Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1011/19. The contractual start date was in November 2011. The final report began editorial review in October 2013 and was accepted for publication in March 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Norma O’Flynn is seconded to the National Clinical Guideline Centre which is funded by NICE to develop clinical guidelines. Tim Stokes does occasional work for pharmaceutical companies on the work of NICE and primary care; any honoraria received are paid directly to the University of Birmingham. Ray Fitzpatrick is a member of the NIHR Journals Board.
Disclaimer
this report contains transcripts of interviews conducted in the course of the research, or similar, and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Ziebland et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Aim
To identify common, core components of patients’ experiences of the NHS to inform the development, and measurement, of National Institute for Health and Care Excellence (NICE) quality standards (QSs) and to examine the reach and limitations of these core components in describing the aspects of care that are important to patients from diverse backgrounds, with experiences of different conditions and NHS care pathways.
Objectives
-
To conduct qualitative secondary analysis of collections of narrative interviews to identify common, core components of patients’ experiences of the NHS.
-
To test these candidate components with (i) further purposive sampling of the interview collections and (ii) a series of focus groups (FGs) with users.
-
To embed the project alongside the development of NICE clinical guidelines (CGs) and QSs.
-
To inform the development of measurement tools on patient experiences.
-
To develop and share resources and skills for secondary analysis of qualitative health research.
In this introductory chapter, we begin by providing a brief overview of the increasing centrality of patient experience in UK health policy, most recently illustrated by the UK coalition government’s White Paper, Equity and Excellence: Liberating the NHS, and the information strategy published by the Department of Health (DH). 1,2 We then describe the process by which NICE produces CGs and QSs, which underpin the development of the proposals outlined in the White Paper. We introduce the Health Experiences Research Group (HERG) interview archive and discuss the methods used in objectives 1 and 2 (secondary analysis of qualitative data and FG research). We discuss how we might understand the ways in which the research knowledge could best be used in practice (objective 3). We also briefly explain the measurement tools used to measure patient experiences and outcomes (objective 4), and, finally, explore the issues surrounding the sharing of qualitative data for secondary analysis (objective 5).
Health policy context: improving patient experience
Improvement of the ‘patient experience’ has been highlighted as a key aim by the DH. The 2012 Health and Social Care Act states that it is the duty of the Secretary of State to ensure continuous improvement in the quality of services including the ‘quality of experience undergone by patients’. 3 The NHS Operating Framework for 2012–13 describes each patient’s experience as ‘the final arbiter in everything the NHS does’. 4 The inquiry into care standards at the Mid Staffordshire Hospitals5 and the subsequent Francis Report6 drew attention to the failures to act on patient and public complaints about poor care, which were recorded, but not acted upon, long before the inquiry.
While the focus of health-care quality improvement appears to have shifted firmly into the territory of patient experience, policies to improve people’s experiences of health care have been introduced by successive governments for decades. These have usually centred on aspects such as the provision of information and patient choice. Other attempts to steer the NHS towards a more patient-centred approach include, for example, the Picker Institute Principles of Patient-Centred Care, which were transformed into the Patient Experience Framework in 2011 by the NHS National Quality Board (NQB). 7 Existing quality frameworks of health care, such as the NICE QS on patient experience in adult NHS services, are formulated as universal statements, describing components of good care that are independent of care setting, condition-specific care pathways or patient characteristics. 8 In a recent critical conceptual synthesis to identify which health-care experiences matter to patients and why, researchers from the Universities of Aberdeen and Dundee reviewed three commonly used health-care quality frameworks: the World Health Organization’s (WHO’s) responsiveness framework, the Institute of Medicine’s domains of health-care quality and the ‘SENSES’ framework of Nolan et al. (Table 1). 9,10 They found that none of these frameworks was sufficiently comprehensive to cover all of the aspects of health-care experience that patients in published research have identified as relevant and important. To catalyse improvements to care, we need a better understanding of why certain aspects of care matter to patients, and how this may differ between individuals, groups and care contexts.
| WHO: responsiveness | |
|---|---|
| Health-care systems ensure | |
| Autonomy | (Of patient/family) via provision of information about health status, risks and treatment options; involvement of individual/family in decision-making if they want this; obtaining of informed consent; existence of rights to treatment refusal |
| Choice | Of health-care providers |
| Clarity of communication | Providers explain illness and treatment options, patients have time to understand and ask questions |
| Confidentiality | Of personal information |
| Dignity | Care is provided in respectful, caring, non-discriminatory settings |
| Prompt attention | Care is provided readily or as soon as necessary |
| Quality of basic amenities | Physical infrastructure of health-care facilities is welcoming and pleasant |
| Access to family and community support | (For hospital inpatients) |
| Institute of Medicine: quality of care | |
| Health services are | |
| Safe | Avoiding injuries to patients from the care that is intended to help them |
| Effective | Providing services based on scientific knowledge . . . avoiding underuse and overuse |
| Patient-centred | Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions |
| Timely | Reducing waits and sometimes harmful delays |
| Efficient | Avoiding waste, including of equipment, supplies, ideas, energy |
| Equitable | Providing care that does not vary in quality because of personal characteristics |
| Nolan et al: SENSES framework | |
| All parties should experience relationships that provide a sense of | |
| Security | To feel safe within relationships |
| Belonging | To feel part of things |
| Continuity | To experience links and consistency |
| Purpose | To have potentially valuable goal(s) |
| Achievement | To make progress towards desired goals(s) |
| Significance | To feel that you matter |
The Health and Social Care Act 2012 was heralded by the UK coalition government’s White Paper, Equity and Excellence: Liberating the NHS, which acknowledges that ‘healthcare systems are in their infancy in putting the experience of the user first’ (p. 13) and many NHS organisations continue to struggle to identify the best way of integrating patients’ experiences into service improvement. 1 The paper proposed ‘an enduring framework for quality and service improvement’ (p. 5). This places patients at the heart of the NHS through ‘an information revolution’ (p. 3), with patients having ‘greater choice and control’ (p. 3). A central component of the government’s vision is the development of national QSs. These provide definitions of good-quality care across a range of clinical pathways and are based on evidence considered during the development of related CGs. The paper states that ‘to achieve our ambition for world-class healthcare outcomes, the service must be focused on outcomes and the quality standards that deliver them’ (p. 4). This ambition was subsequently realised in the Health and Social Care Act 2012, which mandates NICE to develop QSs across a range of health conditions. 3
NICE products
Clinical guidelines
Historically, the DH has commissioned NICE to provide guidance to the NHS and wider public under a number of different programmes. They have produced CGs which set out clear recommendations for the treatment and care of people in England, Wales and Northern Ireland with specific diseases and conditions since 2002. Separate guidelines are produced for Scotland by the Scottish Intercollegiate Guidelines Network (SIGN). NICE commissions guidelines from several National Collaborating Centres (NCCs). The largest of these is the National Clinical Guideline Centre (NCGC) which was established in 2009. The other centres comprise the NCC for Mental Health, the NCC for Women’s and Children’s Health (NCC-WCH) and the NCC for Cancer. NICE also have an internal guidelines programme.
All NICE CGs are based on a review of the best available evidence of the clinical effectiveness and cost-effectiveness of treatments for specific diseases and conditions. There are also generic guidelines, which cover subjects such as patient experience and medicines adherence. As each guideline covers a specific condition, or a specific aspect of a condition, there is also extensive cross-referral between guidelines; for example, the guideline on management of obesity is referred to by guidelines on cardiovascular disease and diabetes. The process and methods of developing a guideline is a pre-specified and lengthy process and is described in the NICE guidelines manual. 11 Guideline topics may be suggested by the DH or Welsh Assembly Government, by health professionals, and by patients and the public. Once a topic is referred to NICE, NICE commissions the guideline development centre, who recruit a chairperson and starts to develop the scope of the guideline. This process involves consulting with stakeholders (who register through the NICE website) to determine what will, and what will not, be covered by the guideline. The scope defines areas of clinical management, the target population and important outcome measures. The stakeholder consultation involves a workshop and a formal written consultation process. The scope is finalised and signed off by NICE. The areas included in the scope are converted to a series of clinical ‘review’ questions during guideline development. The chairperson and a guideline development group (GDG) are recruited for each guideline. These groups comprise health professionals [consultants, general practitioners (GPs), nurses and allied health professionals] and lay members (patients, carers, service users) and are supported by a technical team of an information scientist, a health economist, research fellow(s) and a project manager. All GDG members have an interest or expertise relevant to the topic. A systematic review is performed for each clinical question by the technical team. The quality of the evidence is scored and the cost-effectiveness reported if available or original health economic models developed. The GDG meets every 4 to 6 weeks over a period of 16 months to examine this evidence and to make recommendations based on the evidence and their clinical or personal experience. The wording of these recommendations is chosen carefully to reflect the strength of the evidence. The draft guideline is available for a second period of consultation by stakeholders, after which alterations are made by the GDG if needed. The final guideline is reviewed by NICE and published on the NICE website in different formats: the full version (which lists the methods and evidence and details how the recommendations were derived from that evidence); the NICE version, which lists the recommendations alone; and a lay version. NICE produces ‘pathways’ on its website which present guidance in such a way as to allow easy cross-referral between different guidelines that may be relevant to people with a disease or condition.
Quality standards
Quality standards are a set of specific, concise statements that act as markers of high quality, cost-effective patient care, covering the treatment and prevention of different diseases and conditions. They should be aspirational but achievable and define priority areas for quality improvement. 12
NICE were first tasked to develop QSs for the English NHS in the Darzi Review of 2008. 13 In 2010, the profile of NICE QSs was raised significantly, with the new coalition government emphasising the centrality of NICE QSs in the ‘new NHS’ in its 2010 policy paper Liberating the NHS and in the subsequent 2012 Health and Social Care Act. 1,3 Referrals to NICE for QSs are made by NHS England. QSs are intended for use by health-care professionals (to raise standards of care), patients and the public (so that they are informed of the quality that they should expect of the services provided to them), service providers (to enable performance to be assessed) and commissioners (to help them to purchase high-quality services). Audience descriptors append the QS.
Each quality statement is also accompanied by a ‘quality measure’ which defines the proportion of the target population (as a numerator and denominator) to which it applies (for auditing purposes). To keep the administrative burden manageable, each statement specifies only one measurable metric. QSs inform incentive schemes and payment mechanisms – such as the Clinical Commissioning Groups Outcomes Indicator Set, the Quality and Outcomes Framework for general practice, and the Commissioning for Quality and Innovation payment framework – by linking a proportion of the provider’s income to the achievement of quality improvement goals.
The descriptive statements that constitute QSs are derived from three dimensions of quality: effectiveness, patient experience and safety. Equality issues and resource impact are also considered. The process of QS development is still emerging. The first ‘pilot’ QSs comprised approximately 15 statements which described what good-quality care should look like. As the QS programme rapidly expanded, the need to reduce the administrative burden on service providers was recognised (each statement of each QS has to be measured and audited) and the maximum number of permissible statements was reduced first to 10 and then to between six and eight.
During the lifespan of this study, the process of QS development was as follows (Figure 1): after a QS was referred to NICE, it was developed by a topic expert group (TEG) over three meetings. The TEG, like a GDG, comprised health professionals (consultants, GP, nurses and allied health professionals) and patients and was convened specifically for each QS. During the first meeting, TEG1, the scope of the standard was defined. The scope specified the population groups that would and would not be covered, the health-care settings (primary, secondary, intermediate care and community settings) and areas of care that would and would not be considered. Furthermore, the scope considered economic aspects and designated key development sources (published CGs, guidelines under development, related QSs, other accredited evidence, key policy documents and national audits). Registered stakeholders were invited to comment on the draft scope before it was finalised by NICE.
FIGURE 1.
Overview of the NICE QS development process (at time of fieldwork).
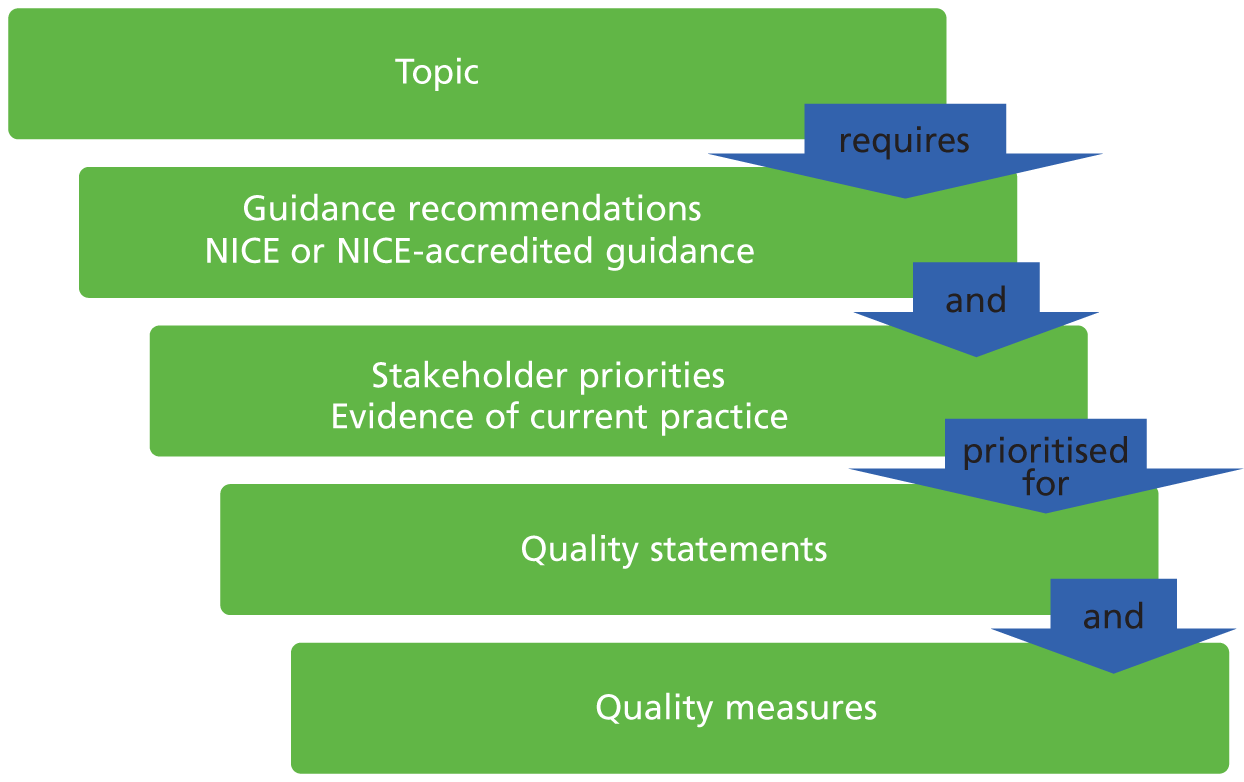
During the second meeting (TEG2), quality statements were discussed and developed with support and guidance from NICE technical teams. The draft QS was also put out to consultation before further development in a third meeting (TEG3). The product was reviewed by NICE before it was finalised and published.
Towards the end of 2012, this process began to be superseded by a standing-committee model. After a topic has been commissioned, a topic overview is developed by a NICE QSs team and published on the NICE website. Registered stakeholders are invited to suggest key areas of care or service provision for quality improvement. A Quality Standards Advisory Committee (QSAC), which again comprises health professionals (consultants, GPs, nurses, allied health professionals), commissioners, experts in quality measurement, NICE representatives, and patient, carer and service user members, meets to prioritise areas for improvement that should be taken forward into draft quality statements. These statements are produced by the QSs team and comment is invited by stakeholders once more. The QSAC meets a second and final time to discuss and modify the draft statements in the light of stakeholder comments. The final product is quality assured and approved by NICE before publication. QSs are reviewed after 5 years. Since April 2013, NICE has an expanded remit to provide guidance and set QSs for social care audiences (further information can be found at www.nice.org.uk/socialcare/).
Although two very different products, the CGs and QSs are related. A major feature of the QS process is agreeing which of the large number of recommendations in a CG should be prioritised for development as a small number of measurable statements. As stated above, the focus is on three dimensions of quality: effectiveness, patient safety and patient experience. There is also a standalone patient experience QS (see Appendix 1), which was developed concurrently with the patient experience CG, with access to the same information. Topic-specific quality statements are not supposed to duplicate material in the patient experience QS. QS development does not include any in-depth discussion of evidence, as this has taken place during the development of the CG, though this may lead to tension when new evidence or changes to practice have emerged in the interim. The NICE manual that was used at the time of our fieldwork contained guidance as to how qualitative evidence might be incorporated into the guidelines development process (see Appendix 2). A detailed figure illustrating the CG development process is appended (see Appendix 3).
The Health Experiences Research Group interview archive: source material for the secondary analysis
The qualitative interviews in the HERG archive are collected as national, purposively sampled collections which aim for maximum variation. The interviews are collected by experienced qualitative social scientists working within HERG. There are currently over 75 collections (60 at the start of the project), each concerning a different health issue (ranging from ‘experiences of pregnancy’ to ‘living with a terminal illness’). Each set comprises 35–50 interviews which are digitally audio or video recorded (depending on the participant’s preference), transcribed, checked by the interview participant and copyrighted to the University of Oxford for a number of non-commercial purposes, including secondary analysis and publication. The research is funded via a peer-reviewed process by bodies including the National Institute for Health Research (NIHR) and the Economic and Social Research Council (ESRC), and research committees of voluntary organisations (including Arthritis Research UK, Wellcome Trust, Marie Curie Cancer Care).
The projects all share a research question (‘What are the experiences, and information and support needs, of people with health condition X?’) and a common interview method that starts with an appropriate variation on an open-ended question intended to invite a narrative response (e.g ‘Could you tell me all about it from when you first thought there might be a problem?’). When the person has completed their account, a semistructured section of the interview includes questions and prompts about any issues of interest that may not have been fully discussed in the narrative. These typically include questions about treatment decisions, information, support and communication with health professionals. All participants are asked if they have anything they would like to tell other people who are starting out on the same journey and if there is anything they would like to pass on to NHS staff, at all levels, who might learn from the participant’s experiences. These questions often add rich, informative data about how services and communication could be improved. 14
Each of the interview studies starts with a literature and field review and sets up a specialist advisory panel including patients, professionals, researchers, clinicians, and representatives from the voluntary sector and (if appropriate) the funding body. The panel advises on the parameters of the project, including selection and recruitment of participants.
A maximum variation sample is sought to help generate as diverse a sample as possible, including those whose experience might be considered ‘typical’ as well as those with more unusual experiences. 15 As this method seeks to achieve representation of the diversity of experiences, it is not appropriate to present results numerically. For each project, recruits are actively sought through a national network of primary care staff, hospital consultants and specialist nurses, advisory panel members, local and national support groups, advertising online and in local newspapers and snowballing through participants’ and personal contacts. Analysis and data collection proceed simultaneously and continue until ‘data saturation’ is reached to ensure that the widest practical range of experiences has been included. Analyses of the data have been published in peer-reviewed journals over the past 10 years. 16–21 Illustrated lay summaries of the research findings are also disseminated via a website, owned by the DIPEx (Database of Individual Patient Experiences) charity: www.healthtalkonline.org. The website has NHS Information Standard approval and the collections are reviewed every 2 years and updated with further interviews if considered necessary, for example to capture the experiences of people who have used new treatments or therapies. The website is the only public source of patient experience evidence cited in the NHS Evidence Process and Methods Manual (www.evidence.nhs.uk/evidence-search-content/process-and-methods-manual), and is already acknowledged as a source of evidence for use by technical staff as part of their review of evidence when they develop a new CG.
Reusing research data
Two developments in prevailing research cultures particularly favour reuse of existing data. First, synthesising published and unpublished research before (or instead of) conducting new research is now mainstream practice. 22–24 Secondly, following the decision in 2000 by the ESRC to require ‘award holders to offer for archiving and sharing copies of both digital and non-digital data to the Economic and Social Data Service’ (p. 256) and to seek the correct permission to do so when collecting data,25 several funding bodies nationally26,27 and internationally28 have followed suit. Many now have explicit expectations that publicly funded research should be shared to maximise the value of data for the public good and ‘to expedite the translation of research results into knowledge, products, and procedures to improve human health’. 29 There has been a debate in the qualitative research community about the legitimacy of secondary analyses. 30 However, the HERG qualitative interview archive has been widely used, under licence by many established research groups, both nationally and internationally, in work funded by the NIHR, the ESRC and the Medical Research Council (MRC) among others. Articles based on secondary analyses of these data have been published in high-impact journals. 31–35 A secondary analysis of HERG data was commissioned by the General Medical Council (GMC) to contribute patients’ perspectives to the guidelines on end-of-life care. 36
Research methods
In this study, we employed the considerable expertise that exists within the HERG to conduct secondary analyses of interview collections covering selected health conditions so as to identify a candidate list of common components of good health care that was grounded in patients’ experiences (objective 1). The reach of this candidate list was tested through further analyses of other data sets from the archive and through FG work (objective 2). In many cases, we were also able to draw upon the expertise of the primary researcher who could provide additional perspective, insight and contextual information.
Secondary analysis
In a modified version of framework analysis, we used charts to make a summary description of data from each of the interviews across a set of categories, which were later developed into themes for analysis. 37 The process was iterative and flexible enough to accommodate anticipated themes (e.g. areas of care that have been identified in the guideline scope) as well as emergent themes. These themes were then compared across cases and between conditions to identify general and specific aspects of good-quality care. Coding and analysis of the interviews was supported by NVivo qualitative data analysis software (version 9, QSR International, Warrington, UK).
Focus group methods
We used FGs to test the candidate core components with people whose views may have been under-represented in the HERG interviews used for the secondary analysis. FGs have been used previously to research the use of health services by seldom heard groups. 38 Being among similar others, in a supportive and reassuring environment, can encourage the sharing of views openly as well as enabling contradictions, personal or private issues to be more easily raised, discussed and sometimes resolved. 39 On the other hand, FGs can be difficult to use with certain groups; for example, those with mental impairments may find conventional FGs harder to participate in than a one-to-one interview. Flexibility in the structure and comportment of the groups is particularly important when one is seeking to engage participants who might not usually take part in research; too rigid an approach may (further) marginalise some participants.
To explore variation in the meaning and importance of components across care settings and social groups, we conducted six FGs with people who we recognise may not be represented in the HERG interview archive (despite striving for maximum variation). In addition to the traditional-format FGs, we designed a webspace in which we held an online discussion forum with patients with long-term conditions (LTCs). The webspace, ‘Good health care’, contained a different forum for each candidate core component and was illustrated with a video clip taken from the archive. The online method allowed us to hear the views of those we could not reach through the FGs, either because of the severity of a LTC or due to a caring role. Our analysis sought to examine and conceptualise the limitations and reach of components of good care and how they may vary between groups.
Knowledge transfer
Our third objective was to embed the project alongside the development of the NICE CGs and QSs. In order to meet this objective, the project team planned a ‘knowledge transfer’ intervention comprising three components:
-
the presentation of HERG secondary analyses to chosen CG and QS groups
-
a training programme for NCGC staff
-
a secondment from HERG to the NCGC.
We studied the intervention using a combination of semistructured interviews with HERG and NCGC/NICE staff, non-participant observation of GDG and TEG meetings and an online survey of NCGC staff who attended the training programme. In keeping with our conceptualisation of the three components as being part of a knowledge transfer intervention, we synthesised and analysed our findings using an existing ‘knowledge to action process’ model which distinguishes ‘knowledge creation’ and ‘action’ as two concepts, with each comprising ideal phases or categories. 40 In the context of our study, ‘knowledge creation’ pertains to the work undertaken by HERG staff to conduct the secondary data analyses, while ‘action’ relates to the process by which we sought to embed this knowledge into the CG and QS development process. As the authors of the model indicate ‘In reality, the process is complex and dynamic, and the boundaries between these two concepts and their ideal phases are fluid and permeable. The action phases may occur sequentially or simultaneously, and the knowledge phases may influence the action phases’ (p. 18). 40 Nonetheless, the model provided a useful heuristic to guide our thinking, data collection and analysis.
Measuring patients’ experiences and outcomes
The identification of a set of core topics that are central to patients’ experiences of the NHS is applicable to the development of quality and outcomes measures for health care. This study sought to inform this measurement (objective 4). Here, we briefly explain the tools used to measure patient experiences and outcomes.
The DH is keen to measure the health status or health-related quality of life from the perspective of the patient so as to assess the quality of care and health outcomes of NHS clinical pathways. The government White Paper, Equity and Excellence: Liberating the NHS, encourages ‘much wider use of effective tools like Patient Reported Outcome Measures’ (PROMs). 1 This includes generic tools such as the Short Form questionnaire-36 items (SF-36)41 and European Quality of Life-5 Dimensions (EQ-5D)42 which can be used across different conditions, as well as more specific measures such as the Oxford Hip and Knee Score. 43 PROMs are validated questionnaires which may be administered before and after a clinical procedure to measure self-reported health changes and hence the effects of care. Results are used to quantify the performance of providers, clinicians, managers and commissioners, to permit clinical auditing and to inform the choices of patients and GPs. PROM development should ideally include consultation with patients to ensure that the measures include outcomes which matter to patients, as well as those which are regarded as clinically important.
Patient-reported experience measures aim to capture patient experiences of a health-care pathway or service. They include the Picker-15 Patient Experience Questionnaire44 and the national GP Patient Survey,45 for example, but can also be on more specific aspects of care experiences, such as the Patient Evaluation of Emotional Care during Hospitalisation (PEECH). 46
Other mechanisms which seek to capture self-reported aspects of patient experience include patient comment and ratings on websites such as NHS Choices and Patient Opinion, real-time feedback devices in hospital, and brief measures such as the Friends and Family Test.
While experience measures are not about health outcomes as such, it is arguable that experience is in itself a form of outcome of the process of care. There is also an emerging body of literature which suggests that patient experience may be linked to or be predictive of health outcomes. 47
In this study, we discussed with key individuals from the PROM and patient-reported experience measure (PREM) academic community whether or not and how our observations about the reach and limitations of the core components of good-quality care might inform the development and interpretation of quantitative data on patients’ experiences.
Sharing of qualitative data for secondary analysis
The qualitative method of conducting relatively unstructured, in-depth interviews with purposive, maximum variation, national sampling of patients is recognised as an important method for ensuring that patients’ views, opinions and perspectives are understood. 48 However, the method is costly and time-consuming to conduct, and some patient groups are hard to include. An alternative to collecting new data is to use secondary analysis of existing qualitative data sets, which can be a highly efficient and cost-effective alternative, provided that the researcher is aware of the challenges and limitations inherent in a secondary analysis and that the original data have been collected with appropriate rigour and in anticipation that they may inform future work. 49,50 Loss of context and lack of contact with the original researcher has often been cited as a reason to question the validity of a secondary analysis. 51,52
The considerable potential of qualitative research has not been fully realised by policy-makers. Owing to the time pressure inherent in the policy-making process, there is often insufficient time to commission, conduct and analyse new qualitative studies to inform a specific policy. In order for the experiences of patients, relatives and carers to be heard, it is, therefore, imperative that use is made of existing data collections. The reticence of policy-makers to translate qualitative data into a means of informing health policy and improving health service provision may relate to a more general lack of awareness of the qualitative paradigm. 53–56
The aim of the fifth objective was to draw on expertise, both within HERG and of archivists, primary researchers and secondary analysts of qualitative data, in health care and in other disciplines, to discuss and develop recommendations for the archiving and preparation of qualitative data for sharing for secondary analysis. Following the workshop, we have developed a 1-day training course on the secondary analysis of qualitative data for inclusion in the HERG programme of qualitative research methods courses.
Chapter 2 Objective 1: qualitative secondary analysis to identify common core components of patients’ experiences of the NHS to inform NICE clinical guidelines and quality standards
As discussed in the previous chapter, existing quality frameworks do not cover all aspects of care that patients have identified as relevant and important. 7,9,57,58 They have a strong focus on safety, effectiveness and equity, and while these are integral components of health care, they could be considered basic rather than good or aspirational aspects of care. Allied to the development of QSs, our interest in the secondary analysis of patient experience data was to identify what patients perceived to be indicators of ‘good care’, which the Francis Report described as ‘enhanced’ care in contrast to fundamental and developmental. 6
To address the first objective, we conducted a qualitative secondary analysis of four interview collections from the HERG archive. Each collection comprised 37–55 narratives from people with experience of a specific health condition. We began with a complete reanalysis of interviews on myocardial infarction (MI). This analysis sought to identify common core components central to patients’ experiences of the NHS; in accord with the focus of QSs, we focused on good or ‘enhanced care’ rather than fundamental care. The HERG interview collections cover patients’ care experiences in both primary and secondary care, in emergency settings and also after hospital discharge, and can therefore provide insights into how core components of good-quality care might vary across different stations of the care pathway. The analysis of subsequent collections added to the components identified from MI as well as seeking to respond to NICE’s specific needs for specific CGs and QSs (see Asthma, Young people with type 1 Diabetes and Rheumatoid arthritis).
Interview collections were carefully selected to ensure that they matched the development schedules of products that had been commissioned by NICE. Considerations included whether or not the topic and the timing of the analysis could feed into NICE processes to:
-
inform NICE products scheduled for development
-
allow observation and assessment of the transfer of knowledge between NICE/NCCs and HERG (through attendance at GDG and TEG meetings) and scrutiny of the final product
-
permit an examination of the different ways and time points at which the analysis might feed into NICE product development
-
permit an examination of whether or not the type of development process (parallel or sequential) affected the degree to which the research findings influenced the final product. (A QS might be developed in parallel with an update of an existing CG or the development of a new CG, or it might be developed sequentially to a CG that was not due for review, through a tertiary review of the evidence.)
A significant limiting factor was that the choice of topics available in the HERG archive was not as large as anticipated due to the lack of fit of QSs and CGs in development by NICE over the study period.
The 18-month project was too short to follow through an entire NICE product lifespan, although we hoped to be able to learn from examining four topics which were at different stages in the process. Furthermore, uncertainty and emergence of the NICE processes for QSs meant that it was not possible to specify input into pre-selected NICE products at the outset. Agreement of the topic areas for collaboration was an iterative process that required consideration of the scope for the guideline alongside the topic as included in the HERG collection and discussion with teams developing guidelines. This resulted in several ‘blind alleys’ where the opportunity for collaboration with specific technical teams was internally explored by the NICE/NCGC co-applicants, without progression beyond an initial expression of interest.
The final four health areas for the qualitative secondary analysis were MI, asthma, rheumatoid arthritis (RA) and young people with type 1 diabetes (Table 2).
| Topic area | Details of HERG collection used in the analysis | NICE products |
|---|---|---|
| MI | Analysis of interviews with 37 people who had experienced MI between 1989 and 2003 (19 after 2001). Nine had been treated with clot-busting drugs, 10 had had angioplasty (2000–4), nine had had a stent (2001–3), and 11 had experience of bypass surgery. The mean interval between diagnosis and interview was 5 years, ranging from < 1 year to 23 years | New guideline on STEMI |
| Updated guideline on secondary prevention after MI | ||
| Asthma | Analysis of interviews with 38 people diagnosed with asthma during 2011–12 | QS (developed in parallel with accreditation of guideline produced by SIGN and the British Thoracic Society) |
| Young people with type 1 diabetes | Analysis of topic summaries (themes from the primary analysis), peer reviewed and published on www.youthhealthtalk.org, and a subset of six interviews from the full data set | Type 1 diabetes in children (NCC-WCH) and type 2 diabetes in adults (internal guidelines team) |
| RA | Analysis of 52 interviews of people diagnosed with RA (and four partners). A wide range of therapies were included; 20 had experience of surgery and two were waiting for an operation at the time of interview | QS (based on guideline developed in 2009) |
Two further interview collections covering adults with autism and people with fertility problems were used to test the reach of the candidate core components (these last two analyses are discussed in objective 2 and were not intended to contribute to QS development).
There was considerable variation in the time available for each topic (a consequence of accommodating NICE product timelines). Based on the feedback received from the NICE/NCGC co-applicants and technical teams, researchers modified their approach on how to present the findings and experimented with a range of formats. These included relatively intensive secondary analysis of both anticipated and emergent themes (MI) (see Appendix 4); a review of existing analytic reports (diabetes); ‘piggybacking’ the analysis onto the primary analysis (by the original researchers) of a project that was very recently collected; and focusing the analysis on 11 specific aspects of care that had already been identified for discussion as part of the development of a QS (RA). The variation in output styles allowed us to compare the work load, contribution and reception of different models of analysis and reporting.
Analysis of the first interview collection on MI adopted an inductive and exploratory approach to coding data that included emergent themes as well as those anticipated from the literature (see Secondary analysis).
In analysing the subsequent three interview collections (asthma, RA and young people with type 1 diabetes), the mode of analysis was increasingly tailored to the scope of the NICE product and the needs of the technical teams.
The four main secondary analyses and how we reported the findings to NICE
Myocardial infarction
The data collection took place in 2002–3 and participant recruitment aimed for diversity. Most were white British and living with a partner or spouse. The sample included fewer women than men and a higher proportion of younger patients (i.e. aged < 55 years at time of diagnosis) compared with the age profile of patients currently experiencing MI in the UK. The diversity in participants’ ages made it possible to explore adjustment to MI and patients’ information and support needs at different ages and stages of the life course. The sample spanned all socioeconomic groups from all parts of the UK, including urban, small town, rural and remote areas. Recruitment routes included GPs, charities and support groups. Analysis explored accounts of experiences of MI and also adjustment and engagement in secondary prevention from different vantage points in the trajectory of illness and recovery.
Presentation of myocardial infarction findings
It was considered likely that the findings from this collection would inform a guideline being developed on ST segment elevation myocardial infarction (STEMI). A review of the content of the collection suggested that it might also inform the update of another guideline: secondary prevention of MI. Both guidelines were being developed at the NCGC and it was initially envisaged that a report of the findings would be presented to the chairpersons and technical teams responsible for these guidelines. NICE processes require that the evidence used to inform the GDG is publicly available, and so the NCGC requested a written report which could be included in an appendix as part of the evidence presented to the GDG and for public consultation.
The scoping consultation for the STEMI guideline had finished in July and the guideline was in development prior to the start of this project. The scope was highly technical and did not include patient experience but it was anticipated that the report might supplement GDG opinion and clinical data in the discussion part of the guideline. The scope for the secondary prevention guideline included barriers to engagement with cardiac rehabilitation services, and, although the scoping phase was almost complete, the guideline was not yet in development.
An extensive report was sent to both the STEMI and secondary prevention technical teams (see Appendix 4). As agreed with the NCGC, the initial report was extended to include three further chapters of greater relevance to the secondary prevention technical team. The content and format were informed through direct discussion. The NCGC anticipated that the process would be iterative, with the technical team feeding back to the HERG in advance of the document being distributed to the GDG.
Asthma
The analysis of this 2012 collection benefited from the insights of the primary researcher who was able to provide additional contextual information. The sample comprised interviews with 38 people (25 women) diagnosed with asthma during 2011–12. Their ages ranged from 16 to 73 years and included 17 participants with childhood-onset (age at diagnosis 6 months to 12 years). Four of those with adult-onset asthma had been diagnosed over the age of 50 years. Length of time since diagnosis ranged from under 1 year to over 30 years.
Presentation of asthma findings
In order to fit with NICE timelines, analysis was based on an initial coding frame that embedded patients’ NHS experiences within their experience of living with asthma more broadly. These findings were presented to fit with the standard NICE briefing paper format for QS development.
The asthma interviews were still in the process of undergoing primary analysis at the time of the project, and this represented an opportunity to draw directly on that primary analysis to address the secondary questions posed by the team working on the NICE QS for asthma. Rather than a complete analysis of components of good care, for TEG1 the researcher was asked to work through the care pathway and identify headline issues that may indicate where a certain aspect of care was currently poor or variable in terms of delivery by health-care professionals. This was to contribute to prioritising which elements of the British Thoracic Society (BTS)/SIGN guideline would be developed into quality statements. In collaboration with NICE co-investigators, this was reduced considerably and presented in bullet point format, using, primarily, headings drawn from the guideline (such as ‘diagnosis’, ‘non-pharmacological management’ and ‘inhaler devices’) but also a new category, ‘emotions and acceptance’ (see Appendix 5).
The researcher then carried out a more expanded analysis of the original bullet points for TEG1 under these headings. Therefore, the text on emotions and acceptance, for example, was now placed under the statement ‘people with asthma are offered self-management education including a personalised action plan’ (see Appendix 6). The asthma technical team added these components into their full briefing paper for TEG2.
Young people with type 1 diabetes
The secondary analysis drew on peer-reviewed topic summaries (themes from the primary analysis) which had already been published on www.youthhealthtalk.org (the sister site of www.healthtalkonline.org for young people). The full data set comprised 37 young people, aged 15–27 years, diagnosed between 1 year and 24 years of age, mostly interviewed in 2006, with updates in 2010 and 2012.
Presentation of diabetes findings
The report was written in consultation with the HERG researcher who had recently updated the diabetes collection. Themes were tested and further developed by coding selected full interview transcripts from the HERG archive. A summary document was produced for the technical team updating the CG on type 1 diabetes in children, which focused on the areas of care that had been highlighted by NICE (see Appendix 7). This was available at the time of scoping of the diabetes guideline but the final scope was very specific and technical, and despite discussion and meetings between the NICE/NCGC investigators and the technical team updating the guideline, it became clear that the secondary analysis would not be incorporated into the process, and so we did not proceed to prepare a full analysis of the data set.
Rheumatoid arthritis
This collection was based on a core set of 38 interviews conducted in 2004–5 and an update of 14 newer interviews from 2012. The interviews included a wide range of ages at diagnosis from 5 to 74 years, and the time that participants had lived with the condition ranged from very recently diagnosed to 46 years. This diversity in participants’ ages and length of illness experience made it possible to explore how the experience of RA and patients’ information and support needs differed at different ages and what the adjustment to living with RA might require practically and emotionally at different stages of life. The sample reflected the diverse severity of the condition across individuals and time periods and included treatment with disease-modifying anti-rheumatic drugs (DMARDS), steroid tablets, injections and intravenous pulses, biological treatments (anti-tumour necrosis factor and B-cell therapies), as well as management with analgesics and non-drug treatments.
Presentation of rheumatoid arthritis findings
A similar model of reporting to that used for the asthma topic was employed following positive feedback from the NICE/NCGC co-investigators. A short summary report was produced after exploratory coding of a subset of interview transcripts (see Appendix 8). Subsequent analysis and coding was focused to generate analytic depth and data saturation in key areas (draft statements) discussed in advance with the NICE technical team. The findings were presented as a second report (see Appendix 9).
Core common components of good health care identified from the four secondary analyses
The analyses of the four health topics allowed us to develop, expand and modify a candidate list of core components of good health care, drawn from the literature (see Table 2) and developed with additions from each collection in turn. In the rest of this section, we describe how these core components were developed through the four secondary analyses.
We begin with a description of the core components of good care identified from the MI interview collection. In subsequent sections on asthma, young people with type 1 diabetes and RA, we consider additional aspects and variations. Results are mapped and summarised in Table 3.
| MI | Asthma | Young people with type 1 diabetes | RA |
|---|---|---|---|
| Being taken seriously (when first presenting with symptoms) | Clarity about when to seek help in event of an asthma attack | Clear rationale for glucose control Also supporting self-care |
Appropriate use of services and referrals Diagnosing the patient’s preferences |
| Kindness and honesty in delivering the diagnosis and implications | Clarity about when a definitive diagnosis has been made (especially adult-onset) | Approachability and friendliness of staff (especially nurses) | Checking knowledge and expectation of the disease |
| Facilitating difficult conversations, e.g. explaining why the MI happened, how to modify life to prevent recurrence | Helping to negotiate responsibilities, e.g. awareness of shifting parent/child dynamics with young people with asthma | Recognition in the consultation of sometimes conflicting agenda between the young person and their parent | Acknowledging uncertainties when seeking effective treatments and the unpredictability of the disease |
| A caring, personal and flexible approach (especially as an inpatient and in early days at home) | Recognising effect on person’s life and relationships as well as the more medical aspects | Helpful if specialist nurses raise topics that may be of concern to young person, e.g. recreational drugs, smoking, alcohol, weight control | Understanding the impact of an unpredictable illness on people’s lives |
| Timely information in a range of formats, including peer support | Repeating information and demonstrating inhaler techniques | Clear, simple but not ‘dumbed-down’ information, given as appropriate over a period of time Peer support important as positive role models and also to exchange tips about living well with diabetes |
Signposting to further information, including peer experiences and support Recognising that younger people have different information and support needs and will use new technologies |
| Building confidence | Recognition of the patient’s own knowledge of their condition | Supporting self-care (also peer support, above) | Entrusting patients with drugs in case of flare-ups, should they wish |
| Continuity of care relationship | Importance of annual reviews Access to specialist asthma nurse |
Back up of personal access to a specialist diabetes nurse | Different consultants known to have different approaches – patients prefer one consultant |
| Smooth transition of information between services | Important if information about diabetes shared when being treated for other illnesses | ||
| Rapid access to specialist advice (especially after leaving hospital) | Access to out-of-hours care in event of an asthma attack | Rapid access to advice and services during hypoglycaemic attacks | Prompt referral from GP to specialist care if needed |
Core components of good health care for patients after a myocardial infarction
People who had had a MI often described feeling shocked and vulnerable and, at least in the short term, lacking confidence in how to manage treatments and other changes to their life. They appreciated kindness and honesty from staff with specialist cardiac knowledge who understood the impact of the illness on the patient’s life. Findings suggested that the relative importance of specific aspects of care varied along the care pathway, reflecting patients’ evolving understanding of, and adjustment to, their condition and their changing information and support needs. We describe below why these aspects of care were important to patients after a MI, with illustrative extracts from the MI interviews.
Being taken seriously when presenting with symptoms
Patients who were later diagnosed as having had a MI were sometimes reluctant to seek help for their symptoms, fearing that they would seem overdramatic. Patients felt well cared for when their GP listened to them, took their concerns seriously and conducted swift and appropriate investigations.
Kindness and honesty in delivering the diagnosis
Myocardial infarction patients usually reported that they had wanted to be fully informed about the possible risks and likely outcomes of their condition and their treatment, but that it was also important to be given hope and encouragement. The following man felt that his consultant gave him a clear explanation as soon as he was admitted to hospital.
He explained [the consultant] – I mean I was very impressed actually because he squatted down and spoke to me at my level. He explained that there were risks attached to this process [. . .] Every intervention was explained to me. [. . .] And, you know, what was very clearly being stated was that, you know, this was the crucial time, you know, that if they were able to intervene successfully now, then my long-term prospects of survival, because I mean, I think there was an explicitness that I wouldn’t necessarily survive.
HA02, male, MI in 2003 aged 54 years
In contrast, another patient described a consultant who was both blunt and pessimistic.
[The consultant] he also wasn’t convinced I’d actually make it through the, the coronary artery bypass. He was surprised that I’d actually made it through that, so like he’s not the sort of guy you want on a football team to gee you up before a game, ‘Hey lads if you keep it down to 10, you’ll do well’. [laughter] He’s not one of those that you want on your team. I think he’s probably going to think he’s trying to give it like it could be, but he probably overdoes how bad it could be.
HA05, male, MI in 2003 aged 37 years
Facilitating difficult conversations
Myocardial infarction patients identified a number of issues that they found difficult to talk to health professionals about, including prognostic information, concern over operation scars and the safety of sexual intercourse after the MI. Patients liked health professionals to guide them through such difficult conversations in a proactive and sensitive manner.
Family members may also be affected by a diagnosis of MI and dynamics may change. Patients sometimes felt ‘mollycoddled’ by an overprotective spouse after returning home. It can be a hard for the patient to explain to other people why they have had a MI and what they can do to avoid another while they are still adjusting to the diagnosis themselves; health professionals can help by including the patients’ partner in discussions about rehabilitation and reassuring them about activities that are safe.
We found that a lot of the stress after the operation derived from the fact that she was more, more worried about, about what I could do than I was. And she was trying to hold me back all the time whereas I was always trying to go. And one of the benefits of joining the support group is precisely this, that the spouse has a chance to speak to other spouses and see you know, what you can do and what you can’t do and that takes away a lot of the stress of rehabilitation. [. . .] [Dr X] was very instrumental in helping me there. He said to my wife, ‘Look he’s got a body and his body’s going to tell him what he can do and what he can’t do’. And my wife took that on board and it was far easier and then from then on we made jokes about it.
HA09, male, MI in 1995 aged 69 years
A caring, personal and flexible approach
After a MI, people often felt very vulnerable and anxious and needed good nursing care. When they were in hospital, people really appreciated feeling that staff were going out of their way to be kind and considerate
I found the staff excellent, you know they said to me ‘you’ll be up and running in a few days you know’. One nurse, an Irish girl if I may say, was on night duty. They used to come down and see me every night about, I used to be awake half the night, and make me a cup of coffee about 3 o’clock in the morning, and we’d have a chat and things like that. They did make life good for me.
HA06, male, MI in 2003 aged 70 years
It was the very attitude of them [that made me feel secure], you know. They were very, they were very caring and they sort of seemed as if they really understood how you were feeling. And I was grateful for that because it wasn’t all this starchy business you know, it was nice.
HA35, female, MI in 2001 aged 77 years
Myocardial infarction means different things to people depending on their awareness of the condition, their life stage, previous health status and caring and work responsibilities. It was appreciated when health professionals showed an understanding of how MI had affected their life, and were willing to be flexible.
The first night I was taken off the monitors, I was actually in little separate room which was fortunate because I’ve a big family and, [um] they thought it’d be, because they’d a room would be easier if I was in that rather than in a general ward, which was lovely of them because it meant that people could come and go.
HA05, male, MI in 2003 aged 37 years
Timely information in a range of formats
Patients usually wanted to understand why they had experienced a MI, whether or not it was likely to happen again and how they might avoid another. Information was not always forthcoming, and some were reluctant to ask busy hospital staff to answer their questions, or were not sure what to ask. It was helpful when health professionals invited questions, provided clear explanations and checked patients’ understanding. A man who had had two MIs had his questions answered but wondered if nursing staff were sometimes a bit cautious about what information they volunteered.
Rushed as they were, they [cardiac ward nurses] always had time to talk to you about what was going on. They would explain procedures to you. I think you have to ask in some cases, but once you have asked, or once I had asked, they were quite willing to go through and tell you. I think they want to be fairly convinced that you aren’t going to panic or misconstrue what they’re saying, so maybe they’ll be a little bit guarded at first.
HA23, male, MIs in 1991 and 1998 aged 49 and 56 years
One woman suggested that a personalised, written record of what exactly had happened to her in hospital, and why, would have been helpful, as it was difficult for her to take in all the information at the time it was given. Having a personal record to revisit over time might also help patients to adjust to their condition, to develop coping strategies and to explain to family and friends.
It was sometimes helpful for patients to hear about how other people had coped. Information about local support groups and recommendations for websites and other resources were appreciated by patients and their families [see Facilitating difficult conversations (HA09)].
Rapid access to appropriate expertise
Myocardial infarction patients usually have to continue to take medicines after being discharged from hospital, but they were not always sure of the purpose of all of their tablets. It was also sometimes hard for them to distinguish between the side effects of treatment and unfamiliar symptoms. Having a telephone number for a cardiac nurse specialist who could be contacted for prompt advice was much appreciated, especially during the early weeks after the MI when the patient and family may have felt particularly anxious.
Building confidence
Health professionals can play a key role in building patients’ confidence after MI and shaping their expectations for the future. This is likely to influence patients’ motivation to make positive lifestyle changes and furnish them with hope for the future. Seeing a rehabilitation exercise class in action was motivating and reassuring for this man and his wife.
Before I was discharged the physiotherapist took me to the gym downstairs and in the gym there were a number of people doing various exercises and she said they were all ex-patients who had had bypass operations and I was, you know, I was pretty impressed. You know, they were doing, they were jumping up and down and they were doing skipping, and they were doing a mild form of press-ups. A number of fairly strenuous looking things and I thought, oh well it must have been 2 or 3 years since they’ve had their bypass and I asked her about that and she said, turned to one of the chaps and she said ‘How long ago have you had your bypass?’ and he said, ‘Oh, just 6 weeks ago now’. So that was, that was a real eye-opener and again something very positive. And really from that moment on I felt, and my wife, we both felt very positive about the whole thing.
HA09, male, MI in 1995 aged 69 years
Smooth information transfer between health professionals and between services
A few patients felt uncertain as to whether or not information about drugs prescribed in primary care reached hospital consultants and vice versa; patients sometimes felt that they needed to take responsibility to ensure smooth information flow between services, but saw it as a marker of good care when information flow was efficient.
Additional perspectives from patients with asthma
Asthma is a chronic condition, often diagnosed in childhood. Below, we describe aspects of good care identified from our interviews with people diagnosed with asthma in childhood or as adults. While many of the components that we have already discussed, such as being taken seriously by health professionals and being treated with kindness and honesty were, of course, also very important to people with asthma, there were particular perspectives on good care that may be more specific to a chronic health issue. These included having one’s own knowledge and experience in managing the condition recognised.
Clarity about when a definitive diagnosis has been made
Patients’ accounts highlighted the need for clarity about when a definite diagnosis of asthma has been made; for example, patients may be required to use inhalers as part of the diagnostic process and this may be confused with the treatment prescribed following diagnosis.
A diagnosis of asthma can come as a surprise to those adults who think of it as a childhood condition; as a result of that perception, some did not take their diagnosis very seriously.
Clarity about when to seek help in event of an asthma attack
An asthma attack can be very alarming to the patient and those around them; people appreciated clear advice about when would be appropriate to seek help from emergency services. Patients sometimes worried that professionals might think they were not using the services appropriately (e.g. if they did not know how to distinguish between a panic attack and an asthma attack).
Access to out-of-hours emergency services
Patients also needed to feel reassured that, if they did require emergency treatment, they knew what to do and that services would be available at any time of the day or night.
Recognition of the patient’s own knowledge of their condition
Information about how their treatment worked and how it could be stepped up or down enabled patients to take a more active role in the management of their condition. Some GPs were willing to pre-prescribe oral steroids for emergency use, thereby showing trust in the patient’s ability to self-manage. Those who had lived with asthma for many years wanted health professionals to respect their expertise and trust them to know when something is wrong, within the context of a regular review.
Repeating information and demonstrating inhaler techniques
‘Good information’ for asthma patients included explanations about the processes leading to a diagnosis, about how oral steroids work and why it is important to take them consistently, as well as when to report side effects. Patients appreciated the repeated provision of information and health professionals taking the time to explain things well. It was helpful when health professionals ‘showed’ rather than just ‘told’, for example demonstrating good inhaler technique.
Patients wanted guidance from health professionals about which sources of information are reliable. Access to specialist primary care asthma nurses was highly valued by those who had experienced it.
Recognising effect on person’s life and relationships
Some asthma patients felt that health professionals could be too focused on medical management at the expense of providing lifestyle advice. Young people appreciated advice on the impact of asthma on their participation in school sports and how to use inhalers preventatively. For adults, consideration of the emotional impact of a diagnosis of asthma was sometimes particularly important.
Helping to negotiate responsibilities and difficult conversations
People who had been diagnosed as children appreciated help from their doctors and nurses in guiding their parents to accept changed responsibilities as they reached young adulthood and the dynamics between the parent and child shifted.
Some health professionals had provided information about asthma and its treatment to schools, and explained to school staff about safety during sports activities and the need for young people with asthma to be able to access medication. This was much appreciated by young people, who had sometimes found it hard to tackle misunderstandings about asthma among school staff.
Additional perspectives on good care from young people with type 1 diabetes
Our analysis of the aspects of good care that were important to young people with diabetes included further parallels with those identified for MI and asthma and also a few topics that were specific to this condition (see Table 3).
Diabetes is a chronic condition which is largely self-managed by patients. All of the young people in this collection had been diagnosed when they were children or young people aged < 25 years and some had experience of the transition from child services to adult services, which raised particular issues for health care.
Communicating a clear rationale for treatment
Getting detailed and intelligible explanations about the condition and its treatment were seen as prerequisites for assuming responsibility for self-management. While type 1 diabetes is a relatively common, chronic condition, there can be long-term complications, such as the amputation of limbs. Hearing about these can frighten young patients (and their parents) rather than motivating them to look after their health. Communication needs to be clear, honest and consistent without being alarmist.
When treatment regimes needed to change, young people liked the doctor (ideally one they had met before) to explain why this was happening.
Information and peer support
Young people sometimes found it hard to raise topics that they were worried about, especially if they were concerned that the nurses and doctors, or their parents, might disapprove. It was helpful if their doctors or specialist nurses raised topics that may be of concern to a young person (e.g. recreational drugs, smoking, alcohol or weight control), rather than waiting until the young person asked or reached 18 years of age.
Hearing about sportspeople who have diabetes could be helpful in providing role models for young people, as could peer support. Patients valued tips and advice about managing the condition from other young people living with diabetes.
Supporting self-care
Young people who had lived with type 1 diabetes for a while were keen for health professionals to recognise their expertise in managing aspects of their own care.
Young people liked health professionals who recognised that it was sometimes a burden to have to monitor their blood glucose and administer insulin. Some staff seemed to be able to empathise with the frustrations of trying to achieve good glucose control. Young people also valued health professionals who recognised changing preferences for autonomy and involvement in decisions as they were growing up and becoming more independent of their parents.
Approachability and friendliness of staff
Genuine friendliness and empathy are very important to young people, some of whom said that they felt guilty or frustrated when their blood sugar levels were not well controlled. It was also helpful if staff recognised that there might sometimes be a conflicting agenda between the young person and their parent, and helped the young person to steer an appropriate course through potential confrontations.
Rapid access to advice and services
Access to specialist support was important especially in the early stages after diagnosis when the young person (and their parent) was learning how to manage the condition. Unforeseen issues sometimes arose; reassurance and reminders about management strategies were needed during hypoglycaemic attacks, especially the first few times they happened.
Access to a specialist diabetes nurse who they knew (especially if they were in mobile, text and e-mail contact) was often greatly appreciated by young people. This was also very useful when they were away from home, for example when travelling abroad.
Additional perspectives on good care from people with rheumatoid arthritis
Rheumatoid arthritis is a condition that affects people very differently, which makes a flexible approach to care, including individual assessment of patients’ information and support needs and tailoring of service level, particularly important. Treatments have changed considerably in recent years, with the result that many patients can now avoid disfiguring damage to joints. People with RA experience pain, stiffness and mobility restrictions, the unpredictable nature of which can cause particular difficulties in their relationships, family, work and social lives. Several of the additional perspectives on good care that we identified from this collection relate to these characteristics of the disease. These perspectives are summarised in relation to the other three conditions in Table 3.
Appropriate use of services and referral
Symptoms were often minor, gradual or non-specific when they began – for example, stiff joints in the morning or painful wrists – and were often initially attributed to sports injuries, chilblains or general ageing. GPs who actively encouraged the patient to come back if the symptoms did not go away, or worsened, were appreciated.
Checking knowledge and expectation of the disease
It was helpful if doctors recognised that patients may have fears about RA based on awareness of older patients who had experienced different treatment regimes. Fear of joint deformity or disability was a common feeling in people diagnosed with RA.
Some patients whose acute symptoms had subsided by the time they saw a rheumatologist found it difficult to accept the chronic and recurring nature of the disease and were reluctant to start treatment.
Treatment explanation and preference diagnosis
Patients with RA emphasised the importance of being involved in decisions about treatments, which might include surgery. A worry for some patients was that when they compared notes with other patients they discovered that different consultants had different treatment preferences.
Patients had different priorities and preferences regarding the acceptability of different types of side effects associated with different drugs (e.g. women of child-bearing age did not want drugs that are contraindicated for pregnancy, but doctors cannot guess whether or not this applies to a particular patient).
Those who did not feel that they knew enough to share decision-making appreciated it when doctors took time to explain the options and rationale, for example why it might be the right time to consider surgery. Several patients felt that surgery was ‘the final resort’ when drug treatments had failed to alleviate problems. It was sometimes difficult for patients to accept the need for surgery when pain or mobility problems were still relatively mild; some sought a second opinion before going ahead with surgery.
Acknowledging uncertainties and understanding the impact of an unpredictable illness
Patients found it reassuring when consultants explained that RA affects people differently and that modern interventions are often successful at preventing joint disfigurement. It was also appreciated when doctors took the time to explain about the variable nature of the disease, acknowledged uncertainties in the diagnostic and treatment process, and reassured patients for whom a suitable treatment might take a little while to identify.
Patients felt that they were being well cared for when health professionals seemed to understand the meaning of RA in the context of their lives. At diagnosis, people were often concerned about how their RA may affect their employment or studies. The unpredictability of RA and the uncertainty about when they might get better has major implications for people of working age, who may need help to explain the nature of RA and its implications.
Signposting to further information and access to peer experiences
People with less secure or manual jobs and those raising young children were particularly worried about their ability to continue supporting their families. Signposting to relevant employment laws, information about assistance at work and available benefits was much appreciated. Information needs and preferences varied, but patients now routinely use the internet for information and appreciate being referred to reliable sites and invited to discuss what they find if they have questions. Support groups and group education sessions were also valued.
Hearing other patients’ experiences of using a drug, in combination with other information about the medicine, helped people to decide whether or not to accept the treatment.
Rapid access to specialist support
When experiencing flare-ups, people with RA have particular information and support needs and require rapid specialist access. However, not all people with RA in the sample had adequate arrangements for this in place. Several people said that they typically received steroid injections from their GP to bridge the time it took to see a consultant who could adjust their medication according to disease activity. In one extreme case, a woman was angry that she had to wait for several weeks for her GP to refer her to her consultant once blood tests had shown increased disease activity, and then had to wait further until that consultation took place to receive the medication she knew she needed all along, despite her symptoms getting worse. This was her third experience of a flare-up.
Several other people reported examples of much more rapid and efficient access systems, for example telephoning a helpline to make a clinic appointment.
Supporting self-care
For health professionals to support patients in self-care, there needed to be mutual trust, as well as sufficient knowledge and confidence on the patients’ side. Patients who had experienced group education sessions found them helpful and particularly valued advice on effective use of painkillers, suggestions for lifestyle changes that might improve their symptoms and finding out about the full range of services available to people with RA. Sessions also provided valued opportunities for peer advice and support.
Summary: sourcing the core components of good health care
After completing the secondary analyses for the four HERG interview collections, the researchers merged the findings and key issues highlighted in the outputs produced for NICE/NCC technical teams. We also mapped the similarities and differences in perspectives of good care on a Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA), which was updated as each secondary analysis was completed (see Table 3).
While many of the core items were common across all conditions, some interesting variations emerged, which will be explored further in a conceptual paper for a social science journal.
Finally, we reduced the total number of core components by collapsing similar or closely linked core components under broader headings, while also maintaining what appeared to be distinct aspects within each.
The final list of candidate core components was intended to be:
-
about good care rather than basic or legal standards (e.g. ‘the doctor is qualified to treat me’/’I’m treated fairly/not discriminated against’)
-
generic, that is apply regardless of health condition or care setting
-
expressed in clear, understandable language from the patient’s perspective.
Further discussion within the Oxford team and feedback from lay steering group members on the candidate list resulted in the following revised list of eight core components (and 20 related ideas). The components were written from the patient viewpoint, and lay representatives of the steering group ensured the use of plain English. These were further tested and modified within the FGs and online discussion forum with ‘seldom heard’ health service users:
-
Involving me in decisions about my care:
-
My health concerns are taken seriously.
-
Health professionals help me to take care of my own health.
-
When choosing a treatment, health professionals listen to what is most important to me.
-
I can refuse a treatment.
-
-
Having a friendly and caring attitude:
-
Health professionals are interested in me as a person.
-
-
Having some understanding of how my life is affected
-
I am asked how my problem affects my work, my hobbies, and so on.
-
Health professionals think about my family and not just me.
-
-
Letting me see the same health professional:
-
I see a health professional who I like and trust.
-
I see a health professional who knows my medical history.
-
-
Guiding me through difficult conversations:
-
I am told bad news with kindness and honesty.
-
I feel at ease to ask about embarrassing things.
-
Health professionals help me to tell other people about my problem.
-
-
Taking time to answer my questions and explain things well:
-
Health professionals explain why I might have developed a problem.
-
I am told what a treatment is supposed to do and what side effects it can have.
-
I am told about the different steps involved in my care.
-
-
Pointing me towards further support:
-
I am told about things like self-help groups, or benefits advice.
-
I am told who to contact in case of unforeseen problems.
-
I am told about other health professionals that can be helpful to me.
-
-
Efficient sharing of my health information across services:
-
Health professionals in different services are up to date about my health problem.
-
I have a written record of what has happened to me, or a care plan.
-
A number of components which patients often described as important aspects of care (including physical comfort, well-trained staff, confidentiality, effective treatment, dignity, access to medical records, access and waiting times, lack of discrimination, prompt attention when needed)9 were not included in the candidate list because these were judged to be features of basic or minimal rather than the ‘good’ health care which is intended to be the focus of NICE QSs. We will come back to several of these issues in the discussion (see Chapter 7) in which we discuss different perspectives on what is considered ‘basic’ or minimal care and what is thought to be good, aspirational or even unattainable to the FG participants.
Chapter 3 Objective 2: testing the reach of the candidate core components across health-care contexts and social groups
Aims
To test the candidate components described in the previous chapter, we undertook (1) further secondary analysis of two interview collections from the HERG interview archive to test whether or not the components held in other health conditions and (2) a series of FGs with users to examine if, how and why the core components of good-quality care differed when discussed with types of participants who are not well covered in the HERG interview archive and who are seldom heard in research of any kind. Some groups, such as people with learning disabilities, illicit-drug users, homeless people or traveller populations, are often left out of health research, unless the focus of the study is on the experiences of that particular group. 59 These omissions leave our understanding of patient experiences incomplete. In the HERG collections of interviews, we were aware that some sociodemographic groups, for example young men and people from ethnic minorities, were not well represented. We therefore sought to test the reach of our core candidate components with people who tend to be less well represented in research.
Testing the core components with further interview collections
The first four collections were selected to accommodate NICE product development timelines. In the second objective, we decoupled from NICE processes and selected two further collections (people with fertility problems and adults with autism) which we considered sufficiently different from the first four chronic conditions to rigorously test the reach of the candidate core components.
Fertility problems
The nature of infertility and its treatment is, in some ways, akin to a chronic condition. The realisation of a problem and getting a diagnosis can take months or years. The average length of time patients reported trying to conceive was 4.7 years (range < 1 year to 20 years). 60 Sometimes there is a clear diagnosis, which can indicate a specific treatment (e.g. blocked Fallopian tubes or hormonal imbalance), but often fertility problems are unexplained. It can affect one or both partners. While initial tests take place in primary care, most treatment takes place at specialist clinics in secondary care. Treatment is provided on the NHS, but is limited. Most treatment in the UK takes place in private clinics (60%). Only around one-quarter of all treatment cycles started result in a live birth.
Individuals who are being treated for fertility problems are rarely ill. They are mostly young and healthy, and their encounters with health services for assisted conception are often the first time that they have been to see specialist doctors. The staff patients come into contact with are GPs, fertility specialists, embryologists, nurses and counsellors.
Adults with autism
Autism is a lifelong neurological condition that manifests in communication and interaction differences, and difficulties in how people make sense of the world around them. It is a spectrum condition, which means that people are differentially affected. Some people are able to lead independent lives, while others may need specialist support. The prevalence of autism is increasing and is estimated to be 1.1% of the UK adult population. 61,62 Diagnosis of autism can be variable and is based on clinical assessment and observation, history from the family and instruments such as the Autism Diagnostic Observation Schedule and the Autism Diagnostic Interview-Revised. Both are in use, albeit with widespread variation. 63
People with autism are not typically physically unwell and, once diagnosed, whether in childhood or as adults, there is no cure. Treatment consists of management strategies which are delivered by specialist services. The multidisciplinary teams (MDTs) include paediatricians and psychologists for children as well as social workers. People with autism may have other psychological and psychiatric diagnoses such as learning disability and mood disorder, and as adults are likely to be seen by psychiatrists and psychologists.
Methods of analysis
The two conditions were analysed thematically by the original researchers who had collected the data. This meant that they were very familiar with the data, thereby overcoming one of the concerns relating to secondary analysis. 30 Each researcher returned to the relevant coding reports from the initial analysis (for infertility: going to the GP, decisions and choices; for autism: autism diagnosis, health and depression, professional support). (In the case of autism, all but two of the participants within the data set were able to articulate their experiences.) These reports were reanalysed and links were made across the codes using a mapping technique. 64 These were interlinked, with codes subsumed or expanded until the core components of good health care were identified. At this stage, the researchers met to discuss and compare findings.
Findings
There were some similarities but also clear differences in what these two groups articulated as good components of health care (Table 4). The main difference between the two groups was the centrality of effective communication to people with autism in the provision of their health care and the importance of empathy to the patients with fertility problems. People with fertility problems valued staff who understood that their experience of infertility was not just about medical treatment, but that the possibility of not being able to have children can have a huge emotional and social impact.
It is a really sensitive area for some people, but I am sure it is a matter of showing just the same skills of empathy and understanding that you would for any other illness. You know it seems life-threatening probably for some people going through it, in the sense that it is their vision of their life that is being threatened.
IFT19, female, aged 36 years
It is not something that they have probably been taught to deal with, at least, on an emotional level or just to understand how important and difficult it is for someone going through this, instead of just being told, ‘Oh go and do this and to do, and go away it has not been long enough’. To actually understand what it means to someone.
IFT16, female, aged 34 years
| Components of good care | People with fertility problems | Autism |
|---|---|---|
| Being taken seriously | Being taken seriously by the GP when first presenting with concerns was important to women and their partners | The importance of being taken seriously was discussed, particularly around getting a diagnosis |
| Having some understanding of how my life is affected | Patients value staff who understand that their experience of fertility problems is not just about medical treatment; patients value understanding of the social/practical context of treatment, in terms of timing and location of appointments and treatment | |
| Letting me see the same health professional | Patients valued connecting with health professionals on an emotional level. Described how important it was to be seen as a person throughout treatment | Some were willing to wait to see a specific GP |
| Guiding me through difficult conversations | There are many ups and downs throughout fertility treatment. While some patients reported support and empathy from clinicians when there was bad news, others were hurt by apparent insensitivity | Very important because people with autism can be very literal. They have specific communication needs |
| Taking time to answer my questions and explain things well | Help in understanding what they are embarking on is appreciated. Preparation for a long journey ahead; that it may well be a ‘rollercoaster’, with regular disappointments | Communication is a key challenge for people with autism. The importance of health professionals understanding these issues and communicating effectively with the patient |
| Pointing me towards further support | This was very important because of the emotional dimension to fertility problems, coupled (sometimes) with a reluctance to discuss with friends and family. Patients wanted to be fully informed about treatment and also directed to support networks | Participants were very practised at searching the internet and researching health issues |
| Efficient sharing of my health information across services | Couples sometimes wondered why the first step in specialist services was often to repeat tests that the GP had already done | This was important for patients with mental health issues as well as a level of learning disability |
| Involving me in decisions about my care | Infertility treatment can involve some difficult decisions around continuing or stopping treatments. Patients valued support and information to help make these decisions |
The importance of being treated as a person rather than a number was also highlighted by the patients with fertility problems.
Remember it’s people . . . and the best doctors and health professionals will probably be the best at whatever field of medicine they’re in because they’re able to connect with somebody at another personal level and acknowledge how difficult it is, how emotionally tiring it is and how horrible it can be at times.
IFT34, male, aged 48 years
This was not articulated within the autism data. For people with autism, empathy was not important, or they did not say it was important. This is perhaps not surprising, given that the condition is characterised by difficulties in social communication. What was important to people with autism was having health-care professionals who understood the communication challenges associated with the condition and, for those people seeking a diagnosis, being listened to and taken seriously. The uncertainty around diagnosis of autism, particularly for women, meant that they valued GPs and health professionals who listened to their concerns and acted on them.
First of all we had to convince the psychiatrist to refer me, a consultant psychiatrist and she actually said she didn’t think I did have it because I was interacting too well [. . .] I was like really, really upset because I knew that, I know that I can.
AUA01b, female, aged 22 years, diagnosed age 21 years
The importance of being taken seriously related not only to the individual person with autism, but also to the condition itself, which was sometimes contested. One woman said that her GP told her she ‘didn’t believe in the condition [Asperger syndrome]’ (AUA06). The contested nature of autism was underpinned at the time of the interviews by discussions and controversy around the development of the Diagnostic and Statistical Manual of Mental Disorders and the planned removal of Asperger syndrome from the new edition.
The lack of knowledge about autism also affected ongoing interactions with health professionals, as people with autism can be very literal or have sensory issues around lighting or sound. With understanding, some situations – such as the distress caused to patients who might be told the doctor will be back ‘in 2 minutes’, and who would expect that to be the literal case – could be avoided. One young man, who was diagnosed with autism in childhood, also flagged up the importance of being listened to and supported by mental health services. There was a lack of integrated care between learning disability and mental health services that could cause people considerable difficulty. As one woman said:
You end up passed between the two which results in just confusion really.
AUA04, female, aged 28, diagnosed age 3 years
The knowledge and competence of health professionals was important to both groups of people. This component was not included in our list of core components, as we had categorised it as something that was a ‘given’ in health care, rather than ‘good’ practice. However, for both groups, feeling that the health professional understood their particular condition (autism or fertility problems) was important. As one man said about his interaction with his GP:
When I had to spell Asperger for him, I knew we weren’t going to get anywhere.
AUT10, male, aged 58, diagnosed age 51 years
For the patients with fertility problems, communication was also important, particularly with regard to being told bad news in a sensitive manner.
I never forget this, because this is the worst bit for me. They opened a book. The nurse was sitting there and she opened a book and it had all our details on, and it just had two lines through it. And it just had the word ‘cancelled’ written on it. And that was how I found out that our IVF [in vitro fertilisation] cycle wasn’t working. I was in the room on my own with the woman. And I was just devastated. I felt like she’d cancelled me.
IFT23, female, aged 41 years
Among the patients with fertility problems, support and signposting to further information was an integral component of good health care.
Our GP’s surgery was really good and very supportive. You know a couple of times I went and they were saying, ‘Well maybe we could explore this and explore that?’
IFT05, female, aged 40 years
This signposting appeared to be less important to the people with autism, many of whom were very comfortable searching for information online.
Ongoing support was important to the patients with fertility problems, especially after treatment failed, as often patients felt abandoned after a failed cycle. For the autism group, social care support was more relevant, as their needs were more social than health related.
You know, they’re all really trying desperately hard to make you pregnant, but there’s a lot of emotional stuff as well. And I think kind of being aware of that, accepting that and making sure that people are offered counselling, that people are given the support network information, that they are told where they can find things out is actually really important. Almost just as important as the rest of it, actually.
IFT04, female, aged 45 years
In summary, conducting a secondary analysis of two further conditions highlighted some condition-specific dimensions to what is considered good health care and made visible some important distinctions in people’s focus on what is important.
Testing the reach of the core components in focus groups
Our next step was to further test the reach of the candidate core components through a series of FGs. By presenting these components for discussion with groups of people who we know to be under-represented in the HERG studies, and more generally in health research, we aimed to explore variations and limitations of the proposed components. This would allow us to develop explanations for why some components might be perceived differently in different service populations.
Between January and April 2013, we ran six FGs (Table 5). We also set up a moderated online discussion forum. It is worth noting that only the learning disabilities group was held before the Francis Report was published (6 February 2013). 6
| Group | Date | Number | Age range | Location | Recruitment route |
|---|---|---|---|---|---|
| FG1: people with learning disabilities | 10 January 2013 | 5 | 35–60 years (approximately) | Oxford | Self-advocacy group |
| FG2: migrant workers with limited English | 15 February 2013 | 6 | 26–47 years | Oxford | Personal contacts |
| FG3: current or former drug users | 7 March 2013 | 13 | 20–60 years (approximately) | Oxford | Contact with charity sector |
| FG4: young men (ethnically diverse) | 13 March 2013 | 10 | 18–19 years | South London | Lay member of steering group |
| FG5: Irish Travellers | 25 March 2013 | 8 | 36–68 years | Liverpool | Lay member of steering group |
| FG6: older adults | 26 March 2013 | 9 | 64–86 years | Midlands | Personal contacts |
| FG7: people with a long term condition | January to April 2013 | 11 | 23–90 years | Online | Personal contacts and social media |
Sampling
Particular efforts were made to include participants who are usually considered seldom heard in research. The nature of the groups were informed through awareness of gaps in the HERG samples, our knowledge of marginalised groups and decided in discussion with the project steering group, in particular the patient and carer members. 59 Participants were recruited through our contacts in voluntary organisations, social media and our patient and carer members. Most of the participants were from pre-existing groups and so were familiar to each other. For example, the older people were recruited from a University of the Third Age (U3A) group, an organisation whose aims are the education and stimulation of retired members of the community. The learning disabled participants were all involved in a self-advocacy group; the young men were pupils at a South London secondary school. A few of the drug user participants knew each other.
Informed consent
Gatekeepers (chairpersons, group conveners, appropriate authorities) circulated an information sheet explaining what was involved in the study. All sessions started with an explanation about the purpose of the group and an opportunity to ask questions. The drug user agency, that helped recruit the drug user group, circulated flyers about the group in various locations including a supported housing initiative and a specialist GP surgery. With this group, we were not aware until the day how many people would participate.
The process of gaining informed consent varied between groups depending on the ability of participants to read, or speak, English. Most groups, including the migrant workers, could read and understand the information sheet, and sign the consent form. In the case of the learning disabled group, minor adaptations enabled participants to give consent.
Several of the Irish Travellers had poor reading and writing skills. We had thought that we would audio record individual consent; however, this proved unnecessary. The session was well resourced, with two researchers and four support staff to help with literacy issues throughout the session. We worked with participants to fill in biography forms, read out the information sheet and check orally for understanding, and then worked on a one-to-one basis with participants to explain the consent form before asking each person to sign or make their mark. It thus became clear at an early stage, without it being made an issue, which participants were comfortably literate. The difficulty in reading and writing was in contrast to the facility the group had with spoken language.
Participants were given £30 shop vouchers for their time, and travel expenses where relevant. Compensation is routinely offered in FGs and there is evidence that it helps to increase participation rates, while not affecting responses to subjective questions. 65,66 The groups were audio (or video) recorded with participants’ permission.
Focus group structure
Each group was held in a venue convenient to participants, as advised by the gatekeeper or personal contact. The groups ran for 90–120 minutes and were facilitated by different combinations of two members of the research team and, in two cases, with the support of the patient and carer members of the steering group. The facilitator guided the discussion, supported the group and aimed to create an environment in which participants felt comfortable and able to share insights and experiences.
The broad structure was:
-
introductions and a warm-up exercise
-
general brainstorming about what good health care looks like
-
small group work ordering and adding to the set of core components
-
discussion of reasons for selecting priorities and less important issues, prompted by the ordering exercise.
After the introductory session, we invited the group to talk about ‘what is important in your health care?’ writing up the points raised on a flip chart. Given the literacy issue in the Irish Traveller group, we read each point out and summarised key points orally at the end of the activity.
The brainstorming discussion, captured on a flip chart, was very much an open discussion. Participants were asked to describe what they thought was good health care and invited to provide examples to illustrate the points they made. The facilitator encouraged participation from all group members as much as possible and encouraged or challenged the groups about the points raised.
Small-group work
One of the tasks for the FGs involved a pair/small-group activity in which participants were asked to order a series of cards each containing one of the eight components of good care, with examples. Blank cards were included and we asked participants to add anything they felt was important that they did not feel was covered.
In designing the FG activities, we recognised the importance of flexibility and willingness to adapt activities before and during a session in response to the needs of the group. For example, in the Irish Traveller group, who had literacy problems, each small group had a facilitator to help with the task. Each of the core components on the cards was read out and discussed by participants and then allocated a position on the table to reflect its priority. We also modified the task for the learning disabled group. Given the small number of people in this group, we asked participants to work together as one group to order the cards. We produced easy-read versions of the components and, drawing inspiration from board games, we placed a sheet of flip-chart paper on the table, with emoticons used to indicate ‘very important’, ‘fairly important’ and ‘not so important’ rankings (Figure 2).
FIGURE 2.
The ordering exercise in the learning disabled group.
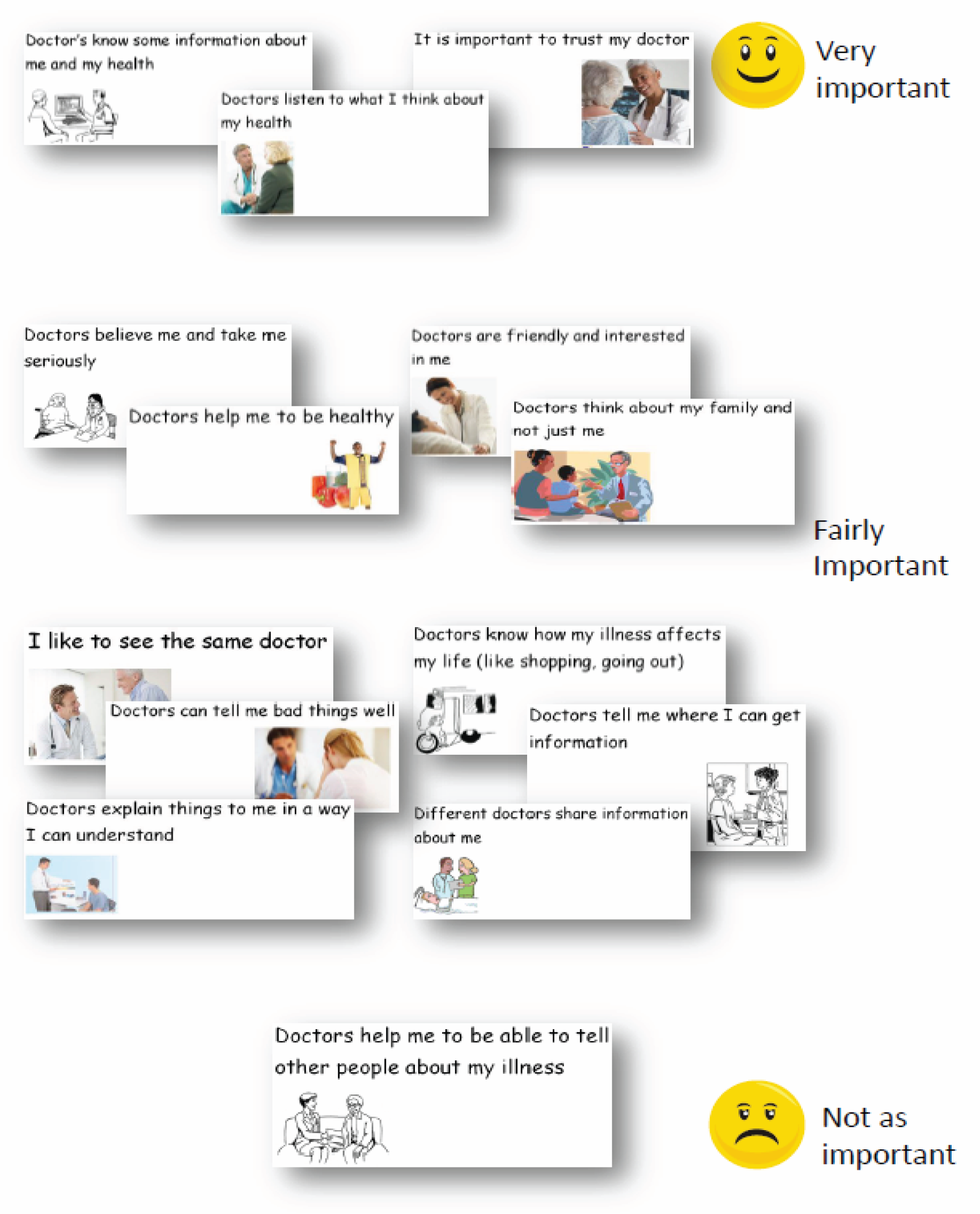
Participants chose a card and then, following discussion, placed it on the chart in terms of its relative importance in their own health care. With guidance from the facilitator and the use of the ‘board game’ approach, the group was able to reach a consensus on what was important to them in health care.
We prepared a set of illustrative video clips to show during the FGs. These were used in the group with learning disabilities (FG1) to generate discussion and, to a lesser extent, in FG2 (migrant workers with limited English) and FG6 (older adults). We decided it was either not appropriate (e.g. due to the language barrier) or unnecessary (because the discussion was going very well) to use the clips in FG3 (current or former drug users), FG4 (young men) and FG5 (Irish Travellers).
Finally, the small groups were asked to talk about what they thought of each component and explain why they thought that some were more important than others. During this, some participants changed their minds about a component and revised their ordering.
In addition to the six face-to-face FGs, we set up an online FG using Ning, a free online platform for creating social networks (Mode Media Corporation, Brisbane, CA, USA) (Figure 3).
FIGURE 3.
The online FG.
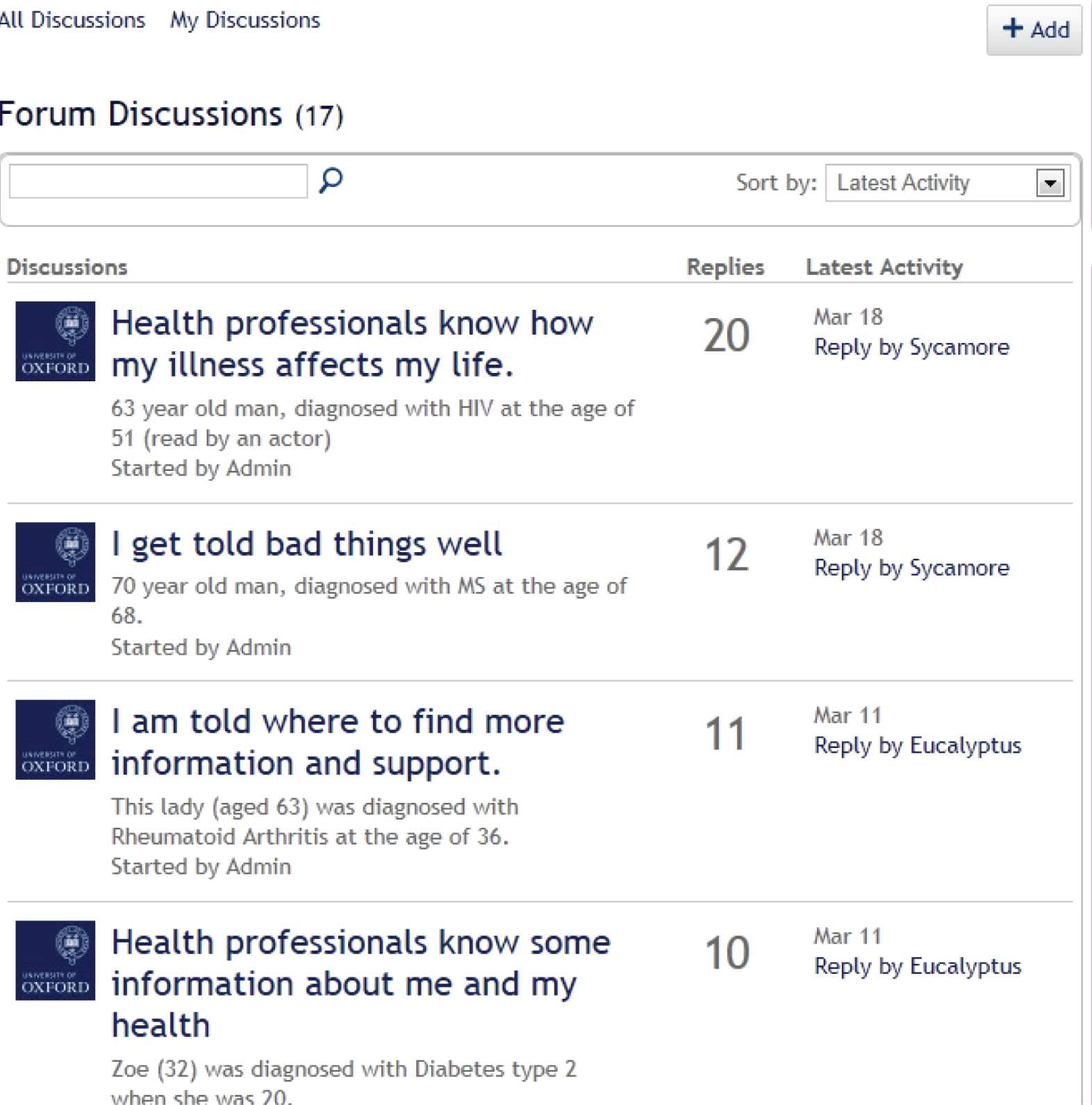
We used social media and personal contacts to recruit participants with LTCs to this group. The details were tweeted and shared via Facebook and the healthtalkonline website. Eleven people volunteered to take part. The webspace ‘Goodhealthcare’ contained a different forum for each candidate core component and was illustrated with a video clip. We invited participants to read the statement, watch the clip and then contribute to a discussion on whether or not that statement was important. Participants were encouraged to return to the webspace to respond to comments that had been left by others (Figure 4). The method allowed us to hear the views of those we could not reach through the FGs, because of the severity of either their own LTC or that of someone they cared for. The facilitator responded to comments and invited further response which generated richer detail. The site remained open for comments for a 6-week period, after which the responses were collated and analysed alongside the six other groups.
FIGURE 4.
Sample extract from the online FG.

Data analysis
A summary of each FG was produced, which included general reflections on the session, selected verbatim quotes and key points of interest that had emerged during discussion.
The data were analysed in two stages. Firstly, the relevant members of the research team watched the video (or, in the case of FG3, current or former drug users, and FG5, Irish Travellers, listened to the audio) together. Researchers made their own notes on each group, and after each, these observations were discussed and comparisons between the groups were noted. We considered whether or not and how the participants’ comments and stories suggested new core components, or could be subsumed under the original eight.
Secondly, these observations were added as notes to the summaries for each group. All summaries were imported into NVivo. Comments were coded according to the health-care setting to which they referred (generic, primary or secondary care), according to whether participants regarded the components as basic, good or aspirational care, and according to whether or not and how the functional, relational or systemic/organisational aspects of care were related.
Findings: testing the breadth and depth of the candidate components across the focus groups
In this section, we first consider the differences and similarities in the FG participants’ responses to each of the eight core components. We then discuss the additional aspects of care that group participants raised as important.
Candidate component 1: ‘involving me in decisions about my care’
Related examples: my health concerns are taken seriously; health professionals help me to take care of my own health; when choosing a treatment, health professionals listen to what is most important to me.
Participants across groups were very clear that they wanted to be involved in decisions about their health care. However, preferences regarding the form such involvement should take, for example having clear explanations about the course of treatment or being asked to choose from different options according to personal values, varied greatly between participants and according to context.
People with learning disabilities (FG1) said that health professionals often steered them towards a particular treatment; this could feel caring and reassuring if done in the right way:
I had my varicose veins done, this doctor in [town], he turned round and said ‘If you were my daughter I’d like you to have it done’. I thought ‘oh my God’, I thought it was really nice.
People with learning disabilities FG1
Migrant workers with limited English (FG2) felt that respect for personal decisions and preferences were very important, particularly with regard to mental health and reproductive health. They perceived the UK as a place where there is choice and genuine concern for achieving good health outcomes. They compared this with their home countries, where they were sure that doctors made treatment recommendations (e.g. for a caesarean section rather than a vaginal delivery) for personal financial gain rather than for the best interests of the patient.
People with LTCs considered their active involvement in decision-making as central to the effectiveness of the treatment:
If I don’t want treatment (or it’s not explained to me) chances are that I am less likely to comply and take the medication/do the exercise etc as prescribed!
Online LTC group, FG7
However, they also acknowledged that not all patients might feel sufficiently equipped to take on an active role in decision-making:
I make treatment decisions in partnership with my doctors: but I am informed, (reasonably) intelligent, and like looking things up on the Internet! Not everyone does. Some patients prefer to have decisions made for them, and those patients also have to be catered for.
Online LTC group, FG7
Current and former drug users (FG3) stressed that part of this ‘involvement’ was that health professionals should listen to patients’ feedback about the treatment they had received.
Involve me in decisions not just for substance misuse but medications in general. They don’t listen to whether it’s working or not. Not just doctors and nurses but dentists too.
Stigma comes along as soon as you mention drug use.
Discussion between current and former drug users, FG3
A few participants in the current and former drug users (FG3) group knew a lot about drug interactions and gave accounts of occasions when health professionals had clearly known less than they did. This provided a strong rationale for the involvement to be a two-way partnership. However, others said that they had sufficient trust in their doctor’s competence to leave decisions about treatment alternatives to them.
If I’ve got faith in the doctor, I might not know what’s the best thing, I’ve got to have trust in the doctor. So it’s not as important.
Current and former drug users, FG3
A few of the young men (FG4) felt that the way in which their doctors involved them in decisions about their care affected their views on their GP’s competence. For example, they were unimpressed if the doctor looked the symptoms up during the consultation, which, as they pointed out, they would have done anyway before the consultation.
My health concerns are taken seriously
Members of all groups thought that it was important that health professionals listened to what the patient was saying. When asked to prioritise, participants across groups said they thought that it was more important to have their views heard and to be treated with professionalism and respect than for health professionals to display warmth or take an interest in their personal life.
I don’t expect them to be caring about me; I want them to do their job. I’d rather have someone who’s cold and clinical who can do a good job.
Current and former drug users, FG3
Listening was also seen as integral to getting the correct diagnosis. Participants across groups linked a caring attitude and creation of a comfortable environment to patients feeling sufficiently at ease to talk about symptoms and hence enable the doctor to reach the correct diagnosis:
I think it should come as second nature. If they want you to confide in them what’s wrong with you.
People with learning disabilities, FG1
It’s important that doctor asks what you think. This is especially important when the illness is not in the body.
Migrant workers with limited English, FG2
Some of the young men (FG4) said that they felt frustrated that they might have to present their symptoms to their GP a number of times before being taken seriously. A young man from an ethnic minority, whose mother was a doctor, told us that she had encouraged him to speak up about what was wrong when he went to his GP.
In my own past experience when I used to go to the doctor’s, outside me and my mum used to have like a pep talk before we walked in, and my mum would be like ‘yeah make sure, make sure you slightly exaggerate what, what is wrong with you to ensure that they actually do something’.
Young men, FG4
The young men (FG4) said that a warm and welcoming approach would help to reassure them that they were not wasting the doctor’s time. The current and former drug users (FG3) were also concerned to feel that staff treated them as appropriate users of services.
Participants across groups felt that health professionals should recognise that patients are experts on their own bodies.
The way I think about it, you know more about your body than anyone and that’s why it’s important. You know how you feel more than anyone else knows.
People with learning disabilities, FG1
Participants in the learning disabled (FG1), current and former drug users (FG3) and older adults (FG6) groups were particularly concerned that their views were taken into account. People with learning disabilities (FG1) said that they resented doctors addressing their carers instead of them. Current and former drug users (FG3) felt that their ‘addict identity’ was foregrounded in interactions with health professionals, who thought that they were always ‘after something’:
Listen to you, actually listen to you and act as if they actually give a shit about you and not just think ‘he’s a drug user’ and fob you off./‘Cos it’s self-inflicted./They fob you off. That’s across the board whether you’re using or not.
Current and former drug users, FG3
One of the online LTC participants (FG7) noted the importance of being taken seriously by the GP to gain access to specialist care.
There are times when I know that I have not been taken seriously and indeed have seen it written in my notes; I have been impressed that this was followed up by the consultant to the relevant doctor. How you are asked questions is important and it is key that medical staff remember the high level of stress involved in attending appointments even for the calmest of folk. Feeling you are being taken seriously is vital.
Online LTC group, FG7
Having the medical staff believe you is key to your own individual care. Patients must be treated as individuals as everyone is different. Half the time if doctors looked at and treated me by my blood results I would rarely be out of hospital. A good doctor will treat the patient and not a set of numbers. Instead doctors ask me how I feel and what has been good and what has been bad and know not to ask me the question on a scale of one to ten. . . . .
Online LTC group, FG7
Candidate component 2: ‘having a friendly and caring attitude’
Related examples: health professionals are interested in me as a person.
Participants’ comments about this component unpicked the different ‘ingredients’ of empathy: warmth, eye contact, smiling, remembering personal things about the patient as well as respect, willingness to listen and taking concerns seriously. Discussions revealed interesting differences between groups and individual participants in the relative importance of the components.
People with learning disabilities (FG1), migrant workers with limited English (FG2), young ethnically diverse men (FG4) and Irish Travellers (FG5) linked a friendly attitude to ease of communication more generally. In particular, FG2 participants emphasised that a genuine desire to understand could help to overcome linguistic difficulties.
One participant from the older adults group (FG6) differentiated between knowing, trusting and liking the doctor:
I do trust my doctor but I don’t particularly like him as a person, but that’s fine – he does his job as a doctor in diagnosing me . . . Although he doesn’t support me but I am finding other sources of that support and information.
Older adults, FG6
Participants of the migrant workers with limited English (FG2) and young men (FG4) groups said that health professionals who made eye contact and greeted them with a welcoming smile had helped to put them at ease and to alleviate feelings of anxiety and insecurity when making first contact with health services. A friendly and caring attitude was important when interacting with reception staff, as well as with doctors and nurses.
Young men (FG4), older adults (FG6) and the online LTC group (FG7) raised concerns over increased ‘efficiency’ coming at the cost of empathy. Not being able to see the same health professional across consultations was seen as detrimental to developing relationships and undermining the possibility of truly personalised and ‘caring’ care.
I can’t imagine personal care like this, [remembering personal details] but would love it! The nurses when I’ve been in hospital have not been interested in you as a person at all, and are so busy that they don’t have time to have a chat with you. It would make you feel so much more cared for and therefore give you strength to manage if you felt that they were interested in you as a person.
Online LTC group, FG7
Candidate component 3: ‘having some understanding of how my life is affected’
Related examples: I am asked how my problem affects my work, my hobbies, and so on; health professionals think about my family and not just me.
Groups and individuals within groups attached very different meanings to this component; this variation may have been encouraged by the examples we gave.
People with learning disabilities (FG1), current and former drug users (FG3) and Irish Travellers (FG5) all emphasised that it was important for health professionals to be aware of the kinds of issues that they were likely to face, but were angry if health professionals made blanket assumptions and resorted to unhelpful stereotypes. They thought that good care should involve a consideration of the social contexts in which people lived (e.g. temporary housing), the social roles they performed (e.g. caring responsibilities) and any special support needs they might have (e.g. providing information to suit literacy).
The mention of ‘work and hobbies’ prompted some participants to suggest that this was a ‘frill’ and worth considering only once more basic needs had been met. As one former drug user commented:
Until you get your main core of problems worked out, you ain’t going to talk about jobs and hobbies. I have to think about whether my tent is going to get flooded and feeding my dog. Nothing like work and hobbies.
Current and former drug users, FG3
This view was echoed by participants in the migrant workers group, one of whom said:
How it affects me in my job is not so important: the main aim is to get better, not to stop working. So it’s the least important thing for me personally.
Migrant workers with limited English, FG2
People with LTCs (FG7) placed considerable importance on this component and described it as central to good care. Two participants from the migrant workers with limited English (FG2) group who had experience of LTCs also rated this component more highly than the other members of that group. Participants in FG7 thought that how their life was affected was part of a holistic care approach that treated people rather than numbers:
Perhaps it [questions about pain] should be related to your daily routine and how it is impacting on that. If I said I’m crippled and am struggling to walk/sleep then that should be enough, rather than being followed by the inevitable ‘on a scale of 1 to 10’ question.
Online LTC group, FG7
People with learning disabilities (FG1) thought that understanding the impact of a condition on patients’ lives was a feature of basic rather than good care – ‘it should come as second nature’ – but acknowledged that this was often not the case in practice. Similar to views expressed by migrant workers with limited English (FG2) and people with LTCs (FG7), FG1 participants thought that primary care clinicians had a tendency to focus on physical symptoms while being prone to overlook patients’ psychological well-being, and linked this tendency to shortened consultation times.
I think they’re too much on what they can see, rather than what you tell them.
He [her husband] doesn’t understand what’s she’s going through. And it’s actually caused her to get depression. She’s on the highest rate of painkillers, the highest rate you can. It is hard not to understand and the GPs should really understand all that but they don’t.
But what’s the point of telling ‘em because they can’t do nothing about it?
They don’t usually have the time. I mean how long are your appointments?
Five or 10 minutes.
Discussion among people with learning disabilities, FG1
Participants across groups talked more about the importance of health professionals’ understanding of the effect of illness on their own lives and less about the need to consider the impact on family members and their information and support needs. It is perhaps interesting to note that the individual interviews included more discussion of the impact on family members; the one-to-one interview gives participants more time to talk about their own illness and the effect on their family.
The young men (FG4) and older adults (FG6) made little reference to this component and, when asked to prioritise components, rated it at the bottom end. The migrant workers with limited English (FG2) and Irish Travellers (FG5) groups also rated the component among the least important.
Candidate component 4: ‘letting me see the same health professional’
Related examples: I see a health professional who I like and trust; I see a health professional who knows my medical history.
Prompt access to health services and continuity of relationship with a specific health professional can be difficult to achieve in service delivery. Participants talked about continuity in different health-care contexts.
Seeing the same health professional in primary care was particularly important to some members of the current and former drug users (FG3) group and to people with learning disabilities (FG1), who said that they often had to see a locum GP. If a locum was unfamiliar with their medical history, the participant had to use up precious time giving background explanations. Good care to them meant that GPs knew them sufficiently well to understand their history and the impact of an illness, and to help them make necessary arrangements as required:
My GP is very good because she helps me if I’m having problems with [husband’s name], she will get in touch with [care provider]. And she’s very good because she knows us. She knows our problems.
People with learning disabilities, FG1
For some of the current and former drug users (FG3), it was important to hold on to a GP with whom they felt they had established a relationship of trust:
I get a build-up of anxiety if I don’t get to see my doctor. There’s a general lack of respect. With my doctor, I feel that he listens to me, respects but I don’t get that off the other doctors, particularly the locums there.
Current and former drug users, FG3
Trust was seen as a two-way street, with doctors knowing patients well enough to trust their motives and not presume their presentation to be made for manipulative ends:
My doctor I’ve had him for years and he knows what I’m like. He knows I don’t blag [try to take advantage of] him. So if I ask him for something, nine times out of 10 he gives it me.
Current and former drug users, FG3
Participants in the migrant workers with limited English (FG2) group said that they appreciated it when a GP remembered them well enough to notice a change, such as weight loss.
Irish Travellers (FG5) and older adults (FG6) said that seeing the same health professional was more efficient (saving time and effort if doctors knew their medical history) and also increased their confidence. While continuity of relationship was seen as less important than continuity of care, there was some discussion in the Irish Travellers (FG5) group about whether or not the latter was achievable without the former.
I belong to a practice that’s a teaching practice and I can go on a Monday and see one doctor and explain my condition, go back on a Wednesday and see an entirely different doctor and have to go through everything again, same story again which is off-putting for me.
Irish Travellers, FG5
Some of the Irish Traveller participants (FG5) attributed poor patient care in hospital, such as leaving food out of the patients’ reach, to frequent turnover of staff and shift changes on hospital wards:
I think it’s because they move staff around a lot – people going on their break – nurses from other wards to cover – they don’t know those patients and their needs.
Irish Travellers, FG5
Another participant in this group pointed out that if the other components of good care are met then it is less important to see the same health professional.
The one that is the least important of our important pile and to the point where I’ve made a note about why that is, is ‘letting me see the same health professional’ because what we said was, if people are doing them and information is shared and people are caring and listening to me and trusting me then actually it’s not so important to see the same person all the time – didn’t we? That’s kind of our thinking on that one so.
Irish Travellers, FG5
They also highlighted special situations in which it might be important to have access to a known health professional for pastoral reasons, such as in the following case of the death of a patient who had to have an autopsy:
We couldn’t get hold of our local doctor and they sent a locum who didn’t know the patient – it just made it so upsetting for the parents – it could have been avoided if we could have contacted the doctor.
Irish Travellers, FG5
Participants in all of the groups, except the young men’s group (FG4), gave reasons why they thought that it was good to see the same health professional. People with LTCs said that continuity of the relationship helped health professionals to develop a more nuanced understanding about how patients’ lives were affected by a particular condition. They also made links between continuity of relationship with health professionals and the likelihood of being taken seriously:
If staff know you then that helps, as they know that when you go and ask you mean you need it!
Online LTC group, FG7
Seeing the same doctor in either primary or secondary care could save time and effort, increase trust and confidence and ensure continuity of treatment approach.
When the condition is long-term, rare and with a complicated medical history, this is great! Otherwise you spend the whole appointment explaining it all to them and not actually getting any further with treatment!
Online LTC group, FG7
Participants in the online group described the frequent turnover of hospital staff as counterproductive to forming empathic relationships.
. . . and when I’ve been in hospital and well enough then I have tried, but when you have a member of staff on duty followed by a new one, followed by a new one etc. it makes it impossible. They don’t have time to stand chatting with you even when you try.
Online LTC group, FG7
Being able to see the same health professional was rated as much less important by the young men. This group, most of whom had little experience of serious health problems, clearly valued prompt access over personal continuity:
If you want to be getting better, it’s not necessarily, if you have to wait a week to see the doctor who you saw a few months ago again, that might not be as good an option. It might be a better option seeing someone different, so then you can get the treatment as soon as possible.
Young men, FG4
That’s not important at all. If you want to see, if you’ve got an illness that bad, if you’ve got an illness and you want to see the same health professional, you’re not really ill, you just want to have a conversation with somebody.
Young men, FG4
Others in the young men’s (FG4) group pointed out that while there was comfort in seeing the familiar ‘family doctor’ they had known since they were children, in some circumstances they might prefer to see a health professional who was unknown to their family and who would treat them more as an independent young adult.
Candidate component 5: ‘guiding me through difficult conversations’
Related examples: I am told bad news with kindness and honesty; I feel at ease to ask about embarrassing things; health professionals help me to tell other people about my problem.
This component was rated as particularly important by migrant workers with limited English (FG2), current and former drug users (FG3) and young men (FG4). Migrant workers with limited English (FG2) relied on health professionals to ‘make an effort’ and have sufficient patience to try to understand their communicative intent in the face of linguistic difficulty. They also relied on health professionals to scaffold their illness accounts in ways that would enable the correct diagnosis to be made. Current and former drug users (FG3), as members of a stigmatised community, appreciated doctors who created a non-judgemental atmosphere and a relationship of trust that would enable mutual openness.
Young men (FG4) appreciated health professionals who put them at ease, reassured them that it was appropriate to be seeking help and asked questions that helped them to talk about potentially embarrassing issues:
Possibly someone that makes you feel at ease and confident about saying what your actual problems are . . . if you’re nervous and shy like.
Is part of that, that you feel okay describing what’s wrong?
Yeah like it’s not embarrassing for you to describe what you have . . .
Discussion between facilitator and participant, young men, FG4
Health professionals help me to tell other people about my problem
In our secondary analysis of the HERG interview collections, patients often said that they wanted health professionals to support them in sharing information about their health problem with partners, children or employers. This could involve helping the patient to think through with whom they wanted to share information, offering to talk to family members on behalf of the patient or recommending websites or other reading material. FG participants considered this topic in relation to confidentiality, as one participant from the people with learning disabilities group (FG1) said, ‘What happens if you don’t want to tell other people?’, while some participants were aware of circumstances in which health professionals had given advice and about who and when to tell about a serious diagnosis.
When my mum had her cancer, they told her not to tell her grandchild because she had an important year in terms of exams.
People with learning disabilities, FG1
Some members of the current and former drug users group (FG3) thought that it would be more efficient for a drugs worker to help to explain things to other people; another agreed, but mainly because of the lack of awareness of drug addiction by GPs.
The doctors shouldn’t help you tell other people, that should be a drug worker. Expensive to get someone who’s been trained for 9 years to do that.
Someone with 6 weeks’ training and some life experience may be able to do that better. It’s not a good use of resources.
GPs don’t have the specialist knowledge to do that, they only have half an hour training on users. It’s a joke.
Comments made by current and former drug users, FG3
In contrast, people with LTCs (FG7) could see a role for health professionals in providing support to explain their condition to others:
For my son with a mental health illness the community nursing support offered to come and talk to his siblings about it (following the long haul to diagnosis). They thought it was a great idea, but not for them, as by time of diagnosis they had an excellent understanding of it and all the implications.
Online LTC group, FG7
Another participant said that her consultant had helped by writing to her employer:
My Consultant recently wrote to my employer and it has made a huge difference. I’d tried talking to my employer and even given them information from the charity that I am a member of who publish leaflets and guidance on how to talk to employers about this condition, but my employer just wasn’t interested. They have had to sit up and take note since the letter from my consultant though.
Online LTC group, FG7
Candidate component 6: ‘taking time to answer questions and explain things well’
Related examples: health professionals explain why I might have developed a problem; I am told what a treatment is supposed to do and what side effects it can have; I am told about the different steps involved in my care.
Participants across groups rated this component as very important. They saw getting sufficient and intelligible information about their illness and its treatment as essential. Having a good understanding about why a health problem occurred, what could be done to recover and/or prevent it happening in future and being prepared for potential side effects of treatment were all highly valued. However, brief appointments in hurried clinics made it difficult for GPs and hospital doctors to convey complex information and answer the patients’ questions.
Irish Travellers (FG5) and people with LTCs (FG7) said that clear explanations about treatment and side effects were necessary for an informed decision.
As patients we felt that every one of these [components] is important. Taking time to answer my questions and explain things well is really important – as [name of other participant] was saying he has medication that has lots of side effects but once it was explained to him he was able to make a choice.
Irish Travellers, FG5
Time to make a decision and being given enough information to make a fully informed decision, in terms of the likely outcome of the treatment and its success rates; the impact it might have on your life etc mean that you feel in control and therefore it is less frightening.
Online LTC group, FG7
Migrant workers with limited English (FG2) and young men (FG4) said that they struggled with medical jargon and appreciated it when health professionals were sufficiently flexible to adapt their explanations to a level that suited their needs. The young men said that they did not want this to result in the ‘dumbing down’ of information to the extent that it stopped being useful; this is a difficult balance, as one young man explained:
Recently, [um] like when I went to the GP, like sometimes they sort of treat you a bit like, in a bit of a stupid way, like they don’t give you, they sort of dumb it down for you when you want to know a bit more, in more detail, and in other cases they sort of do it in a more sort of, [um] like a more explained way. It might like slightly confuse you, like [um] recently when I went to the GP, [um] she started talking [um] in much more detail than any of my other GPs, so it was a bit confusing.
Young men, FG4
Our secondary analysis had suggested that providing information in a range of formats, including written notes, could be very helpful to patients as it allowed them to digest information at their own pace or to return to it at a later point. Some of the young men (FG4), all ‘digital natives’, felt that being given a leaflet or computer printout at the end of a primary care consultation was inadequate and could feel dismissive.
My GP [. . .] all they do is just print out the information and say ‘read this, it’s got everything about your sort of illness’, and if you, and when you do try to ask a question about, about it, they just say ‘oh don’t worry, it’s all on the information sheet’.
Young men, FG4
People with learning disabilities (FG1) rated importance of this component less highly than the other groups. They said that doctors tended to use complicated language and long words without explaining what they meant and that they felt that more use could be made of easy-read materials in primary care practice.
Candidate component 7: ‘pointing me towards further support’
Related examples: I am told about things like self-help groups, or benefits advice; I am told who to contact in case of unforeseen problems; I am told about other health professionals that can be helpful to me.
Groups varied considerably in terms of how much and what kind of signposting they expected from health professionals. They also varied in terms of perceptions about their personal responsibility to educate themselves about their health problem and awareness of the services and sources of support that might be available to them. Participants expected to find certain information for themselves; for example, the young men pointed out that before they went to see the doctor they would probably have looked up their symptoms and possibly also talked to their parents to decide if it was necessary to consult.
People with learning disabilities (FG1), migrant workers with limited English (FG2) and some of the Irish Travellers (FG5) said that receiving written materials or being asked to look up English-language websites would be of little use to them. However, advice on where to go for further information (such as sickness benefit) was appreciated.
Ethnically diverse young men (FG4) and people with LTCs (FG7) said that they welcomed their doctors supplying them with additional sources of information, as long as this was not seen as a way of avoiding questions during the consultation (see Candidate component 6: ‘taking time to answer questions and explain things well’). People with LTCs also valued being told about patient advocacy organisations and local support groups, and thought that it was important for the health professionals involved in their care to consider their information and support needs beyond the purely medical sphere.
My consultant doesn’t get involved in anything that’s not strictly medical, which is hard because being employment is good for my health! I wish they would have signposted me to the relevant charities – it would really help!
Online LTC group, FG7
Signposting to additional information was seen as an important part of encouraging patients’ ability to self-manage. Routine signposting to psychological support was also seen as important by this group:
I think they should provide us with the information to help us make healthy decisions, but at the end of the day we have to take some responsibility for our own health. I do think that they have responsibly for our mental health – especially when it is caused by physical health problems – they should signpost to counselling etc.
Online LTC group, FG7
While the young men (FG4) felt very much at home with using the internet for finding out health information, they felt uncertain about which sources of information could be trusted and thought that browsing web content in an unguided fashion might provoke additional anxieties. They therefore valued the reassurance provided by seeing a health professional in person:
The caring attitude and things like that, you’re not going to get that on Google are you?
Young men, FG4
Current and former drug users (FG3) had different views about whether or not health professionals should be the ones making sure that they had information. Some were already integrated into support networks through other services.
‘Cos of the way we are, we need extra support, whereas some places will be like here you are, take a tablet and see me next week.
You get that information elsewhere from other services like housing.
But I found out about [name] Housing actually when I was in rehab . . . but I never knew about it before . . . I’d be screwed without that.
Putting it [the component] last ‘cos other ones more important. When I was thinking of it, I was thinking you get that information all over the place.
Discussion between current and former drug users, FG3
Older adults (FG6) discussed the importance of signposting to additional support, mainly in terms of community-based services for older people and those with dementia and other specialist needs.
Candidate component 8: ‘efficient sharing of my health information across services’
Related examples: health professionals in different services are up to date about my health problem; I have a written record of what has happened to me, or a care plan.
The importance of this component was widely acknowledged across groups, even if it did not attract ‘top three’ ratings in any of them. Several participants pointed out that one would expect health professionals in different services to be up to date about their patients’ health status and that, therefore, this component should be regarded as a feature of basic rather than good care. The migrant workers with limited English group (FG2) said that the system of electronic health records in the NHS functioned very well and compared it positively with experiences of disjointed care in their home countries.
At least one participant in each of the other groups described instances in which things had gone wrong because vital information had not been communicated between services, between individual doctors and nurses or between hospital wards. Some of those with more experience of dealing with health services [e.g. the LTCs group (FG7) and older people (FG6)] suggested that the only way to make sure that important information was communicated was to do it oneself.
This drives me mad! I’m being seen by two consultants at two hospitals, for related but different issues, and there has been no communication between them due to the GP not passing information on. When I saw one of the Consultants last week I said that I was finding this very frustrating, as I have had to have several tests more than once (with each Consultant wanting them), and he is now going to write direct to the other consultant and just copy the GP in. It’s also really helpful to get copies of all the letters as you can then take things yourself.
Online LTC group, FG7
Confidentiality was raised by the migrant workers with limited English group (FG2); members explained that this was particularly appreciated because they had lived in other countries where this could not be taken for granted. The group of people with learning disabilities (FG1) also raised a concern that ‘efficient sharing of information across services’ might involve professionals gossiping inappropriately about their health and circumstances. This issue of confidentiality was not raised in the other groups, probably because it is a relatively taken-for-granted aspect of NHS care and unlikely to be seen as relevant to our remit.
Additional components proposed by focus group participants
A key aspect of the FG schedule was that we started with a discussion of the participants’ ideas about what ‘good care’ looks like. These thoughts were collected on a flip chart and reviewed by the researchers during the session, often while the sorting task was under way. The online LTC group (FG7) were also invited to comment on other components that were important to them.
Many of the suggestions fitted fairly clearly into the core components that we then invited them to discuss, but it is worth mentioning that some issues were quite specific and did not amalgamate easily with the other topics. For example, fundamental aspects of acceptable health care include that one is able to access treatment, that health professionals are competent and that the environment is fit for purpose. These should be viewed as basic, rather than ‘good’, features of care, but some of the discussion made it clear that there would be dangers in focusing on the ‘aspirational’ without making sure that the basics are soundly covered. People in the FGs also raised several issues that added to our conceptions of what was important and why priorities might vary among individuals and population groups. These included respect and courtesy, confidentiality, and layout and design of health-care facilities.
A point that cropped up more than once in the older adults’ discussion group (FG6) was the need for respect and ‘common courtesy’. Participants stressed how important it was to keep patients informed when appointments were running late (both in GP practices and in hospital) and to avoid ‘overfamiliarity’, for example calling people by their first name (this last point was presented as particularly relevant to their own parents’ generation).
For me it’s about being kept informed, kept ‘in the loop’. I’m in the middle of some investigations and it’s important to me that they let me know what’s happening. The consultants had a meeting about me and it’s about feeding that back to me and nobody has yet.
Older adults, FG6
My mum is over 90 and she fell at home and broke her arm and her hip and I was with her in casualty and this young doctor said, ‘Right Hilda, you’ve broken your arm we’ll get you X-rayed’. He didn’t even look at her. And she hated being called by her first name. And then a Chinese registrar came and she was fantastic – she was so good at talking to her and explaining and I just wondered if it was that the Chinese have a culture of great respect.
Older adults, FG6
While cleanliness was an important issue for the Irish Travellers (FG5) group, the young men (FG4) were the only group to raise wider aspects of the physical environment in waiting rooms and hospitals. One described a late-night emergency visit to accident and emergency (A&E) with a friend, where the loud noises and harsh lights added to the trauma and anxiety. While they were realistic about the fact that making A&E as comfortable as home was unlikely to be feasible, they pointed out that the environment was only likely to make things worse for people who were already very anxious.
Discussion
We arranged FGs with participants who we are aware are under-represented in many studies, including the HERG collections that were the basis for the secondary analysis.
We wanted to see whether or not ideas from the literature about what good care looks like were replicated in HERG interviews on a range of health conditions, four chosen to fit in with NICE QS projects and two (fertility problems and autism) chosen purposively to extend our understanding of the reach of the core components from our collections. Having identified our list of potential core components, we then set out to challenge the list through discussions with five groups who we know are not well represented in our HERG samples: people with learning disabilities, migrant workers with limited English, current and former drug users, young men and Irish Travellers. HERG interviews include many people with LTCs, yet we know that others find it difficult to take part in an interview, for example if their health status varies too much to predict how they will be feeling on a day when a researcher might propose to visit them. We therefore set up an online group, with similar prompts to discussion, so that we could involve people who might find it more difficult to attend a FG or individual interview.
We had hoped to run a sixth group for frail older people living in residential care but that proved too difficult to arrange (mainly due to concerns from the gatekeepers). Through personal contacts, we found another group of ‘older people’, but as a U3A group of people in their 60s and over they did not represent a ‘seldom heard’ category. Nevertheless, they were a very reflective group, with experiences of working in as well as being treated in the NHS and also experience of caring for older relatives, and provided a useful point of contrast in the analysis.
The FG data confirmed that the original set of core components were also important to members of these groups. In interpreting differences in priorities between individuals, it was very evident that the participants drew on their own experiences of (ill) health, caring and interactions with health services, and that these experiences clearly affected what they regarded as most important and also what they thought was ‘basic’, ‘good and ‘aspirational’ aspects of care. Seen in this light, it is understandable that the young men we talked to (a generally healthy group) were not at all concerned about seeing the same doctor, while this was quite important to the people with LTCs. Experiences of care also affected how confident people were that certain aspects of care were indeed ‘fundamental’ and could be taken for granted. This applied to both the trust that people put in their doctor’s specialist training (and consequent interchangeability) and their confidence that the health system would share information appropriately across services. Older adults and those with LTCs were more aware, for example, that health professionals might sometimes be uncertain about what was the best treatment as there would sometimes be a lack of good evidence about what treatments were effective.
We started all of the groups with an open discussion of good care, which helped us to feel confident that the issues we were raising as core components were relevant to them. Given the very different nature of the groups, it would have been inappropriate to run the groups identically, but we found that the sorting task was a useful common addition to the groups. We were interested that, in half of the FGs, the very idea of prioritising between the candidate components was difficult because they were all such important aspects of good care. The main aim of this task was to encourage the group to think and talk about why the aspects were important (or not) rather than to enumerate their priorities. This was a successful approach in stimulating discussion.
The study sheds some light on the aspects of care that may be taken for granted and how and why these vary between these different groups that are less often represented in research. For example, only the migrant workers with limited English group raised ‘confidentiality’ as an aspect of good care in the NHS, although the learning disabled group raised a concern about inadvertent breaches of this, such as overhearing clinical conversations. This does not mean that confidentiality is unimportant to others, of course, but participants may not have been aware of any grounds for doubt that this could be taken for granted.
Participants’ contributions often demonstrated how relational aspects of care were integral to achieving functional aspects. For example, if a GP has an empathic approach and is good at adapting his or her communication style with different patients, this might encourage them to seek help promptly when needed, report symptoms fully and get the correct diagnosis. The groups also illustrated how, in practice, the components of good care are often highly interdependent: doctors who took time to answer questions and explain how treatment works helped patients to manage their own care; knowledge about care pathways and keeping a record of their own health information could safeguard against failings in the transfer of information between health professionals; when the patient was able to take charge of health records this could lead to better continuity of care even if there were frequent staff changes.
Chapter 4 Objective 3: knowledge transfer between Health Experiences Research Group and NICE teams
Aims and objectives
Our third objective was to embed the project alongside the development of NICE CGs and QSs and to address the following research question: how might secondary analyses best be incorporated into NICE CGs and QSs? More broadly, we also sought to identify wider lessons relating to how patient experience data can inform national quality improvement processes. It was not the aim of the project to evaluate the efficacy of the established processes at NICE for developing CGs and QSs per se, nor was it to explicitly explore the role of patient and lay representatives in developing CGs and QSs.
As outlined in the original study protocol, we explicitly conceptualised this third objective as a knowledge transfer intervention comprising three specific elements:
-
the preparation and presentation of secondary analyses of HERG data sets to selected CG and QS development groups
-
a series of expert-facilitated training sessions to encourage take-up of the qualitative findings from the secondary analyses within NICE
-
a part-time secondment to the NCGC for the project’s senior researcher to work with (1) systematic reviewers in use of techniques to analyse qualitative evidence and (2) the NCGC and QS teams in presenting the work of this project to GDGs.
Incorporating secondary analyses of qualitative evidence into NICE product development processes
The first element of the knowledge transfer intervention comprised five ‘cases’ based on secondary analysis of four HERG interview collections (Table 6).
| HERG collection | NICE CG or QS |
|---|---|
| MI | (1) STEMI guideline (2) Update of secondary prevention guideline |
| Asthma | (3) QS (based on the BTS/SIGN guideline) |
| Type 1 diabetes in young people | (4) Type 1 diabetes in children and young people guideline update |
| RA | (5) QS |
In each case except one, secondary analyses of the HERG collections were conducted and the findings were considered as a formal part of the relevant NICE CG or QS development process. In the case of the type 1 diabetes CG, the NCGC investigator met with the clinical codirector of the NCC-WCH and, separately, with the NCC technical team. Having appraised the initial document, the codirector and the technical team informed the NCGC investigator that, although they were interested in the interview transcripts as a source of quotes, they would not require a more detailed secondary analysis.
Training for National Clinical Guideline Centre staff on qualitative research methods and synthesis
The second element of the knowledge transfer intervention comprised three training sessions for staff from the NCGC led by HERG staff during the first half of 2012. During the first 2-hour session, HERG staff invited participants to articulate their criticisms and concerns about qualitative research [so that the session could be built around these (see Appendix 10)]. Participants were introduced to both the ‘enhancement model’ (illustrated through discussion of a number of papers where qualitative research has aided the development of quantitative research) and the ‘difference model’, in which the qualitative research stands alone, but may also have potential to inform health care. The objectives of the second session were to discuss examples of what good qualitative research looks like, to describe commonly used approaches to qualitative research methods and to explore when it is appropriate to use them. The third and final session focused on combining the results of qualitative studies and was a more practical session than the preceding two. Attendees were introduced to the one sheet of paper (OSOP) approach and then applied that approach as a group activity, using migraine and chronic headache as an exemplar topic. 64 The centre had a CG in development on this topic that was using patient experience and the session used papers found in the evidence review.
Secondment to the National Clinical Guideline Centre
It was originally envisaged that the project’s senior researcher would be seconded to the NCGC on a part-time basis. The secondment was envisaged to include some training for NCGC staff; to accommodate NCGC needs, we arranged these training sessions during the early part of the project (see Training for NCGC staff on qualitative research methods and synthesis). The secondment did not take place as intended; we return to this point later (see Problems encountered and limitations).
Methods
The incorporation of secondary analyses of qualitative evidence into NICE product development processes was studied through a combination of one-to-one interviews and non-participant observation at CG (GDG) and QS (TEG) meetings. Fourteen interviews were completed relating to the five ‘cases’, comprising:
-
six HERG staff (exploring issues of knowledge creation, synthesis, tailoring and presentation)
-
four senior NCGC and NICE staff (exploring notions of receptive context, adaptation, barriers and lessons)
-
four GDG and TEG team members (exploring use and outcomes of the presentation of the secondary analyses).
In the three guideline cases, STEMI, secondary prevention of MI and diabetes (see Table 6), the model being explored was to input HERGs secondary analyses into guidelines development (which would subsequently feed into the later QS). In the remaining two cases (asthma and RA), the HERG secondary analyses were available to inform the selection and wording of the QS directly. Non-participant observation of the following nine GDG and TEG meetings was undertaken (Table 7).
| Topic | NICE meetings observed |
|---|---|
| STEMI | GDG |
| Asthma | TEG1 |
| TEG2 | |
| TEG3 | |
| RA | TEG1 |
| TEG2 | |
| TEG3 | |
| Others | Hypertension in pregnancy (TEG3) |
| Routine postnatal care (TEG3) | |
| Heavy menstrual bleeding (QSAC) |
Health Experiences Research Group researchers did not observe any of the diabetes GDG meetings, as the HERG analysis was not presented here. In addition, HERG staff attended three other meetings unrelated to our five ‘cases’ in order to sensitise themselves to emerging NICE QS development processes.
The training provided by HERG staff was assessed by an online survey comprising 21 items, which was administered to NCGC staff who attended at least one of the three training sessions. Approximately 20–25 NCGC staff attended each session; some staff attended more than one of the sessions. The survey (see Appendix 11) explored the knowledge, attitudes and practices of respondents relating to the role of qualitative research in their work and the value of the training they had received. The first invitation to participate in the survey was sent in October 2012, followed by three reminders at fortnightly intervals. A total of 17 responses were received.
Our analytical approach was to consider the embedding of the HERG secondary analyses into NICE processes as a practical problem of transferring knowledge, ‘the process through which one unit . . . is affected by the experience of another’ (p. 151). 67 This required an understanding of the secondary analysis process undertaken by HERG, of the effectiveness of the two elements of the knowledge transfer intervention, and of the overall translation process itself. We specifically sought to evaluate the impact of the intervention in terms of how the final CG and QS were influenced by the secondary analyses, including considering the counterfactual (i.e. what would have happened had the secondary analyses not been undertaken). Our findings were synthesised and analysed using a deductive approach based on the model of knowledge transfer shown in Figure 5.
FIGURE 5.
Knowledge to action process. Reproduced from Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health 2006;26:13–24. 40 Copyright © 2006 Wiley Periodicals, Inc. with permission from John Wiley & Sons.
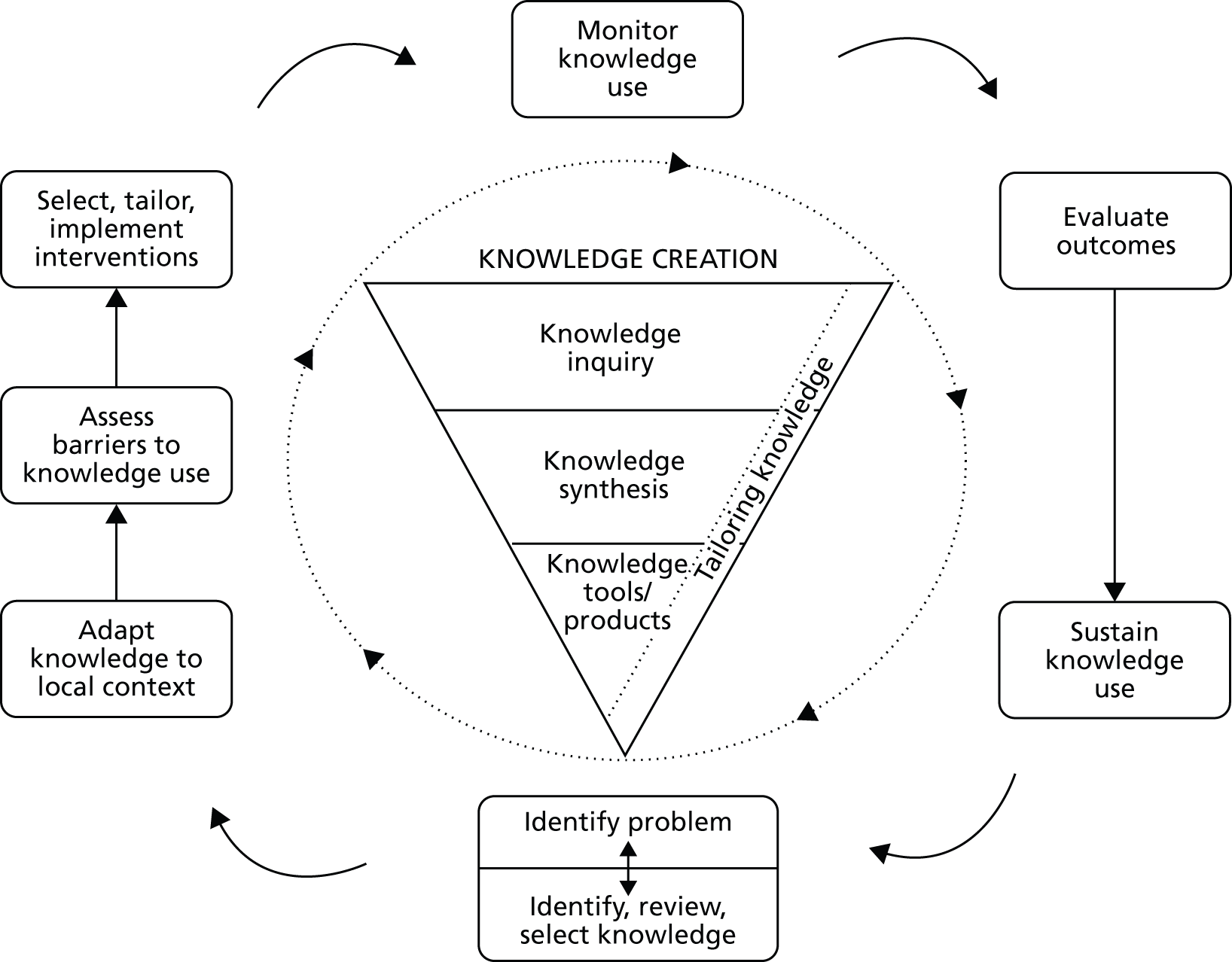
Translating the knowledge arising from health services research into practice remains a key challenge in the drive to improve the quality of health care. Evidence increasingly suggests that organisational and social processes will largely determine whether or not new knowledge is implemented in practice,68,69 and a number of different models of knowledge translation have been proposed in the literature, such as the Stetler model,70 the PARIHS framework,71 the Ottawa model for Research Use72 and the Knowledge to Action framework,73 among others. We selected the model below (see Figure 5) as being the most helpful with which to begin to explore the particular case under study, as its component parts and processes appeared to map closely to the intended approach to transferring and translating knowledge from HERG into the NICE CG and QS development programme.
Our project began with the identification of the problem and selection of the knowledge needed through discussions between the NICE and HERG teams; the inner circle of ‘knowledge creation’ in Figure 5 represents the work undertaken by HERG staff to conduct the secondary analyses (knowledge inquiry and synthesis) and to then ‘tailor’ the findings into ‘knowledge tools/products’ that were presented to NICE teams. The outer circle or ‘action cycle’ represents the process (e.g. adapt knowledge to local context) by which we sought to embed this knowledge into the development of NICE CGs and QSs (our five cases).
A coding framework was developed based on this model and then applied to verbatim transcripts of the 14 interviews and the transcribed observational records of the seven GDG/TEG meetings relating to the asthma, RA and MI topics that were attended by HERG staff.
Incorporating secondary analyses of qualitative evidence into NICE product development processes
The rationale for transferring knowledge between Health Experiences Research Group and NICE
Before presenting our findings relating to the ‘knowledge to action’ process, we first provide the reflections of key actors in that process on the original rationale for the project and why they believed it was worth undertaking. There were certain, albeit isolated, precedents for HERG staff and NICE to work together: for example, a HERG researcher working on a psychosis project had contributed, via a short secondment, to a guideline and a QS. As members of the NICE/NCC teams made clear, there was an element of opportunism underpinning the project which was perceived from the start as being exploratory in nature. The following quotes also underline the difficulties, for staff and team members, of distinguishing between the HERG archive, the HERG peer-reviewed publications and the topics included on the healthtalkonline website (we will come back to this in the discussion).
So I suppose the motivation [for the study] said, ‘Look, very much aware of the importance, or I should say much aware of the profile of the healthtalkonline work,’ it seemed reasonable I think to look at these as something that we could use within our programme in terms of their dataset, and I think looking at ways that that might possibly not only be a good way of improving the quality of our recommendations and making sure we make a difference, using their work, and also it might possibly allow us to think a little bit differently internally about how we prioritise in our areas.
NICE/NCC staff
. . . but if we can demonstrate that the information they have on healthtalkonline can usefully inform the work that we do then that could have some traction . . . I think that there’s such an obvious relationship between what healthtalkonline does and what NICE is trying to do, which ultimately is about improving patient care . . . There just seems to be such an obvious relationship and so, for me, it was really important this project happened as a way of trying to formalise that relationship in some way and if we can demonstrate that it can work, it might well be that it becomes more routine.
NICE/NCC staff
Given this exploratory nature, project team members were aware that a ‘trial and error’ approach was likely to be the most useful in terms of determining whether or not a more formal working relationship between NICE and HERG ought to be established in the longer term:
. . . [we want to] understand the processes whereby we might be able to work with NICE and how secondary analysis of our kind of material could be used to inform. And I suspect in some cases it will add nothing because there will be a really good synthesis of qualitative literature which will say everything that we could possibly say. And in other cases, where there isn’t appropriate literature, there is an opening but whether we can analyse and present and position ourselves such that in that process it really does add I think is a completely different question.
HERG staff
. . . when we understand more about what worked, how it worked, why it didn’t, what the challenges are of adding this type of . . . if as part of this project we could identify ways that our research group could work, so that we can more regularly feed into and help NICE on guidelines and Quality Standards.
HERG staff
In seeking to interpret our findings, it is also crucial to understand the NICE QS development process and the relationship between the CG and QS at the time of our fieldwork (see Figure 1).
It should be noted that the technical team for each guideline play a key role from the beginning of the process as they agree the protocol for the evidence reviews with the GDG and this protocol determines which evidence is relevant and should be presented to the GDG. Nonetheless, it was relatively late in the design of the project that the decision was made to include CGs within the scope of the collaboration:
So when we wrote the grant application it was much more focused initially on informing the quality standards, and then at quite a late stage of the grant application, we turned it into guidelines and quality standards which was largely because our NICE colleagues said, ‘Actually we don’t know where things are going to go with the quality standards, and it just would make it much more potentially useful to us to make it that you would feed into both’.
HERG staff
Despite this, even at the start of the project there were some doubts expressed by NICE/NCC staff as to whether or not it was worth trying to feed the HERG analyses into the later QS stage of the process (although the final NIHR study protocol did encompass both). We will return to this issue later in our findings and proposals for future collaborative work between HERG and NICE.
A final important contextual factor is that while the guidelines programme has an international reputation earned over several years and an established working process, the QS programme has recently been expanded as part of the coalition government’s reforms of the NHS; consequently, working processes, in particular how to develop the number of QSs now required, were still emergent, and how QSs will actually be used remains unclear. 12
the guidelines programme, its international reputation is just a very high quality stable product that’s worldwide recognised. The quality standards work is very much built into part of the coalition government’s reforms of the NHS. We still need more guidance on how these actually are to be used in the system, in the new NHS, and it may be that as we get more clarity on that the nature of the change in terms of their content, their structure. So they’re not a stable product.
NICE/NCC staff
Identify, review, select knowledge
Together, the HERG and NICE/NCC staff identified and selected the topic areas in which HERG should conduct a secondary analysis of their data. The potential choice of topics – in terms of overlap between NICE products and HERG interview collections – was much smaller than anticipated, especially taking into account the intention that the collaboration would deliver results within the term of the project:
So we had discussions with NICE about what was coming up over the next year/18 months of the project and at what stage we might be able to slot in, and we thought it would be a good thing to try slotting in at different stages for different purposes because we could learn more about how this was perceived, what was the best way of delivering it.
HERG staff
The rationale for the four HERG interview collections that were analysed was different. The secondary analysis of the interview data of the first health condition, MI, had the potential to feed into two separate CGs (see Table 6). Unlike the other conditions, the STEMI guideline was largely focused on technical aspects, and much of the development work had already been completed when the HERG analysis was made available to the GDG team:
. . . we came into midway, so the scoping had already been done, they’d already had some of the GDGs and there was not really an element of patient experience incorporated in the scoping stage, but we did hope to influence some of the review questions, somewhat, and just have some sort of influence in the process.
HERG staff member
The second health condition, asthma, was specifically chosen as one where the project could input with a high-level document at the start of QS development (i.e. to influence the scoping exercise) before providing a revised version of the analysis in line with the draft quality statements. The asthma QS was also chosen as one of the NICE products that might benefit, in part because, unusually, it was being informed not by a NICE guideline but by a BTS/SIGN guideline. 74 It was hoped that the HERG secondary analysis would influence the scoping exercise for the QS (which determines which standards might be included or omitted).
Within the constraints imposed by the lack of overlap between commissioned NICE products and the HERG archive, the final two conditions (type 1 diabetes in young people and RA) were purposively selected in order to further test this model by providing (1) a high-level report in advance of the scoping exercise, and (2) a more in-depth analysis focused solely on the key areas identified in the scope and in discussion with the technical team responsible for the delivery of the guideline. The RA QS was being developed from a CG which had included a review of the patient experience literature and followed established NICE processes.
Knowledge creation
The knowledge transfer process began with HERG staff creating the knowledge that was to be transferred to NICE (our five cases). This knowledge creation process comprised three phases which are summarised for each of the four HERG collections (Table 8). Further detail on each of these phases is provided, drawing largely on data from interviews with HERG staff.
| HERG collection | Knowledge inquiry | Knowledge synthesis | Knowledge tools/products | NICE product (1–5) |
|---|---|---|---|---|
| MI | 37 interviews undertaken in 2002–3 | Full secondary analysis undertaken over a 6-month period | One report in two parts prepared for two different CG teams (see Appendix 4) | (1) STEMI guideline (2) Update of secondary prevention guideline |
| Asthma | 38 interviews undertaken in 2011–12 | Interviews analysed in accordance with standard HERG practice Initial high-level summary prepared for NICE. Remit was to identify headline issues that may indicate areas where care is currently poor or variable, without duplicating issues covered in the patient experience QS. The researcher then did a more expanded analysis of the original points under the draft quality statement headings |
Two reports prepared: a high-level summary to feed into the scoping process at TEG1 and a more detailed document for TEG2 (see Appendices 5 and 6) | (3) Asthma QS (including adoption of BTS/SIGN guideline) |
| Type 1 diabetes in young people | 37 interviews (participants aged 16–27 years) undertaken in 2006 (updated 2010 and 2012) | No comprehensive secondary analysis of original data but reanalysis of themes from the primary analysis and a sample of original transcripts. In addition, input/feedback on draft report from researcher who did the topic update | One report prepared: a high-level summary sent to technical team (see Appendix 7) | (4) Type 1 diabetes in children and young people guideline update |
| RA | 38 interviews undertaken in 2004–5 (updated with 14 more in 2012) | A short summary report was produced after exploratory coding of a subset of interview transcripts. Subsequent analysis and coding was focused to inform the draft quality statements | Two reports prepared: a high-level summary to feed into scoping process at TEG1 (see Appendix 8) and a more detailed document for TEG2 (see Appendix 9) | (5) RA QS |
Knowledge inquiry
The primary qualitative data that formed the bodies of knowledge to be synthesised in the second stage of the knowledge creation process were the collections of narrative interviews on various health conditions. Summaries of the primary analysis together with film clips and verbatim extracts are publicly available on the healthtalkonline website. One of the collections was based on interviews undertaken in 2002–3 (MI), while two (type 1 diabetes and RA) had originally been compiled in the period 2004–6 (with subsequent updating). Our original research protocol explicitly stated that we would not use interview collections older than 10 years; the MI data were just within this 10-year window at the start of the project. The age of the collection was discussed as a concern in one of the first project team meetings in November 2011, in particular as the treatment of MI has changed and the STEMI guideline was developing recommendations on interventions that were not commonly used 10 years ago. The consensus of the project team was that insights about what constitutes good-quality care could be gained despite the specific treatments experienced by patients being outdated. The fourth collection (asthma) was a much more recent collection, where secondary analysis proceeded concurrently with the primary analysis. Each of the collections comprised at least 37 interviews.
Knowledge synthesis
The methods and scope of the syntheses of the existing HERG interviews varied significantly by collection. At one extreme, the synthesis of the 37 heart attack interviews took a researcher working 2 days per week approximately 6 months, whereas in the case of the diabetes collection no new synthesis was undertaken; rather, a summary was produced based on a synthesis of the topic summaries already produced for the healthtalkonline website and tested with selected interviews from the full data set.
Knowledge tools/products
In total, HERG staff prepared six reports for various technical teams and groups. In keeping with the exploratory nature of this component of the knowledge transfer process, these reports were structured and presented in different ways and delivered at different points of the NICE product development process.
there will come a point when we can say, ‘We tried these various different ways of presenting evidence and our understanding of how it didn’t work in this area was this, and our understanding of why it worked here was that’.
HERG staff member
There was a great deal of discussion among the project team regarding the best format and style of content of the secondary analyses (e.g. should quotations be presented and, if so, then how, and also how much of the evidence was it necessary to present?). For the high-level reports on asthma, type 1 diabetes and RA, information was presented in the form of bullet points at the request of the NICE consultant clinical adviser and coinvestigator. This was not without residual concerns:
one concern we might have is if we produce something which is too brief it might just look like a couple of anecdotes which can then be very easily ignored. So what is the best way for us to present evidence so that the position of the evidence is clear? And I think if that’s one of the things that we can start trying to untangle over the course of the project that would be extremely helpful to everybody.
HERG staff
Some consideration was given to using short film clips from the HERG archive as a way of illustrating key themes relating to patient experience:
. . . the issue of what our input would look like, whether our input would be somebody coming along to a meeting and showing a few video clips, and saying here are the things which are important to patients . . . that was one model.
HERG staff member
Attitudes to different ways of feeding the HERG qualitative evidence into the process were not homogenous and some NICE/NCC staff appeared much more open to experimentation than others. The technical team for the STEMI and secondary prevention guidelines underwent some personnel changes half way through the process; at one point, the leaders of the secondary prevention team were quite interested in using video data to introduce the material to the GDG. This was not, eventually, taken up.
The steering group also felt that it could be counterproductive in the GDGs to use illustrative examples which might be seen as too individual to inform the process. It was, therefore, decided to present the results of the syntheses in a way that:
looks factual and derived from a big sample . . . [that] conforms more to their idea of what evidence is.
HERG staff member
The consequence of this decision was that the visually engaging, emotional and powerful stories captured by the HERG interviews and used on the healthtalkonline website were, with the exception of the longer MI report, reduced to a few sides of written bullets and presented to members of the GDG or TEG as one small part of a weighty set of meeting papers.
The results of the synthesis of the heart attack collection for the STEMI and updated secondary prevention guidelines were the first to be prepared and presented. The following narrative from a HERG staff member captures the emergent nature of this part of the knowledge transfer process:
I think there was a meeting in March where I’d written a summary on one particular aspect, which was the emotional impact of the diagnosis, because I felt that that was something that was relevant to STEMI, regardless of . . . I mean, there weren’t any questions relating to that in the guidelines. But I thought, ‘Okay, this is all so technical, and this is all around when patients get admitted with this, how they manage, but how do the patients actually feel?’ . . . So I sent them a four-page document where I put key messages if you like, and then what looked more like a topic summary as can be found on the website, with a few points, and then a quote to illustrate this. So we were talking early on about it feels weird for us to write key messages and make these factual statements about, ‘Patients feel this’, without going into further details about how we arrived at this, and showing some of the quotes. . . . We showed them just that summary for the one issue and said, ‘Is that the sort of thing that you want from us? What about the length?’ And the general feedback was, ‘Yeah, continue along those lines’. Then in April we had another meeting, and I said, ‘These are the ten themes I’ve identified, and I’ve loosely mapped it along the care pathway’.
HERG staff member
The NICE/NCGC investigators suggested that the HERG and the NCGC technical teams hold a meeting dedicated to how the data could be presented to the GDGs. While being mindful of NICE processes, the guideline technical teams (who review all the evidence available to them and are independent of the NICE/NCGC investigators) considered how best to accommodate the study within these processes. One area for discussion was whether or not it would be appropriate for a HERG researcher to present material directly or whether or not it would be better if the technical team acted as the channel (for NICE processes on presentation of evidence and competing interests, see Adapt to local context). The HERG and NCGC teams also discussed how best to ensure that the status of the information was transparent; for example, how to indicate whether or not the analysis was supported by other evidence or whether or not there was a gap in the literature, and how a summary description might be useful. The HERG team suggested a broad report structure, which was approved by the NCGC. An extensive report was sent to the STEMI technical team, which was extended to include three further chapters for the secondary prevention technical team as agreed with the NCGC (see Appendix 4 and Presentation of MI findings). The content and format were informed through direct discussion.
Having prepared the report, there remained uncertainty as to quite how it would be used to inform the NICE product development process:
. . . I don’t think the report will be presented to the group at all. That’s my impression. What I think is the report will be digested by the project team, and they will then, I don’t know, possibly pick up something which I present in the PowerPoint slide. That’s how I imagine it . . . I still don’t really know whether it will be at all presented and discussed at a GDG.
HERG staff member
Another HERG staff member reflected:
At the moment the MI document . . . is quite long. And I really don’t know whether something that long is the best use of our time and how they’re going to use it. So I suppose what they’ve got now is some examples of very different ways that we can pull together information boards, and we really need to rely on them to tell us, ‘this is nice but frankly it’s going to be filed and nobody’s going to read it’. And there might be other, better ways of us trying to inform them about what’s most important.
HERG staff
Later syntheses (asthma, diabetes and RA) followed a more common template, although in the case of the asthma QS the summaries produced by HERG were written to follow the themes identified in the BTS/SIGN guideline that was the basis of the QS.
For the asthma topic, the HERG summary report was polished in collaboration with NICE co-investigators. Although it primarily conformed to the guideline headings, it also included a new theme, ‘emotions and acceptance’. The second report was used to populate the patient experience section of the TEG2 briefing paper which was sent out to TEG members and to stakeholder consultation. At least one TEG member plus external stakeholders used the HERG report to bolster their own arguments during the meetings. We consider that the evidence around poor inhaler technique did contribute to the inclusion of a specific statement on inhaler use. However, owing to the limited number of permissible quality statements, it was not possible to draw on the report to inform other areas where patients had reported their experiences.
The full report on RA and the summary report on type 1 diabetes were both viewed by the relevant technical teams but neither was felt to add anything to the existing evidence.
Action cycle
The action cycle in respect of our five cases is summarised in Table 9.
| NICE products | Adapt to local context | Assess barriers to knowledge use | Select, tailor, implement interventions | Monitor knowledge use | Evaluate outcomes |
|---|---|---|---|---|---|
| STEMI guideline | Consultation with NCGC and technical team | No explicit process for including unpublished analysis Lack of peer review of HERG secondary analysis Lack of clarity about the distinction between HERG archive and published data on healthtalkonline TEGs and QS process not place to discuss evidence (asthma and RA) Broader issues of patient experience (e.g. emotions) that are difficult to measure (measurement a requirement for QS), or issues not directly related to the provision of health care and lie outside the scope of NICE’s remit (e.g. social services) In the emerging area of qualitative literature synthesis and secondary analysis there is a lack of agreement about the best way for technical teams and GDGs to incorporate, interpret and use these different types of evidence |
Included ‘key messages’ (see Appendix 4) | Not used | Not used |
| Update of secondary prevention guideline | Consultation with NCGC and technical team | HERG staff discussed areas of interest with technical team who requested additions to the STEMI summary | This was presented to the guideline group but not used in the light of the extensive review conducted for the guideline | Not used | |
| Asthma QS | Consultation with NCC and technical team | The more detailed document for TEG2 addressed specific experiential issues raised at TEG1 Related to draft QS (based on template provided by NICE) |
The HERG summary report (see Appendix 5) was referred to by the technical team in the scoping exercise. The second report (see Appendix 6) was used to populate the patient experience section of the TEG2 briefing paper (sent to TEG members and to external stakeholders) | HERG summary highlighted importance of proper inhaler use and contributed to a quality statement on this. The issue of engaging with patients at an emotional level to enhance self-management was not in the BTS/SIGN guideline and was not included in the final QS | |
| Type 1 diabetes in children and young people guideline update | Consultation with NCGC coinvestigator | No tailoring | Not used | Not used | |
| RA QS | Second report was refined through discussions with technical team; selected aspects of secondary analyses that related to draft quality statements (see Appendix 9) | Not used | Not used |
Adapt to local context
It was challenging for the HERG team members to adapt to the ‘local context’ (the established NICE CG and QS development processes) in which they found themselves working to ‘transfer knowledge’ (the results of their secondary analyses). As the three quotations below illustrate, HERG staff were surprised, and sometimes frustrated, by the constrained nature of their involvement, the requirement to work within the established framework of NICE processes and code of conduct for participation in advisory group work. The code of practice includes the declaration of not only pecuniary interests but also non-pecuniary interests such as involvement in and authorship of research that is presented to advisory groups.
I thought we would have a lot more liberty. I think it does very much feel like they’ve got the system or process of working and we are very much slotting into that.
HERG staff
. . . if I’m completely honest . . . I think it was fairly obvious that unless we were able to work with the way that they [NICE] were going, we were going to have no impact at all, so we had to try and fit with their . . . I felt I was pushing the boundaries even just saying, ‘there’s a section on emotions’.
HERG staff
we are being sort of framed by what they think are the important issues; we’re presenting them with patient experience that is around the things they think are important. So I think within that framework they are giving it due attention but it’s not probably things that they hadn’t thought about before, for the most part.
HERG staff
For example, HERG staff could attend but not speak at the GDG or TEG meetings, where they were non-participant observers, typically sitting not around the meeting table with GDG or TEG members but at the side of the room, and not allowed hard copies of slides shown at the meetings: it was clear that they were external to the discussions. This came as something of a shock to some HERG staff attending their first meeting:
. . . I had understood I was going to be there and available to answer questions and maybe just give them five minutes on what I’d put in the report. And it wasn’t until I was sent a copy of the confidentiality agreement to sign . . . when I looked at what it said, and then realised that I was going to be an observer and not allowed to speak, that was the first I knew of that. So I think we’re an uncomfortable category that they don’t quite know what to do . . . You don’t want to criticise people for that, because it’s [NICE guideline programme] obviously been a very successful process that has meant that they’ve churned out the guidelines on time and to a high standard for many years, and what’s wrong with that. We also have a very rigid process for producing what we produce [. . .] But it does mean that they find it, I think, quite difficult to imagine how they could do anything differently or use evidence in a different way, or different types of evidence.
HERG staff
the fact that this piece of research I’d only literally just done, and it was hot off the press, was possibly going to have some influence. Then going up there and not being able to participate, and feeling as though it was minimal influence. But it was almost like a paper exercise that they’d included patient experience. That’s how it felt to me.
HERG staff member
Assess barriers to knowledge use
Across our five cases, we found six barriers to the use of the HERG syntheses within the development of CGs and/or QSs:
-
There is no explicit process to include secondary analysis performed as part of this study.
-
There is a lack of peer review of HERG secondary analysis.
-
There is a lack of clarity about the distinction between HERG archive and published data on healthtalkonline.
-
The TEGs and QS process are not the places to discuss evidence (asthma and RA).
-
There are broader issues of patient experience (e.g. emotions) that are difficult to measure (measurement a requirement for QSs), or issues that are not directly related to the provision of health care and lie outside the scope of NICE’s remit (e.g. social services).
-
In the emerging area of qualitative literature synthesis and secondary analysis, there is a lack of agreement about the best way for technical teams and GDGs to incorporate, interpret and use these different types of evidence.
There are no protocols or guidance within the existing NICE processes about how to use an unpublished qualitative secondary analysis. While HERG interviews are collected and analysed using a rigorous, documented and peer-reviewed approach, the targeted secondary analyses that were conducted for these reports had not, themselves, been peer reviewed. Perhaps unsurprisingly, there was some confusion and lack of clarity about the status of the reports; it was not clear to members of NICE GDG and TEG teams quite how the HERG interviews could fit within their established working processes:
the Oxford data, the stories, is never going to get any traction as long as it’s considered within the traditional hierarchy of evidence framework because it’s always going to be critiqued for how representative is this, how have you collected the data, it hasn’t been peer reviewed, published, those types of things. So just thinking out loud, if the Oxford data is going to have any kind of place in these processes, it needs to sit outside of that mental model of the hierarchy of evidence and be seen as a completely different type of input to the process, and it may be that there’s simply no space for that.
NICE/NCC staff
so I think there is still quite a lot of work to be done in making not just the incorporation of qualitative evidence as part of what we do every day but actually looking for it in the first place . . . I think there are people at NICE who are trained in doing systematic reviewing and they are trained in analysing randomised controlled trials and they’re trained at looking at other types of evidence if they have to. But there is still a prevailing attitude that qualitative evidence is at the bottom of the hierarchy, whereas I’ve always envisaged it as something that sits alongside the tradition of hierarchy of evidence and informs it at all stages.
NICE/NCC staff
Given the absence of an established process, the HERG secondary analyses faced a credibility problem with NICE/NCC staff. (Although this may have been anticipated, secondary analyses of HERG data had been used previously, for example in the CG on depression.) As reports that had been written to address the specific focus of CGs/QSs, they had not been (and were not likely to be) published, either on the peer-reviewed website (healthtalkonline) or in a peer-reviewed journal. Such unpublished work would not be accepted in any other area of NICE work. The status given to secondary analysis of HERG data was crucial in terms of the contribution that they were likely to make to NICE processes, not just in this project but in the longer term:
The issue certainly in guidelines is very clearly to guideline development groups that actually we are using published data. We were very aware that in all sorts of areas there is stuff out there that never got published and there are whole issues of publication bias and all sorts of things around that. But if we are saying that this data was to be available and to be used in some way, then it would be giving it a status that other data does not get and we have to just think through . . .
NICE/NCC staff
what might be an outcome of this is that [HERG has] a bit more of an explicit procedure for when we are doing secondary analyses to inform NICE quality standards, that we can be more explicit about how we are actually doing that, so we are developing a kind of procedure that then can also, in some way, maybe accredit it or something.
NICE/NCC staff
Given that the work of the NICE technical teams, and GDGs in particular, is very protocol driven, it was suggested that, if the HERG data were to become an integral part of NICE’s working processes, their inclusion and consideration had to be made explicit through revisions to the manuals and templates that the teams and GDG members worked so closely to:
You can advise people all you want and you can say this would be a really good idea and actually your product would be better at the end of the day but that’s not what wins the argument. What wins the argument is saying, ‘Yes, as part of the contracts with the assessment groups your expectation is that they will be looking for the following types of evidence’. And so until it’s in contractual relationships, until it’s in process guides, until it’s in methods guides . . . Until it’s in those various different approaches I think it’s always going to be something that we have to lobby for rather than is integrated.
NICE/NCC staff
Technical teams do, and are encouraged to, search for published qualitative evidence which is included where relevant. The clearest example came from the secondary prevention guideline where a particular issue identified by the technical team related to how patients from ethnic minorities engage with cardiac rehabilitation programmes. The findings from this review were sufficient to inform the guideline development process without the need to draw on the HERG data, which would not have been graded – in evidence-based medicine terms – as highly as a meta-synthesis of published reviews and may not have comprised the relevant patient population in any case. Hence, the HERG data may have had little, if anything, to add to this exercise:
. . . they did a systematic review of the evidence and there was huge amounts of stuff out there, huge amounts of stuff out there. So, for instance, people think there’s an issue around people of certain ethnicities and having engaged in aspects of cardiac rehabilitation and things like that. So people have looked at that very specifically. Whereas the Oxford data didn’t have the older people, didn’t really have many . . . do you know what I mean? And that’s really what happened in the post-MI, they did their own review and found a huge amount of people . . . who’d done systematic reviews of the studies of ethnicity and involvement, who done meta-synthesis of . . . you know, published last year.
NICE/NCC staff
In the case of the STEMI guideline, the highly technical nature of that particular product – allied with the existence of a recent NICE Patient Experience guideline and concerns about whether or not the HERG collection was too old (it had originally been collated in 2002–3) – meant the synthesis had no impact on the development process. 8 As highlighted earlier, the issue of the ‘age’ of the data had been discussed among project team members at an early stage, but differing views about whether or not this was an issue or not remained within the team.
Where the syntheses were presented as a formal part of the GDG or TEG meetings, additional issues arose. HERG staff gave examples from the asthma case where their data revealed significant issues for patients but they simply did not have relevance as far as the remit of the CG or QS:
The other stuff that we’ve got in the data is about relationships, or work and finance, and benefits. You know, that kind of thing, but actually there’s no point in giving them that because it is NICE and it is NHS pathway driven, so there’s little point in giving them a load of stuff about whether people feel they can get a girlfriend or not, if they have an inhaler in their pocket, because they can’t do anything with it in the real world.
HERG staff
Again I felt like our data were really, really . . . there was such strong evidence of people saying that their asthma had been so way out of control for many years, and they’d only realised after years and years of using inhalers that they weren’t doing it right. I felt like that was a really key issue. Again, that wasn’t really pursued, and I wasn’t able to say . . . Yeah. I felt like there were a few missed opportunities to be able to emphasise or reemphasise the part of the data that they applied to what they were talking about. . . . The conversation was all very much geared around the measurability, you know, if you offer somebody something, how do you measure whether they took it up or not, that kind of question . . . If you couldn’t measure it, it wasn’t going to go in there at all. That was what I took from the meeting that I hadn’t actually probably understood beforehand.
HERG staff member
Given the CG and QS development process set out in Figure 1, and in keeping with some reservations expressed by NICE/NCC members at the start of the project, it quickly became apparent that the place to take account of HERG’s secondary analyses of patient experience – if they were to have any influence at all – was most likely in the pre-scoping phase. Only then might there be the possibility of patient experience setting the agenda in the actual scoping phase. TEGs were simply not the right place for secondary analyses:
Guess I saw the primary place for presentation and use of the online data within the guidance production process. Because that is the process at which evidence itself is discussed and used.
NICE/NCC staff
The problem with the quality standards process itself per se is that it isn’t designed to allow an in-depth review of evidence. It’s not designed to do that . . . I think the primary purpose of the quality standard group isn’t so much to know whether those recommendations are valid or of high quality . . . It’s mainly to say, in asthma care, for example, if you’ve got several hundred recommendations in the guidelines across the whole pathway of care, the main aim for the group is to decide which of those areas of care are sufficiently important to scroll down to a relatively small number of statements . . . it might be influenced by a very short summary, say of patient safety information, or the short summary document that was produced for asthma and rheumatoid arthritis, but it isn’t a meeting in which there’s an in-depth discussion of those issues.
NICE senior manager
The same senior manager later added that ‘I also feel the short summary was a very good aid to prioritisation’. One interviewee characterised the work of the TEGs in constructing the QS as a tertiary synthesis; they draw on recommendations from the CGs (themselves drawing on narrow and clearly defined evidence on clinical effectiveness and patient experience) but do not allow in-depth discussion of new (and broader) bodies of evidence:
I guess what we’ve tested so far in the project is, if you like, a kind of blanket approach to using the Oxford data, synthesising it, putting the summaries in to the normal processes, whether it be around guidelines or the quality standards. And I think some of the things you said about the quality standard processes were very interesting. But I guess what’s coming out of quite a few of the interviews that I’ve done recently is that perhaps the main finding of this project, one of the main findings, will be it’s about the targeted use of the Oxford data set to particular guideline topic areas, quality standards, where there is a real felt need for a closer look at patient experience, qualitative data.
NICE/NCC staff
Rather, the focus in the TEG meetings was on determining which statements to include in the QS and which were considered to represent areas for quality improvement, a determination that was often driven by whether or not implementation of the statements could be objectively measured.
Finally, interviewees wondered whether or not there were sufficient skills and capacity for using qualitative research evidence at NICE/NCGC. Qualitative literature synthesis and secondary analysis are emerging areas and there is a lack of agreement about the best way for technical teams and GDGs to incorporate, interpret and use these different types of evidence as part of the core business of developing CGs and/or QSs. None of the research team needed to be convinced about the value of qualitative research but some of our observations, interviews and informal conversations during the project suggested that we would be naive to assume that our team members were representative of many guideline development staff. One interviewee compared the approach in the Danish health technology assessment programme with that of NICE:
And we look at places like Denmark who have whole teams of qualitative researchers in their health technology assessment programmes where they’ve acknowledged that this is a really important area and they‘ve engaged particular analysts with particular skills to make sure that that takes place and we look at those people with absolute envy because it’s such a really good model . . . They’ve acknowledged it as separate expertise, as a valid expertise in its own right, which then confirms the validity on that type of evidence I think. By saying, ‘We take this really seriously, we engage a particular team,’ it says, ‘We take this evidence seriously, that it’s valid evidence in its own right. It’s not the lowest form of evidence we could find. It’s asking a different question’. I think that’s the big philosophical cultural difference.
NICE/NCC staff
Select, tailor, implement interventions
The best opportunity for the HERG and NICE/NCC staff to tailor and implement different forms of intervention during the knowledge transfer process was through interacting with the GDGs and TEGs and – particularly – the technical teams supporting them. As reported earlier, there was no direct interaction between the HERG researcher and the groups at the meetings and no formal role for the researcher (other than as non-participant observers).
. . . We are not actually presenting anything to the guideline discussion group or to the TEG. We are there et al and we are there as observers, and they’re getting a document alongside others . . . that connection might need to be worked up a bit more and it might be difficult to do that in a written format . . . If you could actually have a question and answer with the TEG or the GDG and a discussion to say, ‘Well, this is why we think patient experience is relevant here’ . . . to make those connections. So I think it’s very interesting that they [the technical team] think after looking at [the HERG summary], ‘Oh, this isn’t actually relevant’ . . .
HERG staff
. . . There were three people who worked on the project team for the TEG . . . my understanding is that they are the people who pull together all this evidence which then gets circulated to the TEG members. So they are sort of, the behind the scenes accumulators of evidence. And they are the people who in some ways are the mediators of whatever we come up with. Presumably they are the people who brought the headings together. I don’t know . . . we’ve never met and don’t really engage with them.
HERG staff
The project manager from the STEMI guideline was involved in discussions with the HERG secondary analyst but it was decided not to present the report to the STEMI team. Discussions with members of other technical teams (the team for the secondary prevention guideline update and for the RA QS) were helpful in tailoring the materials prepared for the subsequent meetings:
when we had one of the meetings in London and the project team for myocardial infarction for the secondary prevention, three people came in and then we exchanged e-mails with them, and then X set up a meeting with the three of them . . . when I was chatting to them, and they said, ‘Oh, we would like that, and have you got anything on this?’ You know, just fine tuning what I was doing, and what they were interested in, and that was so helpful from my point of view . . . Because previously we have been feeling a bit like we are working but we are sending things into black space . . .
HERG staff
Other suggested, but not enacted, ways of tailoring the intervention included routinely preparing lay members of the GDG and TEGs to act as ‘agents’ or ‘knowledge brokers’ for the HERG secondary analyses:
I think there has to be somebody, there has to be a role for somebody to draw people’s attention to it to say, ‘This is important, we have to see everything that we’ve looked at so far in the context of this information. Does this change what we would prioritise? Does this change the way we would frame the statements? Does it change anything?’ And it may not but I think that it needs to have its own space, it needs to have its own consideration as part of the group’s work I think in order for it to be taken seriously, not even seriously but for it to be given the air time that it needs. One mechanism might be that the lay members are briefed and they get to talk about what some of the key issues are for it.
NICE/NCC staff
Monitor knowledge use
Two of the technical teams rejected the HERG reports and did not present them to the relevant GDG (see Table 9). In the case of the STEMI team,
. . . they were ending up with a very focused guideline to which most of the stuff around patient experience wasn’t something they were going to or wanted to include.
NICE/NCC staff
they felt that the treatment for [condition] and treatment pathway had changed so much since the interviews that the data was no longer relevant.
Written communication with technical team
Instead, the team stated that the GDG would be referring to the NICE guideline on patient experience and highlighting areas particularly relevant to the specific guideline they were developing:
The group’s response was, ‘This data is too old and doesn’t tell us specifically about . . . it doesn’t give us anything specific that to say the more general patient experience guideline did’. . . . So when you’re doing a guideline like that, when you’re doing any of these guidelines, one of the things you do is look at the quality of the data and one of the issues about the quality would be, ‘Is this the kind of population we’re looking for? Is this relevant?’ And other things may also be excluded for that reason. So it’s not unique to the report from Oxford. It would be the exact same approach.
NICE/NCC staff
The secondary prevention technical team presented the report to the GDG who also provided detailed feedback for their decision not to use the report as a source of data for the guideline. Of interest, the report is again referred to as a ‘healthtalkonline’ report, whereas it was a secondary analysis of HERG data, which is also published on healthtalkonline but, for the purposes of this study, was relatively independent.
The group felt that the data gathered were of great insight into the condition and represented an interesting source of information; however, below is a summary of their thoughts:
-
‘The GDG felt that the data used to develop the report were too old, given recent and substantial changes in [management of the condition], meaning that the data may not always be applicable to the current context.’
-
‘The group were also concerned about the time lag between [onset of condition] and the interview in some cases.’
-
‘The group felt that there may be some bias in how the participants were selected and it was felt that the experiences of those who chose to be interviewed may not be representative of a broader population. Of particular issue is the experience of people from BME [black and minority ethnic] groups . . . and older people.’
-
‘One of the main reasons the GDG decided not to use the data was that in this particular guideline we had conducted our own fairly large review of qualitative data with c500 abstracts reviewed and plenty of included studies. This new work therefore seemed less important than the body of evidence we had already found. Of interest, the findings of the healthtalkonline report were similar to our own review. In this case the GDG did not miss any information by not including this data.’
-
‘Although we reassured the GDG that the work could be included from a NICE perspective, there were some concerns that the analysis was unpublished and by including this work, we would be opening ourselves up the inclusion of any unpublished work identified by GDG members and stakeholders.’
-
‘It was felt that this data would perhaps have been more use in an area where there was less published data available.’
The comment that the GDG had not used the data because the technical team had conducted its own review of qualitative data is an interesting one. The HERG secondary analysis was targeted to examine what constitutes good care for people with MI, whereas the published research literature would likely have taken more specific foci. Individual CGs generally do not address ‘good care’ in a broad sense; they address specific interventions and whether or not they work. As such, their reach is quite limited. The ‘good care’ components are very much about ‘how’ one delivers care, most NICE guideline recommendations are about ‘what’ intervention is delivered: the more focused and technical the guideline, the more likely this is. Therefore, there is a risk that the technical focus will marginalise issues such as support needs, which may not have been addressed in broader guidelines such as the Patient Experience guideline. There is an attempt to include specific non-technical areas in individual guidelines where relevant but it should be acknowledged that this does not always occur.
Evaluate outcomes
The HERG asthma summary report was referred to by the technical team in the scoping exercise. The report highlighted the importance of proper inhaler use, and learning inhaler techniques through demonstration, which contributed to a quality statement. There was little evidence of any of the other HERG secondary analyses having directly (or even indirectly) influenced the five NICE products. For example, engaging with patients at an emotional level to enhance self-management (this issue was not in the BTS/SIGN asthma guideline) was highlighted in the HERG report but the final asthma QS did not include ‘emotional responses’. One further aspect covered in the HERG report for TEG1 related to a proposed statement regarding inhaler use at schools in the proposed QS; however, NICE QSs are intended only for the NHS and this aspect could not, therefore, be included, as NICE has no jurisdiction in schools.
Sustain knowledge use
The task of this component of the knowledge transfer intervention was to explore whether or not it would be possible to effectively incorporate a secondary source of patient experience data into the existing NICE CG and QS development processes. During the course of the project, various approaches were tested and we observed what happened. Beyond the specific recommendations for any future collaboration made in this report, project team members provided some overall reflections:
if you were blue sky, you think, ‘Could we have done something very different?’ There might have been other ways that we could have used it within the process. I think it’s very difficult . . . I find it difficult to think if we were doing it again, I’m still struggling to see how we could have done it differently in terms of the pressures. But it does relate back to my view that I do see the value of the work as being very much upfront and the evidence at this stage rather than downstream in the standards phase, but I think it was a model that we had to test.
NICE/NCC staff
Others reflected that there was a danger of overanalysing what had happened during the course of this component of the knowledge transfer. There are very well-established processes at NICE and the technical staff have been trained to consider ‘hierarchies of evidence’ in assessing the effects of interventions, as reported in peer-reviewed publications. Consequently, key staff on the technical teams clearly struggled to see the value of the HERG secondary analyses, but there is a much simpler explanation for what we observed: the HERG data did not add value for the specific purpose of CG and QS development. Guideline developers ask very specific questions (rather than a general review of patient experience) and for HERG data to be useful they had to be, in the developers’ eyes, both timely and relevant to those specific questions:
the guideline is more the longer process where there’s more immersion of the data, where there’s more immersion of the staff in the work . . . the standards, it is high output, high volume, very . . . quite a focused process, and I think as a result of that we have to go in right from the beginning of saying, ‘Actually to make this work within the context of evidence that we already have, it means that you’ve actually got to request something really focused from Oxford’.
NICE/NCC staff
As NICE/NCC staff put it, ‘we don’t have the luxury not to be focused’. It seems clear that if the HERG data were to be useful to NICE/NCC, a much more targeted process was needed at a very early stage of the process, such as prior to and during scoping and in the establishment of the review questions. Alternatively, the HERG data might have a role in informing future updates of the patient experience CG and QS.
that high level summary could be a synthesising concept, it could be helpful at the early stages of not only the guideline development, but the early stages of guideline development in terms of helping people understand what actual areas of care does the guideline need to focus on? Because we’re not actually – again, in the future – necessarily going to have the resources to develop the guideline that covers every single item of the pathway.
NICE/NCC staff
Training for National Clinical Guideline Centre staff on qualitative research methods and synthesis
Results of online survey
A total of 17 NCGC staff responded to the online survey, representing approximately half of the total number of staff who attended at least one of the three sessions. Of the 17 respondents, 13 were among the 28 staff members who attended the January 2012 ‘Models of qualitative research’ session, 10 were among the 15 attendees at the February 2012 ‘Good practice in qualitative research and applications’ session and 10 attended the July 2012 ‘Practical session’. Six of the respondents identified themselves as a ‘research fellow’, four as a ‘senior research fellow/project manager’, four as a ‘senior reviewer’ or ‘reviewer’, and one each as an ‘operations director’, ‘information scientist’ or ‘guideline lead’.
When asked about their ‘knowledge of qualitative research’, eight stated that they had no previous training, six said that they had received some formal training as part of either a Masters or a Doctorate qualification, and three reported that they had experience of conducting at least one systematic qualitative review as part of their work at the NCGC. Twelve of the 17 respondents reported having used qualitative research findings in their work at NICE in 2012; five respondents had not done so.
Table 10 below summarises the survey findings relating to respondents’ general views as to the value of qualitative research findings in their work. Generally, staff could see the relevance of qualitative research findings for determining the importance of aspects of patient experience, but were less certain of their value in terms of their own work on CGs.
| Survey item | 1 (low) | 2 | 3 | 4 | 5 (high) | Mean |
|---|---|---|---|---|---|---|
| How do you personally rate the value of qualitative research findings in providing evidence of patients’ experiences of health issues? | 0 | 0 | 1 | 2 | 14 | 4.76 |
| Overall, how valuable do you think qualitative research findings are in the work you do at NCGC? | 0 | 4 | 6 | 5 | 2 | 3.29 |
| How do you think the NCGC as an organisation rates the value of qualitative research findings as a source of knowledge relative to randomised controlled trials? | 2 | 6 | 1 | 6 | 1 | 2.88 |
| How do you personally rate the value of qualitative research findings in providing evidence of the effects of treatment? | 1 | 8 | 6 | 1 | 0 | 2.44 |
Figures 6–10 report the main findings from the survey relating to the training that was provided by HERG staff as part of the ‘knowledge transfer’ intervention. The style of teaching (see Figure 6) was positively rated (mean = 3.88); open comments included that the training was ‘extremely well planned, clearly explained and very well presented’ and ‘fantastic – very clear, very helpful’. As described further below, respondents also highlighted session three as being the most helpful of the training sessions.
FIGURE 6.
Responses to question: how would you rate the style of teaching in the HERG training session(s) you attended on qualitative research?
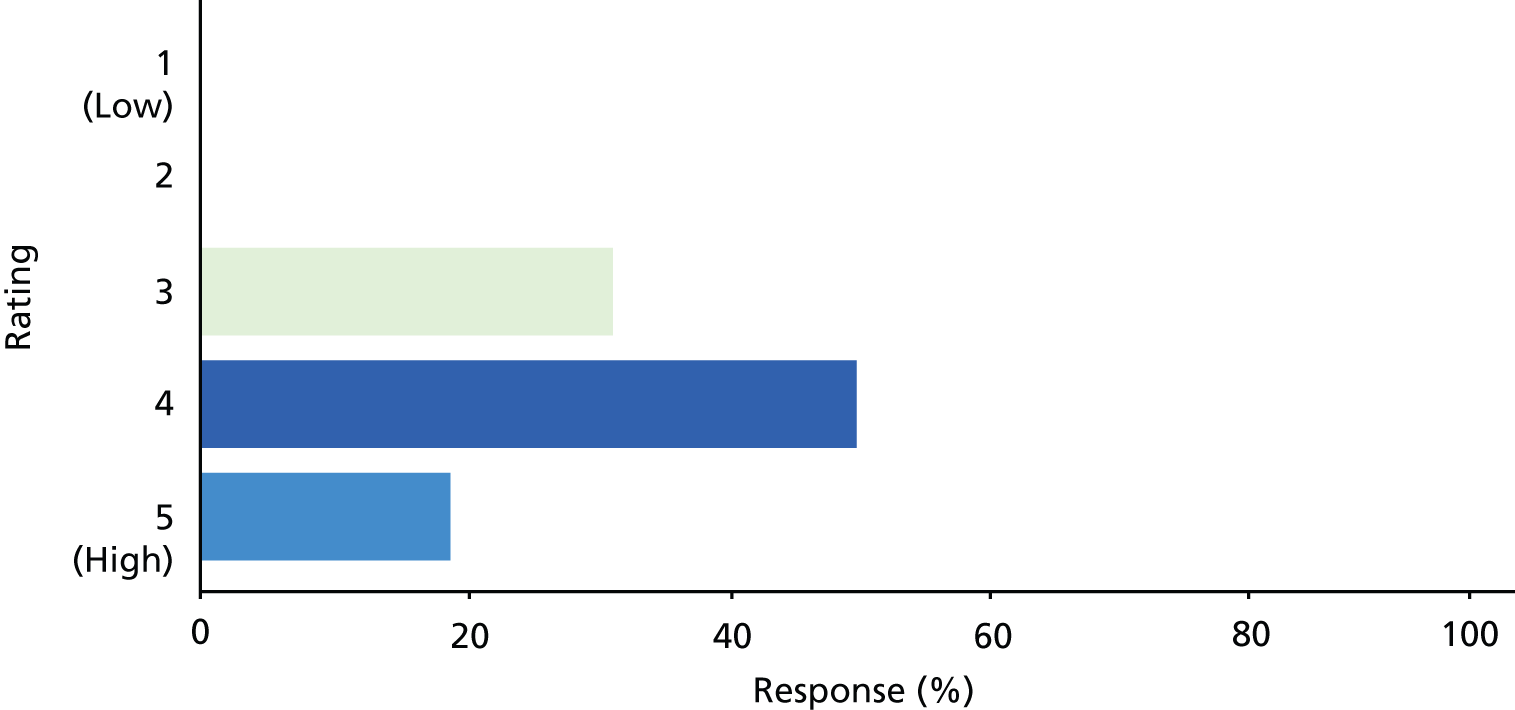
FIGURE 7.
Responses to question: how would you rate the relevance – for your own work at NCGC – of the content of the HERG training session(s) you attended on qualitative research?
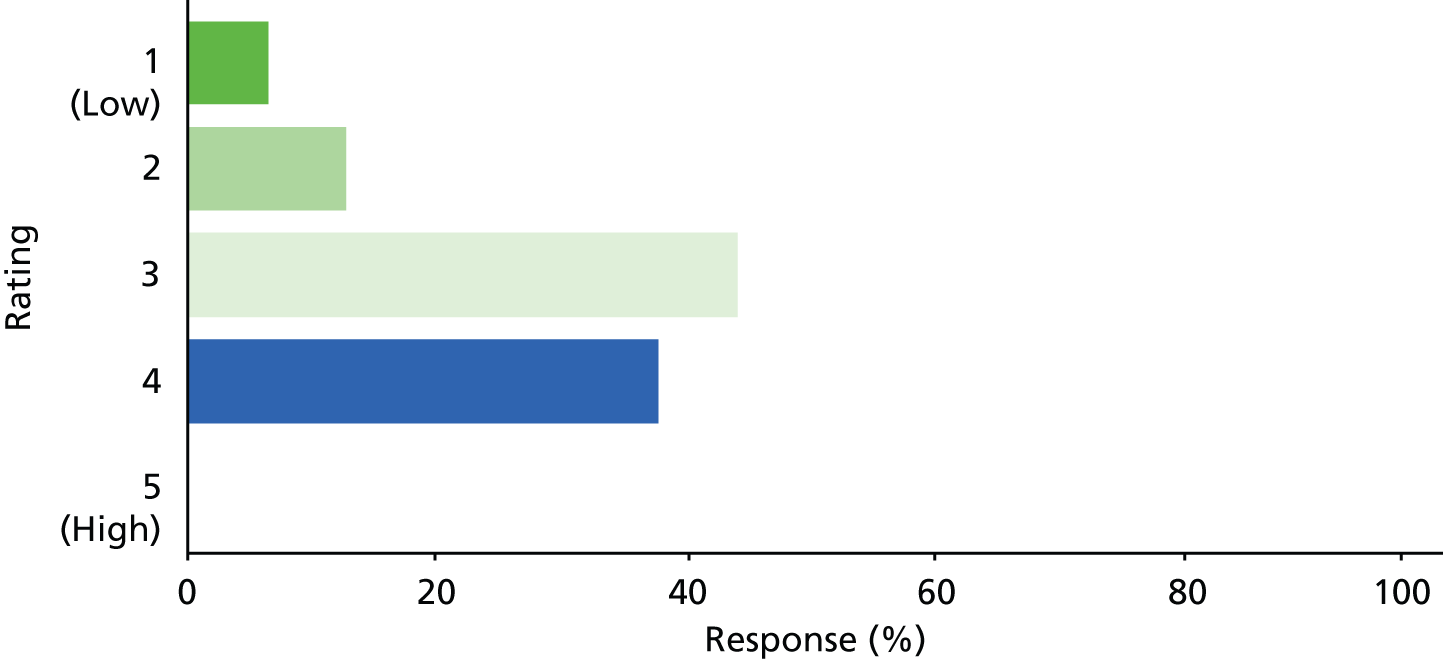
FIGURE 8.
Responses to question: how much impact had the HERG training session(s) you attended on qualitative research had on your own work at NCGC?
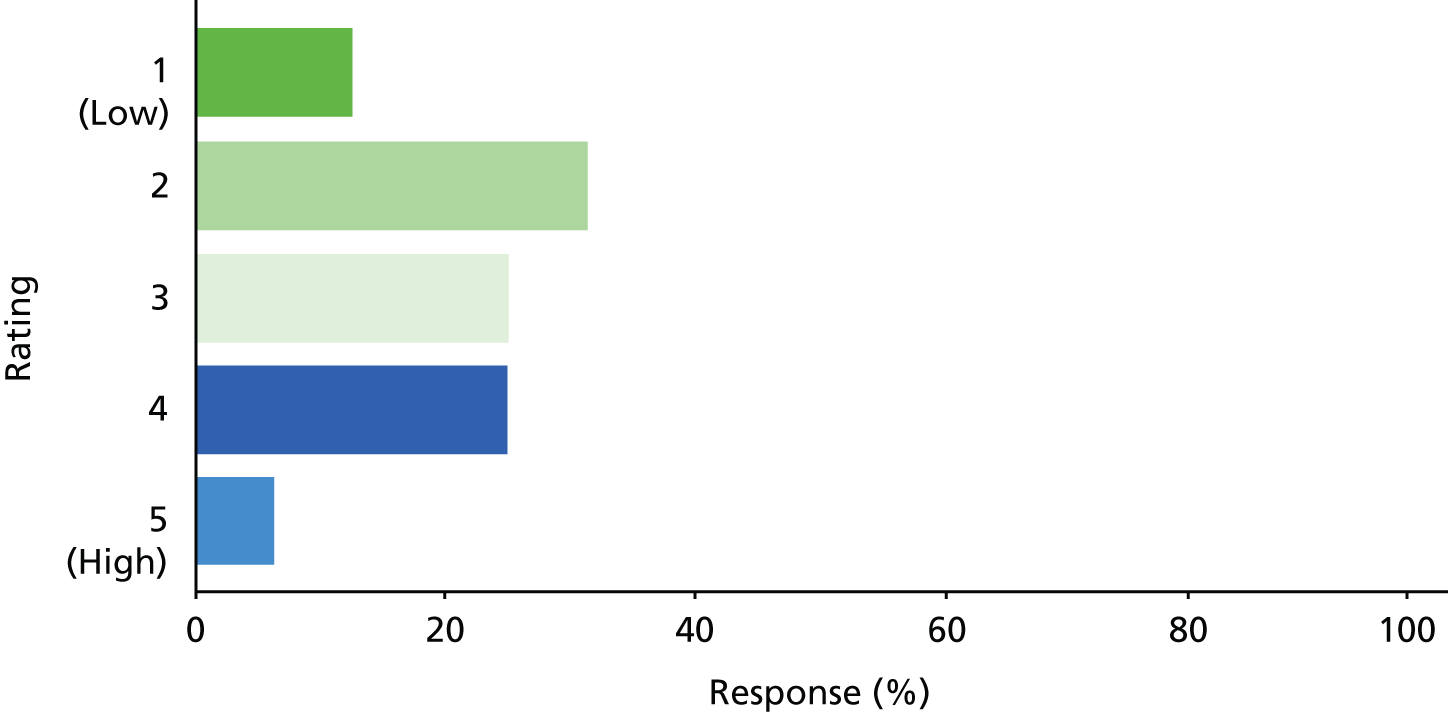
FIGURE 9.
Responses to question: overall, how satisfied where you with the HERG training session(s) you attended on qualitative research?
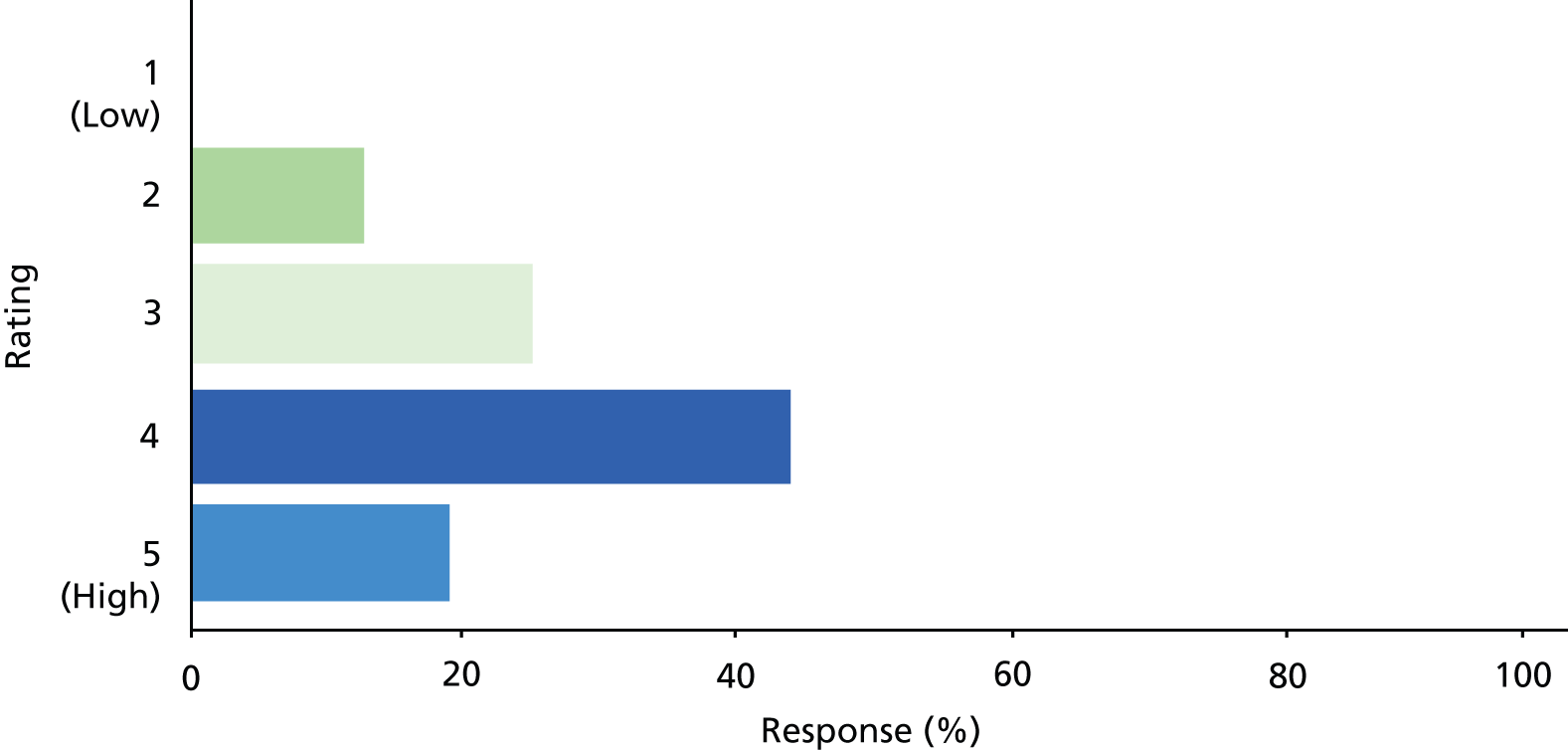
FIGURE 10.
Responses to question: do you think there are any barriers to the greater use of qualitative research findings at NCGC?
The ‘relevance’ of the content of the HERG training sessions (see Figure 7) was rated less positively by respondents (mean = 3.13) but there was a clear distinction in respondents comments between, in particular, the first and third sessions:
the session I attended seemed too academic without much practical application
there did not seem to be an understanding of what NCGC work involved
the first two sessions weren’t particularly helpful
the practical session was very useful in that I now have a good approach to analysing qualitative research
It was good but we may not have the resources to do it in such a thorough way. We have to be specific about what we are looking for and find the balance between the purely academic research side of it and the guideline development work.
The impact of the training on respondents own work at the NCGC (see Figure 8) was also rated as relatively low (mean = 2.81). Two respondents reported that they had applied lessons learnt to qualitative reviews they had subsequently undertaken.
Despite reservations about the relevance and impact of the training, overall satisfaction with the HERG training sessions was high (mean = 3.68) (see Figure 9).
In addition to the findings presented in Figures 6–9, 11 out of 15 of respondents reported that the training was at a suitable level for them personally and eight out of 16 felt that the training covered the aspects of qualitative research that they wanted to learn about. Regarding perceived gaps in the training, the most common suggestion related to how to apply the training in the specific context of guideline development. Eight out of 16 respondents saw qualitative research findings playing a bigger role at NCGC in the future, while the remaining eight respondents saw them as playing the same role. We asked survey respondents to elaborate on what the potential role of qualitative research at NCGC might be, and open comments included the following:
Qualitative research is essential if guidelines are to be responsive to patient needs. At present the role of qualitative research at the NCGC is too small
With new service delivery commissions heading our way, the ability to effectively describe patient experience of services will be really important to our work
I think it is valuable information but we as the NCGC need to find a more efficient way of doing this. We need to try and adapt it to the way we have to do our work, e.g. be very specific in the protocol
It depends if key issues raised during scoping are best addressed by qualitative research and how many of these there are. It looks as though we are going to get more service related guidance. This may mean more issues are answered by qualitative reviews. However, this relies on NCGC technical staff being aware that issues can be answered by this type of research
Finally, most striking of all the survey findings, and most pertinent to this objective, 14 out of 15 respondents felt that there were barriers to the greater use of qualitative research findings at the NCGC (see Figure 10).
All of the respondents to this question provided further feedback in their open comments. Inductive analysis of these comments brought five particular issues to the surface that served as barriers to the greater use of qualitative research findings at the NCGC. These were:
-
a lack of understanding of qualitative research methods:
‘what makes a good and bad qualitative study and how to effectively review these’ / ’quite intimidating to quantitatively oriented people like me (who represent 99% of the research fellows and health economists here) . . . often seem to be in a different language, and are rarely lucid’ / ’lack of understanding on the purpose of qualitative reviews and the areas they have strength compared to RCTs’ [randomised controlled trials]
-
negative perceptions of qualitative research more generally:
‘not seen by GDG as robust evidence’/’Qualitative methods vary and the results are subjective’/’Perhaps well developed and tested questionnaires which have been validated would be acceptable forms of evidence for guidelines’
-
a lack of time to consider qualitative research findings:
‘Time it takes to conduct a qualitative review (intervention reviews are often much quicker, especially if you have RCTs)’/’We work to tight deadline and it is very time consuming as the information is not always easy to find’/’Time constraints and how practical it is to pursue this route for a particular questions. Most guidelines will only have one question where there is the time and the where qualitative research is the most appropriate to answer the review question’/’Resource constraints are a barrier in the use of more qualitative research at NCGC; more resources would help’
-
a lack of ‘felt need’:
‘The type of questions we ask often not answered by qualitative research’/’I think it depends on the questions that we are asking for the guideline. Most of our questions are not about patients’ experiences and so we tend to not look at qualitative reviews or material very often’
-
insufficient training and guidance:
‘[in]ability to confidently use methods to identify, quality assure analyse data within time constraints’/’training on synthesis of qualitative findings keeping the context of guideline development in mind would be useful’/’have a guide on how to do a qualitative review and standardized template for the review’/’needs to be guidance on how qualitative issues can help answer questions. Currently, I think we automatically try and define issues as a quantitative clinical question. This may be the correct/best approach in most cases but we may go down this route as we have always used the quantitative method and we are not ‘in tune’ with qualitative research methods’/’Generally little training offered/available in this area so quality of reviews might not be as good. Output of qualitative reviews not very satisfactory. Often end up with generic common sense recommendations that aren’t specific to the condition’.
Regarding this last issue, the NICE guidelines manual in 2009 did not provide guidance on identifying qualitative evidence and although a revised version was imminent at the end of our fieldwork it was not anticipated that major changes would have been made. 11 Guidance on using patient experience to inform review questions and an appraisal checklist for reviewing qualitative studies of patient experience were provided.
The key points and conclusions arising from our findings in relation to objective 3 are presented in our discussion chapter (see Chapter 7).
Chapter 5 Objective 4: to inform the development of measurement tools on patients’ experiences
Our fourth objective was to contribute to the thinking on the development of PREMs, to help to make measurement more patient-driven. In the PROMs field, it is increasingly common for domains and specific items for questionnaire measures to be informed by qualitative research with patients. PREMs are at an earlier stage of development; while it would seem obvious to use in-depth qualitative understanding of patients’ views on what aspects of experience matter most to them before developing a new measure, in practice this does not always happen. Questions may reflect organisational priorities and assumptions about what aspects of experience it is most important to capture rather than genuine patient priorities. Of course, PROMs may also be driven by professional rather than patient concerns about the effectiveness of treatment; just because outcomes are ‘patient-reported’ does not automatically mean that they are ‘patient important’. An often cited example is the OMERACT75 outcome measure for RA, in which fatigue emerged as an important domain only after patient feedback on the original (professionally led) version. However, in PROMs, the focus remains, essentially, on how well individual patients are able to function with a specific condition, whereas in PREMs there is greater potential for collective organisational priorities to compete with, or even over-ride, patient priorities. In the PROMs field, both generic measures (such as SF-36 or EQ-5D) and condition- or treatment-specific measures such as the Oxford Hip and Knee Score may be used; in the PREMs field, there has tended to be more pressure for generic measures such as national outpatient or GP surveys, with the result that many issues which are very important in specific conditions are lost in the mix.
There has also been debate about what we mean by ‘experience’. One view is that experience is distinct from satisfaction because it is an objective measure of ‘what actually happened’ rather than subjective feelings about care (e.g. how long someone waited or whether or not they were given specific pieces of information). A competing view is that ‘experience’ is inseparable from subjective feelings. The Dr Foster76 Intelligent Board report on patient experience noted:
There is no NHS-wide definition of patient experience. However, there is much jargon, inconsistent use of language and a tendency to confuse concepts that are related but distinct. Our reference group has adopted the following definition: feedback from patients on ‘what actually happened’ in the course of receiving care or treatment, both the objective facts and their subjective views of it. The factual element is useful in comparing what people say they experienced against what an agreed care pathway or quality standard says should happen. The opinion element tells you how patients felt about their experience and helps to corroborate (or otherwise) other quality measures. Some measures that are not derived directly from patients are also used, on the basis that they relate to things known to matter to patients and their experience of care, such as single-sex wards.
Reproduced with permission from Dr Foster Intelligence76 p. 7
Towards the end of the study, emerging findings were presented and discussed as part of a meeting at Nuffield College, Oxford, with a group convened by a coapplicant. The group included key individuals from the PROM and PREM academic community and lay participants. This meeting included both lay and academic members of the steering group for the ‘new models for measuring patient experience’ project, which is jointly led by the Picker Institute and University of Oxford, and funded by the DH’s Policy Research Programme.
The principal investigator presented the main themes from the FGs (see objective 2 and Table 4), with particular attention to how we might understand and interpret differences in priorities and views of the candidate core components in relation to people’s experiences and ‘seldom heard’ status within mainstream health research. We drew attention to (1) the within-group differences, which often clearly related to people’s own experiences of illness or caring for someone who was ill; (2) the between-group differences in what is seen as ‘good’, ‘to be expected’ and ‘aspirational’ care; and (3) the explanations that group members gave for suggesting new components and prioritising the eight candidate core components of good care.
We also discussed how the interdependence between these components and other aspects of care (access, safety, efficiency) and how the relational aspects of care (empathy, communication) were often seen as integral to achieving functional aspects (seeking help, reporting symptoms fully, engaging with treatment).
We were keen to stress that our intention was not to stereotype patients’ priorities but rather to examine the FG and secondary analysis data to help us to understand why different individuals and populations may have particular viewpoints on aspects of care.
The 40-minute presentation, which included some direct quotes from the FGs, was followed by an audio-recorded discussion, lasting 45 minutes, which we draw on below. We particularly invited comment on whether or not and how our observations about the reach and limitations of the core components of good-quality care might inform the development, interpretation or comparisons of quantitative data on patients’ experiences.
Seminar discussion
The work was welcomed as essential in a field where there is a lot of speculation yet little evidence about whether or not (how and why) patients’ ideas about what constitutes good care may differ according to sociodemographic variables, health conditions or care setting.
The testing of the core components in the FGs underlined that, overall, there are few differences in what is seen as important about health care in these seldom heard groups (and certainly no suggestion of a completely different value system). This suggests that the reach of existing outcomes and experience measures may be robust across different groups of patients. The very first comment in the open discussion was that ‘this is of enormous interest to everyone’, especially in the light of the current concerns in NHS England about whether or not services are reaching the populations that they should.
While the study does not suggest new items that should be incorporated into the development of PROMs and PREMs, the results may be very helpful when comparing PREMs scores for different types of services and service populations. The study shows that there are different views on what is important, and should encourage researchers and managers to think carefully about how they analyse and interpret variations in patient-reported data about services.
Part of the discussion focused on the potential impact that the publication of the Francis Report may have had on the focus group discussions (some were conducted just before and some just after its publication). The enquiry and report brought attention to the lack of what most would agree is ‘basic care’, for example safety, cleanliness, food and hydration. The Patient Experience Quality Standard could appear very aspirational in the light of the Francis Report.
Individual and subpopulation experiences
In our presentation, we did not describe the variety of health problems and experiences of the people in the FGs. The discussion turned to how these prior experiences influenced people’s ideas of what good care might look like, and what they might expect. As one workshop participant pointed out, ‘if we want to do better studies of experiences we do need to delve into what is the basis for their comments’. While we are used to comparing experiences with standard sociodemographic data such as age, gender and social class, there are many other, more pertinent factors that shape people’s experiences of care and their ideas about what they need. What any particular patient sees as important can vary enormously from one illness to the next, or at different points during the illness; recognition of what is important in care is, thus, context specific. However, we should be careful not to assume that everyone’s experience is purely individual and ignore patterning by group. For example, people who are homeless share some problems as a group as well as factors that are influenced by the individual. As one patient participant pointed out during the discussion, people who are victims of torture face both different and similar issues; these need to be understood as features of a shared experience as well as reflections of individual agency. The similarities between people who share the same identity, such as drug users or learning disability, combine with other characteristics that are shared with other sectors of the population and which also affect their experiences of care. Our findings have highlighted how inter-relational the different components of good health care can be, with implications for the design and use of generic measurement methods.
One member of the HERG research team drew attention to the differences between groups (e.g. between the older adults and the recent migrants) in their health system literacy, as well as health literacy (both of which are related to education and social class). For example, the older adults were able to use their knowledge, often gained from many years experience of their own care, as well as that of their parents, to talk about organisation and appropriate care.
The discussion turned to the misunderstandings that patients sometimes have about why staff are doing things, for example checking and rechecking a patient’s name. If the health professional does not explain the reasons behind this part of their safety protocol, it could alarm the patients by suggesting that the system is chaotic, prompting low ratings on PREMs.
Expectations, the fresh eye and service redesign
There are pros and cons in involving people who can bring a fresh perspective to service evaluation and redesign. In the interviews and FGs, it is evident that people expect health care to be safe and to see a health professional who is well trained and aware of the best treatments. The confidentiality of the consultation is taken for granted by those who have never had reason to expect it would be otherwise (this had become clear in the FG with migrant workers, who described non-confidential behaviours in another country). It is sometimes only when people have amounted considerable experience of health care that they start to realise the variation in skills and service provision and the lack of a clear evidence base for much treatment.
Members of the public who bring a fresh eye to services can challenge assumptions and bring new insights. Drawing on the FG with young men, who had had relatively little experience of hospital care, could contribute a perspective on service redesign that is relatively invisible to those who have been working in it, or using it, for many years.
One workshop participant described a qualitative study that she had been involved with in four hospitals where different staff members were asked to describe what good care looked like to them; this had found that there was little agreement across teams and roles (e.g. porters, ward clerks or medical staff).
One lay member of the group suggested that future research might ask ‘magic wand’ questions, for example ‘if you were going to design an A&E department, how would you do it?’.
Training health professionals
A workshop participant raised another idea about how the findings from the FG study could be used to improve health care: those involved in training clinical teams often struggle to challenge stereotypes and assumptions about the needs of patients from different population subgroups, and the material collected through the FGs could be very useful for training.
Implications for further research
It was suggested that we could compare the study findings against existing PREMs to check our impression that these findings with seldom heard groups do not challenge the current repertoire.
Some of the group felt that our discussion had underlined the ‘utter uselessness’ of trying to boil it all down to a single question (as in the Friends and Family Test).
We agreed that we need to know more about what is behind the ‘not applicable’ response on questionnaire surveys; ‘Exploring the Not Applicable’ seemed a potential title for a paper.
Finally, it was suggested that a different and potentially insightful set of interviews about what constitutes appropriate/good health care could be gained from interviewing health-care staff who were trained and practised under the ‘old system’; they would have, by now, had time to reflect on what went on in the past and have likely had a chance to make comparisons with current practice in primary care and hospitals, through either personal illness, or caring for children or partners, or acting as carers. Their insights are likely to throw up some different perspectives from those who have never been on the inside of health-care provision. Similarly, the views of health-care staff who have worked in different settings, for example locums, could add further insight and perspective.
Chapter 6 Objective 5: development of resources for secondary analysis
We ran a workshop on qualitative secondary analysis with methodologists, archivists and qualitative researchers who had collected data that others had used for secondary analysis, as well as those who had published secondary analyses themselves.
Proposed outputs from this workshop were:
-
the development of best practice recommendations for the archiving and storage of qualitative interview data as well as preparations for and principles of sharing it with secondary analysts
-
the identification of training needs for researchers wanting to conduct secondary analysis, informing the design of a 1-day course on secondary qualitative analysis.
Background
Secondary analysis of qualitative data is a highly efficient use of existing data (many of which will have been collected with public money). The reuse of existing data sources allow research teams to concentrate their resources on conducting a rigorous analysis and identifying where they can make a contribution to the literature, clinical practice and service delivery. Despite these obvious advantages and recent Research Council encouragement of qualitative secondary analysis as a research methodology, there has been some resistance in the qualitative health research community to contributing and sharing data for secondary analysis. 52,77 While the disciplines of sociology and history, and, more specifically, oral historians, have long recognised the value of archiving their data sets for future use to enable longitudinal comparisons, the archiving of qualitative data in the field of health services research is currently very rare. Obvious obstacles to storing data long term and in formats that would enable their reuse for different analytic purposes from the ones for which they were originally collected are bound up with medical research governance and ethical regulations; these frequently demand the destruction of personal data on completion of a research project and explicit reassurance that data will not be shared as part of the process of consenting participants. Rapidly changing policy contexts and service landscapes in the area of health-care research may also have led to the belief that aged data are a less relevant and useful source of information than is the case in other disciplines.
The HERG collections, held at the University of Oxford, are an exception: they have been licensed for use by several well-established academic colleagues. Studies using secondary analysis of these data include a Service Delivery and Organisation (SDO)-funded project called ‘Information for Choice’, studies of gender and health at the MRC Social and Public Health Research Unit in Glasgow, an ESRC-funded project on comparative keyword analysis in health talk, an ESRC-funded analysis of chronic health issues in young people, studies within a NIHR Programme Grant for Applied Research and a comparison of local and national data on end-of-life care. 30,78–81 These secondary analyses have led to a number of peer-reviewed publications in leading journals. 35,82–88
By bringing together an expert panel of those scholars who have successfully conducted qualitative secondary analysis on the HERG interview collections and other UK data archives, such as the online Economic and Social Data Service (ESDS) Qualidata Archive and the Timescapes Project at the University of Leeds, we aimed to identify practices and principles that would help to promote the sharing and reuse of qualitative data in our field by identifying training needs and providing guidance for academic colleagues who may consider this method for future projects.
The qualitative secondary analysis workshop
A 1-day workshop with key academics from the UK was held at the Department of Primary Care Health Sciences at the University of Oxford in November 2012. The workshop was attended by 17 participants and included presentations by seven scholars with experience of conducting qualitative secondary analysis (see Appendix 13).
Workshop attendees included several HERG researchers who had been involved as primary researchers in the collection and analysis of data sets that had been used for secondary analysis by some of the presenters. This enabled a helpful exchange of perspectives between primary and secondary researchers regarding similarities and differences of primary and secondary analysis processes as well as an identification of specific concerns that primary researchers may have with regard to sharing ‘their’ data.
The debate for and against the reuse of qualitative interview data
Qualitative research is recognised as an important method for including patients’ voices and experiences in health services research and policy-making, yet the considerable potential to analyse existing qualitative data to inform health policy and practice has been little realised to date. This failure may partly be explained by a lack of awareness among health policy-makers of the increasing wealth of qualitative data available and around 15 years of internal debates among qualitative researchers on the strengths, limitations and validity of the reuse of qualitative data.
Mason has summarised the polarisation of the debate into ‘on the one hand a position that says that qualitative data are special and cannot be re-used by others on epistemological or ethical grounds, and on the other a pragmatic or instrumental position that says that data should be open for use by others, not least because they are expensive to produce’. 89 The former position has been well articulated by Parry and colleagues,54,90 who raise issues around ownership and copyright, the coconstruction of data between respondent and researcher, confidentiality, preserving anonymity, and the problematic nature of gaining respondent consent for broader use of the data (particularly as all future potential uses cannot be exhaustively listed). Bishop, by contrast, has argued that there are good suggestive, but not prescriptive, guidelines on how to deal with several of the legal and ethical issues raised (e.g. copyright, ownership, acquiring appropriate consent and protecting confidentiality). 91
An issue that has generated much heat in the debate has been the extent to which the ‘context’, the insights that a researcher has through ‘being there’, can be adequately summarised and captured for use by analysts other than the primary researcher. An interviewer may absorb aspects of the respondent’s life circumstances and biography and become aware of limitations on their willingness and ability to discuss particular issues. Such details may be captured in field notes, but these are often highly individual and difficult for others to make sense of, even if they are shared. Fielding emphasises the need to include as much contextual information as possible when archiving qualitative data, yet there are tensions between this need for detail and requirements to preserve anonymity. 92 Mason argues that ‘the idea that only those involved in initial data generation can understand the context enough to interpret the data is not only anti-historical but it puts enormous epistemological weight onto the notion of “successful reflexivity” ’89 but Parry and colleagues suggest that the ‘recovery of context can only ever be partial’. 54
Attempting to move the debate forwards, Mason has urged qualitative social scientists to be ‘leaders rather than laggards’ in thinking through the challenges of using and ‘re-using’ qualitative data. 89 Others question the clarity of the distinction between ‘reusing’ and ‘using’ qualitative data, emphasising instead that all data are constituted and reconstituted within the research process; that qualitative data are ‘re-contextualised and co-constructed whether reading transcripts or doing an interview in real time’;55 and continuities between ‘primary’ or ‘secondary’ data and the view that ‘secondary analysis’ can be conceptualised as ‘primary analysis of a different order of data’. 56 Irwin and Winterton suggest that
. . . a more productively drawn distinction is between data and evidence . . . both primary and secondary analysts will construct data as evidence in the service of some empirically grounded set of arguments and knowledge claims . . . Presence at the point of data generation is not a final arbiter [of social scientific adequacy].
Irwin and Winterton93 p. 8
Some forms of data are arguably more amenable to secondary analysis than others; for example, video or audio recordings of naturally occurring events differ from an ethnographer’s personal field diaries. Interviews addressing a very focused research question may have less scope for secondary analysis than those eliciting an open narrative. Fitness for purpose is, thus, an important consideration for archivists and ‘reusers’ of qualitative data, and with due consideration of the issues addressed by Bishop, among others, problems are likely to be surmountable in all but a minority of cases. While not all qualitative studies will be equally rich resources for secondary analysis, the same set of video recordings of consultations could, for example, inform quite distinct analyses of topics such as the verbal and non-verbal positioning and performances of identity in clinical encounters. Collections from different eras might illuminate changed orientations to health care or initiatives over time, or in different cultures.
Summary of main discussion points
What makes a suitable data set for secondary analysis?
This issue concerned the quality of the original interview material. Do any qualitative interviews constitute appropriate material? What is the minimal data set needed for contextual information, in terms of study and sample (purpose, participant demographics, settings, recruitment methods, geography) and interviewer details, to maximise value to future users?
Wherever possible, the secondary analyst should assess the original sample and any limitations with regard to the proposed study. In some cases, there may be a comparison group available (e.g. if studying gender and health).
Sampling relevant material
Depending on the nature of the research question and the time frame, it may not be appropriate or feasible to include an original data set in its entirety in the secondary analysis process. Where possible, a conversation with the primary researcher(s) could guide which interviews are most worth including, or focusing on at an early stage.
(How) does secondary qualitative analysis differ from ‘primary’ analysis?
There was general agreement that it is difficult to pin down ‘absolute’ differences between the processes of primary and secondary analysis in terms of coding, iterative development of categories, and so on.
What gets into the ‘methods’ sections of published papers?
A distinction should be made between data and evidence. Secondary analysis requires researchers to describe their own approach to the material and to acknowledge the primary purpose for which the data were collected.
Who owns the data?
When the research has been funded by a research grant this is usually quite clear: the funder, or the researcher’s employer, own the intellectual property in the research. Researchers may feel that the interviews should belong to the research participants who took part in an interview. In HERG studies, this is recognised through inviting interview participants to sign a copyright form and giving them the opportunity to edit sections of the interview. Interview participants may decide to withdraw from the research at a later point, or restrict the purposes for which the interview might be used. Data that are intended for sharing may require some special considerations, for example for consent and copyright.
The researchers who collect the data are also likely to feel some ownership of the data and may hope to be involved in writing papers based on the data. We agreed that the interests of the original researcher should be considered to support career development and not treat researchers (who may be relatively junior, or on short-term contracts) as mere ‘data collectors’.
The primary researcher
Researcher interviewers are coparticipants in the interview conversation. Sometimes, researchers may use self-disclosure as part of the interview process, and, therefore, their identity may need to be protected as part of the anonymisation process, or they might need to be offered the chance to edit their interview contributions before archiving. There is a potential tension between appropriate acknowledgement of the researcher’s role, providing relevant information about characteristics that are important to the context of the study data, and allowing them some influence over the data that are shared.
Some reservations were voiced about how the reuse of qualitative data sets by secondary analysts might impede on a primary researcher’s ability to publish on the same material in future. This concern linked to the issue of when was the best time to archive material – should researchers consider archiving data for sharing with colleagues even if there was a chance that they might want to return to the material themselves in their future work? One possible solution that was proposed was that, wherever possible, primary researchers should be invited to participate in secondary analyses of material that they had coproduced, and, especially, in the write-up of research outputs based on such material.
Best practice recommendations for sharing qualitative data in health services research
Workshop participants identified the UK data archive as a valuable resource for general recommendations and legal requirement on sharing social science data. Within this archive, the ESDS Qualidata online archive presents some helpful examples that can act as guides for best practice.
Aspects of data depositing for sharing and access for reuse covered on the UK data archive website include:
-
research data lifecycle
-
planning for sharing
-
consent and ethics
-
copyright
-
documenting your data
-
formatting your data
-
storing your data
-
strategies for centre.
Gaining participant consent for the future use of qualitative interview data
One frequent obstacle to the reuse of qualitative interview data is that participant consent places restrictions on who is allowed to access transcripts of material, even where they have been fully anonymised. Recontacting research participants to gain consent to share their data with other researchers at a later date can be very time-consuming and difficult, and may also be undesirable for ethical reasons. The best possible solution is, therefore, presented by a multilevel consent form, which specifies a number of options for participants to consent to possible future use of their material at the time of taking consent for the original study.
To facilitate fully informed consent, best practice might involve offering the participant the option of reviewing a copy of their interview (either as transcript or recording) so that they can indicate, edit or delete sections of the material that they do not want to be shared for future research purposes. In the experience of the HERG studies, around 10% of participants take this opportunity to remove some part of their interview at this stage.
Training needs of researchers planning to conduct secondary analysis
We agreed that while junior researchers might gain from being given examples of more experienced researchers’ interviews for analysis practice, learning to collect one’s own data is important for research skills development. Researchers needed to be aware of how the visceral experience of ‘having been there’ in the interview contributes to interpretation of the data. In addition, direct experience of conducting interviews was likely to sharpen awareness of the interview transcript as a recontextualisation of the original conversation and the contents of the interview as a coproduction between interviewer and research participant.
These insights have now been formalised into a 1-day training course to share resources and skills for secondary analysis of qualitative health research, as part of the HERG qualitative research course programme for 2013–14. An outline of the training day programme is included (see Appendix 14).
Why should we conduct qualitative secondary analysis for health services research and policy?
-
It allows focus on a targeted analysis to inform health policy.
-
It is desirable to ‘stand on shoulders’ of existing research (which might not have been published).
-
It is efficient, especially if access and ethics for primary research raise complex issues.
-
It avoids burdening over-researched groups.
-
It may provide access to the perspectives of elusive groups or communities considered hard to engage.
-
It can inform pilot studies; for example:
-
identifying item pools for questionnaire development
-
defining the parameters of a diversity sample.
-
-
It can inform a richer, comparative analysis:
-
between health conditions
-
across time
-
between cultures.
-
Summary
The HERG archive and other UK-based archives and research collections offer a rich and highly cost-effective resource for health policy. Increasingly, as with studies which contribute to the HERG data archive, the potential for secondary analysis needs to be carefully considered from the outset, to ensure that respondents can give appropriate consent for reuse of the data.
The perspectives of researchers whose interviews may be used for secondary analysis have received little consideration in the literature. 30 Researchers in HERG know that the data they collect will be available, under licence, to other researchers. The original researcher has an opportunity to publish key findings first, is often involved as a consultant to a secondary analysis project and may contribute to the resulting papers. While the secondary analysis process can feel somewhat exposing, those in HERG whose data have been used by other researchers emphasise the benefits of approaching the interviews through a new analytical lens, the helpful challenge of a perspective that is more distant from the context of the original data collection and the opportunity to maximise the utility of data (especially if reuse may lead to improvements in services for the patient group).
In conclusion, it is important for policy to be evidence based and that patients’ experiences form a vital part of the evidence about health and social care services. Collecting new qualitative data on people’s experiences is not always achievable within financial or time constraints, yet their exclusion can silence or marginalise the patient voice. We argue for a pragmatic approach that develops appropriate archiving practices and analytic skills among qualitative researchers so that rigorously collected qualitative data sets can be used to establish patients’ perspectives at the centre of health policy.
The workshop has also informed a paper on qualitative secondary analysis as a resource for health policy research. 30
Chapter 7 Discussion
This study was commissioned via a call for research using ‘existing data sources to answer important research questions’. The rationale, stated in the commissioning brief, indicated that much publicly funded data collection is underused. In addition, ‘existing data can often be used more quickly and economically to address a research question than primary research’. 94 The brief also recognised that ‘existing data may have a number of disadvantages too – data quality and completeness can be poor, and researchers have to work within the restrictions of data definitions, coding structures and recording conventions’ which were not designed for the needs of the current research. We will return to these points later.
The project was led by a team including academic researchers and clinicians at NICE and the NCGC and was designed to explore if, and how, a secondary analysis of qualitative interviews might contribute to NICE products, especially new QSs. We reasoned at the outset that if the QSs were to be produced at the anticipated rate, to a process that was still in development, then customised analyses of pre-existing collections of patients’ narratives had the potential either to contribute new insights into patients’ experiences of the pathway or condition or to reassure the development teams that the issues important to patients had been picked up through other means (e.g. existing guidelines and literature reviews). The secondary analysis reports were written and adapted to meet the team’s understanding of NICE requirements for QSs (the process for which was still emerging during the study period). The reports were presented in an unconventional manner for qualitative studies: briefly, they were written without a literature review or methods section and only the MI report included any data extracts. These decisions were influenced by the amount of time available for the secondary analyses and by our combined expectations about how lengthy a report the groups would have time to read. We discuss the implications of the mode of presentation below.
Team members observed NICE product development meetings and conducted interviews to identify the potential and barriers to using secondary analyses from the HERG archive in the development of NICE products.
Drawing on the secondary analyses and the literature, the academic team examined the reach and limitations of the core components of good care through analysis of two further interview collections (infertility and autism). Our aim here was to consider the reasons why ideas about what good care looks like may vary between groups. Our analysis shows that it was the level of intensity or importance attached to these components that differed. Hence, while the core components are broadly applicable across the interview collections, some features were regarded as particularly important due to the nature of the health issue, for example effective communication with people with learning disabilities, or empathy with people going through infertility treatment.
In a further test of the reach of these eight core components, we conducted seven FGs, six of which comprised respondents from ‘seldom heard’ groups. We found that the issues which are important to people who we interviewed in the HERG collections were also relevant to the FG participants [which involved people with learning disabilities, migrant workers with limited English, young men, Irish Travellers, illegal-drug users (some of whom were also homeless) and people with long-term conditions (via the online focus group), all of who are known to be under-represented in HERG studies]. However, patients’ expectations about health care, and, therefore, what was seen as particularly good, or even unattainably good, varied between individuals and groups. This related, in part, to how they felt that they were perceived by health professionals, and included how seriously their health problems seemed to be taken and past experiences of feeling negatively stereotyped or having their ‘moral identity’ questioned by staff. Therefore, the experiences and expectations of older, middle-class adults were very different from those of focus group participants who were homeless, illegal-drug users or Irish Travellers.
As would be expected, we also noted that some perspectives and experiences were discussed more in the individual interviews than in the FGs. For example, in the individual interviews people talked about the impact of their illness on their friends and families, but this was little discussed in the FGs. We think that this is unlikely to constitute a real point of difference between the priorities of the respondents, and is more likely to be an artefact of the different methods and dynamics of group as opposed to individual interviews as well as the fact that the FGs were not centred on people’s accounts of their own illness experiences.
Strengths of the project
While it is quicker than conducting a primary study from scratch, secondary analysis of qualitative data is, nevertheless, generally a time-consuming activity. In this project, we were able to draw on alternative methods of analysis to fit within time scales. This was facilitated by the availability of experienced researchers in qualitative analysis. Different approaches were used in analysing the six data sets and it was apparent that where the researcher doing the secondary analysis had collected the original data there was considerable benefit. This underlines the value of the involvement of the original researcher in secondary analysis projects.
The project also benefited from an engaged group of co-applicants, representing both HERG and NICE, which incorporated different backgrounds, viewpoints and perspectives. The interviews for objective 3 were conducted by another, independent researcher from the team, based at a different university; the team members who were interviewed appeared to speak openly about their experiences of working in collaboration, suggesting that this independence was an important feature of the project. The team met regularly and, throughout the course of the project, there were critically engaged discussions which fed into the research process.
A core strength of the project was the contribution of the patient and carer members, recruited through NICE. As well as attending the steering group meetings and advising us throughout the project, they provided invaluable contacts and helped to set up the FGs with young men and Irish Travellers.
The objective 4 workshop benefited from the connection (through co-applicant RF) with an existing group of key figures working in PROMs and PREMs. The team were also fortunate in being able to attract several prominent figures to take part in the objective 5 secondary analysis workshop. The contributions from those who had direct experience of using, archiving and providing different types of secondary source materials contributed to the success of the workshop.
Problems encountered and limitations
A problem that we encountered in the early months of the project was identifying the most appropriate QS topics. There was not always a close fit between the QS topic and the content of the interviews that were available for secondary analysis. Even when a topic was apparently covered, some of the interview experiences might be several years old and seem (or be) less relevant to the narrow focus of the NICE product under development. This issue of whether or not the available data are fit for the new research purpose is an acknowledged problem of any type of secondary analysis (quantitative or qualitative).
Further research would need to be done to test whether or not these core components (though derived from hundreds of personal experiences of very different health issues) hold for different topics, such as experiences of elective surgery.
The deadlines for the product development meetings also caused some difficulties for the project time lines, but the fact that we were able to call on a larger pool of researchers meant that we were able to prepare the reports simultaneously rather than sequentially, and also allowed us draw directly on the knowledge of the primary researchers.
One aspect of the proposal was not achieved as anticipated: the team did not find a suitable opportunity for the proposed secondment to assist knowledge transfer. We had intended that a senior researcher from the HERG team would be seconded to the NCGC on a part-time basis. Although this was not possible, we were still able to draw on several data sources to inform our findings in relation to the knowledge transfer process: training sessions and observational data from the research team who attended a number of TEGs and GDGs, as well as interviews with the research team and also, more broadly, with individuals from within NICE and the NCGC.
There are three main reasons why the secondment did not happen as envisaged: staffing, the lack of clarity about the secondment role, and timing for dissemination of the findings. We briefly discuss these in the following three sections.
Staffing
We appointed a new senior researcher to this post but for personal reasons their situation changed and they were unable to take up the post. It took us some time to find a replacement, who joined the project for the last 9 months rather than for the entire 18 months as originally envisaged. Staffing has thus been rather more complex than we intended, but continuity through the project has been provided by Kristina Bennert (originally appointed for only 12 months, part-time, to conduct the secondary analysis but whose remit was later extended to the whole project), Angela Martin (project co-ordinator throughout) and Sue Ziebland, the principal investigator (who stepped into the senior research role for the first year, ran the training sessions and has continued to be closely involved in all stages including running FGs, contributing to the analysis and writing the papers and reports).
Lack of clarity about what a secondment might involve
We were not sure what would be the most useful role for a part-time embedded researcher at the NCGC. We therefore left some flexibility in the project staff planning so that if a suitable focus emerged during the course of the project we would be able to field staff accordingly. The subject of a secondment was raised regularly but we did not identify precisely what role might be performed. The technical teams within the NCGC were working on evidence reviews of qualitative evidence intermittently as dictated by individual guideline timelines and it was not feasible to plan these reviews to coincide with a secondment.
Timing for the dissemination of the findings
During the course of the project, we held regular meetings with the members of HERG and the NICE/NCGC colleagues, including three patient and carer members, at which emerging findings were discussed. Part of the proposed knowledge exchange work was for the researcher to present and discuss emerging results with other teams in NICE. As the HERG/King’s College London research team became more familiar with NICE culture and processes, we realised that there would likely be a more receptive audience for the results when the final results were complete and had been peer reviewed. The research team remain willing and able to communicate the results in whichever formats and forums (written, seminar presentations and workshops) are preferred.
Finally, and importantly for a project such as this, knowledge transfer should be a two-way process. NICE processes are well documented, yet total transparency of such a complex process is not possible and at least some organisational knowledge inevitably remains tacit, for example the relative independence of the technical teams/GDGs in deciding on evidence to inform the guidelines. This was not helped by the staffing configuration which meant that knowledge that might have been gained incrementally by a single researcher, especially if that researcher had been able to undertake the planned secondment, was instead distributed among several.
The nature and length of the guideline process means that key decisions about what is included are often made remote from GDG meetings. As a 18-month study, ours was too short to track alongside the entire process. We would recommend that any future work in this area should indentify in advance which NICE products to study and plan the start date and project timing accordingly. Taking a more ethnographic approach, with the researcher embedded within the NICE teams, would help to avoid some of the gaps in knowledge transfer that were evident in this study. There were benefits in working with several products at different stages over the course of the study (e.g. we have realised through trial and error that intervention is feasible only in the initial stages, i.e. during pre-scoping of the guideline) but the approach has highlighted some of the difficulties for knowledge transfer and underlines, hardly uniquely, the necessity for knowledge transfer to work in both directions.
Implications of findings
In this report, our findings are considered in relation to each of our research objectives; where relevant, we have updated the context to take account of recent health policy developments. In summary, we identified eight core components of ‘good care’ from our secondary analysis of people’s experiences of six different health conditions. The components were staff involving the patient in decisions; having a friendly and caring attitude; understanding how the patient’s life is affected; being able to see the same health professional; being guided through difficult conversations; staff taking the time to answer questions and explain; pointing the patient to further support; and efficiently sharing health information across services. We further tested the reach of these components in a series of FGs with people who are often considered hard to engage in research – people with learning disabilities, migrant workers ,illegal-drug users (some of whom were also homeless), Irish Travellers, young men and older people – and also in an online group comprising people with long-term conditions. We found that they, too, valued the same things but that their expectations about their health care varied considerably, in line with their experiences and health-care relationships.
We worked with NICE to see if our reports about what is valued by people with different health conditions might inform their guidelines and ‘quality standards’. We observed meetings and interviewed staff and found that our asthma report had contributed to a ‘quality statement’ on inhaler training. The remaining reports appear not to have added new perspectives. Reports based on existing collections of interviews may contribute to NICE products, especially when there is little published evidence. We conclude that looking at existing interview collections may efficiently fill gaps in understanding, but uncertainty remains about the status of (unpublished) analysis that is conducted specifically to inform a guideline or QS. We plan to share the findings of the report with the guidance-producing teams for NICE’s public health and social care programmes and will follow up as appropriate. We have already made NICE’s QS team aware of the findings.
We presented the findings on the ‘reach’ of the core components to a group of PROMs and PREMs experts who underlined the value of the findings for their field. The study shows that while the core components have reach across many different conditions and types of respondents, including those whose views are rarely captured in research, expectations of care do differ substantially, and relate to previous experience. Researchers and managers should be encouraged to think carefully about how they analyse, compare and interpret variations in patient-reported data about services.
There is a danger, in considering the implications of this study, of conflating the potential contributions and reception of published, peer-reviewed qualitative research studies with those of secondary unpublished qualitative analyses. It is not uncommon (and not regarded as ‘salami publishing’) for unstructured qualitative research to be the basis for several different social science and clinical papers focused on different analytic stories. Some analysts may even revisit their data several times with a different analytic lens for different audiences. These papers sometimes have the potential to inform NICE products and are often incorporated if their relevance is reasonably apparent. The HERG data have been analysed and written up for over 100 research publications, some of which are based on a secondary analysis. Such articles would be readily incorporated into technical team reviews whenever the subject matter coincided; however, it would only be happenstance if a peer-reviewed article on a topic of interest to a specific NICE product had made its way into the literature in time to be used. So, while the very same data could contribute through a conventional route, an unpublished, tailor-made secondary analysis has a problematic and ambivalent status.
Into this mix we also add the complication that the HERG data, on which this particular secondary analysis was based, as well as being written up for publication in peer-reviewed journals, was also analysed and published as topic summaries on the research-based website www.healthtalkonline.org. The HERG interview studies of patients experiences are also used to produce around 25 analyses which are peer reviewed (by another qualitative researcher, an appropriate specialist member of an advisory panel and a patient or lay representative) before being published, using a documented process, on the website www.healthtalkonline.org. The website is the only public source of patient experience evidence cited in the NHS Evidence Process and Methods and is already recommended for use by NICE technical staff as part of their review of evidence when they develop a new CG. This, too, may have added to some of the ambiguity about ‘publication status’ of the data sets we were using.
More broadly, this study has raised questions about the status of critical appraisal of qualitative studies. While it is clear that the thinking on an ‘evidence hierarchy’ has shifted considerably in the last decade, it seems that some of the underlying assumptions of quantitative meta-analysis (e.g. that quality checklists must be used to make sure that one does not skew the meta-analysis by including data from poorly conducted trials) have migrated to qualitative reviews.
The team does not all agree on this, but some of us (principal investigator included) are unconvinced that quality appraising qualitative data for a thematic review is a worthwhile activity, as the themes in the papers either will add to one’s emerging understanding of the topic (which is never divided by the number of studies that reached this conclusion) or will not. If an article does not add this, it may simply be because of the order in which the papers were read, and may have little to do with any aspect of the ‘quality’ of the article that could be discerned by checklist. Most checklists, however, also help to focus the attention of the reader on issues such as the context in which the study took place and the credibility of the finding. These may be relevant when review is conducted by less experienced reviewers. Guidelines and QSs are also often addressing very focused areas, and note general themes, and attention to such aspects of a paper may be relevant when a guideline has to make specific recommendations to a national audience.
We now turn, first, to a discussion of the implications of the study for future knowledge transfer between HERG and NICE, and then to the focus of the commissioning brief and implications for the use of secondary data sources to inform health policy.
Implications for future Health Experiences Research Group and NICE knowledge transfer
In terms of future collaboration, four key issues have emerged from our research. Central to all of them is the issue of how to design and present more persuasive ways of communicating the credibility of findings of targeted, secondary qualitative analyses as a ‘body of evidence’ which fits into existing NICE processes. The four issues are presented below in the form of a series of questions and proposed solutions.
What can be done to establish the appropriate use of the (1) original qualitative data and (2) secondary analysis of the data to inform NICE products?
NICE processes require a quality assessment of each piece of evidence used, and transparency about the evidence and the discussions that inform guideline recommendations and QS statements. A clear concern among NICE/NCC technical staff related to the credibility of the data and/or its analysis without having access to written reports that they could appraise. This was an issue that the project team discussed on several occasions. This is due, in part, to the confusion, mentioned above, about the relationship between the various HERG products, but also to different views about what counts as ‘evidence’.
Table 11 distinguishes between these different HERG products: peer-reviewed articles, peer-reviewed topic summaries on the healthtalkonline website and targeted secondary analyses. Each has potential, in combination with literature reviews and other sources of evidence, to contribute perspectives on patients’ experiences. Two of the three HERG products described are already in a peer-reviewed format that can contribute to CGs/QSs: the challenge is to find a way to utilise the flexibility of a targeted secondary analysis with an approved and transparent process that allows the technical team to make a quality assessment of the evidence.
| HERG products | Peer reviewed? | Focused on patients’ experience of the clinical issue in question? |
|---|---|---|
| Topic summaries on www.healthtalkonline.org | Yes | Sometimes (and could be) |
| Qualitative research papers | Yes | Sometimes |
| Secondary analyses prepared as a report for NICE | No (but could be) | Yes |
How else might qualitative secondary analyses be presented to the clinical guideline and quality standard groups?
A secondary analysis of interviews on patients’ experiences is most likely to add value when there is little published qualitative research in a topic area, or when the evidence from the published qualitative research appears thin or even contradictory. In such circumstances, a targeted secondary analysis, conducted according to the standards required for publication in peer-reviewed journal articles, could add missing perspectives and clarify or triangulate findings that are already evident in the literature. The difficulty of using this is knowing when there is little published evidence available, and this might be identifiable during the scoping process.
With regard to HERG data, another option could be to identify an advocate for the data throughout the process to support how it is introduced to GDGs. NICE already use expert advisors on areas where a guideline does not have much evidence; it would not be inconsistent with current processes to co-opt an expert to present the HERG data (in which case the expert would come to one meeting but not be part of the GDG).
Potentially, this could be a role for lay members on the GDG and on the TEGs in representing the type of data that HERG produces, giving them a broader evidence base to draw upon which goes beyond their own individual experiences. This does raise the question of whether the nature and contribution of lay member participation on the groups is similar to, or different from, data from the secondary analyses and synthesis of the qualitative literature.
What more can be done to facilitate the knowledge transfer process between the Health Experiences Research Group and NICE?
Health Experiences Research Group data are routinely analysed and peer reviewed for dissemination on the healthtalkonline website. The asthma report was written by the primary researcher at a point when the data were still very familiar (and was the only report that can be seen as having directly contributed to a quality statement). Writing one extra report at this stage is a relatively efficient use of a primary researcher’s time and suggests to us that when the HERG researcher is preparing or updating the topic summaries (see Table 11) they might, as part of their analysis, write a brief report on the aspects of care that are particular and important to patients with this condition. In collaboration with NICE, the interview collections could be mapped to the guidelines and QS programme. This could be a promising way to maximise the potential of the collections to inform CG/QS development. HERG interview collections with nationwide samples of around 40 participants typically take around 15 months to recruit, conduct and analyse. Since April 2013, NICE has had a new responsibility, to develop guidance and QSs for social care in England; this may present an opportunity to apply the lessons learnt in this study to broaden the potential influence of qualitative research (whether from primary or secondary analyses).
What is the most appropriate point in the clinical guideline/quality standard development process to consider data from secondary analysis of qualitative data if concerns about its status were to be resolved? Where can it add most value?
Patient-experience evidence, whether from literature synthesis or secondary analysis, is most likely to be useful at the earliest stages in guideline development when the focus of the guideline may still be influenced by the issues that are important to patients and the public. There are two potential roles for this evidence (1) to highlight an area for inclusion by informing what is included in the scope and (2) providing evidence for the guideline itself.
Future training
In terms of any future training provision to NCGC staff, it was very clear from the survey responses that those attending found the third session by far the most useful (‘where we were shown how to pool themes’; ‘outlined how a synthesis of qualitative research may be done’; ‘application of qualitative methods to our work in guideline development’), whereas the first session was seen as the least useful part of the training (‘too basic’; ‘limited relevance . . . for guidelines work’; ‘very general’; ‘not so useful’; ‘far too long’).
In keeping with these findings, participants made the following recommendations for the design and content of future qualitative research courses for NCGC staff:
-
less background information (about the context, methods and design of qualitative studies) and more about how to do a review
-
how to identify sources of qualitative data, gather and interpret and provide some statement of quality
-
expand on the last session and develop ideas on synthesis and presentation of evidence from qualitative studies
-
real examples relevant to our work
-
start with an issue raised in the scope of one of our guidelines, develop this into the kind of questions that can be asked (both qualitative and quantitative), focus on the methods used to answer the qualitative questions, and demonstrate how this might feed into a recommendation
-
extend the practical session into a full day, with more time to work in facilitated groups to see how it is actually done.
Implications for the use of secondary analysis of qualitative data
Finally, we return to the observations in the commissioning brief about the potential for using secondary data sources for new research. There can be little doubt that the use of existing qualitative interviews allows the researcher to engage with a targeted analysis much sooner than would have been feasible if primary research was conducted. Even a relatively low-risk, qualitative interview study can take several months to clear with an ethics committee before the study can begin. To recruit and interview a national, diverse sample of around 40 people would typically take another 12–15 months before the analysis can get under way. 95 Being able to draw on an archive of 75 existing collections (each with around 40 interviews) is certainly quicker than collecting primary research and appears to be a good use of resources. Four initial collections were selected to correspond to NICE products that were in development and another two were used to test the reach of the core components – to gather these data alone might have taken 90 months of researchers’ time to collect (our project was designed to be only 18 months long, with one full-time and one part-time researcher). The achievement of objectives 1 and 2 in identifying and testing the core components of good care illustrates the efficiency of secondary analysis of qualitative interviews.
We also wanted to test whether or not these analyses could be used to inform the development of NICE guidelines and QSs. This part of the study highlighted some of the difficulties (anticipated in the commissioning brief) of working with secondary data. The fit is never likely to compare with data collected to address the precise purpose, and we found that, sometimes, the gap between a set of research interviews designed to elicit patients perspectives and experiences and the more precise focus of the NICE guidelines and QSs was simply too wide for the secondary analysis to contribute. Even when there were potentially useful findings, there were difficulties of timing (which we refer to above) and of the status of an unpublished secondary analysis in relation to peer-reviewed and published papers. As an organisation, NICE promote systematic identification of evidence that is publicly available, and a tailor-made secondary analysis has, therefore, an indeterminate status.
NICE guidelines and QSs staff do not rely on peer review; they also quality appraise any study before it is included as evidence. It is considered that when a data archive is mined, to provide ‘quickly and economically’ answers to a focused policy question, those who are being invited to use this new evidence (which may reinforce, supplement or even contradict what is already known) want reassurance that the secondary analysis has been well conducted on appropriate, relevant and unbiased data. We suggest that this particular aspect of fitness for purpose has received too little attention and may hamper the efficient use of secondary analyses intended to inform policy.
Future research
The study suggests that the NIHR and research community might benefit from research in the following areas (in order of priority):
-
Further testing of the identified core components in other patient groups and health conditions.
-
Working alongside technical teams to establish whether or not it is possible to identify areas of patient experience research where targeted secondary analyses have the most potential to add to qualitative literature synthesis and patient and carer involvement (e.g. in end-of-life care).
-
Consensus on standards for secondary analyses that are fit for purpose.
-
Longitudinal, ethnographic studies of the guideline development processes, including patient and carer influences.
-
Secondary analysis of qualitative data to identify main areas of improvement and potential areas for most improvement.
-
Interviewing staff who are later in their careers (or who have left the health service) and who have recent experiences of personal illness, or caring for children or partners, or acting as carers, about their reflections on past and current practice in primary care and hospitals. Their insights are likely to throw up some different perspectives from those who have never been on the inside of health-care provision. [Note: this suggestion was raised in our dissemination workshop (objective 4).]
Chapter 8 Patient and public involvement
The involvement of patients, the public and service users at multiple points throughout the programme of research has both driven the project and significantly enhanced the results. The project has substantially benefited from the enthusiasm of Victoria Thomas (Associate Director of the PPI Programme at NICE) throughout.
Membership of the project steering group
Lay members who had had experience of sitting on CG development groups or QS TEGs were sought through the NICE PPI programme. A role description and person specification was developed based on that used by NICE but adapted for the project. The lay member role was to ensure that the views, experiences and interests of patients, service users and carers informed the group’s work by:
-
identifying issues of concern to patients, service users and carers
-
highlighting areas where patient preferences and patient choice could be acknowledged and
-
ensuring that patient and carer issues and concerns were taken into account within the final report.
For the person specification, essential criteria included experience of a NICE GDG and/or TEG together with an understanding of, and a willingness to reflect, the experiences and needs of a wide network of patients, service users and their carers (e.g. as a member of a patient organisation or support group). Applicants also had to:
-
have the time and commitment to attend meetings, do background reading and comment on draft documents produced by the group
-
possess good communication skills, including respect for other people’s views, and have the ability to listen and take part in constructive debate
-
have a commitment to the concept of an evidence-based approach
-
have the ability to maintain confidentiality and
-
be able to use the internet and e-mail.
It was desirable to:
-
be familiar with medical and research language, particularly qualitative research and
-
have direct or indirect knowledge or experience (as a patient, service user or carer) of the following topics or conditions: treatment for a heart attack, secondary prevention of a heart attack, asthma or diabetes (types 1 or 2).
Expressions of interest were invited from individuals on the NICE PPI mailing list. Respondents were asked to submit an application (a short supporting statement addressing the criteria outlined in the person specification accompanied by a curriculum vitae).
Fiona Loud had contributed to NICE work previously as a lay member of the groups that developed the chronic kidney disease CG and QS, the hyperphosphataemia CG and the acute kidney injury CG and is currently a member of Patients Involved in NICE on behalf of the Kidney Alliance. She is also leader of a patient team on a quality improvement project funded by The Health Foundation and Kidney Research UK aimed at encouraging self-care in early chronic kidney disease patients, has spoken at numerous patient conferences and is chairperson of both local and national health groups.
David Martin was Vice-Chair of the Patient Assembly, Croydon Health Services NHS Trust. The assembly was a voluntary body committed to being a ‘critical friend’ to the Trust and improving patients’ experiences. He has also been a lay member of the NICE GDG developing a CG titled ‘Patient Experience in adult NHS services’ together with the associated QS and was also a patient member at a national workshop developing a generic Prescribing Competency Framework with the National Prescribing Centre, a NICE collaborating centre. During the course of the project, he also sat on the GDG for a CG entitled ‘GP referral for suspected cancer’.
John Roberts had previously sat on both the type 2 diabetes GDG and, subsequently, the associated TEG. In addition, he is currently a patient representative on the Diabetes Clinical Commissioning Group in Liverpool, is a Health and Social Care Ambassador for Liverpool Heart and Chest, and is involved with Liverpool Local Involvement Network, (LINKS) which aims to give people a stronger voice in how their health and social care services are delivered.
All of the lay members have attended and been actively involved in the three steering group meetings. They provided comment on the timing of the project objectives, on the topics for secondary analysis, on the draft list of core components of good-quality care and on the dissemination plan, and were instrumental in setting up the FGs with the ethnically diverse young men and with the Irish Travellers. Access to these groups would not have been possible without their personal contacts and their enthusiasm for the project. Much time and effort was also given towards attempting to convene a FG with very old and frail people either in residential care, in sheltered housing or through Age UK. Regrettably, individuals were overly protected by their carers or other gatekeepers who were very concerned that the FGs would reflect on the care that they themselves provided rather than in general by the NHS, and a group was not possible within the time frame of the project.
Objective 4
The lay people for objective 4 have all been involved in previous PROM research and are currently advising on the Models of Patient Experience study led by Ray Fitzpatrick. This study aims to develop new models for the collection and use of patient experience information in the NHS.
Dissemination
The three lay steering group members have provided insights and guidance on how best to present the research findings to health professionals, academics, the voluntary sector and others and have also suggested conferences and organisations who would have an interest in the research.
Chapter 9 Dissemination
During the life of the study, the researchers have presented the project and emergent findings at several conferences. One academic article, which has been published in the Journal of Health Services Research and Policy, argues for the development of appropriate archiving practices and analytic skills among qualitative researchers so that patients’ perspectives can be better used to inform health policy. 30 Several more articles are in preparation. The lay members of the steering panel have been very helpful in suggesting other audiences that would be interested in this work and a good range of these will be followed up in the longer term. These include National Voices, INVOLVE (a national advisory group that supports greater public involvement in public health and social care research), Healthwatch and local groups such as Liverpool City Council.
Video and audio clips which illustrate key messages from the secondary analyses were shown to various audiences during the lifetime of the project. Film montages have been assembled and have been placed in the ‘scrapbook’ section of the award-winning website www.healthtalkonline.org together with supportive text. The website has recently been upgraded so that it is possible to harvest video, audio and text material, and produce ‘scrapbooks’ of related material which may be shared with and added to by other professionals. These can be used as teaching and training resources or to generate discussion among professionals. We anticipate that these montages could be a useful resource for NHS staff engaged in service improvement. The scrapbooks and accompanying blog have been tweeted widely, with 51,450 accounts reached within the first 4 days.
We will also feed back to the FG and online discussion forum participants on the findings of the project.
Acknowledgements
The authors would like to thank the following:
The three lay members of the project advisory group, Fiona Loud, David Martin and John Roberts, who were insightful, enthusiastic and very proactive, particularly in setting up and cofacilitating some of the focus groups.. Their passion for improving health care and their willingness to offer guidance and practical help throughout were invaluable.
The participants of the focus groups and the online discussion forum, and also facilitators external to the research team, without whom we would not have had the privilege of hearing the voices of those generally not included in research.
Jenny Hislop, senior researcher at the HERG, who provided expert advice on the format of the focus groups and who helped to facilitate two groups.
Lisa Hinton, senior researcher at the HERG, who conducted further secondary analyses of her data on infertility to further test the reach of the core components as part of objective 2.
Susan Kirkpatrick, senior researcher at the HERG who (as the primary researcher) provided insights into the secondary analysis of the asthma data set, and attended the asthma TEG2 meeting.
Maria Salinas, senior researcher at the HERG, who as the researcher responsible for updating collections, provided insights into the secondary analysis of the ‘young people with diabetes’ and ‘rheumatoid arthritis’ data sets.
Annette Boaz, lecturer in translational research, King’s College London, who contributed to the design of the questionnaires used in objective 3.
Jessy Martinez, Office Support Assistant at the Department of Primary Care Health Sciences, who helped to recruit participants for the migrant workers focus group and acted as translator during the discussion.
Kate Neal, research assistant at the HERG, who observed and made notes on some of the NICE training sessions.
Sophie Pask, research assistant at the HERG, who, in addition to cofacilitating a NICE training session, cofacilitated three of the focus groups and provided editorial assistance for this report.
Jessica Moore, research assistant at the HERG, who cofacilitated one of the focus groups.
Kate Hunt, Social and Public Health Sciences Unit, University of Glasgow, who chaired the workshop on secondary analysis.
Ruth Sanders, from the HERG, who edited the clips used in the focus groups, online discussion forum and www.healthtalkonline.org montages.
Graham Shaw, Adam Barnett and Jo Kidd from the DIPEx charity for developing the online discussion webspace, and for incorporating the montages and text which together illustrate patients’ experiences of health care on to www.healthtalkonline.org.
Nicola Small and Clare Wickings from the Department of Primary Care Health Sciences for financial and administrative support.
We are grateful for funding from the NIHR Health Services and Delivery Research programme (project number 10/1011/19).
This report presents independent research commissioned by the NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of NICE, the NHS, the NIHR, NETSCC, the Health Services and Delivery Research programme or the Department of Health.
Contributions of authors
Sue Ziebland (Director, HERG and principal investigator) led the overall design of the study, led the research, sat on the steering group, conducted two focus groups, contributed to the analysis and led the writing of the final report.
Louise Locock (Knowledge Exchange Director, HERG) contributed to the overall study design, conducted the secondary analysis of the asthma data set (objective 1), contributed to objectives 4 and 5, sat on the steering group, contributed to the final report and gave final approval of the manuscript.
Ray Fitzpatrick (Professor of Public Health) contributed to the design and conduct of objective 4 and gave final approval of the manuscript.
Tim Stokes (Senior Clinical Lecturer in Primary Care, was Consultant Clinical Advisor at NICE) contributed to the overall study design, sat on the steering group, influenced the project from a NICE perspective, contributed to the final report and gave final approval of the manuscript.
Glenn Robert (Professor of Health Care Quality and Innovation) contributed to the overall study design, sat on the steering group, led the knowledge transfer component (objective 3), wrote the corresponding chapter of the final report and gave final approval of the manuscript.
Norma O’Flynn (Clinical Director, NCGC) contributed to the overall study design, sat on the steering group, influenced the project from a NCGC perspective, contributed to the final report and gave final approval of the manuscript.
Kristina Bennert (Senior Researcher, HERG) conducted most of the secondary analyses for objective 1, helped to recruit and design the focus groups and contributed to the analyses (objective 2), contributed to objectives 4 and 5, sat on the steering group, contributed to the final report and gave final approval of the manuscript.
Sara Ryan (Research Director, HERG) led objective 2, recruited and conducted three of the focus groups, contributed to the analysis and objectives 4 and 5, sat on the steering group, contributed to the final report and gave final approval of the manuscript.
Victoria Thomas contributed to the overall study design, sat on the steering group, influenced the project from a NICE perspective, contributed to the final report and gave final approval of the manuscript.
Angela Martin (Operations Manager, HERG) managed and contributed to all objectives, sat on the steering group, contributed to the final report and gave final approval of the manuscript.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publications
Ziebland S, Hunt K. Using secondary analysis of existing qualitative data of patient experiences of health care to inform health services research and policy. J Health Serv Res Policy 2014;19:177–82.
Presentations
Bennert K, Hislop J, Ryan S, Ziebland S. The tellability of good care: how do patients narrate their health service experiences? Oral presentation, BSA Medical Sociology Annual Conference, York, 11–13 September 2013.
Bennert L, Ryan S, Hislop J, Martin A, Ziebland S. Testing the reach of the core components of good quality care with ‘seldom heard’ groups. Poster presentation at ‘The many meanings of ‘quality’ in healthcare’, Cumberland Lodge, Windsor, 4 June 2013.
Hislop J, Ryan S. Enabling inclusion? Reflections on using focus groups with ‘seldom heard’ groups to explore views on good healthcare. Oral presentation, BSA Medical Sociology Annual Conference, York, 11–13 September 2013.
Locock L, Ziebland S. Using health experience narratives to improve care. Oral presentation, Royal College of General Practitioners annual conference, Glasgow, 3–6 October 2012.
Film montages and supportive text have been placed together in the ‘scrapbook’ section of www.healthtalkonline.org.
References
- Public Health White Paper. Equity and Excellence: Liberating the NHS. London: HMSO; 2010.
- The Power of Information: Putting All of Us in Control of the Health and Care Information We Need. London: Department of Health; 2012.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- The Operating Framework for the NHS in England 2012/13. London: NHS; 2011.
- Independent Inquiry into Care Provided by Mid-Staffordshire NHS Foundation Trust 2005–2009. London: The Stationery Office; 2010.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary. London: The Stationery Office; 2013.
- NHS Patient Experience Framework. London: Department of Health; 2011.
- Patient Experience in Adult NHS Services (QS15). London: NICE; 2012.
- Entwistle V, Firnigl D, Ryan M, Francis J, Kinghorn P. Which experiences of health care delivery matter to service users and why? A critical interpretive synthesis and conceptual map. J Health Serv Res Policy 2012;17:70-8. http://dx.doi.org/10.1258/jhsrp.2011.011029.
- Nolan MR, Davies S, Brown J, Keady J, Nolan J. Beyond ‘person-centred’ care: a new vision for gerontological nursing. J Clin Nurs 2004;13:45-53. http://dx.doi.org/10.1111/j.1365-2702.2004.00926.x.
- The Guidelines Manual. London: NICE; 2012.
- Stokes T. NICE quality standards: improving healthcare quality in the English NHS?. Qual Prim Care 2013;13:207-9.
- Darzi A. High Quality Care For All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Herxheimer A, Ziebland S. DIPEx: fresh insights for medical practice. J R Soc Med 2003;96:209-10. http://dx.doi.org/10.1258/jrsm.96.5.209.
- Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries?. J Adv Nurs 1997;26:623-30. http://dx.doi.org/10.1046/j.1365-2648.1997.t01-25-00999.x.
- Barber V, Linsell L, Locock L, Powell L, Shakeshaft C, Colman J, et al. Electronic fetal monitoring during labour and anxiety levels in women taking part in a RCT. Br J Midwifery 2013;21:394-403. http://dx.doi.org/10.12968/bjom.2013.21.6.394.
- Chapple A, Ziebland S, Simkin S, Hawton K. How people bereaved by suicide perceive newspaper reporting: qualitative study. Br J Psychiatry 2013;203:228-32. http://dx.doi.org/10.1192/bjp.bp.112.114116.
- Kirkpatrick S, Locock L, Giles MF, Lasserson DS. Non-focal neurological symptoms associated with classical presentations of transient ischaemic attack: qualitative analysis of interviews with patients. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0066351.
- Kitson AL, Dow C, Calabrese JD, Locock L, Athlin ÅM. Stroke survivors’ experiences of the fundamentals of care: a qualitative analysis. Int J Nurs Stud 2013;50:392-403. http://dx.doi.org/10.1016/j.ijnurstu.2012.09.017.
- Mazanderani F, Locock L, Powell J. Biographical value: towards a conceptualisation of the commodification of illness narratives in contemporary healthcare. Sociol Health Illness 2013;35:891-905. http://dx.doi.org/10.1111/1467-9566.12001.
- Ryan S, Orsini M, Davidson J. Worlds of Autism: Across the Spectrum of Neurological Difference. Minneapolis, MN: University of Minnesota Press; 2013.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20. http://dx.doi.org/10.1258/1355819054308576.
- Petticrew M, Roberts H. Systematic Reviews in the Social Sciences. A Practical Guide. Oxford: Blackwell Publishing Ltd; 2006.
- Pope C, Mays N, Popay J. Synthesising Qualitative and Quantitative Health Research: A Guide to Methods. Maidenhead: Open University Press; 2007.
- Bishop L. Ethical sharing and reuse of qualitative data. Aust J Soc Issues 2009;44:255-72.
- Wellcome Trust . Policy on Data Management and Sharing 2010. www.wellcome.ac.uk/About-us/Policy/Policy-and-position-statements/WTX035043.htm (accessed 3 February 2014).
- Medical Research Council . MRC Policy on Sharing of Research Data from Population and Patient Studies 2011. www.mrc.ac.uk/Ourresearch/Ethicsresearchguidance/datasharing/Policy/PHSPolicy/index.htm (accessed 3 February 2014).
- OECD Principles and Guidelines for Access to Research Data from Public Funding. Paris: OECD Publications; 2007.
- NIH . NIH Data Sharing Policy and Implementation Guidance 2003. http://grants.nih.gov/grants/policy/data_sharing/data_sharing_guidance.htm?print=yes& (accessed 3 February 2014).
- Ziebland S, Hunt K. Using secondary analysis of existing qualitative data of patient experiences of health care to inform health services research and policy. J Health Serv Res Policy 2014;19:177-82. http://dx.doi.org/10.1177/1355819614524187.
- France EF, Hunt K, Ziebland S, Wyke S. What parents say about disclosing the end of their pregnancy due to fetal abnormality. Midwifery 2013;29:24-32. http://dx.doi.org/10.1016/j.midw.2011.10.006.
- France EF, Locock L, Hunt K, Ziebland S, Field K, Wyke S. Imagined futures: how experiential knowledge of disability affects parents’ decision making about fetal abnormality. Health Expect 2012;15:139-56. http://dx.doi.org/10.1111/j.1369-7625.2011.00672.x.
- Almond SC, Salisbury H, Ziebland S. Women’s experience of coronary heart disease: why is it different?. Br J Cardiac Nurs 2012;7:165-70. http://dx.doi.org/10.12968/bjca.2012.7.4.165.
- Seale C, Charteris-Black J, MacFarlane A, McPherson A. Interviews and internet forums: a comparison of two sources of qualitative data. Qual Health Res 2010;20:595-606. http://dx.doi.org/10.1177/1049732309354094.
- Hilton S, Emslie C, Hunt K, Chapple A, Ziebland S. Disclosing a cancer diagnosis to friends and family: a gendered analysis of young men’s and women’s experiences. Qual Health Res 2009;19:744-54. http://dx.doi.org/10.1177/1049732309334737.
- Treatment and Care Towards the End of Life: Good Practice in Decision Making. 2010.
- Ritchie J, Spencer L, Bryman A, Burgess B. Analyzing Qualitative Data. Abingdon: Routledge; 1994.
- Barbour RS. Making sense of focus groups. Med Educ 2005;39:742-50. http://dx.doi.org/10.1111/j.1365-2929.2005.02200.x.
- Wellings K, Branigan P, Mitchell K. Discomfort, discord and discontinuity as data: using focus groups to research sensitive topics. Cult Health Sex 2000;2:255-67. http://dx.doi.org/10.1080/136910500422241.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map?. J Contin Educ Health Prof 2006;26:13-24. http://dx.doi.org/10.1002/chp.47.
- Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-83. http://dx.doi.org/10.1097/00005650-199206000-00002.
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337-43. http://dx.doi.org/10.3109/07853890109002087.
- Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnare on the perceptions of patients about total hip replacement. J Bone Joint Surg 1996;78B:185-90.
- Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care 2002;14:353-8. http://dx.doi.org/10.1093/intqhc/14.5.353.
- Campbell J, Smith P, Nissen S, Bower P, Elliott M, Roland M. The GP Patient Survey for use in primary care in the National Health Service in the UK – development and psychometric characteristics. BMC Fam Pract 2009;10. http://dx.doi.org/10.1186/1471-2296-10-57.
- Williams A, Kristjanson L. Emotional care experienced by hospitalised patients: development and testing of a measurement instrument. J Clin Nurs 2009;18:1069-77. http://dx.doi.org/10.1111/j.1365-2702.2008.02586.x.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-001570.
- Ziebland S, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences. Oxford: Oxford University Press; 2013.
- Heaton J. Secondary analysis of qualitative data. Social Research Update 1998;22:88-93. http://sru.soc.surrey.ac.uk/SRU22.html (accessed 14 October 2013).
- Heaton J. Reworking Qualitative Data. London: Sage Publications; 2004.
- Mauthner NS, Parry O, Backett-Milburn K. The data are out there, or are they? Implications for archiving and revisiting qualitative data. Sociology 1998;32:733-45. http://dx.doi.org/10.1177/0038038598032004006.
- Fielding N. Getting the most from archived qualitative data: epistemological, practical and professional obstacles. Int J Soc Res Methodol 2004;7:97-104. http://dx.doi.org/10.1080/13645570310001640699.
- Hinds PS, Vogel RJ, Clarke-Steffen L. The possibilities and pitfalls of doing a secondary analysis of a qualitative data set. Qual Health Res 1997;7:408-24. http://dx.doi.org/10.1177/104973239700700306.
- Parry O, Mauthner NS. Back to basics: who re-uses qualitative data and why?. Sociology 2005;39:337-42. http://dx.doi.org/10.1177/0038038505050543.
- Bishop L. A reflexive account of reusing qualitative data: beyond primary/secondary dualism. Sociological Res Online 2007;12. http://dx.doi.org/10.5153/sro.1553.
- Moore N. (Re)using qualitative data?. Sociological Res Online 2007;12. http://dx.doi.org/10.5153/sro.1496.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Picker Institute . Principles of Patient-Centred Care Oxford: Picker Institue Europe n.d. http://pickerinstitute.org/about/picker-principles/ (accessed 11 October 2013).
- Ryan S, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and Using Health Experiences: Improving Patient Care. Oxford: Oxford University Press; 2013.
- Human Fertilisation and Embryology Authority . Fertility Treatment in 2010 – Trends and Figures 2011.
- Brugha TS, McManus S, Meltzer H, Smith J, Scott FJ, Purdon S, et al. Autism Spectrum Disorders in Adults Living in Households throughout England: report from the Adult Psychiatric Morbidity Survey 2007. London: NHS Information Centre for Health and Social Care; 2009.
- Brugha TS, McManus S, Smith J, Scott FJ, Meltzer H, Purdon S, et al. Validating two survey methods for identifying cases of autism spectrum disorder among adults in the community. Psychol Med 2012;42:647-56. http://dx.doi.org/10.1017/S0033291711001292.
- Matson JL, Minshawi NF. Early Intervention for Autism Spectrum Disorders: A Critical Analysis. Oxford: Elsevier; 2006.
- Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405-14. http://dx.doi.org/10.1111/j.1365-2929.2006.02467.x.
- Kitzinger J, Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and using Health Experiences. Oxford: Oxford University Press; 2013.
- Martinez-Ebers V. Using monetary incentives with hard-to-reach populations in panel surveys. Int J Public Opin Res 1997;9:77-86. http://dx.doi.org/10.1093/ijpor/9.1.77.
- Argote L, Ingram P. Knowledge transfer: a basis for competitive advantage in firms. Organ Behav Human Decis Process 2000;82:150-69. http://dx.doi.org/10.1006/obhd.2000.2893.
- Dopson S, Fitzgerald L. Knowledge to Action? Evidence-Based Health Care in Context. Oxford: Oxford University Press; 2005.
- Van de Ven AH. Engaged Scholarship: a Guide for Organizational and Social Research. Oxford: Oxford University Press; 2007.
- Stetler CB, Ritchie JA, Rycroft-Malone J, Schultz AA, Charns MP. Institutionalizing evidence-based practice: an organizational case study using a model of strategic change. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-78.
- Rycroft-Malone J. The PARIHS framework – a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual 2004;19:297-304. http://dx.doi.org/10.1097/00001786-200410000-00002.
- Graham K, Logan J. Using the Ottawa Model of Research Use to implement a skin care program. J Nurs Care Qual 2004;19:18-26. http://dx.doi.org/10.1097/00001786-200401000-00006.
- Straus SE, Tetroe J, Graham ID. Knowledge Translation in Health Care: moving from Evidence to Practice. Oxford: Wiley-Blackwell; 2009.
- British Guideline on the Management of Asthma: A National Clinical Guideline. London and Edinburgh: BTS, SIGN; 2011.
- Kirwan J, Heiberg T, Hewlett S, Hughes R, Kvien T, Ahlmèn M, et al. Outcomes from the Patient Perspective Workshop at OMERACT 6. J Rheumatol 2003;30:868-72.
- Intelligent Board 2010 – Patient Experience. London: Dr Foster Intelligence; 2010.
- Corti L, Bergman M, Eberle T. Qualitative Inquiry: Research, Archiving and Re-Use. Bern: Swiss Academy of Humanities and Social Sciences; 2004.
- Wyke S, Entwistle V, France EF, Hunt K, Jepson R, Thompson A, et al. Information for Choice: What People Need, Prefer and Use. Southampton: NIHR SDO programme; 2011.
- Seale C, Ziebland S, Charteris-Black J. Gender, cancer experience and internet use: a comparative keyword analysis of interviews and online cancer support groups. Soc Sci Med 2006;62:2577-90. http://dx.doi.org/10.1016/j.socscimed.2005.11.016.
- Heaton J. Growing Up With Chronic Illness (GUCI) 2011. http://sites.pcmd.ac.uk/guci/ (accessed 11 October 2013).
- Calabrese JD. A Comparison of National and Local Data on Patient Experiences of End of Life Care. Oxford: Green Templeton College, University of Oxford; 2010.
- Charteris-Black J, Seale C. Men and emotion talk: evidence from the experience of illness. Gend Lang 2009;3:81-113.
- Emslie C, Browne S, MacLeod U, Rozmovits L, Mitchell E, Ziebland S. ‘Getting through’ not ‘going under’: a qualitative study of gender and spousal support after diagnosis with colorectal cancer. Soc Sci Med 2009;68:1169-75. http://dx.doi.org/10.1016/j.socscimed.2009.01.004.
- Emslie C, Ridge D, Ziebland S, Hunt K. Exploring men’s and women’s experiences of depression and engagement with health professionals: more similarities than differences? A qualitative interview study. BMC Fam Pract 2007;8. http://dx.doi.org/10.1186/1471-2296-8-43.
- France EF, Wyke S, Ziebland S, Entwistle VA, Hunt K. How personal experiences feature in women’s accounts of use of information for decisions about antenatal diagnostic testing for foetal abnormality. Soc Sci Med 2011;72:755-62. http://dx.doi.org/10.1016/j.socscimed.2010.11.031.
- Hilton S, Hunt K, Emslie C, Salinas M, Ziebland S. Have men been overlooked? A comparison of young men and women’s experiences of chemotherapy-induced alopecia. Psycho-Oncology 2008;17:577-83. http://dx.doi.org/10.1002/pon.1272.
- Hunt K, France EF, Ziebland S, Field K, Wyke S. ‘My brain couldn’t move from planning a birth to planning a funeral’: a qualitative study of parents’ experiences of decisions after ending a pregnancy for fetal abnormality. Int J Nurs Stud 2009;46:1111-21. http://dx.doi.org/10.1016/j.ijnurstu.2008.12.004.
- Lowe P, Powell J, Griffiths F, Thorogood M, Locock L. “Making it all normal”: the role of the internet in problematic pregnancy. Qual Health Res 2009;19:1476-84. http://dx.doi.org/10.1177/1049732309348368.
- Mason J. ‘Re-using’ qualitative data: on the merits of an investigative epistemology. Sociol Res Online 2007;12. http://dx.doi.org/10.5153/sro.1507.
- Parry O, Mauthner NS. Whose data are they anyway? Practical, legal and ethical issues in archiving qualitative research data. Sociology 2004;38:139-52. http://dx.doi.org/10.1177/0038038504039366.
- Bishop L. Protecting respondents and enabling data sharing: reply to Parry and Mauthner. Sociology 2005;39:333-6. http://dx.doi.org/10.1177/0038038505050542.
- Fielding NG, Fielding JL. Resistance and adaptation to criminal identity: using secondary analysis to evaluate classic studies of crime and deviance. Sociology 2000;34:671-89. http://dx.doi.org/10.1177/S0038038500000419.
- Irwin S, Winterton M. Qualitative secondary analysis and social explanation. Sociol Res Online 2012;17. http://dx.doi.org/10.5153/sro.2626.
- Responsive Funding in the NIHR SDO Programme: Call for Proposals from Research Studies. London: NIHR; 2011.
- Reid M, Armstrong D. Guidelines on evaluating qualitative research proposals in health services research. Med Sociol News 2004;30.
- Horne R, James D, Petrie K, Weinman J, Vincent R. Patients’ interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart 2000;83:388-93. http://dx.doi.org/10.1136/heart.83.4.388.
- Cytryn KN, Yoskowitz NA, Cimino JJ, Patel VL. Lay public’s knowledge and decisions in response to symptoms of acute myocardial infarction. Adv Health Sci Educ 2009;14:43-59. http://dx.doi.org/10.1007/s10459-007-9085-z.
- Pattenden J, Watt I, Lewin RJP, Stanford N. Decision making processes in people with symptoms of acute myocardial infarction: qualitative study. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7344.1006.
- Galdas PM, Johnson JL, Percy ME, Ratner PA. Help seeking for cardiac symptoms: beyond the masculine–feminine binary. Soc Sci Med 2010;71:18-24. http://dx.doi.org/10.1016/j.socscimed.2010.03.006.
- Gallagher R, Marshall AP, Fisher MJ. Symptoms and treatment-seeking responses in women experiencing acute coronary syndrome for the first time. Heart Lung 2010;39:477-84. http://dx.doi.org/10.1016/j.hrtlng.2009.10.019.
- O’Brien R, Hunt K, Hart G. ‘It’s caveman stuff, but that is to a certain extent how guys still operate’: men’s accounts of masculinity and help seeking. Soc Sci Med 2005;61:503-16. http://dx.doi.org/10.1016/j.socscimed.2004.12.008.
- Emslie C, Hunt K, Watt G. Invisible women? The importance of gender in lay beliefs about heart problems. Sociol Health Illness 2001;23:203-33. http://dx.doi.org/10.1111/1467-9566.00248.
- Sjöström-Strand A, Fridlund B. Women’s descriptions of symptoms and delay reasons in seeking medical care at the time of a first myocardial infarction: a qualitative study. Int J Nurs Stud 2008;45:1003-10. http://dx.doi.org/10.1016/j.ijnurstu.2007.07.004.
- Nymark C, Mattiasson A-C, Henriksson P, Kiessling A. The turning point: from self-regulative illness behaviour to care-seeking in patients with an acute myocardial infarction. J Clin Nurs 2009;18:3358-65. http://dx.doi.org/10.1111/j.1365-2702.2009.02911.x.
- Allison M, Campbell C. “Maybe it could be a heart attack . but I’m only 31”: young men’s lived experience of myocardial infarction – an exploratory study. Am J Mens Health 2009;3:116-25. http://dx.doi.org/10.1177/1557988307308519.
- Sampson F, O’Cathain A, Goodacre S. Feeling fixed and its contribution to patient satisfaction with primary angioplasty: a qualitative study. Eur J Cardiovasc Nurs 2009;8:85-90. http://dx.doi.org/10.1016/j.ejcnurse.2008.07.003.
- Astin F, Closs SJ, McLenachan J, Hunter S, Priestley C. Primary angioplasty for heart attack: mismatch between expectations and reality?. J Adv Nurs 2009;65:72-83. http://dx.doi.org/10.1111/j.1365-2648.2008.04836.x.
- Höglund AT, Winblad U, Arnetz B, Arnetz JE. Patient participation during hospitalization for myocardial infarction: perceptions among patients and personnel. Scand J Caring Sci 2010;24:482-9. http://dx.doi.org/10.1111/j.1471-6712.2009.00738.x.
- Radcliffe EL, Harding G, Rothman MT, Feder GS. ‘It got right to the spot’: the patient experience of primary angioplasty: a qualitative study. Eur J Cardiovasc Nurs 2009;8:216-22. http://dx.doi.org/10.1016/j.ejcnurse.2009.02.001.
- Schaufel MA, Nordrehaug JE, Malterud K. “So you think I’ll survive?”: a qualitative study about doctor-patient dialogues preceding high-risk cardiac surgery or intervention. Heart 2009;95:1245-9. http://dx.doi.org/10.1136/hrt.2008.164657.
- Emslie C, Hunt K. Men, Masculinities and heart disease: a systematic review of the qualitative literature. Curr Sociol 2009;57:155-91. http://dx.doi.org/10.1177/0011392108099161.
- Altiok M, Yılmaz M. Opinions of individuals who have had myocardial infarction about sex. Sex Disabil 2011;29:263-73. http://dx.doi.org/10.1007/s11195-011-9217-5.
- Arenhall E, Kristofferzon M-L, Fridlund B, Malm D, Nilsson U. The male partners’ experiences of the intimate relationships after a first myocardial infarction. Eur J Cardiovasc Nurs 2011;10:108-14. http://dx.doi.org/10.1016/j.ejcnurse.2010.05.003.
- Arenhall E, Kristofferzon M-L, Fridlund B, Nilsson U. The female partners’ experiences of intimate relationships after a first myocardial infarction. J Clin Nurs 2011;20:1677-84. http://dx.doi.org/10.1111/j.1365-2702.2010.03312.x.
- Mosack V, Steinke EE. Trends in sexual concerns after myocardial infarction. J Cardiovasc Nurs 2009;24. http://dx.doi.org/10.1097/JCN.0b013e318197aaa1.
- Sundler AJ, Dahlberg K, Ekenstam C. The meaning of close relationships and sexuality: women’s well-being following a myocardial infarction. Qual Health Res 2009;19:375-87. http://dx.doi.org/10.1177/1049732309331882.
- Baldacchino D. Long-term causal meaning of myocardial infarction. Br J Nurs 2010;19:774-81. http://dx.doi.org/10.12968/bjon.2010.19.12.48656.
- Brink E. Adaptation positions and behavior among post-myocardial infarction patients. Clin Nurs Res 2009;18:119-35. http://dx.doi.org/10.1177/1054773809332326.
- Schaufel MA, Nordrehaug JE, Malterud K. Hope in action – facing cardiac death: a qualitative study of patients with life-threatening disease. Int J Qual Stud Health Well-Being 2011;6.
- Bethell H, Turner S, Flint EJ, Rose L. The BACR database of cardiac rehabilitation units in the UK. Coron Health Care 2000;4:92-5. http://dx.doi.org/10.1054/chec.2000.0072.
- Tolmie EP, Lindsay GM, Kelly T, Tolson D, Baxter S, Belcher PR. Are older patients’ cardiac rehabilitation needs being met?. J Clin Nurs 2009;18:1878-88. http://dx.doi.org/10.1111/j.1365-2702.2009.02798.x.
- Clark AM, Barbour RS, White M, MacIntyre PD. Promoting participation in cardiac rehabilitation: patient choices and experiences. J Adv Nurs 2004;47:5-14. http://dx.doi.org/10.1111/j.1365-2648.2004.03060.x.
- Jackson AM, McKinstry B, Gregory S, Amos A. A qualitative study exploring why people do not participate in cardiac rehabilitation and coronary heart disease self-help groups, and their rehabilitation experience without these resources. Prim Health Care Res Develop 2012;13:30-41. http://dx.doi.org/10.1017/S1463423611000284.
- O’Driscoll JM, Shave R, Cushion CJ. A National Health Service Hospital’s cardiac rehabilitation programme: a qualitative analysis of provision. J Clin Nurs 2007;16:1908-18. http://dx.doi.org/10.1111/j.1365-2702.2007.01815.x.
- Everett B, Salamonson Y, Zecchin R, Davidson PM. Reframing the dilemma of poor attendance at cardiac rehabilitation: an exploration of ambivalence and the decisional balance. J Clin Nurs 2009;18:1842-9. http://dx.doi.org/10.1111/j.1365-2702.2008.02612.x.
- Wiles R, Kinmonth A-L. Patients’ understandings of heart attack: implications for prevention of recurrence. Patient Educ Couns 2001;44:161-9. http://dx.doi.org/10.1016/S0738-3991(00)00187-7.
- Wiles R. Patients’ perceptions of their heart attack and recovery: the influence of epidemiological “evidence” and personal experience. Soc Sci Med 1998;46:1477-86. http://dx.doi.org/10.1016/S0277-9536(97)10140-X.
- Garavalia L, Garavalia B, Spertus JA, Decker C. Exploring patients’ reasons for discontinuance of heart medications. J Cardiovasc Nurs 2009;24:371-9. http://dx.doi.org/10.1097/JCN.0b013e3181ae7b2a.
- Gregory S, Bostock Y, Backett-Milburn K. Recovering from a heart attack: a qualitative study into lay experiences and the struggle to make lifestyle changes. Fam Practice 2006;23:220-5. http://dx.doi.org/10.1093/fampra/cmi089.
- Newman MA, Ziebland S, Barker KL. Patients’ views of a multimedia resource featuring experiences of rheumatoid arthritis: pilot evaluation of www.healthtalkonline.org. Health Informatics J 2009;15:147-59. http://dx.doi.org/10.1177/1460458209102974.
- Shariff F, Carter J, Dow C, Polley M, Salinas M, Ridge D. Mind and body management strategies for chronic pain and rheumatoid arthritis. Qual Health Res 2009;19:1037-49. http://dx.doi.org/10.1177/1049732309341189.
Appendix 1 Patient experience quality standard
National Institute for Health and Care Excellence. QS15 Patient Experience in Adult NHS Services. London: NICE; 2012. URL: http://guidance.nice.org.uk/QS15 (accessed 24 october 2014). 8 Reproduced with permission.
Statement 1. Patients are treated with dignity, kindness, compassion, courtesy, respect, understanding and honesty.
Statement 2. Patients experience effective interactions with staff who have demonstrated competency in relevant communication skills.
Statement 3. Patients are introduced to all healthcare professionals involved in their care, and are made aware of the roles and responsibilities of the members of the healthcare team.
Statement 4. Patients have opportunities to discuss their health beliefs, concerns and preferences to inform their individualised care.
Statement 5. Patients are supported by healthcare professionals to understand relevant treatment options, including benefits, risks and potential consequences.
Statement 6. Patients are actively involved in shared decision making and supported by healthcare professionals to make fully informed choices about investigations, treatment and care that reflect what is important to them.
Statement 7. Patients are made aware that they have the right to choose, accept or decline treatment and these decisions are respected and supported.
Statement 8. Patients are made aware that they can ask for a second opinion.
Statement 9. Patients experience care that is tailored to their needs and personal preferences, taking into account their circumstances, their ability to access services and their coexisting conditions.
Statement 10. Patients have their physical and psychological needs regularly assessed and addressed, including nutrition, hydration, pain relief, personal hygiene and anxiety.
Statement 11. Patients experience continuity of care delivered, whenever possible, by the same healthcare professional or team throughout a single episode of care.
Statement 12. Patients experience coordinated care with clear and accurate information exchange between relevant health and social care professionals.
Statement 13. Patients’ preferences for sharing information with their partner, family members and/or carers are established, respected and reviewed throughout their care.
Statement 14. Patients are made aware of who to contact, how to contact them and when to make contact about their ongoing healthcare needs.
Appendix 2 Extracts reproduced from ‘The Guidelines Manual’
National Institute for Health and Care Excellence (2012). The Guidelines Manual. London: NICE. URL: http://publications.nice.org.uk/pp-guidelines-manual-pmg6/introduction (accessed 6 October 2014). 11 Reproduced with permission.
Note that CGs being developed in 2011 and 2012 would have been developed in accordance with the 2009 guidelines manual.
Using patient experience to inform review questions
The PICO [population, intervention, comparison, outcome] framework should take into account the patient experience. Patient experience, which may vary for different patient populations (‘P’), covers a range of dimensions, including:
-
patient views on the effectiveness and acceptability of given interventions (‘I’)
-
patient preferences for different treatment options, including the option of foregoing treatment (‘C’)
-
patient views on what constitutes a desired, appropriate or acceptable outcome (‘O’).
The integration of relevant patient experiences into each review question therefore helps to make the question patient-centred as well as clinically appropriate. For example, a review question that looks at the effectiveness of aggressive chemotherapy for a terminal cancer is more patient-centred if it integrates patient views on whether it is preferable to prolong life or to have a shorter life but of better quality.
It is also possible for review questions to ask about specific elements of the patient experience in their own right, although the PICO framework may not provide a helpful structure if these do not involve an intervention designed to treat a particular condition. Such review questions should be clear and focused, and should address relevant aspects of the patient experience at specific points in the care pathway that are considered to be important by the patient and carer members and others on the GDG. Such questions can address a range of issues, such as:
-
patient information and support needs
-
elements of care that are of particular importance to patients
-
the specific needs of groups of patients who may be disadvantaged compared with others
-
which outcomes reported in intervention studies are most important to patients.
As with the development of all structured review questions, questions that are broad in scope and lack focus (for example, ‘what is the patient experience of living with condition X’?) should be avoided. Examples of review questions relating to patient information and support needs are given in box 4.6.
What information and support should be offered to children with atopic eczema and their families/carers?
[From: Atopic eczema in children: management of atopic eczema in children from birth up to the age of 12 years. NICE clinical guideline 57 (2007).]
What elements of care on the general ward are viewed as important by patients following their discharge from critical care areas?
[From: Acutely ill patients in hospital: recognition of and response to acute illness in adults in hospital. NICE clinical guideline 50 (2007).]
Are there cultural differences that need to be considered in delivering information and support on breast or bottle-feeding?
[From: Postnatal care: routine postnatal care of women and their babies. NICE clinical guideline 37 (2006).]
A review question relating to patient experience is likely to be best answered using qualitative studies and cross-sectional surveys, although information on patient experience is also becoming increasingly available as part of wider intervention studies.
6.5 Using patient experience to inform review questions
These questions are described in section 4.3.4.
6.5.1 Assessing study quality
Studies about patient experience are likely to be qualitative studies or cross-sectional surveys. Qualitative studies should be assessed using the methodology checklist for qualitative studies (appendix H). It is important to consider which quality appraisal criteria from this checklist are likely to be the most important indicators of quality for the specific research question being addressed. These criteria may be helpful in guiding decisions about the overall quality of individual studies and whether to exclude certain studies, and when summarising and presenting the body of evidence for the research question about patient experience as a whole.
There is no methodology checklist for the quality appraisal of cross-sectional surveys. Such surveys should be assessed for the rigour of the process used to develop the questions and their relevance to the population under consideration, and for the existence of significant bias (for example, non-response bias).
6.5.2 Summarising and presenting results
A description of the quality of the evidence should be given, based on the quality appraisal criteria from appendix H that were considered to be the most important for the research question being addressed. If appropriate, the quality of the cross-sectional surveys included should also be summarised.
Consider presenting the quality assessment of included studies in tables (see table 1 in appendix H for an example). Methods to synthesise qualitative studies (for example, meta-ethnography) are evolving, but the routine use of such methods in guidelines is not currently recommended.
The narrative summary should be followed by a short evidence statement summarising what the evidence shows. Characteristics of data should be extracted to a standard template for inclusion in an evidence table (see appendix J4).
Appendix 3 The clinical guideline development process
National Institute for Health and Care Excellence (2012). The Guidelines Manual. London: NICE. URL: http://publications.nice.org.uk/pp-guidelines-manual-pmg6/introduction (accessed 6 October 2014). 11 Reproduced with permission.
a, The writing of the guideline is an iterative process that is ongoing throughout the development and consultation phases.
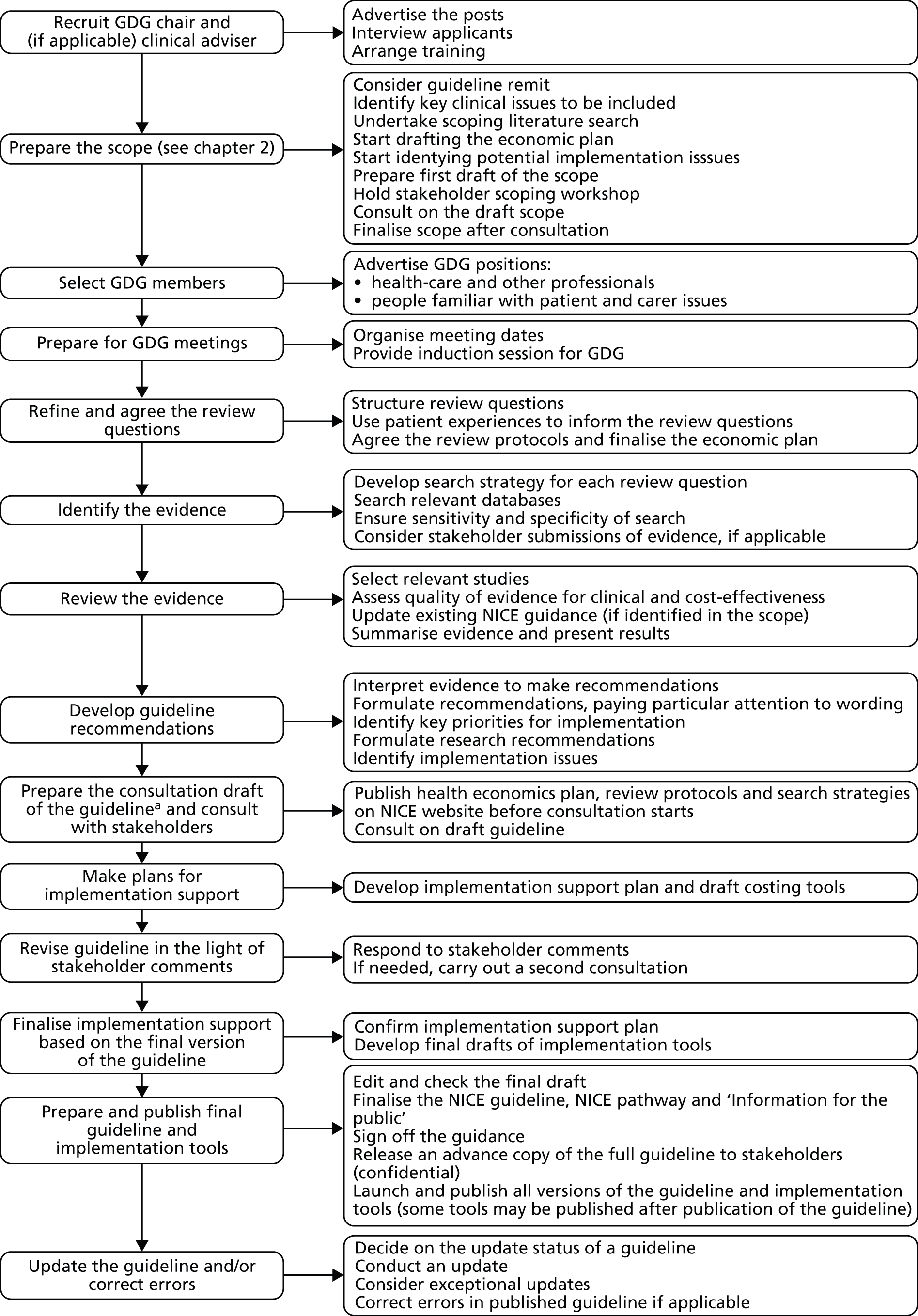
Appendix 4 Myocardial infarction patients’ perspectives of care: a secondary analysis of qualitative interviews
Introduction
This report forms part of a larger project (funded by NIHR HS&DR) between NICE and the University of Oxford, which uses secondary analysis of collections of narrative interviews on various health conditions to identify core components of patients’ experiences of the NHS to inform the development, and measurement, of NICE QSs.
The aim of this report was to answer the question ‘what does good care in myocardial infarction look like from patients’ perspectives?’
We conducted a qualitative secondary analysis of 36 narrative interviews with UK patients who had experienced at least one heart attack. The original data were collected by members of HERG in the Department of Primary Care, University of Oxford, between 2002 and 2003. For further details of how and why the interviews were originally sampled and collected and the implications for the secondary analysis, see Methods of data collection and analysis later in this appendix.
The findings from secondary analysis have been structured into nine sections that map loosely onto the chronological order of the care pathway for patients experiencing MI. They are:
-
the process of seeking help
-
receiving the diagnosis
-
experience of the hospital environment
-
information about diagnostic procedures, surgery and medication
-
preparation for discharge
-
the emotional impact of MI for patients and their families
-
regaining body confidence: patients’ experiences of physical rehabilitation
-
patients’ information and support needs in making lifestyle changes
-
building a supportive environment – MI patients’ ongoing support needs.
To guide the reader into the patient perspective, each section starts with the key questions and emotions that patients describe at the respective points of the care pathway. This is followed by a more detailed narrative account of the findings, illustrated with quotes and contextualised within existing qualitative literature. Naturally, many issues cut across sections and this has been signalled through cross-references.
Executive summary: ‘what does good care in myocardial infarction look like from patients’ perspectives?’
The process of seeking help
To help to avoid delays in admission, health information on MI should:
-
emphasise the breadth of possible symptoms of MI, including that the presentation may be different in women
-
educate about the range of possible causes for MI and the fact that it can occur in young, fit and physically active people with healthy lifestyles
-
recognise that social embarrassment may lead some patients to normalise their symptoms or wait for them to pass even when they suspect a heart attack
-
emphasise that delayed admission reduces treatment options and success.
When patients seek help for MI, health professionals and their gatekeepers need to:
-
Be aware that many patients will use their local surgery and GP as the first port-of-call in an emergency.
-
Patients who seek help from their local surgery or GP risk additional delays in admission due to appointment waiting times and the risk of misdiagnoses.
-
-
Be sensitive to the possibility that patients may understate symptoms.
-
Symptoms may not be those conventionally associated with heart attack; patients may lack knowledge and vocabulary to describe symptoms with confidence. Even patients who suspect a heart attack may be reluctant to self-diagnose out of respect for the medical authority and expertise of doctors.
-
-
Understand why continuity of care is valued by patients.
-
Personal knowledge of patients and their circumstances can enable health professionals to spot emergencies beyond the factual information available at the time.
-
Some patients with a personal GP who had known them for some time reported that they had benefited from their GP’s clinical intuition and were admitted very quickly.
-
-
Bear in mind that patients who live alone may be at particular risk of seeking help late.
-
Partners and family play a vital role in the process of seeking help. Most patients speak to a partner or family member before contacting a health professional, and, frequently, the decision to seek help is made and executed by a partner or family member.
-
Receiving the diagnosis
When communicating the diagnosis of MI, health professionals should:
-
Be mindful that patients may attach very different meanings to diagnosis depending on their unique situation and level of understanding as well as their age and stage of life.
-
Many patients are initially very frightened and think that they might die. At the other extreme, patients with very mild symptoms and no pain may fail to appreciate the severity of MI, especially if they are able to return home very quickly.
-
-
Aim to answer patients’ questions in a manner that conveys hope and empathy alongside medical accuracy.
-
Patients usually appreciate explicit and honest communication about their chances of survival, especially if they are brave enough to have asked the question.
-
-
Offer to talk to the patient’s partner or family members about the diagnosis.
-
Answering their initial questions, recommending websites and other resources (and providing or directing towards emotional support if needed) helps to take pressure off the patient at a time when they are likely to feel very vulnerable.
-
-
Be mindful that patients’ emotional response to diagnosis develops and changes over time.
-
Patients those who appear calm and as if they are coping well may nevertheless require psychological support at a later stage.
-
Experience of the hospital environment
Health professionals can make a positive difference to patients’ experience of the hospital environment by:
-
Being aware that the technical equipment of the cardiac unit might be perceived as threatening by some patients.
-
Simple explanations and allowing patients access to objects or services (such as a mobile telephone) that give them a sense of normality in the unfamiliar environment helps to put patients at ease.
-
-
Providing friendly gestures and words of encouragement.
-
Small things like a chat at the bedside or a cup of tea during the night can help greatly to alleviate anxiety.
-
-
Taking time to explain diagnostic procedures, interventions and drug regimens.
-
Explaining treatment decisions to patients in more detail may provide an additional safeguard against mix-ups due to miscommunication and human error.
-
-
Being observant about how patients may be affected by the presence and behaviours of other patients on the ward.
-
Witnessing and interacting with other MI patients on the ward can be a source of support but also a source of stress for patients, particularly when a fellow patient dies.
-
Information about diagnostic procedures, surgery and medication
To improve patients’ experience of treatment, health professionals should:
-
Routinely provide information about risks, benefits and possible outcomes of treatments, and whether or not there are any alternative treatments.
-
Feeling well informed about what will or might happen can help to alleviate patient fears and uncertainty.
-
-
Consider the possible effects that a patient’s surgery may have on their partner and children.
-
Procedures which last longer than expected can be very worrying for family and friends who are waiting for news. Be aware of their need for information and support.
-
-
Make an effort to answer questions fully and check that explanations are provided at a level that the patient can understand.
-
Make eye contact, avoid talking about patients in the third person in their presence and aim to create an atmosphere that allows for genuine dialogue.
-
Be aware that patients’ information preferences may differ in terms of the amount of technical detail or actual procedures they want to know or see.
Preparation for discharge
When preparing patients for their return home from hospital health professionals should:
-
Provide patients with a written, individualised debrief about what happened to them at the hospital.
-
This may be helpful especially if the care pathway involved complications and uncertainties about treatment alternatives. A better understanding of why they had a heart attack and what happened to them during hospital treatment may be important to help patients explain to family and others what has happened to them (thus improving public understanding about MI) in their emotional adjustment. (See also Part 6: the emotional impact of myocardial infarction for patients and their families. )
-
-
Make sure patients feel confident about their medication regimen and have easy access to someone they can contact in case of problems or questions.
-
Side effects from medicines are not uncommon and are often unexpected. Lack of knowledge about possible side effects causes avoidable anxiety and can lead patients to stop taking their medicines without advice from a doctor.
-
-
Provide opportunities for patients to self-administer sprays or other medications while they are still in hospital.
-
This may help to spot potential problems, especially with devices that are tricky to use, build patients’ confidence and prevent mishaps once they have returned home.
-
-
Exploit opportunities for confidence building and setting up positive expectations for recovery while patients are in hospital.
-
What happens during the time spent in hospital can have an important influence on patients’ orientation to secondary prevention and their motivation to make necessary lifestyle changes once they have returned home.
-
-
Consider the information and support needs of the patient’s partner.
-
Partners are likely to need reassurance about the range of activities which are safe for patients to engage in. Where possible, partners should be involved in rehabilitation and lifestyle advice. (See also Part 8: patients’ information and support needs in making lifestyle changes)
-
-
Inform patients and their partners about peer support, locally and online.
-
Be aware that patients of all ages may have their own caring responsibilities (for children, partners or even parents).
The emotional impact of myocardial infarction for patients and their families
When identifying the support needs of MI patients and their families, health professionals should:
-
Be aware that some individuals may have a great need for repeated reassurance.
-
Patients describe the emotional aftermath of their MI as a severe loss of confidence; reassurance is needed especially in the first days and weeks after returning home.
-
-
Explore patients’ and family members’ possible fears regarding a repeat MI.
-
Unaddressed, such fears may lead patients to avoid physical activities or things they previously enjoyed and lead to negative spiral of avoidance and low mood. (See also Part 7: regaining body confidence: patients’ experiences of physical rehabilitation)
-
-
Prepare patients and their partners about the possible emotional impact of MI on the relationship.
-
Partners and patients may need to be prepared to cope with tensions, short tempers and frustrations due to a combination of anxiety, reactions to treatment and partners who might be perceived as ‘overworrying’.
-
-
Offer reassurance and advice to both partners on the safety of sexual activity.
-
Alongside information, some patients may also need emotional support to rebuild their sexual confidence.
-
-
Ensure that patients’ emotional support needs are routinely assessed as part of their follow-up care.
-
Some patients may need professional psychological support that goes beyond the scope of what health professionals or peer-support groups can provide.
-
Part 1: the process of seeking help
Key questions
What is happening to me?
Could this be a heart attack?
Could someone like me have a heart attack?
Where should I seek help?
Key emotions
Fear, embarrassment, uncertainty.
When experiencing symptoms of MI, patients may delay seeking medical help for a number of reasons:
One main and well-researched reason is misattribution of symptoms: if the experienced symptoms do not fit the patient’s idea of ‘a typical heart attack’ – usually imagined as a sudden-onset severe pain in the left side of the arm and upper body – they may find alternative explanations, such as indigestion or back pain, and wait for symptoms to pass. 96 Women, younger people and those with active lifestyles are especially unlikely to consider themselves as possible candidates for MI.
In this study, only one-third of the patients suspected that their symptoms might be related to heart trouble (Figure 11). Many others ‘normalised’ their symptoms and hoped that they might disappear again given time. (In a few cases, this actually happened and patients only learned weeks or months later that they had previously experienced a ‘silent MI’.) One man told how he ‘tested’ himself for MI by running up and down the stairs and was falsely reassured when this did not affect his symptoms.
I didn’t actually suspect there was anything wrong with my heart; I thought I had a backache, a back problem. [. . .] I was still playing football on a Saturday and I used to get some pain during that but it was across my shoulders and up here, and I’d always – you know you see the films and people have heart attacks, clutch their chest, or their breast and fall to the floor. So looking back I don’t really know whether I really did think there might be a problem and that I’ve just chosen to forget it. Because I do remember at work running up the stairs to see if it got worse because I knew [laughs], I knew that would bring something on and then when it didn’t, I thought, ‘well I must be all right then, it must be my back’.
HA11, male, MI in 1999 aged 42 years
FIGURE 11.
Recognising the symptoms of MI. Number in shape: participant interview ID number. Participant sex is indicated by shape fill colour (blue = male; green = female). Participant age at diagnosis is indicated by shape form (square = diagnosed aged ≤ 40 years; pentagon = diagnosed aged 41–50 years; hexagon = diagnosed aged 51–60 years; heptagon = diagnosed aged 61–70 years; octagon = diagnosed aged 71 years and older). Participant marital status: without shadow = single; with shadow = married or cohabiting. Participant ethnicity: white number = white British; black number = black and ethnic minority background.
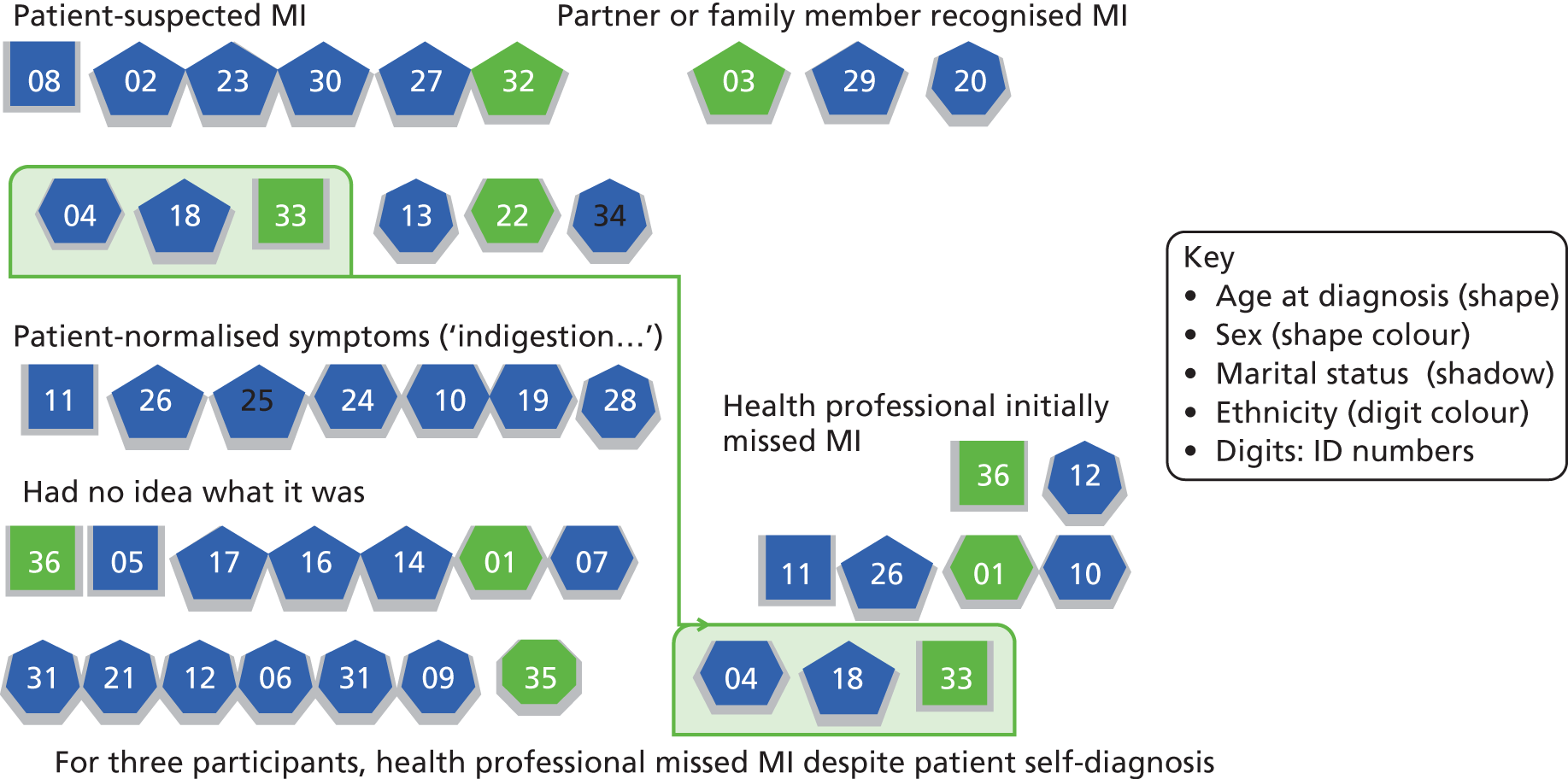
One woman dismissed the possibility of MI because the pain she felt was on the right rather than the left side of her body.
[My husband] and got me some indigestion tablets. It didn’t work. I took a [pain killer] tablet which usually knocks me out. No. So all night I was up with this pain, on and off and he was rubbing my back, and he kept saying to me ‘Are you sure you’re not having a heart attack?’ And I said ‘No, it’s the wrong side’.
HA03, female, MI 1998 aged 53 years
There is a considerable literature about delays in help-seeking, and normalisation and symptom misattribution have been well documented in previous qualitative work. 97
While improved public education about the breadth of possible symptoms of MI and the fact that a broad range of people can be at risk may be helpful, symptom recognition is only one of the factors that accounts for delays in help-seeking. 98 Alongside uncertainties about what a heart attack can feel like, another reason why patients delay seeking help promptly is acute social embarrassment. Having a heart attack constitutes a highly disruptive social event which renders the person experiencing it in the role of a helpless victim. In this study, several patients, all male, said that they had delayed seeking help because they did not want to ‘make a fuss’. The following quote is from a man who described his reluctance to call an ambulance to his holiday hotel.
I suppose in the back of my mind I thought, ‘well, this could be a heart attack but surely it’s worse than that’. Like I said about Rowan Atkinson, that was all I knew about heart attacks. [. . .] So [my wife] said, ‘We’re going to phone NHS Direct. [. . .] After I described the symptoms she said, ‘it sounds to me as if you’ve had a heart attack’, I said, ‘no, no I haven’t, I couldn’t possibly have had a heart attack’ [. . .] and she said ‘I think you better dial 999,’ I said ‘well I’m certainly not doing that’. [. . .] The commotion, the commotion of it and thinking, it was a small guest house type of hotel and you know I could imagine the lights flashing because it was a busy road and there was ambulances flashing all the time you know. It was the drama of it and I didn’t feel it was that bad to be honest. So I left it and [um] slept a bit I suppose and next morning we were going home anyway.
HA14, male, MI in 2003 aged 51 years
Gender differences in seeking help for MI are well documented in previous qualitative research99–101 and interventions to promote prompt help-seeking for MI need to take account of this. Both men and women delay seeking help, but for different reasons. Qualitative research has also explored other gender-specific factors that may delay hospital admission. 33,102,103 Women are more likely to experience atypical symptoms, and are at greater risk of being misdiagnosed. Women may also be taken less seriously by health professionals due to less assertive self-presentation in medical encounters.
One woman told how she was repeatedly admitted to hospital but then discharged without intervention because her electrocardiograms (ECGs) and blood tests appeared normal. She had an angiogram only after her third admission and then promptly received surgery.
And then when I think we went back a third time and went all through the casualty admissions again that there were a set of doctors who were still not prepared to do very much. Then one doctor came along, and I will thank him for the rest of my life, and insisted that three times was too much. And actually he was the one who pushed further in to the problem. [. . .] So I did feel that I wished they’d have listened to me a little more. I felt that three times was enough for them to listen to me. I knew in my heart there was something wrong, oh, that’s a pun isn’t it [laughs]. It just seems as if the nurses were more aware of actual people’s feelings and more aware of what was going on with me.
HA22, female, MI in 2003 aged 63 years
The decision to seek help is a complex and incremental process and the event of an ‘emergency’ is coconstructed by multiple audiences rather than arrived at by the patient in isolation. 104 Partners (or in some cases other family members or coworkers) were described as having played a major role in encouraging the patient to seek help for initial symptoms. Some patients were unaware that delayed admission is likely to result in reduced treatment options and decreased treatment success. Partners frequently pushed their symptomatic spouse to seek medical help or made a call to the GP or emergency service at their own initiative.
Had my tea, didn’t feel well. Went in to the front room. Chest pains started and my arm started the pain and then my wife who was a nurse sort of said to me, ‘lift up your arm over your head’ and ‘did that relieve it?’ ‘No, pain was getting worse’. So I made my way upstairs. Got ready for bed and by that time I got to the bed, my wife had phoned for an ambulance and. I was taken in to [the local hospital].
HA06, male, MI in 1996 aged 70 years
Some patients specifically instructed their partner to call for help, thus effectively relying on someone else to make the case for an emergency response on their behalf. Patients who live alone and do not have this option and support might be at particular risk of delay in getting help.
In this interview study, few patients and spouses directly called for an ambulance. Even in cases where patients themselves suspected MI, several still chose to consult a GP first (Figure 12, yellow-bordered). Some patients who sought help from their local surgery or GP experienced additional delays due to appointment waiting times and the risk of misdiagnoses (see Figure 12, red-bordered).
FIGURE 12.
Delays in hospital admission. Number in shape: participant interview ID number. Participant sex is indicated by shape fill colour (blue = male; green = female). Participant age at diagnosis is indicated by shape form (square = diagnosed aged ≤ 40 years; pentagon = diagnosed aged 41–50 years; hexagon = diagnosed aged 51–60 years; heptagon = diagnosed aged 61–70 years; octagon = diagnosed aged ≥ 71 years). Participant marital status: without shadow = single; with shadow = married or cohabiting. Participant ethnicity: white number = white British; black number = black and ethnic minority background.
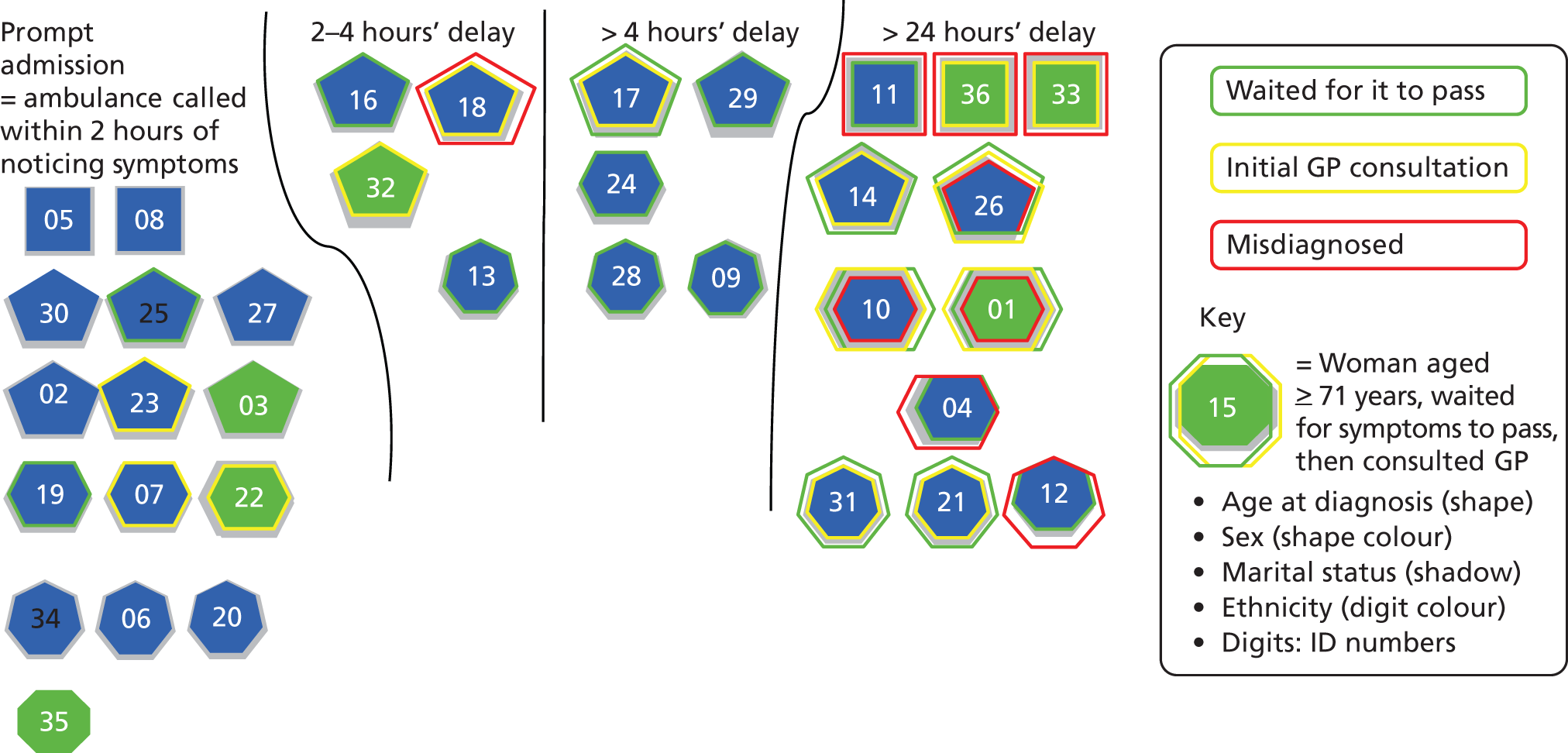
Patients whose GPs knew them well sometimes felt that knowledge of their general health, typical health behaviour and personality had helped the GP to realise that that something could be seriously wrong. In the following account, the GP had picked up that the man’s wife was very worried when they spoke on the phone.
One morning [I was] waking up and just not feeling well at all and of course my wife has always been a person who could recognise when I wasn’t well and she said, ‘You’re not well?’ I says, ‘No’. She says, ‘I’ll get the doctor’. And that was the occasion when the doctor came, dropped everything at his surgery, was in the middle of surgery and came straight round. But in the meantime he’d alerted the paramedics because he did say, ‘that he’d recognised in her voice that there was something seriously wrong’. He got here, the paramedics virtually followed him and they took me in to hospital again.
HA20, male, MI in 2000 aged 66 years
Patients may struggle to accurately describe their symptoms or may understate their impact. People staffing telephone helplines, receptionists and GPs may need to listen to and question patients very carefully to identify when something is seriously wrong. A man who was admitted several days after his initial MI felt that his symptoms were not taken seriously by an unfamiliar GP.
I do appreciate the difficulties that GPs face and that my own case was particularly deceptive, but [. . .] I still think I should have been referred to hospital as a matter of urgency. If a doctor is presented with a sixty-something life-long smoker, not long retired from a responsible and stressful occupation, who seldom attends the surgery and is obviously very concerned about the kind of pain which shouts ‘heart attack’, then, even though other diagnostic features may conflict, he should be given the benefit of the doubt. [. . .] The common cab rank system in larger group surgeries militates against a doctor getting to know patients. Until he retired, I saw the same doctor very infrequently over about twenty years. I am confident that he would have taken me seriously had he still been in practice. I suppose my experience is exceptional, but I do wonder how many people who are referred to hospital expire before their first consultation. I have now moved to another practice and no longer see this doctor.
HA04, male, had MI in 2002 aged 62 years
Symptoms may not be those conventionally associated with heart attack; patients may lack the knowledge and vocabulary to describe symptoms with confidence. Even those who suspect a heart attack may be reluctant to self-diagnose and instead trust that health professionals will recognise the need for urgent action. One woman who said that she had initially suspected that she might be having a heart attack was reassured when, after describing her symptoms, the receptionist gave her a regular GP appointment.
[My ex-husband] came and I told him and he said, ‘Well, phone the doctor straight away’. So I did and I spoke to the triage nurse and she said, ‘Come in at half past eleven’. This was about half past eight in the morning because there weren’t any appointments. She did ask me to describe the symptoms and everything but obviously they weren’t bad and I didn’t have the crushing pain or anything. I just thought, ‘oh I’m going to have [a heart attack]’. But when she said, ‘Come at half eleven’, I thought, ‘oh I must be alright then’. So I went at half eleven and saw the doctor and he said, ‘I think you’d better go down to the hospital. It’ll be quicker if you’re husband takes you, rather than me calling an ambulance’. [. . .] So I went to the hospital and [um] they admitted me. [. . .] When I spoke to the triage nurse, she did ask me what I would consider the right questions. But whether I gave the wrong answer, I don’t know, I could only tell her what I felt and she obviously felt that it didn’t sound serious enough because to me, it didn’t feel serious enough, other than I did say, ‘I felt funny and I’d never felt that before’. And I think your instinct tells you, this is something you’d never had before. I knew I hadn’t had it before. I knew I’d had indigestion before. But she obviously – she misinterpreted what I was saying, I would say.
HA32, female, MI in 2003 aged 53 years
In another example, a woman in her thirties kept seeking help for 5 months because she was concerned about her irregular heartbeat. She was diagnosed with panic attacks before eventually being admitted for MI. The repeated experience of being told her symptoms were imagined made her doubt herself and caused conflict in her relationship as well as shaking her trust in the medical profession.
I never had an ECG done until I had, the day I had the heart attack, never [. . .] I felt like I was, I knew I wasn’t going mad but they made me feel like I was. They made me feel like I wasn’t normal, you know, and I was thinking, ‘God, why do I keep thinking like this?’ You know, thinking that there was something wrong with the way I was thinking because I was being told there was nothing wrong and then I was thinking, well, to me it feels like there’s something wrong. So I felt, I felt hurt, you know, that, and the day when they give me the, the tablets to like calm me down and so when I, I came home and showed my partner those tablets, you know, he started saying to me, ‘you see, they think you’re mad, you know, you’re imagining it. You’ve got to calm down and stop worrying about it and stop freaking out about it because there’s nothing wrong’. So, you know, that, so it’s not only you haven’t got, it’s like everybody’s against you, you know, you feel like no-one’s taking you seriously. [. . .] But I knew there was something wrong.
HA33, female, MI in 2003 aged 36 years
Part 2: receiving the diagnosis
Key questions
Am I going to die?
Why me? Is this my fault?
If I survive, is my life as I know it over now?
Is there any point in making changes to my life or is it hopeless?
Key emotions
Anxiety, shock, denial, despair, disbelief.
Myocardial infarction can be an extremely frightening and life-threatening event, and many patients initially think that they might die.
I was just lying there and they’d given me a lot of morphine so I wasn’t really aware of things going on around me. All I kept saying to people, like ‘can you help me, can you help me?’ I said. And when the doctor come, at first he said, ‘I think it could be pleurisy’, and I was going, ‘oh no, it’s not pleurisy’. But when, actually another doctor come after that and then she told me, ‘Yes, you’re having a heart attack, [name]. We need to get you to coronary care’. And I was going, ‘Am I going to die? Am I going to die?’
HA03, female, MI in 1998 aged 53 years
Before their MI, many said that their understanding of what happens during a heart attack had been very limited, but that the words carried a sense of dread and, if not death, certainly an end to the kind of lives they had led until then. One woman recalled how, after an ECG, her GP told her that she had experienced a silent MI 5 months previously; she felt ill prepared and shocked by the diagnosis.
It was a huge shock. I remember saying to the doctor, I said ‘Do you realise you’ve just given me a death sentence’. And she was ever so sweet. I was, wasn’t very nice to her, I must be honest, because it was such a shock but there we are. [. . .] I burst into tears. She cried because I cried. She was very, very sweet. She gave me a box of tissues and all that. I just couldn’t speak. I felt as though the bottom had dropped out of my world and that I was going to die the next day. I thought she was going to send me to hospital, which immediately panicked me but she didn’t. There’s no way to describe really how I felt apart from being absolutely devastated.
HA01, female, MI in 2003 aged 62 years
One man said that receiving the diagnosis made him feel even worse than he did before he knew what was wrong.
[At] that time I don’t know this heart attack, but the words ‘heart attack’ that’s very heavy words, you know. Everybody is scared. Before I heard this word I was feeling better, but when the doctors told me that, ‘you’ve had a heart attack and you are a heart patient’ and after that my feeling was not better. Because life [is] falling down, you know. You cannot run, you cannot eat of your choice. You cannot work of your choice, like this, like this, you know. Life [is] very badly disturbed.
HA25, male, MI in 2001 aged 49 years
Other patients described themselves as responding more calmly but experienced similar feelings about the threat of dying and the loss of their previous life.
I suppose it was perfectly typical feelings of shock, and of regret that it happened so soon, or that my life was coming to a completely different phase and that I would be disabled as it were for the rest of my life, however long that would be.
HA09, male, MI in 1995 aged 69 years
At the other extreme, patients with very mild symptoms and no pain may fail to appreciate the severity of MI, especially if they are able to return home very quickly. Health professionals should gauge the patient’s view of the severity of their MI so that they can appropriately reinforce the importance of secondary prevention before discharge (see also Preparation for discharge).
I did not feel ill [when I was admitted]. I knew that at that stage I did not feel capable of doing things that I would’ve been capable of doing beforehand but I could wander quite happily around the hospital without feeling out of breath, without feeling the need to sit down. And I suppose the seriousness of what I had suffered just wasn’t evident to me.
HA10, male, MI in 2003 aged 63 years
I found the second attack much more of a pull up, I did take heed of that one. And the fact that I had a really good GP as well, who calls a spade a spade, he doesn’t go around corners, who said, ‘you have two choices,’ he said, ‘you can go back to work and you can die or you can seek medical retirement and hopefully continue a good standard of life’. So I took notice of him as well. I found it very depressing realising that I was not immortal, but as I say we fought through that and came out of the other end, which was wonderful.
HA08, male, mild MI in 1989 aged 40 years and more severe MI in 2001
Patients usually appreciate explicit and honest communication about their chances of survival, especially if they are brave enough to have asked the question. Conscious of the pressures under which health professionals operate, patients sometimes acknowledged that talking about the possibility of death is a difficult conversation to have for doctors and nurses, too.
Some of them, there are one or two who’ve been very good and sat down and explained stuff to me but most of them aren’t too keen, I think that’s mainly a time issue and some of it’s about it’s because they don’t normally do it, there’s a training, there would be a training issue there. But yes, I must admit it’d be a difficult conversation to have with people, because if you know they’re not going to live very long or they’re likely to suffer, would you be the one that’d want to tell them that?
HA05, male MI in 2001 aged 57 years
Patients’ accounts of receiving the diagnosis illustrate some of the aspects of health professionals’ communication style that they experienced as helpful or less helpful. One man spoke very positively about the clear explanations he had received from the consultant straight after his admission to hospital.
A lot of things then happened very quickly. But one of the things that needed to happen I think, was for the consultant to explain (a) what had happened to me but (b) what was required. What he said was that I had had a heart attack and the next few hours were crucial and what was really important, if possible, was to try and attack the clot that would be in my, the part of the heart that the clot would be in. You know I’m not physiologically terribly well-tuned, I’m afraid. He explained – I mean I was very impressed actually because he squatted down and spoke to me at my level. He explained that there were risks attached to this process [. . .] Every intervention was explained to me. [. . .] And, you know, what was very clearly being stated was that, you know, this was the crucial time, you know, that if they were able to intervene successfully now, then my long term prospects of survival, because I mean, I think there was an explicitness that I wouldn’t necessarily survive. My long term prospects of survival and indeed full recovery, were very importantly conditional upon that.
HA02, male, MI in 2003 aged 54 years
Another woman found it reassuring not only to be prepared for the technicalities of the treatment but also to be told that it was normal to feel tearful and emotional.
As soon as I was there [in hospital] they explained to me I was going to be tearful, it’s a big thing, and they explained all my feelings I was going to have. I’m going to do a lot of crying and they explained that they’re going to put this drug in me to get rid of the clot and everything, they just explained every inch of the way what was happening and how I was going to feel. And they was right, everything they said, they was right and they was there, I mean in the night when I was frightened, they was standing at the side of my bed in the middle of night talking to me for an hour or two. They was absolutely brilliant, they was there answering any question.
HA03, female, MI in 1998 aged 53 years
People in the study described feeling reassured by the calm and professional manner in which health professionals had explained the risks and possible consequences of the planned interventions. Patients value health professionals who manage to convey hope and empathy alongside medical accuracy.
Everybody was perfectly civil and, and answered my questions. [. . .] And when the big cheese came in to the ward and I asked him about my prognosis, he smiled and he said, ‘well look,’ he said, ‘you’re here, you’re asking the question. Forty per cent of people who have their first heart attack don’t live to see the day, the next day. So you’ve survived,’ he said, ‘and it appears you’ve survived the previous one as well’. So that was extremely helpful.
HA09, male, MI in 1995 aged 69 years
However, another man described a less positive encounter; he and his wife had nicknamed a certain consultant ‘Dr Death’ due to his brusque manner when describing the possible risks of bypass surgery.
[The consultant] he also wasn’t convinced I’d actually make it through the, the coronary artery bypass. He was surprised that I’d actually made it through that, so like he’s not the sort of guy you want on a football team to gee you up before a game, ‘Hey lads if you keep it down to 10, you’ll do well’. [laughter] He’s not one of those that you want on your team. I think he’s probably going to think he’s trying to give it like it could be, but he probably overdoes how bad it could be. You don’t want an over realistic view but similarly you don’t want to be told that just ‘Well, no it, you could be dead’, because I think everybody knows if it’s heart, you know, if it’s a serious heart problem, yes of course you could be dead, you wouldn’t be here otherwise, [he] just slightly overplayed it.
HA05, male, MI in 2003 aged 37 years
Patients may respond to a diagnosis of MI in very different ways. Health professionals should be mindful of the different meanings the diagnosis can carry depending on the patient’s unique situation, as well as more evident factors such as their age and stage of life. One older woman said that her overwhelming response to receiving the diagnosis was gratitude to still be alive.
I was really pleased I was here you see because lots of people die in the middle of a heart attack. You ask me how I felt, well I felt pleased to be here, still be alive. I think that’s the main thing, I thought ‘well I got over that one and if there’s any more I’m going to get over that’. And as the doctor said an operation could put it right, which it did. It’s strange, it’s a lot to do with the mind, how you tell yourself how you feel.
HA15, female, heart attack in 2000, aged 81 years
HA09 (quoted above) was also aware, because his doctor told him, that he was one of the lucky ones to have survived a first heart attack. However, many of the younger patients felt anger, shock and disbelief to have had a heart attack. Now that many people do not have children until they are in their late twenties and thirties, it is not uncommon for people in their 40s and 50s to still have dependent children at home. Patients may worry about financial and career implications for themselves and their families. They may have different expectations about length and level of recovery than retired patients in their seventies or eighties, although many older patients may also have caring responsibilities. Younger patients talked about a sense of disbelief and the perception that heart attacks were something they associated with their parents’ generation.
I was petrified. Well, part petrified and part believing that they must have it – it must be wrong, you know, I was in the pub yesterday. This all happened on Saturday, I was in the pub yesterday and I’m – and I don’t feel any worse. And then I did start feeling rotten. But I think the whole consequences of it all were dawning on me. And you know, ‘heart attack’, my dad had had a heart attack but he was seventy odd. But it just didn’t – I just didn’t think it could’ve happened.
HA11, male, MI in 1999 aged 42 years
I felt like the world was coming to an end. You feel absolutely shattered, you know really tired and quite depressed really. [. . .] You know, I was only 47 years old. ‘I’ve got a life.’ You know, I have ambitions to reach 97. And you think ‘Well all this is coming to an end; I’m on my way out. This is what my parents should be doing you know, it’s not where I should be. This is for older people, much older people’.
HA18, MI in 1995 aged 47 years
However, health professionals need to consider patients’ individual life circumstances rather than make assumptions based on age alone. The disruption of MI to daily life may be just as severe for older patients as for younger ones, but their horizons of expectation for recovery and their resources for coping and adjustment may be very different.
Those who considered themselves to have led healthy and physically active lifestyles before their MI may particularly struggle to come to terms with the diagnosis. One man, who found it difficult to accept that someone like him could have had a heart attack in his early fifties, explained that it made him feel better when an even younger patient came onto the ward.
I must admit, I felt depressed when I found out I’d had a heart attack. ‘Why me?’ All my life I’d been working on my feet and I thought I was fit. I thought, ‘Why me? There’s other people who sit down at desks, you know bigger than me, so ‘Why me?’ and I was angry as well, it’s hard to explain. You don’t think you’ve survived and thank god you have, but it was a couple of days later when somebody else came in to the hospital who was younger than me, because everyone else in this ward was older and I was the youngest, and when this person came in who was younger than me, I felt a lot better. It’s a terrible thing to say now, but I did.
HA29, male, MI in 1993 aged 54 years
More detailed explanations about the multiple risk factors for MI might help to dispel risk stereotypes as well as provide explanations which can be repeated to family and friends who are curious about why the MI happened.
Conversely, patients with sedentary lifestyles, unhealthy diets and habits may be sensitive to either spoken or unspoken suggestions that they are to blame for their MI and feel very defeatist about diagnosis. These patients may benefit from empathic education that provides encouragement. Previous qualitative research has illustrated how patients’ early sense-making about the possible causes of their heart attack may impact on their motivation for behaviour change and engagement in secondary prevention over time.
Having to tell partners and family members about the diagnosis, and explain why it happened, can be an additional burden for patients. Many patients in this study described having to tell their family as a very difficult and emotional event. While patients themselves feel vulnerable and struggle to make sense of their diagnosis, having to worry about the reactions of their loved ones causes extra stress. Some patients whose parents were still alive decided not to tell them to protect them from worry.
And the worst part was, was telling people. I had to tell my sister. And obviously she was very upset. I was [. . .] Right so and I, then I phoned husband at work and he came home and I phoned, well it was actually my daughter-in-law I spoke to I, I couldn’t get hold of my son – I’ve three boys and – the youngest. Anyway the daughter-in-law came [um] along with my sister and we sat and we talked about it. I was very, very upset. Couldn’t believe, I couldn’t believe it because I felt so well. And I’d had no, no warning, no sign, no anything.
HA01, female, MI in 2003 aged 63 years
HA02 explained that he was particularly worried about his young daughter’s reaction to learning the diagnosis; he and his wife decided to delay telling her until his condition had improved. A couple of patients said they had found it helpful when hospital staff offered to talk to their children.
I suppose the thing that I’m most worried about actually was the impact upon my nine year old daughter [. . .] Over the last 2 or 3 years the only people that she would have been aware of that had had heart attacks; one was her headmistress’s husband that we knew very well, and he just dropped down dead in the street at about my age. And then last summer her best friend’s father, who was a very fit, 64-year-old professor at the university. He just dropped down dead while in Italy, while on holiday in Italy. Therefore, our concerns were that for [my daughter], heart attacks would be seen as being something that killed you. So initially that evening, my wife, didn’t say to, didn’t say to [my daughter] that I’d had a heart attack. She said ‘you know that daddy had a bad pain this morning, well he had to go to hospital but he’s fine now’. So it was about a day later before [my daughter] was aware that I’d had a heart attack.
HA02, male, MI in 2003 aged 54 years
Especially in situations where diagnosis was not straightforward and patients and their families received mixed or changing messages, this could cause strong feelings of anger and guilt among the family.
My husband, because she’d told me there nothing wrong with me and I was fine, I says to my husband, ‘well you might as well go to work’. So he went to work, well he went home, he fetched my daughter and they come back. He didn’t go to work, he come back. Well, he was bitter because he’d left me and I was having a heart attack. So he felt he’d let me down and I felt he’d let me down because he’d gone, he should have stopped, even though I told him to go. And there was all this, but it really upset him to come and see me all wired up and they’d told him there was nothing wrong with me. So you know, they was crying, my daughter and my husband, and I was crying. It’s very emotional.
HA03, female, MI in 1998 aged 53 years
Patients may also feel ill prepared to answer questions from partners and family members, and value the support of staff to explain things accurately and at the appropriate level. Health professionals should check if patients would like support to inform family and friends and answer their initial questions. Recommendations for websites and other resources are also appreciated by patients and families.
Patients’ emotional responses to diagnosis develop over time; those who seem to be coping well initially may nevertheless require psychological support at a later stage. Some patients said that it had taken several weeks or even months for them to emotionally respond to the diagnosis.
I think I was just stunned [um] to the point where I didn’t, I didn’t fully take it in and I’ve spoken to my doctor since and he said, ‘When, when you came to see me,’ he said, ‘you were so calm and you’d had a heart attack, and you were saying, “oh I think it might be a bit of indigestion”, you were very calm,’ he said, ‘and I think it suddenly hit you after a few weeks and that’s why the anxiety came’. It did suddenly hit me that you know I could have died. But it didn’t affect me at the time, I just got on with it.
HA32, female, MI in 2003 aged 53 years
Well with hindsight, you pick up the terminology and I realise now that you just go in to a state of denial, you just don’t accept it. You just refuse to believe that this is happening to me. I enjoyed super health all my life and I worked until I was sixty-five and this happened within three months of me retiring. It just seems so wrong and you refuse to accept it.
HA28, white male, married, MI aged 65 years
Patients with a very stoic and calm response at the time of diagnosis might also be the ones who put up a front towards friends and family and who avoid seeking out peer support. However, maintaining an image of strength and invincibility over a long time is likely to be emotionally exhausting. Previous qualitative research in this area suggests that patients’ ways of coping continue to be influenced by gender stereotypes. 105 Hegemonic ideals of masculinity mean that men may find it especially difficult to come to terms with the feeling of physical vulnerability that the experience of MI brings (see also Part 6: emotional impact of MI for patients and their families and Part 7: regaining body confidence: patients’ experiences of physical rehabilitation).
Part 3: experience of the hospital environment
Key questions
Who and what will keep me safe?
What happens to other MI patients and what does this mean for me?
How long will I need to stay here?
What can I hope for?
Key emotions
Anxiety, worry, lack of familiarity, trust, gratitude, social comparison.
Patients may experience the hospital environment, and especially the technical equipment of the cardiac unit, as reassuring or threatening, depending on their perspective. Health professionals can help put patients at ease in this unfamiliar environment with a reassuring and flexible attitude. Small things can make a big difference, such as access to a telephone.
[In the cardiac ward] I went into a section which is equipped with full monitoring equipment and I was on various drips and goodness knows what else. It’s an intimidating place to find yourself in because all this monitoring equipment is all, emitting all strange sorts of bleeps and noises and it’s very difficult to relax.
HA10, male, MI in 2003 aged 63 years
I was allowed to sit up and have something to eat, make a few phone calls, which was good because it felt a bit like, more like normality. [. . .] I was able to make phone calls to people, although I think people were quite surprised to hear from me, but it was quite therapeutic, hearing somebody else’s voice.
HA11, male, MI in 1999 aged 42 years
Another patient felt grateful that he was given a private room so that his young family could come and visit him without disturbing other patients.
The first night I was taken off the monitors, I was actually in little separate room which was fortunate because I’ve a big family and, [um] they thought it’d be, because they’d a room would be easier if I was in that rather than in a general ward, which was lovely of them because it meant that people could come and go. Because as I say there’s my wife and my young son, well my young daughter as well, my daughter’s only a year older than me son.
HA05, male, MI in 2003 aged 37 years
Several patients in the study said that the first few hours and the first night after their heart attack had been the most difficult and a time when they had felt very worried that they might die alone without anyone noticing. A few said that they had felt so anxious that they had found it difficult to get any sleep. These patients were extremely grateful for friendly gestures from health professionals such as a cup of tea in the middle of the night, someone holding their hand, a chat or words of encouragement, and said these things had made a huge difference to them.
The first night I was taken off the monitors, I was getting panic attacks [pause], because prior, at least if they’re on, I mean in, in reality if you suddenly go crash, the chance of them actually being there watching probably aren’t that strong really [laugh] anyway. The times they do go bing-bing-bing, and nobody comes [laugh], they’d probably look at you and go ‘Oh, forget that, there’s nothing, nothing really wrong because you usually you’ve just pulled it off or something’, 99 times out of 100 it’s just a technical glitch of course. [um] But the first night I didn’t have them I was really quite worried and I called them a couple of times and they were very understanding and very helpful and they actually give me a, a little bit of a sedative to ultimately to sleep, because I just couldn’t sleep, because you’re just so aware of your heartbeat.
HA05, male, MI in 2001 aged 37 years
I found the staff excellent. I found the staff excellent, you know they said to me ‘you’ll be up and running in a few days you know’. One nurse, an Irish girl if I may say, was on night duty. They used to come down and see me every night about, I used to be awake half the night, and make me a cup of coffee about 3 o’clock in the morning, and we’d have a chat and things like that. They did make life good for me.
HA06, male, MI in 2003 aged 70 years
Patients were aware that hospital staff were very busy and often pressurised for time, so they valued it all the more when doctors or nurses provided emotional support by being available to listen or answer questions.
It was the very attitude of them [that made me feel secure], you know. They were very, they were very caring and they sort of seemed as if they really understood how you were feeling. And I was grateful for that because it wasn’t all this starchy business you know, it was nice. And my family were able to come in and they were around me but I was all wired up to everything you know and that is a bit frightening.
HA35, female, MI in 2001 aged 77 years
Many patients spoke very highly of the coronary care specialist staff. By and large, patients felt a great deal of gratitude and trust in the competence of the health professionals who looked after them. Often this was ascribed to personal characteristics and the manner in which they talked to patients, rather than age, seniority or appearance. One man described how the consultant filled him with trust and made him relax despite the fact that the consultant was covered in blood when they first met.
And within about half an hour of arriving, the consultant came in, introduced himself. He’d just, he must’ve come almost straight from surgery because he had – he looked like a butcher. He had a gown on that was covered [laughs] well it had blood all over it. He said, ‘Oh don’t worry, don’t worry, it’s highly unlikely we’ll have to open you up’. But he had this air about him that I was, you know it was just his actions, his voice. I mean he wasn’t very old, he probably wasn’t much older than me, if at all and he was just, I mean it just made me feel relaxed and felt like I was in good hands and that, all the time that meant so much to me that you know, my trust was in these people and as long as I felt that they knew what they were doing, I was going to be all right and that things weren’t going to get any worse.
HA11, male, MI in 1999 aged 42 years
However, some patients thought that the level of information provision during their hospital stay could have been improved. While those who asked a lot of questions usually got answers, others assumed that they would be told what they needed to know without asking. This did not always happen, for example when staff changed. This man was too preoccupied to think of the questions he might need to ask about his stress test.
Another thing that upset me at the time; you’re allocated a nurse when you first get in to the unit. Now then, that nurse after two or three days, her father was taken seriously ill, so she was stood down. Allocated another nurse. So one nurse didn’t know what the other one had told me and now I know I should have asked questions but you’re not, you withdraw in to yourself. You’re angry at being there. ‘Why me at my age?’ I was only 54, coming up for 55 and when I was discharged and went back several weeks’ time for a stress test, I didn’t know what that was. I didn’t know it was a walking machine or a running machine. I didn’t know because I hadn’t been told and I didn’t know to ask.
HA29, male, MI in 1993 aged 54 years
Those who stayed in hospital for longer periods sometimes found that information provision became more patchy as time went on. Patients appreciate health professionals who take the time to explain diagnostic procedures and interventions, even if they are unable to truly share in the decisions. One man observed that the consultants seemed to vary the amount of information they provided to patients. He addressed doctors by their first names to create an equal atmosphere for communication. He appreciated it when a consultant did a drawing of the heart for him to clarify his explanations.
The thing that struck me because you know, hospitals are not private places so although you have screens round, it’s impossible not to hear other conversations going on. And it struck me that there were different levels of information given by doctors. Some of it maybe on the estimation of what the patient will receive and I think some of it is just to do with the assertiveness of the patient. [. . .] I was always fairly questioning and wanted to find out what was going on. I found that actually a very good technique given that the doctors all call you by your Christian name, was I just called them by their Christian name, you know and it’s sort of a – just as a way of getting equality.
HA02, male, MI in 2003 aged 54 years
The asymmetrical power relationship between patients and senior medical staff can be detrimental to the quality of communication. Health professionals can help to redress this power imbalance by making eye contact, talking to patients at the same level (e.g. sitting down by the bedside rather than standing up) and adjusting their manner of speaking in line with patients’ level of understanding.
Change-over of care between different members of staff could mean that changes in drugs were not adequately communicated. HA05 felt it was advisable to double-check with staff that they were getting the correct medication.
Subsequently and while you’re in, when they’re doing the rounds, etc., I don’t think you get an awful lot of information there. I think they just tend to gloss over things and you, you have to ask, you have to check things, because I’ve had one or two instances of problems with wrong dosages of drugs and things being stopped and yet you ask and, ‘Oh no, we shouldn’t be doing that’, Well, you just have’ and you know . . . Not everybody’s necessarily so aware or, or you know, would ask the right questions.
HA05, male, MI in 2003 aged 37 years
Explaining treatment decisions and drug regimens to patients in more detail may thus provide an additional safeguard against mix-ups due to miscommunication and human error.
During their stay on a cardiac ward, patients invariably come into close contact with other coronary care patients. Meeting other patients and witnessing their treatment involved both positive and negative experiences. Several patients said they had found it helpful to talk to others ‘in the same boat’. This man said that even though he would have preferred a room by himself, he experienced the company of other patients on the ward as supportive.
It was quite good being in the ward together [. . .] They were all angina sufferers so it wasn’t quite the same. I sort of leapfrogged them in the scales of who had what wrong, but they understood the pain and the fear of it and it was like suddenly being in a little club. So it was actually quite helpful. I didn’t really like it from the moment I walked in because I’d rather be on my own. But I think it was actually a very good thing because you could actually talk to people you’d never met before in your life about really personal things because they were all in the same boat. So it was actually very good.
HA11, male, MI in 1999 aged 42 years
Another man, who had to return to hospital for a bypass operation, described how the company and atmosphere on the ward helped to improve his experience of the surgery.
They transferred me into a side ward with three young lads in because they thought I would cheer them up. I think the reverse happened, but it was great. There was a 14-year-old with a lung problem who eventually had to get it cut out. There was another young lad with a concave chest, which they were going to take his ribs out and reverse them; a procedure they had never done at the hospital before and there was another chap who was quite an early age to be having bypasses. So we were mixed bag, we settled each other down and the nurses helped. The nurses were quite young, a lot of training nurses, which was surprising. But we were a good mix and we helped each other out and we helped each other to get over their fears, (a) before the surgery and (b) after.
HA12, male, MI in 2003 aged 65 years
Some patients said that comparing their own fate with that of others had helped them to put things in perspective. Seeing other patients make a good recovery gave them hope, but it could also be distressing to realise that fellow patients had died despite being cared for in hospital. Those who were in hospital for several days became aware of the staff behaviour that indicated that someone ‘hadn’t made it’.
But the one thing we, looking round the ward, all had, seemed to have in common is everybody looked most unlike heart problem people in that they all looked fit but to be there they had to be suffering from a heart problem. And I suppose the one very distressing thing was that you soon became aware that, not frequently but on a number of occasions during the time that I was there, people were being admitted and they didn’t make it and we had the all too familiar thing happen where all the curtains were drawn and you knew that somebody else hadn’t made it and they were on their way.
HA10, male, MI in 2003 aged 63 years
Those who are initially in intensive or high-dependency care may find that it is a difficult transition to the ward. The following quote illustrates the difference that a sympathetic nurse made to a patient who was finding it hard to deal with the noise on the ward.
Other people in intensive care had been so quiet and peaceful. Back into a ward, there’s people shouting and there’s a television on, and I, I was frightened, it was horrendous. I can’t explain it. I wasn’t frightened of having another heart attack. It, it was just this tremendous noise; people just shouting across to each other from one bed to another. Turning the television up, any noise at all, was, was horrific. It was, I guess I was seeking peace, peace and quiet. So any noise at all was, was magnified. It was, it wasn’t somebody talking, people to me seemed to be shouting and screaming and I didn’t need that. It was the last thing I wanted; I just purely sought peace and I wasn’t getting it. [. . .] And there was a very sympathetic sister on the ward who realised I was badly affected by the noise, and she moved me into a side ward for a couple of days and then from there into a much quieter ward than the original one.
HA30, male, MI in 1994 aged 53 years
Part 4: information about diagnostic procedures, surgery and medication
Key questions
What are you going to do to me?
What are the possible outcomes? What are the alternatives?
What is my role in this?
Do I have a say? Can I do anything to help?
Key emotions
Uncertainty, worry, anxiety, trust and confidence in health professionals’ competence.
The data analysed in this report were collected in 2002–3. Since then, treatment options for MI have significantly developed, and nowadays many patients will experience minimally invasive procedures and very brief hospital stays. How patients experience these newer forms of treatment could not be explored on the basis of this set of interviews. However, other qualitative research in this area has suggested that while the ‘ “high-tech” procedure of primary angioplasty and fast recovery contributes to high levels of patient satisfaction’, ‘the feeling of being fixed and lack of belief at having had a heart attack may have implications for uptake of rehabilitation and lifestyle changes following hospital discharge’ (p. 85). 106 Patients may tend to see their condition as ‘acute’ rather than ‘chronic’ and their treatment as curative. 107
Involving patients in medical decision-making is now widely regarded as both ethical and beneficial. However, previous qualitative research suggests that health professionals and patients view patient involvement in treatment decisions in coronary care mostly in terms of information provision. 108,109
Many patients will experience feelings of anxiety before having surgical treatment. Health professionals can alleviate fear and uncertainty by keeping patients informed about what will be happening to them and the possible outcomes.
The unknown, the thought of having your chest sliced open, your ribs cut open and your ribs expanded, your heart being handled, being on a life support machine and there’s always a chance even with the best surgeons in the world that you may not come out of it. That really frightened me.
HA17, male, MI in 1980 and 1998 aged 49 years and 67 years, bypass surgery in 1988
When I went in [for the bypass operation] I was very, very apprehensive, I knew he had a 98% success rate and I kept saying to myself I’ve got to be one of the 98 not the 2. I’m a quite positive person really and you know I felt I’m going to be a 98 not a 2, but I was very apprehensive.
HA12, male, MI in 2003 aged 65 years
Health professionals should also consider the possible effects that a patient undergoing surgery may have on partners and other family members.
When I had the bypass, because I was down the theatre 10 ½ hours and [my husband] was expecting me to be back up in 3, he went through hell. He didn’t think I was going to come out of that theatre. And apparently, you know some of the patients’ relatives were saying to me, ‘I’ve never seen a man crying so much’. And every time they went out and said, ‘she’s still in there?’ he’d start crying. He said ‘there’s something wrong, there’s something wrong’. Because the surgeon had told him I’d be out in about 3 hours and when it was 10 ½ hours he . . . and I didn’t know nothing, obviously, I’m asleep. But he went through that. He’s gone through a lot.
HA03, female, MI in 1998 aged 53 years
Previous qualitative research has identified the main existential concerns in surgeon–patient interactions as surviving uncertainty, negotiating responsibility and trusting the doctor’s proficiency. It has also been suggested that when handling uncertainty, doctors are focused on imparting complex information about risk, while for patients, the manner of information provision may serve to establish doctors’ trustworthiness. 110
Positive encounters with staff included those who had made an effort to answer questions fully and provide explanations at an appropriate level. Nurses were usually thought to have more time to talk to patients, and to be better communicators, than surgeons or cardiac consultants.
Rushed as they were, they [cardiac ward nurses] always had time to talk to you about what was going on. They would explain procedures to you. I think you have to ask in some cases, but once you have asked, or once I had asked, they were quite willing to go through and tell you. I think they want to be fairly convinced that you aren’t going to panic or misconstrue what they’re saying, so maybe they’ll be a little bit guarded at first. But generally I think that they’re there to help you get better and if they perceive that what you’re asking is because you want to know and it’s going to help you get better, they’ll give you the right answers.
HA23, male, MIs in 1991 and 1998 aged 49 years and 56 years
There are other barriers to the flow of information between patients and staff, as this woman suggests:
If you ask questions they answer you. If you don’t ask the question, obviously they’re not going to tell you because they don’t know that you want to know. I think probably they could say, ‘Is there anything that you want to know’. I mean they did, they did say that to me sometimes but I know some people are a bit befuddled or a bit in awe of doctors and frightened to ask or they don’t understand the technical terms or what have you.
HA32, female, MI in 2003 aged 53 years
A man voiced his dissatisfaction with the, in his view, disengaged and clipped exchanges he had had with senior clinicians.
What I find so unhelpful is the standard mode of communication with patients that now seems to be adopted by senior clinicians. This is characterised by an absolutely minimalist attitude to factual or explanatory statements that results in a delivery so uninformative and terse that it inhibits any possibility of dialogue. The contrast between consultant--speak and the frank and easy communications that you just take for granted with your GP is stark. [. . .] It’s always possible to find excuses: there’s always the pressure to meet number targets and the chronic shortage of time. It may even be that the high academic intellectual demands of modern hi-tech hardware oriented medicine militates against the selection of good communicators. I recall an elderly lady on the next treadmill to me at a gym session bending my ear unmercifully about some consultant she had taken against in a big way. I hadn’t a clue whom she was talking about until she said, ‘I wouldn’t mind so much if only he would occasionally look me in the eye when he is talking to me’.
HA04, male, MI in 2002 aged 62 years
Patients differed in their information preferences. A number were keen to know as much detail as possible and said that they had been assertive enough to ask the questions. Others were satisfied to have a rough idea of what would happen to them and felt happy to leave the details to medical staff. As the following man observed, providing information at the appropriate level of detail for an individual patient can be challenging for clinicians.
I then enquired as to how [the defibrillator] was fitted. The surgeon actually expressed some surprise that I was interested in the technicalities and he said, and I quite understand and believe what he said, because I’ve found out since a lot patients shut their minds to ‘how’ and ‘why’. It must be a very difficult job for either surgeon or nursing staff to find the right level to pitch the information at, because everybody’s different. In the cath labs where they actually do all these insertions, do all the fancy work with the electrician [laughs], it, I was fascinated to watch it all on the screen and yet there were people who were in the same ward as I was, it was a little four-bedded ward, who asked for their eyes covering because they didn’t want to know.
HA08, male, MI in 1989 aged 40 years
Another man emphasised the difference between the importance of being fully informed about the planned procedure and its attached risks and benefits, and not wanting to be bothered with the full technical details of the operation.
Well, in truth there wasn’t much of a decision to be made [about having the angioplasty]. I had complete confidence in the medical team and they had a clear course of action in mind. There weren’t any options on offer to agonise about. In those circumstances you’d be foolish to do other than go with the flow. Always provided you had fully understood what you had let yourself in for, and subject to the condition, in my fastidious, or just plain nervous case that I wished to be wholly unaware of work in progress. I have never understood this morbid obsession with watching on a display monitor while people poke around your insides. When I next came to I had been fitted with a stent in my left anterior descending artery and diagonal branch. I gather this was thought to be a pretty successful conclusion.
HA04, male, MI in 2002 aged 62 years
One woman acknowledged that it may be difficult to take in all relevant information about the treatments received at the time.
I think sometimes we don’t take things in. It would be useful to be given a sheet, I would like a sheet saying what has actually happened to me. I don’t know what bit of my heart is affected, other than they’ve said it’s the back bit. That’s all, that’s all I heard. They obviously said where in proper technical terms but I didn’t take that in and I would like to know so I think that would be useful for people who want to know.
HA32, female, MI in 2003 aged 53 years
Regardless of their personal information preferences, most patients emphasised that their main concern was the feeling that they could trust the medical staff looking after them and had confidence in their professional expertise and competence. Some patients enquired about the surgeon’s success rates or years of practice in performing a particular procedure. Interpersonal skills were also important in promoting a feeling of trust (see also Part 3: experience of the hospital environment).
One of the things that I wanted to know from the surgeon was how many of these things had he done. Was he, sort of, did he know what he was doing and he told me, this was September, he told me by that time he had done about 140 bypass operations that year. So that was you know, quite reassuring. And I also asked him what the prognosis was and he told me that 95% of all cases of, who have bypass surgery are successful, and 5% are not. So you’ve got a 1 in 20, is it? yes 1 in 20 chance that something might go wrong. And I said ‘what can go wrong?’. He said ‘mostly what can go wrong is that you get some kind of sepsis and we can fix that’. So I thought the odds were pretty good, bearing in mind that my cardiologist said I’ve got to have this done, not much choice.
HA09, male, MI in 1995 aged 69 years
While very few patients described instances of shared decision-making, the case of one elderly patient illustrates how upsetting it can be when patients’ own values and priorities are ignored in the course of deciding treatment options. This woman in her early eighties said that she had been judged to be too old to be operated on. She felt that the medical agenda of minimising risk conflicted with her best interests as a patient.
[I felt] devastated, devastated because they said, ‘oh yes, next week we will be taking you down to the theatre next week’ and when next week came they changed their minds because they brought another somebody else in who said, ‘Oh no, no, she’s too old’. And they said it in front of me, I’m too old and I felt so old, I felt ancient. Really, really I felt about 900 years old and I said, ‘well I don’t mind dying on the table, I won’t know anything about it’. But they said, ‘but we will and we don’t like to lose a patient’. But then I said, ‘you have a chance of saving one, too, haven’t you’. [. . .] I could quite understand they don’t want to lose a patient, it’s not good for them to lose a patient and if the chances are 50/50, I think they’d rather take their 50 on their side and have you die at home than on their table. That is fair enough, but then from the patient’s point of view, who hasn’t got much chance anyway, she would rather take the chance on the other side of the 50 and go ahead. Wouldn’t you?
HA15, female, MI in 2000 aged 81 years
This patient eventually found a consultant who was willing to perform the operation and made a good recovery.
Part 5: preparation for discharge
Understanding as much as possible about why they had a heart attack can be an important stepping stone for patients on the road to recovery. A few patients said that the reasons had never been fully explained to them.
I felt really hurt and angry, angry that, you know, I’d had a heart attack as well and then I was looking back at my life and, you know, thinking, you know, why? Why did I have a heart attack, I didn’t do anything, you know, really bad, to excess. I smoked, that was the only thing that I did really, and worked hard. [. . .] No-one has ever actually sat down with me and spoken to me about the heart attack or why I could have had a heart attack or, or anything like that, really. I, I don’t think there’s enough, well for, for me personally, as a patient, I didn’t feel, think that I was spoken to enough about it. [I would have liked] a lot more reassurance about, you know, about life in general and life after the heart attack and, you know, what I can do and what I can’t do. You know, I think that’s what I need, I think that’s what you need after you’ve had a heart attack is reassurance.
HA32, female, MI in 2003 aged 53 years
One patient suggested that a personalised, written record of what exactly had happened, and why, would have been helpful as it was difficult to take in all the information at the time. Having a personal record to revisit over time might also help patients come to terms with their MI at their own pace and to explain to family, friends and others about what had happened (thus also helping to improve public understanding of MI) (see also Part 6: the emotional impact of MI for patients and their families).
Most MI patients will have to continue taking a range of medications after being discharged. Having to remember to take a mix of different tablets can be difficult. In the study, several participants were unsure what each of the tablets they had been prescribed actually did. This lack of knowledge made it harder for them to self-manage with confidence.
I said ‘What’s this for?’ I asked them what it was for and they said ‘It’s to slow your heart rate down’. I said ‘But I’ve got a slow heart rate,’ and you know, I don’t know anything about the medicine, and I’m just doing what they tell me.
HA13, male, MI in 2002 aged 70 years
Health professionals should make sure that patients can administer their medications with confidence and know what to do and who to contact in case of questions or problems. This man was uncertain about how to apply his spray and passed out after taking an accidental overdose.
When I left the hospital [the spray] came with my pack of pills and another Nitromin spray and the nurse had told me then that if you do feel angina or any chest pain, give yourself a spray under the tongue or she said even two if it’s bad, so I thought two would be all right. But I hadn’t have any experience of using it, you see. When I was in hospital I did have it administered for me. The nurse said ‘hold your tongue up’ and just sprayed it in for me, which was easy. When you do it yourself the aim is a bit doubtful. [. . .] Three or four weeks [after being discharged] I thought I better take a spray here, I’m not feeling too good and then I wasn’t very used to using this spray, you have to aim it under your tongue, you see. And the first one I sprayed mostly on my teeth, I thought well that’s no good. So I sprayed again and it went on my lip and it wasn’t until the third one, I tried again the third time that I actually sort of satisfied myself that I’ve got it on, because I was panicking and thinking about angina and everything else. Gave myself three doses of this spray and I fell over. I completely collapsed, I just couldn’t believe it. It just, it lowers the blood pressure so much that it’s virtually zero.
HA14, male, MI in 2003 aged 51 years
Patients may not necessarily read the supplied information about possible side effects of medication and might be frightened if they experience unexpected symptoms, especially if these resemble the symptoms of MI. If side effects are very uncomfortable, patients may decide to stop medications without consulting a doctor. One woman who worked as an advisor in a peer support group said that she was happy to take her tablets because ‘I understand why you’ve been given them and how much worse I’d feel without them’. She described an encounter with a woman at her class who had stopped taking her diuretic.
[. . .] I have one lady who comes to the class who was prescribed bendrofluazide, small dose and it’s a diuretic. And for mature people, bendrofluazide is the drug of choice to help bring down blood pressure, it’s not just a diuretic. And I was asking this lady about her tablets one day and mentioned that one and she said, ‘Oh I don’t take that’. ‘Why?’ ‘Well because it makes me go to the loo a lot.’ And I had to explain that’s what it’s supposed to and by doing that it brings the blood pressure down.
HA22, female, MI in 2003 aged 63 years
As this quote indicates, peer support (online or in person) might also present a helpful resource for patients to discuss alternative ways of taking medication, strategies for remembering tablets and exchanging information about the range of side effects they might be experiencing.
Health professionals can play a key role in building patients’ confidence after the experience of MI and shaping their expectations for the future once they return home. This in turn is likely to influence their motivation to make positive lifestyle changes. Building these expectations begins straight after diagnosis; time in hospital can be an important influence on the patients orientation to secondary prevention. Explaining to patients the possible causes for their MI may provide opportunities to motivate patients to change their diet or give up smoking. Such attempts can be undermined by hospital catering services – one man commented on the irony of hospital catering serving up crisps on the cardiac unit.
I remember being amused actually because I was hungry on the first day because I’d had nothing to eat and, but equally I wasn’t on the hospital’s food ordering process so they said they’d bring me a sandwich box. And there I was, you know, on a cardiac care unit and this little box comes and the first thing I get when I open it up is a packet of crisps, which struck me as sort of fairly bizarre, you know, this being about the worst sort of thing to eat. And I did sort of talk about that and they said ‘well we can’t change people’s habits overnight’ you know. But for the rest of the time I was able to choose food that was fine, and I was actually quite pleasantly surprised by, you know, that there was a range of reasonably healthy food available if you wanted it.
HA02, male, MI in 2003 aged 54 years
Providing patients with a palpable experience of the prospect of recovery may have even more powerful effects than words. One man told how his speedy improvement on a simple breathing exercise had encouraged him.
The physiotherapist started working on me I think at day two, or thereabouts. The first thing she asked me to do was to have breathing exercises with a little gadget, which she provided me with. You had to not blow, but suck. You had to fill your, your lungs as much as you possibly could and there was a little indicator that showed how much that was. And there was an amazing improvement after a few days. The amount that I could fill, fill my lungs with was increased very dramatically.
HA09, male, MI in 1995 aged 69 years
The same man also talked about how seeing a rehab class in action also had a very motivating and positive effect on him and his wife.
Before I was discharged the physiotherapist took me to the gym downstairs and in the gym there were a number of people doing various exercises and she said they were all ex-patients who had had bypass operations and I was, you know, I was pretty impressed. You know, they were doing, they were jumping up and down and they were doing skipping, and they were doing a mild form of press-ups. A number of fairly strenuous looking things and I thought, oh well it must have been two or three years since they’ve had their bypass and I asked her about that and she said, turned to one of the chaps and she said ‘How long ago have you had your bypass?’ and he said, ‘Oh, just six weeks ago now’. So that was, that was a real eye opener and again something very positive. And really from that moment on I felt, and my wife, we both felt very positive about the whole thing.
HA09, male, MI in 1995 aged 69 years
Part 6: the emotional impact of myocardial infarction for patients and their families
Key questions
Why did I have a heart attack?
Will it happen again?
Can I still be the person I used to be?
Who or what will help me cope with what I feel?
Key emotions
Frustration, grief, loss of confidence, stigma and isolation.
In the days, weeks and months following a heart attack, patients and their families need to adjust to life with a chronic health condition. Besides lifestyle modifications and adoption of new routines such as taking regular medications, patients need to come to terms with the disruption the MI has caused to their sense of identity.
‘Loss of confidence’ was a phrase that was used by almost all patients in the sample when they were asked how the experience of MI had affected them emotionally. ‘Reassurance’ was what they said they most needed from health professionals. For some, the sense of vulnerability and threat was so severe that it led them to abandon activities they had previously enjoyed, leading into a negative spiral of avoidance and depression.
At the moment I don’t feel I ever will be confident enough again. And I, we were going to go on holiday with my sister to Portugal, because last year we went and we had a lovely time and we said we’d go again this year. I won’t fly. I don’t want to go which was a little bit upsetting for my sister. We had a few words because she didn’t understand how I felt. I don’t suppose she ever will understand how I felt, but there is no way I am leaving the country. And there’s no way I’m leaving Wales. It takes me all my time to go to [the local town] because if anything happens to me, I want to go to the hospital, the [local hospital] in [a nearby town].
HA01, female, MI 2003 aged 63 years
Patients who considered themselves in good health and had led an active lifestyle before their MI may feel that they have not only experienced a life-threatening event but have also lost an important part of their previous identity. A loss of confidence in the body can make people afraid to do any kind of exercise – even though most of them were well aware about the importance of physical activity for secondary prevention (see also Part 7: regaining body confidence: patients’ experiences of physical rehabilitation).
A heart attack hits you emotionally as well, that’s what I found. I couldn’t believe it that you know that I’d done all that I could do to be fit, have the right diet, I don’t smoke, I’m not overweight. I just, you know, I just couldn’t believe and if I could have a heart attack, well lots of people said that to me, if you can have a heart attack anybody can. So that made me feel very humble.
HA14, male, MI in 2003 aged 51 years
Patients spoke of a continued sense of stigma surrounding MI and several patients said that they had been selective about who they had told. Those who had made use of peer support and community-based rehabilitation groups spoke very positively about the value of talking to others with similar experiences. However, some patients do not have easy access to this form of support. While some people may benefit from encouragement to use such resources, it is important to recognise that others do not want to meet other people who have had a MI; they may prefer the relative anonymity of websites or telephone helplines. Health professionals should, therefore, give patients addresses for online support groups as well as any locally available resources (see also Part 9: building a supportive environment: myocardial infarction patients’ ongoing support needs).
People in the interviews often said that their partner had been a vital source of emotional support for them in the weeks and months following their heart attack. However, the experience of MI could affect the relationship and bring about a renegotiation of roles within the marriage. This could sometimes be a difficult process.
I suppose having been the breadwinner. I’m from a generation that I never wanted my wife to go out to work. Maybe we were fortunate that we were in such a position that she didn’t have to. And following my initial heart attack, and certainly following my enforced medical retirement some thirteen years ago, I found it difficult, very difficult to come to terms with that and were my wife present, she would tell you that I made life quite difficult for her at that period. Partly related to the job that I had, I was used to being in a position of authority and I found it quite difficult to find a reason for being.
HA08, MI in 1989 aged 40 years
Male patients, in particular, said that they had found it difficult to pass on some of their previous responsibilities, such as driving, to their spouse. A few men who had to take early retirement on medical grounds said that they felt useless and emasculated following their MI. Findings from previous qualitative research confirm that men are at risk of experiencing a crisis of masculinity after MI. 111 For women, on the other hand, it might be difficult to step back from previous domestic tasks and demand additional support from family members.
Some patients also acknowledged that they themselves had become more difficult to be with and a few said that they had become much more short-tempered, possibly as a result of medication side effects.
Well, you know you see the bad side of the thing, you’ve had a heart attack, how bad has it been, what’s the damage, are you going to have another one. If I do this I may have one. I mustn’t do this, I mustn’t do that. In a way it made life a bit hard for my wife. I realised that fully and the treatment I’m on, these various tablets, they do make you a little bit short tempered, I’m understand. And I snap at her sometimes when I shouldn’t. But that may be one of the side effects of it.
HA06, male MI in 1996 aged 70 years
My wife got the, the brunt of my sort of emotional state and it’s something that the consultant had said that you know, I’d have ups and downs and that I might get tearful and if you think you want a good cry to, you know, just let it happen but it will pass. But everybody else was saying how marvellous I was doing and patting me on the back for handling this terrible thing so well. And I mean my wife was getting recognition for the support she’d given me as well but it was, I think it wasn’t fair that everybody was saying how fantastic I was handling it when my wife was getting the dark side.
HA09, male, MI in 1995 aged 69 years
I’m very, very glad that we had such, and still have such a strong marriage [um] because the black moods, the despair and very much out of character after the triple bypass initially had me breaking down and crying for no apparent reason. I could have been talking much as I am now, to either my wife or a friend or a colleague, and I would start to cry and to this day I couldn’t tell anybody why. I then got quite black moods, a case of ‘Why me?’, ‘Why is it happening to me?’ ‘What have I done, what have I done to deserve it?’ All the usual sayings and I think because it’s the nearest and dearest, the only person that’s with you at that time, you take out of them some of your own anguish, some of your own anger.
HA08, MI in 1989 aged 40 years
Health professionals can play a positive role in mitigating the impact of MI on couples’ relationships by helping to prepare patients and their partners for the strains that might occur. Hearing accounts from other patients and partners may also help to understand points of conflict and develop strategies for dealing with marital tensions.
Some patients in the study did not feel able to openly talk about their concerns with their partner because they did not want to worry them.
I don’t think I can fully talk to my wife sometimes about my concerns because [sigh] I think she overly worries about it. On some things she, she gets then frightened and worried about it, and then I only then get upset for her, which doesn’t help me. So the point of trying to share it with somebody helping me, it just defeats, all I’m doing is telling her something that upsets her and I’m thinking where was the benefit in that, that, that’s not to say if there’s something we need to worry about and do something about, that I certainly shouldn’t be hiding something like that from her. But some of the concerns that you might just want to chat to somebody or you know, get off your chest, I wouldn’t do it with my wife now because of having seeing her react.
HA05, male, MI in 2003 aged 37 years
Having a named health professional who is easily accessible (perhaps via e-mail or a telephone messaging service) to provide reassurance on non-urgent concerns was greatly appreciated by patients. Several said that they had benefited from a trusting and supportive relationship with their cardiac nurse.
Partners are likely to worry about the occurrence of a repeat attack, sometimes more than patients themselves, and they might also experience feelings of powerlessness and frustration. Initially after returning home, some patients said that they had felt ‘mollycoddled’ by an overprotective spouse.
She wouldn’t let me out of her sight, that was the main thing. She would have followed me to the toilet if she could. She wouldn’t let me go – there’s a shop 300 yards away from here where I go and buy a paper. Wouldn’t let me go and do that. She was very protective, it worried her a lot, more than I think it did me and I think that is the impact on people.
HA12, male, MI in 2003 aged 65 years
Many patients said they had found it very helpful when a consultant or nurse had talked to their partner to reassure them on the kinds of activities that were safe for patients to engage in during the period of recovery. Involving spouses in rehabilitation could also provide much-needed reassurance.
We found that a lot of the stress after the operation derived from the fact that she was more, more worried about, about what I could do than I was. And she was trying to hold me back all the time whereas I was always trying to go. And one of the benefits of joining the support group is precisely this, that the spouse has a chance to speak to other spouses and see you know, what you can do and what you can’t do and that takes away a lot of the stress of rehabilitation. [. . .] [Also] Dr X was very instrumental in helping me there. He said to my wife, ‘Look he’s got a body and his body’s going to tell him what he can do and what he can’t do’. And my wife took that on board and it was far easier and then from then on we made jokes about it.
HA09, male MI in 1995 aged 69 years
Previous qualitative research has particularly highlighted a need for guidance for both partners on sexual activity. 112–116 One man said that his wife had been more concerned than he was about restarting sexual relations after his heart attack, but openly talking about her worries had helped them to get past it.
Resuming your sex life after a heart attack, it’s quite difficult. It wasn’t so much difficult for me as for my wife actually. She was very concerned that I was going to throw another wobbler when . . . [. . .] What helped was talking. You have to, you have to always, you can tell when things are not quite right, ‘So what is the problem?’ ‘Oh I’m a bit concerned, I don’t want you to hurt yourself, I don’t want you to.’ ‘Okay I’m not going to hurt myself, I’m aware of what I’m doing. If I hurt, you’ll know.’
HA18, male, MI in 1995 aged 47 years
Alongside information about the safety of sexual intercourse, patients may also require emotional support if their body image and sexual confidence have been negatively affected by surgical scars.
Because of the scar on, I didn’t want anybody to look at me, even my legs, you know with the scar all up my leg. I didn’t want anybody, I’d wear trousers all the while. And I didn’t want anybody to see the scar down my chest. It sort of, it’s you know, it was horrible, it was. And I didn’t feel, and I just didn’t feel sexual at all. I just didn’t want to know anything like that.
HA03, female, MI in 1998 aged 53 years.
People also sometimes find positive ways of coping with the emotional impact of MI; for several study participants, the experience of MI had sometimes been a turning point from which to reassess their priorities and make positive changes. Several had become actively engaged in cardiac rehabilitation or peer support groups or embarked on new projects that gave them hope and enjoyment (see also Part 6: building a supportive environment: myocardial infarction patients’ ongoing support needs).
However, some patients may need more intensive psychological support to help them come to terms with their heart attack and to find positive ways forward. The extended extracts below illustrate two cases of patients who experienced prolonged periods of severe depression after their MI before they found help.
Case study 1
One younger woman (HA33, MI in 2003 aged 36 years) developed panic attacks in the aftermath of her MI. After returning home from hospital, she at times felt too anxious to stay at home by herself. She was lucky to have a supportive family and was able to stay with her mother for stretches at a time.
Well I had visitors, everybody sort of kept an eye on me without trying to be too obvious. I did have bouts of anxiety and I would go and stay with my mum. My son would take me over there and I’d stay for a few days and then I’d come back when I felt better. And apparently, this happens quite a lot with people who are reasonably young having a heart attack, you get these anxiety attacks, which again is this wave of feeling which is similar to the heart attack but, but not quite the same. And I would get it for no apparent reason; it was obvious that my brain was doing something that I wasn’t really aware of. Then I would feel dreadful and I couldn’t, I didn’t want to be on my own, so my mum would look after me for a few days and that was nice.
Her depression continued for several months and led her to withdraw from people around her.
I was very, very low and I mean very, very low. Tearful, [um] depressed, depressed is the only word I can describe, really, really depressed. And [um] I didn’t want to go out the door. I didn’t want to go out the door, I didn’t want to do anything. Even after having that done, I still was so depressed and down and I didn’t want to do anything.
She described how she was eventually helped by the dedicated one-to-one support from a cardiac nurse, emphasising that this level of support would not have been possible in a group situation.
It was only [um] [the cardiac nurses] support that got me through it [. . .] Well, I think with [the cardiac nurse] it was her, it was the one-to-one basis, it’s not, it’s not being done in a class and then you can get to speak to somebody and she can, you know, find out more about you and find out why, you know, you’ve had a heart attack and why you’re still feeling down. And so she spent the time with me to get to know why I’d had my heart attack, why I felt so down, so she had something to work on then. And so she just helped me, you know, learn to relax because after you’ve had a heart attack the last thing you want to do is relax. You know, you’re scared to go to sleep in case you don’t wake up again so, you know, she just reassured, she gave me a lot of reassurance and a lot of help, a hell of a lot of help. [. . .] I’m a lot better now, obviously than what I was but I’m still getting there. I, I’ve still got to keep up the relaxation and stress management.
Case study 2
A man (HA30, MI in 1994 aged 53 years) who had previously enjoyed a very active lifestyle developed unstable angina after his heart attack and described how he became very depressed as a result of the constant feeling of physical vulnerability.
I eventually did come out of hospital after I was there for a fortnight. But when I got home, nothing was the same. I wasn’t the same. [Pause 4 seconds] There were days I would quite happily have died. I’d made up my mind, that if I had another heart attack, I wasn’t going to be the one to send for an ambulance because I did not like what was happening to me; it was just so horrific, so depressing, miserable, it was just no way to live. And this of course was only a month after I’d had the original heart attack.
He subsequently developed panic attacks and sank into a deep depression which affected his family life and left him feeling suicidal.
Angina started over the most silly thing. I could watch a programme on television, feel a bit sentimental about something in the programme and I’d get angina. I’d often have to walk out the room. That became [pause 3 seconds] the, the biggest thing in my life this depression, this fear, constant thoughts of suicide, that everything physical seemed to just, didn’t matter. It didn’t matter that I was out of breath when I got to the top of the stairs. Taking tablets, which I hate, to this day I hate, I went through this period where it didn’t matter. I’m supposed to take the tablets so I take the tablets. [. . .] Any confidence I’d had before just drained away. I, from that moment on, I became a failure. I did everybody down, I’d never be good enough to do anything worthwhile again. It was all psychological [um] but it was overwhelming, and from that day I have never been the same. It was quite, quite horrendous.
The turning point came when he asked his GP to sign him off work and he was referred for counselling.
So I ended, had to go to the doctors and say, ‘I’m just not coping’ and they signed me off again and fortunately sent me for counselling. That in itself was another blow to my confidence, the fact that I, of all people, would have to go through counselling. But there was an extremely patient lady, who I was seeing. She was concerned enough that she, she saw me every week, once a week. [. . .] So thrashed all this out and gradually having somebody to talk to in that way did help and I’d recommend to anybody, if they’re offered the chance of counselling, to go for it. Just get it, everything off your mind, get it off your chest as they say, [um] and it did help me.
After the counselling had come to an end, he asked to be referred back to rehabilitation classes. There he managed build a trusting relationship with one of the rehabilitation nurses who suggested that he try Reiki. He was very sceptical initially but now feels this has taught him the essential skill of relaxation and he manages much better than previously.
It was so absolutely wonderful, so refreshing, so relaxing that, yes, I can switch off. I can [pause 3 seconds] sit and watch television, and think of [the nurse], and I don’t go into a trance, but I – everything just washes away. Nothing bothers me, I’m completely at ease with myself. I’m still not the happiest person, I know I’ve got problems, but I can make them go purely because what I learnt during Reiki. And to be able to just switch off, I’m 63; I’ve never been able to do that in my life.
Part 7: regaining body confidence – patients’ experiences of physical rehabilitation
Key emotions
Emasculation and vulnerability.
Worry and uncertainty.
Ambivalence towards exercise.
Empowerment and confidence.
Key questions
Will my body fail me again?
How much physical activity is safe for me to do?
How much exercise is beneficial?
How can I fit exercise into my life?
Insights from previous qualitative research
Previous research on cardiac patients’ engagement in rehabilitation schemes has reported great variation in the type of programmes offered to patients across different NHS localities as well as considerable variation in take-up rates. 120 It has also been suggested that existing schemes do not sufficiently address the needs of particular groups of MI patients who are known to be under-represented among the attendees of cardiac rehab programmes, such as women, people with ethnic minority backgrounds and older people. 121
Several qualitative studies have explored patients’ reasons for and against attending exercise classes and possible structural and personal barriers to accessing such programmes. 122–124 For example, O’Driscoll et al. 124 identified lack of professional training, role confusion among rehab staff and weak communication between secondary and primary care as service-related barriers to successful engagement. They found that staff struggled to prescribe accurate training intensities, had insufficient space/resources to invite partners along and did not transfer information from hospital stress tests, meaning that they were unable to tailor exercise to patients’ individual needs.
Cumulative insights from qualitative work on patients’ experiences of cardiac rehabilitation suggest that non-attendance and attrition from formal programmes are rarely rooted in patients’ lack of knowledge about the importance of exercise and adoption of a healthy lifestyle. Non-engagement should, therefore, not be dismissed as ‘non-compliance’, but is more fruitfully understood as well-reasoned decisions based on patients’ – not necessarily accurate – beliefs and perceptions which can be amenable to intervention122 or as the preliminary result of decisional ambivalence. 125 Instead, patients’ sense of self-efficacy, embarrassment about public exercise and perceptions about other attendees as well as the health professionals involved in delivery have been identified as some of the factors that influence patients’ decision-making about whether or not to attend cardiac rehabilitation schemes. 122,123 Qualitative studies have also shown that patients’ perceptions are subject to change over time123,126 and therefore greater flexibility in the ways rehab schemes are delivered may help to increase their reach. For example, Jackson et al. 123 argue that offering places on rehab schemes for a narrow time window only is likely to result in missed opportunities for those patients who initially may dismiss the need for this type of support but may change their minds when they find that their recovery does not progress as well as they had hoped.
Fears that physical activity will bring on repeat myocardial infarction
All participants in the study were conscious of the importance of regular exercise as a key aspect of secondary prevention. However, many of them said they felt unsure about how much physical activity was safe for them to engage in, and also, how intense and prolonged exercise would need to be to achieve a beneficial effect for their cardiovascular health.
People described their fear of having a repeat attack if they ‘overdid it’ when exercising. The experience of MI could fundamentally alter their relationship with their body: it was no longer trusted to function routinely, but was anxiously monitored for possible signs that another cardiac event was about to happen. This woman’s account illustrates the vicious cycle of fear of repeat attack, avoidance of rewarding physical activities and low mood.
I’m terrified [to go exercising by myself]. I wake up in the morning and I think right now today I will go for a swim. Right, I get my bathing costume, towel, bag, right who can I phone to come with me. So then I phone my sister’s husband, no he can’t come. Right, there’s nobody else I can phone, so I think ‘Well I won’t go, I’ll go tomorrow’. And then for the rest of the day I feel guilty because I haven’t been but I can’t go because I’m scared. What if anything happens to me in the baths. Who’s gonna be there. Whose gonna take me home. You know, if I’m going to die I want to die at home in my bed. I don’t want to go to a hospital and I don’t want to have an operation. So if I’m gonna have this heart attack I’m gonna die at home in my bed, so I’m not going out am I?
HA01, female, MI 2003 aged 63 years
Participants’ experience of formal rehabilitation programmes
The accounts of participants in this study describe a great deal of variation in terms of duration, organisation and content of the types of programmes they were offered. This is likely to reflect both the geographical and temporal range of their experiences (remote, rural, small town and urban settings, and 1989–2003, respectively). In reading the findings presented here, it should be borne in mind that participants were sampled at different stages of the rehabilitation process, allowing some of them to report on recent rehab experiences while others could offer more of a bird’s-eye view of how their experience of exercise classes had shaped their personal engagement in rehabilitation in the longer term.
Figure 13 provides an overview of the types of programmes participants in this study were offered and engaged in. Figure 14 adds information (where available) about whether or not participants continued to engage in regular exercise after completing the initial programme.
FIGURE 13.
Patients’ participation in cardiac rehabilitation programmes. Number in shape: participant interview ID number. Participant sex is indicated by shape fill colour (blue = male; green = female). Participant age at diagnosis is indicated by shape form (square = diagnosed aged ≤ 40 years or younger; pentagon = diagnosed aged 41–50 years; hexagon = diagnosed aged 51–60 years; heptagon = diagnosed aged 61–70 years; octagon = diagnosed aged ≥ 71 years). Participant marital status: without shadow = single; with shadow = married or cohabiting. Participant ethnicity: white number = white British; black number = black and ethnic minority background.
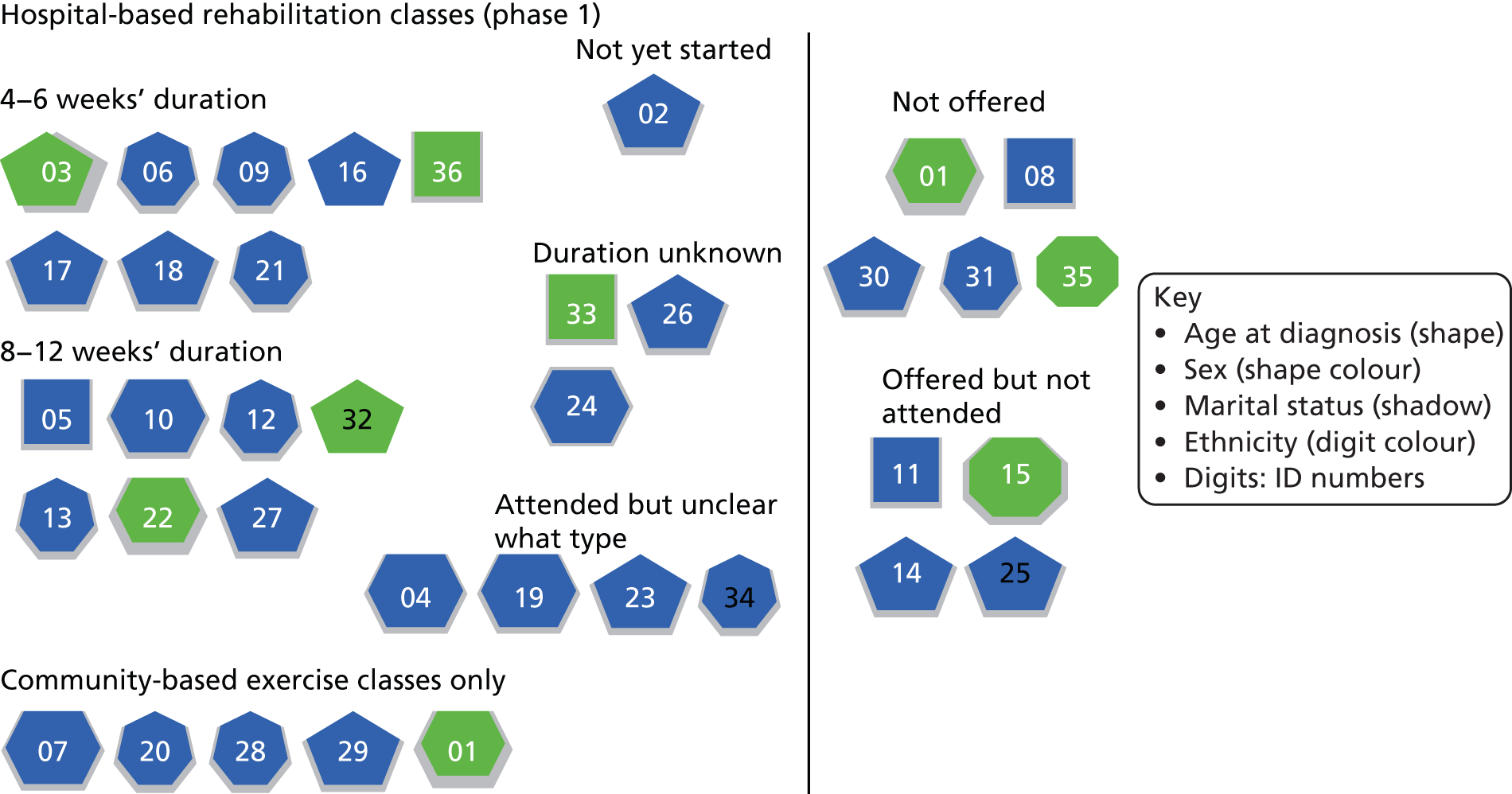
Finding out about rehab schemes and waiting for a place
The majority of participants in this study were offered hospital-based rehabilitation classes in the form of twice- to thrice-weekly classes, running for 4–12 weeks, which combined supervised exercise with education and advice about healthy lifestyle. Most patients said they had been told about hospital-based rehab classes through their cardiac nurse, either just before or just after discharge from hospital. However, several participants said they had to wait for several weeks, and in some cases, months, before the start of the scheme. This could be a very anxious time for patients. This woman described her uncertainty and worry regarding the physical sensations she experienced.
I was frightened to come home. I didn’t want to stop in hospital but I didn’t want to come home. I thought, ‘well my husband’s got to go work, I’m going to be on my own’ and it’s really frightening, that time. From, I think it’s about 8 weeks, that 8 weeks from coming out of hospital to going to the rehabilitation, it’s really frightening because you’re sitting on your own and you have these twinges and you have pain in your chest, you know all these things are happening and I think all it is, is fear. When you’re frightened you tense up, and I think that’s what brings the pain on.
HA03, female, MI in 1998 aged 53 years
A couple of participants said that the offer of a hospital-based rehab place came so late that by then they had already recovered to an extent where they did not think they could gain any more from the programme. One younger man who, unlike many others in the study, felt confident about exercising, but who thought the rehab classes could have helped with his emotional adjustment, regretted that no class was available in the first few weeks after his discharge from hospital.
The fact was that the meetings were so infrequent that, you know, I’d almost fully recovered by then, by the time the aftercare started. But no, had it been in the first few weeks afterwards just possibly I may have got out of my system what caused me to be so horrible to [my wife], I don’t know but may be that would’ve helped.
HA11, male, MI in 1999 aged 42 years
Another man said it was helpful to have been given the Heart Manual with instructions about safe exercise and general lifestyle advice to bridge the time between discharge and the start of the formal programme. He used it like a diary to record his activities and monitor his progress. (HA16, male, MI in 1999 aged 49 years)
These accounts indicate the need to ensure that patients do not feel ‘left hanging’ in the period between discharge from hospital and the start of rehabilitation schemes and to provide them with points of contact and supporting information that can provide guidance on safe physical activities and reassurance in the early stages of recovery.
What do patients value about rehab schemes?
Most participants in the study who had attended an exercise scheme – whether hospital- or community-based – spoke very highly of their experiences. The phrase used by almost everyone who was able to take part was that group-based rehab had ‘rebuilt my confidence’ after the severe sense of vulnerability and loss of physical integrity experienced in the aftermath of MI.
A couple of patients emphasised that they had felt very lucky to promptly get a place on a hospital-based scheme after discharge as they were aware of oversubscription and long waiting times.
Given the widespread uncertainty about how much exercise would be safe and beneficial, one key aspect that participants in this study valued about formal rehab classes was that they provided an opportunity to ‘test the boundaries’ and engage in more strenuous physical activity than they would have dared to by themselves.
One man described how even a relatively short rehab course was sufficient for him to regain confidence in his physical abilities.
From the first day I went to that, it was twice a week for four weeks, I was a different person at the end of it. They showed me what I could do. I was being monitored, I was doing exercises that I wouldn’t have attempted to do and it did give me great confidence. That really prepared me for the complete rehabilitation period.
HA06, male, MI in 1996 aged 70 years
The qualities of programmes that were described by participants as positive and empowering in terms of regaining physical confidence were rehab staff who met their anxieties with empathy, who managed to create a comfortable and caring atmosphere, and who provided a gradual increase in exercise intensity, coupled with frequent feedback and encouragement. Several participants said that they had felt nervous and embarrassed before their first class, but had soon gained in confidence.
I was a bundle of nerves before I went in, and I was shown how to do slight exercises. I was monitored. I was put on a bike for a few minutes to pedal it round and do different exercises, lifting legs and things like that, and very slight the first day. They built that up over the eight days that you were there and by the end of it, it was pretty, you know, my confidence was gone up and I felt that I could do this.
HA06, male, MI in 1996 aged 70 years
The first time you go to the exercise class, it just seems that you know, ‘I can’t do this. I can’t wave my arms about and march round the room,’ but you can, you can do it and now I do not really think about it. Just go once a week and don’t think about it, run up and down, throwing balls to one another and things like that, going on bikes and steps and just don’t think. It’s alright.
HA32, female, MI in 2003 aged 53 years
Patients described their trust into the care and competence and responsiveness of the health professional(s) delivering the scheme as a vital component of what they valued about it. This man emphasised the importance of feeling safe in the presence of qualified health-care staff when attempting more strenuous exercise.
I would advise anybody who has had a heart attack to, if they have the opportunity, to continue the rehabilitation classes because that was one of the things, which shall I say, because you’re being monitored by a qualified person, you extend yourself, you push yourself a bit more and you know that there’s someone there to monitor what you’re doing and if there is a problem they’re there to help you and I think the exercise classes do give you the confidence to do things which you may otherwise not attempt.
HA20, male, MI in 2000 aged 66 years
Another key benefit of attending group-based rehabilitation emphasised by many participants in this study was the emotional and social support they derived from meeting others with the same health condition. This woman described how encouragement from staff and peers had a positive impact on her mood.
It was not just the exercise; it was not just actually doing the physical part. I found the support of the staff, they were great, they were always there for you and they cared for you and checked you and made sure you felt good. They sent me home once when I didn’t feel good and refused to let me do it. But they were always so positive saying, ‘Yes, you’re going to feel better. Every time you come it’s your benefit’. And then you go there and you meet other people who have been in exactly the same situation as you, some worse, some not so bad, and you talk to them and they laugh and smile, and so you end up smiling.
HA22, MI in 2003 aged 63 years
Talking to other MI patients could also provide a useful resource for helping to differentiate which bodily sensations, symptoms and medication effects fell within the normal range of experiences and which were worth talking to a doctor about.
I think it’s good to speak to people that have had the problem that you’ve got because if you don’t and you get this sudden pain, you think ‘oh’. Like just on my left breast, it’s gone all dead round there and I’ve thought ‘why is that all dead,’ and I was thinking about it, well he must have, when he got into my chest, he must have cut some nerves so I won’t worry about it.
HA12, male, MI in 2003 aged 66 years
Most, but not all, of the exercise classes described by participants in this study included education and lifestyle advice alongside the exercise sessions. This was typically delivered by cardiac nurses. Some of the community-based exercise schemes that were run by support groups also regularly invited experts to speak on specialist topics. Many participants said they valued the additional contact and access to clinical expertise and the opportunity to ask questions without a formal GP or hospital appointment (see also Part 9: building a supportive environment: myocardial infarction patients’ ongoing support needs).
One man who took retirement from his job as a PE teacher after his MI, and subsequently trained to become a cardiac rehab instructor, commented on the benefits of including partners in rehab classes and the gradual regain of body confidence over time.
I think what appeals to most people is that they meet a group of people, that they come together socially with and they’re safe and comfortable in the knowledge that these people have been through the same sort of experiences themselves. I think it helps as well that I’ve been through the process, because when I first see them a lot of them are really quite worried about the idea of taking exercise. Their wives and partners, or husbands and partners are also worried because they’re afraid that they’re going to do too much. So I always invite them to come along to the exercise sessions as well, so they can actually see what they’re doing, they can take part as well. They get an idea then of what’s a suitable level of exercise to be doing and they all surprise themselves; they all do more than they thought they could. And as they get fitter and stronger, they’re doing more and more and they look back and think that they never thought they’d be doing this again.
HA23, male, MI in 1998 aged 49 years
To summarise, the aspects of rehabilitation programmes participants in this study said they valued most were:
-
the opportunity to do supervised exercise in a safe and supportive environment
-
knowledgeable, encouraging and caring staff monitoring and providing feedback on their progress
-
ad hoc access to clinical expertise for minor questions and uncertainties
-
emotional and social support from peers for self and partner
-
an orientation about what to expect in terms of normal symptoms, medication effects and rate of recovery
-
a gateway to further sources of information, support and social activities.
Patients’ reasons for non-attendance of group-based programmes
Perception of exercise as insufficiently tailored to individual capabilities
Several participants in our study did not engage in hospital-based rehab schemes. A handful of them said that such a scheme was not available at their hospital or that a place had not been offered to them, though a couple of them had managed to find out about and attend community-based classes instead.
However, there were also a few participants who actively decided against attending a group-based exercise scheme. A couple of men, one of them a fitness instructor, felt sufficiently confident about exercising by themselves and thought that the group had little to offer them in that aspect. Participants’ accounts illustrate the difficulty of getting the exercise balance right for a broad range of ages and fitness levels among participants in the same class.
One man in his early forties, who had been very physically active before his MI, said that he had felt out of place at the hospital-based rehab scheme due to his younger age and greater level of fitness.
I went to one meeting [um] at the hospital for sort of aftercare but everybody else was about thirty years older than me and so we didn’t have a great deal in common because they were older and so they were doing, they had different lifestyles anyway and some of them had other illnesses. And so I didn’t bother going back because I didn’t really feel part of it and I found I was a bit embarrassed actually that was so fit, well and sprightly compared to everybody else, I felt a bit uncomfortable as though I was rubbing it in a bit so I didn’t bother going back.
HA11, male, MI in 1999 aged 42 years
He told how, instead, he had signed up with a personal trainer at a local gym for six lessons to work out an exercise regimen tailored to his needs.
For participants with previous experience of other forms of exercise, the style and pace of cardiac rehabilitation may appear insufficiently challenging and, therefore, unappealing. One man admitted that his initial perception of the exercises as ‘too babyish’ turned out to be unjustified with hindsight, even though they did not match his idea of proper exercise.
The first one [class], I thought it was so babyish that it was going to do me no good. And actually within three or four weeks I was feeling marvellous. And I said to my wife ‘I’m getting fit and I’m hardly doing anything’. Because you were walking around, you were hopping up and down on the trampoline. Now I was jumping up to touch the ceiling but I was still jumping up and down for a minute. Of course that was all a minute, actually for the first one he only lets you do thirty seconds so your first week, then you go forty five, then you go a minute and a half and then one day he says to me ‘You’re on the full two minutes today,’ and I said ‘Cor gee you know two whole minutes’. That was it, that was very good. Obviously the people who design all these things know what they’re doing. If it was left to me, I’d have felt I should do – one of the things I asked him, I said ‘Do we do press ups?’ and he said ‘No, none of these people want to do that, especially those who’ve had bypass surgery’.
HA13, male, MI in 2002 aged 70 years
Time taken to travel to or attend scheme
A couple of participants who had returned to work after their MI mentioned work commitments and a clash of rehab classes with their work schedules as barriers to their participation. Rural living location several miles from the site where a scheme was offered, poor public transport or both were also cited by several participants as factors that had made it difficult to attend sessions regularly, or to continue with regular group-based exercise once the initial programme had finished. This woman explained why she did not go on to attend the ongoing community-based exercise classes once she had completed the initial programme.
There is some classes in the community but if you don’t drive then they’re awkward to get to so then you’ve got to rely on public transport or, you know, to get there. [The person] who runs the rehab class at the [the local hospital], she does a class in [the nearby town] on a Friday morning but to get to [the nearby town] on a Friday morning is a bit, you know, a bit of jaunt for me to get there. [I don’t drive] and then it’s just relying on people for lifts and that, isn’t it? And, you know. And if people don’t like offer, then I’m not going to ask. So . . .
HA33, female, MI in 2003 aged 36 years
Feelings of not fitting in
Given that informal peer support emerged as a crucial element of what participants in this study valued about group-based rehabilitation schemes, it is likely that patients who do not regard other group members as ‘true peers’ are less likely to have a positive experience. In this study, most of those who had experienced MI at a young age commented on the age difference between themselves and other rehab group members, and most of the women commented that the majority of MI patients they encountered were male, but most of them did not describe this as problematic. However, one young woman told how she found it extremely difficult and embarrassing to attend an exercise group with people who were much older than her. Even though she did make a couple of friends among participants, she felt unable to talk about some of the things that greatly mattered to her and that had been affected by her MI, such as her children or her job (not included in this extract). She was grateful that her husband supported her by coming along to the sessions.
When I came home afterwards I had to go to rehab, and that was really hard. Really hard. I made my husband have 6 weeks off work so he could come with me, couldn’t go on my own. They were all old. There were two old ladies, who in time I became very friendly with and still see to this day. But when you have to sit in a circle and say who you are, and that you’d had a heart attack, and how old you were, I was like their grand-daughter then. I used to look at my husband and say, ‘can’t you say,’ even though he’s only a couple of years older than me, ‘can’t you say that you’ve had a heart attack and it wasn’t me’. But that was hard doing exercises, with older people. [. . .] [They were] shocked. ‘She couldn’t have had a heart attack.’ You could see people looking. She’s not old enough to have a heart attack.
HA36, female, MI in 1998 aged 37 years
Experience of the Heart Manual
A few patients who decided against attending group-based exercise were offered the ‘Heart Manual’ instead. For one man, this was a much preferred option that enabled him to engage in rehab activities while returning to work relatively quickly. He valued the toolkit of techniques described and the possibility of revisiting the materials regularly.
I did really [prefer to use the heart manual rather than a programme] because we’re a bit remote here; a few miles from the hospital and so on. And I wanted to get back to normal as soon as I could so my teaching load, although it was, I shed my teaching load completely, I wanted to get back and they wanted me back anyway, so I have, I have gone back teaching so you know I’ve got odd days to teach and I thought well they’ll never fit in with a class at the hospital so I said I’ll go for the manual and that was very good. That was [um] brilliant because I still read the manual [now], I still go back over it. [Um] lots of interesting pages there not only on the relaxation, as I say, pacing out your workload, not trying to do everything. Being able to say no. Lots of techniques like that, really good, really good.
HA14, male, MI in 2003 aged 51 years
One woman in her early eighties also opted for the heart manual in place of group-based rehabilitation. She was unusual among our participants in that her perception of the group setting was as an environment that might involve her in difficult emotions and thus be detrimental to her recovery, rather than provide nurture and support.
I didn’t want to [attend rehab classes]. I felt I could rehabilitate myself, which I did. I didn’t want to be mixed up with other people’s reactions and feelings. I wanted just to have my own and sort my own out and right or wrong, I did it. But no, the doctor asked me and I said, ‘no, I’ll do it,’ I said, ‘I’ll do it myself’. I didn’t want any help to climb the mountain because if somebody fell down I’d fall down with them. I’d rather do it myself.
HA15, female, MI in 2000 aged 81 years
Her case highlights the importance of exploring patients’ expectations around rehabilitation and what they hope to gain from it as well as what they wish to avoid, rather than just assuming the universal appeal of shared experience.
Enabling patients to make physical activity a routine part of life
The majority of participants in this study continued to engage in regular exercise months and even years after their MI and after their initial rehabilitation scheme had come to an end. Those who exercised regularly seemed to share a belief that they had an active role to play in preventing a repeat heart attack and described themselves as empowered by this belief. Many felt that joining a group of people ‘in the same boat’ had been helpful in maintaining the motivation to be regularly physically active, whether this was in the form of a community-based exercise group or as part of the activities organised by peer support groups such as dances or walks.
FIGURE 14.
Patients’ participation in hospital-based rehabilitation classes. Number in shape: participant interview ID number. Participant sex is indicated by shape fill colour (blue = male; green = female). Participant age at diagnosis is indicated by shape form (square = diagnosed aged ≤ 40 years; pentagon = diagnosed aged 41–50 years; hexagon = diagnosed aged 51–60 years; heptagon = diagnosed aged 61–70 years; octagon = diagnosed aged ≥ 71 years). Participant marital status: without shadow = single; with shadow = married or cohabiting. Participant ethnicity: white number = white British; black number = black and ethnic minority background. Green circle indicates participant continued to engage in regular exercise after completing the initial programme, blue circle indicates that they did not.
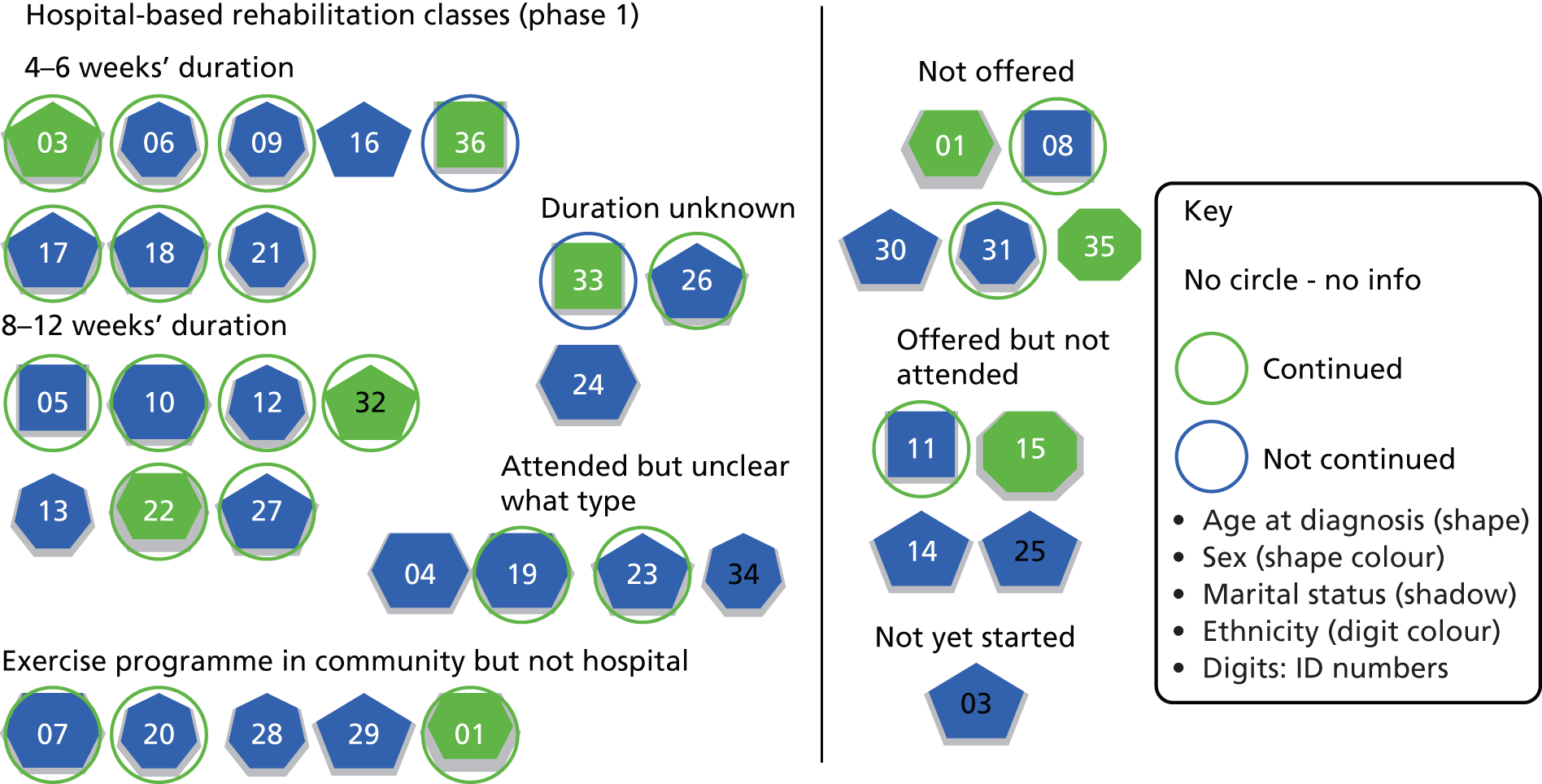
For most of those who attended hospital-based exercise classes, they represented a crucial gateway to further information and support. Most of those who attended community-based exercise schemes after the end of phase 1 rehab had found out about their existence at the hospital-based classes. In a few cases, participants described how the hospital-based group had become a springboard for the setting up of ongoing community-based exercise classes, brought about by the joined initiative of group attendees and committed cardiac rehab staff.
I go to a group, which was set up from the hospital actually, a group of patients that did the exercises because the hospital runs an exercise class for heart patients and we’ve all attended this class and we all wanted to continue. So about five years ago, this group was set up and it’s exercises especially for pumping your heart. They’ve managed to get all sorts of equipment together. They’ve got a defibrillator, in case anybody has problems during the class, so you feel quite safe going to it, in the knowledge that somebody can revive you if something happens [laughs], but I don’t think anything ever has and we just have a good time. That’s, that’s twice a week. I can only go once a week but they do do the class twice a week and it’s good because everybody is glad to be alive and they’re all cheerful and making the most of it.
HA32, female, MI in 2003 aged 53 years
While a small qualitative study cannot establish whether or not those who attend rehab schemes are more likely to continue exercise in the longer term, the accounts of participants in this study highlight the important role that such schemes had played in helping them to make exercise part of their everyday life post MI. Many patients talked about how having a heart attack had caused them to reassess their priorities and make changes to their lifestyle, including new projects and new kinds of leisure activities. Making such far-reaching changes is likely to be easier for patients who have access to local facilities that they can afford and are no longer in full-time employment or with caring responsibilities.
The experiences recounted in this section also highlight some of the possible barriers to engagement in cardiac rehabilitation programmes and some of the challenges faced by those who continue in employment, who live in remote areas with poor public transport or who feel out of place in a group environment due to their age or gender, their approach to dealing with health issues or other personal qualities.
Finally, it should be noted that several participants in this study managed to set up good exercise routines on their own initiative, and all of those who were asked about the Heart Manual said that they had found it helpful, as either a substitute or a complement to group-based rehab.
Cardiac rehab was the best thing that could have happened. You do, you start off very gently, exercise, very gently, very easily and at the end of each session, someone will come and talk to you, the nurses will talk to you, absolutely brilliant. By the end of 6 weeks, I can do anything and it’s continued from there.
HA18, male, MI in 1995 aged 47 years
Part 8: patients’ information and support needs in making lifestyle changes
Key emotions
Helplessness/self-efficacy.
Trust and doubt.
Uncertainty about cause and effect.
Key questions
What can I do to help myself? And will it make a real difference?
What kind of life can I hope for after MI?
Who and what can help me in making changes?
Myocardial infarction as a juncture and turning point in patients’ lives
Patients who have experienced MI typically talk about it as a decisive juncture in their lives (see also Part 2: receiving the diagnosis and Part 6: the emotional impact of myocardial infarction for patients and their families). Many participants in this study used phrases such as ‘it was a wake-up call’ to describe how the realisation that they could have died during the attack had led them to reassess their priorities and make changes to their lifestyle.
A couple of recent studies have suggested that less invasive treatments, shorter hospital stays and quicker recovery rates may lead patients to perceive MI as an acute rather than a chronic health problem and consequently lessen the psychological impact of it as a life-changing experience. 106,107
Understanding the level of seriousness patients attribute to their MI and to what extent they perceive themselves as being able to make a difference to their future health are important preconditions for engaging patients in behaviour change for secondary prevention.
Numerous studies have demonstrated that education – informing patients about the importance of adopting particular health behaviours – is only one piece in the puzzle of affecting behaviour change. Qualitative research has illustrated the complex interactions between patients’ health beliefs, their motivation to change behaviour, their social context and level of support, and how all of these variables may change and develop over time. For example, Wiles127 found that patients’ beliefs about the extent to which they could make a difference to their personal risk were linked to their motivation to adopt health-promoting behaviours, but also that patients’ motivation tended to dwindle with the progress of time, especially if they felt that they were not reaping the benefits that health professionals had led them to expect as a result of their modified behaviours.
This chapter starts by mapping out some of the areas of lifestyle change after MI that are likely to be relevant to patients and that health professionals might want to consider when trying to engage patients in secondary prevention. It then focuses on adherence to medication as a lifestyle change that may appear relatively straightforward from the perspective of health professionals (‘just make sure you take your pills’) but which many participants in this study experienced as a significant burden with far-reaching implications for other areas of their life.
Individual receptiveness for health promotion messages
Most participants in this study described high levels of motivation and adherence to medical advice during the early period following their MI; they felt responsible for their future health, and described the belief that they could actively do something to reduce their risk of a repeat attack as empowering. This man described how his adherence to medical advice and search for information were driven by his desire to ‘fight back’.
I think especially in the first year because you really are doing absolutely everything you’re told to, everything the consultant said to do and more. Everything you’ve read because it’s your way of fighting back. And you pick up every leaflet about heart attacks and look up things on the Internet about angiograms and stents and, but that’s like empowerment, it means that you know this heart attack struck you down but now you’re going to do something about stopping having another one.
HA11, male, MI in 1999 aged 42 years
However, patients who struggle to accept the diagnosis and have a strong sense that they ‘did not deserve this’ may need support to help them adjust emotionally before they can contemplate behaviour changes aimed at secondary prevention. This man took little notice of health promotion messages after experiencing his first MI in his forties, because he found it impossible to reconcile his self-image with being an MI patient.
Because I was quite young, [the MI had] very little [impact on me]. I still hadn’t got over the – if you like, I know I was 40 but as a younger man, as with most younger people, you consider yourself immortal, you’re not ever going to die, nothing can hurt you. I suppose there was still an element of that in my behaviour. In fact you tend, I tended to go the other way, that ‘don’t be silly, I can’t have had a heart attack, I’m going to prove them wrong’. Hence you carry on smoking, hence you don’t reduce your workload and you, you tend effectively to continue, once you get over the initial trauma, you tend to continue your lifestyle exactly as it was.
HA08, male, MI in 1989 when aged 40 years
Return to work or (early) retirement?
The majority of participants in this study were retired from work at the time of interview, but the study included some who had returned to work weeks or sometimes months after their MI. A few had decided to take early retirement following their MI and a couple of others had initially returned to work but found that it had proved too strenuous for them to carry on. It seems important to consider patients’ work status and their feelings about work and retirement when discussing secondary prevention. Several patients said that they felt stress in their job had contributed to their MI. Those who continued in employment sometimes felt reliant on their employers’ good will to allow them a staggered return to their previous workload or time off to attend cardiac rehab schemes.
This woman was grateful that her employer allowed her to return to her job in a gradual fashion.
[My employer was] shocked but very supportive. But they were really, deeply shocked because I’d worked hard for my company for like a good 5 years I’d been there so I’d worked hard. I knew what I was doing and I knew my job and I worked, I did my job well so when I sort of like left to have a heart attack they had to get like somebody else to replace me but they didn’t replace me with one, they had to replace me with two. So that’s how hard I’d worked for them. But they were very supportive to me and they put me on like full pay for all the time that I was off. And obviously, they just wished me well and didn’t want me to go back until I was ready and now they’ve changed my hours so I only work part-time hours at the moment. And you know, I’m slowly building myself back up to do more hours, you know, as time goes by. So at the moment I only do 21 hours a week but I’m slowly building that back up so they’ve been, they’ve been absolutely great. And they’ve sort of like worked my hours around like my hospital appointments and my rehab classes so I must say that they have been brilliant.
HA33, female, MI in 2003 aged 36 years
Several patients of working age said they were concerned about being perceived as ‘disabled’ following their MI and how this might affect their longer-term prospects. Especially younger people of working age and/or with caring responsibilities may struggle to adjust their activity schedules in a way that allows routine integration of health-promoting behaviours. Conversely, suddenly having ‘too much time on your hands’ after MI might also be experienced as difficult and depressing (see also Part 6: the emotional impact of myocardial infarction for patients and their families). One woman talked about her difficulties adjusting to a less busy schedule and finding a new purpose as secretary of a support group after taking early retirement from work following her MI.
When I came out of hospital, I couldn’t settle. I took up cross-stitch, that was a waste of time. I took up making aromatherapy stuff, I was doing all these potions, that was a waste of time. I just couldn’t, I couldn’t settle and I needed to do something because you’ve been busy all your life and you’ve always been active and all of a sudden you’re not doing anything. And I was taking on all these different, and then I says, ‘I think I’ll buy a computer’ and my husband says, ‘look you’ve been buying all these other things which are cheap,’ he said, ‘but a computer is expensive just for a couple of weeks’. I says, ‘no, I want a computer’. So he bought me a computer and I love it, I’ve been using it now for about 4 years and I love it. I am now the secretary of the support group and I do the newsletter and I, you know do all these things. I keep myself quite busy doing things on the computer. I’m quite proud of myself.
HA03, female, MI in 2000 aged 53 years
Many participants in this study had used their experience of MI as an opportunity to reassess their previous lifestyle, had considered the things most important to them and embarked on new projects as a result. This meant that for them, making lifestyle changes such as the adoption of a healthier diet, learning relaxation techniques and engaging in regular physical activity were embedded in a more far-reaching reorientation of their everyday lives. These participants experienced making lifestyle changes for the most part quite positively, as self-directed efforts towards reaching outcomes that they saw as both personally achievable and worthwhile. They were enabled to do so by having good financial, family and peer support, often in the form of ongoing engagement in support groups and regular follow-up care (see also Part 9: building a supportive environment: myocardial infarction patients’ ongoing support needs).
This man initially felt very angry at his forced retirement, but he retrained as a cardiac rehab instructor and successfully managed to build a whole new career with support from his wife and perceptive health professionals who recognised his potential.
I would never have thought that I had the inclination to do some of the things that I do [now]. I was quite angry at first that I’d had to give up [work]. It was a decision that was made for me and I really was quite upset that I had to stop before what I thought was the time I should. I really felt I’d got more to give and I could do more. [. . .] After I was retired, and after a few months of just walking around, doing jobs in the house, getting fed up, I heard about a course of training you can do to get qualified in what they call ‘GP exercise referral’. So I took the course and passed it and when I got back, I was put in touch with the local primary care trust, who asked me to write a scheme for a rural exercise programme, which I did in conjunction with the local surgery and we decided to put on an exercise scheme for people who’ve had heart attacks, bypasses and so on, some years ago who had stabilised and this would be a form of secondary prevention. So I started that nearly three years ago and patients are referred from the surgery. It’s grown quite considerably over that time; we have about fifty patients who come to the classes. I do three sessions a week. Now that my wife’s retired, she comes down and helps as well.
HA23, male, MI in 1998 aged 49 years
Patients’ information and support needs around medication
Qualitative research on the reasons why patients might choose to discontinue prescribed medication has identified adverse effects that are painful and/or interfere with daily life as the most common reason. Other reasons include confusion about why a treatment has been prescribed or of how best to take it, the cost of medication, mistrust in medicines or the health-care system more generally and preferences for alternative therapies. 128 If patients’ information and support needs around taking medication are addressed they may promote better adherence to prescribed treatment regimens.
Acceptance of the burden of medication as the price for improved cardiovascular health
Many participants in this study had experienced adverse effects from the medications they were prescribed at some point after their discharge from hospital. For some, having to put up with the unpleasant side effects had become an accepted part of their life after MI – the lesser of two evils.
I also experience a number of minor reactions; my digestion is upset most of the time to the point of threatening to become inconvenient – I have a small supply of anti-diarrhoea pills just in case but have not yet had to use them; for a good part of the day my fingers are white and cold due to a restricted blood supply but other parts are quite the reverse. Unfortunately this is principally my nose, which lights up like I’m a bottle-a-day man. Apart from the coughing it’s all minor stuff that doesn’t interfere with my life. It’s a small price to pay and I’m not complaining.
HA04, male, MI in 2002 aged 62 years
I’ll have to take [these tablets] for the rest of me life which I’m quite happy to. You know if you came along now and said ‘look, here’s a pill that will guarantee if you take this pill every day you won’t have a heart attack,’ I’d take it. I’d take two. But, there we are. And I know that they don’t guarantee you don’t have one, they’re just helping my blood pressure and my cholesterol.
HA01, female, MI in 2003 aged 63 years
Understanding what medication does and why it is necessary
Most participants in this study had to take 3–5 different pills or sprays several times a day following their MI. Integrating the taking of medication into their daily routines was often achieved with the help of aide memoirs and/or the support of a spouse.
I have a lot of medication, blood pressure and a number of things which fortunately don’t seem to result in any side effects which is a big plus and [my wife], she sees it as her function in life to make sure that I take it. And I do naturally take it in the morning, I take some in the morning as part of my usual routine, shaving and, yes I do shave, and cleaning teeth and so on, and in the evening when we have supper, except then I sometimes forget, but she doesn’t [laughs].
HA09, male, MI in 1995 aged 69 years
Many participants said that they did not like taking their medication, but that they recognised the importance of adhering to the prescribed regimen to keep healthy. However, over time there was a risk that the initial motivation might fade and doubts take hold whether or not the prescribed regimen continued to be truly effective.
I’m fairly organised and methodical and so they [pills] sit on the breakfast table and I always remember them in the morning. We’ve only missed them once in the evening; we’d been out for the evening and we just, well we felt tired and we just went straight to bed. Apart from that I’ve been taking them faithfully. But I said to my wife the other day, I can understand people who would get fed up with taking the pills on a long term basis because this is . . . well 9 months now that I’ve been taking these pills; five a day and you do get fed up with it and you think ‘oh what are they doing?’, you know. ‘Is it doing me any good?’
HA14, male, MI in 2003 aged 51 years
A few patients talked about how they had appreciated being thoroughly briefed at discharge, both verbally and in writing, about the kinds of medicine they needed to take, what each medicine was supposed to do and why this was important. However, there were also several participants whose information needs had not been fully met and who worried about whether or not the combination of medicines they had been prescribed were appropriate for their particular situation. Patients who studied the leaflets supplied with prescription medicines were at times left with more questions than answers, and even those who had an opportunity to raise their concern with a health professional did not always manage to receive answers that they felt were sufficiently in-depth and reassuring.
But this Atenolol is supposed to, I said ‘What’s this for?’ I asked them what it was for and they said ‘It’s to slow your heart rate down’. I said ‘But I’ve got a slow heart rate,’ and you know, I don’t know anything about the medicine and I’m just doing what they tell me.
HA13, male, MI in 2002 aged 70 years
A few participants who felt unsure about why they had been prescribed a particular drug, or whether or not the drug actually showed any beneficial effects, talked about feeling less committed to taking it. This woman was unconvinced about the need for an additional drug that she was concerned might negatively affect her blood pressure.
I’m taking all the heart pills as I said, I don’t know about this Reduxal because it puts your blood pressure up, doesn’t it, but I told her [GP] this, I’ve talked to her about it and she said it’s fine. But it, I can’t see the point of taking it to be honest. I mean I have told her this and she said ‘Well just try it for 3 months,’ which I am doing. But I’ve got a packet there and I haven’t touched them yet so when I go back to see her on the 22nd I’m going to say to her, you know.
HA01, female, MI in 2003 aged 63 years
Symptom or side effect?
Some participants said they found it difficult to know whether to attribute the symptoms they experienced to problems with a particular type of medication, to the range of sensations that should be regarded as ‘normal’ after MI or possibly to an unrelated health problem. They valued follow-up care with health professionals who would take such worries seriously and work with them to find a treatment regimen that might suit them better, as well as pursuing further investigations.
Sometimes I get pins and needles in my feet, and a few aches and pains which I didn’t have before, but whether that’s the tablets or my age, I don’t know. But I did read a leaflet about the blood pressure tablets and it did say that sometimes you get tingling in your feet or your hands. So I’ve put that down to the tablets.
HA01, female, MI in 2003 aged 63 years
However, a couple of patients had struggled to make their GP or consultant understand that a problem that might not be particularly threatening from a clinical point of view could still cause a great amount of personal distress. This woman felt frustrated that after checking that her hair loss was unlikely to be indicative of a serious underlying health problem, her doctor did not feel the need to find an alternative to the medication she suspected to have caused it.
The doctor did say she would do some blood tests just to see if there were any other reasons why my hair was falling out. I think she did some calcium and some iron checks and some other bits and pieces, all of which are normal. So it’s obviously not any other reason so I’m assuming it’s the medicine I’m actually taking. [. . .] The main worry is that if it continues to fall out. I need the medicine for my heart and the doctor said, ‘Well when you stop taking the medicine the hair will grow, it’s not as if it’s a condition where the hair will not regrow back again’. Well, okay it will regrow back again but as long as I’m taking the medicine, it’s not going to regrow back again. So I’d really like to find something to give my hair a chance to regrow back so that I can see if in fact it was going to come back.
HA22, female, MI in 2003 aged 63 years
Shared decision-making, treatment preferences and expert patients
Some of the participants in this study who had been taking medication for several months or years appeared very well informed about possible side effects and drug alternatives. Through participation in support groups and conversations with other MI patients some had become conscious of the risks of polypharmacy (e.g. when they had been prescribed medication for an acute problem that had the potential to interfere with their regular medicine). This woman described how she had become more involved and vigilant about her prescribed medications since her MI.
Like I went to the doctor with this bad chest. I’ve had this cough for three weeks now and I saw him yesterday and I said ‘I can’t breathe,’ I said ‘I don’t know whether it’s my heart or my chest’ and he listened and he said, ‘Oh it’s probably your chest infection’ and he gave me some tablets. Now you see, I get the leaflet out now as soon as I get these tablets – ‘should I take this, what will happen if I take this now?’. So I’m then back in and I’m asking him and he’s saying ‘no it’s okay, you can take your tablets with . . .’ whereas before I would have just taken them. I wouldn’t have read the leaflet. But I do now. I study it very carefully.
HA01, female, MI in 2003 aged 63 years
For MI patients with complex medication regimens, increased involvement in treatment decision-making with non-cardiac health professionals is thus likely to have importance beyond the accommodation of patient preferences as a safeguarding strategy to avoid detrimental drug interactions.
Most patients accepted that there was going to be a trade-off between effects beneficial to their cardiovascular health and undesired side effects. However, they valued health professionals who invested effort into tweaking this balance in favour of reducing the burden of medication on their patients.
There was one beta-blocker I couldn’t take, it was making me really poorly so they had to work really, you know to find one that would suit me. But I think they’re pretty good, if you’re having problems with your tablets, that you go back and say, ‘this isn’t suiting me’ there’s always an alternative. There’s always an alternative to the drugs so you know, you don’t have to suffer side effects; there’s always something else.
HA03, female, MI in 1998 aged 53 years
Participants in this study were conscious that it might be dangerous to experiment with stopping or changing medications by themselves. Several reported very positive experiences with health professionals who were responsive to their dilemmas. This man was grateful to have a consultant who took seriously the problems he had been experiencing with a particular drug and was willing to take the risk of him discontinuing the medication – a decision that he felt had much improved his quality of life.
The drug was called amiodarone. And I felt that the side effects of the drug were in my case worse than the ailment it was treating. So some three months ago, I appealed to the surgeon to look into taking me off of the drug, or at least considering whether I could manage without the drug. And it was decided that since I had the mechanical protection if you like, given by the defibrillator, it would be worth trying to survive without taking this particular drug and I have to say I’ve been in excellent health and spirits ever since. Better spirits because I felt that after coming off of the drug, whether it be part in my head or not, that my mental functions were improved. I didn’t feel as sluggish, I didn’t feel as though I’d lost the ability to think and I found that my memory improved, all of which I found were very noticeable to me personally. Whether this is just me, or whether these are side effects that I am not aware of, I’m not sure.
HA08, male, MI in 1989 aged 40 years
However, in a few cases health professionals insisted on patients ‘giving it a go’ before they were willing to change prescriptions. One man who described himself as ‘having done an awful lot of reading around the problem’ including recent research literature on medication, took the initiative and suggested to his GP that he should be put on an angiotensin-converting enzyme (ACE) inhibitor. His GP followed the suggestion, but was reluctant to let him choose the type of ACE inhibitor at first.
A lot of the ordinary ACE inhibitors will give you a slight dry, irritating cough and when I first suggested to the GP that I should be on an ACE inhibitor, he gave me one of the standard ones and I said, ‘I don’t think that’s a good idea’. And he said, ‘Why?’ and I said, ‘because it’ll give me a dry cough’. And he said, ‘Well try it first’. So a month later I went back and I had the cough so we changed it. That’s not me being clever, it’s just that perhaps I’ve done more reading about it than [the average person].
HA23, MI in 1998 aged 49 years
Clinical necessity and personal meaning of medication
Many participants in the study had been prescribed a nitrate spray to use in case they were experiencing sudden chest pains. While some of them had to use the spray quite regularly, others rarely had any need for it. Nevertheless, the spray fulfilled an important function for them as a ‘safety blanket’ that they carried with them wherever they went – just as many of them said they made sure to always carry a mobile phone.
I feel very reassured by taking the spray, having it with me all the time, you know. [. . .] I was saving it up to start with to sort of for the very, very bad attacks and now I just use it for a mild attack of angina which is what it’s there for really. And I’ve asked the doctor about it and you know I said to him, ‘Does this do any harm?’ and he said, ‘Oh no that’s what it’s there for, it just opens the vessels for a time, just so the angina passes’. And I said, ‘Oh well all right’ and I use it a bit more freely.
HA14, male, MI in 2003 aged 51 years
One man, who initially was told that he was unlikely to need such a spray, but had read up about it in the written information he received at discharge, was grateful that his GP agreed to give him a prescription for additional reassurance.
The medication I’ll be on for life. I mean the cardiac rehabilitation nurse was able to explain, rather somewhat more than maybe the doctors had, some of the implications of those medications. But the other thing that he was stressing and which the booklets tended to stress was GTN [glyceryl trinitrate], which is a spray that you put behind your tongue in the event of pain and discomfort. Anyway, there were very sort of strong messages both on paper and verbally. So when I came to being discharged from hospital, I mean you’re supplied with a month’s medication by the cardiologists, the doctors, I was surprised that I didn’t have any GTN. And I asked the registrar, the specialist registrar why and he said ‘well there’s no indication that you need it because you haven’t had pain and there’s nothing else’ and I said ‘well you know, because there’s such an accent put upon it couldn’t I have it as a comfort blanket?’ and therefore what he suggested was that I just ask my GP for it, which in fact we did on the way back from the hospital.
HA02, male, MI in 2003 aged 54 years
Part 9: building a supportive environment: myocardial infarction patients’ ongoing support needs
Myocardial infarction patients’ experiences of follow-up care
Previous qualitative research has suggested that post MI patients want more consistent follow-up care and ongoing support for help with making lifestyle changes; to meet people with similar experiences; to have regular access to health professionals with cardiac expertise; and to provide reassurance to partners and family members. 129
Follow-up care arrangements varied greatly for participants in the study. While some participants continued to see their hospital consultant at regular intervals for several months, for others their GP became their main point of contact for voicing any concerns about their symptoms or requesting changes to prescriptions. Many patients reported very positive relationships with their GPs.
I have a brilliant GP. I’d vouch for him anytime. He’s caring, he listens, he talks, he checks. If there’s anything wrong he’d send you for an X-ray or anything like that, you know.
HA06, male MI in 1996 aged 70 years
Especially in the early days after discharge from hospital, participants appreciated having access to a designated health professional with specialist cardiac expertise who they were able to contact with concerns or questions between appointments. This woman praised the dedication of her cardiac nurse who phoned her back to check on her well-being.
The rehabilitation Sister’s been my lifeline. I’ve been able to phone her, she’s been phoning me and she’s, to make sure I’m all right when I’ve come home, and things like that. [. . .] And when I had the funny heartbeat I’d phoned her the day before and she’d phoned my GP and I’d seen my GP but he said I was, I was all right. But 9 o’clock the next morning the rehabilitation phoned me and said, ‘how are you?’ and I said, ‘I’ve still got this funny heartbeat’ and she says, ‘come in now’. And she was there like when I got there at the hospital, she’s been a lifeline.
HA03, female, MI in 1998 aged 53 years
Cardiac nurses were usually the health professionals who aided the transition from hospital to home.
I lived by that [the heart manual] for six weeks when I was at home and again saw the doctor every couple of weeks and then I went in to see the cardiac nurse as well. I could ask her lots of questions; [my wife] and I, we both went in to see her, and came out with a few of the answers and a few don’t knows but you know it helps to be able to talk to somebody who has been in the same situation or been with, been with other patients and that was good.
HA14, male, MI in 2003 aged 51 years
Having health professionals proactively checking up on discharged patients may help to reduce barriers towards help-seeking if patients experience symptoms that might suggest a repeat heart attack.
This man felt that having to wait for 3 months for his first specialist appointment after discharge was too long and this caused him and his wife some anxiety.
I then had come home and I’d sort of got an appointment, this was in March and my appointment was for July to see a specialist, which I thought was rather a long time. It was more concern to my wife, I mean she was very worried [um], I couldn’t go out of her sight really. I had to go and buy myself a mobile phone which is something, I don’t want a mobile phone but I always had to carry this mobile phone. And if I was out of her sight more than a minute or two, she was worried about it and I thought well we, I ought to be doing something sooner about this. So we tried to contact the specialist, to say, ‘well it’s a long time July, after a heart attack, to worry about is it going to come back, am I going to get it again’. And I really hadn’t got a great deal of information to work on at this point.
HA12, male, MI in 2003 aged 65 years
In some cases, communication between primary care and consultants at the hospital could be a source of uncertainty, as some participants said that they felt unsure about how much and what kind of information they could rely on to be exchanged between the two systems.
This man was concerned that his GP had decided to treat him with statins even though his cholesterol levels had not been checked in a primary care setting, so he was left wondering whether this was a ‘blanket’ treatment for MI patients or based on actual test results that had been communicated without his knowledge.
The one thing that does surprise me a little bit about the management of the condition I’ve got is the lack of blood tests. In terms of monitoring anything, because some of these problems can be explained by lack of magnesium or overactive whatever thyroid or again cholesterol level, I mean they’ve put me on a statin, but unless I’d been in hospital with a problem they’ve never checked my cholesterol level.
What is it? Why am I still on the statin? That sort of thing. Now, through my GP I get it checked once a year, and I don’t know if they pass that onto the hospital. Every time, they’re interested in my cholesterol because they think I’ve, because of all of this I must have had a horrendous cholesterol level.
HA05, male, MI in 2001 aged 37 years
In contrast, this man explained why he was very satisfied with the follow-up care he had received from his GP and the hospital consultant.
First of all [my GP] seemed to be pretty adept at prescribing the right medication for me. Secondly, I generally only went when I or my wife, usually my wife, felt that something wasn’t quite right and I ought to see doctor X. And so an appointment would be made and doctor X would look at all the papers and look at all the, you know, did some tests and said ‘there’s nothing much wrong with you, you know, you’re alright, you’re doing pretty well’. Might make a few adjustments to the medication and you know that made me feel, you know, better. Also a good thing was that my GP, who’s just here in the village, and doctor X work very well together. There was no professional politics going on which sometimes happens. And my GP was perfectly content to accept doctor X’s prescriptions or his, his recommendations and so on. But now, for some time now, I’m no longer consulting doctor X, (a) he’s moved out of the area and (b) there’s no need.
HA09, male, MI in 1995 aged 69 years
Another man said he had found it useful to write down the list of medications he had been prescribed so he could share this information with his GP without having to worry that he might forget something.
I wrote down everything that had happened to me, typed it up, the tablets I was taking and when I took them and whatever because it was so much easier when you go and see a doctor and we all feel a bit confused with the whole thing, I can refer to it or pass it across to him.
HA12, male, MI in 2003 aged 65 years
Participants’ experiences and perceptions of coronary heart disease support groups
Many of the participants in this study attended support groups for people with heart disease. Some groups were described as focussing predominantly on shared social activities and emotional support, while others also included regular exercise sessions and expert talks. Several groups were run in collaboration with cardiac nurses and consultants, though many were funded from non-NHS sources and relied on the enthusiasm of volunteers and NHS staff giving their spare time to keep going.
Several participants in this study were pleased to find out that a self-help group in their local area provided community-based exercise classes on an ongoing basis, as they felt that the hospital-based rehab schemes they had attended had been too short. They thought that regular attendance of a group was the best way of keeping up the motivation to engage in regular exercise.
Participants’ views on the key benefits of support groups were similar to those described for cardiac rehabilitation schemes (see Part 7: regaining body confidence: patients’ experiences of physical rehabilitation): ‘meeting others in the same boat’; a sounding board for the experience of minor complaints or side effects to find out if they warranted medical consultation or could be regarded as within the normal range of post MI symptoms; regular but informal access to clinical expertise; keeping up to date with medical developments; and opportunities for social comparison allowing participants to make sense of their personal MI experience and recovery against that of other patients.
When we go down to the heart support group, we usually have a doctor, or cardiac nurse, or after care, accident and emergency nurses and resus staff come to give talks and if you want, you can always talk to them if there’s any problem. And usually if anybody has a problem, it’s sorted out in group you know, because somebody’s had that problem and you usually say, ‘well I had that problem but I did this’ and you know, ‘they just went and changed me tablets, or I went to see doctor and he put me on a different tablet sort of thing’. They’ll sort it out between themselves, more or less you know.
HA07, male, MI in 1998 aged 62 years
[The benefit is] actually understanding that you’re not alone, that the feelings that you’re having, the aches that you get, the slight flutters of this and the effects of that drug, you’re not the only person in the world that’s got them. The mere fact that you can go and speak with, in our case, a hundred odd people, and you’re ‘Oh yes, I’ve done that’ ‘Oh yes, that’s exactly what happened to me’ or ‘Have you had this or does this happen?’ The mere fact that it’s a shared experience helps, it really does help [um] and we are quite well supported by very, very caring professionals as well. There’s a nursing sister, a cardiac nursing sister, who really was the guiding light in setting it up. There are two ECG technicians and we’ve had good support from the actual specialist, who considering his extremely busy schedules, has found time for us as well, which was nice.
HA09, male, MI in 1995 aged 69 years
Being a member of the cardiac support group for the last five years . . . they have proved a Godsend. Being able to mix with people who’ve had bypasses, stents, pacemakers and people who’ve had heart attacks and recovered from them, and that’s the situation I am in at the present time. [. . .] There are five ex-patients on the committee, two carers and two sisters from the coronary care. One of the sisters is actually a modern matron. So we get up-to-date knowledge from them what’s happening. We have five cardiologists at the hospital, we’ve had the five of them give us talks. Some of them up to four and five times each over the last five years. The psychologist cardiologist we’ve had her out twice; that’s a new innovation at the local hospital. They’re very entertaining, very knowledgeable and we get a lot of things from that. Also we’ve had the various specialist nurses relating to other diseases who come and are kind enough to give us talks.
HA17, male, MI in 1998 aged 49 years
Support groups were also seen to fulfil a valuable role for the partners of MI patients whose needs might not be addressed to the same extent by NHS services.
One of the biggest helps I think is the spouse. The fact that the spouses is included in everything and doesn’t feel excluded, doesn’t feel as nervous as she started, or he started, when it first happened. That’s a big benefit.
HA09, male, MI in 1995 aged 69 years
We now as a support group, we do lots of exercise classes. We actually run them, we’re doing something like ten a week now as a support group. We’re getting 20 to 25 people in each of these classes. Now we encourage partners and carers if you like, to come along, so out of 20 to 25 people in the class, more than half are actual heart patients. It’s good, good fun. We do all kinds of other things; social activities, we have a dinner dance which we had last week, our annual dinner dance. Wonderful, 100 people all enjoying themselves and I actually had a comment from one lady, ‘How many of these people are actually heart patients?’ ‘Well at least half.’ ‘Wow, you wouldn’t believe it. Look at them dancing rock and roll, wonderful disco, this is the way we go on.’ Life continues, it gets better.
HA18, male, MI in 1995 aged 47 years
FIGURE 15.
Patients’ participation in support groups. Number in shape: participant interview ID number. Participant sex is indicated by shape fill colour (blue = male; green = female). Participant age at diagnosis is indicated by shape form (square = diagnosed aged ≤ 40 years; pentagon = diagnosed aged 41–50 years; hexagon = diagnosed aged 51–60 years; heptagon = diagnosed aged 61–70 years; octagon = diagnosed aged ≥ 71 years). Participant marital status: without shadow = single; with shadow = married or cohabiting. Participant ethnicity: white number = white British; black number = black and ethnic minority background.
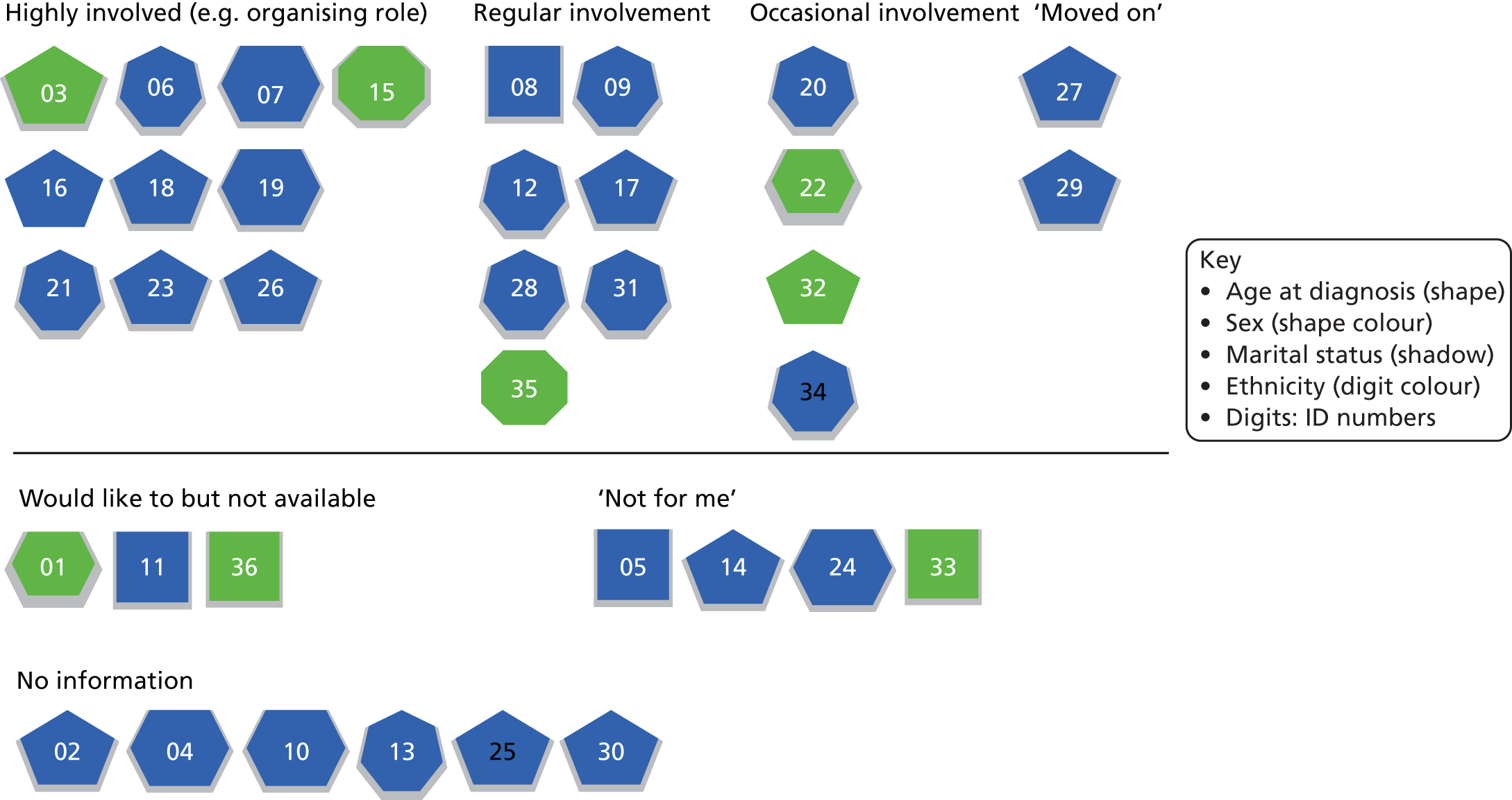
Participants’ engagement with support groups could be seen to develop and change over time, possibly reflecting the amount of psychological work involved in adjusting to their post MI patient identity. (Refer to Figure 15 for a map of support group engagement for participants in this study.) A couple of participants said that they would be keen to meet with other patients of similar age and experience, but had no awareness of a support or self-help group in their local area.
Several others, who had made major lifestyle changes post MI, were highly involved within their local group, for example as chairman or secretary. For some of them, the support group had provided an important and satisfying new role after retirement from work.
A couple of patients several years post MI said they had started to ‘move on’ from regular attendance at support group meetings as they felt well managed in terms of their medication regimen and their contact with health professionals. Living with heart disease and engagement in secondary prevention had started to become a routinely managed background issue for them.
I must admit that I haven’t, I went there for about 6 months and I haven’t since then. Work commitments, and also I suppose one moves on and life’s getting back to sort of the routine before.
HA27, male, MI in 2002 aged 51 years
Many post MI patients will have ongoing information and support needs that could, in principle, be addressed via group attendance. However, groups as the standard delivery format for such support are unlikely to suit all patients. Some people may feel uneasy at social gatherings and others may feel overwhelmed at the prospect of having to engage with other people’s problems and emotions on top of their own. A couple of participants talked about their initial ambivalence about going along to a group meeting.
Then I joined the Heartbeat Club. I hadn’t anticipated joining the Heartbeat Club because I’m not a great one for these type of clubs. I’m not a great one for going to those social things but I thought, ‘well we’ll have a go, if we go and we don’t like it then we don’t have to go again’. But we met some very nice people. The people in charge are fun and encouraging and we met other people and they had stories to tell.
HA22, female MI in 2003 age 63
Another man described an anonymous telephone support system set up by his local support group as an alternative to group attendance.
Another benefit of being part of the support group is what we call ‘ticker talk’. This is the facility for new members, or any members, to get on the phone, to phone numbers and all they know is the Christian name of the person they are phoning. And they can ask questions, and discuss, or make enquiries on anything connected with their condition, anonymously, which I think helps.
HA09, male, MI in 1995 aged 69 years
Another couple of participants said that while they could see the benefits of support groups in principle, they had no interest in attending themselves. Their perception was of support groups being primarily geared towards older people with more time on their hands.
If I could talk to people who had heart attacks while they were fairly young, I felt that [might have] helped more. [. . .] I think it probably would if, if you found people that you were similar with but you know I’m still working and still active as well and I think perhaps the support group would, would probably help people that were retired and had more time on their hands to think about things.
HA14, male, MI 2003 aged 51 years
Another man argued that enough of his life was taken up by cardiology already, and he did not want to become a ‘professional patient’. To him, attendance at support groups equated to ‘wallowing in your own self-pity’. The perceived need for a support group is very much related to patients’ existing resources and support.
You have so much of your time taken up where cardiology is the only subject because that’s what you’re there for and you don’t want to keep adding to this. It’s very tempting for people to almost become a professional patient as it were. I’ll go to that group, I’ll go to that group and I’ll join this group but you don’t want that. You know you’ve got to go and see your cardiologist, the rehab people, your GP. Fine you accept that but it would be very easy if you were that way inclined to become a professional patient. If I didn’t have a stable home relationship and a very good family, I could fill my time with this support group, that support group, which is just wallowing in your own self-pity almost there.
HA24, male, MI in 2002 aged 57 years
Methods of data collection and analysis
This report is based on a qualitative secondary analysis of purposively sampled interviews on experiences of heart attack that were collected by members of the HERG in the Department of Primary Care, University of Oxford, in 2002 and 2003.
Below, we describe how and why the interviews were originally sampled and collected to contribute to the HERG collections. We then provide further details on the participant sample for MI, describe the implications for secondary analysis and outline the process of secondary analysis.
The Health Experiences Research Group interview collections
The qualitative data in the HERG archive were collected as national, purposively sampled interview collections which aimed for maximum variation. The interviews were all collected by experienced qualitative social scientists working with the HERG in Oxford. There are currently over 75 collections of interviews, each concerning a different health issue (ranging from pregnancy to living with a terminal illness) and each set comprising 35–50 interviews. All interviews are tape recorded, transcribed, checked by the interview participant and copyrighted for a number of non-commercial purposes, including secondary analysis and publication.
The projects all share a research question (What are the experiences and information and support needs of people with healthy condition X?) and a common interview method that starts with an appropriate variation on an open-ended question intended to invite a narrative response (e.g. ‘Could you tell me all about it from when you first thought there might be a problem?’). When the person has completed their account, a semistructured section of the interview includes questions and prompts about any issues of interest that may not have been fully discussed in the narrative. These typically include questions about treatment decisions, information, support, communication with health professionals. All participants are asked if they have anything that they would like to tell other people who are starting out on the same journey and if there is anything they would like to pass on to NHS staff at all levels, who might learn from the participant’s experiences. These questions often add rich, informative data about how services and communication could be improved. 64
Each of the interview studies starts with a literature and field review and sets up a specialist advisory panel including patients, professionals, researchers, clinicians, and representatives from the voluntary sector and (if appropriate) the funding body. The panel advises on the parameters of the project, including selection and recruitment of participants.
A maximum variation sample15 of 35–50 people is sought to help generate as diverse a sample as possible, including both people whose experience might be considered ‘typical’ and those with more unusual experiences. For each project, recruits are actively sought through a national network of primary care staff, hospital consultants and specialist nurses, advisory panel members, local and national support groups, advertising online and in local newspapers, snowballing through participants and personal contacts. Analysis and data collection proceed simultaneously and continue until ‘data saturation’ is reached to ensure that the widest practical range of experiences has been included.
The participant sample for myocardial infarction
Narrative face-to-face interviews were conducted with 37 people who experienced a heart attack between 1989 and 2003. Nineteen participants experienced a MI in 2001 onwards. Nine people reported being treated with clot-buster drugs, 10 people reported having had angioplasty (2000–4), nine reported having had a stent fitted (2001–3), and 11 reported experience of bypass surgery.
The mean time gap between diagnosis and interview was 5 years, ranging from 0 to 23 years. This allowed analysis to explore accounts of experiences of MI, adjustment and engagement in secondary prevention from different vantage points in the trajectory of illness and recovery.
| Age range (years) | Total | Male | Female |
|---|---|---|---|
| Under 40 | 2 | 1 | 1 |
| 40–50 | 2 | 1 | 1 |
| 51–60 | 9 | 7 | 2 |
| 61–70 | 18 | 16 | 2 |
| 71–80 | 5 | 5 | 0 |
| 81 and over | 1 | 0 | 1 |
| Total | 37 | 30 | 7 |
FIGURE 16.
Participant sample. Number in shape: participant interview ID number. Participant sex is indicated by shape fill colour (blue = male; green = female). Participant age at diagnosis is indicated by shape form (square = diagnosed aged ≤ 40 years; pentagon = diagnosed aged 41–50; hexagon = diagnosed aged 51–60 years; heptagon = diagnosed aged 61–70 years; octagon = diagnosed aged ≥ 71 years). Participant marital status: without shadow = single; with shadow = married or cohabiting. Participant ethnicity: white number = white British; black number = black and ethnic minority background.
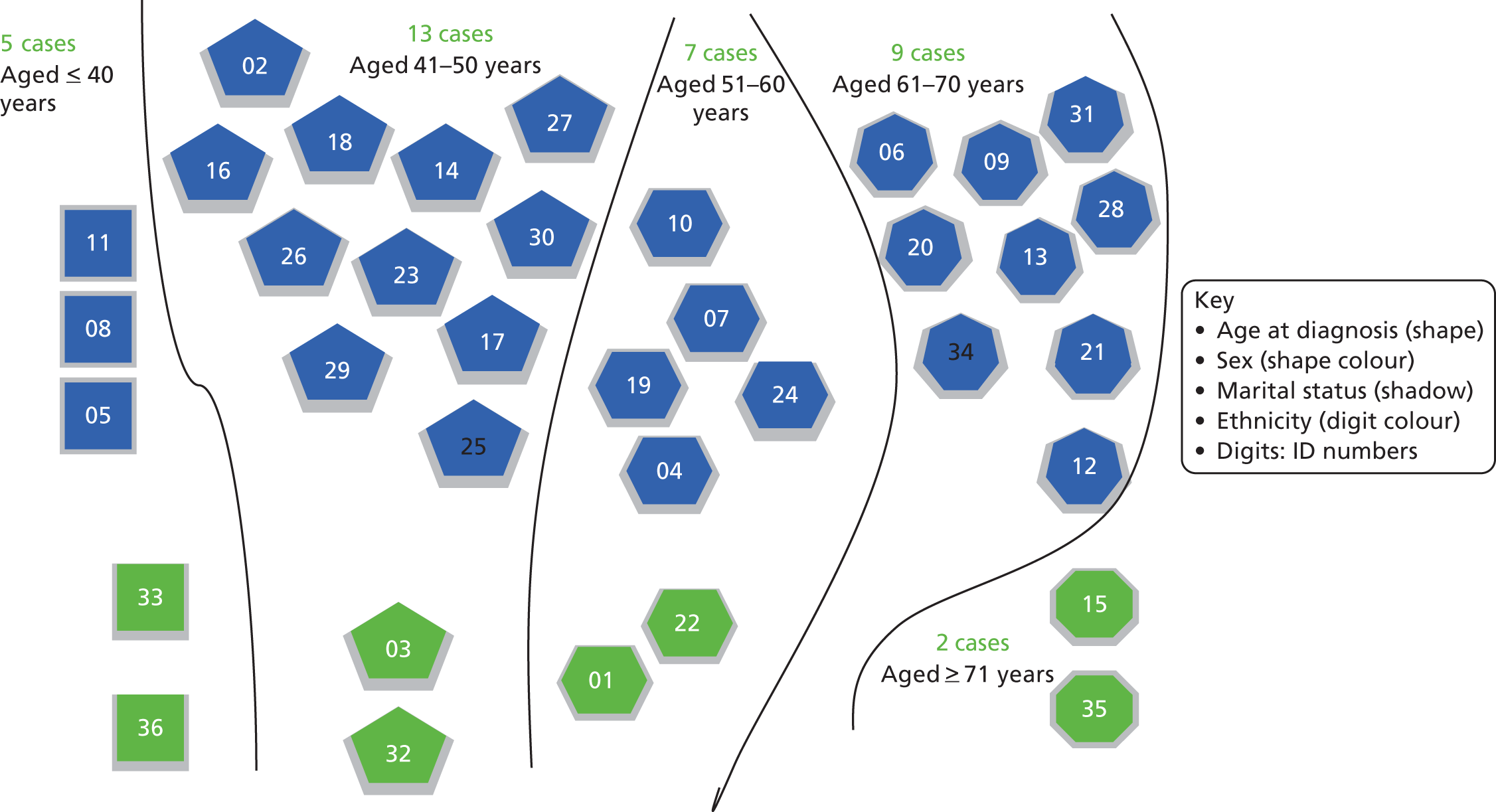
The sampling method aimed for diversity, not numerical representation. However, fewer women than men were interviewed, and all but two of the interviewees were white British. All but three were living with a partner or spouse. The sample also included a higher proportion of younger patients (i.e. aged < 55 at time of diagnosis), compared with the age profile of patients experiencing MI in the UK. The diversity in participants’ ages made it possible to explore how the experience of MI and patients’ information and support needs may differ at different ages and what adjustment to MI might mean practically and emotionally at different stages of the life course.
The sample spanned all socioeconomic groups, but may have included a higher proportion of health-literate patients than the group of MI patients as a whole. Recruitment routes included voluntary and support groups. Participants were thus more likely to be active in peer support, patient organisations and rehabilitation programmes. Participants were sampled from all parts of the UK, including urban, small town, rural and remote areas with different levels of hospital infrastructure and service provision.
Qualitative secondary analysis
A modified framework method was used. 37 This approach uses charts for a summary description of data from each of the interviews across a set of categories, which are later developed into themes for analysis. The process is iterative and flexible enough to accommodate both categorisation of data in terms of pre-existing ideas and organisational principles that have been identified as important to answer the questions at hand (e.g. areas of care that have been identified in the guideline scope) as well as emergent themes that participants themselves identify as relevant and important (e.g. experience of the hospital environment). Anticipated and emergent themes are then compared across cases, and will eventually be compared and collated across the different data sets to identify general and specific aspects of good-quality care.
Coding of the MI interviews proceeded by identifying vignettes from participant narratives that described aspects of the health care they had received and organising these into thematic clusters loosely based on the care pathway for MI. Vignettes were simultaneously coded for emotional response and emotional valence and cross-indexed with recurrent themes in patients’ experience of health care identified in previous literature,9 such as communication quality, trust and confidence, relationships with health professionals and care-givers, information and support needs and preferences, decision-making, autonomy and consent.
This process was supported by NVivo® qualitative data analysis software, which eased the systematic collation of the full range experiences across cases for each of the examined domains (care pathway, emotions, aspects of care, patient evaluation). Findings were structured into nine sections and written up, illustrating key points with verbatim quotations from patients wherever possible.
Appendix 5 Patient experience of asthma: initial briefing note for NICE drawing on Health Experiences Research Group qualitative data analysis
This report was sent to NICE in advance of the first TEG meeting to inform development of the asthma quality standard. It draws on findings from a secondary analysis of 38 qualitative interviews of people with asthma.
Diagnosis
-
Delay in making the connection between allergies and asthma, or that a chest infection or cough that fails to improve could be adult onset asthma – may be partly delay in help-seeking, so public awareness of adult-onset asthma could be improved.
-
Consistent pointers to reliable sources of information/support needed.
-
Clear explanation is needed that trying out an inhaler is part of the diagnostic process, not just a treatment once a diagnosis has already been made.
Non-pharmacological management (including prophylaxis, diet, complementary therapies, environmental factors)
-
Relationship between allergy and asthma not always recognised, need more attention to allergy prevention.
-
Exercise – not always informed that taking reliever inhaler before exercise can help prevent symptoms.
-
Smoking cessation – awareness does not always translate into behaviour change.
-
Vaccination against flu commonly available but practice on pneumococcal vaccine more variable.
-
Focus can tend to be too much on medical solutions rather than lifestyle advice.
Pharmacological management
-
Concern about oral steroid side effects, even while recognising the benefits, may confuse them with anabolic steroids. To prevent suboptimal intervention, patients need clear information about their importance, how to minimise and when to report side effects. Pre-prescribed steroids valued (below).
Inhaler devices
-
A ‘rainbow’ of inhalers described, routinely referred to by colour.
-
More information on what each contains, generic and brand names, how it works and what it is for (preventer, short- or long-acting reliever, combination) could help.
-
Good inhaler technique is essential; specialist asthma nurses can demonstrate and check technique and find alternative delivery modes for those who find standard inhalers difficult.
-
While some report rigorous adherence to their preventer inhaler regime, others see it as something to reduce or stop when their symptoms are back under control.
-
All patients should be advised on stepping treatments up and down, and advised that inhaled steroids do not carry the same risk of side effects as oral steroids.
Management of acute asthma
-
Best strategy to take action before it gets to attack level. Some patients negotiated with their GP to keep pre-prescribed steroid tablets at home for emergency use, and valued this trust in their ability to self-manage. Some also keep a peak flow monitor at home to help them judge when to seek help (but see patient education below).
-
Encouragement needed for people to call ambulance or go to A&E and not feel they are misusing care, and information on timing this.
-
Greater clarity needed for both professionals and patients on what is a panic attack and what is an asthma attack.
-
People report leaving deteriorating symptoms too long hoping they can continue to self-manage and ending up using more hospital resources as a result.
-
Ambulance care generally good. A&E variable – some well-prepared to deal swiftly with asthma patients, others less so, and sometimes staff do not listen to what patient knows of own their condition. When in hospital for another condition, ward staff may not understand asthma.
Adolescence
-
Good support at school is needed – not just in managing medication but also in providing well-informed support and encouragement for taking part in sport.
-
Concerns about schools not allowing children to hold their own medication, or allowing them to take someone else’s inhaler in an emergency.
-
Parents may need advice on how and when to hand over responsibility during teens, and young people on how to manage their own medication and monitoring responsibly.
Organisation of care
-
Specialist asthma nurses in primary care particularly valued but availability and access is inconsistent. Some practices did not have one, or had a practice nurse who was not asthma trained, or there was one but people were not aware of their existence.
-
Regular review of symptoms/medication also inconsistent – some report not being called for annual or regular review.
-
Patchy availability of spirometry.
Patient education and self-management
-
See all sections. Creating an equal partnership with respect for the expertise of people who have had asthma for a long time and trusting them to know something is wrong, but also ensuring they are offered regular review. People need to know their condition may change over time. ‘Please listen’ is one of the most common messages for professionals, along with giving people enough time and patience to answer questions (which they may need to ask several times before they absorb the answer).
-
Peak flow diaries/monitoring at home – not everyone wants this, but can be useful for those who are interested, and may help give people an objective measure to alert them to seek further help.
Emotions and acceptance
-
Adult-onset asthma can be a huge surprise to people. Unwillingness to accept the implications can lead some people to reject medication or stop taking it after a while.
-
Primary care support needs to pay attention to emotional as well as physical responses and explore patient (mis)understandings of living with asthma longer term and the importance of a regular approach to medication.
Appendix 6 NICE draft quality standard: asthma
Supporting information on patient experience by draft quality statement. This report was sent to NICE in advance of the second TEG meeting to inform development of the asthma quality standard. It draws on findings from a secondary analysis of 38 qualitative interviews of people with asthma.
| Draft quality statement | Area of care | Draft quality statements for discussion | Additional information |
|---|---|---|---|
| 1 | Diagnosis | People with asthma have their reasons for diagnosis documented. Diagnosis may follow a number of different trajectories:
|
|
| 2 | Diagnosis of occupational asthma | People with suspected work-related asthma have the diagnosis confirmed using standard objective criteria. Now incorporated in statement 1. Similar issues apply – being unaware occupational asthma is possible and finding it hard to accept. |
May be incorporated into the diagnosis statement and not be a standalone statement. |
| 3 | Self-management education | People with asthma are offered self-management education including a personalised action plan. People with asthma report considerable variation in their experiences of education for self-management and provision of personalised action plans. Key needs (which may be expanded upon in other sections) include:
Action plans: Not all of our interviewees had one; some said they had discussed it with the nurse or doctor but it had not been formalised in writing. The role of specialist asthma nurses in primary care in supporting self-management is particularly valued but availability and access is inconsistent. Some people we talked to said their practice did not have one, or they had a practice nurse who was not asthma trained, or there was one but their existence was not well publicised (for people with complex/severe asthma more specialist secondary care support is better suited to their needs). Emotional responses: Adult-onset asthma can be a huge surprise to people. Unwillingness to accept the implications can lead some people to reject medication or stop taking it after a while. Primary care support therefore needs to pay attention to emotional responses as well as physical management, and explore patient (mis)understandings and fears about living with asthma longer term and the importance of a regular approach to medication. Adolescence: parents may need advice on how and when to hand over responsibility during teens, and young people themselves need tailored support to emphasise the importance of good control and sensible lifestyle choices. |
|
| 4 | Non-pharmacological management (lifestyle) | People with asthma are offered advice on lifestyle modifications to improve asthma control. Some people said they would welcome more attention to lifestyle rather than medical solutions. Weight reduction and exercise: people with exertion-induced asthma may feel advice to take exercise is unrealistic. However, several people recommended taking their reliever inhaler before exercise and felt this strategy should be more widely known. Advice on other forms of exercise should be offered to suit different types of trigger (e.g. indoor for those with hay fever or cold air triggers; less strenuous forms for exercise-induced asthma). Focusing less on the negative aspect of being overweight and more on the positive benefits of increasing lung capacity may help. People feel disheartened if their weight gain is down to increased appetite from steroid use, suggesting more help at an earlier stage with diet and weight control. Children need well informed support and encouragement from schools to participate in sport. Smoking: people may be well aware of the risks from smoking but continue to do it, perhaps because they want to lead a normal life and not feel dominated by the condition, and are therefore unwilling to accept that smoking makes their asthma worse. Again this suggests a need for health professionals to engage with emotional responses to the condition. There were mixed views about how to get the balance right between reassuring people they can live a normal life with asthma but bringing home to them the importance of good control. A few young people wondered whether more stark information from a health professional might help them confront the reality of asthma as they started to take more responsibility for their own health. Breathing exercises: were welcomed by some people, not just as a way to improve their physical breathing but to reduce stress and feelings of panic. Some recommended singing or playing a woodwind instrument. Allergy-related: more advice on allergy prevention would be welcome. However, this needs to be tailored to individual triggers – for example blanket advice not to have a pet would be inappropriate. People spend a lot of money buying hypoallergenic furnishings and adapting their home to reduce dust/dust mites. Evidence for this may be weak but this is counter-intuitive to many people and could undermine wider credibility of advice given. More information on possible food and drink triggers would be welcome. Most people seemed to have discovered this by personal trial and error. |
Lifestyle modifications include weight reduction, smoking and breathing exercises. |
| 5 | Medicines optimisation | People with asthma receive regular medication, adjusted in accordance with disease control. Information: a ‘rainbow’ of inhalers was described, routinely referred to by colour. More information on what each contains, generic and brand names, how it works and what it is for (preventer, short or long acting reliever, combination) could help. This is a fast-changing field so most information providers seem to steer clear of detail on all the types of inhaler, but people would like the option of knowing more about what is available and whether they could try different types. Concern about oral steroid side effects: even while recognising the benefits, people may confuse them with anabolic steroids. To prevent sub-optimal intervention, people need clear information about their importance, how to minimise and when to report side-effects. Pre-prescribed steroids are valued. Some also have misplaced worries about side-effects from inhaled steroids. (Points under ‘review’ are also relevant – there is no easy separation between medicines optimisation and review). |
|
| 6 | Review | People with asthma are offered a review of medicines adherence, compliance and inhaler technique on a regular basis. Good inhaler technique is essential; specialist asthma nurses can demonstrate and check technique and find alternative delivery modes (e.g. spacers) for those who find standard inhalers difficult. People report often not realising how bad their inhaler technique was until someone asked them to demonstrate. Stepping treatment up and down: while some report rigorous adherence to their preventer inhaler regime, others see it as something to reduce or stop when their symptoms are back under control. All patients should be advised on stepping treatments up and down, and encouraged to discuss this with a health professional unless they are very experienced in self-management. As above, clear information on the balance of benefits and side-effects from oral steroids. They can be reassured that inhaled steroids do not carry the same risk of side effects, which is a worry for some. Availability of regular review seems inconsistent – some people do not remember being called. Relationship with a specialist asthma nurse was highly valued for both formal regular review and an informal source of advice in between. (The option of informal telephone contact with both GP and asthma nurse was welcome.) Availability of written personal action plans is also patchy. Acceptability of regular review: while many people valued regular review, some whose asthma is mild and well controlled were unsure they would want regular review. For example, one recently diagnosed young man said regular asthma clinic visits would be depressing. ‘It would feel like it’s getting a grasp on my life. It would feel like it’s controlling me whenever I should be controlling it.’ Making regular review acceptable and explaining its value needs attention. Another person offered helpful advice to others: ‘One of the things I’ve learnt is that it’s important to go back regularly to your asthma clinic, even if you think you don’t need to. Mostly because if you don’t know who they are and they don’t know you and you’re not familiar with it, then if you did get into difficulties it, that’s harder for you’. Acceptability for people with more severe asthma is also an issue – for them it is vital review is conducted by those they perceive as expert enough (see below). Peak flow diaries/monitoring at home: not everyone wants this, but they can be useful for those who are interested, and may help give them an objective measure to alert them to seek further help. |
|
| 7 | Assessment of severity | People with an acute exacerbation of asthma receive a prompt and objective measurement of severity. Understanding exacerbation and seeking help: before severity of an exacerbation can be assessed, the person has to recognise what is happening and seek help. As noted above, some people find home peak flow monitoring and diaries useful to help them know when to get help. Written action plans should also provide indicators that should trigger help-seeking. But people often report leaving deteriorating symptoms too long hoping they can continue to self-manage, and end up with a bad attack. Encouragement is needed to call an ambulance or go to A&E and not feel they are misusing care, and information on the timing of this. People also report finding it hard to make proper decisions during an attack, saying they felt ‘in a fog’, ‘detached’, not wanting to move, and past caring what happened to them. This, combined with the fact that they may not be able to speak to tell people what’s happening, means family, friends and colleagues may have to take action in an emergency. It is vital they know what to look out for and what to do. Ambulance staff: were generally reported to be aware of and responsive to people’s needs for urgent care. People with severe, frequent attacks may benefit from personal registration of their details with the ambulance service. One woman reported that her mobile number was ‘red flagged’ with the ambulance call centre so that an ambulance could be dispatched immediately without her needing to speak. (This contrasted with the ambulance service where she lived previously who had on occasion implied she should get someone to drive her to A&E, against her consultant’s advice). A&E: some had experienced excellent and immediate attention in A&E, but there were also a few encounters with junior staff with limited experience and training who did not realise the need for urgent assessment and treatment. One solution is to carry an emergency admission card to show at reception to ensure quick assessment. One woman also described a patient-held folder developed by her consultant and the community matron containing a detailed management plan which (given the complexity of her condition) does not follow standard protocols. She hands this to the ambulance staff who pass it on to A&E. As this is personalised rather than protocol driven she feels it means she gets appropriate care first time. |
|
| 8 | Treatment for acute asthma | People with an acute exacerbation of asthma are treated in accordance with BTS/SIGN guidance. Oral steroids: some patients negotiated with their GP to keep pre-prescribed steroid tablets at home for emergency use in an acute attack, and valued this trust in their ability to self-manage. Oxygen/nebulisers/ventilation: generally few concerns reported, but one person reported a bad experience where she had to wait in A&E for a nebuliser to be brought. Aminophylline/theophylline: were mostly given in hospital. Side-effects such as vomiting can be very unpleasant and require careful management; tablet form may help. Some people with severe asthma were able to obtain aminophylline/theophylline through their GP surgery, which they welcomed as more convenient. In some cases local minor injuries units were also accessed for acute treatment. (One person with severe asthma and frequent hospital attendances complained on one occasion about having to agree to what she described as an ‘extremely painful blood gas test’ before she could have aminophylline in a hospital where she was not known to the staff, and felt this was down to lack of experience. She contrasted it with excellent care in a ‘village hospital’ where she was immediately nebulised and then given aminophylline with no blood gas tests.) Schools: there is concern about some schools not allowing children to hold their own medication, or allowing them to take someone else’s inhaler in an emergency. |
|
| 9 | Specialist supervision | People admitted to hospital with an acute exacerbation of asthma are seen and treated under the care of a specialist. Specialist care is valued by many people, but particularly those with frequent and severe exacerbations, who need expert input – and recognition of their own expertise. See also sections 7 and 8. There are some concerns for people with asthma admitted for another condition. One woman reported that the nurses had no training in respiratory care and did not understand that she needed medication immediately in an attack. |
|
| 10 | Discharge arrangements | People treated in hospital with an acute exacerbation of asthma receive self-management planning and a written personalised action plan prior to discharge. As with other aspects of self-management planning and written personalised action plans, practice is variable. |
‘People treated in hospital’ includes people treated both in A&E and as an inpatient. |
| 11 | Follow-up | People treated in hospital with an acute exacerbation of asthma are followed up by a clinician with particular expertise in asthma management. As above – access to appropriate level of specialist care is valued but sometimes people feel they are being cared for by someone who is too generalist. People with severe chronic asthma want continuity of care so that they do not have to keep ‘retelling’ their story to new consultants. They want consultants to recognise their past experiences as ‘experts’ on their own condition. |
A clinician may include a primary care nurse or GP with particular skills in asthma management or a respiratory physician. |
| 12 | Difficult asthma | People with difficult asthma are offered an evaluation by a dedicated multidisciplinary difficult asthma service. People with difficult asthma value a highly personalised service, with tailored care instructions and frequent monitoring. See above example of the patient-held folder developed with the consultant and community matron as an exemplar of good practice. |
|
| 13 | Risk stratification | People with asthma have a risk stratification assessment in primary care. Not raised as an issue in interviews. |
Appendix 7 Children and young people’s experiences of type 1 diabetes: initial briefing note for NICE drawing on Health Experiences Research Group qualitative data analysis
This report was sent to the NCC-WCH and to NICE to inform development of diabetes quality standards (type 1 in children and type 2 in adults). It draws on findings from a secondary analysis of 37 qualitative interviews of young people with diabetes.
Interview sample: 37 young people, 15 male, aged 15–27 years, diagnosed with type 1 diabetes aged 1–24 years, interviewed 2006, updated 2010 and 2012.
Diagnosis
-
Parents and children may have diverging information and support needs at diagnosis. Information needs to be easy to understand without being simplistic, followed up by more detailed guidance at patients’ and families’ own pace during the period of adjustment.
-
Parents and patients may self-blame and require reassurance that type 1 diabetes is not a result of bad diet or similar.
-
Receipt of diagnosis during teenage years is likely to affect patient confidence. Give advice and assistance on communicating the diagnosis and implications to school staff and peers.
-
Be aware that newly diagnosed young patients admitted to adult diabetes wards may find it traumatic to be confronted with possible long-term complications of poor glycaemic control such as amputation or loss of eyesight.
Management (insulin, glucose monitoring, diet, exercise)
-
Electronic transmission of glucose test results enables diabetic specialist nurses (DSNs) to spot problems quickly between clinic appointments. However, paper records, while disliked by many young patients, may offer greater opportunities for diabetes staff to educate patients about pattern recognition.
-
‘Controlling diabetes’ has different meanings for young people and clinicians: the priority for the young person is to live life well and achieve their goals within the constraints of managing diabetes. Good glycaemic control may not be experienced as ‘in control’ by the young person if it restricts participation in peer activities and affects their emotional well-being.
-
Provide positive reinforcement that takes into account young patients’ management efforts as well as actual results alongside realistic suggestions for areas of improvement. Be mindful that exam stress, family arguments, periods and illness may detrimentally affect glycaemic control despite patients’ best efforts.
-
Young patients are motivated by diabetes staff who are able to link issues of diabetes management to their interests and aspirations.
Insulin regimen, monitoring and injecting devices (pumps, pens, etc.)
-
Both fixed and more flexible insulin regimes may suit patients’ lifestyles at different developmental ages. A fixed regimen can give a greater sense of security especially in the initial months after diagnosis.
-
Be mindful that the increased freedom of switching to a more flexible regimen as the patient gets older might provide a particular risk period for the development of eating disorders.
-
Administering injections by themselves can provide young patients with a sense of control and independence and is usually experienced as less painful. However, a few young people may require psychological support to overcome fears of injecting themselves. For those diagnosed at an early age, transfer of responsibility for injections may present a key site for tensions around children’s growing sense of independence.
-
Patients and families report having to rely on support groups and other sources external to the diabetes team to access information about insulin pumps. Novice pump users value peer support from more experienced pump users.
Management of hypoglycaemia
-
Despite awareness of its treatment, many patients and families regard hypoglycaemia as the most difficult aspect of diabetes to come to terms with emotionally. Some young patients report that they may keep glucose levels intentionally too high to avoid hypos.
-
Fear of hypos may lead to overly anxious or controlling behaviours on the part of patients and parents.
Management of hyperglycaemia
-
Some patients perceived clinicians as putting too much emphasis on hypos at the expense of discussing hyperglycaemia and its consequences.
-
Ketosticks enable patients to self-monitor for ketoacidosis and may make them feel more in control.
-
Appreciate the impact of ‘highs’ and ‘lows’ on patients’ mood, compounding ‘normal’ teenage moodiness.
Organisation of care
-
DSNs are appreciated for their kindness and accessibility outside of clinic appointments. Supportive and trusting relationships are frequently developed in the transition from hospital to home after initial diagnosis.
-
Young people value being able to contact DSNs via e-mail or text messaging. Especially for teenagers, DSNs can provide a confidential source of information for issues that patients do not want to discuss in the presence of their parents (e.g. sex, drugs, alcohol).
-
Families in rural areas may not have access to medical staff with expert diabetes knowledge outside clinic hours. Lack of access to staff with diabetes expertise is also a problem when patients are admitted to hospital for non-diabetes-related illness or injury.
-
Patients and families value continuity of care within the diabetes team. Young people dislike having to repeat their medical history to changing registrars, etc., if this information could be gleaned from medical records prior to the consultation.
Transition to adult services
-
Flexible consulting structures within paediatric diabetes teams allow patients to gain greater independence stepwise, i.e. the option to consult individually on confidential concerns with the DSN or dietitian while continuing joint visits with parents to discuss less sensitive issues.
Patient education and self-management
-
Many young patients are unclear about the clinical value of frequent finger-prick tests. Understanding fluctuations in glucose levels in the context of their individual lifestyles may increase young patients’ sense of mastering their condition.
-
A focus on HbA1c at clinic appointments results in children perceiving clinical contact as for the benefit of the medical team. To engage young patients, discussions about glycaemic control need to be anchored in patients’ everyday concerns.
-
Education needs to include patients’ school staff (e.g. via visits by the DSN). Teachers may inadvertently penalise patients by excluding them from sports and other class activities due to lack of awareness and overanxious attitudes to risk management.
-
Guidance for schools should cover issues such as provision of easily accessible private space for storing diabetes kits and injecting as well as classroom policies on snacking mid-lesson and visits to the toilet.
Respect for young patients and sensitivity to changing developmental needs
Communication
-
Young patients and families value clinicians with a flexible communication style that is responsive to children’s individual development.
-
Teenagers are likely to disengage from the consultation when talked about in the third person, while younger children may feel put ‘on the spot’ when addressed directly. Attempts at involvement need to feel genuine to the young person.
-
Younger children may be afraid to ask questions of their own but respond well to having information provided at their level of understanding.
Examination
-
Young patients appreciate clinicians treating their bodies with the same respect as adult patients. Female patients may be particularly sensitive to lack of privacy when having their weight measured and recorded.
Psychological support
-
From patients’ and families’ perspectives, psychological support is an integral part of clinical care rather than an add-on specialist service.
-
Glycaemic control is bound up with patients’ self-esteem. Patients may feel despondent and worry about letting clinical staff or parents down if their glycaemic control is poor. Finding an insulin regimen that works can act as a confidence boost.
-
Young patients with eating disorders are generally aware of the damaging consequences of their behaviour, so information and directives by clinical staff are unlikely to improve outcomes. Clinical support needs to address underlying issues such as feelings of isolation, low self-esteem and causes and consequences of dishonesty towards significant others.
-
Some of the problems and difficulties experienced by patients may not be attributable to diabetes but be a ‘normal’ part of being a teenager and families may need to be reminded of this. Rebellion via neglecting injections or testing or eating junk food should be expected. Sometimes ‘straight talk’ from a clinician not usually involved in the young person’s care can make a difference.
Appendix 8 Patient experience of rheumatoid arthritis: initial briefing note for NICE drawing on Health Experiences Research Group qualitative data analysis
This report was sent to NICE in advance of the first TEG meeting to inform development of the RA QS quality standard. It draws on findings from a secondary analysis of 52 qualitative interviews of people with RA (and four partners).
Interview sample: 52 people with RA (and four partners), disease duration: 9 months to 26 years; interviewed 2003–4, updated 2008 and 2012.
Diagnosis
-
The time that patients waited for referral to a hospital specialist was highly variable (sometimes up to eighteen months). Improvement in referral times would result in more timely diagnoses and hence improved patient outcomes. Diagnosis of RA is difficult as clinical signs are similar to conditions such as polymyalgia rheumatic, lupus, etc. Greater awareness that other inflammatory conditions have similar clinical signs may accelerate correct diagnosis.
-
Fear of joint deformity or disability is a common feeling in people diagnosed with RA. Consultants often explained that RA affects people differently and that modern interventions are more successful at preventing joint disfigurement.
-
It is important to tell patients that there are therapies able to modify or halt the physical effects associated with RA in the past. Kindness and reassurance are particularly appreciated by those patients who know older people, maybe relatives, who were considerably disabled through RA.
Pharmacological management
-
Finding the treatment that is appropriate for the individual is a major challenge for RA patients as it can take time and presents a difficult period for the patient and their family. The ‘right’ treatment is one that controls the condition by alleviating symptoms with minimal side effects. During this period patients need appropriately tailored information and emotional support to cope with variable symptoms such as fatigue, stiffness, pain, fears about the future and low moods. Good communication and trust between members of the RA care team and patients is essential to provide the necessary support during this challenging period.
-
Patients on the new biological therapies, who typically attend extra appointments with a specialist nurse, seem to be better informed than patients on DMARDs. Among the people we talked to only those patients on DMARDs said that they sometimes did not take medicines because of concerns about toxicity and side effects.
-
Hearing about other patients experiences of using a drug, in combination with other information about the medicine, helped people to decide whether or not to accept the treatment.
-
Patients who had participated in clinical trials and responded well to the new biological therapies were concerned about whether the funding would be available to continue treatment.
Non-pharmacological management
-
Physiotherapy services in the NHS are restrictive, allowing a limited number of sessions. Lengthy waiting lists meant treatment was often not received when it was most needed and people saw several different physiotherapists.
-
Access to hydrotherapy is also limited, but centres that allowed patients to self-refer for a 3-week course were much appreciated.
-
Experiences of complementary approaches such as massage, acupuncture, etc., were very mixed.
Organisation of care
-
Continuity of care is very important to patients but patients rarely see the same specialist. Continuity of care helps foster trust and confidence in health professionals (different specialists sometimes give different answers to the same questions).
-
Patients who want to play an active role in planning their own treatment nevertheless need time, information and advice from their care team, especially while they are ‘learning the ropes’.
-
The right to exercise informed choice is important to most patients but there are those who prefer to avoid shared decision making. Doctors need to discuss preferences, and recognise that these may change once the patient has learnt more about their condition.
-
Care teams should inform patients about resources for rehabilitation at work and financial/benefits support.
-
Pharmacists are an important source of help, advice and practical support (e.g. dispensing tablets in bottles rather than blister packs). Their supportive role needs highlighting and encouragement.
Self-management
-
People who have attended self-management courses have found them very useful. Patients value additional advice, support and information on a wide-range of issues that due to time constraints may not be comprehensively discussed during consultation, e.g. how to cope with flare-ups, stiffness, medication, painkillers, pacing, long-term effects, side effects of medication, exercise, etc.
Emotional impact
-
People with manual jobs and those raising young children were particularly worried about their ability to continue supporting their families.
-
RA can sometimes put a strain on relationships. Care teams need to consider the patient’s family situation.
-
RA patients reported feeling awkward and embarrassed in public, e.g. opening a bottle or can. Opportunities to learn from other patients’ coping strategies was valued.
Family and friends
-
People worried that they may pass RA to their children. This issue should be addressed during consultation and guidance provided – e.g. on how to explain RA to children and to help them understand early symptoms.
-
Family and friends may need referring to support and information to help them understand the illness, the unpredictability and to appreciate the long term effects of RA.
Young people and young adults
-
Young people have particular concerns such as body image, schooling, leaving home, relationships, alcohol, illicit drugs which they would like to have the opportunity to discuss, confidentially, with their care team.
-
Young people were often shocked to have been diagnosed with RA because they and their peers saw it as an ‘old’ person’s disease.
Information/education needs
-
RA can make sexual activity difficult or impossible. This area is often neglected by health professionals; patients need access to confidential resources for advice and support.
-
Public awareness is needed to counteract the general public view of RA as an illness of ‘old people with crooked hands’. This stereotyped view of RA may prevent young people and young adults from disclosing their illness to others.
Appendix 9 NICE draft quality standard: rheumatoid arthritis
Supporting information on patient experience by draft quality statement. This report was sent to NICE in advance of the second TEG meeting to inform development of the RA quality standard. It draws on findings from a secondary analysis of 52 qualitative interviews of people with RA (and four partners).
Supporting information on patient experience by statement, drawn from secondary analysis of 52 qualitative interviews with people with RA.
| Draft quality statement | Area of care | Draft quality statements for discussion | Important but possibly tangential points |
|---|---|---|---|
| 1 | Referral for specialist assessment | People with suspected synovitis affecting the small joints of the hands or feet or more than one joint receive a specialist opinion within 2 weeks of presentation. OR People with suspected synovitis are referred for a specialist opinion. KEY POINTS Delay in presentation with symptoms. In this interview collection, reasons for delayed presentation included an initial reluctance to seek help, coupled with the hope that minor, gradual or non-specific symptoms (stiff joints in the morning, painful wrists) were due to sports injuries, chilblains or other non-serious causes and might get better by themselves or be put down to general ageing. Occasionally a person may delay consulting because they are fearful about what the symptoms may mean, but those who became suddenly and dramatically ill did not delay consulting. Delay in diagnosis. Several people with RA said that their GPs did not seem to take their symptoms very seriously, even if the GP advised them to return if symptoms persisted. The time that people waited for referral to a hospital specialist was highly variable (sometimes up to 18 months). Issues for public awareness. Younger people said they had previously thought of RA as an ‘old person’s disease’. Most patients had not been aware before diagnosis that accessing treatment quickly could have a significant impact on its effectiveness and avoidance of irreversible damage to their joints.Diagnosis of RA is difficult as clinical signs are similar to conditions such as polymyalgia rheumatic, lupus, etc. Greater public awareness that other inflammatory conditions have similar clinical signs may accelerate correct diagnosis. |
People who had experience of older relatives being severely disabled by RA were frightened to consider the possibility that they might be affected. |
| 2 | Investigations | People with suspected rheumatoid arthritis who are negative for rheumatoid factor are offered anti-cyclic citrullinated peptide antibodies testing. In relation to the possible reluctance of patients to accept drug treatment without a definite diagnosis of RA remarked upon by the GDG, a few people with RA in the HERG interview collection reported a reverse scenario, where they had initially tested negative for rheumatoid factor but were personally convinced that they were experiencing RA and were keen to gain access to RA-appropriate drug treatment. Need for reassurance. As many people with RA seek help at a time when they experience acute inflammation and severe pain, they need reassurance that effective treatments exist and symptoms are unlikely to continue at the same intensity. |
|
| 3 | Initiation of treatment | People with newly diagnosed active rheumatoid arthritis are offered a combination of disease modifying anti rheumatic drugs within 3 months of the onset of persistent symptoms. KEY POINTS Fear of joint deformity or disability is a common feeling in people diagnosed with RA. Patients found it reassuring when consultants explained that RA affects people differently and that modern interventions are often successful at preventing joint disfigurement. Patients whose acute symptoms have subsided by the time they see a rheumatologist may find it difficult to accept the chronic and recurring nature of the disease and therefore be reluctant to commence medication. Patients may also be reassured if doctors explain that it may take time to find the most suitable treatment for an individual. |
RA affects patients in variable and unpredictable ways. RA affects people very differently so requires a flexible approach, individual assessment of patients’ information and support needs and tailoring of service level particularly important. Meaning of diagnosis for patient’s life. At diagnosis people are often concerned about how their RA may affect their employment or studies. Signposting to relevant employment laws, information about assistance at work and available benefits is much appreciated. The unpredictability of RA and the uncertainty about when they may get better has major implications for people of working age who may need assistance in communicating the nature of RA and its implications for their ability to continue in their work role to an employer. People with less secure or manual jobs and those raising young children were particularly worried about their ability to continue supporting their families. Explanation about the nature and causes of RA. Understanding the possible causes of RA and why it happened to them is a key concern for many newly diagnosed patients.Patients like to have an opportunity to ask questions, be listened to respectfully and answered in a way they can understand. Information needs and preferences vary but patients now routinely use the internet for information and appreciate being referred to reliable sites and invited to discuss what they find if they have questions. Drug alternatives and treatment preferences. Patients will have different priorities and preferences regarding the acceptability of different types of side-effect associated with different drugs (e.g. women of child-bearing age may not want drugs that are contra-indicated for pregnancy, but the doctor cannot guess whether this applies to a particular patient). People, including those who did not feel they knew enough to share decision-making, appreciated it when doctors took time to explain drug alternatives, (see also 10. Drug Monitoring). |
| 4 | Access to multidisciplinary team | People with rheumatoid arthritis have ongoing access to a multidisciplinary team. KEY POINTS Access to MTD varies across NHS sites. Ease of access to specialist care within the (multi-disciplinary team) MDT was reported to vary widely by people with RA in the HERG interviews. Experiences ranged from individuals who said they had bi-annual consultant appointments and interim GP monitoring, to others who had their nurse specialist’s phone number, were able to book hospital appointments directly if they had a flare up and were able to self-refer for occupational therapy. Access to physiotherapists (PTs) and occupational therapists (OTs). After diagnosis people usually had contact with a physiotherapists and/or occupational therapists, although sometimes this was a one-off assessment. People liked to be reminded about important practical advice from physiotherapists that had slipped to the back of their minds over the years. Some people said they were able to access PT/OT support directly and valued this, but many patients had no direct access to PTs/OTs and had to wait for needs to be identified at their annual review. Sometimes this meant that the prime period of need had already passed. Lack of continuity of relationship with MDT members. Several people reported a lack of continuity in their relationships with members of the MDT, in particular PTs and OTs. Having to tell their story afresh each time when coming for an appointment can be frustrating especially for people who have lived with RA for many years. Different consultants were perceived to have different treatment preferences which worried some patients who thought they might need to move location. Some patients ask to be transferred to a different consultant because they felt poorly treated or because they had heard very positive accounts about another consultant. Young people may have different needs of the MDT. Young people sometimes have particular concerns such as body image, schooling, leaving home, relationships, alcohol or illicit drugs which they would like to have the opportunity to discuss, confidentially, with their care team. |
Importance of the hospital appointment. When the appointment with the consultant rheumatologist was people’s only access to expert opinion they tended to save up questions to ask. If they did not get a chance to ask their questions or felt replies were rushed or inadequate they were particularly disappointed. Continuity of care is usually valued (for reasons of efficiency as well as relationship), but people with RA may also compare notes with other patients and ask to change to another team if they believe they will be better treated. |
| 5 | Education and self-management | People with rheumatoid arthritis are offered educational activities that include self-management programmes. OR People with rheumatoid arthritis are offered self-management programmes. KEY POINTS Due to time constraints, some important issues such as how to cope with flare ups, stiffness, medication, painkillers, pacing, long-term effects, side-effects of medication, exercise, etc. may not be comprehensively discussed during consultations. Those who had experienced group education sessions found them helpful and particularly valued advice on effective use of painkillers, suggestions for lifestyle changes that might improve their symptoms and finding out about the full range of services available to people with RA. Sessions also provided valued opportunities for peer advice and support. OTs and PTs were reported to be important sources of practical and self-management advice. They were appreciated for providing motivation and encouragement about living with RA, and in some cases, visiting people in their homes to suggest modifications, e.g. to kitchens or bathrooms to ease daily activities. Complementary approaches. Some people said they would like more information about how to identify trustworthy and worthwhile complementary approaches. Several had experimented with modifying their diet, cutting out alcohol or engaging in gentle exercise like swimming or walking. There was some uncertainty as to how much physical activity was beneficial and reports of conflicting messages from different health professionals and a few people felt confused about whether warming or cooling the joints was more beneficial, as both are recommended strategies by physiotherapists. Patients were uncertain how to interpret professionals’ apparently different opinions about the value of regular hydrotherapy. Those who had experience of hydrotherapy tended to like it and report that it helped their RA. Those who were able to self-refer to hydrotherapy felt lucky. |
See above about use of internet – also used to support and inform self-management. The most comprehensive and relevant information often came from charities such as Arthritis Care who run Challenging Arthritis courses. Unmet information needs. Are common, especially in the early years following their diagnosis. Many people wanted to understand the condition and how it differs from other types of joint inflammation, how prescribed medication worked, the best ways of taking drugs and to learn simple things they could do to help themselves. |
| 6 | Measuring disease activity | People with recent-onset active rheumatoid arthritis are offered monthly measurement of disease activity until the disease is controlled. People who have regular monitoring find it reassuring to think that any problems will be picked up early. In the longer term the inconvenience of regular visits may outweigh these advantages but in the initial stages after diagnosis regular testing was usually appreciated. |
|
| 7 | Ongoing disease control | People with rheumatoid arthritis are offered treatment relevant to their disease activity. The opportunity to exercise informed choice is important to most patients but there are those who prefer not to be involved in decision making about drug treatment. Doctors need to discuss drug preferences and recognise that these may change once the patient has learnt more about their condition. Hearing about other patients experiences of using a drug, in combination with other information about the medicine, helped people to decide whether to accept the treatment. |
|
| 8 | Appropriate referral for surgery | People with rheumatoid arthritis who may benefit from surgery are referred for a specialist surgical opinion. KEY POINTS Acceptance of the need for surgery. Several of the HERG respondents who described surgery saw it as ‘the final resort’ when drug treatments had failed to alleviate problems. It was sometimes difficult for patients to accept the need for surgery when pain or mobility problems were still relatively mild, some sought a second opinion before going ahead with surgery. Some chose to delay operations for as long as they could to avoid the need for further surgery if their prosthesis wore out. Patients who did not have the exact nature and extent of the planned surgery explained to them beforehand sometimes felt angry and badly treated (e.g., one man was bitter that both his ‘bad’ and his ‘good’ foot had been operated on under general anaesthetic, when only the operation on the bad foot had been previously discussed with him). Several people remarked that the surgeons they had encountered were poor communicators. Those who had had repeated operations learned what to ask and had more detailed discussions before deciding whether to have an operation. Concerns around undergoing surgery. Patients are sometimes very reluctant to have surgery and can be shocked when it is suggested that they have a series of operations. Those who had undergone several operations said they had greater concerns about the impact of surgery on their everyday lives than about the procedure itself. As surgery was typically followed by several weeks of rehabilitation, this usually meant being unable to fulfil work and family roles in this time. Those who had hand surgery found it difficult to be heavily reliant on help from others, e.g. with personal care, and those with foot surgery found it difficult to be confined at home. In the weeks following an operation, patients could feel depressed and at a loose end, especially as for some it took several months to experience any benefits from surgery. Post-operative pain was not always dealt with effectively. Impact of waiting times. Waiting times of between 9 and 18 months were not uncommon. While some patients thought a 12-month wait was acceptable, coping with pain was frustrating. Patients disliked having to step up their drugs as a result of prolonged waiting times. Loss of mobility was even more difficult to accept as it typically meant that people were unable to engage in a lot of the activities they usually enjoyed. Several patients had opted to have private treatment when pain or loss of function became too intolerable. |
|
| 9 | Symptom control | People with rheumatoid arthritis reporting inadequate pain control are offered analgesics. Several people with RA in the HERG interview collections reported that they had benefited from detailed expert advice on how to use, dose, time and combine analgesics most effectively. The interviews suggest that there are likely to be unaddressed information needs on safe and effective use of analgesics. |
|
| 10 | Drug monitoring (rapid access for flares) | People with satisfactorily controlled established rheumatoid arthritis have ongoing drug monitoring. OR People with satisfactorily controlled established rheumatoid arthritis have access to additional visits for disease flares. OR People with satisfactorily controlled established rheumatoid arthritis know when and how to get rapid access to specialist care. Variability in arrangements for rapid access. When experiencing flares, people with RA have particular information and support needs and require rapid specialist access. However, not all people with RA in the HERG interview collections had adequate arrangements for this place. Several people said they typically received steroid injections from their GP to bridge the time it took to see a consultant who could adjust their medication according to disease activity. In one extreme case, a woman was angry that she had to wait for several weeks for her GP to refer her to her consultant once blood tests had shown increased disease activity and then had to wait further until that consultation took place to receive the medication she knew she needed all along, despite her symptoms getting worse week by week. This was her third experience of a flare. Several other people reported examples of much more rapid and efficient access systems, e.g. phoning a hotline/helpline to make a clinic appointment. Shared treatment decision-making to avoid (severity of) future flares. People with RA in the HERG interview collections were keen to gain information on possible triggers for flares and to discuss their ideas regarding this with consultants. Several said they were willing to accept stronger drugs as a trade-off for preventing severe flares in the future, but a few others said they felt concerned about taking toxic medication once acute effects had subsided. Hearing about other patients experiences of using a drug, in combination with other information about the medicine, helped people to decide whether to accept the treatment. |
Acknowledge the emotional impact of flares. The sudden loss of function associated with a severe flare can be experienced as extremely disabling and frustrating for people with RA. A few people said they felt uncertain about how much physical activity they could/should engage in without worsening their symptoms. A couple of people of working age felt they needed to carry on in their jobs regardless, despite excruciating pains, so as not to risk their job. People with young children also said they had to rely on help from friends and family during flares. However, one woman pointed out that what she felt she needed most during a flare was ‘a chat over a cup of coffee’ as the sudden loss of function and immobility meant that her days became very long and she felt isolated and depressed during such periods. |
| 11 | Annual review | People with rheumatoid arthritis have an annual review that includes assessing disease activity, measuring functional ability and checking for the development of comorbidities. | RA can make sexual activity difficult or impossible yet is little discussed in the consultation. Patients need access to confidential resources for advice and support. |
Additional information on data and methods
This report forms part of a larger project (funded by NIHR HS&DR) between NICE and the University of Oxford, which uses secondary analysis of collections of narrative interviews on various health conditions (referred to as the HERG interview collections) to identify core components of patients’ experiences of the NHS to inform the development, and measurement, of NICE guidelines and QSs.
The aim of this report was to answer the question ‘What does good care in rheumatoid arthritis look like from patients’ perspectives?’ Analysis focused on three areas of patient experience: (1) key concerns, (2) information and support needs and (3) experience of access to specialist services.
For this purpose, we conducted a qualitative secondary analysis of 52 narrative interviews with UK patients with RA. The original interviews were collected in 2004–5 in collaboration with colleagues at the University of Bath (funded by a research grant by Arthritis Research UK) and, following evaluation,130 updated with new interviews in 2012.
The Health Experiences Research Group interview collections
The qualitative data in the HERG archive are collected as national, purposively sampled interview collections which aim for maximum variation. The interviews are collected by experienced qualitative social scientists working with the HERG in Oxford. There are currently over 75 collections of interviews, each concerning a different health issue (ranging from pregnancy to living with a terminal illness) and each set comprising 35–50 interviews. All interviews are tape recorded, transcribed, checked by the interview participant and copyrighted for a number of non-commercial purposes, including secondary analysis and publication. The research is funded via a peer-reviewed process by bodies including NIHR (Research for Patient Benefit), and research committees of voluntary organisations (including Arthritis Research UK, Welcome Trust, Marie Curie and the Economic and Social Science Research Council).
The projects all share a research question (What are the experiences and information and support needs of people with health condition X) and a common interview method that starts with an appropriate variation on an open ended question intended to invite a narrative response (e.g. ‘Could you tell me all about it from when you first thought there might be a problem?’). When the person has completed their account, a semistructured section of the interview includes questions and prompts about any issues of interest that may not have been fully discussed in the narrative. These typically include questions about treatment decisions, information, support and communication with health professionals. All participants are asked if they have anything they would like to tell other people who are starting out on the same journey and if there is anything they would like to pass on to NHS staff at all levels, who might learn from the participant’s experiences. These questions often add rich, informative data about how services and communication could be improved. 64
Each of the interview studies starts with a literature and field review and sets up a specialist advisory panel including patients, professionals, researchers, clinicians, and representatives from the voluntary sector and (if appropriate) the funding body. The panel advises on the parameters of the project, including selection and recruitment of participants.
A maximum variation sample15 is sought to help generate as diverse a sample as possible, including both people whose experience might be considered ‘typical’ and those with more unusual experiences. For each project recruits are actively sought through: a national network of primary care staff, hospital consultants and specialist nurses, advisory panel members, local and national support groups, advertising online and in local newspapers, snowballing through participants and personal contacts. Analysis and data collection proceed simultaneously and continue until ‘data saturation’ is reached to ensure that the widest practical range of experiences has been included. Analyses of the data have been published in peer-reviewed journals, for example Shariff et al. 131
The interview sample for rheumatoid arthritis
Narrative face-to-face interviews were conducted with 38 people with RA in 2004–5. In 2012, following evaluation of the website www.healthtalkonline.org, the project was updated and another 14 interviews were conducted to include more interviews with younger people with RA and experiences of biologic therapies.
The sampling method seeks to achieve representation of the diversity of experiences, rather than numerical representation (so it is not appropriate to present results numerically). Fewer men than women were interviewed, four of the interviewees were from minority ethnic backgrounds, 34 were living with a partner or spouse and 18 lived by themselves.
Age at interview ranged from 21 to 78 years (average age 47 years). Age at diagnosis ranged from 5 to 74 years (average age 35 years). Duration of living with the condition ranged from very recently diagnosed to 46 years (average duration 12.5 years). The diversity in participants’ ages and length of illness experience made it possible to explore how the experience of RA and patients’ information and support needs may differ at different ages and what adjustment to living with RA might require practically and emotionally at different stages of the life course.
Experiences of medication reflected the diverse severity of the condition across individuals and time periods and included treatment with DMARDs, steroid tablets, injections and intravenous pulses, biological treatments (anti-tumour necrosis factor and B-cell therapies), as well as management with analgesics and non-drug treatments. Twenty participants had experience of surgery and another two were waiting for an operation at the time of interview.
Methods of qualitative secondary analysis
A modified framework method37,64 was used. This approach uses charts for a summary description of data from each of the interviews across a set of categories, which are later developed into themes for analysis. The process is iterative and flexible enough to accommodate both categorisation of data in terms of pre-existing ideas and structures (e.g. areas of care as identified in the draft quality standard for RA) as well as emergent themes that participants themselves identify as relevant and important (e.g. concerns about disability and disfigurement). Anticipated and emergent themes were compared across cases, and will eventually be compared and collated across the different data sets to identify general and specific aspects of good-quality care.
Coding and analysis of the RA interviews was supported by NVivo® qualitative data analysis software, which eased the systematic collation of experiences across cases relevant to the areas of care identified in the QS draft.
Findings were grouped under the 11 proposed QS statements and cross-referenced with other areas/statements where applicable.
Appendix 10 Qualitative methods session
Qualitative Methods Session 1
The Royal College of Physicians
Monday 23 January 2012, 2–4 p.m.
Sue Ziebland
Twenty-eight people in attendance.
General views on qualitative research at NICE were collected on arrival.
In groups of 2/3, participants were asked to discuss their criticisms of and concerns about qualitative research, and report back to the group:
-
small sample sizes/no numbers
-
representation not always clear
-
semantics – lack of context when reported/written up
-
problem with interpretation and clarification of meaning
-
subjective (researcher analysis)
-
limited relevance (effects of interventions)
-
hard to combine
-
researcher’s interpretation and then reader’s interpretation (reviewer bias)
-
difficult to summarise data (as numerical analysis inappropriate)
-
can generate more questions than answers
-
hard to replicate
-
only people with something to say join in, therefore representation questionable
-
timing – depends on when you ask question after the event
-
reach of research (age, ethnicity, etc.)
-
time-consuming (little division of labour)
-
resource heavy (potentially takes longer to get through ethics; requires skilled qualitative researcher)
-
how to measure quality?
-
hard to translate once read – quantitative studies provide an answer at the end
-
discussions not conclusions
-
already a summary – interview transcripts not available in paper
-
prefer to have access to full data set
-
concern over ‘leading’ questions; interpretation of body language.
Appendix 11 Qualitative research at the National Clinical Guidelines Centre follow-up survey
Qualitative research at the National Clinical Guidelines Centre follow-up survey (PDF download)
Appendix 12 Participants at workshop to inform objective 4
Sue Ziebland, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Ray Fitzpatrick, Nuffield Department of Population Health, University of Oxford.
Louise Locock, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Kristina Bennert, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Victoria Thomas, NICE.
Elizabeth Gibbons, Nuffield Department of Population Health, University of Oxford.
Crispin Jenkinson, Nuffield Department of Population Health, University of Oxford.
Chris Graham, Picker Institute.
Sophie Staniszewska, University of Warwick.
Jocelyn Cornwell, The King’s Fund, London.
Angela Coulter, Nuffield Department of Population Health, University of Oxford.
Michele Peters, Nuffield Department of Population Health, University of Oxford.
Jenny King, Picker Institute.
Paul Hewitson, Nuffield Department of Population Health, University of Oxford.
Jose Valderas, Department of Primary Care Health Sciences, University of Oxford.
Helen Lloyd, Nuffield Department of Population Health, University of Oxford.
Helen Crocker, Nuffield Department of Population Health, University of Oxford.
Joanne Lloyd, Nuffield Department of Population Health, University of Oxford.
David Morley, Nuffield Department of Population Health, University of Oxford.
Sarah Dummett, Nuffield Department of Population Health, University of Oxford.
Jill Dawson, Nuffield Department of Population Health, University of Oxford.
Laura Kelly, Nuffield Department of Population Health, University of Oxford.
Monica Hadi, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Angela Martin, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Milton Munroe, lay member.
Waveney Munroe, lay member.
Jennifer Bostock, lay member.
Appendix 13 Qualitative secondary analysis workshop
Qualitative Secondary Analysis Workshop.
Health Experiences Research Group, University of Oxford.
7 November 2012 from 10:00 a.m. to 4.30 p.m.
Venue: Nuffield Department of Primary Care Health Sciences.
New Radcliffe House 2nd Floor, Radcliffe Observatory Quarter, Oxford.
Chair: Professor Kate Hunt.
Agenda: We propose a series of talks lasting 10, 20 or 30 minutes interspersed with 15–25 minutes discussion on key questions (suggestions below).
10.00 Introductions and plan for the day.
10.15 A potted and personal history of the reuse of data from qualitative research studies (Sociologist and applied health researcher, University of Exeter).
Proposed discussion points: relationship with primary researcher, co-authorship, responsibilities and obligations, gaining funding for qualitative secondary analysis projects.
11.00 Qualitative secondary analysis in practice: context, working across data sets and qualitative longitudinal analysis (Researchers from Timescapes project, University of Leeds).
Proposed discussion points: The salience of context to secondary analysts’ interpretation of data; Differences and similarities between primary and secondary analysis; what insights can be gained through qualitative longitudinal data?
11.45 Experiences of encouraging Qualitative Secondary Analysis (ESRC, Qualidata).
Proposed discussion points: ESRC funding and data sharing, ethical and practical issues in data sharing; how can we improve access and willingness to share data? What funders need to expect?
1.30 Qualitative Secondary Analysis; opportunities with different types of data, e.g. consultation data, interviews (Professor of Sociology, Brunel University).
Proposed discussion points: why do opportunities for data sharing get missed? What are the great missed opportunities for data sharing? What do primary researchers and archivists need to provide?
2.30 Experiences of sharing data (both sides of story); experiences of using HERG data for secondary analysis and HERG experiences of being the primary researcher when interviews are used for secondary analysis (Lecturer, University of Stirling).
Proposed discussion points: what skills do Qualitative Secondary Analysis need beyond the usual analytic skills? What should a 1-day training course in Qualitative Secondary Analysis cover? Safeguard, e.g. for original researchers – balance of gathering and resource development.
3.15–4.00 General discussion.
Other issues, e.g. transcription, costs and administration, video or audio access, personal nature of field notes and diaries.
4.15 Review conclusions and plans for writing up.
Attended by:
Prof. Kate Hunt, Institute of Health and Wellbeing, University of Glasgow.
Prof. Sue Ziebland, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Libby Bishop, Faculty of Education, Social Sciences and Law, University of Leeds.
Dr Emma France, School of Nursing, Midwifery and Health, University of Stirling.
Dr Janet Heaton, Medical School, University of Exeter.
Dr Sarah Irwin, School of Sociology and Social Policy, University of Leeds.
Dr Mandy Winterton, Faculty of Health Life and Social Sciences, Edinburgh Napier University.
Prof. Clive Seale, School of Social Sciences, Brunel University, London.
Dr Louise Locock, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Kristina Bennert, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Alison Chapple, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Sara Ryan, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Laura Griffith, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Miss Ulla Raisanen, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Jenny Hislop, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Dr Angela Martin, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Miss Laura Kelly, Nuffield Department of Population Health, University of Oxford.
Dr Anne-Marie Boylan, Nuffield Department of Primary Care Health Sciences, University of Oxford.
Appendix 14 Introduction to secondary analysis
| 9.00–9.15 | Registration and coffee |
| 9.15–10.15 | Session 1 Welcome and introduction to secondary analysis: the potential of secondary analysis; some examples of secondary analysis |
| 10.15–11.00 | Session 2 Sourcing data; ethical issues and permissions |
| 11.00–11.15 | Coffee |
| 11.15–12.15 | Session 3 Practical 1: Thinking about the differences between primary and secondary analysis Feedback |
| 12.15–13.15 | Lunch |
| 13.15–13.45 | Session 4 Doing secondary analysis: Analytical approaches, rigour and quality |
| 13.45–14.45 | Session 5 Practical 2: Secondary analysis in practice; coding and first steps Feedback |
| 14.45–15.00 | Coffee |
| 15.00–15.45 | Session 6 Secondary analysis; controversies and debates |
| 15.45–16.30 | Session 7 Practical 3: Secondary analysis in practice; moving to a more conceptual analysis Feedback |
| 16.30–17.00 | Session 8 Questions and answers; using secondary analysis in your projects Conclusion and evaluation |
List of abbreviations
- A&E
- accident and emergency
- ACE
- angiotensin-converting enzyme
- BTS
- British Thoracic Society
- CG
- clinical guideline
- DH
- Department of Health
- DIPEx
- Database of Individual Patient Experiences
- DMARD
- disease-modifying anti-rheumatic drug
- DSN
- diabetic specialist nurse
- ECG
- electrocardiogram
- EQ-5D
- European Quality of Life-5 Dimensions
- ESDS
- Economic and Social Data Service
- ESRC
- Economic and Social Research Council
- FG
- focus group
- GDG
- guideline development group
- GP
- general practitioner
- GTN
- glyceryl trinitrate
- HERG
- Health Experiences Research Group
- LTC
- long-term condition
- MDT
- multidisciplinary team
- MI
- myocardial infarction
- MRC
- Medical Research Council
- NCC
- National Collaborating Centres
- NCC-WCH
- National Collaborating Centre for Women’s and Children’s Health
- NCGC
- National Clinical Guideline Centre
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OT
- occupational therapist
- PPI
- patient and public involvement
- PREM
- patient-reported experience measure
- PROM
- patient-reported outcome measure
- PT
- physiotherapist
- QS
- quality standard
- QSAC
- Quality Standards Advisory Committee
- RA
- rheumatoid arthritis
- RCT
- randomised controlled trial
- SDO
- Service Delivery and Organisation
- SF-36
- Short Form questionnaire-36 items
- SIGN
- Scottish Intercollegiate Guidelines Network
- STEMI
- ST segment elevation myocardial infarction
- TEG
- topic expert group
- U3A
- University of the Third Age
- WHO
- World Health Organization