessions devoted entirely to explaining the trial. This included detailed explanations of equipoise and randomisation. These training materials had been adjusted and routinely delivered and distributed to new teams or new staff when the study was explained. This was changed to help understand randomisation and to support practitioners within therapy delivery teams, as it was observed that the clinical practitioners within these teams were not familiar with research processes such as randomisation, which was seen as a barrier to recruitment.
In total, the study team trained 19 staff members as IPC-A practitioners who all gave consent to take part in the feasibility study. However, subsequently, eight withdrew from the trial. Four consenting IPC-A practitioners were allocated clients. Two IPC-A practitioners delivered the intervention. For those practitioners who did not deliver IPC-A, reasons given were (n = 1) client was offered IPC-A but did not engage with the service and did not attend any IPC-A appointments offered and (n = 1) client was not appropriate for IPC-A due to complexity and risk and was referred for a more appropriate intervention. Staff providing TAU were not consented until they were allocated a client. In total, three staff members providing TAU gave consent to take part in the feasibility trial. Two staff members delivered TAU. One staff member did not deliver TAU as their client withdrew from the study.
Participant flow
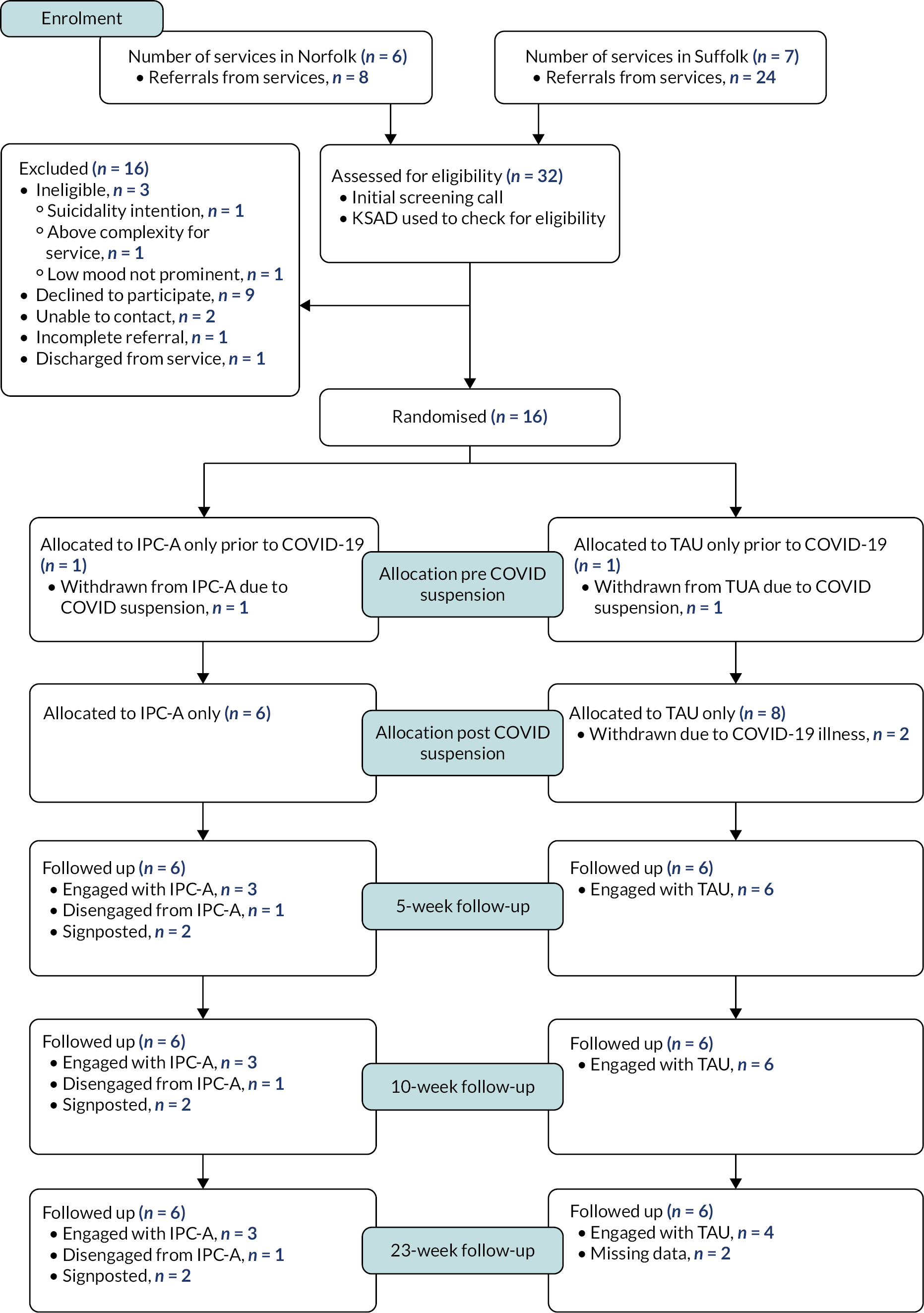
In total, 32 referrals were received, with 16 eligible participants being recruited and randomised (Figure 2). Two of these participants were recruited and randomised before the suspension of the study due to COVID-19. These participants were informed about the decision to discontinue follow-up data collection due to the current COVID-19 crisis causing research to be halted. Therapy (either IPC-A or TAU) continued, but the research practitioner did not contact participants for any more assessments. Of the remaining 14 participants, only 7 received an intervention, with 3 out of 6 participants receiving IPC-A and 4 out of 6 receiving TAU. Among participants who did not complete IPC-A, one did not engage with the service nor attended appointments. Two participants were found inappropriate for ICALM and IPC-A due to complexity and/or risk at rescreening by the IPC-A clinician, highlighting a progression of symptoms between baseline assessment and start of IPC-A. This led to the clients being discharged and signposted to another service. Concerning the two participants who did not complete TAU, not all data were able to be collected as to whether they received any intervention due to staff members not completing the Attendance Questionnaires.
FIGURE 2.
Consolidated Standards of Reporting Trials diagram for feasibility trial (includes two before suspension of study).
Recruitment
Due to remote working, the protocol was changed to allow the young person (or their parent/carer if under 16) to be asked if they are willing to photograph and electronically send a picture of the completed consent form to the research practitioner so that baseline assessments are not delayed by the added complexity caused by postal delivery services. It was also changed to allow interviews/focus groups for the qualitative analysis and treatment and assessment to take place face to face, by telephone/teleconference or videocall/video conference, depending on wishes of participants and safety issues arising from infection risk. Participants were posted copies of the consent form and participant information sheets, with the researcher going through the consent form remotely with the participant. The participant would then take and send a picture of the signed consent form to the research team so further parts of the study could continue. The participant, meanwhile, would post the form back so there was a physical copy for study records. The protocol was changed to accommodate recording online, as this was historically in-person with a dictaphone.
In March 2021, further changes were made in consenting procedures to account for the ongoing changes due to COVID-19. This included having multiple options for carrying out consenting processes, including face to face; via photo and post; and through incorporating the form into the Research Electronic Data Capture system (REDCap) and capturing consent via audio-recording.
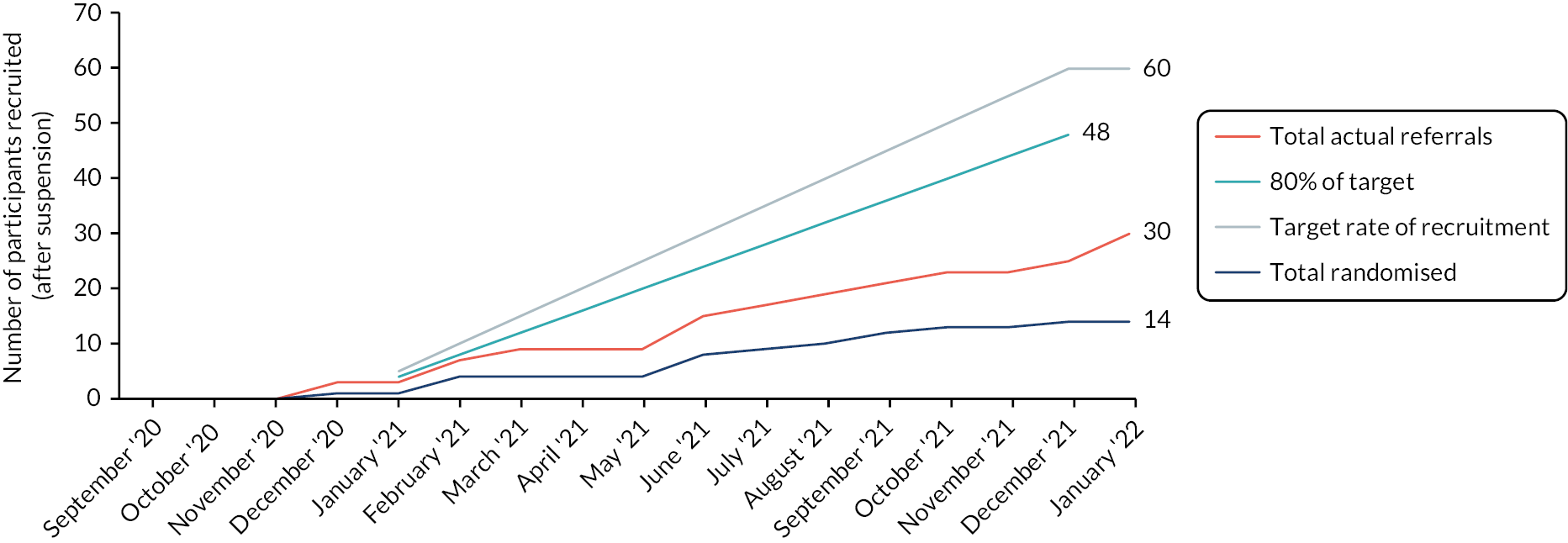
Looking at Figure 3 for those who were recruited after suspension (n = 14), the overall rate of recruitment was slower than anticipated: on average, 1.7 per month (18 months) versus a target recruitment rate of five participants per month (12 months). Recruitment, however, started earlier in September 2020 and ended later than predicted in February 2022, compared to predictions starting in January 2020 and ending in December 2021. The alterations to the referral pathways did not increase the number of referrals made to the study.
FIGURE 3.
Accrual curve for feasibility trial.
Following previous unsuccessful attempts at recruitment, the fast-tracked referral pathway for suitable green-rated cases from Site-10_Central referral point was agreed in November 2021. Prior to this agreement, there were concerns raised from the services around the following areas
Caseloads of therapists
As Early Help managers were aware of the pressures faced by Site-10_Central referral point due to staff shortages and the backlog of cases, they expressed a concern of ‘flooding the services’ by highlighting an incident where approximately 600 cases had been referred from Site-10_Central referral point to another team within a short period of time.
This is an emotive subject for the services because Site-10_Central referral point can see this as a way of offloading cases and may lead to a lot of disquiet. You don’t want to send the message that Site-10_Central referral point is offloading cases. I am concerned that we are not opening the flood gates.
Concerns about the suitability of the cases for their services
The managers felt a number of referrals received from Site-10_Central referral point were not appropriate for their service (even after being advised what the criteria for the service are) and that although they may come through as low mood, there may be other confounding factors which are the cause of this presentation. The main challenge with the referral of cases from Site-10_Central referral point was that there was not a feedback loop which allowed for cases to be returned to the hub if considered inappropriate. The managers of the service therefore felt that there needed to be a feedback loop or support mechanism in place in case the identified cases were beyond the service’s remit.
Site-10_Central referral point not triaging cases before referring
Team managers felt that Site-10_Central referral point did not triage the cases fully, leading to teams not having the full information on the case to decide whether they would be apprioriate for their service. Site-10_Central referral point needed to identify cases that have low-level issues and exclude those that have complexities, for example, violence, safeguarding issues, eating disorders, adoption or learning disabilities.
Usual support
Some teams reported not having TAU for low mood. They would need to ensure provision is made for young people randomised to the TAU arm. This also impacted on practitioners’ willingness to randomise a case they thought suitable for IPC.
Following these concerns from the teams, the plan was to identify a small number of eligible young people (maximum 5) for each of the participating teams based on the capacity of participating therapists and how many cases the practitioners needed to qualify as an IPC-A therapist. The agreed plan was as follows:
Step 1
Site-10_Central referral point clinician to identify potential referrals based on ICALM inclusion and exclusion criteria. Site-10_Central referral point clinician would need to go through the general practitioner (GP) areas to ensure that the cases are being referred to the correct location and right teams. Site-10_Central referral point to refer cases to one of three teams, depending on location: Site-01_Early Help and NEET Team/ Site-02_Early Help and NEET Team/ Site-04_Wellbeing Service to speak to potential participants to see if they would like to find out more about the study:
-
If no – no further action with person for ICALM.
-
If yes – referral is made to the teams.
Step 2
The cases get reviewed by a team manager for appropriateness before assigning them to the team. If appropriate, the team manager will notify Site-10_Central referral point clinician that the case has been assigned to a manager so that it can be closed at the Site-10_Central referral point and noted that it has been assigned to the ICALM study.
Step 3
Team to refer suitable participants to ICALM team for baseline assessment. If they are eligible for ICALM team consent (young person and family), complete baseline measure and randomise participants (this can take up to 3 weeks).
Step 4
ICALM Trial manager to inform the team of the randomisation outcome. When referred to the team, the young people will be in contact with family support practitioners (FSPs) as per usual.
The perceived benefit of the process included reducing the long waiting list for ‘green’ cases while ensuring that services are not inundated with inappropriate referrals.
The Site-10_Central referral point clinician screened 1300 cases, of which only 31 cases were identified as potentially having ‘low mood’.
I filtered out the queues and removed all cases for potential or a diagnosis of ASD or ADHD, l removed learning disabilities, young people suffering from trauma or who are being violent and having anger issues. I also screened the list for the correct GP practices based on the areas of Bury and Ipswich, leaving only 31 cases.
In total I believe there are 19 possible ones for one of the teams and 12 for another – the ones in red (not referring to RAG rating) I am pretty sure on, however this is purely due to a lack of referral info.
For the 1300 referrals that were screened, only 4 young people were then referred to the ICALM team. None of these referrals consented to take part in the study due to not being able to be contacted prior to the recruitment deadline, and one person declined to participate.
Retention
After suspension of the study, of the 14 eligible participants who were randomised to the study, 12 (85.7%) reached the 23-week follow-up, with 2 (14.3%) participants withdrawing from the study at the allocation stage due to testing positive for COVID-19.
Baseline characteristics
Baseline demographic and clinical characteristics of participants recruited to the feasibility RCT are presented in Tables 2 and 3.
| TAU | Intervention | ||
|---|---|---|---|
| n (%) | |||
| Participants randomised n | 9 | 7 | |
| Recruiting site | Norfolk | 5 (56) | 2 (29) |
| Suffolk | 4 (44) | 5 (71) | |
| Gender | Male | 1 (11) | 2 (29) |
| Female | 7 (78) | 5 (71) | |
| Undisclosed | 1 (11) | 0 | |
| Age | 13 | 1 (11) | 2 (29) |
| 14 | 2 (22) | 2 (29) | |
| 15 | 3 (33) | 1 (14) | |
| 16 | 2 (22) | 2 (29) | |
| 17 | 1 (11) | 0 | |
| Ethnicity | British | 1 (11) | 0 |
| White British | 5 (56) | 6 (86) | |
| White European | 1 (11) | 0 | |
| White-Afro-Caribbean | 1 (11) | 0 | |
| Undisclosed | 1 (11) | 1 (14) | |
| Symptom severitya | Low | 6 (67) | 2 (29) |
| High | 3 (33) | 5 (71) | |
| TAU | Intervention | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NEET status | NEET status | |||||||||
| n | Further education | School | Paid work | None | n | Further education | School | Paid work | None | |
| Baseline | 9 | 0 | 6 (67%) | 2 (22%) | 1 (11%) | 7 | 0 | 7 (100%) | 0 | 0 |
| 10 weeks | 6 | 0 | 4 (67%) | 1 (17%) | 1 (17%) | 6 | 0 | 6 (100%) | 0 | 0 |
| 23 weeks | 6 | 0 | 5 (83%) | 1 (17%) | 0 | 6 | 0 | 5 (83%) | 0 | 1 (17%) |
Suitability of outcome measures
Rates of completion
Outcome measures were well completed. Of those successfully followed up at 23 weeks, almost all participants (83%) completed all outcome measures; one RCADS measure was missed at week 23. The Trial Manager/Research Assistant was able to check self-reported measures for missing items and follow up with participants to complete the measures. The researchers then facilitated the assessments at week 10 and week 23, which resulted in no measures being missed.
Descriptive statistics for outcome measures collected
The objective of the study was to assess the feasibility of this study to inform a future RCT. This study was not powered to detect any significant changes in outcomes. Mean changes from baseline by allocated arm are presented in Table 4.
| TAU | Intervention | Estimated treatment effect | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Effect | 95% CI | p | |
| RCADS | |||||||||
| Baseline | 9 | 19.1 | 4.11 | 7 | 15.1 | 5.55 | |||
| 5 weeks | 6 | 18.3 | 5.13 | 6 | 16.7 | 6.50 | –0.10 | –5.39 to 5.18 | 0.966 |
| 10 weeks | 6 | 16.5 | 7.53 | 6 | 13.5 | 5.47 | 1.14 | –5.31 to 7.58 | 0.699 |
| 23 weeks | 6 | 12.5 | 9.77 | 5 | 7.1 | 1.79 | 2.28 | – 7.32 to 11.89 | 0.599 |
| FAD | |||||||||
| Baseline | 9 | 2.3 | 0.20 | 7 | 2.3 | 0.30 | |||
| 5 weeks | 6 | 2.3 | 0.18 | 6 | 2.4 | 0.23 | –0.03 | 0.26 to 0.21 | 0.803 |
| 10 weeks | 6 | 2.5 | 0.19 | 6 | 2.4 | 0.14 | 0.10 | –0.12 to 0.32 | 0.322 |
| 23 weeks | 6 | 2.5 | 0.20 | 6 | 2.4 | 0.12 | 0.10 | –0.13 to 0.33 | 0.341 |
| Cambridge FQ | |||||||||
| Baseline | 9 | 3.3 | 0.49 | 7 | 3.1 | 0.48 | |||
| 5 weeks | 6 | 3.3 | 0.58 | 6 | 3.0 | 0.47 | 0.02 | –0.52 to 0.56 | 0.936 |
| 10 weeks | 6 | 3.5 | 0.32 | 6 | 3.1 | 0.36 | 0.21 | –0.07 to 0.50 | 0.133 |
| 23 weeks | 6 | 3.2 | 0.25 | 6 | 3.2 | 0.70 | –0.20 | –0.88 to 0.48 | 0.521 |
| SWEMWBS (metric) | |||||||||
| Baseline | 9 | 18.0 | 2.58 | 7 | 18.9 | 2.51 | |||
| 5 weeks | |||||||||
| 10 weeks | 6 | 18.7 | 5.09 | 6 | 20.4 | 2.00 | –1.77 | –5.83 to 2.29 | 0.350 |
| 23 weeks | 6 | 21.2 | 5.51 | 6 | 22.3 | 3.22 | –1.25 | –5.36 to 2.85 | 0.508 |
| CHU-9D (score) | |||||||||
| Baseline | 9 | 2.7 | 0.89 | 7 | 2.3 | 0.80 | |||
| 5 weeks | |||||||||
| 10 weeks | 6 | 2.5 | 1.07 | 6 | 1.9 | 0.49 | 0.65 | –0.10 to 1.40 | 0.080 |
| 23 weeks | 6 | 1.9 | 0.87 | 6 | 1.8 | 0.45 | 0.21 | –0.60 to 1.02 | 0.572 |
Safety and adverse events
There was one serious adverse event (SAE) recorded during the feasibility trial. The SAE was in the IPC-A arm and was an instance of a 3-day hospital admission due to urosepsis. The urosepsis was considered to have been caused by a urinary tract infection. Details of the SAE were reported to the Sponsor’s Participant Sub-Committee for independent review. It was deemed not to be related to the study procedures.
There were five adverse events (AEs) recorded during the feasibility trial, four in the TAU arm and one in the IPC-A arm. The AEs in the TAU arm were a positive test result for coronavirus (COVID-19), bereavement due to the death of an uncle and an ongoing investigation for a gluten allergy. The AE in the IPC-A arm was one instance of perceived difficulty breathing due to anxiety a few hours after baseline measures were taken. It was unclear whether this was related to the baseline assessment.
Health economic assessment
Follow-up was obtained on 12 participants at the 10- and 23-week periods. For a CHU-9D score to be generated, it is required that a valid response be given for all nine of the questions. Only in this case can a summary score be generated. It can be seen from the results outlined in Table 5 that scores could be derived in all but one case. For one participant at baseline, there was one answer to one question missing. In all other instances, complete data were obtained. Although sample sizes are small, the data indicate that health, as determined by the CHU-9D, was increasing over time. The use of t-tests suggests that the baseline and 23-week scores were statistically significantly different. There was no statistically significant difference between baseline and 10-week scores or 10-week and 23-week scores.
| Baseline (N = 15) | 10 weeks (N = 12) | 23 weeks (N = 12) | |
|---|---|---|---|
| CHU-9D | 0.716 (0.648–0.784) | 0.78 (0.705–0.855) | 0.833 (0.758–0.909) |
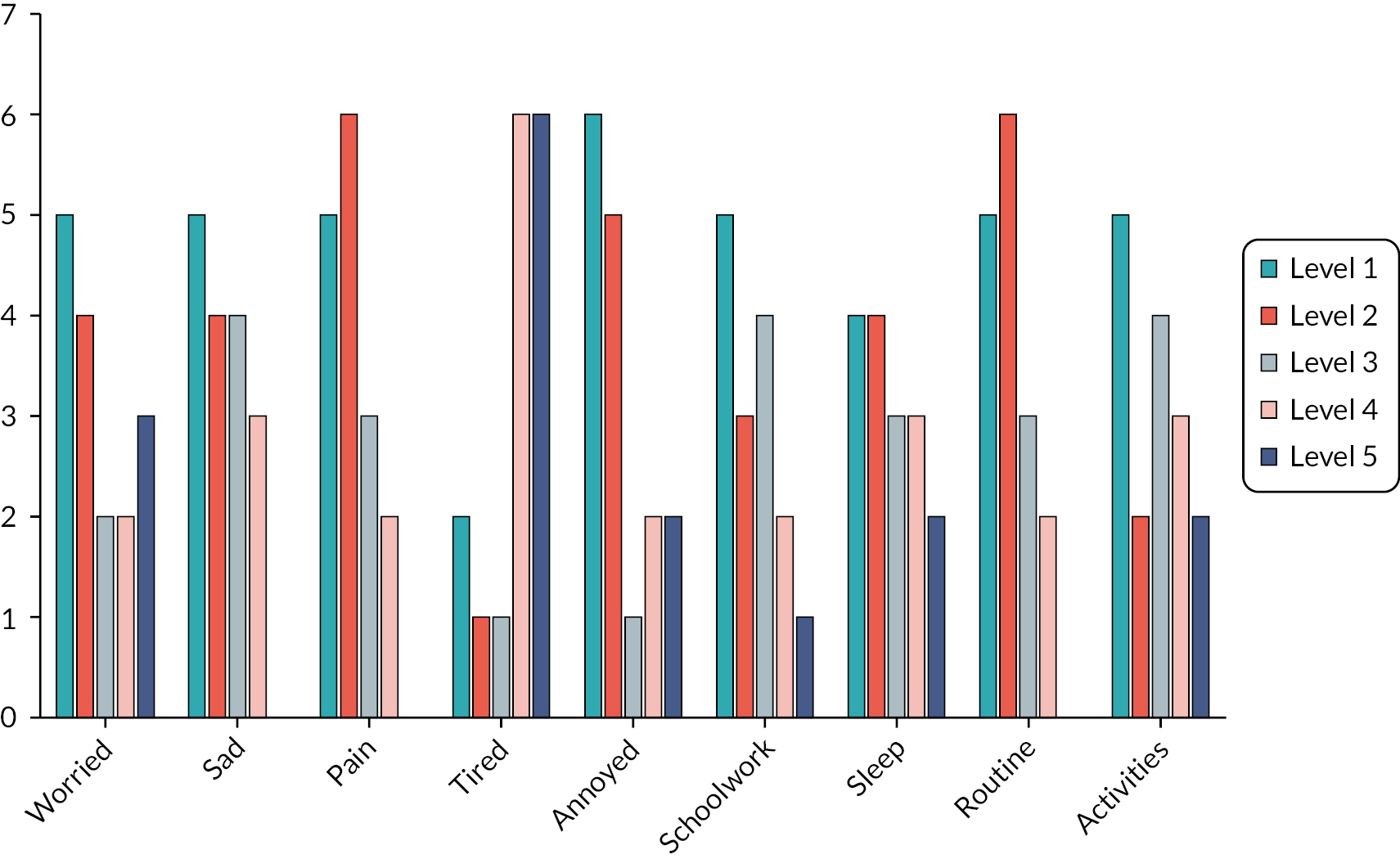
The results of the CHU-9D by individual response to each question are shown in Table 6 and Figure 4 for the baseline responses. The number of responses is given by level for each of the 9 CHU-9D questions. Each question has five possible responses, labelled 1–5 in Table 6 and Figure 4. In all cases, level 1 for each question represents the best response, and level 5 is the worst. Response categories differ by question. For example: level 1 for ‘Worried’ is ‘I don’t feel worried today’, whereas level 1 for ‘Activities’ is ‘I can join in with any activities today’.
FIGURE 4.
Baseline responses by CHU-9D dimension.
| Level | Worried | Sad | Pain | Tired | Annoyed | Schoolwork | Sleep | Routine | Activities |
|---|---|---|---|---|---|---|---|---|---|
| Level 1 | 5 | 5 | 5 | 2 | 6 | 5 | 4 | 5 | 5 |
| Level 2 | 4 | 4 | 6 | 1 | 5 | 3 | 4 | 6 | 2 |
| Level 3 | 2 | 4 | 3 | 1 | 1 | 4 | 3 | 3 | 4 |
| Level 4 | 2 | 3 | 2 | 6 | 2 | 2 | 3 | 2 | 3 |
| Level 5 | 3 | 0 | 0 | 6 | 2 | 1 | 2 | 0 | 2 |
Again, numbers are small, so there are limitations in what can be taken from these data. However, there are some observations that can usefully be made. In most cases, there were responses across the entire range of the possible responses, with only ‘sad’, ‘pain’ and ‘routine’ dimensions recording no responses in the worst state. This indicates that baseline responses in ICALM cover the full range of potential responses in the CHU-9D. This would also indicate that the CHU-9D has the potential to show improvements from baseline in this group of individuals. By contrast, if almost all responses had been at level 1, there would have been little opportunity to show improvements. This may also indicate that the CHU-9D is sensitive to changes caused by depression in adolescents. A second point that could be noted with these data is that the question relating to feeling tired appears to show the most negative responses.
Table 7 shows the completion rates for the CSRI and its various questions at the three time points. At least some sections of the CSRI were completed for 16 participants at baseline, 11 at the 10-week follow-up and 12 at the 23-week follow-up. Responses by category of resource use (individual questions) are shown in Table 7, that is, this shows the number of times this section was completed at each follow-up. Where sections do not appear to be completed, it is likely because a question was left blank. This was particularly common for ‘inpatient stays’ and ‘other drugs’. There were more sections/questions left blank at follow-up than at baseline. There was one CSRI form at the 10-week follow-up that was returned but left blank. Generally, the CSRI appeared to have been completed for participants, particularly at baseline.
| Baseline (N = 16) | 10 weeks (N = 12) | 23 weeks (N = 12) | |
|---|---|---|---|
| Q1 – School-based support | 14 | 11 | 12 |
| Q2 – Drugs relevant to mental health | 16 | 11 | 9 |
| Q3 – Other drugs | 12 | 6 | 3 |
| Q4 – Inpatient | 10 | 6 | 7 |
| Q5 – Other secondary care | 14 | 11 | 12 |
| Q6 – Community-based health and social care | 14 | 11 | 12 |
| Q7 – Residential social care | 14 | 11 | 12 |
| Q8 – Service use by family related to participants' mental health | 14 | 9 | 11 |
| Any category answered | 16 | 11 | 12 |
Resource use at baseline and follow-up, as indicated by the CSRI, is given in Table 8. Here, categories are only given if there was reported use of that type of resource. The ‘education, other’ category includes items such as personal tutors, attendance officers and success centre support workers. The modified CSRI used asked specifically about a number of named mental health drugs (fluoxetine, sertraline, melatonin/circadin, promethazine, citalopram, propranolol). No participant reported any of these drugs at any time period. The ‘other meds’ category in Table 7 gives a count of the number of different drugs reported. Generally, these are not mental health related. There was only one reported inpatient stay in any time period, corresponding to a 3-day stay. For other uses of secondary care, there was some limited use reported, generally for reasons not related to mental health.
| Resource use type | Resource use | ||
|---|---|---|---|
| Baseline | 10 weeks | 26 weeks | |
| School-based support | |||
| Welfare Officer/Well-being Officer/Pastoral Support Worker/Safeguarding lead | 47 | 13 | 3 |
| Classroom assistant | 0 | 0 | 2 |
| Special education needs and disabilities co-ordinator | 1 | 1 | 0 |
| School nurse | 5 | 3 | 4 |
| School counsellor | 4 | 2 | 0 |
| Education, other | 28 | 0 | 1 |
| Other drugs | 13 | 1 | 3 |
| Inpatient stay | 0 | 0 | 1 |
| Other secondary care | |||
| A&E – other | 0 | 0 | 1 |
| Paediatric OP – MH | 0 | 0 | 1 |
| Paediatric OP – not MH | 7 | 0 | 2 |
| Other OP – MH | 0 | 0 | 0 |
| Other OP – not MH | 4 | 0 | 1 |
| Day hospital treatment setting – not MH | 0 | 1 | 0 |
| Community-based health and social care | |||
| School nurse | 4 | 3 | 4 |
| Mental health nurse | 4 | 0 | 0 |
| GP | 18 | 5 | 4 |
| Paediatrician | 4 | 1 | 2 |
| Physiotherapy | 8 | 2 | 2 |
| Other | 16 | 3 | 1 |
| Counselling | |||
| Family therapist | 5 | 0 | 0 |
| Individual therapy | 18 | 22 | 27 |
| Other | 6 | 33 | |
| Support | |||
| After-school club | 17 | 5 | 1 |
| Other | 9 | 1 | 4 |
| Family use of services – total | 47 | 2 | 0 |
The majority of healthcare uses we asked about were not services that were used by any of the respondents. Contacts were reported for: school nurse, mental health nurse, GP, paediatricians, physiotherapy and other healthcare contacts. There was also reported use of therapist services. Generally, this was reported by a small number of individuals reporting multiple contacts. There was no reported use of social care services, though a few individuals used after-school clubs. There were a number of reported contacts with services by participants’ families – this was mostly in the baseline period.
In general, the CSRI appeared to have been completed by most respondents. There were some categories where the response had been left blank and it was not clear if this was ‘missing’ or zero. However, in the majority of cases, a value of zero was used if there was no reported service use. Generally, there were only one or two missing cases in the data for the majority of data types.
There appears to be a clear pattern of reducing service use over the follow-up period. The exception to this appears to be the use of therapy services.
The number in Table 8 generally corresponds to number of visits or contacts or number of stays. The exception is use of ‘other drugs’ where numbers represent prescriptions.
As part of the economic component, we estimated the costs of providing the IPC-A intervention. Given the very small numbers who had the intervention, it was difficult to estimate what the costs may be if this was applied in a larger sample as it would be in any future trial or if the scheme was rolled out into practice. The costs calculated here can be divided into three categories: costs of providing training; costs of supervision; and costs of providing sessions. In all cases, costs are in UK 2020–1 Great British pounds.
The costs of training are given in Table 9. Training was provided for 2 whole days for 19 attenders. It was assumed that two members of staff provided the training; these were grades 8a and a consultant psychiatrist. It was assumed that these receiving training would be equivalent to grade 4 [Agenda for Change (AfC)] NHS staff. In all cases, costs were taken from a published source. 41 The costs of those giving training were a mean of costs for a grade 8a psychologist and for a consultant psychiatrist (£75 and £123 per hour, respectively). The largest cost was the time of the 19 individuals being trained. No cost for accommodation was assumed, but the costs per hour would allow a component for overheads. Based on the 19 individuals trained, a cost per person trained of £636 was estimated. This only includes staff time (with overheads) but does include costs of both trainers and those being trained. There are a number of uncertainties here, so it is very difficult to estimate the training component of the cost of IPC-A. Firstly, it should be noted that of those trained, only two therapists provided intervention sessions. In any future study or routine care, it is likely that a much higher proportion of those trained would go on to practice what they trained, but that this may never be 100%, so the cost per person who goes on to offer IPC-A may be higher than the cost per person trained. However, in this study, there was high turnover of therapists, so it may always be the case in practice that significantly more people need to be trained than will ever provide the intervention. Secondly, in a future trial or in clinical practice, those trained may well provide care for a number of individuals. Also, the training may continue to be relevant for a number of years, so this may also increase the number of individuals to whom training is provided. The 2 staff who provided the intervention gave care to 3 participants or 1.5 participants per therapist. In Table 9, the average cost per person trained (£636) is divided by 1.5 to give an average cost of training per person receiving ICP-A of £42. However, in actual practice, training would enable a person to provide sessions for a larger number of individuals and would presumably be valid for a number of years before retraining was required. So, in a large trial or in clinical practice, the actual costs of training as a component of IPC-A are likely to be considerably lower than the values presented here.
| Hours | Staff | Cost/hour | Total | |
|---|---|---|---|---|
| Cost of trainers | 14 | 2 | £99 | £2772 |
| Cost of trainees | 14 | 19 | £35 | £9310 |
| Total | £12,082 | |||
| Numbers trained | 19 | |||
| Cost/person trained | 19 | £636 | ||
| Numbers trained | 2 | |||
| Interventions provided | 3 | |||
| Cost of training per intervention provided | £424 |
The second component of the therapy cost considered here was that of providing supervision. It was assumed that this was only given to those providing the intervention. To simplify data collection and to reduce burden on participating therapists, no detailed logs of supervision were kept so the costs are based on assumption and expert opinion. Supervision was provided on a weekly basis by two practitioners (a grade 8a and a grade 7) over the course of 6 weeks. This gave an estimate of six sessions of supervision per therapist providing IPC-A. It was assumed that these supervisors provided equal amounts of supervision. Therapists receiving supervision were assumed to be equivalent to AfC grade 4. It was assumed that this would be provided while the therapist was providing the intervention sessions (over a 6-week period) and that no therapist was providing sessions to more than one study participant at any one time. We assumed 18 sessions of supervision were given equally by the two supervisors for the three individuals receiving the intervention. The costs were £75 and 65 for the grade 8a and grade 7, respectively. Assuming 30 minutes gave a cost per supervisory session of £37.5 and £32.5 and a total cost of supervision for the 18 sessions (three sets of 6 weeks) of £630. The cost of the therapist's time for receiving supervision was based on an assumption of 30 minutes and a cost per hour of £35, giving a total cost of receiving supervision of £315 (£35*0.5*18). This gave a total estimated cost of supervision for the therapists providing the three courses of IPC-A of £945 or £315 per person receiving IPC-A.
The third component of costs was the cost of therapists providing the IPC-A sessions. It was assumed that this would be provided by the equivalent of an AfC grade 4. Sessions were assumed to last 55 minutes, and there would be a ratio of contact to non-contact time of 1 to 0.3. 42 For the four participants who received TAU, there was an average of 9.25 sessions per person, giving a total cost of £386 per person. For the three individuals who received the intervention, there was an average of 6.7 sessions per person, giving a total cost per person of £278. The costs of the various components for the IPC-A intervention are given in Table 10, with a total cost of £1017 per person.
| Type of resource | IPC-A |
|---|---|
| Training | £424 |
| Supervision | £315 |
| Sessions | £278 |
| Total | £1017 |
However, it is important to bear in mind that this estimate is subject to large amounts of uncertainty due to the small numbers. In particular, the costs of training per person receiving IPC-A would be much lower if training costs were spread over a much larger number of individuals receiving therapy. This would be the case in a larger trial or in clinical practice.
Chapter 4 Process evaluation
This chapter is adapted from Katangwe-Chigamba et al. 43 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Design
An embedded mixed-methods ethnographic process evaluation to generate an understanding of intervention implementation across services and explore the acceptability of the intervention from the perspective of young people and other key stakeholders.
Objectives
The objectives of the process evaluation were to:
-
provide a description of how IPC-A and TAU were delivered
-
assess implementation and theoretical fidelity to the IPC-A model over time
-
observe how delivery is shaped by the context of differing service models
-
identify any harms arising from treatment (including end of treatment)
-
establish the extent and source of any contamination of the control arm.
Recruitment procedure
Consent for young people and parents to participate in the process evaluation (interviews and having sessions video/audiotaped) was sought during the main consent procedures and ascertained at the 23-week assessment. All parents whose child participated were invited to take part and asked to complete a separate consent form. However, it was not a requirement that a young person/parent consents to the process evaluation in order to take part in the study. IPC-A or TAU YMHWs’ participation in the process evaluation (providing recorded audiotapes of therapy sessions and/or participating in an interview) was also optional; staff were given participant information sheets and asked for informed written consent. Consent to complete the SPQ and participate in an interview was also obtained from managers and/or service leads.
Methods
Data collection methods included SPQ, policy documents, observations of training workshops and supervision, video-/audio-recordings of treatment sessions, fidelity ratings of IPC-A and TAU sessions according to the IPC-A rating scale, interviews with young people (and parents/carer), focus groups with YMHWs’ and wider stakeholders. Data collection aimed to facilitate an understanding of how the delivery of IPC-A was organised within the context of differing service models by setting out macro-, meso- and micro-contextual features relevant to implementation.
Data collected to inform the macro- and meso-contextual features shaping implementation
To understand the macro-contextual features shaping implementation and delivery of the ICALM intervention, we conducted a documentary review of key policy documents to identify contextual features likely to shape implementation of ICALM at the meso and micro levels. To understand the meso-contextual features shaping implementation and delivery of ICALM, we collected SPQ from participating sites. The questionnaires aimed to understand the broader service context in which the intervention is delivered, including TAU for young people with mental health needs; policies, protocols and procedures used by staff; numbers of young people with mental health needs and proportion with depression; training and experience of staff in treating depression in young people; and allocation and distribution of staff to support young people with mental health needs. In conjunction with the SPQ, we planned to also conduct focus groups with key stakeholders (including commissioners, education representatives and service managers) at the end of the study to review study findings and discuss implementation barriers and sustainability of implementation.
Data collected to inform the micro-contextual features shaping implementation
To understand how therapists delivered IPC-A at a micro-contextual level, we collected/conducted:
-
Observations of IPC-A training workshops and supervision: Researchers’ field notes from observations of training and supervision of IPC-A therapists were used to provide a detailed description of process and content of staff training and supervision.
-
Video-/audio-recordings of treatment sessions and fidelity ratings: All therapy sessions were video- or audio-recorded, subject to consent. The recorded therapy sessions were rated by one of the supervisors according to the IPC-A Audio Recording Rating Scale28 to monitor implementation fidelity to the IPC-A treatment model and to assess the degree of contamination. This scale includes ratings of techniques for the assessment (e.g. ‘Complete an interpersonal inventory’), how sessions ended, specific focus areas (e.g. ‘Exploration and discussion of differences in expectations for relationship disputes’) and general IPC techniques to be used for all sessions (e.g. ‘Clear focus on depressive symptoms and interpersonal relationships’). TAU therapists were also asked to submit sessions for rating. The aim was to understand and describe TAU and assess contamination (i.e. evidence of TAU therapists delivering any elements of the IPC-A intervention), rather than to rate the quality of the young person’s therapy.
-
Interviews with participants (and parents/carer) from the IPC-A and TAU arms: Young people participating in the RCT (and their parents) were invited to take part in in-depth interviews after their final assessments (23-week assessment). Subject to consent, a separate interview was also undertaken with a parent/carer. During the interviews, participants were asked about their experience and views of the process of accessing help, the content of intervention sessions, contacts they had in addition to study therapy sessions, whether they felt they had benefitted from receiving the intervention, the experience of ending therapy and suggestions for improvement.
-
Interviews with IPC-A YMHWs (see changes below): Following completion of delivery of the IPC-A and TAU arms, we conducted interviews with YMHWs to understand staff perspectives of each study arm. For IPC-A YMHWs, interviews focused on barriers and facilitators to successful delivery, experiences and views of intervention sessions, additional work required to support delivery of IPC and suggestions for improvement. For TAU YMHWs, interviews focused on how TAU is delivered, the additional support young people in TAU have received and their awareness and perspectives of IPC-A.
Data analysis
A linguistic ethnographic methodology,44,45 which included multiple and mixed methods, was employed to investigate how implementation of ICALM was shaped by the wider context of mental health services and to provide a broad description of intervention delivery. Thematic analysis was used for SPQ, interview and focus group data and populate macro-, meso- and micro-contextual features. Macro, meso and micro levels refer to levels of context, providing an organising structure for our investigation. 46 Along with observational field notes of training sessions, these represented the ethnographic element of this methodology. Conversation analysis was used on the interaction video/audio data to understand interactional sequences that would provide insight into theoretical fidelity of the intervention. The analysis of qualitative data was iterative, moving between session recordings and interviews to test emerging theories. A constant comparison analytical technique, involving triangulating and looking for connections between data, was employed to ensure rigour as the analyst’s interpretations developed.
Thematic analysis
Data sources: site profile questionnaires, interviews, focus groups, observations
To understand how participating organisations were organised to provide mental health services to young people and the interaction between contextual features and intervention delivery, we analysed SPQ and stakeholder interviews/focus groups. Interview/focus group data were transcribed verbatim and thematically analysed together with the questionnaire data to describe the participating services and to set out macro-, meso- and micro-contextual features relevant to implementation within each provider. By framing the analysis of intervention implementation within a macro-, meso- and micro-contextual framework, we aimed to make the transition from the identification of routines and patterns of use in the specific services participating in the current study to theoretical explanations of how different structural relations and mechanisms of the intervention organise moments of delivery, which then impact on specific outcomes. Such insights were particularly evident in highlighting the challenges of conducting key processes for the trial which we report on in detail.
To provide a description of the process and content of therapy sessions, staff training and supervision, researchers’ field notes from observations of training, supervision of IPC-A therapists and interviews with young people, parents/carers and therapists were transcribed verbatim and thematically analysed with the aid of NVivo software. Aspects of speech delivery, such as loudness and changes in pitch, were indicated using symbols (see Appendix 1, Table 24). For intervention arm participants, we developed a coding scheme to evaluate how the process and content of IPC-A as delivered by the YMHWs functioned from the participants’ perspective. In the control arm, we assessed how participants experienced the TAU provided by their YMHW and any other sources of support used. A constant comparison approach was adopted, working iteratively between data obtained from different interviewees within and between implementation sites.
Conversation analysis
Data source: session audio-recordings
Audio-recordings and transcriptions of therapy sessions were analysed to evaluate implementation and theoretical fidelity. To monitor implementation fidelity in the intervention arm and to assess the degree of contamination in the TAU arm, we rated sessions against the IPC-A treatment model. To evaluate theoretical fidelity, a purposive sample of extracts from recorded IPC-A sessions was transcribed according to Jeffersonian conventions and subject to conversation analysis in order to identify how IPC-A components are communicated by therapists and received by young people, including how the mechanisms of the IPC-A intervention function to affect change within and across individual counselling sessions.
Changes to process evaluation
Process evaluation objectives
Due to recruitment and implementation challenges, the funder requested a shift in focus for the study, with greater emphasis being placed on understanding the main barriers to running such trials (i.e. RCTs) within the mental health setting. Therefore, to gain insight into how (or how not) to design future studies, while still reporting on all objectives, the process evaluation places greater emphasis on objectives 1 and 3 in order to highlight the challenges of running this type of research in this setting. Therefore, in the findings, we provide a description of the services, the challenges the services were experiencing and how this impacted ICALM.
Data collection
Low recruitment rates (both for the study and the process evaluation elements) and challenges in obtaining data from participating services negatively impacted the quantity of data collected for the process evaluation and led to changes in data collection methods, as outlined below:
-
Site profile questionnaires: For each site, we originally intended to collect questionnaire data at baseline and at the end of the study. However, due to delays in obtaining data from participating services, we only collected one questionnaire per site at various study time points.
-
Focus group with professional stakeholders: We intended to hold one focus group with professional stakeholders at the end of the study to review study findings and discuss implementation barriers and sustainability of implementation. However, due to the change in key focus outlined above, in-depth stakeholder views were sought by primarily conducting interviews, with commissioners and managers and/or service leads from each participating organisation before the end of the study. We therefore did not conduct focus groups with key stakeholders to review study findings at the end of the study.
-
Interviews with participants and parents: We originally planned to conduct 20 interviews with young people (10 IPC-A and 10 TAU) and 20 interviews with parents/carers (10 IPC-A and 10 TAU). However, only 16 interviews in total were conducted.
-
Young person workers focus groups: We intended to conduct one focus group per arm per service provider with participating young person workers. However, due to some workers moving on from the services and the low number of consenting workers available, we conducted interviews instead. This change allowed us to have an in-depth understanding of implementation and intervention delivery, despite the recruitment limitations.
-
Video-/audio-recordings of treatment sessions and observations of supervision: To evaluate implementation fidelity, we originally planned to randomly select therapy sessions (15% in each arm) for rating by one of the supervisors according to the IPC-A Audio Recording Rating Scale. To evaluate theoretical fidelity, we planned to use the ratings to purposively sample extracts of recorded IPC-A sessions to be transcribed according to Jeffersonian conventions and subject to conversation analysis in order to identify how IPC-A components were communicated by therapists and received by young people, including how the mechanisms of the IPC-A intervention function to affect change within and across individual counselling sessions. However, with only a few participants consenting to their session recordings being analysed for the process evaluation, all sessions were assessed for implementation and theoretical fidelity.
Results
-
Site profile questionnaires: We collected a total of 9 questionnaires out of the 13 participating sites, including 5 from Suffolk (Site-01_Early Help and NEET Team, Site-02_Early Help and NEET Team, Site-03_Early Help and NEET Team, Site-07_Charity and Site-04_Wellbeing Service) and 4 from Norfolk (Site-05_Charity, Site-06_Charity, Site-08_Community NHS Trust and Site-09_Family Support Team). An additional questionnaire was obtained from Site-10_Central referral point.
-
Interviews with professional stakeholders: We conducted eight interviews and one focus group with stakeholders, including: head of service (one), clinical/therapeutic leads (two), clinical managers (two), senior practitioner (one), team managers (four), clinical nurse specialist (one). Stakeholders represented all 13 teams involved in the study as well as Site-10_Central referral point which supported referrals to the Early Help and NEET teams in Suffolk.
-
Interviews with participants and parents: We conducted 16 interviews in total, 8 in the intervention arm (4 young people and 4 parents) and 8 in the TAU arm (3 young people and 5 parents).
-
Young person worker interviews: We conducted eight interviews in total; one with an IPC-A supervisor, six with IPC-A therapists and one with a TAU therapist.
-
Video-/audio-recordings of treatment sessions and observations of supervision: Only four participants (three IPC-A and one TAU) consented to their session recordings being analysed for the process evaluation. Therefore, all recordings were rated and analysed.
-
Observations of IPC-A training workshops and supervision: Two training observations were conducted, and 10 supervision session recordings with 2 IPC-A therapists were provided to the process evaluation team.
Results structure
In order to retain anonymity, organisations and participants involved in the study have been given an ID (Table 11). Firstly, we provide a description of the participating organisations (Tables 11 and 12). Secondly, we report macro-, meso- and micro-contextual features of non-specialist mental health services which had an impact on study and intervention implementation. In Tables 10–13, we set out the macro- and meso-contextual features, with illustrative quotes from SPQ and interviews. Thirdly, we present findings on acceptability and implementation/theoretical fidelity of the intervention. Within this analysis of session recordings, evidence of how macro- and meso-contextual features were made salient by therapists at a micro-contextual level was less evident. However, we provide insight into implementation and theoretical fidelity of the intervention using telling cases to illustrate mechanisms and contextual conditions which appeared key to successful delivery of the intervention. Finally, we then use these findings to make recommendations on (1) how to strengthen mental health services to meet the needs of young people; (2) how to strengthen mental health services to enable new interventions such as ICALM to be implemented (including a consideration of the challenges of taking on research); and (3) how to adapt the intervention content or implementation strategies (e.g. training, referral processes).
| Site ID | Service type | SPQ ID | Stakeholder ID |
|---|---|---|---|
| Site-01 | Early Help and NEET | SPQ-01 | Stakeholder-04 |
| Site-02 | Early Help and NEET | SPQ-02 | Stakeholder-05 |
| Site-03 | Early Help and NEET | SPQ-03 | Stakeholder-10 |
| Site-04 | Wellbeing Service | SPQ-04 | Stakeholder-02 and Stakeholder-07 |
| Site-05 | Charity | SPQ-05 | Stakeholder-09 |
| Site-06 | Charity | SPQ-06 | Stakeholder-11 |
| Site-07 | Charity | SPQ-07 | Stakeholder-08 |
| Site-08 | Community NHS Trust | SPQ-08 | Stakeholder-03 |
| Site-09 | Family Support | SPQ-09 | Stakeholder-06 |
| Site-10 | Central referral point | SPQ-10 | Stakeholder-01 |
| Suffolk | Norfolk | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Site-01_Early Help and NEET Team | Site-03_Early Help and NEET Team | Site-02_Early Help and NEET Team | Site-04_Wellbeing Service | Site-07_Charity | Site-06_Charity | Site-05_Charity | Site-08_Community NHS Trust | Site-09_Family Support Team | |
| Type of agency | Early help and NEET team. 0–19s non-crisis preventative service within Children’s Services | Early help and NEET team. CYP and family non-crisis preventative service within Children’s Services | Early help and NEET team providing non-crisis preventative services within Children’s Services | A tier 2 mental health service for CYP aged 4–18. | A charity providing advice and support to young people. Including counselling provided either independently or under contract with Site-04_Wellbeing Service | A charity funded by the ICB operating under the Point 1 provision umbrella. Providing services for CYP (age 0–18 years) Works closely with Site-05_Charity | A charity funded by the ICB operating under the Point 1 provision umbrella. Providing advice, information, and therapeutic services | Emotional Health Team within an NHS trust. Provide health advice and support for young people at a Universal Services Level across Norfolk | Family Support team. |
| Numbera (or proportion) of young people and/or families with mental health problems in the previous year. | 160–170 young people open; close/open about 5–10 referrals/week, so potentially 390 families/year | Approximately 75% of referrals are around young people with mental health difficulties | 80–85% of referrals have some element of mental health difficulties | Approximately 1250–1500. Eighty per cent of the referrals are for anxiety and depression, with a split of 70/30 between anxiety/low mood | Most common presentation is anxiety | Approximately 100 for intervention. Forty to 50% of the cases are (reactive) low mood owing to friendship fallouts, COVID-19, school avoidance | Approximately 1500 | Ninety per cent of referrals associated with anxiety likely impacted by COVID-19, that is, CYP not wanting to go back to school | Approximately 500 open at any one time, a proportion of these children will have mental health needs |
| Types of mental health difficulties experienced by young people presenting at the services | |||||||||
| Low mood/mild depression | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Anxiety/stress | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Trauma | Y | Y | Y | Y | Y | ||||
| Abuse | Y | ||||||||
| Panic attacks | Y | ||||||||
| Phobias | Y | Y | Y | ||||||
| Low confidence | Y | ||||||||
| Suicidal ideation | Y | Y | |||||||
| OCD | Y | ||||||||
| Emotional dysregulation | Y | Y | |||||||
| EUPD | Y | Y | Y | ||||||
| Selective mutism | Y | ||||||||
| Types of support offered by the services (apart from IPC-A) | Promotion of positive mental health and well-being | Promotion of positive mental health and well-being in young people by YPWs | Promotion of positive mental health and well-being | Anxiety and low mood: Webinars on managing anxiety, low mood, Coming out of lockdown | Counselling for range of presentations, including low mood – enabling young people to develop coping strategies | Low mood support – CBT-informed guided self-help by CWPs | Low mood – counselling involving understanding contributing factors and developing coping | CBT-informed mental health promotion, new emerging mental health difficulties, including low mood, anxiety and emotional dysregulation | Development interventions for anxiety/low mood, for example, talking about emotions and feelings and developing coping strategies |
| Support with self-identity/esteem – personal confidence, bullying, gender, sexuality | Statuary services: supervised contact for CYP in care servicesb | Trauma-Informed Practice | CBT-informed guided self-help for low mood or anxiety by CWPs | Emotional well-being and resilience building | Anxiety support – adolescent-focused (12–18 years) CBT-informed guided self-help by CWPs | Low mood – mental health work to understand causes/develop coping strategies | Emotional health promotion, including working on healthy relationships within the family | Emotional resilience and confidence building | |
| Motivation – for re-engaging with ETE | Graded exposure/ Travel training (school-/college-phobic young people)b | Parenting supportb | CBT-informed work/a brief piece of intervention, if appropriate, by PMHWs | Youth work with a therapeutic foundation, for example, walk and talk group | Processing difficult experiences (mild trauma) (CBT-trained counsellors) | In-call service to offer support for high-level needs (including mental health support) | |||
| Statutory services: supervised contact for CYP in care servicesb | Statutory services: supervised contactb | Behavioural activation by CWPs | Psychoanalytic, trauma-informed practice (counsellors) | Identity workb | |||||
| Graded exposure/travel trainingb | Domestic violence workb | Psychoeducation by CWPs | Psychosocial intervention (counsellors) | Well-being support | |||||
| Bespoke intervention up request from social care for CIN or CP plansb | Bespoke social care request: instead of CAF, only offer six sessionsb | Short-term counselling commissioned via referral to Site-07_Charity | Emotional dysregulation (CBT-trained counsellors) | Exploitation workb | |||||
| Life story work – for CYP that are moving onb | Play/talking therapy (counsellors) | Social work toolboxb | |||||||
| Mediation – household conflictb | |||||||||
| Wishes and feelingsb | |||||||||
| Domestic violence workb | |||||||||
| Location of support (Options flexible to young people and family needs. Virtual delivery commenced during the COVID-19 pandemic) | School/college, | Schools, | Schools | Schools, | Schools, | Schools, | Schools, | Schools | |
| Community venues, for example, children’s services buildings | Community settings | Clinic | Work premises or other venues | Community venues, for example, health and children centres | Work premises/centres | ||||
| Virtual platform | Virtual platform | Virtual platform | Virtual platform | Virtual platform | Virtual platform | Virtual platform | Virtual platform | ||
| Young person’s Home (if no safety concerns with parents | Young person’s Home | Young person’s Home | Young person’s Home | Work premises/centres | Young person’s Home | ||||
| Structure of support: Flexible, based on needs of young people and any safety concerns | Deliver weekly one-to-one sessions for approximately 1 hour p/w | FSP-led interventions often involve the whole family, and YPW-led interventions are one-to-one sessions | One to one with older young people. Approximately 70% of work is with parents (parenting programmes) | One-to-one sessions 8–12 weeks – for CBT, CWP and PMHW interventions. 8–15 sessions – counselling 3 sessions – Assessments |
One-to-one sessions – initially 6 sessions, but can sometimes go up to 8–12 sessions depending on complexity | One to one (6–8 sessions) | Counselling – standard offer 6 sessions, plus 6 extra available on review based on young person’s needs | One to one unless the parents are included. Sometimes have teachers involved towards the end of interventions (6–8 sessions, delivered fortnightly) | One to one with young person – up to 12 weeks, but not capped at this |
| Occasional group sessions where there is a need, for example, skills-based, confidence, etc. | Group sessions with young people at risk of becoming NEET | Group sessions, for example, Elevate (a school-based girl’s group focused on well-being, self-esteem, confidence) | Webinars | For youth work service also offers drop-in sessions; one-to-one, group and activity-based sessions and school-based sessions | Group sessions for anxiety and low mood running for 8 sessions | One to one; YMHW (1–8 sessions) | |||
Description of services involved in the ICALM study
Nine sites across seven organisations, including two County Councils, were involved in the delivery of IPC-A (green) and/or TAU for the study (Figure 5), three in Suffolk and four in Norfolk. Two of the organisations, Norfolk and Suffolk County Council, consisted of several teams, some of which did not (fully) participate in the study (grey). Four of the organisations worked collaboratively to provide either TAU or IPC-A: two in Suffolk (Site-04_Wellbeing Service and Site-07_Charity) and two in Norfolk (Site-05_Charity and Site-06_Charity).
FIGURE 5.
Services involved in the ICALM trial.
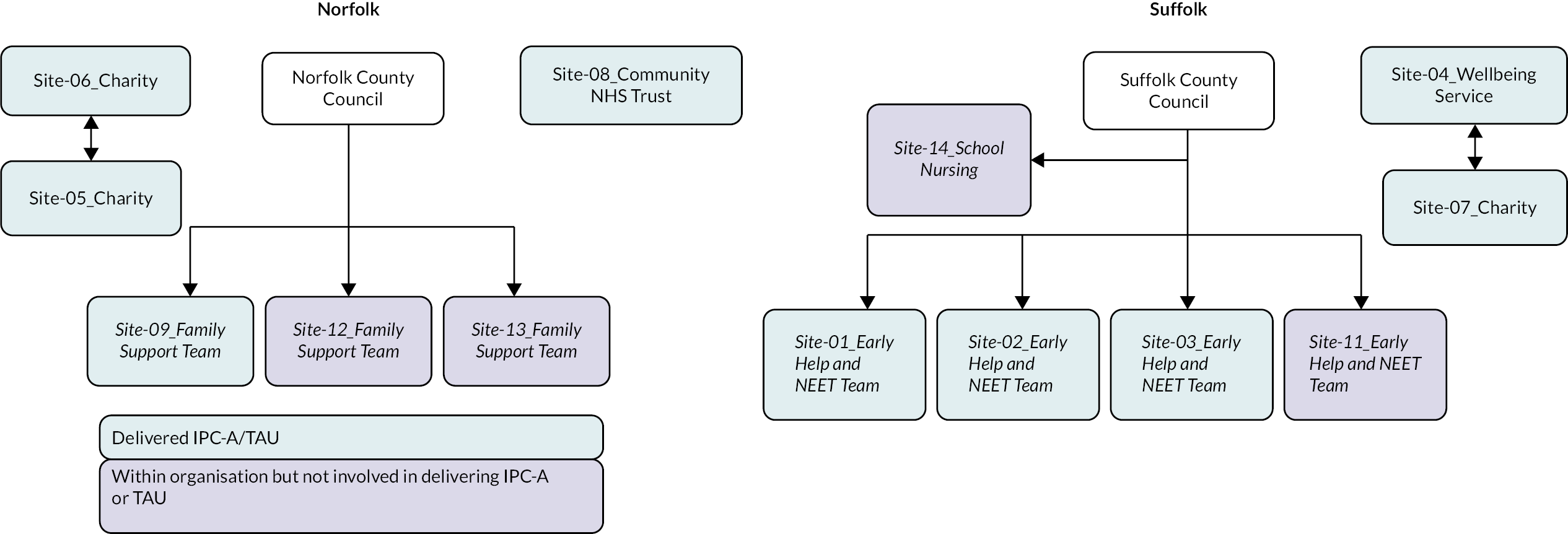
A summarised description of the services involved in the delivery of IPC-A and/or TAU is provided in Table 12. Participating services were tier 2 services, consisting of three charities, three Early Help teams and NEET teams, one wellbeing service and one family support team, each providing a range of support, including mental health interventions for CYPs aged 0–19.
Types of mental health support provided by the services
Tier 2 services (Early Help and targeted services) are designed to offer a range of support, including early and short-term interventions for CYP experiencing mild to moderate mental health problems. Service providers estimated that approximately 40–90% of the cases referred to their services involve some element of mental health difficulty, in particular low mood and anxiety. Other mental health difficulties seen by the services included panic attacks, phobias, suicidal ideation, obsessive–compulsive disorder (OCD), emotional dysregulation, poor emotional literacy and emotionally unstable personality disorder/self-harm (EUPD, also referred to as borderline personality disorder).
While all services included in the study are designed to offer early help, only four services (Site-04_Wellbeing Service, Site-05_Charity, Site-06_Charity, Site-07_Charity) offered targeted services for mild to moderate mental health problems. Targeted services were already providing support other than IPC-A to CYP experiencing mild to moderate mental health difficulties such as anxiety, low mood and mild trauma-type presentations. Types of support target services offered for these presentations included advice, guidance, counselling, treatment/therapeutic interventions [including cognitive behavioural therapy (CBT)-informed interventions] and guided self-help. Interventions offered by the services were typically short-term (six to eight sessions) one-to-one interventions, delivered either virtually (during and post COVID-19) or in various settings according to preference of CYP.
Support offered by Early Help teams and NEET teams in Suffolk focused on supporting families, young people at risk of being NEET and delivery of interventions and support to families in receipt of social care and child protection (CP). Apart from IPC-A, Early Help teams did not offer any specific mental health support but addressed mental health-related issues, for example, peer-related issues, emotional health promotion, motivation, confidence and self-esteem, including low mood occurring within the young person’s life. In Norfolk, support offered by Site-08_Community NHS Trust and Site-09_Family Support Team primarily focused on emotional resilience and confidence building. The teams also depended on targeted services via onward referral for support with specific mental health-related issues, such as low mood.
Mental health is a very small part of what we do but is also very common. Our interventions focussed on safety predominantly but then health and wellbeing is a secondary important focus. We would work alongside any families experiencing any mental health problem, we wouldn’t necessarily take the lead on the mental health part.
SPQ, Site-01_Early Help and NEET Team
There’s no other intervention [apart from IPC-A] that’s specifically focussed on mental health, just our Trauma Informed Practice and our use of Signs of Safety, which is a way to map worries.
SPQ, Site-02_Early Help and NEET Team
Referral pathways into non-specialist services involved in the ICALM study
In Suffolk, young people (and parents) can self-refer either directly to all non-specialist mental health services or through a central referral point (Site-10_Central referral point in Suffolk). Other major gateways into the services include general practice, schools and social care [via common assessment framework (CAF)]. In Norfolk, referrals to the Early Help teams (family support teams) are received from professionals via the Children’s Advice and Duty Service (CADS) or directly from young people and families. Referrals to targeted services (i.e. Site-05_Charity and Site-06_Charity) are received from professionals via a single point of access (SPOA).
Site 10_Central referral point
The majority of CYPs presenting at General Practice with mental health difficulties get referred to the services through Site 10, which is a central referral point for families, professionals and young people (age 0–25) to access mental health services. The referral point consists of a team of 10 staff members, including 7 clinicians, whose role is to screen referrals and triage them by rating them against risk criteria and identifying the right service for them. The referral pathway to and from the referral point is outlined in Figure 6. Each case is RAG (red, amber, green) rated by two qualified clinicians within 24 hours, and the outcome and rationale are recorded.
FIGURE 6.
The referral pathway for Site-10_Central referral point. YP, young people.
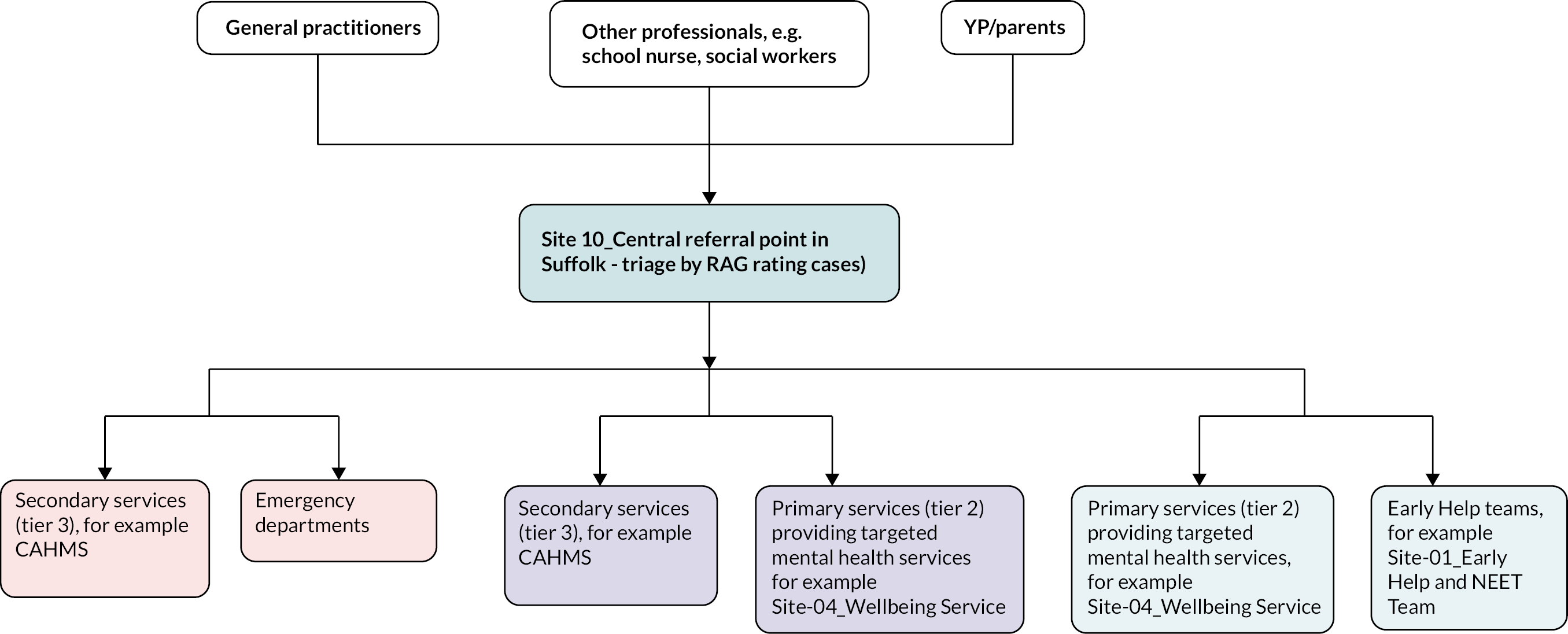
Red cases: High risk of harm to self (and others); severe mental health difficulties, for example, eating disorders, signs of psychosis, actively suicidal (not just thoughts/plans but showing a clear intent), not leaving the house for over a year; and severe OCD. These cases are dealt with within 24 hours by referring them straight to secondary services (tier 3) or emergency departments.
Amber cases: Moderate risk, for example, suicidal ideation – but with lesser intent/ planning, self-harm requiring medical intervention alongside presenting issues and some chronicity/impulsivity, safeguarding concerns, significant phobias, symptoms having a significant impact on daily life or self-care, multiple trauma, significant tics and selective mutism. These cases are seen within 72 hours. These cases may go to secondary services (tier 3) or primary services (tier 2, e.g. Under 18 wellbeing Service).
Green cases: Mild risk, for example, low mood, anxiety due to COVID-19, trauma, bereavement, mild to moderate OCD, attachment difficulties, safeguarding, anger management and emotional dysregulation. These cases are dealt with within 28 days.
The Common Assessment Framework
Schools and social workers can refer CYPs experiencing mental health difficulties directly to early help and targeted services. These referrals usually come through pastoral support, teachers, head teachers and school nurses who identify CYP through self-disclosure or observation, for example, recurring patterns of a problematic behaviour. Referrers complete a CAF, which has a pre-assessment checklist to help identify CYPs with additional needs and decide who would benefit from a common assessment. Schools then put the CAF into a portal which is picked up by the CAF Admin team who then sends them through to the relevant geographical/local teams. The CAF is designed to promote a co-ordinated service provision to meet CYP’s needs. The assessment covers three domains: development of the child or young person; parents and carers; and family and environment. 47
Children’s Advice and Duty Service
In Norfolk, CYP, families, professionals and social workers can refer CYP to Early Help and family support teams directly or through CADS. CADS consists of a team of Consultant Social Workers who provide advice and support to families, social workers and professionals with concerns about a child. The Consultant Social Workers also help with signposting by identifying the correct services to support CYP. CADS also decides whether referrals need a social work assessment or family support.
The single point of access teams
The SPOA in Norfolk is a team of administrators who receive referrals from professionals, parents/carers and young people. The team assesses referrals and signposts them to appropriate clinical teams and services to receive support and guidance. The team is not clinical and does not offer treatments.
Assessment processes for eligibility into the services – Suffolk
Services reported using various assessment processes, frameworks and measures to make decisions on whether referred cases were appropriate for their service or needed signposting/escalation. Assessment processes differed between and within services providing Early Help /family support teams and targeted support services in Norfolk and Suffolk. The services reported holding regular triage or transfer meetings to discuss referrals classed to be outside the service remit or needing escalation. The meetings are attended by representatives from Early Help teams, Point 1 services and well-being (tier 2 Norfolk) services and tier 3 services, for example, Norfolk and Suffolk NHS Foundation Trust (NSFT) and social care who would work together to identify the right services for cases.
Assessment processes for services NOT offering targeted mental health services
Suffolk Early Help and NEET Teams (Site-01, Site-02 and Site-03): Early Help teams within the same organisation, for example, Suffolk County Council had a similar assessment process, which involved three stages (Figure 7): (1) an initial triage involving assessment of the CAF by a practice lead and speaking to CYP or referrer (e.g. parents, school) to identify presenting need, history, etc.; (2) a risk assessment using a threshold matrix to identify whether the service threshold is met. The matrix classifies cases into four categories and gives an indication of the type of support that may be required at each level: level 1 (children with universal needs), level 2 (low risk to vulnerable – early help or targeted support services), level 3 (medium risk/high or complex level of additional needs ranging from targeted early help to CIN) and level 4 (high risk/complex or acute level of additional needs requiring specialist or statutory integrated response). While the matrix serves as a decision-making guide, it recommends professional judgement to always be informed by any known evidence and in consideration of views of children and families and the impact that any risk or uncertainty is likely to have on their safety and well-being. 48 Therefore, the teams reported making case-by-case judgements of CYP suitability for the service and (3) cases meeting the service threshold are assigned to a FSP or a young person’s worker (YPW), who then meets with young person, family and professionals to map Signs of Safety, strengths/protective factors and worries/difficulties using the Signs of Safety and well-being model. This holistic map with family and professionals guides the team to provide a tailored intervention plan. Where there is a safety concern, the teams consult with consultant social workers who offer advice and appropriate next steps. Early Help then develops a family plan (normally CYP-led except where there are safety concerns) in consultation with other professionals. The plans are only individual (not family-oriented) if young person has capacity to be independent. CAF cases last around 6 months from assessment to closure, some longer than a year if complex.
FIGURE 7.
Assessment process for Early Help and NEET Teams (Site-01, Site-02 and Site-03).
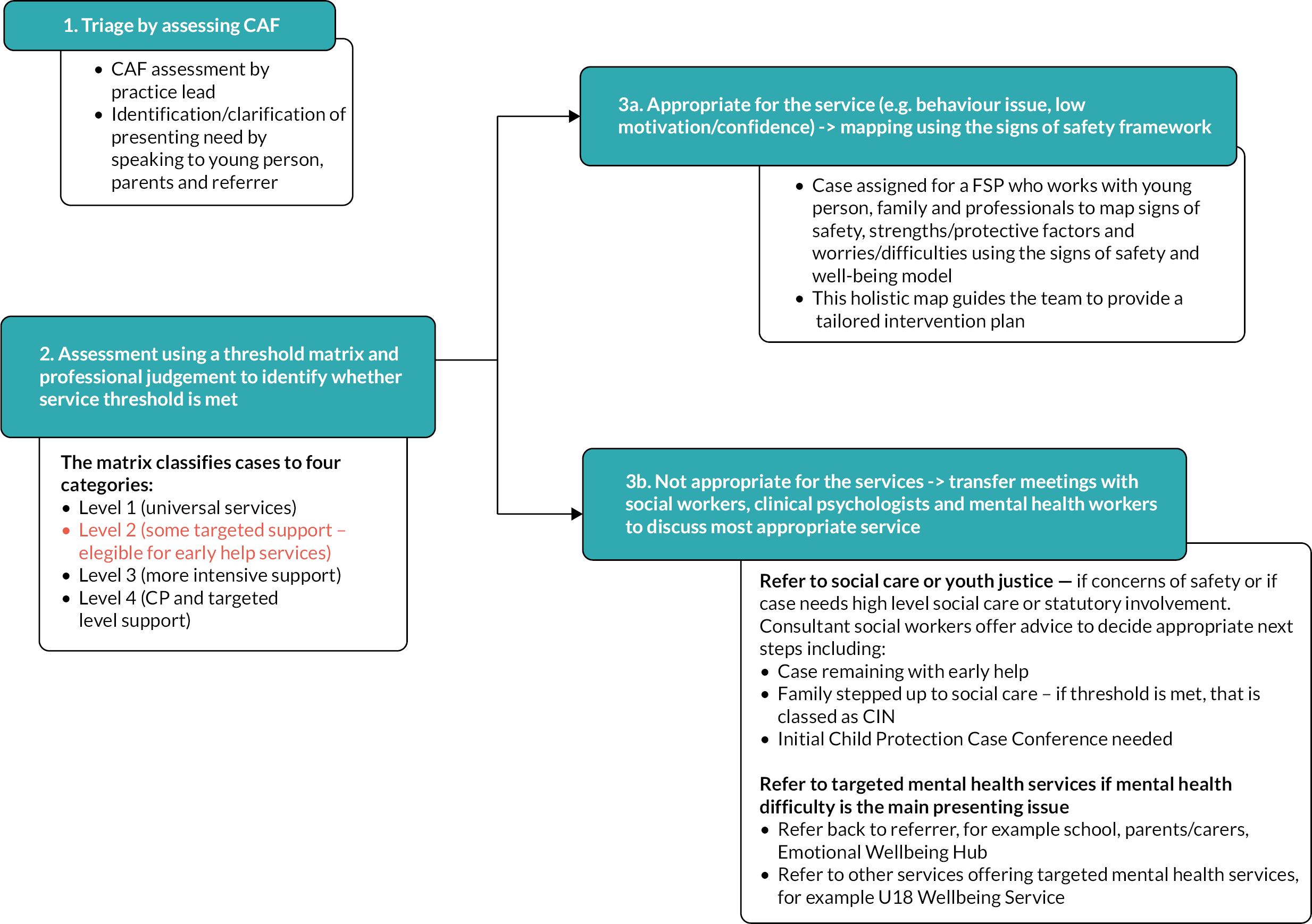
Community NHS Trust (Site-08): The assessment process for Site-08_Community NHS Trust (Figure 8) also involves an initial triage by speaking to the referrer (if necessary) and undertaking a risk assessment. However, unlike the Early Help teams in Suffolk, Site-08_Community NHS Trust uses the RAG rating document to assess risk: green = low risk (appropriate for CCS, e.g. new low mood or anxiety); amber = moderate risk (need further discussion) and red = significant risk (e.g. severe mental health difficulties, low mood associated with other risk factors such as self-harm or suicide plan; ongoing issues (over several years); bereavement; experience of domestic abuse).
FIGURE 8.
Assessment process for Site-08_Community NHS Trust.
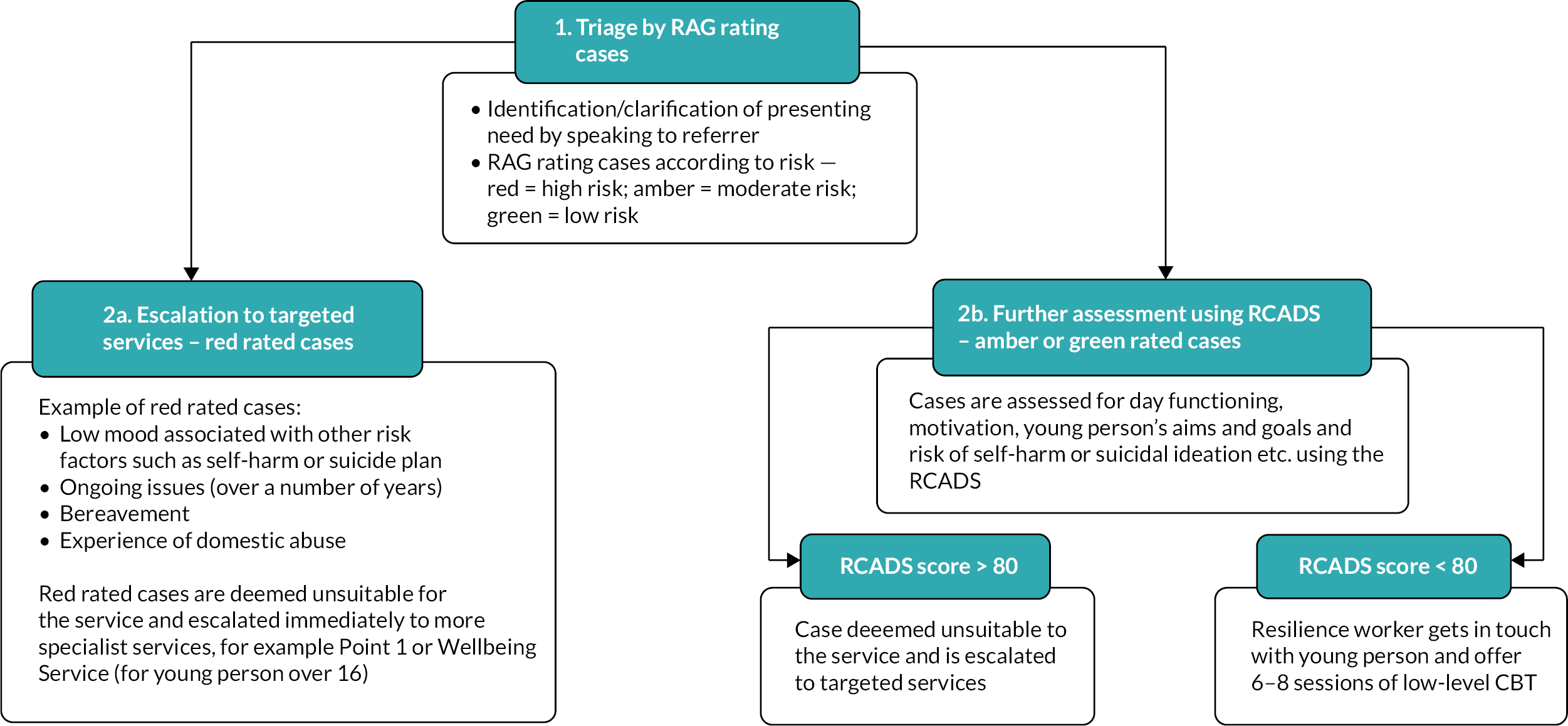
Red cases are deemed unsuitable for the service and escalated immediately to targeted tier 2 services, for example, Point 1 or Wellbeing Service. Point 1 is a tier 2 commissioned service which provides assessment, support and therapeutic help by skilled professionals for CYPs aged 0–18 years old who are experiencing early signs of mild to moderate mental health issues and emotional difficulties. Following the triage, green or amber cases are further assessed for day functioning, motivation, young people’s aims and goals and risk of self-harm or suicidal ideation, etc. using RCADS to decide if appropriate for Site-08_Community NHS Trust pathway. A score over 80 on the RCADS is deemed unsuitable and is escalated to tier 3 CAMH services. If appropriate, a resilience worker gets in touch with young people and offers six to eight sessions of low-level CBT-informed work (not CBT therapists but have some training).
Family Support Team (Site-09): The process for this family support team involves assessing referrals (mainly those coming from CADS) and using professional judgement to decide whether the case falls within the service remit, that is self-esteem and emotional work or if there is an apparent mental health issue. Where there is a mental health issue or CYP identified as requiring a more specialist service and more intrusive treatment (e.g. self-harm), the teams make decisions in consultation with CAMHS and trauma-based workers during a Point 1 group supervision to decide what intervention is needed. Alternatively, they refer young people to general practice so that they can obtain a referral to CAMHS.
Assessment processes for Services offering targeted mental health services (Site-04_Wellbeing Service, Site-05_Charity, Site-06_Charity and Site-07_Charity).
Initial screening processes, including measures and tools used, also differed between services providing targeted mental health interventions (see Figure 7). For example, Site-06_Charity and Site-04_Wellbeing Service tended to carry out an initial triage process to screen cases against risk before carrying out an in-depth assessment, whereas Site-05_Charity and Site-07_Charity did not (Figure 9). Although the in-depth assessment processes for these services involved similar activities (i.e. setting up meetings with young people and parent/carer to look through history, presenting issues, risk and safety planning and identifying suitable treatment), the services described used different measures and tools to further decide on suitability of the cases. For example, while both Site-04_Wellbeing Service and Site-07_Charity described using the RCADS, Site-06_Charity employed the Five P’s formula as an aid to identify both current and historic factors affecting CYP, and Site-05_Charity completed a detailed assessment in collaboration with the young person and his/her family as part of the first session of the treatment package (a specification of pathway) which they use to allocate young people to either youth-centred counselling or youth-centred mental health work, which are standard offers for the service.
FIGURE 9.
Assessment process for teams offering targeted intervention for mental health (Site-04_Wellbeing Service, Site-05_Charity, Site-06_Charity and Site-07_Charity). PHQ, Patient Health Questionnaire.
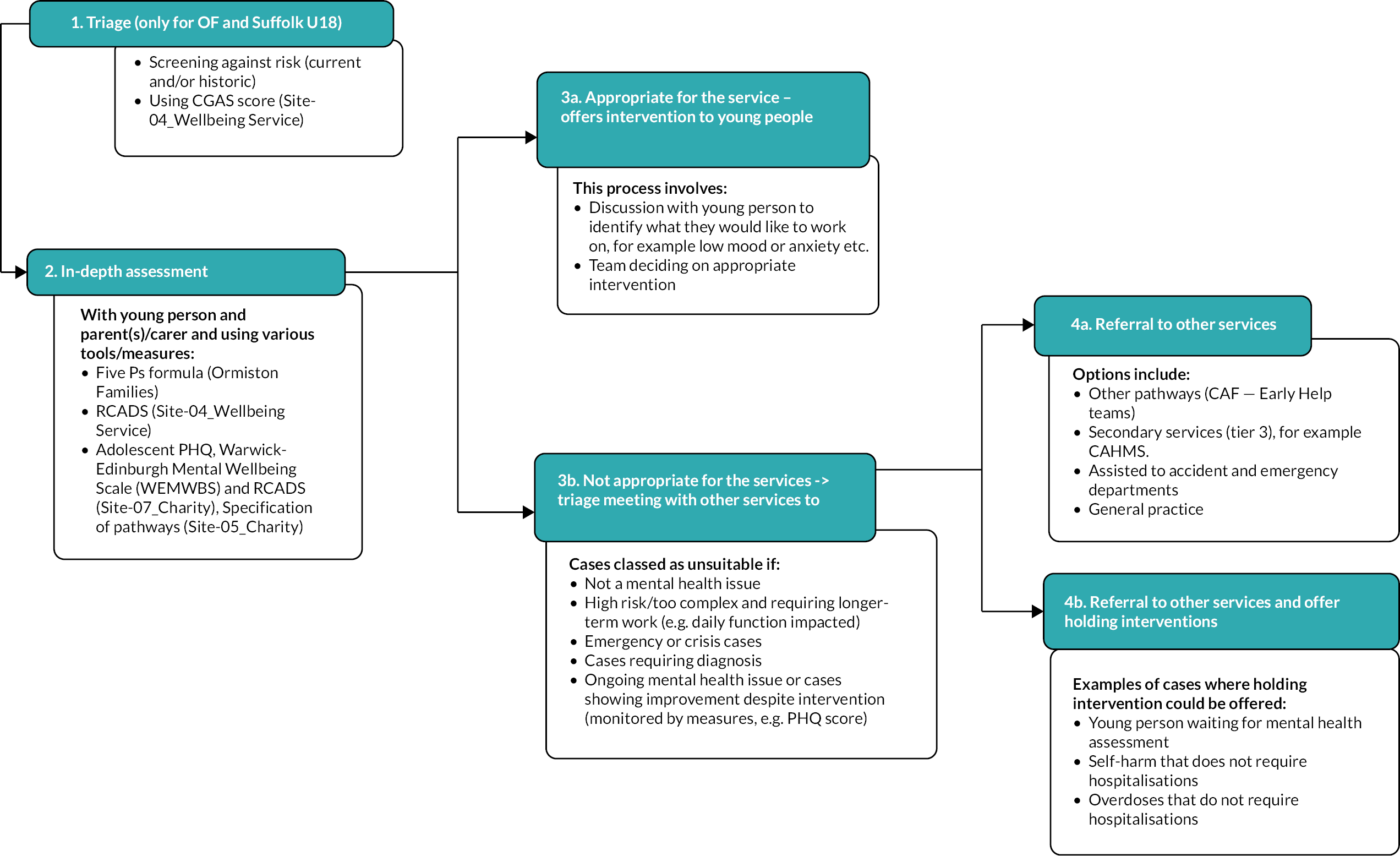
Staff characteristics
A summary of the staff characteristics for the services is presented in Table 13. Most services consisted of a small number of staff members (12–20 staff, including management) employed on a mixture of full- and part-time contracts. Staff expertise differed according to whether the services were offering early help only or targeted mental health services. Generally, Early Help teams tended to primarily consist of staff with no professional mental health backgrounds, whereas targeted service providers consisted of some staff with mental health qualifications.
| Suffolk | Norfolk | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Site-01_Early Help and NEET Team | Site-03_Early Help and NEET Team | Site-02_Early Help and NEET Team | Site-04_Wellbeing Service | Site-07_Charity | Site-06_Charity | Site-05_Charity | Site-08_Community NHS Trust | Site-09_Family Support Team | |
| Total number of staff (FTE) | 14.5 | 16 | 20 | 18.2 | 32 | 12 | 51 | 15 | Approx. 30 |
| Types of contracts | Full-time and part-time | Full-time and part-time | Full-time and part-time | Fixed-term contracts | N/A | Not provided | N/A | Job share – part-time | N/A |
| Type of staff (FTE) | - FSP (9.7) - SFSP (1) - YPW (1.8) - PM (1) - PL (1) |
- FSP (10) - SFSP (1) - YPW (3) - PM (1) - PL (1) |
- FSP (12) - SFSP (1) - YPW (3) - PM (1 - PL (2) |
- CWP (5.6) - PMHW (7) - CBT (3.8) - CTM (1.8) |
- Counsellors (23) - Student placements - Children adolescent trainees |
- CWP (N/A) - Educational Mental Health Practitioners (Counsellors) |
- Counsellors (N/A) - PMHW (N/A) |
- Clinical Psychologists (2) - Health visitors (2) - School nurse (1) - REHP – (9) - CWP (1) |
FSP PM |
| Specific training in supporting young people (and/or their families) with mental health needs (apart from qualifications) | Mental Health Training – YPWs professional development | Mental Health Training – ad hoc training for YPWs professional development | Brief Solution-Focused Therapy (1-year course – manager only) | E-learning and in-house training, for example, ASD/safeguarding | No additional training offered apart from qualifications | No additional training apart from qualifications | Full induction and ongoing CPD – individual and team | All staff have completed a 3-day APT (Accredited Mental Health Training) and CBT training | Most workers are trained in Point 1 and your basic mental health |
| Optional training on trauma-informed practice, attachment and the neglect tool | Consultation with a Clinical Psychologist who can also offer 1:1 work with staff members on their personal/professional issues if needed | Access to 1 : 1 consultation with a Clinical Psychologist for supervision | Suffolk CPD training | Solihull training (2- to 3-day training and annual top-up) – a relationship-based training (the golden standard for health visitor intervention) | |||||
| Resources and tools database on mental health-related issues such as anxiety, low mood | Workshops facilitated clinical psychologists. Topics include mental health and emotional well-being | 2-day Signs of Safety practice (including brief therapy) | Staff receive CBT training from a Clinical Psychologist but are not CBT therapists | ||||||
| Consultation with a Clinical Psychologist | Mental Health First Aid training for FSWs | Online – trauma-based training/understanding the teenage brain | |||||||
| Graded Care Profile training | Staff have completed mindfulness training | ||||||||
Services offering early help primarily consisted of FSP and YPW. FSPs had no professional qualification and came from a mixture of backgrounds, including a qualification in a related subject (e.g. Level 3 qualification in Health and Social Care, Nursery Nursing or Child Development) or relevant experiences (e.g. education, social care, police, health, health visitors, parenting support and Early Childhood Family Service or children centres). YPWs were primarily Joint Negotiating Committee-qualified youth workers (with a degree focused on Youth, e.g. Youth and Community Studies/Youth and Community Development/Youth Work) or had a Level 3 qualification in Health and Social Care. Promotion to Senior FSP was primarily based on experience. Site-08_Community NHS Trust largely consisted of a team of workers known as REHPs (Band 4) who did the bulk of the interventions and had a similar background to FSPs, with some coming from a school/pastoral and children centres' backgrounds. Practice leads and practice management staff also had similar backgrounds as FSPs and YPWs, with promotion based on experience.
Services offering targeted services were primarily made up of a team of CWPs, PMHWs, CBT and counsellors. CWPs do not have a core professional mental health qualification but hold a postgraduate CWP practice qualification (with undergraduate degree in a related field). The CWP qualification is a yearlong course supervised by a trained CWP supervisor and involves working with the clinical team to complete pre-specified clinical hours with CYP/parents and various written tasks, for example, portfolio and reflections on practice. The course teaches various therapeutic interventions, including graded exposure and psychoeducation for young people aged 12 + presenting with anxiety; behavioural activation for young people aged 12 + presenting with low mood; and parent-led graded exposure ‘helping children with fears, worries and feelings of distress’ for children under 12 presenting with either anxiety or low mood.
Primary mental health workers come from a mixture of backgrounds (e.g. nurses, school nurses, social workers, drama therapists), have a core mental health qualification and are registered with respective professional bodies, that is Social Work England, Royal College of Nursing, etc. Cognitive–behavioural therapists are trained and qualified CBTs and registered with British association for behavioural and cognitive behavioural psychotherapists.
Ongoing training and support
There were wide variations in the types of ongoing mental health training and support offered to staff, delivering early help only and targeted services.
Most Early Help practitioners received basic short-term optional mental health training as part of their professional development. The staff also have access to an online database of resources and tools which includes modules on mental health topics such as anxiety, low mood, confidence, self-harm, basic CBT, attachment, etc. Some resources also focus on skill enhancement, including (1) mental health first aid training for family support works (FSWs); (2) trauma-informed practice; (3) the Graded Care Profile training (an assessment tool designed to help workers identify when a child is at risk of neglect by assisting them to measure the quality of care being given to a child in respect of capacity, communication, interaction and well-being); and (4) Brief Solution-Focused Therapy (Yearlong course – manager only) or 2-day Signs of Safety practice (including brief therapy). The team also have access to 1 : 1 consultation with a clinical psychologist who provides clinical supervision, addresses mental health concerns and helps with unsticking stuck cases by considering the mental health issues. Clinical psychologists also facilitate workshops on various mental health and emotional well-being topics.
Site-08_Community NHS Trust team received a 3-day Accredited Mental Health Training (Association for Psychological Therapies) and CBT training from a Clinical Psychologist (although they are not CBT therapists). They also undertook Solihull training; a relationship-based training focused on attachment and brain development with three main principles, including containment, reciprocity and behaviour management. The Solihull training is an initial 2- to 3-day training, followed by an annual top-up. The team also completed mindfulness training and have access to online training, including trauma-based training and understanding of the teenage brain.
Other teams offering targeted mental health services reported receiving very little or no additional mental health-focused training apart from qualifications and their ongoing continuing professional development (CPD).
Contextual features of mental health services
To understand the contextual features shaping implementation, synthesised data from the documentary review, SPQ and stakeholder interviews have been used to map macro-, meso- and micro-contextual features. This analysis considered how national policy, societal contextual features and the COVID-19 pandemic at a macro level impacted the non-specialist mental health services at a meso level, and then ultimately how the ICALM study was impacted at a micro level. The mapping of macro-, meso- and micro-contextual features is a useful heuristic device for conducting process evaluation, but it inevitably led to arbitrary separation of what, in practice, is complex.
A major challenge experienced by the services at a meso level is a huge volume of referrals, exacerbated during the COVID-19 pandemic, firstly leading to backlogs at central referral points such as Site-10_Central referral point in Suffolk and secondly (and consequently) leading to long waiting times. The Site-10_Central referral point in Suffolk received approximately 9000 referrals a year, compounded by increased demand following COVID-19, ranking amongst the top three trusts in the country for referrals. Towards the end of the ICALM study, to resolve the increase in referrals, Site 10 was looking to temporarily increase resources by using agency workers to help clear the backlog. However, similar efforts in the past have flooded other services which were already under pressure, such as the school nursing services. Site 10 was also working to identify bottlenecks in the services, for example, attention deficit hyperactivity disorder (ADHD), and putting more resources to triage them, a process also envisaged to have knock-on effects on capacity of teams aligned to manage those specific conditions.
We have our urgent which, yeah, 24 hours or 72 hours. The target for a green, which will be a low mood, very limited risk, would be 28 days. We are not there at the moment. We are at about five months. But when I started six months ago, we were at 11 months.
Stakeholder-01, Site-10_Central referral point
The [Site-10_Central referral point] model is unsustainable, and they are overwhelmed. The way the [service]works right now, anyone can refer themselves in and everyone must be triaged – they have about 2000 people waiting to be triaged. Because they’re so overwhelmed, they’re now only triaging Red and Amber cases – so the green ones we used to work with aren’t getting referred due to the backlog and prioritising Amber and Red cases.
Stakeholder-02, Site-04_Wellbeing Service
ADHD was a big problem for us. It still remains a big problem for us but we’ve streamlined some of the service. So we’ve just put some people behind the problem in terms of trying to help it … there is a knock-on effect on PMHW, because actually if anxiety is picked up during an assessment for ADHD, anxiety must be tackled first, which then would fall down to the PMHW teams. So as much as we’ve targeted one area, we’ve also pushed it elsewhere …
Stakeholder-01, Site-10_Central referral point
The increased pressure on Site-10_Central referral point and, consequently, services such as Site-04_Wellbeing Service and school nurses resulted in significantly reduced capacity to utilise pathways of referral into ICALM and on the practitioners to undertake and/or complete their IPC-A training due to very limited numbers of mild low mood being accessed and passed onto appropriate services.
Macro-contextual features of mental health services
The findings that follow focus on how societal contextual features, the COVID-19 pandemic and policy at a macro level have shaped the delivery of mental health services and the ICALM intervention at a meso level. Apart from policy documents presented and referenced, this primarily represents views of stakeholders.
Societal contextual features
Stakeholders attributed the high volume of referrals to a combination of (1) social contextual factors (Table 14), including increased population awareness of mental health challenges, inappropriate or changing use of specific mental health language by parents and other health professionals and (2) the COVID-19 pandemic (Table 15).
| Macro-contextual feature | Illustrative quotes |
|---|---|
| Societal shifts in openness about mental health illness and conditions | ‘We’ve seen a huge increase, but I think the numbers are a combination of COVID and the difference in children’s lives, in their teenage lives with parents working, with the use of social media and the internet and actually we’re a lot more open as a society about illness and mental health’ (Stakeholder-06, Site-09_Family Support Team) |
| Mental health education and understanding the role of society in mental health | ‘I think there’s lots of social media, lots of stuff on TV … you look at Panorama when they do my kid has got ADHD. Good watching, I guess for parents of children with ADHD but not overly helpful to us actually. And when I say us I mean health, everybody, because I think a balanced approach would be to say what are you doing as parents to manage this … What are you doing to get the support and guidance you need rather than pushing on to somebody else to get?’ (Stakeholder-06, Site-09_Family Support Team) |
| ‘I think we have to be realistic. I work with parents who may be had their own childhood trauma. Their own education doesn’t put them in a position like you and I where we can make a balanced decision based on research, based on theory, based on fact. They’re making a decision based on what their neighbour told them, or somebody down the road told them, or what they interpreted from TV. That if my son is diagnosed with, I might be entitled to, and it’s that diagnosis to entitlement that I think we probably don’t get right as a society. Why would you get extra money?’ (Stakeholder-06, Site-09_Family Support Team) | |
| ‘… In the last two years probably with COVID there is an ability for some parents to blame – this is because of COVID, this is mental health, this is nothing to do with us and our ability to parent. I think we all have to take responsibility as a society don’t, we. We’re quite rightly say you have to stand up for your child’s rights, if children’s services or health are failing you, you have to bring that to someone’s attention. I guess as a society speaking as a parent you take a choice, do I do the tough job as a parent or do I give it to somebody and take away responsibility. I think we have an increased amount of that. ADHD is a really simple one. What does the label of ADHD get you? For many parents in our service, it gives them that vindication that it’s not their fault. And I don’t think it’s about fault because when you ask health, parents in courses, [town], PPP, all of them about parenting kids with ADHD, tell me what we do different, nothing at all. We approach parents exactly the same. So, I think there’s a misconception that if your child gets labelled you get more’ (Stakeholder-06, Site-09_Family Support Team) | |
| Inappropriate use of mental health language | ‘We get a lot of teenagers; I think I’ve got bipolar … I’m really high one minute then I’m really low … I want a diagnosis. But GPs will send them through. We’re not a service that just gives out a diagnosis because you’d like one’ (Stakeholder-01, Site-10_Central referral point) |
| ‘We’re very quick to put labels on stuff. This kid has got ADHD. This kid is Autistic. Great label but what does it mean for that child … So there’s a difference between mental health and a kid feeling down and low … We’re very cautious not to label young people with mental health, they are people who have ups and downs. I think as a society we’re very quick to say this young person has got mental health rather than they’re just having a real rubbish time. So, it’s about the self-esteem and the network around people. Young people. To identify what their next steps are’ (Stakeholder-06, Site-09_Family Support Team) | |
| ‘But what we’ve also found is they’re asking for an ADHD assessment, and it says, “ADHD diagnosed” and has a date. So, we’re like, well why are they diagnosed? No, what it’ll be is a SENCo (Special Education Needs Coordinator) has said to a parent, “I think your kid’s got ADHD” They go and tell the GP. The GP thinks it’s a diagnosis and records it on their record. That cannot be removed, and they may not even have it. And that ADHD has to go through life. You have to put it on your driving licence. You have to declare it to a lot of adult bodies when you get older. And yet it’s on your record because somebody misinterpreted what was said’ (Stakeholder-01, Site-10_Central referral point) | |
| ‘Sometimes people will say, “I’ve got depression” as opposed to, “I’ve got low mood.” … it’s the language people use, and we try to unpick that … and there’s labels that are, words that are used that are really unhelpful, like when people are saying about this person’s got depression. Well, is this like clinical depression? Is this a diagnosis you’ve got? You know, when people have got generalised anxiety you’re not going to get a seven year old that’s diagnosed with that. There might be some anxious traits that you’re seeing … there might be some low mood … and it’s really important trying to get that common language used across the board in all services’. (Stakeholder-07, Site-04_Wellbeing Service) | |
| Lack of knowledge on the frontline | ‘In mental health there is such a lack of knowledge and resources at the very, very front line that they just tick a box, they literally have just got to put low mood or ADHD, and that’s it, ping, not my problem. You would not be able to do that in any other health field whatsoever. But yet it’s acceptable in mental health …’ (Stakeholder-07, Site-04_Wellbeing Service) |
| ‘… I’m not sure how often it happens, but the GP’s sometimes ticking the psychosis box for really young children. And I mean the evidence base around young children and psychosis is negligible, isn’t it? It’s nothing really. It’s a certain age where presentation’s more common, isn’t it, above 14 I think or something’ (Stakeholder-02, Site-04_Wellbeing Service) | |
| Incomplete referral forms | ‘On the GP form there’s about seven boxes. I mean one of them even is behaviour. It doesn’t mean good behaviour or bad behaviour. It just says “behaviour”. But as far as I’m concerned, any child who has got a behaviour is trying to communicate something to me. But I don’t get to know what that behaviour is. So, they’ll just tick it. Or … you can tick school refusal. The kid doesn’t want to go to school. Oh OK. And that’s a mental health worry’ (Stakeholder-01, Site-10_Central referral point) |
| ‘They’ve got hardly any information, things aren’t ticked properly, risk isn’t explained, so they don’t give us an idea of if they’ve given a young person a safety plan, or even spoken to them about any advice and guidance. So, if that’s not included in the referral and we don’t have adequate information, we will then have to call them as well to gain that information … Sometimes self-referrals can be quite tricky, they don’t really know what we want and what information we sort of need providing’ (Stakeholder-11, Site-06) | |
| ‘Yes, it’s really easy for the GP to tick a box to say somebody might have ADHD, but the result of that is the hub practitioner has got to do so much digging and unpicking and investigating into that, just from the fact that the GP’s ticked a box [based] on something that someone’s said to them’ (Stakeholder-02, Site-04_Wellbeing Service) | |
| Transformation plan | ‘So it will be, a link worker will have two or three or four GP surgeries, and they’ll be the go-to person when there are mental health issues, and they’ll be doing phyco-education with the GP to look at when they need to start being concerned, where can they signpost in early … But also, the link worker will be able to see people within the surgery to say, "Actually this person does need an assessment, so this is what we can do". So, it’s kind of a bit like a, I guess a specialist … that’s going to be educating the GPs and the health practitioners within that surgery. So that is in process … it’s worked well in adult services. It’ll be interesting how it works in under-18s, because they are a very different kettle of fish than dealing with adult services. But it’s a good start (Stakeholder-07, Site-04_Wellbeing Service) |
| Contextual feature | Illustrative quotes |
|---|---|
| Low mood no longer the most frequent presentation | ‘As we’re coming out of COVID, things might change but at the moment we’re seeing lots of anxiety but going forward that might change to low mood’ (SPQ-02, Site-02_Early Help and NEET Team) |
| ‘Anxiety is the major presentation … it’s a problematic thing isn’t it because it is really low mood that is being targeted through IPC. It’s quite unusual to find that presentation of low mood that fits with that right now. Increase in young people who are anxious and not wanting to go out. School refusal is a steadily increasing issue’ (Stakeholder-09, Site-05_Charity) | |
| Increased (and worsening of) mental health difficulties amongst CYP | ‘We became involved with ICALM initially because of the cases we were seeing where wellbeing was one of the main factors, or the major factor. However, since COVID, the need has risen and often the mental health difficulties present in our cases is over and above what the FSP’s can deal with and exceeds the threshold for IPC-A. This was unforeseen really, since COVID specialist MH services have had to become involved with a lot of our cases, whereas, perhaps before coronavirus, they probably would have been OK for IPC’ (SPQ-02, Site-02_Early Help and NEET Team) |
| ‘Our service is meant to be for mild to moderate help requiring “short-term, light touch” interventions however we have seen a huge increase in complexity and risk … we’re seeing more moderate to severe presentations, rather than mild to moderate – young people are presenting with increased suicidal ideation and greater chronicity. We noticed these changes starting in Feb/March 2020 and there was already a capacity/demand issue, but it’s just increased during COVID. We used to be working with green cases, now we rarely see green cases, mainly Amber ones. Assessments used to only be a one-off appointment taking about 90 minutes; now we’re finding that it takes 2–3 sessions to complete an assessment and each appointment is nearing 2 hours – there are more services involved in the young people’s lives so there are more people we have to speak to in order to carry out an assessment’ (SPQ-04, Site-04_Wellbeing Service) | |
| Increase in models of service delivery resulting in variations in CYP engagement with the services | ‘No, we hardly did anything online pre-pandemic but now we are finding some young people are preferring this way, not all of them, but some. I think we’ll keep delivering some stuff online, if young people want it and respond positively to this mode of communication and engagement’ (SPQ-03, Site-03_Early Help and NEET Team) |
| ‘We have now got a mixed offer. And I mean I have to say although that’s a disadvantage there’s also benefits to it because in a rural county when young people might struggle with transport then it has been helpful to some extent to have remote options as well’ (Stakeholder-09, Site-05_Charity) | |
| ‘I don’t think any were successful in regard to the young person wanting the service. And I think it’s got to the point where wellbeing is so severe that they’re at the point where they’re not even at that stage where they can ask for help. And then that’s pretty difficult, how do you engage someone that’s isolating themselves and doesn’t want to engage but needs to engage to get better? And that’s, you know, that’s probably what you’re finding with the emotional wellbeing referrals, they’ve refused because they’re just too overwhelmed, they cannot cope with the professional in their life offering them a service, they just want to hide away and hope it goes away. We all know that’s not how it happens, but you’ve got to be right place, right time, to be able to take up that opportunity’ (Stakeholder-05, Site-02_Early Help and NEET Team) | |
| ‘The impact of COVID has meant some people could not access treatment as engaging virtually was too difficult for them. Some people who had started treatment chose to pause treatment whilst it was offered virtually and will (or have already) resume once we are undertaking face to face more readily’ (SPQ-04, Site-04_Wellbeing Service) | |
| Reduced capacity and resources – higher demand for services | ‘The other major difficulty is that there’s just been such … very high levels of sickness … And obviously … people having to home school and being therefore unable to work because they had children of an age that they couldn’t – they had to look after them basically. So, there were those impacts’ (Stakeholder-09, Site-05_Charity) |
| ‘So, if we’ve got like – OK, we’ve got all these families coming in and then it’s like OK, but we’ve actually got this additional thing that we offer it can feel that sometimes the IPC is an additional thing’ (Stakeholder-10, Site-03_Early Help and NEET Team) | |
| ‘I think COVID has caused us a major problem in the young people world of support, and they report about it on the news, don’t they, about lack of mental health support for kids. Well, they didn’t put anything in, the government. They just left it on the teams that were running just to pick up the backlog as far as I can see. There’s nothing additional put into anything’ (Stakeholder-01, Site-10_Central referral point) | |
| Slowed transformation plans | ‘Within the transformation what’s going to happen is there’s going to be link workers that are going to be attached to GP surgeries, so they’re going to be mental health specialists that are attached to GPs … So, I guess we’re just waiting. I think they were hoping the transformation would be in full swing by middle of last year, but we’re still, because of COVID we’re still trying to put some things in place. So, it’s in progress and in a process’ (Stakeholder-07, Site-04_Wellbeing Service) |
In recent years, the national effort to increase mental health awareness and reduce the stigma around mental illness through national campaigns, television and social media49 has contributed to an increase in people seeking mental health support, in part a desired effect. However, variations in credibility of information sources and differing levels of education amongst the population with respect to mental health have contributed to misinformation and inappropriate use of mental health language at the point of referral to the services. There is also a lack of understanding of the role of society and a lack of or inconsistent guidance for advice and signposting services, in supporting positive well-being and mental health of CYP, leading to an increase in public perception of mental health services providing gold standard interventions or ‘fixes’. Thus, in recent years, the services have experienced a continuously increasing demand for assessments (and ‘a diagnosis’) for certain mental health conditions, for example, ADHD amongst CYPs and parents.
The lack of knowledge of (and support for) front-line staff (e.g. primary health care and school personnel) regarding mental health conditions and support pathways also contributes to the inappropriate use of mental health language and inadequate information provided on referral forms. The Site-10_Central referral point receives referrals from professionals and the general population and has a small team of clinicians who must triage each case before identifying the appropriate service. Having inadequate information on referral forms means that practitioners have to do a lot more information gathering from referrers to aid accurate decision-making, thus creating significant delays in the referral process.
Developing and establishing a common language with regard to mental health difficulties and education with regard to the role of society in supporting positive mental health is therefore crucial in managing some of the current challenges faced by the services. There is also a need for more interventions to help build resilience in CYP and manage emotions. To ameliorate the poor completion of referral forms, some services are in the process of adapting online referral forms to facilitate the completion of all required information. There is also a need to support front-line services, especially general practices where the bulk of the referrals originate, to ensure that referrals made are appropriate and have all the information needed.
Currently, there is a local transformation plan underway which aims to create more streamlined services for CYP. The plan is based on the THRIVE model and aims to create more seamless and closer working between Early Help/Social Care teams, primary mental health services (tier 2 services) and Secondary Services (tier 3 CAMHS). The plans also aim to introduce mental health specialists (link workers) into general practice to support under-18 services. Link workers will offer psychoeducation where needed and signposting and assessment advice to practitioners as well as promote mental health education amongst health practitioners within surgery. The implementation of the transformation plan has, however, been delayed by the COVID-19 pandemic.
The COVID-19 pandemic
The study commenced approximately 1 month before the earliest reported cases of COVID-19 in the UK (January 2020). The impact of the pandemic and ensuing restrictions on mental health services in general and the ICALM study are summarised in Table 15. During the COVID-19 pandemic, from SPQs and interviews, the services reported a sharp increase in mental health difficulties and associated levels of risk amongst CYP with (social) anxiety, low mood, self-harming, OCD-type behaviour, germ-phobic behaviour, emetophobia due to fear of sickness, fear or vomit and agoraphobia. Most services, including those delivering targeted mental health support and interventions, reported receiving referrals that were far beyond their capacity and service threshold with regard to level of need. This created major challenges in identifying suitable cases for IPC-A, with participating services reporting CYP to be more concerned with addressing anxiety than low mood.
We certainly opened it up to where young people were presenting with low mood and anxiety, we certainly did start trying to recruit people. I guess it’s when they’re clearly saying they’re getting tummy ache before school, and in school holidays they’re absolutely fine. It’s literally a worry about going to school. We’ve not offered it (IPC-A) to those young people because I think, you know, there’s not a feeling that their mood is a significant factor, it is really significant and very precise worry about school.
Stakeholder-03, Site-08_Community NHS Trust
For most services, the COVID-19 pandemic also led to reduced capacity to deliver support or interventions due to high levels of staff sicknesses and school closures (and the need for homeschooling). During this time, managers reported having to prioritise the well-being of staff and continuity of service by not participating in activities that were seen as ‘extra’, including research (i.e. ICALM). For some Early Help teams, the focus of the service provision shifted to more safety planning for CYP at home due to the sharp rise in adult mental health challenges and potential safeguarding concerns.
We just had to be quite strict about how we prioritised our time management, all time during the pandemic. And anything additional we just had to be really clear that we weren’t going to take on, for our own wellbeing and therefore the continuity of the service. Nobody has had the capacity I think, or few people have had the capacity to do extra anything, and a trial ends up feeling like extra.
Stakeholder-09, Site-05
At the start of the pandemic, teams also had to adapt to more flexible ways of delivering services, whereby both assessments and interventions were delivered remotely via Zoom, MS Teams or telephone. By the end of the study, most services had adopted a blended model of delivery whereby assessments and interventions were being offered online or face to face depending on CYP preference or need. This mode of delivery increased accessibility, enabling the services to reach CYP living further from the service centres. The virtual delivery of the sessions worked well for some CYPs, with some schools also setting up rooms to support attendance. However, not all CYPs engaged with the virtual sessions due to a preference for face to face and/or increased severity of cases. The COVID-19 restrictions and shift to a virtual way of working also meant that teams had limited access to CYP homes, thus unable to pay close attention to more serious cases that would have ordinarily required intense face-to-face contact and multiple visits. This posed a challenge to the teams in predicting serious incidents, as some families stopped engaging with services or were not allowing professionals in their houses owing to COVID-19.
Policy
A challenge of implementing the different key mental health policies relevant to CYP set out in Table 16 which address some of the social contextual challenges highlighted above, has been a lack of specificity about how to allocate funds to different resources, including the costs for different staff resources. This leads to a disconnect between workforce strategy and policy objectives about meeting different young people’s needs. An additional challenge here is that workforce capacity-building strategies, which are often focused on training and recruiting less experienced clinical staff, do not typically include commissioning senior clinical supervision roles, with senior clinicians typically allocated to seeing high-priority children as a short-term strategy to reduce waiting times, rather than a longer-term view to capacitate the workforce to meet young people’s needs over time.
| Type of policy, discourse relevant to implementation | Description |
|---|---|
| No Health without Mental Health51 (2011) | Underpinned by a philosophy that ‘Mental health is everyone’s business – individuals, families, employers, educators and communities all need to play their part’. Strategy focused on early intervention, cross-sectoral collaboration and measurement of outcomes using the NHS Outcomes Framework domains |
| Future in Mind52 (2015) | The Children and Young People’s Mental Health and Well-being Taskforce identified how to improve CYP’s mental health services across five themes: (1) promoting resilience, prevention and early intervention; (2) improving access to effective support – a system without tiers; (3) care for the most vulnerable; (4) accountability and transparency; (5) developing the workforce |
| The Five-Year Forward View for Mental Health53 (2016) | Taskforce called for recommendations from Future in Mind to be implemented in full. Objective: to provide mental health care to 70,000 more CYP by 2020–1. Waiting times should be substantially reduced, significant inequalities in access should be addressed and support should be offered while people are waiting for care |
| Green Paper on Children and Young People’s Mental Health54 (2017) | Green Paper proposed:
|
| New trials to look at how to strengthen the links between schools and local NHS mental health staff. Major thematic review of children and adolescent mental health services across the country, led by the CQC, to identify what is working and what is not. By 2020–21, at least 1700 more therapists and supervisors will need to be trained and employed to meet additional demand, and the strategy will also outline actions needed to improve retention of existing staff. All localities should work with the existing CYP-IAPT programme to deliver postgraduate training in specific therapies, leading to at least 3400 existing CYP’s mental health service staff being trained by 2020–1 |
|
| NHS Long-Term Plan55 |
|
| Office of Health Improvement (formerly PHE)56 | Focused on specialist treatment and importance of adding capacity to specialist treatment teams and reducing waiting lists across specialist services |
| Status of Mental Health of Children and Young People in July 2020, during the coronavirus (COVID-19) pandemic, and changes since 201757 | Rates of probable mental disorders have increased from one in nine (10.8%) children aged 5–16 years in 2017 to one in six (16.0%) in 2020. The likelihood of a probable mental disorder increased with age, with a noticeable difference in gender for the older age group (17–22 years); 27.2% of young women and 13.3% of young men were identified as having a probable mental disorder |
I think mental health services for young people is very under resourced to meet the need… And so, everybody is really [under] huge pressure, and this is why my service as well as many others are finding themselves picking up cases from the Site-10_Central Referral Pointwaiting list trying to kind of deal with that backlog but it’s often not the services that families want.
Stakeholder-04, Site-01_Early Help and NEET Team
The lack of clarity about how to operationalise mental health policy at a service level is most recently evident in the NHS Long Term Plan, which has objectives to improve access to care by providing a 0–25 service and 24/7 crisis service. However, there is a lack of specificity about how to provide these services, how to implement these services, how many staff are required to support how many children and how senior clinical roles will be deployed to supervise new staff/trainees. Without such specificity, trainees will not be able to develop their skills to build the required specialist workforce over the longer term, perpetuating insufficient capacity across the whole mental health system to meet the ever-increasing demand.
Problems of capacity are not isolated within mental health services, and other service sectors are also overwhelmed with demand for care. As a consequence, young people have experienced being referred across multiple mental health, voluntary, social care and health services, driven by individual providers placing boundaries around which types of problems they treat and do not treat in order to manage that demand. This is reinforced by a lack of system strategy and shared definitions of mental health problems and conditions across services. Oversight, strategy governance and co-ordination of service provision within and across sectors are therefore critical for ensuring young people’s needs are met – a key gap highlighted in the 2017 Care Quality Commission (CQC) report.
A lot of the time it’s [volume of referrals] driven by process and system issues, and the fact that services are overstretched and they’re trying to move people on a lot of the time, and not rightly or wrongly.
Stakeholder-01, Site-10_Central referral point
I will slow think [Signs of Safety term] and I will not take anything on [accept a referral] unless I know my FSP can do it. If it’s just wellbeing [mental health], I won’t take it if it is not on a wellbeing pathway and if it’s not, then my job is to find out why not – talk to the GP, talk to CAMHS and get their input. If, following consultation, with mental health services, we can implement their advice, we will do that. Because once you’ve got their input, they’re responsible for the actions.
Stakeholder-05, Site-02_Early Help and NEET Team
A central policy agenda has been to reduce waiting times in specialist mental health services. However, this agenda set within a context of overwhelming demand has arguably created a public perception that mental health services provide a gold standard set of interventions for young people that are worth waiting for, that all mental problems require specialist support and that the solution lies in enabling access to those services. This suggests that greater effort is required to promote the philosophy of mental health as ‘everyone’s business’,50 namely how effective treatment for mental health problems can be provided across the health and social care system as well as within schools and colleges.
I think we all have to take responsibility as a society don’t, we. We’re quite rightly say you have to stand up for your child’s rights, if children’s services or health are failing you, you have to bring that to someone’s attention. I guess as a society speaking as a parent you take a choice, do I do the tough job as a parent or do I give it to somebody and take away responsibility. I think we have an increased amount of that.
Stakeholder-06, Site-09_Family Support Team
Within this context, the challenge of asking mental health services to implement the IPC-A intervention and feasibility trial becomes clear. While IPC-A as an adaptation of IPT is included within NICE guidance for CYP, it is not a priority of Health Education England, and clinical supervision for CWPs is not available. Targeted investment in IPC-A would be required if IPC-A was to be implemented as a treatment for mild to moderate depression, a significant challenge given the overarching problem of insufficient resources to meet increasing demand. Similarly, evidence-based mental health interventions such as IPC-A are not seen as core elements of Early Help services for CYP or competency/ training and development frameworks for youth services; hence it is difficult to introduce provision in this era of reduced capacity and funding alongside trying to manage increasing demand.
Meso-level contextual features of mental health service provision
The meso-contextual features of mental health services and their impact on ICALM are described below and summarised in Table 17. At a service level, the findings highlight an interaction between enormous demand, unclear service specifications, a lack of capacity and resources, a lack of oversight of service co-ordination and a lack of research prioritisation. The findings reinforce the need to develop an effective workforce strategy, without which services make decisions to minimise risk and manage resources, focusing on those young people with the most severe problems, resulting in young people with mild to moderate mental health problems not being treated or worsening. There is also a need to create more streamlined and co-ordinated service pathways to ensure that CYP are not being passed between multiple services.
| Meso-contextual features | Description | Illustrative quotes |
|---|---|---|
| Increased complexity of cases | ||
| Cases no longer meeting service Early Help thresholds | Long waiting times for green cases have led to increased complexity of cases, and CYP no longer meeting services thresholds. The teams see this as a key barrier to identifying appropriate cases for ICALM | ‘There’s some fairly huge waiting lists for young people that are those types of referrals that you’re talking about … So, they would be the kind of cases that would just sit on this waiting list and the waiting list has been over a year before, you know, that young people just sit on this waiting list, waiting for some sort of mental health service to come about. And it never comes. They never reach the threshold for any sort of therapeutic intervention unless it’s much, much more serious’. (Stakeholder-04, Site-01_Early Help and NEET Team) |
| ‘There are lots of difficulties at the moment with the Site-10_Central referral point. They have a waiting list of 2000 young people who have been RAG Rated as Green and the minimum wait for Green cases is 100 + days for any kind of service. They’re looking at those young people that have gone over 100 days and whether they can come to Early Help. But their green is not necessarily going to be my green. At the moment, I’m not taking any, quite rightly, as they’re not appropriate [i.e. they need a mental health service, not an Early Help service]’ (SPQ-02, Site-02_Early Help and NEET Team) | ||
| Increased complexity of cases referred to Early Help creating a huge demand for targeted services | Despite acknowledging mental health as the biggest underlying need for supporting CYP, the current inability for Early Help to take the lead in providing mental health support has created a huge demand for targeted services which are already under pressure | ‘Mental health is one of our biggest, if not the biggest underlying need for supporting children and young people. And the gaps are that we can’t always access the relevant services as quickly as we’d like to. So, for example, we might do a referral to the Suffolk Wellbeing Hub, but the turnaround might be 12 weeks and then often what happens is people then come back to our service, but we were the original referrers, and not enough support from mental health or special education needs services – all have huge waiting lists’ (Stakeholder-10, Site-03_Early Help and NEET Team) |
| ‘The support that we get from other services is good generally but mental health especially and when children have special educational needs, they’re the two services that we get least support from’ (Stakeholder-04, Site-01_Early Help and NEET Team) | ||
| ‘And I guess sometimes historically there’s been quite a wait for [a service] so when we feel we need to escalate a child or young person sometimes they get told there’s quite a wait. And there’s always that debate around whether or not it would be appropriate for us to offer some low-level psycho education type strategies whilst there’s a wait and sometimes that is appropriate, and sometimes it’s not because of the level of risk or the level – particularly low mood, potentially if the person’s motivations change its maybe impacted then actually it needs a higher tier than us’ (Stakeholder-03, Site-08_Community NHS Trust) | ||
| Increased complexity of cases referred to targeted services creating a huge demand for tier 3 services | Cases referred to targeted services are also getting more complex, with most requiring escalation to tier 3 services. Apart from the huge demand for tier 3 services, targeted services also have challenges in setting up interface meetings with other services to discuss the cases | ‘Because there are long waits. So, for example, if we wish to at the moment refer someone to the NSFT Youth Mental Health Service in the central area there is approximately a year’s wait for a routine assessment. So, this is the main challenge … We come to the end of an intervention … so I’ve referred a young person in October for a routine assessment and I was told that they might get seen in June if I was fortunate, but it might be this October. And of course, having a routine assessment doesn’t mean to say you’ll be accepted for an intervention, and if you are accepted for an intervention, you are then going to have to go on an intervention wait list’ (Stakeholder-09, Site-05_Charity) |
| ‘So, we have daily meetings, or daily interface meetings, with tier three services. So, let’s say there was a quite complex case with a lot of trauma, a lot of self-interest behaviour, that same day or maybe the next day, I could have a conversation with the service in their area and we would discuss the case and see if they would be able to provide support as well. So, the communication is improving between services, which is good. It can be tricky but it is getting a lot better … Because we’re all so busy, you know, it’s trying to actually get hold of people and set up these meetings, and it’s something that we’ve been doing these meetings for just about a year now in a regular capacity, so that’s made it a lot easier to be able to get the young person to the support they need as quickly as we can’ (Stakeholder-11, Site-06_Charity) | ||
| Service specifications and referral pathways | ||
| ** Mental health support not the central focus for Early Help interventions | Despite a large proportion of referrals consisting of mental health difficulties, the Early Help offer is not mental health focused. This means that Early Help teams do not take a lead on mental health issues but work alongside or refer cases to targeted services who take the lead where there is a mental health concern | ‘I don’t even think I could give you a ballpark figure. But recent stats have shown that approximately three quarters of our referrals are around young people’s mental health’. (SPQ-03, Site-03_Early Help and NEET Team) |
| ‘We will co-work alongside mental health services, but we won’t be doing it without the mental health support. Even if it was just low-level low mood or anxiety, I would want the input of health services …’ (SPQ-02, Site-02_Early Help and NEET Team) | ||
| ‘We would work alongside any families experiencing any mental health problem, we wouldn’t necessarily take the lead on the mental health part … It is common for us to have Family Plans that include an element of mental health concern, but in the cases where this is more complex, we would be working alongside more specialist mental health services in the spirit of multi-agency working, and hope that the person is accessing therapy or treatment. The thing we try and avoid is other services stepping away because Early Help are involved’ (SPQ-01, Site-01_Early Help and NEET Team) | ||
| Early Help teams offering both voluntary and statutory services | Early Help teams also taking on more social services roles – further stretching their resources and ‘blurring’ their role in health and mental health | ‘… Early Help will be joining the directorship for Social Care/Youth Justice Services (Statutory). Up until this point we have been very aligned with Health, but the new Direction may choose to take this in a different direction … we may be pulled more into Statutory Services – we are already doing supervised contact for children in care, offering bespoke interventions for CIN or CP plans and we have to balance this with what we can then offer on a voluntary basis under the CAF framework’ (SPQ-01, Site-01_Early Help and NEET Team) |
| ‘There is a review going on about the FSP role, whether that means we’re going to be doing things differently, I don’t know … It’ll likely mean we’re doing more Supervised Contact (of Looked After Children) which will impact what direct work we can do with young people. I find that changes like this with the council happen very quickly … they tend to only look at the “right now” problem, rather than thinking a bit further in the future’ (SPQ-02, Site-02_Early Help and NEET Team) | ||
| Gaps in interventions provided by primary and secondary care | There are treatment gaps between targeted services and tier 3 services, whereby some young people require longer-term interventions (targeted services deliver short-term interventions) but do not reach the criteria for tier 3 services. There are also some gaps whereby, for some conditions, there is no available support either in primary or secondary care | ‘So that’s a real, that’s a challenge for us, because it’s not quite reaching the criteria of secondary, because there isn’t the risk. Sometimes there is the risk and we can step up straightaway, but often there isn’t the risk but there is definitely the complexity. Secondary are also overrun and struggling and they’re almost crisis managing. So their criteria have increased. So the bottom of their criteria, which would not meet our criteria as such, we’re almost rising up to meet that because there’s nowhere else for these people to go, but it’s not short-term primary intervention. That’s just not what it is’. (Stakeholder-07, Site-04_Wellbeing Service) |
| ‘Green cases will often just sit on the Site-10_Central referral point’s waiting list due to the number of referrals they receive. This has had a big impact on our waiting times for both assessment and intervention – our waiting times have changed from 200 days to 400 for CBT … We also get referrals for tics/selective mutism, we don’t offer a service for this, no-one does’. (SPQ-04, Site-04_Wellbeing Service) | ||
| ‘What we tend to do is if we’ve got cases and we’ve tried to step them up and secondary have said no, we’ve got a meeting that we have called patient flow, and it was set up for those cases that get stuck in between teams. We’re saying it’s too complex for us and secondary are saying it’s not complex enough for them or it’s not risky enough, then we take, we present those cases. Then somebody, usually one of the senior managers or somebody above us will say, actually it needs to sit with you, it needs to stay with your team, or it needs to go to this team. They make that decision. But also, with a kind of a formulation that actually if you try this next step, this is the next thing you need to be looking at. If you do this for another six sessions and you’re still not, then secondary will need to accept. So there’s sometimes like a proviso around that acceptance’ (Stakeholder-07, Site-04_Wellbeing Service) | ||
| Outdated or unclear service specifications | As the demands for services rise and the mental health system experiences pressures at every level, service specifications are appearing outdated or unclear | ‘So most teams have got like a service spec, but our service spec is really outdated and hasn’t been updated. So we’ve just ended up holding a lot of these cases, as I’m sure secondary have held cases that probably their team wouldn’t normally take. It would go to a crisis team’ (Stakeholder-07, Site-04_Wellbeing Service). |
| ‘I think our service spec is only considered out of date because of the pressures on the system. I feel like it’s structured as an early intervention service spec, so that is what it is, and I can understand why it hasn’t been amended currently, although we’re going through a transformation, because it looks like an early intervention service spec. It’s not been formal … but we’ve just morphed into a service that adapts and accepts that we need to extend our boundaries a little bit if you know what I mean. It is an early intervention service spec but there’s nowhere else for these patients really to go into the system at the moment. So it’s understandable that they would come to us if they don’t meet other service thresholds. But it’s a challenge’ (Stakeholder-02, Site-04_Wellbeing Service) | ||
| ‘We’ve had so many senior managers try and define what early help actually offer – but it’s such a broad service, it’s really difficult to do. There are 13 locality teams – all do things slightly differently; they have different local partnerships and services and may support families in a variety of different ways. We address lots of the systemic difficulties, all of which will have a knock-on impact on the mental health of young people. It’s easier to list what we don’t do, rather than what we do, do. We’ve become a jack of all trades due to all the difficulties families can present with. The only thing we don’t do is anything to do with family court proceedings’ (SPQ-01, Site-01_Early Help and NEET Team) | ||
| ‘There can be [some ambiguity in using red, amber, green document]. I think we offer a consultation service as well, so within our service we have myself and then three specialist practitioners who can offer consultation to our colleagues, and just kind of try and make sure that we get the referrals to the right place. So, yes, there probably is – we always say it’s case by case’ (Stakeholder-03, Site-08_Community NHS Trust) | ||
| Services having to provide some ‘holding interventions’ while CYP waits for most appropriate support | This knock-on effect has put a lot of pressure on Early Help and targeted service providers, with some reporting having to deliver ‘holding interventions’ or update their service specifications in order to provide support to CYP while they wait for the right services | ‘Sometimes we’re not the right offer for young people and we wish to refer them to see a psychiatrist or psychologist but know they’re going to wait a year for an assessment, that’s a massive challenge. What do we do with that young people when we already know there’s a need? Come to an end of an interventions with young people and want to refer on – routine assessment may take a year and does not mean will be accepted for an intervention, and if are accepted, then have to go on intervention wait list’ (Stakeholder-09, Site-05_Charity) |
| ‘Secondary services (i.e. Tier 3 CAMHS Services) are seeing more and more complex young people (crisis work)–they’ve had to higher their threshold so things that used to automatically go to secondary services, can now sit with us. It used to be that young people who weren’t improving or needed longer term input automatically got transferred to secondary care, but that criteria have changed’ (SPQ-04, Site-04_Wellbeing Service) | ||
| ‘We get CAMHS … through the GP … there are challenges, they’re at crisis point at the moment and the waiting list is absolutely horrific for young people. So, we’re trying to do a lot of that backfilling ourselves, so the way we do it is our consultation with CAMHS. We’ll create a safety plan, and they’ll give some guidance and direction around potential work we can do. I’m cautious because we’re not mental health workers but what we can do is manage the safety around it. And then of course if that continues to escalate then we go back, and then it hits that trigger for crisis which we’ll all try to avoid’ (Stakeholder-06, Site-09_Family Support Team) | ||
| A system- or management-level dysfunction | A system-level dysfunction driving the lack of clarity of treatment pathways between services and causing delays in treatment | ‘Well, I mean some of it is a demand but as I say some of it is just disorganisation … Ten years ago, I asked what the pathways were within (the mental health Trust) that we could refer to. To this day nobody has written down what the pathways are. So, when I’m working with a young person it’s really difficult for me to know what other services there are for them to be referred to. I know there’s a range of different professionals within (the mental health Trust), but I don’t know, for example, if there’s a pathway that’s for acceptance commitment therapy. I don’t know whether there’s one person delivering that therefore it’s unreasonable to think that anyone is going to get that, or whether there’s a team of ten’ (Stakeholder-09, Site-05_Charity) |
| ‘It’s impossible to know the realistic options, yes, because … for some reason … there’s been block contracts in which there’s not been a clarity about the resourcing of the trust I think it’s fair to say, and what exactly they’re doing with the money that they’ve got’ (Stakeholder-09, Site-05_Charity) | ||
| ‘Sometimes that can still feel complex because services can be complex, and families can sometimes feel that they’re being passed – I think that’s always tricky when families feel that they’re being passed between services’. (Stakeholder-03, Site-08_Community NHS Trust) | ||
| ‘A lot of the time it’s driven by process and system issues, and the fact that services are overstretched and they’re trying to move people on a lot of the time, and not rightly or wrongly, but I would say that that’s a huge part of it as well’ (Stakeholder-01, Site-10_Central referral point) | ||
| Training | ||
| Early Help teams receive limited mental health training | Training received by Early Help practitioners does not equip them to provide support to CYPs experiencing mental health difficulties. The lack of knowledge and expertise in Early Help contributed to challenges in identifying suitable cases for IPC-A | ‘All the team do the 2-day Signs of Safety training, some also did a refresher, which was also 2 days. But apart from that, there’s no other training. Suffolk County Council have realised there is a gap, and they say they’re going to do something about it. Hopefully not just a one-day thing but a more extended training, maybe something that gives you a certificate, or something that gives them confidence to intervene with mental health. As a team, we shouldn’t really be dealing with anything more complex than low level low mood or anxiety, anything more complicated should go to a clinician (mental health professional) but at the moment, we’re not even in trained in how to support the low mood and anxiety stuff. I’d love every FSP trained in IPC’ (SPQ-02, Site-02_Early Help and NEET Team) |
| ‘Recently Suffolk County Council seem to have understood that we don’t have any training in supporting young people with their mental health (expanded on below). We do not take on cases which include mental health difficulties without support from wellbeing services and will escalate on if service inappropriate. If we just assume we can handle the wellbeing issue [mental health], we might be doing more harm than good, so the mental health route needs to be followed before we’re going to get involved, because if you don’t, you become accountable. If the wellbeing (mental health) professional tells us what we can do to help, we will go ahead and do that – but we’ll follow what they say, then they’re responsible for the actions’ (SPQ-02, Site-02_Early Help and NEET Team) | ||
| ‘… Because of the lack of knowledge and expertise in a team that isn’t [a] mental health team, it was difficult for people to select the right people … So, for example … we worked with the CWP team … to refer into that team. It’s a very specific offer, you know, CWP work is behavioural activation really. And when we were making referrals to that team … almost all of them were successful. Because we have the expertise to know what young person will work successfully with a structured CBT based behavioural activation model. But other people, if they’re working in early help they wouldn’t necessarily know …. Although I think the intervention [IPC-A] could work well in sort of settings where there are mental health presentations, but the workers are not mental health practitioners … there needs to be support with the triage to ensure that the right young people are selected for that intervention’ (Stakeholder-09, Site-05_Charity) | ||
| ‘Some referrers will just use CAF as a tick box, they think that a service is a service; I don’t agree with that, the right service is the right service. I don’t want to give my FSPs something that is outside of their capabilities because we can do more harm than good. So, when mental health is the only issue on the CAF, I can’t just let them through the gate. It would be like asking a carpenter to do plumbing, you’re just going to end up with leaks’. (SPQ-02, Site-02_Early Help and NEET Team) | ||
| Capacity and funding | ||
| Capacity | Both Early Help and targeted services are facing capacity challenges, which have been exacerbated by the COVID-19 pandemic. Capacity challenges, including staff turnover, have had a significant impact on recruiting into ICALM, as most services were left with a limited number of staff who were able to deliver IPC-A |
‘But for me it’s about resourcing and numbers, you know, and I have a team of 12 people which isn’t huge for the whole of Bury St Edmunds, and like I said earlier 186 something cases’ (Stakeholder-04, Site-01_Early Help and NEET Team) |
| ‘I mean we’ve got a lot of people that can deliver the treatment as usual side of it, but the actual IPC part of ICALM, it’s down to one person that can be the, yeah, be the person that does that … we’re happy to have a discussion with that person and ensure that they focus particularly on the ICALM cases, the IPC ICALM cases and reduces their CWP type caseload to help with the study. But yeah, it’s kind of dependent purely on their ability to get through those people if they’re randomised to treatment, rather than treatment as usual’ (Stakeholder-02, Site-04_Wellbeing Service) | ||
| ‘Difficulty in identifying staff members suitable for it – only 5(ish) out of 80 didn’t have prior mental health qualification. 4 or 5 of the 6 trained then left the organisation; leaving one available to do the intervention. And it was hard because we’ve got so many referrals coming in, their main job at the moment was to do assessments with those young people, call them, you know, do these really in-depth, quite hard, assessments. So, we would just find we didn’t have the capacity for them to be able to do that as well as then do IPCA as well. I think, ICALM was a brilliant opportunity for us to do, just it was unfortunate at the time that we just didn’t have the capacity, really, to really give it our all …’ (Stakeholder-11, Site-06_Charity) | ||
| ‘Cases were identified through the allocated workers and the managers allocating the cases. So, there was a huge burden of responsibility on the poor managers. One of those managers moved on. So, that was down to three. One of those managers took an acting job so that was down to two managers. That was about replacing those managers, but I guess we were so far down the line that never happened.’ (Stakeholder-06, Site-09_Family Support Team) | ||
| ‘The way trainee CWPs were employed in our team contributed to some of the staff not being offered a substantive post as they were only employed on temporary contracts so there was no job security after they finished and eventually, they sought permanent positions elsewhere’ (SPQ-04, Site-04_Wellbeing Service) | ||
| ‘We had some recruit to train positions where we trained, I think six CWPs, and we weren’t able to offer them a permanent contract, which was just such a shame … The CCG wouldn’t pay for those positions. So then we lost them and then we lost some CWPs because they went on mat leave, and then we couldn’t recruit because CWP positions are nationally really difficult to recruit to, because once you get a position and you train within that team, you tend to stay in that team. You don’t tend to move around a lot. So we’ve then had vacant posts within that area as well’ (Stakeholder-07, Site-04_Wellbeing Service) | ||
Increase in complexity of cases initially classed as ‘mild to moderate’
The backlog at the Site-10_Central referral point led to the prioritisation of red and amber cases and long waiting times for green cases, for example, low mood and anxiety. The prioritisation of red and amber cases impacted referrals into the ICALM study by inhibiting referral of green cases into services which had IPC-A-trained staff. In some cases, the delay in obtaining support had led to CYP (and parents) finding other ways of coping or seeking help elsewhere. However, other green cases on the waiting list deteriorate, leading to increased complexity and severity of cases being referred to the services. This consequently leads to an increased need to escalate cases from Early Help teams to targeted services and from targeted services to tier 3 services.
With a large proportion of cases having an element of mental health difficulty, a major challenge for Early Help teams, who currently do not take the lead in delivering mental health support, is the delay in accessing help from tier 2 targeted mental health services. Most early help services, recognising the dangers of waiting lists due to the increased likelihood for cases to deteriorate and increase in complexity, have highlighted the need for transparency with CYP and parents about the likelihood of getting a therapeutic service and the type of support on offer (i.e. short term).
I’ve learnt from 20 years of doing the job that a waiting list is a very dangerous thing to have, because if you have someone on the waiting list who’s got low mood, and they’re tenth on the list, if someone comes in and they’ve got, you know, a more severe sort of need, they trump, so that person goes to 11, then they go to 12. Waiting list gives false hope, what happens in [the] meantime. Waitlists allocate a worker, which looks like they are receiving help when they are not and leads to inability to get other services.
Stakeholder-05, Site-02_Early Help and NEET Team
If families really understood the state of mental health services in Suffolk are such that unless the needs are particularly high the likelihood of you actually getting a therapeutic service is very, very low. I think if families knew that perhaps they would look around to other types of service for support. But I think if they’re just put on a waiting list they’re just there with their fingers crossed just waiting for that phone call, which probably isn’t ever going to come.
Stakeholder-04, Site-01_Early Help and NEET Team
The long waiting times for green cases and increase in complexity were some of the barriers highlighted by the services in identifying appropriate cases for the ICALM study. As such, interventions targeting ‘mild’ presentations, for example, IPC-A, became less helpful to the services owing to the range of mental health issues in young people, including some extremely challenging and/or dangerous behaviours towards themselves or others. The long waiting times also led to poor engagement following the implementation of a new referral pathway for green cases from Site-10_Central referral point to the services.
It didn’t work [new pathway] …out of the people that we identified that could be appropriate [for ICALM], I don’t think any of them wanted to do it or didn’t engage or couldn’t get through by phone. And that’s a large part of the problem when people have got wellbeing issues, they are more likely to be the people that are hardest to engage.
Stakeholder-05, Site-02_Early Help and NEET Team
Restrictive or unclear service specifications and treatment pathways
The primary focus for Early Help interventions is safety, with health and well-being as a secondary focus. Therefore, apart from offering IPC-A (delivered as part of the ICALM study), Early Help teams’ mental health support primarily consists of promotion of mental health and well-being, confidence and motivation-building interventions and re-engaging with community networks and schools. According to the threshold matrix used by Early Help teams to assess whether referred cases fall within the Early Help service remit, CYP displaying signs of deteriorating mental health and episodes (e.g. low mood/mild depression or those with low-level mental health or emotional issues requiring intervention) should be classed as level 2 and are suitable for early help or targeted support services. This recommendation differs from what is happening at a service provision level, whereby Early Help teams refer cases with mental health difficulties, including low mood, to targeted mental health services or work alongside mental health professionals where advice is given on how they can help. The lack of standard treatment for mild to moderate mental health difficulties in some of the services therefore highlighted the challenges of running a RCT in this setting, as at times it was difficult to establish what TAU for low mood was being delivered by the services.
Early Help support is primarily delivered by non-mental health professionals from various backgrounds with basic mental health training; thus, they are currently not fully equipped to deal with a wide range of mental health difficulties. For example, apart from having access to online resources on mental health, some teams described only receiving a 2-day Signs of Safety training course aimed at equipping them to conduct Signs of Safety-based assessments. ICALM adopted a model which aimed to recruit and train Early Help practitioners, who are not professionally trained but work with mental health, to deliver IPC-A. IPC-A, being relational in its focus, should theoretically fit with the philosophy of the Early Help approach. However, the limited knowledge and expertise in teams that were not mental health focused presented challenges in identifying appropriate young people for the IPC-A intervention. Considering that a large proportion of the cases seen by Early Help teams will have some form of mental health difficulty, the lack of training and low involvement in tackling mental health challenges presents a missed opportunity that could help reduce pressures on mental health services, and indeed, Early Help services.
Apart from the limited role in supporting mental health difficulties, the service specification for Early Help is expanding to include more social service roles, for example, supervised contact of Looked After Children. There is also a current review of the role of FSP, which might lead to more social services roles, thus impacting the direct work the services do with young people and other interventions which are not part of their core offer, for example, IPC-A. This provision of both Early Help and statutory services, coupled with the reduced capacity of the workforce, had an impact on ICALM. Managers reported the challenges of protecting time for IPC-A-trained therapists while prioritising delivery of their core offer, which is not specifically mental health focused.
Due to the increased complexity of cases and the variability and subjectivity of assessment processes used, both Early Help teams and targeted services did not appear to be operating using a clear and/or up-to-date service specification with regard to mental health. Targeted services seemed to be more flexible and confident than Early Help teams in supporting CYP that would not ordinarily fall within their remit. These services described offering ‘holding interventions’ until appropriate help was identified through triage/patient flow/transfer meetings where senior managers from different services discuss cases that get stuck between the services. However, even with the transfer meeting, the teams highlighted that there are still gaps in the services whereby CYPs are not falling within any service remit or have a condition/illness which has no clear support pathway. The lack of clarity in referral pathways, which some teams have described as a ‘system level dysfunction’ is therefore a major challenge for the services.
Capacity
Capacity challenges in the mental health sector have been a long-standing issue which has been exacerbated by the COVID-19 pandemic. The numbers of staff varied between the services, with Early Help teams such as Site-01_Early Help and NEET Team having 14 staff members (including managers) supporting 390 families a year and targeted services such as Site-04_Wellbeing Service having 18 practitioners supporting approximately 1250–1500 cases a year. Factors driving the insufficient capacity include lack of funding and recruitment/retention challenges. The teams attributed some of the recruitment challenges to perceptions of some mental health trusts as ‘failing trusts’, perceptions of mental health as being under pressure and understaffed, the nature of the role, stigma around mental health and risk and poor job advertisements leading to audience misunderstanding of what roles involve.
A major challenge for targeted services was the poor retention of CWPs or PMHWs, who are often employed on short-term contracts, thus offering them no job security. This poor retention and high turnover were a significant barrier to the progression of ICALM, where several staff that had received training to deliver IPC-A either left the services or moved on to other roles. For the purposes of the ICALM study, these challenges especially affected services delivering targeted services (i.e. services with mental health support as their core offer), as only a small proportion of their staff members do not have a prior mental health qualification (CWP’s) and hence are eligible to train and deliver IPC-A. For example, Site-04_Wellbeing Service initially trained 12 CWPs to deliver IPC-A, but at the time of the interviews, only one practitioner remained in the service, with others either leaving or moving on to focus on a core profession. The high numbers of referrals also impacted on CWP’s capacity to deliver IPC-A, as they prioritised their primary role within the services, which was to carry out assessments with CYP, parents and referrers.
Conducting randomised controlled trials in non-specialist mental health services – the ICALM study research processes barriers
Given the paucity of RCTs in tier 1/2 services, where most cases of mild depression present in the UK,17–19 the ICALM study set out to address the need for evidence-based interventions in this setting by conducting a feasibility RCT of the IPC-A intervention. Our experiences with implementing the IPC-A intervention and conducting the ICALM feasibility trial highlight some key challenges and learnings (outlined below) in integrating this type of research into tier 1/2 services:
Research prioritisation
At a service level, process evaluation findings highlight a lack of research prioritisation compounded by an interaction between enormous demand for the services, a lack of capacity and resources and a lack of oversight of service co-ordination. Capacity challenges were then exacerbated by the COVID-19 pandemic, during which time managers reported having to prioritise the well-being of staff and continuity of service by not participating in activities that were seen as ‘extra’, including research.
We just had to be quite strict about how we prioritised our time management, all time during the pandemic. And anything additional we just had to be really clear that we weren’t going to take on, for our own wellbeing and therefore the continuity of the service. Nobody has had the capacity I think, or few people have had the capacity to do extra anything, and a trial ends up feeling like extra.
Stakeholder-09, Site-05
Randomisation
The capacity challenges faced by some targeted services posed practical challenges in establishing the delivery of two study arms, that is, for each service to have some practitioners solely delivering IPC-A and others delivering TAU. As such, some targeted services which offered interventions for low mood prior to participating in the ICALM study ended up collaborating with each other to deliver either IPC-A or standard care. For example, Site-06_Charity referred their CYP randomised to the intervention arm to Site-05_Charity, and Site-04_Wellbeing Service referred their CYP randomised to usual care to Site-07_Charity.
The lack of familiarity with research processes, in particular randomisation, was also a barrier to initial study set-up. Observations of the training and feedback noted that practitioners struggled with the concept of randomisation with some managers highlighting practitioners' concerns about putting CYP forward for the ICALM study, knowing that they might not be allocated to the IPC-A arm. It is also important to note that some sites (e.g. Site-03_Early Help and NEET Team) had been involved in the IPC-A pilot study, which was a single-arm study. Stakeholders in these sites felt that the pilot study worked well, as the referral process had been easier and more straightforward compared to the RCT.
Practitioners are struggling with randomisation and the idea that young people might get IPC-A or they might not. [Prompt: Do you think that your team’s involvement with the single arm study might have influenced this?] Yes, that was much simpler because they all got the intervention.
SPQ-03, Site-03_Early Help and NEET Team
Another key lesson was the importance of how equipoise was communicated during the training to services who were not familiar with this type of research and, consequently, how practitioners were introducing the research to potential participants. Initial feedback following the training indicated that, although teams were mostly positive, some felt that the trainers had been overly positive about the success rate of IPC-A. The presentation of the training did include slides on the evidence base for IPT (i.e. first-line treatment in adults and adolescents for moderate to severe depression and persistent mild depression; IPT is better than waiting list/standard treatment and IPT equivalent to CBT) and IPC for adults (remission rates: IPC: 59%/antidepressant: 45%) as well as some findings from the IPC-A pilot study (RCADS) which could have been viewed as positive and might have impacted understanding and communication of equipoise. Following the initial training, and based on the initial feedback, changes were made to the training with emphasis placed on the young person.
Although we do not have access to detailed information about how the research was being communicated to potential participants, interviewed participants allocated to TAU and IPC-A felt that communication about the study, assessment processes and randomisation by the research team was clear and straightforward. Most young people allocated to the IPC-A arm were pleased and indicated that they had hoped for this outcome at the point of randomisation. Although some young people allocated to TAU felt disappointed due to the perceived novelty of IPC-A, most admitted being more concerned about getting the help they needed.
Challenges in establishing treatment as usual
One of the objectives of the process evaluation was to describe TAU for low mood within the participating services. Our findings, highlighting a variation in the types of interventions offered to young people with low mood, with some tier 1/2 services having no standard intervention for low mood, accentuate the complexities in setting up RCTs in this setting as some services were delivering both TAU and IPC-A while others only delivered IPC-A and referred young people randomised to TAU arm to other services (which were also participating in the study). The study team’s perspective at the start of the study was that young people were presenting with low mood at all services that were tasked with addressing the young person’s issues using their service mode and interventions, whether targeting mood or systemic issues. As such, IPC-A was well suited in all services to fit with their treatment philosophies. When under pressure from excessive demand, they resorted to screening out low mood in some services, for example, Early Help, as this was no longer seen as their core business.
If the young person’s issue is only low mood and they are randomised to the TAU then we refer them back to wellbeing specialists e.g., school nurses and wellbeing services and/GP practices. If they are randomised to IPC-A then whatever case they have should be within the early help remit i.e., low mood and other issues, and if the other issues can be dealt with by the Family Support Practitioners, then that’s ok.
Meeting with Site-02_Early Help and NEET Team
Challenges in identifying eligible children and young people
Each team, including those within the same organisation, carried out their own triage and assessments for eligibility. Due to the variation in assessment tools used by the teams and the subjectivity of the assessment, it was difficult to establish whether a case classed as too complex in one service would also be classed as such in another service.
There was also potential for missing some eligible cases, as not all teams in the same organisation were involved or had capacity to deliver ICALM. Other managers carrying out assessments for other sites within the organisation were not aware of the referral criteria for the ICALM study and hence were not looking out for eligible participants who could have been referred to a Family Support Team. There was also a difference in how managers, within the same organisation but with different teams, understood and implemented referral processes, with some delegating the task to practitioners and others taking the task of screening referrals upon themselves and then referring eligible cases to practitioners.
I guess what you need is actually all the managers within our service to understand, you don’t necessarily need them all to be involved but they all need to understand that when a case comes in, they’re looking at it for potential allocation under those parameters to specific workers. So, for you to understand it, each locality and there’s six localities is split up into three teams. So, you have three managers for each locality and those managers are in separate localities, so it may have been lots of cases came into family support that would have been suitable, but they went to different managers, and ICALM managers never had sight of them in the first place. So, say 100 cases went into that locality and they were divided between those three teams only 33 cases would have been checked in your study, whereas 66 may have had them in and went out elsewhere. Logistically I think it was difficult for us, but I think it probably wasn’t set up quite right.
Stakeholder-06, Site-09_Family Support Team
Description of sessions offered to treatment as usual participants
As discussed earlier, not all services had a TAU offer for depression/low mood, in particular teams involved in the provision of social care services who found it difficult to justify TAU for ‘depression’ cases. Therefore, in such services, TAU consisted of referrals to targeted services. As such, recordings of TAU were limited and consisted of three sessions from one therapist and young person. In these observed sessions, TAU used CBT-based approaches – focusing on discussing how the brain develops and how different parts of the brain may relate to the young person’s behaviour. This treatment aimed to retrain the young person’s brain to challenge anxious thought processes. The young people were introduced to strategies which challenged these thoughts, reduced their symptoms and improved their mood. Techniques used within these sessions included breathing and distraction techniques, keeping a diary, rating enjoyment from day-to-day activities and a ‘predictometer’ whereby the young people are asked to predict what they think will happen in a situation and then compare this to what actually happened.
TAU data were also provided by participating services in SPQs and interviews with stakeholders and one TAU therapist. Support provided to young people with low mood by participating in services included: promotion of positive mental health and well-being; emotional well-being and resilience building; CBT-informed work; psychoeducation; and work to develop coping strategies. Numerous services utilised guided self-help to support young person’s needs, for example, using behavioural activation approaches:
Our guided self-help for low mood intervention is mostly based around behavioural activation. So, when there is that lack of motivation, lack of energy, when they’re perhaps not doing as much as they would usually be doing, it’s about getting them to do more and to recognise that when they do more that energy, that motivation, that improvement in mood tends to follow on from that.
Therapist-TAU-01, Site-08_Community NHS Trust
As described by young people’s interviews, TAU sessions most often consisted of eight weekly sessions, lasting from half an hour to an hour, and using virtual or face-to-face delivery. Descriptions from young people on the treatment they received give more insight into how TAU is perceived:
She talked to me about stuff and ways of coping with anxiety, and how to think of it in a different kind of way. Not completely negative and kind of facts instead of what I’m thinking.
YP-TAU-01, Site-08_Community NHS Trust
It was basically, like someone that was there to listen, talk you through everything. It was kind of like having a really good friend, what I needed at the time I guess, like a friend that I could actually talk to. Talk about feelings. That was helpful.
YP-TAU-02, Site-08_Community NHS Trust
I would say ‘hey, today I’m feeling quite sad’ and then she would go ‘I think that you’re feeling a bit sad today’ and that would be the end of the conversation really. [Laughs] I know how I’m feeling, I’m telling you.
YP-TAU-03, Site-04_Wellbeing Service/ Site-07_Charity
In comparison, TAU and IPC-A interventions were similar in duration (6–8 weeks) and session length (up to an hour). With regard to content, while both IPC-A and TAU tended to encourage young people to develop strategies to improve their mood, TAU did not focus on interpersonal relationships to achieve this. Instead, TAU focused on the individual and strategies that young people could carry out alone to reduce their symptoms, for example, keeping a diary or breathing techniques.
Interpersonal counselling for adolescents’ intervention
The acceptability of interpersonal counselling for adolescents
Interpersonal counselling for adolescents was acceptable to both young people and parents, with qualitative data from interviews with four young people and four parents indicating that the intervention was seen to offer positive benefits for young people. Apart from low mood, initial symptomatic experiences of young people receiving IPC-A included isolation, social anxiety and agoraphobia. Following IPC-A, young people reported being more open to family, socialising with friends and being able to engage in ordinary activities such as going shopping, walking the dog, etc. Several parents reported seeing improvements in young people’s well-being after the second or third session, with one feeling that IPC-A had helped to ‘get their child back’.
She’s like a different child in a positive way… I knew it would take time, I know it’s not a magic wand, but we went from being very indecisive, worrying about what time I was coming home from work…to actually being my happy daughter again who would laugh about her indecision. I mean no tears at school…no getting a phone call ‘Can you come and pick her up, she’s so distraught’ nothing. Her friends have started coming here again…tomorrow we’re off to the cinema together, she’s not worried about the open space, and that somebody next to her might cough. So, for me it was like a miracle to be fair.
Parent-IPC-01, Site-08_Community NHS Trust
Structure and delivery
Interpersonal counselling for adolescents was delivered over six to eight 60-minute sessions, either virtually or in person, depending on need or preference of the young person. Key aspects of IPC-A, including its structure, duration and focus on specific areas, received both positive and negative feedback. Young people reported having a positive experience during the sessions and felt that the structure and duration of the sessions were important for providing stability. Some therapists also enjoyed delivering the intervention, with some highlighting the collaborative nature and the structure of the intervention as positive aspects.
I thought they were good [IPC-A sessions], especially the length of them I thought was really good because it was long enough to get something covered but not long enough that I was being drained afterwards. I could still continue with my day.
YP-IPC-01, Site-02
I absolutely love it… I loved the structure. Although there was some flexibility in it, but I liked the fact that we focused on one problem area because often in our service you have one area of problem and other things crop up, and you tend to dive away from the main problem area, so I like the fact that we made it quite clear that we’ve identified the problem area.
Therapist-IPC-01, Site-08
Other therapists and stakeholders, however, felt that the duration of the intervention (six sessions) was too restrictive, especially where young people needed more support. Other stakeholders, particularly those who were already offering other interventions for low mood, also felt that although IPC-A fitted well with young people experiencing specific problems in the four focal areas (i.e. big changes, relationship disputes, grief and loneliness/isolation), the intervention was too narrow as low mood can be impacted by a lot of other factors. These stakeholders felt that selecting a particular area of focus was difficult because young people are changeable each day and struggle to make decisions.
So, your low mood can be impacted by the fact that you’re not eating properly. That you’re not sleeping properly…. we’ve got kids who are sitting on our list, or were sitting on our list, who have multiple things going on. So, when you tell a young person to pick one, they’re going to go ‘What do you mean, I don’t even know which one is the biggest issue today’.
Stakeholder-08, Site-07_Charity
This feedback raises an important point about how the IPC-A model was understood by some stakeholders/managers. The IPC-A model is designed for the practitioner and young people to work together collaboratively in selecting a focus area rather than asking the young people to pick an area. This misinformation around the model of IPC-A might have also contributed to recruitment issues, especially where managers were responsible for screening referrals.
Issues around the structure of IPC-A sessions and their impact on implementation and theoretical fidelity are further discussed below under Implementation and theoretical fidelity.
Content
Three young people felt that the content of IPC-A had contributed to the improvement of their symptoms and helped them to have a better outlook, of which, two described IPC-A as helping them to focus on more positive rather than negatives aspects of their lives. However, one young person who felt that her condition had not improved much since IPC-A, argued that the intervention focused too much on positive aspects, without giving space to understand the negative aspects and support the young people through it. The feedback from this young person highlights the complexity of delivering brief, focused interventions.
I know it sounds kind of weird to say it this way but it’s like they’re focusing too much on the good. They need to try and break down the bad… for example, if I was to say I’ve had an emotionally bad day but there have been a few good highlights, usually my counsellor will talk about mostly the good and a little bit about the bad at the very end. And then of course that would leave me feeling down afterwards. So, it would be better if they were to start off with the bad, go into a bit of detail about it so they’d understand my position and how it affected me during the entire day and how it made those little good things that might not be good things for other people, but may feel like more to me and make me feel a bit uplifted when I leave the session.
YP-IPC-02, Site-04_Wellbeing Service
The young person also reported doing weekly tasks/goals outside the sessions, such as keeping diaries of positive/negative experiences and speaking to their parents or head of year as a way of developing positive relationships. While some young people liked having goals, others reported struggling to complete tasks. Apart from noticing young people doing some tasks at home, most parents were not aware of the contents/discussions of the sessions. However, one parent reported being involved in the sessions, initially at the request of the young person who needed their support in explaining previous experiences. This parent also reported receiving helpful support from the therapist with regard to how best to support the young people at home.
If I’m finding something particularly difficult as well, obviously I say to [name of young person], ‘Oh can you just ask [name of therapist] to grab me for two minutes at the end, there’s just something I need to …’ and I’ll have a chat with [name of therapist] and say, ‘Look, something’s occurred, I don’t know if [name]’s mentioned it, but which is the best way to go?’ And then [name of therapist] will say, ‘Oh I’ll send you an email’, yeah. I’ll leave it a few days and I’ll say, ‘Oh [name of young person], [name of therapist] sent these through, and we need to have a try at these’ and we’ll read through it and whatnot. And then quite often that’s just what I need to be able to broach whatever it is that I’ve got niggling, concerning me, because I’ve noticed it.
Parent-IPC-02, Site-04_Wellbeing Service
Suitability for the services
Some services already delivering interventions for low mood felt that IPC-A was a useful alternative approach for low mood that enabled them to provide the most adequate support for that young people tailored to their need. However, the structure of IPC-A and the need to choose an area of focus were perceived to create some tension in other services whose offer was more general.
It [IPC-A] does involve quite specific work, methodology. And our specialism is much more around meeting young people where they are. We have a range of different kinds of ways of working, including things like cognitive behavioural based things or a creative way of working … It’s not always easy for us to hold a very specific offer within our specialism which is a more general offer as opposed to taking them through a very prescriptive method. There are so many agendas imposed on young people currently from school and other parts of their lives the feedback we get…is that they felt that they were listened to and met exactly where they were. So, that’s our primary offer.
Stakeholder-09, Site-05_Charity
Due to the challenges faced by the services in identifying suitable young people and delivering IPC-A, some Early Help managers felt that interventions such as IPC-A would be more suitable for services set up to tackle mental health, such as U18 Well-being Service and school nurses. Others felt that introducing early interventions such as IPC-A in schools would be a better approach, as Early Help usually refers CYP experiencing mental health difficulties to emotional well-being services or school nurses. Some stakeholders expressed the challenges of implementing an individualised intervention such as IPC-A in a service dedicated to supporting families as a unit. These stakeholders felt that, due to the level of young people engagement required, offering IPC-A at the beginning of a case when FSPs are dealing with the whole family and working to develop an intervention plan that has more to do with safety than therapeutic need was challenging. During the study, Family Support Teams resolved this challenge by ensuring that IPC-A was delivered by practitioners who were not case-responsible (i.e. responsible for the family unit). Practitioners felt that in Family Support Teams, IPC-A could work better if offered at the ‘tail end of a sequence of interventions’ (Stakeholder-04, Site-01) when young people are in a more stable situation and environment. Alternatively, some stakeholders felt that IPC-A could be better suited in a school-based setting where ‘young people are worked with individually, and they have that safe space with a professional where they feel safe’ (Stakeholder-04, Site-01).
We’ve found it’s better used when you’re not case responsible. So, if I’ve got a colleague who is case responsible for a family if – so [name of IPC-A trained therapist] was one of our key people, if say my colleague [name of Family Support Practitioner] is working with a family and he identifies that there’s low mood and depressive symptoms in an adolescent he would be able to refer to [name] and then it’s more effective because the roles aren’t blurred. Otherwise…we have tried being case responsible and doing the IPC and it can just be a bit confusing.
Stakeholder-10, Site-03_Early Help and NEET Team
We could probably put IPC as an intervention for every single child on our caseload, but it probably isn’t an intervention that the child is ready to engage with because there are so many other pressing issues on the intervention plan. And it’s often a result of either other family members or other domestic situations that are going on with that child that is impacting and causing their low mood or their poor mental health.
Stakeholder-04, Site-01_Early Help and NEET Team
Implementation and theoretical fidelity
Fidelity ratings and contamination
Therapists submitted recordings of their sessions to their supervisor to be rated; these sessions included the initial, middle and final sessions (three total). Items were rated on a 0–3 scale: 0 = not attempted, 1 = attempted but incomplete and/or superficial, 2 = completed to a good standard and 3 = completed to an excellent standard. An adequate range of IPC strategies must be demonstrated over training, and for each recorded session, an average score of two or above (for all rated items) was needed for a recording to pass. These ratings indicate how well therapists adhered to the IPC-A manual, which prescribes tasks for each session – differing between initial, middle and final sessions.
Tasks in the initial sessions review the young person’s symptoms, explain depressive symptoms and describe depression as an illness – and not a fault of the young person. The young person’s current coping strategies are also explored, and an interpersonal inventory is conducted. This interpersonal inventory aims to uncover what is going on and who is important to the young person’s life. The therapist and young people may then work together to agree on a problem area to focus on in future sessions by identifying what may trigger and maintain the young person’s depressive symptoms. Middle sessions also involve a review of symptoms and lead to tasks and techniques which are specific to the agreed-upon problem area. The young person’s progress with goals made in each session should also be reviewed and new goals for the next session agreed upon. Final session tasks include reviewing the young person’s progress and improvement by comparing their symptoms and goals across sessions and at the start of IPC-A. Dependent on this progress, the therapist must discuss the possibilities of what should be done once IPC-A has finished. These possibilities range from discharge from the service, maintenance work or referral to more specialist services.
Treatment-as-usual sessions were also rated to assess if IPC-A training led to contamination. No clear systematic use of the principles of IPC-A was identified – suggesting no contamination effects from IPC-A training for the observed TAU therapist, although it is not possible to generalise this with any certainty; see Table 18 for mean ratings for each case, IPC-A and TAU.
Interpersonal counselling for adolescents’ sessions: thematic analysis
Both therapists' and young peoples’ approaches to IPC-A were further explored using a multimethod qualitative approach to identify patterns within the data. Experiences of therapists, young people and parents involved in the ICALM study were considered alongside IPC-A sessions – ‘cases’ refer to the therapist and young people dyads within these sessions; see Table 19 for overview of each case. Thematic analysis was used to explore both session and interview data. Conversational analysis was then used on session data to support findings of the thematic analysis.
| Case number | Treatment | Therapist | Young person | Problem area | Site ID |
|---|---|---|---|---|---|
| 1 | IPC-A | Therapist-IPC-01 | YP-IPC-04 | Big change | Site-08 |
| 2 | IPC-A | Therapist-IPC-01 | YP-IPC-03 | Relationship disputes | Site-08 |
| 3 | IPC-A | Therapist-IPC-03 | YP-IPC-01 | Loneliness and isolation | Site-02 |
One main theme emerged from the data relating to the role of therapist and young peoples’ and interactions between the two in effective delivery of IPC-A: engagement from young people as crucial for successful, collaborative intervention. Within this theme, several subthemes were developed which consider the mechanisms and contextual features of IPC-A sessions and how these can be utilised to encourage engagement and progress for the young person. These subthemes were interactional styles and participation within intervention sessions; importance of feeling heard; orienting discussions to young person’s perspective; and reliability of interpersonal relationships: mini goals and advocacy. It is worth noting the difficulty in defining what is a mechanism of action and what is a contextual feature of IPC-A sessions. Using these terms, we aim to highlight components which are important to the successful delivery of IPC-A. See Table 20 for a summary of findings and recommendations.
| Theme | Subthemes | Recommendations |
|---|---|---|
| Engagement from young people as crucial to successful, collaborative intervention |
|
|
Context for implementation and theoretical fidelity: IPC-A training and supervision
Throughout the findings, the impact of IPC-A delivery on implementation and theoretical fidelity is considered. All therapists in the ICALM study took part in IPC-A training, in which they were trained on how to deliver IPC-A to young people within their service. The main focus of training was to introduce therapists to the structure of IPC-A, followed by supervised practice. Within IPC-A, there are initial, middle and end phases – each of which considers different tasks. During training, therapists are taught the components of and outcomes for each session across each phase. Middle phases require different components depending on the problem area agreed by young person and therapist; however, general IPC-A techniques are utilised across each problem area – all of which are addressed in detail during training.
Perceptions of training were positive from most therapists, with some finding it affirmed their current practices:
It’s done in a different way but ultimately, it’s the same sort of process in the way of offering that young person that containment and trying to stick to the worries. So, yes, but I still got a lot out of it because I felt it was reaffirming some of what I did.
Therapist-IPC-02, Site-09
Training was also described as containing a lot of new information, leading to the suggestion that some perceived training as ‘dense’.
I mean it was two full-on days. I felt there was a lot of jam packed into two days. I did feel a little bit like a rabbit in the headlights when we’d finished. It was like crikey I really don’t know what’s going on now. It was quite daunting. And I thoroughly enjoyed it I have to say.
Therapist-IPC-01, Site-08
I think it would benefit possibly at certain stages for a little bit more participation activities from the trainees, because at certain points there’s quite a long period of information being taken on board.
Therapist-IPC-03, Site-02
I remember it feeling like it’s been long day and it’s a long day of a lot of talking as well. So, it’s not like it’s a long day with right let’s do some break out things, it was just long days of being talked at. So, I did find that really hard at times.
Therapist-IPC-02, Site-09
Density of training and time between training and delivering the intervention appeared to lower therapists’ confidence in being able to deliver IPC-A as described in their training. Many therapists felt they needed to revise their training closer to the delivery owing to delays with referrals and disruption owing to COVID-19 – for whom refresher sessions were arranged.
I mean, the training was good. I’m a person that if I’m not using it, I tend to lose it. Yeah, so it was always agreed that when we have a case, then we’d review that training, so we knew where we were kind of at.
Therapist-IPC-04, Site-09
I was worried actually it’s a very busy world when you’re doing our jobs and my fear was when I’m going to get that referral in and start working with that young person there’s a danger that I’m not going to be able to remember because it’s quite scripted in a way to deliver.
Therapist-IPC-05, Site-01
| Target | Actual | Criteria met (yes/no) |
|---|---|---|
| Recruitment rate is at least 80% of target | 16 out of 60 (26.7%) participants were recruited to the study | No |
| At least 70% of those randomised to receive the intervention attend at least three therapy sessions within the 10-week treatment window | 3 participants (50%) attended three or more sessions | No |
| Follow-up assessments are completed by at least 80% of participants at 10 weeks and 70% of participants at 23 weeks | 100% completed follow-up at 10 and 23 weeks | Yes |
| At least 80% of IPC treatment sessions reviewed meet treatment fidelity criteria | 100% of reviewed treatment sessions met treatment fidelity criteria | Yes |
| Contamination of the control arm can be sufficiently limited for individual randomisation to be justified | No evidence of contamination effects | Yes |
| The mean RCADS depression scores of the IPC-A and TAU groups at 10 weeks are indicative of a clinically significant difference in depression (3 points) | At 10 weeks, there was no clinically significant difference between the two interventions | No |
This latter quote supports the suggestion that this perceived ‘density’ of training and structure of IPC-A may have led to therapists feeling pressured to deliver the IPC-A intervention according to its structure rather than flexibly adapting it to the young people's needs. This therapist goes on to describe the structure of IPC-A as detrimental to their delivery and ability to build rapport with the young people, owing to the pressure of sticking to the structure.
And especially that being the first session as well, you’re beginning to build up that relationship, but at the same time you’re thinking, oh, my goodness, I’ve got – I’ve done this, have I ticked that, have I done that?
Therapist-IPC-05, Site-01
This tension between delivery of IPC-A according to its structure and engaging with the young person’s needs highlights a tension between implementation fidelity and theoretical fidelity. In this case, there appears to be a focus on implementing the intervention as trained (implementation fidelity) over the young person’s needs and desired outcomes from the intervention (theoretical fidelity). Therapists are told within their training that the needs of the client are more important than the needs of the IPC-A. However, therapists’ delivery of these IPC-A sessions is also supervised and subject to feedback from their supervisor. Therapists have weekly supervision sessions alongside their IPC-A sessions, in which to discuss cases and any areas of difficulty. Supervision is seen as ‘an extension of training where therapists continue to learn and are helped with practical implementation of strategies’ (IPC-A Trainer). Once IPC-A sessions have finished, supervisors rate therapists’ IPC-A sessions using the rating system described above (see Fidelity ratings and contamination). These ratings decide if the therapist can pass their IPC-A training, with each therapist needing to pass two case studies to complete their training. Given this context, implementation fidelity may be given priority by therapists, potentially undermining the mechanisms of change the intervention is designed to activate.
Supervision sessions were seen as invaluable by therapists, many of whom were not confident in their delivery of IPC-A – partly owing to the structure and amount of content to be delivered during IPC-A sessions. Through discussion with their supervisors, therapists found validation in their delivery and affirmation that they are delivering IPC-A as needed.
But I just wasn’t confident enough in that session to say I think this is what the problem area is. So, I went away, took some supervision. Had my supervision and I should have gone with my gut feeling because I was absolutely right.
Therapist-IPC-01, Site-08
Increased confidence in their delivery meant that therapists were able to avoid fixating on delivering IPC-A according to the manual and be more flexible in their approach, for example, listening and reacting to the young person’s needs. Guidance from this weekly supervision also allowed therapists to increase their confidence by better understanding young person’s needs through the IPC-A model. Therapists’ perceptions of supervision illustrate the important role it plays in facilitating therapists’ confidence to deliver IPC-A not only well but potentially at all.
And I couldn’t have continued without it in all fairness because I need that for my confidence as well to make sure I was doing the right things.
Therapist-IPC-01, Site-08
She was like my little personal cheerleader for someone to come back and go to ‘I think I did that right, but I’m not sure’, and she’d be like ‘oh yes. And you’ve done this, and you’ve done this’, and yes, I needed [supervisor’s name] in a box, I think, to take around with me.
Therapist-IPC-03, Site-02
Supervisory meetings play an important role in facilitating both implementation and theoretical fidelity by validating therapists’ delivery, increasing their confidence and providing constructive feedback when therapists need redirecting, ‘lots of lovely constructive feedback, and also the feedback when things didn’t go so well, or where I wasn’t sure what I needed to do’ (Therapist-IPC-01, Site-08). By increasing therapists’ confidence in their delivery, supervision allows therapists to avoid focusing on the structure of IPC-A to consider the young person’s perspective and needs – a crucial element in successful interventions. Had therapists been able to take on a higher number of cases, it had been anticipated that confidence in delivering IPC-A would have increased.
Engagement from young people as crucial for successful, collaborative intervention
A key component of IPC-A is collaboration between the therapist and young person. Collaboration is highlighted throughout the IPC-A manual and training and is used as a tool to help young person identify problems and solutions; for example, what their triggers are, how they can recognise the onset of symptoms and find strategies to ease their symptoms. For collaboration to occur, both the therapist and young people need to actively engage with the sessions and tasks. This need for engagement is also reflected in parent and therapist perspectives that young people must be ready to seek help and engage with support before starting these sessions and for support to be effective (see e.g. Appendix 1, Table 22 data extracts).
These perspectives placed young person’s motivation to participate in the intervention as a central component for ensuring effective delivery of the intervention. However, it raises the question of how active engagement might manifest within the sessions themselves and what therapists might do to help young people actively participate in discussions. One of the most beneficial aspects of accessing therapy, as perceived by parents, therapists and young people, was the ability for the young people to talk and have someone listen without judgement.
In contrast, if a young person does not feel heard, there may be a sense that engaging with interventions is pointless, as discussed by one parent describing responses to their child trying to find support in school: ‘That just made his mood just go even lower because he thought what’s the point. If I’m not going to be listened to then I’ll just carry on as I am, and therefore he then wouldn’t talk’ (Parent, Case 2). This capacity for young people to feel heard, and that their voice matters, can start before deciding whether to take part in the ICALM study, as seen here in a discussion between the young person, parent and the young person’s school about support options available to them:
Interactional styles and participation within intervention sessions
Most apparent throughout recorded IPC-A sessions were different interactional styles between therapist and young people, representing different ways that young people respond to the IPC-A intervention. These can broadly be categorised as (1) active participation, young person works with the therapist to find solutions; (2) active resistance, young person resists attempts by the therapist to collaborate, often followed by renegotiation; and (3) passive participation/resistance, young person defers to therapist. Passive participation may reflect an inability to engage with the session or not knowing how to participate, rather than choosing not to engage. For example, the young person may express that they ‘don’t know’ as a form of resistance or an inability to participate owing to their memory or difficulty of the task. It is up to the therapist to navigate these interactional styles to help the young person to engage with IPC-A and improve effectiveness of the intervention.
Contrasts and variations in interactional styles seen across and within sessions for each case suggest that the effectiveness of IPC-A relies on mechanisms which allow the young people to feel comfortable talking and sharing with their therapist. Exploring how and where these interactional types emerge and change throughout IPC-A sessions offers insight into how contextual features and the tools of IPC-A can be used to encourage active participation from young people. One of the main components in encouraging young people to engage with sessions appeared to be therapists’ ability to give the young people space to not only talk but also feel heard, resulting in increased rapport between the two and facilitating the collaborative effort needed for effective IPC-A.
The importance of feeling heard
During their initial session, the therapist and young person in Case 1 illustrate how active participation from the young people facilitates the therapist’s understanding of their symptoms and experiences, enabling a collaborative exchange that leads to them identifying a problem area (‘big change’) to focus on in future sessions. This level of participation was later reflected on by the young person who reported, ‘I cried quite a lot I think, just like for the first one probably when I was just talking about just everything’ (YP-IPC-04, Case 1). An extract from their first session (see Appendix 1, Table 23) illustrates how the therapist works to show the young person that they have heard and understand them – a key mechanism which enabled this young person to actively participate in sessions.
However, to better understand the importance of feeling heard in facilitating active participation from young people, we needed to examine sessions in which young people were more resistant or unable to engage with therapists’ attempts to deliver the intervention session. In Case 3, the young person reported feeling misunderstood by their therapist and the frustration that came with this:
[Interviewer] And how did you get on with the therapist that you were seeing?
[YP] OK. I think I got a bit frustrated with her sometimes but overall, she was all right in the end.
[I] What frustrated you at the beginning then?
[YP] I think that sometimes I’d say things and she’d interpret them a different way which irritated me.
This perception of their sessions may also be reflected in ratings of techniques used by the therapists in Case 3 and Case 1 (and Case 2). For example, Table 7 shows that in the initial session, the therapist in Case 3 averaged lower than the therapist in Case 1 (a score of 2.1 vs. 1.4, which are a pass and fail, respectively). Techniques in which Case 3’s therapist scored lower included not asking the young person about their variation of symptoms (e.g. changes across the week) and creating links between young person’s interpersonal relationships and depressive symptoms. This lack of exploration of the young person’s symptoms may have led to feeling misunderstood, as the complexity of what they had been feeling may not have been fully addressed. Examples of this can be seen in Case 3’s first session, which provides examples of interactional difficulty or tensions between the young person and therapist, locating instances where the young person may have felt misunderstood, or unheard, and the interactional style this led to. These interaction styles included passive participation within the sessions or active resistance towards participating (see Appendix 1, Table 23).
Therapists are rated on their use of exploratory techniques which should be used to actively encourage participation. By showing a sense of curiosity and acknowledging a young person’s contributions, therapists should encourage the young person to expand on productive topics without imposing unnecessary structure. In this case, the therapists’ focus on the structure of IPC-A (and implementation fidelity) and imposition of this may have limited their acknowledgement of the young person’s contributions and exploration of why the young person is unable to describe where their feelings are coming from.
Active resistance is also demonstrated by the young person in Case 3’s initial sessions, which allowed us to explore the difference in context between active and passive resistance. One way in which active resistance appears to be expressed differently from passive resistance is that the young person does not only respond using one-word replies but instead actively responds to the therapist by justifying their reasons for not wanting/being able to engage in an activity. In the observed context of Case 3, this actively resistant interactional style may be prompted by feeling more than misunderstood but also not believed in or even judged by their therapist. This approach, or perceived approach, by the therapist also contrasts with the intended implementation of IPC-A, in which the therapist’s role is to be non-judgemental and on the young person’s side. Further, the rapport between therapist and young person may suffer owing to the misunderstanding in communication between them.
These points of contrast across cases, illustrating varying forms of participation and interactional sequences, reveal the central importance of therapists working to understand and acknowledge young people’s perspectives and the crucial role played by differing interactional styles for facilitating young people’s engagement, with a non-judgemental approach allowing young people to feel heard and share openly without having to defend or justify their disclosures. These points of contrast also illustrate the complex relationship between implementation and theoretical fidelity, in which both may impact the other for better or worse. For example, implementation fidelity does not always ensure theoretical fidelity.
Orienting discussions to a young person’s perspective
One of the most important mechanisms in enabling young people to actively participate in sessions appeared to be the therapists’ ability to be flexible and work to reframe discussions or renegotiate terms in a way that the young people can relate to – orienting discussions to the young person’s perspective.
Therapists’ initial understanding of the young person’s experiences is reliant on how the therapist elicits the young person’s perspectives and how the young person chooses to answer. Depending on the approach taken, misunderstandings may manifest between therapist and young person, creating interactional tension between the two parties. Misunderstandings could also lead to the young person not feeling heard, despite not having shared this information. In Case 1, for example, tension is seen during the initial session when the therapist misinterprets the young person’s relationship with their mum – interpreting their relationship as less close than they are. The young person responds to this by elaborating that their relationship is very close, leading the therapist to readjust their interpretation of the relationship to accommodate this new understanding; in particular, that the young person’s mum is supportive and listens to how they are feeling. See Appendix 1, Table 23 for an example extract showing the consequence of the therapist’s adjustment, with the therapist changing tack.
Listening to the young person’s perspective and reframing the conversation to acknowledge their perspective appears to help the young person actively participate, despite what appears to be a difficult task which requires pauses for thought. Focus then turns to how the young person can change their interactions to discuss their feelings more deeply, for example, going beyond what their feelings are to what has made them feel that way. The young person actively responds to this approach, showing their understanding and the value they see in it – rather than passively accepting the suggestion.
This interaction is followed by an offer to role play this conversation, which is turned down by the young person but later scripted in another session. In this later session, the therapist shows their awareness of young person’s hesitance around ‘role play’: ‘I don’t want to call it role play but it is a little bit like that, just to see how you manage to open up that conversation’. The young person is encouraged to read their script from the screen and have the therapist be their response – rather than starting the conversation on the spot. Again, this therapist can be seen to orient to the young person’s perspective by showing their awareness of issues around ‘role play’ and helping them to script what has been shown to be an uncomfortable, hard conversation for the young person to start. The effectiveness of this technique is seen in the young person’s ability to go on to complete their mini goal. Upon completing this mini goal, the young person is met with praise from the therapist and acknowledgement of its difficulty, ‘I think the more you avoid those emotionally charged situations, the more difficult it becomes for you to then approach those situations and those subjects. So, the fact that you managed to do that, that’s huge, that’s absolutely massive’ (Therapist-IPC-01, Case 1).
Despite the effectiveness of role play, young people appear resistant to trying it out, perhaps owing to their familiarity with talking to the chosen person or the discomfort of improvisation – which scripting conversations appear to relieve. Role play is also offered in Case 2 and again is turned down. The same therapist shows their awareness of hesitation around role play by offering it as a last resort, ‘if you find that you can’t, then what we can do is perhaps do a little bit of – I know this sounds really scary – but a little bit of role play and we can try and sort of act together’ (Therapist-IPC-01, Case 2).
The importance of orienting discussions and sessions to young person’s perspective is also reflected in Case 3. In comparison to the previous case, feelings of misunderstanding for this young person may stem from their inability to relate to the term ‘depressive symptoms’, as they do not think it fits with what they are feeling. Failure of the therapist to recognise and respond accordingly to the young person’s perspective leads to the young person feeling misunderstood, resulting in passive participation from the young person (see e.g. Appendix 1, Table 23).
Initially, the therapist’s response appears inadequate for orienting to the young person’s point of view and enabling the young person to actively engage with the session. This failure to explore and reframe the discussion according to the young person’s perspective appears to result in the young person struggling to actively engage and instead showing passive resistance. This passive resistance is illustrated in their use of unmarked tokens,58 such as ‘yeah’, ‘mhm’ or ‘don’t know’. This interactional style changes within the session when the therapist recognises the issue and renegotiates the terms used with the young person – trying again to orient to the young person’s perspective and successfully enabling the young person to actively engage with the task (see Appendix 1, Table 23).
This renegotiation of terms also highlights a potential tension between implementation and theoretical fidelity for therapists. Implementation fidelity, for example, might encourage the therapist to continue discussing depressive symptoms, owing to the theoretical focus of IPC on the interactional relationship between depressive symptoms and interpersonal relationships. However, for this young person (Case 3), continuing this approach would be inappropriate and result in resistance throughout the sessions and little progress for the young person. Changing these terms shows the therapists’ ability to adapt flexibly to the needs of the young person, helping them to engage and progress with the intervention, and in turn, enhancing theoretical fidelity. Despite the main diagnostic category for the study population being depression/low mood, the therapist’s role is not to diagnose young person with depression. A key mechanism of change within these sessions is the therapist’s ability to work flexibly with the young person to collaborate and work towards a solution on their terms.
Contextualising IPC-A using specific scenarios, relevant to the young person’s experiences, was also seen as another mechanism which involved orienting to the young person’s perspective and encouraging this young person’s (Case 3) engagement. By contextualising IPC-A in this way, the therapist was able to gain information from the young person about their interpersonal relationships, which had proved difficult owing to the young person’s difficulty engaging with previous tasks, for example, creating a timeline of their symptoms.
An important mechanism of IPC-A, therefore, appears to be in the therapist’s ability to orient themselves to the young person’s perspective and reframe discussions accordingly – often requiring flexibility with the structure of IPC-A sessions. Beyond this understanding of the young person’s perspective, therapists must also encourage the young person to change their approach and engage with IPC-A techniques.
Reliability of interpersonal relationships: mini goals and advocacy
Many, if not all, tools of IPC-A rely on active participation from the young people. Most prominent of these are mini goals that are set at the end of each session for the young person to complete before their next session, where they will be reviewed. In accordance with the IPC-A manual, these goals should be agreed on collaboratively, interpersonally and as something the young person has control over. The aim of these goals is to be achievable and help the young person towards their ultimate goals.
Responses to and success in these mini goals can affect the young person’s future engagement with mini goals outside of the sessions. In the cases seen, mini goals were often reliant on others responding appropriately to the young person’s attempts at completing these goals. Engaging in mini goals and not receiving the response they need or expect can be disheartening for the young person and could lead to them feeling less motivated to engage with IPC-A outside of (or within) sessions. This is best illustrated in this example from Case 3, in which the therapist and young person are reviewing the young person’s mini goal to talk more deeply about how they are feeling with their mum (see Appendix 1, Table 23 for extract).
Use of mini goals and advocating for the young person can help to better develop the rapport between the therapist and young person when used effectively. For example, in creating mini goals the young person and therapist make an agreement that the young person will engage with the task outside of the session, and the therapist will follow up with this task in the next session. Following up is a key element of this tool, as much like feeling unheard, if the young person attempts the task but is not asked how it went, they may have little motivation to attempt these mini goals again. Advocating for the young person may also work to reinforce the therapist’s words with actions, going beyond saying that they are listening to their needs to taking steps towards making sure these needs are met by others, where possible. In Cases 2 and 3, both therapists take the opportunity to advocate for the young person by discussing the young person’s needs with important interpersonal relationships (parents and teachers) without revealing details of their sessions.
In Case 2, given the outcome of the previous mini goal, the therapist emphasises the need for the young person to find the right moment to carry out their mini goal: ‘I would like you – if you can – I think it would be a really good idea to, when you’re nice and calm, is to go and visit [teacher’s name] or ask to see him at a certain time’ (Therapist-IPC-01, Case 2). Reframing the context of the mini goal to include finding an appropriate time may foster further consideration of the other person’s perspective, leading to a more balanced view of relationship disputes. The therapist also offers to extend their reach to act as an advocate for the young person to ensure that responses to their reaching out are treated appropriately, in this case by talking to their teacher beforehand in preparation for their chat with the young person. Again, therapist’s ability to act as an advocate for the young person may help the young person feel supported by both their therapist and interpersonal relationships. The latter is crucial to IPC-A’s theoretical fidelity and young person’s progress once their IPC-A sessions have finished. See Appendix 1, Table 23 for an extract from Case 2 which highlights the change in response to the young person's reasons after the therapist is able to advocate for them to their parent.
A key component of the IPC-A is the two-way link between depressive symptoms and interpersonal relationships. Improving young person’s interpersonal relationships through effective advocacy should lead to improved depressive symptoms. Discussing expectations around these interpersonal relationships also appears to be an important tool in understanding the young person’s perspective on IPC-A and how it can work to help them.
Effective use of mini goals and advocacy can change interactional styles and help young people to actively engage in IPC-A, both within and outside of sessions. Use of these tools adheres to the intended implementation of IPC-A and can be seen to foster the theoretical ideals of IPC-A, allowing young people to further develop their interpersonal relationships and the support received from these.
Chapter 5 Discussion
Summary of findings
The aim of the ICALM study was to inform a future trial of the effectiveness and cost effectiveness of IPC-A by answering: (1) Are trial procedures, including recruitment (of participants and therapists), randomisation, research assessments and follow-up, feasible and acceptable? (2) Are IPC-A and TAU delivered and how and why does intervention delivery vary across differing service contexts? (3) To what extent does contamination of the control arm occur and should it be mitigated against in a future trial? (4) Does the interval estimate of benefit of IPC over TAU in depression scores post treatment include a clinically significant effect?1
The aim was to recruit 60 participants for the study. Thirteen different sites participated, and nine SPQs were received. Thirty-two participant referrals were received, of which 16 participants (26.7% of target) were recruited, which is less than the progression criteria of 80% of target. Due to factors related to COVID-19, appointment attendance, increased risk and complexity following baseline assessment and progression of symptoms, only seven participants received an intervention. Three participants received the IPC-A intervention, while four received TAU. Fifty per cent of participants attended at least three therapy sessions within the 10-week treatment window, which was less than the progression criteria target of 70%. Of those that received an intervention, 100% of follow-up assessments were completed, which was above the progression criteria target of 80% at 10 weeks and 70% at 23 weeks. Twelve participants completed the RCADS depression score at the 10-week follow-up. No clinically significant difference was found between the two interventions, meaning the progression criteria were not met; however, this result is likely to have been impacted by three participants not receiving the IPC-A intervention as intended. Eight interviews and one focus group were completed with stakeholders. Sixteen interviews were completed with participants; eight of these were with participants in the intervention arm and eight in the TAU arm. A further eight interviews were completed with YPWs: one IPC-A supervisor, six IPC-A therapists and one TAU therapist. Four participants consented to their recordings being analysed for the process evaluation. One hundred per cent of reviewed treatment sessions met treatment fidelity criteria, which was above the progression criteria target of 80%, and there was no evidence of contamination effects. The feasibility trial was suspended in the first couple of months, for 6 months, due to the COVID-19 pandemic. An extension was applied, and recruitment closed at the end of the agreed recruitment window. The study was not able to randomise the target number of participants; therefore, the data provided were insufficient to answer key research questions regarding the feasibility and acceptability of the intervention.
However, the feasibility of the RCT was accompanied by a mixed-methods ethnographic process evaluation to generate an understanding of intervention implementation across services and explore the acceptability of the intervention from the perspective of young people and other key stakeholders. Following difficulties with recruitment to the main feasibility trial, the funder advised that the process evaluation could refocus on understanding the barriers of running a clinical trial in the various community services that make up CYP’s mental health landscape. We have provided detailed insight into these barriers, with implications for other researchers conducting future research in mental health and community services.
The findings on recruitment, retention, fidelity and contamination are summarised in Chapter 5, Progression Criteria, in relation to the criteria for progression to a definitive RCT. As mentioned above, we assessed the feasibility and acceptability of trial procedures, how intervention delivery varied across the services, how contamination can be mitigated against and whether there is a clinically significant benefit of IPC over TAU.
Results of the feasibility study
Recruitment of participants
Due to low recruitment, potential suitable cases being stuck on a ‘green’ list and services not always having TAU or IPC-A capacity, new pathways were set up which appeared to fit with the changing environment. The new pathways were provided so that services could work together to identify and treat individuals depending on their randomisation to the appropriate service. A fast-track service was also set up from Site-10_Central referral point so that those under a RAG rating of ‘green’ that were potentially suitable could be referred to the ICALM study. The fast track helped with the fact that services were reporting increased complex referrals that were not suitable for ICALM. Although the changes to referral routes were not successful, the different services showed great flexibility and went above expectations to help the study.
As discussed in the process evaluation, due to challenges faced by services in recruiting suitable young people and delivering IPC-A, it was felt by Early Help managers and practitioners that IPC-A may be more suitable for U18 well-being services and school nurses, as they were overtly set up to treat mental health difficulties. The well-being and school services are also normally the first points of call to refer CYP experiencing mental health difficulties.
To encourage recruitment, teams were willing for ICALM to attend allocation, triage and team meetings. This allowed questions to be answered directly, for ICALM to understand referral difficulties, help identify possible referrals and build working relationships across the network. Teams were mostly happy to test alternative procedures and showed a willingness to be involved in the study.
It was also noted that half of participants came from services within NHS Trusts and not Early Help teams. A possible reason for this is due to experience in research studies or a culture of research and evidence-based practice within traditional health services, leading to more confidence and also knowledge/education around the randomisation process. As was suggested by Early Help managers, NHS Trusts are more likely to be set up to identify and screen for mental health, possibly leading to more referrals.
COVID-19 and the recurrent lockdowns impacted clinical presentations of low mood. An increase in presentation of anxiety cases amongst services was noticed with the start and progression of the pandemic. Despite comorbidities between anxiety and low mood, young people expressed greater preference in having their anxiety rather than low mood treated. Since ICALM’s core criterion was to provide IPC-A to young people presenting with low mood, many young people were screened ineligible and were not further referred from services, influencing the number of referrals received in ICALM. Receiving mild to moderate cases of depression is what the study demanded, but such cases appeared to either no longer exist or did not come into the services or to their attention. Ultimately, the study was unable to recruit the required number of participants despite repeated mitigation measures being put in place.
Recruitment of therapists
A high turnover of staff in the services meant that the majority of staff who had received training to deliver IPC-A either left the services or moved on to other roles. By the end of the study, only half of the teams had active therapists who were attending supervision sessions. This reduction meant that regardless of the number of participants coming through, capacity from existing therapists and sites was limited. The previous single-arm study (pre COVID-19) had a high retention rate, and the calculation of the number of trained staff required was based on this study.
A lack of staff trained to deliver IPC-A added pressure to the remaining IPC-A practitioners. This especially affected services delivering targeted services (i.e. services with mental health support as their core offer), as only a small proportion of their staff members do not have a prior professional mental health qualification (CWP qualification). As the study progressed and teams had a reduced number of IPC-A-trained staff, further training sessions were offered, but after the second training offer, no further staff members expressed an interest nor were any put forward by their managers. Future studies may wish to consider funding staff to be trained as IPC-A therapists and deliver the therapy as a core offer, as happened in the initial single-arm pilot.
A major barrier to this trial’s working was existing staff being unable to deliver the trial intervention for multiple reasons. A future study would be more likely to be successful if it also funded staff time for study treatments, training and supervision. We accept this is not normally done for research in NHS services, as such treatment is often considered ‘core business’. However, we have demonstrated the additional barriers to conducting RCTs in tier 1/2 services, which may justify this extra funding.
Randomisation
Initially, staff participants struggled with the concept of randomisation, voicing that they felt it was unfair to refer a young person for the study, knowing that they may not receive IPC-A. This was particularly noticeable within social care settings. One team manager stated that he would not be putting any young person forward as he thought randomisation was unethical. Changes to training were made to include more information on randomisation and less of a focus on IPC-A; however, randomisation continued to be a barrier throughout the study. Once identified as suitable for IPC-A, clinical staff struggled to accept that their standard offer would be of benefit.
Participants in the study expressed concern mostly around the randomisation of the study and getting the help they needed. Some expressed disappointment when randomised to the TAU arm of the study, while one participant was concerned about being allocated to IPC-A as it was an untested intervention without evidence of effectiveness.
Using a cluster randomised trial (CRT) could potentially offer solutions to some of the above-mentioned barriers. In a CRT, there would be dedicated sites for either TAU or IPC-A, meaning all people within a service would receive the same intervention, potentially avoiding staff’s ethical concerns about service users receiving different treatments within the same service. A CRT would also reduce the chance of contamination due to all those within a cluster being treated similarly. 59
Research assessments
The proposed outcome measures appeared to be acceptable to young people. Most measures, researcher-led and self-completed, were completed, and young people did not appear to find the measures to be a burden. One participant found the assessments beneficial as they enabled them to see how their mental health had improved since the start of the study. COVID-19 restrictions led to some complexity in completing measures, which was eventually overcome by incorporating new technological solutions such as video consent procedures.
Acceptability of the intervention
It was reported by a couple of participants that IPC-A focused too much on the positive aspects of their relationships. These young people stated that they would have preferred a greater focus on the more difficult elements and were able to understand these before moving on to positive aspects.
Some parents were not aware of the contents/discussions of the sessions. However, when one parent was included at the request of the young person, the parent had reported this as being helpful to be able to learn how to support the young person at home.
In interviews, IPC-A was acceptable to both young people and parents, with IPC-A being seen as offering positive benefits for young people. As reported in the process evaluation, young people reported being more open to family, socialising with friends and being able to engage in ordinary activities such as shopping. Parents also reported improvements in young people’s well-being after the second or third session.
As reported in the process evaluation, young people reported having a positive experience during sessions and felt that the structure and duration of the sessions were important for providing stability. They felt that the sessions provided a private space which allowed them to open up about the challenges they were facing. They felt that the developing of a positive relationship was an important factor in facilitating discussions, as well as being focused on the positive rather than negative aspects of their lives which helped contribute to the improvement of their symptoms and have a better outlook. Overall, IPC-A as an intervention appeared to be acceptable.
Quantitative analysis
This study was not powered to detect any significant changes in outcomes, and from the data collected there were no clinically significant differences between the two interventions. Half of the participants who were randomised to IPC-A and completed 23-week measures did not receive the intervention; therefore, this would have had an impact on this finding. The mean changes in the outcome measures suggest they are sensitive to change. Therefore, if the intervention was effective, this would be able to detect differences in a future trial.
Health economic analysis
The health economic measures appeared to perform well and were completed. The CHU-9D had a high rate of completion and showed a possible improvement over time. The responses were also spread over a majority of levels. This suggests that there is scope for the CHU-9D to detect differences over time and that there is scope for improvements in health to reflect in the CHU-9D. Similarly, for the CSRI, the majority of fields appeared to have been completed for most cases, showing reduced healthcare use over time. It should be noted, however, that most of the health care was not mental health-related. Due to the CSRI performing well, it would be a potential candidate for use in a future trial of ICALM; however, it would likely benefit from simplification. Owing to the very small number of individuals who had the IPC-A intervention, it was difficult to estimate what the likely cost of the intervention would be. Of particular interest would be turnover of staff. A very high turnover rate, as seen in this study, means that many staff are likely to need to be trained to provide intervention sessions, and much of the benefits of this training may be lost if staff move on to different roles.
Results of the process evaluation
The objectives of the process evaluation were primarily to provide a description of how IPC-A and TAU were delivered and observe how delivery is shaped by the context of differing service models. Few RCTs have been carried out in tier 1/2 mental health services, despite the need to develop evidence-based interventions. The process evaluation findings share some insights into key barriers to conducting research (in particular RCTs) in this setting, while highlighting the current challenges faced by the services in supporting young people experiencing mental health difficulties.
Workforce capacity building strategies and research culture
Workforce capacity challenges were a key recruitment barrier in the ICALM study, as the increased pressure at central referral points led to the prioritisation of urgent cases and consequently long waiting times for ‘green cases’ (e.g. low mood) and low referral rates into services delivering IPC-A. Process evaluation findings also indicate a lack of research culture and research capacity amongst the participating teams, which cannot be isolated from the high demand faced by the services. The findings indicate that some services did not view research as a priority, considering it as something ‘extra’ that could be left out to ease pressure as demand increased, particularly during the COVID-19 pandemic. The IPC-A training sessions and meetings with teams also unveiled a lack of familiarity with research processes, particularly randomisation by the teams, with some teams expressing reluctance to randomise young people.
The low participation in research, fuelled by the need to manage high demand and the lack of processes and frameworks for identifying and implementing evidence-based interventions in this setting, means there is a lack of evidence-based guidance with respect to what should be offered to whom, resulting in local interpretations of best practice. This is especially true for clinical presentations such as low mood, whereby various interventions (e.g. family interventions, behavioural activation, counselling or I-PCA) might equally be used to treat a clinical presentation. This narrow approach of intervention provision which develops naturalistically within this context poses a challenge for local commissioners to establish processes and frameworks for identifying and implementing evidence-based interventions. Such an approach was also to allow individual services to decide whom they treat and how in isolation as demand increased and overwhelmed them. This meant that clarity of who should get what treatment was further disrupted.
There is, therefore, a requirement to develop effective unifying workforce capacity-building strategies, considering areas of greatest need and the professional requirements, training and supervision which will address these needs. To ensure continuity of service, there is also a requirement to develop and implement workforce retention strategies that could incentivise staff to remain in specific posts. As part of wider workforce capacity-building strategy, developing a culture which recognises the value of developing, evaluating and implementing evidence-based interventions will facilitate future research. More practically, teams could be introduced to research processes gradually, through training to increase understanding of specific processes such as randomisation and by initially involving them with lower-level research, for example, single-arm pilot studies, before and after studies, before exposing teams to large RCTs. There is also a need for commissioners and service leads to develop a framework for identifying and delivering evidence-based interventions that could be incorporated within service models, workforce development and supervision. Building such a research culture and incorporating appropriate frameworks may increase success of recruitment and implementation of RCTs in this setting.
Training and review of core service offers
The ICALM study sought to train teams of young people’s workers to deliver IPC-A within tier 1/2 services. While these workers might support CYP with mental health presentations, they do not typically deliver specific mental health interventions. This task-shifting approach, which has had successes in the primary healthcare setting, was met with several barriers in the ICALM study.
Firstly, due to the lack of mental health training, prior experience and confidence in supporting young people with mental health challenges, Early Help teams struggled to identify suitable young people for IPC-A, assessing most referrals with mental health difficulties to be too complex for their service. The lack of system integration in referral pathways, the variations in frameworks and measures used to assess eligibility of cases and the subjectivity of some aspects of the assessment process meant that some cases may have been classed as too complex by one team and eligible by another. Secondly, interviews with Early Help team managers indicated that despite seeing a large proportion of young people with mental health challenges, the teams did not perceive mental health to be part of their core offer. Thirdly, some Early Help teams did not have a standard intervention for low mood, despite the Early Help threshold matrix indicating that CYP displaying signs of deteriorating mental health and episodes (e.g. low mood/mild depression) should be classed as level 2 and are suitable for Early Help or targeted support services. It was anticipated that IPC-A would be a solution to this, in part because of the relational nature of the therapeutic focus. This posed some challenges with respect to setting up the two trial arms in each service, as young people randomised to TAU were being referred to targeted services (also involved in the trial). Consequently, the additional pressure on targeted services to support young people being referred in from multiple routes, including Early Help teams, posed capacity challenges, which resulted in services having to collaborate to either deliver IPC-A or TAU.
Therefore, if Early Help teams are to be involved in supporting young people experiencing mental health challenges, there needs to be an explicit remit to do so. Early Help practitioners also need adequate mental health training/support to help them identify suitable cases at the triage/assessment stage and to enable them to deliver mental health support for CYP experiencing mild to moderate mental health challenges. Equipping Early Help teams to support young people with mental health challenges has a potential to reduce the capacity pressures currently faced by tier 2 mental health services and to prevent young people from being passed around the system, allowing them to build trusting relationships with one service. Arguably, there is a larger piece of work that is needed to map out the core service offers across the tier 1/2 services, including interventions being delivered to support young people experiencing mental health challenges in order to identify gaps in service provision and capacity to support young people with mental health difficulties. This mapping exercise could then guide both commissioners and researchers in identifying and developing new evidence-based interventions that align with core service offers.
The disconnect between policy and practice
The process evaluation findings highlighted a clear disconnect between mental health policy and transformation models and what happens on the ground with practitioners. The current challenges faced by the central referral point, including poor completion of referral forms from front-line services, a lack of knowledge of front-line staff (e.g. GPs and school staff) with regard to mental health treatment pathways and long waiting times, resonate with the 2020 ‘No wrong door’ report, which highlighted how CYP need to navigate through a very complex system and end up either on a waiting list or falling through gaps where there are no services to meet their needs. The experiences captured through the ICALM study indicate a poor implementation of the core recommendation of this report, which was the need for services to wrap around families and provide support wherever young people present, that is school, general practice. It should be noted that this was during the time and aftermath of the COVID-19 pandemic, which significantly increased demand for all services. There is therefore a need to support front-line services, where young people are presenting with mental health difficulties, especially schools and general practices, to ensure that young people receive interventions at the earliest stage or are supported through the mental health system until they receive the support they need. The transformation plan, which is currently underway, is one way of supporting front-line staff in managing under-18s presenting in general practice with mental health difficulties. To ensure successful implementation of the transformation plan, link workers need to be provided with adequate support, training (especially safeguarding) and supervision to work with under 18s. The successful implementation of the transformation plan could reduce backlogs at central referral points and ensure that CYP receive timely help. Link workers could help increase research capacity by providing much-needed access for recruitment of young people into research investigating evidence-based mental health interventions.
Finally, the increased demand for mental health services and the perception of mental health services providing gold-standard interventions suggest that greater effort is required to promote the philosophy of mental health as ‘everyone’s business’. Establishing a common language with regard to mental health difficulties and educating society with regard to their role in supporting positive mental health is therefore crucial in managing some of the current challenges faced by the services. Such education could, for example, focus on the key components of the Thrive model,60 which is a public health approach to promoting good mental and emotional well-being by supporting and educating schools, communities and parents on the key elements of mental health, the importance of self-care, how to build support within families and communities and when to seek help. More investment in prevention work as part of curriculum is needed by including well-being, resilience, managing emotions and developing healthy relationships. The process evaluation also highlights the need to ensure that acceptance criteria and thresholds for treatment are joined up across the system to ensure easy navigation by young people and families and that there is flow to the most suitable service for the right intervention at the right time.
Implementation and theoretical fidelity discussion
| Main theme | Example data extracts |
|---|---|
| Engagement from young people as crucial for successful, collaborative intervention |
|
The IPC-A intervention was acceptable to young people, parents and therapists. However, due to the challenges faced in implementing the study, not all stakeholders felt that the intervention was suitable for Early Help services. The process evaluation findings indicated that evidence-based interventions such as IPC-A can be successfully implemented in tier 1/2 settings, although these services are often overwhelmed with ‘new things to do’ meaning that they struggle to have the capacity to implement new interventions systematically. However, in some cases, there appeared to be a tension between delivery of IPC-A according to its structure and engaging with the young person’s needs and desired outcomes, highlighting a tension between implementation fidelity and theoretical fidelity. Observations of the IPC-A intervention recordings suggest that to meet the aims of IPC-A, practitioners should orientate closely to young person’s needs and perspectives, as a focus on correct delivery alone may not always lead to desired outcomes. Such an approach needs practitioners to be flexible and confident to use IPC-A manual/training as a guide rather than a box-ticking exercise, although if delivered regularly as part of routine care, this confidence should develop. To achieve this level of flexibility and confidence requires long-term investment, ongoing supervision and support of the teams. It is worth noting that despite enthusiasm from services to implement new or research interventions, often services are overwhelmed with the additional tasks these involve and do not always have the capacity to be able to support the implementation of them.
The engagement of young people and collaborating with the practitioner are crucial for achieving desired outcomes from IPC-A. Such engagement and collaboration can be facilitated by the practitioner’s use of terms that the young person is comfortable with, an ability to relate to and empathise with the young person’s experiences and adapting activities to suit the young person’s experiences and abilities. Practitioners need to show they are on the young person’s side by acknowledging the young person’s disclosures and acting as an advocate when needed.
Progression criteria
Below we summarise our findings in relation to the criteria set out at the beginning of the study to inform a future trial of the effectiveness and cost effectiveness of the intervention (IPC-A) (Table 21).
| Sub-themes | Example data extracts | Conversational analysis |
|---|---|---|
| The importance of feeling heard |
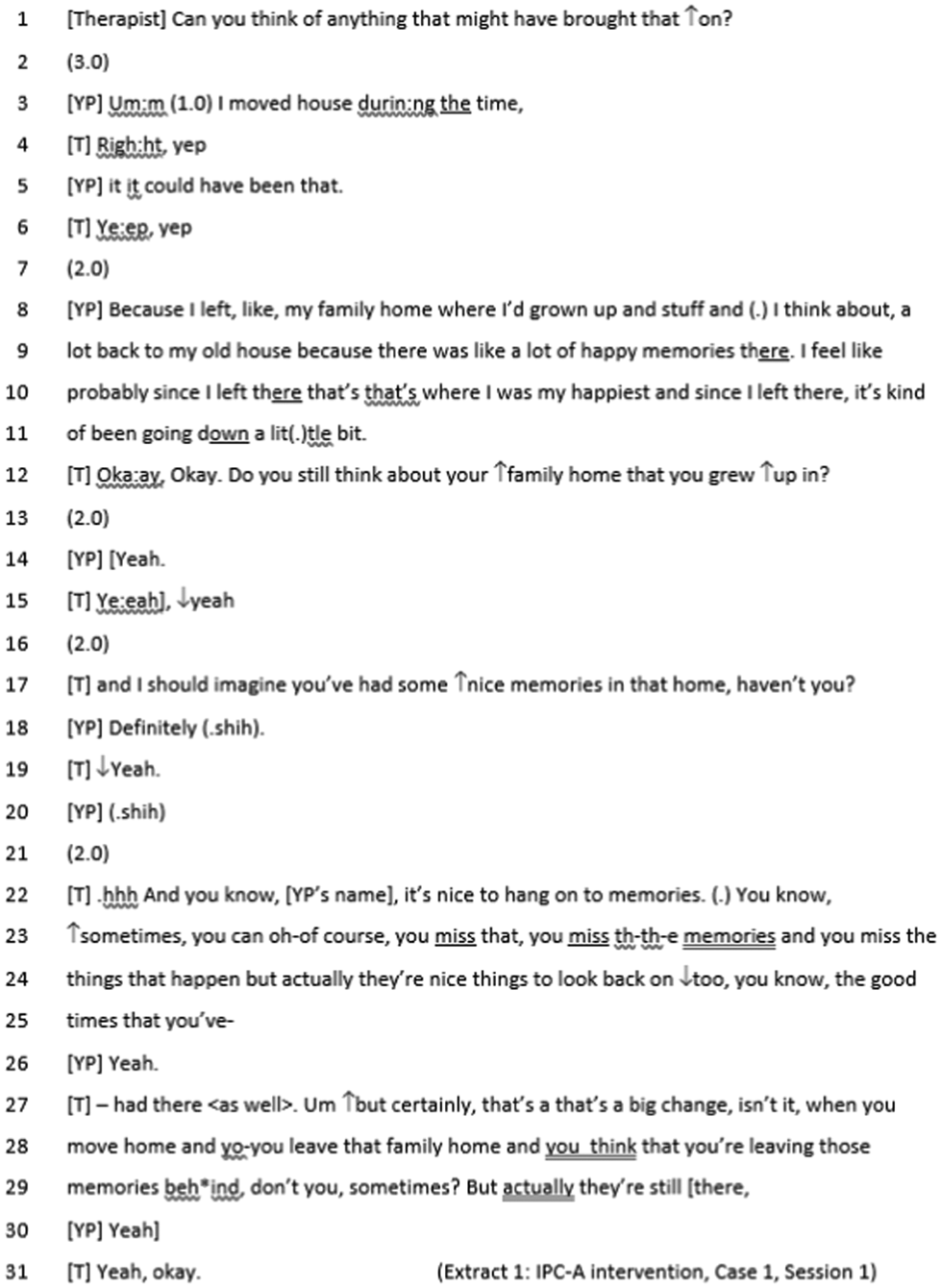
|
Within this extract, the therapist uses both directive and non-directive questions to elicit information from the young person and to emphasise their understanding of what the young person is feeling while sharing this information. Towards the end of each directive question, the therapist can be seen to increase their pitch, which seems to suggest ‘answer if you can’, rather than assuming the young person will be able to answer the question. This approach seems to reassure to the young person who is comfortable answering the question in detail and actively participating in the collaborative search for triggers to their symptoms. After disclosing what they feel might be triggering their symptoms, the young person becomes quieter and more passive, which is responded to with reassurance and acknowledgement from the therapist. Affirmative responses from the young person in response to this reassurance suggests these attempts at reassurance are successful. A non-directive question (‘I should imagine you’ve had some nice memories in that house, haven’t you?’) is asked by the therapist, which appears to aim to give the young person space to share more if they would like or simply spend time on thinking about these memories, rather than seeking information – again without pressure for the young person to answer in a particular way. Whilst the young person’s response does not expand on these memories, they signal a clear message to the therapist that they have understood the young people ‘Definitely (.shih)’. Having established a shared understanding, this approach arguably provides a space for the therapist to offer their own perspective and proposal that a ‘big change’ will be the key problem area. Encouraging the young person to continue to actively participate within the session, by showing that any disclosures they make will be met with acknowledgement, reassurance, and indicating that they have been heard and understood by their therapist enacts the intended implementation of IPC-A, in which part of the therapist’s role is to be positive, encouraging, active, non-judgemental and on the young person’s side |
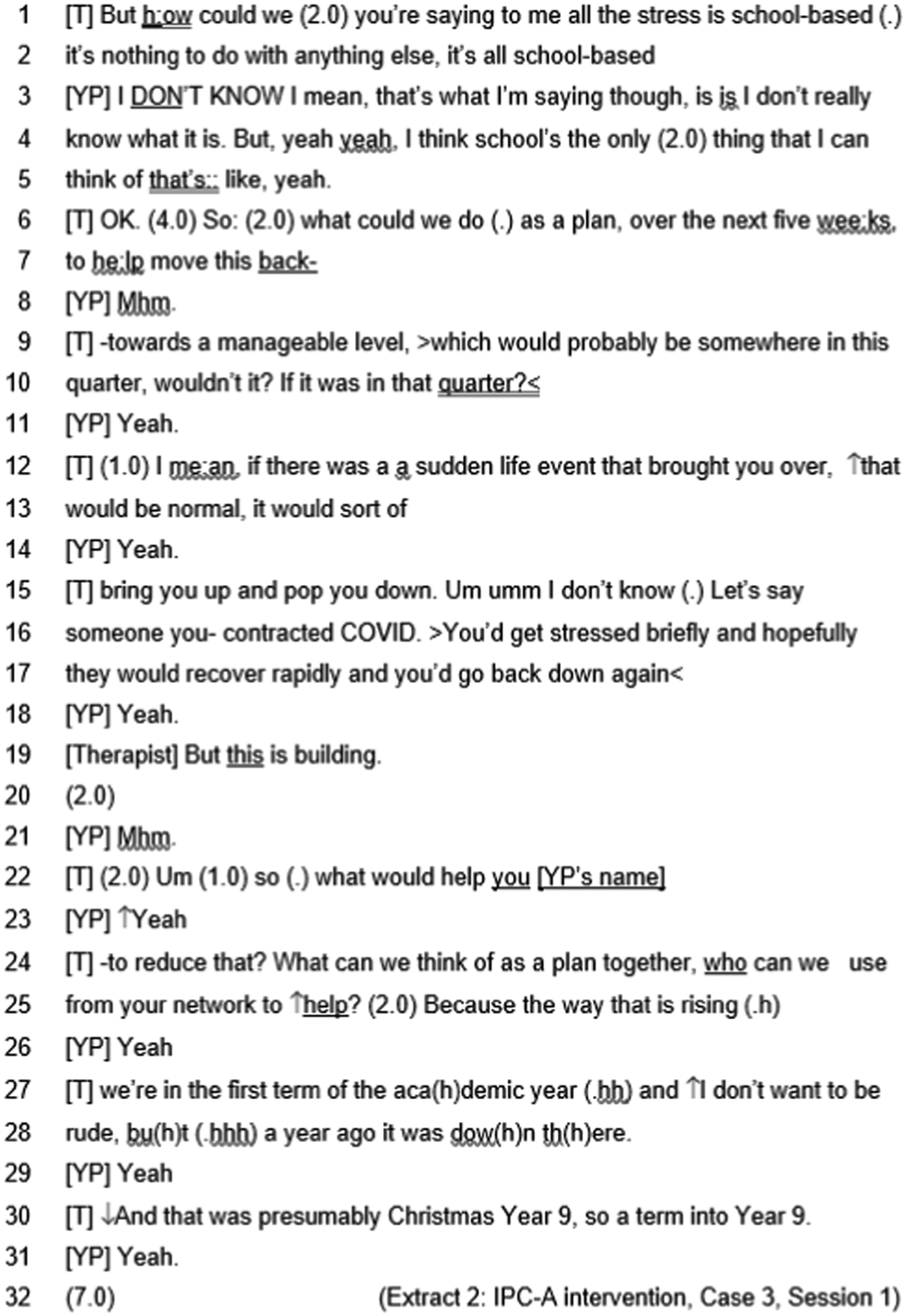
|
In this extract, the therapist and young person are trying to understand what may be causing the young person’s symptoms. The young person repeatedly says that they are unsure of what the cause may be. The young person’s tone appears to shift to illustrate this frustration at having to explain themselves again and the sense of feeling unheard is reinforced by their expression, ‘that’s what I’m saying though’ (line 3). As a culmination of this final disclosure by the young person and not receiving the response they need from the therapist, the young person’s responses illustrate a shift to a form of passive participation, offering one-word responses to show they are listening but not actively engaging with what is being said. In response to this passivity, the therapist attempts to ask direct questions to help the young person re-engage, however these questions fail to acknowledge the uncertainty that the young person has already expressed. Here the young person’s passive participation appears to stem from not knowing how to engage with the task, as expressed by the young person, or resistance to the therapists’ position and approach | |
| Either way, the lack of engagement from the young person appears to be interpreted by the therapist as active resistance, which seems to lead to greater hesitance from the therapist – as shown by their pauses and awkward laughter while trying to emphasize the importance of finding strategies that will help the young person’s symptoms. Towards the end of the extract, the therapist can be seen to try a more collaborative approach, describing making a plan together rather than aiming direct questions for the young person to answer alone. This approach may be undermined by their previous questions which focus on the young person knowing what their triggers are, putting the onus on the young person to know the answer. As a result, this attempt at collaboration is still met with passive resistance, and a long pause before the therapist goes to speak again. This use of direct questions for the young person to answer alone goes against a key component of IPC-A by removing the collaborative element of therapist and young person working together to understand the young person’s triggers. The resulting response highlights the centrality of the young person feeling heard as a mechanism for enabling their active engagement, and the potential for effective and supportive delivery of IPC-A | ||
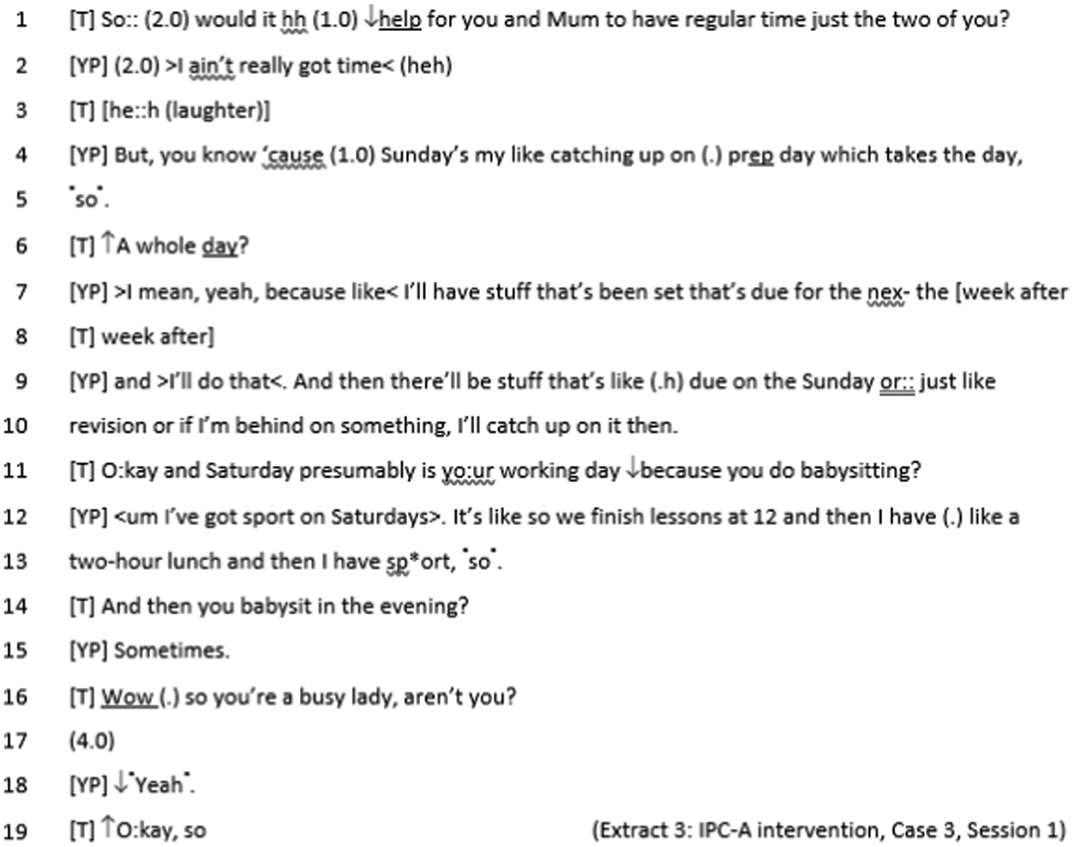
|
By pausing and changing their tone, the therapist appears hesitant in asking the initial question, perhaps in expectation of the young person’s reaction to it. The therapist seems to use this question to test whether the young person’s relationship with their mum is a viable area of exploration in their sessions. The young person’s response gives a clear indication that they have no desire to focus on this area. After a pause, the young person is quick to disclose that they do not have time, followed by laughter which seems to indicate an awareness of how their statement may be perceived as dismissive. This laughter is then shared by the therapist, acknowledging this awareness. Alternatively, the young person’s laughter may be trying to indicate that the therapist has no appreciation of how unrealistic their suggestion was. The young person follows up with a justification of why they cannot, rather than because they do not want to. This is met with a response of disbelief from the therapist, whose questions appear to attempt to find a time when the young person is free, despite the young person expressing that they are not. The young person responds by actively resisting these attempts by the therapist to further describe why they do not have enough time. In these resistant responses, the young person replies very quickly before slowing down to make their point, ‘>I mean, yeah, because like < I’ll have stuff that’s been set that’s due’ (line 8). This speed to respond, suggests the young person is responding reactively, perhaps feeling the need to defend their view, which may explain their active resistance rather than deferring to the therapists’ view. The therapist finally concedes the point by stating that the young person is a ‘busy lady’. Based on their tone and previous discussions with the YP, this seems an attempt at being light-hearted – however, the young person’s response suggests it was not taken in this manner | |
| Orienting discussions to a young person’s perspective |
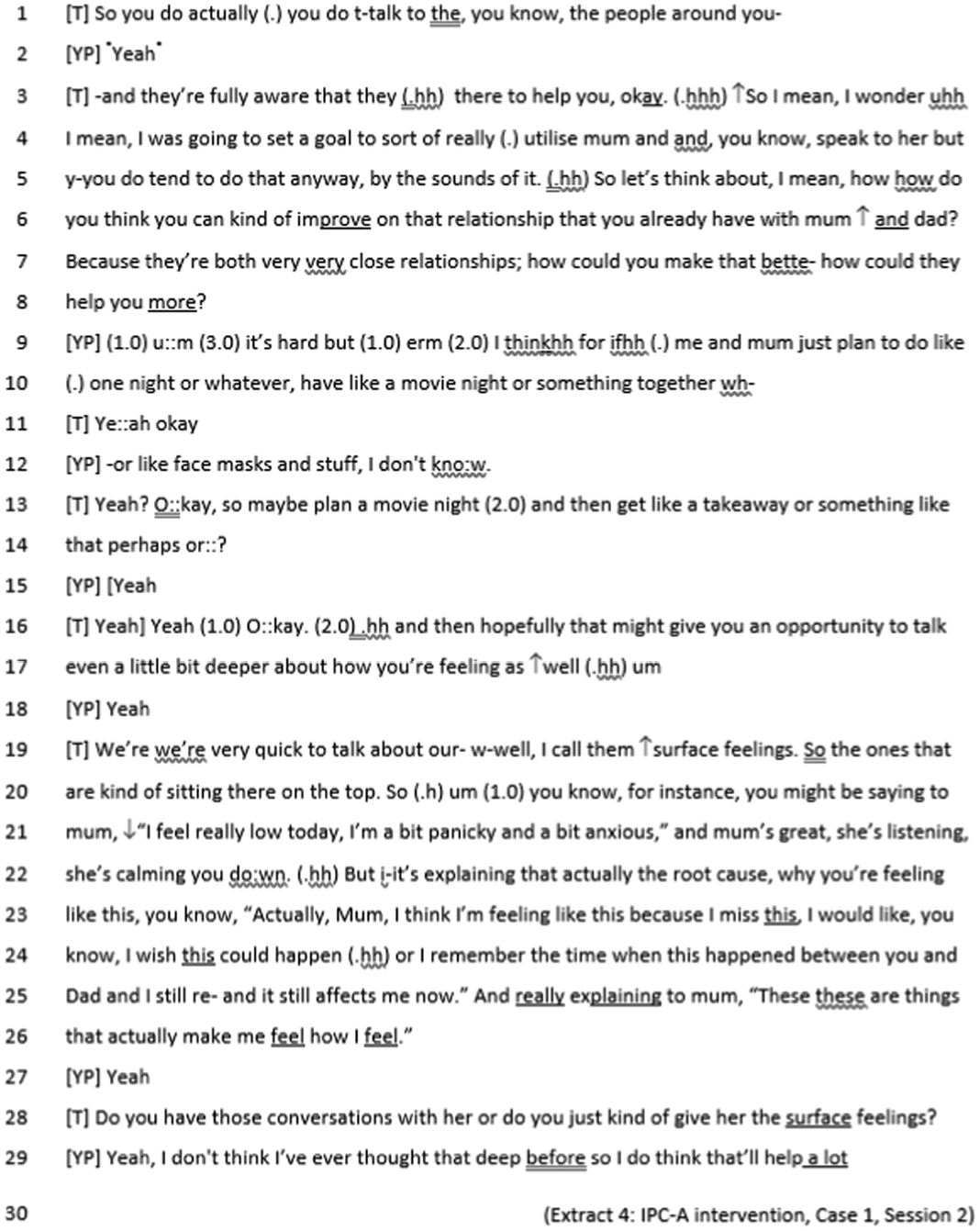
|
In this extract the therapist can be seen to reframe the discussion to reflect the young person’s perspective of their relationship with their mum, ‘because they’re both very very close relationships; how could you make that better, how could they help you more?’ (line 7–9). In doing so, the therapist shows that they are listening to the young person and acknowledges their point of view. This is reinforced in their delivery by putting emphasis on improving the relationship with both mum and dad and getting more help where support already exists. When asking how the young person can feel more supported the therapist can be seen to correct themselves and reframe the question they are trying to ask. In this reframing, they appear to take the onus away from the young person and what they can do alone and back onto the interpersonal relationships and how they can feel supported. This reinforces the theoretical aims of the IPC-A intervention by drawing focus back to how interpersonal relationships can be utilised to help to support the young person |
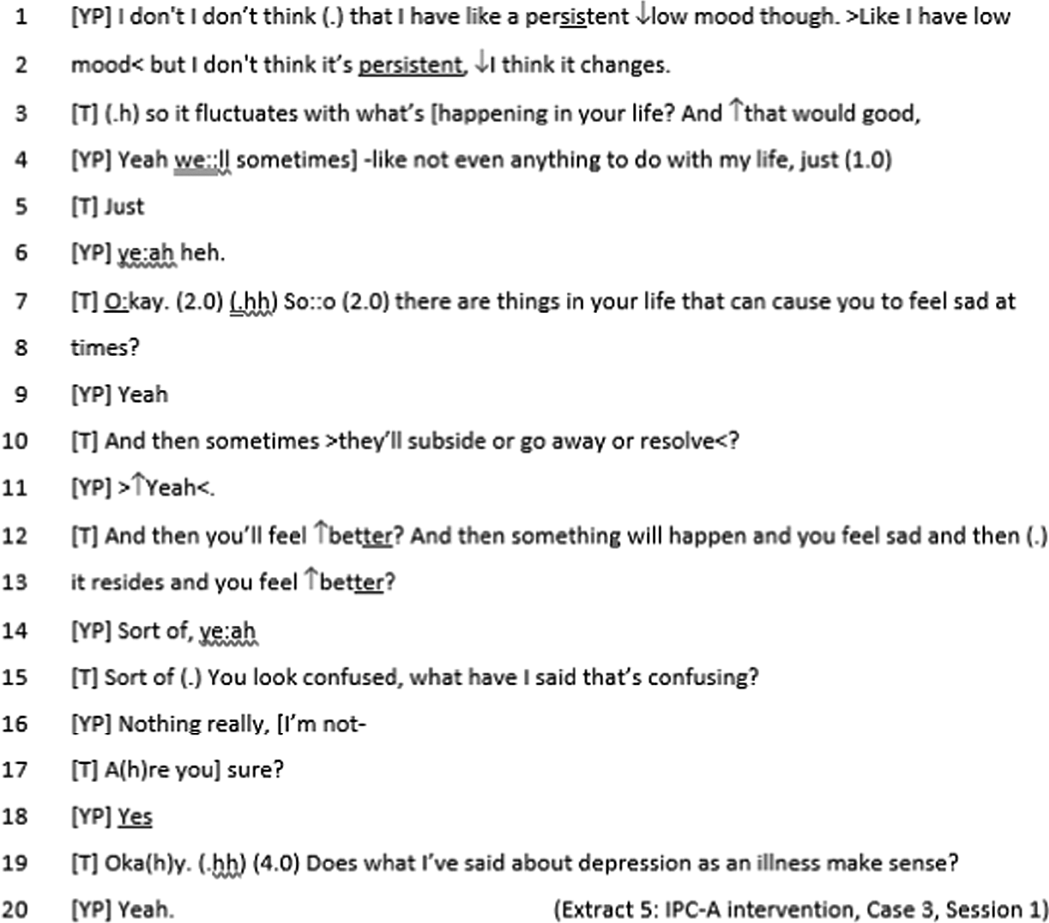
|
The young person can be seen to put emphasis on the aspects of depressive symptoms which do not feel relevant, in this case the persistence of low mood. In response to the young person’s perspective on depressive symptoms, the therapist asks questions aimed at understanding what the young person is feeling, and what may trigger their fluctuations in mood. Throughout the interaction the passivity of the young person’s responses suggests the therapist’s interpretation of what the young person is feeling does not match what the young person is trying to get across. The young person is unable to articulate an alternative suggestion and so unable to actively participate. This potential frustration at being unable to articulate their thoughts may be reflected in the young person’s face and misinterpreted as confusion by the therapist. Unable to resolve this potential misunderstanding or actively engage the young person, the therapist returns to discussing depression despite the young person’s perspective that they do not relate to this term. The young person then appears to defer to the therapist’s approach, acknowledging they understand but without affirming the therapist’s perspective of their symptoms | |
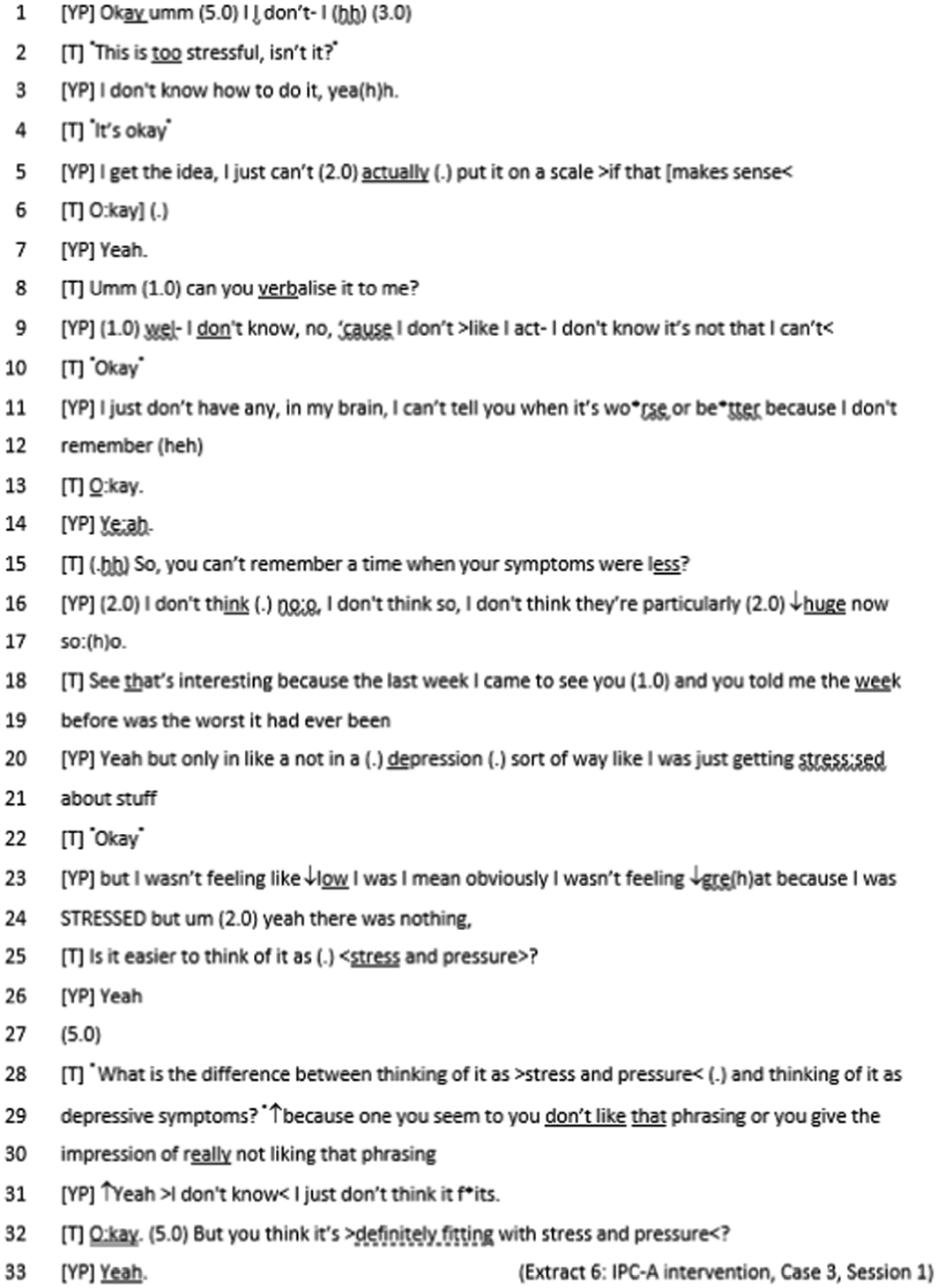
|
In this interaction, the therapist notices the young person’s difficulty in engaging with the task set (start a timeline to track symptoms). This perception is met with openness from the young person who again tries to describe what they are finding difficult – which appears difficult in itself and requires pause. The young person’s pace quickens when they feel uncertain or unable to explain. In response to this uncertainty, the therapist replies quietly and gives the young person the space to explore why they are finding the task difficult. By giving the young person space to talk about their thoughts, the key term ‘stress’ is discovered and leads to collaboration between therapist and young person to renegotiate the terms they use – away from ‘depression’ to ‘stress and pressure’. This renegotiation/reframing of the discussion is a turning point for this session which enables active participation from the young person | |
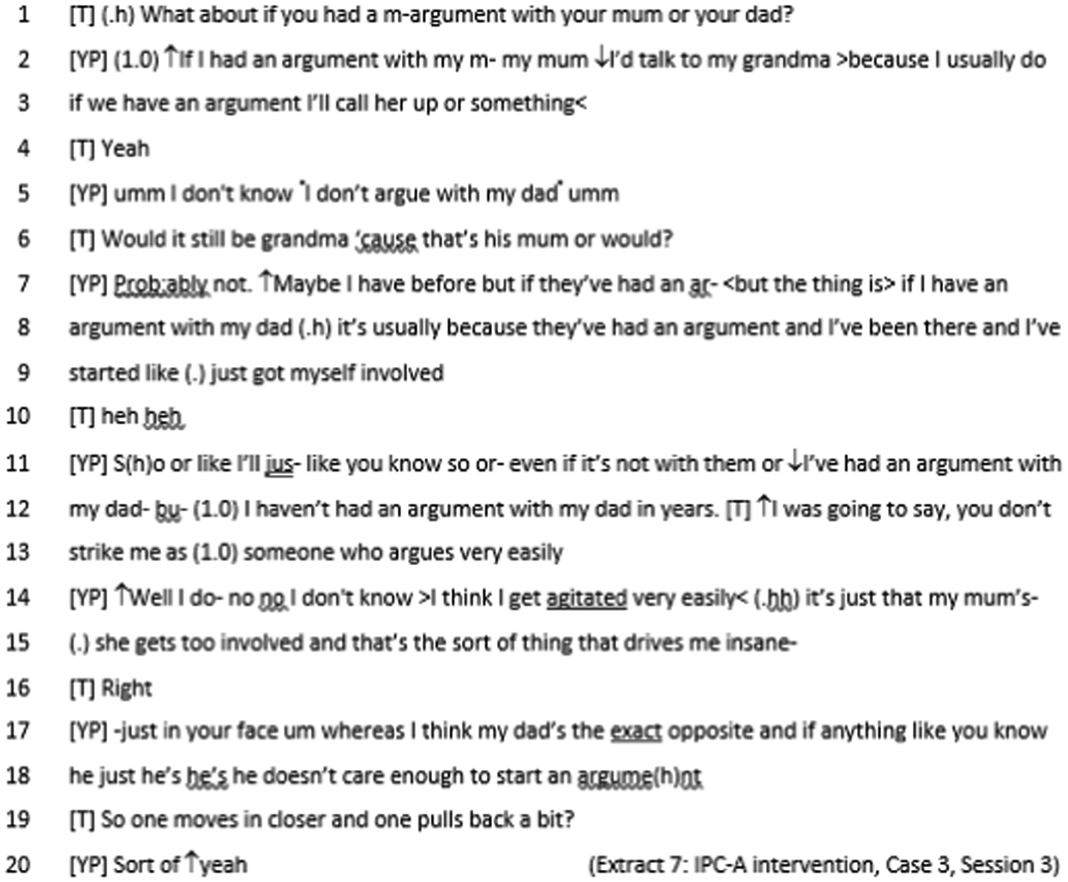
|
In comparison to previous extracts from this pair, active participation is seen in the back and forth of responses between therapist and young person, with fewer pauses and one-word responses. Using specific scenarios may help the young person to engage with the task by allowing them to relate to what is being asked – utilising their perspective to foster engagement. This again requires flexibility from the therapist to adjust questions to the young person’s perspective | |
| This development in interactional style between the pair is further illustrated by the final exchange of this extract. The therapist shares their interpretation of the young person’s parents’ dynamic when arguing and the young person’s response affirms this interpretation as illustrated by the increase in pitch from the young person’s response, ‘Sort of -yeah’ (line 24). The increased level of detail shared by the young person appears to improve the accuracy of the therapists’ interpretations. In contextualising questions to the young person’s experiences, the young person can actively engage and share more information, which the therapist can then use to better understand the young person’s perspective, and further encourage their active participation | ||
| Reliability of interpersonal relationships: mini goals and advocacy |
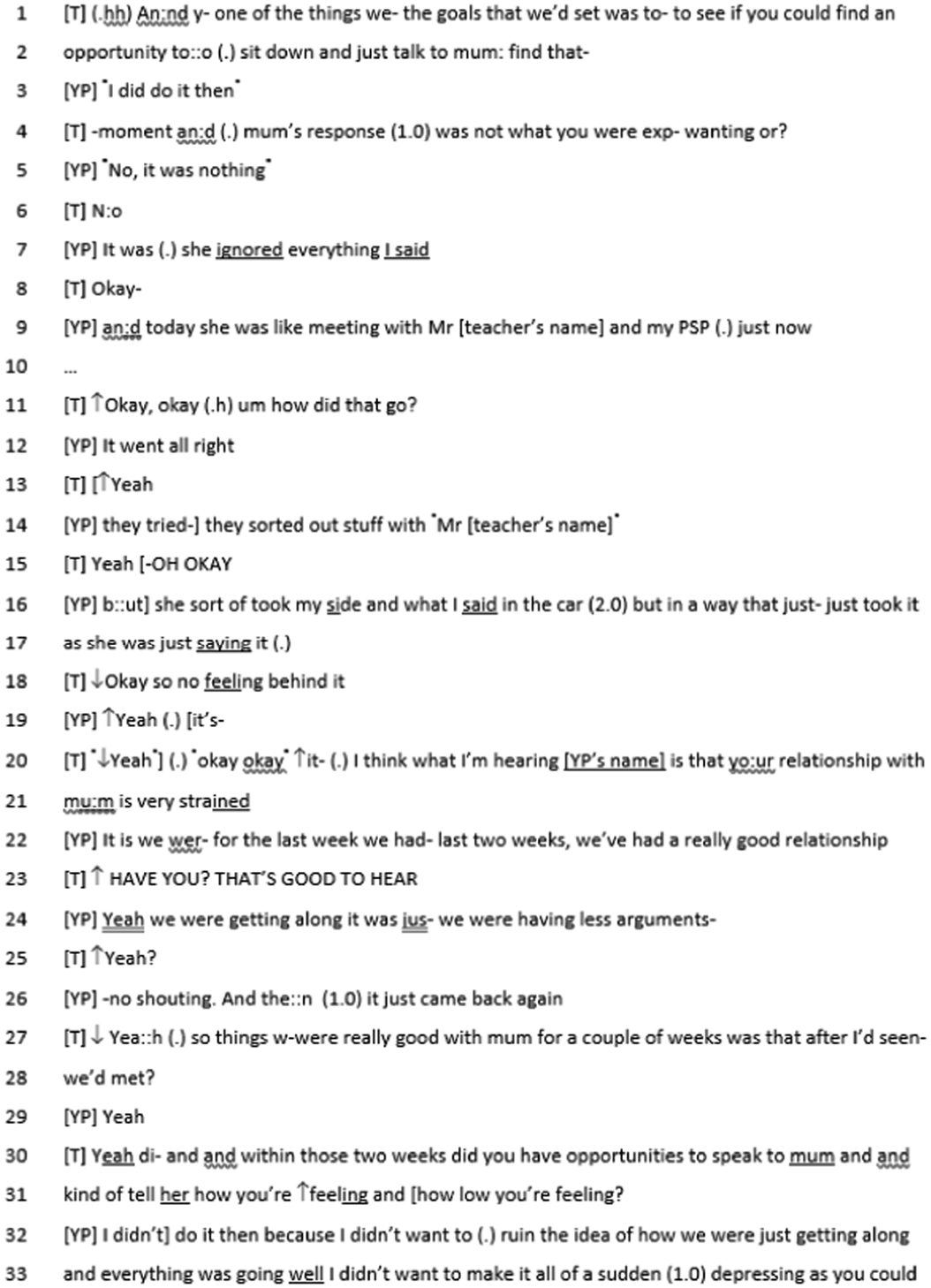
|
Throughout the young person’s explanation of how their mini goal went, and the response received, the therapist reacts and modulates their tone to express their understanding of what the young person is saying – higher pitch for positives, and lower pitch for negatives |
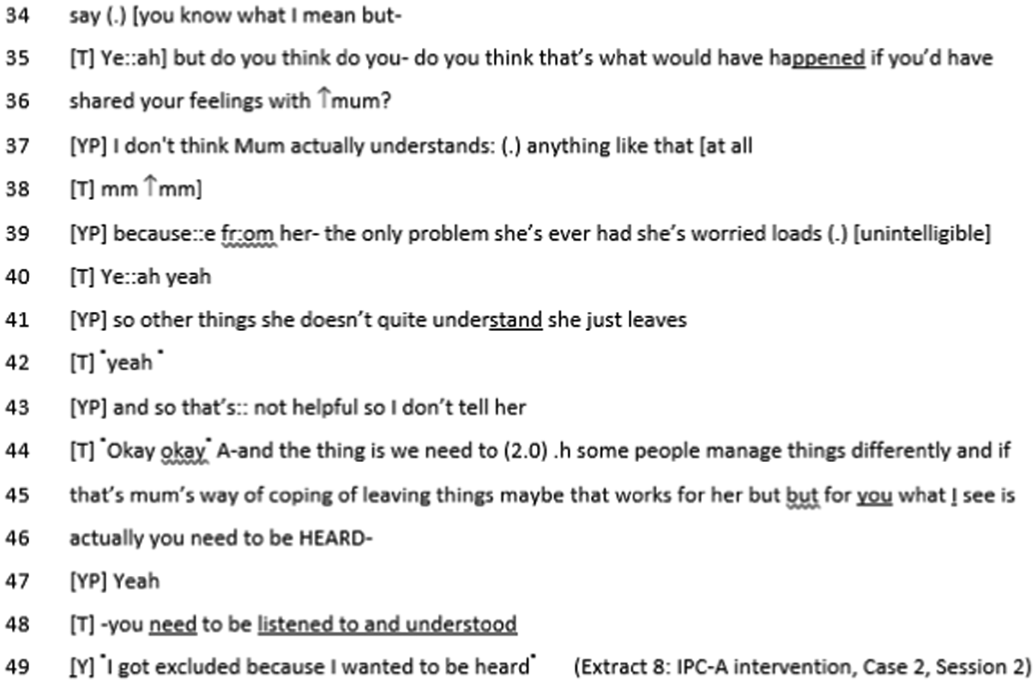
|
The therapist can also be seen to not only listen and respond to the young person, but to also encourage their consideration of others’ perspectives. This consideration is a key theoretical focus of the agreed problem area worked on in Case 2, ‘relationship disputes’. Importantly, the therapist remains non-judgemental while discussing different people’s needs and expectations from relationships but remaining the young person’s advocate, ‘but for you, what I see is actually you need to be heard’ (line 49). In this extract, the therapist’s interpretation of the young person’s needs strikes a particular chord with the young person and leads to a significant disclosure about suicidal thoughts. This response from the young person further emphasises the importance of feeling heard and understood in facilitating young people’s engagement with IPC-A sessions and difficult issues which need to be addressed to enact change for the young people | |
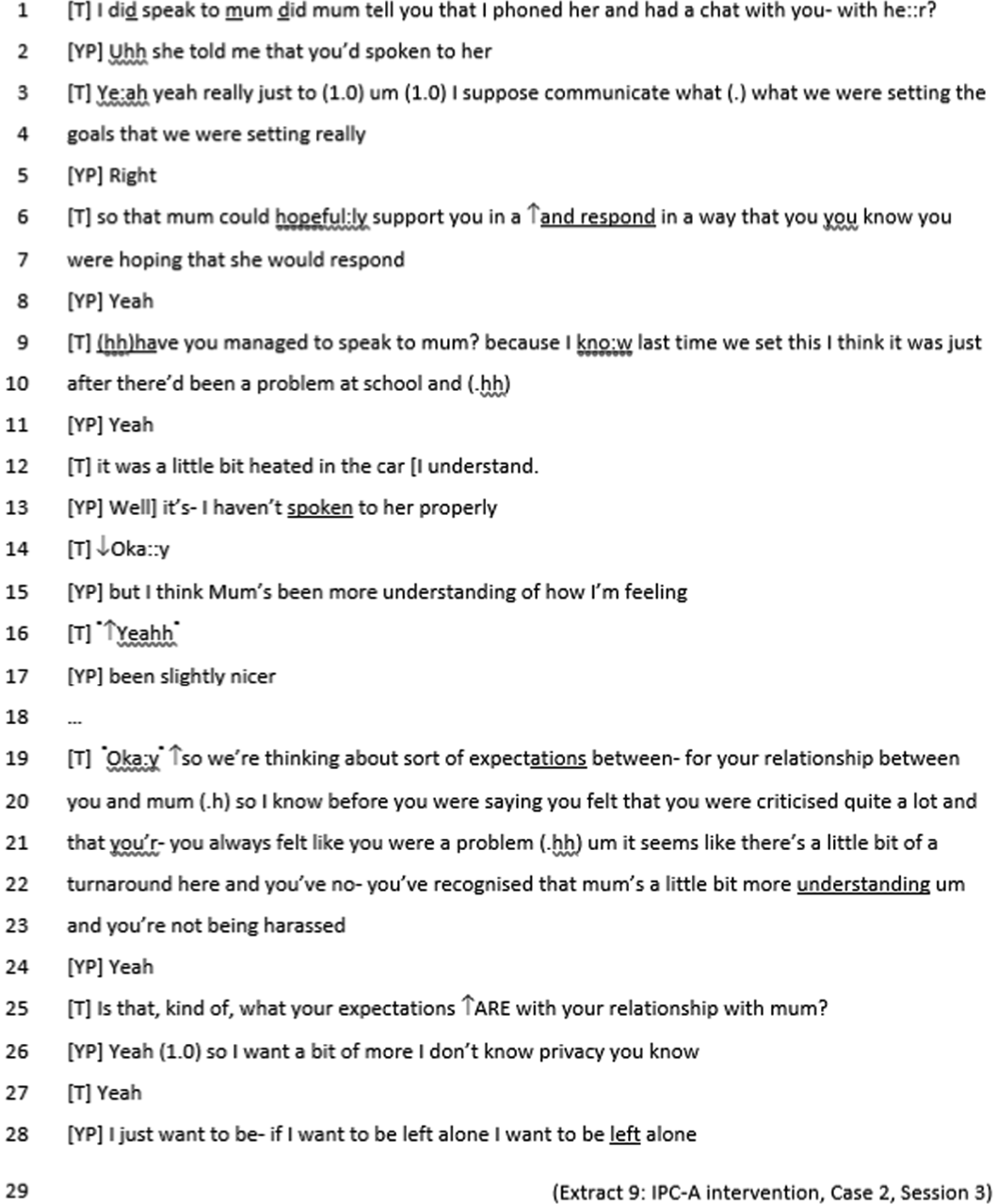
|
This extract highlights the positive impact that having the therapist act as an advocate for the young person can have. The young person’s responses suggest that since having spoken to the therapist, their mother has made changes in the way they respond to the young person. However, the young person also discloses that they have not had a proper discussion with their mother. This suggests that outside of the sessions, the young person may not be fully engaging in or able to enact mini goals. The therapist then focuses the discussion on the young person’s expectations of how they would like their relationship with their mother to be. This may work to focus their sessions to consider what the young person’s desired resolution for this relationship dispute is. This may also allow the therapist to re-orient the discussion to consider what the young person and therapist can work on together, or what mini goals are achievable, to reach this ultimate goal |
| (.) | Just noticeable pause | |
|---|---|---|
| (0.3), (2.6) | Examples of timed pauses | |
| ↑word,↓word | Onset of noticeable pitch rise or fall (can be difficult to use reliably) | |
| A: B: |
word [word [word |
Square brackets aligned across adjacent lines denote the start of overlapping talk. Some transcribers also use ‘]’ brackets to show where the overlap stops |
| .hh, hh | in-breath (note the preceding full stop) and out-breath respectively | |
| wo(h)rd | (h) is a try at showing that the word has ‘laughter’ bubbling within it | |
| wor- | A dash shows a sharp cut-off | |
| wo:rd | Colons show that the speaker has stretched the preceding sound | |
| (words) | A guess at what might have been said if unclear | |
| () | Unclear talk. Some transcribers like to represent each syllable of unclear talk with a dash | |
| A: B: |
word= =word |
The equals sign shows that there is no discernible pause between two speakers’ turns or, if put between two sounds within a single speaker’s turn, shows that they run together |
| word, WORD | Underlined sounds are louder, capitals louder still | |
| ºwordº | Material between ‘degree signs’ is quiet | |
| >word word< <word word> | Inwards arrows show faster speech, outward slower | |
| → | Analyst’s signal of a significant line | |
| ((sniff)) | Transcriber’s effort at representing something hard, or impossible, to write phonetically |
-
Recruitment rate is at least 80% of target.
Recruitment was impacted from the beginning of the study due to COVID-19, with the study being suspended on 18 March 2020. Following the restart of the study in July 2020, meeting the target sample size within the recruitment period required a recruitment rate of five participants per month. To reach 80% of the target, a recruitment rate of four per month would have been sufficient. The recruitment period was extended to 18 months to allow for the additional referral pathways to take effect, which altered the 80% recruitment rate to 2.7. Following the end of the recruitment period, the final recruitment rate was 0.8 per month.
-
At least 70% of those randomised to receive the intervention attend at least three therapy sessions within the 10-week treatment window.
Of the six participants randomised to the IPC-A arm who had come to the end of the 10-week treatment window, three (50%) attended three or more treatment sessions.
-
Follow-up assessments are completed by at least 80% of participants at 10 weeks and 70% of participants at 23 weeks.
Of the 12 participants who had reached the 10-week follow-up, 12 (100%) were followed up at 10 weeks and 23 weeks. All of these visits were conducted remotely with the participants.
-
At least 80% of IPC treatment sessions reviewed meet treatment fidelity criteria.
From the four recordings reviewed, clear systematic use of the principles of IPC-A was identified; therefore 100% of these sessions met the treatment fidelity criteria.
-
Contamination of the control arm can be sufficiently limited for individual randomisation to be justified.
Although there were fewer recordings rated due to lower than anticipated recruitment, there was no evidence of contamination effects from IPC-A training for TAU therapists for the recordings that were provided.
-
The mean RCADS depression scores of the IPC-A and TAU groups at 10 weeks are indicative of a clinically significant difference in depression (3 points).
Of the 12 participants (6 randomised to IPC-A and 6 randomised to TAU) who completed the RCADS depression score at 10 weeks, there was no clinically significant difference between the two interventions. The estimated treatment effect was 1.14 points with a p-value of 0.699. Three of the participants who were randomised to IPC-A did not receive the intervention as intended, which may have had a bearing on this result.
Patient and public involvement
This section is adapted from Abotsie et al. (2020). Interpersonal counselling for adolescent depression delivered by youth mental health workers without core professional training: a feasibility randomised controlled trial study protocol. Pilot Feasibility Stud. https://doi.org/10.1186/s40814-020-00733-8 and is licensed under CC-BY-4.0. 1
This study has been informed by two PPI events attended by 14 young people, most with personal experience of accessing mental health services. The first event was held at a local school, and the second was with members of Suffolk Children and Young People, Action and Transformation (CAT) group. The young people consulted stressed the inadequacy of current mental health provision for young people and supported the idea of extending access to treatment by training existing staff working with young people to deliver IPC-A. They highlighted that knowing workers have appropriate training is important to building trust and that they would prefer to be treated somewhere familiar to them rather than attend a specialist clinic.
A Youth Advisory Group was formed for this study, made up of three to five young people with personal experience of low mood. This group was facilitated by the dedicated PPI lead co-applicant for the trial.
Before the trial commenced, one young person who had received IPC in the first trial also spoke on a Google Hangout (www.youtube.com/watch?v=Q5rTpX8Ko1s&t=2436s) with a colleague in the USA about their experience. This experience was an invaluable part of the decision to do a wider trial.
The advisory group have contributed to the key decisions regarding the conduct of the trial such as helping the study to identify the appropriate wordings and phrases to explain randomisation to young people in the participant information sheets. Further valuable advice was provided when the study team were considering the possibility of moving the face-to-face IPC-A intervention to telephone/video calls during the national social distancing policy for COVID-19. The concerns raised by young people helped the TSC to recommend a costed suspension of the ICALM study during the COVID-19 crisis.
One of the barriers to engagement of PPI was the pandemic. The group that had originally been formed were made up of young people in years 9/10/11, due to the trial having to be extended this meant that that the priorities for the group had changed. For example, some members began studying for their General Certificate of Secondary Education (GCSE) exams or had already moved on to college and therefore moved on to other priorities.
We originally only had one member of the group who had received IPC-A as a therapy due to the low numbers of young people who had received the therapy.
Although the young people within the steering group were able to use their lived experience around mental health support in general, they declined the offer to join the main steering group meetings as they did not feel the information would be relevant to them. They preferred to be presented with a specific set of questions that they could relate to.
Equality, diversity and inclusion
The study population, although targeted towards individuals between 12 and 18 with low mood, did not have a diverse range of participants, with the majority being white British. Although finding individuals with low mood reflects the target population, the results cannot be generalised. One reason for this is that the referrals all come from a central referring point where people self-refer, and the research team is dependent on services for referrals. For a future study, it will be important to consider how to improve inclusion, whether by joining equality, diversity and inclusion groups to discuss inclusion in a RCT or by considering sites with a more diverse population. It will also be important to consider different referral pathways other than self-referral, as this can be known to be biased towards white British individuals. 61
In the case of potential participants who may have difficulty with the English language, information sheets and other materials would have been translated into the preferred language of the potential participants where practically possible. In the case of potential participants with sensory impairment or mild learning disability, information sheets and other materials would be converted into the preferred format (e.g. large print, audio-recording, Easy Read) where practically possible. Where interpretation is necessary for informed consent or other aspects of the study, trained and accredited interpreters would have been used wherever possible. In terms of the research team, characteristics other than age and profession were not included in the study. The research team consisted of a range of professionals from Clinical Psychologist, Psychiatrist, Counselling Psychologist, Research Associates, Head of Children and Young people’s involvement, Research Fellow, Professors of Clinical psychology and of Medical Statistics, Research Assistant Psychologists and a Co-production and engagement lead contributing to a mix of different disciplines at different experience levels.
Ethical considerations
Within the study, ethical considerations were thought about at study design, such as IPC-A having not yet been formally trialled and therefore may not be effective in non-specialist services. It was discussed that it was acceptable for TAU to be given in this study due to no evidence suggesting IPC-A would be better. However, it was not anticipated that at some referral sites there would not be a TAU, resulting in zero treatment being offered. It would be important for future studies to ensure that the TAU is clearly defined for each site, as sites not offering TAU would need to be considered if they are ethically correct to use. Ensuring a TAU could help with barriers to recruitment that came from practitioners feeling that consigning young people to no treatment at all was not appropriate.
Another factor not anticipated with referrals in the trial design, particularly Site-10, was there being no feedback loop allowing for cases to return to the hub if considered inappropriate. Although a lack of system integration in referral pathways was highlighted, it is important for any future studies to clearly identify the referral routes for any potential sites and anticipate any obstacles during this process.
Similarly, the trial was initially hampered by the site's understanding of equipoise and the randomisation process. The trial team supported the sites by including additional information sheets for strategic leaders in an amendment to improve their understanding of the study and attending team meetings to explain research terminology and how this relates to ICALM. Providing this information at the beginning of the study may have resolved some of the difficulties within teams, particularly around the concerns over the randomisation outcomes in TAU, with practitioners communicating a preference for a single-arm study design.
Until a change in Trial Manager in October 2021, the previous Trial Managers were blinded to the randomisation of participants and staff that were providing an intervention for the study. Ideally, in a future RCT, the Trial Manager should be unblinded, as this would resolve issues around participants not taking part in the intervention.
Strengths and limitations
While the study did not meet its aim, certain strengths were acknowledged. Firstly, most methodological elements were acceptable, with participants finding the study procedures and measures easy to understand and complete. Through interviews, staff participants, young people and their parents further acknowledged the usefulness of IPC-A as an intervention to treat low mood. This is of significance as it shows that while we found a definitive trial is not feasible, participants valued the intervention.
Further, training young people’s workers to deliver the intervention was viewed as acceptable, despite this task-shifting strategy being met with a number of challenges in its implementation. Non-qualified practitioners were able to deliver IPC-A, suggesting that such staff could be used to deliver this or similar interventions in the future. Last but not least, one of the main strengths of the study was the in-depth process evaluation, which provided great insight into the barriers to running RCTs in non-specialist mental health services providing clear directions for future research.
A major limitation of the research was the number and complexity of referrals coming through services. This resulted in services with limited capacity prioritising urgent cases, and lower-risk cases, whose presentation would likely be suitable for ICALM, being set aside.
There was a significant impact from COVID-19 due to the recurring lockdowns, causing a delay in recruitment. There was also an impact on the clinical presentation of low mood, with an increase in anxiety cases amongst services from the start and progression of the pandemic. Evidence suggests that the frequency and severity in adolescent mental health presentations increased during the pandemic, and particularly increased for anxiety, which was reflected in the referrals received by services. 62 Despite comorbidities between anxiety and low mood, young people expressed greater preference in treating anxiety than low mood. Consequently, accessing suitable participants was an overarching limitation of the study.
Additionally, the study focused on tiers 1 and 2 services plus Early Help which is provided by social care. As discussed previously, it was suggested by stakeholders that IPC-A may be better suited to services where young people are worked with individually, rather than with the whole family, as is often the case in tier 2 services, although young people with mental health difficulties present in large numbers at all of these services who are set up to address their needs. Likewise, challenges were identified in implementing a RCT in all of these services due to practitioners’ lack of familiarity with research procedures. This indicates the importance of the study team ensuring services are familiar with research processes and implementation of clinical research, something that could have been avoided with further training.
The large turnover of staff delivering IPC-A and TAU and thus the repeated need for training of new staff was another challenge, which had not been anticipated by the research team. This resulted in services being limited on the number of participants they could see, especially under the IPC-A arm, thus creating another potential barrier to recruitment of participants. A larger recruitment of staff and/or services is suggested to prevent such limitations. Concerns over the randomisation outcomes in TAU were a particular challenge, with practitioners communicating a preference for a single-arm study design.
Further, we had intended to provide evidence of the cost effectiveness and potential benefit of IPC-A when compared to TAU. However, due to the low recruitment number, the study was not powered enough to provide any meaningful results on potential benefits of the intervention or the cost effectiveness to be able to comment.
Conclusion
The findings of this feasibility study and the process evaluation indicate that conducting a randomised clinical trial of IPC-A in non-specialist community services is not feasible in the current climate (staff shortages, high staff turnover, high pressure on services making trials a low priority, low familiarity with trials, unclear boundaries between services). It remains unknown if IPC-A is a useful therapeutic addition to universal and mild to moderate services for CYP which should be recommended. This is despite the best efforts of the trial team, clinical teams and commissioners to find ways of making the study succeed. The results did suggest that the data collection and outcome measures were suitable. The intervention was acceptable in all settings, but factors such as high staff turnover, increasing demand for services and increasing complexity of presentations of mental ill heath made it impossible to conduct the feasibility trial within community settings for mild to moderate mental health services.
The impact of COVID-19 was substantial both on services and delivery of the study, and for a full trial to be successful, significant enduring barriers to implementation need to be overcome. It is impossible to know if the original trial design would have been successful, but the process evaluation highlights core complexities within the CYP’s mental health landscape which need to be taken into account for any future trial to be successful. Using the learnings from this study and mapping out the core services in tiers 1 and 2 and the current pathways between them before embarking on any future trials within CYP’s services is critical.
The process evaluation describes in detail the individual elements at macro, meso and micro levels, which ultimately made it impossible for the feasibility trial to meet its progression criteria. While only conducted within two counties within the UK and across multiple systems (health, social care, education and the voluntary sector), it is highly likely that this process evaluation describes issues pertinent to other areas of the UK and the rest of the world. We highly recommend paying specific attention to these issues before setting out on future trials in this clinical area or making assumptions about services involved in clinical trials in the post pandemic era.
Additional information
Contributions of authors
Jon Wilson (https://orcid.org/0000-0002-5279-6237) (Norfolk and Suffolk NHS Foundation Trust) was the study’s Chief Investigator from January 2021. He contributed to study conception and interpretation of results and provided scientific and clinical leadership.
Viktoria Cestaro (https://orcid.org/0000-0003-2340-6735) (Cambridge and Peterborough NHS Foundation Trust) conceived the therapy development with Professor Wilkinson. She contributed to training and supervision of therapists.
Eirini Charami-Roupa (https://orcid.org/0009-0004-5730-6622) (Norfolk and Suffolk NHS Foundation Trust) contributed to analysis of the feasibility study and wrote parts of the first draft of the report.
Timothy Clarke (https://orcid.org/0000-0002-3901-9601) (Norfolk and Suffolk NHS Foundation Trust) contributed to study conception, management and interpretation of the study.
Aoife Dunne (https://orcid.org/0009-0007-1645-7979) (Norfolk and Suffolk NHS Foundation Trust) contributed to analysis of the feasibility study and wrote parts of the first draft of the report.
Brioney Gee (https://orcid.org/0000-0003-0781-7753) (Norfolk and Suffolk NHS Foundation Trust) contributed to study conception, management and interpretation of the study.
Sharon Jarrett (https://orcid.org/0009-0000-0417-994X) (Suffolk County Council) contributed to study conception, management and interpretation of the study.
Thando Katangwe-Chigamba (https://orcid.org/0000-0002-5450-412X) (University of East Anglia) led the process evaluation. She contributed to data collection and analysis of the process evaluation and wrote the first draft of the process evaluation chapter.
Andrew Laphan (https://orcid.org/0000-0003-2343-316X) (Norfolk and Suffolk NHS Foundation Trust) contributed to analysis of the feasibility study and wrote parts of the first draft of the report.
Susie McIvor (https://orcid.org/0009-0000-0546-1330) (Suffolk County Council) was the Co-production Advisor. She was the PPI lead and contributed to the supervision of therapists and interpretation of results.
Richard Meiser-Stedman (https://orcid.org/0000-0002-0262-623X) (University of East Anglia) contributed to study conception, management and interpretation of the study.
Jamie Murdoch (https://orcid.org/0000-0002-9021-3629) (Kings College London) designed and oversaw the process evaluation components of the study and contributed to data analysis and interpretation.
Thomas Rhodes (https://orcid.org/0000-0002-3992-0280) (Norfolk and Suffolk NHS Foundation Trust) was the Trial Manager. He managed the study, co-ordinating recruitment and data management. He collated the contributions and wrote parts of the first draft of the report.
Carys Seeley (https://orcid.org/0009-0002-0451-6330) (University of East Anglia) contributed to data collection and analysis of the process evaluation and wrote parts of the first draft of the report.
Lee Shepstone (https://orcid.org/0000-0001-5524-7818) (University of East Anglia) was the study statistician. He wrote the statistical analysis plan and conducted and reported the analysis.
David Turner (https://orcid.org/0000-0002-1689-4147) (University of East Anglia) was the study’s health economist. He designed the health economic component, conducted analysis and wrote the health economic parts of the report.
Paul Wilkinson (https://orcid.org/0000-0003-3302-9662) (University of Cambridge) was initially the study’s Chief Investigator. He contributed to study conception and provided scientific and clinical leadership. He conceived the therapy development with Mrs Bekeniova-Cestaro.
Acknowledgements
Firstly, our warmest thanks go to the young people, services and staff who participated in the research. We are grateful for your time and commitment to the study. We would also like to thank the Youth Advisory Group who contributed to the development and conduct of the study as PPI representatives.
We gratefully acknowledge the central role in the delivery of the study by the two previous Trial Managers, Gabriel Abotsie and Laura Miles. We are also extremely grateful for the contribution of Kayte Rowe for her work completing outcome assessments and Leanne Hague for editing the final report.
We are extremely thankful to members of the Study Steering Committee and Data Monitoring Committee for contributing their time and expertise to oversee the study.
Finally, we thank the NIHR for supporting this work. Thanks especially to Julie Wright (NIHR Research Manager) for her guidance and support.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
Following the publication of major outputs, we will make anonymised data available to the scientific community wherever possible within the constraints of relevant ethical principles. All data-sharing requests should be submitted to the corresponding author for consideration by the Trial Management Group.
Ethics statement
The study was reviewed by East of England – Cambridge South Research Ethics Committee (19/EE/0300) and received HRA and Health and Care Research Wales (HCRW) approval on 10 December 2019.
Information governance statement
Norfolk and Suffolk NHS Foundation Trust is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation, NSFT is the Data Processor and Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.nsft.nhs.uk/research-compliance-and-policies/
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/GTRV6410.
Primary conflicts of interest: Jamie Murdoch was a member of the HSDR Associate Board from 2014 to 2018 and reports that funding for their role was provided to the University of East Anglia for the duration of the study. Viktoria Cestaro reports that funding for their role was provided to Norfolk and Suffolk NHS Foundation Trust for the duration of the study. Paul Wilkinson reports payment for talks at the British Association of Psychopharmacology on Affective Disorders. There were no declarations by other authors.
Publications
Abotsie G, Cestaro V, Gee B, Wilkinson P. Interpersonal counselling for adolescent depression delivered by youth mental health workers without core professional training: a feasibility randomised controlled trial study protocol. Pilot Feasibility Stud 2020;6:191. https://doi.org/10.1186/s40814-020-00733-8
Katangwe-Chigamba T, Murdoch J, Wilkinson P, Cestaro V, Seeley C, Charami-Roupa E, et al. Doing research in non-specialist mental health services for children and young people: lessons learnt from a process evaluation of the ICALM (Interpersonal Counselling for Adolescent Low Mood) feasibility randomised controlled trial. Pilot Feasibility Stud 2024 Jan 23;10:14. https://doi.org/10.1186/s40814-023-01427-7
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Abotsie G, Cestaro V, Gee B, Murdoch J, Katangwe T, Meiser-Stedman R, et al. Interpersonal counselling for adolescent depression delivered by youth mental health workers without core professional training: a feasibility randomised controlled trial study protocol. Pilot Feasibility Stud 2020;6. https://doi.org/10.1186/s40814-020-00733-8.
- Frith E. CentreForum Commission on Children and Young People’s Mental Health: State of the Nation 2016. http://centreforum.org/live/wp-content/uploads/2016/04/State-of-the-Nation-report-web.pdf (accessed 11 November 2022).
- Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin Psychol Rev 1998;18:765-94. https://doi.org/10.1016/s0272-7358(98)00010-5.
- Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey–adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015;54:37-44.e2. https://doi.org/10.1016/j.jaac.2014.10.010.
- Pickles A, Rowe R, Simonoff E, Foley D, Rutter M, Silberg J. Child psychiatric symptoms and psychosocial impairment: relationship and prognostic significance. Br J Psychiatry 2001;179:230-5. https://doi.org/10.1192/bjp.179.3.230.
- Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry 2010;196:365-71. http://doi.org/10.1192/bjp.bp.109.071191.
- Judd L, Akiskal H, Paulis M. The role and clinical significance of subsyndromal depressive symptoms (SSD) in unipolar major depressive disorder. J Affect Disord 1997;45:5-17. https://doi.org/10.1016/s0165-0327(97)00055-4.
- McLeod GFH, Horwood LJ, Fergusson DM. Adolescent depression, adult mental health and psychosocial outcomes at 30 and 35 years. Psychol Med 2016;46:1401-12. http://doi.org/10.1017/S0033291715002950.
- Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. J Adolesc Health 2007;41:256-62. https://doi.org/10.1016/j.jadohealth.2007.03.015.
- Copeland WE, Wolke D, Shanahan L, Costello J. Adult functional outcomes of common childhood psychiatric problems a prospective, longitudinal study. JAMA Psychiatry 2015;72:892-9. https://doi.org/10.1001/jamapsychiatry.2015.0730.
- Labelle R, Breton JJ, Pouliot L, Dufresne MJ, Berthiaume C. Cognitive correlates of serious suicidal ideation in a community sample of adolescents. J Affect Disord 2013;145:370-7. https://doi.org/10.1016/j.jad.2012.08.027.
- McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026 2008. www.kingsfund.org.uk/sites/default/files/Paying-the-Price-the-cost-of-mental-health-care-England-2026-McCrone-Dhanasiri-Patel-Knapp-Lawton-Smith-Kings-Fund-May-2008_0.pdf (accessed 8 November 2022).
- Bockting CL, Hollon SD, Jarrett RB, Kuyken W, Dobson K. A lifetime approach to major depressive disorder: the contributions of psychological interventions in preventing relapse and recurrence. Clin Psychol Rev 2015;41:16-2. https://doi.org/10.1016/j.cpr.2015.02.003.
- Orchard F, Pass L, Marshall T, Reynolds S. Clinical characteristics of adolescents referred for treatment of depressive disorders. Child Adolesc Ment Health 2017;22:61-8. https://doi.org/10.1111/camh.12178.
- National Institute for Health and Care Excellence . Depression in Children and Young People: Identification and Management 2005. www.nice.org.uk/guidance/ng134 (accessed 8 November 2022).
- Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, et al. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: a systematic review and network meta-analysis. World Psychiatry 2015;14:207-22. https://doi.org/10.1002/wps.20217.
- Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet 2012;379:1056-67. https://doi.org/10.1016/S0140-6736(11)60871-4.
- National Institute for Health and Care Excellence . Addendum to Clinical Guideline 28, Depression in Children and Young People 2015. www.nice.org.uk/guidance/cg28/evidence/addendum-193488882 (accessed 8 November 2022).
- National Institute for Health and Care Excellence . Depression in Children and Young People: Identification and Management in Primary, Community and Secondary Care 2005. www.nice.org.uk/CG028 (accessed 8 November 2022).
- Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. New York, NY: Basic Books; 2000.
- Meyer A. Psychobiology: A Science of Man. Springfield, IL: Charles C. Thomas; 1957.
- Sullivan HS. The Interpersonal Theory of Psychiatry. New York, NY: W. W. Norton; 1953.
- Cuijpers P, Donker T, Weissman MM, Ravitz P, Cristea IA. Interpersonal psychotherapy for mental health problems: a comprehensive meta-analysis. Am J Psychiatry 2016;173:680-7. https://doi.org/10.1176/appi.ajp.2015.15091141.
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 2004;61:577-84. https://doi.org/10.1001/archpsyc.61.6.577.
- Kontunen J, Timonen M, Muotka J, Liukkonen T. Is interpersonal counselling (IPC) sufficient treatment for depression in primary care patients? a pilot study comparing IPC and interpersonal psychotherapy (IPT). J Affect Disord 2016;189:89-93. https://doi.org/10.1016/j.jad.2015.09.032.
- Menchetti M, Rucci P, Bortolotti B, Bombi A, Scocco P, Kraemer HC, et al. DEPICS group . Moderators of remission with interpersonal counselling or drug treatment in primary care patients with depression: randomised controlled trial. Br J Psychiatry 2014;204:144-50. https://doi.org/10.1192/bjp.bp.112.122663.
- Matsuzaka CT, Wainberg M, Norcini Pala A, Hoffmann EV, Coimbra BM, Braga RF, et al. Task shifting interpersonal counselling for depression: a pragmatic randomized controlled trial in primary care. BMC Psychiatry 2017;17:1-11. https://doi.org/10.1186/s12888-017-1379-y.
- Wilkinson PO, Cestaro V, Pinchen I. Pilot mixed-methods evaluation of interpersonal counselling for young people with depressive symptoms in non-specialist services. Evid Based Ment Health 2018;21:134-8. https://doi.org/10.1136/ebmental-2018-300028.
- Singh SP. The great divide: transition of care from child to adult mental health services. Curr Opin Psychiatry 2009;22:386-90. https://doi.org/10.1097/YCO.0b013e32832c9221.
- Markowitz JC, Lipsitz J, Milrod BL. Critical review of outcome research on interpersonal psychotherapy for anxiety disorders. Depress Anxiety 2014;31:316-25. https://doi.org/10.1002/da.22238.
- Wilkinson P. Conceptualization about internalizing problems in children and adolescents. Cien Saude Colet 2009;14:373-81. https://doi.org/10.1590/s1413-81232009000200007.
- Haver A, Akerjordet K, Caputi P, Furunes T, Magee C. Measuring mental well-being: a validation of the short Warwick-Edinburgh mental well-being scale in Norwegian and Swedish. Scand J Public Health 2015;43:721-7. https://doi.org/10.1177/1403494815588862.
- Weissman MM, Hankerson SH, Scorza P, Olfson M, Verdeli H, Shea S, et al. Interpersonal Counselling (IPC) for depression in primary care. Am J Psychother 2014;28:359-83. https://doi.org/10.1176/appi.psychotherapy.2014.68.4.359.
- Kaufman J, Birmaher B, Brent D, Rao U, Ryan N. Kiddie-Sads-Present and Lifetime Version (K-SADS-PL), Version 1.0 1996. https://doi.org/10.1097/00004583-199707000-00021.
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997;36:980-8. https://doi.org/10.1097/00004583-199707000-00021.
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther 2000;38:835-55. https://doi.org/10.1016/s0005-7967(99)00130-8.
- Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. J Marital Fam Ther 1983;9:171-80. https://doi.org/10.1111/j.1752-0606.1983.tb01497.x.
- Goodyer IM, Herbert J, Tamplin A, Secher SM, Pearson J. Short-term outcome of major depression: II. Life events, family dysfunction, and friendship difficulties as predictors of persistent disorder. J Am Acad Child Adolesc Psychiatry 1997;36:474-80. https://doi.org/10.1097/00004583-199704000-00009.
- Chisholm D, Knapp MR, Knudsen HC, Amaddeo F, Gaite L, van Wijngaarden B. Client Socio-Demographic and Service Receipt Inventory – European Version: development of an instrument for international research EPSILON Study 5 European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl 2000;177:s28-33. https://doi.org/10.1192/bjp.177.39.s28.
- Stevens K, Ratcliffe J. Measuring and valuing health benefits for economic evaluation in adolescence: an assessment of the practicality and validity of the child health utility 9d in the Australian adolescent population. Value Health 2012;15:1092-9. https://doi.org/10.1016/j.jval.2012.07.011.
- Jones KC, Burns A. Unit Costs of Health and Social Care 2021. Kent, UK: Personal Social Services Research Unit; 2021.
- Curtis L. Canterbury: Personal Social Services Research Unit; 2010.
- Katangwe-Chigamba T, Murdoch J, Wilkinson P, Cestaro V, Seeley C, Charami-Roupa E, et al. Doing research in non-specialist mental health services for children and young people: lessons learnt from a process evaluation of the ICALM (Interpersonal Counselling for Adolescent Low Mood) feasibility randomised controlled trial. Pilot Feasibility Stud 10. https://doi.org/10.1186/s40814-023-01427-7.
- Rampton B, Tusting K, Maybin J, Barwell R, Creese A, Lytra V. UK Linguistic Ethnography: A Discussion Paper. UK Linguistic Ethnography Forum; 2004.
- Murdoch J. Process evaluation for complex interventions in health services research: analysing context, text trajectories and disruptions. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1651-8.
- Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol 1997;32:513-31. https://doi.org/10.1037/0003-066X.32.7.513.
- Children’s Workforce Development Council . The Common Assessment Framework for Children and Young People: A Guide for Practitioners 2009. https://greatermanchesterscb.proceduresonline.com/pdfs/caf_guidance_practitioners.pdf (accessed 8 November 2022).
- Suffolk SP. Suffolk Threshold Matrix 2022. www.suffolksp.org.uk/assets/Suffolk-Threshold-Matrix-Updated-V2-June-2022.pdf (accessed 8 November 2022).
- NHS . Every Mind Matters. 2021. www.nhs.uk/every-mind-matters/ (accessed 8 November 2022).
- Long R, Parkin E. Support for Children and Young People’s Mental Health. House of Commons Library 2021. https://dera.ioe.ac.uk/38340/1/CBP-7196%20%28redacted%29.pdf (accessed 8 November 2022).
- Her Majesty Government/Department of Health . No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages 2011. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213761/dh_124058.pdf (accessed 8 November 2022).
- Department of Health and NHS England . Future in Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/414024/Childrens_Mental_Health.pdf (accessed 8 November 2022).
- NHS England . Implementing the Five Year Forward View for Mental Health 2016. www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf (accessed 8 November 2022).
- Department of Health and Social Care and Department for Education . Transforming Children and Young People’s Mental Health Provision: A Green Paper 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/664855/Transforming_children_and_young_people_s_mental_health_provision.pdf (accessed 8 November 2022).
- Department of Health and Social Care . NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 8 November 2022).
- Public Health England . PHE Strategy 2020–25 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/831562/PHE_Strategy_2020-25.pdf (accessed 8 November 2022).
- Lifestyles Team, NHS Digital . Mental Health of Children and Young People in England 2020. https://files.digital.nhs.uk/AF/AECD6B/mhcyp_2020_rep_v2.pdf (accessed 8 November 2022).
- Koenig CJ. Patient resistance as agency in treatment decisions. Soc Sci Med 2011;72:1105-14. https://doi.org/10.1016/j.socscimed.2011.02.010.
- Cook AJ, Delong E, Murray DM, Vollmer WM, Heagerty PJ. Statistical lessons learned for designing cluster randomized pragmatic clinical trials from the NIH Health Care Systems Collaboratory Biostatistics and Design Core. Clin Trials 2016;13:504-12. https://doi.org/10.1177/1740774516646578.
- Wolpert M, Harris R, Jones M, Hodges S, Fuggle P, James R, et al. THRIVE: The AFC-Tavistock Model for CAMHS. London: CAMHS Press; 2014.
- Harwood H, Rhead R, Chui Z, Bakolis I, Connor L, Gazard B, et al. Variations by ethnicity in referral and treatment pathways for IAPT service users in South London. Psychol Med 2021;53:1084-95. https://doi.org/10.1017/S0033291721002518.
- Kauhanen L, Wan Mohd Yunus WMA, Lempinen L, Peltonen K, Gyllenberg D, Mishina K, et al. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry 2022;32:995-1013. https://doi.org/10.1007/s00787-022-02060-0.
Appendix 1 Interpersonal counselling for adolescents’ sessions: thematic analysis
Transcription conventions
Basic notation transcription conventions are taken from Charles Antaki’s CA Notation tutorial (https://learn.lboro.ac.uk/ludata/cx/ca-tutorials/notation.htm). Described as a representative list of most widely used symbols stemming from the ‘Jefferson system’ developed by Gail Jefferson (2004).
Engagement from young people as crucial for successful, collaborative intervention
A key component of IPC-A is collaboration between the therapist and young person. Collaboration is highlighted throughout the IPC-A manual and training and is used as a tool to help young person to identify problems and solutions. For example, what their triggers are, how they can recognise the onset of symptoms, and find strategies to ease their symptoms. For collaboration to occur both the therapist and young people need to actively engage with the sessions and tasks. This need for engagement is also reflected in parent and therapist perspectives that young people must be ready to seek help and engage with support before starting these sessions and for support to be effective (see e.g. Appendix 1, Table 22 data extracts).
These perspectives placed young person’s motivation to participate in the intervention are a central component for ensuring effective delivery of the intervention. However, it raises the question of how active engagement might manifest within the sessions themselves and what therapists might do to help young people actively participate within discussions. One of the most beneficial aspects of accessing therapy, as perceived by parents, therapists and young people, was the ability for the young people to talk and have someone listen without judgement.
In contrast, if a young person does not feel heard, there may be a sense that engaging with interventions is pointless, as discussed by one parent describing responses to their child trying find support in school: ‘That just made his mood just go even lower because he thought what’s the point. If I’m not going to be listened to then I’ll just carry on as I am, and therefore he then wouldn’t talk’ (Parent, Case 2). This capacity for young people to feel heard, and that their voice matters, can start before deciding whether to take part in the ICALM study; seen here in a discussion between the young person, parent and the young person’s school about support options available to them:
Interactional styles and participation within intervention sessions
Most apparent throughout recorded IPC-A sessions were different interactional styles between therapist and young people, representing different ways that young people respond to the IPC-A intervention. These can broadly be categorised as: (1) active participation, young person works with the therapist to find solutions; (2) active resistance, young person resists attempts by the therapist to collaborate, often followed by renegotiation; and (3) passive participation/resistance, young person defers to therapist. Passive participation may reflect an inability to engage with the session or not knowing how to participate, rather than choosing not to engage. For example, the young person may express that they ‘don’t know’ as a form of resistance or an inability to participate owing to their memory or difficulty of the task. It is up to the therapist to navigate these interactional styles to help the young person to engage with IPC-A and improve effectiveness of the intervention.
Contrasts and variation in interactional styles seen across and within sessions for each case suggest the effectiveness of IPC-A relies on mechanisms which allow the young people to feel comfortable talking and sharing with their therapist. Exploring how and where these interactional types emerge and change throughout IPC-A sessions offers insight into how contextual features and the tools of IPC-A can be used to encourage active participation from young people. One of the main components in encouraging young people to engage with sessions appeared to be therapists’ ability to give the young people space to not only talk but also feel heard, resulting in increased rapport between the two and facilitating the collaborative effort needed for effective IPC-A.
The importance of feeling heard
During their initial session, the therapist and young person in Case 1 illustrate how active participation from the young people facilitates the therapist’s understanding of their symptoms and experiences, enabling a collaborative exchange that leads to them identifying a problem area (‘big change’) to focus on in future sessions. This level of participation was later reflected on by the young person who reported ‘I cried quite a lot I think, just like for the first one probably when I was just talking about just everything’ (YP-IPC-04, Case 1). An extract from their first session (see Appendix 1, Table 23) illustrates how the therapist works to show the young person that they have heard and understand them – a key mechanism by which enabled this young person to actively participate in sessions. However, to better understand the importance of feeling heard in facilitating active participation from young people, we needed to examine sessions in which young people were more resistant or unable to engage with therapists’ attempts to deliver the intervention session. In Case 3, the young person reported feeling misunderstood by their therapist and the frustration that came with this:
[Interviewer] And how did you get on with the therapist that you were seeing?
[YP] OK. I think I got a bit frustrated with her sometimes but overall, she was all right in the end.
[I] What frustrated you at the beginning then?
[YP] I think that sometimes I’d say things and she’d interpret them a different way which irritated me.
This perception of their sessions may also be reflected in ratings of techniques used by the therapists in Case 3 and Case 1 (and Case 2). For example, Table 7 shows that in the initial session, the therapist in Case 3 averaged lower than the therapist in Case 1 (a score of 2.1 vs. 1.4, which are a pass and fail, respectively). Techniques in which Case 3’s therapist scored lower included not asking the young person about their variation of symptoms (e.g. changes across the week) and creating links between young person’s interpersonal relationships and depressive symptoms. This lack of exploration of the young person’s symptoms may have led to feeling misunderstood as the complexity of what they had been feeling may not have been fully addressed. Examples of this can be seen in Case 3’s first session which provides examples of interactional difficulty or tensions between the young person and therapist, locating instances where the young person may have felt misunderstood, or unheard, and the interactional style this led to. These interaction styles included passive participation within the sessions or active resistance towards participating (see Appendix 1, Table 23).
Therapists are rated on their use of exploratory techniques which should be used to actively encourage participation. By showing a sense of curiosity and acknowledging a young person’s contributions, therapists should encourage the young person to expand on productive topics without imposing unnecessary structure. In this case, the therapists’ focus on the structure of IPC-A (and implementation fidelity) and imposition of this may have limited their acknowledgement of the young person’s contributions and exploration of why it is the young person is unable to describe where their feelings are coming from.
Active resistance is also demonstrated by the young person in Case 3’s initial sessions, which allowed us to explore the difference in context between active and passive resistance. One way in which active resistance appears to be expressed differently to passive resistance is that the young person does not only respond using one-word replies, but instead actively responds to the therapist by justifying their reasons for not wanting/being able to engage in an activity. In the observed context of Case 3, this actively resistant interactional style may be prompted by feeling more than misunderstood, but also not believed of even judged by their therapist. This approach, or perceived approach, by the therapist also contrasts with the intended implementation of IPC-A, in which the therapist’s role is to be non-judgemental and on the young person’s side. Further, the rapport between therapist and young person may suffer owing to the misunderstanding in communication between them.
These points of contrast across cases, illustrating varying forms of participation and interactional sequences, reveal the central importance of therapists working to understand and acknowledge young people’s perspectives and the crucial role played by differing interactional styles for facilitating young people’s engagement, with a non-judgemental approach allowing young people to feel heard and share openly without having to defend or justify their disclosures. These points of contrast also illustrate the complex relationship between implementation and theoretical fidelity, in which both may impact the other for better or worse. For example, implementation fidelity does not always ensure theoretical fidelity.
Orienting discussions to a young person’s perspective
One of the most important mechanisms in enabling young people to actively participate in sessions appeared to be the therapists’ ability to be flexible and work to re-frame discussions or renegotiate terms in a way that the young people can relate to – orienting discussions to the young person’s perspective. Therapists’ initial understanding of the young person’s experiences is reliant on how the therapist elicits the young person’s perspectives and how the young person chooses to answer. Depending on the approach taken, misunderstandings may manifest between therapist and young person, creating interactional tension between the two parties. Misunderstandings could also lead to the young person not feeling heard, despite not having shared this information. In Case 1, for example, tension is seen during the initial session when the therapist misinterprets the young person’s relationship to their mum – interpreting their relationship as less close than they are. The young person responds to this by elaborating that their relationship is very close, leading the therapist to readjust their interpretation of the relationship to accommodate this new understanding; in particular, that the young person’s mum is supportive and listens to how they are feeling. See Appendix 1, Table 23 for an example extract showing the consequence of the therapist’s adjustment, with the therapist changing tack.
Listening to the young person’s perspective and reframing the conversation to acknowledge their perspective appear to help the young person actively participate, despite what appears to be a difficult task which requires pauses for thought. Focus then turns to how the young person can change their interactions to discuss their feelings more deeply, for example going beyond what their feelings are to what has made them feel that way. The young person actively responds to this approach, showing their understanding and the value they see in it – rather than passively accepting the suggestion.
This interaction is followed by an offer to role play this conversation, which is turned down by the young person but later scripted in another session. In this later session, the therapist shows their awareness of young person’s hesitance around ‘role play’: ‘I don’t want to call it role play but it is a little bit like that, just to see how you manage to open up that conversation’. The young person is encouraged to read their script from the screen and have the therapist be their response – rather than starting the conversation on the spot. Again, this therapist can be seen to orient to the young person’s perspective by showing their awareness of issues around ‘role play’ and helping them to script what has been shown to be an uncomfortable, hard conversation for the young person to start. The effectiveness of this technique is seen in the young person’s ability to go on to complete their mini goal. Upon completing this mini goal, the young person is met with praise from the therapist and acknowledgement of its difficulty: ‘I think the more you avoid those emotionally charged situations, the more difficult it becomes for you to then approach those situations and those subjects. So, the fact that you managed to do that, that’s huge, that’s absolutely massive’ (Therapist-IPC-01, Case 1).
Despite the effectiveness of role play, young people appear resistant to trying it out, perhaps owing to their familiarity with talking to the chosen person, or the discomfort of improvisation – which scripting conversations appears to relieve. Role play is also offered in Case 2 and again is turned down. The same therapist shows their awareness of hesitation around role play by offering it as a last resort, ‘if you find that you can’t, then what we can do is perhaps do a little bit of – I know this sounds really scary – but a little bit of role play and we can try and sort of act together’ (Therapist-IPC-01, Case 2).
The importance of orienting discussions and sessions to young person’s perspective is also reflected in Case 3. In comparison to the previous case, feelings of misunderstanding for this young person may stem from their inability to relate to the term ‘depressive symptoms’, as they do not think it fits with what they are feeling. Failure of the therapist to recognise and respond accordingly to the young person’s perspective leads to the young person feeling misunderstood, resulting in passive participation from the young person (see e.g. Appendix 1, Table 23).
Initially, the therapist’s response appears inadequate for orienting to the young person’s point of view and enabling the young person to actively engage with the session. This failure to explore and reframe the discussion according to the young person’s perspective appears to result in the young person struggling to actively engage, and instead showing passive resistance. This passive resistance is illustrated in their use of unmarked tokens,53 such as ‘yeah’, ‘mhm’ or ‘don’t know’. This interactional style changes within the session when the therapist recognises the issue and renegotiates the terms used with the young person – trying again to orient to the young person’s perspective, and successfully enabling the young person to actively engage with the task (see Appendix 1, Table 23).
This renegotiation of terms also highlights a potential tension between implementation and theoretical fidelity for therapists. Implementation fidelity, for example, might encourage the therapist to continue discussing depressive symptoms, owing to the theoretical focus of IPC on the interactional relationship between depressive symptoms and interpersonal relationships. However, for this young person (Case 3), continuing this approach would be inappropriate and result in resistance throughout the sessions and little progress for the young person. Changing these terms shows the therapists’ ability to adapt flexibly to the needs of the young person, helping them to engage and progress with the intervention, and in turn, enhancing theoretical fidelity. Despite the main diagnostic category for the study population being depression/low mood, the therapist’s role is not to diagnose young person with depression. A key mechanism of change within these sessions is instead the therapist’s ability to work flexibly with the young person to collaborate and work towards a solution on their terms.
Contextualising IPC-A using specific scenarios, relevant to the young person’s experiences, was also seen as another mechanism which involved orienting to the young person’s perspective and encouraged this young person’s (Case 3) engagement. By contextualising IPC-A in this way, the therapist was able to gain information from the young person about their interpersonal relationships, which had proved difficult owing to the young person’s difficulty engaging with previous tasks, for example creating a timeline of their symptoms.
An important mechanism of IPC-A, therefore, appears to be in the therapist’s ability to orient themselves to the young person’s perspective and reframe discussions accordingly – often requiring flexibility with the structure of IPC-A sessions. Beyond this understanding of the young person’s perspective, therapists must also encourage the young person to change their approach and engage with IPC-A techniques.
Reliability of interpersonal relationships: mini goals and advocacy
Many, if not all, tools of IPC-A rely on active participation from the young person. Most prominent of these are mini goals that are set at the end of each session for the young person to complete before their next session, where they will be reviewed. In accordance with the IPC-A manual, these goals should be agreed on collaboratively, interpersonal and something the young person has control over doing. The aim of these goals is to be achievable and help the young person towards their ultimate goals.
Responses to and success in these mini goals can affect the young person’s future engagement with mini goals outside of the sessions. In the cases seen, mini goals were often reliant on others responding appropriately to the young person’s attempts at completing these goals. Engaging in mini goals and not receiving the response they need or expect can be disheartening for young person and could lead to them feeling less motivated to engage with IPC-A outside of (or within) sessions. This is best illustrated in this example from Case 2, in which therapist and young person are reviewing the young person’s mini goal to talk more deeply about how they are feeling with their mum (see Appendix 1, Table 23 for extract).
Use of mini goals and advocating for the young person can help to better develop the rapport between the therapist and young person, when used effectively. For example, in creating mini goals, the young person and therapist make an agreement that the young person will engage with the task outside of the session and the therapist will follow up with this task in the next session. Following up is a key element of this tool, as much like feeling unheard, if the young person attempts the task but is not asked how it went, they may have little motivation to attempt these mini goals again. Advocating for the young person may also work to reinforce the therapist’s words with actions, going beyond saying that they are listening to their needs to taking steps towards making sure these needs are met by others, where possible. In Cases 2 and 3, both therapists take the opportunity to advocate for the young person by discussing the young person’s needs with important interpersonal relationships (parents and teachers) without revealing details of their sessions.
In Case 2, given the outcome of the previous mini goal, the therapist emphasises the need for the young person to find the right moment to carry out their mini goal: ‘I would like you – if you can – I think it would be a really good idea to, when you’re nice and calm, is to go and visit [teacher’s name] or ask to see him at a certain time’ (Therapist-IPC-01, Case 2). Reframing the context of the mini goal to include finding an appropriate time may foster further consideration of the other person’s perspective, leading to a more balanced view in relationship disputes. The therapist also offers to extend their reach to act as an advocate for the young person to ensure that responses to their reaching out are treated appropriately, in this case by talking to their teacher beforehand in preparation for their chat with the young person. Again, therapists’ abilities to act as an advocate for the young person may help the young person to feel supported by both their therapist and interpersonal relationships, with the latter being crucial to IPC-A’s theoretical fidelity and young person’s progress once their IPC-A sessions have finished. See Appendix 1, Table 23 for an extract from Case 2 which highlights the change in response the young person reasons after the therapist is able to advocate for them to their parent.
A key component of the IPC-A is the two-way link between depressive symptoms and interpersonal relationships. Improving young person’s interpersonal relationships through effective advocacy should lead to improved depressive symptoms. Discussing expectations around these interpersonal relationships also appears to be an important tool in understanding the young person’s perspective on IPC-A and how it can work to help them.
Effective use of mini goals and advocacy can change interactional styles and help young people to actively engage in IPC-A, both within and outside of sessions. Use of these tools adheres to the intended implementation of IPC-A and can be seen to foster the theoretical ideals of IPC-A, allowing young people to further develop their interpersonal relationships and the support received from these.
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- AE
- adverse event
- AfC
- Agenda for Change
- CADS
- Children’s Advice and Duty Service
- CAF
- common assessment framework
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive–behavioural therapy
- CHU-9D
- Child Health Utility Index 9D
- CIN
- child-in-need
- CP
- child protection
- CPD
- continuing professional development
- CQC
- Care Quality Commission
- CRT
- cluster randomised trial
- CSRI
- Client Service Receipt Inventory
- CTU
- Clinical Trials Unit
- CWP
- children’s wellbeing practitioner
- CYP
- children and young people
- CYP-IAPT
- Children and Young People’s Improved Access to Psychological Therapies
- DMC
- Data Monitoring Committee
- EUPD
- emotionally unstable personality disorder
- FSP
- family support practitioner
- FSW
- family support work
- GP
- general practitioner
- IPC
- interpersonal counselling
- IPC-A
- interpersonal counselling for adolescents
- IPT
- interpersonal psychotherapy
- MDD
- major depressive disorder
- NEET
- not in education, employment or training
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NSFT
- Norfolk and Suffolk NHS Foundation Trust
- OCD
- obsessive–compulsive disorder
- PMHW
- primary mental health worker
- PPI
- patient and public involvement
- RAG
- red, amber, green
- RCADS
- Revised Children’s Anxiety and Depression Scale
- RCT
- randomised controlled trial
- REHP
- resilience and emotional health practitioner
- SAE
- serious adverse event
- SAP
- statistical analysis plan
- SPOA
- single point of access
- SPQ
- site profile questionnaire
- SWEMWBS
- The Short Warwick-Edinburgh Mental Well-being Scale
- TAU
- treatment as usual
- TSC
- Trial Steering Committee
- YMHW
- youth mental health worker
- YPW
- young person’s worker
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/GTRV6410).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
