Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/04/25. The contractual start date was in January 2016. The final report began editorial review in March 2019 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Steve Goodacre is chairperson of the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme Commissioning Committee (2019 to present), deputy director of the HTA programme (2019–present), a member of the HTA Funding Boards Policy Group (2016 to present) and chairperson of the NIHR Clinical Trials Unit Standing Advisory Committee (2019 to present).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Moore et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
The consumption of alcohol causes impairment and, at excessive levels, increased vulnerability to such an extent that medical assistance may be required. 1,2 Alcohol is typically consumed during weekend evenings and at socially significant events. 3 In the UK, alcohol-related emergency department (ED) attendances are accordingly most common around midnight and on Friday and Saturday evenings,4 at which times 70% of all ED attendees are likely to have consumed alcohol. 5–7 At other times it is estimated that 8–15% of ED attendances in the UK are alcohol related. 5,8–10 Approximately 40% of all alcohol-related attendees arrive by ambulance,6 accounting for 3.2% of all ambulance call-outs. A UK study6 found that the most common treatments given during alcohol-related attendances in ED were fluids (67.7%; e.g. saline drip), thiamine hydrochloride (47.9%; to offset malnourishment, which is often comorbid with dependent alcohol use), benzodiazepines (43.6%; for aggression, suicidal ideation, delirium tremens or as a prophylaxis) and, highlighting the airway risks associated with acute alcohol intoxication (AAI), endotracheal intubation (1.3%). Furthermore, 23.2% of patients received some form of radiography, 20.3% received an electrocardiogram and 12.3% received a computed tomography scan of their brain. AAI is preventable but, because of its risks to health, it can require urgent medical attention.
Emergency departments provide specialist health care; therefore, AAI cases will often transit to EDs. This has consequences for the ED environment and ED staff. A survey of 325 emergency care consultants found that 35% felt at risk of physical assault during nightshifts, 42% had been assaulted by someone who was intoxicated one or more times and respondents estimated that 25% of their time was given over to dealing with alcohol-related incidents. Furthermore, a survey of US nurses found that 70% had experienced verbal or physical violence, over half the perpetrators had experienced prolonged waiting times and nearly 70% of the perpetrators were intoxicated. 11 Two of the most prominent predictors of violence in EDs are intoxicated patients and long patient waiting times. 12–16 AAI therefore contributes to a range of related factors that detract from health-care efficiency, including aggression and violence towards staff, increased waiting times and increased use of resources. The effects can induce stress and occupational burnout in ED staff, and other patients can wait longer and experience prolonged pain and reduced satisfaction of care. 16,17
The effects of AAI can also extend beyond the ED, with ambulance services experiencing reduced efficiency. 16 A report ordered by the House of Commons on NHS ambulance services contained the observation that ‘[d]elays in handing over patients from ambulances to hospitals lead to poor patient experience and reduced capacity in ambulance services’ (contains Parliamentary information licensed under the Open Parliament Licence v3.0). 18 Over one-fifth of patient handovers from ambulance crews to ED staff at hospitals take longer than the recommended 15 minutes. If ambulances are queuing at hospitals, they are not available to take other calls, potentially affecting the health of others in the broader community.
Alcohol intoxication management services (AIMSs) (occasionally referred to as alcohol recovery centres, alcohol treatment centres, drunk tanks, safe havens, sobering-up centres, SOS buses or welfare centres) are designed to receive intoxicated patients who would normally attend EDs and, in so doing, lessen the burden that AAI places on emergency services. They are typically located close to areas characterised by excessive intoxication and are open at times when levels of intoxication peak. AIMSs are expected to provide a safe environment in which the intoxicated can be assessed, monitored and treated or referred to EDs as required. They are usually developed through partnerships that include local government, police and health-care services and other agencies that are affected by the problem of AAI. The primary goal is usually to safely divert as many AAI attendees away from EDs as possible and so improve the provision of care in EDs, and provide a facility where police, ambulance and other services can quickly hand over patients to clinical staff. 13
Responses to acute alcohol intoxication around the world
The issues surrounding AAI are not unique to the UK and AIMS-like services have emerged elsewhere. Estimates suggest that the percentage of all ED attendances that are alcohol-related is 1.2% in Belgium,6 2.9% in North America,19 4.5% in Australia20 and 12–15% in the UK. 5,8 The earliest examples of AIMSs are found in Russia. 21,22 As far back as the 18th century there were rooms allocated for sobering up in the quarters of at least one of Russia’s cavalry regiments. However, it was economic concerns over the number of workers who became intoxicated, fell over and died of hypothermia in the Moscow winter that motivated the implementation of vytrezvitels (sobering-up stations) in 1902. 21 By 1959, the number of sobering-up stations, distinct from specialised psychiatric facilities for alcoholics, in Russia was increasing, but these were criticised for not being sufficiently integrated with social facilities and for low standards in the care offered. 22
There is also evidence of services in Europe that divert uncomplicated intoxications away from EDs into specialised sobering-up stations in at least five countries, including the Czech Republic, Poland, Austria23 and Finland. 24 However, the operating procedures for these services vary considerably. Some emphasise the diversion of dependant and chronic alcohol users; the distinction between residential detoxification and field hospitals to counter heavy social drinking is unclear. Some services are open only during the day, such as in Finland;24 some are open only for specific events, such as in New Zealand. 25
The motivations for setting up AIMSs also varies. For example, in North America public drunkenness was defined, until 1971, as a voluntary act of antisocial behaviour and therefore a criminal act,26,27 and the intoxicated were typically held in police-run ‘drunk tanks’. In 1964 it was estimated that in Washington, DC, there were 45,000 alcoholics, of whom 5000 were chronic alcoholics, and of the 28,709 prisoners committed to the DC Department of Corrections two-thirds were committed for intoxication. 26 The implementation of the 1971 Uniform Alcoholism and Intoxication Treatment Act,28 however, shifted the definition of simple intoxication away from criminal justice to public health. 29 In response, a 25-bed detoxification centre was set up in 1971 on the grounds of the District of Columbia General Hospital to deal with ‘simple intoxication’. The service was designed to manage patients at less cost than those of a general hospital and the location was chosen so that the service was accessible to patients and police. 29 The centre had a maximum capacity of 60 patients and was led by a registered nurse assisted by 29 full-time and two part-time staff. 29 Similar services were developed in Massachusetts and San Diego, the latter of which aiming to divert repeatedly intoxicated homeless people away from emergency services including EDs. 30
An aim for the diversionary service in San Diego was to address the frequent use of ED facilities by alcoholics. Data indicate that, prior to the implementation of the service, 308 alcoholic patients attended the ED 2335 times between 2000 and 2003. 30 The San Diego diversionary service was initially a 6-month treatment programme in lieu of custody and those who accepted referral onto and completed the treatment programme demonstrated a 50% reduction in use of the ED. 30 A 24-hours-per-day ‘sobering centre’ was also set up in San Francisco in July 200331 to address the impact of uninsured chronic inebriates on EDs. Although the focus was on the homeless, the service was open to all who were publicly inebriated and who did not require emergency attention. The service did not accept walk-ins and accepted referrals from affiliated services only (mostly mobile assistance patrols and ambulance and police services), including referral from the local ED. The facility in San Francisco is notable for its success not only in diverting patients away from EDs but also for developing into a facility that has become embedded in the community, providing continuity of care to the most vulnerable. 31
In Australia, as in the USA, a series of ‘sobering-up centres’ was established in the 1980s following moves to decriminalise public intoxication. The primary motivation was to alleviate the harms caused by the then custodial response to public drunkenness32 and was partly focused on Aboriginal communities in that the motivation for such services originated from the discovery that a disproportionate number of aboriginal deaths in custody were attributable to alcohol. These centres were therefore established not to address alcoholism or offer long-term rehabilitation but as an alternative to custody to reduce alcohol-related deaths and to offer care in a safe environment. 32
Logic of AIMSs
All AIMSs have in common the need to systematise a process whereby AAI can be appropriately routed to the AIMS or ED based on need. As a result, AIMSs effectively push triage (in EDs triage determines clinical need and therefore priority)33 into the community and in some cases into the remit of non-specialist health-care workers or volunteers with little or no training. This decision to either refer cases of AAI to an ED or divert cases of AAI to an alternative service has received some attention. Cornwall et al. 34 asked emergency medical technicians (EMTs) to complete a 14-item survey concerning the intoxicated patient who they were transporting to ED. Survey items broadly concerned factors that would describe their patient as needing referral to an ED, obviating the opportunity to divert to alternative services. Overall, analyses indicated that EMTs were able to use a simple survey instrument to accurately discriminate between intoxicated patients who required specialist attention and intoxicated patients who would be suitable for diversion, which was based on a comparison of survey results with patient outcomes in EDs. Flower et al. 35 undertook a similar study but with paramedics and found that paramedics might be expected to divert away from EDs 28% of intoxicated patients who might be expected to require emergency attention. Similarly, in Colorado, the evaluation of a nurse-led facility found that 0.6% of those diverted to AIMSs subsequently required referral to an ED and that 58% of those referred to an ED required emergency attention. 36 These studies highlight the central role of ambulance services, which convey a significant proportion of AAI patients to EDs. For AIMSs to be effective, they will require a partnership with ambulance services and need to provide a service of sufficient competence that allows ambulance service staff to safely discharge their patients into AIMSs.
Evaluating the diversion of alcohol-related attendances
As previously outlined in this chapter, those exhibiting AAI can be at significant risk. Although such levels of intoxication are not limited to night-time environments (NTEs) in which people socialise, because of the substantial number of alcohol consumers in these environments the incidence of AAI becomes significant. Any increase in the incidence of AAI will have an impact on front-line services including police, ambulance and health-care services. Impacts include diverting resources into NTEs to manage those who are vulnerable owing to AAI, attracting additional resources in emergency health care. Because AAI is associated with disorder and the involuntary expulsion of body fluids, AAI can also have an impact on those in the local environment. The impact of AAI in the NTE is therefore broad and significant. A number of jurisdictions in the UK have sought to alleviate the impact of AAI through implementing AIMSs to divert AAI patients away from EDs, providing a more convenient facility in which to treat or allow patients to recover and to provide a more convenient and centralised place of safety for police officers and ambulance crews.
The underlying logic of AIMSs is that, of the population in the NTE, a proportion will consume alcohol excessively. Of this group, many will not require assistance; some will require pastoral support from, for example, friends, family or Street Pastors and would be expected to recover; some will require monitoring with a possibility of more extensive assistance; and some will require specialist care. The logic of AIMSs is that a proportion of AAI patients are unnecessarily transferred to an ED. AIMSs provide a facility that facilitates monitored recovery, lessening the burden on EDs. AIMSs are typically situated in NTEs so that those services and groups (e.g. Street Pastors and police and ambulance services) that would otherwise transfer patients to an ED have a convenient facility to which patients can be referred.
No systematic review of the relevant literature was undertaken for this evaluation. This is because this is the first formal evaluation of services such as AIMSs. A narrative review of pertinent literature is provided in this chapter, one we have expanded on elsewhere. 37
Aims
The overarching aim of this evaluation was to examine and estimate the effect of AIMSs, primarily on EDs and ambulance services but encompassing front-line staff generally and considering the impact on police services where possible. The evaluation is a controlled mixed-methods longitudinal observational study with parallel ethnographic evaluation, comparing services in cities where AIMSs have been implemented with services in cities where AIMSs have not been implemented.
Exploratory analyses
Additional exploratory work examining police activity, referrals from AIMSs to EDs and assaults on NHS staff was also considered. These areas of work are not central to the main evaluation but could provide additional insights that reveal how AIMSs work in the NTE more generally. The data used for these additional analyses are known to have significant limitations: they are not available in all jurisdictions, there is considerable variability in how these data are recorded and the validity of the measures is uncertain.
Police activity
Police officers do not routinely record the time that they invest in managing AAI. Instead, key performance indicators are outcome-oriented, such as the number of assaults recorded. We hypothesise that AIMSs will release police resources otherwise invested in caring for those who are vulnerable as a consequence of AAI, and that greater police presence, facilitated by the implementation of AIMSs, will prevent violence escalating to the extent that severe injury is sustained, therefore reducing assault-related ED attendance. Conversely, increased police presence will increase police ascertainment of violence and therefore increase levels of police-recorded violence. Although these data are not specific to police activity, we include these analyses to explore possible associations between AIMSs and police activity.
Referral to emergency departments from AIMSs
Where possible, we considered the proportion of patients admitted to AIMSs and who subsequently transit to an ED for treatment. This requires that patient identifiable information is available both from AIMSs and EDs and that records can be linked.
Emergency department assaults on staff
A key outcome of AAI in EDs is the effect on staff. ED staff can be exposed to verbal, physical and sexual assault. Although there is a statutory obligation under Reporting of Injuries, Diseases and Dangerous Occurrences Regulations (RIDDOR) to record such occurrences, including near misses, guidelines vary across England and Wales and there is no agreed template for either recording occurrences or capturing whether or not the perpetrator of the assault was under the influence of alcohol. This matter is currently being addressed. 38 This analysis is therefore exploratory given the uncertainty in the underlying data.
Patient, public and stakeholder involvement
Patient and public involvement (PPI) is a prominent feature of the current evaluation (see Chapter 7). PPI input guided the revision of research materials so that the materials were better suited to end-users’ needs and represented the demographic of patients likely to be involved in the study. Additional guidance was solicited from the Study Steering Committee (SSC).
Chapter 2 Research approach and methods
Objectives
-
1. Context.
-
1.1. Documentary analysis, interviews and observation to determine variability in study AIMSs.
-
1.2. Survey of UK cities to determine AIMS provision and variation.
-
2. Effectiveness evaluation.
-
2.1. Compare the number of ED attendances (all attendances and stratified by age, patient group, diagnosis and treatment) across control and intervention sites and when AIMSs are and are not operating.
-
2.2. Compare differences between control and intervention ED patient-specific metrics when AIMSs are operating:
-
2.2.1. ED key performance indicators: median and 95th percentile total time in the ED (all attendances and stratified by admission to hospital vs. discharge home); median and 95th percentile time to treatment (all attendances); median and 95th percentile time to initial assessment (ambulance arrivals only).
-
2.2.2. Hospital admissions attributable to alcohol intoxication and attributable to alcohol-related conditions.
-
2.2.3. Ambulance service key performance indicators: proportion of high-priority calls responded to within 8 minutes; proportion of high-priority calls responded to within 19 minutes; median time to arrival of ambulance-dispatched health professional for all calls and high-priority calls; proportion of incidents managed without transport to the ED; proportion of patients who recontacted within 24 hours following treatment and discharge at the scene.
-
2.3. Explore data relating to practitioner well-being (e.g. assaults on staff) and police-recorded violence (under the assumption that these data will be used descriptively owing to poor quality).
-
3. Cost-effectiveness evaluation.
-
3.1. Examine the effects of key items of resource use on ED attendance rates.
-
3.2. Quantify estimates of the costs of an AIMSs model versus usual care.
-
4. Ethnographic study.
-
4.1. Undertake longitudinal non-participant observation of practice to examine the impact of AIMSs on the local work ecology, with specific reference to referral pathways and the management of alcohol intoxication and alcohol-related risks in the NTE.
-
4.2. Explore the division of labour, roles and responsibilities in managing the intoxicated and the impact on practitioners’ working lives (e.g. occupational identity).
-
4.3. Explore related activities, such as care of ED patients, community policing, and transporting patients to hospital.
-
5. Patient evaluation.
-
5.1. Explore the experiences and perceptions of AIMS users using a qualitative study of face-to-face semistructured interviews with AIMS users.
-
5.2. Measure the acceptability of AIMSs using a survey of AIMS users.
-
5.3. Compare rates of acceptability for different models of AIMSs.
-
5.4. Measure differences in ED user experience between areas with AIMSs and control areas without AIMSs (controlled cross-sectional ED survey).
-
5.5. Undertake retrospective analysis of data collected for a national ED survey to measure changes in ED user experience before and after implementation of AIMSs compared with control areas without AIMSs (controlled before-and-after analysis of AIMSs implementation).
Study design
Type of study
A controlled mixed-methods longitudinal observational study with parallel ethnographic evaluation.
Sampling frame
A natural experiment comparing areas in which AIMSs have been implemented (or planned and implemented during the project) against matched areas with no provision (control areas, matched using Home Office iQuanta ‘similar families’). 39
Locations vary by work package. For outcome analyses, economic evaluation and surveys of users’ views, we examine six locations in which AIMSs have been implemented and compare these with six matched control locations. The ethnographic study involved two locations in which a service has been implemented and one control location where a service is not envisaged.
To safeguard the anonymity of places and people, locations are referred to as sites, whereby a site refers to the services in the locale in which the AIMSs are established.
Inclusion and exclusion criteria
Cities included in the study were within the jurisdictions of England and Wales. EDs accepting children only (aged < 18 years) were excluded. Further details on site selection and reasons for some areas dropping out of the study are provided in Appendix 1.
Methods
Protocol and amendments
The Dissemination and Impact Strategy document is available on the project webpage (www.journalslibrary.nihr.ac.uk/programmes/hsdr/140425/#/; accessed 14 February 2020).
Amendments made to the protocol were as follows:
-
13 December 2015 – final proposal, following review.
-
1 November 2015 – workstream 1 (iv): specified sampling process; researcher Laura Gray replaced Penny Buykx.
-
30 November 2015 – workstream 1 (iii): clarified all six AIMSs; added intent to seek verbal permission to conduct telephone questionnaire. Workstream 2: removed intention to collect NHS numbers from AIMS and ED users, instead to examine mechanisms for linking AIMS data to routine NHS data. Reformatted proposal with front sheet and table of contents. Changes reported to the National Institute for Health Research (NIHR) via the National Institute for Health Research Evaluation, Trials and Studies Coordinating Centre (NETSCC).
-
15 January 2016 – workstream 1 (iii): changed telephone to postal survey. Workstream 1 (iv): sample size revised; addressed comments from initial PPI Review submission (09 December 2015) regarding sensitive AIMS patient approach. Terminology: ‘alcohol treatment centre’ changed to ‘alcohol intoxication management service’.
-
16 January 2016 – removed section on dissemination.
-
17 January 2016 – minor revisions.
-
18 January 2016 – workstream 1 (iii): added reference for walk-in centre survey process. Clarified PPI roles, steering committee members and separate advisory group. Cross-referenced all numbered references. Logos added.
-
28 January 2016 – workstream 1 (i, ii): added sample size, recruitment information and potential case study sites. Workstream 2: added provision of Crime and Disorder Act 199840 for facilitated data access.
-
23 March 2016 – amendments in response to Research Ethics Committee (REC) comments (10 March 2016). Addition of statement on limited confidentiality.
-
12 July 2016 – substantial amendment to REC; addition of AIMS staff obtaining consent from AIMS users for workstream 1 (iii) interviews to facilitate recruitment.
Intervention
The intervention to be evaluated is the AIMS, defined as follows:
-
Initiated by local agencies that identify the problems and impacts that AAI is having on services and the wider community.
-
Set up and run by multiple agencies (e.g. ambulance services, local hospital trusts, police, local councils and voluntary sector organisations), so staffing can be a mix of nurses, paramedics, police and volunteers.
-
Located in buildings or mobile units stationed in or near to areas with a high density of licensed premises.
-
Open regularly and at times when AAI is expected to peak (e.g. Friday and Saturday evenings) but may offer additional cover on other evenings such as student nights, evenings of sporting events and national holidays.
-
Users are typically referred in by local ambulance, police or third-sector volunteers (e.g. Street Pastors).
-
Users would typically be triaged by a suitably qualified person, given basic first aid and water, monitored while they sober up and referred to ED if required.
-
Users may be screened for alcohol use problems and offered some form of advice, brief intervention or referral for specialist alcohol support.
-
Users are discharged at the point at which they are deemed safe, usually to the care of friends or family, with plans for safe travel home discussed and arranged.
Procedures
Ethnography
Theoretical framework
Data generation was informed by ecological theories of the division of labour,41 cultural historical activity theory42 and translational mobilisation theory. 43 Ecological theories of the division of labour conceptualise the world of work as a dynamic social system and direct attention to the connections between social groups and institutions and their interdependence in a wider field of action. 41,44,45 For these theorists, the system of work is forever changing in response to economic, technological and social factors that reshape occupations and impact on work content, with a range of implications for professional identity and skill mix. Cultural historical activity theory is concerned with the constellation of people, processes and artefacts oriented towards a shared objective, in this case management of the intoxicated, and the mediated relationship between cognitive processes and practical action. Activities are not regarded as belonging to an individual but as part of a collective endeavour with an associated division of labour, tools, technologies, norms, rules and conventions. Collaboration is achieved by distributing the goals between different actors who align their actions according to the objective of the overall activity. Translational mobilisation theory is a theory that provides a framework for understanding and investigating the emergent organisation of collaborative work practices in institutional contexts and was deployed in the study to analyse the processes, practices, organising logics and materials through which the different actors in the NTE managed individuals with AAI and how this was shaped by the different contexts in which they worked.
Data generation
Data generation was undertaken between May 2016 and November 2017, predominantly on Wednesday, Friday and Saturday nights, when AIMSs and other NTE initiatives were operating. Where possible, nights that were known to be particularly busy, such as pay days, ‘freshers’ events and sports nights were also targeted to get a sense of the overall rhythm of NTE work (i.e. busy nights vs. quieter nights).
In each case, data were generated through non-participant observation of everyday practice with relevant occupational groups (nurses, police, ambulance crews, Street Pastors) and locales (ED, AIMS, street-level work). This was supplemented by ethnographic interviews and the analysis of relevant artefacts, such as policies, protocols and referral systems. Our aim was to understand the related practices, division of labour and artefacts involved in managing the intoxicated and the implications this has for the working lives of staff and their occupational identities. Observations were recorded contemporaneously as low-inference-style field notes that captured what was said and done without interpretation and were later transcribed. Interviews were embedded in the observational process and where possible were digitally recorded. Documents and records were treated as both a resource and a topic. Their content was analysed to inform our understanding of organisational processes and practices. Their form was analysed to develop a better understanding of their role in the wider activity system. A data generation template informed by the theoretical framework was utilised to ensure a consistent focus across all case studies.
Data analysis
All data were transcribed and entered into ATLAS.ti version 8 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany) to augment retrieval and management and coded using a common coding frame. The analysis proceeded as follows:
-
In each case, the various materials collected (field notes, interviews, documents) were used in a triangulating fashion to build up an understanding of the ecology of work; develop concrete descriptions of referral pathways and the management of alcohol intoxication and alcohol-related risks in the NTE; analyse the working lives and occupational identities of staff and the impact of alcohol intoxication work on NTE agents’ other activities.
-
Cross-case comparison was undertaken to examine the commonalities and differences between cases.
Patient evaluation: AIMS user views
Design
A sequential mixed-methods design was adopted whereby qualitative interviews with AIMS users informed the development of a brief questionnaire for an exit survey of AIMS users.
Qualitative interview study
Methods
Semistructured interviews were conducted with 19 AIMS users recruited from four AIMSs that provide different models of service delivery (sites A, B, C and D; see Chapter 3). Our intention had been to interview 16–20 participants from across all six AIMSs to achieve maximum variation of experienced care, age, gender and ethnicity before designing the questionnaire. We reduced this from six to four AIMSs because two AIMSs refused to grant permission for this aspect of the research. Researchers attended the AIMS and approached users to obtain consent to interview towards the end of their stay and when they were sufficiently sober to provide consent. It was anticipated that recruitment from such a participant group would be challenging, which was the case, and we accordingly amended the recruitment process so that AIMS staff could approach users on behalf of the research team at times during which project researchers were unable to attend. Written consent and participant contact details were recorded. Interviews were conducted by telephone within 3 days of consent being obtained.
Researchers made up to three attempts to contact participants by telephone and/or text message. Where contact was established, interviews commenced by reconfirming a participant’s identity and consent to be interviewed. Interviews covered views of using the AIMS in terms of access, treatment, experiences with different staff from different services, discharge, and information and advice about alcohol intoxication.
Interviews were transcribed verbatim and entered into the qualitative data analysis software NVivo version 11 (QSR International, Warrington, UK). Framework analysis was used. 46 The framework approach was appropriate because it allows for the exploration of both a priori and emergent issues. The following steps were taken:
-
Familiarisation – the first three interview transcripts were read (by PB, AI and AOC).
-
Following initial discussion of emerging themes, a thematic framework was developed (by PB, AI and AOC).
-
All transcripts were read and coded according to the framework (by AI).
-
Parallel interview data collection led to an evolving framework to account for additional emergent themes.
-
Discussion of the themes and the connections between them.
-
Short case summaries of individual users were prepared to illustrate the diverse types of AIMS users in the sample.
Data from the first nine interviews, alongside field notes taken by researchers during recruitment and ongoing engagement with the PPI panel, were used to develop a two-sided questionnaire. Initial interviews highlighted as important certain aspects of the care that they had received. These are reflected in the survey service rating scales (e.g. safety, communication, care and compassion). Interviewees talked about being escorted to the AIMS by a variety of associates and services and quantification was therefore sought. Furthermore, commonalities between the AIMS and ED survey were sought so that responses could be compared.
AIMS user questionnaire
The content of the questionnaire was based on analysis of the first nine interviews from two AIMSs (5 interviews at site A and 4 interviews at site B). Drafts were discussed with our PPI group. The questionnaire had sections on referral, reason for being at the AIMS, treatment provided and by whom, seven aspects of care (including comfort and cleanliness), and alternatives to and preference for AIMS care. The overall experience was rated on an 11-point scale that is also used by the Care Quality Commission (CQC) in their ED surveys. 47 This allowed us to compare acceptability of AIMSs with acceptability of EDs. Finally, we asked respondents to write about good aspects of their experience and suggest improvements (see Appendix 2 for the questionnaire).
All AIMS users were handed survey packs by either researchers or AIMS staff during their visit. Survey packs contained a covering letter, a two-sided A4 questionnaire and a reply-paid return envelope. Where possible, AIMS users were encouraged to complete the questionnaire towards the end stages of their treatment or while awaiting discharge, place the completed questionnaires in the pre-paid envelopes and then deposit them in a sealed box before leaving the service. Alternatively, AIMS users could take the questionnaire away and post it back in the reply-paid envelope.
The plan was to undertake the survey in each service for up to 5 weeks to obtain 50 responses in each service. This was based on expectations that AIMSs would see 40 people over one weekend and our response rate would be 25%. This would yield 300 responses and allow us to estimate 80% satisfaction for AIMSs to within 5% and to detect a difference of 10% (70% vs. 80%) at the 5% level with 80% power between two models of AIMSs.
Data were entered into IBM SPSS Statistics version 20 (IBM Corporation, Armonk, NY, USA). The main analysis was descriptive, displaying the proportion of responses for each item on the questionnaire. Prior to starting the study, we were aware of two models of AIMSs: located in a fixed building and located in a mobile van. No other model of AIMSs was apparent during our study, so we tested whether user acceptability varied by fixed and mobile models. We used chi-squared tests for these comparisons but could not use statistical tests for multiple response questions. The overall experience of the AIMS was rated on an 11-point scale. These data violated the assumptions of normality (e.g. were highly skewed) but were analysed using a t-test, which is robust to moderate non-normality. 48
General questions rating the service were converted to a score ranging from one (very poor) to five (very good) and the mean service rating score calculated across all eight questions. Cronbach’s alpha for the scale was high (α = 0.91). Linear regression was used to estimate the effect of the intervention on mean service rating score. We did not expect to see any differences in this comparison. A total of 4914 questionnaires were mailed. The overall response rate was 21.5% after one reminder, which was slightly lower than expected (see Appendix 3). There was no statistically significant difference in overall response rate between intervention and control sites (20.9% vs. 21.9%, respectively; p = 0.41).
Patient evaluation: emergency department users’ views
Rationale
Removing alcohol-related ED users may improve views of the ED environment for other ED users.
Evidence base
The CQC undertakes ED user surveys nationally around every 2 years. They obtained a 38% response rate for their 2012 survey. 47 A review49 of 16 articles assessing ED patient satisfaction reported average response rates for in-department questionnaires/interviews of 74% (range 51–84%) and for postal surveys of 18% (range 9–25%).
Design
Comparison of users’ views in EDs in six areas with AIMSs and six control areas.
Methods
We undertook a survey of patients who attended EDs in cities where our six AIMSs were located and six control cities.
We developed the ED questionnaire to address the research question. We constructed a set of questions about the ED environment, focusing on issues potentially related to the presence of alcohol-intoxicated ED users or associated visitors. We included the question ‘did you feel threatened by other patients or visitors?’, which is used in the CQC ED patient survey, to allow us to compare our findings with those of other ED surveys. We also used their 11-point scale to measure perceptions of overall experience of the ED. We included a set of questions about more generic aspects of the ED visit so that the questionnaire was relevant to all users. We did not expect to see any differences in these generic items. Our aim was to keep the questionnaire short to help us obtain higher response rates. We discussed the questionnaire with members of the Sheffield Emergency Care Forum (SECF), who endorsed it as acceptable and easy to complete with minor changes to the wording of questions.
We obtained permission from the CQC to replicate their ED survey processes, including using their patient covering letter, reminder letter and survey administration procedures. We followed their process except for sending one reminder rather than two.
In each ED, patients who registered between the hours of 20.00 and 04.00 on Fridays and Saturdays in the month of March 2017 were sent a survey pack. Owing to the withdrawal of one of our AIMSs from the research, users were sampled in August 2018 with a replacement AIMS site (site F) and its control site (site J). Friday and Saturday evenings were selected to reflect operational hours of AIMSs. After our data collection we learnt that site B AIMS was open on Wednesday and Saturday nights, so had to remove our Friday night data from site B and its control site in our analysis (see Chapter 4).
We planned to survey 360 users in each ED, with an expected response rate of 25%, yielding around 90 responses per ED. This would result in a total of around 500 responses across all AIMS areas and equivalent numbers across all control areas. We expected a lower response rate than the 38% obtained by the 2014 CQC ED survey47 because it was focused on a narrow aspect of ED experience and may have lacked salience for some ED users.
Analytic strategy
Regression analysis was used to compare the responses from intervention and control sites while adjusting for potentially important covariates (fixed effects) and accounting for potential clustering of data by site (random effect). We planned to adjust for age and waiting time. We were unable to record actual waiting time so used the participant’s estimate of how long they were in the ED. In addition to including all variables, regardless of significance level, in each model forward regression was also applied where the initial model included only AIMSs, and significant variables were added one at a time until there was no change in the goodness of fit of the model.
To limit the number of hypothesis tests we undertook four comparisons between intervention and control sites:
-
Overall mean service rating score – general questions rating the service were converted to a score ranging from one (very poor) to five (very good) and the mean score calculated across all eight questions. Cronbach’s alpha for the scale was high (α = 0.912). Linear regression was used to estimate the effect of the intervention on mean service rating score. We did not expect to see any differences in this comparison.
-
Perception of feeling threatened – logistic regression was used to estimate the effect of the intervention on the odds of responding to the question about feeling threatened by other patients or visitors with ‘yes’ (definitely or to some extent) rather than ‘no’. This question was used by the CQC in its ED surveys.
-
Overall mean negative experiences score – questions relating to potential negative experiences from alcohol-intoxicated patients and visitors were converted to a score ranging from one (strongly disagree) to five (strongly agree) and the mean score calculated across all seven questions. Cronbach’s alpha for the scale was high (α = 0.892). Linear regression was used to estimate the effect of the intervention on mean score for negative experiences.
-
Overall experience score – linear regression was used to estimate the effect of the intervention on the overall experience score measured on a scale of 0 to 10.
We included one open-ended question: ‘how could the time you spent in the emergency department be improved?’. We searched for comments that included ‘alc’, ‘alcohol’, ‘alcoholic’, ‘drink’, ‘drunk’ or ‘drinker’ as potentially related to impact of patients who had used alcohol. We read these responses and coded them using content analysis.
Patient evaluation: controlled before-and-after analysis of emergency department perceptions
The CQC uses the NHS National Patient Survey Programme to regularly gather data on patient experiences of ED care across the NHS. This provides the opportunity to use survey data to retrospectively evaluate the impact of AIMSs on ED user experience. The CQC ED patient survey was run in all English acute trust EDs (≈ 151 EDs) in 2003, 2004, 2008, 2012, 2014 and 2016. A systematic sample of 850 adult patients (aged > 16 years) drawn from a 1-month sample of ED attendees were sent the survey with up to two follow-up reminders. The questionnaire consisted of around 50 questions, divided into 11 sections.
We used two items in the survey in our ED questionnaire because they were potentially relevant to the impact of AIMSs on ED user experience:
-
‘While you were in the emergency department, did you feel threatened by other patients or visitors?’ Available responses: ‘yes, definitely’, ‘yes, to some extent’ and ‘no’.
-
The 0–10 rating of overall ED experience.
We determined that responses to these questions in the CQC survey could be used to undertake a controlled before-and-after analysis of ED user experience if surveys were undertaken before and after AIMS implementation. This involved two separate comparisons:
-
The four English AIMS sites that participated in our ED survey were compared with their control sites. The CQC ED patient survey data were only available for English hospitals; therefore, analysis for the Welsh sites and their matched pairs was not possible.
-
We identified any AIMS across the English NHS that could provide a date from which they commenced operation and then selected a comparator site. A survey of the provision of AIMSs in UK towns and cities was updated in March 2017 and used to identify 15 AIMS sites in England and Wales, along with their nearest ED and the date on which they started operating. Based on the Home Office iQuanta ‘most similar groups’ of cities, each site was matched with a city within the same ‘family’. 39
Data collection
The survey was subject to several changes over time that were relevant to our analysis. Time of attendance was not recorded prior to 2008 and the 2003–2008 surveys contained the question ‘while you were in the emergency department, did you feel bothered or threatened by other patients?’, whereas from 2012 onwards the word ‘bothered’ was removed. We reasoned that ‘bothered’ was not equivalent to ‘threatened’ and, therefore, the results from 2003–2008 and 2012–2016 surveys were not comparable. Because the perception of ‘feeling threatened’ at key times of attendance (Friday and Saturday nights) were key considerations, pre-2012 survey results were not requested, and analysis was limited to the 2012, 2014 and 2016 surveys.
We requested the following data from the CQC data set: trust and ED site identifier (to determine intervention or control groups), age, sex, time and date of ED attendance, reported time spent in ED, response to the ‘feeling threatened’ question and overall experience (0–10 rating). We then used time and date of ED attendance to select surveys from respondents who attended the ED during the hours of AIMS activity (weekend nights).
Analytic strategy
For both analyses (the four study sites only and all AIMSs in England) we used the date of starting operation (defined as being fully operational, open at regular times and not in a pilot phase) to classify whether the survey was undertaken before or after implementation of the AIMS. The same approach was used for control sites, with the start date of the paired intervention site being used to determine whether the survey was before or after implementation.
Regression analysis was undertaken to estimate the effect of AIMS implementation on ED survey responses while adjusting for differences between respondents at intervention and control sites, changes over time and clustering by site. We included age, duration spent in ED, time of arrival, intervention or control site and pre or post intervention as fixed effects, and site and year of survey as random effects. In addition to including all variables regardless of significance level in each model, forward regression was also applied where the initial model included pre/post intervention on its own and significant variables were added one at a time until there was no change in the goodness of fit of the model.
Effectiveness evaluation
We undertook a natural experiment comparing areas in which AIMSs were established with matched areas without AIMS provision. The study population was adults (aged > 14 years) who sought emergency care between 16 November 2010 and 31 March 2016 from providers in the catchment area of the acute trust covering the location of the AIMS or a comparable location in a control city or town (i.e. the main area of activity for the NTE). The population was restricted to those attending during hours of AIMS activity at the intervention sites, or equivalent hours at the intervention sites prior to AIMS implementation. For the control sites the hours corresponded to those of their matched AIMS intervention site. Data were collected before and after implementation of the AIMS (provided that data sources were available before AIMS implementation) at both intervention and control sites so that analysis could estimate the effect of availability while adjusting for baseline differences between AIMS and control sites and changes in emergency care use over time.
Data collection
Data were collected from routine administrative data sources. All data were anonymised (i.e. no personal details were collected).
Key performance indicators and ED attendance data were requested from NHS Digital. The acute hospital trust nearest to the main area of night-time activity in the town or city was identified and available data from all ED attendances were requested. We selected attendances for analysis if they occurred at intervention sites during the regular times of AIMS operation, or during equivalent times before the AIMSs were implemented, or at control sites during the regular times of operation of the matched intervention site. Only adult attendances (aged > 14 years) were analysed.
We were provided with ED data from 1 April 2009 to 31 March 2016 for all cities, but we chose to use only the data from 16 November 2010 because the ED at site F relocated to a new facility on 17 November 2010 (from 00.00), rendering prior data inconsistent and unreliable.
Hospital Episode Statistics (HES) data were requested from NHS Digital. We requested data for all admissions with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision50 (ICD-10) codes potentially related to alcohol intoxication, using an existing method,51 based on classifications used by the Centers for Disease Control and Prevention and the Office for National Statistics. 52 We restricted admissions to adults admitted between midnight on the night that the AIMSs were open (or would have been open) and midnight on the following night. This allowed for delays in the admission process (it was considered unlikely that a patient avoiding admission by presenting to a service at 20.00 would have been admitted to hospital before midnight) and imprecision in the recording of time of admission.
Ambulance service response time data were requested from each ambulance service that agreed to participate. Ambulance services cover large geographical areas, often including more than one study site. We therefore requested data from calls originating in the administrative post codes of the respective city so that ambulance data related to a specific study site. Again, analysis was restricted to calls relating to adults and that occurred during times of actual or assumed AIMS activity.
AIMS activity
We asked each service to provide anonymised data describing attendances to the service during hours of activity. There was substantial variation in the methods used to record attendances, so data varied accordingly. We explored whether or not it was possible to identify if people attending AIMSs subsequently attended a hospital ED. We also asked a member of staff at each service to complete a short survey describing how clinical governance issues were managed.
Outcomes
The primary outcome was all ED attendances occurring during times of AIMS activity.
Secondary outcomes were:
-
Emergency department attendances stratified by age (14–39 years vs. ≥ 40 years), patient group (assault or deliberate self-harm vs. other), diagnosis (poisoning, contusion, laceration or head injury vs. other) and treatment (no investigation or treatment vs. any investigation or treatment). These analyses were planned to determine whether or not AIMSs reduce attendances that are more likely to be related to alcohol intoxication or attendances that result in only observation and/or advice.
-
Emergency department key performance indicators – median and 95th percentile total time in the ED (all attendances and stratified by admission vs. discharge); median and 95th percentile time to treatment (all attendances); median and 95th percentile time to initial assessment (ambulance arrivals only); the proportion leaving the ED before being seen for treatment; and the proportion reattending the ED within 7 days.
-
Hospital admissions attributable to alcohol intoxication (admissions with primary ICD-10 codes F100, T510, T511, T519, X45, Y15, R780, Y90 or Y91) and hospital admissions attributable to alcohol-related conditions (admissions with primary ICD-10 codes F100, T510, T511, T519, X45, Y15, R780, Y90, Y91, E244, F101, F102, F103, F104, F105, F106, F107, F108, F109, G312, G621, G721, I426, K292, K70, K860, K852 or Q860).
-
Ambulance service key performance indicators – proportion of high-priority (category A) calls responded to within 8 minutes; proportion of high-priority (category A) calls responded to within 19 minutes; median time to arrival of ambulance-dispatched health professional for all calls and high-priority calls; proportion of incidents managed without transport to the ED; and proportion of patients who recontacted within 24 hours following treatment and discharge at the scene.
These outcomes were selected because we anticipated that they would be available and reliably recorded for the study period. However, in practice, some measures were not available or reliably recorded. We were therefore unable to examine several planned outcomes:
-
The ED attendance data did not provide enough detail of patient group or diagnosis to allow these stratified analyses.
-
The ED performance data did not accurately report the proportion leaving before being seen or the proportion reattending within 7 days.
-
Ambulance services did not reliably or consistently record if incidents were managed without transport to the ED and were not able to identify recontacts within 24 hours.
-
Ambulance services did not reliably record if calls were potentially related to alcohol intoxication, so we were unable to determine if implementation of the AIMS changed the incidence of such calls compared with control sites.
-
We were unable to obtain data on staff retention, turnover and sick days as human resource records are protected from freedom of information requests.
Furthermore, on undertaking initial descriptive analysis, we found substantial baseline variation between sites for some outcomes or stratification variables (caused by variation in definition or recording of outcomes) that meant that comparative analysis between intervention and control sites was not appropriate. Details are provided alongside the individual analyses. In general, variables used as key performance indicators appeared to be more consistent (at least in the English or Welsh health services) than variables used for other purposes.
Analysis
Primary analysis
Pilot data from site A over a 3-year time period showed that the number of ED attendances and the average time of attendance increased over time and that a time series analysis was the most appropriate method to explore the impact of AIMSs on ED attendances. 53 We used interrupted time series to analyse the influence of the presence of a service on the primary outcome (the number of ED attendances during hours of AIMS activity). An interrupted time series analysis (ITSA) estimates a time series of the outcome of interest and establishes an underlying trend in the data. This underlying trend can then be ‘interrupted’ by an event at a specific point in time. The event, which will interrupt the time series trend, is the date that the AIMS opened for each intervention site or its control. This method allows us to identify the trend in attendances for each site before and after AIMSs became operational. It also allows us to identify any ‘shock’ to this trend when the AIMS opened. For example, if the AIMS opening resulted in a sudden reduction or increase in attendances, then this will be identified in this model. For each intervention site, we estimated this model for only those days that AIMSs were regularly open. These were usually Fridays, Saturday and bank holidays (or the night before bank holidays) but the regular days varied between sites. These nights included data from the following morning (i.e. 20.00 to 06.00). For the control sites we used the equivalent days and times. We included the following explanatory variables: day of the week, ‘Black Friday’ (last Friday before Christmas), Christmas Eve, Christmas Day, Boxing Day, New Year’s Eve, St Patrick’s Day, Halloween and bank holidays (e.g. May Day, Good Friday).
In the first instance, we investigated the trend and interruption using only the intervention sites, individually estimated. Next, we included each site’s control in the ITSA. This allowed us to use the panel element of the data and to control for changes over time in the matched cities. In addition to the ITSA analysis on the matched pairs of intervention and control sites, we also performed additional analyses to check that the results were robust. These included performing ITSA for each intervention site but using pooled control sites (all control cities grouped to form one large control). This allowed us to check that our results are robust to our chosen controls.
We were concerned about the overfitting of the time series models and the violation of time series assumptions in the paired city analysis. Therefore, further models were fitted that included only the usual day of the week that the AIMSs were open (Friday and Saturday or Friday and Wednesday for site B). We excluded bank holidays and day of the week from these models. The results from these are shown in Chapter 4.
Disadvantages of interrupted time series analysis
Although ITSA allows us to take advantage of both the panel and time series elements of the data, there are some drawbacks. It is not possible to include all intervention and control sites in a single model, because each intervention site (and therefore each control site) has a different event date. We considered shifting the time series of each site to align each of the event dates but, because we needed a balanced panel, this would leave us with only 6 months of data that we could use. Therefore, we decided not to use ITSA when looking at all sites together. We planned to fit autoregressive integrated moving average (ARIMA) models to daily ED attendances to compare AIMSs with usual care and different levels of AIMSs and their impact on ED attendances. 54 Exploration of ARIMA models showed lag at day 7, which we were able to adjust for in the ED attendance ITSA model. However, ARIMA models were unable to identify patterns owing to variability and were therefore not used. Alternative ARIMA models were explored, including models fitted to weekly data, monthly data and Saturdays only, but this would have meant not being able to identify when AIMSs were open in model fit.
Secondary analysis
The secondary analyses described here are used to estimate a range of different outcomes. Different analyses are used depending on the type of outcome variable.
Linear regressions
We used linear regressions to estimate the effect of AIMS availability on our primary outcome (ED attendances). This was used as a further robustness check. However, this method has problems in that it does not account for the trend in the data. Linear regression was performed on the secondary outcomes (outlined in Outcomes) if we felt that this was worthwhile and within time restrictions after completing analysis on the primary outcome of interest. The linear regression models used all available dates (but restricted to hours of AIMS activity) rather than only the usual days of opening. This was because this method allowed the inclusion of a binary variable indicating whether or not the service was open. Initially, we took each of the intervention sites and used a linear regression to estimate the effects of AIMSs being in operation on ED attendances at that site. This analysis included a single binary variable to indicate whether or not AIMSs were open on a given day as well as the list of specific days included in the ITSA and was directly comparable to pilot analysis. 53 We then went on to include a further binary variable that indicated whether the data were pre or post AIMS start date. This allowed us to crudely account for the time series element of the data.
Next, we performed linear regression on paired cities to use the panel element of the data. This analysis included three binary variables: the first indicated whether or not the city had an AIMS (intervention vs. control), the second indicating whether the service was open on a given day (allowing an effect on both intervention and control) and the third was an interaction of the previous two. This third variable was our main coefficient of interest, allowing us to estimate the effects of the AIMS in an intervention city over and above any effects in a control site. We also included the indicator of whether the date was pre or post AIMS start date. In addition to the analysis described in Analysis, Primary analysis, we also performed the following to test the robustness of our results:
-
Pooled control sites, such as that described in Analysis, Primary analysis.
-
A single linear regression that included all sites in the study. This was not possible using ITSA but could be used here since we did not include the opening dates.
-
Inclusion of operational days only, such as those used in ITSA. We made assumptions about the days that the AIMS would have been operating prior to its existence in each site.
We also fitted a simplified version of the ordinary least squares (OLS) model as we were concerned about the overfitting of the OLS models. Therefore, further models were fitted that included only the usual day of the week that the service was open. We excluded bank holidays and day of the week from these models; these models were fitted using a generalised linear model (GLM) and allowed for the panel nature of the data.
Disadvantages of linear regression
Linear regression does not automatically account for the panel nature of the data. For this reason, we included a binary variable indicating whether or not each site received the intervention. In addition, linear regression does not consider the time series nature of the data. If there is an upwards trend in the data over time, this could bias the results: the open dates would overpredict (or underpredict) the number of attendances (reduction in attendances) at ED. This is because all the open days will be towards the end of the data collection period, at which time, according to the trend, attendances will be higher regardless. This could result in the linear regression and ITSA giving intuitively different results. The ITSA could show evidence of a shock reduction in ED attendances at the event date, but, conversely, the linear regression could suggest that an AIMS being open is associated with increased attendances in ED. We crudely included a variable indicating pre or post AIMS start date to account for trends in the data.
There is also the potential problem that a linear regression might not be the correct specification. This could cause problems for both linear regressions and ITSAs. We examined plots of the data to determine whether or not other specifications, such as including a squared or quadratic term, might also be appropriate.
Logit models
Proportions should not be estimated using regression models or interrupted time series because of the assumptions that these models make. For this reason, logit models (also known as logistic regression models) were used to analyse data by proportions. A list of these variables is given below:
-
proportion of high-priority ambulance calls responded to within 8 minutes
-
proportion of high-priority ambulance calls responded to within 19 minutes
-
proportion of ED attendances leaving the ED within 4 hours of arrival.
This was in addition to descriptive statistics. All independent variables were the same as for the linear regression models. The impact of AIMSs on number of hospital admissions (attributable to alcohol intoxication) was explored using time series methodology and regression using the same methods described above.
For each primary and secondary analysis there are multicomparisons of analysis for up to eight cities with AIMSs or eight pairs of cities being analysed. Bonferroni correction was used to allow for multicomparison and given that the number of comparisons varied by outcomes. The significance level, after allowing for Bonferroni correction, is given for each outcome. Significance level prior to correction was 0.1. Stata® version 15 (StataCorp LP, College Station, TX, USA) was used for all analysis.
Cost-effectiveness evaluation
The component costs of AIMSs were compared with usual care. Results were presented from the NHS and social care perspective. The set-up and running costs of AIMSs were examined by a standardised costing exercise [which included staffing levels, training, consumables and overheads (building rental, heating and lighting)] and from commissioning documents. We used HES ED data to cost ED services before, during and after AIMS set-up and quantify other potential benefits of the AIMS (e.g. improved ED waiting times, treatment times, time to initial assessment and ambulance response times). We present primary analysis as cost per ED attendance avoided. Ambulance response times and ED waiting times were set alongside evidence on their relationship with risk of harm.
There are three main elements in the economic evaluation study regarding the study sites:
-
effects of AIMSs on service resource use related to key performance indicators
-
costs of services with and without AIMSs
-
potential costs and resource use of national roll-out/uptake scenarios.
Effects of AIMSs on service resource use related to key performance indicators
We examined the effects of key items of resource use on ED attendance rates by including variables on resources measured in the time series models. Resource variables explored included hospital admissions and length of stay for alcohol-related conditions, staffing changes in ED, total time in ED, number of ambulance journeys made and response times, and AIMS attendances. This analysis explains the effect of AIMSs on NHS resources and ambulance and police services.
Costs of services with and without AIMSs
We set out to quantify estimates of the costs of an AIMSs model versus usual care. We undertook a costing exercise to quantify the main components of costs from the six study sites. Set-up and running costs for an AIMS were examined by a standardised costing exercise (a structured request for information on staffing levels and grades, staff time, equipment, consumables, training and overheads) and by examining commissioning documents, including business cases for proposed service developments and actual commissioning contracts. The resource use related to the cost of the ED services during and after set-up of the associated AIMS were obtained from HES ED data and ambulance service dispatch data.
Unit costs for resource use, such as ED attendance and length of stay, were obtained from NHS reference costs55 for HES data and ambulance service data. Staff grades and times had been recorded in the ethnographic analysis and unit costs were obtained from both Agenda for Change56 and Unit Costs for Health and Social Care. 57 Set-up costs were obtained from commissioning documents and business plans. Costs of AIMSs were compared with usual care and results presented for cost per ED admission avoided, and further comparisons compared the costs of types of AIMSs. We also considered costs per avoided ambulance dispatch and examined the consequence of setting up AIMSs at a local level by looking at the displacement costs to local trusts of setting up AIMSs.
Typically, AIMSs are developed through partnerships that can include local government, police, and health-care and other agencies, and set-up costs are likely to be provided across these sectors. In this study the focus is on costs to the health-care sector, though costs to other sectors are important; the main analysis presented here examines costs incurred by the health-care sector. It is expected that the health-care sector will meet some of the costs of the AIMSs; therefore, the sensitivity analysis presents results for scenarios in which the health-care sector meets all the costs and in which the health-care sector meets none of the costs.
Safety considerations
None.
Ethics
The evaluation received a favourable response from the NHS REC (REC 3, Cardiff) [REC reference 16/WA/0065; protocol number v4.6 SPON1472–15; Integrated Research Approval System (IRAS) project identifier: 192273].
Chapter 3 The nature and composition of AIMSs
This section provides an overview of the AIMSs included in the evaluation, providing details on the range of services offered in the UK, how they are configured and funding models. It further considers clinical governance procedures in AIMSs and comments on possible risks associated with various service configurations. Referrals from AIMSs to ED are also explored, although this is mostly limited to summary statistics, with the exception of site A, at which the AIMS uses the ED patient management system, enabling more detailed exposition. This chapter draws together data collected across the evaluation, including the ethnographic component, but which is not reported elsewhere.
Provision of AIMSs in the UK
Cities in the UK were contacted (n = 61; see Appendix 4) to determine service provision. Two or more of the ambulance, police and unscheduled care services, or local government, were contacted in each city. A minimum of two responses from all cities were recorded. Street Pastors (sometimes referred to as Street Angels) were present in 59 cities; AIMSs were present in 18 cities and two subsequently closed (at site D and site I). London was excluded from these data as London previously had an AIMS (the London Alcohol Recovery Centre), which had ceased to operate, although there were opportunities for AIMSs to be set up. Plans for AIMSs and reasons for not implementing AIMSs were obtained from cities (see Chapter 5). Alternative provision was given as the reason for not implementing AIMSs in three cities (typically ambulance paramedics and Street Pastors), one city suggested that it was too small and one city suggested that funding was not available for such a service. Five cities were planning to implement services similar to AIMSs. This matter was explored further in the control cities (see Control cities).
Selection of intervention cities
Six cities were recruited into the evaluation. We were unable to ascertain operational activity from two cities and one city (site E) indicated that they did not have the capacity to contribute to the study and these three cities were replaced. Table 1 summarises the involvement of each site in the study. Site F replaced site I in all analysis, and site G and site H replaced site D and site E, respectively, in selected analyses, as outlined in Table 1. There were no changes to the control sites, which were able to provide all required data. The AIMSs were typically open on Friday and Saturday (except site B, which was open on Wednesday and Saturday) and from late evening (20.00: site A, site E; 21.30: site H; 22.00: site B, site F, site G; 23.00: site C) until early morning (03.30: site H; 04.00: site A, site E, site F, site G; 06.00: site B).
| Site | Group | Type | Study involvement | Data availability | Patients per session | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Workstream 1 | Workstream 2 | Workstream 3 | |||||||||||||||||||||
| Ethnography | Context | AIMS | ED | HES APC/HES ED | Ambulance CAD | AIMS data | Age | Gender | Hour and day of arrival | Arrival by ambulance | Reason for attendance | Length of stay | Tests | Diagnosis | Disposal | Mean | SD | Min. | Max. | ||||
| A | I | F | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | 11.83 | 6.22 | 0 | 38 |
| B | I | F | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | N | N | N | N | Y | 9.54 | 5.36 | 1 | 40 |
| C | I | F | NR | NR | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | Y | 7.98a | 2.86 | 4 | 13 |
| D | I | F | NR | NR | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | NA | NA | NA | NA |
| E | I | M | NR | NR | NA | Y | Y | NA | PAb | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Fc | I | M | NR | NR | Y | Y | Y | Y | Y | Y | N | N | N | N | N | N | N | N | Y | 8.12 | 4.51 | 1 | 27 |
| Gd | I | F | NR | NR | Y | NR | Y | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 2.69 | 1.92 | 1 | 10 |
| He | I | M | NR | NR | Y | NR | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | N | P | 5.25 | 2.88 | 1 | 20 |
| I | I | M | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| J | C | Y | Y | NR | Y | Y | Y | Y | Y | ||||||||||||||
| K | C | NR | NR | NR | Y | Y | Y | Y | Y | ||||||||||||||
| L | C | NR | NR | NR | Y | Y | Y | Y | Y | ||||||||||||||
| M | C | NR | NR | NR | Y | Y | Y | Y | Y | ||||||||||||||
| N | C | NR | NR | NR | Y | Y | Y | Y | Y | ||||||||||||||
| O | C | NR | NR | NR | Y | Y | Y | Y | Y | ||||||||||||||
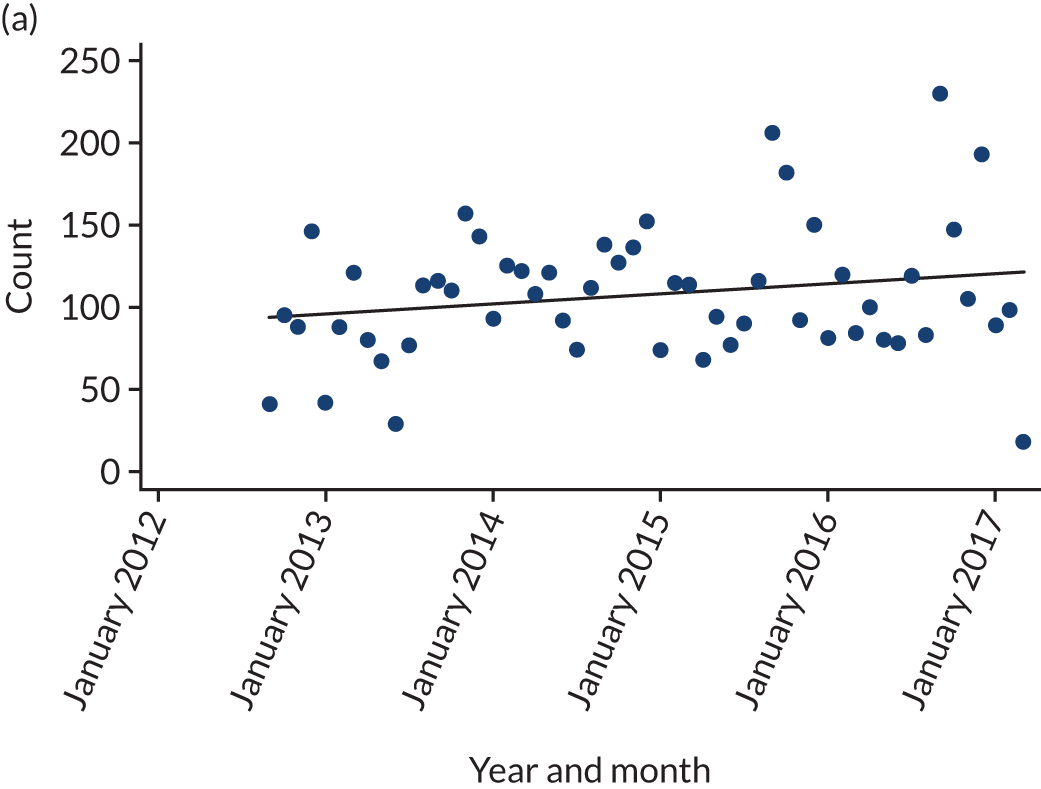
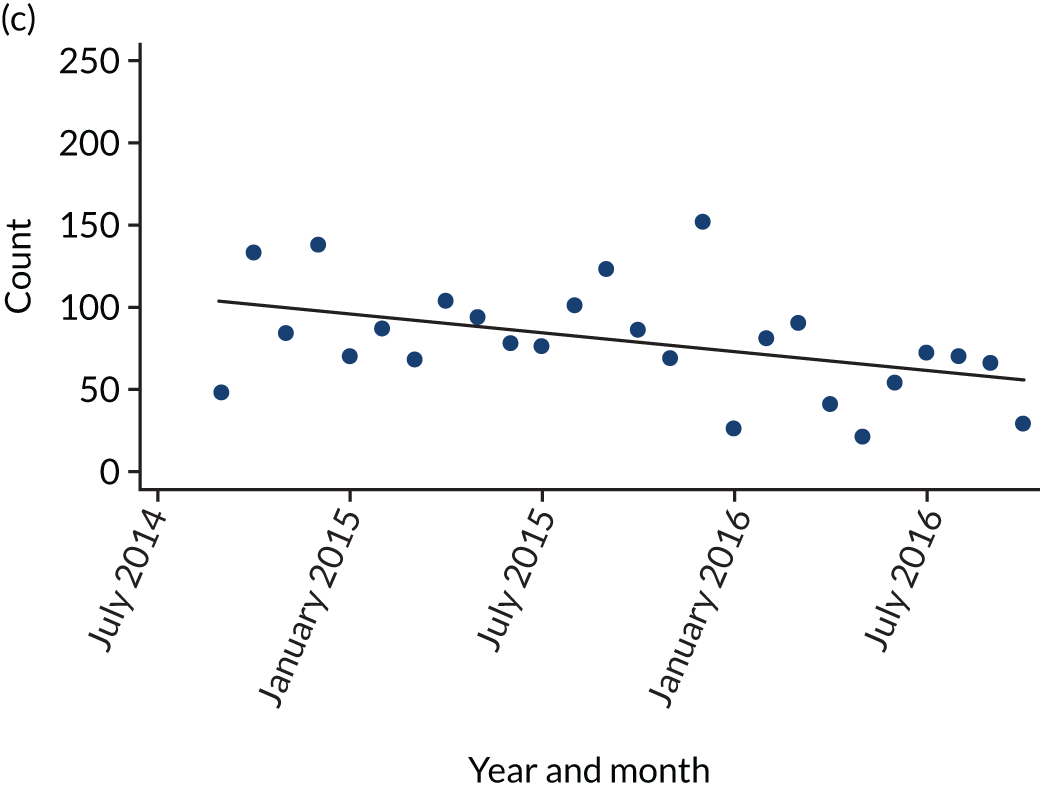
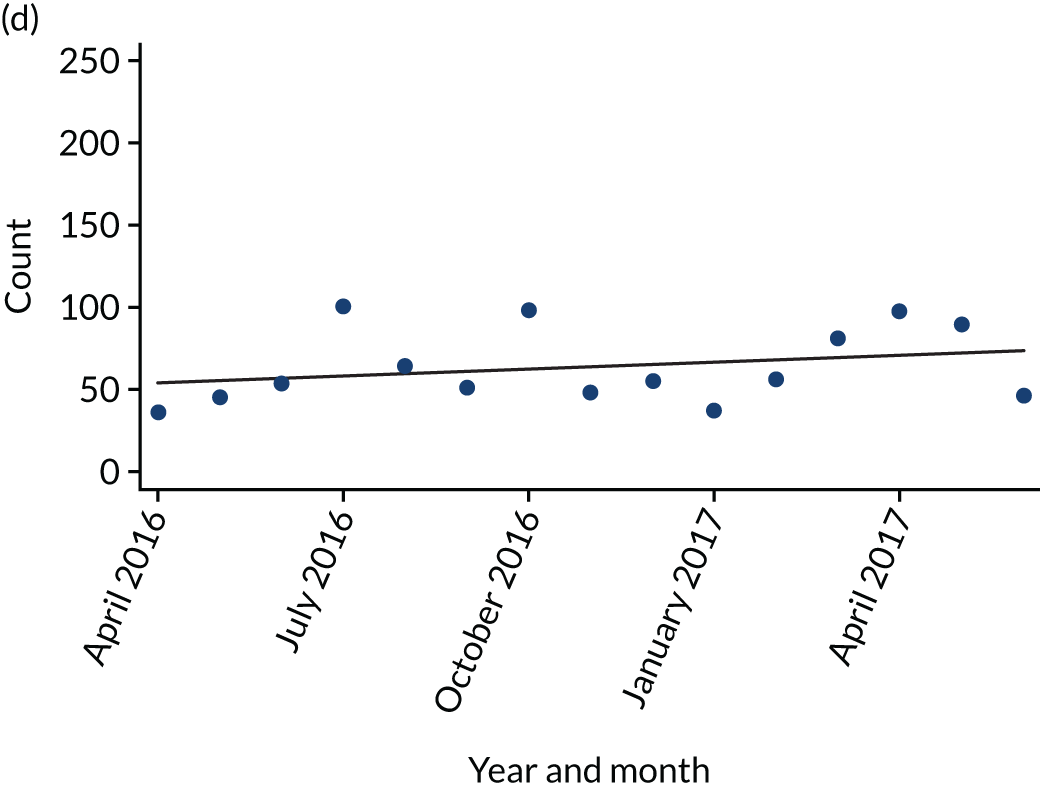
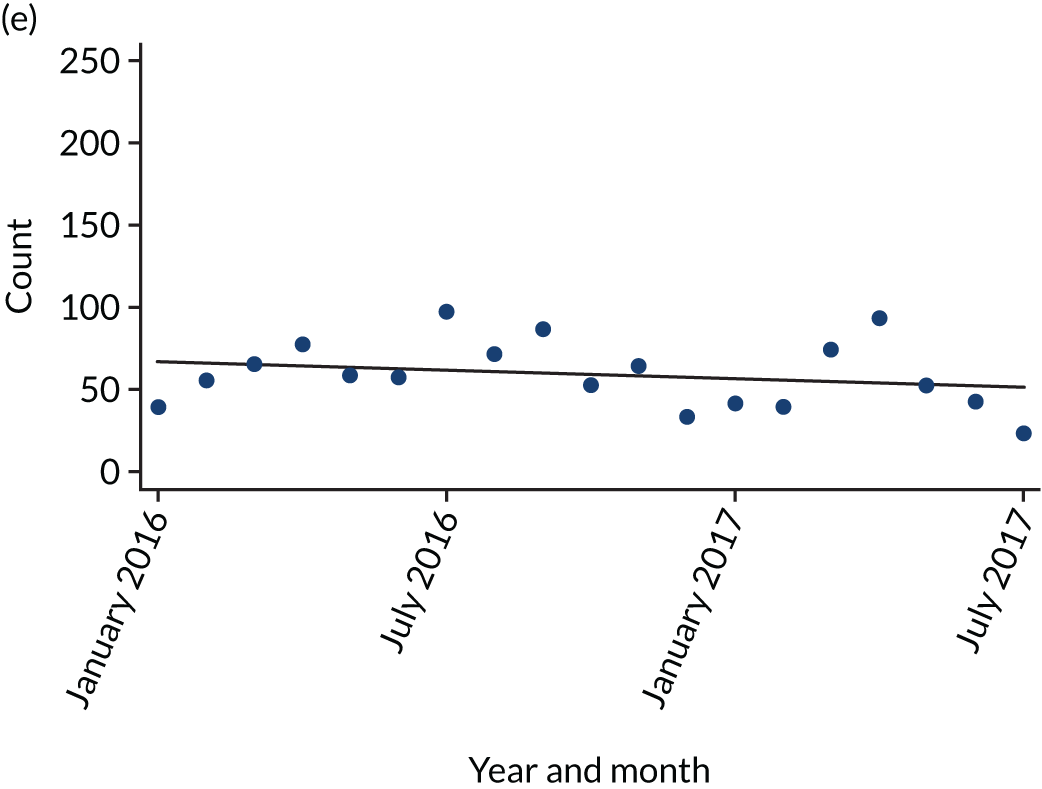
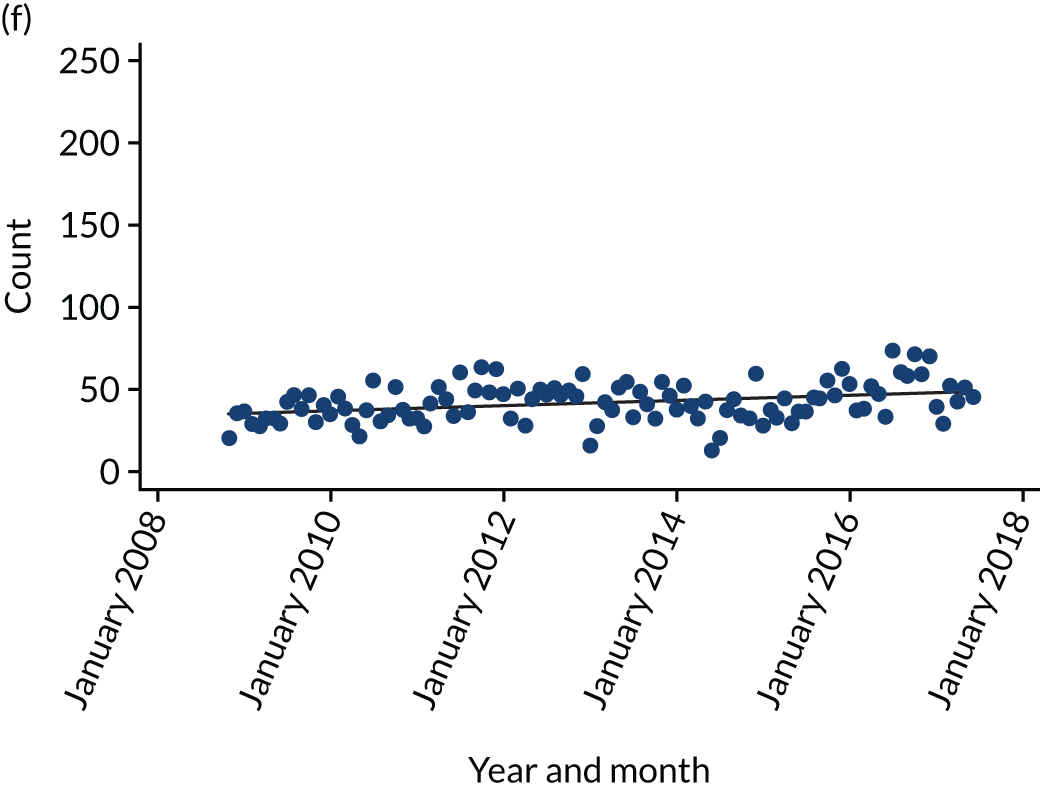
We asked each study AIMS to provide anonymised data on age, gender, hour and day of arrival, arrival by ambulance, reason for attendance, length of stay at the AIMS, tests, diagnosis, treatments and disposal. Table 1 shows which AIMSs were able to provide each type of data. Site E was not able to provide any AIMS activity data. Table 1 provides further attendance summary statistics for the six study AIMS. The mean daily number of attendances were 11.8 at site A, 2.7 at site G, 9.2 at site B, 6.8 at site C, 8.1 at site F and 5.4 at site H. These attendance statistics were explored for any trends for attendance counts increasing or decreasing over time (Figure 1) suggesting that AIMSs were subject to bedding-in periods or wane. No systematic trends were observed (site B experienced a fall in attendances over time and site H experienced an increase).
FIGURE 1.
Monthly AIMS attendance numbers, with estimated linear fits of attendance over time. (a) Site A (b = 0.51, SE 0.34; p = 0.14); (b) site G (b = 0.06, SE 0.1; p = 0.58); (c) site B (b = –1.9, SE 0.8; p = 0.03); (d) site C (b = 1.35, SE 1.37; p = 0.34); (e) site F (b = –0.88, SE 0.86; p = 0.32); and (f) site H (b = 0.13, SE 0.04; p < 0.001). SE, standard error.
All services had, as a minimum, staff able to administer first aid, with many having advanced nurse and paramedic practitioners. Clinical competencies were matched by the facilities offered in each AIMS (Table 2). The services provided met a range of needs associated with AAI. For example, some service users may have become separated from friends and need no more than to charge their phone to find their way home. However, there are some notable differences; for example, only sites A, F and B had facilities to test blood glucose levels and therefore rule out hypoglycaemia, symptoms of which overlap with intoxication and include trembling, confusion and fatigue. Endotracheal intubation6 maintains an open airway and can be required because alcohol is a depressant, which can promote irregular breathing, and an attenuated gag reflex can lead to aspiration of vomitus into the lungs and therefore asphyxiation. The risk of vomitus aspiration is reduced if patients are kept upright. Intravenous saline cannot be prescribed for AAI but can be used in the event of an accelerated heart rate. No AIMS provided pharmacological treatments, such as high-dose thiamine hydrochloride, benzodiazepines or naltrexone.
| Facilities | Site | |||||
|---|---|---|---|---|---|---|
| A | B | C | F | G | H | |
| Tea/coffee | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Phone charging | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Flip flops | ✓ | ✓ | ✓ | |||
| Place to recover | ✓ | ✓ | ✓ | ✓ | ||
| Change of clothes | ✓ | ✓ | ||||
| Transport home | ✓ | ✓ | ||||
| Condoms | ✓ | |||||
| Pregnancy test | ||||||
| Wheelchair | ✓ | ✓ | ✓ | ✓ | ||
| Bandages/plasters | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Breathalyser | ✓ | ✓ | ||||
| Drug test | ✓ | |||||
| Urine test | ✓ | ✓ | ✓ | |||
| Blood O2 level test | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Blood pressure | ✓ | ✓ | ✓ | ✓ | ||
| Prescribe medication | ✓ | ✓ | ✓ | ✓ | ||
| Blood glucose test | ✓ | ✓ | ✓ | ✓ | ||
| Cardiopulmonary resuscitation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Bag valve mask | ✓ | ✓ | ✓ | ✓ | ||
| Glue | ✓ | ✓ | ✓ | ✓ | ||
| Intravenous saline | ✓ | ✓ | ✓ | |||
| Sutures | ✓ | ✓ | ✓ | |||
| Endotracheal intubation | ✓ | ✓ | ✓ | ✓ | ||
Intervention site A
The AIMS at site A opened in September 2012 as a response to the impact on the local ED of patients presenting with AAI. Site A is located in the city centre, 3.5 miles south of the ED and close to an area characterised by many licensed premises and major sporting venues. The space consists of a small seating area, six stretchers in a central treatment area with access to a single-occupancy treatment room, toilets and an additional waiting area. The small seating area is used as a preliminary triage area. Once triaged, patients may be admitted and seated or laid on a bed for observation and treatment; the preference is to keep patients seated to reduce airway risks. The space can be partitioned with screens for privacy and there is seating for friends and family around the periphery of the room. There is a staff room and kitchen that functions as a hub for clinical staff stationed at the service as well as other staff and volunteers working in the NTE, for example local Street Pastors and visiting police officers. The service has capacity for up to seven patients supine and up to 18 patients seated. The service is open from 20.00 to 06.00 on Friday night/Saturday morning and Saturday night/Sunday morning and is also open on other nights/mornings when it is anticipated the NTE will be busy (e.g. during the local university’s student freshers’ fair, pride parades, international sports events, Christmas and New Year). The service is staffed by an emergency nurse practitioner (ENP), one health-care support worker and a senior nurse practitioner. One police officer is stationed at the service during opening hours. The ambulance service has two double-crewed ambulances (four staff) stationed at the service and responds to calls within the city centre. The health board helped to set up the service and secure initial funding from local government for a 1-year pilot of the service. The service’s success resulted in funding from the local government’s Regional Collaboration Fund and it is currently funded through a collaboration between the health board, police, ambulance service and the Substance Misuse Fund. Based on the operational information provided, it is estimated to cost £2170 per session to operate the service.
Governance
The service operates as a satellite site for the local ED and therefore has the same forms, patient records and computer system as the hospital. The senior nurse practitioner takes overall responsibility for clinical governance.
Referrals from AIMS to emergency department
Only this site’s AIMS had available patient identifiers that allowed data from the ED and AIMS to be matched. Patient data (n = 948,742), available from 1 January 2010 to 28 February 2017, comprised data from the AIMS (n = 5721), ED (n = 888,280) and a minor injuries unit (MIU) located in a nearby town (n = 54,741). Data from the MIU were dropped. Of the remaining data, 756 had no age recorded, with patient age ranging from 0 to 111 years [mean 37.08 years, standard deviation (SD) 25.43 years]; 21 records had no gender recorded; and 2709 records did not have a reliable conclusion time (i.e. recorded at the time of attendance), which was therefore marked as missing. Patients who attended the service and were referred to ED could appear in these data twice; once from attending the AIMS and once again through attending ED. However, data describing where patients attending ED were referred from also included patients discharged to ED but who had not attended the AIMS. This occurred, for example, because an ambulance crew sought advice from AIMS staff who deemed that the patient should be referred to ED. In total, 564 patient records were identified in the AIMSs data who had initially attended the AIMS and been discharged to ED. Of the referrals to ED, 38 failed to appear in ED records, suggesting that they did not attend the ED. There were 155 instances of the ED date and time of attendance preceding the AIMS date and time of attendance, leaving 371 records. Two records from the AIMS did not report conclusion date and time and these were replaced with the ED visit date and time. In total, there were 358 unique records for which the AIMS visit date and time could be matched with a subsequent ED visit date and time, representing 6.26% of all attendances recorded in the ED patient management system. The duration, for patients referred to ED from the AIMS, between arrival at the AIMS and arrival at the ED was ≤ 1 hour for 79.3% of patients and > 48 hours for 16.76%. Referrals to ED appeared to comprise two groups: those referred almost immediately on arrival and those referred to ED following a significant delay.
The times for significant stages in patient pathways for those referred to ED within 48 hours of attending the AIMS were as follows: time to first contact (AIMS), 0.18 hours (SD 0.26 hours; n = 175); episode duration (AIMS), 0.86 hours (SD 0.74 hours; n = 304); time to transfer to ED, 0.42 hours (SD 1.05 hours; n = 306); ED arrival to first clinical contact, 2.39 hours (SD 1.69 hours; n = 242); and ED episode duration, 4.76 hours (SD 4.24 hours; n = 305).
The average episode duration for patients attending the AIMS was 1.32 hours (SD 1.46 hours) and for ED patients (who did not first attend the AIMS and during an AIMS session) was 4.27 hours (SD 4.63 hours). These data suggest that those requiring referral into specialist care were referred quickly and that, overall, the episode duration in the AIMS was shorter than the episode duration expected in the ED.
Intervention site B
The AIMS was established by the Police and Crime Commissioner’s Office in response to the demand placed on the ED and police and ambulance services as a result of alcohol-related assaults and AAI in the NTE. The intention was to divert intoxicated people away from the care of police officers and reduce the burden on the ED while also contributing to making the NTE safer. Site B is located in the city centre, 6 miles south of the ED in an area characterised by the high density of premises licensed for the sale and on-site consumption of alcohol. The AIMS is housed in static cabins and contains toilets and areas designated for seating, staff and clinical activity. It is supported by St John Cymru (Cardiff, Wales): it has an operations vehicle and a rapid response vehicle (RRV). Patients may wait in the seating area until triaged. Within the cabin are two clinical treatment rooms with seating and stretcher beds in which patients may receive treatment and recover. There is a small staff room with kitchen facilities. The St John Cymru vehicle is stationed outside and serves as an operations centre receiving 999 calls to the site B ambulance service. All calls to the ambulance service originating from the city centre are redirected to the AIMS, where a response is co-ordinated. Police officers also use the AIMS to take witness statements when it is appropriate to do so. The AIMS has capacity for up to three patients supine and a further five patients seated. Staff can provide treatment and support for minor injuries and support those who are vulnerable. Patients are discharged once it is safe to do so and contact has been made with friends or family members to ensure a safe transit home. The AIMS is open on Wednesdays nights/Thursday mornings (owing to local university student drinking events), and Saturdays nights/Sunday mornings, between 22.00 and 06.00. They also occasionally operate additional periods when significant events are expected to bring additional numbers into the city (e.g. sporting events and bank holidays). A slightly larger proportion of patients were female (51.1%). The majority (72%) of patients were aged 18–24 years. Overall, 14.8% of patients were conveyed (transferred by ambulance) to the local ED. The AIMS is staffed by up to three St John Cymru staff, including volunteer first aiders, an advanced first aider, a nurse practitioner and a paramedic with access to a RRV. In addition, three students from a local university work as police volunteers to support the AIMS team. A police officer is stationed at the AIMS during opening hours. The Police and Crime Commissioner, Home Office Police Innovation Fund and health board currently fund the AIMS. Based on the operational information provided, it is estimated to cost £1345 per session to operate the service.
Governance
A St John Cymru shift leader (paramedic) takes overall responsibly for clinical governance. Patient details are recorded by St John Cymru and collated by the Police and Crime Commissioner, which oversees the running of the AIMS.
Intervention site C
The AIMS opened in November 2014 in a static ambulance. In July 2015 the service moved to premises that could also provide space for patients to recover. The service operates from a building in the city centre, 2.5 miles north of the main hospital, near an area characterised by a number of restaurants and licenced premises. New patients are registered and triaged at the front desk. An open-plan area provides seating for patients, friends and family and functions as the treatment area. Mats and temporary room dividers can be used to partition areas, giving patients an opportunity to lie down. Two treatment beds are present in separate rooms. The AIMS has capacity for approximately 10 patients supine and 10 patients seated. The service is intended to be an alternative pathway for those who have become vulnerable or injured, including those who are exhibiting AAI, in the NTE, but not an alternative to specialist care in the ED. Street marshals collect and escort users into the service by foot or wheelchair. The service provides a space where patients can be monitored until they recover and given treatment for minor injuries and where arrangements can be made for a safe journey home. Typically, patients are seated and offered water and a sick bowl. The service is usually staffed by up to three substance misuse workers, one nurse, two medics provided by Medics UK Ltd (Redcar, UK) and security staff. Two street marshals employed by the city council also operate from the AIMS. We are unable to report on patient demographics, referral routes or discharge destination owing to limitations on the activity data collected. Only monthly data were provided, for April 2016 to June 2017, so we have no data on specific opening dates.
Governance
Medics UK Ltd oversee clinical governance and the disposal of clinical waste in accordance with their policies and procedures. Patient details are recorded electronically on the Safe Haven patient record form. These data are linked directly to a Hospital Intervention and Liaison Team system based in the local hospital. A third-sector organisation local to site C sends the site C Public Health Group and local Clinical Commissioning Group (CCG) monthly Safe Haven data for its records and monitoring purposes. Medics UK Ltd is responsible for the clinical care delivered and the local council is accountable overall. There is no formal relationship with the ED or any means to follow up patients once they have been discharged.
Intervention site F
The AIMS was established in 2010 by the local police and ambulance services to relieve pressure on the ambulance service from AAI on Friday and Saturday nights and as a place of safety. The service is a collection of vehicles: a large mobile St John Ambulance treatment unit, a St John Ambulance ambulance and a police van. The service (as of 19 May 2017) is situated in the city centre, 1 mile south-east of the ED. The St John Ambulance treatment unit provides a space for initial triage, seating for minor injury treatment/waiting and two stretchers for further treatment and recovery. St John Ambulance typically receives calls via the ambulance service and city-linked radio to attend to intoxicated or injured patients and bring them back to the AIMS or provide direct conveyance to ED. The police van provides a space where vulnerable patients can wait in a safe environment. Patients with uncomplicated acute intoxication (initial triage by St John Ambulance) can sit and recover before safe transport home can be arranged. The service has capacity for approximately three patients supine and eight seated. Furthermore, the AIMS provides a service in which people can seek assistance if they are feeling vulnerable or are lost. In addition to medical assistance, people can speak to a police officer in confidence. Typically, patients will receive minor wound care for a brief period and then be offered a place to sit and recover in the police van.
We are unable to report on patient demographics owing to limitations of the activity data provided.
We are unable to report on patients attending the police van who may not have required any medical assistance and so bypassed the treatment unit. Of all patients attending the police van, 8.3% were taken to ED by ambulance and 23% were advised to go to ED.
Typically, the service would be staffed by two to five paid St John Ambulance staff, one St John Ambulance EMT (who assumes the role of clinical lead and takes responsibility for the facility), an emergency transport assistant and up to four other volunteer first aiders (advanced and non-advanced). The police van is run by two police officers. The ambulance trust pays St John Ambulance £1075 per session for the provision of the resources (including staff and non-staff costs). The Police and Crime Commissioner funds their own vehicle and police officers; the value of this funding is undisclosed.
Governance
The service operates in accordance with the St John Ambulance clinical governance standard operating procedures. Patient details are recorded on patient report forms, aggregated and transferred to the ambulance service where they are scanned and stored. The St John Ambulance shift leader takes overall responsibility for patient care, including the suitability of referrals, safe discharge home and referring on to the ED.
Intervention site G
The AIMS was opened in December 2014 as an extension of an existing Street Pastor scheme and in response to the perceived burden that AAI patients from the NTE were placing on ED. In addition, local Street Pastors raised concerns that most of their time was spent on waiting for ambulances and trying to meet the needs of ill and injured people on the street, which is not seen as their core purpose. The AIMS was designed to help vulnerable people in the NTE as well as reduce the impact on emergency services of those who have consumed excessive amounts of alcohol or have used illicit substances. The local ambulance service did not, unlike other sites, refer patients to the AIMS. The service is in a building in the city centre, 0.5 miles west of the ED and close to licensed premises and fast-food outlets. The space consists of a main reception area with seating around the periphery. A partitioned area contains the office equipment, closed-circuit television (CCTV) and a viewing window to an adjoining recovery room. The recovery room contains three crash mats on the floor. There is a small single-occupancy treatment room with a stretcher bed, medical supplies and an additional small room. There is a kitchen and a toilet for staff and patient use. A large people-carrier-style vehicle is stationed outside. The main reception area is used to initially seat and assess patients and for friends and relatives who are waiting. After initial triage, patients may be taken to the recovery room and laid on crash mats or taken to the treatment room for first aid. The additional room may be used for people who may require privacy and emotional support. Staff, patients, friends and visiting Street Pastors use the main reception area to congregate and await referrals. The vehicle is used by staff to pick up patients from the city centre and to transport patients home. The AIMS has capacity for approximately five patients supine and a further five seated. It is open every Saturday night/Sunday morning, some Friday nights/Saturday mornings, Sunday nights/Monday mornings and bank holidays from 22.00 to 04.00. There was a slightly higher proportion of females (53.6%) using the service. The average age of patients was 24 years (median 21 years) and ranged between 16 and 61 years. Overall, 10% of patients were conveyed (transferred by ambulance) to the local ED. The service is staffed by between four and 10 volunteers, including a senior shift leader and a team of local college students, and has managerial and administrative support from the lead organisation. There is no clinical input. The service is run by a Christian charity and is funded by the Police and Crime Commissioner’s Office, a local church, the city council and a local foundation. Based on the operational information provided, it is estimated to cost £1186 per session to operate.
Governance
The shift leader takes overall responsibility for clinical governance. All volunteers are first-aid trained and follow policy and procedures when caring for individuals. Paper reports of all patients seen each night are collated.
Intervention site H
The AIMS was established following the death of three young adults in late 2000: two men drowned in a river during a night out drinking and a third youth was found dead in a city centre nightclub as a result of alcohol intoxication. The service has three vehicles that are intended to keep people safe and reduce unnecessary ambulance call-outs by assisting anyone at risk: a bus, a medical unit and a mobile support vehicle (minibus van). All three vehicles park in a layby in the city centre, 5 miles west of the ED. The bus provides a long, narrow space with bench seating to triage and monitor patients. The medical unit contains two stretcher beds, used when administering treatment, and provides additional space for recovery. The mobile support van usually responds to calls from licensed premises and local street-based volunteers for assistance and returns patients to the bus for assessment. The bus has capacity for two supine and three seated patients but will use public seating outside the bus with appropriate staff support as an additional waiting area. There was a slightly higher proportion of women (51.2%) using the bus. Most patients were aged 18–24 years, with an average age of 24.5 years (median 21 years); 6.9% of patients were conveyed by ambulance to the local ED. The bus team consists of St John Ambulance first-aid volunteers and community first responders, who are supported by an ambulance paramedic and a private security guard. A volunteer shift leader from a charity is supported by other shift support volunteers, including a driver who can operate the mobile unit. The bus receives funds from local CCGs, local businesses and private donations and is run by a registered charity. Based on the operational information provided, it is estimated to cost £1106 per session to operate.
Governance
The paramedic takes overall responsibility for treatment and discharge of patients in accordance with ambulance policy and procedures. The charity shift leader takes overall responsibility for co-ordinating staff and operations. St John Ambulance and ambulance staff use their own patient record forms, which are collated by the bus administrator at the charity.
Funding for AIMSs
All AIMSs were developed in response to front-line staff’s perceptions of the number of people who became vulnerable because of their misuse of alcohol. The rationale was that AIMSs reduce impacts on health-care, ambulance and police services. There is a legal requirement for Crime Reduction Partnerships to produce an annual Crime and Disorder Strategic Assessment. Section 116 of the Local Government and Public Involvement in Health Act 200758 sets out that primary care trusts and partners should produce a Joint Strategic Needs Assessment, revised in the Health and Social Care Act 2012. 59 This requires local authorities, CCGs and other responsible authorities to prepare a strategy and, in addition, consider whether or not needs could be met more effectively by other arrangements under section 75 of the National Health Service Act 2006. 60 Although these strategies include data on alcohol and crime as national performance indicators for public health, the impact of AAI on front-line services is inadequately recorded and strategies are not developed to offset the impact of AAI on police and ambulance services and EDs. In accordance with section 75 of the National Health Service Act 2006,60 changes to functions in the delivery of health care should be considered if there is an improvement ‘in the way in which those functions are exercised’. Improvements attributable to AIMSs, however, are realised across partners, including the police, and not solely by health-care services.
In establishing AIMSs, partnership is key (at all levels); ownership of alcohol-related harm is shared primarily by police and ambulance services and other unscheduled-care services. At the micro level, practitioners work together to manage day-to-day needs of patrons in the NTE. At the meso level, operation of AIMSs requires co-ordination so that all practitioners deliver the AIMS as intended and standard operating procedures are available to determine appropriate referral. At the macro level, funding and governance needs to be in place so that AIMSs can function with appropriate staff and resources. This partnership extends to communication at the front line. Typically, front-line staff will have some formal method of communicating with partners so that resources are appropriately managed. This can be formally realised, such as at site B, where the service was realised as a part of processes designed to manage the intoxicated, or informally realised, for example where private mobile telephones are used to consult across groups. This communication network often extends to taxi drivers, Street Pastors, door security staff and other third-sector organisations. Therefore, AIMSs typically serve as hubs that bring together a range of organisations that can receive patients: ambulance services (including 999-call patients), police, volunteers, Street Pastors, door security staff, friends and family members, the public and self-referral.
Although AIMSs were implemented in response to the impact of intoxicated patrons on services, this awareness was not derived from routine data analysis but from front-line staff reporting informally. For those in health care, this typically focused on AAI patients taking up resources and therefore contributing to bottlenecks in service delivery. Ambulance staff reported on the delays experienced when conveying AAI patients. Police reported on the need to ensure the safety of intoxicated individuals in the NTE and the subsequent drain on resources, having no easy referral route for such individuals, many of whom were not perceived to require care in ED. AIMSs had typically been formally considered in response to a notable event whereby emergency services were able to demonstrate the impact of AAI and so escalate the need to reconsider current patient pathways.
Part 2 of the Police Reform and Social Responsibility Act 201161 allows licensing authorities to make additional charges on those licensed to sell alcohol at night as a contribution towards the costs of policing the NTE. Any decision to enact a levy is expected to be in collaboration with the local Police and Crime Commissioner. The levy is designed to cover the costs of policing associated with the sale of alcohol between midnight and 06.00 and the reduction and prevention of crime and disorder. These funds were not used for any study AIMS.
Clinical risk management
We intended to ask AIMS staff during the study to record critical incidents that could potentially involve a risk to patient safety, such as delayed diagnosis or suboptimal supportive care, and any occasions when an ambulance arriving at the service was redirected to the hospital. However, it became apparent that this would not be feasible because of limitations of critical incident reporting systems, with the exception of site A, and other challenges in ensuring the services’ engagement with the study, such as the need to prioritise recruitment to the AIMS user evaluation. Therefore, we asked the individual responsible for each service to complete a brief survey describing key issues in managing clinical risk. The results are summarised in Appendix 5. Responses were obtained from the six sites participating in the AIMS user survey.
The background of the person with overall responsibility for the service differed between sites, depending on the supporting organisation. The shift staff also varied between AIMSs, with clinical input being variably provided by nurse practitioners, registered nurses, paramedics, ambulance technicians, first aiders and volunteers. The person with clinical responsibility also differed between AIMSs and included a clinical lead, team or shift leader, paramedic, ambulance technician, nurse and first aider.
Training and qualifications for the clinically responsible staff varied between AIMSs, and included nurse practitioners (site A), registered nurses (sites B and C) and St John Ambulance training (site F). Site G provided a bespoke 6-day training package and site H provided on-the-job training. Clinical decisions were documented in patient notes (site A), an AIMS patient report form (sites C and G) or an ambulance patient report form (sites B, F and H).
Policies for reporting untoward incidents also varied across the sites. Site A undertook root cause analysis using data from an incident form. Site G used feedback forms and incident review for adverse events. Sites C and B used standard processes for Medics UK Ltd and St John Ambulance, respectively. Site F used an incident report form and site H used an e-mail or logbook report to the service administrator.
In summary, there were marked variations between service processes for managing clinical risk. We were unable to collect data relating to specific critical incidents during the study period and, thus, unable to assess how clinical risk was managed in practice.
Control cities
Control site M
Alcohol intoxication management services are not planned in this city and the usual pathway is for patients to be taken to ED by the ambulance service. In addition to usual service there is an initiative run by the ambulance service: a paramedic and a police officer travel together in a paramedic car on Friday, Saturday and Sunday nights for a 12-hour shift, responding to issues in the NTE. The initiative runs intermittently because of a lack of police availability. The initiative aims to reduce unnecessary hospital visits via paramedics treating the injured and police de-escalating the situation. The initiative receives calls from both ambulance and police control centres. There are no plans to introduce an AIMS; this is because the NTE is split into six separate areas [student area, café culture area, real ale trail, party zone, LGBT (lesbian, gay, bisexual and transgender) area and lower-income/non-workers area] and there is not the concentration of drinkers found in other cities in which the NTE is centralised. Other reasons include legality, the responsibility involved in caring for people and lack of funding.
Church-led and similar organisations are prominent. Street Angels provide help for the intoxicated and this includes cycle responders: mobile paramedics on bicycles who carry a defibrillator as well as a larger first-aid kit than those carried by Street Angels. Each shift there are typically six Street Angels and two cycle responders. The cycle responders are a Street Angels initiative with additional support from the NHS. The local police provide additional funding and storage for equipment. In addition, a night church opens once per month and provides space for drinkers to take time out and reflect. Staff there can look after intoxicated people and perform basic first aid, although this is not the night church’s primary function.
Street marshals operated from 2008 to 2015 but were withdrawn because of a lack of funding. They were originally taxi marshals and the role developed; they operated every Friday and Saturday, then Saturdays only (usually the busiest weeknights). Street marshals provided pastoral support in the NTE, collected glass from the streets, managed taxi ranks and performed other activities as appropriate. Their role developed and they became a conduit between the intoxicated and the Street Angels. Over a 4-year period, the Street Angels helped > 3000 people directly, most assistance involving first aid. Street Angels are volunteers who receive training in emergency first aid, provide bottles of water and flip flops and carry first-aid kits. They help drinkers to rehydrate, sober up and get a taxi (if they are sober enough) or locate a partner or friend to take the individual home safely. Street Angels try not to send people away in ambulances if they need only sobering up and have no other health issues. If they do feel that they need to call an ambulance, they will wait with the individual for 2–3 hours or more.
Control site L
There are no plans for AIMSs in this city. There are typically 10 police constables and one police sergeant on patrol on Fridays and Saturdays between 13.00 and 06.00. In addition to the usual services, Street Pastors also offer support. In matters of AAI, police will defer to Street Pastors, who stay with the intoxicated individuals and make certain they are safe and that someone can collect them. This releases police officers back to duty. Police-led AIMSs were trialled twice in a church in the city centre, once during a major sporting event and once over the Christmas period. Numbers attending were approximately two or three patients per night. People were instead routed to the local ED, unless the police directed them or took them to the AIMS. The pilot AIMSs were staffed by the local locality manager, one police officer, one advanced paramedic practitioner, one health-care assistant and one nurse practitioner. There were two RRVs and the AIMSs were run in partnership with St John Ambulance, who provided two staffed support vehicles for transportation.
Control site N
The police are investigating options for an AIMS in the city centre. This would be a multiagency setting with volunteers, capable guardians and some form of health service involvement. Currently, Street Pastors help look after intoxicated persons and an ambulance is called if necessary, but often police officers end up taking people to ED. A service was trialled on Millennium Eve in the town hall, staffed by ED doctors and nurses, but this ended because of low demand. A police–ambulance service was trialled from 2009: an ambulance fast-response car staffed by a paramedic and police officer. The ‘polambs’ (ambulances with police officers on board) ran for 4 years but ended as there was nowhere to privately assess the patients. A Dynamic Emergency Care Centre (DECC) was trialled: a partnership between the local council and the police. This was a static unit with an assessment area inside. Referrals to the DECC were mostly by ambulance. The DECC was funded by the local CCG and staffed by two first aiders from St John Ambulance or the British Red Cross (London, UK), one paramedic and one police community support officer. The DECC operated only on key dates (e.g. New Year’s Eve) because there was no call for it on some weekends and funding was limited. Otherwise, AAI was handled by the usual services with additional support from Street Pastors.
Control site K
A clinically-led AIMS is cost prohibitive, with significant resource implications and uncertainty over CQC compliance. Street Pastors have had a ‘Safe Space’ since 2010, where shelter can be given to vulnerable people (not only intoxicated individuals). In addition, there is a service similar to Street Pastors, currently without a base, that uses non-medical intervention or ‘very light’ first aid. Polambs were used for many years but ceased operation because of budget pressures on the ambulance service and safety concerns about solo staffing. Ambulance crews do not use the Street Pastor Safe Space.
Control site J
Proposals for AIMSs, including a mobile bus that provides support and somewhere for people to rest rather than attend ED, were considered but judged financially inviable, and concerns were raised over the level of medical qualifications required. There is a Street Pastor team that provides coverage. There used to be a city centre triage unit, which was a joint venture between the ambulance service and police: an ambulance with police in attendance. This ceased operation because of lack of demand. An AIMS would be useful because it would take pressure off the police and ED, but funding and resources are an issue. The police have a duty of care to the individuals they engage with, so if those individuals are unable to care for themselves, the police need to find someone who can look after them. Street Pastors can stay with the individual, but this is not ideal as the Street Pastors have no base to go back to, so must stay on the street.
Control site O
A mobile medical support bus was launched in 2012 by the local NHS trust in collaboration with the community safety partnership. The vehicle was provided by St John Ambulance and staffed by a paramedic, St John Ambulance first aiders and trained volunteers from Street Pastors. A similar service, operated by Street Pastors, ran from October 2015 to March 2016. The bus was well used but closed in 2013 because of financial constraints. Located in the city centre, it was accessible and well managed. It was open on Friday and Saturday nights, the two busiest nights in the city centre, and freed up the police and ambulance services. Currently, intoxicated people are helped by the police, ambulance patrols and Street Pastors. Owing to heavy demands on ambulance resources, police officers occasionally transport patients to the ED. The bus was larger than an ambulance, with space for people to sit down, lie down and receive treatment and there was a private space at the back.
Summary
The configuration of AIMSs varied considerably. Most services had some formal clinical input, in the form of registered nurses and paramedics, whereas one relied entirely on volunteers. Broadly speaking, nurse practitioners drawn from EDs will have experience of ED triage33 in addition to clinical experience in managing AAI appropriately. Paramedics will also have clinical experience in managing AAI but are less likely to have experience of triage in ED settings. Volunteers have no practical clinical input, only pastoral support value. It is notable that the volunteer-based service was the only service that did not accept patients referred from ambulance services. It is not clear how the more volunteer-oriented services record or respond to adverse events, particularly those that can be identified once patients are discharged from AIMSs.
Alcohol intoxication management services are emerging services, but services that accept patients whose alcohol consumption has placed them at potentially significant risk (see Chapter 1). Given the relatively limited research on how AAI is best managed in NTEs, there is a reasonable expectation that processes should be in place to ensure that activities meet proscribed objectives and that activities are monitored so that service delivery can be assessed against benchmarks. An established audit62 is one option; this would require AIMS practice guidelines63 and data available to inform that process. The stated objective of the AIMSs was to alleviate pressure on front-line services, but some services were unable to provide a count of patients attending.
Alcohol intoxication management services were mostly implemented in response to practitioner-voiced concerns over the effect of AAI on services. This can be partly explained by the lack of routine data that adequately capture the effect of AAI on police and ambulance services and ED practice. Policies related to alcohol are mostly in response to chronic measurable conditions such as alcohol-related liver disease.
Chapter 4 Effectiveness and cost-effectiveness
Hospital EDs and ambulance services can receive a number of people who require health-care assistance as a result of excessive consumption of alcohol, particularly on evenings when large numbers of people socialise in city centres. This places a burden on all emergency services (police, ambulance and unscheduled-care services) as well as on other patients in the health-care system. This chapter summarises the main findings, which are reported in detail in Appendix 6.
Effectiveness
Emergency department attendances
Descriptive statistics
Emergency department attendances were analysed across all sites from 16 November 2010 to 31 March 2016. Table 3 shows the mean number of ED attendances per day during the hours of AIMS activity at each site before and after the AIMS started operating at the intervention site in each matched pair. Pre-intervention data were not available at site H (or site K when matched with site H) because the site H AIMS started operating before 2010. Intervention cities showed a modest increase in ED attendances of 1.38 post AIMS, whereas control cities showed an increase of 5.15, suggesting that matching had failed.
| Intervention site | ED attendances, mean (SD) | Control site | ED attendances, mean (SD) | ||
|---|---|---|---|---|---|
| Pre AIMS | Post AIMS | Pre AIMS | Post AIMS | ||
| H | 66.81 (11.52) | K | 113.01 (15.15) | ||
| A | 87.94 (11.88) | 79.22 (10.81) | N | 47.91 (9.21) | 60.06 (10.11) |
| B | 57.15 (9.88) | 57.54 (9.37) | L | 54.48 (8.73) | 50.55 (7.80) |
| G | 31.04 (6.70) | 32.79 (6.33) | M | 78.65 (10.35) | 80.91 (12.40) |
| F | 70.74 (11.88) | 77.24 (11.73) | J | 91.34 (12.09) | 94.41 (12.27) |
| C | 75.57 (11.46) | 73.16 (11.86) | O | 61.85 (10.26) | 66.37 (9.24) |
| D | 116.72 (17.90) | 120.96 (13.97) | K | 117.06 (14.50) | 127.38 (12.47) |
| E | 112.33 (13.20) | 119.6 (16.59) | M | 69.24 (10.64) | 76.82 (10.70) |
Analysis
We planned to fit ARIMA models to daily ED attendances to compare AIMSs with usual care and different levels of AIMSs and their impact on ED attendances. However, initial explorations using these models on daily data revealed large variability in the data and, subsequently, models were unable to identify any meaningful patterns. Alternative ARIMA models were explored, including models fitted to weekly data, monthly data and Saturday data only, but these would not allow identification of when AIMSs were open. It was therefore decided not to use ARIMA owing to limits on interpretability and, instead, generalised linear models were used. To determine the main effect of AIMSs on ED attendances, all intervention cities and all control cities were included in a single model. Data were restricted to only those days of the week when AIMSs were operational and to the hours they were typically open, and controlled for a linear effect of time to adjust for the known increase in ED attendance over time. Data were realised as a panel and a random-intercept fixed-slope multilevel model was applied, drawing the cities together under the assumption that they are each drawn from a larger population of possible cities. Clustering was by city, to adjust for heteroscedasticity and within panel autocorrelation, but sensitivity analyses were also conducted, clustering on pairs of cities (control–intervention) to better realise the design of the evaluation. No notable differences were observed between models. In the interests of transparency, we have reported all analyses undertaken in Appendix 6.
Consistent with the descriptive statistics (see Table 3), which show a relative decrease, or difference-in-difference, in AIMS sites of 3.85 attendances compared with control sites (excluding site H), AIMSs were associated with a relative decrease in attendance in ED [β = –4.99, 95% confidence interval (CI) –9.44 to –0.54; p < 0.05]. Whereas both control sites and intervention sites exhibited an increase in ED attendance, the increase for intervention sites was less than for control sites. An increase in attendance across all hospitals was observed over time (β = 0.005, 95% CI 0.002 to 0.007; p < 0.001), but this trend did not notably differ across control and intervention groups (z = 0.42; p < 0.34). The model was repeated dropping site D and site E. This model yielded a similar main effect of the intervention (β = –5.30, 95% CI –9.62 to –0.62; p < 0.05). However, stating that this effect is common across all AIMSs in the analyses is not appropriate, particularly given the variability in AIMS configurations (see Chapter 3). Referring to Table 3, this effect is likely to be attributable to a subset of AIMSs.
Interrupted time series analyses were therefore used to understand the underlying effect of AIMSs on a city-by-city basis. These models compare linear trends pre and post intervention. They identify any initial change in the outcome at the time of implementation and any net trend subsequent to implementation.
Models were realised in two ways. First, all dates when an AIMS was open were identified (Table 4) and compared with baseline, controlling for notable dates (e.g. News Year’s Eve, Halloween) and days of the week. Second, the models were restricted to the days when AIMSs were typically open (most commonly Friday and Saturday; Table 5), in an intention-to-treat analysis, and without controlling for notable dates and days of the week (see Table 5). The reason for the sensitivity analyses was that the inclusion of day of week and other notable events risked over-identification in the regression models, particularly given the limited pre- or post-AIMSs data available in some models. Comparisons between intervention cities and control cities, and pooled control sites, were planned; however, these models exhibited significant baseline imbalance, a matter that substantially increases the risk of both type I and type II errors. 64,65
| AIMS site | Effect | Trend | Time (days) | |
|---|---|---|---|---|
| Before | After | |||
| H | 0 | 2019 | ||
| A | –4.89*** | –0.014*** | 728 | 1290 |
| B | –2.41* | 0.008* | 1460 | 557 |
| G | 2.22 | –0.002 | 1533 | 478 |
| F | 4.05 | 0.004 | 1716 | 295 |
| C | 1.29* | –0.011 | 1533 | 485 |
| D | –6.02 | –0.016 | 1680 | 331 |
| E | –5.24 | –0.106 | 105 | 1913 |
| AIMS site | Effect | Trend | Time (days) | |
|---|---|---|---|---|
| Before | After | |||
| H | 0 | 2019 | ||
| A | –4.93*** | –0.013**** | 728 | 1290 |
| B | –2.63 | 0.008* | 1460 | 557 |
| G | 1533 | 478 | ||
| F | 3.32 | 0.008 | 1716 | 295 |
| C | 1.12 | –0.010 | 1533 | 485 |
| D | 1680 | 331 | ||
| E | –0.22 | 0.006**** | 105 | 1913 |
Interrupted time series analysis models including control cities exhibited imbalance between control and intervention cities at baseline, whether the control was the matched site or pooled control sites, and the days available for analysis were unbalanced. Notably, for sites H, F, D and E, ITSA did not include a full calendar year either pre or post intervention, suggesting that any seasonality would not be balanced. Because the AIMS at site H opened in 2001, earlier than the ED attendance data available, it cannot be included in these models. All models corrected for serial autocorrelation. In paired analyses only, the site B–site L pair did not exhibit imbalance at baseline and this model yielded an insignificant effect of AIMSs and post-implementation trend.
Tables 4 and 5 (full model details are available in Appendix 6) provide mostly consistent results, suggesting that the only city demonstrating an initial effect on ED attendances (as opposed to a trend) was site A (Figure 2). Sites G, H and D do not have enough data for the reduced-form single-city analyses. For site H there is no baseline data and sites G and D opened sporadically over the follow-up period. Site A shows a significant initial reduction in ED attendances and a post-implementation trend suggesting that ED attendances would be expected to fall further (see Figure 2), consistent with the view that AIMS effects take time to bed in. This was the only effect that was consistent across single-city analyses (pre and post implementation with no control). Restricting analyses to the total number of ED patients aged between 14 and 39 years reduced the effect observed at site A (–2.71; p < 0.05) with a non-significant post-implementation trend and raised the effect at site B to significance (–2.64; p < 0.01) with a positive post-implementation trend (0.007; p < 0.05), suggesting that the effect of the AIMS on ED attendance numbers may have decreased over time.
FIGURE 2.
Site A ED attendances (dark blue dots) compared with site N (control) ED attendances (light blue dots). Vertical dotted line denotes service implementation.
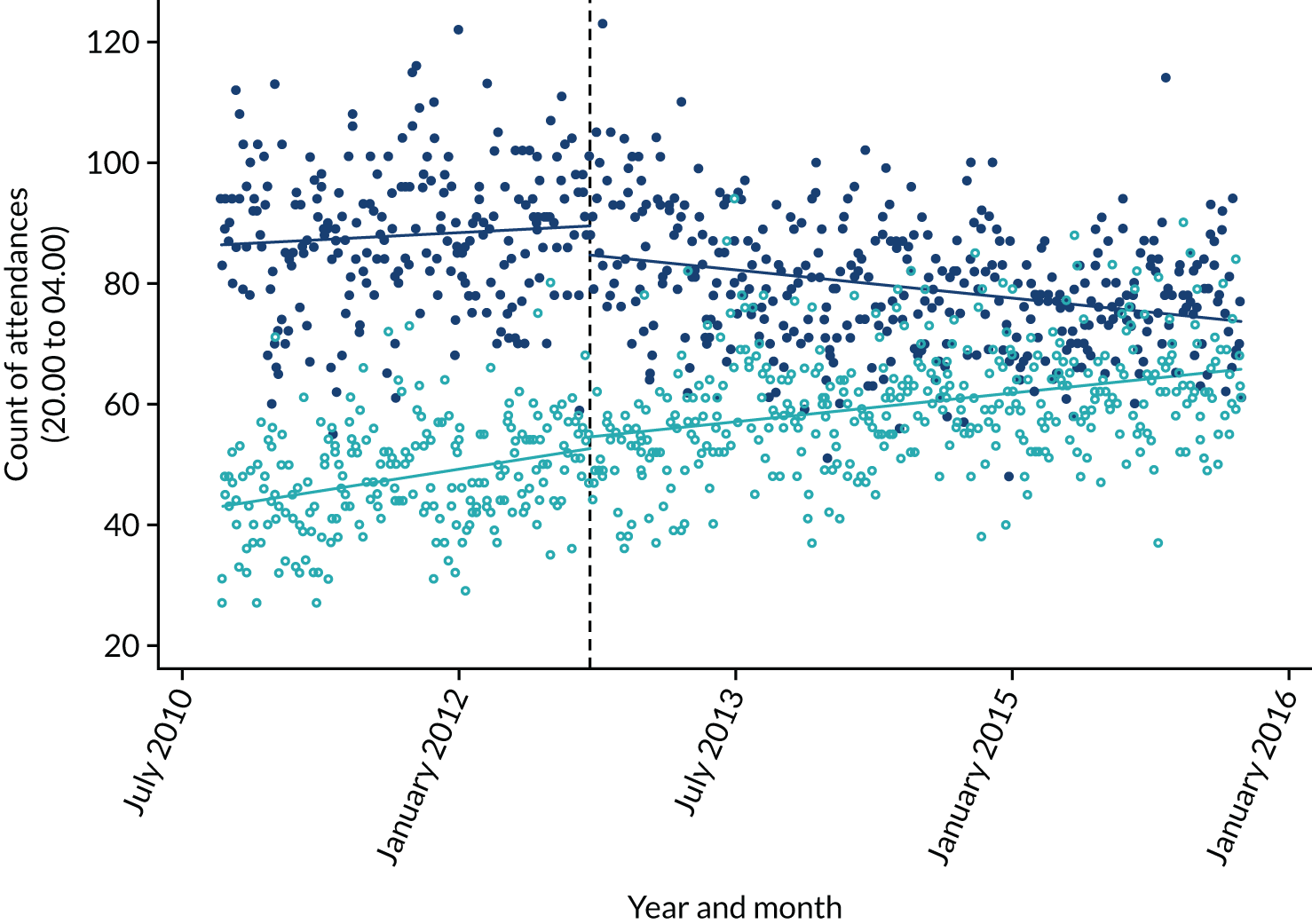
Summary
There is little consistent effect to suggest that AIMSs, overall, reduced ED attendance numbers except at site A, where a reduction in ED attendances was initially observed together with a post-implementation trend, suggesting that site A experienced a bedding-in period. Site A exhibited an initial reduction of approximately 6% in all ED attendances, which increased over time by approximately 1.5 additional diversions or to 8% of all evening attendances by the end of the analytic period.
Emergency department key performance indicators
Total time in ED (time from initial attendance to discharge) is a key performance indicator for EDs. From the individual-level data available we derived a binary indicator of whether or not each patient was seen, treated and discharged within 4 hours. Table 6 presents the percentage of patients with such episode durations of < 4 hours. Over time, performance in EDs declined.
| Intervention site | Pre AIMS | Post AIMS | Control site | Pre AIMS | Post AIMS |
|---|---|---|---|---|---|
| H | 87.6 | K | 85.1 | ||
| A | 71.7 | 70.8 | N | 86.5 | 80.8 |
| B | 61.8 | 45.4 | L | 64.4 | 49.0 |
| G | 87.4 | 64.7 | M | 90.4 | 58.0 |
| F | 95.7 | 88.9 | J | 89.0 | 62.9 |
| C | 91.6 | 86.9 | O | 90.9 | 86.5 |
| D | 89.2 | 86.1 | K | 86.6 | 78.3 |
| E | 92.9 | 88.8 | M | 94.0 | 82.0 |
Pooled analyses were not undertaken because of inconsistencies between English and Welsh data. However, as English data were reported consistently, we undertook a pooled analysis limited to English sites; this showed that intervention sites were more likely, but not significantly, to see patients in the ED within the 4-hour target when an AIMS was open. The marginal effect was 0.015 (95% CI –0.039 to 0.069; p = 0.581) across all sites, 0.005 (95% CI –0.044 to 0.053; p = 0.848) when analysis used the original sites and 0.017 (95% CI –0.062 to 0.095; p = 0.678) when analysis used the replacement sites. In single-city analyses no effect was observed for sites H, A and G. A fall in the number seen within 4 hours was observed for sites F and E. An increase in the number seen within 4 hours was observed for sites B, C and D. Additional analyses were planned for time to treatment and time to initial assessment. However, data were too inconsistent to facilitate analysis, possibly attributable to variable recording practices across EDs.
Summary
It is unclear how the downwards trend in the proportion of patients seen within 4 hours influences results and there is marked variation between sites at baseline. Analyses by city returned no consistent pattern. The effects reported in analyses may therefore be susceptible to the appropriateness of the matching, underlying trends in the time series or noise. It is unlikely that the model can identify a consistent pattern in these data.
Ambulance service key performance indicators
We received ambulance data for sites F, C and O from 1 January 2010 to 31 December 2016, for site H from 1 July 2010 to 31 December 2016, for sites K and N from 1 January 2012 to 31 December 2016, for sites A, B and L from 1 January 2012 to 1 December 2016, for sites J and M from 5 March 2012 to 31 March 2017 and for site D from 1 April 2012 to 31 December 2016. The ambulance services covering sites E and G were unable to provide data; we used data from 16 November 2010 to 31 March 2016 where available. As with the other analyses, site H opened before the start of data availability, so there are no pre-intervention data for this site or its matched control.
From 1 October 2015 the Welsh Ambulance Service changed call categorisation to a three-level red–amber–green system. 66 The high-priority (red) calls were more strictly defined and are therefore not comparable to English or previous Welsh high-priority calls. Prior to this, the English and Welsh services used broadly similar categories, although there are inconsistencies in the way that they are/were operationalised. For example, in Wales the clock starts when the chief complaint has been established, whereas in England the clock starts for the highest priority (‘RED1’) calls when the call is answered.
Descriptive statistics
The mean number of all ambulance calls and high-priority calls per day in each site catchment area pre and post intervention and the percentage of high-priority calls responded to within 8 minutes and 19 minutes are presented in Appendix 6. We noted marked variation in the mean number of all calls and high-priority calls across cities. This was explained by ambulance services interpreting our request for calls originating in the site catchment area in different ways. Only the eight to 10 postal districts nearest to the city centre were provided for sites C and O, whereas all city-region postal districts were provided for sites D and A. We therefore undertook a secondary analysis limiting all sites to the eight postal districts nearest to the city centre. Furthermore, the number of high-priority calls increased after the intervention date at the English sites but decreased at the Welsh sites. This is probably a result of the change in call categorisation instituted by the Welsh Ambulance Service during the project as described in Ambulance service key performance indicators. This observation suggests that the effect of the change in categorisation was substantial and means that pre- and post-intervention data from Welsh sites are not comparable.
Regression models
Pooled analyses were not undertaken because of inconsistencies between English and Welsh Ambulance Service data. However, as the English sites had reasonably consistent call categorisation across the study period, we undertook a pooled analysis limited to English sites. The marginal effect across all English sites for the 8-minute target was 0.003 (95% CI –0.010 to 0.016; p = 0.63) and for the 19-minute target was 0.023 (95% CI 0.018 to 0.029; p < 0.001). When analysis was limited to the original English sites the effect for the 8-minute target was 0.0001 (95% CI –0.013 to 0.013; p = 0.99) and for the 19-minute target was 0.014 (95% CI 0.009 to 0.019; p < 0.001). In additional analyses using replacement sites instead of the original sites, the effect for the 8-minute target was –0.022 (95% CI –0.038 to –0.007; p < 0.01) and for the 19-minute target was 0.025 (95% CI 0.018 to 0.032; p < 0.001).
Discussion
Overall, data quality and model specification limit opportunities to report on AIMS effectiveness. Provisional results suggest some support for AIMSs influencing key performance indicators on aggregate ambulance data. Site A provides the strongest evidence for an effect of AIMSs on ED attendances. Pooled analyses suggest that AIMSs affect urgent ambulance calls, which are responded to within 19 minutes. Performance against all key performance indicators deteriorated over the study and sites varied considerably.
Much of the analytic obstacles to reporting on effectiveness can be resolved with enough AIMSs, a longer time series and a greater number in the counterfactual. However, the number of AIMSs in England and Wales, specifically those opening on regular days, is limited and many have been functional only for a short period of time, the consequences of which are compounded by the varying quality of routine data (primarily due to changes in recording standards).
Cost-effectiveness
Set-up and running costs
The set-up and running costs were collected from six participating AIMSs from which data were available (sites H, A, B, G, F and C) using a standardised costing exercise. An inventory of resources was designed by the team and piloted using information from site A (see Appendix 7). Managers of AIMSs were contacted and asked to provide details of their budget and running costs. Information requested included details on staffing, premises, consumables, equipment and software licensing. For each item we asked for details of which sector met the costs (e.g. NHS, ambulance service, police, charity, voluntary).
No AIMSs provided details on the cost of setting up the service (see Appendix 8); therefore, the following assumptions were made as to what would happen when an AIMS was set up. The decision to set up an AIMS consisted of an initial meeting lasting 2 hours, attended by a hospital consultant, paramedic, police officer, council representative and NHS employee from finance. After the meeting, a manager would be appointed to put forward the business case for an AIMS and oversee its set-up. Appendix 8 provides details of assumptions related to the initial meeting and unit cost source. It was assumed that the manager would be employed for 6 months at 50% full-time equivalent prior to the opening of the AIMS, and management salary costs were assumed to be band 8a of Agenda for Change56 (£10,107). These assumptions were discussed and agreed by the study team. Total staff costs were estimated to be £588.
Most AIMSs are run by NHS staff; therefore, no additional staff training costs were included at this stage. However, site G’s AIMS is run by volunteers and if most of the staff are volunteers then training costs need to be included. Training given to volunteers at the site G service consists of an initial induction and further training if the volunteer wants to be a medical assessor. The induction for drivers, communicators and café befrienders lasts for 2 hours. Medical assessor volunteers receive 6 days’ accredited first aid training and also attend a safeguarding session. The cost of this training is £720 per person, with the volunteer asked to contribute £95 up front and £15 per calendar month for 1 year. Therefore, the AIMS would pay £445 to train each volunteer and the volunteer would pay £275. Hence, if there were to be 10 volunteers the initial cost of training would be £4450.
Running costs were provided at varying levels of detail from each AIMS; these costs are detailed as staff costs, premises-related costs and other costs (see Appendix 7).
Emergency department attendances
The method for estimating the reduction in ED attendances was described in Effectiveness, Emergency department attendances. The cost of an ED admission was taken from NHS reference costs55,67 averaged across all admissions and is £148.36.
Ambulance costs
The proportion of cases that arrived in ED via ambulance was obtained from the ED data for each city. All these cases are assumed to involve ‘see, treat and convey’, with a unit cost of £247.00. The average cost of ED attendance was estimated as the cost of an ED attendance plus the proportion arriving by ambulance multiplied by the cost of conveyance by ambulance.
Inpatient admissions
The inpatient data analysed were for the period 2009–16. A new set of reference costs are released each year based on the latest definitions of Healthcare Resource Group (HRG) codes. HRG codes evolve over time, with some codes being discontinued as their definition changes and new codes being added. For example, what was AA03Z (‘Intracranial procedures from trauma with minor diagnosis’) in 2009/10 became AA03A and AA03B (‘Intracranial procedures for trauma with diagnosis of head injury/skull fracture with and without complications and comorbidities’) for 2010/11. These definitions were reclassified again in 2012/13. These changes could create additional noise in the cost data because some of the variation in cost could be due to how the HRG code was defined. Therefore, different methods of costing were used to estimate the cost for each episode. The first method costed the HRG code recorded in the data set; the second method estimated a HRG code based on the 2015/16 NHS reference cost definitions. 67 The percentage brought in as inpatients is defined following the HES ED data and is the percentage of those seen when an AIMS was regularly open who were coded as admitted as inpatient (for English data this was those coded 1 or 2 for the ‘aeattenddisp’ variable and for Welsh data coded 01 or 02 for the ‘outcomeofattendancecode’ variable).
Method 1: inflated costs
A data set was constructed that contained all HRG codes between 2008/09 and 2015/16 (the latest reference costs available); reference costs for 2012/13 were excluded because they were split by specialty and not recorded as a combined total. If the cost was not available for the latest NHS reference costs (2015–16)67 then costs were inflated using the Hospital and Community Health Services Index. 57 A separate data set contained the latest trim points for each HRG code. Each unit cost is based on a defined length of stay for each HRG code (the trim point); if the episode length exceeds the trim point then additional days are costed based on the excess bed-day cost for the HRG code. The inpatient data set was then merged with the unit cost data set and trim point data set. From this an episode cost was estimated based on the unit cost of the HRG code and any excess bed-days.
Method 2: 2015/16 Healthcare Resource Group codes
To make HRG codes comparable by year and NHS trust, the 2015/16 reference cost grouper was used to generate a HRG code. The provider spell number was also not provided, so HRG codes generated by the reference cost grouper related only to the episode level, not to the spell level. After the HRG codes had been generated, the unit cost could be assigned to each episode from the NHS Reference Costs 2015–16. 67 Excess bed-days were costed the same way as in method 1.
Creating inpatient spells from episodes
The York Centre for Health Economics method68 was used to create inpatient spells from inpatient episodes. Spells were created based on patient identifier, provider code, admission date, discharge method, episode start date and episode end date. A spell cost was then estimated based on the combined cost of all episodes in the spell. This method can only create spells for patients who remain in the same hospital (or in the same NHS trust for the English data); this is known as a provider spell. Analysis was limited to alcohol-related admissions (primary diagnosis codes: F100, T510, T511, T519, X45, Y15, R780, Y90, Y91, E244, F101, F102, F103, F104, F105, F106, F107, F108, F109, G312, G621, G721, I426, K292, K70, K860, K852 and Q860).
Analysis
Duplicates were removed from both ED and inpatient data prior to analysis. The primary analysis used ED and ambulance costs. A sensitivity analysis included inpatient admission costs for those patients who were admitted with an alcohol-related code. The average cost per ED attendance avoided was estimated for each city and overall. The number of ED attendances avoided per night for an AIMS to be cost-effective was calculated by dividing the average service cost per session by the average cost per ED attendance. If the number is less than the reduction in ED attendances, then the AIMS is cost saving. Unit costs were obtained for the 2016/17 financial year; any unit costs that were based on a financial year prior to 2015 were inflated to the latest price levels using the Hospital and Community Health Services Index. 69 Sites D and E dropped out of the study and did not provide AIMS set-up or running costs so are not included in this analysis.
Results
Set-up and running costs
The cost of the initial set-up meeting was estimated at £588 and management costs were £10,107. Thus, the estimated set-up cost for a NHS-run AIMS was £10,695 and for a volunteer-run AIMS was £15,145.
The running costs for AIMSs have been broken down into staffing costs, premises-related costs and other costs (see Appendix 8) and overall costs per session varied from £1075 to £2170 (see Appendix 8). The only AIMS not to provide a breakdown of costs was site F, which provided a cost per weekend of service provision. Costs per session ranged from £1075 for site F to £2170 for site A. Site A’s AIMS had higher staff costs than any other AIMS and included managerial and administration staff, police, paramedics, nurses and a first aider, but also paid staff overtime, which no other unit did.
Table 7 presents the average cost per attendance in an AIMS; this was lowest at site F (mean £132) and highest at site G (£584) which, on average, saw the fewest people per night. Given that sites H, A, B and G reduced ED attendances, they produced some cost savings to the NHS. However, for the AIMSs to break-even they would need to divert between seven and 15 ED attendances per session if the only cost savings related to reduced ED attendances.
| Variable | Site | Overall | |||||
|---|---|---|---|---|---|---|---|
| H | A | B | G | F | C | ||
| Measure of effectiveness | |||||||
| Reduction in ED attendances (per night AIMS open) | –1.05 | –6.39 | –1.75 | –1.05 | 3.93 | 0.00 | –1.05 |
| Lower limit on reduction in ED attendances | –1.26 | –6.40 | –1.96 | –1.26 | 3.59 | –1.22 | –1.26 |
| Upper limit on reduction in ED attendances | –0.84 | –6.37 | –1.54 | –0.84 | 4.28 | 1.22 | –0.84 |
| Cost analysis | |||||||
| Cost of AIMS per annum (£) | 126,820.00 | 253,643.00 | 158,654.00 | 61,389.00 | 109,650.00 | 165,279.00 | 145,906.00 |
| Mean number of AIMS attendances per night | 5.392 | 11.838 | 9.242 | 2.696 | 8.121 | 6.800 | 7.348 |
| Average cost per session (£) | 1208.00 | 2265.00 | 1442.00 | 1574.00 | 1075.00 | 1476.00 | 1635.00 |
| Average cost per attendance in AIMS (£) | 224.04 | 191.33 | 156.03 | 583.83 | 132.37 | 217.06 | 222.50 |
| ED attendance costa (£) | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 |
| Saving in ED attendance (reduction in ED attendances × cost per ED attendance) (£) | –155.78 | –948.02 | –259.63 | –155.78 | 583.05 | 0.00 | –155.78 |
| Net incremental costs per session (£) | 1052.22 | 1316.98 | 1182.37 | 1418.22 | 1658.05 | 1476.00 | 1479.22 |
| Incremental cost-effectiveness of implementing AIMS compared with pre implementation | |||||||
| Mean incremental cost per ED attendance avoided (£) | 1002.00 | 206.00 | 676.00 | 1351.00 | –422.00 | n/a | 1409.00 |
| Lower limit of mean incremental cost per ED attendance avoided (£) | 808.34 | 205.45 | 586.72 | 1098.20 | –448.05 | 1060.41 | 1146.50 |
| Upper limit of mean incremental cost per ED attendance avoided (£) | 1290.90 | 207.20 | 789.03 | 1726.97 | –399.71 | –1357.13 | 1799.65 |
| Threshold analysis for effectiveness of AIMS to be entirely cost-saving | |||||||
| Number of ED attendances needed per session for AIMS to break-even | 8.14 | 15.27 | 9.72 | 10.61 | 7.25 | 9.95 | 11.02 |
Sensitivity analysis
Cost of conveyance by ambulance was included in a sensitivity analysis (Table 8). Including ambulance conveyance resulted in the average cost per ED attendance ranging from £256 to £276 per attendance. AIMSs at sites H, A, B and G reduced ED attendances and produced some cost savings to the NHS. However, for AIMSs to break-even they would need to divert between 4.0 and 8.6 ED attendances per session if the only cost savings related to reduced ED attendances.
| Variable | Site | Overall | |||||
|---|---|---|---|---|---|---|---|
| H | A | B | G | F | C | ||
| Measure of effectiveness | |||||||
| Reduction in ED attendances (per night AIMS open) | –1.05 | –6.39 | –1.75 | –1.05 | 3.93 | 0.00 | –1.05 |
| Percentage brought in by ambulance | 48.08 | 45.90 | 51.75 | 46.92 | 51.41 | 43.60 | 48.08 |
| Mean number of AIMS attendances per night | 5.392 | 11.838 | 9.242 | 2.696 | 8.121 | 6.800 | 7.348 |
| Cost analysis (£) | |||||||
| Cost of AIMS per annum | 126,820.00 | 253,643.00 | 158,654.00 | 61,389.00 | 109,650.00 | 165,279.00 | 145,906.00 |
| Average cost per session | 1208.00 | 2265.00 | 1442.00 | 1574.00 | 1075.00 | 1476.00 | 1635.00 |
| Average cost per attendance in AIMS | 224.04 | 191.33 | 156.03 | 583.83 | 132.37 | 217.06 | 222.50 |
| ED attendance costa | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 |
| Ambulance cost per see, treat and conveya | 247.00 | 247.00 | 247.00 | 247.00 | 247.00 | 247.00 | 247.00 |
| Cost per ED attendance including ambulance costs | 267.12 | 261.73 | 276.18 | 264.25 | 275.34 | 256.05 | 267.12 |
| Saving in ED attendance (reduction in ED attendances × cost per ED attendance) | –280.74 | –1671.41 | –483.32 | –277.73 | 1082.64 | 0.00 | –280.74 |
| Net incremental costs per session | 927.26 | 593.59 | 958.69 | 1296.27 | 2157.64 | 1476.00 | 1354.26 |
| Incremental cost-effectiveness of implementing AIMS compared with pre implementation | |||||||
| Mean incremental cost per ED attendance avoided (£) | 882.26 | 92.95 | 547.82 | 1233.37 | –548.74 | n/a | 1288.54 |
| Threshold analysis for effectiveness of AIMS to be entirely cost-saving | |||||||
| Number of ED attendances needed per session for AIMS to break-even | 4.52 | 8.65 | 5.22 | 5.96 | 3.90 | 5.76 | 6.12 |
Costs of admissions were included in a sensitivity analysis (Table 9). The proportion of admissions that were alcohol attributable (from HES data for admissions that were alcohol attributable seen on days that the AIMS was regularly open; there was no time stamp for time of admission) was obtained and ranged from 21% at site A to almost 50% at sites G and C. Between 15% and 27% of admissions were either fully or partially due to alcohol. Including these costs in the cost of attendance increased the ED costs from £420 (site A) to £628 (site G).
| Variable | Site | Overall | |||||
|---|---|---|---|---|---|---|---|
| H | A | B | G | F | C | ||
| Measure of effectiveness | |||||||
| Reduction in ED attendances (per night AIMS open) | –1.05 | –6.39 | –1.75 | –1.05 | 3.93 | 0.00 | –1.05 |
| Percentage brought in by ambulance | 48.08 | 45.90 | 51.75 | 46.92 | 51.41 | 43.60 | 48.08 |
| Percentage brought in as inpatient | 40.76 | 21.45 | 28.43 | 49.81 | 46.09 | 49.94 | 40.76 |
| Percentage of those admitted who are alcohol attributable | 26.70 | 19.72 | 17.72 | 24.27 | 24.14 | 15.05 | 20.85 |
| Mean number of AIMS attendances per night | 5.392 | 11.838 | 9.242 | 2.696 | 8.121 | 6.800 | 7.350 |
| Cost analysis (£) | |||||||
| Cost of AIMS per annum | 126,820.00 | 253,643.00 | 158,654.00 | 61,389.00 | 109,650.00 | 165,279.00 | 145,906.00 |
| Average cost per session | 1208.00 | 2265.00 | 1442.00 | 1574.00 | 1075.00 | 1476.00 | 1635.00 |
| Average cost per attendance in AIMS | 224.04 | 191.33 | 156.03 | 583.83 | 132.37 | 217.06 | 222.50 |
| ED attendance costa | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 | 148.36 |
| Ambulance cost see, treat and conveya | 247.00 | 247.00 | 247.00 | 247.00 | 247.00 | 247.00 | 247.00 |
| Average inpatient cost (method 1) | 2763.32 | 3723.13 | 3156.09 | 2954.29 | 2925.84 | 2579.06 | 2994.50 |
| Average inpatient cost (method 2) | 2438.42 | 2471.34 | 2497.03 | 2601.44 | 2173.74 | 2365.16 | 2423.75 |
| Method 1 (£) | |||||||
| Cost per ED attendance including ambulance costs and inpatient costs | 567.85 | 419.22 | 435.18 | 621.39 | 600.88 | 449.89 | 521.60 |
| Saving in ED attendance (reduction in ED attendances × cost per ED attendance) | –596.81 | –2677.13 | –761.56 | –653.08 | 2362.64 | 0.00 | –548.21 |
| Net incremental costs per session | 611.19 | –412.13 | 680.44 | 920.92 | 3437.64 | 1476.00 | 1086.79 |
| Incremental cost-effectiveness of implementing AIMS compared with pre implementation | |||||||
| Mean incremental cost per ED attendance avoided (£) | –581.53 | 64.54 | –388.82 | –876.23 | 874.27 | n/a | –1034.06 |
| Threshold analysis for effectiveness of AIMS to be entirely cost-saving | |||||||
| Number of ED attendances needed per session for AIMS to break-even | 2.13 | 5.40 | 3.31 | 2.53 | 1.79 | 3.28 | 3.13 |
| Method 2 (£) | |||||||
| Cost per ED attendance including ambulance costs and inpatient costs | 532.49 | 366.27 | 401.98 | 578.74 | 517.20 | 433.82 | 473.10 |
| Saving in ED attendance (reduction in ED attendances × cost per ED attendance) | –559.65 | –2339.00 | –703.46 | –608.25 | 2033.61 | 0.00 | –497.23 |
| Net incremental costs per session | 648.35 | –74.00 | 738.54 | 965.75 | 3108.61 | 1476.00 | 1137.77 |
| Incremental cost-effectiveness of implementing AIMS compared with pre implementation | |||||||
| Mean incremental cost per ED attendance avoided (£) | –616.89 | 11.59 | –422.02 | –918.88 | 790.59 | n/a | –1082.56 |
| Threshold analysis for effectiveness of AIMS to be entirely cost-saving | |||||||
| Number of ED attendances needed per session for AIMS to break-even | 2.27 | 6.18 | 3.59 | 2.72 | 2.08 | 3.40 | 3.46 |
Using method 1 (inflate costs) to estimate inpatient costs resulted in an average cost per ED attendance of £521.60, ranging from £419.22 at site A to £621.39 at site G. The number of attendances needed for AIMSs to break-even ranged from 1.79 to 5.40, with only site A observing a greater reduction in ED attendances (n = –6.39) per night. Using method 2 (HRG costs from 2015–16) to estimate inpatient costs resulted in an average cost per ED attendance of £473.10, ranging from £366.27 at site A to £578.74 at site G. The number of attendances needed for AIMSs to break-even ranged from 2.07 to 6.18, with only site A observing a greater reduction in ED attendances (n = –6.39) per night.
National roll-out of AIMSs
Although the site A AIMS was the most expensive to set up, it was the only service to show potential cost-effectiveness and that would break-even (assuming ED, ambulance and inpatient costs were accounted for). If this model of AIMS was rolled out across England and Wales (assuming 207 EDs in England and Wales), the NHS would need to invest £52.5M per year.
A cost–utility analysis was not possible with the data available.
Discussion
Alcohol intoxication management services would need to divert an average of 11 attendances per session (ranging from 7.3 to 15.3 attendances per session depending on service configuration) from the ED to break-even from the perspective of the ED. Sensitivity analysis included ambulance and inpatient admission costs and suggested that AIMSs may break-even if 3.5 patients (ranging from 2.1 to 6.2 depending on service configuration) are diverted. It is interesting to note that the site G volunteer-led service was not the least expensive service. The most expensive service, site A’s, was led by nurse practitioners.
Overall, AIMSs received, on average, 7.3 patients per session. Analysis of individual AIMSs found that attendance varied considerably, from an average of 2.7 to 11.8 patients per session. Given evidence that AIMSs attract unmet need that would not otherwise be expected to require attendance in ED (see Chapter 6), it is reasonable to assume that the average attendance at AIMSs does not reflect the total number of patients who are diverted away from ED. Therefore, it is unlikely that AIMSs are cost-effective from the perspective of the ED.
Analyses are hindered in several ways. Key performance indicators are noisy and, therefore, accurately identifying what is likely to be a small effect of AIMSs in highly variable ED and ambulance data is difficult. Key performance indicators are prone to seasonality, for example varying in frequency weekly (e.g. increases at weekends), monthly (e.g. pay day) and annually (e.g. summer compared with winter). Without balance before and after implementation, any observed effect could be due to characteristics of the time series. Underlying trends, if not accounted for, can further obscure estimates. Given that the expected effect of AIMSs is relatively small, models can be subject to overfitting, where noise drives the results more than the effect of AIMSs themselves. These issues are particularly prominent where sample sizes are reduced, such as in the single-city analyses.
Although there is agreement across analyses suggesting that AIMSs significantly affect ED attendance numbers and ambulance response times, it is similarly clear that such effects cannot be attributed to each AIMS. Site G, for example, has no formal relationship with the local ambulance service and it is not feasible to attribute changes in ambulance response times to the effect of site G. The high variability in AIMS design therefore precludes opportunities for a general statement on effectiveness and cost-effectiveness. However, a model led by a nurse practitioner incurs the greater cost but is also more likely to successfully divert patients away from the emergency health-care system.
Exploratory analyses
Assaults on emergency department staff
Freedom of information requests to all participating EDs sought data concerning assaults on staff working in ED. These data were collected in a variety of formats and for a variety of time periods across sites. To make comparisons, all data were aggregated to quarterly time periods and all assault categories combined. The latter was necessary because some hospitals, for example, used several defined categories (e.g. sexual, physical, verbal) to describe events. Mean number of assaults by control site and intervention site is presented in Figure 3. This figure suggests that EDs with a locally implemented AIMS maintained a more modest number of assaults on staff than EDs without a locally implemented AIMS. To assess this relationship statistically, a simple random effects negative binomial regression was used, including time as a covariate, regressing the status of whether or not an AIMS was operational (0 or 1) in the city for all cities supplying data (n = 13) and the sum of all forms of assault as the outcome variable. The model performed better than chance (Wald χ2 = 11.77; p < 0.01), with the incident rate ratio (IRR) suggesting that EDs with operational AIMSs have fewer assaults than control sites (IRR 0.86, 95% CI 0.79 to 0.94). These data must be viewed with some scepticism; they are aggregated and, therefore, cannot distinguish between evenings when AIMSs are operational from other times of day, nor whether assaults were alcohol related or due to other reasons.
FIGURE 3.
Mean total (with standard error bars) number of assaults on ED staff, by quarter, year and groups, by cities with AIMSs (intervention) and without (control).
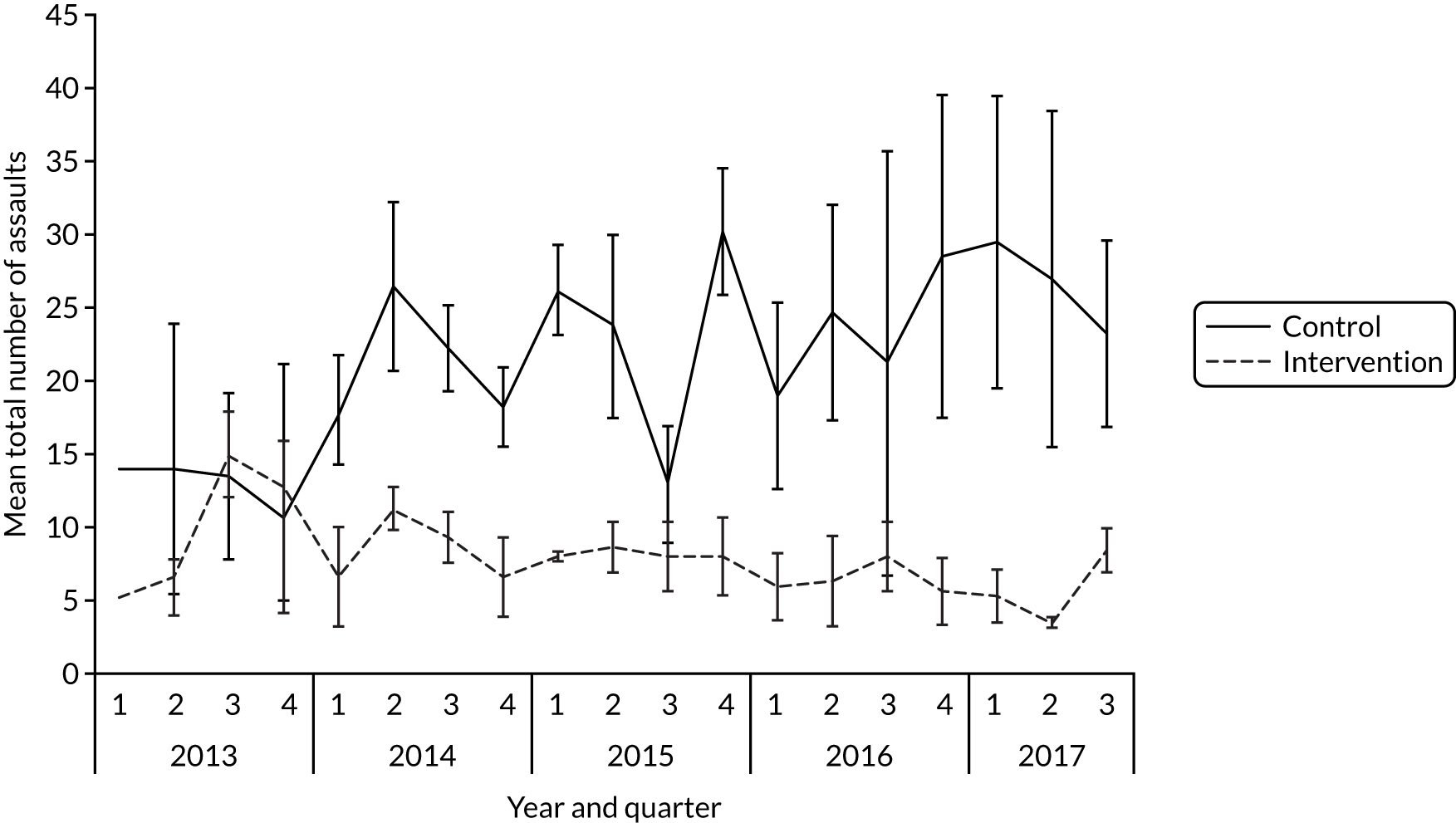
Police-recorded violence
Data concerning police-recorded violence was accessed from the UK Police open data portal (https://data.police.uk; accessed 11 February 2020) and grouped by city: nine cities known to have AIMSs and six control cities. Data recorded total number of sexual assaults, total number of assaults resulting in injury and total number of assaults resulting in no injury, by time (year and quarter). Figure 4 presents the total count of all assaults by time, for cities with AIMSs and cities without AIMSs, and suggests that trends diverge: cities with AIMSs show a greater increase in assaults than control cities. A conditional fixed-effects Poisson regression was used to determine any effect of AIMSs being operational (0 or 1; 0 for control cities) on police-recorded violence over time and for each of the crime categories. In each of the three models there was a significant influence of time on the outcome variable (sexual: IRR 1.05, z = 46.83, p < 0.001; with injury: IRR 1.02, z = 39.49, p < 0.001; with no injury: IRR 1.05, z = 111.40, p < 0.001). For each of the crime types, an operational AIMS was associated with a greater ascertainment of crime (sexual: IRR 1.05, z = 2.52, p < 0.05; with injury: IRR 1.03, z = 3.80, p < 0.001; with no injury: IRR 1.21, z = 23.38, p < 0.001). Possible reasons for this divergence include more police in NTEs able to record incidents that would otherwise have been missed. However, the quarterly nature of these data mean that attribution to AIMSs is not feasible and the effects could be an artefact of other changes locally.
FIGURE 4.
Police-recorded violenceb for control and intervention cities. a, Recording processes and counting rules for ‘violence against the person’ changed substantially from 2012 onwards and accounts for the upward trend evident here; b, violence without injury, violence with injury, and sexual offences.
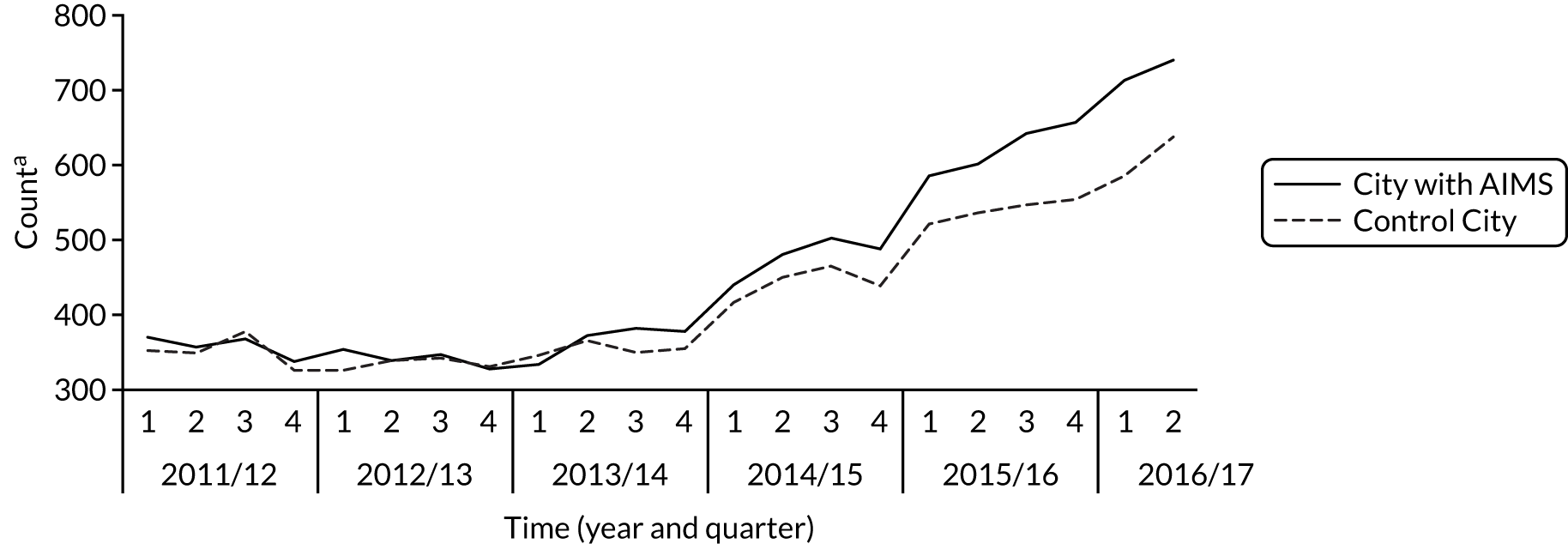
Chapter 5 Ethnographic case studies
This section analyses the work of managing AAI and alcohol-related risk and harm in the NTE. It compares the two AIMS case studies (sites A and B) with the non-AIMS case study (site J; see Appendix 9). Analyses are presented thematically to draw out points of commonality and difference between the cases. The services covered in this study are described in Chapter 3.
Case studies
Case study 1: site A
The site A NTE (Figure 5) has a high density of premises licensed for the on- and off-site sale of alcohol. It has a large student population and is a destination city, attracting people from surrounding areas and across the UK every weekend. The central actor in managing the acutely intoxicated is the AIMS, which is based in a permanent location in the city centre. Established in September 2012 through a partnership between the health board, the police and the ambulance service, the AIMS was a response to the growing challenge of managing acutely intoxicated individuals in the ED and the stress that it was causing staff and patients. Its primary aim was to divert individuals with AAI and/or minor injuries away from the ED on Friday and Saturday nights. Personnel were funded initially by grants from the Substance Misuse Area Fund and the Regional Collaboration Fund and volunteered to work in the AIMS on an overtime basis. Grants reduced and although hospital staff, paramedics and EMTs continue to volunteer to work in the service on an overtime basis, the shift now forms part of the core duties of health-care workers and police officers.
FIGURE 5.
Ethnographic infographic for case study 1.
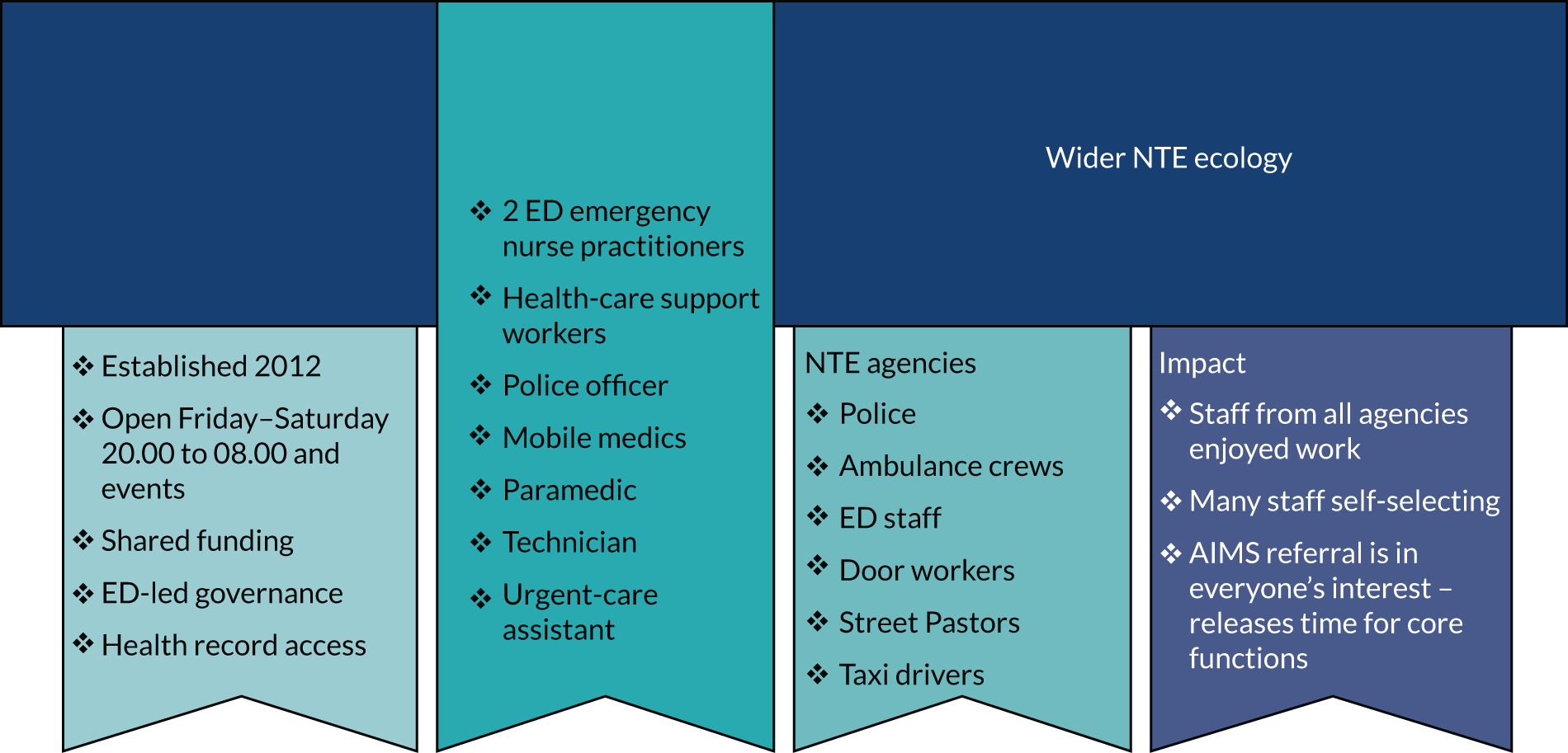
Case study 2: site B
Site B has a compact, densely populated NTE (Figure 6). It has a large student population and, like site A, it attracts people from the surrounding areas, including for hen and stag parties. The central actor in managing the NTE is the AIMS. Located in two portable buildings in a city centre car park, the service was established in September 2014 through a partnership between the health board, St John Ambulance, ambulance service, local authority, police and a local university. Founded on a number of partnership initiatives that had been operating in the NTE since the early 2000s, the service’s primary aims are to alleviate the demand on emergency services (police and ambulance services and ED) and to create a safer NTE by diverting individuals who may be acutely intoxicated, injured and/or vulnerable to an alternative facility. The AIMS is led by St John Ambulance.
FIGURE 6.
Ethnographic infographic for case study 2.
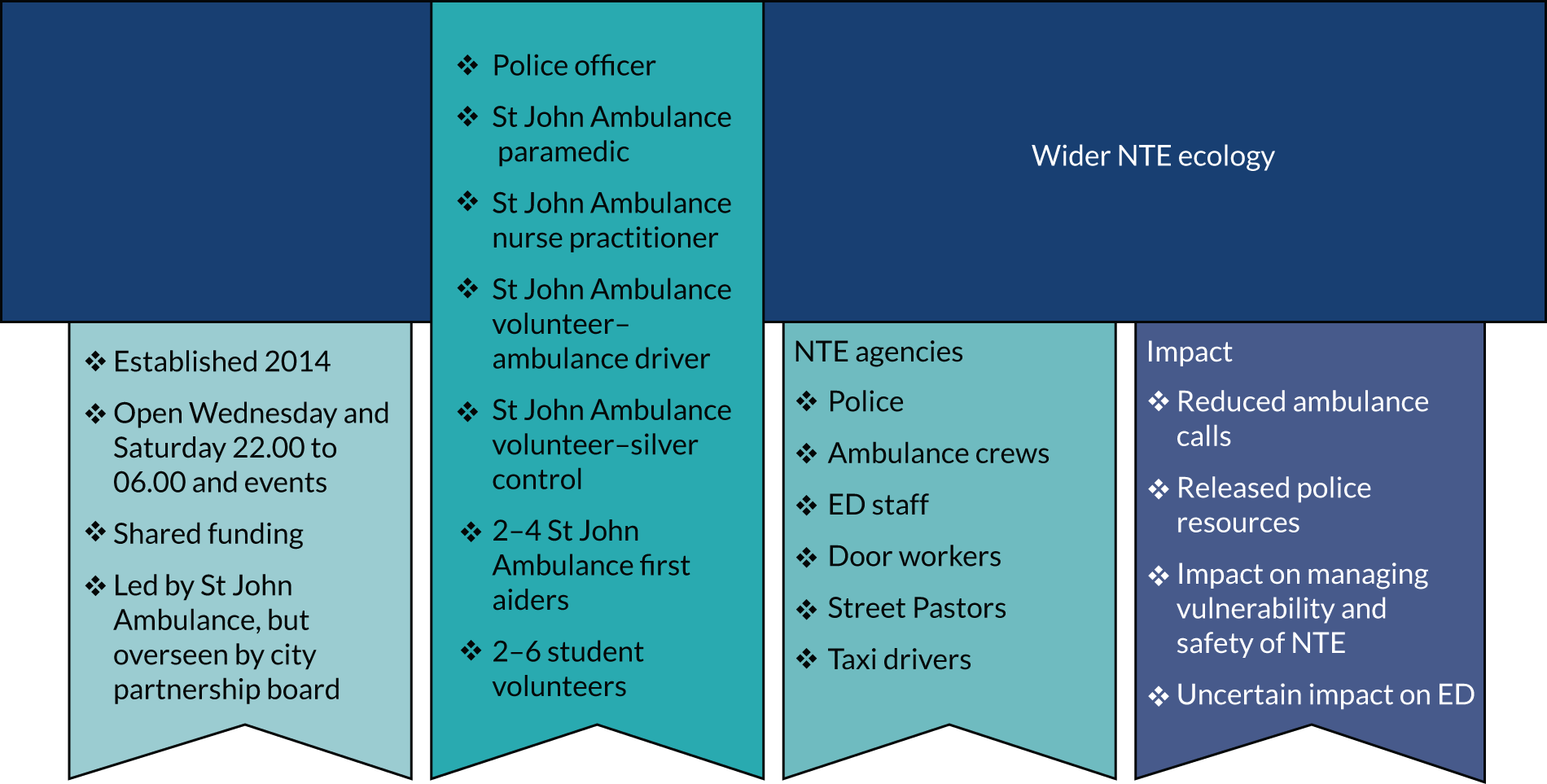
Case study 3: site J
The site J NTE (Figure 7) is characterised by a large student population and is a destination for drinkers across the UK. Unlike sites A and B, the city does not tend to attract people from surrounding areas, perhaps owing to the number of other large cities nearby, nor does it have a reputation as a destination city attracting stag and hen parties. The NTE does not have an AIMS but operates a number of partnership initiatives designed to improve the safety of its NTE through promoting best practice among bars and clubs. It also runs K-responder, a joint initiative between the police and the ambulance service intended to reduce the demand on these services in the city centre over Friday and Saturday nights, which has been in operation for around 6 years. A paramedic practitioner (on overtime) and one or two special constables (police volunteers with power to arrest) respond to calls predominantly from licensed premises in and around the city centre on Friday and Saturday nights in a RRV.
FIGURE 7.
Ethnographic infographic for case study 3. Resus, resuscitation area.
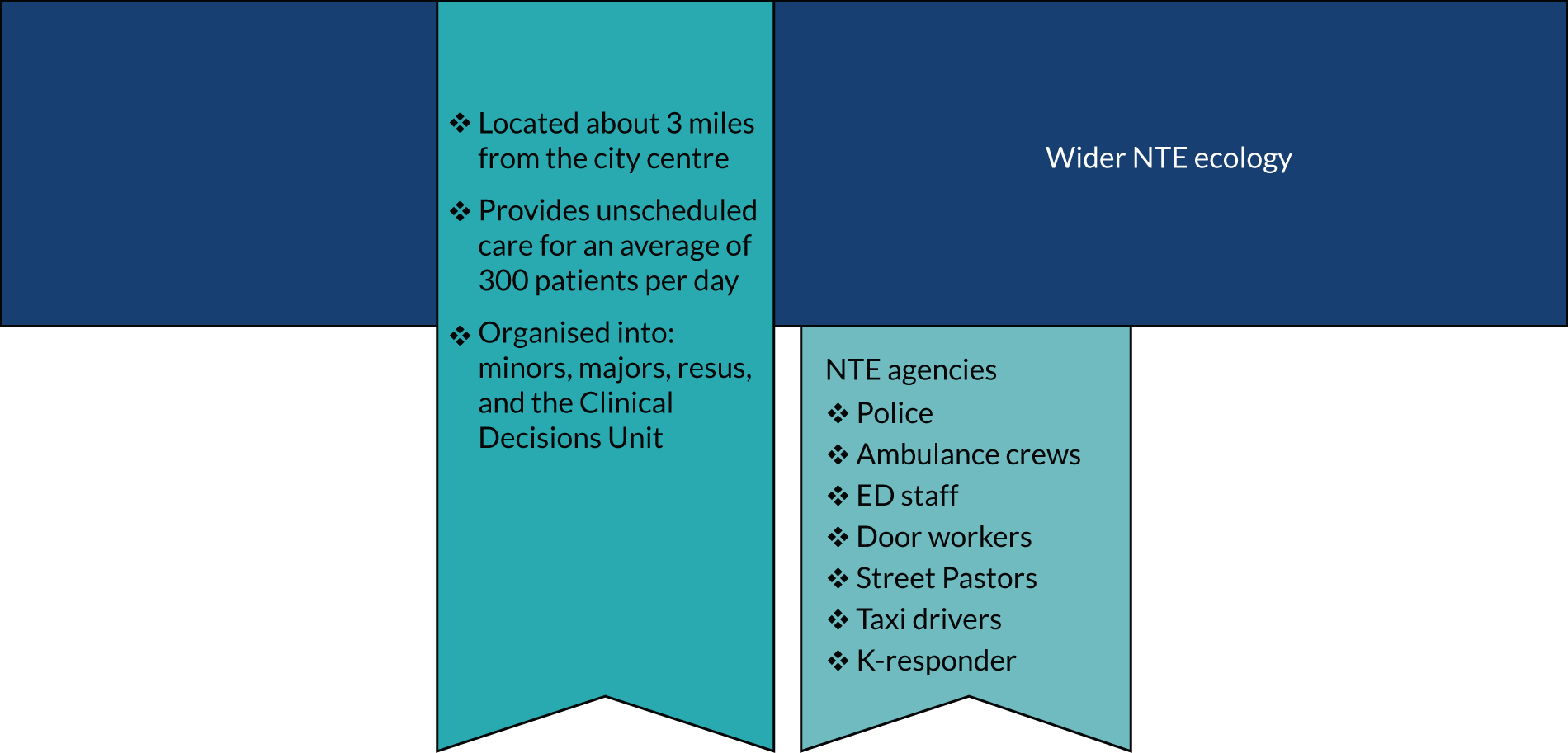
Alcohol-related risk and the night-time environment: the ecology of work
The work of managing alcohol-related risk in the NTE is multifaceted and involves a range of preventative and responsive strategies divided between the police, ambulance crews, health-care providers, Street Pastors, door workers, the public and taxi drivers. The management of alcohol-related risk is undertaken alongside the core work of front-line emergency services, be that preventing crime, responding to acute medical emergencies or providing charitable support. With no single agency responsible for managing alcohol-related risk, AIMSs operate as central actors in co-ordinating activity in the NTE. In the absence of an AIMS, the ED functions as the central actor, exerting power at a distance on the work of police and ambulance crews whose work is driven by an organising logic aimed at avoiding inappropriate ED attendances.
Public services
Police
The primary focus of police work in the NTE is to deal with perpetrators and victims of crime and alcohol-related crime. Police work in the NTE was organised differently than at other times of the day. It aims to be preventative rather than reactive and is designed to ensure high visibility to enhance safety, deter criminal activity and facilitate early intervention to prevent issues escalating. In all sites, police work entailed active and friendly engagement with patrons of the NTE and the use of dispersal notices to manage antisocial behaviour. Arrests were avoided where possible, because this involves additional administrative work and takes officers away from the front line if they are required to place someone in custody. Police work also involved intervening with individuals who were intoxicated and/or vulnerable or injured, although this varied across the sites. In the sites with AIMSs, there was more proactive police engagement with this population and referral of cases to the AIMS either directly or via a third party (e.g. ambulance, Street Pastors). At site J, in the absence of an AIMS and with no referral pathway available to them, officers displayed a disinclination to engage with the acutely intoxicated because their management could be protracted and took them away from their core duties. At sites A and B, a police officer also worked in the respective AIMS, primarily to protect health-care staff, intervene in any incidents and interview victims of crime. Officers also assisted with AIMS work, such as information gathering, handing out vomit bowls, tidying and cleaning up after patients, helping nurses to contact friends or family and interacting with patients and/or their friends or family.
Ambulance crews
Ambulance crews play a key role in managing alcohol-related risk in the NTE, but this varied across sites. At site A, a mobile medics crew operated from the AIMS and responded to all city centre 999 calls plus radio calls generated from street-level agents. At site B, all city centre 999 calls were directed to the AIMS, leaving ambulance crews to deal with other emergency calls outside the city. At both sites, city centre 999 calls were triaged by ambulance operatives. At site A, mobile medics were the resource of choice to respond to city centre calls, but other ambulance resources would be dispatched if the mobile medics were not available. At site B, if an 8-minute response was indicated, an ambulance resource would be dispatched prior to the call being transferred to the AIMS if St John Cymru resources were unavailable, but usually the Welsh Ambulance Services NHS Trust (WAST) resource was ‘stood down’ for AIMS staff to attend. At site J, city centre calls were managed by either the K-responder or regular crews.
The work of ambulance crews is to assess the case and make a disposal decision. In the case studies with AIMSs they could treat at scene, refer to AIMS or refer to ED. At site J, in the absence of an AIMS, the only options were to treat at the scene or refer to ED.
Health-care providers
Health-care workers have a key role in managing alcohol-related harm and risk. This entails clinical assessment and triage, attending to minor injuries, care of individuals who have lost control of bodily functions, assisting people to sober up, dispatching individuals into the care of friends and family and identifying those with a more serious underlying health condition such as head injury or health need (such as assistance with maintaining an airway). At sites A and B, much of this work was carried out by AIMS staff, with only serious cases referred to ED (such as individuals with a potential head injury or requiring radiography or treatment for minor injuries that were either beyond the scope of practice of AIMS staff or dependant on resources that were not available). Both AIMSs also functioned as a place of safety for people who were intoxicated and/or vulnerable. Only nurses with enough experience of working weekend nights in the ED were considered for AIMS shifts because they would be experienced in dealing with the AIMS patient population and have the skills to identify risk.
Volunteers
Street Pastors
Street Pastors, one of the many volunteer initiatives run by the Ascension Trust (London, UK), operated in each of the three case study sites. Pastors understood their NTE work to fulfil their responsibilities as good Christians by helping the vulnerable. Pastors tailored their work to each locale and the needs of individuals. In city centres this is generally understood to mean helping individuals who are intoxicated, although their work extends beyond intoxicated individuals to anyone who was vulnerable. Although not clinically qualified, all Street Pastors had undergone drug and alcohol training and, at site A, basic life support training was also provided by one of the ED nurses as a direct result of the Street Pastors’ involvement in the AIMS partnership.
Street Pastors worked at street level and intervened in a number of ways to ensure the safety and well-being of the patrons of the NTE by, for example, interacting with homeless people and providing them with chocolate, water and/or blankets; handing out water and/or flip flops; offering assistance to those who appeared to be intoxicated and/or vulnerable and/or injured; collecting glass bottles and safely disposing of them to prevent glass injuries and their use in potential assaults; and assisting individuals into taxis to get home or those who were lost.
The role of Street Pastors in the NTE varied across the case study sites. In all cases they were actively involved in managing intoxicated and/or injured individuals. At sites A and J they responded to calls for assistance from other agents in the NTE (door staff, police, taxi ambassadors, mobile medics) and at site A they made referrals to the AIMS. At site B, Street Pastors were less integrated into the management of alcohol intoxication and alcohol-related risk in the wider NTE ecology, possibly because of the availability of student volunteers aligned with the AIMS who fulfilled the functions performed by Street Pastors in other cases. At site J, of the four agencies shadowed, the Street Pastors and the K-responder teams were the only agencies that understood dealing with intoxicated individuals to be one of the core purposes of their work and not a distraction from it.
St John Cymru
St John Cymru, the Welsh arm of St John Ambulance, is a third-sector organisation operating across Wales. It provides first aid, training, first aid equipment and resources, patient transport and first aid cover for events. It is the lead organisation in the operation of the AIMS at site B.
Metropolitan Police Service student volunteers
The site B AIMS is supported by two to six Metropolitan Police Service (MPS) student volunteers (male or female) depending on availability and anticipated demand. All student volunteers attend a local university and are given the opportunity to volunteer at the AIMS as part of their undergraduate degree in public services. Students who choose to do this commit for the entire 3 years of their course. All volunteers undertake training in first aid (provided by St John Cymru), manual handling, vulnerability training and violence and aggression training. MPS volunteers retrieved patients, brought them to the AIMS and undertook proactive patrols in the city centre looking for potentially injured, intoxicated and/or vulnerable individuals who needed assistance and/or referral to the AIMS.
Private agencies
Door workers
Door workers, typically employed by licensed premises, also have a role in managing alcohol-related risk in the NTE. They can refuse entry to individuals who appear acutely intoxicated and intervene in cases where an individual’s behaviour suggests intoxication. Sometimes intoxicated individuals were managed inside the venue by being moved into a separate first aid area and their needs (e.g. receiving water, calling friends) met. Door staff also referred cases to other NTE agents as appropriate.
Taxi drivers
Taxi drivers in the NTE often have a role in transporting intoxicated patients to and from the city centre in exchange for a fare. Intoxicated individuals are considered to be risky customers. If someone vomits in the back of a taxi, this costs the driver time and lost earnings because of the need to clean the vehicle. Nonetheless, intoxicated individuals are an important source of income for drivers. Taxi drivers who chose to work these nights mitigated these risks by attempting to judge how intoxicated individuals appeared before allowing them into their cabs. Some male drivers were also wary of accepting lone female passengers because they did not want to be accused of sexual assault.
Site B made extensive use of taxis to transport people to ED and home, although the site B city centre Street Pastors were more cautious about taxi use. Site A staff used taxis to transport individuals with minor injuries to ED and home but relied on known drivers only. At site J, NTE agents used taxis to get people home and to attend ED for minor injuries but reported that drivers often refused to transport an intoxicated passenger. Site J Street Pastors described how they tried to stay out of sight when escorting individuals to a taxi rank to avoid being a ‘red flag’ to taxi drivers, because many taxi drivers refused to take intoxicated individuals. Ambulance crews identified the refusal of taxi drivers to transport intoxicated individuals to ED as a reason for inappropriate use of ambulance resources. At both site A and site B, the city council runs a taxi ambassadors (council employees) scheme to oversee the taxi rank, directing patrons into taxis, ensuring that taxis take patrons or, in cases where drivers refuse to take an intoxicated patron, radioing the AIMS for assistance. At site J there were only taxi drivers, no taxi ambassadors. Taxi drivers sometimes refused to transport intoxicated patrons to ED, leaving the task to other services:
That’s half the battle really; if the taxis would take them we wouldn’t have to take them, but we have no choice but to take them to A&E [accident and emergency department].
M (emergency care assistant)
(Quotation attributions minimally describe respondents’ roles while ensuring anonymity, but with sufficient detail to link data with the original transcripts.)
Alcohol-related risk in the night-time environment
The challenges of managing alcohol-related risk
Alcohol-related risk and harm in the NTE presents in diverse ways. It includes those who have sustained minor or major injury either through accident or assault, individuals who are ‘worse for wear’ (often unable to control bodily functions) and require support to sober up, individuals who are unresponsive (‘flat out’), the acutely vulnerable (such as intoxicated young women who had become separated from friends) and others with longer-term vulnerabilities such as mental ill health, homelessness and alcoholism and other addictions.
People who are intoxicated present several challenges to workers in the NTE. They are often difficult to reason with and considered to have the potential to become violent and aggressive; they may also be reluctant to wait in ED to be seen. Dealing with alcohol intoxication is also ‘dirty’ work, with acutely intoxicated individuals likely to lose control of their bodily functions. Arguably, the most important challenge is assessing if an individual simply needs time to sober up or there is a more serious reason for their symptoms, such as a head injury requiring specialist care:
It’s too risky to discharge on scene. I don’t doubt some do, but you have to be really careful, they could have a head injury, or they could choke on their vomit.
Ambulance crew member (site B)
Acutely intoxicated people are often unable to offer an account of what has happened to them, with agents having to rely on friends and other observer accounts. At sites A and B, the presence of an AIMS allows such assessments to be undertaken over a longer time frame than at site J, at which such assessments will result in ambulance crews or police being involved for a protracted length of time or, depending on the other demands on services, a referral to ED:
Like with drunks, they don’t need to be in ED, but if we discharge on scene and their friends don’t look after them properly, and they die, then it’s our fault and not theirs for getting so drunk. So I’ll only ever discharge if they actually seem fine, you know, talking and walking, and with people who can look after them, but if they’re out of it, it’s too risky. Plus alcohol can mask stuff like head injury, so it’s better just to be safe.
Paramedic (site B)
Much of the work of managing AAI also involves managing vulnerability, particularly of women. AIMSs operate as places of safety in such cases, but this option is not available at site J.
Organising logics and ways of working
Street-level work
At all three case study sites the different agents in the NTE worked flexibly and responsively to identify and manage alcohol-related risk. Activity was underpinned by an organising logic that emphasised prioritisation of activity in relation to demand, using resources judiciously given agents’ wider responsibilities, and the avoidance of inappropriate use of emergency services. At site J, in the absence of an alternative to ED, ambulance crews acted as gatekeepers to ED:
I manage it by trying to discharge on scene if I can. Now, that will take more time, but if it saves a bed up there it’s more cost-effective and a better outcome because they [the intoxicated] are hard to manage, aren’t they?
Advanced EMT (site J)
Agents at all three sites were connected by radio; this facilitated reflexive monitoring of the NTE and situational awareness of shifting patterns of demand. Radio can be used to alert agents about incidents where intervention is required and negotiate referrals based on agents’ availability and wider priorities:
The AIMS mobile medics received a call from the Street Pastors to attend to a ‘paralytic female’ who they could not get ‘off the floor’. The mobile medics agreed to attend, leaving the AIMS to respond to the call. However, en route they received what they felt was a higher priority call (an unresponsive female) from door staff so they decided to defer their attendance to the first call, informing the Street Pastors that they were attending a ‘higher priority call’ and advising them to radio police for assistance.
Field notes
Maintaining situational awareness appeared to be more challenging at site J owing to the geographical spread of the NTE. Outside the primary areas of night-time activity the NTE was distributed across many streets, some of which had only one large venue. K-responders fulfilled an important role, linking on-the-ground intelligence of the demands in the NTE to ambulance control. Ambulance dispatch used the K-responder paramedic to ‘quickly eyeball’ cases in the city centre before determining what resource was required, as information from calls was often limited. Furthermore, because calls were often from the same vicinity, and for similar kinds of complaints, dispatch could also make use of the K-responder paramedic to verify how many patients were on scene, to prevent dispatching too many resources unnecessarily.
Referral pathways in the NTE can be complex. A referral might begin with a member of door staff first noticing an intoxicated individual inside or outside the premises and deciding if they should handle the issue themselves, contact the police, Street Pastors or ambulance services or do nothing. To some extent, referral pathways were informed by the availability of other agents. When an agent arrived at the scene, they had to decide on the appropriate action. The police at all sites were encouraged to use the Street Pastors (or, at site B, MPS volunteers) where this was appropriate to avoid being distracted from their core work.
In the presence of an obvious injury, determining the requirement for ED or AIMS referral or treatment on the scene was usually straightforward. In cases of acute intoxication and absence of an injury, or where individuals were ‘flat out’, reaching a disposal decision was more complicated, reflecting the need to manage risk and use resources appropriately. Decision-making was often based on situated judgements taken on the ground, in the light of the perceived state of the individual, whether they were alone or with friends, and at what stage of the night the agent encountered the individual. For example, if an individual appeared very intoxicated but was in the care of friends who were acting in the individual’s ‘best interests’, then assisting the individual and their friends into a taxi home was viewed as a satisfactory outcome. In cases where this was not possible, the AIMS provided a useful facility where they could be kept safe and monitored until sobering up. At site J, in the absence of an AIMS, agents had to remain on the scene until they were able to discharge or had to take the individual to ED. Site J Street Pastors reported that they spent more time dealing with individuals who were vulnerable, particularly lone females, than individuals who were acutely intoxicated. They also reported sometimes using the 24-hour McDonald’s (McDonald's Corporation, San Bernardino, CA, USA) on the edge of the city as a safe space where lone females could wait until they could get a train or bus home in the morning.
AIMSs
Although organised and structured differently, the successful operation of both the AIMSs hinged on negotiating the management of intoxicated individuals to consider the core roles of each of the agents involved while working flexibly to mitigate some of the risks to which individuals in the NTE are exposed. Although there was a strong sense that nurses are the overall authority on patient care, during busy periods roles and responsibilities become more fluid. The need to manage patient flow was an important organising logic in both AIMSs, but this appeared to be driven by the need to maintain capacity rather than meeting performance targets (such as in the EDs).
An individual attending an AIMS was first assessed by a nurse and a decision was made about whether they could be treated or should be referred to ED. Although referral pathways to the site B AIMS were open, the site A service had formal referral criteria. Nevertheless, we observed that NTE agents regularly referred individuals to the site A service who did not meet the referral criteria; ED nurses were happy to assess and make the ED referral if this was indicated.
The site A AIMS was formally aligned with the ED; thus, the management and progress of referred patients reflects the fact that they have been triaged in the AIMS. Minor injury patients were transported to ED by taxis or the urgent care service; in more serious cases (e.g. head injury), ambulance crews were involved. Operating within the same governance structures as the ED also enabled the AIMS nurses to refer patients to mental health or social services when necessary. Unlike ED, the AIMS also had direct access to PARIS (mental health services database) and indirect access to the police database (via the officer in the AIMS). Access to the PARIS database enabled ENPs to establish whether a patient presenting with potential mental health concerns was known to mental health teams or a new referral was required. Irrespective of whether or not the patient was known to mental health services, if they displayed suicidal behaviour or expressed suicidal thoughts then they were referred to the ED for observation.
There was no formal relationship between the AIMS and the ED at site B. In instances where the nurse was unable to fully assess or treat the patient, the patient was advised to attend the ED following their assessment. An informal agreement between St John Cymru and the ED enabled St John Cymru patients to be offloaded quickly to allow the crew to return to the city centre. AIMS staff also made extensive use of taxis to transport less serious cases to ED.
Emergency department
In the absence of AIMSs or when the AIMS was not operating, acutely intoxicated patients were referred to ED. Here, intoxicated patients were cared for in the context of the wider spectrum of ED work and prioritised according to need and clinical risk. All ED work in the case studies was driven by waiting-time targets, where the aim is to see, treat and discharge patients within 4 hours. During the fieldwork, the effects of this were most marked at site J where, unlike in Wales, there are financial penalties for failing to meet these targets. The structure of EDs in all cases included the areas minors, majors and resus (resuscitation area), with additional areas such as a Clinical Decision Unit (site J) or Ambulatory Care Unit where patients could be placed if they did not require a trolley and/or were likely to be discharged after a period of observation and assessment.
At site J, all patients arriving by ambulance were admitted initially into majors or resus but, depending on the demands on the service, could be reallocated to minors by the nurse who triaged patients on arrival. The management of patient flows and the effective utilisation of beds was a nursing responsibility, but pressures on admissions and downstream blockages in the hospital meant that sometimes there was no option but to attend to patients in the corridors and in the middle of ward areas. Fieldwork at site J revealed nurses to be working under considerable pressure and feeling dissatisfied by how the demands on the system compromised their ability to provide dignified care. In this context, nurses tended to perceive intoxicated patients as inappropriate users of the service.
According to the lead nurse at site J, most of the intoxicated patients in the ED were not acutely intoxicated but had sustained a minor injury under the influence of alcohol. These patients would be seen in minors and treated for their presenting complaint. Most sobered up while waiting to be treated and had a degree of sobriety when seen. Acutely intoxicated patients in majors tended to arrive by ambulance and during the fieldwork presented with a combination of intoxication and a head injury or a fall or a mixture of recreational drug and alcohol use. Patients unable to maintain their own airway, presenting a low Glasgow Coma Scale (GCS) score, who had aspirated vomit or who were violent and aggressive were admitted to resus. Patients considered too intoxicated to be discharged were moved to the Clinical Decisions Unit where they could be observed before discharge. This was also a mechanism for managing waiting-time targets.
Intoxication management
Street level
At all case study sites, much of the work of managing alcohol intoxication and risk took place at street level. Door workers, police, Street Pastors, MPS volunteers and ambulance crews worked hard to deal with situations on the scene. This might involve assisting someone who is unwell, providing water or helping people to contact friends and/or supporting individuals to get a taxi home. At sites A and B, the AIMS provided an alternative place of safety to enable individuals to recover, whereas at site J intoxication management could occupy street-level agents for prolonged periods of time and/or result in ED admission.
AIMS
Staff at site A and site B AIMS worked actively to manage intoxication. During the fieldwork there were relatively few occasions where a patient’s stay extended beyond 2 hours, and both services worked with an organising logic designed to sober up patients and/or discharge patients into the care of family and friends. Observed strategies for achieving this included:
-
putting intoxicated patients on a chair rather than on a stretcher/bed to prevent them from falling asleep
-
repeatedly assisting patients to sit upright
-
giving intoxicated patients water
-
attempting to engage intoxicated patients in conversation to keep them awake
-
enlisting friends and family into the care and management of intoxicated patients
-
proactively contacting friends and family at the earliest opportunity to expedite discharge.
Emergency department
At all case study sites the active management of intoxicated patients in AIMSs contrasted with the management of intoxicated individuals in ED. On the one hand, intoxicated ED attendees who were not deemed to be at risk tended to be left to sober up in the waiting room, with staff privately hoping that they would self-discharge, particularly when ED was busy. Unlike AIMSs, EDs did not have the resources for staff to proactively contact friends and family to enable discharge. On the other hand, ED staff observed that ‘flat out’ patients tended to be overinvestigated by doctors. Pressures of work on staff, a target-driven culture and the very real challenges of undertaking an assessment on someone who is unconscious or uncooperative meant that intoxicated attendees were often sent for computerised tomography (CT) scans to exclude a possible head injury before a full clinical assessment had been carried out. At site J, patients required a nurse to accompany them to a CT scan and one consequence of this was to deplete ED nurse staffing levels, which undermined the quality of care nurses felt able to provide.
A member of staff from the site J ED highlighted that one advantage of an AIMS would be to improve the quality of care received by intoxicated patients in the ED:
I think people just expect too much. The more you give, the more they’ll take. One patient annoyed me the other day, an intoxicated one – she was asking me if I could get her a mirror so she could look at her hair [pulls a face of disbelief]. I felt so angry with her. As if we have time to do that?! So I just told her she could go and look in the bathroom. But if I was a staff nurse in an AIMS I think I’d feel different because that’s what the service is there for, so I would feel like I could provide better quality care for these intoxicated patients, without feeling bad about it taking me away from giving quality care to my other patients. I think it would be a win-win. Non-intoxicated patients in here would get better care, because we would be able to give them our complete focus, and intoxicated patients would get better care because we wouldn’t have to be worried about caring for our more serious patients.
Staff nurse
Follow-up and interventions
There was little evidence of services deploying short-term interventions to address alcohol consumption. A brief alcohol intervention – in the form of videoing people when they were intoxicated – was built into the site A AIMS design but later abandoned because it was impractical. At the time of the fieldwork, AIMS staff shared patient details with Taith (Barry, UK) (a third-sector drug and alcohol open access and engagement service) who contacted each patient that had attended the AIMS to carry out a welfare check within 72 hours.
Interventions at the site B AIMS were less about alcohol consumption and more about encouraging individuals to take responsibility for themselves, and for each other, when on nights out. Over freshers’ week, AIMS staff handed out wristbands to service users on their discharge. The wristbands informed patients that they had visited the AIMS and highlighted the local ‘#wheresyourmates?’ campaign, run by a local university to enhance student safety in the NTE by reminding students to remain in contact with their friends on nights out.
At site J, staff informed us that they tended to offer brief interventions only to those who repeatedly attended the ED for intoxication/alcohol-related incidents and this entailed provision of a leaflet on alcohol services.
Treatment milieu
The organisational culture of the two AIMSs contrasted markedly to the clinical culture of all three EDs and this had important implications for staff interactions with the acutely intoxicated. In both facilities, service users were generally young, out enjoying the NTE and accompanied by friends in the clinical areas. Most staff in the AIMS had chosen to work in the AIMS and saw the management of intoxicated individuals as their core work, whereas in the three EDs such patients tended to be viewed as distractions from the ‘real’ work of ED staff:
If it’s a purely intoxicated patient, they don’t need to be here really, they don’t need urgent emergency care, I mean we don’t really provide any clinical care, and I just end up feeling like I’m their mother, looking after them, like a babysitting service, and I’m not here for that. Imagine when it’s busy and we have an intoxicated patient, an intoxicated patient with injuries, and then all your other urgent patients. It’s an ethical thing too. It costs £250 just for an ambulance. It’s a ridiculous waste of resources.
Staff nurse
Compared with work roles in the ED, work roles in the AIMS were more fluid [‘everyone mucks in’ (staff nurse)], albeit with clear demarcation in relation to clinical decisions. In addition, other NTE agents dropped in to catch up with staff or to deliver food and drinks to staff, particularly if the city centre was quiet. Staff would share stories and discuss the politics of their respective jobs. For the various agents of the NTE, these opportunities for ‘chatter’ were viewed as a valuable resource for learning and better understanding each other’s work, and sharing their knowledge of the NTE in general.
The above qualities had the effect of making the AIMS environment feel more informal than the ED. The revelry of the NTE seemed to seep into the service, and the AIMS staff appeared to enjoy this. For example, at site A, staff collected and kept the various fancy-dress props left behind or given to them by patients, and spent time talking with patients. AIMS staff seemed to enjoy opportunities to exchange stories with their patients. Because there was less concern that an intoxicated patient’s behaviour would have a negative impact on the experiences of their fellow patients, who were also likely to be patrons of the NTE and thus out to have a good time, staff were able to engage with patients ‘on their level’, whereas in the ED intoxicated patients whose behaviour was inappropriate were challenging to manage within the prevailing interactional norms.
Working with the acutely intoxicated
Staff orientation to acute alcohol intoxication
At all three case study sites, emergency services staff regarded AAI as normal behaviour and for the most part staff were non-judgemental in their interactions with patients:
I mean we’ve all been there.
Paramedic (site B)
We’ve all been like it.
Police officer (site B)
Nevertheless, although AAI was accepted as normal behaviour, it was not condoned. Although AIMS staff were happy to engage and interact with patients on friendly terms, this did not extend to what, at site A, they termed ‘there, there nursing’, that is, anything that made the patient too comfortable. Indeed, anyone exhibiting such behaviours, for example, by rubbing a person’s back or providing blankets, was reminded that this was not how things should be done.
At street level, the primary complaint was not that people became intoxicated but that responsibility for looking after them fell to the emergency services:
Problem is, people won’t take responsibility for themselves anymore and no one will take responsibility and turn inappropriate people away either.
Paramedic (site B)
We used to get ‘em [drunks] all the time before the AIMS. Trouble is, it’s too easy to call an ambulance and people don’t like to take responsibility. [. . .] People don’t seem to have any common sense anymore. Friends won’t just put their mate in a taxi or look after them. It’s just too convenient to call us and have someone else look after them.
Paramedic (site B)
In the ED there was ambivalence about the care of intoxicated patients. On the one hand, being deemed responsible for their own condition, they were regarded as undeserving and inappropriate users of the service. For example, nurses referred to the care given to those sleeping off the effects of intoxication as ‘babysitting’. On the other hand, it was also recognised that individuals were vulnerable and presented clinical risks. The care of intoxicated patients in majors and resus represented dilemmas for staff; intoxicated patients were regarded as an illegitimate demand on resources that should be left available for other emergencies:
Why are they here if they’re just intoxicated? There’s nothing wrong with them?
As a place of safety, you can’t just leave them on the street, can you? They’re vulnerable.
Right, I get it, but there should be somewhere else you can take them.
I know.
I mean, there’s over a 4-hour wait to see a doctor.
Well, they’re not really here to see a doctor, are they, they’re here to sober up.
I’d say she’s just smashed, and he is too by the look of his eyes. They all say they’ve been spiked but the consultant tells us that that’s pretty much urban myth for the most part. You can tell the difference between someone who has been spiked and someone who is just pissed. I mean, if I’d had that many drinks I’d be on the floor. It’s funny really.
Yeah, spiked on Jägerbombs more like, that’s what I said.
But yeah, they don’t really need to be here, and they’re taking up beds, so it is annoying, but what else can you do with them? There’s nowhere else for them to go. We had one here in resus last week, only 16!
Do you think there’s a need for it [an alcohol intoxication management service]?
Definitely. It’s a joke. Every weekend between 2 and 3 [o’clock] that’s all we get, but it’s all the time really, y’know, we’ll have someone intoxicated in most days.
Impact on staff
AIMS
Many staff had self-selected to work in the AIMS. At site B, for the St John Cymru paramedics and nurses whose core day-to-day roles were either working for WAST or the health board, working in the AIMS reportedly offered an easy way to make a ‘bit of extra’ money, providing a break from some of the pressures they experienced day-to-day:
I love it up there [in ED], but it’s so full-on all the time, so this place is a nice way to get a bit of extra, although it can be mental too.
K (St John nurse/senior ED nurse)
The St John first aid volunteers and MPS volunteers, on the other hand, freely offered up their time to work in the AIMS, and reportedly enjoyed their time there. Furthermore, unlike in the ED, where interaction with intoxicated patients was viewed as a distraction from work, interaction with patients was a central component of the work in AIMSs. The volunteers appeared to enjoy engaging with their patients. Police officers, usually based in Community Safety Teams, do one AIMS shift per month. Officers reported to ‘like’ these shifts and appeared to enjoy their time chatting with other staff members and patients.
Similarly, at site A the AIMS shift seemed to provide ED staff with light relief and entertainment after what had usually been an intense, and almost always fast-paced, working week in the ED. Furthermore, unlike the seriousness and complexity of some of the conditions of patients in the ED, intoxication was for the most part viewed as straightforward to treat and the unintended outcome of some fun and frivolity rather than anything more serious. Ambulance crews saw the AIMS shift as an easy way to accrue overtime, and the paramedic and EMT seemed to enjoy the general revelry of the NTE, and the varied pace of the work (some nights it would be quiet; other nights they would be working non-stop), which contrasted with their day-to-day work, where the volume of calls was almost always high, with little time for pause. For the urgent-care assistants (UCAs), the mobile medics shift was part of core duties and this group expressed more mixed perspectives; some found intoxicated patients difficult to manage and did not enjoy dealing with bodily fluids and aggressive behaviour. Police officers’ views of their work in AIMSs also varied. For some, it was ‘a welcome reprieve’ from their normal duties in the NTE, whereas for others it was viewed as dull in comparison. Nevertheless, all officers seemed to understand that police presence in AIMSs was necessary for nurses to feel safe while conducting their work and understood that without their presence the service would no longer function. AIMS shifts were therefore accepted as a necessary part of their work in the NTE.
Street-level workers
At the street level, acutely intoxicated individuals were regarded as just one example of numerous inappropriate demands made on front-line emergency services. Agents in the NTE talked about how the growing volume of their work related to the care of cases that challenged their sense of professional jurisdiction:
Our bread and butter, our top five, I’d say, is drug, alcohol, assaults, chest pain, mental health and falls.
Yep, we get a lot of unnecessary calls, your mental health, your drug and alcohol, they’re just difficult patients because you don’t know what to do with them – they’ll keep coming back again and again. A lot of the young ones don’t like it.
Why?
I don’t know. They don’t want the bread and butter for some reason, but this is the job, this is the world we live in.
I don’t mind working overtime when it’s for someone genuine, but when it’s not [sighs] – I’m losing my patience I think. [. . .] I don’t think I could do this job full-time [having just returned from maternity leave]. There’s just too many social calls.
Paramedic (site B)
Emergency department staff
Emergency department staff recognised that some intoxicated patients had a legitimate need for treatment and/or presented serious clinical risks (e.g. head injury). However, those who attended ED to sober up were generally viewed as inappropriate admissions that used scarce resources (e.g. nursing time, trolleys). Although intoxication was regarded as normal behaviour, those who ended up in the ED were considered to have taken it too far and had failed to take responsibility for themselves (or their family and friends had failed to take responsibility for them). Nurses were observed to work under pressure that caused them to struggle to give the quality of care they aspired to. In this context, care of intoxicated patients was an unwelcome additional demand on an overstretched team.
Who benefits from AIMSs?
Both site A and site B AIMSs were established in the context of wider strategic initiatives designed to increase the safety of the NTE and had developed against the backdrop of growing pressure on emergency services (police, the ambulance service and ED).
Impact on the emergency department
Long-serving ED staff at site A described the AIMS as a ‘godsend’ and claimed that it has had a huge impact on the ED, relieving some of the strain on staff and other patients:
The AIMS is an absolute godsend. We really feel it on those nights when it’s busy, like when there’s an event on or something. We just really can’t manage the intoxicated patients here [in the ED]. We had a few in off the ambulances last week, flat out they were, it was an initiation night, and they’d been drinking all afternoon. [. . .] But that doesn’t tend to happen so much now anyhow. It used to be a massive issue on weekends before the AIMS was open. We’ll get some during the week in term-time but mostly it’s the alcohol-related injuries we get in the week now.
Senior nurse (site A ED)
At site B, ED practitioners tended to be positive about the AIMS, reporting that they dealt with fewer alcohol-related attendances on the nights it was operational. However, because the AIMS served only a small part of the overall area that the ED served and was not able to treat certain conditions, staff reported that they still had intoxicated patients presenting in the ED most days:
The AIMS has really helped. We’d be lost without it because we’re just so busy, but we still get intoxicated patients in here most days, even over the weekends. We’ll have those the AIMS can’t treat, like your head injuries, or anything that needs an X-ray. But we’ll also get intoxicated patients from [location], y’know, people out drinking there or those from their home addresses.
Nurse in charge
Emergency department staff who worked in the AIMS as St John Cymru nurses were particularly positive about the service. They had witnessed the value of the service first-hand and could not envisage returning to a time when the service did not exist. Indeed, a few nurses recalled Saturday nights before the service, when half of the department’s trolley bays were taken up with acutely intoxicated individuals. Since the AIMS had opened, this was reportedly a rare occurrence. For nursing staff, the value of the service was that it ensured that resources were used more appropriately. It also served to reduce the volume of a category of patients who could be volatile and difficult to manage:
The AIMS is brilliant, it’s made such a difference. You can see how busy we are. Well, before, about 50% of our trolleys used to be taken up with drunks, just waiting to sober up, so it’s massively helped us here. It was horrible before. People spewing everywhere.
Staff nurse
A senior health board respondent was less certain about whether or not the AIMS had reduced ED alcohol-related attendances. The data collected by the AIMS could not show whether care in the service had diverted an ED attendance. From the perspective of the health board, many AIMS attendees would not be referred to the ED anyhow. Although it was acknowledged that the service had value and was fulfilling a previously unmet need in relation to managing vulnerability, the health board (as the funders of the service) argued that the AIMS needed to better demonstrate its effectiveness at reducing unnecessary ED attendances. At the time of the study, the health board was in discussion with St John Cymru about implementing a shared information technology (IT) system whereby those who attended the AIMS are logged onto an ED IT system to allow the health board to see whether or not AIMS attendees later attended the ED.
At site J, the ambivalence of staff towards management of the intoxicated – that they were undeserving but also presented potential clinical risks – was also reflected in their views about the value of an AIMS. On the one hand, they were keen to remove intoxicated people from the ED to an alternative facility. On the other hand, many expressed concerns about how risks would be managed. Some saw the value of a MIU located in the city centre but expressed concerns about a sobering-up facility because of the perceived risks of acute intoxication and the difficulty of differentiating between individuals who needed to be supported to sober up and individuals whose symptoms were indicative of an underlying condition or injury that required medical intervention.
Impact on ambulance services
At site A, mobile medics were highly valued because they freed other ambulance crews to respond to emergency calls in the surrounding area. Although most ambulance crews were overwhelmingly positive about the service, the service was not an additional resource but drew on existing resources, so outside the NTE the ambulance service operated with reduced resources. Nevertheless, the general view was that the overall benefits of the AIMS outweighed these costs.
At site B, all city centre calls were managed through the AIMS. WAST crews reported that the AIMS had greatly reduced the volume of alcohol-related calls that they attended, freeing them up to respond to other emergency calls in their respective localities:
Ask any crew and they’ll say that they barely go into the city centre when it’s open [. . .]. Before, the police could be with people for hours because the calls would often get downgraded if someone was with them, so it’s helped them massively too. When I’ve been on the RRV when the AIMS is not open, I’ve been with patients for hours waiting for a vehicle to convey.
Paramedic (site B)
In addition, AIMSs offered a referral option in cases where the assessment of risk or the management of vulnerability would otherwise place demands on emergency crew resources. In the absence of an AIMS, site J ambulance crews had limited options. For ambulance crews, the main benefit of an AIMS was that it would offer an alternative pathway to refer intoxicated individuals (without feeling a sense of guilt about inappropriate use of ED resources) and would also take some burden off decision-making, as discharging patients who were intoxicated was viewed by some crew members as a potentially risky strategy:
I think it’s a good idea. It’s embarrassing taking people in who essentially just need babysitting. Because the problem is, we can’t leave them either. We’ve had people die because whoever we have left them with hasn’t kept an eye on them, and they’ve choked on their own vomit. And whose fault is it then? Ours, of course!
Paramedic (site J)
Impact on police
Police officers at sites A and B valued the AIMS because it provided them with a place to refer individuals who were vulnerable or who needed more intervention than they were equipped to give. In both cases, police proactively engaged with the AIMS to refer intoxicated and/or at-risk individuals. This relieved the pressure on the core work of policing:
There’s not enough resources for us to do everything properly, it’s like spinning plates. This week has been unusually quiet though, so it’s given us some time to catch up a bit, but it’s rare it’s like that. [. . .] On these shifts [after dark], we’re expected to be doing everything, but we can’t do it, we can’t go and check on every person who might be a bit vulnerable – CCTV is handy in that sense though. [. . .] But, basically, we can’t be everywhere at once and we’re expected to be, but there’s not the resource to do it.
Police officer (site B)
The Street Pastors will tend to deal with D&Is [drunk and incapables], but if it’s a Saturday or a Wednesday we can send them to the AIMS.
Police sergeant (site B)
Although the police were unable to place a quantitative value on the impact of the site B AIMS on police demand, both a senior source and practitioners in the field were positive about the service and its impact. Officers felt that the AIMS had greatly reduced the amount of time they spent dealing with acutely intoxicated individuals, allowing them to focus on their core work of policing. Police officers spoke of occasions prior to the AIMS where they had spent hours with intoxicated individuals waiting for an ambulance crew to arrive, and of times when they had resorted to taking individuals to the ED themselves because the wait was so long. Furthermore, the role of the MPS volunteers at the AIMS was also felt to be of value for police officers, particularly in respect of tackling vulnerability, since intervening before something escalated prevented it from becoming a police matter in the first place (e.g. preventing a potential sexual assault on a vulnerable female by providing somewhere safe for her to sober up before she made her way home).
At site A, police officers believed it was good to have somewhere to take intoxicated people, but most interviewed for the study were new and were not able to compare their work in the NTE with a time before the AIMS was in place. At site J, in the absence of an AIMS, dealing with cases of alcohol intoxication and risk could take up police resources:
The other week, I dealt with a teacher, a female, who was drunk, but I reckon she’d also taken something. She were in a right state, she couldn’t even speak, and we just didn’t have anywhere to take her. I stayed with her for 3 hours waiting for an ambulance, and that wouldn’t have even been recorded as an incident, so yeah, it does take up a lot of our time.
Police officer (site J)
Indeed, the absence of an alternative referral option to ED, and the risks of resources being tied up on the ground, meant that police officers at site J were disinclined to get involved in the management of alcohol intoxication, even if this meant reduced confidence in the management of risks:
Traditionally the police are the first line of response, but we can’t be anymore. The night-time environment is particularly hard to police because there’s so much we should be doing that we can’t. If we come across someone who is shit-faced for example, ideally they should probably go somewhere safe to sober up and then make their way home, as sometimes we can spend hours with them trying to get them sober and home, or if we can’t get them up, we’re just there waiting for an ambulance, and all we can do really is assess whether they vaguely look alright, and if they’re with someone just ask them if they’re alright looking after them and going on their way basically. It’s not great gold-star service.
Police sergeant (site J)
I mean, with vulnerable women, I mean with anyone who is drunk really, we have to constantly make judgements as to whether to intervene. Like last week there was quite a muscly bare-chested guy carrying a female over his shoulder, like he were taking home his conquest sort of thing, and she were completely out of it. I had to stop them and check his intentions. He said he knew her, and that he were taking her back to her flat, but how do I really know what his intentions are? How long do I question him for to find out, and do I believe him or not? Anyway, he understood but he were mortified at my suggestion that something more sinister were going on, so I gave him the benefit of the doubt and sent him on his way. She would have been a perfect diversion candidate, somewhere neutral I could have directed them to get her sobered up before taking her home.
Police sergeant (site J)
Impact on volunteers
Alcohol intoxication management services were positively evaluated by volunteers. For Street Pastors at site A, having somewhere to refer patients and quickly hand them over enabled them to help more people in the NTE. At site B, the AIMS functioned as a learning environment, developing the skills of volunteers. For example, the relationship between St John Cymru paid staff and St John Cymru first aid volunteers resembled that of a mentor and mentee. There were a couple of instances where, while overseeing the work of the first aid volunteers, the nurse or paramedic on duty would take the time to explain to the first aid volunteers how to perform certain assessments, such as assessing a patient’s GCS score or how to establish capacity (although this tended to happen more when the service was less busy). For the MPS volunteers, their work at the AIMS was reported to have provided them with a valuable learning experience, giving them unique insight into the work of city centre police officers and partnership working. Indeed, the majority of MPS volunteers volunteered specifically to gain work experience for the police force, with the relationships they built up with city centre officers over the 3 years being understood to potentially aid their future employment.
Conclusion
The management of alcohol intoxication and alcohol-related risk is a profoundly distributed activity. With no single responsible agency, AIMSs operate as central actors in the NTE. In sites A and B, the partner agencies had already developed a close working relationship before the implementation of the AIMS, but this had been further strengthened by the AIMS at strategic and operational levels, with agents in the NTE working together more closely than they would ordinarily, for example sharing the same space and/or the same communication network. Field observations revealed that agents worked together almost seamlessly to mitigate the risks that individuals are exposed to in the NTE, be that handing out flip flops to prevent foot injuries, alerting relevant agents to attend to individuals who were vulnerable, steering intoxicated individuals into a taxi or, depending on an individual’s state and/or injuries, referring them to AIMS or ED. Thus, the AIMSs appear to have been intrinsic to the development of a wider work ‘ecology’ in which agents in the NTE work together to manage alcohol-related risk in the context of shifting patterns of demand. In the absence of AIMSs, at site J the ED functions as the central actor, exerting power at a distance on the work of police and ambulance crews who seek to manage risk and avoid inappropriate attendances. Unlike sites A and B, site J did not have a taxi ambassadors scheme at the time of the study and drivers could not be relied on to transport intoxicated individuals home: another factor that increased the risk of an ED attendance.
The case studies suggest that from a workforce perspective the most immediate beneficiaries of AIMSs are street-level agents. When dealing with individuals who were acutely intoxicated and/or injured, all NTE agents had an interest in making a referral to AIMS. This is because alternative approaches [transporting the individual to the ED (involving ambulance crew and sometimes the police), spending time managing the case at the scene or waiting with the individual for an ambulance to arrive and transport the individual to the ED (involving police, door staff, Street Pastors)] diverted street-level agents from their primary function when demand was at its highest and could leave them responsible for a situation that they did not feel adequately trained to deal with. Thus, for street-level agents, enrolment in AIMSs resulted in the alignment of all interests and perhaps accounts for why perspectives on AIMSs were so positive. ED staff also reported positive benefits of AIMSs in reducing (but not eliminating) the requirement to care for intoxicated individuals in the ED.
Alcohol intoxication management services in both cases relied heavily on self-selecting staff: either staff working on an overtime basis or volunteers (e.g. K-responders at site J). This may be one factor contributing to the success of the services, because staff willingly engaged with the typical service user. For those who work in AIMSs as part of their core duties (UCAs and police) there is some evidence that the work was not regarded as positively. This has important implications for future service design.
We observed limited follow-up care in either the AIMSs or ED. At site B, this is something that the MPS volunteer manager wanted to change, the idea being to establish arrangements with the city’s universities, whereby repeat attenders would be offered the opportunity to engage with university support services, because, in her view, repeat attenders often had underlying mental health problems. Thus, as presently constituted, AIMSs are driven by an acute care function but have potential to fulfil a wider public health function, particularly by working more closely with universities with regards to the student population, for which poor mental health is a growing concern.
A further important finding is the value of AIMSs in supporting vulnerability in the NTE. This was one argument for having an AIMS at site J. Findings suggest that AIMSs should have a wider remit than simply diverting ED attendances and should also be evaluated on this basis.
Chapter 6 Experiences and perceptions of AIMS users and emergency department users
AIMS users
Care offered in the NHS must be acceptable to users. 70 AIMS users may not want to return to an AIMS if they find treatment unsatisfactory and may instead opt to attend an ED. This must be balanced with concerns that AIMSs may normalise the use of emergency services for alcohol intoxication.
Interviews
Description of interviewees
It was not feasible to select different types of user to maximise diversity, as initially planned. Recruitment was difficult because the number of people using the AIMSs were sometimes very low, and many people attending the AIMSs were too intoxicated to approach or chose to leave quickly before contact was made. Recruitment was achieved from four AIMSs. The sample was therefore a convenience sample. Overall, consent from 49 participants was obtained across four AIMSs and 19 telephone interviews were undertaken. The 30 participants not interviewed did not respond to attempts to contact them. Interviews were shorter than planned, lasting 10–35 minutes, because they reached a natural conclusion in less time than anticipated, possibly owing to users’ poor recall of their experience with the AIMS. To protect interviewees’ anonymity, a detailed table of participant characteristics is excluded. Summary statistics are that interviews were conducted with seven women and 12 men. Interviewee age groups were late teen (n = 3), early 20s (n = 10), mid-20s (n = 4) and > 40 years (n = 2).
Overview of themes
The interview topic guide (see Appendix 10) followed a broadly chronological exploration of an individual’s evening: how they came to be in an AIMS, their experience of treatment given, their views of different staff and their experiences of discharge. The themes were:
-
i. reason for attending the AIMS
-
ii. who made the decision to attend the AIMS
-
iii. care and treatment provided in the AIMS
-
iv. staff and communication in and around the AIMS
-
v. preference for AIMSs or alternative care.
In addition, there were two conceptual themes:
-
vi. risk and safety (emerged from the data)
-
vii. normalisation.
We were interested in the possible normalisation of using health care to offset the risks from excessive alcohol consumption and whether or not doing so encouraged excessive alcohol consumption. Case summaries of four patients are provided in Appendix 11.
Circumstance: reasons for using an AIMS
The circumstances surrounding the use of an AIMS varied in our sample. Five interviewees had been involved in university student nights out, three were working in or around the NTE, three had attended sporting events and eight had participated in mixed drinking occasions including special occasions and birthdays.
In our sample, the university student nights were usually related to freshers’ week when interviewees said they went out with new friends and drank alcohol. First-year students often described very high levels of alcohol intoxication, being separated from friends and being unfamiliar with their new city of residence:
I just got too, too intoxicated. And ended up there. I was on my own as well, so I think [the people who found me] may have been concerned because I had no idea how to get home.
Interviewee iv (male, late teens)
Becoming separated from friends was a feature of several interviewees’ circumstances and appeared to heighten both their own sense of vulnerability and the concerns of the staff in licensed premises who found them. Interviewee iv talked about being taken home by a special minibus provided by the university.
Those working in the NTE described being injured while discharging duties relating to their employment, including injuries related to handling glassware and hot food, slips and trips, and aggressive and unpredictable customers. Time appeared to be important for workers in the NTE, who valued being checked in a local facility and not having a long wait for treatment, so they could return to work quickly.
Big sporting events, such as the international rugby union competition Six Nations Championship, attract very large numbers to licensed premises. Often these events occur in the afternoon. Our interviewees suggested that the timing of the event meant that they could drink alcohol from the early afternoon onwards and drank more than they usually would over a longer period of time. Some were consequently involved in fights that resulted in minor injuries:
A friend of mine started, well, seemed to be in a fight with one of his friends. I tried to intervene, erm, not really sure how I ended up on the floor but I think it was sort of, I don’t know, sort of got pushed or something, I’m not a hundred percent how. I don’t think I was hit but then ended up with a couple of, well, a big gash on the top of my head and lost one of my teeth.
Interviewee xiii (male, early 20s)
Decisions to attend an AIMS
Some of our interviewees chose to attend the AIMS themselves, whereas others had the choice made for them by friends, workers in the NTE, volunteers or Street Pastors:
I think it was my girlfriend as well as the bouncer, they all kind of said ‘listen, let’s get him in, let’s get him somewhere safe, somewhere inside’.
Interviewee viii (male, early 20s)
Occasionally AIMS staff themselves influenced the decision to attend, for example when an incident occurred in the immediate vicinity of an AIMS or where the AIMS staff went into the city centre to pick people up, by either wheelchair or vehicle, having been contacted by premises staff. Interviewees did not express any negative opinions about others making the decision for them to attend an AIMS.
Police officers were also involved in the decision to attend an AIMS. The AIMS was a place police officers could take a statement if a criminal offence was suspected, or a place of safety for the intoxicated or those otherwise vulnerable. One interviewee described being asked to leave the premises of a nightclub because of a fight. Attendance at an AIMS may have been an alternative to arrest and spending time in police custody:
They put me in the back of a van, in the back of a police van like, and then next thing I knew, they opened the door and said ‘we’re taking you here to sober up’.
Interviewee xiv (male, mid-20s)
All but two interviewees were unaware of the AIMS before attendance. Those that were aware knowingly attended the AIMS either as an alternative to calling 999 or because they weren’t seeking advice on their condition (i.e. were aware that alcohol intoxication was the cause of their symptoms). Other interviewees relied on the knowledge of friends, Street Pastors, premises staff or health-care professionals. Indeed, some interviewees highlighted the importance of improved public awareness:
I’ve been in [city name] all my life. I didn’t know it was there.
Interviewee x (male, mid-20s)
I think it was last year a boy killed himself. He chucked himself in the river [. . .] so I think more people should know about it, because when people get drunk they do tend to get very depressed.
Interviewee i (female, early 20s)
Care and treatment in AIMSs
Interviewees described what happened to them while at AIMSs. Patients recalled a wide range of treatments, including a saline drip to treat dehydration. Other treatments included water, ambulatory assessment, bandages, plasters, ice packs and analgesics. Investigations included an initial assessment, a physical examination, blood sugar test, body temperature test, blood pressure test, being breathalysed and a mouth swab test for drugs. Other activities included receiving a blanket, being reassured, being referred to other health-care providers (e.g. their GP), receiving an intervention around alcohol use and receiving leaflets and advice on, for example, wound care and personal safety.
Most interviewees described receiving simple, supportive care, such as being sat or laid down, having a physical examination, receiving wound care and being provided with water and a sick bowl as required:
They took all my details, name, address, what happened to me, where I was at the time and they gave me water to sober me up. They put an ice pack on my foot, they checked over my foot and chatted to me, really.
Interviewee vii (female, early 20s)
Descriptions of care were matter of fact, with little discernible value ascribed to the technical aspects of the care they received:
I’d got the bandage, I talked to them, I thanked them. And then I left.
Interviewee v (male, early 20s)
Patients recalled treatment durations from 20 minutes to 3 hours. Short treatment durations appeared to be associated with minor injuries that required only simple first aid with no other complicating factors, and where patients could be discharged on foot with friends rather than waiting for a taxi or other transport home. Longer treatment durations appeared to be associated with heightened levels of intoxication through alcohol consumption or suspected involuntary drug use (e.g. ‘spiking’), requiring lengthier times to monitor recovery, for sleep and rehydration, and for plans to be put in place for a safe discharge:
They wouldn’t just let me go out, [a friend] had to come back to actually sign me out sort of thing but then they made sure I was fit enough to leave before I did.
Interviewee xvi (male, mid-20s)
Interviewees valued the quality of their interactions with staff more highly than the medical checks and treatments provided to them. They accepted and appreciated the firm directive approach taken by AIMS staff in enrolling friends and family in their care to ensure their safety.
Referral to other health-care providers
A small number of interviewees in our sample were advised to seek care from other health-care providers by AIMS staff. One interviewee was taken to an AIMS having suffered a blackout while drinking. She was advised to see her GP as soon as possible but she expressed concern that she did not have the information she needed from the AIMS for a fruitful consultation with her GP:
I was hoping that it would have said on there, was what my blood pressure was at the time and what treatment I had received, like I know I was on a drip, but obviously I don’t know, to put fluids back in my body, but when I was going to see the doctor, myself then on the following Monday, I would like to have been able to say what my blood pressure was because obviously my own doctor wanted to know exactly what happened.
Interviewee vi (female, late teens)
Two interviewees were advised to go to the local ED for radiography. Interviewee i (female, early 20s) was sent directly in a taxi. She felt that this was helpful and was pleased that the radiography form had been filled in by the AIMS staff in advance because this enabled her to avoid triage in ED and go straight to radiology. Interviewee xvii was advised to have his assault-related injury radiographed but chose not to go immediately to the ED. He expressed the view that this was not necessary and only agreed to seek further care to satisfy AIMS staff and his friends’ wishes:
Yeah [laughs] they probably did. [. . .] I ended up going home and sleeping. And then going up the next day for the X-ray.
Interviewee xvii (male, mid-20s)
Information or advice about alcohol use
One interviewee described being ‘a bit surprised’ to receive a phone call from an agency offering some advice around drug and alcohol use a few days after attending an AIMS:
I got a call this morning actually. [. . .] I can’t remember what he said but I think it’s basically an attachment to that [AIMS]. And they just told me that they were, just to make sure I was OK, and they were going to give me advice about drinking loads of water and things like that.
Interviewee ii (female, late teens)
None of the interviewees received advice or information around alcohol use and did not question this. Views on whether or not it would be a good idea for staff in AIMSs to talk to AIMS users about alcohol use were mixed. Most interviewees characterised themselves as social drinkers who, although highly intoxicated on this occasion, generally know their limits and so would not have wanted or needed any intervention. Interviewees felt that the utility of any advice, information or brief intervention would depend on the patient or should be focused on a specific population (e.g. repeat AIMS users):
If someone’s been in three times in the last 2 weeks then definitely need to have a word with them and say ‘look, we realise that you’re not a machine, you are gonna get hurt if you drink too much’ [. . .] You know you would be a bit more, you know, susceptible to advice from someone who’s just, you know, potentially saved their lives.
Interviewee xiii (male, early 20s)
Staff and communication
Alcohol intoxication management service users recalled being cared for by various staff members, some of whom were identified confidently as police officers, paramedics (St John Ambulance and NHS) and nurses:
That’s what they said they were, they said they were nurses and they wore a blue top to [. . .] assign that they are nurses.
Interviewee xix (male, early 20s)
Interviewees spoke about others involved in their care from the first contact through to discharge. They mentioned premises staff and volunteers such as Street Pastors, and then volunteers working in the AIMS. They did not always know the roles of the people they had contact with due to poor recall:
I can’t really remember much about the evening, to be fair about it, but I remember they identified what they were and what they were doing.
Interviewee xvi (male, mid-20s)
Most interviewees in our sample were very positive about the care they received from staff. They appreciated the amount of communication offered by staff in the AIMS, the calmness of the atmosphere and the informality of communication:
They’re telling you exactly what they’re doing, when they’re doing it, you know, they’re like ‘now I’m gonna get this, now I’m gonna do this’ and it’s just like, as they’re going along, because they’re stood in front of you, is that you’re doing it yourself, yeah, and because there’s a few doctors and nurses there, that was quite nice as well because it was just one on one then, it wasn’t like that awkward, you know, atmosphere, there was loads of people there like you said. The policeman as well, I don’t know what his name was, he was like joking around with everyone there, even the nurses, and it was just nice, I enjoyed it, was stupid to say, but I enjoyed being there.
Interviewee vii (female, early 20s)
I don’t really know the word, just all like, you don’t feel under pressure or anything, it’s just really, not formal like whatsoever.
Interviewee x (male, mid-20s)
Preferences for AIMSs
When asked where they preferred to be treated, all the interviewees said they preferred AIMSs because it fitted their level of need, they would be low priority at an ED and treatment at an ED would be a waste of both their and the ED’s time:
I was still happy to be at the [AIMS] just because I know I was bleeding from my hand but I know it wasn’t bad enough to go to a hospital. It was more that I just wanted to get it checked over but I wouldn’t have wanted to go all the way to the hospital to waste anyone’s time when it wasn’t as serious as it looked.
Interviewee xi (male, early 20s)
If you go into A&E as a result of drinking you’re a low priority most of the time, because it’s self-inflicted.
Interviewees ix (female, early 20s)
Some interviewees suggested that they preferred AIMSs because they did not feel judged for their alcohol intoxication:
They are really helpful actually, really polite, no matter how drunk you come in!
Interviewee vii (female, early 20s)
Nobody was angry or annoyed.
Interviewee v (male, early 20s)
Some interviewees also felt that the quality of service at the AIMS surpassed their expectations or experience in the ED:
You’re waiting in A&E for a long time whereas there, as soon as I went in, they were with me and they were with me the whole time I was there and there wasn’t like a period of time I was left on my own. Whereas you don’t get that kind of service in an A&E.
Interviewee ix (female, early 20s)
Risk and safety
When interviewees described how they ended up in an AIMS it was clear that either they or others were concerned about their personal safety. They were incapacitated or alone and therefore vulnerable. They had lost their friends, lost the means to communicate via their mobile phone, were unfamiliar with the location or were disoriented because of AAI. The AIMS acted as a place of safety for them while they recovered, and friends were contacted to take them home (see Appendices 11 and 12).
A small number of interviewees believed that their drinks had been spiked (see Appendices 11 and 12). Spiking is associated with a heightened risk of sexual assault. Our interviewees who suspected spiking were with friends so did not feel at risk of sexual assault. Instead, they felt that they had been at risk and that there might be health risks associated with the drugs. They wanted tests to reassure them that they were not at risk of any drug-related health problems. One interviewee found the calm atmosphere, the informal communication with staff and the attentiveness of staff helpful in terms of calming them down and making them feel safe after feeling at risk.
Some interviewees had injuries that were minor enough to be treated at AIMSs. However, some interviewees identified potential risks associated with attending an AIMS. One wanted AIMS to be aware of their limits in terms of the severity of injury they attempted to treat, and the other was concerned about the potential of being discharged too early with a head injury:
For what I required they were brilliant. I mean, I can’t say what it would have been like if someone had come in with, I dunno, a head injury or, you know, I suppose that they know their limitations on what they would accept and what would be referred to a hospital.
Interviewee vi (female, late teens)
The only thing that I would possibly question is obviously I was, the nurse asked like, she was cleaning my wound and obviously go through questions and give me leaflets about head trauma, things like that. But I was told I could go and I walked home, which in hindsight probably wasn’t the right idea after actually banging my head.
Interviewee xiii (male, early 20s)
Normalisation of alcohol intoxication
There is the risk that AIMSs could normalise emergency health care for alcohol intoxication in NTEs and, with this additional safety net, encourage alcohol misuse. There was little evidence of this in our data. Some interviewees expressed distress, regret and embarrassment around their use of AIMSs:
I’ve never drunk like that, I’ve never been that drunk in my life. [. . .] I am really mortified about this, it was the most embarrassing thing that ever happened.
Interviewee ix (female, early 20s)
Other interviewees viewed alcohol intoxication, as well as the violence associated with it in clubs, as a normalised behaviour:
Everybody’s drinking in Britain, let’s be honest, especially where I’m from and where I know, it’s sort of part of growing up.
Interviewee xiii (male, early 20s)
I got caught up in a bit of, well, bit of a fight in one of the nightclubs so, um, I got, well, a few of us got kicked out, as you do.
Interviewee xiv (male, mid-20s)
Some concerns were expressed by our interviewees about the normalisation of formal health care for intoxication, asking that AIMSs are not made too appealing in case they attract users to them. The opposite stance was taken by others, who dismissed the possibly of this occurring. In our data there was only one example of complacency around using AIMSs, with AIMSs being described as a place of convenience enabling friends to relinquish their role of caring for each other, rather than as a place of safety or source of treatment:
You don’t want to make it overly comfortable, like a cafeteria, otherwise we’ll all be walking in anyway.
Interviewee xv (female, mid-50s)
It made it a lot easier. I didn’t have to try and recover too quickly. I wouldn’t have been in the right state to stay there and it would’ve been a pain going home at that time because I’d only just gone and it would have then been a hassle with friends looking after me.
Interviewee xvi (male, mid-20s)
Survey of AIMS users
Recruitment
The number of responses from some AIMSs was much lower than planned, partly because AIMSs had small numbers of attendees and partly because of the difficulty recruiting users. The recruitment period was increased to mitigate the slower-than-anticipated rate of recruitment. In practice, staff in some AIMSs rarely handed out questionnaires, or questionnaires taken out of an AIMS were not returned. It was not possible to calculate response rates because we relied on staff handing out questionnaires. The sample obtained is best described as a convenience sample with a risk of non-response bias. Participants were recruited from all six AIMSs.
Description of sample
A total of 208 completed questionnaires were received from the six AIMSs (see Appendix 12).
Results
Circumstances surrounding attendance
Respondents were asked three questions about the circumstances surrounding their attendance at the AIMS: the reason for their attendance, who accompanied them and what they thought they would have done had the AIMS not been available.
Care received at the AIMS
Care was most commonly received from ambulance paramedics, nurses and volunteers, although it seemed that care was more frequent from nurses at fixed sites and from paramedics and volunteers at mobile sites. The type of care received at fixed and mobile sites was similar despite differences in staffing (see Appendix 12).
Referral to emergency department
A total of 13.4% of AIMS users (26/194) reported being referred to an ED by staff in the AIMS. One in five AIMS users (21.3%; 10/47) who said that they would have gone to the ED if AIMSs were unavailable were referred to ED (compared with 10.7% of AIMS users [16/149] who did not say that they would have gone to the ED).
Satisfaction with different aspects of AIMSs
Overall, AIMSs were rated highly. When asked whether or not they ‘thought a service like this was a good idea?’, only one person responded ‘no’. In response to eight five-point Likert scale items rating different aspects of the service or care they received in the AIMS from ‘very good’ to ‘very poor’, each aspect was endorsed as ‘very good’ by > 80% of respondents (all sites combined; Table 10). ‘Safety’ and ‘comfort and cleanliness’ were endorsed as ‘very good’ by > 90%. No aspect of care was rated as ‘fairly poor’ or ‘very poor’ by > 2% of respondents. When ratings were compared for fixed and mobile sites, no statistically significant differences (at α < 0.006 following Bonferroni adjustment) were found in the proportion endorsing each aspect as ‘very good’.
| Characteristic | Endorsed as ‘very good’, n (%) | χ 2 | p-value | ||
|---|---|---|---|---|---|
| Site(s) | |||||
| All | Fixed | Mobile | |||
| Service location | 190 (81.1) | 124 (77.4) | 66 (87.9) | 3.07 | 0.06 |
| Safety | 194 (92.3) | 128 (89.8) | 66 (97.0) | 3.10 | 0.06 |
| Comfort and cleanliness | 191 (90.1) | 125 (87.2) | 66 (95.5) | 3.29 | 0.05 |
| Communication | 193 (83.9) | 128 (81.3) | 65 (89.2) | 2.04 | 0.11 |
| Care and compassion | 194 (89.7) | 128 (88.3) | 66 (92.4) | 0.81 | 0.26 |
| Tests and treatment | 181 (82.3) | 119 (81.5) | 62 (83.9) | 0.16 | 0.43 |
| Advice or information | 185 (83.2) | 121 (82.6) | 64 (84.4) | 0.09 | 0.47 |
| How was discharged | 154 (88.3) | 100 (87.0) | 54 (90.7) | 0.48 | 0.34 |
Preference for place of treatment
When asked about where they would have preferred to go, more than three-quarters (77.5%) of respondents indicated that they were happy to have been treated in the AIMS. However, about one in seven people indicated they would have preferred to go home. Only 8% would have preferred to go to the ED and preferences did not differ by fixed or mobile site (n = 187, χ2(3) = 1.35; p = 0.72) (see Appendix 12).
Overall satisfaction with AIMSs
Respondents rated their overall experience of attending the AIMS on an 11-point scale from 0 (‘I had a very poor experience’) to 10 (‘I had a very good experience’). Two-thirds (67%) rated their experience at 10 and 2.2% rated it as ≤ 5 (mean 9.35, SD 1.39). There was no difference between fixed and mobile sites (mean rating 9.28 and 9.47, respectively; t < 1).
About three-quarters of respondents provided an answer when asked what was good about the service. These mostly referred to the helpfulness and friendliness of staff (e.g. ‘staff polite, friendly, caring’, ‘people are friendly and not judgemental’) or were very generally positive (e.g. ‘everything’). A few people commented on the speed and convenience of the service (e.g. ‘quick medical attention, no long wait. Staff were very helpful’).
When asked what could be improved, most responses were ‘nothing’. The very few suggestions for improvement included opening later or on other nights, publicising the service, scope of service provision (suggestions to include providing food, medication, sexual health advice) and help getting home. However, these were expressed by a only small number of respondents. One person commented that the service provision is a waste of public funding.
Discussion
Based on the samples in our interview study and survey, it appears that AIMSs offer a service to workers in the NTE, people who have suffered injuries and those presenting with AAI. Users’ perceptions of AIMSs were positive regardless of the AIMS model (fixed or mobile). The caring and friendly approach of staff in AIMSs was appreciated. One-quarter of respondents to the survey reported that they would have been unsafe without the service and interviews suggested that the personal safety of some was at risk prior to attending. One-third of respondents to the survey reported that they would have contacted emergency services or gone to the ED if AIMSs had not been available. This highlights the possibility that only a minority of AIMS users were potentially diverted from ED (accepting that survey respondents may not be representative of all AIMS users, with the most intoxicated less likely to respond), and some AIMS users were referred by the AIMS to ED.
Context of other research
There is little relevant research available to draw on and none directly relevant to evaluation of AIMS users’ perceptions and experiences. This may reflect the difficulties in engaging patients with alcohol intoxication in this type of research. We identified one study71 in which interviews were undertaken with similar cases to those in our study: five binge drinkers who were admitted to hospital, three of whom were described as injured or assaulted, having consumed excessive amounts of alcohol. In this study, the authors described the issue of ‘spiked drinks’ as a common way of explaining extreme levels of intoxication or embarrassing events despite very low police estimations of actual drink spiking (< 1% of suspected drinks tested). A 2013 online survey72 found that over one-third of site B university students thought that they had been spiked when socialising in the city centre. In another study,73 which explored the notion of safety in relation to women’s use of alcohol and fear of drink spiking in the NTE, participants described situations in which the influence of alcohol had placed them at significant risk of personal harm. Our study identifies similar heightened perceptions of risk associated with alcohol intoxication.
Strengths and limitations
This is the first study to our knowledge to explore the views of AIMS users, and is therefore novel, not only because of the successful recruitment to interview and survey of those experiencing AAI despite this being a difficult population from which to recruit. 71 The materials were developed with strong PPI involvement, and so too were the interpretation of the findings (see Chapter 1, Patient, public and stakeholder involvement). Finally, the mixed-methods design ensured a detailed understanding of users’ experiences, a questionnaire based on the experiences of the target population and the ability to compare different models of AIMSs.
There were limitations. There were fewer than anticipated respondents in the survey. This was due to the small number of attendances at some AIMSs coupled with difficulties recruiting users. There was also a risk of bias as those with AAI may have been less likely to participate. Caution is therefore required when generalising findings to all users of AIMSs.
Implications for research and practice
The implications of this work include that AIMSs appear to offer an acceptable service to users. There was little evidence that users would avoid an AIMS, although our samples may have excluded unhappy users. There was also little evidence that AIMSs contributed to the further normalisation of AAI through the provision of additional care in the NTE and thereby contributed to an increase in risky alcohol use.
Alcohol intoxication management services appear to offer a place of personal safety as well as treatment for injuries for some users. Only a minority of users reported that they were likely to be diverted from ED. This raises the concern that AIMSs may not necessarily affect EDs to the extent anticipated. In this sense, AIMSs may provide an additional service that meets a previously unmet social need rather than an alternative diversionary service from emergency services. Finally, some use of AIMSs was made by workers in the NTE due to their knowledge of the service and its location. Further publicity of these services may increase their use, although this may have a greater impact on unmet need than ED diversion.
Perspectives of emergency department users
If AIMSs reduce the number of patients attending ED due to AAI, users of EDs may be more satisfied with their experiences of care because they find the environment more pleasant in terms of being quieter and feeling safer. This section reports findings from a postal survey developed for the study to measure differences in ED user experience between areas with AIMSs and control areas without AIMSs, and a retrospective analysis of data collected for a national ED survey to measure changes in ED user experience before and after implementation of AIMSs compared with control areas without AIMSs.
Controlled cross-sectional emergency department survey
Response rates
Although the survey was intended for people attending ED between 20.00 and 04.00, a proportion of respondents stated that they had attended outside these times (see Appendix 13). Furthermore, the site B AIMS did not open on Friday nights. We did not consider an effect on the ED user experience to be plausible outside AIMS opening hours, so we excluded responses from users attending outside the period of 20.00 to 04.00 at all sites and excluded Friday night attendances at sites B and L (the control site paired with site B). The number of attendances remaining after these exclusions was 340 (41%) at intervention and 492 at control sites (59%).
Respondent characteristics
The respondents had a mean age of 52.9 years (range 16 to 98 years) and 408 (49%) were female. There were no significant differences in respondent age (p = 0.16), in respect of gender (p = 0.96), arrival time (p = 0.64), time in department (p = 0.23) or the person who completed the survey (the patient or someone on behalf of the patient (p = 0.72; see Appendix 13).
General service ratings
Full details of the responses are provided in appendices (see Appendices 13 and 14). Service ratings were generally high, with 45–67% of respondents rating the service in ED at the highest level of ‘very good’. There was some variation between dimensions, with care and compassion and tests/treatments being rated high (rated very good by more than 60%) and communication low (rated very good by < 50%). There were no obvious differences between intervention and control sites. Regression analysis of service rating is reported in Appendix 13. There was no significant association between AIMSs and general service rating in any model.
Perception of threat
In response to the question ‘While you were in the emergency department, did you feel threatened by other patients or visitors?’, 21 out of 319 (6.6%) ED users in AIMS sites responded ‘yes definitely’, 49 out of 319 (15.4%) responded ‘yes to some extent’ and 249 out of 319 (78.1%) responded ‘no’. The corresponding figures for the control group were 16 out of 462 (3.5%), 54 out of 462 (11.7%) and 392 out of 462 (84.9%).
The results of regression analysis of threat perception are presented in Appendix 14. People arriving between midnight and 04.00 were more likely to feel threatened than those arriving between 20.00 and midnight. Older people were less likely to feel threatened than younger people. However, there was no significant difference between intervention and control sites on feelings of threat.
Perception of negative experiences
Overall, 31% agreed or strongly agreed that patients and visitors affected by alcohol shouted and made a lot of noise, 35% that the emergency department felt very crowded, 23% that the emergency department felt chaotic, 33% that patients and visitors affected by alcohol caused problems, 24% that staff spent a lot of time with patients or visitors affected by alcohol and 14% that it did not feel safe in the emergency department. The results of regression analysis are presented in Appendix 13. There was no significant difference between intervention and control sites.
Overall experience
The mean rating was 7.06 (95% CI 6.77 to 7.35) across the intervention sites and 7.24 (95% CI 7.01 to 7.47) across the control sites on a scale ranging from 0 (very poor experience) to 10 (very good experience). Appendix 13 presents the regression analysis of overall experience score. Those waiting 1–2 hours or > 2 hours reported the worst experiences. Mean overall experience levels increased with age and those arriving between midnight and 04.00 reported worse experiences than those arriving between 20.00 and midnight. However, there was no significant difference between intervention and control sites.
Secondary analysis
Alcohol intoxication management services activity analysis (see Chapter 6) showed that activity at the site D service was low and decreasing. The service at site D ultimately closed in 2017 after the ED survey was undertaken. The low and decreasing activity suggested that an effect on ED user experience at site D would not be plausible. We therefore repeated the analysis with site D and its paired control site (site K) excluded. The results are reported in Appendix 13. The secondary analysis findings were essentially unchanged from the primary analysis. There was no evidence of AIMSs being associated with any difference in ED general service rating, perception of threat, perception of negative experiences or overall ED experience rating.
Alcohol-related comments
Of the 1055 respondents, a large proportion (n = 704; 67%) responded to the open-ended question, of which 65 (9%) comments were related to alcohol (34 from intervention sites, 31 from control sites). Comments were overwhelmingly negative in tone. Some of the language respondents used about intoxicated patients and associated friends and family were ‘rude’, ‘abusive’, ‘shouting’, ‘noisy’, ‘arguing’, ‘fighting’, ‘falling over’, ‘vomiting’ and ‘threatening’. This made patients feel ‘stressed’, ‘unsafe’, ‘vulnerable’, ‘uncomfortable’, ‘upset’ and ‘annoyed’. Several respondents highlighted groups of patients who felt particularly unsafe: children, those attending with mental health problems and elderly patients:
It was really bad and surrounded by shouting drunks tripping over and falling into me, throwing up and fighting with the police. I left at 03.30 as I couldn’t cope anymore.
Suggestions for improving the situation caused by alcohol intoxication were grouped into three categories.
Security
Those who mentioned feeling unsafe felt that the ED should have more visible security staff present:
The amount of people who were drunk or under arrest is an issue. I understand funding is an issue but some visible security would help.
However, some patients noted that the presence of security and police heightened the sense of fear:
Police were present, but it made us feel very uneasy and could do without it.
‘Make them pay’
Patients who commented about charging people who were intoxicated felt that this would reduce the numbers attending ED and therefore improve the environment:
Charge people who are drunk to put people off drinking too much.
Separate them from other patients
Most patients who suggested an improvement said that they thought that people affected by alcohol should be separated from other patients. Some suggested having different areas in the hospital. Others explicitly suggested having separate facilities away from the ED, such as AIMSs:
If patients are assessed as drunk move them to another area. It was very distressing.
Drunks would be better treated outside A&E maybe in a bus away from people who did not want drunken louts making a traumatic experience worse than it already was.
Other
Other significant comments conveyed a sense of admiration for ED despite the difficulties caused by people affected by alcohol:
Full of admiration for staff and police who had to deal with alcohol-related incidents with professionalism and cool compassion.
The hospital staff were competent, professional and caring and worked like sheepdogs to cut out the drunk and unstable and keep me safe – brilliant.
Controlled before-and-after analysis of emergency department perceptions
English study cities
Care Quality Commission data are available only for English EDs. Therefore, data from the four AIMSs in English cities and their matched controls were analysed.
Perception of threat
For the four English sites, respondents’ perceptions of threat decreased significantly as age increased. However, there was not a significant difference in perception of threat either with or without AIMSs or pre or post intervention (see Appendix 15). Time in department was removed from this model as the model would not converge if it was included.
Overall experience
There was no significant difference in mean experience for those in AIMSs and those in control sites and there was no significant difference in mean experience pre or post introduction of AIMSs in any of the models fitted (see Appendix 16).
All AIMS cities
Overall, 7036 records were received, with complete data from 100 trusts. Appendix 15 presents the number of survey responses at each site during the relevant hours in 2012, 2014 and 2016 (in 2016 the survey sample month was September; in 2012 and 2014 the survey sample month was January, February or March). Overall, the mean age of respondents was 56.6 years and 54.1% were female. Appendix 6 includes further details of the survey responses.
Respondents’ perceptions of threat decreased significantly as age increased. Those waiting > 2 hours were more likely to perceive threats than those waiting for shorter periods. However, there was no significant difference in perception of threat with or without AIMSs or pre or post intervention across all models.
Mean experience ratings increased significantly (i.e. experiences were rated more positively) with age and experiences were more positive for male respondents than for female respondents. Overall, experiences were rated significantly more positively in 2014 and 2016 than in 2012. Those who spent > 2 hours in the department had significantly worse experience than those who spent less time there. However, there was no significant difference in mean experience between those in ED where an AIMS had been implemented locally and those in control sites, nor was there a significant difference in mean experience pre or post introduction of AIMSs (see Appendix 16).
Discussion
There was no evidence that the presence of AIMSs influenced the experience of ED users. One-quarter of ED users did not feel safe in ED and the open-ended question in our survey revealed that a number of ED users had strong feelings about the detrimental effects of alcohol-intoxicated users on their experience in the ED. However, most ED users reported feeling no threat to their safety and most responses to the open-ended question did not mention alcohol-related attendances.
Context of other research
Both the CQC and our ED patient survey found that most ED users rated their experiences in ED as positive. Across CQC survey years, about one-quarter rated their experience of the ED as very good. Across survey years the CQC also found that scores on overall experience were consistently lower for people attending in the evening between 21.00 and midnight. It is therefore unsurprising that our ED survey found that a lower proportion (19.2–20.4%) of ED users rated their experience as very good.
In contrast, using the same CQC rating scale as that used in our ED survey, we found that a significantly higher proportion (67%) of AIMS users rated their experience as very good. AIMS users highlighted the high-quality and frequent staff communications in their experience of care, with 83.9% of survey respondents rating communication as very good. In comparison, less than 50% of ED users in our survey endorsed this aspect of care as very good. These findings raise questions around inequity of health care and whether or not those who may be acutely intoxicated in AIMSs are receiving a higher standard of care and attention than ED users. Alternatively, these findings may reflect differences in the way that the AIMS and ED populations were selected, surveyed and responded; it is notable that AIMS respondents were likely to be intoxicated while using the service.
The 2016 CQC ED patient survey73 found that 8% of respondents felt ‘definitely’ or ‘to some extent’ threatened. Focusing on Friday and Saturday evenings only, our survey found that double that figure (18.6%) felt definitely or to some extent threatened. In contrast, over 90% of our AIMS users felt that the ‘safety’ aspect of their care was very good, compared with 58.5% of ED users in our survey.
Evidence suggests that alcohol-related ED attendances, especially at weekends, can make patients more fearful12,14,16,53,74 and have a negative impact on staff, to the detriment of overall care. 75 Issues around safety in the ED are reflected in the CQC’s inspection report (2014–16),76 which states that ‘protecting staff and patients from abuse and avoidable harm’ remains the biggest concern, with four out of five acute trusts needing improvement. Our findings suggest that, although some ED users report negative experiences related to concerns about safety and alcohol-related attendances, most report a positive experience, with no major concerns about safety.
The ED survey findings also need to be considered in the context of the AIMS activity data and AIMS user survey. The former show that mean nightly attendances varied across AIMSs (see Chapter 3, Study cities). The latter found that only a minority of AIMS users who responded to the survey said that they would have attended the ED if the AIMS had not been available. These findings suggest limited potential for AIMSs to have a measurable general effect on ED user experience, which may be reflected in the negative findings of the ED user survey. It could be argued that the diversion of a small number of highly disruptive patients with alcohol intoxication away from ED could have a substantial impact on the ED environment, and that the AIMS activity data and user survey do not consider the potential impact of intoxicated friends and relatives. Either way, the ED survey found no evidence of an effect of AIMSs on ED user experience.
We should also consider ED user survey findings in the context of the ethnographic component (see Chapter 5); ED staff in case study sites with nearby AIMSs reported positive benefits for the ED environment. We found no evidence that these perceived benefits led to an improved ED patient experience. This may be because diversion to AIMSs of ED attendances affects only staff, or because the study was insufficient to produce a measurable general effect on patients, or because the study was not sufficiently powered to detect small but worthwhile benefits at specific times or related to specific AIMSs. It is worth noting that the two sites included in the ethnographic study were the two most active AIMSs and that Welsh sites were not included in the controlled before-and-after analysis of AIMS implementation using CQC survey data.
Strengths and limitations
We used two different approaches to measure the impact of AIMSs on the experiences of ED users. One was a controlled cross-sectional design using our six AIMS sites and six control sites, with the strength of large numbers and the limitation of not being a controlled before-and-after design. The other, using analysis of existing data, was a stronger design in that we could measure change over time, but it had the limitation of small numbers of users per ED per year and it excluded the two Welsh AIMS sites and their control sites. The response rate to all surveys was low, consistent with expectations. This creates potential for non-response bias. The number of responses from each site was too small to allow meaningful analysis of individual sites, so we were unable to determine whether or not a specific AIMS or a specific type of AIMS had an effect that was not observed across all sites.
Implications for research and practice
The implications of our findings are that policy-makers should not expect the establishment of an AIMS to influence ED user experience. We cannot rule out the possibility that a specific AIMS could have an effect, particularly if it was active in diverting the most disruptive patients, but we found no evidence of a general effect. We found that ED user experience in our survey was generally positive but not as positive as general ED surveys undertaken at other times of the day and not as positive as the experience reported in the AIMS user survey (although not directly comparable). A small but significant proportion of ED users felt unsafe or threatened in the ED at times associated with alcohol-related attendances. These findings suggest that, although the ED during weekend nights may not be the entirely negative environment that is sometimes perceived, there is still potential for improvement. Ways of improving the ED environment during weekend nights could be explored.
Conclusion
The AIMSs in this evaluation catered for more than alcohol-intoxicated people; they also provided care to workers in the NTE and people who were injured. In this convenience sample, AIMS users were satisfied with the care they received, particularly valuing the quality of communication with AIMS staff. Users’ perceptions of AIMSs were largely positive regardless of the AIMS model (fixed or mobile). One-quarter of respondents to the survey reported that they would have been unsafe without the AIMS and the interviews suggest that the personal safety of some users attending the AIMS was at risk. One-third of respondents to the survey reported that they would have contacted emergency services or gone to the ED if the AIMS had not been available. This shows that only a minority of AIMS users were potentially diverted from the ED. Some of these people were then referred to the ED by the AIMS, further reducing the potential for AIMSs to reduce the use of EDs. There was no evidence that AIMSs reduced negative experiences of the environment in EDs.
Chapter 7 Patient and public involvement
Overview
Patient and public involvement was a critical feature of the evaluation. The Research Governance Framework for Health and Social Care77 states that research should be ‘pursued with the active involvement of service users and carers, including, where appropriate, those from ‘hard-to-reach groups’, and that patients should be involved at every stage of the research process where appropriate. Hard-to-reach groups (also termed ‘seldom heard’ groups) may be defined as minority or socially disadvantaged groups, for example minority ethnic, LGBT or homeless people, people with chronic mental illness, drug users or criminal offenders. 78
Patient and public involvement groups
Health and Care Research Wales public involvement community
This network is a group of people interested in being actively involved in health and social care research and it is based in Wales. The network was set up in 2006 as part of the Clinical Research Collaboration Cymru and since 2010 has been incorporated into the National Institute for Social Care and Health Research Clinical Research Centre. The network is made up of over 200 patients, carers, service users and members of the public interested in a range of areas including dementia, children and young people, cancer, diabetes mellitus, arthritis, stroke and public health. We engaged with the Involving People Network in Wales in the early stages of proposal development, which recruited one member from South Wales to act as independent lay advisor to the SSC. The Welsh member had been a victim of an alcohol-related assault and had an interest in health service research.
The Sheffield Emergency Care Forum
The SECF founding members were formerly part of the Community Health Council and Sheffield Patient Forum before SECF was formed in 2009. The group takes a special interest in research related to urgent and emergency care and has worked closely with teams from the Medical Care Research Unit and Centre for Urgent and Emergency Care Research of the School of Health and Related Research (ScHARR), University of Sheffield. The group was represented on the Strategic Local Priority Group for Public and Patient Involvement for South Yorkshire and the Humber and has links with other local and national PPI forums. 79,80 One member of the SECF volunteered to join the project advisory group because she was interested in the impact of alcohol on pre-hospital and urgent care.
Sheffield Addiction Recovery Research Panel
The Sheffield Addiction Recovery Research Panel (ShARRP) is a PPI group receiving support from the Clinical Research Office of Sheffield Teaching Hospitals NHS Foundation Trust. The group comprises former and current service users for drug and alcohol treatment and family and carers of people who have had experience of drug and alcohol misuse. The group represents most of the main providers of local drug and alcohol treatment and support groups, including known national agencies such as Alcoholics Anonymous (New York, NY, USA), Turning Point (London, UK), Addaction (London, UK), Phoenix Futures (London, UK) and Change, Grow, Live (formerly Crime Reductions Initiatives) (Brighton, UK). Members are also networked with local and national service users and recovery groups, allowing the facility to demonstrate how research can engage and promote PPI.
Two of the founding members of the ShARRP joined the project lay advisory group (LAG) because they had experience of drug- and alcohol-related harms and were keen to see how AIMSs cared for people affected by alcohol.
Patient and public involvement coordinator
Developing good relationships and having a dedicated PPI co-ordinator, either internal or external to the team, is significant in providing effective PPI. 81 A named lead for PPI in the research team worked closely with members of the SECF and ShARRP from the outset to form a LAG. This method of involvement provided an efficient single point of accountability and communication between project team and PPI members.
Proposal stage
The provision of PPI in research has been mostly medical and injury focused with no long-term opportunities for people with personal and familial experience of alcohol or drug use and associated harms to be involved in the research process. Therefore, members of the SECF patient and public advisory group were given the opportunity to review an early draft of the project proposal. Comments motivated us to capture the views of all patients in the ED, not just the intoxicated, and helped us formulate research questions:
If there is a way to divert the intoxicated public to a place of safety for their own good and where they can be observed and treated as necessary, then steps should be taken to do this. The idea of AIMSs is sound and should benefit everyone.
E (SECF member)
This sounds like a fantastic project! In order to get the maximum out of it, I would say interviews would need to be conducted with a lot of different people.
J (SECF member)
On methods (including proposed data collection, inclusion and exclusion criteria):
I have been in A&E at [hospital name] on a Friday evening and the disruption caused by the behaviour of intoxicated patients was very upsetting.
A (SECF member)
The SECF further advised on the Plain English summary. However, the complexity of the area to be examined demanded that we involve multiple PPI groups that would be able to provide diverse cultural and geographic perspectives, including experiences related to alcohol use and the impact of alcohol-related harm.
Project development and implementation stage
Lay advisory group involvement activities
The main aim of LAG involvement was to achieve insight into the methodology most likely to be well received by the intended participants (users of AIMSs and EDs). ShARRP members advised on survey design and provided revisions so that surveys could be read and understood by participants.
The normal mechanism for PPI in the Evaluating the Diversion of Alcohol Related Attendances (EDARA) project has been face-to-face meetings between the LAG and PPI lead. Meetings have been held at regular intervals throughout the project but with flexibility to enable more intensive periods of work and around various PPI-related events. In meetings and by e-mail correspondence, the LAG was invited to review all project documentation, review and comment on patient-friendly recruitment and consent processes, and review and suggest improvements on patient information sheets and consent forms.
The SECF has a long history and expertise in urgent and emergency care research and so was consulted specifically around ED users’ views. 79 Researchers attended regular SECF meetings to update on progress. Researchers also attended regular ShARRP meetings to discuss preliminary findings and to solicit feedback on data on AIMS users’ views.
Study Steering Committee
A fully independent member of the public was invited onto the SSC. Independent of the ‘hands-on’ LAG, the PPI SSC member represented patient and public interests at these meetings, specifically around adherence to the protocol and any issues around participant safety. The PPI SSC member ensured that the safety, well-being and rights of participants were considered. 82 The SSC member was kept informed of LAG activities outside SSC meetings via e-mail to ensure that PPI-related issues could be raised when required.
Specific tasks
Four specific tasks that could usefully include PPI were identified:
-
advise on the AIMS user interviews, recruitment and consent processes, interview question wording and interview format and design
-
advise on the analysis of AIMS user interview data (within the bounds of confidentiality) and the development of the AIMS exit survey
-
input into the design and content of the ED user questionnaire
-
co-production of guidance on AIMS development and implementation.
One of the early project management group and LAG discussions centred on what were to be the inclusion criteria of the AIMSs, what term would be applied and what the definition of these centres should be. Members were keen to avoid the word ‘treatment’ in the name for services, because this was felt to be misleading insofar as no obvious treatment for alcohol use as a disorder is provided. Similarly, ‘recovery’ was highlighted as a term to avoid because no support for recovery is provided and this phrase often connotes long-term support for abstinence in the drug and alcohol service user and research community.
Development of the AIMS exit survey
-
Lay advisory group members highlighted the need to ‘ask about comparisons’, for example ‘are you glad you came to AIMS, or prefer to have gone to ED?’.
-
Researchers suggested that it would be useful to ask AIMS users ‘in principle, do you think people who use this service should be asked to pay for it?’. The LAG challenged the inclusion of this question, claiming it ‘doesn’t feel fair, appropriate, or relevant’ and that the ‘question could stoke up resentment, which may colour answers to the following questions’. Based on the objections raised, the question was removed. ShARRP LAG members asserted that the questionnaire should not appear judgemental or moralistic.
-
Bigger tick boxes were suggested and implemented to make the responses easier for people who may be unwell or intoxicated.
-
Easy-to-read, colour-coded faces, happy to sad, were suggested and applied to help people understand the scale ‘very good’ to ‘very poor’.
-
Thinking about the sentence in the protocol about ‘concerns that AIMSs may normalise alcohol intoxication’, LAG members asked ‘did they [AIMS users] know their local AIMS existed? If so, did knowing the safety net was there affect their level of drinking?’.
-
Incentives to improve survey completion rate: LAG members discussed the initial problems and poor response rate to the AIMS survey and the advantages and disadvantages of using a small monetary incentive. The LAG raised no objection to the use of incentives in principle but felt that it was unnecessary for a short questionnaire and would be practically very difficult to implement. Based on the issues raised, incentives were not implemented.
AIMSs data interpretation
AIMS users’ interviews
The LAG reviewed three de-identified interview transcripts and offered preliminary thoughts. The ‘hazy recollections’ of interviewees was highlighted as an issue. LAG members asked, ‘what about the friends and family members of those who attend AIMSs?’; because these individuals are less likely to be intoxicated, we should interview and survey them to understand their experiences. Although it is important to consider friends and family members as significant in the referral process, project ethics approval permitted interaction with the users of AIMSs only. Ideas were taken forward into the development of the AIMS survey question around ‘who accompanied you to this service?’. In addition, LAG members discussed the issues raised in these transcripts and informed the initial coding framework.
AIMS survey
Preliminary results of the AIMS survey were presented to the LAG for discussion and comments on the future analysis. LAG members were keen for further analysis to explore if the experiences varied by gender. This analysis was undertaken. No significant differences were found and this was fed back to the group. LAG members were asked to consider the extensive use of ‘other’ as a question response option and the free text in the comments sections of the questionnaire. LAG members grouped ‘other’ responses by extant response options that were subsequently re-coded by researchers. LAG members suggested ways of grouping the additional comments thematically, which sometimes converged with themes emerging from parallel interview data analysis.
Lay advisory group members were surprised that there was a lack of intervention to address alcohol use. LAG members raised concerns that not delivering some brief advice to people who were intoxicated to the point of requiring assistance represented a ‘missed opportunity’ and were keen to explore this further:
We felt strongly that the opportunity for this [intervention and brief advice] should be taken advantage of. Also, the need to signpost treatment agencies when appropriate. I feel, personally, that this would also help allay some criticism around the provision of AIMSs condoning this type of behaviour.
Implications for service development and delivery will be explored further with patient and public input in future engagement and dissemination activities.
Development of the emergency department users’ questionnaire
-
The LAG members agreed that the ED survey should match parts of the AIMS survey for comparability of results.
-
The SECF members suggested that we should be interested in hearing from people in our sampling frame who attended an ED but walked out, because this may be because of finding the ED unpleasant in some way. This suggestion was discussed and reflected in the ED survey guidance documents, which directed participating EDs to include all those registered at the ED, including those who subsequently walked out without being seen.
-
One SECF member commented that ‘I think your survey needs to be sent out as soon as possible after the visit to A&E; memories are very short!’. The research team considered the current instructions manual issued to hospitals. Prompt mail-out was highlighted.
-
A draft version of the ED survey was presented to a SECF meeting for mock completion and comments. One member commented that ‘the questions all seem reasonable and straightforward and should give a good insight into people’s experience of weekend A&E’.
Emergency department survey response and interpretation
Despite having a robust process for checking ED survey patient sample lists for deaths before mailing, a small number were returned and marked as ‘patient deceased’. Our comprehensive review of procedures and report to the REC included feedback from the LAG. In this review, members suggested that text be added to the survey cover letter (and reminder) such as ‘if there has been any change in circumstances in the health of the intended recipient, please accept our apologies for this mailing and disregard this letter and survey’. The REC was satisfied with other corrective and preventative action taken by the research team and so this sentence was not used.
Sheffield Emergency Care Forum and Sheffield Addiction Recovery Research Panel meeting feedback
Project researchers capitalised on good relationships with both PPI groups to attend their regular meetings to provide updates on project progress and garner any additional feedback required. Preliminary findings were presented to both groups. SECF members were surprised by the apparent lack of any impact of AIMSs on ED users’ views. This may be the result of the general assumptions that AIMSs would divert large numbers of intoxicated patients and that the ED environment, especially at weekends, is unpleasant. These thoughts are reflected in the main discussion.
Evidence of impact
Impact on lay advisory group members
I feel that being involved in the study has been very informative and has hopefully equipped me to be able to contribute to other studies and related projects. Indeed, [En], [Mg] and I recently wrote a letter to [the REC] in support of a related follow-up research application. Looking at consenting people, especially vulnerable people, has been particularly interesting and an experience that will be useful in many future studies. Being involved with EDARA has also dispelled many stereotypes and confirmed that things are not always as reported in the press.
Ln (LAG and SECF member)
Ln’s comments highlight the personal benefits of the involvement activities and in enabling her to positively contribute to further research:
Being involved in the EDARA project has been a positive experience. I have felt at all times our comments have been valued and acted up. For example, the PPI group debated the suitability of including a financial charge question to service users in the AIMS survey: ‘would they be prepared to pay for future services?’. The group thought this was inappropriate. This resulted in it being removed from the questionnaire. The EDARA PPI members regularly feed back to the quarterly ShARRP group to enable us to gain a wider perspective from people who have real-life experiences of problematic alcohol use. I do not have any experience of formal research. My involvement with EDARA has helped my personal development and enabled me to gain an understanding of research methodology. In addition, I have been interested in learning about the work of the AIMS.
Md (LAG and ShARRP member)
Overall, the contribution of the LAG has been valuable not only in the research process but as an enjoyable and useful experience for members working closely with the research team at site J. Managing public involvement across two research centres (sites A and J) created some challenges, which have been reflected on:
I feel I would have benefited from one direct meeting with the site J PPI group as I felt quite isolated in the SSC situation. I did arrange a personal visit to the Site A AIMS which was very informative and I reported on this in the newsletter. I found the protocol of my role within the SSC rather difficult to grasp – I found the meetings worthwhile but was unsure of the value of my contribution.
Hn (SSC lay advisor)
The lay SSC member’s role was to represent patient and public interests at SSC meetings, specifically around any issues of participant safety. The disconnect between the LAG and SSC member was necessary and unavoidable but created challenges for LAG work to inform SSC input. In hindsight, a member of the site A team would have been well placed to offer Hn face-to-face advice and support on his role as SSC member.
Impact on public involvement groups
The Sheffield Addiction Recovery Research Panel
The ShARRP was formed partly to meet the public involvement needs of the EDARA project and to address the gap in the provision of drug- and alcohol-related PPI. Throughout the EDARA project, ShARRP has grown and is now well recognised as a source of relevant PPI, supporting several other drug- and alcohol-related research projects:
I have been pleased to be part of the LAG. Initially I was concerned that our involvement may have been a tick box exercise, but I am pleased to say that I always felt that our comments and suggestions were valued and acted on. I thought that our input to the format of the questionnaire was important. It ensured the questions and information was explained clearly to service users.
Md (LAG and ShARRP member)
Involvement activities with clear results reassured ShARRP members that their input was worthwhile. Contrary to the often self-stigmatising views of (former or current) drug and alcohol users and their friends and family, this project has reinforced the fact that people with experience of drug and alcohol use are valued contributors.
The Sheffield Emergency Care Forum
The SECF continues to provide a well-respected source of public involvement in urgent and emergency care research. EDARA has brought two very different PPI groups (SECF and SHARRP), with often quite different life experiences, together. Ln’s comment ‘dispelled many stereotypes’ related to the fact that most of the people attending AIMSs seemed to be appreciative and quite apologetic, clearly divergent from stereotypes referred to in the press around abusive and unruly intoxicated members of the public out on a Friday and Saturday night.
Conclusion
Patient and public advisors have had a positive impact on each stage of the EDARA research process. The challenges and achievements of managing multiple PPI contributors across sites and diverse PPI groups provide a good example for other drug- and alcohol-related research.
Chapter 8 Discussion and conclusions
To our knowledge, this is the first formal controlled evaluation of AIMSs. The underlying assumption behind AIMSs is that bespoke city-centre facilities that can safely manage those who have consumed too much alcohol alleviate pressure on front-line services operating in NTEs. The primary approach of this evaluation was to undertake a natural experiment by comparing cities with an AIMS with cities without an AIMS, with ED attendances as the primary outcome. EDs are one of the few locations that can safely receive those who have become vulnerable because of their alcohol use, and ambulance services and the police are involved with the management and transport of intoxicated patients to ED. If AIMSs successfully divert patients away from EDs, this should result in a measurable change in ED attendance rates and related key performance indicators across front-line services compared with cities without an AIMS. This mixed-method evaluation was well suited to the anticipated complexity of NTEs and has brought to the fore aspects of AAI management not previously captured in the literature, notably the broad-reaching impact of AAI across services and the community generally. Each substantive chapter in this report includes a summary of principal findings specific to that chapter. The role of this discussion is to integrate and discuss results.
Effectiveness
There were consistent results on pooled measures for ED attendance numbers, ambulance response times and the quarterly number of assaults on ED staff, suggesting that AIMSs have a positive effect. However, it is inappropriate to infer that all AIMSs have an equal impact. Site G, for example, does not receive patients from their local ambulance service and it is therefore implausible that this AIMS contributes to improved ambulance response times. Furthermore, attendance in AIMSs was variable and on average low for most AIMSs and it is not plausible that these AIMSs could divert many patients away from ED and contribute to improvements related to other key performance indicators. Therefore, it is likely that these main effects are attributable to the site A AIMS; we estimate that the service diverted approximately six patients away from ED out of an average attendance of 11 patients. The potential discrepancy between the variable (and often low) levels of AIMS activity and the evidence of an effect on ED attendances and emergency care key performance indicators associated with AIMSs could be explained by concurrent interventions or changes in the emergency care system. We did not identify specific interventions that were introduced alongside AIMSs, although our discussion of control cities found, unsurprisingly, that AAI attracted resources in its management, and practitioners, typically without the competency to do so, avoided referral to ED. Street-level actors working to prevent the referral of patients to ED suggest that AIMSs may influence the risk profile of the NTE and the nature of the treatment available to patrons. Furthermore, it is conceivable that AIMSs may have been introduced in response to a perceived problem of AAI in the intervention sites and may have been part of a wider intervention to address the problem. Moreover, comparisons assume that overall demand for ED is unaffected by AIMSs. It is feasible that diversion of AAI out of EDs frees resources and this in turn encourages referral of patients to ED from elsewhere, a matter that cannot be addressed without AAI-specific routine data. Finally, the divergent qualitative accounts from staff, where a benefit of AIMSs at sites A and B were reported, might be attributable to effectiveness being blunted in aggregate. These services showed variable attendance, from 0 to 40 attendances per evening, and effectiveness might therefore be more apparent during the busier evenings, which are less common.
Cost-effectiveness
The cost per session of an AIMS was approximately £1000–2200 and cost-effectiveness modelling was completed primarily from the ED perspective. Analyses indicate that an AIMS should divert approximately six attendances away from an ED for the more expensive model at site A, once savings from reduced ambulance journeys and admissions are included, and as few as two attendances for the less expensive model at site F. From the ED perspective alone, none of the services approached cost-effectiveness. It is noteworthy that services relying purely on volunteers, such as the service at site G, are not the cheapest services. Ambulance-led AIMSs were the least expensive and therefore needed to divert fewer patients than the nurse-led model at site A. The ethnographic study found that the impact of AAI was far broader than the ED.
Although we were unable to make definitive statements on whether or not an AIMS is cost-effective, it is feasible that the model at site A may become cost-effective once the post-implementation trend (the effect of site A AIMS on ED attendance numbers increased over time) is accounted for and savings associated with ambulance service transfer of patients are accounted for. Furthermore, these thresholds for cost-effectiveness are likely to fall further as additional savings (to the police) are factored in. There may also be additional costs that are not included. Notably, the motivation for several AIMSs was to provide a facility that improved the safety of patrons in the NTE. Several cities had experienced serious sexual assaults and deaths. These are high-value but rare events that only a national study would be likely to capture.
Cost-effectiveness has relevance to AIMS funding and, therefore, to the partners involved in supporting AIMSs. It is notable that a beneficiary of AIMSs, as revealed in the ethnographic study, was the police force. However, we were unable to include estimates on how AIMSs benefit the police service because routine data that describe the impact of AAI on police resources is not available. However, this does suggest that, should an observable effect be apparent on police resources that is attributable to AIMSs (including effects on ED), ambulance services and police would substantially alter the presumed cost-effectiveness estimates for AIMSs. Given the evidence that all emergency services may benefit from AIMS, consideration should be given to AIMSs models that share the financial burden among the services involved.
Patient and staff experiences
Against a backdrop of positive perceptions of care received in ED from patients attending ED, we found no evidence that AIMSs were associated with a change in ED patient experiences. A total of 67% of respondents to the ED survey responded to open-ended questions. Of these responses, 9% concerned other patients who were visibly intoxicated, and these comments were overwhelmingly negative in tone. This confirms that AAI patients are perceived negatively by other ED patients and builds on observations in the ethnographic study in which practitioners also reported that AAI negatively affects usual working roles. The effect of AAI on ED staff did not go unnoticed in the ED patient survey, with one patient stating that they were ‘[f]ull of admiration for staff and police who had to deal with alcohol-related incidents with professionalism and cool compassion’. The survey data collected from ED patients are broadly consistent with the ED analyses on AIMS attendance rates; there was little consistent evidence that AIMSs divert a substantial number of patients away from ED. However, for site A, at which there was evidence of diversion, no effect on ED patients was observed. There are at least two possible reasons for this. First, it is feasible that AAI was still present and the diversionary effects away from ED were not entirely realised. Second, the impact of AAI may be felt more by staff than by patients, the latter being passive viewers while staff manage AAI to reduce its impact. The ethnographic study presented some evidence that AAI may be overinvestigated in ED and that, therefore, these patients might be more likely to be taken out of the ED waiting area for assessment.
Alongside typical implementation outcomes, the acceptability of new services to users and the extent to which they are adopted are increasingly regarded as important evaluation outcomes. 70 Alongside efforts to increase patient choice in health care,83 it is notable that we found evidence of a preference among AIMS patients for receiving treatment in an AIMS over ED coupled with high levels of acceptability of AIMSs to patients.
AIMS provision
A full description of the services offered at each AIMS is available in Chapter 3 and offers insights into possible mechanisms underlying AIMSs effectiveness. First, provision varied considerably, from ED-type care at site A to paramedic-led services to volunteer-led services. It was the intention of this evaluation to capture this variability, with the expectation that doing so would highlight differences in effectiveness. However, in so doing, an unexpectedly large variation was discovered, suggesting that there exists no consensus on how AAI should be managed in the night-time context or what procedures should be adopted to determine and mitigate risk. In cities with AIMSs and without AIMSs there was evidence of informal volunteer-based services ascertaining risk and the appropriate care pathway for those who were vulnerable. The site A ED is led by ENPs with the competency to see, treat and discharge patients. These nurse practitioners also have experience of triage (the process used to determine a patient’s clinical need in ED), can consult with colleagues in ED and can refer direct to specialty (obviating the need for patients to go through ED triage a second time). Conversely, the site G service was staffed primarily by volunteers and is unusual in that it is the only AIMS evaluated that did not receive patients from the local ambulance service. Notable differences in AIMSs configuration beyond staffing include capacity.
Static AIMSs, such as at sites G, C and A, have greater capacity for patients to recuperate than mobile units such as those at sites E and H. Limited capacity would suggest less opportunity to observe patients over a period and that any decision to refer to ED must therefore be made according to presenting symptoms. In respect of alcohol, the concern is that inebriation is comorbid with other underlying issues,33 including hypoglycaemia. Accordingly, there are several tests available to help decision-makers rule out underlying conditions. Not every AIMS evaluated had all tests available (see Table 2) or the professional competency to identify the symptoms of head injury. Once other causes are ruled out, a discriminating feature between AAI and a loss of neurological function not wholly attributable to alcohol is that neurological function is expected to improve with AAI. 33 No specialist skill is required to help someone sober up; there is skill in identifying someone who is exhibiting complicated intoxication. Thus, facilities without appropriate tests or clinical staff able to assess patient need, or facilities in which patients cannot be adequately monitored for recovery, should be expected to refer patients to ED.
Impact on front-line staff
The ethnographic study found that the management of AAI was highly distributed, and that AAI placed significant burden on all front-line services. Because of the perceived high-risk nature of AAI, and because ambulance crews and police frequently have to manage demanding AAI-related incidents in the NTE, front-line staff can find it challenging to determine whether or not to take someone to ED, particularly as they do not want to increase the burden on ED unnecessarily. In relation to this issue of required expertise, the ethnographic study’s findings suggest that there already exists an informal process of street-based triage irrespective of the presence of an AIMS and that, therefore, one potential outcome of appropriately staffed AIMSs could be the reduction of risk.
The ethnographic study found no agency to be solely responsible for AAI and suggests that AIMSs operate as central actors in the NTE. At sites A and B, partner agencies had already developed a close working relationship with the AIMS before AIMS implementation, which was further strengthened by the AIMS at strategic and operational levels. Although enthusiasm for AIMSs was particularly notable from police officers, we did not consider routine data on how AIMSs might directly affect police operations. For the police, although AAI remains a criminal justice matter, it is more of a social issue than one involving crime, and if AIMSs are able to free up police resources from managing AAI then it may provide opportunities to reduce deployment numbers and adverse events (operations outside police remit).
The data captured for this evaluation primarily focused on routine health data. However, there is evidence that the impact of AIMSs is much broader than ED. AIMSs are particularly popular with front-line police officers and ambulance staff. Police officers are required to stay with anyone that they regard as vulnerable until they are safe (e.g. handed over to a Street Pastor or paramedic). We uncovered examples of officers having to take the very intoxicated to ED or stay with them for prolonged periods of time. These events require officers to become involved in what are ostensibly social issues that are outside their remit and which they do not necessarily have the expertise to manage. Some evidence indicates that, in response, police officers may not risk taking responsibility for some time-consuming cases. Although public drunkenness remains in the remit of the criminal justice system in the UK, it is clear from the work presented here that it is primarily the health service that is leading in this area and that it is an inconvenience for police officers. The UK is unusual in this respect; in Australia and the USA public intoxication has shifted from a criminal justice matter to a public health matter.
One of the main, but unmeasurable, advantages of AIMSs was that they provided a hub that brought police, ambulance and health service personnel closer together in their efforts to manage the NTE. There was evidence of collaborations emerging that better suited the complex relationship between partners. An example of this is AIMSs with facilities that allowed a police officer to interview patients without having to do so in police custody or in the ED. This meant that clinical needs could be addressed in parallel, with the option of transport to ED if required. Overall, a consistent finding is that the management of AAI is shared across all three blue-light services. The narrow focus of the current evaluation on ED attendances fails to capture this interdependency or related intangible benefits. Future work in this area should consider the broader benefits of AIMSs and costs of AAI, notably the reduction of risk for rare events such as sexual assault.
Equity
There are costs involved in setting up and running AIMSs and it is unclear whether or not those resources would be better spent elsewhere. AIMS patients reported that they found AIMSs satisfactory and preferred their treatment there over a referral to ED. ED patients also reported very positive views of their time in ED, irrespective of whether or not an AIMS was implemented locally. The question remains of whether or not the money spent on AIMSs could be spent elsewhere with greater impact on patients. The ED patient survey found neither a positive nor a negative effect of AIMSs on ED patients’ experiences. This suggests, and particularly so for site A, at which ED resources are used to support the AIMS, that ED patients did not experience inequity through the diversion of resources to AIMSs.
The decision to implement AIMSs
Only one AIMS has had funding included in partners’ routine budgets. The rest require applications for funding from a variety of sources. These sources include CCGs, local authorities, police and crime commissioners and others. These funding streams are typically short term and as such are unreliable. One potential reason for this short-term approach concerns how AAI is presented in the evidence available to decision-makers. There is a requirement in law for local Crime Reduction Partnerships to produce an annual Crime and Disorder Strategic Assessment. Section 116 of the Local Government and Public Involvement in Health Act 200758 sets out that primary care trusts and partners should produce a Joint Strategic Needs Assessment, revised in the Health and Social Care Act 2012. 59 This requires local authorities, CCGs and other responsible authorities to prepare a strategy to consider whether or not needs could be more effectively met by other arrangements under section 75 of the National Health Service Act 2006. 60 Although these strategies include data on alcohol and on crime, as national performance indicators for public health, AAI as it affects front-line services is inadequately recorded and, as a result, it is unclear how strategies can be developed to offset the impact of AAI on police and ambulance services and ED.
There is general acceptance that the ED data set, one source of data available to decision-makers for understanding the effect of AAI, which was developed in the 1970s, is not fit for purpose. Only about 5% of ED patients have a meaningful reason recorded for their attendance. In addition, 40% of diagnosis codes are absent and half of the remainder are either vague or symptoms. The system cannot be used to accurately determine the cause of problems that the ED handles. The new Emergency Care Data Set (ECDS) is being introduced; it has been implemented in England in type 1 EDs (consultant-led 24-hour care with resuscitation facilities) and specialist type 2 EDs. There are plans to implement the ECDS in minor injury units and urgent care centres (type 3 and 4 EDs, respectively), and in walk-in centres, by October 2018. A pilot comparing diagnosis codes pre and post ECDS found that 74% of ‘diagnoses’ were invalid pre ECDS but that all diagnoses were valid post ECDS. Currently, there is no national measure of acuity, and EDs use many different measures, for example triage or the National Early Warning Score. ECDS specifies that acuity must be measured on a 5-point scale, with category 1 being the highest acuity. If acuity is not formally assessed, it will be inferred from the intended physical destination of the patient (e.g. minors at 4 and resuscitation at 1). There are plans to use the ECDS template for use in ambulatory emergency care and ambulance services.
The list of 138 items in the new ECDS, which is based on a well-validated Canadian list of presenting complaints, has been used successfully in several centres in the UK and many countries around the world. The ECDS now includes data items that were not universally adopted in UK EDs, including place of injury (latitude and longitude), injury intent, injury mechanism, whether or not injury was due to alcohol or drug involvement and whether or not those presenting to EDs presented with alcohol withdrawal symptoms. The new data set will improve understanding of the impact of alcohol and domestic violence and pick up safeguarding issues. Better data will ensure that the services commissioned are services that patients will use and that services provide definitive, cost-effective care that is safe and of good quality. It has been proposed that Wales adopts the ECDS that has been implemented in England.
The issue is that the impact of alcohol, particularly AAI, in NTEs has not been adequately recorded across all front-line services. It is also characteristic of a larger issue that explains the origin of many AIMSs. All AIMSs were developed primarily in response to front-line staff’s calls for AIMSs to be implemented. None was directly commissioned. This is not surprising; if there are no data available to describe the impact of AAI, it is not feasible to expect commissioners and other decision-makers to respond in the same way that they do in the case of, for example, alcohol-related liver cirrhosis, which is well recorded in routine data. This is compounded somewhat by the observation that legislation in this area remains service specific. For example, in relation to Section 75 of the National Health Service Act 200660 and delivering health care, agreements should be considered if in so doing there is an improvement ‘in the way in which those functions are exercised’. Improvements attributable to AIMSs, however, are realised across partners, and consideration should be given to the place of AAI in the relevant legislation, which is complicated by the fact that AAI remains a criminal justice matter.
A result of the variable routes through which AIMSs were developed resulted in variable service provision and a lack of consensus on standard operating procedures. Lead services included police, ambulance, ED and third-sector services. Some services had capacity to observe patients, whereas many did not. Most services, but not all, had some form of clinical input, and some did not receive patients from the ambulance service. This variability was problematic for the evaluation insofar as this variation in design reduced opportunities to make a general statement on the effectiveness of AIMSs, but it also highlights the degree of uncertainty about what would be effective in NTEs. This matter needs to be addressed.
Funding
Alcohol intoxication management services are truly cost-effective if ED can reduce costs in response to diversion to AIMSs, and this raises questions about how AIMSs are funded. The measure adopted here is the cost of patients attending ED, and, even where ED attendance rates decline, there is not necessarily a mechanism on which EDs are able to capitalise and through which EDs are able to reduce costs. We did not consider funding further than recognising the source of funding for each AIMS. Nevertheless, ‘who pays?’ was a matter that was raised across our extensive stakeholder engagement and has implications for cost-effectiveness estimates. Broadly, there are three possible sources of funding: (1) public funds (e.g. health commissioners), (2) private funds, including the alcohol industry, and (3) those who allow themselves to become acutely intoxicated with alcohol and require assistance. Point 3 was raised by a small number of patients in the ED survey, who candidly suggested that AAI patients should be ‘made to pay’. This is antithetical to the free-at-point-of-delivery health-care arrangement in the UK; the balance between public and private funds, however, is worth considering.
In the NTE, licensed premises compete for profit from the sale of alcohol to customers. As is well described, this has negative consequences in the form of alcohol-related harms. These harms are traditionally known as externalities because, typically, the costs of these harms are not borne by those who supply the alcohol but are instead covered by society (e.g. police, EDs, ambulance services and even individuals in communities who must wait longer for an ambulance). Such externalities are not unique to the alcohol industry and have been discussed in the field of welfare economics for a number of years. 84,85 One response is that a tax could be levied that offsets these costs to society. For example, the tobacco industry profits from the sale of cigarettes but UK health services cover the costs for treating those with smoking-related disease. Tax can be applied per unit of production (e.g. pack of cigarettes) to cover these externalities. Applying such a tax to premises in NTEs is problematic, however. It is not clear what the unit of production is (there exists a dose–response relationship between alcohol consumed and vulnerability but very few consumers drink to the point at which assistance is required), and imposing a per-unit cost may adversely disincentivise across all levels of consumption. 85 Nevertheless, legislation is available to impose a Pigouvian-like charge on businesses in NTEs: the late-night levy.
The late-night levy was introduced as a part of the Police Reform and Social Responsibility Act 201161 and affords localities options to offset police costs associated with NTEs by placing a charge on licensed premises in an annual charge that is set nationally for businesses operating between midnight and 06.00. The levy has proven to be contentious with industry-affiliated groups, which suggest that it disincentivises businesses from operating beyond midnight to limit production, which is similar to criticisms of such taxes generally. 85 The levy also fails to take into account that the harms associated with NTEs are distributed across partners and include health, ambulance and police services, and it therefore appears to be directed more towards generating a revenue stream and complicating administrative processes than responding to and disincentivising externalities. 86
One opportunity arises from related work concerned with assault-related injury, a prominent harm associated with NTEs. 87,88 EDs across the UK are now encouraged to record features of an assault (where, when, who was involved) as patients attend ED. These data are passed to partners who can then allocate resources to challenge the causes of violence. This model represents an important step in aligning health costs with police resourcing decisions and subsequent deterrence activities, providing a model in which health services can inform resource allocation decisions through which the causes of ED attendance can be addressed for one significant category of patient. An extension of this approach is evidenced at the site A AIMS. At site A the place of last drink for those attending the AIMS is recorded and passed to local licensing committees. This extends the opportunity for partnerships to communicate the identity of premises that may be engaged in the inappropriate sale of alcohol (under UK law it is an offence to serve those already intoxicated), thus levying co-payments proportionately and in a manner that communicates the significance of AAI to licensed premises, effectively bringing the costs of AAI into the operating costs of those who gain from the sale of alcohol.
Future research
There is considerable variance in AIMS design. This study further identified considerable uncertainty across the distributed networks of those involved in managing AAI in NTEs. Individuals would often balance perceived risk against a referral into ED. Research could contribute to National Institute for Health and Care Excellence guidance that details the minimum requirements for the best management of AAI and contribute to agreed AIMS standard operating procedures.
It remains a fact that the routine data available to characterise the impact of AAI on services and determine strategies to counter the cause of AAI-related costs are lacking. Methodological innovation, together with improvements to routine data capture, could contribute to a more complete picture of the costs of AAI, including the previously unmet need that AIMSs captured. This would benefit evaluations in this area and inform service delivery.
The impact of AAI on front-line staff in routine data is poorly captured. Research could be undertaken to better capture data on sexual, verbal and physical assaults on staff, so that the true cost of AAI on front-line staff can be determined.
The costs associated with AAI need to be understood more broadly, as costs that detract from the community generally and as costs that affect and are managed by all front-line services. Future work in operations research and evaluations in this area need to be conducted from this perspective rather than narrowly focusing on ED.
Co-payments by licensed premises should be explored, including possible opportunities for charges to be made to licensed premises under the late-night levy. Opportunities for a ‘market of harm’ that both incentivises harm reduction and provides for service innovation could be investigated.
Conclusion
Alcohol intoxication management services may provide additional unmeasured benefits in the management of NTEs for practitioners, AIMS patients and those with otherwise unmet needs. They provide an accessible facility in which those who become vulnerable can be cared for, they are preferred to ED by those who use them and they are popular with front-line staff. Their impact is broader than diversion from ED and they are likely, in some examples, to reduce risk and vulnerability in NTEs. There is limited evidence that AIMSs improve service delivery in respect of key performance indicators but that services led by nurse practitioners, although more expensive, are more likely to provide a tangible return on investment, in addition to an intangible return in improving staff well-being. The service aligned with the local ED and led by nurse practitioners, who would typically determine clinical need in the ED, may be better placed to judge whether or not AAI patients require specialist care and have the competence to appropriately manage risk over volunteer-led services. Being familiar with the local ED also allowed the referral of patients directly into specialty, avoiding triage again at ED. AIMSs should be understood as a partnership across the police, ambulance services and ED. Health care in the context of the NTE is diffuse and managed by many organisations with varying levels of competency. Qualitative accounts indicate that AIMSs may facilitate better use of resources in managing AAI (notably with nurse-practitioner-led services) and reduce risk of more high-value but low-frequency outcomes, including sexual assault. Further developments in the UK need to be formally evaluated, appropriate governance decided and minimum service provision agreed. Funding models should be explored that both disincentivise AAI and offset the costs of AIMSs to society. Work needs to be undertaken to improve the measurement of alcohol-related intoxication as it effects on front-line services.
Acknowledgements
We acknowledge the support and willingness to engage of all those who have contributed to this work, including staff in EDs, ambulance services and the police, as well as the patients and members of the public who selflessly gave their time. This work uses data provided by patients and collected by the NHS as part of their care and support and would not have been possible without access to these data. The NIHR recognises and values the role of patient data, securely accessed and stored, both in underpinning and leading to improvements in research and care. We also acknowledge the Welsh Government for funding an earlier pilot study from which this project developed. We also recognise the patience of our colleagues at the NIHR and their continued support.
Contributions of authors
Simon C Moore (https://orcid.org/0000-0001-5495-4705) was project lead and contributed to data interpretation and the writing of the final report.
Davina Allen (https://orcid.org/0000-0002-6729-7502) was ethnographic lead and contributed to the writing of the final report.
Yvette Amos contributed to data collection and interpretation and the writing of the final report.
Joanne Blake (https://orcid.org/0000-0001-7471-1620) was ethnographic researcher and contributed to the writing of the final report.
Alan Brennan (https://orcid.org/0000-0002-1025-312X) contributed to cost-effectiveness modelling and the writing of the final report.
Penny Buykx (https://orcid.org/0000-0003-4788-4002) contributed to survey design and data collection and analysis.
Steve Goodacre (https://orcid.org/0000-0003-0803-8444) was effectiveness lead and contributed to the writing of the final report.
Laura Gray (https://orcid.org/0000-0001-6365-7710) contributed to data analysis and interpretation.
Andy Irving (https://orcid.org/0000-0002-1175-716X) contributed to project management and data collection and interpretation.
Alicia O’Cathain (https://orcid.org/0000-0003-4033-506X) was patient views lead and contributed to the writing of the final report.
Vaseekaran Sivarajasingam (https://orcid.org/0000-0001-9812-6100) contributed to the writing of the final report.
Tracey Young (https://orcid.org/0000-0001-8467-0471) contributed to data analysis, effectiveness modelling and the writing of the final report.
Publications
Irving A. Managing Alcohol-related Attendances in Emergency Care: Can Diversion to Bespoke Services Lessen the Burden? International Roundtable in Community Paramedicine, Warwickshire, 10 February 2017.
Moore S, Irving A. Alcohol Intoxication Management Services in the Night-time Economy are Highly Acceptable to their Users but they may not Reduce Demand on Emergency Services: A Mixed Methods Study. European Emergency Medical Services Congress, Copenhagen, 16 February 2017.
Irving A, Goodacre S, Blake J, Allen D, Moore SC. Managing alcohol-related attendances in emergency care: can diversion to bespoke services lessen the burden? Emerg Med J 2018;35:79–82.
Allen D, Blake J, Moore SC. The impact of alcohol intoxication management services on frontline work in the night-time economy: an ethnographic study. Health Services Research UK Conference, Manchester, 2–3 July 2019.
Goodacre S, et al. EDARA: Evaluating the Diversion of Alcohol-Related Attendances. Royal College of Emergency Medicine, Gateshead, 2 October 2019.
Irving A, Allen D, Blake J, Moore S, Goodacre S. Managing Alcohol Intoxication in the Night-time Economy: Staff and Patient Perspectives. Abstract accepted for oral presentation at the 45th Annual Alcohol Epidemiology Symposium of the Kettil Bruun Society (KBS 2019), Utrecht, 5 June 2019.
Irving A, Buykx P, Amos Y, Goodacre S, Moore SC, O’Cathain A. The acceptability of Alcohol Intoxication Management Services to users: a mixed methods study. Drug and Alcohol Review 2019;39:36–43.
Moore S. Oral Presentation by Professor Simon Moore. Lisbon Addictions Conference, Lisbon, 23 October 2019.
Data-sharing statement
The data used for the primary analyses undertaken were accessed from ambulance service trusts, NHS Digital and the NHS Wales Informatics Service. These data are available to other bona fide researchers following appropriate application. These data are not available from the authors. All other data are available to other researchers once appropriate anonymity can be assured and from the lead researcher in each area [patient view (AoC); ethnography (DA)]. For more information please contact the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Vonghia L, Leggio L, Ferrulli A, Bertini M, Gasbarrini G, Addolorato G. Alcoholism Treatment Study Group . Acute alcohol intoxication. Eur J Intern Med 2008;19:561-7. https://doi.org/10.1016/j.ejim.2007.06.033.
- Perham N, Moore SC, Shepherd J, Cusens B. Identifying drunkenness in the night-time economy. Addiction 2007;102:377-80. https://doi.org/10.1111/j.1360-0443.2006.01699.x.
- Lloyd B, Matthews S, Livingston M, Jayasekara H, Smith K. Alcohol intoxication in the context of major public holidays, sporting and social events: a time-series analysis in Melbourne, Australia, 2000–9. Addiction 2013;108:701-9. https://doi.org/10.1111/add.12041.
- Young DJ, Stockwell T, Cherpitel CJ, Ye Y, Macdonald S, Borges G, et al. Emergency room injury presentations as an indicator of alcohol-related problems in the community: a multilevel analysis of an international study. J Stud Alcohol 2004;65:605-12. https://doi.org/10.15288/jsa.2004.65.605.
- Parkinson K, Newbury-Birch D, Phillipson A, Hindmarch P, Kaner E, Stamp E, et al. Prevalence of alcohol related attendance at an inner city emergency department and its impact: a dual prospective and retrospective cohort study. Emerg Med J 2016;33:187-93. https://doi.org/10.1136/emermed-2014-204581.
- Verelst S, Moonen PJ, Desruelles D, Gillet JB. Emergency department visits due to alcohol intoxication: characteristics of patients and impact on the emergency room. Alcohol Alcohol 2012;47:433-8. https://doi.org/10.1093/alcalc/ags035.
- Drummond C, Phillips T, Coulton S, Barnaby B, Keating S, Sabri R, et al. Saturday Night and Sunday Morning: The 2003 Twenty-four Hour National Prevalence Survey of Alcohol-related Attendances at Accident and Emergency Departments in England. London: Department of Addictive Behaviour and Psychological Medicine, University of London; 2003.
- Pirmohamed M, Brown C, Owens L, Luke C, Gilmore IT, Breckenridge AM, et al. The burden of alcohol misuse on an inner-city general hospital. QJM 2000;93:291-5. https://doi.org/10.1093/qjmed/93.5.291.
- Newton A, Sarker SJ, Pahal GS, van den Bergh E, Young C. Impact of the new UK licensing law on emergency hospital attendances: a cohort study. Emerg Med J 2007;24:532-4. https://doi.org/10.1136/emj.2007.046094.
- Hoskins R, Benger J. What is the burden of alcohol-related injuries in an inner city emergency department?. Emerg Med J 2013;30. https://doi.org/10.1136/emermed-2011-200510.
- Crilly J, Chaboyer W, Creedy D. Violence towards emergency department nurses by patients. Accid Emerg Nurs 2004;12:67-73. https://doi.org/10.1016/j.aaen.2003.11.003.
- Baboolal K, Griffiths JD, Knight VA, Nelson AV, Voake C, Williams JE. How efficient can an emergency unit be? A perfect world model. Emerg Med J 2012;29:972-7. https://doi.org/10.1136/emermed-2011-200101.
- Knight VA, Harper PR. Modelling emergency medical services with phase-type distributions. Health Systems 2012;1:58-6. https://doi.org/10.1057/hs.2012.1.
- Stirling G, Higgins JE, Cooke MW. Violence in A.E departments: a systematic review of the literature. Accid Emerg Nurs 2001;9:77-85. https://doi.org/10.1054/aaen.2000.0204.
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med 2008;52:126-36. https://doi.org/10.1016/j.annemergmed.2008.03.014.
- Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med 2000;35:63-8. https://doi.org/10.1016/S0196-0644(00)70105-3.
- Brewster-Liddle J, Parsons W, Moore S. Setting up an alcohol treatment centre. Emerg Nurse 2013;21:14-8. https://doi.org/10.7748/en2013.10.21.6.14.s17.
- House of Commons Committee of Public Accounts . Transforming NHS Ambulance Services: Forty-Sixth Report of Session 2010–12 2011.
- McDonald AJ, Wang N, Camargo CA. US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Arch Intern Med 2004;164:531-7. https://doi.org/10.1001/archinte.164.5.531.
- Indig D, Copeland J, Conigrave KM, Rotenko I. Why are alcohol-related emergency department presentations under-detected? An exploratory study using nursing triage text. Drug Alcohol Rev 2008;27:584-90. https://doi.org/10.1080/09595230801935680.
- Russiapedia . Of Russian Origin: Vytrezvitel n.d. http://russiapedia.rt.com/of-russian-origin/vytrezvitel/ (accessed 16 September 2016).
- Wortis J. Alcoholism in the Soviet Union: public health and social aspects. Am J Public Health Nations Health 1963;53:1644-55. https://doi.org/10.2105/AJPH.53.10.1644.
- Mravčík V, Burešová Z, Popov P, Miovský M. Sobering-up stations in the Czech Republic in the context of analogous models of care for acute intoxications in Europe. Cas Lek Cesk 2013;152:129-34.
- Säilä SL. An experimental detoxification center in Helsinki from a cross-national perspective. Ann N Y Acad Sci 1986;472:161-7. https://doi.org/10.1111/j.1749-6632.1986.tb29618.x.
- Swain AH, Weaver A, Gray AJ, Bailey M, Palmer SG. Ambulance triage and treatment zones at major rugby events in Wellington, New Zealand: a sobering experience. N Z Med J 2013;126:12-24.
- Grant M, Tatham RJ. The District of Columbia’s experiences with the alcoholic. JAMA 1967;202:931-4. https://doi.org/10.1001/jama.1967.03130230057007.
- Fagan RW, Mauss AL. Padding the revolving door – an initial assessment of the Uniform Alcoholism and Intoxication Treatment Act in practice. Social 1978;26:232-46. https://doi.org/10.2307/800285.
- National Conference of Commissioners on Uniform State Laws . Uniform Alcoholism and Intoxication Treatment Act. 1973.
- Tatham RJ. Detoxification center: a public health alternative for the drunk tank. Fed Probation 1969;33.
- Dunford JV, Castillo EM, Chan TC, Vilke GM, Jenson P, Lindsay SP. Impact of the San Diego Serial Inebriate Program on use of emergency medical resources. Ann Emerg Med 2006;47:328-36. https://doi.org/10.1016/j.annemergmed.2005.11.017.
- Smith-Bernardin S, Schneidermann M. Safe sobering: San Francisco’s approach to chronic public inebriation. J Health Care Poor Underserved 2012;23:265-70. https://doi.org/10.1353/hpu.2012.0144.
- Brady M, Nicholls R, Henderson G, Byrne J. The role of a rural sobering-up centre in managing alcohol-related harm to Aboriginal people in South Australia. Drug Alcohol Rev 2006;25:201-6. https://doi.org/10.1080/09595230600644657.
- Mackway-Jones K, Marsden J, Windle J. Emergency Triage: Manchester Triage Group. Chichester: John Wiley & Sons; 2013.
- Cornwall AH, Zaller N, Warren O, Williams K, Karlsen-Ayala N, Zink B. A pilot study of emergency medical technicians’ field assessment of intoxicated patients’ need for ED care. Am J Emerg Med 2012;30:1224-8. https://doi.org/10.1016/j.ajem.2011.06.004.
- Flower K, Post A, Sussman J, Tangherlini N, Mendelson J, Pletcher MJ. Validation of triage criteria for deciding which apparently inebriated persons require emergency department care. Emerg Med J 2011;28:579-84. https://doi.org/10.1136/emj.2009.089763.
- Ross DW, Schullek JR, Homan MB. EMS triage and transport of intoxicated individuals to a detoxification facility instead of an emergency department. Ann Emerg Med 2013;61:175-84. https://doi.org/10.1016/j.annemergmed.2012.09.004.
- Irving A, Goodacre S, Blake J, Allen D, Moore SC. Managing alcohol-related attendances in emergency care: can diversion to bespoke services lessen the burden?. Emerg Med J 2018;35:79-82. https://doi.org/10.1136/emermed-2016-206451.
- Dixon D. A Five Year Analysis of Physical Assaults Against NHS Staff in England: SIRS RPA Violence Report 2010–15. 2016.
- Crime Statistics Advisory Committee (CSAC) . Statistical and Analytical Guidance on Crime and Policing Statistics: For Analysts Working for Police and Crime Commissioners 2013.
- Great Britain . Crime and Disorder Act 1998 1998.
- Hughes EC. The Sociological Eye. London: Transaction Books; 1984.
- Engeström Y. Activity theory as a framework for analyzing and redesigning work. Ergonomics 2000;43:960-74. https://doi.org/10.1080/001401300409143.
- Allen D, May C. Organizing practice and practicing organization: an outline of translational mobilization theory. SAGE 2017;7. https://doi.org/10.1177/2158244017707993.
- Abbott A. The System of Professions: An Essay on the Division of Expert Labor. Chicago: University of Chicago Press; 1988.
- Freidson E. The division of labour as social interaction. Social Problems 1976;23:304-13. https://doi.org/10.2307/799776.
- Spencer L, Ritchie J, Burgess RG, Bryman A. Analyzing Qualitative Data. London: Routledge; 2002.
- Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from inpatient surveys in five countries. Int J Qual Health Care 2002;14:353-8. https://doi.org/10.1093/intqhc/14.5.353.
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health 2002;23:151-69. https://doi.org/10.1146/annurev.publhealth.23.100901.140546.
- Trout A, Magnusson AR, Hedges JR. Patient satisfaction investigations and the emergency department: what does the literature say?. Acad Emerg Med 2000;7:695-709. https://doi.org/10.1111/j.1553-2712.2000.tb02050.x.
- World Health Organization (WHO) . International Statistical Classification of Diseases and Related Health Problems 2004.
- Fone D, Dunstan F, White J, Webster C, Rodgers S, Lee S, et al. Change in alcohol outlet density and alcohol-related harm to population health (CHALICE). BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-428.
- Baker A, Rooney C. Recent trends in alcohol-related mortality, and the impact of ICD-10 on the monitoring of these deaths in England and Wales. Health Stat Q 2002;17:5-14.
- Moore SC, Heikkinen M. Commentary on Lloyd et al. (2013): Secondary harms and opportunities for moderation. Addiction 2013;108:710-11. https://doi.org/10.1111/add.12072.
- Janacek GJ. Practical Time Series (Arnold Texts in Statistics). Abingdon: Hodder Education; 2001.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2012–13 2013.
- Health Careers NHS. Agenda for Change – Pay Rates n.d. www.nhscareers.nhs.uk/working-in-the-nhs/pay-and-benefits/agenda-for-change-pay-rates/ (accessed 1 June 2018).
- Curtis L. Unit Costs for Health and Social Care 2013. London: Personal Social Service Research Unit; 2013.
- Great Britain . Local Government and Public Involvement in Health Act 2007 2007.
- Great Britain . Health and Social Care Act 2012 2012. https://doi.org/10.12968/eqhe.2012.1.7.5.
- Great Britain . National Health Service Act 2006 2006.
- Great Britain . Police Reform and Social Responsibility Act 2011 2011.
- Esposito P, Dal Canton A. Clinical audit, a valuable tool to improve quality of care: General methodology and applications in nephrology. World J Nephrol 2014;3:249-55. https://doi.org/10.5527/wjn.v3.i4.249.
- Grimshaw J, Freemantle N, Wallace S, Russell I, Hurwitz B, Watt I, et al. Developing and implementing clinical practice guidelines. Qual Health Care 1995;4:55-64. https://doi.org/10.1136/qshc.4.1.55.
- Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J 2015;15:480-50. https://doi.org/10.1177/1536867X1501500208.
- Linden A. Challenges to validity in single-group interrupted time series analysis. J Eval Clin Pract 2017;23:413-18. https://doi.org/10.1111/jep.12638.
- Welsh Government . Quality Report: Ambulance Services in Wales 2016 n.d. https://gov.wales/docs/statistics/2016/160302-ambulance-services-quality-report-en.pdf (accessed 1 July 2018).
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2015–16 2016.
- Bojke C, Castelli A, Grasic K, Howdon, DDH, Street AD, Rodriguez Santana IDLN. Productivity of the English NHS: 2014/15 Update. York: Centre for Health Economics, University of York; 2017.
- Curtis L. Unit Costs for Health and Social Care 2015. London: Personal Social Service Research Unit; 2015.
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65-76. https://doi.org/10.1007/s10488-010-0319-7.
- Benger J, Carter R. Pilot Study of Inter-Agency Working to Reduce Binge Drinking and Acute Healthcare Demand. Bristol: Alcohol Education and Research Council; 2006.
- Flynn C. 1 in 3 Students Say They’ve Been Spiked 2013. http://waterfrontonline.co.uk/news/1-in-3-students-say-theyve-been-spiked (accessed 1 August 2018).
- Care Quality Commission (CQC) . NHS Patient Survey Programme: 2016 Emergency Department Survey Statistical Release 2017.
- Bischof G, Grothues JM, Reinhardt S, Meyer C, John U, Rumpf HJ. Evaluation of a telephone-based stepped care intervention for alcohol-related disorders: a randomized controlled trial. Drug Alcohol Depend 2008;93:244-51. https://doi.org/10.1016/j.drugalcdep.2007.10.003.
- Department of Health and Social Care (DHSC) . Healthcare Sector Staff Wellbeing, Service Delivery and Health Outcomes 2014.
- Care Quality Commission (CQC) . The State of Care in NHS Acute Hospitals: 2014 to 2016. Findings from the End of CQC’s Programme of NHS Acute Comprehensive Inspections 2017.
- Department of Health and Social Care (DHSC) . Research Governance Framework for Health and Social Care 2009.
- Lambert EY. The Collection and Interpretation of Data from Hidden Populations. Rockville, MD: US Department of Health and Human Services; Public Health Service; Alcohol, Drug Abuse, and Mental Health Administration; National Institute on Drug Abuse; 1990.
- Hirst E, Irving A, Goodacre S. Patient and public involvement in emergency care research. Emerg Med J 2016;33:665-70. https://doi.org/10.1136/emermed-2016-205700.
- Weber EJ, Hirst E, Marsh M. The patient’s dilemma: attending the emergency department with a minor illness. BMJ 2017;357. https://doi.org/10.1136/bmj.j1941.
- Wilson P, Mathie E, Keenan J, McNeilly E, Goodman C, Howe A, et al. ReseArch with Patient and Public invOlvement: a RealisT evaluation: the RAPPORT study. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03380.
- National Institute for Health Research . Research Governance Guidelines: Trial Steering Committees and Study Steering Committees n.d. www.nihr.ac.uk/documents/research-governance-guidelines/121542014 (accessed 3 March 2020).
- Appleby J, Dixon J. Patient choice in the NHS. BMJ 2004;329:61-2. https://doi.org/10.1136/bmj.329.7457.61.
- Pigou A. The Economics of Welfare. London: Routledge; 2017.
- Carlton DW, Loury GC. The limitations of Pigouvian taxes as a long-run remedy for externalities. Q J Econ 1980;95:559-66. https://doi.org/10.2307/1885093.
- Barthold TA. Issues in the design of environmental excise taxes. J Econ Perspect 1994;8:133-51. https://doi.org/10.1257/jep.8.1.133.
- Boyle AA, Snelling K, White L, Ariel B, Ashelford L. External validation of the Cardiff model of information sharing to reduce community violence: natural experiment. Emerg Med J 2013;30:1020-3. https://doi.org/10.1136/emermed-2012-201898.
- Florence C, Shepherd J, Brennan I, Simon T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: experimental study and time series analysis. BMJ 2011;342. https://doi.org/10.1136/bmj.d3313.
- NHS England . A&Amp;E Attendances and Emergency Admissions n.d. www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ (accessed 5 January 2019).
- Welsh Government . Time Spent in NHS Accident and Emergency Departments n.d. https://gov.wales/statistics-and-research/time-spent-nhs-accident-emergency-departments (accessed 5 January 2019).
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2019. Kent: Personal Social Services Research Unit; 2019.
- Heslin M, Callaghan L, Packwood M, Badu V, Byford S. Decision analytic model exploring the cost and cost-offset implications of street triage. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009670.
Appendix 1 Site selection
We planned to compare six areas in which AIMSs have been implemented or are planned with six control areas. As a natural experiment we anticipated that the lack of experimental control over the implementation of the intervention would present a challenge.
A preliminary scoping survey of AIMS provision in the UK identified a number of sites. We selected six sites (Table 11) that had an active AIMS covering a defined geographical region and that expressed an interest in participation. The sites (and paired control sites) were: site I (site J), site A (site N), site D (site K), site C (site O), site E (site M) and site B (site L).
| Number | Site | Workstream 1 | Workstream 2 | Workstream 3 | |||||
|---|---|---|---|---|---|---|---|---|---|
| (i) Ethnography | (ii) Context | (iii) AIMS | (iv) ED | HES APC/HES ED | Ambulance CAD | AIMS data | |||
| 1 | A (I; CS): fixed AIMS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2 | B (I; CS): fixed AIMS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 3 | Ia (I): mobile AIMS | NA | NA | NA | NA | NA | NA | NA | NA |
| 4 | C (I): fixed AIMS | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 5 | Db (I): fixed AIMS | NR | NR | NA | ✓ | ✓ | ✓ | ✓ | ✓ |
| 6 | Ec (I): mobile AIMS | NR | NR | NA | ✓ | ✓ | NR | d | NR |
| 7 | F (I): mobile AIMS | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 8 | G (I): fixed AIMS | NR | NR | ✓ | NR | ✓ | NR | ✓ | ✓ |
| 9 | H (I): mobile AIMS | NR | NR | ✓ | NR | ✓ | ✓ | ✓ | ✓ |
| 10 | J (C; CS) | ✓ | ✓ | NR | ✓ | ✓ | ✓ | ✓ | ✓ |
| 11 | K (C) | NR | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ |
| 12 | L (C) | NR | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ |
| 13 | M (C) | NR | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ |
| 14 | N (C) | NR | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ |
| 15 | O (C) | NR | NR | NR | ✓ | ✓ | ✓ | ✓ | ✓ |
Workstreams
The evaluation was originally described according to three primary workstreams, which are referred to in this appendix.
Workstream 1
-
Ethnographic studies of the impact of AIMSs on the front-line work setting (lead: DA).
-
Context.
-
AIMS users’ views.
-
ED users’ views.
Workstream 2
Outcome evaluation.
Workstream 3
Economic evaluation.
Challenges
Site I
Despite initial positive responses from the AIMS at site I and its associated ambulance service, support for EDARA was withdrawn because of uncertainties around the operation of the AIMS and concerns over pressures on staff time and capacity to support workstream 1 work and undertake workstream 2 data extraction requests. Site I was therefore unable to take part in any element of the evaluation.
We identified site F as a replacement for site I, which matched site J as a control site. Site F was able to participate in workstream 1 (iii) and (iv), workstream 2 and workstream 3. Administration of the ED survey was delayed at both site F and site J to accommodate the change of site (the paired survey ran in August 2017; all other ED paired surveys ran in March 2017). Delays in setting up site F meant late engagement with the ambulance-service-run AIMS in workstream 1 (iii) and (iv), yielding no interviews and very few survey responses. Site B replaced site I as a workstream 1 (i) case study site.
Site D
Early recruitment visits to site D (May–July 2016) were unsuccessful owing to very low or zero clients that could be recruited. Despite initial approval from the AIMS lead organisation (site D police), site D withdrew their support for workstream 1 (iii) owing to ethical concerns over approaching vulnerable adults for the purposes of research. This notwithstanding, we were able to confirm the operational dates of the AIMS and therefore kept this site in workstream 1 (iv), workstream 2 and workstream 3.
Site E
Despite preliminary approvals from site E ambulance service and AIMS staff, site E withdrew support owing to significant operational demands and concerns over staff capacity to support the study. We were able to confirm the operational dates of the AIMS and therefore kept this site in workstream 1 (iv) and workstream 2. We identified site H and site G as sites to replace site D and site E in workstream 1 (iii), workstream 2 and workstream 3. However, for the reasons outlined above, the ambulance service for site G was unable to provide data, so we could not include this site in the workstream 2 ambulance data analysis and workstream 3.
Additional information
-
Given the problems with recruitment, we amended the study protocol (v4.6, 12 July 2016) to allow volunteers and AIMS staff to facilitate interview and survey recruitment at times when a member of the research team was not present, thus increasing the number and diversity of AIMS users we were able to recruit.
-
Following ethics approval (July 2016), additional volunteers and local collaborators were identified at site A and site B who were able to support recruitment visits.
-
In summer 2017, the project team carried out last attempts to boost the numbers of AIMS survey responses by sending site-specific results from the survey to each AIMS saying that if they had higher numbers then the information might be of more use to them, as well as by conducting the last round of site visits to those sites that had the lowest numbers of responses.
Appendix 2 The AIMS user survey
Appendix 3 Emergency department user survey
Appendix 4 UK cities
Bangor, Bath, Birmingham, Bradford, Brighton and Hove, Bristol, Cambridge, Canterbury, Cardiff, Carlisle, Chelmsford, Chester, Chichester, Colchester, Coventry, Derby, Durham, Ely, Exeter, Gloucester, Hereford, Kingston upon Hull (Hull), Lancaster, Leeds, Leicester, Lichfield, Lincoln, Liverpool, City of London, Manchester, Newcastle upon Tyne, Newport, Norwich, Nottingham, Oxford, Peterborough, Plymouth, Portsmouth, Preston, Ripon, Reading, St Albans, St Asaph, St David’s, Salford, Salisbury, Sheffield, Southampton, Stoke-on-Trent, Sunderland, Swansea, Truro, Wakefield, Wells, City of Westminster, Winchester, Wolverhampton, Worcester, York, Glasgow and Belfast.
Appendix 5 Clinical risk survey results
| Site | Response |
|---|---|
| Who is the person with overall responsibility of the AIMS site? | |
| A | Shift lead/senior nurse for unscheduled care |
| G | Third-sector CEO |
| C | A third-sector organisation local to site C, commissioned by [site C] Public Health, with support from Medics UK Ltd, and additional funding from the local CCG |
| F | St John Ambulance station manager/ambulance service head of risk, quality and safety/police and crime commissioner |
| H | Shift leader, OPEN [site H] Youth Trust (local charity) |
| B | Police & Crime Commissioners Office |
| What are the job titles held by staff members working an AIMS shift? | |
| A |
ENPs Health-care support workers Police officer |
| G |
Shift lead First aider Volunteers |
| C |
A third-sector organisation (local to site C) substance misuse worker Security Street marshals Medics UK Ltd nurse and medic |
| F |
(Alcohol recovery centre) All St John Ambulance First Aiders Emergency transport attendants Ambulance technicians Advanced first aiders (occasionally) Volunteers (occasionally) |
| H |
AIMS shift leader Paramedic or health-care practitioner St John Ambulance member Shift support worker Support vehicle driver SIA registered security Community first responders |
| B |
Advanced paramedic St John Ambulance nurse practitioner St John Ambulance advanced first aider St John Ambulance volunteers Police officer Student volunteers |
| Who decides if a person has any medical needs, for example if they should go home or if they need to go to hospital? | |
| A | Clinical lead |
| G | Team leader and supervisor |
| C | Medics UK Ltd |
| F | First aider treating |
| H | Paramedic, St John Ambulance and shift leader |
| B | St John Ambulance nurse and St John Ambulance paramedic |
| How are these decisions recorded? | |
| A | Documented in the patient’s notes on ED patient record system |
| G | Recorded on in-house patient record form |
| C | Patient data and decisions stored electronically by a third-sector organisation local to site C |
| F | St John Ambulance patient record form and team leader report form |
| H | Client contact sheet and/or ambulance service and St John Ambulance paperwork |
| B | St John Ambulance patient report form |
| Who does the person responsible for making these decisions report to? | |
| A | Lead nurse and clinical director |
| G | Project manager, CEO or safeguarding lead |
| C | Medics UK Ltd clinical lead |
| F | St John Ambulance/shift lead |
| H | Ambulance service co-ordinator, St John Ambulance co-ordinator or Youth Trust CEO |
| B | St John Ambulance officer in charge |
| Does the person responsible for making these decisions have any training for this role? If so, what? | |
| A | All staff are qualified ENPs or advanced nurse practitioners or will have equivalent to a clinical patient assessment qualification |
| G | Bespoke 6-day training package |
| C | |
| F | St John training: emergency transport attendant, 6-week course; ambulance technician, 5-week course |
| H | On-the-job training and mentoring from established shift leaders |
| B | Registered nurse with additional training |
| What qualifications does this person have, if any? | |
| A | Relevant professional registration |
| G | None |
| C | In accordance with NMC and HCPC governance, managed by Medics UK Ltd |
| F | St John Ambulance internal accreditation |
| H | None |
| B | Relevant professional registration |
| Do you have a system for reporting unintended outcomes, things that might have gone wrong or near misses? | |
| A | Incident form and root cause analysis on any adverse incidents |
| G | Feedback form at the end of every shift and lean on me incident review for adverse events |
| C | Medics UK Ltd accountable for clinical error |
| F | Incident report form |
| H | E-mail or logbook report to administrator |
| B | Recorded as per St John Ambulance policy |
| Is there a procedure for dealing with complaints or negative feedback? | |
| A | Yes |
| G | Yes |
| C | Yes |
| F | Yes |
| H | Yes |
| B | Yes |
Appendix 6 Detailed effectiveness evaluation
Emergency department attendances (primary outcome)
Descriptive statistics
Emergency department attendances were analysed across all sites from 16 November 2010 to 31 March 2016. Table 12 shows the mean number of ED attendances per day during hours of AIMS activity at each site before and after the service started operating at the intervention site in each matched pair. Pre-intervention data were not available at site H (or site K when matched with site H) because the site H AIMS started operating before 2010. The number of ED attendances per night ranged from 31 at site G pre intervention to 127 per night at site K post intervention. Emergency department attendances decreased after intervention at sites A and C, and at site L post intervention at its paired site (site B), but increased after intervention at all other sites.
| Variable | Mean attendances (SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Site | ||||||||
| Intervention | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 87.94 (11.88) | 57.15 (9.88) | 31.04 (6.70) | 70.74 (11.88) | 75.57 (11.46) | 116.72 (17.90) | 112.33 (13.20) |
| Post AIMS | 66.81 (11.52) | 79.22 (10.81) | 57.54 (9.37) | 32.79 (6.33) | 77.24 (11.73) | 73.16 (11.86) | 120.96 (13.97) | 119.60 (16.59) |
| Control | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 47.91 (9.21) | 54.48 (8.73) | 78.65 (10.35) | 91.34 (12.09) | 61.85 (10.26) | 117.06 (14.50) | 69.24 (10.64) |
| Post AIMS | 113.01 (15.15) | 60.06 (10.11) | 50.55 (7.80) | 80.91 (12.40) | 94.41 (12.27) | 66.37 (9.24) | 127.38 (12.47) | 76.82 (10.70) |
Tables 13 and 14 show the percentage of male patients (see Table 13) and mean patient age in years (see Table 14) in the same format. The mean percentage of male patients across all sites was 51.9% pre intervention and 51.1% post intervention, with little evidence of men or women being over-represented at any site before or after implementation. The mean age of patients across all sites was 42.4 years pre intervention and 44.3 years post intervention. All sites except site D showed a small increase in mean age post intervention.
| Variable | Percentage of male patients | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 52.86 | 52.70 | 51.27 | 53.19 | 51.00 | 52.03 | 54.99 |
| Post AIMS | 49.41 | 51.09 | 52.06 | 51.47 | 51.98 | 49.77 | 51.01 | 53.55 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 52.88 | 51.51 | 51.95 | 51.52 | 51.09 | 51.28 | 53.60 |
| Post AIMS | 50.98 | 50.32 | 50.42 | 51.04 | 51.02 | 48.85 | 50.42 | 51.53 |
| Variable | Mean age of patients (years) | |||||||
|---|---|---|---|---|---|---|---|---|
| Site | ||||||||
| Intervention | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 40.08 | 43.25 | 44.85 | 39.29 | 43.01 | 36.68 | 39.83 |
| Post AIMS | 48.26 | 41.54 | 46.42 | 48.75 | 41.73 | 45.45 | 36.45 | 40.73 |
| Control | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 43.58 | 42.89 | 43.50 | 44.31 | 44.07 | 42.01 | 42.25 |
| Post AIMS | 42.97 | 44.78 | 44.78 | 45.83 | 45.33 | 46.14 | 43.78 | 45.10 |
Interrupted time series analysis
Tables 15–17 show the results of ITSA using intervention-site-only analysis (see Table 15), controlling for (not shown) day of week and significant dates (e.g. Halloween, bank holidays, Black Friday), paired analysis with single control sites (see Table 16) and paired analysis with pooled control sites (see Table 17). Bonferroni correction across each set of seven ITSA tests resulted in a p-value of ≤ 0.0143 for statistical significance.
| Site | Constanta (p) | t (p) | x (p) | xt (p) | Post-trend difference (p) | F (p) |
|---|---|---|---|---|---|---|
| Hb | – | – | – | – | – | – |
| A | 76.12 (< 0.001) | 0.005 (0.144) | –4.89 (0.005) | –0.014 (< 0.001) | –0.009 (< 0.001) | 77.6 (< 0.001) |
| B | 46.68 (< 0.001) | 0.0005 (0.630) | –2.41 (0.099) | 0.008 (0.052) | 0.008 (0.034) | 110 (< 0.001) |
| G | 31.57 (< 0.001) | 0.0001 (0.922) | 2.22 (0.217) | –0.002 (0.713) | –0.002 (0.720) | 2715 (< 0.001) |
| F | 62.45 (< 0.001) | 0.002 (0.036) | 4.05 (0.061) | 0.004 (0.763) | 0.006 (0.644) | 142 (< 0.001) |
| C | 76.25 (< 0.001) | –0.0004 (0.760) | 1.29 (0.537) | –0.011 (0.086) | –0.012 (0.072) | 9.4 (< 0.001) |
| D | 106.20 (< 0.001) | 0.013 (< 0.001) | –6.02 (0.075) | –0.016 (0.286) | –0.003 (0.861) | 51,160 (< 0001) |
| E | 97.48 (< 0.001) | 0.112 (0.066) | –5.24 (0.237) | –0.106 (0.082) | 0.006 (< 0.001) | 12.6 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | K | – | – | – | – | – | – | – | – | – | – |
| A | N | 37.42 (< 0.001) | 43.29 (< 0.001) | –0.009 (0.039) | 0.014 (< 0.001) | 1.61 (0.271) | –0.005 (0.110) | –6.34 (0.006) | –0.008 (0.074) | –0.018 (< 0.001) | 150 (< 0.001) |
| B | L | 52.28 (< 0.001) | 1.32 (0.234) | 0.002 (0.158) | –0.001 (0.141) | –3.99 (0.002) | 0.004 (0.182) | 1.60 (0.402) | 0.003 (0.565) | 0.005 (0.328) | 28.2 (< 0.001) |
| G | M | 78.34 (< 0.001) | –44.39 (< 0.001) | –0.004 (0.012) | 0.004 (0.003) | –6.47 (0.001) | 0.018 (0.062) | 8.59 (0.007) | –0.019 (0.089) | –0.024 (0.036) | 315 (< 0.001) |
| Fc | J | 82.83 (< 0.001) | –19.85 (< 0.001) | –0.001 (0.526) | 0.003 (0.004) | 5.03 (0.034) | –0.034 (0.005) | –1.12 (0.726) | 0.037 (0.030) | 0.036 (0.034) | 94 (< 0.001) |
| C | O | 60.00 (< 0.001) | 18.97 (< 0.001) | –0.007 (< 0.001) | 0.007 (< 0.001) | –2.22 (0.228) | –0.002 (0.734) | 3.42 (0.260) | –0.009 (0.320) | –0.017 (0.075) | 40.4 (< 0.001) |
| D | K | 111.95 (< 0.001) | –5.19 (0.035) | 0.006 (0.022) | 0.008 (< 0.001) | 2.32 (0.467) | 0.002 (0.872) | –8.78 (0.047) | –0.019 (0.329) | –0.013 (0.496) | 12.6 (< 0.001) |
| E | M | 57.65 (< 0.001) | 43.21 (< 0.001) | –0.002 (0.977) | 0.111 (0.062) | –1.21 (0.776) | –0.109 (0.068) | –3.89 (0.499) | 0.006 (0.937) | 0.004 (0.015) | 153.9 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | All control sites | – | – | – | – | – | – | – | – | – | – |
| A | All control sites | 65.23 (< 0.001) | 14.82(< 0.001) | –0.002 (0.597) | 0.007 (< 0.001) | 0.137 (0.885) | –0.002 (0.441) | –5.04 (0.013) | –0.012 (0.006) | –0.014 (< 0.001) | 26.5 (< 0.001) |
| B | All control sites | 47.88 (< 0.001) | –6.34 (< 0.001) | –0.002 (0.098) | 0.003 (0.002) | –3.20 (0.065) | 0.003 (0.533) | 1.04 (0.681) | 0.005 (0.524) | 0.002 (0.756) | 86.8 (< 0.001) |
| G | All control sites | 74.32 (< 0.001) | –43.12 (< 0.001) | –0.005 (< 0.001) | 0.005 (< 0.001) | –2.23 (0.104) | 0.005 (0.250) | 4.60 (0.041) | –0.007 (0.316) | –0.013 (0.090) | 608 (< 0.001) |
| Fc | All control sites | 67.84 (< 0.001) | –2.94 (0.006) | –0.004 (0.001) | 0.006 (< 0.001) | 1.70 (0.287) | –0.008 (0.296) | 2.06 (0.440) | 0.013 (0.382) | 0.009 (0.525) | 45.9 (< 0.001) |
| C | All control sites | 70.78 (< 0.001) | 4.36 (< 0.001) | –0.007 (< 0.001) | 0.006 (< 0.001) | –1.68 (0.162) | 0.002 (0.590) | 3.04 (0.205) | –0.013 (0.084) | –0.020 (0.008) | 21.9 (< 0.001) |
| D | All control sites | 74.79 (< 0.001) | 30.73 (< 0.001) | 0.009 (< 0.001) | 0.004 (< 0.001) | 1.21 (0.342) | 0.0002 (0.970) | –6.93 (0.050) | –0.021 (0.221) | –0.011 (0.804) | 117 (< 0.001) |
| E | All control sites | 0.0004 (0.775) | 36.68 (< 0.001) | 0.086 (0.259) | 00010 (0.793) | 0.098 (0.965) | –0.004 (0.912) | –4.55 (0.384) | –0.086 (0.261) | 65.08 (< 0.001) | 228 (< 0.001) |
The intervention-site-only analysis (see Table 15) showed no obvious trend, with effects ranging from six fewer to four more ED attendances per night. There was a significant decrease in ED attendances at site A.
The paired analysis with a single control (see Table 16) showed effects ranging from eight to nine fewer to eight to nine more ED attendances per night. The decrease in ED attendances at site A and the increase in ED attendances at site G was statistically significant after Bonferroni correction.
We could not do a pooled analysis for all English/Welsh/all cities because paired intervention-site AIMSs opened at different times. The effect of opening the AIMS ranged from 7.0 fewer to 4.6 more ED attendances per night. There was a significant decrease in ED attendances at site A but no other statistically significant effects after Bonferroni correction.
Linear regression analysis (estimated using ordinary least squares)
Tables 18–20 show the results of linear regression analysis using intervention-site-only analysis (see Table 18), paired analysis with a single control (see Table 19) and paired analysis with pooled control sites (see Table 20). Bonferroni correction across eight tests resulted in a p-value of ≤ 0.0125 for statistical significance.
| Site | Constanta (p) | Open (p) | Post AIMS (p) | F (p) | R 2 | Root MSE |
|---|---|---|---|---|---|---|
| Ha | 75.34 (< 0.001) | –4.53 (0.003) | n/a | 27.85 (< 0.001) | 0.172 | 10.71 |
| A | 74.52 (< 0.001) | –4.04 (< 0.001) | –3.26 (< 0.001) | 40.18 (< 0.001) | 0.243 | 9.96 |
| B | 50.90 (< 0.001) | –0.90 (0.299) | 1.55 (0.001) | 38.71 (< 0.001) | 0.236 | 8.26 |
| G | 32.84 (< 0.001) | 1.06 (0.389) | 2.33 (< 0.001) | 20.69 (< 0.001) | 0.142 | 6.17 |
| F | 80.47 (< 0.001) | 0.52 (0.689) | 6.16 (< 0.001) | 86.88 (< 0.001) | 0.409 | 9.50 |
| C | 82.79 (< 0.001) | –2.36 (0.041) | –0.15 (0.809) | 27.94 (< 0.001) | 0.182 | 10.33 |
| D | 121.52 (< 0.001) | 0.67 (0.838) | 3.98 (< 0.001) | 25.90 (< 0.001) | 0.171 | 16.61 |
| E | 124.35 (< 0.001) | 1.56 (0.580) | 4.61 (0.007) | 30.81 (< 0.001) | 0.197 | 14.90 |
| Site | Constant (p) | Intervention site β (p) | Post AIMS β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | K | 121.70 (< 0.001) | –44.21 (< 0.001) | n/a | –2.27 (0.008) | 907 (< 0.001) | 0.793 | 11.90 |
| A | N | 54.05 (< 0.001) | 21.53 (< 0.001) | 4.02 (< 0.001) | –1.62 (0.057) | 250 (< 0.001) | 0.528 | 10.63 |
| B | L | 49.52 (< 0.001) | 2.07 (< 0.001) | –0.31 (0.351) | 2.07 (< 0.001) | 59.48 (< 0.001) | 0.210 | 8.03 |
| G | M | 82.95 (< 0.001) | –46.65 (< 0.001) | 2.13 (< 0.001) | –0.02 (0.993) | 1784 (< 0.001) | 0.889 | 8.39 |
| F | J | 102.05 (< 0.001) | –22.85 (< 0.001) | 4.93 (< 0.001) | 4.30 (0.001) | 360 (< 0.001) | 0.617 | 10.39 |
| C | O | 69.78 (< 0.001) | 10.85 (< 0.001) | 2.93 (< 0.001) | –3.99 (< 0.001) | 99.6 (< 0.001) | 0.308 | 10.08 |
| D | K | 122.36 (< 0.001) | –1.02 (0.028) | 6.75 (< 0.001) | –2.95 (0.324) | 62.2 (< 0.001) | 0.218 | 14.69 |
| E | M | 82.46 (< 0.001) | 39.35 (< 0.001) | 5.96 (< 0.001) | 3.45 (< 0.001) | 628 (< 0.001) | 0.737 | 84.70 |
| Site | Constant (p) | Intervention site β (p) | Post AIMS β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | All control sites | 82.43 (< 0.001) | –8.466 (< 0.001) | n/a | –0.94 (0.435) | 47.11 (< 0.001) | 0.054 | 22.22 |
| A | All control sites | 78.03 (< 0.001) | 1.57 (0.008) | 3.97 (< 0.001) | 0.42 (0.756) | 28.60 (< 0.001) | 0.035 | 22.22 |
| B | All control sites | 79.66 (< 0.001) | –21.08 (< 0.001) | 4.09 (< 0.001) | 1.10 (0.571) | 116 (< 0.001) | 0.128 | 22.09 |
| G | All control sites | 80.75 (< 0.001) | –45.37 (< 0.001) | 4.01 (< 0.001) | –2.68 (0.538) | 444 (< 0.001) | 0.361 | 21.93 |
| F | All control sites | 82.07 (< 0.001) | –5.93 (< 0.001) | 5.67 (< 0.001) | 2.95 (0.245) | 48.78 (< 0.001) | 0.059 | 22.10 |
| C | All control sites | 81.41 (< 0.001) | –0.18 (0.749) | 3.63 (< 0.001) | –5.82 (0.003) | 34.16 (< 0.001) | 0.042 | 22.14 |
| D | All control sites | 81.98 (< 0.001) | 35.88 (< 0.001) | 4.19 (< 0.001) | 1.86 (0.652) | 279 (< 0.001) | 0.262 | 22.58 |
| E | All control sites | 77.85 (< 0.001) | 41.09 (< 0.001) | 5.27 (< 0.001) | –4.84 (< 0.001) | 378 (< 0.001) | 0.325 | 22.41 |
The single-site analysis showed effects ranging from 4.0–5.0 fewer to 1.6 more ED attendances per night. The decrease in ED attendances at site A and increase in ED attendances at site B were statistically significant after Bonferroni correction.
The paired analysis with single control sites showed effects ranging from 4.0 fewer to 4.3 more ED attendances per night. The increases in ED attendances at sites B, E and F and the decreases in ED attendances at sites H and C were statistically significant after Bonferroni correction.
The paired analysis with pooled control sites showed effects ranging from 5.8 fewer ED attendances per night to 3.0 more ED attendances per night. The decreases in ED attendances at sites C and E were statistically significant after Bonferroni correction.
The overall pooled analysis across all sites showed markedly different results depending on whether all sites, the original sites (i.e. including sites D and E) or the replacements sites (i.e. including sites H and G) were used. The substantial variation between sites in the ED attendance rate also meant that the overall estimate across sites was subject to substantial uncertainty, with much less precise estimates than those for the individual sites. The estimated effect of implementing the AIMSs was 8.89 additional ED attendances per night (95% CI –14.44 to 32.22; p = 0.405) when all cities were used, 14.83 additional ED attendances per night (95% CI –6.91 to 36.58; p = 0.146) when the original cities were used and 0.59 additional ED attendances per night (95% CI –13.98 to 15.16; p = 0.924) when the replacement cities were used. Overall, there was no evidence of an effect from AIMSs on ED attendances, but CIs were wide.
Figure 8 shows paired comparisons between intervention and control sites of the rate of ED attendances per night over time. This provides further insight into the findings for individual sites.
FIGURE 8.
Graphs of ED attendance by intervention site and paired control site (dark blue, intervention site; light blue, control site). (a) Site E and control site; (b) site A and control site; (c) site G and control site; (d) site D and control site; (e) site C and control site; (f) site F and control site; (g) site H and control site; and (h) site B and control site.
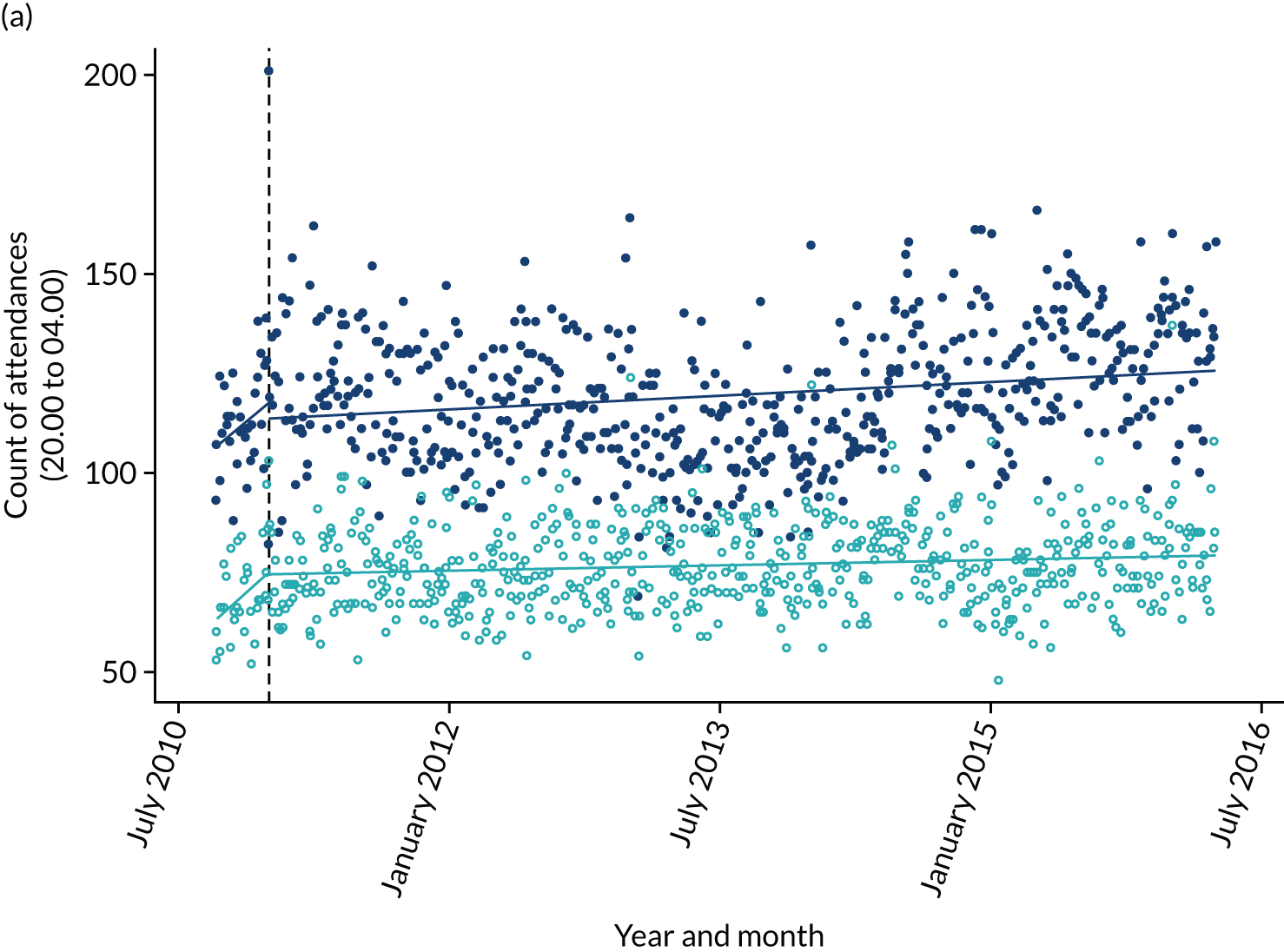
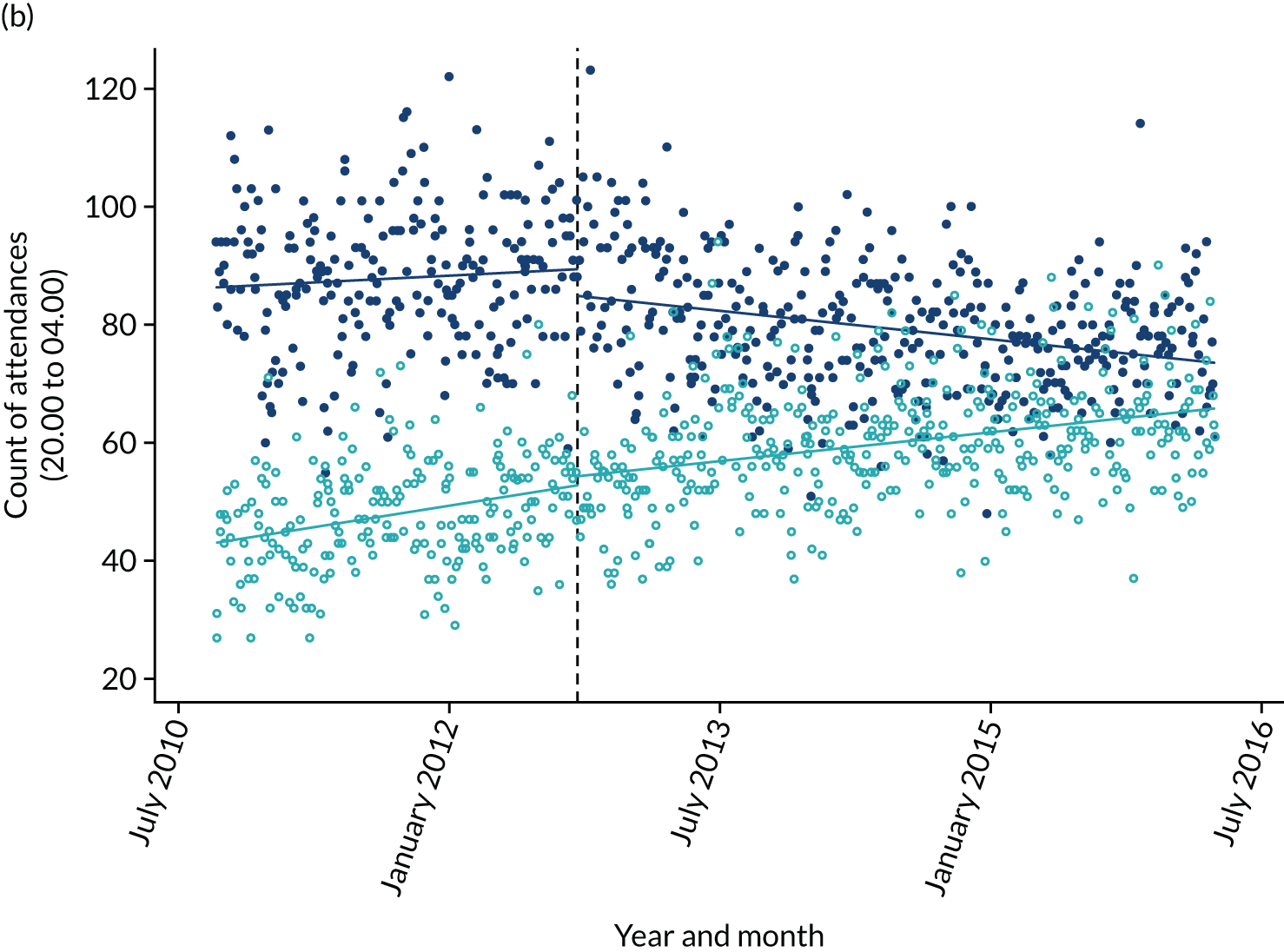
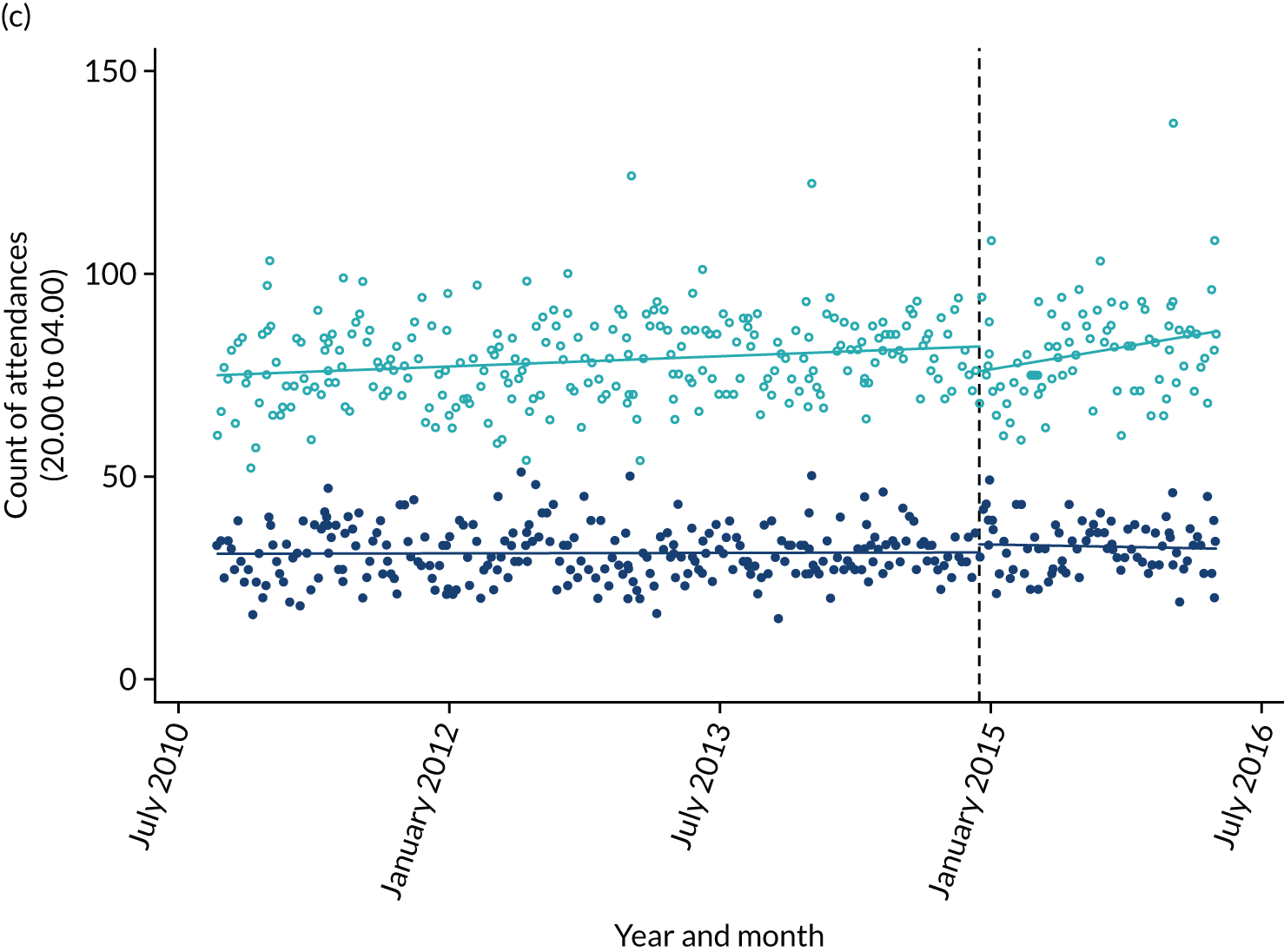
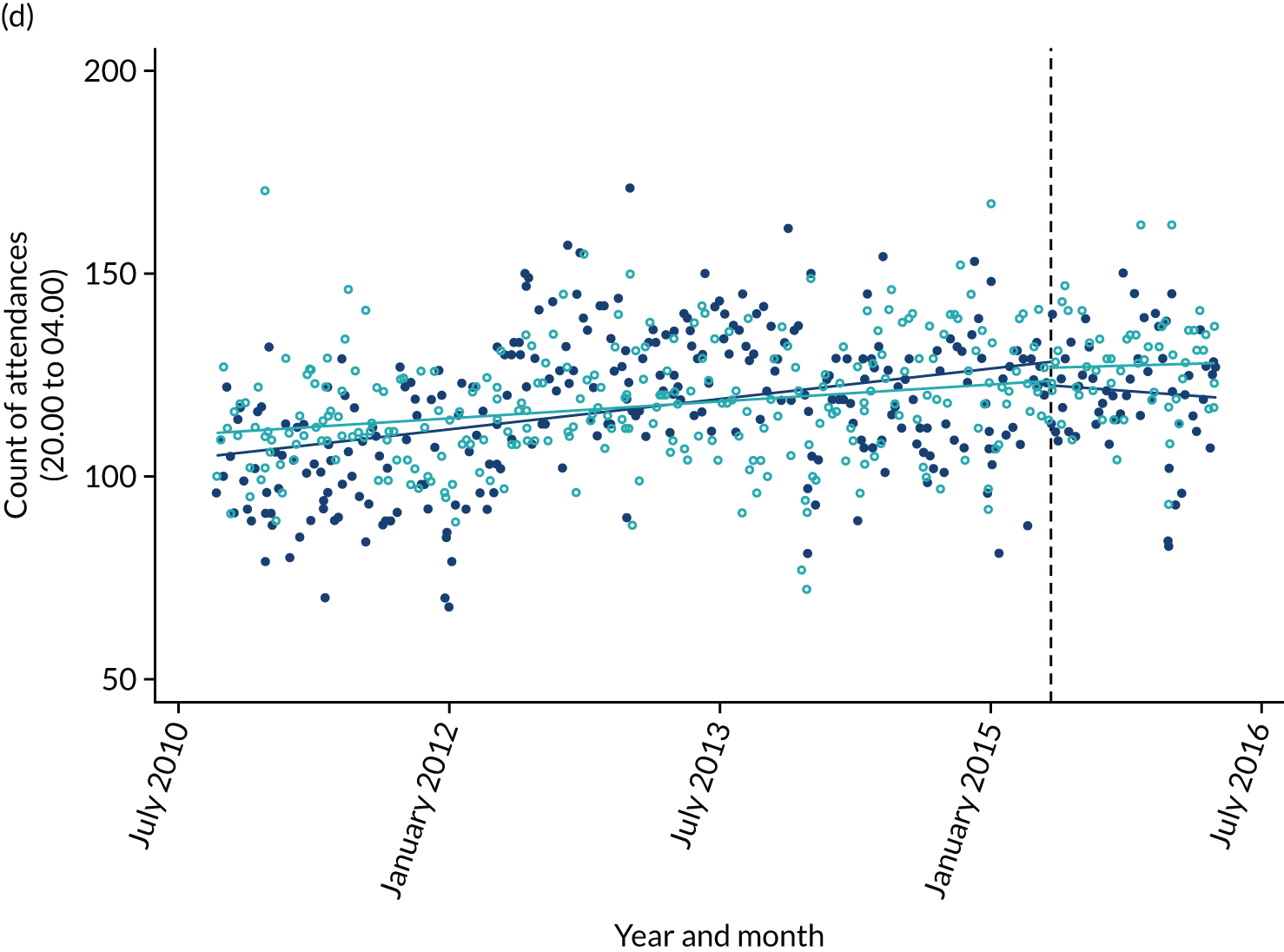
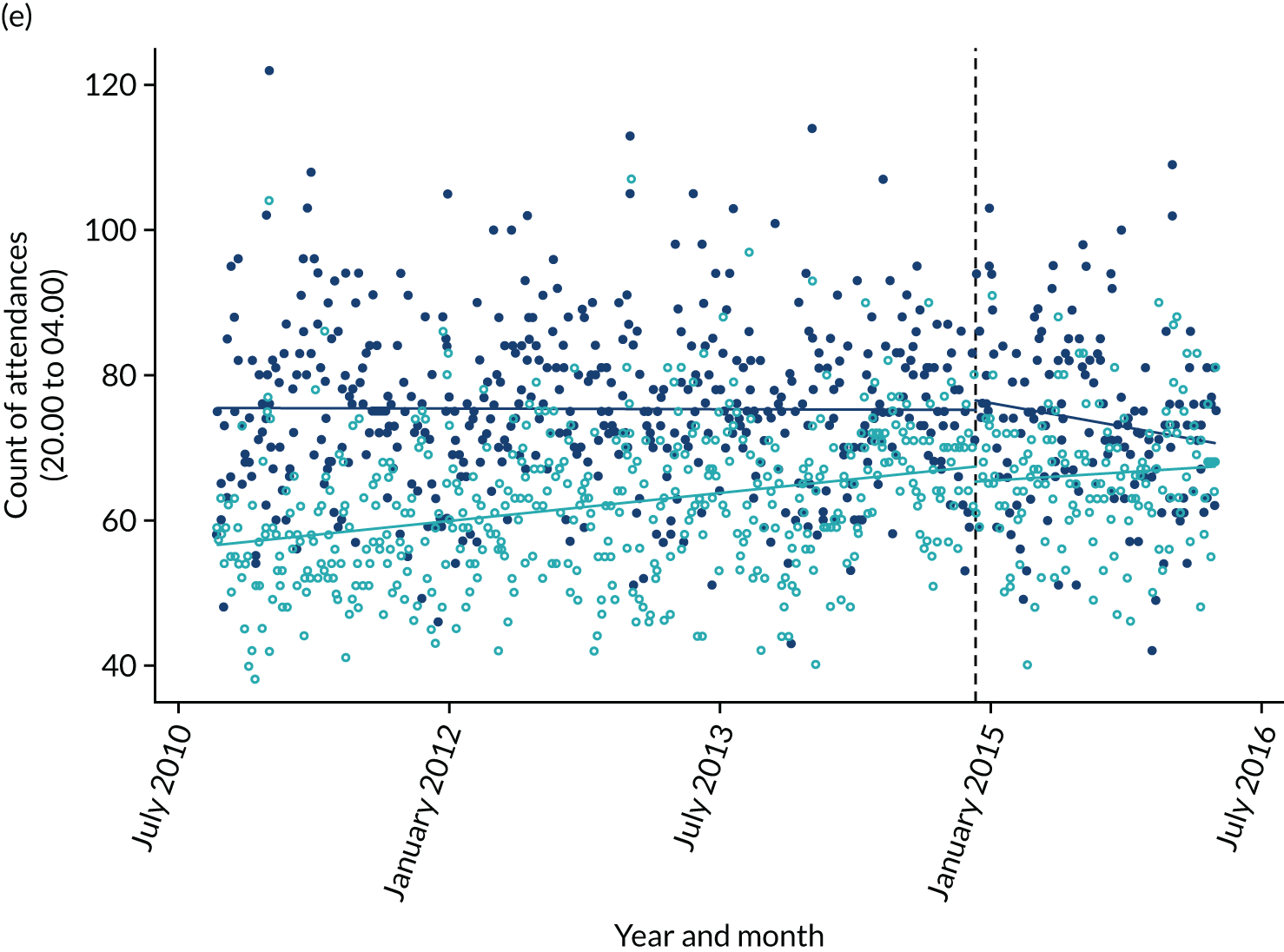
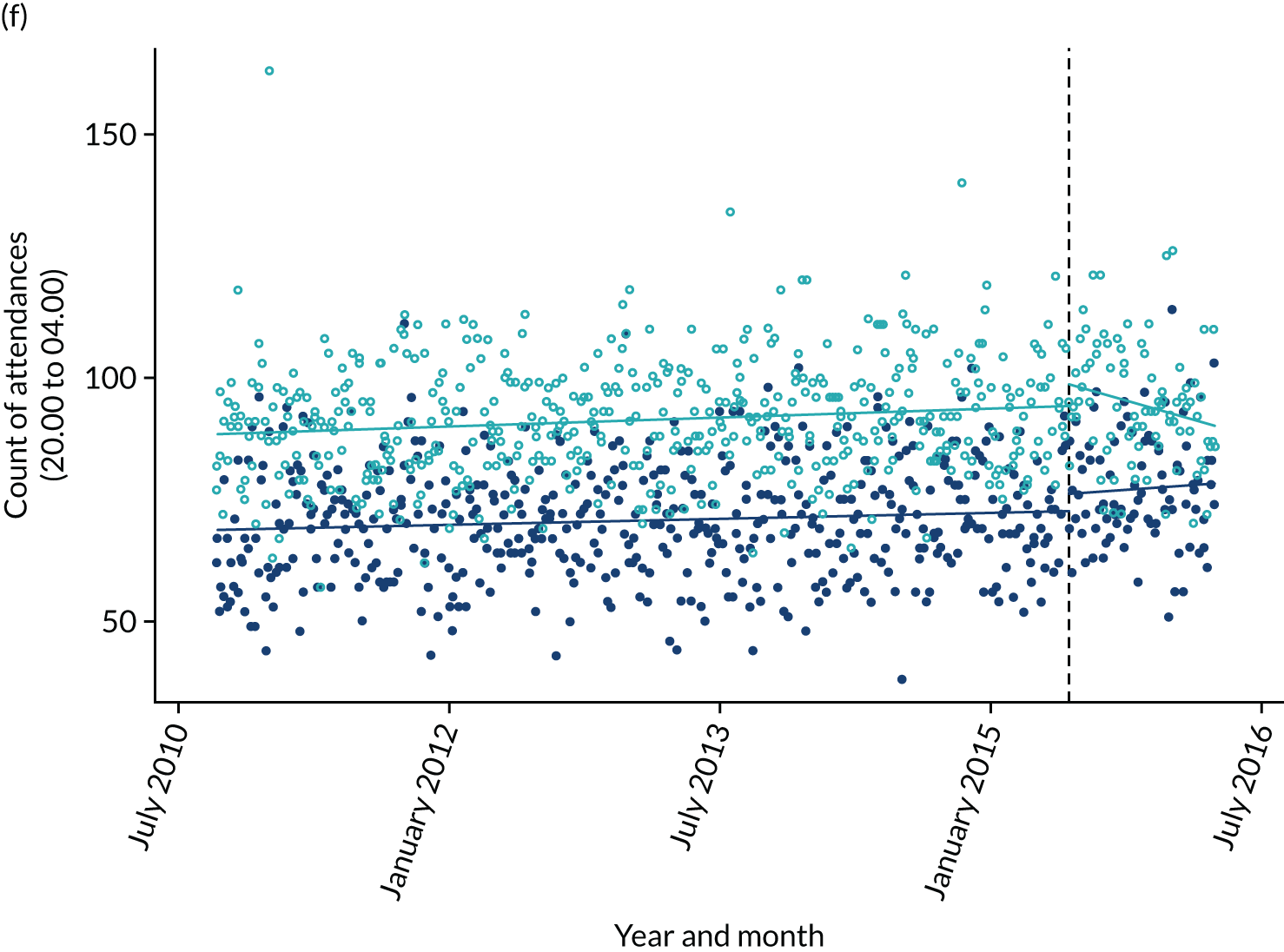
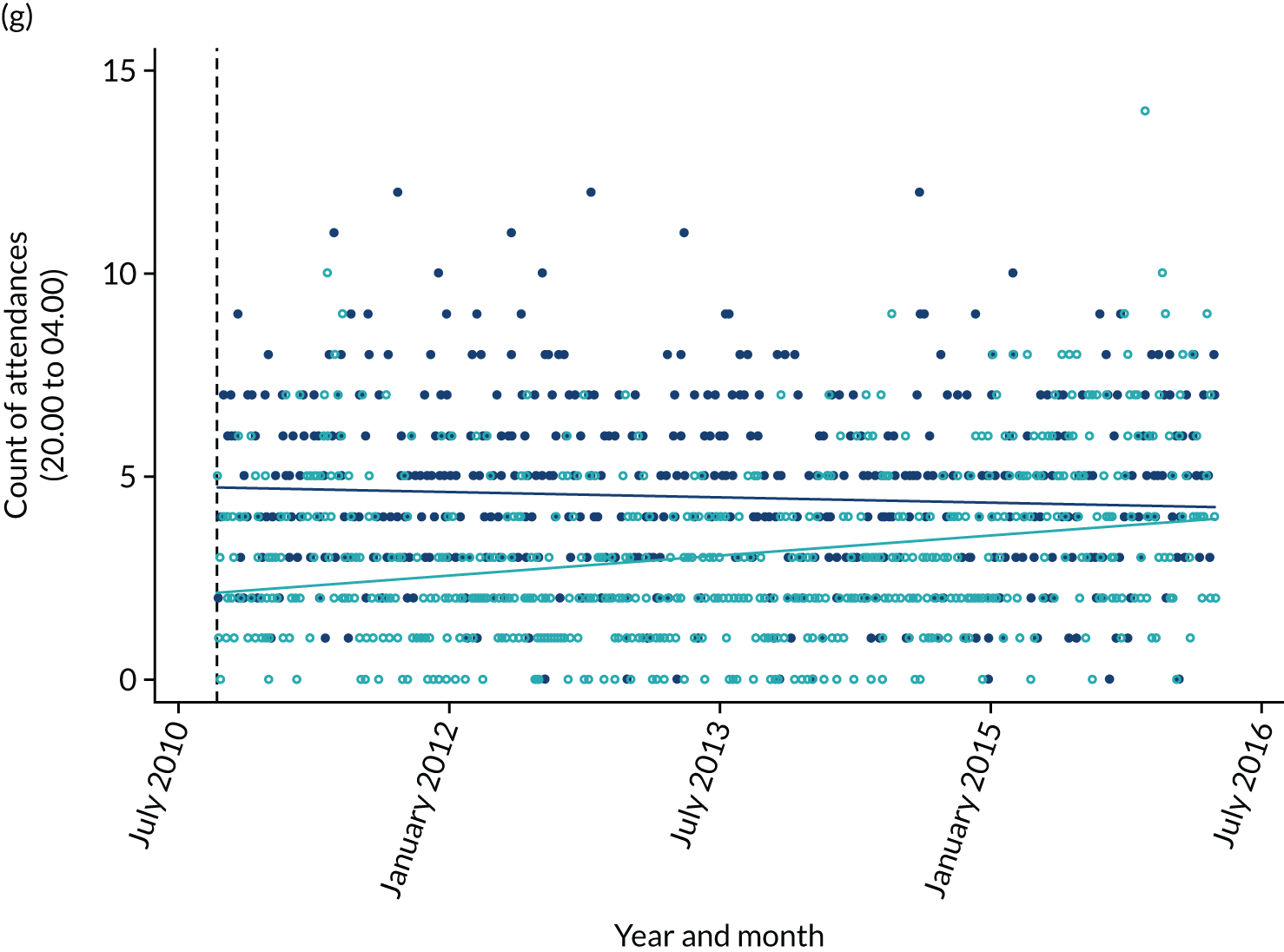
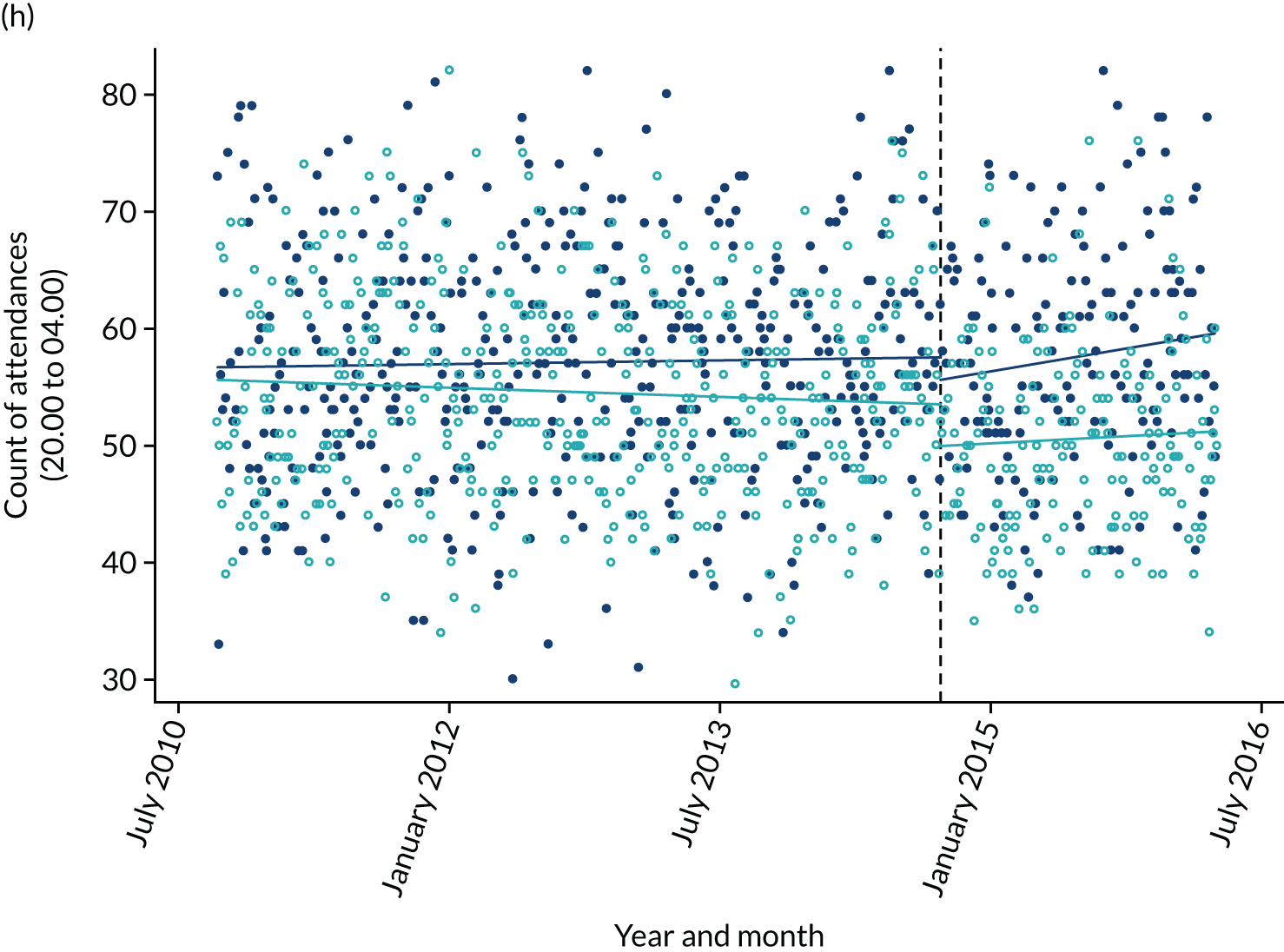
Individual sites’ results are inconsistent owing to the noise in the data and violation of ITSA assumptions [paired analysis showed that there was a difference in ED attendances between intervention and control sites (Z) and a difference in the change in ED attendances over time between intervention and control sites (Zt)].
Figure 8 suggests that there is a decrease in ED attendances for site A post AIMS, which continues to decrease over time. This decrease was not reflected in the ITSA analysis but was observed in the single-city regression analysis. Other results for site A suggested an increase in ED attendances ranging between 2.5 and 4.0 ED attendances.
The site B AIMS was associated with variable effects across the analysis, ranging from four fewer to six more ED attendances per night, and had no obvious effect in the figure.
The site G AIMS was associated with increased ED attendances on ITSA but had no obvious effect in linear regression or in the figure. This suggests that matching site G with site M was inappropriate, at least in terms of ED attendances, because site G had much fewer ED attendances throughout the study.
The site F AIMS was associated with variable effects across the analyses, ranging from one fewer to four more ED attendances per night, and had no obvious effect in the figure. The site C AIMS also showed variable effects, being associated with one to three additional ED attendances on ITSA but two to seven fewer ED attendances on linear regression. The figure suggests no obvious explanation for this inconsistency.
The site D AIMS was associated with six to nine fewer ED attendances per night on ITSA but had no obvious effect in logistic regression or in the figure. The finding of a reduction in ED attendances on ITSA is inconsistent with the low level of activity we observed in the AIMS.
The site E AIMS had very inconsistent effects across the analysis and no obvious effect in the figure. We were unable to obtain any activity data from site E to determine whether or not activity would be consistent with an effect on ED attendances.
The lack of pre-intervention data for the site H AIMS meant that this could be assessed only in the linear regression, which suggested that it was associated with reduced ED attendances, ranging from four to five per night in the single-site analysis to one per night in the pooled analysis.
In summary, the findings suggest that the effects of AIMSs on ED attendance is variable, inconsistent and uncertain. Given that some of the ITSA assumptions are violated, further analysis using a simplified model is explored in Tables 21 and 22.
| Variable | All sites | ||||
|---|---|---|---|---|---|
| Observations | 8092 | ||||
| Groups | 16 | ||||
| Observations per group | |||||
| Minimum | 289.0 | ||||
| Mean | 505.8 | ||||
| Maximum | 578.0 | ||||
| R 2 | |||||
| Within | 0.046 | ||||
| Between | 0.035 | ||||
| Overall | 0.005 | ||||
| Variable | Coefficient | SE | z | p-value | 95% CI |
| Attendance | |||||
| AIMS | –4.991 | 2.271 | –2.200 | 0.028 | –9.443 to –0.540 |
| Time | 0.005 | 0.001 | 3.820 | < 0.001 | 0.002 to 0.007 |
| Constant | –12.611 | 23.027 | –0.550 | 0.584 | –57.743 to 32.521 |
| sigma_u | 25.420 | ||||
| sigma_e | 11.777 | ||||
| Rho | 0.823 | ||||
| Variable | dy/dx | SE | z | p-value | 95% CI |
| Marginal effects | |||||
| Control sites | 0.005 | 0.001 | 3.430 | 0.001 | 0.002 to 0.007 |
| Intervention sites | 0.006 | 0.002 | 2.470 | 0.014 | 0.001 to 0.010 |
| Variable | All sitesa | ||||
|---|---|---|---|---|---|
| Observations | 6358 | ||||
| Groups | 12 | ||||
| Observations per group | |||||
| Minimum | 289.0 | ||||
| Mean | 529.8 | ||||
| Maximum | 578.0 | ||||
| R 2 | |||||
| Within | 0.040 | ||||
| Between | 0.000 | ||||
| Overall | 0.010 | ||||
| Variable | Coefficient | SE | z | p-value | 95% CI |
| Attendance | |||||
| AIMS | –5.300 | 2.378 | –2.230 | 0.026 | –9.962 to –0.639 |
| Time | 0.004 | 0.002 | 2.660 | 0.008 | 0.001 to 0.007 |
| Constant | –8.529 | 29.057 | –0.290 | 0.769 | –65.480 to 48.422 |
| sigma_u | 20.985 | ||||
| sigma_e | 10.856 | ||||
| rho | 0.789 | ||||
| Variable | dy/dx | SE | z | p-value | 95% CI |
| Marginal effects | |||||
| Control sites | 0.004 | 0.002 | 2.230 | 0.026 | 0.000 to 0.007 |
| Intervention sites | 0.007 | 0.003 | 2.600 | 0.009 | 0.002 to 0.012 |
Stratified by age and treatment
Aged 14–39 years
The assumption behind this analysis was that people aged 14–39 years would be more likely than those aged ≥ 40 years to attend the ED with alcohol-related attendances during hours of AIMS activity. We therefore present analysis for the strata aged 14–39 years only. Table 23 shows the mean ED attendances per day during hours of AIMS activity among those aged 14–39 years for each site pre and post intervention. In general, just over half of the individuals attending ED during hours of AIMS activity were in the age group of 14–39 years. In contrast to the primary analysis, in which most sites showed increases in ED attendance post intervention, ED attendances for those aged 14–29 years tended to decrease at most sites post intervention.
| Variable | Mean ED attendances | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | ||||||||
| H | A | B | G | F | C | D | E | |
| Pre intervention | – | 51.77 | 30.08 | 15.31 | 42.60 | 39.51 | 76.10 | 64.61 |
| Post intervention | 29.21 | 44.53 | 26.77 | 14.12 | 42.99 | 35.33 | 79.63 | 67.52 |
| Variable | Control site | |||||||
| K | N | L | M | J | O | K | M | |
| Pre intervention | – | 24.67 | 28.67 | 41.03 | 46.58 | 31.04 | 64.58 | 37.58 |
| Post intervention | 60.37 | 29.58 | 24.88 | 39.48 | 46.10 | 31.18 | 66.77 | 37.98 |
Tables 24–26 show the results of ITSA using intervention-site-only analysis (see Table 24), paired analysis with single control sites (see Table 25) and paired analysis with pooled control sites (see Table 26). Bonferroni correction across all 21 ITSA tests resulted in a p-value of ≤ 0.0048 for statistical significance.
| Site | Constanta (p) | t (p) | x (p) | xt (p) | Post-trend difference (p) | F (p) |
|---|---|---|---|---|---|---|
| Hb | – | – | – | – | – | – |
| A | 44.57 (< 0.001) | –0.003 (0.306) | –2.71 (0.045) | –0.003 (0.255) | –0.006 (< 0.001) | 398 (< 0.001) |
| B | 27.37 (< 0.001) | –0.003(< 0.001) | –2.64 (0.008) | 0.007 (0.011) | 0.004 (0.106) | 22.47 (< 0.001) |
| G | 18.29 (< 0.001) | –0.003 (< 0.001) | 1.01 (0.391) | 0.003 (0.351) | 0.0006 (0.867) | 772 (< 0.001) |
| F | 38.55 (< 0.001) | –0.002 (0.018) | –0.40 (0.826) | 0.018 (0.087) | 0.016 (0.121) | 34.9 (< 0.001) |
| C | 42.80 (< 0.001) | –0.004 (< 0.001) | 0.68 (0.624) | –0.003 (0.443) | –0.007 (0.099) | 15.3 (< 0.001) |
| D | 71.46 (< 0.001) | 0.007 (< 0.001) | –1.18 (0.686) | –0.009 (0.450) | –0.003 (0.815) | 64,114 (< 0.001) |
| E | 53.81 (< 0.001) | 0.050 (0.319) | –0.94 (0.793) | –0.049 (0.326) | 0.0007 (0.419) | 12.0 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | K | – | – | – | – | – | – | – | – | – | – |
| A | N | 18.28 (< 0.001) | 30.04 (< 0.001) | –0.008 (0.014) | 0.005 (0.003) | –0.16 (0.878) | –0.001 (0.739) | –2.53 (0.147) | –0.002 (0.525) | –0.010 (< 0.001) | 133 (< 0.001) |
| B | L | 26.89 (< 0.001) | 2.16 (0.012) | –0.001 (0.306) | –0.002 (0.016) | –3.20 (0.001) | 0.004 (0.125) | 0.63 (0.646) | 0.003 (0.377) | 0.002 (0.534) | 35.4 (< 0.001) |
| G | M | 44.07 (< 0.001) | –25.06 (< 0.001) | –0.001 (0.439) | –0.002 (0.027) | –1.84 (0.225) | 0.010 (0.058) | 2.60 (0.176) | –0.006 (0.373) | –0.007 (0.302) | 197 (< 0.001) |
| Fc | J | 40.70 (< 0.001) | –2.04 (0.056) | –0.002 (0.033) | 0.001 (0.376) | 1.58 (0.375) | –0.018 (0.055) | –2.08 (0.413) | 0.035 (0.011) | 0.033 (0.017) | 42.5 (< 0.001) |
| C | O | 30.18 (< 0.001) | 12.45 (< 0.001) | –0.005 (< 0.001) | 0.002 (0.008) | –1.97 (0.097) | 0.002 (0.687) | 2.66 (0.165) | –0.005 (0.407) | –0.010 (0.076) | 36.5 (< 0.001) |
| D | K | 64.45 (< 0.001) | 6.21 (0.001) | 0.006 (0.001) | 0.0001 (0.904) | 2.69 (0.222) | –0.002 (0.822) | –3.69 (0.277) | –0.008 (0.563) | –0.002 (0.896) | 27.3 (< 0.001) |
| E | M | 27.68 (< 0.001) | 27.80 (< 0.001) | –0.014 (0.809) | 0.060 (0.172) | –1.28 (0.660) | –0.063 (0.157) | 0.57 (0.891) | 0.017 (0.772) | 0.003 (0.007) | 157 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | All control sites | – | – | – | – | – | – | – | – | – | – |
| A | All control sites | 32.64 (< 0.001) | 14.11 (< 0.001) | –0.004 (0.188) | 0.002 (0.240) | –0.40 (0.552) | –0.0007 (0.636) | –2.42 (0.118) | –0.003 (0.451) | –0.007 (< 0.001) | 43.1 (< 0.001) |
| B | All control sites | 23.19 (< 0.001) | –2.25 (0.009) | –0.002 (0.013) | –0.0003 (0.685) | –1.60 (0.139) | 0.001 (0.670) | –0.93 (0.562) | 0.006 (0.169) | 0.004 (0.404) | 76.4 (< 0.001) |
| G | All control sites | 41.25 (< 0.001) | –23.96 (< 0.001) | –0.003 (< 0.001) | 0.0002 (0.734) | –1.62 (0.114) | 0.006 (0.121) | 2.75 (0.086) | –0.002 (0.661) | –0.006 (0.301) | 419 (< 0.001) |
| Fc | All control sites | 5.03 (< 0.001) | –0.002 (0.012) | 0.0005 (0.270) | 2.19 (0.017) | –0.007 (0.155) | –2.73 (0.169) | –2.73 (0.169) | 0.026 (0.025) | 0.023 (0.040) | 31.97 (< 0.001) |
| C | All control sites | 37.27 (< 0.001) | 3.71 (< 0.001) | –0.005 (< 0.001) | 0.001 (0.008) | –1.59 (0.053) | 0.004 (0.107) | 2.32 (0.145) | –0.007 (0.146) | –0.012 (0.013) | 24.7 (< 0.001) |
| D | All control sites | 41.76 (< 0.001) | 28.77 (< 0.001) | 0.007 (< 0.001) | –0.0005 (0.411) | 2.21 (0.009) | –0.003 (0.510) | –3.19 (0.293) | –0.007 (0.617) | –0.0001 (0.999) | 164 (< 0.001) |
| E | All control sites | 33.60 (< 0.001) | 23.50 (< 0.001) | 0.070 (0.191) | –0.033 (0.306) | 2.20 (0.191) | 0.034 (0.293) | –2.78 (0.486) | –0.070 (0.236) | –0.0003 (0.703) | 203 (< 0.001) |
As with the primary analysis, there were no obvious trends. The effect of intervention ranged from 1.0 more to 2.7 fewer ED attendances per night in the intervention-site-only analysis, with only the decrease in ED attendances at site B being significant. The paired analysis showed an effect ranging from 2.7 more to 3.7 fewer ED attendances per night saved, with no significant results. The paired analysis with pooled control sites showed an effect ranging from 2.7 more to 3.1 fewer ED attendances, with no significant results.
Tables 27–29 show the results of linear regression analysis using intervention-site-only analysis (see Table 27), paired analysis with a single control (see Table 28) and paired analysis with pooled control sites (see Table 29). Bonferroni correction across all 24 tests resulted in a p-value of ≤ 0.0143 for statistical significance.
| Site | Constant (p) | Open (p) | Post AIMS (p) | F (p) | R 2 | Root MSE |
|---|---|---|---|---|---|---|
| Ha | 35.83 (< 0.001) | –3.24 (< 0.001) | n/a | 37.23 (< 0.001) | 0.218 | 6.55 |
| A | 41.73 (< 0.001) | –2.87 (< 0.001) | –3.34 (< 0.001) | 52.45 (< 0.001) | 0.295 | 7.60 |
| B | 24.69 (< 0.001) | –1.55 (0.011) | –1.32 (< 0.001) | 51.58 (< 0.001) | 0.292 | 5.80 |
| G | 16.50 (< 0.001) | 0.59 (0.459) | –0.28 (0.194) | 30.63 (< 0.001) | 0.196 | 4.01 |
| F | 50.81 (< 0.001) | –0.48 (0.643) | 1.02 (0.063) | 92.75 (< 0.001) | 0.425 | 7.51 |
| C | 46.21 (< 0.001) | –1.69 (0.037) | –2.48 (< 0.001) | 45.86 (< 0.001) | 0.268 | 7.26 |
| D | 81.54 (< 0.001) | –0.40 (0.862) | 3.19 (< 0.001) | 43.05 (< 0.001) | 0.256 | 11.61 |
| E | 78.18 (< 0.001) | 2.64 (0.180) | –1.05 (0.382) | 48.19 (< 0.001) | 0.278 | 10.41 |
| Site | Constant (p) | Intervention site β (p) | Post site β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | K | 68.03 (< 0.001) | –29.62 (< 0.001) | n/a | –1.81 (0.002) | 928 (< 0.001) | 0.797 | 8.00 |
| A | N | 29.46 (< 0.001) | 14.16 (< 0.001) | 0.51 (0.073) | 1.24 (0.041) | 235 (< 0.001) | 0.512 | 7.59 |
| B | L | 25.04 (< 0.001) | –0.03 (0.856) | –2.01 (< 0.001) | 1.99 (0.002) | 76.2 (< 0.001) | 0.254 | 5.70 |
| G | M | 43.72 (< 0.001) | –24.13 (< 0.001) | –0.93 (< 0.001) | 0.19 (0.898) | 1059 (< 0.001) | 0.826 | 5.76 |
| F | J | 55.15 (< 0.001) | –5.45 (< 0.001) | 1.01 (0.007) | 1.32 (0.183) | 148 (< 0.001) | 0.399 | 7.79 |
| C | O | 37.51 (< 0.001) | 7.29 (< 0.001) | –0.46 (0.090) | –3.19 (< 0.001) | 125 (< 0.001) | 0.358 | 6.84 |
| D | K | 70.18(< 0.001) | 11.31 (< 0.001) | 2.97 (< 0.001) | –0.71 (0.738) | 156 (< 0.001) | 0.410 | 10.37 |
| E | M | 47.92 (< 0.001) | 27.62 (< 0.001) | 0.08 (0.907) | 1.91 (0.002) | 653 (< 0.001) | 0.745 | 8.87 |
| Site | Constant (p) | Intervention site β (p) | Post site β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | All control sites | 44.38 (< 0.001) | –8.32 (< 0.001) | n/a | –1.61 (0.022) | 115 (< 0.001) | 0.122 | 12.96 |
| A | All control sites | 43.03 (< 0.001) | 4.17 (< 0.001) | 0.18 (0.492) | 1.82 (0.024) | 66.1 (< 0.001) | 0.078 | 13.18 |
| B | All control sites | 43.12 (< 0.001) | –11.71 (< 0.001) | 0.33 (0.252) | 0.40 (0.727) | 133 (< 0.001) | 0.144 | 13.00 |
| G | All control sites | 43.88 (< 0.001) | –24.67 (< 0.001) | 0.269 (0.303) | –1.04 (0.683) | 416 (< 0.001) | 0.346 | 12.83 |
| F | All control sites | 44.78 (< 0.001) | 2.37 (< 0.001) | 1.54 (< 0.001) | 0.91 (0.542) | 84.2 (< 0.001) | 0.097 | 13.06 |
| C | All control sites | 44.53 (< 0.001) | 0.46 (0.153) | –0.08 (0.781) | –4.29 (< 0.001) | 68.6 (< 0.001) | 0.080 | 13.02 |
| D | All control sites | 44.83 (< 0.001) | 33.13 (< 0.001) | 1.04 (0.001) | 2.81 (0.253) | 656 (< 0.001) | 0.455 | 13.42 |
| E | All control sites | 44.61 (< 0.001) | 27.35 (< 0.001) | 0.54 (0.281) | –2.87 (< 0.001) | 503 (< 0.001) | 0.391 | 13.27 |
There were some significant changes at individual sites following intervention, in most cases involving a decrease in attendances. However, the findings were inconsistent, with some sites showing an increase in attendances in one analysis and a decrease in attendances in another analysis. The effect of intervention ranged from 2.6 more to 3.2 fewer ED attendances per night in the intervention-site-only analysis, with significant decreases at sites A, B and H after Bonferroni correction. The paired analysis showed an effect ranging from 2.0 more to 3.2 fewer ED attendances per night, with significant increases at site E and significant decreases at sites B, H and C. The paired analysis with pooled control sites showed an effect ranging from 4.2 more to 4.1 fewer ED attendances per night, with significant decreases at sites C and E after Bonferroni correction.
As with the primary analysis, the pooled analysis across all sites showed markedly different results depending on whether the original sites (sites D and E) or the replacements sites (sites H and G) were used, and the overall estimate across sites was much less precise than estimates for individual sites. The estimated effect of implementing AIMSs was 3.16 additional attendances per night (95% CI –12.96 to 19.27 attendances per night; p = 0.663) across all sites, 7.35 additional attendances per night (95% CI –7.22 to 21.92 attendances per night; p = 0.263) when the original sites were used and 1.65 fewer attendances per night (95% CI –11.36 to 8.05 fewer attendances per night; p = 0.692) when the replacement cities were used. Overall, there was no evidence of an effect from AIMSs on ED attendances in those aged 14–39 years, but CIs were wide.
No investigation or treatment
The assumption behind this analysis was that AIMSs would be more likely to divert attendances that did not require ED investigation or treatment. Therefore, we present analysis only for the strata with no ED investigation or treatment. Table 30 shows the mean ED attendances per day during hours of AIMS activity among those with no ED investigation or treatment recorded at each site pre and post intervention. There was substantial variation between sites in ED attendances with no investigation or treatment, with some sites reporting no such attendances during the pre-intervention period. This is likely to be the result of sites defining or recording investigations or treatments in different ways, for example whether observation in the ED or provision of written advice are recorded as treatments. The subsequent analysis was not interpretable in the light of this variation and is therefore not presented.
| Mean attendances at ED per night | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 25.00 | 32.52 | 7.59 | 0.29 | 2.64 | 12.45 | 0.00 |
| Post AIMS | 0.003 | 52.60 | 55.00 | 0.89 | 8.36 | 1.03 | 10.41 | 5.86 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.00 | 3.83 | 13.54 | 0.004 | 24.35 | 2.88 | 7.55 |
| Post AIMS | 2.47 | 0.13 | 0.00 | 13.77 | 10.77 | 4.39 | 2.09 | 13.04 |
Key performance indicators
Total time in the ED is widely reported as the main key performance indicator for ED waiting times. 89,90 During the EDARA study the target for this measure was that 95% of attendances should spend no more than four hours in the ED. We therefore decided that total time in the ED should be the main analysis and should focus on whether the 4-hour target was achieved, as there is evidence that EDs manage patients (and thus influence total ED time) in relation to this target.
Data for ED-related key performance indicators revealed a number of inconsistencies, particularly between English and Welsh data. The English data reported time to initial assessment, time to treatment and total time in the ED; the Welsh data reported time to first clinical contact, time to treatment and time to completion of treatment. Examining the data suggested that time to completion of treatment was the most consistently recorded variable in the Welsh data and appeared to be consistent with total time in the ED in the English data. Therefore, we used time to completion of treatment in the Welsh data alongside total time in the ED in the English data to estimate the effect of the intervention on the proportion achieving the 4-hour target for total time in the ED.
Total time in the emergency department
Table 31 shows the median total time in the ED for each pair of sites pre and post AIMS implementation at the intervention site. Median times increased markedly at all sites except at sites E and D, which showed little change, and at site H, which had no pre-intervention data.
| Total time (minutes) in ED, median (5th to 95th centiles) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 156 (1 to 656) | 215 (28 to 746) | 159 (20 to 502) | 166 (45 to 239) | 140 (27 to 304) | 176 (23 to 432) | 168 (43 to 290) |
| Post AIMS | 192 (56 to 358) | 174 (1 to 623) | 269 (42 to 987) | 217 (37 to 813) | 197 (58 to 348) | 159 (31 to 324) | 178 (34 to 498) | 166 (38 to 342) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 178 (29 to 410) | 223 (41 to 858) | 185 (41 to 357) | 162 (44 to 336) | 141 (16 to 316) | 181 (37 to 399) | 186 (45 to 310) |
| Post AIMS | 183 (38 to 428) | 195 (34 to 600) | 253 (48 to 958) | 232 (52 to 699) | 218 (60 to 584) | 159 (22 to 354) | 194 (43 to 565) | 195 (43 to 488) |
Table 32 presents the percentage seen within 4 hours by site. Percentages are lower post intervention and are lowest for Welsh sites, at which the 4-hour target had a lower priority than at English sites.
| Percentage of ED attendances of < 4 hours’ total duration | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 71.7 | 61.8 | 87.4 | 95.7 | 91.6 | 89.2 | 92.9 |
| Post AIMS | 87.6 | 70.8 | 45.4 | 64.8 | 88.9 | 86.9 | 86.1 | 88.8 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 86.5 | 64.4 | 90.4 | 89.0 | 90.9 | 86.6 | 94.0 |
| Post AIMS | 85.1 | 80.8 | 49.1 | 58.0 | 62.9 | 86.5 | 78.3 | 82.0 |
Tables 33 and 34 show the results for logistic regression in the intervention-site-only analysis (see Table 33) and paired analysis (see Table 34). After Bonferroni correction, results are statistically significant if p < 0.014. In the intervention-site-only analysis there were statistically significant reductions in those meeting the 4-hour target for sites F and E and a significant increase in those for sites C and D. In the paired analysis, sites G, F and D were significantly more likely and site C was significantly less likely to meet the 4-hour target when an AIMS was open.
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 |
|---|---|---|---|
| Ha | 0.011 (0.006; 0.065) | 824 (< 0.001) | 0.008 |
| A | –0.004 (0.004; 0.373) | 361 (< 0.001) | 0.002 |
| B | 0.014 (0.007; 0.030) | 2551 (< 0.001) | 0.017 |
| G | –0.002 (0.011; 0.822) | 3824 (< 0.001) | 0.068 |
| F | –0.019 (0.003; < 0.001) | 1905 (< 0.001) | 0.033 |
| C | 0.013 (0.004; < 0.001) | 750 (< 0.001) | 0.008 |
| D | 0.027 (0.006; < 0.001) | 614 (< 0.001) | 0.004 |
| E | –0.019 (0.007; 0.003) | 399 (< 0.001) | 0.002 |
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|
| Intervention | Control | |||
| Ha | K | 0.029 (0.015; 0.059) | 2033 (< 0.001) | 0.007 |
| A | N | –0.061 (0.027; 0.022) | 5517 (< 0.001) | 0.019 |
| B | L | 0.056 (0.037; 0.131) | 4839 (< 0.001) | 0.017 |
| G | M | 0.154 (0.048; 0.001) | 21496 (< 0.001) | 0.108 |
| F | J | 0.043 (0.005; < 0.001) | 20700 (< 0.001) | 0.093 |
| C | O | –0.025 (0.004; < 0.001) | 1619 (< 0.001) | 0.009 |
| D | K | 0.064 (0.008; < 0.001) | 4051 (< 0.001) | 0.012 |
| E | M | –0.004 (0.013; 0.759) | 4580 (< 0.001) | 0.015 |
Pooled analysis showed that sites were more likely to report ED attendance durations of < 4 hours when an AIMS was open. The marginal effect was 0.015 (95% CI –0.039 to 0.069; p = 0.581) across all sites, 0.005 (95% CI –0.044 to 0.053; p = 0.848) when analysis used the original sites and 0.017 (95% CI –0.062 to 0.095; p = 0.678) when analysis used the replacement sites.
Time to treatment
Table 35 shows median time to treatment at the English sites, Table 36 shows the percentage of ED attendances with a time to treatment of 0 minutes and Table 37 shows the percentage of ED attendances with missing time to treatment data. There are marked inconsistencies, particularly between the English and Welsh sites, and between time to treatment and time to completion of treatment at the Welsh sites. At site B the median time to treatment was 239 minutes post intervention. Time to treatment is not used to judge performance in the same way as total time in ED (there is no specified target and no financial implications for failing to achieve a target), so this may be reflected in the rigour of recording. Given the inconsistencies in both recording and using time to treatment as a performance indicator, we decided not to proceed with using this measure to evaluate the effect of AIMS implementation.
| Time (minutes) to treatment, median (5th and 95th centiles) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 155 (1 to 672) | 238 (32 to 441) | 62 (3 to 239) | 76 (4 to 1101) | 60 (1 to 204) | 93 (11 to 223) | 92 (15 to 206) |
| Post AIMS | 105 (11 to 228) | 195 (0 to 691) | 239 (239 to 239) | 83 (10 to 340) | 102 (11 to 223) | 55 (0 to 188) | 89 (11 to 218) | 81 (10 to 198) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 93 (8 to 251) | 197 (36 to 750) | 97 (8 to 217) | 71 (0 to 207) | 60 (0 to 198) | 76 (7 to 183) | 104 (4 to 225) |
| Post AIMS | 77 (8 to 185) | 118 (9 to 709) | 211 (43 to 873) | 119 (9 to 306) | 129 (5 to 384) | 63 (3 to 200) | 83 (9 to 194) | 101 (8 to 238) |
| Percentage with a time to treatment of 0 minutes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 2.3 | 0.1 | 2.7 | 0.02 | 4.7 | 0.7 | 0.1 |
| Post AIMS | 1.2 | 1.8 | 0.0 | 0.2 | 0 | 8.0 | 1.2 | 0.2 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.5 | 0.2 | 1.2 | 7.5 | 5.0 | 0.9 | 3.2 |
| Post AIMS | 0.9 | 0.2 | 0.1 | 0.8 | 3.0 | 0.9 | 0.8 | 1.0 |
| Percentage with missing time to treatment data | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 28.4 | 60.5 | 22.9 | 0.5 | 3.2 | 11.3 | 0.0 |
| Post AIMS | 0.00 | 67.1 | 95.4 | 2.5 | 9.8 | 1.5 | 8.6 | 5.0 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.01 | 6.1 | 16.4 | 0.0 | 37.0 | 2.3 | 11.4 |
| Post AIMS | 2.2 | 0.2 | 0.0 | 17.4 | 10.8 | 5.9 | 1.8 | 16.9 |
Time to initial assessment
Table 38 shows the median time to initial assessment, Table 39 shows the percentage reporting 0 minutes for time to initial assessment and Table 40 shows the percentage with missing data for time to initial assessment. The Welsh sites did not report time to initial assessment and some English sites reported high rates of missing or no data. This probably reflects a lack of consistent use of this measure as a performance indicator with a specified target and financial implications. Given the inconsistencies, we decided not to proceed with analysis to determine whether or not AIMS implementation would affect time to initial assessment in the ED.
| Time (minutes) to initial assessment, median (5th to 95th centiles) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | – | – | 4 (1 to 58) | 12 (3 to 1273) | 6 (0 to 148) | 5 (0 to 37) | 4 (1 to 52) |
| Post AIMS | 0 (0 to 14) | – | – | 17 (3 to 77) | 73 (9 to 211) | 0 (0 to 46) | 7 (0 to 40) | 5 (0 to 33) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 9 (1 to 53) | – | 4 (0 to 33) | 0 (0 to 38) | 15 (1 to 62) | 15 (3 to 48) | 25 (3 to 125) |
| Post AIMS | 16 (3 to 53) | 16 (2 to 91) | – | 18 (2 to 235) | 7 (0 to 75) | 12 (1 to 56) | 23 (6 to 68) | 5 (0 to 120) |
| Percentage with a time to initial assessment of 0 minutes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | – | – | 3.8 | 0.04 | 39.4 | 24.7 | 4.3 |
| Post AIMS | 59.4 | – | – | 0.1 | 0.00 | 61.0 | 20.1 | 7.7 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 1.0 | – | 13.0 | 66.3 | 4.3 | 1.5 | 0.5 |
| Post AIMS | 1.4 | 0.4 | – | 1.8 | 26.0 | 2.1 | 0.8 | 10.8 |
| Percentage with missing time to initial assessment data | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 100 | 100 | 3.7 | 0.4 | 2.2 | 6.4 | 0.0 |
| Post AIMS | 0.01 | 100 | 100 | 8.8 | 8.8 | 0.4 | 5.3 | 1.0 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 1.3 | 100 | 12.3 | 1.0 | 10.6 | 3.2 | 50.2 |
| Post AIMS | 3.5 | 2.4 | 100 | 8.4 | 7.7 | 2.9 | 5.0 | 9.4 |
Hospital admissions potentially related to alcohol intoxication
Attributable to alcohol intoxication
Table 41 shows the mean number of admissions with AAI per day (starting at midnight) during hours of AIMS activity. This is shown for intervention sites before and after AIMS implementation and for control sites before and after AIMS implementation at the paired intervention site. Numbers of admissions were low, with admission rates varying from less than one admission per week to an admission every 1 or 2 days. There was no obvious trend towards admissions increasing or decreasing across intervention or control sites.
| Mean number admitted with AAI per day | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 0.12 | 0.16 | 0.03 | 0.07 | 0.15 | 0.26 | 0.45 |
| Post AIMS | 0.27 | 0.12 | 0.09 | 0.00 | 0.09 | 0.13 | 0.35 | 0.52 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.02 | 0.40 | 0.19 | 0.09 | 0.40 | 0.56 | 0.67 |
| Post AIMS | 0.64 | 0.06 | 0.44 | 0.16 | 0.04 | 0.27 | 0.89 | 0.21 |
Interrupted time series analysis
Tables 42 and 43 show the results of ITSA using intervention-site-only analysis (see Table 42) and paired analysis with pooled control sites (see Table 43). Bonferroni correction across seven ITSA tests resulted in a p-value of ≤ 0.0142 for statistical significance. We were unable to fit a time series model for the paired analysis with single control sites because the data were not balanced. Caution should be exercised in the interpretation of ITSA results; some of the models have poor model fit (F-statistic). Autocorrelation was explored and, in all cases excluding site C, no lags were significant; therefore, autocorrelation was not adjusted for.
| Site | Constanta (p) | t (p) | x (p) | xt (p) | Post-trend difference (p) | F (p) |
|---|---|---|---|---|---|---|
| Hb | – | – | – | – | – | – |
| A | –0.033 (0.800) | 0.0001 (0.477) | 0.039 (0.615) | –0.0002 (0.175) | –0.0001 (0.059) | 858 (< 0.001) |
| B | 0.133 (0.621) | –0.0001 (0.096) | –0.015 (0.783) | 0.0001 (0.672) | –0.00 (0.897) | 2.05 (0.011) |
| G | –0.002 (0.929) | 0.00002 (0.595) | –0.051 (0.181) | –0.00001 (0.737) | 0.00 (0.520) | 0.48 (0.899) |
| F | 0.060 (0.025) | 0.00002 (0.301) | –0.054 (0.374) | 0.0004 (0.346) | 0.0004 (0.313) | 3.38 (< 0.001) |
| C | 0.074 (0.649) | –0.00001 (0.758) | –0.031 (0.617) | 0.0002 (0.529) | 0.0001 (0.562) | 4.03 (< 0.001) |
| D | –0.064 (0.474) | 0.0003 (< 0.001) | 0.244 (0.228) | –0.003 (0.002) | –0.002 (0.006) | 16,580 (< 0.001) |
| E | 0.346 (0.498) | –0.007 (0.244) | 0.693 (0.008) | 0.006 (0.263) | –0.0003 (< 0.001) | 8.44 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | All control sites | – | – | – | – | – | – | – | – | – | – |
| A | All control sites | 0.198 (0.011) | –0.127 (0.030) | –0.00003 (0.864) | 0.0001 (0.177) | 0.087 (0.105) | –0.0002 (0.034) | –0.056 (0.550) | 0.00003 (0.877) | –0.000 (0.993) | 8.84 (< 0.001) |
| B | All control sites | 0.258 (0.108) | –0.127 (0.037) | –0.00005 (0.426) | –0.00002 (0.621) | –0.011 (0.881) | 0.0002 (0.442) | –0.005 (0.958) | –0.0001 (0.717) | –0.0002 (0.572) | 6.64 (< 0.001) |
| G | All control sites | 0.258 (< 0.001) | –0.274 (< 0.001) | 0.00002 (0.694) | 0.00 (0.947) | 0.009 (0.887) | 0.0001 (0.633) | –0.055 (0.430) | –0.0001 (0.633) | –0.0001 (0.689) | 114 (< 0.001) |
| F | All control sites | 0.278 (< 0.001) | –0.217 (< 0.001) | –0.00002 (0.520) | 0.00004 (0.061) | 0.133 (0.028) | –0.001 (< 0.001) | –0.188 (0.028) | 0.002 (0.001) | 0.002 (0.001) | 17.2 (< 0.001) |
| C | All control sites | 0.240 (0.011) | –0.086 (0.037) | –0.00001 (0.044) | 0.00008 (0.003) | –0.058 (0.222) | –0.0001 (0.506) | 0.026 (0.733) | 0.0002 (0.317) | 0.0002 (0.527) | 9.85 (< 0.001) |
| D | All control sites | 0.193 (< 0.001) | –0.235 (< 0.001) | 0.0003 (0.0001) | 0.000 (0.792) | 0.125 (0.040) | –0.0006 (0.074) | 0.116 (0.581) | –0.002 (0.027) | –0.002 (0.053) | 7.84 (< 0.001) |
| E | All control sites | 0.153 (0.442) | 0.394(0.367) | –0.003 (0.611) | –0.002 (0.301) | 0.188 (0.181) | 0.002 (0.295) | 0.420 (0.096) | 0.003 (0.646) | –0.0003 (< 0.001) | 5.01 (< 0.001) |
The intervention-site-only analysis suggested a significant increase in admissions after intervention at site E. The effects across other sites were non-significant trends towards both increases and decreases in admissions. The paired analysis with pooled control sites showed a non-significant increase in admissions at site E and a decrease at site F that was not significant with Bonferroni correction. Again, the effects across other sites were variable and non-significant.
Linear regression analysis (estimated using ordinary least squares)
Tables 44–46 show the results of linear regression analysis using intervention-site-only analysis (see Table 44), paired analysis with single control sites (see Table 45) and paired analysis with pooled control sites (see Table 46). Bonferroni correction across sites and eight tests resulted in a p-value of ≤ 0.0125 for statistical significance.
| Site | Constant (p) | Open (p) | Post AIMS (p) | F (p) | R 2 | Root MSE |
|---|---|---|---|---|---|---|
| Ha | 0.062 (0.772) | –0.143 (0.108) | n/a | 0.68 (0.795) | 0.016 | 0.551 |
| A | 0.008 (0.956) | –0.045 (0.531) | 0.049 (0.494) | 3.58 (< 0.001) | 0.085 | 0.360 |
| B | 0.105 (0.674) | –0.028 (0.777) | –0.051 (0.589) | 1.31 (0.199) | 0.030 | 0.377 |
| G | 0.011 (0.793) | –0.005 (0.931) | –0.031 (0.337) | 0.19 (0.999) | 0.012 | 0.162 |
| F | 0.080 (< 0.001) | –0.408 (0.033) | 0.420 (0.026) | 0.74 (0.697) | 0.015 | 0.266 |
| C | 0.067 (0.649) | –0.024 (0.495) | Omitted collinearity | 0.97 (0.478) | 0.023 | 0.368 |
| D | 0.193 (0.092) | 0.255 (0.088) | –0.065 (0.572) | 1.12 (0.343) | 0.044 | 0.528 |
| E | 0.037 (0.909) | 0.271 (0.734) | –0.175 (0.829) | 2.85 (< 0.001) | 0.067 | 0.780 |
| Site | Constant (p) | Intervention site β (p) | Post AIMS β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | K | 0.695 (0.001) | –0.250 (0.022) | n/a | –0.132 (0.267) | 5.20 (< 0.001) | 0.066 | 0.733 |
| A | N | –0.025 (0.777) | 0.077 (0.005) | 0.048 (0.188) | –0.002 (0.957) | 3.27 (< 0.001) | 0.050 | 0.302 |
| B | L | 0.191 (0.436) | –0.250 (< 0.001) | 0.128 (0.128) | –0.077 (0.274) | 6.16 (< 0.001) | 0.076 | 0.521 |
| G | M | 0.076 (0.205) | –0.154 (< 0.001) | –0.038 (0.358) | –0.076 (0.606) | 2.38 (0.003) | 0.065 | 0.368 |
| F | J | 0.099 (< 0.001) | –0.022 (0.228) | –0.052 (0.147) | 0.057 (0.242) | 0.69 (0.775) | 0.008 | 0.286 |
| C | O | 0.269 (0.072) | –0.253 (< 0.001) | –0.173 (0.003) | 0.113 (0.109) | 5.31 (< 0.001) | 0.071 | 0.528 |
| D | K | 0.476 (< 0.001) | –0.344 (< 0.001) | 0.269 (0.002) | 0.059 (0.705) | 4.52 (< 0.001) | 0.095 | 0.673 |
| E | M | 0.462 (0.028) | –0.206 (0.195) | –0.306 (0.523) | 0.519 (0.002) | 7.29 (< 0.001) | 0.093 | 0.655 |
| Site | Constant (p) | Intervention site β (p) | Post AIMS β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | All control sites | 0.341 (< 0.001) | 0.038 (0.611) | n/a | –0.075 (0.356) | 0.81 (0.676) | 0.004 | 0.610 |
| A | All control sites | 0.338 (< 0.001) | –0.155 (< 0.001) | 0.048 (0.329) | –0.045 (0.415) | 3.68 (< 0.001) | 0.018 | 0.589 |
| B | All control sites | 0.218 (0.144) | –0.155 (< 0.001) | 0.122 (0.046) | –0.073 (0.213) | 3.58 (< 0.001) | 0.021 | 0.542 |
| G | All control sites | 0.235 (< 0.001) | –0.267 (< 0.001) | 0.021 (0.611) | –0.071 (0.671) | 3.56 (< 0.001) | 0.037 | 0.535 |
| F | All control sites | 0.313 (< 0.001) | –0.233 (< 0.001) | 0.044 (0.227) | 0.008 (0.917) | 6.71 (< 0.001) | 0.026 | 0.583 |
| C | All control sites | 0.352 (< 0.001) | –0.156 (< 0.001) | –0.016 (0.640) | –0.025 (0.681) | 2.88 (< 0.001) | 0.014 | 0.589 |
| D | All control sites | 0.281 (0.001) | 0.013 (0.740) | –0.030 (0.305) | 0.175 (0.145) | 3.39 (< 0.001) | 0.016 | 0.610 |
| E | All control sites | 0.234 (0.024) | 0.234 (0.054) | 0.050 (0.327) | –0.117 (0.353) | 6.67 (< 0.001) | 0.029 | 0.648 |
As with the time series analysis, the results were inconsistent and largely non-significant across the sites. Only the increase in admissions at site E on the paired analysis with single control sites was significant with Bonferroni correction.
The effect of AIMSs across all sites was 0.090 additional admissions per day (95% CI –0.175 to 0.356 additional admissions per day; p = 0.466). The effects when only the original sites were used was 0.233 additional admissions per day (–0.029 to 0.494 additional admissions per day; p = 0.074) and when the replacement sites were used was –0.097 additional admissions per day (–0.180 to –0.014 additional admissions per day; p = 0.029). In summary, the results were inconsistent across sites and showed no overall effect from AIMSs on hospital admissions for alcohol intoxication.
Alcohol-related hospital admissions
Table 47 shows the mean number of alcohol-related admissions on days that started at midnight during hours of AIMS activity. Admission rates varied from less than an admission per week to an admission every one or two days. There was no obvious trend towards admissions increasing or decreasing across intervention or control sites.
| Mean number of alcohol-related admissions per day | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 0.43 | 0.58 | 0.51 | 0.85 | 0.75 | 1.04 | 1.94 |
| Post AIMS | 0.86 | 0.54 | 0.53 | 0.45 | 0.76 | 0.68 | 1.07 | 1.76 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.61 | 1.02 | 0.87 | 1.36 | 1.38 | 1.72 | 1.36 |
| Post AIMS | 1.79 | 0.62 | 1.24 | 0.54 | 1.51 | 1.37 | 2.16 | 0.86 |
Interrupted time series analysis
Tables 48 and 49 show the results of ITSA using intervention-site-only analysis (see Table 48) and paired analysis with pooled control sites (see Table 49). Bonferroni correction across the seven sites in each ITSA resulted in a p-value of ≤ 0.0142 for statistical significance. Caution should be exercised in the interpretation of ITSA results; some of the models have poor model fit (F-statistic). We were unable to fit a time series model for the paired analysis with single control sites because the data were not balanced. Autocorrelation was explored and, in all cases excluding sites D (lag 3) and E (lag 6), no lags were significant; therefore, autocorrelation was not adjusted for.
Both analyses showed inconsistency across the sites, with some being associated with increased admissions and others with decreased admissions. There was a statistically significant decrease in admissions at sites B and F in the pooled analysis, which was still evident after Bonferroni correction.
| Site | Constanta (p) | t (p) | x (p) | xt (p) | Post-trend difference (p) | F (p) |
|---|---|---|---|---|---|---|
| Hb | – | – | – | – | – | – |
| A | 0.583 (0.003) | 0.0003 (0.248) | 0.041 (0.752) | –0.0003 (0.219) | –0.00 (0.668) | 144 (< 0.001) |
| B | 0.466 (0.417) | 0.0001 (0.220) | –0.295 (0.027) | 0.0005 (0.207) | 0.0006 (0.103) | 25.5 (< 0.001) |
| G | 0.650 (< 0.001) | –0.0002 (0.110) | 0.292 (0.192) | –0.0007 (0.275) | –0.0009 (0.151) | 27.8 (< 0.001) |
| F | 0.818 (< 0.001) | 0.0001 (0.299) | –0.306 (0.070) | 0.0007 (0.395) | 0.0008 (0.329) | 188 (< 0.001) |
| C | 1.014 (0.004) | –0.0001 (0.171) | 0.087 (0.540) | –0.00007 (0.882) | –0.0002 (0.670) | 3.14 (< 0.001) |
| D | 0.606 (0.007) | 0.0005 (< 0.001) | –0.081 (0.797) | –0.002 (0.072) | –0.002 (0.147) | 14,906 (< 0.001) |
| E | 3.150 (< 0.001) | –0.014 (0.101) | 1.193 (0.042) | 0.014 (0.114) | –0.0005 (< 0.001) | 7.3 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | All control sites | – | – | – | – | – | – | – | – | – | – |
| A | All control sites | 1.16 (< 0.001) | –0.702 (< 0.001) | –0.00001 (0.966) | 0.003 (0.089) | 0.033 (0.744) | –0.0003 (0.124) | 0.016 (0.923) | –0.00005 (0.881) | –0.0001 (0.638) | 22.53 (< 0.001) |
| B | All control sites | 1.03 (0.005) | –0.727 (< 0.001) | 0.0002 (0.085) | –0.0001 (0.227) | 0.314 (0.068) | –0.0002 (0.630) | –0.608 (0.005) | 0.0007 (0.219) | 0.0009 (0.103) | 15.25 (< 0.001) |
| G | All control sites | 1.01 (< 0.001) | –0.377 (0.001) | –0.0004 (0.010) | 0.0002 (0.055) | 0.012 (0.937) | –0.0004 (0.332) | 0.280 (0.292) | –0.0001 (0.933) | –0.0004 (0.567) | 108 (< 0.001) |
| F | All control sites | 1.17 (< 0.001) | –0.320 (0.001) | –0.0001 (0.583) | 0.0001 (0.001) | 0.230 (0.079) | –0.002 (0.003) | –0.538 (0.012) | 0.003 (0.007) | 0.003 (0.008) | 8.41 (< 0.001) |
| C | All control sites | 1.23 (< 0.001) | –0.239 (0.009) | –0.0003 (0.004) | 0.0002 (0.002) | 0.066 (0.552) | –0.0006 (0.095) | 0.004 (0.984) | 0.0007 (0.239) | 0.0004 (0.507) | 9.86 (< 0.001) |
| D | All control sites | 1.02 (< 0.001) | –0.421 (< 0.001) | 0.0004 (0.004) | 0.00007 (0.187) | 0.196 (0.110) | –0.001 (0.075) | –0.233 (0.487) | –0.001 (0.352) | –0.001 (0.505) | 4.50 (< 0.001) |
| E | All control sites | 1.66 (< 0.001) | 1.14 (0.033) | –0.005 (0.589) | –0.006 (0.120) | 0.393 (0.117) | 0.006 (0.112) | 0.531 (0.353) | 0.004 (0.639) | –0.0007 (< 0.001) | 7.16 (< 0.001) |
Linear regression analysis (estimated using ordinary least squares)
Tables 50–52 show the results of linear regression analysis using intervention-site-only analysis (see Table 50), paired analysis with single control sites (see Table 51) and paired analysis with pooled control sites (see Table 52). Bonferroni correction across eight tests resulted in a p-value of ≤ 0.0125 for statistical significance. The results were again inconsistent, with some sites associated with increased admissions and others associated with decreased admissions, and generally non-significant.
| Site | Constant (p) | DiD (open) (p) | Post AIMS (p) | F (p) | R 2 | Root MSE |
|---|---|---|---|---|---|---|
| Ha | 1.35 (0.001) | 0.054 (0.739) | n/a | 0.94 (0.520) | 0.022 | 1.00 |
| A | 0.656 (0.025) | –0.119 (0.394) | 0.218 (0.118) | 1.90 (0.024) | 0.047 | 0.70 |
| B | 0.518 (0.297) | –0.186 (0.341) | 0.110 (0.556) | 1.30 (0.202) | 0.030 | 0.74 |
| G | 0.531 (0.001) | 0.127 (0.568) | –0.103 (0.408) | 0.61 (0.834) | 0.038 | 0.63 |
| F | 0.901 (< 0.001) | –0.212 (0.741) | 0.099 (0.876) | 0.61 (0.819) | 0.012 | 0.89 |
| C | 0.916 (0.006) | –0.056 (0.479) | Omitted collinearity | 1.28 (0.216) | 0.029 | 0.837 |
| D | 0.990 (< 0.001) | 0.036 (0.899) | –0.011 (0.959) | 0.96 (0.486) | 0.038 | 0.998 |
| E | 2.49 (< 0.001) | 1.33 (0.346) | –1.39 (0.332) | 1.94 (0.017) | 0.047 | 1.38 |
| Site | Constant (p) | Intervention site β (p) | Post AIMS β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | K | 2.17 (< 0.001) | –0.84 (< 0.001) | n/a | –0.081 (0.690) | 11.22 (< 0.001) | 0.132 | 1.25 |
| A | N | 0.65 (0.002) | –0.16 (0.014) | 0.175 (0.041) | 0.093 (0.288) | 2.30 (0.002) | 0.036 | 0.71 |
| B | L | 0.74 (0.082) | –0.45 (< 0.001) | 0.335 (0.021) | –0.265 (0.029) | 8.47 (< 0.001) | 0.102 | 0.90 |
| G | M | 0.81 (< 0.001) | –0.31 (< 0.001) | –0.244 (0.006) | 0.229 (0.465) | 2.31 (0.004) | 0.063 | 0.78 |
| F | J | 1.38 (< 0.001) | –0.504 (< 0.001) | 0.197 (0.124) | –0.242 (0.165) | 6.87 (< 0.001) | 0.074 | 1.02 |
| C | O | 1.41 (< 0.001) | –0.633 (< 0.001) | 0.032 (0.782) | –0.049 (0.725) | 7.53 (< 0.001) | 0.097 | 1.05 |
| D | K | 1.67 (< 0.001) | –0.734 (< 0.001) | 0.430 (0.005) | –0.161 (0.559) | 5.71 (< 0.001) | 0.117 | 1.19 |
| E | M | 1.68 (< 0.001) | 0.588 (0.040) | –1.314 (0.128) | 0.309 (0.294) | 12.03 (< 0.001) | 0.145 | 1.18 |
| Site | Constant (p) | Intervention site β (p) | Post AIMS β (p) | DiD (open) (p) | F (p) | R 2 | Root MSE | |
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||
| Ha | All control sites | 1.42 (< 0.001) | –0.284 (0.049) | n/a | –0.104 (0.504) | 4.02 (< 0.001) | 0.019 | 1.17 |
| A | All control sites | 1.28 (< 0.001) | –0.698 (< 0.001) | 0.071 (0.446) | –0.046 (0.669) | 13.23 (< 0.001) | 0.062 | 1.13 |
| B | All control sites | 0.89 (0.003) | –0.584 (< 0.001) | 0.181 (0.134) | –0.155 (0.183) | 10.06 (< 0.001) | 0.056 | 1.07 |
| G | All control sites | 1.09 (< 0.001) | –0.664 (< 0.001) | 0.108 (0.211) | –0.031 (0.930) | 4.95 (< 0.001) | 0.051 | 1.12 |
| F | All control sites | 1.31 (< 0.001) | –0.370 (< 0.001) | 0.149 (0.037) | –0.180 (0.246) | 6.44 (< 0.001) | 0.025 | 1.15 |
| C | All control sites | 1.32 (< 0.001) | –0.467 (< 0.001) | 0.105 (0.109) | –0.146 (0.216) | 6.96 (< 0.001) | 0.033 | 1.15 |
| D | All control sites | 1.18 (< 0.001) | –0.070 (0.346) | 0.057 (0.314) | –0.039 (0.866) | 2.27 (0.002) | 0.011 | 1.17 |
| E | All control sites | 1.18 (< 0.001) | 0.877 (< 0.001) | 0.160 (0.095) | –0.450 (0.058) | 8.69 (< 0.001) | 0.037 | 1.22 |
The effect of AIMSs across all sites was 0.310 additional admissions per day (95% CI –0.364 to 0.983 additional admissions per day; p = 0.330). The effects when only the original sites were used was 0.629 additional admissions per day (–0.112 to 1.370 additional admissions per day; p = 0.086) and when the replacement sites were used was –0.160 additional admissions per day (–0.313 to –0.008 additional admissions per day; p = 0.042). In summary, the results were inconsistent across sites and showed no overall effect from AIMSs on hospital alcohol-related admissions.
Ambulance service key performance indicators
Descriptive statistics
We received ambulance service data for sites F, C and O from 1 January 2010 to 31 December 2016, for site H from 1 July 2010 to 31 December 2016, for sites K and N from 1 January 2012 to 31 December 2016, for sites A, B and L from 1 January 2012 to 1 December 2016, for sites J and M from 5 March 2012 to 31 March 2017 and for site D from 1 April 2012 to 31 December 2016. The ambulance services for sites E and G were unable to provide data; the results for site E and site G (paired with site M) are therefore missing from this analysis. We used data from 16 November 2010 to 31 March 2016, where available. As with the other analyses, the site H AIMS opened before the start of data availability, so there are no pre-intervention data for site H or its matched pair.
From 1 October 2015 the Welsh Ambulance Service66 changed call categorisation to a three-level, red/amber/green system. High-priority (red) calls were more strictly defined and are therefore not comparable to English or previous Welsh high-priority (category A) calls. Prior to the introduction of this system, the English and Welsh services used broadly similar categories, although there are inconsistencies in the way they were operationalised. For example, in Wales the clock starts when the chief complaint has been established, whereas in England the clock starts for the highest priority (Red1) calls when the call is answered.
Tables 53 and 54 show the mean number of all ambulance calls (see Table 53) and high-priority calls (see Table 54) per day in each site catchment area pre and post intervention. We noted the marked variation between the mean number of all calls and mean number of high-priority calls. This was explained by ambulance services interpreting our request for calls originating in the site catchment area in different ways. Only the 8–10 post districts nearest to the city centre were provided for sites C and O, whereas all city-region postal districts were provided for sites D and A. Therefore, we undertook a secondary analysis limiting all sites to the eight postal districts nearest to the city centre.
| Mean number of ambulance calls per day | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 172.5 | 120.8 | 77.8 | 28.2 | 179.9 |
| Post AIMS | 93.6 | 189.5 | 131.8 | 80.6 | 30.5 | 191.3 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 70.3 | 90.2 | 88.3 | 28.6 | 135.7 |
| Post AIMS | 135.6 | 70.4 | 96.7 | 88.0 | 30.2 | 135.5 |
| Mean number of high-priority calls per day | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 84.8 | 55.8 | 28.8 | 11.0 | 71.3 |
| Post AIMS | 34.9 | 80.5 | 43.6 | 39.4 | 15.3 | 81.9 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 27.7 | 44.9 | 32.6 | 10.0 | 55.6 |
| Post AIMS | 57.6 | 30.6 | 30.3 | 36.4 | 14.6 | 65.2 |
The number of high-priority calls increased after the intervention date at the English sites but decreased at the Welsh sites. This was probably due to the change in call categorisation instituted by the Welsh Ambulance Service during the project as described above. This observation suggests that the effect of the change in categorisation was substantial and means that Welsh-site pre- and post-intervention data are not comparable.
Tables 55 and 56 show the percentage of high-priority calls relating to male patients (see Table 55) and mean patient age (see Table 56). Mean age tended to be higher post intervention in most sites and mean age tended to be higher in the control sites.
| Percentage of calls relating to male patients | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 50.0 | 50.4 | 50.0 | 48.9 | 50.1 |
| Post AIMS | 49.0 | 48.7 | 50.2 | 51.1 | 47.8 | 49.7 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 49.4 | 48.4 | 48.7 | 49.4 | 48.5 |
| Post AIMS | 48.5 | 47.7 | 47.6 | 49.5 | 47.4 | 48.4 |
| Mean age (years) of patients | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 52.66 | 55.26 | 49.76 | 50.39 | 48.43 |
| Post AIMS | 56.14 | 53.79 | 57.12 | 48.22 | 48.16 | 48.91 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 52.77 | 55.27 | 52.07 | 53.93 | 55.35 |
| Post AIMS | 55.60 | 55.06 | 57.36 | 52.62 | 53.10 | 56.51 |
Tables 57 and 58 show the percentage of high-priority calls responded to within 8 minutes (see Table 57) and within 19 minutes (see Table 58). All sites show a decrease in performance against both key indicators over time.
| Percentage of high-priority calls responded to within 8 minutes | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 48.31 | 50.26 | 66.29 | 63.61 | 62.34 |
| Post AIMS | 56.19 | 39.79 | 44.11 | 51.77 | 51.69 | 54.67 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 68.01 | 42.50 | 54.87 | 61.65 | 57.96 |
| Post AIMS | 54.95 | 49.81 | 40.17 | 47.74 | 53.01 | 45.68 |
| Percentage of high-priority calls responded to within 19 minutes | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 89.55 | 90.88 | 98.50 | 97.80 | 96.06 |
| Post AIMS | 90.52 | 83.39 | 86.18 | 95.21 | 94.51 | 90.82 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 95.37 | 85.84 | 95.92 | 98.33 | 95.06 |
| Post AIMS | 93.99 | 89.17 | 82.05 | 94.91 | 95.68 | 90.70 |
Tables 59 and 60 show the median response time [and interquartile range (IQR)] for high-priority calls (see Table 59) and all calls (see Table 60). Median response times generally increased after intervention, reflecting worsening performance over time. Median times at Welsh sites were longer for high-priority calls, probably owing to the different approaches to the categorisation of high-priority calls in England and Wales. At the English sites the median response time was < 8 minutes (i.e. meeting the 8-minute target), which means that > 50% of calls were responded to within 8 minutes. Response times for all calls were slightly longer than for high-priority calls only.
| Response time (minutes), median (IQR) | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 8.7 (4.4–13.1) | 6.6 (4.4–10.9) | 6.6 (4.4–8.7) | 6.6 (4.4–8.7) | 6.6 (4.4–8.7) |
| Post AIMS | 6.6 (4.4–10.9) | 8.7 (6.6–15.3) | 8.7 (4.4–13.1) | 6.6 (4.4–10.9) | 6.6 (4.4–10.9) | 6.6 (4.4–10.9) |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 6.6 (4.4–8.7) | 8.7 (6.6–13.1) | 6.6 (4.4–10.9) | 6.6 (4.4–8.7) | 6.6 (4.4–10.9) |
| Post AIMS | 6.6 (4.4–10.9) | 8.7 (4.4–10.9) | 8.7 (6.6–15.3) | 8.7 (6.6–10.9) | 6.6 (4.4–10.9) | 8.7 (6.6–13.1) |
| Response time (minutes), median (IQR) | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 10.9 (6.6–21.8) | 8.7 (6.6–17.5) | 10.9 (6.6–30.6) | 10.9 (6.6–28.4) | 8.7 (6.6–19.7) |
| Post AIMS | 10.9 (6.6–19.7) | 13.1 (6.6–28.4) | 13.1 (6.6–26.2) | 13.1 (6.6–43.7) | 10.9 (6.6–32.8) | 10.9 (6.6–28.4) |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 8.7 (4.4–15.3) | 13.1 (6.6–24.0) | 10.9 (6.6–24.0) | 10.9 (6.6–32.8) | 10.9 (6.6–24.0) |
| Post AIMS | 10.9 (6.6–24.0) | 10.9 (6.6–24.0) | 15.3 (8.7–37.1) | 10.9 (6.6–28.4) | 10.9 (6.6–37.1) | 13.1 (6.6–30.6) |
Key performance indicators analysis
The following results show the marginal effect of an AIMS being open on the proportion of high-priority calls responded to within each time limit (8 or 19 minutes). They provide an estimate of the effect of AIMSs on the proportion of calls achieving the relevant target. Bonferroni correction across all six tests per set of analyses resulted in a p-value of ≤ 0.017 for statistical significance.
Sites E and G are excluded from this analysis because the site E ambulance service was unable to provide data. The change in categorisation of high-priority calls in the Welsh Ambulance Service meant that Welsh and English data were not comparable and that pairing a Welsh site with an English site would not be appropriate for ambulance data. Because we had data from only one Welsh control site, we decided to pair site A with site L instead of site N in the paired analysis. This at least meant that the Welsh sites were paired with a control site that had undergone the same change in categorisation of high-priority calls.
Tables 61 and 62 show the results of analysis of the 8-minute target on single sites (i.e. without using the control sites; see Table 61) and the analysis on paired sites (in which each intervention site is paired with its control site; see Table 62). In the intervention-site-only analysis, the marginal effect at each site ranged from a 4.3% improvement to a 1.7% deterioration in performance, but the only statistically significant effect was the 4.3% improvement seen at site D. The paired analysis produced more varied results, with marginal effects ranging from a 9.2% improvement to a 20.8% deterioration in performance. Only the improvements at sites D and A were statistically significant.
| Site | Marginal effect post AIMS (SE) | Marginal effect if AIMS open (SE) | Likelihood ratio χ2 (p) | Pseudo R2 |
|---|---|---|---|---|
| Ha | n/a | 0.018 (0.159) | 57.63 (< 0.001) | 0.0007 |
| A | –0.088 (< 0.001) | 0.010 (0.199) | 380.51 (< 0.001) | 0.0046 |
| B | –0.062 (< 0.001) | 0.002 (0.835) | 190.25 (< 0.001) | 0.0032 |
| F | –0.136 (< 0.001) | –0.004 (0.695) | 907.37 (< 0.001) | 0.014 |
| C | –0.109 (< 0.001) | –0.017 (0.245) | 366.17 (< 0.001) | 0.013 |
| D | –0.080 (< 0.001) | 0.043 (< 0.001) | 980.57 (< 0.001) | 0.007 |
| Site | Marginal effect post AIMS (SE) | Marginal effect if AIMS open (SE) | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Ha | K | n/a | –0.005 (0.936) | 260.72 (< 0.001) | 0.0013 |
| A | N | –0.088 (< 0.001) | 0.060 (0.021) | 409.00 (< 0.001) | 0.0048 |
| B | L | –0.044 (< 0.001) | –0.208 (0.269) | 527.51 (< 0.001) | 0.0054 |
| F | J | –0.102 (< 0.001) | –0.018 (0.078) | 1,974.01 (< 0.001) | 0.0170 |
| C | O | –0.093 (< 0.001) | 0.005 (0.753) | 589.68 (< 0.001) | 0.0111 |
| D | K | –0.099 (< 0.001) | 0.091 (< 0.001) | 2,673.19 (< 0.001) | 0.0104 |
Tables 63 and 64 show the results of analysis of the 19-minute target on single sites (see Table 63) and paired sites (see Table 64). In the intervention-site-only analysis, the marginal effect at each site ranged from a 1.5% improvement to a 0.3% deterioration in performance, with statistically significant improvements seen at sites D and C. The paired analysis produced more varied results. The improvement at site D was again statistically significant, as were the changes at sites F and C.
| Site | Marginal effect if AIMS open (SE) | p | Likelihood ratio χ2 (p) | Pseudo R2 |
|---|---|---|---|---|
| H | 0.002 (0.008) | 0.801 | 135.46 (< 0.001) | 0.0101 |
| A | –0.039 (0.008) | < 0.001 | 90.55 (< 0.001) | 0.004 |
| B | –0.029 (0.010) | 0.004 | 78.11 (< 0.001) | 0.008 |
| F | –0.007 (0.004) | 0.077 | 175.97 (< 0.001) | 0.040 |
| C | 0.041 (0.011) | < 0.001 | 114.82 (< 0.001) | 0.044 |
| D | –0.001 (0.004) | 0.743 | 251.83 (< 0.001) | 0.016 |
| Site | Marginal effect if AIMS open (SE) | p | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Ha | K | –0.040 (0.003) | < 0.001 | 398.18 (< 0.001) | 0.014 |
| A | N | –0.020 (0.005) | < 0.001 | 114.33 (< 0.001) | 0.004 |
| B | L | 0.024 (0.007) | < 0.001 | 107.18 (< 0.001) | 0.006 |
| F | J | 0.006 (0.003) | 0.031 | 217.93 (< 0.001) | 0.023 |
| C | O | –0.005 (0.004) | 0.300 | 171.72 (< 0.001) | 0.038 |
| D | K | 0.0002 (0.004) | 0.960 | 364.01 (< 0.001) | 0.012 |
Further results
Emergency department attendances (primary outcome)
Descriptive statistics
Emergency department attendances were analysed across all sites from 16 November 2010 to 31 March 2016. Table 65 shows the mean number of ED attendances per day during hours of AIMS activity at each site before and after the AIMS started operating at the intervention site in each matched pair. Pre-intervention data were not available at site H (or site K when matched with site H) because the site H AIMS started operating before 2010. The number of attendances per night ranged from 31 at site G pre intervention to 127 at site K post intervention when paired with site D. Attendances decreased after intervention at sites A and C and at site L after intervention at its paired site (site B), but increased after intervention at all other sites.
| Attendances at ED per night on days when the AIMS was regularly open, n (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 88.89 (11.25) | 57.56 (9.75) | 30.79 (6.49) | 70.74 (11.88) | 74.91 (10.89) | 116.87 (16.71) | 117.80 (8.27) |
| Post AIMS | 66.51 (11.36) | 79.85 (10.52) | 57.60 (9.47) | 32.41 (6.49) | 77.24 (11.73) | 72.65 (11.77) | 120.90 (14.11) | 125.03 (15.51) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 47.72 (9.12) | 54.54 (8.84) | 78.05 (9.30) | 91.34 (12.09) | 61.02 (9.56) | 117.06 (13.82) | 71.53 (10.22) |
| Post AIMS | 112.68(14.85) | 59.71 (9.95) | 50.20 (7.86) | 79.34 (10.68) | 94.41 (12.27) | 66.08 (9.11) | 127.47 12.48) | 78.72 (9.49) |
Tables 66 and 67 show the percentage of male patients (see Table 66) and mean patient age (see Table 67). The mean percentage of male patients across all sites was 52.0% pre intervention and 50.9% post intervention; there is therefore little evidence of men or women being over-represented at any site pre or post implementation. The mean age of patients across all sites was 42.3 years pre intervention and 44.3 years post intervention. All sites excluding site D showed a small increase in mean age post intervention.
| Percentage of patients who were male | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 53.05 | 52.85 | 51.19 | 53.19 | 51.00 | 52.17 | 56.58 |
| Post AIMS | 49.48 | 51.15 | 52.10 | 51.76 | 51.98 | 49.52 | 51.23 | 53.63 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 52.83 | 51.71 | 51.87 | 51.52 | 51.20 | 51.42 | 53.53 |
| Post AIMS | 51.04 | 50.38 | 50.73 | 50.79 | 51.02 | 48.84 | 50.51 | 51.51 |
| Mean age (years) of patients | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 39.97 | 43.22 | 44.69 | 39.29 | 43.10 | 36.47 | 39.00 |
| Post AIMS | 48.24 | 41.41 | 46.32 | 48.75 | 41.73 | 45.60 | 36.56 | 40.16 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 43.54 | 42.80 | 43.41 | 44.31 | 44.10 | 41.87 | 41.89 |
| Post AIMS | 42.95 | 44.80 | 44.63 | 45.82 | 45.33 | 46.17 | 43.80 | 44.09 |
Interrupted time series analysis
Tables 68–70 show the results of ITSA using intervention-site-only analysis (see Table 68), paired analysis with single control sites (see Table 69) and paired analysis with pooled control sites (see Table 70). It was not possible to fit ITSA models for sites G and D owing to irregular opening dates. Bonferroni correction across each set of seven ITSA tests resulted in a p-value of ≤ 0.0143 for statistical significance.
| Site | Constant (p) | t (p) | x (p) | xt (p) | Post-trend difference (p) | F (p) |
|---|---|---|---|---|---|---|
| H | – | – | – | – | – | – |
| A | 87.37 (< 0.001) | 0.004 (0.237) | –4.93 (0.008) | –0.013 (0.001) | –0.009 (< 0.001) | 48.3 (< 0.001) |
| B | 57.20 (< 0.001) | 0.0005 (0.670) | –2.63 (0.108) | 0.008 (0.085) | 0.008 (0.059) | 1.27 (0.285) |
| Ga | – | – | – | – | – | – |
| F | 68.74 (< 0.001) | 0.002 (0.032) | 3.32 (0.176) | 0.006 (0.702) | 0.008 (0.586) | 9.10 (< 0.001) |
| C | 75.07 (< 0.001) | –0.0004 (0.731) | 1.12 (0.623) | –0.010 (0.175) | –0.010 (0.152) | 1.55 (0.201) |
| Da | – | – | – | – | – | – |
| E | 108.47 (< 0.001) | 0.05 (0.572) | –0.22 (0.972) | –0.04 (0.622) | 0.006 (< 0.001) | 13.76 (< 0.001) |
| Site | Constant (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| H | K | – | – | – | – | – | – | – | – | – | – |
| A | N | 43.04 (< 0.001) | 44.33 (< 0.001) | –0.009 (0.052) | 0.013 (< 0.001) | 1.36 (0.368) | –0.004 (0.223) | –6.29 (0.009) | –0.009 (0.060) | –0.018 (< 0.001) | 389 (< 0.001) |
| B | L | 55.46 (< 0.001) | 1.74 (0.193) | 0.002 (0.261) | –0.001 (0.230) | –3.98 (0.007) | 0.003 (0.390) | 1.35 (0.538) | 0.004 (0.449) | 0.006 (0.278) | 15.3 (< 0.001) |
| Ga | M | – | – | – | – | – | – | – | – | – | – |
| F | J | 88.59 (< 0.001) | –19.85 (< 0.001) | –0.001 (0.580) | 0.003 (0.005) | 4.44 (0.102) | –0.03 (0.027) | –1.12 (0.760) | 0.04 (0.069) | 0.036 (0.075) | 124 (< 0.001) |
| C | O | 55.86(< 0.001) | 19.21 (< 0.001) | –0.007 (< 0.001) | 0.007 (< 0.001) | –1.90 (0.265) | –0.001 (0.841) | 3.02 (0.289) | –0.009 (0.342) | –0.016 (0.076) | 69.67 (< 0.001) |
| Da | K | – | – | – | – | – | – | – | – | – | – |
| E | M | 63.36 (< 0.001) | 43.11 (< 0.001) | 0.001 (0.992) | 0.048 (0.301) | 3.48 (0.246) | –0.045 (0.327) | 3.70 (0.586) | 0.003 (0.979) | 0.004 (0.020) | 461 (< 0.001) |
| Site | Constant (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| H | All control sites | – | – | – | – | – | – | – | – | – | – |
| A | All control sites | 71.20 (< 0.001) | 16.05 (< 0.001) | –0.003 (0.490) | 0.007 (< 0.001) | –0.29 (0.766) | –0.002 (0.440) | –4.72 (0.024) | –0.012 (0.009) | –0.014 (< 0.001) | 59.19 (< 0.001) |
| B | All control sites | 74.31 (< 0.001) | –17.10 (< 0.001) | –0.004 (0.003) | 0.005 (< 0.001) | –1.66 (0.244) | 0.002 (0.559) | –1.11 (0.609) | 0.006 (0.307) | 0.002 (0.767) | 273 (< 0.001) |
| G | All control sites | 74.24 (< 0.001) | –43.42 (< 0.001) | –0.005 (< 0.001) | 0.005 (< 0.001) | –3.10 (0.021) | 0.007 (0.128) | 6.04 (0.013) | –0.012 (0.118) | –0.018 (0.026) | 1435 (< 0.001) |
| F | All control sites | 71.73 (< 0.001) | –2.94 (0.017) | 0.006 (< 0.001) | –0.004 (0.004) | 1.29 (0.315) | –0.007 (0.252) | 2.06 (0.456) | 0.013 (0.415) | 0.009 (0.554) | 46.39 (< 0.001) |
| C | All control sites | 71.32 (< 0.001) | 3.90 (0.003) | –0.007 (< 0.001) | 0.007 (< 0.001) | –2.00 (0.066) | 0.003 (0.457) | 3.20 (0.206) | –0.012 (0.127) | –0.019 (0.014) | 32.55 (< 0.001) |
| D | All control sites | 74.84 (< 0.001) | 31.08 (< 0.001) | 0.009 (< 0.001) | 0.004 (< 0.001) | 1.88 (0.163) | –0.004 (0.487) | –7.96 (0.031) | –0.014 (0.456) | –0.005 (0.804) | 264 (< 0.001) |
| E | All control sites | 72.60 (< 0.001) | 37.97 (< 0.001) | 0.047 (0.612) | –0.028 (0.362) | 2.83 (0.164) | 0.033 (0.271) | –1.99 (0.758) | –0.046 (0.615) | 0.0004 (0.770) | 540 (< 0.001) |
The intervention-site-only analysis showed no obvious trend, with effects ranging from 6.3 fewer to 4.0 more ED attendances per night. There was a significant decrease in ED attendances at site A.
The paired analysis with single control sites showed effects ranging from 4.9 fewer to 4.0 more ED attendances per night. There was no obvious trend across cities, though there was a significant decrease in attendances at site A.
After pooling the control sites, the effect of opening AIMSs ranged from eight fewer to six more ED attendances per night. Site G had a significant increase in attendances when Bonferroni correction was applied.
Linear regression analysis (estimated using generalised least squares)
Tables 71 and 72 show the results of linear regression analysis using paired analysis with single control sites (see Table 71) and paired analysis with pooled control sites (see Table 72). Model results do not make sense; for example, site G has an average of 30 ED attendances per night, so it does not make sense for the reduction in ED attendances to be 25 per night when the AIMS sees, on average, less than five cases per night. Bonferroni correction across eight tests resulted in a p-value of ≤ 0.0125 for statistical significance.
| Site | Constant (p) | Open (p) | Marginal effect of open AIMS (p) | Wald χ2 (p) | Overall R2 | |
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| H | M | –50.54 (0.001) | –42.57 (< 0.001) | 0.009 (< 0.001) | 2418 (< 0.001) | 0.677 |
| A | N | 148.26 (< 0.001) | 17.20 (< 0.001) | –0.009 (< 0.001) | 218 (< 0.001) | 0.159 |
| B | L | 105.57 (< 0.001) | 4.77 (< 0.001) | 0.008 (0.103) | 33.53 (< 0.001) | 0.028 |
| G | K | –28.44 (0.422) | –25.21 (< 0.001) | –0.011 (0.767) | 22.89 (< 0.001) | 0.038 |
| F | J | –18.20 (0.274) | –9.19 (< 0.001) | 0.014 (0.486) | 42.71 (< 0.001) | 0.036 |
| C | O | 46.08 (0.001) | 4.00 (0.001) | –0.004 (0.534) | 24.77 (< 0.001) | 0.021 |
| D | K | –62.19 (< 0.001) | 2.05 (0.474) | 0.011 (0.710) | 139 (< 0.001) | 0.108 |
| E | M | 78.84 (< 0.001) | 44.73 (< 0.001) | 0.003 (0.075) | 1435 (< 0.001) | 0.714 |
| Site | Constant (p) | Open (p) | Marginal effect of open AIMS (p) | Wald χ2 (p) | Overall R2 | |
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| H | All control sites | –34.74 (< 0.001) | –8.89 (< 0.001) | 0.009 (< 0.001) | 144.25 (< 0.001) | 0.037 |
| A | All control sites | 24,24 (< 0.001) | 2.26 (0.097) | –0.009 (0.013) | 22.25 (< 0.001) | 0.006 |
| B | All control sites | –41.38 (< 0.001) | 19.98 (< 0.001) | 0.008 (0.521) | 133.46 (< 0.001) | 0.034 |
| G | All control sites | –30.05 (< 0.001) | –42.15 (< 0.001) | –0.011 (0.784) | 91.91 (< 0.001) | 0.026 |
| F | All control sites | –19.93 (< 0.001) | –1.37 (0.604) | 0.014 (0.644) | 53.91 (< 0.001) | 0.014 |
| C | All control sites | –12.86 (< 0.001) | –6.23 (0.002) | –0.004 (0.750) | 47.04 (< 0.001) | 0.013 |
| D | All control sites | –15.10 (0.306) | 36.53 (< 0.001) | 0.011 (0.833) | 112.16 (< 0.001) | 0.029 |
| E | All control sites | –6.56 (0.635) | 49.20 (< 0.001) | 0.003 (0.302) | 1074 (< 0.001) | 0.237 |
As with the primary analysis, the paired analysis with pooled control sites showed markedly different results to the paired analysis with single control sites.
The overall pooled analysis showed markedly different results depending on whether all sites, the original sites (i.e. including sites D and E) or the replacements sites (i.e. including sites H and G) were used. The substantial variation between sites in the ED attendance rate also meant that the overall estimate across sites was subject to substantial uncertainty, with much less precise estimates than for the individual sites. The estimated effect of implementing AIMSs was 5.15 fewer attendances per night (95% CI –10.79 to 0.51 attendances per night; p = 0.074), with a marginal effect of 0.6% (p = 0.020), when all cities were used; 5.02 fewer attendances per night (95% CI –11.98 to 1.93 attendances per night; p = 0.157), with a marginal effect of 0.2% (p = 0.248), when the original cities were used; and 5.46 fewer attendances per night (95% CI –11.79 to 0.88 attendances per night; p = 0.091), with a marginal effect of 0.7% (p = 0.017), when the replacement cities were used. Overall, there was no evidence of an effect from AIMSs on ED attendances.
Stratified by age and treatment
Emergency department attendances aged 14–39 years
The assumption behind this analysis was that people aged 14–39 years would be more likely than those aged ≥ 40 years to attend the ED for alcohol-related reasons during hours of AIMS activity. Therefore, we present analysis for the strata aged 14–39 years only. Table 73 shows the mean ED attendances per day during hours of AIMS activity among those aged 14–39 years at each site pre and post intervention. In general, just over half of ED attendances during hours of AIMS activity were in the age group of 14–39 years. In contrast to the primary analysis, in which most sites showed increases in attendances after intervention, ED attendances for those aged 14–29 years tended to decrease at most sites after intervention.
| Mean ED attendances per night during hours of AIMS activity: aged 14–39 years | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 52.53 | 30.38 | 15.29 | 42.60 | 39.05 | 76.47 | 69.73 |
| Post AIMS | 29.08 | 45.00 | 26.89 | 13.85 | 42.99 | 34.98 | 79.25 | 72.19 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 24.60 | 28.79 | 40.82 | 46.58 | 30.59 | 64.93 | 38.93 |
| Post AIMS | 60.23 | 29.44 | 24.87 | 38.62 | 46.10 | 31.00 | 66.73 | 40.38 |
Tables 74–76 show the results of ITSA using intervention-site-only analysis (see Table 74), paired analysis with single control sites (see Table 75) and paired analysis with pooled control sites (see Table 76). Bonferroni correction across ITSA tests resulted in a p-value of ≤ 0.0143 for statistical significance.
| Site | Constanta (p) | t (p) | x (p) | xt (p) | Post-trend difference (p) | F (p) |
|---|---|---|---|---|---|---|
| Hb | – | – | – | – | – | – |
| A | 53.41 (< 0.001) | –0.002 (0.425) | –2.94 (0.056) | –0.003 (0.323) | –0.006 (< 0.001) | 38.23 (< 0.001) |
| B | 32.43 (< 0.001) | 0.0003 (0.001) | –2.74 (0.019) | 0.008 (0.021) | 0.005 (0.132) | 14.00 (< 0.001) |
| Gc | – | – | – | – | – | – |
| F | 43.81 (< 0.001) | –0.001 (0.123) | –0.90 (0.639) | 0.018 (0.102) | 0.017 (0.130) | 1.56 (0.197) |
| C | 41.76 (< 0.001) | –0.004 (< 0.001) | 0.505 (0.741) | –0.002 (0.705) | –0.006 (0.223) | 14.09 (< 0.001) |
| Dc | – | – | – | – | – | – |
| E | 63.87 (< 0.001) | –0.004 (0.943) | 3.39 (0.410) | 0.005 (0.936) | 0.001 (0.536) | 1.68 (0.170) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | K | – | – | – | – | – | – | – | – | – | – |
| A | N | 22.87 (< 0.001) | 30.54 (< 0.001) | –0.007 (0.046) | 0.005 (0.012) | –0.037 (0.973) | 0.00009 (0.996) | –2.90 (0.121) | –0.003 (0.393) | –0.011 (< 0.001) | 299 (< 0.001) |
| B | L | 29.87 (< 0.001) | 2.55 (0.014) | –0.001 (0.264) | –0.001 (0.067) | 3.29 (0.003) | 0.003 (0.281) | 0.55 (0.734) | 0.004 (0.315) | 0.003 (0.465) | 15.71 (< 0.001) |
| Gc | M | – | – | – | – | – | – | – | – | – | – |
| F | J | 45.86 (< 0.001) | –2.04 (0.118) | –0.002 (0.078) | 0.001 (0.347) | 1.17 (0.608) | –0.017 (0.156) | –2.08 (0.487) | 0.035 (0.031) | 0.033 (0.043) | 8.31 (< 0.001) |
| C | O | 29.31 (< 0.001) | 12.45 | –0.005 | 0.002 (0.026) | –1.65 (0.190) | 0.001 (0.718) | 2.16 (0.276) | –0.003 (0.601) | –0.009 (0.154) | 42.49 (< 0.001) |
| Dc | K | – | – | – | – | – | – | – | – | – | – |
| E | M | 35.43 (< 0.001) | 28.44 (< 0.001) | –0.034 (0.632) | 0.030 (0.413) | 1.17 (0.585) | –0.032 (0.380) | 2.23 (0.631) | 0.037 (0.605) | 0.003 (0.011) | 394 (< 0.001) |
| Site | Constanta (p) | Z (p) | Zt (p) | T (p) | X (p) | Xt (p) | Zx (p) | Zxt (p) | Post-trend difference (p) | F (p) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||||
| Hb | All control sites | – | – | – | – | – | – | – | – | – | – |
| A | All control sites | 38.48 (< 0.001) | 14.77 (< 0.001) | –0.004 (0.256) | 0.002 (0248) | –0.68 (0.341) | –0.0006 (0.719) | –2.34 (0.167) | –0.003 (0.427) | –0.007 (< 0.001) | 62.76 (< 0.001) |
| B | All control sites | 42.04 (< 0.001) | –9.61 (< 0.001) | –0.003 (0.019) | –0.0002 (0.760) | –0.73 (0.499) | 0.003 (0.406) | –2.17 (0.172) | 0.006 (0.214) | 0.003 (0.487) | 181 (< 0.001) |
| G | All control sites | 41.89 (< 0.001) | –24.29 (< 0.001) | –0.003 (0.001) | 0.00009 (0.887) | –2.33 (0.026) | 0.007 (0.063) | 3.70 (0.028) | –0.006 (0.265) | –0.009 (0.091) | 1030 (< 0.001) |
| F | All control sites | 38.87 (< 0.001) | 5.03 (< 0.001) | –0.002 (0.036) | 0.0007 (0.147) | 1.87 (0.023) | –0.007 (0.131) | –2.73 (0.193) | 0.026 (0037) | 0.023 (0.055) | 8.4 (< 0.001) |
| C | All control sites | 38.58 (< 0.001) | 3.33 (0.001) | –0.005 (< 0.001) | 0.001 (0.024) | –1.80 (0.034) | 0.005 (0.086) | 2.38 (0.173) | –0.006 (0.230) | –0.012 (0.029) | 12.24 (< 0.001) |
| D | All control sites | 42.35 (< 0.001) | 29.02 (< 0.001) | 0.007 (< 0.001) | –0.0008 (0.169) | 2.97 (0.001) | –0.008 (0.123) | –6.18 (0.023) | 0.006 (0.643) | 0.013 (0.317) | 371 (< 0.001) |
| E | All control sites | 41.28 (< 0.001) | 24.83 (< 0.001) | 0.029 (0.652) | –0.066 (0.020) | 4.62 (0.011) | 0.067 (0.019) | –0.08 (0.985) | –0.029 (0.649) | –0.0002 (0.822) | 418 (< 0.001) |
As with the primary analysis, there were no obvious trends. The effect of intervention ranged from 3.4 additional to 2.9 fewer attendances per night in the intervention-site-only analysis, with no statistically significant results. The paired analysis with single control sites showed an effect ranging from 2.2 additional to 2.9 fewer attendances per night, with no significant results. The paired analysis with pooled control sites showed an effect ranging from 3.7 additional to 6.2 fewer attendances per night, with no significant results.
Tables 77 and 78 show the results of generalised linear regression using paired analysis with single control sites (see Table 77) and paired analysis with pooled control sites (see Table 78). The results do not make sense and are not commented on further here.
| Site | Constant (p) | Open (p) | Marginal effect of being open (p) | Wald χ2 (p) | Overall R2 | |
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| H | M | 33.45 (0.002) | –28.81 (< 0.001) | 0.003 (< 0.001) | 2059 (< 0.001) | 0.641 |
| A | N | 139.47 (< 0.001) | 13.20 (< 0.001) | –0.005 (0.004) | 243 (< 0.001) | 0.174 |
| B | L | 90.32 (< 0.001) | 0.84 (0.231) | 0.004 (0.283) | 72.35 (< 0.001) | 0.050 |
| G | K | 43.68 (0.027) | –12.68 (< 0.001) | –0.009 (0.645) | 21.59 (< 0.001) | 0.036 |
| F | J | 42.91 (< 0.001) | –1.55 (0.205) | 0.021 (0.096) | 1.75 (0.416) | 0.002 |
| C | O | 74.30 (< 0.001) | 2.50 (0.003) | –0.002 (0.661) | 18.89 (0.001) | 0.016 |
| D | K | 21.01 (0.010) | 11.70 (< 0.001) | 0.015 (0.532) | 46.15 (< 0.001) | 0.039 |
| E | M | 115.79 (< 0.001) | 30.82 (< 0.001) | –0.002 (0.065) | 1373 (< 0.001) | 0.705 |
| Sites | Constant (p) | Open (p) | Marginal effect of being open (p) | Wald χ2 (p) | Overall R2 | |
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| H | All control sites | 21.07 (0.005) | –9.62 (< 0.001) | 0.003 (0.002) | 223 (< 0.001) | 0.056 |
| A | All control sites | 63.23 (< 0.001) | 5.77 (< 0.001) | –0.005 (0.016) | 50.54 (< 0.001) | 0.013 |
| B | All control sites | 20.16 (0.011) | –11.40 (< 0.001) | 0.004 (0.598) | 85.63 (< 0.001) | 0.022 |
| G | All control sites | 24.68 (0.005) | –22.55 (< 0.001) | –0.009 (0.685) | 47.93 (< 0.001) | 0.014 |
| F | All control sites | 37.23 (< 0.001) | 3.90 (0.015) | 0.021 (0.248) | 6.55 (0.039) | 0.002 |
| C | All control sites | 34.95 (< 0.001) | –3.94 (0.001) | –0.002 (0.792) | 10.61 (0.005) | 0.003 |
| D | All control sites | 31.96 (0.002) | 35.19 (< 0.001) | 0.015 (0.665) | 116 (< 0.001) | 0.030 |
| E | All control sites | 39.95 (< 0.001) | 33.32 (< 0.001) | –0.002 (0.210) | 1308 (< 0.001) | 0.274 |
As with the primary analysis, the pooled analysis across all sites showed markedly different results depending on whether the original sites (sites D and E) or the replacements sites (sites H and G) were used, and the overall estimate across sites was much less precise than those for the individual sites. The estimated effect of implementing AIMSs was 3.0 fewer attendances per night (95% CI –6.07 to 0.06 attendances per night; p = 0.055), across all cities a marginal increase of 0.1% (p = 0.511); 3.15 fewer attendances per night (95% CI –6.84 to 0.54 attendances per night; p = 0.094) when the original cities were used; and 3.53 fewer attendances per night (95% CI –6.72 to –0.35 attendances per night; p = 0.030), with a marginal increase of 0.2% (p = 0.136), when the replacement cities were used. Overall, there was no evidence of an effect of AIMSs on ED attendances in those aged 14–39 years, but CIs were wide.
Emergency department attendances with no investigation or treatment
The assumption behind this analysis was that AIMSs would be more likely to divert attendances that did not require any ED investigations or treatments. Therefore, we present analysis for the strata with no ED investigation or treatment only. Table 79 shows the mean ED attendances per day during hours of AIMS activity among those with no ED investigation or treatment recorded at each site pre and post intervention. There was substantial variation between sites in ED attendances with no investigation or treatment, with some sites reporting no such attendances during the pre-intervention period. This is likely to be the result of sites defining or recording investigations or treatments in different ways, for example whether or not observation in the ED and/or provision of written advice are recorded as treatments. The subsequent analysis was not interpretable in the light of this variation and is therefore not presented.
| Mean attendances at ED per night receiving no investigation or treatment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 24.51 | 32.77 | 7.48 | 0.29 | 2.55 | 12.51 | 0.00 |
| Post AIMS | 0.003 | 53.06 | 55.00 | 0.94 | 8.36 | 1.02 | 10.16 | 5.80 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.00 | 3.89 | 13.43 | 0.004 | 24.10 | 2.84 | 8.00 |
| Post AIMS | 2.44 | 0.12 | 0.00 | 13.90 | 10.77 | 4.26 | 2.08 | 13.84 |
Key performance indicators
Total time in the emergency department (including bank holidays): sensitivity analysis
Table 80 shows the median total time in the ED for each pair of sites before and after AIMS implementation at the intervention site. Median times increased markedly at all sites except at sites E and D, which showed little change, and at site H, which had no pre-intervention data.
| Total time (minutes) in ED, median (5th to 95th centiles) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 164 (1 to 554) | 212 (28 to 710) | 152 (20 to 370) | 160 (44 to 238) | 139 (27 to 297) | 175 (24 to 386) | 164 (42 to 262) |
| Post AIMS | 188 (55 to 326) | 177 (1 to 556) | 259 (41 to 969) | 218 (38 to 729) | 196 (57 to 333) | 155 (31 to 313) | 180 (34 to 432) | 163 (37 to 338) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 173 (26 to 328) | 222 (40 to 836) | 183 (39 to 357) | 156 (43 to 315) | 138 (17 to 293) | 181 (35 to 361) | 185 (42 to 239) |
| Post AIMS | 183 (37 to 384) | 1892 (35 to 434) | 239 (49 to 933) | 228 (44 to 649) | 217 (63 to 542) | 155 (22 to 332) | 193 (42 to 496) | 192 (40 to 472) |
Table 81 presents the percentage of attendances seen within 4 hours by site. Percentages are lower post intervention and are lowest for the Welsh cites, at which the 4-hour target had a lower priority than at English sites.
| Percentage of ED attendances of < 4 hours’ total duration | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 71.1 | 62.8 | 90.9 | 97.0 | 92.0 | 90.4 | 94.3 |
| Post AIMS | 90.4 | 70.7 | 47.1 | 66.8 | 89.6 | 88.7 | 86.7 | 89.2 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 90.9 | 65.4 | 90.4 | 90.6 | 92.6 | 88.2 | 95.7 |
| Post AIMS | 86.7 | 85.6 | 50.8 | 59.0 | 63.7 | 88.8 | 80.1 | 82.3 |
Tables 82 and 83 show the results for logistic regression in the paired analysis with single control sites (see Table 82) and paired analysis with pooled control sites (see Table 83). After Bonferroni correction results are statistically significant if p < 0.014. In the paired analysis with single control sites, sites H, B, F and C were significantly less likely and sites A and D were significantly more likely to meet the 4-hour target when an AIMS was open. In the paired analysis with pooled control sites, sites H, G, F, D and E were significantly more likely and sites A, G and C were significantly less likely to meet the 4-hour target when an AIMS was open.
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|
| Intervention | Control | |||
| Ha | K | –0.021 (0.004; < 0.001) | 1678 (< 0.001) | 0.069 |
| A | N | 0.066 (0.007; < 0.001) | 188 (< 0.001) | 0.003 |
| B | L | –0.011 (0.009; 0.220) | 1041 (< 0.001) | 0.023 |
| G | M | 0.018 (0.010; 0.065) | 879 (< 0.001) | 0.115 |
| F | J | –0.050 (0.005; < 0.001) | 620 (< 0.001) | 0.043 |
| C | O | –0.052 (0.006; < 0.001) | 120 (< 0.001) | 0.005 |
| D | K | 0.025 (0.004; < 0.001) | 378 (< 0.001) | 0.009 |
| E | M | –0.015 (0.009; 0.108) | 298 (< 0.001) | 0.012 |
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|
| Intervention | Control | |||
| Ha | K | 0.034 (0.002; < 0.001) | 3127 (< 0.001) | 0.041 |
| A | N | –0.113 (0.004; < 0.001) | 1136 (< 0.001) | 0.013 |
| B | L | –0.014 (0.006; 0.023) | 2275 (< 0.001) | 0.003 |
| G | M | 0.042 (0.008; < 0.001) | 4221 (< 0.001) | 0.149 |
| F | J | 0.044 (0.002; < 0.001) | 2100 (< 0.001) | 0.036 |
| C | O | –0.012 (0.003; < 0.001) | 175 (< 0.001) | 0.004 |
| D | K | 0.048 (0.004; < 0.001) | 1796 (< 0.001) | 0.019 |
| E | M | 0.067 (0.003; < 0.001) | 3177 (< 0.001) | 0.070 |
Pooled analysis showed that sites were more likely to see patients in the ED within the 4-hour target when an AIMS was open. The marginal effect was 0.005 (95% CI –0.060 to 0.069; p = 0.884) across all sites, –0.017 (95% CI –0.108 to 0.074; p = 0.708) when analysis used the original sites and –0.006 (95% CI –0.091 to 0.079; p = 0.892) when analysis used the replacement sites.
Time to treatment
Table 84 shows the median time to treatment at the English sites, Table 85 shows the percentage reporting 0 minutes for time to treatment and Table 86 shows the percentage with missing data for time to treatment. There are marked inconsistencies, particularly between the English and Welsh sites, and between time to treatment and time to completion of treatment at the Welsh sites. At site B the median time to treatment was 239 minutes post intervention. Time to treatment is not used to judge performance in the same way as total time in the ED (there is no specified target and no financial implications for failing to achieve a target), so this may have affected the rigour of recording. Given the inconsistencies in both recording and using time to treatment as a performance indicator, we decided not to proceed with using this measure to evaluate the effect of AIMS implementation.
| Time (minutes) to treatment, median (5th to 95th centiles) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 165 (1 to 563) | 237 (34 to 420) | 61 (3 to 219) | 74 (5 to 1154) | 61 (1 to 199) | 91 (10 to 220) | 84 (14 to 204) |
| Post AIMS | 99 (10 to 216) | 199 (0 to 654) | 239 (239 to 239) | 89 (11 to 296) | 99 (11 to 217) | 52 (0 to 183) | 89 (10 to 222) | 74 (10 to 196) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 83 (7 to 232) | 197 (35 to 715) | 97 (7 to 220) | 65 (0 to 200) | 55 (0 to 184) | 73 (7 to 183) | 108 (5 to 221) |
| Post AIMS | 74 (7 to 184) | 110 (9 to 700) | 210 (44 to 845) | 113 (7 to 319) | 129 (6 to 390) | 59 (3 to 176) | 81 (9 to 193) | 100 (7 to 249) |
| Percentage reporting 0 minutes for time to treatment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 2.1 | 0.1 | 2.7 | 0.02 | 4.6 | 0.7 | 0.1 |
| Post AIMS | 1.3 | 1.7 | 0 | 0.1 | 0 | 8.7 | 1.3 | 0.3 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.5 | 0.2 | 1.2 | 7.1 | 4.4 | 1.0 | 2.5 |
| Post AIMS | 1.0 | 0.2 | 0.04 | 0.6 | 2.8 | 0.8 | 0.9 | 1.0 |
| Percentage with missing data for time to treatment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 27.4 | 56.9 | 24.3 | 0.4 | 3.4 | 11.3 | 0.0 |
| Post AIMS | 0.01 | 66.3 | 95.5 | 2.9 | 10.8 | 1.4 | 8.4 | 4.6 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.0 | 7.1 | 17.2 | 0.0 | 39.5 | 2.3 | 11.2 |
| Post AIMS | 2.2 | 0.2 | 0 | 17.5 | 11.4 | 6.4 | 1.5 | 17.6 |
Time to initial assessment
Table 87 shows the median time to initial assessment, Table 88 shows the percentage reporting 0 minutes for time to initial assessment and Table 89 shows the percentage with missing data for time to initial assessment. The Welsh sites did not report time to initial assessment and some English sites reported high rates of missing or zero data. This probably reflects a lack of consistent use of this measure as a performance indicator with a specified target and financial implications. Given the inconsistencies, we decided not to proceed with analysis to determine whether or not AIMS implementation would affect time to initial assessment in the ED.
| Time (minutes) to initial assessment, median (5th and 95th centiles) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | – | – | 4 (1 to 52) | 11 (3 to 1274) | 6 (0 to 145) | 4 (0 to 34) | 4 (1 to 51) |
| Post AIMS | 0 (0 to 14) | – | – | 17 (2 to 79) | 69 (9 to 207) | 0 (0 to 42) | 6 (0 to 39) | 5 (0 to 33) |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 9 (1 to 53) | – | 4 (0 to 37) | 0 (0 to 36) | 14 (1 to 58) | 15 (3 to 49) | 23 (3 to 154) |
| Post AIMS | 16 (3 to 53) | 16 (2 to 88) | – | 17 (2 to 230) | 7 (0 to 68) | 12 (1 to 54) | 24 (6 to 67) | 5 (0 to 106) |
| Percentage with a time to initial assessment of 0 minutes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | – | – | 2.9 | 0.05 | 39.7 | 26.6 | 3.4 |
| Post AIMS | 58.2 | – | – | 0.2 | 0.02 | 61.2 | 21.9 | 7.0 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 1.0 | – | 11.7 | 64.9 | 4.0 | 1.4 | 0.6 |
| Post AIMS | 1.3 | 0.4 | – | 1.5 | 26.7 | 2.0 | 0.8 | 9.7 |
| Percentage with missing time to initial assessment data | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 100 | 100 | 3.3 | 0.4 | 2.3 | 5.9 | 0.0 |
| Post AIMS | 0.02 | 100 | 100 | 8.3 | 9.6 | 0.5 | 5.2 | 1.0 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 1.4 | 100 | 13.6 | 0.9 | 10.6 | 3.4 | 48.8 |
| Post AIMS | 3.8 | 2.3 | 100 | 8.6 | 7.9 | 3.6 | 5.3 | 10.6 |
Hospital admissions attributable to alcohol intoxication
Table 90 shows the mean number of admissions with AAI on days (starting at midnight) during hours of AIMS activity. This is shown for intervention sites before and after AIMS implementation and for control sites before and after AIMS implementation at the paired intervention site. Numbers of admissions were low, with admission rates varying from less than an admission per week to an admission every one or two days. There was no obvious trend towards admissions increasing or decreasing across intervention or control sites.
| Mean number admitted with AAI per day | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 0.12 | 0.15 | 0.04 | 0.07 | 0.15 | 0.29 | 0.47 |
| Post AIMS | 0.27 | 0.13 | 0.09 | 0.00 | 0.09 | 0.13 | 0.34 | 0.42 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.02 | 0.41 | 0.22 | 0.09 | 0.41 | 0.58 | 0.53 |
| Post AIMS | 0.65 | 0.05 | 0.43 | 0.18 | 0.04 | 0.27 | 0.88 | 0.19 |
Interrupted time series analysis
As the number of admissions were low and infrequent it was decided not to fit ITSA models because the ITSA assumptions were violated and data were not balanced.
Linear regression analysis (estimated using generalised linear models)
Tables 91 and 92 show the results of generalised linear models using intervention-site-only analysis (see Table 91) and paired analysis (see Table 92) to allow for the panel nature of the data. Bonferroni correction across sites and eight tests resulted in a p-value of ≤ 0.0125 for statistical significance. Models fitted poorly and the results were inconsistent and non-significant across the sites and should be treated with caution.
| Site | Constant (p) | Open (p) | Marginal effect of AIMS being open, % (p) | Wald χ2 (p) | Overall R2 |
|---|---|---|---|---|---|
| H | –2.81 (< 0.001) | –0.36 (< 0.001) | 0.007 (0.175) | 91.37 (< 0.001) | 0.075 |
| A | 0.44 (0.220) | 0.07 (0.003) | –0.01 (0.048) | 8.71 (0.013) | 0.009 |
| B | 0.16 (0.782) | –0.22 (< 0.001) | –0.0005 (0.984) | 20.48 (< 0.001) | 0.018 |
| G | 1.48 (0.020) | –0.090 (0.447) | –1.4e-14 (0.999) | 6.01 (0.050) | 0.013 |
| F | –0.24 (0.437) | –0.015 (0.681) | 0.02 (0.500) | 1.06 (0.588) | 0.001 |
| C | 0.69 (0.270) | –0.13 (0.017) | 0.01 (0.652) | 10.04 (0.007) | 0.009 |
| D | –4.48 (< 0.001) | –0.21 (0.123) | –0.2 (0.097) | 24.31 (< 0.001) | 0.040 |
| E | 2.92 (0.001) | 0.22 (< 0.001) | –0.01 (0.039) | 26.16 (< 0.001) | 0.044 |
| Site | Constant (p) | Open (p) | Marginal effect of AIMS being open (p) | Wald χ2 (p) | Overall R2 |
|---|---|---|---|---|---|
| H | –0.22 (0.517) | –0.05 (0.098) | 0.008 (0.108) | 5.20 (0.074) | 0.001 |
| A | –0.33 (0.332) | –0.19 (< 0.001) | –0.01 (0.302) | 27.60 (< 0.001) | 0.008 |
| B | –0.19 (0.571) | –0.23 (< 0.001) | –0.0006 (0.986) | 18.03 (< 0.001) | 0.005 |
| G | –0.16 (0.667) | –0.32 (0.077) | 4.2e-15 (0.999) | 4.35 (0.113) | 0.001 |
| F | –0.38 (0.260) | –0.23 (0.001) | 0.02 (0.745) | 12.24 (0.002) | 0.003 |
| C | –0.35 (0.306) | –0.19 (< 0.001) | 0.01 (0.677) | 13.91 (0.001) | 0.004 |
| D | –0.30 (0.405) | 0.13 (0.247) | –0.2 (0.062) | 4.78 (0.092) | 0.001 |
| E | 0.19 (0.603) | 0.11 (0.006) | –0.01 (0.049) | 7.83 (0.020) | 0.002 |
The marginal effect of AIMSs across all sites was –0.0002% additional admissions per day (95% CI –0.01% to 0.01%; p = 0.975). The effects when only the original sites were used was –0.01% (95% CI –0.01% to –0.006%; p < 0.001) and when the replacement sites were used was 0.004% (95% CI –0.003% to 0.001%; p = 0.279). In summary, the results were inconsistent across sites and showed no overall effect of AIMSs on hospital admissions for alcohol intoxication.
Alcohol-related hospital admissions
Table 93 shows the mean number of alcohol-related admissions on days that started at midnight during hours of AIMS activity. Admission rates varied from less than an admission per week to an admission every one or two days. There was no obvious trend towards admissions increasing or decreasing across intervention or control sites.
| Mean number of alcohol-related admissions per day | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention site | H | A | B | G | F | C | D | E |
| Pre AIMS | – | 0.44 | 0.57 | 0.51 | 0.85 | 0.73 | 1.07 | 1.53 |
| Post AIMS | 0.83 | 0.53 | 0.51 | 0.44 | 0.76 | 0.70 | 1.08 | 1.64 |
| Control site | K | N | L | M | J | O | K | M |
| Pre AIMS | – | 0.61 | 1.04 | 0.89 | 1.36 | 1.36 | 1.69 | 0.86 |
| Post AIMS | 1.78 | 0.53 | 1.24 | 0.49 | 1.51 | 1.37 | 2.16 | 0.79 |
Interrupted time series analysis
As the number of admissions were low and infrequent it was decided not to fit ITSA models because the ITSA assumptions were violated and data were not balanced.
Linear regression analysis (estimated using generalised linear models)
Tables 94 and 95 show the results of generalised linear models using intervention-site-only analysis (see Table 94) and paired analysis (see Table 95) to allow for the panel nature of the data. Bonferroni correction across cities and eight tests resulted in a p-value of ≤ 0.0125 for statistical significance. Models fitted poorly and the results were non-significant across the sites and should be treated with caution.
| Site | Constant (p) | Open (p) | Marginal effect of AIMS being open (p) | Wald χ2 (p) | Overall R2 |
|---|---|---|---|---|---|
| H | –4.51 (< 0.001) | –0.86 (< 0.001) | 0.02 (0.025) | 158.68 (< 0.001) | 0.124 |
| A | –0.67 (0.417) | –0.07 (0.184) | –0.005 (0.649) | 2.83 (0.242) | 0.003 |
| B | –2.56 (0.015) | –0.51 (< 0.001) | 0.06 (0.231) | 29.51 (< 0.001) | 0.026 |
| G | 4.80 (< 0.001) | –0.017 (0.942) | –0.2 (0.271) | 11.26 (0.004) | 0.024 |
| F | –2.33 (0.041) | –0.55 (< 0.001) | 0.08 (0.536) | 18.85 (< 0.001) | 0.017 |
| C | –1.03 (0.403) | –0.49 (< 0.001) | –0.01 (0.853) | 19.30 (< 0.001) | 0.017 |
| D | –7.03 (< 0.001) | –0.70 (0.004) | –0.3 (0.198) | 25.42 (< 0.001) | 0.041 |
| E | 6.62 (< 0.001) | 0.84 (< 0.001) | –0.02 (0.052) | 85.34 (< 0.001) | 0.129 |
| Site | Constant (p) | Open (p) | Marginal effect of AIMS being open (p) | Wald χ2 (p) | Overall R2 |
|---|---|---|---|---|---|
| H | –0.93 (0.151) | –0.38 (< 0.001) | 0.02 (0.016) | 57.22 (< 0.001) | 0.016 |
| A | –1.96 (0.003) | –0.71 (< 0.001) | –0.005 (0.776) | 113.79 (< 0.001) | 0.031 |
| B | –1.83 (0.005) | –0.75 (< 0.001) | 0.06 (0.329) | 61.33 (< 0.001) | 0.017 |
| G | –0.80 (0.251) | –0.76 (0.025) | –0.1 (0.463) | 12.17 (0.002) | 0.004 |
| F | –1.19 (0.070) | –0.53 (< 0.001) | 0.08 (0.574) | 22.74 (< 0.001) | 0.006 |
| C | –1.25 (0.057) | –0.56 (< 0.001) | –0.01 (0.862) | 35.38 (< 0.001) | 0.010 |
| D | –1.07 (0.116) | –0.20 (0.353) | –0.3 (0.180) | 11.42 (0.003) | 0.003 |
| E | –0.16 (0.821) | 0.41 (< 0.001) | –0.02 (0.067) | 33.97 (< 0.001) | 0.010 |
The marginal effect of AIMSs across all sites was 0.002% additional admissions per day (95% CI –0.02% to 0.03%; p = 0.873). The marginal effects when only the original sites were used was –0.002% (95% CI –0.03% to –0.006%; p = 0.004) and when the replacement sites were used was 0.012% (95% CI –0.0006% to 0.02%; p = 0.063). In summary, the results were inconsistent across sites and showed no overall effect from AIMSs on hospital alcohol-related admissions.
Ambulance service key performance indicators
Descriptive statistics
Tables 53 and 54 show the mean number of all ambulance calls (see Table 53) and high-priority calls (see Table 54) per day in each site catchment area pre and post intervention. We noted the marked variation between the mean number of all calls and mean number of high-priority calls. This was explained by ambulance services interpreting our request for calls originating in the site catchment area in different ways. Only the 8–10 post districts nearest to the city centre were provided for sites C and O, whereas all city-region postal districts were provided for sites D and A. Therefore, we undertook a secondary analysis limiting all sites to the eight postal districts nearest to the city centre.
The number of high-priority calls increased after the intervention date at the English sites but decreased at the Welsh sites. This is probably due to the change in call categorisation instituted by the Welsh Ambulance Service during the project as described above. This observation suggests that the effect of the change in categorisation was substantial and means that Welsh-site pre- and post-intervention data are not comparable.
Tables 96 and 97 show the percentage of high-priority calls relating to male patients (see Table 96) and mean patient age (see Table 97). Mean age tended to be higher post intervention in most sites and mean age tended to be higher in the control sites.
| Percentage of calls relating to male patients | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 51.73 | 51.09 | 50.80 | 49.42 | 51.31 |
| Post AIMS | 50.24 | 50.49 | 51.19 | 50.71 | 48.91 | 51.10 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 51.82 | 48.64 | 50.46 | 49.43 | 49.36 |
| Post AIMS | 49.40 | 49.57 | 49.01 | 50.86 | 46.78 | 49.55 |
| Mean age (years) of patients | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 50.18 | 53.19 | 46.37 | 47.85 | 45.65 |
| Post AIMS | 52.67 | 50.81 | 55.58 | 44.73 | 45.66 | 46.22 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 48.53 | 53.98 | 49.50 | 51.36 | 52.19 |
| Post AIMS | 52.57 | 51.95 | 55.73 | 49.72 | 50.96 | 53.94 |
Tables 98 and 99 show the percentage of high-priority calls responded to within 8 minutes (see Table 98) and within 19 minutes (see Table 99). All sites show a decrease in performance against both key indicators over time.
| Percentage of high-priority calls responded to within 8 minutes | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 47.84 | 49.59 | 66.62 | 61.52 | 60.32 |
| Post AIMS | 56.42 | 40.28 | 43.28 | 51.47 | 47.71 | 53.83 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 70.63 | 40.37 | 52.91 | 60.62 | 56.46 |
| Post AIMS | 53.40 | 52.28 | 39.39 | 47.55 | 50.97 | 43.88 |
| Percentage of high-priority calls responded to within 19 minutes | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 86.14 | 90.20 | 98.21 | 96.39 | 95.29 |
| Post AIMS | 89.85 | 80.09 | 85.14 | 94.74 | 92.81 | 90.40 |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 95.61 | 82.93 | 94.80 | 97.84 | 94.45 |
| Post AIMS | 93.17 | 90.68 | 80.14 | 94.00 | 94.38 | 89.18 |
Tables 100 and 101 show the median response time (and IQR) for high-priority calls (see Table 100) and all calls (see Table 101). Median response times generally increased after intervention, reflecting worsening performance over time. Median times at Welsh cities were longer for high-priority calls, probably owing to the different approaches to the categorisation of high-priority calls in England and Wales. At the English sites the median response time was < 8 minutes (i.e. meeting the 8-minute target), which means that > 50% of calls were responded to within 8 minutes. Response times for all calls were slightly longer than for high-priority calls only.
| Response time (minutes), median (IQR) | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 8.7 (4.4–13.1) | 8.7 (4.4–13.1) | 6.6 (4.4–8.7) | 6.6 (4.4–8.7) | 6.6 (4.4–8.7) |
| Post AIMS | 6.6 (4.4–10.9) | 8.7 (4.4–15.3) | 8.7 (4.4–15.3) | 6.6 (4.4–10.9) | 8.7 (6.6–10.9) | 6.6 (4.4–10.9) |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 6.6 (2.2–8.7) | 8.7 (6.6–15.3) | 6.6 (4.4–10.9) | 6.6 (4.4–8.7) | 6.6 (4.4–10.9) |
| Post AIMS | 6.6 (4.4–10.9) | 8.7 (4.4–10.9) | 8.7 (6.6–15.3) | 8.7 (6.6–10.9) | 6.6 (4.4–10.9) | 8.7 (6.6–13.1) |
| Response time (minutes), median (IQR) | ||||||
|---|---|---|---|---|---|---|
| Intervention site | H | A | B | F | C | D |
| Pre AIMS | – | 10.9 (6.6–24.0) | 10.9 (6.6–17.5) | 10.9 (6.6–30.6) | 10.9 (6.6–30.6) | 8.7 (6.6–21.8) |
| Post AIMS | 10.9 (6.6–19.7) | 13.1 (6.6–30.6) | 13.1 (6.6–26.2) | 10.9 (6.6–43.7) | 10.9 (6.6–37.1) | 10.9 (6.6–28.4) |
| Control site | K | N | L | J | O | K |
| Pre AIMS | – | 8.7 (4.4–15.3) | 13.1 (6.6–28.4) | 10.9 (6.6–26.2) | 10.9 (6.6–35.0) | 10.9 (6.6–24.0) |
| Post AIMS | 10.9 (6.6–26.2) | 10.9 (6.6–21.8) | 17.5 (8.7–39.3) | 13.1 (6.6–30.6) | 10.9 (6.6–39.3) | 13.1 (6.6–30.6) |
Key performance indicators analysis
The following results show the marginal effect of an AIMS being open on the proportion of high-priority calls responded to within each time limit (8 or 19 minutes). They provide an estimate of the effect of AIMSs on the proportion of calls achieving the relevant target. Bonferroni correction across all six tests per set of analyses resulted in a p-value of ≤ 0.017 for statistical significance.
Sites E and G are excluded from this analysis because the site E ambulance service was unable to provide data. The change in categorisation of high-priority calls in the Welsh Ambulance Service meant that Welsh and English data were not comparable and that pairing a Welsh site with an English site would not be appropriate for ambulance data. Because we had data from only one Welsh control site, we decided to pair site A with site L instead of site N in the paired analysis. This at least meant that the Welsh sites were paired with a control site that had undergone the same change in categorisation of high-priority calls.
Tables 102 and 103 show the results of analysis of the 8-minute target on single sites (i.e. without using the control sites; see Table 102) and the analysis on paired sites (in which each intervention site is paired with its control site; see Table 103). In the intervention-site-only analysis, the marginal effect at each site ranged from a 4.6% improvement to a 7.1% deterioration in performance. The only statistically significant effects were the 4.6% improvement in performance seen at site D and the 7.1% and 5.1% deteriorations in performance seen at sites F and A, respectively. The paired analysis produced more varied results, with marginal effects ranging from a 7% improvement to a 2.4% deterioration in performance. Only the improvements at sites D and B were statistically significant.
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 |
|---|---|---|---|
| H | 0.006 (0.013; 0.626) | 296.35 (< 0.001) | 0.011 |
| A | –0.051 (0.010; < 0.001) | 67.98 (< 0.001) | 0.0023 |
| B | –0.008 (0.015; 0.601) | 64.21 (< 0.001) | 0.0034 |
| F | –0.071 (0.012; < 0.001) | 379.12 (< 0.001) | 0.016 |
| C | 0.012 (0.021; 0.590) | 186.31 (< 0.001) | 0.020 |
| D | 0.046 (0.010; < 0.001) | 422.74 (< 0.001) | 0.009 |
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|
| Intervention | Control | |||
| H | K | 0.003 (0.005; 0.506) | 752.11 (< 0.001) | 0.011 |
| A | N | –0.005 (0.006; 0.418) | 65.81 (< 0.001) | 0.002 |
| B | L | 0.041 (0.011; < 0.001) | 97.78 (< 0.001) | 0.003 |
| F | J | 0.018 (0.009; 0.046) | 581.64 (< 0.001) | 0.014 |
| C | O | –0.024 (0.013; 0.063) | 267.55 (< 0.001) | 0.015 |
| D | K | 0.070 (0.009; < 0.001) | 839.75 (< 0.001) | 0.010 |
Tables 104 and 105 show the results of analysis of the 19-minute target on single sites (see Table 104) and paired sites (see Table 105). In the intervention-site-only analysis, the marginal effect at each site ranged from a 4.1% improvement to a 3.9% deterioration in performance, with statistically significant improvements seen at site C and significant deteriorations at sites B and A. The paired analysis produced more varied results, ranging from a 2.4% improvement to a 4% deterioration in performance. There were statistically significant improvements at site B and significant deteriorations at sites A and H.
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 |
|---|---|---|---|
| H | 0.002 (0.008; 0.801) | 135.46 (< 0.001) | 0.0101 |
| A | –0.039 (0.008; < 0.001) | 90.55 (< 0.001) | 0.004 |
| B | –0.029 (0.010; 0.004) | 78.11 (< 0.001) | 0.008 |
| F | –0.007 (0.004; 0.077) | 175.97 (< 0.001) | 0.040 |
| C | 0.041 (0.011; < 0.001) | 114.82 (< 0.001) | 0.044 |
| D | –0.001 (0.004; 0.743) | 251.83 (< 0.001) | 0.016 |
| Site | Marginal effect if AIMS open (SE; p) | Likelihood ratio χ2 (p) | Pseudo R2 | |
|---|---|---|---|---|
| Intervention | Control | |||
| Ha | K | –0.040 (0.003; < 0.001) | 398.18 (< 0.001) | 0.014 |
| A | N | –0.020 (0.005; < 0.001) | 114.33 (< 0.001) | 0.004 |
| B | L | 0.024 (0.007; < 0.001) | 107.18 (< 0.001) | 0.006 |
| F | J | 0.006 (0.003; 0.031) | 217.93 (< 0.001) | 0.023 |
| C | O | –0.005 (0.004; 0.300) | 171.72 (< 0.001) | 0.038 |
| D | K | 0.0002 (0.004; 0.960) | 364.01 (< 0.001) | 0.012 |
We did not undertake pooled analysis across all sites because of the inconsistency between English and Welsh Ambulance Service data. However, as the English sites had reasonably consistent call categorisation across the study period, we undertook a pooled analysis limited to English sites. The marginal effect across all English sites for the 8-minute target was –0.0145 (95% CI –0.0209 to –0.0082; p < 0.001) and for the 19-minute target was –0.0310 (95% CI –0.0345 to –0.0275; p < 0.001). When analysis was limited to the original English sites, the effect for the 8-minute target was 0.0241 (95% CI 0.0133 to 0.0350; p < 0.001) and for the 19-minute target was 0.0067 (95% CI 0.0026 to 0.0109; p = 0.002). When the replacement sites instead of the original sites were used, the effect for the 8-minute target was –0.0254 (95% CI –0.0324 to –0.0183; p < 0.001) and for the 19-minute target was –0.0389 (95% CI –0.0429 to –0.0350; p < 0.001).
In summary, we found some evidence of an effect from AIMSs on the 8-minute and 19-minute targets. However, effects for individual sites were varied and inconsistent.
Appendix 7 Cost-effectiveness
| Intervention site | Number of ambulance calls per day, mean (% designated high priority) | Control site | Number of ambulance calls per day, mean (% designated high priority) | ||
|---|---|---|---|---|---|
| Pre intervention | Post intervention | Pre intervention | Post intervention | ||
| H | 93.60 (37.29) | K | 135.60 (42.48) | ||
| A | 172.50 (49.16) | 189.50 (42.48) | N | 70.30 (39.40) | 70.40 (43.47) |
| B | 120.80 (46.19) | 131.80 (33.08) | L | 90.20 (49.78) | 96.70 (31.33) |
| F | 77.80 (37.02) | 80.60 (48.88) | J | 88.30 (36.92) | 88.00 (41.36) |
| C | 28.20 (39.01) | 30.50 (50.16) | O | 28.60 (34.97) | 30.20 (48.34) |
| D | 179.90 (39.63) | 191.30 (42.81) | K | 135.70 (40.97) | 135.50 (48.12) |
| Intervention site | Percentage of priority calls responded to, within 8 minutes (within 19 minutes) | Control site | Percentage of priority calls responded to, within 8 minutes (within 19 minutes) | ||
|---|---|---|---|---|---|
| Pre intervention | Post intervention | Pre intervention | Post intervention | ||
| H | 56.19 (90.52) | K | 54.95 (93.99) | ||
| A | 48.31 (89.55) | 39.79 (83.39) | N | 68.01 (95.37) | 49.81 (89.17) |
| B | 50.26 (90.88) | 44.11 (86.18) | L | 42.50 (85.84) | 40.17 (82.05) |
| F | 66.29 (98.50) | 51.77 (95.21) | J | 54.87 (95.92) | 47.74 (94.91) |
| C | 63.61 (97.80) | 51.69 (94.51) | O | 61.65 (98.33) | 53.01 (95.68) |
| D | 62.34 (96.06) | 54.67 (90.82) | K | 57.96 (95.06) | 45.68 (90.70) |
| Staff member | Cost (£) | Source/notes | |
|---|---|---|---|
| Per hour | Total | ||
| Consultant | 135 | 270 | PSSRU.91 Consultant: medical with qualifications |
| Paramedic | 45 | 90 | Agenda for Change band 6; estimated from PSSRU.91 Hospital-based scientific and professional staff |
| Police | 58 | 116 | Heslin, et al.92 |
| Finance (NHS band 4) | 28 | 56 | Estimated from PSSRU.91 Hospital-based nurses band 4. Using this as estimation as average salary is similar |
| Council representative | 28 | 56 | Site J council: team leader, grade 7 (£28,485 per annum); business support officer, grade 3 (£16,123–17,772 per annum). Assuming to be same as finance band 4 in NHS |
| Total | 588 | ||
| Site | Source |
|---|---|
| A | Budget 2014/2015 (estimated after the third quarter) |
| G | 2016 and 2017 actual spend/budget |
| C | Returned costing template |
| F | Average cost per weekend service provision |
| H | 2017/2018 budget |
| B | Figures collated from economic evaluation of the site B city-centre AIMS scheme |
| Staff | Cost (£) | ||||
|---|---|---|---|---|---|
| Site | |||||
| A | G | C | H | B | |
| Management and administration | |||||
| Management/administration services | 22,229 | 14,516 | 1120 | 25,130 | 15,000 |
| Clerical | 5000 | ||||
| Total | 22,229 | 14,516 | 11,200 | 25,130 | 20,000 |
| Medical | |||||
| Nurses | 79,399 | 56,472 | |||
| Paramedics/ambulance | 69,149 | 33,500 | |||
| St John Ambulance | 7750 | ||||
| Health-care support workers | 33,600 | ||||
| First aiders | 16,416 | ||||
| Combined medical staff (where individual costs not available) | 62,400 | ||||
| Total | 164,964 | 0 | 90,072 | 41,250 | 62,400 |
| Security | |||||
| Police | 24,021 | 22,464 | |||
| Security | 12,656 | 8250 | |||
| Total | 24,021 | 0 | 12,656 | 8250 | 22,464 |
| Other | |||||
| Street marshalsa | 12,656 | ||||
| Street Pastorsa | 10,133 | ||||
| Volunteer support staff | 3080 | ||||
| Total | 10,133 | 0 | 12,656 | 0 | 3080 |
| Voluntary | |||||
| Volunteers | 12,209 | ||||
| Combined total | |||||
| Excluding volunteers | 231,325 | 14,516 | 126,584 | 74,630 | 107,944 |
| Including volunteers | 231,325 | 14,516 | 126,584 | 74,630 | 120,153 |
| Source of cost | Cost (£) | ||||
|---|---|---|---|---|---|
| Site | |||||
| A | G | C | H | B | |
| Premises costs | 11,623 | 5400 | 15,000 | 1500 | 16,668 |
| Business rates | 13,000 | (included in premises costs) | |||
| Service costs | 1388 | 720 | 8976 | ||
| Combined total | 11,623 | 6788 | 28,000 | 2220 | 25,644 |
| Source of cost | Cost (£) | ||
|---|---|---|---|
| Site | |||
| G | H | B | |
| Advertising | 840 | 1200 | |
| Audit/accountancy/bank charges | 429 | 5500 | |
| Consumables | 480 | 2100 | 2162 |
| Consumables (testing equipment) | 2100 | ||
| Data systems | 116 | ||
| Insurance | 4888 | 4950 | |
| Insurance (vehicle) | 3800 | ||
| Office-related consumables | 772 | (included elsewhere) | |
| Other costs | 4560a | 11,450b | |
| Related to staffing | 9555 | 3775 | |
| Vehicle related | 1200 | 6500 | |
| Combined total | 24,940 | 39,275 | 2162 |
| Site | Cost (£) | Number of nights open | Average cost (£) per session | |||
|---|---|---|---|---|---|---|
| Staff | Premises | Other | Total | |||
| A | 231,325 | 11,623 | 242,948 | 112 | 2170 | |
| G | 14,516 | 6788 | 24,940 | 46,244 | 39 | 1186 |
| C | 126,584 | 18,000 | 144,584 | 112 | 1380 | |
| F | 55,900a | 102 | 1075 | |||
| H | 74,630 | 2220 | 39,275 | 116,125 | 105 | 1106 |
| B | 107,944 | 25,644 | 2162 | 135,750 | 110 | 1345 |
Appendix 8 The AIMS resource inventory
For all resources we need to know who meets the costs (e.g. NHS, public sector, private sector, charity).
Business plan/budget.
Staffing.
Premises (including any new premises).
Communication: information required for information gathering and sharing, for example funding required for patient record systems or sending information on attendances to other systems such as general practice or emergency departments.
In addition, whether or not brief intervention/evaluation is being carried out and whether or not any support services are needed for this.
| Staff costs: everyday running of the AIMS | ||||
|---|---|---|---|---|
| Average number of people | % of WTE | Grade | Funder (e.g. NHS, public sector, voluntary) | |
| Management and administration of services | ||||
| Clerical | ||||
| Data systems | ||||
| Staff costs: staff employed now – full-time/whole time equivalent/shifts and grade | |||||
|---|---|---|---|---|---|
| Staff | Average number per session | WTE | Grade | Funder (e.g. NHS, public sector, voluntary) | Shifts worked |
| Security | |||||
| Police | |||||
| Paramedics | |||||
| Consultants | |||||
| Nurses | |||||
| Street Pastors | |||||
| St John Ambulance staff | |||||
| Health-care support workers | |||||
| First aiders | |||||
| Other | |||||
Facilities.
What is provided by whom?
Consumables (what are they and how often are these replenished?).
Equipment (e.g. computers, trolleys; may be included in the business case).
Accommodation (may be included in the business case).
Data systems, licences, software and hardware.
Appendix 9 Ethnographic data set
| Case | Site | Date | Number of participants | Observations | Number of interviews | Documents |
|---|---|---|---|---|---|---|
| 1 | A | June 2016 to October 2016 | 49 | 20 fieldwork episodes with AIMS staff, ED staff, ambulance crew, police, Street Pastors and other NTE agents, totalling ≈ 125 hours | 16 transcribed interviews (plus interviews conducted in the field as part of the fieldwork) | AIMS SOP, AIMS injury pro forma, ambulance crew documentation, ED patient documentation |
| 2 | B | August 2017 to December 2017 | 48 | 16 fieldwork episodes with AIMS staff, ED staff, ambulance crews, police, Street Pastors and other NTE agents, totalling ≈ 118 hours | Five transcribed interviews (plus interviews conducted in the field as part of the fieldwork) | AIMS SOP, AIMS patient documentation, AIMS communications materials, ED patient documentation |
| 3 | J | February 2017 to June 2017 | 45 | 16 fieldwork episodes with ED staff, ambulance crews, police, Street Pastors and other NTE agents, totalling ≈ 120 hours | Six transcribed interviews (plus interviews conducted in the field as part of fieldwork) | ED patient documentation, ambulance crew documentation, police NTE maps showing resource allocation and plan for shift |
Appendix 10 The AIMS users interview topic guide
Thank you for agreeing to the interview.
Check again that the person still consents to the interview and it being recorded.
I’d like to talk to you about the visit you had to the [alcohol intoxication management service (use local name)] on [date].
| 1 | Tell me about the decision to go to the service |
| Prompt: Who made the decision? What transport was used? What time, approximately, was this? | |
| 2 | Tell me about what happened to you while you were there |
| Prompt: tests and treatments? | |
| Prompt: interactions with doctors, nurses, reception, police, other staff? | |
| Prompt: what was the environment like? | |
| Prompt: was it comfortable? Welcoming? | |
| 3 | Did you get any information or advice about drinking alcohol while you were there? |
| If yes: what was it? Who gave it? When was it given? What did you think about it? | |
| If no: is it a good idea to do this? | |
| 4 | Tell me about being discharged/sent home/being told you may leave the service |
| Prompt: what time, approximately, did you leave the AIMS? | |
| Prompt: did you feel it was the right time to leave? | |
| Prompt: were you offered any help getting home? | |
| Prompt: were you encouraged to stay longer? Were staff happy for you to leave? | |
| 5 | Do you think these types of services are a good idea? |
| Prompt: what is good about them? | |
| Prompt: do you think there are any problems with them? | |
| Prompt: what improvements would you like to see? | |
| 6 | What do you think about the alternatives to AIMSs? |
| Prompt: how do AIMSs compare with A&E? | |
| Prompt: would you have preferred to have been taken to A&E/another service? If so, why? | |
| 7 | Anything else you want to say? |
THANK YOU FOR YOUR TIME.
WE WILL SEND THE VOUCHER TO YOU AT THIS ADDRESS [CHECK THIS].
Appendix 11 The AIMS users: case studies
We expected AIMS users to be young people who had drunk too much alcohol and were either incapacitated, had injured themselves or had been victims of violence. We identified a broad range of users and offer a detailed case summary of four, selected to showcase this heterogeneity: young people found intoxicated by workers or volunteers in the NTE (see Case 1 and Case 4), workers in the NTE who had been either in an accident or a victim of violence caused by alcohol-intoxicated customers (see Case 2) and people who were concerned that their drinks had been spiked (see Case 3).
Case 1
Young male found acutely intoxicated by Street Pastors in an alleyway by large chain pub.
Circumstances
A local male in his early 20s found by Street Pastors just before midnight in an alleyway next to a large chain pub where he had been with friends. He vomited in the street and was offered water and tissues. The Street Pastors offered further treatment at a local AIMS. The patient was picked up by an AIMS roving vehicle and escorted by AIMS staff and friends.
AIMS treatment
On arriving at around midnight, the patient was taken into the ‘recovery room’, which had mattresses on the floor. An AIMS volunteer took his blood pressure, heart rate and temperature and breathalysed him. He was also given bottles of water and a sick bowl before being allowed to sleep for a while.
Discharge
About 3 hours later the patient was sufficiently sober to provide contact details of a friend to collect him and take him home. AIMS staff called a taxi and discharged him home with a friend. No advice or information was given on alcohol use.
Patient view
At interview, this person expressed gratitude towards the friendly staff and was highly satisfied with the service. He commented that if the AIMS had not been there it would have been a ‘hassle’ for friends to have to look after him:
I’d have probably have been ill in a taxi, so I’d have probably had to pay a lot of money, so probably, worse scenario, I’d probably have had to go to the A&E to get sorted out there, but I’m not sure.
Case 2
Bartender in a club injured while working behind the bar.
Circumstances
Shortly after midnight, a male bartender in his early 20s at a local nightclub refused service to a male who then punched the bartender in the face. He was aware of the AIMS and its location (less than 2 minutes’ walk away). His manager and attending police recommended he attend the AIMS for treatment at the end of his shift.
AIMS treatment
A physical examination of the head was undertaken by an onsite paramedic to check for concussion. His blood pressure and heart rate were taken, and painkillers and water offered. The patient was advised by AIMS staff to attend the ED for radiography to check whether or not his cheekbone was broken.
Discharge
At about 03.00 the patient called a friend who collected him by car. Although advised to go directly to the ED for radiography, the patient opted to go home and instead attended the ED later that day.
Patient view
At interview, this person indicated that he was very grateful for the care given and impressed by the service in general and was particularly struck by the compassion of the staff:
A woman that came in and she was absolutely annihilated from drinking too much and the [AIMS staff] was asking her if she had any way home, a friend to call or a taxi and potentially even the police driving her back to her place, so that was pretty cool to see.
The compassion, the compassion and the help, the lengths that the council, volunteers and police are willing to go.
Case 3
Young male out with friends at university suspected that his drink had been ‘spiked’.
Circumstances
A young male in his early 20s was out at a nightclub with friends. At around midnight he suddenly complained of feeling extremely dizzy and nauseated, with very slurred speech, and fell over in the club. Club staff thought that he was very drunk and took him into a first aid room. The young man recalled that this first aid room was very noisy and stressful. He was taken the very short distance to the local AIMS by wheelchair.
AIMS treatment
The young male was sat on a chair and given water and encouraged to steady his breathing to calm down. A blood test was undertaken.
Discharge
At around 01.00 AIMS staff felt that it was an appropriate time for him to be discharged and called a taxi, which took him and a friend home.
Patient view
At interview this person was adamant that his drink had been spiked and suggested that this could have been flunitrazepam. He felt that he had been discharged too early:
I was still in quite a bad state. I was struggling to walk, my vision was still blurry, but they let me go anyway and let me get in a taxi just with my girlfriend on her own. At this point I just, I didn’t really know what was happening. If I was in any sober state, I’d have never got in the taxi.
Overall, the patient felt that he would have preferred to have been treated at the AIMS rather than at the noisy nightclub first aid room or at ED, which he thought would be busy and stressful.
Case 4
Young female out drinking on a mid-week student night out.
Circumstances
A young woman in her early 20s was drinking at home first and then drinking with friends in a nightclub. Having drunk too much alcohol, she went to the toilet where she was sick and fell asleep. Her friends assumed that she had gone home and they left the club. When staff checked the toilets after the club closed at around 03.30 they discovered her slumped in the cubicle. The manager of the club called the local AIMS, which sent volunteers with a wheelchair to collect her. The young woman felt disoriented because she had lost her friends and had no phone signal.
AIMS treatment
The paramedic, police and volunteers at the AIMS provided reassurance and gave the woman water and a sick bowl. They kept her talking and awake, asking her about the circumstances of her night out and her use of alcohol. They also gave her advice on how to stay safe with friends in future.
Discharge
After about 1 hour, the patient was strongly encouraged by AIMS staff to contact a friend and for this friend to pick her up. A taxi was called by the staff to collect the patient and her friend.
Patient view
This person was very grateful to be seen in an AIMS rather than an ED, ‘because if you go into A&E as a result of drinking, you’re a low priority most of the time, because it’s self-inflicted’.
Furthermore, the patient expressed humiliation about the situation and was very grateful for the AIMS and for its staff taking good care of her: ‘I am really mortified about this; it was the most embarrassing thing that ever happened’.
She imagined that if the AIMS had not been there, she would have been taken out of the club by the club staff and left to find a taxi, which she felt she may not have managed as she was not familiar with the city: ‘Without the [AIMS], God knows where I would’ve ended up’.
Appendix 12 The AIMS survey sample
| Site | Number of survey responses |
|---|---|
| Fixed sites | |
| A | 59 |
| B | 39 |
| C | 22 |
| G | 17 |
| Mobile sites | |
| F | 28 |
| H | 43 |
| All | 208 |
| Age (years) of respondents | Number of survey responses | ||
|---|---|---|---|
| Male respondents | Female respondents | Total | |
| 17–24 | 57 | 51 | 108 |
| 25–34 | 27 | 21 | 48 |
| ≥ 35 | 16 | 16 | 32 |
| Total | 100 | 88 | 188a |
| Service provided | Number of people who received care | Percentage of attendees who received care | ||
|---|---|---|---|---|
| Site | ||||
| Fixed | Mobile | Alla | ||
| Who looked after person while at AIMS | (n = 134) | (n = 68) | ||
| Paramedic | 79 | 32.8 | 51.5 | 39.1 |
| Nurse | 73 | 52.2 | 4.4 | 36.1 |
| Volunteer | 69 | 19.4 | 63.2 | 34.2 |
| Police | 26 | 15.7 | 7.4 | 12.9 |
| Doctor | 7 | 4.5 | 1.5 | 3.5 |
| Otherb | 33 | 23.1 | 2.9 | 16.3 |
| Treatment, tests or advice received | (n = 130) | (n = 64) | ||
| General support | 112 | 53.1 | 67.2 | 57.7 |
| Water to drink | 107 | 56.9 | 51.6 | 55.2 |
| Injury care | 46 | 20.8 | 29.7 | 23.7 |
| Advice about safer alcohol use | 33 | 16.9 | 17.2 | 17.0 |
| Referral to ED/hospital | 26 | 13.1 | 14.1 | 13.4 |
| Medication | 13 | 8.5 | 3.1 | 6.7 |
| Information about alcohol support services | 12 | 6.2 | 6.3 | 6.2 |
| Fluids via drip | 6 | 3.8 | 1.6 | 3.1 |
| Breathalysed/urine tested | 5 | 3.8 | 0.0 | 2.6 |
| Otherc | 26 | 11.5 | 12.5 | 11.9 |
| Preferred place of treatment | n | Percentage of total | ||
|---|---|---|---|---|
| All sites (N = 187) | Fixed sites (N = 122) | Mobile sites (N = 65) | ||
| I was happy to be treated here | 145 | 77.5 | 75.4 | 81.5 |
| Home | 26 | 13.9 | 14.8 | 12.3 |
| Local ED/hospital | 15 | 8.0 | 9.0 | 6.2 |
| Different treatment/health service | 1 | 0.5 | 0.8 | 0.0 |
Appendix 13 Details of the emergency department user survey results
This appendix details the responses of intervention and control site ED users to the patient experience survey and the results of secondary analysis excluding sites D (intervention) and K (control).
Service ratings
Tables 118–125 outline responses to questions to rate aspects of the service. There were no obvious differences between intervention or control sites for any question.
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 187 | 83 | 32 | 7 | 6 | 315 |
| % | 59.4 | 26.4 | 10.2 | 2.2 | 1.9 | 100 |
| Control | ||||||
| n | 248 | 138 | 53 | 17 | 9 | 465 |
| % | 53.3 | 29.7 | 11.4 | 3.7 | 1.9 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 184 | 93 | 21 | 9 | 7 | 314 |
| % | 58.6 | 29.6 | 6.7 | 2.9 | 2.2 | 100 |
| Control | ||||||
| n | 261 | 138 | 31 | 14 | 4 | 448 |
| % | 58.3 | 30.8 | 6.9 | 3.1 | 0.9 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 153 | 92 | 35 | 22 | 9 | 311 |
| % | 49.2 | 29.6 | 11.3 | 7.1 | 2.9 | 100 |
| Control | ||||||
| n | 236 | 144 | 47 | 24 | 6 | 457 |
| % | 51.6 | 31.5 | 10.3 | 5.3 | 1.3 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 141 | 84 | 32 | 31 | 25 | 313 |
| % | 45.1 | 26.8 | 10.2 | 9.9 | 8.0 | 100 |
| Control | ||||||
| n | 220 | 116 | 54 | 46 | 26 | 462 |
| % | 47.6 | 25.1 | 11.7 | 10.0 | 5.6 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 209 | 63 | 18 | 11 | 15 | 316 |
| % | 66.1 | 19.9 | 5.7 | 3.5 | 4.8 | 100 |
| Control | ||||||
| n | 313 | 95 | 30 | 13 | 13 | 464 |
| % | 67.5 | 20.5 | 6.5 | 2.8 | 2.8 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 201 | 64 | 28 | 14 | 8 | 315 |
| % | 63.8 | 20.3 | 8.9 | 4.4 | 2.5 | 100 |
| Control | ||||||
| n | 293 | 107 | 32 | 15 | 13 | 460 |
| % | 63.7 | 23.3 | 7.0 | 3.3 | 2.8 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 164 | 75 | 34 | 21 | 15 | 309 |
| % | 53.1 | 24.3 | 11.0 | 6.8 | 4.9 | 100 |
| Control | ||||||
| n | 253 | 118 | 42 | 30 | 16 | 459 |
| % | 55.1 | 25.7 | 9.2 | 6.5 | 3.5 | 100 |
| Site | Very good | Fairly good | Neither good nor poor | Fairly poor | Very poor | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 144 | 77 | 47 | 19 | 22 | 309 |
| % | 46.6 | 24.9 | 15.2 | 6.2 | 7.2 | 100 |
| Control | ||||||
| n | 244 | 115 | 52 | 24 | 23 | 458 |
| % | 53.3 | 25.1 | 11.4 | 5.2 | 5.0 | 100 |
Perception of threat by other patients or visitors
Table 126 outlines the number and percentage of respondents who felt threatened by other patients or visitors. There were no obvious differences between intervention and control sites.
| Site | Yes, definitely | Yes, to some extent | No | Total |
|---|---|---|---|---|
| Intervention | ||||
| n | 21 | 49 | 249 | 319 |
| % | 6.6 | 15.4 | 78.1 | 100 |
| Control | ||||
| n | 16 | 54 | 392 | 462 |
| % | 3.5 | 11.7 | 84.9 | 100 |
Perception of negative experiences
Tables 127–132 outline the number and percentage of respondents agreeing or disagreeing with negative statements about ED experience. There were no obvious differences between intervention and control sites.
| Site | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 33 | 72 | 54 | 82 | 70 | 311 |
| % | 10.6 | 23.2 | 17.4 | 26.4 | 22.5 | 100 |
| Control | ||||||
| n | 53 | 82 | 75 | 136 | 112 | 458 |
| % | 11.6 | 17.9 | 16.4 | 29.7 | 24.5 | 100 |
| Site | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 57 | 71 | 41 | 84 | 58 | 311 |
| % | 18.3 | 22.8 | 13.2 | 27.0 | 18.6 | 100 |
| Control | ||||||
| n | 67 | 73 | 78 | 131 | 112 | 461 |
| % | 14.5 | 15.8 | 16.9 | 28.4 | 24.3 | 100 |
| Site | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 33 | 37 | 54 | 91 | 68 | 283 |
| % | 11.7 | 13.1 | 19.1 | 32.2 | 24.0 | 100 |
| Control | ||||||
| n | 41 | 49 | 83 | 131 | 124 | 428 |
| % | 9.6 | 11.5 | 19.4 | 30.6 | 29.0 | 100 |
| Site | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 59 | 49 | 53 | 68 | 62 | 291 |
| % | 20.3 | 16.8 | 18.2 | 23.4 | 21.3 | 100 |
| Control | ||||||
| n | 62 | 69 | 65 | 119 | 117 | 432 |
| % | 14.4 | 16.0 | 15.1 | 27.6 | 27.1 | 100 |
| Site | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 44 | 42 | 66 | 70 | 67 | 289 |
| % | 15.2 | 14.5 | 22.8 | 24.2 | 23.2 | 100 |
| Control | ||||||
| n | 43 | 47 | 92 | 130 | 120 | 432 |
| % | 10.0 | 10.9 | 21.3 | 30.1 | 27.8 | 100 |
| Site | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Total |
|---|---|---|---|---|---|---|
| Intervention | ||||||
| n | 19 | 17 | 47 | 95 | 110 | 288 |
| % | 6.6 | 5.9 | 16.3 | 33.0 | 38.2 | 100 |
| Control | ||||||
| n | 27 | 41 | 61 | 125 | 179 | 433 |
| % | 6.2 | 9.5 | 14.1 | 28.9 | 41.3 | 100 |
Overall experience
Table 133 shows how the overall experience of the ED visit was rated on a scale from 0 (very poor experience) to 10 (very good experience).
| Site | Rating | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Intervention | |||||||||||
| n | 8 | 9 | 8 | 11 | 8 | 39 | 26 | 32 | 62 | 49 | 60 |
| % | 2.6 | 2.9 | 2.6 | 3.5 | 2.6 | 12.5 | 8.3 | 10.3 | 19.9 | 15.7 | 19.2 |
| Control | |||||||||||
| n | 13 | 11 | 4 | 14 | 20 | 39 | 42 | 55 | 96 | 73 | 94 |
| % | 2.8 | 2.4 | 0.9 | 3.0 | 4.3 | 8.5 | 9.1 | 11.9 | 20.8 | 15.8 | 20.4 |
Appendix 14 Emergency department user survey: additional results
Response rates
| Site | Number sent first mailing | Number sent reminders | Number returned | Response rate (%) | Number remaining after exclusions |
|---|---|---|---|---|---|
| Intervention | |||||
| A | 286 | 252 | 73 | 25.5 | 60 |
| B | 360 | 300 | 115 | 31.9 | 44 |
| C | 261 | 227 | 65 | 24.9 | 59 |
| F | 387 | 351 | 69 | 17.8 | 61 |
| D | 490 | 467 | 65 | 13.3 | 56 |
| E | 400 | 375 | 70 | 17.5 | 60 |
| All | 2184 | 1972 | 457 | 20.9 | 340 |
| Control | |||||
| L | 287 | 247 | 73 | 25.4 | 26 |
| K | 517 | 436 | 123 | 23.8 | 117 |
| O | 550 | 489 | 85 | 15.5 | 81 |
| M | 600 | 520 | 145 | 24.2 | 124 |
| N | 276 | 258 | 67 | 24.3 | 57 |
| J | 500 | 448 | 105 | 21.0 | 87 |
| All | 2730 | 2398 | 598 | 21.9 | 492 |
Respondent characteristics
| Characteristic | Site | |
|---|---|---|
| Intervention | Control | |
| Mean age (years) | 51.6 | 53.7 |
| Female, n (%) | 165 (51.7) | 243 (51.9) |
| Arrival time, n (%) | ||
| 20.00 to midnight | 206 (69.6) | 297 (68.0) |
| Midnight to 04.00 | 90 (30.4) | 140 (32.0) |
| Time (hours) in department, n (%) | ||
| < 1 | 25 (7.9) | 23 (5.0) |
| 1–2 | 52 (16.5) | 72 (15.7) |
| > 2 | 238 (75.6) | 363 (79.3) |
| Who completed the questionnaire? n (%) | ||
| Patient | 250 (80.1) | 375 (81.0) |
| Friend or relative | 27 (8.7) | 45 (9.7) |
| Both | 31 (9.9) | 36 (7.8) |
| Patient with health professional | 4 (1.3) | 7 (1.5) |
| Total | 340 | 492 |
Perception of threat
| Model | Coefficient (SE) | z | p-value |
|---|---|---|---|
| I | |||
| AIMS | –0.40 (0.258) | –1.55 | 0.122 |
| Constant | –0.89 (0.41) | –2.17 | 0.030 |
| II | |||
| AIMS | –0.36 (0.248) | –1.44 | 0.149 |
| Age (years) | –0.01 (0.005) | –2.58 | 0.010 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | 0.74 (0.208) | 3.55 | < 0.001 |
| Female | 0.41 (0.207) | 1.97 | 0.049 |
| Constant | –1.20 (0.588) | –2.03 | 0.042 |
| III | |||
| AIMS | –0.37 (0.249) | –1.51 | 0.132 |
| Age (years) | –0.01 (0.005) | –2.68 | 0.007 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | 0.73 (0.209) | 3.48 | 0.001 |
| Time (hours) spent in ED | |||
| < 1 | Reference | Reference | Reference |
| 1–2 | –0.19 (0.543) | –0.36 | 0.722 |
| > 2 | 0.36 (0.473) | 0.76 | 0.499 |
| Female | 0.39 (0.208) | 1.87 | 0.062 |
| Constant | –1.37 (0.705) | –1.95 | 0.052 |
General service ratings
| Model | Coefficient (SE) | z | p-value |
|---|---|---|---|
| I | |||
| AIMS | 0.09 (0.08) | 1.11 | 0.267 |
| Constant | 4.13 (0.13) | 32.66 | < 0.001 |
| II | |||
| AIMS | 0.06 (0.06) | 0.93 | 0.350 |
| Age (years) | 0.01 (0.001) | 5.11 | < 0.001 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | –0.15 (0.146) | –1.05 | 0.296 |
| Female | –0.51 (0.129) | –3.98 | < 0.001 |
| Constant | 4.21 (0.17) | 25.36 | < 0.001 |
| III | |||
| AIMS | 0.06 (0.07) | 0.89 | 0.372 |
| Age (years) | 0.01 (0.001) | 4.87 | < 0.001 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | –0.08 (0.065) | –1.18 | 0.237 |
| Time (hours) spent in ED | |||
| < 1 | Reference | Reference | Reference |
| 1–2 | –0.14 (0.146) | –0.93 | 0.352 |
| > 2 | –0.49 (0.130) | –3.80 | < 0.001 |
| Female | –0.08 (0.061) | –1.34 | 0.181 |
| Constant | 4.35 (0.19) | 22.51 | < 0.001 |
Perception of negative experiences
| Model | Coefficient (SE) | z | p-value |
|---|---|---|---|
| I | |||
| AIMS | –0.147 (0.112) | –1.31 | 0.189 |
| Constant | 2.75 (0.182) | 15.12 | < 0.001 |
| II | |||
| AIMS | –0.138 (0.09) | –1.46 | 0.145 |
| Age (years) | –0.006 (0.002) | –3.14 | 0.002 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | 0.481 (0.206) | 2.34 | 0.019 |
| Female | 0.844 (0.185) | 4.55 | < 0.001 |
| Constant | 2.33 (0.24) | 9.62 | < 0.001 |
| III | |||
| AIMS | –0.147 (0.113) | –1.29 | 0.196 |
| Age (years) | –0.006 (0.002) | –2.77 | 0.006 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | 0.156 (0.089) | 1.76 | 0.079 |
| Time (hours) spent in ED | |||
| < 1 | Reference | Reference | Reference |
| 1–2 | 0.446 (0.206) | 2.16 | 0.030 |
| > 2 | 0.795 (0.187) | 4.25 | < 0.001 |
| Female | 0.158 (0.082) | 1.93 | 0.054 |
| Constant | 2.06 (0.287) | 7.17 | < 0.001 |
Overall experience
| Model | Coefficient (SE) | z | p-value |
|---|---|---|---|
| I | |||
| AIMS | 0.272 (0.293) | 0.93 | 0.352 |
| Constant | 6.74 (0.472) | 14.29 | < 0.001 |
| II | |||
| AIMS | 0.262 (0.30) | 0.88 | 0.378 |
| Age (years) | 0.012 (0.005) | 2.46 | 0.014 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | –0.45 (0.20) | –2.19 | 0.028 |
| Time (hours) spent in ED | |||
| < 1 | Reference | Reference | Reference |
| 1–2 | –1.043 (0.45) | –2.31 | 0.021 |
| > 2 | –1.971 (0.40) | –4.88 | < 0.001 |
| Constant | 7.98 (0.63) | 12.57 | < 0.001 |
| III | |||
| AIMS | 0.25 (0.324) | 0.77 | 0.440 |
| Age (years) | 0.011 (0.005) | 2.37 | 0.018 |
| Time of arrival in ED | |||
| 20.00 to midnight | Reference | Reference | Reference |
| Midnight to 04.00 | –0.45 (0.204) | –2.19 | 0.029 |
| Time (hours) spent in ED | |||
| < 1 | Reference | Reference | Reference |
| 1–2 | –1.00 (0.45) | –2.21 | 0.027 |
| > 2 | –1.92 (0.41) | –4.74 | < 0.001 |
| Female | –0.28 (0.19) | –1.49 | 0.136 |
| Constant | 8.40 (0.72) | 11.62 | < 0.001 |
Appendix 15 Care Quality Commission survey analysis: characteristics
Characteristics of the respondents
Table 140 compares the characteristics of respondents at intervention and control sites across all 3 years. Mean age is lower for intervention sites than control sites. Slightly more females responded to the survey than males. There were more attendances on Fridays and Saturdays than on Sundays, with no difference between intervention sites and control sites. Over 70% of attendances were between 20.00 and midnight, with people at intervention sites being more likely to be seen between midnight and 04.00 than those in control sites, though this pattern was not observed when all sites were included. Most people waited more than 2 hours at intervention sites; waiting times were slightly higher at control sites, but when looking at all sites or those in the survey, the pattern was reversed.
| Characteristic | Survey sites only | All sites | ||
|---|---|---|---|---|
| Intervention (N = 173) | Control (N = 198) | Intervention (N = 724) | Control (N = 627) | |
| Mean age (years) | 53.5 | 57.8 | 55.6 | 57.9 |
| Female, n (%) | 97 (56.1) | 100 (50.5) | 382 (52.8) | 351 (56.0) |
| Day of attendance, n (%) | ||||
| Friday | 67 (38.7) | 88 (44.4) | 277 (38.3) | 241 (38.4) |
| Saturday | 76 (43.9) | 82 (41.4) | 344 (47.5) | 293 (46.7) |
| Sunday | 30 (17.3) | 28 (14.1) | 103 (14.2) | 93 (14.8) |
| Time of attendance, n (%) | ||||
| 20.00 to midnight | 122 (70.5) | 148 (74.8) | 539 (74.5) | 464 (74.0) |
| Midnight to 04.00 | 51 (29.5) | 50 (25.2) | 185 (25.5) | 163 (26.0) |
| Time (hours) in department, n (%) | ||||
| < 1 | 17 (10.3) | 23 (10.1) | 65 (9.7) | 54 (9.6) |
| 1–2 | 25 (15.2) | 37 (16.3) | 107 (15.9) | 108 (19.2) |
| > 2 | 123 (74.6) | 167 (73.6) | 500 (74.4) | 402 (71.3) |
Table 141 compares the characteristics of respondents in each year across the survey sites and across all sites. Mean age was greater in later years, and the percentage of females responding was < 50% in 2014. Generally, there were slightly more attendances on Saturdays than on Fridays; however, in 2016 this was reversed, with more Friday than Saturday attendances. The number of attendances between 20.00 and midnight was lowest in 2014. There was no obvious difference in time in ED by year, although the percentage does appear to increase in 2016 for those in the survey.
| Characteristic | 2012 | 2014 | 2016 |
|---|---|---|---|
| Survey sites | |||
| Total | 101 | 144 | 126 |
| Mean age (years) | 52.6 | 56.9 | 57.2 |
| Female, n (%) | 55 (54.5) | 69 (47.9) | 73 (57.9) |
| Day of attendance, n (%) | |||
| Friday | 41 (40.6) | 55 (38.2) | 59 (46.8) |
| Saturday | 45 (44.6) | 63 (43.8) | 50 (39.7) |
| Sunday | 15 (14.9) | 26 (18.1) | 17 (13.5) |
| Time of attendance, n (%) | |||
| 20.00 to midnight | 73 (72.3) | 102 (70.8) | 95 (75.4) |
| Midnight to 04.00 | 28 (27.7) | 42 (29.2) | 31 (24.6) |
| Time (hours) in department, n (%) | |||
| < 1 | 12 (12.5) | 11 (8.5) | 11 (9.2) |
| 1–2 | 18 (18.8) | 23 (17.7) | 16 (13.5) |
| > 2 | 66 (68.8) | 96 (73.9) | 92 (77.3) |
| All sites | |||
| Total | 440 | 422 | 489 |
| Mean age (years) | 54.1 | 56.6 | 59.1 |
| Female (%) | 254 (57.7) | 209 (49.5) | 270 (55.2) |
| Day of attendance, n (%) | |||
| Friday | 157 (35.7) | 136 (32.2) | 225 (46.0) |
| Saturday | 219 (49.8) | 209 (49.5) | 209 (42.7) |
| Sunday | 64 (14.6) | 77 (18.3) | 55 (11.3) |
| Time of attendance, n (%) | |||
| 20.00 to midnight | 320 (72.7) | 293 (69.4) | 390 (79.8) |
| Midnight to 04.00 | 120 (27.3) | 129 (30.6) | 99 (20.3) |
| Time (hours) in department, n (%) | |||
| < 1 | 37 (9.3) | 40 (10.3) | 42 (9.4) |
| 1–2 | 73 (18.3) | 67 (17.2) | 75 (16.8) |
| > 2 | 290 (72.5) | 389 (72.5) | 330 (73.8) |
Details of the results
Responses to the question ‘While you were in the ED, did you feel threatened by other patients or visitors?’ are outlined in Table 142. There are no obvious changes in the proportion of those who felt threatened pre and post intervention at the intervention sites.
| Site | Yes, definitely | Yes, to some extent | No | Total | |
|---|---|---|---|---|---|
| Survey sites only | |||||
| Intervention | |||||
| Pre intervention | n | 1 | 8 | 82 | 91 |
| % | 1.1 | 8.8 | 90.1 | ||
| Post intervention | n | 3 | 5 | 72 | 80 |
| % | 3.8 | 6.3 | 90.0 | ||
| Control | |||||
| Pre intervention | n | 3 | 8 | 84 | 95 |
| % | 3.2 | 8.4 | 88.4 | ||
| Post intervention | n | 5 | 7 | 89 | 101 |
| % | 5.0 | 6.9 | 88.1 | ||
| All sites | |||||
| Intervention | |||||
| Pre intervention | n | 7 | 20 | 276 | 303 |
| % | 2.3 | 6.6 | 91.1 | ||
| Post intervention | n | 10 | 29 | 362 | 401 |
| % | 2.5 | 7.2 | 90.3 | ||
| Control | |||||
| Pre intervention | n | 7 | 18 | 217 | 242 |
| % | 2.9 | 7.4 | 89.7 | ||
| Post intervention | n | 11 | 33 | 331 | 375 |
| % | 2.9 | 8.8 | 88.3 | ||
Table 143 shows how the overall experience of the ED visit was rated on a scale from 0 (very poor experience) to 10 (very good experience). There is no difference in rating of overall experience pre and post intervention and between intervention sites and control sites.
| Site | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Mean | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Survey sites | |||||||||||||
| Intervention | |||||||||||||
| Pre intervention | n | 1 | 2 | 0 | 2 | 3 | 6 | 9 | 8 | 20 | 16 | 19 | 7.6 |
| % | 1.2 | 2.3 | 0.0 | 2.3 | 3.5 | 7.0 | 10.5 | 9.3 | 23.3 | 18.6 | 22.1 | ||
| Post intervention | n | 0 | 2 | 3 | 2 | 2 | 3 | 6 | 8 | 17 | 14 | 22 | 7.7 |
| % | 0.0 | 2.5 | 3.8 | 2.5 | 2.5 | 3.8 | 7.6 | 10.1 | 21.5 | 17.7 | 27.9 | ||
| Control | |||||||||||||
| Pre intervention | n | 0 | 2 | 3 | 4 | 1 | 3 | 8 | 13 | 22 | 13 | 21 | 7.6 |
| % | 0.0 | 2.2 | 3.3 | 4.4 | 1.1 | 3.3 | 8.9 | 14.4 | 24.4 | 14.4 | 23.3 | ||
| Post intervention | n | 0 | 2 | 1 | 3 | 2 | 3 | 10 | 8 | 23 | 17 | 25 | 7.9 |
| % | 0.0 | 2.1 | 1.1 | 3.2 | 2.1 | 3.2 | 10.6 | 8.5 | 24.5 | 18.1 | 26.6 | ||
| All sites | |||||||||||||
| Intervention | |||||||||||||
| Pre intervention | n | 2 | 2 | 6 | 9 | 8 | 19 | 19 | 32 | 66 | 52 | 71 | 7.7 |
| % | 0.7 | 0.7 | 2.1 | 3.2 | 2.8 | 6.6 | 6.6 | 11.2 | 23.1 | 18.2 | 24.8 | ||
| Post intervention | n | 3 | 11 | 8 | 9 | 10 | 20 | 24 | 33 | 90 | 67 | 108 | 7.6 |
| % | 0.8 | 2.9 | 2.1 | 2.4 | 2.6 | 5.2 | 6.3 | 8.6 | 23.5 | 17.5 | 28.2 | ||
| Control | |||||||||||||
| Pre intervention | n | 2 | 6 | 5 | 9 | 6 | 14 | 15 | 26 | 46 | 40 | 56 | 7.5 |
| % | 0.9 | 2.7 | 2.2 | 4.0 | 2.7 | 6.2 | 6.7 | 11.6 | 20.4 | 17.8 | 24.9 | ||
| Post intervention | n | 2 | 10 | 6 | 8 | 15 | 10 | 29 | 31 | 89 | 67 | 87 | 7.7 |
| % | 0.6 | 2.8 | 1.7 | 2.3 | 4.2 | 2.8 | 8.2 | 8.8 | 25.1 | 18.9 | 24.6 | ||
Details of the regression analysis
Tables 144–146 show the responses (n = 367) to the perception of threat question at survey sites in England, with models involving pre–post intervention only (see Table 144), pre–post intervention and significant variables (by forward selection) only (see Table 145) and all variables regardless of significance (see Table 146). There was no significant difference in perception of threat with or without intervention or pre or post intervention across all models. Perception of threat decreased significantly as respondent age increased.
| Perception of threat | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.032 | 0.353 | 0.09 | 0.928 |
| Constant | –2.12 | 0.254 | –8.33 | < 0.001 |
| Perception of threat | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.078 | 0.339 | 0.23 | 0.818 |
| Respondent age | –0.022 | 0.008 | –2.78 | 0.005 |
| Constant | –0.99 | 0.445 | –2.22 | 0.027 |
| Perception of threat | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| AIMS | –0.26 | 0.349 | –0.74 | 0.460 |
| Post intervention | 0.03 | 0.517 | 0.07 | 0.947 |
| Respondent age | –0.023 | 0.008 | –2.85 | 0.004 |
| Survey year | ||||
| 2012 | Baseline | |||
| 2014 | –0.53 | 0.431 | –1.22 | 0.222 |
| 2016 | –0.21 | 0.596 | –0.35 | 0.725 |
| Weekday | ||||
| Sunday | Baseline | |||
| Friday | –0.29 | 0.851 | –0.35 | 0.730 |
| Saturday | –0.42 | 0.749 | –0.56 | 0.573 |
| Female | –0.11 | 0.346 | –0.31 | 0.758 |
| Time of attendance: midnight to 04.00 | –0.63 | 0.688 | –0.91 | 0.361 |
| Constant | –0.01 | 0.965 | –0.01 | 0.988 |
Tables 147–149 show the full details of regression analysis for responses (n = 1221) to the perception of threat question across all survey sites, with models involving pre–post intervention only (see Table 147), pre–post intervention and significant variables (by forward selection) only (see Table 148) and all variables regardless of significance (see Table 149). There is no significant difference in perception of threat with or without AIMS or pre or post intervention across all models. Perception of threat decreased significantly as respondent age increased. Those waiting > 2 hours are more likely to perceive threats than those waiting ≤ 2 hours.
| Perception of threat | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.16 | 0.209 | 0.70 | 0.485 |
| Constant | –2.34 | 0.187 | –12.50 | < 0.001 |
| Perception of threat | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.274 | 0.224 | 1.23 | 0.221 |
| Respondent age | –0.019 | 0.005 | –4.19 | < 0.001 |
| Time (hours) in department | ||||
| < 1 | Baseline | |||
| 1–2 | 0.999 | 0.654 | 1.53 | 0.127 |
| > 2 | 1.73 | 0.600 | 2.88 | 0.004 |
| Constant | –2.94 | 0.654 | –4.49 | < 0.001 |
| Perception of threat | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| AIMS | –0.21 | 0.273 | –0.80 | 0.426 |
| Post intervention | 0.27 | 0.302 | 0.88 | 0.379 |
| Respondent age | –0.02 | 0.005 | –4.19 | < 0.001 |
| Survey year | ||||
| 2012 | Baseline | |||
| 2014 | 0.05 | 0.255 | 0.19 | 0.848 |
| 2016 | 0.03 | 0.317 | 0.08 | 0.936 |
| Weekday | ||||
| Sunday | Baseline | |||
| Friday | –0.42 | 0.450 | –0.93 | 0.354 |
| Saturday | –0.29 | 0.388 | –0.75 | 0.451 |
| Female | 0.16 | 0.198 | 0.83 | 0.408 |
| Time of attendance: midnight to 04.00 | –0.32 | 0.346 | –0.93 | 0.353 |
| Time (hours) in department | ||||
| < 1 | Baseline | |||
| 1–2 | 1.02 | 0.655 | 1.56 | 0.118 |
| > 2 | 1.75 | 0.601 | 2.91 | 0.004 |
| Constant | –2.56 | 0.805 | –3.18 | 0.001 |
Tables 150–152 show the full details of regression analysis for responses (n = 367) to the overall experience question at the survey sites in England, with models involving pre–post intervention only (see Table 150), pre–post intervention and significant variables (by forward selection) only (see Table 151) and all variables regardless of significance (see Table 152). There was no significant difference in mean experience rating for those in AIMS and those in control sites, nor was there a significant difference in mean experience rating pre or post intervention in any of the models fitted. Mean experience rating increased significantly with respondent age. Those who spent > 2 hours in the ED had a significantly worse experience than those who spent ≤ 2 hours in the ED.
| Overall experience | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.23 | 0.250 | 0.91 | 0.361 |
| Constant | 7.58 | 0.181 | 41.93 | < 0.001 |
| Overall experience | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.258 | 0.272 | 0.95 | 0.341 |
| Respondent age | 0.016 | 0.006 | 2.80 | 0.005 |
| Time (hours) in department | ||||
| < 1 | Baseline | |||
| 1–2 | –0.828 | 0.491 | –1.69 | 0.092 |
| > 2 | –1.70 | 0.411 | –4.14 | < 0.001 |
| Constant | 8.01 | 0.550 | 14.55 | < 0.001 |
| Overall experience | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| AIMS | 1.06 | 0.248 | 0.43 | 0.670 |
| Post intervention | 0.10 | 0.370 | 0.27 | 0.784 |
| Respondent age | 0.016 | 0.006 | 2.72 | 0.007 |
| Survey year | ||||
| 2012 | Baseline | |||
| 2014 | 0.10 | 0.321 | 0.32 | 0.746 |
| 2016 | 0.21 | 0.456 | 0.45 | 0.652 |
| Weekday | ||||
| Sunday | Baseline | |||
| Friday | –0.89 | 0.573 | –1.56 | 0.118 |
| Saturday | –0.81 | 0.493 | –1.65 | 0.099 |
| Female | –0.38 | 0.247 | –1.60 | 0.126 |
| Time of attendance: midnight to 04.00 | –0.71 | 0.445 | –1.54 | 0.111 |
| Time (hours) in department | ||||
| < 1 | Baseline | |||
| 1–2 | –0.76 | 0.496 | –1.54 | 0.123 |
| > 2 | –1.70 | 0.416 | –4.08 | < 0.001 |
| Constant | 9.00 | 0.783 | 11.50 | < 0.001 |
Tables 153–155 show the full details of regression analysis for responses (n = 1159) to the overall experience question across all survey sites, with models involving pre–post intervention only (see Table 153), pre–post intervention and significant variables (by forward selection) only (see Table 154) and all variables regardless of significance (see Table 155). There was no significant difference in mean experience rating for those in AIMs and those in control sites, nor was there a significant difference in mean experience rating pre or post intervention across all models. Mean experience rating increased significantly with respondent age and was higher for male than female respondents. Overall, experience ratings were significantly higher in 2014 and 2016 than in 2012. Those who spent > 2 hours in the ED had a significantly worse experience than those who spent ≤ 2 hours in the ED.
| Overall experience | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | 0.09 | 0.136 | 0.69 | 0.493 |
| Constant | 7.65 | 0.105 | 72.61 | < 0.001 |
| Overall experience | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| Post intervention | –0.231 | 0.187 | –1.23 | 0.218 |
| Respondent age | 0.017 | 0.003 | 5.55 | < 0.001 |
| Survey year | ||||
| 2012 | Baseline | |||
| 2014 | 0.36 | 0.169 | 2.11 | 0.035 |
| 2016 | 0.58 | 0.211 | 2.76 | 0.006 |
| Female | –0.29 | 0.132 | –2.23 | 0.026 |
| Time (hours) in department | ||||
| < 1 | Baseline | |||
| 1–2 | –0.568 | 0.265 | –2.15 | 0.032 |
| > 2 | –1.58 | 0.226 | –6.99 | < 0.001 |
| Constant | 7.94 | 0.308 | 25.77 | < 0.001 |
| Overall experience | Coefficient | SE | z | p-value |
|---|---|---|---|---|
| AIMS | 0.21 | 0.167 | 1.27 | 0.206 |
| Post intervention | –0.23 | 0.196 | –1.18 | 0.239 |
| Respondent age | 0.017 | 0.003 | 5.48 | < 0.001 |
| Survey year | ||||
| 2012 | Baseline | |||
| 2014 | 0.36 | 0.169 | 2.14 | 0.032 |
| 2016 | 0.59 | 0.215 | 2.75 | 0.006 |
| Weekday | ||||
| Sunday | Baseline | |||
| Friday | –0.01 | 0.304 | –0.03 | 0.973 |
| Saturday | –0.03 | 0.263 | –0.10 | 0.921 |
| Female | –0.29 | 0.132 | –2.17 | 0.030 |
| Time of attendance: midnight to 04.00 | –0.10 | 0.227 | –0.44 | 0.661 |
| Time (hours) in department | ||||
| < 1 | Baseline | |||
| 1–2 | –0.57 | 0.266 | –2.14 | 0.033 |
| > 2 | –1.58 | 0.226 | –6.99 | < 0.001 |
| Constant | 7.87 | 0.425 | 18.49 | < 0.001 |
Appendix 16 Details of the Care Quality Commission survey analysis
Controlled before-and-after analysis of AIMS implementation
| Site | Year of survey | ||||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | 2012 | 2014 | 2016 | |||
| Intervention | Control | Intervention | Control | Intervention | Control | ||
| Study sites | |||||||
| C | O | 15 | 12 | 10 | 18 | 9 | 20 |
| D | K | 28 | 14 | 10 | 16 | 16 | 20 |
| G | M | 22 | 8 | 16 | 21 | 15 | 21 |
| F | J | 14 | 16 | 16 | 21 | 11 | 11 |
| H | K | 0 | 14 | 26 | 16 | 19 | 20 |
| E | M | 20 | 8 | 13 | 21 | 16 | 21 |
| Non-study sites | |||||||
| Portsmouth | Plymouth | 16 | 23 | 15 | 14 | 16 | 25 |
| Brighton and Hove | Northampton | 0 | 20 | 17 | 15 | 16 | 18 |
| Exeter | Cambridge | 18 | 20 | 20 | 15 | 25 | 22 |
| Chelmsford | York | 28 | 11 | 19 | 17 | 12 | 30 |
| Colchester | Lancaster | 20 | 22 | 18 | 13 | 21 | 19 |
| Oxford | Watford | 31 | 0 | 10 | 16 | 14 | 20 |
| Reading | Coventry | 19 | 16 | 23 | 17 | 25 | 16 |
| Southampton | Derby | 23 | 24 | 17 | 12 | 23 | 27 |
| Total | 254 | 208 | 230 | 232 | 238 | 290 | |
Analysis at four sites in England
| Coefficient | SE | z | p-value | |
|---|---|---|---|---|
| Sites | ||||
| Control | Reference | |||
| Intervention | –0.26 | 0.349 | –0.74 | 0.460 |
| Study period | ||||
| Pre intervention | Reference | |||
| Post intervention | 0.03 | 0.517 | 0.07 | 0.947 |
| Age of respondent | –0.023 | 0.008 | –2.85 | 0.004 |
| Survey year | ||||
| 2012 | Reference | |||
| 2014 | –0.53 | 0.431 | –1.22 | 0.222 |
| 2016 | –0.21 | 0.596 | –0.35 | 0.725 |
| Weekday | ||||
| Sunday | Reference | |||
| Friday | –0.29 | 0.851 | –0.35 | 0.730 |
| Saturday | –0.42 | 0.749 | –0.56 | 0.573 |
| Gender | ||||
| Male | Reference | |||
| Female | –0.11 | 0.346 | –0.31 | 0.758 |
| Time of attendance | ||||
| 20.00–23.59 | Reference | |||
| 00.00–04.00 | –0.63 | 0.688 | –0.91 | 0.361 |
| Constant | –0.01 | 0.965 | –0.01 | 0.988 |
| Coefficient | SE | z | p-value | |
|---|---|---|---|---|
| Sites | ||||
| Control | Reference | |||
| Intervention | 1.06 | 0.248 | 0.43 | 0.670 |
| Study period | ||||
| Pre intervention | Reference | |||
| Post intervention | 0.10 | 0.370 | 0.27 | 0.784 |
| Age of respondent | 0.016 | 0.006 | 2.72 | 0.007 |
| Survey year | ||||
| 2012 | Reference | |||
| 2014 | 0.10 | 0.321 | 0.32 | 0.746 |
| 2016 | 0.21 | 0.456 | 0.45 | 0.652 |
| Weekday | ||||
| Sunday | Reference | |||
| Friday | –0.89 | 0.573 | –1.56 | 0.118 |
| Saturday | –0.81 | 0.493 | –1.65 | 0.099 |
| Gender | ||||
| Male | Reference | |||
| Female | –0.38 | 0.247 | –1.60 | 0.126 |
| Time of attendance | ||||
| 20.00–23.59 | Reference | |||
| 00.00–04.00 | –0.71 | 0.445 | –1.54 | 0.111 |
| Time (hours) in ED | ||||
| < 1 hour | Reference | |||
| 1–2 hours | –0.76 | 0.496 | –1.54 | 0.123 |
| > 2 hours | –1.70 | 0.416 | –4.08 | < 0.001 |
| Constant | 9.00 | 0.783 | 11.50 | < 0.001 |
Analysis involving all AIMS sites
| Coefficient | SE | z | p-value | |
|---|---|---|---|---|
| Sites | ||||
| Control | Reference | |||
| Intervention | –0.21 | 0.273 | –0.80 | 0.426 |
| Study period | ||||
| Pre intervention | Reference | |||
| Post intervention | 0.27 | 0.302 | 0.88 | 0.379 |
| Age of respondent | –0.02 | 0.005 | –4.19 | < 0.001 |
| Survey year | ||||
| 2012 | Reference | |||
| 2014 | 0.05 | 0.255 | 0.19 | 0.848 |
| 2016 | 0.03 | 0.317 | 0.08 | 0.936 |
| Weekday | ||||
| Sunday | Reference | |||
| Friday | –0.42 | 0.450 | –0.93 | 0.354 |
| Saturday | –0.29 | 0.388 | –0.75 | 0.451 |
| Gender | ||||
| Male | Reference | |||
| Female | 0.16 | 0.198 | 0.83 | 0.408 |
| Time of attendance | ||||
| 20.00–23.59 | Reference | |||
| 00.00–04.00 | –0.32 | 0.346 | –0.93 | 0.353 |
| Time (hours) in ED | ||||
| < 1 hour | Reference | |||
| 1–2 hours | 1.02 | 0.655 | 1.56 | 0.118 |
| > 2 hours | 1.75 | 0.601 | 2.91 | 0.004 |
| Constant | –2.56 | 0.805 | –3.18 | 0.001 |
| Coefficient | SE | z | p-value | |
|---|---|---|---|---|
| Sites | ||||
| Control | Reference | |||
| Intervention | 0.21 | 0.167 | 1.27 | 0.206 |
| Study period | ||||
| Pre intervention | Reference | |||
| Post intervention | –0.23 | 0.196 | –1.18 | 0.239 |
| Age of respondent | 0.017 | 0.003 | 5.48 | < 0.001 |
| Survey year | ||||
| 2012 | Reference | |||
| 2014 | 0.36 | 0.169 | 2.14 | 0.032 |
| 2016 | 0.59 | 0.215 | 2.75 | 0.006 |
| Weekday | ||||
| Sunday | Reference | |||
| Friday | –0.01 | 0.304 | –0.03 | 0.973 |
| Saturday | –0.03 | 0.263 | –0.10 | 0.921 |
| Gender | ||||
| Male | Reference | |||
| Female | –0.29 | 0.132 | –2.17 | 0.030 |
| Time of attendance | ||||
| 20.00–23.59 | Reference | |||
| 00.00–04.00 | –0.10 | 0.227 | –0.44 | 0.661 |
| Time (hours) in ED | ||||
| > 1 hour | Reference | |||
| 1–2 hours | –0.57 | 0.266 | –2.14 | 0.033 |
| > 2 hours | –1.58 | 0.226 | –6.99 | < 0.001 |
| Constant | 7.87 | 0.425 | 18.49 | < 0.001 |
Glossary
- Acute alcohol intoxication
- A state of vulnerability caused by physiological consequences of ingestion of alcohol and defined by the consumer’s dependence on assistance to remain safe and well.
- Alcohol intoxication management services
- The generic nomenclature for bespoke services in night-time environments implemented to manage the needs of people who are vulnerable owing to excessive consumption of alcohol. Such services are also occasionally referred to as alcohol recovery centres, alcohol treatment centres, drunk tanks, safe havens, sobering-up centres, SOS buses or welfare centres.
- Alcohol intoxication management service session
- An alcohol intoxication management service session refers to a period during which an alcohol intoxication management service is open (i.e. the period between the opening and closing of the service). Analyses are typically undertaken on data restricted to one alcohol intoxication management service session, for example only data generated by patients attending an emergency department during the period between the opening and closing of the local alcohol intoxication management service.
- Clinical Commissioning Group
- In England, a Clinical Commissioning Group is a clinically led statutory NHS body responsible for planning and commissioning health services in their jurisdiction. They typically work closely with local authority health and well-being boards to manage public health. In Wales, NHS trusts and Local Health Boards plan and provide health care; matters concerning substance use typically fall within the remit of local authority Area Planning Boards. Health and health services are devolved to the National Assembly for Wales.
- St John Ambulance
- St John Ambulance (London, UK) is a volunteer-led charity providing tutelage in first aid and first-aid cover at public events. Services provided include clinical staff (e.g. physicians, nurses and paramedics), cycle responders, mobile treatment centres and ambulances.
- St John Cymru
- St John Cymru (Cardiff, UK) is the Welsh arm of St John Ambulance.
- Street marshal
- A role accredited and approved by the Security Industry Authority under the Community Safety Accreditation Scheme. A street marshal has similar authority to a police constable in uniform [see Section 50 of the Police Reform Act 2002 (Great Britain. Police Reform Act 2002. London: The Stationery Office; 2002)] and can require a person to give their name and address [see Section 1 of the Crime and Disorder Act 1998 (Great Britain. Crime and Disorder Act 1998. London: The Stationery Office; 1998)]. Street marshals aim to promote positive community relationships and encourage good behaviour.
- Street Pastor/Street Angel
- Street Pastors and Street Angels are non-denominational church-led groups of volunteers who provide care to those in need. In night-time environments this primarily concerns acute alcohol intoxication, assault, personal distress and related needs. As volunteers their care is pastoral.
List of abbreviations
- A&E
- accident and emergency department
- AAI
- acute alcohol intoxication
- AIMS
- alcohol intoxication management service
- ARIMA
- autoregressive integrated moving average
- CCG
- Clinical Commissioning Group
- CCTV
- closed-circuit television
- CI
- confidence interval
- CQC
- Care Quality Commission
- CT
- computerised tomography
- DECC
- Dynamic Emergency Care Centre
- ECDS
- Emergency Care Data Set
- ED
- emergency department
- EDARA
- Evaluating the Diversion of Alcohol Related Attendances
- EMT
- emergency medical technician
- ENP
- emergency nurse practitioner
- GCS
- Glasgow Coma Scale
- HES
- Hospital Episode Statistics
- HRG
- Healthcare Resource Group
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- IQR
- interquartile range
- IRR
- incident rate ratio
- IT
- information technology
- ITSA
- interrupted time series analysis
- LAG
- lay advisory group
- LGBT
- lesbian, gay, bisexual and transgender
- MIU
- minor injuries unit
- MPS
- Metropolitan Police Service
- NIHR
- National Institute for Health Research
- NTE
- night-time environment
- OLS
- ordinary least squares
- PPI
- patient and public involvement
- REC
- Research Ethics Committee
- resus
- resuscitation area
- RRV
- rapid response vehicle
- ScHARR
- School of Health and Related Research
- SD
- standard deviation
- SECF
- Sheffield Emergency Care Forum
- ShARRP
- Sheffield Addiction Recovery Research Panel
- UCA
- urgent-care assistant
- WAST
- Welsh Ambulance Services NHS Trust
