Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 13/05/12. The contractual start date was in March 2014. The final report began editorial review in April 2014 and was accepted for publication in May 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Turner et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This rapid evidence synthesis has been written in response to a request by NHS England to further examine the evidence around the delivery of congenital heart disease (CHD) services. The purpose of the evidence synthesis is to support the ongoing NHS England service review about how CHD services should be best organised.
Services for children with CHD have been the subject of scrutiny for a number of years. In 2012, following an extensive review as part of the Safe and Sustainable work programme, a series of recommendations were made for the reconfiguration of cardiac services for this patient group. 1 The rationale for change was based on the view that clinical expertise was spread too thinly and that providing CHD surgery in a smaller number of units would ensure a critical mass of cases, access to associated specialist staff and the ability to provide a safe 24/7 emergency service. At the time of the review CHD surgery for children was carried out in 11 centres.
The Safe and Sustainable CHD review (Review of Children’s Congenital Cardiac Services in England)1 recommended that CHD services be provided by seven managed clinical networks centred on seven units. However, these recommendations were challenged and subsequently became the subject of a judicial review (JR) and an independent reconfiguration panel (IRP) inquiry, which concluded that processes of the review were flawed. Consequently, service reconfiguration was not implemented and these services are subject to a new review which will consider the whole lifetime pathway for CHD.
The JR and IRP identified a number of issues of concern with the Safe and Sustainable review process including the use and interpretation of the existing evidence base on surgical services for CHD and patient outcomes. In particular, they questioned the reliance on evidence around the relationship between volume of cases and outcomes. A literature review undertaken in 2009 by Ewart2 had examined this evidence in detail and, although confirming the existence of a relationship between volume and outcome, cautioned that this relationship alone was not sufficient to make recommendations on the size of units needed. The review was not able to identify any reliable evidence on the cut-off points in terms of the minimum annual numbers of cases needed for a centre. Ewart2 also highlighted that probable contributory effects of other system and process factors on the relationship between volume and outcome in the published literature were unclear.
As it is now almost 5 years since the publication of the Ewart review, it is timely to reassess the evidence base for CHD services to support the current service review. The purpose of this evidence synthesis, in the form of a rapid review, is to examine what evidence there is for a relationship between organisational features and patient outcomes in CHD services.
This rapid review of published research on the relationship between volume, proximity and patient outcomes is just one of the sources of evidence which has been commissioned to inform the NHS England CHD service review. The overall aim of this service review was to ensure that services for people with CHD are provided in a way that achieves the highest possible quality within the available resources. This will involve consideration of a very wide range of types of evidence including published research, but also audit and other service quality-related data from CHD services and information based on the experiences of clinicians, patients and families.
Chapter 2 Hypotheses tested in the review (research questions)
Because this is a rapid review, it focuses on two key organisational features: volume and proximity. The rationale for this is based on the existing, evidence-based consensus that there may be a relationship between the volume of CHD procedures (both by institution and by surgeon) and patient outcomes and the clinical consensus that reconfiguration which includes the colocation (or increased proximity) of specialist services may be related to better patient outcomes. The research questions also reflect the view that there are mediating factors that influence the relationship between patient outcomes and volume and proximity.
The research questions are as follows:
-
What is the current evidence for the relationship between institutional and surgeon volume and patient outcomes and how is that relationship influenced by complexity of procedure and by patient case mix?
-
How are patient outcomes influenced by proximity to/colocation with other specialist clinical services (e.g. colocation of services such as specialist cardiac paediatric intensive care)?
Chapter 3 Review methods
Rapid review methods
Owing to the need to complete this review within a very short timeframe (12 weeks including a 3-week protocol development stage) rapid review methods were used to ensure the efficient identification and synthesis of the most relevant evidence.
Rapid review methods are still in their relative infancy, in comparison with the more established systematic review. Harker and Kleijnen3 examined a number of rapid reviews in order to develop understanding and definition of what a rapid review was. Rapid reviews are undertaken over a short time frame with a streamlined methodology. This streamlined methodology is a necessary compromise from a standard systematic review. Although Harker and Kleijnen3 found considerable variation in the methodologies adopted by rapid reviews, acknowledging that there is not a ‘one size fits all’ methodology, they advise ‘clear and transparent description and discussion of methodology utilised and acknowledge any limitations’. This advice has informed our choice of methods and report writing.
Our review did not attempt to identify all relevant evidence or to search exhaustively for all evidence that meets the inclusion criteria; the search approach aimed to identify the key evidence of most relevance to the review question.
The scope to both search for and review related evidence, reflecting the multiple dimensions of the topic, was considerable and, thus, was considered prohibitive within the given time frame. The rapid review therefore focused on the most relevant evidence from CHD services for children and adults. The rapid review was based on a proposed conceptual framework included in the study protocol. This allowed us to:
-
define the scope of the search strategy
-
define inclusion and exclusion criteria to specify what types of studies were to be included in the final report
-
construct summary tables of all included studies to present key information and findings
-
synthesise the evidence from the included studies.
Protocol development
The protocol for the review was developed iteratively between the School of Health and Related Research (ScHARR), NHS England and the National Institute for Health Research (NIHR) Health Services and Delivery Research (HS&DR) programme. In addition, comments were sought from key stakeholders, who were part of the NHS England Clinical Advisory Panel for the CHD review. The protocol development started on 7 January 2014 and was published on the NHS England website on 10 February 2014. 4
Use of the conceptual framework
There is an extensive health services research evidence base documenting associations between a range of organisational factors, particularly factors related to location, nature and size of specialist facilities and outcomes, in both elective and emergency service provision. There is also a major field of research that has explored, both quantitatively and qualitatively, the impact of different aspects of service organisation and delivery which influence patient safety and may reduce the risk of adverse outcomes for patients. In order to make the relationship between this wider evidence base and the, relatively limited, scope of this commissioned rapid review more explicit, a logic model (or conceptual framework) was developed for the study protocol and this is included in Appendix 1. This figure shows the relationship between the specific inclusion criteria for this review and the much wider context of factors of known relevance which were considered for inclusion in the review if there were relevant data within the included studies. This approach was chosen based on the need to both limit the scope of the review to the most relevant evidence, while not ignoring the very wide range of organisational, cultural and patient-related factors already known to be important predictors of outcome. The conceptual model was used to inform (1) the literature search, (2) development of inclusion and exclusion criteria, (3) data extraction and (4) evidence synthesis.
Literature searching
A range of search methods, as outlined below, were used in order to identify evidence to answer the rapid review research questions in a timely fashion:
-
Stage 1 – search of health and medical databases.
-
Stage 2 – citation searching.
-
Stage 3 – call for evidence from topic experts.
-
Stage 4 – scrutiny of reference lists of published reviews/key evidence.
-
Stage 5 – scrutiny of reference lists of included papers.
The search process was undertaken with reference to the protocol, in particular to the conceptualisation of the different subareas within which to identify relevant evidence (Figure 1).
FIGURE 1.
Conceptualisation of the evidence base.
A systematic search of medical and health-related databases [MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), The Cochrane Library and Web of Science] was undertaken for the years 2009–14 together with citation searching, reference list checking and recommendations from stakeholders to identify evidence for 2003–14. The rationale for limiting the review to 2003–14 was that this was in line with the dates used by Ewart2 and would limit the body of evidence to a manageable but meaningful number of studies.
Stage 1: search of health and medical databases
The starting point of our search strategy was Ewart. 2 We modified search terms from the previous review to capture a wider evidence base around the population (adults and children), interventions (surgical and interventional) and outcomes (mortality, complications and related outcomes).
The search strategy used a combination of free text and medical subject headings (MeSH) and can be found in Appendix 2. The search was around key terms for the population (CHD), the intervening variables (volume and proximity) and outcomes (mortality, death, survival).
We searched MEDLINE and EMBASE via OvidSP, The Cochrane Library via Wiley Online Library, Web of Science via Web of Knowledge and CINAHL via EBSCOhost. MEDLINE, EMBASE, CINAHL and The Cochrane Library are commonly considered the core databases for identifying evidence relating to clinical topics. 5
The search strategy was limited to 2009–14 with the rationale that relevant evidence from 2003–8 would be cited in later papers or in later reviews retrieved by the database search and, therefore, identified via stages 2–5.
The searches were undertaken in January 2014 and an updated search was undertaken in March 2014. The search results were downloaded into Reference Manager (version 12; Thomson Reuters, New York City, NY, USA) where they were assessed for inclusion in the review. Additional detail on this process is available later in Chapter 3, Assessment according to inclusion and exclusion criteria.
Stage 2: citation searching
A search was undertaken to identify any published articles that have cited any of the articles included in the Ewart review. 2 This search was undertaken via Google Scholar, using the Publish or Perish software [Harzing AW (2007); available from www.harzing.com/pop.htm] to manage the references identified. These references were then imported into Reference Manager.
We also undertook citation searching using included papers in areas not included within the scope of the original Ewart review2 (i.e. adult and paediatric proximity and adult volume).
Stage 3: call for evidence from topic experts
A call for evidence for potential inclusion in the review was made via the NHS England CHD blog,4 directly at the NHS England patient and public group and via e-mail to the NHS England Clinical Advisory panel. Evidence was forwarded to ScHARR via NHS England. Papers suggested by topic experts and the wider group of interested parties are listed in Appendix 2.
Stage 4: scrutiny of reference lists of published reviews/key evidence
In order to identify additional published evidence that was not retrieved by the database searches, the team undertook scrutiny of reference lists of published reviews of services, guideline documents and reports as identified through stages 1, 2, 3 and 5. Reviews that informed this stage of the search are listed in Appendix 2.
Stage 5: scrutiny of reference lists of included papers
Reference lists of all papers identified for inclusion were examined. Any titles considered to be relevant were then scrutinised at an abstract level via PubMed. Any relevant full papers were considered for inclusion by a reviewer. Where papers were identified for inclusion, their reference lists were subsequently checked.
Inclusion/exclusion criteria
The inclusion or exclusion of studies in the review was according to the criteria in Table 1.
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Population | Adults and children undergoing treatment (surgical or interventional) for CHD | |
| Intervention | Measurement of outcomes based on at least one of the following: volume of activity or colocation with other related services | |
| Outcome | Patient outcomes | Process/service outcomes (these will be included only if studies report at least one patient outcome) |
| Study type | Quantitative studies (observational evidence and evidence from trials). Publication date 2003–14. Published, peer-reviewed evidence | Qualitative evidence, evidence from surveys of views/experiences, editorials, opinions, non-English-language papers, non-OECD countries |
Assessment according to inclusion and exclusion criteria
References identified from stages 1 and 2 were downloaded into Reference Manager, version 12, to be sifted for inclusion in the review. All potential titles were examined for inclusion by one reviewer. Any titles that did not meet the inclusion criteria were excluded. Following the examination at the title level, any remaining references were scrutinised at the abstract level. For any references where possible inclusion was unclear, a second reviewer independently examined the corresponding full text.
Ten per cent of the titles and abstracts of these citations identified by the searches were checked by a second reviewer (and a check for consistency undertaken).
For stages 3, 4 and 5 references were checked following the same three-stage process as for stages 1 and 2 (title, abstract and full text).
Assessment for inclusion of conference abstracts identified from all stages of the search was undertaken by one reviewer and checked by a second. Both reviewers assessed each conference abstract based on three criteria, namely whether or not:
-
the abstract fulfilled the inclusion criteria, in terms of the explanatory variables and outcomes
-
the evidence in the abstract was included within an already included paper
-
there were sufficient data in the abstract to be able to use the data in a meaningful manner to address the aims of the review.
Data extraction, including development of the data extraction tool
The aim of the data extraction process was to focus on the most critical information for evidence synthesis rather than exhaustively extracting and critiquing all available information within individual papers. Owing to the rapid nature of the review, data extraction was undertaken by five reviewers.
A standardised data extraction form was developed using the following process. The initial draft of the data extraction tool was designed as a comprehensive way to capture all relevant information from the studies on a broad range of factors related to CHD services that may affect patient outcomes following interventions. Four members of the ScHARR review team tested this initial draft on three studies. 6–8
It became apparent that these studies, which focused on the relationship between volume and mortality, considered complexity of the underlying cardiac condition and other patient-level factors in their analysis, but did not include details of relevant organisational factors such as staffing and proximity of related services. Similarly, mortality was the only outcome considered in these studies and other relevant outcomes such as morbidity, complications, length of stay (LOS) and readmissions were not included.
The data extraction tool was therefore revised in the light of this initial data extraction. The revision also included reference to data tables included in other reviews in this area: Ewart2 and Bazzani and Marcin. 8 The final layout was determined to explicitly include the following key details, in addition to the information included as standard on a data extraction form:
-
where data were obtained from a database, whether contribution to the database was voluntary (to indicate potential bias in reporting) and whether the purpose of the database was administrative or clinical (to highlight the potential limitations of the details available)
-
whether volume was considered as a continuous or categorical variable and, if categorical, what were the thresholds determined by the study for the different categories
-
the covariates used in the analysis
-
in the quantitative assessment of the relationship between volume/proximity and mortality, a breakdown of the crude association and the adjusted association (for case mix ± other covariates).
-
where an association was identified, what was the nature of this relationship (linear or non-linear)?
A sample data extraction form is available in Appendix 3.
Quality assessment
Rather than using a standard checklist approach, the focus was on an assessment of the overall usefulness of the included evidence in answering the research questions. The assessment of usefulness was based on a number of factors which included:
-
whether the study adjusted for severity of condition
-
whether the study adjusted for age
-
whether the study was multicentre
-
whether the study included more than one intervention/condition
-
whether the contribution to the database used to collect the data was voluntary and whether data were collected comprehensively or collectively.
Assessment of the limitations of included studies was also undertaken using the limitations reported by study authors in the included studies.
Synthesis
Data were extracted and tabulated. This tabulation was used to inform the narrative synthesis in the results section. A meta-analysis was not considered given that the review was a rapid review and there was considerable heterogeneity in the design, methods and setting of the included studies making the clinical value of such a formal statistical analysis open to debate.
Chapter 4 Studies included in the review
Results of the literature search
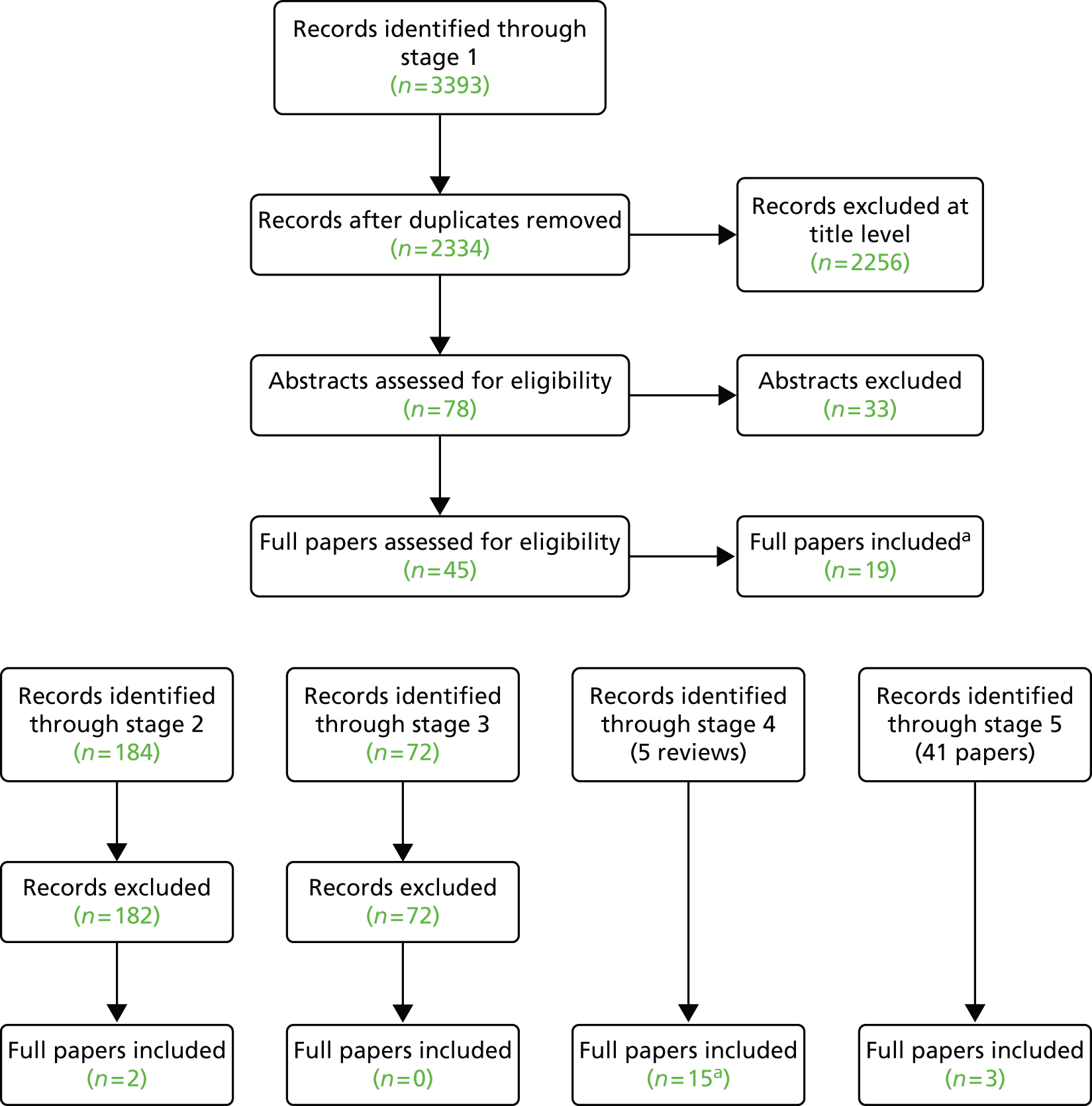
The full papers and conference abstracts identified as a result of the literature search are described in the modified Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram in Figure 2.
To summarise Figure 2, 39 full journal articles and four conference abstracts met the inclusion criteria. Four additional abstracts met the inclusion criteria; however, the evidence included in them was already included in a full paper. Upon scrutiny, the information included in the abstracts was insufficient for full data extraction and could not be used in a meaningful manner to address the aims of the review. Therefore, a decision was made to extract as much data as possible from these abstracts and include this information for reference in the report appendix but to not include this evidence in the analysis. The tables can be found in Appendix 3.
Second screening of retrieved references
In order to check the screening consistency of the single reviewer a second reviewer screened approximately 10% of the references (n = 300). Reviewer 2 tagged 5 out of 292 (1%) references excluded by reviewer 1 as potential includes and tagged 1 out of 8 (12.5%) references included by reviewer 1 as probable excludes. This gave a kappa statistic of 0.77, generally acknowledged as good agreement. The three additional potential includes identified by reviewer 2 were tenuous includes (two review articles potentially relevant as background, and an article for which only a title was available), whereas the one article tagged as ‘include’ by reviewer 1 and ‘exclude’ by reviewer 2 was subsequently checked for inclusion at the full-text stage. Therefore, it was unlikely that any relevant primary studies were overlooked in the 10% sample checked and this result can be extrapolated to the remainder of the screening process.
List of studies included in the review
Box 1 lists the studies that met the criteria for inclusion for review.
-
Arenz et al. , 2011. 9
-
Arnaoutakis et al., 2012. 10
-
Bazzani and Marcin, 2007. 8
-
Benavidez et al., 2007. 11
-
Berry et al., 2007. 12
-
Berry et al., 2006. 13
-
Burstein et al., 2011. 14
-
Chang et al., 2006. 7
-
Checcia et al., 2005. 15
-
Davies et al., 2011. 16
-
Dean, 2013. 17
-
Dinh and Maroulas, 2010. 18
-
Eldadah et al., 2011. 19
-
Fixler, 2012. 20
-
Gray et al., 2003. 21
-
Hickey et al., 2010. 22
-
Hirsch et al., 2008. 23
-
Hornik et al., 2012. 24
-
Karamlou et al., 2013. 25
-
Karamlou et al., 2008. 26
-
Karamlou et al., 2010. 27
-
Kazui et al., 2007. 28
-
Kim et al., 2011. 29
-
McHugh et al., 2010. 30
-
Mery, 2014. 31
-
Morales et al., 2010. 32
-
Oster et al., 2011. 33
-
Pasquali et al., 2012a. 34
-
Pasquali et al., 2012b. 35
-
Petrucci et al., 2011. 36
-
Pinto et al., 2012. 37
-
Sakata et al., 2012. 38
-
Seifert et al., 2007. 39
-
Tabbutt et al., 2012. 40
-
Vinocur, 2013. 41
-
Welke et al., 2010. 42
-
Welke et al., 2009. 43
-
Welke et al., 2008. 6
-
Welke et al., 2006. 44
List of conference abstracts included in the review
Table 2 lists the conference abstracts that met the criteria for inclusion in the review.
Chapter 5 Studies excluded from the review
A full list of the full-text studies and conference abstracts excluded from the review is available in Appendix 2. In addition, the evidence suggested by topic experts and assessed for inclusion by the review team is also available in Appendix 2.
Chapter 6 Results of the review
Detailed summary tables of included papers are provided in Appendix 3. We also identified four relevant published conference abstracts and a summary of these is provided in Appendix 2 for reference. However, we have not considered these in our analysis.
Characteristics of included studies
Thirty-nine full-text papers were included in the review. The characteristics of these papers are summarised in Table 3.
| Study characteristics | Number (%) |
|---|---|
| Total number of full-text papers included | 39 (100) |
| Variables | |
| Paediatric volume and mortality relationship (all conditions) | 18 (46) |
| Paediatric volume and outcome relationship (specific conditions/procedures) | 14 (36) |
| Variables other than volume or non-mortality outcomes | 7 (18) |
| Country | |
| USA/Canada | 35 (90) |
| Japan | 2 (5) |
| Germany | 1 (2.5) |
| Sweden | 1 (2.5) |
| Centre type | |
| Multicentre | 36 (92.4) |
| Single centre | 3 (7.6) |
| CHD condition/procedure type | |
| All CHD conditions/procedures | 25 (64) |
| Single CHD condition/procedure | 14 (36) |
| Data sources | |
| Voluntary (STS-CHD, HCUP-KIDS, PCCC and UHC databases) | 21 (53) |
| Involuntary/registry (PHIS, NIS, OSHPD, UNOS, Texas birth defects registry) | 13 (33) |
| Study specific | 5 (13) |
| Patient population | |
| All children (0–20 years) | 22 (56.4) |
| Newborns and infants only | 14 (36.9) |
| Adults | 3 (7.6) |
| Outcomes measured | |
| Survival/mortality only | 29 (74.5) |
| Survival/mortality and other outcomes | 8 (20.5) |
| Other outcomes only (e.g. morbidity, complications) | 2 (5) |
| Design | |
| Retrospective cohort | 33 (82) |
| Cross-sectional analysis | 5 (13) |
| Before and after | 1 (2.5) |
No UK studies were identified and 36 out of 39 studies (92%) included only paediatric patients. The majority of studies (90%) were conducted in the USA and most were multicentre (92%). We have classified included studies in to three broad groups: those where the primary objective was to explore the relationship between volume of service and mortality outcome for a range of CHD conditions (18/39); those where the focus was on the relationship between volume and mortality outcome for specific single conditions or procedures (14/39); and those where the focus was on the impact of a variable other than volume or where non-mortality outcomes only were reported (7/39). For studies involving specific conditions or procedures these were mainly complex conditions, such as hypoplastic left heart syndrome (HLHS), pulmonary atresia and/or procedures including the Norwood procedure, arterial switch operation (ASO), transposition of great arteries (TGA) and Blalock–Taussig shunt procedure (BTSP) (10/14); heart transplant (2/14); ventricular septal defect (VSD) repair cases only (1/14); and ventricular assist devices (VADs) only (1/14).
Two studies included a paediatric CHD population as a subgroup in studies that examined a range of cardiothoracic procedures38,28 and one a range of common paediatric operations. 12 For these studies only the findings related to the CHD population are reported here. Three procedure-based studies for heart transplant10,16 and VAD32 included patients with conditions other than CHD.
The majority of studies used routine data sets (35/39) and, among these, voluntary clinical or mixed clinical and administrative data sources predominated (21/39), with 13 studies utilising involuntary administrative data. Descriptions of these data sets are provided in Appendix 4. Five studies used study-specific data including one using data from a clinical trial. 40
Half of the studies included children of all ages (age range 0–20 years), 14 out of 39 included only newborns and infants and three studies included adults.
Mortality was the primary outcome measure used, with two studies reporting only morbidity outcomes. The use of routine data is reflected in the types of study design used. There were no primary clinical trials with retrospective observational designs being the predominant feature. There was one before-and-after study assessing the impact of a cardiac paediatric intensive care unit (cPICU). 19
Study populations and settings
Table 4 provides a summary of the dates, inclusion dates, study settings and sample sizes. Where reported, numbers of centres and centre volumes are included. In-hospital mortality is death during the admission for the procedure.
| Study | All (A) or specific (S) casesa | Study period | Sample size,b number of centres | Lowest and highest reported centre volumes per yearc | Mortality/survival end point |
|---|---|---|---|---|---|
| Arenz et al. 20119 | A | 2006–9 | 1828 | Single centre mean 457 cases per year | In hospital within 30 days |
| Arnaoutakis et al. 201210 | S | 2000–10 | 18,226,141 centres | ≤ 7 to > 15 transplant cases | 30 days and 1 year |
| Bazzani and Marcin 20078 | A | 1998–2003 |
|
Lowest 20 < 75, > 75 cardiac surgery cases | Within 30 days |
| Benavidez et al. 200711 | A | 2000 | 10,032, 100 centres | < 150 to > 450 CHD surgery admissions | Morbidity only |
| Berry et al. 200712 | S | 2003 | 2301, 113 centres | ≤ 4 to ≥ 10 VSD repair cases | In hospital |
| Berry et al. 200613 | S | 1997 and 2000 | 754 in 1997, 880 in 2000 | 1 to 10 HLHS cases | In hospital |
| Burstein et al. 201114 | A | 2007–9 | 20,922, 47 centres | < 150 to ≥ 350 CHD surgery cases | In hospital |
| Chang et al. 20067 | A | 1989–99 | 25,402, 500 centres | ≤ 100 cases to > 100 cases CHD surgery cases | In hospital, 30, 90 and 365 days |
| Checcia et al. 200515 | S | 1998–2001 | 801, 29 centres | < 16 to > 30 Norwood procedure cases | In hospital |
| Davies et al. 201116 | S | 1992–2007 | 4647, 136 centres | < 19 to ≥ 63 transplants in preceding 5 years | In hospital, 1 year |
| Dean 201317 | S | 1998–2007 | 1949, 48 centres | Not specified | In-hospital mortality |
| Dinh 201018 | A | 1985–2004 | 80,000, 47 centres | Not specified | In hospital |
| Eldadah et al. 201119 | A | 2004–8 | 199 before, 244 after | Single centre | In hospital |
| Fixler 201220 | A | 1996–2003 | 1213 | Distance not volume | 1 year |
| Grey et al. 200321 | A | 1992 | 284 admissions, 261 patients, four centres | 47 to 85 complex CHD surgery cases | 30 days post operation |
| Hickey et al. 201022 | A | 2005–6 | 19,736, 38 centres | 47 to 764 CHD surgery cases | In hospital |
| Hirsch et al. 200823 | S | 2003 | 547, 74 centres | 1 to 31 Norwood procedure 1 to 24 ASO |
In hospital |
| Hornik et al. 201224 | S | 2000–9 | 2555 patients, 53 centres | ≤ 10 to > 20 Norwood procedure cases | In hospital |
| Karamlou et al. 201325 | A (ECMO only) | 2000–9 | 3867, 207 centres | Annual ECMO cases < 15 to > 30 |
In hospital |
| Karamlou et al. 200826 | A | 1988–2003 | 30,250 | Not specified Continuous variable |
In hospital |
| Karamlou et al. 201027 | S | 1987–2000 | 2421, 33 centres | 1 to 47 (per surgeon) of four complex groups | In hospital |
| Kazui et al. 200728 | A | 2000–4 | 11,197, 135 | ≤ 1–4 to > 20 cases of open heart surgery of newborns and infants | In hospital |
| Kim et al. 201129 | A | 2000–8 | 97,563 all CHD, 3061 adults, 42 centres | < 10 to > 20 adults admitted for CHD surgery < 200 to > 400 all cases including children |
In hospital |
| McHugh et al. 201030 | S | 1998–2007 | 9187, 118 centres | 10-year study period: HLHS palliation procedures < 20 to > 64 procedures |
In hospital |
| Mery 201431,49 | A | 2004–11 | 77,777, 43 centres | Not volume | Complication only |
| Morales et al. 201032 | S | 2006 | 187, 67 centres | 1 to > 5 VAD placements | In hospital |
| Oster et al. 201133 | A | July 2006–8 | 49,792, 24,112 subgroups, 39 centres | Not specified Continuous variable |
In hospital |
| Pasquali et al. 2012a34 | S | 2000–9 | 2557, 53 centres | ≤ 10 to > 20 Norwood procedure cases | In hospital |
| Pasquali et al. 2012b35 | A | 2006–9 | 35,776 patients, 68 centres | < 150 to > 350 CHD surgery cases | In hospital |
| Petrucci et al. 201136 | S | 2002–9 | 1273, 70 centres | Not specified | In hospital |
| Pinto et al. 201237 | A | 2005–June 2006 | 271 | Distance not volume. Single centre | Post discharge |
| Sakata et al. 201238 | A | 2005–9 | 13,074, 220 centres | Not specified – CHD subgroup of eight cardiothoracic procedures | 30 days |
| Seifert et al. 200739 | A | 2000 | 10,282 | Not specified Continuous variable |
In hospital |
| Tabbutt et al. 201240 | S | 2005–8 | 549 cases, 15 centres | ≤ 15 to > 30 Norwood procedure cases | In hospital, 30 days |
| Vinocur 201341 | A | 1982–2007 | 10,945, 85,023 subgroups, 49 centres | ≤ 10 to 500 CHD surgery cases | In hospital |
| Welke et al. 201042 | A | 2000–5 | 21,709, 161 centres | Modelling | In hospital |
| Welke et al. 200943 | A | 2002–6 | 32,413, 48 programmes | < 150 to ≥ 350 CHD surgery cases | In hospital |
| Welke et al. 20086 | A | 1988–2005 | 55,164, 307 centres | < 200 to < 300 CHD surgery cases | In hospital |
| Welke et al. 200644 | A | 2001–4 | 12,672 procedures, 11 centres | 103–801 CHD surgery cases | In hospital |
Most of the included studies were conducted after 2009 (29/39, 74%), with 14 studies conducted before 2009. The latter comprised the seven studies included in the Ewart review2 and an additional seven studies identified as a consequence of our broader search strategy and inclusion criteria to include adult studies and those concerned with non-mortality outcomes or the impact of factors other than volume. Fifteen studies (38%) covered time periods of greater than 5 years. Just over half (8/14) of the studies for specific conditions or procedures, in which case numbers will be smaller, utilised data from more than 5 years compared with 28% of studies where all conditions were included. Unsurprisingly, there is a marked difference in sample sizes between studies including all CHD conditions compared with those including highly selected populations based on single conditions or procedures and single-centre studies. Where reported, there are also differences in the centre volumes with studies on specific conditions or procedures having lower-volume thresholds. Among these 14 studies, nine included centres with 20 or fewer cases per year. For studies including all CHD cases, 10 out of 25 had centres with ≤ 200 cases per year and five of these had < 100 cases per year, including two studies with very low-volume centres with < 10 cases per year. 41,28
The primary end point for measuring mortality outcome was within the post-operative period, with 31 out of 37 (84%) studies reporting in-hospital mortality. Seven studies measured mortality at 30 days and four studies measured mortality up to 1 year.
Study analyses: adjustment for confounders and risk
The CHD population is highly complex and varied in terms of both the range of conditions it encompasses and the associated severity and risk of mortality for different conditions. Three CHD risk scores that take account of surgical complexity and associated risk of mortality have been developed for risk adjustment in CHD: Society of Thoracic Surgeons–European Association for Cardio Thoracic Surgery (STS-EACTS), Risk Adjusted classification for Congenital Heart Surgery (RACHS-1) and the Aristotle Complexity score. A detailed description of each score is provided in Appendix 4. Other risk scores do exist for CHD, but have not been used in the studies that have been included in the review. Outcome is also dependent on a range of patient, demographic and service factors that need to be taken into account in study analyses. We extracted details of all covariates used in the analyses of each included study and identified 67 different types of covariate (excluding subgroups within types). Thirty-one (79%) of the studies included a covariate that accounted in some way for the patient’s condition. Of these, 18 used a risk score for surgical complexity, eight a condition descriptor, three a procedure descriptor and two an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic code. Of other covariates, the most commonly used were age (18/39), comorbidity (14/39), sex (13/39) and ethnicity (9/39). Some studies of highly selected groups of patients did not always adjust for common covariates such as complexity (where a single condition was the subject) or age (where the study population was all neonates).
A detailed summary of the 32 covariate types reported in at least 2 of the 39 included studies is provided in Appendix 4.
Overview of main findings
We have summarised the main findings of each included study in terms of whether or not a measurable effect of volume on mortality outcome was reported. Effect is defined as an inverse relationship between volume and mortality, that is increasing volume results in decreasing mortality (or, conversely, low volume is associated with higher mortality). Where survival is reported, the effect relationship is increasing survival with increasing volume and vice versa. Kazui et al. 28 reported an inverse relationship between volume and mortality with higher mortality in low-volume centres, and Sakata et al. 38 found no relationship between volume and morbidity for the CHD subgroup. Both reported wide variation in mortality rates across all volumes and both concluded that risk-adjusted measures are needed to explore this relationship more robustly.
Relationship between volume and mortality for all coronary heart disease conditions
We identified 19 studies that examined the relationship between centre volume and mortality. A single-centre study by Arenz et al. 9 examined unit performance over 4 years using a composite measure including mortality, but did not directly test the relationship between volume and mortality. Thirteen studies examined this relationship as the primary objective of the study, two examined the effect of adult CHD operative management by paediatric services or surgeon and two examined the relationship as part of a more general study to identify risk factors for mortality or surgical performance. One study examined the relationship between volume and mortality and the impact of specialist nursing skills. A summary of the findings is given in Table 5. Note that the estimates of effect size are not comparable between studies because of the different inclusion criteria (procedures, time periods, institutions), different definitions for volume categories, different definitions for mortality outcomes and adjustment for different confounding factors. Detailed analysis for each included study is available in Appendix 3.
| Study | Adjusted analysis of volume and mortality/survival outcome | Notes and headline message | |
|---|---|---|---|
| No effect detected (estimate of effect size and/or p-value) | Effect detected (estimate of effect size and/or p-value) | ||
| Arenz et al. 20119 | N/A | Basic and comprehensive performance score increased from 100% at baseline to 124.9% and 132.9% respectively. Volume increased from 407% to 487% over the same time period | Composite measure of performance including mortality showed performance over 3 years maintained despite increasing complexity and volume |
| Bazzani and Marcin 20078 | Continuous
|
Effect weaker using new expanded data set than replicated analysis of four previous studies. Effect lost by removing single highest-volume centre. Scatterplot of volume vs. outcome showed no clear cut-off For each 100-patient increase in annual volume, there was a 13.9% decrease in the odds of dying |
|
| Dinh and Maroulas 201018 | Mortality
1990–4: p = 0.016 1995–9: p = 0.043 2000–4: p = 0.045 |
Modelling study. Inverse relationship between volume and mortality. Small and medium-sized centres had higher mortality than high-volume centres In small and medium-sized centres, the smaller the volume, the higher the risk of dying |
|
| Gray et al. 200321 | All patients Volume/mortality: ORs = 0.24,a 0.12,b 0.32c (p = 0.0001) |
Comparison between four centres in 1 year Differences in mortality in centres was not consistent with smaller-volume centres, having lower mortality than the highest-volume centre |
|
| Hickey et al. 201022 | Volume/mortality: OR 0.93/increase of 100 cases, 95% CI 0.90 to 0.96 | Also looked at effect of specialist nursing staff For each 100-patient increase in annual volume, there was a 7% decrease in the odds of dying |
|
| Kazui et al. 200728 | Newborns: OR 2.20, 95% CI 0.95 to 5.09 Infants: OR 3.69, 95% CI 2.02 to 6.73 |
Higher mortality in lowest-volume centres than in highest-volume centres for subgroup of cardiothoracic procedures No adjustment for risk |
|
| Oster et al. 201133 | p = 0.41 low risk; p = 0.067 high risk | SMR calculated from previous performance. Stratified cases no significance in low-risk cases, borderline for high risk Previous hospital mortality was more significantly associated with future mortality than volume, indicating that factors other than volume have an effect |
|
| Pasquali et al. 201235 | Continuous
|
Complex analysis comparing cases with and without complications. Association highest in cases of highest surgical risk Mortality greatest in low-volume centres for all cases and those with complications |
|
| Sakata et al. 201238 | Pearson’s correlation coefficient Newborns: –0.108 (p = 0.273) Infants: –0.151 (p = 0.149) |
No relationship between volume and mortality for subgroup of paediatric cardiothoracic procedures
No adjustment for risk |
|
| Vinocur 201341 | OR 0.84/increase of 100 cases, 95% CI 0.78 to 0.90; p < 0.0001 | Inverse relationship for each 100 cases added to volume. 10-fold decrease in mortality in teaching hospitals over time For each 100-patient increase in annual volume, there was a 16% decrease in the odds of dying |
|
| Welke et al. 201042 | Only 8% of hospitals had minimum case load required to detect a 5% difference in mortality | Compared case volumes with thresholds needed to detect 5% and doubling a decrease in mortality Paediatric cardiac surgery operations are performed too infrequently or have mortality rates that are very low. Mortality rates are a poor measure for comparing hospital performance |
|
| Welke et al. 200943 | Low-difficulty operations: p = 0.29 | Difficult operations (Aristotle score > 3)
|
There is no relationship between volume and mortality for low-difficulty operations but mortality decreases as volume increases for complex procedures |
| Welke et al. 20086 | Small/medium hospital vs. large hospitals OR 1.85, 95% CI 1.56 to 2.20 vs. OR 1.48, 95% CI 1.24 to 1.77 respectively | Age and complexity better predictors of mortality than volume Mortality rates significantly better for hospitals performing > 200 operations per year, but volume–mortality relationship was not linear with variability in different volume groups |
|
| Welke et al. 200644 | Volume not predictor of mortality; c-statistic 0.55 | Mortality most associated with case-mix and not volume | |
| Karamlou et al. 200826 | Non-paediatric vs. paediatric surgeons
|
Study looked at adult CHD surgery by paediatric surgeons Adult patients operated on by paediatric surgeons have lower mortality and this decreases further as surgeon volume increases |
|
| Kim et al. 201129 | Total CHD volume. High volume (≥ 400 cases) vs. low volume (< 200 cases): adjusted OR 1.6, 95% CI not reported | Adult volume high vs. low adult CHD surgery volume (< 10 cases annually)
|
Study looked at adult CHD in paediatric hospitals Adult CHD patients have lower mortality in the highest-volume group compared with two lower-volume groups |
| Studies identifying predictors of mortality or other indirect measures | |||
| Chang et al. 20067 | No difference for post-discharge mortality | Total mortality (in hospital and post discharge)
|
One risk factor for mortality examining a range of variables Lower-volume hospitals had higher mortality for all cases combined (in hospital and post discharge), but no difference in post-discharge-only deaths |
| Seifert et al. 200739 | Highest vs. lowest-volume quartile
|
Main objective was to assess effect of sex on mortality. Volume used as one of a number of covariates Mortality lower in highest-volume centres and may be one factor influencing outcome |
|
A number of studies detected no effect of volume on mortality. Oster et al. 33 calculated standardised mortality rates from previous performance and found no strong effect with borderline significance for all cases and high-risk cases and no effect for low-risk cases and concluded that it is whole-hospital performance, rather than volume, that produces impact on outcome. Welke et al. has conducted a series of studies examining the relationship between volume and mortality. The earliest study44 found no effect of volume on mortality although complexity increased and mortality decreased over the study period. The 2008 study6 found high-volume hospitals performed better than other groups, but complexity (RACHS-1) and age were better discriminators for mortality than volume, which was only just significant (receiver operating curve area 0.5). This general relationship was repeated in the 2009 study,43 which found an inverse relationship between volume and mortality, but this was only significant for high-risk groups with no effect in low-risk groups. The most recent study42 examined the threshold needed to detect changes in mortality as a consequence of differences in volume and found that mortality was too low or individual procedures too rare to detect the true relationship between volume and performance.
Two studies included volume as a variable in broader studies designed to identify predictors of mortality in CHD, but were not designed to explore this relationship as a primary objective. Chang et al. 7 analysed the effect of a range of variables and found no association between volume and mortality for post-discharge deaths, but an association when in-hospital deaths are included, and that age and procedure type were better predictors of mortality risk. The objective of the study by Seifert et al. 39 was to examine the influence of sex on outcome. Volume was used as a covariate in the analyses and an association between volume and outcome was detected, but this was one of a number of variables that were also associated with increased risk of mortality. Both of these studies highlight that volume is just one factor influencing outcome.
Of studies reporting an effect of volume on outcome, Bazzani and Marcin8 conducted a comprehensive set of analyses replicating four previous studies and developing a new model using a larger, more contemporary data set. A significant effect was found when volume was analysed as both a categorical and continuous variable, with mortality decreasing for every 100 additional cases per year. However, the effect detected was weaker than that reported in the previous studies and after sensitivity analysis, in which the single highest-volume hospital was removed, the effect was reduced for the continuous analysis and disappeared for the categorical analysis. Dinh and Maroulas18 conducted a modelling study and found an inverse relationship between volume and mortality that held for both low- and high-risk patients in low- and medium-volume units and suggested this relationship was strong enough that it should be possible to identify a threshold for unit size. The study by Gray et al. ,21 published in 2003, used data from a single year 10 years previously (1992). The study found no consistent relationship between volume and outcome in four centres with variable rates in the three lower-volume centres compared with the highest, suggesting there is also a centre effect but the relevance to current services is questionable. Pasquali et al. 35 conducted a complex set of analyses examining the relationship between volume and mortality and mortality in patients with complications. An effect was found in the relationship between volume and mortality in all patients and was stronger in those with complications. There was no difference in complication rates between high- and low-volume centres but low-volume centres had higher mortality in patients with complications, suggesting high-volume hospitals may be better at managing complications. Vinocur41 analysed data from a 25-year period (1982–2007) and found an inverse relationship between volume and mortality for every 100 extra cases per year. However, the study also found that mortality decreased 10-fold over this time period, indicating improving care and that individual centre effect contributed more than volume to the risk model. A number of studies used data over a time period of 10 years or more and, while these remain of value in contributing to the evidence base, it is also the case that over time there has been substantial change in the management of CHD so relevance to current service provision or performance needs to be considered when interpreting results.
Two studies examined the effect of managing adult CHD in paediatric services or by paediatric surgeons. The study by Karamlou et al. 26 found that adults operated on by paediatric heart surgeons had lower mortality rates than those operated on by non-paediatric heart surgeons and that mortality was also associated with surgeon volume. Kim et al. 29 examined the relationship between volume and mortality among adults undergoing operation in paediatric centres. They found no effect of total CHD volume on mortality, but did find that mortality was lower in centres that had higher volumes of adult cases.
Relationship between volume and mortality for all selected conditions or procedures
We identified 14 studies of the relationship between volume and mortality for selected conditions or procedures. The findings are summarised in Table 6.
| Study | Adjusted analysis of volume and mortality/survival outcome | Notes and headline message | |
|---|---|---|---|
| No effect detected (estimate of effect size and/or p-value) | Effect detected (estimate of effect size and/or p-value) | ||
| Arnaoutakis et al. 201210 | 30-day mortality
|
Heart transplants including non-CHD (CHD only 3% of cases) Mortality lower in high-volume centres at 30 days and 1 year. High-risk patients had higher mortality in low-volume centres, suggesting higher volume moderates the effect of risk |
|
| Berry et al. 200712 | Highest vs. lowest mortality rate (1.7% vs. 1.1%) OR 1.59, 95% CI 0.2 to 12.7 | Surgery for VSD is a subgroup in a study of common paediatric operations. No relationship between volume and mortality, but VSD surgery concentrated in children’s hospitals resulted in better outcome | |
| Berry et al. 200613 | Low volume vs. high volume: OR 3.1, 95% CI 1.1 to 8.3 | HLHS. Effect in low (one to three cases per annum) quartile. Operation at teaching hospital was also an effect Comparing mortality in four volume groups found mortality was worse in the lowest-volume group but no difference between the other three groups |
|
| Checcia et al. 200515 | Surgeon, p = 0.312 | Volume r 2 = 0.18; p = 0.02 Survival increased 4% (95% CI 1% to 7%) per 10 additional procedures |
The Norwood procedure. Number of cases per surgeon too small to detect an effect For each additional increase in volume of 10 cases per year there is a 4% improvement in survival |
| Davies et al. 201116 | Low- vs. high-volume centres: OR 1.60, 95% CI 1.13 to 2.24 Medium- vs. high-volume centres: OR 1.24, 95% CI 0.92 to 1.67 |
Heart transplants including non-CHD Measure is observed vs. expected mortality In low- and medium-volume centres mortality is worse than expected when compared with mortality in high-volume centres |
|
| Hirsch et al. 200823 | Significant inverse associations for institutional volume/in-hospital mortality for the Norwood procedure (p ≤ 0.001) and ASO (p = 0.006) | The Norwood procedure vs. ASO. Inverse relationship of volume to mortality As volume of cases per year increases mortality decreases |
|
| Hornik et al. 201224 | Continuous lower centre volume associated with higher inpatient mortality (p = 0.03). Surgeon volume associated with higher inpatient mortality (p = 0.02) Categorical lowest vs. highest category: OR 1.56, 95% CI 1.05 to 2.31; p = 0.03 Lowest vs. highest surgeon volume: OR 1.6, 95% CI 1.12 to 2.27; p = 0.01 |
The Norwood procedure. Analysed centre and surgeon volume. Effect held for both Both high-volume centres and high-volume individual surgeon case load have lower mortality than low-volume centres and low case load surgeons |
|
| Karamlou et al. 201027 | Centre volume on adjusted mortality: p = 0.17 for the Norwood procedure and p = 0.07 for PAIVS Surgeon total case volume: p = 0.4 for the Norwood procedure |
Centre volume impact on adjusted mortality: p < 0.001 for TGA and IAA Surgeon total case volume: p = 0.002 for TGA |
Complex CHD (four groups). Centre and surgeon volume. Variable performance – good outcomes for one group did not translate to all groups No relationship between centre or surgeon volume for the Norwood procedure and PAIVS. but higher-volume centres had lower mortality for TGA and IAA and higher surgeon volume had lower mortality for TGA only |
| McHugh et al. 201030 | Stage 2: medium volume vs. highest and stage 3: low volume vs. highest, not significant but no values given | Stage 1
|
HLHS. Longitudinal study, so it also looked at early vs. late-era surgery. Late era also had an effect A complex pattern emerges with higher mortality in both low- and medium-volume centres compared with high-volume centres for stage 1, but mixed results for stages 2 and 3. Mortality reduced over time independently of volume |
| Morales et al. 201032 | OR 0.07, 95% CI 0.02 to 0.24 | Use of VAD – patients other than CHD. Effect was in large-volume teaching hospitals vs. rest Placement of VAD at large-volume teaching hospitals reduces the risk of mortality when compared with lower-volume and non-teaching hospitals |
|
| Pasquali et al. 201234 | Volume as continuous variable p = 0.04; categorical lowest vs. highest category > 20; OR 1.54, 95% CI 1.02 to 2.32; p = 0.04 | The Norwood procedure. Volume mortality effect, but when volume adjusted between-centres, variation remained Overall higher volumes are associated with lower mortality, but there is variation in individual centre mortality rates that do not reflect this relationship |
|
| Studies identifying predictors of mortality | |||
| Dean 201317 | Stage 2 and 3 palliation | Stage 1 palliation
|
HLHS. Volume split is top five vs. the rest (42) Volume is one variable examining a range of risk factors for mortality For stage 1 palliation mortality is lower in the highest-volume centres, but mortality in medium-volume centres is not investigated. No relationship between volume and mortality for stages 2 and 3 |
| Petrucci et al. 201136 | OR per 10-unit increase in average volume = 0.98, 95% CI 0.85 to 1.13; p = 0.78 | BTSP. Total case volume and BTSP volume included No relationship between volume and mortality was found |
|
| Tabbutt et al. 201240 | Mortality – no effect, but values not reported | Morbidity
|
The Norwood procedure. Centre and surgeon volume No relationship between volume and mortality was found, but lower-volume centres and surgeon procedures were associated with higher rates of morbidity outcomes and LOS |
Studies of the volume and mortality relationship were predominantly centred on complex and relatively rare conditions and associated procedures (9/14 studies). In general, these studies did demonstrate an effect of volume on mortality, but the relationship is not straightforward. In two studies of HLHS palliation, Dean17,50 found an effect for stage 1 palliation but not for stage 2, and McHugh et al. 30 also found that the association between low volume and higher mortality was strongest for stage 1, with variable effects for stages 2 and 3. The study by Karamlou et al. 27 looked at volume and outcome for five conditions and procedures, and found that the volume and outcome effect was present for only one group (TGA). Four of the six studies on the Norwood procedure found an association between volume and mortality15,23,24,34 and two found no association,27,40 although Tabbutt et al. 40 did find that low volume was associated with higher morbidity and LOS in hospital. A single study identifying risk factors for mortality after BTSP found no relationship between volume and mortality, with condition severity and weight being the most significant predictors for mortality.
One of the advantages of using these highly selected and standardised patient groups is that the potential effects of other factors on outcome may also be identifiable. Indeed the findings of these studies highlight this complexity. Highly specialised and complex surgery requires clinical expertise. Four studies also measured the effect of individual surgeon volume. For the Norwood procedure, Hornik et al. 24 reported decreasing mortality with increasing surgeon volume, while Tabbutt et al. 40 and Checcia et al. 15 found no effect of surgeon volume, although in the latter study it was acknowledged that the number of cases per surgeon may have been too small to detect an effect. Karamlou et al. 27 found increasing surgeon volume improved outcome, but only for TGA and not for other groups within that study.
These studies also acknowledged the effect that individual institutions may have on mortality. The study by Karamlou et al. 27 on five different but complex patient groups found that there was wide between-centre variation in performance for the different conditions and that good performance for one condition was not necessarily translated to all conditions within a centre. McHugh et al. 30 also identified substantial between-centre variation and found that, although, overall, mortality was higher in low-volume centres, some low- and medium-volume centres were also achieving good outcomes. Similarly, the study by Pasquali et al. 34 identified an effect of volume on outcome, but volume accounted for only 14% of between-centre variation in risk of mortality, indicating that there is a range of other factors that are also having an impact.
Included studies also demonstrate the potential effects of changes in clinical advances and service provision. The study by McHugh et al. 30 used data over a 10-year period and a dichotomised analysis of early- and late-era surgery found that mortality improved over time. There has also been a move to centralisation or regionalisation of services, which is reflected in these studies. The primary objective of the study by Berry et al. 13 was to assess the impact of management at teaching compared with non-teaching centres and found over a 3-year period that stage 1 palliation surgery for HLHS in non-teaching hospitals reduced from 20% to 2%. In another study, Berry et al. 12 explored the relationship between volume and outcome for four common paediatric operations including repair of VSD. For this subgroup no effect was detected between volume and mortality but VSD surgery was much more centralised to specialist children’s hospitals than the other three operations, which the author considered may have provided a protective effect. A study by Morales et al. 32 of patients receiving a VAD found an effect of volume on mortality where the comparator was not just high volume but high-volume teaching hospitals compared with other centres. We included two studies of cardiac transplant and both identified lower mortality rates in high-volume hospitals. However, one study included only adults,10 the other16 focused on children, and both included a range of conditions other than CHD. These studies add to the already substantial evidence on centralisation of transplant services but are of limited relevance to the evidence base on specialist paediatric CHD service provision.
Relationship between proximity and distance on mortality and volume on non-mortality outcomes
The provision of good CHD surgical care requires not just surgical expertise but also provision of the associated services that provide pre- and post-operative care. It has been suggested that the proximity of these services, for example by having them all available on one site rather than having to transfer patients at critical times for specialist care, may also be a factor that contributes to outcome in CHD. In addition, although the emphasis of volume on outcome is dominated by mortality, it can be argued that there may also be an effect on non-mortality patient outcomes such as morbidity and quality of life and service consequences such as LOS in hospital and associated costs. We identified seven studies that explored relationships other than volume and mortality for CHD. The findings of these studies are summarised in Table 7.
| Study | Impact on outcome | Notes and headline messages | |
|---|---|---|---|
| No effect detected (estimate of effect size and/or p-value) | Effect detected (estimate of effect size and/or p-value) | ||
| Effect of proximity of associated services or distance from specialist centres | |||
| Burstein et al. 201114 | No overall difference between CICU and PICU: OR 0.88, 95% CI 0.65 to 1.19 | For STS-EACTS 3: OR 0.47, 95% CI 0.25 to 0.86 in favour of CICU | Paediatric cardiac intensive care unit vs. other ICUs Overall, there was no relationship between mortality rates and the type of ICU caring for patients but for one group of mid-complexity cases, where mortality was lower in paediatric ICU |
| Eldadah et al. 201119 | Mortality declined from 3.5% to 0.8%; p < 0.05 | Paediatric cardiac intensive care unit before and after. Decrease in mortality and morbidity Outcomes following paediatric cardiac surgery improved after the introduction of a dedicated paediatric cardiac ICU |
|
| Karamlou et al. 201325 | Highest category of volume for ECMO: OR 0.51, 95% CI 0.30 to 0.87; p < 0.01 | ECMO case volume. Lowest mortality in patients requiring ECMO associated with highest ECMO volume centres Patients requiring ECMO have a lower mortality rate if they are cared for in units that manage a high volume of ECMO cases |
|
| Fixler 201220 | Mortality not significantly related to distance 50–100 miles vs. < 50 miles: HR 0.83, 95% CI 0.57 to 1.22; for > 100 miles vs. < 50 miles: HR 1.08, 95% CI 0.86 to 1.36 | Distance to cardiac centre not related to unadjusted first-year survival The distance to a specialist cardiac centre does not appear to have any impact on mortality following CHD surgery |
|
| Pinto et al. 201237 | Mortality for those living 90–300 minutes away vs. those < 90 minutes away: HR 2.1; 95% CI 0.7 to 5.7 | Effect detected for adverse events in patients 90–300 minutes from centre, but not for patients < 90 minutes or > 300 minutes The distance to a specialist cardiac centre does not appear to have any impact on mortality following CHD surgery |
|
| Effect of volume on non-mortality outcomes only | |||
| Benavidez et al. 200711 | Complications – increased risk of death if complications: OR 2.4; p < 0.001 | High-volume hospitals had more complications, higher complexity but lower mortality Patients with complications after CHD surgery have a higher mortality rate, but this is reduced if they are cared for in high-volume centres |
|
| Mery 201431 | Complications – highest-volume quartile lower incidence of chylothorax: OR 0.49, 95% CI 0.42 to 0.58 vs. lowest volume | Chylothorax complication Patients cared for in lowest-volume centres are more likely to develop this specific complication when compared with the highest-volume centres |
|
We identified two studies that specifically looked at proximity of associated specialist services and both examined the effect of a specialist cPICU. In a multicentre study, Burstein et al. 14 compared care in cPICU with other intensive care units (ICUs) and found no effect on mortality except for STS-EACTS level 3 cases and primarily in patients undergoing atrioventricular repair and ASOs, suggesting that potential benefits may only be applicable to specific patient groups. Eldadah et al. 19 conducted a single-centre before-and-after study evaluating the impact of introducing a cPICU and found a reduction in mortality and a bigger effect in reducing morbidity (wound infection and chest re-exploration).
One study by Karamlou et al. 25 explored the relationship between centre extracorporeal membrane oxygenation (ECMO) case volume and mortality in paediatric patients requiring ECMO and found a decreased mortality rate in the highest-volume ECMO centres, supporting the concept of regionalising highly specialist services.
In a related study discussed earlier, Hickey et al. 22 examined the effect of volume on not only mortality but also ICU nursing staffing and skill mix. They found no relationship between nursing staffing and skill mix and mortality but did find that high nursing workload was associated with volume. They concluded that it is possible that nursing staffing levels may already be above the threshold needed to detect an effect on mortality.
Two studies examined the relationship between distance from specialist cardiac centres and mortality20,37 and both found no relationship between distance and mortality, although Fixler20 found higher mortality in specific geographical areas where there was no identifiable cardiac centre. This effect may be as dependent on demographic factors as distance. Pinto et al. 37 did find a higher rate of adverse events in one group, although this was the mid-distance (and not nearest or furthest) and the paper raised the possibility that the effect may be a consequence of follow-up and monitoring policies related to proximity to a centre rather than distance itself.
We found two studies in which the primary outcomes in relation to volume were complication rates. The study by Benavidez et al. 11 primarily looked at complication rates, although mortality rates were also measured. The main findings were that higher-volume centres had higher complication rates but lowest-volume centres had higher mortality rates. They acknowledged that this may be a consequence of better reporting of complications in high-volume centres but also suggested that better mortality outcome, despite higher complication rates in high-volume centres, may be because high-volume centres are better at managing and rescuing patients with complications. The study by Mery31,49 looked at risk factors for one specific complication – chylothorax – and found a relationship with a reduced rate of chylothorax in the highest-volume centres compared with other centres. Nevertheless, the same study also observed that some low-volume centres had comparable complication rates to high volume, again highlighting variability between centres.
A small number of the other studies we have included also examined non-mortality outcomes. In addition to the Eldadah et al. 19 and Pinto et al. 37 studies mentioned above, Tabbutt et al. 40 and Davies et al. 16 both found lower complication rates in high-volume centres following the Norwood procedure. Burstein et al. ,14 Berry et al. 12 and Pasquali et al. 35 all found no association between volume and complication rates. Karamlou et al. 26 and Davies et al. 16 both found that low-volume centres were associated with longer LOS. Two studies26,32 also assessed costs, and both found a relationship of higher costs associated with low-volume centres. Mery31 found that chylothorax complication increased both LOS and costs. Although these variables were not explicitly tested in conjunction with volume in this study, this does provide some indication, given the relationship of lower complication rates in high-volume units, that there is likely to be an association. There is a more substantial literature on costs and volume, but this was outside the scope of our review.
Chapter 7 Discussion
Summary of the evidence about the relationship between volume and outcomes
The evidence reviewed did not include any UK-based studies and is predominantly based on outcomes in paediatric patients. Overall, we have found that although the evidence does demonstrate a relationship between volume and outcome in the majority of studies this relationship is not consistent. Instead there is a mixed picture with both effect and no effect being reported. Studies on single conditions or procedures were more likely to identify an effect of volume on mortality but, given that the focus of these studies was populations of patients with complex conditions and associated surgical procedures that require highly specialised care and expertise, this in itself is unsurprising. The findings from these studies were not unequivocal as even within these highly selected groups there was considerable variation in effect depending on procedure type and individual centre performance. What these studies do indicate is the potential value of centralising or regionalising highly specialised services for very rare and complex cases. However, it cannot be assumed that comparable effects can be achieved for a much broader range of conditions and, therefore, used to define CHD centre volume. It is possible that surgeon volume may be as important as centre volume for these complex cases.
The findings from studies that did consider broader CHD populations were more equivocal. In some studies where an effect was identified, the effect was weak or only demonstrable for specific subgroups of patients. There was no clear indication that the evidence for the volume and mortality relationship was substantially stronger than the evidence for a no effect relationship in these broader groups. The findings further highlight the complex relationship between volume and outcome and the range of other factors which also have an effect. Some of these, such as condition severity, are well established but the effect of association of processes, systems and individual clinical effects on outcome remain unknown.
We also searched for evidence from studies on adult CHD, but this yielded only three papers. One of these studies was concerned exclusively with cardiac transplantation for a range of conditions, not just CHD, so is of limited value other than to provide more general evidence of the potential value of centralising specialist services. The main focus of the other two studies was the effect of surgeon type and both found that adult CHD patients had better outcomes when operated on by paediatric surgeons in specialist children’s centres. Karamlou26 found that outcome was associated with surgeon volume and Kim et al. 29 found a similar association with adult procedure volume indicating the influence of expertise on outcome.
The previous systematic review conducted by Ewart2 included studies published up until 2009. We have included studies considered by that review in this rapid review together with related studies published from 2009 to March 2014. The review by Ewart2 included seven studies and concluded that, while the evidence did suggest there is a relationship between volume and outcome, it is likely that volume is a surrogate marker that encompasses other processes and system factors, the effects of which are unknown. The additional evidence included in this review primarily adds further to our understanding of the complexity of the relationship between volume and outcome. While there is now a larger number of studies reporting a relationship between volume and outcome, these studies also increase the evidence that this is unlikely to be a simple, independent and purely directly causal relationship. The effect of volume on outcome relative to the effect of other, as yet undetermined, health system factors remains a complex and unresolved research question.
Summary of the evidence about the relationship between proximity and outcomes and volume and non-mortality outcomes
We also attempted to identify studies that explored factors related to influencing outcomes in CHD other than the relationship between volume and mortality. This yielded only a small number of relevant papers. Two studies found a benefit in terms of reducing mortality and morbidity in patients cared for in specialist ICUs. One study identified lower mortality for patients requiring ECMO who were cared for in high-volume ECMO units. Two studies on distance to specialist cardiac care found no relationship to mortality. Similarly, we found only two studies in which the primary objective considered the effect of volume on complications. However, a small number of the studies that examined the volume–mortality relationship also measured morbidity as a secondary outcome. Such a small number of relevant studies does not provide a robust evidence base on related factors but collectively they do highlight that the overriding emphasis of research studies on CHD services has been dominated by measurement of the relationship between volume and mortality and mainly short-term, in-hospital mortality. Care is the product of a complex set of processes, of which volume of activity in any given centre or unit is only one contributor. There appears to be relatively little evidence from studies that attempt to measure the effect of related processes on outcome. The consequences of care, and hence outcomes, are also greater than may be captured by data on short-term mortality. Long-term mortality is also important, as are a range of other important short- and long-term outcomes for survivors including morbidity (for example, complications) physical and neurological functioning and quality of life, and service consequences such as LOS and costs, that seem to have received scant attention. As a consequence, the available evidence base that can inform CHD service design is seriously limited and does not reflect the complex features and relationships that contribute to service provision.
What are the issues that have emerged from the evidence?
We have not conducted a systematic review but in assessing a broader topic range and more current literature we have identified some key themes.
-
There are a range of factors which influence mortality in CHD, and centre volume is only one of them. In our data extraction we recorded variables within studies that were also identified as associated with mortality. This process revealed a wide range of patient, demographic and service factors that also have an impact on outcome. The most influential risk factor for mortality by far is the severity of the condition and the associated surgical complexity needed to treat that condition. Where an effect of volume on mortality was measured, in general, this tended to be greater in high-risk patients, as illustrated by the studies on complex single conditions. This is further supported by some of the studies that included broader CHD populations. It is reasonable to assume that complex high-risk surgery requires high-level surgical expertise. A small number of studies have attempted to try to disentangle the effects of individual surgeon performance on outcome but with mixed results. This requires further exploration as this complex relationship of what has an effect – a high volume of complex procedures in a centre or a high volume of complex procedures by an individual surgeon – is still unclear. Furthermore, there is some evidence27 that it cannot be assumed that a high level of technical competence in one complex procedure translates across a range of conditions.
-
Medicine moves forward and clinical advances, training, increasing expertise and changes in service provision mean outcomes for CHD have also changed over time. Five studies that analysed data over long time periods (≈ 10 years) measured changes in mortality over time and found that, irrespective of other factors including volume, mortality decreased despite increasing complexity8,18,30,41,44 illustrating ongoing clinical improvement. What this also means is that the relevance of findings from historical studies or more recent studies that have used historical data will not reflect current care and clinical improvements, so relevance to contemporary services needs to be considered. This observation also has implications for future research. The most recent study by Welke et al. 42 attempted to establish the case volume thresholds needed to detect changes in mortality and concluded that some individual procedures occurred too infrequently or mortality rates were too low to reliably use mortality as a measure of between-centre performance. If clinical advances continue to improve survival, this principle will need to be borne in mind.
-
Although aggregated data may show a difference in mortality rates between low- and high-volume centres, such aggregation may mask between-centre variation. The studies by Gray et al. ,21 Pasquali et al. ,34 Karamlou et al. 27 and McHugh et al. 30 all identified variation between centres, with some low- or medium-volume centres performing equally as well as those with high volume. These studies acknowledged that there are likely to be other centre effects such as training, management protocols, expertise, teaching hospitals, availability of services, composition of care teams and quality programmes that influence outcome. As a result it is unclear whether it is volume or these other effects that are influencing outcome.
-
The evidence base available to guide UK decisions on service design and configuration for CHD is dominated by retrospective and uncontrolled studies conducted within the USA. A noteworthy absence is the lack of any relevant large, well-designed UK multicentre studies. The extent to which the reported findings are generalisable and relevant to the UK setting is therefore limited. In the USA, services are organised very differently to the UK. Key differences include geography and, therefore, distances to specialist care; multiple providers of health care, which means variation in organisation of services, for example numbers of units within different counties and states; and complex health service financing models. Many of the studies have analysed centres with very low volumes of cases – for very rare complex cases the volume of cases may be less than five a year and for broader CHD services some studies have included centres treating fewer than 20 cases a year.
-
Elsewhere and in line with other specialist services there has been a move to centralisation or regionalisation of CHD services, particularly in Europe. 51,52 In the UK, CHD services for children are already regionalised, so evidence on the relationship of very low-volume centres on mortality has little relevance to decision-making about services which are already highly centralised. However, CHD services for adults are less centralised, so decision-making relating to service provision may be informed by evidence relating volume and outcomes.
-
It is axiomatic that, with this centralisation, there is also a corresponding increase in volume as more cases are concentrated in fewer centres but centres will also be characterised by the range of factors associated with service provision discussed previously. It remains unclear whether the impact of volume on outcome is largely a consequence of higher-volume units organising and providing a complex service and high-quality service with all the right components that would be expected to reduce risk, or an independent factor directly related to the advantages of dealing with a larger number of cases. For example, staff may have more experience of specific procedures and potential complications. It is the individual and combined effects of these complex factors on clinical outcomes for patients that remain to be unpicked. Without this better understanding the appropriate interpretation of the observed volume–outcome relationship remains unclear. There is also a lack of evidence about the effects of service factors such as proximity to specialist services and the impact of care on outcomes other than mortality.
-
Despite the growing number of studies on the relationship between volume and outcome, few studies have suggested what the optimum size of a CHD centre in terms of volume should be. Fewer than half of the included studies analysed volume as a continuous variable (14/35 relevant studies), which would provide the most robust evidence from which to consider volume thresholds. Analyses conducted with volume as a categorical variable carry several limitations in informing decisions about volume thresholds in terms of both decisions about within study thresholds and the questionable robustness of the findings. This is particularly the case when comparisons have been made between very high- and very low-volume centres only. Dinh and Maroulas18 suggested that the inverse relationship between volume and outcome detected in their modelling study on 10 years of data was sufficiently robust to allow calculation of volume thresholds. However, these authors did not go as far as identifying what this should be. Hirsch et al. 23 suggested that a reasonable threshold for referral of children requiring the Norwood procedure is centres doing at least 20 procedures a year and 10 procedures a year for ASO. Bazzani and Marcin8 constructed scatterplots of volume against mortality and found no obvious threshold for centre volume. The review by Ewart2 considered the data presented by Welke et al. 6 and suggested a possible threshold of 200–250 cases per year. Welke et al. 6 clearly expressed the view that volume is likely to be a surrogate for the processes and characteristics of care systems that produce outcomes and that centre-specific quality measures would be more informative than volume thresholds. Pasquali et al. 34 and Vinocur41 concurred with this view and suggested that service design decisions should be guided by a range of individual centre performance measures and not volume. There are consistent and clear messages within the literature we have reviewed about the danger of viewing volume in isolation. Furthermore, included studies also caution concerning the likely, but as yet poorly understood, interaction of volume with the numerous other clinical and structural dimensions that contribute to delivering high-quality services and, hence, good outcomes. Finally, questions still remain concerning what volume should be the item of consideration: is it whole-service volume, complex procedure volume or individual surgeon volume that should direct decisions?
Methodological limitations of the included studies
Quality assessment and methodological limitations
As this is a rapid review we have not conducted a quality appraisal of individual included studies. However, we have considered the collective methodological limitations of these studies in order to provide an overview of study quality and have assessed the usefulness of these studies in answering the research questions. Appendix 4 provides a simple summary of key items for each paper that relate to the usefulness of studies on CHD services. Items relate to whether or not studies have conducted analyses that have adjusted for the two key risk factors for mortality, severity/complexity and age, whether they are single-centre or multicentre studies and whether they included at least two CHD conditions or procedures. In summary, 37 out of 39 studies adjusted for severity, 28 out of 39 adjusted for age, although some studies on specific groups of patients were confined to specific age groups or, for example, neonates; 35 out of 39 were multicentre studies, with just three single-centre studies; and 25 out of 39 studies included a population with more than one condition or procedure.
Author assessments of study limitations
Many authors of included studies take great care to point out the methodological limitations of their studies and caution against overinterpretation of their findings. Included studies are predominantly retrospective and observational in nature. There were no prospective studies. Such design features make it very problematic when trying to establish a direct inverse relationship of cause (volume) to effect (mortality). Many of the source databases are limited in being primarily created for administrative purposes, for example claims data collection and billing. 6,17,23,26,29,42,50 As a consequence, we can have little confidence in the clinical coding,42 although several studies seek to ascertain accuracy by comparing the coding for diagnosis with the coding for the surgical procedure42 in order to establish internal coherence and consistency.
Information bias might be introduced through ‘miscoding of information provided, missing data, or misinterpretation of data’. 23 Incompleteness of data is considered problematic, for example even where records are available, large numbers of surgeon identifiers may be missing. 12 Other data sources were voluntary, which introduces problems of selection bias as they may be selective in their coverage27,36,41,43 or according to predefined membership or explicit criteria. 40 Changes or indeed inconsistency in institutional characteristics, such as coding for teaching status, may result in one hospital being coded differently across different points of an interrupted time series. 13 Welke6 considered that in large data sets errors in quality are likely to be random rather than systematic, although it could also be argued that for data on rare conditions errors may then be systematic.
A key concern of this report relates not simply to the surgical performance of different sized units but also to the personnel and structural characteristics of the observed surgical units. On these latter matters, administrative source databases have few contextual data to offer. 14 Important contextual details are thought to include institutional factors such as team composition, individual surgeon training and experience, type of facility (e.g. freestanding children’s hospital, general hospital), transfusion practices, infection control, and care pathways. 41 Indeed several commentators also bemoan the lack of even basic clinical contextual details such as certain anatomical features13 or accompanying non-surgical procedures. Critical details such as non-intervention, transfer to another institution and pre-operative mortality are frequently unavailable. 15 Furthermore, some clinical data features rely on subjective judgement, while perioperative details are frequently missing. 36 It is essential to recognise that not all in-hospital mortality will have an underlying surgical cause. 39
A further consideration occurs where the research question is deliberately prescribed, i.e. where data relate to a single institution, a single year or, as with a substantial proportion of studies, a single procedure. Data relating to a single institution are unlikely to be generalisable, particularly in the absence of details of the pattern of referrals to that location. 37 While analysing data from a single year circumvents concerns relating to structural changes or improvements in procedures over time,39 it carries the attendant danger of placing inordinate and inappropriate emphasis on an isolated time point. Finally, in the case of study reports of a single surgical procedure, the insights to be gained by a more extended examination of a discrete area of surgical practice involving typically more rare and complex conditions are outweighed, at least for the question that is the focus of this report, by neglecting overall surgical volume. Such studies thus provide a negligible contribution to the ‘evidence’ that relates to optimal volumes for entire CHD services.
The well-reported characteristic of paediatric cardiac surgery as covering a wide range of conditions and associated procedures poses a further threat to accurate interpretation. While it is helpful to consider an overall portfolio of procedures, the data for rare conditions necessarily involve small numbers of procedures. 14 Combining this statistical characteristic with the decreasing numbers of events of interest (i.e. mortality), particularly as cardiac surgical procedures improve, further limits the value of the reported results. 33,42 Numbers of procedures and numbers of deaths are particularly limited in low-volume units meaning that low-volume units are particularly vulnerable to even very small errors in the data.
With the ongoing development of methods for analysing the volume/outcome conundrum comes increasing recognition of the unsuitability of certain methods of investigation and analysis. For example, recent papers carry almost universal acknowledgement of the inappropriateness of any analysis that does not take into account any adjustments for risk38 and complexity. Handling data on number of procedures as a continuous, rather than a categorical, variable is now considered essential while approaches that seek to establish a threshold that represents a stepwise change in outcome are frequently criticised for being unsophisticated and misleading. 26
It would be negligent to overlook the considerable advances in methodology that have occurred during the time period charted by these included studies. The increasing sophistication of the tools that seek to score for complexity are just one such example, as documented in Appendix 4. However, while evolution and improvement of such tools and scores is to be welcomed such ongoing modification adds further to the complexity of a research area already characterised by considerable clinical heterogeneity. It is arguable whether or not the ongoing debates regarding the optimal configuration for volume/outcome are likely to be resolved in the absence of a comprehensive and accurate national database that provides sufficient information for risk stratification, complexity scoring and adequate contextual detail on clinical context as well as on structural and personnel-related factors.
Chapter 8 Conclusions
We have conducted a rapid review of the evidence on the relationship between volume and outcome, and other service factors and outcomes, for CHD. We found a large proportion of papers which analysed the relationship between volume and mortality for paediatric CHD surgery, but very limited evidence in relation to the other factors of interest or for adult populations. It is noteworthy that so much evidence is available in what is a relatively small clinical specialty. No UK-based studies or cross-country comparisons were identified. This review identified a substantial number of studies reporting a positive relationship between volume and outcome, but the complexity of the relationship and of the evidence underpinning it requires careful interpretation. The mixed picture emerging from the 39 included studies increases our understanding of the complexity of this relationship and highlights variation in both methods and findings across individual studies, the potential effects of a range of other factors that may interact with volume and influence outcome, and the methodological limitations imposed by the research approaches taken.
Even though our systematic, yet time-limited, searches have revealed a substantial number of studies on CHD outcomes, the existing data sources carry major limitations, particularly given the absence of information on clinical and service-related processes and outcomes, which are consistently recognised as important to patient care and safety. As a consequence, it is problematic to interpret the current evidence for the relationship between volume and outcome, as the impact this relationship may be having cannot be disentangled from the effects of other factors. The limitations of the rapid review approach mean that we could not consider conducting a meta-analysis of the evidence on volume and outcome, but this is an option that could be considered and which may further enhance the evidence available. Further evidence review of the broader fields of cardiac surgery (rather than just CHD) may also contribute to identifying some of the clinical and service-related processes and outcomes that may be relevant to CHD and provide a framework for future data collection and new studies.
The design, development and delivery of consistently good-quality and safe services require an understanding of the complex components and interactions that constitute a service and how these influence patient outcome. There is a clear evidence gap that needs to be addressed with regard to better understanding of the relationships between the wide range of organisational factors in CHD services; how these relationships can potentially predict a number of outcomes of relevance to patients and families; and the causal pathways between organisational factors and outcomes. The development and validation of clinical and administrative databases which can be used for observational studies of the relationship between organisational factors and outcomes would clearly be a valuable resource. There is scope to expand the National Institute for Cardiovascular Outcomes Research (NICOR) database to consistently collect information on a wider range of processes, organisational factors and outcomes related to quality of care that are not captured at present. It is our considered opinion that this should be the target at which future research efforts should be directed. This would support the design and conduct of UK studies and help address the clear lack of evidence relevant to service provision in the NHS.
Acknowledgements
We would like to thank the NIHR HSDR team for their support and the stakeholders and clinical experts who suggested evidence for the inclusion in the review.
Contributions of authors
Ms Janette Turner (Senior Research Fellow) contributed to proposal writing, undertook data extraction and led on the evidence synthesis.
Dr Louise Preston (Research Associate) contributed to the proposal writing, designed and ran the literature search, contributed to report writing and managed the project.
Dr Andrew Booth (Reader) undertook citation searches, contributed to the proposal writing, assessed evidence for inclusion in the review, proofread the final report, constructed summary tables, assessed the methodological limitations of the included studies and was the chief methodologist on the review.
Mr Colin O’Keeffe (Research Fellow) undertook data extraction and contributed to evidence synthesis through the production of summary tables and other key tables.
Mrs Fiona Campbell (Research Fellow) undertook data extraction and contributed to the construction of summary tables.
Dr Amrita Jesurasa (Honorary Clinical Lecturer in Public Health) undertook data extraction and report writing.
Dr Katy Cooper (Research Fellow) undertook the double-sifting and contributed to the proposal writing and construction of summary tables.
Professor Elizabeth Goyder (Professor of Public Health) was the senior lead on the project, contributed to the proposal writing and undertook the sifting of conference abstracts and construction of summary tables.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publications
There are currently no publications associated with this rapid review.
References
- Review of Children’s Congenital Cardiac Services in England. London: NHS Specialised Services; 2012.
- Ewart H. The Relation Between Volume and Outcome in Paediatric Cardiac Surgery. Oxford: Public Health Resource Unit; 2009.
- Harker J, Kleijnen J. What is a rapid review? A methodological exploration of rapid reviews in health technology assessments. Int J Evid Based Healthc 2012;10:397-410. http://dx.doi.org/10.1111/j.1744-1609.2012.00290.x.
- Holden J. The New Congenital Heart Disease Review: 17th update – John Holden. NHS England; 2014.
- Sampson M, Barrowman NJ, Moher D, Klassen TP, Pham B, Platt R, et al. Should meta-analysts search EMBASE in addition to MEDLINE?. J Clin Epidemiol 2003;56:943-55. http://dx.doi.org/10.1016/S0895-4356(03)00110-0.
- Welke KF, Diggs BS, Karamlou T, Ungerleider RM, Welke KF, Diggs BS, et al. The relationship between hospital surgical case volumes and mortality rates in pediatric cardiac surgery: a national sample, 1988–2005. Ann Thorac Surg 2008;86:889-96. http://dx.doi.org/10.1016/j.athoracsur.2008.04.077.
- Chang RK, Rodriguez S, Lee M, Klitzner TS, Chang RK, Rodriguez S, et al. Risk factors for deaths occurring within 30 days and 1 year after hospital discharge for cardiac surgery among pediatric patients. Am Heart J 2006;152:386-93. http://dx.doi.org/10.1016/j.ahj.2005.12.016.
- Bazzani LG, Marcin JP. Case volume and mortality in pediatric cardiac surgery patients in California, 1998–2003. Circulation 2007;115:2652-9. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.678904.
- Arenz C, Asfour B, Hraska V, Photiadis J, Haun C, Schindler E, et al. Congenital heart surgery: surgical performance according to the Aristotle complexity score. Eur J Cardiothorac Surg 2011;39:e33-7. http://dx.doi.org/10.1016/j.ejcts.2010.11.062.
- Arnaoutakis GJ, George TJ, Allen JG, Russell SD, Shah AS, Conte JV, et al. Institutional volume and the effect of recipient risk on short-term mortality after orthotopic heart transplant. J Thorac Cardiovasc Surg 2012;143:157-67. http://dx.doi.org/10.1016/j.jtcvs.2011.09.040.
- Benavidez OJ, Gauvreau K, Del NP, Bacha E, Jenkins KJ, Benavidez OJ, et al. Complications and risk factors for mortality during congenital heart surgery admissions. Ann Thorac Surg 2007;84:147-55. http://dx.doi.org/10.1016/j.athoracsur.2007.02.048.
- Berry JG, Lieu TA, Forbes PW, Goldmann DA, Berry JG, Lieu TA, et al. Hospital volumes for common pediatric specialty operations. Arch Pediatr Adolesc Med 2007;161:38-43. http://dx.doi.org/10.1001/archpedi.161.1.38.
- Berry JG, Cowley CG, Hoff CJ, Srivastava R, Berry JG, Cowley CG, et al. In-hospital mortality for children with hypoplastic left heart syndrome after stage I surgical palliation: teaching versus nonteaching hospitals. Pediatrics 2006;117:1307-13. http://dx.doi.org/10.1542/peds.2005-1544.
- Burstein DS, Jacobs JP, Li JS, Sheng S, O’Brien SM, Rossi AF, et al. Care models and associated outcomes in congenital heart surgery. Pediatrics 2011;127:e1482-9. http://dx.doi.org/10.1542/peds.2010-2796.
- Checchia PA, McCollegan J, Daher N, Kolovos N, Levy F, Markovitz B, et al. The effect of surgical case volume on outcome after the Norwood procedure. J Thorac Cardiovasc Surg 2005;129:754-9. http://dx.doi.org/10.1016/j.jtcvs.2004.07.056.
- Davies RR, Russo MJ, Hong KN, Mital S, Mosca RS, Quaegebeur JM, et al. Increased short- and long-term mortality at low-volume pediatric heart transplant centers: should minimum standards be set? Retrospective data analysis. Ann Surg 2011;253:393-401. http://dx.doi.org/10.1097/SLA.0b013e31820700cc.
- Dean PNM. Effects of race, ethnicity, and sex on surgical mortality in hypoplastic left heart syndrome. Pediatr Cardiol 2013;34:1829-36. http://dx.doi.org/10.1007/s00246-013-0723-3.
- Dinh K, Maroulas V. Statistical modelling of mortality risk for congenital heart defects. J Appl Quantit Methods 2010;5:670-8.
- Eldadah M, Leo S, Kovach K, Ivan, Pepe J, Fakioglu H, . Influence of a dedicated paediatric cardiac intensive care unit on patient outcomes. Nurs Crit Care 2011;16:281-6. http://dx.doi.org/10.1111/j.1478-5153.2011.00455.x.
- Fixler DEN. Effect of acculturation and distance from cardiac center on congenital heart disease mortality. Pediatrics 2012;129:1118-24. http://dx.doi.org/10.1542/peds.2011-3114.
- Gray DT, Louhimo I, Ahonen J, Emanuelsson Br. Inter-institutional variation in risk-adjusted paediatric cardiac surgical outcomes. Prog Pediatr Cardiol 2003;18:33-42. http://dx.doi.org/10.1016/S1058-9813(03)00074-2.
- Hickey P, Gauvreau K, Connor J, Sporing E, Jenkins K, Hickey P, et al. The relationship of nurse staffing, skill mix, and Magnet recognition to institutional volume and mortality for congenital heart surgery. J Nurs Admin 2010;40:226-32. http://dx.doi.org/10.1097/NNA.0b013e3181da3f71.
- Hirsch JC, Gurney JG, Donohue JE, Gebremariam A, Bove EL, Ohye RG, et al. Hospital mortality for Norwood and arterial switch operations as a function of institutional volume. Pediatr Cardiol 2008;29:713-17. http://dx.doi.org/10.1007/s00246-007-9171-2.
- Hornik CP, He X, Jacobs JP, Li JS, Jaquiss RD, Jacobs ML, et al. Relative impact of surgeon and center volume on early mortality after the Norwood operation. Ann Thorac Surg 2012;93:1992-7. http://dx.doi.org/10.1016/j.athoracsur.2012.01.107.
- Karamlou T, Vafaeezadeh M, Parrish AM, Cohen GA, Welke KF, Permut L, et al. Increased extracorporeal membrane oxygenation center case volume is associated with improved extracorporeal membrane oxygenation survival among pediatric patients. J Thorac Cardiovasc Surg 2013;145:470-5. http://dx.doi.org/10.1016/j.jtcvs.2012.11.037.
- Karamlou T, Diggs BS, Person T, Ungerleider RM, Welke KF, Karamlou T, et al. National practice patterns for management of adult congenital heart disease: operation by pediatric heart surgeons decreases in-hospital death. Circulation 2008;118:2345-52. http://dx.doi.org/10.1161/CIRCULATIONAHA.108.776963.
- Karamlou T, McCrindle BW, Blackstone EH, Cai S, Jonas R, Bradley SM, et al. Lesion-specific outcomes in neonates undergoing congenital heart surgery are related predominantly to patient and management factors rather than institution or surgeon experience: a Congenital Heart Surgeons Society Study. J Thorac Cardiovasc Surg 2010;139:569-77. http://dx.doi.org/10.1016/j.jtcvs.2008.11.073.
- Kazui T, Osada H, Fujita H. Committee for Scientific Affairs . An attempt to analyze the relation between hospital surgical volume and clinical outcome. Gen Thorac Cardiovasc Surg 2007;55:483-92. http://dx.doi.org/10.1007/s11748-007-0172-0.
- Kim YY, Gauvreau K, Bacha EA, Landzberg MJ, Benavidez OJ, Kim YY, et al. Risk factors for death after adult congenital heart surgery in pediatric hospitals. Circulation 2011;4:433-9. http://dx.doi.org/10.1161/CIRCOUTCOMES.110.958256.
- McHugh KE, Hillman DG, Gurka MJ, Gutgesell HP, McHugh KE, Hillman DG, et al. Three-stage palliation of hypoplastic left heart syndrome in the University HealthSystem Consortium. Congenital Heart Dis 2010;5:8-15. http://dx.doi.org/10.1111/j.1747-0803.2009.00367.x.
- Mery CMM. Incidence and treatment of chylothorax after cardiac surgery in children: analysis of a large multi-institution database. J Thorac Cardiovasc Surg 2014;147:678-86. http://dx.doi.org/10.1016/j.jtcvs.2013.09.068.
- Morales DL, Zafar F, Rossano JW, Salazar JD, Jefferies JL, Graves DE, et al. Use of ventricular assist devices in children across the United States: analysis of 7.5 million pediatric hospitalizations. Ann Thorac Surg 2010;90:1313-18. http://dx.doi.org/10.1016/j.athoracsur.2010.04.107.
- Oster ME, Strickland MJ, Mahle WT, Oster ME, Strickland MJ, Mahle WT. Impact of prior hospital mortality versus surgical volume on mortality following surgery for congenital heart disease. J Thorac Cardiovasc Surg 2011;142:882-6. http://dx.doi.org/10.1016/j.jtcvs.2011.04.011.
- Pasquali SK, Jacobs JP, He X, Hornik CP, Jaquiss RD, Jacobs ML, et al. The complex relationship between center volume and outcome in patients undergoing the Norwood operation. Ann Thorac Surg 2012;93:1556-62. http://dx.doi.org/10.1016/j.athoracsur.2011.07.081.
- Pasquali SK, Li JS, Burstein DS, Sheng S, O’Brien SM, Jacobs ML, et al. Association of center volume with mortality and complications in pediatric heart surgery. Pediatrics 2012;129:e370-6. http://dx.doi.org/10.1542/peds.2011-1188.
- Petrucci O, O’Brien SM, Jacobs ML, Jacobs JP, Manning PB, Eghtesady P, et al. Risk factors for mortality and morbidity after the neonatal Blalock–Taussig shunt procedure. Ann Thorac Surg 2011;92:642-51. http://dx.doi.org/10.1016/j.athoracsur.2011.02.030.
- Pinto NM, Lasa J, Dominguez TE, Wernovsky G, Tabbutt S, Cohen MS, et al. Regionalization in neonatal congenital heart surgery: the impact of distance on outcome after discharge. Pediatr Cardiol 2012;33:229-38. http://dx.doi.org/10.1007/s00246-011-0116-4.
- Sakata R, Kuwano H, Yokomise H, Sakata R, Kuwano H, Yokomise H. Hospital volume and outcomes of cardiothoracic surgery in Japan: 2005–9 national survey. Gen Thorac Cardiovasc Surg 2012;60:625-38. http://dx.doi.org/10.1007/s11748-012-0128-x.
- Seifert HA, Howard DL, Silber JH, Jobes DR, Seifert HA, Howard DL, et al. Female sex increases the risk of death during hospitalization for pediatric cardiac surgery. [Erratum appears in J Thorac Cardiovasc Surg. 2007;134:333–4.]. J Thorac Cardiovasc Surg 2007;133:668-75. http://dx.doi.org/10.1016/j.jtcvs.2006.11.014.
- Tabbutt S, Ghanayem N, Ravishankar C, Sleeper LA, Cooper DS, Frank DU, et al. Risk factors for hospital morbidity and mortality after the Norwood procedure: a report from the Pediatric Heart Network Single Ventricle Reconstruction trial. J Thorac Cardiovasc Surg 2012;144:882-95. http://dx.doi.org/10.1016/j.jtcvs.2012.05.019.
- Vinocur JMM. Surgical volume and center effects on early mortality after pediatric cardiac surgery: 25-year North American experience from a multi-institutional registry. Pediatr Cardiol 2013;34:1226-36. http://dx.doi.org/10.1007/s00246-013-0633-4.
- Welke KF, Karamlou T, Ungerleider RM, Diggs BS, Welke KF, Karamlou T, et al. Mortality rate is not a valid indicator of quality differences between pediatric cardiac surgical programs. Ann Thorac Surg 2010;89:139-44. http://dx.doi.org/10.1016/j.athoracsur.2009.08.058.
- Welke KF, O’Brien SM, Peterson ED, Ungerleider RM, Jacobs ML, Jacobs JP, et al. The complex relationship between pediatric cardiac surgical case volumes and mortality rates in a national clinical database. J Thorac Cardiovasc Surg 2009;137:1133-40. http://dx.doi.org/10.1016/j.jtcvs.2008.12.012.
- Welke KF, Shen I, Ungerleider RM, Welke KF, Shen I, Ungerleider RM. Current assessment of mortality rates in congenital cardiac surgery. Ann Thorac Surg 2006;82:164-70. http://dx.doi.org/10.1016/j.athoracsur.2006.03.004.
- Karamlou T, Jacobs M, Pasquali S, He X, Hill K, O’Brien S, et al. Influence of Surgeon and Center Volume on Early Morbidity and Mortality Following Arterial Switch Operation for Transposition of the Great Arteries: An Analysis of the STS Congenital Heart Surgery Database n.d.
- Kochilas L, Maroulas V, Rood K, Larson V, Moller J. In-hospital mortality for surgical repair of congenital heart defects is inversely related to hospital surgical volume. Circulation 2009;120:S568-9.
- Scheurer M, Gauvreau K, Laussen PC, Mayer J, Atz AM, Newburger JW. The impact of a designated cardiac intensive care unit on outcomes after the Norwood procedure. J Am Coll Cardiol 2011;57. http://dx.doi.org/10.1016/S0735-1097(11)60405-1.
- Welke KFK, Karamlou T, He X, Jacobs M, Jacobs J, Pasquali S. Surgeon volume is associated with operative mortality after congenital cardiac surgery. Circulation 2012;126.
- Mery CMM. Incidence and treatment of chylothorax after cardiac surgery in children: analysis of a large multi-institution database. J Thorac Cardiovasc Surg 2014;147:678-86. http://dx.doi.org/10.1016/j.jtcvs.2013.09.068.
- Dean PNM. Effects of race, ethnicity, and sex on surgical mortality in hypoplastic left heart syndrome. Pediatr Cardiol 2013;34:1829-36. http://dx.doi.org/10.1007/s00246-013-0723-3.
- Daenen W, Lacour-Gayet F, Aberg T, Comas JV, Daebritz SH, Di DR, et al. Optimal structure of a congenital heart surgery department in Europe. Eur J Cardiothorac Surg 2003;24:343-51. http://dx.doi.org/10.1016/S1010-7940(03)00444-5.
- Lundström NR, Berggren H, Björkhem G, Jögi P, Sunnegårdh J. Centralization of pediatric heart surgery in Sweden. Pediatr Cardiol 2014;21:353-7. http://dx.doi.org/10.1007/s002460010079.
- Tsang VT, de LM, Utley M, Tsang VT, de Leval M, Utley M. Paediatric cardiac surgery. Scand Cardiovasc J 2009;43:4-6. http://dx.doi.org/10.1080/14017430802422387.
- Caldarone CA, Al-Radi O. The limits of confidence: at what price a baby’s life?. Pediatr Cardiol 2008;29:704-5. http://dx.doi.org/10.1007/s00246-008-9218-z.
- Hilton CJ, Hamilton JRL, Vitale N, Haaverstad R. Effects of Bristol on surgical practice in the United Kingdom. Interact Cardiovasc Thorac Surg 2005;4:197-9. http://dx.doi.org/10.1510/icvts.2004.102137.
- Hudsmith LE, Thorne SA. Transition of care from paediatric to adult services in cardiology. Arch Dis Child 2007;92:927-30. http://dx.doi.org/10.1136/adc.2006.103812.
- Lacour-Gayet F, Clarke D, Jacobs J, Gaynor W, Hamilton L, Jacobs M, et al. The Aristotle score for congenital heart surgery. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2004;7:185-91. http://dx.doi.org/10.1053/j.pcsu.2004.02.011.
- Report of the Taskforce on Paediatric Cardiac Services. Brisbane, QLD: Queensland Government; 2006.
- Mellis C, Cartmill T, Dobson A, Gentles T, Shann F. Review of Paediatric Cardiac Services in Queensland. Brisbane, QLD: The State of Queensland (Queensland Health); 2006.
- The Report of the Public Inquiry into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–1995: Learning from Bristol. London: The Stationery Office; 2001.
- Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, et al. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 2004;113:e197-205. http://dx.doi.org/10.1542/peds.113.3.e197.
- Welke KF, Peterson ED, Vaughan-Sarrazin MS, O’Brien SM, Rosenthal GE, Shook GJ, et al. Comparison of cardiac surgery volumes and mortality rates between the Society of Thoracic Surgeons and Medicare databases from 1993 through 2001. Annals Thorac Surg 2007;84:1538-46. http://dx.doi.org/10.1016/j.athoracsur.2007.06.022.
- Concentration of Congenital Heart Surgery and Catheter Interventions. Leiden: Commission for Paediatric Heart Interventions; 2009.
- O’Brien SM, Jacobs JP, Clarke DR, Maruszewski B, Jacobs ML, Walters HL, et al. Accuracy of the Aristotle basic complexity score for classifying the mortality and morbidity potential of congenital heart surgery operations. Ann Thorac Surg 2007;84:2027-37. http://dx.doi.org/10.1016/j.athoracsur.2007.06.031.
- Moons P, Meijboom FJ, Baumgartner H, Trindade PT, Huyghe E, Kaemmerer H. Structure and activities of adult congenital heart disease programmes in Europe. Eur Heart J 2010;31:1305-10. http://dx.doi.org/10.1093/eurheartj/ehp551.
- Proclamation of a Resolution of the Federal Joint Committee Regarding a Guideline Over Quality Assurance Measures Over Cardiac Surgery Care for Children and Teenagers in Accordance with 137 Paragraph 1 Number 2 of the Fifth Book Of Social Security Statute Book (Sgb V), Guidelines for Paediatric Cardiac Surgery. Berlin: Federal Ministry of Justice; 2010.
- Surgery for Children: Delivering a First Class Service. London: The Royal College of Surgeons of England; 2007.
- Specialized Paediatric Services Review – Report of the Minister’s Advisory Committee. Toronto, ON: Ministry of Health and Long Term Care; 2002.
- Giamberti A, Chessa M, Abella R, Butera G, Carlucci C, Nuri H, et al. Morbidity and mortality risk factors in adults with congenital heart disease undergoing cardiac reoperations. Ann Thorac Surg 2009;88:1284-9. http://dx.doi.org/10.1016/j.athoracsur.2009.05.060.
- Centre for Maternal and Child Health . Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006–8. BJOG 2011;118:1-203. http://dx.doi.org/10.1111/j.1471-0528.2010.02847.x.
- Hickey PA, Gauvreau K, Curley MA, Connor JA, Hickey PA, Gauvreau K, et al. The effect of critical care nursing and organizational characteristics on pediatric cardiac surgery mortality in the United States. J Nurs Admin 2013;43:637-44. http://dx.doi.org/10.1097/NNA.0000000000000005.
- Hickey PA, Gauvreau K, Jenkins K, Fawcett J, Hayman L, Hickey PA, et al. Statewide and national impact of California’s Staffing Law on pediatric cardiac surgery outcomes. J Nurs Admin 2011;41:218-25. http://dx.doi.org/10.1097/NNA.0b013e3182171b2e.
- Chang RK, Klitzner TS. Can regionalization decrease the number of deaths for children who undergo cardiac surgery? A theoretical analysis. Pediatrics 2002;109:173-81. http://dx.doi.org/10.1542/peds.109.2.173.
- Jenkins KJ, Newburger JW, Lock JE, Davis RB, Coffman GA, Iezzoni LI. In-hospital mortality for surgical repair of congenital heart defects: preliminary observations of variation by hospital caseload. Pediatrics 1995;95:323-30.
- Hughes GC, Zhao Y, Rankin JS, Scarborough JE, O’Brien S, Bavaria JE, et al. Effects of institutional volumes on operative outcomes for aortic root replacement in North America. J Thorac Cardiovasc Surg 2013;145:166-70. http://dx.doi.org/10.1016/j.jtcvs.2011.10.094.
- Lange R, Hoerer J, Schreiber C. What are the obstacles to training in surgery for congenital heart disease in Germany?. Thorac Cardiovasc Surg 2013;61:273-7. http://dx.doi.org/10.1055/s-0033-1345024.
- Holden J. The New Congenital Heart Disease Review: 18th Update. NHS England; 2014.
- Der Deutscher Herzbericht. Frankfurt: The German Heart Foundation; 2011.
- Funkat A, Beckmann A, Lewandowski J, Frie M, Schiller W, Ernst M, et al. Cardiac surgery in Germany during 2011: a report on behalf of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg 2012;60. http://dx.doi.org/10.1055/s-0032-1326724.
- The World Heart Congress, Cape Town 2013. http://livestreamsa.co.za/wcpccs/presentations/?step=4&l_id=320&p_id=308&a_id=2090 (accessed 6 March 2014).
- Dudley R, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: Estimating potentially avoidable deaths. JAMA 2000;283:1159-66. http://dx.doi.org/10.1001/jama.283.9.1159.
- Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 2002;137:511-20. http://dx.doi.org/10.7326/0003-4819-137-6-200209170-00012.
- Hannan EL, Siu AL, Kumar D, Kilburn H, Chassin MR. The decline in coronary artery bypass graft surgery mortality in New York State. The role of surgeon volume. JAMA 1995;273:209-13. http://dx.doi.org/10.1001/jama.1995.03520270043029.
- Sowden A, Deeks J, Sheldon T. Volume and outcome in coronary artery bypass graft surgery: true association or artefact?. BMJ 1995;311:151-5. http://dx.doi.org/10.1136/bmj.311.6998.151.
- Ho JG, Cohen MD, Ebenroth ES, Schamberger MS, Cordes TM, Bramlet MT, et al. Comparison between transthoracic echocardiography and cardiac magnetic resonance imaging in patients status post atrial switch procedure. Congenit Heart Dis 2012;7:122-30. http://dx.doi.org/10.1111/j.1747-0803.2011.00571.x.
- Sinzobahamvya N, Kopp T, Photiadis J, Arenz C, Schindler E, Haun C, et al. Surgical management of congenital heart disease: correlation between hospital costs and the Aristotle complexity score. Thorac Cardiovasc Surg 2010;58:322-7. http://dx.doi.org/10.1055/s-0030-1249866.
- Catchpole KR. Task, team and technology integration in the paediatric cardiac operating room. Progress in Pediatric Cardiology 2011;32:85-8. http://dx.doi.org/10.1016/j.ppedcard.2011.10.005.
- Catchpole KR, Giddings AEB, Wilkinson M, Hirst G, Dale T, de Leval MR. Improving patient safety by identifying latent failures in successful operations. Surgery 2007;142:102-10. http://dx.doi.org/10.1016/j.surg.2007.01.033.
- Catchpole KR, Giddings AEB, de Leval MR, Peek GJ, Godden PJ, Utley M, et al. Identification of systems failures in successful paediatric cardiac surgery. Ergonomics 2006;49:567-88. http://dx.doi.org/10.1080/00140130600568865.
- Catchpole KR, de Leval MR, McEwan A, Piggott N, Elliott M, McQuillan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Pediatr Anesth 2007;17. http://dx.doi.org/10.1111/j.1460-9592.2006.02239.x.
- Wahr JA, Prager RL, Abernathy JH, Martinez EA, Salas E, Seifert PC, et al. Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation 2013;128:1139-69. http://dx.doi.org/10.1161/CIR.0b013e3182a38efa.
- Carthey J, de Leval MR, Reason JT. The human factor in cardiac surgery: errors and near misses in a high technology medical domain. Annals Thorac Surg 2001;72:300-5. http://dx.doi.org/10.1016/S0003-4975(00)02592-3.
- Catchpole K, Godden P, Giddings A, Hirst G, Dale T, Utley M, et al. Identifying and Reducing Errors in the Operating Theatre 2005. www.birmingham.ac.uk/Documents/college-mds/haps/projects/cfhep/psrp/finalreports/PS012FinalReportDeLeval.pdf (accessed 26 August 2014).
- Eggli YH. Surgical safety and hospital volume across a wide range of interventions. Med Care 2010;48:962-71. http://dx.doi.org/10.1097/MLR.0b013e3181eaf9f6.
- Allen SW, Gauvreau K, Bloom BT, Jenkins KJ. Evidence-based referral results in significantly reduced mortality after congenital heart surgery. Pediatrics 2003;112:24-8. http://dx.doi.org/10.1542/peds.112.1.24.
- Ashburn D, McCrindle BW, Tchervenkov CI, Jacobs ML, Lofland GK, Bove EL, et al. Outcomes after the Norwood operation in neonates with critical aortic stenosis or aortic valve atresia. J Thorac Cardiovasc Surg 2003;125:1070-82. http://dx.doi.org/10.1067/mtc.2003.183.
- Austin CR, Wood AE, Graham ANJ. Can low volume adult congenital surgery be delivered safely in a high volume adult cardiac surgery unit?. Ir J Med Sci 2013;182.
- Bennett TD, Klein MB, Sorensen MD, De Roos AJ, Rivara FP, Bennett TD, et al. Influence of birth hospital on outcomes of ductal-dependent cardiac lesions. Pediatrics 2010;126:1156-64. http://dx.doi.org/10.1542/peds.2009-2829.
- Boucek DY. Does surgeon training or hospital (pediatric vs. adult) affect survival after heart transplant in adults with congenital heart disease?. J Heart Lung Transplant 2013;32:S240-1. http://dx.doi.org/10.1016/j.healun.2013.01.617.
- Cabrera AGP. Interhospital transport of children requiring extracorporeal membrane oxygenation support for cardiac dysfunction. Congenit Heart Dis 2011;6:202-8. http://dx.doi.org/10.1111/j.1747-0803.2011.00506.x.
- d’Udekem Y, Galati JC, Konstantinov IE. Intersurgeon variability in long-term outcomes after transatrial repair of tetralogy of Fallot: 25 years’ experience with 675 patients. J Thorac Cardiovasc Surg 2014;147:880-6. http://dx.doi.org/10.1016/j.jtcvs.2013.11.010.
- Davies RR, Pasquali SK, Jacobs ML, Jacobs JJ, Wallace AS, Pizarro C, et al. Current spectrum of surgical procedures performed for Ebstein’s malformation: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg 2013;96:1703-9. http://dx.doi.org/10.1016/j.athoracsur.2013.05.005.
- DeCampli WM. Joint programmes in paediatric cardiothoracic surgery: a survey and descriptive analysis. Cardiol Young 2011;21:159-64. http://dx.doi.org/10.1017/S1047951111001740.
- Dimick JB, Welch HG, Birkmeyer JD. Surgical mortality as an indicator of hospital quality: the problem with small sample size. JAMA 2004;292:847-51. http://dx.doi.org/10.1001/jama.292.7.847.
- Freeman CL, Bennett TD, Casper TC, Larsen GY, Hubbard A, Wilkes J, et al. Pediatric and neonatal extracorporeal membrane oxygenation: does center volume impact mortality?. Crit Care Med 2014;42:512-19. http://dx.doi.org/10.1097/01.ccm.0000435674.83682.96.
- Hannan ELC. Regulatory efforts to assess and improve the quality of pediatric cardiac surgery in New York State. Prog Pediatr Cardiol 2011;32:111-19. http://dx.doi.org/10.1016/j.ppedcard.2011.10.009.
- Jacobs JP, O’Brien SM, Pasquali SK, Jacobs ML, Lacour-Gayet FoG, Tchervenkov CI, et al. Variation in outcomes for risk-stratified pediatric cardiac surgical operations: an analysis of the STS Congenital Heart Surgery Database. Ann Thorac Surg 2012;94:564-71. http://dx.doi.org/10.1016/j.athoracsur.2012.01.105.
- Kang GS, Soh YF, Kofidis T, Lee CN, Kang GS, Soh YF, et al. Five-year experience with congenital cardiac surgery at National University Heart Centre, Singapore. Singapore Med J 2010;51:570-5.
- Mahle WT, Kirshbom PM, Kanter KR, Kogon BM. Cardiac surgery in adults performed at children’s hospitals: trends and outcomes. J Thorac Cardiovasc Surg 2008;136:307-11. http://dx.doi.org/10.1016/j.jtcvs.2008.04.020.
- Mascio CEA. Perioperative mechanical circulatory support in children: an analysis of the Society of Thoracic Surgeons congenital heart surgery database. J Thorac Cardiovasc Surg 2014;147:658-65. http://dx.doi.org/10.1016/j.jtcvs.2013.09.075.
- Morris SAE. Prenatal diagnosis, birth location, surgical center, and neonatal mortality in infants with hypoplastic left heart syndrome. Circulation 2014;129:285-92. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.003711.
- Nykanen DW. Prospective risk stratification of pediatric cardiac catheterization procedures: a simple scoring system. Catheter Cardiovasc Intervent 2013;81.
- Raj S, Tosi L, Rotta A. The incidence of cardiopulmonary resuscitation as an outcome variable in a pediatric cardiovascular critical care program. Crit Care Med 2011;39.
- Rhee DP. Comparison of pediatric surgical outcomes by the surgeon’s degree of specialization in children. J Pediatr Surg 2013;48:1657-63. http://dx.doi.org/10.1016/j.jpedsurg.2012.12.048.
- Sinzobahamvya NA. Minimal requirements for a congenital heart surgery programme: Contribution of the Aristotle complexity score. Thorac Cardiovasc Surg 2012;60. http://dx.doi.org/10.1055/s-0031-1297437.
- Jacobs JP, Jacobs ML, Maruszewski B, Lacour-Gayet FG, Tchervenkov CI, Tobota Z, et al. Initial application in the EACTS and STS Congenital Heart Surgery Databases of an empirically derived methodology of complexity adjustment to evaluate surgical case mix and results. Eur J Cardiothorac Surg 2012;42:775-80. http://dx.doi.org/10.1093/ejcts/ezs026.
Appendix 1 Final protocol
Appendix a: conceptual framework
Appendix b: proposed search strategy (based on Ewart2)
Appendix c: references
Appendix 2 Literature search
Appendix a: stage 1 – database search strategy
MEDLINE
Via OvidSP.
Searched on 29 January 2014.
Search strategy
-
exp Child/ or exp Infant/ or exp Infant, Newborn/
-
(infan* or newborn* or neonat*).tw.
-
(child* or pediatric* or paediatric*).tw.
-
1 or 2 or 3
-
thoracic surgery/
-
exp Cardiac Surgical Procedures/ or exp Cardiac Care Facilities/
-
((heart or cardiac or cardiol* or thoracic or cardiothoracic) adj5 (surge* or procedure* or intervent* or defect*)).tw.
-
5 or 6 or 7
-
4 and 8
-
exp Heart Defects, Congenital/su, th [Surgery, Therapy]
-
Heart Diseases/cn [Congenital]
-
(congenital adj (heart or cardiac)).tw.
-
9 or 10 or 11 or 12
-
workload/
-
Physician’s Practice Patterns/
-
"Personnel Staffing and Scheduling"/
-
(caseload* or case load* or workload* or work load*).tw.
-
volume*.tw.
-
activit*.tw.
-
14 or 15 or 16 or 17 or 18 or 19
-
((proximity or close* or locat* or near or adult or pediatric or paediatric or child*) adj3 (facilit* or site or hospital* or service* or specialis* or specializ*)).tw.
-
(rationali* or streamlin* or centralis* or centraliz* or colocation or co-locate or (single adj site)).tw.
-
(Distance* or travel* or transport or regionali*).tw.
-
21 or 22 or 23
-
exp Mortality/
-
Survival/
-
exp "Outcome Assessment (Health Care)"/ or exp Treatment Outcome/
-
(mortality or death or survival or outcome* or complication*).tw.
-
25 or 26 or 27 or 28
-
13 and (20 or 24) and 29
-
limit 30 to yr= "2009 - 2014"
-
Limit to Humans and language= English
The Cochrane Library
Via Wiley Online Library.
Searched on 29 January 2014.
Search strategy
#1 MeSH descriptor: [Child] explode all trees
#2 MeSH descriptor: [Infant] explode all trees
#3 infan* or newborn* or neonat*:ti,ab,kw (Word variations have been searched)
#4 child* or pediatric* or paediatric:ti,ab,kw (Word variations have been searched)
#5 #1 or #2 or #3 or #4
#6 MeSH descriptor: [Thoracic Surgery] explode all trees
#7 MeSH descriptor: [Cardiac Surgical Procedures] explode all trees
#8 MeSH descriptor: [Cardiac Care Facilities] explode all trees
#9 ((heart or cardiac or cardiol* or thoracic or cardiothoracic) near/5 (surge* or procedure* or intervent* or defect*)):ti,ab,kw (Word variations have been searched)
#10 #6 or #7 or #8 or #9
#11 #5 and #10
#12 MeSH descriptor: [Heart Defects, Congenital] explode all trees
#13 congenital near (heart or cardiac):ti,ab,kw (Word variations have been searched)
#14 #12 or #13
#15 #11 or #14
#16 MeSH descriptor: [Workload] explode all trees
#17 MeSH descriptor: [Physician Practice Patterns] explode all trees
#18 MeSH descriptor: [Personnel Staffing and Scheduling] explode all trees
#19 case load or caseload or work load or workload:ti,ab,kw (Word variations have been searched)
#20 volume or activity:ti,ab,kw (Word variations have been searched)
#21 #16 or #17 or #18 or #19 or #20
#22 ((proximity or close* or locat* or "near" or adult or pediatric or paediatric or child*) near/3 (facilit* or site or hospital* or service* or speciali*)):ti,ab,kw
#23 (rationali* or streamlin* or centrali* or colocation or co-locate or colocation or colocate or (single near/2 site) or distance* or travel* or transport or regionali*):ti,ab,kw
#24 #22 or #23
#25 MeSH descriptor: [Mortality] explode all trees
#26 MeSH descriptor: [Survival] explode all trees
#27 MeSH descriptor: [Outcome Assessment (Health Care)] explode all trees
#28 MeSH descriptor: [Treatment Outcome] explode all trees
#29 (mortality or death or survival or outcome* or complication*):ti,ab,kw
#30 #25 or #26 or #27 or #28 or #29
#31 #21 or #24
#32 #15 and #31 and #30 from 2009 to 2014
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
Via EBSCOhost.
Search strategy
S25 (S22 AND S23 AND S24)
S24 (S14 OR S17)
S23 S9 OR S10
S22 S18 OR S19 OR S20 OR S21
S21 TX mortality or death or survival or outcome* or complication*
S20 MH outcome assessment
S19 MH survival
S18 MH mortality
S17 S15 OR S16
S16 TX (rationali* or streamlin* or centralis* or centraliz* or colocation or co-locate or (single site) or distance* or travel* or transport or regionali*)
S15 TX ((proximity or close* or locat* or near or adult or pediatric or paediatric or child*) N3 (facilit* or site or hospital* or service* or specialis* or specializ*))
S14 (S11 OR S12 OR S13)
S13 TX volume* or activit*
S12 TX caseload* or case load* or workload* or work load*
S11 MH workload
S10 TX congenital N1 (heart or cardiac)
S9 S5 AND S8
S8 S6 OR S7
S7 TX ((heart or cardiac or cardiol* or thoracic or cardiothoracic) N5 (surge* or procedure* or intervent* or defect*))
S6 MH thoracic surgery
S5 (S1 OR S2 OR S3 OR S4)
S4 TX child or pediatric or paediatric
S3 TX (infant* OR newborn or neonat*)
S2 MH infant
S1 MH child
Web of Science
Via Web of Knowledge.
Search strategy
# 8 #6 AND #5 Refined by: PUBLICATION YEARS= ( 2013 OR 2010 OR 2012 OR 2009 OR 2011 )
# 7 #6 AND #5
# 6 TITLE: ((caseload* or case load* or workload* or work load* or volume or activity or ((proximity or close* or locat* or adult or pediatric or paediatric or child*) near (facilit* or site or hospital* or service* or specialis* or specializ*)) or (rationali* or streamlin* or centralis* or centraliz* or colocation or co-locate or (single site) or distance* or travel* or transport or regionali*)))
# 5 #4 OR #3
# 4 #2 AND #1
# 3 TITLE: ((congenital NEAR (heart or cardiac)))
# 2 TITLE: (((heart or cardiac or cardiol* or thoracic or cardiothoracic) NEAR (surge* or procedure* or intervent* or defect*)))
# 1 TI= (infan* or newborn* or neonat* or child* or pediatric* or paediatric*)
Appendix b: stage 2 – citation searching
Citation searches were conducted on Google Scholar (14 February 2014) for any references citing any of the following eight studies included in the Ewart review:
-
Bazzani and Marcin8
-
Chang et al. 7
-
Checchia et al. 15
-
Hirsch et al. 23
-
Tsang et al. 53
-
Welke et al. 44
-
Welke et al. 6
-
Welke et al. 43
One hundred and eight-four individual citations (from an initial combined set of 366) remained following de-duplication and removal of non-English references.
Appendix c: stage 3 – evidence suggested by stakeholders and reasons for inclusion/exclusion
| Source and date | Type of evidence | Bibliographic details | Reviewer? | Outcome |
|---|---|---|---|---|
| Jo Glenwright (personal communication), NHS England, 9 January 2014 | List of references from the Safe and Sustainable Review of Children’s Congenital Cardiac Services(any references that are dated 2002 or earlier have not been included in this table for reasons of clarity) | Ewart 20092 | LP | Exclude: study type – review |
| Caldarone and Al Radi 200854 | LP | Exclude: study type – discussion paper | ||
| Hilton et al. 200555 | LP | Exclude: study type – discussion paper | ||
| Hirsch et al. 200823 | LP | Include (already identified by ScHARR) | ||
| Hudsmith and Thorne 200756 | LP | Exclude: study type – review | ||
| Lacour-Gayet et al. 200457 | LP | Exclude: study type – no data on outcomes | ||
| Queensland Government 200658 | LP/AB | Exclude: not peer reviewed. No original data on volume/mortality. Reports findings of earlier Mellis review59 and other international reviews, e.g. Kennedy report.60 However, these are pre-2003 | ||
| Reid et al. 200461 | LP | Exclude: topic | ||
| Welke et al. 200762 | LP | Exclude: topic – no cardiac subgroup for CHD | ||
| Welke et al. 20086 | LP | Include | ||
| Jo Glenwright (personal communication), NHS England, 9 January 2014 | Additional references in consultation document | Commission for Paediatric Heart Interventions 200963 | AB | Potentially relevant data on volumes and outcomes, but has not been subject to peer review. Translation not freely available. Includes five relevant papers – two of which were excluded after the full text was reviewed (Daenen et al. 2003,51 O’Brien et al. 200764). One is an abstract – exclude but use as source of evidence (Moons et al. 2009).65 One is outside the date range of the review (Lundström 2000)52 and one was already identified for inclusion (Welke et al. 2009)47 |
| Federal Ministry of Justice 201066 | AB | Translation not freely available | ||
| Daenen et al. 200351 | AB | Provides suggested standards for number of procedures, etc. Not evidence-based standards but may be useful for discussion. No original data; therefore, exclude. Identifies a number of relevant references but all of these are outside the date range of the review | ||
| Analysis undertaken of the Hospital Episodes Statistics data by National Cancer Services Analysis Team, September 2010 (John Waring, Central Manchester University Hospitals NHS Foundation Trust, personal communication, 2014) | LP | Exclude: not peer-reviewed evidence | ||
| The Royal College of Surgeons of England67 | LP | Exclude: not peer-reviewed evidence | ||
| Ontario Ministry of Health and Long-Term Care 200268 | AB | Considers volume data, but no data on outcomes and has not been subject to peer review. Cites selected published evidence (but not within date range of the review) | ||
| Welke et al. 200943 | LP | Include (already identified by ScHARR) | ||
| Standard C9, National Specialised Commissioning Team, Safe and Sustainable: Children’s Congenital Cardiac Services in England Service Standards, March 2010. (John Waring, Central Manchester University Hospitals NHS Foundation Trust, personal communication, 2014) | LP | Exclude: not peer-reviewed evidence | ||
| John Wareing, Central Manchester University Hospitals NHS Foundation Trust, 4 March 2014 | Giamberti et al. 200969 | AJ | Exclude: data – neither volume nor proximity appears to be variables under assessment in this study. It is an analysis of pre-operative and operative factors and their relationship to outcome variables, one of which is mortality, in one institution. The pre-operative factors are demographic and patient-level clinical factors. The conclusion in both the abstract and main paper that ‘Reoperations in ACHD . . . were associated with a low mortality rate if performed in a centre with a considerable activity and a dedicated program’69 does not appear to relate to the results of the study | |
| Kim et al. 201129 | LP | Include | ||
| John Wareing, Central Manchester University Hospitals NHS Foundation Trust, 3 March 2014 | We note that the current list of references does not refer to pregnancy outcomes in women with CHD. While there is limited literature on the subject the above reference70 contains a specific recommendation from the cardiac disease chapter that ‘Women with a known history of cardiac disease must be referred to consultant-led obstetric care in a maternity unit where there is a joint obstetric/cardiology clinic or a cardiologist with expertise in the care of women with heart disease.’ The last sentence of this chapter examining maternal mortality is ‘Some women with known heart disease before pregnancy are not offered or referred to appropriate multidisciplinary care in specialist units.’ Heart disease has been the leading cause of maternal death in the last two triennial reports | Centre for Maternal and Child Health 201170 | LP | The chapter on cardiac disease was examined. There is no evidence in this chapter linking either volume or proximity to outcomes for pregnant women |
| Robert Craig (personal communication), Royal Brompton & Harefield NHS Foundation Trust, 3 March 2014 | Report commissioned by RB&H on the impact on RB&H of the proposed decommissioning of cardiac surgery under the ‘Safe & Sustainable’ Review (FH Partnership, January 2013). The report is marked ‘strictly confidential’ but was released to the IRP in January 2013. Pages 39–42 discuss the relationship between surgical volumes and outcomes | Pasquali et al. 201234 | LP | Include (already identified by ScHARR) |
| Welke et al. 201248 | LP | Include (conference abstract already identified by ScHARR) | ||
| Letter from Professor Pascal Vouhe (Paris) – undated, but received late 2012 – citing the 2003 EACTS paper51 on the ‘Optimal structure of a congenital heart surgery department’, which falls within the wider time horizon (2003–14) identified in the ScHARR proposal | Daenen 200351 | LP | Exclude: paper about standards. Not evidence based | |
| Pedro Del Nido, Children’s Hospital Boston/Harvard Medical School, 21 February 2014 | Hickey and Gavreau 201371 | LP and project team | Exclude: topic – organisational factor under consideration is critical care nursing (i.e. clinical experience). There are no variables relating to either volume or proximity. While skill mix of staff is a variable for data extraction, this would only be extracted when there is evidence about volume or proximity as the main organisational variable | |
| Hickey et al. 201172 | LP and project team | Exclude: topic – organisational factor under consideration is staffing numbers and staffing ratios. There are no variables relating to either volume or proximity. While skill mix of staff is a variable for data extraction, this would only be extracted when there is evidence about volume or proximity as the main organisational variable | ||
| David Barron, Birmingham Children’s Hospital, 14 February 2014 | ‘Publications on the experience with reconfiguration in Sweden and Netherlands that would be important to trace’ | LP | The literature search did not identify any publications from either of these countries that were peer-reviewed evidence that included evidence on the relationship between either volume or proximity and outcomes | |
| Karamlou et al. 201445 | LP | Include as conference abstract | ||
| Pasquali et al. 201235 | LP | Include (already identified by ScHARR) | ||
| Welke et al. 200943 | LP | Include (already identified by ScHARR) | ||
| Oster et al. 201133 | LP | Include (already identified by ScHARR) | ||
| Chang and Klitzner 200273 | LP | Exclude: date | ||
| Jenkins et al. 199574 | LP | Exclude: date | ||
| Pasquali et al. 201234 | LP | Include (already identified by ScHARR) | ||
| Tabbutt et al. 201240 | LP | Include (already identified by ScHARR) | ||
| Hornik et al. 201224 | LP | Include (already identified by ScHARR) | ||
| Karamlou et al. 201325 | LP | Include (already identified by ScHARR) | ||
| Hughes et al. 201375 | EG | Exclude: population – not CHD | ||
| Arnaoutakis et al. 201210 | LP | Include (already identified by ScHARR) | ||
| Karamlou et al. 200826 | LP | Include (already identified by ScHARR) | ||
| Lange et al. 201376 | EG | Exclude: no outcomes data reported in the paper | ||
| David Barron, Birmingham Children’s Hospital, 27 February 2014 | E-mail in response to list of 22 references circulated via NHS England’s new CHD Review Blog post on 24 February 2014.77 References were 2009–14 only | Welke et al. 200943 | LP | Include (already identified by ScHARR) |
| Karamlou et al. 200826 | LP | |||
| Lange et al. 201376 | LP | Exclude: no outcomes data reported in the paper | ||
| Hughes et al. 201375 | EG | Exclude: population – not CHD | ||
| Arnaoutakis et al. 201210 | LP | Include (already identified by ScHARR) | ||
| Karamlou et al. 201445 | LP | Conference abstract. Not identified by original search or in the list of references as abstract not obtained when the list was drawn up. On scrutiny of the reference, include in conference abstract table | ||
| Bob Ward, 13 February 2014 | Included in letter supplied to ScHARR team, under paragraph 2 | The German Heart Foundation 201178 | AB | Exclude: relevant population but no data linking volume and outcome |
| Funkat et al. 201279 | AB | Table 31 reports distribution of units by number of procedures. However, this is not linked to outcome anywhere within the report. Despite the high quality and completeness of the data, the report (published in a peer-reviewed journal) is unable to address the volume/proximity–outcome question | ||
| Press statement 18 May 2012 following inspection of RHSC Yorkhill by Sir Ian Kennedy’s team (Bob Ward, Leeds, personal communication, 2014) | LP | Exclude: not peer-reviewed evidence | ||
| Daenen et al. 200351 | Exclude: paper about standards. Not evidence based | |||
| Chang and Klitzner 200273 | LP | Exclude: date | ||
| Included in e-mail | Pasquali et al. 201234 | LP | Include (already identified by ScHARR) | |
| ‘We recently came across some interesting data from 50 of the largest centres in USA – and have plotted the results in Excel. This shows scarcely any variation of volume and outcome’ (Bob Ward, Leeds, personal communication, 2014) | http://health.usnews.com/best-hospitals/paediatric-rankings/cardiology-and-heart-surgery/data?sort_by = surgical_mortality (accessed 15 February 2014) | LP | Exclude: this is not data from a peer-reviewed source. The topic is relevant as it does link volume and outcome | |
| Bob Ward, 6 March 2014 | Link to two presentations given at the World Heart Congress, Cape Town, 201380 Presentations include a number of references which were assessed for inclusion/exclusion |
Daenen et al. 200351 | LP | Exclude: paper about standards. Not evidence based |
| Dudley et al. 200081 | LP | Exclude: date | ||
| Halm et al. 200282 | LP | Exclude: date | ||
| Hannan et al. 199583 | LP | Exclude: date | ||
| Sowden et al. 199584 | LP | Exclude: date | ||
| Ho et al. 200085 | LP | Exclude: date | ||
| Sinzobahamvya et al. 201086 | LP | Exclude: topic – relationship in question is costs for congenital heart surgery as related to the Aristotle Complexity Score | ||
| Pasquali et al. 201235 | LP | Include (already identified by ScHARR) | ||
| Hornik et al. 201224 | LP | Include (already identified by ScHARR) | ||
| Welke et al. 200943 | LP | Include (already identified by ScHARR) | ||
| Welke et al. 201248 | LP | Include (already identified by ScHARR) | ||
| Ken Catchpole, Cedars-Sinai Medical Centre, Los Angeles, CA, USA, 10 February 2014 | Extract from e-mail ‘The hypothesis – supported by the attached papers – is that performance in congenital heart surgery is defined by the interactions between people and systems’ (Ken Catchpole, personal communication, 2014) | Catchpole 201187 | LP | Exclude: does not include evidence that links volume or proximity to outcomes |
| Catchpole et al. 200788 | LP | Exclude: does not include evidence that links volume or proximity to outcomes | ||
| Catchpole et al. 200689 | LP | Exclude: does not include evidence that links volume or proximity to outcomes | ||
| Catchpole et al. 200790 | LP | Exclude: does not include evidence that links volume or proximity to outcomes | ||
| Wahr et al. 201391 | LP | Exclude: does not include evidence that links volume or proximity to outcomes | ||
| Carthey et al. 200192 | LP | Exclude: does not include evidence that links volume or proximity to outcomes | ||
| Catchpole et al. 200593 | LP | Exclude: does not include evidence that links volume or proximity to outcomes |
Appendix d: stage 4 – references of reviews and other reports used as a source of evidence
Eggli 2010. 94
Ewart 2009. 2
Moons et al. 2010. 65
Queensland Government 2006. 58
Tsang and Utley 2009. 53
Appendix e: list of full-text excludes and reasons for exclusion
| Bibliographic information | Reviewer? | Reason |
|---|---|---|
| Allen et al. 200395 | JT | Is about the efficacy of the referral process, rather than outcomes based on centre volume |
| Ashburn et al. 200396 | FC | Comparison of institutions, insufficient data reported |
| Austin et al. 201397 | EG | Data on case-mix, single centre compared with database but no comparison of case mix or outcome data from any other centre (so zero mortality impossible to interpret – could have just been all very low risk – only say ‘20 different ops’/’different complexity’) |
| Bennett et al. 201098 | Team | Paper looks at the influence of location of birth hospital on outcomes |
| Boucek 201399 | LP | Explanatory variables were the type of surgeon (no detail given on actual volume of procedures on children or adults) and the hospital (again no detail given on volume) |
| Cabrera 2011100 | JT | ECMO and transportation |
| d’Udekem et al. 2013101 | LP | Surgeon volume and centre volume are not variables. Outcome measure is reoperation not mortality |
| Davies et al. 2013102 | CO | No measure of volume or colocation of services – measure of regional factors |
| DeCampli 2011103 | LP | Data are via survey instrument therefore will not be sufficient to address the volume/proximity and outcome relationship |
| Dimick et al. 2004104 | FC | The study reported mortality rates but no relationship with unit size was reported |
| Freeman et al. 2014105 | CO | The population is a combination of seven different diagnostic indications. While some of these seven were CHD, the volume/mortality relationship was measured for the seven indications as a whole |
| Giamberti et al. 200970 | AJ | Neither volume nor proximity appears to be a variable under assessment in this study. It is an analysis of pre-operative and operative factors and their relationship to outcome variables, one of which is mortality, in one institution. The pre-operative factors are demographic and patient-level clinical factors. The conclusion in both the abstract and main paper that ‘Reoperations in ACHD . . . were associated with a low mortality rate if performed in a centre with a considerable activity and a dedicated program’ does not appear to relate to the results of the study |
| Hannan 2011106 | LP | This is an article on the regulatory system. It is not an article that contains data on outcomes associated with explanatory variables – it just addresses how these data are collected |
| Jacobs et al. 2012107 | CO | No analysis based on volume or proximity. Data analysis for benchmarking |
| Kang et al. 2010108 | LP | Exclude as evidence is from an non-OECD country |
| Mahle et al. 2008109 | JT | This is a descriptive paper – it reports volume but does not test the relationship between volume and outcome |
| Mascio 2014110 | JT | Paper does not look at the relationship between volume and outcome, rather the relationship between volume and likelihood of using mechanical circulatory support |
| Morris 2014111 | Team | Paper looks at the influence of location of birth hospital on outcomes |
| Nykanen 2013112 | EG | Conference abstract. Methods paper with no data on volume or other organisational factors (states ‘risk and volume adjusted’) |
| Raj et al. 2011113 | EG | Conference abstract. Not relevant – testing the hypothesis that CPR rates predict mortality |
| Rhee 2013114 | Team | Surgical experience cannot be used as a proxy for surgical volume |
| Sinzobahamvya 2012115 | EG | Conference abstract. Methods paper on impact of using ‘complexity score’. Insufficient data on explanatory variables |
Appendix 3 Data extraction
Appendix a: list of criteria included on data extraction form
-
Ref ID study (author, year, country).
-
Aim of study.
-
Data source/type of data/study design.
-
Dates of study.
-
Sample size.
-
Population characteristics.
-
Unit characteristics.
-
Procedures included.
-
Definition of volume/proximity.
-
Type of risk adjustment (none, administrative data, clinical data, clinical data with robust prediction model).
-
Covariates used.
-
Relation of volume/proximity to mortality.
-
Crude.
-
Adjusted (case mix ± other).
-
Age adjusted.
-
Non-linear versus linear relationship.
-
-
Relation of other characteristics to mortality (covariates used).
-
Other outcomes.
-
Comments.
-
Headline/key messages.
Appendix b: study groupings
| Group 1: volume and mortality – all CHD conditions | Group 2: volume and mortality – specific CHD conditions/procedures | Group 3: other – proximity, distance, non-mortality outcome | |
|---|---|---|---|
| Arenz et al. 20119 | Welke et al. 200943 | bArnaoutakis et al. 201210 | dBenavidez et al. 200711 |
| Bazzani and Marcin 20078 | Welke et al. 20086 | Berry et al. 200712 | cBurstein et al. 201114 |
| Chang et al. 20067 | Welke et al. 200644 | Berry et al. 200613 | cEldadah et al. 201119 |
| Dinh 201018 | Checcia et al. 200515 | cFixler 201220 | |
| Grey et al. 200321 | Davies et al. 201116 | dKaramlou et al. 201325 | |
| Hickey et al. 201022 | Dean 201317,50 | dMery 201431 | |
| Kazui 200728 | Hirsch et al. 200823 | cPinto et al. 201237 | |
| aKaramlou et al. 200826 | Hornik et al. 201224 | ||
| aKim et al. 201129 | Karamlou et al. 201027 | ||
| Oster et al. 201133 | McHugh et al. 201030 | ||
| Pasquali et al. 2012b35 | Morales et al. 201032 | ||
| Sakata 201238 | Pasquali et al. 2012a34 | ||
| Seifert et al. 200739 | Petrucci et al. 201136 | ||
| Vinocur 201341 | Tabbutt et al. 201240 | ||
| Welke et al. 201042 | |||
Appendix c: Study descriptive tables
| Study, country | Study design | Population included | Data source and study dates | Sample size |
|---|---|---|---|---|
| Arenz et al. 2011,9 Germany | Longitudinal study | Paediatric patients undergoing any CHD surgery. Surgical closure of patent ductus arteriosus in premature newborns and primary ECMO cannulation (excluded) | International study developing a composite complexity score (Aristotle complexity score) and mortality data (2006–9) | 1828 patients (single centre) |
| Bazzani and Marcin 2007,8 USA | Retrospective cohort (five separate analyses) | Paediatric cardiac surgery patients (< 18 years) identified by diagnosis and procedure codes | OSHPD Discharge database (1998–2003) | 12,801 cases four analyses. 13,917 cases one analysis |
| Chang et al. 2006,7 USA | Retrospective cohort study | Infants and children undergoing Norwood operation, VSD closure, ASD closure | OSHPD Discharge database (1989–99) | 25,402 cardiac surgery cases from over 500 acute centres |
| Dinh and Maroulas 2010,18 USA and Canada | Retrospective cohort | Paediatric cardiac surgeries | PCCC Database (1985–2004) | Approximately 80,000 consecutive surgeries from 47 small and medium-sized centres from different areas across the USA and Canada |
| Gray et al. 2003,21 Sweden | Cross-sectional cohort | Primary or one-stage procedures, multistage procedures and major procedures performed to correct earlier procedure failures or to treat major operative complications. Excluded heart transplants, group 1 procedures (closed heart procedures) and straightforward open heart procedures (e.g. open correction of primum and secundum atrial septal defects, simple VSDs) | Hospital medical records | 284 admissions involving 261 patients from four centres |
| Hickey et al. 2010,22 USA | Retrospective cohort (patient and staffing analysis) | Patients < 18 years, all hospital discharges indicating surgical repair of a congenital heart defect Institutions < 25 cases in study period, heart transplants, premature infants or neonates with patent ductus arteriosus closure as only congenital heart surgery and cases that could not be assigned to a RACHS-1 risk category were excluded |
PHIS Database (2005–6) for patient data National Association of Children’s Hospitals and Related Institution data (staffing data) |
19,736 congenital heart surgery cases from 38 paediatric centres |
| Kazui et al. 200728 Japan | Retrospective cohort | Open heart surgery in newborns and infants | Survey data collected by Japanese Association for Thoracic Surgery (2000–4) | 11,197 open heart surgeries (n = 2611 in newborns; n = 8586 in infants) |
| Oster et al. 2011,33 USA | Retrospective cohort | Children (0–18 years) undergoing surgery for CHD | PHIS database (2006–8) | 49,792 hospital encounters from 39 centres |
| Pasquali 2012 et al.,35 USA | Retrospective cohort | Children 0–18 years undergoing cardiothoracic surgery | STS-CHD database | 35,776 patients from 68 centres |
| Sakata 2012, Japan38 | Retrospective cohort | Newborns and infants with CHD | Survey data collected by Japanese Association for Thoracic Surgery (2005–9) | 13,074 patients with CHD (2825 newborns and 10,249 infants undergoing open heart surgery in 105 and 115 hospitals respectively) |
| Seifert et al. 2007,39 USA | Retrospective cohort study | Ages 0–20 years undergoing cardiac surgery (all procedures except closure of patent ductus arteriosus) | HCUP-KIDS (2000) | 10,282 patients |
| Vinocur 2013,41 USA | Retrospective cohort | All paediatric cardiac operations (except isolated ductal ligation in preterm infants weighting < 2.5 kg). Excluded centres outside North America, or centres contributing incomplete data or performing < 10 operations | PCCC Database (1982–2007) | 109,475 operations for volume calculations and 85,023 admissions for detailed statistical analysis from 49 centres |
| Welke et al. 2006,44 USA | Retrospective cohort | All paediatric cardiac surgical procedures that could be risk scored on RACHS-1 | Study data collected from 29 CHSS member institutions (2001–4) | 12,672 (out of 16,805 procedures = 76%) could be placed into RACHS-1 categories from 11 CHSS institutions |
| Welke et al. 2008,6 USA | Retrospective cohort | Paediatric (< 18y) cardiac operations identified by diagnosis and procedure codes | NIS database (1988 –2005) | 55,164 operations from 307 hospitals |
| Welke et al. 2009,43 USA | Retrospective cohort | Patients 18 years of age or less undergoing cardiac operation, which could be categorised by RACHS-1 or Aristotle risk categories Patients weighing ≤ 2500 g, undergoing patent ductus arteriosus ligation as primary procedure or missing age and/or weight data were excluded |
STS-CHD database (2002–6) | 32,413 operations from 48 programmes |
| Welke et al. 2010,42 USA | Retrospective cohort | Congenital cardiac surgical procedures performed on patients < 18 years of age identified by ICD-9-CM diagnosis and procedure codes | Nationwide Inpatient Sample Database (2000–5) | 21,709 operations from 161 hospitals |
| Study, country | Study design | Population included | Data source and study dates | Sample size |
|---|---|---|---|---|
| Karamlou et al. 2008,26 USA | Retrospective observational study | Adults with CHD for open heart or thoracic aorta procedures | NIS (1988–2003) | 30,250 operations |
| Kim et al. 2011,29 USA | Retrospective cohort | Admission ages 18–49 years with ICD-9-CM codes indicating at least one congenital heart surgery procedure. Excluded cardiac transplants, transcatheter interventions and pacemaker placements if it was the sole surgical procedure coded. Upper age limit was < 50 years to minimise inclusion of acquired heart disease | PHIS (2000–8) | 3061 admissions from 42 centres |
| Study, country | Study design | Population included | Data source and study dates | Sample size |
|---|---|---|---|---|
| Berry et al. 2006,13 USA | Retrospective cohort study | Children with HLHS undergoing stage 1 palliation (mitral stenosis, aortic atresia/stenosis, or aortic hypoplasia systemic to pulmonary arterial shunt). Exclusions were right ventricle to pulmonary artery conduit (Sano modification, cardiac transplantation) Stage 2 surgical palliation or stage 3 surgical palliation |
HCUP-KIDS Database (1997 and 2000) | 754 in 1997 880 in 2000 |
| Berry et al. 2007,12 USA | Retrospective cohort | Children 0–18 years having VSD surgery with cardiopulmonary bypass | HCUP-KIDS database (2003) | 2301 patients from general children’s hospitals, children’s hospitals within an adult teaching hospital or children’s speciality hospitals |
| Checcia et al. 2005,15 USA | Retrospective cohort | Principal diagnosis of HLHS and age on admission of 30 days or less undergoing the Norwood procedure | PHIS Database (1998–2001) | 801 patients from 29 hospitals |
| Davies et al. 2011,16 USA | Retrospective cohort | Paediatric heart transplants in patients aged under 19 years | United Network for Organ Sharing Standard Transplant and Research Data set (1992–2007) | 4647 transplants from 136 centres |
| Dean et al. 2013,17 USA | Retrospective cohort study | Patients with a diagnosis of HLHS undergoing three palliative procedures:
|
University Health System Consortium Database (1998–2007) | 2761 patients |
| Hirsch et al. 2008,23 USA | Cross-sectional analysis | Neonates undergoing either the Norwood procedure for HLHS and ASO for d-TGA | HCUP-KIDS database (2003) | 547 patients with the diagnosis of d-TGA undergoing an ASO in 74 hospitals624 patients with the diagnosis of HLHS undergoing the Norwood procedure in 60 hospitals |
| Hornik 2012, USA24 | Retrospective cohort | Infants (median age 6 years) undergoing the Norwood procedure | STS-CHD database (2000–9) | 2555 patients, 53 centres and 111 surgeons |
| Karamlou et al. 2010,27 Canada/USA | Retrospective cohort | Four groups of neonates, either undergoing the Norwood procedure or with one of three conditions: TGA; IAA; PAIVS | STS-CHD database. Dates for each of four groups vary from 5 to 10 years’ worth of data during years 1987–2000 | Total of 2421 operations (the Norwood procedure 710; TGA 829; IAA 474; PAIVS. 408) from between 24 and 33 CHSS institutions |
| McHugh et al. 2010,30 USA | Retrospective cohort | All paediatric hospital admissions with a diagnosis of HLHS. Included procedures were stage 1–3 palliation (S1P–S3P), cardiac transplant, biventricular repair, coarctation of the aorta repair, percutaneous valvuloplasty and balloon atrial septostomy | UHC database (1998–2007) | 9187 hospital admissions (5416 patients) from 118 institutions; 1949 S1Ps were performed at 48 institutions 1279 S2Ps were performed at 48 institutions 1084 S3Ps performed at 47 institutions |
| Morales et al. 2010,32 USA | Retrospective cohort study | All patients aged 20 years or younger undergoing VAD discharged from hospital for cardiac conditions including cardiomyopathy (40%), CHD (21%), myocarditis (12%) | HCUP-KIDS database (2006) | 187 patients from 67 centres |
| Pasquali et al. 2012,34 USA | Retrospective cohort | Infants (median age 6 years) undergoing the Norwood procedure regardless of underlying anatomy | STS-CHD database (2000–9) | 2557 infants, 53 centres |
| Petrucci et al. 2011,36 USA | Retrospective cohort | Neonates who received a MBTS with or without cardiopulmonary bypass, and with or without concomitant ligation of a patent ductus arteriosus; aged < 30 days; weight > 1.5kg | STS-CHD database (2002–9) | 1273 operations from 70 hospitals |
| Tabbutt et al. 2012,40 USA | Analysis of randomised controlled trial data | Children undergoing either the Norwood procedure with right ventricular–pulmonary artery shunt or MBTS | 2005–8 (extracted from randomised controlled trial, clinical and outcome data) | 549 cases in 15 centres |
| Study, country | Study design | Population included | Data source and study dates | Sample size |
|---|---|---|---|---|
| Arnaoutakis et al. 2012,10 USA | Retrospective cohort | Adult (> 18 years) OHT recipients | UNOS Standard Transplant and Research Dataset (2000–10) | 18,226 OHT recipients at a total of 141 unique centres |
| Study, country | Study design | Population included | Data source and study dates | Sample size |
|---|---|---|---|---|
| Burstein et al. 2011,14 USA | Retrospective cohort analysis of volume and proximity | Patients were 0–18 years. All CHD-related surgery except children weighing < 2.5 kg and undergoing patent ductus arteriosus ligation | Two data sources
|
20,922 patients from 47 centres |
| Eldadah et al. 2011,19 USA | Before-and-after study (single centre) of proximity | All paediatric post-operative cardiac admissions to the general ICU and then to cardiac ICU | Hospital records (September 2004–8) | 443 cases (199 with general ICU compared with 244 in the cardiac ICU) |
| Fixler 2012,20 USA | Retrospective cohort | Inclusion infants with estimated first-year mortality > 25%, having the diagnoses of HLHS, single ventricle, pulmonary valve atresia and PAIVS, pulmonary valve atresia with VSDs, tricuspid atresia, interrupted aortic arch, Ebstein’s malformation of the tricuspid valve, and truncus arteriosus, born in Texas. Exclusion: infants with trisomy 13 and 18 | Texas Birth Defects Registry (1996–2003) | 1213 patients from multiple paediatric hospitals and birthing centres in Texas |
| Pinto et al. 2012,37 USA | Cross-sectional cohort | Neonates < 30 days of age at the time of surgery undergoing congenital heart surgery. Patients who died before discharge from the surgical hospital or who had inoperable CHD and patients who underwent minor surgical procedures were excluded from the study | Clinical data (2005–6) | 271 patients (status unknown for 15) from single large paediatric referral hospital |
| Study, country | Study design | Population included | Data source and study dates | Sample size |
|---|---|---|---|---|
| Benavidez et al. 2007,11 USA | Cross-sectional study | Congenital heart surgery admissions aged < 18 years that could be assigned to a RACHS-1 risk category. Excluded transcatheter closure of atrial septal defects, VSDs, patent ductus arteriosus and balloon atrial septectomy, vessel repair, or occlusion | HCUP-KIDS Database (2000) | 10,032 congenital heart surgical admissions from 100 centres |
| Karamlou et al. 2013,25 USA25 | Retrospective cohort | Paediatric patients (< 20 years) undergoing ECMO of cardiac indication which could be scored on RACHS-1 risk categories | HCUP-KIDS database (2000–9) | 4954 (86%) cardiac cases mapped to RACHS-1 categories |
| Mery 2014,31 USA | Retrospective cohort study | All patients younger than 18 years who underwent congenital heart surgery | PHIS (2004–11) | 77,777 patients included from 43 tertiary care paediatric hospitals |
Appendix d: data tables
| Study, country | Main question/objective | Definition of volume/proximity | Results – volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Arenz et al. 2011,9 Germany | To measure if surgical performance changes over time in relation to complexity and case volume | None | Volume/mortality
|
Paper does not correlate volume/outcome. It does show that as volume increases, so does complexity of cases but performance can be maintained and improved. Very complex cases are rare (1%) |
| Bazzani and Marcin 2007,8 USA | Replicated four previous studies and developed own model based on previous studies | Volume treated as a continuous variable and then model rerun with annual volume dichotomised to 75 paediatric congenital open heart surgeries/year. (California guidelines on minimum volume/year.) Excluded hospitals. < 20 cases/year | Volume/mortality
|
|
| Chang et al. 2006,7 USA | To characterise the epidemiology of post-discharge death among infants and children undergoing cardiac surgery and to identify risk factors for early and late post-discharge death | Hospital average annual case volume used to define the hospitals as low volume (≤ 100 cases per year) and high volume (> 100 cases per year) | Volume/mortality
|
Findings suggest that predictors of mortality post-discharge may be different from risk factors for in-hospital mortality. In this population, lower hospital volume was associated with higher overall mortality but did not show an effect on post-discharge mortality |
| Dinh and Maroulas 2010,18 USA and Canada18 | To determine if hospital surgical volume is related to better patient outcomes in terms of in-hospital mortality, and whether or not there are differences for both high and low complexity paediatric cardiac procedures. To determine evidence for a hospital surgical volume threshold | Volume = continuous variable | Volume/mortality
|
|
| Gray et al. 2003,21 Sweden | To conduct institutional comparison of risk-adjusted 30-day post-operative mortality | Total number of admissions in 1992. Largest hospital used as a referent in analyses | Volume/mortality
|
Higher institutional volumes of complex procedures not consistently associated with increased survival. Adjusting for pre-operative risk significantly altered institutional mortality ORs Risk-adjusted analysis addressed concerns that hospitals might be ‘penalised’ for treating patients with more complex disease |
| Hickey et al. 2010,22 USA | To examine the relationship of nurse staffing, skill mix, and Magneta recognition to institutional volume and mortality for congenital heart surgery in children’s hospitals | Institution cardiac surgery volume = annual number of CHD procedures at each paediatric hospital over 2 years (2005–6) | Volume/mortality
|
After risk adjustment using RACHS-1 method, higher annual cardiac surgery volume associated with lower mortality Nursing characteristics varied in ICUs in children’s hospitals treating congenital heart surgery but were not associated with mortality ICU nurse staffing levels (in children’s hospitals in study) may be above threshold to find difference for outcome of mortality |
| Kazui et al. 2007,28 Japan | To investigate the relationship between hospital volume and outcome for 10 cardiac, lung and oesophageal surgical procedures. Open heart surgery in newborns and infants of relevance | Categorical Newborn group; 1–4 cases, 5–9 cases, 10–19 cases, ≥ 20 cases per year Infant group; 1–4 cases, 5–19 cases, 20–49 cases, ≥ 50 |
Volume/mortality
|
An inverse correlation was noted between hospital volume and operative mortality, although there were wide variations in clinical outcome among the very low-volume hospitals. Further analysis is warranted using risk-adjusted data |
| Oster et al. 2011,33 USA | To assess the relationships of a hospital’s past adjusted in-hospital mortality and surgical volume with future in-hospital mortality after surgery for CHD | Surgical volume and SMR (SMR = observed number of deaths/expected number of deaths adjusted for surgery type) calculated for January 2004 to June 2006 and July 2006 to Dec 2008 separately | Volume/mortality
|
After adjusting for multiple factors including prior hospital surgical mortality, prior surgical volume tended towards significant for higher-risk operations for CHD but was not significant for lower risk operations for CHD Prior in-hospital mortality was significantly associated with future in-hospital mortality after surgery for CHD across all risk strata, even after adjusting for multiple factors including prior hospital surgical volume Prior hospital mortality may be an appropriate consideration in the referral process – target quality improvement efforts and not just expansion efforts |
| Pasquali et al. 2012,35 USA | Measurement of relationship between:
|
Categorical and continuous variables for volume (four categories: < 150 operations, 150–250 operations, 250–350 operations and > 350 operations) | Volume/mortality:
|
Lower mortality in high-volume centres in part due to lower mortality in patients with a post-operative complication. Quality improvement should be aimed at not only reducing complications, but also recognising and managing complications that occur |
| Sakata et al. 2012,38 Japan | Measurement of relationship between hospital volume and cardiothoracic outcome (30-day mortality) | Case volume calculated as mean number of cases per year for 5 years | Volume/mortality
|
Wide variation in 30-day mortality between low- and high-volume hospitals. Need to evaluate performance in low-volume hospitals using risk adjustment |
| Seifert et al., USA,39 2007 | To determine if sex is a determinant of in-hospital mortality after CHD surgery and identify other associated factors | Annual number of paediatric cases used to calculate quartiles. Lowest quartile was reference | Volume/mortality
|
Although study aims were to determine the relationship with sex, findings suggest hospital volume is independent predictor of in-hospital mortality |
| Vinocur 2013,41 USA | To analyse relationship of surgical volume and other risk factors on post-operative mortality in all operations performed for paediatric CHD over five time periods between 1992 and 2007 | Surgical volume modelled as continuous and categorical (divided into approximate tertiles) | Volume/mortality
|
Over study period RACHS-1 score remained best predictor of post-operative mortality Increased surgical volume significant positive impact on post-operative mortality. The effect was clinically relevant (relative odds reduction generally 10–30%) but modest compared with that of other variables. Volume/mortality relationship varied significantly by risk category (no effect at lowest risk) Volume is a relatively weak predictor of a centre’s mortality rate and volume should not be used in insolation to predict quality at the level of individual institutions |
| Welke et al. 2006,44 USA | To evaluate whether or not published and widely quoted mortality rates for paediatric cardiac surgery accurately reflect current expectations. Hypothesises that (1) mortality rates at high-quality paediatric cardiac programmes are lower than published national results despite (2) change in case mix with shift away from low complexity operations. Hypothesises that, unlike RACHS-1 category, hospital volume is poor discriminator of mortality | Hospital volume – average number of RACHS-1 categorised procedures performed per year over 4 years of study
|
Volume/mortality
|
Mortality was most related to case mix – mortality rates declined, despite an increase in case mix complexity. Lack of association for hospital surgical volume/mortality suggests that other factors determine outcomes at high-quality institutions |
| Welke et al. 2008,6 USA | To determine the relationship between hospital surgical volume and mortality after paediatric cardiac surgery | Volume evaluated as continuous variable. Then, volume groups created using the following criteria: (1) natural cut-off points in the data, (2) previously studied volume thresholds, and (3) maintenance of a sufficient number of hospitals in each volume group to minimise impact of any individual hospital. All volume thresholds from 1 to 300 cases per year were investigated | Volume/mortality
|
|
| Welke et al. 2009,43 USA | To determine the association between paediatric cardiac surgical volume and mortality using sophisticated case-mix adjustment and a national clinical database | Volume: number of admissions for which the index operation was cardiovascular. (Surgical volumes: total number of cardiovascular operations.) Categorical – small, < 150 cases per year; medium, 150–249 cases per year; large, 250–349 cases per year; and very large, ≥ 350 cases per year. Categories chosen to ensure adequate sample size. Volume/mortality explored as categorical, single continuous linear variables and to explore nonlinear volume effects | Volume/mortality
|
|
| Welke et al. 2010,42 USA | To demonstrate that case volumes and mortality rates present in paediatric cardiac surgery are too low to allow the use of mortality to, statistically, differentiate between hospitals | Hospital annual surgical volumes = number of operations performed in a year. Actual volumes compared with thresholds necessary to detect doubling and a 5 percentage point increase in mortality rate | Volume/mortality
|
|
| Study, country | Main question/objective | Definition of volume/proximity | Results – volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Karamlou et al. 2008,26 USA | To assess whether or not outcomes for adult CHD surgery vary between paediatric and non-paediatric surgeons | Volume defined as percentage of paediatric operations performed annually by a surgeon (continuous variable) | Volume/mortality
|
Lower adjusted mortality for adult CHD cases operated on by surgeons with greater paediatric CHD experience |
| Kim et al. 2011,29 USA | To assess relationship between adult CHD surgery mortality and (1) adult CHD surgery volume and (2) total (adult and paediatric) CHD surgery volume | Annual adult CHD surgical volume – low (< 10 operations per year), medium (10–19 operations per year) or high (≥ 20 operations per year) Total (adult + paediatric) CHD surgery volume – low (< 200), medium (200–399) or high (≥ 400) |
Volume/mortality
|
Adult CHD surgery associated with lower risk of inpatient mortality in paediatric hospitals with higher adult CHD surgery volumes. No relationship for total (adult and paediatric) CHD surgery volume and adult CHD mortality |
| Study, country | Main question/objective | Definition of volume/proximity | Results – volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Berry et al. 2006,13 USA | To evaluate mortality of HLHS in children undergoing stage I surgical palliation in teaching and non-teaching hospitals | Four volume categories based on annual HLHS stage I palliation volume. Median institutional stage I volume did not vary by teaching status in 1997; in 2000, teaching hospitals had a higher median volume vs. non-teaching hospitals | Volume/mortality
|
Hospitals performing a low volume of stage I palliation were associated with increased adjusted mortality in 1997 (not assessed for year 2000) In-hospital mortality for stage I palliation higher in non-teaching hospitals in 1997 |
| Berry et al. 2007,12 USA | To describe hospital volumes for common paediatric speciality operations and evaluate outcomes from hospital volumes | Volume – number of annual surgical cases per hospital for operation type. Case load quartiles calculated for each procedure and hospitals in lowest quartile designated as low volume | Volume/mortality
|
No relationship for volume/mortality for VSD |
| Checcia et al. 2005,15 USA | To quantify the relative effects of institution and surgeon experience on patient outcome | Institutional volume measured as continuous and categorical variables. Categorical measure of institutional volume (for 4-year total case volume). Three groups (1) low < 16 cases, (2) medium 16–30 cases, (3) higher > 30 cases. Surgeon volume measured continuously | Volume/mortality
|
Greater association for risk-unadjusted survival and institutional surgical volume of Norwood procedures vs. individual surgeon volume. Small number of cases seen by most surgeons may mean inadequate power to detect surgeon effect. Data suggest that regionalisation of individual, high-risk procedure might improve outcome |
| Davies et al. 2011,16 USA | To assess the volume of paediatric heart transplants performed at each centre in the USA over 10-year period (1998–2007) and estimate the influence of centre volume on outcomes | Transplants assigned to one of three categories determined by the 25th and 75th percentiles of volume (based on the number of paediatric heart procedures in the previous 5 years at transplant centre). Categories were: high-volume (≥ 63 procedures in the preceding 5 years), medium volume (19–62 procedures) or low volume (< 19 procedures) | Volume/mortality
|
Adjusted analysis (multivariate logistic regression) showed volume remained a significant predictor of post-operative mortality. The volume of transplants performed at any one centre has a significant impact on outcomes. Regionalisation of care is one option for improving outcomes in paediatric cardiac transplantation |
| Dean 2013,17 USA | To investigate the effect of race, ethnicity and sex on the in-hospital mortality for three palliative procedures commonly used in the management of HLHS procedures: stage 1, stage 2 and stage 3 palliation (S1P, S2P and S3P) | For each of the three surgical procedures, the five institutions that performed most procedures are ‘large-volume institutions’. The remaining institutions are ‘small volume institutions’ | Volume/mortality
|
Identified other risk factors which might influence in-hospital mortality – for one procedure admission from home was a risk factor; for two procedures ethnicity was a significant predictor of mortality |
| Hirsch 2008,23 USA | To determine the effect of institutional volume on hospital mortality for the Norwood and ASO as representative high-complexity neonatal cardiac procedures | Institutional volume as a continuous variable, but for descriptive purposes specific point estimates are highlighted on the continuum of data points | Volume/mortality
|
Inverse relation for in-hospital mortality/institutional volume for both the ASO and the Norwood procedures |
| Hornik et al. 2012,24 USA | Relative impact of (1) surgeon volume and (2) centre volume on inpatient mortality following the Norwood procedure | Centre and surgeon volume calculated as categorical and continuous variables. Centre volume 0–10, 11–20, > 20 annual Norwood procedures. Surgeon volume 0–5, 6–10, > 10 annual procedures | Volume/mortality
|
Centre and surgical volume significantly associated with inpatient mortality and both need to be taken into account when considering policy. Further study of factors in addition to volume need to be undertaken, i.e. training, availability of personnel, composition of care teams |
| Karamlou et al. 2010,27 Canada/USA | To identify impact of institution and surgeon factors on 5-year survival from complex CHD surgery | Five domains for centre volume: (1) total case volume over study period; (2) total number of years procedure done for; (3) cases per year per institution; (4) rank order of cases; and (5) case velocity over time. Surgeon volume calculated for same five domains for the Norwood procedure and TGA only | Volume/mortality
|
Institution and surgeon experience are not the only factors influencing outcome in complex CHD. Overall no clear relationship for volumes/outcome. Excellence in one area not translated to others. Experience should be composite measure not just volume. One institution with improved Norwood procedure outcomes had neutralised effect of low birth weight suggesting institutional management protocols may play a part |
| McHugh et al. 2010,30 USA | To assess the impact of institutional volume and surgical era for patients undergoing surgery for HLHS over a 10-year period (1998–2007) | Hospitals categorised as small (< 20), medium (20–64), or large (> 64) on number of procedures for HLHS performed during the 10-year study period. Categories determined independently for S1P, S2P and S3P | Volume/mortality
|
Inverse relationship for institution surgical volume/mortality for S1P of HLHS. Large-volume centres generally had low mortality rates. However, large range of mortality rates present for medium-sized centres, and some smaller centres achieved excellent results |
| Morales et al. 2010,32 USA | To characterise the use of VAD in children in the USA | For VAD, high volume characterised as five or more procedures per year | Volume/mortality
|
Increasing use of VAD may be best served in terms of outcomes and resource use by being centralised to high-volume teaching hospitals |
| Pasquali et al. 2012,34 USA | (1) Evaluating whether or not risk status of patients impacts on relationship between centre volume and outcome. (2) Extent to which differences in centre volume account for between-centre variation in outcome | Annual Norwood procedure volume (continuous variable), Also categorical outcome with three categories of volume 0–10 annual Norwood procedures (34 centres), 11–20 (13 centres), > 20 (six centres) | Volume/mortality
|
Centre volume modestly associated with inpatient mortality (regardless of pre-operative risk status, centre volume accounts for only a small proportion of between-centre variation (centre-specific risk-adjusted outcome may be more appropriate than centre volume as marker of quality) |
| Petrucci et al. 2011,36 USA | To identify potential risk factors (including centre volume) for morbidity and mortality in neonates undergoing MBTS | Continuous only | Volume/mortality
|
Mortality rate after the neonatal MBTS remains high, particularly for infants weighing < 3 kg and those with the diagnosis of PAIVS. Patient-specific factors play a more important role than system factors in this population |
| Tabbutt et al. 2012,40 USA | To identify risk factors for mortality and morbidity after performance of the Norwood procedure for ventricular reconstruction | Centre volume defined as patients with single RV screened per centre per year. Categorised as ≤ 15 (lowest volume), 16–20, 21–30 or > 30 (highest volume) patients per centre per year. Surgeon volume defined as patients with single RV scheduled for the Norwood procedure screened per surgeon per year. Categorised as ≤ 5 (lowest volume), 6–10, 11–15, > 15 (highest volume) patients per surgeon per year | Volume/mortality
|
While centre and surgeon volume was not associated with mortality in this population, a range of patient- and procedure-related variables were associated with mortality Lower centre and surgeon volume were associated with some causes of post-operative morbidity and poorer clinical outcomes |
| Study, country | Main question/objective | Definition of volume/proximity | Results – volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Arnaoutakis 2012,10 USA | To develop a recipient risk index predicting short-term mortality OHT. To examine the relationship between institutional volume and recipient risk on post-OHT mortality Note: only 3% CHD; mean age 52 years |
Annual centre volume categorised as low (seven OHT procedures), medium (8–15 procedures) or high (> 15 procedures) | Volume/mortality
|
For OHT (3% CHD; mean age 52 years), adjusted 30-day and 1-year mortality was higher for medium and low-volume vs. high-volume centres. Effect was more pronounced for high-risk patients |
| Study, country | Main question/objective | Definition of volume/proximity | Results – volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Burstein et al. 2011,14 USA | To identify if there are differences in post-operative outcomes in children cared for in dedicated CICU vs. other ICU | Proximity – CICU ‘a stand-alone unit dedicated to care of paediatric patients with congenital and acquired heart disease’.14 Volume – median number of operations per year stratified as < 150 operations; 150–249 operations; 250–349 operations; ≥ 350 operations | Proximity/mortality
Volume/other outcomes:
|
A dedicated CICU does not appear to have an impact on mortality, LOS or post-operative complications following surgery for CHD. Potential benefits for specific subgroups of patients. Probably a complex pattern of structure, training, surgeon performance and protocols contribute to outcome |
| Eldadah et al. 2011,19 USA | To determine whether the designation of a separate, dedicated cardiac ICU affected outcomes (morbidity and mortality) for post-operative cardiac care in children | Proximity – introduction of an on-site dedicated paediatric cardiac care unit, instead of just general PICU. Volume not a variable as unchanged over time | Proximity/mortality Mortality declined from 7 of 199 (3.5%) to 2 of 244 (0.8%); p < 0.05 Volume/other outcomes:
|
|
| Fixler 2012,20 USA | To determine the effect of home distance to a cardiac centre, or having a Latin American-born parent, on first-year mortality in infants with severe CHD | Distances stratified as: 50 miles, 50–100 miles and > 100 miles | Proximity/mortality
|
Neither home distance to a cardiac centre nor race, ethnicity or parental birth country were related to unadjusted first-year survival. Survival was lower in Texas counties bordering Mexico (which have high rates of poverty) and in Hispanic infants with HLHS |
| Pinto et al. 2012,37 USA | In neonates undergoing congenital heart surgery, to determine association between patient travel time and post-discharge mortality and adverse events | Distance to surgical centre calculated as car travel time from patient’s primary residence | Proximity/mortality
|
Patients living 90–300 minutes from centre were less likely to have unplanned readmissions or reinterventions vs. those living < 90 minutes away, though the relationship was non-linear (no difference for those > 300 minutes away) |
| Study, country | Main question/objective | Definition of volume/proximity | Results – Volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Benavidez et al. 2007,11 USA | To examine association of an occurrence of complication during congenital heart surgery admissions on risk of death | Categorical < 150, 150–299, 300–449, > 450 (CHD surgery cases per year) | Volume/mortality
|
Hospitals with < 150 CHD surgical cases per year had threefold higher adjusted odds of death vs. hospitals with ≥ 450 cases. Hospitals with intermediate volumes had higher mortality vs. those with high volumes |
| Karamlou et al. 2013,25 USA | To measure the association between centre volume of cases of ECMO and survival in patients requiring ECMO | Annual ECMO volume calculated as continuous variable and three categories: < 15 patients/year, 15–30 patients/year and > 30 patients/year | Volume/mortality
|
Higher annual ECMO volume associated with improved outcomes in paediatric cardiac cases requiring ECMO. Regionalisation of care in which majority of cardiac ECMO support is provided should be considered |
| Mery et al. 2014,31 USA | To determine the incidence, risk factors, current treatment strategies and outcomes of children with chylothorax after heart surgery | Median annual RACHS procedure volume was calculated for each hospital and hospitals divided into quartiles according to cumulative median volumes. A similar analysis was done for median surgeon volume | Volume/mortality
|
Hospitals in the highest quartile for volume had half the incidence of chylothorax of those in the lowest quartile after adjustment for procedure complexity Development of chylothorax consistently associated with greater risk of in-hospital mortality, even after adjustment for hospital volume. Differences in specific complication rates may therefore mediate relationship for volume/mortality Unclear whether or not relationship is related to better pre-operative selection, differences in post-operative patient care and feeding protocols, differences in reporting between centres, or differences in surgical technique. May suggest that certain practices, not identified in this study, prevalent in high-volume centres and some lower-volume centres, are responsible for lower incidence of chylothorax |
Appendix e: conference abstracts descriptive table
| Study, country | Population included | Data source | Study dates | Sample size |
|---|---|---|---|---|
| Welke et al. 2012,48 USA | Congenital cardiac operations performed on patients < 18 years | Society of Thoracic Surgeons Congenital Heart Surgery Database | 2005–10 | 71,745 operations, 197 surgeons at 85 hospitals |
| Scheurer et al. 2011,47 USA | Neonates undergoing the Norwood procedure | Paediatric Health Information System database | 2004–8 | 2051 neonates who underwent the Norwood procedure at 29 freestanding paediatric hospitals |
| Karamlou et al. 2014,45 USA | Neonates undergoing ASO for d-TGA with or without VSD repair | Society of Thoracic Surgeons Congenital Heart Surgery Database | 2005–12 | 2404 patients (84 centres, 155 surgeons) |
| Kochilas et al. 2009,46 USA | Children (paediatric cardiac procedures) | Paediatric Cardiac Care Consortium | 2000–4 | 22,148 surgical procedures in 29 centres |
Appendix f: conference abstracts data table
| Study, country | Main question/objective | Definition of volume/proximity | Results – Volume/proximity and mortality; volume/proximity other outcomes; other variables associated with mortality | Key findings and messages |
|---|---|---|---|---|
| Welke et al. 2012,48 USA | To test the hypothesis that surgeon volume is associated with mortality after accounting for hospital volume | Annual volume hospitals low (< 150 cases per year), medium (150–249 cases per year), high (≥ 250 cases per year). Surgeons low (< 75 cases per year), medium (75–124 cases per year), high (≥ 25 cases per year) | Both surgeon and hospital volume inversely associated with mortality (p < 0.0001). Surgeons – low vs. high (OR 1.6, 95% CI 1.3 to 1.9; p = 0.0001). Hospitals low vs. high (OR 1.4, 95% CI 1.2 to 1.8) Low-volume surgeons had higher adjusted mortality rates regardless of hospital volume The addition of surgeon volume to the hospital volume models attenuated, but did not mitigate, the association of hospital volume with mortality (relative attenuation of OR 53% in low and 22% in medium-volume hospitals) |
Hospital and surgeon volume associated with in-hospital mortality when adjusting for case mix |
| Scheurer et al. 2011,47 USA | To explore the impact of dedicated paediatric intensive care units on high-risk neonatal populations (after the Norwood procedure) | Presence or absence of CICU | Patients undergoing the Norwood procedure treated at hospital with CICU did not differ in terms of mortality (OR 0.91, 95% CI 0.57 to 1.45), duration of mechanical ventilation (MF 0.85, 95% CI 0.58 to 1.23) log ICU LOS (MF 0.95, 95% CI 0.66 to 1.36) or log hospital LOS (MF 0.92, 95% CI 0.76 to 1.1) Centres with a CIU had decreased variability in outcomes (decreased median SD for: ventilation time 13 hours vs. 18 hours (p = 0.04), ICU LOS 19 days vs. 27 days (p = 0.04), hospital LOS 22 days vs. 28 days (p = 0.13) |
Presence of CICU is not associated with better patient outcomes at freestanding paediatric hospitals |
| Karamlou et al. 2014,45 USA | Association of surgeon and centre volume with early outcome following ASO | Categorical – annual centre volume 2 cases, 5 cases or 7 cases vs. 10 cases. Annual surgeon volume 1 case, 3 cases or 5 cases vs. 6 cases | Lower centre volume (2 cases vs. 10 cases: OR 2.08, 95% CI 1.34 to 3.24) and lower surgeon volume (1 case vs. 6 cases: OR 2.00, 95% CI 1.33 to 3.24) associated with composite end point (adjusted) Centre volume + surgeon volume attenuated OR by 31%. Surgeon volume + centre volume attenuated OR by 7% |
Surgeon and centre volume affect outcomes following ASO. Surgeon volume appears to be more important than centre volume |
| Kochilas 2009,46 USA | Whether or not surgical volume is a determinant of centre-specific differences in surgical mortality for CHD | < 100 procedures per year (9 centres), 101–200 procedures per year (10), 201–290 procedures per year (7), > 290 procedures per year (3) | Significant inverse relationship between in-hospital mortality and surgical volume (p = 0.0001). Similar results when grouping surgeries by risk category |
Appendix 4 Supporting evidence
Appendix a: data source description table
| Database | Type | Database description |
|---|---|---|
| The NIS database | Administrative, involuntary | An administrative database developed by the HCUP, NIS is the largest all-payer inpatient care database in the USA. It is a stratified, cross-sectional sample taken from the State Inpatient database (SID) comprising approximately 20% of all community (non-Federal) hospital discharges in the USA. It contains discharge data on approximately 8 million hospital stays between 1988 and 2011 from over 1000 hospitals, drawn from 46 states. The NIS contains both clinical and resource-use information including primary and secondary diagnoses; admission and discharge status; patient demographics; hospital characteristics; discharge status; severity and comorbidities |
| The STS-CHD database | Clinical registry, voluntary | This was set up to facilitate quality improvement and patient safety. The STS-CHD database is a clinical register collecting operative, perioperative and outcomes information on all patients at participating institutions undergoing paediatric and congenital heart surgery from 1989 to the present day. Approximately 85% of all US paediatric heart surgery centres voluntarily participate in these databases. This equates to outcomes data on > 250,000 patients from 105 participating hospitals. Data quality and reliability are ensured through intrinsic verification of data and a process of site visits and data audits. Data collected include patient demographics (including age, sex, weight and ethnicity), diagnoses, pre-operative risk factors including non-cardiac abnormalities, procedures undertaken, post-operative data and complications, and discharge status |
| HCUP-KIDS database | Predominantly administrative with limited clinical data | Sponsored by the Agency for Healthcare Research and Quality, KIDS is the only national, all-payer database for inpatient paediatric care in the USA (represents 36 states). It contains a systematic random sample of paediatric discharges from all community, non-rehabilitation hospitals participating in the HCUP. The sampling frame for the KIDS is approximately 97% of all hospital discharges in the USA and the sample of data approximates a 20% stratified sample of US community hospitals. It contains data from approximately 8 million inpatient episodes and when weighting is applied it estimates data on over 40 million episodes. Hospitals are stratified by geographic region, location (urban vs. rural), teaching status, bed size and ownership/control (government vs. private, not-for-profit status, etc.). Key data items collected include: primary and secondary diagnoses and procedures, admission and discharge status, patient demographics (e.g. sex, age, race, median income for ZIP code), hospital characteristics (e.g. ownership, size and teaching status), expected payment source, total charges, LOS and severity and comorbidity measures |
| The PHIS | Administrative | PHIS is a large multicentre administrative database containing inpatient, emergency department, ambulatory surgery and observational data from not-for-profit paediatric tertiary care hospitals that are members of the Child Health Corporation of America (CHCA). Member hospitals contribute information on demographics, diagnoses, procedures, interventions and outcomes for all inpatient episodes. The database currently holds data on over six million inpatient episodes from 44 tertiary care centres. Forty-two of these hospitals also submit resource utilisation data (e.g. pharmaceutical, imaging and laboratory resources) into PHIS. Data are collected directly from each participating hospital’s electronic medical and financial record systems. Data are subjected to reliability and validity checks between participating hospitals and the CHCA |
| The PCCC | Clinical registry, voluntary | This database contains data from approximately 137,000 consecutive surgeries from up to 57 small and medium-sized (≤ 300 surgeries per year) centres from different areas across the USA and Canada for the period 1982–2007. Founded in 1982, centres participate voluntarily and membership has varied over the time span with 35 centres contributing at least 10 years’ worth of data. The PCCC prospectively collects detailed clinical data on cardiac operations (except isolated ductal ligation for prematurity). The PCCC classifies operations into six categories based on expected early mortality rates using the RACHS-1, a validated and widely used system |
| UHC clinical database | Clinical database, voluntary | UHC is an alliance of 101 academic medical centres and 178 of their affiliated hospitals sharing diagnostic, demographic, procedural and outcome data on all hospital discharges. The Clinical Database/Resource Manager provides an expanded set of comparative data by combining patient encounter level and line-item transactional detail to yield information on patient outcomes and high-impact resource utilisation |
| The UNOS STAR data set | Clinical registry, involuntary | The UNOS is an organisation that manages the organ transplant system, the Organ Procurement and Transplant Network, in the USA. UNOS collects information on every organ donation and transplant event occurring in the USA since 1 October 1987 on a secure internet-based transplant information database. The database allows individual centres to register patients for transplants, match donated organs to waiting patients and manage the time-sensitive, life-critical data of all patients, before and after their transplants. The STAR data set contains data variables on transplant recipients collected on UNOS data forms and contains patient-level data for all kidney, pancreas, liver and thoracic transplant candidates and/or recipients. The data set includes > 500 variables from most UNOS forms, a number of calculated variables and extensive documentation of data variables |
| OSHPD Discharge database | Administrative and clinical registry, involuntary | This database includes data on all discharges collected from all licensed California hospitals (> 500 acute care hospitals), including inpatient, emergency care, and ambulatory surgery data, hospital emergency departments, and licensed stand-alone ambulatory surgery clinics in the state. OSHPD data contains ICD-9-CM discharge, diagnosis and procedure codes assigned by California hospitals to each individual discharge during the year. Among other variables, the data set includes primary procedure and diagnosis and up to 20 secondary procedures and 24 secondary diagnoses |
| Texas Birth Defects Registry | Population registry | The Birth Defects Epidemiology and Surveillance Branch of the Texas Department of State Health Services manages this population-based active registry. Data are collected from a variety of medical facilities in the state to identify instances of major birth malformations in offspring of Texas-resident mothers (structural malformations and chromosomal disorders). Through these multiple sources of information, the Registry monitors all births in Texas (approximately 400,000 births each year) and identifies cases of birth defects. Once identified, detailed demographic and diagnostic data are abstracted and entered into the electronic registry |
Appendix b: risk adjustment for congenital heart surgery (based on Jacobs et al. 2012116)
Complexity stratification tools have seen increasing popularity in the analysis of outcomes associated with congenital and paediatric cardiac surgery, reflecting the fact that so many different distinct types of operations are performed. Since 2002, complexity stratification has been used extensively by the STS-CHD database and the EACTS Congenital Heart Surgery Database.
Aristotle Complexity Score
The Aristotle Basic Complexity Score defines the complexity of an operation through three factors: potential for mortality, potential for morbidity, and technical difficulty of the operation.
When designed in 2000, the Aristotle Complexity Score was entirely based on subjective probability. This approach, based on the opinion of experts, was considered a good solution owing to the limited number of data available at that time. The Aristotle score evaluates basic surgical performance and more complex surgical performance through two complexity scores: 1) the basic complexity score (1.5–15 points), which is a procedure-adjusted complexity comprising four levels of complexity, and 2) the comprehensive complexity score (1.5–25 points), which adds patient-adjusted complexity (0–10 points) to the procedure-adjusted complexity and comprises six categories.
Risk Adjustment for Congenital Heart Surgery-1
The RACHS-1 is a mortality risk-adjustment methodology based on paediatric cardiac procedures for CHD. The method was created to adjust for differences in case mix when examining in-hospital death rates after congenital heart surgery. RACHS-1 was developed using a consensus approach involving a nationally representative panel of paediatric cardiologists and surgeons in the USA. The focus of RACHS-1 is on short-term mortality after surgery with inpatient mortality as the indicator for this outcome, as it is easily available in administrative data and other data sets.
The RACHS-1 method involves the grouping of different cardiac procedures with similar risks for in-hospital mortality into six risk categories, several of which are stratified by age or diagnosis. The procedures are organised into the six categories to form an ordinal scale of increasing risk for inpatient mortality, where category 1 has the lowest risk of death and category 6 the highest. In instances where a patient is undergoing multiple cardiac surgical procedures, the procedures are placed in the category corresponding to the single highest risk procedure. The risk categories were created by consensus judgement of the panel primarily using common coding systems such as ICD-9-CM. The allocation of procedures was subsequently refined by using mortality data from two large multicentre data sets. In order to measure case mix as accurately as possible, the risk categories are usually included in multivariable models with other key variables such as age, prematurity and the presence of a major non-cardiac structural anomaly, such as cleft lip/palate or anal atresia.
Society of Thoracic Surgeons – European Association for Cardio-Thoracic Surgery Congenital Heart Surgery Mortality Categories
The STS-EACTS Congenital Heart Surgery Mortality Score, an objective, empirically based index used to identify the statistically estimated risk of in-hospital mortality by procedure and to group procedures into risk categories. When modelled with three patient-level factors (age, weight and pre-operative LOS) STS-EACTS has a c-statistic of 0.816. The tool was developed using primarily objective data with minimal use of subjective probability. The risk of mortality prior to discharge from the hospital after cardiac surgery was estimated for 148 types of operative procedures by using actual data from 77,294 patients entered into the Congenital Heart Surgery Databases of the EACTS (33,360 patients) and the STS (43,934 patients) between 2002 and 2007. Procedure-specific mortality rate estimates were calculated using a Bayesian model that adjusted for small denominators. Each procedure was assigned a numeric score (the STS-EACTS Congenital Heart Surgery Mortality Score). Claimed advantages of the STS-EACTS Mortality Score and Categories include that it is based on objective evidence, rather than expert opinion, that it is able to classify more procedures than RACHS-1 or Aristotle Complexity Score and that it demonstrates a higher correlation with outcome (observed mortality) by c-statistic.
Appendix c: table of covariates of included studies
| Patient factors | Study |
|---|---|
| Age | Chang et al. 2006,7 Bazzani et al. 2007,8 Benavidez et al. 2007,11 Burstein et al. 2011,14 Dean 2013,17 Eldadah et al. 2011,19 Hornik et al. 2012,24 Karamlou et al. 2013,25 Karamlou et al. 2008,26 Kim et al. 2011,29 Mery 2014,31 Morales et al. 2010,32 Oster et al. 2011,33 Pasquali et al. 2012,34 Pasquali et al. 2012,35 Seifert et al. 2007,39 Tabbutt et al. 2012,40 Welke et al. 200943 |
| Sex/gender | Chang et al. 2006,7 Benavidez et al. 2007,11 Dean 2013,17 Eldadah et al. 2011,19 Hirsch et al. 2008,23 Hornik et al. 2012,24 Karamlou et al. 2013,25 Karamlou et al. 2013,26 Kim et al. 2011,29 McHugh et al. 2010,30 Pasquali et al. 2012,34 Seifert et al. 200739 |
| Race/ethnicity | Chang et al. 2006,7 Benavidez et al. 2007,11 Dean 2013,17 Fixler 2012,20 Hirsch et al. 2008,23 Kim et al. 2011,29 Oster et al. 2011,33 Pinto et al. 2012,37 Seifert et al. 200739 |
| Prematurity | Benavidez et al. 2007,11 Berry et al. 2006,13 Dean 2013,17 McHugh et al. 201030 |
| Weight at surgery | Burstein et al. 2011,14 Hornik et al. 2012,24 Pasquali et al. 2012,34 Pasquali et al. 2012,35 Petrucci et al. 2011,36 Pinto et al. 2012,37 Welke et al. 200943 |
| Insurance status | Chang et al. 2006,7 Benavidez et al. 2007,11 Berry et al. 2007,12 Oster et al. 201133 |
| Family income | Chang et al. 2006,7 Seifert et al. 200739 |
| Gestational age | Arnaoutakis et al. 2012;10 Tabbutt et al. 201240 |
| Category (of covariates) | Covariates | Studies (adjusting for covariates) |
|---|---|---|
| Cardiac diagnosis | CHD; single ventricle; double ventricle; pulmonary atresia; intact ventricular septum; aortic atresia; endocardial cushion defect; pulmonary venous return; arrhythmia; double outlet right ventricle; dominant ventricle | Berry et al. 2006,13 Burstein et al. 2011,14 Davies et al. 2011,16 Hornik et al. 2012,24 McHugh et al. 2010,30 Pasquali et al. 2012,34 Petrucci et al. 201136 |
| Comorbidities/other non-cardiac abnormalities | Genetic syndrome; risk factor; abnormality; chromosomal anomaly | Berry et al. 2006,13 Burstein et al. 2011,14 Hornik et al. 2012,24 Kim et al. 2011,29 McHugh et al. 2010,30 Oster et al. 2011,33 Pasquali et al. 2012,34 Pasquali et al. 2012,35 Tabbutt et al. 201240 |
| Renal abnormalities | Morales et al. 2010,32 Welke et al. 2009,43 Petrucci et al. 201136 | |
| Major non-cardiac structural anomaly | Benavidez et al. 2007,11 Berry et al. 200613 | |
| ICD-9-CM diagnostic code | Bazzani et al. 2007,8 Berry et al. 200613 |
| Category (of covariates) | Covariates | Studies (adjusting for covariates) |
|---|---|---|
| Year (or era) in which procedure undertaken | Davies et al. 2011,16 Dean 2013,17 Hornik et al. 2012,24 Karamlou et al. 2013,25 Pasquali et al. 2012,34 Welke et al. 200943 | |
| Surgical complexity | STS-EACTS RACHS 1 Aristotle Basic Complexity Other |
Bazzani et al. 2007,8 Arenz et al. 2011,9 Benavidez et al. 2007,11 Burstein et al. 2011,14 Dinh and Maroulas 2010,18 Eldadah et al. 2011,19 Gray et al. 2003,21 Hickey et al. 2010,22 Karamalou et al. 2010,27 Kim et al. 2011,29 Oster et al. 2011,33 Pasquali et al. 2012,34 Pasquali et al. 2012,35 Pinto et al. 2012,37 Vinocur 2013,41 Welke et al. 2010,42 Welke et al. 2009,43 Welke et al. 200644 |
| Procedure | Chang et al. 2006,7 Checchia et al. 2005,15 Mery 2014,31 Oster et al. 2011,33 Welke et al. 200943 | |
| Admission type – planned or emergency | Bazzani et al. 2007,8 Berry et al. 2007,12 Dean 2013,17 Seifert et al. 200739 | |
| Pre-operative LOS | Hornik et al. 2012,24 Pasquali et al. 2012,34 Pasquali et al. 2012,35 Welke et al. 200943 | |
| Ventilator use/support | Burstein et al. 2011,14 Eldadah et al. 2011,19 Petrucci et al. 2011,36 Welke et al. 200943 | |
| Pre-operative mechanical ventilation support | Hornik et al. 2012,24 Pasquali et al. 2012,34 Petrucci et al. 201136 | |
| Use of ECMO | Karamlou et al. 2013,25 Tabbutt et al. 2012,40 Morales et al. 201032 | |
| Characteristics of donor | Arnaoutakis et al. 2012,10 Davies et al. 201116 | |
| Cardiopulmonary support/bypass | Bazzani et al. 2007,8 Eldadah et al. 201119 | |
| Acidosis | Petrucci et al. 2011,36 Welke et al. 200943 | |
| Post-operative sepsis | Burstein et al. 2011,14 Morales et al. 201032 | |
| Re-exploration of the chest/reoperative sternotomy | Davies et al. 2011,16 Eldadah et al. 201119 |
| Hospital factors | |
|---|---|
| Surgeon volume (including volume by procedure and volume by adult/paediatric) | Kim et al. 2011,29 Mery 2014,31 Tabbutt et al. 201240 |
| Hospital type (teaching or non-teaching) (rural or urban) | Hirsch et al. 2008,23 Karamlou et al. 2013,25 Karamlou et al. 200826 Morales et al. 2010,32 Seifert et al. 200739 |
| Distance from patient’s home to hospital/travel time | Fixler 2012,20 Pinto et al. 201237 |
| Bed size of hospital | Karamlou et al. 2013,25 Mery 201431 |
Appendix d: assessment of relevance table
| Study | Adjusted for severity of condition? | Adjusted for age? | Multicentre? | Included > 1 intervention/condition? |
|---|---|---|---|---|
| Arenz et al. 20119 | Yes | Yes | No | Yes |
| Arnaoutakis et al. 201210 | Yes | Yes | Yes | No |
| Bazzani and Marcin 20078 | Yes | Yes | Yes | Yes |
| Benavidez et al. 200711 | Yes | Yes | Yes | Yes |
| Berry et al. 200712 | No | No | Yes | No |
| Berry et al. 200613 | Yes | No | Yes | No |
| Burstein et al. 201114 | Yes | Yes | Yes | Yes |
| Chang et al. 20067 | Yes | Yes | Yes | Yes |
| Checcia et al. 200515 | No | No | Yes | No |
| Davies et al. 201116 | Yes | Yes | Yes | No |
| Dean 201317,51 | No | No | Yes | No |
| Dinh and Maroulas 201018 | Yes | Yes | Yes | Yes |
| Eldadah et al. 201119 | Yes | Yes | No | Yes |
| Fixler 201220 | Yes | Yes | No | Yes |
| Grey et al. 200321 | Yes | Yes | Yes | Yes |
| Hickey et al. 201022 | Yes | Yes | Yes | Yes |
| Hirsch et al. 200823 | Yes | No | Yes | No |
| Hornik et al. 201224 | Yes | Yes | Yes | No |
| Karamlou et al. 201325 | Yes | Yes | Yes | Yes |
| Karamlou et al. 200826 | Yes | Yes | Yes | Yes |
| Karamlou et al. 201027 | Yes | Yes | Yes | No |
| Kazui et al. 200728 | No | No | Yes | Yes |
| Kim et al. 201129 | Yes | Yes | Yes | Yes |
| McHugh et al. 201030 | Yes | No | Yes | No |
| Mery 201431 | Yes | Yes | Yes | Yes |
| Morales et al. 201032 | Yes | No | Yes | No |
| Oster et al. 201133 | Yes | Yes | Yes | Yes |
| Pasquali et al. 201234 | Yes | Yes | Yes | No |
| Pasquali et al. 201235 | Yes | Yes | Yes | Yes |
| Petrucci et al. 201136 | Yes | No | Yes | No |
| Pinto et al. 201237 | Yes | Yes | No | Yes |
| Sakata et al. 201238 | No | No | Yes | Yes |
| Seifert et al. 200739 | Yes | Yes | Yes | Yes |
| Tabbutt et al. 201240 | Yes | No | Yes | No |
| Vinocur 201341 | Yes | Yes | Yes | Yes |
| Welke et al. 201042 | Yes | Yes | Yes | Yes |
| Welke et al. 200943 | Yes | Yes | Yes | Yes |
| Welke et al. 20086 | Yes | Yes | Yes | Yes |
| Welke et al. 200644 | Yes | Yes | Yes | Yes |
List of abbreviations
- ASO
- arterial switch operation
- BTSP
- Blalock–Taussig shunt procedure
- CHD
- congenital heart disease
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- cPICU
- cardiac paediatric intensive care unit
- EACTS
- European Association for Cardio-Thoracic Surgery
- ECMO
- extracorporeal membrane oxygenation
- HLHS
- hypoplastic left heart syndrome
- HS&DR
- Health Services and Delivery Research
- ICD-9-CM
- International Classification of Diseases, Ninth Revision, Clinical Modification
- ICU
- intensive care unit
- IRP
- independent reconfiguration panel
- JR
- judicial review
- LOS
- length of stay
- MeSH
- medical subject heading
- NIHR
- National Institute for Health Research
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RACHS-1
- Risk Adjusted classification for Congenital Heart Surgery
- ScHARR
- School of Health and Related Research
- STS-EACTS
- Society of Thoracic Surgeons–European Association for Cardio-Thoracic Surgery
- TGA
- transposition of great arteries
- VAD
- ventricular assist device
- VSD
- ventricular septal defect