Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1017/04. The contractual start date was in January 2013. The final report began editorial review in January 2018 and was accepted for publication in September 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Manthorpe et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Introduction to the report
This report presents the findings of the first UK study of older homeless people living with memory problems or memory problems associated with the disabilities of dementia. It contains findings from literature reviews, and primary data collected from older people living in hostels and hostel staff supporting them. We discuss the prevalence of memory problems among older people accommodated in hostels, a form of temporary accommodation in which they have no security of tenure. We compare the services used by hostel residents with memory problems and services used by those without, using a categorisation developed for this study.
Our first three chapters follow the sequence of presenting the research questions and background to the study (see Chapter 1), the findings from two literature reviews (see Chapter 2) and the study methods (see Chapter 3). The next chapters report our findings: Chapter 4 profiles the research participants and the study sites, Chapter 5 reports our definitions and classifications of memory problems, Chapter 6 reports hostel residents’ health and social care needs and Chapter 7 presents data on their use of health and care services. Chapter 8 forms our discussion chapter and our final chapter (see Chapter 9) outlines the study’s implications for service development, commissioners, providers, practice and researchers.
Background
This unique study investigated four under-researched question areas:
-
To what extent are hostel staff aware of memory problems among their older residents and their prevalence? What impact does this have on their practice or service? How do hostel staff respond to residents’ memory problems?
-
What ‘service pathways’ exist for an older homeless person with memory problems? What are their experiences of these services?
-
What are the gaps in service provision for such individuals, and what are the costs of providing services for them?
-
How do older homeless people with memory problems perceive their quality of life (QoL), and how can this be evaluated? Does this differ from other older people and other older homeless people? What are the implications of this for agreeing desirable outcomes from services?
The background to the study is formed by three different domains: (1) the imperatives of dementia policy and practice, (2) equalities legislation and efforts to reduce health inequalities among older people with long-term conditions, including dementia, and (3) the impact of homelessness on older people with memory problems, including dementia, and their service needs. Little research has been conducted about the problems faced by older homeless people with memory problems (such as dementia), the services and support that they receive and the extent to which their needs are met. Our conversations with different stakeholders working in dementia services and in homelessness services as part of the development of the study proposal revealed that some older homeless people are deemed hard to engage and reluctant to work with services, and are perceived as difficult to assess and help because of persistent alcohol use. We were also told about other problems experienced by professionals in supporting homeless older people; these included accounts of distressed behaviour, complications of physical ill health, and self-neglect. We found little information about any help available to staff working with this client group in homelessness services in the UK and little research evidence about their contacts with other sectors. There were also few reported experiences of working constructively with health and social care services. In our consultations as part of our preparation for this study, professionals from all sectors expressed a desire to gain a greater understanding of this area of practice. These discussions helped frame our study so that it would explore implications for service design through an evidence-based analysis of the barriers to diagnosis, service access, support, treatment and unmet need, and exploration of ways to address the many challenges envisaged. This study, therefore, was designed to investigate these areas. The next section provides more detail of the threefold context to the study.
Dementia
Two major policy documents have shaped dementia services and provide the background to the emerging interests in dementia recognition at patient and society levels in England: the National Dementia Strategy,1 superseded by the Prime Minister’s Challenge on Dementia. 2 Both emphasise the need for earlier or more timely recognition of dementia. Commenting on the progress made under the National Dementia Strategy and the Prime Minister’s Challenge, Knapp et al. 3 reported that the provision and use of memory assessment services (sometimes referred to as memory clinics) has increased, although it is hard to detect what changes there have been and where they have occurred. The development of memory service accreditation has been slow, meaning that commissioners cannot rely on strong evidence of how best to deliver memory services. Knapp et al. 3 added:
Local services will and should respond to local circumstances and be more person-centred, but the wide variations currently seen in staff-mix, methods of clinical assessment and provision of post-diagnostic care are unacceptable if the aim is to equalise access to diagnosis and post-diagnostic support.
P. 2.
Although the National Dementia Strategy1 addressed issues of equalities, generally there has been a lack of focus on people who are homeless who have memory problems or cognitive problems that are indicative of a dementia syndrome. The Ministerial Advisory Group on Dementia Research4 recommended that public and professional awareness and understanding of dementia should be improved. However, whereas it made reference to caring for people with dementia at home, in hospital and in care homes, it contained no mention of those who are homeless or socially excluded from settled accommodation. It also recommended that health and social care staff working in care homes with residents who have dementia should receive appropriate training and continuous professional development, and that community mental health teams (CMHTs) working with older people should provide specialist services to care homes; however, practitioners working in homelessness services were not mentioned. The Ministerial Advisory Group on Dementia Research advised that everyone with dementia should have access to a pathway of care services, including specialist assessment, treatment, care and support, and that this pathway should be responsive to individual need and preferences. It made no reference to possible difficulties in providing care and support to older people with dementia who are homeless, or to the staff groups working with them.
Policy has also promoted broad public health and community development approaches to responses to dementia. Knapp et al. 3 noted the considerable emphasis on improving awareness about and attitudes towards dementia through campaigns such as Dementia Friends and the development of dementia-friendly communities. Such initiatives have generally focused on people living in their own homes. 5
Equalities
Part of the justification for a National Dementia Strategy1 was that dementia has long been overlooked as a health problem, despite its often devastating impact in human terms and its impact on public expenditure. There have been arguments that this lack of priority reflects dementia’s associations with old age and the impact of ageist beliefs and stereotypes; that the condition is stigmatised; and that there is therapeutic nihilism – or a feeling that nothing can be done. 6 There is increasing interest in seeing dementia as needing a rights-based dimension, building on the ideas of the disability movement. 7,8 A report from the Mental Health Foundation suggested that this would bring several benefits, such as greater legal protection and improved service entitlement, thereby promoting cultural shifts to how dementia is perceived that will have benefits to society as well as people with dementia. 9
Thomas and Milligan10 have argued that adapting the social model of disability to people with dementia also encourages us to think beyond the social and institutional disadvantages that may be experienced by people with dementia, and instead notice the impact this can have on the places they live. As people with dementia may lose their sense of orientation of time and space, formerly familiar places may start to seem unfamiliar or frightening to them. 10 The premise that people with dementia may lose their memories of settled and familiar locations overlooks people without settled accommodation or who are unfamiliar with their present neighbourhood.
The premise that people with dementia may lose their memories of settled and familiar locations overlooks people without settled accommodation or who are unfamiliar with their present neighbourhood.
More recently, there has been greater interest in the heterogeneity of the ‘dementia population’ and the possible impact of social inequalities being sustained when a person has dementia or of such inequalities being reproduced or enhanced. Research, for example, has investigated differences in service responses, such as prescriptions of ‘anti-dementia’ medication, by socioeconomic group,11 variations in symptom recognition between ethnic groups,12 fear of prejudice about revealing sexual orientation13 and gender disparities affecting women throughout the dementia trajectory. 14,15 Concluding their literature review, Ludwin and Parker15 observed:
As we have seen throughout the material we reviewed, individuals with dementia are marked by the social locations and identities they occupied prior to diagnosis; these axes of identity may form important parts of individual sense of self. Failing to recognise them in interactions and provision of support may thus contribute to an erosion of personhood and perpetuate marginalisation.
P. 2015
The importance of considering equalities in respect of people who are homeless is not generally recognised, despite the very poor health and QoL of this population. 16 According to the Equality and Human Rights Commission,17 this population is among the most disadvantaged groups in UK society. Although the Equality Act 201018 provides a legal imperative to ensure that ‘protected characteristics’ are addressed in assessments of service impact (many of which are relevant to people with dementia2), homelessness is not readily translated into the ‘characteristics’ for which there is legal protection. Some advocates from the homelessness sector have suggested that the NHS Constitution instead may be an effective lever to ensure the rights of homeless people to health services. 19
Housing people with dementia
There has been growing interest in the living accommodation and housing choices of people with dementia. Much has focused on how to design new accommodation and how to modify existing accommodation so that people with dementia can stay in their own homes or move to better accommodation offering choices over patterns of care and tenure. 20 Several organisations (e.g. the National Federation of Housing21) have argued that dementia-friendly housing must be an integral part of dementia care. Research has also begun to explore particular housing needs of some groups of people with dementia; for example, Lipman and Manthorpe22 investigated how social housing providers (housing associations) were beginning to respond to tenants with dementia from black and minority ethnic groups.
As Knapp et al. 3 reported, local authorities have been encouraged to develop, in collaboration with the Homes and Communities Agency and the Greater London Authority, partnerships with housing associations (social housing providers that may offer housing and care services) and private builders to meet the needs of older people with long-term conditions, including dementia. However, the focus of such developments has been on people with dementia who already have homes, some of whom have considerable assets from home ownership and who are potentially attractive new purchasers to ‘housing with care’ providers.
Older homeless people
The problems and needs of older homeless people and of the effectiveness of services for them were summarised in a review article by Crane and Joly16 and the responses of statutory housing bodies by Alden. 23 There has been little research in the UK about the circumstances and needs of older people who are homeless and have memory problems, although the subject has received some attention in other developed countries, such as the USA24,25 (see Chapter 2 of this report for our review of the relevant literature).
This present study used the former UK Coalition on Older Homelessness26 definition of ‘older’ homeless people as those aged ≥ 50 years, because many homeless people in their fifties have chronic health problems and disabilities normally associated with old age. Those in their fifties who are single and without dependent children are often not regarded by statutory services as ‘elderly’ or particularly vulnerable, meaning that these authorities’ responsibilities may be fulfilled by temporary hostel placement with, increasingly, shorter stays only being permitted. Moreover, at least two-thirds of older homeless people are men in respect of whom problems have been reported if they are rehoused in care homes, which tend to be occupied predominantly by very elderly women. 27 Care home staff have reported difficulties in managing formerly homeless men’s drinking and/or chaotic behaviour, such that some are ‘evicted’ from care homes,27 although there is little direct evidence about this from more recent times.
The number of older homeless people is rising, as is the number of homeless people in England generally, although data quality is not sufficient to provide accurate numbers. 28 In 2017, Homeless Link reported a total of 36,540 bed spaces in 1253 hostels and second-stage accommodation across England. London has the greatest number of projects in total, at 183, and the most bed spaces, with 9647 beds. Reporting on the 1121 accommodation projects for single homeless people in England, Homeless Link29 noted that levels of support, access and inclusion criteria varied between projects. Services that offered lower-level support tended to be for those who were homeless or in need of housing, but deemed to otherwise be capable of living independently. Some other services offered more support for those who had support needs alongside their accommodation needs, and faced many barriers to living independently.
There are expectations that hostel residents will move on from first-stage hostels (those that provide intensive support in a 24-hour hostel) to other accommodation often within 6 to 12 months. 29 (Stage 2 hostels involve shared accommodation and a lower level of support and stage 3 often involves a move to independent living.) Yet some older homeless people with increasing memory impairment and other vulnerabilities may remain in hostels for years, with growing frailty, as there is no suitable alternative accommodation. Most hostels are not designed or staffed to provide long-term housing or a high level of support for this client group or others. In addition, many older homeless people are reported to dislike staying in hostels, fearing intimidation and violence from younger residents. 30
Audits conducted over 20 years ago by homeless sector staff in Blackburn, Brighton, Cambridge, Liverpool, Oxford and Westminster26 suggested that 10–16% of older homeless people known to them had ‘serious memory problems’ or ‘have memory problems/are prone to wander’. Other reports have noted the presence of dementia among older homeless people31 but have not given any estimates of its prevalence. Many of such audits relied on the observations of non-clinical staff, and not on mental health workers’ clinical examinations or tests; various lower age limits were applied (from 45 to 60 years); and profiles of the residents were not collected or not reported. The lack of clinical input in such audits may account for difficulties in analysing what might be contributing to the problems reported: alcohol misuse resulting in vitamin B12 and folate deficiencies, for example, or untreated human immunodeficiency virus (HIV) infection, vascular disease, or chronic or long-standing brain or head injury. There is a strong association between long-standing heavy alcohol consumption and alcohol-related brain damage (ARBD) or injury. 32 Moreover, studies of hostel residents of all ages have revealed multiple health needs; for example, a comprehensive survey of residents in a London hostel for homeless women collected demographic data, and information on past and present psychiatric and social morbidity and on current and premorbid cognitive functioning. 33 This reported that over half of the residents surveyed had ‘severe mental illness’. The associations between poor health and homelessness are becoming better recognised. 19
Quality of life of older homeless people
The research discussed in the previous section is problem focused and does not engage with the individuals of concern and their situations. Thus, although several measures of social functioning and wider QoL have been developed for use with people with long-term mental illnesses,34,35 their development for use with people with dementia is more recent, although there is a long history of measurement of stress and coping among family carers. Work has been undertaken to design measures that better address the social circumstances of older people who are homeless (e.g. the focus group discussions of QoL in a Canadian study included older homeless participants36). These confirm the necessity of taking into account all of the social factors that this marginalisation generally brings (such as lack of family contact or meaningful activities). The QoL measures being developed in social psychiatry are embedded within a strong conceptual framework, including medical and multidimensional, holistic models of functioning,37 wider health and psychosocial needs-based and life satisfaction models,34 but these generally take ‘home’, ‘occupation’ and ‘social contacts’ for granted. The development and use of a robust measurement of QoL among homeless people with dementia may need to take into account the literature on QoL among people with mental illness who are homeless (emphasising maintenance of stable housing, food and clothing, health and risk of victimisation38), and among homeless people per se (emphasising food, shelter, necessities, respect, choice and relationships39). Two particular studies have validated such scales among homeless people: Riley et al. 40 used the SF-36 (Short Form Questionnaire-36 items), although this was confined to a particular subgroup of people infected with HIV who were homeless or marginally housed, whereas Auquier et al. 41 used the same measure with homeless people with schizophrenia living in urban France. These highlighted the need for QoL measures to reflect the priorities of the target population, enabling better understanding of the need for any QoL instrument for those with dementia and who are homeless or ‘hard to house’ to reflect their own needs and priorities. The first part of the present study was therefore designed to examine the appropriateness of existing QoL instruments in reflecting the needs and priorities of this group (see Chapter 2).
Workplace contexts
The subsequent and major part of the present study sought to remedy, in part, the current lack of research evidence and knowledge of the extent of memory problems (used as a general term suggestive of possible dementia and to make a distinction between learning disability-related memory problems and any other mental illnesses) and service use among older homeless people resident in hostels. Other studies have investigated specific health conditions among this group (e.g. Hill et al. ,42 who focused on dental problems). Little is known about how staff working in hostels are involved in identifying memory problems and steering residents into memory services, or how they manage symptoms of possible or recognised dementia among hostel residents in the current context in which dementia is a policy and practice imperative.
The hostel workforce is an under-researched group. 43 In England, most of those working in hostels are employed by not-for-profit or commercial organisations that provide ‘temporary’ accommodation for homeless people. Funding is mainly through local authority housing-related support payments (previously through the Supporting People programme) but also through other income streams and fundraising. Staffing levels in accommodation projects for single homeless people run at an average of nine full-time-equivalent staff,44 although hostels vary greatly in resident numbers, staffing deployment and resources. Staff working in homelessness services generally undertake a range of duties but, in general, receive little continuing professional development and support compared with health-care professionals. 45 They are reported to be uncertain of their positions in local health networks,46 yet they are considered to have much to offer health-care services locally in terms of skills and knowledge. 47 Fitzpatrick and Wygnanska48 argued that hostel staffing and support arrangements can be even more critical to residents’ QoL and future prospects than physical standards, but noted that hostel staff can be poorly qualified, often needing only a basic vocational (non-university) qualification.
Chapter summary
This chapter has located this study in the contexts of policy and practice relating to dementia and homeless older people. It has drawn attention to policy contexts of health inequalities and to the lack of knowledge about the workforce in organisations supporting older homeless people. The discussion of QoL among older homeless people highlights the general lack of information about this important matter, and draws together the contextual themes by noting the importance of this to the individuals concerned, despite difficulties in defining it. The next chapter moves to discuss previous work on this subject on which the present study draws.
Chapter 2 The literature reviewed: the prevalence of memory problems among older people who are homeless and quality of life
Introduction
The previous chapter described the overall aim of this research project as being to investigate service responses to older homeless people with memory problems (consistent with mild cognitive impairment or dementia) and the experiences of those so defined. This chapter presents findings from our two reviews of the literature to set the context for the data collected and analysed. Literature review A aimed to address objective 1 of the study by investigating the prevalence of memory problems among older homeless people. Literature review B aimed to address objective 4 of the study: how homeless people with memory problems perceive their QoL. This has been published49 and so is briefly summarised.
There is emerging, if, at times, varied, UK evidence about the circumstances and needs of older people who are homeless and have memory problems, although, as we report below, the subject has received sustained attention in other developed countries, such as the USA, Canada and Australia. A recent paper commented that ‘(R)eported rates of mild and moderate cognitive impairment in older people experiencing homelessness range from 5–80%’. 50 One explanation for such a vast range may be that several different interpretations of three key terms are being used, namely homelessness, older/old (usually by chronological age, which can start at 45 years) and memory problems (or disability or dementia). International comparisons are rendered even more difficult by national arrangements and terminology relating to locations, with the functions and roles of hostels, flophouses (a term mainly used in North America), shelters (North America in the main) and boarding houses (Australia and North America in the main and approximately equivalent to UK hostels) being variable or overlapping. Other national considerations include whether homeless people are covered by universal health services or systems that are based on insurance (e.g. see Brown et al. 51). There are also differences between people who have been homeless for several years and are reaching older ages, and people who have become homeless for the first time in later life. 52,53
Relatively few homeless people live long. A recent audit of mortality data concerning homeless people in East London who were registered with two specialist primary care practices54 found that the average age at death was 47 years and concluded that most deaths were very premature and preventable. The UK Coalition on Older Homelessness26 defined ‘older’ homeless people as those aged ≥ 50 years, because many people who are homeless at this age already have long-term health problems and disabilities that are normally associated with (very) old age. In Canada, Grenier et al. 55 concluded that ≥ 50 years would be an appropriate threshold. Similarly, Alden23 adopted the age of ≥ 50 years on the basis of evidence that poor health and ‘premature ageing’ are inevitably associated with ‘rooflessness’.
Although official UK statistics on homelessness are acknowledged to be limited in their accuracy,28 approximately one-fifth of homeless people living on the streets and in hostels are aged ≥ 50 years (around 8% are aged ≥ 60 years). 56 The audits reported in Chapter 1 by the former UK Coalition on Older Homelessness26 relied on the observations of staff only, and various lower age limits were applied (from 45 to 60 years), and profiles of the residents were not supplied. Around two-fifths of older homeless men and one-fifth of older homeless women have long histories of alcohol misuse, and there is a strong association between long-standing heavy alcohol consumption and brain damage or Korsakoff syndrome, which is characterised in part by short-term memory loss. 57
Little is known about the problems faced by older homeless people with memory problems, the services and support that they receive, and the extent to which their needs are met. Some are reported to be hard to engage, reluctant to work with services, and difficult to assess and help because of persistent heavy drinking or other challenges and experiences. There are the added problems among some of distressing behaviour, multiple physical health problems and self-neglect. However, Johnson and Chamberlain58 pointed out that it is difficult to help homeless people with their mental health or other problems if they are living in substandard accommodation, such as boarding houses (as noted previously, this term is used in Australia to refer to facilities approximately equivalent to UK hostels), in which they may be at risk of violence and lack control over their environment. There is little information about the help available to homeless-sector staff working with this group, and their knowledge and experiences of accessing health and social care services. Rather than pathologising the older homeless person, there is a perceived need, which many in the homelessness sector acknowledge,59 to gain a greater understanding of these problems, identify the barriers to diagnosis, service access and unmet need, and find out ways in which these might be addressed in services that should be characterised by respect and dignity for older homeless people. 60
Literature review A: a scoping review of prevalence of dementia in older homeless people
Methods
Search strategy
For this scoping review of what is known about the prevalence of dementia among homeless people, we conducted a comprehensive, cross-disciplinary, systematic search of the conceptual and empirical literature across clinical and social sciences, and health, housing and social care. We searched for any type of English-language literature published or written from 1980 to the end of 2016. We included observational studies, controlled evaluations and randomised controlled trials of health and social care interventions relevant to older homeless populations with dementia or memory problems.
Process of the review
The process of the review was that two reviewers independently screened all titles and abstracts that had been retrieved for relevance; disagreements were resolved by consensus. If relevant, the full-text article or publication was obtained. The full text of obtained articles was judged to be potentially relevant by the two reviewers. A list of key questions was generated, and a pro forma (data extraction tool) was developed to address these from the included papers. These were piloted on a small number of selected papers. Owing to the few papers identified, unlike Burra et al. 61 and Ennis et al. 62 we did not adopt a critical appraisal approach to rating the quality of studies, thereby following procedures generally categorised as scoping reviews. 63 One key reason for this is that such an approach risks overlooking studies with small sample sizes and, thus, might exclude individual case study or whole-hostel research if the numbers of older residents were not sizeable. Ennis et al. 62 considered a sample size of over 100 to be ‘good’, but, as discussed below, we found few studies reporting such numbers.
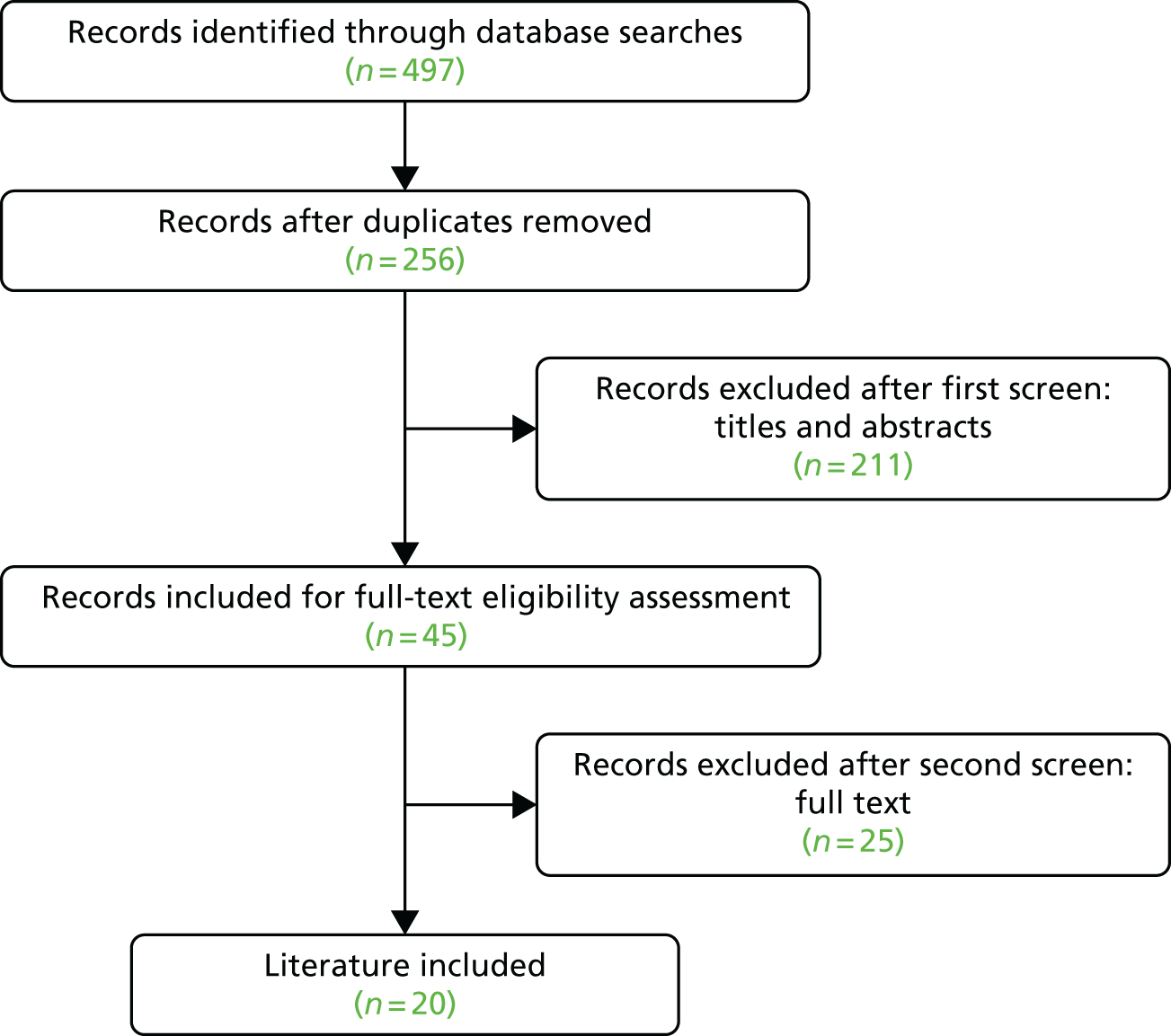
We identified 20 articles for inclusion in the review, after screening 260 articles retrieved from our database searches (the searches were run in May 2016). We searched English-language databases only (Web of Science, Scopus, Social Care Online, PubMed and The Cochrane Collaboration) for material published from 1980 to 2016, including ‘grey’ literature [Figure 1 shows the flow chart – a modified PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram – for the process of literature review].
FIGURE 1.
Literature review A flow chart (a modified PRISMA diagram).
We cross-checked our findings with a recent (2014) literature review from Australia conducted by a researcher at La Trobe University,64 in which the period 2004–14 had been searched for items from English-language literature, using the terms cognitive impairment, dementia, care needs and illness of homeless people. Chenco undertook one search for ‘dementia’ and ‘homeless’ and another for ‘illness’ and ‘homeless’, and then combined the findings into a single larger list. 64 This resulted in the location of 344 references, once Chenco had removed duplicates. Of these, 35 were deemed directly relevant for the purposes of Chenco’s Australian review, which, as noted previously, took a much broader scope than our study by including the term ’illness’. 64 In this search of four main databases, Chenco located the following numbers of items:
-
Social Services Abstracts (via ProQuest) (n = 241)
-
AgeLine (via EBSCOhost) (n = 24)
-
Australian Family & Society Abstracts Database (via Informit) (n = 84)
-
Health & Society Database (via Informit) (n = 73).
In addition to comparing our searches with Chenco’s findings,64 we took particular account of the findings of other scoping and systematic reviews of similar subjects. In the review by Spence et al. ,65 for example, the following terms were searched for in the titles, abstracts and any subject heading fields: ‘homeless*’ or ‘roofless*’ or ‘fixed abode*’ or ‘hostel*’ or ‘bed and breakfast*’ or ‘night shelter*’ or ‘hotel*’ or ‘housing benefit*’ or ‘street dwell*’ or ‘tramp’ or ‘tramps’ or ‘vagrant*’ or ‘vagabond*’ AND ‘cognit*’ or ‘executive function’. We did not search for the terms ‘tramp’ or ‘vagabond’, but it is interesting to note that such terms were evidently in use just over a decade ago in the UK. There are wide variations between services that provide hostel accommodation and night shelters, both internationally and in the UK and in terms of their residents or user profiles; these need to be taken into account in any comparison and are mentioned in Findings.
Findings
Our searches found a small number of studies covering homelessness and memory problems/deficit/dementia and Appendix 1 contains a full table of the studies included in the second literature review. Of these studies, one of the earliest to examine these subjects in terms of prevalence was undertaken in Australia by Teeson and Buhrich. 66 Over 20 years ago, these researchers used the Mini Mental State Examination (MMSE),67 which is still commonly used in UK dementia services, and estimated that severe memory problems affected 25% of one hostel’s 65 residents, and another 40% showed signs of mild memory problems.
To establish if the high prevalence of severe memory problems was more commonly borne out in other hostels, and because no women had been included in their 1993 research,66 Buhrich et al. 68 later conducted a broader study of homeless people, again in inner-city Sydney, NSW, Australia. Using the MMSE67 with 204 participants (155 men and 49 women) in seven hostels, they found that 10% (20 people) had some form of memory problems. Of the 14 men with memory problems, five had severe memory problems. The six women had mild memory problems:
The prevalence of cognitive impairment among the homeless subjects in this sample was 10 percent . . . the prevalence of cognitive impairment in the general adult population is 1.7 percent . . .
Buhrich et al. 68
In this study, MMSE scores of 0–17 were interpreted as indicative of severe impairment and scores of 18–23 were interpreted as mild impairment (although six people were not included in these figures as they were unable to complete the MMSE, were deaf, or could not speak English). The researchers found that people with memory problems were likely to stay in the hostel accommodation for longer than those without, postulating that this might be because ‘move on’ accommodation was much harder for them to find, or because their motivations to move on were compromised. 68
Measurements and assessments
Ennis et al. ’s62 review found 11 studies that measured memory impairment among homeless people (of any age) using validated neuropsychiatric tools. They excluded those studies in which memory was assessed by the MMSE,67 as they argued that this does not produce a unique score for items of memory. Eight distinct studies contained unique samples of people who were homeless, a total of 436 participants. The mean age of the studies’ participants was 40.75 years and most participants were male. Most studies had been conducted in the USA. The authors commented that older homeless people were not adequately represented in the studies they reviewed (neither were women, young people or children). They suggested that studies that collect data about ‘memory’ problems without using validated tools are virtually impossible to compare. In respect of their findings of prevalence of memory impairment, they expressed caution in making firm estimates as there were so many variations of assessment, scoring and sample populations. They also highlighted a need for further research on traumatic brain injury, which they concluded is often misdiagnosed or mistaken for other problems. Despite their reservations about using the MMSE, and as the findings reported below show, many other researchers have used this assessment.
Other modes of assessment have explored the presence of serious mental disorders among homeless people. A systematic review (not focusing on older people) identified 29 surveys in which 5684 homeless people had participated through clinical examination or interviews using validated instruments, many of which had good participation or response rates, mostly above 70%. 69 Inner-city Sydney, NSW, Australia, is one research site where several studies with older populations have been undertaken. For example, Rogoz et al. 70 found that 67% of participating homeless older people showed evidence of memory problems. Rogoz and Burke’s later study of 171 older (aged ≥ 45 years) homeless people in inner-city Sydney screened them for memory problems using the MMSE (taking a score of ≤ 26 as indicative of memory problems), or asked them to complete a clock-drawing test, a verbal fluency test and the Trail Making Test (this was the most sensitive). 50 This screening found that 78% (134 out of 171) were cognitively impaired, with 75% showing marked impairment of their frontal lobe functioning. This study recruited from a wide range of sources, including people living on the streets, in temporary accommodation and in marginal or shared facilities. The researchers commented that using one neuropsychological test was easy to administer and appeared acceptable.
In a US study that explored the presence of ‘geriatric syndromes’ among older (age range 50–69 years) homeless people in eight homeless shelters in Boston, MA, USA, Brown et al. 71 found that memory problems (measured by a MMSE score of ≤ 24) were present among 24.3% (n = 247). Other health problems were frequently mentioned, such as incontinence (49.8%), self-reported hearing loss (29.7%), major depression (39.8%) and visual impairment (30%). Comparisons with the general population revealed a higher presence of health problems among the homeless population. Interestingly, to make such comparisons more accurate, the researchers excluded the three eligible participants who were aged ≥ 70 years, meaning that the definition of ‘older’ should not always concentrate on the minimal age of this category (45 years, 50 years, and so forth) but should also enquire about other exclusion criteria on the basis of age.
In a further analysis of the data, Brown et al. 51 explored the factors associated with ‘geriatric syndromes’ among older homeless adults who had participated in the data collection through interviews and physical examinations. These included assessment using the MMSE and the Trail Making Test Part B to measure executive function by the time taken to complete tasks. Joyce and Limbos24 similarly used the MMSE but also used the 15-item Geriatric Depression Scale (GDS-15) among 49 users of a community-based homeless shelter for older men in Toronto, ON, Canada. Study participants were ≥ 55 years of age (mean age 66.4 years) who had been homeless for an average of 8.8 [standard deviation (SD) 10.2] years. The oldest was 89 years. There was a refusal rate of 40.8%; thus, only 29 people completed the depression measures (GDS-15) and the MMSE. One person had a recorded dementia diagnosis before moving to the shelter but within 6 months of moving in another seven people had been so diagnosed (the researchers generally confirmed this) by primary health services. The researchers found a further four participants with mild impairment (MMSE score of 23–27) and one with dementia (MMSE score of ≤ 22) who had not been previously diagnosed. They concluded that brief screening tools seemed to be effective in identifying memory problems (and depression) among this client group. 24
While focusing on ARBD among homeless hostel-dwellers (aged > 34 years, mean age 53 years) in Glasgow, Scotland, Gilchrist and Morrison57 also collected data relating to memory problems using the Addenbrooke’s Cognitive Examination (ACE). Of their sample, 82% had memory problems as measured by a score of < 88 on the ACE (the researchers estimated that ARBD affected 21%). This study helpfully describes the type of hostels participating, which ranged from large hostels for men and one for women, to a hostel with ‘rapid turnover’. Similarly, in Sydney, NSW, Australia, Conroy et al. 72 found that among the 50 homeless clients of one service they interviewed (average age of ≥ 50 years), all had a history of alcohol abuse and early cognitive decline. They estimated that 39% had scored similarly to people with dementia in their assessments.
In a US study undertaken in California, Brown et al. 73 recruited older homeless people (aged ≥ 50 years) from a variety of homelessness providers, thereby expanding the more usual recruitment source, which, as illustrated above, has often been from shelters and their sometimes transient and heterogeneous populations. They used the Modified MMSE74 to assess cognition and defined memory problems as a score below the seventh percentile or when a participant was unable to complete the assessment. 73 Among their 350 participants, one-quarter (25.8%) had memory problems as measured in this study. However, Rota-Bartelink25 cautioned against using the MMSE with older homeless people, despite it being easy and quick to administer. She considered it an insensitive indicator of memory problems and observed that this may account for the wide variations in detection of memory problems among homeless populations.
Summing up, a recent review of cognitive functioning among homeless people (aged ≥ 18 years) located 24 studies that had tested for cognitive functioning, including performance in the MMSE, abbreviated Mental Test or ACE. 75 The authors observed many inconsistencies across the studies in terms of data collection, definitions, reporting and diagnoses. They pointed to the difficulties of determining associations between homelessness and cognition. Despite this, the authors estimated that among the adults who participated in the studies reviewed (mean age 46 years), the ‘average prevalence of cognitive impairment was about 5–8 times greater than the rate of memory problems in the US population older than 70 years’. 75
However, caution is needed when generalising from this estimate, as difficulties remain in assessing whether or not cognition impairment overlaps with what might be termed dementia. In one of the few studies of homeless people (published in English) from Japan, Nishio et al. 76 explored the overlap between cognitive disability and mental illness in a sample of 114 people living on the streets or in a temporary residence and recruited via a support centre at mealtimes. Although ages ranged from 20 to 78 years, 84% were aged > 50 years (31 were aged 50–59 years, 33 were aged 60–69 years and 10 were aged > 70 years). Their measurements of cognitive disability covered lifelong (congenital) and acquired impairment. In this study, standardised cognitive testing, including reading, was undertaken during semistructured diagnostic interviews. Relevant to the present study was the researchers’ finding of cognitive disability among 34.2% of their sample; but they concluded that half of this group’s cognitive problems were not the result of congenital disability but were age related or had arisen with mental illness. 76
Summary of prevalence studies
This review first sought to determine the prevalence of older homeless people, with and without memory problems, by synthesising audits published as ‘grey’ literature and surveys. The literature suggests a consensus that older homeless people are more likely to have memory problems than other older people and probably more so than younger homeless people. However, there are limitations to each study, as described previously, meaning that an overall prevalence estimate is hard to determine. These complications render comparisons of prevalence near impossible. Although this may be frustrating, it is likely to be more helpful to service providers and service funders to accept that ‘prevalence’ will be affected by the nature of the service from which participants are recruited, their clientele, the definitions of impairment, and the measurements or tests chosen.
We also explored the range of definitions of memory problems used in these studies. Overall, the term cognitive impairment was prominent, but, as noted above, this was largely synonymous with cognitive dysfunction or cognitive deficit. 25 The use of the term dementia is a fairly recent addition to the literature, reflecting perhaps a more social model of dementia but also the wider user of this term in public and health services settings. Alzheimer’s disease is not generally used in the existing research, possibly because the classifications of dementia were broad or simply not considered. In some discussions arising from the reviews’ analyses, the term memory problems appears to be more mild than dementia, as Chenco64 described people with dementia as a group who will need more specialised support or treatment than others with memory problems. The next section of this review discusses the literature related to service models and staffing.
Services
One point implicitly raised by Rota-Bartelink25 was whether or not memory problems matter in the context of providing services to homeless people. She suggested that they do indeed matter because they affect people’s ability to keep or get stable housing and to benefit from support. The person may need support to make decisions and judgements, regulate their behaviour, and build and keep social relationships. A person’s ability to benefit from interventions has to take into account their cognitive abilities and disabilities. Services should beware of devising or agreeing to outcomes that do not reflect these challenges. The thesis that memory problems bring extra vulnerability was echoed in Grenier et al. ’s55 review, which pointed to the likely needs of older homeless people as being for safety and, by extension, the heightened vulnerabilities if a homeless person has dementia.
Two further reviews of the service needs of older homeless people were found. Stergiopoulos and Herrmann77 noted that some researchers had concluded that older homeless people are likely to be missed by studies that recruit from large services because they are ‘hidden’ or do not use such services and sometimes do not access other related services, such as primary health care. The service needs in their review were mainly indicated by reports of surveys and interview-based studies that pointed to the range of problems commonly found among older people who are homeless or the ‘chronically mentally ill elderly’. 77 They noted that better understanding of the events that precipitate homelessness might inform prevention measures or the pathways to homelessness. However, they also suggested that there exist ‘age-specific unmet physical and mental health needs among homeless seniors, particularly among those with mobility and memory problems’. 77 They proposed that it would be helpful to think about services for all homeless people as well as those for older homeless people; the latter experience particular barriers to accessing some services, such as physical inaccessibility, and often have a legacy of dissatisfaction with services and lack of health card identification (proof of entitlement). One concrete suggestion was that local consideration should be given to day centre programmes to engage older homeless people and to provide more acceptable and accessible assistance.
Stergiopoulos and Herrmann’s study77 was one of the few found that collected data from multiple sources, obtaining data from local health and community services in Toronto, ON, Canada, and surveying 11 hostel directors (eight responded) (in addition to completing a literature review). The directors reported that although older (aged > 65 years) male hostel residents were a very small minority of hostel users, and likely to have been homeless long term, the problems that gave rise to most concern among hostel staff were older residents’ memory difficulties, verbal aggression and alcohol misuse. Fewer in number, older female hostel residents were more likely, in the directors’ experiences, to have memory problems, symptoms of paranoia and depression. The directors expressed concern that overall they were not meeting older residents’ memory and mobility needs.
Burra et al. 61 systematically reviewed studies of cognitive deficits in homeless adults, and discussed their implications for services. They found that, among the studies that had administered the MMSE, between 4% and 7% of homeless people were reported as having global cognitive deficits. The consequent implications for services were thought to lie in problems with clients’ adherence to treatment regimes, their difficulties following rehabilitation programmes and their lack of participation in ‘training’.
Likewise, Brown et al. ,73 whose study included older homeless people living in a variety of environments, concluded that there were few differences in the mental and physical health status of older homeless people by location (temporary or rooflessness), many of whom had disproportionately high levels of long-term conditions compared with the general older population, and even when compared with older people living in poverty. These authors suggested that current service efforts in areas such as rehabilitation, environmental adaptation and addressing polypharmacy may not have much traction with older homeless people, whose key need seems to be for permanent supportive housing.
Some researchers concluded that homeless people not only need stable housing but also need support. For example, Lippmann78 argued that older homeless people need to be able to access more of mainstream older people’s (aged care in Australia) resources and funding. Van Wormer79 similarly proposed that older homeless people need assistance with gaining and retaining housing. A review of the literature on housing options for older people80 reported the wide spectrum of housing services, noting the importance of distinguishing between supported and supportive housing, for example the different models of shelters, and the growing evidence base for the ‘housing first’ approach that sees housing as a necessary preliminary for rebuilding people’s lives.
For older people, it is reported to be even more difficult to provide care and resources if they are living on the streets. 81–83 O’Connell et al. 84 noted that diagnosing dementia is difficult ‘on the streets’ as assessment necessitates access to tests and the ability to take details of a person’s history. In this unique longitudinal study of older homeless people in Boston, MA, USA, where the authors followed up 30 people aged ≥ 60 years for 4 years, multidisciplinary teams of health professionals undertook outreach work regularly.
There have been few evaluations of services for older people with dementia or similar conditions who have been rehoused in care facilities. One of the few is of the Wicking Project in Melbourne, VIC, Australia, a model of residential care for older people with dementia and challenging behaviour arising from alcohol-related brain injury. This started in 2006, as described by Rota-Bartlink and Lipmann60 (Lipmann is the chief executive of the provider organisation, Wintringham, a not-for-profit homeless service for people aged ≥ 50 years). Using a household model with an emphasis on harm minimisation and on meeting the needs of people who ‘shuffle transiently between organisations that cannot provide long-term care management solutions,’60 this facility offers individual care plans and specialist case management.
Findings from interviews with 50 stakeholders in Sydney, NSW, Australia, about possible best practice for older homeless people were summed up by Conroy et al. 72 as suggesting the need for persistent engagement with individuals, taking a harm minimisation approach, targeting people for assessment of possible mild cognitive impairment, and improving links and referrals systems between agencies. 72 Backer and Howard85 had earlier noted that, although prevalence estimates of cognitive problems varied, the effects of such impairments were that older homeless people could find it difficult to access help and support or to sustain engagement with services when their housing was at risk.
Barrett et al. ,83 reporting on older homeless service provision in Florida, USA, claimed that there was an increasing need to understand and work on the different ways in which older homeless people gain access to services and the pathways designed. Unsurprisingly, perhaps, they suggested that better collaboration between services and agencies was needed.
In one of the few discussions about distressing or challenging symptoms of dementia that may be experienced in service settings supporting previously homeless older people, the homelessness provider mentioned previously, Wintringham,78 welcomed proposals for a funding supplement to cover the extra costs needed to provide such support. It commended an approach that was ‘behaviour based’, although it queried whether or not the proposed assessment tool would be appropriate for people who had been homeless. Furthermore, it suggested that a wider range of staff be approved to undertake such assessments, noting that, in homelessness services, members of staff were not generally clinically qualified. It further speculated that some people’s behaviour might be so challenging that a ‘top-up’ or an upload to the funding supplement should be considered. Such detailed considerations of cost-effectiveness and service models are rarely encountered in the literature.
Staff training and skills have been considered in some studies, although there does not appear to have been any evaluation of skills development or of training packages or workforce models. Concurring with the conclusions of other studies,81,86,87 Rogoz et al. 70 suggested that improved access and delivery of services to homeless older people with memory problems should be undertaken by specialist, multidisciplinary teams of health professionals. The skills reportedly needed were summarised as spanning the areas of outreach, assessment and multimorbidity management. In addition to advocating for more research on older homeless people following her review, Chenco64 argued the importance of better understanding of the educational, training and resource needs of health professionals who work with homeless older people.
More specifically related to the content of clinical services, Andersen et al. 88 recommended screening for traumatic brain injury after finding that this seemed to explain the poor performance in cognitive testing among a sample of 34 homeless people in Canada, whose average age was 58.8 years. Further related to health services, Abdul-Hamid et al. 89 had earlier raised questions about whether clinical services for older homeless people should be under the responsibility of geriatricians or psychogeriatricians.
However, as reported by other commentators, some older homeless people refuse to be assessed or evaluated, and questions of competency and decision-making autonomy may forestall service engagement. 84 The legal position of having a proxy or court-appointed decision-maker is not generally addressed in most studies, although the first report of the Wicking Initiative60 mentioned briefly that some residents had an administrator appointed to make decisions (in England and Wales this would perhaps be an appointee for benefits because other provisions of the Mental Capacity Act 200590 would apply only if decision capacity was substantially impaired).
Backer et al. ,85 among others, have pointed to the need for services to prevent homelessness by addressing its causes and risk factors. The skills to follow that path are not delineated, nor is how to change service commissioning. The Wicking Initiative, discussed above, remains one of the few service examples of tertiary provision described in any detail. We do not know much about what happens over time to older homeless people in other settings who are recognised as having memory problems or a dementia. As one example of the importance of this, of the 15 older homeless people with dementia contacted by an outreach initiative91 in the city of Tel Aviv, Israel, 11 later moved to a nursing home, with unreported outcomes. More generally, this study recommended intensive outreach and case management to effectively assist older homeless people.
Ending the ‘invisibility’ of memory problems among older homeless people
According to Lipmann,78 founder and chief executive of Wintringham, Australia’s largest aged care provider for homeless people, being homeless limits access to many of the supports that most other people take for granted. He argued that homeless people are often not included in support services because of their sometimes fierce independence and reluctance to push their ‘rights’; in effect, they become invisible or marginalised. Likewise, he observed that homeless people do not come to the attention of ‘aged care’ (the term used in Australia) services and, to some extent, they also remain invisible here. Lipmann78 acknowledged that considerable Australian government funding is provided for dementia research and services for people with dementia, but observed that little of such funding reaches homeless people with dementia. In his view, the reason for this rests on the stigma associated with homelessness and the ‘fact’ that homeless people do not engage with services, particularly the aged care services to which the mainstream funding is allocated. Lipmann argued that funding should be directed towards Australian welfare organisations, such as his own, that provide services to older homeless people. 78
Literature review B: how homeless people with memory problems perceive their quality of life
Although several measures of social functioning and wider QoL have been developed for use with people with long-term mental illnesses,34,35 their development for use with people with dementia has been slower, although stress and coping among carers have been widely studied. None appears to be relevant to the social circumstances of older people who are homeless, with all of the factors that this living situation generally brings (lack of family contact or meaningful activities, and poor health overall). This literature review49 investigated the evidence on how older homeless people with memory problems perceive their QoL, and the potential appropriateness of existing QoL instruments in reflecting the needs and priorities of this group.
Literature review B49 comprised a narrative systematic review and an evidence synthesis of QoL instruments used in assessing people with dementia (all types) to assist investigators and service providers in selecting the optimal measures for their aims and to specifically address issues and life areas that are of particular importance to homeless older people. It noted the presence of a large body of literature in this area (QoL and dementia), and so a narrative review and critical discussion, with tabulated evidence, were undertaken to compare the measurement properties of the QoL instruments identified, their appropriateness for assessing the QoL of homeless people with dementia, and by type and severity of dementia, and sensitivity to the type, organisation, delivery and use of health service interventions.
The objectives of this review were to:
-
assess the scope and domains included in the QoL measures, theoretical and conceptual frameworks, and the extent of user involvement in their development, by type of user
-
assess their sensitivity to different models and settings of care, the process, organisation, delivery and take-up, and outcomes of services (including service skill mix and voluntary-sector interventions)
-
assess how perceived QoL influences decisions about the care of people with dementia, including homeless groups
-
identify the factors that affect reported QoL, and QoL outcomes of people with dementia, including among homeless groups
-
examine the relevance of existing dementia QoL measures, and their appropriateness, in relation to people who are/have been homeless
-
summarise the current data on the QoL of people with dementia, including homeless groups
-
identify research gaps and the need for further primary research.
The findings of this review were published in 201549 and informed our study data collection instruments.
Chapter summary
In summary, literature review A found that studies of the physical and mental health of older people who are homeless or have experienced recent homelessness have collected data on memory problems using different definitions and in different ways either as a focus or in combination with other conditions. As a scoping review, the publications reviewed were not assessed or graded for quality, but a narrative approach has drawn attention to the key features of the studies or descriptive accounts. The review has not only identified the several varied estimates of prevalence and some debate about the most appropriate means of assessment, but, by providing details of the study populations and approaches, it offers a means of interpreting the variations.
Scoping reviews also facilitate understanding of where gaps in the evidence may lie. Notably, service evaluations and trials of interventions are few. The future of homelessness research with older people may need to shift from estimates of prevalence, as there is international consensus that older homeless people experience multiple health problems but we have far fewer data establishing what is effective in care and support or how to implement the findings. Interestingly, there are few personal accounts or qualitative studies of personal experiences and, with one exception from the Melbourne service (Wintringham), very few accounts of practice, service commissioning and outcomes. This review has set the scene for this study; Chapter 3 presents the methods used in the research.
Chapter 3 Study methods
This chapter describes the methods used to conduct the fieldwork that was planned and undertaken to address the research objectives. The chapter begins with an explanation of what was originally planned in the study design during the preparation for the grant application in 2011, including the potential study sites identified and the proposed data collection methods for the two phases of the study. The various challenges that arose during the implementation of the study design are then discussed. The details of data sources are presented. The last section of the chapter provides accounts of the different methods of data analysis undertaken. This includes a descriptive analysis of the participants’ profiles, the analysis of the cognitive assessments, an economic analysis of participants’ service use and an analysis of participants’ intermittent pathways through health and social care services.
The study design
The study was designed to have two distinct phases: (1) a quantitative element to examine the prevalence of memory problems among older homeless people living in hostels and the extent to which homeless-sector staff are aware of and respond to these problems, and (2) a longitudinal case study phase to investigate:
-
the pathways by which older homeless people with suspected cognitive problems are referred to memory assessment services
-
the services and support that this user group receives for cognitive problems, and the cost of these services
-
how existing services can be developed to address any gaps in service provision or unmet need
-
how homeless people with memory problems perceive their QoL and available support.
Phase 1 design
The first phase of the study aimed to recruit and conduct short ‘screening’ interviews with up to 200 older homeless people aged ≥ 50 years living in hostel accommodation in England, with a maximum of 50 people in each of four diverse study sites. These were the Midlands (five hostels), Central London and South London (three hostels) and the North East of England. As noted in Chapter 1, we used the former UK Coalition on Older Homelessness definition of ‘older’ homeless people as those aged ≥ 50 years.
At the time the study was being designed, managers of several hostels in the sample areas were contacted to find out if they had any residents aged ≥ 50 years and to ascertain their interest in participating in the study. There was an enthusiastic response, with the managers welcoming the need for the research as they perceived the needs of older homeless people to be growing. In the North East of England, however, the numbers of older homeless people were thought to be small in the areas approached, and, consequently, four further hostels were identified in the North East of England that potentially could supplement numbers.
The recruitment and screening interviews of older homeless people aimed to obtain a profile of each participant and an overall assessment of their problems and needs. These also aimed to enable the research team to consider whether or not a participant had any memory problems and, if so, to determine whether or not depression was an influencing factor. This enabled participants to be selected for the case study phase (phase 2). These interviews were designed using a semistructured interview schedule to collect the following information: (1) demographic factors (age, gender, ethnicity); (2) brief histories of homelessness (i.e. length of time homeless, duration of stay in present hostel); (3) previous and current employment, education, income and welfare benefits; (4) use of time and family and social contacts; (5) support received with personal care and household tasks, such as obtaining meals and personal hygiene; (6) past and current physical and mental health problems (including administration of a validated depression tool), substance misuse problems, histories of head injuries and other accidents or traumas, other diagnoses including chronic or long-term conditions, past hospitalisations, and medication and treatment; (7) concerns about memory and support or treatment received, and administration of the MMSE; (8) the use of different health services; and (9) QoL, and hopes and plans for the future in terms of housing and support.
We were conscious that older people with memory problems and in marginal living conditions could be a vulnerable group in terms of research as well as in much of their lives. In our application for ethics approvals, we addressed the risks that they might feel obliged to co-operate in the study, might find the questions intrusive or upsetting and might have expectations of more help. Two senior researchers (MC and LJ) had considerable experience of research and practice in the homelessness sector and they supported the wider research team in fieldwork. One ethical challenge was how to acknowledge participants’ time in study participation. We decided that, at the end of each interview, older homeless participants would be offered £5 to thank them for their time, either in cash or as a shopping voucher: the type of incentive was negotiated with each hostel manager.
Once participant baseline interviews were completed in each hostel, each person’s key worker was contacted and invited to take part in the study. An information sheet about the study was designed for hostel workers, and workers were shown the consent form signed by the hostel resident that gave consent for the worker to be interviewed about them. Hostel workers were also required to provide written consent to be interviewed. This interview included questions on (1) the characteristics of the hostel resident; (2) how the worker assessed and planned support for the resident; (3) their perspective on any physical, mental health, substance misuse and memory problems and the support and treatment provided; (4) what assistance, prompting or supervision was provided on a day-to-day basis by hostel staff or other services; and (5) future plans for the hostel resident. If a worker suspected that the participant had memory problems, they were then asked, based on the informant interview questions in the General Practitioner assessment of Cognition (GPCOG) tool,92 the reasons for this, such as whether the person (1) had problems remembering things that had happened recently, (2) could not recall conversations a few days later or (3) had difficulty finding the right word or tended to use the wrong words.
To gain an understanding of the hostel staff’s training and experience, a short structured questionnaire was also designed to be administered at the first interview with each practitioner. Topics were (1) current role, length of time working in the hostel and hours of work; (2) previous experience of working with homeless people; (3) other work experience; (4) training related to working with homeless people and training on supporting someone with mental health or memory problems; and (5) training that was/would be helpful in working with older hostel residents.
To collect background information about the hostel and the services it provided, an interview was also planned with the manager or senior practitioner in each hostel. An interview schedule was designed to collect information about (1) the hostel management, facilities and funding; (2) client groups and access policies; (3) tenure policies; (4) staffing levels and training available for staff; (5) help and support provided to hostel residents; and (6) characteristics of residents with memory difficulties, support provided and services available.
After the baseline interviews were completed with hostel residents and hostel staff, data were summarised so that each participant could be discussed by the research team psychiatrists to enable participants to be allocated to observation or control groups. It was initially intended that decisions regarding allocation to the observation or control group would be made with the 30 hostel residents suspected of having memory problems and a random selection of eight residents not suspected of having memory problems being invited to take part in an interview with the research psychiatrists using the Addenbrooke’s Cognitive Examination tool version R (ACE-R),93 which would be used to confirm the group allocation. This tool was later replaced by the Addenbrooke’s Cognitive Examination III (ACE-III) following further discussion. The ACE-III is one of the most popular and commonly used cognitive tests in dementia clinics and in the assessment of other neurological disorders. It provides a sensitive, reliable, secure and easy-to-administer clinical tool to assess cognition as part of the process of assessing for dementia. The ACE-III has five subdomains, which provide a cognitive score out of a maximum of 100: (1) attention, 18 scores; (2) memory, 26 scores; (3) fluency, 14 scores; (4) language, 26 scores; and (5) visuospatial, 16 scores. The assessment also involves asking participants if they have problems with face recognition, remembering names of people or objects, and problems with their short- or long-term memory. As with other hostel residents who participated in interviews, £5 was given for participation.
Phase 2 case study design
The 6-month longitudinal case study phase aimed to conduct case studies of 60 older homeless people – 30 with memory problems and 30 without memory problems – divided between the study sites with the samples matched on age and duration of their stay in the hostel. These 60 participants would be selected from the 200 participants recruited in phase 1. A case study methodology was chosen as it would enable an in-depth exploration of the predominant factors and challenges that staff in homelessness services face in a real-time context,94 which can be especially useful in researching practice settings. 95
Interviews with hostel residents
The case study phase of the study involved interviews being conducted 3 and 6 months after the first ‘screening’ interview with the 60 hostel residents described above. In both interviews, the aim was to collect information relating to their situations during the previous 3 months. Questions covered (1) their use of time and social contacts; (2) courses, training and voluntary work undertaken; (3) contact and support received from hostel staff; (4) everyday tasks and help given; (5) changes to physical, mental health, memory, alcohol and drug use and any associated treatment or support; (6) referrals and use of health, substance misuse and other services including hospital admissions, hospital outpatient drug and alcohol detoxification and rehabilitation services, services accessed from a general practice, urgent and emergency care; and (7) help that they would have liked to have had, but did not receive.
Interviews with hostel staff
Interviews were also planned to be conducted at 3 and 6 months with hostel staff in relation to the participating hostel residents they supported. These interviews focused on the same subject areas as covered in their first interview conducted in phase 1, in particular any changes perceived by the worker in the resident’s physical or mental health, substance misuse or memory problems, the services used by the resident, the support provided by hostel staff or other services and how long they spent providing this support.
It was initially proposed that information about the length of time workers spent supporting an individual could be collected using a self-completion diary sheet. This was piloted in one hostel by members of staff supporting two residents over a 2-day period. Staff were asked to document hourly any support or attention they gave these residents and how many minutes this took. This included help with finances, social activity and personal care, as well as any activities they undertook on a resident’s behalf, such as arranging appointments and dealing with rent payments. However, this proved not to be a very accurate way of collecting these data, as support often involved checking on or keeping an eye on people to monitor their well-being rather than being a specific task, and, as residents often spent large amounts of time in communal areas, such ‘support’ was not provided to a single person. The diary element was, therefore, not pursued.
The final interview with hostel staff at 6 months contained additional questions regarding (1) effective ways of engaging with the hostel resident and any strategies or techniques used, (2) their challenges and difficulties in working with the resident and attempts to overcome the difficulties, (3) experiences of working with other agencies to support the hostel resident and (4) implications for hostel staff and other workers in helping older homeless people with similar problems.
Interviews with other support workers
To obtain as much relevant information about the support needed and provided to each participant, interviews were also planned with other workers providing support. At their 6-month interview, hostel resident participants who received support from a service such as an alcohol misuse or community mental health team were to be asked to provide permission for the worker to be invited to take part in a semistructured interview about the support they provided. Interviews were intended to last about 45 minutes and would be digitally recorded and transcribed. The topic areas were (1) current role and experience in working with older homeless people, (2) help and support provided to the participant, (3) working arrangements with other services to provide this support, (4) challenges or difficulties in providing this support and (5) unmet needs of the participant.
Data collection from participants’ hostel records
It was also planned that, following the 6-month interviews with residents, data would be collected from participants’ hostel records. Information would be collected about (1) length of time in the hostel; (2) welfare benefits received and rent paid to the hostel; (3) mental and physical health conditions, substance use issues and treatment programmes; (4) medication; (5) use of different health services, including general practitioner (GP) and other health-care services, such as emergency department [accident and emergency (A&E)] use and hospital admissions; (6) frequency and duration of receipt of social care services, including domiciliary care/home care; and (7) other service use, such as voluntary services (e.g. day centres).
Data collection from participants’ medical records
At the end of the case study period, data would also be requested from the medical records held by the named GP for each resident. These data would comprise all medical records for the 6-month study period, including active health problems, previous health problems, current medication, hospital admissions and discharges, responses to referrals, use of urgent care and out-of-hours services and hospital outpatient department reports.
Study implementation
This section discusses the challenges involved in implementing the study design and the responses to these.
Recruitment of study sites and participants
Ethics approval was obtained from the London and South East Research Ethics Committee in April 2014 (14/LO/09373) and fieldwork began in May 2014. Once fieldwork for phase 1 commenced, however, the recruitment plan for the study sites changed substantially in some areas. This was due to the closures of some hostels that had initially agreed to participate, and changes to the resident profiles. The team contacted many hostels, considered other areas to try to supplement numbers and attempted to identify replacement sites. A summary of the changes to the sites, the nomenclature used and the numbers of participants recruited is shown in Table 1.
| Original site | Other attempts to recruit to site | Total number of hostels as recruitment sites | Total number of residents recruited | Final site name |
|---|---|---|---|---|
| London | Also recruited from this locality | 2 | 24 | Central London |
| London | None | 2 | 19 | South London |
| North East | Tried to recruit one large hostel but it had closed. Recruited another location | 3 | 19 | North England |
| Midlands | Not able to recruit from initial hostel:
|
1 | ||
| Total | 8 | 62 |
Central London and South London
Recruitment began in May 2014 with the hostel identified during the study design period that had a large number of residents aged ≥ 50 years. In this hostel, 17 residents were recruited. To supplement numbers, two additional hostels were contacted. One hostel manager met with members of the research team but later declined permission for the hostel to take part (reason unspecified). The other participated and seven out of its eight eligible residents were recruited.
The other two hostels identified in the study design stage agreed to participate. Here, 19 participants were recruited (10 in one hostel in October/November 2014 and nine in the other in February 2015).
The North East
Once recruitment began in this region in June 2014, the need for supplemental hostels became even more evident from the unexpectedly small numbers of participants. An additional hostel in the area was identified and agreed to take part; however, of the handful of other, smaller local hostels, only three became involved and, from these, only four residents were recruited: one hostel was not able to recruit any participants. Of the four hostels that did not participate, the manager of one hostel declined to be involved, the manager of two hostels was reluctant to allow access to residents’ records, and one had only a few older residents. Attempts were made to contact the two hostels previously identified in the region in 2011. One had been demolished, and the other had closed and been replaced with three smaller units with a total of 40 beds. These units either did not have any residents aged ≥ 50 years or had such small numbers (one had one resident and the other had three) that it was not feasible to recruit there. Instead, a hostel in another locality participated, from which 11 residents were recruited.
The Midlands
Although three hostels were identified as suitable in one locality during the design stage of the study, once fieldwork commenced in 2014 they were found to currently have very few older hostel residents. As there were such small numbers in this locality, we looked further afield for a potential fourth site in this region. In one potential area, a hostel with > 200 beds supported many residents aged ≥ 50 years and, when visited in 2011, was very willing to participate. However, by May 2014 this hostel had closed. Residents in another hostel in the locality were being required to move from the hostel after about 3 months; therefore, it was not suitable for the study’s needs. In another nearby locality, five hostels were identified in 2011 as potentially suitable; however, only one worked with homeless people aged ≥ 50 years. By 2014, this hostel was providing only short-term emergency accommodation, which also made it unsuitable for the study. Having failed to find suitable hostels in the Midlands, the potential for creating a cluster in an adjacent region was explored. In August 2014, two hostels were identified that appeared suitable initially. However, although one of these hostels had 16 residents aged ≥ 50 years, the high turnover of these residents made follow-up over 6 months untenable. The hostel in the other locality had very few residents aged ≥ 50 years. Finally, one hostel was contacted in another locality, which had four residents aged ≥ 50 years. All four eligible participants in this hostel were recruited in September and October 2014.
Recruiting, obtaining consent and interviewing older hostel residents
Once the initial sites had agreed to participate, three members of the research team (MC, LJ and KS) met with the site managers to further explain the study and provide information sheets for residents and staff. A few days before the team visited each hostel, hostel staff spoke to residents aged ≥ 50 years, provided them with an invitation letter and study information sheet, and sought their permission to tell the interviewers if they were interested in taking part. When the interviewers visited the hostel, residents who had expressed an interest were contacted. The researcher explained what was involved, specifically that (1) participation was voluntary and they could withdraw at any time or refuse to answer any question; (2) that they would be seen three or four times by a researcher over the following 6 months, one of whom would be the research team psychiatrist for some questions related to memory and concentration; (3) that their consent was needed to collect information from hostel staff, their hostel records and their medical records; and (4) if they said something that indicated that they or someone else was at risk of harm, the interviewer would be obliged to take appropriate action. Permission was also sought for the researchers to make enquiries about participants’ whereabouts from hostel staff, and nominated services, family or friends if they could not be contacted for future interviews.
Written consent was obtained before the first interview, with verbal consent obtained before subsequent interviews. Only hostel residents who gave informed and written consent were recruited. Participants’ capacity to give informed consent was determined before each subsequent interview. It was planned that, should a participant lose capacity during the following 6 months, they would be kept in the study and, in accordance with the Mental Capacity Act 2005, a nominated consultee would be involved. This, however, was not necessary. For participants who were heavy daily drinkers of alcohol, interviews were arranged in the morning before they became intoxicated or fell asleep.
There were several challenges in recruiting residents to the study. Despite numerous visits to hostels, recruitment took much longer than planned and a greater number of older people than anticipated declined to take part. One problem was that the title of the study led to misunderstandings. Some hostels persistently referred to the study as the ‘dementia study’ and at times staff perceived that only people with memory problems were needed. Consequently, some residents were reluctant to take part as they felt that they did not have memory problems or dementia. Repeated efforts were made by the research team to challenge these misconceptions but it is likely that this had a negative effect on participation.
Being reliant on staff to initially speak to residents and explain the study brought other challenges. Some members of staff were very interested in the study, discussed it with residents, encouraged them to take part, and readily liaised with the research team. In other hostels it was more difficult. This was largely because of work pressures but insufficient interest in and unfamiliarity of being involved in research may have also influenced the way in which the study was explained and the extent to which residents were encouraged to take part. In one hostel in North England, only 2 out of the 16 eligible residents agreed to participate.
Practical aspects also affected when interviews could take place as the research team had to work around the shifts of hostel staff, staff handover meetings and other activities, such as resident meetings and groups run by visiting alcohol/addictions or health workers. In two hostels, members of staff were only on site until 4 p.m. so, for safety reasons, researchers could not visit after this time. Another hostel only permitted researchers to visit once per week.
Arranging and conducting interviews were also complex tasks. As outlined previously, many hostel residents were heavy consumers of alcohol and illicit drugs. On two occasions, interviews had to be completed at a second visit: one person fell asleep in their first interview and another had to attend an unexpected case review. Some participants had been homeless for many years and were vague about past details. Therefore, capturing the required information was often difficult. Some questions had to be rephrased and asked in different ways, and details needed to be checked at different points during the interview if contradictory information was provided.
Nonetheless, a total of 62 older homeless participants aged ≥ 50 years were recruited to the study. Fifteen people (24%) were lost to follow-up and 47 were included in the case study analysis. Several reasons were offered as to why people either dropped out of the study or could not be followed up. These are shown in Table 2.
| Reason why participant was lost to follow-up | Number of participants |
|---|---|
| Died | 1 |
| Moved to another hostel managed by different organisation; it was not feasible to follow up as this would have involved having to negotiate access and permissions again | 4 |
| Evicted/moved from hostel and contact lost | 2 |
| Relocated out of the UK | 1 |
| Went to drug and alcohol detoxification centre and then abandoned rehabilitation | 1 |
| Declined to participate further at point of ACE-III or when contacted for 3-month interview | 5 |
| Did not consent to collection of information from medical records | 1 |
Undertaking cognitive assessments
Changes were made to the study design in relation to the various cognitive assessments undertaken in both phases of the study. In phase 1, the MMSE was replaced by the Six-Item Cognitive Impairment Test (6-CIT). This was because it was felt that the 6-CIT was more achievable to conduct as an initial screening tool, as it was shorter than the MMSE and did not involve a requirement to draw.
Although the study was designed so that only some participants would receive further cognitive assessment by the research team psychiatrists, by the time the data of the first group of residents were discussed by the research team it was apparent that recruiting up to 50 participants per site was not feasible and that it would be a challenge to obtain 60 participants for the case study phase. It was therefore decided that (1) all participants would be taken into the case study phase and (2) to ensure consistency in allocation to observation or control group, all participants would be invited for cognitive assessment. Appointments were consequently arranged with each participating hostel resident for a psychiatrist or a psychologist (RN, Tanya Walton and Elspeth Dustagheer) to conduct a short (20-minute) assessment of cognition with them where they lived. Although it was planned that the ACE-R would be used, this was replaced by the Addenbrooke’s Cognitive Examination tool III (ACE-III) as copyright permissions were needed for the ACE-R.
On reviewing the first set of residents’ data, the research team noted that some participants struggled to answer the 6-CIT questions about memory and concentration and therefore might struggle with the ACE-III. It was therefore proposed that the shorter Montreal Cognitive Assessment (MoCA),96 which captures executive function of memory more succinctly, should be used with participants for whom the ACE-III could be too burdensome. This would theoretically enable all participants to undertake a cognitive assessment and reduce the number of missing data. The ACE-III was considered to still be useful for any subanalysis but the MoCA would give a good indication of whether or not an individual had memory problems. An application for a substantial amendment to ethics permissions was made and accepted at the end of July 2014. Nonetheless, 48 ACE-III assessments were conducted and the MoCA was attempted with only one participant.
Interviewing hostel staff
There were challenges in completing interviews with hostel staff. They were often very busy and found it hard to make time and, in a few cases, long-term illness meant that some could not be interviewed as planned. Consequently, on some occasions baseline questions were combined with 3-month interviews. In one hostel, members of staff were interviewed only once at 6 months. When possible, the same member of staff was interviewed each time; however, the high turnover of agency/locum staff in one hostel meant that different staff were acting as key workers for residents at baseline and at 3 and 6 months. Even when appointments with workers had been arranged, at times interviews were cancelled if there was a crisis in the hostel. Nonetheless, interviews were held with 44 hostel workers. All were recorded with consent, transcribed and analysed thematically, and linked to any relevant resident for whom the staff member acted as a key worker (see Data sources).
Data sources
Extensive attempts were made to obtain a ‘complete’ data set that included participants’ self-reports, hostel worker reports and information from hostel and medical records. However, the challenges in conducting the fieldwork explained previously meant that this was not possible in many cases. Although the majority of hostels provided full access to electronic and paper records, ensuring that all relevant information could be collected, in a few cases staff either completed the extraction themselves or acted as gatekeepers to data, making it difficult to be certain whether or not all of the relevant information had been provided.
Health centres were also difficult to contact, and, although medical records were obtained for 30 participants, nine participants’ GPs did not respond to data requests, one hostel resident did not have a GP and another’s GP was contacted only to find that the resident had not used the practice during this time; four practices reported that they were unable to provide the data as the resident was no longer registered with them. In one case, the hostel resident changed his GP in the last month of the case study period. Efforts were made to contact the second practice, but it did not respond. Not being able to pay general practices for the provision of data was a stated barrier to their willingness to provide data, but this did not appear to be the only factor. The different data sources and the number of participants for whom data were collected are shown in Table 3.
| Data source | Interviews (n) | ||
|---|---|---|---|
| Baseline | 3 months | 6 months | |
| Older homeless people (aged ≥ 50 years) | 62 | 37 | 37 |
| Hostel staff (key workers); 43 SWs participated. Some were interviewed about more than one participant | 44 | 15 + 4 combined with baseline questions | 30 + 9 combined with baseline questions |
| External workers | 4: tenancy SW, alcohol worker, clinical psychologist and community mental health nurse | ||
| Hostel managers | Interviews with manager(s)/senior staff were completed at eight hostels | ||
| Hostel records | Data were collected from records of all 47 case study participants | ||
| Medical records | Data were collected for 30 case study participants and partial data were collected for one participant (31 in total) | ||
Data analysis
Descriptive analysis of the sample
Quantitative data from the interviews with hostel residents and staff were entered into a SPSS database. Open-ended responses from interviews with hostel residents and staff were entered into a NVivo database. A straightforward process of thematic analysis was applied to these responses so that categories and themes could be identified. Most of the answers related to the questions asked of participants. Drawing on the data collected in baseline interviews with hostel residents and staff, the profiles of the 62 older homeless people recruited to the study were analysed using descriptive statistics. These included age, sex, ethnicity, education and work history, housing and homelessness history, activities and family/social contacts, income, management of everyday tasks, physical and mental health problems, head injuries, use of alcohol and drugs, and use of services in the 3 months prior to baseline interview. These findings are presented in Chapter 4.
Analysis of cognitive assessments
The allocation of each case study participant into the observation or control group was conducted throughout the case study period once the relevant data had been collected. Although it was proposed that each participant in the case study phase would be categorised, as far as possible, as either having memory problems (suggestive of some form of dementia) or not having memory problems, it was not possible to allocate all participants precisely into these two groups. Consequently, a third group was created: those with borderline memory problems. Each case was examined by the team, with decisions regarding the allocation into each group made by the research team psychiatrist (RN) with reference to the ACE-III scores, participant self-report, hostel staff perceptions of whether or not an individual had memory problems and information obtained from participants’ hostel and medical records (when available). A cut-off point of ≥ 82 out of 100 was considered to categorise participants with memory problems (in clinical terms, cognitive decline). We also examined the history of declining activities of daily living for those who scored < 82 out of 100 points. Considering that many of these individuals had a history of alcohol abuse at the point of cognitive assessment, it was not possible to rely very heavily on the score from the ACE-III. To make a diagnosis of dementia in a clinical setting, a clinician usually interviews the patient, tries to gather information from family and relatives, and then reviews the person’s medical record. Clinicians often use a series of biomarkers, such as blood tests, brain imaging and neuropsychiatric testing, to confirm a diagnosis. As most of that information was not available, the research team, supervised by Ramin Nilforooshan, examined the medical record and other information available for each case carefully to categorise the resident to each subcategory. These findings are presented in Chapter 5.
Economic analysis
To enable the costs of service use to be calculated, and to explore the pathways of participants through different health and social care services, the service use of each participant during the 6-month period following recruitment was collected and documented, as precisely as the available data would allow, in a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet. The utilisation of a large number of services was included. Categories were informed by the Client Service Receipt Inventory, which is a well-validated and widely used instrument that captures the full range of health (primary, community, hospital A&E, outpatient and inpatient), social and voluntary sector provision. 97 Incidences of did-not-attend (DNA) appointments were also noted.
Data were collected from several sources: participant self-report, hostel staff accounts, hostel records and medical records. When dates were recorded for specific aspects of service use, these were documented, as were the reasons for service use and outcomes. The sources of each occurrence of service use were also recorded. This allowed accounts of the same episode of service use from different sources to be cross-checked and for any discrepancies to be identified and considered. Where there were discrepancies in accounts, the most reliable source was selected. Medical records, when available, were considered to be the most accurate source, followed by hostel records, hostel staff reports and participant self-report. For example, if a hostel record showed that a resident had said that they were going to see their GP but the GP record did not have details of any contact, this would not have been counted as a GP contact.
The number of times each service was used was recorded for months 1–3 and for months 4–6 and subsequently amalgamated so that frequencies of use could be calculated over the full 6-month follow-up period. Frequencies of use for each service were tabulated. Some services were not used at all, or were used relatively infrequently, so groupings were created: GP and other general practice staff (nurse, care navigator) contacts in surgery, hostel or on the telephone; other primary care (i.e. chiropodist, dentist, optician); drug (including pharmacist for opiates) and alcohol services; community psychiatric/mental health nurse, counsellor, team/memory service; social care (social worker, social care allied health professionals in clinic, hostel and day centre); A&E and out-of-hours walk-in/urgent care, ambulance; hospital outpatient appointments (psychiatric and other), tests, treatments; and hospital inpatient days and stays, including intermediate care (psychiatric and other) and voluntary. In addition, all psychiatric and mental health service use was collected together in one category (community services, outpatient and inpatient) for separate consideration.
The unit costs of all services (2014–15) were obtained from validated national sources, primarily Unit Costs of Health and Social Care 201598 and NHS Reference Costs 2014–15,99 and applied to each service for each participant and summed to give a total service use per participant over the 6-month period. Summary statistics were calculated (mean, SD, median, minimum and maximum) across all participants for each service use item and for groupings of services, and overall. Proportions of zero utilisation were shown for each item. DNA (or missed) appointments were costed as if the contact had taken place, and proportions of DNA appointments were reported.
Two approaches were used to test the association between memory problems and service use costs. With costs being non-normally distributed, non-parametric tests were used. First, the Kruskal–Wallis test, a rank-based non-parametric test, was used to determine if there were statistically significant differences in the mean costs of service utilisation (each item and groupings of items) between participants grouped according to memory problems (no memory problems, borderline, and memory problems present). The Mann–Whitney U-test (a rank-based, non-parametric test for comparing only two groups) was then used for pairwise comparisons, where the Kruskal–Wallis test was significant. The level of significance was set at a p-value of 0.05. Memory problems groupings were determined by the research psychiatrist (RN), based on scores from the ACE-III (range 0–100 points, with lower scores indicating more memory problems), participant self-report, hostel staff perceptions of whether or not an individual had memory problems, and information obtained from hostel and medical records. As noted previously, it had been intended to categorise each participant as having memory problems or not, but this was not possible, so a ‘borderline’ category was introduced. Second, associations were explored between service groupings and memory problems as indicated solely by ACE-III scores using Spearman’s rank-order correlation. As ACE-III scores were not available for all participants, and service use for some groups was low, correlations were not conducted for individual service use items.
Ten other participant characteristics with potential to influence service use costs were identified: sex, ethnicity (white British/other), literacy problems (yes/no), current (within the last 3 months) illegal drug use (yes/no), frequency of alcohol consumption (< 6–7 times per week/6–7 times per week), location (north/south, i.e. London), number of comorbidities, number of prescribed medications and number of head injuries. When more than one indicator of a particular characteristic was available (e.g. different measures of drug and alcohol use), the variable with least missing information was selected. Associations between the baseline values of each of these participant characteristics were calculated using Spearman’s rank-order correlations (for pairs of continuous variables), Mann–Whitney U-tests (for continuous and categorical variables) and chi-squared or Fisher’s exact tests (for pairs of categorical variables). Then the associations between each characteristic and each cost grouping were explored using Spearman’s rank test (continuous variables), and Mann–Whitney U-test and Kruskal–Wallis tests (two and three or more category discrete variables, respectively). Finally, all 10 variables were included in backward stepwise regression modelling to explore independent predictors of each cost item. The decision to carry out linear modelling was driven by inspection of the cost variable. Hence, social care was excluded from the modelling exercise because of the small number of participants who accessed social care services. Logistic regression approaches were not considered suitable because of the small sample size and low proportions of participants in some categories.
Analysis of service needs and use
The service needs and use of all three case study groups were examined. Each potential ‘case’ was considered individually to decide whether or not there was sufficient information to understand the participant’s pathway through services, and to calculate their service use. When 3-month interviews were not conducted with a participant or key worker, at the 6-month interview it was ensured that as much information was collected about the previous 6 months. In some cases it was not possible to conduct a 6-month interview with a hostel worker and/or a participant; in one hostel, for example, three participants who had lived in the hostel for almost all of the 6-month case study period could not be interviewed at 6 months as two were in hospital and one had been evicted. However, in these cases the hostel and medical records provided a clear account of what had happened and the range of services used, enabling the cases to be suitable to be retained. In other cases in which a participant was relatively independent, hostel records held sparse information about their service use, yet hostel staff and participant self-report provided reliable data.
Chapter summary
This chapter has set out the original study design as planned prior to the submission of the grant application and then explained the challenges of implementing the design. We have shown that undertaking research with older homeless people with or without memory problems is possible, despite the continually changing landscape of homelessness services in England, and have outlined the difficulties of conducting a longitudinal study within hostels for homeless people that are supporting individuals with complex health and social care needs and in collecting data from other sources. This chapter provides detail of the adaptations made in response to the challenges of the study.
Chapter 4 Profile of hostels and their staff
This is the first chapter reporting study findings. It describes the study sites, namely the hostels that agreed to participate in the research, and the hostel staff. We have anonymised the hostels, and some details that would risk making them or their residents easily identifiable are not reported. Information reported here was collected from (1) interviews with hostel managers about the characteristics of each hostel and (2) interviews with hostel staff, namely residents’ key workers.
Study sites
A total of eight study sites were included: four in the London area and four in North England. Table 4 contains details of the sites in the London area and Table 5 contains details of sites in North England; information was obtained in interviews with hostel managers and researcher observations and enquiries.
| Characteristic | Hostel | |||
|---|---|---|---|---|
| Central London hostel 1 | Central London hostel 2 | South London hostel 1 | South London hostel 2 | |
| Gender (maximum number) of occupants | Male only (40–50) | Male and female (20–30) | Male only (40–50) | In main building, both men and women (60–70) |
| Number and type of bedrooms | All single rooms | All single rooms | Majority single rooms (two with shared bathroom) | All single rooms |
| Bedroom facilities | Each room has a bed, wardrobe, sink, chest of drawers and coffee table | Each room has a bed, wardrobe, dressing table and chair | Bed, en-suite bathroom (for two residents), washbasin | Each room has a bed, wardrobe, cabinet, underbed storage, sink, clock and kettle |
| Number of floors and accessibility | Two floors; has a lift | Three floors; has a lift | Two floors; has a lift | Four floors; has a lift |
| Accessibility or disabled facilities | Some accessible bathrooms with chairs for showering; grip rails in the toilets. Three wider rooms and all bathrooms and toilets suitable for wheelchair use | Wheelchair access at side of building; ongoing building works had closed this access at time of study. Hostel can make adaptations if necessary for residents. Bathrooms have chairs for people to sit on when showering | Two large rooms for wheelchair users. Half rooms on the ground floor. Wide corridors for wheelchairs. Disabled access to bathrooms in most rooms | Three accessible rooms, accessible toilet on most floors |
| Meals included | Breakfast, lunch and evening meal included in service charge | Cooked breakfast and cooked evening meal, both included in service charge. Sandwiches donated every week night to the hostel for residents’ use | Cooked meals three times a day, included in service charge | All meals available if so chosen |
| Cooking facilities | Shared kitchen on ground floor and second floor | Microwave for heating up food or drinks and basic snacks | Shared kitchen. Can make themselves sandwiches or ask staff to help them | None. Communal kitchens for those preparing to move on |
| Laundry facility? | Yes | Yes | Yes, on each floor | Yes |
| Referral system | Minimum age 21 years, no maximum age. Referrals only through other hostels or outreach teams | Minimum age 18 years, maximum age 65 years. Referrals only through other hostels or outreach teams | Minimum age 40 years, no maximum age. Referrals through local authority | Referrals through Vulnerable Adults Pathway filtered through local authority |
| Needs profile of residents (low, medium, high, as described by hostels) | All | High | Medium and high | All |
| Drinking of alcohol permitted? | Yes, only in own room | Yes, anywhere | Yes, in bedroom, in garden, not in communal lounge rooms | Yes, in bedroom |
| Number of paid staff | One manager; one assistant manager (FT); nine SWs (FT); one cleaner (FT); one drug and alcohol worker (PT); two night staff (FT); three night concierges (one FT and two PT); and two kitchen staff (PT) | One manager and one assistant manager (FT); five SWs (FT); one support assistant (FT); one cleaner (FT); one cook (FT); and two night staff (PT, agency staff) | One manager and one assistant manager (FT); 11 SWs (FT); two night support workers (FT); five cleaning/catering staff (three FT and two PT); and two porters/security staff (FT) | One manager, two senior practitioners, one case worker, four lead SWs, four assistant SWs, three administrators, four cleaning/catering staff, two porter/night staff, one head chef, two other night workers and four trainees/apprentices Staff per shift: three management, four social workers |
| Key worker status for residents | Five residents per key worker; meet once a week; action plan meeting every 3 months; look at Outcomes Star to set goals with clients | Expected to meet once every 4 weeks | Five on average (range from 3 to 6). Meet once a week or fortnight | Varies from 1 to 9 depending on seniority of role; details recorded in case files |
| Life skills training | Move-on training: adult cooking groups, budgeting training | Stopped because of budget cuts | Stopped because of budget cuts | Yes – but need more volunteers to help with budgeting, cooking, employment |
| Other support | Massage/reiki/alternative therapist visits weekly | Complex needs worker visits twice a week | Art workshops, gardening groups, film group, bingo night, gentle exercise classes | Activity every night, psychologists support group, therapy-based arts |
| Total hostel rent (rounded to nearest £) | £267 (£242 rent plus £25 service charge) | £295 (£270 rent plus £25 service charge) | Information not provided (£35 service charge) | £270 (£230 rent plus £40 service charge) |
| Funding source | 100% local authority in documentation but manager not sure | 50% local authority plus 50% donations/grants | Manager did not know details of funding arrangements as just started role | Local authority main source, but manager did not know specific proportions met by other agencies |
| Characteristic | Hostel | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Gender (maximum number) of occupants | Male and female (40–50) | Male only (40–50) | Male only (20–30) | Male and female (50–60) |
| Number and type of bedrooms | All single rooms | All single rooms | Four shared rooms, the rest all single | All single rooms; 15 en-suite rooms |
| Bedroom facilities | Each room has a bed, wardrobe, safe, set of drawers, sink with cupboard underneath it and curtains | Each room has a bed, bedside table, wardrobe and hand basin | Each room has a bed, bedside table, wardrobe, sink, table, chairs and kettle | Each room has a bed, wardrobe, sink and chest of drawers |
| Number of floors and accessibility | Four floors; no lift | Four floors; no lift | Three floors; no lift | Four floors, with lift |
| Disabled facilities | Nine rooms on the ground floor; one room has disabled access with a wet room, toilet and shower. Lounge and dining area are all on ground floor and accessible | None | None | Accessible toilet, pull cord ramp at front door, panic alarms around hostel |
| Meals included | Breakfast and evening meals only in main house. Both meals included in service charge. Resettlement home is self-catering | All three meals | Breakfast and evening meal | Breakfast and evening meal |
| Cooking facilities | Each landing has a kitchenette with microwave, kettle, fridge and cupboards; for quick meals rather than preparing from scratch. No cookers of any type allowed in rooms | Snack kitchen, kettle and fridge (required by local authority) | Can use kitchen, fridge, microwave and toaster | Each floor has lounge, microwave, kettle and electric hobs; one floor has a fridge |
| Laundry facility? | Yes | No; but service charge includes one load of washing a week done by hostel | Yes | Yes |
| Referral system | Minimum age 18 years; no upper age limit. Any referrals welcome: agencies, self, local authority referrals are prioritised | 21 years minimum age; no upper age limit; referrals through adult social services, probation officers, self-referrals, NHS CMHT | 35 years minimum age, no upper age limit; ‘older drinkers’ largest group, history of arson excluded; mostly through self-referrals, also mental health team and council homelessness unit | 18 years minimum age, no upper age limit; all needs levels; majority mental health and substance abusers, complex needs; no formal exclusion criteria, consider referrals on case-by-case basis; referred via Housing Support Pathway |
| Needs profile of residents (low, medium, high) | All | All; those with high levels of risk excluded | Medium-high | All |
| Tenure agreement with residents | Licence | Licence | Licence | Licence |
| Access times | 24 hours | 24 hours; 6 p.m. to 7 a.m., let in and out by staff | 24 hours | 24 hours; allowed two nights out per week with prior notification to staff |
| Drinking of alcohol permitted? | No | No | Yes, but not in communal areas | No |
| Number of paid staff | One manager and one programme co-ordinator (FT); five SWs (FT); one facilities manager and admin (FT); three cleaners (one FT and two PT); night staff (four FT, no security staff); two assistant support workers (FT); one chaplain; and five kitchen staff (two FT and three PT) |
10 (two managers, two assistant managers, SWs, cleaner, chef, night staff) and two volunteers Staff per shift: 2–4 staff, manager always on call |
Two managers, three SWs, and one catering/cleaning staff and residents help Staff per shift: five; manager on-call at night |
One service manager, one programme co-ordinator, one facilities and admin, five SWs, two security staff, two assistant SWs for night shifts; and one regular volunteer Staff per shift: three managers and two SWs |
| Key worker status for residents | 10 residents per key worker; meet once per week; review support plan every 4–6 weeks | Varies from 2 to 22 depending on seniority of role; see formally every 8 weeks, informally daily; details in case file | 20 get Supporting People funding so 20 have key worker; this entails the worker seeing them daily | 10–12; formal contact every 3–4 weeks, informal daily |
| Life skills training | A little – budgeting, cooking, rights and responsibilities of a tenancy, form-filling – in house course | None | Daily input from key worker | External agency to do budgeting, form-filling, crafts, ICT, English and maths |
| Other support |
|
None | In-hostel activities: quiz, art class, photography | In-hostel activities: movie night, pool tournament, day out in summer |
| Total hostel rent | £238.99 in the main hostel (£204.47 rent + £34.52 service charge). £178.83 in the resettlement house (£157.30 rent + £21.55 service charge) | £80 rent + £10 or £35 (includes meals and one washing load) service charge | £178 per week (£112.35 housing benefit rent + £43 service charge). For 20 clients receiving Supporting People funding, rent is £135 | £155 per week (£112.35 housing benefit rent + £43 service charge). For 20 clients receiving Supporting People funding, rent is £135 |
| Funding source | 80% local authority + 20% residents’ rents | Local authority 100%, top-up from residents’ chargesBig drop in funding from £240 pw [per week], clients now only pay £80 pw with same service being provided. In dispute with council for last 16 months, as not enough service is seen as being provided. If hostel does not win tribunal regarding not getting enhanced Housing Benefit, management will have to rethink how hostel is run and what service is provided – even less support, more signposting |
Local authority 100% Changes to funding: |
Local authority Supporting People money 33%, Housing Benefit 40%, rest top up from charity Changes to funding: |
Sites
We outline in this chapter the salient characteristics of the hostels participating in this study. We have grouped together some identifying features, such as the exact numbers of beds, and some other details that might be easily recognisable and so compromise anonymity. We have divided the hostels into three groups for ease of reading – the Central London group (two hostels), the South London group (two hostels) and the North England group (three hostels). This does not mean that the hostels were totally representative of these geographical areas. Data from the interviews with managers are used to further set out the context of the participating hostels.
Key characteristics relevant to this study
Duration of resident stay
In this section, we report on the salient characteristics of the participating hostels. As outlined in Chapter 1, there is an increasing trend for hostels to require residents to move on ‘quickly’, and hence the average length of stay or maximum period of stay was of interest, in particular in noting whether or not the participating hostels made exceptions for certain residents or groups. We found considerable variation in how long residents were able to stay in each hostel. The reasons for longer stays were multifactorial, and appeared to include lack of housing options, increasing care needs, and whether or not the hostel owners/managers considered themselves as offering a ‘home’. For example, in one of the London hostels (Central London hostel 1), although the maximum stay was 2 years, we were told that if a resident is not able to cope independently with their alcohol problem or is ‘elderly’, or ‘does not fit into categories [for move on], or can’t look after themselves’ – or they are in ‘limbo’, for example not being ‘ill enough for a care home’ (not meeting local authority eligibility criteria), then they ‘may be able to stay’. Central London hostel 2 declared a maximum 18 months’ stay, whereas South London hostel 2 cited a maximum of 3–4 months but then acknowledged that this might be ‘flexible’. Although still aspiring to a 2-year maximum stay, in South London hostel 3 about 15 residents had been living in the hostel for some years, and the staff reported that suitable housing with care to move them on had not been found for half of them. According to the manager:
Those on older contracts predating 3 years ago, this is generally when no other service can meet their need adequately. And, in some cases, it is when social services has come in, assessed the person, and despite very obvious high needs have deemed them as not needing another place of care. Social services know we provide a lot of support to clients here so they are happy to leave us to it, but it goes against our contract and it increases our workload when social services avoid their duty of care.
Manager, South London hostel 3
Even more variations were evident in the hostels outside London. In North England hostel 1, although there was a limit of 140 days’ (4–5 months’) stay, there were two long-term residents, one of whom had been living in the hostel for nearly 20 years and was said to have a mild learning disability and no close family; ‘this is his home’, declared the manager, who added ‘when he first moved in, there would have been no pressure to move’. The other long-term resident had been living in the hostel for over a decade. In North England hostel 2, the official stay was a maximum of 24 months and we found no exceptions to this. In North England hostel 3, the maximum stay was stated to be 3 years but the manager declared being under no pressure to move residents as there was ‘nowhere for them to go’. By contrast, in North England hostel 4, stays were limited to 6–12 months, with a very high turnover of residents; staff reported that they helped ‘move on’ 8–10 residents each month.
Housing options
Similar variations were found in the housing options open to hostel residents. The metaphor of ‘fighting’ with other agencies was used in a couple of London hostels to emphasise that interagency working was not always smooth-running. In Central London hostel 1, the manager reported that, of their older residents:
A few go into care [homes], especially if doubly incontinent. Few continue to remain in hostel. One is awaiting supported housing; have to fight for it. We have to fight to get them into registered care homes. It can take 1–2 years to get them in. In the meantime we get carers [care workers] in and then we see the person gradually go down. It is cheaper for them to remain here, but then sometimes if they end up in hospital we have to then say we won’t take them back as their needs are too high and we have to fight not to take them back.
Manager, Central London hostel 1
South London hostel 1 reported similar tensions, here described more as a ‘constant battle’, in respect of the local authority adult services department (social services). Its manager explained:
This has been a big bone of contention with social services, as I explained before. They tend to view us as a care home and leave us to look after clients who get ever more frail and needy. We try and fight for nursing home placements for the most vulnerable but it doesn’t always work. We had social services come in and assess our most vulnerable clients as not needing another placement when he had a carer [care worker] come in once a day, needed his food cut up, needed help feeding, was having difficulties swallowing, zero mobility, very, very vulnerable, and obviously needed nursing care that we are not trained to provide. Since I started, I have asked our commissioners to step in three times – they have spoken to the relevant head of social services and clients have been reassessed and rehoused. The one whom I mentioned before went from ‘not needing any more care’ to requiring the highest level of care. So it’s a constant battle that we have to fight.
Manager, South London hostel 1
In Central London hostel 2, moves for older residents were more often to sheltered accommodation, but sometimes to other hostels. The manager here commented that the presence of memory problems among residents constituted a ‘big stumbling block to finding appropriate housing’.
South London hostel 2, the hostel site with the highest turnover and most restricted length of stay, declared itself not suitable for those with memory problems; its manager considered that such residents would need a smaller, semi-independent service with greater support.
Central London hostel 1 reported more day-to-day working with the local authority adult services department than with the local authority housing department. The manager commented that, for its older residents:
Referrals often come via social services and alternative housing for people with memory problems is most often found through social services.
Manager, Central London hostel 1
However, in North England hostel 3, the manager considered that local cost pressures meant that rehousing for older residents was limited:
Care home costs are too high compared to hostels (£550 per week) so the local authority is reluctant to move them.
Manager, North England hostel 3
He added that some residents did not want to move to locations such as care homes because ‘drinking [of alcohol] will not be allowed’. This led to an unsatisfactory situation for residents who, in his view, should not be living in hostels:
There’s nothing, it’s us or nothing. We try our best, not really equipped to deal with it, [we] try and help as best we can.
Manager, North England hostel 3
Experience in North England hostel 4 was that of fairly rapid turnover and most residents moved to ‘own tenancy or try social housing with support, e.g. sheltered or tenancy support and any other possible support’. However, the amount of support for individuals following moves was thought to be shrinking; the manager here reported:
Due to lack of funding, [we’re] looking at church-based community groups for support to plug the gap.
Manager, North England hostel 4
Support for residents with memory problems
Despite their differences in locations and policies, the accounts of hostel managers in describing the extent of support provided by some members of staff for residents with memory problems were similar, and at times such support was considerable. The manager of Central London hostel 1 reported:
We have to escort them everywhere, sometimes we have to do missing persons reports. They [residents] get upset when they realise what’s going on and they get frustrated and if you speak to them about it they can get very angry with you as they don’t believe you . . . If it gets very bad and we can’t cope we get social services in for assessment for a care package. Some are reluctant to get help and say they are OK. We constantly have to update the risk assessment. They also have unrealistic expectations at action plan meetings. For example, one man thinks he will be able to go back to work. How they think they are is very different to what we see. Their relationship with alcohol doesn’t help.
Manager, Central London hostel 1
In Central London hostel 2, substantial support could be provided inside the hostel, as the manager reported:
If they have appointments you have to keep knocking for them. They say – give me 5 minutes and then you have to go back again and again. They forget the real time. You would think your body would tell you. Not being able to do simple tasks.
Manager, Central London hostel 2
In this hostel, staff obtained appointeeship (authority to manage welfare benefits and pensions) for some residents. This indicates the high level of need among some residents in activities of daily living and also illustrates the extent of staff engagement with budgeting and money management. South London hostel 1 also reported having:
. . . a harm minimisation programme, which I think is unique to us. So what we do, with the voluntary agreement of clients, we hold their money, we hold their bank card and we give them a daily allowance. We also buy them and give them alcohol – this is always less than 6% (alcohol) beer or cider and give them in stages – so three times a day and two cans only. We are essentially working with them to avoid them spending all their money in one go and bingeing on potent alcohol and harming themselves. Many feel this is controversial as we are then buying them alcohol, but we feel it reduces the risk of overuse and bingeing.
Manager, South London hostel 1
The manager of South London hostel 1 listed some of the manifestations of memory problems among its residents as confusion, forgetfulness, aggressions, falling, wandering and getting lost, and again spoke of the complexities when such behaviours were hard to differentiate from the impact of drinking; they do ‘virtually everything, ensuring safety, minimising risk, try and arrange memory assessments’. A couple of residents who were ‘wandering and getting lost’ were supplied with wrist bands (at a cost of £20 each) by the hostel containing their identification details. Concerns about safety and adult safeguarding (protection from abuse and exploitation) were also noted in South London hostel 2, where managers reported that staff needed to be alert because certain residents were ‘forgetting they are vulnerable’ and that their lack of judgement meant that others took advantage of them. All of this was complicated by general difficulties in engaging with certain residents, particularly if their behaviour was challenging to staff or others or distressing, or if they were difficult to motivate or slowing down in their progress to resettlement. In North England hostel 2, the manager reported that residents with memory problems required ‘more intense support, reminding appointments, time spent on routine tasks, going to appointments with them’.
Other forms of surveillance or monitoring were evident; for example, the manager of North England hostel 1 reported that staff:
[H]ad to keep a closer eye on and make sure one person had meals – but then he’d forget he had already eaten. We can’t keep any medication for people we don’t have any form of care provision. We do help them to get a dosette box (for pills) and remind them about meals.
Manager, North England hostel 1
However, this was exceptional as the practice in this hostel was to move such people on:
If we do get someone with memory problems, we get them moved on as quickly as we can.
Manager, North England hostel 1
North England hostel 3 similarly reported encouraging residents to eat and complete routine tasks but also efforts to maintain hygiene; as someone’s poor self-care worsened, this could be accompanied by lack of motivation and energy, or, on the other hand, a resident could become non-compliant and aggressive. Several managers commented on the complications of substance misuse, which sometimes excluded people from receiving support from other services but could also mask the extent of memory problems and confusion.
Referral routes for residents with memory problems
As noted above, there were some accounts of accessing specific help for residents with memory problems, who, in addition to needing more time for support than other residents, had higher support requirements. Some needed prompting and frequent reminders, particularly in terms of managing appointments, and generally tailoring the approach to their support. The process for referral to support with memory problems was generally to advise the resident to contact their GP or to do this on their behalf:
We refer them to the GP for a referral to the memory clinic.
Manager, Central London hostel 2
However, Central London hostel 1’s manager had one experience following making a referral of a resident to the local memory service, when the resident ‘turned up drunk’ for his appointment. In his view:
They didn’t cater for homeless people. Now we refer to alcohol services and are happy about it. We also have to refer people to the continence service as well.
Manager, Central London hostel 1
Similarly, in Central London hostel 2 referrals were made to the resident’s GP or alcohol services, who decided whether or not a referral for dementia assessment was needed. The difficulties of accessing help for residents who consumed large amounts of alcohol regularly were again voiced by South London hostel 1’s manager, who knew that, theoretically, residents with memory problems or similar could be directly referred to the local CMHT for assessments, but for this to happen the resident needed to be sober, which the manager observed was not always possible to arrange. Likewise, North England hostel 3’s manager summed up the lack of referral pathway as being again related to ‘alcohol acceptability’, stating more generally that there were:
No services, nothing for them. Can’t be assessed in memory clinic until they’re dry.
Manager, North England hostel 3
Only one out of the four North England hostels had a referral route for residents with memory problems, indicating their generally weaker links with secondary NHS services.
Primary care input
In this section, we report on the variations of primary care services’ input to the hostel as summarised by the hostel managers. North England hostel 3 was an outlier, in that no input from primary care was reported by its staff or observed on our visits or in the records. Other hostels had different types and levels of engagement that varied from proactive to reactive. In the London hostels, overall, there was more regular and planned input from primary care teams to the hostels, although in Central London hostel 1 a GP surgery and a walk-in centre were also located nearby. In this hostel, a nurse from the local drug misuse service also visited weekly to undertake health assessments and to see new residents. A different model of primary health care operated in Central London hostel 2, as staff from a specialist primary care intervention for homeless people visited the hostel weekly.
A similarly separated and specific approach was evident in South London hostel 1, where there was a weekly GP visit, a weekly visit from a nurse from an integrated care pathway service, and, in addition, weekly visits from staff from a Homeless Intermediate Care Project (described by its staff as providing ‘wrap around’ care for the most vulnerable residents, including taking them to appointments and helping hostel staff support them). This was similar to North England hostel 2, where a weekly visit to the hostel was made by a local health outreach team; a nurse visited weekly (for 3 hours) and a nurse prescriber visited weekly for a full day. Although not part of any specialist service or new NHS configuration, the health-care practice local to South London hostel 2 held a weekly clinic (full day) in the hostel; a nurse visited weekly (for a full day) and a further specialist nurse prescriber made a weekly visit (for a full day). A similar pattern operated in North England hostel 4, where the local GP made a weekly visit, and a community nurse was described as coming in when needed. Similarly, in North England hostel 1, a local general practice held a clinic every week (lasting 3 hours) in the hostel; a nurse from a well-being team visited weekly (3 hours) to undertake hepatitis injections and apply dressings, although this seemed to be a new specialist initiative as she was not attached to a general practice.
Mental health team input
Hostels could be busy places once primary care input and other services were viewed together. In Central London hostel 1, a member of the CMHT visited weekly, and an alcohol worker visited once or sometimes twice per week. This hostel was unique in our sample in employing its own part-time drug and alcohol worker. In sharp contrast, Central London hostel 2 reported that its local CMHT was reluctant to work with the hostel because of residents’ drug and alcohol problems. In its stead, a local mental health charity had been visiting regularly and had accepted self-referrals, and another voluntary sector service had formerly provided drop-in mental health support. Both had recently ceased at the time of our study. North England hostel 1 reported that it could not make direct referrals to the CMHT; these had to be made by a GP or by the local authority adult services department (social services). North England hostel 4 reported no contact with mental health services, whereas North England hostel 3 reported that a CMHT worker visited weekly or monthly, depending on the worker; its residents had often been referred to the CMHT following their hospital A&E visits. In this hostel, a drugs or alcohol worker used to make weekly visits to the hostel but this had recently ceased following funding cuts.
Further different patterns of engagement with mental health services were evident in South London hostel 1, where some residents were ‘live’ cases with the local CMHT, although sobriety was required before the CMHT would engage with a resident; this was described, optimistically, as offering opportunities for residents to give up or reduce alcohol consumption. More unusually, a psychologist was available for consultations every weekday in South London hostel 2, where the local intermediate care (rehabilitation) project staff were also available daily. In this hostel, an alcohol worker ran a weekly alcohol support group, and a drugs worker visited the hostel weekly to carry out one-to-one work with some residents.
Hostel staff
Background demographics
Forty-three hostel key workers were interviewed for this study (some did not supply full demographic details). Table 6 presents background information about them. All but two were employed full-time and worked shifts, each shift typically lasting 6 hours. Shifts changed weekly and the hours of work were not always consistent. Their job titles ranged from project worker and support worker (SW) to lead case worker, all of which incorporated many elements of the same job descriptions. Six were assistant managers, a role that SWs undertook alongside their resident caseload as key workers. In some cases, the SW was identified as having a specialist role, such as ‘substance misuse worker’ or ‘lead worker in medication and health and support’, the duties of which were in addition to their caseload.
| Characteristic | Hostel staff (n) |
|---|---|
| Gender | |
| Male | 18 |
| Female | 25 |
| Ethnicity | |
| White British/Irish | 26 |
| Black/African/Caribbean | 6 |
| Other | 9 |
| Age group (years) | |
| 18–24 | 2 |
| 25–34 | 10 |
| 35–44 | 8 |
| 45–54 | 16 |
| 55–65 | 4 |
The length of time participants had worked in their current hostel ranged from 1 month to 26 years. Twelve participants had worked in their current hostel for < 12 months, seven had worked there between 1 and 2 years and 12 had worked there for > 5 years.
Current roles and experiences
Descriptions of their roles essentially covered the same functions. Most described having a caseload of six or seven clients, for whom they provided a range of support, including supporting them with day-to-day tasks, such as keeping themselves clean, tidying rooms and laundry assistance; managing money and budgeting; managing their health in terms of appointments, medication and attending to chronic problems; identifying and helping them achieve manageable goals; drawing up support plans; undertaking risk assessments; and checking on each client every day or as frequently as necessary. Such a role was often described as being the resident’s key worker.
Previous roles
Eighteen SWs had not previously worked with homeless people before their current job. Their prior work experience varied; one had been a restaurant manager, another a hotel manager, one had managed laboratories, one had been a personal assistant in a technology company, one had worked in retail, two trained in nursing and one had previously worked as a designer/photographer. Three participants had started as apprentices in the homeless sector, and one as a housing officer in a local authority. The remaining participants had started work as project workers and SWs in hostels, shelters and day centres in the homelessness sector.
Training undertaken and training needs
Hostel staff described undertaking a wide range of training. Some training was described as mandatory, but several voiced enthusiasm for signing up to training as a way of developing their skills. Most appeared to be in-house training, being organised either by individual hostels themselves or by an overarching hostel provider in the not-for-profit sector. This was the case in Central London hostel 1, which ran a comprehensive mandatory training programme for all staff. This covered drug and alcohol use, key working and ‘emotional intelligence’. For any staff commencing apprenticeships, there was an opportunity to take a qualification [National Vocational Qualification (NVQ) level 2] in health and social care. There was also one-off training available on ‘care of the elderly’ and dementia, and ‘end-of-life’ training. In contrast, another hostel put great reliance on being able to access local authority training covering safeguarding, managing dual diagnoses and managing complex needs.
Across the hostels, staff reported recently accessing training in adult safeguarding, working with vulnerable people, first aid, fire training, equality and diversity, risk assessment, mental health, alcohol and substance use, emotional care, health and safety, rehabilitation, debt and benefits advice, dealing with challenging behaviour (their phrase), dealing with difficult families, working with complex clients, administering medication and caseload management. Training specific to this study’s focus included working with older adults, mental health, dementia training, hoarding, managing ‘challenging behaviour’, capacity and decision-making, and the Mental Capacity Act 2005. 90
Although most participants felt that the training they required was available and accessible, when probed several identified specific areas in which more training might be helpful. Two talked about the value of more dementia-specific training, especially identifying early symptoms and supporting people with ‘everyday’ memory problems. One described needing more refresher courses rather than only day-long training courses. A senior member of staff in South London hostel 1 commented that training was not always available to meet the changing needs of their hostel resident profiles:
Dementia training is very hard to access and very expensive. We can’t always get everyone on the course, nor is it easy or cheap to get someone to come here and deliver training. So we send someone with the understanding that they will come back and disseminate the information to the rest of us. Which is not the best way to do it! I would really like us all to have some training in managing behaviours in dementia. There are so many challenging behaviours we come across, that we can never know whether it’s dementia, or their alcohol or their personality and how to deal with it. I saw this lovely clip about someone with dementia presenting with aggressive behaviour and how staff dealt with it, and it was fascinating! Wish we had access to more training like that.
Senior member of staff, South London hostel 1
There was some indication of training being carried out online as e-learning. In one North England hostel, staff accessed some courses online. In this hostel, there was particular emphasis on addictions and mental health; its managers undertook diploma courses, and other staff undertook a 2-day mental health ‘first aid’ course covering suicide intervention skills training, and some had completed a foundation unit in men’s health to help them identify early mental health problems and self-harm and how to guide someone to the right services. However, no specialist training was accessed here that covered memory problems.
Across the hostels, 16 staff participants had obtained NVQs levels 2 and 3. The majority of these were in health and social care (nine participants), followed by mental health (three), vulnerable adults (two), promoting independence (one) and counselling (one). These had been achieved either during the course of their employment at the hostel or prior to their current role. Overall, there seemed low expectations of regular training except in the hostels that had their own in-house provision. High staff turnover clearly affected the extent to which more experienced staff could support new colleagues; this affected one North England hostel in particular, which relied more than others on what it called ‘on-the-job learning’.
Chapter summary
This first chapter reporting the study findings paints a picture of the case study hostels and their residents, providing further information about the hostel staff. The physical conditions of the hostels varied, together with their accessibility and services for resident groups. Some staff had substantial experience but others were new to this area of work, reflecting the sector’s high staff turnover, particularly in London. Linkages with primary care and mental health services varied considerably between hostels. This reflects others’ findings that CMHTs for older people vary considerably in their engagement or outreach activities with local services. 100 There were very wide variations in training availability, suggesting that health-care professionals should not assume that hostel staff possess high-level skills, although they should not underestimate their competence. Differences were also found in the extent to which hostel staff were permitted to access courses arranged by the local statutory sector. The background of hostel staff in front-line SW roles varied and the staffing complement of hostels could encompass staff with considerable experience as well as those new to the sector.
Important variations in the physical fabric of hostels were found, and in the support that they provided to residents. This suggests that care is needed in overestimating or underestimating services available to residents, such as cooking facilities and laundry. Accounts of needing local authority-arranged social care services to support hostel residents with their care illustrate the high level of disability or self-care needs among some residents and the difficulties of providing them with adequate care in hostel environments (such problems have recently been observed in respect of hostel residents who are at the end of life101). The next chapter turns to residents themselves to discuss the study findings in relation to individuals and the research team’s assessments of the extent and impact of any memory problems.
Chapter 5 Profiles of the hostel residents and assessments of their memory problems
Sixty-two older homeless people were interviewed for the first phase of the fieldwork. This chapter first summarises their demographic details, education and employment history, homelessness history, and physical health, mental health and substance misuse problems. It then examines memory problems among the group as reported by the older residents interviewed and hostel staff, and presents findings from cognitive assessments undertaken by the research team’s clinicians.
Demographic and background details
Age, sex and ethnicity
Among the 62 older homeless people, 24 were staying in hostels in Central London when they were first interviewed, 19 were staying in hostels in South London and 19 were staying in hostels in North England. The majority (n = 54) were men; just eight were women. One-third (34%) were aged 50–54 years, 29% were aged 55–59 years, 21% were aged 60–64 years, 8% were aged 65–69 years and 8% were aged ≥ 70 years. Their ages ranged from 50 to 82 years, and the median age was 56.5 years. Hence, the sample was relatively young compared with older people generally, but was comparable with the age distribution of ‘older’ homeless people in Western countries. According to statistics from England, Canada and the USA, the majority of older homeless people are aged in their fifties; just 5–10% of homeless adults are in their sixties or older. 16 There was no significant difference in age according to the cluster site of their hostel.
Most residents were white British (76%) or white Irish (8%), and 16% were from other ethnic groups. There were, however, differences among the cluster sites. All in the North England sample were white British, and most originated from the local area. By comparison, slightly fewer (71%) in the Central London cluster and just 58% in the South London one were white British. The findings are not surprising given the ethnic mix of the general population in London.
Education and employment histories
Just under half (45%) of residents said that they had an educational or vocational qualification, mainly GCSEs (General Certificates of Secondary Education), NVQs or City & Guilds certificates. Those in the North England cluster were most likely to have a qualification (68%); and those aged 50–54 years were least likely to have a qualification (29%). More than one-third of participants (37%) reported literacy difficulties, including some who had dyslexia. Reports of literacy problems were less common among the North England cluster (26%) and most common among those aged 50–54 years (48%). Several participants who reported literacy problems described the struggles that they experienced with reading and writing, including some who had left school at an early age:
I’m a bit dyslexic – have problems with writing and spelling, but not reading. I had a misspent youth. I should have gone to school but I got picked on a lot. So I’d go into school, get a mark, and then leave again.
Can’t read or write – I struggle to read a sentence. Left school aged 13.
Difficulty reading. They kicked me out of school.
The employment histories of the participants varied greatly. Three-fifths (61%) said that they had been mostly employed during their adult lives, one-quarter (25%) had been ‘in and out’ of work, and 14% had been mostly unemployed. The last group included one man who had never been in employment. Among the 59 residents who were able to provide more detailed information, 31% had worked until they were aged in their fifties or older, and 29% had been unemployed since aged in their twenties or thirties. Participants’ types of employment also varied greatly. Using the Office for National Statistics’ Standard Occupational Classification (2010),102 most residents (46%) had either been in skilled trades, such as painters and decorators, carpenters, chefs or similar, or they had been in elementary occupations (34%), as security guards, cleaners, postal workers, shelf fillers or similar (Table 7). Just one person had employment at the time of their interview.
| Occupational classificationa | Age group (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| Skilled trades | 57.9 | 33.3 | 41.7 | 50.0 | 45.8 |
| Elementary occupations | 42.1 | 22.2 | 33.3 | 40.0 | 33.9 |
| Sales and customer services | 0.0 | 22.2 | 0.0 | 0.0 | 6.8 |
| Caring, leisure, other services | 0.0 | 16.7 | 8.3 | 0.0 | 6.8 |
| Administrative and secretarial | 0.0 | 0.0 | 16.7 | 0.0 | 3.4 |
| Process, plant and machine operatives | 0.0 | 5.6 | 0.0 | 10.0 | 3.4 |
| Number of residents | 19 | 18 | 12 | 10 | 59 |
The great variation in their employment histories is apparent from their accounts (some roles have been slightly modified to maintain anonymity):
-
Worked for the civil service for 40 years, until the age of 57 years.
-
Worked as a delivery man for 10 years from the age of 15 years, and then as a street cleaner for a few years. Not worked since the age of 40 years.
-
Worked as a manual labourer for 16 years, then as a machine operative for 20 years, and then as a semiskilled engineer for 10 years. Retired aged 65 years.
-
Worked in a supermarket filling shelves from 16 to 26 years. Not worked since.
History of homelessness
Age first homeless
The age at which residents first became homeless varied greatly. According to 54 people who were able to give details, almost one-quarter (24%) had first become homeless as teenagers or when they were aged in their twenties. By comparison, 22% had first become homeless when they were aged in their fifties and 15% were aged ≥ 60 years at the time. As shown in Table 8, more than one-third (37%) of those aged in their early fifties had first become homeless before the age of 30 years. By contrast, most of those aged ≥ 60 years had experienced late-onset homelessness; 70% had first become homeless after the age of 50 years.
| Age first homeless (years) | Age when interviewed (years) (%) | Total (%) | ||
|---|---|---|---|---|
| 50–54 | 55–59 | ≥ 60 | ||
| ≤ 19 | 10.5 | 13.3 | 5.0 | 9.3 |
| 20–29 | 26.3 | 6.7 | 10.0 | 14.8 |
| 30–39 | 26.3 | 13.3 | 10.0 | 16.7 |
| 40–49 | 31.6 | 33.3 | 5.0 | 22.2 |
| 50–59 | 5.3 | 33.3 | 30.0 | 22.2 |
| ≥ 60 | N/A | N/A | 40.0 | 14.8 |
| Number of residents | 19 | 15 | 20 | 54 |
The age at which residents first became homeless differed by cluster site (Figure 2). Almost three-fifths (59%) of those in North England first became homeless after the age of 50 years. This compares with just 39% in the South London hostels and 25% in the Central London cluster. Many in the two London sites had become homeless when they were in their thirties or forties.
FIGURE 2.
Participants’ age when they first become homeless, by cluster site.
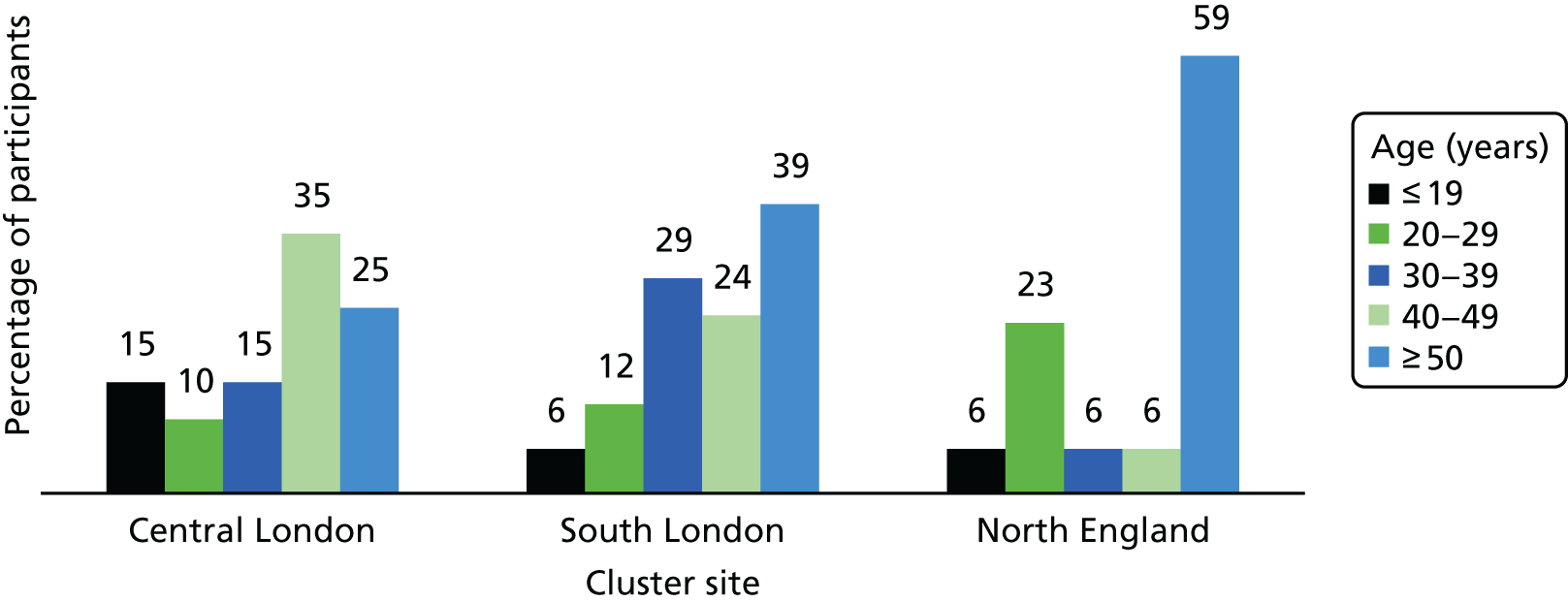
Length of time homeless
It is very difficult to collect accurate histories from homeless people about the length of time that they had been homeless, as ‘homelessness’ is often not a continuous state. Many frequently move between homelessness and insecure housing. For our study, collecting this information was more problematic given that some residents had memory problems, and several had moved between homelessness and insecure housing for many years. Data about the length of time homeless are drawn from residents’ accounts and those of hostel staff, and from hostel records, when available. In some cases, the data refer to the minimum time spent homeless, as hostel records had information only about the length of time that residents had been using hostels run by that particular organisation. Therefore, the findings have to be interpreted cautiously.
Residents’ length of time as homeless varied, but many had been living on the streets or in hostels continuously or intermittently for several years. Among 57 people for whom some details were available, 7% had been homeless for < 1 year, and nearly half (47%) had been homeless for > 10 years, including 21% who had been homeless for > 20 years. There were differences by cluster site. Almost one-fifth (19%) in the North England site had been homeless for < 1 year, compared with just 5% in South London and none in Central London (Table 9). The corresponding figures for those who had been homeless for > 10 years were 50%, 58% and 36%.
| Length of time (months) | Cluster site (%) | Total (%) | ||
|---|---|---|---|---|
| Central London | South London | North England | ||
| Homeless | ||||
| < 12 | 0.0 | 5.3 | 18.8 | 7.0 |
| 12–60 | 22.7 | 5.3 | 25.0 | 17.5 |
| 61–120 | 40.9 | 31.6 | 6.2 | 28.1 |
| 121–240 | 18.2 | 31.6 | 31.2 | 26.3 |
| ≥ 241 | 18.2 | 26.3 | 18.8 | 21.1 |
| Number of residents | 22 | 19 | 16 | 57 |
| In current hostel | ||||
| ≤ 6 | 25.0 | 31.6 | 15.8 | 24.2 |
| 7–12 | 33.3 | 21.1 | 15.8 | 24.2 |
| 13–24 | 16.7 | 10.5 | 15.8 | 14.5 |
| 25–60 | 20.8 | 15.8 | 5.3 | 14.5 |
| 61–120 | 4.2 | 21.1 | 26.3 | 16.1 |
| ≥ 121 | 0.0 | 0.0 | 21.1 | 6.5 |
| Number of residents | 24 | 19 | 19 | 62 |
Duration of stay in current hostel
There were variations in the length of time that residents had been staying in their current hostel. Nearly half (48%) had been in the hostel for ≤ 12 months, and nearly one-quarter (23%) for > 5 years. Those in North England tended to have been in their hostel longer; nearly half of them (47%) had been so housed for > 5 years (see Table 9). By contrast, those in the two London clusters were more likely to have been so accommodated for ≤ 12 months. These differences may partly reflect the contractual arrangements imposed on homelessness organisations by local authorities rather than the needs of homeless people. Since 2010, there have been several changes to housing and welfare policies and practice in England, and the length of stay in hostels imposed by some local authority contracts has reduced substantially. Some hostels now have maximum durations of ≤ 6 months, and people are moved from one hostel to another. 103
Health and substance misuse
This section describes the health of the residents when they were first interviewed, and their use of alcohol and illegal drugs or novel psychoactive substances. It does not include memory problems, which are addressed in the following section. It draws on various sources: the accounts of the residents and hostel staff and, when available, hostel and medical records. In some instances, residents may not have mentioned or may have denied health or substance misuse problems, but the problems were clearly reported by hostel staff and/or documented in their medical records. This section, therefore, presents the ‘best evidence’ available.
Residents were asked to rate their general health; 35% described it as ‘good’ or ‘very good’, 35% described it as ‘fair’ and 30% described it as ‘bad’ or ‘very bad’. Interestingly, those aged in their fifties were least likely to describe their health as good: 43% rated it as ‘bad’ or ‘very bad’, whereas none over the age of 65 years described their health in this way. Half (50%) of those who had been homeless for ≤ 5 years described their health as good or very good, compared with only 37% of those who had been homeless for > 10 years.
Most residents smoked cigarettes or other forms of tobacco, and they were much more likely than the general older population to be smokers. In 2014, just 17.7% of people in England aged 50–64 years, and 9.2% of those aged ≥ 65 years, were smokers. 104 This compares with 87% in our study.
Physical health problems
Nearly all residents (97%) had one or more physical health problems. As shown in Table 10, the most common problems were musculoskeletal conditions, followed by respiratory problems, eye conditions, hypertension and gastrointestinal problems. The reported figures are the minimum percentages of residents with each problem, as some people may have had conditions that they did not report, and data from their medical records were not always obtained or obtainable.
| Physical health problem | Age group (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| Musculoskeletal (e.g. arthritis) | 52.4 | 61.1 | 61.5 | 40.0 | 54.8 |
| Respiratory (e.g. asthma, COPD) | 19.0 | 55.6 | 61.5 | 40.0 | 41.9 |
| Eye problems (e.g. glaucoma, cataracts) | 28.6 | 61.1 | 38.5 | 20.0 | 38.7 |
| Hypertension | 33.3 | 44.4 | 30.8 | 40.0 | 37.1 |
| Gastrointestinal (e.g. gastritis) | 42.9 | 38.9 | 46.2 | 10.0 | 37.1 |
| Blackouts, epilepsy, alcohol-induced fits | 61.9 | 22.2 | 30.8 | 0.0 | 33.9 |
| Cardiovascular disease (e.g. clots, strokes, transient ischaemic attacks) | 33.3 | 16.7 | 38.5 | 40.0 | 30.6 |
| Angina or heart disease | 23.8 | 16.7 | 38.5 | 40.0 | 27.4 |
| Liver problems (e.g. cirrhosis, hepatitis C) | 38.1 | 16.7 | 30.8 | 40.0 | 27.4 |
| Skin conditions (e.g. eczema, leg ulcers) | 14.3 | 44.4 | 23.1 | 30.0 | 27.4 |
| Renal/urinary problems | 19.0 | 22.2 | 23.1 | 10.0 | 19.4 |
| Hearing problems | 9.5 | 16.7 | 23.1 | 20.0 | 16.1 |
| Diabetes mellitus | 4.8 | 5.6 | 15.4 | 10.0 | 8.1 |
| Number of residents | 21 | 18 | 13 | 10 | 62 |
Head injuries
Three-fifths (61%) of residents reported having had a head injury, including 11% who described having had three or more such injuries. In some cases, the head injuries dated back years, but for others the injuries had occurred in recent years. Most were the result of accidents or assaults and were often linked to heavy drinking and fighting. A small percentage of residents (7%) had sustained a head injury during an epileptic seizure. The situations leading to head injuries were described by two men:
I used to be a very heavy drinker and drug taker. I’d regularly fight and fall about. One time I had an axe on my head because of a fight.
A guy knocked me out – I was away with the fairies . . . [another time] I keeled over and knocked my head when I was pissed.
Most residents who reported a head injury (88%) had received hospital treatment on at least one occasion, including 68% who were admitted into hospital. One man aged in his fifties, for example, first sustained a head injury as a teenager when he was playing rugby. He described being ‘knocked out’ but was not taken to hospital. As an adult, he worked on building sites and in factories, and said that he had suffered a head injury on two occasions when items fell on him at work. The first time he was in his early thirties and was taken to hospital but ‘sent home to rest’. The second injury occurred a few years later and he was kept in hospital for 4 days. He sustained a fourth head injury about 7–9 years ago during an epileptic seizure, and was taken to hospital but discharged the next day. He had subsequently experienced further head injuries during epileptic seizures.
Mental health problems
Nearly two-thirds (63%) of residents reported a history of mental health problems, and 44% described current mental health problems. These percentages do not include memory problems, which are described in Memory problems. When information from staff and from medical and hostel records is also considered, a higher prevalence of mental health problems was apparent: 81% of residents had a history of mental health problems, and 74% had current mental health problems.
The main problem both identified by residents and recorded by GPs was depression, sometimes accompanied by anxiety. Almost seven-tenths (69%) of residents were reported to have suffered from depression, including five people who had attempted suicide in the past. According to the medical records, two residents had been diagnosed with personality disorder, and six with schizophrenia or ‘alcoholic psychosis’ or ‘alcohol-induced hallucinations’. One-fifth (22%) of residents described having first experienced mental health problems when they were teenagers or young adults. For some, the problems had continued over many years. Several associated the onset of mental health problems with traumas and stressful events that had taken place before they became homeless, such as marital or family breakdown, the death of their mother or a child, or the loss of a job:
[Mental health problems] started when I was aged 14 when I was badly beaten up at school. Was in hospital 7 months. Was bullied at school.
It was when things were all going wrong for me – marital problems, work problems. I was a heroin addict at the time as well.
So much depression – I can’t forget my family . . . they were killed. When I sleep I see my mother and brothers and gran dead. I have no future.
My parents divorced when I was 15, and I was diagnosed with anxiety and depression.
Drawing on scores from the depression tool administered during the baseline interview (described in Chapter 3), although 54.1% of residents were assessed as having no depression, 6.6% had mild depression, 26.2% had moderate depression and 13.1% had severe depression. There were age differences. Those aged in their fifties were more likely to have moderate or severe depression than those above this age (affecting 42.9% aged 50–54 years, 58.8% aged 55–59 years, 30.8% aged 60–64 years and just 10% aged ≥ 65 years). Residents living in hostels in Central London were more likely to have moderate or severe depression (52.2%) than those living in hostels in South London or North England (31.6% for both areas).
Residents with moderate or severe depression were more likely than those with mild or no depression to rate their general health as ‘bad’ or ‘very bad’ (52.1% and 13.9%, respectively), and their QoL as ‘poor’ or ‘very poor’ (34.8% and 10.8%, respectively). There were also associations between depression and alcohol and drug use. Those who drank alcohol daily or almost daily (6 days per week) were more likely to be moderately or severely depressed than those who drank less frequently or not at all (47.2% compared with 28%, respectively). Likewise, 64.7% who had used illegal drugs in the preceding 3 months were assessed as having moderate or severe depression, compared with 30.3% who had not used illegal drugs during this period [χ2 = 6.03; degrees of freedom (df) = 1; p = 0.014]. Further details of their drinking habits and use of drugs are provided in the following sections.
Alcohol use
Three-quarters (76%) of residents said that they had been a heavy drinker at some time or had had alcohol problems. This increased to 85% when reports from staff and information from medical records were included. Twenty-six residents (42%) said that they had started to drink heavily before the age of 20 years. Among those who had been heavy drinkers, 26% said that one of their parents had also drunk heavily, and an additional 10% said that both parents had been heavy drinkers. A history of heavy drinking was common among all age groups, but particularly prevalent among those aged 50–54 years (95% of this age group). It was also more common in the two London cluster sites, affecting 91% of participants in London, compared with 74% in North England.
When current drinking habits are examined, 13% of residents said that they did not drink alcohol and this was confirmed in hostel staff accounts. Almost three-fifths (58%), however, drank alcohol on 6 or 7 days per week (Table 11). Some had a few days of heavy drinking when they received their welfare benefits, followed by periods of light drinking or abstinence when they had no money. Although relatively few people drank spirits or wines, a high proportion (57%) regularly had super-strong lager (such as Tennent’s, which is 9% alcohol by volume) or extra-strong beers or ciders, such as White Ace (7.5% alcohol by volume). Most people (83%) who drank alcohol daily tended to consume extra-strong beers and lagers.
| Use of alcohol | Age groups (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| Frequency of drinking | |||||
| Not at all | 4.8 | 16.7 | 23.1 | 10.0 | 12.9 |
| Monthly or less | 0.0 | 5.6 | 7.7 | 10.0 | 4.8 |
| 2–4 times a month | 9.5 | 11.1 | 7.7 | 10.0 | 9.7 |
| 2 or 3 times a week | 0.0 | 11.1 | 0.0 | 10.0 | 4.8 |
| 4 or 5 times a week | 0.0 | 0.0 | 7.7 | 0.0 | 1.6 |
| 6 or 7 times a week | 71.4 | 44.4 | 53.8 | 60.0 | 58.1 |
| Binge patterna | 14.3 | 11.1 | 0.0 | 0.0 | 8.1 |
| Type of alcoholb | |||||
| Standard beers/lagers | 42.9 | 35.3 | 46.2 | 70.0 | 45.9 |
| Super-strength beers/lagers | 81.0 | 47.1 | 38.5 | 50.0 | 57.4 |
| Spirits | 14.3 | 17.6 | 7.7 | 30.0 | 16.4 |
| Wine | 4.8 | 11.8 | 23.1 | 0.0 | 9.8 |
| Number of residents | 21 | 18 | 13 | 10 | 62 |
It is difficult to calculate the number of units of alcohol the residents consumed each week because their drinking patterns fluctuated. Some drank spirits when they had money but consumed cheap, extra-strong lager or beer at other times. Hostel staff were also unable to say how much alcohol some residents consumed as they tended to drink either in their bedroom or away from the hostel. The average number of units of alcohol consumed by residents per week has been calculated as accurately as possible from the information they provided. Among 52 residents for whom information is available, 63.5% were regularly drinking in excess of the Department of Health and Social Care recommended weekly guidelines of no more than 14 units per week. Moreover, 48% were drinking > 50 units each week, including 25% who were drinking, on average, > 100 units per week.
Those aged in their early fifties were more likely than other age groups to drink excessively. Among those aged 50–54 years, 71% had alcohol most days and 81% consumed extra-strong beers and lagers (Table 12). They were also the age group most likely to be far exceeding the Department of Health and Social Care recommended weekly guidelines for alcohol consumption; 71% were consuming > 50 units of alcohol per week (see Table 12).
| Weekly alcohol intake (units) | Age groups (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| > 14 | 82.4 | 60.0 | 45.5 | 55.6 | 63.5 |
| > 50 | 70.6 | 33.3 | 36.4 | 44.4 | 48.1 |
| > 100 | 41.2 | 20.0 | 9.1 | 22.2 | 25.0 |
| Number of residents | 17 | 15 | 11 | 9 | 52 |
There were differences in drinking habits by cluster site. Residents in the North England cluster were less likely than those in the two London clusters to consume alcohol most days (Table 13). The former were significantly less likely to drink strong beers or lagers (21%, compared with 71% in Central London and 78% in South London; χ2 = 15.1; df = 2; p = 0.001). They were also less likely to exceed the Department of Health and Social Care recommended guidelines of no more than 14 units of alcohol per week (χ2 = 6.7; df = 2; p = 0.034). Residents in the Central London cluster were most likely to be drinking excessively, with nearly half (48%) drinking, on average, > 100 units each week (Table 14).
| Use of alcohol | Cluster site (%) | Total (%) | ||
|---|---|---|---|---|
| Central London | South London | North England | ||
| Frequency of drinking | ||||
| Not at all | 8.3 | 10.5 | 21.1 | 12.9 |
| Monthly or less | 4.2 | 0.0 | 10.5 | 4.8 |
| 2–4 times a month | 4.2 | 5.3 | 21.1 | 9.7 |
| 2 or 3 times a week | 4.2 | 5.3 | 5.3 | 4.8 |
| 4 or 5 times a week | 4.2 | 0.0 | 0.0 | 1.6 |
| 6 or 7 times a week | 70.8 | 68.4 | 31.6 | 58.1 |
| Binge patterna | 4.2 | 10.5 | 10.5 | 8.1 |
| Type of alcoholb | ||||
| Standard beers/lagers | 33.3 | 38.9 | 68.4 | 45.9 |
| Super-strength beers/lagers | 70.8 | 77.8 | 21.1 | 57.4 |
| Spirits | 20.8 | 27.8 | 0.0 | 16.4 |
| Wine | 16.7 | 5.6 | 5.3 | 9.8 |
| Number of residents | 24 | 19 | 19 | 62 |
| Weekly alcohol intake (units) | Cluster site (%) | Total (%) | ||
|---|---|---|---|---|
| Central London | South London | North England | ||
| > 14 | 76.2 | 73.3 | 37.5 | 63.5 |
| > 50 | 57.1 | 60.0 | 25.0 | 48.1 |
| > 100 | 47.6 | 13.3 | 6.2 | 25.0 |
| Number of residents | 21 | 15 | 16 | 52 |
Among residents whose weekly alcohol intake was > 14 units, three-quarters (76%) acknowledged that they had felt the need to cut down on their drinking, half (50%) had felt guilty about their drinking and most (84%) said that they had sometimes needed a drink first thing in the morning to steady their nerves or get rid of a hangover. There was no significant association between drinking excessively each week and current mental health problems. As described in the following accounts, however, a few participants believed that there was a link between their mental health problems and heavy drinking:
Something inside me doesn’t want to go on . . . that’s why I’m binging [drinking] more. I have made threats to kill myself. But when I’m sober I don’t want to kill myself.
My depression can’t stop. I’ve asked my GP for treatment for depression but he said I have to stop drinking first.
Use of illegal drugs
Just over half (55%) of residents said that they had used illegal drugs at some time, although many fewer (16%) reported having taken drugs during the previous 3 months. These findings increase to 57% for past drug use and 29% for drug use in the previous 3 months when reports from hostel staff are also included. Most residents who had used drugs in the previous 3 months reported having taken cannabis or crack-cocaine. Just two people said that they had taken heroin. In most cases, they had started taking drugs when they were in their teens or early twenties.
Three-quarters (76%) of residents aged in their early fifties reported a history of illegal drug use, and just over half (52%) said that they had taken drugs in the previous 3 months (Table 15). This age group was most likely to report this behaviour. There were also differences by cluster site. Two-thirds (67%) of Central London participants had used illegal drugs in the past, and 37.5% had taken drugs in the previous 3 months. Slightly lower figures were reported for the South London participants (57% and 28%, respectively), and even lower figures were reported for the North England cluster (47% and 21%, respectively).
| Illegal drug use | Age group (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| History of illegal drug use | 76.2 | 50.0 | 50.0 | 40.0 | 57.4 |
| Used illegal drugs in previous 3 months | 52.4 | 27.8 | 7.7 | 11.1 | 29.5 |
| Number of residents | 21 | 18 | 12 | 10 | 61 |
Memory problems
At the baseline interview, all residents were asked about their memory and whether or not they were experiencing any difficulties, and the 6-CIT was administered by the researchers. Hostel staff were also interviewed and their views were sought about each resident’s memory. Finally, the ACE-III was administered to all residents who consented to this by the research team’s consultant psychiatrist, a psychiatric registrar or a psychologist. This section reports the findings from the various sources and examines the extent to which hostel staff identified memory problems compared with the findings of the psychiatry team.
Reports of memory problems by hostel residents
Among the 62 residents, more than half (54.8%) reported having memory difficulties, 25 (40.3%) reported no problems, and three were unsure. As shown in Table 16, those aged in their early fifties and early sixties were most likely to describe memory problems, and older residents aged ≥ 65 years were least likely to report a problem. This may be a surprising finding in the light of the strong association of such problems with advancing age; however, caution has to be taken when interpreting these findings because of small numbers.
| Any memory problems | Age group (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| Yes | 66.7 | 44.4 | 76.9 | 20.0 | 54.8 |
| No | 33.3 | 44.4 | 23.1 | 70.0 | 40.3 |
| Unsure | 0.0 | 11.1 | 0.0 | 10.0 | 4.8 |
| Total number of residents | 21 | 18 | 13 | 10 | 62 |
When the 34 residents who reported memory problems were asked how they were affected, the most common responses were:
-
unable to remember appointments and other tasks (41.2%)
-
unable to remember names (20.6%)
-
unable to remember the day and date (17.6%)
-
unable to remember yesterday’s activities (14.7%)
-
loses things (14.7%).
When the residents who reported memory problems were asked how long they had experienced such difficulties, 21.2% said < 1 year, 27.3% said between 1 and 5 years, 12.1% said > 5 years, and 39.4% were unable to say.
The accounts from three residents illustrate the ways in which they felt they were being affected by their poor memory:
I can go to the shops and forget what I’ve gone for and forgotten to take my money with me . . . small things like that.
I mislay things all the time. When I have a conversation about sport I know the answer but it’s slow coming to me. I used to be able to answer immediately but now my brain is not ticking over as much.
It’s [memory loss] annoying. It will stop me talking to someone as I can’t recall their name and it’s embarrassing.
Reports of memory problems by hostel staff
Hostel staff were asked whether or not they believed that certain residents had memory problems and, if so, the reasons why. Information was obtained about 60 residents from their key workers (some key workers were responsible for more than one study participant). As shown in Table 17, hostel staff believed that nearly half (46.7%) of residents had a memory problem and that 40% of residents did not have a memory problem, and they were unsure about the remainder (13.3%). Staff in Central London were less certain about their residents than were staff in the other two cluster sites.
| Any memory problems | Cluster site (%) | Total (%) | ||
|---|---|---|---|---|
| Central London | South London | North England | ||
| Yes | 45.5 | 36.8 | 57.9 | 46.7 |
| No | 27.3 | 57.9 | 36.8 | 40.0 |
| Do not know | 27.3 | 5.3 | 5.3 | 13.3 |
| Total number of residents | 22 | 19 | 19 | 60 |
Members of staff gave many reasons as to why they suspected or were aware that the residents had memory problems. For example, among the residents in whom memory problems were suspected, staff said that 77.8% had difficulty remembering recent happenings and appointments, 74.1% had difficulty recalling conversations a few days later, and 37% had difficulty finding the correct words. A selection of staff’s accounts illustrate this further:
He repeats himself a lot; asks everyone the same questions all the time.
He can’t remember anything. Quite severe. He can’t remember conversations we had 2 minutes ago. Tell him what he needs from the shop, ask him to repeat it 2 minutes later, and he can’t.
He doesn’t remember some things, like the other day he went out of the hostel. He could not remember this and thought he was here in the hostel all day.
Hostel staff explained that it was difficult to determine the extent to which alcohol was responsible for memory difficulties among some residents. As two workers summarised:
He often forgets what he needs to do but that could be due to alcohol. He would often ask what we had spoken about . . . but he knew when meal times were.
I give her all letters and reminders . . . is it early dementia or alcohol?
According to staff, six residents had been diagnosed as having Korsakoff syndrome, vascular dementia or alcohol-related dementia. A further six had been referred by their GP to the local memory clinic or to other services for an assessment of their memory. For some, assessments were in progress, and one resident had been initially assessed at a memory clinic but could not be assessed further because he was still drinking heavily. Another resident with memory problems was being monitored by his GP and, according to the staff, was to be referred for specialist help if his memory difficulties worsened.
Making a diagnosis of cognitive decline/dementia
The study aimed to identify individuals with memory problems. To be able to assess an individual in order to make a diagnosis of dementia or related memory problems, clinicians across different services in England follow a fairly similar care pathway. It usually starts with an individual or their family reporting concerns about the person’s memory to the person’s GP. After basic blood tests and initial memory assessments are carried out in primary care, the patient may be referred to secondary care services for further assessment and diagnosis. The majority of memory assessments in secondary care in England are carried out by CMHTs or at memory clinics for older adults; some of those assessments are carried out by geriatricians, neurologists and clinicians working in private centres. After a person is referred to a secondary care service, they will be seen in an outpatient department, or in their home, with the aim of gathering detailed information about their difficulties, and also collateral information will be gathered from their relatives, friends or carers.
The majority of people who are seen in memory services will be offered a type of brain imaging (computerised tomography scan or magnetic resonance imaging) to exclude a brain-occupying lesion or another reason for their cognitive presentation. Brain imaging data are helpful to confirm some dementia syndromes. Only a small percentage of those people require further imaging, such as a PET (positron emission tomography) or DaT (dopamine transporter) scan. This would usually be requested by a specialist. Almost all of those who attend a memory clinic will have memory assessment tests, and, if required, they will be referred to a neuropsychologist for further detailed memory and cognitive assessment. A simple memory assessment takes between 5 and 20 minutes to complete and a detailed assessment takes up to 3 hours. After the results of imaging and memory assessments are reviewed by clinicians, individuals with memory problems will be seen again to receive their results and possibly be given their diagnosis during the same session. The entire process may take up to 6 months to complete.
Formal assessments
In this study, it was not possible to follow the routine care pathway of the NHS to identify people with memory and cognitive difficulties; therefore, we tried to gather as much information as possible during visits and interviews with individuals and the staff from hostels. We used ACE-III as a memory test. 93 The tests were undertaken by the research team’s consultant psychiatrist, psychiatric registrar and psychologist.
The ACE-III test has been widely used in memory clinics to assist clinicians to assess individuals’ cognition. It has been validated, and the maximum score is 100 points. The cut-off point of 88 is 100% sensitive and 96% specific. There is also another cut-off point of 82 out of 100; in this case it is 93% sensitive and 100% specific for dementia. This test usually takes 20 minutes to be completed and requires a rater who has been trained to complete this memory assessment. 105 This scale includes five subdomains, with a total maximum score of 100 points. The five domains are visuospatial (out of 16 points), attention (out of 18 points), memory (out of 26 points), fluency (out of 14 points) and language (out of 26 points).
Cognitive scores from Addenbrooke’s Cognitive Examination III
Of the 62 residents interviewed at baseline, the ACE-III was completed with 42. Among those who did not complete the ACE-III, five left their hostel before it could be administered, one resident died, another could not complete it because of language difficulties, and another could not complete it because of literacy difficulties and therefore the MoCA96 was administered to this person. The remaining 12 residents either refused to take part or were not in the hostel when the psychiatrist visited (despite several visits).
Of the 42 residents who completed the ACE-III, total scores ranged from 29 to 89 points. Just 28.6% scored ≥ 80 points, and 30.9% scored < 60 points. The mean of their total ACE-III scores was 66.81 points, with a SD of 16.64 points. As shown in Table 18, there were differences by age group, although the findings must be treated cautiously because of small numbers. Half of those aged in their early fifties scored between 60 and 79 points, just over one-third scored ≥ 80 points and just 14.3% scored 40–59 points. None in this age group scored < 40 points. By contrast, half of residents aged 55–59 scored ≤ 59 points, including 10% who scored < 40 points. Those aged in their early sixties had the highest scores, and those aged ≥ 65 years had the lowest scores.
| Total ACE-III score (points) | Age groups (years) (%) | Total (%) | |||
|---|---|---|---|---|---|
| 50–54 | 55–59 | 60–64 | ≥ 65 | ||
| ≤ 39 | 0.0 | 10.0 | 0.0 | 22.2 | 7.1 |
| 40–59 | 14.3 | 40.0 | 11.1 | 33.3 | 23.8 |
| 60–79 | 50.0 | 30.0 | 33.3 | 44.4 | 40.5 |
| ≥ 80 | 35.7 | 20.0 | 55.6 | 0.0 | 28.6 |
| Total number of residents | 14 | 10 | 9 | 9 | 42 |
Classifying whether or not residents had memory problems
Owing to the small numbers of hostel residents who were interviewed at baseline, it was agreed that all who were willing and available would be included in the ‘case study’ element of the study. The next step was to classify residents according to whether or not they had memory problems. Several team meetings reviewed all of the data with the psychiatrist, and participants were allocated to groups according to whether or not there was enough information about them to make a judgement.
Based on all of the information, residents were assigned to one of three groups: ‘memory problems’, ‘borderline’ and ‘no memory problems’. We decided to use these three groups based on the data we had after reviewing each participant’s study profile, such as age, physical health problems, weekly alcohol intake and use of illegal drugs, reports and diagnoses of memory problems, and the duration of this complaint. We used these data, alongside their score on the ACE-III, to identify participants with memory problems. All data relating to individuals were reviewed by the consultant psychiatrist and his team to make sure that people were accurately placed in a subgroup. We also examined the subdomains of ACE-III scores to help us identify individuals with memory problems. We categorised each subdomain into three parts to help us analyse the data relating to individuals, before placing individuals in one of the three categories related to memory problems. Although the subcategory score of each subdomain is not validated and not tested, it has been used widely by clinicians to make decisions about an individual’s memory problems based on their scores on subcategories.
We explained earlier the process and the time needed to make an accurate diagnosis of dementia through the NHS (see Making a diagnosis of cognitive decline/dementia). We had to adapt the system to improve the accuracy of our diagnostic criteria and it was impossible to rely on only the cut-off point of ACE-III as an inclusion or exclusion criterion for memory problems. Other factors, as explained previously, played an important role in assessing this group.
Many of the residents reported having had one or several head injuries in the past. We were not in a position to request any brain imaging for this group, and therefore we relied on the data that we had to make a decision about the cognition of these participants. One of the major problems we faced when assessing cognition was that many of these participants were under the influence of alcohol and so it was not possible to conduct a memory assessment at that point. We had to repeat some of the visits to be able to complete those assessments. Such efforts are not generally undertaken in routine NHS services in our experience.
Cognitive groups and their scoring
Based on all of the information, 23 out of the 47 case study participants were allocated to the ‘memory problems’ group, seven were allocated to the ‘borderline’ group and 17 were allocated to the ‘no memory problems’ group. However, only 42 residents completed the ACE-III, of whom 14 were allocated to the ‘no memory problems’ group (mean of their ACE-III score 83.79 points, SD 4.09 points), eight were in the ‘borderline’ group (mean 71 points, SD 6.78 points) and 20 were in the ‘memory problems’ group (mean 53.25 points, SD 12.49 points) (Table 19). Their scores for the subdomains are in Table 20. One of the residents in the borderline group was subsequently evicted from the hostel and therefore could not be included as a case study.
| Cognitive group | Group (n) | Mean score (points) | SD (points) |
|---|---|---|---|
| No memory problems | 14 | 83.79 | 4.098 |
| Borderline | 8 | 71.00 | 6.782 |
| Memory problems | 20 | 53.25 | 12.489 |
| Total | 42 | 66.81 | 16.643 |
| Cognitive domain scores (points) | Cognitive group (%) | Total (%) | ||
|---|---|---|---|---|
| No memory problems | Borderline | Memory problems | ||
| Visuospatial | ||||
| 0–8 | 0.0 | 12.5 | 35.0 | 19.0 |
| 9–12 | 0.0 | 37.5 | 50.0 | 31.0 |
| 13–16 | 100.0 | 50.0 | 15.0 | 50.0 |
| Attention | ||||
| 0–10 | 0.0 | 0.0 | 30.0 | 14.3 |
| 11–14 | 21.4 | 62.5 | 50.0 | 42.9 |
| 15–18 | 78.6 | 37.5 | 20.0 | 42.9 |
| Memory | ||||
| 0–9 | 0.0 | 0.0 | 60.0 | 28.6 |
| 10–16 | 35.7 | 62.5 | 40.0 | 42.9 |
| 17–25 | 64.3 | 37.5 | 0.0 | 28.6 |
| Verbal fluency | ||||
| 0–4 | 0.0 | 25.0 | 70.0 | 38.1 |
| 5–8 | 42.9 | 62.5 | 20.0 | 35.7 |
| 9–14 | 57.1 | 12.5 | 10.0 | 26.2 |
| Language | ||||
| 0–16 | 0.0 | 0.0 | 20.0 | 9.5 |
| 17–22 | 0.0 | 50.0 | 55.0 | 35.7 |
| 23–26 | 100.0 | 50.0 | 25.0 | 54.8 |
| Total number of residents | 14 | 8 | 20 | 42 |
Hostel staff’s reports of memory problems compared with formal assessments
One of the study’s objectives was to determine the extent to which hostel staff were aware of memory problems among their older hostel residents. As shown in Table 21, hostel staff identified memory problems for most residents who were formally assessed as having memory problems; out of 23 residents with memory problems, hostel staff identified memory problems in 70%. They were unsure for two residents, and did not identify memory problems in just five residents (22%) in whom there were memory problems in our judgement. At the same time, among 17 residents who did not have memory problems, the staff reported this correctly in 59%. Among the five residents whom the hostel staff suspected had memory problems but were found not to have memory problems by the psychiatrist, one was undergoing tests at a memory clinic, and another was a former heavy drinker and, according to the hostel staff, ‘may be a little bit degenerative’.
| Hostel staff’s reports | Cognitive group (formal assessment) (n) | Total (N) | ||
|---|---|---|---|---|
| No impairment | Borderline | Impairment | ||
| Has memory problems | 5 | 2 | 16 | 23 |
| Does not have memory problems | 10 | 5 | 5 | 20 |
| Unsure | 2 | 1 | 2 | 5 |
| Total | 17 | 8 | 23 | 48 |
Chapter summary
The backgrounds of older homeless people vary greatly, as described in this chapter. Some residents interviewed for this study had relatively stable histories, had worked for years, and became homeless for the first time in later life. Others had unsettled histories, had left school at an early age without qualifications, and had subsequently experienced long periods of unemployment and homelessness. Our sample tended to be ‘young-elderly’ homeless people, with the majority being aged in their fifties. Despite their relatively young age in terms of the general population, there was a high prevalence of physical ill-health, depression, and alcohol and drug problems among them. For some, mental health and substance misuse problems dated back to their teens or to early adulthood and preceded their entry into homelessness. Some associated these problems with traumas and stressful events that they had experienced as youths or young adults, while some had been raised in households in which one or both of their parents were heavy drinkers.
There were differences by age. Those aged in their early fifties tended to be particularly disadvantaged in that many had left school early without qualifications and had literacy difficulties. They were more likely than those in other age groups to have first become homeless as teenagers or when they were in their twenties, and very heavy drinking and the use of illegal drugs were characteristic of this age group. A high percentage of this age group consumed super-strength lagers and beers, drinking > 50 units of alcohol per week. By contrast, many aged in their sixties or older had worked for years and tended to have first become homeless in later life. Although several drank alcohol most days, they were less likely to drink standard-strength lagers and beers, and fewer consumed > 50 units of alcohol per week. Those in this age group were also less likely to be current illicit drug users.
There were also differences by cluster site. Those in North England were more likely to have had stable histories and to have become homeless for the first time after the age of 50 years, whereas many in the London sites had experienced homelessness intermittently or continuously since early adulthood. Heavy drinking and the consumption of super-strength alcohol were characteristic of participants in the two London clusters but less so among those in North England. Many in the latter group could be regarded as ‘settled’ in that they had remained in their hostel for several years.
Age is the greatest risk factor for developing dementia, and around 16% of adults in the UK experience increasing confusion or memory loss (Alzheimer’s Society, 2016106). This study clearly found, however, that memory problems were much more prevalent among older homeless people in the hostels participating in this study; nearly half (47.6%) of hostel residents were assessed as having memory problems, and a further 19% were deemed to be borderline. The median age for those with memory problems (memory problems or borderline) was just 60.4 years. Hostel staff were relatively proficient at identifying hostel residents who were having memory difficulties. Regular contact with residents enabled them to recognise when residents were more confused or were struggling with everyday activities. As we will discuss at the end of this report, there is perhaps a strong case for currently seeing hostel staff as part of the ‘dementia care workforce’. The next chapter examines the health and social care needs of all 47 residents who were involved in the case study element of this research project.
Chapter 6 Residents’ health and social care needs and quality of life
This chapter focuses on the health and social care needs of the hostel residents in the case studies, and on their QoL and housing outcomes. It draws on information gathered over 6 months (the course of the case study element). It first summarises the key characteristics of the residents with and without memory problems, and then examines their health needs and how these were met, followed by their personal and social care needs. The chapter then describes the residents’ activities and how they spend their time, and their self-ratings of QoL and the factors that enhance this. Finally, their housing outcomes over the study period are summarised.
Key characteristics of the residents with and without memory problems
Thirty out of the 47 hostel residents who were included in the case studies were found to have memory difficulties (23 had memory problems and seven were borderline). All except one were men. The majority were either aged in their early fifties (33.3% were aged 50–54 years) or aged ≥ 65 years (30.0%). They were fairly evenly spread across the three cluster sites: 36.7% were in hostels in Central London, 33.3% were in hostels in South London and 30.0% were in hostels in North England. As shown in Figure 3, those residents with memory problems were more likely than those without to have been homeless for many years; this applied to 67% and 29%, respectively.
FIGURE 3.
Length of time homeless, by cognitive or memory problem group.
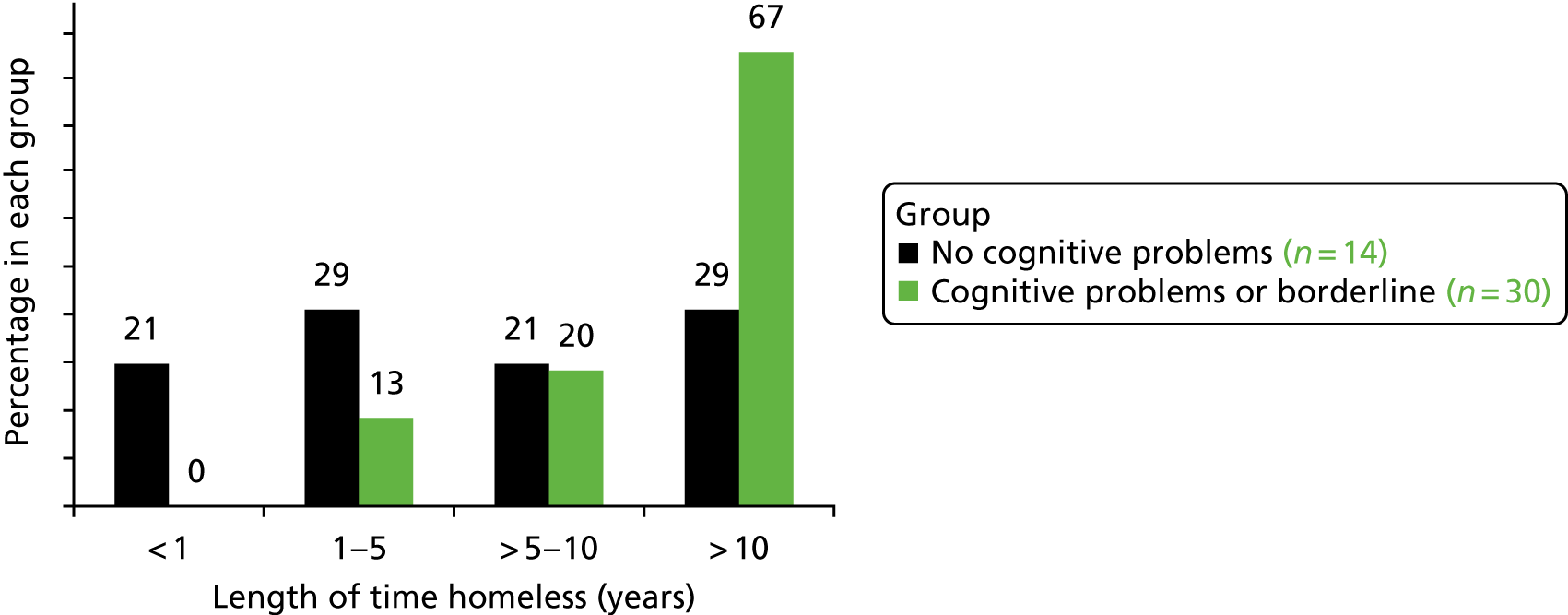
Those residents with memory problems were also more likely to have been in their hostel longer than those without memory difficulties. One-third (33%) with memory problems had been so housed for ≥ 5 years, compared with just 18% with no memory problems (Figure 4). By contrast, 53% of residents without memory problems had moved into the hostel fairly recently (within the past year). This compares with just 37% of those with memory problems.
FIGURE 4.
Length of time in current hostel, by cognitive or memory problem group.
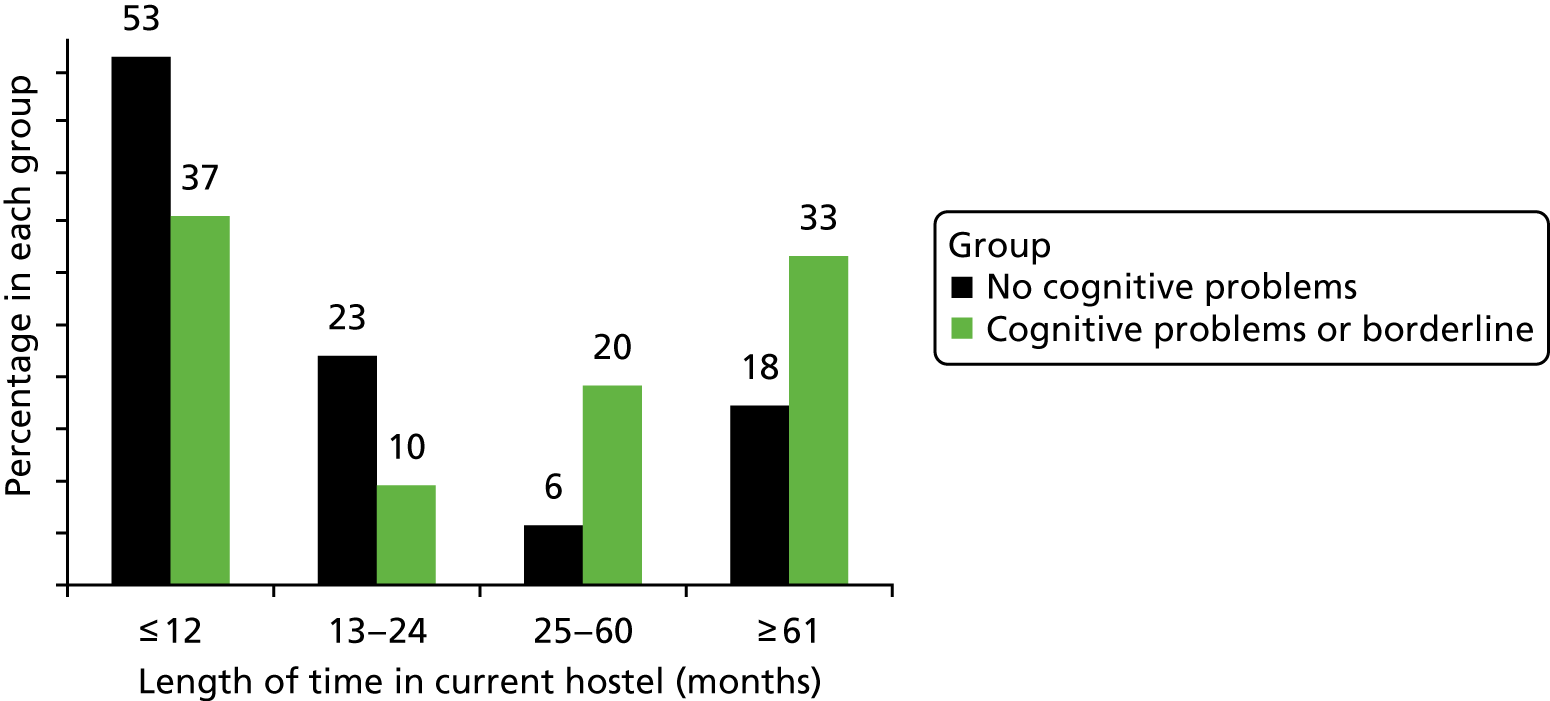
Drawing on scores from the depression tool administered during the baseline interview, there was no difference between levels of depression and whether or not residents had memory problems. There was also no significant difference between reports of recent or past head injuries and the presence of memory problems. There was also little difference between past and present alcohol use and memory problems. Overall, 67% of residents who had ever been a heavy drinker, and 50% with no history of heavy drinking, had memory problems. A slightly higher percentage with memory problems (60.9%) currently drank on 6 or 7 days per week, compared with 47.1% with no memory problems. A slightly higher proportion of residents without memory problems had a history of illicit drug use (68.8%, compared with 52.2% with memory problems).
Health needs
As described in the previous chapter, most residents had physical health problems, and nearly all of these people (98.2%) were receiving medication from their GP. During the 6 months of the case study period, virtually all residents (93.6%) had contact with their GP at least once, including 34% who had eight or more GP contacts. Many (59.6%) also had contact with primary care nurses or other health staff from a general practice. Similarly, a high proportion (68.1%) had contact with one or more allied health professionals such as podiatrists, dentists or opticians. During the course of the study, eight people (17%) were admitted to hospital because of physical health problems.
Almost three-quarters (73.8%) of residents in the case studies had mental health problems, and many of these received treatment (medication) from their GP. Nearly half (48.4%) also had at least one contact with mental health services during the course of the study. This included one person who was visited in the hostel by a psychiatrist from a memory clinic. Just one person was admitted to a mental health inpatient unit during the study period. One-third of residents were prescribed medication for depression, usually citalopram (Celexa®, Teva UK) or mirtazapine (Remeron®, Teva UK). When this is examined further in relation to the severity of depression scored at the baseline interview, the following groups were prescribed antidepressant medication:
-
37% without depression
-
50% with mild depression
-
38.5% with moderate depression
-
25% with severe depression.
Caution has to be taken when interpreting these findings regarding depression, as the number of residents in each group is small. For example, only four residents were in the ‘severe depression’ group, and only one of these was prescribed antidepressants. In addition, although several with current mild or no depression were receiving treatment, it could be that their depression had improved because of the medication.
The majority of residents who were drinking heavily or had past alcohol problems were being prescribed one or more vitamin supplements by their GP. Of those who consumed > 14 units of alcohol per week, 91.3% were prescribed vitamins. Among this group, 87% were prescribed thiamine (vitamin B1) and 82.6% were prescribed vitamin B compound strong tablets. Ten residents also had contact with alcohol services during the study period; this included six (22.2%) out of the 21 residents who were drinking daily or nearly every day. In some hostels, staff restricted, to some extent, the amount of alcohol that residents who were heavy drinkers could have each day, either by having a budget plan with the resident and limiting the amount of money that was handed to the person each day, or by agreeing the number of ‘cans of beer’ that would be given to the resident each day. The following two illustrative cases, compiled from the research records, describe the help that was given to residents with alcohol problems and the difficulties of helping some who were reluctant to stop drinking:
Participant 201 (borderline memory problems) was reluctant to give up alcohol. His keyworker SW11 was keen for 201 to engage with alcohol services and described working very hard to change his attitude by taking the following approach: ‘keep chipping away regarding alcohol use, try to get him [201] to engage with services, [I] worry for his future’. Six months later, SW11 said that the hostel staff had ‘put in place a daily alcohol diary as he won’t engage with professional alcohol services, we review diary monthly and will encourage him to accept professional treatment’.
Participant 118 (no memory problems) was similarly reluctant to give up alcohol and drugs. He was supported by staff member SW19 who again was trying to encourage him to engage with drug and alcohol services, but described feeling that his job role was restricted. ‘Encouragement is as far as I can go. Our work is client-centred so if [118] says no to offers of support; all I can do is to say it will affect their move on’.
Personal and social care needs
All hostels participating in this study provided older residents with basic assistance, when needed, with everyday tasks, such as bathing, washing clothes and keeping their bedrooms tidy. Some staff assisted residents with budgeting and managing money, with collecting and supervising medication and by taking them shopping to buy clothes and other essentials. The type of assistance ranged from prompting to do the domestic chore to giving a great deal of assistance with it. In some cases, residents required regular and extensive help with tasks such as bathing and managing continence, which was beyond the remit of hostel staff and the support that they could provide. Some residents had been referred to social services (adult services) and arrangements were in place for a care worker to assist with self-care and daily living activities.
As shown in Table 22, residents with memory problems were more likely than those without memory problems to require assistance across a range of personal and social care needs. Two-thirds with memory problems required assistance with personal hygiene and bathing, and some were occasionally incontinent (the latter was mainly associated with heavy drinking). Residents without memory problems tended to require help because of physical health and mobility problems. Overall, a relatively high proportion (36.2%) of residents received help from a care worker (organised by social services); this included 50% of those with memory problems and 11.8% of those without (see Table 22). In a few instances, a ‘care package’ was arranged but residents refused to accept help. One man, for example, regularly left the hostel when he knew that his care worker was coming to help him with bathing.
| Prompting or assistance with . . . | Cognitive group (%) | Total (%) | |
|---|---|---|---|
| No memory problems | Memory problems or borderline | ||
| Personal hygiene/bathing | 29.4 | 66.7 | 53.2 |
| Managing incontinence | 5.9 | 30.0 | 21.3 |
| Personal laundry | 29.4 | 70.0 | 55.3 |
| Cleaning bedroom/changing bedsheets | 52.9 | 83.3 | 72.3 |
| Budgeting/managing money | 25.0 | 66.7 | 52.2 |
| Ordering/collecting medication | 29.4 | 76.7 | 59.6 |
| Managing/administering medication | 17.6 | 46.7 | 36.2 |
| Shopping for clothes and toiletries | 28.6 | 40.7 | 36.6 |
| Has regular input from care worker (organised by social services) | 11.8 | 50.0 | 36.2 |
| Number of residents | 17 | 30 | 47 |
In addition to providing support with everyday self-care needs, hostel staff spent a great deal of time arranging appointments and contacting services on behalf of residents, and accompanying them to various appointments such as with the Jobcentre or the GP. In one hostel, arrangements were in place for peer advocates to escort residents to GP and hospital appointments when needed. During the study period, high percentages of both residents with and residents without memory problems received assistance from hostel staff with contacting services and with arranging and by accompanying them to appointments (Table 23).
| Task undertaken by hostel staff on behalf of residents | Cognitive group (%) | Total (%) | |
|---|---|---|---|
| No memory problems | Memory problems or borderline | ||
| Contacted services/arranged appointments | 64.3 | 88.9 | 80.5 |
| Accompanied residents to appointments | 50.0 | 50.0 | 50.0 |
| Number of residents | 17 | 30 | 47 |
Supporting and monitoring residents
All residents had a key worker and many hostel staff described adopting an individual or tailored approach with each resident. Over time, they became acquainted with the residents and learned how best to engage them in care and support. In some cases, this involved the staff making themselves available whenever a particular resident wanted to speak to them. In some other cases, staff sought out residents who would not seek help. For example, one man with memory problems would get anxious if too many questions were asked of him in a short period of time. Consequently, the key worker approached him gently and asked questions one at a time, sometimes over the span of a day.
The hostel staff described a need to ‘keep an eye on’ some residents, which applied to 34% of residents in the study (43.3% with, and 17.6% without, memory problems). It involved checking on them two or three times a day to find out how they were feeling, asking if they needed anything, and prompting them to eat or to attend to their personal hygiene or clean their room. For some residents, this was required at certain times, such as when they were intoxicated or when they appeared to be ‘out of sorts’ or physically unwell. In one hostel, the most vulnerable residents were allocated bedrooms near the staff office so that staff could be alerted to any problems. A few hostel residents were aware of the intensity of the support they received, and most were grateful for this. As one man described, ‘the beauty of living here, you’re in a bubble and you feel safe, you’re under their wing, they watch out for you, you feel secure and safe’.
Activities and use of time
Residents were asked an open-ended question regarding how they spent their time. This elicited a range of responses. Many described watching television or listening to the radio, either in their own rooms or in communal areas. Several mentioned going to the shops, which was often linked to buying cigarettes and/or alcohol. A small proportion described going for walks or to the local library, or going to day centres or drop-in centres (for homeless people). Only a small number said that they liked doing activities (organised in the hostel), or reading or browsing the internet.
A high proportion of residents (72.3%) said that they were in contact with family or relatives. This included 88.2% of people without cognitive problems and 63.3% of those with memory problems. Their main contacts were with a child or a sibling, usually a sister. Many fewer, however, regularly saw a family member; just 14.9% saw at least one family member monthly or more often. Just over one-quarter (27.7%) said that they did not have any family or relatives. Those in this last group tended to be older residents (aged ≥ 65 years).
The residents’ comments describe their various activities and the diverse ways in which they spent time:
Reading, lot of walking. Go to nature reserves. Have freedom pass [free travel card] so go out most days . . . I like cooking so I cook upstairs [in the hostel].
Get a four-pack [four cans of beer or lager] and drink. Don’t go out the hostel much. I don’t use the TV room – I like to be private.
Watch telly, relax, sleep a lot. My son visits me . . . I can’t go far because of my legs. I have no power in my legs anymore.
Walk to [locality] and back – that’s 5 miles. See friends, go to their flats or a café or the library. Drink with friends.
Quality of life
Residents’ ratings of quality of life
Residents were asked at baseline to rate their QoL; they could respond ‘very good’, ‘good’, ‘neither good nor poor’, ‘poor’ or ‘very poor’. Almost half rated their QoL as ‘very good’ or ‘good’, 31.1% described it as neither good nor poor, and 20% described it as ‘poor’ or ‘very poor’ (Table 24). There were slight differences, however, between those with and those without memory problems (see Table 24). Fewer residents with memory problems were likely to say that their QoL was ‘very good’, although a relatively high percentage described it as ‘good’. By contrast, a high proportion without memory problems rated their QoL as ‘neither good nor poor’.
| Rating | Cognitive group (%) | Total (%) | |
|---|---|---|---|
| No memory problems | Memory problems or borderline | ||
| Very good | 17.6 | 7.1 | 11.1 |
| Good | 17.6 | 50.0 | 37.8 |
| Neither good nor poor | 47.1 | 21.4 | 31.1 |
| Poor | 11.8 | 17.9 | 15.6 |
| Very poor | 5.9 | 3.6 | 4.4 |
| Number of residents | 17 | 28 | 45 |
There were differences by age groups in ratings of QoL, although the figures must be treated cautiously because of the small numbers in each age group. Those aged ≥ 65 years were most optimistic and four-fifths described their life as ‘good’ or ‘very good’ (Figure 5). Residents aged 50–59 years were most likely to describe their QoL as ‘neither good nor poor’. Those who were depressed were less likely than those who were not depressed to rate their QoL in positive terms. Among those with depression, 27.8% described their QoL as ‘good’ or ‘very good’ and 33% described it as ‘poor’ or ‘very poor’. The corresponding figures for those without depression were 62.9% and 11.1%. There were also marked differences in relation to whether or not they were drinking heavily. As shown in Figure 6, those who were drinking very heavily (≥ 50 units of alcohol per week) were less likely to be optimistic about their QoL.
FIGURE 5.
Residents’ ratings of QoL, by age group.
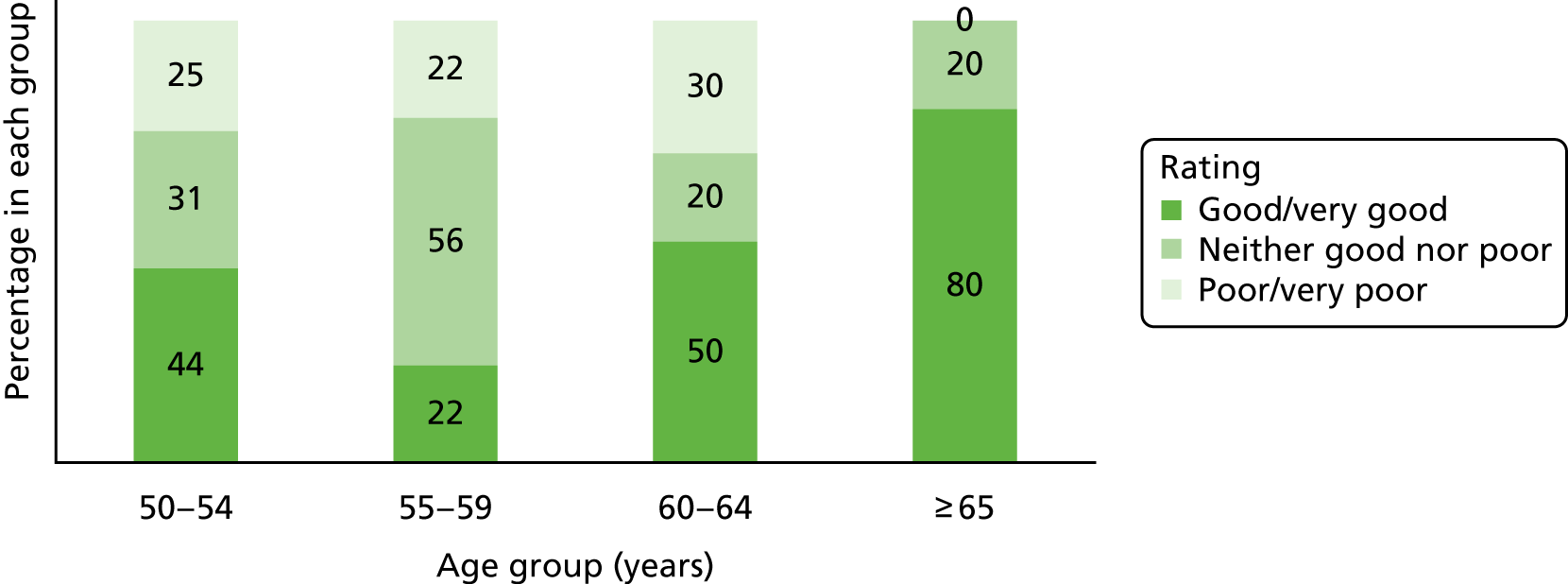
FIGURE 6.
Residents’ ratings of QoL, by weekly alcohol consumption.
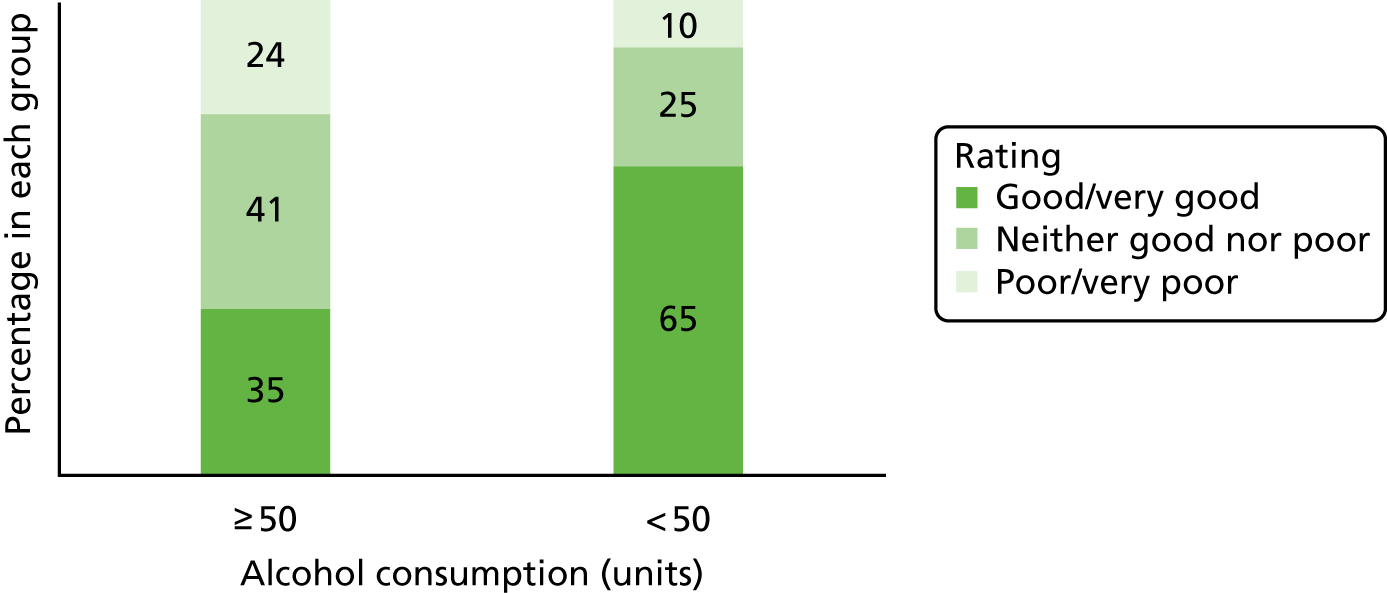
Factors contributing to quality of life
When asked what factors contributed to their QoL, most residents described one or more factor. However, 19% were unable to answer or could not identify anything that added quality to their life. This included 17.6% of those without memory problems and 20.1% with memory problems (or who were borderline). There were large differences between those with and those without memory problems in relation to their responses about the factors that gave quality to their life (Table 25). The residents without memory problems were most likely to identify being healthy and engaging in various activities, such as reading, watching television and going for walks, as important factors in enhancing their QoL. By contrast, those with memory problems were most likely to say that socialising with other hostel residents and drinking alcohol were the most important factors.
| Factor | Cognitive group (%) | Total (%) | |
|---|---|---|---|
| No memory problems | Memory problems or borderline | ||
| Socialising with friends/other residents | 5.9 | 20.1 | 15.2 |
| Being healthy and able to get up in the morning | 29.4 | 6.9 | 15.2 |
| Watching television, listening to music | 17.6 | 10.3 | 13.0 |
| Going out/going for walks | 23.5 | 6.9 | 13.0 |
| Reading, activities in the hostel | 17.6 | 6.9 | 10.9 |
| Drinking alcohol | 0.0 | 13.8 | 8.7 |
| Family contact | 5.9 | 6.9 | 6.5 |
| Feeling confident/trusted/happy | 5.9 | 6.9 | 6.5 |
| Hope and plans for the future | 5.9 | 3.4 | 4.3 |
| Having somewhere to stay/the hostel | 5.9 | 3.4 | 4.3 |
| Number of residents | 17 | 30 | 47 |
The following accounts are examples of activities that residents said added to their QoL:
Able to get out and about. Chat with people. Make a fuss of people’s dogs. Chat to shopkeepers and people on the streets.
‘Borderline’ group
I love music. I used to write songs and lyrics and I used to be in a band. I like being creative and doing paintings. I’ve done several courses at college.
‘No memory problems’ group
Don’t know. Going to the pub.
‘Memory problems’ group
Factors that would improve quality of life
When the residents were asked what factors would improve their QoL, there were again differences depending on whether or not they had memory problems. The most commonly reported factor by far, in both groups, was being rehoused and moving out of the hostel (Table 26). Overall, 34.9% of residents identified this, including 58.8% of those without memory problems. Those residents without memory problems also mentioned having more money, getting a job and having better health as important factors. Those with memory problems identified having more money, having better health and stopping drinking or using drugs as important factors. Only a small proportion in both groups (4.7% overall) said that more contact with family and relatives would improve their QoL.
| Factor | Cognitive group (%) | Total (%) | |
|---|---|---|---|
| No memory problems | Memory problems or borderline | ||
| Moving/being rehoused | 58.8 | 19.2 | 34.9 |
| More money | 23.5 | 11.5 | 16.3 |
| Better health | 11.8 | 11.5 | 11.6 |
| Getting a job | 11.8 | 7.7 | 9.3 |
| Stop drinking/using drugs | 0.0 | 11.5 | 7.0 |
| More contact with family/relatives | 5.9 | 3.8 | 4.7 |
| Going on holiday/travelling | 5.9 | 3.8 | 4.7 |
| Number of residents | 17 | 30 | 47 |
Housing outcomes during the study period
Most residents remained in their present hostel during the study period (Table 27). A few were rehoused, taking up their own tenancy; these tended to be residents without memory problems. One person with memory problems was also rehoused in a tenancy but was unable to cope and moved back to the hostel. Although, as described in the previous section, many residents wanted to move on from their hostel, the majority would require accommodation with flexible levels of support. The lack of suitable alternative housing options was evident. This is discussed further in Chapter 7.
| Housing outcome | Cognitive group (%) | Total (%) | |
|---|---|---|---|
| No memory problems | Memory problems or borderline | ||
| Remained in original hostel | 76.5 | 90.0 | 85.1 |
| Moved to another hostel | 5.9 | 0.0 | 2.1 |
| Rehoused in own tenancy | 17.6 | 0.0 | 6.4 |
| Othera | 0.0 | 10.0 | 6.4 |
| Number of residents | 17 | 30 | 47 |
Chapter summary
This chapter has summarised the health and social care needs of the hostel residents who agreed to provide us with this information, and their self-ratings of QoL. It has revealed that many older homeless people in hostels require substantial help and support to manage their everyday needs and health problems. This was particularly the case for people with memory problems. It has illustrated how hostel staff often provide considerable support to some older residents, which is beyond the traditional remit of a ‘hostel worker’ in a homeless setting. They were acting as advocates and taking on the role that family members or social care staff generally provide to older people with health and support needs living in the community. For some residents, the local authority had undertaken an assessment and organised a care package, mainly personal care delivered by a home care agency. This was not always the case, however, partly as a result of the lack of engagement of some residents with support services and the high threshold for local authority support. The challenges identified in this study of helping older homeless people to access health and social care services, and their unmet needs, are addressed in the next chapter.
Chapter 7 Cost of services, unmet needs and challenges in providing services
This chapter draws on the context provided in Chapter 6 regarding the health and social care needs of hostel residents. It presents findings that cover four main topics: (1) costs of the use of health and social care services, (2) hostel staff’s reports of residents’ unmet needs, (3) challenges along the health and social care pathway and (4) housing options.
Costs of the use of health and social care services
This section reports on the data collected about service utilisation and the calculation of costs of provisions. The relationships between participant characteristics and costs are explored.
Sample for the economic analysis
The analysis of costs was based on complete cases. Data on service use were available for 47 (75.8%) out of the 62 study participants.
Frequency of service use
Data were recorded for a large number of services, many of which were used by small proportions of the participants (see Appendix 2). GP services were the most frequently accessed. Non-attendance at GP appointments was > 15%, and it was 44% for appointments with allied health professionals (see Appendix 3). Table 28 presents frequency of service use data.
| Service groupings: number of participants who had . . . | Frequency of use, n (%) | |||||
|---|---|---|---|---|---|---|
| Never used | 1–3 times | 4–7 times | 8–15 times | 16–30 times | ≥ 31 times | |
| Contacts with a GP | 3 (6.4) | 14 (29.8) | 14 (29.8) | 12 (25.5) | 3 (6.4) | 1 (2.1) |
| Contacts with other GP staff (nurse, care navigator) | 19 (40.4) | 21 (44.7) | 5 (10.6) | 1 (2.1) | 0 (0.0) | 1 (2.1) |
| Contacts with other primary care (chiropodist, dentist, optician)a | 15 (31.9) | 20 (42.6) | 9 (19.2) | 3 (6.4) | 0 (0.0) | 0 (0.0) |
| Contacts with community psychiatric/mental health services | 35 (74.5) | 8 (17.0) | 1 (2.1) | 3 (6.4) | 0 (0.0) | 0 (0.0) |
| Alcohol and drug service contacts | 29 (61.7) | 8 (17.0) | 4 (8.5) | 3 (6.4) | 2 (4.3) | 1 (2.1) |
| Community pharmacist contacts (supervision of opiate substitute) | 45 (95.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (4.3) |
| Contacts with social care services (AHP, social worker) | 31 (66.0) | 14 (29.8) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Social services funded carer visiting at hostel | 30 (63.8) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 2 (4.3) | 14 (29.8) |
| Half days at AHP centre | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Full days at AHP centre | 42 (89.4) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 2 (4.3) | 2 (4.3) |
| Contacts with emergency and out-of-hours services | 25 (53.2) | 13 (27.7) | 5 (10.6) | 4 (8.5) | 0 (0.0) | 0 (0.0) |
| Hospital outpatient consultations and treatments/tests | 15 (31.9) | 17 (36.2) | 8 (17.0) | 7 (14.9) | 0 (0.0) | 0 (0.0) |
| Days as a hospital inpatient (includes day and intermediate care) | 38 (80.8) | 4 (8.5) | 2 (4.3) | 0 (0.0) | 2 (4.3) | 1 (2.1) |
| Admissions, in-hospital stay (psychiatric) | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Admissions, in-hospital stay (non-psychiatric) | 39 (83.0) | 8 (17.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Contacts with voluntary helper | 41 (87.2) | 3 (6.4) | 2 (4.3) | 1 (2.1) | 0 (0.0) | 0 (0.0) |
| Contacts with all psychiatric servicesb | 32 (68.1) | 10 (21.3) | 2 (4.3) | 3 (4.3) | 0 (0.0) | 0 (0.0) |
When services were grouped (Table 29), 94% of participants had appointments for contact with a GP during the 6-month period, 60% had appointments with other general practice staff, 68% had a hospital outpatient appointment, 47% had used emergency or out-of-hours services, 38% had used alcohol and drug services and 32% had had contact with any psychiatric or secondary mental health service (such as a member of a CMHT).
| Service | Cost (£) per participant of services used during months 0–6 | ||||||
|---|---|---|---|---|---|---|---|
| Mean | Median | % of non-zeros | SD | Interquartile range | Minimum | Maximum | |
| GP contacts | 324.43 | 220.00 | 93.6 | 262.81 | 132–468.50 | 0.00 | 990.00 |
| Other GP staff contacts | 67.00 | 14.50 | 59.6 | 263.77 | 0–43.50 | 0.00 | 1816.30 |
| Other primary services (chiropodist, dentist, optician) | 98.29 | 63.90 | 68.1 | 110.78 | 0–160 | 0.00 | 440.40 |
| Psychiatric/mental health services | 56.60 | 0.00 | 25.5 | 129.84 | 0–42 | 0.00 | 546.00 |
| Alcohol and drug services | 442.64 | 0.00 | 38.3 | 1055.83 | 0–244 | 0.00 | 4603.56 |
| Social care services | 775.95 | 19.00 | 51.1 | 1337.19 | 0–1086 | 0.00 | 5824.00 |
| Emergency and out-of-hours services | 175.60 | 0.00 | 46.8 | 317.88 | 0–225.59 | 0.00 | 1381.95 |
| Hospital outpatient services | 285.03 | 118.00 | 68.1 | 366.43 | 0–485.84 | 0.00 | 1416.00 |
| Hospital inpatient services | 738.36 | 0.00 | 19.1 | 2382.44 | 0–0 | 0.00 | 11,083.56 |
| Voluntary helper | 11.49 | 0.00 | 12.8 | 37.70 | 0–0 | 0.00 | 200.00 |
| All services | 2975.39 | 1454.50 | 0.0 | 3300.16 | 631.86–1454.50 | 163.90 | 13,280.92 |
| All psychiatric servicesa | 128.06 | 0.00 | 31.9 | 403.47 | 0–118 | 0.00 | 2646.00 |
Service use costs
The cost for each service for each participant was calculated by applying 2014/15 unit costs (see Appendix 2) to utilisation data, including for appointments that were not attended. Summary statistics for the service groupings are shown in Table 30. All participants incurred a cost from at least one service group. The mean (median) cost during the 6-month period was £2975 (£14,550), of which £128 (£0) was for psychiatric services; however, there is considerable variability between participants, as shown by the SDs and ranges. The most costly grouping (means of > £700 for the 6 months) were social care services, owing to 12 participants having a care worker making frequent visits to the hostel to provide personal care and support to specific residents (five participants had daily visits and seven had several visits per week), and in-hospital stays (one day case, one psychiatric/mental health stay, and nine non-psychiatric stays including one participant having two hospital episodes). The next most costly items were alcohol and drug services (mean £443) and GPs (mean £324).
| Service group cost | Total cost | Service use cost | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP | Other GP | All GP | Other primarya | Psychiatric/mental health | Alcohol and drugs | Social care | Emergency and out of hours | Hospital outpatient | Hospital inpatient | All psychiatricb | ||
| Spearman’s coefficient | –0.150 | –0.34 | 0.344 | –0.159 | –0.062 | –0.011 | 0.061 | –0.145 | –0.339 | –0.143 | –0.051 | –0.043 |
| p-value | 0.349 | 0.03 | 0.028 | 0.320 | 0.699 | 0.946 | 0.706 | 0.365 | 0.03 | 0.371 | 0.75 | 0.789 |
| Association | Not significant | Worse cognition = higher costs | Worse cognition = lower costs | Not significant | Not significant | Not significant | Not significant | Not significant | Worse cognition = higher costs | Not significant | Not significant | Not significant |
Associations between memory problems and service use costs
When all services were considered individually, there was only one significant difference in costs between participants in whom memory problems were present, participants who were borderline and participants in whom memory problems were not present. This was for the visiting home care workers, for which all costs were incurred by participants with memory problems either present or borderline (data not shown). When comparisons were conducted for groups of services, the costs for people without memory problems were significantly higher than those for people in whom memory problems were present or borderline for other GP services (i.e. nurses, care navigators in general practices), but not for any other service grouping (see Appendix 4). The difference in service patterns between memory problem groups should not be interpreted as identifying specific impact of memory problems, as the three groups of homeless people also differ in a number of other characteristics.
There were 41 participants who had undergone cognitive testing with the ACE-III (range 0–100 points, with lower scores indicating worse cognition). The mean ACE-III score was 65.76 points (SD 16.85, median 66, interquartile range 29–81.5 points). There were significant correlations between the ACE-III scores and costs of three groups of services. Higher costs of GP services and emergency and out-of-hours services were associated with lower scores; higher costs of other GP services (nurses, care navigators) were associated with higher scores. There was no significant association between all GP services (GPs and other practice staff together) or any other cost grouping, or total costs, and cognition as measured by ACE-III scores (see Table 30).
Associations between participant characteristics and costs
Tests of association between participant characteristics revealed significant (positive) correlations between number of named medications and number of comorbidities and number of head injuries reported by participants. Illegal or illicit drug use in the previous 3 months was also associated with more head injuries. Location in London, rather than North England, was associated with non-white British ethnicity and more frequent alcohol consumption (see Appendix 5).
Associations between costs and other participant characteristics (sociodemographic and medical) revealed that higher total costs were associated with location in London, and having more comorbidities and more prescribed medications; higher psychiatric costs were associated with more head injuries. Higher costs of all GP services were associated with being in London, more alcohol use, and having more comorbidities, prescribed medications and head injuries. Hospital stays were associated with more comorbidities and prescribed medications. Out-of-hours costs were associated with number of medications and number of head injuries (Table 31).
| Sociodemographic characteristic | Type of service | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All services | GP and other GP staff | Other primary | Psychiatric/mental health | Alcohol and drug | Social care | Emergency, out of hours | Hospital outpatient | Hospital inpatient | All psychiatrica | |
| Sex | ||||||||||
| Male (n = 42), median (mean) | 1441.64 (2819.51) | 274.93 (381.87) | 63.90 (102.60) | 0 (63.33) | 0 (354.06) | 0 (665.43) | 0 (176.70) | 116.50 (236.88) | 0 (826.26) | 0 (132.07) |
| Female (n = 5), median (mean) | 5709.09 (4284.77) | 431.90 (471.78) | 0 (62.08) | 0 (0) | 488 (1186.72) | 1064 (1704.30) | 140.59 (166.35) | 625 (689.53) | 0 (0) | 0 (94.40) |
| Mann–Whitney p-value | 0.228 | 0.409 | 0.336 | 0.319 | 0.202 | 0.058 | 0.242 | 0.049 | 0.449 | 0.725 |
| Age when first interviewed (n = 47); mean 59.3 years, median 57 years | ||||||||||
| Spearman’s coefficient | –0.068 | –0.192 | 0.087 | –0.156 | –0.048 | 0.145 | –0.17 | –0.053 | 0.029 | –0.143 |
| p-value | 0.650 | 0.197 | 0.562 | 0.296 | 0.75 | 0.332 | 0.254 | 0.721 | 0.848 | 0.337 |
| Ethnicity | ||||||||||
| White British (n = 37), median (mean) | 1675.77 (3245.84) | 290.50 (406.34) | 63.90 (102.21) | 0 (58.27) | 0 (401.45) | 41 (834.26) | 0 (190.44) | 118 (312.82) | 0 (925.99) | 0 (149.05) |
| Other (n = 10), median (mean) | 1290.77 (1974.74) | 306.90 (336.31) | 63.90 (83.77) | 0 (50.40) | 61 (595.06) | 0 (560.20) | 49.50 (120.68) | 27.50 (182.20) | 0 (44.13) | 0 (50.40) |
| Mann–Whitney p-value | 0.465 | 0.908 | 0.99 | 0.828 | 0.53 | 0.274 | 0.949 | 0.117 | 0.53 | 0.888 |
| Literacy problems | ||||||||||
| No (n = 31), median (mean) | 1539.29 (3034.90) | 290.50 (376.35) | 63.90 (98.52) | 0 (65.71) | 0 (495.02) | 41 (798.69) | 0 (149.04) | 118 (275.26) | 0 (765.99) | 0 (166.45) |
| Yes (n = 16), median (mean) | 1441.64 (2860.09) | 332.03 (420.65) | 83.90 (97.84) | 0 (38.94) | 0 (341.16) | 0 (731.88) | 49.50 (227.06) | 118 (303.97) | 0 (684.84) | 0 (53.69) |
| Mann–Whitney p-value | 0.686 | 0.406 | 0.493 | 0.792 | 0.355 | 0.676 | 0.387 | 0.681 | 0.883 | 0.408 |
| Number of comorbidities (n = 47); mean 5.3, median 5 | ||||||||||
| Spearman’s coefficient | 0.403 | 0.294 | 0.239 | 0.181 | 0.286 | 0.104 | 0.235 | 0.136 | 0.287 | 0.1 |
| p-value | 0.005 | 0.045 | 0.106 | 0.224 | 0.051 | 0.487 | 0.111 | 0.362 | 0.05 | 0.503 |
| Number of named medications (n = 47); mean 7.4, median 5 | ||||||||||
| Spearman’s coefficient | 0.516 | 0.607 | –0.127 | 0.284 | 0.323 | 0.228 | 0.502 | 0.357 | 0.327 | 0.172 |
| p-value | > 0.0005 | > 0.0005 | 0.395 | 0.053 | 0.027 | 0.124 | > 0.0005 | 0.014 | 0.025 | 0.249 |
| Total number of head injuries (n = 47); mean 1.4, median 1 | ||||||||||
| Spearman’s coefficient | 0.156 | 0.319 | 0.115 | 0.44 | 0.142 | –0.202 | 0.357 | –0.019 | 0.028 | 0.322 |
| p-value | 0.294 | 0.029 | 0.44 | 0.002 | 0.34 | 0.174 | 0.014 | 0.898 | 0.853 | 0.027 |
| Illegal drug use in the previous 3 months | ||||||||||
| No (n = 32), median (mean) | 1165.63 (2632.63) | 237.15 (312.40) | 63.90 (115.53) | 0 (47.25) | 0 (346.97) | 31.50 (637.83) | 0 (102.72) | 118 (324.62) | 0 (725.70) | 0 (148.53) |
| Yes (n = 15), median (mean) | 2819.20 (3706.61) | 381.05 (540.85) | 40 (61.50) | 0 (76.53) | 122 (646.74) | 0 (1070.60) | 198 (331.08) | 115 (200.59) | 0 (765.37) | 0 (84.40) |
| Mann–Whitney p-value | 0.193 | 0.132 | 0.170 | 0.800 | 0.155 | 0.923 | 0.042 | 0.377 | 0.561 | 0.679 |
| How often participant drinks alcohol | ||||||||||
| < 6 times/week (n = 19), median (mean) | 1429.60 (1875.14) | 176 (253.12) | 127.80 (133.44) | 0 (62.45) | 0 (319.61) | 0 (608.45) | 0 (85.71) | 88.56 (258.29) | 0 (150.92) | 0 (105.92) |
| 6 or 7 times/week (n = 28), median (mean) | 1631.23 (3721.99) | 406.48 (485.29) | 45.65 (74.44) | 0 (52.53) | 61 (526.13) | 31.50 (889.61) | 99 (236.59) | 118 (303.18) | 0 (1136.99) | 0 (143.09) |
| Mann–Whitney p-value | 0.146 | 0.008 | 0.057 | 0.966 | 0.094 | 0.426 | 0.112 | 0.284 | 0.57 | 0.564 |
| Location | ||||||||||
| South England (London) (n = 32), median (mean) | 2038.53 (3641.99) | 317.53 (436.83) | 40 (80.58) | 0 (66.39) | 0 (596.35) | 98.50 (882.36) | 99 (207.24) | 118 (304.53) | 0 (1050.85) | 0 (149.23) |
| North England (n = 15), median (mean) | 921 (1553.32) | 146.50 (294.60) | 80 (136.07) | 0 (35.70) | 0 (114.73) | 0 (548.93) | 0 (108.10) | 88.56 (243.44) | 0 (71.73) | 0 (82.90) |
| Mann–Whitney p-value | 0.015 | 0.004 | 0.063 | 0.216 | 0.064 | 0.104 | 0.008 | 0.561 | 0.397 | 0.629 |
Backward stepwise regression modelling was used to explore the independent predictors of each category of costs. Characteristics describing participants were entered into the models and the least significant were removed one by one (if a p-value > 0.1). Sex (gender) was excluded from the analysis because of an underlying relationship with location (there were only five women in the sample, four of whom were in the south of England). Final models are shown in Table 32. The number of medications was an important predictor of several cost categories. Memory problems were a significant factor in predicting emergency and out-of-hours care, but not any other cost category. Over one-third (37.5%) of the total service use cost (which does not include the cost of prescribed medications) was explained by number of comorbidities and number of prescribed medications. Each extra prescribed medication that a participant reported added £309 to the 6-month service use costs; each additional comorbidity added £393.
| Cost category | Variable | Unstandardised coefficients | Standardised coefficients | Significance p-value | aAdjusted R2 | Durbin–Watsonb | ANOVA p-valuec |
|---|---|---|---|---|---|---|---|
| Total cost of all services | (Constant) | –1380.899 | 0.157 | 0.375 | 2.091 | < 0.0005 | |
| Number of comorbidities | 392.662 | 0.280 | 0.045 | ||||
| Number of different named medications | 308.521 | 0.443 | 0.002 | ||||
| Total cost of all GP services | (Constant) | 0.629 | 0.994 | 0.315 | 2.186 | < 0.0005 | |
| Number of different named medications | 28.631 | 0.399 | 0.003 | ||||
| Illegal drug use in previous 3 months (1 = yes) | 226.926 | 0.315 | 0.013 | ||||
| How often drink alcohol (1 = at least 6 or 7 times a week) | 178.589 | 0.261 | 0.042 | ||||
| Total cost of community psychiatric/mental health services | (Constant) | 0.680 | 0.974 | 0.273 | 1.780 | < 0.0005 | |
| Total number of head injuries | 39.819 | 0.538 | < 0.0005 | ||||
| Total cost of emergency and out-of-hours services | (Constant) | –209.792 | 0.031 | 0.297 | 1.995 | < 0.0005 | |
| Memory problems (1 = yes, including borderline) | 196.768 | 0.301 | 0.021 | ||||
| Illegal drug use in previous 3 months (1 = yes) | 265.673 | 0.394 | 0.003 | ||||
| Number of different named medications | 23.231 | 0.346 | 0.008 | ||||
| Total cost of hospital outpatient services | (Constant) | 29.831 | 0.743 | 0.181 | 1.737 | 0.002 | |
| Number of different named medications | 34.467 | 0.445 | 0.002 | ||||
| Total cost of hospital inpatient services | (Constant) | –937.603 | 0.117 | 0.185 | 2.486 | 0.002 | |
| Number of different named medications | 226.352 | 0.450 | 0.002 | ||||
| Total cost of all psychiatric services | (Constant) | –242.318 | 0.078 | 0.150 | 1.927 | 0.004 | |
| Number of comorbidities | 70.193 | 0.410 | 0.004 |
Hostel staff’s reports of residents’ unmet needs
During each interview, hostel staff were asked whether or not the resident they were being interviewed about had any unmet needs. Their responses were combined during the 6-month study period so that any unmet need during this time could be identified. Out of the 47 case study participants, 35 (74%) were considered to have one or more unmet needs. Table 33 shows the distribution by cognitive group.
| Hostel staff report | Cognitive group (formal assessment), n (%) | Total (n) | ||
|---|---|---|---|---|
| No memory problems | Borderline | Memory problems | ||
| Has unmet needs | 12 (70.6) | 5 (71.4) | 18 (78.3) | 35 |
| Does not have unmet needs | 5 (29.4) | 2 (28.6) | 5 (21.7) | 12 |
| Total (N) | 17 | 7 | 23 | 47 |
Table 33 shows that while almost four-fifths of those with memory problems had unmet needs from the perspective of hostel staff, there were also high levels of reported unmet need among residents with no memory problems. The types of unmet need were then categorised into six broad groups, relating to mental ill health or memory problems, physical health needs, alcohol problems, drug problems, social, welfare or housing needs, and personal care needs. These findings are shown in Table 34.
| Hostel staff reporta | Cognitive group (formal assessment) (n) | Total (n) | ||
|---|---|---|---|---|
| No memory problems | Borderline | Memory problems | ||
| Physical health | 1 | 0 | 2 | 3 |
| Mental health or memory problems | 6 | 3 | 8 | 17 |
| Alcohol use | 5 | 1 | 8 | 14 |
| Drug use | 2 | 1 | 2 | 5 |
| Social, welfare benefit, housing | 5 | 3 | 11 | 19 |
| Personal care | 0 | 0 | 5 | 5 |
| Total (N) | 19 | 8 | 36 | 63 |
Nineteen residents were reported by hostel staff to have unmet social, welfare benefit or housing needs. In many cases, staff felt that residents would benefit from more social activities, including befriending services, social support and opportunities to get out of the hostel periodically. There were various reports as follows:
He is isolated and needs a befriender. I’ve also tried to get him more involved in social activities to reduce isolation.
A befriender would be nice to come sit with him and talk to him.
With more support he could have used the swimming baths more.
Going to a day centre . . . would benefit him hugely to get out and meet other people.
He likes to venture out, supported day trips would be good.
Although the role of hostel staff included helping people to manage their finances, there were occasions when this remained an unmet need, particularly when the need was more complex, as in the following quotation:
He [needs] . . . support for budget of his finances – we are fighting to get appointeeship, but there are many hoops to go through.
Some hostel staff felt that residents needed more suitable accommodation, as shown in the following quotation:
[He needs] more suitable housing. Should be somewhere where staff have more time to prompt and try and stimulate his brain.
Seventeen residents were reported to have unmet mental health or memory needs, and 14 had unmet alcohol needs. These were often closely associated, as shown in the following examples:
He needs more dementia support. He needs more support to stay off the alcohol so he can get dementia support.
He needs help with his mental health, his Korsakoff and in being seen by the memory clinic. [Also had unmet alcohol needs.]
Counselling – going to approach it with him when he has less alcohol, he might be more open to it.
Hostel staff reported three main reasons why residents did not receive the help they needed (for some, there was more than one reason why they did not receive help). Lack of engagement was reported as a problem for just over half of hostel residents whose needs were not met (54.3%). Eleven (31.4%) were not receiving help as they were deemed not eligible to receive the support, although for some this was disputed by hostel staff. Ten residents (28.6%) were not receiving help as either the type of service they needed did not exist or the service was unavailable as it was not the type of service offered by the hostel they were staying in.
When this is considered by cognitive group, although lack of engagement was evident in both those with and those without memory problems, this suggests that factors other than cognition affected engagement. Hostel workers provided many examples illustrating non-engagement, as described in the following comments about individual residents:
He didn’t attend appointments with the counsellor.
No willingness to do anything. He’ll agree to things but won’t take them up.
He refused help for his drinking.
He refuses help [with his drinking and cannabis use].
He denies his hygiene is neglected. He does not engage with carers. He lets the carer clean his room, but nothing else.
He was referred to a dementia group, which he went to once and didn’t go to again.
He refuses to engage with mental health services and refused to fill in the form to claim PIP [Personal Independence Payment – welfare benefit].
Refuses help. There is nothing out there for him until he has sorted out his drinking.
He won’t engage or is too intoxicated to engage. He only engages when he needs something.
He doesn’t want to go to any social activities, he can’t be bothered.
The second reason residents did not receive the help hostel staff felt that they needed was because they were not deemed eligible by services external to the hostel. Ongoing alcohol and/or illicit drug use was one reason services would not accept referrals. Mental health services, in particular, were reported as not being able to work with some people because of their substance use, as shown in the following four examples:
[He] had drug and alcohol problems – [he was] not able to be referred to counselling as the drug and alcohol team felt it was due to alcohol and so he didn’t get the counselling.
He needs psychological input due to his entrenched lifestyle, crime, homelessness and drug use for a number of years but it is not offered to that kind of client group. Deal with drug use first, then mental health later.
The alcohol services say they cannot work with him due to his Korsakoff’s – he can’t retain information. He is just left. He’ll just go from hostel to hostel. He has been thrown from one service to another. He is lost in the system. Services don’t take him seriously . . . they are just waiting for him to get worse and only when he is very bad will they get him into a care home. I thought counselling would help but the GP said it wouldn’t as he needs to be able to remember what has been said in order for counselling to be of any help. There is nothing I can do until he addresses his alcohol issues. His memory is getting worse every day.
He needs a mental health or dementia assessment, but they won’t see him as [he is] drinking.
Some residents underwent assessment during the study period to assess their eligibility for local authority-funded social care packages of support with activities of daily living. In contrast to those who received support with personal care, the outcome of such assessments did not always lead to a care package being provided. One resident, for example, was referred to social services for help with cleaning his room and doing laundry, but on the day of assessment he presented himself as clean and tidy and was in a good mood. The consequence was the social worker said that he did not need help. In North England, two residents underwent an assessment period of several weeks to determine their eligibility for domiciliary social care at the hostel. At the end of the study period, hostel staff reported that the care package had been withdrawn because hostel staff were not on site 24 hours per day and the hostel was not considered safe for care workers to visit residents when staff were not on site. Other unmet needs relating to eligibility included residents who were reported to be ineligible for sheltered housing or care home accommodation because they were too young.
The final reason residents were not able to have their needs met was the lack of particular services, or the inability of the hostel they were staying in to provide specific support. In Central London, for example, staff felt that the care needs of one resident were becoming too high to manage. Elsewhere in London, another person’s specific cultural needs (for worship) could not be met as there were no nearby services he could access.
Limitations of the hostel staff role and the amount of time they could spend with individual residents also had an impact on their ability to provide help. One resident was believed to be potentially able to benefit from access to a day centre; however, staff were unable to accompany him to and from the centre. Similarly, another worker felt that although it would be positive for the resident they supported to go out, their part-time hours limited what they could do. Other barriers to receipt of help included that some alcohol services delivered their support through group work only rather than through the one-to-one support preferred by residents.
This section has shown that there were unmet needs across all cognitive groups. Although hostel staff and other workers provided significant support to residents, the limitations of hostel workers’ roles and the criteria for service access by external agencies, alongside the reluctance of some residents to engage in addressing their needs, all contributed to challenges in ensuring that hostel residents were able to access the help they needed.
Challenges along the health and social care pathway
Two main challenges were identified along the health and social care pathway: (1) identifying memory problems and getting a diagnosis and (2) challenges in making referrals to health and social care services.
Challenges in identifying memory problems and getting a diagnosis
As presented in Chapter 5, there were discrepancies between the reports of residents about their memory problems and hostel staff’s perception of these. Some residents were aware of their memory problems; for example, participant 110 described their problems thus: ‘I put it down to my head getting old’. Participant 122 acknowledged:
Some days I wake up and I don’t know what day it is when I’ve been on a binge. So I have to go and buy a newspaper to find out what day it is. It’s when I’ve had too much booze.
Qualitative responses may shed some light on these discrepancies. Residents described a number of everyday tasks for which they received help from hostel staff, including budgeting, arranging appointments, prompting, and assisting with hygiene and self-care tasks. Some of this assistance may have supported hostel residents who, if living independently, would have otherwise struggled to cope.
‘Prompting’ was often cited by many hostel staff as the support they provided to some residents who were able to complete daily tasks fairly independently, but might forget to do them. In the case of participant 207 (borderline), for example, hostel staff maintained his daily diary of appointments, details of his medication regime and ‘things coming up’ that needed attending to. His key worker, SW14, said about participant 207 that ‘he couldn’t live on his own; he would forget to eat, or run out of clean clothes, etcetera. He would forget what day it is’, indicating the extent of participant 207’s problems with activities of daily living.
Participant 207 was himself aware of the help he was getting in supporting what may have otherwise manifested as memory problems:
If I was not living here [in hostel], it [his memory problems] would be serious; but I am living here so it’s not that serious as I’ve got help.
He referred to the hostel as ‘my home’, was very satisfied with the support he received from hostel staff, and described this support as just ‘assistance’ and not ‘care’.
Some staff felt that it was not always evident why residents needed prompting. In the case of participant 109 (borderline memory problems), his key worker, SW06, thought that he had early memory problems, which, combined with alcohol, resulted in his needing a great deal of prompting. SW06 described his view of participant 109:
Yes [he has] memory difficulties. A little. Because he’s drinking alcohol. Forgets laundry loads – hard to know why. We prompt him to do things because of hygiene and his drinking, not memory problems.
Difficulties in keeping appointments
In cases in which older homeless residents had moderated their alcohol drinking and hostel staff had managed to get an appointment for an older homeless resident who was willing to engage with services, another challenge arose in that the residents sometimes found it difficult to keep their appointments. The level of support hostel staff were able to offer residents with appointments varied between hostels as previously mentioned (see Table 23); some staff were able to remind and prompt residents about appointments and others were able to accompany a resident to an appointment to ensure that they arrived, while in other hostels residents were assumed to be able to manage their appointments independently. In one hostel, peer workers from a local charity volunteered to take residents to hospital appointments. There were several reports that residents struggled with follow-up appointments and, even after appointments had been made, some changed their minds about attending.
At times, hostel staff could make the case or advocate for residents who found it difficult to make appointments, and rearrange their missed appointments or accompany them to a fresh appointment. This could be possible after negotiations with some agencies, such as the NHS or local authority. However, two residents described the serious consequences of missing appointments or failing to arrive punctually at social security offices (Department of Work and Pensions or Jobcentres), which had affected their incomes.
However, it often was hard for staff to rearrange missed appointments, especially if this happened on a regular basis. Indeed, if residents had other health conditions in addition to the presenting problem, it made it doubly hard to find the time to reschedule another appointment. Hostels in the study had varying relationships with local primary care practices. In some hostels, staff were able to discuss residents frequently with GPs for support. While appointments with primary care professionals were usually local, or, in the case of two hostels, doctors and nurses routinely ran clinics in the hostels, only some hostels had staff or volunteers able to accompany residents to hospital appointments. This would often take several hours and staff did not always feel that it was possible for them to be spared from the hostel.
Comorbidity and alcohol problems
A significant theme discussed by hostel staff was the inability to tell whether a resident’s memory problems were attributable to their drinking alcohol or to growing problems with cognition or memory. Such uncertainties were illustrated in the case of participant 101 (borderline), whose key worker, SW05, was asked whether or not the participant had memory problems, and responded:
I don’t know. He often forgets what he needs to do, but that could be due to alcohol. He would often ask what we had spoken about. He knew when meal times were. He would sometimes ask about when he had an appointment.
The amount of support hostel staff provided to some residents may have also masked the level of memory problems among some residents.
Variability in presentation
Another challenge encountered by hostel staff when referring a resident to the NHS in respect of memory problems or confusion was the variability in how these presented themselves. A new health problem could manifest itself quite suddenly among some. In one instance reported, a resident keen to seek medical attention for a health condition was happy for staff to call an ambulance, but changed their mind about leaving the hostel once the ambulance arrived. In relation to memory problems, staff member SW04 felt that they had encountered several difficulties with getting an assessment appointment for participant 104 (memory problems), whom he suspected had memory problems:
I think he has memory problems – I’d have a conversation with him and he couldn’t remember what I’d said 5 minutes later. Yet he let the GP do a memory test on him and the GP said he was OK.
This had not reassured the staff member, who continued to be concerned about the resident:
But he does appear to have memory problems but then he remembers something – I can’t put two and two together. I wonder if it’s linked to his drinking and falling?
One resident [105 (memory problems)], who, in the view of the hostel staff, required a great deal of support from them, was in an atypically positive mood when interviewed in this research study at baseline. He stated that during a recent visit from the social worker to review his case, he had inflated his abilities to manage independently, and declined the care package offered. Responsibility for continuing to look after this resident therefore continued to fall on hostel staff. The researcher noted in her visit to the hostel:
Staff were managing most everyday tasks for 105, either by doing them themselves or by needing to prompt him. 105 had been told he had borderline Korsakoff and (staff member) SW09 was struggling to get another appointment to see if it had progressed, as he suspected. SW09 had contacted social services as 105 needed a care worker to help with budgeting and benefits, cleaning his room, doing his laundry and assisting with bathing. 105, in his interview, said he did all of these tasks independently. The staff member reported ‘(105) Was referred to social services but he was in a good mood the day the social worker came to do an assessment. He was clean and tidy. The social worker said he did not need it’.
Researcher field notes
Completing a full memory assessment and giving a diagnosis could present challenges for several parties, as SW08 said about participant 108 (memory problems):
He disappeared for one night in April and when he came back to the hostel he couldn’t remember where he’d been. I went with him to the GP for a memory test but he covered up – said he could remember and we shouldn’t worry.
The staff member added:
[The health team] tried to assess (when 108 first came to hostel) but 108 was rude and stopped the interview. They [managed to diagnose him] with dementia but could not do a proper assessment as he would not engage.
Lack of flexible dementia support and treatment
Alongside the difficulty of assessing a resident with problems such as memory loss or decreasing ability to function independently was the added problem of accepting and taking prescribed medication for some, and resident acceptance of other therapeutic options. Participant 123 had apparently received a diagnosis of alcohol-related dementia but refused to engage with services for any further help. SW24 said about this participant:
[He] Refuses help. Refuses to go to memory clinic and refuses to take thiamine [vitamin B1].
Abstaining from alcohol in order to be prescribed medication added another layer of complexity to the challenges encountered in providing care and treatment for older hostel residents. This was illustrated in one case in which the resident’s dementia had been acknowledged several years previously, as noted by the researcher:
SW23 said about participant 111 (memory problems): ‘[He was] diagnosed with dementia many years ago. They won’t prescribe medication to him till he has abstained from alcohol for at least six months.’ Adding ‘He managed to abstain for a good long time once, but gave up just before the six months were up, so he’s on no medication at all now’.
Researcher field notes
Hostel staff also highlighted the lack of dementia-specific therapeutic options and the lack of reviews of residents with dementia. In respect of the case of participant 111 mentioned above, who was atypical in having had his dementia diagnosed some years previously, there was general concern about whether or not suitable support could be provided to people in his position:
He [participant 111] needs more dementia support . . . He was referred to a dementia group, which he went to once and didn’t go to again. I feel like that should be offered to him again . . . He refused it the first time, but I wish more was being done to review his condition and to see how his memory is doing. Because it’s getting worse, but nothing is being done about it.
Staff member SW23
Challenges in making referrals to health and social care services
Many challenges were described by staff in several of the hostels concerning local referral systems to health and social care services for hostel residents whom staff felt needed more support. These ranged from the requirement to not be drinking at the time of assessments, how the personalised approach adopted by hostel support staff did not seem possible to replicate in formal services, the refusal of older residents to engage with services and services’ refusals to engage with residents.
Requirement to not be drinking at the time of assessments
Just over half of all case study participants with memory problems drank alcohol. Patterns of drinking, the amount of alcohol, and the strength of alcohol consumed varied among them. All of the hostels included in the study allowed residents to drink alcohol in communal areas. Some hostels also allowed residents to drink in their own rooms. Most hostel staff described their residents’ drinking habits as a significant impediment to receiving support from the NHS and local authority adult services. Staff described some residents as often falling into dangerous cycles of addiction, spending their daily or weekly allowance on alcohol as soon as they received money, and then having no resources or needing to beg for alcohol by the end of the week. Local GP services were reluctant to refer people to memory clinics, as memory clinics require those attending to be dry (i.e. to not drinking alcohol) for 3 months before presenting for any assessments related to their increasing or apparent problems with cognitive functioning. Hostel staff often said that this was difficult or impossible for some residents to achieve.
Several hostel residents appeared not to wish to reduce the amount of alcohol they were consuming. During interviews, although some residents talked of wanting to reduce or give up alcohol, their key worker sometimes reported the opposite perspective. One interviewer noted in her field notes:
Interview with SW30 about their participant 202 (memory problems): ‘[Hostel alcohol worker] talks to 202 about other agencies that help regarding alcohol; 202 agrees just to shut [the worker] up and then afterwards says he has no problem with alcohol’.
Similarly, hostel staff reported several residents being referred to detoxification services and agreeing to accept help to cut back on drinking, but then refusing to go when the time of the appointment came round:
When staff member SW21 signed up participant 112 (borderline) to a drug and alcohol service he recalled that: ‘[121] agreed and signed the paperwork, but then he refused to go. After three Did-Not-Attends, they took him off their books. He said he liked drinking. He didn’t think it affected him and had no intention to change’.
Similarly, staff member SW04 said about participant 104 (memory problems):
The first year here (I) was doing some good work with [104]. I got [him] a detox in place [treatment for detoxification], got the money for it, he initially agreed, but then refused when a place became available. He’s too attached to this place; he wants to live here forever.
Even if a resident had willingly signed up to and then attended one therapy or detoxification session, it did not always mean that they were willing to go through with the recommendations of giving up and abstaining from alcohol. Staff member SW34 said about participant 133:
She attends the weekly support group [for alcohol] but doesn’t really want to stop drinking. So it feels like she comes more for the socialising.
Inflexibility of services
It was evident from interviews that almost all hostel staff endeavoured to support their residents through as personal an approach as possible and that personalising support was a dominant motive in describing their interventions and the purpose of the service. For instance, staff member SW30 said of participant 202 (memory problems) that he did not ‘do official’, and that he had to be approached in a friendly, non-threatening manner. His key worker, SW30, chose to phrase things in a jocular way to engage him. Similarly, staff member SW09 said about participant 101 that he was simply unable to attend appointments ‘first thing’ in the morning. Health services, he acknowledged, were not traditionally ready to engage with patients in such roundabout ways or have sufficient flexibility of timing. Seeing patients at a predesignated appointment was described as generally the way in which residents were responded to, and it was evident that many hostel staff felt that many older homeless residents were likely to be dismissed by local health services if they failed to attend.
Some residents described the format of the therapy or other support sessions on offer as one that did not appeal to them. For instance, most of the alcohol support services appeared to offer group sessions, which participant 210 (no memory problems) said he did not like. No other services, such as one-on-one sessions, were available in the locality, as noted by staff member SW03, who commented in relation to participant 210:
He doesn’t want to do group work and that’s what you have to do at alcohol support.
Practitioners working in the local NHS secondary mental health services were also encouraging participant 210 to enrol for ‘detox’, but unsuccessfully. It was not clear if this reluctance was related to participant 210’s increasing memory problems or if there was another reason behind his wish to avoid group sessions.
Reluctance of services to engage with homeless clients
Several staff talked about the difficulties they experienced in getting local authority adult services and staff from other agencies to engage with the hostel and its residents. Staff member SW32 reported contacting adult services about resettlement for participant 132 (borderline) and estimated that he had made 10–15 telephone calls to various officers, followed by additional repeat calls, and had been speaking to five or six different people about this resident. The manager of another hostel felt that the reluctance of services to address the needs of homeless people living in hostels was perhaps because residents were not perceived as requiring urgent care or because they were not seen as particularly vulnerable because they were being looked after in the hostel.
In some cases, when local authority adult services had been called and an assessment appointment had been made for a resident, a care package did not always follow as the resident did not meet the eligibility criterion of having sufficiently high unmet needs for care and support. In other cases, as with participant 108, a local authority-funded care package had been put in place but the resident kept refusing access to the care workers when they visited. Eventually the service was withdrawn, leaving hostel staff with the responsibility of supporting the resident. Key worker SW08 said:
I send e-mails to the social worker but she never replies; he has had three social workers, it’s been a nightmare. It makes the process slow as we have to start all the way from the beginning again. I put 108 through the social services panel (to agree to fund the care package) and they agreed to the home care . . . he’s (over 80) years old. Now agreed he cannot live independently. He was supposed to be in this hostel for just 10 days but social services just left him here.
Similarly, staff member SW05 made several efforts to get an assessment for participant 107 (memory problems), who needed increasing help with his personal care:
It was hard to get the personal care worker set up. It took 4–5 months to sort it out as I had to make a strong case. I got fed up. The social services’ older persons unit didn’t want to do anything. I had to provide lots of evidence about his needs. We had got to the stage where he didn’t do anything.
There was very little mention of regular communication with local adult services’ departments, more a sense of individual residents being referred to them for assessment, which resulted sometimes in a care plan and services and sometimes in an assessment that concluded that the person did not have eligible care needs. Residents’ needs for information and advice about care appeared to be met by hostel staff. As with participant 107, hostel staff felt that it was their responsibility to pass on information to adult services and other bodies; at one level this seemed to be because they held valuable information and were a credible source, and in other cases it seemed to be because the resident was not able to convey the details of their own circumstances accurately for reasons that included their confusion, memory loss and sometimes misuse of substances such as alcohol.
Reluctance of residents to engage with services
A further challenge encountered by hostel staff in referring older homeless residents with suspected memory problems for assessment or support was the reluctance of residents to engage with health and other services. Reasons reported ranged from apathy and a lack of motivation to seek help to an active distrust of services and professionals.
A general sense of apathy and distrust of formal services was apparent in interviews with several older hostel residents. Some older homeless residents described ‘hating’ the hostel, resenting hostel staff and generally having no trust in authority or professionals working in health and care services. In some instances, such feelings were more muted and were evident only when the reluctance to go to services was revealed. For example, staff member SW42 felt that participant 123 (no memory problems) made ‘empty promises’ that he did not keep and would lie about attending appointments that he had deliberately missed. Similarly, staff member SW21 said that participant 112 (borderline) would say ‘all right’ to suggestions but then consistently find excuses to not follow them through.
In some cases, when hostel staff had tried to encourage a resident to engage with health and social care services to get more appropriate support, they reported that the resident had not been interested and had disregarded their encouragement. Some hostel staff felt that they understood why residents were behaving this way and were willing to work around this lack of engagement and distrust. Many staff considered that some residents’ drinking patterns were often reflective of a troubled past and a long-standing chaotic lifestyle. In respect of participant 201 (discussed previously), his key worker noted that this resident suffered from low self-esteem and had problems with anger management; as a result, in the key worker’s view, he refused to cut down on drink or engage with services. Staff in this hostel worked hard to reinforce the messages to him about the risks of his alcohol use and described their general approach as being to ‘keep chipping away regarding alcohol use, try to get him to engage with services, worry for his future’. By 6 months, staff member SW11 said that the staff had:
put in place a daily alcohol diary as he won’t engage with professional alcohol services, we review diary monthly and will encourage him to accept professional treatment.
Some residents were openly reluctant to try cutting down their alcohol use, citing their experiences with different abstaining services over the years and how none had worked for them. Participant 137 (no memory problems) acknowledged:
There is an alcohol counsellor here but I don’t go – I’ve done all that before and it didn’t work. Been to a hundred AA [Alcoholics Anonymous] meetings and it didn’t help.
Similarly, participant 113 (no memory problems) said that he ‘didn’t go back to drug and alcohol programme as I didn’t like the other people in the group’. He revealed, ‘I don’t trust the GP, they are not very helpful’, adding:
Doctor told me to sort out some anger management issues I had, but I told them I don’t need it – only when I’m drunk.
Anger and challenging behaviour were described by staff in relation to several hostel residents and some of these residents also acknowledged that they could become angry in situations they found threatening. For example, participant 101 (borderline) routinely refused to engage with health services to help him reduce his alcohol use, yet he blamed all his outbursts and challenging behaviour on drink and his irritable bowel syndrome. Staff member SW09 described being supportive of participant 101’s irritable bowel syndrome, but said of his behaviour:
I wanted him to engage with a counsellor. He’d say yes and then didn’t engage. X was a really good worker and was very firm with clients. But they closed 101’s case. He’d put it down to anxiety. We are not paid to be abused.
Case study
It is challenging to identify trends in service pathways when each participant’s ‘patient journey’ has been complex, with many repeat referrals and rescheduled appointments, and no trajectory has been straightforward. We therefore adopted a case study methodology for the next part of this chapter to provide an illustrative example of service pathway or patient journey through care encountered by this group of participants. Case studies are not generalisable, but are typical and representative of the experiences of other participants in some form or another. This case study was presented to and discussed by the study advisory group, and their views and feedback are also presented.
Case study of ‘John’ (name anonymised)
Background
John was in his early sixties and had lived in the hostel for 18 months when he was first interviewed. His first homelessness experience had been in his early thirties and he had spent at least 12 of these years sleeping rough. He had no contact with his family. He was interviewed twice by the research team and his key worker was also interviewed twice. We also obtained information about John’s health and social care needs from hostel records and medical records. For the purposes of the study, an ACE-III memory test had been completed with John by the research psychiatrist.
Perception of memory problems
John reported that he did not have any concerns about his memory. However, while the memory test was being conducted, he said that he had some issues with short- and long-term memory. Staff reports were, however, different. The key worker reported that John knew that he was experiencing memory problems and had started to leave himself reminder notes. He had problems remembering recent events and would forget to take his medication if staff did not give it to him. He also forgot his resolve to drink lower-strength alcohol and that he had given up drinking fortified wine. He would worry about, and repeatedly ask about, appointments, as he struggled to retain information. His key worker felt that his problems had become worse over the 6 months.
Memory assessment by research team
On the 6-CIT, John scored 15 out of 28 points. On the ACE-III, he scored 48 out of 100 points, with the following subscores:
-
attention, 10 out of 18 points
-
memory, 14 out of 26 points
-
fluency, 1 out of 14 points
-
language, 17 out of 26 points
-
visuospatial, 6 out of 16 points.
He was allocated to the ‘memory problems’ group.
Memory support
John reported not seeing anyone about his memory; however, staff felt that his symptoms reflected an early stage of Korsakoff syndrome. However, his medical records noted that John had ‘dementia in Alzheimer’s disease, atypical or mixed type (mixed type = vascular and alcohol related)’, corroborated by a head scan.
Support from hostel staff
John was provided a range of support from hostel staff, including prompting to get meals, and budgeting (they held his money and had an agreement that he would get £10 per day); a member of staff checked on him twice per shift (three shifts per day); ordered, collected and gave him his medication; reminded him about his appointments and gave him a notebook to write things down; and bought him clothing when needed. Care workers from the local authority also supported John by helping with personal hygiene twice per day, changing incontinence pads, laundry, cleaning his room and changing bed clothes when needed; they visited for 14 hours per week.
Health and social care use over 6 months
Table 35 details some of the health and social care services John used during the study period (excluding home care). This includes the number of times a specific service was used during the 6-month period.
| Service | Number of times used during 6-month period |
|---|---|
| GP: home visit | 2 |
| GP: telephone call with worker | 8 |
| GP: seen at general practice | 2 (includes 1 DNA) |
| Nurse: seen at general practice | 1 |
| District nurse visit at hostel | 4 |
| Out-of-hours GP visit to hostel | 2 |
| NHS 111 service | 1 |
| Ambulance service | 3 |
| Chiropody | 3 |
| Outpatient investigations (with hostel worker) | 3 |
| Outpatient appointments (with hostel worker) | 4 |
| Other | 3 (TB screening; social worker; memory service) |
Challenges in providing/obtaining support as reported by hostel staff
Over time, John’s physical health problems deteriorated and his memory and mobility worsened. John’s support needs were proving too high for the hostel and during the 6 months of the study hostel staff tried to find a suitable care home for him. John visited several housing schemes where he could still drink alcohol but turned them all down. The local funding panel of adult services decided that his needs were being met and that he could stay in the hostel. He continued to refuse help even when very unwell. After the study period ended, we learned that he had been admitted to hospital for several months and then moved to a care home, but only after the hostel refused to have him back.
Feedback from study advisory group members (anonymised to preserve confidentiality)
Member 1 expressed surprise at how much service input John had received. He that said it was atypical of what a lot of other hostels and services would provide, and he was impressed by how hard the hostel had worked towards getting the right kind of care for John. Member 2 agreed with this view and also speculated that, were John living in his own home, placement in a care home would have taken place a lot sooner, as a Best Interests Assessment would have taken place and a placement would have been deemed necessary. Member 2 also said that mental health services had not been involved in John’s care at all, atypical for any client who lived in the community.
Member 3 also said how she could see that funding would have been an issue, as those living in their own homes as owner-occupiers had greater access to money, making it easier for them to access and receive services. Member 4 concurred and said that adaptations to the home would perhaps have been the first starting point, which is unlikely to happen in a hostel.
Member 5 remarked on how individual decision-making had meant that John was able to make unwise decisions, such as refusing to move to a care home even if it was better for him to do so.
Both the advisory group chairperson and member 3 discussed the level of staff involvement and that there appeared to be far greater tolerance of challenging or distressing behaviour by hostel staff than by care home staff. Discussion ensued regarding whether or not this was because the hostel was a large provider, which meant that staff were available to accompany residents to hospital appointments and care home visits (as in the case of John). Member 1 considered this to be atypical, as a specific charity at this hostel had been set up for this very reason, namely to take hostel residents to necessary appointments.
Member 2 remarked that it would be interesting to find out how John was doing in the care home. Was he using fewer services, as care homes generally provide some services anyway (e.g. chiropody)? Had his health and cognition stabilised? The researchers said that it was not possible to follow up this individual in this study, but that it might be a good idea for future studies to compare hostel service use and outcomes with care home service use and outcomes.
The advisory group discussed how John’s outcomes might have been different had he received different services. If John had been referred by a GP, member 2 thought that he would have been given less time at a memory clinic. At a memory clinic assessment, he would have been given 5 minutes of ‘cajoling’ to participate in the assessment and then the clinician would have left to see the next patient. The research clinician, on the other hand, was thought to have made more effort and spent more time in carrying out an assessment with him. Member 5 remarked that this was worrying, as some residents may be more reticent to engage with, and maybe be in even greater need of, services.
This case example also highlighted how different services had to work effectively together to provide care for John. Member 1 wondered whether or not ‘bad’ care in hostels where services were not so good would have been highlighted in our study. The research team reassured him that ‘bad’ care would have been reported and that there was no evidence of negligence or very poor services in the fieldwork, something the research team would have reported and dealt with immediately.
Member 2 thought that it was common, as in John’s case, for someone to be dropped off at A&E and for hospital services to be forced to take over their care and find a placement for them. Thus, whereas care home managers might have refused to take a client who drinks, a hospital might have been able to have arranged for his detoxification and then been able to place him in a care home.
Lack of appropriate housing options
Chapter 4 describes how long residents were able to stay in each of the hostels in the study. In several cases, hostel staff described the problems they encountered in terms of finding somewhere appropriate for residents to move to following their hostel stay. For residents who were alcohol dependent, staff thought that care homes were unsuitable, even if funding for a care home place had been agreed by the local authority and if the care home had agreed to accept the person. Similarly, other long-term care settings, such as sheltered housing or extra care, were not generally an option, as staff predicted that many residents were unlikely to cope independently because of their alcohol dependence, learning difficulties and/or behaviour or lifestyle. In some cases, the problems of agreeing funding and then finding a placement for a resident limited the range of options that were deemed feasible.
The example of participant 203 (memory problems) illustrates the lack of housing and care options for older people with a history of homelessness combined with deteriorating health and increasing memory problems. Participant 203 also had learning disabilities, and, although at the time of data collection he was managing daily self-care tasks independently, he had never lived on his own or managed a budget. Left to live in a flat on his own, staff were certain that he would not cope. Sheltered housing was seen to provide too little support, and a care home would have provided too much in terms of restricting the lifestyle he chose; therefore, there seemed to be nowhere for him to go.
In respect of one of the few female residents who participated in this study, participant 133 (memory problems), SW34 said:
Ideally, we would like some sheltered accommodation for her. The biggest barrier to that will be her drinking, and that she can’t manage money or shopping or cooking on her own. So the options of where she can move on to are limited. She wants to move, she’s ‘maxed out’ on the 2 years she should be living here, but we’re being realistic about what is and isn’t possible. We talk about her moving on a lot – but we’re trying to make smaller steps towards independence, as finding suitable accommodation for her is going to be tricky.
This cautious approach from hostel staff indicated how such discussions were sometimes ‘in-house’ and did not involve NHS or other public bodies. As with other residents who were ‘overstaying’ their allotted time in a hostel, there were particular concerns that alcohol use and misuse significantly reduced their likelihood of finding other forms of accommodation.
Some staff and residents described very specific needs that affected the type of accommodation required if a move from the hostel was being considered; for example, participant 201 (borderline) described himself as having very specific needs, as he had a history of seizures:
A warden-aided flat near my current hostel so I can pop back in and see friends and staff. It’ll need to be warden-aided.
Staff member SW14 described the very specific needs of participant 207 (borderline) as being for ‘specialist supported housing – with cognitive therapy, 24-hour staff support, more hands-on support, such as being taken out shopping when needed’ – but explained that ‘he’s too well for nursing care and independent living is not suitable’. This view of a care home with nursing as being for people with physical health needs and other complex needs for care and support was not always voiced in relation to how these care homes often catered for older and frailer people. However, it was frequently mentioned that the age bracket of care home residents did not always fit with older homeless people.
For example, staff member SW28 felt quite strongly that accommodating young and older residents together in the same hostel was not a good idea because there were ‘different attitudes, falling out, older people were brought up to show respect and don’t get it back’. He added that the older residents were ‘open to financial abuse [in these environments]’.
Another staff member, SW13, also felt that residents such as participant 209 (no memory problems) were at risk of exploitation and that this person needed to be in ‘his own flat, maybe sheltered with older people, not younger people as they could take advantage of him’. The language of adult safeguarding services was not generally used by hostel staff, but they were aware of the vulnerability of some older residents to exploitation from some younger residents or others in their social circles.
Life skills and independence
Some residents with borderline memory problems were supported by hostel staff and managed to live mostly independently, with many of their everyday needs for care and support met in a relatively informal way. However, once individuals left the hostel and moved to more independent living situations or sheltered accommodation, this low-level but continuous support was not always available. In the case of participant 129 (memory problems), for example, staff member SW39 observed that in the hostel:
Here he’s [participant 129] fine and managing OK – but for moving-on purposes, he will need a carer [care worker], who sees him at least once a day for medication and self-care.
The hostel worker thought that this would be an unlikely development.
Similarly, staff member SW04 said about participant 104 (memory problems):
He’s been here [in the hostel] over the allotted time. I’d like to see him in a care home where he gets the support he needs. I need help from social services with this. He’s been allowed to stay on here because the manager wants him to have a positive move on. The level of support he needs will take money and that’s the problem. If he was put in a flat he wouldn’t last – he has no life skills. It’s difficult to prove his case – I’ve sent in medical assessments to X housing options but they say he doesn’t fit the criteria.
In this case, the hostel was able to continue to support participant 104 but this appeared to rely on the goodwill of the manager and of the hostel’s ability to be able to secure funding for participant 104 even though he did not meet the criteria set out in the hostel’s funding contract. This was not the only example of hostels ‘holding’ residents who they thought would deteriorate substantially if they moved on to locations that proved unable to support them.
Residents being reluctant to move
Staff in several hostels reported finding it difficult to engage residents and to encourage them to move from their present location. Several explanations were provided for such reluctance. For example, participant 108 (memory problems) could not find housing that was acceptable to him or suitable for his needs. Staff member SW08 said that this was not for want of effort; indeed, he had accompanied participant 108 to at least five locations to view potential new accommodation. However, each was rejected with the following reasons:
One place was in [the area] but was too far away; another was nice but the waiting list was too long; another was [name of house] but he didn’t like it. Also another in [name of area] but it was too independent. Also [name of house]. Nothing has worked out.
Although some of these reasons could be linked to the participant’s possible fear of not managing in more independent living and of being some distance away from his support or social networks, they were not as firmly linked to declining functional ability as in the case of participant 106. Here, hostel staff described their great and continuing difficulties in finding appropriate housing for him to move on to. Box 1 summarises what happened to participant 106 (memory problems).
Throughout 2015, participant 106 was shown round other hostels with a SW (who was not from the hostel he was staying in), but he declined to consider these alternatives, saying:
They have sent me to see a lot of hostels not suitable for me. One said you can drink three cans [of beer] a day – it’s not much. One place didn’t have a lift. One was in [X area], another in [street name far away]. I’ve seen most and refused them. I had my reasons for each one.
The specific difficulties for staff seeking to move 106 were his needs for nursing care, which hostel staff were finding increasingly difficult to provide. The hostel staff said that their referral of participant 106 to local authority adult services had not worked, and one voiced some anger at this rejection:
He needed more care. I referred him to the review panel for a place in a registered care home and they turned him down. We were concerned about him not being able to leave the building quickly enough if there was a fire . . . But the panel thought he was OK to stay here. They said we should put a fire extinguisher in his room – but that was not the point.
Eventually, participant 106 was admitted to hospital, which resulted in his condition deteriorating further. His SW described the difficulties of not being adequately supported by NHS staff:
When he went into hospital, we had to decline him coming back here. We suggested he went instead to the hospital discharge unit that was downstairs at the time. His needs were too high for the hospital discharge place. I had one or two calls from the hospital saying they were ready to discharge him. He was in hospital for 3–4 months. We weren’t trying to get rid of him. We were ready to argue it out and the hospital was told to sort it out.
Chapter summary
This chapter has provided the opportunity to consider individual residents in the context of the data previously presented. As might have been expected, the variety of hostels means that there is unlikely to be a ‘typical older hostel resident’. Common among many of the accounts reported above, and others that are similar but not illustrated, was the lack of suitable housing with care options for this vulnerable group. Access to other services in the community could be complicated or limited by thresholds or rules that meant that these older people were not deemed suitable for or potentially responsive to support. The situation of social care staff coming to hostels to provide care and support has not generally been conveyed in the UK literature on social care or on homelessness.
Chapter 8 Discussion
In this chapter, we discuss the study’s main findings. We note the limitations and strengths of this study. We have referred to the multiple sources of evidence – from residents, from staff and from medical records – as providing the ‘best evidence’ available. Such evidence will provide a baseline for other studies and service development. Although the focus of this study is on England, in many developed countries the single homeless population is ageing and increasing numbers of older people are homeless. Just under half (23/47; 49%) of those in our sample for whom substantial data were collected had ‘memory problems’ and a further 15% (7/47) were considered ‘borderline’. Their cognitive status had not generally been collected previously.
Homelessness is described as a ‘silent killer’, the average age of death among UK homeless people being 47 years. 54,107 Therefore, many do not live long enough for memory problems to emerge or be identified. This present study took place at a time when homelessness and rough sleeping were of great and increasing policy concern in the UK. Owing to a multitude of reasons, in 2015/16 local authorities in England responded to the threat of, or to actual, homelessness among 327,390 households (254,320 households in 2009/10). The situation of single homeless people, particularly older people, is caught up in these wider trends, and in the gaps between housing need and affordable housing supply. 27 Although none of this present study’s participants was currently rough sleeping, several had done so during earlier episodes of homelessness (see Chapter 4). Today’s rough sleepers may be future hostel residents; others will not survive. 108 Homelessness among older people is increasing internationally,109 offering new challenges to health and social care services that have traditionally focused on community-dwelling (i.e. housed) older people and now need to address the shifting age profile of homeless people.
The Homelessness Reduction Act 2017110 has placed further responsibilities on local authorities to help prevent homelessness (its main provisions amend Part VII of the Housing Act 1996111). They are mandated to take reasonable steps to help secure accommodation for any eligible person who is homeless. The impact of this Act on hostel residents’ health and well-being will need to be ascertained.
Internationally, the subject of homelessness and ageing is being argued as representing a challenge to services,73 and specific attention to homelessness and dementia has been evident in Australia, building on the Chenco review64 and informed by consultations with front-line homelessness services and advocacy organisations. The discussion paper from Wintringham offered a variety of reasons why homeless people fail to access dementia assessment pathways. 112 Similar to our findings, this organisation pointed out that homelessness services staff often have to act on clients’ behalf yet they are not being supported in this work by wider health agencies.
The next section draws on our study’s findings that should be set in this context of dementia pathways, both the explorations of a person’s memory problems and the pathways or their access to appropriate care, accommodation and services.
Physical health problems
Although the focus of our study was on memory problems, the extent of physical health problems among the hostel residents participating in this study was substantial, and this is likely to have been under-reported. A recent US study of older people (aged ≥ 50 years) who were homeless summarised their findings as that the homeless group experienced health and disability problems that were generally experienced by people who were 20 years their senior. 73 The sample group in our study had at least one long-term condition. Participating hostels were not generally well equipped to support people whose health was in decline and whose disabilities were likely to worsen and accelerate if not well controlled. Some hostels were more accessible (in terms of physical facilities and adaptations) than others but overall they faced challenges in accommodating residents with increasing needs for care and long-term health problems. Our data on the physical conditions of hostels add considerably to the picture of what is available to residents and the wide variety of living conditions. Overall, the implications of this for our study research question about ‘pathways’ are that memory problems may be one among many health-related problems facing older hostel residents and that pathways are not necessarily helpful if they are disease specific.
Sight and hearing problems may mask early or mild symptoms of memory problems, and they were commonly reported. This has implications for the provision of information, for the keeping of appointments and for the mode of assessments, and, of course, for the physical fabric of hostels and their accessibility. Hostels without or with very limited key worker systems appeared to find it especially difficult to respond to residents with multiple problems covering physical and mental health, and their contacts with local health and care services appeared to be more tenuous. Furthermore, hostels without key workers were not generally equipped with good records of residents’ physical health problems. The presence of key workers should not be presumed by other professionals external to a hostel.
Head injuries
Our findings of the level and extent of head injury among older hostel residents in this study have implications for any assessments of cognition as well as longer term effects of such injuries. It is likely that among this group not all head injuries had been reported to NHS professionals or were on patient records. Among hostel staff, their knowledge of residents’ head injuries was partial; thus, their role as possible informants in assessments or monitoring would be limited, although better than no-one.
Mental health problems
Chapter 6 reported that nearly three-quarters of case study participants had a history of mental health problems and three-quarters had current mental health problems, particularly depression. Here, our study design of combining data from hostel residents and from staff interviews, hostel and medical records was particularly helpful. For example, the staff reports and hostel/medical records showed much higher percentages (81% from medical records vs. 63% self-reports) of a history of mental health problems than were found in self-reports. Using a depression tool, as described in Chapter 4, enabled us to ascertain current details of the extent and severity of depression among residents. Not surprisingly, depression was associated with poor physical health. There were also associations between depression and excessive alcohol use and the use of illicit substances.
Homeless Link’s audit19 of > 2500 homeless people found that the proportion of homeless people with mental health problems (45%) was nearly twice that among the general population (approximately 25%). Most significantly, the audit found that just over one-third (36%) had depression (compared with 3% of the general population) with further higher rates of bipolar disorder, personality disorder, schizophrenia and post-traumatic stress disorder. Such findings are in line with this present study’s data.
Mental health and well-being are prominent in the government’s recent Homelessness Prevention Programme. The development of Social Impact Bonds is intended to support a group who are described as the most complex and entrenched, namely rough sleepers, including personalised mental health support. Older hostel residents may no longer be rough sleepers but are likely to have survived these experiences and share many of their characteristics.
Alcohol use
Heavy alcohol use is not unusual among people who have a history of homelessness or are currently homeless, particularly men. 19 Similarly, the high weekly alcohol intake among the residents who participated in this study (see Chapter 4) indicates that heavy drinking is not unusual; indeed, one-quarter of the 52 hostel residents who provided details of their alcohol consumption were consuming > 100 units of alcohol each week. Alcohol use varied by hostel, particularly as some hostels permitted drinking on their premises. There are implications for memory assessment and other services from these data. First, assessments that require patients to be sober or abstinent for a period may exclude certain groups from their services. Second, regularly high levels of alcohol consumption may mean that certain times of day are best for professional assessments and conversations (and for researchers). Some days of the week may be better than others for accessing individuals who drink heavily or ‘binge drink’ after receiving their welfare benefits. Third, the researchers asked questions carefully to elicit ideas about what was being drunk and, methodologically, this collected a more accurate picture of consumption than just numbers of drinks. Finally, it is not easy to calculate what individuals drink; in this study we relied on self-reports. Hostel staff admitted that they did not know too much about the amounts being drunk; indeed, several residents informed us that they consumed their alcoholic beverages outside the hostel.
Use of illicit drugs
The growth in number of older drug users and the ageing of ‘baby boomers’, whose rates of illicit drug use are higher than those of previous older cohorts, combined with improved health care for drug users so that they are living longer, all need to be taken into account as relevant changes to the practice and service contexts. 19
We relied on self-reports and staff reports about illicit drug use in this study. Although of course there are limits to this, our findings suggested that many hostel residents have a history of drug misuse (in this study over half) and that some (nearly one-third in this study) still regularly consume drugs (see Chapter 6). Among our participants, this consumption was mainly of cannabis and crack-cocaine; these were long-standing patterns of behaviour. The implications of this for memory assessment are similar to those in respect of alcohol consumption; behaviour and responses to tests may be affected by substance use. Similarly, staff working in hostels may not have accurate information about residents’ substance use.
Literacy problems
We noted in Physical health problems that sight and hearing problems may affect communication. The level of literacy among some hostel residents is also relevant. Literacy problems were, of course, long-standing; more than one-third reported such problems (see Chapter 5). Unsettled early lives and leaving formal education at an early age to move to unskilled work or unemployment were characteristic of some residents. The impact of this on dementia pathways was that hostel staff often acted for these residents in communication with health and care services, ‘proving their case’ and making exceptions about moving residents on, and accompanying them to appointments and to ‘move on’ possibilities. Not all hostels were able to provide this level of support.
The next section focuses on the hostels and the wider systems in which the difficulties of following routine care pathways to identify people with memory problems or cognitive difficulties were prominent.
Hostel provision
Our study focused on people aged ≥ 50 years who were living in hostels; in other jurisdictions this population might be described as ‘provisionally sheltered’. 113 The case study approach of this study revealed the wide variety of UK hostels and also their risks of non-sustainability. Whereas large not-for-profit hostels have a range of services and contracts with statutory sectors and appear more organisationally resilient, smaller and single-ownership hostels are highly vulnerable to changes in their external environment and also to the decisions made by owners about sustainability. The differences encountered, as reported in Chapter 4, reflect this heterogeneity and this too affected their resident group. In one hostel, for example, some residents were ‘settled’ as they had lived there for many years. However, this situation may not continue, and so the attention being given by the social care sector to risks of care home closures114 and resident resettlement could be expanded to other provision such as hostels.
Hostel staff were generally helpful and engaged in the study, and freely gave their time and views in the context of being busy and sometimes short-staffed. There is a risk of bias in that those hostels that participated in this study may have been exceptional. These risks were mitigated by the research team explaining that this was an independent study and that data would be confidential and not reported to commissioners. High staff turnover is common in social care services;115 the extent of it in homelessness services should be acknowledged in interagency communications as well as in research. Completing a diary was not feasible, not only because staff were busy but also because communal facilities meant that ‘checking’ or monitoring was done in relation to several residents and could not be easily linked to individuals. Hostel staff’s descriptions of ‘prompting’ residents may seem an easy task but our interviews revealed that this work was skilled in making such assistance acceptable and not disempowering. The range of support in hostels was potentially extensive (see Tables 4 and 5). However, laundry and cleaning provision varied, budgeting assistance was infrequent, and collection or management of medication was provided in some hostels but not in others. Each of these activities was identified and interrogated in this study, providing a rich set of data about hostel provision and experiences. The expositions of these multiple differences highlighted the value of data collected from meticulously conducted semistructured interviews and structured survey questions.
In our interviews with hostel staff, several expressed a wish for more training and this may be a reflection of the high levels of resident need that they are encountering. As noted, whereas some hostel staff had relevant skills and training in mental health, other staff lacked such experience. Almost all acknowledged that some hostel residents were not trusting of other professionals or lacked motivation to seek further involvement in services. For some of the most disabled residents, the extent to which hostel workers acted as their advocates was substantial. The mixed presentation of hostel residents, with multiple problems and apparent reluctance to access support, further complicated interagency networking.
It is important to stress, however, that the hostel residents were homeless and that housing (for many this needed to be accompanied by care of some form) was a primary need. This is particularly the case at a time when the length of hostel stays is becoming shorter, when hostels are vulnerable to closure or to having to accept residents with multiple needs, and when wider system pressures are evident, such as increased pressure on hospital beds. 116 Although much has been said about social care being at a ‘tipping point’116 and that local authority funding is declining,117 provision in the homelessness sector for people who have care and support needs is similarly affected by instability and resource limitations. Despite the best efforts of their staff, on the basis of our findings hostels are not suitable accommodation for older homeless people with memory problems. As we shall highlight in the implications of this study, suitable, accessible and acceptable long-term accommodation needs to be available; our literature review identified some examples of care homes run by homelessness-sector organisations for older homeless people with memory problems, some of whom are heavy drinkers. Such a model could be developed in England, and the current context of moves to more integrated care might foster such developments.
It is seemed inappropriate for older homeless people with memory problems and often comorbid or other long-term conditions to be in hostels with transient resident populations, young and middle-aged drug or alcohol misusers or other residents in troubled circumstances. Some of the ‘checking’ tasks carried out by hostel staff were protective and risk managing in intent. Although older homeless people generally do not like living in hostels with younger people – they may feel or be threatened and intimidated – in other circumstances this work would be seen as addressing safeguarding concerns. As a recent report from St Mungo’s118 suggested, homeless people on the streets are at risk of harm, including violent attacks; thus, safety and well-being in hostels also need to be addressed as safeguarding matters when adults have care and support needs under the Care Act 2014119 and are unable to protect themselves.
There is currently strong emphasis on a policy of only short stays in hostels for all age groups. 44 This rests on a belief that hostels are not suitable accommodation other than for a short period. Older homeless people with memory problems are probably more difficult to rehouse than others and, as our study found, sometimes remain in hostels because of a lack of suitable accommodation (see Chapter 7). This is not an argument for them staying in hostels. As gerontological researchers such as Grenier et al. 120 have argued, homelessness in later life may newly occur or, for some, may have been experienced on several occasions. An implication of our study is that ‘older homelessness’ needs to be part of local strategic thinking for public services.
Strengths and limitations of the study
To our knowledge, this is the first study of cognitive problems, dementia and older homeless people in the UK. We were able to assess clinically the extent of memory problems among a sample of hostel residents, using a test (ACE-III) that appeared to work well in not being too intrusive, time-consuming or onerous (48 such assessments were conducted). We were able to adjust our study to categorise residents into three rather than two groups for analysis according to their memory problems (memory problems, no memory problems and ‘borderline’). Our work on unit costs broke new ground in linking (or attempting to link) sources of self-report, hostel staff accounts, medical and hostel records. Medications were not included in the costing data and no comparison was made of service use and costs with another comparator group (e.g. non-homeless or long-term care residents). Despite the challenges of interviewing hostel residents, out of 62 participants at baseline, 37 were interviewed at 3 months and 37 were interviewed at 6 months. Only six residents declined to participate further in the study for reasons other than being unavailable, moving away or relocation. Over half of those interviewed (25 out of 47) considered that they had difficulties with or concerns about their memory. Notably, we acquired data on the impact of this on their everyday life but also on their ability to provide information about themselves; a total of 18 residents were not able but perhaps not willing to tell the research team if they had stayed in a hostel prior to their current stay. Among participants in this study, most spent their days in the hostel with visits to shops their most frequent outing, and made very limited use of day centres or drop-in facilities. In many ways, several were living a life that was close to living in a long-term care facility, except that community contact was possibly even more restricted and that care quality inspection, regulation and monitoring are absent from the hostel sector.
Finally, in terms of the strengths of this study, the assistance of an study advisory group from different perspectives, including people with experience of homelessness, offered insights and deepened understanding. The group was involved in discussions of the research design, decisions following recruitment challenges and dissemination. Those with lived experience of homelessness were involved as full members of this group and made very insightful comments; for example, it was on their advice that we collected data not only on how much alcohol might be consumed by study participants but also on the type of alcohol. They drew attention to the low cost of super-strength alcohol, such as lager or cider. As older people with lived experience, they were very helpful in the study; sadly, one member died during the study. Representatives from the homelessness service provider St Mungo’s and from the Alzheimer’s Society who attended the Advisory Group have agreed to actively help with study dissemination.
There are, of course, several limitations to this study. We accessed hostels in urban environments and the needs and circumstances of rural homeless people were not addressed, important though these are. 121 We were not able to access NHS data for several residents, although for some this was understandable as contact had ceased or been temporary. In any future study we would seek funding for incentivising of GPs and would collect data on medication prescription and use (and on over-the-counter medications). We took care not to refer to this as the ‘dementia’ study, but this is how this study became known to hostel staff and residents; this may have affected not only recruitment (see Chapter 3) but also responses. We have previously noted the volatility of hostel provision in some areas and unpredictability in their contractual arrangements. There were fewer contacts with other professionals than we anticipated, bearing in mind the level of need for care and support of the hostel residents. We further noted in our review of the literature that there is little on social care provision for homeless people, and that much of the earlier evidence of the outcomes of their moves to care homes focused on the problems for care homes and is now dated. 27 These gaps in the evidence base remain. Few studies and other literature have identified that older homeless people may experience inequities of provision, ageist and discriminatory behaviours and systems, and that their human rights are hard to uphold in settings such as hostels.
Our work on service use also broke new ground. Information on the service use of homeless people is rarely available and not triangulated with different reports of what is taken up. This was a small sample of older homeless people, but the information was meticulously collected. Much variability in service use was found among the sample. The median cost of service use over the 6-month period was £1454, but the mean was much higher than this (£2975), reflecting a small number of high users of social care services and inpatient care.
One of the original aims of this study was to compare access to services of older homeless people with memory problems with that of their peers without memory problems. Just under half (49%) of the sample for whom service use was available had memory problems, and a further 15% were considered borderline. The proportion of the group with memory problems (the ‘cognitively impaired’ group) who had used some form of psychiatric or mental health service during the 6-month study was higher than for those in the borderline or no memory problems groups (39%, 29% and 24%, respectively). However, the proportion of total costs accounted for by psychiatric or mental health services was < 5%. Moreover, the reason for accessing psychiatric or mental health care is not known, and it may have been for depression or another psychiatric morbidity rather than for memory problems. Contact with the memory assessment services was recorded for only one participant (a hostel visit). For many participants, it was only through the research project that cognitive status was assessed. Without any formal diagnosis before the study, it is perhaps to be expected that there is little evidence of memory service input.
Participants with memory problems (the memory problems group) used NHS emergency and out-of-hours services more than did those without such problems, but there was no other association between cognitive status and service use cost categories. However, there was much variability in service utilisation at the individual level and a larger sample would be required to gain definitive results.
A limitation of the study noted previously is that medications were not included in the costing study. More generally, the lack of a comparison group means that it is not possible to comment on the extent to which the service utilisation of homeless people differs from that of the non-homeless population.
The final chapter of this study outlines the implications of our study.
Chapter 9 Implications
The previous chapters have reported unique data in the UK context that we have used to construct a set of implications for four main audiences: commissioners, providers, practitioners and researchers. We also frame these implications for the attention of the wider dementia stakeholder community, and in the context of equalities in mental health services and services for older people, particularly those who are disadvantaged socially. Although some of the implications overlap, they are a unique set of implications coming from the analysis of the experiences of people who are homeless, some of whom have received a diagnosis of dementia and some who have not, and of those who support them as practitioners and managers in homelessness services.
Early or timely recognition of dementia was a key policy goal of the National Dementia Strategy. 1 Older people who are homeless were not considered in this policy and practice imperative despite their risk factors. Indeed, we identified barriers to their assessment for possible memory problems. Overall, the system of memory assessment is not only far from patient-centred for this group but also largely inaccessible. Older people living in hostels are very likely to have several long-term conditions, including mental health needs. Thus, the issues arising for people with possible dementia who are homeless may be similar to those for other older people but they may also be experienced to a greater degree and cover different aspects of life and well-being. Experiences of declining cognitive abilities were reported in this study, and some people with a diagnosis of dementia were living in hostels. To the best of our knowledge, no other study and no policy document acknowledges these as ‘dementia communities’.
These confounding effects of dementia and homelessness may need to be investigated further so that health care, social care and housing support practices can be better tailored to support older homeless people. Although undertaking interviews with older hostel residents, and in particular those consuming a large amount of alcohol, could take several attempts, our study showed that psychiatric assessments can be conducted; however, it may be more productive for parts of assessments to be conducted at a hostel rather than at a memory service. It is interesting that several hostel staff were able to determine which residents had suspected memory problems (although there were also several ‘false positives’) and this suggests that their role as informants is potentially significant and may partially compensate for a lack of family informants. In this context, the following implications are drawn out for the consideration of different groups.
Implications
In this section we outline some of the emerging implications from this study.
Implications for the consideration of commissioners
-
There is a need for local strategies to create and agree a plan(s) for the support of older homeless residents in hostels, which should be undertaken in partnership with the hostel staff. This might be usefully informed by public health expertise. Such specific planning and anticipation of need will help to ensure that current reactive care is part of a co-ordinated plan. Local work on integration may be the vehicle for such developments, but only if older homeless people are identified as a priority.
-
Are hostels providing another form of ‘housing with care’ in the local health and care economy? The implications of our findings that some hostel residents have substantial care and support needs merits exploration of whether or not the use of such terminology might help integrate funding and provide better continuity of care and support. Furthermore, the closure of a hostel or change to its contracted funding arrangements may have substantial implications for older residents with high or growing support needs. Our study suggests that hostel provision might be encompassed in the new market shaping responsibilities of local authorities under the Care Act 2014119 and its wider responsibilities for local citizens’ well-being.
-
We suggest that local health and care agencies’ training and education be welcoming to hostel staff. Such shared learning might also forge greater contact between hostel staff and statutory services to the benefit of their shared clients or residents.
Implications for the consideration of practitioners
-
We do not know what social care staff supporting older hostel residents with or without memory problems find to be the most effective and acceptable elements of their practice. This study suggests that they may have a wider role in ‘bridging’ the different sectors, or at least their managers being able to communicate with other professionals if a care plan is not working well. As with hostel staff who are key workers, we do not know if and how care workers are engaged in care planning and anticipatory care. The implications of this study are that home care workers who provide care and support to hostel residents are potentially underused as a monitoring system, particularly in hostels without key worker systems.
-
Living alone with dementia but not on one’s own is a situation highlighted by this study. People who are living alone or are isolated are not generally thought of as living in a congregate environment such as a hostel. However, increasing frailty and the needs of other residents may affect socialisation within a hostel. Hostel residents themselves and those who work with them may have relevant insight into the needs of people who are used to being on their own and person-centred experiences of how to help support be accessible and acceptable. These could be usefully explored by other practice communities working with older people who are lonely or unwillingly isolated. The implication of this study is that societal commitment to reducing the loneliness and isolation of older people should be inclusive of older people who have a history of homelessness.
-
The practice evidence about the relative merits and benefits of different resources and supports for homeless people wishing to sustain their abilities and memory is thin. Memory support, environmental modifications and technology are variously suggested and appreciated among some people with dementia. A stronger evidence base for these in diverse settings might be developed so that health-care practitioners can better support people who are not usually seen as benefiting from them, such as older homeless people.
-
This study found that many hostel staff would like more training. This is a broad topic; but in respect of ageing and memory problems, evidence of most effective and cost-effective ways to support older residents could be collated into good practice guidelines that could underpin training. Training resources for practitioners could be developed by the homelessness sector with the support of dementia practice communities.
-
For clinical practice this study has identified several barriers to memory assessment that could be addressed by flexibility in terms of appointments, assessment practices and liaison with hostel staff. Records of individual health status and history are not always complete among people with histories of homelessness. One important implication of this study is that the presence of head injury or a history of trauma may merit particular consideration in assessments, but that records of such an injury may not be available or may not have been taken. Another clinical implication is our finding of high levels of depression among residents. Although this was being treated in some residents, its presence may merit greater preventative efforts, taking a public health approach.
Implications for the consideration of hostels
-
Hostel staff are a key resource, and many were informed, supportive and committed to resident well-being. Providers may wish to encourage and assist them to access local training and practice development opportunities.
-
Key working was a very effective way of supporting residents with high-level needs in hostels and some key workers undertook case management roles. Not all hostels run their service with key workers and their managers or owners may wish to consider this staffing arrangement.
-
Hostel staff and hostel records may be the main sources of information about some residents. Practice varies widely in terms of record keeping and how such records are maintained. Hostels facing difficulties in this activity should work with partners in local authorities and health services to seek assistance so that such valuable data are not lost. The implication of this study’s finding that hostels may close quickly means that there is substantial risk of unique information about residents being lost. For those with memory problems, this is of great concern to future person-centred care that takes a life history approach.
-
Hostels are not traditionally seen as dementia communities; but this research shows that they are supporting people with such conditions, diagnosed or not. The difficulties faced by hostels supporting people with memory problems are substantial and are compounded at a system level by demands for short stays and resettlement. Even those hostels whose facilities are more suitable for people with physical health conditions are not the optimal environment for living well with dementia. The implication of this study is that hostel providers will need to continue to advocate for their residents to move to more appropriate accommodation in general and that the appropriateness of this takes into account declining cognition or memory problems. Hostel providers may wish to build up local alliances or to join dementia community initiatives to improve the lives of their residents with memory problems and to supplement their advocacy on residents’ behalf.
Implications for the consideration of the research community
-
Multiple research methods were used in this study. Not surprisingly, interviews were more productive than questionnaires or surveys among people whose recall levels might fluctuate. Our interviews with older homeless people seemed to be encouraging of discussion and facilitated recall in some instances; however, they were only partially successful (see Chapter 3) in providing factual information. A few records were incomplete or partial; as noted above, these could cover clinical histories but sometimes chronologies or biographies. Research with older homeless people needs more time and resource than is the case with other homeless people, and compared with studies of other housed older people with or without dementia. Further longitudinal research would be helpful in considering ways to support older homeless people with memory problems across the trajectory of multiple conditions and challenges.
-
The funders of research are in a strong position to enable researchers to accommodate the efforts of data collection and may have a helpful role in the developing of researcher capacity to work in this sector when investigating health and social care questions, especially those related to addressing inequalities. The building up of experience of research participation in hostels, particularly those that are small and not part of larger charitable bodies, could be part of this capacity building. There are risks of bias in recruiting only from large hostels or day centres whose funders or central offices are committed to research but even in such locations this needs to be fostered locally. The professional or service backgrounds of researchers in homelessness studies assist greatly in understanding the subject, the approach and communications; if they are not available, then greater preparation and induction will be needed. An expert advisory group is strongly recommended, including people with lived experience of homelessness. Such capacity could be fostered and funded.
Conclusion
Our study has presented new information about the lives and circumstances of older people with memory problems, about older hostel residents and about services for both groups. We have established baseline information and tested out different methods and data collection approaches. On the basis of the evidence, the implication of this study is that hostels are not suitable accommodation for older people with memory problems, such as those associated with dementia. Nevertheless, the study found much evidence of the skills and competence among some hostel staff who provided support to residents for whom memory problems were having a negative impact on their lives and well-being. Inequalities of support for people with dementia or memory problems include the exclusion of some older people from a place to call home and the security that this brings.
Acknowledgements
We are most grateful to all participants who willingly shared their views with us, to hostel managers who facilitated recruitment and allowed us to use their premises for interviews and to St Mungo’s for support with public and patient involvement in this study. We offer particular thanks to members of the Study Advisory Group; to Stephen Martineau of the National Institute for Health Research Health and Social Care Workforce Research Unit for help with searches; and to Tanya Walton and Elspeth Dustagheer, who assisted in assessments.
Contributions of authors
Professor Jill Manthorpe (Professor of Social Work) was chief investigator, designed the study, reviewed the background literature, provided supervisory support and co-wrote the report.
Dr Kritika Samsi (Research Fellow) was co-investigator, conducted recruitment, data collection and data analysis, and co-wrote the report.
Dr Louise Joly (Research Fellow) designed the study and the interview documents, conducted recruitment, data collection and data analysis, and co-wrote the report.
Dr Maureen Crane (Reader in Applied Social Research) was co-investigator, designed the study and interview documents, conducted recruitment, data collection and data analysis, and co-wrote the report.
Professor Heather Gage (Professor of Health Economics) was co-investigator and conducted the economic aspects of the study; for this, she developed study instruments, conducted the analysis and wrote the relevant chapter.
Professor Ann Bowling (Visiting Professor in Health Sciences) was co-investigator and conducted the systematic review for the study; for this, she designed the review, conducted the searches, analysed the data and co-wrote the relevant chapter.
Dr Ramin Nilforooshan (Consultant Psychiatrist) designed the clinical investigations of the study, identified suitable cognitive instruments, conducted assessments with his colleagues, analysed the relevant data and co-wrote the relevant chapter.
Publications
Manthorpe J, Samsi K, Crane M, Joly L, Timms P, Gage H, et al. Dementia & homelessness: starting to make the links. Journal of Dementia Care 2013;21:39.
Bowling A, Rowe G, Adams S, Sands P, Samsi K, Crane M, et al. Quality of life in dementia: a systematically conducted narrative review of dementia-specific measurement scales. Aging and Ment Health 2015;19:13–31.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Living Well With Dementia: A National Dementia Strategy. London: Department of Health and Social Care; 2009.
- National Dementia Strategy: Equalities Action Plan. London: Department of Health and Social Care; 2011.
- Knapp M, Black N, Dixon J, Damant J, Reihill A, Tan S. Independent Assessment of Improvements in Dementia Care and Support Since 2009. London: Report from the Policy Innovation Research Unit and the NIHR School for Social Care Research; 2014.
- Headline Report. London: Department of Health and Social Care; 2011.
- Prior P. Knowing the Foundations of Dementia Friendly Communities for the North East. Newcastle upon Tyne: North East Dementia Alliance; 2012.
- Rockwood K. For how long should we use symptomatic therapies to treat people with Alzheimer disease?. Can J Psychiatry 2014;59:615-17. https://doi.org/10.1177/070674371405901201.
- Mittler P, Batsch N, Mittelman M. World Alzheimer Report 2012 – Overcoming the Stigma of Dementia. London: Alzheimer’s Disease International; 2012.
- Ensuring a Human Rights-Based Approach for People Living with Dementia. Geneva: World Health Organization; 2015.
- Dementia, Rights and the Social Model of Disability. London: Mental Health Foundation; 2015.
- Thomas C, Milligan C. How Can and Should UK Society Adjust to Dementia?. York: Joseph Rowntree Foundation; 2015.
- Cooper C, Lodwick R, Walters K, Raine R, Manthorpe J, Iliffe S, et al. Observational cohort study: deprivation and access to anti-dementia drugs in the UK. Age Ageing 2016;45:148-54. https://doi.org/10.1093/ageing/afv154.
- Giebel C, Challis D, Worden A, Jolley D, Bhui KS, Lambat A, et al. Perceptions of self-defined memory problems vary in South Asian minority older people who consult a GP and those who do not: a mixed-method pilot study. Int J Geriatr Psychiatry 2016;31:375-83. https://doi.org/10.1002/gps.4337.
- Westwood S. Dementia, women and sexuality: how the intersection of ageing, gender and sexuality magnify dementia concerns among lesbian and bisexual women. Dementia 2016;15:1494-514. https://doi.org/10.1177/1471301214564446.
- Bamford S. Women and Dementia: Not Forgotten. London: International Longevity Centre UK; 2011.
- Ludwin K, Parker G. Women and Dementia: All But Forgotten? A Literature Review. York: Social Policy Research Unit, University of York; 2015.
- Crane M, Joly L. Older homeless people: increasing numbers and changing needs. Rev Clin Gerontol 2014;24:255-68. https://doi.org/10.1017/S095925981400015X.
- England’s Most Disadvantaged Groups: Homeless People. London: Equality and Human Rights Commission; 2016.
- Equality Act 2010. London: The Stationery Office; 2010.
- The Unhealthy State of Homelessness. London: Homeless Link; 2014.
- Andrews J, Molyneux P. Dementia: Finding Housing Solutions. London: National Federation of Housing; 2013.
- Dementia: Finding Housing Solutions Looks at the Role Housing Associations can Play in Allowing People with Dementia to Live Independently. London: National Federation of Housing; 2013.
- Lipman V, Manthorpe G. Social housing provision for minority ethnic older people with dementia: findings from a qualitative study. Dementia 2017;16:750-65. https://doi.org/10.1177/1471301215616539.
- Alden S. Public-sector service provision for older people affected by homelessness in England. Ageing Soc 2017;37:410-35. https://doi.org/10.1017/S0144686X15001233.
- Joyce DP, Limbos M. Identification of cognitive impairment and mental illness in elderly homeless men: before and after access to primary health care. Can Fam Physician 2009;55:1110-11.e6.
- Rota-Bartelink A. The influence of cognitive capacity on the efficacy of early intervention and prevention strategies among older homeless. Parity 2009;22:25-6.
- Audit of Older Homeless People September 2007: Summary of Findings. London: Housing Learning and Improvement Network; 2007.
- Crane M, Warnes A. The outcomes of rehousing older homeless people: a longitudinal study. Ageing Soc 2007;27:891-918. https://doi.org/10.1017/S0144686X07006319.
- Communities and Local Government Committee: Homelessness. Third Report of Session 2016–17, HC 40, 18 July. London: House of Commons; 2016.
- Support for Single Homeless People in England: Annual Review 2017. London: Homeless Link; 2017.
- Gorton S, Borrill A. Guide to Resettling Older Residents from Hostels. London: Homeless Link; 2007.
- Parnell J, Palmer G. Coming of Age: Opportunities for Older Homeless People under Supporting People. London: UK Coalition on Older Homelessness; 2004.
- Ridley NJ, Draper B, Withall A. Alcohol-related dementia: an update of the evidence. Alzheimers Res Ther 2013;5. https://doi.org/10.1186/alzrt157.
- Adams CE, Pantelis C, Duke PJ, Barnes TR. Psychopathology, social and cognitive functioning in a hostel for homeless women. Br J Psychiatry 1996;168:82-6. https://doi.org/10.1192/bjp.168.1.82.
- Bowling A. Measuring Health: A Review of Quality of Life Measurement. Scales. Maidenhead: Open University Press; 2005.
- Thornicroft G, Tansella M. Mental Health Outcome Measures. Berlin: Springer; 1996.
- Palepu A, Hubley AM, Russell LB, Gadermann AM, Chinni M. Quality of life themes in Canadian adults and street youth who are homeless or hard-to-house: a multi-site focus group study. Health Qual Life Outcomes 2012;10. https://doi.org/10.1186/1477-7525-10-93.
- International Classification of Functioning, Disability and Health. Geneva: World Health Organization; 2001.
- Sullivan G, Burnam A, Koegel P, Hollenberg J. Quality of life of homeless persons with mental illness: results from the course-of-homelessness study. Psychiatr Serv 2000;51:1135-41. https://doi.org/10.1176/appi.ps.51.9.1135.
- Russell LB, Hubley A, Palepu A. What is Important to the Quality of Life of Homeless or Hard-to-house Canadian Adults and Street Youth? A Multi-site Study. Vancouver, BC: University of British Columbia, for REACH Research Team; 2005.
- Riley ED, Bangsberg DR, Perry S, Clark RA, Moss AR, Wu AW. Reliability and validity of the SF-36 in HIV-infected homeless and marginally housed individuals. Qual Life Res 2003;12:1051-8. https://doi.org/10.1023/A:1026166021386.
- Auquier P, Tinland A, Fortanier C, Loundou A, Baumstarck K, Lancon C, et al. Toward meeting the needs of homeless people with schizophrenia: the validity of quality of life measurement. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0079677.
- Hill KB, Rimington D. Investigation of the oral health needs for homeless people in specialist units in London, Cardiff, Glasgow and Birmingham. Prim Health Care Res Dev 2011;12:135-44. https://doi.org/10.1017/S1463423610000368.
- Allan T, Filsak L. Homelessness and Adult Social Care Workforce: Scoping Study. Leeds: Skills for Care; 2014.
- Support for Single Homeless People in England, Annual Review 2015. London: Homeless Link; 2015.
- Maguire N. Training for front-line homeless workers: practicalities and ethics of teaching cognitive behavioural and dialectical behavioural psychological therapeutic techniques. Housing Care Support 2012;15:177-85. https://doi.org/10.1108/14608791211288589.
- Cornes M, Joly L, O’Halloran S, Manthorpe J. Rethinking Multiple Exclusion Homelessness: Implications for Workforce Development and Interprofessional Practice. Summary of Findings. Swindon: Economic and Social Research Council; 2011.
- Cameron A. The contribution of housing support workers to joined-up services. J Interprof Care 2010;24:100-10. https://doi.org/10.3109/13561820903012065.
- Fitzpatrick S, Wygnanska J. Harmonising hostel standards: comparing the UK and Poland. Eur J Homelessness 2007;1:41-66.
- Bowling A, Rowe G, Adams S, Sands P, Samsi K, Crane M, et al. Quality of life in dementia: a systematically conducted narrative review of dementia-specific measurement scales. Aging Ment Health 2015;19:13-31. https://doi.org/10.1080/13607863.2014.915923.
- Rogoz A, Burke D. Older people experiencing homelessness show marked impairment on tests of frontal lobe function. Int J Geriatr Psychiatry 2016;31:240-6. https://doi.org/10.1002/gps.4316.
- Brown RT, Kiely DK, Bharel M, Mitchell SL. Factors associated with geriatric syndromes in older homeless adults. J Health Care Poor Underserved 2013;24:456-68. https://doi.org/10.1353/hpu.2013.0077.
- Petersen M, Parsell C. Homeless for the first time in later life: an Australian study. Housing Studies 2015;30:368-91. https://doi.org/10.1080/02673037.2014.963522.
- Rothwell D, Sussman D, Grenier A, Mott S, Brogeois-Guerin V. Patterns of shelter use among men new to homelessness in later life: duration of stay and psychosocial factors related to departure. J Appl Gerontol 2017;36:71-93. https://doi.org/10.1177/0733464815624154.
- Hassanally K, Asaria M. Homeless mortality data from East London. London J Prim Care 2018;10:99-102. https://doi.org/10.1080/17571472.2018.1458443.
- Grenier A, Barken R, Sussman T, Rothwell D, Brogeois-Guerin V, Lavoie JP. Literature Review: Aging and Homelessness. Hamilton, ON: Gilbrea Centre for Studies in Aging, McMaster University; 2013.
- Homeless Households Accepted by Local Authorities, Table 781. London: Ministry of Housing, Communities and Local Government; 2014.
- Gilchrist G, Morrison DS. Prevalence of alcohol related brain damage among homeless hostel dwellers in Glasgow. Eur J Public Health 2005;15:587-8. https://doi.org/10.1093/eurpub/cki036.
- Johnson G, Chamberlain C. Are the homeless mentally ill?. Aus J Soc Issues 2011;46:29-48. https://doi.org/10.1002/j.1839-4655.2011.tb00204.x.
- Lipmann B. Opinion. Parity 2008;21.
- Rota-Bartelink A, Lipmann B. Older people with alcohol-related brain injury and associated complex behaviors: a psychological model of residential care (the Wicking Project). Care Manage J 2010;11:112-21. https://doi.org/10.1891/1521-0987.11.2.112.
- Burra T, Stergiopoulos V, Rourke S. A systematic review of cognitive deficits in homeless adults: implications for service delivery. Can J Psychiatry 2009;54:123-33. https://doi.org/10.1177/070674370905400210.
- Ennis N, Roy S, Topolovec-Vranic J. Memory impairment among people who are homeless: a systematic review. Memory 2015;23:695-713. https://doi.org/10.1080/09658211.2014.921714.
- Orellana K, Manthorpe J, Moriarty J. What do we know about care home managers? Findings of a scoping review. Health Soc Care Community 2017;25:366-77. https://doi.org/10.1111/hsc.12313.
- Chenco C. Homelessness and Dementia in Australia: A Literature Review. Melbourne, VIC: Victoria & Tasmania Dementia Training Study Centre; 2014.
- Spence S, Stevens R, Parks R. Cognitive dysfunction in homeless adults: a systematic review. J R Soc Med 2004;97:375-9. https://doi.org/10.1258/jrsm.97.8.375.
- Teesson M, Buhrich N. Prevalence of cognitive impairment among homeless men in a shelter in Australia. Hosp Community Psychiatry 1993;44:1187-9. https://doi.org/10.1176/ps.44.12.1187.
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. https://doi.org/10.1016/0022-3956(75)90026-6.
- Buhrich N, Hodder T, Teesson M. Prevalence of cognitive impairment among homeless people in inner Sydney. Psychiatr Serv 2000;51:520-1. https://doi.org/10.1176/appi.ps.51.4.520.
- Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLOS Med 2008;5. https://doi.org/10.1371/journal.pmed.0050225.
- Rogoz A, Burke D, Price P, Hickie I. Cognitive impairment in the elderly homeless in the inner-city of Sydney: a preliminary report on a study in progress. Parity 2008;21.
- Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. J Gen Intern Med 2012;27:16-22. https://doi.org/10.1007/s11606-011-1848-9.
- Conroy E, Burns L, Wilson S. Alcohol Use Disorder and Cognitive Impairment Among Older Homeless Persons and Implications for Service Delivery. Sydney, NSW: Foundation for Alcohol Research and Evaluation; 2013.
- Brown RT, Hemati K, Riley ED, Lee CT, Ponath C, Tieu L, et al. Geriatric conditions in a population-based sample of older homeless adults. Gerontologist 2017;57:757-66. https://doi.org/10.1093/geront/gnw011.
- Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3MS) as a screen for dementia. Can J Psychiatry 2001;46:506-10. https://doi.org/10.1177/070674370104600604.
- Depp CA, Vella L, Orff HJ, Twamley EW. A quantitative review of cognitive functioning in homeless adults. J Nerv Ment Dis 2015;203:126-31. https://doi.org/10.1097/NMD.0000000000000248.
- Nishio A, Yamamoto M, Horita R, Sado T, Ueki H, Watanabe T, et al. Prevalence of mental illness, cognitive disability, and their overlap among the homeless in Nagoya, Japan. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0138052.
- Stergiopoulos V, Herrmann N. Old and homeless: a review and survey of older adults who use shelters in an urban setting. Can J Psychiatry 2003;48:374-80. https://doi.org/10.1177/070674370304800603.
- Lipmann B. Elderly homeless men and women: aged care’s forgotten people. Aus Soc Work 2009;62. https://doi.org/10.1080/03124070902792454.
- Van Wormer R. Homelessness among older adults with severe mental illness. J Hum Behav Soc Environ 2005;10:39-4. https://doi.org/10.1300/J137v10n04_03.
- McGhie L, Barken R, Grenier A. Literature Review: Housing Options for Older Homeless People. Hamiltion, ON: Gilbrea Centre for Studies in Aging, McGill/McMaster University; 2013.
- Crane M, Warnes A. Older homeless people with complex problems and needs: the British experience. Parity 2008;21:20-1.
- Ploeg J, Hayward L, Woodward C, Johnston R. A case study of a Canadian homelessness intervention programme for elderly people. Health Soc Care Community 2008;16:593-605. https://doi.org/10.1111/j.1365-2524.2008.00783.x.
- Barrett B, Fogel SJ, Garrett J, Young SC. Accessing health care needs among street homeless and transitionally housed adults. J Soc Serv Res 2011;37:338-50. https://doi.org/10.1080/01488376.2011.564073.
- O’Connell JJ, Roncarati JS, Reilly EC, Kane CA, Morrison SK, Swain SE, et al. Old and sleeping rough: elderly homeless persons on the streets of Boston. Care Manag J 2004;5:101-6. https://doi.org/10.1891/cmaj.5.2.101.66284.
- Backer TE, Howard EA. Cognitive impairments and the prevention of homelessness: research and practice review. J Prim Prev 2007;28:375-88. https://doi.org/10.1007/s10935-007-0100-1.
- Green DM. History, discussion and review of a best practices model for service delivery for the homeless. Soc Work Ment Health 2005;3:1-16. https://doi.org/10.1300/J200v03n04_01.
- Yang JA, Garis J, McClure R. Clinical mental health outreach to older adults: serving the hard to serve. Clin Gerontol 2006;29:71-9. https://doi.org/10.1300/J018v29n02_08.
- Andersen J, Kot N, Ennis N, Colantonio A, Ouchterlony D, Cusimano MD, et al. Traumatic brain injury and cognitive impairment in men who are homeless. Disabil Rehabil 2014;36:2210-15. https://doi.org/10.3109/09638288.2014.895870.
- Abdul-Hamid W, Holloway F, Silverman M. Psychiatric care needs of elderly graduates – unanswered questions. Aging Ment Health 1998;2:167-70. https://doi.org/10.1080/13607869856632.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Barak Y, Cohen A. Characterizing the elderly homeless: a 10-year study in Israel. Arch Gerontol Geriatr 2003;37:147-55. https://doi.org/10.1016/S0167-4943(03)00043-8.
- Brodaty H, Pond D, Kemp NM, Luscombe G, Harding L, Berman K, et al. The GPCOG: a new screening test for dementia designed for general practice. J Am Geriatr Soc 2002;50:530-4. https://doi.org/10.1046/j.1532-5415.2002.50122.x.
- Hsieh S, Schubert S, Hoon C, Mioshi E, Hodges JR. Validation of the Addenbrooke’s Cognitive Examination III in frontotemporal dementia and Alzheimer’s disease. Dement Geriatr Cogn Disord 2013;36:242-50. https://doi.org/10.1159/000351671.
- Yin RK. Enhancing the quality of case studies in health services research. Health Serv Res 1999;34:1209-24.
- Crabtree B, Miller W. Doing Qualitative Research. London: Sage; 1999.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
- Chisholm D, Knapp M, Knudsen H, Amaddeo F, Gaite L, van Wijngaarden B, et al. Client socio-demographic and service receipt inventory – European version: development of an instrument for international research Epsilon study 5. Br J Psychiatry 2000;177:s28-33. https://doi.org/10.1192/bjp.177.39.s28.
- Curtis L. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS Reference Costs 2014–15. London: Department of Health and Social Care; 2015.
- Tucker S, Wilberforce M, Brand C, Abendstern M, Challis D. All things to all people? The provision of outreach by community mental health teams for older people in England: findings from a national survey. Int J Geriatr Psychiatry 2014;29:489-96. https://doi.org/10.1002/gps.4031.
- Shulman C, Hudson BF, Low J, Hewett N, Daley J, Kennedy P, et al. End-of-life care for homeless people: a qualitative analysis exploring the challenges to access and provision of palliative care. Palliat Med 2018;32:36-45. https://doi.org/10.1177/0269216317717101.
- Standard Occupational Classification. ONS; 2010.
- Crane M, Joly L, Manthorpe J. Rebuilding Lives: Formerly Homeless People’s Experiences of Independent Living and Their Longer-term Outcomes. London: NIHR Health and Social Care Workforce Research Unit, The Policy Institute, King’s College London; 2016.
- Table 7 Cigarette Smokers by Age Group by Country, 2010 to 2014. Newport: Office for National Statistics; 2015.
- Crawford S, Whitnall L, Robertson J, Evans JJ. A systematic review of the accuracy and clinical utility of the Addenbrooke’s Cognitive Examination and the Addenbrooke’s Cognitive Examination – Revised in the diagnosis of dementia. Int J Geriatr Psychiatry 2012;27:659-69. https://doi.org/10.1002/gps.2771.
- Factsheet Risk Factors for Dementia, Factsheet 450LP. Alzheimer’s Society; 2016.
- Homelessness: A Silent Killer. London: Crisis; 2011.
- Homelessness: Applying All Our Health. London: Public Health England; 2016.
- Culhane D, Metraux S, Byrne T, Stino M, Bainbridge J. The age structure of contemporary homelessness: evidence and implications for public policy. Anal Soc Issues Public Policy 2013;13:228-44. https://doi.org/10.1111/asap.12004.
- Homelessness Reduction Act 2017. London: The Stationery Office; 2017.
- Housing Act 1996. London: The Stationery Office; 1996.
- The Dementia and Veterans’ Supplement in Aged Care, Consultation Paper (April 2013) Wintringham’s Comments and Feedback. Melbourne, VIC: Wintringham; 2013.
- Canadian Homeless Research Network . Definition of Homelessness 2016. www.homelessresearch.net/canadian-definition-of-homelessness/ (accessed 11 June 2018).
- Glasby J, Robinson S, Allen K. Achieving Closure: Good Practice in Supporting Older People During Residential Care Closures. London: Adass; 2011.
- The State of the Adult Social Care Sector and Workforce in England, 2016. London: Skills for Care; 2016.
- The State of Adult Social Care Services 2014 to 2017. London: Care Quality Commission; 2017.
- Impact of Funding Reductions on Local Authorities. London: National Audit Office; 2014.
- Nowhere Safe to Stay: The Dangers of Sleeping Rough. London: St Mungo’s; 2016.
- Care Act 2014. London: The Stationery Office; 2014.
- Grenier A, Barken R, Sussman T, Rothwell D, Bourgeois-Guerin V, Lavoie JP. Homelessness and aging in Canada: defining the parameters of a policy and practice relevant research agenda. Can J Aging 2016;35:1-14. https://doi.org/10.1017/S0714980815000616.
- Snelling C. Right to Home? Rethinking Homelessness in Rural Communities. London: Institute for Public Policy Research; 2017.
- Stergiopoulos V, Cusi A, Bekele T, Skosireva A, Latimer E, Schütz C, et al. Neurocognitive impairment in a large sample of homeless adults with mental illness. Acta Psychiatr Scand 2015;131:256-68. https://doi.org/10.1111/acps.12391.
- User Guide: Reference Costs 2017/18. A Guide to Using the Data. London: NHS Improvement; 2018.
- PayScale . Average Pharmacist Salary n.d. www.payscale.com/research/UK/Job=Pharmacist/Salary (accessed 21 February 2019).
- Net Salary Calculator UK . Pharmacist Salary 2017 2019. www.netsalarycalculator.co.uk/pharmacist-salary/ (accessed 21 February 2019).
- C4 Sightcare . Optical Coherence Tomography (OCT) n.d. www.c4sightcare.com/page87aa.html (accessed 21 February 2019).
Appendix 1 Table summarising the 20 items included in the second literature review
| Author(s), year | Country | Methods | Study aims | Study population | Findings/content |
|---|---|---|---|---|---|
| Abdul-Hamid et al.,89 1998 | International | Literature review using three databases | To identify the needs of ‘elderly graduates’ (defined as people who started using mental health services before the age of 65 years and continue to do so) and models and methods of services they use | ‘Elderly graduates’ and their needs assessments | The review concluded that the needs of the ‘elderly graduates’ of mental health/psychiatric services are under-researched; this particularly applied to nursing home residents but also to the homeless. Questions that require further research have been highlighted |
| Andersen et al.,88 2014 | Canada | Quantitative and qualitative | To examine cognitive performance among a sample and compare cognitive performance between those with and those without traumatic brain injury; using qualitative methods to explore their situations | Sample of men (aged ≥ 18 years) from a residential unit – an urban homeless shelter (n = 34) | A history of TBI was associated with generally poorer cognitive performance in the study sample. Improved awareness of TBI and cognitive dysfunction among service providers is recommended |
| Backer and Howard,85 2007 | USA | Literature review and discussion paper | To examine the forms of cognitive impairment and how many homeless people are cognitively impaired | N/A | More research is needed to document the prevalence of cognitive impairment among people who are homeless and at risk of homelessness, about the origins and severity of their impairments, and about the consequences of these impairments for the effectiveness of the service process |
| Barak and Cohen,91 2003 | Israel | Examination of all elderly homeless people in Tel Aviv by a psychiatrist over a 10-year period | To characterise the ‘new’ homeless – defined as non-‘skid row’ | Over a 10-year period each homeless person aged ≥ 65 years was assessed by a psychiatrist (old number = 98; general homeless population number = 2567) | The main conclusion is that the ‘new’ elderly homeless are typically male and suffering from frequent psychiatric morbidity and physical comorbidity. Of the 44 who were diagnosed with a psychiatric disorder, 15 had dementia |
| Brown et al.,71 2012 | USA | Cross-sectional. 247 homeless people (aged 50–69 years) interviewed and examined. Known as project MUSE | To determine prevalence of common geriatric syndromes in a sample of older homeless adults and compare these with population-based cohorts | Population drawn from homeless facilities for single adults aged ≥ 50 years in Boston, MA | Cognitive impairment present in 24.3% of participants. Geriatric syndromes that are potentially amenable to treatment are common in older homeless adults, and are experienced at higher rates than in the general older population |
| Brown et al.,51 2013 | USA | Used multivariable regression models to estimate association of individuals’ characteristics with number of ‘geriatric syndromes’. Geriatric syndromes included falls, cognitive impairment, frailty, major depression, sensory impairment and urinary incontinence. Data had been collected in in-person interviews and physical examinations | To extend previous work describing prevalence of geriatric syndromes in cohort of 250 homeless people aged ≥ 50 years | As in Brown et al.,71 recruited from eight shelters (six emergency, five transitional, five day centres) in Boston, MA, serving single adults aged ≥ 50 years (of 387 eligible, 250 were recruited) | A higher total number of ‘geriatric syndromes’ was associated with having less than a high school education, medical comorbidities (diabetes mellitus and arthritis), alcohol and drug use problems, and difficulty performing one or more activities of daily living. Average MMSE score of 26; 61% scored < 24 in MMSE, indicating impairment. Overall high number of geriatric syndromes (e.g. falls in past year 53.4%; 41.6% mobility impaired; 49.1% sensory impairment) |
| Brown et al.,73 2017 | USA | Interviews with 350 homeless adults aged ≥ 50 years | As only a minimum of homeless adults stay in shelters, the prevalence of geriatric conditions among older homeless people in other environments is unknown; this study aimed to address this gap | Older homeless people in Oakland, CA, were recruited by population-based sampling from unsheltered locations; shelters/hostels; intermittent stayers with family/friends; and renters who were recently homeless | A total of 25.8% of interviewees had cognitive impairment. Geriatric conditions were common among older homeless adults living in diverse environments, and the prevalence of these conditions was higher than that seen in housed adults who are 20 years older |
| Buhrich et al.,68 2000 | Australia | 204 homeless adults were interviewed and assessed using the MMSE | To assess the prevalence of cognitive impairment among a cohort of homeless men and women in inner Sydney, NSW | A cohort of homeless men and women (n = 155/n = 49) were selected randomly from larger hostels in Sydney and assessed | 10% of sample showed evidence of cognitive impairment (prevalence of cognitive impairment in general adult population is 1.7%) |
| Conroy et al.,72 2013 | Australia | Data were collected on physical/mental health, alcohol use and acquired brain injury. Used MoCA and PRMQ and interviews with 11 key stakeholders | To conduct a pilot study to examine needs of older homeless people with a history of problematic alcohol use and cognitive decline | 50 people (aged ≥ 45 years) (39 male) who had been homeless within past 6 months were interviewed. Recruited from a centre and a clinic. Stakeholders were providers and professionals | Prevalence of mild cognitive impairment among the sample was high (i.e. 77%) |
| Depp et al.,75 2015 | US-based review of international literature | Literature review; items located through PubMed and PsycInfo from 1980 to 2013 | To estimate frequency of cognitive impairment among homeless populations | Found 24 studies measuring cognition in homeless adults | Among the 24 studies, there are indications that cognitive impairment is common among homeless adults and may be a ‘transdiagnostic’ problem. Average prevalence of cognitive impairment was about 5–8 times greater than the rate of cognitive impairment in the US population aged > 70 years (mean age across the samples was 46.1 years). Notes lack of data on women and the ‘unsheltered’ population |
| Ennis et al.,62 2015 | Canadian-based review of the international literature | Systematic review using MEDLINE and CINAHL (excluded studies only using MMSE assessment) | To systematically review literature on memory deficits among homeless people to gain better understanding of their nature, causes and prevalence | All age groups studied. Notes that of 11 studies the mean age of participants was 40–75 years (the range 30–58 years = mean) | Identifies 11 studies of memory deficits among people who are homeless and of all adult ages. Across the studies, memory deficits were common among the samples of homeless persons studied. However, conclusions difficult to draw because of variation in measures used to assess |
| Gilchrist and Morrison,57 2005 | Scotland | Used ACE to assess prevalence of ARBD in hostel-stayers | To assess prevalence of ARBD among homeless people staying in hostels | Survey of 266 homeless people staying in hostels in Glasgow (Scotland). Mean age 53 years (95% CI 51 to 54 years) | 82% of sample had cognitive impairment. Prevalence of ARBD was 21%. Hostel-dwellers were aged ≥ 34 years |
| Joyce and Limbos,24 2009 | Canada | Cross-sectional study; used MMSE and Geriatric Depression Scale | To describe occurrence of mental health problems and cognitive impairment in a group of older homeless men and how clinical examination and screening in a shelter context might help with their identification | 49 homeless men aged ≥ 55 years in a homeless shelter in Toronto, ON | Of the 29 men who were assessed, 37.9% had cognitive impairment |
| Nishio et al.,76 2015 | Japan | Semistructured interviews conducted by psychiatrists. Wechsler Adult Intelligence Scale used to diagnose intellectual/cognitive disability | To comprehensively address the prevalence of mental illness and cognitive disability and their overlap in a homeless population in Nagoya (fourth largest city in Japan) | 114 homeless people, 84% aged > 50 years (age range 20–78 years; mean 44 years), were assessed in Nagoya. Recruited in co-operation with local support centre that had proposed the study with other voluntary sector providers. An earlier study had reported high prevalence of mental illness, cognitive disability and their overlap but was limited to 18 participants | 34.2% of whole sample demonstrated cognitive disability (for half this was likely to be congenital; for the other half this had come later in life); 42% had mental illness. This is much higher than in the general population. Some of the cognitively impaired group did not seem likely to take up support leading to leaving their homeless life. High rates of smoking, drinking alcohol and gambling were noted relative to participants’ limited incomes |
| Rogoz and Burke,50 2016 | Australia | Screening for cognitive impairment with MMSE | To determine prevalence and characteristics of cognitive impairment in older homeless people in inner Sydney | 144 men and 27 women aged 45–93 years were screened; those with MMSE scores of ≤ 26 undertook a semistructured interview | 78% of sample manifested cognitive impairment |
| Rota-Bartelink,25 2009 | Australia | Evidence review in homelessness sector journal mentioning the ongoing Wicking Project in Melbourne, VIC | To explore the influence of cognitive capacity on the efficacy of early intervention and prevention strategies among older homeless people | General homelessness with focus on experience of Melbourne services | General account of significance of cognitive impairment among homeless people, appropriate instruments for assessing it and strategies for supporting people with it |
| Rota-Bartelink and Lipmann,60 2010 | Australia | Description of intervention (the Wicking Project, a specialist residential care project using a psychosocial model of care) with older people with alcohol-related brain injury and associated complex behaviours | Outlines the aim of the Wicking Project: to provide services with opportunity to develop and trial a specialist service for older homeless men and women aged ≥ 50 years. Sets out service values and operating processes (e.g. rules of the residential care facility) | Descriptive report of the residential model used in the Wicking Project (in Melbourne) and its clientele | Discussion of the synthesis, design and key features of the Wintringham model. Mentions that Wicking trial was completed in 2009 |
| Stergiopoulos and Herrmann,77 2003 | International review and survey in Canada | Literature review using MEDLINE, AgeLine and PsycINFO; survey of directors of shelters in Toronto, ON; analysis of shelter-use data for Toronto | Survey of 11 hostel directors (eight responses) seeking information of reasons for clients’ shelter use, problem behaviours and mental health needs. Reporting of data and some secondary data analysis of shelter usage completed from 1997 (start of this data collection) | Studies reviewed indicate high prevalence of mood and psychotic disorders and cognitive impairment among older homeless people. Service use data showed that about 2% of Toronto’s shelter users are aged ≥ 65 years (= about 450 people annually). Homeless older people are most vulnerable of shelter users. Geriatric psychiatrists should play a more active role with this population | |
| Stergiopoulos et al.,122 2015 | Canada | Assessment of 1500 homeless adults enrolled in the At Home/Chez Soi study (homeless people with mental illness) who provided neuropsychological, sociodemographic and clinical information. Analysis using linear regression to examine factors associated with neurocognitive performance | To characterise neurocognitive performance of large sample of homeless people with mental illness using a battery of tests and to test hypothesis that psychosis, alcohol abuse/dependence, history of traumatic brain injury and longer homeless would be associated with greater neurocognitive deficits | Sample recruited from a multisite (five sites across Canada) randomised controlled trial of a Housing First intervention in Canada. Mean age of sample was 41 years (SD 10.9 years). 67.3% were male; 31.8% were female | Overall, 72% of participants demonstrated neurocognitive impairment and 71% experienced problems with verbal learning and 67% with recall; 38% experienced problems with executive functioning |
| Teesson and Buhrich,66 1993 | Australia | Cognitive assessment of hostel residents, one-quarter of whom were randomly selected and asked to complete the MMSE and a schizophrenia assessment | To establish prevalence of cognitive impairment in a representative sample of residents of a large refuge for homeless men in Sydney | In the sample from the hostel containing 450 beds for male residents, 185 completed the MMSE | Of the sample residents, 28% (n = 18) had severe cognitive impairment (mean age 57 years, SD 10.7 years) and 13% (n = 10) had mild cognitive impairment (mean age 59 years, SD 7.8 years). The mean age of the cognitively impaired group was 55 years |
Appendix 2 Unit costs used in the costing analysis
| Service | Unit cost (£) | Source |
|---|---|---|
| Visit GP at surgery | 44/visit | PSSRU98 section 10.8b, general practitioner – unit costs – £44 per patient contact lasting 11.7 minutes, length of a consultation at surgery |
| See GP at hostel | 70.75/visit | PSSRU98 sections 10.8a and 10.8b, general practitioner – cost elements and unit costs, respectively – £225 per hour of patient contact for 11.4 minutes, length of a home visit consultation, plus £140 per hour of General Medical Services activity for 12 minutes, average travel time per home visit |
| Speak to GP over telephone | 27/call | PSSRU98 section 10.8b, general practitioner – unit costs – £27 per telephone consultation lasting 7.1 minutes |
| Visit nurse (non-psychiatric) at surgery | 14.50/visit | PSSRU98 section 10.6, nurse (GP practice) – £56 per hour of face-to-face contact lasting 15.5 minutes, duration of surgery consultation |
| See nurse (non-psychiatric) at hostel | 27.30/visit | PSSRU98 section 10.1, community nurse – £67 per hour of patient-related work lasting 15.5 minutes, assumed consultation length, plus £50 per hour lasting 12 minutes, assumed travel time |
| Speak to nurse (non-psychiatric) over telephone | 7.90/call | PSSRU98 section 10.1, community nurse – £67 per hour of patient-related work lasting 7.1 minutes, assumed consultation length |
| See nurse (psychiatric) at hostel | 45.50/visit | PSSRU98 section 10.2, nurse (mental health) – £75 per hour of face-to-face contact lasting 30 minutes, assumed consultation length, plus £40 per hour lasting 12 minutes, assumed travel time |
| Use care navigator at GP practice | 14.50/use | PSSRU98 section 10.6, nurse (GP practice) – £56 per hour of face-to-face contact lasting a duration of 15.5 minutes |
| Use health trainer at GP practice | 14.50/use | PSSRU98 section 10.6, nurse (GP practice) – £56 per hour of face-to-face contact lasting a duration of 15.5 minutes |
| Visit AHP clinic | 19/visit | PSSRU98 section 13.2, hospital occupational therapist – £38 per hour with an assumed consultation length of 30 minutes |
| See AHP at hostel | 22/visit | PSSRU98 section 11.5, community occupational therapist (local authority) – £44 per hour lasting an assumed consultation length of 30 minutes |
| Use AHP day centre (half-days) | 28/half day | PSSRU98 section 2.4, local authority social services day care for people with mental health problems – £28 per client session lasting 3.5 hours |
| Use AHP day centre (full days) | 56/day | PSSRU98 section 2.4, local authority social services day care for people with mental health problems – £28 per client session lasting 3.5 hours, assume a full day lasts 7 hours |
| Visit walk-in clinic | 85/visit | NHS Reference Costs99 – service code T02NA, currency code VB11Z (emergency medicine, no investigation with no significant treatment). Use national average unit cost of £85 |
| Visit urgent care centre | 85/visit | NHS Reference Costs99 – service code T02NA, currency code VB11Z (emergency medicine, no investigation with no significant treatment). Use national average unit cost of £85 |
| Visit A&E but not admitted | 140.59/visit | NHS Reference Costs99 – total outpatient attendances, service code 180 (A&E). Use ‘total’ unit cost of £140.69 |
| In-hospital stay (non-psychiatric) | NHS Reference Costs99 – non-elective (admitted via A&E) and elective (otherwise) long stays. If the stay was at or below the trim point, a cost per day was applied, calculated by dividing the national average unit cost by the average length of stay (days). If the stay was over the trim point, the ‘spell cost’ (national average unit cost) was used plus an excess bed-day cost for each day beyond the trim point.a For specific costs, see Table 38 | |
| In-hospital stay (psychiatric) | NHS Reference Costs99 – mental-health-care clusters – unit cost per occupied bed-day. For specific costs refer to Table 38 | |
| Day cases in hospital | 704/day case | PSSRU98 section 7.1, NHS reference costs for hospital services – national average of day cases, weighted average of all stays (£704) |
| Use intermediate care unit (post hospital discharge) | 119/day | NHS Reference Costs99 – service code IC, currency code IC01 (intermediate care, crisis response and early discharge services). Use national average unit cost of £119 |
| Attend outpatient consultation (non-psychiatric) | 118/visit | PSSRU98 section 7.1, NHS Reference Costs99 for hospital services – national average of consultant-led outpatient attendances (£118) |
| Attend outpatient consultation (psychiatric) | 118/visit | PSSRU98 section 7.1, NHS Reference Costs99 for hospital services – national average of consultant-led outpatient attendances (£118) |
| Have outpatient treatment | See Table 37 | |
| Have outpatient test | ||
| Use ambulance | 99/use | PSSRU98 section 7.1, NHS Reference Costs99 for hospital services – national average of all ambulance services (£99) |
| Attend alcohol services | 122/visit | PSSRU98 section 2.1, NHS Reference Costs99 for mental health services – mean of alcohol services – community (per care contact) (£122) |
| Attend alcohol/drug services | 123/visit | PSSRU98 section 2.1, NHS Reference Costs99 for mental health services – combination of alcohol (£122) and drug (£124) services |
| Attend drug services | 124/visit | PSSRU98 section 2.1, NHS Reference Costs99 for mental health services – mean of drug services – community (per care contact) (£124) |
| Use community pharmacist (for supervised opiate substitute) | 7.58/visit | PSSRU98 section 10.7, advanced nurse (similar salariesb) – £91 per hour of client contact with an assumed visit duration of 5 minutes |
| Use social worker | 39.50/use | PSSRU98 section 11.2, social worker (adult services) – £79 per hour of client-related work lasting 30 minutes, assumed duration |
| Have carer visit hostel, arranged by social services | 12/visit | PSSRU98 section 11.6, home care worker – £24 per hour weekday of face-to-face contact, assuming 30 minutes duration per visit |
| Visit dentist | 51.30/visit | PSSRU98 section 10.12, NHS dental charges – band 2 treatment (£51.30) |
| Visit chiropodist | 40/visit | NHS Reference Costs99 – service code AHP, currency code A09A (Podiatrist, Tier 1, General Podiatry). Use national average unit cost of £40 |
| Visit optician | 63.90/visit | NHS Reference Costs99 – total outpatient attendances, service code 130 (ophthalmology). Use non-consultant unit cost of £63.91 |
| Use community mental health services crisis team | 189/use | PSSRU98 section 12.3, crisis resolution team for adults with mental health problems – mean average cost for a crisis resolution team per team contact (£189) |
| Receive counselling | 42/use | PSSRU98 section 12.1, NHS CMHT for older people with mental health problems – £42 per hour per team member where duration of a visit is 60 minutes |
| Use older people’s mental health team | 42/use | PSSRU98 section 12.1, NHS CMHT for older people with mental health problems – £42 per hour per team member where duration of a visit is 60 minutes |
| Use memory service visiting at hostel | 42/use | PSSRU98 section 12.1, NHS CMHT for older people with mental health problems – £42 per hour per team member where duration of a visit is 60 minutes |
| Phone out-of-hours call handler | 7/call | PSSRU98 section 7.1, NHS Reference Costs99 for hospital services – national average of calls within ambulance services (£7) |
| Phone NHS 111 | 7/call | PSSRU98 section 7.1, NHS Reference Costs99 for hospital services – national average of calls within ambulance services (£7) |
| Have voluntary helper as advocate for health appointments | 20/use | PSSRU98 section 10.5, clinical support worker nursing (community) – £20 per hour with an assumed duration of 60 minutes |
| Outpatient treatment/test | Unit cost (£) | Directory | Description |
|---|---|---|---|
| Treatment | |||
| Diabetes mellitus prevention group | 111.19 | Total Outpatient Attendances – Service code 307 | Diabetic medicine – non-consultant |
| Dysport® (Galderma Laboratories) injections, Botulinum toxin clinic | 133.98 | Total Outpatient Attendances – Service code 400 | Neurology – non-consultant |
| Laser treatment to hair on face | 78.94 | Total Outpatient Attendances – Service code 160 | Plastic surgery – non-consultant |
| Cast fitted to fractured leg | 92.47 | Total Outpatient Attendances – Service code 110 | Trauma and orthopaedics – non-consultant |
| Cardiac rehabilitation | 60.68 | Total Outpatient Attendances – Service code 327 | Cardiac rehabilitation – non-consultant nt |
| Cardiac dietary advice | 93.05 | Total Outpatient Attendances – Service code 327 | Cardiac rehabilitation – consultant led |
| Cardiac exercise programme | 60.68 | Total Outpatient Attendances – Service code 327 | Cardiac rehabilitation – non-consultant |
| Fitted leg brace | 92.47 | Total Outpatient Attendances – Service code 110 | Trauma and orthopaedics – non-consultant |
| Fitting of shoes, orthotics | 129.57 | Total Outpatient Attendances – Service code 658 | Orthotics – consultant led |
| Collecting shoes from orthotics | 112.04 | Total Outpatient Attendances – Service code 658 | Orthotics – non-consultant |
| Test | |||
| Abdominal aortic screening (ultrasound) | 55 | Diagnostic Imaging – Department code IMAGOP – Currency Code RD40Z | Ultrasound scan with duration of < 20 minutes, without contrast (duration and contrast assumed) – national average |
| Blood test | 3.46 | Total Other Currencies – Currency code DAPS08 | Phlebotomy – ‘total’ unit cost |
| Chest X-ray | 17 | Non Consultant Led – Currency code WF01D | Service code 811 – interventional radiology – national average unit cost |
| CT scan | 93 | Diagnostic Imaging – Department code IMAGOP – Currency Code RD20A | CT scan of one area, without contrast, ≥ 19 years (contrast assumed) – national average |
| MRI scan | 137 | Diagnostic Imaging – Department code IMAGOP – Currency code RD01A | MRI scan of one area, without contrast, ≥ 19 years (contrast assumed) – national average |
| Bronchoscopy | 98 | Outpatient Procedures – Service code 120 – Currency code DZ69A | Diagnostic bronchoscopy, ≥ 19 years – national average |
| Retinopathy screening | 117 | Outpatient Procedures – Service code 130 – Currency code BZ89A | Digital retinal photography, ≥ 19 years – national average |
| Abdomen ultrasound | 60 | Diagnostic Imaging – Department code IMAGOP – Currency code RD42Z | Ultrasound scan with duration of ≥ 20 minutes, without contrast (duration and contrast assumed) – national average |
| Bladder ultrasound | 55 | Diagnostic Imaging – Department code IMAGOP – Currency Code RD40Z | Ultrasound scan with duration of < 20 minutes, without contrast (duration and contrast assumed) – national average |
| Testicle ultrasound | 55 | Diagnostic Imaging – Department code IMAGOP – Currency Code RD40Z | Ultrasound Scan with duration of < 20 minutes, without contrast (duration and contrast assumed) – national average |
| Eye slit lamp screening | 88.56 | Total Outpatient Attendances – Service code 662 | Service description optometry – ‘total’ unit cost |
| Flexible cystoscopy | 167 | Outpatient Procedures – Service code 100 – Currency code LB72A | Diagnostic flexible cystoscopy, ≥ 19 years – national average |
| OCT of maculae (eye) | 35a | ||
| Leg ultrasound to check for DVT | 61 | Diagnostic Imaging – Department code IMAGOP – Currency code RD43Z | Ultrasound scan with duration of ≥ 20 minutes, with contrast (duration and contrast assumed) – national average |
| Endoscopy | 223 | Outpatient Procedures – Service code 100 – Currency code FZ42A | Wireless capsule endoscopy, ≥ 19 years – national average |
| Breast ultrasound (gynaecomastia) | 60 | Diagnostic Imaging – Department code IMAGOP – Currency code RD42Z | Ultrasound scan with duration of ≥ 20 minutes, without contrast (duration and contrast assumed) – national average |
| X-ray of hip and knee | 17 | Non Consultant Led – Currency code WF01D | Service code 811 – interventional radiology – national average unit cost |
| Mammogram | 33.98 | Total HRG – Currency code WH15Z | Special screening, examinations or other genetic disorders – ‘total’ unit cost |
| In-hospital stay | Further description | Currency description (code) | Cost per day (spell) (£)a |
|---|---|---|---|
| Non-elective | |||
| Epigastric bleeding | Following recent alcohol binge | Gastrointestinal bleed without interventions – average of all CC scores (FZ38M-FZ38P) | 406.94 |
| COPD exacerbation | COPD of bronchitis, without Interventions – average of all CC scores (DZ65F-DZ65J) | 373.83 | |
| Admitted to HDU | Participant shouting at receptionist, police involved | Admission related to social factors without interventions – average of all CC scores (WH17B-WH17C) | 430.43 |
| Transient ischaemic attack | Transient ischaemic attack – average of all CC scores (AA29C-AA29F) | 434.35 | |
| Thrombus | Acute cholecystitis | Deep-vein thrombosis – average of all CC scores (YQ51A-YQ51E) | 253.91 (2763) |
| Seizure | From alcohol withdrawal | Muscular, balance, cranial or peripheral nerve disorders, epilepsy or head injury, with CC score 0–2 (AA26H) | 441.33 |
| COPD exacerbation and congestive cardiac failure | COPD or bronchitis, without Interventions – average of all CC scores (DZ65F–DZ65J)/heart failure or shock– average of all CC scores (EB03A–EB03E) (average taken of both) | 388.49 | |
| Scabies and cellulitis | Skin disorders without Interventions – average of all CC scores (JD07E-JD07K) | 382.31 | |
| Elective | |||
| Respiratory unit | Respiratory failure | Respiratory failure without interventions – average of all CC scores (DZ27S-DZ27U) | 634.15 |
| Fractured leg/ankle | Problem related to the fracture | Foot fracture without interventions – average of all CC scores (HE31D-HE31G) | 371.93 |
| Psychiatric | |||
| Psychiatric hospital | Cluster 03: non-psychotic (moderate severity) (MHCC03) | 345 | |
Appendix 3 Frequency of use of services over a 6-month period
| Service group | Number of . . . | Number of times, n (%) | Notesa | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2–4 | 5–10 | 11–25 | 26–75 | 76–150 | ≥ 151 | |||
| GP | GP appointments made at surgery | 17 (36.2) | 5 (10.6) | 15 (31.9) | 8 (17.0) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 15.9% DNA |
| GP appointments made at hostel | 27 (57.5) | 4 (8.5) | 6 (12.8) | 8 (17.0) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2.0% DNA | |
| Contacts with GP by telephone | 31 (66.0) | 5 (10.6) | 3 (6.4) | 6 (12.8) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Other GP | Non-psychiatric nurse appointments made at surgery | 32 (68.1) | 6 (12.8) | 8 (17.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5.9% DNA |
| Non-psychiatric nurse appointments at hostel | 33 (70.2) | 7 (14.9) | 4 (8.5) | 2 (4.3) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 1.1% ‘accompany’ | |
| Contacts with non-psychiatric nurse by telephone | 45 (95.7) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Contacts with care navigator at GP practice | 46 (97.9) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Contacts with health trainer at GP practice | 46 (97.9) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Other primary | Dentist visits | 41 (87.2) | 2 (4.3) | 3 (6.4) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Chiropody appointments made | 28 (59.6) | 5 (10.6) | 11 (23.4) | 3 (6.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 16.1% DNA | |
| Optician appointments made | 28 (59.6) | 14 (29.8) | 5 (10.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3.8% DNA | |
| Community psychiatric/mental health | Contacts with psychiatric nurse at hostel | 45 (95.7) | 1 (2.1) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Community mental health services crisis team | 44 (93.6) | 3 (6.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Counselling/psychotherapy appointments made | 41 (87.2) | 1 (2.1) | 2 (4.3) | 1 (2.1) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 8.1% DNA; 2.7% ‘elsewhere’ | |
| Older people’s mental health team | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Memory service visiting at hostel | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Alcohol and drugs | Bookings made for alcohol services | 35 (74.5) | 4 (8.5) | 4 (8.5) | 1 (2.1) | 1 (2.1) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 1.0% were DNAs |
| Bookings made for alcohol/drug services | 43 (91.5) | 2 (4.3) | 0 (0.0) | 1 (2.1) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10.5% were DNAs | |
| Contacts with drug services | 45 (95.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 1 (2.1) | 0 (0.0) | 0 (0.0) | ||
| Community pharmacist (opiate substitute) | 45 (95.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 1 (2.1) | ||
| Social care | Appointments made with AHP at clinic | 41 (87.2) | 4 (8.5) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 44.4% were DNAs |
| Contacts with AHP at hostel | 44 (93.6) | 2 (4.3) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Social worker/care manager | 39 (83.0) | 4 (8.5) | 3 (6.4) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Social service carer visiting at hostel (hours) | 30 (63.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 7 (14.9) | 4 (8.5) | 5 (10.6) | ||
| Half day at AHP centre | 46 (97.9) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Full day at AHP centre | 42 (89.4) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 2 (4.3) | 1 (2.1) | 0 (0.0) | ||
| Emergency and out of hours | Walk-in clinic visit | 43 (91.5) | 4 (8.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Urgent care centre visit | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| A&E but not admitted | 35 (74.5) | 6 (12.8) | 5 (10.6) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Ambulance trips | 30 (63.8) | 7 (14.9) | 7 (14.9) | 3 (6.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Out-of-hours call handler | 41 (87.2) | 5 (10.6) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| NHS 111 service | 41 (87.2) | 5 (10.6) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Hospital outpatient | Non-psychiatric OP consultations made | 25 (53.2) | 7 (14.9) | 11 (23.4) | 3 (6.4) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 27.1% were DNAs |
| Attendances to psychiatric OP consultation | 42 (89.4) | 4 (8.5) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| OP treatment | 40 (85.1) | 2 (4.3) | 4 (8.5) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| OP test appointments made | 31 (66.0) | 6 (12.8) | 9 (19.2) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 15.8% were DNAs | |
| Hospital inpatient | Day cases (in-hospital) | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Days’ intermediate care (post hospital discharge) | 46 (97.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Admissions, in-hospital stay (psychiatric) | 46 (97.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Admissions, in-hospital stay (non-psychiatric) | 39 (83.0) | 7 (14.9) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Nights in other (psychiatric in-hospital stay) | 46 (97.9) | 0 (0.0) | 0 (0.0) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Nights in other (non-psychiatric in-hospital stay) | 39 (83.0) | 3 (6.4) | 1 (2.1) | 1 (2.1) | 2 (4.3) | 1 (2.1) | 0 (0.0) | 0 (0.0) | ||
| Voluntary | Voluntary service advocate for appointments | 41 (87.2) | 1 (2.1) | 3 (6.4) | 2 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
Appendix 4 Associations between service use costs and cognitive impairment grouping
| Service | Cognitive impairment group | Cost (£) of services per participant in months 1–6 | Kruskal–Wallis test | Mann–Whitney U-test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Quartile 1 | Median | Quartile 3 | n (%) zeroa | Mean | p-value | Rankingb | None vs. (borderline and present) | (None and borderline) vs. present | ||
| GP services | None | 79.50 | 212.25 | 330.88 | 2 (11.8) | 225.10 | 0.191 | N/A | 0.071 | 0.139 |
| Borderline | 132 | 212.50 | 912.75 | 0 (0) | 397.96 | |||||
| Present | 132 | 331 | 610 | 1 (4.3) | 375.47 | |||||
| Other GP staff contacts | None | 7.25 | 54.60 | 85.85 | 4 (23.5) | 153.28 | 0.012c | None > borderline, presentc |
0.006 None > borderline and presentc |
0.212 |
| Borderline | 0 | 0 | 27.30 | 5 (71.4) | 7.80 | |||||
| Present | 0 | 14.50 | 29 | 10 (43.5) | 21.25 | |||||
| Other primary (chiropodist, dentist, optician) | None | 0 | 63.90 | 163.90 | 5 (29.4) | 107.10 | 0.888 | N/A | 0.875 | 0.845 |
| Borderline | 0 | 40 | 120 | 2 (28.6) | 86.64 | |||||
| Present | 0 | 80 | 183.90 | 8 (34.8) | 95.32 | |||||
| Psychiatric/mental health services | None | 0 | 0 | 0 | 14 (82.4) | 30.88 | 0.650 | N/A | 0.355 | 0.462 |
| Borderline | 0 | 0 | 126 | 5 (71.4) | 51 | |||||
| Present | 0 | 0 | 42 | 16 (69.6) | 77.30 | |||||
| Alcohol and drugs services | None | 0 | 0 | 612.50 | 9 (52.9) | 443.33 | 0.406 | N/A | 0.249 | 0.189 |
| Borderline | 0 | 0 | 244 | 4 (57.1) | 662.43 | |||||
| Present | 0 | 0 | 122 | 16 (69.6) | 375.24 | |||||
| Social care services | None | 0 | 0 | 1120.50 | 10 (58.8) | 912.15 | 0.706 | N/A | 0.423 | 0.455 |
| Borderline | 0 | 22 | 1086 | 3 (42.9) | 528.50 | |||||
| Present | 0 | 331 | 1131.50 | 10 (43.5) | 750.59 | |||||
| Emergency and out-of-hours services | None | 0 | 0 | 106 | 12 (70.6) | 59.75 | 0.158 | N/A | 0.059 | 0.101 |
| Borderline | 0 | 0 | 732.77 | 4 (57.1) | 290.96 | |||||
| Present | 0 | 99 | 345.59 | 9 (39.1) | 226.12 | |||||
| Hospital outpatient services | None | 0 | 67.96 | 301.92 | 8 (47.1) | 257.35 | 0.286 | N/A | 0.215 | 0.803 |
| Borderline | 55 | 472 | 690.94 | 1 (14.3) | 431.08 | |||||
| Present | 0 | 118 | 510 | 6 (26.1) | 261.04 | |||||
| Hospital inpatient services | None | 0 | 0 | 0 | 15 (88.2) | 194.71 | 0.174 | N/A | 0.342 | 0.698 |
| Borderline | 0 | 0 | 9951.38 | 4 (57.1) | 3058.12 | |||||
| Present | 0 | 0 | 0 | 19 (82.6) | 434.18 | |||||
| All services | None | 485.53 | 1173.75 | 3923.67 | 0 (0) | 2389.54 | 0.312 | N/A | 0.288 | 0.966 |
| Borderline | 905.80 | 2907.86 | 12,231.90 | 0 (0) | 5520.21 | |||||
| Present | 831.30 | 1546.05 | 4321.92 | 0 (0) | 2633.90 | |||||
| All psychiatric servicesd | None | 0 | 0 | 63 | 13 (76.5) | 58.65 | 0.683 | N/A | 0.414 | 0.418 |
| Borderline | 0 | 0 | 126 | 5 (71.4) | 396 | |||||
| Present | 0 | 0 | 118 | 14 (60.9) | 97.83 | |||||
Appendix 5 Characteristics of 47 participants in the economic analysis and associations (p-values) between them
| Characteristic | Mean | SD | Characteristic (p-valuea) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age when first interviewed | Number of comorbidities | Total number of head injuries | Number of different medications | Sex | Ethnicity | Literacy problems | Illegal drug use | Memory problems: yes/(borderline and no) | Memory problems: (yes and borderline)/no | Location | How often participant drinks alcohol | |||
| Age when first interviewed (years) | 59.3 | 7.77 | 0.904 | 0.083 | 0.841 | 0.242 | 0.159 | 0.212 | 0.732 | 0.495 | 0.218 | 0.714 | 0.879 | |
| Number of comorbidities | 5.28 | 2.36 | 0.904 | 0.099 | < 0.0005b | 0.88 | 0.07 | 0.865 | 0.173 | 0.129 | 0.937 | 0.782 | 1 | |
| Total number of head injuries | 1.4 | 1.75 | 0.083 | 0.099 | 0.015b | 0.167 | 0.075 | 0.169 | 0.024b | 0.629 | 0.406 | 0.054 | 0.238 | |
| Number of different medications | 7.4 | 4.74 | 0.841 | < 0.0005b | 0.051b | 0.287 | 0.144 | 0.684 | 0.963 | 0.74 | 0.349 | 0.186 | 0.073 | |
| Sex, male (vs. female) | 42 | 89.4 | 0.242 | 0.88 | 0.167 | 0.287 | 1c | 1c | 0.648c | 0.348c | 0.051c | 1c | 1c | |
| Ethnicity: white British (vs. other) | 37 | 78.7 | 0.159 | 0.07 | 0.075 | 0.144 | 1c | 0.068c | 0.704c | 1c | 0.46c | 0.019b,c | 0.496c | |
| Literacy problems: yes (vs. no) | 16 | 34.0 | 0.212 | 0.865 | 0.169 | 0.684 | 1c | 0.068c | 0.211 | 0.051 | 0.074 | 0.164 | 0.769 | |
| Illegal drug use in last 3 months: yes (vs. no) | 15 | 31.9 | 0.732 | 0.173 | 0.024b | 0.963 | 0.648c | 0.704c | 0.211 | 0.831 | 0.305 | 0.742c | 0.968 | |
| Memory problems: yes (vs. borderline and no) | 23 | 48.9 | 0.495 | 0.129 | 0.629 | 0.74 | 0.348c | 1c | 0.051 | 0.831 | <0.0005b | 0.831 | 0.859 | |
| Memory problems: no (vs. borderline and yes) | 17 | 36.2 | 0.218 | 0.937 | 0.406 | 0.349 | 0.051c | 0.46c | 0.074 | 0.305 | <0.0005b | 0.708 | 0.485 | |
| Location: North (vs. South/London) | 15 | 31.9 | 0.714 | 0.782 | 0.054 | 0.186 | 1c | 0.019b,c | 0.164 | 0.742c | 0.831 | 0.708 | 0.012b | |
| How often participant drinks alcohol: < 6 (vs. 6 or 7) times a week | 19 | 40.4 | 0.879 | 1 | 0.238 | 0.073 | 1c | 0.496c | 0.769 | 0.968 | 0.859 | 0.485 | 0.012b | |
Appendix 6 Hostel resident baseline interview
Appendix 7 Hostel resident case study interview at 3 and 6 months
Appendix 8 Hostel staff case roles and experiences
Appendix 9 Hostel manager interview
List of abbreviations
- 6-CIT
- Six-Item Cognitive Impairment Test
- ACE
- Addenbrooke’s Cognitive Examination
- ACE-III
- Addenbrooke’s Cognitive Examination III
- ACE-R
- Addenbrooke’s Cognitive Examination tool version R
- A&E
- accident and emergency
- ARBD
- alcohol-related brain damage
- CMHT
- community mental health team
- DNA
- did not attend
- GP
- general practitioner
- MMSE
- Mini Mental State Examination
- MoCA
- Montreal Cognitive Assessment
- NVQ
- National Vocational Qualification
- QoL
- quality of life
- SD
- standard deviation
- SW
- support worker
