Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1007/53. The contractual start date was in May 2012. The final report began editorial review in November 2013 and was accepted for publication in May 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by O’Hara et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
The delivery of emergency health care within the NHS embodies challenges for risk management and patient safety. Circumstances can be demanding for patients and staff, with multiple decisions being made that often involve crossing professional and organisational boundaries. Front-line ambulance service staff routinely make critical decisions about the most appropriate care to deliver in a complex system characterised by significant variation in patient case mix, care pathways and linked service providers. Before the commissioning of this research very little research had been carried out within ambulance service settings to identify areas of high risk associated with decision-making about patient care options or to examine ways in which working across boundaries can affect patient care.
The patient’s journey from calling an ambulance to a decision about subsequent discharge by ambulance service staff is complex and can involve being assessed over the telephone by a clinician to having clinical assessment and initial emergency treatment at the scene of an emergency. The National Institute for Health Research commissioned this primary research to explore safe decision-making by ambulance service staff around transitions through the pre-hospital care system.
The ambulance service system and decision-making
To address the patient safety issues associated with decisions around transitions in patient care, it is necessary to examine the influence of the wider system, taking into account ongoing developments such as changes to service configurations, patient care options and staff roles.
The ambulance service control room represents the initial point of contact for patients making 999 calls. Critical decisions regarding the prioritisation of calls and the most appropriate responses must be made based on information provided by the caller. Two UK studies that have specifically examined the safety and accuracy of call prioritisation systems1,2 found that the risk of serious under-triage (i.e. assigning a low-priority response to a high-priority call) is low, whereas over-triage to high priority levels for lower-level priority calls is high. Decisions also need to be made regarding the type of emergency response to send and what information needs to be conveyed to health-care staff. In recent years the initial call-handling process has been enhanced to represent an emergency care response in its own right (‘hear and treat’), which entails decisions made by qualified clinicians such as nurses and paramedics over whether or not to dispatch other resources to the patient. However, there is little evidence on patient safety issues and what is needed to ensure safe decision-making by staff dealing with the varied case mix of patients seeking emergency care. 3
Ambulance services have made increasing use of specialist paramedic roles [variously termed emergency care practitioners (ECPs), paramedic practitioners (PPs) or community paramedics according to the specific nature of the role and the training provided], equipped with the enhanced knowledge and skills needed to make complex decisions about patient care. Decisions about patient management will involve assessment, diagnosis, treatment, including medication, and discharge or referral. The available evidence indicates that these specialist roles have provided service delivery benefits in terms of enhanced efficiency of patient care, increased patient satisfaction and a reduction in costs associated with ambulance journeys, accident and emergency (A&E) attendances and hospital admissions. 4–7 However, there remains a lack of research examining the safety of these new roles and the care pathways in which they operate, despite the recommendation that the safety of ambulance service staff to discharge patients at scene or decide on appropriate referral should be assessed before being widely adopted. 8 Studies employing expert review of patient care from PPs and ECPs9–11 suggest that the care provided by staff in these new roles was appropriate. However, these were small-scale reviews and provide a limited assessment of the care provided, with little insight into the various influences on care decisions. Other studies evaluating the safety of enhanced roles have focused on the risk associated with specific skill acquisition, for example pre-hospital thrombolysis. 12
Not transporting patients to the nearest A&E requires ambulance service staff to make clinical decisions in a system in which A&E has traditionally been the default option for decision-making. Safety concerns have been raised about decisions not to convey patients to hospital. Snooks et al. 13 followed up emergency (999) calls for older people who had experienced a fall but who were not subsequently conveyed to hospital and found a high rate of subsequent emergency health-care contacts and increased risk of death and hospitalisation.
Although ambulance services have polices and protocols to guide staff in making appropriate decisions about whether to leave a patient at the scene of care, one UK study points to a disparity between policy and practice. 14 This study of ambulance service staff views on decisions to transport or leave at scene highlighted the complexity of the decision-making involved. For example, decisions about non-transportation often involved negotiation between the ambulance service staff and the patient but this was not easily accommodated in the policies and procedures. 14 This study highlights the important issue of patient choice in decisions about their care. Halter et al. 15 conducted a qualitative study of the assessment and referral of older people who have fallen and identified a predominance of informal decision-making processes. They concluded that further research is needed to look at how new care pathways offering an alternative to A&E may influence decision-making around non-conveyance.
Patient safety models
Decisions in the context of emergency care are challenging for staff, are often time critical and are based on limited information, but wrong decisions in this context could have serious consequences. Researching how people make tough clinical decisions under difficult conditions involves examining how people assess situations and problems, plan, make choices and take actions. 16 In line with ‘an organisation with a memory’, which highlights that threats to safety are rarely due to the behaviour of one individual,17 this research examines the influences on patient care and safety within the context of the wider emergency care system. Reason18 describes the systems approach to patient safety as concentrating on ‘the conditions under which individuals work’ (p. 768). The safety culture of an organisation is also well recognised as an important aspect of patient safety and is identified as the first step in the National Patient Safety Agency’s (NPSA) ‘seven steps to patient safety’. 19 It refers to the shared safety-related values, beliefs and behaviours of the members of an organisation. 20
A common approach to addressing patient safety is to retrospectively review adverse events and target action at preventing such events in the future. For example, the National Reporting and Learning System (NRLS) managed by the NPSA collects reports of patient safety incidents from NHS organisations to assist in improving patient safety in England and Wales. The statistics for ambulance services in England (October 2011–September 2012) identify a number of types of incidents that may be connected with system influences on decision-making and transitions in care: access/admission/transfer/discharge (24%), medical device/equipment (11%), treatment/procedure (9%), implementation of care and ongoing monitoring/review (6%), consent/communication/confidentiality (5%), medication (5%), infrastructure – staffing, facilities, environment (4%), clinical assessment – diagnosis, scans, tests, assessment (4%) and documentation – records, identification (1%). 21 However, the actual number of incident reports received from ambulances services (n = 4506) is regarded as relatively low compared with those received from other care settings and therefore this approach is likely to provide only a limited insight into safety issues. This study adopts a more proactive approach to identifying potential threats to patient safety within the whole emergency care system, not just where an adverse event has happened.
The increase in demand for emergency care over the last decade has led to significant changes in the way that pre-hospital emergency care is delivered. 22 These changes, involving the introduction of new services, staff roles and associated patient care pathways, along with increasing demands to meet operational standards and performance targets, have increased the complexity of the system. Although some developments, such as patient care protocols, are intuitively designed to reduce the possibility for error by providing decision support for emergency care staff, it is by no means clear that safety has been enhanced.
Patient safety in an evolving system
Research that enhances our understanding of the challenges that decision-making in emergency care situations presents, and contributes to ways in which these decisions can be made more safely, is even more crucial when we consider the continually evolving role of the ambulance service and its staff. In the Department of Health report High Quality Care for All: NHS Next Stage Review, Lord Darzi presented a compelling argument for saving lives by creating specialised centres for major trauma, heart attacks and strokes. 23 These changes create a number of specific issues which relate to centralisation of services that are of particular relevance to the ambulance service. These include the safety and reliability of pre-hospital triage systems, decisions whether to ‘treat and leave’ or to bypass the nearest hospital and go straight to the facility most capable of providing definitive care for the patient.
Department of Health-funded research conducted by the 999 Emergency Medical Services Research Forum involved a prioritisation exercise to identify research topics relevant to pre-hospital care followed by a rapid review of current evidence on the prioritised topics. 3,24 One of the three main themes identified in the prioritisation exercise was managing increased demand for emergency care by safely managing increased workloads, safely reducing A&E admissions for minor conditions and safely bypassing A&E for some major conditions. 24 The review of evidence highlighted a lack of studies taking a whole-systems approach to examining the provision of pre-hospital care that took into account call categorisation, assessment, response and clinical management options, including services across the entire emergency ambulance call profile. 3 This evidence gap undermines attempts to fully understand the issues around alternatives to ambulance response or transportation to A&E, as well as the skills needed to deliver services.
The need for research investigating the safety of enhanced roles allowing ambulance service staff to discharge patients at scene or decide on appropriate referral or transport destinations was expressed by Cooke et al. 8 Their National Institute for Health Research Service Delivery and Organisation (SDO) programme-funded systematic review of innovations to reduce attendances at, and waits in, A&E departments recommended that this research should be prioritised before changes were widely adopted. 8 A more recent review and Delphi consultation exercise to identify priorities for research in pre-hospital care identified the ‘safety, costs and benefits of alternatives to conveyance to hospital’ as the top priority (p. 10). 24 Research examining enhanced roles identified decisions to leave patients at scene as a particular safety concern warranting attention. 13 Vincent25 also highlights the importance of research which establishes that innovations intended to maximise access and reduce costs do not undermine the safety of patients.
The current study examines system influences on decision-making by ambulance service staff around transitions in patient care. The study builds on previous research examining service delivery innovations in emergency care, including SDO programme-funded research conducted by members of the research team evaluating the ECP role11 and the management of low-priority ambulance calls by NHS Direct. 26
Dixon-Woods27 reviewed four ethnographic studies of patient safety in hospitals conducted as part of the UK Patient Safety Research Programme and highlighted the valuable insight that this approach can provide. The review concluded that there are multiple interacting influences on safety and solutions need to be based on a sound understanding of the nature of the problems. The studies revealed a number of patient safety challenges common to the four different organisations. This approach appears to be ideally suited to exploring system influences on decision-making by ambulance service staff.
Aim and objectives
Aim
To explore the various influences on safe decision-making by ambulance service staff to identify areas in which interventions are needed to improve patient safety during transitions and areas in which further research is needed.
Objectives
-
To map the ambulance service system, care pathways, linked services and decisions that are critical for safe care in a sample of ambulance services in England.
-
To conduct an ethnographic investigation of factors influencing decision-making by ambulance service staff directly involved in patient care to identify threats to patient safety (risk factors) and how these threats are managed.
-
To feed back the study findings to participating ambulance services and local stakeholders to elicit their views and identify areas in which strategies are needed to improve patient safety and further research is needed.
Chapter 2 Methods
Justification for the study design
The study adopted a multisite design in three ambulance service trusts using multiple qualitative methods to examine the various influences on decision-making by ambulance service staff, particularly concerning transitions in the care process and the safety implications for patient care. This approach involved data collection and analysis techniques that support a detailed elucidation of issues needed to understand complex systems, work settings and decision-making.
It is now well accepted that qualitative methods have much to offer those conducting health services research. 28 The use of multiple methods permitted the collection of a richer and stronger range of evidence than would have been possible using any single method. The methods were chosen to enhance our understanding of the emergency system and in particular ambulance service care in relation to decision-making and patient safety.
Methodological approaches
The systems approach
The study adopted a systems approach to explore influences on safe decision-making in the ambulance service. This involved consideration of the clinical microsystem of the paramedic team attending the patient in an emergency vehicle, the clinical mesosystem involving an ambulance service call centre, response and transport or referral to other services (when these occurred) and the wider emergency care system in which these operated. It considered all aspects of the system, consistent with a human factors framework, to explore the following factors identified as influencing patient care: patient characteristics, task factors, individual (staff) factors, team factors, the work environment and organisational and management factors. 29 This framework is based on established human factors theory and knowledge including Reason’s18 model of organisational accidents, which has been widely used in health care.
The multisource approach
Multisource methodology requires the collection and cross-referencing of data from a range of sources. In this study we included documentation, interviews, focus groups, observations, digital diaries and workshops. The aim in our study was to build up and record aspects of decision-making and their link to risk so that corroboration or contradictions could be identified from information gathered within and between each source of data. Triangulation was one way that study findings could be validated as the same concepts were assessed from different perspectives. Contradictions between data sources provided an opportunity for analytical development and these were actively sought out. 30
Study setting
The selection of three ambulance service trusts sought to ensure that the study represented the variety of contextual factors in the pre-hospital emergency care system (e.g. care pathways, staff roles, service configuration) and that the issues identified had relevance to the other ambulance service trusts in England. Having three case study organisations enabled the examination of variations in system characteristics and how these relate to delivering safe care. It was also an opportunity to examine similarities and differences in safety culture across the three organisations. The three participating trusts operate across diverse geographical areas, including densely populated urban areas and sparsely populated rural areas. They also serve socioeconomically diverse populations and provide a variety of emergency care responses [e.g. paramedics or paramedics with advanced training and skills such as ECPs or critical care paramedics (CCPs)]. Specific operational areas within the three participating ambulance services were identified that would be best suited for the ethnographic part of the study. The aim was to include a range of different patients encompassing different transitions in care, for example ‘treat and leave’ at scene; bypass of A&E and direct transfer to specialist units; and transfer through other care pathways to community services.
Purposive sampling31 of staff and service users aimed to ensure a broad representation in terms of service delivery and use relevant to addressing the study objectives.
Components of the study
Patient safety was examined in relation to the broad spectrum of care pathways and associated decisions in three different ambulance services. The study comprised three phases.
Phase 1: mapping the system
An initial mapping exercise in participating ambulance services was carried out to provide an understanding of the system in which ambulance service care is delivered. Phase 1 was designed to inform the planning of work in phase 2, including identifying issues for attention.
Recruitment
Members of the project team with ambulance service posts and other trust staff assisted researchers in gaining access to appropriate informants. We were particularly interested in speaking to members of the ambulance service who could provide an overview of the service, such as managerial staff. Interviews at each site (total n = 16) were carried out with a range of personnel including clinical governance leads, directors of operations, medical directors or clinical leads and health-care professionals involved in leadership or management roles, as well as other staff members who were regarded as good informants in relation to the issues of interest. Written consent was obtained by the researcher before each interview, following a discussion of the study aims and the information sheet (see Appendix 1).
Project team members, trust staff and interviewees also assisted in the identification of potentially useful documents that might assist in our understanding of each ambulance service. One control room at each site was visited to gain an understanding of the context and working environment as well as the triage system.
Data collection: documentation
Key documentary information was examined, for example geographical maps of the region covered, minutes of board meetings, annual reports and relevant protocols, guidance or standards that influence decisions over patient care. A range of information was obtained from websites related to the three sites. Data from discussions, documents and web pages were used to develop a profile of each site.
Data collection: interviews
Using the interview as a means of data collection allows in-depth exploration of individual experiences or complex situations. The one-to-one approach is more suited to gaining a detailed understanding of phenomena than, for example, a focus group. 32 For the mapping aspect of our study this method was therefore appropriate to gain an understanding of specific roles within the service and how different aspects of the service link together, as well as some information about potential risks at transition points. Combining this method with a range of complementary approaches in our study allowed data to be compared so that views obtained through interview could be verified or contradicted by the other data.
A total of 16 semistructured interviews of 50–90 minutes’ duration took place in ambulance service premises. Interviews were conducted with the aid of a topic guide (see Appendix 2). The interviews identified examples of transition in care, from the initial 999 call to the final disposition (conveyance, referral or discharge), and explored factors that might influence these decisions. Interviews were audio recorded and then transcribed verbatim.
Data analysis
Transcripts were analysed by two members of the study team to identify preliminary themes, which were then reviewed with the wider project team. Discussion of the themes allowed clarification of key concepts and informed the focus group discussions in phase 2 of the study.
Phase 2: exploring influences on decision-making and safety
The examination of decision-making by ambulance service staff entailed an in-depth inductive exploration using an ethnographic approach33 to identify key influences on safety in patient care.
Ethnographic observation
Ethnographic methods involve the participation of the researcher in the daily life of others, observing and listening as well as questioning participants, either formally, through interviews, or informally. They can also involve the collection of documents and artefacts, and therefore can include a range of sources. The format of data collection and analysis is usually unstructured and allows meanings, functions and consequences of actions or practices to be examined for their implications in other contexts. 33
Observation in natural surroundings can be viewed as an appropriate way to assess complex social phenomena within their natural contexts. Such phenomena can be difficult to articulate, for example in interviews, and are more accessible when directly observed. The actions of health-care professionals have been assessed previously using observation, which derived insights that could not be obtained by other methods. 34 A limitation of the method is the risk of observed individuals behaving differently from normal because of the presence of the observer. However, in our study this risk was reduced as crews are observed frequently by health-care professional trainees.
Recruitment
Research access can be complicated by considerations of safeguarding patients and staff as well as other ethical concerns. In our study we aimed to observe ambulance staff in action, and therefore patients who were receiving care, as well as their relatives and friends, would be within the frame of observation. It was specified that no patient-identifying information would be recorded nor any information from other individuals who had not consented to be observed, including other health-care professionals.
The ethnographic component of the study aimed to involve at least two operational areas (e.g. ambulance stations) that transported patients to two different emergency departments within each ambulance service. Selection of ambulance stations aimed to ensure representation of a range of paramedic staff roles and associated skill sets and responsibilities in terms of the care pathways that they could offer. The operational areas were selected as being large enough to have a range of paramedic roles. The researchers shadowed a range of staff across a variety of shifts.
At each site the ambulance service researcher facilitated access to potential participants and identified other gatekeepers within the organisation who could assist with access. The gatekeepers’ relationship with the participants was an important link – crew were more likely to agree to participate if there was trust than if there was distance. Similarly, the observers needed to be aware that they might be viewed with suspicion if appearing to take on the role of expert or critic. 33 Time needed to be allowed for delays in responses from paramedics, who had limited access to e-mail whilst on duty.
Each site had a different observer protocol in place, specifying requirements for observers shadowing ambulance service staff (e.g. viewing a training DVD). The aim of observer protocols was to protect all parties, patients, staff and researchers. For example, observers, in particular the university researcher, needed to be aware of the hazards associated with accompanying ambulance service staff. For the paramedics, there needed to be reassurance that they would be able to carry out their activities without undue intrusion from the observer.
Written consent was obtained by researchers before observations, following a discussion of the study aims and the information sheet (see Appendix 3).
Data collection: observations
Initial piloting observation shifts with an ambulance service crew were carried out by the ambulance service and university researchers to allow familiarisation with the process before data collection and so that initial findings could be discussed and a framework developed for future observations. The observation framework (see Appendix 4) included demographic information such as setting, date and time of the shift, as well as the qualifications of the crew. It was further reviewed following initial data collection.
A total of 34 shift observations of 10–12 hours’ duration were carried out by one university and four ambulance service researchers across the three ambulance service trusts: 13 at site 1, 12 at site 2 and nine at site 3. Across the sites, 155 attendances were carried out during the observation periods. A total of 57 crew members representing a range of staff roles were observed (see Appendix 5). Because of unforeseen circumstances, the university researcher was not able to carry out observational shifts at the third site within the study time frame. The ambulance service researcher carried out three additional observation shifts at the station where the university researcher would have been observing. This resulted in less observation data from one site and an inability to make comparisons between ‘insider’ and ‘outsider’ observations. However, we were able to explore differences between practices at two stations within the same region, as viewed by the same researcher.
During the shift observations, paramedics were asked about the rationale behind the decisions they were making at each patient contact. Conversations were also carried out at quiet times to identify general issues about the shift or recollections of previous shifts, dilemmas or instances in which decisions had been difficult to make. In some instances, short interviews were carried out with crew members when there was time to explore in-depth issues that affect decisions. These were audio recorded when appropriate or recoded in note form.
Observational data were recorded through a combination of field notes and audio recordings of conversations with crew members between calls. Consistent with ethnographic tradition, oral accounts were solicited by the observer asking for explanations about the decisions that had been made with respect to each patient decision. Prompts for solicited conversations were developed and piloted by the researchers during the familiarisation stage and on the initial data collection shift. Reflections on the observation process and any other relevant information were also recorded separately during quiet times.
The observer role has been referred to as an ‘acceptable incompetent’ (p. 79)33 in that there is a need to make sense of what is going on in settings hitherto unfamiliar. Hammersley and Atkinson33 write about an initial ‘culture shock’ as the observer steps into an unknown environment. There may also be a sense of feeling let down if expectations about the way that the organisation or culture is perceived from reading the literature are not borne out in reality.
In contrast, observing in one’s own environment may make it difficult to see clearly the events that are occurring, because of their familiarity. To balance the advantages and disadvantages of observing as an ‘outsider’ or as an ‘insider’, researchers from both perspectives carried out the observer role so that data could be analysed for consistencies and inconsistencies. The extent to which observers are positioned as ‘outsider’ or ‘insider’ is dynamic, that is, can shift, so that outsiders become more (or even too) familiar with the field over time. 34
A related pitfall that needs to be considered when carrying out observations is developing too much rapport with participants, which can result in ‘going native’, in which the observer starts to identify with a particular group. This can affect the ability to report from a neutral position. Observers in the field may feel that they have to report from the perspective of those being observed, or give information about themselves to increase the rapport. 33 One way of limiting this pitfall was to observe a range of people in different settings so that familiarisation was curtailed at each shift.
Digital diaries
The diary method allows events and experiences to be recorded and reported in their natural context. There is a shorter time lapse between experiences and their reporting than in most other data collection methods. However, the method can place a burden on the participant in terms of expectations and commitment. Expectations therefore need to be clarified before participation. 35
Recruitment
Recruitment to the digital diary aspect of the study was carried out in parallel with that for observations, interviews and focus groups. Ambulance crews were invited to specify which of the four methods they were interested in participating in. A total of 18 digital audio recorders were distributed across the three sites and 10 digital diaries were completed (three at site 1, three at site 2 and four at site 3).
An event-based design was used to identify calls that were salient to staff participants in terms of their decision-making, for example when decisions were difficult or staff felt that their decision-making was being challenged. Staff were asked to identify events over a 4-week period and record these using digital audio recorders as soon as possible following the event. A guidance sheet was provided along with instructions on how to operate the digital recorder (see Appendix 6). It was expected that events deemed worth reporting would be relatively uncommon compared with the overall number of calls attended. Time constraints might also restrict the number of events recorded.
A total of 141 diary entries were recorded by the 10 diary participants across the three sites. Table 1 shows the staff roles of those who completed the digital diaries.
| Staff role | Site 1 (n = 3) | Site 2 (n = 3) | Site 3 (n = 4) |
|---|---|---|---|
| Paramedic | 3 | 2 | 1 |
| Paramedic team leader | – | – | – |
| ECP | – | 1 | – |
| PP | – | – | 1 |
| CCP | – | – | 1 |
Data collection
The digital recorders were returned to a named individual within each ambulance service trust. Audio files were transferred to the university researchers via an encrypted data stick and/or via encrypted files. Audio recordings were transcribed verbatim.
Data analysis
Data transcripts from the phase 2 observations, interviews and diaries were examined for key issues and themes by two researchers. Following initial familiarisation and review of the data, more detailed thematic analysis was conducted using qualitative data analysts software (ATLAS.ti 7; ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). Transcripts were initially coded for the types of decisions made at each patient contact with regard to patient disposition. Findings were also reviewed with the wider project team.
The rationale behind each decision made during observations and the influences on the decisions made were charted. A typology was developed of types of decision and each observed patient contact was assigned one position in the typology. This was checked against digital diary data for any new types of decision. The human factors framework provided a basis for further analysis. 29 Issues from observations and digital diaries mainly related to the wider organisation, the work environment, task factors and patient factors. A major aspect of this data was the process of decision-making in the context of these factors and patient safety, as staff were clearly looking to protect patients and themselves from harm. A narrative structure was developed that helped to describe this process and the influences on decision-making observed and recorded during the study.
Ambulance service staff focus groups
The focus group differs from the interview approach in that interactions between members of the group are permitted. However, information offered can be influenced by the presence of others in the group. Focus groups also enable the collection of data from several participants over a short duration, which is an advantage over more time-consuming methods such as observation and individual interviews. 36
Recruitment
Recruitment of staff was carried out by the ambulance service researcher in each trust. As with the observations, the emphasis was on recruiting staff in paramedic roles. Venues for the focus groups were chosen for convenience of access for members of staff across each trust. All members of staff who had shown an interest in participating in the focus groups were provided with an information sheet for phase 2 of the study (see Appendix 3). Informed consent was documented with each participant before the session or prior to the discussion.
Data collection
Three focus groups were conducted, one in each trust, with a total of 21 paramedics, including some in specialist roles. Table 2 shows the staff roles represented across the groups.
| Staff role | Site 1 (n = 8) | Site 2 (n = 8) | Site 3 (n = 5) |
|---|---|---|---|
| Paramedic | 4 | 7 | 4 |
| Paramedic team leader | 2 | – | – |
| Community paramedic | 1 | – | – |
| ECP | 1 | – | – |
| PP | – | 1 | – |
| CCP | – | – | 1 |
Paramedic experience among participants ranged from 6–12 months to > 20 years, with the majority having at least 2 years’ experience as a paramedic. A number of participants had worked in the ambulance service for longer, for example as technicians. The groups also comprised a mix of staff who had trained through the ‘newer’ graduate route or the ‘older’ apprenticeship route.
The staff focus groups commenced with an introduction to the study and an outline of themes from phase 1. The focus group discussions consisted of two parts. The first part explored the structural, technical and sociotechnical system influences on decision-making and the potential risks for patient care. In the second part the Manchester Patient Safety Framework (MaPSaF)20 (see Appendix 7) was used to stimulate and structure the discussion of patient safety culture within each ambulance service trust. MaPSaF is a tool designed to help NHS organisations and health-care teams assess their progress in developing a safety culture. It consists of a typology of nine critical dimensions of patient safety that are proposed to relate to areas in which attitudes, values and behaviours about patient safety are likely to be reflected in an organisation’s working practices, for example how patient safety incidents are investigated, staff education and training in risk management. 37 The staff focus group topic guide is provided in Appendix 8.
The MaPSaF tool can be used to profile organisations and teams across the dimensions and to represent a level of maturity in relation to organisational safety culture. For the purposes of our study the focus was on exploring and understanding respondents’ perspectives on ambulance service safety culture issues within and across the participating trusts. The dimensions and associated criteria were used to prompt discussion. During the focus group discussions, participants were asked to reflect on their experiences where possible and without compromising patient or staff anonymity.
Two researchers were present at each session, one to facilitate and the other to take notes. Digital audio recorders were used to record the discussions. Written notes enabled the researchers to identify the specific contributions of individuals but anonymity was maintained by allocating a number to each participant.
Data analysis
The focus group discussions were transcribed. Following initial familiarisation with the data by two researchers a more detailed thematic analysis was conducted. The focus group transcripts were uploaded into computer software for coding (ATLAS.ti 7). The study team service user representative also reviewed the focus group transcripts to identify key themes and met with the researchers to explore similarities and differences in themes across the three sites. Findings were also reviewed with the wider project team. All project team members had access to anonymised focus group transcripts to permit verification of the findings.
Phase 2: service user focus groups
The involvement of service users in identifying and prioritising research issues is important to make practice and policy more relevant to their needs. 38 Their experiences and knowledge can complement those of clinicians, health professionals and researchers. 39 A focus group approach was used to explore service users’ concerns about patient safety in emergency care.
Recruitment
The study team service user representative assisted in the recruitment of participants for one of the groups and patient and public involvement (PPI) managers assisted in the recruitment of participants in the other trust locations. Potential participants were contacted through existing PPI networks. To understand the relative importance of safety for patients accessing the ambulance service, service users were recruited who had a specific interest in, or experience of, ambulance service care.
Settings for the focus groups were chosen for their convenience in terms of travel. Arrangements were made for participants to claim transport expenses and a £10 voucher was distributed to each participant as an appreciation of his or her time and effort (see Appendix 9 for the participant information sheet).
Data collection
In total, 23 service users took part in the focus groups across the three sites. Two focus groups were attended by eight participants each and the other by seven. The characteristics of the group participants are shown in Table 3.
| Characteristic | Site 1 (n = 7) | Site 2 (n = 8) | Site 3 (n = 8) |
|---|---|---|---|
| Age (years) | |||
| 18–24 | 1 | – | – |
| 25–34 | – | 1 | – |
| 35–44 | – | 2 | – |
| 45–54 | 1 | 1 | 1 |
| 55–64 | 3 | 2 | 4 |
| 65+ | 2 | 2 | 3 |
| Gender | |||
| Male | 3 | 5 | 4 |
| Female | 4 | 3 | 4 |
Men and women were fairly equally represented overall (11 women, 12 men). All age ranges were represented at least once across the three groups, although two-thirds of participants were aged > 55 years. In one group all participants were aged > 45 years.
Some of the participants were experienced in public involvement within their respective ambulance service trust and therefore had a greater understanding of service delivery issues. Other participants who had had previous contact with the ambulance service but not in any formal capacity are possibly more representative of the wider public. Both types of service user contributed informative and complementary insights. Participants across the three groups had personal experience of mobility issues, communication issues and the management of chronic health conditions and so were able to represent specific concerns in connection with these.
At the start of the focus groups a brief introduction to the study and an outline of themes from phase 1 were provided. The focus groups explored views on the issues that had been identified in phase 1 of the study, with an emphasis on the service user perspective (see Appendix 10 for the topic guide). For example, the transitions from the initial 999 call through to disposition were used as prompts to encourage service users to share their experiences and views.
The approach to data collection was largely the same as that for the staff focus groups except that the topic guide was somewhat different and the emphasis was on the service user perspective and experience rather than on the staff perspective and experience. The topic guide for the discussions was reviewed by members of a local emergency care PPI group. It was not expected that the discussions would strictly follow the topic guide, rather that the guide would facilitate discussion that might bring up new issues that could be followed up.
Data analysis
The approach to data analysis was the same as that for the staff focus groups, detailed in the previous section.
Phase 3: feedback workshops
Feedback workshops were conducted within each of the ambulance service trust regions. The aim of the workshops was to present the main findings from the study to ambulance service staff, service users and local stakeholders to provide an opportunity to comment on the findings. Feedback was also elicited from attendees regarding potential areas for future intervention and research. Discussions were audiotaped with consent from the attendees. In addition, attendees were asked to complete a simple prioritisation task to rank the issues arising from the study in terms of their perceived importance for future attention.
Workshop attendees
All study participants (staff and service users) who had consented to be recontacted were invited to attend a workshop within their trust catchment. Lead investigators at the three ambulance services were free to invite additional internal and external participants whose attendance they felt would be useful. The invitation letter advised attendees that the feedback from the workshop would be included in the study report (see Appendix 11). The secondment period for the ambulance service researchers had ended by the time that we were recruiting to the workshops, which made the task more challenging. Numbers were limited to approximately 25 participants at each venue because of resource constraints. A total of 45 individuals attended across all of the workshops in addition to study team members, including 28 ambulance service staff and 17 service users or lay/public representatives. Table 4 provides details of the attendees at each workshop.
| Role | Site 1 (n = 15) | Site 2 (n = 18) | Site 3 (n = 12) |
|---|---|---|---|
| Ambulance service staff – participants | 5 | 3 | 4a |
| Service user/public – participants | 3 | 5 | 5 |
| Ambulance service staff – new to study | 7 | 9 | – |
| Service user/public – new to study | – | 1 | 3 |
In total, 12 of the ambulance service staff attendees had participated in some aspect of the study and 13 of the service users had participated in a service user focus group (see Appendix 12 for more details). Members of the study team employed by the trusts participated in the workshop discussion but were excluded from the analysis of the prioritisation data to avoid potential bias.
Prioritisation task
The interviews, observations, diaries and focus groups produced a rich and detailed insight into system influences on decision-making by crews and the potential risk for patient safety. The thematic analysis performed on these data sets revealed that the findings could be characterised with reference to a common set of key issues. The strength of this analysis was that it allowed conclusions to be drawn regarding how and in what ways respondents characterised the role of each issue, and the implications for associated attitudes and behaviour, including shared understandings and cultural impacts. Beyond this, it was possible to go some way towards characterising the degree of consensus over salient issues, and draw some more tentative conclusions over their relative salience. It was decided that the qualitative findings would be strengthened through further triangulation, achieved by adopting a more formal, quantitative and systematic approach to assessing issues of relative salience and consensus over key priorities for the delivery of care by the ambulance service.
To address this, as a component of the feedback sessions conducted with ambulance staff and service user representatives, participants undertook a ranking task designed to elicit views on priorities for future attention in relation to the delivery of emergency care by ambulance services.
The issues selected for ranking were derived from a synthesis of findings across the various study methods (interviews, observations, diaries and staff focus groups) and were presented to workshop attendees (see Chapter 4, Synthesis of findings).
Method
A range of options with regard to the method for ranking the entities was considered, including direct ordinal ranking and the use of subjective rating scales. The method of paired comparisons was selected as it is simple to administer and embodies the capacity to statically test both the reproducibility of responses and the degree of agreement between respondents. A further desirable feature is that it produces a ratio scale. This provides more information than a simple ordinal ranking in that it shows the relative distance (importance/salience) between each issue and the rest of the set. 40,41 This approach to deriving a ranking of priorities for patient safety risk management reflects guidance on good practice in risk assessment42 and has been widely applied in in public policy and regulatory contexts. 43,44 The ranking task involved each respondent independently comparing the issues in pairs, for all permutations of pairings. For each pairing, respondents were asked to rank the priorities for future attention in relation to the delivery of emergency care by ambulance services. The task was a desktop exercise, with the issues presented in a randomised order in a booklet format (see Appendix 13). In total, 44 of the workshop participants completed the ranking task (27 ambulance service staff and 17 service users). Data analysis is described in Chapter 6 (see Prioritisation task) along with the findings.
Ethical and research governance approval
The study received ethics approval from the National Research Ethics Service Committee Yorkshire and the Humber – South Yorkshire (12/YH/0327) for research involving service users (phases 2 and 3). Ethics approval for research involving staff (phases 1–3) was received from the University of Sheffield Research Ethics Committee [School of Health and Related Research (ScHARR) REC ref. 0530/KW). Additional ethics approval was obtained for all aspects of the study from the University of Surrey (EC/2012/88/FHMS), as required by one of the study co-applicants.
Ethics approval for observation of ambulance service staff was obtained on the basis that no patient-identifying information would be collected and the researchers would not have direct contact with or elicit any information from patients.
Research governance (research and development) approval was granted at each of the three participating sites for all aspects of the study. Specific local requirements to permit researchers to travel as observers in ambulance service vehicles were adhered to.
Chapter 3 Phase 1 findings: mapping the system
Mapping the ambulance system was challenging because of the shifting nature of the environment in terms of policies and procedures across time and across even small areas of service delivery. It was also limited to the time frame allowed for this part of the study. The following is a brief overview of the context within which the participating trusts are delivering care.
Institutional and organisational context
This study was carried out within the context of the government’s Health and Social Care Bill 2011 and an overall financial aim to ‘reduce the deficit’ (p. 10). 45 For its part, the NHS was expected to achieve efficiency savings of up to £20B by 2015, including ambulance service efficiencies of around £75M per year. 46 To focus on achievable savings, the National Audit Office was commissioned to report on the cost-efficiency of the service. 46 It found variations in the costs of calls and incidents between services and also recommended that some savings could be achieved by maximising ‘hear and treat’, ‘see and treat’ and other alternative care options.
Ambulance services in England are regulated by the Care Quality Commission (CQC) against a number of quality indicators. One indicator is performance, which includes the achievement of target response times. There is now awareness by government that quality of care has a broader remit than target response times. The new NHS Outcomes Framework has three quality dimensions: clinical and patient-reported effectiveness outcomes; patient safety; and broader patient-related outcomes including patient experience. 45 Achieving a balance between performance and ‘a more rounded response model’ (p. 10)46 will be a challenge for future policy makers.
The government is also focusing on patients as advocates for their own care decisions so that choice of care options is optimal. Patients are encouraged to share their experiences of health care to inform other individuals who are choosing services and to inform health-care organisations about their strengths and weaknesses. 45
The extension of quality indicators to include patient reports and broader assessment of performance comes in the aftermath of the Mid Staffordshire NHS Foundation Trust inquiry, which found poor attendance to patient and staff concerns and an overemphasis on achieving targets. 47
As well as shifts to increase cost-efficiency and patient-centred care, the government is reorganising the commissioning of NHS services. The responsibility for commissioning is being transferred from primary care trusts (PCTs) to a number of general practice consortia. Again, this change was in process during the data collection period of this study.
The following sections present the organisational context within which the three ambulance service sites are working, based on current publicly available information as well as data from phase 1 interviews (see Appendix 14 for details of the roles of the phase 1 participants).
Funding and commissioning
Government aims to reduce funding were reported to be occurring at the same time as expectations remain high that organisations will achieve targets and the number of calls to the ambulance service continues to rise:
I think the NHS is like a handful of sand and the tighter you squeeze, the more it slips through your fingers and the difficulty we are going to have is you can only squeeze so much efficiency out of the system before the system starts to crack and if, I think our activity is rising something like 5% year on year with a 0.1% in real terms budget increase, yes there are efficiencies to be had, there are often efficiencies to be had but I think there is an argument to be had of diminishing returns with those efficiencies savings; the tighter you squeeze it you know.
Int14
In April 2013, changes to the commissioning of NHS services, which were outlined in the Health and Social Care Act 2012,48 were implemented. An important change in the context of this study was that responsibility for commissioning urgent and emergency services within local geographical areas was transferred from PCTs to Clinical Commissioning Groups (CCGs) under the supervision of the NHS Commissioning Board. Urgent and emergency services include A&E departments and the direct call line 111 as well as ambulance services. Out-of-hours facilities (not including local services funded by the general practice contract) are also commissioned by CCGs.
Care quality and performance measurement
Ambulance service performance is currently audited against 11 National Ambulance Clinical Quality Indicators:49
-
outcome from acute ST segment elevation myocardial infarction (STEMI)
-
outcome from cardiac arrest – return of spontaneous circulation
-
outcome from cardiac arrest – survival to discharge
-
outcome following stroke for ambulance patients
-
proportion of calls closed with telephone advice or managed without transport to A&E (when clinically appropriate)
-
recontact rate following discharge of care (i.e. closure with telephone advice or following treatment at the scene)
-
call abandonment rate
-
time to answer calls
-
service experience
-
category ‘A’ 8-minute response time
-
time to treatment by an ambulance-dispatched health professional.
Commissioning for Quality and Innovation (CQUIN) is a national framework that rewards excellence and service improvement (see http://aace.org.uk/national-performance/; accessed 25 September 2014). Improvement schemes are agreed locally with commissioners and outcomes have an impact on a proportion of local funding.
Performance can be assessed and compared across services using the National Clinical Dashboard. To meet the requirements of quality indicators, numbers of available operational staff and their working hours are maximised, as performance shortfalls have an effect on funding. Overtime is offered to operational staff to maintain the number of crews on the road.
Since publication of the Francis report,47 an increased focus on patient-centred care is evident across NHS trusts. Recommendations from the report are being identified to form part of future ambulance service quality care outcomes with the support of organisations such as the CQC (see www.cqc.org.uk; accessed 10 October 2014) and Monitor (see www.monitor-nhsft.gov.uk; accessed 10 October 2014), a regulatory organisation that aims to protect the interests of patients. Monitor will also take on a commissioning role moving forward, with the aim of increasing access to integrated care.
A particular concern in the ambulance service at the moment is that the ambulance service forms only part of a large NHS system and that the parts that make up the NHS are being funded differently. This variation in funding leads to different agendas in the organisation of services. As the ambulance service lies at the interface with a number of NHS services, this issue can impact on decisions made by staff. For example, a decision to treat a patient at scene and refer follow-up care to another service requires that service to be available and accessible at the time of referral.
The increasing burden on A&E departments has been recognised in a recent review of urgent and emergency care services. 50 In line with the fifth National Ambulance Clinical Quality Indicator, in some areas of the country this burden is being addressed by setting targets for PPs or ECPs regarding the percentage of patients who can be discharged or referred to alternative pathways when safe and appropriate.
Reorganisation and restructuring
UK ambulance service trusts have over recent years experienced a series of reorganisation and restructuring processes. In 1990 there were 46 separate ambulance services in England. By 2006, because of the merging of smaller ambulance trusts to increase efficiency and limit the duplication of resources, this had reduced to 31. 22 Currently, there are 10 ambulance service trusts, with each now responsible for a much larger geographical coverage. From phase 1 interviews it appeared that some idiosyncratic working practices persisted within each of the former smaller trusts despite these mergers.
There was evidence from phase 1 interviews that restructuring aspects of each service was a continual process and that ambulance service staff are constantly having to familiarise themselves with these changes. Reorganisation of staffing structures to create a ‘leaner’ system was evident in two of the sites, for example:
The ambulance service is going through a big transition at the moment, we have got a new Chief Executive, we have got less money, we have got to have a leaner management structure so we are going down from five divisions to three divisions.
Int2
Related to this was a sense of uncertainty evident among some managers regarding their future roles.
Foundation trust status
NHS trusts that gain foundation trust (FT) status are able to make decisions about the care that they deliver independently of the government. FTs are accountable to the communities that they serve, having members and governors from those communities. FTs hold contracts with a range of commissioners and are responsible for delivering annual reports to Parliament. FTs require a licence through the organisation Monitor, the independent regulator for NHS FTs, which has a role in assessing applications for FT status, and these are audited to comply with requirements of the CQC, the overall independent regulator of health and adult social care in England.
Of the three sites participating in the study, one had already achieved FT status and two were in the process of submitting applications. From phase 1 interviews, views about FT status were more positive in the site that had already achieved it than in those sites pursuing it. FT status was associated with a business model and, although this was reported as a concern by one interviewee, its reported advantages included the independence to be creative in designing care provision, for example local pathways that are tailored to the needs of the population might be more achievable.
My understanding is that it gives us the freedom to be able to pursue things that would perhaps be considered outside the box, and I think that if you actually want innovation, you have to give people the opportunity to do things outside the box.
Int14
Another reported advantage was an increased engagement with pre-hospital care research. A concern was that if a trust did not achieve FT status the future became more uncertain and the regions could split off and become more fragmented. There was a sense that applying for FT status was essential to prevent such fragmentation. Managers commented on the time and effort that it took to apply for FT status.
Policies, procedures and guidelines
Policies are actions that an organisation advises whilst procedures are a stepwise sequence of activities that are carried out to achieve the aims of the policy. Standing operating policies are developed to standardise the way that an activity is carried out, to reduce risk.
The current policies and procedures of each ambulance trust include a vast amount of information, and, although principles were similar, the policies and procedures were not identical across sites, either in number or content. However, within trusts, procedural documents are bound by their own policy to ensure that they are structured consistently and are regularly monitored.
Ambulance service policies and procedures include content relating to equality and diversity, procurement, health and safety and infection control. Policies and procedures are supplemented by guidelines that have been established from available evidence. Joint Royal Colleges Ambulance Liaison Committee (JRCALC) 2006 guidelines are used by ambulance service staff to identify how best to deal with particular circumstances, whether it be administering a drug to a patient or assisting with a birth (see www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/prehospitalcare/jrcalcstakeholderwebsite/guidelines; accessed 25 September 2014). The latest JRCALC guidelines (2011) were in the process of being published whilst this study was being carried out, showing a backlog of 2 years in disseminating this information. Guidelines allow for some deviation according to circumstances but such deviations need to be justifiable. Justification of one’s actions was reported to be more likely if the guidelines are out of date. However, in some cases, when deviation by an individual can be shown to improve outcomes, a protocol can be revised.
Incident reporting
In the ambulance service, adverse incidents are reported using the incident report form (IR1) system, the format of which has recently altered, from completing paper forms to telephone reporting. The latter was developed to assist reporting while on the road, as expecting staff to complete forms following a shift runs the risk of non-reporting.
An incident can be described as patient related, staff related or equipment related. Missing equipment should ideally be reported verbally to the team leader and logged; however, if that missing equipment results in deficient care, this should be formally reported.
Relatively minor incidents can usually be dealt with at a local level, usually by the team leader. However, more serious incidents will require more senior involvement and further investigation. An increased focus on patient safeguarding encourages staff to report incidents that they have witnessed in which other staff members appear not to be delivering appropriate care. Such incidents can result in the Health Care Professionals Council (HCPC) becoming involved.
I know of a few incidents that went on at the moment where fellow professionals have gone as back up to a single responder or a single responder has gone as back up to the crew and the job has not been dealt with or managed effectively. It may be the deficiency that’s perceived and the delivery of what the paramedic or the technician is delivering and then it gets reported.
Int2
Incident reporting appears to occur to the extent that staff members feel supported in their reporting. For example, a ‘blame culture’ may inhibit reporting for fear of repercussions. It was noted that an increase in reporting is therefore not necessarily a sign that more incidents are occurring. Incident reporting is being encouraged to increase openness and the opportunity for learning; however, the need for staff to feel that they are getting feedback from their reporting was emphasised, otherwise this may be another disincentive.
Complaints procedures
Ambulance service trusts are proactive in obtaining both negative and positive patient and carer views about their care experiences through patient surveys and through the Patient Advice and Liaison Service (PALS). In addition, complaints can be made formally by service users, and the extent to which complaints are made against a trust is regarded as both a detriment, in that care quality may have been breached, and a learning/training opportunity.
Patient complaints can now be made in relation to discharge decisions by ambulance service crews in a similar way to those made against hospitals. Historically, ambulance staff were not responsible for discharging patients from ambulance service care, instead transferring them to another part of the health service, usually A&E. It was noted that experiencing complaints in relation to such decisions has the potential to deter clinicians from leaving patients at the scene at future calls, thereby increasing unnecessary attendance at hospital.
The extent to which patients or carers submit complaints is perceived to be related to public expectations of the ambulance service. For example, the change towards using fast response vehicles may cause concern for patients if they are expecting an ambulance. Non-conveyance may be a cause for complaint if conveyance was expected. Other complaints appear to be related to the interaction between ambulance staff and patients:
So it may be that you just didn’t communicate and you did all these things to the person without actually saying I am going to do this, this might hurt you know. And it is not that you are actually rude because you may be caring but you are not showing it.
Int5
Complainants are often visited by the ambulance service to explore any issues. The content of complaints is analysed to identify common themes from reported incidents. This allows patterns to be recognised to facilitate learning. Serious incidents arising from complaints are investigated. It is regarded as important for the service to identify and address shortfalls as well as good practice in care quality in a timely manner to avoid the situation that arose at the Mid Staffordshire NHS Foundation Trust.
Professional roles and responsibilities
Across the three sites a range of ambulance service roles are apparent; some are common across sites whereas others are associated with a particular site. The main roles are described in the following sections.
Emergency operations centre staff
Emergency call handlers
Emergency operations centre (EOC) staff at all three sites utilise a computerised algorithm that takes the call taker through stages of inquiry, the action at each stage being dependent on previous responses. In an emergency, a rapid response will be generated at the outset whilst call takers continue to communicate with the caller and provide advice for life support and care of the patient while help is on its way. Computerised triage systems can vary between trusts; however, the only two systems used in England, and therefore in sites participating in this study, were the Advanced Medical Priority Dispatch System (AMPDS) and NHS Pathways.
Advanced Medical Priority Dispatch System
The AMPDS is licensed for use in the UK to provide caller interrogation and pre-arrival advice or instructions. Calls are categorised into prioritisation groups. Category A is life-threatening and triggers an immediate response at dispatch as well as an 8-minute performance target. Category C calls are subdivided into four categories; they are urgent and require face-to-face assessment but are not immediately life-threatening. 51 Category C calls are therefore often referred to clinicians within the control room.
The AMPDS works by coding information received from the caller through interrogation and therefore a narrative is formed of the event. As with any triage system, accurate information is required as well as accurate coding. Inaccurate coding or a coding-related flaw in the AMPDS can result in under- or over-response to the situation. The inflexibility of the system, although being an advantage in terms of standardised coding and instruction that ensures quality through managing calls in the same structured way, can also be a disadvantage in terms of assessing the nuances of individual circumstances.
NHS Pathways
NHS Pathways triage is carried out by computerised clinical assessment using a set of > 700 symptom pathways that are systematically linked to determine the next set of questions to be asked of the caller. The combined pathways result in a defined care plan over a defined time frame for the patient.
The system is linked to a Directory of Services to assist call takers or crews in supplying appropriate and available care for the condition within the patient’s locality (see http://systems.hscic.gov.uk/pathways/comms/corenav.pdf; accessed 18 July 2013).
The system is also used for NHS 111, a new resource for non-999 calls.
Therefore, both systems can result in dispositions ranging from a 999 call (when the call taker deems this is appropriate) to advice to seek help at a walk-in centre, pharmacy or general practice.
Emergency medical dispatchers
Dispatch teams assess available resources and match these to calls in the area, taking into account the urgency of the situation and the expertise of available crews.
Triage nurses
Within the EOC, clinically qualified staff assess non-emergency cases over the telephone to identify an appropriate disposition. For example, a caller could be advised that a walk-in centre or an out-of-hours team is the most appropriate route, rather than an ambulance.
Operational staff
Emergency care assistants and emergency support workers
Emergency care assistants (ECAs) and emergency support workers drive ambulances under emergency conditions and provide support for qualified paramedics. They are usually trained in-house whilst carrying out their job. ECAs may have previous experience working with patient transport services.
Emergency medical technicians
Emergency medical technicians (EMTs) can undertake intensive courses in basic life support. They support paramedics in the assessment and diagnosis of patients. EMTs may have previous experience working with patient transport services.
Paramedic qualifications
Traditionally there has been a history of movement through the career path from patient transport services or ambulance technician (with 5 weeks of clinical training as well as 3 weeks of emergency driving training) to paramedic, by undertaking extra training. This is changing towards a more global 2- or 3-year higher education course that can be accessed straight from school with the required GCSE and A-level (or equivalent) qualifications. The 2-year course is a foundation-level (level 5) course whereas the 3-year course can lead to a BSc degree (level 6) (see www.collegeofparamedics.co.uk/downloads/Paramedic_Higher_Education.pdf; accessed 15 July 2013).
Completion of either course allows registration by the HCPC. Paramedics who wish to obtain a degree-level qualification can do so by attending higher education courses. Paramedics are required to have a driving licence that includes category C1 vehicles (heavy vehicles). In-house training in driving an emergency vehicle is then provided.
Paramedics respond to emergency and complex urgent calls, often with the support of an ECA, support worker or technician. They make decisions regarding patient referrals, admissions and discharges.
Specialist paramedic roles
The work that paramedics carry out has evolved over recent decades, from conveying patients to hospital to more diagnostics and treatments being carried out on scene. The number of patients who require urgent care has risen at a greater rate than calls for emergency care, which have remained relatively stable. Therefore, specialist roles have been developed, for example with a focus on primary care practice (ECPs and PPs) and critical care (CCPs).
Emergency care practitioners
The ECP role was piloted in Sheffield in 2004 with the aim of bridging the gap in expertise between paramedic practice and that of the medic. The pilot developed from calls by the Changing Workforce Programme to create a new role where professional boundaries can be merged to serve increasing demands in health and social care. 52 The role includes enhanced skills such as minor illness assessment, treatment for minor injuries and antibiotic therapy. ECPs can be registered with the HCPC, General Medical Council or Nursing and Midwifery Council and, although trained through higher education by the ambulance service, will not necessarily work in the ambulance service setting. For example, ECPs also care for patients at walk-in-centres, minor injury units and general practices.
A major advantage of the ECP role is that conveyance to A&E can be avoided in appropriate cases because of enhanced training that includes treating minor ailments and dressing minor injuries on scene. Although the cost of employing ECPs is greater than the cost of employing paramedics, an economic evaluation showed that this cost is compensated for by a reduction in conveyance to hospital. 53 A 12-month mixed-methods case study showed that 62% of patients attended by ECPs were not conveyed to hospital. 5 ECPs can be deployed directly by the EOC or referrals can be made by other clinicians when conveyance is deemed to be inappropriate.
The paramedic practitioner
In some sites the PP (or advanced practitioner or community paramedic) role is being developed to equip paramedics, through higher education, with knowledge and skills in assessment, diagnosis and referral of undifferentiated illness, previously part of the primary care domain. In one study site the role of the ECP is not recognised and the PP has instead been developed as the only primary care role.
The objective of the PP role is similar to that of the ECP role with respect to reducing conveyance rates. The major difference is that the PP is always a paramedic governed by the HCPC. A randomised controlled trial of PPs specifically trained to care for older people showed that, although the PP role incurred more contact time with patients, it was more cost-effective than usual care and reduced conveyance rates by > 30%. 54
The critical care paramedic
The CCP role was conceived in 2005 out of the recognition that intensive therapy unit nurses were being brought out of their setting to care for patients requiring critical care during transfers between hospitals. In 2007 the first UK CCP course was implemented in Hertfordshire, closely based on an established Australian model [MICA (Mobile Intensive Care Ambulance) – see www.colacambulance.com/colac_mica.htm; accessed 25 September 2014]. The CCP role consists of distinct care sets for (1) the retrieval of patients on scene and (2) the transfer of critically ill patients. CCPs often make use of air ambulances as well as road vehicles. Dedicated dispatch of CCPs, who are extensively trained in complex competencies, has been shown to improve outcomes for trauma patients. 55,56 The additional resource of an experienced medic, either attending with a CCP or accessible via telecommunication, enhances the combined level of experience available for care.
Hazardous area response team
A hazardous area response team (HART) is trained and equipped to safely locate, stabilise, treat and rescue casualties from dangerous environments such as collapsed buildings or crashed vehicles.
Air ambulances
Helicopters are dispatched for speedy access and conveyance or if the emergency cannot be reached easily by road. They may have a paramedic crew or a doctor and a paramedic crew.
Cycle response units
Specially adapted bicycles that can carry life-saving equipment are used by paramedics to access congested areas more easily. Motorcycles are used in some areas.
Other supportive roles
Community first responders
Volunteer support is provided by responders who have basic life support skills and carry kit bags comprising an automated external defibrillator, oxygen, oropharyngeal airways and a standard set of first aid equipment. They provide basic levels of intervention before the arrival of an ambulance crew.
British Association for Immediate Care doctors
British Association for Immediate Care (BASICS) doctors, specially trained in pre-hospital emergency care, can provide support to ambulance crews at serious road accidents and other trauma calls.
Documentation and communication
Each patient attendance is documented by the attending crews. The date and time of attendance and the ambulance ID, as well as patient assessment, treatment and disposition (or death), are recorded manually on a paper patient record form (PRF) or electronically using an electronic patient record form (ePRF), which is accessed via a purpose-built ‘laptop’. On both systems, each attendance is allocated an incident number for future reference.
Patient record forms
The PRF holds > 700 fields of information on an A3 size paper form in triplicate. One copy is handed to the hospital administrator or other referral agency or left with the patient in the case of treatment at scene. A second copy is filed in a secure box at the ambulance station, which is collected regularly by the audit team. Trusts can use both paper PRFs and ePRFs, as is the case with site 1.
Electronic patient record forms
Paramedics using the ePRF system log on at the beginning of each shift using their personal ID. The ePRF allows dispatch personnel to communicate details of the incident directly to crews on the road. It also serves as a portal for information such as available NHS services, JRCALC guidelines, Toxbase (a guide to dealing with the effects of toxic substances) and the British National Formulary (for information regarding medications). The system also allows e-mail communication. Information about attendances can be transferred via the system to other paramedic teams or to emergency departments.
Computerised databases
Computerised databases such as the Intelligence Based Information System (IBIS) are being developed that allow crews to access patient information provided by community specialists, for example during the care of patients with chronic conditions. This information, generated by a matching process that begins with a postcode and then address, can assist crews in their decision-making regarding the disposition of the patient as more contextual information is available than would otherwise be the case. Decisions about conveyance are often based on whether a particular sign or symptom is normal for that patient; this type of information can be identified using IBIS. 57 An additional benefit is a reduction in the duplication of information when patients receive care from a range of health professionals.
Characteristics of participating sites
Site 1
Geographical coverage of services
Site 1 currently serves populations across six counties. Within the region there are 11 acute trusts and seven mental health trusts as well as a large number of general practices and community health service providers. The six counties and the organisations within them each have a separate identity, which creates complex fulfilling requirements.
Population
The region covered by site 1 includes areas of severe deprivation. The population is growing and the number of elderly in the population is also increasing.
Restructuring of services
This research project was carried out during a time of restructuring at the site. Plans include the reduction in the number of regional divisions from five to three. The reported rationale for restructuring is to reduce unnecessary costs as well as increase quality of care. The five divisions are reported to no longer serve a useful operational purpose yet perpetuate reported cultural divisions that are historically linked to the five separate county ambulance services.
In carrying out the plan, the trust aims to disestablish one line of management (around 46 posts) as well as the general manager role. An important factor behind the restructuring plans is the loss of the patient transport service contract, which will impact on future resource planning. In addition, many of the ambulance service bases are reported to be outdated and for much of the time vacant. Therefore, a larger number of smaller bases called tactical deployment points, supported by 13 hubs (four to five in each division), are planned. The small bases will provide staff with essential amenities to support standby duties such as toilets and drink facilities. Hubs will provide space for meetings and will have Make Ready facilities. Make Ready facilities include a team that carries out cleaning of vehicles, with deep cleaning of interiors to comply with infection prevention and control indicators. The team also check that the vehicle is serviceable before the shift begins and that it is carrying the correct (tested) equipment and that it is stored in the correct way.
Service delivery model
Currently, there is one level of response to all types of call, regardless of the clinical requirements. At least one paramedic is required for each attendance, either responding alone (paramedic or ECP) or assisted by a technician or an ECA. The new model proposes three levels of response, to be implemented by 2014:
-
Urgent care ambulance crewed by two ECAs, available for urgent transport in cases in which a paramedic is not required. The vehicles will all have bariatric capabilities. The crew will still be able to respond to emergency (category A) calls in the first instance if they are close to an incident.
-
A paramedic and ECA/technician in an ambulance or a sole responding paramedic in a fast response vehicle. In both cases the paramedic will assess the case and make decisions about the most appropriate pathway. In both cases it is envisaged that this service will form the core response to 999 calls.
-
An ECP, following assessment by the urgent care hub and a subsequent decision that further assessment is required, to potentially allow the patient to remain on scene or be referred to community health care. ECPs will still be able to respond to any call category but will focus on admission avoidance.
Divisional operations structure
Each division has a service delivery manager who oversees the operational support managers and paramedic team leaders. A clinical quality manager is responsible for delivering clinical strategy against clinical indicators within the division. Operational support managers can oversee groups of ambulance stations or one station and are responsible for managing staff and budget issues. Paramedic team leaders facilitate personal development as well as managing staff and their working arrangements. They also carry out operational roles when demand is high. Restructuring will disestablish 144 paramedic team leader posts and replace them with 90 team leaders and 30 locality team supervisors. Further new roles resulting from restructuring include a divisional director, a head of performance, a paramedic consultant and a service improvement manager for each division.
Strategies
Risk management
The risk management policy is reviewed by the trust board once a year. Potential risk is registered at local and divisional levels. A risk evaluation model is used to score risk for its potential impact.
Staff profile
Emergency operations centre
The EOC includes non-clinical health advisors who use the AMPDS to assess incoming calls. A clinical hub is staffed by qualified paramedics and nurses who assess non-life-threatening calls and provide self-care advice or referral to other health-care professionals. Clinicians also provide a telephone clinical assessment and advice service for patients who do not require admission to A&E.
Operational staff
As well as employing ECAs, paramedics and ECPs, three consultants paramedic posts were appointed during the course of this study. Site 1 supports three air ambulances in the area. The HART comprises 40 members of staff. Site 1 is also supported by a range of voluntary community first responders (CFRs) across the region.
Documentation and communication
Site 1 was the first ambulance service in England to roll out the use of the ePRF in one of its divisions in 2011. It is now in operation across all divisions, although paper PRFs are also used.
The Directory of Services was recently introduced to allow front-line staff access to information about alternative pathways in the local area.
Site 2
Geographical coverage of services
Site 2 covers a geographical area of approximately 6000 square miles, across five regions. The area includes a total of 62 ambulance stations and seven administration/training centres. The area includes remote moorland and coastal areas as well as towns and cities.
Population
The population across the area is diverse, with many of the major towns and cities reported as having higher deprivation levels than the average for England, although some have relatively low levels of deprivation. The area has the third most ethnically diverse population in England. Site 2 reports a Muslim population that is twice the national average according to the 2001 census. A CFR scheme has been initiated to address the tendency towards late reporting of incidents in this population. Around 40% of site 2 emergency services are used by the elderly (> 65 years).
Alternative referral pathways
A number of referral pathways are being developed as an alternative to conveyance to A&E. These include end of life, mental health, social care and alcohol/substance misuse.
Staff profile
Emergency operations centre
The EOC includes non-clinical health advisors who use the AMPDS to assess incoming calls. Recently, a clinical hub has been developed that is staffed by qualified paramedics and nurses. Clinicians assess non-life-threatening calls and provide self-care advice or referral to other health-care professionals. The clinical hub also provides clinical information and advice to ambulance crews on the road, for example crews may require information about a specialist pathway in an unfamiliar area.
Operational staff
Site 2 employs nearly 1900 paramedics, EMTs and ECPs across the region. ECPs work in a number of areas; over 500 referrals to ECPs were made in the year 2012–13. 58
The site introduced the ECA as a new role within this service during the course of this study.
The air ambulance service currently has two charity-funded helicopters based in the area. A HART has been in operation since 2009.
To improve service delivery for residents in rural areas, a pilot scheme is in progress to assess the use of community paramedics working within a local general practice in a rural area. The paramedic works alongside the general practitioners (GPs) and district nurses.
Thirty BASICS doctors are currently supported by the service and 960 volunteer CFRs work within the site.
Documentation and communication
Site 2 uses paper PRFs to record attendances. Up to 20,000 forms are completed each week across the trust. Forms are stored securely at each ambulance station before collection and delivery to one of five clinical business units for electronic scanning into the OnBase system (ProcessFlows Ltd, Winchester, Hampshire). The system allows key words to be searched within the documents so that clinical audit can take place.
Site 3
Geographical coverage of services
Site 3 covers an area of 3600 square miles; it is therefore smaller than the two other sites yet the number of calls that it receives per year is comparable. The population covered is around 4.3 million. The trust operates from 70 ambulance stations.
Service delivery model
Site 3 is developing a front-loaded service model which ensures that initial patient assessment is carried out by an allied health professional, preferably with advanced training (such as a CCP or a PP).
The trust makes clear distinctions between critical care (emergency – convey) and primary care (urgent – referral) elements of pre-hospital care. Practitioner roles reflect this distinction. The ideal is that these two elements would function seamlessly to provide overall pre-hospital care.
In site 3 the ECP role is not recognised as the role is not regulated by one professional body.
Strategies
Risk management
The trust claims to aim to integrate risk management into other trust functions. Locally identified risks to service users, staff or other stakeholders are entered onto a Directorate Risk Register and trust-wide risks are entered onto a Corporate Risk Register. The register is reviewed every 2 months by the Risk Management and Clinical Governance Committee, every 3 months by the Audit Committee and every 6 months by the board to ensure compliance with the CQC.
Staff profile
As of March 2013, site 3 employed whole-time equivalents of 318 EOC staff, who commenced utilisation of the NHS Pathways triage system in 2011. The system was developed to provide links to a broader range of health and social care pathways. It includes facilities for clinical assessment and patient call backs, as well as ‘hear and treat’.
Site 3 employs 1728 operational staff. Of these, 51% hold professional qualifications, including specialist paramedics, managers and team leaders, and 49% are technicians and support workers. The service employs a HART comprising 73 members of staff.
The role profile includes ECAs, emergency support workers, ambulance technicians (although this role is now being phased out), paramedics, PPs, CCPs and a HART. The service is also supported by 500 CFRs.
Documentation and communication
Site 3 is implementing the procurement of the ePRF system to replace paper PRFs.
The site is developing IBIS to improve clinical information sharing. IBIS has three elements:
-
It holds information from specialist community resources regarding patients with long-term conditions. The information is shared with ambulance staff, triggered by a 999 call for that patient.
-
It collates information about non-conveyance to hospital and can assist in more effective management of care for regular callers.
-
Clinical summaries of care can be forwarded to GPs following an episode of care delivered by a PP.
Themes from phase 1 interviews
As well as allowing us to map the ambulance services in terms of organisational and institutional processes, data from the phase 1 interviews highlighted a number of issues that may influence decision-making and patient safety. Although there were some organisational differences between the three sites participating in this study, there were also differences within each site that most likely are associated with historical boundaries prior to regional mergers. We have therefore mainly reported common issues that are relevant to all three NHS ambulance trusts.
Increasing demand
The number of 999 calls in England is reported to have increased by between 5% and 7% annually,59 with an increase of 6.9% between 2012 and 2013. 60 Demand can rise at particular times of the week or year in certain areas but generally remains high and peaks in demand cannot always be planned for. There was recognition that, although high-acuity emergency calls have remained relatively stable in relation to population size, the impact of low-acuity calls to the service has increased demand year on year as they form the majority of incidents and are more complex to deal with. Reported reasons for this increase include the growing elderly population, changes in the attitude of the general public towards accessing services, frequent callers and the use of mobile phones, which makes calling much easier than in the past.
Demand impacts on the whole NHS system; reducing demand in one area creates more demand in another and outstrips available resources. Although there are particular days and times of the day when demand increases, such as Mondays, Fridays and out of hours, predicting demand was regarded as difficult to achieve. Demand on ambulance services is rising even with the development of services that aim to improve access to health care through alternative routes, such as NHS Direct. The impact of NHS 111 on ambulance service demand was unclear as it was in the process of being rolled out at the time that the interviews were being carried out.
Yes, and this is when there are more services available. So it is bizarre to think you have got all these other people available like NHS Direct, out-of-hours doctors and all that stuff and it is still getting busier, because it is not as though the population is increasing.
Int9
Regular callers have an impact on ambulance service demand and their needs may require special consideration. As stated already, demand and lack of capacity at other services creates backlog in the ambulance service, which affects performance. Demand can be increased by public lack of awareness about other options such as walk-in-centres, or lack of understanding of services such as NHS Direct or NHS 111.
When demand is high in a particular geographical area, crews can be called from other areas to provide cover. Demand peaks can impact on the likelihood of crews obtaining release from their operational work to carry out training.
Prioritisation
All three participating sites take 999 calls from the public at two or three control centres within the region. Each centre tends to focus on calls from the local area, although centres take over a proportion of calls from other areas when demand is high. Centres at all three sites have a clinical hub where qualified clinicians (nurses or paramedics) can assist call takers in their decisions, call patients and carers back to give advice and advise operational staff on the road.
The majority of calls are taken by non-clinically trained call takers, who respond to calls in the order that they are put through by the operator. They are not aware of the nature of the calls so at this stage there can be no prioritisation as calls come in. The AMPDS or NHS Pathways triage system is used by call takers to assess the situation and prioritise the response. For example, a category A 8-minute response will immediately be prompted by a call that describes a cardiac arrest.
The call taker reassures the caller if necessary and, if appropriate, delivers advice on how to manage the patient until help arrives. The extent to which a call taker remains on the telephone with a caller is dependent on the severity of the incident; for a life-threatening event the call taker remains in communication with the caller until the crew arrives on scene, to monitor any change in the patient’s condition. For less serious incidents the call can be ended sooner.
The dispatch team receives coded information from the algorithm and makes decisions around which vehicle(s) to deploy. There can be around 40 resources at any given time and deployment will depend on the severity of a patient’s condition and the distance needed to travel, as well as the extent and whereabouts of available crews.
Communication: information accuracy
The importance at the triage stage of receiving accurate information was reported. The severity of a patient’s condition can be determined only using information received during the call; therefore, the clarity and accuracy of this information is important with respect to the appropriate response. Many callers are anxious and this can affect their ability to communicate information. Callers may also have language barriers or communication difficulties that can affect the interpretation of information. This may then have an effect on the response that is made to a call.
Time for assessment: appropriate decisions
Paramedic crews are increasingly spending more time with patients to accurately assess or diagnose their condition as well as provide holistic care. Many patients have more complex health and social care needs, for example they have comorbidities or live alone. Referrals also take time to complete because of difficulties in getting through to the appropriate professional on the telephone. Documentation is time-consuming because of the complexity of many situations that paramedics assess and treat.
Decision-making processes aim for an outcome that is appropriate for the patient. It is no longer the case that all patients need to be conveyed to hospital. Paramedics, particularly those with enhanced training such as PPs and ECPs, are able to treat patients on scene and refer or discharge; however, this involves complex decision-making to maintain the ongoing safety of the patient. The time taken to achieve these objectives can be at odds with response time and turnaround targets, depending on distance. A range of clinical and quality measures also have to be considered when assessing patients, which can impact on time on scene.
Staff roles: skills and training
As already described previously, a range of roles is evident within the ambulance service. All three sites employ qualified paramedics and specialised paramedics (such as ECPs, PPs and CCPs) as well as emergency support workers, ECAs or EMTs. There are differences in the specific role combinations that are employed at each site, for example up until recently one site did not train ECAs and another site does not employ ECPs.
For ongoing learning and professional development, training sessions are provided by the ambulance service. These are either mandatory or optional. Mandatory training often focuses on aspects of practice that could directly impact on patient safety, such as infection control and safeguarding. Training is also required for the safe assessment and decision-making necessary for patients who might not be conveyed or who may be conveyed unnecessarily. However, a key part of training is identifying gaps in individual practice and addressing how to overcome these. This could involve spending time in a hospital unit to understand a particular aspect of care. Particular aspects of care that might be enhanced include how best to deliver care for patients with learning disabilities or for children.
Training is carried out at specified training centres or through outreach sessions by the training team at ambulance stations. Some educational courses use simulation as a training tool. Crews are allocated a clinical supervisor for continued training support, although, as clinical supervisors also have an operational role, the time available to support staff can be compromised by operational demands.
Feedback is available for ambulance staff on gaps in care identified from analysing PRFs, feedback from incident forms and patient service evaluation or complaint data. In the control room, calls are monitored and trends are picked up for which learning might be required by an individual or by a team. Such learning is then related not only to clinical practice but also to professional behaviour, which includes attitudes towards patients. Similarly, reflection is encouraged when decisions are being made so that previous decision-making experiences can be used as a guide for learning.
Protocols compared with flexibility over decisions
Interviews highlighted the extent of policy, procedural and guideline information available to ambulance service employees. The broad nature of operational work in terms of possible events and conditions that can be encountered is one reason for this. Lengthy documents are difficult to assimilate, particularly within a time-bound occupation. At one site presentation of protocols is being reviewed to increase readability.
Sometimes protocols can conflict with decision-making; those utilised by the ambulance service allow for some deviation according to circumstances but such deviations need to be justifiable. This becomes more likely when guidelines are out of date. In some cases, deviation by an individual may lead to new learning for the organisation and a protocol can be revised as a result.
Policies also exist that govern practitioners’ scope of practice, for example ECPs have access to a greater range of pathways for patients. Specialist pathways for stroke, acute myocardial infarction, trauma, etc., are protocol based, with expectations that they will be followed. They can also protect staff in their decisions to bypass the local hospital. There is a trade-off between standardised pathway protocols that can be used across regions and localised protocols that allow for the nuances of service and resource availability.
Ambulance service resources
The main resources mentioned by interviewees in phase 1 were funding, staff, vehicles and equipment. A shortage of resources could in principle lead to patients waiting longer for a response. For example, short staffing in the EOC would mean longer waiting times for calls to be answered. Although demand can be predicted using a range of factors such as time of year, it can also be unpredictable, which may result in a shortage of staff to cover an increase in demand.
There needs to be a sufficient number of working vehicles available for crews; a broken-down vehicle or vehicle part that needs a repair may prevent crews from operating. Similarly, a lack of available crews and/or vehicles will cause calls to stack at dispatch and lead to extended waiting times.
Lack of equipment stock because of breakages and loss can be detrimental to patient care and safety, and so reporting of this is encouraged. Recently, with a rise in the prevalence of obesity, vehicles and equipment designed to meet the needs of bariatric patients have become necessary and in demand. Assessing and treating larger patients can take more time and/or crew members, particularly if a patient requires moving and handling.
Computer equipment is required to aid documentation and communication. Interviews highlight problems in obtaining and maintaining up-to-date information technology resources.
Availability of local community pathways and out-of-hours care
Pre-hospital care has evolved over recent years to respond to a broader range of needs than emergency and life-threatening calls. The majority of calls require more complex decision-making in terms of assessment, treatment and appropriate disposition for the patient. Part of the decision relates to the condition of the patient and immediate circumstances such as the presence of carers. However, the decision is also based on available services in the wider community. The emergency department is open 24 hours a day but it may not be the most appropriate option. Conversely, more appropriate services may not be available at the time of need.
Availability of out-of-hours care and alternative (primary care or community) referral pathways varies according to local provision, time of day, admission criteria and capacity. For example, end-of-life care and mental health services may not be accessible after 1700 or an intermediate care bed may admit only patients who fulfil strict criteria. When care options are known to exist, for example for chronic obstructive pulmonary disease (COPD) and diabetes, it is not always possible for crews to make contact with those services or to speak to a GP at an appropriate time to discuss patient disposition. Therefore, for some paramedics, access to alternative care can be limited.
Sort of virtual ward, community bed type pathways because there are so many patients, we have an older person here with a dehydration who is physically not in danger, but they can clearly not look after themselves and again may end up in A&E.
Int12
For ambulance crews, patients are located across wide geographical locations with associated variation in local available services and out-of-hours provision. Decisions are therefore made in the context of the best available knowledge, which may be sought from a central clinical hub or a Directory of Services. Paramedics can call the hub to identify the appropriate local service and associated referral criteria for its use.
Paramedics with specialised primary care skills such as ECPs and PPs are in theory able to admit patients directly to medical, surgical or orthopaedic units, with the benefit that patients bypass A&E when appropriate. However, this capability is dependent on the relationship that the member of staff has with the specialist unit. An increase in crew expertise might avoid patient admissions: a patient’s condition, although appearing serious, may be identified as being normal for him or her and may require a GP or nurse visit rather than attendance at hospital. However, as already stated, sometimes limited access to community services can restrict full use of this expertise:
because decision-making is only as good as the system, but it operates within another system which compose this mosaic of not quite feral, but quite divergent other services from a number of different suppliers that is totally quite a, quite an issue for us.
Int13
For pre-hospital care one of the main concerns will be whether CCGs will be more or less likely to commission services that could mean a reduction in demand at A&E and an increase in options for crews and patients. For crews there can be dilemmas when service provision out of hours is poor; the only alternative might be to convey a patient inappropriately to A&E.
Delays in response and handover
Operationally, although every attempt is made to reach patients within the desired time frame, this must also be achieved safely. Delays in response can occur when demand outstrips available resources. Crews can be delayed at any of the transitional stages, mainly because of geography, traffic situations or the complexity of assessing and referring patients. Using a specialist pathway can increase the time taken to convey a patient if this necessitates bypassing the local A&E.
Paramedic crews interact with A&E frequently and there can be delays here at busy times that impact on pre-hospital performance. Delays at A&E can be due to high patient demand combined with competing priorities that are affected by targets such as the 4-hour waiting time limit at A&E. Guidance states that patient handover to another service should take no more than 15 minutes46 and there is an expectation that the service will reduce turnaround times (the time between an ambulance arriving at and leaving A&E). However, these targets can be impacted by the demands on, and targets of, other parts of the health service.
Targets
Since April 2011, immediately life-threatening cases have been categorised as category A calls requiring an emergency response within 8 minutes 75% of the time and a vehicle to transport patients if necessary within 19 minutes 95% of the time. Category A calls are monitored using an additional set of clinical quality indicators. The remaining calls are categorised as non-life-threatening. 46 Performance is impacted by the number of calls that are inaccurately categorised as category A calls as well as multiple calls from patients. It is therefore beneficial to avoid these situations as much as possible through accurate assessment at the level of both triage and care.
Historically, performance measures based on response time targets have been linked to (performance-related) payments for the service. Response time performance is maintained partly by dispatching rapid response vehicles (RRVs) to the scene before a dual crew ambulance and by recruiting and training local volunteers who can arrive at an incident very quickly. Local services are particularly important in rural areas where the distances needed to travel from the ambulance station to a patient can be very long compared with those in cities.
However, overemphasis on response times can conflict with the achievement of other clinical quality indicators and can place both ambulance staff and the public at risk from road traffic collisions because of speeding vehicles. More recently it is being recognised that focusing mainly on a narrow indicator of performance such as response times is not consistent with the broad aims of the service and that patient safety and patient experience are also important quality indicators.
Targets that focus on performance can also impact on staff well-being as staff may find it difficult to take an adequate break during a busy shift. They also impact on training:
when money is tight, the first thing to go is training and education. Very often you will book persons on courses but if performance is dipping then pull them away from the course, putting them back on the road again to try and get performance back up there again because they keep coming back to this.
Int2
There is now encouragement from the government to avoid unnecessary A&E attendances as the burden on A&E departments continues to increase. Specialist paramedics such as ECPs and PPs are trained in primary care assessment and treatment so that they can assess and treat a wider range of patients on scene and avoid conveyance when this is considered safe and appropriate. A range of alternative referral services exists for patients who require follow-up visits but the availability of such services varies across localities.
Transfers/handover to other services
An issue that was reported at the interface with other providers is a mismatch in expectations of responsibilities. Paramedic crews may be perceived in their traditional role as conveyers to hospital, with their assessments being duplicated on arrival there. Referral to other services appears also to be hampered by the perception of the paramedic role by other health professionals.
Communication between staff and services
Clear communication is important as patients are handed over to a new team of health professionals at A&E or in other health-care facilities. Research suggests that weaknesses exist in the handover processes that may be the result of cultural and communication issues. One interviewee in our study referred to SBAR as a tool to aid communication. SBAR is an acronym for situation, background, assessment and recommendation; information about patients is structured in this order to standardise the way that details are handed over, rather than it being ad hoc. The system aims to improve safety through better communication. 61
Good communication channels and relationships between the ambulance service and community health professionals can facilitate the referral process, which in turn allows for a reduction in conveyance to A&E. For example, when general practices are made aware of recurring ambulance calls for certain patients, this will flag up a need for a specific package of care. IBIS is a tool that allows information about patients to be shared between community health services and the ambulance service. For example, crews can obtain a patient’s medical history and particular wishes that he or she may have in relation to future care.
Feedback on decisions
Although paramedics often make complex decisions when attending patients, the outcomes of such decisions are not usually available so paramedics may feel that they cannot learn from strengths or weaknesses in their previous decision-making.
Feedback is available for ambulance staff on gaps in care identified from analysing PRFs, feedback from incident forms and patient service evaluation or complaint data. In the control room, calls are monitored and trends picked up for which learning might be required by an individual or by a team. Such learning is then related not only to clinical practice but also to professional behaviour, which includes attitudes towards patients. Similarly, reflection is encouraged when decisions are being made, so that previous decision-making experiences can be used as a guide for learning.
Geography/distance: time
For ambulance service crews, a major part of the working day takes place out on the road. The ability to maintain performance is dependent on access into and out of busy areas as well as on distances between patient and disposition. Crews work across rural and urban areas, particularly now that divisions have merged to create larger regions. Workload may vary depending on the area, with there being less demand but more uncertainty regarding the whereabouts of patients in rural areas as well as generally longer distances to travel to health-care units. In contrast, cities are busier and travel times are relatively short.
The relatively recent development of specialised pathways for STEMI, stroke and major trauma has also altered the landscape of travel, with nearby hospitals being bypassed to apply the pathway protocol. This can add to travel time and to geographical uncertainty, although these disadvantages are balanced against the provision of specialised care for the patient.
NHS changes: Clinical Commissioning Groups
Interviewees in phase 1 of the study had no experience of fully implemented primary care CCGs, most of which formally began in April 2013, although some were becoming involved in negotiations with their local CCGs. There were mixed views about the potential impact of CCGs on services. A positive view was that the development of CCGs could raise opportunities for developing relationships between the ambulance service and GPs and could lead to more localised tailoring of services, increased options for alternative appropriate patient disposition and direct referrals from paramedics. This could lead to fewer 999 calls and A&E attendances. Relationships between GPs and PPs could be particularly enhanced by the formation of CCGs, as their objectives are similar. The closeness of GPs to patient care compared with PCT policy makers was also stated as a possible advantage when making decisions about services.
However, concerns were also raised regarding the development of CCGs. There was a perception that fragmented commissioning decisions could impact on existing pathways and also create confusion for operational staff working with a range of services in different areas, as the profile of available services might differ geographically to an even greater extent than at present. Other concerns were that differing attitudes of GPs towards the ambulance service and CCGs would be an obstacle to the two services working together. Also, GPs may not feel confident in making commissioning decisions, leaving individuals who historically have been making those decisions to continue doing so.
Specific patient groups
It was reported in the phase 1 interviews that increased demand for ambulance services was being generated partly by a new generation of people who cannot cope with incidents without professional intervention. In contrast, older people were reported to be reticent about calling 999 as they are concerned about using scarce resources. However, older people made up a significant proportion of service users because of the ageing population, the greater incidence of chronic disease in older people, the decreased mobility and mental capacity of older people and the greater risk of falling in this age group. Alternatives to A&E varied in their availability and accessibility across regions. Groups reported to be at greater risk because of limited access to appropriate services in the community, particularly out of hours, include those with mental health, alcohol and drug abuse problems.
Patients who required special consideration include those at the end of life, for whom A&E or hospital was not deemed an appropriate place to be cared for because repeated surveys have found that most people would prefer to die at home. The increase in the prevalence of obesity is also a challenge for the ambulance service in terms of requiring appropriate equipment, moving and handling, as well as transportation. Difficulties can also arise when assessing people who have communication difficulties or language barriers. LanguageLine facilitates communication between ambulance staff and patients for whom English is not their first language.
Frequent callers were identified as a group who risk not being taken seriously and who require a particular community care package rather than recurrent visits from an ambulance. People from rural areas were reported to be less frequent users as they are used to having fewer resources in the area and tend to self-manage. Close-knit communities such as coal mining areas and immigrant communities were also reported to self manage as well as pass on advice within the community about how to manage health, only using 999 as a last resort.
Public awareness and understanding of the service
Data from phase 1 interviews suggested that raising public awareness and understanding of the service is an important factor for future development of the service:
So I am standing up there waving my flag saying ‘I think people need to understand a bit more’, public information about what happens when you call 999. That you will not always get someone turning up at your front door within 8 minutes.
Int7
The development of NHS 111 within the three sites raised concerns that the public may not understand how to effectively use the new system, despite advertising campaigns that aimed to raise public awareness before its launch. There were challenges in understanding how the service worked for people for whom English was not their first language or for patients or carers who have learning disabilities or communication difficulties.
Comparisons across sites
Comparisons across the three sites were difficult because of the significant geographical and operational variation within each of the sites. These within-site differences were most likely the result of historical boundaries between ambulance service regions prior to 2006, when they merged into larger NHS ambulance service trusts. Between sites, site 3 differed from sites 1 and 2 in terms of its proximity to busy transport networks. Although site 3 included rural areas, these were not as remote as some areas in sites 1 and 2. Sites 1 and 2 were also more similar in their staffing profile than site 3.
The following chapter presents findings from phase 2 of the study, which builds on the themes discussed above.
Chapter 4 Phase 2 findings: observations and digital diaries
Ethnographic observations and interviews
A total of 34 observations of operational shifts were carried out by ambulance service and university researchers across the three participating organisations between November 2012 and August 2013. Consenting crews were observed during a range of different shifts including different days of the week and day/evening/night shifts. Crews consisted of solo RRV responding paramedics (n = 11), ECPs (n = 3) and dual manned ambulance (DMA) crews (n = 20). Two of the DMA crews included a CCP and one included a PP. A minimum of 100 hours of observation was carried out at each site, comprising a total of 155 patient attendances.
Five researchers carried out the observations, one university researcher as well as one or more researchers from each of the three sites. Data collection involved a combination of audio recording and handwritten notes. The latter was more suitable when high levels of background noise made audio recording less feasible. However, audio recordings were used at other times, for example when crews were on standby.
Although the approach to data gathering was designed to be naturalistic and relatively unstructured, a topic protocol was configured to maintain the focus within the scope of the research aim. Contextual data were also recorded (crew type, time of day, nature of emergency, location, patient characteristics and circumstances, crew decisions about care and the rationale given for this).
Written and audio-recorded data were transcribed into an electronic format. An analysis chart (matrix) was developed to summarise and characterise the data gathered (see Appendix 15). This was used to classify the types of decisions made by crews and the reasons for those decisions.
Digital diaries
In addition to the above, 10 ambulance service staff completed a digital diary to record their rationale for their decision-making during patient contacts. An initial appraisal revealed that:
-
some participants recorded a small number of entries in great detail whereas others recorded a large number of entries with not as much detail
-
data that were recorded focused on challenging attendances in terms of decision-making or represented decisions associated with particular roles, or a series of consecutive attendances, for example over two shifts
-
the role of the staff member had a bearing on the decisions made (e.g. PPs and ECPs tended towards non-conveyance).
These differences were acknowledged during analysis as clinicians with more specialised skills were more likely to decide not to convey patients to hospital. We did not request participating practitioners to randomly select the events that were recalled as we were interested in data that would inform us about challenges to decision-making.
The recordings provide an insight into decision-making processes at the time that decisions were made. The strength of this supplementary data set is held to be that it is less subject to hindsight biases, lapses in recall and observation effects. The diary entries therefore compensated for cognitive constraints that may have inhibited detailed recall about specific decision-making instances in interviews and focus groups.
Decision-making typology
From the observation data charts it became clear that some decisions that crews were making were more complex than others and that patient safety was a key factor in making decisions. Observation data charts revealed a typology of decisions comprising nine key ‘types’ of decision (Table 5).
| Code | Decision | Presenting condition/factors |
|---|---|---|
| 1 | Emergency conveyance: condition-specific pathway | STEMI, stroke, major trauma |
| 2 | Emergency/urgent conveyance: A&E | For example, meningitis, breathing difficulty, fracture, trauma, low Glasgow Coma Scale score |
| 3 | Conveyance to maternity, oncology or another hospital unit | Patient admitted to see a specialist via own existing care pathway or to hospital in a different area (e.g. whilst on holiday) or by direct referral from paramedic (e.g. medical assessment unit) |
| 4 | Decision to convey to hospital already made by another clinician (e.g. GP or another attending paramedic) | Attending physician deems that patient requires hospital assessment and/or treatment |
| 5 | Conveyance to A&E, call for back-up to convey to A&E or patient advised to attend A&E for further assessment (not category A) | Uncertainty of condition, comorbidities, atypical presentation, abnormal observation(s), unrelieved pain, history of a severe condition, medication a risk factor |
| 6 | Conveyance of patient: A&E as place of safety | Psychosocial factors |
| 7 | Conveyance rather than referral to a community practitioner | Patient requires minor wound care, antibiotics or mental health/out-of-hours assessment and there is no access to facilities at the time of attendance |
| 8 | Decision based on preference of patient or family | Conveyance/non-conveyance/refusal to travel/location of conveyance is negotiated by paramedic(s) and patient/family |
| 9 | Non-conveyance: ‘treat and leave‘ at scene (residential or self-care) or referral to another service are regarded as safe options, or safer options than conveyance | Uncomplicated or long-standing condition; patient/carers understanding of condition; availability of referral options (e.g. ECP or out-of-hours services) Presence of infectious condition or risk of hospital-acquired infection |
The typology was subsequently reviewed against the digital diary entries sample to identify any new or conflicting data. The typology excluded any transfers between health-care facilities (arranged before attendance) or attendances in which the patient had died as these instances were regarded as not falling within the scope of crew decision-making and as such fell outside the focus of the study.
According to Ritchie et al. ,62 typologies often combine two or more dimensions. In this study the dimensions include the types of decisions made and staff attributions regarding the underpinning rationale. The key defining feature of a typology is that a characteristic can be assigned to only one category. Thus, in this study decisions made at each attendance, whether recorded during an observation or via digital diary, are accounted for in only one of the nine elements of the typology. This was achieved by an iterative process of coding the data, updating the typology and rechecking for inconsistencies.
The typology presents the nine types of decision encountered in the field and detailed in digital diary accounts along with examples from the data. At first it appeared that some decisions were ‘clear-cut’ but it was later decided that, although some decisions are less complex than others, mainly at the higher-acuity end and when another practitioner has already made a decision, few can be classed as completely unequivocal. The following sections detail the nine types of decision that were encountered in the ethnographic data and how each decision was exhibited in the field in relation to patient safety.
Emergency conveyance: condition-specific pathway
Specialist pathways have recently been developed to enhance care for patients who are suspected to have experienced a stroke or a STEMI or to have suffered major trauma. In these cases timely and specialised care can make a difference to patient outcomes. In practice, this means travelling to a unit that can provide the appropriate expertise and equipment. From the interviews carried out for this study it would appear that specialist pathways were fairly straightforward in terms of paramedic decision-making as there is a protocol to follow for each pathway.
For suspected stroke the FAST (face, arms, speech, time) assessment is made, with the outcome being either FAST-positive or FAST-negative. FAST-positive patients may be admitted to a specialist stroke unit for further assessment to identify the cause and appropriate treatment.
Patients with chest pain will be assessed by a paramedic using a 12-lead electrocardiogram (ECG) to check for the presence of a STEMI. Suspected positive cases can be admitted along the STEMI pathway to a specialist unit where a primary percutaneous coronary intervention (PPCI) can be performed. The procedure is performed to relieve blockages in the arteries, which can then be kept open with metal stents.
Major trauma can include a range of injuries but the common decision criterion is that they are serious enough to pose a potential threat to life or to cause disability. The type of cases treated on a major trauma pathway include serious head injury, gunshot wounds and wounds sustained from an accident such as a fall or a road traffic collision.
Not all hospitals provide specialist pathway facilities; some provide one but not all or provision is not 24/7 and therefore crews needed to be aware of the appropriate centre to convey patients. As this is often not the local hospital, travelling times can be longer than to A&E.
Emergency/urgent conveyance: accident and emergency
During the observations approximately one-third of decisions to convey to A&E were influenced by the severity of the patient’s condition. Decision-making in these cases was regarded as fairly straightforward as patient safety rested on emergency treatment; conveyance was swift, often on ‘blue lights’, with a pre-alert to the A&E department.
Conditions that required a decision to ‘load and go’ on blue lights were considered time critical; they included breathing problems, often in elderly people or small children, or cases of chest pain in which the ECG did not suggest STEMI but there was suspicion of acute myocardial ischaemia.
In one case a patient was resuscitated from cardiac arrest using cardiopulmonary resuscitation and was transported to the resuscitation unit at the local A&E. A low Glasgow Coma Scale score without recovery is also an indicator for emergency conveyance to A&E when the airway is compromised and the cause cannot be determined. Any incident that results in a life-threatening haemorrhage would also be treated as an emergency.
Many patients, when life was not immediately threatened, were conveyed to A&E for further assessment. These cases were deemed to require swift assessment or treatment that could not be carried out in the pre-hospital setting and included severe abdominal pain and fractures. The decision about where to convey might be based on the locality of appropriate follow-on services (e.g. the patient might require PPCI or surgery following hospital assessment). Decisions were therefore made about the immediate safety of the patient but longer-term care was also considered. One scenario that paramedics tried to avoid was re-conveyance to a second more distant unit following the A&E assessment.
Conveyance to maternity, oncology or another hospital unit
Occasionally, patients were attended who had a well-defined condition for which care had already been established at a particular unit and for whom the decision to convey was certain. Continuation of that care package was regarded as beneficial to the patient and therefore the aim was to obtain a referral to that unit. An example of this from observations was a pregnant woman who presented with abdominal pain and vaginal bleeding. The woman was conveyed to a maternity unit with the agreement of staff working at that unit. Another example was a patient who was experiencing symptoms related to his cancer diagnosis and who had received regular care from a particular hospital:
The decision to convey to the MAU [medical assessment unit] instead of A&E was made due to the patient’s ill condition as well as his historical relationship with staff at that hospital.
Ob1
Some patients with chronic conditions such as COPD and diabetes were receiving ongoing support; however, access to direct pathways, either in hospital or within the community, were limited out of hours. In such conditions exacerbations were usually transient and it was stated by paramedics that care could be better addressed by specialist teams who were already known to the patient than by an A&E department.
Specialist paramedics such as ECPs and PPs can refer patients directly for admission to medical, surgical or orthopaedic units as new cases if this is deemed to be a more appropriate option than A&E. However, the lack of this option for all paramedics was a source of debate in relation to providing the most appropriate care for patients as well as lessening the burden on A&E departments.
Decision to convey to hospital already made by another clinician
In a number of observations paramedics had no scope for decision-making as the decision to convey to hospital had already been made before the call. In many cases the decision was made by a GP who had visited the patient, or the patient was attending the GP practice. In these cases the paramedics generally conveyed patients as requested because the risk to patients was usually small.
The decision to convey the patient to A&E was made by the GP so was ‘out of our hands’. The paramedic stated later that he would have been happy to leave her at home had she had the backing of the GP for her pain relief and if the patient had wanted this.
Ob14
In some cases GPs had made the decision to convey without attending the patient. In one such case the ECP challenged the GP decision as the patient was receiving end-of-life care. A negotiation between the two practitioners resulted in the patient remaining at scene with the GP agreeing to visit and develop a care plan for future exacerbations of the patient’s condition.
In one digital diary entry, a paramedic reported a case in which the GP had been called to request an attendance for a patient who was dying rather than convey the patient to A&E. The GP could not attend and the paramedic remained with the patient for 2 hours until death.
Non-urgent conveyance/referral
In a large proportion of observed attendances it was apparent that decisions about conveyance could be quite complex. This was usually because of uncertainty regarding a patient’s condition; crews did not have access to patient records apart from documents that remain with the patient. These include copies of PRFs from previous ambulance service visits as well as carer documentation. Without this information, much of the decision-making made by paramedics was based on a snapshot of the patient’s situation at the time of the visit. Therefore, a key element of decision-making relates to proficiency and skill in eliciting as much information about the patient as possible before making a decision. In a number of digital diary entries, paramedics called the patient’s GP to ask for more information and to discuss available options.
The presence of a carer was useful in terms of accessing verbal information about historical conditions that may not be communicated through the initial call. For example, chest pain may be assessed to be non-cardiac in origin but a cardiac medical history might convince the paramedic that further assessment is required. Caution is required in such decision-making because of the uncertainty inherent in diagnosing without technologies such as radiography, scanning and blood testing.
Risk [is] always there . . . we never get the full picture
Ob30
Information regarding certain medications that patients are prescribed serves as a ‘red flag’ to paramedics in the course of history taking. One such example from observations was a patient who had fallen in the street and incurred minor grazes. The paramedic decided to convey the patient to A&E because the assessment revealed that she was taking warfarin and the full extent of her injuries was not certain.
Often the decision about whether to convey a patient to A&E relied on features which meant that the crew did not feel comfortable leaving the patient at the scene. For example, one abnormal test result, such as raised blood pressure, or a combination of factors, such as comorbidities, particularly in elderly people, strengthened the decision to convey.
Conveyance of patients to accident and emergency as a place of safety
In some cases the over-riding factor for conveyance was not entirely medical. Many conditions can be safely self-managed providing that the patient and/or carer is able to understand the health implications of the condition and how to deal with them. There is more challenge in decision-making when patients live alone. Many elderly people who were attended by ambulance crews were at risk from falling because of limited mobility. In addition, patients diagnosed with dementia were at risk because of a limited ability to self-care.
Looking around the flat there were signs that the patient was at risk if she was left alone; she smoked, and the cleaner had arrived to find one of the cooker hotplates switched on. Due to her inability to mobilise unaided, her status of living alone and her confusion . . . the decision was made to convey the lady to A&E to be assessed.
Ob7
Elderly patients may not choose to be transferred to hospital but would be vulnerable if left alone. One observation was of a night-time visit to an elderly female patient who had called 999 because she ‘felt funny’. It emerged that it was not usual for this lady to call 999 and she appeared quite anxious. Decision-making for the crew was difficult because they could not find anything medically wrong with the patient. However, she was living alone, her mobility was limited, she had no family in the area and her carers were not due to visit until the next day. The paramedics were concerned about her being able to get to the toilet during the night and the risk of her falling. There was no alternative service that could be accessed at that time of night in the locality and so there appeared to be no other option but to convey to A&E to ensure that she was not left alone.
However, there are safety implications in conveying patients to A&E and the crew did indicate that these were considered. Particularly for elderly patients there may be a risk of increased confusion and falling or other adverse consequences in an unfamiliar environment. They also considered the risk of acquiring an infection whilst in hospital.
Conveyance rather than referral to a community practitioner
In many observed instances as well as in diary entries conveyance to A&E was not regarded as necessary despite patients having conditions that required specialised attention. For example, some people had sustained minor injuries that could be treated at the scene by an ECP or at a minor injuries unit. Others had typical signs and symptoms of a urinary tract infection and required antibiotics. ECPs and PPs are trained to assess and treat patients safely in these instances and reduce the risk of hospital admission, but they are a limited resource:
Ideally an ECP job would have been perfect, but he hadn’t re-registered, he used to live in [area] miles away and he hadn’t re-registered yet for a GP locally, so there was no way of getting him analgesia without going somewhere else.
DD4
Limited access to out-of-hours services had an impact on decision-making in these cases, as out-of-hours GPs or nurses could potentially provide the care required.
Decision based on the preference of the patient or family
Whatever course of action paramedics considered, the decision had to be agreed with the patient and, if present, the family/carers. Some patients preferred not to be conveyed to hospital but came to the understanding after assessment that it was safer to have a more thorough assessment. In two cases paramedics decided that the best disposition was for the patient to remain at the scene with some self-care advice, yet the patient preferred to be admitted. An example of this was a young adult with abdominal pain that was associated with a combination of diarrhoea and menstruation. It was judged that these two conditions could have been self-managed with appropriate treatment, particularly as her parents were present, but the patient was considered to be too anxious to stay at home with the pain that she was experiencing. It was decided that, if left at the scene, the patient would be more at risk of increased pain because of anxiety. Paramedics tended to convey in cases in which a patient had a strong preference to be conveyed because of the perceived risk that leaving them at the scene would incur further calls to the ambulance service and attendance by another crew.
Afterwards the paramedic told me that he had been in two minds about what to do, but if the patient wants to go then he usually goes along with that, especially as in this case it was a new situation for her that was also creating anxiety, which in turn could exacerbate her breathing difficulties.
Ob18
At times observation and digital diary data showed that families were influential in making the decision, for example when a patient was at the end of life his or her family often wanted to care for him or her at home. When a patient had communication or mental capacity issues, the family had to make what they felt to be the safest decisions on the patient’s behalf.
Digital diary entries showed that families also had a preference for where the patient was conveyed based on the distance to the hospital and/or historical links with a particular health-care unit. Paramedic crews reported that whenever possible they take family preferences into account. If a preference does not appear to unduly affect patient safety or predicted outcomes, it was reported that this can usually be accommodated.
The most challenging cases for crews can be when a patient refuses to travel. This was apparent in one of the observed attendances. A woman who lived alone and was clearly quite ill refused to go to hospital because she didn’t want to leave her dog alone. A significant amount of time was spent by the paramedics trying to persuade her that hospital was the safest place and that she may well die if she stayed at home. They also made ‘frantic’ attempts to find someone to look after the patient’s dog whilst she was away. Once a carer for the dog had been arranged, the patient was more willing to travel. Diminished mental capacity was also cited as a reason for admitting a patient who refused to travel, but this has to be established by psychiatric assessment. Otherwise a patient who refuses to travel and has mental capacity to make that decision cannot be conveyed.
Non-conveyance: ‘treat and leave’ at scene (residential care/self-care) regarded as safe options or safer options than conveyance
In total, 30 patients who were observed and 52 cases reported in digital diaries were not transported to hospital following a 999 call. The main reason for non-conveyance (referral or discharge) was that the patients’ conditions were not judged to be serious enough to warrant transfer to hospital. Admission avoidance was widely held to be beneficial to patients, providing that there were safe alternatives.
Some patients were not conveyed but were referred to another service for follow-up care. This could include a GP, out-of-hours service, a falls team, an end-of-life care team, a mental health team or another community service. In these cases the decision criterion appeared to be that the condition was established to be long-standing or at risk of recurrence.
Paramedics mentioned having a ‘safety net’ in place to ensure that patients are not at risk as a consequence of making a decision not to convey. Referral to a falls team or mental health crisis team allowed paramedics to hand clinical responsibility over to another set of professionals in a similar way to handover at A&E.
When patients resided in a home that includes 24-hour nursing care, paramedics were more reassured about the safety implications of leaving them, provided that further clinical investigations or interventions were not required.
Initially when you go in [nursing home] you always think that they are probably quite safe to leave, if there are any problems that there is someone that can check on them every hour and usually have their own protocols to document head injury signs for the next 24 hours.
DD5
Digital diary entries identified continuous care as a factor in making a decision not to convey. Similarly, when patients were living with a carer who understood the implications of the patient’s condition and the care advice given, as well as the need to contact services in the event of a recurrence or deterioration of the patient’s condition, admission avoidance was more likely to be considered.
Data from the observations and digital diaries showed a difference in the rate of ‘treat and leave’ decisions between paramedics and those specialising in primary care such as PPs and ECPs. This is perhaps not surprising as specialised primary care roles are designed to reduce rates of unnecessary conveyance to A&E, and training of staff in these enhanced roles allows for more complex assessment and treatment to support discharge at the scene.
Staff acknowledged the move towards avoiding admission to A&E when possible, particularly at one site where there are targets for non-conveyance. However, the data indicate a concern that decisions should not be overly influenced by such policies. As one observed paramedic stated:
If they need to go to hospital they go, if they don’t, they don’t.
Ob28
As well as forming a typology of decisions, the observation and digital diary data were examined for factors that influenced these decisions.
Influences on decision-making
Communication from emergency operations centres
Observations and digital diary entries showed that, to some extent, decision-making starts before the crew arrives on scene, based on communications from the control room. These are usually brief summaries of the patient’s age and condition as well as location, which can be read on a screen above the vehicle dashboard. As one paramedic stated, the information can appear vague, particularly as EOC staff are reliant on the information being given to them by the caller.
In some instances, initial perceptions of a patient’s condition, formed during communication with the EOC, were altered on arrival at the scene, in the light of the presenting status and circumstances. On one occasion a woman with abdominal pain was attended; the communication from the EOC did not include information that the patient was pregnant, which changed the potential treatment and disposition. In another instance, on arrival it was discovered that a physician had requested transport to the medical assessment unit. This information had not been received by the crew so medical assessment unit staff had to be contacted to ascertain whether they were prepared to receive the patient.
A further observation highlighted that if a crew had been informed that a patient was lying on the floor they would not have spent so long attempting to get a response at the front door. Therefore, although initial impressions are being formed on the journey to the location, it is acknowledged that these are subject to verification on arrival. One crew member reported that there was no point in thinking about the scene beforehand as ‘you don’t know what you are going to’ (Ob8).
The NHS 111 service had been implemented in some, but not all, areas where observations were carried out. Paramedics perceived this as adding to uncertainty following initial communication, as, particularly in its initial phase, they claimed it resulted in overtriage from NHS 111 through to 999. One paramedic described the perceived difficulties in interpreting calls.
But I can understand that the way the job comes through those on the end of the phone can’t really tell what’s going on so they’re safety netting and calling an ambulance, you know. Back pain, back pain could be anything from pulled muscle to a triple A so they’re going to send, aren’t they. It’s difficult on the phone. I wouldn’t do phone triage, not in a million years.
Ob23
Patient assessment
What is the situation? ‘Looking for clues’
Although EOC communication gave some idea of the seriousness of a patient’s condition, most information was determined on arrival at an incident. Immediately, crews began ‘detective work’ to determine what was going on. The patient’s immediate safety in terms of life-threatening conditions was the first consideration so that an appropriate quick response could be made:
Basically I attended this, no history from the patient due to the amount of confusion that there was, the lady was laid on her back on the floor, pointing in the air at things that weren’t there and picking at things that weren’t there. On first appearance, looking at her it was evident that this lady was not staying at home.
DD5
When a patient’s life were not immediately threatened, paramedics looked for factors that might have contributed to the incident, such as the cause of a fall. According to one paramedic, crews use their experience to ‘pick up on clues around the scene’ (Ob22) as well as non-verbal clues from the patient to formulate a diagnosis and a plan of action. For example, anxiety was reported to be a factor that could influence patients’ perceptions about the severity of their condition.
When a patient was unable to offer his or her own version of events, information was sometimes obtained from a carer, who was often the first person on the scene. This information would help in making a decision about whether to leave a patient at the scene or convey to hospital, based on how safe the patient might be if non-conveyance was an option.
When calls were made from the home environment, assessment would include looking for potential risk. For example, the physical environments in two homes attended were judged to be hazardous because of hoarding behaviour. On another occasion the crew noted that there was no further space to continue signing for prescribed drugs on a patient’s drug chart. In this instance the patient remained at home but the GP was informed so that the medication chart could be revised.
When signs are not so obvious, crews describe a ‘sixth sense’ – when no precise reason for non-coping is available, but they have a hunch that there are probably social issues that needed addressing. There were several examples in the data in which patients living alone did not have relatives living close by, or relatives were not willing to attend. For example:
There was some other aspects of her care that made me wonder whether the care package she was receiving at home was sufficient, because she described her own meds regime as disorganised.
DD7
Conversely, the presence of a full-time carer such as a spouse or nurses at a residential home was a positive sign in non-conveyance decisions.
Initially when you go in [nursing home] you always think that they are probably quite safe to leave, if there are any problems that there is someone that can check on them every hour.
DD5
It was reported that the option of treating patients at home to avoid conveyance to the emergency department was a consideration on arrival at scene: ‘it’s always in the back of my mind when it comes to treating the patient at home and non-conveying’ (Ob34). Another positive situation reported was when a patient has a good relationship with his or her GP so that self-referral can be considered.
What is ‘normal’? Identifying a change in condition
Crews were generally not familiar with patients who they attended and therefore decision-making required some idea of their usual disposition to determine whether presenting symptoms represented a significant change in status. Crews attempted to derive this insight by questioning the patient, family members, carers or others with contextual knowledge, for example neighbours. Other reference sources included notes left by health and social care professionals from previous visits.
However, there were times when such secondary sources were not available and the patient was unable to provide an account, either because of their presenting status or because of some underlying condition, for example confusion or dementia:
The fact that she couldn’t quite remember all events although she did remember opening the window but couldn’t tell me if she had tripped or whether she had felt dizzy and gone over so there was a little bit of a gap in decision-making.
DD4
Such situations increased the difficulty of judging whether patient assessment (FAST) showed positive or negative signs of the patient having had a stroke. For admission to a stroke pathway the time since onset of symptoms needs to be certain, and < 12 hours:
We were unable to ascertain onset time of CVA [cerebrovascular accident] so the thrombolysis protocol could not be followed as the last time the lady was seen was over a day ago.
DD2
Language barriers can also limit the information obtained from the patient and/or attendant others, which can also increase uncertainty regarding the patient’s condition:
Bit of a language problem here, mum and dad, although they can speak English it wasn’t very clear, not very understandable either so difficult to take a history as the patient can’t tell us how she feels.
DD4
On one visit a patient’s brother was attempting to speak for his non-English-speaking sister. However, the paramedics judged his account to be at odds with their assessment of the patient. Thus, although bystander accounts can potentially enhance the clinical decision-making, there is also the potential for misleading information. An unreliable history from the patient or others present was reported to be more likely to lead to conveyance. Vague information such as the ‘patient is “not quite herself” ‘ or ‘the patient is feeling “generally weak” ‘ were also said to be likely to lead to conveyance as the former indicates a change in condition over time and the latter a general inability to cope. Both indicate a potential risk to patient safety.
One patient population often mentioned during observations was those described as ‘regular callers’. When attending patients who called 999 frequently, the notion of ‘what is normal’ had to be considered more carefully as crew were usually familiar with the callers. The challenge to decision-making here was to try to ignore impressions that a patient’s reason for calling might not be ‘genuine’, particularly if calls were being made on a daily basis.
What is abnormal? Using diagnostics
As well as recourse to visual clues and questioning techniques, a range of diagnostic tests was available to crews, including an ECG and blood glucose, temperature and oxygen saturation measurements, although in one trust thermometers were not routinely available on vehicles to support decision-making. Paramedics used the results of such tests to rule out or diagnose conditions that might require treatment. For example, ST segment elevation on an ECG would indicate immediate conveyance to a PPCI unit.
Paramedics with specialist skills in primary care (ECPs, PPs) have an enhanced range of diagnostics at their disposal, for example the ability to detect a urinary tract infection from a urine test can result in treatment at the scene with antibiotics that ECPs and PPs carry in the vehicle. This element of testing is not available to paramedics, although a referral to an ECP or a PP can be made if the paramedic suspects a urinary tract infection, leading at least one paramedic to propose that:
perhaps if there were more referral abilities and perhaps to test urine and things like that to try and find out where infections are it might be quite useful but currently that’s limited to ECPs.
DD1
In some instances no abnormalities were found, yet symptoms persisted, adding to the complexity of diagnosis. It was acknowledged that, although substantial information can be obtained from available tests, the ‘risk is always there . . . we never get the full picture’ (Ob30), as access to definitive clinical assessments such as radiography and full blood counts were available only in hospital. Lack of access to full blood counts was regarded as contributing to risk when discharging patients at scene, compared with discharge at hospital.
What is needed? Identifying definitive care
At all attendances, the aim of safe decision-making for crews was to identify and implement definitive care for that particular patient in that situation. When necessary, crews were keen to hand over clinical responsibility to the most appropriate available resource. As one paramedic stated:
decision-making involves ‘what can I do for this person?’ ‘where do they need to go?’ ‘what do they need?’
Ob13
Influences on this decision-making include having available information about the patient as described earlier as well as access to information about the pathways that are available to the patient. Decisions about where to convey a patient can be supported by other health professionals or by algorithms, as described in Decision support systems. During observation shifts and in digital diaries, the initial decision that was being made was generally whether or not to convey the patient to a hospital. As already discussed, serious conditions – ‘Patient “poorly . . . big sick” ’ (Ob27) and unsafe environments – ‘he couldn’t be managed in the community in his current state’ (Ob30) – were a trigger for conveyance.
Most patients were conveyed, including patients ‘readmitted’ if they had been recently discharged from hospital. Similarly, patients who were already receiving care at a hospital unit would often be conveyed to that unit. Patients presenting with multiple physical, psychological and/or social problems were also usually conveyed to A&E. Age was another factor influencing conveyance; very young and ageing patients were regarded as being more vulnerable, with conditions that could be unpredictable and that could change quite suddenly:
It being a kid that was weak and floppy . . . kids can be that much more time critical.
Ob32
Specialist pathways have been developed within all participating sites for major trauma, stroke and STEMI; these were regarded as the definitive option for patients meeting specific criteria as professional expertise and equipment are channelled into these specialist centres. Paramedics stated during observations that conveying a patient who fits the criteria for specialist care to A&E might save journey time but could ultimately result in a secondary transfer, thus delaying care and increasing morbidity and mortality: ‘The difference between going to university or being wheelchair bound’ (Ob29).
Location of the incident with regard to available resources can also influence decision-making. Often, paramedics reported a choice of hospitals that were equidistant from the scene. In such instances, criteria applied included a judgement over which hospital could offer the highest level of expertise for the patient’s condition. This judgement was complicated in instances in which attended patients had a combination of issues, for example respiratory and cardiac problems, and in which one hospital specialised in respiratory conditions and the other in cardiac conditions. Crews reported that their judgement in this area could be challenged once at the hospital:
you can’t get it right in these situations – i.e. if you take the patient to one hospital, they [hospital staff] will tend to say that you should have gone to the other.
Ob21
Decisions may also be influenced by previous experience, for example a crew being turned away from a hospital that was perceived to be the most appropriate for a patient because of a lack of capacity. Although no cases of this were observed, this situation was reported twice in conversations with crews.
When opinions differ, some decisions are negotiated with other health-care professionals or the patient/carer. In one trauma incident, crews from two different sites attended the scene. The patient’s address and its proximity to an major trauma centre was an influence on the final decision of where to convey. In other cases, negotiations may be more difficult:
there was a little bit of a power struggle, I had to try harder than I usually do to stamp my authority on the job just to make sure that we all functioned as one team.
DD9
For some, definitive care could be to allow the patient to remain at the scene. For example, in non-serious or chronic condition cases in which out-of-hours care was not likely to assist the patient because of a lack of patient information, care was deferred until the following day:
Out of hours was not able to provide more than the ambulance service in some cases – own GP has patient’s notes and can be more informative during hours.
Ob21
Conveyance and/or referral was often deemed unnecessary for patients residing in a nursing home, as nurses were able to arrange a referral if they felt that it was appropriate. The reassurance of clinical handover as a back-up for decision-making was evident from the data; referrals were a way of ensuring that patients who were not conveyed continued to be monitored by a health-care professional. In one case of a patient who was himself a health-care professional, advice was given that ‘injuries not present, however “must be excluded by clinician” ’ (Ob32). In another borderline case for non-conveyance, it was reported that:
Reasons for non-conveyance and referral to GP due to the fact something was going on, a second opinion was needed . . . no definite diagnosis, therefore a GP was needed.
Ob25
In some instances the decision for non-conveyance was influenced by the ease of GP access for clinical handover of the patient. Paramedics now have options that include calling for an ECP or a PP referral rather than calling the patient’s GP. A final decision might be based on the time of day, as was the case in one observed attendance in which, although a paramedic practitioner worked in the area, it was decided that the GP had more information about the patient:
due to time of day and weekday it was felt that the GP was the ‘better choice’.
Ob27
Decisions were therefore made on the basis of access criteria, for example GPs are not available 24/7 and ECPs and PPs work within their scope of practice. For example, referrals to ECPs to treat and dress a wound could be made only if the wound was minor (< 2 inches in length). Sometimes the extent of an injury cannot be known until a paramedic arrives on scene, which is a limitation to the EOC directly dispatching an ECP to the scene. On one observation attendance an ECP had been dispatched directly to assess the patient but could not attend to the wound. The patient was also displaying the effects of concussion and so required assessment at A&E. However, praramedic practitioners are more likely to discharge patients at scene because of their enhanced skills and scope of practice, supported by guidelines and safety netting procedures:
Because I can . . . As a PP I can medically diagnose and discharge. Very minimum should be the gold standard. NICE [National Institute for Health and Care Excellence] guidelines; policies for fallers > 65 years of age.
Ob28
Praramedic practitioners also considered the wider picture when caring for the patient; one ECP also negotiated district nurse care for a spouse who was caring for his terminally ill wife.
Paramedics also had to make decisions about definitive care that met the specific needs of patients once on scene. For example, obese patients may require a specially designed and equipped vehicle. At one attendance a combination of the patient’s size and inaccessibility within the home meant that the HART was requested to stand by. The HART can use specialised skills to remove windows if necessary to obtain access to the patient.
Observed solo responders (in RRVs) had to decide whether to call for a DMA to back up their visit and transport a patient to hospital. There were reports of concerns when requesting a DMA to arrive within 2 hours – that the solo responder would have had to leave the scene by the time the DMA arrived. Such instances potentially have a negative impact on the quality and completeness of the transfer of patient information, although this situation was not observed. We observed cases, however, in which there was uncertainty around the duration of the delay between requesting a DMA and the time of arrival. In one observed visit the DMA was delayed because of a road closure:
It took an hour for the crew to arrive. During this time the patient’s colour started to improve and her temperature rose slightly. It was quite a challenging time as we were conscious that other patients would need assistance and until the crew arrived we could not leave the scene.
Ob2
Solo responders reported that they have sometimes transported patients in the rear seat of their vehicle. This was seen as an acceptable practice when the hospital was very close to the incident and the estimated time for a DMA to arrive would mean that the patient would have a long wait. This option was considered only when the patient’s condition was stable enough to permit travel by car.
Hospital was not always regarded as the most appropriate care option for patients with an infectious condition that could be passed on to other patients or patients who were at risk of developing an infection in hospital because of their compromised immunity. Such risks had to be balanced against the risk to the patient of non-conveyance. One observed attendance to a patient with diarrhoea and vomiting resulted in conveyance because of a reported collapse. It was reported afterwards that the collapse could have been syncope associated with a virus, but crews were not prepared to take the risk. Hospital admission was not always deemed the most appropriate disposition for those whose main problem was their mental health or intoxication; however, there was a reported lack of options available for these groups.
One barrier to decision-making for definitive care, as noted in more detail in the next chapter, was the lack of feedback available from previous decisions:
Do not know what happens to people after a referral (or conveyance), whether they have done the right thing or not.
Ob13
Occasionally, patients will tell crews what happened to them when they revisit, but there was not enough information on which to base future decisions.
What does the patient want? Patient preferences
Despite the complexity of decision-making influences, paramedics emphasised the importance of patient preference. It was reported and observed that patients often know what they want before the crew arrives:
An important point is what does the patient want, what is their agenda – they can be walking out of the door with their bag packed. Nine out of ten patients know what they want before the paramedic gets there.
Ob13
When decisions over whether to convey/not convey were ambiguous, patient preference assumed salience. The rationale for this was that not conveying a patient who prefers to go to A&E might create anxiety and possibly another 999 call. Similarly, some patients prefer to remain at home and these wishes can be accommodated more easily when there is no evidence of risk in this decision and/or the patient can be referred to community services. Patients have to give their consent before some referrals can be made, for example to a falls team.
However, patient preference can be considered only when the patient is deemed by the crew to have the mental capacity to make an informed choice, and when the choice is judged to be safe for the patient. The exact process of assessing mental capacity appeared, from speaking to paramedics, to remain something of an uncertainty. Capacity is not just about cognitive functioning; making an informed decision requires some level of health/medical understanding. Language barriers can again be a barrier to such understanding; one report was received of a patient being conveyed to hospital because the paramedic did not feel confident that the advice offered had been understood.
Patient preference might also conflict with the paramedic’s idea of definitive care for the patient, with the risk of creating a difficult situation on scene. In one observed instance a patient refused to be conveyed unless it was to the local cottage hospital, which was not judged by the paramedics to be appropriate to meet the patient’s needs. The patient’s GP was contacted and he agreed to visit the patient.
This was a classic example of a scenario where there is no black and white protocol, you are having to think on the hoof as the situation unfolds.
Ob25
Patient preference takes its most challenging form when a patient refuses to travel despite an apparent need for medical assistance. Refusal requires an accompanying acknowledgement of the implications of this action, as well as a signature to denote this acknowledgement:
This lady was confirmed regular known alcoholic, who regularly falls, called out 100 times plus in the past year. On arrival patient was by her bed and had fallen out as she was trying to use her commode. Was heavily intoxicated but rousable, all obs within normal ranges. Patient just described that she wanted to be put into bed, we obliged. She refused to sign a non-conveyance.
DD9
A number of instances were observed in which patients initially refused to travel; in all observed cases negotiation with the patient resulted in conveyance, as the risks were made clear. In some cases a patient’s relatives can have an influence on decisions:
Sometimes the relatives are at you more. You are having to justify yourself to the relatives more often than in the past. They are expecting it. They think you are a miracle worker. You are here, now sort everything out.
Ob9
This is also the case when decision-making is not so much about whether to convey a patient but about where to convey a patient. With some specialist centres being further afield than A&E, there is evidence of resistance, with relatives wanting to limit the distance that they will need to travel to visit the patient. In addition, in rural areas, sometimes the distance needed to travel will affect the patient’s or the relatives’ decision:
Patient’s wife was adamant that patient be conveyed to different hospital as she was not able to get to the one they were proposing, 30 miles away. However, the local hospital would not have accepted the patient due to his presenting abdominal pain.
Ob13
Relatives were observed to be resistant to conveyance when the patient was at the end of life and had a care package in place. However, care packages do not always include a statement from the patient and relatives regarding conveyance or emergency intervention. One visit resulted in an extended conversation with a GP to allow a patient to remain at home at the wishes of his family. A living will was planned to avoid recurrence of the situation as the patient’s condition deteriorated.
Related to patient preference was public expectation – it was reported by one ECP that callers often expect something, anything, to be done, a ‘magic pill’, and do not expect to be given advice only. Conversely, many patients expressed their embarrassment at having an ambulance attend, particularly if they were expecting a GP following an NHS 111 call.
Decision support systems
One aspect of crew activities that was mentioned several times during the study was isolation. This is in marked contrast to colleagues working in hospitals. Paramedics routinely have to make important decisions at scene without direct, readily available access to the opinions of clinicians. It has, for example, been hypothesised that this could fuel a risk-averse orientation on the part of paramedics.
To assist paramedics in their decision-making, a range of support systems were consulted, such as pathway algorithms (‘trauma trees’). These decision aids for paramedics guide assessments to identify the most appropriate pathway for patients with suspected stroke or STEMI or patients with major trauma. Similarly, specific guidelines and criteria, such as those pertaining to children under the age of 2 years, reduce the scope for decision-making by paramedics:
she’s under 2 so she goes into ED [emergency department] anyway, so it takes the decision-making out of your own hands even though she was just a snotty child.
DD4
Control rooms also serve as a source of secondary clinical advice, through a clinical hub staffed by qualified nurses, physicians or specialist paramedics, which staff found helpful as they can be contacted for advice on the appropriate way to address a specific condition or appropriate destination for a patient in a particular locality. The ePRF is currently being developed as a portal for crews to access information about local services and JRCALC guidelines.
Often crews arrive at the scene following attendance by a solo RRV responder or voluntary first responder. We observed that, in the case of RRV attendances, a decision regarding conveyance had usually been made, as the dispatch of an ambulance essentially communicated a judgement over the need for conveyance. However, there were occasions when a back-up DMA was requested but the decision became less certain whilst waiting for its arrival. This tended to result in discussions between the DMA and RRV crews. However, as one observed crew member stated: ‘If one person in crew thinks A&E, then A&E should be the choice’ (Ob26). There was evidence from observations that it was not regarded as good practice to argue in favour of non-conveyance in the presence of the patient.
Paramedics used their own peer network as a source of advice when faced with difficult decisions, for example a specialist paramedic may be contacted for support and/or advice. During our observations, one visit resulted in conveyance because the ECP advised over the telephone that a new medication might be putting the patient’s well-being at risk. At another incident, in which a PP was already at the scene, the crew were guided by his decisions as he was perceived to be ‘more experienced’.
Perhaps worthy of note, one CCP reported that paediatrics was an area in which paramedics can become emotional:
Due to the emotive nature of the job, crews tend to grab and run, therefore primary survey, examination and airway control is not carried out when it is really needed . . . paeds is one area where colleagues really do appreciate back-up.
Ob32
Observation and digital diary data showed that crews often attempt to telephone the patient’s GP to seek advice to support decision-making. However, some paramedics reported finding it difficult to gain access to GPs directly and were not confident that indirect access such as a fax message would reach the GP or be acted on promptly. Similarly, requesting a call back from the GP, although an option, has time implications.
Alternatives to accident and emergency
As already discussed, policies and paramedic roles have been developed across the ambulance service to reduce rates of conveyance. However, one paramedic claimed that decisions were not unduly influenced by the trust target for non-conveyance: ‘If they need to go to hospital they go, if they don’t, they don’t’ (Ob31).
Non-conveyance decisions that required referral were reliant on support from other services so that clinical handover could be carried out. There were positive reports of local referral pathways, particularly in city centres. However, in rural areas and some smaller towns, alternative pathways to A&E such as walk-in-centres, minor injuries units, out-of-hours GPs and referral teams for falls were reported to be fragmented, to have unclear availability or to be not available at all: ‘I can discuss them [pathways] within a minute . . . there ain’t any’ (Ob31).
Particular areas of health need were identified for which access to referrals was considered very limited, including out-of-hours care and options for patients with mental health or substance misuse issues, patients with an exacerbation of a chronic condition and those requiring end-of life-care.
Gentleman has been transported to local hospital due to the fact that there are no emergency mental teams available. I thought that this could possibly be one that we could have been left at home if we had outreach mental health teams in this area but there are none apart from the ones at the hospital which do require to be sober and have no injuries.
DD3
The RRV had made a decision to convey before the DMA arrived; the patient did not want to go to hospital. However, she had exacerbated COPD and there was no option in the city for short-term monitoring (subject to certain criteria) and care.
Ob19
There was a notable consensus that A&E was not appropriate for these groups, yet often there was said to be no alternative. For example, it was reported by an ECP that there used to be more than six resource centres in the city where patients could be admitted for short-term monitoring, but only two of these remained open. It was also reported that the local Community Intermediate Care Services team was at full capacity because patients were being directly referred as they were discharged from hospital. Respite care was also reported to be difficult to arrange as criteria varied across different facilities.
For PPs this presents a dilemma as their focus is primarily on reducing A&E admissions, yet ‘there are few options, particularly out of hours, to conveyance. The PP role is not being used as intended’ (Ob14). PPs and ECPs can, however, refer patients directly to some hospital units rather than conveying patients to A&E, an option that is not available to all paramedics.
Referral to a GP was also a varied experience and depended on accessibility. The main barrier was lack of 24-hour availability; some areas provide out-of-hours GP services that were helpful, although currently there is no access to patients’ past medical history. One crew believed that contacting an out-of-hours GP would lead only to the GP advising that the patient be conveyed to A&E if the word ‘seizure’ was mentioned. They had previous experience of out-of-hours GPs referring patients to A&E to ‘cover their backs’. However, there were reports of positive experiences of out-of-hours services and falls teams and of relationships being developed between the services.
Summary
Observation and digital diary data have highlighted the complexity of decisions made when attending 999 calls. A number of ‘types’ of decision have been described as well as influences from the scene and available support from within and outside the ambulance service.
Phase 2 findings: staff focus groups
Three focus groups were conducted with ambulance service crew members, one group at each of the three study sites, representing a total of 21 staff. The following sections present the findings from the focus group discussions in relation to the themes identified as key influences on decision-making and the potential risks for patient safety.
Control room: triage and dispatch information
Emergency call handlers in the control centre are the first point of contact for 999 callers to the ambulance service. Participants discussed how initial triage decisions can impact on their decision-making. Some participants commented that the initial triage decision and information conveyed to crews can set up expectations about the call that they are responding to, which in the case of the priority category is quite explicit. Participants were also conscious that sometimes implicit expectations may be generated, for example when attending frequent callers. They did acknowledge the need to be aware of the risk of bias in prejudging situations and the importance of maintaining an open mind, particularly as the patient information received is often too limited to permit any reliable judgement of the situation.
Going back to pre-dispatch information . . . I’ll take it with a pinch of salt what the patient’s presenting with; I’ll go in with an open mind. I’ll start from the beginning, you know, interrogate the patient, assess the patient, ‘cos nine times out of ten it’s not what it appeared.
Staff focus group (STFG) 2
Participants commented that the limited information that they receive from the control room can mean that they are not mentally prepared for the case that they are attending and may be unsure of what equipment is most appropriate to take in.
It can often be misleading as well, ‘cos if you get to a job were, say young person with chest pain you might not take the full resus bag in, you might only take the oxygen, the defib and essential kit. And you get there and the information is completely incorrect. So your whole decision-making is based on the information given. If they just spent a little bit more time getting that information for you and then giving it to us correctly.
STFG5
Instances were also cited in which information had not been conveyed about a situation that posed a personal safety risk to the ambulance crew.
Response vehicles get dispatched on address with no information. You could walk into anything, on someone with a knife and they’ve not told you. I walked into a heroin overdose and they were waving a needle, I don’t accept they’re too busy because if the information is there with the dispatcher, why aren’t I getting it. The times you will pull up at a door and a message will come up ‘do not enter this property – risk to you’. If you’d been 5 minutes quicker you’d have been walking into it but that’s an acceptable risk they give to staff on a daily basis.
STFG13
Paramedics recognised the challenging role of the emergency call handlers who are not medically trained and have to make quick triage decisions based on information provided over the telephone with the aid of a computerised algorithm. However, it was claimed that the rigidity of decision-making at this stage tends to lead to over-triage, which contributes to system pressures and impacts negatively on staff.
The triage is a very limited system anyway because you’re not face-to-face, you’re faced with information that you’re getting via one route, verbally, so you’re unable to take subconscious markers or indicators accordingly. There are instances where you as the clinician arrived on scene and you ask a particular question and they give you an answer which is totally contradictory to the one given the call handler in the call taken before. Very minor things such as past medical history, medication, how long have you had the problem before, things like that. And that can give you a level of despondency so that can probably influence your decision-making as well.
STFG3
Of particular concern are the cases in which calls are categorised as high priority, such as chest pain, but which, when crews attend, turn out to be a minor ailment. During periods of high demand this is perceived as diverting limited resources from cases that do require an emergency response. This can create a sense of conflict as all of the required documentation still needs to be completed and to respond to another call perceived as being more urgent would carry considerable risk for them as professionals even when there is no apparent risk to the patient they are with.
It is and I agree. Whilst I’m there dealing with a job that could have been dealt with elsewhere, i.e. primary care or out of hours GP. I am conscious that I’m dealing with that one person but certainly in the back of your mind you are always conscious that two doors down somebody could be having a major STEMI and because you’re tied up there and we’ve got limited resources; I think it does influence you.
STFG12
It was suggested that greater investment in time and expertise at the call-handling stage could improve triage decisions, provide better information for crews and free up resources.
I know we’re trying to get away from that with clinical-based outcomes, etc. But that’s still the thing that ultimately drives our funding from the government. Have we got to that mis-categorised/mis-triaged call within 8 minutes.
STFG12
Changing service demands
Participants discussed the significant increase in demand for emergency care from the ambulance service in recent years. When asked about trends and causal influences they identified an apparent change in public orientation regarding what constitutes an emergency. Specifically, they cited an increase in demand from younger people with minor illnesses and injuries and the growing elderly population rather than an increase in emergencies such as stroke, STEMI or major trauma. The ever-increasing demand is perceived as impacting significantly on ambulance services in terms of ensuring that there are sufficient resources and capacity to maintain expected levels of service performance. This change in demand also has specific implications for staff in terms of increasing the scope of their clinical decision-making, thus creating a need for additional training to deal with a more diverse patient population. The increased demand from patients with minor illnesses and injuries is also perceived as diluting the exposure of staff to the less frequent life-threatening emergencies. Both situations potentially increase the risk to patients, with staff expected to make decisions on a wide range of possible conditions, with the more critical conditions being encountered less often.
The big jobs we used to deal with on a regular basis are now diluted and we’re receiving less training than we did 2 years ago.
STFG13
Whereas coming across sepsis or meningitis at an early stage, if you don’t see it very often, they’re at more risk. Especially if we don’t have some of the simple equipment.
STFG9
Staff across all of the groups spoke of a shift in focus from emergency care decision-making to primary care decision-making, as well as having to consider psychosocial (non-clinical) issues to a greater extent. Decisions around primary care and psychosocial issues are regarded as less clear-cut (lower-acuity decisions) as non-conveyance is more likely to be an option relative to emergencies such as stroke, STEMI, major trauma or critical illness (higher-acuity decisions), which normally require conveyance to hospital.
From the outside, if you don’t work in here, the hardest decisions are heart attacks and road traffic accidents and cardiac arrest when in actual fact if you’re a paramedic, en route you know that if someone’s crashed their car, having a heart attack, been shot or whatever they probably are going to go to hospital, 90% of the decision is already made. Whereas like you say it’s down to as basic as can this old lady go to the toilet next time she gets the urge to use the loo and they become more the decisions rather than the trauma.
STFG11
I find the most difficult decisions I make aren’t clinical ones at all. It’s the psychosocial. Allowing patients to make their own decisions about their own destiny and I’m getting more confident about getting people to sign statements on the patient report form recording the informed consent process.
STFG19
Enhanced roles such as the CCP were perceived by staff in one trust as relatively ‘easier’ in terms of decision-making because the staff have directly relevant training in advanced patient assessment and are more likely to have to take the patient to hospital.
Participants considered that the increasing demand for an ambulance service response is driven by a number of factors. One such factor was limited public awareness of alternative options for non-urgent health care as well as actual or perceived difficulties in accessing alternative such as primary care, particularly out-of-hours care.
Everyone talks about ‘we’re busy, we’re busy’ and there’s clearly not been an increase in heart attacks, an increase in road traffic accidents, just an increase in access to 999 paramedics. We’ve all heard that phrase time and time again – ‘we thought it was best to just get it checked out’. But they’re [patients/callers] now moving on to that next stage of we’re happy if you say they’re all right, we don’t want them to go to hospital. They want that peace of mind. They’ve given up accessing some other avenues, GPs, NHS Direct, and that makes the decision more complicated.
STFG11
Service delivery priorities and pressures
Staff felt that ambulance service targets such as the 8-minute response contributes to the claimed tendency to over-triage at the call-handling stage and to poor resource utilisation. An example was provided of a paramedic in a fast response vehicle dispatched for an 8-minute response for a patient who was assessed as being a lower priority but who needed conveyance to hospital. The paramedic can face a lengthy wait at the scene until an ambulance arrives and may have to decide to prioritise the patient to get a faster response. Although not regarded as ideal, the rationale for this is that it will free the paramedic up as a resource to respond to other calls. Alternatively, the paramedic can decide to leave the patient to wait for the ambulance if it is considered safe to do so. This latter option is perceived as carrying greater risk both for the patient and for the member of staff. It was felt that in most cases the risk in conveyance by fast response vehicle was too great.
I’ve had a couple of cases recently where I’ve been to the patient and have said yes they do need to go into hospital but they’ve had this for a couple of days, they need to go in. Then control will say what you want a hot or a cold response . . . if you get a hot response you have to justify a crew travelling at elevated speed in emergency conditions to your patient who you’re sitting with and have done for the last hour or a cold response where they can wait up to 2 hours. Then you’ve got moralistic issue and decision-making of do I feel compelled to upgrade this to an immediate response because of time or am I happy to sit here for up to 2 hours and wait for a vehicle while I’m out of the system. So for patient safety, that is a decision where you say this patient is going to be safe to be left for 2 hours knowing that they can go into hospital and you may safety net with ‘if it gets worse phone 999’. And do you risk that. Do you make that decision and assume that responsibility or do you fear that if that if you leave them the ‘what if’ factor may kick in and then they could go into cardiac arrest.
STFG4
Some staff also discussed their experiences of feeling pressure to ‘come clear’ while they are still with a patient, that is, to finish with that person and indicate that they are available for another call. Some appear to feel this pressure more intensely than others, even though all paramedics recognised that they had to be thorough and complete the necessary assessments and documentation. It was also noted that a more detailed assessment takes longer but decisions may be better as a result.
If I have an elderly faller, assist only. I’m going to spend time properly documenting and that takes time. I get criticised for my turnaround at hospital because you’ve been with the patient and haven’t documented everything. If I’m preoccupied with writing up my notes, I’m not looking after the patient so I get to hospital I then sit down and write up my notes. If that takes me half an hour it takes me half an hour, it shouldn’t be well, I’ve only got 15 minutes.
STFG21
As far as I’m concerned, whatever’s outside that front door is irrelevant to me. ‘Cos if you’re thinking like that you’re going miss something, put yourself at risk, put the patient at risk. The other 999s, it’s the service responsibility to manage those.
STFG13
Calls for a reduction in rates of conveyance to A&E have increased in prominence for the ambulance service in recent years and this is perceived as a greater priority by staff with specific roles such as PPs and ECPs, who are equipped with enhanced training and referral options.
Participants indicated that they would consider the actual need for conveyance and the potential risks associated with conveyance to A&E, for example the risk of contracting a hospital-acquired infection or the risk posed to others from diarrhoea and vomiting. Sometimes the decision to convey is made by another health professional and the paramedic has to convey the patient even when they feel that it is not appropriate.
Over the last few weeks, the amount of calls we’ve had to people with D&V [diarrhoea and vomiting] and . . . I don’t want to be taking this patient to hospital . . . You try and get out-of-hours GP involved or the majority of them have actually come directly from GPs themselves. The patient’s phoned the GP and the GP has phoned us. Then we’ve got to take them. The risk then is infection of everybody else.
STFG14
Although staff were conscious of organisational pressures to meet the 8-minute target, reduce ‘on-scene’ time and reduce rates of conveyance to A&E, they were clear that their decisions are not unduly influenced by these targets such that they might increase the risk to patients.
Alternative care options for patients
The discussion highlighted that non-conveyance decisions are more likely when there are alternative care options available, including GP referral. Some examples were provided of effective alternative care pathways, for example the Falls Risk Assessment Tool. However, the prevailing picture was of considerable variation in the availability and accessibility of alternative care pathways within each of the participating trusts.
It’s not just the risk from people falling. In [area 1] we are on the [area 2] border, we have pathways for fallers and elderly but if you go across to [area 2], they have a different pathway than ours. In [area 1] there’s definitely a care pathway for people with diabetes but go into the other county and there’s nothing.
STFG7
When pathways are available, staff reported that there is limited or no access during out of hours, weekends and bank holidays.
I think the biggest risk in my decisions that I make for my patients today are that between midnight and 6 a.m. there aren’t as many options and often I would like to leave an old lady at home but the ECPs finish at 2. So she’s not getting the very best decision for her. She’s gonna have to go to A&E and it’s Friday night and it’s full of intoxicated individuals.
STFG15
A number of instances were recounted in which staff had decided that A&E was not the most appropriate option for their patients but then had to convey them there as it was the only option available.
The targets affect my decision-making as a PP in the sense that I do turn up and think not do they need to go to hospital but how can I keep them at home . . . Trouble is I’ve also had times where by trying to keep the patient at home, I’ve just spent ages on scene and they’ve ended up going in anyway. ‘Cos I’ve exhausted so many avenues trying to keep them at home, like the lady that just needs someone to sit. Ringing the GP, ringing intermediate care, ringing social workers or mental health teams. Trying to keep them out of hospital and then an hour and a half down the line, I’ve had to say ‘actually can I have that crew now’, which I sent away initially.
STFG10
Participants provided examples of cases in which they had struggled to get other health professionals to accept the referral of a patient, for example requests for a GP follow-up or a hospital admission. Quite often this meant that they gave up and took the patient to A&E. Staff in enhanced roles with more experience appeared to be more confident about challenging such resistance to ensure that their patients received the care that they deemed most appropriate. Participants indicated that when they had negative experiences of trying to access a certain service this would deter them from trying to access that service in the future.
I tried to get an admission one day at about 1 o’clock in the morning, a urology admission for a guy who was in retention and I spoke to the Urology Reg who said send him to A&E, I’m not accepting him and I said ‘in all fairness doctor I’m not selling you this patient, he’s coming in whether you like it or not, he’s in distress and can I just trouble you for your name’ . . . ‘Why?’ . . . ‘so when the consultant asks me why as an ECP I didn’t refer to Urology when he clearly knows that I can, I’m going to give him your name’. ‘Oh you’d better send him in then’.
STFG4
Delays in follow-up action from services following referral can mean that staff have to decide whether it is safe to leave the patient alone over the intervening period. This was perceived as a risk for both the patient and the crew member because of the potential for deterioration. In the event of something going wrong, it was considered that the paramedic would most likely be held accountable by the trust and blamed for their decision. The importance of ensuring that there is a ‘safety net’ in place in such circumstances was mentioned, for example locating a relative or friend to stay with the patient, but this can be time-consuming.
It’s that initial time from us saying, we’re leaving now and we’ve done x, y and z to refer you on to another service and from when that other health-care professional takes over it’s that time that we are at most risk and it is the forefront of our mind when we make these decisions about whether it’s safe or not and whether it impacts on us and our professional registration.
STFG10
A number of specific patient populations and conditions were identified as being more likely to need referral to an alternative care pathway as the most appropriate care option: mental health, end-of-life care, elderly fallers, chronic conditions – diabetes/hypoglycaemia. However, staff reported that they often struggled to find suitable alternative care options to A&E.
Mental health is for me, my biggest problem. That is where, if you’re talking about patient risk, that’s where I think there’s a massive risk because you take a mental health patient, whether it be alcohol, drugs or a pure mental health episode . . . They’ve tried ringing their crisis line that they’ve got the number for and it goes to answer machine. So you try ringing the crisis line and eventually you get through and they say, ‘well are you with the patient at the moment?’ – ‘yes’; ‘do you think they’re vulnerable?’ – ‘yes’; ‘well take them to A&E then’.
STFG21
An increase in the distances travelled by ambulance service crews, including transporting patients to specialist centres for conditions such as STEMI, stroke and major trauma, often takes staff beyond the boundary of the trust area where they are normally based. A lack of local knowledge regarding care pathway options in other areas can impact negatively on rates of A&E conveyance, that is, knowledge of alternatives tends to be absent or incomplete. Services exist to support crews in accessing local information (e.g. clinical hubs) but participants reported variable experiences of using such services, rating them from good to poor.
Which also goes back to the crews going into different areas. Crews can have critically ill patients on a lot longer, going to designated trauma centres elsewhere, purely because of the restructure of the trauma networks and you have crews going well out of area and again not knowing the locality.
STFG5
Staff in specialist roles appear to have access to a wider range of information sources and referral options.
Up in [area] we’ve got a thing called the single point of access hub [SPUR], which is a community hub that everybody rings to refer to community teams. I’ll use the same falls referral as paramedics for falls but if it’s not a fall I’ll ring that SPUR hub and see what else I can do for that patient. It’s not outside of my professional remit but it’s outside of what the trust specifically has.
STFG10
Although some areas have a restricted range of alternative care pathways, staff report that some areas have an overwhelming number of pathways, which can make it difficult to decide which is the most appropriate for a patient. Participants also cited occasions when they had tried to access pathways only to find that they no longer existed. This would seem to highlight the need to provide crews with up-to-date information on care options in a given area.
Risk perception and avoidance
Staff across all of the focus groups identified their concerns regarding decisions about patient care that they perceived as presenting the greatest risk to their patients and to them as professionals. Some participants specifically referred to the need to ‘cover yourself’, for example the importance of documenting decisions, whether crew or patient decisions.
You get paranoid about putting things down on paper. Write everything out, patient refused this, this was considered but refused. You are almost going into a ridiculous level of risk management, which actually isn’t to do with patient care.
STFG21
A&E is considered the default place of safety for patients and staff when alternative care options are unavailable and when there are concerns about leaving a patient alone, even when conveyance to hospital is not considered to be the most appropriate option. A&E is perceived as the safest (lowest personal risk) option for a paramedic, as all alternatives require a justification for the decision made in the event of a negative outcome for the patient.
That’s [A&E] our default safety net and that’s what negates our risk. What makes us risky is when you get external pressures saying try and keep them out of hospital.
STFG10
And then you get the flipside that you get the paramedics that refuse to leave patients at home because you don’t lose your job from taking a patient to hospital. Everybody goes in.
STFG1
A common concern was that, if an incident occurred, respondents did not feel that they would be backed by their employer. It would appear that some ambulance service staff seek to reduce feelings of personal vulnerability through the strategy of ensuring that clinical responsibility for all patients not conveyed to hospital is transferred to another service or health-care professional. Others felt that this was not necessary in every instance and was likely to be very time-consuming, with negative impacts on ambulance service resources and service delivery.
It’s so much more now about covering yourself . . . I was speaking to a paramedic and he went ‘every single patient, I will refer. Even if it’s just be ringing up their doctor and saying I went out to this patient’. Which is not necessarily a bad thing but then I think well why do we need to do that with every single patient, for example someone that’s just cut their finger.
STFG17
There was some indication that the desire to minimise personal/professional risk may vary by level of experience and confidence and may also be affected by negative experiences or stories relating to the experiences of others. A particular consideration is the action taken by the trust in the event of an incident. Some staff discussed instances in which they felt that what was best for the patient conflicted with service policy and they feared the ramifications of not adhering to guidelines or policy.
It was commented that perceptions of risk and willingness to accept a degree of risk are contributory factors in the increased demand for ambulance service care, including nursing homes that have no lift policies and call 999 for assistance when residents fall, GPs asking patients to call 999 when they cannot see them straight away and the public seeking immediate reassurance on health problems that are not life-threatening or time critical.
That happens right at the point of initial triage, doesn’t it? Everyone seems to need almost too much, erring on the side of caution.
STFG2
I think that’s true of other health-care professionals that work in nursing homes that have no lift policies, nursing homes that rings us and when we’d first go round, they’d say we just wanted to you to lift ‘cos we’ve got a no lift policy.
STFG5
Staff training and skills
A number of participants identified the beneficial impact of additional training and qualifications on their decision-making. Some felt that it made them more confident in their decisions, that it increased their awareness of the risk and therefore they were able to make better-informed decisions. Additional training was also considered to aid interprofessional communication for referrals, for example communication with GPs and hospital clinicians.
I am so much more happier with my decision-making and referral because I know that my patient assessment has been taken that one step further. Possibly frustrating for my crew mate because I probably take longer on patient assessment. You have that different edge because you had additional training.
STFG21
Some paramedics felt that they were not getting to use their training and skills to the best effect. This was particularly the case for those staff who had trained for more specialist roles but who were not employed in those roles.
The more knowledge you get you actually might even have a tendency to seek more advice because you’re much more aware so you may contact the out-of-hours GP or you may contact the emergency care practitioners. But I think it bolsters, it’s a better quality referral to be able to, when the GP does say what about this, what about that, you can have a more informed discussion. It’s safer.
STFG11
Advanced training is optional and relies on the personal investment of time by staff. A consequence of this is that staff in the same role within trusts may have quite different levels of training. Concerns were voiced about staff not engaging with any additional training, particularly those longer-standing staff who trained when there was a greater focus on the delivery of emergency care. Participants questioned how well equipped these staff may be to deal with the changes in the patient population and decision options.
The more I’ve learnt the more I’ve learnt about different conditions that I wasn’t aware of before or was not as aware of so it is enlightening . . . But I do worry about a lot of other people who haven’t done those courses and that will be encouraged to leave people at home but perhaps not with the knowledge or not referring people on to the correct pathways because they have not got the knowledge or training to do so.
STFG14
Similarly, the exposure of newly qualified staff to the full range of calls was identified as an area of potential risk, particularly when paramedics may be working alone or accompanied by staff with very limited training. The impact of operational demands on staff training within the ambulance service was a source of concern for staff across the three trusts, based on their experiences of training being cancelled because of operational demands.
To put it in context, I haven’t had any education input from the organisation, any mandatory/statutory study days. I might have done little bits of paper but every time you get nearly due your update it gets cancelled because of operational demands. It’s very short-term management where people say we’ll make better decisions with more training but there just isn’t the investment. ‘Cos we can’t invest because we won’t get the money if we don’t make the 8 minutes.
STFG11
Training was also identified as important to ensure that staff are kept up to date with developments and maintain competence in dealing with situations encountered infrequently.
We’re just saying give us the opportunity to practice from time to time. Like intraosseous, I think I did my training 2 years ago and 2 years after you’ve got a drill and a person. If you empower us and train us, the patient will get excellent care . . . There are so many small things they can do already that’s not going to cost anything.
STFG9
Staff roles
Paramedics discussed the changes in ambulance service staff roles in recent years, including professional registration and roles that are more focused on non-conveyance. Although they described themselves as autonomous practitioners in that they often make decisions in isolation with limited access to peer or senior support, they did refer to making decisions that are in line with organisational policies, protocols and guidelines (e.g. JRCALC guidelines). Staff with more advanced training appeared to be more confident about deviating from guidelines when it was deemed appropriate.
I thought it was interesting what you said earlier about flexibility in the context of guidelines and I guess certainly I maybe step outside guidelines more as a CCP than I did as a paramedic. That might be partly because of the situation that the job puts me in. It might be because I’ve now got the education to do so confidently. But actually I find the more risky situation I’m in the more closely I tend to try and stick to the protocols because I know that stepping outside the guidelines inherently caries risk anyway.
STFG20
Attention was drawn to variations in the implementation of roles across the different ambulance service trusts, for example one site has implemented the CCP role whereas the other two have ECPs. Some staff expressed frustration at this inconsistency, which was perceived as limiting the scope for them to use their skills acquired from CCP training as well as constraining their career progression.
whilst it’s in the NHS plan for critical care paramedics to do the longer distances to critical care centres, the ambulance service has chosen not to implement that. It’s in the NHS plan but we’re gonna be years before that comes in. That’s frustrating.
STFG5
There appeared to be mixed views about the impact of professional registration for ambulance service staff. Some regarded it as enhancing their professional status, whereas others considered it made them more vulnerable. The latter view appears to have been reinforced in the early days of registration by their respective organisations emphasising the possibility of being reported to the HCPC.
One of my bugbears is, I feel becoming professionally registered for paramedics is one of the worst things that’s happened to us because although the ambulance service retains vicarious liability for our actions they use our professional registration as a method for devolving responsibility . . . And there’s no concept of their ‘system failure’ that might actually cause you to get into situations.
STFG18
Despite the significant changes in ambulance service roles associated with advanced training and increased scope for decision-making, it was felt that perceptions of paramedics by other health-care professionals have not kept pace with these changes. It was claimed that paramedics are regarded by some as passenger transport providers rather than as care providers. The persistence of this traditional view of their role was said to negatively impact on their credibility at the point of patient referral and handover. Participants recounted experiences of struggling to get referrals accepted by GPs and hospital clinicians. This was a source of tension and anxiety for paramedics, but it also has the potential to lead to delays and other negative impacts on patient care.
I sit in a station that is right in the middle of a whole number of hospitals so generally speaking, on a shift, I could go to three, four, five different hospitals. It’s really interesting to see the difference between those hospitals and the ones where you have to work harder to make sure that your patient is properly looked after . . . it doesn’t matter how much knowledge you’ve got if the only thing the nurse will take from you or if the nurse considers you an ambulance driver and not a fellow health-care professional there’s only so far you can go and you just have to hope that somebody at some point looks at the notes.
STFG21
It was also discussed that paramedics in specialist roles may not always be able to use their skills because of the difficulties in ensuring that they are dispatched to patients with whom they can use their skills, for example cases in which ‘treat and leave’ is likely to be an option.
at the minute, there’s no difference between my role [paramedic practitioner] and a paramedic in the sense that I’m going to specific jobs to facilitate non-transport, it’s just pot luck whether I turn up and can use my practitioner skills for non-transport. ‘Cos there are times when a paramedic would take a patient in and I’ve managed to refer them on safely. There are differences.
STFG10
Information and support
The discussions revealed a common theme in relation to the approach to, and volume of, internal communications from the trust. Participants talked of feeling ‘overloaded’ by the amount of information communicated to them, for example policies, procedures, protocols and updates. It was considered extremely challenging to both access and keep up to date with information communicated to them through various routes, including e-mail, notice boards, posters and newsletters. Staff indicated that they try to prioritise and pay greater attention to information perceived as having greatest relevance to them, their role and their location. However, they did cite concerns that this carries the risk of missing something important that may have been skimmed over.
If there’s a high amount of clinical updates and a reduced amount of time. I think there’s a safety issue in that you’ll look at the red ones and then miss the green ones because you have not got much time or there’s so many of them that you cannot become versed with them all and therefore you will miss opportunities to be made aware or increase your knowledge about pathways.
STFG4
Some of the staff with more advanced training queried the usefulness of information (protocols, policies and procedures) that is written for the ‘the lowest common denominator and does not take account of the additional higher education that a lot of us are doing at either masters or degree level’ (STFG5).
Staff across the three trusts indicated that they would feel uninhibited from communicating directly with the medical/clinical director in their respective organisations, with some citing examples of sending e-mails about specific issues and having received a reply. Although this was cast as a positive feature of the prevailing management communication system, it was suggested that the ability to circumvent lower and middle levels of management was not indicative of a good communication system. Middle management was identified by some as a ‘bottleneck’ in the communication system, which impacts on information sharing, feedback and learning lessons.
That’s great, you can talk to the boss but actually if you talk to your CTL [clinical team leader], which is the route you should go, through your team leader. That team leader doesn’t have an easy route up because at various points people will block it so although there is a system where you can talk directly to the boss it then bypasses everybody in between so it’s not from the team, it’s an opinion going to the boss with a reaction coming back down again and maybe there’s someone being told you must do this because I’ve heard from your staff that this isn’t working. That’s not to me a good communication system. If you’re doing good communication and you are saying there’s a safety issue, I should be able to pass that to my CTL who should be able to make a localised decision to solve that problem there and then, who could then pass it up to the COM [clinical operations manager] to check they are happy with that decision, who can look at that decision encompassing the whole of the area and it then cascades outwards and upwards.
STFG21
Paramedics recounted various experiences of the availability and usefulness of decision support services, for example clinical hubs, ECPs and PPs. As with alternative care pathways, having a negative experience can deter future use. This could mean that crews are making decisions about patient care options with limited knowledge of potentially appropriate local pathways. Given the varied patient case mix and patient care options, having to make decisions in isolation without access to advice or support places considerable pressure on staff and puts patients at risk of not receiving the care that best suits their needs. This also highlights that it is not sufficient to simply have services in place; their use and effectiveness also need to be monitored.
I’ve tried the clinical hub but it’s a waste of time. Even though they’re paid B6 and I am band 5 and they’ve got a computer in front of them with loads of information, they’ll say, ‘well you’re there with the patient, you have to make the decision’. Yes, I do but I’m asking you for some help. They were no help whatsoever so it’s just put me off.
STFG14
Access to feedback
Participants identified a lack of routine feedback or debriefing as potentially having a negative impact on their decision-making by limiting the opportunity to reflect on practice and learn how to improve.
I worry about some decisions that I’ve made because we never get feedback and I never ever get told whether I made the right decision to either leave somebody at home or take them to hospital and whether what treatment I did was right. If you take them to A&E it’s hard to get feedback.
STFG14
There was considerable agreement across the staff groups that they tend to receive feedback when things go wrong, such as when a complaint is received, whereas success is greeted with silence and compliments take a lot longer to be communicated. There appeared to be some local variations in experiences of feedback on vulnerable adult forms and IR1s.
Whereas now we’ve got much better feedback systems in terms of, if you fill out a vulnerable adult form, you get told what became of it . . . IR1s as well, possibly as a result of a new team leader.
STFG20
Staff raised concerns that a lack of feedback in relation to these forms promotes apathy among staff with regard to reporting. Some participants discussed variations in levels of staff reporting and cited examples of staff who submit high numbers of reports, many of them perceived to be trivial, and staff who rarely report anything. In the absence of constructive feedback on report forms such behaviour was considered likely to persist. Staff sought feedback regarding the outcomes of their reports and clarity over what they should or should not report as a way of ensuring consistency. It was also suggested that a lack of feedback and information sharing, particularly in relation to clinical incidents, leaves greater scope for the organisational ‘grapevine’ to fill the void, often with negative stories that may contribute to perceptions of vulnerability and promote a risk-averse orientation.
Ambulance service resources: equipment, vehicles and staff
Ambulance service resources were identified on a number of occasions as a factor in decision-making about patient care. The tension between service demands and availability of resources to meet the demand can place pressure on staff.
We’re often under-resourced. We often don’t know where we can refer and what we can do. But also, there’s always that pressure that they need you to come clear for the next job so you’re rushing jobs. There’s always that element where you feel vulnerable because you’ve not got the time to do everything properly.
STFG5
The impact on ambulance service resources was identified as a consideration when making conveyance decisions.
I think possibly because I work on an ambulance the majority of the time, it’s so busy on an ambulance. When you’re on a RRV and you’re deciding does this patient really need to go or not, it makes your decisions harder because you’re thinking how busy they are on the ambulances.
STFG14
The availability of ambulances during busy periods can create challenges and, as mentioned earlier, can pose a dilemma for staff, such as whether to wait with a patient or leave to attend to another incident. Accessing specialist vehicles such as bariatric ambulances can be particularly difficult because of limited availability and because they may be located a considerable distance away from the area where they are needed.
It’s like the bariatric ambulance. You’ll ask for the bariatric ambulance in North [area] and you’re told its somewhere in South [area]. What do you do, wait for 2 hours?
STFG2
The absence of some basic equipment in vehicles was mentioned (e.g. thermometers, blankets), with some staff reporting that they resorted to purchasing their own equipment such as thermometers to avoid situations in which they are making decisions about patient care with limited information. Participants also cited occasions when they had been working on a vehicle and they were not trained to use some of the equipment or drugs available on that vehicle.
I’m conscious that I’ve been on a vehicle this week and the equipment on there, had things like a splint, that I’d never used before and I’m working with someone who is junior, who has been trained in it. You get those sorts of things. You also get that ambulance service staff are now purchasing their own equipment.
STFG11
Ambulance service patient safety culture
The extent to which patient safety is prioritised and supported is to some extent reflected in the other findings from the study. Using MaPSaF dimensions permitted a more focused exploration of the perceived safety culture within each trust. Analysis examined the individual MaPSaF dimensions and assessments of progression towards achieving a mature safety culture. The findings are structured according to three predominant aspects of safety culture that encompass what were felt to be more related dimensions. To address each of the nine dimensions individually would involve considerable repetition. Areas of relative strengths and weaknesses are also identified. Staff worked in pairs to discuss safety culture issues and some of the transcript notes identify the pairs rather than individual speakers; therefore, the quotations provided in the following sections do not have individual numerical designations as with the other quotations.
Patient safety as a priority
Staff across all three sites did acknowledge that patient safety is regarded as a priority by their trust but added that the extent to which it is prioritised is constrained by resources (e.g. funding) and the demands placed on the ambulance service.
We felt that risks are accepted to contain costs; it’s more down to funding.
STFG
Some staff referred to the organisational challenges of balancing service delivery demands and organisational resources:
They’ve only got so many resources and demand is high so what can you do?
STFG
A discussion of commitment to continuous safety improvement revealed perceptions of improvement as being driven largely by pressure from external sources such as targets, the CQC or the ombudsman.
Within the organisation I certainly think they have a reactive way of doing things. The CQC, for example, they know they’re coming in – better chuck a better ambulance out, better check the drugs, better make sure they’re all right today because the CQC are in. Everything revolves around the targets, which is the outside influence.
STFG
Participants did express the belief that their respective trusts want to improve and are trying to do so but that only partial progress has been made. However, they regarded their organisations as having a tendency towards being reactive rather than proactive, as characterised by ‘knee-jerk’ responses to situations. This tendency to be reactive rather than proactive was identified on a number of occasions as problematic in terms of improving patient safety.
There’s a disparity between where the organisation would like to be and where they have managed to get to so far.
STFG
We did feel there was a culture of just responding to incidents but despite the problems we are steadily getting an increase in care pathways, which is part of an improvement agenda.
STFG
Discussion of staff engagement with the improvement agenda within each trust indicated that paramedics feel somewhat distant from the wider organisation and management on a day-to-day basis unless there is a problem that brings them into direct contact. A lack of proactive engagement with staff to support improvement was perceived as a limiting factor.
The only time that we actually get organisational input into day-to-day running of the station is when things are going wrong, when your tough book numbers are down, your sickness is up. It’s a knee-jerk reaction by the organisation to make sure something that’s failing is working. The majority of the time our station works and when it doesn’t work that’s when we see the managers and it’s normally things that are outside of our control and threats when the organisation has to get involved.
STFG
Front-line staff are not engaged in some of the stuff they want us to do.
STFG
From the discussion, it appears that risk management systems are in place but that staff are of the opinion that they are not really integral to all activities. Again, the trusts were characterised as being reactive in prioritising patient safety following an incident rather than proactively seeking weaknesses and areas for improvement. Variable levels of awareness were apparent regarding trust activity in engaging with PPI groups to support an improvement agenda.
When you talk about foundation service users, I’ve never seen any actual minutes in connection with that so my perception is that it doesn’t take place.
STFG
Organisational learning from patient safety incidents
The discussion of organisational learning from patient safety incidents considered the safety culture in relation to incident reporting, investigation of the causes of incidents and dissemination of lessons learned. Participants talked about variations in the levels of incident reporting by staff as well as variations in organisational responses to reports submitted. Concerns about reporting appeared to be fuelled by the anticipated organisational response. A common expectation was that the focus in relation to exploring the perceived causes of patient safety incidents would be on identifying individuals to blame rather than identifying cause and system failures. Comments from staff indicated that they feel that the organisation is more likely to blame them than support them ‘so patient safety issues are not being reported because of fear’.
The organisation says that it has an open and fair culture but it is not perceived in that way by staff.
STFG
Although staff feel that they are encouraged by the trusts to report incidents, the organisational response, such as lack of feedback, attributing blame to individuals and lack of support, is perceived as a barrier to reporting.
It does have a reporting system and does try to encourage people to use it, whether the reporting system is ‘fit for purpose’ because it is not anonymous and there is a kind of a blame return from reporting. The higher-level management would encourage you to report but lower down the reaction doesn’t encourage you.
STFG
Concern was expressed that some incident investigations can be quite superficial such that they do not identify root causes or they place too much emphasis on failures in procedures and the associated audit trail of documentation, for example the PRF. This was perceived among respondents as contributing to a focus on the individual rather than the system when investigating patient safety incidents, including complaints. Some staff cited instances of investigations that had considered system issues, but what they described as a drive by trusts to find a ‘quick fix solution’ to the problem tended to result in an individual focus predominating, with an emphasis on accountability and blame.
I think there’s a genuine involvement in trying to investigate but it gets bogged down in seeking the pound of flesh.
STFG
Rather than thinking let’s prevent this happening again, its apportioning individual blame.
STFG
The discussion of organisational learning as an aspect of their organisation’s patient safety culture identified considerable scope for improvement. Staff indicated that any lessons that are learned from incidents are often not shared with all staff.
There’s not really lessons learned from an incident, it’s not shared throughout the organisational areas or even amongst stations to prevent it happening again.
STFG
When there is learning following an incident, respondents believed that it was too restricted to the local trust area concerned so other areas and trusts could not benefit from learning about the issues and solutions.
I think they do try to do organisational learning, there are some systems in place but I would say it was more localised learning.
STFG
I think you have to ask a question which is, if two events occur that are the same, occur separately at different locations, could we have done something about it? And therefore, is risk management integral. A mechanism would be in place to stop that happening. I wonder if that’s because it takes so long for these processes to get put into action.
STFG
Participants talked of a tendency for ‘knee-jerk’ reactions to incidents rather than changes being based on investigation. They also commented that staff are not really involved in making changes following incidents. Some examples were provided of organisational developments intended to improve organisational learning. At one of the trusts, an in-house magazine published reflections on clinical cases, but respondents were critical that the format was not consistent with that advocated for reflective practitioners and the reflections were therefore not as informative as they might have been. Staff at another trust mentioned that they now have a clinical manager/supervisor role specifically intended to promote learning from patient safety incidents. The introduction of a fortnightly e-mail from the clinical director was welcomed.
This e-mail now is good [from Clinical Director]. This time it was a person who was having a cerebral bleed and got left at home. You can learn from that and its valuable and that’s what the aviation industry have been doing for decades.
STFG
Finding effective ways of communicating information appears to be one of the challenges for learning from incidents, as highlighted by the following statement: ‘Communication systems are in place, but no-one checks whether they are working. I think that sums it up’.
Participants described a reliance on formal communication systems that overload them with significant amounts of information, as described in Information and support and Access to feedback. Staff identified concerns about the amount of information that they are expected to process and the possibility of missing something important, which leaves them feeling vulnerable.
Everything comes back to communication. People forget that we get to work at say 6 o’clock in the morning and are out on the road. Sometimes you might see a locality manager three times in a year. The systems are there but they forget that we’re away from computers, away from staff. We literally go 6–7 hours, have something to eat, another 3 or 4 hours and go home.
STFG
Electronic communication methods such as e-mail are used within each of the trusts but these are not easily accessible, particularly for staff who have no electronic data access when they are out on a vehicle.
They do put loads of posters up everywhere, every time you turn on your e-mail there’s something else, clinical updates. They do communicate with you but only in certain ways, no-one talks to you. You find locality managers putting up lots of notices but it’s more of a team than organisational thing.
STFG
Staff support and development
Some staff spoke of feeling unsupported, for example participants from one of the sites stated that the organisation was punitive rather than supportive over sickness absence.
The lack of support for training was also considered relevant and indicative of organisational commitment to staff who are involved in the delivery of safe care. Organisational targets were perceived as a greater priority in terms of allocating additional resource.
Staffing levels seem to change in response to problems. For example, end of the month or year, to meet targets.
STFG
Some participants felt that their staff development and appraisal system is treated as a ‘tick-box exercise’ rather than making any real contribution to their development.
The discussion of staff education and training in the context of safety culture was consistent with the findings presented in Staff training and skills. Staff felt that training is a low priority, with cancellation of training because of operational demands a consistent feature across all sites. This is viewed as conflicting with a commitment to continuous improvement.
The continuous improvement thing, it seems that they are saying ‘yes, we want to improve our staff’, but when it comes to giving training days they’re not. It seems like they’re paying lip service to it.
STFG
An example was also cited of a lack of involvement in identifying and addressing training needs, which meant that valuable training time was not considered to be beneficial.
They put in a key skills training session and rather than saying let’s look at what needs to be put across, we were told, these are things you need to do for key skills and then they dumb it down to the lowest common denominator and say, this is what you need to know. So there isn’t actual learning, just, don’t do this, don’t do this, do do this, do do this, that’s wrong, that’s right, go.
STFG
One of the CCPs felt that the trust was investing in staff to a certain extent and spoke favourably about the investment in this role by the trust.
I don’t think there’s anywhere else in the country where we could clinically specialise to this level.
STFG
Participants discussed teamworking as an aspect of the safety culture that potentially impacted on patient care. However, many of the participants struggled to identify with a specific team, which reflects the view of paramedics being autonomous practitioners expressed in Staff roles.
I don’t understand how you work as a team in this job. In my experience I don’t really have a team, you get an ambulance, you go out and you come back.
STFG
It was apparent that experiences of teamworking were very different for staff working in different areas within each site. Those participants who did clearly identify with a specific team tended to view their team as performing better in terms of its patient safety culture: ‘We’re a bit more proactive in the team’ (STFG).
Areas of relative strength and weakness
For each of the safety culture dimensions, the groups attempted to reach a consensus on their assessments of progression towards a mature culture. This entailed a process of individual assessments, discussion in pairs and group discussion. Consensus was not always achieved but for most of the dimensions there was reasonable agreement within and across groups. There were some specific exceptions in relation to the perceived strengths and weaknesses.
The safety culture across the trusts was characterised as predominantly bureaucratic (i.e. have systems in place to manage patient safety), with elements of reactive and proactive approaches to safety. Dimensions in relation to staff education, training and safety were identified as weaker in terms of progression towards a mature culture. The prioritisation of operational demands over training was a notable factor. The limited investment in specialist roles and the wider implementation of roles with very limited clinical training (ECAs) was also a consideration. Investment in the CCP role was perceived as an indicator of commitment to safety whereas staff at trusts not implementing this role or perceived to be down-skilling saw this as revealing a lack of commitment. The dimension relating to how incidents are reported and viewed (an opportunity to blame or improve) was regarded as a particular strength in one of the trusts. In contrast, it was identified as an area of relative weakness in one of the others.
Synthesis of the findings
The findings from the phase 2 staff interviews, observations, digital diaries and focus groups were reviewed and classified using a human factors framework29 to identify system risk factors and the associated issues based on our data (see Appendix 16 for examples). A further review of the framework was conducted to synthesise related issues into a more concise set of system influences on decision-making that reflected consistent issues identified across the various methods. This iterative process produced seven overarching system influences and risk factors potentially influencing paramedic decision-making. These are:
-
Meeting the increasing demand. The changing nature of demand for ambulance service care has shifted the scope of decision-making from emergency care decisions to primary care and psychosocial decisions. These decisions are less clear-cut and can take more time. In addition, exposure to emergencies is diluted.
-
Performance regime and priorities. Over-triage of calls requiring an 8-minute response places pressure on resources (staff/vehicles). Time pressures conflict with conducting detailed triage/assessment, which can take longer but may result in a better decision.
-
Access to appropriate care options. Considerable variation exists between areas and regions in the availability and accessibility of alternatives to A&E, which is often not the best option for patients (e.g. those with mental health issues, those at the end of life, the elderly and those with chronic conditions). Increased distances travelled by staff can impact on staff awareness of relevant local pathways and protocols.
-
Disproportionate risk aversion. Varying levels of risk tolerance among staff appear to be influenced partly by competence, confidence and negative experiences. Professional risk is a concern in relation to a perceived blame culture. Transfer of clinical responsibility is viewed by many as key to reducing vulnerability.
-
Staff education, training and development. Operational demands constrain opportunities for education, training, development and skill use (specialist paramedic roles). Some staff invest personal time in advanced training and cite benefits (competence and confidence) but this can lead to skill variations within staff roles/grades.
-
Communication and feedback to crews. Staff feel overloaded by organisational communications (e.g. policies, procedures, protocols) and fear missing something important. This contrasts with limited constructive feedback on performance. Limited patient information conveyed from the control room and access to decision support are also concerns.
-
Ambulance service resources (staff, vehicles and equipment). Continual high demand for an ambulance service response puts a strain on resources. Variations in the availability of specialist paramedic roles (e.g. ECPs, CCPs) and in the availability of equipment, drugs and vehicles can potentially impact on care.
Safety culture and the extent to which patient safety is prioritised and supported are reflected in the seven influences identified above (e.g. perceived blame culture, communication, teamworking, training and resources).
Chapter 5 Phase 2 findings: service user focus groups
The following sections present the findings from the service user group discussions, which explored perceptions of the care options available to ambulance service staff and any concerns about the potential risk for patients.
Call handling: communication and triage
Service users discussed the risk associated with triage decisions at the initial call-handling stage. The risk was considered to be higher when callers have communication difficulties or impairments.
You have to consider that if someone has multiple issues, so if your language isn’t English first, you are disabled, one of your impairments is that your communication is difficult, you are old, you are at end of life and you are vulnerable. Who is going to decide which one of those is the most important? That’s a massive thing for someone to have to make a decision on over the phone. Especially over the phone.
Service user focus group (SUFG) 12
The significance of obtaining appropriate information at this stage was emphasised as this forms the basis for decisions in relation to categorisation and prioritisation of the patient and whether or not to dispatch a response vehicle. Therefore, such decisions need to be well informed. Participants did recognise the challenging nature of telephone triage and considered the training and skills of call handlers to be essential in ensuring that they are equipped to communicate with anxious callers and make appropriate triage decisions.
It seems to be that unless the people who are taking the calls are properly trained and do have the sense to realise that certain bits of information are essential then it is going to make it even harder for that triage to take place and for priorities to be made.
SUFG15
Personal experiences were recounted that highlighted how callers’ lack of understanding of the call-handling process can add to their anxiety, for example when a caller perceives the questioning to be delaying a response. This may then impact on the information provided.
Well from my experience, my wife has dialled 999, explained to the operator, you know, symptoms and she asked the wife you know quite a few questions and wife was like . . . but what do you want to know about that for. I want an ambulance. And then afterwards she said that the receiver of the 999 call had already dispatched an ambulance and she was trying to confirm to the wife that everything was all right.
SUFG9
When a decision is made to dispatch a vehicle, communicating the appropriate information to the crew is also regarded as important. However, the experiences of some participants gave them the impression that this did not always happen. The need to avoid pre-judgement based on limited information was mentioned as this could lead to possible misdiagnosis, for example assuming that the problem is alcohol related because of the context.
Participants regarded shared access to patient information as important in supporting good decision-making at the initial triage stage and at the scene. Service users at one of the sites were aware of the history marking procedure within their trust whereby the ambulance service records relevant clinical or non-clinical information, which is highlighted by the computer-aided dispatch system when a call is received from that address.
But the thing is that history marking system is not universal throughout the NHS and if the patient is transferred the alerts that are in the history marking system are not necessarily already in the receiving department and are not necessarily transferred with the patient.
SUFG21
Involvement in decisions
There was a consensus of opinion that patients, and carers when appropriate, should have a say in decisions about whether or not to go to hospital. Participants felt that it was important that relatives and carers are recognised as potentially valuable sources of information and patient advocates. For some patients who are reliant on carers or relatives (e.g. because of communication or mental capacity impairments), being separated during the transfer to hospital can increase vulnerability.
He said he would never, ever want to go in unless it was an absolute emergency and he would want autonomy on that . . . It may well be the best thing is that you are going to hospital, but even the best thing is not the best thing for us. He said just say how difficult the scenario was when he went in. Five hours in A&E with no-one having any understanding whatsoever of what a PA [personal assistant] or a support worker does. No concept of facilitating. No real understanding that that might be the chair that has been made especially for him but he doesn’t want to sit in it for 5 hours. And then when you are in there, when we went to visit, this [communication board] was in the cupboard. Regardless of what’s wrong with you, you would rather be ill at home and not have that on top of it. To be over-ruled and say oh well you need to go in.
SUFG12
Participants revealed varying levels of understanding in relation to their rights as patients to have a say in the decisions being made about their care, including the refusal of conveyance to hospital. Some participants felt that patient decisions can be over-ridden in end-of-life care by GPs and ambulance service crews, for example when they think that it would be better for a patient to go to hospital.
I certainly think there is a risk around the out-of-hours service and the emergency services and the interface between the agencies and the way that they communicate. End-of-life care is one example of the way GPs are over-riding the decision of the patient because they think it is better for them to go into hospital.
SUFG8
It was suggested that hospital may be perceived as the safest option by the health professional and this appears to highlight a tension between safety and dignity. One participant did query whether such decisions are driven by concerns over professional safety as much as patient safety although the two are very much interlinked.
By the time they had got her into the ambulance she was sitting up and saying I’m fine now but they were very, very persuasive that she had to go to A&E to be checked even though she didn’t really want to go . . . So it meant a lot of NHS staff time was used unnecessarily. I did wonder if they were doing it to cover their own backs so to speak.
SUFG10
Some of the participants identified participation in PPI advisory groups as a way of increasing their involvement in decision-making at the organisational level, representing the needs of patients, including safety, and contributing to policy.
I am a member, as are several people here, of the inclusion advisory group, or IHAG [Inclusion Hub Advisory Group]. And the advisory group aims to have representation from as many different groups as possible. [. . .] And I think it is this sort of thing that ambulance services need because we are talking as people, either service users or people outside of the service, and that is what the ambulance services need, otherwise if they are all sort of internal looking and get very tunnel vision on this is how it should be, this is how it should be, and I think you do need to have this sort of hierarchy as we are now. We are quite high there aren’t we.
SUFG20
Balancing demand and resources
Demand
The increasing demand for ambulance service resources was perceived as a risk to patients, as articulated by one of the participants:
Surely a major risk factor for all potential patients is a mismatch between an ever-growing demand and the resources.
SUFG20
The increasing demand for 999/ambulance service care was attributed in part to difficulties in accessing urgent care. Specific barriers identified included limited opening hours for GP surgeries, the perceived difficulty of accessing appointments and a lack of home visits, combined with limited awareness of and confusion over the various alternative options for urgent care. It was also suggested that the ambulance service was ‘filling the gap for home visits’.
In the community in which I live there is a consensus that with the GPs’ surgeries, there’s no faith whatsoever with them and other services are too far away. There is a large part of the community that don’t have access to vehicles and sometimes even relatives to give them lifts anywhere and the safest bet would be 999. I am not just talking about seniors I am talking about across the board.
SUFG23
It was also suggested that primary care and other services are contributing directly to the increase in 999 calls. Participants shared experiences of relatives being advised by GPs and NHS Direct to call 999 when they did not feel that it was necessary. Some participants expressed optimism that GPs’ involvement in commissioning services will improve awareness of the ambulance service.
She fell down and hit her head, about 6 months ago. Phoned the doctor up at 6 o’clock at night. He says phone the ambulance. All she had was some bruises to her face and he said phone the ambulance. Whereas 20 odd years ago the GP would have come out.
SUFG1
Service users also discussed with apparent frustration the impact on limited ambulance service resources of having to deal with social problems such as alcohol abuse. Some innovative examples were cited across the groups of attempts to address alcohol-related demand at weekends, including buses and tents that focus on treating people at the scene and keeping them out of A&E.
Educating people to be more proactive in taking responsibility for managing their health was proposed as a way of managing the demand for care. This includes expanding patient education programmes to enable those with a chronic condition to better manage their condition and reduce the need for urgent or emergency care.
That then goes into the realm of expanding and ensuring the expert patient programme is incorporating everybody who has chronic conditions because both they and their carer should know what that condition is, what the treatments are, what the risks are and what the response is that they should seek.
SUFG21
Education of the general public in relation to calling 999 and highlighting the role of the ambulance service was also suggested. It was felt that the latter option would be harder to achieve but that focusing on the education of young people in schools could be desirable.
The difficulty there is that mostly until they need it, information, whether it was leaflets or whatever, they wouldn’t read it. But it is really more when they need it. That’s when they will start taking notice and that is a difficulty with getting the message out to people.
SUFG19
Resources
Accommodating the specific needs of patient groups such as wheelchair users and bariatric patients, including carers, was a concern. Participants were aware that the limited availability of vehicles and increasing need may result in delays. Wheelchair users felt that there was a lack of clarity over whether they should wait for a special vehicle or be transferred to a stretcher for transport.
I am coming across lots of different scenarios with wheelchair users and conveyance policies and whether they are in keeping with what the needs of the patient might be. For example, in an emergency context my understanding is that patients have to be transferred onto a stretcher, no questions asked, because the vehicles can’t accommodate wheelchair users in their own wheelchairs. So I would flag that up as a possible risk to patients because sometimes there can be a delay there in the debate about whether someone can transfer, or if they are fit to transfer or not, and whether the vehicle is actually suitable for conveying them to the emergency department or maybe centre of excellence. Likewise the issue about the carer. Sometimes the carer wants to go with the person, who might be in the wheelchair, or the carer might be a wheelchair user and their spouse or partner might be another wheelchair user. Sometimes the lack of clarity about whether the two parties can go in the same vehicle when someone has to go separately. And what happens to the individual who needs the care of the person who is ill. So I would really like to suggest that something is done around that.
SUFG8
Participants discussed the issue of receiving a fast response that is not necessarily the most appropriate response, and which in some instances may give the impression that specific requirements were not communicated. Participants in one of the groups were asked, ‘What is most important to a patient, is it the speed of a response or the most appropriate person turning up with perhaps a bit of a delay?’ The group indicated a preference for ‘speed of the response’, but then added ‘the outcome’.
It doesn’t matter if the first responder isn’t a specialist or qualified in that area as long as they can give assistance. And then the proper, that sounds wrong doesn’t it? The qualified response turns up afterwards.
SUFG18
When Make Ready ambulances were used they were perceived to be safer on the basis that all of the equipment was available. Participants were less in favour of voluntary and private ambulances. The scope for community pharmacists to play a greater role in providing unscheduled care to reduce the burden on the ambulance service was also mentioned in one of the groups, with a view to freeing the ambulance service to deal with emergencies and reducing the risk of not getting emergency care to the people who need it most.
The goal has to be that the emergency services deal with emergencies otherwise that is piling more demand onto the ambulance service. If you are overstretched that puts some patients at risk of not getting emergency help as quickly as they need. A hidden risk factor.
SUFG20
Concerns were expressed that expectations of ambulance service crews are too high. Participants questioned whether it was reasonable to increase the training of one individual to deal with the full range of 999 calls and whether specialism is preferable (e.g. a paramedic specialising in strokes being sent to stroke calls).
Service users at one of the sites were particularly knowledgeable about staff issues such as training and feedback. The lack of time for staff training, because of high service demands, was regarded as a significant risk in terms of safe decision-making and patient care.
Now as a patient, if two guys turn up in an ambulance I expect them to be up to date on all their training techniques and practices and to find that there are that many hours that had to be made up and the consequence of having to make that up and the cost of it because it’s an accumulative cost because if two people turn up who are not able to deal with it, they have got to seek back-up. That delays it whilst someone else arrives and so you have got two vehicles, four people and possibly a line manager turning up as well for the one call.
SUFG21
Service users queried the potential impact of work demands (e.g. long hours, solo working) on the well-being and performance of staff in terms of patient care, particularly if they do not have adequate support.
You work individually, there is no support there and it just concerns me that there is not enough back-up for crew or for individuals working. They could be under a lot of pressure all the time. Can they carry on working like that or is this just a short space model and they are finding it can’t work?
SUFG18
Access to care
The possibility of a delay in accessing A&E when arriving by ambulance was identified as a concern across all groups in relation to the potential impact on the safety of individual patients. The potential impact on the wider patient population and public of already limited ambulance service resources (staff and vehicles) being unavailable was also mentioned.
But A&E gets that crowded at times that the poor person on the ambulance might be sitting outside for an hour and a half. The ambulance can’t move. They can’t take the patient in and say ‘stay out there and they’ll fetch you, I’ve got to go to another call’.
SUFG8
In terms of alternatives to hospital, some participants expressed a preference for remaining at the scene unless it was absolutely necessary to go to hospital, stating that ‘it’s not unstressful to go to hospital’. It was also noted that older patients may be fearful of going to hospital and it may not always be the safest care option for them. However, participants were concerned that ambulance service staff decision-making should take into account access to appropriate support for patients left at the scene.
Conversely, it was mentioned that there may be times when a patient really wants to be conveyed to A&E, to seek the reassurance of being checked at hospital, even though the crew consider it unnecessary. In this scenario it was plausible that no additional checks would take place beyond what paramedics with advanced training could do, which begs the question of whether public confidence in alternative care is an issue.
Service user anxieties about decisions to refer patients to alternative pathways appeared to be centred on the risk of delays in accessing other services or referrals not being acted on at all, for example being unable to see a GP the next day or get a home visit.
If they’re signposted somewhere else other than hospital, who makes sure that happens? Who will follow that up? Twenty-five years ago it would have been the GP, wouldn’t it. Who does make sure that the patient actually receives the appropriate treatment?
SUFG1
Limited awareness of ambulance service roles and competencies also appears to be a factor in relation to concerns over non-conveyance, including ‘treat and leave’ and referral to alternative pathways. Some of the participants were not aware of the specialist paramedic roles and ‘just thought a paramedic was a paramedic’.
The need for more community care options was discussed in relation to accommodating patients who did not need to be in hospital but who would not be safe to return home without appropriate support. One of the focus group participants worked in a residential care home that offered respite care/beds and shared examples of this working effectively as intermediate care, in particular for older patients. The difficulty from the ambulance service perspective is that this service can be accessed only through GP referral. For paramedics seeking to secure intermediate care for a patient, the potential delay created by having to go through a GP may result in a decision to take the patient to hospital instead.
Participants felt that the urgent care system was very fragmented and confusing in terms of identifying where and how to access local services. A specific instance was recounted in which one of the service users had experienced significant difficulty in accessing out-of-hours care and found that the information in leaflets and online was incorrect and that the walk-in centre required an appointment.
We could not find the walk-in service, which was what we were looking for. We asked a porter where to go and he said down the corridor there and you will see a sign. We did see a sign and we went in and the person there in the reception said ‘Oh we can’t see you. You have to go outside and phone for an appointment. Have you got a mobile? Go outside then and phone in for an appointment’. As I say, went outside, phoned in and she said 4 o’clock this afternoon. So with that I went in and said ‘No, I have just brought him 20 miles in my car. If you think I am going 20 miles in my car and coming back again at 4 o’clock, I am not’. Anyway, they did see him in A&E and treated him.
SUFG22
Although more positive experiences of out-of-hours care were shared by others, it was acknowledged that negative experiences are likely to deter people from trying to use these services again.
Risk aversion
Some of the service users recounted situations in which they felt that behaviour was possibly influenced by risk averseness, for example GPs asking patients to call 999 and crews taking patients to hospital when it was perceived to be unnecessary and more about fear of what might happen if they were left at the scene to wait for a pathway service to call. The behaviour of the public was also perceived to reflect risk averseness, for example calling 999 for a non-emergency condition to be checked over rather than waiting to access other services. Participants were concerned about the impact of this behaviour on both the service and patients.
I suppose at the end of the day ambulance service personnel are only human and sometimes you make a personal judgement, don’t you, whether somebody is safe, isn’t safe or whatever. They might look after someone and by the time the ambulance men leave they might look perfectly safe but then perhaps something else could happen, it creates a greater problem than there was originally. Sometimes it has to be a sensible judgement. I get very annoyed with lots and lots of compensation claims being made because it does make people paranoid. It makes the health service paranoid. And also, you’ve got to think about the service as a whole. So you’ve got to consider not just the risk to that patient but also the risk to the other patient.
SUFG6
One person had experienced being chastised by a hospital clinician for apparently being admitted unnecessarily after her GP had advised her to call 999 and the ambulance crew made the decision to convey her to hospital. It was also felt that mutual respect for decisions by different health professionals was important in ensuring that the best decisions are made, including respect for decisions of ambulance service staff.
Geographical location
Participants discussed the impact of geographical location on their experience of care options. There appeared to be an acceptance that in rural areas travelling times are longer and an awareness that this may result in slower responses and take vehicles out of service for quite some time. It was also noted that the perception of time in emergency situations may mean that service users perceive the wait for a response to be longer than it actually is.
I think it just feels like a long time when you’ve got this emergency and you’re thinking where are you, where are you? But actually when they arrive and you look at the clock you realise it wasn’t that long after all.
SUFG8
Local voluntary first responders were felt to be working well in getting someone on the scene faster than an ambulance may be able to get there.
That’s why they brought out a lot of the ‘lives first responders’ because that counts for the 8 minutes. They’re so busy and sometimes have to wait 45 minutes for an ambulance because some of the places they go are so rural, they’re not gonna make it in time anyway.
SUFG2
On the other hand, it was mentioned that travel times through busy urban areas can be long because of traffic congestion, and that these are generally the location of specialist centres. Concerns were expressed over the increased centralisation of services, resulting in patients having long distances to travel to specialist centres, even if they are initially taken to the nearest A&E department.
Cross-boundary working between ambulance service trusts was identified as a concern for patients who live close to the boundary between two trusts. They queried how information is communicated between trusts to ensure that patients get the fastest response rather than waiting for a vehicle from their ambulance service area.
Although there is an ambulance station within 4 miles of where I live, it belongs to [area x], and the ambulance came from [further end of area y] and it took 20 minutes or something to arrive. Do neighbouring ambulance services communicate?
SUFG14
Vulnerable patients
A number of patient populations were regarded as being particularly vulnerable at care transitions. Some of these have already been identified:
-
patients with communication difficulties, including language barriers
-
patients requiring special vehicles (e.g. bariatric vehicles)
-
patients with mental health and mental capacity problems
-
patients taking multiple medicines
-
patients requiring end-of-life care (mentioned in the context of the tension between dignity and safety).
Chapter 6 Phase 3 findings: workshops and prioritisation
A total of 45 individuals attended across all of the workshops in addition to study team members. At the start of the workshops the study team provided attendees with an outline of the study and a summary of the findings. This included the types of decisions being made, a synthesis of key influences on decision-making by crews based on data from the observations, diaries and staff focus groups, staff perceptions of the patient safety culture in their trust and service users’ views on decision-making by ambulance service staff. Attendees were asked to comment on the findings and to consider what they felt were priorities for future attention. They were then asked to carry out an individual prioritisation task, which involved ranking the issues in terms of their assigned priority for future attention. Finally, attendees were asked to identify potential areas for intervention and areas for further research relevant to the issues identified.
Feedback from attendees: comments on findings
Attendees were asked to comment on the findings and to consider what they felt were priorities for future attention. They discussed the findings in small groups and fed back their comments to the larger group. The discussions were audio recorded and transcribed for analysis. Feedback from each workshop was collated and the content was reviewed to identify common or specific issues. There was considerable consistency in the feedback across the three workshops. The following section provides details.
Participants across the three sites commented that they felt that the findings were ‘reflective and relevant’ and that there were ‘no surprises’ in terms of the issues raised. It was suggested that a larger sample could have enhanced the findings, for example including a wider range of staff within the participating trusts or exploring the issues with other ambulance service trusts and the various linked services.
Prioritisation task
Findings
Tests of within-respondent (internal) consistency were performed to establish whether participants were able to discriminate between the issues in a reliable and reproducible manner, that is, to test for the presence of logically inconsistent ratings of the type A > B > C > A. This revealed high levels of within-respondent consistency, with 84% of respondents (n = 44) demonstrating a coefficient (K) of > 0.70. 63 It was therefore concluded that the issues were meaningful to respondents and that the judgements made were stable and reliable.
The extent of agreement between respondents was also calculated, using the coefficient of concordance (W). This revealed a moderate global level of concordance (W = 0.30). Further exploration revealed slightly higher within-group concordance when the ambulance staff (W = 0.32) and service user groups (W = 0.40) were explored separately. However, the degree of agreement between the two groups over the ranked order of issues was found to be high (rho = 0.91) (Table 6). It was therefore concluded that the response set from the two groups could be pooled and treated as a single data set.
| Ambulance staff | Service users | Combined |
|---|---|---|
| High | ||
| Education, training and professional development for crews | Education, training and professional development for crews | Education, training and professional development for crews |
| Gaining access to appropriate care options | Gaining access to appropriate care options | Gaining access to appropriate care options |
| Ambulance service resources (staff, vehicles and equipment) | Communication of information and feedback to crews | Ambulance service resources (staff, vehicles and equipment) |
| Communication of information and feedback to crews | Ambulance service resources (staff, vehicles and equipment) | Communication of information and feedback to crews |
| Disproportionate risk aversion | Meeting the increasing demand for emergency care | Meeting the increasing demand for emergency care |
| Meeting the increasing demand for emergency care | Disproportionate risk aversion | Disproportionate risk aversion |
| Impacts of performance regime and priorities on service delivery | Impacts of performance regime and priorities on service delivery | Impacts of performance regime and priorities on service delivery |
| Low | ||
As noted above, a key strength of the method of paired comparisons is that the rankings are based on judgement proportions, which can be transformed to standard (Z) scores to produce an interval scale. This provides a means of describing the relative prominence by plotting the distance between the issues on a single continuum. This produced the scale presented graphically in Figure 1.
FIGURE 1.
Relative importance/salience by plotting the distance between the entities on a single continuum.
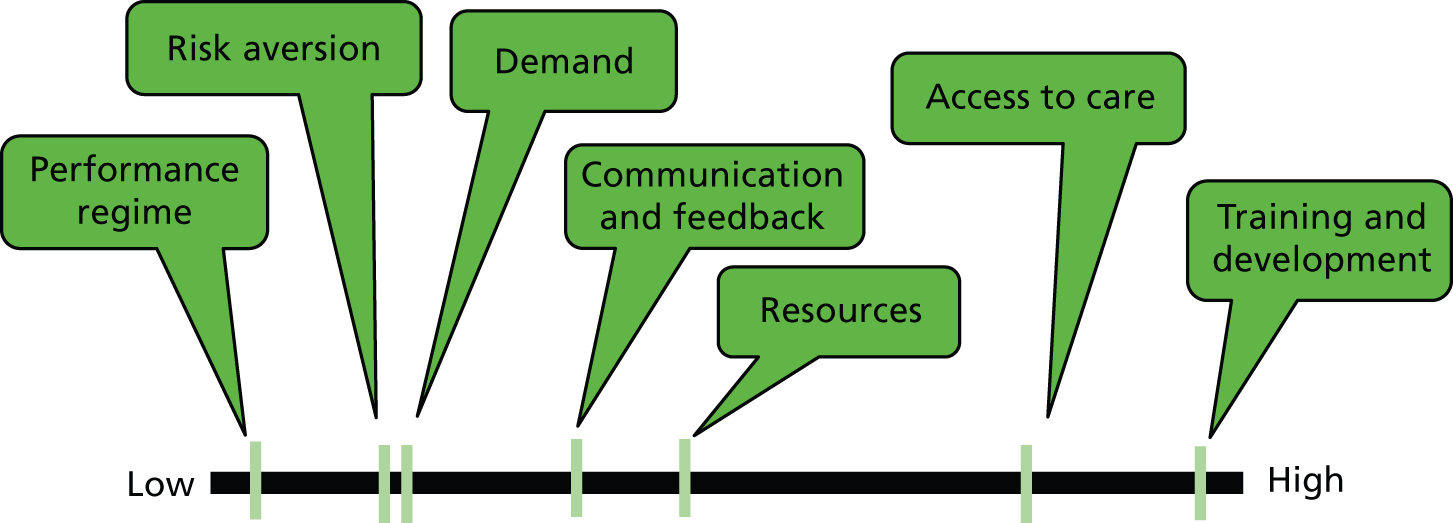
Although it seems that ratings for the set of issues reflect two, or possibly three, clusters, it would be inappropriate to view issues that rank at the lower end of the scale as unimportant. It should be kept in mind that each of the issues included in the ranking task had earlier been identified as having high salience for respondents (see Chapter 4, Synthesis of the findings). The scale is therefore most appropriately interpreted as relating to a prioritisation of the most significant aspects from a list of high-priority issues. Of the set of future priorities, staff training and development and access to care occupy a prominent position that is notably discrete from ratings for the other important issues.
In conclusion, the analysis indicates that the set of variables identified was meaningful to participants and produced a reliable ranking of future priorities. Although the within-group consensus was modest, the level of agreement between the primary stakeholder groups was high. Confidence in the generalisability of the results presented here would be enhanced if corroborated by findings from a larger sample of stakeholders.
Suggestions for potential interventions and research
Workshop attendees were also asked to suggest potential areas for intervention and for further research. They discussed their ideas in small groups and then fed back to the larger group. This section presents suggestions from across the three workshops, which have been grouped into common themes. There was greater variation in some of the potential research areas identified.
Interventions
The suggested interventions presented here are those that workshop participants identified. They represent what attendees regard as the implications of the study findings for health care. They largely relate to actions that are considered feasible to undertake. However, it is apparent that many of the suggested areas for intervention also have implications for research, for example trialling or evaluating innovations. Implications for health care based on the overall study findings are presented in Chapter 8.
Health and social care options
Suggested interventions to address the current difficulties in gaining access to appropriate care options target three key areas: availability, access and effectiveness, including safety. Workshop participants identified a number of potential interventions to support improved availability of effective alternative care pathways, for example 24-hour access to services and direct referral for hospital admission. It was also suggested that there is a need to streamline the existing pathways. This could include monitoring how well they are functioning and identifying how they could be improved. Addressing the needs of populations who are poorly served in terms of current access to pathways was regarded as crucial as many of these patient populations are the least appropriate for conveyance to A&E (e.g. those with mental health and alcohol abuse issues and the elderly).
To address the need for more robust ways of ensuring that staff are aware of and can access pathways, it was suggested that a single point of access for referrals could be trialled. A single point of contact and number nationally could refer callers to a local referral support service. Such a service could potentially facilitate access to services in the local area, not just provide information. This would address the problem of lack of awareness of local referral options when crews are working outside their own area. Increased use of digital technology was also mentioned, for example having access to an up-to-date digital database.
Participants also identified the need for intervention to reduce the variation in referral protocols and the frequency of changes in requirements to reduce the risk of error, particularly when crews go out of their local area.
Effective cross-boundary working
In support of improved access, it was suggested that there is a need to increase awareness and understanding of ambulance service roles among other health professionals to enable improved interprofessional and interservice communication. Joint training on emergency simulations and scenarios was suggested as one way of enhancing cross-disciplinary/cross-service working. Related to this, it was remarked that trusts need to be more active in supporting staff to challenge front-line resistance to referrals so that referral protocols and agreements in place are respected.
Improved two-way information sharing between the ambulance service and other services was regarded as key to supporting effective clinical decision-making and feedback on patient care. However, there are a number of structural barriers and, quite possibly, attitudinal barriers. For example, not all GP surgeries have software to enable data sharing from the ePRF. Shared records across services could improve the safety of decision-making as staff would have access to more patient information, and paramedics consider this to be preferable to patient-held records. One of the sites has developed its own system for improving access to relevant information about patients to support better decision-making (IBIS).
Managing the demand for care
Staff in more managerial roles identified a need for improved business intelligence and feedback to trusts on the availability of and access to pathways. This would ideally include feedback on instances in which the needs of patients are not being met (e.g. conveyance to A&E because of a lack of alternatives). This should ensure that pathways are set up where need exists. One trust had set up a telephone line for staff in one area to feed back on problems with availability and access to pathways, but a lack of awareness among staff at the time meant that this was not used.
Staff training and development
Improving access to education and training for staff was considered to be a key area for intervention. This could include exploring different models of training that may be appropriate for certain training needs (e.g. distance learning, informal workshops and information sharing with colleagues). Access to training may require trusts to consider how they can free up resource for staff to engage in professional development. One option is for better long-term planning and sustainability assessment of anticipated demands against resources to avoid knee-jerk reactive responses to situations, such as cancelling all training.
To meet the changing needs of the patient population it is considered important for ambulance service trusts to develop a strategy to invest in specialist paramedic roles (e.g. ECPs). This will support urgent care and non-conveyance and ensure the appropriate use of staff with advanced training to avoid skill degradation.
Improving information and feedback
Ambulance service staff identified the need to develop improved ways of delivering feedback to staff that conveys positive and not just negative messages. (e.g. individualised face-to-face feedback, peer-to-peer and supervisor feedback within clinical teams, more informal educational activities such as workshops). Linked to this there is a need for trusts to identify ways of obtaining feedback on patients to support reflective practice and improved decision-making that fits with Caldicott requirements. 64 The example was given of one hospital starting to provide 24-hour data feeds on the diagnosis, treatment and admission of patients, which can help when assessing the appropriateness of transfers to A&E. The provision of opportunities for access to decision support for crews was also suggested, for example peer or supervisor support.
Input on commissioning decisions
Ambulance service clinicians, managers and service users emphasised the need to become embedded in CCGs to ensure that service and patient issues are understood. Service users want commissioners to listen to the patient voice and to ambulance service staff who can often be a proxy for patient needs.
Research
Based on the study findings and discussion, workshop attendees identified a range of potential areas for further research. These represent what attendees regard as key areas for future research to address potential influences on paramedic decision-making and patient safety (see Appendix 17).
Chapter 7 Discussion
Introduction
The aim of this study was to explore system influences on decision-making by ambulance service staff and potential risk factors for patient care. The study considered all aspects of the system using a human factors framework to inform data collection and analysis; patient characteristics, task factors, individual/staff factors, team factors, the work environment and organisational and management factors were all considered. 29
A range of qualitative methods was used to explore paramedic decision-making in relation to patient safety, with contributions from ambulance service staff and service users across three ambulance services in England. The initial interviews, mainly with management-level ambulance service staff, identified a range of system issues potentially impacting on decisions about patient care. These issues, and other issues identified as relevant, were explored in more detail in the staff focus groups. Observation and digital diary data were combined to illustrate the types of decisions that are made by paramedics within the context of a number of real-time patient attendances. Potential system influences on these decisions were extrapolated from all available data, showing a complex arena of factors within which paramedics and crews perform their decision-making.
Principal findings
This section will examine the main findings from the study with reference to relevant theoretical and empirical literature.
Typology of decisions and system influences
Boxes 1 and 2 outline the main findings from the study in relation to paramedic decision-making and system influences.
-
Emergency conveyance: condition-specific pathway (e.g. stroke).
-
Emergency/urgent conveyance: A&E.
-
Conveyance to maternity, oncology or another hospital unit.
-
Decision to convey to hospital already made by another clinician (e.g. GP, other attending paramedic).
-
Conveyance to A&E, call for transport to convey to A&E or patient advised to attend A&E for further assessment (not category A).
-
Conveyance of patient: A&E as place of safety (e.g. psychosocial factors).
-
Conveyance rather than referral to community practitioner (e.g. no access).
-
Decision based on preference of patient or family.
-
Non-conveyance: ‘treat and leave’ at scene (residential or self-care) or referral to another service are regarded as safe or safer options than conveyance.
-
Staff training and development – operational demands constrain opportunities for training, development and skill use.
-
Access to appropriate care options – considerable variation exists (areas/regions) in availability and accessibility of alternatives to A&E.
-
Ambulance service resources – continual high demand places a strain on staff, vehicles and equipment resources.
-
Communication and feedback to crews – staff overloaded by operational information in contrast to more limited decision feedback and support.
-
Meeting increasing demand from a more diverse case-mix – increased scope of decision-making, from emergency care decisions to primary care and psychosocial decisions.
-
Disproportionate risk aversion – staff risk tolerance influenced by competence, confidence, previous experiences and perceived blame culture.
-
Performance regime and priorities – the 8-minute response in particular places pressure on resources.
Safety culture
The extent to which patient safety is prioritised and supported is reflected in the above influences. Staff assessments of progression towards a mature safety culture were broadly consistent – predominantly bureaucratic with elements of reactive and proactive approaches to safety.
The order reflects the prioritisation derived from phase 3 workshops.
Analysis of observation and digital diary data led to the development of a nine-item typology reflecting the types of transitional decisions made by paramedics when attending patients (see Box 1). These ranged from fairly clear-cut decisions, for example in emergencies, to protocol-driven decisions, such as those made in the context of trauma and STEMI pathways, and less clear-cut decisions in more complex cases, in which decisions are mitigated by social circumstances and comorbidities. It is the last type of decision that created most uncertainty and risk for paramedics as well as patients, as certainty about handover of clinical responsibility for patients to an appropriate health or social care provider was perceived as critical to high-quality care in most cases. The typology reflects the wide scope of decision-making that paramedics encounter.
Analysis of phase 2 staff interview, observation, digital diary and focus group data resulted in the identification of seven overarching system influences and risk factors that potentially influence paramedic decision-making (see Box 2). The various influences identified are not mutually exclusive and can potentially impact on any situation in which paramedics are making decisions about patient care. They are therefore relevant to all types of decisions. The study findings identify areas of potential risk associated with each of these influences. These are discussed in the following sections.
The changing nature of ambulance service care and decisions
Ambulance services are managing care delivery in the context of continual policy changes, increasing demand and decreased resources. Demand is increasing in part because of an ageing population, more of whom are living with chronic conditions. 59 Mason et al. 65 reported that between 12% and 21% of visits to A&E are made by older people (aged ≥ 60 years), who are more likely to arrive by ambulance than their younger counterparts. Alcohol misuse poses another rising demand on services; a study in the north-east of England66 showed that > 3% of calls were related to alcohol. Our study confirms previous findings that a combination of rising public expectations and service users often not knowing which care options they can access are also factors contributing to rising demand. 59,67 Our findings also highlight that the management of increasing demand for emergency care and the changing nature of the care required for an increasingly diverse set of clinical needs are key issues impacting on front-line staff. Within this context, crews strive to meet patients’ needs as well as develop their own potential.
Supporting self-care in the population has been identified as a way of reducing demand on NHS services. This includes raising awareness of self-treatment options as well as standardising care planning so that health-care professionals can better advise patients about individualised self-care. 68 Within services, changes in delivery design in A&E and in urgent care settings also aim to cope with rising demand by targeting care more appropriately to specific groups.
The study findings highlight the influence of the current performance regime and priorities within the ambulance service. The most notable is the effect of the 8-minute response time target, which was designed to improve outcomes in life-threatening conditions. However, the proportion of attendees who require a category A response remains relatively low compared with non-emergency cases and, with the exception of out-of-hospital cardiac arrest, there is no evidence to support the current 8-minute response time target. 69 The tension between meeting performance targets and providing appropriate care is apparent from our data, which highlight a more recent move towards encouraging non-conveyance. Wankhade69 identifies prioritisation of the 8-minute response as a distraction from holistic care and other areas of perfomance (e.g. clinical outcomes) that emphasises short-term over long-term benefits, local rather than organisational objectives and stifles innovation. Our findings show that shifts in the demand profile and trust operational requirements mean that crews are under increasing pressure to combine complex decision-making and timeliness in the context of developing and maintaining the quality and safety of care.
The increased volume of 999 calls was regarded as placing a considerable strain on staff, vehicle and equipment resources. This is reinforced by findings from an ethnographic study of changes in the paramedic role, which identified work intensification and a target culture as placing huge pressures on ‘road staff’. 70
Staff roles, skills and development
Changes to service delivery associated with ‘taking healthcare to the patient’22 resulted in the introduction of new specialist paramedic roles (e.g. PPs, ECPs) and new patient care pathways to increase the scope for treat and refer decisions. However, our study highlights the limited and variable availability of these roles and pathways, both within and across services. A further challenge identified was the lack of understanding of these roles by other health professionals and service users, which can act as a barrier to ensuring appropriate care. Despite some resistance to new specialist roles,71 ECPs and PPs in our study were optimistic that this is being reduced through building trusting relationships with other practitioners. This is needed at a service level not just at the level of individual practitioners to ensure consistency in the operation of these new roles. Appropriate non-conveyance appears to be based on adequate training as well as confidence. Formal decision-making techniques can be taught to paramedics, but there is also evidence that experience and intuition come into play when first assessing patients,72 which despite being efficient can sometimes lead to errors because of cognitive bias. 73,74
A major issue for crews, identified as a priority in phase 3, was education and training. Our data highlight the range of roles and educational levels among crews. An increasing number of paramedics are educated to degree and masters level, with some undertaking specialist skills courses that were developed to address particular gaps in primary care and critical care provision. However, this higher level of education and training represents a minority of paramedics. There is some evidence that ECPs can deliver quality care safely75 and are having an impact on non-conveyance rates, with discharge rates upward of 20% greater than those for usual care,6,76,77 although the evidence for subsequent readmission or appropriateness of care is generally lacking. 77
The interface with other health and social care services
From a human factors and patient safety perspective,29 latent organisation-level system failures can lead to compromised work conditions. In our study, one of the main threats to decision-making about patient care, which was evident across all sites and all data collection methods, was a lack of other options for patient referral or assessment when A&E attendance was deemed unnecessary or inappropriate. When options were accessible, criteria for admission varied between organisations; therefore, variance of provision was more evident within sites than between them. For example, some geographical areas provided accessible out-of-hours services whereas others did not. Conveyance to A&E was often the default option to avoid delays or making an unsafe decision to leave a patient at the scene. Fragmentation of provision, as evidenced in our study, is acknowledged in recently published reports that emphasise the need for 24/7 seamless urgent and emergency care, mainly delivered by primary care services including pharmacies and outreach provision. 59,67
There is little existing evidence regarding the alternative community pathways that support non-conveyance to A&E. 3 However, there is evidence that conveyance rates are declining and that more alternatives are required. Snooks et al. 78 focused on the needs and outcomes of patients for whom emergency (999) calls to the ambulance service are made, showing that up to 52% of these patients do not require immediate medical care. Triage systems at the EOC and on scene that identify self-care or community-based care as a potential disposition carry significant safety risks. 78 For example, a controlled study of protocols for non-conveyance of patients showed no difference in conveyance rates between the intervention group and the control group but highlighted the complexity of implementation of protocols, suggesting that further development is required. 79 The use of protocols required more time on scene and safety concerns were identified in both the intervention group and the control group for patients not conveyed. However, Gray and Wardrope80 report that the risk to patients as well as the ambulance trust is increased by the lack of a coherent clinical governance framework for non-conveyance.
Non-conveyance has previously been studied with regard to what paramedics consider to be the perceived risks to their job when decisions to discharge patients at the scene are challenged. 14 Our findings also highlight concerns about the lack of options available, and there is evidence that some paramedics are fearful of the consequences if a referral does not proceed to plan. Past experience of impeded access and communication channels when paramedics try to hand over patient responsibility to community services exacerbates the situation as it engenders a reluctance to try these services again, resulting in low uptake of pathways. A related issue is the risk to patients of unnecessary transportation when there is little or no chance of survival. 78 Our findings highlighted the decision-making challenges associated with attending patients at the end of life when there is no clear plan or care package agreed with the primary provider. Paramedics in these situations feel bound to remain with the patient when an alternative referral cannot be made immediately, despite operational demands. This has a potential impact on other individuals using the ambulance service as it limits the resources available. In most cases it is deemed inappropriate to convey patients who are terminally ill to A&E. However, when well-designed and developed referral systems exist, clinical handover can mitigate against anxieties about patient safety following attendance as well as fears of potential litigation.
Communication and feedback to support decision-making
At the human factors level of teams, communication between management and crews generally appeared to be limited according to our data, mainly because of operational pressures and also a sense of distance between the two groups. Information was, at the same time, both overwhelming yet difficult to access because of pressure to be out on the road. This issue could be followed up in future research as meetings between professional levels are an important way of minimising risk through information sharing: ‘The greater emphasis placed on arrangements for formal communication, the lower the risk of adverse events’ (p. 27). 81 However, there was no evidence to suggest that crews were abandoning protocols or making decisions that were without clinical or academic reasoning or knowledge of the environment. It could be that information is shared in a less formal way, for example Waring and Bishop82 suggest that information sharing between colleagues can occur ‘backstage’ from clinical work. Participants in our study did suggest that shortcomings in feedback and information sharing, particularly in relation to clinical incidents, leave greater scope for the organisational ‘grapevine’ to fill the void, with negative stories often having greater currency.
Waring et al. 83 explored patient safety in operating theatres, describing the theatre setting as ‘closed off’ but with links to other departments. Adverse events could affect other departments and vice versa. The ambulance service setting differs from the operating theatre setting in that, although the ambulance and crew may appear ‘closed off’ in transit, they are also open in the sense of being mobile between a broad range of settings and in communication with a range of professionals. The operating theatre setting was also described as ‘chaotic’ at the boundaries, or interface between patient attendances and between departments, in that so much is going on at the same time and clinical staff might be attending to several tasks at once. 83 In the ambulance service setting, services that paramedics relied on for patient referrals were, apart from A&E departments, lacking in any kind of standardisation across the geographical area covered. This situation could be described as chaotic; however, decision-making at the scene appeared to follow the logical progression of a deductive approach.
Decisions were made at the scene without the opportunity to learn through constructive feedback about the outcomes of previous decisions. Feedback from incident reports has attracted more attention17 but crews remained ambivalent about reporting incidents; they recognised the importance of doing so but reported that they rarely had time to compete documentation after a shift. Communication about patients is important for safe continuous care, especially when patient care is transferred between services. Patients who cannot communicate effectively are particularly at risk when communication between clinicians is not clear. Risk can also be introduced when PRFs are illegible. 84 Our study shows that such issues are being addressed by using new technology such as the ePRF and IBIS. This electronic interface also has the potential to increase the extent of information shared by practitioners to allow more appropriate assessments and diagnosis, as well as standardising the form that the information takes.
Risk perception and management
In our study paramedics worked alone or in teams of two, often with a less qualified colleague; therefore, responsibility was not ‘diffused’ between professionals. 81 Clinicians spoke of the fear of losing their job or their licence to practice based on a decision that might, at a later date, be perceived as incorrect or inappropriate. When blame is attributed, West81 states that it is more likely to be aimed at operational clinicians at the mid-level of the organisation rather than at those at the top level or the bottom level because the decision-makers and the decisions made are more visible.
Some participants in our study had experienced the impact of complaints or disciplinary hearings, or witnessed similar incidents happening to colleagues, which were identified as potential influences on decision-making. Consequently, many paramedics conveyed patients to A&E rather than take the risk of leaving them without expert clinical care. Conveying as a default option to avert risk appeared to decrease with increased levels of training and experience, particularly as some specialist paramedic roles were developed to avoid unnecessary admission to hospital. However, for all paramedics, decisions not to convey patients were accompanied by an acute sense of accountability, resulting in rationalising, safety netting and documenting the reasons for that decision to mitigate personal risk.
Porter et al. 14 also report mistrust of managerial support from their participant crew members should anything go wrong following a decision to non-convey. The need for support in this area was voiced in our focus groups. Risk aversion was reported as driving crews to carry out lengthy documentation to support their decisions, an issue highlighted by Porter et al. 85 However, the main institutional impetus to develop a culture of safety has been around facilitating greater incident reporting. 17
Cook et al. 86 recommend that health-care providers proactively attempt to identify and bridge gaps that might appear in continuity of care, particularly following changes in the system. For example, providing the means by which paramedics can produce clear documentation may be one way of ensuring a patient’s smooth transition through different modes of care.
Findings from the ethnographic study of McCann et al. 70 into changes in the paramedic role are consistent with findings from our study; they comment that, contrary to the notion of paramedics having a degree of decision autonomy, fear of litigation, lack of support from managers and concerns over making errors and causing harm to patients result in self-limiting actions. The authors also emphasise the need for allocating resources to build on service improvements, for example more advanced training, new patient pathways and more sophisticated vehicles and information technology systems.
Safety culture reflects the extent to which patient safety is prioritised and supported. 87 Safety culture was a feature of the specific system influences identified in the study findings, for example reporting and learning from incidents. In addition, we used the MaPSaF tool to permit a more explicit and focused discussion of the safety culture in relation to various dimensions and levels of maturity. This also highlighted the variation regarding experiences of teamworking. Staff assessments were broadly consistent across sites, with the level of safety culture maturity across the various dimensions being characterised predominantly as bureaucratic but with aspects of reactive and proactive cultures on specific dimensions. The safety culture in relation to the three staff-related dimensions, including teamworking, was regarded by many as relatively less mature. A change to the staffing model at one of the sites (the introduction of the lower-skilled ECA) was felt quite strongly by some to reflect a shift towards a less mature safety culture.
The MaPSaF tool provided insights into perceptions of safety culture and the staff discussion did reflect the development of safety culture over time,37 as many staff felt that safety culture had become more of a priority and more systems were in place to support this. It also highlighted the perceived impact of organisational change.
The service user perspective
Service user concerns were largely consistent with those of staff but with more of a focus on the patient perspective and experience. One difference from the staff findings relates to the desire for patient involvement in decision-making, first, at the level of individual patient care, which can be challenging for staff when patient decisions are at odds with staff recommendations, and, second, at the level of commissioning services, to ensure that patient interests in relation to safe care are represented and that issues of dignity and acceptability are considered.
Strengths of the study
A major strength of this study was the use of a range of data collection and analysis methods that identified similar issues from different perspectives and, in the main, across sites. The various methods provided service users and ambulance service staff with a voice and this appeared to be valued by them. Ethnographic methods enabled patient contacts to be observed in real time, which verified many of the issues identified during staff focus groups. A number of ethnographic studies have examined patient safety issues;27,82,83 however, these are largely situated in the hospital context. These studies similarly highlight multiple interacting influences on safety. The current study provides new and in-depth understanding around decision-making. This is particularly important given the recent emphasis on developing the ambulance service to provide care closer to home. 68 If these objectives are to be achieved, the issues raised in our findings need to be considered.
The participation of three ambulance service sites in England allowed findings to be compared across staff and service user groups and across research methods. The three sites provided evidence associated with operating across rural, urban and coastal geographical areas as well as within a range of ambulance service management teams. Our findings show that there was much more variation in perceptions and practices between regions within the individual trusts than between the three trusts. The main issues raised from the qualitative enquiry applied cross-regionally and so it is probably fair to assume that these issues are national. However, we acknowledge that there may be idiosyncrasies, for example within central London there may be issues that relate to operating within the capital city compared with the provinces.
A team of researchers with varied backgrounds collected and analysed data for the study, including ambulance service and non-ambulance service staff. The aim was to allow comparison of data collected from ‘insider’ and ‘outsider’ perspectives to limit the bias that might arise from paramedics alone observing their peers. In practice, there was little difference between the forms of data produced except that registered paramedics reported observations using language that could be attributed to their paramedic training and experience. Each individual observer recorded data in a slightly different way, with some including more detail and/or quotations from the crews than others.
The study team comprised multidisciplinary expertise including academics with experience in risk research, paramedics, a GP, an A&E consultant, a nurse and members of the public. We ensured that there was strong service user involvement at all stages, from designing the study to recruitment, data collection and analysis of data, including editing the report. Many of the team members have carried out previous research in the field of emergency services and pre-hospital care. Others had experience of working within the ambulance service. The study benefited from the combined expertise and guidance of this team. Data were presented to the team at regular intervals for their feedback and input.
Limitations of the study
This was a relatively small-scale study employing qualitative methods to explore potential influences on decision-making and system risk factors. It did not include any measures of patient safety. The scope of the study was also limited in terms of its focus on front-line professionally registered ambulance staff. Although this provided a great deal of complex data, views from non-registered staff as well as health professionals providing services on the various referral pathways would have provided more balance in terms of perspective as well as adding to the explanatory ability of the findings. The study included staff in specialist paramedic roles although these represent a relatively small proportion of the overall sample. Phase 1 provided a limited management perspective on issues for further exploration in phase 2. Phase 3 focused on feedback from study participants as well as non-participant staff and service users; a wider range of views from ambulance service staff and stakeholders from linked service providers could have been sought.
Although the study focused on system influences on decision-making, the scope of the study did not include observations within the control room, nor were we able to obtain the views of NHS staff working alongside the ambulance service, such as GPs and A&E staff.
Participants in the study were generally a self-selected group who were possibly more proactive in terms of engagement with training and research. Similarly, participating service users had a specific interest in this topic. This limitation was difficult to control and is a common characteristic of the recruitment process. It was not possible to examine the complete patient journey from call taking to triage and handover, referral or discharge. The study has focused on part of the journey and transitions arising from decisions made by paramedics.
At one site the university researcher was not able to carry out observations because of unforeseen circumstances. This meant that extra shifts were taken on by the ambulance service researcher; this was challenging as the shifts needed to be completed within a part-time secondment to the study. The principal investigator maintained regular contact with the ambulance service researcher during data collection and the university researcher was available for data analysis. As far as could be discerned, there did not appear to be a significant variation between the nature of the data collected by the researcher at this site and the nature of the data collected at the other two sites.
Challenges
Although we acknowledge the strengths of using a range of data collection methods, which produced a large volume of data, this had to be managed within a finite timespan. Transcribing and analysing data was time-consuming as well as complex. Many of the issues raised in the data were intertwined, making distinct themes difficult to identify.
The practicalities of data collection were challenged by the multisite and multiresearcher design, particularly with regard to the digital diaries. In total, five researchers were distributing audio recorders out in the field; this required close monitoring of where audio recorders were at any given time. Data protection was managed by the use of encrypted data sticks and a shared document folder that was set up within the University of Sheffield computer network.
At times, potential participants were obliged to focus on operational commitments, particularly during winter, which meant that they were no longer able to take part in the study. The recruitment of paramedics for observations and focus groups was a challenge, mainly because of the time-bound and mobile nature of shift work. In addition, carrying out observations for the study was competing, in terms of arranging shifts with the requirements of other observers, such as student paramedics.
Having office-based individuals responsible for contacting crews was a strength at two sites, particularly in recruiting non-participant workshop attendees. Setting up observation shifts required familiarisation with different protocols at each site and logistically was challenging for researchers because of the duration and timing of shifts and having to travel away from home.
Chapter 8 Conclusions and recommendations
The aim of this study was to explore the range and nature of influences on safety in decision-making by ambulance service staff (paramedics). A qualitative approach was adopted using a range of complementary methods. The study has provided insights on the types of decisions that staff engage in on a day-to-day basis. It has also identified a range of system risk factors influencing decisions about patient care. Although this was a relatively small-scale exploratory study, confidence in the generalisability of the headline findings is enhanced by the high level of consistency in the findings, obtained using multiple methods, and the notable consensus among participants.
The seven predominant system influences identified should not be considered discrete but as overlapping and complementary issues. They also embody a range of subthemes that represent topics for future research and/or intervention.
The apparently high level of consistency across the participating trusts suggests that the issues identified may be generic and relevant to other ambulance service trusts.
In view of the remit of this study, aspects relating to system weaknesses and potential threats to patient safety dominate in the account of findings. However, it should be noted that respondent accounts also provided examples of systems that were said to be working well, for example specific care management pathways, local roles and ways of working and technological initiatives such as IBIS and the ePRF.
Implications for health care
The NHS system within which the ambulance service operates is characterised in our study as fragmented and inconsistent. For ambulance service staff the extent of variation across the geographical areas in which they work is problematic in terms of knowing what services are available and being able to access them. The lack of standardisation in practice guidelines, pathways and protocols across services and between areas makes it particularly challenging for staff to keep up to date with requirements in different parts of their own trust locations and when crossing trust boundaries. Although a degree of consistency across the network is likely to improve the situation, it is also desirable to have sufficient flexibility to accommodate the needs of specific local populations. There was some concern over the potential for further fragmentation with the increased number of CCGs.
Ambulance services are increasingly under pressure to focus on reducing conveyance rates to A&E; this arguably intensifies the need to ensure that crews are appropriately skilled to be able to make effective decisions over the need to convey or not to convey if associated risks to patients are to be minimised. Our findings highlight the challenges of developing staff and ensuring that their skills are utilised where they are most needed within the context of organisational resource constraints and operational demands. Decisions over non-conveyance to A&E are moderated by the availability of alternative care pathways and providers. There were widespread claims of local variability in this respect. Staff training and development, and access to alternatives to A&E, were identified as priorities for attention by workshop attendees.
One of the difficulties for ambulance services is that they operate as a 24/7 service within a wider urgent and emergency care network that, beyond A&E, operates a more restricted working day. The study findings identify this as problematic for two reasons. First, it fuels demand for ambulance service care as a route to timely treatment, when alternatives may involve delay. Second, it contributes to inappropriate conveyance to A&E because more appropriate options are unavailable or limited during out-of-hours periods. Ultimately, this restricts the scope for ensuring that patients are getting the right level of care at the right time and place. Study participants identified some patient populations as particularly poorly served in terms of alternatives to A&E (e.g. those with mental health issues, those at the end of life, older patients and those with chronic conditions).
The effectiveness of the paramedic role in facilitating access to appropriate care pathways hinges on relationships with other care providers (e.g. primary care, acute care, mental health care, community health care). An important element relates to the cultural profile of paramedics in the NHS, specifically, the extent to which other health professionals and care providers consider the clinical judgements/decisions made by paramedics as credible and actionable. Staff identified this as a barrier to access where the ambulance service is still viewed primarily as a transport service. Consideration could be given to ways of improving effective teamworking and communication across service and professional boundaries.
Although paramedics acknowledged the difficulties of telephone triage, they also identified how the limitations of this system impact on them. Over-triage at the initial call-handling stage places considerable demands on both staff and vehicle resources. A related concern is the limited information conveyed to crews following triage. Initial triage was suggested as an area that warrants attention to improve resource allocation.
The findings highlight the challenges faced by front-line ambulance service staff. It was apparent that the extent and nature of the demand for ambulance conveyance represents a notable source of strain and tension for individuals and at an organisational level. For example, there were widespread claims that meeting operational demands for ambulance services limits the time available for training and professional development, with this potentially representing a risk for patients and for staff. Staff perceptions of risk relating to patient safety extend to issues of secondary risk management, that is, personal and institutional liabilities, in particular risks associated with loss of professional registration. The belief that they are more likely to be blamed than supported by their organisation in the event of an incident was cited by staff as a source of additional anxiety when making more complex decisions. This perceived vulnerability can provoke excessively risk-averse decisions. These issues merit further attention to examine the workforce implication of service delivery changes, including how to ensure that staff are appropriately equipped and supported to deal effectively with the demands of their role.
Paramedics identified a degree of progress in relation to the profile of patient safety within their organisations but the apparent desire within trusts to prioritise safety improvement was felt to be constrained by service demands and available resources. Attempts to prioritise patient safety appear to focus on ensuring that formal systems are in place (e.g. reporting and communication). Concerns were expressed over how well these systems function to support improvement, for example how incident reports are responded to and whether lessons learned are communicated to ambulance staff within and between trusts. Consideration could be given to identifying ways of supporting ambulance service trusts to develop the safety culture within their organisation.
Service users attributed the increased demand for ambulance services to difficulties in identifying and accessing alternatives. They were receptive to non-conveyance options but felt that lack of awareness of staff roles and skills may cause concern when patients expect conveyance to A&E.
Recommendations for research
The workshop attendees identified a range of areas for attention in relation to intervention and research, which are provided in Chapter 6 (see Suggestions for potential interventions and research). The following recommendations for research are based on the study findings:
-
Limited and variable access to services in the wider health and social care system is a significant barrier to reducing inappropriate conveyance to A&E. More research is needed to identify effective ways of improving the delivery of care across service boundaries, particularly for patients with limited options at present (e.g. those with mental health issues, those at the end of life and older patients). Research should address structural and attitudinal barriers and how these might be overcome.
-
Ambulance services are increasingly focused on reducing conveyance to A&E and they need to ensure that there is an appropriately skilled workforce to minimise the potential risk. The evidence points to at least two issues: (1) training and skills and (2) the cultural profile of paramedics in the NHS, that is, whether others view their decisions as credible. Research could explore the impact of enhanced skills on patient care and on staff, for example the impact of increased training in urgent rather than emergency care. This would also need to address potential cultural barriers to the effective use of new skills.
-
Research to explore the impact of different aspects of safety culture on ambulance service staff and the delivery of patient care (e.g. incident reporting, communication, teamworking, and training) could include comparisons across different staff groups and the identification of areas for improvement, as well as interventions that could potentially be tested.
-
The increased breadth of decision-making by ambulance service crews with advanced skills includes more diagnostics; therefore, there is a need to look at the diagnostic process and potential causes of error in this environment.
-
There is a need to explore whether there are efficient and safe ways of improving telephone triage decisions to reduce over-triage, particularly in relation to calls requiring an 8-minute response. This could include examining training and staffing levels, a higher level of clinician involvement or other forms of decision support.
-
There is a need to explore public awareness of, attitudes towards, beliefs about and expectations of the ambulance service and the wider urgent and emergency care network and the scope for behaviour change interventions, for example communication of information about access to and use of services; empowering the public through equipping them with the skills to directly access the services that best meet their needs; and informing the public about the self-management of chronic conditions.
-
A number of performance measures were identified engendering perverse motivations leading to suboptimal resource utilisation. An ongoing NIHR Programme Grant for Applied Research (RP-PG-0609–10195; ‘Pre-hospital Outcomes for Evidence-Based Evaluation’) aims to develop new ways of measuring ambulance service performance. It is important that evaluations of new performance metrics or other innovations (e.g. Make Ready ambulances, potential telehealth technologies or decision-support tools) address their potential impact on patient safety.
Acknowledgements
We would like to thank the following for their contribution to the study: staff participants at the three ambulance service trusts; service user participants from the three ambulance service trust areas; the Sheffield Emergency Care Forum (public and ambulance service representatives) for their advisory input and contribution to study progression, including ethics submissions and feedback on findings (Rosemary Harper, Beryl Darlison, Maggie Marsh, Jessica Abouzeid, Shan Bennett, Lisa Ashley, Simon Brown, Andy Pike, Thomas Drake, Daniel Bradbury and Chris Richmond); Annie Palmer (East Midlands Ambulance Service), Anita Smith (South East Coast Ambulance Service) and Angela Rayner (South East Coast Ambulance Service) for assistance in recruiting service users; Samantha Smithson (Yorkshire Ambulance Service) for assistance in arranging observation shifts; Jo Byers and Julia Williams (South East Coast Ambulance Service) and Anne Spaight (East Midlands Ambulance Service) for advice and assistance to support study progress; and Dr Joanne Fisher (University of Warwick) for feedback on SDO-funded project 10/1008/12 (Patient Safety in UK Ambulance Services – a Scoping Review).
Contribution of authors
Dr Rachel O’Hara (Lecturer, Public Health) was the lead investigator with regard to the conception, design and overall management of the study, including data analysis and report writing. She managed the staff and service user focus groups (data collection and analysis).
Dr Maxine Johnson (Research Fellow, Public Health) was the lead researcher for phase 1 and phase 2 ethnographic data collection and analysis. She contributed to project management activities, the feedback workshops and report writing.
Mrs Enid Hirst (PPI/service user representative) was a co-investigator. She contributed to the original proposal, service user recruitment and data collection, analysis of staff and service user focus group data and report writing.
Dr Andrew Weyman (Senior Lecturer, Psychology) was a co-investigator. He contributed to the original proposal, the staff focus groups (data collection and analysis), the prioritisation task development and analysis and report writing.
Miss Deborah Shaw (Research Manager, Ambulance Service) was an ambulance service researcher. She led on local staff recruitment and data collection and contributed to data analysis and report writing.
Mr Peter Mortimer (Research and Development Manager, Ambulance Service) was an ambulance service researcher. He led on local staff recruitment and data collection and contributed to data analysis and report writing.
Mr Chris Newman (Paramedic) was an ambulance service researcher. He led on local staff recruitment and data collection and contributed to data analysis.
Mr Matthew Storey (Paramedic) was an ambulance service researcher. He assisted with local staff recruitment and data collection and contributed to data analysis.
Ms Janette Turner (Senior Research Fellow, Emergency Care) was a co-investigator. She contributed to the original proposal, the service user focus groups and workshops, the analysis and report writing.
Professor Suzanne Mason (Professor of Emergency Medicine) was a co-investigator. She contributed to the original proposal and supported various aspects of study development and progression.
Professor Tom Quinn (Professor of Clinical Practice) was a co-investigator and lead local investigator. He contributed to the original proposal, supported local project management, reviewed the data analysis, provided input to the feedback workshop and contributed to report writing.
Mrs Jane Shewan (Head of Research and Development, Ambulance Service) was a co-investigator and lead local investigator. She contributed to the original proposal, supported local project management, reviewed the data analysis and provided input to the feedback workshop.
Professor Niroshan Siriwardena (Professor of Primary and Prehospital Health Care) was a co-investigator and lead local investigator. He contributed to the original proposal, supported local project management, reviewed the data analysis, provided input to the feedback workshop and contributed to report writing.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Nicholl JP, Gilhooley K, Parry G, Turner J, Dixon S. The Safety and Reliability of Priority Dispatch Systems. Final Report to the Department of Health. Sheffield: Medical Care Research Unit, University of Sheffield; 1996.
- Deakin CD, Sherwood DM, Smith A, Cassidy M. Does telephone triage of emergency (999) calls using advanced medical priority dispatch (AMPDS) with Department of Health (DH) call prioritisation effectively identify patients with an acute coronary syndrome? An audit of 42,657 emergency calls to Hampshire Ambulance Service NHS Trust. Emerg Med J 2006;23:232-5. http://dx.doi.org/10.1136/emj.2004.022962.
- Turner J. Building the Evidence Base in Pre-Hospital Urgent and Emergency Care: A Review of Research Evidence and Priorities for Future Research. London: Department of Health; 2010.
- Mason S, Coleman P, Keeffe C, Ratcliffe J, Nicholl J. The evolution of the emergency care practitioner role in England: experiences and impact. Emerg Med J 2006;23:435-9. http://dx.doi.org/10.1136/emj.2005.027300.
- Cooper S, O’Carroll J, Jenkin A, Badger B. Collaborative practices in unscheduled emergency care: role and impact of the emergency care practitioner. Quantitative findings. Emerg Med J 2007;24:630-3. http://dx.doi.org/10.1136/emj.2007.048058.
- Mason S, O’Keeffe C, Coleman P, Edlin R, Nicholl J. Effectiveness of emergency care practitioners working within existing emergency service models of care. Emerg Med J 2007;24:239-43. http://dx.doi.org/10.1136/emj.2006.035782.
- Gray JT, Walker A. Is referral to emergency care practitioners by general practitioners in-hours effective?. Emerg Med J 2009;26:611-12. http://dx.doi.org/10.1136/emj.2008.059956.
- Cooke M, Fisher JD, Dale J, McLeod E, Szczepura A, Walley P, et al. Reducing Attendances and Waits in Emergency Departments: A Systematic Review of Present Innovations. London: National Co-ordinating Centre for NHS Service Delivery and Organisation R&D; 2005.
- Halter M, Ellison G. Evaluation of the Emergency Care Practitioner Role in London: A Study of the Processes and Outcomes of Clinical Decision-Making. London: Faculty of Health and Social Care Sciences, University of London; 2008.
- Mason S, Knowles E, Freeman J, Snooks H. Safety of paramedics with extended skills. Acad Emerg Med 2008;15:607-12. http://dx.doi.org/10.1111/j.1553-2712.2008.00156.x.
- Mason S, O’Keeffe C, Coleman P, O’Hara R, Dixon S, Rick J, et al. A Multi-Centre Community Intervention Trial to Evaluate the Clinical and Cost Effectiveness of Emergency Care Practitioners. London: National Coordinating Centre for the Service Delivery and Organisation (NCCSDO) research programme, managed by the London School of Hygiene & Tropical Medicine; 2009.
- McPherson K, Kersten P, George S, Lattimer V, Ellis B, Breton A, et al. Extended Roles for Allied Health Professionals in the NHS. London: National Co-ordinating Centre for NHS Service Delivery and Organisation R&D; 2004.
- Snooks HA, Halter M, Close JCT, Cheung WY, Moore F, Roberts SE. Emergency care of older people who fall: a missed opportunity. Qual Saf Health Care 2006;15:390-2. http://dx.doi.org/10.1136/qshc.2006.018697.
- Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. ‘Should I stay or should I go?’ Deciding whether to go to hospital after a 999 call. J Health Serv Res Policy 2007;12:32-8. http://dx.doi.org/10.1258/135581907780318392.
- Halter M, Vernon S, Snooks H, Porter A, Close J, Moore F, et al. Complexity of the decision-making process of ambulance staff for assessment and referral of older people who have fallen: a qualitative study. Emerg Med J 2011;28:44-50. http://dx.doi.org/10.1136/emj.2009.079566.
- Klein G. Naturalistic decision-making. Hum Factors 2008;50:456-60. http://dx.doi.org/10.1518/001872008X288385.
- An Organisation with a Memory: Report of an Expert Group on Learning from Adverse Events in the NHS. London: Department of Health; 2000.
- Reason J. Human error: models and management. BMJ 2000;320:768-70. http://dx.doi.org/10.1136/bmj.320.7237.768.
- Seven Steps to Patient Safety. London: National Patient Safety Agency; 2004.
- Kirk S, Parker D, Claridge T, Esmail A, Marshall M. Patient safety culture in primary care: developing a theoretical framework for practical use. Qual Saf Health Care 2007;16:313-20. http://dx.doi.org/10.1136/qshc.2006.018366.
- Quarterly Data Summaries. London: National Patient Safety Agency; 2012.
- Taking Healthcare to the Patient: Transforming NHS Ambulance Services. London: Department of Health; 2005.
- Darzi A. High Quality Care for All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Snooks H, Evans A, Wells B, Peconi J, Thomas M, Archer F, et al. What are the highest priorities for research in pre-hospital care? Results of a review and Delphi consultation exercise. J Emerg Prim Health Care 2008;6.
- Vincent C. Patient Safety. London: Elsevier; 2006.
- Turner J, Snooks H, Youren A, Dixon S, Fall D, Gaze S, et al. The Costs and Benefits of Managing Some Low Priority 999 Ambulance Calls by NHS Direct Nurse Advisers 2006.
- Dixon-Woods M. Why is patient safety so hard? A selective review of ethnographic studies. J Health Serv Res Policy 2010;15:11-6. http://dx.doi.org/10.1258/jhsrp.2009.009041.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154-7. http://dx.doi.org/10.1136/bmj.316.7138.1154.
- Patton MQ. Qualitative Reserach and Evaluation Methods. Thousand Oaks, CA: Sage; 2002.
- Mays N, Pope C, British MJ. Qualitative Research in Health Care. Oxford: Wiley Online Library; 2000.
- Legard R, Keegan J, Ward K, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Hammersley M, Atkinson P. Ethnography; Principles in Practice. London: Routledge; 1995.
- Walshe C, Ewing G, Griffiths J. Using observation as a data collection method to help understand patient and professional roles and actions in palliative care settings. Palliat Med 2012;26:1048-54. http://dx.doi.org/10.1177/0269216311432897.
- Bolger N, Davis A, Rafaeli E. Diary methods: capturing life as it is lived. Annu Rev Psychol 2003;54:579-616. http://dx.doi.org/10.1146/annurev.psych.54.101601.145030.
- Morgan DL. Focus Groups as Qualitative Research. London: Sage; 1997.
- Parker D. Managing risk in healthcare: understanding your safety culture using the Manchester Patient Safety Framework (MaPSaF). J Nurs Manag 2009;17:218-22. http://dx.doi.org/10.1111/j.1365-2834.2009.00993.x.
- Richards T. Patients’ priorities. BMJ 1999;318. http://dx.doi.org/10.1136/bmj.318.7179.277.
- Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach. Health Technol Assess 2004;8. http://dx.doi.org/10.3310/hta8150.
- Bock RD, Jones JV. The Measurement and Prediction of Judgment and Choice. San Franciso, CA: Holden-Day; 1968.
- David HA. The Method of Paired Comparisons. London: Charles Griffin; 1988.
- Comer MK, Seaver DA, Stillwell WG, Gaddy CD. Generating Human Reliability Estimates Using Expert Judgment. Volume 2. Appendices. Albuquerque, NM: Sandia National Laboratories; 1984.
- Weyman A, Clarke DD. Investigating the influence of organizational role on perceptions of risk in deep coal mines. J Appl Psychol 2003;88:404-12. http://dx.doi.org/10.1037/0021-9010.88.3.404.
- Weyman A, Pidgeon NF, Walls J, Horlick-Jones T. Exploring comparative ratings and constituent facets of public trust in risk regulatory bodies and related stakeholder groups. J Risk Res 2006;9:605-22. http://dx.doi.org/10.1080/13669870600799812.
- Equity and Excellence: Liberating the NHS. London: The Stationery Office; 2010.
- Transforming NHS Ambulance Services. London: Department of Health; 2011.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Health and Social Care Act 2012. London: The Stationery Office; n.d.
- Association of Ambulance Chief Executives . Measuring Patient Outcomes: Clinical Quality Indicators n.d. http://aace.org.uk/national-performance/ (accessed 2 September 2014).
- High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England. The Evidence Base from the Urgent and Emergency Care Review. Leeds: NHS England; 2013.
- AMPDS Call Categorisation Version 11. London: Her Majesty’s Stationery Office; 2005.
- Right Skill, Right Time, Right Place. The ECP Report. London: Department of Health; 2004.
- Widiatmoko D, Machen I, Dickinson A, Williams J, Kendall S. Developing a new response to non-urgent emergency calls: evaluation of a nurse and paramedic partnership intervention. Prim Health Care Res Dev 2008;9:183-90. http://dx.doi.org/10.1017/S1463423608000765.
- Dixon S, Mason S, Knowles E, Colwell B, Wardrope J, Snooks H, et al. Is it cost effective to introduce paramedic practitioners for older people to the ambulance service? Results of a cluster randomised controlled trial. Emerg Med J 2009;26:446-51. http://dx.doi.org/10.1136/emj.2008.061424.
- von Vopelius-Feldt J, Benger J. Who does what in prehospital critical care? An analysis of competencies of paramedics, critical care paramedics and prehospital physicians [published online ahead of print 21 August 2013]. Emerg Med J 2013. http://dx.doi.org/10.1136/emermed-2013-202895.
- von Vopelius-Feldt J, Wood J, Benger J. Critical care paramedics: where is the evidence? A systematic review [published online ahead of print 26 September 2013]. Emerg Med J 2013. http://dx.doi.org/10.1136/emermed-2013-202721.
- Collen A. IBIS – anticipatory care planning when patients call 999. Breath Matters 2012;12:1-3.
- ProcessFlows Ltd . Information Gathered Today Will Ultimately Improve Patient Care Tomorrow 2013. http://processflows.co.uk/data-capture (accessed 10 October 2014).
- A Vision for Emergency and Urgent Care: The Role of Ambulance Services. London: NHS Confederation; 2008.
- Ambulance Services, England – 2012–13. Leeds: Health and Social Care Information Centre; 2013.
- Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf 2006;32:167-75.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: a Guide for Social Science Students and Researchers. London: Sage; 2003.
- Ferguson GA. Statistical Analysis in Psychology and Education. New York: McGraw-Hill; 1959.
- Report on the Review of Patient-Identifiable Information. The Caldicott Report. London: Department of Health; 1997.
- Mason S, Wardrope J, Perrin J. Developing a community paramedic practitioner intermediate care support scheme for older people with minor conditions. Emerg Med J 2003;20:196-8. http://dx.doi.org/10.1136/emj.20.2.196.
- Martin N, Newbury-Birch D, Duckett J, Mason H, Shen J, Shevills C, et al. A retrospective analysis of the nature, extent and cost of alcohol-related emergency calls to the ambulance service in an English region. Alcohol Alcohol 2012;47:191-7. http://dx.doi.org/10.1093/alcalc/agr158.
- Fernandes A. Guidance for Commissioning Integrated Urgent and Emergency Care: A ‘Whole System’ Approach. London: Royal College of General Practitioners Centre for Commissioning; 2011.
- Keogh B. High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England – Urgent and Emergency Care Review End of Phase 1 Report. London: NHS England; 2013.
- Wankhade P. Performance measurement and the UK emergency ambulance service: unintended consequences of the ambulance response time targets. Int J Public Sector Manag 2011;24:384-402. http://dx.doi.org/10.1108/09513551111147132.
- McCann L, Granter E, Hyde P, Hassard J. Still blue collar after all these years? An ethnography of the professionalization of emergency ambulance work. J Manag Stud 2013;50:750-76. http://dx.doi.org/10.1111/joms.12009.
- Squires JP, Mason S. Developing alternative ambulance response schemes: analysis of attitudes, barriers, and change. Emerg Med J 2004;21:724-7. http://dx.doi.org/10.1136/emj.2004.016923.
- Snooks HA, Kearsley N, Dale J, Halter M, Redhead J, Foster J. Gaps between policy, protocols and practice: a qualitative study of the views and practice of emergency ambulance staff concerning the care of patients with non-urgent needs. Qual Saf Health Care 2005;14:251-7. http://dx.doi.org/10.1136/qshc.2004.012195.
- Kahneman D. Thinking, Fast and Slow. London: Allen Lane/Penguin Books; 2011.
- Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 2003;78:775-80. http://dx.doi.org/10.1097/00001888-200308000-00003.
- O’Hara R, O’Keeffe C, Mason S, Coster JE, Hutchinson A. Quality and safety of care provided by emergency care practitioners. Emerg Med J 2012;29:327-32. http://dx.doi.org/10.1136/emj.2010.104190.
- Hill H, McMeekin P, Price C. A systematic review of the activity and impact of emergency care practioners in the NHS [published online ahead of print 13 July 2013]. Emerg Med J 2013. http://dx.doi.org/10.1136/emermed-2013-202660.
- Tohira H, Williams TA, Jacobs I, Bremner A, Finn J. The impact of new prehospital practitioners on ambulance transportation to the emergency department: a systematic review and meta-analysis [published online ahead of print 15 November 2013]. Emerg Med J 2013. http://dx.doi.org/10.1136/emermed-2013-202976.
- Snooks HA, Kingston MR, Anthony RE, Russell IT. New models of emergency prehospital care that avoid unnecessary conveyance to emergency department: translation of research evidence into practice?. Sci World J 2013. http://dx.doi.org/10.1155/2013/182102 (accessed 9 September 2014).
- Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung WY. Towards primary care for non-serious 999 callers: results of a controlled study of ‘treat and refer’ protocols for ambulance crews. Qual Saf Health Care 2004;13:435-43. http://dx.doi.org/10.1136/qshc.2003.007658.
- Gray JT, Wardrope J. Introduction of non-transport guidelines into an ambulance service: a retrospective review. Emerg Med J 2007;24:727-9. http://dx.doi.org/10.1136/emj.2007.048850.
- West E, Walshe K, Boaden R. Patient Safety: Research into Practice. Buckingham: Open University Press; 2006.
- Waring J, Bishop S. ‘Water cooler learning’: knowledge sharing at the clinical ‘backstage’ and its contribution to patient safety. J Health Organ Manag 2010;24:325-42. www.emeraldinsight.com/doi/abs/10.1108/14777261011064968.
- Waring J, McDonald R, Harrison S. Safety and complexity: inter-departmental relationships as a threat to safety in the operating department. J Health Organ Manag 2006;20:227-42. http://dx.doi.org/10.1108/14777260610662753.
- Redfern E, Brown R, Vincent CA. Improving communication in the emergency department. Emerg Med J 2009;26:658-61. http://dx.doi.org/10.1136/emj.2008.065623.
- Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. Covering our backs: ambulance crews attitudes towards clinical documentation when emergency (999) patients are not conveyed to hospital. Emerg Med J 2008;25. http://dx.doi.org/10.1136/emj.2007.050443.
- Cook RI, Render M, Woods DD. Gaps in the continuity of care and progress on patient safety. BMJ 2000;320:791-4. http://dx.doi.org/10.1136/bmj.320.7237.791.
- Research Scan: Does Improving Safety Culture affect Patient Outcomes?. London: The Health Foundation; 2011.
- Manchester Patient Safety Framework–Ambulance. 2006.
Appendix 1 Phase 1 information sheet
Decision-making and safety in emergency care transitions: phase 1
Information sheet
You are being invited to take part in a research study. Before you decide it is important for you to understand why the research is being done and what it will involve. Please take time to read the following information carefully and decide whether or not you wish to take part. Discuss it with others if you wish and ask the research team if anything is not clear or if you would like more information.
1. What is the purpose of the study?
A team of researchers from the Universities of Sheffield, Lincoln, Surrey and Bath are carrying out research to explore the influences on safe decision-making by emergency care staff. The aim is to understand how staff make tough clinical decisions and to identify areas where safety could be improved and where there are examples of good practice. This research is funded by the National Institute for Health Research (NIHR).
You are being invited to take part in phase 1 of this three-phase study.
Phase 1 aims to gain an understanding of the emergency care system, care pathways, linked services, safety critical decisions and organisational characteristics that may affect patient safety in ambulance services.
Phase 2 will explore the various influences on decision-making around specific transition points in patient care (e.g. control room response; treat and leave at scene; pre-alerts during transport to the emergency department; bypass of the emergency department and direct transfer to specialist units; and transfer through other care pathways to community services).
Phase 3 will feed back findings to those involved.
2. Why have I been invited to take part?
We are asking key staff and representatives of different staff roles in three different ambulance services to take part in interviews to help us gain an understanding of the range of factors that may influence patient safety in ambulance services. You are being invited to take part because it is considered that you could provide us with relevant information.
3. Do I have to take part?
It is up to you to decide whether or not to take part. If you do decide to take part you will be given this information sheet to keep (and be asked to sign a consent form). You are free to withdraw at any time.
4. What will happen if I take part in an interview?
You will be invited to attend an interview with a researcher, who will ask questions about the key transition points in pre-hospital emergency care and about aspects of the organisation that may influence decisions about patient care, for example resources (e.g. funding; facilities; staffing – numbers, training), service demands (e.g. patient numbers; geographical coverage; performance targets) and the organisation of service delivery (e.g. network of providers; protocols and guidelines).
The interview may be conducted face-to-face at your workplace or over the telephone, at a time that is convenient to you. It is expected to last no longer than 1 hour. With your permission the interview will be audio recorded. The recordings will be transcribed and analysed before being destroyed. If you do not want to be recorded the researcher will take notes instead.
5. What about confidentiality?
As the interviews will involve a relatively small number of key staff and staff representatives in each organisation to provide an understanding of service delivery we cannot guarantee confidentiality or anonymity.
In the event that the information you provide identifies a significant safety concern (e.g. not reporting serious equipment malfunctions), the local collaborator for the research team may decide to report this information via the local reporting system.
6. What will happen to the information that I provide?
The information from the interviews will be transcribed and analysed by members of the research team and findings will be included in a research report for the funders and additional publications to communicate the study findings. The findings may include quotations.
Phase 3 of this study includes a workshop where key findings from phases 1 and 2 will be presented. At the end of the overall study a full copy of the report will be available on the NIHR website.
All research information will be stored on password-protected university computers/laptops, on encrypted data sticks or in a locked cupboard on university premises and will be accessible only to members of the research team. Any personal details will be stored separately and will be destroyed at the end of the overall research study. Paperwork and audio recordings will be destroyed 12 months later. One copy of the electronic data set (with identifying information removed) will be kept in secure university storage for the purposes of research audit/monitoring and will be destroyed 7 years after the study ends.
7. Who has ethically reviewed the project?
Phase 1 of the study ‘Decision-making and safety in emergency care transitions’ has been ethically approved by the School of Health and Related Research (ScHARR), University of Sheffield.
8. Contact for further information.
For further information, please contact:
Maxine Johnson (Research Fellow)
E-mail:
Telephone:
Address:
If you have any concerns about the study or any aspect of the way you have been approached or treated during the course of this study, please contact:
Dr Rachel O’Hara (Principal Investigator)
E-mail:
Telephone:
Address:
Appendix 2 Phase 1 interview topic guide
Decision-making and safety in emergency care transitions: phase 1
Interview topic guide
Introduction
-
Thank you for seeing me today and offering to take part in this study.
-
I would like first to outline the study so that you are able to decide whether you wish to proceed further (recap information sheet).
-
Sign consent form × 2 (one for participant and information sheet, one for interviewer).
-
I have a list of topics that I want to address.
-
Feel free to ask questions at any stage during the interview.
-
I might make a few notes in case I want to come back to something later.
Topics/questions
-
Background information on the interviewee.
-
Current and any prior relevant roles/responsibilities, training, duration in employment.
-
-
Identify and elicit details on the key transition points in pre-hospital emergency care in their organisation (elicit any examples of increased and reduced risk for patients).
For example:
-
control room response
-
treat and leave at scene
-
pre-alerts during transport to emergency department
-
bypass of the emergency department and direct transfer to specialist units
-
transfer through other care pathways to community services
-
others . . .
-
-
Identify and elicit details on specific patient characteristics/conditions where there is increased risk and where risk has been reduced.
For example:
-
head injury or falls;
-
suspected respiratory conditions (asthma or respiratory infection, COPD)
-
cardiovascular conditions (chest pain or weakness)
-
abdominal (pain or urinary) symptoms
-
others . . .
-
-
Identify and elicit details on aspects of the emergency care system in their organisation that may influence decisions about patient care and safety (elicit any examples of increased and reduced risk for patients).
For example:
-
resources (e.g. funding; facilities; staffing – numbers, training; teams; work environment)
-
task/service demands (e.g. patient numbers; geographical coverage; performance targets)
-
organisation and management of service delivery (e.g. care pathways, linked services, network of providers; protocols and guidelines)
-
others . . .
-
-
Identify and elicit details on perceived threats to the delivery of safe patient care.
-
Areas where strategies are needed to improve patient safety.
-
-
Identify and elicit details on perceived strengths in relation to the delivery of safe patient care.
-
Examples of good practice.
-
Lessons that can be learned/shared.
-
-
Identify potential areas to focus on in phase 2 of the study.
-
Areas where further research is needed.
-
-
Anything else that the interviewee feels has been missed and anything that they did not get a chance to discuss fully.
-
Anyone else that would be useful to speak to.
End of interview – thank you.
Appendix 3 Phase 2 staff information sheet
Decision-making and safety in emergency care transitions: phase 2
Information sheet
You are being invited to take part in a research study. Before you decide it is important for you to understand why the research is being done and what it will involve. Please take time to read the following information carefully and discuss it with others if you wish. Ask the research team if anything is not clear or if you would like more information. Take time to decide whether or not you wish to take part.
1. What is the purpose of the study?
A team of researchers from the Universities of Sheffield, Lincoln, Surrey and Bath are carrying out research to explore decision-making by ambulance service staff. The aim is to understand how staff makes tough clinical decisions, to identify influences on these decisions and patient safety. This research is funded by the National Institute for Health Research (NIHR).
The second stage of this research is an exploratory study of what influences decisions made at key transition points in patient care (e.g. control room response; treat and leave at scene; pre-alerts during transport to emergency department; bypass of the emergency department and direct transfer to specialist units; and transfer through other care pathways to community services).
We are seeking volunteers from a range of staff involved in the delivery of care across three different ambulance services and would welcome your participation.
2. Do I have to take part?
It is up to you to decide whether or not to take part. If you decide to take part you will be given this information sheet to keep and asked to sign a consent form before participating in any research activities. You are free to withdraw from the study at any time, without giving a reason and without it affecting you in any way.
3. What will taking part involve?
You are invited to take part in any or all of the following study activities:
Observation: This will involve observing (shadowing) staff carrying out their normal day-to-day activities. It will also include asking questions about decisions where possible, but will not interfere with your work activities. Handwritten notes will be used to record observations. Answers to questions may be audio recorded with permission. Researchers will not record any patient-identifying information. Staff being observed can determine situations when observation is not appropriate.
Interview: This will involve further exploration or clarification of information relevant to observations. An interview will last 30–50 minutes as appropriate and take place on ambulance service premises.
‘Digital diary’: A digital audio recorder will be provided to record your thoughts about key decisions made about patient care over several shifts and any issues or concerns. Staff and patient-identifying information should not be recorded. The diary (recorder) will be collected by the researcher on site.
Focus group: This will involve taking part in a group discussion with around seven other operational staff from your ambulance service. The discussion will explore influences on decisions about patient care and associated risks. You will also be asked to complete a brief patient safety questionnaire to stimulate a discussion of the strengths and weaknesses in your ambulance service. The focus group will last about 4 hours in total and take place on ambulance service premises.
All interviews and focus groups will be audio recorded with your permission. If you do not want to be recorded the researcher will take notes instead. Recordings and information from the ‘digital diaries’ will be transcribed and analysed before being destroyed. Personal details will be deleted from transcripts to ensure that individuals are not identified.
4. What will happen to the information that I provide?
Information from the study will be analysed by the research team and findings will be included in a report for the funders and additional publications to communicate the findings. The findings may include quotations but information that could identify individuals will be removed. Your name will not be linked with the information you provide, and you will not be identifiable in the research report or other publications.
Any personal information will be stored separately and destroyed at the end of the overall study (31 October 2013). Paperwork and audio recordings will be destroyed 12 months later. One electronic copy of the data (minus identifying information) will be securely stored and destroyed 7 years after the study.
The final stage of this study includes a workshop where key findings will be presented to participants. When the overall study is completed a copy of the research report will be available on the funder’s website: http://www.netscc.ac.uk/hsdr/project.php.
5. What about confidentiality?
As researchers we will follow ethical and legal practice to manage all information. Regulatory authorities (e.g. funders) may review project documents to check that correct procedures have been followed but any identifying information would be removed.
In the event that the information you provide identifies a significant safety concern (e.g. not reporting serious equipment malfunctions), the local collaborator <name> for the research team may decide to report this information via the local reporting system.
6. Who has ethically reviewed the project?
Before any research starts it is checked by a research ethics committee to ensure that the research is acceptable. This study has been approved by the University of Sheffield Research Ethics Committee.
7. Contacts for further information
If you want further information or want to take part, please contact:
Ms Maxine Johnson (Research Fellow) A. S Researcher
E-mail:
Telephone:
Address:
If you have any concerns about the study or any aspect of the way you have been approached or treated during the course of this study, please contact the lead researcher:
Dr Rachel O’Hara (Principal Investigator)
E-mail:
Telephone:
Address:
Appendix 4 Phase 2 staff observation guide
Decision-making and safety in emergency care transitions: phase 2
Observational data prompt sheet
(Note: do not record any personal identifying information)
For each shift, note the following:
Background information:
-
Shift – time/day
-
Setting – rural, urban, mixed
-
Crew characteristics – single, double, etc.
-
Any issues around vehicle availability, etc.
For each response designated to the crew, note the following:
Calls:
-
Initial response to call – response/category
-
Context of event (where event took place)
-
Has any other health professional attended the patient before the crew
-
Patient characteristics:
-
age, disabilities, etc.
-
level of consciousness
-
alone or with carer
-
other
-
-
Initial information taken – assessments, documentation (PRF/ePRF?)
Decisions/actions/behaviour:
Describe and explore:
-
What decision was made regarding disposition
-
Reasons for the decision
-
What has influenced the decision
-
Risks associated with the decision
Other relevant information (e.g. communication at the emergency department or with other professionals, etc.)
Appendix 5 Phase 2 staff observation participants
| ID | Site | Area | Role | Solo or dual crew |
|---|---|---|---|---|
| 1 | 1 | 1 | Paramedic and ECA | Dual |
| 2 | 1 | 1 | Paramedic and ECA | Dual |
| 3 | 1 | 1 | Paramedic tutor and ECA | Dual |
| 4 | 1 | 1 | Paramedic and ECA | Dual |
| 5 | 1 | 1 | Paramedic – RRV | Solo |
| 6 | 1 | 1 | ECP | Solo |
| 7 | 1 | 2 | Paramedic × 2 | Dual |
| 8 | 1 | 2 | Paramedic | Solo |
| 9 | 1 | 2 | Paramedic and ECA | Dual |
| 10 | 1 | 2 | Paramedic and ECA | Dual |
| 11 | 1 | 2 | Paramedic | Solo |
| 12 | 1 | 2 | Paramedic × 2 | Dual |
| 13 | 1 | 2 | ECP | Solo |
| 14 | 2 | 1 | Paramedic and technician | Dual |
| 15 | 2 | 1 | Paramedic and assistant practitioner | Dual |
| 16 | 2 | 1 | Paramedic × 2 | Dual |
| 17 | 2 | 1 | ECP | Solo |
| 18 | 2 | 1 | Paramedic and ECA | Dual |
| 19 | 2 | 1 | Paramedic – RRV | Solo |
| 20 | 2 | 2 | Paramedic × 2 | Dual |
| 21 | 2 | 2 | Paramedic carrying out PP training | Solo |
| 22 | 2 | 2 | Paramedic and EMT | Dual |
| 23 | 2 | 2 | Paramedic and ECA | Dual |
| 24 | 2 | 2 | Paramedic | Solo |
| 25 | 2 | 2 | Paramedic and EMT | Dual |
| 26 | 3 | 1 | Paramedic × 2 | Dual |
| 27 | 3 | 1 | Paramedic and advanced technician | Dual |
| 28 | 3 | 1 | PP | Solo |
| 29 | 3 | 1 | Paramedic and advanced technician | Dual |
| 30 | 3 | 1 | Paramedic and advanced technician | Dual |
| 31 | 3 | 1 | Paramedic and advanced technician | Dual |
| 32 | 3 | 2 | CCP and emergency care support worker | Dual |
| 33 | 3 | 2 | CCP and emergency care support worker | Dual |
| 34 | 3 | 2 | Paramedic | Solo |
Appendix 6 Phase 2 digital diary guidance
Decision-making and safety in emergency care transitions: phase 2
‘Digital diary’
Thank you for agreeing to take part in the ‘digital diary’ activity as part of the above study.
Before taking part you should have read the information sheet for this study (dated 6 July 2012) and signed copies of the relevant consent form.
You are being provided with a digital audio recorder to record your thoughts about key decisions made about patient care over two to four shifts (ideally at different times – day or night). You can use the ‘digital diary’ to record your thoughts during shifts as time permits when cases/events may be clearer.
We would particularly like any information on the following:
-
Decisions made at different stages of your emergency care response (e.g. treat and leave, transfer to emergency department/specialist centre, pre-alert hospital and referral to community pathways).
-
What has influenced the decisions made? (e.g. patient, resources, training, time/day, location, targets).
-
Potential risks for the patient (e.g. delays, lack of follow-up).
-
Anything you feel increases/reduces the risk.
-
Anything else you feel is relevant.
You can provide some general information on the nature of calls and the context but staff and patient-identifying information should not be recorded. All information will be treated confidentially.
If you have any questions or when you are ready to return your recorder, please contact either <insert ambulance service researcher details> or Maxine Johnson (Researcher), m.johnson@sheffield.ac.uk, 0114 2220850.
Please turn over for instructions on the use of the digital recorder.
Appendix 7 Manchester Patient Safety Framework: ambulance
Nine dimensions of patient safety
| Dimension | Description |
|---|---|
| 1. Commitment to continuous improvement | How much is invested in developing the quality agenda? What is seen as the main purpose of policies and procedures? What attempts are made to look beyond the organisation for collaboration and innovation? |
| 2. Priority given to safety | Where does responsibility lie for patient safety issues? |
| 3. What causes patient safety incidents? | How are they identified? What sort of reporting systems are there? How are reports of incidents received? How are incidents viewed – as an opportunity to blame or improve? |
| 4. Investigating patient safety incidents | Who investigates incidents and how are they investigated? |
| 5. Organisational learning following a patient safety incident | What happens after an event? What mechanisms are in place to learn from the incident? How are changes introduced and evaluated? |
| 6. Communication – what communication systems are in place? | What are their features? What is the quality of record keeping like? |
| 7. Staff and safety issues | What is the work environment like? How are staff problems managed? What are the recruitment and selection procedures like? |
| 8. Staff education and training and safety issues | How are education and training programmes developed? What do staff think of them? |
| 9. Teamworking and safety issues | How and why are teams developed? How are teams managed? How much teamworking is there around service user safety issues? |
Five levels of safety culture maturity
| Level | Description |
|---|---|
| 1. Pathological | Why do we need to waste our time on patient safety issues? |
| 2. Reactive | We take patient safety seriously and do something when we have an incident |
| 3. Bureaucratic | We have systems in place to manage patient safety |
| 4. Proactive | We are always on the alert/thinking about patient safety issues that might emerge |
| 5. Generative | Managing patient safety is an integral part of everything we do |
Appendix 8 Phase 2 staff focus group topic guide
Decision-making and safety in emergency care transitions: phase 2
Staff focus group – topic guide
-
Background information on the participants.
-
Current roles/responsibilities, duration in employment.
-
-
What are your main decisions (transitions) in relation to patient care? (e.g. control room; treat and leave; pre-alerts to the emergency department; bypass of the emergency department to specialist units).
-
What are the risks to patients associated with your decisions?
Prompts:
-
– Which patients are at greatest risk?
-
– Specific characteristics of patient population where there is increased risk (e.g. communication difficulties; geographical location; age – older; chronic conditions; mental health).
-
-
What influences your decisions about patient care – increase/reduce risk? (e.g. skills/training; procedures/protocols; resources; pathways; equipment; task/service demands; ambulance service organisation and management).
Prompts:
-
– How have targets (e.g. 8-minute call-out) impacted on your behaviour (i.e. do you feel it on a day-to-day basis)?
-
– What are the consequences if they are not met?
-
– How is information about risk communicated to you (risk assessments)?
-
– Has there been an increase in procedures in recent times?
-
– What do you see as the basis for this (e.g. line managers feeling vulnerable)?
-
– How has this impacted on your behaviour (e.g. does it result in impracticable/unworkable procedures that invite infringement)?
-
-
What are your concerns about the risk involved?
Prompts:
-
– Under what circumstances do you feel vulnerable [i.e. when do you feel exposed (personally) – in the sense of repercussions rather than exposure to violence, etc.]?
-
– What do you worry about when you get home?
-
-
How do you manage the risk involved?
Prompts:
-
– How much do you trust (i) your line managers and (ii) senior managers to support your decisions in the field (or do you become ‘lightening rods’ when things go wrong)?
-
– Do you feel alone with all this – or part of a robust and cohesive team?
-
-
What could be done differently?
Prompts:
-
– What aspect of the job would you change if you could and why?
-
– How could it be reconfigured to address this?
-
-
Anything else relevant to the risk(s) associated with decisions about patient care?
Manchester Patient Safety Framework
-
Introduction to MaPSaF (use MaPSaF materials)
-
Evaluation and discussion of dimensions of the framework (for ambulance service):
-
Commitment to continuous improvement.
-
Priority given to safety.
-
What causes patient safety incidents? How are they identified?
-
Investigating patient safety incidents.
-
Organisational learning following a safety incident.
-
Communication (How do you feel about feedback?).
-
Staff and safety issues (How involved are you in risk assessments?).
-
Staff education and training and safety issues (Do you get to use your skills?).
-
Teamworking and safety issues (To what extent is there a hierarchy – at what levels? What impact does this have?).
-
-
How does this safety culture influence your decisions about patient care?
-
What could be done differently?
-
What would you like to see done to improve the patient safety culture?
-
Anything else relevant to patient safety culture and the risk(s) associated with decisions about patient care?
Appendix 9 Phase 2 service user information sheet
Decision-making and safety in emergency care transitions: phase 2
Information sheet
You are being invited to take part in a research study. Before you decide it is important for you to understand why the research is being done and what it will involve. Please take time to read the following information carefully and discuss it with others if you wish. We are happy to provide more information if anything is not clear.
1. What is the purpose of the study?
A team of researchers from the Universities of Sheffield, Lincoln, Surrey and Bath are carrying out research that aims to understand the influences on safe decision-making by ambulance service staff. This research is funded by the National Institute for Health Research (NIHR).
As part of this study we are inviting members of the public (service users) from three areas in England to take part in group discussions (focus groups) to obtain your views on the different care choices available to ambulance service staff (e.g. whether to treat and leave patients or transport them to hospital). If you have any views or experiences about this topic, we would like to hear them.
2. Do I have to take part?
It is entirely up to you; this information sheet is designed to help you decide. If you decide to take part we will discuss this information again and ask you to sign a consent form to show you have agreed to take part. You are free to leave the study at any time, without giving a reason. This would not affect in any way the care you receive from the NHS.
3. What will happen if I take part in a focus group?
A researcher will contact you to arrange your participation along with seven other service users. The focus group will last between 1.5 and 2 hours and take place in a local public building. It will be run by an experienced researcher who will talk about different care choices available to ambulance service staff and ask for your views, any experience of ambulance service care and any concerns you may have about the safety of different care choices.
With your permission, we will audio record the discussion. The recording will be transcribed into written form by a member of the research team and analysed before being destroyed.
As a thank you for your time and effort you will be offered a £10 gift voucher. Reasonable travelling expenses will be reimbursed.
We are aware that using the ambulance service may have been a worrying time. If you feel this makes it hard for you to continue to take part in the discussion, you can leave the group at any time or ask the researcher for a brief break. If appropriate, the researcher can contact a family member or friend for you.
4. Are there any benefits in taking part?
We cannot promise the study will help you personally but the information will be useful and will contribute to a larger study exploring safety in ambulance service care. In the long term we hope that this research will contribute to improved care.
5. What will happen to the information that I provide?
Information from the focus groups will be analysed by the research team and findings will be included in a report for the funders and additional publications to communicate the findings. The final stage of this study includes a workshop where key findings will be presented to participants.
At the end of the overall study we can provide a summary of the findings if requested. A full copy of the research report will be available on the funder’s website (http://www.netscc.ac.uk/hsdr/project.php).
Your name will not be linked with the information you provide and you will not be identifiable in the research report or other publications. Any personal information will be stored separately and destroyed at the end of the overall study (31 October 2013). Paperwork and audio recordings will be destroyed 12 months later. One electronic copy of the data (minus identifying information) will be securely stored and destroyed 7 years after the study.
6. What about confidentiality?
As researchers we will follow ethical and legal practice to manage all information. Regulatory authorities (e.g. funders) may review project documents to check that correct procedures have been followed but any identifying information would be removed.
7. Who has ethically reviewed the project?
Before any research starts it is checked by a research ethics committee to ensure that the research is acceptable. This study has been checked and approved by the Yorkshire and the Humber NHS Research Ethics Committee.
8. What if there are any problems?
We do not expect there to be any problems, but if there are we will deal with these promptly. If you have any concerns about the study or any aspect of the way you have been approached or treated during the course of this study, please contact the lead researcher:
Dr Rachel O’Hara
E-mail:
Telephone:
Address:
Appendix 10 Phase 2 service user focus group topic guide
Decision-making and safety in emergency care transitions: phase 2
Service user focus group – topic guide
Before focus group – give pack as participants arrive:
-
Information sheet
-
Consent form
-
Slides
-
Expenses claim form
-
Gift voucher (need to sign for receipt)
Introduction
-
Housekeeping
-
Introductory slides
-
Focus group format
Topics/questions
-
What are your views on the risk of harm for ambulance service patients?
-
Which patients are at greatest risk? (e.g. communication difficulties; older; chronic conditions; mental health)
-
What are your experiences of ambulance service care (positive or negative)?
-
What are your main areas of concern?
-
Have you any suggestions for how the risk could be reduced?
-
Are there any other areas of concern we have not identified?
End of focus group
-
Thank participants
-
‘What next’ – workshop
-
Report
Appendix 11 Phase 3 workshop invitation letter
Appendix 12 Phase 3 workshop attendees
| Role | Participant status |
|---|---|
| Paramedic | Previous participant (phase 2 focus group) |
| Paramedic | Previous participant (phase 2 observation) |
| Paramedic | Previous participant (phase 2 digital diary) |
| Paramedic | Previous participant (phase 2 observation, focus group) |
| Paramedic team leader | Previous participant (phase 2 observation) |
| ECP (n = 2) | New to study |
| Paramedic | New to study |
| Paramedic team leader | New to study |
| Paramedic clinical advisor | New to study |
| Operations manager (paramedic) | New to study |
| Service improvement manager | New to study |
| Service user (n = 3) | Previous participants (focus group) |
| Total = 15 | |
| Role | Participant status |
|---|---|
| Paramedic | Previous participant (phase 2 observation, digital diary) |
| Paramedic (n = 2) | Previous participants (phase 2 focus group) |
| Paramedic (n = 8) | New to study |
| Clinical supervisor/paramedic | New to study |
| Service user (n = 5) | Previous participants (phase 2 focus group) |
| Service user | New to study |
| Total = 18 | |
| Role | Participant status |
|---|---|
| EOC manager/paramedic | Previous participant (phase 1 interviews) |
| Clinical development manager | Previous participant (phase 1 interviews) |
| Paramedic | Previous participant (phase 2 focus group) |
| Paramedic | Previous participant (phase 2 digital diary, focus group) |
| Service user (n = 5) | Previous participants (phase 2 focus group) |
| Service user (n = 3) | New to study – representatives from Healthwatch and the trust governors |
| Total = 12 | |
Appendix 13 Phase 3 prioritisation booklet
Decision-making and safety in emergency care transitions
What are the priorities for future attention?
-
This booklet asks you to rank the priorities for future attention in relation to the delivery of emergency care by ambulance services.
-
To make the task easier you are asked to compare each issue against every other issue two at a time.
-
For each pairing you have to decide which of the two issues you consider to be the highest priority for future attention. Indicate your choice by placing a tick in the box beside what you consider the higher priority (please do not tick both).
-
Please make sure that you complete the whole booklet.
| What is your role? (Please tick) Ambulance service staff □ Public/service user □ Other □ (please state) _____________________________________________________________________________________ |
Please turn to the next page to start
| 1. Tick the highest priority | |||
| □ | Impacts of performance regime and priorities on service delivery | Disproportionate risk aversion | □ |
| 2. Tick the highest priority | |||
| □ | Communication of information and feedback to crews | Gaining access to appropriate care options | □ |
| 3. Tick the highest priority | |||
| □ | Education, training and professional development for crews | Meeting the increasing demand for emergency care | □ |
| 4. Tick the highest priority | |||
| □ | Gaining access to appropriate care options | Education, training and professional development for crews | □ |
| 5. Tick the highest priority | |||
| □ | Impacts of performance regime and priorities on service delivery | Ambulance service resources (staff, vehicles and equipment) | □ |
| 6. Tick the highest priority | |||
| □ | Disproportionate risk aversion | Communication of information and feedback to crews | □ |
| 7. Tick the highest priority | |||
| □ | Communication of information and feedback to crews | Ambulance service resources (staff, vehicles and equipment) | □ |
| 8. Tick the highest priority | |||
| □ | Gaining access to appropriate care options | Impacts of performance regime and priorities on service delivery | □ |
| 9. Tick the highest priority | |||
| □ | Ambulance service resources (staff, vehicles and equipment) | Disproportionate risk aversion | □ |
| 10. Tick the highest priority | |||
| □ | Ambulance service resources (staff, vehicles and equipment) | Meeting the increasing demand for emergency care | □ |
| 11. Tick the highest priority | |||
| □ | Communication of information and feedback to crews | Impacts of performance regime and priorities on service delivery | □ |
| 12. Tick the highest priority | |||
| □ | Meeting the increasing demand for emergency care | Gaining access to appropriate care options | □ |
| 13. Tick the highest priority | |||
| □ | Education, training and professional development for crews | Communication of information and feedback to crews | □ |
| 14. Tick the highest priority | |||
| □ | Disproportionate risk aversion | Meeting the increasing demand for emergency care | □ |
| 15. Tick the highest priority | |||
| □ | Impacts of performance regime and priorities on service delivery | Education, training and professional development for crews | □ |
| 16. Tick the highest priority | |||
| □ | Disproportionate risk aversion | Gaining access to appropriate care options | □ |
| 17. Tick the highest priority | |||
| □ | Ambulance service resources (staff, vehicles and equipment) | Education, training and professional development for crews | □ |
| 18. Tick the highest priority | |||
| □ | Meeting the increasing demand for emergency care | Communication of information and feedback to crews | □ |
| 19. Tick the highest priority | |||
| □ | Meeting the increasing demand for emergency care | Impacts of performance regime and priorities on service delivery | □ |
| 20. Tick the highest priority | |||
| □ | Education, training and professional development for crews | Disproportionate risk aversion | □ |
| 21. Tick the highest priority | |||
| □ | Gaining access to appropriate care options | Ambulance service resources (staff, vehicles and equipment) | □ |
The end.
Thank you for completing the booklet.
Appendix 14 Phase 1 participants
| Interviewee number | Role |
|---|---|
| Int1 | Deputy medical director |
| Int2 | ECP/clinical champion |
| Int3 | Acting clinical quality manager |
| Int4 | Head of clinical governance |
| Int5 | Head of safety and risk management |
| Int6 | Clinical education manager |
| Int7 | Head of quality and patient experience |
| Int8 | Registered nurse/triage manager |
| Int9 | Operational team leader |
| Int10 | Deputy medical director |
| Int11 | Locality manager |
| Int12 | Clinical development manager |
| Int13 | Clinical director of operations |
| Int14 | CCP co-ordinator |
| Int15 | Emergency centre operations manager |
| Int16 | Emergency centre operations manager |
Appendix 15 Phase 2 observation data analysis matrix
| Shift | Patient details | Practitioner details | Disposition | Comments | ||||
|---|---|---|---|---|---|---|---|---|
| Gender | Age | Incident/call (as reported by control) | Role/gender | Solo/dual | Disposition | Reason stated for disposition | ||
| Total number of hours: | ||||||||
Appendix 16 System influences on decision-making: human factors framework
| Key system influences | Specific issues |
|---|---|
| Institutional context | |
| Health and Social Care Act 201248 | CCGs |
| FT status | |
| Increase in demand and non-emergency calls |
|
| Availability and access to alternative care pathways (to A&E) |
|
| Increase in geographical area covered |
|
| Organisational and management factors | |
| Resources – capacity (staff, vehicles) |
|
| Performance measures |
|
| Service delivery change – non-conveyance |
|
| Communication of information |
|
| Incident reporting |
|
| Support for training/education and skills development |
|
| Safety culture |
|
| Work environment | |
| Crew health, safety and well-being |
|
| Interface between crew members and control/dispatch staff |
|
| Interface/relationship between crew members across trusts |
|
| Interface/relationship between crew members and other health and social care staff – primary care, A&E |
|
| Access to feedback on performance/decisions |
|
| Reporting and feedback |
|
| Team factors | |
| Supervisor and coworker support |
|
| Identification with teams |
|
| Individual (staff) factors | |
| Staff roles and responsibilities |
|
| Professional development – individual training and skills |
|
| Staff risk perception and management |
|
| Increased scope of clinical decision-making |
|
| Task factors | |
| Patient assessment and types of decisions |
|
| Public and patient characteristics | |
| Public awareness and expectations of the service |
|
| Patient/carer preference |
|
| Specific populations at increased risk |
|
Appendix 17 Areas for future research identified by workshop participants
-
Explore why the public are making so many 999 calls and what their expectations are of the ambulance service.
-
Explore what are the most efficient and safe ways of improving telephone triage decisions, for example greater clinician involvement. One of the sites was piloting GP input on secondary triage but it is a very costly way of making better decisions.
-
Establish if there are effective ways of increasing public awareness of ambulance service roles and alternative urgent care options (e.g. public education campaigns).
-
Establish how best to empower the public with the skills to directly access the appropriate services and reduce the use of 999 calls (e.g. self-management of chronic conditions).
-
Define what demand is and identify how this might change over time and how resources might change (disease patterns, technological developments).
-
Explore evidence-based quality outcomes that could form a range of performance measures as an alternative to the current response time measure.
-
Explore if patient involvement in the commissioning process and service development leads to more patient-centred and efficient care.
-
What are the perceptions of other health-care professionals of the ambulance service and what are their expectations.
-
Education, training and professional development.
-
Explore the impact of variations in skill mix on staff and patient care.
-
Assess the impact of increasing training for urgent rather than emergency care.
-
Assess the impact of paramedic experience and training on patient outcomes.
-
The increased scope of decision-making by ambulance service crews includes more diagnostics; therefore, there is a need to look at the diagnostic process and errors in the pre-hospital emergency environment.
-
Explore why communication with staff is not working and identify how to improve it.
-
Explore effective strategies for reducing sickness absence.
-
Explore staff perceptions of how they are valued by the organisation.
-
Explore the scope for increasing the use of technologies (e.g. telehealth).
-
Explore the impact of Make Ready ambulances on staff ways of working and on patient care.
Glossary
- Alternative pathways
- Pathways that provide an alternative to accident and emergency, for example minor injuries unit, out-of-hours services, walk-in centre, emergency care practitioner or paramedic practitioner.
- Ambulance service crew
- When references to ambulance service crew or crew members are used they refer to staff in response vehicles (e.g. ambulances, cars), including solo (single) responders.
- Caldicott review
- Guidelines on the storage of, maintenance of and access to patient information.
- Digital diary
- Digital recording of events and experiences whilst in the natural setting.
- Dispatch
- Allocation of ambulance service resources to cover demands placed on the service.
- FAST
- Stroke assessment tool: face, arms, speech, time.
- ‘Hear and treat’
- Clinician gives advice to a patient/carer over the telephone.
- Make Ready ambulances
- Make Ready is a vehicle preparation system that employs specialist teams of staff to clean, restock and maintain vehicles, to allow clinical staff more time to treat patients.
- Monitor
- Regulator for the protection of patient interests.
- NHS 111
- Resource for medical help (non-emergency).
- NHS Direct
- Digital health and advice service.
- NHS Pathways
- Computerised triage system.
- Non-conveyance
- A decision is made not to convey a patient to accident and emergency or another health-care facility.
- Pre-alert
- Call made to a health-care unit to advise about a patient transfer.
- ‘See and treat’
- Practitioner provides treatment at the scene.
- Toxbase
- Guide to dealing with the effects of toxic substances.
- Trauma tree
- Algorithm to aid decision-making when assessing trauma patients.
- ‘Treat and leave’
- Patient is assessed and treated at the scene and a decision is made not to convey him or her to accident and emergency or another health-care facility.
- Triage
- Prioritisation for treatment according to the seriousness of the condition.
- Typology
- Classification of types.
List of abbreviations
- A&E
- accident and emergency
- AMPDS
- Advanced Medical Priority Dispatch System
- BASICS
- British Association for Immediate Care
- CCG
- Clinical Commissioning Group
- CCP
- critical care paramedic
- CFR
- community first responder
- COPD
- chronic obstructive pulmonary disease
- CQC
- Care Quality Commission
- DMA
- dual manned ambulance
- ECA
- emergency care assistant
- ECG
- electrocardiogram
- ECP
- emergency care practitioner
- EMT
- emergency medical technician
- EOC
- emergency operations centre
- ePRF
- electronic patient record form
- FAST
- face, arms, speech, time
- FT
- foundation trust
- GP
- general practitioner
- HART
- hazardous area response team
- HCPC
- Health Care Professionals Council
- IBIS
- Intelligence Based Information System
- IR1
- incident report form
- JRCALC
- Joint Royal Colleges Ambulance Liaison Committee
- MaPSaF
- Manchester Patient Safety Framework
- NPSA
- National Patient Safety Agency
- PCT
- primary care trust
- PP
- paramedic practitioner
- PPCI
- primary percutaneous coronary intervention
- PPI
- patient and public involvement
- PRF
- patient record form
- RRV
- rapid response vehicle
- SBAR
- situation, background, assessment, recommendation
- SDO
- Service Delivery and Organisation
- STEMI
- ST segment elevation myocardial infarction
- STFG
- staff focus group
- SUFG
- service user focus group