Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1014/04. The contractual start date was in April 2012. The final report began editorial review in June 2013 and was accepted for publication in December 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Gemma Pearce received expenses from the World Stroke Organization to present this research at their international conference. Hilary Pinnock chairs the self-management evidence review group for the British Thoracic Society/Scottish Intercollegiate Guideline Network Asthma Guideline. No other author has any competing interest to declare.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Taylor et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 The brief and overview of the project
This study was formulated in response to the National Institute for Health Research (NIHR) Health Services and Delivery Research (HS&DR) commissioning brief (NIHR HS&DR project: 11/1014/04): ‘A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions’ (LTCs),1 and took place during 2012 and 2013.
Commissioning brief
The HS&DR brief highlighted that despite the growing interest in supporting self-management for people with LTCs, the ‘huge range of self-care activities’ makes it difficult for decision-makers to identify what works. 2 Some conditions (such as asthma and diabetes) have a reasonable evidence base, whereas other patient groups are relatively overlooked. In addition, the literature on self-management is often condition-specific, making it difficult to generalise from one disease area to another.
The brief called for a single evidence synthesis on key findings on self-management, specifically focusing on the information needs of commissioners to identify effective strategies to support people with LTCs at a population level, and covering:
-
Models of care: who for?
-
At a population level, what models work best and for whom? What is the impact on service use?
-
-
Skill mix: who by?
-
What is the role of specialists, generalists, case managers or peer-led facilitators in providing self-management support?
-
-
Intervention: what?
-
From the broad range of interventions, what works to improve outcomes? What is the role of telehealthcare?
-
-
Delivery of care: how?
-
How should interventions be delivered? How can professionals be motivated to support effective self-management?
-
The brief stated that the completed synthesis should describe the key components of effective programmes to support self-management for people with LTCs, and identify gaps in the existing knowledge base.
The project in relation to the brief
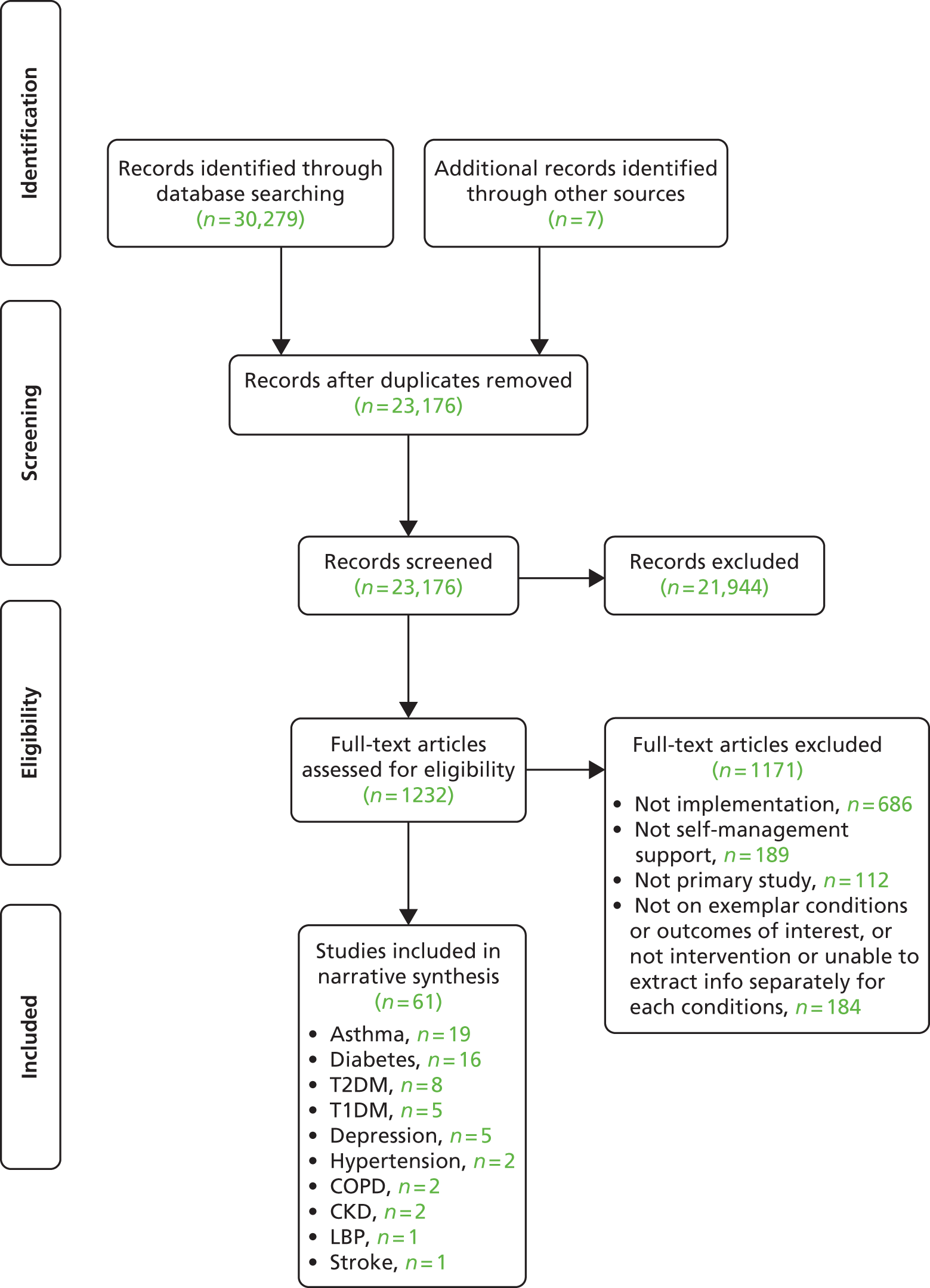
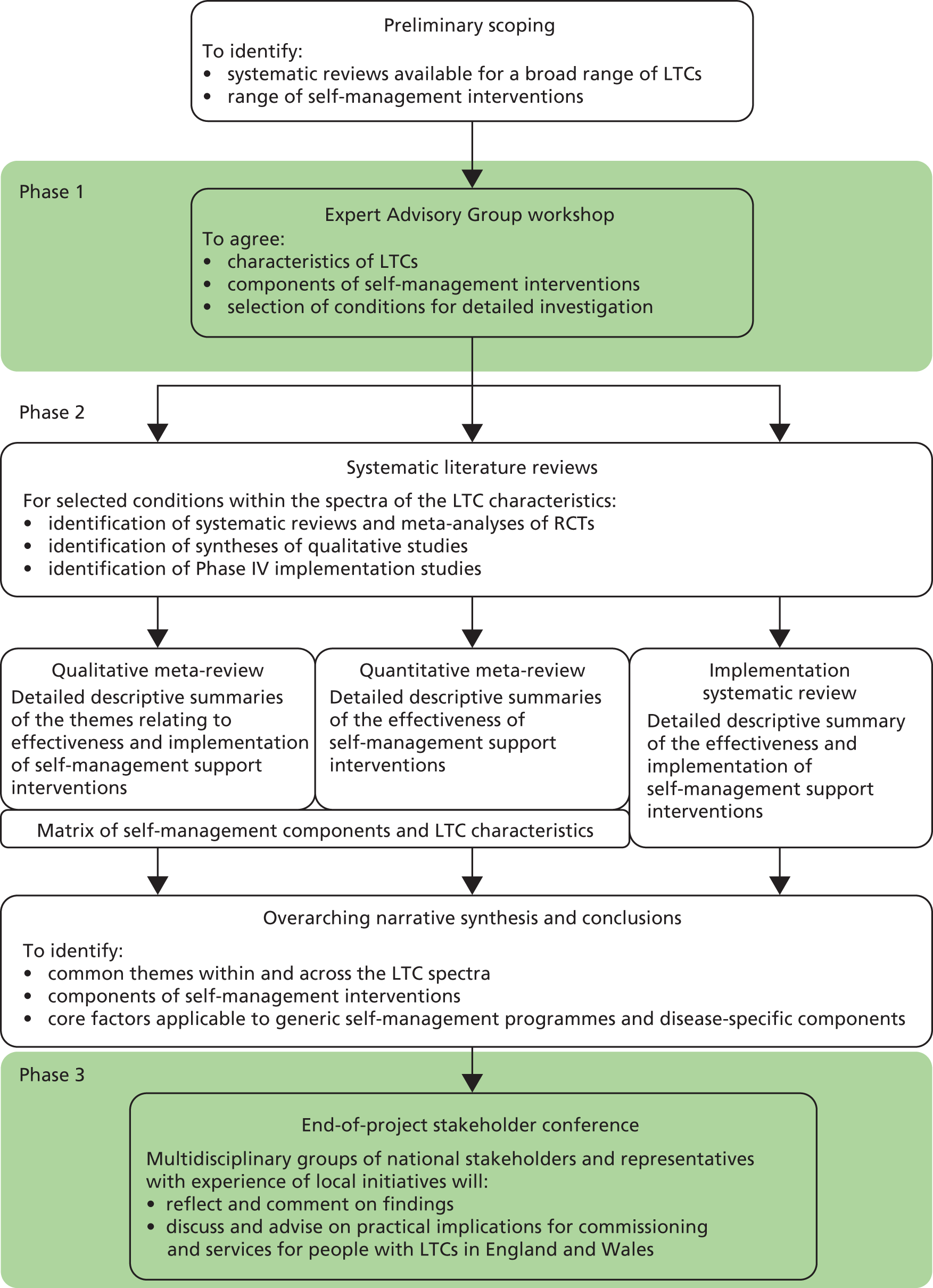
Our systematic overview of self-management support interventions had three phases (Figure 1):
-
Phase 1 involved an External Advisory Group workshop to identify potential components and important characteristics of self-management support interventions (to assist the development of a taxonomy of self-management support interventions), to agree the clusters of LTCs with similar features and to identify the best representative LTCs within each cluster for detailed study in phase 2.
-
Phase 2 involved extracting effectiveness evidence and other relevant evidence from systematic reviews, qualitative syntheses and Phase IV implementation studies on the LTCs identified for detailed study. We then used a series of matrices of LTC clusters and self-management support interventions in an attempt to synthesise the evidence from these sources. Following this, we conducted an overarching narrative synthesis of all this material and developed provisional summaries and recommendations for commissioners.
-
Phase 3 involved a second stakeholder conference at which we presented our findings and recommendations to be discussed and refined by the multidisciplinary delegates.
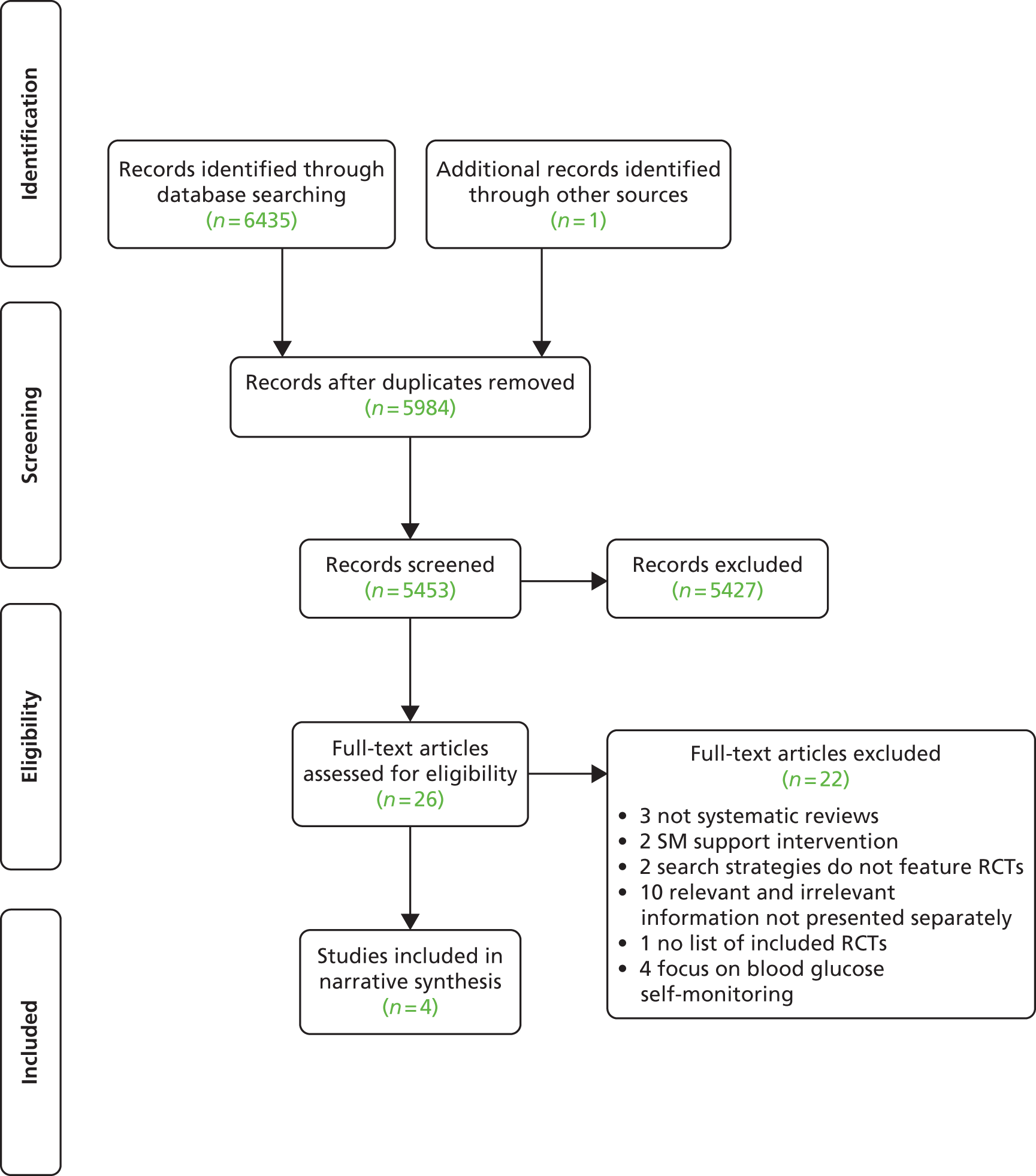
FIGURE 1.
Overview of study design. RCT, randomised controlled trial.
Rationale for changes from the original protocol
Some iterative changes to our original protocol were made during the project; these are described in relation to the original protocol in Table 1.
| Change | Description |
|---|---|
| Taxonomy of self-management interventions (see Chapter 4) | As a result of our preparations for the Expert Advisory Group workshop, it became clear that it would not be feasible to create a taxonomy for self-management interventions at the beginning of this project. We therefore set out to collate a descriptive list of self-management components and features from workshop attendees and the reviews |
| LTCs (see Chapter 4) | It became clear from the first Expert Advisory Group workshop that LTC characteristics should be considered as spectra rather than absolutes enabling more flexible classification. Additionally, the experts at the workshop helped us to pick the LTCs on which to focus our review. Following this we identified four priority LTCs for more in-depth systematic meta-reviews, and an additional 10 LTCs for more rapid and focused systematic meta-reviews |
| Implementation review (see Chapter 21) |
|
| Collaboration with RECURSIVE | We anticipated a high level of collaboration with Professor Peter Bowers and his Reducing Care Utilisation through Self-management Interventions (RECURSIVE) review team. Although we did invite the team to both of the PRISMS workshops, and liaised via regular teleconference, we did not achieve the level of collaboration which we would have liked. This is a result of the time pressures which both teams were under |
Chapter 2 Background
The policy context
As the population ages,3 the prevalence of LTCs is increasing,4,5 resulting in major challenges to the adequate provision of health and social care. 6 Promotion of self-care is a core response of health-care systems globally to this challenge. 7–10
In England and Wales, self-care is promoted by leading health organisations, including The King’s Fund and the Health Foundation,11 as an indispensable component of modern health care. The intense interest in support for self-care, driven by a desire to reduce unscheduled care, shrink costs and improve patient outcomes, has contributed to a plethora of Department of Health (DH) policies and initiatives including the Expert Patients Programme,12 the Quality, Innovation, Productivity and Prevention workstream,13 the whole-system demonstrator telehealth project,14 the annual national Self Care Week,15 NHS Direct,16 NHS Choices (including, for example, a library of downloadable ‘health apps’, see http://apps.nhs.uk/),17 and personalised care planning. 18 Implementation of these initiatives, however, remains patchy or disjointed. 19 Indeed, the Secretary of State for Health regards current systems as inadequate to meet growing burden from LTCs, and called recently for the development of a more proactive approach, definitions and scope of self-management support. 20
The fluidity of terminology in this area21 and the diversity of definitions are symptomatic of the current lack of clarity about what constitutes a clinically effective and cost-effective self-management programme. The diversity of the LTCs that may benefit from self-management, the spectrum of disease severity, and range of professional and lay contexts in which these complex interventions might be delivered, are further challenges to defining self-management.
Self-care and self-management
Although the DH sometimes appears to use the terms ‘self-care’ and ‘self-management’ interchangeably, they are commonly seen as different. In this report we have maintained the distinction adopted by Parsons et al. :22
. . . we give preference to the term ‘self-management’ in order to refer to those actions individuals and others take to mitigate the effects of a long term condition and to maintain the best possible quality of life. ‘Self-care’ refers to a wider set of behaviours which both the healthy and the not so healthy take to prevent the onset of illness or disability, and, again to maintain quality of life.
We have thus adopted the definition of self-management proposed by the US Institute of Medicine. 23
Self-management is defined as the tasks that individuals must undertake to live with one or more chronic conditions. These tasks include having the confidence to deal with medical management, role management and emotional management of their conditions.
This is echoed by the DH who describe their Expert Patients Programme as being ‘based on developing the confidence and motivation of patients to use their own skills and knowledge to take effective control over life with a chronic illness’ and ‘not simply about educating or instructing patients about their condition’. 12
Tasks, skills and self-efficacy
The tasks of medical, role and emotional management were outlined by Corbin and Strauss as the core components of chronic disease self-management. 24 To facilitate these tasks, Lorig and Holman identified five core self-management skills: problem-solving; decision-making; appropriate resource utilisation; forming a partnership with a health-care provider; and taking necessary actions. 25
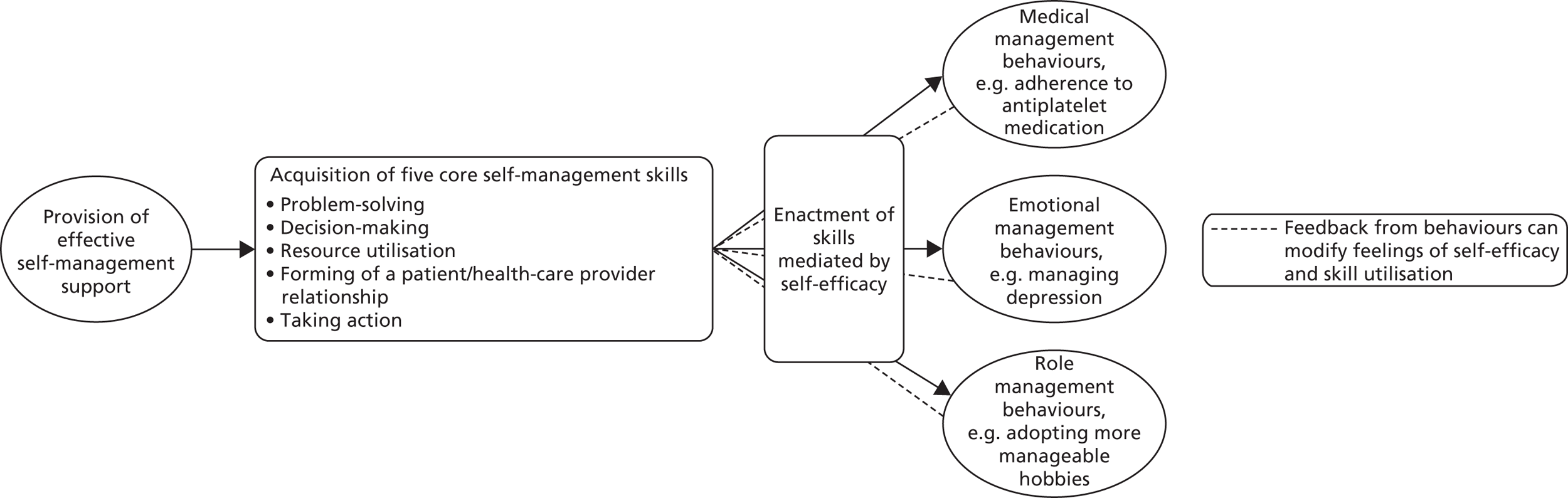
Self-efficacy is commonly viewed as the mediator between the acquisition of self-management skills, and the enactment of self-management behaviours,26 as illustrated in Figure 2. Self-efficacy, one of the core concepts of Bandura’s social–cognitive theory, focuses on increasing an individual’s confidence in their ability to carry out a certain task or behaviour, thereby empowering the individual to self-manage. 27
The range of self-management interventions
Self-management support may range from the provision of disease-specific information via a website or leaflet, to extensive generic programmes such as the Expert Patients Programme which aim to promote behavioural change by building the confidence of individuals to manage their condition and the biopsychosocial effects of LTCs. 12 ‘Personalised Care Planning’ is an ambitious programme involving improved access to, and provision of, information for the 15 million people living with LTCs,28 which emphasises personal involvement and choice in health care (‘no decisions about me without me’). 29,30 A key component of personalised care planning is support for self-management.
Other initiatives include interactive educational projects, complex interventions involving repeated contact with health-care professionals (HCPs) from a variety of disciplines in a range of settings (home, clinic, physician’s office). Telemonitoring for a broad range of LTCs is seen as a means of promoting self-management,31 though the inter-relationship is complex. 32
The inter-relationship between professional and self-management
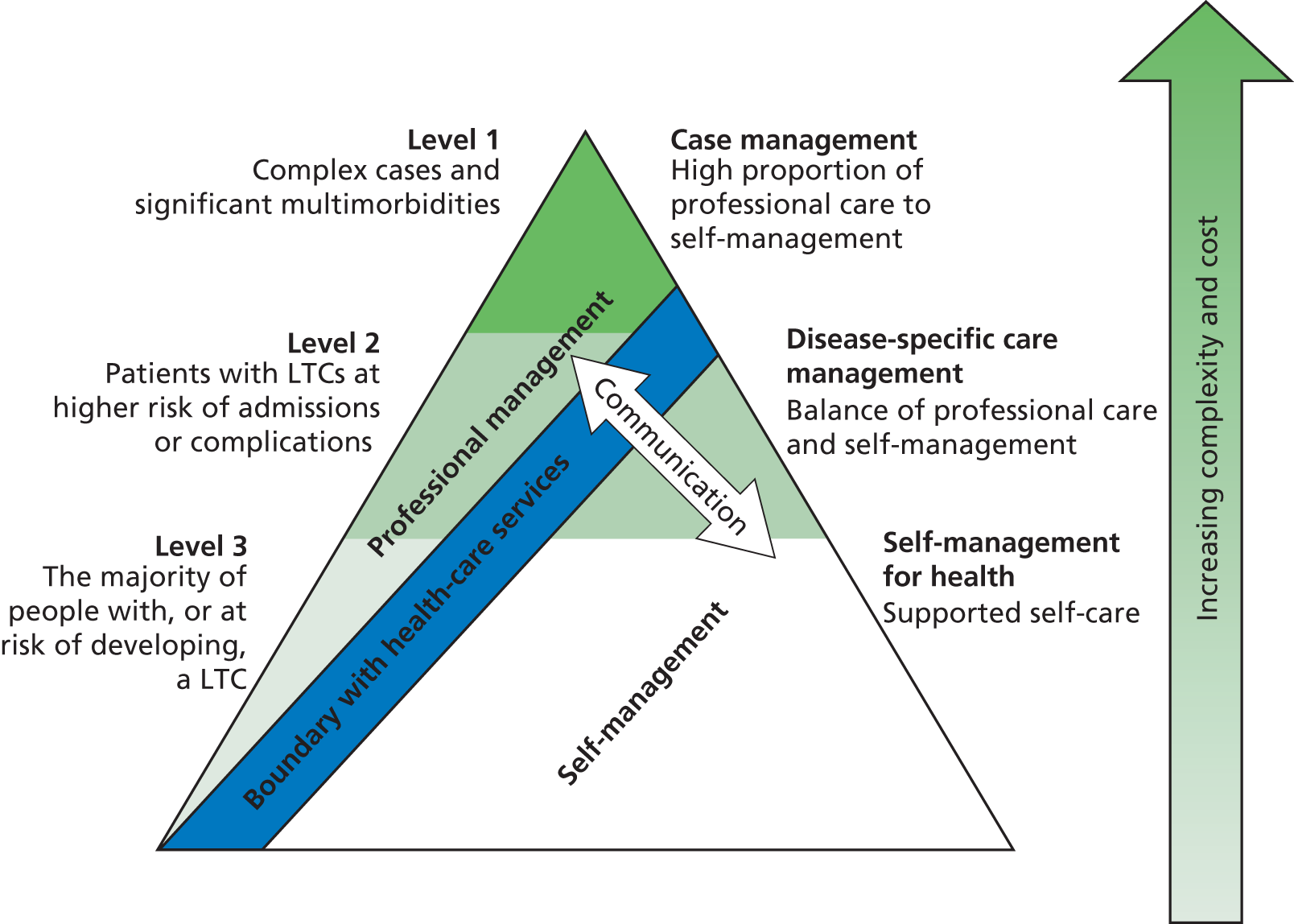
The DH has developed and refined a generic LTC model which stratifies the local population into three levels of need, often depicted using the ‘Kaiser pyramid’ (Figure 3). 33 Level 1 focuses on those with complex needs and accounts for around 5% of people. Level 2 in the middle has a medium level of need (around 25%) and the bottom level represents the 70% of patients with a typically low level of need and well controlled LTCs. The relative importance of self-management compared with professional care at each level has been proposed as low for those with complex problems, and high for those with well-controlled LTCs, with ‘equally shared care’ in the middle level. 34
The inter-relationship at an individual level
Central to our thinking is the concept that patients are de facto responsible for day-to-day lifestyle choices, adhering (or not) to medication advice, monitoring their condition, recognising deterioration and deciding on the action(s) they will take. The role of professionals within the health service is to inform and support the patient so that positive behaviours are enabled and decisions are (clinically) appropriate and enacted with increased confidence.
This is exemplified in the specific context of monitoring by the theoretical model developed by Glasziou et al. 35 that describes the complementary and evolving roles of periodic professional reviews and on-going patient self-monitoring. A newly diagnosed condition is assessed and brought under control with professional support before the patient assumes responsibility for self-management as the stable maintenance phase is established. If symptoms or a physiological measurement subsequently fall outside pre-defined limits, the patient is empowered to act (either by initiating treatment or seeking appropriate professional advice) in order to regain control. Self-management programmes aim to ensure that the patient has the knowledge and confidence to take appropriate and timely action.
A whole-systems approach at population level
Kennedy et al. 36 argue for a whole-systems approach to the provision of effective support for self-care, yet most of the evidence supporting self-management is derived from Medical Research Council Phase III randomised controlled trials (RCTs) of complex interventions delivered to individual patients. 37 Phase IV implementation studies which accommodate the diversity of patient, professional and structural contexts are relatively uncommon. Echoing Kennedy et al. ’s framework, qualitative data in the context of chronic respiratory disease highlight the importance of availability of relevant information for patients and a patient-centred attitude from trusted professionals working within a health-care service. This enables flexible access to professional advice in order to support self-management. 38,39
Commissioning systems to support self-management
The DH estimates that around 15 million people in England (including half of all those aged > 60 years) are living with at least one LTC. 40 There is, however, no definitive list of LTCs, and the potential range of diseases of interest is both extensive and diverse. Commissioners face the daunting challenge of developing commissioning briefs that facilitate the development of services to support self-management across the full range of LTCs. A key goal of our synthesis is therefore to make the task of commissioners easier by summarising the key components of effective programmes to support self-management for people with LTCs.
Chapter 3 Aim and objectives
Aim
To undertake a systematic overview of the evidence on self-management support in people with one or more exemplar LTCs in order to inform commissioners and health-care providers about what works, for whom, in what contexts, how and why.
Objectives
Workshop: phase 1
To agree in discussion with our Expert Advisory Group:
-
a taxonomy of LTCs based on the presence, variability and persistence of symptoms, the risk of exacerbations and the risk of LTCs
-
a taxonomy of self-management support interventions for people with LTCs based on consideration of models of care, skill-mix, components of the intervention and process of delivery of care
-
the selection of exemplar conditions for detailed investigation in phase 2.
Systematic reviews: phase 2
To undertake meta-syntheses of the evidence around interventions for self-management support in the exemplar conditions (for both priority and additional LTCs identified as a result of the workshop) from:
-
published systematic reviews of RCTs
-
syntheses of qualitative studies
-
primary studies specifically concerned with the implementation of interventions in populations with one or more LTCs (i.e. Phase IV implementation trials).
To synthesise these meta-reviews in an overarching narrative synthesis, to determine what is known about their likely effectiveness with respect to health service resource use (including unscheduled use of health-care services and hospital admission rates), health outcomes [including quality of life (QoL), symptoms and biological markers of disease] and equity (including different ethnic populations, minority groups and hard-to-reach groups).
National end-of-project workshop: phase 3
To organise a national, multidisciplinary workshop as a result of the work undertaken in phases 1 and 2. This will enable us to discuss, debate and derive practical recommendations for commissioners and providers seeking to implement effective population level self-management support services for people with a range of LTCs.
To identify research gaps for future primary research or research synthesis.
Chapter 4 Expert Advisory Group workshop
In the first phase of our study we worked with an Expert Advisory Group both to inform our understanding of self-management support for LTCs and to reach consensus on an appropriate focus for our reviews. The three specific objectives of the workshop were to:
-
group LTCs according to characteristics that influence the type of self-management support they might need
-
identify features of self-management support interventions that might reflect these needs
-
select exemplar LTCs for the project reviews.
Preliminary scoping of the literature
We undertook a preliminary scoping of the literature to inform the content and process of the Expert Advisory Group workshop. We obtained national/international clinical guidelines for a range of common LTCs in order to identify whether (or not) self-management interventions were promoted as potentially useful management techniques in that disease area, and any recommendations on component parts of those self-management interventions. The extent and nature of the supporting research evidence were also assessed.
Recruitment of the Expert Advisory Group
We invited a range of stakeholders encompassing a broad range of LTCs to be members of a multidisciplinary Expert Advisory Group. We sent invitations to a total of 83 people (including both representatives of relevant organisations and named individuals) representing a wide range of experts, policy-makers, commissioners, self-management providers, HCPs, academics, patients and people from charities, professionals from the NIHR Service Delivery and Organisation Network (now the NIHR HS&DR Programme Network) and colleagues from the parallel health economics project led by Professor Peter Bower at Manchester University. The experts were invited specifically to contribute to a pre-workshop open round and attend the workshop, but also to attend the end-of-project stakeholder conference.
Pre-workshop open round
In the pre-workshop open round, members of the Expert Advisory Group were invited to complete a survey consisting of three tasks in line with the three workshop objectives (see Appendix 1). Respondents were asked to:
-
list characteristics that they felt should be taken into account when grouping LTCs from the perspective of health-care services seeking to support self-management
-
list components of self-management support they thought should be taken into account when developing services for people with LTCs
-
compile a list of common and/or important LTCs.
We collated the free-text suggestions for characteristics of LTCs and components of self-management support using thematic analysis. Themes were abstracted separately by each member of the team and then discussed as a group. They formed the basis of the introduction to the workshop and the exercises carried out throughout the day.
Workshop methods
The 1-day workshop, held at a central London venue, aimed to reach consensus on the three tasks to inform and direct the subsequent foci of the project (for the agenda see Appendix 2).
Presentations incorporating definitions of key terms, explanations of the rationale and usefulness of each activity and feedback from the pre-workshop survey were used to set the scene for the day and as introductions to each of the tasks. Delegates were then allocated to one of three groups ensuring that each group included members with different professional or lay backgrounds and experiences.
Building on the themes emerging from the pre-workshop open round and in line with the three workshop objectives, delegates were asked to consider from the perspective of commissioners and providers of services:
-
the significance of identified LTC characteristics for the design of services to support self-management and the (lack of) potential for these to be used to cluster LTCs
-
the components of self-management interventions which could be considered for inclusion in services to support self-management and their importance with regard to the proposed clusters of LTCs
-
exemplar LTCs representing the proposed LTC clusters for our review.
Group work was designed to allow participants to provide judgements, discuss, clarify and/or evolve ideas before rating the relative importance of items with a view to moving towards a consensus. The ethos of the workshop was to encourage an iterative process that enabled perceptions to be refined in the light of participants’ diverse views. For example, the specific details of the task for the final session (selection of exemplar LTCs), were not finalised until the outcomes of the earlier discussions (on characteristics of LTCs and components of self-management interventions) were known.
Task one: identification of characteristics of long-term conditions of relevance to the provision of self-management support
-
The LTC characteristics suggested in the pre-workshop open round were presented to the whole group (see Appendix 3).
-
Delegates then completed a score sheet (see Appendix 4) on which they individually rated the importance (one = not important, five = crucially important) of each characteristic in terms of potential relevance to designing services to support self-management. Responses were collated and numerical scores entered onto a Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA) which calculated the median score for each item.
-
In a 50-minute facilitated group discussion, delegates shared their perceptions of the LTC characteristics suggested during the open round.
-
At the end of the group discussions, the original score sheets, to which the median scores for each LTC characteristic had been added, were returned to delegates. They were then asked to revise their original score in the light of the workshop delegates’ median score and the outcomes of the group discussion.
-
The revised scores were entered onto an Excel spreadsheet and the degree of consensus calculated. Consensus was defined as 60% agreement using a five-point Likert scale, with higher scores representing higher levels of importance. These results were used to inform task three (selection of exemplar LTCs).
Task two: identification of components of self-management support interventions
-
The components of self-management interventions suggested in the pre-workshop open round were presented to the whole group (see Appendix 5).
-
Delegates were asked to form informal groups of between three and six people to complete a worksheet (see Appendix 6). They scored the importance (one = not important, five = crucially important) of self-management components for four different example LTCs (epilepsy, arthritis, dementia and heart failure). The example LTCs were derived from the list suggested in the pre-workshop open round and were selected to reflect a range of LTC characteristics (e.g. potential self-management, variability, complexity and severity of symptoms). A free-text box was provided to highlight any additional components which might be important when developing self-management interventions for people with LTCs.
-
After the workshop, median scores were calculated for the relevance of each component in each of the four conditions: epilepsy, arthritis, dementia and heart failure. The degree of agreement was assessed by counting the proportion with scores of four or five across the four disease areas.
Task three: selection of exemplar long-term conditions
-
The results from task one (characteristics of LTCs) and task two (components of self-management interventions) were presented to the workshop. The LTC characteristics that reached consensus were presented as the agreed ‘primary’ characteristics, with the remaining presented as ‘secondary’ characteristics (see Appendix 7).
-
Working in the same three multidisciplinary groups as the first session, the groups were asked to decide which exemplar LTCs should be used as topics for the systematic overviews. In order to inform discussion, groups were provided with the long list of LTCs suggested in the pre-workshop open round (see Appendix 8). This was annotated with UK prevalence, outline demographics, a brief summary of symptoms and management and an estimate of the extent of the literature on self-management.
-
Delegates were asked to select LTCs that reflected the high and low extremes of the primary characteristic’s continuum. For example, the highest ranking characteristic was ‘potential of (self)-treatment/management (in this chapter shortened to self-management) to improve symptoms’. Groups were asked to identify LTCs which stood to gain substantial benefit from self-management, and those where benefits might be limited. Factors to consider when deciding which LTCs to select included the burden of disease and the availability of evidence for that LTC.
-
Initially, group facilitators attempted to gain consensus on between three and five LTCs which could represent each end of the spectrum for the primary characteristics. Once this task was completed, the groups considered if they could allocate their selected LTCs to populate the spectra for any/all of the secondary LTC characteristics.
Results
Response rate
The pre-workshop open round was completed by 19 out of the 83 invited (23%) people, 14 of whom attended the workshop. A total of 27 (33%) delegates attended the conference, encompassing health-care managers, commissioners, policy-makers, patients and HCPs (Table 2).
| Sector | Role of delegatea | LTC(s) represented |
|---|---|---|
| Policy-makers | Head of Respiratory, Diabetes, Liver and Kidney Programmes, DH | Asthma, COPD, diabetes, chronic liver disease, CKD |
| DH | All | |
| Commissioner | Director of Public Health, NHS East London and The City Alliance | All |
| Self-management providers | (Clinician) Clinical Lead for the Year of Care project | Diabetes |
| (Social Enterprise Organisation) Social Action for Health | All | |
| Self-management support providers | (Training of HCPs) Education for Health | All |
| Chairman, Expert Patients Programme Community Interest Company | All | |
| Patients | Patient | Not supplied |
| Patient representative | Not supplied | |
| Professional stakeholder | Professional stakeholder | Not supplied |
| PPI expertise/HCP | PPI in Research Advisor, RCN | All |
| Voluntary sector | Service Improvement Manager, Diabetes UK | Diabetes |
| Chef Executive, The Stroke Association | Stroke | |
| Head of Research, British Lung Foundation | Asthma, COPD | |
| Social enterprise | Tuke Institute | All |
| HCP | LTC Adviser, RCN | All |
| Academic/HCP | Professor of Clinical Diabetes, Director of Research and Development | Diabetes |
| Academics | Project Manager, Irish College of General Practitioners | All |
| Senior Research Analyst, Social Care Institute for Excellence | All | |
| Senior Research Fellow, Applied Research Centre in Health and Lifestyle Interventions | All | |
| Senior Lecturer in Health Policy Research, QMUL | All | |
| Senior Lecturer, Medical Sociology, QMUL | All | |
| Health Foundation Self-Management Support Fellow | All | |
| Reader, NPCRDC, University of Manchester | All | |
| Senior Research Fellow, NPCRDC, University of Manchester | All | |
| Senior Research Fellow, QMUL | All | |
| Research Assistant, QMUL | All |
Results of task one: identification of the long-term conditions characteristics of relevance to the provision of self-management support
Pre-workshop open round
The characteristics of LTCs suggested by respondents during the open round as important considerations when developing services to support self-management were grouped thematically into 16 characteristics (Table 3). For the workshop we listed each characteristic across a spectrum to illustrate how they might be expressed to very different extents in different conditions. We also included delegates’ comments from the pre-workshop exercise to aid understanding and illustrate the different perspectives on the characteristics (see Appendix 3).
| Themes | Subthemes |
|---|---|
| Presence or absence of ongoing symptoms |
|
| Impact of symptoms on lifestyle |
|
| Risk of future progression/mortality necessitating self-monitoring |
|
| Risk of significant complications or comorbidity needing self-monitoring |
|
| Significant variability/risk of (serious/high-cost) exacerbations |
|
| Potential of self-management to improve symptoms |
|
| Potential of self-management to be disease modifying |
|
| Impact on ability to self-manage and/or requiring significant assistance from (informal) carers |
|
| Who provides care: predominantly self-management or reliant on professional input |
|
| Degree of complexity of medical/clinical/social/lifestyle self-management regimes |
|
| Genetics/familial nature of condition |
|
| Age at onset |
|
| Presence of comorbidities (including depression) |
|
| Stigma/social class/medically unexplained symptoms |
|
| Prevalence (burden to health-care system/society) |
|
| Evidence base/existing tools/skills required |
|
Consensus process
Following discussion and two rounds of scoring, consensus was reached for two characteristics: ‘the potential of self-management to improve symptoms’ and ‘the impact of symptoms on lifestyle’ (Table 4). There was then a substantial gap before a group of characteristics scoring 24–34% agreement. Many of these scored highly when the data were reanalysed using consensus for scores of four or five (see final column in Table 4). Two were particularly poorly scored: ‘the age at onset’, and ‘the genetics/familial nature of condition’.
| Characteristic | Spectrum | Proportion (%) awarded a score of five | Proportion (%) awarded scores of four or five | ||
|---|---|---|---|---|---|
| Achieved pre-defined consensus | |||||
| Potential of self-management to improve symptoms | Very effective treatment | ← → | Limited benefit | 72 | 90 |
| Impact of symptoms on lifestyle | Normal activities (including work) | ← → | Severely limited (including housebound) | 62 | 90 |
| Did not achieve pre-defined consensus | |||||
| Significant variability/risk of (serious/high cost) exacerbations | Highly variable | ← → | Minimal variability | 34 | 79 |
| Degree of complexity of clinical/social/lifestyle self-management regimes | Simple tasks | ← → | Complex daily regimes | 34 | 66 |
| Risk of significant complications or comorbidity necessitating self-monitoring | Unlikely/not serious | ← → | Likely/significant | 31 | 93 |
| Presence of comorbidities (including depression) | No comorbid conditions | ← → | Significant comorbidity | 31 | 86 |
| Potential of treatment/self-management to modify disease | Very effective treatment | ← → | Limited benefit | 31 | 83 |
| Prevalence (burden to health-care system/society) | Common condition | ← → | Rare condition | 31 | 72 |
| Risk of future progression/mortality necessitating self-monitoring | Unlikely/not serious | ← → | Common/potentially fatal | 28 | 79 |
| Who provides care: predominantly self-management or reliant on professional input | Largely self-care | ← → | High level of professional care | 28 | 66 |
| Impact on ability to self-manage and/or requiring assistance from (informal) carers | Self-caring | ← → | Highly dependent | 25 | 79 |
| Presence or absence of ongoing symptoms | Asymptomatic | ← → | Persistent symptoms | 24 | 76 |
| Evidence base/existing tools/skills required | No evidence about self-management | ← → | Extensive evidence base | 14 | 76 |
| Stigma/social class/medically unexplained symptoms | No stigma/inequity issues | ← → | Stigma | 14 | 59 |
| Age at onset | Onset in childhood | ← → | Onset as adult | 7 | 28 |
| Genetics/familial nature of condition | No significant familial component | ← → | Clear genetic condition | 3 | 17 |
Results of task two: prioritisation of components of self-management support interventions
Pre-workshop open round
Potential components of self-management support suggested by the respondents as important to the open round were collated and analysed thematically into 10 categories (Table 5; for respondents’ verbatim comments see Appendix 5). We recognised that the respondents had in fact suggested both components and features of self-management support intervention in this exercise.
| Themes | Subthemes |
|---|---|
| Training and education |
|
| Access to information | |
| Monitoring |
|
| Environmental adaptations | |
| Care planning | |
| Access to specialist team | |
| Emotional/social/psychological support |
|
| Users having financial control |
|
| Large-scale public initiatives |
In addition, respondents also highlighted the importance of considering the following features of a self-management support intervention: patient centredness, complexity, multidisciplinary approach, disruption to the individual, involvement of carer/families, generic/disease-specific, duration, accessibility, integrated care and monitoring of outcomes.
Workshop exercise
The components of self-management support interventions considered by the delegates as most important with a median score of five (highest priority) for all four diseases were ‘training and education’; ‘access to information’ and the overarching characteristic of ‘patient centredness’ (Table 6).
| Component of self-management support interventions | Epilepsy | Arthritis | Dementia | Heart failure | Total with median score four or five |
|---|---|---|---|---|---|
| Training and education | 5 | 5 | 5 | 5 | 4 |
| Access to information | 5 | 5 | 5 | 5 | 4 |
| Patient centredness | 5 | 5 | 5 | 5 | 4 |
| Care planning | 4 | 5 | 5 | 5 | 4 |
| Emotional/social/psychological support | 4 | 5 | 5 | 5 | 4 |
| Accessibility | 5 | 4 | 4 | 5 | 4 |
| Involvement of carers/family | 4 | 4 | 5 | 4 | 4 |
| Integration into mainstream health care | 4 | 4 | 5 | 4 | 4 |
| Duration | 4 | 4 | 4 | 4 | 4 |
| Generic/disease-specific | 4 | 4 | 4 | 4 | 4 |
| Access to specialist team | 4 | 3 | 4 | 4 | 3 |
| Multidisciplinarity | 4 | 4 | 4 | 3 | 3 |
| Environmental adaptations | 2 | 5 | 5 | 3 | 2 |
| Monitoring | 4 | 2 | 3 | 5 | 2 |
| Users having financial control | 2 | 3 | 4 | 3 | 1 |
| Large-scale public health initiatives | 3 | 3 | 3 | 4 | 1 |
| Complexity | 2 | 2 | 4 | 2 | 1 |
| Disruption to individual | 3 | 3 | 3 | 3 | 0 |
| Financial incentives | 2 | 2 | 2 | 2 | 0 |
Results of task three: selection of exemplar long-term conditions
A list of over 100 LTCs was compiled during the pre-workshop open round (see Appendix 9). Using the characteristics identified in the first workshop exercise, delegates allocated potential exemplar LTCs to these characteristics.
The LTCs highlighted by the three groups as exemplar conditions for the meta-reviews and implementation systematic review were asthma, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), dementia, depression, epilepsy, hypertension, inflammatory arthropathies (IAs) [rheumatoid arthritis (RA), psoriatic arthritis, ankylosing spondylitis and systemic lupus erythematosus (SLE)], irritable bowel syndrome (IBS), low back pain (LBP), progressive neurological disorders (PNDs) [motor neurone disease (MND), multiple sclerosis (MS) and Parkinson’s disease (PD)], stroke, type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM).
Conclusions from the workshop
Final decision on the exemplar long-term conditions with selection of four priority conditions
The team reviewed the recommendations of the three groups, taking into account:
-
the frequency with which they were suggested by the groups (e.g. asthma was suggested by all three groups)
-
the extent of the evidence base for each LTC identified in our scoping of the literature
-
the potential of individual LTCs to represent a number of the characteristics of LTCs (e.g. asthma was not only applicable to the spectrum ‘potential of (self)-treatment/management to improve symptoms’ as a condition with ‘very effective treatment’, but was also ‘highly variable’, ‘common’ and ‘largely self-caring’) (see Table 4)
-
where possible, the advantage of ensuring a range of LTCs from various disease areas.
In this way a final list of four priority LTCs was derived and used to inform the ‘priority meta-reviews’ (stroke, T2DM, asthma and depression). Table 7 maps the LTCs to the two LTC characteristics that reached consensus, and the next five highest scoring characteristics, all of which are presented as spectra. We recognise that our positioning of conditions on these spectra is subjective and that at different stages in the natural history of some LTCs they might be placed at different positions on the spectra. We carried out a slightly simplified version of the meta-reviews, ‘additional reviews’, to test our emerging themes by examining the literature from the other 10 highlighted disease areas [COPD, CKD, dementia, epilepsy, hypertension, IAs, IBS, LBP, PNDs (MND, MS and PD) and T1DM]. The implementation review covers all 14 LTCs.
| Low ◄––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Stroke | T2DM | Epilepsy | Depression | T1DM |
| Dementia | CKD | IAs | IBS | Asthma |
| PNDs | COPD | LBP | ||
| Hypertension | ||||
| Low ◄––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Hypertension | T2DM | Epilepsy | IAs | Dementia |
| CKD | Asthma | IBS | Stroke | |
| LBP | PNDs | |||
| T1DM | COPD | |||
| Depression | ||||
| Low ◄––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Stroke | T2DM | IBS | Epilepsy | COPD |
| Dementia | CKD | IAs | Depression | Asthma |
| PNDs | LBP | T1DM | ||
| Hypertension | ||||
| Low ◄–––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Hypertension | CKD | IBS | IAs | T1DM |
| Epilepsy | Stroke | T2DM | ||
| LBP | Dementia | PNDs | ||
| Depression | COPD | |||
| Asthma | ||||
| Low ◄–––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Stroke | Depression | CKD | IAs | T1DM |
| IBS | Epilepsy | PNDs | Hypertension | T2DM |
| Dementia | LBP | Asthma | COPD | |
| Low ◄–––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Epilepsy | Depression | CKD | Stroke | COPD |
| Asthma | Hypertension | LBP | T1DM | T2DM |
| PNDs | IBS | Dementia | ||
| IAs | ||||
| Low ◄–––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––► high | ||||
|---|---|---|---|---|
| Epilepsy | Hypertension | LBP | T1DM | T2DM |
| Stroke | IBS | Depression | Asthma | IAs |
| PNDs | Dementia | COPD | CKD | |
Components of self-management support interventions
The components and features of self-management support interventions suggested by the respondents were incorporated in our search strategies for all of the reviews, and the components contributed to our proposed taxonomy of components of self-management support interventions which was used in the final overarching synthesis. We revisited some of the proposed features of self-management support interventions when considering the results of our meta-reviews and our implementation review.
Chapter 5 Methods
We undertook a systematic overview of the evidence related to self-management support in the exemplar LTCs. Papers identified through a common search strategy were analysed in three parallel streams.
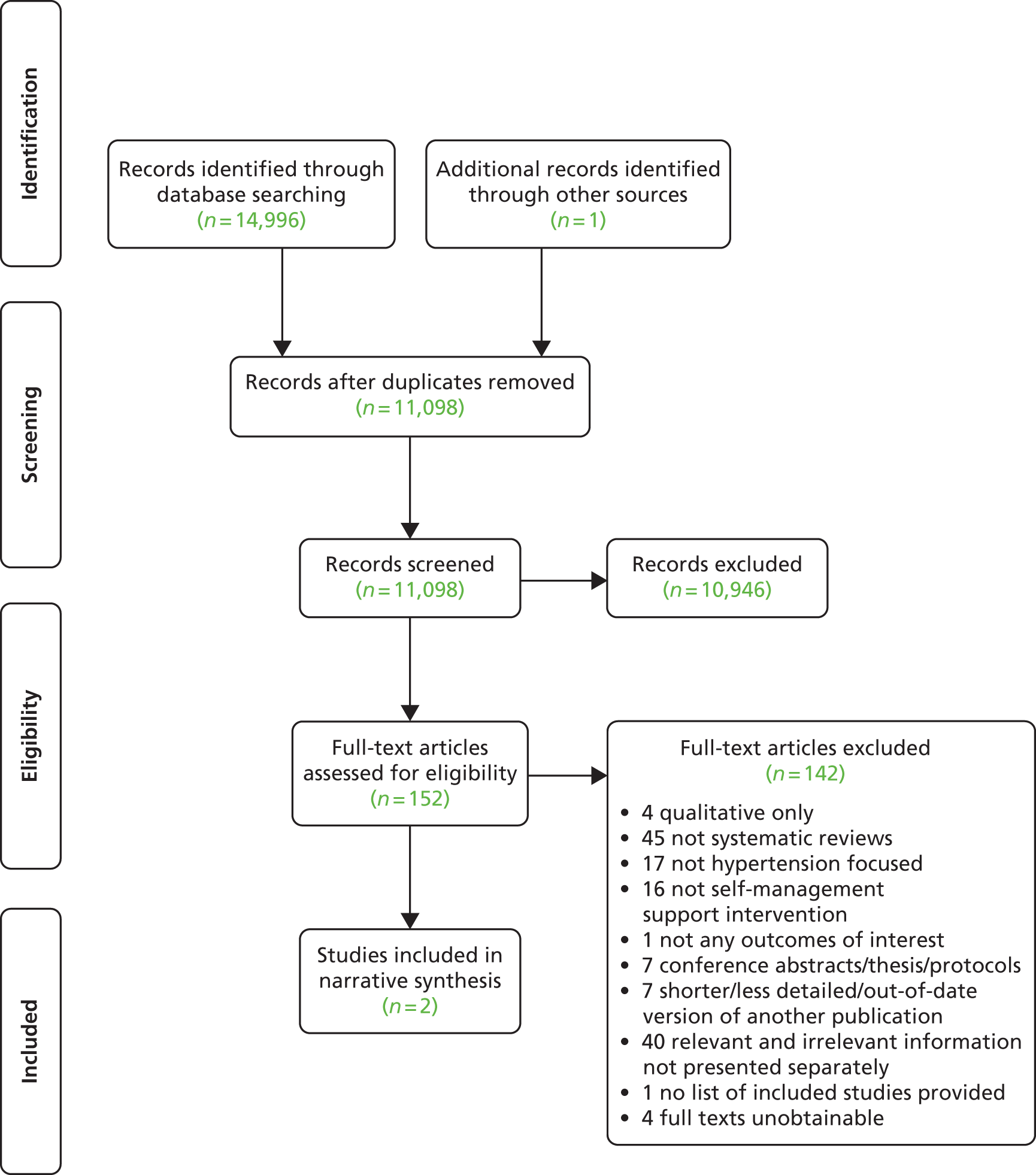
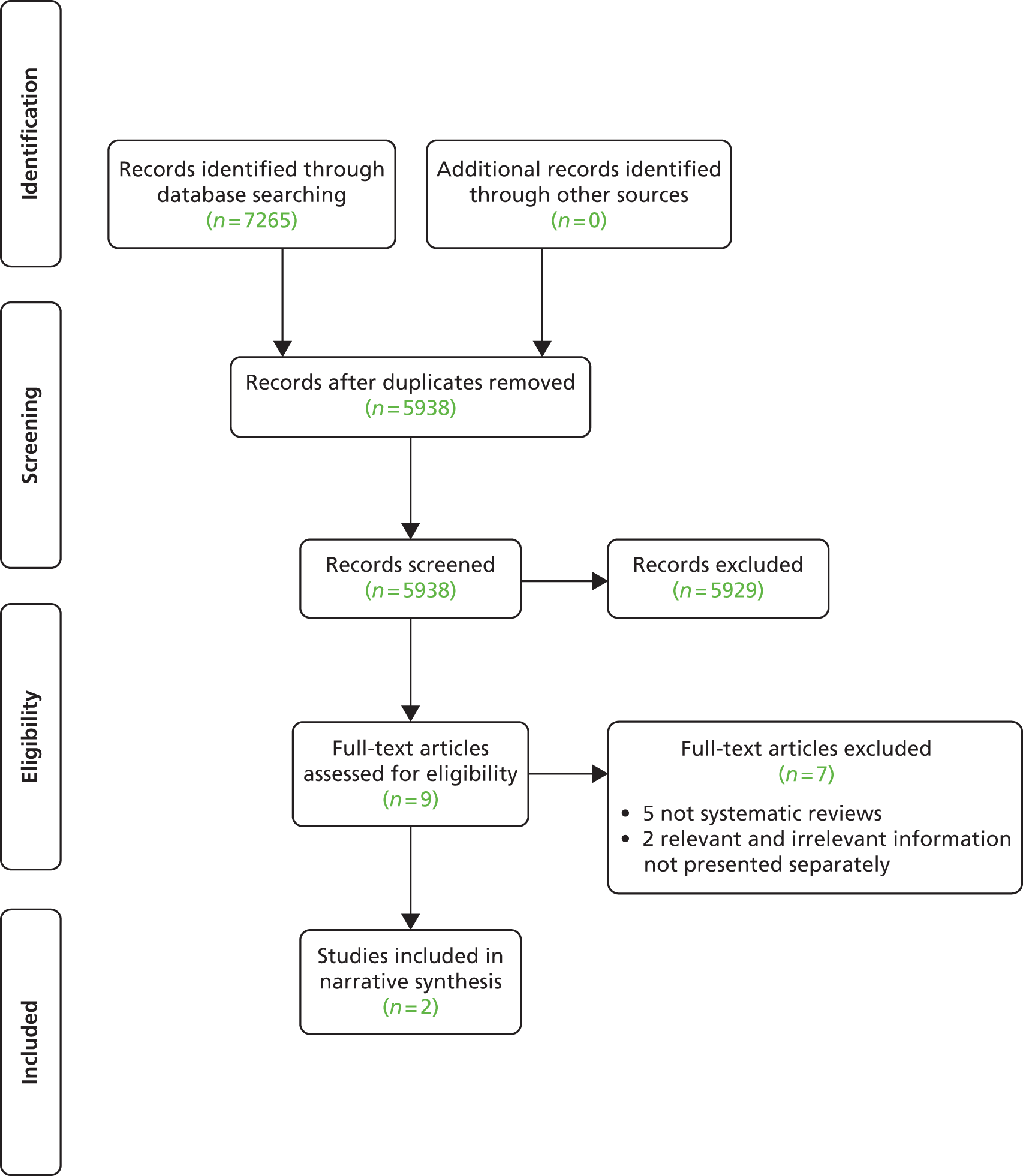
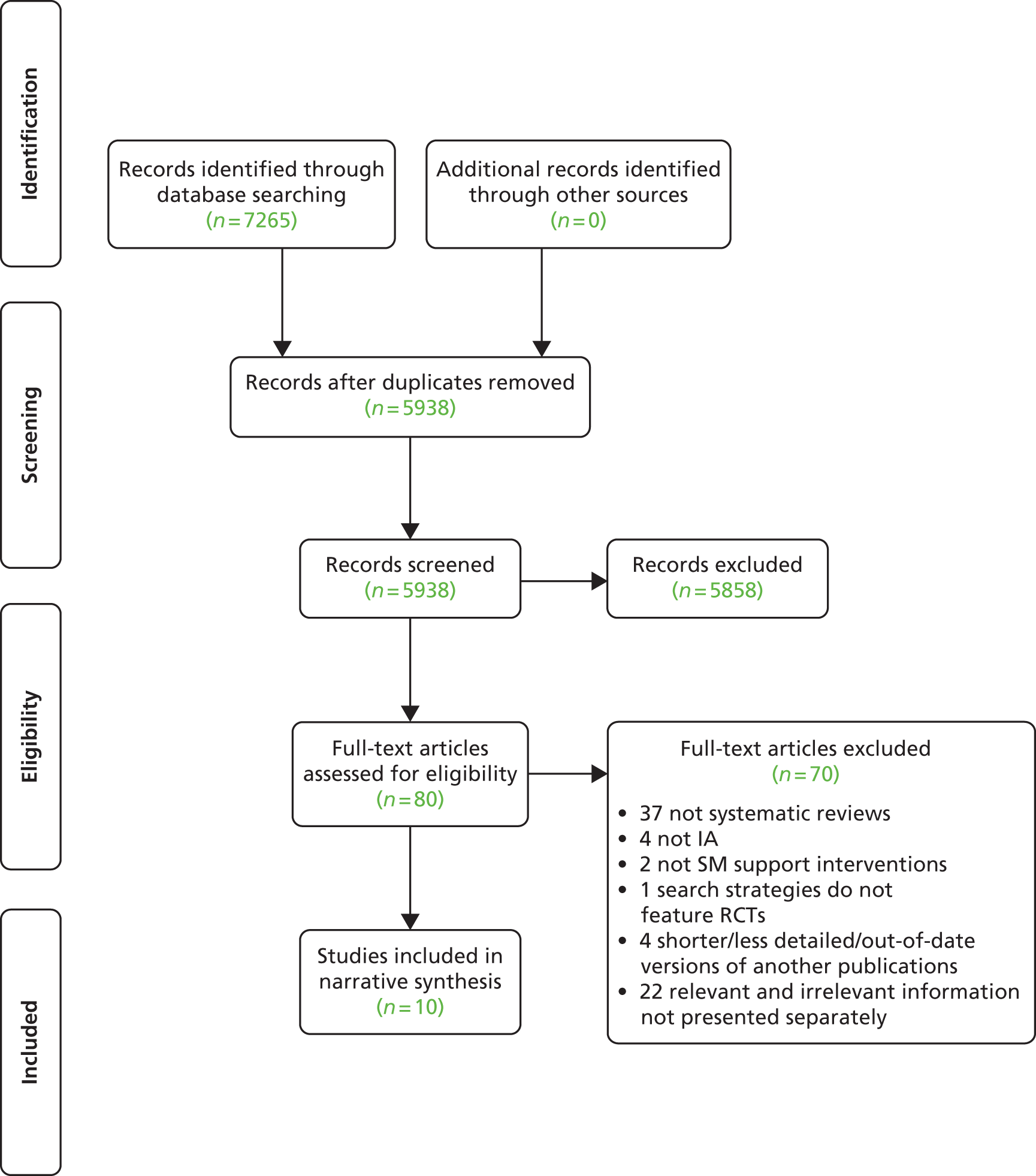
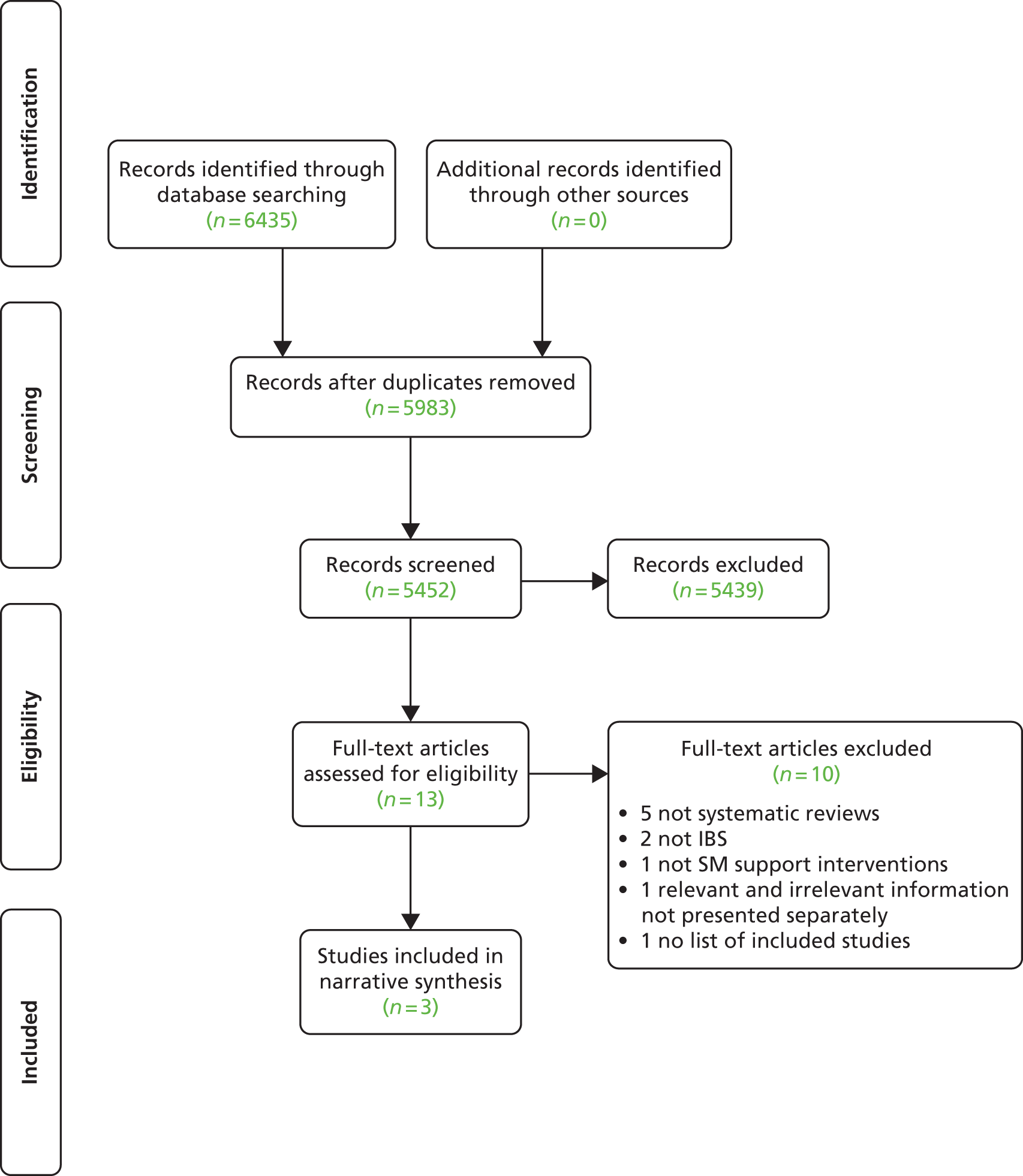
Priority meta-reviews Includes two types: quantitative and qualitative meta-reviews. A quantitative meta-review is an overview of systematic reviews of RCTs. A qualitative meta-review is an overview of systematic syntheses of qualitative studies. These were carried out for the four LTCs identified as priority conditions (stroke, T2DM, asthma and depression).
Additional meta-reviews Simplified versions of the quantitative and qualitative meta-reviews for the remaining 10 conditions (COPD, CKD, dementia, epilepsy, hypertension, IAs, IBS, LBP, PNDs and T1DM).
Implementation review Systematic review of Phase IV implementation studies for all 14 exemplar conditions.
Our overarching analysis synthesised the findings of all the above streams into the spectra of LTC characteristics produced in the Expert Advisory Group workshop (see Chapter 23). Additionally, the self-management components identified in the initial workshop were developed into a taxonomy of self-management interventions based on the evidence collated from the existing literature, the two Expert Advisory Group workshops and the Practical Reviews of Self-Management Support (PRISMS) reviews (see Chapter 6).
We adapted established systematic review and qualitative synthesis methodology for the quantitative and qualitative meta-reviews41,42 and the systematic implementation review. 43 The protocol for the systematic implementation review was registered with PROSPERO (registration number: CRD42012002898). Meta-reviews cannot be registered with PROSPERO but all the protocols are available on the PRISMS website (http://blizard.qmul.ac.uk/research-generation/609-prisms.html).
Search strategy
Search strategy and databases
The priority meta-reviews used a tailored ‘PICOS’ (patients/population; intervention; comparison; outcome; setting) search strategy43 (Table 8). Our basic search strategy was: ‘self-management support’ and ‘LTC’ and ‘systematic review’ terms. Self-management support search terms included ‘confidence’, ‘self-efficacy’, ‘responsib*’, ‘autonom*’, ‘educat*’, ‘knowledge’, ‘(peer or patient) ADJ1 (support or group)’ and ‘(lifestyle or occupational) ADJ1 (intervention* or modification* or therapy)’ as well as relevant medical subject heading (MeSH) terms (see Appendix 10 for the full search strategy). The additional meta-reviews had a simplified version of this search strategy (see Appendix 11).
| Priority meta-reviews | Additional meta-reviews | Implementation review | |||
|---|---|---|---|---|---|
| Quantitative | Qualitative | Quantitative | Qualitative | ||
| Population | Priority exemplar LTCs: stroke, T2DM, asthma and depression | Additional exemplar LTCs: COPD, CKD, dementia, epilepsy, hypertension, IAs, IBS, LBP, PNDs and T1DM | All 14 exemplar LTCs | ||
| Studies were included if self-management support was delivered to populations with one or more of the exemplar LTCs. Generic self-management support was included if one or more of the exemplar LTCs were specified and subgroup data for that condition was provided. As appropriate, we included adults and/or children, ethnic minorities and groups who were perceived as finding services ‘hard to reach’ | |||||
| Intervention | We were interested in any systematic review which focused on, or incorporated, strategies to support self-management | We were interested in any qualitative primary studies that either informed or provided feedback for interventions which focused on, or incorporated, strategies to support self-management | We were interested in any systematic review which focused on, or incorporated, strategies to support self-management | We were interested in any qualitative primary studies that either informed or provided feedback for interventions which focused on, or incorporated, strategies to support self-management | We were interested in any Phase IV implementation intervention which focused on, or incorporated, strategies to support self-management, and which were delivered as part of routine clinical service |
| Comparator | Typically ‘usual care’. The nature of the control service was noted and accommodated within our analysis, but papers were not excluded on this basis | N/A | Typically ‘usual care’. The nature of the control service was noted and accommodated within our analysis, but papers were not excluded on this basis | N/A | Typically ‘usual care’, though definition of ‘usual care’ will vary between trials. The nature of control service was noted and accommodated within our analysis |
| Outcomes | Use of health-care services (including unscheduled use of health-care services and hospital admission rates), health outcomes (including biological markers of disease), symptoms, health behaviour, QoL or self-efficacy | N/A | The reviews’ primary outcome (if supplied), use of health-care services (if supplied), and the two most important health outcomes for each condition (usually a disease-specific outcome, and a measure of patient experience or process outcome) | N/A | Use of health-care services (including unscheduled use of health-care services and hospital admission rates), health outcomes (including biological markers of disease), symptoms, health behaviour, QoL or self-efficacy |
| Settings | Any health-care setting: hospital (inpatient or outpatient), community or remote (e.g. web-based) settings | ||||
| Study design | Systematic reviews which had explicitly searched for RCTs. To be classified as a systematic review the following must be present:
|
Systematic reviews which had explicitly searched for qualitative primary studies | Systematic reviews which had explicitly searched for RCTs. To be classified as a systematic review the following must be present:
|
Systematic reviews which had explicitly searched for qualitative primary studies | Phase IV implementation studies. Where possible, we prioritised cluster randomised trials, quasi-experimental studies, interrupted time series, case–control, controlled before-and-after studies. If these more robust designs were not available, we included uncontrolled before-and-after studies and observational studies |
For the implementation review we used the same self-management and LTC search terms used in the priority meta-reviews along with implementation design terms, i.e. ‘real world’, ‘routine clinical care’, ‘Phase IV’ (see Appendix 12). For the implementation review we also completed a search for unpublished and in-progress studies using general self-management terms.
For the priority and additional meta-reviews, database searches commenced in 1993 (the year in which The Cochrane Collaboration was established; this marked the widespread initiation of high-quality systematic reviews). The end dates of the searches are given in Table 9. No limits in publication year were applied for the implementation review. We searched nine databases for the priority meta-reviews and eight for the implementation review (see Table 9). For reasons of efficiency in the additional meta-reviews, we selected the two databases with the highest sensitivity and specificity (see Appendix 11 for details of the rationale for this decision). Snowball searches and manual searches were applied in all reviews. Forward citation searches were also run for the implementation review and the priority meta-reviews, but not for the additional meta-reviews because of their rapid methodology.
| Priority meta-reviews | Additional meta-reviews | Implementation review | |||
|---|---|---|---|---|---|
| Quantitative | Qualitative | Quantitative | Qualitative | ||
| Databases | MEDLINE, EMBASE, CINAHL, PsycINFO, AMED, BNI, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects and ISI Proceedings (Web of Science) | MEDLINE, CINAHL, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects | MEDLINE (1980 onwards), EMBASE (1974 onwards), CINAHL (1982 onwards), PsycINFO, AMED (1985 onwards), BNI, Database of Abstracts of Reviews of Effects and ISI Proceedings (Web of Science) | ||
| Dates | All from January 1993 Stroke to June 2012 Asthma to July 2012 T2DM to August 2012 Depression to October 2012 |
All from January 1993 COPD, CKD, dementia, epilepsy, IBS, LBP, PND and T1DM to January 2013 Hypertension to October 2012 IAs to November 2012 |
Database searches were completed between 7 and 13 August 2012; searches for unpublished and in-progress studies were completed between 21 and 28 November 2012 | ||
| Manual searching | Systematic Reviews, Health Education and Behaviour, Health Education Research, Journal of Behavioural Medicine and Patient Education and Counseling | Patient Education and Counseling, Health Education and Behaviour and Health Education Research | |||
| Forward citations | A forward citation search was performed on all included systematic reviews using ISI Proceedings (Web of Science). The bibliographies of all eligible studies were scrutinised to identify additional possible studies | None | A forward citation search was performed on all included papers using ISI Proceedings (Web of Science). The bibliographies of all eligible studies were scrutinised to identify additional possible studies | ||
| Unpublished and in-progress studies | N/A | UK Clinical Research Network Study Portfolio (www.clinicaltrials.gov) and the Meta Register of Controlled Trials (www.controlled-trials.com) | |||
Inclusion and exclusion criteria
We excluded papers not published in English (translation was impractical within the time scale of the project), or if we were unable to extract data on self-management support in one or more of the exemplar conditions. Reviews of multiple interventions were included where the focus of the review incorporated self-management, and where data from the RCTs of self-management interventions could be extracted separately, regardless of how many RCTs had this focus. For all of the meta-reviews, we excluded papers published before 1993, or papers which were a shorter and less detailed version of another included review, or if a more recent updated version had been published. The quantitative meta-reviews only included systematic reviews of RCTs (or mixed-method reviews in which the RCT data were presented separately), the qualitative meta-reviews only included systematic reviews reporting a qualitative synthesis (or mixed-method reviews in which the qualitative data were presented separately), and the implementation review only included Phase IV primary studies in which the self-management support intervention was implemented in routine practice. From a practical perspective, when screening papers this meant the studies had to include outcomes from whole populations, define eligibility to the service (not the research), recruit patients to the new service (as opposed to consenting to research), report uptake and attrition, be delivered by service personnel (though they could be trained specifically to deliver the intervention). For the implementation review qualitative studies and RCTs were not included as they were considered to be included in the meta-reviews. The detailed exclusion process for the meta-reviews is detailed in Appendix 13 and for the implementation review in Appendix 14.
Training and quality control
Three reviewers (EE, GPe and HLP) and the joint lead applicants (ST and HP) independently reviewed a sample of 100 titles and abstracts from the searches. The team then compared which titles and abstracts had been selected for further scrutiny. Any disagreements were resolved by discussion and consultation with the Steering Group, if required. This process was repeated on further samples of 100 titles and abstracts until the level of agreement between the joint leads and all reviewers was deemed satisfactory.
Screening of titles and abstracts
Following training, one reviewer (HLP, GPe, EE, SJ, AS or NP) reviewed titles and abstracts from the literature searches and selected possible relevant studies addressing our research question. A random 10% sample of titles and abstracts were examined by a second reviewer (ST or HP) working independently as a quality check. The agreements for the meta-reviews were stroke = 96%; T2DM = 96%; asthma = 97%; depression = 98%; hypertension = 99%; IAs = 99%; and the remaining additional reviews together = 95%. In the case of any disagreements between reviewers, this was resolved by discussion between the two reviewers; in the case of consensus not being reached, a third reviewer (ST or HP) became involved and, if necessary, arbitrated.
Full-text screening
The full texts of all potentially eligible studies were retrieved and assessed against the exclusion criteria (see Appendices 13 and 14) by one reviewer (EE, HLP, GPe, AS or NP). At this stage a 10% check was again implemented (ST or HP). The agreements were stroke = 81%; T2DM = 89%; asthma = 83%; depression = 88%; hypertension = 67%; IAs = 67%; and the remaining additional reviews together = 86%. Disagreements were resolved by discussion with a third reviewer (ST or HP) arbitrating if necessary.
Dealing with multiple publications
Multiple papers may be published for a number of reasons, including translations, results at different follow-up periods or reporting of different outcomes. In the meta-reviews, we only included either the most recent or most comprehensive version of the research (based on exclusion criteria 10), but may make reference to other relevant publications where considered useful.
Implementation review
A random 25% control check was implemented where a second reviewer working independently examined the sample. Disagreements between the reviewers were resolved by discussion between them and sometimes with a third reviewer arbitrating if deemed necessary. Due to the challenges in identifying Phase IV implementation studies, all papers considered relevant to the review were rescreened by ST or HP. Any disagreements or uncertainties between the reviewers were resolved but if deemed necessary a third reviewer arbitrated. The percentage of agreement was calculated separately for diabetes, asthma and depression due to the high volume of relevant papers and a joint percentage of agreement was implemented for the remaining conditions.
Assessment of methodological quality
Meta-reviews
The quality of a systematic review is assessed at two levels:41
-
Quality of systematic review: this reflects the quality of the review process, including an assessment of the methodology of searching, selection of studies, data extraction and synthesis. 44
-
Quality of evidence included within systematic review: this reflects the rigour with which the reviews assessed the quality of the studies included in each of the reviews, looking for potential bias, conflicting results across individual studies, sparse evidence or a lack of relevance to the review question. 41
We used the Revised Assessment of Multiple Systematic Reviews (R-AMSTAR) quality appraisal tool to assess the methodological quality of all included systematic reviews45 (see Appendix 15). Assessment of Multiple Systematic Reviews (AMSTAR) has good face and content validity but is unable to produce quantifiable assessments of quality. 46,47 R-AMSTAR is a revised version of the AMSTAR instrument which can quantify the quality of systematic reviews. 45 Due to the dearth of tools to assess quality of qualitative systematic reviews, we adapted the R-AMSTAR for this purpose (see Appendix 16). The qualitative tool was assessed out of 40 and papers were judged to be high quality if scored as ≥ 30 and low quality if scored < 30.
Quality assessment was undertaken by one reviewer (GPe, HLP, SJ, AS or NP), with a random 10% conducted independently by a second reviewer (EE, GPe, HLP, ST or EH). Disagreements were resolved by discussion and, if necessary, with the involvement of a third reviewer.
Implementation review
We used the checklist described by Black and Downs,48 which was developed to assess the methodological quality of both randomised and non-randomised studies of health-care interventions (see Appendix 17). This checklist was chosen on the basis of being one of the best in assessing non-randomised controlled studies. 49 Quality assessment was undertaken by one reviewer (EE), with a random 10% conducted independently by a second reviewer (HP). Disagreements were resolved by discussion and, if necessary, with the involvement of a third reviewer.
Extraction of data
Meta-reviews
Data were extracted by one reviewer (GPe, HLP, SJ, AS or NP) using a piloted data extraction table and 10% of the completed data extraction tables were checked by a second reviewer (HP or ST) for integrity and accuracy. We resolved any disagreements by discussion between reviewers; in the case of consensus not being reached, a third reviewer (HP or ST) became involved and, if necessary, arbitrated.
We extracted data under the headings of review rationale, research question(s), inclusion criteria, definition of self-management support component reviewed, definition of the LTC(s) reviewed, completeness of search strategy, screening procedure, method of data analysis, number and reference of all relevant primary studies included (either RCTs or qualitative studies), participant demographics, study details, descriptive results and synthesised results. Additionally, the quantitative meta-reviews extracted specific information reported in the reviews on the range of comparison groups, settings, service arrangements, delivery modes of intervention, duration and intensity of self-management component(s), and follow-ups within the included RCTs. We extracted the findings and conclusions as synthesised by the authors of the systematic reviews, and specifically avoided going back to the individual primary studies.
Implementation review
Data were extracted by one reviewer (EE) using a piloted data extraction table and the completed data extraction tables were checked by a second reviewer (HP or ST) for integrity and accuracy. We resolved any disagreements by discussion between reviewers; in the case of consensus not being reached, a third reviewer became involved and, if necessary, arbitrated.
We extracted data under the headings of: at whom the intervention is directed (HCPs, patients, carers, mixture); setting; mode of delivery (group, individual, professional, lay led, joint led, face to face, telehealthcare); group allocation (if applicable); components (education, action plans, techniques to support behaviour change); (tele)monitoring; support materials (written/electronic information); duration and intensity of components; follow-up (frequency and mode); service arrangements (‘usual’ primary/additional care, dedicated service); and any cost-effectiveness data.
Data analysis
Priority quantitative meta-reviews
Detailed description
The initial step was to compile a detailed descriptive summary of the evidence for self-management support in each of the priority exemplar LTCs (stroke, T2DM, asthma and depression).
Synthesis
Meta-analysis is inappropriate at the meta-review level due to the overlap of included RCTs between reviews. However, for any primary outcomes where three or more systematic reviews present pooled statistics, results were displayed graphically by creating ‘meta-forest plots’. These graphical representations do not attempt to create overall pooled statistics, as this would require going back to the original RCTs. They provide a visual representation of results instead, allowing for more straightforward interpretation of data. Where there was heterogeneity between the included reviews for each LTC, we undertook a narrative synthesis. Interpretation of results was facilitated by discussion among the multidisciplinary study team. Interpretation of systematic review results was weighted by consideration of study quality and the total number of participants included in the systematic review.
Priority qualitative meta-reviews
Levels of interpretation
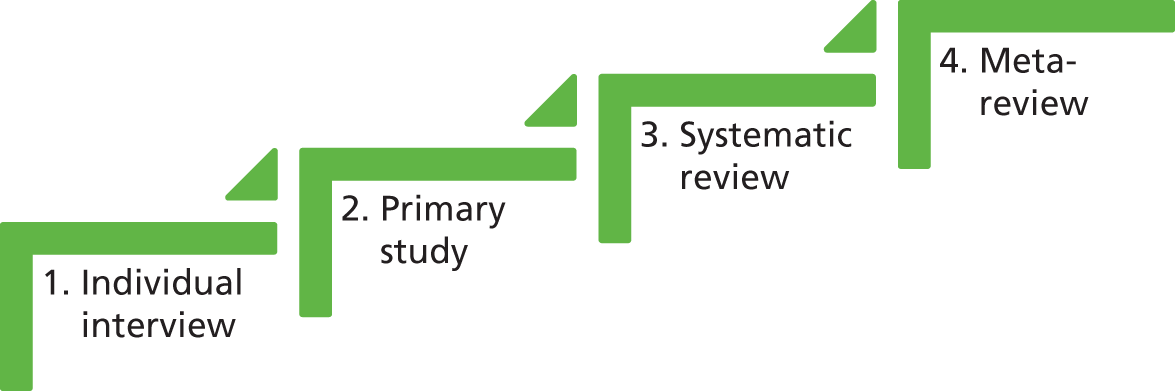
It is important to acknowledge the four main levels of interpretation and hermeneutic philosophy50 (a quadruple hermeneutic) involved when carrying out a meta-review of qualitative reviews. The first is the participant’s interpretation of their own experiences when discussing them during the interview in the course of the primary research project; the second relates to the researcher’s reflections and report in the primary study; the third level involves the synthesis of all the findings from the primary studies included in a systematic review; and the last is the meta-review level (Figure 4). For this final level, our aim was to only analyse the summaries and syntheses of the existing evidence in the included reviews [i.e. the second (as reported in the systematic reviews) and third hermeneutic levels], rather than to investigate or analyse data from the primary studies or individual interviews.
FIGURE 4.
Levels of interpretation: the four levels of collected data, of which the meta-review is the fourth. It aims to synthesise the systematic reviews’ findings and conclusions only, and not to examine the individual interview or primary study level of data.
A meta-ethnographic framework
We were concerned not only to examine the arising patterns within these data, but also to integrate the findings together in relation to our aim of informing the commissioning of health services. As a result, we employed a meta-ethnographic framework to meta-synthesise these data. 51 Our qualitative meta-review questions were (i) how can people with a specific LTC be effectively supported in their self-management; and (ii) how can this inform commissioners and health-care providers about what works, for whom, in what contexts, how and why?
In order to address the first question, reciprocal translation51 was used to examine patterns and identify arising metaphors within the included reviews. In meta-ethnographic framework, reciprocal translation is specifically focused on translating similarities across data in order to organise the concepts taking place. This was followed by a lines-of-argument synthesis51 to examine the second question. Lines-of-argument synthesis is a technique used to interpret and infer at a whole level, such as at an organisational or cultural level. In these particular meta-reviews the key purpose of the lines-of-argument synthesis was to translate the findings into a broader understanding about their meaning in the commissioning context. The analysis and quality assessment were carried out by two reviewers (GPe, SJ, EH, ST or HP) working independently; findings were cross checked and discrepancies resolved through discussion.
Data saturation
In meta-reviews where the data arising reached a point where no additional data were being found and each arising theme was a repetition of a previous one, a conclusion of data saturation was made. 52
Additional meta-reviews
This analysis was similar to the priority meta-reviews, but for the additional exemplar LTCs (COPD, CKD, dementia, epilepsy, hypertension, IAs, IBS, LBP, PND and T1DM) a more focused approach to analysis was adopted.
In order to simplify the quantitative data extraction and analysis, we focused on:
-
the primary outcome as defined by the systematic review (if supplied)
-
any measures of health-care utilisation (if supplied)
-
a disease-specific outcome – this was usually a measure of disease control (e.g. number of seizures in epilepsy, number of hospitalisations in COPD)
-
a measure of patient experience or process measure of self-management (e.g. QoL, ownership of action plans or self-efficacy).
We synthesised the quantitative and qualitative data, focusing on (though not limited to) issues raised by the analysis of our priority meta-reviews. We specifically looked for evidence which confirmed or refuted our conclusions from previous analyses.
Implementation review
Detailed description
The initial step was to compile a descriptive summary of the evidence for implementing self-management support in each of the exemplar LTCs.
Narrative synthesis
The eligible trials were characterised by a substantial heterogeneity and thus meta-analysis was not appropriate. We used narrative analysis53 and adopted the whole-systems approach as a framework for the analysis. 36 This considers interventions from a multilevel perspective, engaging patients, professionals and the organisation in a collaborative approach.
Over-arching synthesis
We then developed matrices that mapped the evidence for, and where possible the components of, effective self-management support interventions, to the characteristics of the exemplar LTCs as defined by the Expert Advisory Group. The highlighted areas where there was a paucity of evidence enabled us to see any patterns of evidence for effectiveness and ineffectiveness of self-management support interventions.
Interpretation of the findings
Multidisciplinary discussion
Throughout the process of undertaking the reviews, the multidisciplinary team met regularly (normally weekly) to discuss the emerging findings. The monthly Steering Group meetings provided further opportunities to discuss and refine preliminary conclusions. Regular teleconferences with Professor Bower enabled synergy with the findings of the complementary HS&DR programme-commissioned health economics project. 54
This enabled the analysis to develop iteratively as the work progressed. For example, the outcomes of the priority quantitative meta-reviews dictated the primary outcomes for our additional quantitative meta-reviews. Building on the findings of the quantitative meta-reviews, the Phase IV implementation review sought evidence of effectiveness (or not) of models of supported self-management which had been shown to be effective in RCTs.
End-of-project workshop
The findings and over-arching conclusions from our programme of reviews were presented to 34 multidisciplinary stakeholders (including the initial Expert Advisory Group) at an end-of-project stakeholder conference. Small discussion groups reflected on findings and discussed and advised on practical implications for commissioning and providing services for people with LTCs in England and Wales. The conclusions of the discussion groups were used to refine the priorities for practice, research and policy, and to inform the final report and publications.
Long-term condition-specific methods
In some LTCs, methods varied from those described previously (Table 10).
| LTC | Condition-specific methods |
|---|---|
| Stroke | The aims of both the included systematic reviews and the studies they included did not always completely match the aims of our review. To address this, we assessed the potential relevance of the individual studies to our aim and used this, in combination with the quality assessment results, to guide the weight we attached to the conclusions of each review |
| T2DM – qualitative | After the completion of full-text screening for qualitative reviews exploring T2DM, we were left with the decision about whether to only include those explicitly including T2DM only, or whether to include those that did not separate types of diabetes as well (e.g. not separately including or analysing T1DM and T2DM, or insulin-dependent diabetics with non-insulin-dependent diabetics). As there was only one paper fitting the description of the former, the team decided to include the latter as well to add depth and breadth to the findings. This was based on Campbell et al.’s rationale that ‘qualitative health research synthesis should not be driven by medical considerations but should rather concern itself with the way in which patients experience disease and illness’.55 We included all of the findings from the included reviews unless the paper explicitly referred to an aspect specific to T1DM, such as children and families learning to use insulin. However, comparing these findings with each other was carried out with caution. The following exclusion criteria were revised to explicate the changes: Exclude 5. Exclude if the review does not focus on or include adults’ self-management of diabetes mellitus or self-management by those that have been diagnosed with T2DM (include diabetes mellitus papers that mix T1DM and T2DM or insulin- and non-insulin-dependent diabetes together if they focus on self-management in populations that are relevant to adults with diabetes mellitus). As the review was not focusing on T1DM alone, we excluded reviews that focused on T1DM only Exclude 11. Exclude if unable to data extract the information on qualitative primary studies in the selected LTCs separately from the rest of the findings (unless it is between T1DM and T2DM or insulin- and non-insulin-dependent diabetes: these will be included) |
| T2DM – quantitative | Although the focus of this meta-review was T2DM, and reviews combining data for T1DM and T2DM were excluded, an exception was made for reviews of interventions specifically targeting self-management in foot ulcer care or DKD as these two conditions require broadly the same self-management regardless of whether the individual has a diagnosis of T1DM or T2DM56 A significant number of retrieved reviews were concerned exclusively with SMBG. NICE guidelines recommend offering SMBG to individuals newly diagnosed with T2DM as an integral part of self-management education.57 A recent Cochrane review on this subject observed that the efficacy of SMBG in T2DM has been the focus of a large number of systematic reviews and meta-analyses over time, most including RCTs only. This most recent review reached similar conclusions to the NICE guidelines, finding SMBG to be beneficial in individuals newly diagnosed with T2DM, but finding less effect when diabetes mellitus duration was over 1 year.58 The research team decided to exclude all reviews focusing purely on SMBG as it is a thoroughly researched area with up-to-date clinical recommendations already in place. Furthermore, where SMBG formed part of a self-management package which included other components such as education, peer support, counselling, etc., we hoped that studies would be picked up by reviews with a broader self-management support focus |
| T1DM – quantitative | As discussed with regards to T2DM, we acknowledge SMBG as an important aspect of self-management support. However, due to the huge body of evidence which already exists to support the effectiveness of this single aspect of self-management in T1DM, the review team decided to exclude reviews which focused solely on SMBG. This is in keeping with our decision not to review monocomponent self-management support interventions, apart from education. Where reviews explored SMBG alongside other self-management support components they were still considered for inclusion in our meta-review |
| Depression | After removing duplicates, a total of 8570 titles and abstracts were identified through systematic searching of the following databases: AMED, BNI, CINAHL, EMBASE, MEDLINE and PsycINFO. In addition, 2865 titles and abstracts were identified through searching the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects. All databases were searched from 1993 onwards To familiarise the review team with the emerging forms of self-management delivered within the context of depression, scoping of a randomly selected 1000 titles and abstracts was performed. This scoping was undertaken concurrently with title and abstract screening, and involved the reviewer (GPe) keeping an open mind as to what self-management support might mean within the context of depression. The idea behind this broad and inclusive screening of 1000 titles and abstracts was to facilitate discussion between the review team, and to ensure reviewers were in agreement before further screening continued. A basic search of the EndNote file (Thomson Reuters, CA, USA) containing all references was also undertaken, searching for the key words ‘self-management’ and ‘self management’ In addition to the screening of a random sample of 1000 titles and abstracts and the basic key word search, all 2865 titles and abstracts identified from the search of the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects were screened |
| Hypertension and IAs | Although these were additional meta-reviews, the search strategy and screening process carried out for them were the same as for the priority reviews. The analysis remained at the level of the additional meta-reviews |
Layout of the rest of this report
The next chapter describes the development of a proposed taxonomy for self-management support – this work was conducted in parallel with the reviews which comprise the main bulk of this report.
The four priority meta-review chapters follow (see Chapters 7–10). Each chapter reports a meta-review of qualitative systematic reviews with a line of argument synthesis, followed by a meta-review of quantitative systematic reviews. The overall quantitative evidence on self-management support and the effective components of multicomponent interventions, any evidence about context and how and by whom such interventions should be delivered is summarised in a figure and this is followed by a mixed-methods synthesis which combines the quantitative and qualitative meta-review findings.
Ten additional chapters on different LTCs follow (see Chapters 11–20). Again, each chapter reports a meta-review of qualitative systematic reviews, but this simply presents key themes arising from the qualitative systematic reviews, rather than attempting a line of argument synthesis. Each chapter also presents a quantitative meta-review, but this is limited to two or three carefully chosen health outcomes rather than examining all possible health-related outcomes. Again, any evidence including that about context and how and by whom such interventions should be delivered is summarised in a figure and this is followed by a mixed-methods synthesis which combines the quantitative and qualitative meta-review findings.
The report is deliberately structured so that those interested in self-management support in a particular LTC can get a detailed summary of the systematic review evidence on that LTC in the respective chapter.
The next chapter (see Chapter 21) is an original systematic review of implementation research relating to all the conditions studied in the earlier chapters.
This is followed by an overarching synthesis chapter (see Chapter 22) which attempts to bring all the review findings together. The final chapter (see Chapter 23), includes our conclusions in relation to the brief and recommendations for future research.
Chapter 6 Proposed taxonomy for self-management support interventions
Background and rationale
One of the problems encountered when searching for, or analysing, literature related to self-management is recognising it. We have already described the lack of a universally accepted definition for self-management support (see Chapter 2). Similarly, there is no universally accepted classification, or taxonomy, for types of self-management support interventions. Barlow et al. 59 produced a list of self-management components in their seminal 2002 overview of self-management approaches for people with LTCs, Fisher et al. 60 produced a useful list of ‘resources and supports for self-management’ and the American Heart Association has produced a disease-management taxonomy61 in which self-management is one component; however, we wanted to focus on self-management support components. We wanted to apply such a taxonomy to the research evidence to better explore ‘what works, for whom in what setting?’. We initially attempted to use Michie et al. ’s behaviour change taxonomy,62 but found that this provided a level of sophistication and detail that we were unable to apply to the accounts of self-management support interventions gleaned from the systematic reviews and implementation studies. Furthermore, Michie et al. ’s62 taxonomy deals with behaviour change techniques whereas we were interested in classifying interventions simply by components which might themselves comprise a number of different techniques. Ultimately, we believe that describing self-management support interventions by both components and the behaviour change technique using Michie et al. ’s62 taxonomy would be most helpful but we were unable to do this for this review.
We present our proposed taxonomy before we present the meta-reviews in this report. In practice, the taxonomy was actually developed iteratively across the duration of the PRISMS study.
Development of the proposed taxonomy
Following on from the suggestions from our Expert Advisory Group workshop and informed by the sources described above and the systematic reviews included early on in the PRISMS meta-analyses, we propose a layered taxonomy of self-management support interventions that recognises that these complex interventions may have the following dimensions:
-
Different recipients: patients, carers, HCPs, organisations.
-
Different components.
-
Different modes of delivery: face to face, remote, telehealthcare, web based.
-
Different personnel delivering or facilitating the support: lay people (with or without training), different types of HCPs.
Furthermore, on top of all these, interventions may be generic, culturally specific or tailored to individuals.
It is also apparent from the PRISMS meta-reviews that self-management support interventions have very varied durations and intensity, but we have not proposed these features as part of the taxonomy.
The recipients and the components
It is important to clarify that self-management support interventions are commonly complex interventions and usually include more than one of these components (indeed our reviews did not examine isolated self-management support components other than education).
Patients and/or carers as recipients
We identified 14 different types of components of self-management support, which might be directed at the patient and/or carer level. These are listed with some elaboration and examples taken from the PRISMS work in Table 11.
| Taxonomy | Elaboration | Examples from RCTs included within the meta-reviews or considered for the implementation review |
|---|---|---|
| Direct components (delivered directly to patients and/or carers) | ||
| 1. Education about condition and management | – |
|
| 2. Information about available resources | Including:
|
|
| 3. Provision of/agreement on specific action plans and/or rescue medication | Definition:
|
|
| 4. Regular clinical review | – |
|
| 5. Monitoring of condition with feedback to the patient | Including:
|
|
| 6. Practical support with adherence (medication or behavioural) | Including:
|
|
| 7. Provision of equipment | – |
|
| 8. Safety netting | Including:
|
|
| 9. Training/rehearsal to communicate with HCPs | – |
|
| 10. Training/rehearsal for ADL | – |
|
| 11. Training/rehearsal for practical self-management activities | – |
|
| 12. Training/rehearsal for psychological strategies | Including:
|
|
| 13. Social support | Including:
|
|
| 14. Lifestyle advice and support | Including:
|
|
| Indirect components: health or social care professional level (delivered to individual HCPs or social care professionals) | ||
| Education and training | Including:
|
|
| Equipment | Including:
|
|
| Prompts | Including:
|
|
| Feedback and review | Including:
|
|
| Financial incentives | Including:
|
|
| Indirect components: organisational level (delivered at an organisational level) | ||
| Education and training | Including:
|
|
| Equipment | – |
|
| Prompts | Including:
|
|
| Feedback and review | – |
|
| Financial incentives | – |
|
Chapter 7 Priority meta-review: self-management support for stroke survivors
Meta-review of qualitative systematic reviews
Systematic reviews identified
There were 13,058 citations identified by the searches, including 658 duplicates (Figure 5). Following title and abstract screening, 18 full-text reports were reviewed and seven syntheses were included in the meta-review. 64–70 Across all the LTCs examined, the qualitative systematic reviews often failed to comment on the countries of origin of their included original studies or give further details about the context of the studies so this is not routinely reported for the qualitative meta-reviews.
FIGURE 5.
Stroke: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for qualitative meta-review. 63
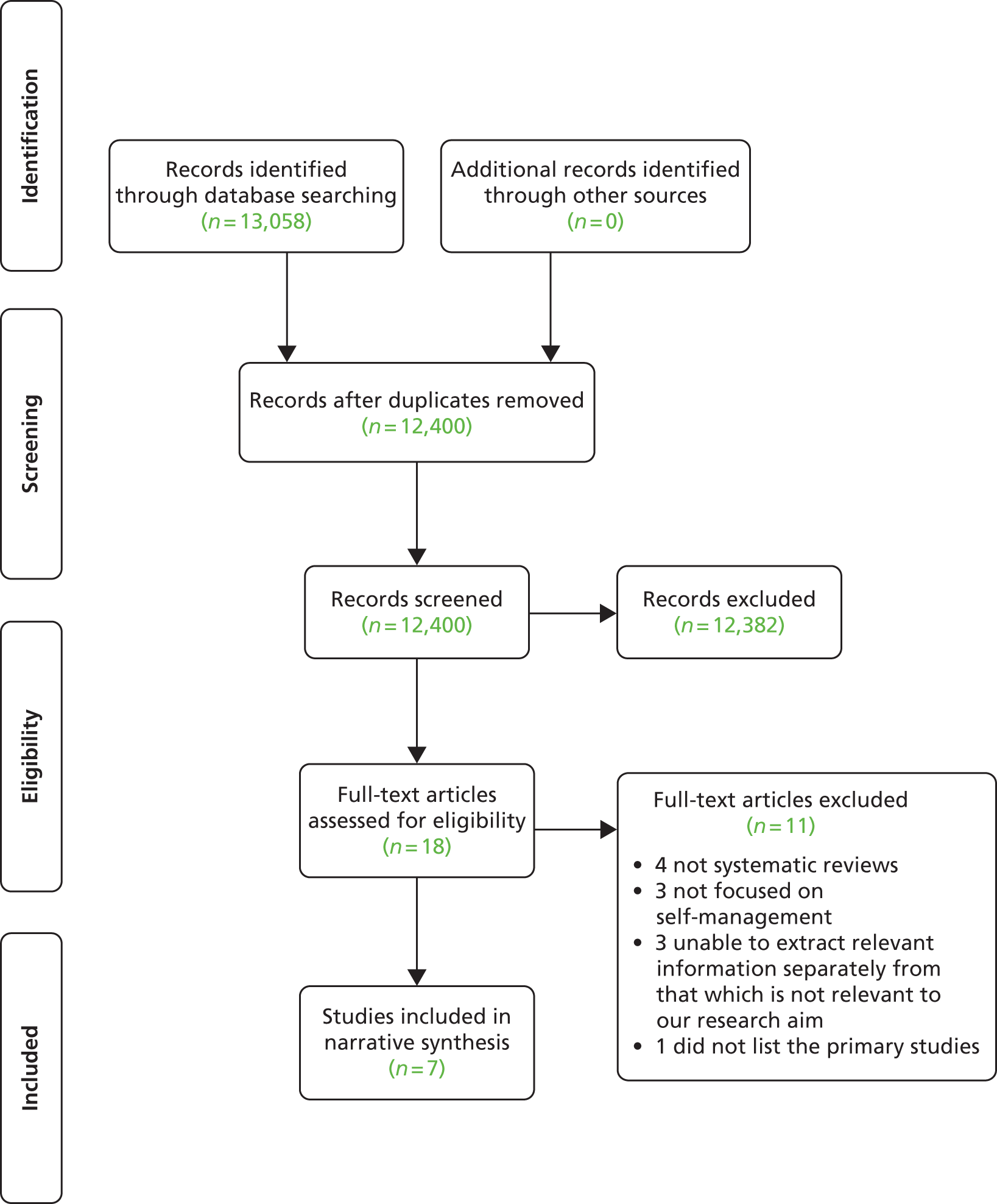
Of the seven syntheses (published 2003–12), six exclusively included qualitative studies and one included a range of study designs but reported qualitative studies separately. 70 Some of the primary qualitative studies were included in more than one review (Table 12), but there were 130 unique qualitative studies (1974–2008) included in the reviews overall.
| Study | Lamb 200864 | Lui 200570 | McKevitt 200465 | Murray 200366 | Peoples 201167 | Reed 201268 | Salter 200869 |
|---|---|---|---|---|---|---|---|
| Lamb 200864 | 27 | ||||||
| Lui 200570 | 0 | 2 | |||||
| McKevitt 200465 | 16 | 2 | 95 | ||||
| Murray 200366 | 3 | 2 | 15 | 23 | |||
| Peoples 201167 | 3 | 0 | 4 | 0 | 12 | ||
| Reed 201268 | 5 | 0 | 7 | 2 | 0 | 18 | |
| Salter 200869 | 5 | 0 | 8 | 3 | 0 | 3 | 9 |
No systematic reviews specifically examined the qualitative evidence on self-management support in stroke; instead they captured broader concepts and aspects of this topic (Table 13). There were two clear foci of qualitative review included in this meta-review as a result of our selection criteria. One revolved around patients’ experiences of being a survivor of stroke, either more generally or with a specific focus on psychosocial experiences in the elderly population. 64,65,67,69 The second was based on reviews examining people’s views of services offered to those who had experienced a stroke, investigating challenges faced and potential solutions found. 65–68,70
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary of key findings |
|---|---|---|---|
| Lamb 200864 (Qualitative) |
To appraise and synthesise the best available evidence on the psychosocial spiritual experience of elderly individuals recovering from stroke | 27 | Four main themes:
|
| Lui 200570 (Mixed quantitative and qualitative) |
To identify and review studies that have examined the effectiveness of teaching problem-solving skills to caregivers in stroke care to improve patient outcomes, highlight gaps in the evidence base and recommend avenues for additional research | 2 | This supports the view that the goal-setting process is complex, and there is a need to develop clearer guidelines to help nurses and family caregivers to set realistic and achievable goals |
| McKevitt 200465 (Qualitative) |
To identify the scope of published qualitative studies of stroke, consider their relevance to the development and delivery of services for people with stroke, and make recommendations for future work | 95 | Findings were discussed in four main categories:
|
| Murray 200366 (Qualitative) |
To identify the most frequently encountered longer-term problems experienced by stroke patients and their informal carers. This will provide a platform for the development of a patient-centred, primary care-based stroke service | 23 | The review identified 203 problem areas, which were categorised into five domains:
|
| Peoples 201167 (Qualitative) |
To obtain the best available knowledge on stroke survivors’ experiences of rehabilitation | 12 | One theme, ‘Power and Empowerment’ and six subcategories were identified:
|
| Reed 201268 (Qualitative) |
To identify the key factors to account for in planning and developing rehabilitation and community services for stroke, based on users’ perspectives | 18 | The main interconnected themes, or third-order constructs, relate to how the impact of stroke is influenced by the person, close social relationships and the social environment, as well as the interactions between all three The key factors to be considered in supporting stroke survivors and helping them maintain an active and positive presence in their unique social world are to:
|
| Salter 200869 (Qualitative) |
To examine the contribution of the published qualitative literature to our understanding of the experience of living with stroke | 9 | Five inter-related themes were identified as follows:
|
Four reviews focused on the experiences of stroke survivors,64,67–69 and three included both stroke survivors and others involved in their lives, such as caregivers, family and friends. 65,66,70 Most reviews carried out syntheses using extraction matrices, with only three describing their analytical approach (clustering technique,66 meta-summary,67 and meta-synthesis and lines-of-argument synthesis with a meta-ethnographic approach68).
Quality assessment
More weight was applied to the results of the four papers that scored highly (30+) during the quality assessment,64,66,68,69 and less weight applied to the three lower (< 30) scoring papers65,67,70 (Table 14). A high level of data saturation emerged around the arising themes, suggesting similar experiences being discussed in the majority of qualitative studies.
| R-AMSTAR criteria | Lamb 200864 | Lui 200570 | McKevitt 200465 | Murray 200366 | Peoples 201167 | Reed 201268 | Salter 200869 |
|---|---|---|---|---|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 3 | 3 | 2 | 4 | 1 | 4 | 4 |
| Was a comprehensive literature search performed? | 2 | 3 | 4 | 4 | 4 | 3 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 4 | 2 | 2 | 2 | 2 | 3 | 1 |
| Was a list of studies (included and excluded) provided? | 4 | 1 | 2 | 2 | 2 | 4 | 2 |
| Were the characteristics of the included studies provided? | 1 | 4 | 2 | 4 | 2 | 4 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 1 | 1 | 1 | 1 | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 4 | 1 | 4 | 2 | 4 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 3 | 4 | 4 | 4 | 4 | 4 |
| Was the conflict of interest stated? | 2 | 1 | 2 | 1 | 4 | 3 | 1 |
| Total score/40 | 32 | 26 | 24 | 30 | 26 | 37 | 30 |
| Quality rating (low = < 30; high = ≥ 30) | High | Low | Low | High | Low | High | High |
Findings
The synthesis revealed a paucity of explicit evidence around stroke survivors’ experience of self-management and self-management support. However, three central metaphors were identified that could be used to inform self-management support: impact of stroke; needs as a result of stroke; and impact and feedback of treatment (Table 15). The qualitative syntheses provided a useful overview of a stroke survivor’s journey: from suffering an acute stroke, to rehabilitation after a stroke, to being a stroke survivor and looking towards the future.
| Central metaphors | Themes | Reference | Illustrative quotation |
|---|---|---|---|
| Impact of stroke | Shock | Lamb 2008 (p. 177)64 |
|
| Salter 2008 (p. 597)69 |
|
||
| Negative change | Lamb 2008 (p. 177)64 |
|
|
| McKevitt 2004 (p. 1500)65 |
|
||
| Murray 2003 (pp. 138/140)66 |
|
||
| Peoples 2011 (p. 167)67 |
|
||
| Reed 2012 (p. 558)68 |
|
||
| Salter 2008 (p. 597)69 |
|
||
| Salter 2008 (pp. 597–8)69 |
|
||
| Salter 2008 (p. 598)69 |
|
||
| Ambiguity | Lamb 2008 (p. 177)64 |
|
|
| McKevitt 2004 (p. 1501)65 |
|
||
| Salter 2008 (p. 599)69 |
|
||
| Murray 2003 (p. 140)66 |
|
||
| New self | Lamb 2008 (p. 177)64 |
|
|
| Reed 2012 (p. 558)68 |
|
||
| Salter 2008 (p. 597)69 |
|
||
| Salter 2008 (p. 600)69 |
|
||
| Environment vulnerability | Reed 2012 (p. 558)68 |
|
|
| Needs as a result of stroke | Physical | Lamb 2008 (p. 177)64 |
|
| Peoples 2011 (p. 168)67 |
|
||
| Reed 2012 (p. 558)68 |
|
||
| Salter 2008 (p. 597)69 |
|
||
| Informational | Lamb 2008 (p. 189)64 |
|
|
| McKevitt 2004 (p. 1502)65 |
|
||
| Murray 2003 (p. 138)66 |
|
||
| Peoples 2011 (p. 168)67 |
|
||
| Reed 2012 (p. 560)68 |
|
||
| Reed 2012 (p. 561)68 |
|
||
| Psychological | Lamb 2008 (p. 177)64 |
|
|
| McKevitt 2004 (p. 1502)65 |
|
||
| Peoples 2011 (p. 168)67 |
|
||
| Reed 2012 (p. 558)68 |
|
||
| Salter 2008 (p. 600)69 |
|
||
| Murray 2003 (p. 138)66 |
|
||
| Social | Murray 2003 (p. 140)66 | ||
| Lamb 2008 (p. 177)64 |
|
||
| McKevitt 2004 (p. 1502)65 |
|
||
| Peoples 2011 (p. 168)67 |
|
||
| Peoples 2011 (p. 169)67 |
|
||
| Reed 2012 (p. 558)68 |
|
||
| Reed 2012 (p. 561)68 |
|
||
| Salter 2008 (p. 599)69 |
|
||
| Salter 2008 (p. 600)69 |
|
||
| Impact and feedback of treatment | Recovery plateau | McKevitt 2004 (p. 501)65 |
|
| Salter 2008 (p. 600)69 |
|
||
| Respect and value | Lamb 2008 (p. 177)64 |
|
|
| McKevitt 2004 (p. 1502)65 |
|
||
| Peoples 2011 (p. 168)67 |
|
||
| Salter 2008 (p. 600)69 |
|
||
| Communication | Lamb 2008 (p. 177)64 |
|
|
| Lui 2005 (p. 2519)70 |
|
||
| McKevitt 2004 (p. 1501)65 |
|
||
| Murray 2003 (p. 138)66 |
|
||
| Peoples 2011 (p. 168)67 |
|
||
| Proactivity | Lamb 2008 (p. 177)64 |
|
|
| Lui 2005 (p. 2519)70 |
|
||
| McKevitt 2004 (p. 1501)65 |
|
||
| Murray 2003 (p. 138)66 |
|
||
| Peoples 2011 (p. 168)67 |
|
||
| Peoples 2011 (p. 169)67 |
|
||
| Reed 2012 (p. 561)68 |
|
||
| Salter 2008 (p. 600)69 |
|
Impact of stroke
This metaphor relates to the disruptive change of having a stroke and the impact this has on a person’s life, including the feelings of shock, negative change and ambiguity, adapting to the new self and feelings of vulnerability in external or unknown environments. Having a stroke is a sudden, shocking event that the stroke survivors perceived as having disrupted their previously anticipated life trajectory. 64,69 Stroke survivors reported this event as being a negative change in their lives, associated with feelings of loss, grief, frustration, embarrassment, shame due to changed physical and social feeling, appearance, ability, power64–69 and helplessness. 64,69 They now viewed their bodies as unreliable and their futures uncertain. As a result of this feeling of ambiguity, they compared themselves with their pre-stroke selves and abilities, leading to further feelings of frustration and anxiety. 64–69 Additionally, in Reed et al. ’s68 review stroke survivors reported feeling safe in their home environment, whereas outside they felt unsafe and vulnerable, making them feel separated from the outside world. Stroke survivors reported that the stroke event had resulted in a new self, with recovery involving the acceptance of the changes in their lives and self-image, and the role reassessment and reconstruction of their identity. 64,66,68,69 This adjustment to the new self is an important phase in psychological recovery after the stroke that needs to be supported. HCPs can enable the stroke survivor to adaptively cope with the changes and positively adjust to their new identity and help them to feel empowered. They can involve family and friends in these changes so that the stroke survivor feels supported in their self-management by family and friends as well as HCPs.
Needs as a result of stroke
Inherent in this metaphor were four main needs stroke survivors reported as a result of their stroke: physical, informational, psychological and social. Initial recovery was predominantly focused on physical rehabilitation and medical management. Stroke survivors felt that the simplest aspects of life they had previously taken for granted, such as getting out of bed, walking and talking, now involved a conscious effort that mediated everything in their lives. 64,67–69 The reviews found that after early discharge patients felt more in control, enabling them to assess their needs and carry out their own routines, as opposed to waiting passively on health-care staff’s schedules. 65,67,68 All the reviews recommended that support should be personalised to help the individual carry out daily tasks to increase feelings of confidence, independence and hope, and in turn further motivate the survivor to set and achieve new realistic challenges. 64–70
Stroke survivors reported a lack of understanding about having a stroke and life afterwards, and requested further guidance and information on what they were experiencing at different stages of the stroke survival process and how best to self-manage. 64–69 In some cases, stroke survivors reported feeling afraid of having another stroke and limited their abilities to an extent that could derail their recovery. 64 HCPs can therefore be specifically trained to effectively enable self-management and empower stroke survivors by learning how best to explore their understanding of stroke, identify barriers to adjusting and self-managing, and provide them with patient-specific information at all stages of recovery after a stroke. 64–69
Stroke survivors discussed their observation that rehabilitation from HCPs was very focused on functional rehabilitation and did not support psychological and emotional needs, such as adaptation and coping with being a survivor, and building confidence, motivation, faith and hope. 64–69 Goal-setting and problem-solving should be patient centred, educating the stroke survivor on how to set realistic goals themselves and take steps to achieve these. This, in turn, provides the stroke survivor with the self-efficacy to apply these skills when faced with new challenges. 64–70 It is also recommended that stroke survivors are encouraged to learn or develop new skills in areas in which they did not excel prior to their stroke. Stroke survivors often found it frustrating trying to relearn something they were once highly skilled at, whereas new or developing skills were perceived from afresh and could be seen as a productive and enjoyable challenge. 64
There was a clear deterioration in stroke survivors’ social lives after their stroke, with a need to rebuild this as physical aspects improved. 64 All the reviews identified that, after having a stroke, many felt isolated as they missed their previous social lives and felt that they were not around people who understood what they were going through. Stroke survivors often felt the need to manage the impressions they gave other people. In the wider public, they tried to match other people’s impressions of what a ‘normal’ person should be like, which could be emotionally draining, in order to avoid negative perceptions due to stigma. 69 This, in turn, could lead to further feelings of isolation as part of a vicious cycle. Social support groups with other stroke survivors and groups of people who were understanding and supportive were reported as valuable provision to exchange experiences and coping strategies. These were useful to encourage comparison with other people in similar situations, rather than comparison with their pre-stroke selves or people who have not had a stroke. 64–69 This reduced feelings of isolation, concerns of impression management and social vulnerability, and increased feelings of self-efficacy in social situations.
Some stroke survivors reported that carers could be overprotective and, in turn, reduce the survivor’s autonomy. 66 Self-management support should not only be given to the stroke survivor, it should also consider the informal carers, family, friends and the social world external to the home environment. Self-management support should be delivered to the whole unit revolving around and including the stroke survivor. A positive outcome of stroke should be perceived when the stroke survivor is comfortable within their social world regardless of what stroke effects still exist. 68 Rebuilding these social links and psychological (and sometimes spiritual) strength can help increase feelings of belonging and connectedness, confidence, independence and hope, enabling the stroke survivor to refocus their life and look towards their future. 64–69
Figure 6 is a visual representation of a stroke survivor’s needs, beginning with a high amount of functional needs and some psychosocial needs after the acute stroke event. At this point, rehabilitation is appropriate alongside addressing the first stages of adjustment to their new life. As functional needs decrease, the stroke survivor reaches a recovery plateau and they are discharged from therapy services, they are faced with a lack of support and increased psychosocial needs of adjustment to their new selves and to address feelings of social isolation.
FIGURE 6.
Visual representation of stroke survivor’s needs over recovery pathway.
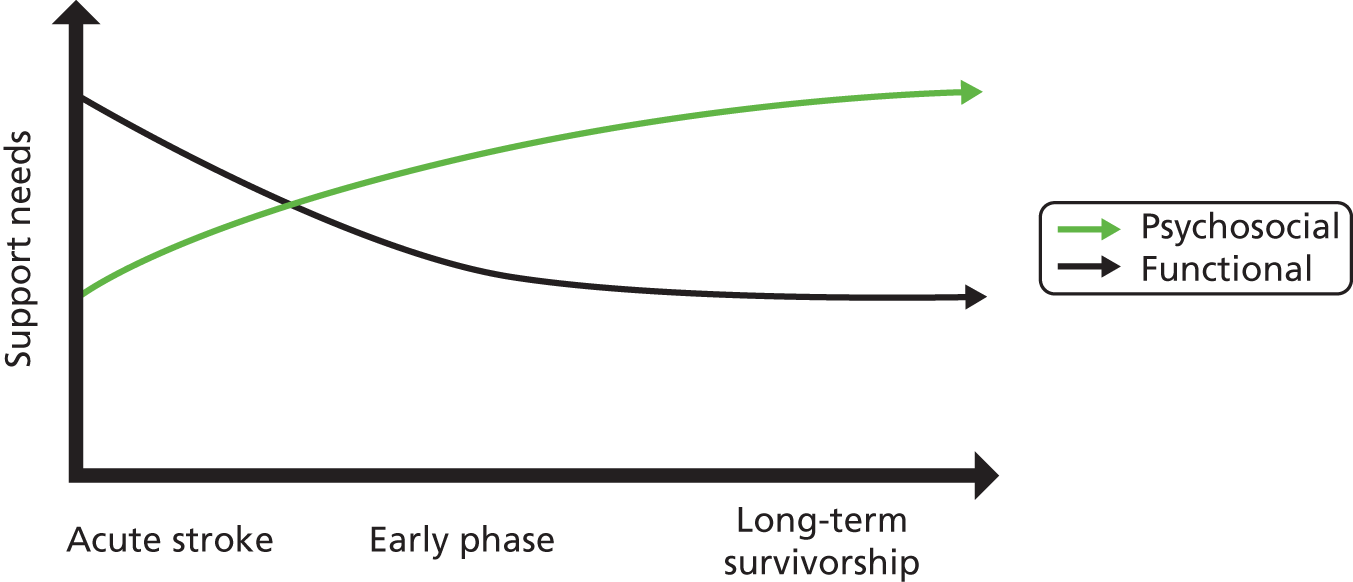
Impact of, and feedback on, treatment
Within this metaphor, stroke survivors’ discussed four aspects relating to their experiences of treatment and the impact this had on their recovery: the recovery plateau, communication, respect and proactivity. The recovery plateau is a result of treatment focusing on the physical and medical aspects of recovery. Stroke survivors were provided with rehabilitative support all the time they were improving physically, but they perceived that support ceased when they were no longer viewed as a medical patient needing rehabilitation. 65,69 A plateau in physical recovery often occurs simultaneously with the stroke survivor’s realisation that they were not going to reach what they perceived to be a full recovery (returning back to their pre-stroke self). 65,69 However, there is a lack of psychological and social support to enable them to cope and accept these changes to their self-perception and identity. 64,66,68,69 The relationship with the HCP should be a collaborative and educational one, with the professional listening to the patients’ and carers’ needs, giving expert advice, providing information and answering questions. 64–68,70 One of the most commonly reported issues was a mismatch of goals or different perceptions of the same goals between the stroke survivor and the HCP. All the studies highlighted that these were often caused by differing views of the concept of recovery, how it could be attained and how progress towards it might be measured. Stroke survivors also reported receiving a mixture of messages from different professionals about what to do and not do, which led to patient confusion and feelings of guilt if they were not doing something or progressing at a certain speed. 67 However, they did feel that being taught skills that enabled more proactive engagement, such as goal-setting, resulted in autonomy, control and empowerment. 64–70 Self-management education would enable the stroke survivor to not only understand stroke, the different challenges they might face, and the meaning of life after stroke to them, but it also teaches the stroke survivor skills to proactively problem-solve and goal set when future challenges arise.
Stroke survivors tended to view the professional as the expert and expected them to take on a controlling role, whereas they took on the role of a ‘patient’ and adopted a passive role. Therefore, care routines could constrain autonomy and stroke survivors reported feeling as though they were waiting passively for treatment. 67 Even those who felt that their self-management skills were improving reported that they missed the support offered by the professional when they were not present. 64 Generally, stroke survivors discussed the need to feel valued, and reported that this was hindered whenever carers and professionals treated them with a lack of respect and dignity. 64,65,67,69 This resulted in feelings of subordination and a lack of control over their own lives (although this was sometimes seen as a positive aspect that relieved patients from the burden of decision-making in the early stages after having a stroke). 64,67 Stroke survivors reported feeling invisible and isolated to those around them, yet paradoxically they also felt that they were very visible as a stigmatised burden to others who were caring for their vulnerable selves. 64,65,67,69 Stroke survivors need to feel respected and valued by the professional in order to help build communication between the professional and the survivor. Feeling emotionally and socially supported (rather than an isolated burden) can enable the survivor to feel self-efficacious in their recovery and encourage them to take a proactive approach in self-management. It is important that all those involved with the stroke survivor’s management (e.g. informal carers) are involved in this process and come to a consensus about realistic targets in the short and long term. 64–69 This, in turn, will encourage the stroke survivor to be more in control of their goal-setting and recovery, while using the support of the professionals to help them with their self-management needs.
Support for self-management
The lines-of-argument synthesis enabled these findings to be integrated to provide a broader picture to inform future commissioning of self-management support.
-
Confusion, memory and communication problems can influence a stroke survivor’s self-management behaviours and therefore their support needs. Stroke survivors’ fear of having another stroke can limit their activities and impair their recovery.
-
Stroke survivors feel the need to manage the impressions they give other people. To professionals they might try and appear more motivated than they actually are in order to elicit support. To the wider public they may try and match other people’s impressions of ‘normality’, which can be emotionally draining, to avoid negative perceptions and stigma.
-
Early discharge after an acute stroke can be beneficial to the stroke survivor’s autonomy, as long as they feel supported and understand what services are available to them, should they need them.
-
Guidance and information should be specific to the stage of recovery. Patients may feel guilty if they are only making small improvements (often due to lack of information/understanding about their condition and unrealistic goal-setting).
-
Individually tailored psychological, behavioural and emotional support from the early stages after suffering a stroke may enable stroke survivors to cope with specific life barriers and encourage them to accept this new life stage.
-
Goal-setting and problem-solving including others involved in the stroke survivor’s care may address mismatches (between patients and professionals) in concepts of recovery and aims. Stroke survivors reported receiving mixed messages from different professionals so communication between professionals regarding goal-setting might need to be addressed.
-
Collaborative relationships with HCPs enable stroke patients to feel respected, valued and in control of the decisions made about their lives.
-
Encouraging stroke survivors to focus on new or developing skills can be seen as a productive and enjoyable challenge.
-
Social groups with other stroke survivors, and groups of people who are understanding and supportive, may encourage useful comparison with other people in similar situations, rather than comparison with pre-stroke selves or people who have not had a stroke. Rebuilding social links and psychological (and sometimes spiritual) strength can help increase feelings of confidence, independence and hope, enabling the stroke survivor to refocus their life and look towards their future. Support should also consider the informal carers, family, friends and the social world external to the home environment.
-
Commissioners need to be aware of the potential for inequalities in services in real-life settings (e.g. professionals may offer less provision to older, or less motivated, patients, or language barriers may result in a lack of communication/understanding).
Meta-review of quantitative systematic reviews
Systematic reviews identified
Of 12,400 titles and abstracts, 13 systematic reviews were identified for inclusion in our meta-review of self-management support interventions for stroke survivors. 70–82 (Figure 7). These reviews collectively represented 101 individual RCTs, 29 of which were included in more than one review (Table 16). Year of review publication ranged from 2003 to 2012, although the year of publication of RCTs included within these reviews dated back to 1981. Trials were conducted in seven countries (details of study location were absent in some reviews): UK, USA, China, Australia, the Netherlands, Sweden and Denmark.
FIGURE 7.
Stroke: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for quantitative meta-review. 63
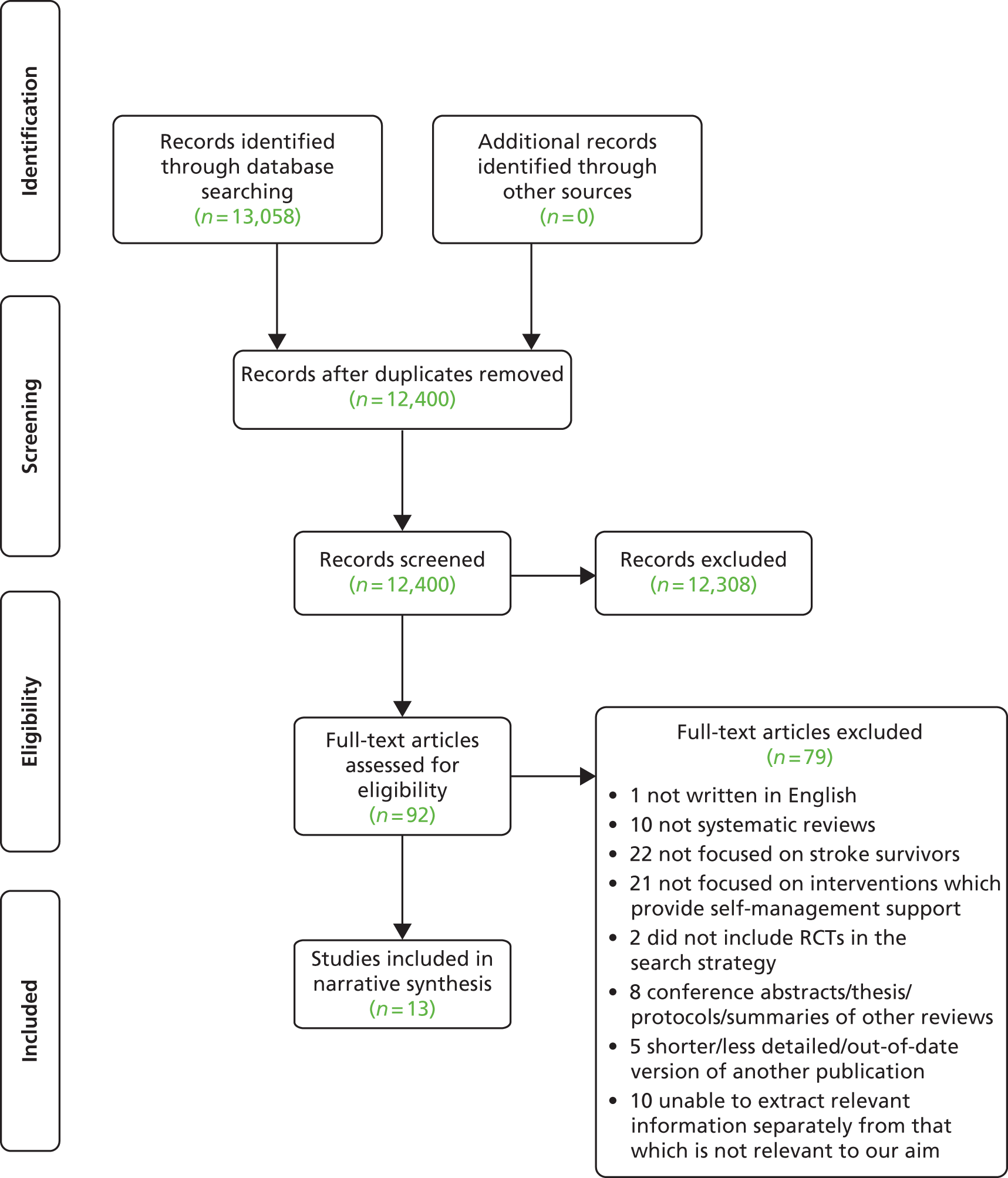
| Study | Aziz 200871 | Hoffman 201072 | Legg 200673 | OST 200374 | Poulin 201275 | Steultjens 200376 | Walker 200477 | Ellis 201078 | Ko 201079 | Korpershoek 201180 | Lui 200570 | Rae-Grant 201181 | Smith 200882 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aziz 200871 | 5 | ||||||||||||
| Hoffman 201072 | 0 | 1 | |||||||||||
| Legg 200673 | 0 | 0 | 9 | ||||||||||
| OST 200374 | 0 | 0 | 7 | 14 | |||||||||
| Poulin 201275 | 0 | 0 | 0 | 0 | 3 | ||||||||
| Steultjens 200376 | 0 | 1 | 6 | 6 | 0 | 18 | |||||||
| Walker 200477 | 0 | 0 | 7 | 8 | 0 | 6 | 8 | ||||||
| Ellis 201078 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 16 | |||||
| Ko 201079 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| Korpershoek 201180 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 4 | |||
| Lui 200570 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 6 | ||
| Rae-Grant 201181 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Smith 200882 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 17 |
The term ‘self-management’ was rarely used, but by reference to our definition and the underlying theoretical basis for self-management (see Chapter 2) we identified interventions which provided components of self-management support (albeit not by name). Table 17 summarises the scope of interventions included in each review, an explanation of why we considered that these interventions represented components of self-management support, and the characteristics of the RCT interventions extracted from each review (see Appendix 18 for further clarity on why these reviews are considered to explore self-management support interventions).
| Review | Summary of relevant aim(s) | Inclusion criteria for interventions | Why this is self-management support | Characteristics of RCT interventions identified for inclusion from primary review | |||
|---|---|---|---|---|---|---|---|
| Setting, service arrangements, delivery mode | Components included | Timing of delivery | Duration and intensity | ||||
| Therapy rehabilitation | |||||||
| Aziz 200871 | Do therapy-based rehabilitation services influence stroke survivor outcomes 1 year or more after the index stroke? | Outpatient-based rehabilitation, provided by physiotherapist, OT or multidisciplinary staff, working with patients to improve task-orientated behaviour. The intervention must require an organisational and staffing structure, and must be delivered 1 year post stroke | All trials showed an approach based on problem-solving, aiming to reduce disability by altering task-orientated behaviour and goal-orientated activities | Patients’ own home or in outpatient rehabilitation centres. Part of therapists’ usual work. Intervention performed by established community physiotherapy service | Approaches adopted by trials were single or multidisciplinary interventions, some using problem-solving approaches | 1 year post stroke | Trials adopted fixed or flexible structures. Programmes ranged in duration from 12 weeks to 1 year, and varied in their intensity |
| Hoffman 201072 | Is OT for people with cognitive impairment after a stroke effective in improving functional and cognitive abilities? | OT interventions for cognitive impairment in people with stroke. These interventions may take either a remedial or a compensatory approach, or both. A remedial approach involves training for specific cognitive deficits, while the compensatory approach may include training skills for daily activities, advising and educating about the use of assistive devices, educating patients, families and caregivers about strategies to overcome patients’ cognitive impairment. The dynamic interactional approach is an integrated approach which encompasses both remedial and compensatory elements | Compensatory approach included training skills using compensatory strategies, advising and educating about the use of assistive devices, educating patients, families and caregivers about strategies to overcome patients’ cognitive impairment | Inpatients. Delivered on an individual basis | Cognitive skills remediation training | Hospital-based post-acute stroke | Training administered 30–40 minutes three times a week for an average of 3–4 weeks |
| Legg 200673 | Do interventions provided by OTs, which aim to facilitate personal ADL, improve outcomes for stroke survivors? | OT interventions which either focused on practice of personal ADL or were targeted towards improving the patient’s ability to perform personal ADL. OTs working as part of a multidisciplinary team were excluded | Aims to enable people to achieve health, well-being and life satisfaction. Promotes recovery through the use of purposeful activities. Targeted towards improving the patient’s ability to perform personal ADL | Home based. Delivery on an individual basis | A range of OT interventions including one or more of: OT based on leisure activities; OT based on ADL; teaching new skills; support with adaptive equipment use; carer involvement; goal-setting; information provision; referring to, or liaison with, other services; facilitating return of function | Various. Mainly post admission to or discharge from inpatient facilities | Duration of programmes was between 6 weeks and 6 months. Number of visits ranged from 2.5 to 18 |
| OST 200374 | Do therapy-based rehabilitation services influence stroke survivor outcomes? | Therapy-based rehabilitation service interventions delivered to stroke patients resident in the community. Interventions must be provided or supervised by qualified physiotherapy, OT or multidisciplinary staff, who work with the patient to improve task-orientated behaviour primarily aiming to reduce disability | Included problem-solving and education aimed at reducing disability | Mostly home based, some delivered in rehabilitation centres. Delivery mainly on an individual basis, face to face | Physiotherapist, OT or multidisciplinary team input. Components including teaching skills; facilitating return of function; information provision to patient and carer; provision of equipment; adaptations; advice on obtaining financial assistance and transport; liaison with specialist organisations; providing physical assistance, identifying and managing psychosocial stressors affecting patients and carers | Various. Mainly at discharge from inpatient facilities | Intervention periods ranged from 5 weeks to 6 months. Intensity ranged from one visit every day during study period, to an average of one visit every 8 weeks |
| Poulin 201275 | Do executive function interventions improve executive functions and functional abilities in daily life? | Cognitive interventions to remediate executive function impairments or improve functional tasks compromised by impairments in executive function. Attentional processes were excluded as they had been previously reviewed. Interventions involving components such as computerised cognitive training, problem-solving, strategy formation techniques, goal management training, or other compensatory strategies and external aids for overcoming every day executive problems were all considered | Involved components such as problem-solving, strategy formation techniques, goal management training, and other compensatory strategies and external aids for overcoming every day executive problems | All interventions were delivered remotely to individuals in a home-based setting except in one subgroup where strategy training was delivered face to face by therapists | Heterogeneous interventions. Working memory: computerised tasks, involved presentations of auditory and visuo–spatial stimuli. Strategy training: problem-solving, planning, multitasking and goal management. External compensation: electronic prompts to carry out self-selected tasks, e.g. taking medication, remembering appointments | Chronic (> 6 months post stroke) | Interventions lasted between 5 and 20 weeks. Sessions (where applicable) lasted between 40 and 45 minutes, and occurred between one and five times a week |
| Steultjens 200376 | Do OT interventions improve outcomes for stroke survivors? | OT interventions in clinically diagnosed adult stroke patients, of which six categories are defined: (1) training of sensory–motor functions; (2) training of cognitive functions; (3) training of skills such as dressing, performing domestic activities; (4) advice and instruction in the use of assistive devices; (5) provision of splints and slings; and (6) education of family and primary caregivers. Comprehensive OT was an additional category which involved all six specific intervention categories | Interventions aimed to facilitate task performance by improving relevant skills or developing and teaching compensatory strategies to overcome lost skills. Included advice, education and sharing of information | Unclear descriptions, suggests that the majority were home based and delivered on an individual basis, others were delivered in an inpatient setting | Components included: client-centred OT; enhanced OT; teaching new skills; facilitating independence in ADL and return of function; enabling use of equipment; counselling of patient and caretaker; intellectual training; and strategy training | Various. Lack of some detail. Generally, less than 1 year since stroke | Sessions lasted between 30 and 52 minutes each and occurred between once and twice a week. Duration was between 6 weeks and 6 months |
| Walker 200477 | What is the efficacy of community OT? | Home-based OT intervention in patients with a clinical diagnosis of stroke. Two approaches to the OT intervention are defined: (1) ADL interventions encouraging patients to participate in personal and extended ADL; (2) leisure therapy interventions aiming to improve leisure participation | Primarily concerned with the reablement and resettlement of individuals into their chosen home environment | Delivered by research OTs or clinicians in a home-based setting (including care or nursing homes) | Components included training in ADL, leisure therapy and both | Not synthesised | Between 5 and 10+ sessions delivered over 6 weeks to 6 months |
| Other self-management support | |||||||
| Ellis 201078 | What is the efficacy of stroke liaison workers for stroke survivors in increasing participation and improving well-being? | Referral to a stroke liaison worker. These individuals provide a multifaceted service including more than one of education and information provision, social support and liaison with other services. Often this intervention is provided from the point of patient discharge from hospital. Studies were excluded where the intervention was judged to be single faceted | Aim to increase participation and improve well-being for patients and carers. Typically provide emotional and social support and information | Mostly with urban populations. Delivery home based: face to face or via telephone | Interventions were either proactive or reactive, and adopted a structured, flexible or focused approach | Various. Mainly 2–6 weeks since stroke onset | Between 3 and 15 contact sessions, lasting between 15 and 90 minutes each. Intervention delivered for a maximum of 9 months |
| Ko 201079 | Do patient-held medical records improve clinical care, patient outcomes or satisfaction? | Paper-based, patient-held medical record. The patient or carer is given a copy of the record to keep, take to health appointments, help manage health-care tasks and communication. May be with or without other interventions such as additional education for staff, reminder posters in clinics and/or dedicated patient held record co-ordinating staff. This review excluded electronic health records, including electronic health records that are controlled by the patient | Aim to help manage health-care tasks and communication, to enable continuity and improve quality of care. They include key patient and health-care information and blank sections to enable patient note-taking | No RCTs identified in stroke survivors | N/A | N/A | N/A |
| Korpershoek 201180 | What self-efficacy enhancing interventions influence mobility, ADL, depression and HRQoL of stroke survivors? | Self-efficacy enhancing interventions for stroke patients. Interventions must aim to increase confidence in one’s ability to perform a task or specific behaviour. Interventions must also be feasible and suitable to be delivered in nursing practice | Self-efficacy is the confidence in one’s ability to perform a task or specific behaviour. A high sense of self-efficacy leads to desired outcomes | Community or hospital rehabilitation settings | A heterogeneous group of four interventions judged to enhance self-efficacy: psychosocial intervention; computer-generated tailored written information; the Chronic Disease Self-Management Program education; task-oriented walking intervention | Various. Ranges from acute to within 1 year of stroke onset | The walking intervention was delivered three times a week for 6 weeks. Insufficient detail provided for the remaining three RCTs |
| Lui 200570 | Is teaching problem-solving skills to caregivers in stroke care effective? | Educational interventions for problem-solving delivered to family caregivers in stroke care. Interventions involve teaching family caregivers to cope with problems and to relieve stress | Teaching family caregivers to cope with problems. Problem-solving strategies included positive problem orientation and goal-setting | Delivery varied encompassing class training, home visits and telephone contact. Most teaching was given to stroke patients and caregivers in their home on an individual basis by HCPs | Problem-solving strategies taught included positive problem orientation, confronting the problem, analysing the problem and goal-setting | Mostly applied in the early post-stroke period | The duration of interventions ranged from 2 to 12 months. On average, each home visit lasted 1–2 hours |
| Rae-Grant 201181 | What is the efficacy of self-management programmes in individuals with chronic neurological conditions? | Self-management interventions for neurological disorders. Interventions collaboratively help patients and families acquire skills and confidence to manage their illness, providing self-management tools, and routinely assessing problems and accomplishments | Collaboratively helping patients and families acquire the skills and confidence to manage their chronic illness, providing self-management tools, and routinely assessing problems and accomplishments | No RCTs identified in stroke survivors | N/A | N/A | N/A |
| Smith 200882 | What is the effectiveness of information strategies provided with the intention of improving outcomes for stroke survivors or their caregivers? | Information intervention delivered to stroke patients, their caregivers, or both. Information must be provided with the intention of improving outcomes of patients, their caregivers, or both. Information may be active (following information provision there was a purposeful attempt to allow participants to assimilate information and subsequently clarify/consolidate) or passive (single occasion of information provision with no follow up or consolidation). Trials were excluded in which information giving was only one component of a more complex rehabilitation intervention | Information strategies provided with the intention of improving the outcome for stroke patients or their identified caregivers or both | Delivery setting varied and included home-based, outpatient, inpatient and rehabilitation units | Active interventions (n = 9) included programmes of lectures; opportunities to ask questions or to contact specialist nurses for further information; hands on training; telephone calls; interactive workbooks; regular reviews; personalised records detailing risk factors and targets; counselling. Passive interventions (n = 8) included written generic information; and information tailored to the individual | Prior to discharge in eight trials. Between 1 and 24 months post discharge in the remaining nine | Between one and eight contact sessions, lasting between 30 minutes and 2 hours each. Intervention length varied from a one-off to 6 months. In some studies there was no contact |
Seven reviews explored interventions based on therapy rehabilitation,71–77 though the focus of the interventions varied. Two reviews looked at interventions designed specifically for people with cognitive impairment. 72,75 The remaining reviews explored therapy rehabilitation generally,71,74 or occupational therapy (OT) specifically. 73,76,77 Components relevant to our definition of self-management support in the therapy-based reviews included problem-solving; remediation training; goal-setting; information provision; support with adaptive equipment; liaison with other services; and training in activities of daily living (ADL). The majority of interventions were home based and delivered to individuals on a face-to-face basis, though other models included delivery in an outpatient rehabilitation centre, or group setting. Delivery of the therapy rehabilitation was initiated soon after the acute stroke event in five reviews,72–74,76,77 and later in stroke recovery (6 months to more than 1 year) in two reviews. 71,75 Outcomes were measured between 1 week and 12 months after the end of the intervention period.
The remaining six reviews looked at various self-management support interventions. Ellis et al. 78 explored referral to stroke liaison workers who provided multifaceted services including social support, liaison with other services, education and information provision. Smith et al. 82 focused on the effects of active and passive information provision, Korpershoek et al. 80 examined self-efficacy enhancement, and Lui et al. 70 explored interventions targeting caregiver problem-solving. Ko et al. 79 reviewed interventions providing patient-held records and Rae-Grant et al. 81 explicitly examined self-management programmes.
Quality and relevance assessment
The R-AMSTAR scores ranged from 24 to 42 out of a possible total of 44. Ten of the reviews are classified as higher quality (score of ≥ 31), whereas the remaining three reviews are classified as lower quality (score of ≤ 30) (Table 18).
| R-AMSTAR criteria | Therapy rehabilitation | Other self-management support | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aziz 200871 | Hoffman 201072 | Legg 200673 | OST 200374 | Poulin 201275 | Steultjens 200376 | Walker 200477 | Ellis 201078 | Ko 201079 | Korpershoek 201180 | Lui 200570 | Rae-Grant 201181 | Smith 200882 | |
| Was an a priori design provided? | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 2 | 3 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 4 | 4 | 1 | 3 | 4 | 3 | 1 | 3 | 3 | 4 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 3 | 2 | 3 | 3 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 4 | 4 | 4 | 4 | 3 | 3 | 4 | 4 | 2 | 2 | 2 | 2 | 4 |
| Was a list of studies (included and excluded) provided? | 3 | 4 | 4 | 4 | 4 | 4 | 1 | 4 | 2 | 1 | 1 | 1 | 4 |
| Were the characteristics of the included studies provided? | 4 | 4 | 4 | 4 | 3 | 1 | 4 | 3 | 3 | 2 | 4 | 2 | 4 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 4 | 4 | 3 | 3 | 4 | 3 | 4 | 2 | 1 | 3 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 1 | 4 | 3 | 4 | 4 | 2 | 3 | 4 | 3 | 4 | 4 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 3 | 3 | 3 | 3 | 3 | 4 | 3 | 4 | 4 | 1 | 1 | 1 | 3 |
| Was the likelihood of publication bias assessed? | 3 | 1 | 4 | 4 | 1 | 1 | 4 | 1 | 1 | 1 | 2 | 1 | 3 |
| Was the conflict of interest stated? | 3 | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 3 | 3 | 1 | 3 | 2 |
| Total score/44 | 40 | 35 | 42 | 41 | 32 | 32 | 35 | 35 | 31 | 24 | 24 | 27 | 40 |
Table 19 details the results of the R-AMSTAR quality assessment as well as the judgements made on the relevance of the individual RCTs included within the reviews. The majority of RCTs were deemed to be self-management interventions and so the review findings were judged to be highly relevant to the aim of our meta-review.
| Study | Primary study designs identified to answer relevant review question (only RCT data are included in this meta-review) | Total number of RCTs extracted | Number of extracted RCTs judged to include self-management support | R-AMSTAR total score/44 |
|---|---|---|---|---|
| Therapy rehabilitation | ||||
| Aziz 200871 | RCTs | 5 | 5 | 40 |
| Hoffman 201072 | RCTs | 1 | 0 | 35 |
| Legg 200673 | RCTs | 9 | 8 | 42 |
| OST 200374 | RCTs | 14 | 11 | 41 |
| Poulin 201275 | Controlled and uncontrolled designs | 3 | 1 | 32 |
| Steultjens 200376 | Controlled and uncontrolled designs | 18 | 6 | 32 |
| Walker 200477 | RCTs | 8 | 8 | 35 |
| Other self-management support | ||||
| Ellis 201078 | RCTs | 16 | 16 | 35 |
| Ko 201079 | None identified | 0 | 0 | 31 |
| Korpershoek 201180 | RCTs | 4 | 2 | 24 |
| Lui 200570 | Quantitative and qualitative designs | 6 | 6 | 24 |
| Rae-Grant 201181 | None identified | 0 | 0 | 27 |
| Smith 200882 | RCTs | 17 | 9 | 40 |
Relevance of the interventions reported in the RCTs included in the reviews was assessed on the basis of the detail provided in the review report. The quality of reporting details about the interventions varied between the reviews so that some judgement was required.
Outcomes
Table 20 outlines the relevant outcome measures included in our review.
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Primary outcomes | ||
| Primary ADL | Typically limited to functional ability and personal care (e.g. feeding, bathing and dressing measures) | Barthel Index or alternative global dependency scale |
| Extended ADL | Encompasses more complex tasks necessary for community and domestic participation (e.g. shopping, cooking and transportation use) | Frenchay Activities Index, Nottingham Extended ADL scale, Lawton Instrumental ADL scale, other unspecified extended ADL scales |
| Self-efficacy | The confidence that an individual has in their own ability to perform a specific task or behaviour | Recovery efficacy, self-efficacy to perform, self-efficacy scale |
| Community reintegration | The ability of individuals to reintegrate into their society, including participation in leisure or social activities or work, where relevant | Patient Personal Adjustment and Role Skills scale, Nottingham Leisure Questionnaire, London Handicap Scale, activity limitation |
| QoL | QoL or subjective health status | COOP, Nottingham Health Profile, the SIP |
| Secondary outcomes | ||
| Cognitive function | Functioning in cognitive areas including problem-solving, attention, memory, orientation and executive function | CFQ64 cognitive failures in daily life, category test for problem-solving, various (unspecified) measures |
| Mood | Anxiety, depression or general mood | HADS, Beck Depression Inventory, GHQ |
| Service use | Use of health-care services | Hospital admissions, service contacts or health professional contacts, cost to health and social services |
| Compliance | Modification of health behaviours, risk reduction and performance of required tasks | Miller’s Health Behaviour scale |
| Poor outcome(s) or death | Deterioration in ADL, a label of dependency (above or below a defined cut-off point on an ADL scale), requiring institutional care or death | ADL measures as above, dichotomous institutional care measure, or death |
Findings
Table 21 documents the relevant results for each review as well as our interpretation of these results. The only review that searched specifically for self-management interventions,81 did not identify any RCTs delivered to stroke survivors, suggesting that there is a paucity of evidence exploring the concept of ‘self-management’ within stroke care.
| Review intervention focus | RCTs, n (n relevant) | Total participants, n | R-AMSTAR score | Time of outcome measure | Primary and secondary outcomes | Narrative | Meta-analysis | Significant findings | Interpretation |
|---|---|---|---|---|---|---|---|---|---|
| Therapy rehabilitation | |||||||||
| Aziz 200871 Therapy rehabilitation 1 year post stroke |
5 (5) | 487 | 40 | 3–12 months | 1o ADL | 0 | Difference in poor outcome or death (51% vs. 76%) (95% CI 3% to 48%; p = 0.03) | The only positive finding is based on a single study. Inconclusive evidence whether or not therapy-based rehabilitation intervention 1 year after stroke was able to influence any relevant patient outcome | |
| Extended ADL | 0 | ||||||||
| QoL | 0 | ||||||||
| 2o Mood | 0 | ||||||||
| Poor outcome(s) or death | + | ||||||||
| Hoffman 201072 OT rehabilitation for cognitive impairment |
1 (0) | 33 | 35 | NR | 1o ADL | 0 | No significant findings to report | There is a paucity of RCTs evaluating cognitive rehabilitation in stroke survivors as only one RCT was identified | |
| Legg 200673 OT rehabilitation |
9 (8) | 1258 | 42 | 3–12 months | 1o ADL | ++ | Increased ADL scores (SMD 0.18, 95% CI 0.04 to 0.32; p = 0.01). Increased extended ADL scores (SMD 0.21, 95% CI 0.03 to 0.39; p = 0.02). Reduction in the odds of a poor outcome or death (OR 0.67, 95% CI 0.51 to 0.87; p = 0.003). Reduction in the odds of deterioration or death (OR 0.60, 95% CI 0.39 to 0.91; p = 0.02) | OT rehabilitation has positive outcomes on personal ADL | |
| Extended ADL | + | ||||||||
| QoL | 0 | ||||||||
| 2o Mood | 0 | ||||||||
| Poor outcome(s) or death | + | ||||||||
| OST 200374 Therapy rehabilitation |
14 (11) | 1617 | 41 | 3–12 months | 1o ADL | + | Increased ADL scores (SMD 0.14, 95% CI 0.02 to 0.25; p = 0.02). Increased extended ADL scores (SMD 0.17, 95% CI 0.04 to 0.30; p = 0.01). Reduction in odds of a poor outcome or death (OR 0.72, 95% CI 0.57 to 0.92; p = 0.009) | Both positive outcomes indicate therapy-based rehabilitation to have a positive effect on personal ADL | |
| Extended ADL | ++ | ||||||||
| QoL | 0 | ||||||||
| 2o Mood | 0 | ||||||||
| Service use | 0 | ||||||||
| Poor outcome(s) or death | ++ | ||||||||
| Poulin 201275 Therapy rehabilitation for cognitive impairment |
3 (1) | 109 | 32 | NR | Working memory training: | Working memory training subgroup (chronic): positive effect on cognitive failures in daily living (ES = 0.80; p = 0.005). Strategy training subgroup (chronic): positive effect on extended ADL (p < 0.01). More improvement in problem-solving self-efficacy for face-to-face training vs. intervention delivered via computer-assisted training, or online though video conferencing (F = 6.45; p = 0.003). External compensation subgroup (chronic): positive effect on compliance in activities achieved (z = 2.953, p = 0.003) | All findings are based on a single study so are taken with caution. Strategy training is the only intervention which meets our definition of self-management support. The review offers some support for the effectiveness of strategy training on improving extended ADL. All RCTs involved individuals in the chronic phase of recovery, highlighting need for research into cognitive rehabilitation at early stages | ||
| 2o Cognitive function | ++ | ||||||||
| Strategy training: | |||||||||
| 1o Extended ADL | ++ | ||||||||
| External compensation: | |||||||||
| 2o Compliance | ++ | ||||||||
| Steultjens 200376 OT rehabilitation |
18 (6) | 1825 | 32 | NR | Comprehensive OT: | Comprehensive OT subgroup: small but significant ESs on ADL (SMD 0.31, 95% CI 0.03 to 0.60). Training of skills subgroup: significant effect on ADL in one study (SMD 0.46, 95% CI 0.05 to 0.87) and a significant effect on extended ADL in another study (SMD 2.29, 95% CI 1.26 to 3.32) | Comprehensive OT (only subgroup we define as self-management support) positively affected more outcomes than any other subgroup. Outcomes reported for comprehensive OT are composite of six RCTs. Isolated OT elements were less effective than comprehensive OT; only training of skills found any beneficial effects based on single study so must be taken with caution. No RCTs explored education of family/caregivers by OT. Education provision is an important role of OT, but is unlikely to be done in isolation, this may explain the paucity of RCTs in this area | ||
| 1o ADL | +* | ||||||||
| Extended ADL | 0 | ||||||||
| Community reintegration | 0 | ||||||||
| Cognitive function: | |||||||||
| 1o ADL | 0 | ||||||||
| Training of skills: | |||||||||
| 1o ADL | +* | ||||||||
| Extended ADL | +* | ||||||||
| Cognitive function vs. training of skills: | |||||||||
| 1o ADL | 0 | ||||||||
| Extended ADL | 0 | ||||||||
| 2o Cognitive function | 0 | ||||||||
| Advice and instruction regarding assistive devices: | |||||||||
| 1o QoL | 0 | ||||||||
| Walker 200477 OT rehabilitation |
8 (8) | 1143 | 35 | End of intervention 1.25–6 months. End of trial 4.5–12 months | 1o ADL | +* | Positive effect on ADL (OR 0.71, 95% CI 0.52 to 0.98) at intervention end, and positive effect on extended ADL (WMD 1.30 points, 95% CI 0.47 to 2.13 points) and community reintegration (WMD 1.51 points, 95% CI 0.24 to 2.79 points) at trial end. OT emphasising ADL subgroup: improved extended ADL (WMD 1.61 points, 95% CI 0.72 to 2.49 points). OT emphasising leisure subgroup: improved community reintegration (WMD 1.96 points, 95% CI 0.27 to 3.66 points) | Effect of ADL-based intervention on extended ADL varied by patient age; older patients appeared to benefit more than younger ones (interaction term between age and intervention; p = 0.01). Patients with lower levels of dependency appeared to benefit more in leisure scores (WMD 2.86 points, 95% CI 0.70 to 5.02 points). Duration and intensity of intervention did not appear to mediate effect on primary outcome (data not shown). Review provides support for OT rehab, showing positive effects on extended ADL and leisure scores. Subgroup analysis highlights lack of generalisability between OT interventions targeting ADL or leisure | |
| Extended ADL | +* | ||||||||
| Community reintegration | +* | ||||||||
| 2o Mood | 0 | ||||||||
| Poor outcome(s) or death | 0 | ||||||||
| OT emphasising ADL: | |||||||||
| 1o Extended ADL | +* | ||||||||
| Community reintegration | 0 | ||||||||
| OT emphasising leisure: | |||||||||
| 1o Extended ADL | 0 | ||||||||
| Community reintegration | +* | ||||||||
| Other self-management support | |||||||||
| Ellis 201078 Stroke liaison |
16 (16) | 4759 | 35 | NR | 1o ADL | 0 | Education and information subgroup: positive subgroup result for QoL (SMD –0.24, 95% CI –0.44 to –0.04; p = 0.02) Barthel Index 15–19 (mild to moderate disability): significant reduction in dependence (OR 0.62, 95% CI 0.44 to 0.87; p = 0.006), death or dependence (OR 0.55, 95% CI 0.38 to 0.81; p = 0.002). Significant subgroup heterogeneity found for Barthel Index 15–19 group (χ2 p < 0.05) |
No positive overall effects were demonstrated for stroke liaison. Post-hoc analysis found positive effects for those individuals with mild to moderate disability | |
| Extended ADL | 0 | ||||||||
| Community reintegration | 0 | ||||||||
| QoL | 0 | ||||||||
| 2o Mood | 0 | ||||||||
| Poor outcome(s) or death | 0 | ||||||||
| Education and information emphasis: | |||||||||
| 1o QoL | + | ||||||||
| Barthel Index 15–19: | |||||||||
| 2o Poor outcome(s) or death | ++ | ||||||||
| Ko 201079 Patient-held medical records |
0 (0) | 0 | 31 | Found no RCTs – no outcomes to report | Found no RCTs – no outcomes to report | Found no RCTs – no outcomes to report | No RCTs were identified which studied the use of patient-held medical records in stroke survivors. This highlights an area of potential stroke self-management where more primary research is required | ||
| Korpershoek 201180 Self-efficacy enhancing |
4 (2) | 630 | 24 | 6 and 12 months (chronic disease self-management), NR for others | Task-oriented walking: | Chronic disease Self-management course subgroup: significant positive effect on HRQoL outcomes, including mobility (p < 0.01), self-care (p < 0.001), thinking (p < 0.01) and social roles (p < 0.001). Computer-generated tailored information subgroup: anxiety scores changed significantly in favour of control (95% CI 0.2 to 2.8; p = 0.03) | Results must be taken with caution: each subgroup represents a single study. From descriptions provided by the review authors we can only be confident of chronic disease self-management course meeting our definition of self-management support. We reject information provision intervention as self-management support because it was a relatively passive intervention. The chronic disease self-management course shows positive results on a range of HRQoL outcomes, but results from one RCT must be interpreted with caution | ||
| 1o Self-efficacy | 0 | ||||||||
| Chronic disease self-management course: | |||||||||
| 1o Self-efficacy | 0 | ||||||||
| Community reintegration | 0 | ||||||||
| QoL | ++ | ||||||||
| 2o Mood | 0 | ||||||||
| Psychosocial intervention: | |||||||||
| 1o Self-efficacy | 0 | ||||||||
| Computer-generated tailored information: | |||||||||
| 1o Self-efficacy | 0 | ||||||||
| QoL | 0 | ||||||||
| 2o Mood | – | ||||||||
| Lui 200570 Caregiver problem-solving |
6 (6) | 1676 | 24 | 2 weeks–12 months | 1o ADL | 0 | Better patient adjustment at 12 months after stroke (p < 0.01). Improvement of social outcome in patients with mild disability at 6 months (p = 0.03) | Inconclusive evidence. The reported positive results represent only one study each. There is a paucity of evidence exploring caregiver problem-solving that report outcomes on stroke survivors (only three of six RCTs reported outcomes for stroke survivors) | |
| Self-efficacy | 0 | ||||||||
| Community reintegration | + | ||||||||
| 2o Mood | 0 | ||||||||
| Rae-Grant 201181 Self-management programmes |
0 (0) | 0 | 27 | Found no RCTs – no outcomes to report | Found no RCTs – no outcomes to report | Found no RCTs – no outcomes to report | There is an absence of RCTs explicitly investigating stroke self-management | ||
| Smith 200882 Information provision |
17 (9) | 2831 | 40 | 1 week–1 year | 1o ADL | 0 | Clinically small evidence of benefit of information provision on depression scores (WMD –0.52, 95% CI –0.10 to 0.93; p = 0.01, for continuous data outcomes) Active information vs. passive information: active information significantly more effective than passive for patient depression (p < 0.02 for trials reporting dichotomous or continuous data), and anxiety (p < 0.05 dichotomous data, p < 0.01 continuous data) |
We take active, but not passive, information provision to be self-management support. This review provides evidence that active information has a positive impact on anxiety and depression in stroke survivors | |
| Community reintegration | 0 | ||||||||
| QoL | 0 | ||||||||
| 2o Mood | ++ | ||||||||
| Service use | 0 | ||||||||
| Compliance | 0 | ||||||||
| Poor outcome(s) or death | 0 | ||||||||
Therapy rehabilitation: secondary outcomes
The composite measure of poor outcome (including deterioration in ADL, dependence, institutional care or death) was reported in the three highest-quality reviews, together encompassing interventions delivered in both the early and later stage of stroke recovery, finding significant beneficial effects. 71,73,74 Death itself as an outcome was not reduced.
Summary of effectiveness of therapy rehabilitation in supporting self-management
In summary (Figure 8), there is strong evidence that therapy rehabilitation delivered soon after the index stroke has beneficial effects on basic and extended ADL and the composite outcome of poor outcome(s) or death. There is also some evidence that early rehabilitation benefits reintegration into the community. There is less evidence to support therapy rehabilitation delivered 1 year or more after the Index stroke, but some evidence that these interventions may benefit extended ADL and reduce poor outcome(s) or death. There is no evidence to suggest that therapy rehabilitation, either early or late, has an impact on mood.
FIGURE 8.
Stroke: summary of the quantitative evidence.
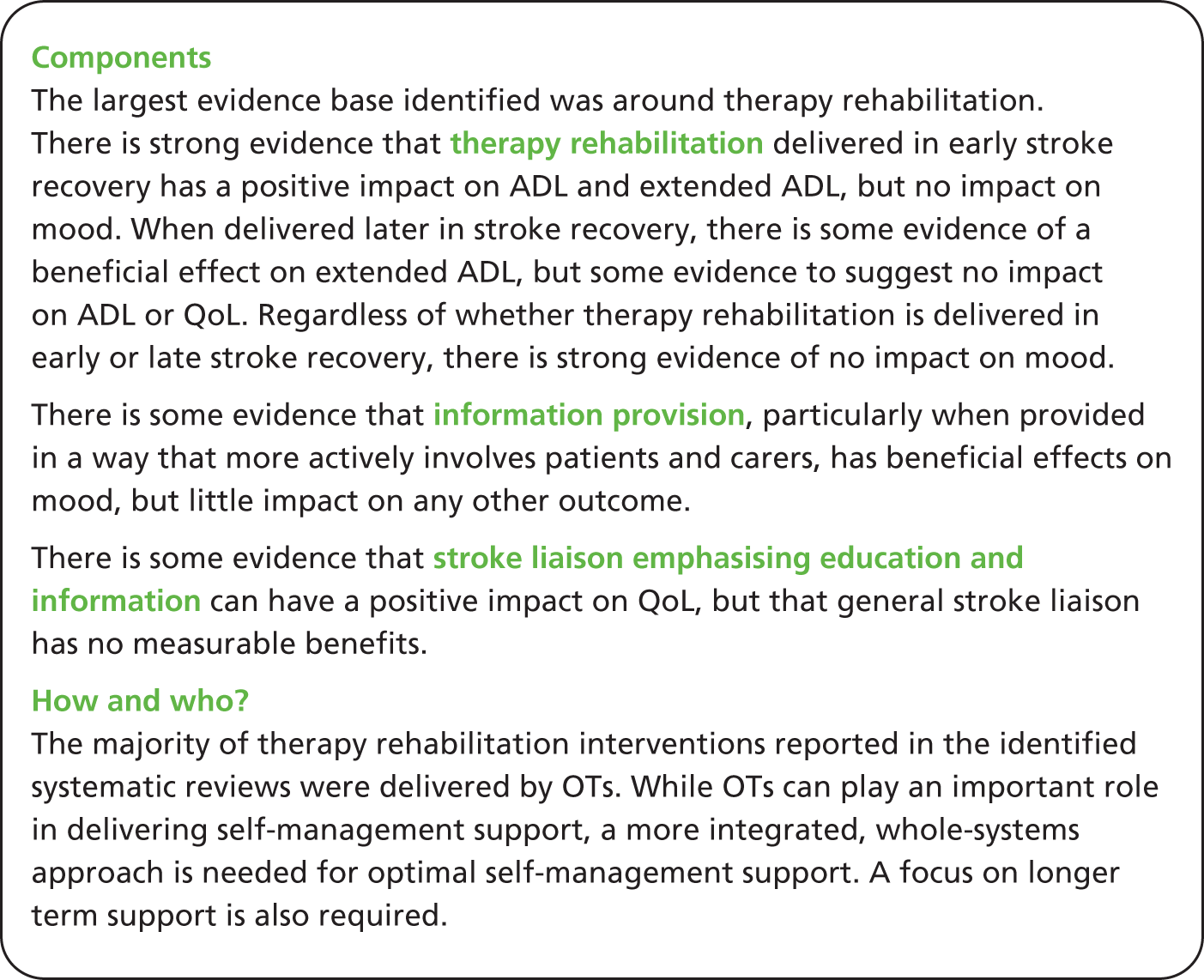
Other self-management support
One beneficial significant outcome effect was suggested by the lower-quality review of interventions to enhance self-efficacy, which found that a chronic disease self-management course had a significant positive effect on QoL. 80
A lower-quality review exploring problem-solving delivered to caregivers identified positive influences on community reintegration. Better patient adjustment and improved social outcomes were found; however, both outcomes were based on only one RCT. 70
A high-quality review of information provision found strong evidence that the intervention had a small beneficial impact on mood. This review also found strong evidence to suggest that active information provision was more effective than passive information interventions in improving mood outcomes. These benefits were, however, of limited clinical significance. 82 The remaining two reviews identified no RCTs of stroke survivors. 79,81
Subgroup results
Subgroups of therapy-based interventions that appeared to have most impact on primary outcomes included comprehensive OT (as opposed to specific skills training) on ADL,76 and face-to-face training groups (as compared with interventions delivered via self-paced computer-assisted training, or online through video conferencing with a therapist) on problem-solving self-efficacy. 75 Interventions targeted at improving ADL (or leisure scores) were associated with significant increases in the outcome of primary focus, but tended not to be associated with benefits in other domains. 77 All the subgroup results reported here are from reviews of a reasonable quality.
Walker et al. ’s77 high-quality review of therapy rehabilitation found the effect of ADL-based interventions to vary by age; older patients appeared to gain more benefit in extended ADL skills than those who were younger.
Effect also appeared to vary by the severity of stroke. The reasonable quality and high relevance review of stroke liaison workers found no intervention effects overall, but a significant reduction in dependence, or the composite of dependence or death, for the subgroup of individuals with a Barthel Index score of 15–19 (mild to moderate disability). 78 Similarly, Walker et al. ’s77 review of therapy rehabilitation suggested that patients with lower levels of dependency gained more improvement in community reintegration scores than those with higher levels of dependency, although findings were not statically significant. 77 In both cases, those with the most severe disability were found to gain least from the support interventions.
Ellis et al. 78 identified a significant effect on QoL for the subgroup of interventions with an emphasis on education and information provision. 78 Walker et al. concluded that the duration and intensity of treatment sessions had little impact on outcomes, but the power of this analysis was reduced due to limited data. 77
The review of stroke liaison workers, although finding no overall benefit in subjective health status, did find a positive subgroup result where the emphasis of the intervention was education and information provision. This suggests that the contrast between education and information provision and the other aspects of the stroke liaison role reflects a real difference in the intervention. 78 Similarly, in information provision a positive health outcome was found for the subgroup of active information, suggesting a real difference between active and passive information interventions. 82
Our results are in agreement with a recent review by Jones and Riazi,83 which concluded that there is evidence that increased self-efficacy has a positive effect on outcomes after stroke including QoL, health status, depression and ADL, but that evidence of effective interventions to support self-management in stroke is sparse. (This review was not formally included in our meta-review because the RCT evidence was not summarised separately in the review.)
Mixed-methods discussion
We discovered the term ‘self-management’ to be poorly recognised and infrequently used in both the quantitative and qualitative literature on stroke. Although self-management (see Chapter 2 for definitions) was not explicitly described in the reviews of therapy-based rehabilitation, it is fundamental to the work of OTs and other allied therapists, and may therefore be implicit in the therapy-based interventions. 84 The commonalities between stroke rehabilitation programmes and self-management support have also been recognised by Jones,85 who noted that the aims of such rehabilitation often involve increasing problem-solving self-efficacy, constructing action plans and making decisions, all prominent elements of self-management support. A stated goal of OT is to promote a sense of self-efficacy:84 this is an acknowledged mediator of self-management. 86
Another self-management skill described by Lorig and Holman is the ability to find and utilise resources. 25 The provision of such information is a prominent feature of stroke liaison interventions,78 and has been identified by stroke survivors and their caregivers as a useful service. 87
In the absence of qualitative syntheses explicitly exploring self-management, recommendations to inform self-management support were extrapolated from reviews examining experiences of stroke and feedback on services. Specialised provision is necessary over the different stages of recovery from suffering an acute stroke, to rehabilitation after a stroke, to being a stroke survivor and looking towards the future. This should address the stroke survivors’ informational, physical, psychological and social needs as a result of both the stroke and the treatment provided.
The main beneficial effects identified in the quantitative meta-review came from the therapy rehabilitation. These interventions principally addressed role management tasks, producing improvements in ADL, extended ADL and reducing poor outcomes (physical dependence). These improvements in basic functional outcomes reflect the needs of stroke survivors in the early phase of adjustment and the majority of RCTs included within the rehabilitation reviews explored the early phase of stroke recovery, with few delivering rehabilitation interventions after the first year of stroke survival. Although the evidence endorses the value of therapists, particularly OTs, in supporting self-management, optimal self-management delivery should be integrated across all HCPs and embedded within care pathways. Cultural and organisational change is required to gain maximal benefit from such initiatives. 36,88
Emotional tasks involve being able to deal with common psychological responses such as post-stroke depression; only one systematic review found a (clinically small) significant benefit on mood. 82 The failure of therapy rehabilitation interventions to impact on mood suggests that current interventions may not be adequate to enable individuals to self-manage their emotional tasks, and future interventions should consider this gap. Our qualitative findings corroborate this, finding evidence which suggests stroke survivors continue to struggle once their physical recovery has plateaued and their rehabilitation therapy is withdrawn. This may be because survivors have not become self-efficacious in their recovery and are uncertain how to approach future challenges that may arise.
Self-management support could focus on building self-efficacy to help stroke survivors feel more empowered. 89 As social modelling is a source of self-efficacy, social support groups could benefit stroke survivors, especially as physical recovery plateaus. Building these social relationships can help reduce concerns around the stigma associated with having a stroke,90 and survivors’ need for impression management. 91–93 We suggest that the early focus mediated by rehabilitation therapists on basic role-related goals could be gradually replaced by interventions which support reintegration into society through the adoption of meaningful social roles. Data from the quantitative meta-review provide less clear evidence as to what format this late phase support should take, though some positive effects on community reintegration and mood have been identified in shorter-term interventions.
Medical tasks were less commonly explored in the included reviews, but such tasks provide the foundation of secondary stroke prevention and modification of risk factors is an important element of self-management. Lawrence et al. 94 found lifestyle interventions such as diet modification and smoking cessation to affect positive behavioural change in stroke survivors; more explicit support to enable individuals to adopt such behaviours should therefore be considered in future self-management support interventions.
Chapter 8 Priority meta-review: self-management support for people with type 2 diabetes mellitus
Meta-review of qualitative systematic reviews
Systematic reviews identified
There were 10,298 unique citations identified by the searches (Figure 9). Following title and abstract scrutiny, 23 full texts were reviewed, including 15 mixed-method reviews and eight qualitative reviews. All the mixed-methods reviews were excluded: one was not a systematic review, and it was not possible to extract the qualitative data separately from the remaining 14. Of the eight qualitative reviews, we excluded three as being unidimensional (n = 1) or exclusively focused on T1DM (n = 2), and five were included in the meta-review. 55,95–98 Of those included, only one explicitly focused on adults with T2DM,96 whereas the others considered adults (although age was not actually specified in all the reviews) with a combination of both T1DM and T2DM. 55,95,97,98 Paterson et al. 98 describes the majority of their participants as educated, married women with insulin-dependent diabetes. Fleming and Gillibrand95 only included studies where the majority were of first- or second-generation South Asian ethnicities.
FIGURE 9.
Type 2 diabetes mellitus: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for qualitative meta-review. 63
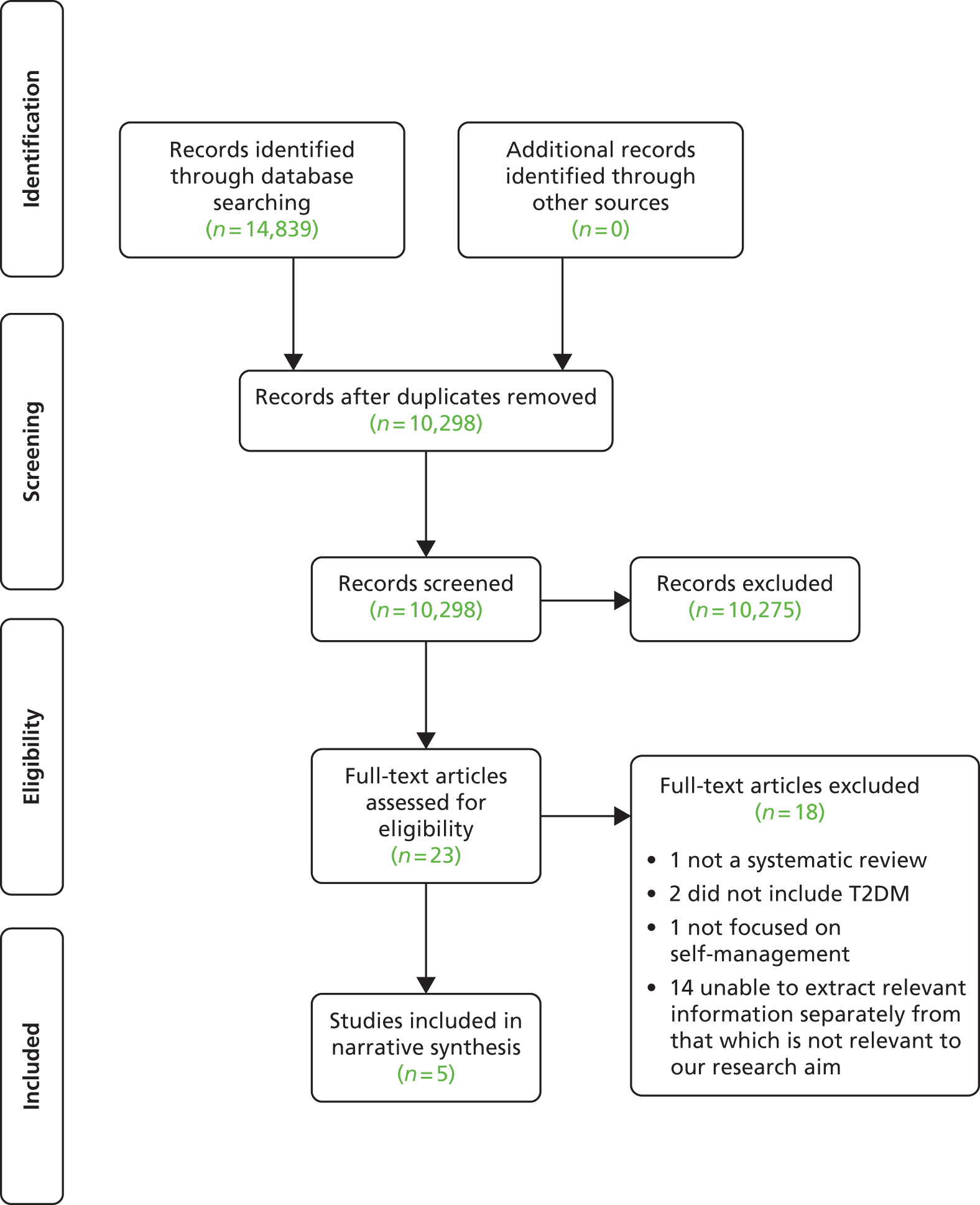
Out of 108 included qualitative studies, only four occurred in more than one systematic review (Table 22). One primary study was included in both Ho et al. 97 and Fleming and Gillibrand,95 and the remaining three were included in both Paterson et al. 98 and Campbell et al. 55 There was, however, some repetition of authors, for example, there were seven primary studies by Lawton et al. , five included in Gomersall et al. ,96 one in Ho et al. ,97 and one in Fleming and Gillibrand95 with no overlap. The lack of overlapping studies between reviews highlights potential issues with their searching or screening methods.
| Study | Paterson 199898 | Campbell 200355 | Fleming 200995 | Ho 201097 | Gomersall 201196 |
|---|---|---|---|---|---|
| Paterson 199898 | 43 | ||||
| Campbell 200355 | 3 | 7 | |||
| Fleming 200995 | 0 | 0 | 11 | ||
| Ho 201097 | 0 | 0 | 1 | 9 | |
| Gomersall 201196 | 0 | 0 | 0 | 0 | 38 |
All reviews detailed their approach to meta-synthesising the data. Fleming and Gillibrand95 used the method of theory explication, Campbell et al. ,55 Paterson et al. 98 and Ho et al. 97 used interpretations of the meta-ethnographic framework proposed by Noblit and Hare,51 and Gomersall et al. 96 drew on the data synthesis method of grounded theory (Strauss and Corbin)24 and the meta-ethnographic approach to theory development (Noblit and Hare). 51 Each review’s aims and key findings are detailed in Table 23.
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary of key findings |
|---|---|---|---|
| Paterson 199898 (Qualitative) |
To advance understanding of the lived experience of diabetes as described in published research and theses. Meta-analysis extends the analysis of individual research studies beyond individual experience to incorporate dominant system beliefs and health system ideologies | 43 | ‘Balance has emerged as the predominant metaphor of the lived experience of diabetes. Individuals learn to balance their diabetes and its management through experience (Nyhlin, 1990a, 1990b, 1991; Paterson & Sloan, 1994).’ Learning to balance involves both the decision to assume control and assuming control: knowing the body, learning how to manage diabetes and fostering supportive, collaborative relationships |
| Campbell 200355 (Qualitative) |
To report on the findings from a synthesis of qualitative research studies on patients’ perspectives of diabetes mellitus using the meta-ethnographic approach | 7 | Six key concepts were identified from all seven papers as being important in enabling a person with diabetes to achieve balance in their life and to attain a sense of well-being and control. These included: time and experience, trust in self, a less subservient approach to care providers, strategic non-compliance with medication, effective support from care providers and an acknowledgement that diabetes is serious. None of the studies included in the synthesis referenced any of the early papers nor did they appear to have taken account of, or built on, previous findings |
| Fleming 200995 (Qualitative) |
To (a) analyse the findings presented in research papers in relation to how South Asian people self-manage diabetes and (b) synthesise the current research data to provide a coherent indication for nursing practice | 11 (reporting 9 studies) | The results comprise four themes: health beliefs, individuality, context and shared experiences. The first three themes are concerned with how people interpret and negotiate culture alongside diabetes self-management at an individual level. The fourth theme highlights the importance of shared experiences across ethnic and cultural groups. This demonstrates how people from different cultures have parallel self-management experiences, and that culture is just one of many factors that individuals incorporate into their self-management processes |
| Ho 201097 (Qualitative) |
To contribute to a deeper understanding of what patients perceive as being important in an effective empowerment strategy for diabetes self-management. How can persons with diabetes be effectively empowered? | 9 | Four central metaphors that influenced empowerment were identified: trust in nurses’ competence and awareness, striving for control, a desire to share experiences, and nurses’ attitudes and ability to personalise. The lines-of-argument synthesis suggested the need for an evaluation system to appraise clients’ diabetes knowledge, health beliefs and negative emotions, as well as the outcome of interventions |
| Gomersall 201196 (Qualitative) |
The aim of this article is the integration and critical interrogation of the contemporary qualitative research on patient perspectives on the self-management of T2DM | 38 | Culturally mediated experiences of T2DM in terms of ethnic/cultural groups and in the context of gender and contrasting circumstances and milieu; perspectives of newly diagnosed patients; development and testing of interventions to improve diabetes control; the ways in which people with diabetes perceived health care professionals and service delivery, ways of facilitating patient autonomy and patients’ diabetes-related goals; the social construction of diabetes management; movement along the illness trajectory: from oral medication to insulin; the impact of being sleepy; the impact of illness trajectory on causation accounts; and perspectives of people with diabetes following a cardiac event. Although the content of the articles, as outlined above, is not synonymous with the conceptual themes developed below, there is some overlap. Four conceptual themes ensued from the analysis of the findings. These are: (a) self-management in context – the self of diabetes management exists in particular cultural milieus which might have both facilitating and constraining aspects for self-management; (b) gender and self-management – the social and historical positioning of women as caregivers for children and husbands impacts on how diabetes management is understood and enacted by the whole family; (c) self under attack – the idea that one must control oneself to be a successful self-manager of diabetes was common but diabetes self-management is influenced by multiple contexts and sociocultural factors outside the control of the individual. A perspective that obscures the relevance of such factors might therefore increase the possibility of patient self-blame and sense of personal failure and, paradoxically, undermine people’s agency in managing their illness; and (d) intervention and regulation of the self – interventions tend to be viewed as a means to achieving regulation of the self |
Quality assessment
Overall, all papers included in this diabetes meta-review scored low levels (< 30) and were all in close range of quality to each other (ranging from 24–28/40) (Table 24).
| R-AMSTAR criteria | Gomersall 201196 | Paterson 199898 | Campbell 200355 | Fleming 200995 | Ho 201097 |
|---|---|---|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 3 | 2 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 1 | 4 | 4 | 2 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 | 3 | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 4 | 2 | 1 | 2 | 2 |
| Was a list of studies (included and excluded) provided? | 3 | 1 | 2 | 2 | 1 |
| Were the characteristics of the included studies provided? | 3 | 2 | 2 | 2 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 1 | 1 | 4 | 2 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 1 | 2 | 1 | 1 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 | 4 | 4 |
| Was the conflict of interest stated? | 3 | 2 | 3 | 1 | 2 |
| Total score/40 | 28 | 25 | 26 | 24 | 26 |
| Quality rating (low = < 30; high = ≥ 30) | Low | Low | Low | Low | Low |
Findings
Overall, the reviews were heterogeneous in nature with some themes more saturated than others (Table 25). From these themes, two central metaphors (adjustment and balance) were identified that encapsulate the impact that being diagnosed and living with diabetes has on a person’s life.
| Central metaphors | Themes | Reference | Illustrative quotation |
|---|---|---|---|
| Adjustment | Sense of self | Gomersall 2011 (p. 865)96 |
|
| Gomersall 2011 (p. 867)96 |
|
||
| Paterson 1998 (p. 60)98 |
|
||
| Responsibility and control | Gomersall 2011 (p. 863)96 |
|
|
| Gomersall 2011 (p. 863)96 |
|
||
| Gomersall 2011 (p. 864)96 |
|
||
| Gomersall 2011 (p. 865)96 |
|
||
| Paterson 1998 (p. 59)98 |
|
||
| Paterson 1998 (p. 58)98 |
|
||
| Paterson 1998 (p. 59)98 |
|
||
| Campbell 2003 (p. 678)55 |
|
||
| Knowledge, beliefs and attitude towards condition | Paterson 1998 (p. 59)98 |
|
|
| Campbell 2003 (p. 679)55 |
|
||
| Campbell 2003 (p. 680)55 |
|
||
| Campbell 2003 (p. 680)55 |
|
||
| Fleming 2009 (p. 149)95 |
|
||
| Fleming 2009 (p. 150)95 |
|
||
| Fleming 2009 (p. 151)95 |
|
||
| Ho 2010 (p. 261)97 |
|
||
| Social/emotional support | Paterson 1998 (p. 60)98 |
|
|
| Paterson 1998 (p. 60)98 |
|
||
| Ho 2010 (p. 262)97 |
|
||
| Psychological support | Campbell 2003 (p. 679)55 |
|
|
| Ho 2010 (p. 261)97 |
|
||
| Ho 2010 (p. 262)97 |
|
||
| Balance | Identity | Gomersall 2011 (p. 863)96 |
|
| Campbell 2003 (p. 678)55 |
|
||
| Fleming 2009 (p. 152)95 |
|
||
| Collaboration of expertise | Gomersall 2011 (p. 865)96 |
|
|
| Campbell 2003 (p. 679)55 |
|
||
| Campbell 2003 (p. 680)55 |
|
||
| Ho 2010 (p. 263)97 |
|
||
| Lifestyle and the body | Gomersall 201196 |
|
|
| Paterson 1998 (pp. 58–59)98 |
|
||
| Paterson 1998 (p. 59)98 |
|
||
| Paterson 1998 (p. 59)98 |
|
||
| Campbell 2003 (p. 694)55 |
|
||
| Campbell 2003 (p. 679)55 |
|
||
| Campbell 2003 (p. 681)55 |
|
||
| Fleming 2009 (p. 150)95 |
|
||
| Using services to support needs | Gomersall 2011 (p. 864)96 |
|
|
| Fleming 2009 (p. 152)95 |
|
||
| Fleming 2009 (p. 153)95 |
|
||
| Ho 2010 (p. 263)97 |
|
Adjustment
This first central metaphor is a result of being diagnosed with diabetes and includes the themes: sense of self; responsibility and control; knowledge; beliefs and attitude towards condition; and psychological support. It is important to note that adjustment does not necessarily happen straight away and can take different amounts of time depending on the individual. It involves the individual adjusting to their new self in comparison to their pre-diabetic self, reassessing their identity and learning (and accepting) the new behaviours that they need to incorporate into their lives. 96,98 Part of this is taking responsibility for their own health, including diet, exercise and information, and overcoming any barriers to that. For example, if a woman always cooks food for her husband and he is diagnosed with diabetes, then the HCP should not only advise him about how to change his diet, but help him think about how this can actually be applied at home. 96 However, this may be less effective if the individual believes that managing diabetes is out of their control, for example if they think that their prescribed medicine is a cure rather than a management tactic, or have a religious belief that they are passive in their relationship to their illness and it is in the hands of God. 96
A key turning point to a person’s adjustment is the decision to take control over their life. 55,96,98 Being in control is not just about medical management, but about the strategic management (and balance) of applying medical advice while still feeling they have a good QoL. 55 The decision to take control was sometimes reported to be a result of negative experiences with HCPs, such as not feeling listened to, being accused of ‘cheating’ if readings were high or they had been experimenting with their diet, or realising that compliance with medical advice does not always prevent diabetes-related complications. 98 This may lead to distrust in HCPs and a lower use of services being provided to support self-management. Therefore, it is important for HCPs to encourage, enable and support people with diabetes to take control. This is not just control of blood sugar, but of the psychological and social aspects, for example supporting people to cope with the emotions and role implications of being diagnosed with diabetes. 55,96,98
An individual’s attitude towards diabetes, such as how serious the condition is and their level of control,55 knowledge and beliefs 55,95,97,98 were reported to influence their self-management. Support for self-management should help to improve the patient’s knowledge about the biological mechanisms and treatments of diabetes, and how to monitor and respond to their bodies. Learning to cope with the new self with diabetes can be emotional, and building a group of ‘allies’, such as family, friends, professionals and other people with diabetes, can help provide social support. 97,98 It is useful to have people with whom to share experiences and tips97 and if ‘allies’ understand the individual, the condition and how best to support self-management. 98 Education may therefore not only be useful for those diagnosed with diabetes, but also for those ‘allies’ involved in their lives. 98 Additionally, psychological distress was a common problem reported by people who had diabetes, as they often felt frustrated about lifestyle changes, unable to control sugar levels, and/or fearful of the future. Gomersall et al. 96 point out that an emphasis on individual responsibility for control of diabetes while failing to recognise the effect of the individual’s personal circumstances and the societal milieu may paradoxically increase a sense of failure and undermine patients’ confidence. Psychological support and skills training, such as problem-solving exercises, should therefore also be implemented to help the individual achieve overall well-being, as opposed to just medical health. 55,97
Balance
Within the reviews, balance was a central metaphor that arose in many forms, including the balancing of identity, collaboration of expertise, lifestyle and the body, and the use of services to support needs. The achievement of balance is largely an outcome of adjustment, and should be the goal that is strived for when supporting self-management while an individual is adjusting to their life after being diagnosed with diabetes. The first is to aim for the balance between the individual’s perceived identity before they were diagnosed with diabetes (e.g. a mother, a Muslim, a healthy person), and the newer part of their identity as someone with diabetes. The attempt to incorporate this new identity into their pre-diabetic identity can cause disruption to their lives, especially when knowledge, beliefs and attitudes contradict each other. 55,95,96 It is therefore important that HCPs discuss this incorporation with the individual.
The balance of collaboration between the HCP and the individual with diabetes is vital to facilitate and support self-management. Reported issues with this communication include lack of empathy from the HCP, differing perceptions on health and well-being between the HCP and the patient, and different goals and focus when managing the condition. 55,97 The meeting between the patient and the HCP should be viewed as a meeting between two collaborating experts, the HCP as an expert in medicine and the overall condition, and the patient as the expert in their own body and how they live with the condition as an individual.
A large part of an individual learning how to manage their diabetes is learning the different bodily cues and how best to react to them. This involves trial and error with different aspects of lifestyle. This is a key part of management that enables the individual to transform from a passive patient relying on HCP advice and prescription, to an active informed self-manager. This can help the individual know when it is all right to take a ‘break’ and relax from the prescribed lifestyle in order to maintain QoL, and how best to correct and maintain fluctuations in blood sugar over time. 55,95,96,98 They understand that this is a LTC that needs to be managed as opposed to cured with medicine. 55 This knowledge of the condition and their body allows them to collaborate as experts with HCPs to discuss the best pathway of care. To enable this collaboration between patient and services, they need to be made easily available and accessible to people with diabetes. 95–97 For example, information and advice should be delivered in lay terms and accessible to those who do not speak English.
Support for self-management
The lines-of-argument synthesis enabled these findings to be integrated to provide a broader picture to inform future commissioning of self-management support.
-
Education, guidance and support should be personalised and in lay terms, taking into account the person’s lifestyle and culture. People with T2DM should be encouraged and educated to take responsibility for their own health (e.g. diet and exercise), and use other sources to build on their understanding and psychological skills (e.g. internet and problem-solving exercises).
-
Education should also be provided for those who directly influence the person’s lifestyle to avoid potential tension between social/familial pressure and to help encourage them to incorporate the recommended changes into their lives.
-
Education should encourage understanding of the condition so that when/if people with T2DM deviate from lifestyle recommendations, it is in a strategic, thoughtful and intelligent way associated with a feeling of confidence, less guilt, acceptance of the diabetes and improved glucose levels. Encourage the person with diabetes to listen to their body and to validate their interpretation of bodily cues to make sure they understand it correctly. Acknowledge that ‘taking a break’ from proactive experimentation or prescribed lifestyle is not a temporary failure, but a choice. Those who are enabled to be experts in their condition are better able to judge the appropriateness of these breaks and how these can be corrected in the long term.
-
Education for HCPs on how to support self-management. The aim of the professional should be to understand how the individual can be supported, not just physiologically, but psychologically and socially as well. They need to be careful how they perceive compliance and respect, and facilitate autonomy while still providing support.
-
Interventions should include elements of social support from families, multidisciplinary HCPs and others with diabetes. It is useful for the person with T2DM to recruit allies in supporting self-management (e.g. family members) who understand the condition and what to do in an emergency, or other people with diabetes who can share experiences and tips (being around other people with T2DM may create a social situation where it is the norm to eat healthy diabetic foods), or professionals who encourage a collaborative relationship where they offer advice and the individual chooses how best to use it based on their knowledge of their body and condition.
-
Delivery of self-management support services should also address shared experiences and problems (e.g. need for services in ‘real-life’ settings with ‘real’ relevance rather than in external medical settings, delaying attending the doctor, misdiagnosis, late diagnosis, a lack of patient-centred care, restricted availability of specialist diabetes services and knowledge of which foods to eat).
-
Coping is an important aspect from the initial stage after diagnosis to living with the condition after adjustment. Maladaptive coping relates to poor glycaemic control and psychological/emotional distress so psychological training to encourage adaptive coping mechanisms would help to support self-management.
-
Being diagnosed with T2DM was often perceived as a threat to identity and sense of self and individuals needed to be supported in their adjustment to this change. This means supporting the initial stage after being diagnosed with diabetes where the individual reaches a ‘turning point’ and an active role in the management of their diabetes. Rather than the turning point being due to distrust of the health professional, this change should be encouraged by the health professional so that the individual with diabetes is empowered to take control of their condition. Patients who realise the seriousness of their condition were more likely to change their ‘daily routines necessary to manage diabetes and to achieve a “new normal” routine’. This can take a long time after diagnosis but support for this is needed from the beginning.
-
Professionals need to have positive and optimistic messages (positive reinforcement) for those with diabetes to encourage them to be proactive about establishing a balance in their lives, not just a control of their blood glucose. The emphasis should be on empowerment and facilitation rather than negatively focused on threat.
Meta-review of quantitative systematic reviews
Systematic reviews identified
We identified 14,841 references for screening, of which 17 were included in this meta-review99–115 (Figure 10). A total of 322 RCTs were included within these 17 systematic reviews. However, only 179 RCTs were unique, with the remaining number accounted for by 78 RCTs appearing in multiple reviews (Table 26). The most frequently included RCT was captured in nine reviews. RCTs were conducted across at least 21 different countries (details were omitted in some reviews): the UK, Spain, the Netherlands, Sweden, Denmark, Italy, Germany, Austria, Finland, Turkey, Croatia, Israel, Australia, New Zealand, Japan, Hong Kong, the Republic of Korea, Thailand, Mexico, the USA and Canada. Year of review publication ranged from 2001 to 2012, and the earliest included RCT dated back to 1981. Of the 17 reviews, nine presented statistical estimates of benefit aggregated over the included studies. The remaining eight only presented results narratively.
FIGURE 10.
Type 2 diabetes mellitus: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for quantitative meta-review. 63 SMBG, self-monitoring of blood glucose.
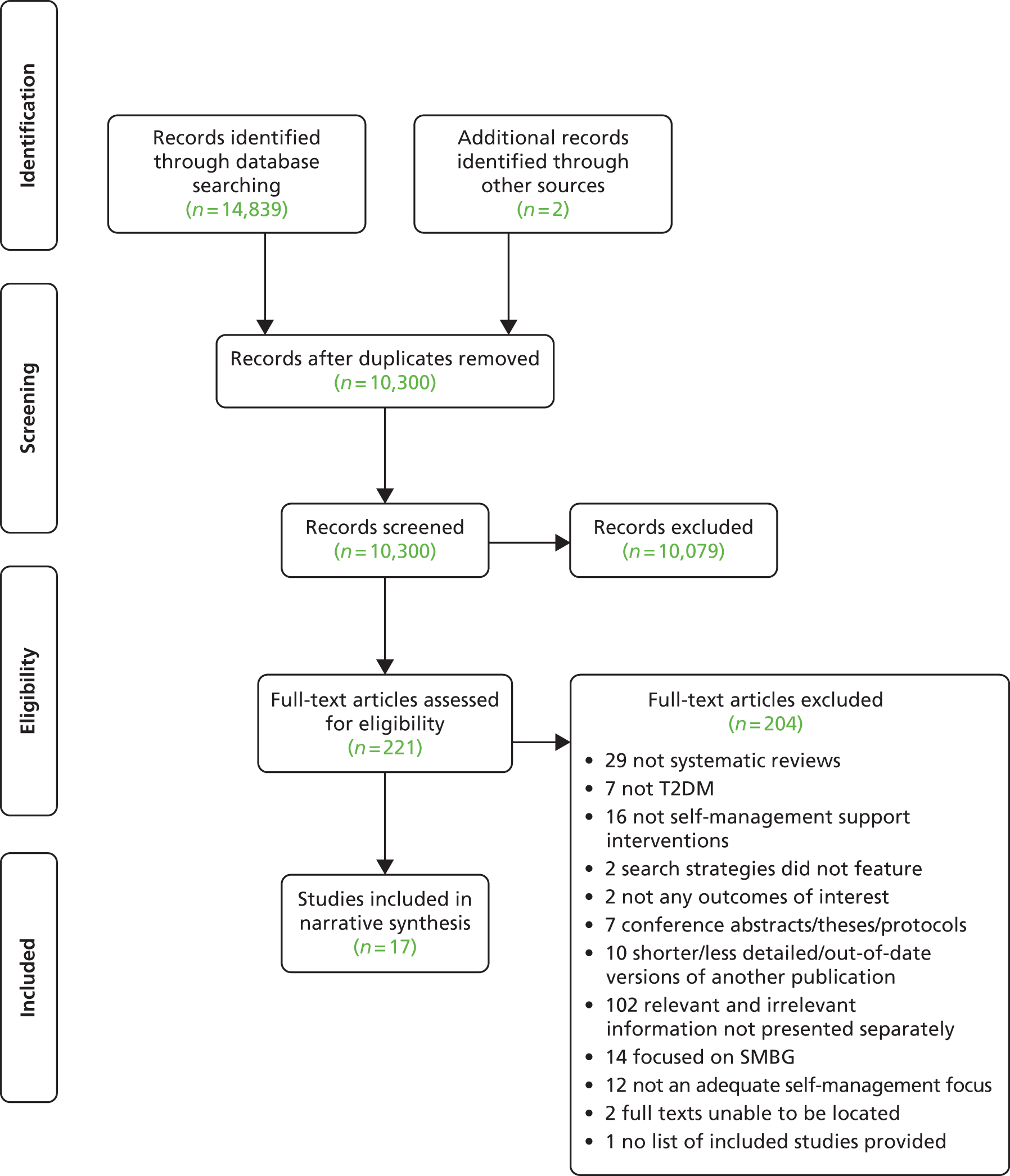
| Study | Chodosh 200599 | Dorrejstein 2010100 | Duke 2009101 | Gary 2003102 | Hawthorne 2008103 | Heinrich 2010104 | Khunti 2008105 | Li 2011106 | Minet 2010107 | Nam 2012108 | Newman 2004109 | Norris 2001110 | Norris 2002111 | Pérez-Escamilla 2008112 | Sigurdardottir 2007113 | Steinsbekk 2012114 | Van Dam 2005115 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chodosh 200599 | 26 | ||||||||||||||||
| Dorresteijn 2010100 | 0 | 11 | |||||||||||||||
| Duke 2009101 | 1 | 0 | 9 | ||||||||||||||
| Gary 2003102 | 4 | 2 | 2 | 18 | |||||||||||||
| Hawthorne 2008103 | 2 | 0 | 2 | 1 | 11 | ||||||||||||
| Heinrich 2010104 | 1 | 0 | 2 | 0 | 2 | 14 | |||||||||||
| Khunti 2008105 | 0 | 0 | 2 | 0 | 4 | 0 | 5 | ||||||||||
| Li 2011106 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | |||||||||
| Minet 2010107 | 2 | 0 | 8 | 1 | 5 | 8 | 0 | 1 | 43 | ||||||||
| Nam 2012108 | 1 | 0 | 2 | 1 | 9 | 2 | 3 | 0 | 4 | 12 | |||||||
| Newman 2004109 | 4 | 0 | 2 | 2 | 3 | 0 | 0 | 0 | 5 | 1 | 21 | ||||||
| Norris 2001110 | 16 | 10 | 4 | 9 | 3 | 0 | 1 | 0 | 6 | 3 | 3 | 72 | |||||
| Norris 2002111 | 8 | 4 | 4 | 7 | 3 | 0 | 1 | 0 | 6 | 3 | 3 | 30 | 31 | ||||
| Pérez-Escamilla 2008112 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | |||
| Sigurdardottir 2007113 | 2 | 0 | 4 | 0 | 1 | 1 | 0 | 0 | 7 | 2 | 5 | 3 | 3 | 0 | 18 | ||
| Steinsbekk 2012114 | 1 | 0 | 0 | 0 | 3 | 4 | 1 | 0 | 7 | 2 | 2 | 3 | 3 | 1 | 4 | 21 | |
| Van Dam 2005115 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 2 | 2 | 1 | 0 | 1 | 1 | 6 |
The types of interventions in the reviews were self-management programmes or multicomponent interventions aimed at self-management; education, both group and individual based; behavioural or counselling strategies; and social support. Duration and intensity of these interventions was highly variable, ranging from a one-off contact session, to intensive interventions involving residential retreats as well as regular meetings over an extended period (Table 27). The content of these interventions was also highly variable, and included a diverse range of components including education on dietary change; meal demonstrations; exercise groups; counselling sessions; workbooks; goal-setting; stress management; monetary incentives; family involvement; and provision of foot care supplies.
| Review | Intervention of interest | Participant demographics | Setting, delivery mode and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Chodosh 200599 | Chronic disease self-management programmes, interventions which aim to improve active participation in either self-monitoring or decision-making or both | NR | NR | NR | NR |
| Duke 2009101 | Individual patient education systematic programmes, delivered face to face that address a wide range of self-management issues | All trials except one recruited both men and women. Mean age 52–65 years. One study focused on education in a migrant population with a low level of literacy | Majority of the interventions carried out by diabetes educators and dieticians. One study trained a link worker (with no previous medical background) to deliver the education | Education typically covered pathophysiology of diabetes, diabetes control through diet and exercise, compliance with medication, glucose self-monitoring, diabetic complications, foot care, services available, motivation and behavioural strategies | Variable: most studies involved 2–4 hours face-to-face time. Two studies < 2 hours contact time and two studies > 5 hours of contact time |
| Gary 2003102 | Clear behavioural or counselling component aimed at improving long-term diabetes self-care behaviour | Mean age of participants = 57 years | Outpatient clinic setting (96%) Delivered by nurse (39%), dietitian (26%), physician (17%), psychologist (9%), exercise physiologist (9%), health educator (4%) |
Only three RCTs included more than one intervention. Focus was diet (70%), exercise (57%), foot care (35%), medication adherence or regimen changing (33%). Other topics included SMBG, pathophysiology and education Most used group and/or individual patient counselling. Some employed telephone outreach, clinician prompting or clinician education, also computer programmes, instruction packets and audiovisual materials |
Duration 1–19 months (median 5 months). Overall median number of visits nine (range 2–52 visits) |
| Heinrich 2010104 | Multicomponent interventions aimed at self-management. Interventions had to target at least two behaviours or had to be focused on diabetes in general | Three studies had specific target populations: African-American adults and Latino/Hispanic adults Three studies only included women |
Most commonly delivered by PhD student/researcher, also patients’ usual health-care providers or other HCPs (e.g. nurses and dieticians) One study took place during usual care; other interventions were additional to usual care |
Four interventions consisted of learning only, seven included learning and planning, and three used learning, planning and practising Focus of interventions varied: a broad range of diabetes-related topics including self-management (six studies); a narrower focus on self-management behaviours (five studies), very specifically targeted lifestyle changes (three studies)Six studies described one-on-one interventions; six evaluated group interventions; two combined both intervention types |
Large variation in intervention intensity. Low intensity: patients only had a pre-intervention visit in addition to usual care, where a computer-based lifestyle assessment took place. High intensity: a 2.5-day retreat followed by 6 months of weekly 4-hour meetings |
| Minet 2010107 | Self-care management interventions using educational or behavioural strategies | Pooled mean age of participants in studies using behavioural psychosocial techniques was 60.7 years, 59.3 years for studies using educational techniques | NR | Studies providing educational interventions: didactic-oriented interventions focusing on knowledge acquisition, skills and information in order to improve diabetes self-management Studies providing behavioural psychosocial interventions: based on cognitive, behavioural or motivational approaches, or receiving psychologically centred counselling involving relaxation, problem-solving, or motivational interviewing |
NR |
| Newman 2004109 | Interventions that aim to increase patients’ involvement and control in their lives with chronic illness | NR | Most interventions led by HCPs | Focused on various behavioural changes including both lifestyle and cognitive components Individual and group settings were used in roughly similar proportions. Almost all programmes were delivered face to face, although the telephone was also used in some |
Duration of interventions varied. Maximum 58 hours |
| Norris 2001110 | Educational interventions, or multicomponent interventions where the effects of the educational component could be examined separately | Studies were heterogeneous with respect to patient population | NR | NR | NR |
| Norris 2002111 | Teaching individuals to manage their diabetes through self-management education | Average age of participants = 55 years (range 35–67 years). Average baseline HbA1c 9.4 (range 6.1–12.9) | Majority set in clinic, also home and senior centre Delivered by nurse 13%; dietitian 13%; physician with team 25%; team (nurse, dietitian, etc.) 20%; lay health-care worker 3%; self (e.g. computer-assisted instruction) 7%; NR 20% |
Majority focus on lifestyle and knowledge. Skills (SMBG and foot care) uncommon Mode of instruction: individual (32%); collaborative (87%); theory based (39%); computer-assisted instruction (6%); interface with primary care (13%) |
Median duration 6 months (range 1–27 months) Median number of contacts six (range 1–36 contacts) Median total contact time 9.2 hours (range 1–28 hours) |
| Sigurdardottir 2007113 | Education that aims to enhance diabetes-related self-care | NR | Delivered by nurses, physicians, team of health-care providers and dieticians | All interventions apart from one used collaborative teaching methods, e.g. goal-setting, problem-solving and cognitive reframing. Content mostly teaching basic diabetes knowledge and self-care skills, e.g. diet and exercising, medication adherence, SMBG and psychosocial aspects. Thirteen studies included teaching emotional aspects. Group education in combination with individual education was most commonly used (13 studies). The most common delivery method was face to face (17 studies) | Twelve interventions used more than 11 hours of intervention. Duration of interventions: 8 weeks–12 months |
| Steinsbekk 2012114 | Group-based diabetes education | 40% male. At baseline the pooled average age = 60 years (SD 9.5), BMI 31.5 kg/m2 (SD 5.6), diabetes duration was 8.1 years (SD 7.0), HbA1c 8.23% (SD 1.80%), 81.9% used insulin and/or oral hypoglycaemic agents | Set in primary care (12 studies), hospital diabetes centres (five studies), NR (four studies). Educators were all HCPs, except in two studies – lay health advisors or community workers Most frequently delivered by physicians in association with other HCP; dietitian and nurse ± community workers and other HCP; or diabetes specialist nurses with other HCP. Less frequently delivered by dieticians, nurses or nutritionists working alone |
Four studies reported that a family member or friend was invited to attend the programme | Duration varied, least intensive = 3 hours/year for 2 years. In 10 trials programmes ranged 6–20 hours of group-based education over a period of 4 weeks–10 months Most intensive programme was 96 hours over 6 months |
| Van Dam 2005115 | Social support interventions which may be emotional support, appraisal support, informational support or tangible assistance | The mean age of participants was 59.3 years (range 52.4–68 years) | Delivered by physician, peer counsellor, personal coach | Support from peer patients in group visits to a physician, peer group support with telephone calls from peer counsellor, organised internet peer group with personal coach support, support from spouse by participation in diabetes education, peer support group following diabetes education, and support from family and friends in diabetes education | Delivered weekly or monthly, duration ranged from five sessions to a 2-year intervention period |
| Focused on a specific target group | |||||
| Medically specific | |||||
| Dorresteijn 2010100 | Educational programmes that aim to promote foot self-care and to prevent the occurrence of foot lesions | In three RCTs participants were at high risk of foot ulceration, in four RCTs participants were at low or medium risk of foot ulceration, and risk was undetermined in the remaining four. All patients were diagnosed as having T1DM or T2DM | Mixed settings: community-based care; primary care; secondary care; and ED | Patient education programme on diabetes including a component of foot care education (three studies); education tailored to patients’ individual needs only directed at improving foot care (two studies); intensive foot care education programme (six studies) Mode of instruction included one-to-one education, group sessions, hand-outs, reminder telephone calls, lectures and viewing a videotape |
Variable: from a single 15-minute session to 14 hours of group education |
| Li 2011106 | Educational programmes (or programmes which include education) used for people with DKD | Average age of participants 63.0 ± 13.5 years and 60.9 ± 11.7 years, intervention and control groups respectively. More men than women were included overall. All patients were diagnosed as having T1DM or T2DM. Duration of diabetes in intervention and control groups = 20.5 ± 13.0 years and 22.0 ± 11.7 years respectively. All patients in stage V of CKD. All patients on dialysis therapy > 30 months | Set in dialysis units, haemodialysis unit or PD clinic (one study); inner city hospital outpatient clinics (one study) Delivered by diabetes specialist nurses and dieticians (one study); diabetes care manager (one study) |
Self-management and self-monitoring common to both, motivational coaching included in one study while general discussion about living with diabetes featured in the other Mode of instruction was group-based programme (one study); NR (one study) |
12 months duration with self-management education three times a week for patients in haemodialysis units, monthly for patients in PD clinic. Motivational coaching every 1–2 weeks for haemodialysis participants, monthly for PD participants. Weekly sessions lasting 2.5 hours for 5 weeks plus one booster session of 2.5 hours held 3 months after intervention end (one study) |
| Culturally specific | |||||
| Hawthorne 2008103 | Education tailored to the cultural or religious beliefs and linguistic skills of the community being approached | Four studies looked specifically at African Americans in the USA, two explored Hispanic Americans in the USA, three looked at South Asians in the UK, one study was based on Surinam Asians in the Netherlands and one study was based on Portuguese Canadians | Various combinations of HCPs; most commonly dieticians, diabetes nurses or link workers. Also podiatrists, psychologists, exercise physiologists. One study used a non-professional link worker as the main health educator. If communication other than in English was needed, educators, the link workers or both spoke the relevant languages fluently | Variable content: group education sessions, group discussion sessions, support group work, flashcards, dietary booklets, home visits and individual counselling Focus was weight reduction, increasing PA, diabetes knowledge, attitudes and self-management, healthy living, diabetes-related knowledge Group-based interventions, one-to-one interventions, and a combination of both were used. Education generally combined both interactive patient-centred methods with semistructured didactic formats |
Duration: from one session to 12 months. Many of the studies used a prolonged, repeated intervention lasting between 6 and 12 weeks |
| Khunti 2008105 | Any educational intervention for migrant South Asian populations | South Asian populations living in western countries were mainly mixed. However, two studies looked only at one population – Surinamese and Pakistani | Delivered by link workers | Tailored clinic sessions including education, enhanced care with education sessions, educational programme, structured education, flashcards, culture-specific care (including educational resources) Four studies describe one-on-one intervention, one study evaluated group interventions |
NR |
| Nam 2012108 | Culturally tailored diabetes education interventions | The mean age of participants was 63.6 years. 68% female participants, four studies included African Americans, three studies included Hispanic Americans, four studies included Asians, and one study included others (e.g. Portuguese Canadians). The mean baseline HbA1c level was 8.6% (SD 1.4%; median 8.5%) | Set in hospital-based outpatient department or hospital diabetes education centres (58%) and community-based settings (42%) Delivered by nurses (36%) and dieticians (36%). Remaining by certified diabetes educators, other professionals (e.g. pharmacists, physiotherapists and non-professional staff) Bilingual/bicultural professional educators or non-professional workers provided the education |
Culturally appropriate teaching about dietary and activity change; delivery of intervention in the preferred language; attendance by family member to elicit home-based support (encouraged in two-thirds of the studies); and use of visual aids to tailor to low-literacy needs Main focus: diabetes knowledge, diabetes self-management (including diet, PA, SMBG). Other topics included psychosocial strategies, risk management of cardiovascular diseases 84% used either group education sessions or a combination of group sessions and individual patient counselling. 16% of studies used only individual sessions |
Ranged from one-off to 12 months (median 3 months), with up to 25 weekly or biweekly sessions. Intervention was provided for ≤ 1 month in three studies; 1–3 months in eight studies; and 12 months in one study. Contact hours: from approximately 1 to > 30 hours, but most studies did not describe contact hours |
| Pérez-Escamilla 2008112 | Peer nutrition education and counselling to Latinos delivered by community | Puerto Rican and Mexican origin living in the USA | Delivered by bilingual/bicultural Puerto Rican CHWs living in the target community and who had previously volunteered in a diabetes clinic (one study). Bilingual clinic employees who received 60 hours of training in diabetes self-management (one study) | CHWs acted as liaison with medical providers, reminded about upcoming appointments, reinforced self-care instructions and nutrition education (one study) Classes and follow-up calls following American Diabetes Association curriculum guidelines. The nutrition component only included a discussion of the food guide pyramid and reading food labels (one study). CHWs attended clinic session with their assigned clients (one study); group classes and follow-up calls (one study) |
Eight weekly 2-hour group classes, for 6 months, frequent follow-up contact telephone contact (one study) |
The identified interventions can be broadly divided into those that were focused on a specific target group, and those that were not. However, this categorisation is not mutually exclusive as 53 of the RCTs included within the culturally specific reviews have also been included in the more general reviews.
Interventions focused on a specific target group
Two reviews explored clinically specific interventions. 100,106 Dorrejstein et al. 100 looked for educational programmes which focused on reducing foot lesions, while the review by Li et al. 106 only included educational programmes for people with diabetic kidney disease (DKD). All participants had a diagnosis of either T1DM or T2DM. In Dorrejstein et al. ,100 participants included those at high, medium, low and undetermined risk of foot ulceration. In Li et al. 106 all participants were in stage V CKD (end-stage kidney failure), and had been on dialysis for more than 30 months. As well as being the only two reviews in this meta-review to look at individuals with both T1DM and T2DM, these reviews are also unique in the setting of their interventions. Dorrejstein et al. 100 examined interventions delivered in a range of settings including secondary care and emergency departments (EDs), while Li et al. 106 included interventions delivered in dialysis clinics.
Four reviews were identified which focused on culturally specific interventions. 103,105,108,112 Two of these looked at a specific ethnic minority: South Asians living in western countries105 and Latinos living in the USA. 112 The remaining two reviews looked more broadly at interventions which were culturally or religiously tailored. 103,108 The RCTs identified in these two reviews overlapped significantly, exploring interventions with African American, Hispanic American, British South Asian, Surinam Asian and Portuguese Canadian populations. These culturally specific interventions were most often delivered by link workers, bilingual/bicultural community health workers (CHWs), or bilingual/bicultural professional or non-professional educators.
Other interventions
The remaining 11 systematic reviews explored interventions targeted at individuals with T2DM. Where stated, most participants were middle aged (mean age 55–60 years). Interventions were delivered by a range of individuals, including dieticians, nurses, diabetes specialist nurses, physicians, psychologists, researchers/students, CHWs, peer counsellors, multidisciplinary teams and remote (e.g. computer assisted). Due to the diverse nature of health-care systems both within and between countries, the exact settings in which interventions were delivered are difficult to ascertain. However, it is clear that no interventions were delivered on an inpatient basis, and that the most commonly used settings were primary care/community care, outpatient clinics and home.
Quality assessment and weighting
The quality of the 17 included reviews ranged from 23111 to 41,105,108 out of a possible total of 44. A total of 11 reviews were assessed as being higher quality (scoring ≥ 31), while six were deemed lower quality (scoring ≤ 30) (Table 28). Total numbers of participants included within the reviews ranged from 207108 to 7677. 109 We classified three reviews as smaller (< 1000 participants per review). A star system of weighting was applied to all included reviews, taking into consideration both quality and size (Table 29). Nine reviews received an overall evidence weighting of three stars, seven were allocated a weighting of two star, and one review was weighted at one star (Table 30).
| R-AMSTAR criteria | Chodosh 200599 | Dorresteijn 2010100 | Duke 2009101 | Gary 2003102 | Hawthorne 2008103 | Heinrich 2010104 | Khunti 2008105 | Li 2011106 | Minet 2010107 | Nam 2012108 | Newman 2004109 | Norris 2001110 | Norris 2002111 | Pérez-Escamilla 2008112 | Sigurdardottir 2007113 | Steinsbekk 2012114 | Van Dam 2005115 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 3 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 3 | 4 | 4 | 1 | 4 | 4 | 4 | 1 | 1 | 1 | 1 | 1 | 1 | 4 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 | 3 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 3 | 4 | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 4 | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 3 | 3 |
| Was a list of studies (included and excluded) provided? | 3 | 4 | 4 | 2 | 4 | 2 | 1 | 4 | 3 | 2 | 1 | 1 | 3 | 4 | 2 | 3 | 1 |
| Were the characteristics of the included studies provided? | 2 | 3 | 4 | 4 | 4 | 3 | 4 | 4 | 2 | 4 | 3 | 2 | 2 | 3 | 2 | 4 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 4 | 4 | 4 | 2 | 1 | 4 | 4 | 4 | 2 | 4 | 3 | 3 | 4 | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 1 | 2 | 4 | 4 | 4 | 1 | 3 | 4 | 3 | 3 | 4 | 3 | 4 | 2 | 4 | 3 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 | 2 | 4 | 1 | 4 | 4 | 4 | 4 | 1 | 4 | 4 | 1 | 1 | 4 | 4 |
| Was the likelihood of publication bias assessed? | 4 | 3 | 1 | 3 | 3 | 1 | 1 | 4 | 4 | 4 | 1 | 1 | 2 | 1 | 1 | 1 | 1 |
| Was the conflict of interest stated? | 3 | 3 | 3 | 2 | 3 | 3 | 2 | 3 | 3 | 3 | 1 | 2 | 2 | 2 | 2 | 3 | 2 |
| Total score/44 | 34 | 39 | 36 | 36 | 41 | 24 | 30 | 41 | 37 | 35 | 23 | 27 | 31 | 25 | 26 | 37 | 31 |
| Weighting the evidence | Higher quality (R-AMSTAR ≥ 31) | Lower quality (R-AMSTAR ≤ 30) |
|---|---|---|
| Larger sample size (≥ 1000 participants) | *** | ** |
| Smaller sample size (< 1000 participants) | ** | * |
| Systematic review | Total population size | Quality score | Weighting |
|---|---|---|---|
| Chodosh 200599 | 2579 | 34 | *** |
| Dorresteijn 2010100 | 3144 | 39 | *** |
| Duke 2009101 | 1359 | 36 | *** |
| Gary 2003102 | 2720 | 36 | *** |
| Hawthorne 2008103 | 1603 | 41 | *** |
| Heinrich 2010104 | 1778 | 24 | ** |
| Khunti 2008105 | 1004 | 30 | ** |
| Li 2011106 | 207 | 41 | ** |
| Minet 2010107 | 7677 | 37 | *** |
| Nam 2012108 | 1495 | 35 | *** |
| Newman 2004109 | 2032 | 23 | ** |
| Norris 2001110 | NR | 27 | * |
| Norris 2002111 | 4263 | 31 | *** |
| Pérez-Escamilla 2008112 | 214 | 25 | * |
| Sigurdardottir 2007113 | 4293 | 26 | ** |
| Steinsbekk 2012114 | 2833 | 37 | *** |
| Van Dam 2005115 | 712 | 31 | ** |
Outcomes
The primary outcomes selected were those we felt it most important for a self-management intervention to impact on (Table 31), namely (1) blood glucose – preference given to HbA1c (a measure of glycated haemoglobin), other measures of HbA1c accepted, with fasting blood glucose as the least favoured outcome; and (2) QoL – general or diabetes mellitus-specific. Secondary outcomes of interest were self-efficacy; psychological well-being; self-management behaviours; biomedical markers; body mass index (BMI) or weight; complications; health-care use; and death (death is obviously the most important outcome for patients but is never the primary outcome of self-management studies or reviews because it is, fortunately, a relatively rare event within the typical duration of follow-up of studies).
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Primary outcomes | ||
| Blood glucose | Biochemical marker of blood glucose control | HbA1c (synonyms HbA1; GHb; total GHb), fasting blood glucose |
| QoL | QoL or subjective health status | General (e.g. SF-36 mental and physical scales); diabetes mellitus-specific (e.g. QoL in diabetes instrument); components of QoL instruments |
| Secondary outcomes | ||
| Self-efficacy | The confidence that an individual has in their own ability to perform a specific task or behaviour | Self-efficacy; specific task self-efficacy; personal control; DES-SF |
| Psychological well-being | Psychological and social functioning, mental health | Anxiety; effective coping; psychosocial functioning; depression scale |
| Self-management behaviours | Measures of self-management behaviour adoption, including behaviours relating to SMBG, PA, diet and foot care | Health behaviour questionnaire; behaviour assessment scores; self-care behaviours; achievement of behavioural goals; eye examination attendance; seeking treatment for smoking cessation; smoking cessation; increased frequency of SMBG; increased accuracy of readings; adherence to wearing socks and shoes; checking feet; washing and drying feet; foot care routine adherence; trimming toenails; general and specific diet; carrying carbohydrate; energy from total sugars; energy from carbohydrate; energy from fat; fruit and vegetable consumption; food intake |
| Biomedical markers | BP and lipids | SBP; DBP; cholesterol; triglycerides; HDL; LDL |
| BMI or weight | BMI or weight | BMI = weight (kg)/height (m); weight (kg) |
| Complications | Shorter- and longer-term complications of T2DM | Foot ulcers; fungal infection; nail dystrophy; retinopathy; cardiovascular disease (includes amputation, intermittent claudication); neuropathy, nephropathy (includes kidney death, initiation of RRT) |
| Health-care use | Use of health-care services | Number and duration of hospital admissions and readmissions; acute hospital admissions; average LOS; visits to the GP; ED visits; medication use |
| Death | Mortality | |
Although frequently reported in systematic reviews, we did not consider outcomes of knowledge to be of interest for this meta-review. This is because there is, at best, only a weak correlation between increased participant knowledge and subsequent behaviour change. 116 We also excluded outcomes of attitudes or beliefs, as these outcomes were reported using a variety of tools, many not validated.
Findings
Results have been classified into two categories: (1) headline statistical results from meta-analyses (Table 32); and (2) other results which include narrative syntheses, subgroup meta-analyses and results from one RCT only (Table 33). The quantitative results are then summarised in Figure 11 in relation to components and delivery.
| Reference and weighting | Outcome | Time | Sample size | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Chodosh 200599*** | Primary outcomes | ||||
| HbA1c | NR | 20 RCTs | +a | –0.36 (–0.52 to –0.21) | |
| Fasting blood glucose | NR | 13 RCTs | +b | –0.28 (–0.47 to –0.08) | |
| Secondary outcomes | |||||
| Weight | NR | 17 RCTs | 0 | –0.04 (–0.16 to 0.07) | |
| Duke 2009101*** | Comparison (1): individual education vs. usual care | ||||
| Primary outcomes | |||||
| HbA1c | < 12 months | Three RCTs; 295 participants | 0 | WMD –0.2% (–0.5% to –0.03%); p = 0.08 | |
| HbA1c | ≥ 12 months | Four RCTs; 632 participants | 0 | WMD –0.1% (–0.3% to 0.1%); p = 0.33 | |
| Secondary outcomes | |||||
| SBP | ≥ 12 months | Three RCTs; 625 participants | 0 | WMD –2 mmHg (–5 to 1 mmHg); p = 0.19 | |
| DBP | ≥ 12 months | Three RCTs; 624 participants | 0 | WMD –2 mmHg (–3 to 0 mmHg); p = 0.05 | |
| Cholesterol | ≥ 12 months | Three RCTs; 627 participants | 0 | WMD –0.03 mmol/l (–0.2 to 0.1 mmol); p = 0.66 | |
| BMI | ≥ 12 months | Two RCTs; 312 participants | 0 | WMD –0.2 kg/m2 (–1.0 to 0.62 kg/m2); p = 0.62 | |
| Comparison (2): individual education vs. group education | |||||
| Primary outcomes | |||||
| HbA1c | < 12 months | Two RCTs; 148 participants | +++ | WMD 0.8% (0.3% to 1.3%); p = 0.0007 | |
| HbA1c | ≥ 12 months | Two RCTs; 112 participants | 0 | WMD 0.03% (–0.02% to 0.10%); p = 0.22 | |
| Secondary outcomes | |||||
| SBP | ≥ 12 months | Two RCTs; 95 participants | 0 | WMD 4 mmHg (–4 to 12 mmHg) | |
| DBP | ≥ 12 months | Two RCTs; 95 participants | 0 | WMD 2 mmHg (–4 to 7 mmHg) | |
| BMI | < 12 months | Two RCTs; 169 participants | 0 | WMD –0.1 kg/m2 (–0.9 to 0.7 kg/m2); p = 0.77 | |
| BMI | ≥ 12 months | Two RCTs; 123 participants | 0 | WMD –0.01 kg/m2 (–0.8 to 0.7 kg/m2); p = 0.98 | |
| Gary 2003102*** | Primary outcomes | ||||
| GHb (total GHb, HbA1, HbA1c) | NR | 18 RCTs | ++ | –0.43 (–0.71 to –0.14); p = 0.003 | |
| Fasting blood glucose | NR | 12 RCTs | 0 | WMD –12.22 mg/dl (–25.1 to 0.67 mg/dl) | |
| Total GHb | NR | Six RCTs | 0 | WMD –0.4% (–0.73% to 0.08%) | |
| HbA1 | NR | Seven RCTs | 0 | WMD –0.77% (–1.88% to 0.34%) | |
| HbA1C | NR | Five RCTs | + | WMD –0.52% (–0.96% to –0.08%); p = 0.02 | |
| Secondary outcomes | |||||
| Weight | NR | Seven RCTs | 0 | WMD –4.64 lb (–9.95 to 0.66 lb) | |
| Minet 2010107*** | Primary outcomes | ||||
| HbA1c | Overall | 43 RCTs; 7677 participants | +b | MD 0.36% (0.207% to 0.509%) | |
| Norris 2002111*** | Primary outcomes | ||||
| GHb | Immediate | 20 RCTs | +b | –0.76% (–0.34% to –1.18%) | |
| GHb | 1–3 months | Nine RCTs | 0 | –0.26% (–0.73% to 0.21%) | |
| GHb | ≥ 4 months | Eight RCTs | +b | –0.26% (–0.48% to –0.05%) | |
| bSigurdardottir 2007113** | Primary outcomes | ||||
| HbA1c | NR | NR | ++ | p = 0.008 | |
| Steinsbekk 2012114*** | Primary outcomes | ||||
| HbA1c | < 12 months | 13 RCTs; 1827 participants | +++ | MD –0.44% (–0.69% to –0.19%); p = 0.0006 | |
| HbA1c | 12 month | 11 RCTs; 1503 participants | +++ | MD –0.46% (–0.74% to –0.18%); p = 0.001 | |
| HbA1c | 2 years | Three RCTs; 397 participants | +++ | MD –0.87% (–1.25% to –0.49%); p < 0.00001 | |
| Fasting blood glucose | < 12 months | Three RCTs; 401 participants | 0 | NR | |
| Fasting blood glucose | ≥ 12 months | Five RCTs | +++ | MD –1.26 mmol/l (–1.69 to –0.83 mmol/l); p < 0.00001 | |
| QoL | < 12 months | Three RCTs; 473 participants | 0 | SMD 0.31 (–0.15 to 0.78); p = 0.19 | |
| Secondary outcomes | |||||
| Self-efficacy | < 12 months | Two RCTs; 326 participants | ++ | SMD 0.28 (0.06 to 0.5); p = 0.01 | |
| Self-management behaviours | < 12 months | Four RCTs; 534 participants | ++ | SMD 0.55 (0.11 to 0.99); p = 0.01 | |
| SBP | < 12 months | Five RCTs; 815 participants | 0 | –0.34 mmHg (–5.19 to 4.51 mmHg) | |
| DBP | < 12 months | Five RCTs; 815 participants | 0 | –0.46 mmHg (–2.31 to 1.39 mmHg) | |
| SBP | ≥ 12 months | Two RCTs | 0 | –3 mmHg (95% CI –7 to 2 mmHg) | |
| DBP | ≥ 12 months | Two RCTs | 0 | 0.17 mmHg (–4.46 to 4.80 mmHg) | |
| Total cholesterol | < 12 months | Seven RCTs; 1161 participants | 0 | –0.06 mmol/l (–0.23 to 0.12 mmol/l) | |
| Triglycerides | < 12 months | Seven RCTs; 1161 participants | 0 | –0.05 mmol/l (–0.19 to 0.08 mmol/l) | |
| Total cholesterol | ≥ 12 months | Four RCTs | 0 | 0.07 mmol/l (–0.09 to 0.20 mmol/l) | |
| Triglycerides | ≥ 12 months | Four RCTs | 0 | 0.03 mmol/l (–0.42 to 0.48 mmol/l) | |
| HDL | < 12 months | Six RCTs; 932 participants | 0 | 0.01 mmol/l (–0.05 to 0.03 mmol/l) | |
| LDL | < 12 months | Six RCTs; 932 participants | 0 | 0.05 mmol/l (–0.2 to 0.1 mmol/l) | |
| Body weight | < 12 months | Three RCTs; 433 participants | 0 | –2.08 kg (–5.55 to 1.39 kg); p = 0.24 | |
| BMI | < 12 months | Seven RCTs; 1159 participants | 0 | 0.21 kg/m2 (–0.86 to 0.43 kg/m2); p = 0.51 | |
| Body weight | ≥ 12 months | Four RCTs; 492 participants | + | MD –1.66 kg (–3.07 to –0.25 kg); p = 0.02 | |
| BMI | ≥ 12 months | Seven RCTs; 1092 participants | 0 | –0.22 kg/m2 (–1.13 to 0.69 kg/m2); p = 0.63 | |
| Mortality | NR | NR | 0 | OR 1.10 (0.37 to 3.29) | |
| Culturally specific | |||||
| Hawthorne 2008103*** | Primary outcomes | ||||
| HbA1c | 3 months | Five RCTs | +b | WMD –0.3% (–0.6% to –0.01%) | |
| HbA1c | 6 months | Six RCTs | +b | WMD –0.6% (–0.9% to –0.4%) | |
| HbA1c | ≥ 12 months | Three RCTs | 0 | WMD –0.1% (–0.4% to 0.2%) | |
| QoL | < 12 months | Three RCTs | 0 | NR | |
| Secondary outcomes | |||||
| Self-efficacy | NR | Three RCTs | 0 | NR | |
| BP | Overall | Four RCTs | 0 | NR | |
| Total cholesterol | < 12 months | NR | 0 | NR | |
| HDL | < 12 months | NR | 0 | NR | |
| LDL | < 12 months | NR | 0 | NR | |
| Total cholesterol | ≥ 12 months | Three RCTs | +b | WMD –0.39 g/dl (–0.64 to –0.14 g/dl) | |
| Triglyceride | < 12 months | Three RCTs | 0 | NR | |
| BMI | Overall | Three RCTs | 0 | NR | |
| Nam 2012108 *** | Primary outcomes | ||||
| HbA1c | Overall | 12 RCTs | +b | –0.29 (–0.46 to –0.13) | |
| HbA1c | 3 months | Eight RCTs | 0 | –0.21 (–0.47 to 0.05) | |
| HbA1c | 6 months | Five RCTs | +b | –0.41 (–0.61 to –0.21) | |
| HbA1c | ≥ 12 months | Two RCTs | 0 | –0.14 (–0.39 to 0.11) | |
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusion (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Chodosh 200599*** | Chronic disease self-management programmes, interventions that aim to improve active participation in either self-monitoring, or decision-making, or both | 26 RCTs; 2579; 1983–2004 | Meta-analysis | Compared with control, a statistically significant reduction in HbA1c (ES –0.36) and blood glucose (ES –0.28) were found. Interventions were not found to impact on weight when compared with control | Chronic disease self-management programmes improved glycaemic control Feedback associated with improvement in HbA1c Possible publication bias |
| Additional | Feedback the only factor associated with a significant improvement in HbA1c. Did not identify any other elements significantly associated with greater efficacy of self-management programmes | ||||
| Duke 2009101*** | Individual patient education systematic programmes, delivered face to face which addressed a wide range of self-management issues | Nine RCTs; 1359; 1996–2007 | Meta-analysis | Individual education interventions had no significant effect on HbA1c, BP, cholesterol or weight compared with usual care Compared with individual education, group education had a greater impact on HbA1c reduction in the short term (WMD 0.8%). No differences in BP or BMI outcomes were found between individual and group education |
Group education more effective than individual education in reducing HbA1c short term. However, for people with higher baseline HbA1c, individual education may be more effective Included studies were generally poor quality with the majority having a high risk of bias |
| Additional | For people with HbA1c > 8%, individual education suggested to be most effective Impact on QoL unclear, small tentative suggestion that group education may produce greater improvements in QoL than individual education |
||||
| Gary 2003102*** | Clear behavioural or counselling component aimed at improving long-term diabetes self-care behaviour | 18 RCTs; 2720; 1984–97 | Meta-analysis | Strong evidence on GHb reduction compared with control (ES –0.43). Also evidence of reduction in HbA1c (WMD –0.52). No effect was found on other measures of glycaemic control or weight | Educational or behavioural interventions improved glycaemic control. Physician-led interventions may cause greater improvements in HbA1c; however, authors suggest this may be due to manipulation of medical regimens Possible publication bias |
| Additional | Physician led interventions may cause larger improvements in HbA1c than those led by nurses or dieticians | ||||
| Heinrich 2010104** | Multicomponent interventions aimed at self-management. Interventions had to target at least two behaviours or had to be focused on self-management or diabetes in general | 14 RCTs; 1778; 2001–9 | Narrative synthesis | Dietary changes appear to be the outcome most responsive to interventions, regardless of intervention form Interventions most successful in increasing PA focused on self-management behaviours and lifestyle changes SMBG frequency appears reactive to interventions regardless of intervention form |
Dietary change and SMBG appear reactive to multicomponent interventions. Suggests interventions aiming to increase PA should focus on self-management behaviours and lifestyle changes |
| Minet 2010107*** | Self-care management interventions using educational or behavioural strategies | 43 RCTs; 7677; 1988–2007 | Meta-analysis | Evidence of benefit in HbA1c reduction compared with control (MD 0.36%) | Self-care management interventions improve glycaemic control. Greater improvements found in those RCTs with shorter follow-up, suggesting reduced impact long term. More compact interventions may also be of greater benefit Three studies had several intervention groups, with each intervention arm compared with the control group and considered as an individual study |
| Additional | Interventions with shorter follow-up found larger improvements in HbA1c Some suggestion that educational techniques are more effective than behavioural or psychosocial techniques for improving HbA1c. In addition, suggestion that interventions of shorter duration are more effective than those lasting more than 9 months |
||||
| Newman 2004109** | Interventions that aim to increase patients’ involvement and control in their lives with chronic illness | 21 RCTs; 2032; 1997–2002 | Narrative synthesis | Majority of interventions reduce HbA1c at some point, evidence suggests that reductions can be sustained after 6 months Little effect on QoL found No difference in psychological well-being between intervention and control, evidence suggests cognitive–behavioural components to be most effective for improving psychological well-being Interventions identified positive changes in self-management behaviours compared with control Few interventions assessed outcomes long term, and in those that did, many found benefits not to be sustained at long-term follow-up. Of those interventions that had long-term effectiveness, design varied, suggesting there is no one correct approach |
Interventions improve glycaemic control and self-management behaviours Little effect on QoL, and no difference in psychological well-being Long-term effectiveness unclear |
| Norris 2001110** | Educational interventions, or multicomponent interventions where the effects of the educational component could be examined separately | 72 RCTs; NR; 1981–99 | Narrative synthesis | Evidence shows improved short-term glycaemic control compared with usual care. Less evidence to support improvements longer term. Group support meetings focusing on coping skills may be beneficial in improving glycaemic control Beneficial effects were found for weight loss, dietary change, and frequency and accuracy of SMBG Benefits for psychological outcomes, QoL, BP, cholesterol and PA were all mixed, as were interventions focusing on foot care Characteristics of interventions demonstrating greater effect: shorter follow-up periods; collaborative; repetitive; ongoing; interactive; individualised. It remains unclear if the use of computers and videos for education is advantageous |
Interventions improve glycaemic control short term. Also benefits for weight loss, and self-management behaviours |
| Norris 2002111*** | Teaching individuals to manage their diabetes through self-management education | 31 RCTs; 4263; 1981–99 | Meta-analysis | Evidence of benefit in GHb after 4 months or more compared with control (ES –0.26%) | Self-management education interventions improve glycaemic control short term No study fulfilled all reviewer quality criteria for bias |
| Additional | On average, 23.6 hours of contact between the educator and patient are needed to achieve a 1% reduction in GHb Duration of contact time between educator and patient was the only significant predictor of effect |
||||
| Sigurdardottir 2007113** | Education which aims to enhance diabetes-related self-care | 18 RCTs; 4293; 2001–5 | Meta-analysis | Strong evidence of reduction in HbA1c compared with control | Educational interventions improve glycaemic control. Greater reduction in those with high baseline HbA1c |
| Additional | There is strong evidence to suggest greater reduction in HbA1c in individuals with baseline HbA1c ≥ 8% compared with individuals with baseline HbA1c < 8% | ||||
| Steinsbekk 2012114*** | Group-based diabetes education | 21 RCTs; 2833; 1988–2007 | Meta-analysis | Very strong evidence of effect on HbA1c short term (SMD –0.44%), at 12 months (SMD –0.4%) and long term (SMD –0.87%). Also strong evidence of reduction in fasting glucose long term (SMD –1.26 mmol/l). Some evidence of benefit on self-efficacy (SMD 0.28) and self-management behaviours (SMD 0.55). Suggestive evidence of benefit on body weight long term (SMD 1.66 kg). No evidence of benefit on QoL, BP, cholesterol or mortality | Group-based education improves glycaemic control short and long term. Some evidence of benefit on self-efficacy, self-management behaviours and body weight Two studies were classified as having a low risk of bias, 12 studies as having moderate risk of bias, and seven studies were classified as having a high risk of bias |
| Additional | Suggests the following factors to be associated with reduced effectiveness: reporting theoretical model; combination of different educator types; baseline HbA1c ≥ 7%; include follow-up; completed education delivery in 12 months; 9–12 hours education; family member or friend invited to participate; fewer than 6 or more than 10 sessions Suggests the following factors to be associated with increased effectiveness: diabetes specialist nurse or dietitian as only educator; conducted in primary care settings; lasting 1–10 months; provide 19–52 hours education; between 14–18 participants per group; between 6 and 10 sessions |
||||
| Van Dam 2005115** | Social support interventions which may be emotional support, appraisal support, informational support or tangible assistance | Six RCTs; 712; 1991–2002 | Narrative synthesis | No beneficial effect of social support on glycaemic control Findings suggest social support to help increase self-management behaviours, lifestyle adjustments and psychosocial functioning Support from spouse may help weight loss in women, but not in men |
Social support does not improve glycaemic control, but may increase self-management behaviours, weight loss and psychosocial well-being |
| Focused on a specific target group | |||||
| Medically specific interventions | |||||
| Dorresteijn 2010100*** | Educational programmes which aim to promote foot self-care and to prevent the occurrence of foot lesions | 11 RCTs; 3114; 1986–2008 | Narrative synthesis | Found foot education interventions not to be associated with increased self-management behaviours. However, small but inconclusive suggestion that intensive educational interventions or foot education tailored to individual needs are associated with increased self-management behaviours | Foot education not found to be effective; interventions should be tailored or intensive to increase likelihood of changing behaviour |
| Li 2011106** | Educational programmes (or programmes which include education) used for people with DKD | Two RCTs; 207; 2002–5 | Narrative synthesis | Suggest that interventions may improve some aspects of QoL Unclear effects on self-efficacy, some suggestion of benefits for specific forms of self-efficacy Some suggestion of improvement in self-management behaviours No effect on mortality found |
Educational programmes for people with DKD may improve some aspects of QoL and self-management behaviours |
| Culturally specific interventions | |||||
| Hawthorne 2008103*** | Education tailored to the cultural or religious beliefs and linguistic skills of the community being approached | 11 RCTs; 1603; 1997–2007 | Meta-analysis | Positive effect of intervention compared with control on HBA1c short term (WMD –0.6%) and total cholesterol long term (WMD –0.39 g/dl). No evidence of benefit on QoL, self-efficacy, BP or BMI | Education tailored to cultural or religious beliefs improves glycaemic control short-term and cholesterol long-term. Better outcomes found when combinations of providers and approaches used Possible publication bias |
| Additional | Health educator type appears to make no difference Better outcomes with combinations of provider and approaches No difference found between one to one and one to one plus group |
||||
| Khunti 2008105** | Any educational intervention for migrant South Asian populations | Five RCTs; 1004; 1997–2006 | Narrative synthesis | Suggestion of benefit for improved glycaemic control in the short term, less evidence of benefit longer term Some suggestion of improved BP outcomes Mixed findings for cholesterol, suggests some benefit Mixed findings for weight/BMI, inconclusive No difference between group and one to one |
Educational interventions for migrant South Asian populations improved glycaemic control in the short term, but not long term. Also some suggestion of improved BP |
| Nam 2012108*** | Culturally tailored diabetes education interventions | 12 RCTs; 1495; 1997–2009 | Meta-analysis | Overall reduction on HbA1c compared with control (ES –0.29). No evidence of benefit long term | Culturally tailored interventions improve glycaemic control short term. Community-based interventions may have larger benefits than hospital or clinic based |
| Additional | Suggestion that community-based interventions may lead to larger benefits than hospital based Suggestion of marginally increased benefit in individual with lower baseline HbA1c |
||||
| Pérez-Escamilla 2008112* | Peer nutrition education and counselling to Latinos delivered by community | Two RCTs; 214; 1997–2007 | Narrative synthesis | Inconclusive mixed effects CHWs associated with greater completion rates |
Peer nutrition education had inconclusive mixed effects |
FIGURE 11.
Type 2 diabetes mellitus: summary of the quantitative evidence.
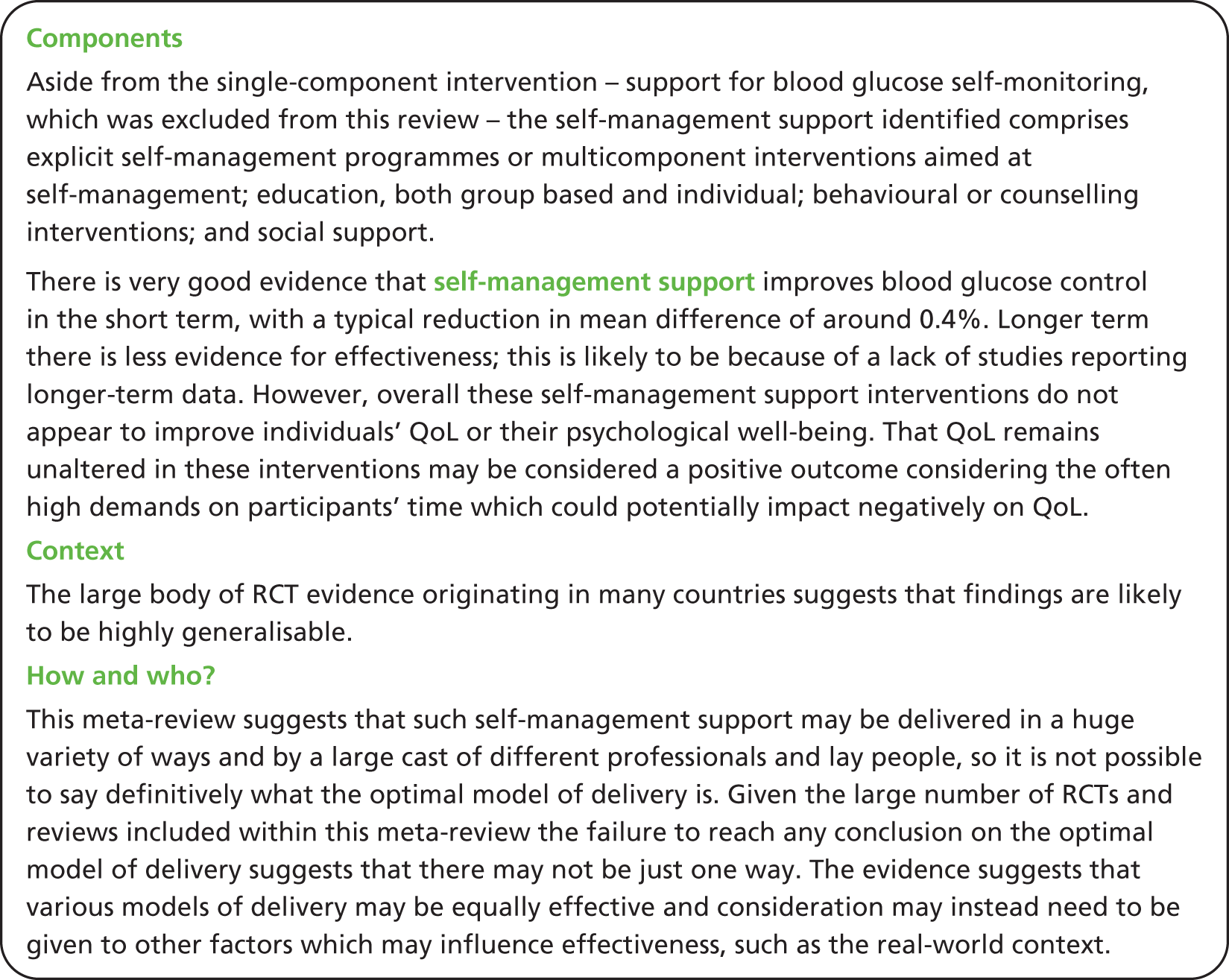
Overall intervention results from all included reviews
Primary outcomes
Meta-analysed data for blood glucose control was presented in eight systematic reviews. All eight presented pooled statistics for blood glucose in the short term (< 12 months after intervention end), but only four of these reviews also presented pooled statistics for long-term effect (≥ 12 months after intervention end). The effectiveness of interventions in improving blood glucose control < 12 months after intervention end is convincing, with all but one review finding a statistically significant result favouring the intervention. However, the evidence for the effectiveness of such interventions in affecting any long-term improvement in blood glucose control is less strong, with only one review finding a statistically significant result favouring the intervention,114 and the remaining three reviews suggesting a tendency to benefit from the intervention which failed to reach significance. 101,103,108 However, the only review to find a significant benefit long term114 pooled data from 11 RCTs, whereas the other three reviews exploring long-term effectiveness included data from between two and four RCTs. Thus, the absence of significant findings may be due to a lack of statistical power (Figures 12 and 13).
FIGURE 12.
Type 2 diabetes mellitus: forest plot of pooled statistics for blood glucose control < 12 months after intervention end.
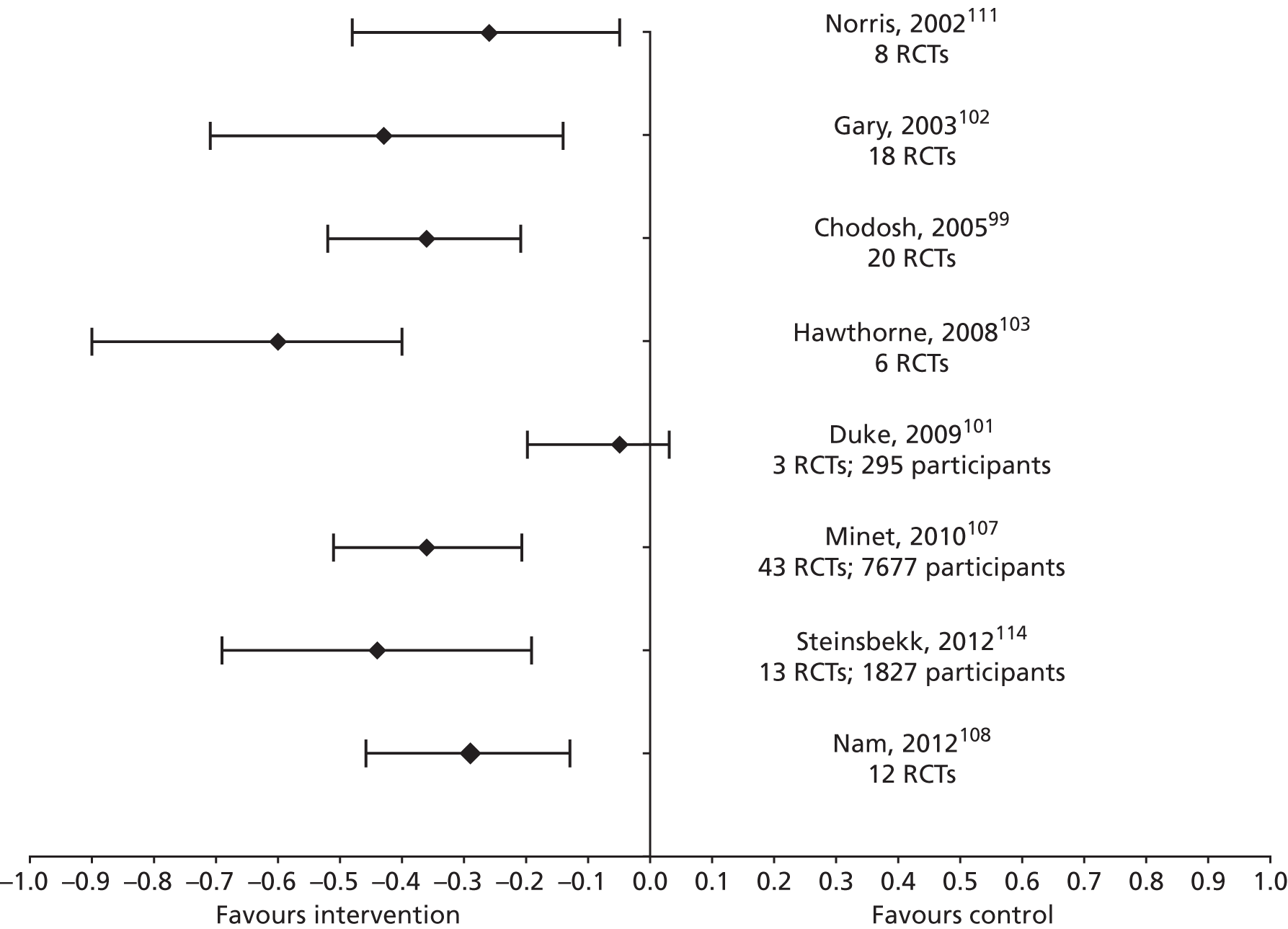
FIGURE 13.
Type 2 diabetes mellitus: forest plot of pooled statistics for blood glucose control ≥ 12 months after intervention end.
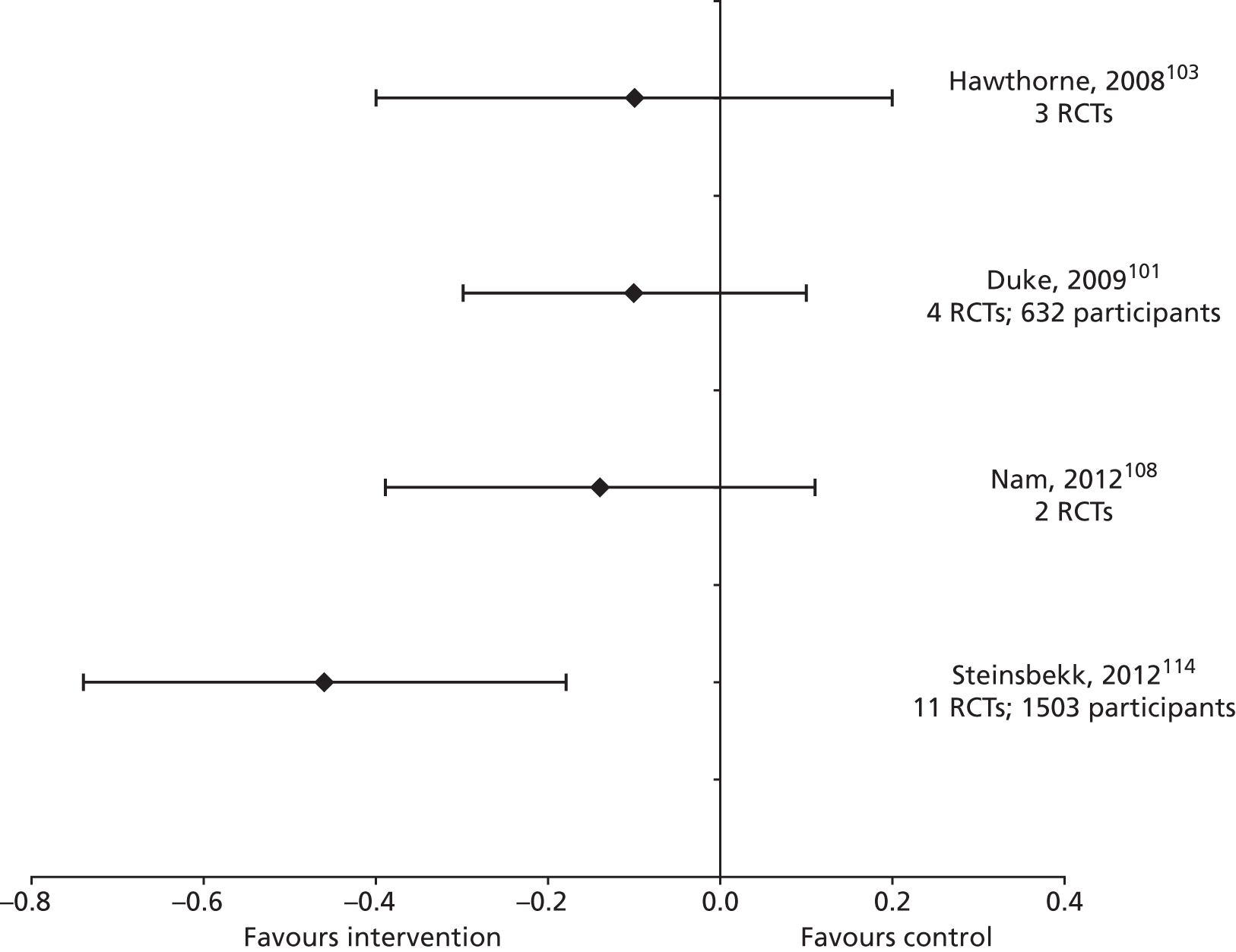
Additionally, five systematic reviews presented narrative findings on blood glucose control. 105,109,110,112,115 These reviews broadly support the finding from meta-analyses regarding shorter- and longer-term effectiveness. Newman et al. 109 reports sustained improvements in HbA1c beyond 6 months in four of the seven studies which report on the outcome. Norris et al. 110,111 found that studies with a follow-up period of < 6 months tended to demonstrate greater effectiveness than those with longer follow-up. This review also notes a paucity of studies with follow-up periods of > 1 year after intervention end, and reports that those RCTs that do have longer-term results show mixed effectiveness on glycaemic control. Khunti et al. 105 also found suggestion of reduced effectiveness over time.
Many reviews aimed to characterise optimal conditions for improving blood glucose control. The only characteristic associated with improved control not contradicted by another review within the meta-review was the provision of feedback. 99 Considering factors found not to affect outcomes, both Chodosh et al. 99 and Minet et al. 107 found no difference in blood glucose control outcomes when comparing a psychosocial approach with a non-psychosocial approach. For all other characteristics, findings either came from one review only, or there were conflicting findings from two reviews. For example, Gary et al. 102 concluded that group-based interventions had larger effect sizes (ESs), while Chodosh et al. 99 reported no difference in outcomes between group and individual delivery.
Two reviews presented meta-analysed data for QoL,103,114 with an additional four reviews presenting purely narrative results on the outcome. 101,106,109,110 No statistically significant effects were found for QoL compared with control in the two meta-analyses performed. From the narrative syntheses, there was a small amount of evidence to suggest some improvements in QoL, or aspects of QoL, in particular from group-based or intensive interventions. 101,106,110,114 However, these findings come from very small numbers of RCTs. As acknowledged by Newman et al. ,109 the absence of a decline in QoL for participants in the interventions could be regarding as a positive finding, as it provides evidence that participating in these often time- or labour-intensive interventions does not impair QoL.
Secondary outcomes
Self-efficacy outcomes were reported in two meta-analyses. 103,114 One review found strong evidence of short-term benefit compared with control,114 whereas the other, culturally specific review, found no evidence of effect. 103 Self-efficacy was also reported in a narrative way in one review, with suggestion of some short-term benefit, but these conclusions were based on only one RCT. 106
No meta-analysed data were reported for the outcome of psychological well-being, but narrative synthesis of the outcome was performed in three reviews. 109,110,115 Overall, there is little evidence to suggest that self-management interventions improve psychological well-being. There is, however, some evidence to recommend interventions which include cognitive–behavioural components as more likely to improve psychological well-being.
Although self-management behaviours were not included in any meta-analysis, they were reported narratively in nine reviews. 100,101,104,106,109,110,112,114,115 The four most commonly reported self-management behaviours were diet, physical activity (PA), self-monitoring of blood glucose (SMBG) and foot care behaviours. Three reviews found strong evidence to support the role of self-management interventions in facilitating dietary change. 104,109,110 There was also evidence to suggest that self-management interventions can have beneficial effects on PA levels, although the evidence for this was less strong than for that of dietary change. 104,109,110 Furthermore, evidence suggests self-management interventions can increase the frequency or accuracy of SMBG,104,109,110,114 with large ESs found in one review,104 and a corresponding improvement in HbA1c levels found in another. 110 Foot-care behaviours were reported in four narrative syntheses, all reporting mixed results. 100,104,106,109 Dorrejstein et al. 100 focused specifically on foot care and found evidence to suggest that tailored and intensive education can produce beneficial behaviour change, whereas basic foot education was not found to produce any improvements in foot-care behaviour.
The biomedical markers reported in the reviews were blood pressure (BP) and cholesterol. Meta-analysis of BP was performed in three reviews. One found some suggestion of beneficial changes long term in diastolic blood pressure (DBP) compared with usual care, although not statistically significant,101 while the other two detected no change. 103,114 Narrative results were mixed. 105,110 The same three reviews to perform meta-analyses on BP outcomes also synthesised cholesterol outcomes, looking at high-density lipoprotein, low-density lipoprotein (LDL) and triglyceride values as well as total cholesterol. Only Hawthorne et al. 103 noted any significant changes, finding total cholesterol to be significantly reduced long term compared with control. This finding must be interpreted cautiously as the more highly powered review by Steinsbekk et al. 114 found no significant changes in any marker of cholesterol, long or short term. However, Khunti et al. ’s narrative synthesis105 does offer some evidence of small suggestive improvements in cholesterol, presenting an overall mixed and inconclusive picture.
Body mass index or weight outcomes were reported in eight of the reviews. Of the meta-analyses, four found no significant effects on either BMI or weight at any time point compared with control. 99,101–103 Steinsbekk et al. 114 found some evidence to suggest interventions reduced weight long term compared with control; however, this was based on a relatively small sample size and no effects were found for the more highly powered outcome of BMI. Three reviews described narrative findings for weight or BMI, with one review finding mixed but overall minimal effects,105 whereas Norris et al. 110 found positive effects on weight loss in 13 studies, with an average weight loss of 2 kg. Norris et al. 110 states interventions with very short follow-up periods to be associated with more positive results, suggesting that any beneficial effects are likely to be short term. The Van Dam et al. 115 review of social support suggests that although spousal support may act positively for weight loss in women, it can have a negative effect on weight loss in men.
Complications of T2DM, mortality and health-care utilisation were infrequently reported in the review. Complications were only explored in three reviews. 100,110,114 Dorrejstein et al. ’s 100 review of foot-care interventions found some evidence to suggest that intensive educational interventions are associated with greater reductions in complications compared with brief educational interventions, and that standard foot education interventions are not associated with reduced complications. Steinsbekk et al. ’s114 review identified just one RCT which explored T2DM complications, finding no changes at 2 years, but strong evidence that diabetic retinopathy was progressed more slowly in the intervention compared with control groups at 4 years. Norris et al. ’s110 review found two RCTs to report cardiovascular disease outcomes, neither finding any significant differences in outcome. Mortality was reported in three reviews, with none finding any overall effect. 106,110,114 One review, Norris et al. ,110 reported on health-care utilisation outcomes, finding a positive outcome in reduced ED visits, which was based on the results of one RCT only. The relative absence of positive outcomes on complications, health-care utilisation and mortality, may be explained by the lack of RCTs measuring longer-term outcomes.
Culturally specific interventions
Of the two reviews of culturally specific interventions which performed meta-analyses, positive effects on HbA1c were found in the short term, but both failed to demonstrate any long-term benefits. 103,108 These findings are also echoed by Khunti et al. ,105 who found some evidence of reduced impact of interventions on HbA1c outcomes in the long term.
Aside from HbA1c, the only other outcome for which benefit was reported at meta-analysis was cholesterol levels after ≥ 12 months. 103 Some suggestion of improved cholesterol levels compared with control was also found in Khunti et al. ’s105 narrative synthesis.
The evidence from these culturally specific reviews suggests that certain intervention characteristics may be associated with greater benefits: more than one type of health education provider;103 multiple approaches adopted within the interventions;103 attending two or more group self-help meetings;105 community based. 108 With regards to participant characteristics which may be associated with greater benefit, results are mixed. One review found a larger ES for those with baseline HbA1c < 8.5%,108 whereas results from a single study contained within the review by Khunti et al. 105 found participants with baseline HbA1c > 9.5% to be the only participants to benefit from the intervention.
Mixed-methods discussion
Both the quantitative and qualitative evidence presented here focus predominantly on the short term. The qualitative synthesis explores the processes which follow a diagnosis of diabetes, from tackling adjustment to achieving a sense of balance. There is a notable omission of issues that may be faced concerning long-term maintenance once balance has been achieved. Likewise, there is a short-term focus within the quantitative data, with few outcomes reported 12 months or more after intervention end.
Our qualitative findings suggest that during the period of adjustment, self-management support should aim to improve individuals’ knowledge and understanding of their diabetes. Evidence from the quantitative meta-review supports this: although it is difficult to identify the individual components of the self-management interventions in the quantitative reviews, education is by far the dominant component and there is strong evidence to suggest that this education has a positive impact on HbA1c values. Qualitative work also advocates the involvement of ‘allies’ in this education. Some of the included quantitative reviews report that a number of RCTs invited family or friends to attend the interventions alongside the individual with diabetes; however, we cannot make specific conclusions on the effectiveness of this tactic due to a lack of data.
A prominent finding from the qualitative reviews was the importance of achieving psychological as well as medical well-being. Psychological support is advocated as a means of achieving this. The evidence obtained from quantitative reviews supports the importance of psychological support to an extent, with evidence suggesting psychological or behavioural strategies can lead to improvements in HbA1c. However, these strategies were often part of wider multifaceted self-management support, and therefore positive effects cannot be directly attributed to any single component. Importantly, the self-management interventions identified do not appear to improve individual’s QoL or their psychological well-being. Any measurable benefits from psychological forms of support appear to manifest as improved diabetic control rather than improved psychological well-being or QoL.
Qualitative evidence also emphasises the importance of tailoring interventions, particularly around information provision. The reviews focusing on culturally specific interventions found strong evidence to suggest a short-term reduction in HbA1c from interventions, supporting the effectiveness of tailored interventions. These interventions go beyond simple language issues to consider cultural issues, such as how best to provide culturally competent dietary change support, how to promote exercise in a culturally acceptable way, and delivery by individuals from the same cultural group.
The included qualitative reviews suggested several reasons why patients with diabetes mellitus might fail to maintain good diabetic control, in particular the importance of the personal circumstances and milieu of the diabetic patient, and the quantitative reviews found little evidence that these educational self-management strategies result in weight loss, increased PA, or better BP control.
Chapter 9 Priority meta-review: self-management support for people with asthma
Meta-review of qualitative systematic reviews
Systematic reviews identified
Following the title and abstract screening, 15 full texts were reviewed (Figure 14). Of those 15, 11 were mixed-methods reviews and four were qualitative reviews. All of the mixed-methods reviews were excluded as one was not classed as a systematic review, one did not include asthma, one was not considered to be about self-management and there were eight where reviewers were unable to extract the qualitative data separately from other irrelevant data. Out of the four qualitative reviews, one was not classed as a systematic review, two did not include asthma, leaving only one included in the meta-review to be analysed. 117 As a single study cannot be synthesised, this report will summarise the included paper and report the findings from the quality assessment.
FIGURE 14.
Asthma: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for qualitative meta-review. 63
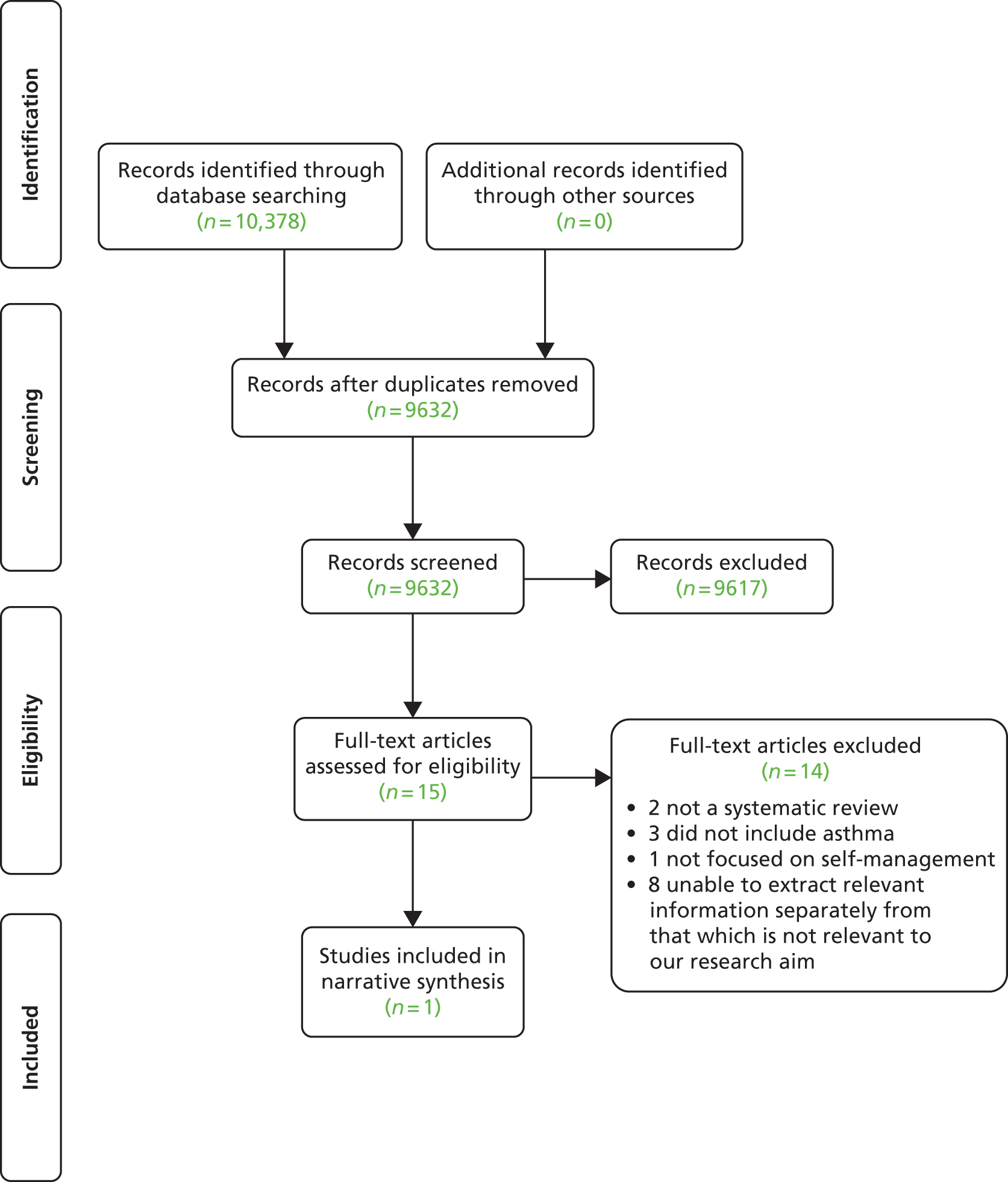
The included paper by Ring et al. 117 was recently published (2011) in Patient Education and Counseling. Ring et al. 117 included 19 primary studies published between 1998 and 2009, and synthesised the findings using a meta-ethnographic approach (see Table 34 for aims and key findings).
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary of key findings |
|---|---|---|---|
| Ring 2011117 (Qualitative) |
To obtain qualitative insight into what helps or hinders action plan implementation from the perspective of health professionals and patients/carers | 19 (in 20 papers) | Seven main influences on action plan implementation were identified, including perceived unhelpfulness and irrelevance of the plans. Translation and synthesis of the original authors’ interpretations suggested that action plan promotion and use was influenced by professionals’ and patients’/carers’ asthma beliefs and attitudes, and patient/carer experiences of managing asthma. Action plan use is hindered because professionals and patients/carers have different explanatory models of asthma, its management and their respective roles in the management process. Patients/carers, based on their experiential knowledge of their condition, perceive themselves as capable, effective in managing their asthma, but health professionals do not always share this view |
Quality assessment
The review scored at high level on quality assessment with a score (35/40) that compared favourably with the reviews in the other qualitative meta-reviews. It provided explicit detail of the review process from searches to analysis, reflected on the different levels of interpretation involved, and discussed findings in relation to the literature and practice (Table 35).
| R-AMSTAR criteria | Ring 2011117 |
|---|---|
| Was an appropriate and detailed design provided? | 4 |
| Was there duplicate study selection and data extraction? | 4 |
| Was a comprehensive literature search performed? | 3 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 2 |
| Was a list of studies (included and excluded) provided? | 3 |
| Were the characteristics of the included studies provided? | 4 |
| Was the scientific quality of the included studies assessed and documented? | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 |
| Was the conflict of interest stated? | 3 |
| Total score/40 | 35 |
| Quality rating (low = < 30; high = ≥ 30) | High |
Findings
The first stage of their analysis found seven themes identified as helping or hindering the promotion and/or use of action plans. Each theme was represented in the majority of studies (bullet points copied as written in review pp. 133–7):117
-
Variable support for, and use of, action plans, for example, professionals saw them as mainly useful for the educated, the motivated or those with good asthma control, and patients saw action plans as a tool for those with serious asthma or as unnecessary because they felt they knew what to do.
-
Asthma decision-making processes ‘were often based on their subjective assessment, yet some had difficulty recognising asthma and/or its symptoms, resulting in uncertainty about when to respond to worsening asthma.’ These were also affected by the next three themes.
-
Asthma management practices were mainly based around treating acute episodes rather than the prevention of future attacks, and managing strategies in order to ‘live with’ the effects of asthma.
-
Asthma perceptions differed between professionals and patients. Professionals perceived asthma as a chronic condition needing long-term prevention, aiming for an asymptomatic life; whereas patients/carers generally regarded asthma as an acute, intermittent condition requiring episodic treatment and were more prepared to tolerate symptoms and a restricted lifestyle while using the inhaler less to appear ‘more normal’. This difference was reflected in goal-setting.
-
Role perception with patients and carers seeing themselves as experts in their condition and, conversely, self-management, and professionals viewing themselves as the experts who could ‘allow patients to take responsibility for their condition’.
-
Use of asthma services was determined by the patients’/carers’ attitudes towards the service; for example, they often went straight to hospital if they felt that an exacerbation could not be dealt with by the GP or if they had had a previous unacceptable experience.
-
Communication was often affected by differences in uses of terminology between patients and professionals. Patients also felt it was important to feel respected by the professional and that their knowledge and experience was recognised.
After providing a descriptive summary and thematic analysis of the studies in the review, the reviewers only included those they considered to be ‘conceptually rich’ in the next stage. These were eight studies that provided an in-depth interpretation of their findings. These underwent a ‘reciprocal translational analysis’, ‘involving concept mapping, identifying clusters of related studies, extracting data and identifying themes’ (p. 133). They reported ‘two separate but over-lapping clusters – (i) beliefs and attitudes; (ii) asthma management’ (p. 137). 117
Beliefs and attitudes:
Translation highlighted differences in how patients/carers and professionals see and understand asthma and their roles in its management. These differences were reflected in the language used, decision-making processes, asthma management goals and behaviours. Patients/carers commonly see themselves as an expert on their asthma, actively managing their condition (including assessing and altering prescribed medication), and making decisions based on their past experience. By comparison, many professionals appear to under-acknowledge the patients’/carers’ asthma expertise and instead focus on compliance with prescribed asthma medication.
p. 137117
Asthma management:
For many patients/carers, ‘learning to manage’ asthma was a dynamic process involving a number of stages over time. Personal competence and confidence in asthma self-management was based on their acquired experience of managing their symptoms in the context of their wider lives/family and experimenting with different asthma management strategies. From the patients’/carers’ perspective, good working relationships with health professionals (with partnership and trust) were vital for encouraging progression through these asthma management stages. Translation also highlighted that some patients/carers can feel – or are perceived by others such as their professionals to be – ‘out of control’, in terms of asthma management, a position often associated with anger towards, or denial of, the condition.
p. 137117
The same eight papers were then combined in a ‘line of argument’ synthesis for the third and final stage of analysis, which centred on the reviewer’s interpretation of what helps or hinders action plan implementation. This section provides two main recommendations for supporting action plan implementation:
Professionals seem to be continuing to work solely within a medical model of asthma care, providing action plans that often do not ‘fit’ with the patients’/carers’ views of asthma or their asthma management strategies. So, when patients/carers are provided with a traditional medically focused action plan, they either perceive it as unhelpful – as it does not reflect their personal asthma model – or they adapt it to suit their understanding of the condition and their management practices. Health professionals then interpret patients’/carers’ adaptation of action plans as evidence these plans are ineffective or unsuitable rather than welcoming the mutual iterative learning process they might offer.
p. 140117
Health professionals need to recognise patients’/carers’ own explanatory models, expertise and knowledge, appreciating that patients’/carers’ management strategies may be quite different from their own. For some patients/carers, a level of asthma symptoms or restricted activity may be acceptable if this means they are able to ‘balance’ the condition within the rest of their lives. Patients/carers and professionals must therefore collaborate to agree asthma goals and develop action plans tailored to the needs of the individual patient at that time. This requires effective communication during consultations with greater partnership working, shared decision-making and patient-centred asthma care.
p. 141117
Support for self-management
Although a lines-of-argument synthesis could not be carried out, a summary of how the findings from this review might inform self-management support is suggested below:
-
Provide personalised guidance and support, not just taking the individual’s medical situation into context, but also their own knowledge as the expert on their own experiences and life. An action plan should be viewed as a joint negotiation with those involved as experts of different aspects working in collaboration. This cannot be done without a shift in the power relationship between the professional and the patient/carer.
-
Education for professionals is needed to help ‘address the “tensions” they may experience “between patient autonomy and professional responsibility” as they encourage patients to self-care’ (p. 141). 117
-
Communication is an important aspect to work on between professionals and patients, ensuring that ideas about asthma, what needs to be managed, how asthma is perceived (long term or acute bouts), terminology and lifestyle priorities (such as taking medicine vs. appearing normal), need to be discussed.
-
Who benefits from an action plan is an important aspect to clarify for both professionals and patients/carers. There are differing views about who should use action plans, with professionals thinking that educated and motivated people with good management skills need them, and patients feeling that only those with serious asthma, and those who do not understand or manage their condition well, need them. This means that professionals may be trying to provide action plans to those who do not feel they need them and not providing them for those who may feel they need them.
-
Action plans may be most useful just after diagnosis of asthma when patients/carers (including school teachers) are learning about what does and does not work for them, and learning about their new condition. An action plan can therefore be used as a supportive educational guidance tool, although this is still being debated.
-
Asthma is a variable condition that has several dynamic stages, and even an experienced asthma patient may have to adapt to and learn new aspects of their condition. An action plan can be a useful tool to support adaptation to change.
-
Asthma plans tend to focus on the medical management of acute exacerbations. However, this means that often important wider issues are not being addressed, such as psychological coping with lifestyle changes and the QoL of a person living with asthma. More holistic action plans could include health promotion, such as increasing PA and smoking cessation.
Meta-review of quantitative systematic reviews
Systematic reviews identified
A total of 9632 unique references were identified for screening, with 18 systematic reviews included in this meta-review (Figure 15). 109,118–134 These reviews included 217 RCTs, of which 157 were unique (Table 36). The RCTs were carried out in at least 16 different countries (details were omitted in some reviews): Sweden, Norway, the UK, Belgium, Finland, the Netherlands, Italy, Switzerland, Denmark, Spain, France, Australia, New Zealand, Canada, the USA and Brazil. Year of review publication ranged from 1995 to 2012, and included RCTs dated from 1979 to 2010. Of the 18 systematic reviews, half presented statistical estimates from aggregated data, and half presented narrative syntheses.
FIGURE 15.
Asthma: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for quantitative meta-review. 63
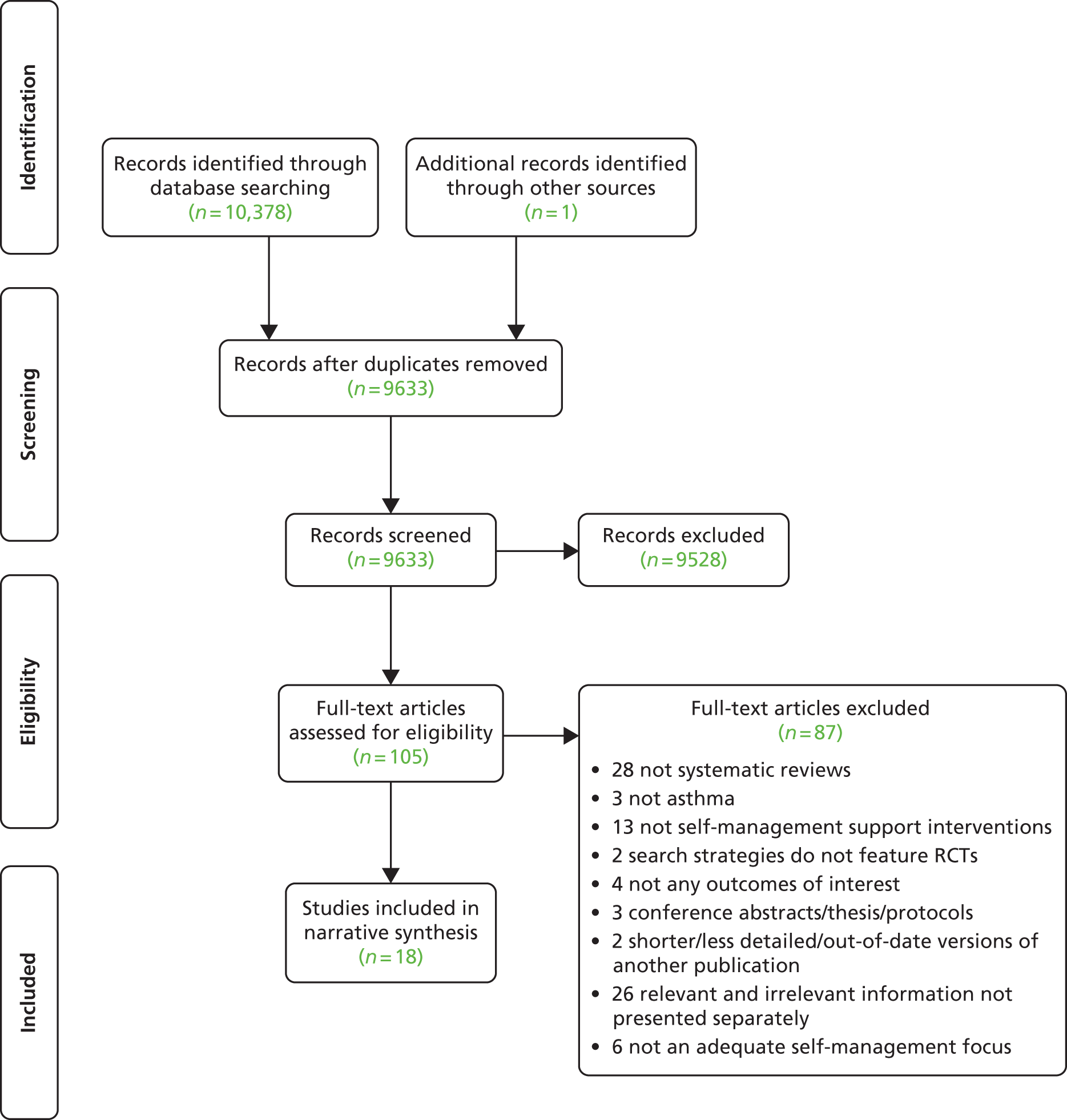
| Study | Bhogal 2006;118 Zemek 2008119 | Bailey 2009120 | Bernard-Bonnin 1995121 | Boyd 2009122 | Bussey-Smith 2007123 | Chang 2010124 | Coffman 2009125 | Gibson 2002,126 2004127 | Moullec 2012128 | Newman 2004109 | Postma 2009129 | Ring 2007131 | Tapp 2007132 | Toelle 2004133 | Welsh 2011134 | Powell 2002130 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bhogal 2006;118 Zemek 2008119 | 3 | |||||||||||||||
| Bailey 2009120 | 0 | 3 | ||||||||||||||
| Bernard-Bonnin 1995121 | 0 | 0 | 5 | |||||||||||||
| Boyd 2009122 | 1 | 0 | 2 | 17 | ||||||||||||
| Bussey-Smith 2007123 | 0 | 0 | 1 | 1 | 2 | |||||||||||
| Chang 2010124 | 0 | 0 | 0 | 0 | 0 | 0 | ||||||||||
| Coffman 2009125 | 0 | 0 | 1 | 1 | 0 | 0 | 2 | |||||||||
| Gibson 2002,126 2004127 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 33 | ||||||||
| Moullec 2012128 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 19 | |||||||
| Newman 2004109 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 8 | 6 | 24 | ||||||
| Postma 2009129 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Ring 2007131 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 3 | 2 | 1 | 0 | 14 | ||||
| Tapp 2007132 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 2 | 2 | 0 | 2 | 11 | |||
| Toelle 2004133 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 2 | 0 | 0 | 0 | 13 | ||
| Welsh 2011134 | 0 | 0 | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 7 | |
| Powell 2002130 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 2 | 4 | 0 | 2 | 0 | 6 | 0 | 21 |
Interventions identified
The types of interventions identified in this review were self-management programmes; written action plans (WAPs); interactive teaching; education; environmental interventions; interventions to increase medication adherence; and interventions to increase promotion of action plan use. A range of settings were explored which included school-based, home-based or a health-care settings. Interventions were delivered to both individuals and groups. Personnel delivering the interventions included asthma nurses, social workers, case managers, CHWs, physicians, physiotherapists and licensed psychologists. The content of these interventions was also varied and included a diverse range of components, including inhaler techniques; access to 24-hour hotlines; education on triggers; emphasising the importance of regular review; referral to services (e.g. smoking cessation); monitoring of symptoms; motivational interviewing; and instruction on the correct usage of medications.
There are various ways in which these 18 systematic reviews could be categorised. We decided on two ways of organising the evidence: (1) by the population they targeted, and (2) considering if they focused on understanding the components of self-management support, the context in which self-management support is delivered, or the mode of self-management support delivery. For the purposes of this meta-review we have divided reviews based on the target population, though our analysis is informed by both classification systems.
Three reviews specifically explore culturally tailored interventions for ethnic minority groups. 120,124,129 Six look at interventions targeted towards asthmatic children or adolescents. 118,119,121,122,125,134 The remaining nine target less specific populations and include children, adolescents, adults, HCPs, and ethnic majorities and minorities. 109,123,126–128,130–133 Four reviews are linked: Zemek et al. 119 provides an update of Bhogal et al. 118 and both reports were included as the earlier publication was deemed to contain useful information not reported in the later update. Additionally, Gibson and Powell127 provide a more focused review based on the data presented in Gibson et al. 126 As the two publications present different analysis and findings, both were included here.
Interventions focused on a specific population group
Three reviews looked at culturally specific interventions. 120,124,129 Bailey et al. 120 looked at broad asthma programmes, whereas Chang et al. 124 explored education specifically, and Postma et al. 129 focused on environmental interventions. All three included interventions undertaken with any ethnic minority, and identified the following groups: Puerto Rican; African American; Hispanic; and Indian subcontinent. In one review, all population groups resided in the USA. 129 Interventions were delivered by asthma educators fluent in participants’ own dialect,120 indigenous health-care workers (IHWs)124 and CHWs who generally lived or worked in the same community as participants. 129 As well as interventions being delivered by culturally or linguistically competent personnel, culturally relevant issues were also addressed within these interventions, and all were home based. These included culturally tailored workbooks which contained illustrations of people of the same ethnicity as participants, reference to famous people of the same ethnicity who have asthma and could serve as role models, reference to stressors common to individuals of the given ethnic group, and addressing misconceptions and myths commonly held by people of the specific ethnic group.
Six systematic reviews explicitly focused on interventions for asthmatic children or adolescents. 118,119,121,122,125,134 The age range of the included populations varied between reviews. Two reviews included infants,121,122 and in three reviews the youngest children were aged 4–6 years). 118,119,125 The remaining review did not explicitly state the age of the youngest participants. 134 The upper age limit was relatively consistent and ranged from 17 years125 to 19 years. 118,119 The focus of these reviews varied, with four looking at education in various formats121,122,125,134 and two118,119 focusing on WAPs. Of the educational interventions, Bernard-Bonnin et al. 121 explored interactive teaching conducted in both one to one or group settings; Coffman et al. 125 studied school-based education; Welsh et al. 134 looked at home-based self-management education programmes; and Boyd et al. 122 explored educational interventions more generally. It should also be noted that in addition to these six reviews, two of the culturally specific reviews are also focused on a paediatric population.
Other interventions
The remaining nine reviews include a diverse range of populations, including children, adolescents, adults, HCP, and ethnic majorities and minorities. 109,123,126–128,130–133 Self-management support, or self-management education, were the explicit focus in three reviews. 109,126,130 WAPs were the focus in two. 127,133 Education was the focus in two. 123,132 The remaining two reviews explored interventions to improve inhaled corticosteroid (ICS) use128 and interventions to promote action plan use. 131 Interventions were delivered in a wide range of settings, including self-administered; group setting; one to one; primary care; tertiary hospitals; and asthma clinics. Delivery personnel included asthma nurses, ED nurses, physiotherapists and non-health-care workers (Table 37).
| Review | Intervention of interest | Participant demographics | Setting, delivery and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Culturally specific interventions | |||||
| Bailey 2009120 | Specifically developed culturally orientated asthma programmes | Both adult and paediatric populations. Minority groups identified: Puerto Rican, African-American, Hispanic, Indian subcontinent | Home visits, hospital, others unspecified. Group sessions or one-to-one sessions Delivered by asthma educators fluent in participants’ own dialect |
Programmes covered education; action plans; identifying triggers; environmental adaptation; emphasis on collaboration between children, parents and HCPs; practical demonstrations; videos | Number of sessions ranged from one session plus reinforcement to eight sessions. Duration of sessions ranged from 40 minutes to 1 hour. Follow-ups occurred at 3, 4, 6 and 12 months post intervention |
| Chang 2010124 | IHWs in asthma education programmes | Children aged 1–17 years. Mean age approximately 7 years. More boys than girls | After the initial consultation, all visits were made to the home Delivered by trained IHWs |
Personalised, child-friendly booklet given during initial consultation. Reinforcement of asthma education by IHW. Culturally appropriate paediatric asthma education materials were used with parents and children | Three visits from health-care worker (1, 3 and 6 months after clinical consultation). Outcomes collected at baseline and at 12 months (last visit) when all children had another clinical consultation and outcome measures recollected |
| Postma 2009129 | Environmental interventions for paediatric asthma delivered by CHWs | Participants aged 5–9 years, were generally of low income, were ethnic minorities (mainly African American and Hispanic), and all lived in the USA. Atopy status reported in five RCTs, 28–75% of participants tested positive to at least one allergen | All interventions were delivered by home visit, two RCTs also included follow-up telephone calls Delivered by CHWs who generally came from, lived, or worked in the same community as participants |
All delivered education on asthma triggers and avoidance techniques. All studies also provided at least one resource, e.g. pillow encasement, rodent traps, vacuum bags. Almost all studies provided individually tailored interventions (incorporating caregiver preferences; responding to individual allergic sensitivity; responding to triggers identified during home assessment). Most studies focused solely on environmental triggers. Additional content included general information about asthma and education around medication use and devices. Participants were also offered referrals to services, e.g. smoking cessation, social service agencies | Intervention generally consisted of between three and nine home visits. Visits on average 60 minutes long. Intervention period ranged from 6 weeks to 1 year. Length of follow-up ranged from 4 months to 2 years, five studies followed participants for 1 year |
| Child or adolescent interventions | |||||
| Bernard-Bonnin 1995121 | Interactive teaching on asthma self-management | Age 1–18 years | One-to-one basis or group settings | Interactive teaching sessions | NR |
| Bhogal 2006118 | WAPs for asthma management | Age 6–19 years. Larger proportion of males recruited (53.2–63.9%). Asthma severity mild–severe | Primary and secondary care | Asthma education provided in every study. Action plans formatted to target both parents and children. Generally contained three steps. Three studies associated the steps with traffic light colours | Monitoring either daily or when symptomatic. Most trials required completion of daily diary. Duration of intervention was 3 months in three studies, 24 months in one study. Telephone follow-up interview after 1 year in one study |
| Zemek 2008119 | WAPs for asthma management | In addition to above, one study of school-aged children with moderate asthma severity | In addition to above, a three-step written plan based on peak flow when symptomatic | In addition to above, one study with a 3-month study duration | |
| Boyd 2009122 | Educational intervention targeted at asthmatic children, their parents or both | Children (0–18 years of age) who had attended the emergency room for asthma within the previous 12 months | Setting (most frequent to least frequent): home; combination of hospital/clinic and home; hospital; outpatient clinic; community education centre; school Delivery (most frequent to least frequent): nurses; trained health educators; social workers; case manager; via computer game |
All interventions involved interactive transfer of information. Components included self-monitoring; medical therapy review; WAPs; education on environmental triggers | Duration of intervention ranged from one 20-minute session at time of discharge, to a programme of visits or reinforcement over 12 months. Follow-up was conducted from 12 weeks to 2 years post intervention |
| Coffman 2009125 | School-based asthma education | Children aged 4–17 years. Where reported, percentage with moderate-to-severe asthma 9–62%. Boys outnumbered girls in most studies. Where reported, majority of participants black or Latino | Mostly group-based interventions. Delivered by a range of personnel including (most frequent to least frequent): nurses; peer counsellors; teachers; interactive computer programme; physicians; and health educators | In almost all, education covered four areas: basic facts about the pathophysiology of asthma; correct usage of medications; techniques for monitoring symptoms; and the importance of avoiding triggers. The majority also incorporated components for parents, school personnel and classmates without asthma | Where reported, number of sessions ranged from 2 to 34 (median 6). Time period ranged from 2 weeks to 1 year (median 6 weeks). Follow-up from immediately after intervention completion to 1 year |
| Welsh 2011134 | Self-management education programmes delivered in the home of an asthmatic child/adolescent | Asthma severity ranged from mild to severe. All studies except one included patients who had a health-care utilisation visit in the past year. The majority of participants were children (up to 12 years of age) rather than teenagers (aged 12–18 years). In eight studies high numbers of participants were on public insurance/attending subsidised community clinics. Eight studies included > 50% participants from ethnic minorities; one study was in a predominantly white population. Ten studies were in urban or suburban settings involving vulnerable populations | Setting: home visits, mainly in urban or suburban settings involving vulnerable populations. Some with additional telephone sessions Delivery: nurses; social workers; bilingual, bicultural health educators; pulmonary therapists; licensed psychologists or master’s level psychology students; bilingual bicultural home visitors |
All provided basic education on asthma disease process, and all reviewed asthma medications along with inhaler technique and strategies for self-management. WAPs were reviewed and/or provided in 10 out of 12 studies. All but one study reviewed asthma triggers, measures to reduce environmental allergens or both. Six studies provided printed materials and/or homework to complete after the educational sessions. Additional components included electronic devices to provide objective feedback on medication adherence or nebuliser use; active disease monitoring and management via scheduled telephone calls and access to a 24-hour hotline | The majority of interventions consisted of between four and six visits, each lasting 30–60 minutes. Visits generally occurred weekly or monthly. One study was of higher intensity than this range, and three were of lower intensity The shortest follow-up was 3 months; most studies collected follow-up data for 9–24 months |
| Wider population interventions | |||||
| Bussey Smith 2007123 | Interactive computerised educational asthma programmes | Patients aged 3–75 years. Seven RCTs focused on children, two on adults. Four RCTs evaluated urban or inner-city populations | NR | Few features in common. Included games tailored to specific features of asthma in the individual; web-based education; personal interactive communication device | Length of follow-up ranged from 4 to 12 months. Four studies had a 1-year follow-up period, three studies had a 12-week follow-up period |
| Gibson 2002126 | Asthma self-management and educational programmes | Recruited from a variety of settings including hospital; emergency room; outpatient department; community setting; general practice | NR | Education (100%); self-monitoring of symptoms and/or peak expiratory flow (92%); regular review of treatment and asthma severity by a medical practitioner (67%); WAP (50%). These studies fell into five subgroups:
|
NR |
| Gibson 2004127 | WAPs for asthma management | Individualised complete action plans (17 RCTs, 15 also included education, self-monitoring and regular medical review incorporated into the self-management programme); incomplete individualised action plans (four RCTs); non-specific action plans (five RCTs) | |||
| Moullec 2012128 | Interventions for improving ICS use among adult asthma patients | 17/18 studies conducted in moderate–severe asthma patients. 14/18 studies included age range 35–50 years. Women over-represented in most studies | Setting: most RCTs delivered individual interventions, four conducted both individual and group interventions | All studies included a self management component (education, behaviour therapy, motivational interviewing). Additional components included in some RCTs were decision support; delivery system design; clinical information systems. The remaining CCM components, i.e. ‘healthcare organization’ and ‘community resources’, were not included in the studies selected in the current review | Duration of the intervention ranged from one 30 minute session to 12 hours or more (mean 3 hour; median, 2 hour). Follow-up ranged from 1 week to 2 years (mean 10 months; median 9 months) |
| Newman 2004109 | Self-management interventions for asthma | NR | Setting: individual and group settings in roughly similar proportions Delivery: almost all delivered face to face, telephone was also used in some. One RCT self-administered with workbook and audiotape. HCPs led most |
Tended to focus specifically on monitoring symptoms and better adherence to medication to decrease hospital admissions. Other behaviours targeted included inhaler technique and avoidance of triggers. Generally information based/instructional; only a few incorporated techniques to address barriers to effective self-management | Duration: < 12 hours total contact time |
| Powell 2002130 | Asthma education and self-management | Adults with asthma | NR | Asthma education (100%); self-monitoring of symptoms and/or peak expiratory flow (100%); regular review of treatment and asthma severity by a medical practitioner (96%); WAP (88%) | NR |
| Ring 2007131 | Interventions encouraging health professionals (or others) to promote/encourage action plan use | People with asthma (or their parents); doctors; general practice teams. Studies included adults; children; health professionals. Most participants had moderate-to-severe asthma or were recruited following medical care for acute asthma | Setting: most studies conducted in a non-hospital setting. Intervention delivered via telephone consultation; postal prompt; asthma clinics; asthma management systems; and practice-based quality improvement Delivery: most used HCPs; non-health-care workers also used |
Interventions were varied, could be categorised as educational; reinforcing or prompting; asthma clinics; asthma management systems; and quality improvement | NR |
| Tapp 2007132 | Asthma education provided to adults while attending the ED for an asthma exacerbation | More females than males. Participants recruited either within the ED/hospital setting following asthma exacerbation, or subsequent to the event | Delivery: mostly asthma or ED nurses, also respiratory specialists; physiotherapist; respiratory therapist | Mixed educational interventions. Education included one or more of written self-management plans; education on symptoms and triggers; information booklet or card; teaching on use of medication and inhalers (including peak flow metres); importance of follow-up | Average follow-up time was 7.4 months (range 6–18 months) |
| Toelle 2004133 | Individualised WAPs for asthma management | All included participants with well-established asthma. Only one study recruited children. Mean age of adults 28–45 years | Setting: tertiary hospitals; primary care | Peak flow-based WAPs or symptom-based WAPs | Intervention duration: three trials = 6 months; four trials = 12 months |
Quality assessment and weighting
Quality of the 18 systematic reviews, as assessed by the R-AMSTAR, ranged from 23109,129 to 41118,119,134 out of a total possible score of 44. A total of 12 reviews were classified as being of higher quality (R-AMSTAR ≥ 31),118–120,122,124,126,127,130–134 whereas six were classed as lower quality (R-AMSTAR ≤ 30). 109,121,123,125,128,129 The total number of participants included within the reviews ranged from 113124 to 8077. 125 Twelve reviews were of larger total size (≥ 1000) (Table 38).
| R-AMSTAR criteria | Culturally specific | Child or adolescent | Wider population interventions | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baile, 2009120 | Chan, 2010124 | Postma 2009129 | Bernard-Bonni, 1995121 | Zemek 2008;119 Bhogal 2006118 | Boyd 2009122 | Coffman 2009125 | Welsh 2011134 | Bussey-Smith 2007123 | Gibson 2002;126 2004127 | Moullec 2012128 | Newman 2004109 | Powell 2002130 | Ring 2007131 | Tapp 2007132 | Toelle 2004133 | |
| Was an a priori design provided? | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 3 | 4 | 3 | 4 | 4 | 3 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 1 | 1 | 4 | 4 | 3 | 4 | 2 | 4 | 2 | 1 | 4 | 1 | 4 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 | 2 | 4 | 4 | 4 | 2 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 4 |
| Was the status of publication used as an inclusion criterion? | 3 | 3 | 1 | 3 | 3 | 2 | 1 | 4 | 1 | 4 | 1 | 2 | 3 | 3 | 4 | 4 |
| Was a list of studies (included and excluded) provided? | 4 | 4 | 1 | 3 | 4 | 4 | 2 | 4 | 1 | 4 | 2 | 1 | 4 | 3 | 4 | 4 |
| Were the characteristics of the included studies provided? | 4 | 4 | 4 | 1 | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 3 | 2 | 4 | 4 | 4 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 2 | 4 | 4 | 4 | 4 | 4 | 1 | 4 | 1 | 2 | 4 | 4 | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 1 | 4 | 2 | 2 | 4 | 4 | 3 | 4 | 2 | 4 | 3 | 4 | 2 | 4 | 3 | 2 |
| Methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 | 3 | 2 | 3 | 2 | 4 | 4 | 4 | 3 | 1 | 3 | 4 | 3 | 3 |
| Was the likelihood of publication bias assessed? | 1 | 3 | 1 | 1 | 4 | 3 | 3 | 2 | 1 | 1 | 2 | 1 | 1 | 2 | 2 | 2 |
| Was the conflict of interest stated? | 3 | 2 | 1 | 1 | 4 | 3 | 2 | 3 | 3 | 3 | 2 | 1 | 3 | 3 | 3 | 3 |
| Total score/44 | 36 | 40 | 23 | 27 | 41 | 39 | 29 | 41 | 26 | 39 | 27 | 23 | 34 | 35 | 39 | 38 |
Taking into consideration both quality and total population size, one review received an overall evidence weighting of one star,123 10 are weighted two stars,109,118–121,124,125,128,129,133 and seven have an evidence weighting of three stars122,126,127,130–132,134 (see Table 39 for weighting and Table 29 for the explanation on how this weighting was reached).
| Review | Total number participants | Quality score | Weighting |
|---|---|---|---|
| Zemek 2008119 (and Bhogal 2006118) | 365 | 41 | ** |
| Bailey 2009120 | 617 | 36 | ** |
| Bernard Bonnin 1995121 | 1290 | 27 | ** |
| Boyd 2009122 | 7845 | 39 | *** |
| Bussey Smith 2007123 | 957 | 26 | * |
| Chang 2010124 | 113 | 40 | ** |
| Coffman 2009125 | 8077 | 29 | ** |
| Gibson 2002126 (and Gibson 2004127) | 6090 | 39 | *** |
| Moullec 2012128 | 3006 | 27 | ** |
| Newman 2004109 | 2004 | 23 | ** |
| Postma 2009129 | 2316 | 23 | ** |
| Ring 2007131 | 4588 | 35 | *** |
| Tapp 2007132 | 2157 | 39 | *** |
| Toelle 2004133 | 967 | 38 | ** |
| Welsh 2011134 | 2342 | 41 | *** |
| Powell 2002130 | 2460 | 34 | *** |
Outcomes
Table 40 outlines the relevant outcome measures included in our review.
| Outcomes | Definitions | Measures reported in reviews |
|---|---|---|
| Primary outcomes | ||
| Health-care utilisation | Use of health-care services | Hospital admissions; LOS; unscheduled doctor visits; ED visits |
| Lung function | Airway calibre | Baseline % predicted FEV1; FEV1; PEFR |
| QoL | Asthma-specific or generic QoL | Asthma specific: AQOL; SG-RQ; PACQLQ; PAQLQ; ITG-CASF Generic: PedsQL; carer/parent QoL (for very young children only) |
| Secondary outcomes | ||
| Symptoms and exacerbations | Experienced exacerbations or symptoms of poorly controlled asthma | Sleeping problems: nocturnal awakening; nocturnal asthma; night-time wheezing; night-time coughing Psychosocial difficulties: emotional problems; social problems Number of days per week with symptoms/symptom score/LASS; frequency of asthma attacks |
| Activity limitation | Limitation to usual activities caused by asthma | Work/school absenteeism; functional impairment |
| Self-efficacy | The confidence that an individual has in their own ability to perform a specific task or behaviour | Likert scales of self-efficacy |
| Self-management behaviours | Measures of self-management adoption behaviour | Possession of action plan; use of/adherence to action plan; frequency of peak flow metre use; peak flow metre technique; adherence to ICSs; inhaler technique; recognition and appropriate use of rescue medications; avoidance or prevention of triggers: smoking in home; vacuuming; use of provided environmental resources (e.g. pillow encasements); HCP behaviours to encourage self-management |
Findings
Results have been classified into two categories: (1) headline statistical results from meta-analyses of intervention compared with control (Table 41); and (2) other results which include narrative syntheses, subgroup meta-analyses and results from one RCT only (Table 42).
| Reference and weighting | Outcome | Time (from initiation of intervention) | Sample size | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Culturally specific interventions | |||||
| Bailey 2009120 ** Culturally orientated programmes vs. control |
Asthma specific QoL | NR | Two RCTs; 293 | +* | WMD 0.25 (0.09 to 0.41) |
| Child- and adolescent-specific interventions | |||||
| Bernard-Bonnin 1995121 ** Interactive teaching on asthma self-management vs. control |
School absenteeism | NR | Five RCTs; 706 | 0 | 0.04 (SE ± 0.08) |
| Asthma attacks | NR | Three RCTs; 225 | 0 | 0.09 (SE ± 0.14) | |
| Hospital admissions | NR | Five RCTs; 701 | 0 | 0.06 (SE ± 0.08) | |
| Hospital days | NR | Five RCTs; 594 | +* | –0.11 (SE ± 0.08) | |
| ED visits | NR | Five RCTs; 522 | +* | 0.14 (SE ± 0.09) | |
| Boyd 2009122 *** Educational interventions for paediatrics vs. control |
ED visits | 12 weeks–2 years | 17 RCTs; 3008 | +* | RR 0.73 (0.65 to 0.81) NNT ranged from 7 to 53 |
| Hospital admissions | NR | 18 RCTs | +* | RR 0.79 (0.69 to 0.92) | |
| Unscheduled doctor visits | NR | Seven RCTs | +* | RR 0.68 (0.57 to 0.81) | |
| FEV1 predicted | NR | Two RCTs | 0 | 0.24% (–5.25% to 5.73%) | |
| QoL | NR | Two RCTs | 0 | WMD 0.13 (0.73 to 0.99)a | |
| Welsh 2011134 *** Home-based education vs. usual care or less intensive non-home-based education |
ED visits | 6 months | Two RCTs; 430 | 0 | MD 0.4 (–0.20 to 0.27) |
| Child- and adolescent-specific interventions: comparisons between two types of active intervention | |||||
| Bhogal 2006118 ** Symptom-based action plans vs. peak flow-based action plans |
Unscheduled doctor or ED visits | NR | Five RCTs; 353 | +* | RR 0.72 (0.55 to 0.99); favours symptom based NNT to prevent one acute visit is 9 (5 to 138) |
| Requiring systemic steroids | NR | Three RCTs; 185 | 0 | RR 0.40 (0.05 to 3.40) | |
| Hospital admissions | NR | Three RCTs; 296 | 0 | RR 1.51 (0.35 to 6.65) | |
| School absenteeism | NR | Two RCTs; 245 | 0 | RR 0.81 (0.58 to 1.12) | |
| Acute care visits per activation of step 2 of the action plan | NR | Two RCTs | 0 | RR 0.86 (0.68 to 1.09) | |
| Average % predicted FEV1 | 3 months | Two RCTs; 257 | 0 | MD –0.73% (–4.75% to 3.28%) | |
| Child QoL | 3 months | Two RCTs; 257 | 0 | MD –0.25 (–0.55 to 0.05) | |
| Wider population interventions | |||||
| Gibson 2002126 *** Asthma self-management and educational programmes vs. control |
Hospital admissions | NR | 12 RCTs; 2418 | +++ | RR 0.64 (0.50 to 0.82); p = 0.0003 |
| ED visits (dichotomous) | NR | 13 RCTs; 2902 | ++ | RR 0.82 (0.73 to 0.94); p = 0.003 | |
| ED visits (mean number) | NR | Eight RCTs; 731 | +* | SMD –0.36 (–0.50 to –0.21) | |
| Unscheduled doctor visits (dichotomous) | NR | Seven RCTs; 1556 | +* | RR 0.68 (0.56 to 0.81) | |
| Unscheduled doctor visits (mean number) | NR | Seven RCTs; 1042 | 0 | SMD –0.07 (–0.19 to 0.06) | |
| Work/school absenteeism (dichotomous) | NR | Seven RCTs; 732 | +* | RR 0.79 (0.67 to 0.93) | |
| Work/school absenteeism (mean number) | NR | 13 RCTs; 1728 | +* | SMD –0.18 (–0.28 to –0.09) | |
| Nocturnal asthma | NR | Five RCTs; 1136 | +* | RR 0.67 (0.56 to 0.79) | |
| FEV1 | NR | Seven RCTs; 1072 | 0 | SMD 0.10 (–0.02 to 0.22) | |
| PEFR | NR | 10 RCTs; 1346 | +* | SMD 0.18 (0.07 to 0.29) | |
| QoL | NR | Six RCTS; 515 | +* | SMD 0.29 (0.11 to 0.47) | |
| Powell 2002130 *** Asthma education and self-management vs. control |
Mean FEV1 | NR | Three RCTs | 0 | SMD 0.19 (–0.05 to 0.25) |
| PEFR | NR | Three RCTs | +* | SMD 0.16 (0.01 to 0.31) | |
| Tapp 2007132 *** Education vs. control |
Hospital admissions | NR | Five RCTs; 572 | +* | RR 0.50 (0.27 to 0.91) Average NNT = 9 Stratified by risk: lower risk NNT = 20, moderate risk NNT = 8, high risk NNT = 4 |
| ED visits | NR | Eight RCTs; 946 | +* | RR 0.66 (0.41 to 1.07) | |
| Scheduled clinic attendance | NR | Two RCTs; 198 | +* | RR 1.73 (1.17 to 2.56) | |
| Lung function, PEFR | NR | Three RCTs | 0 | 16.89 l/minute (–11.59 to 45.73 l/minute) | |
| Work/school absenteeism | NR | Two RCTs; 171 | 0 | RR 0.88 (0.44 to 1.73) | |
| Wider population interventions: comparisons between two types of active intervention | |||||
| Toelle 2004133 ** Peak flow-based action plans vs. symptom-based action plans |
Unscheduled doctor visits | NR | Two RCTs; 207 | +* | RR 1.34 (1.01 to 1.77) NNT: 7 favours symptom based |
| Hospital admissions | NR | Three RCTs; 283 | 0 | RR 1.17 (0.31 to 4.43) | |
| ED visits | NR | Three RCTs | 0 | RR 0.86 (0.44 to 1.67) | |
| Reference and weighting | Comparison | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author |
|---|---|---|---|---|---|
| Bailey 2009120 ** | Culturally orientated programmes vs. usual care or limited/non-specific education | Four RCTs; 617; 2000–8 | Meta-analysis | A significant benefit in asthma QoL was found in intervention compared with control | The available evidence suggests that culturally orientated education programmes for adults and children from minority groups are effective in improving asthma QoL in both adults and children, and rates of asthma exacerbations and asthma control in children. Authors theorise that culturally specific programmes allow participants to fully engage in education, which has positive effects on QoL This review is limited by a small number of studies and small sample sizes in two of the studies |
| Other | No differences between intervention and control were found in any measure of adult exacerbation In the paediatric population, significant benefits were found for rates of asthma control and number of hospitalisations in intervention compared with control. Evidence for ED visits was conflicting |
||||
| Bernard-Bonnin 1995121 ** | Interactive teaching on self-management vs. standard care | 11 RCTs; 1290; 1981–91 | Meta-analysis | Significant reductions were found for number of hospital days and emergency visits in intervention vs. control. No effect was found on school absenteeism, frequency of asthma attacks and hospitalisation. (See comment below) | This meta-analysis shows a modest impact of self-management teaching programmes on paediatric asthma morbidity. Intermediate outcomes should be explored and interventions should be designed for targeted audiences. Overall asthma severity was classified as mild to moderate, limiting the possible reduction in morbidity. This may account for the modest impact which these interventions had Although stratification was not impossible, review authors speculate that individual teaching is more adapted to the patient and more easily understood, with a higher impact on outcome than group sessions Authors state that inclusion of preschoolers in many studies may have reduced overall impact of interventions The understanding of different phenotypes of childhood asthma was in its infancy when this review was done. Viral associated wheeze – the cause of most wheezing in under-fives does not respond to asthma treatment and therefore PAAPs are ineffective For each outcome of interest, data were pooled from five studies or fewer |
| Other | It was among children with high baseline numbers of hospitalisations and emergency visits that the greatest subsequent reduction in morbidity was observed | ||||
| Zemek 2008119 ** | Symptom-based WAP vs. peak flow-based WAP Additionally, WAP vs. no action plan |
Four RCTs; 355; 1990–2004, one additional RCT | Meta-analysis | A significant reduction in acute care visits was found for those receiving symptom-based action plans compared with peak flow-based plans (NNT = 9). No difference was found between groups for hospital admissions, exacerbation requiring steroids, school absenteeism, FEV1 and QoL | There is a gap in the evidence to support the recommendation of action plans for children as no studies comparing the use of an action plan with no action plan in children were identified In a plan recommending daily maintenance steroids with step-up therapy using β2-agonist and increased steroids before urgent medical consultation, the use of symptom-based plans is more effective than peak flow-based plans. Review authors recommend reserving peak flow monitoring for children who are poor perceivers of their asthma symptoms The small number of trials identified in this review limited the power of detecting significant difference in secondary outcomes, and hindered the authors’ conduct of subgroup and sensitivity analyses |
| Other | No significant difference between three-step WAP without graphics, and three-step streetlight WAP Significantly fewer children assigned to symptom-based WAP required acute care compared with peak flow monitoring only when symptomatic. No group difference when comparing symptom-based with daily peak flow monitoring. Compared with symptom monitoring, children assigned to peak flow monitoring had a significantly greater reduction in the change of number of days per week of symptoms recorded |
||||
| Other | A significant reduction in acute care events, school days missed, nocturnal awakening and symptom scores was found in the intervention group compared with control | Data were too limited to firmly conclude that provision of a WAP compared with none reduces acute care visits and symptoms | |||
| Boyd 2009122 *** | Educational intervention targeted children/parents/both vs. low intensity/basic/routine education | 38 RCTs; 7843; 1985–2007 | Meta-analysis | Significantly fewer ED visits (NNT = 55–57), hospital admissions and unscheduled doctor visits in those receiving educational interventions vs. control No effect on FEV1 predicted and QoL found |
Asthma education aimed at children and parents present in the ED for acute exacerbations is effective in reducing risk of future ED presentation and hospital admission. The long-term effect of education on other markers of asthma morbidity is uncertain. The most effective type, duration and intensity of educational packages remains unclear Future work in this area should focus on whether or not there are important differences between teams delivering interventions Many of the outcomes of interest were not reported in the studies, limiting the conclusions reached by the authors. There was also significant heterogeneity between the results |
| Other | Subgroup analysis to investigate if type and timing of intervention, timing of outcome assessment, or age of participants, affected results did not produce any significant findings. Challenges associated with managing adolescent asthma remain. Research assessing the effect of intervention delivery by physician and other allied health teams is not well represented in the analyses | ||||
| Bussey-Smith 2007123 * | Interactive computerised educational programmes vs. routine care/traditional self-management education and monitoring | Nine RCTs; 957; 1986–2005 | Other | Five out of nine studies found a positive impact on at least one of the following: hospitalisation; acute care visits; short-acting bronchodilator use; lung function. Five studies found statistical improvements in asthma symptoms compared with control. No single computerised educational programme was superior in all outcomes. Some beneficial effects were seen only within a limited time frame or in a subset of patients. In several trials improvements were seen in both intervention and control groups. Clinical outcomes, including short-acting β2-agonist use and lung function, do not appear to correlate with programme time | Overall, interactive computerised programmes appear to improve patient asthma symptoms. There is less evidence to support the effect of these interventions on objective clinical outcomes No obvious link between the different formats or components of the programmes and outcomes. None of the programmes stands out as the best vehicle to provide self-management education for asthmatic children or adults |
| Chang 2010124 ** | IHWs in education programmes vs. routine education | One RCT; 113; 2010 | Other | All results here are from a single RCT. Significant improvements were found in parents’ asthma skills, possession and interpretability of action plans, and school absenteeism. There was a suggestion that carer QoL was improved in the intervention group compared with control; however, this did not reach statistical significance. No statistically significant improvement was found in the number of acute presentations to health facilities or hospitalisations | No difference was found in exacerbations between groups; however, in all other outcomes, the group with IHW involvement either had significantly or suggestively better outcomes compared with the control group. Authors state that the inclusion of IHW in asthma education programmes for indigenous children and adults with asthma is justified, unless new data suggest otherwise This review is considerably limited by the very small sample size and the presence of only a single study |
| Coffman 2009125 ** | School-based asthma education vs. usual care | 18 RCTs; 8077; 1987–2007 | Other | Statistically significant effects on self-efficacy were found in five of six RCTs. Self-management behaviours were significantly improved in all six RCTs reporting this outcome. Statistically significant improvements in QoL were found in four of six RCTs. Days with symptoms were significantly reduced in three of eight RCTS. Nights with symptoms improved in one of three RCTs. School absences significantly reduced in 5 of 13 RCTs reporting the outcome | Asthma education was associated with improvements in self-efficacy and self-management behaviours. Asthma education was also associated with a statistically significant increase in QoL Some of the cluster RCTs may have overstated the impact of the interventions as seven studies failed to use appropriate statistical methods |
| Gibson, 2002;126 *** | Self-management and educational programmes vs. usual care | 36 RCTs; 6090; 1986–2001 | Meta-analysis | A significant impact was found on hospitalisation rates, emergency hospital visits, unscheduled doctor visits, days off work/school, nocturnal asthma, PEFR and QoL in the intervention group compared with control. No differences in FEV1 values were found between intervention and control | Self-management educational programmes delivered to adults with asthma result in clinically important improvements in asthma health outcomes including reduced health-care utilisation, improvement in nocturnal asthma and reduced days off work. These benefits are most pronounced with interventions which involve a WAP, self-monitoring and regular medical review. Interventions which are less intensive, especially those that do not include a WAP, are less effective |
| Other | Subgroup analysis found optimal self-management (involving provision of WAPs) led to significant reductions in asthma-related hospitalisations and ED visits. Two interventions which included regular review of medication also found significantly reduced ED visits. Six studies reported on unscheduled doctor visits, with none finding a significant effect between groups. Nocturnal asthma was explored in four studies, three finding a significant improvement whereas one found no significant change. Oral corticosteroids and QoL were both assessed in four studies with mixed effects | ||||
| Gibson 2004127 | Further, WAPs vs. usual care | 26 RCTs; 1987–2002 | Other | Hospital admissions were significantly reduced in participants using action plans based on both personal best PEFR and % predicted PEFR compared with control. Emergency room visits were significantly reduced, and airway calibre improved, in intervention arms using personal best PEFR compared with control; however, no significant benefit was seen with plans based on % predicted PEFR. Benefits were found for any number of action points (two to four). Traffic light system not consistently better than conventional presentation. Use of inhaled and oral steroids were both consistently beneficial. Efficacy of incomplete and non-specific action plans was inconclusive | The findings of this review strongly support the use of individualised complete WAPs. Effective action plans can be based on symptoms or PEFR and use two, three or four action points. PEFR-based plans should use personal best PEFR and not % predicted PEFR for the action point. Treatment instruction should include both inhaled and oral steroids In some cases there were insufficient studies to allow a comparison and hence a type II error is possible. However, review authors report that they were cautious in their interpretation of the data |
| Moullec, 2012128 ** | Interventions for improving ICS use vs. usual care | 18 RCTs; 3006; 1990–2010 | Other | Subgroup analysis found the smallest pooled ES in adherence measures for interventions with only one component of the CCM. ES for adherence measures were larger for interventions with two CCM components, and larger still for interventions with four CCM components. All adherence effects were statistically significant. Out of 13 studies exploring one CCM, three found significant effects, two out of five studies exploring two CCM components found significant effects, and two out of three studies exploring four CCM components found significant effects. One study compared joint decision-making negotiated between clinician and patient, with decision made by physician alone. This study found a significant effect to support joint decision-making | This review concludes that the more CCM components included within interventions, the greater the effects on ICS adherence outcomes. This review also suggests that interventions which include motivational support, such as through joint decision-making, may show the greatest promise in improving adherence. However, more research is needed to confirm this A small number of studies were included, particularly for subgroup analysis on interventions with four CCM components. Also, the review authors acknowledge that a small number of CCM component combinations were tested, which limits the ability to determine which components were most important for success |
| Newman 2004109 ** | Self-management interventions vs. standard care/basic information, or direct comparison between self-management interventions | 18 RCTs; 2004; 1997–2002 | Other | 8 out of 14 studies showed some improvement in lung function. Most of these used education with an action plan, but others that used this approach did not find any improvements. A writing intervention for emotional expression and a stress management intervention also improved lung function, suggesting methods directed at stress and emotions can improve lung function. Half of the studies measuring QoL reported significant benefits. There was no particular pattern between those that did and did not impact on QoL. Of those interventions targeting some aspect of behaviours, 57% reported a significant change in behaviour. 7 out of 11 interventions showed reduction in health-care use; all but one used education and action plans. Only one study to use this approach did not find any reduction. No differences seen with or without action plans. Little difference recorded between use of symptoms or PEFR to guide use of medication | Review authors conclude that it should be recognised that one therapy or programme might not be suitable for all patients Evidence suggests importance of action plans in combination with education for improved lung function and reduced health-care utilisation. However, no clear patterns can be established as to the optimal self-management provision Review authors state a potential limitation of their review to be their decision to only include papers published between 1997 and 2002. They also report that not all outcomes (in particular all clinical outcomes) were included in this review |
| Postma 2009129 ** | Environmental interventions for children delivered by CHWs vs. usual care | Seven RCTs; 2316; 2004–8 | Other | Six studies reported unscheduled asthma-related clinical utilisation; results favoured intervention group and were generally statistically significant. There were mixed results in terms of which allergens or exposures significantly decreased over time. Behaviour change was measured in four studies with mixed results, finding positive changes to be tied to resource provision. Changes in medication use and lung function were measured in four studies with mixed effects. Child QoL did not improve in the one study that measured it. Asthma-related health outcomes were reported in six out of seven studies, with consistent and significant decreases in caregiver reported asthma symptoms. Benefits persisted 1 year after intervention end in one study Interventions with higher intensity and frequency reported the most positive health outcomes |
Authors conclude that the evidence for the effectiveness of CHW-led interventions provided here supports ongoing development of this CHW role. Studies consistently identify positive outcomes associated with CHW-delivered interventions Evidence from this review suggests that social, behavioural and environmental dimensions of asthma management are necessary to consider when designing and evaluating asthma intervention programmes This is very difficult review to interpret because there are two interventions: allergen avoidance (generally considered to be ineffective – see BTS-SIGN guidelines) and education delivered by CHWs. The description of the education component suggests that it was typically focused on allergen avoidance and the behaviours changed are focused on compliance with allergen avoidance |
| Powell, 2002130 *** | Asthma education and self-management vs. usual care or one element of self-management (regular review/basic education/self-monitoring only) | 15 RCTs; 2460; 1990–2001 | Meta-analysis | Those in the intervention had significantly better PEFR than those in the control arm. There was no significant difference in mean FEV1 between intervention and control | Optimisation of asthma control by adjustment of medications may be facilitated either by self-adjustment with the aid of a WAP or by regular medical review Individualised WAPs based on PEFR are equivalent to action plans based on symptoms These findings are clinically important as they enable interventions to be tailored to patient preference, patient characteristics and the resources available Reducing the intensity of self-management education or level of clinical review may reduce its effectiveness |
| Other | Optimal self-management vs. regular medical review was explored in six RCTs with no difference in asthma outcomes found. PEFR action plans vs. symptom-based action plans were also explored in six RCTs. Action plans based on PEFR were found to be equivalent to symptom-based action plans for hospitalisations and unscheduled visits to the doctor, with mixed effects found for other outcomes Optimal self-management vs. modified optimal self-management was studied in three RCTs, with one study finding regular medical review to be associated with better FEV1, while another study found intensive education to be associated with improved symptoms and fewer unscheduled doctor visits. A third study found no difference on any outcome between verbally instructed and WAPs | ||||
| Ring 2007131 *** | Interventions encouraging use of action plans vs. usual care | 14 RCTs; 4588; 1993–2005 | Other | Self-management education interventions were explored in five RCTS: four reported a significant increase in the number of people/parents with action plans; one reported significantly higher action plan use. Telephone consultation to reinforce action plan use was investigated in two RCTS: one study reporting a significant increase in people having action plans; both RCTs reporting greater understanding of how to use their plans. Asthma clinics were used in two interventions, both reporting increased ownership at 6 months post intervention, although only one was statistically significant. Asthma management systems were used in two studies: one finding more children received action plans (NNT = 5); the other reporting significantly higher action plan use. Two studies looked at interventions aimed at HCPs. One study educated HCPs, with results suggesting this may facilitate action plan use for up to 2 years post intervention. Another RCT implemented quality improvement and found no overall effect | Primary care professionals could encourage the ownership and use of action plans through the implementation of proactive practice-based organisational systems Highlights the lack of robust evidence on the best ways for GPs and practice nurses to sustain action plan use among patients in the long term. Patient self-management education, reinforcement and prompting, school asthma clinics and asthma management systems all increase patient ownership or initial use of action plans up to 1 year post intervention. However, more research is needed to determine use of action plans over the longer term Some interventions used nurses with specialist asthma training; however, not all clinical nurses providing asthma care have received such training. Research interventions may also have extra resources not otherwise available. These factors may mean reduced effectiveness in a ‘real-world’ setting The authors acknowledge the possibility of publication bias in their review; however, they state that steps were taken to minimise this possibility |
| Tapp 2007132 *** | Asthma education after acute asthma exacerbation event vs. usual care | 13 RCTs; 2157; 1979–2009 | Meta-analysis | Significant benefits in terms of hospital admission rates, ED attendance and scheduled clinic attendance were reported in the intervention group compared with the control. No statistically significant difference was found for PEFR or days off work/school | Although the evidence is supportive of educational interventions to reduce readmission following an episode of acute asthma in adults, the review does not provide evidence to suggest that other important markers of long-term asthma morbidity are affected Adults may have limited opportunities to attend educational sessions in practice due to work and child care commitments, and the format, content and uptake of educational interventions still requires quantitative and qualitative evaluation Review authors acknowledge the possibility of publication bias, although steps were taken to avoid this |
| Other | Two RCTS detected no difference in QoL between education and control in any domain. One RCT found no difference between intervention and control in various symptom measures. One RCT found suggestive improvements in inhalation technique and awareness of PEF readings | ||||
| Toelle 2004133 ** | Individualised WAP vs. no plan; or symptom-based plan vs. peak flow-based plan | Seven RCTs; 967; 1990–2001 | Meta-analysis | Participants in intervention arms had significantly fewer unscheduled doctor visits compared with control. No significant effects were found on hospitalisation or ED visit rates | Authors state that it is not possible to conclude whether or not use of written management plans alone leads to an improvement in asthma management behaviours. They go on to comment that in order to deliver benefit to the patient, programmes must be comprehensive and include education, a written self-management plan and regular review Authors acknowledge that the small number of included studies that contributed data for the meta-analysis and the small number of patients recruited in the studies have limited the ability to draw conclusive findings |
| Other | Two of three RCTs found increased adherence in the peak flow-based plan compared with the symptom-based plan. Oral corticosteroid use was reported in two RCTs comparing peak flow with symptom-based plans, finding mixed results. Days lost from school/work were reported in two studies, with no significant difference found | ||||
| Welsh 2011134 *** | Self-management education delivered in the home of child/adolescent vs. routine care or general asthma education | 12 RCTs; 2342; 1986–2010 | Meta-analysis | No significant difference was found in the frequency of acute visits for asthma between intervention and control | Authors conclude that the effect of home-based education is context dependent. Inconsistent evidence was found for these interventions, and the review does not contribute further information on the fundamental content, intensity or optimum setting for such educational interventions High clinical heterogeneity across included studies Context in most of the trials was a vulnerable urban population of North American children with asthma |
| Other | Overall, no effect on QoL was found from five studies. From four RCTs, there is suggestion of benefit on symptoms in intervention compared with control which did not reach statistical significance. Hospitalisation rates were reported in five studies, two finding a significant difference favouring intervention, whereas the remaining found no difference. Six RCTs explored frequency of ED visits, with one significantly favouring controls over intervention. Number of school days missed was reported in one study with no significant result found. One RCT found rates of decrease in mean courses of oral corticosteroids were faster for intervention compared with control over 18 months follow-up. When comparing education with less intensive education, a small reduction in ED visits and hospitalisations was found from one study |
Primary outcomes
The earlier included systematic review by Bernard-Bonnin et al. 121 is not presented or discussed here for reasons explained in Table 42.
Health-care utilisation
Four of the seven systematic reviews to conduct meta-analysis of intervention compared with control presented at least one overall ES from pooled data on health-care utilisation. 122,126,132,134
Pooled results for hospital admissions were presented in four reviews. A forest plot of ESs is provided from the three reviews that presented risk ratios. 122,126,132 All three reviews were of high quality, and all found a significant effect to favour intervention. Boyd et al. 122 focused specially on paediatric asthma, whereas the other two reviews explored intervention with the general asthmatic population126,132 (Figure 16).
FIGURE 16.
Asthma: forest plot for hospital admissions.
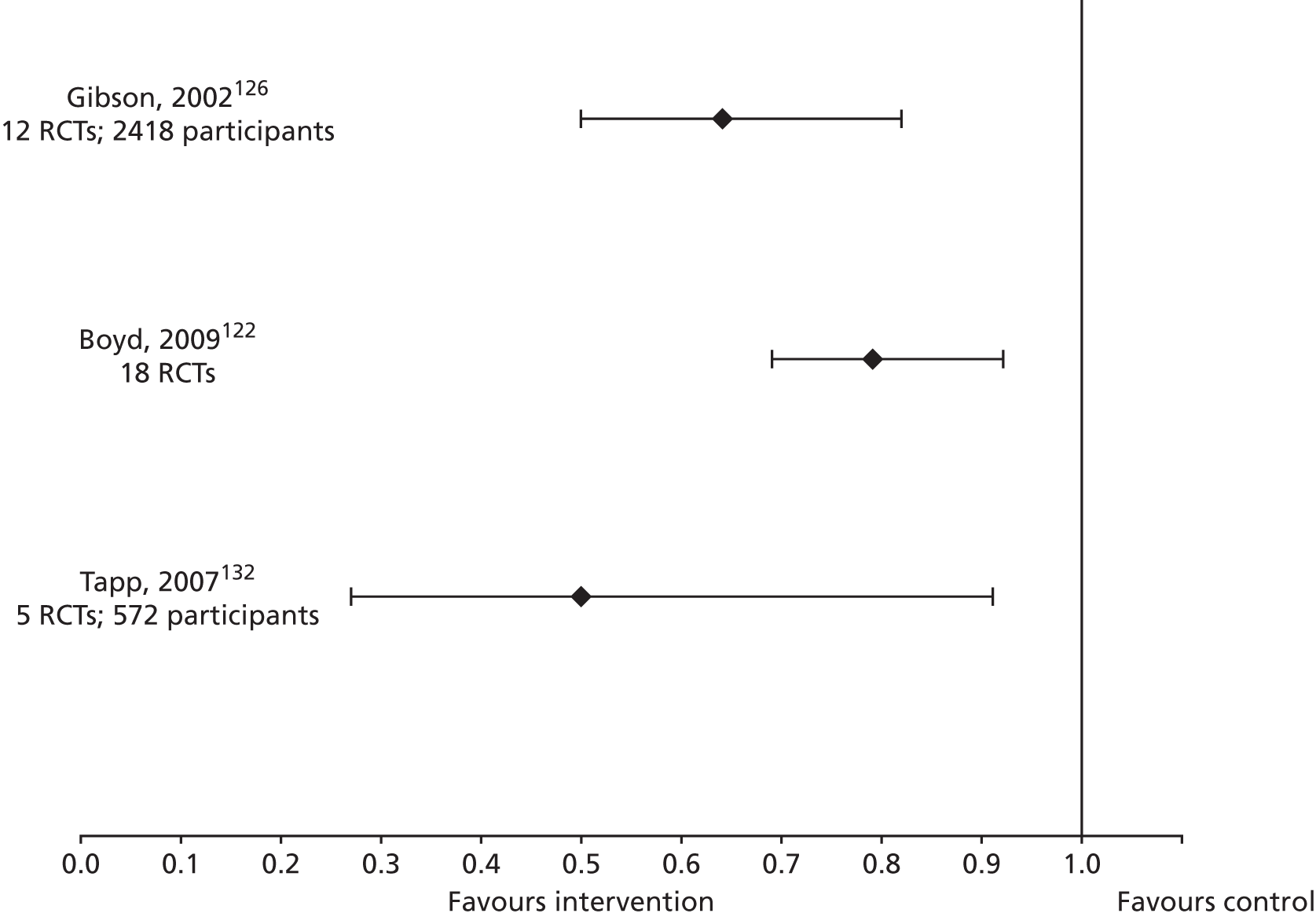
Five reviews also presented pooled data for ED visits. Again, a forest plot was compiled using only the three reviews to use risk ratio. The two more highly powered, high-quality reviews found a significant effect-to-favour intervention,122,126 whereas the smaller, high-quality review showed a very wide confidence interval (CI) which spans the point of no effect132 (Figure 17). ED visits were reported to be unaffected in one review from pooled estimates with two RCTs. 134
FIGURE 17.
Asthma: forest plot for ED visits.
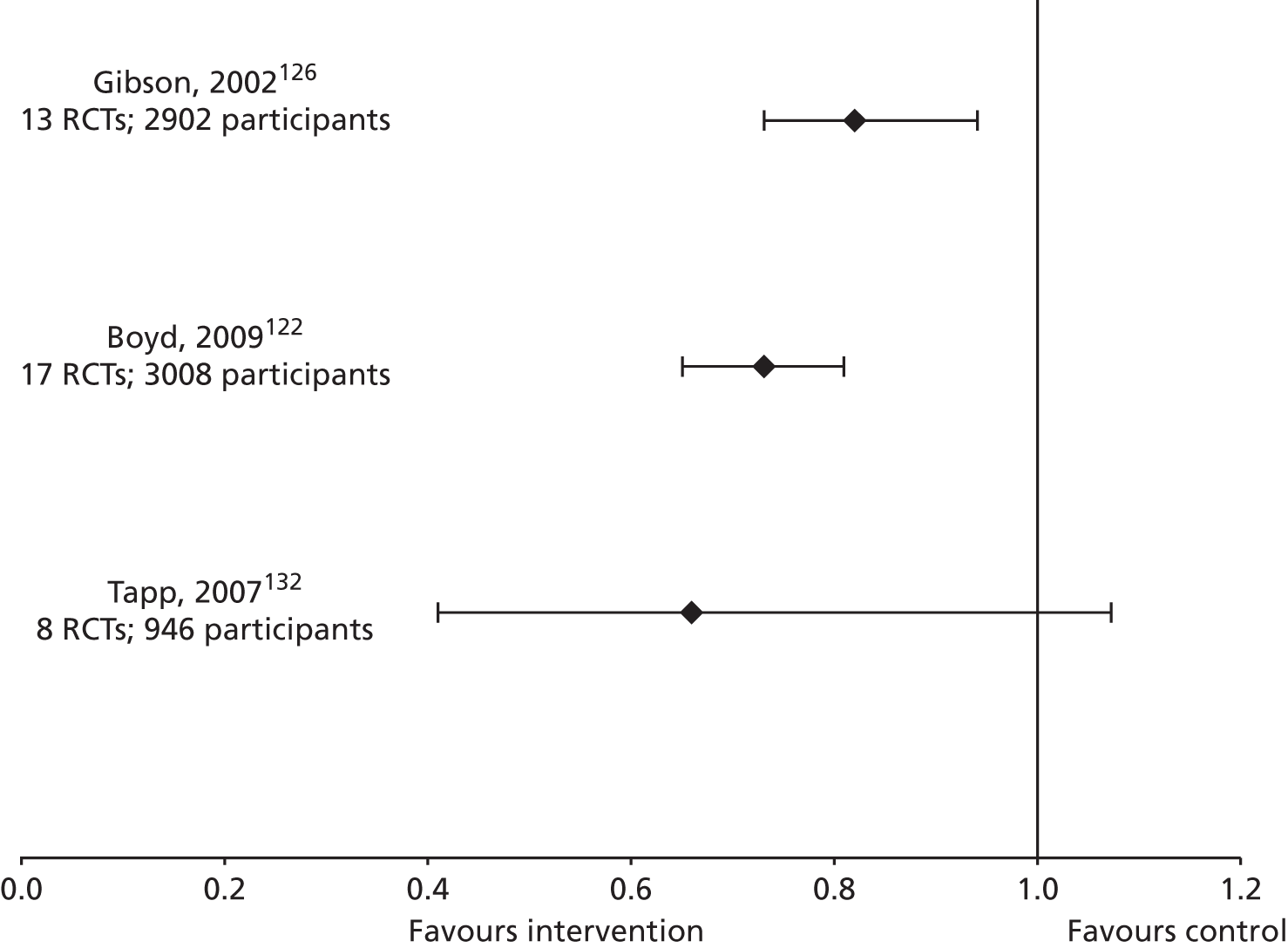
Unscheduled primary care was reported in two meta-analyses, both finding a risk ratio of 0.68 to favour intervention, which was statistically significant in both cases. 122,126 Length of hospital stay was reported in one review.
In addition to meta-analysis results on health-care utilisation, narrative synthesis of health-care utilisation comparing intervention with control was presented in six reviews. 109,119,120,127,129,134 Hospital admissions were significantly reduced in two high-quality reviews,120,127 with Bailey et al. 120 specifying this effect to be with the paediatric population only, whereas a third high-quality review focusing on home-based self-management education for paediatric asthma education found mixed effects from five RCTs. 134 Evidence for effect on ED visits was conflicting in one high-quality review,120 whereas another high-quality review found a significant beneficial effect of the intervention. 127 Acute care visits, taken to encompass both ED attendances, and acute visits to the GP, were found to be significantly reduced in one review. 134 Two lower-quality reviews reported health-care utilisation outcomes more generally. Newman et al. ’s review109 of self-management interventions found 7 of 11 RCTs to show a reduction in health-care use, whereas Postma et al. ’s129 culturally specific environmental interventions for children reported results from six RCTs to favour intervention for unscheduled asthma-related clinical utilisation, and to be clinically significant.
Quality of life
Pooled estimates on QoL from meta-analysis comparing intervention with control were presented in three high-quality reviews. 120,122,126 Bailey et al. ’s review120 of culturally orientated programmes and Gibson et al. ’s review126 of self-management and educational programmes, both detected a significant difference between intervention and control to favour intervention, whereas Boyd et al. ’s review122 focusing on educational interventions in children or their parents found no significant difference (Figure 18).
FIGURE 18.
Asthma: forest plot for QoL.
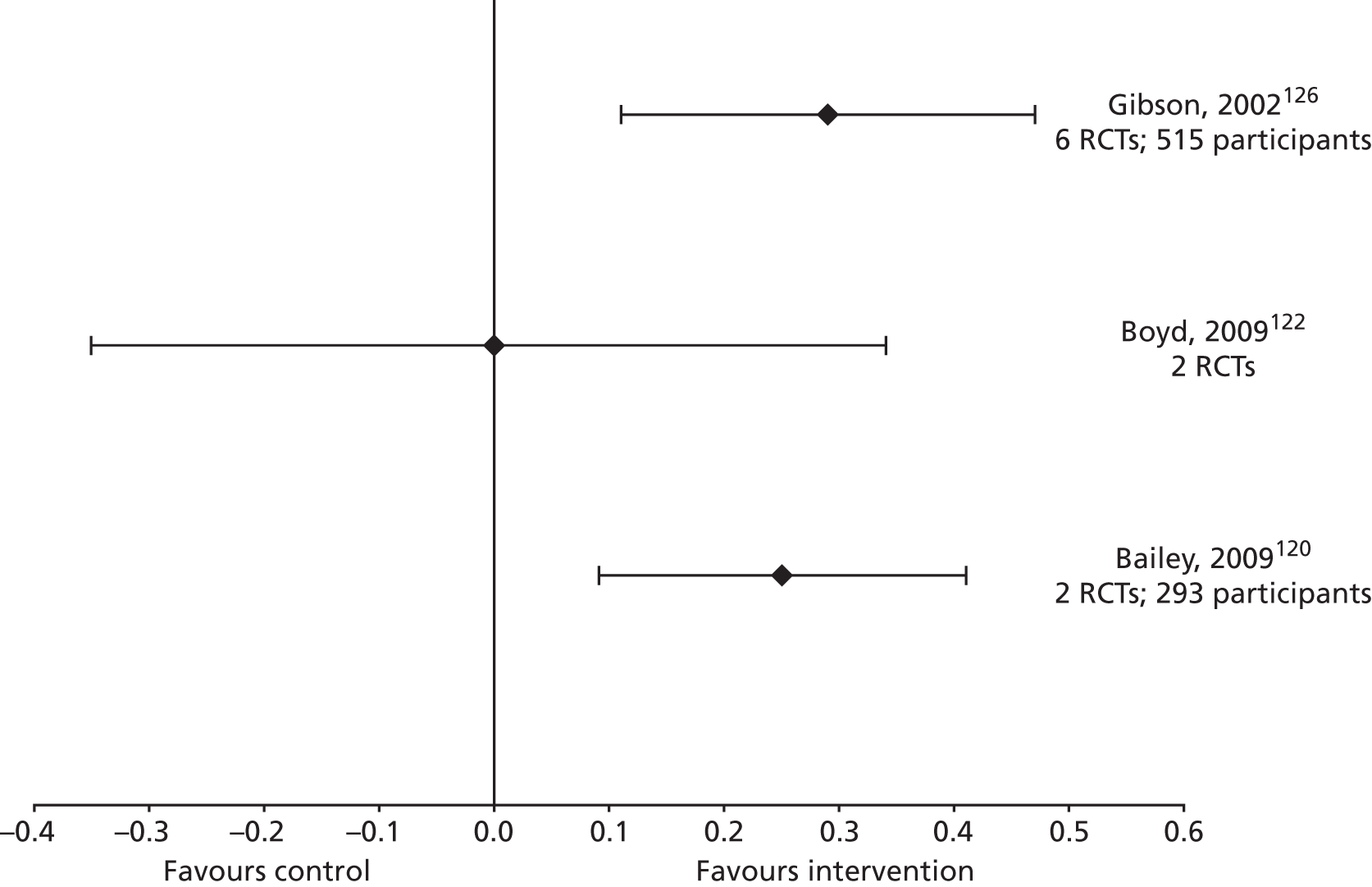
In addition, QoL was reported narratively in six reviews, which present an overall mixed picture. Promising results on QoL are reported in two reviews. Coffman et al. ’s125 lower-quality review of school-based interventions reports a statistically significant improvement in QoL in four of six RCTs, whereas Newman et al. 109 found half of studies measuring QoL to detect significant benefits. The review by Chang et al. 124 which explored education programmes delivered by IHWs found a trend suggesting improvement in carer QoL in the one RCT included in the review, but this did not reach statistical significance. The suggested benefits for QoL are not supported by three other reviews,129,132,134 which report no overall evidence of benefit in QoL from between one and five RCTs.
Lung function
Pooled outcomes for forced expiratory volume in 1 second (FEV1) were reported in three high-quality reviews122,126,130 and peak expiratory flow rate (PEFR) was also pooled in three high-quality reviews. 126,130,132 Neither of the outcomes could be presented as forest plots due to the use of different units in the presented ESs. All three reviews suggested that their interventions were associated with benefit in PEFR; these effects reached statistical significance in two reviews. 127,130 Intervention was not associated with a significant improvement in FEV1 in any of the three reviews reporting on the outcome, although two did demonstrate trends towards a beneficial effect. 127,130 Three reviews present narrative synthesis of lung function outcomes. 109,127,129 Gibson et al. 126 found mixed results, with improved airway calibre only in a subgroup of the intervention which used action plans based on personal best PEFR, and not on plans based on per cent predicted PEFR. Newman et al. 109 found an improvement in lung function in 8 of 14 RCTs. Postma et al. 129 found mixed effects on lung function from four RCTs.
Secondary outcomes
Symptoms and exacerbations
Meta-analysed results for asthma symptoms were reported in one review, reporting on nocturnal asthma. 126 A significant improvement in nocturnal asthma was found in the intervention compared with control. Furthermore, seven reviews of mixed quality present narrative results. 119,120,125,126,129,132,134 Significant reductions were found for paediatric asthma symptoms120,129 and nocturnal awakening and symptom scores. 119 Coffman et al. 125 reported a significant reduction in days with symptoms in three of eight RCTs, and a reduction in nights with symptoms in one of three RCTs. Symptoms were reported in only one RCT in Tapp et al. ,132 finding no difference in various symptom measures. Lack of effect was also reported for adult exacerbations in one review. 120 Additionally, the use of oral corticosteroids was assessed in two reviews: mixed effects were reported in one review from four RCTs126 and evidence from just one RCT found rates of decrease in mean courses of oral corticosteroids were faster for intervention compared with control over 18-month follow-up. 134
Activity limitation
School or work absenteeism was the most frequently reported measure of activity limitation, with pooled ESs presented in two meta-analyses. 126,132 Gibson et al. 126 reported a statistically significant reduction in days off work or school, while findings by Tapp et al. 132 showed a trend towards reduced risk of absenteeism that did not reach statistical significance.
Four reviews presented narratively synthesised data on activity limitation with mixed findings. Chang et al. 124 found a significant improvement in school absenteeism in the only RCT included within the review, whereas Coffman et al. 125 found school absences to be significantly reduced in 5 of the 13 RCTs reporting on the outcome. Toelle and Ram133 and Welsch et al. 134 found no significant reduction in absenteeism; however, these findings come from a total of two RCTs and one RCT respectively.
Self-efficacy
Self-efficacy was very infrequently reported in the reviews, and was not pooled in any meta-analysis. Narrative results were presented in just one review, with statistically significant effects found in five of six RCTs. 125
Self-management behaviours
Scheduled clinic attendance was the only self-management behaviour to be pooled in meta-analysis, with a significant benefit in the behaviour reported. 134 Narrative syntheses provide more evidence of the effect of interventions on self-management behaviours. The only RCT identified by Chang et al. 124 demonstrated significant improvement in parents’ asthma skills, possession and interpretability of action plans. Self-management behaviours were found to be significantly improved in all six RCTs reporting on the outcome in Coffman et al. 125 Newman et al. 109 found that of those interventions to target some aspect of behaviour, 57% reported a significant change in behaviour. Behaviour change was measured in four studies in Postma et al. ,129 finding mixed effects with positive changes tied to resource provision. Tapp et al. ’s132 review of high-quality studies found a suggestive improvement in inhalation technique and awareness of PEFR readings from one RCT.
Two reviews looked at interventions that were specifically designed to enhance a certain self-management behaviour, and therefore reported on no outcome other than the self-management behaviour of interest. 128,131 Ring et al. ’s131 high-quality review, which explored the promotion of action plan use, found self-management education interventions to be associated with a significant increase in the number of people/parents with action plans in four of five RCTs, and with significantly higher action plan use in one RCT. One of two RCTs exploring the role of telephone consultations reported a significant increase in the number of people with an action plan, and both RCTs reported greater understanding on how to use the action plan. Asthma clinics were associated with increased ownership in both RCTs, but this difference only reached statistical significance in one study. Two studies explored asthma management systems, one finding more children to receive action plans, the other finding significantly higher action plan use. Education of HCPs was explored in one study, which found that the intervention may facilitate action plan use. Last, one RCT examined a quality improvement intervention and found no overall effect.
Moullec et al. ’s128 lower-quality review of interventions for improving adherence to ICSs found the smallest pooled effect in adherence measures for interventions which contained only one component of the Chronic Care Model (CCM). ESs for adherence measures were larger for interventions with two CCM components, and larger still for interventions with four CCM components. All adherence effects were statistically significant. One RCT compared joint decision-making negotiated between clinician and patient with decisions made by physicians alone, and found a significant effect to support joint decision-making.
Comparisons between self-management support interventions
One review included within the meta-review focuses on comparing two forms of action plans: those based on symptoms and those based on peak flow readings. 118 A subsection of Toelle and Ram133 also explored this same question. In addition, a number of reviews attempted to characterise the effective components of interventions through subgroup analysis or meta-regression.
Symptom-based written action plans versus peak flow-based written action plans
Bhogal et al. ’s118 high-quality review of WAPs for children reports pooled estimates in comparisons between WAPs based on symptoms and WAPs based on peak flow readings. A significant difference was detected for the outcome of at least one acute visit, favouring symptom-based WAPs. For the other outcomes of hospital admissions, school absenteeism, requiring systemic steroids, acute care visits per activation of step 2 of the action plan, average % predicted FEV1 and child QoL, no significant difference was found between WAPs based on symptoms and those based on peak flow.
Toelle and Ram’s133 high-quality review also compared the use of WAPs based on symptoms with those based on peak flow readings. This review also found a significant difference in unscheduled doctor visits which favoured symptom-based WAPs, but found no difference in hospitalisation or ED visit rates.
Another high-quality review that compared WAPs based on symptoms with those based on PEFR found the two forms to be equivalent for hospitalisations and unscheduled doctor visits, with mixed effects found for other outcomes. 130
When comparing symptoms or PEFR to guide medication use, Newman et al. ’s109 review detected little difference in outcome measures.
Detailed nature of self-management support
Bhogal et al. 118 also made comparisons between different types of WAPs. Using WAPs with more than three steps but no graphics, significantly fewer children assigned to symptom monitoring required acute care visits. There was no group difference with a three-step streetlight WAP. However, there was no significant difference between the two subgroups. Significantly fewer children assigned to symptom-based WAPs required acute care visits compared with a group engaged in peak flow monitoring only when symptomatic. When comparing symptom-based to daily peak flow monitoring there was no significant difference.
A high-quality review focused on educational interventions targeted at children or their parents performed subgroup analysis to investigate if type and timing of interventions (or timing of outcome assessment), affected results but found no significant effects. 122
The lower-quality review of interactive computer educational programmes makes some observations on the optimal nature of the interventions. The review authors found no single intervention to be superior in all outcomes, but noted some beneficial effects were seen only within a limited time frame, or in a subset of patients. They stated that clinical outcomes did not appear to be correlated with programme time. 123
A high-quality review of explicit self-management found that optimal self-management (defined as involving a WAP for self-management of medications for exacerbations, together with self-monitoring and regular medical review) led to significant reductions in asthma-related hospitalisations and ED visits. Two interventions which included regular review of medication also found significant reduced ED visits. 126 Additionally, the follow-on publication127 found the benefits of a WAP to be consistent for any number of action points (two to four), but that a traffic light presentation was not consistently better than a conventional presentation. The efficacy of incomplete and non-specific action plans was inconclusive.
Newman et al. 109 observes that although most studies used education with an action plan to show some improvement in lung function, others that used this approach did not find any improvements.
The lower-quality review of environmental interventions for children observed that the interventions with higher intensity and frequency reported the most positive health outcomes. 129
Who benefits most?
One high-quality review exploring educational interventions targeted at children or their parents performed subgroup analysis to investigate whether or not age of participants affected results. The analysis did not produce any significant findings122 (see Figure 19 for a summary of the quantitative evidence).
FIGURE 19.
Asthma: summary of the quantitative evidence.
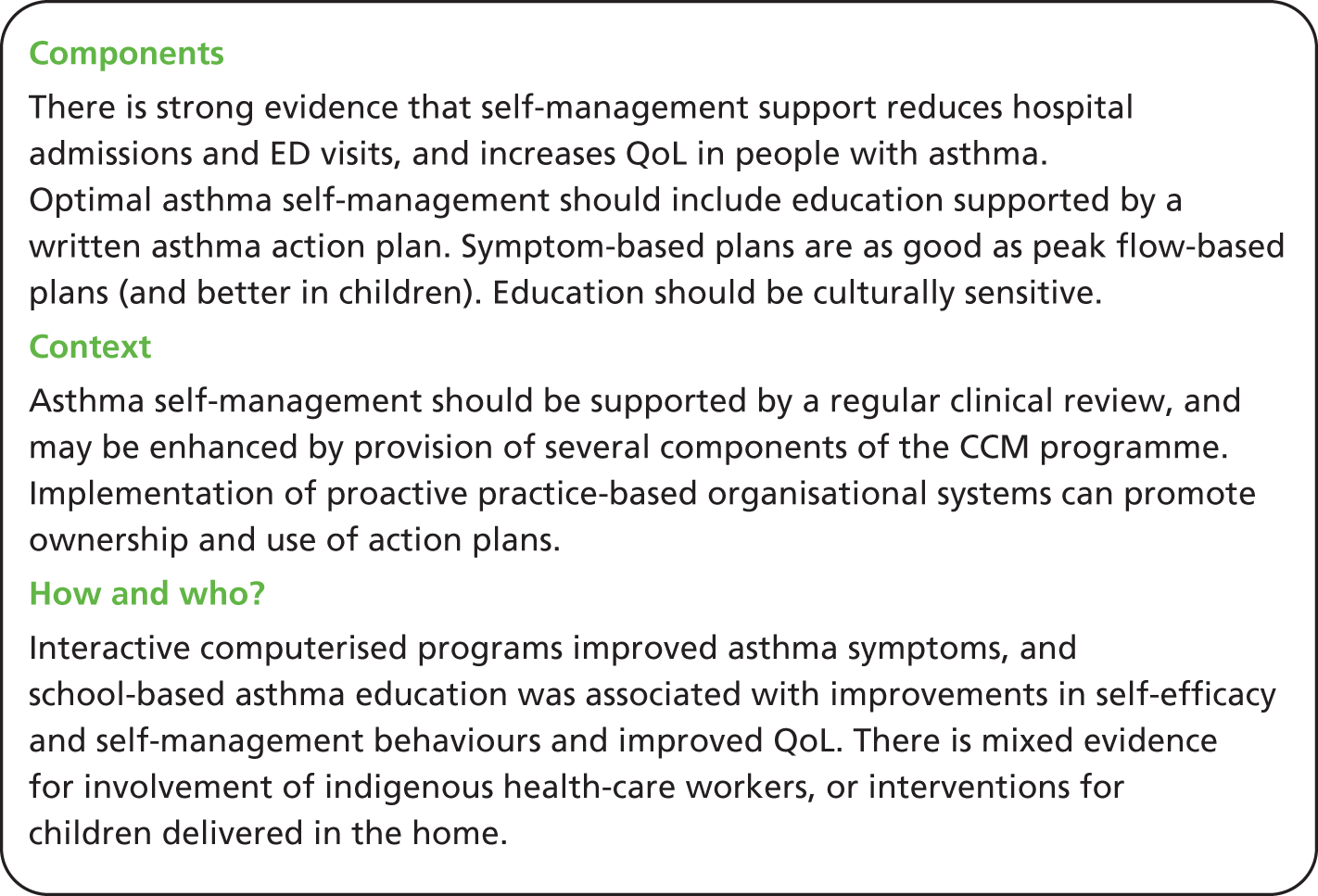
Mixed-methods discussion
The quantitative evidence for self-management support in asthma is highly developed. The reviews identified provide high-level evidence to inform optimal self-management support design and delivery. In contrast, only one qualitative review was identified which could inform self-management support. Although this lack of qualitative evidence limits a mixed-methods synthesis, there are some conclusions which can be reached by considering both the quantitative and qualitative evidence together.
Quantitative evidence demonstrates the value of action plans in reducing health-care utilisation and improving airway calibre. However, qualitative work identifies some potential barriers to the optimal use of these action plans. HCPs and patients hold opposing views as to who should be using action plans. This mismatch in ideas highlights the need for more education on action plan use for both professional and patient groups. The qualitative work also highlights the concern that HCPs may not be providing action plans to some patients who feel that they would benefit from them. This suggests a change in culture is needed to promote action plan use, particularly considering the strong evidence to support the effectiveness of action plans. Evidence from interventions promoting action plan use provides evidence to support the use of proactive practice-based organisational interventions to ensure that these effective interventions are properly implemented.
Qualitative work also revealed a contrast in perceptions of asthma between professionals and patients, with patients viewing their asthma as an acute intermittent condition rather than a chronic condition requiring long-term prevention. Such beliefs are likely to lead to suboptimal asthma self-management. This may help explain a key quantitative finding: that education on the nature of asthma and its management has beneficial effects on health-care utilisation, QoL and absenteeism.
A central message emerging from the qualitative literature is the need for HCPs to acknowledge the expertise that the patient holds, and to understand that a divergence from a strictly medical model of management does not necessarily equate to a non-compliant patient. Effective self-management support must always have the patient at its centre; effective partnerships between HCPs and patients are required in order to achieve this. The quantitative evidence supporting the value of regular clinical review may support the development of this patient-centred collaborative partnership.
Chapter 10 Priority meta-review: self-management support for people with depression
Meta-review of qualitative systematic reviews
Systematic reviews identified
From 8488 papers eligible for screening, three papers fulfilled the inclusion criteria135–137 (Figure 20). The reviews included 26 primary studies of which three overlapped between two reviews135,136 (Table 43). Four of the 11 primary studies in Malpass et al. 136 were published in more than one paper.
FIGURE 20.
Depression: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for qualitative meta-review. 63
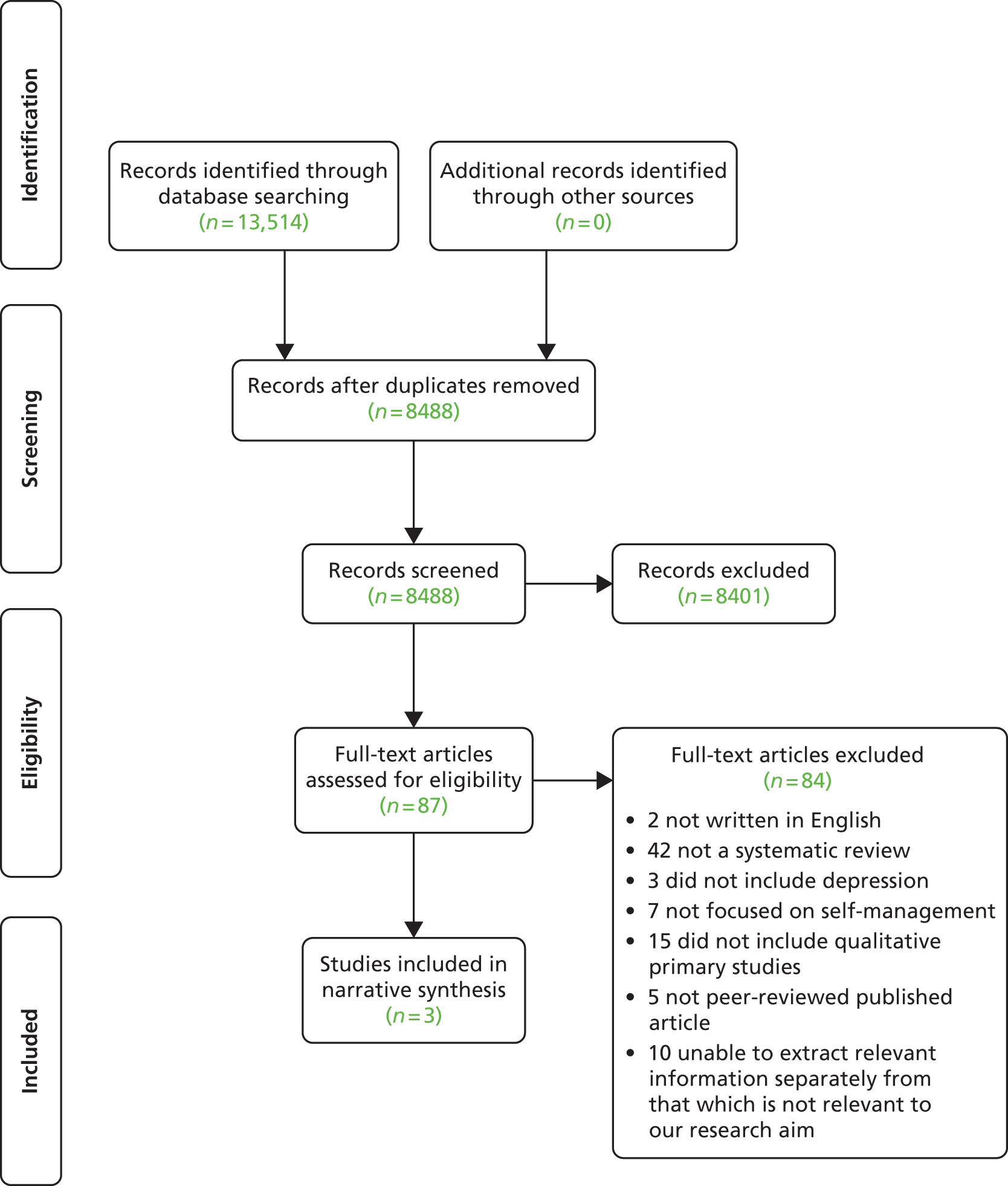
| Study | Dundon 2006137 | Khan 2007135 | Malpass 2009136 |
|---|---|---|---|
| Dundon 2006137 | 6 | ||
| Khan 2007135 | 0 | 9 | |
| Malpass 2009136 | 0 | 3 | 11 |
The three reviews were published between 2006 and 2009 in the UK135,136 and the USA. 137 In addition to published qualitative primary studies, Dundon137 included two unpublished dissertations. The three included reviews all purported to use a meta-ethnographic approach but focused on different aspects of depression: adolescents’ experiences (Dundon137), patients’ experience of depression management in primary care, support groups, self-help clinics (Khan et al. 135) and patients’ experience of antidepressant medication (Malpass et al. 136) (Table 44).
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary of key findings |
|---|---|---|---|
| Dundon 2006137 (Qualitative) |
The aim of this study was to unify the voices of the adolescents who have participated in qualitative research in order to contribute to the theoretic base of the experience of adolescent depression, affect future research and guide clinical practice | 6 | Six themes that outline the course of adolescents who struggle with depression:
|
| Khan 2007135 (Qualitative) |
The study aimed to identify qualitative studies of patient experience of depression management in primary care, synthesise these studies to develop an explanatory framework, and then apply this framework to the development of a guided self-help intervention for depression | 9 | The synthesis revealed a number of themes, including the nature of personal experience in depression; help seeking in primary care; control and helplessness in engagement with treatment; stigma associated with treatment; and patients’ understandings of self-help interventions |
| Malpass 2009136 (Qualitative) |
The main aim in this synthesis was to derive new conceptual understandings of patients’ experiences of antidepressants to inform a future longitudinal qualitative study that will examine the extent to which doctors and patients achieve concordance over the prescription of antidepressants for depression | 11 | Patients’ experience of antidepressants is characterised by the decision-making process and the meaning-making process, conceptualised in the review as the ‘medication career’ and ‘moral career’ |
Quality assessment
Only one paper scored high136 (30/40) and one paper scored just under the cut off (< 30) with 27/40. 135 A third lower-quality paper137 performed a less comprehensive literature search and failed to assess and document the quality of its included studies. Therefore, less weight was applied to this paper and the results were read with caution (Table 45).
| R-AMSTAR criteria | Dundon 2006137 | Khan 2007135 | Malpass 2009136 |
|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 1 | 1 | 2 |
| Was a comprehensive literature search performed? | 3 | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 2 | 1 | 1 |
| Was a list of studies (included and excluded) provided? | 1 | 2 | 2 |
| Were the characteristics of the included studies provided? | 4 | 3 | 4 |
| Was the scientific quality of the included studies assessed and documented? | 1 | 2 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 2 | 2 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 |
| Was the conflict of interest stated? | 1 | 4 | 1 |
| Total score/40 | 23 | 27 | 30 |
| Quality rating (low = < 30; high = ≥ 30) | Low | Low | High |
Findings
The papers did not explicitly focus on self-management support, suggesting a gap in the research. However, the emerging themes had a high degree of saturation and had the potential to inform self-management support.
Two metaphors, ‘control’ and ‘tension’, arose from the reviews and are considered the central metaphors of this meta-review. Many of the themes encompassed by these two metaphors were described at multiple junctures in the timeline of depression. The concept of depression as an individually unique experience emerged as a salient theme overarching both central metaphors, with patient’s experiences often extending beyond typical definitions of depression (Table 46).
| Central metaphors | Themes | Reference | Illustrative quotation |
|---|---|---|---|
| Control | Language | Dundon 2006 (p. 386)137 |
|
| Khan 2007 (p. 207)135 |
|
||
| Self-concept | Dundon 2006 (p. 386)137 |
|
|
| Khan 2007 (p. 207)135 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Malpass 2009 (p. 164)136 |
|
||
| Malpass 2009 (p. 166)136 |
|
||
| Emotions | Dundon 2006 (p. 386)137 |
|
|
| Dundon 2006 (p. 388)137 |
|
||
| Dundon 2006 (p. 389)137 |
|
||
| Khan 2007 (p. 207)135 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Malpass 2009 (p. 161)136 |
|
||
| Malpass 2009 (p. 165)136 |
|
||
| Isolation | Dundon 2006 (p. 388)137 |
|
|
| Dundon 2006 (p. 388)137 |
|
||
| Khan 2007 (p. 207)135 |
|
||
| Coping strategies | Dundon 2006 (p. 391)137 |
|
|
| Khan 2007 (p. 207)135 |
|
||
| Malpass 2009 (p. 164)136 |
|
||
| Seeking help | Dundon 2006 (p. 390)137 |
|
|
| Dundon 2006 (p. 390)137 |
|
||
| Khan 2007 (p. 207)135 |
|
||
| Malpass 2009 (p. 164)136 |
|
||
| Contact with health services/previous experiences | Khan 2007 (p. 207)135 |
|
|
| Malpass 2009 (p. 162)136 |
|
||
| Malpass 2009 (p. 163)136 |
|
||
| Patient–professional relationship | Dundon 2006 (p. 390)137 |
|
|
| Khan 2007 (p. 209)135 |
|
||
| Malpass 2009 (p. 162)136 |
|
||
| Malpass 2009 (p. 163)136 |
|
||
| Information, resources and education | Dundon 2006 (p. 390)137 |
|
|
| Dundon 2006 (p. 391)137 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Khan 2007 (p. 210)135 |
|
||
| Malpass 2009 (p. 162)136 |
|
||
| Individuality/beyond the typical (themes spans both control and tension metaphors) | Dundon 2006 (p. 386)137 |
|
|
| Tension | Khan 2007 (p. 209)135 |
|
|
| Malpass 2009 (p. 163)136 |
|
||
| Responsibility and duty | Dundon 2006 (p. 388)137 |
|
|
| Khan 2007 (p. 207)135 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Malpass 2009 (p. 164)136 |
|
||
| Support network | Dundon 2006 (p. 389)137 |
|
|
| Dundon 2006 (p. 390)137 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Stigma | Dundon 2006 (p. 386)137 |
|
|
| Dundon 2006 (p. 386)137 |
|
||
| Dundon 2006 (p. 390)137 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Khan 2007 (p. 209)135 |
|
||
| Malpass 2009 (p. 164)136 |
|
||
| Malpass 2009 (p. 164)136 |
|
Control
This metaphor covered patients’ feelings of loss of control, the language they used to convey this and pathways they took to regain it. The language used by individuals provided a sense of struggle or battle,137 with patients feeling defenceless and powerless,137 trying to fight and conquer135 the ‘enemy or intruder’137 of the symptoms and life with depression that is taking control. 135–137 Loss of control was also attributed to taking ‘unnatural’136 antidepressants resulting in individuals feeling that their sense of self had been threatened135–137 and that depression and antidepressants had changed their identity135 and personality. 135,137 In terms of antidepressants, individuals either felt a new corrected self was ‘revealed’, that their pre-depressive self was ‘restored’ or that an ‘enhanced self’ had replaced their ‘authentic self’. 135
The symptoms of depression, such as unprovoked anger and low motivation and energy,135,137 caused some individuals to feel abnormal136,137 and socially isolated. 135,137 Associated with this were feelings of self-deficiency,135 ‘weakness and vulnerability’136 and shame135–137 that their illness did not allow them to fulfil their social roles and duties. 135–137 In order to counter this and regain control, some patients tried to normalise their thoughts and behaviour. 136,137 Other coping strategies included ‘substance abuse, smoking or cutting’137 as well as more positive techniques such as ‘distraction’135 and the use of safe places. 135 Failure of these was a key trigger for seeking help,135–137 more so than the symptoms of the illness. 135
Some individuals found that seeking help led to further loss of control,135 as their hesitancy to divulge their feelings and question information given to them,135–137 led to them taking a more passive role and accepting treatment without full comprehension. 135,136 There was also an element of uncertainty about the role of health professionals in the management of depression and how active they, as the patient, could be. 135,136 However, others experienced that ‘acquiring a safe place to express and admit feelings’ and ‘joining support groups’137 allowed them to regain control. This was achieved through greater involvement, shared decision-making and regular follow-up, which created more positive and concordant relationships. 135,136 Patients felt more confident, useful and had a ‘sense of ownership of recovery’. 136 This was due to their improved expectations and understanding136 coupled with reduced misconceptions135 leading to better adherence. 135,136
Some patients sought to regain control from medication by stopping treatment early136 and those participating in guided self-help often altered the prescribed guidelines and activities to fit into their lives. 135 Improved information and resources were found to be extremely supportive and valuable for individuals to understand their experiences and the management options available to them135–137 in order to take back control. Importantly, education about depression and helpful resources were also necessary for health professionals, friends, family and educators of people with depression and to society in general as a means of improving public perception. 137
Tension
This metaphor encompassed the concepts of constant evaluation, problem-solving and decision-making evident throughout an individual’s experiences of depression. For example, there was tension between the barriers and the necessity to seek help. The barriers included negative self-concepts and perceived ‘lack of legitimacy’135 and stigma135–137 associated with having a psychological illness135 and a label of depression. 135,137 The need for help was considered because of feelings of guilt about the effect on others, a sense of responsibility135–137 and a ‘duty to be well’. 136 This was related to the tension between individuals feeling distant, isolated and misunderstood135,137 by friends and family because of the symptoms of depression and being encouraged and supported by them to recognise these symptoms and seek help. 135–137
The decision to seek help was balanced against individuals’ reliance on their own and others previous experiences and low expectations of the helpfulness of health services. 135–137 Accepting help involved tensions between individuals’ existing health beliefs, and the biomedical135,136 and psychological135 causal models on which antidepressant treatment and cognitive–behavioural therapy (CBT) are based. Though patients accepted aspects of these models, their beliefs tended to vary or extend beyond them135,136 and included significant life events, current circumstances and stressors. 135–137 However, the knowledge acquired from previous experiences and existing health beliefs was used as a tool for understanding interventions135 and a measure to compare136 and complement135 information received from health professionals.
Accepting treatment led to tension between the individual’s perceptions of reduced and doubled stigma. 135,136 Accepting treatment was an acceptable action to counter their symptoms136 and provided legitimacy to their illness. However, taking medication was simultaneously believed to indicate weakness and a failure to cope, and added to the perceived stigma of having depression. 135,136 Similarly, individuals experienced tension between a sense of relief at being able to ‘return to function’136 and the sense that they were reliant on the support of medication to do so. 135,136 This in turn was associated with individual’s balancing ‘feeling’ healthy due to the control of medication with ‘being’ healthy due to personal control of their symptoms. 135
Support for self-management
The synthesis enabled these findings to be integrated to provide a broader picture to inform those who commission self-management support:
-
Support should be individually tailored, incorporate the language used by individuals, and recognise the importance of their own coping strategies and extend these into self-management interventions. Self-awareness and the desire to regain control could be incorporated as a mechanism for change and self-management.
-
The attitudes and experiences of patients and health professionals regarding the management of depression could be explored and used to inform education. This in turn might be used to facilitate the individual in taking an active role in their management and regaining control with support from the professional.
-
Information and resources should be specific and appropriate, and health services and professionals accessible and approachable.
-
Education and training in problem-solving and decision-making skills may support patients with the constant tensions they experience.
-
Support and services might include both the person with depression and others closely involved in their lives. This could help individuals balance their sense of responsibility and duty and support them through feelings of isolation and perceived stigma, and promote positive outcomes.
Meta-review of quantitative reviews
After scoping the quantitative review literature, it was decided that a quantitative meta-review of depression self-management support would not be undertaken. The remainder of this chapter provides our rationale for this conclusion.
Systematic reviews identified
After screening a total of 3865 titles and abstracts, 71 articles were included for team discussion, with the view of potentially including for full-text screening. Of the 71 articles, 27 were identified as focusing specifically on CBT. The remaining 44 articles broadly explored three areas felt to be most closely allied to self-management support: psychological therapies not explicitly labelled CBT (including mindfulness-based therapy, behavioural therapies, psychotherapeutic and psychosocial treatments); system-level organisational interventions (including chronic disease management models, case management, team care approaches and shared care); and telehealth applications (including tele- and mobile-mental health). In addition to these categories, a small number of reviews exploring self-help, and mutual help or peer support, were identified.
What is self-management support in depression?
Cognitive–behavioural therapy
As CBT was so dominant in the literature, it was important to ascertain whether or not this well-recognised form of treatment in depression met our definition of self-management support. According to the British Association for Behavioural & Cognitive Psychotherapies, CBT involves:
the identification of personalised, usually time-limited therapy goals and strategies which are continually monitored and evaluated. The treatments are inherently empowering in nature, the outcome being to focus on specific psychological and practical skills aimed at enabling the client to tackle their problems by harnessing their own resources . . . Thus the overall aim is for the individual to attribute improvement in their problems to their own efforts, in collaboration with the psychotherapist.
Emphasis added 138
Lorig and Holman identify five core self-management skills which self-management support should aim to develop: taking necessary actions; problem-solving; making decisions; forming a partnership with a health-care provider; and appropriate resource utilisation. 25 Many of these skills are supported within the practice of CBT, for instance, taking action can involve goal-setting, a prominent feature of CBT. The psychological and practical skills developed in CBT aim to develop an individual’s ability to problem-solve and make decisions, two further core skills highlighted by Lorig and Holman’s work. Furthermore, the emphasis on collaboration between the individual and the psychotherapist reflects the core self-management skill of partnership formation. We therefore view CBT as used in depression as a form of self-management support.
Other psychological therapies
We explored other psychological therapies to determine whether or not these also fell within our broad self-management support definition. We found many of the therapies identified within our searches to be built on, or to contain elements of, CBT. This challenged our initial distinction between CBT-based interventions and non-CBT interventions, and a broad spectrum of CBT and related psychotherapies was felt to be a more appropriate form of classification.
System-level organisational interventions
On closer inspection, these reviews were felt to have a broader scope than just self-management support, and although some elements of such high-level interventions may have supported aspects of self-management, this was not felt to be the main focus of such reviews.
Telehealth applications
Telehealth interventions are a way of delivering a service or information remotely and a large variety of interventions can be delivered via this modality. Although self-management support could be delivered through telehealth applications, the reviews we identified did not focus specifically on self-management support and instead looked at a broad range of interventions targeted at improving the care of people with depression.
Self-help and mutual help
Several reviews of self-help for people with depression were identified. These reviews tended to identify a heterogeneous group of interventions, including bibliotherapy, alternative medicine, massage and other unicomponent interventions which we would not consider self-management support. Other self-help interventions had a more behavioural focus and overlapped considerably with CBT-based interventions.
Two reviews explored mutual help, or peer support interventions. One review distinguished mutual help from group-based CBT, excluding any group-based psychotherapy; methodology was unclear in the other review.
The focus for our meta-review
After considering the possible forms of self-management support explored at review level, it was decided that CBT and CBT-related psychological therapies formed the vast majority of the relevant evidence base for this meta-review.
However, there is a strong and established evidence base for the use of psychological therapies involving CBT for managing depression. Current National Institute for Health and Care Excellence (NICE) guidelines, updated in 2010, provide detailed recommendations on CBT and other therapies which involve CBT. 139 These guidelines were developed through extensive searches for systematic reviews alongside other sources including guidelines, primary studies and expert consensus. It was therefore felt that an additional meta-review on this subject was unlikely to contribute further to the established evidence base.
The current NICE guidelines recommend CBT in various forms, and in combination with other therapies, across a wide clinical spectrum of depression. CBT is a recommended part of therapy in persistent subthreshold depressive symptoms; mild to moderate depression; moderate and severe depression; and relapse prevention. NICE state CBT to have the best evidence base for efficacy of all psychological treatments for people with depression. 139
A meta-review of computerised cognitive–behavioural therapy (cCBT) conducted in 2011 acknowledged and built on the NICE guidelines, commenting that while evidence for CBT was established, the novel delivery mode was less researched. 140
In efforts to avoid duplication of work, and to ensure that limited resources were used to maximum effect, the review team decided not to progress any further with the quantitative review of depression self-management support.
Areas for further research
Although NICE offers a comprehensive review of the evidence on CBT and related psychotherapies, the guidelines are specifically tailored to the requirements of the NHS in England and Wales.
The evidence of psychotherapies in low- and middle-income countries have been reviewed in a recent meta-analysis; however, review authors highlight the need for implementation studies to understand the effectiveness of implementing such interventions in resource-limited settings, and the potential barriers which might be faced in these contexts. 141 Furthermore, a recent commission by The Lancet on technologies for global health highlights the need for more research on cCBT in low- and middle-income settings where the current evidence base comes only from high-income countries. This is especially important as such low-cost forms of CBT delivery may be particularly advantageous in resource-constrained settings. 142
Discussion based on the qualitative meta-review
In summary, the knowledge of different aspects of a person’s experience of depression allowed a holistic picture to develop and a range of findings to be revealed. In the context of adolescents with depression,137 primary care, support group, and self-help clinic users135 and patients taking antidepressants,136 the experience of depression was characterised by loss of control and contending with numerous tensions. Therefore, for such individuals, self-management support that is tailored to their particular needs and understands the importance of these characteristics is recommended.
Individuals’ experience of depression management, such as taking antidepressants and ‘guided self-help’, was fraught with an array of emotions. 135 These included confusion about the symptoms they were experiencing, the effects of management on their sense of self and ambiguity about the role of health-professionals. Therefore, improving changes in self-concept and encouraging the positive effects of a concordant relationship are key factors that can be accomplished as part of self-management support.
The significance of the views of family, friends, health professionals and other people who individuals with depression come in contact with was a pertinent finding. Negative views and relationships were attributed to worsening the symptoms of depression,135,137 acting as barriers to seeking help135–137 and continuing with management. 135,136 Positive relationships allowed individuals to gain a better understanding of their experience and encouraged help-seeking and confidence to maintain their management. 135–137 Therefore, a vital component of self-management support is the inclusion of the individual’s social network and health professionals in order to develop more positive relationships and a better understanding of depression in society.
Chapter 11 Additional meta-review: self-management support for individuals with chronic obstructive pulmonary disorder
Meta-review of qualitative systematic reviews
Systematic reviews identified
The COPD qualitative meta-review included three reviews143–145 (published in peer-reviewed journals between 2007 and 2009) reporting 25 unique qualitative primary studies (published between 1990 and 2006) [see Figure 21 for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram].
FIGURE 21.
Chronic obstructive pulmonary disorder: PRISMA flow diagram for qualitative meta-review. 63
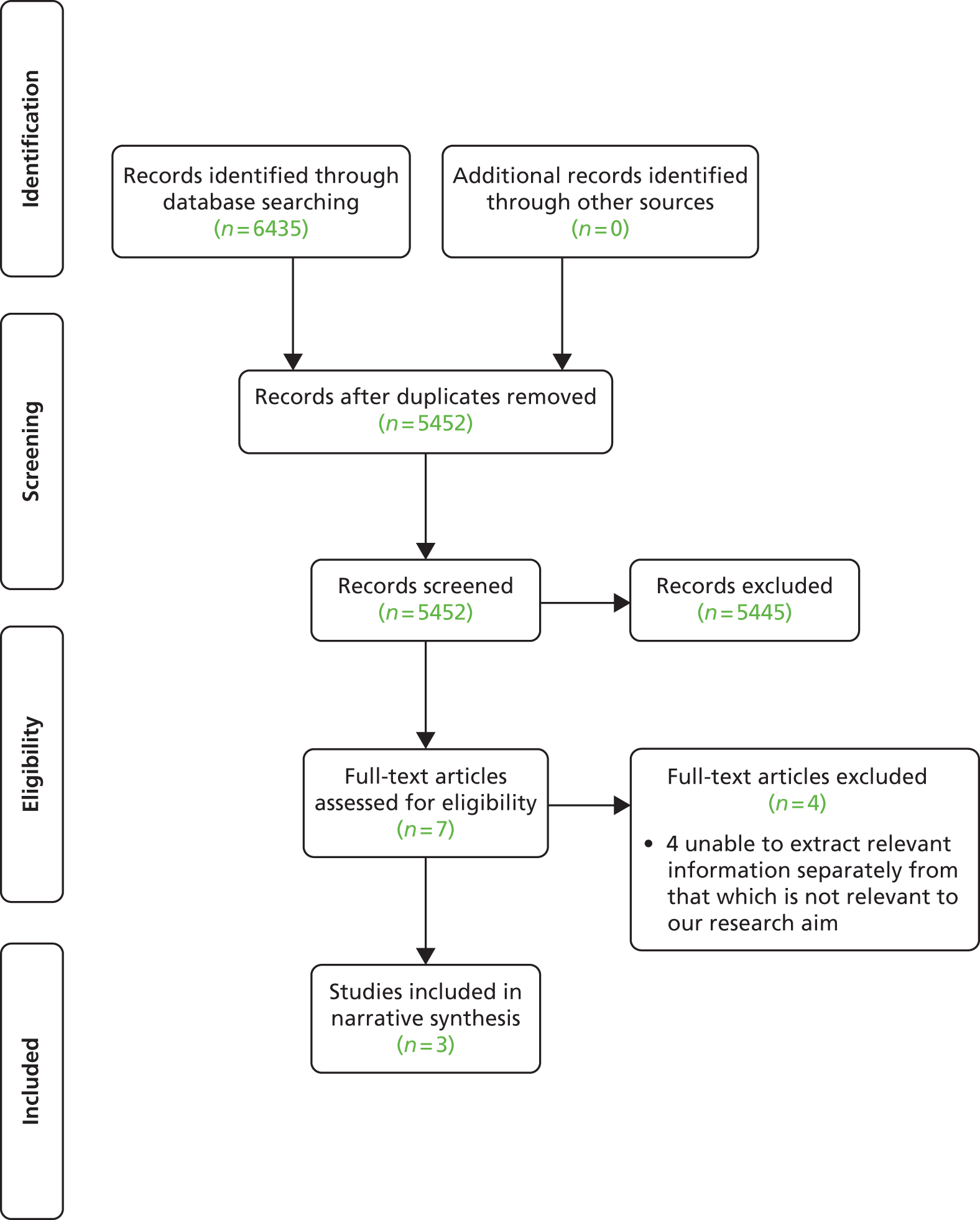
Two reviews were qualitative syntheses: one on COPD patients’ experiences of breathlessness143 and the other on experiences of long-term oxygen therapy (LTOT)144 (Table 47). The remaining review was a mixed-methods synthesis examining telemedicine services for patients with COPD. 145
| Authors, year | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Gysels 2007143 | To review and assess the evidence on breathlessness not within the boundaries of COPD but as a symptom in the context of different conditions that lead to breathlessness | 19 on COPD (out of 22) | Studies on COPD (19) outnumbered ‘all other conditions’ (3), one of which had COPD and cancer patients and so these were analysed separately. Within the COPD category most studies (17) considered the experience of breathlessness from the perspective of the patient, one study from the informal carer and one from the professional carer. Most studies sought to understand the meaning of the symptom in the patient’s daily life. The other papers distinguished the experience of acute exacerbations and the patient’s view on care. The studies explored the subjective component of breathlessness, as part of human experience and social life. The papers showed the influence that the meaning the symptom has on the patients’ ability to cope and on their management |
| Cullen 2009144 | To obtain qualitative research studies, describe the findings and synthesise patients’ experiences surrounding the use of LTOT. The specific review question is ‘What are the experiences of persons using LTOT?’ | Four (one on COPD, three on LTOT with majority of participants with COPD – results not separated) | Twelve findings formulated into four themes: adapting oxygen to life’s circumstances, living in a restricted world, self-management is fostered by oxygen, and submission and dependency. From the four themes, meta-synthesis resulted in two overarching themes: (i) persons prescribed oxygen rationalise its use while negotiating the interference with lifestyle; and (ii) the drive to care for one’s self is conflicted [sic]. Oxygen users face tremendous physical, psychological and emotional challenges which affect their ability to adhere to LTOT treatment guidelines. They strive to adapt and maintain mastery but eventually oxygen dependency results. These barriers and challenges are seldom addressed. Clinicians need to be aware and work with the patients to facilitate their use of oxygen. Inclusion of the patients’ perspective could guide practice and assist with the development of new interventions and management strategies |
| Bartoli 2009145 | To conduct a systematic literature review focused on telemedicine services for patients affected by COPD. In particular, it addresses (1) which telemedicine applications and related organisational models have been adopted for patients affected by COPD and (2) the impact of these applications | 2 qualitative on COPD out of 40 | 40 articles were considered. The adoption of telemedicine resulted in the reconfiguration of the existing practices and sociomaterial relationships. Roles may be redistributed (1) in the relationship between specialists and primary care physicians, (2) within the disease management programme between the clinical team and the patient, and (3) within the clinical team between nurses and specialists. These organisational changes must be understood and addressed The patient-centred approach promoted self-management as adoption of telemedicine services promoted awareness in patients with chronic conditions |
Quality assessment
All three reviews scored relatively low ranging from 23 to 27 out of 40 (Table 48).
| R-AMSTAR criteria | Gysels 2007143 | Cullen 2009144 | Bartoli 2009145 |
|---|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 2 | 1 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 | 3 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 2 | 1 |
| Was a list of studies (included and excluded) provided? | 2 | 2 | 3 |
| Were the characteristics of the included studies provided? | 2 | 2 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 3 | 1 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 3 | 3 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 2 | 4 | 3 |
| Was the conflict of interest stated? | 3 | 2 | 3 |
| Total score/40 | 27 | 27 | 23 |
| Quality rating (low = < 30; high = ≥ 30) | Low | Low | Low |
Findings
Support for self-management
Synthesis of these findings provides a broad picture to inform the context within which self-management may be supported.
-
There were many negative emotions listed in association with living with COPD and breathlessness, including isolation, vulnerability, uncertainty, loss and frustration, alongside regret and anger as a result of causing the illness themselves by smoking. Positive thoughts included deepened spiritualty and acceptance potentially facilitated by psychosocial support.
-
Breathlessness resulted in reduced activity (sometimes exacerbated by the lack of portability of treatment such as LTOT) leading to ‘misery and isolation, especially alongside stigma and guilt’ (p. 144). 144 The nature of the progression of COPD often led to a ‘fear of dying’ (p. 298),143 and was related to a vicious cycle of anxiety and dyspnoea. Alternative forms of activity and social support might improve the experience of living with COPD.
-
There was an ongoing tension between the constant need to monitor/manage symptoms in order to retain control and maintain their sense of self and a fear of dependence on medical treatment or social support. There was a conflict, for example, between adherence to LTOT to promote self-mastery of ADL and improved mobility, and non-adherence because of fear of addiction and dependence on the oxygen. Self-management support should facilitate and encourage self-mastery while discussing fears of dependence.
-
Tailored education to address the individual’s needs, condition and coping strategies was important and considered to promote adherence to treatment. Adherence to drug regimens was often better than adherence to lifestyle changes because of the fear of distressing dyspnoea and vulnerability associated with non-adherence to medication. Poor-quality information was perceived as adversely affecting adherence to lifestyle and management.
-
The relationship between a patient and their GP was viewed as important, and potentially facilitated adherence to treatment, promoted changes in health behaviour and enabled prompt medical advice rather than emergency hospital admission. There was a reported mismatch between the patient’s needs and the services received, as well as between primary and secondary care services. Specialist community nurses were viewed as potentially successful in meeting patient’s social, psychological and physical needs, and liaising with secondary care.
-
HCPs should encourage patients to discuss the complexities of their subjective experiences and their preferred model of self-management support. For example, some patients appreciated regular surveillance by a HCP, especially if they had a good relationship with their GP. Others cited negative experiences with impersonal and changing health-care systems; in this context additional ‘surveillance’ regimens (p. 285)143 could be perceived as troublesome and a challenge to the person’s autonomy.
-
Education for HCPs is important to enable optimal implementation of self-management support, for example adequate training on the efficient use of equipment and facilitate positive attitudes towards its use.
Meta-review of quantitative systematic reviews
Systematic reviews identified
Following the title and abstract screening, 39 articles were screened for eligibility, five of which were included in the COPD quantitative meta-review146–150 (Figure 22).
FIGURE 22.
Chronic obstructive pulmonary disorder: PRISMA flow diagram for quantitative meta-review. 63
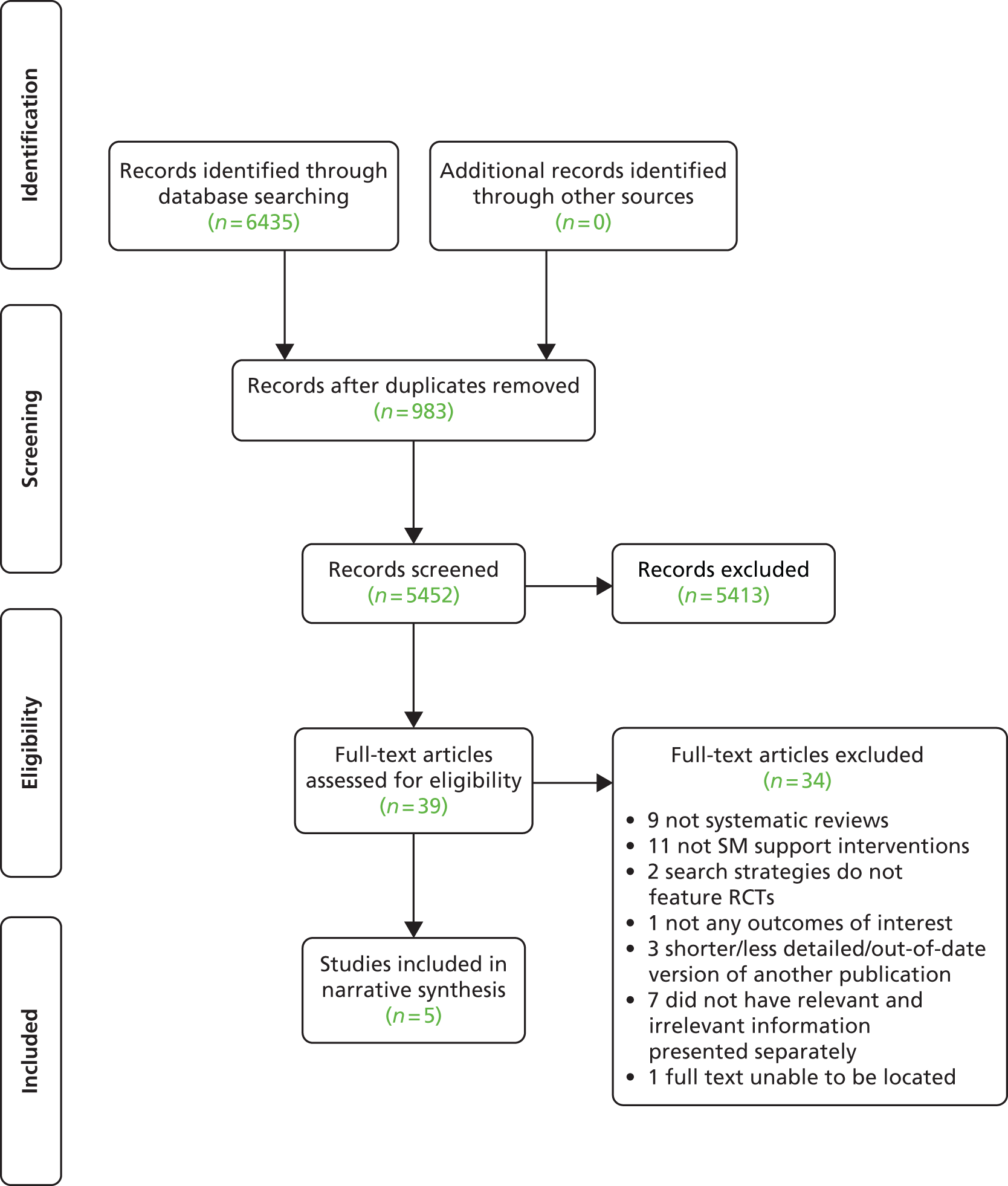
There were five reviews included, three of which were Cochrane reviews and two in peer-reviewed published journals. There were 41 RCTs included in the reviews overall; however, there was some overlap, so only 28 were unique RCTs. RCTs were carried out in at least eight different countries: Canada, the Netherlands, Sweden, France, USA, UK, Australia and Hong Kong.
The reviews were published between 2005 and 2012, with the included RCTs ranging from 1987 to 2011. One review evaluated self-management interventions; two were on education, one on action plans and one on outreach nursing (Table 49).
| Review | Intervention of interest and comparison | Participant demographics | Setting, delivery and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow up |
|---|---|---|---|---|---|
| Bentsen 2012146 | Self-management inventions vs. usual care | The mean age of the patients was between 60 and 70 years. All studies included both male and female subjects and both ex and current smokers | Usual care included normal clinical care from a chest physician, family physician and/or home-care nurse | The self-management interventions included patient education (group and individual), exercises (group and individual), a self-help book, an individual action plan and discussion therapy groups |
|
| Effing 2007147 | Self-management education and usual care | NR | Recruitment from outpatient clinics (seven RCTs); general practice (four RCTs), community (one RCT) and a combination of settings (two RCTs) Delivery by group (four RCTs), individual (nine RCTs) and written education material (one RCT) |
Action plans for self-treatment of exacerbations (six RCTs) | Overall, the follow-up time was 12 months in eight studies, 10 months in one study, 6 months in three studies, 12 weeks in one study and 2 months in one study. One study also evaluated the outcome ‘hospital admissions’ after 24 months |
| Tan 2012148 | Disease-specific education and usual care | NR | Recruited from outpatient clinics (seven RCTs); general practice (four RCTs), community (one RCT), or from a mix of these settings (two RCTs) | Group education (four RCTs), individual education (nine RCTs) and written education material only (one RCT). The use of an action plan for self-treatment of exacerbations was also assessed (six RCTs) | The follow-up time was 12 months in eight studies, 10 months in one study, 6 months in three studies, 12 weeks in one study and 2 months in one study. One study also evaluated the outcome ‘hospital admissions’ after 24-months |
| Turnock 2005149 | Action plans and usual care | Adults with severe/moderate COPD. All fitted the criteria of smoking history of ≥ 10 pack-years, and FEV1/FVC ratio < 70%. There were more male participants in all studies. The proportion of current smokers in each group varied from 23% to 53% | All studies recruited through primary care. One RCT was delivered by a nurse | All studies used action plans with an information booklet. Education provided with action plans included an individual education session with a health-care worker (two RCTs) | One RCT recorded measures at baseline, 3, 6, 9 and 12 months, whereas the other two recorded measures at baseline, 6 and 12 months Follow-up: one RCT was 6 months, and two RCTs were 12 months (one of which also recorded some outcomes at 6 months) |
| Wong 2012150 | Home care by outreach nursing vs. usual care, without respiratory nurse/health worker input | Participants classed as having moderately severe COPD | Home visits were provided by a respiratory nurse or similar respiratory health worker to patients with COPD | The home-based intervention represented a respiratory nurse providing care, education and support in a patient’s home | Included only trials with at least 3 months of follow-up. Two studies followed up the effect of the intervention at 3 months, one at 4 months, four at 6 months, one at 9 months and five at 12 months |
Quality assessment and weighting
Four of the five reviews scored ≥ 31 out of 44 (defined as higher quality), with Bentsen et al. 146 scoring 26 (defined as lower quality) (Table 50). The total sample size of the RCTs included in Bentsen et al. 146 and Turnock et al. 149 was under 1000 participants, with the remaining three reviews having over 1000 participants. As a result, these three were weighted with the highest levels of evidence in this meta-review (Table 51).
| R-AMSTAR criteria | Bentsen 2012146 | Effing 2007147 | Tan 2012148 | Turnock 2005149 | Wong 2012150 |
|---|---|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 2 | 4 | 1 | 4 | 2 |
| Was a comprehensive literature search performed? | 3 | 4 | 4 | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 1 | 3 | 1 | 4 |
| Was a list of studies (included and excluded) provided? | 1 | 4 | 2 | 4 | 4 |
| Were the characteristics of the included studies provided? | 3 | 3 | 4 | 4 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 2 | 3 | 3 | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 3 | 3 | 3 | 4 | 3 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 | 4 | 4 |
| Was the likelihood of publication bias assessed? | 1 | 1 | 3 | 3 | 2 |
| Was the conflict of interest stated? | 2 | 3 | 2 | 3 | 3 |
| Total score/44 | 26 | 34 | 33 | 39 | 37 |
Outcomes
The outcomes of interest chosen for this meta-review were health-related quality of life (HRQoL), which was an outcome included in all five reviews, and hospital admissions, which was included in all bar Bentsen et al. 146 These were considered key outcomes by the review team to inform commissioners, and at least one of the two was considered a primary outcome in each of the included reviews (Table 52).
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Hospital admissions | COPD-related admissions where possible, if not general hospital admissions | COPD-related; general hospital admissions |
| HRQoL | HRQoL | SG-RQ; CRQ; SIP; SF-36; Health Survey Questionnaire; HSQ 2.0; GHQ; III; COOP |
Findings
Our meta-review suggests that COPD self-management education reduces COPD-related hospital admissions. 147,148 Consistent and clinically significant positive effects of self-management education on QoL and HRQoL were much less obvious across the reviews. 147,148 Outreach nursing programmes were not associated with a reduction in health-care resource use but there was a tendency for improved HRQoL with this intervention, although this may not be clinically significant. 150 There are few studies of the use of action plans in COPD and no evidence from these that they decrease health-care resource use or increase HRQoL149 (see Table 53 for results from meta-analyses, Table 54 for an overall summary of findings and Figure 23 for a summary of the quantitative evidence).
| Reference and weighting | Outcome | Time | Sample size | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Effing 2007147 *** | Hospital admissions | ||||
| COPD-related hospital admissions vs. regular care | – | Seven RCTs | ++ | OR 0.64 (0.47 to 0.89); p = 0.007 | |
| HRQoL | |||||
| SG-RQ total vs. usual care | – | Seven RCTs | + | WMD –2.58 (–5.14 to –0.02); p = 0.05 | |
| SG-RQ impact vs. usual care | – | Seven RCTs | +* | WMD –2.83 (–5.65 to –0.02) | |
| SG-RQ symptom score vs. usual care | – | Seven RCTs | 0 | WMD –1.45 (–4.41 to 1.51) | |
| SG-RQ PA vs. usual care | – | Seven RCTs | 0 | WMD –2.88 (–5.90 to 0.13) | |
| Tan 2012148 *** | Hospital admissions | ||||
| COPD-related admissions vs. usual care | 12 months | Four RCTs | +++ | OR = 0.55 (0.43 to 0.71); p < 0.00001 | |
| HRQoL | |||||
| SG-RQ impact vs. usual care | 12 months | Six RCTs | + | WMD –3.78 (–6.82 to –0.73); p = 0.02 | |
| SG-RQ total and other domains vs. usual care | 3 and 6 months | Six RCTs | 0 | NR | |
| Turnock 2005149 ** | Hospital admissions | ||||
| Hospital admissions vs. usual care | 12 months | Two RCTs | 0 | WMD 0.16 (–0.09 to 0.42) | |
| HRQoL | |||||
| SG-RQ overall vs. usual care | 6 months | Two RCTs | 0 | WMD –1.91 (–5.46 to 1.63) | |
| SG-RQ symptoms vs. usual care | 6 months | Two RCTs | 0 | WMD –4.78 (–10.81 to 1.24) | |
| SG-RQ activity vs. usual care | 6 months | Two RCTs | 0 | WMD –2.43 (–7.37 to 2.50) | |
| SG-RQ impact vs. usual care | 6 months | Two RCTs | 0 | WMD –0.62 (–4.45 to 3.21) | |
| SG-RQ overall vs. usual care | 12 months | Two RCTs | 0 | WMD –0.32 (–3.34 to 2.70) | |
| SG-RQ symptoms vs. usual care | 12 months | Two RCTs | 0 | WMD 1.87 (–3.27 to 7.00) | |
| SG-RQ activity vs. usual care | 12 months | Two RCTs | 0 | WMD –2.82 (–6.84 to 1.19) | |
| SG-RQ impact vs. usual care | 12 months | Two RCTs | 0 | WMD 1.16 (–2.21 to 4.53) | |
| Wong 2012150 *** | Hospital admissions | ||||
| Hospitalisations vs. routine care | – | Five RCTs | 0 | Peto OR 1.01 (0.71 to 1.44); p = 0.95 | |
| HRQoL | |||||
| SG-RQ total vs. routine care | – | Four RCTs | + | MD –2.60 (–4.81 to –0.39); p = 0.02 | |
| SG-RQ activity vs. routine care | – | Three RCTs | 0 | NR | |
| SG-RQ impact vs. routine care | – | Three RCTs | 0 | NR | |
| SG-RQ symptoms vs. routine care | – | Three RCTs | 0 | NR | |
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Bentsen 2012146 * | Self-management interventions that improve COPD patients’ HRQoL | Four RCTs; 529; 2003–11 | Narrative | Self-management interventions reduced the burden on patients and improved patient activity and total health | Self-management interventions tend to improve QoL of patients with COPD. Further RCTs are recommended to confirm these benefits. Involvement of nursing in health-care services is suggested to develop these interventions Narrative synthesis broad and unclear on how RCT findings are related to conclusions made. Potential bias towards nurses rather than general HCPs |
| Effing 2007147 *** | Settings, methods and efficacy of COPD self-management education programmes on health outcomes and use of health-care services | 13 RCTs; 1580; 1987–2005 | Meta-analysis | Hospital admissions: there was a clinically and statistically significant reduction in the probability of at least one hospital admission among patients receiving self-management education compared with those receiving regular care [OR 0.64 (95% CI 0.47 to 0.89)] HRQoL: the SG-RQ total and domain scores in the self-management groups were all lower (indicating a better HRQoL) or equal to the scores in the usual care groups. The differences on the SG-RQ total [WMD –2.58 (95% CI –5.14 to –0.02)] and impact scores [WMD –2.83 (95% CI –5.65 to –0.02)] reached statistical significance at the 5% level, but did not reach the clinically important difference of 4 points. No significant relevant difference was found on the SG-RQ symptom score [WMD –1.45 (95% CI –4.41 to 1.51)] or the SG-RQ domain PA [WMD –2.88 (95% CI –5.90 to 0.13)] |
Self-management education is associated with reduction in hospital admissions with no indication of detrimental effects on other outcomes. Because of heterogeneity in interventions, study populations, follow-up time and outcome measures, data are insufficient to formulate clear recommendations regarding form and contents of self-management education programmes in COPD. There is an evident need for more large RCTs with a long-term follow-up, before more conclusions can be drawn Publication bias was not measured |
| Narrative | Hospital admissions: in the three studies which could not be meta-analysed no significant differences were found between the two arms. In the three studies which could not be meta-analysed, no significant differences were found between the two arms, though 24-month results on hospital admission (all causes) in one of the trials showing a significant reduction of –0.44 hospitalisations per patient/year in favour of the self-management education group HRQoL: no differences in SG-RQ scores after 12 months of follow-up were found. With the CRQ, two out of four HRQoL dimensions (fatigue and mastery) showed a significant improvement after a follow-up of 12 months General QoL: evidence showed significant improvement in total function measured by the SIP in the control group, better physical function and total function in favour of the intervention group. There is also a suggestion of significantly improved scores for the well-being dimension and the perceived III in one of the intervention groups (nurse-assisted collaborative management) compared with usual care |
||||
| Tan 2012148 *** | Disease-specific education in COPD | 12 RCTs; 2103; 1997–2010 | Meta-analysis | Hospital admissions: there was a significant reduction in hospital admission rates among patients receiving a disease-specific education programme compared with those receiving usual care [fixed effects model, OR 0.55 (95% CI 0.43 to 0.71); p < 0.00001] HRQoL: the SG-RQ total and domain scores in the disease management groups were all lower (indicating higher HRQoL) or equal to the usual care groups scores at the 12-month intervention period. At 12-months follow-up only SG-RQ impact was significantly better, with no significant differences in other SG-RQ scores Results after a 3- or 6-month intervention: no statistically significant changes were observed in any of the SG-RQ scores. The statistical heterogeneity for the outcome (SG-RQ impact scores after 6-month intervention) may be related to the outlying effects reported in one study. Its removal led to a lower statistic (59% vs. 0%). One trial could not be used in the meta-analysis because of a lack of data |
A meta-analysis on these studies revealed a positive relationship between disease-specific education programmes and HRQoL scores (as measured by the SG-RQ). Although significant effects were not detected across all HRQoL, findings suggest that education programmes have the potential to be a valuable intervention for COPD patients. Results provide a foundation for future research in this area, with more rigorously designed, large, randomised studies |
| Turnock 2005149 ** | Action plans for the management of COPD | Three RCTs; 367; 1997–2004 | Meta-analysis | Hospital admissions: no evidence of a significant effect on the number of hospital admissions over 12 months from two studies [WMD 0.16 (95% CI –0.09 to 0.42)] HRQoL (at 6 months): no statistically significant differences between groups for HRQoL. Overall HRQoL [WMD –1.91 (95% CI –5.46 to 1.63)]; symptoms [WMD –4.78 (95% CI –10.81 to 1.24)]; activity [WMD –2.43 (95% CI –7.37 to 2.50)]; impacts [WMD –0.62 (95% CI –4.45 to 3.21)] HRQoL (at 12 months): no statistically significant difference between groups for HRQoL. Overall HRQoL [WMD –0.32 (95% CI –3.34 to 2.70)]; symptoms [WMD 1.87 (95% CI –3.27 to 7.00)]; activity [WMD –2.82 (95% CI –6.84 to 1.19)]; impacts [WMD 1.16 (95% CI –2.21 to 4.53)] |
Action plans to date have not shown any significant reduction in the use of health-care resources, or improved clinical outcomes. However, the lack of evidence to support the role of action plans in COPD management should not be necessarily seen as the evidence of lack of efficacy, at this time a WAP without a broader self-management plan cannot be recommended for widespread adoption in primary care |
| Wong 2012150 *** | Outreach respiratory health-care worker programmes for COPD patients | Nine RCTs; 1498; 1987–2006 | Meta-analysis | Hospital admissions (meta-analysis): no significant change in the number of hospitalisations with the intervention [Peto OR 1.01 (95% CI 0.71 to 1.44)] Hospital admissions (subgroup analysis): after excluding an outlying study, a statistically significant increase in the number of hospitalisations in patients receiving the intervention was reported [Peto OR 1.59 (95% CI 1.02 to 2.47)] HRQoL: significantly improved with the intervention [MD –2.60 (95% CI –4.81 to –0.39)]. No statistically significant reductions in SG-RQ subscores of activity, impact and symptoms |
Outreach nursing programmes for COPD improved disease-specific HRQoL. However, the effect on hospitalisations was heterogeneous, reducing admissions in one study, but increasing them in others, therefore we could not draw firm conclusions for this outcome. Other narrative findings regarding HRQoL were more heterogeneous |
| Narrative | HRQoL: across other individual studies that could not be pooled, there were heterogeneous findings for the ‘physical score’ in the SIP and a range of HRQoL scores |
FIGURE 23.
Chronic obstructive pulmonary disorder: summary of the quantitative evidence.
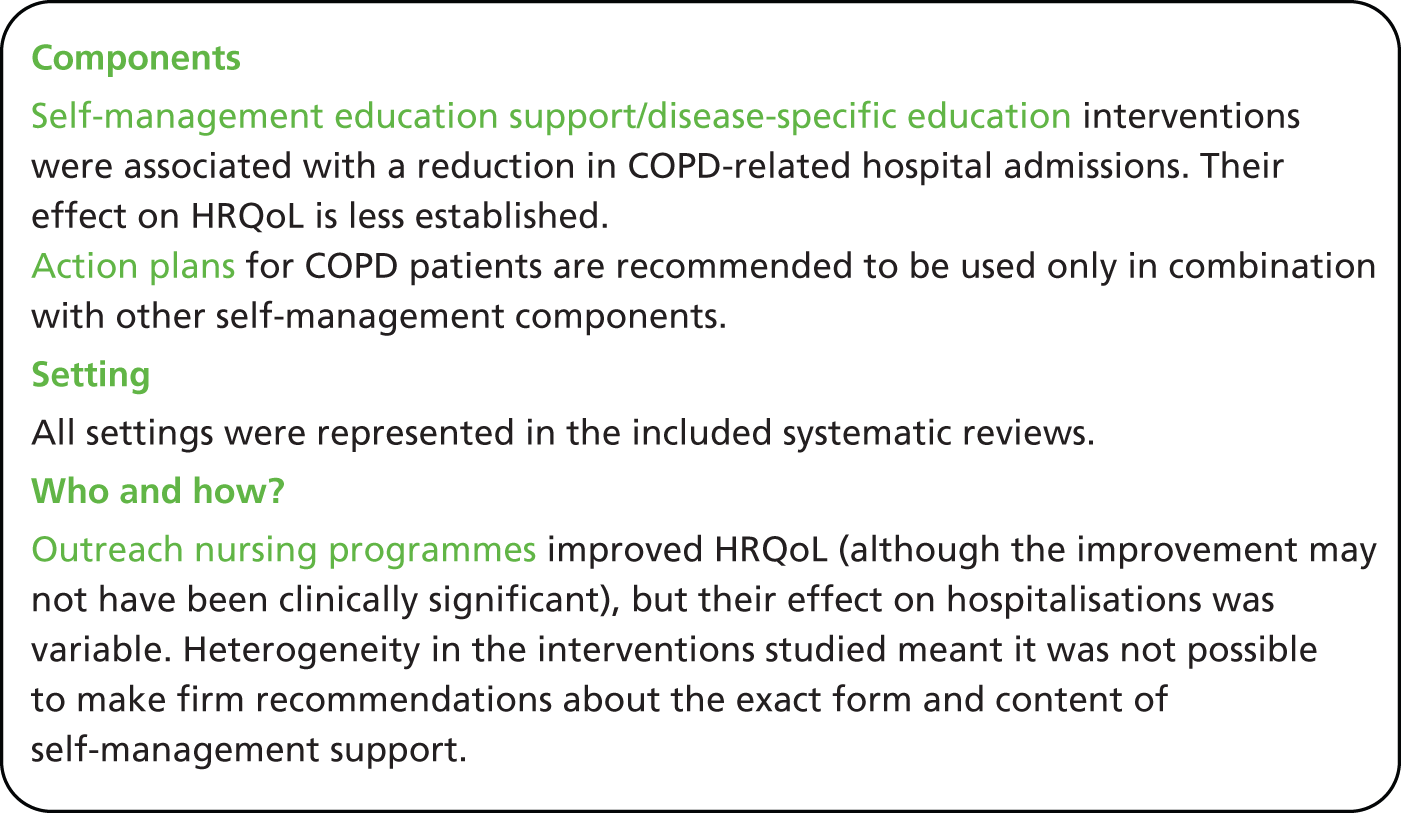
Mixed-methods discussion
Both the qualitative and quantitative evidence presented here focus on the importance of incorporating COPD-specific education as a core component of self-management support for patients with COPD. The qualitative synthesis explores the importance of tailored education to address needs and increase treatment adherence to avoid dyspnoea and vulnerability. Evidence from the quantitative meta-reviews shows that COPD-specific education equips COPD patients with the knowledge to understand their condition, manage symptoms and medication in order to reduce hospitalisations. Consequently, we conclude that COPD-specific education is an important component of self-management support intervention programmes.
A prominent finding from qualitative reviews was the importance of supporting the patient as they adjusted to illness-related physical and psychological symptoms and the consequent need for illness-related therapy. Psychological support to discuss and explore patients’ feelings of uncertainty, frustration and loss and work for a better adjustment to illness is advocated as a means to achieve this. Evidence from quantitative reviews shows how difficult it is to produce a clear, demonstrable improvement in HRQoL in COPD patients.
Qualitative evidence emphasises the importance of the relationship patients have with their health-care provider as a contributory factor in affecting health behaviour change, promoting treatment adherence and reducing hospital admissions. However, the only systematic review which explored the role of a specific professional (outreach nursing programmes) found very equivocal results. No other reviews explored this issue in depth in order to identify aspects of a patient/professional relationship which were beneficial to health utilisation and patients’ QoL.
Evidence from quantitative reviews shows that, despite increasing the recognition and reactions to exacerbations, action plans per se did not improve HRQoL, or reduce health-care utilisation and patients’ actual and perceived symptoms, an observation that existing qualitative reviews do not explain. Action plans, were, however, components of some successful programmes.
Chapter 12 Additional meta-review: self-management support for individuals with chronic kidney disease
Meta-review of qualitative systematic reviews
Systematic reviews identified
There were two reviews included in the CKD qualitative meta-review,151,152 both published in 2012 in peer-reviewed journals (Figure 24). There were no repeated studies across the reviews, resulting in 30 qualitative primary studies (published between 1971 and 2011).
Both included reviews were qualitative syntheses: one on experiences of those with kidney failure151 and the other specifically focusing on the dialysis experiences of children with kidney failure152 (Table 55).
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Makaroff 2012151 (Qualitative) |
The purpose of this study was to examine the qualitative nursing research focused on individuals’ experiences of kidney failure. The research question was, ‘What are the experiences of people living with kidney failure?’ | 13 | Meta-synthesis of the texts suggests individuals with kidney failure have experiences of paradoxical nature, including occurrences of restricted freedom that bring about distant connection, dependent autonomy, abnormal normalcy and uncertain hope |
| Tjaden 2012152 (Qualitative) |
This systematic review aimed to synthesise qualitative studies on the perspectives of children and adolescents of living on dialysis; these findings can be used to inform health service delivery and policy to improve the medical, health and psychosocial outcomes for young patients on dialysis | 17 | A total of 17 studies, which reported the experiences of 143 children receiving dialysis, were included. Five major themes were identified: loss of control (high reliance on carers, parental overprotectiveness, unrelenting dependence on a machine, impaired body integrity), restricted lifestyle (limited socialisation opportunities, academic struggle), coping strategies (hope for kidney transplant and medical advances, social support, positive determination and self-awareness, engaging in activities, denial), managing treatment (ownership, proactive involvement, adherence to fluid and diet restrictions) and feeling different (abnormal physical appearance, injustice, being a burden) |
Quality assessment
Makaroff151 and Tjaden et al. 152 scored similarly, with scores of 29 (low) and 31 (high) respectively (Table 56). It is also worth noting that Makaroff151 did not score on criteria relating to quality assurance, as none were reported, or team discussion, as there was only one review author.
| R-AMSTAR criteria | Makaroff 2012151 | Tjaden 2012152 |
|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 |
| Was there duplicate study selection and data extraction? | 1 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 2 | 1 |
| Was a list of studies (included and excluded) provided? | 2 | 2 |
| Were the characteristics of the included studies provided? | 3 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 3 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 3 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 |
| Was the conflict of interest stated? | 3 | 3 |
| Total score/40 | 29 | 31 |
| Quality rating (low = < 30; high = ≥ 30) | Low | High |
Findings
Support for self-management
The synthesis enabled these findings to be integrated, providing a broader picture to inform future commissioning of self-management support:
-
Autonomous self-management was pursued by patients in order to promote good care, retain responsibility and control, become long-term survivors and engage in self-advocacy. It is important that patients feel supported in their self-management pursuit.
-
Psychological support for adaptation to the perceived restrictions that accompany kidney failure, such as dialysis and the change from ‘normalcy’ to a state of ‘dependent autonomy’ (p. 27). 151 Concerns of illness/anxiety can be addressed and restrictions can often be reframed to focus on freedom. For example, dialysis can be considered a treatment that sustains life, rather than a burden.
-
Patients tended to prefer being in a comfortable environment for their dialysis. This provided ‘a counterbalance to the dehumanizing objectification that comes with dependence on technology’,151 so this choice should be offered and supported when appropriate.
-
Patients depend (a) on the treatment to keep them alive; and (b) on the HCP to provide information and education to help them make informed decisions. However, patients felt they had shallow relationships with the HCPs including unmet expectations. Therefore, this is an area where active education provision and collaborative relationships between the expert patient and the expert HCP can be developed to support self-management.
-
Social and emotional support, including spirituality, was viewed as important for decision-making processes, providing strength and motivation, and enhanced feelings of connectedness while establishing distance (autonomy) from HCPs. Access to peer support from others with similar experiences may be helpful, whether in person or through online social networks.
-
Where carers are involved, it is important to encourage communication between them and the person with CKD. A fine balance between dependence and independence is necessary in this relationship. The carer needs to be there to support and provide for them, but must allow them to feel that they are not a burden and are in control of monitoring and managing their own treatment and diet/fluid intake.
-
Children with CKD reported that the treatment interfered with their school lives, especially in relation to social and physical activities. Some were put in a special educational needs class and felt that this segregated them further from others. They felt disappointed that they were ‘left out’ (p. 399)152 from society. Providing information to the school on potential barriers to activities, guidance on how best to overcome them, or alternative activities that would include the child with CKD with other children may help provide social support from an organisational level.
-
Experiences of kidney failure are diverse and multifaceted, and although HCPs ‘clearly have many demands on their time, acknowledging each person’s individuality and showing interest in what might be of importance to each person may significantly impact the QoL for those living with kidney failure’ (p. 26). 151
Meta-review of quantitative systematic reviews
Systematic reviews identified
A total of three systematic reviews were identified for inclusion in this meta-review of self-management support for people living with CKD. 153–155 The three reviews were published between 2008 and 2012 and included a total of 32 RCTs, five of which were included in more than one review. RCTs were carried out in six countries: USA (the majority of studies), Canada, UK, Scotland, the Netherlands and Taiwan. 155 Publication dates of the included RCTs ranged from 1981 to 2005 (Figure 25).
The three reviews all focused on a different form of self-management support: Mason et al. 153 focused on educational interventions; Matteson and Russell154 explored interventions specifically aimed at increasing adherence to lifestyle and treatment; and Strand and Parker155 studied multidisciplinary care (MDC). However, despite the varied focuses, all interventions tended to include one or more of the following three components: education about CKD and its management; psychological strategies; or lifestyle advice and support.
In one review, all patients were receiving dialysis. 154 In another, the majority of studies involved dialysis patients, with a small minority of studies including only pre-dialysis patients (CKD stages four and five). 153 The remaining review included only pre-dialysis patients, with CKD stage ranging from stage 3 to stage 5155 (Table 57).
| Review | Intervention of interest and comparison | Participant demographics | Setting and delivery | Content and focus | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Mason 2008153 *** | Educational interventions that were structured and involved both informational and psychological components | Men and women, mean age 55 years (range 19–82 years). Five RCTs with pre-dialysis patients (CKD stages 4 and 5); remaining 17 RCTs involved dialysis patients | Majority of studies (82%) used an individual format to deliver the intervention. All interventions took place in hospitals. Trained or experienced professionals were used in all except one study, which used peers to teach and mentor fellow patients | Aimed at improving both knowledge and motivation. Components were used in various combinations and formats ranged in terms of complexity Pre-dialysis care: written material plus patient-centred group intervention based on problem-solving; collaborative role learning Dialysis care: dietary and interdialytic fluid management; educational interventions aimed at coping with dialysis therapy; exercise interventions |
Sessions ranged in number from 1 to 12 and in duration from 15 minutes to 4 hours per session. Pre-dialysis follow-up: one study with 4-week follow-up, four longer-term studies with follow-up from 18 months to 20 years. Remaining studies follow-up ranged from 1 to 6 months, a single study had a 12-month follow-up period |
| Matteson 2010154 * | Interventions aimed at enhancing adherence to fluid, diet, medications and treatment | Adult haemodialysis patients. Time on dialysis ranged from 14 to 79 months. Non-adherent patients were the subjects of study in five of the eight RCTs | Interventionist most commonly registered was dietitian, also included a trainee clinical psychologist, a psychologist, nephrology nurse specialists and a team of a hypnotherapists. One study did not identify the interventionist | The haemodialysis adherence enhancing interventions focused in three areas: cognitive (three RCTs), cognitive/behavioural (four RCTs) and hypnotherapy/coaching (one RCT) interventions | The dose of the interventions spanned from a few minutes to hours and the duration of the intervention from one time to 6 months. Follow-up time ranged from 10 weeks to 6 months |
| Strand 2012155 * | MDC vs. traditional medical care | Two studies only: CKD stages 3–5 CKD sages 4 and 5 |
Two studies only: CKD clinic, MDC care included nephrologist, renal nurse, renal dietitian, social worker Hospital-based renal clinic, delivery by lecture and take-home booklet, supportive follow-up calls from health educators |
Two studies only:
|
Two studies only:
|
Quality assessment and weighting
One review was classified as high quality153 (scoring ≥ 31), whereas the remaining two were classified as being of lower quality154,155 (scoring ≤ 30) (Table 58). Considering both quality and size of the reviews, Mason et al. 153 was considered the review to carry the largest weight of evidence with a three star rating, whereas both Matteson and Russell154 and Strand and Parker155 received a weight of just one star (Table 59).
| R-AMSTAR criteria | Mason 2008153 | Matteson 2010154 | Strand 2012155 |
|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 2 | 1 |
| Was a comprehensive literature search performed? | 4 | 3 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 1 | 1 |
| Was a list of studies (included and excluded) provided? | 3 | 1 | 2 |
| Were the characteristics of the included studies provided? | 4 | 4 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 2 | 2 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 2 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 1 | 4 |
| Was the likelihood of publication bias assessed? | 1 | 1 | 1 |
| Was the conflict of interest stated? | 3 | 1 | 1 |
| Total score/44 | 36 | 22 | 25 |
Outcomes
Only two outcomes were selected to be of interest in this meta-review: clinical markers of CKD control or progression; and QoL (Table 60).
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Clinical markers | Any important clinical markers of CKD associated with the control or progression of the disease | Phosphorous levels; interdialytic weight gain; BP; eGFR; time to RRT |
| QoL | Either disease-specific QoL or generic QoL measures | SF-36 |
Findings
Mason et al. ’s153 high-quality review of educational interventions, predominantly with dialysis patients, but also including pre-dialysis patients, reported that 18 of the included 22 studies demonstrated significant improvement in at least one outcome. However, in the majority of cases these significantly improved outcomes were not our selected outcomes of interest. Of those RCTs involving pre-dialysis patients, no results for either of our selected outcomes were reported. However, it is important to acknowledge that a significant reduction in mortality was reported in one large RCT at 20 years follow-up. Of the RCTs involving dialysis patients, in the short term there were mixed, inconclusive findings on the effect on health status. In the medium term, two of the three interventions focusing on diet found significant improvement in either serum phosphorus level or interdialytic weight gain. Both exercise interventions were associated with significantly improved QoL and the remaining interventions that involved peer mentoring were also associated with improved QoL. Only one study reported long-term outcomes, demonstrating improved psychosocial skills.
Matteson and Russell’s154 lower-quality review, which explored adherence promoting interventions in patients on dialysis, reported statistically significant results for either serum phosphorus level or another marker of treatment adequacy in six of the eight included RCTs.
The lower-quality review by Strand and Parker,155 which investigated MDC, found no evidence to suggest an overall beneficial effect of the interventions on BP or estimated glomerular filtration rate (eGFR). Some evidence was found to suggest MDC interventions can delay the time to renal replacement therapy (RRT) compared with control, and can improve metabolic and anaemia control (see Table 61 and Figure 26 for summaries of quantitative results).
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Mason 2008153 *** | Education | 22 RCTs; 1967; 1981–2005 | Narrative | Predialysis care: short term (one study), no relevant outcomes reported. Long-term (four studies), initial follow-up reported significant improvement in delayed onset of dialysis therapy. At 20 years, there were significant increases in survival rates Dialysis care: short term (four dietary and interdialytic fluid management interventions; two other educational interventions), one of the two studies to assess psychological outcomes found some significant improvement in health status at 4 weeks. Medium term (eight diet and/or fluid interventions, two exercise interventions, three others), of three diet interventions to report relevant outcomes, one found no affect on phosphorous levels, whereas in another study decreased interdialytic weight gain was demonstrated, and a third found significantly improved phosphate levels. Both exercise interventions were successful, with significantly improved QoL. The three other interventions in this category involved peer mentoring which led to improved QoL. Long term (one study), at 1 year demonstrated improvement in psychosocial skills |
Eighteen studies reported significant improvements for at least one of the outcomes of clinical, psychological, behavioural and knowledge, indicating that educational interventions were applied successfully. However, despite including only true RCTs, methods generally were suboptimal, mainly because of poor reporting, small sample sizes, high dropout rate and inconsistency in the delivery of interventions In general, the findings of the present study show promising results for dialysis educational interventions aimed at improving dialysis and/or fluid concordance, exercise and coping/adaptation. However, many studies lacked rigorous evaluation |
| Matteson 2010154 * | Adherence promoting | Eight RCTs; 594; 2000–5 | Narrative | Statistically significant results in the main outcomes of either phosphorous or a marker of treatment adequacy (Kt/V) or interdialytic weight gain were noted in six of the eight studies. Of these six studies, all had a cognitive component, with three studies utilising cognitive/behavioural interventions to increase diet/medication (phosphorus) or fluid adherence | Six of eight RCTs (75%) resulted in statistically significant improvement in adherence outcomes with the intervention compared with control. The limitations of the reviewed studies include short intervention dose and duration, no long-term outcome data, small sample sizes with a lack of adequately powered studies, no paediatric interventional studies, lack of theoretical basis for the intervention and varied instruments to measure adherence outcomes |
| Strand 2012155 * | MDC | Two RCTs; 734 participants; 1998–2005 | Narrative | BP was reported in three studies. Two reported no significant benefit in intervention compared with control. The third study found a significant reduction in both SBP and DBP among patients with no diabetes compared with the group with diabetes as comorbidity. eGFR was reported in three studies, two failed to show any statistically significant differences between groups over time. The third demonstrated a statistically significant decline in the progression of CKD pre vs. post intervention. No comment is made on significance when comparing intervention with control. Time to RRT was reported in two of the four studies. In one study the intervention group had a statistically significant delay of RRT compared with the control group. The other study reported only on risk for and time to RRT as related to the CKD stage at the time of referral to clinic. Metabolic and anaemia control showed increased values and signs of improved control in three studies; however, statistical significance was only reported to be reached in one RCT | More well-conducted RCTs are required to definitely claim that MDC is more effective than usual care in adults with pre-dialysis CKD No evidence to support a significant effect of MDC interventions on BP. Suggestion that intervention is more effective in patients without T2DM compared with those with T2DM on BP outcome. No evidence to support a significant effect of MDC interventions on eGFR in intervention compared with control. Some evidence to support the role of MDC interventions on delaying the time to RRT compared with control. Some evidence to support the role of MDC interventions on improving metabolic and anaemia control |
FIGURE 26.
Chronic kidney disease: summary of the quantitative evidence.
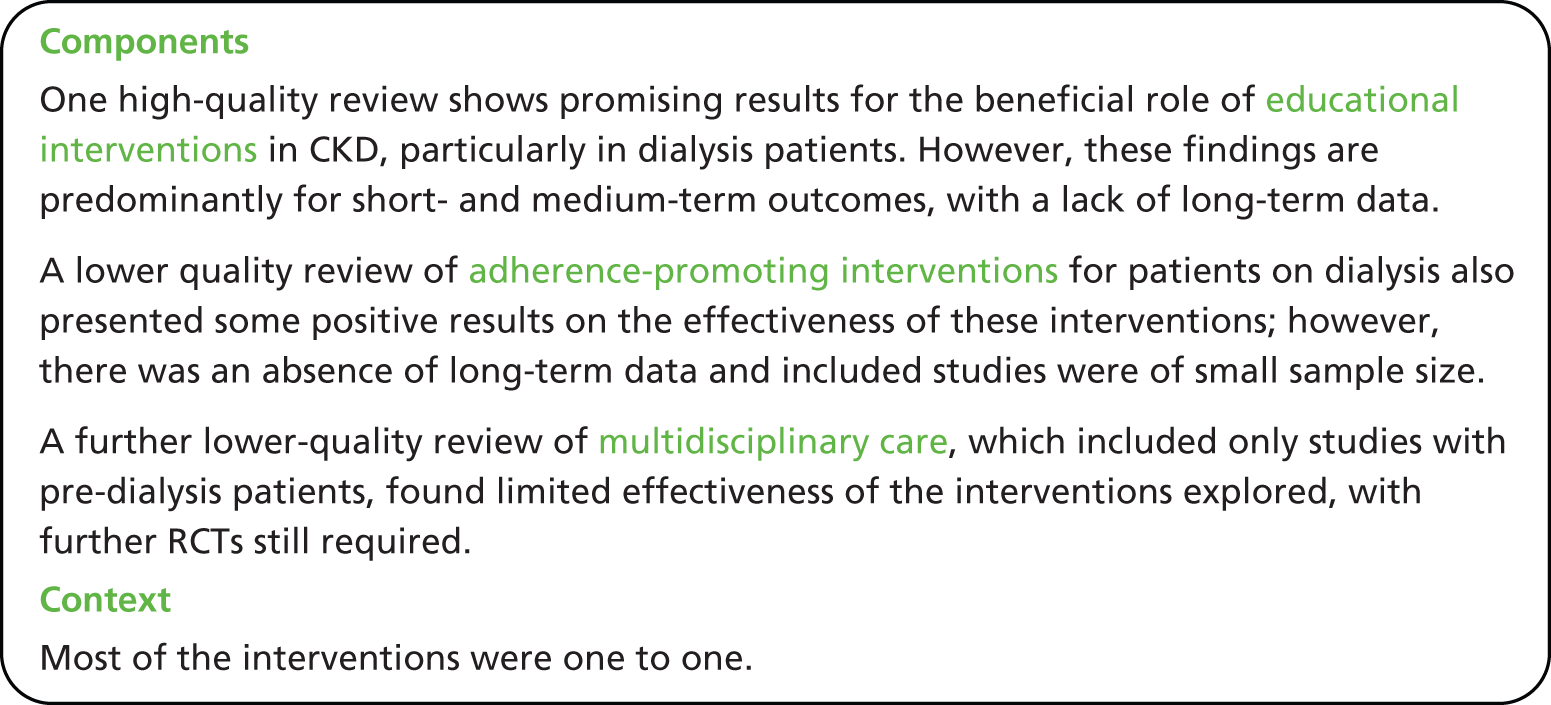
Mixed-methods discussion
Self-management in CKD is highly demanding, with complex treatment regimens and strict dietary and fluid intake guidelines. It is unsurprising, therefore, that the majority of interventions identified included education about CKD and its management and/or lifestyle advice and support as key components of self-management support, with some promising results identified. This emphasis on informational needs is supported by qualitative work which describes individuals with CKD striving towards self-management, and the importance of HCPs assisting in this transformation by providing the needed support.
In addition to informational needs, psychological support was frequently the focus of the identified interventions, again with some promising results reported. This emphasis on psychological support is also supported by the qualitative syntheses, which discuss feelings of anxiety experienced by those living with CKD and the loss of autonomy associated with dialysis treatment.
A third dimension identified by the qualitative research was the need for social support, particularly in relation to providing strength and sustaining the motivation of the individual with CKD. Peer education, or peer support, is advocated as one way of providing this. Involvement of carers (where appropriate) in self-management support is also suggested to be helpful. There is no quantitative evidence specifically focusing on social support, although it did feature in a number of the included RCT interventions. The qualitative evidence suggests that social support may be an important feature to consider in future self-management support for this group of patients.
Despite some promising results in delivering educational and psychological interventions for patients with CKD, more robust RCTs are required with larger sample sizes, longer follow-up intervention assessments, adequate intervention delivery and consistent intervention delivery. Furthermore, the reviews discussed highlight the importance of the above characteristics for both in studies with adults and children with CKD.
Chapter 13 Additional meta-review: self-management support for people with dementia
Meta-review of qualitative systematic reviews
Systematic reviews identified
There were two reviews156,157 (published in peer-reviewed journals in 2006 and 2007) included in the dementia qualitative meta-review (Figure 27). Some primary qualitative studies were included in both of the reviews, but overall there were 55 unique studies.
No systematic reviews specifically examined the qualitative evidence on self-management support in dementia; instead they captured broader concepts and aspects of this topic. Both of the included reviews aimed to examine the subjective experiences of people living with dementia, including management and social interaction involved in their lives,156 and analysis aimed at informing an inventory of subjective needs157 (Table 62). We have only included people living at home with dementia in this review (although they include a wide range of Mini Mental State Examination scores) as support for self-management may be a less relevant, or somewhat different, concept for people whose dementia has resulted in their requiring residential care.
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Steeman 2006156 (Qualitative) |
To advance understanding of the ways in which people with early stage dementia come to understand, account for, take action, and otherwise manage their daily life with the condition, and the ways in which social interaction is involved in this process | 28 studies (in 33 articles) | Living with dementia is described from the stage a person discovers the memory impairment, through the stage of being diagnosed with dementia, to that of the person’s attempts to integrate the impairment into everyday life. Memory loss often threatens perceptions of security, autonomy and being a meaningful member of society. At early stages of memory loss, individuals use self-protecting and self-adjusting strategies to deal with perceived changes and threats. However, the memory impairment itself may make it difficult for an individual to deal with these changes, thereby causing frustration, uncertainty and fear. Results support integration of proactive care into the diagnostic process, because even early stage dementia may challenge QoL. Moreover, this care should actively involve both the individual with dementia and their family so both parties can adjust positively |
| van der Roest 2007157 (Qualitative) |
To provide an overview of the literature on subjective needs of people with dementia living in the community, in various types of research reported between January 1985 and July 2005 with the aim to develop a customised care | 34 | Subjective needs were found in 34 studies with various research aims, such as awareness and coping. Few studies aimed to measure needs of people with dementia. The most frequently reported needs of people with dementia were the need to be accepted and respected as they are, the need to find adequate strategies to cope with disabilities, and the need to come to terms with their situation. Explicit wants or demands were reported less frequently than needs. The high number of reported needs and the limited number of wants and demands show that people with dementia do not frequently mention how they want their needs to be met. Most reported needs are not instrumental, but are related to well-being and coping |
Quality and relevance
Both reviews scored 28 in the quality assessment; however, they scored differently in different aspects of the criteria (Table 63). For example, Steeman et al. 156 had a lack of detail about the study selection and conflict of interest but did assess quality of the included studies, whereas van der Roest et al. 157 provided more details of the review process but did not mention any quality assessment.
| R-AMSTAR criteria | Steeman 2006156 | van der Roest 2007157 |
|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 |
| Was there duplicate study selection and data extraction? | 1 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 3 | 2 |
| Was a list of studies (included and excluded) provided? | 1 | 1 |
| Were the characteristics of the included studies provided? | 3 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 1 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 3 | 1 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 |
| Was the conflict of interest stated? | 1 | 4 |
| Total score/40 | 28 | 28 |
| Quality rating (low = < 30; high = ≥ 30) | Low | Low |
Findings
Support for self-management
The synthesis enabled these findings to be integrated to provide a broader picture to inform future commissioning of self-management support.
-
Services need to be available with information not just for those diagnosed with dementia, but also for those who are concerned about any associated symptoms that they or their loved ones are experiencing (e.g. memory loss). Due to the negative ‘stigma’ (p. 732)156 surrounding this condition and its progressive nature, this can be a difficult concern to face and discuss with others. The individual’s desire to acknowledge the ‘problem may be triggered by several needs: the need for an explanation, the need to relieve the pressure of maintaining a normal appearance, and the need to feel supported’ (p. 730). 156
-
Psychological support is important to aid adjustment to the diagnosis and what this means to the person’s life. ‘Avoidance’/’denial’ (p. 731)156 may be a coping strategy employed at first with a ‘vague’ idea of their ‘self-image’ and a ‘fear of loss of identity’ (p. 731). 156 It is important that family members are encouraged not to ‘cover up’ (p. 731)156 or avoid discussing any problems regarding dementia, as such encouragement can aid the person with dementia address their own denial.
-
When supporting a person to reach acceptance, it is important to consider potential perceptions of loss, incompetence, intimacy, control, independence, confused reality, burden, role and/or self-identity as a valuable person. These can often be accompanied with feelings of frustration, uncertainty, embarrassment, worthlessness and/or stupidity. There is sometimes a mix of positive and negative feelings simultaneously, especially if they have high feelings of competence from their selves prior to diagnosis, whereas now they are unsure about their competence. ‘Self-protective’ and ‘integrative strategies’ (p. 733)156 can be employed to aid self-maintenance and adjustment.
-
Acceptance tended to come in two forms, either from a ‘positive attitude’ (p. 733),156 hope and/or ‘faith’ (p. 581),157 or from ‘accepting loss and relieving pressure’ (p. 733)156 and reprioritising the future and remaining enjoyment, for example pleasure from sensory awareness by appreciating ‘aesthetic’ (p. 581)157 aspects of life such as nature, music and art. Either way, it is important that it is perceived as only one part of the person’s life, and future psychological ups and downs are prepared for and supported.
-
Social support is an important consideration for people with dementia as they often reported feeling misunderstood, unsupported and alienated. This could lead to feelings of sadness and anger, which are also accompanied by the fear that this will only get worse as their condition progresses. ‘People commonly view the following as supportive: having a sense of belonging and being loved; of being understood, accepted and valued as an individual; of being included in enjoyable and meaningful activities and of feeling supported’ (p. 734). 156 There is a want to feel normal and so depending on the stage of acceptance the person is at, being around people who have similar experiences to them could help or hinder this. This needs to be addressed on an individual basis.
-
‘People experiencing early stage dementia have an increased need to be comforted and to feel secure and valued, empathetic caregivers are needed to fulfil this burgeoning need’ (p. 734). 156 The person with dementia needs to feel that they are treated seriously and are not ignored or treated like a child. As communication is difficult but important, it is important that carers look for ways beyond verbal communication that helps them to learn about the person with dementia’s experience.
-
Support should consider ‘physical disabilities’ and not only ‘focus on memory problems’ for people who have dementia. 157
-
Disruption to daily living and concern for ‘danger’ (p. 579)157 were discussed. People with dementia may benefit from having written plans or prompts for what to do in certain situations if they experience memory issues, such as driving the car and forgetting where you are going or where you are.
-
People with dementia often prefer to live in their own homes but are concerned about being a ‘burden’ (p. 732;156 p. 580157) to their loved ones. Adequate support is needed to allow people to ‘stay in their homes while also supporting their informal carers to alleviate care tasks’ (p. 581). 157
Meta-review of quantitative reviews
Systematic reviews identified
Following the title and abstract screening, 64 articles were screened for eligibility, three of which158–160 (all published in 2012) were included into the dementia quantitative meta-review. However, on full data extraction we identified major flaws and inconsistencies in the reporting of Corbett et al. ,159 and after discussion this review was also excluded leaving two reviews included (Figure 28). One review evaluated OT and one explored non-pharmacological interventions (Table 64).
| Review | Intervention of interest and comparison | Participant demographics | Setting and delivery | Content and focus | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Kim 2012160 | OT compared with usual activity, routine care or no treatment | The number of women and men was similar. Average age varied from 77.78 to 83.8 years. All participants diagnosed with dementia based on the DSM IV. Participants in one intervention were persons with early stage Alzheimer’s disease, the remaining two interventions did not specify the type of dementia | OT | OT interventions were all functional task-based activities:
|
The first intervention was a 60-minute session, one time/week for 8 weeks. The second intervention was a 90-minute session, six home visits, a 15-minute session, two telephone contacts eight times for over 4 months. The third intervention was a 45-minute session, two times/week for 8 weeks |
| Cooper 2012158 | Non-pharmacological inventions focusing on QoL/well-being. Controls included no treatment, usual care and waiting list control | Divided into interventions for those living at home and for those living in care homes (not included in this meta-review) | Three out of six with OTs, one was an education-based group setting | Types of interventions: family carer interventions; combined patient and family carer interventions; cognitive stimulation; individual cognitive rehabilitation | Two RCTs followed up at ‘post intervention’, one at 1 and 7 weeks post intervention, one at 5 months and two at 6 months post intervention |
There were 24 RCTs included in the reviews overall, not all with outcomes relevant to this meta-review. Nine of the quantitative primary studies were included in both reviews leaving 15 unique studies, of which nine were relevant to this review. Neither included review indicted the countries where their included studies were conducted.
Quality assessment and weighting
The two reviews scored ≥ 31, meeting our classification as higher-quality reviews158,160 (Table 65).
| R-AMSTAR criteria | Kim 2012160 | Cooper 2012158 |
|---|---|---|
| Was an a priori design provided? | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 1 |
| Was a list of studies (included and excluded) provided? | 2 | 2 |
| Were the characteristics of the included studies provided? | 3 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 1 |
| Was the likelihood of publication bias assessed? | 3 | 4 |
| Was the conflict of interest stated? | 1 | 3 |
| Total score/44 | 34 | 33 |
The total sample sizes of the RCTs included in the reviews were both under 1000 participants and therefore neither were given a maximum weight of three stars in this meta-review (Table 66).
Outcomes
The outcomes of interest chosen for this meta-review was QoL. This was considered a key outcome by the review team (Table 67).
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| QoL | QoL | Self-report measures: QOL-AD, ADQRL, DEMQOL, Quality of Life assessment, EuroQOL Observer-rated measures: DCM; QUALID; depression and anxiety |
Findings
‘Self-management’ does not appear to be a widely used term in the dementia literature, but supporting self-management is fundamental to many of the interventions in the reviews we included. Although many studies report affects on carers’ own QoL we attempted to dissect out information on patient’s QoL. In some cases this was a proxy measurement provided by the carer.
We identified potential problems with analysis in the systematic reviews identified. Our included systematic reviews, in turn, reported weaknesses in many of the RCTs in this area. There was some evidence that coping-based strategies for carers of people living at home with dementia, with or without activity interventions directed at the patient with dementia, may improve patients’ QoL.
There is some evidence to suggest that OT interventions based on promoting functional task activity do not improve depression in patients with dementia living at home. There is currently very little available review level evidence, and none positive, that discussion groups or cognitive rehabilitation improve the QoL of patients living at home with dementia (see Table 68 for statistical results, Table 69 for an overall summary of findings and Figure 29 for a summary of the quantitative evidence).
| Reference and weighting | Outcome | Time | Sample size | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Kim 2012160 ** | OT delivered functional task activity on depression | NR | Three RCTs | 0 | 0.15 (−0.17 to 0.47); p > 0.05 |
| Cooper 2012158 ** | Family carer interventions on patient QoL | NR | Four RCTs, 420 | +a | WSES 0.24 (range 0.03–0.45)a |
| Combined patient and family carer interventions on patient QoL | NR | Two RCTs, 191 | +a,b | WSES 0.84 (range 0.54–1.14)a,b |
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (meta-review author) |
|---|---|---|---|---|---|
| Kim 2012160 ** | OT for persons with dementia | Three RCTs; 203; 2008–10 | Meta-analysis | Effects of OT intervention based on functional task activity on depression Three studies involving 203 people were analysed to examine the effect of OT intervention based on functional task activity. Meta-analysis reported no significant effects |
The number of studies included in this review is limited. More research is needed to enable evidence-based OT for dementia patients |
| Cooper 2012158 ** | Non-pharmacological inventions on QoL of people with dementia | Seven RCTs examining patients living at home; 2007–10 | Some attempt quantitative synthesis and narrative | QoL Coping-based strategies for carers four studies including: two manualised interventions for carers of people with dementia focusing on coping and behavioural strategies designed for low- and middle-income countries (Peru, Russia). Five 30-minute sessions; OT-tailored educational intervention directed at carers with up to 12 OTs or nurse home or telephone contacts in 4 months. Eight weekly sessions and four telephone calls; HCP manualised intervention based on behavioural management based on communication and increasing pleasant events. No individual studies showed an effect on care QoL but pooled SES suggests benefit Activity programmes for people with dementia and family carer coping strategy combined interventions: two RCTs of individual tailored activity interventions delivered by OTs, patients and carers, involved 10 1-hour sessions over 5 weeks, six weekly home visits and two telephone calls People with dementia in the intervention group had higher QoL compared with the usual care group, 1 and 7 weeks after the end of the intervention in one study, unclear results for the other study, reviewer pooled ES significant Discussion groups: one RCT of nine weekly 1.5 hour manualised, structured groups provided by support group volunteer facilitators for people with dementia and their carers – results unclear as review authors disagree with study authors Individual cognitive rehabilitation: cognitive rehabilitation by an occupational therapist did not improve patient or carer-rated QoL in one higher-quality study |
There is a lack of definitive evidence for any intervention that increases QoL or well-being of people with dementia. Nonetheless, lack of evidence of efficacy is not evidence of lack of efficacy. Preliminary evidence indicated that coping strategy-based family carer therapy with or without a patient activity intervention improved QoL of people with dementia living at home. Future research should explore the longer-term impact of interventions on, and devise strategies to increase, life quality of people with dementia living in care homes or at home without a family carer |
FIGURE 29.
Dementia: summary of the quantitative evidence.
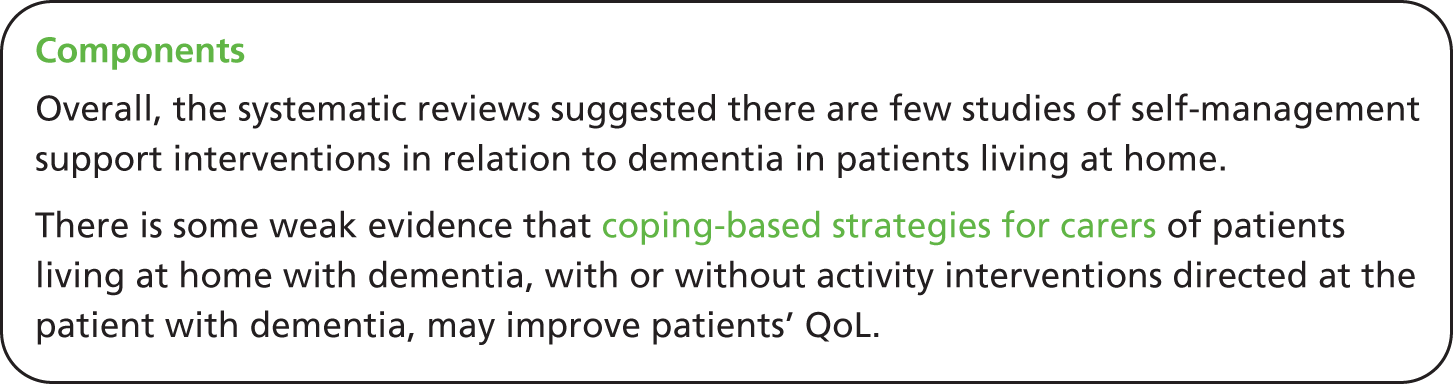
Mixed-methods discussion
Being diagnosed with dementia is often accompanied by fear and uncertainty due to gradual memory loss and loss of autonomy. It is important for professionals to provide patient-centred information and advice. Social support is advocated to reduce feelings of isolation. Being around people who can understand them, feel accepted and valued as individuals is important. Evidence from the quantitative meta-review shows that group discussions to talk about dementia, discuss future plans and personal relationships did not significantly improve patients’ QoL. As support and feeling valued and accepted is important for patients with dementia, further research in this area is needed.
Preliminary quantitative evidence indicated that coping strategy-based family carer therapy, with or without a patient activity, improved QoL of people with dementia living at home. A potential benefit from written plans or prompts about specific situations when danger is imminent emerged from the qualitative studies. Goal-setting and environmental adjustments including carer training in problem-solving strategies were components of these family carer interventions. Future interventions perhaps could focus to identify different action plan content and explore their effectiveness for patients’ QoL.
Last, qualitative studies indicate the importance of psychological support for patients with dementia to aid adjustment to the diagnosis and deal with issues such as potential perceptions of loss, incompetence, intimacy, control and independence. Unfortunately, the quantitative evidence does not provide information on the nature of effective psychological self-management support components.
There has been a previous qualitative meta-review on the subjective experiences of people with dementia,161 which had a broader inclusion criterion for review types than our meta-review. For quality control, we only included reviews that were considered to be systematic (see Chapter 5). Although some reviews included in the previous meta-review were also included in our present meta-review, the former meta-review included additional reviews that we did not consider to be systematic. Our meta-review updates von Kutzleben et al. ’s161 meta-review (as their searches were completed in June 2010) and builds on this literature by focusing on how this information can be used to inform self-management support in combination with a quantitative meta-review examining what self-management interventions are effective.
To avoid bias, we did not read the results of von Kutzleben et al. ’s161 meta-review until after our synthesis was complete. Our meta-review findings agree with von Kutzleben et al. ’s meta-review that ‘people with dementia experience a whole range of emotions’ when ‘coming to terms with the disease and maintaining normality’ (p. 378). 161 They concluded that ‘with regard to expectations from the side of professional health care, the need for accompanying, continuous support and counselling appeared to be central. Furthermore, disclosure of diagnosis represents a critical stage . . . but our findings indicated that they prefer to be included in this process’ (p. 378). 161 However, von Kutzleben et al. ’s meta-review does conclude that people with dementia’s ‘needs and demands do not differ significantly from those of other groups of patients with chronic conditions’ (p. 378). 161 Although we agree that there are similar needs and issues arising across the LTCs from these PRISMS reviews (e.g. communication with HCPs, active education, informed decision-making and holistic biopsychosocial support), we have found that self-management support needs are condition-specific and should be individually tailored [e.g. managing physical disabilities and/or memory loss, considering the impact of a progressive condition (compared with an asymptomatic, stable or variable one) and the changing needs involved with living with dementia from the early to late stages]. We have identified the need for higher-quality reviews and reporting in this field, and for further investigation of interventions for self-management support for patients with dementia.
Chapter 14 Additional meta-review: self-management support for people with epilepsy
Meta-review of qualitative systematic reviews
Systematic reviews identified
Our search did not identify any relevant qualitative systematic reviews regarding support for self-management (see Appendix 19 for PRISMA chart).
Meta-review of quantitative systematic reviews
Systematic reviews identified
Following the title and abstract screening, 12 articles were screened for eligibility, four of which were included into the epilepsy quantitative meta-review162–165 (Figure 30). All four were Cochrane reviews published between 2008 and 2011. Thirty-five RCTs were included in the reviews of which 29 were unique RCTs, published between 1980 and 2009. The country settings of the individual RCTs were very inconsistently reported in the four systematic reviews but appear to have included the UK, Scotland, Norway, Germany, Switzerland, Austria, the USA, South Africa and Zimbabwe.
One review examined medication adherence interventions for adults, one explored psychological treatments and two reviewed care delivery and self-management strategies (one with children and the other with adults) (Table 70).
| Review | Intervention of interest and comparison | Participant demographics | Setting, delivery mode, and service arrangement | Content, focus, and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Al-aqeel 2011162 | Medication adherence interventions in comparison with usual care (‘no intervention’) | Five RCTs targeted adult epileptic patients (total n = 222); one RCT targeted parents of children with epilepsy (n = 51) | Primary care, outpatient or other community setting. No synthesised data about details of those included | Five RCTS of behavioural and educational interventions for adults. One RCT examined educational mothers’ discussion group meetings for parents of children with epilepsy | Follow-up time from 4 weeks to 6 months |
| Ramaratnam 2008165 | Psychological treatments, control NR (some quasi-randomised studies included) | Extremely varied, e.g. for CBT (five studies): adults; depressed adults; institutionalised adults; day worker adults attending an epilepsy centre in South Africa; and newly diagnosed adolescents | NR | CBT, education, self-management and relaxation combined with behavioural therapy are included within this meta-review. Thirteen studies (some quasi-randomised) | NR |
| Lindsay 2010164 | Care delivery and self-management strategies for children in comparison with usual care | One study included children only, one included children and parents, and one involved teenagers and parents | No included study investigated specialist teams of health or social care professionals either in hospital or community settings | All of the included studies investigate interventions for improved self-management: these interventions were identified by the review authors as either education, counselling or training | NR |
| Bradley 2008163 | Care delivery and self-management strategies for adults in comparison with usual care | Adults | They included the following settings:
|
Self-management education; strategies to improve patient compliance; self-management through screening; alternative models of outpatient care delivery; specialist nurse practitioners; lifestyle interventions; guideline implementation; and patient intervention | NR |
Quality assessment and weighting
All four reviews scored 31 or more out of 44, classifying all four as higher quality (Table 71).
| R-AMSTAR criteria | Al-aqeel 2011162 | Ramaratnam 2008165 | Lindsay 2010164 | Bradley 2008163 |
|---|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 4 | 4 |
| Was a comprehensive literature search performed? | 3 | 4 | 4 | 3 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 1 | 1 | 1 |
| Was a list of studies (included and excluded) provided? | 4 | 4 | 4 | 4 |
| Were the characteristics of the included studies provided? | 3 | 2 | 2 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 3 | 3 | 2 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 4 | 4 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 | 4 |
| Was the likelihood of publication bias assessed? | 1 | 1 | 1 | 1 |
| Was the conflict of interest stated? | 2 | 2 | 2 | 2 |
| Total score/44 | 34 | 33 | 33 | 31 |
Both Ramaratnam et al. 165 and Bradley and Lindsay163 contained data on over 1000 participants, these reviews were therefore weighted the highest levels of evidence in this meta-review (Table 72).
Outcomes
The outcomes of interest chosen for this meta-review were seizure frequency (an outcome included in all four reviews), medication adherence and QoL (each included in two of the reviews). These were considered key outcomes by the review team to inform commissioners and at least one of the three was considered a primary outcome in each of the included reviews (Table 73). (Health-care resource use was not reported by any review although two include costs of care and one reports on cost-effectiveness of the interventions, not presented here.)
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Seizure frequency | Frequency of seizures | Seizure frequency/severity; seizure index (frequency times duration); seizure reduction (50% or greater, seizure free and percentage change); seizure diaries; seizure frequency graded scale |
| Medication adherence | Adherence to medication | Percentage of doses taken; percentage of correct doses taken; percentage of doses taken on schedule; a combination average of the previous three scores |
| QoL | Global and HRQoL | CAS; SWLS; WHO QOL-BREF; SF-36; QoL QOLIE-31 and QOLIE-89 (these are epilepsy-specific QoL measures); POMS; Rosenberg Self-esteem Scale; ESES; Sherer Self-Efficacy Scale; physical self-concept and vigour (PSDQ) |
Findings
All four reviews reported narrative results due to heterogeneity (see Table 74 and Figure 31 for summaries of quantitative results).
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Al-aqeel 2011162 ** | Strategies for improving adherence to antiepileptic drug treatment in patients with epilepsy | Six RCTs; 273; 1980–2009 | Narrative | Adherence (all results below from single studies):
|
Education and counselling of patients with epilepsy have shown mixed success. Behavioural interventions such as the use of intensive reminders and implementation intention interventions provided more positive effects on adherence |
| Ramaratnam 2008165 *** | Psychological treatments for epilepsy | 13 RCTs; 1267; 1985–2009 | Narrative | CBT vs. no active treatment Seizure frequency: no significant effect in one study. Another found a statistically significant reduction in seizure frequency and seizure index. The remaining two studies did not investigate the effect of CBT on seizuresQoL: one study found no significant differences between intervention and control. In another study of the use of CBT in people with epilepsy and a depressed affect, significantly greater reduction in dysphoria and depression in the treatment group compared with controls were reported. There was also a significant decrease in self-reported anxiety, stress and anger. A third study found significant improvements in the SWLS at 6 months (p < 0.05) and 12 months (p < 0.001) after intervention, and QoL at 1-year follow-up in the intervention group (p < 0.05). Last, one study found subthreshold depressive disorder and QoL significantly improved at follow-up (at 6 and 9 months) in intervention compared with control group (p < 0.05) CBT vs. yoga Seizure frequency: one study reported no significant difference in number of participants seizure free; seizure frequency; seizure duration QoL: no data presented directly comparing intervention with control Educational interventions Seizure frequency: in one study the treatment group demonstrated a significant decrease in fear of seizures and significant decreases in hazardous medical self-management practices QoL: from one study no significant improvement in SF-36, depression or other epilepsy-specific measures such as self-esteem, fear, stigma, mobility and leisure Combined use of relaxation and behaviour therapy Seizure frequency: one RCT found sustained reduction in the median seizure index for the behaviour modification group at 1 and 8 years. In control groups there was an increase in seizure index at the end of 1 year. ES not reported in the other study exploring this outcome Explicit self-management interventions QoL: one RCT found no significant differences in overall QoL. Another reported non-significantly higher levels of self-efficacy and seizure management in intervention group |
In view of methodological deficiencies and the limited number of individuals studied, we have found no reliable evidence to support the use of psychological treatments and further trials are needed. Since the last version of this review, none of the new relevant studies have provided additional information to change the conclusions |
| Lindsay 2010164 ** | Care delivery and self-management strategies for children with epilepsy | Three RCTs; 665; 1990–2002 | Narrative | Seizure frequency: a child-centred model for children with chronic illness reported a significant difference between groups in epileptic seizures at 12 months favouring this intervention (p = 0.036) Medication adherence: at 6 months an evaluation of video conference-based family counselling and speakerphone family counselling found no differences in outcome measures between groups for medication issue frequency for teenagers or parents, or adherence to treatment QoL: at 3 months an evaluation of a modular education programme found no impact on QoL |
Every intervention showed some benefit, but impacts were extremely variable. No intervention showed benefits across all outcomes. No study demonstrated detrimental effects. Currently not possible to recommend one intervention over another |
| Bradley 2008163 *** | Care delivery and self-management strategies for adults with epilepsy | 13 RCTs; 3234; 1984–2005 | Narrative | Self-management education Seizure frequency: at 4 months no significant difference reported in one RCT Medication adherence: significantly increased compliance in intervention group compared with the control (subgroup only) MOSES Seizure frequency: suggestion of reduction in seizure frequency. Between group comparisons not reported Strategies to improve patient compliance Seizure frequency: significant reduction in seizure frequency in intervention but not control group. Between group comparisons not reported Medication adherence: significant differences in one measure of patient compliance at 6 months in one study. Significantly increased compliance to prescription refill frequency at 6 months. No significant changes were seen in measures of clinic appointment keeping Prompt and reminder cards Seizure frequency: no significant changes in the proportion of seizure-free patients in doctor-held card practices or in patient-held care practices Self-management through screening Seizure frequency: no significant differences in change in seizure frequency QoL: change in QoL not significantly different between groups Alternative care delivery in outpatient clinics Seizure frequency: one study found no significant difference between groups in seizure frequency at 3, 6 and 12 months Specialist nurse practitioners Seizure frequency: one study found no significant difference in seizure frequency at 6 months. Another study found no difference in the number of people having no seizures, or one or less seizures per month between intervention and control at 6 months Medication adherence: no between-group comparison for, or outcomes of interest, presented in one study. Another study found no difference between study and intervention groups in self-reported non-compliance with medication and attendance at epilepsy clinic QoL: intervention group participants significantly more likely than controls to have improved QoL score (p = 0.019). Another RCT reported some promising improvements in QoL before and after, but no between group comparisons presented. Another study found no significant changes in perceived QoL at 1 and 2 years Lifestyle interventions Seizure frequency: no statistical difference in seizure frequency from one RCT QoL: at 12 weeks no significant differences between the groups were reported for the QoL, mood state, self-esteem scale or PSDQ scores (physical self-concept and vigour domains) Guideline implementation and patient information QoL: no significant difference in SF-36 at 6 and 12 months |
Specialist epilepsy nurse and self-management education have some evidence of benefit. No clear evidence that other service models substantially improve outcomes. It is possible that benefits are situation specific and may not generalise to other settings. At present it is not possible to advocate any single model of service provision |
FIGURE 31.
Epilepsy: summary of the quantitative evidence.
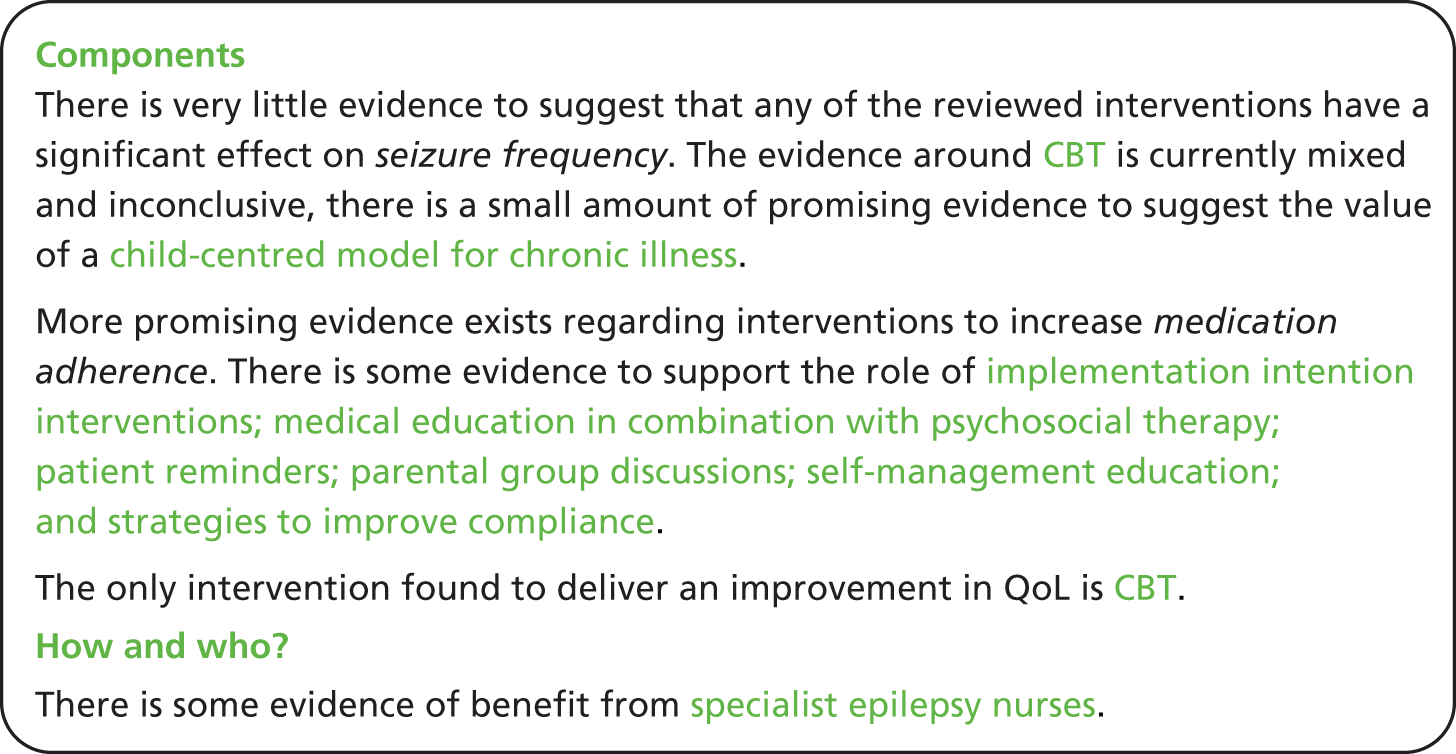
Seizure frequency
Only one intervention described in one study across these reviews found a reduction in seizure frequency, although this outcome was not reported by all the included RCTs. Lindsay and Bradley164 report a significant reduction in seizure frequency from the study of a child-centred model of chronic illness.
The two studies within Al-aqueel and Al-sabhan’s162 higher-quality review of interventions to improve adherence to antiepileptic medication reporting on seizure frequency failed to find any significant effect. Ramaratnam et al. 165 reports inconclusive effects of CBT on seizure frequency from two studies. Bradley and Lindsay’s163 review of care delivery and self-management strategies for adults with epilepsy found evidence to suggest no impact on seizure frequency from single studies on the following interventions: self-management education; prompt and reminder cards; self-management through screening; alternative care delivery in outpatient clinics; and lifestyle intervention. Two studies on specialist nurse practitioner interventions were also found not to have any significant impact on seizure frequency. There was some suggestion of beneficial effect from other interventions but these were based on pre–post effects and did not present comparisons between intervention and control.
Medication adherence
Al-aqueel and Al-sabhan’s162 review of interventions to improve adherence to antiepileptic medication report promising findings from a single study. An implementation intention intervention (which involves the completion of a simple worksheet by patients, linking the intention of taking medication with a particular time, place and other routine activity) was found to be effective in enhancing medication adherence. Motivational interviewing was not found to be associated with any positive effects in one study. An intervention delivering medical education alongside psychosocial therapy reported significant improvements in one measure of antiepileptic medication adherence. The use of patient reminders (reminders for prescription refill and appointments together with a counselling leaflet) was associated with a significant improvement in intervention compared with control in only one of three measures of adherence. Provision of educational materials was not associated with any significant effect on adherence in one study, whereas an educational mothers’ discussion group was associated with a significant improvement in adherence in one study. Lindsay and Bradley164 report no significant effect on adherence outcomes from one study of family counselling for children with epilepsy.
Bradley and Lindsay’s163 review of care delivery and self-management strategies for adults with epilepsy found self-management education to be associated with significantly increased adherence in intervention compared with control in a subgroup of participants. Strategies to improve compliance were also found to have significant positive effects on adherence measures. Two studies exploring specialist nurse practitioner interventions both reported no significant effect on medication adherence.
Quality of life
Evidence from Ramaratnam et al. 165 suggests CBT to be associated with an overall beneficial effect on QoL. From the same review, there is evidence from one study to suggest education has no effect on QoL. QoL outcomes were only reported for four of the interventions explored in Bradley and Lindsay,163 with no significant differences detected for self-management through screening; lifestyle interventions; and guideline implementation and patient information. There was, however, some evidence to support a positive impact of specialist nurse practitioners on QoL.
Chapter 15 Additional meta-review: self-management support for people with hypertension
Meta-review of qualitative systematic reviews
Systematic reviews identified
A total of 11,098 quantitative and qualitative unique references were identified for screening. Following title and abstract screening, four qualitative reviews and two mixed reviews were reviewed for exclusion separately on both qualitative and quantitative criteria. After full-text screening, two reviews166,167 (published 2007 and 2012 in peer-reviewed journals) were included in the hypertension qualitative meta-review (Figure 32). The reviews reported a total of 64 primary qualitative studies (published between 1980 and 2011). Seven of these were included in both of the reviews, leaving a total of 57 unique studies.
Both reviews focused on lay perspectives about hypertension and medication adherence (Table 75).
| Authors, year | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Marshall 2012166 | We carried out a systematic review and narrative synthesis of qualitative studies on hypertension. Specifically, we examined lay understandings about the causes of hypertension and perspectives on drug taking. We also investigated how patients’ perspectives varied among different cultures and ethnic groups | 53 (in 59 papers) | 59 papers reporting on 53 qualitative studies were included in the synthesis. These studies came from 16 countries (USA, UK, Brazil, Sweden, Canada, New Zealand, Denmark, Finland, Ghana, the Islamic Republic of Iran, Israel, the Netherlands, the Republic of Korea, Spain, Tanzania and Thailand). A large proportion of participants thought hypertension was principally caused by stress and produced symptoms, particularly headaches, dizziness and sweating. Participants widely intentionally reduced or stopped treatment without consulting their doctor. Participants commonly perceived that their blood pressure improved when symptoms abated or when they were not stressed, and that treatment was not needed at these times. Participants disliked treatment and its side effects and feared addiction. These findings were consistent across countries and ethnic groups. Participants also reported various external factors that prevented adherence, including being unable to find time to take the drugs or to see the doctor; having insufficient money to pay for treatment; the cost of appointments and healthy food; a lack of health insurance; and forgetfulness |
| Schlomann 2007167 | The purpose of this interpretive synthesis is to explore lay beliefs about high blood pressure and its treatment, as described in qualitative research, in order to develop a foundation for better partnering with clients. This analysis is rooted in the naturalistic perspective and the assumption that qualitative research would provide the richest data and most accurate portrayal of lay beliefs | 11 | Professional and lay beliefs about hypertension are not congruent. Historical factors, lack of congruence between belief systems and poor relationships with providers lead many clients, especially African Americans, to distrust providers and impede the effectiveness of treatment plans. The most problematic discrepancies were related to beliefs about (a) the presence of symptoms, (b) the need to take medications for the rest of one’s life, and (c) race-specific treatment plans. The interactions between nurse practitioners and hypertensive clients have not been explored. Implications for practice: professional–client interactions based on partnership models, with specific consideration for the above-stated discrepancies in beliefs, are necessary to improve hypertension control |
Quality assessment
Marshall et al. ’s166 review was high quality with clear, explicit details about the review process, methods to reduce biases (e.g. no language restriction), how the quality impacted the findings (including a sensitivity analysis) and what this meant for research and practice. Schlomann and Schmitke’s167 review was more focused (e.g. only USA-based studies included) and scored low on our assessment of quality (Table 76).
| R-AMSTAR criteria | Marshall 2012166 | Schlomann 2007167 |
|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 4 | 1 |
| Was a list of studies (included and excluded) provided? | 1 | 1 |
| Were the characteristics of the included studies provided? | 3 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 1 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 |
| Was the conflict of interest stated? | 1 | 1 |
| Total score/40 | 33 | 22 |
| Quality rating (low = < 30; high = ≥ 30) | High | Low |
Findings
The synthesis enabled these findings to be integrated to provide a broader picture to inform future commissioning of self-management support.
-
There was a mixture of beliefs regarding the aetiology of hypertension and what hypertension is, including regarding high BP and hypertension as separate conditions. These beliefs can cause confusion for someone diagnosed with hypertension if their understanding does not match their sense of self, for example if they believe it is hereditary and no one else in their family has it, or if they believe it is caused by eating certain foods when they do not eat those foods.
-
The role of stress was discussed extensively as a major cause, exacerbating factor and consequence of hypertension. A range of life stressors were reviewed; for example, a busy job may not only cause psychological stress, but also act as a barrier to medication adherence and healthy lifestyle choices. Finance, family problems and racism were also discussed as examples of stressors and some people even felt that particularly stressful life stories or even individual life events may have caused their hypertension.
-
The potential consequences of hypertension caused fear about what this meant for the future. Patients also judged the seriousness of their hypertension based on the amount of symptoms they were experiencing. There was often a belief among patients who hypertension is symptomatic and therefore if they did not have symptoms then they could not have the condition. Taking medication was reported to be motivated by periods of experiencing symptoms or periods of high stress, rather than the perception of having a chronic condition needing regular medication. Some patients were very adherent to their treatment, whereas others were more concerned about the long-term effect of taking medication or side effects. Alternative remedies, such as garlic, were sometimes perceived as a more effective option with fewer side effects. Relapse from taking medication and feeling ill again may lead to the realisation that the hypertension still exists. There was a reported need for more information about the complications caused by hypertension.
-
There was a conflict between HCPs’ provision of information that hypertension was asymptomatic and people’s beliefs that for it to be a disease, it must have symptoms. Similarly, in the perceived discrepancy in information provided by HCPs that making lifestyle changes could ‘treat’ the condition and yet, regardless of any changes made, lifelong medications might also be needed. There is a reported need for HCPs to address the underlying concerns of people (such as the safety of long-term medications, presence of symptoms and the need for lifestyle change) and work within their lay understanding of the disease rather than assuming people have little knowledge of the condition or trying to ‘correct’ their knowledge to a biomedical model.
-
People who were more adherent to medication described their HCP as caring and listening, and their relationship with them as a partnership, with joint goal-setting and holding individuals accountable for their behaviour. Without this, distrust was reported, with some patients believing that medication was the easier option for HCPs to prescribe, compared with diet and lifestyle advice. Support and information regarding lifestyle change is important. Barriers to dietary change included culturally specific ones, such as patients feeling that they are being asked to stop eating food from their culture, and start eating food from another. It also included more general reasons, such as cost, food preparation or the simple difficulty of making a change. Questioning the diagnosis, advice and prescription from the HCP led to the patient deciding if they should, or should not, take medication without necessarily understanding the potential consequences.
Meta-review of quantitative systematic reviews
Systematic reviews identified
A total of 11,098 unique references were identified for screening (Figure 33). Only systematic reviews in which information on people with diagnosed hypertension was presented and synthesised separately, or from which it could easily be extracted for synthesis, were included (for more detail see Chapter 5). Similarly, only reviews from which evidence from RCTs alone could be extracted were included. Reviews focusing solely on monocomponent interventions such as meditation, relaxation, exercise or stress-management were excluded. In keeping with the rest of this meta-review, professional education was included when it formed part of a wider search for interventions to support self-management. Despite multiple approaches, including contacting authors and British Library searches, four reviews were not obtainable (one of these was not yet published). These titles and abstracts were reviewed again and it was felt that it was unlikely that they would be of relevance to the final review thus, in view of this and the rapid nature of this meta-review, they were excluded on this basis. After full-text screening, there were 10 systematic reviews included in this quantitative review99,168–176 (see Figure 33).
A total of 233 references were captured within these systematic reviews, of which 151 were unique references and the remaining were duplicates appearing in more than one review. The year of review publication ranged from 1998170 to 2011176 and included RCTs dating from 1973 to 2010, published in peer-reviewed journals. Total numbers of participants in the RCTs were not synthesised in several of the reviews, but we were able to calculate that they ranged from 382168 to more than 87,000171 (in which the number of participants in all RCTs was not given). Of the 10 reviews, six presented statistical estimates from aggregated data and the remaining four presented data synthesised narratively alone. Not all systematic reviews recorded where individual RCTs had been conducted; of those that did, the greatest number was from the USA. The majority of the rest were from Europe, including France, UK, Turkey, Finland, Norway, Spain, Holland, Switzerland and Germany, whereas others were from Canada, Australia and South Africa.
Half the included reviews (five) searched for all self-management support interventions (Chodosh et al. ,99 Glynn et al. ,171 Ebrahim,170 Schroeder et al. 174 and Takiya et al. 175). Chodosh et al. 99 focused on chronic disease self-management programmes for osteoarthritis and diabetes mellitus as well as hypertension, in which it reviewed their effect on BP. Although the RCTs in this review were varied, they were based on the principle that they should be tailored, conducted in the group setting, involve patient feedback, involve care from physicians or primary care providers and have a psychological emphasis. Nevertheless, some did involve individual interventions and many were complex, involving multiple support components such as self-monitoring, contracts and education.
The remaining four reviews that looked at general interventions for self-management support were all specific to hypertension. Glynn et al. 171 looking at control of BP, divided the interventions into ‘self-monitoring’, ‘educational interventions directed to the patient’, ‘educational interventions directed to the physician’, ‘health professional (nurse or pharmacist)-led care’, ‘organisational interventions that aimed to improve the delivery of care’ and ‘appointment reminder systems’.
Ebrahim170 looked at the effect of interventions on adherence and BP but gave limited synthesised information on the interventions in the RCTs it reviewed. Although they were divided into ‘education’, ‘home-monitoring’, ‘self-monitoring’, and ‘miscellaneous’ by the authors, it is clear from the individual RCTs included that many of the interventions were complex and involved multiple other interventions, including doctor, nurse, counsellor and psychologist-led care, group and individual work, contracts, computer support, appointment reminders and medication changes.
Schroeder et al. 174 and Takiya et al. 175 focused primarily on adherence as their outcome, although the former also reviewed any BP changes as a secondary outcome. Schroeder et al. 174 divided the types of interventions it reviewed into ‘simplification of dosage regimens’, ‘patient education’ (including an educational programme, group education, written educational material, visual aids, lectures, tests and postal information), ‘patient motivation, support and reminders’ (including self-monitoring) and ‘complex health and organisational interventions including interventions in combination’ (also encompassing allied professional-led care). Finally, Takiya et al. 175 divided the interventions it reviewed into ‘behavioural interventions’ (such as packaging and schedule changes and reminders), ‘educational interventions’ and ‘combined interventions’, which included education and behavioural interventions, as well as other tools such as self-monitoring of BP.
Several reviews focused solely on the use of technology in supporting self-management of hypertension. Ogedegbe and Schoenthaler172 looked at the effect of home BP monitoring on medication adherence the majority of the RCTs were complex interventions that also delivered education, counselling and other support (such as home visits or medication reminders). Verbek et al. 176 focused on telecare in the management of hypertension, these were interventions where patients measured their BP at home and transmitted these data to health-care providers, often alongside educational and behavioural interventions delivered by nurses or pharmacists. Finally, Saksena173 explored the use of computer-based education for patients, involving computer education programmes, website-based interactive technology and BP monitoring. It should also be noted that many of the general systematic reviews above also included technological interventions as part of their review.
Bosch-Capblanch et al. 168 focused on contracts as a support intervention to improve people’s adherence to treatment. These trials predominantly utilised education, behavioural strategies, relaxation techniques and BP monitoring, delivered in group settings that were supported by the use of contracts.
The final systematic review, Dickinson et al. ,169 analysed the effect of lifestyle interventions to reduce BP in hypertensive patients; we only focused on combined interventions from this systematic review, as the aim of this meta-review was to look at multidimensional self-management support interventions. The combined interventions reviewed included combinations of group exercise, diet, salt restriction and relaxation. The authors note that about 60% of all the active interventions in the combined trials brought participants together regularly in groups and most trials of diet enrolled overweight people, although no further information regarding the lifestyle interventions reviewed was described by the authors so it is hard to know what form these interventions took (Table 77).
| Review | Intervention of interest | Participant demographics | Setting, delivery mode and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Bosch-Capblanch 2009168 | Whether or not contracts between practitioners and patients really improve the patients’ adherence to treatment or their health status | Any age, gender and any health setting | Four trials examined the effects of contracts on a variety of outcomes, in the context of hypertension management | Studies varied in content:
|
NR |
| Chodosh 200599 | Do chronic disease self-management programmes result in improved disease-related outcomes for specific chronic diseases of high prevalence in older adults? If self-management interventions are effective, are there specific components that are most responsible for the effect? | Older adults | All RCTs that assessed the effects of an intervention or interventions relative to either a group that received usual care or a control group among the elderly | Most studies compared their intervention with usual care or with a control intervention designed to account for the added attention received in the intervention (such as attending classes on vehicle safety instead of attending classes on self-management) Multiple designs including exercise, education, psychological support, relaxation, anxiety management, self-monitoring and lifestyle support |
NR |
| Dickinson 2006169 | To quantify the effects of lifestyle interventions for hypertension | For combined interventions alone: mean baseline BP = 144/91 mmHg; mean age = 52 years; mean % male = 66%; mean % white = 75% | NR | Two trials provided interventions combining group exercise and diet; two also included salt restriction; one trial further included relaxation; one trial combined a weight loss diet, relaxation and salt restriction. Control groups received no intervention or placebo medication | Median treatment = 26 weeks (range 9–52 weeks); median follow-up = 26 weeks (range 9–78 weeks) |
| Ebrahim 1998170 | The (relevant) objectives were to find out the most effective methods of improving patient adherence with treatment and improving control of BP | NR | NR | Not summarised by authors but evident that multiple different interventions have been reviewed including: education, self-monitoring, complex interventions, different health professional-led care, medication changes and reminders, and organisational change interventions | NR |
| Glynn 2010171 | To determine the effectiveness of interventions whose objective was to improve follow-up and control of BP in patients taking BP-lowering drugs | The population of interest comprised adult patients (aged ≥ 18 years) with essential hypertension (treated or not currently treated with BP lowering drugs) in a primary care, outpatient or community setting | NR | Interventions aimed at improving control of BP or clinic attendance, classified as:
|
NR |
| Ogedegbe 2006172 | The effects of HPBM on adherence to prescribed antihypertensive medications among hypertensive patients | NR | Trials conducted in various settings, including shopping malls, community/retirement centres, worksites, hospital-based clinics/tertiary care centres. Three studies conducted in primary care practices and study setting NR for two trials | 82% trials were complex interventions where effects of HBPM on medication adherence was tested in combination with other adherence-enhancing strategies such as patient education; counselling on medication adherence by nurses, pharmacists or through a telephone-linked system; use of timed medication reminders (such as special vials); monthly home visits; and nurse case management. The remaining two trials were simple interventions (they used HBPM alone) | Median duration: 6 months (range 1.5–12 months) |
| Saksena 2010173 | To evaluate the effectiveness of computer-based interventions for hypertensive patient education. Only one RCT assessed BP as an outcome | NR for the RCT alone | Two studies developed software-based programmes which participants completed on site, under guidance of a moderator. The other studies used interactive websites that participants could access over a number of months. It was expected that participants would access websites in their own time, and work through the information independently | Only one trial reported BP as an outcome: this three-arm trial compared usual care, access to a website with health information, and access to the same website with pharmacist assistance in using the website and creating a management plan. Both intervention groups also received a home BP monitor. The third arm of the trial received telephone and web communication from a pharmacist who helped create a care plan | This intervention lasted 12 months |
| Schroeder 2004174 | Any intervention designed to enhance medication adherence, including:
|
Study participants fell into a number of different categories that included newly diagnosed patients, patients with established hypertension on medication, patients with controlled or uncontrolled hypertension, patients adherent or non-adherent to medication or infrequent attendees at clinic. All studies examined both men and women in varying proportions | NR other than details already given |
|
NR but, where stated, ranged from 1 day to 1 year |
| Takiya 2004175 | To identify adherence tools and methods evaluated in RCTs targeted to improve adherence with antihypertensives and determine the net and individual effects of the tools and methods on adherence using meta-analytic techniques | 54% (n = 13) did not report age, 63% did not report gender. Of the cohorts reporting gender and age, 91% (10/11) consisted of adults (aged 18–65 years) and 56% (5/9) had more than 50% male patients. However, target study population was not always clear. In many cases the medication would be prescribed for a geriatric patient; however, the intervention was directed at the caregiver, not the patient | 46% of the interventions were conducted in the physician’s office. Other settings were long-term care facility, pharmacy, MCOs and ‘other’ | Of the 16 citations, two included distinctly different study populations with different interventions (behavioural interventions, educational interventions, and combined behavioural and educational interventions) and three studied more than one intervention in different patient groups in parallel. The majority of the interventions (14/24; n = 1531) focused on behavioural interventions to improve adherence; however, some (7/24; n = 708) studied the effect of behavioural and educational interventions. The most common behavioural intervention studied was a dosing schedule change (8/14); for educational interventions, it was oral education (2/3) | The median duration of the various interventions was 3 months (mean 3.8 months; range 1–6 months) |
| Verbek 2011176 | The usefulness of telecare for the management of hypertension | The patient characteristics were similar between both groups (usual care and telecare). Total population (n = 2501), age (years) 61.4 (SEM ± 0.6), male 42.3 (SEM ± 2.7). Patient population involved mild to moderate treated and untreated hypertensive patients | There was a large difference in study design. Some studies made websites available such that patients could check their own data and easily contact a health-care member by e-mail. In other studies, telecare patients also received extra support from a nurse or pharmacist In some studies patients had to have a computer and access to the internet |
Included designs: website; weekly lifestyle recommendations; reminding beep to measure BP; HBPM training and training on how to use the website and other utilities; pharmacist assistance; home visits; data feedback provided by telephone call; a weekly report; antihypertensive drugs adjusted through a telephone call and/or visit, if necessary; education and motivation counselling; a two-step self-management algorithm; how to adjust medication according to self-measured BP data; two group training sessions; telephone number available for trial-related questions | Study duration (days): mean 198 days (range 56–365 days) |
Quality assessment and weighting
Quality of the 10 systematic reviews, as assessed by R-AMSTAR, ranged from 24 to 35, out of a total possible score of 44. Half of the reviews (five) were classified as being of higher quality (R-AMSTAR ≥ 31),99,168,169,174 whereas five were classified as lower quality (R-AMSTAR ≤ 30)170,172,173,175,176 (Table 78).
| R-AMSTAR criteria | Bosch-Capblanch 2007168 | Chodosh 200599 | Dickinson 2006169 | Ebrahim 1998170 | Glynn 2010171 | Ogedegbe 2006172 | Saksena 2010173 | Schroeder 2004174 | Takiya 2004175 | Verbek 2011176 |
|---|---|---|---|---|---|---|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 1 |
| Was a comprehensive literature search performed? | 3 | 4 | 3 | 3 | 4 | 3 | 4 | 4 | 4 | 2 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 4 | 1 | 1 | 1 | 4 | 2 | 4 | 4 | 1 | 1 |
| Was a list of studies (included and excluded) provided? | 4 | 3 | 3 | 4 | 3 | 3 | 3 | 4 | 1 | 3 |
| Were the characteristics of the included studies provided? | 3 | 2 | 4 | 2 | 3 | 3 | 3 | 2 | 3 | 4 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 4 | 4 | 4 | 3 | 1 | 4 | 2 | 1 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 1 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 1 | 1 |
| Were the methods used to combine the findings of the studies appropriate? | 1 | 4 | 4 | 1 | 4 | 1 | 1 | 1 | 4 | 2 |
| Was the likelihood of publication bias assessed? | 1 | 4 | 4 | 1 | 1 | 1 | 2 | 2 | 3 | 4 |
| Was the conflict of interest stated? | 3 | 3 | 2 | 2 | 3 | 2 | 1 | 3 | 2 | 1 |
| Total score/44 | 32 | 34 | 35 | 28 | 35 | 27 | 28 | 34 | 29 | 24 |
A weight of evidence was then applied by considering both the quality assessment scores and the total number of participants represented in the review (Table 79). Three systematic reviews were found to have three star ratings99,171,174 and seven studies were weighted as two stars. 168–170,172,173,175,176 Glynn et al. 171 was the strongest systematic review, with the overall highest R-AMSTAR score and largest number of patients reviewed, whereas Verbek et al. 176 had the lowest AMSTAR score.
| Review | Quality | Total population size | Weighting |
|---|---|---|---|
| Bosch-Capblanch 2007168 | 32 | 382 | ** |
| Chodosh 200599 | 34 | 1557 | *** |
| Dickinson 2006169 | 35 | 413 | ** |
| Ebrahim 1998170 | 28 | > 32,000a | ** |
| Glynn 2010171 | 35 | > 87,000a | *** |
| Ogedegbe 2006172 | 27 | 1550 | ** |
| Saksena 2010173 | 28 | 1319 | ** |
| Schroeder 2004174 | 34 | 15,519 | *** |
| Takiya 2004175 | 29 | 2446 | ** |
| Verbek 2011176 | 24 | 2501 | ** |
Outcomes
The main outcomes of interest in the included reviews were adherence and BP [DBP and systolic blood pressure (SBP)]. Health-care resource use was rarely reported in the constituent systematic reviews. Therefore this review of self-management interventions for hypertension focused on these two outcomes; other outcomes including self-efficacy, self-care behaviour and knowledge,173 were not extracted further (Table 80).
| Primary outcomes | Definition | Measures reported in reviews |
|---|---|---|
| BP | Changes in BP (mmHg) | DBP, SBP, meeting BP control targets |
| Adherence | Adherence to antihypertensive medication | Included self-report, direct questioning, pill counts and the MEMS |
Findings
We present a synthesis of our findings below (see Table 81 for the statistical findings, Table 82 for the narrative findings and Figure 34 for a summary), divided into categories of interventions and, in each case, considering the two primary outcomes of adherence and BP. All CIs were at 95% level unless stated otherwise.
| Reference and weighting | Outcome | Time | Sample size | Significancea | ES (95% CI) |
|---|---|---|---|---|---|
| Glynn 2010171 *** | Self-monitoring | ||||
| Mean SBP change | NR | 12 RCTs | ++ | –2.5 mmHg (–3.7 to –1.3 mmHg) | |
| Mean DBP change | NR | 14 RCTs | ++ | –1.8 mmHg (–2.4 to –1.2 mmHg) | |
| BP control achieved | NR | Six RCTs | 0 | OR 0.97 (0.81 to 1.16) | |
| Educational interventions directed to the patient | |||||
| BP control achieved | NR | Eight RCTs | + | OR 0.83 (95% CI 0.75 to 0.91)b | |
| Educational interventions directed to the physician | |||||
| Mean SBP change | NR | NR | 0 | –0.4 mmHg (–1.1 to 0.2 mmHg) | |
| Mean DBP change | NR | NR | 0 | –0.4 mmHg (–1.1 to 0.3 mmHg) | |
| Appointment reminder systems | |||||
| BP control achieved | NR | Two RCTs | + | OR 0.54 (0.41 to 0.73)b | |
| Verbek 2011176 ** | Telecare intervention vs. control | ||||
| Mean SBP change | NR | NR | +++ | –5.2 mmHg (p < 0.001) | |
| Mean DBP change | NR | NR | ++ | –2.1 mmHg (p < 0.01) | |
| Percentage meeting BP targets | NR | NR | 0 | 2.7% (p = 0.6) | |
| Intervention but without antihypertensive drug modification vs. control | |||||
| Mean SBP change | NR | NR | 0 | –8.6 mmHg (no p-value provided) | |
| Mean DBP change | NR | NR | 0 | –3.6 mmHg (no p-value provided) | |
| Intervention with antihypertensive drug modification based on measured BP values vs. control | |||||
| Mean SBP change | NR | NR | 0 | –5.1 mmHg (p = 0.07) | |
| Mean DBP change | NR | NR | 0 | –2.2 mmHg (p = 0.22) | |
| Chodosh 200599 *** | Self-management programme | ||||
| SBP change | NR | NR | + | –0.39 (–0.51 to –0.28) | |
| DBP change | NR | NR | + | –0.51 (–0.73 to –0.30) | |
| Dickinson 2006169 ** | Combinations of interventions (improved diet, exercise, alcohol restriction, sodium restriction) | ||||
| Mean SBP change | NR | Six RCTs; 374 participants | +++ | –5.5 mmHg (–8.8 to –2.3 mmHg) | |
| Mean DBP change | NR | Six RCTs; 374 participants | +++ | –4.5 mmHg (–6.9 to –2.0 mmHg) | |
| Takiya 2004175 ** | Behavioural interventions | ||||
| Adherence (different measures converted to ES) | NR | NR | 0 | 0.04 (–0.01 to 0.09) | |
| Ebrahim 1998170 ** | Home monitoring | ||||
| Mean DBP change | NR | NR | 0 | –0.5 mmHg (–0.7 to 0.7 mmHg) | |
| Self-monitoring | |||||
| Mean DBP change | NR | NR | + | –1.5 mmHg (–2.7 to –0.3 mmHg) | |
| Patient education | |||||
| Mean SBP change | NR | NR | +++ | –7.6 mmHg (–8.5 to –6.7 mmHg) | |
| Mean DBP change | NR | NR | +++ | –4.2 mmHg (–4.6 to –3.8 mmHg) | |
| Patient education without the Hypertension Detection and Follow-up Program | |||||
| Mean SBP change | NR | NR | 0 | –0.7 mmHg (–2.8 to 1.4 mmHg) | |
| Mean DBP change | NR | NR | 0 | –0.6 mmHg (–1.6 to 0.4 mmHg) | |
| Professional education | |||||
| Mean DBP change | NR | NR | + | –1.9 mmHg (–3.3 to –0.5 mmHg) | |
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Bosch-Capblanch 2007168 ** | Contracts between practitioners and patients | Four RCTs; 382; 1980–8 | Narrative synthesis |
|
There is not enough evidence to recommend the widespread introduction of patient contracts into health services |
| Chodosh 200599 *** | Chronic disease self-management programmes and any specific components that are most effective | 13 RCTs; 1557; 1977–2003 | Meta-analysis |
|
Overall pooled results from 13 studies show a statistically and clinically significant reduction in SBP and DBP Unaccounted for heterogeneity, may be due to publication bias, pooled results must be viewed with caution |
| Dickinson 2006169 ** | Lifestyle interventions | Six RCTs; 413; 1985–2002 | Meta-analysis |
|
Despite the likelihood of achieving only a small reduction in BP, some patients with mild hypertension may wish to change their lifestyle in an effort to delay or prevent starting antihypertensive drug therapy. In people with more severe hypertension, lifestyle changes may complement the BP lowering effect of drugs and thereby reduce the number of medications needed to control BP |
| Ebrahim 1998170 ** | Methods for improving adherence and control | 46 RCTs (from 56 references); > 32,000; 1975–95 | Meta-analysis |
|
Evidence is lacking to support any specific approaches to improving patient adherence with antihypertensive drugs or lifestyle changes Evidence to support nurse-led care compared with doctor-led care as a better option in achieving BP control is very sparse |
| Narrative synthesis |
|
||||
| Glynn 2010171 *** | Models of care that improve BP control or follow-up care of patients | 77 studies from 72 unique RCTs; unclear n participants but > 87,000 (from those recorded); 1975–2007 | Meta-analysis |
|
Effective delivery of hypertension care in the community requires a rigorous approach in terms of identification, follow-up and treatment with antihypertensive drugs. This systematic review shows that such an approach is likely to translate into reductions in cardiovascular mortality and morbidity. Supplementary and alternative models of care, including self-monitoring of BP by patients, BP management by allied HCPs and computer-based clinical decision support systems require further development and evaluation. Educational interventions directed to either patients or health professionals alone are unlikely to produce clinically important reductions in either SBP or DBP |
| Additional narrative synthesis |
|
||||
| Ogedegbe 2006172 ** | The effects of home BP monitoring on adherence | 11 RCTs; 1550; 1976–2004 | Narrative synthesis |
|
The data on the effects of home BP monitoring on patients’ medication-taking behaviour are mixed, given that only a little over half of the studies reviewed reported a statistically significant improvement in medication adherence between intervention and control. The reported improvement in adherence was greater in the trials that tested home BP monitoring along with other adherence-enhancing strategies such as patient counselling, patient reminders and the use of nurse case managers. Home BP monitoring could be considered a useful adherence-enhancing strategy in combination with other strategies such as patient counselling |
| Saksena 2010173 ** | The effectiveness of computer-based interventions | Four RCTs; 1319; 1995–2008 | Narrative synthesis |
|
Computer-based interventions in isolation were insufficient to change health behaviours. There is promising evidence that computer-based interventions with additional pharmacist care can improve BP control |
| Schroeder 2004174 *** | Interventions designed to enhance medication adherence | 38 RCTs; 15,519; 1975–2000 | Narrative synthesis |
|
Findings suggest that introducing simpler dosing regimens can be effective in improving adherence, but the effect on subsequent BP reduction has not been established and may not be clinically important. The results of various motivational and more complex interventions are promising, although there is insufficient evidence to suggest a single approach The results of this review should be interpreted with caution due to the poor methodological quality and heterogeneity of trials included in this review |
| Takiya 2004175 ** | Adherence tools and methods to improve adherence | 16 RCTs; 2446; 1973–2000 | Meta-analysis |
|
There is no single intervention that improves adherence to antihypertensives over others; therefore a patient-specific approach should be modelled |
| Verbek 2011176 ** | Telecare for the management of hypertension | Nine RCTs; 2501; 1996–2010 | Meta-analysis |
|
Telecare leads to a greater decrease in SBP and DBP than is obtained with usual care. Telecare may be particularly useful for increasing patients’ awareness, which may lead to improved adherence to treatment and lifestyle advice |
FIGURE 34.
Hypertension: summary of the quantitative evidence.
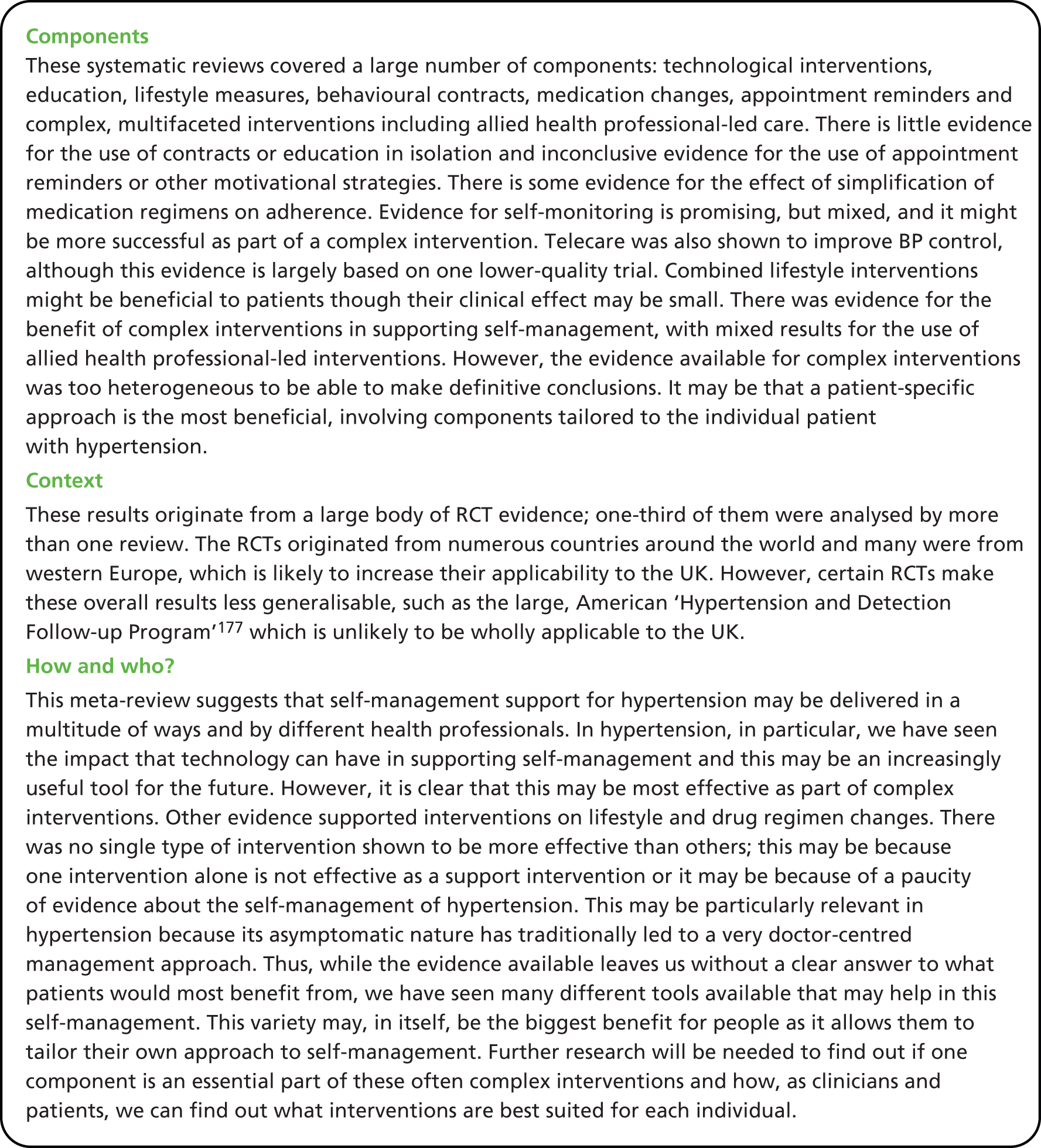
Technological interventions: self-monitoring of blood pressure, telecare and computer-based education
Self-monitoring: outcomes
Multiple studies included self-monitoring as part of multicomponent interventions and this will be discussed further below (see Complex interventions, including allied health professional-led care). However, Glynn et al. 171 Ebrahim,170 and Ogedegbe and Schoenthaler172 also synthesised results for self-monitoring as the primary intervention in hypertension support. Out of these, only Glynn et al. 171 was weighted as a three star review.
Only Ogedegbe and Schoenthaler172 studied the effect of self-monitoring on adherence. This review was focused solely on home BP monitoring, although many of the RCTs it reviewed were part of complex interventions and, more specifically, usually included education. In fact, 82% of the 11 trials reviewed were ‘complex interventions’, with only two trials using home BP monitoring alone. Although the results were too heterogeneous to pool together, 54% (six) of the RCTs reported statistically significant improvements in medication adherence, with five of these being complex and one including home BP monitoring alone. Interestingly, the authors also found that none of the studies set in primary care settings (three) showed any statistically significant benefit from this intervention. Overall, the authors concluded that the results of RCTs reviewing the effect of self-monitoring were ‘mixed at best’ and that the greatest effects were seen when monitoring was used alongside other ‘adherence-enhancing strategies’. 172
All three studies also reviewed the effect of monitoring on BP control. Ogedegbe and Schoenthaler172 found that only 4 trials out of 11 showed statistically significant improvements in both adherence and BP. Glynn et al. ,171 the highest-quality review, assessed 18 RCTs that looked at self-monitoring of BP and pooled the data from 12 RCTs that reported differences in mean SBP. This showed a significant reduction of –2.5 mmHg (95% CI –3.7 to –1.3 mmHg) in SBP and –1.8 mmHg (95% CI –2.4 to –1.2 mmHg) in DBP from the 14 studies that measured this outcome. However, they noted significant between-group heterogeneity for mean SBP. There was also no significant improvement in BP control in the six RCTs that reported on this. They therefore concluded that self-monitoring was associated with a decline in BP but might be a most useful tool in combination with other interventions, as the improvement seen was clinically small. It should be noted that Glynn et al. 171 did not explicitly state whether or not these interventions involved more than self-monitoring alone, but it is clear from their descriptions of studies that many did involve additional education and home visits.
In a much older review, Ebrahim170 found that self-monitoring of BP had a small but significant effect on DBP control [–1.5 mmHg (95% CI –0.3 to –2.7 mmHg)], whereas the effect of home monitoring on DBP (which included the effects of family monitoring too) was not significant [–0.5 mmHg (CI –0.7 to 0.7 mmHg)]. The study concluded that the evidence base to support self-monitoring was small but that ‘simpler techniques of self-monitoring may be effective’. 170 Although it should be noted that this study was weighted as two star-quality due to its high number of participants, it had a lower R-AMSTAR score and was the oldest review in our meta-review.
Telecare interventions: outcomes
One review, by Verbek et al. ,176 looked at the use of telecare interventions in the management of BP; the authors assessed BP but not adherence as an outcome. This review had the lowest-quality rating in this meta-review. This systematic review found that there was a significant decrease in both SBP (–5.2 mmHg; p <0.001) and DBP (–2.1 mmHg; p < 0.01) when compared with usual care. The authors also acknowledged that, after adjustment for publication bias, this decrease would have been less, though still significant. There was a higher percentage of patients reaching their BP target in the three studies that measured this outcome, although this was not a significant difference. Just over half of the studies (five out of nine) also adjusted medications during the course of the study and the remaining four made no changes. Verbek et al. 176 found that the average decrease difference in BP between treatment and usual care tended to be greater when antihypertensive medications were not changed. The authors conclude from this that the decrease in BP may be due to other factors such as lifestyle improvements or adherence. Again, it should be noted that many of the RCTs reviewed also included education and behavioural training as part of the telecare intervention.
Computer-based education: outcomes
Saksena173 only included one RCT that measured BP as an outcome; note, this RCT had also been reviewed as part of Verbek et al. 176 This RCT showed no statically significant improvement in BP control from computer-based education (website) alone. Improvement was only seen when pharmacist care was also used with computer-based education. The authors concluded that evidence does not support computer-based education for changing health behaviours nor as a sole intervention for BP. However, they did feel that this result supported the use of computer-based education when used ‘in concert with traditional provider-based education’. 173
Summary of effectiveness of technological interventions in supporting self-management
On the basis of the three reviews included, there is some evidence for the effectiveness of self-monitoring on adherence and BP. There was higher-quality evidence for a clinically small improvement in BP control with self-monitoring; however, it was most likely to be of benefit when used as part of more complex interventions to support the self-management of hypertension. There was also lower-quality evidence that telecare leads to a greater decrease in BP than usual care. The sparse evidence available did not suggest that computer-based education alone improves BP, though it might be beneficial if used with other interventions.
The evidence for the use of technological interventions for self-management is therefore mixed, with some evidence suggesting that telecare and self-monitoring might be promising. However, most of the RCTs used these technologies alongside education or other traditional support interventions; indeed telecare in itself is often simply a modality for aiding these interventions to occur. As the authors of all these studies have suggested, it may be that technological interventions are most beneficial when used as part of complex, multicomponent interventions.
Education interventions towards the patient and the physician
Patient education: outcomes
Three of the reviews included the use of education on its own as a self-management support intervention for hypertension (Ebrahim,170 Glynn et al. 171 and Schroeder et al. 174), although education was also a feature of many of the complex interventions seen in the other systematic reviews. Saksena173 also looked at the role of computer-based education (see above).
Two of these studies looked at the effect of education on adherence. Schroeder et al. 174 was a three star-weighted study; it concluded that education interventions alone were largely unsuccessful in improving adherence to medications, although one small RCT that used group education and postal information did improve adherence without having an effect on BP. Similarly, Ebrahim170 concluded that educational interventions are unlikely to be effective on their own in improving adherence.
All three studies also reviewed education interventions on BP. Ebrahim170 found evidence that patient education showed a large reduction in BP but this result was dominated by the results of one study (the Hypertension Detection and Follow-up Program177) which was a multifaceted US intervention that involved several approaches, including free care. Ebrahim170 therefore concluded that the statistically insignificant improvements in BP seen in the other RCTs reviewed were more likely to be representative of the benefit of educational interventions [–0.7 mmHg (95% CI –2.8 to 1.4 mmHg) SBP and –0.6 mmHg (95% CI –1.6 to 0.4 mmHg) DBP]. Glynn et al. 171 also found a trend towards improved BP control that was significant for educational interventions, though they noted that the result of the mean difference (MD) in BP was too heterogeneous to be pooled and the results were of marginal clinical importance. They therefore concluded that education alone would be unlikely to influence control of BP. Saksena173 also found no significant improvement with computer-based education alone, though it was felt that it could be a useful adjunct alongside other interventions.
Professional education: outcomes
Ebrahim170 reviewed professional education and found that this produced a statistically significant reduction in mean DBP, though the effect of this was small. He concluded that this improvement is more likely to have been a result of medication changes in intervention groups, rather than increased patient adherence or other approaches. Glynn et al. 171 also looked at interventions directed towards the physician and found that they were not associated with either a decrease in SBP or DBP and that the results for BP control were heterogeneous.
Summary of effectiveness of education in supporting self-management
On the basis of these four studies there appears to be limited evidence of the effectiveness of patient educational interventions alone in improving either adherence or BP control. However, it may form an important part of more complex interventions. Education of professionals had mixed results but higher-quality review evidence suggested that it would be unlikely to have any beneficial effect on BP.
Lifestyle interventions
Lifestyle interventions: outcomes
Dickinson et al. 169 reviewed the effect of complex lifestyle interventions on BP. The authors found a statistically significant reduction in SBP of –5.5 mmHg (95% CI –8.8 to –2.3 mmHg) and DBP of –4.5 mmHg (95% CI –6.9 to –2.0 mmHg) with combinations of interventions (exercise, alcohol restriction, salt restriction). However, they noted that reductions varied considerably between trials and that the overall reduction from lifestyle interventions was small. Nevertheless, they concluded that, despite these caveats, hypertensive patients should be encouraged to make lifestyle changes to complement other methods used to lower their BP.
Summary of effectiveness of lifestyle interventions in supporting self-management
The evidence for lifestyle interventions is based on the findings of only one systematic review, but this has illustrated that combined lifestyle interventions, aimed at improving diet, reducing salt and alcohol, and increasing exercise, most of which also included weight advice, are likely to improve BP. However, this may be by only a clinically small amount and we have no further information as to what form these interventions should take.
Motivational interventions: contracts, medication regime changes and reminders and appointment system reminders
Interventions involving contracts: outcomes
Bosch-Capblanch et al. ’s168 systematic review, which was of higher quality, looked at the effects of using contracts to improve adherence in the management of hypertension. There was significantly better adherence to relaxation practices in one review but worse adherence to treatment in another review. Similarly, one RCT showed no difference in BP outcomes, whereas one RCT showed statistically improved DBP only. The authors therefore concluded that ‘the evidence from the included trials supporting the use of contracts for hypertension was very weak. 168
Medication packaging, regimen changes and reminders: outcomes
Three systematic reviews assessed dosing regimen simplification and medication packaging changes as a support intervention. 170,174,175
Ebrahim170 concluded that ‘while simpler drug regimens are likely to improve adherence, simple reminder packaging does not improve adherence or control’. 170
Takiya et al. 175 reviewed the effects of ‘behavioural interventions’ that altered packaging and dosing and gave medication reminders. They found that these changes led to a small but non-statistically significant improvement in adherence [ES 0.04 (95% CI –0.01 to 0.09)]. No difference in impact was found depending on the setting of the intervention and they did not find any one intervention tool that was significantly more effective than the others, although blister packaging was the most successful. They therefore concluded that there was no one particular intervention that improved adherence significantly.
Schroeder et al. 174 looked at simplification of dosing regimens as a separate synthesis and found that it improved adherence in seven out of nine RCTs. Seven RCTs also reviewed BP changes but no information is given as to the effect of these, except that one study demonstrated an improved adherence and decreased SBP. Thus, the authors question whether or not any effect seen from increased adherence on BP may be small. Other interventions, such as special compliance dispensers and drug reminder charts, were also reviewed as part of ‘patient motivation, support and reminder interventions’. Although extraction of specific intervention results from this was impossible, the authors state that ‘there was inconclusive evidence for the effect of motivational interventions’. 174
Appointment system reminders: outcomes
Glynn et al. 171 looked at appointment reminder systems and found an improvement in follow-up in five out of eight RCTs, though only two RCTs looked at BP changes. These showed very heterogeneous results for SBP and DBP but, overall, a significant improvement in BP control [odds ratio (OR) 0.54 (95% CI 0.41 to 0.73)]. The authors did not feel this intervention area demonstrated clear evidence of change in BP, though they might have an effect on improving follow-up. Schroeder et al. 174 also reviewed appointment reminders as part of motivational interventions (see above) but found inconclusive evidence for their effect. 174
Summary of effectiveness of motivational interventions in supporting self-management
There is some evidence for the simplification of medication regimens and packaging changes from good-quality reviews, although the clinical effect of this may be small and was not supported by all the studies. The evidence for the use of appointment reminder systems is mixed with no clear improvement seen for BP, although there might be a positive effect on follow-up and control. The evidence supporting the use of contracts in hypertension is weak.
Complex interventions, including allied health professional-led care
Complex interventions: outcomes
Five systematic reviews looked generally at interventions to support self-management of hypertension and looked at complex interventions. 99,170,171,174,175 Three of these were the highest-quality reviews in this meta-review (Chodosh et al. ,99 Glynn et al. 171 and Schroeder et al. 174). Complex interventions were also reviewed in the systematic reviews by Ogedegbe and Schoenthaler172 and Verbek et al. ,176 and to some extent by Bosch-Capblanch et al. ,168 Dickinson et al. 169 and Saksena. 173
There is evidence from Ebrahim170 that complex interventions can improve adherence. The review concluded that ‘complex interventions may improve adherence and control in difficult patients’170 and felt that no single intervention alone would make this difference; however, no meta-analysis could be performed on the evidence due to data heterogeneity. Although further information on the nature of these interventions was not summarised, the author felt that worksite, nurse-led, protocol-guided care might be beneficial for younger men.
Takiya et al. 175 also aimed to review combined interventions that would improve adherence but they found the results too heterogeneous to pool and therefore did not analyse them further.
Schroeder et al. 174 reviewed complex health and organisational interventions including interventions in combination, such as worksite-based care, home visits, education and dosing devices, and pharmacist and nurse-led care. Adherence was increased in 8 out of 18 study interventions; they found overall that there was inconclusive evidence for more complex interventions, although they felt they were promising.
Ogedegbe and Schoenthaler’s172 review should also be noted for reviewing complex interventions (see above) as the monitoring interventions it reviewed were largely complex. It found that the greatest effects on adherence were seen when monitoring was used alongside other ‘adherence-enhancing strategies’172 supporting the evidence for complex interventions.
Several systematic reviews also looked at intervention effects on BP. Ebrahim170 found that a ‘stepped-care approach’, as seen in the ‘Hypertension Detection and Follow-up Program’177 which included education, guidelines and free drugs and clinics, would be helpful in controlling BP. He also noted contradictory evidence for the benefit of nurse-led clinics.
Chodosh et al. 99 of three star-rated quality, reviewed self-management programmes for hypertension in older adults; these were multifaceted interventions and included education. There was no information provided about the details of these interventions. The authors found a statistically significant reduction in SBP [ES –0.39 (95% CI –0.51 to –0.28)] equivalent to about 5 mmHg, and DBP [ES –0.51 (95% CI –0.73 to –0.30)]. However, the authors also stressed that their results were very heterogeneous, which might be as a result of publication bias, and therefore felt that the overall results needed to be viewed with caution.
Although Glynn et al. 171 did not summarise complex interventions together, the review’s categories of ‘health professional-led care’ and ‘organisational interventions to improve the delivery of care’ seemed similar to the complex interventions reviewed by other authors and used a multifaceted approach. They found that nurse- and pharmacist-led care might be promising, as the majority of RCTs were associated with improved BP control, although results were very heterogeneous. Evidence supporting organisational interventions was mixed, with findings dominated by the results of the ‘Hypertension Detection and Follow-up Program’. 177
Other systematic reviews also found some evidence for complex interventions on BP. Schroeder et al. 174 found weak and limited evidence for the benefit on BP of a patient-centred pharmaceutical model. However, it also noted a net reduction in DBP in a complex intervention involving nurse-led care at the worksite. Saksena173 found that adding in pharmacist care to computer education led to an improvement in BP. Dickinson et al. 169 found that combined lifestyle interventions were likely to improve BP by a clinically small amount. Verbek et al. 176 also found an improvement in BP using telecare, in what were effectively complex interventions, although the authors themselves did not highlight this conclusion.
Summary of effectiveness of complex interventions in supporting self-management
Evidence for complex interventions is promising but inconclusive, largely because of the inherently heterogeneous nature of the RCT results, which meant comparisons were difficult. Indeed, some authors did not try to evaluate these interventions further because of their varied nature. The systematic reviews that looked at all interventions in general were largely of higher quality which adds weight to their findings. One of these, Chodosh et al. ,99 found a statistically significant improvement in BP with complex interventions, although it noted heterogeneity in its results. Several of the systematic reviews’ findings were also dominated by the results of the ‘Hypertension Detection and Follow-up Program’177 which, though useful, is unlikely to be relevant in the UK. There was some evidence that nurse- or pharmacist-led care was associated with improved BP control but, overall, the results for this were very mixed. Of note, several of the reviews that looked at technological interventions found improved results when they were part of complex interventions. In general, many authors felt that complex interventions were some of the most promising interventions tested but that no conclusive evidence could be drawn on their effect because of the paucity of evidence about the individual components of them. 170,172,174
Mixed-methods discussion
Hypertension stands alone in this overarching review as a ‘silent’ disease that is asymptomatic until, for some, potentially devastating sequelae present. This also makes hypertension unique for people to manage as there may be little obvious motivation for controlling BP effectively and often no consequences from poor self-management until many years later. The qualitative evidence from this meta-review supports this: it has shown that people struggle to understand that hypertension is a disease because of its asymptomatic nature and that they may base their medication taking on the presence or absence of symptoms. Indeed, people feel confused over its cause. They feel that stress is intrinsically linked to hypertension and information that it is inherited or related to poor lifestyle can often feel irrelevant to them and mean they struggle to identify why they are affected at all. This may result in health beliefs that conflict with those of health professionals and may leave them unable to understand their patients. This is particularly important to note in the management of hypertension because the condition’s asymptomatic nature has traditionally led to a very doctor-centred management approach. It also makes the need to improve our knowledge of how we can empower people to understand and manage their hypertension all the greater.
There are relatively few systematic reviews on self-management support interventions with hypertension as their focus, both in the qualitative and quantitative literature. Unlike in other conditions, such as asthma or diabetes, self-management support is not well defined; there are no well recognised programmes that have set out to do this and most authors did not use this term themselves. There are more, yet still few, reviews that assess interventions that follow the ethos of self-management. Thus, thinking around the term self-management, we looked for interventions that could offer support, even when the original authors had not specifically discussed this. In order to limit this potential area of review weakness, screening decisions were taken by a multidisciplinary team and through consensus. The initially lower consensus on full-text screening reflects this difficulty and all reviews that were included and excluded were therefore extensively discussed again after this first consensus check.
We felt that the focus of the included reviews had to be on multifaceted interventions that empowered the patient to self-manage. Thus, certain possibly relevant reviews, such as Capuccio et al. ’s review of self-monitoring of BP,178 were excluded as they did not fit this ethos. Where unidimensional interventions, such as drug reminders, were presented as part of mixed reviews, we did include them for further analysis as the focus of the overall review was multifaceted. Lifestyle changes were a difficult area to assess as, although there are multiple reviews showing the benefit of lifestyle changes on BP, few assessed the benefits of the interventions themselves. Even Dickinson et al. 169 gave limited information regarding the interventions discussed. In view of the stated aims of this meta-review, we focused on the combined, complex interventions that it reviewed.
One of the greatest difficulties faced by all the systematic reviews was the lack of good-quality evidence on self-management in hypertension. Many authors noted publication bias and poor-quality design in primary papers. Half of the quantitative systematic reviews in this meta-review were of higher quality but studies by Ogedegbe and Schoenthaler,172 Saksena173 and Verbek et al. ,176 which were unique in providing information on certain types of interventions, were of lower quality. There was one qualitative study of higher quality and one of lower quality. The primary studies reviewed originated from around the world and included many from Western Europe; however, it should be noted that the unique nature of the NHS may make some of these less applicable to this health system. In particular, several reviews’ findings were dominated by the results of the ‘Hypertension Detection and Follow-up Program’177 which may be less applicable to the UK as it included offering free health care as one of its interventions.
Perhaps the greatest difficulty faced by authors of the systematic reviews, and by this meta-review, was the lack of division of different parts of complex interventions so that limited conclusions could be made as to each part of them. Some reviewers used broad types of interventions, categorised them differently, or failed to make any synthesis of their results, which made further analysis hard. The majority of the reviews also found that the data they had collected were too heterogeneous to pool, which may reflect the many different types of interventions used. It is not possible to know conclusively if the inability to identify one intervention as most effective in the self-management of hypertension is because there is no one most effective intervention or because it results from a paucity of evidence.
This meta-review demonstrates that self-management support for hypertension may be delivered in a multitude of ways. It is also clear that no single type of intervention stands out for its efficacy, with mixed evidence for the interventions that are most beneficial in the self-management of hypertension. A large number of people now use technology in the management of their BP, for example through self-monitoring at home. Although the evidence for the use of technology is still mixed, there is evidence that self-monitoring might be promising for the future, particularly when used in combination with other interventions. Similarly, there was some evidence to show that simplification of drug regimens and packaging changes might increase adherence and lower-quality evidence to support telecare interventions. Interventions to improve lifestyle were recommended, although their benefit is likely to be small; this result should be seen alongside our qualitative evidence, which has suggested that people need support and information in terms they can understand, in order to change their lifestyles.
There was considerable evidence around the use of complex interventions to support self-management in hypertension. This has suggested that complex interventions tailored to individuals and delivered in partnership with health professionals, may be some of the most beneficial interventions in helping people to self-manage their BP. However, the heterogeneous nature of these complex interventions, wherein may actually lie their greatest strength, also makes them most difficult to evaluate and this evidence therefore remains inconclusive. Although it is likely that technological interventions, lifestyle and drug regimen changes may play a crucial part in them, we currently have no clear answer as to which components of complex interventions people would most benefit from or whether or not it is in fact their inherent complexity that is crucial.
The qualitative evidence from this meta-review also emphasises the need for supporting patients to understand and manage their hypertension. It also stresses the important part that a good relationship between health professionals and patients can play in encouraging understanding of and adherence to treatments. However, although it is clear from our quantitative evidence that some form of educational or psychological support formed a part of most of the complex interventions that had been effective in our review, there was limited evidence for education alone. This apparent paradox was initially hard to understand. However, it was also interesting to note from our qualitative review that people had very different approaches and motivations towards taking their medications: some took their medications regularly, others were less adherent as they felt more concerned about medication side effects, and some patients only took their medications when life stressors or symptoms prompted them too. Perhaps this then can offer a potential explanation as to why standard education programmes have not shown quantitative evidence of benefit; interventions may need to be tailored, basing them on a person’s individual motivations and health beliefs.
This meta-review has demonstrated multiple and varied tools that can form part of self-management interventions for people with hypertension; it may be this variety that is of biggest benefit as it allows people to tailor their own approach into self-management. We have also seen that people who trusted their health professionals and felt that they were working with them were most likely to take medications and to make lifestyle changes. Indeed, perhaps we should not be surprised that an asymptomatic condition with potentially frightening, though distant, consequences requires multicomponent support, in partnership, to effectively promote self-management. Further research will be needed to find out if one component is an essential part of these often complex interventions and how, together, we can identify which interventions are best suited for each individual.
Chapter 16 Additional meta-review: self-management support for people with inflammatory arthropathies
Meta-review of qualitative systematic reviews
Systematic reviews identified
There were two reviews179,180 (published 2011 and 2012) included in the IAs qualitative meta-review, both published in peer-reviewed journals (Figure 35).
The reviews reported a total of 43 primary qualitative studies; however, five of these were included in both of the reviews resulting in 38 unique studies.
Both reviews focused on RA, precluding general conclusions about IAs (Table 83).
| Author, year | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Stack 2012179 | This review synthesised the literature regarding the drivers of, and barriers to, help-seeking behaviour in people with new onset RA | 21 | Interacting themes included: the early experience of symptoms, minimising the impact of symptoms, speaking to others, gathering information and seeking alternative treatments, and issues related to accessing health services, and attitudes towards health-care professionals. Pre-diagnosis RA was often perceived as a mild condition that affected older people. Normalising and ignoring symptoms led to delay help-seeking until symptoms impacted on daily activities. Interpretations of symptoms are both drivers of and barriers to help seeking. Targeted public health interventions are required to inform symptom interpretation and reduce delays [sic] |
| Campbell 2011180 | Our meta-review used only part of this broader HTA report: a synthesis of studies exploring patients’ experiences of living with RA | 22 (in 25 papers) | Most studies were concerned with the everyday experience of living with RA. The final synthesis was presented as a textual distillation of the findings supported by novel tabular summaries of the needs of people with RA and the general and specific coping strategies that they deployed to accommodate the disease. This synthesis did not produce significant new insights, probably because the early papers in the area were substantial and theoretically rich, and later papers were mostly confirmatory |
Quality assessment
Campbell et al. ’s180 review scored high in quality as it provided explicit detail on most areas of the review process. Stack et al. 179 mainly scored low for not reporting a quality assessment (Table 84).
| R-AMSTAR criteria | Stack 2012179 | Campbell 2011180 |
|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 |
| Was there duplicate study selection and data extraction? | 2 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 2 | 4 |
| Was a list of studies (included and excluded) provided? | 2 | 4 |
| Were the characteristics of the included studies provided? | 2 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 1 | 3 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 2 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 |
| Was the conflict of interest stated? | 3 | 3 |
| Total score/40 | 26 | 34 |
| Quality rating (low = < 30; high = ≥ 30) | Low | High |
Findings
Support for self-management
The synthesis enabled integration of findings to provide broad themes to inform implementation of self-management support.
-
People with RA reported delaying seeking help until multiple joints were affected or the pain became troublesome, rather than appreciating the potential to prevent escalation by presenting early. The slow onset caused uncertainty about whether early symptoms were due to illness, a different more temporary cause (ageing/general aches), or a different pre-existing condition. The need for more information and increased public awareness of the importance of early intervention in RA was highlighted.
-
People often searched for information, and/or tried alternative therapies or self-medication before seeking professional advice. People reported trying to self-manage the symptoms and minimise life disruption but sought help when they became concerned or their strategies were not helping. It is important that people have the information on effective culturally/lifestyle-appropriate methods of self-management, and understand what support services are available to them.
-
People with RA searched for an understanding of disease aetiology, which became personal in reflection of their self, body and society in relation to a chronic illness. Some viewed the condition as a mechanical breakdown of the body due to ageing or injury, or caused by an external agent/illness. Aspects of lifestyle (e.g. certain foods) were often perceived to exacerbate pain. Active discussion and information provision may help understanding of the disease process.
-
Barriers to seeking professional advice included concern about wasting the professionals’ time, fear that they might be advised to change their lifestyle, or that their early symptoms might not be taken seriously. First experiences of medical help often reinforced these concerns, as the condition was misdiagnosed or dismissed as not serious. Practical barriers included lack of continuity of care and difficulties making appointments. Patient’s often believed that little could be done to relieve their pain. In contrast, some people with a good relationship with their HCP had a proactive approach to the use of services and recognised the benefit of rapid help-seeking, reinforced if they had been advised to return if symptoms persisted/changed.
-
The main concerns centred around exacerbations and progression of pain, associated with feelings of fatigue and a ‘reduction in personal resources’. This caused disruption to physical, psychological and social functioning, including aspects that were once ‘taken for granted’ norms. Support should address an individual’s specific concerns in these social/lifestyle domains.
-
Barriers to support from family/friends were discussed, with some not disclosing a problem because of a fear of being judged as ‘moaning’, not being taken seriously or lacking empathy. The invisibility of the condition was perceived to be the cause of this and meant that people had to ‘disclose’ the condition in order to gain support. This is a problem if people are concerned about how others will react or are in denial regarding the condition.
-
Psychological support for people with, or who may have, RA is important to help with acceptance of the diagnosis and the lifestyle implications. Denial of the diagnosis is often accompanied by fear of permanent negative lifestyle change and medical regimes. As a result exhaustion, anger, depression, despair, self-pity, perception of loss of control, low confidence and sexual difficulties often occur as secondary symptoms.
Meta-review of quantitative systematic reviews
Systematic reviews identified
A total of 10 systematic reviews (published between 1997 and 2012) met the inclusion criteria and were included in this meta-review. 181–190 These reviews represented a total of 132 RCTs, though after excluding overlaps this represented 66 unique RCTs, published between 1981 and 2010 (Figure 36).
Six of the reviews181,182,184,186–188 looked at RA exclusively, one looked at SLE190 and three looked at multiple LTCs (not exclusively IAs) but reported results for RA separately (Table 85). 183,185,189
The interventions included in the systematic reviews were all multimodal; with at least one psychological or educational/training component associated with each. The interventions were wide ranging and hence we grouped them broadly into the following categories.
Psychological interventions:181–184,190 CBT, counselling, disclosure therapy, psychotherapy, self-regulation programmes (goal-setting, planning, self-monitoring, feedback and relapse prevention), writing or talking disclosure of experiences and the Arthritis Self-Management Program (ASMP) were all grouped under this category.
Patient education and training:185,187–189 classic education, providing information about the disease and medication, interactive instructional computer programs, computerised health assessment and history-taking, computerised information support networks, mailed leaflets, skill building and training, and OT were grouped in this category.
Complementary and alternative medicine therapies:186 relaxation, biofeedback, meditation and mindfulness (the interventions were multimodal associated with either a psychological or educational/training component).
The delivery and content of the interventions varied significantly. Most were outpatient- or community-based programmes, delivered by both lay people and trained professionals.
| Review | Intervention of interest | Participant demographics | Setting, delivery mode and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Psychological interventions | |||||
| Astin 2007181 | Multimodal CBT, psychotherapy, biofeedback, written or oral disclosure | NR | Average length of time that patients had the disease was 10.6 years | Thirteen RCTs were either described or could be characterised as multimodal, CBT. Interventions typically involved some combination of relaxation, imagery, stress management or the teaching of cognitive coping skills. Five studies also included biofeedback. Five studies employed more traditional psychotherapeutic interventions, both group based and individual. The intervention in two studies involved subjects’ writing or speaking about difficult emotional or stressful experiences | Length of the interventions varied from 3 days to 9 months with a mean of 9.8 weeks. One study utilised a ‘refresher’ course following the actual intervention. 19 of the 25 RCTs collected follow-up data with follow-up time periods ranging from 2 to 18 months (mean of 8.6 months) |
| Dissanayake 2010182 | Psychological interventions such as biofeedback, relaxation, disclosure, counselling, psychotherapy, meditation and mindfulness and CBT | NR | NR | Interventions varied greatly: biofeedback (involves providing patients with access to physiological information in order to gain control of processes under autonomic control); CBT; psychotherapy (aims to alleviate difficulties through the development of a therapeutic relationship to encourage insight); disclosure (private disclosure either verbally or written); counselling; mindfulness meditation; relaxation training | CBT-based interventions group was further divided according to the duration of treatment as short (< 6 weeks) (six studies), long (> 6 weeks) (six studies) and CBT with maintenance therapy throughout the follow-up period |
| Iverson 2010183 | Cognitive and behavioural strategies using SCT and CBT | NR | Mainly hospital based Clinical psychologists using CBT combined with education via the use of leader manuals, staff training in SCT/CBT Three studies recruited people with well-established disease (average 12–15 years) and two with early to established disease |
All provided information about the disease and medication. Only two included regular exercise CBT combined with education From multidisciplinary team members using ‘more traditional didactic approaches’ for physical strategies |
Programme duration varied from 12 to 52 hours, over 6 weeks to 9 months, with three including booster sessions (3–9 months after the programme). Three had longer-term follow-up at 12 months |
| Knittle 2010184 | Face-to-face psychological interventions for adults with RA | Adults with RA | Setting NR All face to face Provider varied: OT, physiotherapist, medical doctor, psychologist, doctoral student, lay person |
Included CBT, ASMP, education, coping skills, relaxation and biofeedback – multimodal interventions | Varied from 2 weeks to 6 months. Average, 1–2 hours per week |
| Zhang 2012190 | Psychological interventions vs. control group (treatment as usual, wait list or placebo) | Adults aged ≥ 18 years with a clinical diagnosis of SLE | Individuals and groups | Psychological interventions in which verbal communication between therapist and participant was the core element, or in which a psychological treatment was delivered in a self-administered written format with some personal support from a therapist (by telephone, e-mail or otherwise) Two RCTs explored CBT; two supportive therapy; one multiple psychological interventions; and one psychoeducational interventions |
12 days to 6 months duration. Follow-ups were for a maximum of 12 months only |
| Patient education and training | |||||
| Krishna 1997185 | Interactive instructional computer programs, computerised health assessment and history-taking, and computerised information support networks | Population aged 12–91 years. Of the 19 studies that included adults, two included only male subjects and three included only female subjects. Eight RCTs provided data on educational level of participants, but only two reported testing computer experience of participants | Interactive computer programs, interactive multimedia (interactive computer programmes that combine audio, video, text and graphics to communicate educational messages) | Educational information was provided using interactive computer programs, about general health-related problems, diseases or a specific diagnosis. The instructional programs were menu-driven and offered self-paced learning by allowing users to input data or respond to prompted questions | The average duration of computer-assisted intervention was 30 minutes (range 10–210 minutes) A self-paced instruction programme on RA lasted up to 3.5 hours |
| Niedermann 2004187 | Education, CBT. One study tested the effects of mailed educational leaflets | NR | NR | Patient education interventions to teach knowledge and specifically needed skills, CBT with focus on coping strategies and psychological support | Programme duration ranged between 4 and 15 weeks (median seven interventions) Eight programmes were organised as weekly 1.5–2-hour sessions; two with subsequent reinforcement; three programmes included an initial 1-week hospital stay plus a 12-month support programme of nine afternoon sessions and an educational leaflet mailing Follow-ups ranged from 6 to 15 months |
| Riemsma 2003188 | Three categories:
|
Adult participants aged ≥ 18 years with clinically confirmed diagnosis of RA | NR | ‘Information only’ included all interventions aimed primarily at the exchange of information, by means of persuasive communication or informational brochures. These interventions do not include a behavioural component and are not aimed at supporting self-management ‘Counselling’ included interventions mainly aimed at social support and giving patients the opportunity to discuss their problems ‘Behavioural treatment’ refers to interventions that included techniques aimed at behavioural change, such as behavioural instruction, skills training and biofeedback |
Follow-up of 3–18 months |
| Wilkins 2003189 (one RCT only) | OT intervention | The population included people aged ≥ 65 years, both well and with chronic conditions | Delivered at home by a therapist Intensive for the first 6 weeks, then less frequent |
OT intervention delivered at home by a therapist | 6 and 12 weeks |
| Complementary and alternative medicine therapies | |||||
| Leverone 2010186 | Multimodal treatments, with at least one component being psychologically based, ranging from coping strategies for pain to relaxation techniques or meditation | NR | Most interventions were delivered in person, two were conducted by telephone and one over the internet | An active treatment that included some psychological/psychosocial component beyond simply providing information about the disease | Total study time ranged from 2 weeks to 1 year with all follow-up being less than 15 months |
Quality assessment and weighting
Quality was assessed using the R-AMSTAR scoring system and scores ranged from 21 to 39 out of a possible 44. Five studies181,182,184,188,190 are of higher quality with a scores ≥ 31 and five studies183,185–187,189 are of lower quality with a score < 31 (Table 86).
| R-AMSTAR criteria | Psychological | Education and training | CAM | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Astin 2007181 | Dissanayake 2010182 | Iverson 2010183 | Knittle 2010184 | Zhang 2012190 | Krishna 1997185 | Niedermann 2004187 | Riemsma 2003188 | Wilkins 2003189 | Leverone 2010186 | |
| Was an a priori design provided? | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 3 | 2 | 4 | 4 | 3 | 4 | 4 | 4 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 | 3 | 4 | 4 | 2 | 3 | 4 | 4 | 2 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 2 | 2 | 3 | 2 | 1 | 1 | 2 | 1 | 2 |
| Was a list of studies (included and excluded) provided? | 3 | 4 | 3 | 3 | 3 | 3 | 3 | 4 | 3 | 2 |
| Were the characteristics of the included studies provided? | 4 | 3 | 4 | 3 | 3 | 3 | 3 | 4 | 3 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 2 | 2 | 4 | 4 | 4 | 4 | 1 | 1 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 3 | 3 | 2 | 3 | 3 | 2 | 3 | 3 | 1 | 1 |
| Were the methods used to combine the findings of the studies appropriate? | 3 | 3 | 3 | 4 | 4 | 1 | 1 | 4 | 1 | 1 |
| Was the likelihood of publication bias assessed? | 4 | 1 | 1 | 4 | 2 | 1 | 1 | 4 | 1 | 1 |
| Was the conflict of interest stated? | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 2 | 2 | 3 |
| Total score/44 | 35 | 32 | 27 | 35 | 35 | 25 | 28 | 39 | 25 | 21 |
The included systematic reviews were then weighted, taking into consideration both quality as assessed by the R-AMSTAR and size represented by the total number of participants included in the review (Table 87).
| Review | Total number participants | Quality score | Weighting |
|---|---|---|---|
| Psychological interventions | |||
| Astin 2007181 | 2171 | 35 | *** |
| Dissanayake 2010182 | 2021 | 32 | *** |
| Iverson 2010183 | 731 | 27 | * |
| Knittle 2010184 | 1675 | 35 | *** |
| Zhang 2012190 | 537 | 35 | ** |
| Patient education and training | |||
| Krishna 1997185 | NR | 25 | * |
| Niedermann 2004187 | 931 | 28 | * |
| Riemsma 2003188 | 14,249 | 39 | *** |
| Wilkins 2003189 | 105 | 25 | * |
| CAM therapies | |||
| Leverone 2010186 | 2206 | 21 | ** |
Outcomes
For this review we chose two key outcomes – disability and QoL (Table 88).
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Disability | Functional loss, pain-related disability, ADL | Health Assessment Questionnaire; AIMS; AIMS2-physical function scale |
| QoL | QoL, psychological status | Center for Epidemiological Studies Depression Scale; the Beck Depression Inventory; AIMS; Self-Rated Global Health Scale; AIMS2; SCL-90-R; Psychological Well-Being Scale; Mindfulness Attention Awareness Scale; HADS |
Although pain is another possible outcome, we opted to focus to the closely linked outcome of disability as that reflects the impact of the disease on lifestyle and thus represents a primary target for self-management interventions. Successful self-management support interventions would be expected to deliver improvements in disability and functional limitation, thus positively effecting QoL. As QoL was infrequently reported, we also chose to report on measures of psychological status as a proxy measure.
Findings
We present a synthesis of our findings below, divided into psychological interventions, patient education and training-based interventions, and complementary and alternative medicine therapies (see Table 89 for results from meta-analyses, Table 90 for narrative summaries and Figure 37 for a summary of quantitative results).
| Reference and weighting | Outcome | Time | Sample size; n RCTS; n participants (where available) | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Psychological interventions | |||||
| Astin 2007181 *** Psychological interventions |
Functional disability | Post intervention | 12 RCTs | +++ | 0.27 (0.12 to 0.42); p = 0.00001 |
| Follow-up | Seven RCTs | ? | Assume error | ||
| Psychological status | Post intervention | 12 RCTs | + | ES –0.15 (p = 0.03, 95% CI –0.31 to –0.01) | |
| Follow-up | Five RCTs | ++ | ES –0.33 (p = 0.01; 95% CI –0.59 to –0.07) | ||
| Knittle 2010184 *** Psychological interventions |
Disability | Post treatment | 12 RCTs | +++ | 0.417 (0.179 to 0.655); p = 0.001 |
| Follow-up (2–14 months post treatment) | 12 RCTs | + | 0.145 (0.002 to 0.288); p = 0.047 | ||
| Depression | Post treatment | 12 RCTs | + | 0.279 (0.054 to 0.504); p = 0.015 | |
| Follow-up (2–14 months post treatment) | 12 RCTs | +++ | 0.318 (0.160 to 0.475); p < 0.001 | ||
| Anxiety | Post treatment | NR | 0 | 0.121 (–0.064 to 0.306); p = 0.201 | |
| Follow-up | NR | 0 | 0.122 (–0.065 to 0.308); p = 0.200 | ||
| Zhang 2012190 ** Psychological interventions |
Physical function | NR | Three RCTs; 196 | 0 | MD 7.65 (0.16 to 15.13); p = 0.05 |
| 6 months | Three RCTs | ++ | MD 10.29 (2.59 to 17.98); p = 0.01 | ||
| 12 months | Two RCTs | 0 | MD 8.35 (–3.26 to 19.95); p = 0.16 | ||
| Anxiety | NR | Three RCTs; 223 | ++ | SMD –0.95 (95% CI –1.57 to –0.34; p = 0.00) | |
| Depression | NR | Four RCTs; 282 | ++ | SMD –1.14 (–1.84 to –0.44); p = 0.00 | |
| Patient education and training | |||||
| Riemsma 2003188 *** Patient education |
Disability | First follow-up | 2275 | +++ | SMD –0.17 (–0.25 to –0.09); p = 0.00007 |
| Final follow-up | 1308 | 0 | SMD –0.09 (–0.20 to 0.02); p = 0.10 | ||
| Psychological status | First follow-up | 1138 | ++ | SMD –0.15 (–0.27 to –0.04); p = 0.010 | |
| Final follow-up | NR | 0 | Not stated in main body of text | ||
| Depression | First follow-up | 1770 | ++ | SMD –0.14 (–0.23 to –0.05); p = 0.004 | |
| Final follow-up | NR | 0 | Not stated in main body of text | ||
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Psychological interventions | |||||
| Astin 2007181 *** | Psychological interventions for RA | 25 RCTs; 2171; 1981–2001 | Meta-analysis |
|
The results suggest psychological approaches (e.g. relaxation, biofeedback, CBT, stress management) may be effective and important components of self-management support in RA |
| Dissanayake 2010182 *** | Psychosocial interventions for RA | 31 RCTs; 2021; 1981–2008 | Narrative synthesis |
|
This review shows consistent supportive evidence for the use of disclosure therapy and CBT with maintenance therapy as adjunct therapies in patients with RA It also highlights methodological limitations in the current literature and the need for future research in this area |
| Iverson 2010183 * | Education with psychological intervention | Five RCTs; 731; 2003–8 | Narrative synthesis |
|
Little is known about outcomes 12 months or more after the end of intervention |
| Knittle 2010184 *** | Psychological interventions for RA: self-regulation | 27 RCTs; 1675; 1984–2007 | Meta-analysis |
|
Psychological interventions are beneficial for many patients with RA |
| Zhang 2012190 ** | Psychological interventions for SLE | Six RCTs; 537; 2002–10 | Meta-analysis |
|
The present data indicate that psychological interventions are promising treatments for patients with SLE. The findings were based on only six RCTs, some of which were relatively small, so more methodologically rigorous large-scale RCTs are required to confirm these preliminary findings |
| Patient education and training | |||||
| Krishna 1997185 * | Interactive, computerised patient education for chronic conditions | NR | Narrative synthesis |
|
Limited conclusions from one RCT, did not report on our primary outcomes of interest |
| Niedermann 2004187 * | Patient education for RA | 11 RCTs; 931; 1987–99 | Narrative synthesis |
|
There is limited evidence of patient education influencing psychological health status or physical health status |
| Riemsma 2003188 *** | Patient education | 31 RCTs; 14,249; 1981–2000 | Meta-analysis |
|
Patient education as provided in the studies reviewed here had small short-term effects on disability, psychological status and depression. There was no evidence of long-term benefits in adults with RA |
| Wilkins 2003189 * | Community-based OT education and functional training for chronic conditions | One RCT; 105; 1991 | Narrative synthesis |
|
Results are from one RCT only so conclusions are limited |
| CAM therapies | |||||
| Leverone 2010186 ** | Non-pharmacological interventions: mind–body medicine for RA | 16 RCTs; 2206; 1986–2008 | Narrative synthesis |
|
Across studies, statistically significant improvements were found (clinical significance is open to interpretation). The RA patients had generally maximised pharmacological treatments. The authors conclude that mind–body medicine may be a helpful adjunct to conventional therapy to enhance treatment response and possibly reduce the use of more risky pharmacological therapies |
FIGURE 37.
Inflammatory arthropathies: summary of the quantitative evidence.
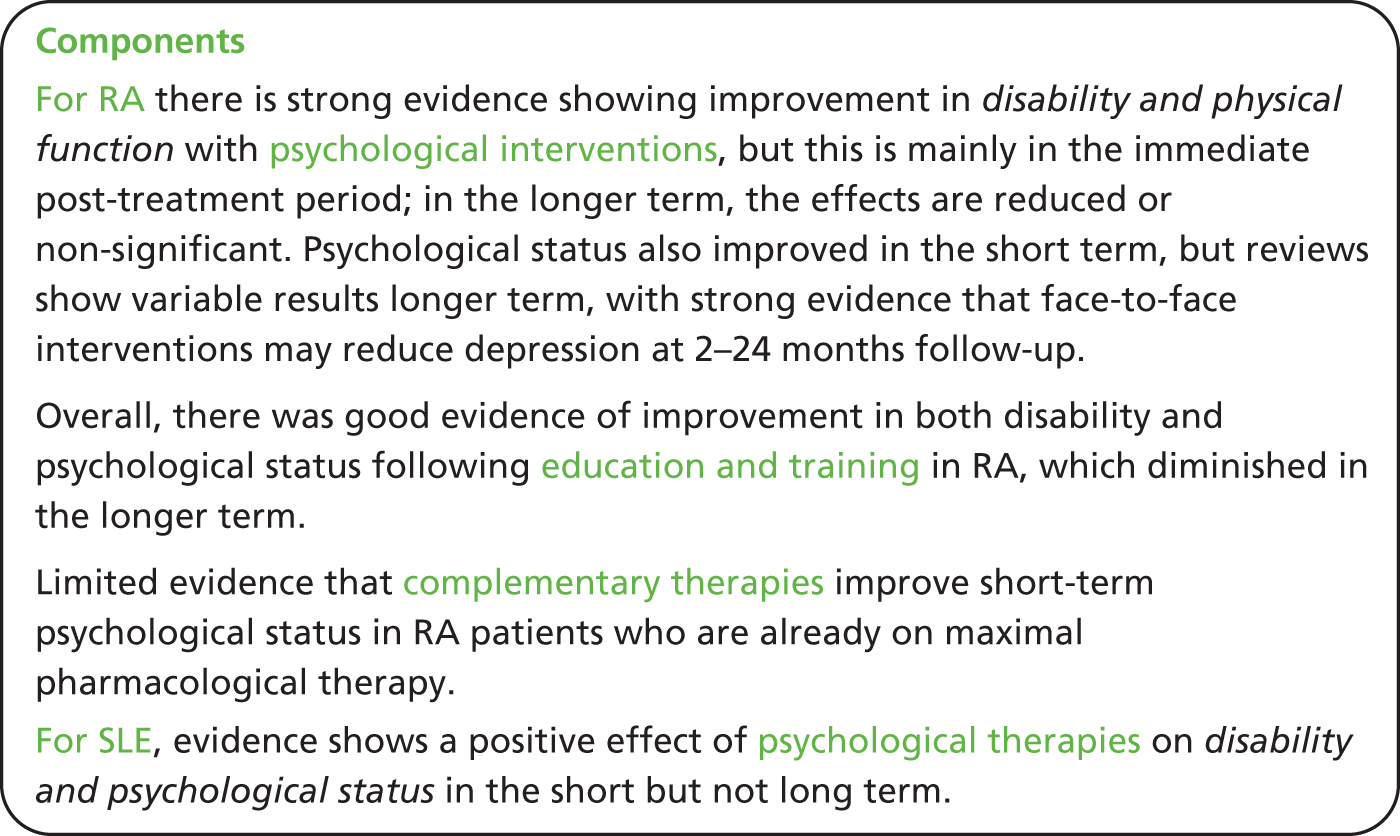
Psychological interventions
Five systematic reviews looked at psychological therapies out of which four focused on RA181–184 and one looked at SLE. 190
Two reviews181,184 show strong evidence of benefit in functional disability immediately post-intervention, but the effect disappeared at follow-up. Psychological status, however, improved immediately post treatment and persisted at follow-up in one high-quality review181 but decreased in the other, more recent high-quality review. 184
Another high-quality review182 concluded that there was consistent evidence that CBT with maintenance therapy throughout the follow-up period, resulted in positive outcomes for both reduction in depression and stress. There was also some evidence that although disclosure therapy may initially increase negative emotions it may improve physical function at follow-up.
Iverson et al. 183 (a lower-quality review) showed some evidence of short-term benefits in physical function, mood and self-efficacy with CBT and social cognitive therapy delivered alongside education.
Zhang et al. 190 reported a short-term improvement in depression and stress (which diminished at follow-up), but no change in fatigue and physical function. Reflecting the paucity of published research regarding self-management in SLE, the other results were inconclusive with few relevant to our meta-review aims.
Patient education and training
Four systematic reviews185,187–189 focused on education and training. Reissma et al. ,188 a higher-quality review, found strong evidence of benefits in terms of both disability and psychological status at first follow-up; this had diminished by the final follow-up. Neidermann et al. 187 looked at seven RCTs which (apart from one study) did not show any significant evidence of change in psychological status, short- or long-term. Neither did this review show any consistent evidence of improvement in disability short- or long-term. Wilkins et al. 189 looked at home-based OT for RA, reporting evidence from one RCT that may be suggestive of a short-term improvement in physical function. Krishna et al. 185 looked at computerised education in patients with RA, reporting some evidence of an improvement in hopefulness and self-belief.
Complementary and alternative medicine therapies
There is some evidence from a relatively low-quality review,186 of improvement in psychological status in the short term, but no consistent evidence for disability or functional status. The participants included in this review were on maximal pharmacological therapy, so the authors considered that any additional benefit could be clinically significant.
Mixed-methods discussion
Although we searched broadly for IAs (specifically including RA, psoriatic arthropathy, ankylosing spondylosis and SLE), the available evidence focuses on RA with only one review in SLE highlighting a gap in the current evidence base.
The qualitative reviews show that people with RA delay seeking help as they initially believe that symptoms are temporary and not illness-related. Programmes to raise awareness of IAs may facilitate early presentation, prompt diagnosis and early provision of effective disease-modifying management and self-management support. Lack of public awareness of the illness may exacerbate the difficulty, highlighted by one qualitative review,179 that friends and family may have in understanding the impact of chronic pain and disability. Paradoxically, however, a RCT included within one quantitative review183 showed a worsening of self-efficacy and fatigue when partners attended a cognitive strategy self-management programme with the patient.
Education is a key component of self-management support and evidence from quantitative reviews in IAs suggests that education effectively improves disability and patients’ psychological status in the short term. Qualitative reviews, however, show that patients feel poorly informed about the disease, supporting a focus on providing patient education and training shortly after diagnosis.
In the longer term, qualitative evidence reflects the strain of living with an IA (depression, exhaustion, etc.). Specific concerns identified by qualitative reviews include misconceptions on the causes of pain and disease, worries about exacerbations and disease progression. Psychological interventions including goal-setting, planning, self-monitoring, feedback and relapse prevention discussed in a high-quality review showed significant long-term effects to patients’ depression and disease-related stress. 184 Evidence from another high-quality review shows that CBT including maintenance support is related to significant reductions in fatigue, depression, mood and daily stress. 182 Psychological interventions including relaxation, stress management and teaching cognitive coping may be important components of self-management support for sustaining benefit in the longer term. ‘Long-term’ in the context of the reviews, however, ranged from 6 to 18 months. In the context of informing self-management support interventions for LTCs, there is a need to extend this time scale to understand the implications for maintenance of effect over the lifetime of the condition.
Chapter 17 Additional review: self-management support for people with irritable bowel syndrome
Meta-review of qualitative reviews
Systematic reviews identified
There were no relevant qualitative systematic reviews identified by our searches (see Appendix 20).
Meta-review of quantitative reviews
Systematic reviews identified
Following the title and abstract screening, 13 articles were screened for eligibility, three of which were included into the IBS quantitative meta-review191–193 (Figure 38). The reviews were all recent (published 2009–10) and their included RCTs were published between 1991 and 2010.
One review191 examined self-management support interventions and the remaining two reviews included psychological treatments for IBS (Table 91). Seven of the nine RCTS in Dorn191 took place in the USA and studies in the Ford et al. 192 review came for a variety of countries, including India (one study) and the Islamic Republic of Iran (two studies). Zijdenbos et al. 193 did not supply these data.
| Review | Intervention of interest and comparison | Participant demographics | Setting, delivery and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Zijdenbos 2009193 | Psychological treatments Control: ‘usual care’ and ‘waiting list conditions’ or placebo intervention |
Middle-aged adults | Often unclear, most studies were carried out in a secondary or tertiary care setting. Three studies were carried out wholly or in part in a primary care setting Most were delivered on an individual basis, with three RCTs using a group setting |
Cognitive therapy (four RCTs), behavioural therapy (seven RCTs), a combination of CBTs (six RCTs). CBT includes systemic desensitization, problem-solving therapy, social skills training, imagery and homework exercises. Two RCTs combine relaxation and CBT | Overall, for all psychological treatments, duration and follow-up time varied from 6 weeks to 12 months but separate information for CBT studies was not provided |
| Ford 2009192 | Psychological treatments Control: physician’s ‘usual management’ |
Adults (aged ≥ 16 years) | Primary, secondary and tertiary care | Multicomponent psychological therapy (three RCTs), CBT (six RCTs), CBT with relaxation therapy (one RCT) and self-administered CBT (one RCT) | Range from 6 weeks to 6 months, with between 5 and 12 sessions. Inclusion criteria had a minimum criterion for follow-up of 7 days but details were not provided in results |
| Dorn 2010191 | Self-management-related interventions Control: usual care (four RCTs – one had single-session brief self-management programme); waiting list control (four RCTs – two were three-arm RCTs with a third arm given cognitive therapy); IBS booklet (one RCT) |
Adult patients (aged > 18 years) | Primary, secondary and tertiary care, community and one Health Maintenance Organisation. One of the nine RCTs did not describe the setting | Self-management interventions including education (one RCT), self-administered CBT (one RCT), self-help guidebooks (two RCTs), self-management programmes (three RCTs), support groups (two RCTs) Due to the two reviews above on psychological treatments, the authors did not include this type of intervention unless the psychological therapy was primarily self-administered as a means of strengthening self-care |
Stated duration ranged from 6 weeks to 3 months (one RCT did not describe the duration) |
Ford et al. 192 included ‘psychological therapies’ of at least 7 days duration, whereas Zijdenbos et al. 193 included ‘(cognitive)–behavioural therapy’ provided by a therapist either at the individual or group level. Interventions in Ford et al. 192 were between 6 weeks and 6 months duration, and fell somewhere between 6 weeks and 12 months in Zijdenbos et al. 193 In Dorn’s191 review the interventions were heterogeneous in their nature, but were grouped into the following five categories: patient education; self-help guidebooks; self-administered CBT; self-management programmes; and support groups. Among these RCTs, intervention duration varied from the provision of a guide book (duration of this intervention not given) to 12 weeks, but the majority lasted 10–12 weeks. Follow-up periods were not consistently recorded in this review.
Dorn191 identified 11 studies which addressed self-management, only nine were RCTs. Both reviews of psychological interventions192,193 included some monocomponent interventions not considered self-management support for the purposes of this review, but both also separately presented results for CBT or multicomponent psychological support interventions separately and it is these 11 RCTS192 and 17 RCTS193 that are considered here. There is huge overlap between Ford et al. 192 and Zijdenbos et al. ,193 with only two papers in Ford et al. 192 not included in Zijdenbos et al. ,193 but the more broadly self-management focused Dorn191 has only one RCT in common with Ford et al. 192 and two with Zijdenbos et al. 193
Quality assessment and weighting
All three reviews scored above 30 (out of 44) on our assessment of quality (Table 92).
| R-AMSTAR criteria | Zijdenbos 2009193 | Ford 2009192 | Dorn 2010191 |
|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 3 | 3 | 2 |
| Was a list of studies (included and excluded) provided? | 4 | 2 | 1 |
| Were the characteristics of the included studies provided? | 3 | 3 | 2 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 4 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 3 | 4 | 4 |
| Was the likelihood of publication bias assessed? | 1 | 4 | 4 |
| Was the conflict of interest stated? | 2 | 3 | 1 |
| Total score/44 | 36 | 39 | 31 |
The total number of participants in the RCTs included in Zijdenbos et al. 193 and Dorn191 exceeded 1000, therefore these studies were weighted as offering the highest level of evidence in this meta-review (Table 93).
Outcomes
The outcomes of interest chosen for this meta-review were self-reported symptoms and QoL, which were key outcomes in the included reviews and we considered the most helpful to inform commissioners (Table 94). Health-care resource use was not reported by the included reviews.
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Symptoms | Adequate relief, symptoms, abdominal pain | Symptoms scores: a CPRS, BSSS, VAS-scale, adequate relief, CAS (a symptom score, acronym not explained), McGill pain score, diary, IBS scale, IBS-SSS, global symptom improvement, composite GI symptom score, global relief |
| QoL | QoL | QoL scores: SF-36, IBS-QoL, GI-QoL |
Findings
Only the two reviews of psychological therapies could be statistically synthesised (Table 95). Essentially, Zijdenbos et al. 193 meta-analysed the studies in smaller, more homogenous groups and failed to identify much evidence of benefit from CBT for IBS in terms of abdominal pain, QoL or symptom scores. 193 The authors conclude ‘CBT is better than usual care or waiting list for improving symptoms and QoL at 3 months, but is not superior to placebo’ and question the clinical significance of this result. They point out a placebo response is relatively pronounced in IBS, the poor quality of the included trials and the lack of studies with longer follow-ups. In contrast, Ford et al. 192 appears to offer more evidence to support CBT, but the studies in their analysis are exactly the same as in the Cochrane review so this outcome may have arisen from their meta-analysing a larger group of more heterogeneous studies than Zijdenbos et al. 193 Ford et al. 192 identifies evidence of publication bias and in a sensitivity analysis ‘when the three studies conducted in the same centre were excluded from the analysis, the beneficial effect of CBT on symptoms of IBS disappeared’ but still goes on to endorse CBT as ‘efficacious in the treatment of IBS in the short-term’.
| Reference and weighting | Outcome (comparison group) | Time | Sample size; n RCTS; n participants (where available) | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Zijdenbos 2009193 *** | CBT | ||||
| Symptom score (vs. usual care/waiting list) | 2 months | Four RCTs, 133 | 0 | SMD 0.75 (–0.20 to 1.70) | |
| 3 months | Five RCTs, 378 | ++a | SMD 0.58 (0.36 to 0.79) | ||
| 6 months | Two RCTs, 170 | + | SMD 0.56 (0.06 to 1.07) | ||
| Symptom score (vs. placebo) | 2 months | Two RCTs, 44 | 0 | SMD 0.68 (–0.01 to 1.36) | |
| 3 months | Two RCTs (one in twice due to three arms), 230 | 0 | SMD –0.17 (–0.45 to 0.11) | ||
| Abdominal pain (vs. usual care/waiting list) | 2 months | Three RCTs, 80 | 0 | SMD 0.45 (0.00 to 0.91) | |
| 3 months | Seven RCTs, 359 | 0 | SMD 0.22 (–0.04 to 0.49) | ||
| Abdominal pain (vs. placebo) | 3 months | Four RCTs (one in twice due to three arms), 395 | 0 | SMD 0.33 (–0.16 to 0.82) | |
| QoL (vs. usual care/waiting list) | 2 months | Two RCTs, 97 | +a | SMD 0.44 (0.04 to 0.85) | |
| Ford 2009192 ** | CBT | ||||
| Symptoms persisting (vs. usual management) | NR | Seven RCTs, 491 | ++b | RR 0.60 (0.42 to 0.87) NNT = 3 (2 to 7) |
|
| Multicomponent psychological therapy | |||||
| Symptoms persisting (vs. usual management/control therapy) | NR | Three RCTs, 211 | ++a | RR 0.69 (0.56 to 0.86) NNT = 4 (3 to 8) |
|
In Dorn’s191 review, the primary outcomes of the RCTs were also heterogeneous but nearly always involved symptom scores and nearly every study reported a positive primary outcome result favouring, or tending to favour, the intervention. In view of the heterogeneity (which included heterogeneity in study size, diagnostic criteria, setting and quality, in addition to intervention and outcome measures), Dorn191 did not attempt a meta-analysis – instead presenting results of each individual studies narratively.
Dorn191 concludes that self-management support interventions do benefit patients with IBS; ‘and in some cases these benefits exceed those seen in IBS drugs and psychological intervention studies’, but noted that the studies were frequently of poor quality. ‘The most convincing benefit was seen with self-administered cognitive–behavioural interventions (72% vs. 7% achieved adequate relief)’, followed by a study of a self-help guidebook. Evidence on patient support groups was of poor quality and inconclusive. He notes that although self-management support is probably key to managing IBS it is difficult to deliver in ‘real-world’ settings, at least in the USA, and concludes ‘Thus, the next key challenge is to develop practical self-management interventions that can be applied across various clinical settings, and to then test them in well-designed clinical trials’ (see Figure 39 for an overall summary).
FIGURE 39.
Irritable bowel syndrome: summary of what the quantitative evidence shows.
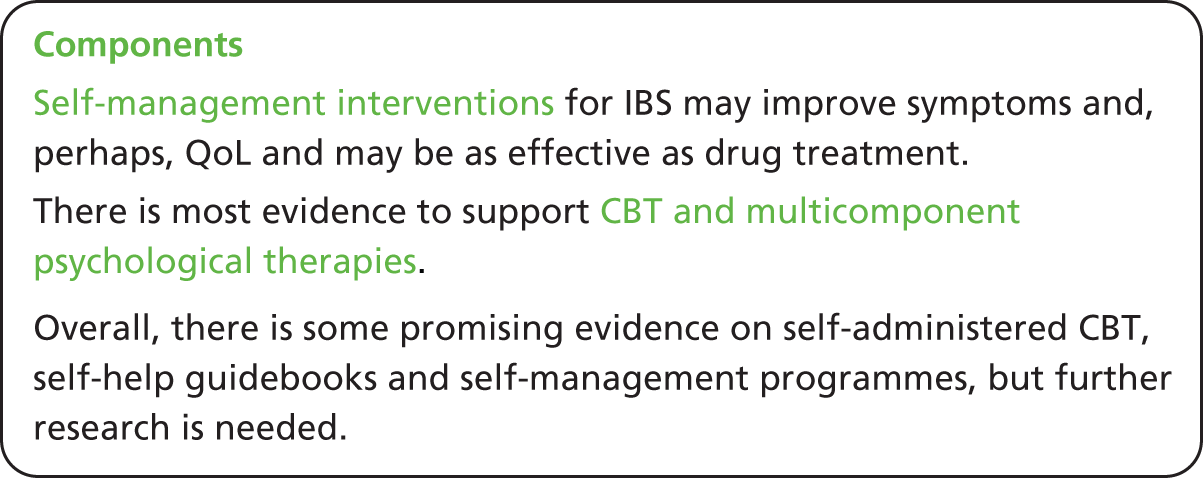
Discussion
Overall, there is some evidence for the effectiveness of CBT and multicomponent psychological therapies; however, this has mainly been measured within the first 2- to 6-months post-intervention and so findings can only be generalised to the short term. Often there was only one study per intervention component and therefore this heterogeneity created problems pooling or synthesising interventions types that were not CBT or multicomponent psychological therapy. There is some promising evidence on self-administered CBT, self-help guidebooks, self-management programmes and structured patient education, but further evidence on each intervention type, and much better quality studies, are needed to assess effectiveness. Self-management support appears to be potentially very important in the management of patients with IBS but more evidence on low cost, feasible, effective and acceptable interventions is needed.
Chapter 18 Additional meta-review: self-management support for individuals with low back pain
Meta-review of qualitative syntheses
Systematic reviews identified
From a total of 6435 papers we included one review194 (published in 2004) in the LBP qualitative meta-review (Figure 40).
The review included both qualitative and quantitative evidence from primary studies examining patients with LBP on their expectations and satisfaction with treatment as part of practice guideline development. Only the 12 qualitative primary studies (published between 1998 and 2001) were extracted for this meta-review. The review included a range of primary studies examining both acute and chronic LBP, defining chronic as pain lasting more than 3 months. The studies were based in UK (3), USA (2), Australia (2), Sweden (2), the Netherlands (1), Norway (1) and Switzerland (1). They included feedback on the following treatments: care from chiropractor, rheumatologist, GP, other medical doctors, physiotherapist, general diagnostic tests and rehabilitation (Table 96).
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Verbeek 2004194 (Mixed methods) |
To summarise evidence from studies among patients with LBP on their expectations and satisfaction with treatment as part of practice guideline development | 12 | This review included 12 qualitative and 8 quantitative studies. Qualitative studies revealed the following: patients want a clear diagnosis of the cause of their pain, information and instructions, pain relief, and a physical examination. Next, expectations are that there are more diagnostic tests, other therapy or referrals to specialists, and sickness certification. They expect confirmation from the health-care provider that their pain is real. Like other patients, they want a confidence-based association that includes understanding, listening, respect, and being included in decision-making |
Quality assessment
The review scored 30/40 for quality (Table 97).
| R-AMSTAR criteria | Verbeek 2004194 |
|---|---|
| Was an appropriate and detailed design provided? | 4 |
| Was there duplicate study selection and data extraction? | 4 |
| Was a comprehensive literature search performed? | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 |
| Was a list of studies (included and excluded) provided? | 1 |
| Were the characteristics of the included studies provided? | 2 |
| Was the scientific quality of the included studies assessed and documented? | 2 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 |
| Was the conflict of interest stated? | 4 |
| Total score/40 | 30 |
| Quality rating (low = < 30; high = ≥ 30) | High |
Findings
Support for self-management
The review reported that there were two ‘treatment aspects’ (p. 2310)194 that occurred most frequently. These were that (i) patients want to know the cause of their pain and (ii) patients want information or instruction. As a synthesis cannot be carried out from one review, instead a summary of how the evidence can be used to inform future commissioning of self-management support is provided.
-
Self-management support needs to address ‘noncongruence’ (p. 2313)194 between patients and professionals. This includes differences in opinions about the definition and cause of LBP and how it should be identified and treated. Communication in a collaborative style creates a greater chance of congruence. People with LBP reported feeling that they were not believed, not treated with respect and not listened to by HCPs.
-
To aid this congruency, it is important to actively involve participants in their education about LBP and include them in the decision-making process. (Especially those that are more experienced in their condition. The review did provide distinctions between papers looking at acute or chronic LBP and the conclusion of experience may have been influenced by the comparison between acute and chronic treatment. All of the other conclusions are made from studies focusing on chronic LBP.) People with LBP reported that there was an inadequacy in diagnosis and consultation, and felt many questions remained unanswered. They were frustrated when they were not involved in decision-making processes. Authors of the review suggested that physicians could explore patients’ expectations through motivational interviewing so that during the interview, or in future interviews, their expectations are met.
-
People with LBP tended to initially seek help from a HCP to alleviate pain/symptoms, but as they became more experienced with their condition, they expected this less and were more concerned with treatment to decrease difficulties with normal activities. Authors suggested that perhaps those who had adjusted to the need to manage the pain, rather than cure it, were more realistic and less dissatisfied with treatment and therefore better able to self-manage. Tailored psychological support for this adjustment may be an important aspect of self-management support.
-
One study in the review found the need for better continuity of care, for example improvement in referrals, investigations, results, appointments, surgery and clinics.
Meta-review of quantitative systematic reviews
Systematic reviews identified
A total of 14 reviews were identified for inclusion in this meta-review (Figure 41). 195–208 These reviews reported on a total of 255 RCTs, of which 114 were included in more than one review. Reviews were published between 1995 and 2012 and included RCTs published from 1977 to 2010.
Of the 14 reviews, two had an explicit focus on self-management; seven explored multicomponent rehabilitation; three studied psychological therapies; and two examined educational interventions (Table 98).
| Review | Intervention of interest (definition) | Participant demographics | Setting, delivery and service arrangements | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Explicit self-management | |||||
| Du 2011195 ** | Self-management programmes Eight essential elements: self-efficacy building; self-monitoring; goal-setting and action planning; decision-making; problem-solving; self-tailoring; partnership between the views of patients and health professionals; and community based and close to home. Must also focus on managing pain and minimising disability |
Three RCTs:
|
Three RCTs:
|
Three RCTs:
|
Duration: range 6–12 weeks Three RCTs:
|
| Oliveira 2012196 *** | Self-management Where indicated by primary RCT authors by naming the intervention ‘self-management’ or ‘self-care’. Intention of the intervention is for the participant to manage their own condition with minimal oversight or active involvement of the health care provider |
61% women | Delivered by health-care providers or lay-trained leaders | Trials used written information, discussion sessions and audiovisual resources (i.e. audiotape, videotape, or web site) as self-management strategies | Amount of support given by health-care providers or lay-trained leaders, varied between 1 and 13 sessions |
| Multicomponent rehabilitation | |||||
| Brox 2008197 ** | Back schools, brief education and fear-avoidance training Back schools: consists of an education and skills programme, including physical exercises Brief education: brief contact with HCPs, self-management patient-led groups, provision of educational booklets and internet discussion groups which aim to encourage active self-management and to reduce concerns Fear-avoidance training: addressing fears and encouraging normal activities and physical exercise |
Non-specific back pain and/or lower limb pain of more than 12 weeks duration | Set in primary care; out-patient; OT department; rehab department. Delivered by physiotherapists; OTs; physical education instructor; lecturers; psychologists | Interventions included brief education: examination; information; reassurance; advice to stay active; neurophysiology education; fear-reducing techniques; cognitive intervention; and exercises | NR |
| Di Fabio 1995198 ** | Comprehensive rehabilitation programmes and back schools Back schools: provided patient education for proper bending and lifting activities and a passive or active back exercise programme Comprehensive rehabilitation programme: back school plus worksite visit, operant conditioning, cognitive–behavioural group therapy, or intensive physical training |
Age range, 18–61 years; mean age, 42 years 53% chronic LBP; 27% acute/subacute LBP; 20% mixed chronicity |
57% outpatient; 24% inpatient (controlled residential environment at least 5 days per week) | NR | NR |
| Guzmán 2002199 *** | Essential physical dimension (assessed for physical causes of back pain and offered pharmacological or exercise/physical therapy if indicated), plus either psychological dimension (assessed regarding psychological factors and received group or individual counselling as necessary) or social/occupational dimension (assessed regarding family, social and/or occupational environment, followed by appropriate intervention) | Mostly workers selected from insurance listings or patients referred to pain centres | Inpatient and outpatient settings | All contained three components: physical, psychological and social/occupational | Programme duration fell into two main categories: daily intensive programmes with more than 100 hours of therapy; once or twice a week programmes with less than 30 hours of therapy. Most programmes had standard duration and interventions, allowed limited individualisation |
| Heymans 2004200 *** | Back school Consisting of an educational and skills acquisition programme, including exercises, in which all lessons were given to groups of patients and supervised by a paramedical therapist or medical specialist |
LBP without radiation (four RCTs); mixed with and without radiating symptoms (eight RCTs); unspecified (seven RCTs). Acute/subacute LBP (four RCTs); chronic (12 RCTs); mixed (three RCTs) | Delivered to groups, supervised by a paramedical therapist or medical specialist | Educational and skills acquisition programme, including exercises | Interventions varied from a very intensive 3-week programme to an intervention of four lessons totalling 3 hours |
| van Geen 2007201 ** | Multidisciplinary back training Physical dimension essential, plus at least one other component: psychological, behavioural, educational or social. The main objective of the training is to restore the daily functioning of participants for the longer term |
Time from onset of LBP until baseline ranged from at least 6 months to over 2 years; intensity of LBP varied from perceived minor restrictions to not being able to work for at least 90 days | Involved several disciplines, e.g. psychologists, physiotherapy, OTs, medical specialists | Interventions ranged from four elements (physical, educational, psychological and social) to two elements (physical and educational or psychological) | Ranged from 2 hours to 35 hours a week |
| van der Giessen 2012202 ** | GA Consisted of four components: measurements of functional capacity; a workplace visit; back school education; and an individual, submaximal, gradually increased exercise programme |
The mean age of participants ranged from 38–42 years. The duration of complaints ranged from 1 to a maximum of 24 weeks. The percentage of female participation in the studies ranged from 5.9% to 64% | NR | Every study used operant conditioning, provided back school education and an individual submaximal gradually increasing exercise programme | Durations and frequencies differed, including:
|
| van Middelkoop 2011203 *** | Physical and rehabilitation interventions Behavioural treatments: operant, cognitive and respondent treatments or a combination Back school: educational and skills acquisition programme, including exercises Patient education: one or more methods which influence the way the patient experiences their illness and/or their knowledge and health behaviour Multidisciplinary treatment: minimally one physical dimension and one other dimension (psychological or social or occupational) |
NR | NR | Four invention categories of interest to the meta-review: behavioural treatments; back school; patient education; multidisciplinary treatment | NR |
| Psychological therapy | |||||
| Henschke 2010204 *** | Behavioural treatment Treatment based on behavioural therapy which aims to alter maladaptive thoughts, feelings and behaviours as well as dysfunctional sensory phenomena |
NR | NR | Treatments based on behavioural therapy principles; three broad categories: operant, cognitive and respondent | Variable follow-up: short term (immediately post-treatment); intermediate term (6-month follow-up); long term (12-month follow-up) |
| Hoffman 2007205 ** | Psychological interventions Adopted a broad definition of psychosocial interventions, not limited by theoretical orientation |
Mean percentage of male subjects 41.69% (range 8.33–68.82%). Mean subject age 42.70 years (range 35.50–49.70 years). Mean pain duration 90.86 months (range 4.60–154.80 months) | NR | Psychological and multidisciplinary treatment | NR |
| Scheer 1997206 * | Cognitive–behavioural interventions Return to work interventions which emphasise or include cognitive or behavioural approaches |
NR | NR | Components include: cognitive strategies; relaxation; physical therapy; fitness; biofeedback; education; coping skills; operant conditioning; back schools; ergonomics; cognitive pain control; risk reduction; home exercise | Five RCTs:
|
| Education | |||||
| Engers 2008207 *** | Individual education Any advice or information (verbal, written or audiovisual) given by a HCP to improve patients’ understanding of their back problems and what they should do about them |
Acute/subacute LBP (14 studies); chronic LBP (four studies); mixed chronicity (six studies) | Delivered exclusively by HCP, individual basis | Written educational materials (17 studies); pamphlets containing biopsychosocial information (three studies); a variety of booklets (12 studies); book and videotapes (one study); oral individual education (14 studies) | NR |
| Liddle 2007208 *** | Advice All the information that the patient receives verbally, in written, audiovisual, or electronic format during the course of treatment |
Males and females between the ages of 16 and 79 years, one trial exclusively used 57-year-old women | Advice could be received verbally, in written, audiovisual or electronic format | Advice as an adjunct to exercise most commonly used in acute LBP (8/13 RCTs) and chronic LBP (8/19 RCTs). Advice as part of a back school most commonly used in subacute LBP (3/7 RCTs) | NR |
Randomised controlled trials were conducted in the following countries (not reported in all reviews): the Netherlands, Sweden, Denmark, Norway, Finland, Germany, Switzerland, UK, Israel, Hong Kong, USA, Canada and Australia. Four were Cochrane reviews (Engers et al. ,207 Guzmán et al. ,199 Henschke et al. 204 and Heymans et al. 200).
Explicit self-management
Du et al. 195 reported strict inclusion criteria, with all RCTs needing to meet eight essential criteria to be classed as a self-management programme. These rigorous criteria led to the inclusion of just three RCTs on LBP, one of which focused on pregnancy-related LBP 3 weeks after delivery. Oliveira et al. ,196 on the other hand, included 13 RCTs; just one RCT was common to both reviews. These two reviews included a diversity of self-management support components in various combinations, including fear-avoidance techniques; education; behavioural rehearsal; discussion sessions; and audiovisual resources. Education, usually supported by a book, was a very common component across the interventions.
Other multicomponent interventions including ‘back schools’ and biospsychosocial approaches
Three reviews (Brox et al. ,197 Heymans et al. 200 and van Middelkoop et al. 203) examined ‘back schools’, defined by Heymans et al. 200 as an ‘educational and skills acquisition program, including exercises, in which all lessons were given to groups of patients and supervised by a paramedical therapist or medical specialist’.
Other interventions explored include comprehensive rehabilitation programmes, multidisciplinary biopsychosocial rehabilitation (MBPSR)199 and graded activity (GA), defined as ‘developed by Lindstrom, [and consisting of] . . . four parts: (i) measurements of functional capacity; (ii) a work-place visit; (iii) back school education, and (iv) an individual, submaximal, gradually increased exercise program . . .’. In at least three of these reviews, participants included those with acute or subacute LBP as well as chronic LBP.
We would define these interventions as self-management support due to their multicomponent nature which in all cases included education as a key component, thereby helping empower individuals (to a lesser or greater extent) (see Chapter 7).
Psychological
There were considerable similarities in the focus of the three reviews, with Henschke et al. 204 exploring behavioural treatments, Hoffman et al. 205 looking at psychological interventions and Scheer et al. 206 reporting on cognitive–behavioural interventions. These similarities are reflected in the overlap in the studies included. Seven RCTs were included in both Henschke et al. ’s review204 of behavioural treatments and Hoffman et al. ’s review205 of psychological treatments. Three RCTs were common to both Henscke et al. ’s204 and Scheer et al. ’s206 reviews of cognitive–behavioural interventions. Just one study was common to both reviews. The interventions explored in these three reviews included relaxation therapies; operant therapy; cognitive therapy; and multidisciplinary treatment. Components included cognitive strategies, relaxation, physical therapy, education, biofeedback and coping skills.
We would consider some forms of psychological therapy, in particular CBT, to represent a form of self-management support (see Chapter 10).
Educational
The two educational reviews207,208 were the two largest reviews in terms of total size: both with more than 7000 participants. Despite their large size, only seven RCTs were common to both. In both reviews, the focus was not exclusively on chronic LBP, but also included RCTs with acute, subacute, or mixed chronicity LBP. In fact, in Engers et al. ’s207 review only three studies examined chronic LBP exclusively. Interventions included education in a variety of formats (pamphlets, books, videotapes and oral). In some RCTs education was an adjunct to exercise, or back schools.
Education is the only unidimensional intervention that we considered to represent self-management support. However, we believe education to support self-management best when delivered in an ‘active’ way, i.e. when education engages participants in its delivery and comprehension and is not a didactic and passive process (see Chapter 7).
Quality assessment and weighting
The two reviews identified which focused explicitly on self-management195,196 were both assessed as high quality (scoring ≥ 31). The seven multicomponent rehabilitation reviews varied in their quality, with three defined as lower quality197,198,201 and four classed as being of a higher quality. 199,200,202,203 The assessed quality in the reviews of psychological therapies varied, with one higher quality review204 and two reviews of lower quality. 205,206 Both reviews of educational interventions were classed as high quality (Table 99).
| R-AMSTAR criteria | Explicit self-management | Multicomponent rehabilitation | Psychological therapy | Education | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Du 2011195 | Oliveira 2012196 | Brox 2008197 | Di Fabio 1995198 | Guzmán 2002199 | Heymans 2004200 | van Geen 2007201 | van der Giessen 2012202 | van Middelkoop 2011203 | Henschke 2010204 | Hoffman 2007205 | Scheer 1997206 | Engers 2008207 | Liddle 2007208 | |
| Was an a priori design provided? | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 2 | 1 | 4 | 4 | 1 | 1 | 4 | 4 | 4 | 2 | 4 | 4 |
| Was a comprehensive literature search performed? | 4 | 3 | 1 | 3 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 4 | 4 |
| Was the status of publication used as an inclusion criterion? | 1 | 1 | 1 | 1 | 4 | 2 | 1 | 2 | 2 | 4 | 2 | 1 | 2 | 1 |
| Was a list of studies (included and excluded) provided? | 3 | 3 | 1 | 4 | 4 | 4 | 2 | 3 | 2 | 4 | 1 | 1 | 4 | 4 |
| Were the characteristics of the included studies provided? | 4 | 3 | 3 | 4 | 4 | 4 | 4 | 4 | 1 | 1 | 1 | 1 | 4 | 4 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 4 | 1 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 4 | 2 | 1 | 4 | 3 | 3 | 3 | 4 | 3 | 2 | 2 | 3 | 4 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 4 | 4 | 4 | 2 | 2 | 4 | 2 | 4 | 3 | 3 | 4 | 4 |
| Was the likelihood of publication bias assessed? | 1 | 4 | 1 | 2 | 2 | 2 | 1 | 1 | 3 | 1 | 4 | 1 | 2 | 2 |
| Was the conflict of interest stated? | 2 | 1 | 2 | 1 | 3 | 3 | 3 | 3 | 3 | 3 | 1 | 2 | 3 | 3 |
| Total score/44 | 35 | 35 | 25 | 26 | 41 | 36 | 29 | 33 | 32 | 36 | 30 | 24 | 38 | 38 |
Taking into account both the quality of the included reviews, and the total number of participants which the reviews included, a weighting of evidence was applied to all reviews (Table 100).
| Review | Quality score | Total number participants | Weighting |
|---|---|---|---|
| Du 2011195 | 35 | 286 | ** |
| Oliveira 2012196 | 35 | 3063 | *** |
| Brox 2008197 | 25 | 4949 | ** |
| Di Fabio 1995198 | 26 | 2373 | ** |
| Guzmán 2002199 | 41 | 1964 | *** |
| Heymans 2004200 | 36 | 3584 | *** |
| van Geen 2007201 | 29 | 1958 | ** |
| van der Giessen 2012202 | 33 | 680 | ** |
| van Middelkoop 2011203 | 32 | 3831 | *** |
| Henschke 2010204 | 36 | 3438 | *** |
| Hoffman 2007205 | 30 | 1747 | ** |
| Scheer 1997206 | 24 | 679 | * |
| Engers 2008207 | 38 | 7049 | *** |
| Liddle 2007208 | 38 | 7347 | *** |
Outcomes
The two outcomes selected to be of interest in this meta-review were any measure of participant pain and any measure of functional status. In the case that no measure of function was reported, return-to-work measures were used instead (Table 101).
| Outcomes | Definition | Examples of measures reported within systematic reviews |
|---|---|---|
| Pain intensity/severity | Any measure of participant pain intensity or severity | VAS; NRS; McGill pain questionnaire; Body Pain Scale of the SF-36; symptom bothersomeness scale |
| Disability/functional status (or if absent: return to work/occupational status) | Any measure of participant disability or functional status, or if this is not reported, then a measure of return to work or occupational status | Back pain-specific functional status/disability: Roland–Morris Questionnaire; Oswestry Disability Index Generic functional status/disability: SIP; SF-36; EuroQol; ADL; self-reported reduced activity |
| Days off work; days of cut-down work; work status; time to return to work |
Findings
Explicit self-management
Although no significant effect on pain was reported by Du et al. ,195 Oliveira et al. 196 found evidence to support a small, statistically significant effect at short- and longer-term follow-up. The impact of the interventions on disability was more consistently positive across the two reviews, with two of the three RCTs included in Du et al. ’s review finding significant, small benefits (Du et al. calls these ‘moderate’) in the medium term (6 months),195 and Oliveira et al. 196 reporting small, significant effects in the short and longer term.
Other multicomponent interventions
Back schools
The evidence to support a beneficial impact of back schools on the outcome of pain or disability (or functional status where disability was not reported) is limited. Brox et al. ,197 Heymans et al. 200 and van Middelkoop et al. 203 all found conflicting evidence for back schools when compared with no intervention/wait list control at any time point. There was more evidence for the effectiveness of back schools in occupational settings in one high-quality review, but the clinical relevance of their findings were questioned by reviewers.
Multidisciplinary back training, comprehensive rehabilitation, graded activity
Evidence for multidisciplinary back training, which in this review overlapped with biopsychosocial and GA) is also lacking, with one lower-quality review concluding that there was no demonstrable long-term effect on pain or functional status. 201 Comprehensive rehabilitation programmes were found to be more effective than back schools at reducing pain in one older and lower-quality review. 198
The available systematic review evidence does not support the use of GA (here there was an overlap with back school interventions), with a higher-quality review finding that only one of four RCTs reported a significant effect on pain compared with usual care,202 and all four RCTs detecting no significant difference for the outcome of disability.
Biopsychosocial approaches
There is strong evidence to suggest that intensive MBPSR significantly reduces pain compared with usual care, and moderate evidence that it improves function (although there was no evidence that less intensive interventions benefited pain-related disability) in a high-quality review. 199
Psychological interventions
Henscke et al. ’s204 high-quality review found all behavioural treatments to confer a significant benefit on short-term pain only with no difference in the long term on pain or on functional measures. Similarly, Hoffman et al. ’s205 lower-quality review found a significant reduction in pain post-treatment but no significant differences at longer-term follow-up. For the outcome of disability or functional status, Henscke et al. 204 found no significant benefit from cognitive, operant or combinations of therapies, but did find a significant short-term benefit from progressive relaxation. Hoffman et al. 205 reports overall beneficial effects at follow-up and long-term follow-up, but gives no indication of the actual duration of follow-up in the included studies. Scheer et al. ’s206 low-quality review reports mixed, inconclusive findings regarding return to work, with no overall trend suggesting effectiveness.
Educational interventions
The high-quality review by Engers et al. ,207 identified only three studies that examined chronic LBP: there was moderate evidence of no difference between individual educational interventions and non-educational interventions (yoga, physiotherapy, exercises and spinal manipulation) for pain and back pain-specific function; and strong evidence that written educational interventions were inferior to such non-educational interventions.
Liddle et al. ’s high-quality review208 found evidence to suggest a favourable outcome for advice when delivered as part of a back school and also found a positive result in 14 of 19 RCTs investigating the use of advice in chronic LBP trials (see Table 102 for results from meta-analyses, Table 103 for narrative summaries and Figure 42 for an overall summary).
| Reference and weighting | Outcome | Time | Sample size; n RCTS; n participants (where available) | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Oliveira 2012196 *** Self-management* negative values favour self-management* |
Self-management vs. minimal intervention | ||||
| Pain | Short term | 10 RCTs, 2700 | + | –3.2 points (–5.1 to –1.3 points) | |
| Long term | 10 RCTs, 2700 | + | –4.8 points (–7.1 to –2.5 points) | ||
| Disability | Short term | 10 RCTs, 2700 | + | –2.3 points (–3.7 to –1.0 points) | |
| Long term | 10 RCTs, 2700 | + | –2.1 points (–3.6 to –0.6 points) | ||
| Sensitivity analysis: self-management interventions fulfilling six core components vs. minimal intervention | |||||
| Pain | Short term | Eight RCTs | + | –3.1 (–5.1 to –1.1) | |
| Long term | Eight RCTs | + | –5.7 (–8.2 to –3.3) | ||
| Disability | Short term | Eight RCTs | + | –3.0 (–5.2 to –0.8) | |
| Long term | Eight RCTs | + | –4.7 (–7.5 to –1.9) | ||
| van Middelkoop 2011203 *** Physical and rehabilitation interventions* negative values favour self-management* |
Behavioural treatment: respondent therapy (progressive relaxation) vs. no treatment control | ||||
| Pain intensity | Post treatment | Three RCTs | + | –19.74 (–34.32 to –5.16) | |
| Disability | Post treatment | Three RCTS | + | –5.24 (–8.42 to –2.06) | |
| Behavioural treatment: respondent therapy (EMG biofeedback) vs. no treatment control | |||||
| Pain intensity | Post treatment | Three RCTs | + | –8.67 (–13.59 to –3.74) | |
| Disability | Post treatment | Two RCTS | 0 | –7.33 (–21.38 to 6.73) | |
| Behavioural treatment: operant therapy vs. no treatment control | |||||
| Pain intensity | Post treatment | Three RCTs | + | –7.00 (–12.33 to –1.67) | |
| Disability | Post treatment | Three RCTs | 0 | –2.87 (–7.15 to 1.41) | |
| Behavioural treatment: combined respondent and cognitive therapy vs. no treatment control | |||||
| Pain intensity | Post treatment | Four RCTs | + | –12.74 (–24.10 to –1.37) | |
| Disability | Post treatment | Four RCTs | 0 | –2.60 (–6.48 to 1.27) | |
| Behavioural treatment: cognitive therapy vs. no treatment control | |||||
| Pain intensity | Post treatment | Two RCTs | + | –12.67 (–20.26 to –5.08) | |
| Back schools vs. no treatment control | |||||
| Pain | Post treatment | Two RCTs | 0 | –4.64 (–13.65 to 4.37) | |
| Disability | Short term | Two RCTs | 0 | –13.04 (–37.04 to 10.95) | |
| Multidisciplinary treatment vs. no treatment control | |||||
| Pain intensity | Short term | Two RCTs | + | –9.47 (–13.87 to –5.07) | |
| Disability | Short term | Two RCTs | 0 | –8.84 (–18.49 to 0.82) | |
| Pain intensity | Long term | Two RCTs | 0 | –9.27 (–27.86 to 9.12) | |
| Disability | Long term | Two RCTs | 0 | –0.77 (–4.62 to 3.08) | |
| Hoffman 2007205 ** Psychological interventions |
Psychological or multidisciplinary intervention vs. any control | ||||
| Pain intensity | Post treatment | 614 | + | (0.06 to 0.48); p = 0.01 | |
| Follow-up | 939 | 0 | (–0.27 to 0.59); p = 0.47 | ||
| Disability: working | Follow-up | 245 | + | (0.06 to 0.65); p = 0.02 | |
| Long-term follow-up | 609 | + | (0.19 to 0.86); p = 0.03 | ||
| Multidisciplinary intervention vs. control | |||||
| Pain intensity | Post treatment | 284 | 0 | (–0.13 to 0.38); p = 0.33 | |
| Follow-up | 393 | 0 | (–0.29 to 0.59); p = 0.51 | ||
| Disability: working | Follow-up | 245 | + | ES 0.36 (0.06 to 0.65; p = 0.02) | |
| Long-term follow-up | 609 | + | ES 0.53 (0.19 to 0.86; p = 0.03) | ||
| Psychological intervention vs. control | |||||
| Pain intensity | Post treatment | 352 | + | (0.23 to 0.82); p = 0.00 | |
| Cognitive–behavioural intervention vs. control | |||||
| Pain intensity | Post treatment | 256 | + | (0.25 to 0.98); p < 0.01 | |
| Self-regulatory intervention vs. control | |||||
| Pain intensity | Post treatment | 202 | + | p < 0.001 | |
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Explicit self-management | |||||
| Du 2011195 ** | Self-management programmes | Three RCTs; 286; 2004–8 | Narrative | None of the three RCTs showed significant positive effect in reducing back pain. Only one study showed a short-term positive trend and another study showed a medium-term positive trend in reducing pain. Of the three RCTs, only one reported that self-management programmes had a short-term (3 months) significant positive effect in improving disability. Two studies reported that self-management programmes had a medium-term (6 months) positive trend in improving disability | Further research is needed on self-management for chronic back pain |
| Oliveira 2012196 *** | Self-management | 13 RCTs; 3063; 1989–10 | Meta-analysis | Self-management vs. minimal intervention: moderate quality evidence that self-management interventions have small but statistically significant effects compared with minimal interventions, on pain and disability at short- and long-term follow-up Sensitivity analysis for self-management interventions fulfilling six core components: statistically significant beneficial effect on pain and disability at short- and long-term follow-up. ES slightly larger than for all self-management interventions combined |
There is moderate-quality evidence that self-management has small effects on pain and disability in people with LBP. These results challenge the endorsement of self-management in treatment guidelines |
| Narrative synthesis | Self-management vs. other interventions: two trials reported self-management equally or less effective than comparison (massage, acupuncture, yoga, exercise). Third trial reported self-management more effective than 60-minute educational session on pain at short-term follow-up and on disability at short- and long-term follow-up | ||||
| Multicomponent rehabilitation | |||||
| Brox 2008197 ** | Back schools, brief education and fear-avoidance training | 23 RCTs; 4949; 1983–2006 | Narrative synthesis | Back schools: conflicting evidence on pain and disability vs. waiting list/no intervention/placebo. Limited evidence for effectiveness vs. exercises, usual care, cognitive–behavioural-based back school Brief education: moderate evidence for the short-term effectiveness vs. usual care on disability. Limited evidence when compared with back school or exercises. Five studies compared back book or internet education with eight different interventions. Evidence of effectiveness limited compared with yoga, massage, exercises, stabilising exercises, manipulation and acupuncture, and conflicting compared with waiting list/no intervention for both pain and disability Fear avoidance: one large high-quality trial – limited evidence that an intervention in primary care and physiotherapy setting incorporating fear-reducing techniques is more effective than usual care in reducing pain or disability. Moderate evidence that fear-avoidance training incorporated in a rehabilitation programme consisting of cognitive intervention and exercises is equal to spinal fusion on back pain and disability |
Consistent recommendations are given for brief education in the clinical setting. Fear-avoidance training should be considered as an alternative to spinal fusion and back schools may be considered in the occupational setting |
| Di Fabio 1995198 ** | Comprehensive rehabilitation programmes and back school | 19 RCTs; 2373; 1977–92 | Meta-analysis | Due to lack of details, not presented in meta-analysis results table Overall found an ES favouring control for the outcome of pain and a very small positive ES for the outcome of disability Comprehensive rehabilitation had an overall ES d index = 0.28. Back school overall ES d index = –0.14. Comprehensive rehabilitation programmes were more effective at reducing pain with back school alone; no difference between the two intervention types in effect on disability |
Back schools in general yield no benefit beyond that of control interventions Comprehensive rehabilitation does yield benefit beyond control interventions |
| Narrative synthesis | |||||
| Guzmán 2002199 *** | MBPSR | 10 RCTs; 1964; 1989–97 | Narrative | Moderate evidence that intensive MBPSR with a functional restoration approach reduces pain compared with outpatient non-multidisciplinary rehabilitation or usual care. Strong evidence that intensive MBPSR with a functional restoration approach improves function compared with inpatient/outpatient non-multidisciplinary treatments | Provides evidence that intensive MDBPSR with a functional restoration approach improves pain and function. Less intensive interventions did not show improvements in clinically relevant outcomes |
| Heymans 2004200 *** | Back school | 19 RCTs; 3584; 1977–2002 | Narrative | Back schools vs. other treatments (exercises, spinal or joint manipulation, myofascial therapy, instructions or advice): moderate evidence that back school is more effective than other treatments for pain and functional status at short- and intermediate-term follow-up. Moderate evidence that there is no difference in effect on these outcomes in long term Back schools vs. waiting list controls or ‘placebo’ interventions: conflicting evidence on pain and functional status at short-, intermediate- and long-term follow-up Back schools in occupational settings vs. other treatments: moderate evidence that back school is more effective than other treatments for pain and functional status at short- and intermediate-term follow-up. Conflicting evidence at long-term follow-up Back schools in occupational settings vs. waiting list controls or ‘placebo’ interventions: moderate evidence that a back school is more effective than waiting list controls for pain and return to work (short- and intermediate-term follow-up) |
Moderate evidence suggests that back schools, in an occupational setting, reduce pain and improve function in the short and intermediate term, compared with exercises, manipulation, myofascial therapy, advice, placebo or waiting list controls |
| van Geen 2007201 ** | Multidisciplinary back training | 10 RCTs; 1958; 1988–2002 | Narrative synthesis | Only one of seven studies reported a positive effect on experienced pain or functional status. No demonstrable long-term effect in terms of these outcome measures, regardless of the quality of the study and the intensity of the intervention | Pain and functional status of people with chronic LBP cannot be improved with multidisciplinary back training |
| van der Giessen 2012202 ** | GA | Five RCTs; 680; 1992–2008 | Narrative synthesis | Pain: four RCTs reported on the effect of GA on pain; all studies except one reported no statistical significant differences between the control group and GA on the outcome measure of pain Disability: four RCTs reported on disability due to non-specific LBP. No statistically significant differences were found between GA and usual care |
The best-evidence synthesis showed either no or insufficient evidence for the effect of GA on pain or disability |
| van Middelkoop 2011203 *** | Physical and rehabilitation interventions | 33 RCTS; 3831; 1982–2008 | Meta-analysis | Progressive relaxation had significant beneficial effects on both pain and disability in the short term. The following interventions had significant effects on pain short term but no effect on disability: EMG biofeedback; operant therapy; cognitive therapy; combined respondent and cognitive therapy; multidisciplinary treatment. Back schools had no effect on either outcome | Behavioural: all types of behavioural therapy were more effective in reducing pain intensity than waiting list controls Back schools: no statistically significant short or intermediate difference on pain and disability Patient education: no difference in intermediate- and long-term effect on pain and disability Multidisciplinary treatment Found to be significantly more effective in reducing pain intensity compared with controls and active treatments |
| Narrative synthesis | Behavioural treatments: all types of behavioural therapy were more effective in reducing pain intensity than waiting list controls. Operant therapy more effective in improving functional status than cognitive therapy (one study). Mixed inconclusive results between CBT and operant therapy No significant findings on pain or disability between:
Patient education: mixed, generally non-significant effects of patient education compared with physiotherapy, Swedish Back School and exercise/yoga exercises. Beneficial effect on disability where education focused on neurosystem vs. anatomy (one study) Multidisciplinary treatment: significant benefit on short- but not long-term pain compared with no treatment (three studies). Significant benefit on short- but not long-term pain compared with other kinds of active treatment (four studies). No difference found when comparing outpatient to inpatient setting (one study) |
||||
| Psychological therapy | |||||
| Henschke 2010204 *** | Behavioural treatment | 30 RCTs; 3438; 1983–2007 | Narrative synthesis | Behavioural treatment vs. waiting list controls: respondent therapy (progressive relaxation or EMG biofeedback), operant therapy, or a combination of behavioural therapies all found to be effective for short-term pain relief. Respondent therapy (progressive relaxation) found to confer significant benefit on functional status in the short term. Cognitive therapy, operant therapy, or a combination of behavioural therapies all found to have no significant benefit on function in the short term Comparison among different types of behavioural treatment: little or no difference between cognitive therapy and operant therapy, or operant therapy and a combination of behavioural therapies, on pain relief over a short- to intermediate-term follow-up. Suggestion from very low-quality evidence that respondent therapy using EMG biofeedback is more effective than respondent therapy using progressive relaxation for pain relief in the short term Behavioural treatment vs. other kinds of treatment: moderate-quality evidence that behavioural treatment is more effective than usual care for pain relief in the short term, but no difference in the intermediate term. No significant difference found between behavioural therapy and group exercise for pain in the short, intermediate and long term. No significant difference between behavioural treatment and usual care for improved back-specific functional status in the short to intermediate term, or compared with surgical stabilisation for back-specific functional status in the long term Behavioural treatment in addition to another treatment vs. other treatment alone: low-quality evidence that adding behavioural treatment to physiotherapy and back education was no more effective for pain or function in short to intermediate term than physiotherapy and back education alone. Moderate-quality evidence that adding behavioural treatment to inpatient pain rehabilitation was no more effective for short-term pain relief than inpatient rehabilitation alone |
There is moderate-quality evidence that in the short term, operant therapy is more effective than waiting list and behavioural therapy is more effective than usual care, for pain relief. No specific type of behavioural therapy is more effective than another. In the intermediate- to long-term, there is little or no difference between behavioural therapy and group exercises for pain |
| Hoffman 2007205 ** | Psychological interventions | 22 RCTs; 1747; 1982–2003 | Meta-analysis | Overall beneficial effects on disability at follow-up and long-term follow-up, and pain at post treatment Multidisciplinary interventions had significant benefit on disability but not pain. Psychological interventions all had benefit on pain intensity post treatment |
Provides support for the efficacy of psychological interventions in reducing self-reported pain and disability among persons with chronic LBP |
| Scheer 1997206 * | Cognitive–behavioural interventions | Five RCTs; 679; 1982–92 | Five RCTs: mixed findings regarding return to work outcomes. No overall trend suggesting effectiveness | Best evidence based on available RCTs does not support the idea that cognitive and operant strategies are effective in affecting vocationally relevant outcomes | |
| Education | |||||
| Engers 2008207 *** | Individual education | 24 RCTs; 7049; 1987–2006 | Narrative | Individual patient education vs. non-educational interventions: strong evidence that written educational material was less effective than non-educational interventions for LBP (i.e. spinal stabilisation, physiotherapy, yoga, exercises, modified Swedish Back School). Moderate evidence of no difference between individual education and non-educational interventions for LBP (i.e. spinal stabilisation, physiotherapy, yoga and exercises). No difference in return to work between written educational material vs. modified Swedish Back School (one study) Individual patient education vs. other types of patient education: individual educational session of 3 hours was more effective for functional status when the focus was on the nervous system than when the focus was on the lower back (anatomy, posture, endurance) at short-term (3-day) follow-up (one study) |
For patients with chronic LBP, the effectiveness of individual education is still unclear |
| Liddle 2007208 *** | Advice | 39 RCTs; 7347; 1986–2004 | Narrative | Advice as an adjunct to exercise: most effective for improving pain and back-specific function in chronic LBP (compared with acute or subacute LBP) Advice as part of a back school: 22 (56%) reported a result favouring intervention, 16 (41%) reported no difference, and one reported a negative outcome (acute, subacute and chronic LBP) The relevance of advice content to LBP phase: a positive result was obtained in 74% (14/19) of chronic LBP trials. Most common experimental interventions resulting in a positive outcome in chronic LBP trials were advice as an adjunct to exercise (n = 5), or as part of a functional restoration approach (n = 5) The influence of advice at follow-up: six (43%) chronic LBP trials with a positive result incorporated advice into follow-up; advice incorporated into short-term follow-up was predominantly used. A further six positive chronic LBP trials provided advice throughout treatment only; only one of these trials did not maintain its positive results at all follow-up points |
For chronic LBP there is strong evidence to support the use of advice to remain active in addition to specific advice relating to the most appropriate exercise, and/or functional activities to promote active self-management. More investigation is needed into the role of follow-up advice for chronic LBP patients |
FIGURE 42.
Low back pain: summary of the quantitative evidence.
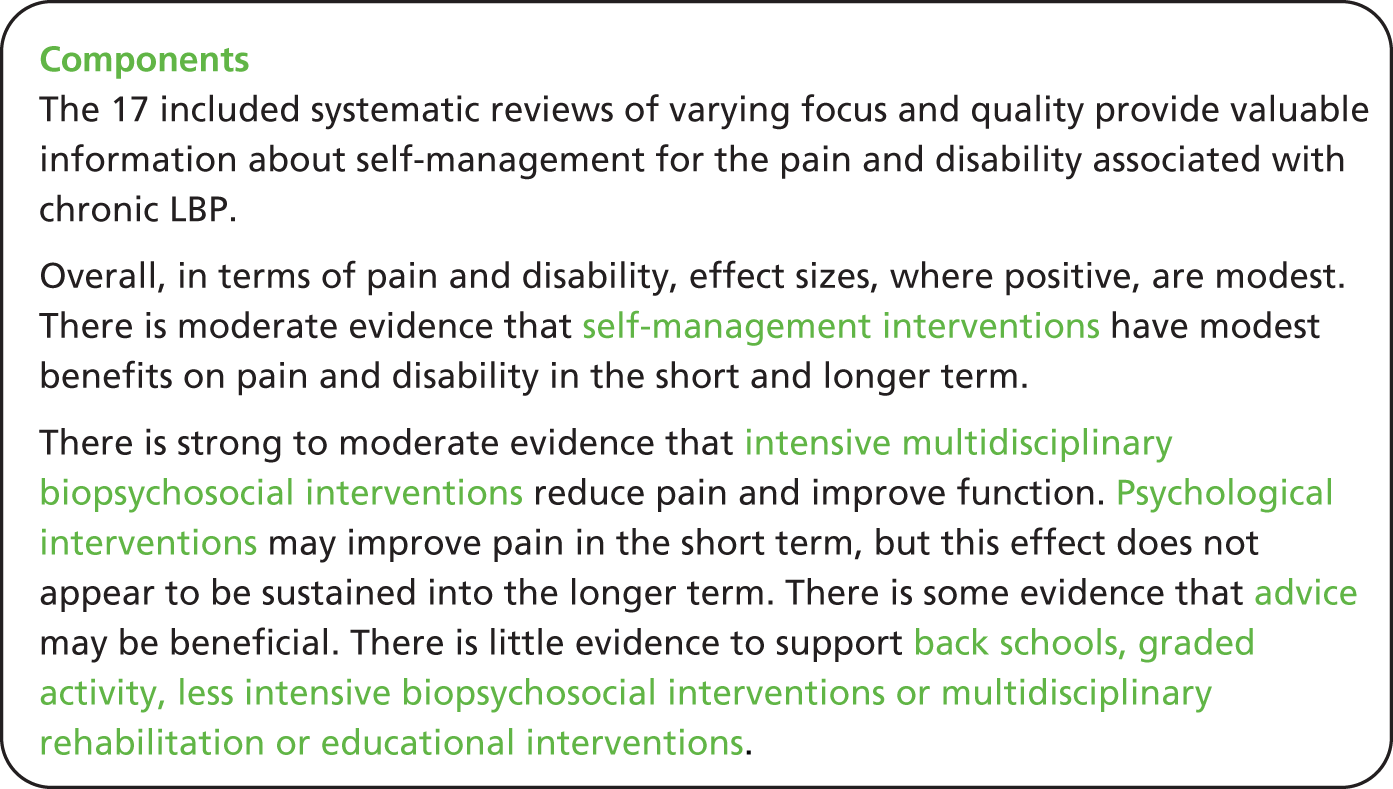
Mixed-methods discussion
The importance of psychological support emerges from both the qualitative and quantitative evidence. The qualitative synthesis discusses the difference in expectations between patient and HCP, with the patient initially seeking a ‘cure’ for their pain. Psychological support is highlighted as a means of assisting individuals in the adjustment process as they begin to manage their expectations more realistically. The qualitative evidence states that this is most helpful in the initial stages of LBP, whereas some patients with longer-standing pain tend to have more realistic expectations which are more congruent with those held by HCPs.
Another important issue emerging from the qualitative reviews is the importance of actively involving individuals in their education. This should include actively involving individuals in decision-making processes, aiming to increase independence and facilitate self-management. Evidence from quantitative studies aiming to enable patients to manage their own condition with minimal oversight or active involvement of the health-care provider showed small effects on pain and disability in people with LBP.
Despite the substantial number of RCTs focusing on the management of chronic LBP, supporting self-management in this condition remains a problem, with the majority of effective interventions showing small or moderate evidence in the short term.
Chapter 19 Additional meta-review: self-management support for people with a progressive neurological disorder
Meta-review of qualitative reviews
Systematic reviews identified
There were no relevant qualitative systematic reviews concerning PNDs identified by our searches (see Appendix 21).
Meta-review of quantitative reviews
Systematic reviews identified
Four reviews were identified for inclusion in this meta-review81,209–211 (Figure 43). Three were Cochrane systematic reviews. Twenty RCTs in total were included within the reviews, with no overlapping studies between reviews. Only one of the four included systematic reviews described the country setting for its included studies (Ng and Khan210 four studies: Italy, Ireland, Cuba and the Netherlands).
The reviews were published between 2006 and 2011, and included RCTs published between 1984 and 2008.
Each review explored interventions for different PNDs: Dixon et al. 209 explored PD; Ng and Khan210 examined MND; Thomas et al. 211 looked at MS; and Rae-Grant et al. 81 reviewed neurological disorders more generally. (Rae-Grant et al. 81 is also included in our stroke meta-review.)
The types of interventions explored were OT,209 MDC,210 psychological interventions211 and explicit self-management support. 81
The review exploring MDC for MND failed to identify any RCTs for inclusion. The setting for the other three reviews included home based and/or community. Components of these interventions were diverse and included general mobilisation activities; socialisation; promoting dexterity; functional activities; educational activities; visual and auditory cues; participation in arts and crafts; dancing; games; motivational interviews; goal-setting; telephone counselling sessions; individualised exercise programmes; and encouragement via a telephone call. The duration and intensity of interventions varied, with the longest follow-up reported at 12 months (Table 104).
| Review | Intervention of interest and comparison | Participant demographics | Setting, delivery and service arrangements | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Dixon 2007209 ** | OT vs. placebo or no intervention for PD | Patients with PD | Delivery to an individual or group. Delivered by OT in one study, unclear in the other | One explored OT in combination with physiotherapy. OT components: general mobilisation activities; socialisation; promoting dexterity; functional activities; educational activities; visual and auditory cues. The other explored occupational therapy alone. OT components: handicrafts; picture drawing; basketry; folk singing; dancing and games | Duration in one study: 20 hours over 5 weeks; the other: 12 hours over 1 month. Follow-up after 1 year or immediately at end of therapy |
| Ng 2009210 ** | MDC for MND | No RCTs identified | – | – | – |
| Rae-Grant 201181 * | Self-management in neurological disorders | Patients with MS and PD, residing in the community | Home-based/community setting | One study provided a motivational interview and goal-setting meeting (MS) followed by a series of telephone health promotion counselling sessions. Another was a home-based exercise programme to reduce falls in PD: an individualised exercise programme plus a telephone call to encourage continuing the exercises A third was of a professionally guided self-care programme for individuals with MS living in the community |
In one study: one meeting and a series of five follow-up sessions over 12 weeks In the other: home-based exercise programme, monthly telephone call In the third: not given |
| Thomas 2006211 *** | Psychological interventions for MS | Four categories of people: with MS; with MS and moderate/severe disability; with MS and depression; with MS and cognitive impairment | Highly heterogeneous | Highly heterogeneous | Highly heterogeneous |
Quality assessment and weighting
The quality of the reviews using the R-AMSTAR tool was generally good, with three reviews classed as high quality,209–211 and only one lower-quality study81 (Table 105).
| R-AMSTAR criteria | Dixon 2007209 | Ng 2009210 | Rae-Grant 201181 | Thomas 2006211 |
|---|---|---|---|---|
| Was an a priori design provided? | 4 | 4 | 3 | 4 |
| Was there duplicate study selection and data extraction? | 4 | 4 | 4 | 4 |
| Was a comprehensive literature search performed? | 4 | 4 | 3 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 4 | 2 | 4 |
| Was a list of studies (included and excluded) provided? | 4 | 4 | 1 | 4 |
| Were the characteristics of the included studies provided? | 4 | 4 | 2 | 3 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 4 | 3 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 4 | 4 | 4 | 2 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 4 | 1 | 4 |
| Was the likelihood of publication bias assessed? | 2 | 2 | 1 | 1 |
| Was the conflict of interest stated? | 3 | 4 | 3 | 3 |
| Total score/44 | 38 | 42 | 27 | 37 |
A weighting of evidence was then calculated by considering both quality and total population size included within the reviews (Table 106).
Outcomes
The two outcomes of interest selected for this review were QoL and disability (to include any measure of motor impairment/disability, or ADL) (Table 107). (Health-care utilisation was only included, as a secondary outcome, in one review. 211)
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| QoL | Preference given to disease-specific QoL, but generic QoL also accepted | PDQ-39; MSIS-29; MSQLI; SF-36 |
| Disability | Measure of disability or motor impairment, or ADL | Kurtzke Expanded Disability Scale; Guy’s Neurological Disability Scale; Unified Parkinson’s Disease Rating Scale motor score |
Findings
Meta-analyses on our outcomes of interest were not performed in any of the reviews, therefore all data comes from narrative syntheses (Table 108 and Figure 44). Dixon et al. ’s review209 of OT for PD identified two RCTs. Both trials claimed some positive effects of OT in PD; however, the improvements were small and their clinical or statistical significance was unclear.
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Dixon 2007209 ** | OT vs. placebo or no intervention for PD | Two RCTs; 84; 1987–97 | Narrative | Motor impairment (one RCT): MD 0.04 ADL (two RCTs): MD of –4.6 and –6.5 QoL (one RCT): MD –2.5 Statistical significance not provided for any result |
Both trials claimed some positive effects of OT in PD; however, the improvements were small and it is doubtful whether they were clinically or statistically significant. The authors felt that they were unable to draw any firm conclusions about the efficacy and effectiveness of occupational in PD |
| Ng 2009210 ** | MDC for MND | 0 RCTs, 0 | Narrative | No RCTs identified for inclusion | The absence of proof that MDC is effective must not be interpreted as proof that this approach is ineffective. This review has highlighted a significant gap in the current literature |
| Rae-Grant 201181 * | Self-management in neurological disorders | Two RCTs; NR; 2007–8 | Narrative | Review’s primary outcomes Health Promoting Lifestyle Profile II Inventory – MS (one RCT): self reported health promotion activities significantly increased in the treatment group and were stable in the control group. Specific areas of change included PA, spiritual growth and stress management Fall rate – PD (one RCT): a trend towards reduced fall rate in the treatment group that did not reach statistical significance |
Limited but promising evidence supporting the value of programmes designed to promote self-management. Demonstrates an existing need for more strictly designed and performed studies of self-management strategies in this population |
| Thomas 2006211 *** | Psychological interventions for MS | 16 RCTs; 1006; 1984–2004 | Narrative | People with MS with cognitive impairment MS-specific QoL subscales (one RCT): immediately post-treatment percentage improvement in mental health subscale significantly better in the cognitive rehabilitation group vs. placebo group. No significant difference for the cognitive subscale. Short-term follow-up percentage improvement in mental health subscale was not significantly different in cognitive rehabilitation vs. placebo and there was no significant difference for the cognitive subscale People with MS with moderate to severe disability No relevant outcomes identified People with MS QoL (three RCTs)
Measures of disability (one RCT): immediately post treatment, statistically significant difference between coping skills and peer support group, but direction of difference is not reported People with MS with depression No relevant outcomes identified |
Considerable creativity has gone into developing and adapting interventions. The downside of this is that, in general, interventions have been evaluated in single studies only (and often with limited sample size). Although this review has identified 16 relevant studies, they are very diverse and there are large gaps in the evidence base for the use of psychological interventions for people with MS |
FIGURE 44.
Progressive neurological disorders: summary of the quantitative evidence.
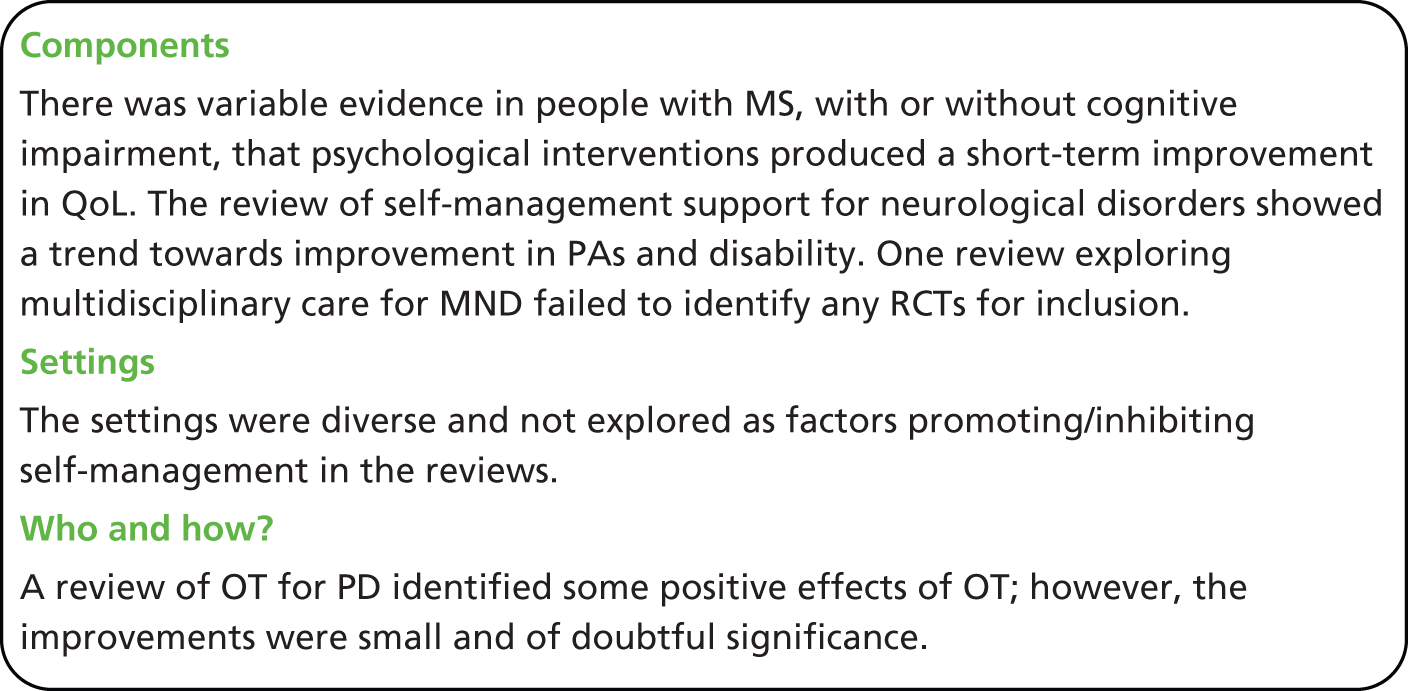
The broader review of self-management support for neurological disorders identified three RCTs. Of the two RCTs judged to be high quality, one was delivered to people with PD, and the other to people with MS. 81 These studies provided limited evidence, with significant results in self-reported, self-care activities in only one study (MS) and a trend to reduced falls in the PD study.
Last, the review of psychological interventions for MS is the largest included review and received the highest weighting of evidence in this meta-review. 211 The 16 included RCTs were very diverse, preventing meta-analyses and limiting the conclusions which could be drawn from narrative synthesis. Only one of the three RCTs in uncomplicated MS (i.e. MS without depression, cognitive impairment or significant disability), detected an improvement in QoL and this was only present immediately post treatment. Similarly, in the group of people with MS and cognitive impairment, a significant improvement in QoL was found immediately post treatment in one RCT, but not at 4 months follow-up after baseline. 211
Chapter 20 Additional meta-review: self-management support for individuals with type 1 diabetes mellitus
Type 1 diabetes mellitus meta-review of qualitative syntheses
Systematic reviews identified
We included two reviews 212,213 in the T1DM qualitative meta-review; these were published between 2010 and 2012 in peer-reviewed journals (Figure 45). Some of the primary qualitative studies were included in both reviews, with an overall total of 22 unique studies (published from 1994 to 2009).
Both Spencer et al. 213 and Palladino and Helgeson’s212 reviews examined experiences of T1DM in adolescents, with Palladino and Helgeson’s review212 specifically focusing on the influence of peers (Table 109).
| Authors, year (type) | Review aim | Qualitative studies included, n | Summary key findings |
|---|---|---|---|
| Spencer 2010213 (Qualitative) |
To review empirical qualitative research exploring the experiences of adolescents with T1DM and their parents | 20 studies (in 28 papers); however, only 18 were listed in the table | Four sets emerged from the integration of studies:
|
| Palladino 2012212 (Mixed methods) |
To examine the influence of peers on T1DM self-care and glycaemic control. This article will address: (a) the behaviours peers exhibit that help or hinder self-care and glycaemic control (qualitative research) and (b) how these behaviours relate to self-care and glycaemic control (quantitative research) | 7 out of 24 were qualitative | Mixed-methods summary: Qualitative studies revealed that teens believe peers have an impact on diabetes behaviours, but quantitative findings are inconclusive. We found more evidence that social conflict was harmful than that it was helpful. Associations were more likely in studies that measured specific support and specific self-care variables. Studies addressing how individual differences interact with social context had promising findings |
Quality assessment
Spencer et al. 213 scored high with 31 out of 40, but Palladino and Helgeson212 scored low with 20 out of 40 and was therefore given lower weighting in informing the findings of this meta-review212 (see Table 110 for detailed description of quality scoring). Specifically, Palladino and Helgeson212 did not explicitly state which studies were qualitative and quantitative so assumptions had be made by the meta-reviewer based on statements in the text. Additionally, the included studies were summarised descriptively rather than synthesised into a set of findings; this made it difficult to extract findings in order to inform future self-management support212 (Table 110).
| R-AMSTAR criteria | Spencer 2010213 | Palladino 2012212 |
|---|---|---|
| Was an appropriate and detailed design provided? | 4 | 4 |
| Was there duplicate study selection and data extraction? | 3 | 1 |
| Was a comprehensive literature search performed? | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 3 | 2 |
| Was a list of studies (included and excluded) provided? | 2 | 1 |
| Were the characteristics of the included studies provided? | 4 | 1 |
| Was the scientific quality of the included studies assessed and documented? | 4 | 1 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 2 | 1 |
| Were the methods used to combine the findings of the studies appropriate? | 4 | 2 |
| Was the conflict of interest stated? | 1 | 3 |
| Total score/40 | 31 | 20 |
| Quality rating (low = < 30; high = ≥ 30) | High | Low |
Findings
Support for self-management
The synthesis enabled these findings to be integrated to provide a broader picture to inform future commissioning of self-management support:
-
Support for the development of emotional and psychological strength, such as the need for confidence to become more independent and gain factual, experiential knowledge and problem-solving skills. Diabetes camps and school trips provided safe environments to gain such experience away from home; however, being away from home also caused stress for some. Coping mechanisms included implementing routines for diabetes management, carrying supplies in preparation for potential blood glucose fluctuations, asking parents for help and thinking ahead regarding the possible implications of non-compliance.
-
Support from HCPs needs to ensure that the person with diabetes can be an informed decision-maker in their self-management. Often adolescents reduced their attendance with HCPs as they became adults and did not completely trust them. Patients responded more positively when HCPs made suggestions to them and planned their management collaboratively with them. Adolescents felt that they needed information to be provided to them on a more understandable level, consultations should be directed towards them rather than their parents, should treat them as a person rather than a disease, and should listen to their individual needs and try to help incorporate treatments into their lives.
-
Adolescent girls incorporated diabetes into their identities more than boys, for whom mothers took on most of the responsibility for their care. It is therefore a key point to acknowledge potential gender differences when implementing self-management support.
-
The relationship between the adolescent with T1DM and the adult is a vital one with regards to helping or hindering autonomy. It is important that adults play a supportive role and that the person with T1DM feels in control of their condition. Those that perceived poor control were likely to ignore reminders from adults rather than utilise the support. Parents often felt guilty about the burden placed on the adolescent. Diabetes management was especially of concern if the adolescent did not act responsibly in other aspects of their lives. Adolescents with diabetes responded more positively to reassuring feedback from parents. It is important to facilitate communication within this relationship and educate the person with T1DM to self-manage and the adult how best to support their self-management.
-
Psychosocial support can help people cope with aspects of living with diabetes. For example, making decisions and managing conflicts, following their management plan and being truthful about their self-care, telling others about their diabetes, and asking for help.
-
Peers can provide obstacles and/or support to a person with T1DM’s self-management. It is therefore important to focus on reducing those obstacles and encouraging peers to play a supportive role in their lives, for example provide verbal reminders, monitor symptoms of hyper/hypoglycaemia, refrain from drawing attention to their diabetes, behaviours that provide assistance or resources for solving a problem and emotional support (i.e. behaviours that provide comfort, affirmation or communicate caring). It was helpful when a person’s friends knew they had T1DM and what to do in an emergency; this enabled the person with T1DM to feel more relaxed and ‘safe’ when with those friends in social situations.
-
Self-management may be easier to complete as part of a routine that fits well with the family and others involved. Parents/carers should frame this life change positively as it may increase the health behaviours of the family as a whole (e.g. better diet, more exercise).
-
Practical group education (not didactic) was viewed as beneficial by people with T1DM. Refresher courses were not seen as beneficial as they did not learn anything new. The use of technology was discussed as a method of encouraging participation.
-
Schools were sometimes a barrier to self-management; specifically, some teachers’ lack of knowledge and questioning of a pupil’s need to inject or eat, as well as the school canteen food options, meant that pupils with T1DM struggled to meet school rules. School level education would be useful to ensure that school policies and provisions meet their needs.
Meta-review of quantitative systematic reviews
Systematic reviews identified
Four reviews were identified for inclusion in this meta-review, published between 2006 and 2010 (Figure 46). 214–217 The four reviews include a total of 67 RCTs, of which 11 appeared in more than one review, with 56 unique studies in total. Only one of the four included systematic reviews mentioned the country setting for its included studies (McBroom and Enriquez:215 USA and Sweden). Publication date of RCTs ranged from 1985 to 2008.
The focus of the four reviews varied. The earliest identified systematic review explored psychological interventions for adults or children and adolescents. 217 The next of our four reviews to be published explored family centred interventions. 215 Two reviews were published in 2010, one studying adherence promoting factors214 and the other investigating educational, psychosocial and family therapy interventions. 216
The setting of the interventions included clinic and home based, and were delivered in group, individual, family and multiple family settings. Components within these reviews were diverse and included components which could be viewed as directly related to core self-management skills, as defined by Lorig and Holman:25 problem-solving; blood glucose monitoring; instruction; and coping skills training. Although other components supported self-management in a slightly more peripheral way: automated text-messaging support; motivational games; behavioural family systems therapy; motivational interviewing; a diabetes personal trainer; CBT; and counselling. Maximum reported time to follow-up was 18 months (Table 111).
| Review | Intervention of interest | Participant demographics | Setting, delivery and service arrangement | Content, focus and mode of instruction | Duration, intensity and follow-up |
|---|---|---|---|---|---|
| Hood 2010214 | Adherence promoting interventions | Two studies reported inclusion of poor glycaemic control only. Average age = 13.6 years. Average proportion of non-white individuals = 27.0%. Mean duration of T1DM ranged from 2.7 to 8.7 years, average = 5.89 years | Clinic or home based. Delivered in group, individual and family settings | Direct or combined interventions. Direct interventions focused on direct, behavioural processes. Combined interventions focused on one or several behavioural tasks but the emphasis of the intervention was on promoting coping or problem-solving skills, or a family process involved in T1DM management. These included problem-solving, coping skills, motivational games, instruction, behavioural family systems therapy, home upload of blood glucose monitoring | Time to follow-up ranged from 12 to 52 weeks, average = 29.5 weeks |
| McBroom 2009215 | Family centred interventions | All studies focused on adolescents, some also included school-aged children. Three studies enrolled participants with a wide age range (8–18 years). In all studies, children had been diagnosed with T1DM for at least 1 year, six studies reported mean duration of T1DM of 5 years | Seven interventions were conducted with one family at a time. Two interventions conducted groups of families simultaneously. One intervention formed a parent’s group and a children’s group, whereas the other intervention formed groups that included the children together with parents | Teamwork: education and discussion focused on parent–teen responsibility, sharing of diabetes tasks and avoiding conflicts that undermine teamwork Multisystemic therapy: intensive, individually tailored, family centred, community-based treatment, targeting adherence-related problems within the family system, peer network and community Self-management training: training included written lessons, discussion, modelling and role-playing exercises used to conduct behaviour-change projects for behaviour modification for self-management skills related to diabetes health care Family therapy: psychiatric sessions that aimed to identify and change dysfunctional family interaction patterns rather than focusing on an individual family member’s idiosyncrasies; concentrated on hierarchical organisation of the family, coalitions between family members and clarification of family rules of interaction Multifamily groups: parents and their children were included in groups that discussed diabetes management and attitudes towards diabetes, and received guidance and support from each other and group leaders Behavioural family systems therapy: therapy tailored to individual family’s treatment needs, including problem-solving training, communication skills training, cognitive restructuring, and functional and structural family therapy with behavioural homework assigned and reviewed |
Not synthesised |
| Savage 2010216 | Education, psychosocial and/or family therapy interventions | Not synthesised | Not synthesised | Education, psychosocial (included automated text-messaging support, motivational interviewing, diabetes personal trainer, coping skills training) and family therapy interventions | Not synthesised |
| Winkley 2006217 | Psychological interventions | Adults: clinical subgroups were suboptimal glycaemic control, new onset diabetes, complications and obesity. Mean duration of T1DM = 14.1 years. Children and adolescents: mean duration of T1DM = 5.6 years | Adults: eight studies used either group format or a combination of group and individual formats. Children and adolescents: most common mode of delivery was multiple family or parent group | Adults: most trials examined CBT, two examined psychoanalytical techniques, two examined counselling. Children and adolescents: seven studies examined CBT, six studies were of counselling and three studies used family systems therapy | Adults: mean duration of follow-up = 7.2 months. Children and adolescents: mean duration of follow-up = 11.4 months |
Quality assessment and weighting
The overall quality of these four systematic reviews was poor, with three categorised as lower quality (scoring ≤ 30),214–216 and one classed as higher quality (scoring ≥ 31) with a R-AMSTAR score of 41217 (Table 112).
| R-AMSTAR criteria | Hood 2010214 | McBroom 2009215 | Savage 2010216 | Winkley 2006217 |
|---|---|---|---|---|
| Was an a priori design provided? | 4 | 3 | 4 | 4 |
| Was there duplicate study selection and data extraction? | 2 | 1 | 1 | 4 |
| Was a comprehensive literature search performed? | 3 | 4 | 4 | 4 |
| Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 1 | 2 | 1 | 4 |
| Was a list of studies (included and excluded) provided? | 2 | 1 | 3 | 3 |
| Were the characteristics of the included studies provided? | 4 | 4 | 3 | 4 |
| Was the scientific quality of the included studies assessed and documented? | 1 | 1 | 3 | 4 |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | 2 | 2 | 2 | 3 |
| Were the methods used to combine the findings of the studies appropriate? | 3 | 2 | 4 | 4 |
| Was the likelihood of publication bias assessed? | 1 | 2 | 1 | 4 |
| Was the conflict of interest stated? | 3 | 1 | 3 | 3 |
| Total score/44 | 26 | 23 | 29 | 41 |
All included reviews were then given a weight of evidence based on quality scores and total population represented by the reviews (Table 113).
Outcomes
The two key outcomes of interest selected in this meta-review were glycaemic control and QoL. Where QoL was not reported, a marker of psychological distress was taken as a proxy of QoL (Table 114).
| Outcomes | Definition | Measures reported in reviews |
|---|---|---|
| Glycaemic control | Percentage of HbA1c | HbA1c, HbA1 |
| QoL or psychological distress | Disease-specific or generic QoL | Diabetes-specific QoL, psychological distress |
Findings
Winkley et al. 217 provide weak evidence for the effectiveness of psychological treatments in improving glycaemic control and reducing psychological distress in children and adolescents, but not in adults.
The meta-analysis performed by Hood et al. ,214 exploring adherence promoting factors, shows a very modest beneficial pooled effect on glycaemic control. Mean ES in this meta-analysis was three times smaller than that reported by Winkley et al. 217
The review of family centred interventions provides weak evidence to suggest some benefit from these interventions. Of the subcategories of family centred interventions included within this review, strongest evidence currently exists for teamwork interventions. Teamwork interventions are characterised by the review authors as interventions which include ‘education and discussion focused on parent-teen responsibility sharing of diabetes tasks and avoiding conflicts that undermine teamwork’. 215
Evidence from the review exploring effectiveness of educational, psychosocial and family therapy interventions shows promising results for some intervention types, with evidence suggesting that education offers less potential for improving T1DM-related health outcomes compared with psychosocial or family therapy216 (see Table 115 for meta-analyses results, Table 116 for narrative summaries and Figure 47 for summary of quantitative evidence).
| Reference and weighting | Outcome | Time | Sample size; n RCTS; n participants (where available) | Significance | ES (95% CI) |
|---|---|---|---|---|---|
| Hood 2010214 * | Improvement in GHb | NR | 15 RCTs | 0 | 0.11 (–0.01 to 0.23) |
| Winkley 2006217 *** | GHb | NR | 21 RCTs | + | SMD –0.26 (–0.47 to –0.05) |
| GHb (child/adolescent) | NR | 10 RCTs; 543 participants | + | SMD –0.35 (–0.66 to –0.04); p = 0.03 | |
| GHb (adult) | NR | 11 RCTs; 516 participants | 0 | SMD –0.17 (–0.45 to 0.10); p = 0.22 | |
| Psychological distress | NR | 10 RCTs; 417 participants | + | SMD –0.35 (–0.54 to –0.15) | |
| Psychological distress (child/adolescent) | NR | Four RCTs | + | SMD –0.46 (–0.83 to –0.10); p = 0.013 | |
| Psychological distress (adult) | NR | Six RCTs | 0 | SMD –0.25 (–0.51 to 0.01); p = 0.059 |
| Reference and weighting | Focus | RCTs, n; participants, n; date range | Synthesis | Main results | Main conclusions (review author); important quality concerns (review author or meta-review author) |
|---|---|---|---|---|---|
| Hood 2010214 * | Adherence promoting interventions | 15 RCTs; 997; 1994–2007 | Meta-analysis | Modest evidence of improved GHb control which does not reach statistical significance | This meta-analysis shows that the pooled effect on glycaemic control of these 15 interventions was very modest. Mean ES in this meta-analysis was three times smaller than that reported by Winkley et al.217 |
| Narrative | The correlation between whether the intervention targeted direct, behavioural processes alone or had combined targets was significant, indicating that multicomponent interventions (i.e. those that targeted direct and indirect processes together) were associated with larger effects on glycaemic control | ||||
| McBroom 2009215 * | Family centred interventions | Nine RCTs; 631; 1985–2007 | Narrative | Behavioural family systems therapy: two RCTs reported this outcome but neither present data comparing intervention with control Family therapy: two RCTs – one did not report on our selected outcomes, the other very small RCT shows a small suggestion of possible beneficial effect on blood glucose control Multifamily group intervention: one RCT – small suggestive effect of benefit on blood glucose control Multisystemic therapy: one RCT – reports significant decrease in child blood glucose Self-management training: one RCT – improved blood glucose control in both intervention and control Teamwork interventions: two RCTs – both showed improved blood glucose control, only statistically significant in one RCT |
Provides some evidence to suggest some benefit from family centred interventions, strongest evidence currently exists for teamwork interventions |
| Savage 2010216 ** | Education, psychosocial and/or family therapy interventions | 14 RCTs; 1511; 2004–8 | Narrative | A structured group education programme for children and parents, supported by computer-assisted consultations with adolescents directing them to useful education links, improved QoL A group-based family centred education programme integrated into clinic consultations reduced HbA1c by 0.29%; however, this was the only educational intervention to improve HbA1c levels Statistically significant reductions in HbA1c at 12 months follow-up were evident in three psychosocial interventions: automated text-messaging support combined with intensive insulin therapy; personal trainer; and motivational interviewing. Family therapy was also found to improve HbA1c levels significantly following completion of intervention, but was maintained long term (18 months) in one RCT only |
The evidence from this review suggests that education offers less potential for improving T1DM-related health outcomes compared with psychosocial, or family therapy interventions |
| Winkley 2006217 *** | Psychological interventions | 29 RCTs; 1709 participants; 1985–2005 | Meta-analysis | A significant effect found to support a real reduction in GHb and psychological distress which is increased further when looking at children and adolescents only, and which is not significant when analysing data for adult populations only | This review provides weak evidence for the effectiveness of psychological treatments in improving glycaemic control and reducing psychological distress in children and adolescents but not in adults |
| Narrative | Restriction to family therapy interventions delivered to children and adolescents slightly increased the pooled ES [SMD –0.41 (95% CI –0.79 to –0.03); p = 0.03]. Restriction to group CBT delivered to adults further attenuated the pooled ES [SMD 0.02 (95% CI –0.41 to 0.44); p = 0.95] |
FIGURE 47.
Type 1 diabetes mellitus: summary of what the quantitative evidence shows.
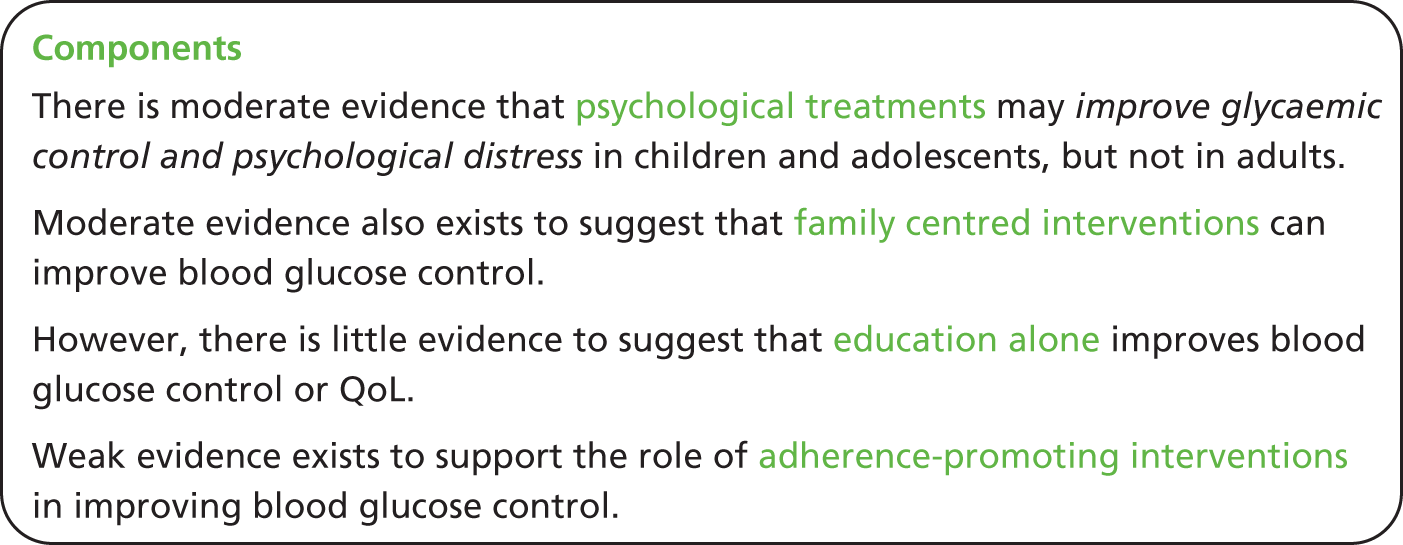
Mixed-methods discussion
The qualitative evidence presented in this meta-review only identified evidence relating to adolescents with T1DM and not adults. Although the quantitative evidence identified was also focused on children and adolescents, some evidence was reported for interventions involving adults with T1DM.
Qualitative evidence emphasises the importance of psychological and emotional support in adolescents with T1DM. Adolescents need to become confident in order to self-manage successfully; this requires becoming emotionally and psychologically strong. This is reflected in the quantitative findings, which report moderate evidence that psychological treatments may improve glycaemic control in children and adolescents with T1DM. That these findings were not true for the adult population with T1DM suggests that psychological support may be less of a pressing issue in this population.
As the focus of the qualitative literature was on adolescents, much of the work discussed relationships with parents/carers, peers and school teachers. The qualitative evidence highlights the importance of ensuring that these groups, with whom the adolescent is in close and frequent contact with, are aware of how to best support the adolescent in their self-management. It is suggested that involving parents/carers in the delivery of self-management support may be important, and that education of teachers and peers would also be helpful. To an extent, these conclusions are reflected in the quantitative evidence, with moderate evidence identified to support a beneficial effect of family centred interventions on blood glucose control.
Chapter 21 Implementation systematic review
Findings
Studies identified
The papers identified, the screening process and the final number of studies included, are detailed in the PRISMA flow diagram (Figure 48). On title and abstract screening, the 10% reliability check showed 93% agreement between reviewers (EE and GPe, HLP or HP). Disagreements were discussed and resolved, leaving 1225 papers for full-text screening, of which 12 could not be obtained (either the libraries we used, including The British Library, did not carry the journals or relevant issues were missing).
Quality assurance
For full-text screening, a quality control check of 25% of papers using Downs and Black checklist,48 achieved agreement of 89% between the first reviewer (EE) and the second (HP). Initially, we included 73 papers for diabetes, 29 for asthma and 11 for depression, but were concerned about poor reporting and unclear design of many of the papers. A third reviewer (ST) therefore checked these 113 papers with 61%, 93% and 82% agreement respectively. Disagreements were resolved by discussion between the three reviewers.
Overview of results
Because of the diversity of interventions and study design, a meta-analysis was not possible in any of the disease areas. We used the whole-systems approach as a framework for our narrative analysis. 53 This considers interventions from a multilevel perspective engaging patients, professionals and the organisation in a collaborative approach36 (Tables 117–124 provide details of all the included studies and their key findings). Tables 117–124 are organised by condition and the studies are classified according to whether or not the intervention was:
-
primarily professional training, with or without organisational change
-
primarily patient education, with or without organisational changes
-
primarily organisational change
-
a whole-systems approach with components operating at patient, professional and organisational level.
| LTC, study, country, setting | Study design | Participants | Service implementation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Design, underpinning evidence, theory | Aim | Eligibility criteria | Total eligible population | Number (%) participating | Participating population characteristics | Attrition | Intervention and strategy for implementation | Duration, intensity, frequency | |
| Primarily professional training | |||||||||
| Asthma, Cleland 2007,218 UK, primary care | Cluster RCT, informed by RCTs | To assess the effectiveness in real-life primary care of training designed to support practice nurses in implementing PAAPs | 13 practices: using a compatible electronic health record, patients aged 18–55 years with asthma for > 1 year receiving regular preventative asthma therapy | Identified as having poor asthma control, n = 667 | Routine data, n = 629; questionnaire, n = 177 | No demographic data on total eligible population. Questionnaire responders were older, more likely to be female and used fewer β2-agonists and courses of oral steroids than those who consented to use of routine data | No practice attrition Poorly controlled asthmatics invited to (a) allow access to routine data, and (b) complete questionnaires. Non-response at follow-up Intervention = 31 (24%) Control = 28 (26%) |
Intervention focused on practice nurse training. Doctors aware, but no attempt to facilitate incorporation into practice procedures. Professionals’ training: focused on clinical and communication skills, case studies to practise formulation and review of individualised PAAPs, role play with actors with feedback, communication strategies and patient resources | Duration of follow up: 6 months Intensity and frequency: 1 day, 3-hour seminar |
| Asthma, Homer 2005,219 USA, primary care | Cluster RCT based on national asthma guidelines and evidence-based behavioural change theory | To implement and test a quality improvement intervention intended to improve care and outcomes for patients with childhood asthma | Practices: providing paediatric asthma care. Patients: children aged 2–16 years with asthma and using asthma medication in the previous year | 13,878 | 631 | Mean age: intervention group = 8.5 years; control group = 9 years. Gender: intervention group = 64% male; control group = 60% male | Three intervention practices withdrew (one just after randomisation and two during study year). Attendance at the learning sessions declined progressively. Only 42% of the practices submitted data. Patients: 490 of 631 (78%) provided follow-up interviews | A theoretically based quality improvement intervention, designed to engage and support the practice team to achieve change. Professional teams (doctor, nurse and administrator) participated in a learning collaborative project to facilitate asthma management based on the CCM. Provision of additional learning tools regular support | Duration: 12 months. Three 1-day learning sessions + additional learning sessions + biweekly conference calls |
| Primarily patient education | |||||||||
| Asthma, Bunting 2006,220 USA, managed care | Time series analysis, based on previous RCTs | To assess the clinical and economic outcomes of a pharmacist-driven medication therapy management programme for patients with asthma | All patients with a diagnosis of asthma covered by the participating employers’ health plans, and who had accessed at least one aspect of the programme | Not stated | 207 | Mean age: 42 years (men 40 years; women 42 years). Gender: 72% female | 39 had withdrawn by the end of the study period: 30 because of changes in employment and/or insurance status. Nine ‘failed to meet the requirements of the programme’ | Based on a diabetes programme, the insurance-based intervention was financially supported by employers who waived fees for patients who attended the programme Patients chose a pharmacist care manager who provided regular review of medication, inhaler technique, triggers and environmental control and individual asthma education including a PAAP review |
Duration: 5 years. (Included patients were in the programme for at least a year.) 60- to 90-minute sessions, every 3 months |
| Asthma, Chini 2011,221 Italy, primary schools | Before-and-after study, based on evidence from systematic reviews | To evaluate a comprehensive school-based asthma programme in which health-care actions beginning at school are followed up with child’s family at home | School children with asthma (identified by questionnaire) | Six primary schools (total population n = 2765): n = 135 with asthma | 135 | 2765 school children, aged 6–10 years. n = 135 with asthma | NR | A comprehensive asthma programme, based on a strong family–physician–school relationship, provided an educational intervention to families, school staff and pupils, as well as questionnaire identification of children with asthma, individual diagnosis and management, and provision of extracurricular activities | Duration: set-up in each school 2 months, then 7-month individual and group work with children with asthma Each year two schools participated in the 1 year programme |
| Asthma, Delaronde 2005,222 USA, managed care | Preference trial (‘opt-in’, ‘opt-out’, ‘probably’ group were randomised, and ‘non-responders’) informed by national guidelines | To assess the effectiveness of an asthma management programme on the Asthma Medication Index (ratio of preventer/reliever medication: optimal prescribing is ≥ 0.50) | Members of the ConnectiCare Inc & Affiliates programme for at least 3 months, aged 13–65 years, excluding those whose Asthma Medication Index was already optimal | 836 | 399, 28 ‘opt-in’, 52 ‘opt-out’, 67 allocated to intervention, 67 allocated to control, 185 ‘non-responders’ | Age: mean = 45 years. Gender: 51% female | 27% of the intervention group and 68% of the opt-in group completed four or more contacts | Centrally led initiative. Administration of the scheme and nurse educators funded and undertaken by the MCO. Intervention: telephone self-management education including review of asthma and asthma knowledge, with feedback about different asthma behaviours and provision of personalised educational materials | Duration: 6 months Intensity and frequency: one telephone call every 6 months |
| Asthma, Forshee 1998,223 USA, managed care | Prospective with four assessments post-intervention | To evaluate an intensive education programme for high-risk patients | People with poorly controlled asthma (aged 5–65 years) | NR | 201 patients from four managed care plans | Mean age = 34 years. Gender: 74% female | NR | The programme consisted of one-to-one nurse-to-patient (‘nurse champion’) education | Duration: 24 weeks Intensity and frequency: four contacts every 6 weeks |
| Asthma, Gerald 2006,224 USA, inner city elementary schools | Cluster randomised trial [the intervention was delivered in a (random) third of the schools each year]. Underpinning theory, guidelines not discussed | To evaluate a comprehensive school-based asthma management programme designed to address the higher rates of asthma morbidity in African-American children from low-income backgrounds | Children with asthma (previously diagnosed and newly diagnosed by questionnaire + spirometry with exercise test) | 54 elementary schools (total 13,247 pupils) | 736 children with asthma of whom 603 (82%) attended the physician assessment. 610 were still at the same school for the final assessment | 46% female, 97% African American. First to fourth grade pupils (no age given) | Substantial turnover in school register (12% transferred out of the school system and were lost to follow-up: another 5% transferred between immediate and delayed intervention group schools) | Comprehensive programme which provided training for school staff, classroom education for all school children about asthma and specific group education to students with asthma as well as an individual session with a physician who reviewed medication and developed a PAAP | Duration: 1 school year. Intensity and frequency: staff training one in-service. One 30-minute classroom lesson for whole school. Asthma children: six 30-minute sessions + one consultation |
| Asthma, Vollmer 2006,225 USA, managed care | RCT based on guidelines | To test the ability of an automated telephone outreach intervention to reduce acute health-care utilisation and improve QoL among adult asthma patients in a large MCO | Adults on regular medication, or considered to be at high risk (e.g. because of using four or more inhalers a year). COPD patients were excluded | 6948 (patients were able to opt out of the service) | All patients were randomly allocated to intervention or control, with 192 given ‘live’ telephone calls | Age: mean = 52 years (range = 18–99 years). Gender: 65% female | 38% participated in the first call, 32% in the second and 18% in the third. Overall, 47.0% of intervention participants completed at least one intervention call and 12% completed all three calls | Centrally led initiative. Recruitment and set-up undertaken by the MCO. Automated telephone calls to patients: assessing asthma control, providing tailored information. Patients at risk of exacerbations were flagged for the attention of their usual health-care provider. Patients not regularly reviewed were allocated a primary care physician. 192 members were randomly chosen to receive the call from a real person | Duration: 10 months Frequency and intensity: three rounds of calling, lasting 10 minutes |
| Primarily organisational change | |||||||||
| Asthma, Kemple 2003,226 UK, primary care | RCT based on evidence for self-management and regular review | To assess whether or not a mailed review reminder with a personalised WAP improves patients’ understanding and use of self-management | Patients aged ≥ 16 years, due an asthma review, excluding people with COPD | 1209 (663 excluded because not using regular therapy) | 545 | Median age by group: 38 years, 44 years, 43 years Gender: 58%, 60%, 56% in the three groups Current smokers: 34%, 25%, 26% |
N/A | Initiative undertaken at practice organisational level. Apart from the GP author, involvement of other professionals in the practice is not described. Three groups:
|
Single intervention. Duration of follow-up = 12 months |
| Asthma, Lindberg 2002,227 Sweden, primary care | Cross-sectional audit of routine clinical records + prospective patient survey. Based on the literature on nurse-led asthma clinics | To compare the care of patients with asthma in a primary health-care centre with an ANP with traditional models of delivering asthma care in primary care | Asthma patients ≥ 7 years of age, who visited the centres during the 3-month period | Prevalence: 4.1% in ANP practice and 2.2% in the seven control practices | Records: random sample of 20 per practice Survey: ANP centre 186 (82%); responses control centres 161 (53%) response |
Median age: ANP centre 55 years; control centres 51 years Gender: ANP centre 53% female; control centre 55% females |
N/A Eight patients were excluded from the control centres (no record of a confirmed diagnosis of asthma), one centre was excluded from the survey (only one response) |
The specially trained ANP had her own practice with regular patient follow-ups. She provided regular review, patient asthma education, including a PAAP, use of inhalers, avoidance of environmental triggers | The ANP had been in post for 1 year at the time of the study |
| Asthma, Pinnock 2007,228 UK, primary care | Controlled implementation trial, building on the evidence from a RCT | To evaluate the effectiveness of a telephone option as part of a routine structured asthma review service | All patients on the ‘active’ asthma register (defined as patients with a diagnosis of asthma and prescribed asthma medication in the previous year) | 1809 people with active asthma | 1809 were eligible for the service. Subgroup of 822 responded to survey | Age, mean (SD) TC 43.0 (24.8) FtF 42.3 (24.4) UC 45.4 (24.1) Gender Female, n (%) TC 309 (55.8) FtF 363 (55.1) UC 285 (55.3) |
There was a 20% turnover in patients with ‘active asthma’ in the course of the year | Patient review: asthma review included assessment of control, adjustment of treatment and provision of self-management. Three groups:
|
Duration: 12 months Intensity and frequency: clinics offered a range of appointment times throughout the week. Telephone calls could be booked or made opportunistically to non-responders |
| A whole-systems approach | |||||||||
| Asthma, Andrade 2010,229 Brazil, primary health-care network | Real-life historical cohort study. Informed by national guidelines | To assess the effectiveness of a paediatric asthma management programme (including provision of self-management education) on unscheduled health service utilisation by children and adolescents | Children aged 4–15 years from low-income families, with history of two or more exacerbations in the previous year, under a paediatrician, and responsive to asthma therapy | 582 | 470 (80.8%) intervention group and 112 controls | Cases: mean age 6.8 years. 291 (61%) male Controls: mean age 6.6 years. 62 (57%) male Cases were more likely to have persistent asthma |
NR | City-wide public health initiative: unclear who was involved/consulted in the process. Pharmacists and health workers (training not described) provided self-management education reinforced by a PAAP and emphasised the importance of regular medication which was then provided free of charge. Comprehensive educational activities provided for patients and caregivers | Follow-up: 12 months |
| Asthma, Bunik 2011,230 USA, secondary care paediatric clinics | Retrospective before-and-after study using 4 years of routine data based on quality improvement literature | To determine if the quality improvement intervention was associated with improved asthma-related outcomes | Clinic attendees (2006–9) aged > 2 years with a diagnosis of asthma. Children with comorbidity were excluded | 1797 | 1797 | Age: 90% were aged < 13 years. Gender: 58% female | No mention of attrition | Quality improvement programme designed by a multidisciplinary team which met biweekly. Pre-consultation patient questionnaires, provider alerts and electronic templates within the health record were combined into a highly collaborative intervention | Duration: 6 months to implement the project Intensity and frequency: monthly professional training + biweekly discussion at staff meetings |
| Asthma, Findley 2011,231 USA, community day-care centres for pre-school children | Before-and-after study. Based on evidence from similar programmes in other contexts | To evaluate the impact of a comprehensive, multilayered intervention throughout 2003–8 | Pre-school children with asthma (identified by questionnaire) | 9279 children: 5938 parents completed the baseline assessment of whom 1908 had symptoms consistent with asthma | 1374 parents participated in at least one educational event. 871 enrolled in the programme | Age: mean = 4.1 years. Gender: 56% male | HCPs, centre staff, parents and children were able to participate in any or all of the activity. Only 249 (29%) of parents completed the final assessment | Multilayered intervention offering educational activities to centre staff, parents and children, and PACE training to physicians in 31 pre-school day-care centres | Intensity and frequency: centre staff attended a 4-hour training session. Mentors had a 24-hour ‘train the trainer’ teaching Parents: two 1-hour parent workshops Physicians could attend a 4-hour PACE training |
| Asthma, Haahtela 2006,232 Finland, primary, secondary and community settings | Longitudinal evaluation over the 10 years of the programme. Interventions were based on international guidelines | To implement a national asthma care programme to improve care of asthma and thus lessen burden to individuals and the society and prevent an increase in costs | All people in Finland with asthma | 225,000 in 1994 rising to 350,000 in 2004 | N/A | All people with asthma in Finland | N/A | The Finnish programme is ‘comprehensive and reaches deep into the structures of health care’. Goals included:
|
Duration: 1994–2004 Frequency and intensity: ongoing programme for all HCPs involving professional bodies, patient organisations |
| Kauppi 2013233 | This publication reports follow-on data from Haahtela et al.235 All the descriptive information is therefore the same | ||||||||
| Asthma, Polivka 2011,234 USA, deprived community | Before-and-after study using routine anonymised data collected by the service personnel. Based on a ‘Health Homes’ policy initiative | To evaluate the impact of an urban Healthy Homes intervention that included educational home visits to reduce asthma morbidity in children | Areas with high levels of asthma, and poor housing. Properties had to have families with low-household income. Families had to include a child aged < 18 years with physician diagnosed asthma | NR | 243 families were recruited, but data on 84 after 159 (65.4%) were lost to follow-up | Mean age = 6.9 (SD 4.8) years. Gender: 62% males | 159 (65.4%) of the original 243 subjects were lost to follow-up. Follow-up was better in those with a high school diploma (87% vs. 76%; p = 0.05) | Environmental assessment, followed by educational home visits for parents of children with asthma designed to support housing remediation work to reduce asthma triggers (such as damp, moulds, cockroaches, air fresheners), provide asthma education and PAAPs | Duration: 36 months Frequency and intensity: one environment assessment, one education visit (2–3 hours), two community outreach worker visits 2 and 6 weeks after the education visit |
| Asthma, Souza-Machado 2010,235 Brazil, community | Controlled longitudinal study over 9 years (4 before and 5 after the programme). Based on evidence and policy initiatives | To evaluate the impact of a ‘Programme for Control of Asthma’ in the city of Salvador on hospitalisations | Severe asthma as defined by global guidelines | All people in Salvador with severe asthma | 1895 people registered with the programme (but data are from hospital registries) | NR | N/A | A public health intervention project, supported by the Brazilian Ministry of Health, which provided free asthma care including individual and group asthma education, free access to specialist care and medication | Data over 9 years: 4 before and 5 after introduction of the programme |
| Asthma, Swanson 2000,236 Scotland, primary care | Controlled before-and-after study. Based on national guidelines | To evaluate the impact of the introduction of a HBP of asthma care in general practice | People with asthma diagnosis between the ages of 2 and 50 years, registered with the practice since January 1992 | All eligible patients in participating practices (HBP = intervention vs. non-HBP = control) | Case note survey of 400 asthma patients + a patient satisfaction survey of 532 asthma clinic attendees | Mean age = 20.8 years in intervention practices and 21.3 years in control practices | N/A (routinely collected data). Normal turnover in practices | Professional training in implementing the BTS asthma guidelines (including protocol for asthma assessment, follow-up record cards, peak-flow diaries) | Duration: 1991–4 |
| LTC, study, country, setting | Study | Intervention | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|
| Design and duration | Quality score | Patient | Professional | Organisation | Health service utilisation | Disease control and QoL | Process | |
| Primarily professional training | ||||||||
| Asthma, Cleland 2007,218 UK, primary care | Cluster RCT Follow-up: 6 months Intervention practices and waiting list controls |
24 | – | Intervention: one 3-hour interactive seminar vs. control | – | – | Routine data: SABA use: NR Oral steroids: NR Subgroup: QoL: I: 6.49 vs. C: 6.33 (p = 0.03) (less than the minimum clinically important difference of 0.5) Asthma control: NR |
– |
| Participants: 13 practices Adults aged 18–55 years with poorly controlled asthma I: 373; C: 256 |
Implementation strategy: exclusive focus on professional training; no facilitation of integrating into routine practice Fidelity: inconsistent coding meant it was not possible to ascertain whether or not practice nurses in the intervention arm used PAAPs more than nurses in the control arm |
|||||||
| Author’s reflections and lessons learned: inconsistent coding meant routine data were frequently missing in the electronic health record. For example, whether a nurse-led review had occurred, or whether a PAAP had been issued A one-off intervention may be insufficient to teach and reinforce behaviour change; the authors comment they had underestimated the complexity of the support required |
||||||||
| Asthma, Homer 2005,219 USA, primary care | Cluster RCT Follow-up: 12 months |
18 | – | Three 1-day group training sessions + two additional sessions + biweekly conference calls | Intended implementation of CCM | Admissions: no between-group difference (both groups improved) | Asthma attacks: no between-group difference (both groups improved) | Ownership of WAP I: 54% vs. C: 41% (but large baseline difference) |
| 43 practices (13,878 children with asthma) Subgroup of 631 children provided interviews |
Implementation strategy: a theoretically based quality improvement intervention, but organisational barriers impeded the process Fidelity: considerable lack of engagement, e.g. substantial attrition from training (only 42% of practices submitted performance data) |
|||||||
| Author’s reflections and lessons learned: implementation in primary care practices is challenging. Specific organisational barriers encountered included: changing practice networks, financially challenged managed care plans, and changes in staffing and contracts for providers | ||||||||
| Primarily patient education | ||||||||
| Asthma, Bunting 2006,220 USA, managed care | Time series analysis. Routinely collected outcomes at annual intervals over 1–5 years | 17 | One-to-one education + PAAP by a hospital-based asthma educator. Sessions lasted 60–90 minutes + regular follow-up for 5 years by pharmacists | Certified asthma educators and trained pharmacists | Pharmacist costs reimbursed by health plans. Waived medication co-payments on asthma-related medications | From insurance claims Hospitalisations/ED attendances: event rates for the 3 years before enrolment were much higher at 21.3, 22.2 and 22.3 events/100 patients/year than during the 5 years of the programme, which averaged 5.4, 2.6, 1.9, 5.4 and 0 events/100 patients/year |
Compared with baseline, at most recent follow-up the proportion of patents with:
|
PAAP ownership increased from 63% at baseline to 99% at follow-up (p < 0.0001) |
| 207 adults covered by employer’s health plans | Implementation strategy: the programme was implemented through an employers’ insurance-based scheme. The cost to the employers of providing financial incentives was offset by the reduction in absenteeism Fidelity: unclear. Nine were reported as dropping out for ‘failure to meet the requirements of the programme’ |
|||||||
| Author’s reflections and lessons learned: there was no attempt to determine the contribution of the various interventions (asthma education, long-term follow-up, financial incentives); the authors concluded that a combination of these factors led to the observed outcome improvements At a time of rising health-care costs, it is extremely important to determine whether or not preventative approaches are cost-effective |
||||||||
| Asthma, Chini 2011,221 Italy, primary schools | Before-and-after study. Each year two schools participated in the 1 year programme | 15 | Children with asthma had a clinical assessment and were given a PAAP at 2 months with follow-up review at end of the year Age-appropriate groups taught cognitive techniques and breathing control |
– | Lessons aimed at teachers, school personnel, parents and school children to improve their knowledge of asthma | Compared with baseline, at the end of the school year:
|
||
| 2765 school children, aged 6–10 years. 135 with asthma | Implementation strategy: a comprehensive asthma programme based on an existing strong family–physician–school relationship Fidelity: no data on attendance at groups, uptake of assessments |
|||||||
| Author’s reflections and lessons learned: the programme also encouraged a close relationship between families, children, school staff and physicians through numerous meetings and lessons addressed to all participants and represent a model for combining health care with social care forming a ‘health-care chain’ system | ||||||||
| Asthma, Delaronde 2005,222 USA, managed care | Preference trial (‘opt-in’, ‘opt-out’, ‘probably’ group were randomised, and ‘non-responders’) Follow-up: 12 months |
20 | 6 month programme of nurse-led individualised telephonic case management vs. usual care | – | – | There were no significant differences in the numbers of physician office visits, ED visits or hospitalisations | QoL improved in the intervention group (p = 0.04) though not by the minimum clinically important difference, but not in the control group | Ratio of preventer/reliever medication improved in all groups. Increase in intervention group (0.176) was twice that in the control group (0.091); p = 0.04. The increase in the ‘opt-in’ group was even larger at 0.285 |
| 399 adults not using a recommended asthma medications regime | Implementation strategy: administration of the scheme and nurse educators funded and undertaken by the MCO Fidelity: intervention delivered by certified asthma trainers – no description of any quality checks. 27% of the intervention group and 68% of the opt-in group completed four or more contacts |
|||||||
| Author’s reflections and lessons learned: self-motivation is an important indicator of readiness to initiate and maintain asthma self-management | ||||||||
| Asthma, Forshee 1998,223 USA, managed care | Before-and-after study with four assessments over 24 weeks | 15 | Tailored individualised education + videos + handouts | Nurse champions were educated about asthma | Compared with baseline, at follow-up over 24 weeks adults and children had:
|
Compared with baseline, at follow-up over 24 weeks adults and children had:
|
Monthly reviews increased for both adult and children (p ≤ 0.05) and specialist referrals (p ≤ 0.05) | |
| 201 adults and children with poorly controlled asthma from four managed care plans | Implementation strategy: training of a nurse champion Fidelity: no information |
|||||||
| Author’s reflections and lessons learned: training an existing employee to deliver the intervention enabled intervention implementation compared with training a contractor who did not already have a relationship with the patients | ||||||||
| Asthma, Gerald 2006,224 USA, inner city elementary schools | Cluster randomised trial with immediate and delayed groups | 18 | Six 30-minute group education sessions for pupils with asthma + a consultation with a paediatric allergist who (if necessary) confirmed the diagnosis, reviewed medication and developed a PAAP | Asthma education was provided for school staff in an ‘in-service’ meeting | A 30-minute classroom lesson was given to all children in grades one to four in the school | Compared with baseline, at the end of the school year children had:
|
Compared with baseline, at the end of the school year children had:
|
Compared with baseline, post-school education there was a statistically significant increase in knowledge (p < 0.0001) |
| 736 children with asthma from 54 schools. Due to attrition (e.g. moving schools) data on 610 were available for the final analysis | Implementation strategy: a comprehensive collaboration between school and health services Fidelity: the authors describe significant difficulty in maintaining the fidelity of the programme. Students frequently changed schools, there was a high turnover of school staff, workload meant that staff were unable to provide the planned in-school education, the trained volunteer staff proved too costly to supervise and time constraints meant that the education sessions had to be shortened |
|||||||
| Author’s reflections and lessons learned: connecting children with a regular source of health care in this inner city African-American population was difficult. More intensive methods of medical management, such as school-based health centres or supervised asthma therapy, might prove more effective in inner-city schools | ||||||||
| Asthma, Vollmer 2006,225 USA, managed care | RCT, 3581 telephone outreach (192 had live calls). 3367 usual care | 18 | Three 10-minute automated calls providing asthma review and personalised feedback | – | This was a service implemented by the MCO | Health-care utilisation: no difference in proportion of patients with unscheduled care (I = 10.9 vs. C = 10.00; p = 0.14), or proportion attending ED/hospitalisation (I = 4.1 vs. C = 4.0; p = 0.88) | Asthma control: no difference in QoL (p = 0.56) or asthma symptoms | Medication use: no difference in ICS use (p = 0.20) or short-acting β2-agonist use (p = 0.86). (In a post-hoc per-protocol analysis, intervention patients were more likely to received ICS and less to request SABA) |
| 6948 people with asthma | Implementation strategy: recruitment and set-up of the intervention undertaken by the MCO Fidelity: automated telephone call. 47.0% of intervention participants completed at least one intervention call, and 12.1% completed all three calls 59.9% of live-caller participants completed at least one call and 27.6% completed all three calls vs. automated-caller (46.3% and 11.2% respectively) |
|||||||
| Author’s reflections and lessons learned: common reasons for non-participation were unwillingness to talk to a computer, lack of time and ‘my asthma is already well controlled’ The intervention had a broad remit: a more focused intervention (such as promoting medication adherence in patients who have not refilled a prescription for preventer medication) might be more effective |
||||||||
| Primarily organisational change | ||||||||
| Asthma, Kemple 2003,226 UK, primary care | RCT, three groups:
|
20 | – | – | Organisational intervention enclosing PAAPs with invitations to review | There were no significant differences in use of health-care resources over the subsequent 12 months | There were no significant differences in prescriptions of short-acting β2-agonists | Proportion attending for an asthma review increased (group 1: 70%, group 2: 82%, group 3: 84%; p = 0.002) (OR 2.33, 95% CI 1.37 to 3.93) Personalised plan increased knowledge of using a PAAP (OR 2.58, 95% CI 1.24 to 5.36) |
| 545 with asthma on regular medication | Implementation strategy: administration was at organisational level. Involvement of other professionals in the practice is not described Fidelity: content of mailing were controlled but no check on content of the subsequent review |
|||||||
| Author’s reflections and lessons learned: personalised prompts can help, but many patients only respond to prompts and access help when they realise they have a problem | ||||||||
| Asthma, Lindberg 2002,227 Sweden, primary care | Cross-sectional audit of routine clinical records + prospective patient survey | 16 | The ANP provided regular review, patient asthma education including a PAAP, use of inhalers, avoidance of environmental triggers | The ANP had specialist asthma training | With the exception of emergency visits and the yearly follow-up visit to their physician, all visits were made to the asthma nurse | Survey Patients from ANP centre had:
|
Survey Patients from ANP centre were:
|
Clinical records ANP centre was:
Patients from ANP centre were:
|
| Records: random sample of 20 per practiceSurvey: ANP centre 186 (82%) responses; control centres 161 (53%) response | Implementation strategy: this was an evaluation of an existing service. The ANP had been providing the majority of routine asthma care in one of the primary health-care centres for at least 1 year Fidelity: N/A as this was an existing service |
|||||||
| Author’s reflections and lessons learned: ANP strategy in primary care can improve asthma care and has economic advantages. However, the result may only be generalised to other practices working with asthma nurses in the same way | ||||||||
| Asthma, Pinnock 2007,228 UK, primary care | Controlled implementation trial over 1 year. Reminders about review: comparing telephone option with face to face only, and a ‘usual care’ group | 21 | Asthma review according to clinical need, including assessment of control, adjustment of treatment, and provision (or review) of self-management (with PAAP) | Asthma nurses who had an accredited diploma on asthma care | Three reminders to patients due a review, with an option to book a telephone or face-to-face review. Opportunistic telephone calls to non-responders | Compared with the face-to-face-only group, patients in the telephone option group had:
|
Routine asthma review was provided for 397/598 (66.4%) in the telephone option group and 352/654 (53.8%) in the face-to-face option group [risk difference 12.6% (95% CI 7.2% to 17.9%); p < 0.001] Compared with the face-to-face-only group, patients in the telephone option group had:
|
|
| Routine data from 1809 people with ‘active asthma’ Subgroup of 822 responded to survey |
Implementation strategy: implemented within the context of the newly introduced quality and outcome framework which rewarded the provision of routine asthma reviews. This provided an incentive for the practice to send out reminders and undertake opportunistic telephone calls. Senior practice staff were involved in the design of the interventions Fidelity: standardised training was provided for all administrative and nursing staff. The process was monitored on a monthly basis to assess the number of reviews undertaken and the content of the review (including provision of self-management education |
|||||||
| Author’s reflections and lessons learned: the study coincided with the introduction of the UK GP contract (2004) which rewards practices who achieve clinical standards, including a target of 70% for the annual review of people with asthma The data suggest that opportunistic calls should be provided for enhancing access rather than accepting non-response as an exclusion criterion |
||||||||
| A whole-systems approach | ||||||||
| Asthma, Andrade 2010,229 Brazil, primary health-care network | Historical cohort Follow-up: 12 months |
19 | Individual and group educational activities, including PAAP | Patient education provided by pharmacists and health workers but no details of their training | Free medication | Health service use: at 12 months 23/470 (5%) of cases used the Municipal Health System for acute asthma compared with 38/112 (34%) of controls (p ≥ 0.01) | – | The use of BDP was higher in cases than controls: 68% of cases were BDP users. All users of the service had a PAAP |
| 582 children aged 4–15 years (470 cases, 112 controls). (Cases were slightly younger and more severe than controls) | Implementation strategy: city-wide public health initiative; no description of the process or who was involved Fidelity: all intervention children had accessed the programme at least once and had been given a PAAP. No information on subsequent attendances. For cost reasons unlikely to have sought medical attention/prescriptions elsewhere |
|||||||
| Author’s reflections and lessons learned: asthma programmes in low-to-middle income settings should provide antiasthmatic reliever and controller medicines (free, when possible) as well as a comprehensive educational framework because of their synergistic effect in reducing the burden on health services by acute asthma | ||||||||
| Asthma, Bunik 2011,230 USA, secondary care paediatric clinics | Retrospective study using routine data from before, the year after and 4 years after the intervention | 15 | Asthma educators provided asthma education about medications and devices, assisted in creating of PAAPs, and provided telephone calls 2 weeks after unscheduled care | Monthly 1-hour education sessions for junior medical staff and nurses. Familiarisation with the project for all new staff Computer and paper prompts to facilitate structured review, appropriate prescribing and provision of PAAPs |
Organisational strategies included pre-consultation questionnaires for families, paper alerts and computer templates for asthma reviews, respiratory therapist support for providing education and PAAPs | There was a trend towards fewer ED visits and hospitalisations from 2006 to 2009, but this was not statistically significant | – | Compared with those seen in 2006, children seen 2 years after the intervention were more likely to:
|
| 1797 clinic attendees over 4 years | Implementation strategy: quality improvement programme designed by a multidisciplinary team which met biweekly throughout the 6-month project Fidelity: process outcomes (such as provision of PAAPs) suggest that protocols were followed, though the volume of patients seen meant that some strategies such as completion of the pre-consultation forms did not always occur |
|||||||
| Author’s reflections and lessons learned: collaborative practice change can be achieved with demonstrable and sustainable effects on important outcomes, but need allocated time for regular meetings and working through several plan/do/study/act cycles while addressing implementation problems | ||||||||
| Asthma, Findley 2011,231 USA, community day-care centres for pre-school children | Before-and-after study in 35 pre-school centres | 17 | Parent education workshops: delivered by mentors (parents who have children with asthma and managed asthma well). Parents received asthma education and a PAAP, and were encouraged to talk with their child’s physicians. Children played activities and games on asthma triggers and signs | Professionals of children enrolled in the programme were offered. PACE training | The centre staff received training on asthma and asthma management (including creating an ‘asthma-friendly centre’), identifying children with asthma, arranging a PAAP and handling emergencies | Compared with baseline, at 9–12 months assessment the proportion of children with:
|
Compared with baseline, at 9–12 months assessment the proportion of children with:
|
Compared with baseline, at 9–12 months assessment:
|
| 1374/1908 (72%) parents participated in at least one educational event. 871 enrolled in the programme. 249 completed the final assessment | Implementation strategy: a multilayered approach as day-care centre staff made the centres more asthma-friendly, and centre staff educated parents about asthma management and the community’s paediatric providers received training to provide state-of-the-art care Fidelity: 31/35 centres completed training and engaged in at least one activity. 871 (46%) of parents enrolled in the programme. 183 (59%) of the childrens’ health-care providers attended PACE training. No reported assessment on how interventions were implemented |
|||||||
| Author’s reflections and lessons learned: a multilayered approach can improve asthma outcomes among pre-school children with a combination of parent and provider education having the greatest impact A key element of the ABC strategy was linking asthma education activities in the day-care setting with improving the quality of asthma care by health-care providers |
||||||||
| Asthma, Haahtela 2006,232 Finland, primary, secondary and community settings | Longitudinal evaluation over the 10 years of the programme | 10 (note: many of the criteria did not apply) | Patient organisations arranged direct patient counselling and distributing information and resources free of charge | Education was provided for: respiratory specialists (n = 5300); primary/secondary care professionals (n = 3700); all HCPs (n = 25,500); pharmacists (n = 695) | The Ministry of Social Affairs and Health recognised asthma as an important public health issue and set up the national programme. Finnish health-care were committed to the programme | Over the 10-year programme:
|
Over the 10-year programme:
|
Over the 10-year programme:
|
| All people with asthma in Finland | Implementation strategy: the Finnish programme is ‘comprehensive and reaches deep into the structures of health care’ Fidelity: a network of asthma co-ordinators (a doctor and nurse in each health-care centre) promoted the initiative and monitored quality |
|||||||
Author’s reflections and lessons learned:
|
||||||||
| Kauppi 2013233 | This publication reports follow on data from the Haahtela et al. study.232 All the descriptive information is therefore the same | In the 10 years from 2000 to 2010 (i.e. covering 6 years after the end of the Finnish programme):
|
In the 10 years from 1996 to 2007 (i.e. covering 3 years after the end of the Finnish programme):
|
|||||
| Asthma, Polivka 2011,234 USA, deprived community | Before-and-after study over 2 years using routine anonymised data collected by the service personnel | 18 | Environmental assessment home repairs, educational home visits to reduce asthma triggers (such as damp, moulds, cockroaches, air fresheners), and provide asthma education and PAAPs | Professionals completed the National Centre for Healthy Homes practitioners’ course and the American Lung Association of Ohio’s asthma educator course | Costs included repair work, contractors, supplies for assessment and education provided to participants | Compared with baseline, at 2-year follow-up children had:
|
Compared with baseline, at 2-year follow-up children had:
|
Compared with baseline, at 2-year follow-up:
|
| 243 families were recruited, 84 (35%) completed | Implementation strategy: a comprehensive home visitation intervention programme delivered by a multidisciplinary team (programme manager, health educator, sanitarians, community outreach workers) and which provided practical remediation for unhealthy housing as well as asthma health education Fidelity: barriers: many clients were highly transient, their housing arrangements or status changed unexpectedly from month to month |
|||||||
| Author’s reflections and lessons learned: the cost of interventions averaged $1242 per unit not including start-up, staffing, training and overhead costs. These cost considerations point to the difficulty in sustaining efforts like these without grant funding or other support. A related sustainability issue is the ongoing need for home maintenance and repair | ||||||||
| Asthma, Souza-Machado 2010,235 Brazil, community | Controlled longitudinal study over 9 years (4 before and 5 after the programme) | 11 (note: many of the criteria did not apply) | Patient training: individual asthma education + monthly group sessions discussing asthma prevention and treatment | Experienced staff trained 512 primary health-care physicians, nurses, pharmacists, social workers and managers on the prevention and management of asthma and rhinitis | Centres offered specialist care and free medication to patients with severe asthma | Over the 9 years of data collection:
|
In-hospital mortality which had been rising from 1998 to 2002, decreased after introduction of the programme from 23 deaths in 2003 to only one in 2006. In Recife (the control city), the in-hospital mortality rate increased from five deaths in 2003 to six deaths in 2006) | From 2003 to 2006, the programme dispensed 220,889 units of inhaled medication for asthma control (ICS and/or SABA/LABA). There was a strong inverse correlation between hospitalisation rates and drug dispensation (–0.801; p = 0.001) |
| 1895 people registered with the programme (but data are at population level using routine hospital registries) | Implementation strategy: the major role of the programme has been to catalyse an initiative that combines contributions of all levels of public health administration (city, state and Ministry of Health) into a programme that involves health care, capacity building and research Fidelity: not reported |
|||||||
| Author’s reflections and lessons learned: we speculate that the most important factors that determined our favourable results were (1) a considerable proportion of patients with severe asthma with no access to good-quality care, including affordable medication at baseline; (2) establishment of treatment with the most effective and safe medications; (3) an education programme to increase compliance to medication use; and (4) a referral system made easy for patients and the health services | ||||||||
| Asthma, Swanson 2000,236 Scotland, primary care | Controlled before-and-after study | 16 | Asthma self-management education in asthma clinic | Professional training in implementing the BTS asthma guideline | Provision of paper-based templates | Compared with control practices, at follow-up patients in Health Board intervention practices were:
|
Compared with patients in control practices, patients who had attended Health Board intervention practice clinic reported:
|
Compared with control practices, at follow-up patients in intervention practices were:
|
| 400 people with asthma (aged 2–50 years) registered with the practice since 1992 + 532 responders to the survey of asthma clinical attendees | Implementation strategy: Health Board initiative Fidelity: findings report adherence to guidelines as judged by retrospective audit of clinical records |
|||||||
| Author’s reflections and lessons learned: some practices were reluctant to take part in the study which may have reflected poor standards of asthma care, whereas those who participated might represent an overoptimistic picture of asthma care. Similarly, patients responding to the survey were those attending the asthma clinics likely to hold more positive perceptions of clinics and proactive care than non-attendees | ||||||||
| LTC, study, country, setting | Study design | Participants | Service implementation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Design underpinning evidence, theory | Aim | Eligibility criteria | Total eligible population | Number participating | Participating population characteristics | Attrition | Intervention and strategy for implementation | Duration, intensity, frequency | |
| Primarily professional training | |||||||||
| Diabetes, Stevens 2010,237 USA, secondary care | Prospective monthly collection of routine data | To (1) redesign resident practices based on the CCM; (2) implement and test educational strategies based on the CCM; and (3) evaluate changes in the clinical processes and outcomes of care | Volunteer resident teams | All resident teams in 400 US teaching hospitals were invited | 57 teams from 37 teaching hospitals | – | NR | Professional teams used PDSA cycles to implement the CCM, working collaboratively to learn from each team’s successes, learn how to overcome barriers and exchange programme redesign tips | Duration: 2004–6 Intensity: three 2-day learning sessions + one all-day web-mediated meeting + monthly telephone conferences for support and report |
| Primarily patient education | |||||||||
| Diabetes, Albisser 2001,238 USA, managed care | Controlled longitudinal observational study. Based on guidelines and modelling of interventions | To compare changes in outcomes from three distinct diabetes disease management initiatives | Registered with the MCO | 8000 | First 978 patients to enrol into one of three initiatives | Mean age (of the 978 studied): 58 years. Gender: 51% male | NR | ‘Standard’ diabetes education for all patents (ED only). This was supplemented by daily automated telephone self-monitoring or self-management education from a diabetes educator | Education ± 15–30 minutes instruction on using the daily automated telephone call, or 15 hours of SM education |
| Diabetes, Harris 2000,239 USA, community | Before-and-after study. Limited references to support the programme which is based on addressing social inequalities | To offer education to underserved population of patients with diabetes | Adults with diabetes. The clinic served patients with mental illness, homeless, illiterate, non-English-speaking and indigent individuals. All these patients were offered the programme | Not reported | 85 completed at least one session | Mean age: 50 years (59%), between 41–65 years. Gender: 35 (41%) males | 29% completed all four education sessions. Many had transport problems, did not have a telephone or permanent address making follow-up difficult | Implementation of a patient education system in a deprived community using volunteer health educators many of whom have substantial psychosocial needs and poor literacy | Duration: 1 year Intensity: four sessions, 1.5 hours each |
| Diabetes, Jordan 2011,240 UK, primary care | Retrospective cohort study comparing cases with matched controls from the General Practice Research Database | To evaluate the effectiveness of a telephone-based nurse-delivered motivational coaching and support for self-management and lifestyle change for patients with poorly controlled diabetes | Adults with poorly controlled diabetes with at least one complication and with access to a telephone. Referred by their GP | 1195 enrolled after GP referral | 473 had at least 90 days in the rolling programme | Mean age: 62 years. Gender: 55.6% male | NR, as only people with a 90-day follow-up were included | A telephone-based ‘bespoke’ disease management programme which supports individuals with diabetes, cardiovascular disease and heart failure to change their daily behaviour to improve their health and use of NHS services. Supported by NHS organisations, NHS Direct and a private health-care provider | Patient intervention: duration 9 months Frequency: one to two calls every month of varying length according to need Case managers: 6-week training process |
| Diabetes, Kelly 2005,241 Australia, community | Before-and-after study. Based on ‘an extensive literature review’ of coaching skills | To support people with diabetes to improve self-management and utilise more effectively existing local health services | Specific targeted strategies implemented to recruit older men and members from the Chinese community | Unknown | 343 enrolled population | 43% male, 10% Chinese | 145 completed measures at baseline, 6 and 18 months | Telephone coaching to support the setting of realistic goals, making lifestyle changes and developing care plans for discussion with GP. Coaches’ training: motivational interviewing | Duration: 12-month programme Coaches training: 2-day course in motivational interviewing |
| Diabetes, Lowe 2008,242 Australia, secondary care | Prospective observational study. Based on RCT evidence | To describe the short-term outcomes of an already established programme to teach patients to match insulin dose to carbohydrate intake | English speaking patients with insulin requiring diabetes (T1DM or T2DM) | 154 patients were invited to participate in the programme | 137 patients attended in 2001–2. (A total of 800 diabetics have attended over 13 years of the programme) | Mean age: 47 years Gender: 55% female |
All who started the 4-day programme completed it | Existing educational programme combining training to adjust insulin dosage to carbohydrate intake + self-management skills (i.e. problem-solving, goal-setting, communication with HCPs) + empowerment programme | Duration: 4 days running as a rolling programme once a month |
| Diabetes, Lowe 2009,243 Australia, secondary care | Historical cohort | To compare the long-term outcomes of the skills training + empowerment programme (see Lowe et al.242) with the skills training only | Attendees on the combined programme in 2001–2 vs. attendees on the basic course only | 119 on the combined programme vs. 383 on the basic course | N/A (routinely collected data) | Age of the type 1 diabetics on both courses was similar (40 years vs. 37 years). Type 2 diabetics were older (57 years vs. 61 years) | People who had attended both courses were excluded, and those not resident in the area | Combined programme taught adjustment of insulin dosage to carbohydrate intake + self-management skills (i.e. problem-solving, goal-setting) + empowerment programme. Basic training course included didactic insulin education | Duration: 45 hours combined programme vs. 20-hour didactic course |
| Diabetes, Roblin 2007,244 USA, MCO (primary care) | Case–control using routinely collected data. Based on RCTs | To estimate the impact of participation in a multifactorial diabetes health education programme on glycaemic and lipid levels | Adults (aged > 25 years) with diabetes who participated in the organisation’s diabetes education programme during 2003–4, registered with a primary care practice | 1991 participants + 12,741 matched controls | Final HbA1c sample 1864 (93.6%). Final LDL sample 1681 (84.4%) | Mean age: 64 years | – | Cases Patient education: diabetes education and self-management training Control: usual care |
Duration: 2-hour class programme Frequency: offered during day, evening and Saturday sessions |
| Diabetes, Welch 2006,245 USA, managed care | Before-and-after survey data. Based on RCT evidence | To evaluate the impact of an existing DDMP in a MCO on use of preventative services and adoption of diabetes self-management behaviours by race/ethnicity | Adults with high risk diabetes enrolled in a MCO for 2 years (a year before and the year after joining the diabetes programme) | 19,483 members of the MCO. 6433 returned the baseline survey prior to joining the diabetes programme | 5174 were sent a survey at the end of the year-long programme. 1961 valid responses | Mean age: 61.7 years Gender: 58.3% male |
1259 were not sent a follow-up survey because they were no longer members. 1319 of the 3369 were excluded because enrolment dates were inconsistent | All participants received educational materials. Graded support depending on risk:
|
Duration: the programme lasted a year with telephone calls lasting between 30 and 60 minutes |
| Diabetes, Banister 2004246 USA, community clinic | Before-and-after study. Based on RCT evidence | To assess the clinical outcomes when providing diabetes self-Management training to the ‘working poor’ | Patients with diabetes at the low poverty level | 127 attendees at the clinic | 70 (55%) | Gender: 46 (65.7%) female Ethnicity: 55.7% Hispanic Weight: 45 (64.3%) obese |
Of the 127 attendees, 18 had no baseline HbA1c, or written consent. Eight had T1DM | Patient education: group and individual diabetes education followed by support meetings | One 4-hour group session + at least one individual session + monthly support meetings |
| Diabetes, Joshu 2007,247 USA, primary care | Before-and-after study. Based on RCTs | To describe the integration of a promotora (i.e. CHWs)-led self-management component into a system of care | Patients with T2DM | NR | 301 | Mean age: 60.3 years Gender: 73.1% female |
81% completed 7 out of 10 educational sessions | The self-management intervention, consisting of self-management education classes, support groups, individual follow-up, and monitoring by promotores, was incorporated into the system of patient care | Duration: 10 weekly sessions Intensity: 2.5 hours + weekly telephone calls by promotores |
| Diabetes, Micklethwaite 2012,248 USA, secondary care | Before-and-after study. Based on RCT evidence | To describe and evaluate an educational/self-management intervention for persons with T2DM in a community general hospital | Diabetes, and ‘at-risk’ (i.e. no other access to education) | 969 were referred to the service. 505 (52%) enrolled in the programme | 81 (of 505) with an A&E attendance and/or admission were analysed in this study | Mean age: 53.7 years Gender: 72% female |
NR | 3-year programme which aimed to provide, free of charge, diabetes education, self-management skills training and diabetes case management services, plus a range of other support activities (food tasting, ‘diabetes days’, weight management) | Duration: 3 years. Individual consultations, five 2-hour group sessions on a rolling basis + other optional ‘events’ |
| Diabetes, Rasekaba 2012,249 Australia, secondary care | Before-and-after study. Based on national guidelines | To evaluate the effectiveness of a multidisciplinary disease management programme that incorporates self-management in a culturally and linguistically diverse population | Patients with T2DM who had HbA1c data available at programme enrolment and at 12-month follow-up | 967 enrolled in the programme | 545 (56.4%) (HbA1c available at baseline and 12-month follow-up) | Mean age: 60 years Gender: 53% male |
Excluded patients (incomplete data) attended the programme less frequently (mean 8 visits vs. 17 visits for the included group) | Integrated programme which optimises medical management to improve glycaemic control and prevent complications, and provide training in diabetes self-management and lifestyle modification. A diabetes nurse educator works with the patient to set treatment goals and strategies to implement lifestyle modifications. Referrals to the other team members are made as needed | The programme ran for 4 years, but individual patients are enrolled for an average of 12 weeks and attend an average of 13 (range 1–52) appointments |
| Diabetes, Sedlak 2005,250 Austria, secondary care | Before-and-after. Based on the ‘well-established’ diabetes teaching programme but which had not been tested in elderly patients | To compare metabolic control and patient survival in patients enrolled with the programme and able to self-monitor vs. those whose monitoring was performed by community nurses | T2DM patients aged > 80 years who started insulin therapy in the hospital | 43 patients commenced insulin | 21 (49%) were judged able to self-monitor and enrolled in the programme | Age and gender were similar in the two groups Mean age: 85 years (range 80–90 years) in both groups Gender: female : male 15 : 6 in the programme group vs. 12 :10 |
No attrition | Self-monitoring group received a structured educational programme adjusted for the patient’s age and needs which enabled blood glucose self-monitoring and adjustment of insulin doses vs. information about diabetes, but blood glucose monitoring and insulin dosing performed by community nurses with the help of patients’ relatives | 5-day education programme |
| Diabetes, Bott 2000,251 Germany, secondary care | Before-and-after study. Based on RCTs and uncontrolled studies | To assess an intensive inpatient programme for patients with T1DM who already been trained on insulin therapy but have not achieved therapeutic goals | Patients with T1DM who had completed insulin training but were unable to achieve their therapeutic goals | 83 were enrolled in the programme in the study time frame | 76 had been reassessed at 18 months (range 12–24 months) | Mean age: 35 years (SD 10) Gender: 41% female |
Seven patients were lost to follow up:
|
The programme extends previous training by providing intensive group discussions and individual counselling, including motivational aspects, coping strategies and psychological issues | Duration: 5-day inpatient programme Group sessions with four to six patients Intensity: 20 hours of teaching |
| Diabetes, Pieber 1995,252 Austria, secondary care | Before-and-after study. Based on RCT evidence | To determine the efficacy and safety of a structured educational programme in patients with insulin-dependent diabetes in an outpatient setting | Adults with insulin-dependent diabetes for > 12 months; and able and willing to follow the structured 5-day diabetes programme for intensive insulin therapy | 243 referred by GPs or specialists usually because of poor control on existing regimes | 210 (86%) participated in the programme. 205 were followed up at 3 years | Age: mean = 40 years (range 18–74 years) Gender: 53% female |
Reasons for not participating were: 12 already trained; four severe comorbidity; 12 unwilling to change regime Losses to follow-up were due to moving, or otherwise uncontactable |
Based on existing intensive programmes, initial assessment and optimisation of treatment is followed by training in small groups delivered by a specialist nurse and dietitian. The focus is on adjusting insulin dosages according to the anticipated amount of carbohydrate intake and the actual blood glucose | Duration: 5-day course Intensity: 24 hours of group teaching |
| Diabetes, Sämann 2005,253 Germany, secondary care | 10-year longitudinal quality assurance project in 96 centres | To evaluate the implementation of a course teaching flexible, intensive insulin therapy on glycaemic control and severe hypoglycaemia in routine care | Patients with T1DM without advanced late complications and resident within 100 km of the diabetes centre | 96 centres each reviewed 50 consecutive patients one year after education. 11,135 patients invited | Over 10 years (1993, 1996–2004) 9583 patients with baseline and 1-year follow-up assessment responded | Mean age: 38 years | Loss to 1-year follow-up of 15% | The 5-day structured inpatient training course for intensive insulin therapy, teaches patients to match insulin doses to their food choices, while keeping blood glucose close to normal | Duration: one 5-day course involving 20 hours teaching |
| Sämann 2006254 | This publication reports data from a subgroup of patients from Sämann et al.253 All the descriptive information is therefore the same. It reports the impact of the intervention in a subgroup of 341 people with T1DM and a history of repeated or unexplained severe hypoglycaemia, or hypoglycaemia unawareness, or a history of repeated ketoacidosis | ||||||||
| Sämann 2008255 | This publication reports data from a subgroup of patients from Sämann et al.253 All the descriptive information is therefore the same. It reports the impact of the intervention in a subgroup of 1592 teenagers and young adults (aged 12–24 years) with T1DM | ||||||||
| Primarily organisational change | |||||||||
| Diabetes, Glasgow 2002,256 USA, community-managed care or hospitals | Observation of change management. Based on the CCM | To integrate self-management support into broader health-care systems for diabetes or heart failure | Organisations willing to make major change to either diabetes or heart failure care | 24 organisation | Seven organisation focused on diabetes | Four of the seven were MCOs. Average of 256 diabetics on their registers | Two organisations initially planned to address both heart failure and diabetes, but opted to focus on heart failure | PDSA cycles as part of a collaborative to enable organisations to implement patient-centred self-management support as part of CCM | Duration: 13 months, 2-day group session + national congress and a series of PDSA cycles |
| Diabetes Hargraves 2012,257 USA, community health-care teams | Paired health-care teams (based on previous collaborative performance) randomly allocated to intervention or control | To assess the impact of involving CHWs assigned to health-care teams in training patients to set self-management goals | Participation in a previous collaborative which used PDSA cycles to improve care for patients with diabetes | 12 centres paired and randomised | 12 centres. serving 1415 patients (494 in intervention + 921 in control) | Intervention: mean age = 54.9 years; 53.2% female; ethnicity = 52.6% white Control: mean age = 52.3 years; 51.3% female; ethnicity = 35.5% white |
NR | CHWs on health-care teams supported patients to be activated participants in health-care consultations, assisted in diabetes education, and building self-efficacy | Duration of intervention: 13 months |
| A whole-systems approach | |||||||||
| Diabetes Anderson 2008,258 USA, primary care | Longitudinal before-and-after study. Based on RCTs and change management theory | To provide self-management education to underserved, largely Hispanic population of patients with diabetes and to meet the specific language, culture, and literacy level needs | Hispanic patients with diabetes | 2389 registered diabetics | 488 (20.4%) | Ethnicity: 63% Hispanic (of which 32% were monolingual) | NR, but follow-up HbA1c only available for 263 patients | Implementation was through a series of PDSA cycles and involved culturally specific group/individual patient education, detection and management of comorbid depression, staff training/support to provide self-management, monitoring of goal attainment | Duration: 4-year ongoing programme Staff training: half-day session + ongoing support and monitoring |
| Diabetes, Dettori 2005,259 USA, primary and secondary care clinics | Before-and-after study | To improve diabetes care in rural settings | Patients with diabetes registered with practices in Montana | Estimated 588 people with diabetes (based on national prevalence rates) | 213 (36.2%) | Age: mean = 65 years Gender: 57% female |
NR | A quality improvement intervention with state diabetes control programme support to the primary care practices including establishing registries, promoting improvement through regular site visits, providing technical support and establishing a diabetes education programme through the American Diabetes Association | Duration: 3-year programme (2000–3) |
| Diabetes, Gruesser 1993,260 Germany, primary and secondary care | Physician survey and ‘before-and-after’ data from patient records | To evaluate the impact of a training programme for physicians and the practicability and efficacy of the education they provided for T2DM patients in routine primary care | Physicians who had attended training + data from records of patients who had attended education | 139 physicians | 127 (91%) + 179 patients of 17 physicians who had attended education programme | Of the 127 physicians, 42% were internists and 58% GPs. The mean patient age was 67 years (SD 9.6) 65% were female |
Nationwide implementation of a structured treatment and education programme for T2DM patients in Germany. Seminars for trainers, who lead training courses for physicians who are then reimbursed for providing education programmes for their patients | Physician training was over 2.5 days. Patient education groups of four sessions/week (90–120 minutes each) | |
| Diabetes, Korsatko 2007,261 Austria, primary care | Before-and-after study. Based on guidelines | To assess effectiveness of a free structured educational programme for patients with T2DM | Patients with T2DM not using insulin for glycaemic control | 120 physicians + 52 diabetes educators taught 4396 patients | 2122 (48%) attended follow-up assessment | Age: 63.8 years (SD 10.7) Gender: 55% female |
Less than half (48%) attended the follow-up session | Patient education: group diabetes education + role play techniques + refresher course | Duration: 4 years Intensity: four sessions (16 hours) 90–120 minutes each + 2-hour refresher course after 1 year |
| Diabetes, Liebman 2007,262 USA, community health centre | Longitudinal data for 3 years before and the 3 years of the programme | To implement the CCM + and a self-management intervention to improve diabetes care in a deprived Latino population | Latino participants with diabetes | 1188 on the centre database by the end of the 3-year programme | 580 (48.8%) participated in some aspects of the programme | 86% Latino. About two-thirds were obese | Variable attendance at the range of educational events | Self-management activities as part of a CCM of MDC implemented over a 3-year programme offering experiential learning in culturally and linguistically appropriate ways | Duration: programme ran for 3 years, rolling programme of classes, drop-in events and access to support |
| Diabetes, Senior 2008,263 Canada, five community clinics | Quality improvement report. Based on RCTs | To determine whether community-based teams could deliver a multifactorial intervention to promote good health and reduce the risk of cardiovascular and renal complications | Adults (aged > 17 years) with diabetes + hypertension or albuminuria | 570 referrals, 464 had scheduled visits in the time frame of the study | 424 (74.4%) attended the first visit | Mean age: 59 years (SD 13) Gender: 52.8% male |
37 (8%) did not attend the first appointment | Individualised education from a trained nurse and dietitian focusing on diabetes, lifestyle changes, pharmacotherapy, barriers to self-care, adherence to lifestyle recommendations and current therapy. Professionals’ undertook a 5-day training programme covered specialist clinical knowledge, principles of teaching adult learners + and were supported with mentoring | Programme duration: 2004–5. Two patient home visits: 2 hours and 1 hour |
| Diabetes, Musacchio 2011,264 Italy, secondary care diabetes clinic | Before-and-after study using routine data. Based on RCTs and recognised frameworks | To assess the impact of the intervention on clinical outcomes (maintaining stability) while reducing the number of face-to-face encounters | People with optimised treatment and stable T2DM (i.e. a steady level of HbA1c ≤ 7.0%) and able to follow the programme | NR | 1004 (referred to the programme and with clinical data for the preceding year) | Mean age: 66.6 years (SD 6.2) Gender: 54.1% male |
NR | Based on the CCM, the education programme aims to shift care from regular specialist review to supported self-management. The core components are education of the whole diabetes team; initial specialist assessment; referral to the educational programme; and follow-up with the specialist nurses and dieticians | 1-year follow-up for clinical data Intensity of programme: no detail but involves group, individual and follow-up consultations |
| LTC, study, country, setting | Study | Intervention | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|
| Design and duration | Quality score | Patient | Professional | Organisation | Health service utilisation | Disease control and QoL | Process | |
| Primarily professional training | ||||||||
| Diabetes, Stevens 2010,237 USA, secondary Care | Prospective monthly collection of routine data | 11 | – | Teaching practice teams, faculty, residents and staff participated in collaboratives by attending monthly calls and regular 2-day face-to-face meetings with the other teams | Teams used rapid cycle PDSA cycles to implement aspects of the CCM. There was ‘strong moral and financial support’ from the institutions. Teams reported performance measures monthly | – | Compared with baseline, at the 12-month follow-up more patients from participating teams had:
|
Compared with baseline, at the 12-month follow-up participating teams reported that more patients had:
|
| 57 teams from 37 teaching hospitals | Implementation strategy: collaborative application of PDSA cycles Fidelity: monitored as part of the improvement programme and markers improved over time |
|||||||
| Author’s reflections and lessons learned: implementation of the CCM in these settings required a substantial redesign effort even for these highly motivated teams The collaborative strategy was effective for team learning. For example, high-performing teams developed benchmarks and implementation strategies that have been reported elsewhere as a ‘tool kit’ for developing the CCM in an academic environment |
||||||||
| Primarily patient education | ||||||||
| Diabetes, Albisser 2001,238 USA, managed care | Controlled longitudinal observational study | 14 | Standard diabetes education for all patents (ED only), supplemented by daily automated telephone self-monitoring or self-management education from a diabetes educator | Multidisciplinary team – all trained to deliver diabetes care | – | Costs to the organisation were:
|
Compared with baseline, at 12-month follow-up HbA1c had:
|
|
| First 978 patients to enrol into one of three initiatives: ED-only n = 151, +TC n = 238, +SM n = 589 | Implementation strategy: initiative offered by the MCO. Recruitment not described. Unclear if there were any incentives provided. One case worker was dedicated to the telephone self-monitoring self-care initiative: 45 MDC providers supported the self-management education initiative Fidelity: not reported |
|||||||
| Author’s reflections and lessons learned: both the automated telephone self-monitoring and the self-management education initiatives improved HbA1c. Therefore, in choosing a DDMP, it would appear that costs should be the primary consideration and methodologies that control body weight should be a priority Findings suggest the use of computer technology and modern telemedicine to play an important role in future disease management initiative for diabetes |
||||||||
| Diabetes, Harris 2000,239 USA, community | Before-and-after study | 13 | Patient education: group diabetes education and one-to-one instruction in monitoring blood glucose, administering insulin, meal planning | – | Programme supported by a clinic set up to provide care for a homeless community often with no regular health-care provider | No data (many of the patients had no regular health-care providers) | Of the 22 people who had HbA1c measured before and after the intervention, 16 (73%) had improved, five (23%) were worse and one had stayed the same | Of the change goals identified by the 25 people who completed the course, all were rated as being at least 50% successful |
| 85 people with diabetes from a deprived community. Only 25 patients completed all follow-ups | Implementation strategy: community-based teaching sessions run by volunteer educators Fidelity: poor, mainly because of the psychosocial problems of the community being targeted |
|||||||
| Author’s reflections and lessons learned: barriers included (1) transportation, as many patients depended on public transportation or family and friends; (2) referrals, marketing the programme better; (3) empowerment, empowering patients who avoid responsibility is challenging; and (4) resources, most dietary substitutions and medications are expensive which can impede people from maintaining behaviour change | ||||||||
| Diabetes, Jordan 2011,240 UK, primary care | Retrospective cohort study comparing cases with matched controls from the General Practice Research Database | 18 | A diabetes trained nurse developed a personalised care plan with the patient using decision-support software. Motivational coaching with counselling and support for self-management and lifestyle change delivered during pro-active telephone calls | Specialist nurses trained in case management and diabetes education | – | NR | Compared with baseline, at follow-up intervention patients had reductions in:Measurements in the General Practice Research Database controls remained stable. Greater improvements were seen in those with worse baseline scores | NR |
| 473 (out of 1195 enrolled) with outcome data at 90 days or more (mean 332 days) | Implementation strategy: organised by a collaboration of NHS and private provider Fidelity: not reported |
|||||||
| Author’s reflections and lessons learned: the intervention targeted deprived communities who are traditionally hard to reach and seemed to benefit patients with poor outcomes from deprived populations The use of telephone intervention overcomes barriers related to non-participation in self-management programmes |
||||||||
| Diabetes, Kelly 2005,241 Australia, community | Before-and-after study | 10 | Telephone coaching to support the setting of realistic lifestyle and to develop care plans for discussion with GP | Nurse of other HCPs trained to provide coaching using motivational interviewing | Three monthly reports to the primary care practice | No outcomes reported | No outcomes reported | Improvement in a number of self-reported general health outcomes (‘fearful of health’, ‘health worries’, ‘frustrated with health’, shortness of breath’, ‘pain’) |
| 343 enrolled, 145 completed measures at baseline, 6 and 18 months | Implementation strategy: referral service for primary care using telephone coaching Fidelity: not assessed |
|||||||
| Author’s reflections and lessons learned: this project demonstrates an augmentation of the traditional role of the GP seeing patients on an intermittent basis and having the GP’s advice and management reinforced between visits | ||||||||
| Diabetes, Lowe 2008,242 Australia, secondary care | Prospective observational study | 18 | 4-day educational programme to teach patients to adjust their insulin dosage to their carbohydrate intake + self-management skills (i.e. problem-solving, goal-setting) + empowerment programme | Delivered by a professional team of a physician and a diabetes educator | – | – | Compared with baseline, at 12 months:
|
Compared with baseline, at 4 months:
|
| 137 insulin requiring diabetic patients attending the programme in 2001–2 | Implementation strategy: the programme, which has been running for the last 13 years, uses a collaborative approach in which a medical officer and a dietitian (who is a credentialed diabetes educator) cofacilitate a programme aimed at helping people build up the knowledge and psychosocial skills to develop an advanced diabetes self-care plan Fidelity: not assessed |
|||||||
| Author’s reflections and lessons learned: an intensive diabetes self-management programme led to improvements in HbA1c, empowerment and QoL that were largely sustained at 1 year. This is all the more remarkable given that the intervention was once only, entailed no long-term follow-up and took place in normal clinical operations | ||||||||
| Diabetes, Lowe 2009,243 Australia, secondary care | Historical cohort study | 18 | 4-day programme to teach patients to adjust their insulin dosage to their carbohydrate intake + self-management skills (i.e. problem-solving, goal-setting) + empowerment programme vs. didactic training on insulin management | Delivered by a professional team of a physician and a diabetes educator | – | Compared with those who had attended basic training, attendees on the combined course were:
|
Compared with those who had attended basic training, attendees on the combined course were:
|
– |
| 119 on the combined training + empowerment programme vs. 383 on the basic training course | Implementation strategy: both the combined programme and the basic training had been running for many years Fidelity: not assessed |
|||||||
| Author’s reflections and lessons learned: a one-time, complex intervention was able to enhance diabetes care and postpone hospital admissions/visits as much as 5 years later. Whether this is because of increased education contact time by enthusiastic and motivated HCPs or the specifics of the programme will need further research | ||||||||
| Diabetes, Roblin 2007,244 USA, MCO (primary care) | Case–control using routinely collected data | 16 | 2-hour class programme of diabetes education and self-management training | – | – | – | Compared with controls, at 6-month follow-up cases had:
|
– |
| 1991 cases + 12,741 matched controls | Implementation strategy: routinely available diabetes education offered to all newly diagnosed diabetics in the MCO Fidelity: not assessed |
|||||||
| Author’s reflections and lessons learned: participation in a multifactorial diabetes health education programme significantly improved glycaemic and lipid levels in the short term | ||||||||
| Diabetes, Welch 2006,245 USA, managed care | Before-and-after survey data | 15 | Telephone calls to provide patient education on diabetes, meal planning, managing hypo- and hyperglycaemias, medication and sick days. Supporting education materials, graded support (including case management and telemonitoring according to risk) | – | – | Blacks and Hispanics reported more annual health-care visits (average of 6.2 and 6.5 respectively) compared with whites (average of 5.0); p < 0.0001 | – | At follow-up, both blacks and whites were more likely than at baseline to report up-to-date status of influenza and pneumococcal vaccination (p ≤ 0.0001). The racial/ethnic gap in self-management behaviours observed at baseline had reduced |
| 1961 members with high-risk diabetes | Implementation strategy: high-risk diabetes patients, stratified for centrally delivered, graded education + support programme Fidelity: no report on the fidelity of the programme delivery |
|||||||
| Author’s reflections and lessons learned: the largest improvement was in closing the racial/ethnic gap in self-management behaviours | ||||||||
| Diabetes, Banister 2004,246 USA, community clinic | Before-and-after study | 16 | Patient education: group and individual diabetes education followed by support meetings | – | – | The cost of the intervention was $280 per person/year: $185 for each point reduction in HbA1C | Compared with baseline, at 12-month follow-up participants had:
|
54 (77%) met the dietitian. 29 (41%) attended at least one follow-up support meeting; 75% of patients who attended support meetings reported daily home glucose testing |
| 70 patients with T2DM at the low poverty level | Implementation strategy: introduction of structured education within a community clinic Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: barriers identified to follow-up were work schedules, lack of transportation and family commitments | ||||||||
| Diabetes, Joshu 2007,247 USA, primary care | Before-and-after study | 16 | Patients referred to the self-management course, were seen by the promotores who provided self-management information | – | Monthly promotores meetings were held with physicians to discuss and address patient self-management issues | – | Compared with baseline, 12 months post education participants:
|
On average patients attended 8 out of the 10 sessions: 25% attended support groups |
| 301 patients with T2DM | Implementation strategy: CHWs (promotores) were integrated into the clinic in order to support self-management Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: a team approach among providers, clinical staff, and promotores is essential for successful programme outcomes and continual improvements to patient care | ||||||||
| Diabetes Micklethwaite 2012,248 USA, secondary care | Before-and-after study | 12 | The team worked with individual patients to set goals, monitor progress and help improve coping skills. They also offered five 2-hour group sessions on a rolling basis | – | Programme was provided free of charge | Admissions dropped from 22 prior to programme to 1 post programme. This resulted in a net saving of $43,417 | Compared with baseline, latest reading post enrolment showed:
|
– |
| 81 diabetics with an A&E attendance and/or admission | Implementation strategy: free provision of self-management education led by a dietitian and nurse as part of a multidisciplinary team Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: a programme with unreimbursed expenses is competing for shrinking resources with services that may bring a positive return on the investment. Grant funding can provide valuable seed money to develop, test and implement a beneficial new programme, but grants are not a reliable or permanent source of funding | ||||||||
| Diabetes, Rasekaba 2012,249 Australia, secondary care | Before-and-after study | 17 | A diabetes nurse educator works with the patient to set treatment goals and strategies to implement lifestyle modifications. Referrals to the other team members are made as needed | – | – | – | Compared with baseline, 12 months post enrolling in the programme patients had:
|
The median number of contacts was 13 (range 1–52) in the group with good glycaemic control at enrolment; 16 (range 1–52) in the suboptimal control group, and 20 (range 4–52) in the poor control group |
| 545 people with diabetes with HbA1c available at baseline and 12 months follow-up) | Implementation strategy: integrated programme which optimises medical management to improve glycaemic control and prevent complications, and provide training in diabetes self-management and lifestyle modification Fidelity: not reported for content of the education programme. Patients attended an average of 13 (range 1–52) appointments over 12 weeks |
|||||||
| Author’s reflections and lessons learned: there is a known shortage of GPs and endocrinologists in the catchment area of this programme. The programme attempted to address this need by providing patients with expert endocrinologist review and development of a medical management plan aimed at achieving optimal glycaemic control | ||||||||
| Diabetes, Sedlak 2005,250 Austria, secondary care | Before-and-after study | 13 | Structured educational programme adjusted for the patient’s age and needs which enabled blood glucose self-monitoring and adjustment of insulin doses vs. information about diabetes and community nurse care | – | Community nurses undertook blood glucose monitoring and insulin dosing for the patient unable to undertake the training programme | Compared with control group, 2 years after starting insulin patients in the programme had:
|
Compared with control group, patients in the programme had:
|
Compared with control group, 2 years after starting insulin patients in the programme:
|
| 43 T2DM patients aged > 80 years who had started insulin therapy in the hospital | Implementation strategy: age-appropriate version of the standard training programme introduced for patients with T2DM who had just commenced insulin Fidelity: no attrition from the programme |
|||||||
| Author’s reflections and lessons learned: the programme was not suitable for about half of all newly insulin-treated patients over the age of 80 years normally because of reduced cognitive capacity | ||||||||
| Diabetes, Bott 2000251 Germany, secondary care | Before-and-after study | 14 | In addition to addressing knowledge deficits, the 5-day inpatient programme provides intensive group discussion, individual motivational counselling and addresses psychosocial problems and coping strategies | – | – | There was no significant difference in number of admissions per patient/year | Compared with baseline, 18 months post inpatient programme patients had:
|
Blood glucose self-monitoring: 82% vs. 88% (not significant) |
| 76 patients with T1DM who had completed insulin training but were unable to achieve their therapeutic goals | Implementation strategy: intensive inpatient programme addressing psychosocial issues and coping strategies Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: a more individualised programme suggested by patients and which included psychological support, along with counselling, problem-focused strategies and emotional support seems to be important | ||||||||
| Diabetes, Pieber 1995,252 Austria, secondary care | Before-and-after study | 17 | Initial assessment and optimisation of treatment + small group training in adjusting insulin dosages according to the anticipated amount of carbohydrate intake and the actual blood glucose level | – | – | Compared with baseline, 3 years post programme patients had:
|
Compared with baseline, 3 years post programme patients had:
|
Compared with baseline, 3 years post programme patients were:
|
| 205 adults on insulin for > 12 months, able to switch to an intensive regime, and to be followed up at 3 years | Implementation strategy: based on existing intensive programmes, initial assessment and optimisation of treatment is followed by small group training to enable adjustment of insulin dosages according to the anticipated carbohydrate intake and the blood glucose level Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: implementing in an outpatient setting may be more beneficial since hospitalisation usually interrupts patients’ daily lifestyle, meal plans and meal times | ||||||||
| Diabetes, Sämann 2005,253 Germany, secondary care | 10 year longitudinal quality assurance project in 96 centres | 15 | The 5-day structured inpatient training course for intensive insulin therapy, teaches patients to match insulin doses to their food choices, while keeping blood glucose close to normal | – | – | – | Compared with baseline, 1-year post-programme patients had:
|
– |
| 9583 people with uncomplicated T1DM | Implementation strategy: national programme of inpatient self-management education to teach people with T1DM to adjust insulin dose according to expected food intake and pre-meal blood sugar Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: a liberated diet for patients with T1DM seems to be related to significant positive clinical outcomes as it improves patients’ self-management skills and confidence in managing their insulin and their ability to manage difficult situations | ||||||||
| Sämann 2006254 | This publication reports data from a subgroup of patients from Sämann et al.253 (see previous entry). All the descriptive information is therefore the same. It reports the impact of the intervention in a subgroup of 341 people with T1DM and a history of repeated or unexplained severe hypoglycaemia, or hypoglycaemia unawareness, or a history of repeated ketoacidosis | Compared with baseline, 1-year post-programme patients with a history of three or more episodes of severe hypoglycaemia the preceding year had:
|
||||||
| Author’s reflections and lessons learned: patients at high risk for severe hypoglycaemia or severe ketoacidosis may benefit from participation in a standard training programme for intensive insulin therapy and dietary freedom. Likely explanations for the observed effects are that the education improves self-management skills | ||||||||
| Sämann 2008255 | This publication reports data from a subgroup of patients from Sämann et al.253 (see entry above). All the descriptive information is therefore the same. It reports the impact of the intervention in a subgroup of 1592 teenagers and young adults (aged 12–24 years) with T1DM. The mean age was 19 years (SD 3) | Compared with baseline, 1-year post-programme teenagers and young adults with T1DM had:
|
||||||
| Author’s reflections and lessons learned: adolescents and young adults with T1DM benefit from participation in a standard training course for flexible, intensive insulin therapy and dietary freedom | ||||||||
| Primarily organisational change | ||||||||
| Diabetes, Glasgow 2002,256 USA, community, managed care or hospitals | Observation of change management | 9 (note: many of the criteria did not apply) | Not specified, as this was determined by individual teams, but focused on setting self-management goals | Commitment to collaborating in the change process to develop skills for implementing self-management | PDSA cycles as part of a collaborative to enable organisations to implement patient-centred self-management support as part of CCM | NR | NR | Compared with baseline, during last 3 months of follow-up proportion of patients reporting documentation of self-management goals increased from 3% to 23% |
| Seven organisations focused on diabetes (mean 256 patients with diabetes) | Implementation strategy: PDSA cycles as part of a collaborative with a specific focus on implementing patient-centred self-management support as part of CCM Fidelity: no formal count of the number of self-management PDSA cycles, but it was estimated that each team implemented at least 15–20 throughout the collaborative |
|||||||
| Author’s reflections and lessons learned: the Improving Chronic Illness Care Collaborative appears to be one mechanism of structuring and supporting necessary system changes It is our impression that the improvement teams that were most successful at self-management in the Collaborative adopted self-management as part of their philosophy as opposed to an optional extra), embarked on frequent PDSA cycles, identified specific staff to be responsible for delivery of each of the key aspects of the self-management model and integrated self-management support with other components of chronic illness care |
||||||||
| Diabetes Hargraves 2012,257 USA, community health-care teams | Paired health-care teams randomly allocated to intervention or control | 18 | Recipients of the CHW intervention. No specific patient programme | CHWs training: duration 48 hours (16 × 3-hour modules) + monthly support calls + three learning sessions | All the health-care centres were part of a collaborative programme of diabetes improvement | NR | No consistent pattern of improvement in clinical measures was observed for the 12 months before and 12 months after the CHW intervention | CHWs completed 1198 encounters with 540 patients in the six health centres (63% included recording or discussing a self-management goal). Compared with baseline, at 13-month follow-up more patients from intervention (but not control) centres had a documented self-management goal |
| 12 centres serving 1415 patients (494 in intervention + 921 in control) | Implementation strategy: the CHWs were implemented as part of a collaborative programme of PDSA cycles Fidelity: key aspects of the intervention that were monitored were the number of consultation with the CHW and the proportion of patients with a documented action plan |
|||||||
| Author’s reflections and lessons learned: CHWs were also critical to efforts to get patients to make and keep appointments We found that CHWs were frequently asked to work with patients not in their assigned population, which is an indication of their value to the centre Practice transformation that is team-based and patient-centred is extremely difficult without changes in the reimbursement system (e.g. reimbursement for CHW services on a fee-for-service basis) |
||||||||
| A whole-systems approach | ||||||||
| Diabetes Anderson 2008,258 USA, primary care | Before-and-after study | 12 | Individual + group self-management education about diabetes, plus setting and attaining realistic goals | Professionals were trained (with ongoing support) to provide self-management goal-setting | Implementation was through a series of PDSA cycles | NR | Mean HbA1c dropped by 0.9%/year (p < 0.0001). LDL cholesterol dropped by 23.3 mg/dl/year. Proportion achieving a BP of 130/80 increased from 121 (28.8%) to 206 (42.3%) | Total number of goals set = 2139. 1612 were assessed at follow-up; 72% had made significant progress towards their goals |
| 488 (of 2389) people with diabetes | Implementation strategy: a series of PDSA cycles involving staff training and ongoing monitoring and support Fidelity: ability of the newly trained staff to provide self-management using goal attainment was monitored and supported |
|||||||
| Author’s reflections and lessons learned: training professionals in proper self-management education techniques takes time and ongoing monitoring. There is a strong tendency for medical staff to revert back to more didactic modes of education. A method of oversight and frequent review is necessary to maintain fidelity with the self-management model | ||||||||
| Diabetes, Dettori 2005,259 USA, primary and secondary care clinics | Before-and-after study | 16 | Redesigned patient education using standardised resources, local (free) group education sessions. The diabetes nurse in each clinic provided one-on-one diabetes education | Provision of diabetes educators and training for local clinical staff in the practices | Support for identifying people with diabetes, establishing a register, recording recent care. Support for implementing proactive care and prompts to highlight outstanding procedures | Compared with baseline, at 3-year follow- up proportion of diabetics with:
|
Compared with baseline, at 3-year follow-up:
|
Compared with baseline, at 3-year follow-up the proportion of diabetics with:
|
| Routine clinical data and telephone survey of people with diabetes at baseline (59% response) and 3 years (62% response) | Implementation strategy: centrally organised and supported quality improvement programme involving the State Diabetes Control Program and the American Diabetes Association Fidelity: considerable investment in support for local practices, and monitoring process measures (such as immunisation rates, foot checks provided) |
|||||||
| Author’s reflections and lessons learned: system changes in primary care practices and the implementation of accessible diabetes education can improve care and reduce barriers for rural patients with diabetes on a countywide level For rural communities, one of the key barriers is access to diabetes education. This could be accomplished through distance communication strategies, such as telemedicine, or through the provision of educational support and resources to assist local health professionals to improve their diabetes education skills |
||||||||
| Diabetes, Gruesser 1993260 Germany, primary and secondary care | Physician survey and ‘before-and-after’ data from patient records | 13 | Patient education comprises four weekly group sessions covering basic information, self-monitoring, treatment, diet, foot care, PA, sick day rules and late complications. Teaching was practical, experimental and theoretical | Standardised training for office-based physicians (2.5 days) includes information about the patient education programme, basic methods of adult education | Supported national programme of structured diabetes education | – | Compared with baseline, 5–6 months post practice-based education:
|
Of the 127 physicians, 78 (61%) had performed at least one structured treatment and patient education course in their practice by the time of re-evaluation |
| 127 physicians + 179 patients of 17 physicians | Implementation strategy: nationwide implementation of a structured treatment and education programme for T2DM patients in Germany Fidelity: the Central Institute is responsible for quality control and the organisation of trainer seminars |
|||||||
| Author’s reflections and lessons learned: patient education, which is an obligatory and most effective part of diabetes treatment, has been introduced with a fee comparable with a very low salary Barriers in implementing the structured course included staff who had attended the course no longer being available, lack of time to organise the teaching, insufficient number of interested patients |
||||||||
| Diabetes, Korsatko 2007,261 Austria, primary care | Before-and-after study | 13 | The programme covers basic information, self-monitoring, treatment, diet, foot care, PA, sick day rules, and late complications | Structured roll-out of professional education | Provision of the course is reimbursed | All target parameters (HbA1c, BMI, BP, LDL cholesterol) improved significantly at 1-year compared with baseline; p < 0.001 | ||
| 2122 patients with T2DM who attended the follow-up assessment | Implementation strategy: a national programme of diabetes education Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: patients do not attend follow-up because of loss of motivation, a guilty conscience because they did not modify their behaviour after the training course, or because they do not see the sense of a follow-up, having already heard everything in the initial course | ||||||||
| Diabetes, Liebman 2007,262 USA, community-based health centre | Longitudinal data for 3 years before and the 3 years of the programme | 17 | Culturally appropriate counselling to increase diabetes knowledge; improve goal-setting, problem-solving and self-efficacy. In addition, drop-in sessions + support from CHWs | Training for professionals to implement self-management support | Wide range of options available from a multidisciplinary team | NR | Over 3 years prior to self-management programme, HbA1c had remained stable (between 8.1 and 8.4). During the subsequent 3 years of the self-management programme, the average HbA1c declined to 7.5 Proportion well controlled increased from 30% to 46% Proportion with very poor control decreased from 19% to 11% |
Participation in activities at least once:
|
| 1188 on the centre database: 580 (48.8%) participated in some aspects of the programme | Implementation strategy: a culturally appropriate programme of educational and supportive events delivered by a multidisciplinary professional team supported by community workers Fidelity: uptake of the range of educational options allowed for personal preference and varied (as was intended) |
|||||||
| Author’s reflections and lessons learned: involving more patients was challenging largely because of staff and space resources, rather than a lack of interest from patients The ability to engage patients has been largely due to the CHWs who developed personal relationships with patients, promoted self-management, and created the important linkages between patients’ home situations, participation in self-management activities and the patients’ clinical care. Their involvement as peers rather than professionals enables them to motivate patients |
||||||||
| Diabetes, Senior 2008,263 Canada, community clinics | Quality improvement report | 18 | Individualised education by a nurse dietitian focusing on diabetes, lifestyle changes, pharmacotherapy, barriers to self-care, adherence to lifestyle recommendations and current therapy | Professionals’ training covered diabetes, hypertension, cardiovascular protection, principles of teaching adult learners + training sessions + telehealth sessions + mentoring | Twice yearly supporting visits from consultant endocrinologist | – | Compared with baseline, at 9 months follow-up participants had:
|
Compared with baseline, at 9 months follow-up participants were more likely to be taking ACE-inhibitors, antiplatelets and lipid lowering drugs (60% vs. 37%); p < 0.001 |
| 412 adults (aged ≥ 17 years) with diabetes + hypertension or albuminuria | Implementation strategy: community-based diabetes education provided by a trained nurse and dietitian Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: the clinics were most warmly received in communities where there were few existing services; difficulties arose if the role of the new clinic was perceived to overlap with existing programmes The nurse and dietitian need to develop trust and overcome concerns with patients and local physicians before implementing any programme |
||||||||
| Diabetes, Musacchio 2011,264 Italy, secondary care diabetes clinic | Before-and-after study using routine data | 16 | Tailored diabetes education + empowerment incorporating problem-solving and addressing cultural and psychosocial needs + routine follow-up + accessible support via telephone or e-mail | Professional education of staff operating in the clinic to provide high-quality care to patients | All professionals with whom the patient interacted to implement the empowerment philosophy | Diabetologist consultations reduced from median 2.8 (IQR 2.3–3.4) to 2.3 (IQR 1.9–2.7) (p < 0.0001) visits per patient/year | Compared with baseline, a year post enrolment the proportion of patients with:
|
Proportion of patients treated with insulin was unchanged (from 5.2% to 5.9%). Use of antihypertensive drugs unchanged from 37.1% to 37.8% |
| 1004 people with stable diabetes and data from 1 year before to 1 year after enrolment in the programme | Implementation strategy: based on the CCM, the education programme aims to shift care from regular specialist review to supported self-management. The core components are education of the whole diabetologic team; initial specialist assessment; an educational programme; and follow-up with the specialist nurses and dieticians Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: transferring the responsibility to the patient with the professional’s support when needed was not associated with detrimental effect, but continuous contact with professionals when necessary is important. The synergic relationship between the patient and the professional encourages the patient to be their own ‘case managers’ and maintain good metabolic control in the long term in the absence of particular problems | ||||||||
| LTC, study, country, setting | Study design | Participants | Service implementation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Design underpinning evidence, theory | Aim | Eligibility criteria | Total eligible population | Number (%) participating | Participating population characteristics | Attrition | Intervention and strategy for implementation | Duration, intensity, frequency | |
| Primarily patient education | |||||||||
| Depression, Cavanagh 2011,265 UK, service user-led, third sector self help clinic | Before-and-after study. RCTs of the computer programs | To provide evidence on the generalisability and effectiveness for a cCBT programme in a widely accessible context | Adults, referred by GP or self-referred | 510 referrals to the service, 432 attended first appointment of whom 351 were clinically suitable for cCBT | 295 commenced the programme | 66% female. Mean PHQ 14.46, GAD7 12.8 | 295 started CBT, 265 completed two sessions, 156 completed all eight sessions. No reasons provided | Evidence-based cCBT for depression and anxiety. Initial video, then eight interactive 50-minute therapy sessions normally taken at weekly intervals with minimum supervision. ‘Homework’ between sessions (e.g. problem diaries, thought records, behavioural experiments). Clinical progress reports, including suicide risk indicators, were prepared after each session | Duration: eight weekly sessions Intensity and frequency: 50 minutes each session, first session 30–60 minutes |
| Depression, Farrand 2008,266 UK, primary care | Uncontrolled before-and-after study. Based on pilot work | To examine patient attendance and dropout in paraprofessional primary care clinics utilising the 2 + 1 model of service delivery and to examine efficiency and effectiveness of guided self-help | All patients were aged ≥ 16 years, had mild-to-moderate levels of anxiety or depression | 1162 referred to the service. 951 attended for the assessment. 823 were clinically eligible | 658 undertook the GMHW supported self-help programme | 36% male, mean age 40 years; 64% female, mean age 39 years | 76% attended final support session and 39% attended follow-up support session. Non-attendance at final session: being young, having lower levels of depression and anxiety, being unemployed or a student | Patient training: patients chose a self-help book with a GMHW who supported problem-solving and helped to overcome any difficulties | Initial assessment followed by two sessions, 1 week apart lasting 20 minutes each followed by a third session at 3 months |
| Depression, Learmonth 2008,267 UK, secondary care | Before-and-after study. Based on guidelines | To determine the effectiveness of cCBT in secondary mental health-care services | Adults suffering from anxiety and/or depression who had been referred to a CBT therapist for clinical assessment | Number of patients referred not reported | 104 | Mean age: 39.5 years (range 19–70 years) Gender: 63.4% female |
71 (63%) completed the eight sessions | Evidence-based cCBT for depression and anxiety. Initial video, then eight interactive 50-minute therapy sessions normally taken at weekly intervals with minimum supervision. ‘Homework’ between sessions (e.g. problem diaries, thought records, behavioural experiments). Clinical progress reports, including suicide risk indicators, were prepared after each session | Duration: eight weekly sessions Intensity and frequency: 50 minutes each session, first session 30–60 minutes |
| Depression, Learmonth 2008,268 UK, specialist CBT clinic | Before-and-after study. Based on guidelines | To develop and evaluate an cCBT service which could meet the increased demands for specialist CBT services | Adults suffering from anxiety and/or depression who had been referred to a CBT therapist for clinical assessment | 829 | 555 (67%) | Mean age: 39.8 years Gender: 63.1% female |
Of those who started the programme, 394 (71%) completed all eight sessions | Evidence-based cCBT for depression and anxiety. Initial video, then eight interactive 50-minute therapy sessions normally taken at weekly intervals with minimum supervision. ‘Homework’ between sessions (e.g. problem diaries, thought records, behavioural experiments). Clinical progress reports, including suicide risk indicators, were prepared after each session | Duration: eight weekly sessions Intensity and frequency: 50 minutes each session, first session 30–60 minutes |
| Depression, Marks 2003,269 UK, community CBT clinic | Before-and-after study | To evaluate a primary care clinic’s use of four cCBT self-help systems | Adults with anxiety or depression, motivated to use self-help; and no substance misuse, psychosis or active suicidal plans | 355 were referred, 210 were assessed as suitable for cCBT | 168 (80%) enrolled on the cCBT, 108 (51%) completed | Gender: 54% female | 60 (29%) did not complete. Reasons for withdrawing included hard to attend clinic; the therapy was unhelpful; wanting face-to-face help; low motivation; help offered elsewhere; problem improved | Patients used a computerised programme for depression and anxiety at least six times over 12 weeks. Six brief therapist contacts (telephone or face to face) were scheduled. Assessments made with an automated telephone call populated a review to assess suicide risk | Duration: 12 weeks |
| Primarily organisational change | |||||||||
| Depression, Newnham 2010270 Australia, secondary care CBT service | Historical cohort design. Based on RCTs | In the context of group CBT, to assess the effectiveness of monitoring patient progress with a measure of well-being (WHO-5), and feeding back the score to clinicians and patients | English-speaking patients with anxiety and/or depression who participated in the hospital’s 2-week CBT programme | 1308 participants in the CBT service between 2005 and 2009 | 1137. Groups in three time phases were matched so that 379 participants in each group | Mean age: 39.8 years (range 16–76 years) Gender: 63.1% female |
6.9% dropped-out of the control cohort, 10.3% in the no feedback cohort and 10% in the feedback cohort. No characteristics are provided | Group CBT intervention. Three cohorts: Group 1 (2005–6): no feedback Group 2 (2006–7): monitored with WHO-5, but no feedback until end of course Group 3: feedback at the mid-point enabling discussion and goal reassessment |
Duration: 10 working days Intensity and frequency: run ‘9–5’ each day |
| LTC, study, country, setting | Study | Intervention | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|
| Design and duration | Quality score | Patient | Professional | Organisation | Health service utilisation | Control and QoL | Process | |
| Primarily patient education | ||||||||
| Depression, Cavanagh 2011,265 UK, service user-led, third sector self-help clinic | Before-and-after study | 18 | Eight interactive computerised CBT sessions at weekly intervals + ‘homework’ (e.g. problem diaries, thought records, behavioural experiments) | Professional worker for the initial assessment, then centres are staffed by volunteer workers | – | – | Compared with baseline, at the end of the cCBT patients were less likely to meet ‘caseness’ criteria for depression or anxiety: 226 (85%) vs. 123 (46%)
|
295 started cCBT, 265 completed two sessions, 156 completed all eight sessions |
| 295 adults, referred by GP or self-referred | Implementation strategy: cCBT provided to people with anxiety/depression referred by their GP or self-referred as part of routine service Fidelity: cCBT is standardised |
|||||||
| Author’s reflections and lessons learned: cCBT can be effectively implemented in a service user-led, third sector self help clinic, increasing access to psychological therapies to meet local needs for interventions for depression and anxiety | ||||||||
| Depression, Farrand 2008,266 UK, primary care | Uncontrolled before-and-after cohort study | 16 | Patients chose to use a self-help book (brief behavioural activation/self-help approaches) with a GMHW who supported problem-solving and helped overcome any difficulties with using the book | GMHW have been associated with supporting and developing a range of interventions, though self-help currently forms the most significant aspect of the role | – | – | Compared with baseline, at the 3-month follow-up:
|
– |
| 658 patients who undertook the GMHW supported self-help programme | Implementation strategy: service provision to meet the increasing need for mental health treatments Fidelity: no report of the fidelity with which the intervention was delivered |
|||||||
| Author’s reflections and lessons learned: clinics on average employed three rather than two support sessions, possibly because patients were being referred into the guided self-help clinic with more complex difficulties than the clinics were originally established to deal with | ||||||||
| Depression, Learmonth 2008,267 UK, secondary care | Before-and-after study | 16 | Eight interactive cCBT sessions at weekly intervals + ‘homework’ (e.g. problem diaries, thought records, behavioural experiments) | – | – | – | Compared with baseline, at the end of the course patients had:
|
– |
| 104 adults suffering from anxiety and/or depression referred for cCBT | Implementation strategy: people on a waiting list for CBT were offered the computerised programme as an immediate alternative Fidelity: cCBT is standardised |
|||||||
| Author’s reflections and lessons learned: these preliminary findings suggest a potential role for cCBT within secondary care as a first step, self-help treatment tool for anxiety and depression | ||||||||
| Depression, Learmonth 2008,268 UK, specialist CBT clinic | Before-and-after study | 18 | Eight interactive cCBT sessions at weekly intervals + ‘homework’ (e.g. problem diaries, thought records, behavioural experiments) | – | – | At the end of the course, 72 (19%) of those who completed cCBT were referred for face-to-face CBT and 13 to other services. At the end of the course, 144 (90%) of those who did not complete the cCBT were referred to face-to-face CBT, and 9 to other services | Compared with baseline, at the end of the course patients had:
|
– |
| 555 adults suffering from anxiety and/or depression who had been referred to a CBT therapist for clinical assessment | Implementation strategy: people on a waiting list for CBT were offered the computerised programme as an immediate alternative Fidelity: cCBT is standardised |
|||||||
| Author’s reflections and lessons learned: adherence to the programme appears to be independent of age, gender, duration or severity of anxiety and/or depression The service capacity of the CBT specialist centre was increased by approximately 50% over the 5 years that CBT was used as part of the treatment options within the centre |
||||||||
| Depression, Marks 2003,269 UK, CBT clinic | Before-and-after study | 15 | Patients used a cCBT programme for depression and anxiety at least six times over 12 weeks. They had six brief scheduled therapist contacts (telephone or face to face). Automated telephone assessments populated a review to assess suicide risk | – | – | – | Compared with baseline, at the end of the course patients had:
|
– |
| 108 adults with anxiety or depression, motivated to use self-help | Implementation strategy: people on a waiting list for CBT were offered the computerised programme as an immediate alternative Fidelity: cCBT is standardised |
|||||||
| Author’s reflections and lessons learned: it can take a long time for sociopolitical processes to be worked through to make new technologies a routine aspect of health services The programme gives patients immediate rather than delayed access to CBT, unrestricted access, easier disclosure of sensitive information and removal of the need to travel to a therapist |
||||||||
| Primarily organisational change | ||||||||
| Depression, Newnham 2010,270 Australia, secondary care CBT service | Historical cohort design | 17 | Group intervention covering management of anxiety and depression, CBT techniques, communication skills and self-esteem. Each group member set treatment goals in homework tasks | – | Three cohort:
|
– | Feedback to staff and patients about scores on the WHO-5 did not significantly improve patients’ well-being by the end of the course (day 9) The subgroup of patients with poor well-being at the mid-point in the programme who received feedback exhibited relatively greater improvements in depression scores (vitality and role emotion domains) |
– |
| 1137 participants (379 in each of three groups) | Implementation strategy: routine monitoring with WHO-5 and feedback mid-course were integrated in the CBT service from 2007 Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: monitoring and feedback presents an opportunity to improve safety issues, increase the reliability of outcome measurement and foster a collaborative relationship between clinician and patient | ||||||||
| LTC, study, country, setting | Study design | Participants | Service implementation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Design underpinning evidence, theory | Aim | Eligibility criteria | Total eligible population | Number (%) participating | Participating population characteristics | Attrition | Intervention and strategy for implementation | Duration, intensity, frequency | |
| Primarily patient education | |||||||||
| COPD, Pushparajah 2006,271 UK, community | Before-and-after study. Based on RCTs | To provide a hospital-initiated community-based programme to improve chronic management of COPD at home, and thereby to reduce readmissions with exacerbations of COPD, and LOS | Patients admitted with exacerbation of COPD, resident in the area | 255 admissions, 109 not eligible/died. Total eligible = 146 | 95 (65%) received the intervention | Gender: 46% male | 21 had no accurate contact details, 20 declined, 10 discharged before assessment | Home visit immediately after discharge to provide COPD self-management, medication review, assessment of coping ability and referral to other services when required | Duration: November 2000–March 2002 (excluding 18 weeks between March 2001 and July 2001) |
| CKD, Chen 2008,272 Taiwan, peritoneal dialysis unit | Retrospective audit of health-care records. Based on guidelines | To determine whether or not training for new peritoneal dialysis patients meets Taiwan standards and reduces peritonitis | New peritoneal dialysis patients | NR | Data from 100 new patients | Mean age: 52.7 years (SD 16.1) Gender: 58% female |
NR | Individualised intervention including attending lectures, receiving printed materials (signs and symptoms of peritonitis and complications, and troubleshooting) and practice dialysis procedures | Intensity and frequency: a qualified peritoneal dialysis nurse spends 25–40 hours to train each new patient |
| CKD, Loos-Ayav 2008,273 France, dialysis unit | Before-and-after study. Based on RCTs | To investigate changes in HRQoL observed during the first year of RRT, comparing patients on self-care dialysis with patients on in-centre dialysis | Patients aged 18–70 years, starting dialysis in 1997–9 and still on dialysis a year later | 277 patients commenced dialysis: 49 died during the first year of dialysis, and 33 had a kidney transplant | 195 were still on dialysis at 1 year | NR for the whole population. Mean age for those who achieved autonomy = 50 years vs. 56 years for those who did not | – | Individualised structured training in self-care dialysis provided by specialist nurses, including education about CKD, dialysis and its complications, training in the necessary skills safely to implement dialysis, and ongoing supervision to establish home dialysis | Patient training: three sessions/week. Peritoneal dialysis training lasted 1 week; haemodialysis training lasted 3–6 months; staff training involved a 4-day training course |
| LBP, van Hoof 2010,274 the Netherlands, secondary care clinic | Before-and-after study. Based on guidelines | To evaluate the 1-year follow-up results of a programme based on the cognitive–behavioural approach in patients with chronic LBP | Adults (aged 20–65 years). LBP for > 6 months, off work for < 2 years, no planned surgical, medical or pain treatment, motivated and willing to follow the 2-week, hotel-based programme | 155 referred, 107 were assessed | 59 after exclusions and withdrawals | Mean age: 44.1 years (range 23–60 years) Gender: 57% female |
19 (12%) failed to meet the inclusion criteria, 17 (11%) decided not to join the programme, 12 (8%) postponed participation for diverse reasons | Structured programme including CBT, education and physical activities. Patients aimed to achieve their own goals and to return to an active lifestyle by using activity-based planning and pacing strategies, alongside CBT techniques to endorse more adaptive behaviours and beliefs | Duration: 100 hours over 10 days + 2 days follow-up Intensity and frequency: 50 hours of CBT, 35 hours of PAs and 15 hours of education |
| Primarily organisational change | |||||||||
| COPD, Deprez 2009275 USA, rural primary care | Before-and-after study. Based on guidelines | To improve standards of care for COPD (specifically including self-management) | Practices in rural state of the USA | NR | 18 practice teams (25 physicians), 584 (pre-) and 626 (post-) patients + focus groups of patients | NR | NR | Using a collaborative model the emphasis was on developing goals and action plans at the practice level. Teams reported their practices’ progress, including accomplishments, challenges and barriers faced, so that others could learn from their experiences | Duration: each collaborative lasted 9 months |
| A whole-systems approach | |||||||||
| Hypertension, Gruesser 1997,276 Germany, primary care | Survey of physicians and before-and-after study. Based on RCTs | To evaluate the practicability and efficacy of the structured treatment and teaching programme for patients with hypertension in routine primary health care | Primary care physicians who had participated in the training and the patients trained | 111 practices trained, 466 patients | 272 (58%) patients of 43 of the participating physicians | Age: 59 years (SD 12) Gender: 55% female |
NR | A national initiative to promote self-management for people with hypertension. Training courses were run for primary care physicians who were then reimbursed for providing standardised education to people with hypertension | Patient training: Intensity and frequency: four sessions at weekly intervals, 90–120 minutes Staff training: Intensity and frequency: 1 day; adult education 1.5 days |
| Hypertension, Bosworth 2011,277 USA, managed care | Before-and-after study. Based on previous work in MCOs | To evaluate the implementation of a multifaceted programme, tailored to patients and administered by nurse care managers to improve adherence to medication as measured by prescription fill patterns | Adults with hypertension, enrolled with North Carolina Medicaid for 12 months before and for duration of the study, enrolled with a primary care provider and receiving hypertensive medication | 4550 were approached by the case managers | 558 participated | Mean age: 51.1 years Gender: 68% female |
Programme to improve care of Medicaid patients following the principles of the CCM The intervention comprised telephone calls to provide:
|
Duration: 6-months Intensity and frequency: 10 calls during the 6 months (approximately 3-weekly) |
|
| Stroke, Mosimaneotsile 2000,278 Hawaii, secondary care | Observational study using routinely collected, longitudinal data | To evaluate the integrated delivery model of care over time | People referred to the unit < 30 days after a stroke, and who were in the unit for < 30 days | 1526 referred to the unit: 287 were excluded because they were outside the time scales for the unit | 1239 | Over the 4 years, demography was stable (mean age 68 years; gender 52% male). Baseline disability (FIM score) decreased over the 4 years | Phased introduction of an integrated model of care in a stroke unit which engages all members of the team in supporting the patient to achieve their goals and achieve re-entry into the community | Inpatient programme of rehabilitation until ready for discharge | |
| LTC, study, country, setting | Study | Intervention | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|
| Design and duration | Quality score | Patient | Professional | Organisation | Health service utilisation | Disease control and QoL | Process | |
| Primarily patient education | ||||||||
| COPD, Pushparajah 2006,271 UK, secondary care | Before-and-after study | 19 | Home visit within 5 days of discharge to provide COPD self-management, medication review, assessment of coping ability and referral to other services when required | – | – | Compared with the previous year, in the year after the intervention:
|
– | Medication errors were detected in 47 (59%) of the 80 patients. 23 (29%) were referred to other agencies for medication changes, medicines management or provision of aids |
| 95 (65%) adults discharged after a COPD admission (80 with complete data) | Implementation strategy: patients recruited during an admission and reviewed at home within 5 days Fidelity: intervention delivered by one specialist physio, process measures following the assessment are reported |
|||||||
| Author’s reflections and lessons learned: we were able to demonstrate that a community programme is effective and may be more beneficial in patients with more severe COPD who are high users of health care | ||||||||
| CKD, Chen 2008,272 Taiwan, peritoneal dialysis unit | Retrospective audit of health-care records | 13 | Individualised intervention including attending lectures, receiving printed materials (signs and symptoms of peritonitis and complications, and troubleshooting) and dialysis procedures | – | – | – | During the (not specified) study period, there were 19 episodes of peritonitis, 18 episodes of exit-site infection and three episodes of tunnel infection The risk of peritonitis was not related to the post-training scores (p = 0.8) |
Post training, 70% of the knowledge questions were answered correctly. Patients with a lower education level tended to have worse scores |
| 100 new dialysis patients | Implementation strategy: structured education programme delivered by nurses in a peritoneal dialysis unit Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: the learning abilities of patients, as judged by test scores, does not correlate with the risk for peritonitis suggesting that even patients with a minimum educational background can learn to perform peritoneal dialysis. Every dialysis patient, therefore, needs to know the early symptoms and signs of peritonitis and other complications | ||||||||
| CKD, Loos-Ayav 2008,273 France, dialysis unit | Before-and-after study | 22 | Individualised structured training in self-care dialysis including education about CKD, dialysis and its complications, training in the necessary skills safely to implement dialysis, and ongoing supervision to establish home dialysis | Professionals’ training: qualified nurses took a 4-day training course and took 2 months of clinical training in an authorised peritoneal dialysis training centre | – | – | At baseline, patients who achieved autonomy were younger with fewer comorbidities Several dimensions of the HRQoL were significantly higher in autonomous patients at 12 months: less burden of kidney disease (51.7 vs. 37.3), fewer effects of kidney disease (65.9 vs. 54.0), better cognitive function (72.0 vs. 62.7) and role emotional (53.0 vs. 34.5) |
At a year, 48 patients were considered autonomous and 147 non-autonomous |
| 195 patients aged 18–70 years, on dialysis for at least a year | Implementation strategy: structured education programme delivered by a dialysis unit Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: the patient’s active participation in disease management, the motivation of the nephrology team and the resources devoted to patient education are of utmost importance | ||||||||
| LBP, van Hoof 2010,274 the Netherlands, secondary care clinic | Before-and-after study | 20 | Structured programme (CBT + activity based) focusing on returning to an active lifestyle, using planning and pacing techniques + CBT to endorse more adaptive behaviours and beliefs | – | – | – | Compared with baseline, patients at 12 months had:
|
– |
| 59 adults with chronic LBP | Implementation strategy: patients referred by orthopaedic surgeons for 10 hours of CBT- and activity-based programme Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: the participants of this evidence-based programme learned to manage chronic LBP, improved in daily functioning and QoL Comparisons with other studies seem to indicate that the intensity, duration and frequency of a CBT pain management programme may be the most important key to success Factors such as mood, fear of movement, catastrophising, coping strategies and self-management seem to be important factors |
||||||||
| Primarily organisational change | ||||||||
| COPD, Deprez 2009,275 USA, rural primary care | Before-and-after study | 13 | Practices focused on providing self-management education to patients in their care | Professional education and training on guidelines was part of the collaborative | Implementation of health-care improvement teams, in-practice reminders to prompt physicians and staff to use the evidence-based guidelines, implementation of a COPD registry | – | – | Compared with baseline, at the end of the collaborative, documentation of:
|
| 18 practice teams (25 physicians), 584 (pre-) and 626 (post-) patients + focus groups of patients | Implementation strategy: collaborative approach. Practice barriers and patient barriers were identified through focus groups and were then addressed at the learning sessions and through direct contact with the practices Fidelity: practice self-reported assessment of process outcomes |
|||||||
| Author’s reflections and lessons learned: participants reported that the collaborative nature of the project allowed for mutual learning, provided teams with support to identify and overcome barriers and fostered teamwork to find solutions to shared problems We learned that tools must fit within the current care system and be tailored to the goals of the collaborative. Although the COPD registry system was useful to provide feedback to providers, there must be motivation for providers to use this tool, particularly for small practices with few COPD patients Success requires strong clinical leadership in the practice and/or at the system level. Clinical intervention programmes have limited impact without physician buy-in and active participation. Equally important, however, is that individual team members see value in the effort and feel that it warrants their time and commitment Although we brought some community resources into the collaborative (e.g. pulmonary rehabilitation centres, tobacco helpline), it would be helpful to have a greater focus on system-level collaboration and system-level changes to accompany the work of practices |
||||||||
| A whole-systems approach | ||||||||
| Hypertension, Gruesser 1997,276 Germany, primary care | Survey of physicians and before-and-after study from patient records | 14 | Patient education: group discussion on hypertension and their experience; learned to practise BP measurement; methods of achieving satisfactory BP through lifestyle changes were discussed | Professionals’ training: staff informed about the programme, received training on adult education, received guidelines and information on their responsibilities in implementing the programme in their practice | Training courses were provided for primary care physicians. Reimbursed for providing the education courses was proposed, but not implemented during the time of this study | – | Compared with baseline, after the intervention patients had:
|
63(57%) of the 111 practices performed at least one structured treatment and patient education course during 8 months |
| Survey of 111 physicians and retrospective data from the records of 272 patients from 43 of the practices | Implementation strategy: a national initiative to promote self-management for people with hypertension Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: the results of the study demonstrate the practicability and efficacy of the implementation of the programme for patients with hypertension into routine primary health care Barriers to implementing the programme in routine clinical care included (a) lack of time to organise the group teaching in the practice; (b) staff missed the training course; (c) the staff who attended the training were no longer available; (d) dislike of the programme; (e) insufficient number of interested patients; (f) practical equipment problems; and (g) lack of time on the part of the patients |
||||||||
| Hypertension, Bosworth 2011,277 USA, MCO | Before-and-after study. Administrative data provided feedback on the quality of care | 15 | Telephone-administered tailored hypertension education, focus on medication adherence, side effects and improving medication adherence | The care managers received training, but were also supported by computerised scripts | The three locations were the most enthusiastic about the programme and had identified hypertension as a problem in their organisations | – | – | Compared with baseline, a year after the programme:
|
| 558 people with hypertension | Implementation strategy: programme to improve care of Medicaid patients following the principles of the CCM Fidelity: patients received 4.5 calls over 6 months |
|||||||
| Author’s reflections and lessons learned: the most common challenges the care managers experienced were locating and tracking down patients, particularly given their other responsibilities Motivation is an important aspect of implementing routine clinical care. The study included implementation sites volunteering to participate, active feedback being requested from care managers and primary responsibility for the programme resting with the care mangers |
||||||||
| Stroke, Mosimaneotsile 2000,278 Hawaii, secondary care | Observational study using longitudinal data | 13 | Comprehensive assessment and tailored rehabilitation programme to learn the skills required for independent living | All the multidisciplinary team members were involved in providing or supporting care | Organisational strategy to improve integration of care and improve efficiency | Compared with 1994, in 1997:
|
Compared with 1994, in 1997:
|
– |
| Routinely collected data on 1239 people referred to the unit < 30 days after a stroke | Implementation strategy: phased introduction of an integrated model of care in a stroke unit which engages all members of the team in supporting the patient to achieve their goals and achieve re-entry into the community Fidelity: NR |
|||||||
| Author’s reflections and lessons learned: the system integrates a number of components – use of collaborative care maps, integrated documentation, collaborative team assessment and follow-up, cross-functional training of rehabilitation technicians, and integrated patient/caregiver education. The authors consider that it was not possible to identify which aspect of the integrated delivery model of care was most important | ||||||||
Asthma
Description of the studies
We included 19 papers reporting 18 studies (see Table 116 for details) nine of which were conducted in the USA,219,220,222–225,230,231,234 four from the UK,218,226,228,236 two from Brazil,229,235 one (two reports) from Finland232,233 and two from other European countries. 221,227 The majority (n = 9) were conducted in primary care or community settings,218,219,226,228,229,234–236 four in managed care organisations (MCOs),220,222,223,225 one in secondary care,230 three in schools221,224,231 and one (two reports) was a national multisetting initiative. 232,233
Quality assessment and weighting of the evidence
Study designs varied, with five cluster randomised trials,218,219,224–226 a preference trial with randomised groups222 or controlled implementation. 228 Seven were based on longitudinal data,220,223,230–235 one with a control cohort,229 and two uncontrolled before-and-after221,236 or cross-sectional studies. 227
This resulted in substantial variation in quality assessment, ranging from 10 to 24 out of a possible score of 28. 48 Common reasons for low quality included lack of information on participants lost to follow-up (n = 15) and/or whether participants were representative of the whole eligible population (n = 11). Defined whole eligible populations ranged from 135 to 6984. One study232,233 reported a national initiative and an estimated population of 350,000 people with asthma. Participating populations ranged from 84 to 1895 participants.
Intervention description and results
Primarily professional training with or without organisational change
Two studies described interventions primarily directed at professionals. 218,219
Cleland et al. ,218 in a high-quality UK cluster RCT, provided asthma education, including communication skills and advice on formulating action plans, to primary care asthma nurses in a single workshop. The intervention had no impact on process or clinical outcomes, and the authors considered that they had underestimated the complexity of the support required to enable the nurses to make the organisational changes necessary to implement self-management in practice. The authors also reflected that inconsistent coding made it impossible to ascertain whether patients in the intervention arm received more or fewer action plans than the patients in the control arm.
In a US cluster RCT (n = 43 practices), Homer et al. 219 implemented a quality improvement intervention for children and adolescents with asthma by training and educating professionals from the practices. Results showed an increase in the proportion of children in the intervention practices with action plans from 37% to 53%, but no impact on clinical outcomes. The training aimed to support implementation, but the authors observed that there was considerable lack of engagement with the programme (only 9 of the 22 practices attended all the training sessions, and even fewer submitted any performance data).
These two studies thus reach similar conclusions: professional training is insufficient on its own to achieve successful implementation of a new intervention. There is a need to support trained professionals by addressing the organisation’s strategic priorities and the logistical barriers to achieving change.
Primarily patient education, with or without organisational changes
Six studies described interventions directed primarily at educating patients: four in US MCOs,220,222,223,225 and two in schools. 221,224
The health-care studies were two trials of good quality,222,225 a time series analysis220 and a before-and-after study. 223
In Delaronde et al. ,222 the US MCO offered adult members a 6-month programme of nurse-led individualised telephone calls reinforced by educational material which focused on improving asthma knowledge and supporting self-management, reviewing adherence, revising action plans. In a preference design, patients who ‘opted-in’ were compared with those who ‘opted out’ and to those who expressed no preference and were randomised to intervention or control. Twenty-seven per cent of the intervention group and 68% of the opt-in group completed the programme. The ratio of preventer to reliever treatment improved in both groups receiving the education, but to a greater degree in the ‘opt-in’ group. The authors concluded that self-motivation was an important indicator of readiness to initiate and maintain asthma self-management. 222
Vollmer et al. 225 provided an automated telephone intervention designed to identify risk, provide self-management information and alert their HCP to half the 7000 members with asthma in an MCO. Overall, the intervention showed no significant difference in medication use, asthma control or health-care utilisation, but only 12% of the intervention group completed all three automated calls. Completion rate in a subgroup of 192 patients who received telephone calls from a live-caller was 28%, suggesting that direct interaction with the professional is important.
In Bunting et al. ’s study,220 self-management education from an asthma educator and regular review from a community pharmacist improved control and reduced use of health-care resources in a time series analysis over 5 years.
In a before-and-after study, Forshee et al. 223 demonstrated that delivery of tailored asthma education to high-risk patients by nurse champions was associated with improved control and reduced unscheduled consultations. Implementation was more effective in centres where the nurse champion was an existing member of staff.
These four studies were all promoted and funded by MCOs which provided health care to their insured members. This relationship may have had an impact on the uptake of and adherence to the initiatives.
The remaining two patient education interventions were implemented in schools and provided teaching for families, children and staff as well as systematic identification of children with asthma. 221,224 In a before-and-after study in Italian primary schools, Chini et al. 221 demonstrated improved morbidity from an intervention which aimed to foster relationships between parent, school and health-care services. In a good-quality cluster randomised trial, Gerald et al. 224 targeted low-income African-American children, and showed no differences in school absences, or use of emergency health care. Challenges were the high turnover in staff and pupils at the inner-city schools, and limited parental involvement. 224
Primarily organisational change
Three interventions targeted the organisation with the aim of improving asthma reviews including self-management education. 229,236,251 The common approach was the promotion of structured routine reviews with an asthma trained nurse whose remit included self-management education and the provision of personalised asthma action plans (PAAPs).
Two high-quality trials in UK primary care facilitated asthma reviews by sending action plans with postal reminders,236 or offering telephone reviews. 229 Kemple and Rogers226 showed that, compared with just sending an invitation letter, enclosing an action plan increased the proportion of patients responding to the invitation to a review and facilitated discussion of self-management at the review. Partially completing the plan improved patients understanding of self-management. In a controlled implementation trial, Pinnock et al. 228 provided a telephone option for people due an asthma review, and opportunistic calls for non-responders to invitations. More patients were reviewed in the group with the telephone option and enablement and confidence in asthma care were greater. There was no difference in either trial in asthma control or use of health-care resources. 229,236
Lindberg et al. 227 reports a cross-sectional audit of an existing nurse-led asthma service in Sweden and compared it to seven neighbouring practices. The nurse-led clinic was associated with greater ownership of PAAPs, and fewer asthma symptoms, though more days lost from work than the control group.
A whole-systems approach with components operating at patient, professional and organisational levels
Seven studies implemented a whole-systems approach addressing patient-, professional- and systems-level interventions. Three studies used population data to observe the impact of multifaceted public health programmes on admissions,229,232,233,235 two quality improvement projects aimed to promote asthma self-management230,236 and two complex interventions targeted low-income communities in US cities. 231,234
A national programme to improve asthma care in Finland232,233 included a strong focus on self-management education, in the context of widespread professional education- and systems-level expectations of raising the quality of asthma diagnosis and management. Routine data over the decade of the intervention showed increased use of preventer medication and a reduction in hospital admissions and emergency visits,232 which was maintained after the end of the programme. 233 The authors attributed the success of the initiative to positive attitudes from a committed health-care system, training of all professionals coming into direct patient contact and implementation of guided self-management.
Souza-Machado et al. 235 report a public health intervention project supported by the Brazilian Ministry of Health and the Salvador city authorities, which promoted individual/group patient education, training for GPs and pharmacists, and free consultations and prescriptions. 235 The intervention was associated with a rapid reduction in asthma admissions and reversal of the previously increasing mortality rate in contrast to rising mortality and a small reduction in admissions in a similar control city. A historical cohort study of a similar intervention in another Brazilian city reported a similar dramatic reduction in admissions. 229
Two moderate-quality studies described initiatives specifically designed to promote self-management. Bunik et al. 230 used longitudinal data to evaluate a quality improvement programme in US secondary care. The intervention was led by a multidisciplinary team which met biweekly throughout the 6-month implementation phase, promoted professional training, patient education and decision support strategies, was associated with an increase in the number of action plans but did not improve any clinical outcomes. Volume of work meant that some of the strategies (such as completing pre-consultation reminders) were not completed. Repeated Plan Do Study Act (PDSA) cycles could help overcome such barriers. 230 Swanson et al. 236 undertook a survey of asthma patients to assess the impact of a programme to promote self-management in UK primary care. Compared with practices who did not participate in the programme, patients from intervention practices were more likely to have attended a review and to have an action plan. The intervention was associated with improvement in markers of control and reduced hospitalisations.
Two studies targeted deprived communities with multilevel interventions including self-management education. In the context of pre-school centres, Findley et al. 231 provided educational activities for parents and training for community professionals (social workers, teachers) in implementing ‘asthma-friendly’ initiatives and physician asthma care education training to the childrens’ physicians. The intervention was associated with improved markers of asthma control and a reduction in hospitalisations, but the greatest benefits were in children exposed to a combination of pre-school centre, parent and physician components of the intervention. Similarly, Polivka et al. 234 showed improved morbidity after a complex intervention including self-management education and attention to home environment (with funding for repairs).
Summary and conclusions
The evidence from these asthma self-management implementation studies suggests that complex whole-systems interventions which address patient education, professional training and facilitate a supportive organisation are associated with improvement in process outcomes,229–232,234–236 markers of control231,232,234–236 and use of health-care resources. 229,231–236 Large-scale initiatives which include collaborations with national or regional authorities and health services can reduce admissions,229,232,233,235 deaths232,235 and time off work. 232 Quality improvement programmes in individual practices or services can improve ownership of PAAPs230,231,234,236 and reduce morbidity. 231,234,236 Key facilitators highlighted by the authors are commitment of the health-care system229,232,235 and local practice or clinic,236 professional training in self-management,230–232 with ongoing evaluation,232 collaborative multidisciplinary working,230,232 with good communication and referral systems between professionals,235 effective patient education supported by regular reviews,231,235 and partnership with patients. 231
Individually these components are not sufficient. Improving professionals’ knowledge is a core component of effective self-management programmes, but on its own does not improve patient outcomes. 218,219 Just targeting the organisation to facilitate structured reviews including self-management support intervention improves process outcomes, but in trials shows no impact on clinical outcomes. 226,228 Targeting the patient is related to significant changes in some process outcomes,222 with inconsistent effects on clinical outcomes. 220,223,225 Authors highlighted the need to support professional education with integrating new behaviour into practice,218 the challenges of staff turnover,219 importance of involving senior staff in the design of interventions. 228
Routinely collected data were used in a number of these implementation studies,218,220,222,224–226,228,230,232,233,235 and the authors comment on the limitations of clinical records as a source of information which may be incomplete or misleading. 218,224,228,231 Improving procedures for standardising the routine recording of clinical data would facilitate collection of outcomes in implementation studies,279 but might also act as an intervention if, for example, a template prompted action. Similarly, school records have been criticised as being unreliable with some being influenced by external factors or motivators such as organisational expectations. 231
Diabetes
Description of the studies
We included 28 papers reporting 26 studies which evaluated the implementation of self-management support interventions for patients with diabetes (see Table 118 for details). Five papers reporting three studies focused on T1DM,251–255 eight focused on T2DM,246–250,260,261,264 the remaining 15 included mixed populations. 237–245,256–259,262,263
Thirteen of the studies were conducted in the USA,237–239,244–248,256–259,262 one in the UK,240 three from Germany (in five papers),251,253–255,260 three from Austria,250,252,261 four from Australia,241–243,249 and one each from Canada263 and Italy. 264 About half (n = 12) were conducted in primary care or community settings,239–241,246,247,257–263 four in MCOs238,244,245,256 and 10 (in 12 papers) in secondary care. 237,242,248–250,252–255,264
Quality assessment and weight of evidence
Study designs varied, with only one cluster randomised trial. 257 Six (eight reports) were based on longitudinal data,237,238,253–255,258,262,263 two case–control studies,240,244 fourteen before-and-after studies,239,241,242,245–252,259,261,264 one with a control cohort,243 one observation of change management256 and one physician survey. 260
Study quality was generally assessed as moderate to poor (scores 9–18 out of a total of 28) with failings related to lack of information on patient characteristics (n = 6), confounding variables (n = 24), characteristics of patients lost to follow-up (n = 24) and representativeness of participants (n = 21). Participating populations ranged from 85 to 9583 participants. One study in three papers,253–255 reported a decade of data on nearly 10,000 patients involved in a national programme of inpatient self-management education to teach people with T1DM to adjust insulin dose according to expected food intake and pre-meal blood sugar.
Intervention description and results
See Table 120 for detailed findings.
Primarily professional training with or without organisation support
One study focused on training professionals to deliver self-management support, within the context of implementation of the CCM. Self-management is one of the key components of the CCM. Rapid cycles of the PDSA cycle resulted in improved documentation of self-management goals, but only modest improvements in HbA1c. 237 Authors highlighted the substantial effort required to redesign services, even in the context of a highly motivated US secondary care clinic. 237
Primarily patient education, with or without organisational changes
Sixteen studies (reported in 18 papers) focused on educating patients about diabetes through group and/or individual educational sessions. 238–255 Education programmes encompassed interventions delivered by MCOs,238,240,244,245 in primary241 or secondary care,249,250 complex interventions in deprived US inner cities239,246–248 and intensive training on flexible insulin regimes. 242,243,251–255
Managed care
In a longitudinal study in a US MCO, Albisser et al. 238 compared outcomes in patients who had selected education alone, or supported by individual self-management training or computer-assisted self-care. At 12 months post-intervention, HbA1c had not changed in the ‘education-only’ group, but had fallen in the other two groups. The authors emphasised that education alone is not enough to improve outcomes and that it should always be supported with self-management training, regular follow-up, or (as in this study) computer-aided self-care. Roblin et al. 244 reports that a free, 2-hour self-management education group was associated with improvements in HbA1c and cholesterol at 6 months compared with matched controls in a US MCO.
The before-and-after study reported by Welch et al. 245 used telephone calls to members of a US MCO in order to assess risk of hypo- or hyperglycaemia and target education and support accordingly. Support ranged from educational resources to case management and telemonitoring. There were racial/ethnic disparities in service utilisation: blacks and Hispanics had lower utilisation rates than whites for six of the eight available preventative services.
In the UK, a collaboration between the NHS and a managed care initiative provided self-management supported by telephone base case management for people with poorly controlled diabetes from deprived communities. 240 The significant reductions in HbA1c, BP and weight represented clinically important benefits which were not observed in a large matched cohort from the General Practice Research Database. The authors observed that the use of the telephone intervention overcame barriers to participation in self-management programmes.
Deprived communities
Four before-and-after studies observed the impact of complex interventions in deprived ethnic minority communities in US cities,239,246–248 and one in a Chinese community in Australia. 241
Community-based teaching sessions led by volunteer educators provided diabetes group education on lifestyle behaviours, diabetes complications and medication, and individual sessions addressed blood glucose monitoring and insulin administration. 239 Of the 22 patients who provided data before and after the intervention, 16 (73%) had lower HbA1c levels and 5 (23%) had increased levels. Barriers to participation included poor public transport links, while expensive dietary changes and the cost of medication inhibited sustained behaviour change.
Diabetes educators provided free group teaching (in Spanish or English) on diabetes, supported by individual sessions with a dietitian to discuss self-monitoring and goal-setting. 246 Informal support meetings provided ongoing support. Overall, HbA1c levels improved in the 70 patients with before-and-after data, especially in those patients who participated in the ongoing support. Logistical barriers that need to be addressed to enhance participation and retention in the programme included clashes with work schedules, lack of transportation and family commitments.
A dietitian and a nurse led a multidisciplinary team which implemented an educational and self-management intervention in a deprived community setting. 248 To increase attendance, the programme was offered free to 969 patients, although only 81 patients remained in the programme for ≥ 6 months. HbA1c improved between baseline and 6 months and costs reduced because of a reduction in emergency care. Authors highlighted the practical funding issues associated with instigating and sustaining a complex intervention.
Promotores (CHWs) supported the provision of self-management education, collaborative goal-setting and problem-solving for 301 patients in a Hispanic community. 247 More than 80% completed the course and the majority achieved their personal goals 12 months post-intervention. The intervention was associated with a significant reduction in HbA1c and cholesterol at 3 and 12 months post-intervention. The team approach involving the community as well as health-care workers was seen as essential to the success of the project.
Inpatient training for flexible insulin regimes
Five papers reported the outcomes of national programmes (in Germany251–255 and Austria252) to train patients to adjust their insulin to their carbohydrate intake. The 5-day training was provided to a standard protocol by nurse educators and dieticians within well-established diabetic services. All of the studies report post-intervention improvements in HbA1c and reduction in episodes of severe hypo- or hyperglycaemia
Three papers present outcomes from the national database which monitored the German inpatient programme on an annual basis over a decade. Sämann et al. 253 demonstrated improved glycaemic control and reduced incidence of ketoacidosis, without increasing the risk of severe hypoglycaemia in the whole population of 9583 patients. In subgroup analyses, of the 341 patients with a history of three or more episodes of severe hypoglycaemia in the previous year, 56% had no episodes post-intervention, despite a small reduction in HbA1c. 254 The final paper assesses the impact of the programme in 1592 teenagers and young adults255 and demonstrates similar improvements in diabetic control. The authors considered that the flexible regime seemed to be related to significant positive clinical outcomes as it improved patients’ self-management skills and confidence in managing their insulin. 253
The addition of motivation and empowerment training for patients who had already participated in the intensive programme did not improve HbA1c, but reduced severe hypoglycaemia and days off work. 251
In a similar programme from Austria, Pieber et al. 252 demonstrated that similar outcomes could be achieved when the teaching was provided to outpatients and was less disruptive to the patients normal lifestyle.
In more recent studies, Lowe et al. 242,243 report a similar well-established programme including psychosocial support delivered in Australian secondary care settings. 242,243 The intervention reported significantly reduced HbA1c 12 months post-intervention and increased self-efficacy at 4 but not 12 months. 242 Compared with those on the basic insulin training course, patients with T2DM trained in flexible insulin dosage had reduced hospitalisations, reduced cardiac events and death. 243
Other primary and secondary care interventions
Telephone coaching in an Australian community aimed to augment traditional GP services by reinforcing information, improving self-management, reviewing goals and training ‘hard to reach’ people with diabetes to use community services effectively. 241 Between 6 and 8 months post-intervention there were significant improvements in attitudes and perceptions about diabetes.
Rasebaka et al. 249 reports before and 12-month follow-up data from 545 of the 967 people who had attended their multidisciplinary self-management programme led by an endocrinologist and a diabetes nurse educator. 249 HbA1c improved in 68% of patients; the multivariate analysis showed that the number of contacts with the programme was significantly associated with the magnitude of HbA1c change.
An Austrian study specifically observed the outcomes of insulin training in the elderly (aged > 80 years). 250 Two years after the initiation of insulin, patients considered to be able to undertake the self-management programme had a similar HbA1c and number of hospitalisations as those managed by a community nurse. The most common reason for inability to undertake the programme was cognitive impairment. 250
Primarily organisational change
Two US studies evaluated the use of PDSA cycles to achieve organisational change in the context of diabetes self-management. 256,257
In an observation of change management, Glasgow et al. 256 recorded an increase in the proportion of patients with documented self-management goals as seven clinical teams focused on improving their diabetes care over a year. Factors facilitating a successful implementation of self-management were a more favourable attitude towards self-management, HCPs’ intention to change, and the organisation’s intention to integrate self-management into different elements of its delivery system.
In a cluster randomised design, Hargreaves et al. ,257 allocated CHWs to participate in the PDSA organisational change process by providing a link with community services in 12 clinical teams. Involvement of CHWs increased the proportion of patients with a recorded self-management goals including in ethnic groups, but had no impact on HbA1c. The close supervision of the intervention and documentation of study fidelity was important to avoid dilution. The authors considered the challenges of achieving change that is team-based and patient-centred, unless reimbursement system change to reflect new ways of working.
A whole-systems approach with components operating at patient, professional and organisational level
Implementing national programmes
Three studies reported national programmes promoting implementation of diabetes self-management education in the USA,259 Austria261 and Germany. 260 Common features were organisational support for establishing registers,259 reimbursement of costs,259–261 professional training260,261 or provision of trained educators,259 and a structured patient education programme with provision of resources. 259–261
Gruesser et al. 260 reported the experience of physicians from 127 practices in Germany who had undertaken training the previous year. Nearly two-thirds had implemented at least one structured patient education course. Barriers to implementation were staff attending the training course no longer working in the practice, lack of time to organise the group teaching, or insufficient number of interested patients in small practices. Before-and-after patient data from a random sample of practices showed a reduction in HbA1c.
Korsatko et al. ,261 in Austria, reports the outcomes in the 2122 patients who attended for the 12-months follow-up (48% of those who attended the education). 261 HbA1c, BMI and BP were all improved post-intervention.
A quality improvement programme in a rural US setting, supported clinical teams to set up a disease registry, trained them to enable deliver free local diabetes education and self-management support. 259 Telephone calls from diabetes nurses and regular information about diabetes supported the initiative. HbA1c and BP fell post-intervention with no changes in LDL cholesterol. Improvements in process outcomes such as foot examination, influenza and pneumococcal immunisation were also reported.
Other implementation projects
Anderson and Christison-Lagay258 reported a community-based project in which professional staff from a US primary care centre were trained, and supported, to provide self-management education. Using PDSA cycles, self-management was integrated into the organisation and tools were developed to help professionals assess patients’ goals. Post-intervention data on 488 (out of 2389) diabetics showed improvements in HbA1c, LDL cholesterol and BP with the majority of patients making progress towards their goals their goal. One of the challenges identified was changing providers’ mentality in following a ‘didactic mode’ and this required regular oversight and frequent review to ensure intervention fidelity.
Leibman et al. 262 reported 6 years of routinely collected data during the implementation of the CCM in a US community centre. A key component was the involvement of CHWs who helped patients set goals, develop strategies to overcome barriers, use the support of their peers, and create important links between the patient, the clinical care team and home situations. Professionals received clinical protocols and had access to a patient registry to track patient progress and clinical outcomes. Seventy-six per cent of patients had at least one individual session with a nurse educator. When the CCM was first introduced, the HbA1c remained constant, but when self-management was added into the programme HbA1c levels fell significantly. The authors highlighted that patient engagement was largely due to the CHWs who developed personal relationships with patients and created links in self-management activities, patients and clinical care. Their involvement as peers rather than professionals enabled them to motivate patients.
Senior et al. 263 instigated a multidisciplinary quality improvement intervention in a Canadian community setting which included staff training in diabetes education with ongoing mentoring, regular visits from an endocrinologists and patient education from a nurse or dietitian. Post-intervention there was improvement in HbA1c, BP and cholesterol. The authors highlighted that implementation is hindered when the new intervention is perceived to overlap with existing programmes and thus individuals are less motivated to change. The nurse and dietitian needed to develop trust and overcome concerns with patients and local physicians before implementing any programme.
Musacchio et al. ,264 in Italy, explored the effectiveness of a multifaceted intervention based on the CCM. The programme aimed to engage all professionals with whom the patient interacted to implement the empowerment philosophy. Following individual assessment and development of a management plan by a physician, the patient consulted with other professionals who provided tailored diabetes education and training in problem-solving and addressing psychosocial needs. Accessible support was available via telephone or e-mail. HbA1c and LDL cholesterol improved. There was no effect on BP. Transferring the responsibility to the patient was not associated with detrimental effect, but accessible contact with professionals when necessary is important.
Summary and conclusions
The evidence from these diabetes self-management implementation studies supports the provision of self-management for people with diabetes as they show consistent improvement in process outcomes,237,239,241,242,247,252,256–259,262–264 improved markers of control such as HbA1c,238,240,244,246–249,252–255,258,259,261–264 cholesterol,244,258,261,263,264 BP,240,258,259,261,263,264 diabetic crises251–255 and use of health-care resources. 243,245,248,252,254 Many of these studies, however, are uncontrolled before-and-after studies with the inherent methodological limitations. The only cluster randomised trial, in the very specific context of including CHWs in multidisciplinary collaborative programmes for diabetes improvement, showed improved process outcomes (documented self-management goals) but no difference in clinical outcomes. 257
A series of large-scale evaluations of national programmes promoting diabetes education consistently demonstrated clinical benefit. In a whole-systems approach, primary care physicians were reimbursed to attend training enabling them to deliver standardised diabetes education including self-management. Analysis of the routine data collected to monitor the services in Austria (n = 2122 patients),261 showed that all target parameters (HbA1c, BMI, BP, LDL cholesterol) improved significantly at 1-year compared with baseline. Other longitudinal databases include Leibman et al. 262 who reported 6 years of routinely collected data (n = 1188) before, during and after the implementation of the CCM in a US community centre, and demonstrated that the previously stable HbA1c fell when the self-management programme was introduced. Albisser et al. 238 used a database of 978 patients from a managed care network and demonstrated that education alone is not enough to improve outcomes: it should always be supported with self-management training and supported by regular follow-up.
Following the promotion of flexible insulin dosage regimes, national programmes have promoted and evaluated 5-day courses. In a database of 9583 patients collected over 10 years, Samann 2005 demonstrated improved glycaemic control and reduced incidence of ketoacidosis, without increasing the risk of severe hypoglycaemia. 253 Smaller data sets from similar projects in Austria252 and Australia241–243 reach similar conclusions.
Many of the authors provided insights into the barriers and the facilitators they encountered during the implementation of their projects. Achieving change is a challenge, even in well-motivated teams,237 and the need to build relationships with existing services263 and the need for regular oversight and frequent review to ensure intervention fidelity. 258 A team approach involving the community as was seen as essential to the success of projects in deprived, minority communities,247 the involvement of health-care workers as peers rather than professionals enabled them to motivate patients. 262 Practical issues such as sufficient and ongoing funding to enable complex interventions to be instigated and sustained, were highlighted. 248,257 Achieving good uptake of programmes seen as beneficial for the minority who engaged was discussed by several studies. Barriers identified included clashes with work schedules and family commitments,246 lack of transportation,239,246 and the cost of medication and expensive dietary changes. 239 The use of telephone interventions may overcome some of these barriers to participation in self-management programmes. 240
Depression
Description of the studies
Six implementation studies were included for depression (see Table 121 for details): five from the UK,265–269 and one from Australia. 270 All the studies dealt with strategies for implementing CBT but in different settings: two specialist CBT centres,267,268 one private psychiatric hospital270 and three community-based clinics. 265,266,269
Quality assessment and weighting of the evidence
Five of the papers reported uncontrolled before-and-after studies,265–269 only one included a (non-randomised) historical control. 270 Study quality was poor (range 15–18), failings being due to lack of information on intervention (n = 3), description of principal confounders (n = 6) and whether or not treatment was representative of treatment the majority of patients received (n = 6). Eligible populations ranged from 510 to 1308 participants, while the population included in the studies ranged from 108 to 1137 patients.
Intervention description and results
Primarily patient education, with or without organisational changes
Five of the studies implemented strategies for efficiently delivering CBT to the increasing number of patients being referred. Four implemented interactive cCBT programmes undertaken in six or eight sessions at the local centre with homework tasks (e.g. problem diaries, thought records, behavioural experiments). 265,267–269 Trained mental health workers were available to support the cCBT and to assess progress at the end of each session, alerting senior therapists in the event of concerns (e.g. suicide risk). Farrand et al. 266 provided behavioural advice in the form of a self-help book supported by a graduate mental health worker to people on the waiting list for CBT. All studies reported improved depression and anxiety post intervention, both in terms of changes in mean score greater than the defined clinically important difference and in the proportion of people who improved during the course. 265–269
At the end of the course, approximately one in five of those who completed the cCBT were referred on to face-to-face therapy. 268 Authors concluded that offering cCBT as a first step was an effective way to manage demand,265,267,268 provide timely access to therapy269 and could be supported by volunteer support workers (as opposed to mental health professionals). 266
Primarily organisational change
Newnham et al. 270 describe a group CBT intervention in a private hospital in Australia, which introduced monitoring of the service with the outcomes of the World Health Organization well-being scale. 270 Initially, this was used to monitor the effectiveness of the service, but in the course of the study was provided as feedback to patients and the therapist at the mid-point of the CBT programme. Patients not improving at the mid-point who received feedback had greater improvements in depression at the end of the programme (p < 0.001), though not in well-being, stress, mental health status or anxiety scores. 270
Summary and conclusions
These uncontrolled before-and-after studies suggest that innovative approaches to delivering CBT (using interactive computer programs,265,267–269 or self-help books supported by mental health workers266) may be efficient strategies for increasing access to psychological therapies, though randomised trials will be needed to confirm their effectiveness.
Hypertension
Description of the studies
Two studies in hypertension were included (see Table 122 for details):276,277 one from a primary care setting in Germany276 and one from a managed care programme in the USA. 277
Quality assessment and weight of evidence
Both studies analysed before and after data, and the quality assessment scores (14 and 15 out of a total of 28) reflected the limitations of this methodology. Studies failed to report (a) patients lost to follow-up, (b) the characteristics of patients lost to follow-up, and (c) confounders.
Intervention description and results
See Table 123 for detailed findings.
A whole-systems approach with components operating at patient, professional and organisational levels
Both studies reported national, or state-level interventions which addressed organisational issues as well as training professionals to teach and support patient self-management.
Gruesser et al. 276 report a national initiative in Germany, analogous to the national diabetes training programme,260,261 which trained primary care professionals to provide self-management education. The study reported improvements in SBP, DBP and BMI. 276 Although the programme was considered to be practical, the authors identify a number of practical barriers: lack of time to organise the group teaching in the practice; staff missing the training course, or were not available at the time of the course; dislike of the programme; insufficient number of interested patients; lack of time on the part of the patients.
The intervention in the US study reported by Bosworth et al. 277 was a tailored multifaceted programme delivered during regular telephone by a registered nurse with the aim of increasing medication adherence. Compared with baseline, adherence to medication improved a year post-intervention. No clinical outcomes were reported. The authors observed that the voluntary character of the programme aided its implementation as participating practices were motivated to deliver the programme and the motivated care managers had full responsibility for its delivery. In addition, using telephones to implement the intervention provided an opportunity to reach more patients and allowed individualised, personal interaction without time and transportation barriers.
Chronic obstructive pulmonary disease
Description of the studies
We included two studies,271,275 both delivered in the community, but one led by primary care physicians in rural USA,275 and the other led from secondary care immediately after an admission (see Table 122 for details). 271
Quality assessment and weight of evidence
Both studies analysed before-and-after data and the quality assessment scores (13 and 19 out of a total of 28) reflected the limitations of this methodology.
Intervention description and results
See Table 123 for detailed findings.
Primarily patient education, with or without organisational changes
Pushparajah et al. 271 report a physiotherapy-led service which provided home visits within 5 days of a hospital discharge with an exacerbation of COPD with the aim of supporting self-management to reduce future admissions. The process evaluation identified referrals and medication errors corrected as a result of the visit, but there was no change in frequency or duration of admissions.
Primarily organisational change
Deprez et al. 275 reports a quality improvement programme among primary care professionals in rural USA. Professionals were encouraged to work collaboratively to develop practice-level goals and monitor progress. Regular meetings facilitated mutual support between teams, enabling identification of barriers and fostering of teamwork to find solutions to shared problems. Practices made some infrastructure changes (e.g. developing COPD registries) and process markers improved (e.g. documented respiratory education and discussion of self-management goals). No clinical outcomes were measured.
The authors were positive about the collaborative nature of the project but observed that to be adopted new processes must fit within the current care system, be promoted by strong clinical leaders (typically physicians) and be perceived as relevant (and thus valued) by all staff members. 275 Wider system-level resources were helpful.
Summary and conclusions
There is a very sparse evidence base to inform the implementation of self-management support in COPD. Strong clinical leadership within collaborative quality improvement programmes275 and individual specialist provision of care,271 both improved process outcomes in these before-and-after studies, but neither study provided evidence of clinical effectiveness.
Chronic kidney disease
Description of studies
Two observational studies were included in our review (see Table 122 for details), both reporting structured education provided by dialysis units to train CKD patients to undertake self-dialysis. 272,273 One study, from Taiwan, included patients starting on peritoneal dialysis;272 the other from France, included both peritoneal and haemodialysis. 273
Quality assessment and weight of evidence
Both studies used before-and-after methodology, but although Loos-Ayav et al. scored 22 (out of a possible 28),273 Chen et al. only scored 13,272 mainly because the report did not describe the statistical tests used, calculate the influence of confounding variables or provide descriptions of patient characteristics, reasons for patients lost to follow-up or information on patient representativeness.
Intervention description and results
See Table 123 for detailed findings.
Primarily patient education, with or without organisational changes
Both studies report the outcomes of individualised training, delivered by a specialist nurse which covered education about CKD, dialysis and its complications, training in the necessary skills safely to implement dialysis and ongoing supervision to establish home dialysis. 272,273 These were intensive courses, extending to 25–40 hours for training each patient,272 or three sessions a week for 3–6 months. 273
Chen et al. 272 demonstrated improved knowledge post-intervention with scores reflecting patients’ college/high school educational standards. The occurrence of peritonitis, however, was not related to the post-training scores.
In Loos-Ayav et al. ,273 patients who achieved autonomy in home dialysis were younger and had less comorbidity than the non-autonomous group. Multivariate analysis showed that greater improvement in ‘role-emotional’ and ‘burden of kidney disease’ dimensions of HRQoL was associated with success in achieving autonomy. The authors highlight that the patient’s active participation in disease management, the motivation of the nephrology team and the resources devoted to patient education are of utmost importance.
Summary and conclusions
Evidence around the implementation of self-management support interventions in CKD appears to be very sparse. Intensive training programmes delivered by motivated nephrology teams may enable patients to achieve autonomy in dialysis and this is associated with greater improvement in ‘role-emotional’ and ‘burden of kidney disease’ dimensions of HRQoL. 273 The acquisition of knowledge about CKD is probably not related to the occurrence of peritonitis. 272
Low back pain
Description of studies
One study from the Netherlands was eligible for inclusion in our review (see Table 122 for details). 274 The setting was a secondary care-led residential course.
Quality assessment and weight of evidence
The before-and-after study scored 20 out of a total of 28 on the quality assessment checklist. 274
Intervention description and results
See Table 123 for detailed findings.
Primarily patient education, with or without organisational changes
A 10-day, hotel-based residential course, offered a structured programme including CBT, education and physical activities. Patients aimed to achieve their own goals and to return to an active lifestyle by using activity-based planning and pacing strategies, alongside CBT techniques to endorse more adaptive behaviours and beliefs. 274 A year after the course, patients had reduced functional disability, improved pain self-efficacy, improved QoL and improved daily functioning.
Summary and conclusions
Based on a single before-and-after study, an intensive CBT-based approach to train patients with chronic LBP to manage their pain and minimise its impact on lifestyle may improve functional ability, pain self-efficacy and QoL. 274
Stroke
Description of studies
Only one paper, which evaluated an integrated model of care in a Hawaiian in-patient setting, was included (see Table 122 for details). 278
Quality assessment and weighting of the evidence
The longitudinal observational study scored 13 out of a total of 28 on quality assessment. 278
Intervention description and results
See Table 123 for detailed findings.
A whole-systems approach with components operating at patient, professional and organisational levels
The study evaluates the phased introduction of an integrated model of care in a stroke unit which engaged all members of the team in supporting the patient to achieve their goals and achieve re-entry into the community. 278 A key driver was organisational efficiency. Although demographic data over the 4 years was stable, patients admitted in later years were less disabled by their stroke, though had more comorbidities than patients admitted in the early years. Length of stay decreased significantly with the introduction of the integrated care model but the change (improvement) in functional ability was less.
Summary and conclusions
This low-quality paper suggests that an integrated delivery model may improve efficiency in stroke units,278 though changes in disease severity and comorbidity at admission make interpretation of the clinical outcomes difficult. It is not clear which aspects of the intervention were more effective in achieving earlier discharge.
Discussion
The Medical Research Council framework for the design and evaluation of complex interventions recognises that Phase IV implementation studies may utilise a range of methodologies. 37 In our systematic review of implementation studies we therefore did not specify the methodology and anticipated that the studies we would find would be diverse. Thirty of the 61 papers we included reported before-and-after studies, though some had sought comparison with other local practices,251 matched controls from national data,240,244 or historical controls. 270 Many were single centre studies and relatively small: none provided power calculations. Their findings need to be interpreted with caution.
Weight of evidence
The most robust evidence comes from studies in asthma (n = 18) and diabetes (n = 26) which included examples of more rigorous methodologies including cluster randomised trials and large/longitudinal database studies. The other conditions had a paucity of data (six in depression, two in hypertension, two in COPD, two in CKD, one in LBP and one in stroke). We did not find any implementation studies evaluating self-management in dementia, epilepsy, IAs, IBS or PNDs.
Randomised trials
In all we found eight randomised trials: seven in asthma218,219,222,224–226,228 and one in diabetes. 257
Two cluster RCTs in asthma,217,218 tested the effectiveness of training professionals to deliver self-management education. They were both negative, though both authors highlighted the probability that the professionals were not sufficiently supported by their organisation to enable them to change their practice. The need for organisational support, practical resources and the benefits of achieving buy-in from the (ideally multidisciplinary) team is a common theme in many of the studies. 237,247,248,258,262,263 The only cluster randomised trial in diabetes endorses the benefits of teamwork, in the specific context of including CHWs in multidisciplinary collaborative programmes for diabetes improvement. Intervention centres showed improved process outcomes (documented self-management goals) though there was no difference in clinical outcomes. 257
A RCT226 and a randomised implementation study,228 evaluated interventions designed to increase the proportion of people with asthma who had a routine review, a core component of which is the provision of self-management education. 280 Both succeeded in their aim of facilitating asthma reviews, Kemple and Rogers226 increased the proportion people with PAAPs, but neither improved clinical outcomes or use of health-care resources. The practices in these studies had asthma trained nurses, but the intervention did not offer specific training to enhance self-management skills.
Two trials conducted by US MCOs targeted educational initiatives at their members with asthma. 222,225 Delaronde et al. 222 used preference methodology and was thus able to compare the group randomised to receive the nurse-led telephone management with the group who opted for the service. Effects (acceptance of calls, use of inhaled steroids, improved QoL) were enhanced in the ‘opt-in’ group leading the authors to highlight the importance of self-motivation to initiate and maintain asthma self-management. Poor uptake of programmes was a problem for many studies in all the disease areas, and some studies discussed strategies for addressing the challenge. For example, overcoming the barriers of clashes with work schedules and family commitments,246 lack of transportation,239,246 and the cost of medication and the expensive of dietary changes239 have all been highlighted as priorities. The use of telephone interventions may overcome some of these barriers to participation in self-management programmes. 240 Vollmer et al. 225 used automated telephone calls and showed no clinical benefit, but observed that many patients were unhappy with ‘talking to a computer’ and preferred a live call.
In a cluster randomised trial in 54 US inner city schools, Gerald et al. described similar problems. 224 The challenging social context, and a high turnover of both staff and pupils made it very difficult to maintain the fidelity of the programme and establish a meaningful relationship with the children and their families. Many studies reported self-management initiatives deprived, inner city, culturally diverse communities, and echoed the challenges of maintaining fidelity,239,240,246 high turnover of staff,262 poor recruitment rates246 and high levels of attrition,234,239,246 but were nevertheless able to demonstrate an impact on process outcomes234,246,257 and clinical benefits. 229,234,235,240,246,262 Multifactorial intervention addressing the management of disease in the context of substantial psychosocial problems231,234,239 and the benefits of involving community workers were common themes. 234,235,247,257
Large and/or longitudinal database studies
A number of studies in asthma and diabetes used routinely collected data from whole populations, often in longitudinal databases, in order to evaluate national or regional initiatives. 230,232,233,235,237,253–255,261,262 The largest example is the national programme in Finland which prioritised self-management as a core component of improving asthma care. 232,233 Reported in Haahtela et al. ,232 the intervention was multifactorial, addressing barriers in the system, training professionals and engaging with patients through their charities. National statistics on an estimated 350,000 people with asthma, showed a substantial and sustained reduction in asthma admissions, ED visits and deaths over the decade of the programme. In the resource-poor environment of a Brazilian city, Souza-Machado et al. 235 describes a regional intervention which combined staff training, patient education and provision of free asthma care which reduced asthma admissions and deaths at population level.
In the 1990s, diabetes education was actively promoted at a national level in Germany and Austria, with a programme of physician training and reimbursement for providing group education for patients. Before-and-after data collected from 2012 people showed a significant improvement in diabetes control and BP. 261 An analogous national programme promoting self-management for hypertension reported improvements in SBP, DBP and BMI. 276 Using a longitudinal database of 1188 people over 6 years, Leibman et al. 262 followed the implementation of the CCM in a large US community centre. The previously stable HbA1c fell when the self-management programme was introduced.
More recently, in an analysis of a 10-year database of 9583 people who had attended the nationally promoted self-management training for flexible insulin dosage regimes, Sämann et al. 253 demonstrated improved diabetic control.
The whole-systems approach
The key message from these studies is that implementation in the real world is complex, fraught with barriers which impact on patients’ uptake of education, professionals’ engagement with discussing and creating personalised action plans, and health-care organisations’ prioritisation of self-management as a core component of care. Most randomised trials have focused on one or two aspects of a whole-systems approach – most clearly demonstrated in the asthma studies, but echoed by the evidence in other conditions. Large-scale initiatives suggest that programmes which are most likely to succeed are:
-
promoted by policy ensuring meaningful adoption (and ideally provision of resources, reimbursement of costs) by health services
-
provide training programmes for professionals, and
-
focus on structured self-management education for patients in the context of overall disease management and are sufficiently flexible to address local, cultural and personal variation.
A recent cluster RCT, which sought to implement self-management for people with diabetes, COPD and IBS, introduced as a whole-systems intervention in UK primary care, had no impact on any clinical outcomes. 281 The authors conclude that although the practices were engaged, and training was well received, implementation in routine practice remained challenging. Another factor may have been that self-management in IBS and COPD have less of an evidence base than other conditions and existing structured programmes may have reduced the potential for improvement in diabetes.
There remains, therefore, a need to explore and refine the components of a whole-systems approach in a Phase IV intervention. The complex intervention framework currently illustrates a cycle of development and evaluation which includes implementation as a final step. 37 We propose that the research underpinning implementation should be visualised as a second inter-related cycle. 282 Just as the ‘Phase III cycle’ includes the iterative steps of development and piloting, a similar process may be needed to translate the intervention into a practical service which can be tested in a Phase IV implementation study. Lessons from authors of the diverse implementation studies included in our review may inform this process.
Lessons learned
We identified important practical lessons from authors’ reflections on the process of implementing complex self-management support interventions in routine clinical care.
-
Effective patient education needs to be supported by regular reviews,231,235 underpinning a partnership with patients. 231 In addition to education, psychological support, along with counselling, problem-focused strategies and emotional support seems to be important. 251 Teenagers and young people can benefit from self-management education,255 and old age is not a necessarily a barrier to learning self-management skills,250,268 unless there is cognitive impairment. 250
-
There is a distinction between knowledge and skills: one does not necessarily predict the other. 272
-
Only a proportion of people accepted the offer of self-management education and all studies reported an attrition rate. For some interventions, especially those delivered in deprived communities, recruiting and retaining patients was a major challenge. 234,239–241,246 Practical barriers identified included clashes with work schedules and family commitments,246 lack of transportation239,246 and the cost of medication and expensive dietary changes. 239 Some patients may avoid follow-up because they feel they have not succeeded in achieving the recommended behaviour change. 261
-
The use of telephone interventions may overcome some of the practical barriers to participation in self-management programmes240 and in one study was credited with ‘closing the racial/ethnic gap in self-management behaviours’. 245
-
Achieving change is a challenge, even in well-motivated teams. 237 There is a need to support professionals as they integrate new behaviour into practice. 218 Promising approaches include collaboratives, PDSA cycles237,256,275 and introduction of self-management support as a component of improved chronic care (e.g. the CCM). 256,278
-
There is a need for regular oversight and frequent reviews to ensure intervention fidelity. 239,240,246,258 Frequent staff turnover can be a particular challenge which needs to be addressed,219,260,262 to ensure that skills are not lost.
-
Professional training in supporting self-management,230–232,259 collaborative multidisciplinary working,230,232 with good communication and referral systems between professionals,235 and the involving staff members in the design of interventions228,275 are potentially important ingredients of implementing self-management support.
-
There is a need to build relationships with existing services263 and integrate innovation with existing practice. 275 New initiatives were most warmly received by communities where there were few existing services. 263
-
A team approach involving the community was seen as essential to the success of projects in deprived, minority communities. 247 Patients perception of community health-care workers as peers (as opposed to professionals) enabled them to form relationships and motivate patients to engage with their (self-) care. 257,262
-
A key facilitator highlighted by several authors is the commitment of the health-care system229,232,235,253,261,262,275 and/or local practice or clinic236,277 with ongoing evaluation. 232
-
There are practical barriers if ongoing funding or resources (including time) are insufficient to enable complex interventions to be sustained. 248,257,260,262,273,276
-
Technological solutions (such as cCBT programmes, automated telephone calls) are being explored and show some promise. 225,238,265,267,269,271
-
The only study which specifically explored duration of intervention and effect found evidence of benefit as much as 5 years after a one-off intensive insulin training course. 243 Intensive courses in diabetes and LBP seem to be more effective than less intensive programmes. 274
Conclusions
Multidisciplinary, complex self-management support interventions delivered in routine clinical care require the involvement of individuals from all levels, the patient, the professional and the organisation. Success requires strong clinical leadership in the practice and/or at the system level such that self-management is integrated in routine care. Delivering the intervention is challenging, thus procedures for assessing intervention fidelity and robust implementation are required.
Chapter 22 Overarching synthesis
Summary of findings from the quantitative systematic reviews in the individual meta-review chapters
Types of self management support or components
Stroke
There was strong evidence that therapy rehabilitation delivered in early stroke recovery has a positive impact on ADL and extended ADL. When delivered later in stroke recovery, there was some evidence of a beneficial effect on extended ADL, but no impact on ADL or QoL. Regardless of whether therapy rehabilitation was delivered in early or late stroke recovery, there was strong evidence it had no impact on mood.
There was some evidence that information provision, particularly when provided in a way that more actively involved patients and carers, had beneficial effects on mood, but little impact on any other outcome.
There was some evidence that stroke liaison emphasising education and information could have a positive impact on QoL, but that general stroke liaison had no measurable benefits.
Type 2 diabetes mellitus
Aside from the single-component intervention – support for blood glucose self-monitoring (excluded from this review) – there is very good evidence that self-management support improved blood glucose control in the short term, with typical reduction in mean difference in glycosylated haemoglobin of around 0.4% in the intervention group compared with the control group. Longer term, there was less evidence for effectiveness; probably due to a lack of studies reporting longer-term data. However, overall, these self-management support interventions do not appear to improve individuals’ QoL or their psychological well-being. That QoL remained unaltered in these interventions may be considered a positive outcome considering the often high demands on participants’ time which could potentially impact negatively on QoL.
Asthma
There was well-established evidence that self-management support reduces hospital admissions and ED visits and increases QoL in people with asthma. Optimal asthma self-management should include education supported by a WAP. Symptom-based plans were as good as peak-flow-based plans (and better in children).
Education should be culturally sensitive.
Asthma self-management should be supported by regular clinical review, and may be enhanced by provision of several components of the CCM programme. Implementation of proactive practice-based organisational systems can promote ownership and use of action plans.
Interactive computerised programmes improved asthma symptoms and school-based asthma education was associated with improvements in self-efficacy and self-management behaviours and improved QoL.
There was mixed evidence for interventions for children delivered in the home.
Chronic obstructive pulmonary disease
Self-management education support/disease-specific education interventions were associated with a reduction in COPD-related hospital admissions. Their effect on HRQoL was less established. Heterogeneity in interventions studied meant it was not possible to make firm recommendations about the exact form and content of self-management support, many of these educational interventions included action plans.
Action plans for COPD patients were recommended to be used only in combination with other self-management components.
Outreach nursing programmes improved HRQoL (although the improvement may not have been clinically significant), but their effect on hospitalisations was variable.
Chronic kidney disease
One high-quality review showed promising results for the beneficial role of educational interventions in CKD, particularly in dialysis patients. However, these findings were predominantly for short- and medium-term outcomes, with a lack of long-term data.
A lower-quality review of adherence-promoting interventions for patients on dialysis also presented some positive results on the effectiveness of these interventions; however, there was an absence of long-term data, and included studies were of small sample size.
A further lower-quality review of MDC, which included only studies with pre-dialysis patients, found limited effectiveness of the interventions explored, with further RCTs still required.
Dementia
Overall, the systematic reviews suggested there were few studies of self-management support interventions in relation to dementia in people living at home.
There was some weak evidence that coping-based strategies for carers of people living at home with dementia, with or without activity interventions directed at the patient with dementia, may improve patients’ QoL.
Epilepsy
There was very little evidence to suggest that any of the reviewed interventions had a significant effect on seizure frequency. The evidence around CBT was mixed and inconclusive. There was a small amount of promising evidence to suggest the value of a child-centred model for chronic illness.
More promising evidence existed regarding interventions to increase medication adherence. There was some evidence to support the role of implementation intention interventions; medical education in combination with psychosocial therapy; patient reminders; parental group discussions; self-management education; and strategies to improve compliance.
The only intervention found to deliver an improvement in QoL was CBT.
Hypertension
There was little evidence for the use of contracts or education in isolation and inconclusive evidence for the use of appointment reminders or other motivational strategies. There is some evidence for the effect of simplification of medication regimens on adherence. Evidence for self-monitoring is promising but mixed and it might be more successful as part of a complex intervention. Telecare was also shown to improve BP control, although this evidence was largely based on one lower-quality trial. Combined lifestyle interventions might be beneficial to patients though their clinical effect may be small. There was evidence for the benefit of complex interventions in supporting self-management, with mixed results for interventions led by allied health professionals. However, the evidence available for complex interventions was too heterogeneous to be able to make definitive conclusions. It may be that a patient-specific approach is the most beneficial, involving components tailored to the individual patient with hypertension.
Rheumatoid arthritis
There was strong evidence showing improvement in disability and physical function with psychological interventions, but this was mainly in the immediate post-treatment period. In the longer term, the effects were reduced or non-significant. Psychological status was also improved short term, but reviews showed variable results longer term with strong evidence that face-to-face interventions may reduce depression at 2- to 24-month follow-up.
Overall, there was good evidence of improvement in both disability and psychological status following education and training in RA, which diminished in the longer term.
There was only limited evidence that complementary therapies improved short-term psychological status in RA patients who were already on maximal pharmacological therapy.
Systematic lupus erythematosus
There was evidence of a positive effect of psychological therapies on disability and psychological status in the short term but not long term.
Irritable bowel syndrome
Self-management interventions for IBS may improve symptoms and, perhaps, QoL, and may be as effective as drug treatment.
There is most evidence to support CBT and multicomponent psychological therapies.
Overall, there is some promising evidence on self-administered CBT, self-help guidebooks, self-management programmes, but further research is needed.
Low back pain
Overall, in terms of pain and disability, ESs, where positive, were modest. There was moderate evidence that self-management interventions have modest benefits on pain and disability in the short and longer term.
There was strong to moderate evidence that intensive multidisciplinary biopsychosocial interventions reduce pain and improve function. Psychological interventions may improve pain in the short term, but this effect did not appear to be sustained into the longer term. There was some evidence that advice may be beneficial. There was little evidence to support back schools, GA, less intensive biopsychosocial interventions, multidisciplinary rehabilitation or educational interventions.
Type 1 diabetes mellitus
There is moderate evidence that psychological treatments may improve glycaemic control and psychological distress in children and adolescents, but not adults.
Moderate evidence also exists to suggest that family centred interventions can improve blood glucose control.
However, there is little evidence to suggest that education alone improves blood glucose control or QoL.
Weak evidence exists to support the role of adherence-promoting interventions in improving blood glucose control.
Self-management support, how and who?
Stroke
The majority of therapy rehabilitation interventions reported in the identified systematic reviews were delivered by OTs. Although OTs can play an important role in delivering self-management support, a more integrated, whole-systems approach is needed for optimal self-management support. A focus on longer-term support is also required.
Type 2 diabetes mellitus
This meta-review suggests that such self-management support may be delivered in a huge variety of ways and by a large cast of different professionals and lay people, so it is not possible to say definitively what the optimal model of delivery is. Given the large number of RCTs and reviews included within this meta-review, the failure to reach any conclusion on the optimal model of delivery suggests that there may not be just one way. The evidence suggests that various models of delivery may be equally effective and consideration may instead need to be given to other factors which may influence effectiveness, such as the real world context.
Asthma
There was mixed evidence for involvement of IHWs.
Epilepsy
There was some evidence of benefit from specialist epilepsy nurses.
Hypertension
This meta-review suggests that self-management support for hypertension may be delivered in a multitude of ways and by different health professionals. In hypertension in particular, we have seen the impact that technology can have in supporting self-management and this may be an increasingly useful tool for the future. However, it is clear that this may be most effective as part of complex interventions. Other evidence supported interventions on lifestyle and drug regimen changes. There was no single type of intervention shown to be more effective than others; this may be because one intervention alone is not effective as a support intervention or it may be because of a paucity of evidence about the self-management of hypertension.
Components of self-management support and the taxonomy
It was not possible to map all the results from the individual quantitative meta-reviews perfectly on to our proposed taxonomy of self-management support components as the constituent systematic reviews on which our meta-reviews were based had very often combined multicomponent interventions under a single heading. For example, many of the studies classed as disease-specific education for COPD also had components involving action plans (and these would be two separate components in the proposed taxonomy). Indeed, sometimes in the meta-reviews we could only talk about ‘interventions providing self-management support’. In addition, in line with our definition, we excluded systematic reviews examining monocomponent interventions such as home monitoring of BP or blood sugar, unless it was clear that the patient was expected to use the measurements to manage their own condition (as opposed, for example, to reporting the readings to a clinician who then took the management decisions). The exception to this was education, which we included, though we later came to distinguish passive provision of information from an active process of learning new skills. Finally, it should be noted that the taxonomy was derived from the work of conducting the meta-reviews and looking at their description of their contributing RCTs and did not exist when the reviewers were originally conducting their reviews. Our use of terms may differ from the included systematic reviews. For example, we make a clear distinction between education and the provision of information (see Chapter 6); however, some of the systematic authors used the terms interchangeably.
Summary of findings from the qualitative systematic reviews in the individual meta-review chapters
The main themes arising from the priority LTC qualitative meta-reviews are summarised graphically in the in Figure 49. (The findings of the one qualitative synthesis on asthma, which was around the specific role of action plans, is not repeated here.)
FIGURE 49.
The main themes arising from the priority LTC qualitative meta-reviews.
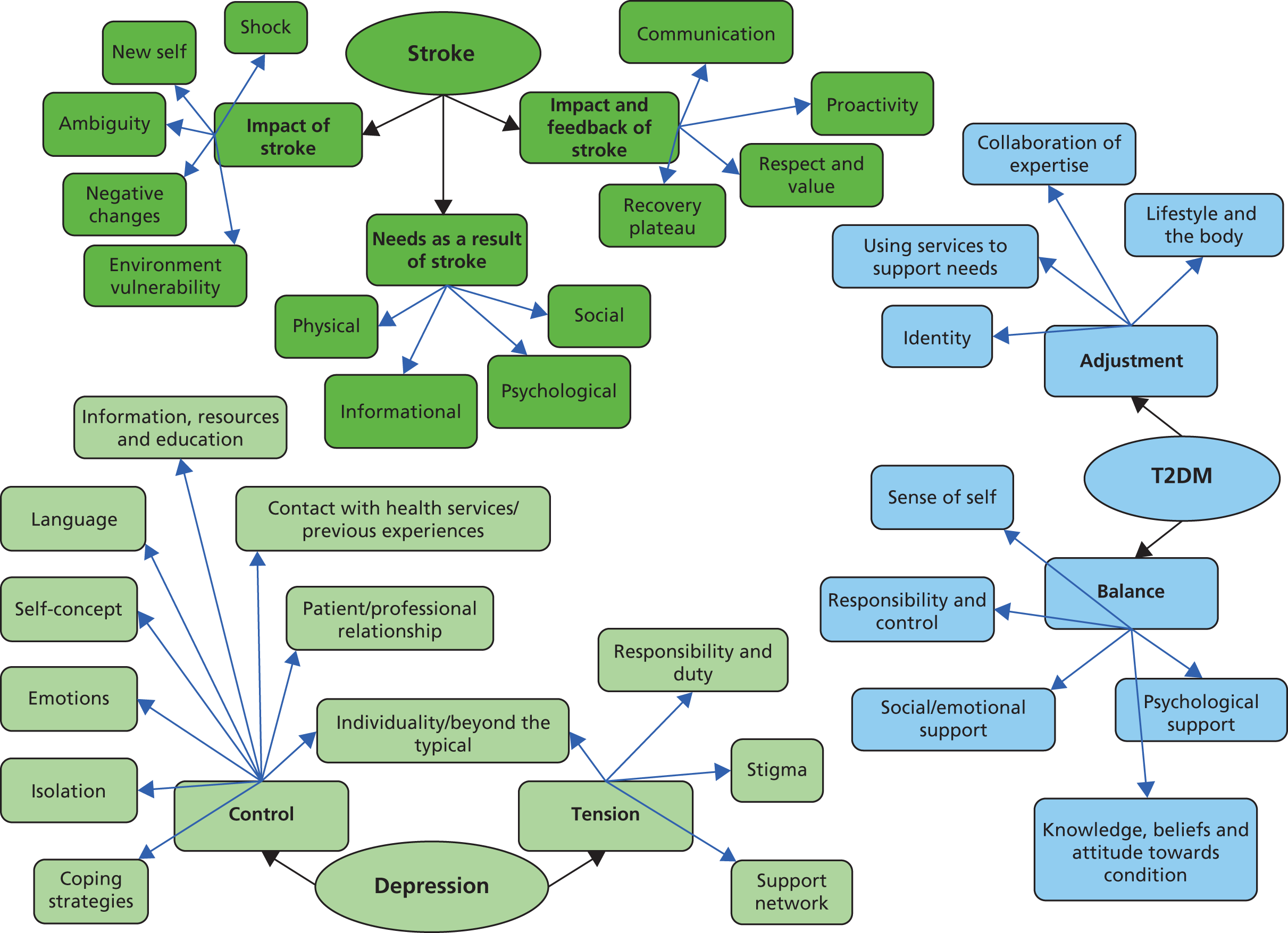
The qualitative systematic reviews included in the additional meta-reviews, were synthesised thematically, their findings relating to self-management support are summarised in Table 125. All the themes arising from this qualitative work arose in several LTCs. The need for education about their disease, and the importance of good, collaborative relationships between patients and HCPs arose in the meta-reviews for all but one LTC and are probably common across all LTCs.
| Themes arising | COPD | CKD | Dementia | Hypertension | RA | LBP | T1DM |
|---|---|---|---|---|---|---|---|
| Need for collaborative relationships with HCPs | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Need for social and emotional support/helpful peer support | ✗ | ✗ | ✗ | ||||
| Individuality of the experience of illness | ✗ | ✗ | |||||
| Importance of striking a balance with carers between support and autonomy | ✗ | ✗ | |||||
| Need for information and education or explanation about condition from HCP | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Psychological support may be important to help adjustment | ✗ | ✗ | |||||
| There may be issues around adherence to medication or treatment regimes | ✗ | ✗ | ✗ |
Conclusions from the quantitative and qualitative meta-reviews
[Note: this section synthesises the findings of the meta-reviews and systematic review reported in previous chapters. In order to cite these meta-reviews we have adopted the following convention:
quantMR: asthma: the finding is derived from the asthma quantitative meta-review
qualMRs: stroke, COPD: the finding is derived from the stroke and COPD qualitative meta-reviews
implSR: the finding is derived from the implementation systematic review (sometimes qualified by disease).
In the interests of brevity we have used the following abbreviations in the citations: IBS, LBP, PNDs, CKD, IAs, T2DM, T1DM, COPD.]
Overall, there appears to be a great deal of evidence, much of it favourable, relating to self-management support across most of the LTCs studied, but it is clear that not everything works. Many of the authors of included systematic reviews noted that some poor-quality studies and the short follow-up times commonly studied, limited their findings. To this we might add that the fact that the systematic review authors usually did not, or were unable to, tease out the individual components in the complex interventions studied also limits their findings. Despite this, in the most commonly studied conditions, like diabetes, asthma and hypertension, the large body of RCT evidence originating in many countries suggests that their findings are likely to be highly generalisable.
The matrix of characteristics of long-term conditions and components of self-management
Although acknowledging the fact that the components emerging from the quantitative meta-reviews did not map perfectly onto the components in our proposed taxonomy (see Chapter 6), we attempted to map them to the characteristics of the exemplar LTCs as defined by the Expert Advisory Group (see Appendix 23 for the full matrix). Together with the results of the individual quantitative and qualitative meta-reviews, this enabled identification of core components common to self-management support of most of the LTCs, and specific components which were linked to specific characteristics.
Core components
-
Education was invariably included in the effective multicomponent self-management support interventions for most LTCs, but there was evidence that it was not effective as an isolated intervention (see Information and education for further details). The only conditions about which there was no evidence, or equivocal findings of benefit from education were LBP and IBS, both of which responded well to psychosocial management interventions. quantMRs: IBS, LBP
-
Psychological support was mentioned as potentially helpful in the qualitative meta-reviews (where available) for virtually all the conditions, and the majority of self-management interventions included an element of psychological support. Overall, there was variable evidence for the effectiveness of these components across the different conditions, with strong evidence in some conditionsquantMRs: LBP, IAs, T1DM and there is an established role for CBT in depression. 138 In some conditions, benefit was not sustained long term. quantMRs: LBP, IAs
-
Interventions to support adherence with medication or treatment had a positive effect in some conditions,quantMRs: CKD, HT, T1DM but overall there was little evidence to support these sort of interventions in epilepsy.
Identifying likely disease/characteristic-specific self-management components
-
Action plans were associated with conditions in which there was significant variability or risk of (serious/high-cost) exacerbations. The evidence for PAAPs is particularly strong,quantMR: asthma and as an integral component of asthma self-management support they are associated with reduced exacerbations, ED visits and hospitalisations. In COPD, action plans increased recognition of exacerbations but had no impact on hospitalisation except as part of a multifaceted intervention. quantMR: COPD The other condition subject to marked variability and necessitating urgent action is T1DM. The term ‘action plan’ is not used here, though the effective intensive diabetes education programmes include training on responding to emergencies such as hypoglycaemia, and actions for ‘sick days’.
-
Therapy rehabilitation was a feature of several of the disabling conditions. Although the term self-management was not used, key aspects of therapy addressed coping with disability, goal-setting and rehearsing ADL. This was an effective strategy, at least in the short term, in most conditions where it was evaluated,quantMRs: stroke, PND, IAs though not in dementia,quantMR: dementia and it was only effective in LBP as part of a complex psychosocial intervention. quantMR: LBP
-
The only LTC which was reported as benefiting from monitoring and feedback was hypertension, an asymptomatic condition in which progress could only be measured by BP readings. quantMR: hypertension
-
Intensive education may have a particular role in complex medical conditions (such as T1DM, or home dialysis in severe CKD) when specific training can enable patients to self-manage clinical tasks. quantMRs: CKD, T1DM
The other characteristics identified by the Expert Advisory Group at the initial workshop (potential of treatment/self-management to be disease modifying, presence of comorbidities, or risk of complication necessitating monitoring) were not associated with any particular disease/characteristic-specific self-management components.
Summary of findings from the implementation systematic review
The most robust evidence comes from studies in asthma (n = 18) and diabetes (n = 26), which included examples of more rigorous methodologies including cluster randomised trials and large/longitudinal database studies. The other conditions had a paucity of data [depression (n = 6), hypertension (n = 2), COPD (n = 2), CKD (n = 2), LBP (n = 1) and stroke n = 1)]. We did not find any implementation studies evaluating self-management in dementia, epilepsy, IAs, IBS or PNDs.
Asthma
Complex whole-systems interventions which address patient education, professional training and are facilitated by a supportive organisation are associated with improvement in process outcomes, markers of control and use of health-care resources. Large-scale initiatives which include collaborations with national or regional authorities and health services can reduce admissions, deaths and time off work. Quality improvement programmes in individual practices or services can improve ownership of PAAPs, and reduce morbidity.
Individually these components are not sufficient. Improving professionals’ knowledge is a core component of effective self-management programmes, but on its own does not improve patient outcomes. Just targeting the organisation to facilitate structured reviews including self-management support intervention improves process outcomes, but in trials shows no impact on clinical outcomes. Targeting the patient is related to significant changes in some process outcomes, with inconsistent effects on clinical outcomes. Authors highlighted the need to support professional education by facilitating integration of new behaviours into practice, the challenges of staff turnover and the importance of involving staff in design of interventions.
Diabetes
Implementing self-management for people with diabetes consistently improves process outcomes, markers of control such as HbA1c, cholesterol, BP, diabetic crises and use of health-care resources. Many of these studies, however, are uncontrolled before-and-after studies with the inherent methodological limitations. The only cluster randomised trial, in the very specific context of including CHWs in multidisciplinary collaborative programmes for diabetes improvement, showed improved process outcomes (documented self-management goals) but no difference in clinical outcomes.
A series of large-scale evaluations of national/regional programmes promoting diabetes education consistently demonstrated improved control of HbA1c, BMI, BP and cholesterol. In a whole-systems approach, primary care physicians were reimbursed to attend training enabling them to deliver standardised diabetes education including self-management.
National programmes promoting training for flexible insulin dosage regimes improved glycaemic control and reduced incidence of ketoacidosis, without increasing the risk of severe hypoglycaemia post-intervention. Implementation of supported self-management in the context of the CCM reduced HbA1c.
Depression
The uncontrolled before-and-after studies suggest that innovative approaches to delivering CBT (using interactive computer programs, or self-help books supported by mental health workers) may be efficient strategies for increasing access to psychological therapies, though randomised trials will be needed to confirm their effectiveness.
Hypertension
In the routine care of people with hypertension, a whole-systems approach to supported self-management, combining patient-, professional- and system-level interventions, was effective in improving adherence to mediation and reducing BP.
Chronic obstructive pulmonary disease
There is a very limited evidence base to inform the implementation of self-management support in COPD. Strong clinical leadership within collaborative programmes to improve general standards of care, and individual specialist provision of care, both improved process outcomes in these before-and-after studies, but neither study provided evidence of clinical effectiveness.
Chronic kidney disease
Intensive training programmes delivered by motivated nephrology teams can enable patients to achieve autonomy in dialysis and this is associated with greater improvement in ‘role-emotional’ and ‘burden of kidney disease’ dimensions of HRQoL.
Low back pain
Based on a single before-and-after study, an intensive CBT-based approach to train patients with chronic LBP to manage their pain and minimise its impact on lifestyle may improve functional ability, pain self-efficacy and QoL.
Stroke
One low-quality paper suggests that an integrated delivery model can improve efficiency in stroke units, though changes in disease severity and comorbidity at admission make interpretation of the clinical outcomes difficult.
Lessons learned
Achieving change is a challenge, even in well-motivated teams. Key facilitators highlighted by the authors are commitment of the health-care system and local practice or clinic; professional training in self-management, with ongoing evaluation; collaborative multidisciplinary working with good communication and referral systems between professionals; effective patient education supported by regular reviews and partnership with patients. A team approach involving the community was seen as essential to the success of projects in deprived, minority communities. Regular oversight is important to ensure intervention fidelity. Practical issues such as sufficient and ongoing funding to enable complex interventions to be instigated and sustained were highlighted. Barriers to participation include clashes with work schedules and family commitments, lack of transportation, and the cost of medication and expensive dietary changes. The use of telephone interventions may overcome some of these barriers to participation in self-management programmes.
Key themes emerging form the meta-reviews and the implementation review
Supporting self-management is inseparable from high-quality care of people with long-term conditions
The key theme from all our qualitative and quantitative meta-reviews and the implementation systematic review is that supporting self-management is inseparable from high-quality care of people with LTCs. Commissioners and providers of services for people with LTCs should consider how they can promote a culture of actively supporting self-management as a normal, expected, monitored and rewarded aspect of the provision of care.
In the exemplar conditions that we studied, the qualitative meta-reviews emphasised the information needs of people with LTCs,qualMRs: T1&2DM, depression, stroke, COPD the importance of psychological support to enable adjustment to living with a LTC, qualMRs: diabetes, IAs, asthma, depression, dementia, LBP and advice/training/resources to overcome physical disabilities. qualMRs: stroke, COPD Although not always identified as ‘self-management’ support, interventions that provided information, supported psychosocial adjustment and enabled practical coping strategies provided at least short-term benefit in several of the exemplar conditions.
These self-management support interventions, however, were not a substitute for high-quality care. Indeed, in a high-quality systematic review included in the asthma meta-review, Gibson et al. 126 demonstrated the synergy between the benefits of self-management education and regular clinical review. Far from feeling abandoned and left to look after themselves, supported self-management empowered patients to access best care and support, though potentially (and paradoxically) reducing health-care resource use especially in asthma and COPD. This echoes the findings of the RECURSIVE health economic analysis which highlights the reduced hospitalisations associated with self-management of respiratory conditions. 54
Supported self-management must be tailored to the individual, their culture and beliefs, and the time point in the condition.
A recurring theme from the meta-analyses was the importance of tailoring the self-management support to the individual and their condition. There was abundant evidence from the qualitative meta-reviews suggesting that individuals’ existing health beliefs frame their understanding of their condition, and they will tailor medical regimes and self-management strategies to fit into their own lives and beliefs. MRs: asthma, T2DM, depression, hypertension, stroke, COPD Gomersall et al. ,96 a qualitative systematic review included in the diabetes meta-review, observed that an emphasis on individual responsibility for control of diabetes while failing to recognise the effect of the individual’s personal circumstances and the societal milieu may paradoxically increase a sense of failure and undermine patients’ confidence. Quantitative meta-reviews in both T2DM and asthma identified the benefits of providing culturally specific interventions.
The nature of the LTC emerged as an important factor in determining the self-management priorities. For example, a stroke survivor has suffered a sudden, disabling event and an initial priority is to encourage and support the patient to regain control over ADL. As functional recovery plateaus, psychosocial needs become more important as the patient struggles to adjust to a new ‘normal’ with the realisation that they are not going to recover all their pre-stroke abilities. In contrast, in conditions where there is less functional disruption (e.g. diabetes), psychosocial interventions to aid acceptance of the diagnosis may need to be the initial focus before the patient is able to relate to the clinical self-management advice that will enable them to achieve the balance that is the hall-mark of effective self-management. Identifying and delivering self-management appropriate to the individual patient at a particular time point is a professional responsibility and a core skill required of HCPs.
Communication
Echoing the forming of a patient/health-care provider partnership described by Lorig and Holman,25 as an element of self-management support, a common theme in most of the qualitative meta-reviews, is the importance of enhancing communication between HCPs and patients. qualMRs: T1&2DM, asthma, COPD, CKD, hypertension, stroke, LBP
It is recognised in the context of cancer survivorship, that strong collaborative relationships between patients and professionals are a pre-requisite to creating mutually agreed care plans that promote self-efficacy. 283 Our qualitative meta-reviews concluded that an ongoing collaborative/communicative relationship – evolving through the phases of accepting and learning to deal with a LTC was highly valued, though not always a reality. qualMRs: stroke, T2DM, CKD, COPD, asthma, LB
A sense of ‘not being listened to’ runs throughout the qualitative reviews, with examples of mismatch between professionals’ and patients’ understanding and aims for self-management behaviours. Examples include a professional focus on medical ‘action plans’ in asthma contrasting with the patients’ need for broader advice on ‘living with asthma’; patients’ disbelief that they have diabetes may preclude adherence to clinical advice on diet, exercise and tablets; the functional goals of a therapist may contrast sharply with the goals of the stroke patient who hopes to return to their pre-stroke level of functioning. It is the responsibility of the HCP to identify the patients’ needs/beliefs and wishes and tailor self-management accordingly. Underlining this there was also a strong suggestion that trust in the individual health-care provider may directly influence self-management behaviours and health-care resource use in the qualitative meta-reviews. QualMRs: T1&2DM, asthma, COPD CKD, hypertension
The inter-related components of self-management support
Self-management support is a complex intervention and although many components were described and trialled in the systematic reviews no one component stood out as more important than any other. Importantly, the more successful interventions were multicomponent. quantMRs: asthma, LBP, stroke, diabetes, hypertension (We noted the quantitative systematic reviews we included often struggled to identify effective single intervention components – sometimes highlighting a component which was actually delivered in association with a number of other components in the included RCTs. In other cases the same RCTs appeared in different systematic reviews as representing different components.)
Information and education
Education, provision of knowledge and information about the LTC, was a component of all the interventions included in the quantitative systematic reviews. A variety of formats were used (groups, individual, lay-led, computerised, school/workplace) and it was not possible to differentiate the effectiveness of one mode compared with another – indeed many interventions included more than one mode. For example, diabetes group education was often complemented by individual sessions with a dietitian and/or specialist nurse. There was some evidence that interactive learning was more effective than didactic lectures,quantMRs: stroke, T1DM and in at least three conditions there was evidence that education provided in isolation was not effective. quantMRs: LBP, hypertension, T1DM
The meta-reviews suggested the potential benefits of providing education/information extended beyond the person affected by the LTC to informal carers,qualMRs: stroke, diabetes, depression, dementia schoolsquant MR: asthma and workplace colleagues. quantMRs: LBP, hypertension
Practical support for physical care
The nature and focus of support for physical aspects of self-management varied according to the characteristics of the LTC.
Coping with ADL was a key challenge for people with disabling conditions (such as stroke, IAs, LBP, COPD, PNDs) and occupational and physiotherapists played an important role in enabling patients to self-manage their disabilities and maintain as much independence as possible. Complex medical conditions (such as T1DM, or home dialysis in severe CKD) involved specific – and often intensive – training to enable patients to self-manage clinical tasks. Conditions subject to marked variation, or at risk of exacerbations (such as asthma and COPD), typically involved provision of action plans to advise on recognition of deterioration and prompt appropriate action. In hypertension (an asymptomatic condition), there was some evidence of benefit from practical support with adherence strategies and/or BP self-monitoring with feedback.
Support with psychological impact of long-term conditions
Psychological training encompasses a range of strategies to support people adjusting to life with a LTC. As mentioned above, many of the qualitative meta-reviews highlighted the importance of including psychological support to help the individual achieve overall well-being, as opposed to just medical health. qualMRs: stroke, asthma, dementia, IAs, LBP, diabetes
Bury’s284,285 theory of biographical disruption emphasises the practical consequences and symbolic significance of chronic illness and highlights the need to reconstruct one’s identify by adjusting to the physical, emotional and societal implications of illness. A thread through most of the qualitative meta-reviews was how the condition had disrupted ‘normal’ life which not only had practical consequences,qualMRs: stroke, IAs, PND, but was also of symbolic significance as the person becomes a ‘patient’,qualMRs: T2DM, stroke, depression invoking fears of dependence on medicationqualMRs: T2DM, asthma, COPD, depression or the support of carers. qualMRs: stroke, COPD Identities were threatenedqualMRs: stroke, dementia, T2DM and roles within society changed. qualMRs: depression, IAs, stroke
Components of psychological skills training were included in many of the effective self-management support interventions such as problem-solving exercises with some specifically using CBT,quantMRs: depression, IAs, T2DM, IBS though the effect was often only seen in the short term and the evidence was limited or equivocal in other conditions.quantMRs: CKD, epilepsy, PND
Social support
The need for social support was a major issue highlighted in the qualitative reviews of some conditions such as stroke, where once physical improvement had plateaued the stroke survivor could be left with the challenge of returning to society with a significant disability. The carers of people with dementia highlighted the need for increasing social support.
More broadly, the need to adopt a new lifestyle was a self-management challenge highlighted by people with T2DM and severe CKD as dietary restrictions impacted on social behaviours. Action plans for people with asthma were clinically focused and did not address social issues of living with the variable condition.
Other components
It is not possible to comment on the specific role of some of the components in our proposed taxonomy, in particular the provision of equipment, as some individual components, although likely to have been included in many of the included RCTs, were not highlighted in the systematic reviews included in our meta-reviews.
Health or social care professional level
The interventions in the RCTs included in the systematic reviews, and thus our quantitative meta-analyses, were delivered by many different professionals and it is not possible to identify a ‘preferred professional’. Specialist nurses were often involved, but so too were therapists, physicians, pharmacists. In addition, in some conditions support was provided by lay educators/mentors.
Training to provide the self-management support for the HCP/lay mentor was common to all the interventions, but, crucially, professional training as an isolated intervention was not effective. implSR The need to provide consistent, ongoing self-management support demands a cultural shift in the relationship between the patient/professional and in the culture of the organisation.
Organisational level
Culture of the organisation
Organisational support is crucial. Without the support of their health-care organisation, professionals struggle to integrate self-management support into their routine clinical care. implSR Promotion of effective self-management support requires a health-care setting in which everyone (including leaders, professional and administrative staff) believes that care should be based on shared decision-making, and patients need to be equipped with the skills and knowledge to self-manage and supported be their own ‘self-managers’. implSR The organisation is responsible for providing the means (both training and time/material resources) to enable professionals to implement self-management support, regularly evaluating self-management process and clinical outcomes and providing ongoing encouragement to maintain good practice.
The need for a public story
More widely there is a societal need to address public understanding of LTCs. The lack of public story for many of our exemplar conditions, and the impact this has on patient help-seeking behaviour and public perceptions of need emerged from the qualitative reviews.
For conditions in which symptoms develop slowly, there is a pre-diagnosis phase in which people may be aware that something is potentially wrong but before they have decide that they need to seek medical advice. qualMRs: T2DM, COPD, IAs Delay may compromise the potential benefits of early treatment, so that public awareness of the implication of symptoms, when to seek help and accessibility to health services are important in this initial phase of self-management.
A common qualitative theme was patients’ perceived need to ‘manage’ the image that they presented to the world,qualMRs: stroke, depression, IAs which could be problematic in conditions for which there was little public understanding of the nature of (for example) breathlessness in COPD, pain in IAs and mood in depression.
Implementing a whole-systems approach to self-management support
The implementation systematic review not only endorses the whole-systems approach to providing self-management support, but also sees self-management support services as a core component of high quality, proactive care for people with LTCs. Finally, it offers insight into effective strategies for achieving the organisational changes necessary to implement self-management support.
The pivotal role of organisational support
In keeping with the broad range of components of self-management support included in the meta-reviews, the implementation systematic review highlighted that effective interventions were multifaceted and multidisciplinary; actively engaging patients, and training and motivating professionals within the context of an organisation which prioritised and actively supported self-management. Although all three components are important, the culture of the organisation underpins and enables integration of self-management principles into routine clinical care, such that the process and clinical impact of patient/professional interventions are realised/enhanced. implSR: asthma, diabetes, hypertension Evidence from the implementation review, including evidence from the researchers’ insights, shows that the organisation’s readiness to change and implement a new intervention, its competence to motivate patients and professionals, ability to offer regular and quality support to professional teams, and capacity to adopt regular monitoring and evaluations may facilitate or hinder the intervention implementation. As we found in the quantitative meta-reviews, a range of professionals led self-management initiatives and diverse modes of delivery, including telehealthcare, were employed. implSR: asthma, depression, diabetes
The broader setting of high-quality long-term condition care
Many of the interventions were introduced in the context of developing services generally to improve the care of people with LTCs. Specific examples which provide evidence of the effectiveness of this approach are a major national programme to improve asthma in Finland,232 an initiative to improve asthma care in Brazil,235 a programme to improve asthma care in Scotland,236 COPD quality improvement programme in the USA,275 diabetes quality improvement programmes in the USA259 and Canada,263 integrated stroke care in Hawaii,278 and four studies which implemented self-management for diabetes in the context of the CCM. 237,256,262,264 Moullec et al. ’s review128 specifically addressed the role of setting in the context of adherence to asthma treatment by comparing RCTs which had provided one of more components of the CCM. The review concluded that the more CCM components included within interventions, the greater the effects on ICS adherence.
Leadership and implementing long-term condition support
Several studies described strategies for achieving the necessary organisational change to implement effective self-management support. Key messages were the need for strong clinical leadership and commitment at the highest level to ensure that a self-management support was prioritised, involving stakeholders to ensure that professionals are motivated and ‘bought in’ to the process of change, training to ensure all staff have appropriate skills, availability of resources to enable ongoing delivery of self-management programmes, and regular oversight and evaluation to sustain the programme. Impl SRs: diabetes, COPD, asthma
Successful programmes have used PDSA cycles and similar collaborative approaches to harness and build on professional/organisational motivation in order to achieve the desired service redesign. 237,256–258
Phase 3 end-of-project workshop
Towards the end of our study we organised a national, multidisciplinary end-of project workshop. The three specific objectives of this workshop were to:
-
enable us to present and discuss the preliminary results of the work undertaken in phases 1 and 2
-
help us derive practical recommendations for commissioners and providers seeking to implement effective population-level self-management support services for people with LTCs
-
advise us about the best ways to disseminate our findings to commissioning groups and health service managers.
Recruitment of workshop participants
We invited the 87 people originally invited to our first workshop, irrespective of whether they attended that event or not, though in some cases e-mails ceased to exist or roles had changed. Where people had changed post, we attempted to invite their replacement if appropriate. We were very keen to invite commissioners so in addition we invited the Clinical Commissioning Group (CCG) chairpersons or, where possible, the designated CCG LTC leads, for all the CCGs in the greater London area. However, our meeting was held at a very difficult time of year from the point of view of the CCG commissioning cycle and only a few CCG representatives responded to our invitation. Our final acceptance list of the 32 delegates and their roles is included in Appendix 24, almost all of whom attended on the day of the workshop, or sent colleagues as replacements. Delegates included people with previous primary care trust commissioning experience, new CCG members including at least one lead commissioner, health service managers, policy-makers, academics, third sector representatives, self-management training providers and representatives from professional bodies. Several delegates had other relevant roles such as patient or carer.
Workshop methods
Preliminary results from the phases 1 and 2 were presented to the delegates and were discussed at two multidisciplinary, small group sessions. Professor Bower presented preliminary results from his RECURSIVE study. The full agenda is shown in Table 126.
| Workshop | |||
|---|---|---|---|
| 9.30 | Registration, coffee | ||
| 10.00 | Milton lecture theatre (LT) | Introductions and aims of the day The PRISMS project |
Stephanie Taylor, Hilary Pinnock |
| 10.30 | Milton LT | Qualitative meta-review | Gemma Pearce |
| 10.50 | Milton LT | Quantitative meta-review | Hannah Parke |
| 11.10 | Milton LT | Implementation review | Eleni Epiphaniou |
| 11.30 | Tea/coffee | ||
| 11:45 | Milton LT | Taxonomy of self-management support components | Stephanie Taylor |
| 12.00 | Break out rooms | Discussion of findings: Do our findings resonate with your experience? |
In discussion groups |
| 12.45 | Lunch – Senor Common Room (above the Milton LT) | ||
| 13.45 | Milton LT | RECURSIVE review | Peter Bower |
| 14.05 | Milton LT | Introduction to the matrix | Hilary Pinnock |
| 14.25 | Break out rooms | Discussion of practical application: How can our findings be useful to the NHS? |
In discussion groups |
| 15.10 | Milton LT | Brief discussion and next steps | Hilary Pinnock, Stephanie Taylor |
| 15.30 | Close and thank you! | ||
Conclusions from workshop
The delegates were very interested in the preliminary results which overall appeared to resonate with their experience. They considered that our proposed taxonomy made sense and suggested a few refinements (which for the purposes of clarity we have already incorporated in the version appearing in this report). In particular, they agreed that education delivered in isolation was unlikely to be successful and that self-management support should be seen as part of the ethos of good-quality care throughout health-care services, rather than as a stand-alone activity which was the responsibility of a single health service manager or a small group of individuals.
The delegates felt that the PRISMS work would be very useful to commissioners and suggested a number of ways the findings might be disseminated, including a suite of different documents of varying degrees of detail.
Chapter 23 Discussion, conclusions and implications
Discussion in relation to the key aims of the brief
Models of care: who for?
The most compelling evidence for reduction in health service use is in the context of respiratory LTCs. Asthma self-management education, including action plans and supported by regular clinical review, reduces exacerbations including ED attendances and hospitalisations. In the context of COPD, it is clear that to be effective, action plans need to be given in the context of multifaceted self-management support. Intensive training can enable people with CKD to undertake home dialysis.
Improved glycaemic control in diabetes and BP control in hypertension have the potential to reduce complications and the associated health-care costs. Other important outcomes include improved coping with disabilities in stroke as a result of rehabilitation therapy. Psychological strategies can improve coping in RA, reduce symptoms in IBS, improve QoL in MS and, as part of a multifaceted intervention, reduce disability due to LBP.
Skillmix: who by?
The interventions in the RCTs included in the systematic reviews and thus our quantitative meta-analyses were delivered by many different professionals and it is not possible to identify a ‘preferred professional’. Specialist nurses were often involved, but so too were therapists, physicians, pharmacists, and in some LTCs support was provided by lay educators/mentors.
The need to provide consistent, ongoing self-management support demands a cultural shift not only in the relationship between the individual patient and a trusted professional, but in the culture of the organisation such that all professionals involved in providing care embrace the same principles of supporting self-management.
Intervention: what?
The more successful self-management support interventions were multicomponent and although many components were described and trialled in the systematic reviews no one component stood out as more important than any other. Crucially, the support needs to be tailored to the patients’ existing health beliefs, preferred lifestyle and cultural background.
Mapping the components of self-management support to the characteristics of LTCs revealed some core components likely to be important in any self-management support intervention. These were:
-
Education, provision of knowledge and information about the LTC. A variety of formats were used (groups, individual, lay-led, computerised, school/workplace) and it was not possible to differentiate the effectiveness of one mode compared with another – indeed many interventions included more than one mode. There was some evidence that interactive learning was more effective than didactic lectures, intensive training may be important to enable patients to self-manage complex clinical tasks and there was evidence that education provided in isolation was not effective.
-
Psychological training encompasses a range of strategies to support people adjusting to life ‘disrupted’ by a LTC. This adjustment process has a time scale influenced by the nature of the disease and the beliefs/attitudes/experience of the patient. Identifying and delivering self-management appropriate to the individual patient at a particular time point is a professional responsibility and a core skill required of HCPs.
-
Practical support for physical care needs to reflect the requirements of individual LTCs. Maintaining independent living and coping with ADL was a key challenge for people with disabling conditions, whereas action plans to facilitate timely response to deterioration can reduce use of health-care resources in conditions subject to exacerbations.
-
Practical social support is an important component for helping patients cope with the effects of disabling LTCs and, more broadly, social adjustments may be needed to enable effective lifestyle changes.
Delivery of care: how?
The implementation systematic review highlighted the importance of a whole-systems approach. Effective interventions were multifaceted and multidisciplinary; actively engaging patients, training and motivating professionals within the context of an organisation which prioritised and actively supported self-management. Although all three components are important, the culture of the organisation underpins and enables integration of self-management principles into routine clinical care, such that the process and clinical impact of patient/professional interventions are realised/enhanced. A range of professionals-led self-management initiatives and diverse modes of delivery, including telehealthcare, were employed.
The key theme from all our qualitative and quantitative meta-reviews and the implementation systematic review is that supporting self-management is inseparable from high-quality care of people with LTCs. Many of the interventions were introduced in the context of developing services generally to improve the care of people with LTCs.
Strategies for achieving the necessary organisational change to implement effective self-management support, include strong clinical leadership and commitment at the highest level to ensure that a self-management support is prioritised, involvement of professionals to ensure they are motivated and ‘bought in’ to the process of change, training to ensure all staff have appropriate skills, availability of resources to enable ongoing delivery of self-management programmes, and regular oversight and evaluation to sustain the programme.
Strengths and limitations of our methods
An important strength of this meta-review was the thorough search process: seven databases were searched using a comprehensive search strategy; relevant journals were checked manually; reference lists of all included reviews were scrutinised; and experts in the field were contacted. An additional strength was the regular meetings between team members, whose multidisciplinary backgrounds encompassed public health, general practice and health psychology, enabling a balanced perspective.
The obvious strength of our approach was our ability to encompass a huge volume of evidence across 14 carefully chosen, diverse LTCs. The 132 unique systematic reviews we appraised, analysed and synthesised contained 1484 unique studies. We believe no other approach could have delivered such a rapid, balanced, systematic overview of this vast amount of research literature.
Qualitative research is notoriously difficult to identify systematically in research databases and this was evident in the lack of overlap between most of the qualitative syntheses within our individual LTC qualitative meta-reviews – even when the syntheses had a similar focus. By synthesising all the available qualitative syntheses in an area together, we were able to get a more complete picture of the available qualitative research. Data saturation between reviews based on different bodies of evidence within the same LTC was quite common in our meta-reviews suggesting the findings were valid and potentially transferable. We believe the qualitative meta-reviews helped give patients and carers ‘a voice’ alongside the findings of the quantitative meta-reviews and the implementation review. However, in acknowledgement of hermeneutic philosophy, the interpretations made in this meta-review were further away from the expressed views of individuals at interview.
There were many challenges to identifying papers for the implementation systematic review, not least the lack of clear definitions of implementation studies and the design and reporting standards to which they should adhere. 286 We applied specific tests (inclusion/exclusion criteria are in Appendix 14) to establish whether or not a study was actually implementation. From a practical perspective, when screening papers this meant the studies had to include outcomes from whole populations, define eligibility to the service (not the research), recruit patients to the new service (as opposed to consenting to research), report uptake and attrition, be delivered by service personnel (though they could be trained specifically to deliver the intervention). 282 Given the lack of reporting guidelines in this area, it was not always possible to be sure of the status of a report and we may have rejected relevant papers because key information was not available, though doubtful papers were not rejected without discussion.
A second challenge was the plethora of terms used to refer to implementation research making it challenging to identify terms for our search strategy. In some instances, even some terms closely related to implementation research, i.e. ‘effectiveness trials’, ‘routine clinical care’, ‘pragmatic’, were used arbitrarily for a wide range of study types rather than only for implementation studies. We tried to be as broad as possible in our search strategy (and screened 30,279 ‘hits’) but we acknowledge that we may have missed some implementation studies.
Combining the findings from our qualitative and quantitative meta-reviews together helped generate insights into why some interventions might succeed or fail and, perhaps more commonly, what type of self-management support interventions patients might want. Our implementation review attempted to generate evidence from a real-world settings and considering 14 different conditions enabling us to extrapolate our findings into real-life provision of care.
Meta-reviews have some intrinsic limitations. We were reliant on the authors of our included systematic-reviews providing accurate and detailed descriptions of RCTs, and the resynthesis of materials already synthesised risks further loss of detail and a consequent potential for erroneous assumptions. As a result, our conclusions are sometimes broadly descriptive rather than detailed.
We appraised the quality of all reviews using R-AMSTAR and used these scores alongside relevance scores to inform the weighting of evidence. The R-AMSTAR has limitations – although it provides a single score which was very convenient for our purposes. However, the generation of a score implies that the different items in the R-AMSTAR have similar weight with respect to quality – which is unlikely to be the case in reality. We recognise that the R-AMSTAR is a very approximate tool and our quality assessments of the quantitative systematic reviews were likely to be very imprecise There are no published quality appraisal tools for qualitative syntheses (as opposed to individual studies). We adapted the R-AMSTAR (detailed in Appendix 15), but this was an imperfect tool for this task and, again, our quality assessments are approximate.
We paid careful attention to studies that overlapped between reviews in order not to exaggerate the amount of evidence and scrutinised interpretation of the studies common to different reviews. In the event of systematic reviewers differing in their interpretation of the same body of literature, we attempted to understand from the reviews why this might have arisen. Inevitably, our reviews will not be completely up to date (and some were very old), so recent evidence is not included. For example, the systematic reviews did not include the findings of the recently published whole-system demonstrator study14 nor a recent trial of a whole-systems approach to implementing self-management. 281
This overarching review was a commissioned, policy-focused rapid review, meaning that screening and data extraction was conducted by one reviewer, and not two reviewers working independently. Although we acknowledge this as a potential weakness, we ensured all the reviewers were trained before commencing each stage of the review and by instituting random 10% checks at every stage of the meta-reviews, and a 25% check for the implementation review (because poor reporting often made it difficult to decide on eligibility).
A widely encountered problem for many systematic review authors was the heterogeneity of RCTs which limited, or prevented, meta-analysis. This also presented challenges for our meta-review.
We excluded reviews where we were unable to extract RCTs separately from other study designs. This restricted the number of reviews we were able to include, and may have resulted in the omission of important evidence. On the other hand, our strict inclusion criterion ensured that included reviews provided a high level of relevant evidence. Our approach did not allow us specifically to consider multimorbidity, although it is inevitable that most of the adult patients include within the systematic reviews would have had more than one LTC. We would have liked to consider this important issue of multimorbidity but, unfortunately, it was not discussed in any detail in any of our included systematic reviews, perhaps because it has only recently become an area of particular concern to health services.
The original brief mentioned telehealth, but although telehealth interventions were included in many of the interventions in our included systematic-reviews it was only in one area, hypertension, that the review authors had much to say about telehealth. Our taxonomy recognises telehealth as a mode of delivery but our synthesis – and thus our conclusions – was based around content of interventions and the characteristics of LTCs.
Much of the evidence for the implementation review comes from studies of poor quality. Many report before-and-after data and lacked a control group. The results of these studies therefore need to be interpreted with caution. To help the reader to gauge the weight than can be placed on individual findings, we frequently describe the methodology in our description of the findings, so that outcomes from randomised trials, or from large longitudinal databases may be given more credence than small single-centre observational studies.
Finally, as one of our reviewer’s has pointed out, It might have been a useful approach to use the qualitative and quantitative themes and results to frame the extraction and synthesis in the implementation review, but due to the time scale of this review these pieces of work were conducted in parallel so this was not possible.
Conclusions and considerations for commissioners
Effective self-management support interventions are multifaceted, should be tailored to the individual (their culture and beliefs) and specific condition, and underpinned by a collaborative/communicative relationship between the patient and a trusted HCP within the context of a health-care organisation that actively promotes self-management.
Self-management support is a complex intervention and although many components were described and trialled in the systematic reviews no one component stood out as more important than any other, or was effective in isolation. Core components include:
-
Provision of knowledge and information about the LTC.
-
Psychological strategies to support people adjusting to life with a LTC.
-
Practical support for physical care tailored to the specific LTC. Disease/characteristic-specific self-management components include coping with ADL for people with disabling conditions; action plans to advise on prompt appropriate action in the event of deterioration in conditions subject to marked exacerbations; (intensive) disease-specific training to enable self-management of specific clinical tasks.
-
Social support as appropriate.
-
Other potentially effective components include self-monitoring with feedback and practical support with adherence strategies.
Implementation requires a whole-systems approach which intervenes at the level of the patient, the professional and the organisation. The health-care organisation is responsible for providing the means (both training and time/material resources) to enable professionals to implement and patients to benefit from self-management support, regularly evaluating self-management processes and clinical outcomes.
More widely, there is a societal need to address public understanding of LTCs. The lack of public story for many of our exemplar conditions impacted on patient help-seeking behaviour and public perceptions of need.
Supporting self-management is inseparable from high-quality care of people with LTCs. Commissioners and providers of services for people with LTCs should consider how they can promote a culture of actively supporting self-management as a normal, expected, monitored and rewarded aspect of the provision of care.
Recommendations for research
-
Research is needed to understand how health-service managers and staff can change the culture in their health-care organisations to enable a whole-systems approach to self-management support.
-
Most research on self-management support interventions has only short-term follow-up periods. There is a need for studies with longer-term follow-up and, in particular, for studies which examine the maintenance of the benefits from self-management support.
-
Dementia is a LTC which did not seem to ‘fit’ into our predictions from other conditions of what self-management support might be effective. Furthermore, the quantitative systematic review evidence suggested there is a paucity of research in this area. We recommend research exploring how the self- (and carer-) management of patients with dementia living at home may best be supported.
-
Research is needed to understand the evolution of self-management support needs across the trajectory of different LTCs.
-
The quality of the implementation studies in our review was very variable. There is a need to develop quality standards for the design and reporting of implementation studies.
-
We identified a number of areas where we felt new qualitative systematic reviews would be helpful, in some cases the lack of such an existing review may indicate the lack of primary qualitative research in the area, but it is not possible to conclude this from our meta-review searches. A table explaining our rationale for these recommendation is presented in Appendix 25. In summary the areas are
-
– Asthma: there is a need for a qualitative syntheses on the lived experience of asthma and the wider aspects of self-management support, other than action plans.
-
– COPD: there is a need for higher-quality qualitative synthesis examining self-management support for people with COPD.
-
– Dementia: there is a need for higher-quality qualitative synthesis examining self-management support for people with dementia living at home and their carers.
-
– CKD: there is a need for qualitative synthesis examining self-management support for those at earlier stages of CKD.
-
– Epilepsy: there is a need for a qualitative synthesis on self-management support for people with epilepsy.
-
– IBS: there is a need for a qualitative synthesis on self-management support for people with IBS.
-
– LBP: there is a need for a focused qualitative synthesis examining self-management support for people with chronic LBP.
-
– PNDs: there is a need for a qualitative synthesis on self-management support for people with PNDs.
-
-
We suggest our proposed taxonomies of the characteristics of LTCs and of self-management support might be a useful framework for others researching in the area to consider when developing, describing and analysing interventions.
Acknowledgements
John Ribchester.
Alison Powell.
Andrea Takeda.
David Salisbury.
Shahid Mahmood.
Paula Broome.
Sharon Dabrowa.
Attendees at May 2012 and May 2013 workshops.
Contribution of authors
Stephanie JC Taylor (Professor in Public Health and Primary Care, Queen Mary University of London) and Hilary Pinnock (Reader, Allergy and Respiratory Research Group, University of Edinburgh): joint principal investigators, involved in conception, design, analysis and interpretation of the study and drafting the manuscript. Responsible for the integrity of the work as a whole.
Eleni Epiphaniou (PRISMS Senior Research Assistant), Gemma Pearce [Centre for Technology Enabled Health Research (CTEHR), Coventry University, UK; PRISMS Research Assistant] and Hannah L Parke (PRISMS Research Assistant): substantial contributions to the design and conduct of the study, the acquisition, analysis and interpretation of data, and drafting the manuscript.
Anna Schwappach (GP Specialist Trainee Year 4), Neetha Purushotham (GP Specialist Trainee Year 4) and Sadhana Jacob (Global Public Health and Primary Care Student): substantial contributions to the acquisition, analysis and interpretation of data, and drafting the manuscript.
Chris J Griffiths (Professor of Primary Care), Trisha Greenhalgh (Professor of Primary Health Care) and Aziz Sheikh (Professor of Primary Care Research and Development): substantial contributions to the conception and design of the project and revising the manuscript critically for important intellectual content.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- NIHR Health Services and Delivery Research . Commissioning Brief (NIHR HS&Amp;DR Project: 11 1014 04): A Rapid Synthesis of the Evidence on Interventions Supporting Self-Management for People With Long-Term Conditions n.d. www.netscc.ac.uk/hsdr/projdetails.php?ref=11-1014-04 (accessed April 2014).
- Research Evidence on the Effectiveness of Self-Care Support (2005–07). London: Department of Health; 2007.
- Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, et al. Healthy life expectancy for 187 countries, 1990–2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet 2012;380:2144-62. http://dx.doi.org/10.1016/S0140-6736(12)61690-0.
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163-96. http://dx.doi.org/10.1016/S0140-6736(12)61729-2.
- Murray CLM, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197-223. http://dx.doi.org/10.1016/S0140-6736(12)61689-4.
- Wanless D. Securing our Future Health: Taking a Long-Term View. London: Department of Health; 2002.
- Innovative Care for Chronic Conditions: Building Blocks for Action. Geneva: WHO; 2002.
- Improving Chronic Disease Management. London: Department of Health; 2004.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: The Stationery Office; 2006.
- Designed for Life: Creating World Class Health and Social Care for Wales in the 21st century. Cardiff: Welsh Assembly Government; 2005.
- Co-Creating Health Briefing paper. London: The Health Foundation; 2008.
- The Expert Patient: A New Approach to Chronic Disease Management for the 21st Century. London: Department of Health; 2001.
- Quality, Innovation, Productivity and Prevention (QIPP) Work-Stream for Patients with LTCs. London: Department of Health; 2010.
- Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Hirani S, et al. Effect of telehealth on use of secondary care and mortality: findings from the whole systems demonstrator cluster randomised trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3874.
- Review of National Self Care Week 15–21 November 2010. London: Department of Health; 2011.
- National Health Service . NHS Direct n.d. www.nhs.uk/nhs-direct/Pages/NHS-Direct-legacy-enquiries.aspx (accessed September 2014).
- National Health Service . Your Health, Your Way: Your NHS Guide to Long-Term Conditions and Self Care n.d. www.nhs.uk/Planners/Yourhealth/Pages/Yourhealth.aspx (accessed April 2014).
- Supporting People with Long Term Conditions: Commissioning Personalised Care Planning – A Guide for Commissioners. London: Department of Health; 2009.
- Baseline Study of Activity and Development in Self Care Support in PCTs and Local Areas. London: Department of Health; 2005.
- Hunt J. Primary Care and the Modern Family Doctor n.d. www.gov.uk/government/speeches/primary-care-and-the-modern-family-doctor (accessed April 2014).
- Ring N, Pinnock H, Wilson C, Hoskins G, Jepson R, Wyke S, et al. Understanding what asthma plans mean: a linguistic analysis of terminology used in published texts. Prim Care Respir J 2011;20:170-7. http://dx.doi.org/10.4104/pcrj.2011.00012.
- Parsons S, Bury M, Carter S, Hurst P, Magee H, Taylor D. Self Management Support Amongst Older Adults: The Availability, Impact and Potential of Locally Based Services and Resources. London: HMSO; 2010.
- Adams K, Greiner AC, Corrigan JM. The 1st Annual Crossing the Quality Chasm Summit: A Focus on Communities. Washington, DC: The National Academic Press; 2004.
- Corbin JM, Strauss AL. Unending Work and Care: Managing Chronic Illness at Home. San Francisco, CA: Jossey-Bass Publishers; 1988.
- Lorig K, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1-7. http://dx.doi.org/10.1207/S15324796ABM2601_01.
- Marks R, Allegrante JP. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part II). Health Promot Pract 2005;6:148-56. http://dx.doi.org/10.1177/1524839904266792.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Adv Behav Res Ther 1978;1:139-61. http://dx.doi.org/10.1016/0146-6402(78)90002-4.
- Gheera M. Direct Payments and Personal Budgets for Social Care 2012. www.parliament.uk/briefing-papers/SN03735 (accessed April 2014).
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Miles A, Hall H. Long-Term Conditions Care Planning Commitment. London: Department of Health; 2010.
- Hunt J. UK To Be ‘World Leader’ on Health Technology, says Hunt. London: Department of Health; 2012.
- Fairbrother P, Pinnock H, Hanley J, McCloughan L, Sheikh A, Pagliari C, et al. Exploring telemonitoring and self-management by patients with chronic obstructive pulmonary disease: a qualitative study embedded in a randomized controlled trial. Pat Educ Counsel 2013;93:403-10. http://dx.doi.org/10.1016/j.pec.2013.04.003.
- Department of Health . Generic Long Term Conditions Model, October 2010 n.d. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Healthcare/Longtermconditions/DH_120915 (accessed September 2014).
- Self Care – A Real Choice: Self Care Support – A Practical Option. London: Department of Health; 2005.
- Glasziou P, Irwig L, Mant D. Monitoring in chronic disease: a rational approach. BMJ 2005;330:644-8. http://dx.doi.org/10.1136/bmj.330.7492.644.
- Kennedy A, Rogers A, Bower P. Support for self care for patients with chronic disease. BMJ 2007;337:968-70. http://dx.doi.org/10.1136/bmj.39372.540903.94.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Pinnock H, Huby G, Powell A, Kielmann T, Price D, Williams S, et al. The Process of Planning, Development and Implementation of a General Practitioner with a Special Interest Service in Primary Care Organisations in England and Wales: A Comparative Prospective Case Study. London: HMSO; 2008.
- Kielmann T, Huby G, Powell A, Sheikh A, Price D, Williams S, et al. From support to boundary: a qualitative study of the border between self care and professional care. Pat Educ Counsel 2010;79:55-61. http://dx.doi.org/10.1016/j.pec.2009.07.015.
- Department of Health . Ten Things You Need to Know About Long Term Conditions n.d. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Healthcare/Longtermconditions/DH_084294 (accessed September 2014).
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Library. England: John Wiley & Sons Ltd; 2008.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Method 2009;9. http://dx.doi.org/10.1186/1471-2288-9-59.
- Systematic Reviews. CRD’s Guidance for Undertaking Reviews in Healthcare. York: University of York; 2008.
- Oxman AD. Systematic reviews: checklists for review articles. BMJ 1994;309:648-51. http://dx.doi.org/10.1136/bmj.309.6955.648.
- Kung J, Chiappelli F, Cajulis OO, Avezova R, Kossan G, Chew L, et al. From systematic reviews to clinical recommendations for evidence-based health care: validation of revised assessment of multiple systematic reviews (R-AMSTAR) for grading of clinical relevance. Open Dent J 2010;4:84-91. http://dx.doi.org/10.2174/1874210601004020084.
- Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Method 2007;7. http://dx.doi.org/10.1186/1471-2288-7-10.
- Shea BJ, Bouter LM, Peterson J, Boers M, Andersson N, Ortiz Z, et al. External validation of a measurement tool to assess systematic reviews (AMSTAR). PLOS ONE 2007;2. http://dx.doi.org/10.1371/journal.pone.0001350.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377-84. http://dx.doi.org/10.1136/jech.52.6.377.
- Woolf SH, Johnson RE. The break-even point: when medical advances are less important than improving the fidelity with which they are delivered. Ann Fam Med 2005;3:545-52. http://dx.doi.org/10.1370/afm.406.
- Heidegger M. Being and Time. London: Wiley-Blackwell; 1962.
- Noblit GW, Hare RD. Meta-Ethnography: Synthesizing Qualitative (Qualitative Research Methods Volume 11). Newbury Park, CA: Sage Publications; 1988.
- Glaser B, Strauss A. The Discovery of Grounded Theory. New York, NY: Aldine Publishing Company, Hawthorne; 1967.
- Reid PP, Compton WD, Grossman JH, Fanjiang G. Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC: National Academies Press (US); 2005.
- Bower P, Murray E, Kennedy A, Newman S, Richardson G, Rogers A. Self-Management Support Interventions to Reduce Health Care Utilisation Without Compromising Outcomes: A Rapid Synthesis of the Evidence n.d. www.netscc.ac.uk/hsdr/projdetails.php?ref=11-1014-06 (accessed April 2014).
- Campbell R, Pound P, Pope C, Britten N, Pill R, Morgan M, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med 2003;56:671-84. http://dx.doi.org/10.1016/S0277-9536(02)00064-3.
- Diabetic Foot Problems – Inpatient Management (CG119). London: NICE; 2011.
- Type 2 Diabetes – Newer Agents (Partial Update of CG66). London: NICE; 2009.
- Malanda UL, Welschen LMC, Riphagen II, Dekker JM, Nijpels G, Bot SDM. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database Syst Rev 2012;1.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Pat Educ Counsel 2002;48:177-87. http://dx.doi.org/10.1016/S0738-3991(02)00032-0.
- Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. J Public Health 2005;95:1523-35. http://dx.doi.org/10.2105/AJPH.2005.066084.
- Krumholz HM, Currie PM, Riegel B, Phillips CO, Peterson ED, Smith R, et al. A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation 2006;114:1432-45. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.177322.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically-clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Med 2009;6.
- Lamb M, Buchanan D, Godfrey C. The psychosocial spiritual experience of elderly individuals recovering from stroke: a systematic review. Int J Evidence-Based Healthcare 2008;6:173-205. http://dx.doi.org/10.1111/j.1744-1609.2008.00079.x.
- McKevitt C, Redfern J, Mold F, Wolfe C. Qualitative studies of stroke: a systematic review. Stroke 2004;35:1499-505. http://dx.doi.org/10.1161/01.STR.0000127532.64840.36.
- Murray J, Ashworth R, Forster A, Young J. Developing a primary care-based stroke service: a review of the qualitative literature. Br J Gen Pract 2003;53:137-42.
- Peoples H, Satink T, Steultjens E. Stroke survivors’ experiences of rehabilitation: a systematic review of qualitative studies. Scand J Occup Ther 2011;18:163-71. http://dx.doi.org/10.3109/11038128.2010.509887.
- Reed MC, Wood V, Harrington R, Paterson J. Developing stroke rehabilitation and community services: a meta-synthesis of qualitative literature. Disabil Rehabil 2012;34:553-63. http://dx.doi.org/10.3109/09638288.2011.613511.
- Salter K, Hellings C, Foley N, Teasell R. The experience of living with stroke: a qualitative meta-synthesis. J Rehabil Med 2008;40:595-602. http://dx.doi.org/10.2340/16501977-0238.
- Lui MHL, Ross FM, Thompson DR. Supporting family caregivers in stroke care a review of the evidence for problem solving. Stroke 2005;36:2514-22. http://dx.doi.org/10.1161/01.STR.0000185743.41231.85.
- Aziz NA, Leonardi-Bee J, Phillips MF, Gladman J, Legg LA, Walker M. Therapy-based rehabilitation services for patients living at home more than one year after stroke. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.CD005952.pub2.
- Hoffmann T, Bennett S, Koh CL, McKenna KT. Occupational therapy for cognitive impairment in stroke patients. Cochrane Database Syst Rev 2010;9. http://dx.doi.org/10.1002/14651858.CD006430.pub2.
- Legg L, Drummond A, Langhorne P. Occupational therapy for patients with problems in activities of daily living after stroke. Cochrane Database Syst Rev 2006;4.
- Outpatient Service Trialists . Therapy-based rehabilitation services for stroke patients at home. Cochrane Database Syst Rev 2003;1.
- Poulin V, Korner-Bitensky N, Dawson R, Bherer L. Efficacy of executive function interventions after stroke: a systematic review. Top Stroke Rehabil 2012;19:158-72. http://dx.doi.org/10.1310/tsr1902-158.
- Steultjens EMJ, Dekker J, Bouter LM, van de Nes JCM, Cup EHC, van den Ende CHM. Occupational therapy for stroke patients: a systematic review. Stroke 2003;34:676-88. http://dx.doi.org/10.1161/01.STR.0000057576.77308.30.
- Walker MF, Leonardi-Bee J, Bath P, Langhorne P, Dewey M, Corr S, et al. Individual patient data meta-analysis of randomized controlled trials of community occupational therapy for stroke patients. Stroke 2004;35:2226-33. http://dx.doi.org/10.1161/01.STR.0000137766.17092.fb.
- Ellis G, Mant J, Langhorne P, Dennis M, Winner S. Stroke liaison workers for stroke patients and carers: an individual patient data meta-analysis. Cochrane Database Syst Rev 2010;5. http://dx.doi.org/10.1002/14651858.CD005066.pub2.
- Ko H, Turner T, Jones C, Hill C. Patient-held medical records for patients with chronic disease: a systematic review. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.037531.
- Korpershoek C, van der Bijl J, Hafsteinsdottir B. Self-efficacy and its influence on recovery of patients with stroke: a systematic review. J Adv Nurs 2011;67:1876-94. http://dx.doi.org/10.1111/j.1365-2648.2011.05659.x.
- Rae-Grant AD, Turner AP, Sloan A, Miller D, Hunziker J, Haselkorn JK. Self-management in neurological disorders: systematic review of the literature and potential interventions in multiple sclerosis care. J Rehabil Res Dev 2011;48:1087-100. http://dx.doi.org/10.1682/JRRD.2010.08.0159.
- Smith J, Forster A, House A, Knapp P, Wright JJ, Young J. Information provision for stroke patients and their caregivers. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.CD001919.pub3.
- Jones F, Riazi A. Self-efficacy and self-management after stroke: a systematic review. Disabil Rehabil n.d.;33:797-810. http://dx.doi.org/10.3109/09638288.2010.511415.
- Radomski MV, Latham CAT. Occupational Therapy for Physical Dysfunction. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
- Jones F. Strategies to enhance chronic disease self-management: how can we apply this to stroke?. Disabil Rehabil 2006;28:841-7. http://dx.doi.org/10.1080/09638280500534952.
- Dishman RK, Motl RW, Sallis JF, Dunn AL, Birnbaum AS, Welk GJ, et al. Self-management strategies mediate self-efficacy and physical activity. Am J Prevent Med 2005;29:10-8. http://dx.doi.org/10.1016/j.amepre.2005.03.012.
- Greveson G, James O. Improving long-term outcome after stroke – the views of patients and carers. Health Trends 1991;23:161-2.
- Co-Creating Health: Evaluation of the First Phase. London: The Health Foundation; 2012.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Rev 1977;84:191-215. http://dx.doi.org/10.1037/0033-295X.84.2.191.
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York, NY: Simon and Schuster; 1963.
- Goffman E. The Presentation of Self in Everyday Life. Garden City, AT: Doubleday; 1959.
- Jones EE. Ingratiation: A Social Psychological Analysis. New York, NY: Appleton-Century-Croft; 1964.
- Leary M. Self-Presentation: Impression Management and Interpersonal Behaviour. Oxford: Westview Press; 1995.
- Lawrence M, Kerr S, McVey C, Godwin J. A systematic review of the effectiveness of secondary prevention lifestyle interventions designed to change lifestyle behaviour following stroke. JBI Library Syst Rev 2011;9:1782-827.
- Fleming E, Gillibrand W. An exploration of culture, diabetes, and nursing in the South Asian community: a metasynthesis of qualitative studies. J Transcult Nurs 2009;20. http://dx.doi.org/10.1177/1043659608330058.
- Gomersall T, Madill A, Summers L. A metasynthesis of the self-management of type 2 diabetes. Qual Health Res 2011;21. http://dx.doi.org/10.1177/1049732311402096.
- Ho AYK, Berggren I, Dahlborg-Lyckhage E. Diabetes empowerment related to Pender’s Health Promotion Model: a meta-synthesis. Nurs Health Sci 2010;12:259-68. http://dx.doi.org/10.1111/j.1442-2018.2010.00517.x.
- Paterson BL, Thorne S, Dewis M. Adapting to and managing diabetes. Image J Nurs Sch 1998;30:57-62. http://dx.doi.org/10.1111/j.1547-5069.1998.tb01237.x.
- Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Improving patient care. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 2005;143:427-40. http://dx.doi.org/10.7326/0003-4819-143-6-200509200-00007.
- Dorresteijn JAN, Kriegsman DMW, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev 2010;5. http://dx.doi.org/10.1002/14651858.CD001488.pub3.
- Duke SS, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.CD005268.pub2.
- Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabet Educ 2003;29:488-501. http://dx.doi.org/10.1177/014572170302900313.
- Hawthorne K, Robles Y, Cannings-John R, Edwards AGK. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev 2008;3.
- Heinrich E, Schaper NC, de Vries NK. Self-management interventions for type 2 diabetes: a systematic review. Eur Diabet Nurs 2010;7:71-7. http://dx.doi.org/10.1002/edn.160.
- Khunti K, Camosso-Stefinovic J, Carey M, Davies MJ, Stone MA. Educational Interventions for Migrant South Asians with Type 2 Diabetes: A Systematic Review. Leicester: Department of Health Sciences, University of Leicester; 2008.
- Li T, Wu HM, Wang F, Huang CQ, Yang M, Dong BR, et al. Education programmes for people with diabetic kidney disease. Cochrane Database Syst Rev 2011;6. http://dx.doi.org/10.1002/14651858.CD007374.pub2.
- Minet L, Møller S, Vach W, Wagner L, Henriksen JE. Mediating the effect of self-care management intervention in type 2 diabetes: a meta-analysis of 47 randomised controlled trials. Pat Educ Counsel 2010;80:29-42. http://dx.doi.org/10.1016/j.pec.2009.09.033.
- Nam S, Janson SL, Stotts NA, Chesla C, Kroon L. Effect of culturally tailored diabetes education in ethnic minorities with type 2 diabetes: a meta-analysis. J Cardiovasc Nurs 2012;27:505-18. http://dx.doi.org/10.1097/JCN.0b013e31822375a5.
- Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet 2004;364:1523-37. http://dx.doi.org/10.1016/S0140-6736(04)17277-2.
- Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabet Care 2001;24:561-88. http://dx.doi.org/10.2337/diacare.24.3.561.
- Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabet Care 2002;25:1159-72. http://dx.doi.org/10.2337/diacare.25.7.1159.
- Pérez-Escamilla R, Hromi-Fiedler A, Vega-López S, Bermúdez-Millán A, Segura-Pérez S. Impact of peer nutrition education on dietary behaviors and health outcomes among Latinos: a systematic literature review. J Nutr Educ Behav 2008;40:208-26. http://dx.doi.org/10.1016/j.jneb.2008.03.011.
- Sigurdardottir AK, Jonsdottir H, Benediktsson R. Outcomes of educational interventions in type 2 diabetes: WEKA data-mining analysis. Patient Educ Counsel 2007;67:21-3. http://dx.doi.org/10.1016/j.pec.2007.03.007.
- Steinsbekk A, Rygg L, Lisulo M, Rise M, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-213.
- Van Dam HA, Van Der Horst FG, Knoops L, Ryckman RM, Crebolder HFJM, Van Den Borne BHW. Social support in diabetes: a systematic review of controlled intervention studies. Pat Educ Counsel 2005;59:1-12. http://dx.doi.org/10.1016/j.pec.2004.11.001.
- Glasgow RE, Osteen VE. Evaluating diabetes education. Are we measuring the most important outcomes?. Diabet Care 1992;15:1423-32. http://dx.doi.org/10.2337/diacare.15.10.1423.
- Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A, et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Pat Educ Counsel 2011;85:e131-43. http://dx.doi.org/10.1016/j.pec.2011.01.025.
- Bhogal SK, Zemek RL, Ducharme F. Written action plans for asthma in children. Cochrane Database Syst Rev 2006;3.
- Zemek RL, Bhogal SK, Ducharme FM. Systematic review of randomized controlled trials examining written action plans in children. What is the plan?. Arch Pediatr Adolesc Med 2008;162:157-63. http://dx.doi.org/10.1001/archpediatrics.2007.34.
- Bailey EJ, Cates CJ, Kruske SG, Morris PS, Brown N, Chang AB. Culture-specific programs for children and adults from minority groups who have asthma. Cochrane Database Syst Rev 2009;2.
- Bernard-Bonnin AC, Stachenko S, Bonin D, Charette C, Rousseau E. Self-management teaching programs and morbidity of pediatric asthma: a meta-analysis. J Allergy Clin Immunol 1995;95:34-41. http://dx.doi.org/10.1016/S0091-6749(95)70150-8.
- Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M. Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009;2. http://dx.doi.org/10.1002/14651858.CD001290.pub2.
- Bussey-Smith KL, Rossen RD. A systematic review of randomized control trials evaluating the effectiveness of interactive computerized asthma patient education programs. Ann Allergy Asthma Immunol 2007;98:507-16. http://dx.doi.org/10.1016/S1081-1206(10)60727-2.
- Chang AB, Taylor B, Masters IB, Laifoo Y, Brown ADH. Indigenous healthcare worker involvement for Indigenous adults and children with asthma. Cochrane Database Syst Rev 2010;5. http://dx.doi.org/10.1002/14651858.CD006344.pub3.
- Coffman JM, Cabana MD, Yelin EH. Do school-based asthma education programs improve self-management and health outcomes?. Pediatrics 2009;124:729-42. http://dx.doi.org/10.1542/peds.2008-2085.
- Gibson PG, Powell H, Wilson A, Abramson MJ, Haywood P, Bauman A, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2002;3.
- Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax 2004;59:94-9. http://dx.doi.org/10.1136/thorax.2003.011858.
- Moullec G, Gour-Provencal G, Bacon SL, Campbell TS, Lavoie KL. Efficacy of interventions to improve adherence to inhaled corticosteroids in adult asthmatics: impact of using components of the chronic care model. Respir Med 2012;106:1211-25. http://dx.doi.org/10.1016/j.rmed.2012.06.001.
- Postma J, Karr C, Kieckhefer G. Community health workers and environmental interventions for children with asthma: a systematic review. J Asthma 2009;46:564-76. http://dx.doi.org/10.1080/02770900902912638.
- Powell H, Gibson PG. Options for self-management education for adults with asthma. Cochrane Database Syst Rev 2002;3.
- Ring N, Malcolm C, Wyke S, Macgillivray S, Dixon D, Hoskins G, et al. Promoting the use of personal asthma action plans: a systematic review. Prim Care Respir J 2007;16:271-83. http://dx.doi.org/10.3132/pcrj.2007.00049.
- Tapp S, Lasserson TJ, Rowe BH. Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007;3.
- Toelle B, Ram FSF. Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev 2004;1.
- Welsh EJ, Hasan M, Li P. Home-based educational interventions for children with asthma. Cochrane Database Syst Rev 2011;10. http://dx.doi.org/10.1002/14651858.CD008469.pub2.
- Khan N, Bower P, Rogers A. Guided self-help in primary care mental health: meta-synthesis of qualitative studies of patient experience. Br J Psychiatry 2007;191:206-11. http://dx.doi.org/10.1192/bjp.bp.106.032011.
- Malpass A, Shaw A, Sharp D, Walter F, Feder G, Ridd M, et al. ‘Medication career’ or ‘Moral career’? The two sides of managing antidepressants: a meta-ethnography of patients’ experience of antidepressants. Soc Sci Med 2009;68:154-68. http://dx.doi.org/10.1016/j.socscimed.2008.09.068.
- Dundon E. Adolescent depression: a metasynthesis. J Pediatr Health Care 2006;20:384-92. http://dx.doi.org/10.1016/j.pedhc.2006.02.010.
- British Association for Behavioural and Cognitive Psychotherapies . CBT: Therapy Worth Talking About n.d. www.babcp.com/Public/What-is-CBT.aspx (accessed April 2014).
- Depression: The NICE Guideline on the Treatment and Management of Depression in Adults (Updated Edition). London: The British Psychological Society and The Royal College of Psychiatrists; 2010.
- Foroushani PS, Schneider J, Assareh N. Meta-review of the effectiveness of computerised CBT in treating depression. BMC Psychiatry 2011;11. http://dx.doi.org/10.1186/1471-244X-11-131.
- van’t Hof E, Cuijpers P, Waheed W, Stein DJ. Psychological treatments for depression and anxiety disorders in low- and middle-income countries: a meta-analysis. Afr J Psychiatry 2011;14:200-7. http://dx.doi.org/10.4314/ajpsy.v14i3.2.
- Howitt P, Darzi A, Yang GZ, Ashrafian H, Atun R, Barlow J, et al. Technologies for global health. Lancet 2012;380:507-35. http://dx.doi.org/10.1016/S0140-6736(12)61127-1.
- Gysels M, Bausewein C, Higginson IJ. Experiences of breathlessness: a systematic review of the qualitative literature. Palliat Support Care 2007;5:281-302. http://dx.doi.org/10.1017/S1478951507000454.
- Cullen DL, Stiffler D. Long-term oxygen therapy: review from the patients’ perspective. Chronic Respir Dis 2009;6:141-7. http://dx.doi.org/10.1177/1479972309103046.
- Bartoli L, Zanaboni P, Masella C, Ursini N. Systematic review of telemedicine services for patients affected by chronic obstructive pulmonary disease (COPD). Telemed E-Health 2009;15:877-84. http://dx.doi.org/10.1089/tmj.2009.0044.
- Bentsen SB, Langeland SB, Holm AL. Evaluation of self-management interventions for chronic obstructive pulmonary disease. J Nurs Manag 2012;20:802-13. http://dx.doi.org/10.1111/j.1365-2834.2012.01469.x.
- Effing T, Monninkhof EM, van der Valk PD, van der Palen J, van Herwaarden CL, Partidge MR, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2007;4.
- Tan JY, Chen JX, Liu XL, Zhang Q, Zhang M, Mei LJ, et al. A meta-analysis on the impact of disease-specific education programs on health outcomes for patients with chronic obstructive pulmonary disease. Geriatr Nurs 2012;33:280-96. http://dx.doi.org/10.1016/j.gerinurse.2012.03.001.
- Turnock AC, Walters EH, Walters JAE, Wood-Baker R. Action plans for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2005;4.
- Wong CX, Carson KV, Smith BJ. Home care by outreach nursing for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;4. http://dx.doi.org/10.1002/14651858.CD000994.pub3.
- Makaroff KLS. Experiences of kidney failure: a qualitative meta-synthesis. Nephrol Nurs J 2012;39:21-9.
- Tjaden L, Tong A, Henning P, Groothoff J, Craif JC. Children’s experiences of dialysis: a systematic review of qualitative studies. Arch Dis Child 2012;97:395-402. http://dx.doi.org/10.1136/archdischild-2011-300639.
- Mason J, Khunti K, Stone M, Farooqi A, Carr S. Educational interventions in kidney disease care: a systematic review of randomized trials. Am J Kidney Dis 2008;51:933-51. http://dx.doi.org/10.1053/j.ajkd.2008.01.024.
- Matteson ML, Russell C. Interventions to improve hemodialysis adherence: a systematic review of randomized-controlled trials. Hemodialysis Int 2010;14:370-82. http://dx.doi.org/10.1111/j.1542-4758.2010.00462.x.
- Strand H, Parker D. Effects of multidisciplinary models of care for adult pre-dialysis patients with chronic kidney disease: a systematic review. Int J Evid Based Health 2012;10:53-9. http://dx.doi.org/10.1111/j.1744-1609.2012.00253.x.
- Steeman E, De Casterle BD, Godderis J, Grypdonck M. Living with early stage dementia: a review of qualitative studies. J Adv Nurs 2006;54:722-38. http://dx.doi.org/10.1111/j.1365-2648.2006.03874.x.
- van der Roest HG, Meiland FJM, Maroccini R, Comijs HC, Jonker C, Dröes R. Subjective needs of people with dementia: a review of the literature. Int Psychogeriatr 2007;19:559-92. http://dx.doi.org/10.1017/S1041610206004716.
- Cooper C, Mukadam N, Katona C, Lyketsos CG, Ames D, Rabins P, et al. Systematic review of the effectiveness of non-pharmacological interventions to improve quality of life of people with dementia. Int Psychogeriatr 2012;24:856-70. http://dx.doi.org/10.1017/S1041610211002614.
- Corbett A, Stevens J, Aarsland D, Day S, Moniz-Cook E, Woods R, et al. Systematic review of services providing information and/or advice to people with dementia and/or their caregivers. Int J Geriatr Psychiatry 2012;27:628-36. http://dx.doi.org/10.1002/gps.2762.
- Kim S, Yoo E, Jung M, Park S, Park J. A systematic review of the effects of occupational therapy for persons with dementia: A meta-analysis of randomized controlled trials. NeuroRehabilitation 2012;31:107-15. http://dx.doi.org/10.3233/NRE-2012-0779.
- von Kutzleben M, Schmid W, Halek M, Holle B, Bartholomeyczik S. Community-dwelling persons with dementia: What do they need? What do they demand? What do they do? A systematic review on the subjective experiences of persons with dementia. Aging Ment Health 2012;16:378-90. http://dx.doi.org/10.1080/13607863.2011.614594.
- Al-aqeel S, Al-sabhan J. Strategies for improving adherence to antiepileptic drug treatment in patients with epilepsy. Cochrane Database Syst Rev 2011;1. http://dx.doi.org/10.1002/14651858.CD008312.pub2.
- Bradley PM, Lindsay B. Care delivery and self-management strategies for adults with epilepsy. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.CD006244.pub2.
- Lindsay B, Bradley PM. Care delivery and self-management strategies for children with epilepsy. Cochrane Database Syst Rev 2010;12. http://dx.doi.org/10.1002/14651858.CD006245.pub2.
- Ramaratnam S, Baker GA, Goldstein LH. Psychological treatments for epilepsy. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.CD002029.pub3.
- Marshall IJ, Wolfe CDA, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3953.
- Schlomann P, Schmitke J. Lay beliefs about hypertension: an interpretive synthesis of the qualitative research. J Am Acad Nurse Prac 2007;19:358-67. http://dx.doi.org/10.1111/j.1745-7599.2007.00238.x.
- Bosch-Capblanch X, Abba K, Prictor M, Garner P. Contracts between patients and healthcare practitioners for improving patients’ adherence to treatment, prevention and health promotion activities. Cochrane Database Syst Rev 2007;2.
- Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens 2006;24:215-33. http://dx.doi.org/10.1097/01.hjh.0000199800.72563.26.
- Ebrahim S. Detection, adherence and control of hypertension for the prevention of stroke: a systematic review. Health Technol Assess 1998;2.
- Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010;3.
- Ogedegbe G, Schoenthaler S. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens 2006;8:174-80. http://dx.doi.org/10.1111/j.1524-6175.2006.04872.x.
- Saksena A. Computer-based education for patients with hypertension: a systematic review. Health Educ J 2010;69. http://dx.doi.org/10.1177/0017896910364889.
- Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev 2004;3.
- Takiya LN, Peterson AM, Finley RS. Meta-analysis of interventions for medication adherence to antihypertensives. Ann Pharmacother 2004;38:1617-24. http://dx.doi.org/10.1345/aph.1D268.
- Verbek WJ, Kessels AGH, Thien T. Telecare is a valuable tool for hypertension management, a systematic review and meta-analysis. Blood Pressure Monitor 2011;16:149-55. http://dx.doi.org/10.1097/MBP.0b013e328346e092.
- Hypertension detection and follow-up Program Cooperative Group . The effect of treatment on mortality in ‘mild’ hypertension. Results of the Hypertension Detection and Follow-up Program. New Engl J Med 1982;307:976-80. http://dx.doi.org/10.1056/NEJM198210143071603.
- Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ 2004;13:145-51. http://dx.doi.org/10.1136/bmj.38121.684410.AE.
- Stack RJ, Shaw K, Mallen C, Herron-Marx S, Horne R, Raza K. Delays in help seeking at the onset of the symptoms of rheumatoid arthritis: a systematic synthesis of qualitative literature. Ann Rheum Dis 2012;71:493-7. http://dx.doi.org/10.1136/ard.2011.155416.
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess 2011;15. http://dx.doi.org/10.3310/hta15430.
- Astin JA, Beckner W, Soeken K, Hochberg MC, Berman B. Psychological interventions for rheumatoid arthritis: a meta-analysis of randomized controlled trials. Arthrit Rheum 2007;47:291-302. http://dx.doi.org/10.1002/art.10416.
- Dissanayake RK, Bertouch JV. Psychosocial interventions as adjunct therapy for patients with rheumatoid arthritis: a systematic review. Int J Rheum Dis 2010;13. http://dx.doi.org/10.1111/j.1756-185X.2010.01563.x.
- Iversen MD, Hammond A, Betteridge N. Self-management of rheumatic diseases: state of the art and future perspectives. Ann Rheum Dis 2010;69:955-63. http://dx.doi.org/10.1136/ard.2010.129270.
- Knittle K, Maes S, De Gucht V. Psychological interventions for rheumatoid arthritis: examining the role of self-regulation with a systematic review and meta-analysis of randomized controlled trials. Arthrit Care Res 2010;62:1460-72. http://dx.doi.org/10.1002/acr.20251.
- Krishna S, Balas EA, Spencer DC, Griffin JZ, Boren SA. Clinical trials of interactive computerized patient education: implications for family practice. J Fam Prac 1997;25:25-33.
- Leverone D, Epstein BJ. Nonpharmacological interventions for the treatment of rheumatoid arthritis: a focus on mind–body medicine. J Pharm Prac 2010;23:101-9. http://dx.doi.org/10.1177/0897190009360025.
- Niedermann K, Fransen J, Knols R, Uebelhart D. Gap between short- and long-term effects of patient education in rheumatoid arthritis patients: a systematic review. Arthrit Rheum 2004;51:388-98. http://dx.doi.org/10.1002/art.20399.
- Riemsma RP, Kirwan JR, Taal E, Rasker HJJ. Patient education for adults with rheumatoid arthritis. Cochrane Database Syst Rev 2003;2.
- Wilkins S, Jung B, Wishart L, Edwards M, Norton SG. The effectiveness of community-based occupational therapy education and functional training programs for older adults: a critical literature review. Can J Occup Ther 2003;70:214-25. http://dx.doi.org/10.1177/000841740307000405.
- Zhang J, Wei W, Wang CM. Effects of psychological interventions for patients with systemic lupus erythematosus: a systematic review and meta-analysis. Lupus 2012;21:1077-87. http://dx.doi.org/10.1177/0961203312447667.
- Dorn SD. Systematic review: self-management support interventions for irritable bowel syndrome. Aliment Pharmacol Ther 2010;32:513-21. http://dx.doi.org/10.1111/j.1365-2036.2010.04374.x.
- Ford AC, Talley NJ, Schoenfeld PS, Quigley EMM, Moayyedi P. Efficacy of antidepressants and psychological therapies in irritable bowel syndrome: systematic review and meta-analysis. Gut 2009;58:367-78. http://dx.doi.org/10.1136/gut.2008.163162.
- Zijdenbos IL, de Wit NJ, van der Heijden GJ, Rubin G, Quartero AO. Psychological treatments for the management of irritable bowel syndrome. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.CD006442.pub2.
- Verbeek L, Sengers MJ, Riemens L, Haafkens J. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine 2004;29:2309-18. http://dx.doi.org/10.1097/01.brs.0000142007.38256.7f.
- Du S, Yuan C, Xiao X, Chua J, Qiu Y, Qian H. Self-management programs for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Pat Educ Counsel 2011;85:e299-310. http://dx.doi.org/10.1016/j.pec.2011.02.021.
- Oliveira VC, Ferreira PH, Maher CG, Pinto RZ, Refshauge KM, Ferreira ML. Effectiveness of self-management of low back pain: systematic review with meta-analysis. Arthrit Care Res 2012;64:1739-48. http://dx.doi.org/10.1002/acr.21737.
- Brox JI, Storheim K, Grotle M, Tveito TH, Indahl A, Eriksen HR. Systematic review of back schools, brief education, and fear-avoidance training for chronic low back pain. Spine J 2008;8:948-58. http://dx.doi.org/10.1016/j.spinee.2007.07.389.
- Di Fabio RP. Efficacy of comprehensive rehabilitation programs and back school for patients with low back pain: a meta-analysis. Phys Ther 1995;75:865-78.
- Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low-back pain. Cochrane Database Syst Rev 2002;1.
- Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev 2004;4.
- van Geen JW, Edelaar MJA, Janssen M, van Eijk JTM. The long-term effect of multidisciplinary back training: a systematic review. Spine 2007;32:249-55. http://dx.doi.org/10.1097/01.brs.0000251745.00674.08.
- van der Giessen RN, Speksnijder CM, Helders PJM. The effectiveness of graded activity in patients with non-specific low-back pain: a systematic review. Disabil Rehabil 2012;34:1070-6. http://dx.doi.org/10.3109/09638288.2011.631682.
- van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011;20:19-3. http://dx.doi.org/10.1007/s00586-010-1518-3.
- Henschke N, Ostelo RW, van Tulder MW, Vlaeyen JW, Morley S, Assendelft WJ, et al. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev 2010;7. http://dx.doi.org/10.1002/14651858.CD002014.pub3.
- Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007;26:1-9. http://dx.doi.org/10.1037/0278-6133.26.1.1.
- Scheer SJ, Watanabe TK, Radack KL. Randomized controlled trials in industrial low back pain. Part 3. subacute/chronic pain interventions. Arch Phys Med Rehabil 1997;78:414-23. http://dx.doi.org/10.1016/S0003-9993(97)90235-5.
- Engers AJ, Jellema P, Wensing M, van der Windt DAWM, Grol R, van Tulder MW. Individual patient education for low back pain. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.CD004057.pub3.
- Liddle SD, Gracey JH, Baxter GD. Advice for the management of low back pain: a systematic review of randomised controlled trials. Manual Ther 2007;12:310-27. http://dx.doi.org/10.1016/j.math.2006.12.009.
- Dixon L, Duncan D, Johnson P, Kirkby L, O’Connell H, Taylor H, et al. Occupational therapy for patients with Parkinson’s disease. Cochrane Database Syst Rev 2007;3.
- Ng L, Khan F. Multidisciplinary care for adults with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev 2009;4.
- Thomas PW, Thomas S, Hillier C, Galvin K, Baker R. Psychological interventions for multiple sclerosis. Cochrane Database Syst Rev 2006;1.
- Palladino BS, Helgeson VS. Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. J Pediatr Psychol 2012;37:591-603. http://dx.doi.org/10.1093/jpepsy/jss009.
- Spencer J, Cooper H, Milton B. Qualitative studies of type 1 diabetes in adolescence: a systematic literature review. Pediatr Diabet 2010;11:364-75. http://dx.doi.org/10.1111/j.1399-5448.2009.00603.x.
- Hood KK, Rohan JM, Peterson CM, Drotar D. Interventions with adherence-promoting components in pediatric type 1 diabetes meta-analysis of their impact on glycemic control. Diabet Care 2010;33:1658-64. http://dx.doi.org/10.2337/dc09-2268.
- McBroom LA, Enriquez M. Review of family-centered interventions to enhance the health outcomes of children with type 1 diabetes. Diabet Educ 2009;35. http://dx.doi.org/10.1177/0145721709332814.
- Savage E, Farrell D, Mcmanus V, Grey M. The science of intervention development for type 1 diabetes in childhood: systematic review. J Adv Nurs 2010;66:2604-19. http://dx.doi.org/10.1111/j.1365-2648.2010.05423.x.
- Winkley K, Landau S, Eisler I, Ismai K. Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ 2006;333:65-8. http://dx.doi.org/10.1136/bmj.38874.652569.55.
- Cleland JA, Hall S, Price D, Lee AJ. An exploratory, pragmatic, cluster randomised trial of practice nurse training in the use of asthma action plans. Prim Care Respir J 2007;16:311-18. http://dx.doi.org/10.3132/pcrj.2007.00063.
- Homer CJ, Forbes P, Horvitz L, Peterson LE, Wypij D, Heinrich P. Impact of a quality improvement program on care and outcomes for children with asthma. Arch Pediatr Adolesc Med 2005;159:464-9. http://dx.doi.org/10.1001/archpedi.159.5.464.
- Bunting BA, Cranor CW. The Asheville Project: long-term clinical, humanistic, and economic outcomes of a community-based medication therapy management program for asthma. J Am Pharm Assoc 2006;46:133-47. http://dx.doi.org/10.1331/154434506776180658.
- Chini L, Iannini R, Chianca M, Corrente S, Graziani S, La Rocca M, et al. Happy air, a successful school-based asthma educational and interventional program for primary school children. J Asthma 2011;48:419-26. http://dx.doi.org/10.3109/02770903.2011.563808.
- Delaronde S, Peruccio DL, Bauer BJ. Improving asthma treatment in a managed care population. Am J Manag Care 2005;11:361-8.
- Forshee JD, Whalen EB, Hackel R, Butt LT, Smeltzer PA, Martin J, et al. The effectiveness of one-on-one nurse education on the outcomes of high-risk adult and pediatric patients with asthma. Manag Care Interface 1998;11:82-9.
- Gerald LB, Redden D, Wittich AR, Hains C, Turner-Henson A, Hemstreet MP, et al. Outcomes for a comprehensive school-based asthma management program. J School Health 2006;76:291-6. http://dx.doi.org/10.1111/j.1746-1561.2006.00114.x.
- Vollmer WM, Kirshner M, Peters D, Drane A, Stibolt T, Hickey T, et al. Use and impact of an automated telephone outreach system for asthma in a managed care setting. Am J Manag Care 2006;12:725-33.
- Kemple T, Rogers C. A mailed personalised self-management plan improves attendance and increases patients’ understanding of asthma. Prim Care Respir J 2003;12:110-14.
- Lindberg M, Ahlner J, Ekström T, Jonsson D, Möller M. Asthma nurse practice improves outcomes and reduces costs in primary health care. Scand J Caring Sci 2002;16:73-8. http://dx.doi.org/10.1046/j.1471-6712.2002.00054.x.
- Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A. Accessibility, clinical effectiveness, and practice costs of providing a telephone option for routine asthma reviews: phase 4 controlled implementation study. Br J Gen Prac 2007;57:714-22.
- Andrade WC, Camargos P, Lasmar L, Bousquet J. A pediatric asthma management program in a low-income setting resulting in reduced use of health service for acute asthma. Allergy 2010;65:1472-7. http://dx.doi.org/10.1111/j.1398-9995.2010.02405.x.
- Bunik M, Federico MJ, Beaty B, Rannie M, Olin JT, Kempe A. Quality improvement for asthma care within a hospital-based teaching clinic. Acad Pediatr 2011;11:58-65. http://dx.doi.org/10.1016/j.acap.2010.10.004.
- Findley SE, Thomas G, Madera-Reese R, McLeod N, Kintala S, Andres Martinez R, et al. A community-based strategy for improving asthma management and outcomes for preschoolers. J Urban Health 2011;88:S85-99. http://dx.doi.org/10.1007/s11524-010-9479-8.
- Haahtela T, Tuomisto LE, Pietinalho A, Klaukka T, Erhola M, Kaila M, et al. A 10 year asthma programme in Finland: major change for the better. Thorax 2006;61:663-70. http://dx.doi.org/10.1136/thx.2005.055699.
- Kauppi P, Linna M, Martikainen J, Mäkelä MJ, Haahtela T. Follow-up of the Finnish Asthma Programme 2000–2010: reduction of hospital burden needs risk group rethinking. Thorax 2013;68:292-3. http://dx.doi.org/10.1136/thoraxjnl-2011-201028.
- Polivka BJ, Chaudry RV, Crawford J, Bouton P, Sweet L. Impact of an urban healthy homes intervention. J Environ Health 2011;73:16-20.
- Souza-Machado C, Souza-Machado A, Franco R, Ponte EV, Barreto ML, Rodrigues LC, et al. Rapid reduction in hospitalisations after an intervention to manage severe asthma. Eur Respir J 2010;35:515-21. http://dx.doi.org/10.1183/09031936.00101009.
- Swanson V, Wright S, Power KG, Duncan B, Morgan J, Turner E, et al. The impact of a structured programme of asthma care in general practice. Int J Clin Prac 2000;54:573-80.
- Stevens DP, Bowen JL, Johnson JK, Woods DM, Provost LP, Holman HR, et al. A multi-institutional quality improvement initiative to transform education for chronic illness care in resident continuity practices. J Gen Intern Med 2010;25:S574-80. http://dx.doi.org/10.1007/s11606-010-1392-z.
- Albisser AM, Harris RI, Albisser JB, Sperlich M. The impact of initiatives in education, self-management training, and computer-assisted self-care on outcomes in diabetes disease management. Diabet Technol Therapeut 2001;3:571-9. http://dx.doi.org/10.1089/15209150152811199.
- Harris F, Chamings P, Piper S, Levick FR. Development and initiation of a diabetes self-management program for an underserved population. Diabet Educ 2000;26:760-4.
- Jordan RE, Lancashire RJ, Adab P. An evaluation of Birmingham Own Health telephone care management service among patients with poorly controlled diabetes. A retrospective comparison with the General Practice Research Database. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-707.
- Kelly J, Crowe P, Shearer M. The Good Life Club project. Telephone coaching for chronic disease self management. Aus Fam Phys 2005;34:31-4.
- Lowe J, Linjawi S, Mensch M, James K, Attia J. Flexible eating and flexible insulin dosing in patients with diabetes: results of an intensive self-management course. Diabet Res Clin Prac 2008;80:439-43. http://dx.doi.org/10.1016/j.diabres.2008.02.003.
- Lowe JM, Mensch M, McElduff P, Fitzgerald M, Attia J. Does an advanced insulin education programme improve outcomes and health service use for people with type 2 diabetes? A 5-year follow-up of the Newcastle Empowerment Course. Diabet Med 2009;26:1277-81. http://dx.doi.org/10.1111/j.1464-5491.2009.02858.x.
- Roblin DW, Ntekop E, Becker ER. Improved intermediate clinical outcomes from participation in a diabetes health education program. J Ambulat Care Manag 2007;30:64-73. http://dx.doi.org/10.1097/00004479-200701000-00009.
- Welch VL, Oster NV, Gazmararian JA, Rask K, Schild L, Cutler C, et al. Impact of a diabetes disease management program by race and ethnicity. Dis Manag Health Outcomes 2006;14:245-52. http://dx.doi.org/10.2165/00115677-200614040-00007.
- Banister NA, Jastrow ST, Hodges V, Loop R, Gillham MB. Diabetes self-management training program in a community clinic improves patient outcomes at modest cost. J Am Diet Assoc 2004;104:807-10. http://dx.doi.org/10.1016/j.jada.2004.02.027.
- Joshu CE, Rangel L, Garcia O, Brownson CA, O’Toole ML. Integration of a promotora-led self-management program into a system of care. Diabet Educ 2007;33:151S-8S. http://dx.doi.org/10.1177/0145721707304076.
- Micklethwaite A, Brownson CA, O’Toole ML, Kilpatrick KE. The business case for a diabetes self-management intervention in a community general hospital. Popul Health Manag 2012;15:230-5. http://dx.doi.org/10.1089/pop.2011.0051.
- Rasekaba TM, Graco M, Risteski C, Jasper A, Berlowitz DJ, Hawthorne G, et al. Impact of a diabetes disease management program on diabetes control and patient quality of life. Popul Health Manag 2012;15:12-9. http://dx.doi.org/10.1089/pop.2011.0002.
- Sedlak M, Raml A, Schmekal B, Grafinger P, Biesenbach G. Metabolic control in insulin-treated type 2-diabetic patients aged over 80 years and without participation in a structured diabetic teaching program. Wiener Medizinische Wochenschrift 2005;155:26-9. http://dx.doi.org/10.1007/s10354-004-0133-5.
- Bott U, Bott S, Hemmann D, Berger M. Evaluation of a holistic treatment and teaching programme for patients with type 1 diabetes who failed to achieve their therapeutic goals under intensified insulin therapy. Diabet Med 2000;17:635-43. http://dx.doi.org/10.1046/j.1464-5491.2000.00345.x.
- Pieber TR, Brunner GA, Schnedl WJ, Schattenberg S, Kaufmann P, Krejs GJ. Evaluation of a structured outpatient group education program for intensive insulin therapy. Diabet Care 1995;18:625-30. http://dx.doi.org/10.2337/diacare.18.5.625.
- Sämann A, Mühlhauser I, Bender R, Kloos Ch, Müller UA. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Diabetologia 2005;48:1965-70. http://dx.doi.org/10.1007/s00125-005-1905-1.
- Sämann A, Mühlhauser I, Bender R, Hunger-Dathe W, Kloos C, Müller UA. Flexible intensive insulin therapy in adults with type 1 diabetes and high risk for severe hypoglycemia and diabetic ketoacidosis. Diabet Care 2006;29:2196-9. http://dx.doi.org/10.2337/dc06-0751.
- Sämann A, Lehmann T, Kloos C, Braun A, Hunger-Dathe W, Wolf G, et al. Flexible, intensive insulin therapy and dietary freedom in adolescents and young adults with type 1 diabetes: a prospective implementation study. Diabet Med 2008;25:592-6. http://dx.doi.org/10.1111/j.1464-5491.2008.02406.x.
- Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams. Ann Behav Med 2002;24:80-7. http://dx.doi.org/10.1207/S15324796ABM2402_04.
- Hargraves JL, Ferguson WJ, Lemay CA, Pernice J. Community health workers assisting patients with diabetes in self-management. J Ambulat Care Manag 2012;35:15-26. http://dx.doi.org/10.1097/JAC.0b013e31822cbe35.
- Anderson D, Christison-Lagay J. Diabetes self-management in a Community Health Center: Improving health behaviors and clinical outcomes for underserved patients. Clin Diabet 2008;26:22-7. http://dx.doi.org/10.2337/diaclin.26.1.22.
- Dettori N, Flook BN, Pessl E, Quesenberry K, Loh J, Harris C, et al. Improvements in care and reduced self-management barriers among rural patients with diabetes. J Rural Health 2005;21:172-7. http://dx.doi.org/10.1111/j.1748-0361.2005.tb00078.x.
- Gruesser M, Bott U, Ellermann P, Kronsbein P, Joergens V. Evaluation of a structured treatment and teaching program for non-insulin-treated type II diabetic outpatients in Germany after the nationwide introduction of reimbursement policy for physicians. Diabet Care 1993;16:1268-75. http://dx.doi.org/10.2337/diacare.16.9.1268.
- Korsatko S, Habacher W, Rakovac I, Plank J, Seereiner S, Beck P, et al. Evaluation of a teaching and treatment program in over 4,000 type 2 diabetic patients after introduction of reimbursement policy for physicians. Diabet Care 2007;30:1584-6. http://dx.doi.org/10.2337/dc06-2095.
- Liebman J, Heffernan D, Sarvela P. Establishing diabetes self-management in a community health center serving low-income Latinos. Diabet Educ 2007;33:132S-8S. http://dx.doi.org/10.1177/0145721707304075.
- Senior PA, MacNair L, Jindal K. Delivery of multifactorial interventions by nurse and dietitian teams in a community setting to prevent diabetic complications: a quality-improvement report. Am J Kidn Dis 2008;51:425-34. http://dx.doi.org/10.1053/j.ajkd.2007.11.012.
- Musacchio N, Lovagnini Scher A, Giancaterini A, Pessina L, Salis G, Schivalocchi F, et al. Impact of a chronic care model based on patient empowerment on the management of type 2 diabetes: effects of the SINERGIA programme. Diabet Med 2011;28:724-30. http://dx.doi.org/10.1111/j.1464-5491.2011.03253.x.
- Cavanagh K, Seccombe N, Lidbetter N. The implementation of computerized cognitive behavioural therapies in a service user-led, third sector self help clinic. Behav Cogn Psychother 2011;39:427-42. http://dx.doi.org/10.1017/S1352465810000858.
- Farrand P, Confue P, Byng R, Shaw S. Guided self-help supported by paraprofessional mental health workers: an uncontrolled before-after cohort study. Health Soc Care Community 2008;17:9-17. http://dx.doi.org/10.1111/j.1365-2524.2008.00792.x.
- Learmonth D, Rai S. Taking computerized CBT beyond primary care. Br J Clin Psychol 2008;47:111-18. http://dx.doi.org/10.1348/014466507X248599.
- Learmonth D, Trosh J, Rai S, Sewell J, Cavanagh K. The role of computer-aided psychotherapy within an NHS CBT specialist service. Counsel Psychother Res 2008;8:117-23. http://dx.doi.org/10.1080/14733140801976290.
- Marks IM, Mataix-Cols D, Kenwright M, Cameron R, Hirsch S, Gega L. Pragmatic evaluation of computer-aided self-help for anxiety and depression. Br J Psychiatry 2003;183:57-65. http://dx.doi.org/10.1192/bjp.183.1.57.
- Newnham EA, Hooke GR, Page AC. Progress monitoring and feedback in psychiatric care reduces depressive symptoms. J Affect Disord 2010;127:139-46. http://dx.doi.org/10.1016/j.jad.2010.05.003.
- Pushparajah S, McClellan R, Henry A, Kuitert LM. Use of a chronic disease management programme in COPD to reduce hospital admissions. Chron Respir Dis 2006;3:187-93. http://dx.doi.org/10.1177/1479972306070371.
- Chen TW, Li SY, Chen JY, Yang WC. Training of peritoneal dialysis patients-Taiwan’s experiences. Peritoneal Dialysis Int 2008;28:S72-5.
- Loos-Ayav C, Frimat L, Kessler M, Chanliau J, Durand PY, Briançon S. Changes in health-related quality of life in patients of self-care vs. in-center dialysis during the first year. Qual Life Res 2008;17:1-9. http://dx.doi.org/10.1007/s11136-007-9286-1.
- van Hooff ML, van der Merwe JD, O’Dowd J, Pavlov PW, Spruit M, de Kleuver M, et al. Daily functioning and self-management in patients with chronic low back pain after an intensive cognitive behavioral programme for pain management. Eur Spine J 2010;19:1517-26. http://dx.doi.org/10.1007/s00586-010-1435-5.
- Deprez R, Kinner A, Millard P, Baggott L, Mellett J. Improving quality of care for patients with chronic obstructive pulmonary disease. Popul Health Manag 2009;12:209-15. http://dx.doi.org/10.1089/pop.2008.0043.
- Gruesser M, Hartmann P, Schlottmann N, Lohmann FW, Sawicki PT, Joergens V. Structured patient education for out-patients with hypertension in general practice: a model project in Germany. J Hum Hypertens 1997;11:501-6. http://dx.doi.org/10.1038/sj.jhh.1000508.
- Bosworth HB, Dubard CA, Ruppenkamp J, Trygstad T, Hewson DL, Jackson GL. Evaluation of a self-management implementation intervention to improve hypertension control among patients in Medicaid. Translation Behav Med 2011;1:191-9. http://dx.doi.org/10.1007/s13142-010-0007-x.
- Mosimaneotsile B, Braun KL, Tokishi C. Stroke patient outcomes: does an integrated delivery model of care make a difference?. Phys Occup Ther Geriatr 2000;17:67-82.
- Fernando B, Kalra D, Morrison Z, Byrne E, Sheikh A. Benefits and risks of structuring and/or coding the presenting patient history in the electronic health record: systematic review. BMJ Qual Saf 2012;21:337-46. http://dx.doi.org/10.1136/bmjqs-2011-000450.
- Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshon J, Price D, et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010;19:75-83. http://dx.doi.org/10.4104/pcrj.2010.00006.
- Kennedy A, Bower P, Reeves D, Blakeman T, Bowen R, Chew-Graham C, et al. Implementation of self management support for long term conditions in routine primary care settings: cluster randomised controlled trial. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f2882.
- Pinnock H, Epiphaniou E, Taylor SJC. Phase IV implementation studies: the forgotten finale to the complex intervention methodology framework. Annals ATS 2014;11:S118-22. http://dx.doi.org/10.1513/AnnalsATS.201308-259RM.
- McCorkle R, Ercolano E, Lazenby M, Schulman-Green D, Schilling LS, Lorig K, et al. Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin 2011;61:50-62. http://dx.doi.org/10.3322/caac.20093.
- Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982;4:167-82. http://dx.doi.org/10.1111/1467-9566.ep11339939.
- Bury M. The sociology of chronic illness: a review of research and prospects. Sociol Health Illn 1991;13:451-68. http://dx.doi.org/10.1111/j.1467-9566.1991.tb00522.x.
- Pinnock H, Taylor S, Epiphaniou E, Sheikh A, Griffiths C, Eldridge S, et al. Developing Standards for Reporting Phase IV Implementation Studies n.d. www.equator-network.org/ (accessed March 2014).
- NHS Choices n.d. www.nhs.uk (accessed April 2014).
- RC Psych . Alcohol and Drugs Misuse Subgroup of the Changing Minds Campaign. Drugs and Alcohol – Whose Problem Is It Anyway? Who Cares? 2003. www.rcpsych.ac.uk/pdf/whocares.pdf (accessed September 2014).
- Institute of Alcohol Studies . Alcohol Concern’s Information and Statistical Digest 2008. www.ias.org.uk/uploads/pdf/Women/Women%20factsheet.pdf (accessed September 2014).
- Goddard E. Smoking and Drinking Among Adults, 2006. Newport: Office for National Statistics; 2008.
- Alcohol-Use Disorders: Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence. London: NICE; 2011.
- Scadding GK, Durham SR, Mirakian R, Jones NS, Leech SC, Farooque S, et al. Guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy 2008;38:19-42. http://dx.doi.org/10.1111/j.1365-2222.2007.02888.x.
- Arthritis Research UK n.d. www.arthritisresearchuk.org (accessed April 2014).
- The Information Centre for Health and Social Care. Disease Prevalence. Quality and Outcomes Framework (QOF) for April 2010–March 2011. England: NHS; 2011.
- Atrial Fibrillation: The Management of Atrial Fibrillation. London: NICE; 2006.
- Rowland AS, Lesesne CA, Abramowitz AJ. The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view. Ment Retard Dev Disabil Res Rev 2002;8:162-70. http://dx.doi.org/10.1002/mrdd.10036.
- Rosenblatt M. I Exist: The Message From Adults with Autism in England. London: The National Autistic Society; 2008.
- Whiteley P, Todd L, Carr K, Shattock P. Gender ratios in autism, asperger syndrome and autism spectrum disorder. Autism Insights 2010;2:17-24. http://dx.doi.org/10.4137/AUI.S3938.
- HM government . Fulfilling and Rewarding Lives. The Strategy for Adults With Autism in England 2010. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_113369 (accessed September 2014).
- Bipolar Disorder. London: NICE; 2006.
- CancerStats – Key Facts. London: Cancer Research UK; 2012.
- About Cancer n.d. www.cancerresearchuk.org/about-cancer/ (accessed September 2014).
- Updates Advice on Cerebral Palsy Operation. London: NICE; 2010.
- National Institute for Health and Care Excellence (NICE) . Clinical Knowledge Summaries. Constipation in Children n.d. http://cks.nice.org.uk/constipation-in-children (accessed September 2014).
- Wessely S, Chalder T, Hirsch S, Wallace P, Wright D. The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a prospective primary care study. Am J Public Health 1997;87:1449-55. http://dx.doi.org/10.2105/AJPH.87.9.1449.
- Health Inequalities and Chronic Kidney Disease. London: NHS Kidney Care; 2011.
- Snively CS, Gutierrez C. Chronic kidney disease: prevention and treatment of common complications. Am Fam Phys 2004;70:1921-8.
- DePalma MJ, Ketchum JM, Saull TR. Multivariable analyses of the relationships between age, gender, and body mass index and the source of chronic low back pain. Pain Med 2012;13:498-506. http://dx.doi.org/10.1111/j.1526-4637.2012.01339.x.
- Dementia UK . A Report into the Prevalence and Cost of Dementia Prepared by the Personal Social Services Research Unit (PSSRU) at the London School of Economics and the Institute of Psychiatry at King’s College London, for the Alzheimer’s Society 2007. file:///C:/Users/sjctaylor/Downloads/Dementia_UK_Full_Report-1%20(1).pdf (accessed September 2014).
- Diabetes UK . Diabetes in the UK 2011 2012: Key Statistics on Diabetes n.d. www.diabetes.org.uk/documents/reports/diabetes-in-the-uk-2011-12.pdf (accessed September 2014).
- Department of Health . Publications, Policy and Guidance. Who Gets Diabetes n.d. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/browsable/dh_4899972 (accessed September 2014).
- n.d. www.patient.co.uk/search.asp?searchterm=endometriosis&searchcoll=All (accessed September 2014).
- Booth L, Thompson G. House of Commons Library. Epilepsy Statistics 2010. file:///C:/Users/sjctaylor/Downloads/SN05691.pdf (accessed September 2014).
- Arthritis Research UK n.d. www.arthritisresearchuk.org/arthritis-information/conditions/gout.aspx (accessed September 2014).
- World Health Organization . Hepatitis B Factsheet n.d. www.who.int/mediacentre/factsheets/fs204/en/ (accessed April 2014).
- The Hepatitis C Trust . About Hepatitis C n.d. www.hepctrust.org.uk/Hepatitis_C_Info/About%2bHepatitis%2bC/About%2bHepatitis%2bC.html (accessed 8 December 2014).
- Health Protection Agency . HIV in the United Kingdom: 2011 Report n.d. www.ivecic.com/uploads/7/5/4/1/7541913/hiv_in_the_uk_2011_report.pdf (accessed September 2014).
- Public Health England . Modelled Estimate of Prevalence of Hypertension in England 2011. www.apho.org.uk/resource/item.aspx?RID=111119 (accessed September 2014).
- Thyroid UK n.d. www.thyroiduk.org.uk/tuk/ (accessed September 2014).
- Emerson E, Hatton C. CEDR Research Report 2008(1): People with Learning Disabilities in England. Working Paper. Lancaster: Lancaster University; 2008.
- NHS Commissioning Support for London . Executive Summaries for General Practitioners n.d. www.londonhp.nhs.uk/wp-content/uploads/2011/03/Executive-Summary-for-General-Practitioners.pdf (accessed April 2014).
- The NHS. Statistics on Obesity, Physical Activity and Diet n.d. http://data.gov.uk/dataset/statistics_on_obesity_physical_activity_and_diet_england (accessed September 2014).
- Parkinson’s UK n.d. www.parkinsons.org.uk (accessed April 2014).
- Symmons D, Turner G, Webb R, Asten P, Barrett E, Lunt M, et al. The prevalence of rheumatoid arthritis in the United Kingdom: new estimates for a new century. Rheumatology 2002;41:793-800. http://dx.doi.org/10.1093/rheumatology/41.7.793.
- National Rheumatoid Arthritis Society n.d. www.nras.org.uk (accessed April 2014).
- Royal Free London n.d. www.royalfree.nhs.uk (accessed April 2014).
- National Institute for Health and Care Excellence (NICE) n.d. www.nice.org.uk (accessed April 2014).
- Stroke Association n.d. www.stroke.org.uk (accessed April 2014).
- St. Thomas’ Lupus Trust n.d. www.lupus.org.uk (accessed April 2014).
Appendix 1 Pre-workshop questionnaire
Appendix 2 Agenda for workshop
Appendix 3 Characteristics of long-term conditions
Appendix 4 Long-term condition scoring sheet
Appendix 5 Components and characteristics of self-management
Appendix 6 Components and characteristics self-management score sheet
Appendix 7 Exemplar long-term conditions post scoring
Appendix 8 Long-term condition information aid
| LTC | UK prevalence | Summary description | Number of systematic reviews |
|---|---|---|---|
| Agoraphobia | 3%287 | Demographic: agoraphobia is twice as common in women as in men, usually starts between age 18 years and 35 years | |
| Effect on individual: a cluster of phobias related to being in unfamiliar, public, or crowded places. Physical (e.g. rapid heart rate, dizziness, trembling), behavioural (e.g. avoiding driving, being far away from the house or PA) and psychological (loss of self-esteem, depression, anxiety) symptoms may be experienced. Treatment can be psychological therapy or medication, although individuals are often reluctant to seek treatment287 | |||
| Alcohol dependence | 7%288 | Demographics: average weekly alcohol consumption for men, 18.7 units; women 9.0 units.289 Men are more likely to exceed the daily benchmark at least 1 day of the week.290 Men and women with higher income are more likely to consume alcohol289 | |
| Effect on individual: associated with cravings, tolerance and preoccupation with alcohol. Also related to increased criminal activity and domestic violence, increased physical and mental problems. A chronic and relapsing course291 | |||
| Allergic rhinitis (e.g. hay fever) | 20%292 | Demographics: starts early in childhood | 2 |
| Effects to the individual: a collection of symptoms, mostly in the nose and eyes, including sneezing, congestion and rhinorrhoea. Oral medication, sprays and drops can be used to control symptoms. Prevented by avoidance of the allergen causing the response, e.g. dust, pollen287 | |||
| Amputation | Demographics: people with diabetes are 15 times more likely to need an amputation than the general population. Planned amputations usually occur in older patients | ||
| Effect on individual: surgical removal of a body part, usually a leg or an arm. Prosthetics are often fitted. Trauma can cause psychological and emotional impact287 | |||
| Ankylosing spondylitis | 7.3%293 | Demographics: onset usually 15–35 years | |
| Effect on individual: back pain and stiffness, can result in long-term disability. Chronic and progressive, treatment aims to relieve symptoms and delay disease progression. Systemic disease means that the whole body and internal organs may also be affected287 | |||
| Asthma | 5.9%294 | Demographics: more common in children and women and runs in families | 29 |
| Effect on individual: acute episodes of coughing, wheezing, shortness of breath and tightness of chest. Successful prevention is achieved through the combination of medication and lifestyle changes and also the avoidance of potential asthma attacks287 | |||
| Atrial fibrillation | 1.4%294 | Demographics: more prevalent in males. People of aged ≥ 85 years more likely to be diagnosed | 1 |
| Effect on individual: symptoms include chest pain, breathlessness, weakness and tiredness. Regular electrocardiograms for patients with irregular pulse are suggested295 | |||
| ADHD | 2–18%296 | Demographics: usually diagnosed between ages 3 years and 7 years, more commonly in boys | |
| Effect on individual: short attention span, restlessness, easily distracted. Medication in combination with therapy, can be lifelong and two-thirds of children with ADHD still have symptoms at age 25 years287 | |||
| Autism | 1%297 | Demographics: boys are more likely to be diagnosed with autism than girls (4 : 1)298 | |
| Effect on individual: a lifelong developmental disability. A spectrum condition which affects people in different ways, usually through social communication, interaction and imagination. Some people live independent lives, others may need a lifetime of specialist support. No cure, but interventions include learning and development techniques299 | |||
| Bipolar disorder | 0.3–4.0%300 | Demographics: onset usually at age 15–19 years | |
| Effect on individual: a cyclical mood disorder where people fluctuate between abnormally elevated mood and depressed mood. Key features include mania, depression, hypomania and mixed states. Usually managed with combination of psychological and pharmacological therapies, regular reviews of weight and physical health300 | |||
| Burns injuries | 13,000 people/year287 | Demographics: highest rates in children aged ≤ 5 years and elderly aged ≥ 75 years | |
| Effect on individual: burns can be very painful, may alter feeling and look of skin, and will initially be at increased risk of infection. The trauma can cause shock, followed potentially by emotional/psychological coping issues, especially if changed appearance/scarring287 | |||
| Cancer | 1.6%294 | Demographics: more common in older people (aged ≥ 65 years). 1% occur in children, teenagers and young adults301 | |
| Effect on individual: people experience symptoms such as unexplained pain and weigh loss, breathlessness, skin changes abnormal bleeding, etc. During treatment patients may experience symptoms such as nausea and vomiting, hair loss, fatigue and tiredness, constipation or diarrhoea302 | |||
| Cerebral palsy | 1800 diagnosed each year303 | Effect on individual: covers a number of neurological conditions that affect a child’s movement and co-ordination. May include curvature of the spine, muscle stiffness, learning difficulties and affect balance and depth perception. Can also cause epilepsy, sensory impairment and incontinence. Cerebral palsy is not a progressive condition. A range of treatments can help relieve symptoms and increase independence and self-esteem287 | |
| Childhood constipation | Up to 30%304 | Demographics: most commonly in children aged 1–4 years | 0 |
| Effect on individual: pain and discomfort, possibility of anal fissure development. A third of children with chronic constipation continue to have problems beyond puberty304 | |||
| Chronic fatigue syndrome or myalgic encephalomyelitis | 2.6%305 (0.5% if comorbid psychological disorders excluded) | Demographics: more common in women, usually develops early twenties to mid-forties | 1 (as part of larger systematic review on chronic disease in children) |
| Effect on individual: main symptom is severe fatigue, both physical and mental. May also include muscular pain, headaches, insomnia. Treatment is mainly therapy based, but medication can help alleviate specific symptoms. For most people, symptoms improve over time. Many people make a full recovery, others may have symptoms that persist for long periods287 | |||
| CKD (ages ≥ 18 years) | 4.3%294 | Demographics: in people aged ≥ 75 years, CKF is present in 1 : 2 people; 31% men and 36% women aged ≥ 75 years have CKD.288 Stages 3–5 is higher in women (7% women; 5% men)306 | 7 |
| Effect on individual: a progressive condition. Regular follow-ups and medical management can delay disease progression. Behaviour change interventions such as healthier dietary habits and smoking cessation are essential307 | |||
| Chronic LBP | 1%304 | Demographics: older people and women, and individuals with high BMI are more likely to have chronic LBP308 | 2 (LBP) 14 (chronic pain) |
| Effect on individual: pain, stiffness, often a chronic problem in which the symptoms follow an irregular course. Periods of little pain or disability are interrupted by acute episodes of severe pain which may be disabling304 | |||
| COPD | 1.6%294 | Demographics: usually affects ≥ 35 year olds. More men than women | 10 |
| Effect on individual: experience cough, shortness of breath, sputum and chest infections. Limits physical exertion. Inhalers can provide symptom relief287 | |||
| Chronic pelvic pain | 17%287 (women) | Demographics: predominantly women (usually gynaecological) | |
| Effect on individual: pelvic pain which may be episodic or continuous. More intense than ordinary period pain, and lasts for longer. Usually a symptom of other gynaecological, bladder, musculoskeletal or digestive problems287 | |||
| Coeliac disease | 0.8–1.9%287 | Demographics: females are about twice as likely as males to be diagnosed with coeliac disease | |
| Effect on individual: GI symptoms are common, and malabsorption may lead to nutritional complications such as anaemia, weight loss, and (in children) failure to thrive. Symptoms controlled by adhering to a gluten-free diet287 | |||
| Congestive heart failure | 0.7%294 | Demographics: average age at diagnosis is 76 years | 19 |
| Effect on individual: people may experience extreme tiredness, breathlessness or swollen feet. Life-threatening condition which can lead to sudden death287 | |||
| Coronary heart disease | 3.4%287 | Demographics: 1 in 5 men and 1 in 7 women die from coronary heart disease | |
| Effect on individual: may cause angina, heart attacks or heart failure287 | |||
| Crohn’s disease | 145 per 100,000 people287 | Demographics: presents most commonly in adolescence and early adulthood | 3 (inflammatory bowel disease) |
| Effect on individual: a chronic, lifelong condition with unpredictable relapses and remissions. Mortality is higher than in the general population, and complications include bowel cancer, anaemia, growth failure, ulcers, osteoporosis and malnutrition287 | |||
| Cystic fibrosis | Demographics: a recessive genetic condition | 1 | |
| Effect on individual: causes recurrent chest infections, poor growth and related health problems, such as diabetes and infertility. There is no cure for cystic fibrosis, but many treatments and therapies can make cystic fibrosis easier to live with. Half of all people with cystic fibrosis can expect to live beyond the age of 38 years287 | |||
| Dementia | 0.5%294 | Demographics: 1 in 3 people aged ≥ 65 years will die from dementia. 10% of deaths in men aged ≥ 65 years, and 15% of deaths in women aged ≥ 65 years may be attributable to dementia.294 Young onset of dementia more likely for men | 8 |
| Effect on individual: a progressive and largely irreversible condition characterised with impaired mental function. Including memory loss, changes in personality and disorientation309 | |||
| Depression (age ≥ 18 years) | 11.2%294 | Demographics: prevalence is higher for women than men. Likely to be less educated and belong to a lower social class296 | 20 |
| Effect on individual: low mood, loss of pleasure and difficulty in concentration.296 Can vary from feeling mildly low to severely suicidal. Can occur consistently or in episodic bouts | |||
| T1DM and T2DM | 4.5%310 (15% T1DM; 85% T2DM) | Demographics: 98% of T1DM diagnosed in childhood. T2DM is more prevalent in adults (90%). More prevalent in men; however, women are more likely to die from diabetes than men. People from less affluent populations are more likely to be diagnosed with diabetes311 | T1DM: 15; T2DM: 40 + 5 related Both: 58 + 15 related |
| Effect on individual: may be managed through careful diet control and insulin treatment. Complications of poor control include visual damage and foot problems287 | |||
| Drug misuse | 2% drug dependent288 | Effect on individual: highly stigmatised. Associated with blood borne viruses transmitted by sharing needles, individuals are often susceptible to other infectious disease due to poor health or inadequate housing288 | |
| Eating disorders (e.g. anorexia nervosa, bulimia) | Demographics: usually develops around ages 16–19 years, majority female | ||
| Effect on individual: abnormal attitudes towards food cause individuals to change eating habits and behaviour. Can affect individuals physically, psychologically and socially. Treatment usually involves monitoring physical health while deal with underlying psychological causes287 | |||
| Eczema | 15–20% children 2–10% adults | Demographics: more common in children. Eighty per cent cases occur before 5 years of age | 1 (severe skin conditions) |
| Effect on individual: chronic, relapsing itchy skin. An episodic disease of flares, which may occur as frequently as two or three times each month, and remissions. In severe cases may be continuous. A tendency to gradual improvement in adult life. Associated with other atopic conditions | |||
| Endometriosis | 2–22%312 | Demographics: women of reproductive age, usually mid-thirties. Unusual in the under-twenties | |
| Effect on individual: chronic pelvic pain and sometimes infertility. No cure but treatment can help reduce symptoms. Higher risk of developing ovarian cancer, breast and other cancers, autoimmune and atopic disorders. 5 years post treatment, 20–50% will have a recurrence312 | |||
| Epilepsy (age ≥ 18 years) | 0.8%294 | Demographics: usually diagnosed in people aged < 20 years or > 60 years313 | 4 |
| Effect on individual: affects the brain and causes recurrent seizures. Frequency and severity of epileptic episodes depends on the individual, but most cases can be managed with medication | |||
| Fibromyalgia | 3%287 | Demographics: effects more women than men, and usually between age 30 years and 60 years but can affect any age | |
| Effect on individual: LTC in muscles, ligaments and tendons. Can cause all over body pain, fatigue, muscle stiffness, sleep problems, headaches, and IBS. Unknown cause. Treatment includes physical and psychological therapy and lifestyle changes287 | |||
| GORD | One in five people will have at least one episode of GORD a week287 | Demographics: twice as common in men as women | |
| Effect on individuals: a common condition where stomach acid leaks out of the stomach and into the oesophagus. Symptoms include heartburn, regurgitation and difficulty swallowing. Most people respond well to treatment with medication, but relapses are common. Some people may need long-term medication to control symptoms. A few individuals do not respond to medication and need surgery287 | |||
| Generalise anxiety disorder | 5%287 | Demographics: most common in people in their twenties | |
| Effect on individual: anxiety experienced most days about a range of issues, can cause psychological and physical symptoms. Psychological therapy and medication may help address or alleviate symptoms287 | |||
| Gout | 1.4%314 | Demographics: three to four times more prevalent in men. Age at onset 40–60 years in men, 60–80 years in women | |
| Effect on individual: painful swelling and inflammation in one or more joint, usually the big toe. Treatment involves symptom relief and prevention of further episodes, over time people may no longer experience any symptoms287 | |||
| Haemophilia (A + B) | A: 1 : 5000 males B: 1 : 30,000 males |
Demographics: almost always occurs in males | |
| Effect on individual: a genetic (inherited) condition that affects the blood’s ability to clot. Treatment uses synthetic clotting agents that can be taken when needed. Severe cases use these preventatively. Asymptomatic when treatment managed effectively287 | |||
| Hepatitis B (chronic infection) | Demographics: individuals infected as young children are most at risk of chronic infection. Most common transmission through i.v. drug use and sexual activity. Occupational hazard of health workers | ||
| Effect on individual: chronic liver infection can develop into cirrhosis of the liver or liver cancer315 | |||
| Hepatitis C (chronic infection) | 0.5% carriers | Demographics: i.v. drug users at increased risk | |
| Effect on individual: non-specific symptoms may be present, e.g. fatigue, muscle aches and nausea. Often remains asymptomatic until liver disease is advanced. Most develop cirrhosis of the liver over 20–40 years316 | |||
| HIV | 91,500 in the UK317 | Demographics: injecting drug users and men who have sex with men are at higher risk | 4 |
| Effect on individual: individuals may experience stigma. Careful medical management means HIV infection can be effectively controlled | |||
| Hypertension | 32% (England, aged ≥ 16 years) | Demographics: slightly more prevalent in males, most common in white English people | 15 |
| Effect on individual: asymptomatic, a risk factor for cardiovascular disease318 | |||
| Hypothyroidism | 3.0%287 | Demographics: most commonly women aged 40–50 years. Ten times more common in women than men | |
| Effect on individual: uncontrolled will cause symptoms including weight gain, difficulty swallowing and constipation. Daily oral medication can offer complete control319 | |||
| IBS | 20% | Demographics: symptoms first occur between ages 20 and 30 years | 1 |
| Effect on individual: episodic bouts of stomach cramps, bloating, diarrhoea and constipation. Symptom relief by diet and lifestyle modification as well as medication287 | |||
| Learning disability (e.g. Down syndrome) | 2% England320 | Demographics: lifelong, diagnosed in childhood | |
| Effect on individual: affects the way a person understands information and how they communicate. Many children diagnosed with profound and multiple learning disability will also have a sensory or physical disability, complex health needs or mental health difficulties287 | |||
| Medically unexplained symptoms | 1% (London only)321 | Effect on individual: poorly understood and costly to the individual. Currently no clear pathway and individuals end up being frequently referred to secondary care. Many people present to the GP or practice nurse and can consume a large amount of resources with little evident benefit321 | |
| Migraine | 12% | Demographics: three times more common in women than men | 1 |
| Effect on individual: episodic severe headaches with associated symptoms such as nausea, vomiting and sensitivity to light or sound. Management of migraines dependent on type and severity. Can be in response to attack or preventative. Medication and lifestyle changes can help reduce migraines but no cure294 | |||
| MND | 0.002%287 (England) | Demographics: most cases develop in late fifties or early sixties. Slightly more common in men than women. Family history in 10% of cases | |
| Effect on individuals: progressively damages the nervous system causing muscle wasting. Affects walking, speaking, breathing and swallowing. Treatment aims to make person more comfortable and increase QoL. People generally survive 2–5 years after symptoms start287 | |||
| MS | 0.16%287 | Demographics: onset of symptoms typically at age 20–40 years. Twice as common in women as men | 4 |
| Effect on individual: a lifelong condition with gradual deterioration. 20% of patients have shortened life. Symptoms can include numbness, blurring of vision, problems with mobility and balance and muscle weakness. Long-term treatment may be required to control symptoms and day to day functioning may need to be adapted294 | |||
| Muscular dystropy (e.g. Duchenne muscular dystropy) | 0.12% (muscle disease or related condition) | Demographics: more common in males and usually diagnosed at a young age | |
| Effect on individual: a genetic condition that causes gradual and progressive muscle weakness. There are more than 30 types of MD, each with slightly different symptoms. Not all types of MD cause severe disability. There is no cure, but there are treatments that can help with physical disabilities and heart problems287 | |||
| Obesity | 28%322 children 23%322 adults |
Demographics: more prevalent in children and older adults. More common in low SES | |
| Effect on individual: can cause a number of health problems including heart disease, stroke and diabetes. Addressed through lifestyle modification, surgery and drugs287 | |||
| Obstructive sleep apnoea/hypoapnoea syndrome | 3%294 | Demographics: 30–60 years of age. More in men and elderly | |
| Effect on individual: interrupted breathing at night. This often causes excessive daytime sleepiness. Variety of medical treatments and lifestyle changes that can reduce symptoms294 | |||
| Osteoarthritis | 2.4%314 | Demographics: mainly in the over 45 year olds | 15 |
| Effect on individual: pain, stiffness and swelling in joints. In most cases a slow process developing over many years | |||
| Osteoporosis | 3 million people in the UK287 | Demographics: commonly associated with post-menopausal women | |
| Effect on individual: causes bones to become weak, fragile and more likely to break287 | |||
| PD | 28%287 | Demographics: most aged ≥ 50 years | 3 |
| Effect on individual: parkinson’s is a progressive disease and symptoms, which include tremor, rigidity and slowness of movement, which will worsen over time. Drugs can help offer symptom control323 | |||
| Peripheral vascular disease | 2.5% aged < 60 years 8.3% aged 60–70 years 19% aged > 70 years287 |
Demographics: more in elderly and men | |
| Effect on individual: build-up of fatty deposits in the arteries restricts blood supply to leg muscles. This can cause painful cramping in the legs brought on by walking. Associated with cardiovascular disease287 | |||
| Polycystic ovarian syndrome | 6–7%287 | Demographics: overweight and positive family history | |
| Effect on individual: can affect a woman’s menstrual cycle, fertility and aspects of her appearance. May also increase risk of long-term health problems such as diabetes, hypertension, heart disease and endometrial cancer287 | |||
| Post-traumatic stress disorder | 3% | Demographics: all ages | 1 |
| Effect on individual: episodic re-experiencing of symptoms including flashbacks or intrusive images or thoughts294 | |||
| RA | 1.16% in women and 0.44% in men324 | Demographics: onset usually at age 40–60 years, affects three times more women than men | 7 |
| Effect on individual: chronic and progressive. Joint swelling, pain, morning stiffness and unpredictable flares of inflammation. Ultimately will affect an individual’s ability to carry out everyday tasks. Systemic disease means that the whole body and internal organs may also be affected325 | |||
| Sarcoidosis | 0.03%326 | Demographics: onset age 20–40 years | |
| Effect on individual: in most cases the disease will go away without treatment after a few years. Usually, symptoms are not crippling and do not affect everyday life. However, some individuals are severely affected, with gradual worsening of symptoms and organ damage287 | |||
| Schizophrenia | Between 0.4–1.4%327 | Demographics: typically presents in adolescence and young adulthood | 6 |
| Effect on individual: symptoms include hallucinations and delusions, loss of motivation, social withdrawal and a lack of insight by the person into their condition. With medical treatment symptoms may fully resolve, recur intermittently with periods of remission, or persist continually294 | |||
| Sickle cell anaemia | 0.02%287 | Demographics: recessive genetic condition most prevalent in black Caribbean, black African and black British people | |
| Effect on individual: some people only have mild symptoms, while others have frequent attacks of pain and experience a wide range of complications. Average life expectancy to be 53–60 years of age287 | |||
| Spina bifida | 0.1% | Demographics: a developmental abnormality which an individual will be born with | |
| Effect on individual: birth defect affecting spine and central nervous system development. Surgery performed soon after birth. Individuals may have partial or total paralysis of the lower limbs, bowel and urinary incontinence, loss of skin sensation, cognitive symptoms and muscle weakness287 | |||
| Stroke | 1.7%287 | Demographics: most common in over 65 years of age | |
| Effect on individual: one in three survivors will make a significant recovery within a month. Two in three will have long-term problems such as weakness and paralysis, visual problems, depression and difficulty with speech. Long-term rehabilitation aims to improve or manage symptoms328 | |||
| SLE | 0.1–0.4%329 | Demographics: 90% of cases occur in women, most of childbearing age (15 years to 50 years) | |
| Effect on individual: many people will experience long periods of time with few or no symptoms, and sudden flare-ups. May cause serious complications, e.g. kidney and heart disease. Most individuals have a normal, or near normal, life expectancy329 | |||
| Urinary incontinence | 9% | Demographics: increases with advanced age. Twice as common in women as men | |
| Effect on individual: can be an uncomfortable and upsetting condition, can be improved by conservative treatment, e.g. weight loss, muscle training287 |
Appendix 9 List of long-term conditions
| Original | Additional | ||
|---|---|---|---|
| 1 | Allergy/anaphylaxis | 1 | Addictions – substance and alcohol, etc. |
| 2 | Asthma | 2 | ADHD |
| 3 | Atrial fibrillation | 3 | Allergic rhinitis/rhinitis/sinusitis/rhinosinusitis |
| 4 | Childhood constipation | 4 | Amnesia |
| 5 | Chronic fatigue syndrome/ME | 5 | Amputations |
| 6 | Chronic kidney disease | 6 | Anaemia |
| 7 | Chronic obstructive pulmonary disease | 7 | Angina |
| 8 | Chronic pain | 8 | Angiooedema |
| 9 | Congestive heart failure | 9 | Anklosing spondylitis (and other arthritic conditions) |
| 10 | Dementia | 10 | Antenatal screening for haemoglobinoapthies – sickle cell and thalassemia, Downs |
| 11 | Depression | 11 | Anxiety and stress disorders (including complex and post-traumatic stress disorders) |
| 12 | Diabetes: Type I | 12 | Aphasia |
| 13 | Diabetes: Type II | 13 | Ataxia’s |
| 14 | Endometriosis | 14 | Autism |
| 15 | Epilepsy | 15 | Autoimmune disorders (e.g. lupus, Sjögrens syndrome) |
| 16 | Hypertension | 16 | Blood disorders |
| 17 | Hepatitis B | 17 | Brain injuries (including stroke and TIAs) |
| 18 | Hepatitis C | 18 | Bronchopulmonary dysplasia (chronic lung disease of infancy) |
| 19 | HIV | 19 | Burn injuries |
| 20 | Inflammatory bowel disease | 20 | Cancer |
| 21 | Irritable bowel disease | 21 | Cardiac arrhythmias |
| 22 | Low back pain | 22 | Cerebral palsy |
| 23 | Migraine | 23 | Crohn’s disease |
| 24 | Multiple sclerosis | 24 | Coeliac disease |
| 25 | Osteoarthritis | 25 | Connective tissue diseases |
| 26 | Parkinson’s disease | 26 | Coronary heart disease |
| 27 | Cystic Fibrosis | ||
| 28 | Digestive conditions, stomach ulcers, oesophagus, reflux | ||
| 29 | Dizziness | ||
| 30 | Dyslexia or dyspaxia | ||
| 31 | Eating disorders (anorexia/bulimia) | ||
| 32 | Eczema | ||
| 33 | Endocrine disorders (thyrotoxicosis, hypothyroidism, hypogonadism, Cushing syndrome, Addison’s disease) | ||
| 34 | Fibromyalgia/chronic widespread pain | ||
| 35 | Gout | ||
| 36 | Gynaecological problems, chronic pelvic pain | ||
| 37 | Haemophilia and other coagulation disorders | ||
| 38 | Heart failure | ||
| 39 | Learning disabilities | ||
| 40 | Lung fibrosis | ||
| 41 | Lupus | ||
| 42 | Malaria | ||
| 43 | Medically unexplained symptoms | ||
| 44 | Mood disorders (not only depression, but mania and bipolar disorders) | ||
| 45 | Motor neurone disease | ||
| 46 | Multimorbidity | ||
| 47 | Multisystem autoimmune diseases (MSAIDs, including lupus) | ||
| 48 | Muscular dystrophy(ies) | ||
| 49 | Neuralgias (including, head and back pain) | ||
| 50 | Newborn screening programme diseases, including thyroid disease, hearing loss | ||
| 51 | Obesity | ||
| 52 | Obstructive sleep apnoea | ||
| 53 | Occupational lung disease (various) | ||
| 54 | Osteoporosis | ||
| 55 | Other slowly degenerative neurological conditions | ||
| 56 | Peripheral vascular disease | ||
| 57 | Personality disorders | ||
| 58 | Phobias | ||
| 59 | Physical disabilities | ||
| 60 | Polycystic ovary disease | ||
| 61 | Post-traumatic stress | ||
| 62 | Progressive supranuclear palsy | ||
| 63 | Psoriasis | ||
| 64 | Rare disease, genetic disorders | ||
| 65 | Sarcoidosis | ||
| 66 | Sensory problems/disabilities (deafness/blindness) | ||
| 67 | Severe skin conditions | ||
| 68 | Sickle cell disease | ||
| 69 | Skin conditions | ||
| 70 | Sleep disorders | ||
| 71 | Speech deficits | ||
| 72 | Spina bifida | ||
| 73 | Spinal injuries | ||
| 74 | Stroke/transient ischaemic attacks | ||
| 75 | Tuberculosis | ||
| 76 | Urinary Incontinence | ||
| 77 | Urticarial | ||
Appendix 10 Priority meta-review search strategy
Basic search strategy for all databases
General self-management support terms or LTC specific self-management support terms.
AND
LTC terms.
AND
Quantitative or qualitative review filter.
AND
Apply human, English and published 1993 onwards limits.
All searches in [Title/Abstract].
Detailed search terms: general self-management support terms
| General self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Exp Self care/ | Exp Self care/ | Exp Self care/ | Exp Self care skills/ |
| #2 | Exp Communication/ | Exp Education professional/ | Exp Health education/ | Exp Self management/ |
| #3 | Exp Professional Family Relations/ | Exp Education nonprofessional/ | Exp Patient education/ | Exp Health behavior/ |
| #4 | Exp Telephone/ | Exp Human activities/ | Exp Telehealth/ | Exp Self efficacy/ |
| #5 | Exp Professional Patient Relations/ | Exp Self concept/ | Exp Interpersonal communication/ | Exp Self help techniques/ |
| #6 | Exp Health education/ | Exp Self help groups/ | Exp Empowerment/ | Exp Coping behavior/ |
| #7 | Exp Attitude of health personnel/ | Exp Telemedicine/ | Exp Self concept/ | Exp Behavior modification/ |
| #8 | Exp Cellular phone/ | Exp Communication/ | Exp Patient participation/ | Exp Self monitoring/ |
| #9 | Exp Patient education as topic/ | Exp Rehabilitation/ | Exp Health knowledge/ | |
| #10 | Exp Handheld computer/ | Exp Professional patient relations/ | Exp Health education/ | |
| #11 | Exp Self efficacy/ | Exp Professional family relations/ | Exp Telemedicine/ | |
| #12 | Exp Activities of Daily Living/ | Exp Client education/ | ||
| #13 | Exp Self help devices/ | |||
| #14 | Exp Community health services/ | |||
| #15 | Exp Rehabilitation/ | |||
| #16 | (Self ADJ2 (car* or manag* or help or administ* or monitor* or medicat*)) or self-car* or self-manag* or self-help or self-administ* or self-monitor* or self-medicat* or selfcar* or selfmanagement or selfhelp or selfadminist* or selfmonitor* or selfmedicat* | |||
| #17 | SM or SMS | |||
| #18 | Responsib* or Autonom* | |||
| #19 | Manag* or copes or coping | |||
| #20 | “Disease management” | |||
| #21 | “expert patient” | |||
| #22 | (professional or clinician) ADJ2 development | |||
| #23 | Educat* or training or skill* or knowledge | |||
| #24 | Confidence or self-efficacy | |||
| #25 | (Access* or provi*) ADJ3 (information or records or results) | |||
| #26 | Monitor* or self-monitor* or selfmonitor* | |||
| #27 | ((patient or individual* or person* or client*) ADJ3 (remind* or feedback)) | |||
| #28 | (Tele ADJ2 (health or medicine or care)) or tele-health or tele-medicine or tele-care or telehealth or telemedicine or telecare | |||
| #29 | “Short message service” or SMS or “mobile phone” or “text message*” | |||
| #30 | (home or environment* or living or assistive) ADJ2 (adaptation or modif* or equipment or technolog*) | |||
| #31 | “Care plan*” | |||
| #32 | “Action plan*” | |||
| #33 | Hypno* ADJ1 (self or home) | |||
| #34 | (cognitive or psychological or interpersonal or relaxation or biofeedback) ADJ3 (therap* or intervention* or program*) | |||
| #35 | CBT | |||
| #36 | Psychoeducation* | |||
| #37 | (Peer or patient or emotional or social or psychosocial) ADJ1 (support or group) | |||
| #28 | “Expert patient” | |||
| #39 | Financial ADJ1 control | |||
| #40 | “personal health budget*” | |||
| #41 | (Financial or monetary or payment* or discount or service*) ADJ5 incentiv* | |||
| General self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Exp Self care/ | Exp Self care/ |
| #2 | Exp Self medication/ | Exp Self concept/ |
| #3 | Exp Patients: education/ | Exp Patient education/ |
| #4 | Exp Personal care/ | Exp Health education/ |
| #5 | Exp Self help groups/ | Exp Attitude of Health Personnel/ |
| #6 | Exp Patients: empowerment/ | Exp Telehealth/ |
| #7 | Exp Interpersonal relations/ | Exp Communication skills/ |
| #8 | Exp Technology in health care/ | Exp Assistive technology devices/ |
| #9 | Exp Disabilities: aids and appliances/ | Exp Support groups/ |
| #10 | Exp Telemedicine/ | Exp Rehabilitation/ |
| #11 | Self ADJ2 (car* or manag* or help or admistrat* or monitor* or medicat*) | Self ADJ2 car* |
| #12 | or self-car* or self-manag* or self-help or self-adminisrat* or self-monitor* or self-medicat* | Self ADJ2 manag* |
| #13 | SM or SMS | Self ADJ2 help |
| #14 | Responsib* or Autonom* | Self ADJ2 administrat* |
| #15 | Manag* or copes or coping | Self ADJ2 monitor* |
| #16 | “Disease management” | Self ADJ2 medicat* |
| #17 | “expert patient” | self-car* |
| #18 | (professional or clinician) ADJ2 development | self-manag* |
| #19 | Educat* or training or skill* or knowledge | SM |
| #20 | Confidence or self-efficacy | SMS |
| #21 | (Access* or provi*) ADJ3 (information or records or results) | Autonom* |
| #22 | Monitor* or self-monitor* or selfmonitor* | Responsib* |
| #23 | ((patient or individual* or person* or client*) ADJ3 (remind* or feedback)) | Manag* |
| #24 | (Tele ADJ2 (health or medicine or care)) or tele-health or tele-medicine or tele-care or telehealth or telemedicine or telecare | copes |
| #25 | “Short message service” or SMS or “mobile phone” or “text message*” | coping |
| #26 | (home or environment* or living or assistive) ADJ2 (adaptation or modif* or equipment or technolog*) | “Disease management” |
| #27 | “Care plan*” | “expert patient” |
| #28 | “Action plan*” | Professional ADJ2 development |
| #29 | Hypno* ADJ1 (self or home) | Clinician ADJ2 development |
| #30 | (cognitive or psychological or interpersonal or relaxation or biofeedback) ADJ3 (therap* or intervention* or program*) | Educat* |
| #31 | CBT | knowledge |
| #32 | Psychoeducation* | skill* |
| #33 | (Peer or patient or emotional or social or psychosocial) ADJ1 (support or group) | training |
| #34 | “Expert patient” | self-efficacy |
| #35 | Financial ADJ1 control | Confidence |
| #36 | “personal health budget*” | Access* ADJ3 information |
| #37 | (Financial or monetary or payment* or discount or service*) ADJ5 incentiv* | Access* ADJ3 records |
| #28 | Access* ADJ3 results | |
| #39 | Monitor* | |
| #40 | Patient ADJ3 remind* | |
| #41 | Patient ADJ3 feedback | |
| #42 | Individual* ADJ3 remind | |
| #43 | Individual* ADJ3 feedback | |
| #44 | Tele ADJ2 health | |
| #45 | Tele ADJ2 medicine | |
| #46 | Tele ADJ2 care | |
| #47 | “text message*” | |
| #48 | Home ADJ2 adaptation | |
| #49 | Home ADJ2 modif* | |
| #50 | Assistive ADJ2 technolog* | |
| #51 | “Care plan*” | |
| #52 | “Action plan*” | |
| #53 | Hypno* ADJ1 self | |
| #54 | Cognitive ADJ3 therap* | |
| #55 | Psychological ADJ3 intervention* | |
| #56 | Relaxation ADJ3 program* | |
| #57 | CBT | |
| #58 | Psychoeducation* | |
| #59 | Peer ADJ3 support | |
| #60 | Patient ADJ3 group | |
| #61 | “Expert patient” | |
| #62 | Financial ADJ1 control | |
| #63 | “personal health budget*” | |
| #64 | Financial ADJ5 incentiv* | |
| #65 | Monetary ADJ5 incentiv* | |
Detailed search terms: long-term condition-specific self-management support terms
| Stroke self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | |
|---|---|
| #1 | Exercise or training or rehabilitati* |
| #2 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) |
| #3 | “Speech and language therapy” |
| Stroke self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
|
Exp Stroke: rehabilitation/ | |
|
Exp Stroke: Services/ | |
|
Exercise or training or rehabilitati* | Exercise |
|
(Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | rehabilitati* |
|
“Speech and language therapy” | training |
|
Lifestyle ADJ1 intervention* | |
| Lifestyle ADJ1 modification* | ||
|
“Speech and language therapy” | |
| COPD and asthma self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | |
|---|---|
| #1 | Exercise or training or rehabilitati* |
| #2 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) |
| #3 | Action plan* |
| #4 | (Reduce or remove) ADJ2 (dust or mite) |
| #5 | Buteyko or “breathing technique*” |
| #6 | (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) |
| COPD and asthma self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Exercise or training or rehabilitati* | Exercise |
| #2 | (Reduce or remove) ADJ2 (dust or mite) | training |
| #3 | Buteyko or “breathing technique” | rehabilitati* |
| #4 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | Lifestyle ADJ1 intervention* |
| #5 | (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) | Lifestyle ADJ1 modification* |
| #6 | Reduce ADJ2 dust | |
| #7 | Buteyko | |
| “breathing technique” | ||
| #8 | Smok* ADJ3 cessation | |
| Diabetes mellitus self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | ||
|---|---|---|
| MEDLINE | EMBASE | |
| #1 | Exp Blood Glucose Self Monitoring/ | Exp Diabetes education/ |
| #2 | Exercise or training or rehabilitati* | |
| #3 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | |
| #4 | Foot care | |
| #5 | (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) | |
| #6 | Diet* | |
| Diabetes mellitus self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| Exp Diabetes: Health promotion/ | Exp Diabetic diet/ | |
| Exp Diabetic foot/ | ||
| Exp Diabetes Education/ | ||
| “Foot care” | “Foot care” | |
| (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) | Smok* ADJ3 cessation | |
| Diet* | Diet* | |
| Depression self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | |
|---|---|
| Exercise or training or rehabilitati* | |
| (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | |
| Depression self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| Exercise or training or rehabilitati* | Exercise | |
| rehabilitati* | ||
| (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | Lifestyle ADJ1 modification* | |
| Lifestyle ADJ1 therapy | ||
| Hypertension self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | |
|---|---|
| #1 | (Reduc* or restrict* or control* or limit* or avoid) ADJ (alcohol or coffee or caffeine or salt) |
| #2 | (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) |
| #3 | Exercise or training or rehabilitati* |
| #4 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) |
| Hypertension self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| Exercise or training or rehabilitati* | Exercise | |
| (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | rehabilitati* | |
| (Reduc* or restrict* or control* or limit* or avoid) ADJ1 (alcohol or coffee or caffeine or salt) | training | |
| (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) | Lifestyle ADJ1 intervention* | |
| Lifestyle ADJ1 modification* | ||
| Restrict* ADJ1 alcohol | ||
| Restrict* ADJ1 salt | ||
| Smok* ADJ3 cessation | ||
| CKD, IBS, IAs and LBP self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | |
|---|---|
| MEDLINE | |
| #1 | Exp Dependent Ambulation/ |
| #2 | Exp Health Services for the Aged/ |
| #3 | (Reduc* or restrict* or control* or limit* or avoid) ADJ1 (protein or potassium or phosphate or salt or diet) |
| #4 | (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) |
| #5 | Exercise or training or rehabilitati* |
| #6 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) |
| #7 | Diet* |
| #8 | Exercise or training or rehabilitati* |
| #9 | Gerotechnolog* |
| #10 | ((mobility* or ambulat* or walk* or orthop?dic) ADJ3 (device* or technolog* or aid* or equipment*)) |
| #11 | (“Manual therapy” or “spinal manipulation” or “spinal mobilisation”) ADJ3 (self or home or education) |
| CKD, IBS, IAs and LBP self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Exercise or training or rehabilitati* | Exercise |
| #2 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | rehabilitati* |
| #3 | (Reduc* or restrict* or control* or limit* or avoid) ADJ1 (protein or potassium or phosphate or salt or diet) | training |
| #4 | (Smok* or nicotine or tobacco) ADJ3 (cessation or quit*) | Lifestyle ADJ1 intervention* |
| #5 | Diet* | Lifestyle ADJ1 modification* |
| #6 | ((mobility* or ambulat* or walk* or orthop?dic) ADJ3 (device* or technolog* or aid* or equipment*)) | Restrict ADJ1 protein |
| #7 | Gerotechnolog* | Restrict ADJ1 potassium |
| #8 | (“Manual therapy” or “spinal manipulation” or “spinal mobilisation”) ADJ3 (self or home or education) | Restrict ADJ1 salt |
| #9 | Smok* ADJ3 cessation | |
| #10 | Diet* | |
| #11 | Mobility* ADJ3 aid* | |
| #12 | Orthop?dic ADJ3 equipment* | |
| #13 | Mobility ADJ3 device* | |
| #14 | Gerotechnolog* | |
| #15 | “Manual therapy” ADJ3 education | |
| #16 | “spinal manipulation” ADJ3 education | |
| Dementia, epilepsy and PNDs self-management support terms: MEDLINE, AMED, EMBASE, PsycINFO | |
|---|---|
| #1 | Exercise or training or rehabilitati* |
| #2 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) |
| #3 | (self-administered or home or self) ADJ3 (aromatherapy or “multisensory stimulation” or massage or music or dancing) |
| #4 | “Ketogenic diet” |
| #5 | “Speech and language therapy” |
| #6 | “Linoleic acid” |
| #7 | Immunisation* or vaccination* |
| Dementia, epilepsy and PNDs self-management support terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Exercise or training or rehabilitati* | Exercise |
| #2 | (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) | rehabilitati* |
| #3 | (self-administered or home or self) ADJ3 (aromatherapy or “multisensory stimulation” or massage or music or dancing) | training |
| #4 | “Speech and language therapy” | Lifestyle ADJ1 intervention* |
| #5 | “Linoleic acid” | Lifestyle ADJ1 modification* |
| #6 | “Ketogenic diet” | self-administered ADJ3 aromatherapy |
| #7 | Immunisation* or vaccination* | Home ADJ3 music |
| #8 | Home ADJ3 dancing | |
| #9 | “Speech and language therapy” | |
| #10 | “Linoleic acid” | |
| #11 | “Ketogenic diet” | |
| #12 | Immunisation* | |
Detailed search terms: long-term condition terms
| Stroke LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Stroke/ | Cerebral infarction/ | Stroke/ | Cerebrovascular accidents/ |
| #2 | Brain ischemia/ | Cerebral ischemia/ | ||
| #3 | Stroke/ | |||
| #4 | Cerebrovascular accident/ | |||
| #5 | (Stroke or poststroke or post-stroke or cerebrovascu* or “brain vasc*” or “cerebral vasc*” or cva* or apoplexy* or sah) | |||
| #6 | ((brain* or Cerebr* OR vascular OR cerebell* or intracran* or intracerebral* or subarachnoid) ADJ1 (accident OR isch?mi* OR infarct* or thrombo* or emboli* or occlus* or h?morrhage or h?matoma* or bleed*)) | |||
| Stroke LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Stroke/ | Stroke/ |
| #2 | (Stroke or poststroke or post-stroke or cerebrovascu* or “brain vasc*” or “cerebral vasc*” or cva* or apoplexy* or sah) | Stroke |
| #3 | ((brain* or Cerebr* OR vascular OR cerebell* or intracran* or intracerebral* or subarachnoid) ADJ1 (accident OR isch?mi* OR infarct* or thrombo* or emboli* or occlus* or h?morrhage or h?matoma* or bleed*)) | poststroke |
| #4 | post-stroke | |
| #5 | cerebrovascu* | |
| #6 | “brain vasc*” | |
| #7 | “cerebral vasc*” | |
| #8 | cva* | |
| #9 | sah | |
| #10 | apoplexy* | |
| #11 | Brain adj1 accident | |
| #12 | Brain adj1 infarct* | |
| #13 | Intracran* adj1 infarct* | |
| #14 | Cerebr* adj1 accident | |
| #15 | Subarachnoid adj1 h?morrhage | |
| #16 | Intracerebral* adj1 h?morrhage | |
| Asthma and COPD LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Exp Asthma/ | Asthma/ | Asthma/ | Asthma/ |
| #2 | Bronchial Spasm/ | |||
| #3 | Bronchoconstriction/ | |||
| #4 | Exp Pulmonary Disease, Chronic Obstructive/ | Exp Pulmonary Disease Chronic Obstructive/ | Chronic Obstructive Lung Disease/ | Exp Chronic Obstructive Pulmonary Disease/ |
| #5 | ((bronchial* or respiratory or airway* or lung*) ADJ3 (hypersensitive* or hyperreactiv* or allerg* or insufficiency)) | |||
| #6 | Bronch* ADJ3 (constrict* or spas*) | |||
| #7 | Asthma* | |||
| #8 | Wheez* | |||
| #9 | Bronchoconstrict* | |||
| #10 | Antiasthma* | |||
| #11 | Anti-asthma* | |||
| #12 | “Respiratory sounds” | |||
| #13 | “Bronchial hyperreactivity” | |||
| #14 | Bronchospas* | |||
| #15 | (Obstruct* ADJ3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)) | |||
| #16 | Chronic* ADJ3 bronchiti* | |||
| #17 | “Chronic Obstructive Pulmonary Disease” | |||
| #18 | “Chronic Obstructive Airways Disease” | |||
| #19 | “Lung disease*” | |||
| #20 | Emphysema* | |||
| #21 | COPD or CAL or COAD or COLD or COBD or AECB | |||
| Asthma and COPD LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Asthma/ | Exp Asthma/ |
| #2 | COPD/ | Exp Pulmonary Disease, Chronic Obstructive/ |
| #3 | ((bronchial* or respiratory or airway* or lung*) ADJ3 (hypersensitiv* or hyperreactiv* or allerg* or insufficiency)) | Bronchial* ADJ3 hypersensitiv* |
| #4 | Bronch* ADJ3 (constrict* or spas*) | Bronchial* ADJ3 hyperreactiv* |
| #5 | Asthma* | Airway* ADJ3 hypersensitiv* |
| #6 | Wheez* | Respiratory ADJ3 insufficiency |
| #7 | Bronchoconstrict* | Airway* ADJ3 hyperreactiv* |
| #8 | Antiasthma* | Bronch* ADJ3 spas* |
| #9 | Anti-asthma* | Bronch* ADJ3 constrict* |
| #10 | “Respiratory sounds” | Asthma* |
| #11 | “Bronchial hyperreactivity” | Wheez* |
| #12 | Bronchospas* | Bronchoconstrict* |
| #13 | (Obstruct* ADJ3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)) | Antiasthma* |
| #14 | Chronic* ADJ3 bronchiti* | Anti-asthma* |
| #15 | “Chronic Obstructive Pulmonary Disease” | “Respiratory sounds” |
| #16 | “Chronic Obstructive Pulmonary Disease” | “Bronchial hyperreactivity” |
| #17 | “Lung disease*” | Bronchospas* |
| #18 | Emphysema* | Obstruct* ADJ3 respirat* |
| #19 | COPD or CAL or COAD or COLD or COBD or AECB | Obstruct* ADJ3 lung* |
| #20 | Obstruct* ADJ3 airway* | |
| #21 | Chronic* ADJ3 bronchiti* | |
| #22 | “Chronic Obstructive Pulmonary Disease” | |
| #23 | “Chronic Obstructive Airways Disease” | |
| #24 | “Lung disease*” | |
| #25 | Emphysema* | |
| #26 | COPD | |
| #27 | COAD | |
| Diabetes mellitus LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Diabetes mellitus, type 1/ | Exp Diabetes Mellitus/ | Diabetes Mellitus/ | Diabetes Mellitus/ |
| #2 | Diabetes mellitus, type 2/ | |||
| #3 | Insulin resistance/ | |||
| #4 | Diabetic ketoacidosis/ | |||
| #5 | (diabet* or dm) ADJ5 (typ* ADJ3 (one or 1 or I)) | |||
| #6 | (diabet* or dm) ADJ5 (typ* ADJ3 (two or 2 or II)) | |||
| #7 | (Insulin or noninsulin or non-insulin) ADJ2 (resistan* or depend*) | |||
| #8 | Diabet* | |||
| #9 | DM or DM1 or DM2 or T1D or T1DM or T2D or T2DM or NIDDM or IDDM or MODY | |||
| #10 | “Glucose ?tolerance” | |||
| Diabetes mellitus LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Diabetes/ | Diabetes mellitus, type 1/ |
| #2 | Diabetes mellitus, type 2/ | |
| #3 | Diabetic patients/ | |
| #4 | diabet* or dm | Diabet* ADJ5 1 |
| #5 | (Insulin or noninsulin or non-insulin) ADJ2 (resistan* or depend*) | Diabet* ADJ5 I |
| #6 | DM1 or DM2 or T1D or T1DM or T2D or T2DM or NIDDM or IDDM or MODY | Diabet* ADJ5 one |
| #7 | DM ADJ5 I | |
| #8 | Diabet* ADJ5 2 | |
| #9 | Diabet* ADJ5 II | |
| #10 | Diabet* ADJ5 two | |
| #11 | DM ADJ5 II | |
| #12 | Insulin ADJ2 resistan* | |
| #13 | Insulin ADJ2 depend* | |
| #14 | Non-insulin ADJ2 depend* | |
| #15 | Diabet* | |
| #16 | DM | |
| #17 | DM1 | |
| #18 | DM2 | |
| #19 | “Glucose ?tolerance” | |
| Depression LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Depression/ | Depression/ | Depression/ | Exp Major Depression/ |
| #2 | Exp Depressive Disorder/ | |||
| #3 | Depress*or Dysthymi* | |||
| #4 | “Major Depressive Disorder” or MDD | |||
| #5 | “Unipolar Depression” | |||
| #6 | (Adjustment or mood or affective) adj1 (disorder or symptoms) | |||
| Depression LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Depression/ | Depression/ |
| #2 | Dysthymic Disorder/ | |
| #3 | Depress*or Dysthymi* | Depress* |
| #4 | “Unipolar Depression” | Dysthymi* |
| #5 | “Major Depressive Disorder” or MDD | “Major Depressive Disorder” |
| #6 | (Adjustment or mood or affective) adj1 (disorder or symptoms) | MDD |
| #7 | “Unipolar Depression” | |
| #8 | Adjustment ADJ1 disorder | |
| #9 | Mood ADJ1 disorder | |
| #10 | Affective ADJ1 disorder | |
| Hypertension LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Hypertension/ | Hypertension/ | Hypertension/ | Exp Hypertension/ |
| #2 | Hypertens* | |||
| #3 | Blood adj1 pressure | |||
| Hypertension LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Blood pressure/ | Hypertension/ ??unsure-exp to renal hypertension, pulmonary hypertension |
| #2 | Hypertens* | Hypertens* |
| #3 | Blood adj1 pressure | Blood adj1 pressure |
| CKD, IBS, IAs and LBP LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Kidney Failure, Chronic/ | Kidney Failure Chronic/ | Chronic kidney disease/ | Kidney disease/ |
| #2 | Exp Renal replacement therapy/ | Arthritis Rheumatoid/ | Chronic kidney failure/ | Lupus/ |
| #3 | Irritable bowel syndrome/ | Irritable bowel syndrome/ | Irritable bowel syndrome/ | Irritable bowel syndrome/ |
| #4 | Arthritis, Rheumatoid/ | Low back pain/ | Rheumatoid Arthritis/ | Exp Arthritis/ |
| #5 | Arthritis, psoriatic/ | Lupus Erythematosus Systemic/ | Psoriatic arthritis/ | |
| #6 | Spondylitis, Ankylosing/ | Spondylitis Ankylosing/ | Ankylosing Spondylitis/ | Back pain/ |
| #7 | Exp Lupus Erythematosus, Systemic/ | Systemic Lupus Erythematosus/ | ||
| #8 | Low back pain/ | Low back pain/ | ||
| #9 | ((Kidney or renal) ADJ2 (disease* or failure or insufficien* or dialysis)) | |||
| #10 | (kidney or renal) ADJ chronic | |||
| #11 | H?mofiltration | |||
| #12 | Dialysis | |||
| #13 | Predialysis | |||
| #14 | H?modialysis | |||
| #15 | “Renal replacement therapy” | |||
| #16 | CKD or CAPD or CCPD or APD or CRF or CRD or ESKD or ESRD or ESFF or ESRF | |||
| #17 | ((Irritable or functional or spastic) adj1 (bowel or colon)) | |||
| #18 | IBS | |||
| #19 | “Mucous colit*” | |||
| #20 | “Gastrointestinal syndrome*” | |||
| #21 | “Functional gastrointestinal” | |||
| #22 | ((r?umatoid or r?umatic or rheumat* or reumat*) ADJ3 (arthrit* or artrit* or diseas* or condition* or nodule*)) | |||
| #23 | RA | |||
| #24 | “Still* disease” | |||
| #25 | (psoria* ADJ1 (arthriti* or arthropath*)) | |||
| #26 | “Ankylosing Spondylitis” | |||
| #27 | Lupus | |||
| #28 | SLE | |||
| #29 | “Low* back pain*” | |||
| #30 | Lumbago | |||
| #31 | “Low* backache*” | |||
| #32 | Sciatica or Lumbosacral or Dorsalgia or Spondylosis | |||
| #33 | Lumbar ADJ2 pain | |||
| #34 | Back ADJ2 pain | |||
| CKD, IBS, IAs and LBP LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Dialysis/ | Exp Kidney failure, chronic/ |
| #2 | Kidney Disorders/ | Irritable bowel syndrome/ |
| #3 | Irritable bowel syndrome/ | Exp Arthritis, Rheumatoid/ |
| #4 | Arthritis and rheumatism/ | Arthritis, psoriatic/ |
| #5 | Systemic Diseases/ | Low back pain/ |
| #6 | Back pain/ | #Lupus Erythematosus, Systemic/ |
| #7 | ((Kidney or renal) ADJ2 (disease* or failure or insufficien* or dialysis)) | Kidney ADJ2 failure |
| #8 | Chronic ADJ1 (kidney or renal) | Kidney ADJ2 disease* |
| #9 | H?mofiltration | Renal ADJ2 failure |
| #10 | ((Irritable or functional or spastic) adj1 (bowel or colon)) | Renal ADJ2 disease* |
| #11 | IBS | Kidney ADJ2 insufficien* |
| #12 | “Mucous colit*” | Chronic ADJ1 kidney |
| #13 | “Gastrointestinal syndrome*” | Chronic ADJ1 renal |
| #14 | “Functional gastrointestinal” | H?mofiltration |
| #15 | ((r?umatoid or r?umatic or rheumat* or reumat*) ADJ3 (arthrit* or artrit* or diseas* or condition* or nodule*)) | Dialysis |
| #16 | RA | Predialysis |
| #17 | “Still* disease” | H?modialysis |
| #18 | (psoria* ADJ1 (arthriti* or arthropath*)) | “Renal replacement therapy” |
| #19 | “Ankylosing Spondylitis” | CKD |
| #20 | Lupus | CRF |
| #21 | SLE | CRD |
| #22 | “Low* back pain*” | Irritable ADJ1 colon |
| #23 | Lumbago | Irritable ADJ1 bowel |
| #24 | “Low* backache*” | IBS |
| #25 | Sciatica or Lumbosacral or Dorsalgia or Spondylosis | “Mucous colit*” |
| #26 | Lumbar ADJ2 pain | “Gastrointestinal syndrome*” |
| #27 | Back ADJ2 pain | “Functional gastrointestinal” |
| #28 | Rheumatoid ADJ3 arthrit* | |
| #29 | Rheumatoid ADJ3 diseas* | |
| #30 | Rheumatoid ADJ3 condition* | |
| #31 | RA | |
| #32 | “Still* disease” | |
| #33 | Psoria* ADJ1 arthriti* | |
| #34 | Psoria* ADJ1 arthropath* | |
| #35 | “Ankylosing Spondylitis” | |
| #36 | Lupus | |
| #37 | SLE | |
| #38 | “Low* back pain*” | |
| #39 | Lumbago | |
| #40 | “Low* backache*” | |
| #41 | Sciatica | |
| #42 | Lumbosacral | |
| #43 | Dorsalgia | |
| #44 | Spondylosis | |
| #45 | Lumbar ADJ2 pain | |
| #46 | Back ADJ2 pain | |
| Dementia, epilepsy, PND LTC terms: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | Exp Dementia/ | Exp Dementia/ | Dementia/ | Exp Dementia/ |
| #2 | Delirium/ | Multiple Sclerosis/ | ||
| #3 | Delirium/ | Exp Neurodegenerative Diseases/ | ||
| #4 | ||||
| #5 | Exp Epilepsy/ | Epilepsy/ | Epilepsy/ | Exp Epilepsy/ |
| #6 | Seizures/ | Exp Seizures/ | Motor Neurons/ | |
| #7 | Motor Neuron Disease/ | Motor Neuron Disease/ | Motor Neuron Disease/ | Nervous System Disorders/ |
| #8 | Multiple Sclerosis/ | Multiple Sclerosis/ | Multiple Sclerosis/ | |
| #9 | Parkinson Disease/ | Parkinson Disease/ | Parkinson Disease/ | |
| #10 | ((Cerebr* or brain or cogniti*) ADJ2 (deteriorat* or insufficient* or disease or syndrome or impair*)) | |||
| #11 | “Mild cognitive impairment” | |||
| #12 | ((memory* or mental*) ADJ2 (declin* or deteriorat* or impair* or los*)) | |||
| #13 | Pick* ADJ2 disease | |||
| #14 | Lewy* ADJ2 bod* | |||
| #15 | Dement* | |||
| #16 | Deliri* | |||
| #17 | Alzheimer* | |||
| #18 | “Primary progressive aphasia” | |||
| #19 | Binswanger* | |||
| #20 | “Benign senescent forgetfulness” | |||
| #21 | Epilep* | |||
| #22 | Seizure* | |||
| #23 | Aura* | |||
| #24 | Convulsion* | |||
| #25 | “Motor neuron* disease*” or MND | |||
| #26 | “Multiple Sclerosis” or MS | |||
| #27 | “Demyelinating disease*” | |||
| #28 | “Parkinson* disease” or PD | |||
| #29 | Parkinson* | |||
| Dementia, epilepsy and PND LTC terms: BNI, CINAHL | ||
|---|---|---|
| BNI | CINAHL | |
| #1 | Dementia/ | Exp Dementia/ |
| #2 | Epilepsy/ | Exp Epilepsy/ |
| #3 | Seizures/ | Seizures/ |
| #4 | Motor Neurone Disease/ | Motor Neuron Diseases/ |
| #5 | Multiple Sclerosis/ | Multiple Sclerosis/ |
| #6 | Parkinson Disease/ | Parkinson Disease/ |
| #7 | ((Cerebr* or brain or cogniti*) ADJ2 (deteriorat* or insufficient* or disease or syndrome or impair*)) | Cerebr* ADJ2 insufficiency |
| #8 | “Mild cognitive impairment” | Cogniti* ADJ2 deteriorat* |
| #9 | ((memory* or mental*) ADJ2 (declin* or deteriorat* or impair* or los*)) | Cogniti* ADJ2 impair* |
| #10 | Pick* ADJ2 disease | “Mild cognitive impairment” |
| #11 | Lewy* ADJ2 bod* | Memory ADJ2 loss |
| #12 | Dement* | Mental* ADj2 declin* |
| #13 | Deliri* | Mental* ADJ2 deteriorat* |
| #14 | Alzheimer* | Pick* ADJ2 disease |
| #15 | “Primary progressive aphasia” | Lewy* ADJ2 bod* |
| #16 | Binswanger* | Dement* |
| #17 | “Benign senescent forgetfulness” | Deliri* |
| #18 | Epilep* | Alzheimer* |
| #19 | Seizure* | “Primary progressive aphasia” |
| #20 | Aura* | Binswanger* |
| #21 | Convulsion* | “Benign senescent forgetfulness” |
| #22 | “Motor neuron* disease*” or MND | Epilep* |
| #23 | “Multiple Sclerosis” or MS | Seizure* |
| #24 | “Demyelinating disease*” | Aura* |
| #25 | “Parkinson* disease” or PD | Convulsion* |
| #26 | Parkinson* | “Motor neuron* disease*” |
| #27 | MND | |
| #28 | “Multiple Sclerosis” | |
| #29 | MS | |
| #30 | “Demyelinating disease*” | |
| #31 | PD | |
| #32 | Parkinson* | |
Quantitative and qualitative review filter
| Quantitative and qualitative review filter: MEDLINE, AMED, EMBASE, PsycINFO | ||||
|---|---|---|---|---|
| MEDLINE | AMED | EMBASE | PsycINFO | |
| #1 | meta-analysis/ | meta-analysis/ | systematic review/ | meta-analysis/ |
| #2 | meta analysis as topic/ | meta-analysis/ | literature review/ | |
| #3 | review literature as topic/ | |||
| #4 | MEDLINE | |||
| #5 | (systematic review* or meta-analy* or metaanaly* or "research synthesis" or “literature review”) | |||
| #6 | systematic ADJ3 literature | |||
| #7 | data ADJ2 extract* | |||
| #8 | ((information or data) ADJ3 synthesis) | |||
| #9 | cochrane | |||
| #10 | (qualitative or narrative or thematic or evidence or realist or interpret* or induct* or refutational or framework or systematic or textual) adj2 (approach or review* or synthes* or meta-summary or “meta summary” or summary) | |||
| #11 | Meta adj1 (summary or narrative or synthesis or ethnograph* or study or data or interpretation or aggregation or needs-assessment or ‘needs assessment’) | |||
| #12 | meta-summary or meta-narrative or meta-synthesis or meta-ethnograph* or meta-study or meta-data-analysis or meta-data-synthesis or meta-interpretation or meta-aggregation | |||
| #13 | ‘reciprocal translational analysis’ | |||
| #14 | ‘lines-of-arg?ment synthesis’ or ’lines of arg?ment synthesis’ | |||
| #15 | ‘LOA synthesis’ | |||
| #16 | ‘grounded formal theory’ | |||
| #17 | ‘grounded theory synthesis’ | |||
| #18 | ecological adj2 (triangulation or sentence or synthesis) | |||
| #19 | Phenomenography | |||
| #20 | ((mixed or multi* or cross) adj1 (method* or design* or research or strategy)) adj2 (synthesis or review) | |||
| #21 | (mixed-method* or multi-method* or mixed-design or multi-design or multiple-methods or multi-strategy or cross-design) adj2 (synthesis or review) | |||
| #22 | Bayesian adj1 (meta-analysis or ’meta analysis’) | |||
| #23 | ‘case survey’ | |||
| #24 | “qualitative comparative analysis” | |||
| #25 | Or/ 1-25 | |||
| #26 | letter.pt. | Letter.pt | letter.pt | – |
| #27 | comment.pt. | Comment.pt or commentary.pt | – | – |
| #28 | editorial.pt. | editorial.pt. | editorial.pt | – |
| #29 | Or/26-28 | |||
| #30 | 25 not 29 | |||
Example search: MEDLINE stroke
#1 Self care/
#2 Communication/
#3 Professional Family Relations/
#4 Telephone/
#5 Professional Patient Relations/
#6 Health education/
#7 Attitude of health personnel/
#8 Cellular phone/
#9 Patient education as topic/
#10 Handheld computer/
#11 Self efficacy/
#12 Activities of Daily Living/
#13 Self help devices/
#14 Community health services/
#15 Rehabilitation/
#16 (Self ADJ2 (car* or manag* or help or admistrat* or monitor* or medicat*)) or self-car* or self-manag* or self-#help or self-adminisrat* or self-monitor* or self-medicat* or selfcar* or selfmanagement or selfhelp or #17 selfadministrat* or selfmonitor* or selfmedicat* or SM.ti/ab.
#17 Responsib* or Autonom*.ti/ab.
#18 Manag* or copes or coping.ti/ab.
#19 “Disease management”.ti/ab.
#20 “expert patient”.ti/ab.
#21 (professional or clinician) ADJ2 development.ti/ab.
#22 Educat* or training or skill* or knowledge.ti/ab.
#23 Confidence or self-efficacy.ti/ab.
#24 (Access* or provi*) ADJ3 (information or records or results).ti/ab.
#25 Monitor* or self-monitor* or selfmonitor*.ti/ab.
#26 ((patient or individual* or person* or client*) ADJ3 (remind* or feedback)).ti/ab.
#27 (Tele ADJ2 (health or medicine or care)) or tele-health or tele-medicine or tele-care or telehealth or telemedicine or telecare.ti/ab.
#28 “Short message service” or SMS or “mobile phone” or “text message*”.ti/ab.
#29 (home or environment* or living or assistive) ADJ2 (adaptation or modif* or equipment or technolog*).ti/ab.
#30 “Care plan*”.ti/ab.
#31 “Action plan*”.ti/ab.
#32 Hypno* ADJ1 (self or home)ti/ab.
#33 (cognitive or psychological or interpersonal or relaxation or biofeedback) ADJ3 (therap* or intervention* or program*).ti/ab
#34 CBT.ti/ab.
#35 Psychoeducation*.ti/ab.
#36 (Peer or patient or emotional or social or psychosocial) ADJ1 (support or group) .ti/ab.
#37 “Expert patient”.ti/ab.
#38 Financial ADJ1 control.ti/ab.
#39 “personal health budget*”.ti/ab.
#40 (Financial or monetary or payment* or discount or service*) ADJ5 incentiv*.ti/ab.
#41 Exercise or training or rehabilitati*.ti/ab.
#42 (Lifestyle or occupational) ADJ1 (intervention* or modification* or therapy) .ti/ab.
#43 “Speech and language therapy”.ti/ab.
#44 Or/1-43
#45 Stroke/
#46 Brain ischemia/
#47 (Stroke or poststroke or post-stroke or cerebrovascu* or “brain vasc*” or “cerebral vasc*” or cva* or apoplexy* or sah).ti/ab.
#48 ((brain* or Cerebr* OR vascular OR cerebell* or intracran* or intracerebral* or subarachnoid) ADJ1 (accident OR isch?mi* OR infarct* or thrombo* or emboli* or occlus* or h?morrhage or h?matoma* or bleed*)).ti/ab.
#49 Or/45-48
#50 meta-analysis/
#51 meta analysis as topic/
#52 Review literature as topic/
#53 MEDLINE.ti/ab.
#54 (systematic review* or meta-analy* or metaanaly* or "research synthesis" or literature review) .ti/ab.
#55 systematic ADJ3 literature.ti/ab.
#56 data ADJ2 extract*.ti/ab.
#57 ((information or data) ADJ3 synthesis).ti/ab.
#58 Cochrane.ti/ab.
#59 (qualitative or narrative or thematic or evidence or realist or interpret* or induct* or refutational or framework or systematic or textual) adj2 (approach or review* or synthes* or meta-summary or “meta summary” or summary)
#60 Meta adj1 (summary or narrative or synthesis or ethnograph* or study or data or interpretation or aggregation or needs-assessment or “needs assessment”)
#61 meta-summary or meta-narrative or meta-synthesis or meta-ethnograph* or meta-study or meta-data-analysis or meta-data-synthesis or meta-interpretation or meta-aggregation
#62 “reciprocal translational analysis”
#63 RTA
#64 “lines-of-arg?ment synthesis” or “lines of arg?ment synthesis”
#65 “LOA synthesis”
#66 “grounded formal theory”
#67 “grounded theory synthesis”
#68 ecological adj2 (triangulation or sentence or synthesis)
#69 Phenomenography
#70 ((mixed or multi* or cross) adj1 (method* or design* or research or strategy)) adj2 (synthesis or review)
#71 (mixed-method* or multi-method* or mixed-design or multi-design or multiple-methods or multi-strategy or cross-design) adj2 (synthesis or review)
#72 “research synthesis”
#73 Data ADJ2 extract*
#74 ((information or data) ADJ3 synthesis)
#75 Bayesian adj1 (meta-analysis or “meta analysis”)
#76 “case survey”
#77 “qualitative comparative analysis”
#78 Or/50-77
#79 letter.pt
#80 comment.pt
#81 editorial.pt
#82 Or/79-81
#83 78 not 82
#84 44 and 49 and 83
Appendix 11 Search strategy for additional meta-reviews
Additional meta-reviews of the quantitative and qualitative literature were carried out for the following LTCs: COPD, CKD, dementia, epilepsy, IBS, LBP, PNDs and T1DM.
Method
Owing to time constraints, it was decided that searches would be limited to databases likely to yield results of reasonable relevance. Databases producing large numbers of irrelevant hits would be excluded, thereby ensuring optimal efficiency given limited resources.
Using database records from previous searches of self-management support interventions in two other LTCs (T2DM and stroke), the individual databases were explored to determine the sensitivity/accuracy and specificity/precision of the search results in relation to our final list of included quantitative reviews.
As a review team, it was decided that we would search the databases with highest sensitivity/accuracy. This was to ensure comprehensiveness in our review results. However, due to time constraints, we did not want to search databases with low specificity/precision, creating large volumes of work for little gain.
The databases identified to have highest sensitivity/accuracy were EMBASE, MEDLINE and CINAHL. Of these three databases, EMBASE had the lowest specificity. It was therefore decided that we would search both MEDLINE and CINAHL for these additional meta-reviews.
In addition, Cochrane Database of Systematic Reviews and Database of Abstracts of Reviews for Effectiveness were searched. A forward citation search was performed on all included systematic reviews using ISI Proceedings (Web of Science), and all included publication reference lists were screened.
| AMED | BNI | CINAHL | EMBASE | MEDLINE | PsycINFO | |
|---|---|---|---|---|---|---|
| Stroke: quantitative | ||||||
| Aziz 200871 | ||||||
| Hoffman 201072 | ||||||
| Legg 200673 | ||||||
| Outpatient Service Trialists 200374 | ||||||
| Poulin 201275 | ||||||
| Steultjens 200376 | ||||||
| Walker 200477 | ||||||
| Ellis 201078 | ||||||
| Ko 201079 | ||||||
| Korpershoek 201180 | ||||||
| Rae-Grant 201181 | ||||||
| Smith 200882 | ||||||
| Stroke: qualitative | ||||||
| Lamb 200864 | ||||||
| Reed 201268 | ||||||
| Salter 200869 | ||||||
| Peoples 201167 | ||||||
| McKevitt 200465 | ||||||
| Murray 200366 | ||||||
| Stroke: quantitative and qualitative | ||||||
| Lui 200570 | ||||||
| AMED | BNI | CINAHL | EMBASE | MEDLINE | PsycINFO | |
|---|---|---|---|---|---|---|
| T2DM: quantitative | ||||||
| Chodosh 200599 | ||||||
| Dorresteijn 2010100 | ||||||
| Duke 2009101 | ||||||
| Gary 2003102 | ||||||
| Hawthorne 2008103 | ||||||
| Heinrich 2010104 | ||||||
| Khunti 2008105 | ||||||
| Li 2011106 | ||||||
| Minet 2010107 | ||||||
| Nam 2012108 | ||||||
| Newman 2004109 | ||||||
| Norris 2001110 | ||||||
| Norris 2002111 | ||||||
| Pérez-Escamilla 2008112 | ||||||
| Sigurdardottic 2007113 | ||||||
| Steinsbekk 2012114 | ||||||
| Van Dam 2005115 | ||||||
| T2DM: qualitative | ||||||
| Campbell 200355 | ||||||
| Fleming 200995 | ||||||
| Gomersall 201196 | ||||||
| Ho 201097 | ||||||
| Paterson 199898 | ||||||
| Database | Sensitivity/accuracy (%), n relevant identified/total relevant identified | Specificity/precision (%), n relevant identified/total hits | ||
|---|---|---|---|---|
| Stroke | Diabetes | Stroke | Diabetes | |
| AMED | 26 | 5 | 1.8 | 1.6 |
| BNI | 26 | 23 | 9.6 | 6.0 |
| CINAHL | 74 | 68 | 1.7 | 1.6 |
| EMBASE | 79 | 86 | 0.3 | 0.3 |
| MEDLINE | 84 | 82 | 0.6 | 0.5 |
| PsycINFO | 26 | 32 | 1.5 | 1.6 |
Appendix 12 Implementation search strategy
Database search
Generic LTC search terms OR specific exemplar LTC keywords.
AND Phase IV implementation studies search terms OR MeSH terms for each database.
AND generic self-Management search terms OR self-Management components.
NOT guidelines NOT drug.
All searches in [Title/Abstract].
Phase IV search terms
| #1 | ((implement* or effectiveness or clinical or ‘Phase IV’ or ‘Phase 4’ or efficacy or real-world or ‘real world’ or ‘field effectiveness’ or field-effectiveness or population or pragmatic or evidence-based or ‘evidence based’ or evaluation* or real-life or ‘real life’) adj1 (trial* or stud* or research or intervention*)) |
| #2 | ((case-control or quasi-experimental or ‘quasi experimental’ or ‘interrupted time series’ or ‘uncontrolled before and after’ or ‘controlled before and after’ or before-and-after or ‘before and after’ or cluster-randomi* or ‘cluster randomi*’) adj1 (trial* or stud* or research or intervention*)) |
| #3 | (Real-world or ‘real world’ or routine or normal or nationwide) adj1 (setting* or practice or context*) |
| #4 | “Routine clinical care” |
| #5 | “quality improvement” |
| #6 | “nationwide context” |
Medical subject heading terms
| MEDLINE/PubMed | #Clinical trials, phase IV as topic/ |
| #Evidence-Based Practice/ | |
| #Evidence-Based Medicine/ | |
| #Evidence-Based Nursing/ | |
| #Comparative effectiveness research/ | |
| #Disease management/ | |
| #Patient education as topic/ | |
| AMED | #exp Patient education/ |
| #exp Quality of health care/ | |
| #Chronic Disease/ | |
| #Disease management/ | |
| #Evidence based medicine/ | |
| BNI | None |
| CINAHL | #Prospective studies/ |
| #Nonrandomised trials/ | |
| #Behavioral research/ | |
| #Disease management/ | |
| #Outcomes research/ | |
| #Quality of care research/ | |
| #Summative Evaluation Research/ | |
| #Evaluation research/ | |
| #exp Clinical research/ | |
| #Medical practice, evidence-based/ | |
| #Professional practice, evidence-based/ | |
| #Nursing practice, evidence-based/ | |
| EMBASE | #disease management/ |
| #treatment outcome/ | |
| #diabetes education/ | |
| #patient education/ | |
| #Outcomes research/ | |
| #Outcome assessment/ | |
| PsyclNFO | #Client education/ |
| #Evidence based practice/ | |
| #Evidence based medicine/ | |
| #Telemedicine/ | |
| #Disease management/ | |
| #Cohort analysis/ | |
| #Educational program evaluation/ |
Journal search
Health education and behaviour
Search:
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’
AND
self-manag* OR "self care" OR tele-health OR tele-medicine OR telemedicine OR ‘Action plan*’OR ‘text message*’ OR ‘mobile phone’
Health education research
Search:
Routine clinical practice OR Nationwide context OR Real-world OR Self-management OR Self-care OR Self care OR Tele-health OR Tele-medicine OR Telehealth OR Telemedicine OR Action plan
Patient education and counselling
Search:
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND self-manag*
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND ‘self care’
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND tele-health
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND tele-medicine
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND telemedicine
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND ‘action plan*’
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND ‘text message’
implement* OR ‘real world’ OR ‘Phase IV’ OR pragmatic OR “Routine clinical setting” OR “nationwide context” OR “Routine clinical context” OR ‘Phase 4’ AND ‘mobile phone’
Registries search
Online registry, URL: www.clinicaltrials.gov
Search:
# Self-manag* OR self-management OR selfmanagement OR self-care
# tele-health OR tele-medicine OR telehealth OR telemedicine OR tele-care OR telecare
# selfmonitoring OR self-monitor OR selfmonitor OR self-monitoring
# education OR training OR skill OR knowledge AND self-management
# empower OR empowerment OR self-efficacy
# real-world OR pragmatic OR real-life OR nationwide OR routine care
Online registry, URL: www.controlled-trials.com
Included:
-
ISRCTN Register (international) – copy of ISRCTN Register.
-
Action Medical Research (UK) – subset from ISRCTN Register.
-
The Wellcome Trust (UK) – subset from ISRCTN Register.
-
UK Trials (UK) – subset from ISRCTN Register, UK trials.
Search:
# Self management OR self-management OR self-care
# tele-health OR tele-medicine OR telehealth OR telemedicine OR tele-care OR telecare
# selfmonitoring OR self-monitor OR selfmonitor OR self-monitoring
# empower OR empowerment OR self-efficacy
# phase IV OR real-world OR pragmatic OR real-life OR nationwide OR routine care
Appendix 13 Exclusion criteria for meta-reviews
Exclusion criteria must be applied in order, so papers are excluded on the first of these criteria that applies.
For example, if not a systematic review or about self-management then it is excluded on 4 rather than 6.
If the paper cannot be excluded on any criteria, then it is included into the meta-review.
Exclude 1
Exclude if the review is not written in English.
Exclude 2
Exclude if the review does not include human participants.
Exclude 3
Exclude reviews published before 1993.
Exclude 4
Exclude if the review is not a systematic review of the literature.
Searches at least two sources, one of which must be an electronic database (e.g. Cochrane database, MEDLINE, EMBASE, PsycINFO, BNI, CINAHL), the other may be a second electronic database, or one of the following: manual searching of one or more journal(s), checking reference lists; and consulting with experts.
Provides reasoning for the inclusion/exclusion of studies.
Provides some explanation of how they synthesised the data (e.g. systematic data extraction, meta-analysis, narrative synthesis meta-ethnography).
Exclude 5
Exclude if the review does not focus on or include one or more of the LTCs you are interested in.
Exclude 6
Exclude if the focus of the review is not about:
Quantitative: self-management support interventions, or
Qualitative: the lived experience of the condition that can be used to inform self-management support, the experience of self-management of the condition, or the experience/feedback of self-management services/provision either as an intervention or in the real-world community.
Exclude 7
Exclude if the systematic review does not attempt to identify:
Quantitative: RCTs, or
Qualitative: qualitative primary studies.
Exclude 8
Exclude if the review does not:
Quantitative: measure one of the following outcomes: use of health-care services; health outcomes (including biological markers of disease); symptoms; health behaviours; QoL; self-efficacy/empowerment, or
Qualitative: if findings cannot be used to inform self-management support.
Exclude 9
Exclude if the paper is a published conference abstract, thesis, protocol, book, book chapter or summary of other reviews.
Exclude 10
Exclude if the paper is a shorter and less detailed version of a review or if there has been an updated version of the review published.
Often authors do one review, publish it as a Cochrane review first and then about 1 year later exactly the same thing gets published in a journal article. However, this is in less depth because of the restricted word limit for journals. Therefore the journal article version gets excluded on criteria 10 for being a shorter, less detailed version of a review.
If there is a Cochrane review that includes a mixture of designs, such as RCTs, controlled clinical trials and observational studies, and does not separate them out in the results but there is a journal article version of the same thing that only writes up the RCTs, exclude the Cochrane review on criteria 11 and keep the journal article version in.
A review is considered being an updated review if it includes an updated re-search, so, for example, if a Cochrane review is done in 2002 and then the same thing is re-searched in 2006, the 2002 version is excluded under criteria 10.
Exclude 11
Exclude if unable to data extract.
Different study designs: where systematic reviews include a range of study designs these reviews will only be included in our meta-review if they report or comment the findings of the RCTs/qualitative studies separately, either under separate subheadings, or in separate paragraphs, or in whole sections of text. Where results across the RCT/qualitative design studies are not clearly distinguished from those of other study designs in the results or conclusions sections – for example necessitating referral to a table to identify the actual study design of individual studies or where the findings from studies of different designs are combined or interdigitated – these reviews will not be included in the meta-review.
Different LCTs: where systematic reviews include both the condition of interest and other conditions these reviews will only be included in our metareview if they report or comment the findings of the RCTs/ qualitative studies on our index conditions separately, either under separate subheadings, or in separate paragraphs, or in whole sections of text. Where it is not possible to easily extract results for our conditions of interest from those for other conditions – for example necessitating referral to a table to identify the underlying condition in a particular study, or where the findings from studies on different conditions are combined or interdigitated – these reviews will not be included in the meta-review.
Exclude 12
Exclude if the review does not report somewhere in the review the list of studies included. If the review provides references in the text, and includes the studies in a reference list at the end of review, this is fine.
Appendix 14 Implementation exclusion criteria
Exclude 1
Exclude if it is not written in English.
Exclude 2
Exclude if not a primary empirical study (do not include if review of literature or conceptual/philosophical papers).
Exclude 3
Exclude if the paper does not focus on or include one or more of the exemplar LTCs.
Exclude 4
Exclude if the study is not an intervention.
Exclude 5
Exclude if the focus is not about self-management support interventions.
Exclude 6
Exclude if the paper is not an implementation trial (i.e. delivered as part of routine service to populations of people). Do not include Phase III RCTs or qualitative studies as these are included in the two other PRISMS reviews).
Exclude 7
Exclude if does not measure one of the outcomes of interest (use of health-care services, health outcomes, symptoms, health behaviour, QoL or self-efficacy).
Exclude 8
If more than one LTCs included, exclude if unable to data extract the information for the selected LTCs separately from the rest of the findings for the other LCTs.
Appendix 15 Revised Assessment of Multiple Systematic Reviews quality appraisal tools
Appendix 16 Qualitative meta-review quality assessment tool
These decisions were based on the information provided in the published report; no further information was sought from the reviewers. It was therefore considered to be the judgement of the quality and explicitness of their reporting. Each main question has smaller subquestions to guide the answer to the main question. Each question is positively worded so if the answer is yes, it will be considered as a positive towards the assessment of the review’s quality.
Appropriate and detailed design provided?
-
Does the review specify their original protocol with details of any iterative changes made explicit and the rationale for these changes explained?
-
Do they provide a statement of inclusion criteria?
-
Do they use PICOS to guide their research question(s)?
Duplicate study selection and data extraction?
-
Did they have at least two independent data extractors?
-
Did they have a consensus procedure for disagreements?
-
Were disagreements resolved properly?
Did they carry out a comprehensive literature search?
-
Did they search at least two electronic sources?
-
Did they state both the years and databases that they searched?
-
Did they state key words/MeSH terms and were you able to trace the filtering of articles for inclusion, for example a flow diagram?
-
Were textbooks/experts/references of included reviews consulted?
-
Did they hand-search/manual-search journals?
Was status of publication used as an inclusion criterion?
-
Did they state whether or not they searched for reports regardless of publication type?
-
Did they state if they excluded reports based on publication status, language, etc.?
-
Did they state whether or not non-English papers were translated?
-
Did they include all languages in the review (have no language restriction)?
Was a list of included and excluded studies provided?
-
Did they provide a table/list of included studies?
-
Did they include a table/list of excluded studies after full-text screening?
-
Do they state the reason for exclusion of studies at the full-text screening stage?
-
Are you able to retrace included and excluded papers through references?
Were characteristics of included studies provided?
-
Did they provide summarised information on participants, methods, contexts?
-
Did they provide ranges of relevant characteristics provided (e.g. age, gender, ethnicity)?
-
Did the information provided appear to be complete and accurate?
Was scientific quality of included studies assessed and documented?
-
Did they have an a priori method of assessment?
-
Did the scientific quality of included studies appear meaningful?
-
Did they include a discussion/awareness of levels of evidence?
-
Did they score the quality of included studies using a set instrument/technique?
Was scientific quality of included studies used appropriately in formulating conclusions?
-
Were the results of quality and credibility considered in the analysis and conclusions?
-
Were the results of quality and credibility explicitly stated in formulating recommendations?
-
Do the conclusions drive towards a clinical consensus statement/summary of evidence?
-
Does this clinical consensus statement drive towards a recommendation for practice?
Were appropriate methods used to combine findings of studies?
-
Did they provide a description of how the primary studies were analysed?
-
Was the type of analysis appropriate to answer the research questions/achieve the aims?
-
Do they discuss convergence within the primary study’s findings?
-
Do they discuss divergence within the primary study’s findings?
Was conflict of interest stated?
-
Was a statement of sources or support provided?
-
Did they state that there was no conflict of interest?
-
Did they state an awareness of conflict of interest in the inclusion of primary studies, i.e. providing a discussion on author reflexivity?
All 10 sections marked out of 4 same as R-AMSTAR in Appendix 15, therefore giving a total of 40.
Appendix 17 Implementation quality checklist
| Checklist | Items | Scale |
|---|---|---|
| Reporting (10 items) Is the information in the paper enough to help the reader make an unbiased assessment of findings? |
1. Is the hypothesis/aim/objective of the study clearly described? | Yes = 1; no = 0 |
| 2. Are the main outcomes to be measured clearly described in the introduction or methods section? | Yes = 1; no = 0 | |
| 3. Are the characteristics of the patients included in the study clearly described? | Yes = 1; no = 0 | |
| 4. Are the interventions of interest clearly described? | Yes = 1; no = 0 | |
| 5. Are the distributions of principal confounders in each group of subjects to be compared clearly described? | Yes = 2; partially = 1; no = 0 | |
| 6. Are the main findings of the study clearly described? | Yes = 1; no = 0 | |
| 7. Does the study provide estimates of the random variability in the data for the main outcomes? | Yes = 1; no = 0 | |
| 8. Have all important adverse events that may be a consequence of the intervention been reported? | Yes = 1; no = 0 | |
| 9. Have the characteristics of patients lost to follow-up been described? | Yes = 1; no = 0 | |
| 10. Have actual probability values been reported (e.g. 0.035 rather than < 0.05) for the main outcomes except where the probability value is < 0.001? | Yes = 1; no = 0 | |
| External validity (three items) Are the results generalisable to the population from which participants were derived? |
1. Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | Yes = 1; no = 0; unable to determine = 0 |
| 2. Were those subjects who were prepared to participate, representative of the entire population from which they were recruited? | Yes = 1; no = 0; unable to determine = 0 | |
| 3. Were the staff, places and facilities where the patients were treated representative of the treatment the majority of patients receive? | Yes = 1; no = 0; unable to determine = 0 | |
| Bias (seven items) Bias in the measurement of intervention and outcomes? |
1. Was an attempt made to blind study subjects to the intervention they have received? | Yes = 1; no = 0; unable to determine = 0 |
| 2. Was an attempt made to blind those measuring the main outcomes of the intervention? | Yes = 1; no = 0; unable to determine = 0 | |
| 3. If any of the results of the study were based on ‘data dredging’, was this made clear? | Yes = 1; no = 0; unable to determine = 0 | |
| 4. In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or in case–control studies, is the time period between the intervention and outcome the same for cases and controls? | Yes = 1; no = 0; unable to determine = 0 | |
| 5. Were the statistical tests used to assess the main outcomes appropriate? | Yes = 1; no = 0; unable to determine = 0 | |
| 6. Was compliance with the intervention/s reliable? | Yes = 1; no = 0; unable to determine = 0 | |
| 7. Were the main outcome measures used accurate (valid and reliable)? | Yes = 1; no = 0; unable to determine = 0 | |
| Confounding (six items) Bias in the selection of study participants? |
1. Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited from the same population? | Yes = 1; no = 0; unable to determine = 0 |
| 2. Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited over the same period of time? | Yes = 1; no = 0; unable to determine = 0 | |
| 3. Were study subjects randomised to intervention groups? | Yes = 1; no = 0; unable to determine = 0 | |
| 4. Was the randomised intervention assignment concealed from both patients and health-care staff until recruitment was complete and irrevocable? | Yes = 1; no = 0; unable to determine = 0 | |
| 5. Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | Yes = 1; no = 0; unable to determine = 0 | |
| 6. Were losses of patients to follow-up taken into account? | Yes = 1; no = 0; unable to determine = 0 | |
| Power (one item) Are negative effects of intervention due to chance? |
1. Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is < 5%? | Yes = 1; no = 0 |
Appendix 18 Why the included reviews are self-management support
| Review | Relevant aim(s) | Why this is self-management support |
|---|---|---|
| Therapy rehabilitation: interventions which are delivered by therapists (may include OTs and physiotherapists) working to rehabilitate individuals after a stroke | ||
| Aziz 200871 | To determine whether or not therapy-based rehabilitation services influence stroke patient and carer outcomes 1 year or more after the index stroke, and which outcomes are influenced |
|
| Hoffman 201072 | To determine the effectiveness of OT for people with cognitive impairment after a stroke in improving functional performance of basic and instrumental ADL and cognitive abilities |
|
| Legg 200673 | To determine whether or not any intervention provided by an OT (or under the supervision of an OT) with the specific aim of facilitating personal ADL improves the outcomes for patients following stroke |
|
| OST 200374 | To determine whether or not therapy-based rehabilitation services influence stroke patients and carer outcomes, and which outcomes are influenced. Furthermore, to examine which components of therapy-based rehabilitation services are effective |
|
|
||
| Poulin 201275 | To determine whether or not executive function intervention are more effective than no intervention or an alternative intervention in improving executive functions and functional abilities in daily life in the acute, subacute and chronic stages of stroke recovery |
|
| Steultjens 200376 | To determine whether or not OT interventions improve outcome for stroke patients |
|
| Walker 200477 | To address the efficacy of community OT using individual patient data from RCTs |
|
| Other self-management support: a heterogeneous group of interventions delivered by various persons and of various modalities which aim to support stroke survivors/caregivers | ||
| Ellis 201078 | To determine the efficacy of stroke liaison workers for patients with stroke and their caregivers in increasing participation and improving well-being for patients and carers |
|
| Ko 201079 | To determine whether or not in patients with chronic disease, a patient-held medical record, compared with usual care, improves clinical care, patient outcomes or satisfaction |
|
| Korpershoek 201180 | To determine which self-efficacy enhancing interventions influence mobility, ADL, depression and HRQoL of patients with a stroke |
|
| Lui 200570 | To examine the effectiveness of teaching problem-solving skills to caregivers in stroke care |
|
| Rae-Grant 201181 | To review the current body of evidence supporting the efficacy of self-management programmes in individuals with MS and other chronic neurological conditions |
|
| Smith 200882 | To examine the effectiveness of information strategies provided with the intention of improving the outcome for stroke patients or their identified caregivers or both |
|
Appendix 19 Epilepsy qualitative Preferred Reporting Items for Systematic Reviews and Meta-Analyses chart
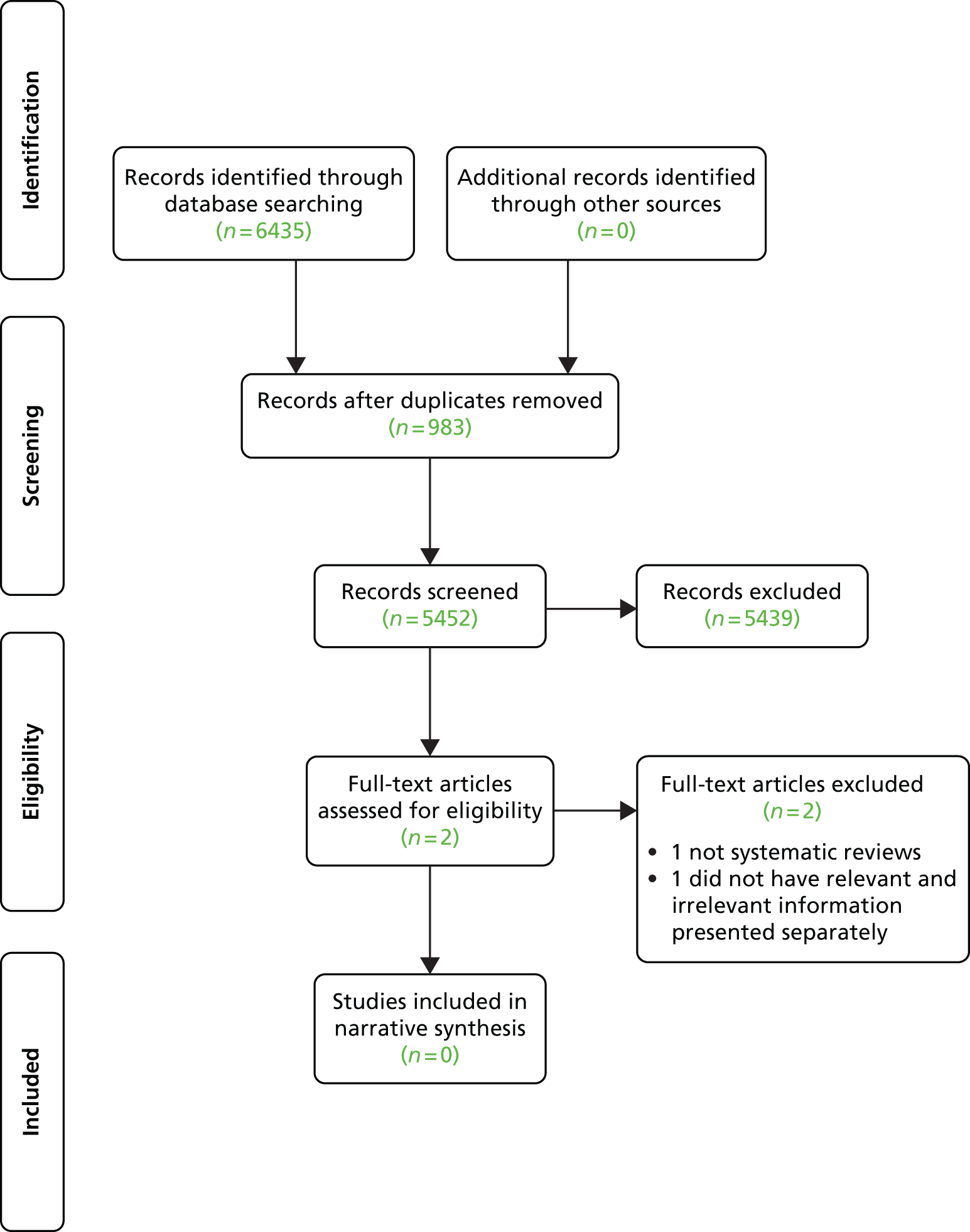
Appendix 20 Irritable bowel syndrome qualitative Preferred Reporting Items for Systematic Reviews and Meta-Analyses chart
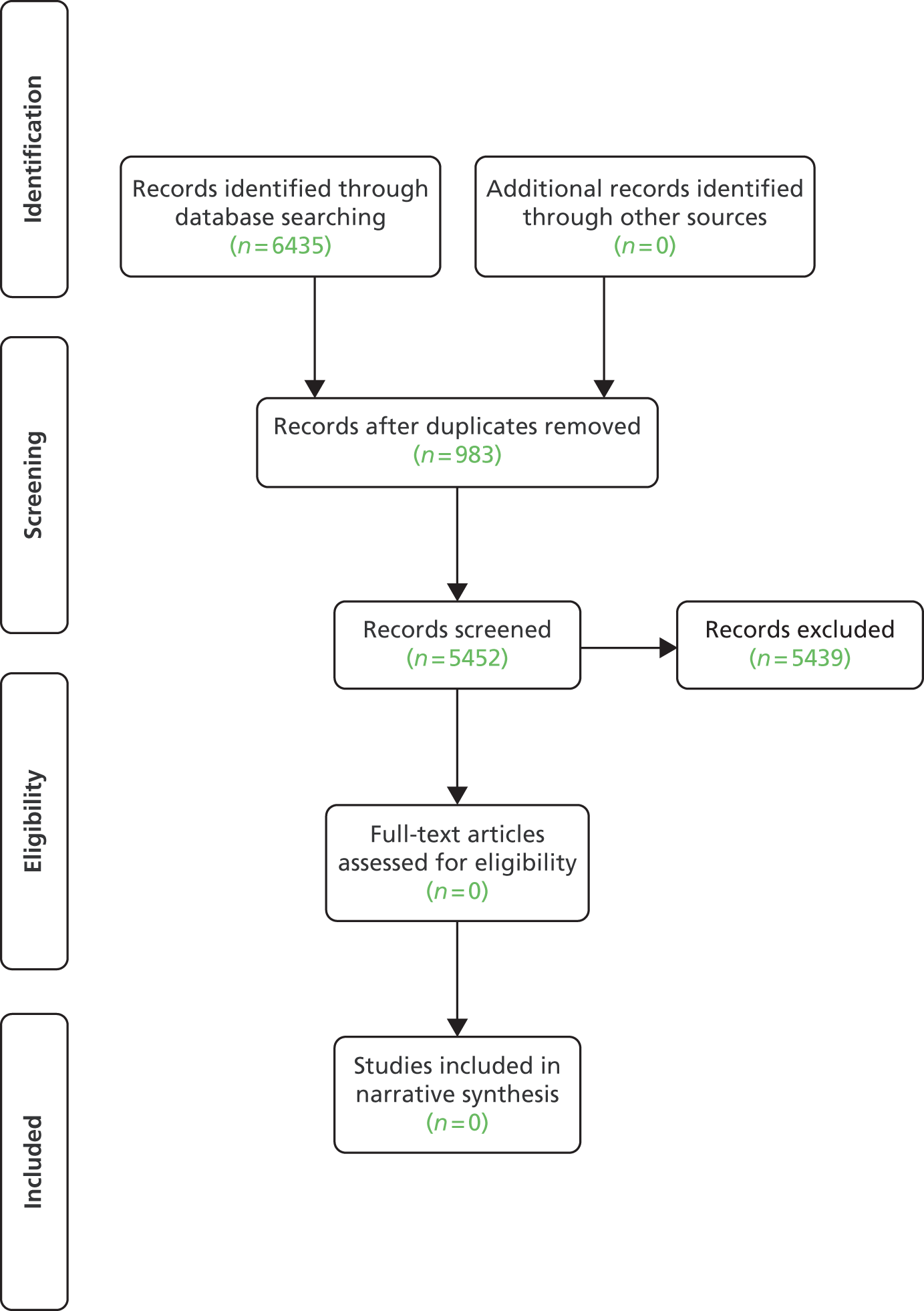
Appendix 21 Progressive neurological disorder qualitative Preferred Reporting Items for Systematic Reviews and Meta-Analyses chart
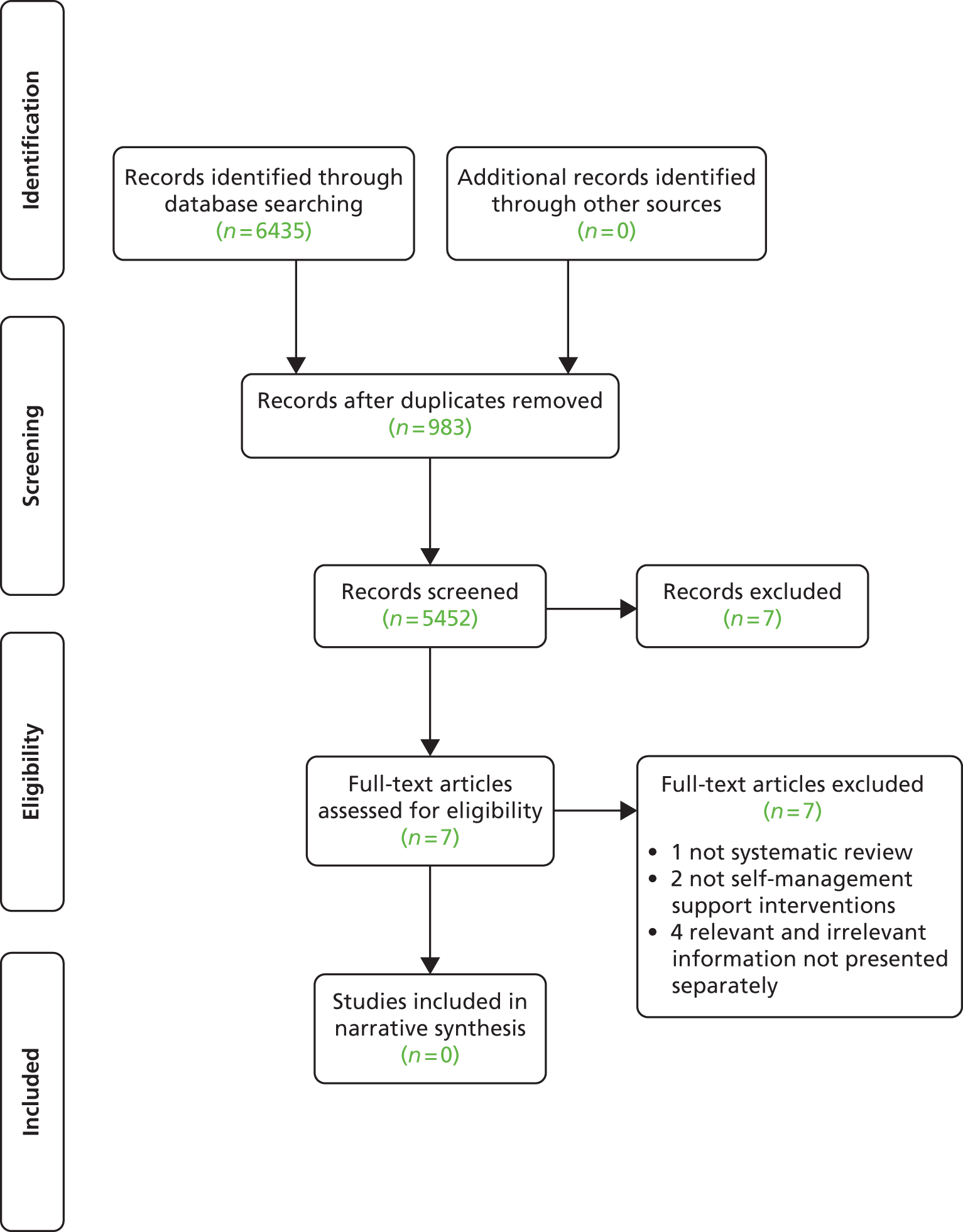
Appendix 22 Abstract for implementation systematic review
Background: Medical Research Council Phase IV studies which accommodate the diversity of patient, professional and health-care contexts in order to inform implementation in real-life settings are relatively uncommon. We undertook a systematic review of implementation studies of self-management support interventions in 14 exemplar conditions to explore what works for whom and why.
Methods: We searched and screened records from seven electronic databases, and performed snowball and manual searches. We quality assessed all eligible papers, extracted, and synthesised. Outcomes of interest included condition-related symptoms, process outcomes and use of health services.
Results: Sixty-one studies (1998–2012) satisfied eligibility criteria and were included in the review. The health-care contexts included primary, secondary, community and private care settings and targeted patients, professionals and organisations. Strategies encompassed individual, group, telephone interventions with some studies using telehealthcare. Evidence shows that, in the conditions included in our review, delivering patient education and professional training with the organisation’s support is related to significant changes in clinical and process outcomes. Although all three components are important, the culture of the organisation underpins and enables integration of self-management principles into routine clinical care, such that the process and clinical impact of patient/professional interventions are realised/enhanced.
Conclusions: Multidisciplinary, complex self-management support interventions delivered in routine clinical care require the involvement of individuals from all levels, the patient, the professional and the organisation. Success requires strong clinical leadership in the practice and/or at the system level such that self-management is integrated in routine care. However, results need to be interpreted with caution since evidence focused predominantly on the short term and emerges from poor study designs with the majority of studies scoring low for quality, and the possibility of publication bias, with studies with positive results being more likely to be published, is acknowledged.
Appendix 23 Matrices of characteristics of long-term conditions versus components of self-management support
-
Significant variability/risk of (serious/high cost) exacerbations.
-
Impact of symptoms on lifestyle.
-
Degree of complexity of medical/clinical/social/lifestyle self-care regimes.
-
Potential of treatment/(self-) management to improve symptoms.
-
Risk of significant complications or comorbidity necessitating (self-) monitoring.
-
Presence of comorbidities (including depression).
-
Potential of treatment/(self-) management to be disease modifying.
Appendix 24 Delegates list
Appendix 25 Summary of qualitative research foci and qualitative research
Recommendations
| LTC | Included reviews, n | Research focus |
|---|---|---|
| Stroke | 7 | There were two clear foci of qualitative review included in this meta-review as a result of our selection criteria. One revolved around patients’ experiences of being a survivor of stroke, either more generally or with a specific focus on psychosocial experiences in the elderly population.64,66,68,70 The second was based on reviews examining people’s views of services offered to those who had had a stroke, investigating challenges faced and potential solutions found62,64–67 |
| T2DM | 5 | Of those included, only one explicitly focused on adults with T2DM,95 whereas the others considered adults (although age was not actually specified in all the reviews) with a combination of both T1DM and T2DM.55,94,96,97 Paterson et al.’s review98 describes the majority of their participants as educated, married women with insulin dependent diabetes. Fleming and Gillibrand95 only included studies where the majority were of first or second generation South Asian ethnicities |
| Asthma | 1 | What helps or hinders action plan implementation from the perspective of health professionals and patients/carers117 |
| Depression | 3 | They focused on different aspects of depression: adolescents’ experiences,137 patients’ experience of depression management in primary care, support groups, self-help clinics135 and patients’ experience of antidepressant medication136 |
| COPD | 3 | Two reviews were qualitative syntheses; one on COPD patients’ experiences of breathlessness143 and the other on experiences of LTOT.144 The remaining review was a mixed-methods synthesis examining telemedicine services for patients with COPD145 |
| CKD | 2 | One review focused on experiences of those with kidney failure151 and the other specifically focused on the dialysis experiences of children with kidney failure152 |
| Dementia | 2 | Both of the included reviews aimed to examine the subjective experiences of people living with dementia (at home, not in residential care), including management and social interaction involved in their lives156 and analysis aimed at informing an inventory of subjective needs.157 Both were of lower quality on AMSRAR and only some of the studies they included were relevant to our meta-review |
| Epilepsy | 0 | N/A |
| Hypertension | 2 | Both reviews focused on lay perspectives about hypertension and medication adherence166,167 |
| IAs | 2 | Both reviews focused on RA, precluding general conclusions about IAs. One was about the drivers and barriers to help-seeking behaviour in people with new onset RA,179 and the other about experiences of living with RA180 |
| IBS | 0 | N/A |
| LBP | 1 | Mixed-methods review examining patients with both chronic and acute LBP on their expectations and satisfaction with treatment as part of practice guideline development |
| PNDs | 0 | N/A |
| T1DM | 2 | Both reviews212,213 examined experiences of T1DM in adolescents, with Palladino et al.’s review212 specifically focusing on the influence of peers |
Based on this table, we have systematically identified a list of key areas where there is still a need for a (high-quality) qualitative synthesis on self-management support for the relative LTC:
-
Asthma: there were no qualitative synthesis on self-management support (other than action plans) or the lived experience of asthma found in this review.
-
COPD: the reviews in this condition scored between 23/40 and 27/40 with 30/40 being the quality cut off for high quality, therefore there is a need for higher-quality qualitative synthesis examining self-management support for people with COPD.
-
Dementia: an important area with only two relevant lower-quality (28/40) systematic reviews identified which did not entirely map onto our area of interest; there is a need for higher-quality qualitative synthesis examining self-management support for people with dementia living at home and their carers.
-
CKD: there is a need for qualitative synthesis examining self-management support for those at earlier stages of CKD as at the moment the syntheses focus on kidney failure.
-
Epilepsy: there is a need for a qualitative synthesis on self-management support for people with epilepsy.
-
IBS: there is a need for a qualitative synthesis on self-management support for people with IBS.
-
LBP: there is a need for a focused qualitative synthesis examining self-management support for people with chronic LBP.
-
PNDs: there is a need for a qualitative synthesis on self-management support for people with PNDs.
Glossary
- +/–
- 0.05 ≥ p > 0.01, some evidence of effect in favour of intervention/control.
- ++/– –
- 0.01 ≥ p > 0.001, strong evidence of effect in favour of intervention/control.
- +++/– – –
- p ≤ 0.001, very strong evidence of effect in favour of intervention/control.
- +*
- No p-values provided, there is at least some evidence of effect, but + may underestimate true effect size.
- *
- Lower quality (Revised Assessment of Multiple Systematic Reviews score of < 31) and smaller sample size (< 1000 participants).
- **
- Lower quality (Revised Assessment of Multiple Systematic Reviews score of < 31) and larger sample size (≥ 1000 participants), or higher quality (Revised Assessment of Multiple Systematic Reviews score of ≥ 31) and smaller sample size (< 1000 participants).
- ***
- Higher quality (Revised Assessment of Multiple Systematic Reviews score of ≥ 31) and larger sample size (≥ 1000 participants).
List of abbreviations
- ADL
- activities of daily living
- AMSTAR
- Assessment of Multiple Systematic Reviews
- ASMP
- Arthritis Self-Management Program
- BMI
- body mass index
- BP
- blood pressure
- CBT
- cognitive–behavioural therapy
- cCBT
- computerised cognitive–behavioural therapy
- CCG
- Clinical Commissioning Group
- CCM
- Chronic Care Model
- CHW
- community health worker
- CI
- confidence interval
- CKD
- chronic kidney disease
- COPD
- chronic obstructive pulmonary disease
- DBP
- diastolic blood pressure
- DH
- Department of Health
- DKD
- diabetic kidney disease
- ED
- emergency department
- eGFR
- estimated glomerular filtration rate
- ES
- effect size
- FEV1
- forced expiratory volume in 1 second
- GA
- graded activity
- GHb
- glycated haemoglobin, glycosylated haemoglobin, synonym: haemoglobin A1c
- GP
- general practitioner
- HbA1c
- haemoglobin A1c synonyms: glycated haemoglobin, glycosylated haemoglobin, GHb
- HCP
- health-care professional
- HRQoL
- health-related quality of life
- HS&DR
- Health Services and Delivery Research
- IA
- inflammatory arthropathy
- IBS
- irritable bowel syndrome
- ICS
- inhaled corticosteroid
- IHW
- indigenous health-care worker
- LBP
- low back pain
- LDL
- low-density lipoprotein
- LTC
- long-term condition
- LTOT
- long-term oxygen therapy
- MBPSR
- multidisciplinary biopsychosocial rehabilitation
- MCO
- managed care organisation
- MD
- mean difference
- MDC
- multidisciplinary care
- MeSH
- medical subject heading
- MND
- motor neurone disease
- MS
- multiple sclerosis
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- OT
- occupational therapist/occupational therapy
- PA
- physical activity
- PAAP
- personal asthma action plan
- PD
- Parkinson’s disease
- PDSA
- Plan Do Study Act
- PEFR
- peak expiratory flow rate
- PICOS
- patients/population; intervention; comparison; outcome; setting
- PND
- progressive neurological disorder
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRISMS
- Practical Reviews of Self-Management Support
- QoL
- quality of life
- RA
- rheumatoid arthritis
- R-AMSTAR
- Revised Assessment of Multiple Systematic Reviews
- RCT
- randomised controlled trial
- RRT
- renal replacement therapy
- SBP
- systolic blood pressure
- SEM
- standard error of mean
- SLE
- systemic lupus erythematosus
- SMBG
- self-monitoring of blood glucose
- T1DM
- type 1 diabetes mellitus
- T2DM
- type 2 diabetes mellitus
- WAP
- written action plan