Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/09/04. The contractual start date was in January 2019. The draft manuscript began editorial review in December 2022 and was accepted for publication in February 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 McDermott et al. This work was produced by McDermott et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 McDermott et al.
Chapter 1 Background
Introduction
There is worldwide concern about the prevalence of young people’s mental health problems and the COVID-19 pandemic has catapulted young people’s mental health to the top on the global health agenda. UNICEF’s The State of the World’s Children 2021: On My Mind report concentrated for the first time on promoting, protecting and caring for children’s mental health. They argue that mental health is a global issue and little attention has been paid to either the problem or its potential solutions. 1
The consensus from the UN, UNICEF and WHO is that there is a fundamental relationship between human rights and mental health. UNICEF (UK) argue that ‘it is key that local government, services and professionals frame good mental health as a basic human right, one all children and young people are entitled to’. 1,2 In addition, the consensus posits that the most effective, human-rights-enhancing approach to young people’s mental health care should be based on public health and psychosocial support rather than overmedicalisation and institutionalisation. 3 WHO Comprehensive Mental Health Action Plan (2013–30) states:4
Children and adolescents with mental disorders should be provided with early intervention through evidence-based psychosocial and other non-pharmacological interventions based in the community, avoiding institutionalization and medicalization. Furthermore, interventions should respect the rights of children in line with the United Nations Convention on the Rights of the Child and other international and regional human rights instruments. (p.11)
This report presents the results of a multi-methods study conducted between 2019 and 2022, examining mental health early intervention services and self-care support for LGBTQ+ young people with common mental health problems in the UK. The aim was to generate evidence about what works, why, for whom and in what context.
First, we provide an overview of evidence concerning mental health inequalities for LGBTQ+ young people in the UK and the paucity of existing evidence concerning how services can best meet the needs of this population. Chapter 2 covers the methodology for this multi-methods study in detail, describing the three distinct stages of the research. The following chapters focus on the results of each of these distinct stages. Chapter 3 details the meta-narrative review (MNR) conducted to synthesise existing evidence, from which we produced an initial theoretical model of what works to effectively support, at an early point, LGBTQ+ young people’s mental health. This chapter presents an in-depth review of the evidence on early intervention mental health support for LGBTQ+ young people. In Chapter 4, we map the services identified providing mental health early intervention and self-care support for LGBTQ+ young people in the UK and present a resulting typology of service provision. Chapter 5 provides details of the collective case study evaluation conducted and the model for effective support developed based on data from 12 case study sites that provided mental health support to LGBTQ+ young people. The concluding chapter brings together the results of each stage of the study to deliver our overarching arguments, outline recommendations for policy, practice and future research, and provide details of the impact and dissemination of the research.
Mental health inequalities and LGBTQ+ young people
Lesbian, gay, bisexual, trans, queer/questioning, plus young people report significantly higher rates of depression, self-harm, suicidality and poor mental health than cisgender and heterosexual youth. 5–8 The evidence demonstrating this mental health prevalence inequality has been consistent in the UK over the last 20 years. In 2003, findings were published for the first large-scale UK study examining mental health and quality of life for lesbians and gay men living in England and Wales. These findings highlighted greater levels of psychological distress among lesbians and gay men compared to heterosexual women and men respectively, across age brackets, including young people aged 16–24 years. 9
This mental health inequality continues to be reported in subsequent research. In 2019, an analysis of online survey data from 677 UK participants aged 16–25 years in the ‘Youth Chances’ community study highlighted higher rates of poor mental health, suicidality and experiences of victimisation among trans and non-binary young people than in the wider population. 10 A 2016 pooled analysis of 12 UK population surveys showed that lesbian, gay and bisexual identified people under the age of 35 years were twice as likely to report symptoms of poor mental health compared with heterosexual peers. 8 As the severity of mental health problems worsens, this disparity between LGBTQ+ youth and cisgender youth increases. A recent meta-analysis of studies comparing suicidality in youth found that compared to cisgender and heterosexual youth, trans youth were six times, bisexual youth five times and LG youth four times more likely to report a history of attempted suicide. 11 Longitudinal evidence also demonstrates that in the UK, these mental health disparities start as early as 10 years old increasing throughout adolescence and peaking between the ages of 13 and 19 years. 6
Explaining LGBTQ+ poor mental health
The most prominent model in explaining these mental health inequalities is ‘minority stress’12 whereby experiences of stigma, prejudice and discrimination create hostile environments, leading to mental health problems. Being LGBTQ+ means young people do not conform to expectations or ‘norms’, that is, that you are heterosexual and cisgender (non-transgender). LGBTQ+ young people are marginalised through lack of mainstream visibility, discrimination, (micro)aggression, bullying and victimisation they experience. 13,14 Even within LGBTQ+ communities, young people may come up against assumptions and pressures about the ‘right’, ‘normal’ or ‘best’ ways to be LGBTQ+, such as stereotypes about bisexual people,15,16 or what it means to be ‘trans enough’. 17,18 Young people may also experience the erasure of their identities within service settings and in their interactions with adults, that is, where it is not considered that they could be LGBTQ+ and cis-heterosexuality is presumed. 19
A 2020 systematic review of qualitative research into LGBTQ+ young people’s mental health identified isolation and rejection, LGBTQ+ phobic victimisation and discrimination, and marginalisation as key factors impacting mental health. 20 Parent/carer and family rejection has been identified as a profound factor informing depression21 and suicidality. 22 Parental rejection has also been identified as an important factor driving elevated rates of homelessness among LGBTQ+ young people, with experiences of homelessness being associated with hopelessness, depression and post-traumatic stress disorder (PTSD). 23 These mental health risks are often compounded by intersecting minority stressors of racism and poverty. 24 The negative mental health impacts of family rejection have been exacerbated for LGBTQ+ young people during COVID-19. 25,26
School and education are also key sites of exclusion and victimisation for LGBTQ+ young people. A 2021 systematic review identified victimisation as a key factor impacting self-harm and suicidality among LGBTQ+ young people. 20,27 A quarter of the LGBTQ+ young people surveyed for Stonewall’s 2017 School Report experienced being ignored and isolated as a pattern of bullying. 28 Experiences of victimisation and discrimination at school have been identified as a prominent risk factor for depression, self-harm, suicidality, PTSD and school absence. 21,27,29,30
Unsurprisingly, evidence regarding protective factors for LGBTQ+ young people’s mental health indicates safe and supportive school environments,21,29,31 and parent/carer and family support and affirmation29,32,33 can protect mental health. In addition, social connectedness and belonging20,21,29 (including the presence of LGBTQ+ support movements and communities),33,34 and being able to talk to a trusted adult32,35 are key factors promoting resilience and reducing poor mental health for LGBTQ+ young people.
The mental health inequalities faced by LGBTQ+ young people have been exacerbated by COVID-19 and the impact of national and regional lockdowns, with evidence emerging that lockdowns have led to high levels of stress and depressive symptoms reported by LGBTQ+ people, especially young people. 36,37 Among 1140 LGBTQ+ young people surveyed for research commissioned by the charity organisation ‘Just Like Us’, 68% reported that their mental health worsened during the pandemic; 55% reported worrying daily about their mental health, rising to 65% for black LGBTQ+ young people, trans and gender-diverse young people, and disabled LGBTQ+ young people. 37
Underutilisation of mental health services
Despite this mental health inequality, LGBTQ+ young people have elevated unmet mental health needs compared to their cis-heterosexual peers and underuse mental health services. 38–42 Findings from a UK study indicated that in a sample of 789 LGBTQ+ young people, only one-fifth of participants had sought help for their mental health difficulties. 42 Through interviews and survey data, the study found that LGBTQ+ young people were reluctant to access statutory or third-sector mental health services because of experiences of homophobia, biphobia and transphobia; cis-heteronormativity (fear their sexual orientation or gender identity would be scrutinised or blamed for their mental health problems); difficulties disclosing their sexual and/or gender identity; fears of being misunderstood or judged by adults because they were young; and stigma related to having mental health problems. 41–44
Importantly, studies show that LGBTQ+ youth will seek mental health help online and from peers13,41,45 and prefer accessing LGBTQ+ organisations for mental health support. 42,46 There is a limited understanding of why asking for help for mental health problems is problematic for LGBTQ+ youth.
Poor mental health service experience
In addition to the underutilisation of mental health services,47 studies suggest LGBTQ+ young people have poor overall experience of mental health services and school-based support. 10,13,38,43,48,49 Discriminatory and marginalising experiences include service staff using the incorrect name or pronouns for the young person, it being assumed that every young person is cisgender and heterosexual by default, and service staff asking inappropriate questions. 49,50
Limited staff awareness and understanding of LGBTQ+ issues and minority stresses is a problem raised by both LGBTQ+ young people and staff working in mental health services. 42 A 2020 study involving data produced with a sample of 2064 LGBTQ+ young people aged 14–25 years found that practitioners’ lack of knowledge was perceived as increasing the risk that LGBTQ+ identities would be pathologised and framed as a ‘cause’ or ‘symptom’ of mental health problems. 51 Evidence indicates that, in response to this inadequate knowledge base, LGBTQ+ young people feel responsible for educating professionals and practitioners about LGBTQ+ identities, taking up time during which they should be receiving support. 50,52
Lacking knowledge and awareness within services also means that some LGBTQ+ young people feel unable to be open about their experiences, identities and emotions as a whole, detracting from the efficacy of mental health support. 42,50 This self-censorship is connected to fears of negative response53 and being ‘outed’ by the service to parents/carers or other family, peers, or other services. 51 LGBTQ+ young people’s experiences of mental health services are also characterised by a profound loss of autonomy and exclusion from decisions about their own support. 42,51
Research suggests the competence of healthcare staff to provide appropriate care to LGBTQ+ young people is a vital factor in ensuring access. For example, a 2020 EU study found that the barriers to health care for LGBTQ+ people are exacerbated by two related assumptions held by healthcare professionals. First, the assumption that patients are heterosexual and cisgender and, second, the assumption that LGBTQ+ people do not experience significant problems due to their LGBTQ+ identity, meaning that LGBTQ+ identity is viewed as incidental or irrelevant to the delivery of appropriate health care. 19
While it is unhelpful (and harmful) for the importance of the LGBTQ+ experience to be dismissed, it is also damaging for mental health practitioners to overemphasise LGBTQ+ identities in excessive or pathologising ways. When staff have limited understanding and awareness about LGBTQ+ identities, this can manifest as the attribution of mental distress and poor mental health exclusively to a young person’s being LGBTQ+, particularly when the young person is trans or gender diverse. 13,49
Newman et al. 52 suggest that it is necessary to pay attention to the ‘affective dimensions of healthcare engagement’ (p. 1) in order to understand how to develop inclusive health care for LGBTQ+ youth. The authors argue for a model of care that goes beyond ‘tolerant inclusivity in which sexually and gender-diverse people are framed as different in spaces governed by normative practices, concepts, representations, language, and hierarchies’ (p. 2). Their research suggests ‘belonging’ is important to inclusive health care for LGBTQ+ youth, where there is an unconditional acceptance and recognition of gender and sexual diversity. 13
Despite the recognition that LGBTQ+ youth are less likely to access mainstream mental health services and have a poor experience, the evidence base examining LGBTQ+ youth mental health support needs and service preferences is very limited. A systematic review found that research was more likely to identify barriers to accessing mental health support rather than facilitators to encourage engagement. 20 In addition, there is an absence of focus on intersectional factors such as ethnicity, socioeconomic status and disability in LGBTQ+ youth mental health care. 14,52,54
The current study aims to address this knowledge gap by examining ‘what works best?’ for supporting the mental health of LGBTQ+ young people with common mental health problems at an early stage.
Rationale for the current study
According to the Early Intervention Foundation, the central principle of early intervention is effectively identifying and providing early and preventive support to children and young people who are more at risk of poor mental health outcomes. 55 This strategy has been emphasised further in light of COVID-19 and the impacts on children and young people’s mental health since the first UK lockdown in early 2020. 56–58
The importance of early and preventive support for the long-term development of young people is included in the UK government’s Health and Social Care (HSC) Committee’s 2021 report on children and young people’s mental health, which advocates for radical action to focus mental health provision on early intervention and prevention. 56 Drawing on research conducted by the National Children’s Bureau and UCL59 and by the charity Stonewall,28 the HSC committee affirms the need for targeted strategies to increase protective factors for LGBTQ+ young people.
Ensuring better mental health outcomes for LGBTQ+ young people requires long-sighted, innovative and creative approaches. Here, we use ‘early intervention’ to refer to mental health services that LGBTQ+ young people can access before reaching a crisis point. While the focus of the Queer Futures 2 project was young people aged 12–25 years, there is evidence that mental health inequalities for LGBTQ+ young people start as early as age 10 years. 6 Early intervention more broadly covers all stages of a child’s development from birth onwards.
The UK evidence base examining LGBTQ+ young people’s early intervention mental health support needs and services is very limited. Consequently (and despite this manifest inequality and underutilisation of mental health services), there is no research in the UK on how to develop appropriate mental health early intervention and supported self-care provision to this vulnerable group. This study delivers rigorous evidence to fill this gap, address this inequality and fulfil the requirements of NHS mental health strategic direction.
Research objectives
-
To produce a synthesis of the evidence on mental health early intervention services and self-care support to LGBTQ+ young people.
-
To identify service models for mental health early intervention and supported self-care which are accessible and acceptable to LGBTQ+ young people.
-
To develop a programme theory of how, why and in what context mental health early intervention services and self-care support work for LGBTQ+ young people.
-
To increase understanding of LGBTQ+ young people’s access to and navigation of formal and informal mental health early intervention services and self-care support.
-
To generate commissioning guidance (including service costs) on mental health early intervention and supported self-care services for LGBTQ+ young people.
Research questions
-
What evidence exists on mental health early intervention services and supported self-care for LGBTQ+ young people?
-
What type of service models for mental health early intervention and supported self-care to LGBTQ+ young people are currently provided?
-
How, why and in what context do mental health early intervention services and supported self-care work for LGBTQ+ young people?
-
In what ways do LGBTQ+ young people access and navigate formal and informal mental health early intervention services and self-care support?
-
How can LGBTQ+ young people be encouraged to access and engage with mental health early intervention services and self-care support?
Chapter 2 Methodology
Sections of this chapter have been reproduced with permission from McDermott et al. 60 and Pattinson et al. 61 These are Open Access articles distributed under the terms of the Creative Commons Attribution Licence (https://creativecommons.org/licenses/by-nc-nd/4.0/).
This research project is a multi-methods theory-led case study evaluation with three distinct stages answering the key study objectives:
-
Stage 1. A systematic review of existing literature concerning early mental health interventions and self-care support for LGBTQ+ young people.
-
Stage 2. A service mapping study to identify existing UK LGBTQ+ youth-specific mental health interventions and support.
-
Stage 3. A theory-led case study evaluation of 12 case study sites (CSS) to establish the components of appropriate, quality early intervention mental health and self-care support for LGBTQ+ young people.
In this chapter, the rationale for a multi-methods approach is provided, followed by a description of the review, mapping and case study evaluation stages of the research. This chapter also contains details of the study’s research governance and ethics approval, and an overview of patient and public involvement (PPI).
Study design
The study used a theory-driven evaluation methodology, as appropriate when there is little evidence on the effectiveness or acceptability of services and interventions. 62,63 There is a paucity of UK research examining mental health early intervention services and supported self-care provision for LGBTQ+ young people. Consequently, we designed a study that recognises we are at the first stage of understanding the ways in which mental health services might support LGBTQ+ young people. This initial ‘innovation stage’ required evaluation methods capable of ‘discovering’, ‘describing’ and providing a theoretical understanding of why, how and in what context a service might work. 64
Experimental designs are excellent for assessing the effectiveness of services and interventions, but they cannot assess how or why services achieve particular outcomes in a variety of contexts. 65,66 Theory-driven evaluation approaches seek to not only understand why a service may work but also detail the underlying logic or theory of why it may work. 63,66 In order to develop health services which are likely to be effective, sustainable and scalable, evaluations need to understand not just whether, but how, why and in what contexts a service has a particular outcome. 64,67 Theory-led evaluation methods acknowledge that healthcare delivery takes place in complex social systems with potentially multiple pathways to the provision of services that work. 67,68
It is now widely recognised that theory is important to health services research because it aids the development of generalisable and robust knowledge and builds a scientific understanding of healthcare quality. 68 Case study design has been criticised because of concerns regarding external validity, that is that a single case study is a poor basis for generalising. However, the Medical Research Council, among others,62,69,70 have argued it is possible to generate ‘cumulative knowledge’ about the factors that influence healthcare delivery by adopting a theoretically driven method. We utilised Yin’s62 ‘analytical generalisation’ approach whereby the programme theory established in an evidence synthesis is ‘tested’ during the case study data analysis. This means a case study evaluation research design does not generalise results to the population as a whole but generalises to theoretical propositions on how or why a service/intervention may work. 62 We used a case study evaluation to generate a theoretical understanding of the mechanisms by which mental health early intervention services and self-care provision can support LGBTQ+ young people with common mental health problems.
Theoretical framework
The lack of research on LGBTQ+ young people and their use of mental health services has resulted in few theoretical explanations for why current services may be inappropriate. Members of the research team have been at the forefront of developing theories to explain why LGBTQ+ populations have elevated rates of mental health problems. 13,71 This work builds on Meyer’s72 minority-stress model that explains LGBTQ+ individual mental health and well-being in terms of experiences of discrimination/victimisation/stigma and is a plausible explanation for poor experiences of mental health service provision. 13
McDermott (CI) and Johnson’s (CA) theoretical perspective uses the concept of cis-heteronormativity (the dominance of cis-heterosexuality where gender identities and bodies align and everyone is assumed heterosexual)73 as a central lynchpin to understanding why LGBTQ+ young people may face additional burdens on their mental health. Young people, particularly in the early stages of non-normative gender and sexual identity development, can feel alienated from traditional forms of support (family, friends)72 and at odds with normative expectations of cis-heterosexuality. 13,74,75 This isolation will often be underpinned by deep feelings of shame which are implicated in both poor mental health and a reluctance to access formal support services. 71,76,77
The study is theoretically framed using an intersectional perspective and draws on Collins’78 definition of intersectionality, which positions race, class, gender, sexuality, ethnicity, nation, ability and age as interconnected phenomena that produce and shape social inequalities. When thinking about the experience and impacts of oppression, identity categories are often conceived as discrete from each other and static. LGBTQ+ identities are often represented in homogeneous ways, structured by homo- and trans norms that centre whiteness, heterosexuality, class privilege and being non-disabled in relation to the ‘right’ ways to be LGBTQ+. 79,80 We utilised Collins and Bilge’s 81 intersectional approach to centre relations of power across structural, cultural, disciplinary and interpersonal domains in our understanding and operationalisation of intersectionality.
Theories and models that explain why LGBTQ+ young people are hesitant to ask for help for their mental health problems are crucial to the development of early intervention mental health service models that are acceptable and accessible to LGBTQ+ youth. We utilised models of young people’s help-seeking for mental health problems that go beyond the barriers/facilitators model that is commonly used in research. Our approach drew from Biddle et al. ’s82 ‘cycle of avoidance’ model that conceptualises help-seeking in relation to normalising and coping. McDermott’s development of this model13,40,41 posits that LGBTQ+ young people are hesitant to ask for help because they are afraid of being judged and humiliated in relation to normative expectations of adolescent development, cis-heteronormativity and mental health, and, as a result, they minimise their mental health problems and try to cope alone. 13,40–42,76 However, LGBTQ+ young people will look for support from places/people where they feel they are not judged, such as peers, LGBTQ+ individuals/organisations and online,40,42 and this provides some initial evidence for the development of appropriate service models.
Thus, theories for understanding the need for appropriate mental health early intervention services for LGBTQ+ young people were informed by models of youth help-seeking,13,40,41 youth psychology,74 theories of sexuality and gender13,71 and developmental approaches to identity,71 rather than narrowly defined sexual orientation labels. 83
The study has worked with the definition of early intervention and supported self-care that included any health, social care or educational intervention, service or technology provided by the public, private or third sectors that aims to facilitate LGBTQ+ young people (or carers) taking action to address their mental health problems. This included services that specifically target both the LGBTQ+ young people and the services that have adapted their delivery to meet the mental health needs of LGBTQ+ young people. Throughout the report, we use ‘mental health support’ as shorthand for ‘early mental health intervention and supported self-care’.
Stage 1: systematic review method
The first stage of the study addressed research question 1:
-
What evidence exists on mental health early intervention services and supported self-care for LGBTQ+ young people?
And objective 1:
To produce a synthesis of the evidence on mental health early intervention services and self-care support to LGBTQ+ young people
Scoping review
An initial scoping review conducted by the research team confirmed the nascent nature of existing research on early intervention support for mental health of LGBTQ+ youth. The primary aim of the scoping review was to assess the size of the available published literature on LGBTQ+ youth mental health early intervention services/support research. Scoping review methodology can be used to identify knowledge gaps, scope a body of literature and provide a roadmap for a subsequent full systematic review. 84 We searched four main databases, from 2005, for research examining LGBTQ+ youth and mental health services, and research on mental health interventions aimed at LGBTQ+ youth. We located 55 relevant studies and no systematic reviews on the topic. The scoping review revealed a body of literature from divergent research paradigms such as medicine, clinical psychology, psychiatry, sociology, cultural studies, education, youth studies, social work and queer theory.
For this reason, a configuring systematic review methodology68,85 was utilised rather than hypothesis testing systematic review methodology. A configuring approach is suitable as our scoping review did not find any randomised control trials and very few large-scale studies that are used to test causal hypotheses and ask ‘what works’?86 Use of a configuring rather than aggregative approach to the systematic review87,88 is appropriate for reviews with heterogenic literature, and it specifically aims to broaden understanding of particular services/interventions, asking instead, ‘what happens?’. 86 This discovery informed our decision to utilise the MNR method because it offers a strategy to make use of a conflicting body of research from diverse research paradigms. 89
Meta-narrative review rationale
Research on LGBTQ+ youth mental health early intervention services and self-care support is an emerging field of investigation. The nascent nature of existing literature, and limited theoretical explanations of why existing interventions and services are inappropriate for LGBTQ+ young people, guided our view that a theory-led systematic review methodology will be more fruitful than the traditional Cochrane and Campbell collaborations approach which are typically focused on forms of a meta-analysis. 90 Theory-driven approaches seek to detail the underlying logic or theory of how, why and in what contexts a service or intervention may work,63,68 which is necessary to ensure they are effective, sustainable and scalable. This underlying theoretical explanation is often overlooked but is, in fact, crucial to ensure that interventions that have been successful in their original contexts can be ‘meaningfully replicated’68 in other settings.
We chose to utilise the MNR method rather than other theory-led review methods (e.g. realist review, meta-ethnography, thematic synthesis) for two reasons. First, the scoping review revealed a heterogeneous body of literature consisting of disparate research paradigms with different epistemological and ontological perspectives that have produced a disjointed empirical evidence base. Second, our aim was to produce a theoretical explanation of mental health early intervention support for LGBTQ+ youth that could be tested within a case study evaluation methodology. A MNR is a distinct systematic theory-driven technique developed by Greenhalgh et al. 91 that is used to generate understanding from heterogeneous, complex, often contradictory evidence across diverse disciplines. 89,92
There are six guiding principles that inform MNR, and these were incorporated into each step of the review process from the outset. These are listed below (taken from Greenhalgh and Wong;93 Wong et al. 85):
-
Pragmatism – being guided by evidence most likely to promote sense-making.
-
Pluralism – explored from multiple perspectives and the quality appraised according to the discipline of origin.
-
Historicity – attention to how the tradition within which the research evidence was generated has unfolded over time.
-
Contestation – analysis and sense-making about conflicting evidence.
-
Reflexivity – individual and team of reviewers continually reflect on emerging findings.
-
Peer review – testing findings with external reviewers.
In addition to the six guiding principles, quality standards and training materials92,93 have been developed to ensure MNR are conducted in a systematic way ‘according to an explicit, rigorous and transparent method’91 (p. 418).
Specifically, MNRs make sense of complex interventions/services by exploring the implications of different conceptualisations of a given topic across a range of research paradigms over time. The underlying assumption is that key constructs, in our case ‘sexual orientation’, ‘gender identity’, ‘mental health’, ‘youth’ and ‘help-seeking’, are conceptualised, theorised and empirically studied differently among research paradigms. A MNR is premised upon a constructivist epistemological approach that suggests that knowledge is produced within particular research traditions (e.g. sociological, psychological, biomedical). Consequently, a MNR aims to make sense of heterogeneous bodies of literature by identifying, comparing and analysing the belief systems that exist within different research paradigms. The aim of this MNR was to obtain a theoretical understanding of how early intervention mental health services can support LGBTQ+ youth with common mental health problems. The review questions addressed were:
-
What empirical studies have been undertaken on mental health early intervention services and self-care support for LGBTQ+ young people?
-
What are the theoretical propositions for how and why these services may work?
Multidisciplinary team
Consultation throughout the review process with a wider team for the purposes of reflexivity and peer review of findings are central principles in a MNR. 93 A multidisciplinary research team is important to conducting MNR because it enables pluralism of approaches and an appreciation of distinct research traditions. 89 The Queer Futures Research Team included people from a variety of disciplines (such as clinicians, mental health nursing, psychology, public health, health economics, health science, sociology) and were involved throughout the MNR.
We also took the view that user involvement is key to conducting systematic reviews to ensure they will produce meaningful outcomes for all stakeholders. 90 The Queer Futures 2 study Project Advisory Group was consulted about the review at regular intervals. The Project Advisory Group comprised health service staff and commissioners; clinicians; voluntary sector practitioners who work with the population group; and a service user representative. We also conducted extensive PPI with LGBTQ+ young people recruited from different sites across the UK.
Search strategy
The aim of the search strategy, consistent with the MNR, is to identify documents that are conceptually or empirically relevant to the research questions. 85 Using the RAMESES85 standards for MNRs the protocol was registered with PROSPERO (CRD42019135722). The search terms (Table 1) were developed in four domain categories: (1) sexual orientation and gender identity, (2) age, (3) mental health and (4) intervention/service. Searching was then undertaken via relevant electronic databases including both discipline-specific databases and multidisciplinary databases to increase the scope. These included, for example, MEDLINE, CINAHL, PsycInfo, Academic Search Ultimate, Web of Science, British Education Index, NHS Evidence, Social Care Online (see Appendix 1, Tables 17 and 18). The electronic database search was supplemented by expert informants, journal hand searching, citation tracking, and informant-led grey literature online searches. All identified papers were then subject to the review procedure.
| Sexual orientation and gender identity | Age | Mental health | Intervention/service |
|---|---|---|---|
| lesbian OR | Youth OR | “mental health” OR | Support OR service OR program* OR |
| gay OR | adolescen* OR | “mental disorder” OR | “early intervention” OR |
| bisexual OR | teen* OR | “mental* ill*” OR | “help seeking” OR |
| transgend* OR | “young people” OR | “mental* distress*” OR | CAMHS OR |
| same-sex OR | “young adult” OR | wellbeing OR | “Child and adolescent mental health service*” OR Thrive OR “CYP-IAPT” OR |
| “sexual minorit*” OR | “young person” | “well being” OR | IAPT OR mindfulness OR “primary care” OR outpatient OR |
| homosexual* OR | psycholog* OR | “cognitive therapy” OR CBT OR | |
| “sexual orientation” OR | psychiatr* OR | “behavio# * therapy” OR | |
| sexualities OR | depress* OR | Therap* OR | |
| queer* OR | “low mood” OR | counselling OR | |
| “gender atypicality” OR | anxiet* OR | school OR college OR | |
| “sexual identit*” | “self injur*” OR | university OR “higher education”? OR | |
| “self-harm” OR | “community–based” OR | ||
| “emotional problem*” OR | “social care” OR “social work” OR | ||
| “emotional difficult*” OR | “youth group” OR “youth service” OR | ||
| “emotional* distress*” OR | “peer support” OR “self manag*” OR | ||
| “emotional dysregul*” | “self car*” OR “self help*” OR | ||
| online OR virtual OR web OR internet OR | |||
| digital OR cyber OR “social media” OR | |||
| technolog* |
Inclusion/exclusion criteria
The inclusion/exclusion criteria (Table 2) were based upon the Population, Intervention, Comparison, Outcomes, Study (PICOS) framework. However, in comparison to other forms of systematic reviews, MNR does not pre-define a ‘preferred’ study design. This is consistent with the principle of pragmatism, that is, that evidence most likely to promote sense-making about the phenomenon (LGBTQ+ youth mental health support) and be most useful to the ‘intended audience’, is selected. 93 Thus, Table 2 represents PICOS criteria adapted to capture the diversity of possible search results that is acceptable for inclusion within a MNR.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Findings |
|
|
| Study details |
|
|
The selection of papers for a MNR is an interpretative process that attempts to make sense of the literature to produce an account of how the research traditions develop over time. This MNR selection process was iterative, that is, it required a series of judgements within the research team about the relevance of particular research within that tradition. Papers published before 1990 were excluded because research published before this date were unlikely to be relevant given substantial changes in attitudes, policies and laws towards LGBTQ+ populations. The United Nations94 defines ‘youth’ as referring to people aged 15–24 years, but the age definition of youth varies across nations, disciplines and policies. Research written in English, Spanish, Portuguese, Italian and French were included because these languages are spoken within the research team. The inclusion/exclusion criteria were applied independently by two members of the research team.
Quality assessment
The systematic review methodology does not have a standard quality appraisal framework. We drew on the EPPI-Centre ‘Weight of Evidence Framework’95 and recommendations for theory-led systematic reviews96 to devise a quality appraisal tool (Table 3) that focused on the relevance to the review question and the quality standard in relation to the discipline of origin. The tool was applied by two members of the research team.
| Relevance to the review question |
|
| Quality standard in relation to the discipline of origin |
|
Data extraction
Data extraction and synthesis were simultaneously conducted using the data analysis software Atlas.ti. Three members of the research team developed a data extraction and synthesis coding schema (Table 4), and this was applied to the included studies. The use of Atlas.ti enabled easy comparison and contrast of the extracted data across the included studies for the synthesis of the literature.
| Data extraction code and definition | Subcodes |
|---|---|
| Synthesis code and definition | Subcodes |
| Context: Describes the setting in which the research or discussion about mental health support takes placeFinding: Any findings in the papersStudy design: Explicit research design statedTheoretical perspective: Explicit statement about the theoretical orientation of the studyIntervention/service: The intervention or support service that the study involves | Clinical, Community, Online, Other, SchoolConceptual, EmpiricalQuantitative, Qualitative, Mixed Method, Systematic Review, Other, for example clinical case |
| Help-seeking: Conceptualization of help-seeking LGBTQ+ Identities: Conceptualization of relationship between LGBTQ+ identities and mental healthMental Health: Conceptualization of mental healthYouth: Conceptualization of youth | Access, Autonomy, Barriers, Cycle of avoidance, Health behaviour, Health information, Other, Power(lessness), StigmaDecompensation model, Essentialist, Heteronormativity, Homophobia, Intersectionality, Marginalisation, Minority Stress, Psychological Mediation Framework, VictimizationBiomedical, Critical, Individualising, Other, Pathologising, Psychological, Psycho-social. Adolescent psychological development, Autonomy, Biological, Other |
Data synthesis
It is usual in the synthesis stage of a MNR to have two interpretative phases. In the first phase, reviewers aim to identify and map out specific meta-narratives for each research tradition, focusing in particular on the concepts, theories, methods and instruments, which have characterised the tradition. The second stage involves comparing the meta-narratives asking what insights can be drawn by combining and contrasting findings from different traditions. 85 We outline the two phases below.
In stage one of the synthesis, multiple research team members used the extracted data to identify the research paradigms and map each meta-narrative. In this way, the different research traditions ‘become the unit of analysis’. 89 For each research paradigm, we asked key questions:
-
How has each tradition conceptualised the topic?
-
What theoretical approaches and methods did they use?
-
What are the main empirical findings?85
The synthesis process was informed ‘a priori’ by the research team’s familiarity with the key concept areas of the research project: (1) LGBTQ+ identities, (2) youth, (3) mental health and (4) help-seeking. Therefore, theoretical understandings of these concept areas were used analytically to inform an interpretive reading of all the research tradition meta-narratives created. Emergent theories were recorded transparently as with other stages of the MNR process. 85
Stage 2 of the synthesis compared the key dimensions across the research paradigms to generate a higher-order theoretical understanding of how and why interventions/services might work. In particular, we attended to the conflicts that arise between the theories, concepts and findings underpinning research from different traditions. This is consistent with the principle of ‘contestation’ – the commitment of MNR ‘to engage in disagreements’97 (p. 732). This second phase of the synthesis was conducted iteratively, using five distinct analytical steps that were guided by the principles of a MNR: pragmatism, pluralism, historicity, contestation, reflexivity, and peer review91 (Table 5). We moved between these five steps and the key question we asked across the research paradigms was ‘what are the implications of the contested concepts for developing early intervention mental health support for LGBTQ+ youth?’
| Step | Analytical strategy | Description |
|---|---|---|
| 1 | Historical theory building | Identification for each meta-narrative of the theories and models that seek to explain poor mental health in LGBTQ+ populations. From these we generated a draft theoretical framework for the entire stage 2 synthesis |
| 2 | Contestation | The key concepts (mental health, youth, LGBTQ+ identities, help-seeking interventions/services and findings) were compared across the meta-narratives. Attending to the conflicts that arose between the theories, concepts and findings underpinning the meta-narratives, and then comparing these to the draft theoretical framework |
| 3 | Pragmatism | As a result of the ‘contestation’ of the research traditions, we asked ‘what are the implications of the contested concepts for developing early intervention mental health support for LGBTQ+ youth?’ |
| 4 | Reflexivity | Reflecting both individually and as a team, we iteratively moved between ‘contestation’ and ‘pragmatism’ steps, the raw data (literature), the research questions and the draft theoretical framework. To supplement this thinking, we performed three additional cross-sectional analyses of the included data with a focus on LGBTQ+ youth of colour, trans and gender diverse youth, and bisexual youth |
| 5 | Peer review | The draft theoretical framework was further developed through discussion with the research team (including LGBTQ+ youth) and practitioners from the health, education, and voluntary sector |
The multidisciplinary research team developed a robust theory68 consistent with the pluralism and peer review principles of MNR. 93 The theoretical explanation of mental health early intervention services and self-care support for LGBTQ+ young people with common mental health problems derived from the MNR was then ‘tested’ during the case study data analysis in stage 3 of the overall study design.
Stage 2: service mapping method
The second stage of the study addressed research question 2:
-
What type of service models for mental health early interventions and supported self-care to LGBTQ+ young people are currently provided?
And objective 2:
-
To identify service models for mental health early intervention and supported self-care which are accessible and acceptable to LGBTQ+ young people
Method overview
This stage of the study drew on the successful mapping methods used in Pryjmachuk et al. ’s children and young people mental health self-care research. 98 Between February 2019 and February 2020, we employed systematic online and offline search strategies to identify services of various types for example self-care, peer-support, digital support, clinical; in a range of service settings for example health, local authority, third sector. Data collection was desk based and basic details (e.g. target population, mode of delivery, theoretical approach) of potential services obtained from any source were extracted and entered into an Excel spreadsheet. The service mapping data were tested against inclusion criteria in the information extraction phase and a final typology was generated to describe service provision across the UK. A full summary of the mapping data then produced a typology of services which was used to inform the selection of the CSS in stage 3 evaluation.
Search strategy
The search strategy was devised as both online and offline to identify services in the UK where youth, sexuality or gender identity, and mental health were a focus.
Online search strategy
During online searching, Google (the internationally most used search engine) and Bing (the default search engine for the respective organisation’s IT systems) were used to locate websites of interest using the following search phrases:
-
LGBTQ+ Young People Mental Health Services [ADD GEOGRAPHICAL AREA].
-
LGBTQ+ CAMHS [ADD GEOGRAPHICAL AREA].
-
LGBTQ+ Youth Group [ADD GEOGRAPHICAL AREA].
These search phrases were selected and piloted with LGBTQ+ young people and service providers, to ensure they reflected the type of search term used when looking for mental health support for themselves or a service user. The rationale for this search strategy was that current active services would need to be discoverable to potential service users in a basic web search and therefore these phrases should illuminate most of the available service options. The first 10 sites yielded through these search terms were checked for available services. Information about the service and provision offered was also gathered through specific websites, forums, blogs, and relevant social networking sites. Online searches were also conducted for local Children and Adolescent Mental Health Services (CAMHS) transformation plans, which were likely to detail current and planned services for LGBTQ+ young people. In addition, a search for LGBTQ+-associated charter marks (e.g. Stonewall Champions, The Rainbow Flag Award to identify potential school services) was undertaken. The online search was supplemented by standard systematic search strategies including expert informants (academics and service providers) and subject-specific hand searching of print media (March 2019 issues of DIVA, Attitude and Gay Times). 87
Services that clearly offered support for LGBTQ+ youth mental health and those which were likely to support LGBTQ+ youth mental health were recorded. In the latter case, ‘likely’ meant that there was good reason to think the service supports LGBTQ+ youth mental health in some capacity including:
-
LGBTQ+ youth services, many of which had basic websites or Facebook groups and did not give detailed account of their activities in online information, including how they offer mental health support.
-
LGBTQ+ mental health services that did not explicitly state they offered targeted work to young people but were available to under 26-year-olds.
-
Youth mental health services that did not advertise LGBTQ+ specific work but are important providers of mental health support to this age group (e.g. Young Minds).
-
Services known through expert informants to support the mental health of LGBTQ+ young people.
Offline search strategy
The offline search included the use of print-only media such as magazines, newspapers and free periodicals that do not necessarily have an online format to facilitate in-depth search at a local level. The use of offline print media allows for the identification of any potential smaller, more marginalised groups or services that may utilise small advertising for discretion. The offline search will also be facilitated through the following key contacts and networks such as:
-
LGBTQ+ third sector service providers, for example MindOut, Viva LGBTQ+ youth (Wales), Gendered Intelligence, The Proud Trust
-
LGBTQ+ third sector national umbrella organisations, for example National LGB&T Partnership, Stonewall, Stonewall Cymru, LGBTQ+ Foundation, LGBTQ+ Consortium, LGBTQ+ Youth Scotland, Cara-friend [Northern Ireland (NI)]
-
Key third sector youth organisations, for example 42nd Street, Barnardo’s
-
Key third sector mental health organisations for example Young Minds, Self Harm UK
-
Key expert informants, that is professionals developing LGBTQ+ youth mental health services
-
Professional groups such as the Royal Colleges of Nursing, General Practice and Psychiatrists, Schools and Students Health Education Unit, CAMHS Nurse Consultants network, British Psychological Society
-
NIHR clinical research networks, for example primary care, mental health
-
All primary care trusts and mental health trusts
-
All directors of children’s services in local authorities
-
National third sector umbrella organisations, for example, NCVO (The National Council for Voluntary Organisations), National Youth Agency.
We made a Freedom of Information (FOI) request directly to all NHS trusts delivering CAMHS in the UK (n = 79) to enquire about any LGBTQ+ youth-specific mental health service provision as CAMHS have a minimal online presence, and we were unable to obtain service information via webpages. FOI request contained the following questions:
-
Does your trust provide a specific mental health service for LGBTQ+ young people?
-
Are your staff offered LGBTQ+ awareness training?
-
Do you deliver the training in house or is it provided by an external partner?
-
Do you have a specific policy for working with LGBTQ+ people?
Trusts were asked to provide contact details for a staff member who would be able to provide more information about any services identified.
Inclusion/exclusion of services
The identified services were considered against inclusion and exclusion criteria. Determining whether services meet the inclusion criteria was an iterative process, dependent on the information available through the website and informal conversations with expert informants and the services directly. This was applied by two research team members. The inclusion/exclusion criteria are detailed in Table 6.
| Domain | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Mental health | Provide support for common mental health conditions for example depression, anxiety, self-harm | Crisis servicesNo mental health problems |
| Age | Targeted to 12- to 25-year-olds | Services for exclusively under 12 years oldServices exclusively for over 25 years old |
| Sexuality/gender | Targeted to LGBTQ+ young peopleYouth mental health support within gender identity services | No LGBTQ+ youth provisionGender identity services (physical health services) |
| Service operation | Moderated by an agent, for example service staff memberActive during February 2019–February 2020Delivered in the UK (England, Scotland, Wales, NI) | Services where no agent/staff were involved, for example self-help appsNot active between 1 February 2019 and 31 December 2019Delivered exclusively outside the UK |
Data extraction
Detailed information (Table 7) about the operation of the eligible mental health services was collected using the service website, online resources, key contacts, and direct contact with the service via telephone or e-mail and entered into an Excel spreadsheet by two members of the study team.
| Data type | Definition |
|---|---|
| Service name | All names the service has operated under |
| Service provider | NHS, Local Authority, School, Private, Voluntary/Charity, Community Interest Company |
| Sexual orientation | Lesbian, Gay, Bisexual, Queer, Questioning, Asexual, Aromantic, Fluid, Pansexual, Skoliosexual; and any other sexual orientations |
| Gender identity | Transgender, Gender Fluid, Non-Binary, Agender, Bigendered, Genderqueer, Intersex, Transman, Transwoman; and any other gender identities |
| Target group | Demographic details of who attends the services |
| Mental health condition | Common mental health conditions: Anxiety, depression, obsessive-compulsive disorder, self-harm, PTSD, emerging personality disorders |
| Theoretical approach | This will be determined by grouping the services at the end of the mapping exercise |
| Mode of delivery | How is the service delivered? For example, face-to-face, online, groups, one-to-one |
| Tools/techniques | What tools/techniques does the service use to provide mental health support? For example, counselling, arts therapy, sports, exercise |
| Self-care element | What is done by the service user to improve their mental health (usually an activity of some sort, for example reading materials, practising an action, learning a technique) |
| Support element | What is done by the staff member to support the improvement of young people’s mental health (coaching, facilitating, giving feedback and encouragement) |
| Setting | Where is the service delivered? For example, clinic, community, home, online |
| Rural/urban | What is the geographic location of the service? Urban or rural |
| Length of contact | What is the average length of time a young person is involved in the service? |
| Frequency of contact | How often on average is a young person involved in the service? |
| LGBTQ+ training | Does the service offer LGBTQ+ training? Is it voluntary or mandatory? |
| LGBTQ+ policy | Does the service have a specific LGBTQ+ policy? |
| Facility adaptations | Have there been any adaptions to the facility to make it more suitable for LGBTQ+ young people? For example, gender-neutral toilets |
| Country/county | Where is the service based? Country (England will be split into counties) |
| Duration running | How long has the service been operational? |
| Commissioned specifically? | Is the LGBTQ+ mental health support specifically funded as part of somebody’s job description? |
Frequently it was difficult to determine from the information available during the searching phase (e.g. via websites) whether a service definitely met the inclusion criteria. In these cases, services were contacted via telephone or e-mail by the researchers for further information. Thus, the searching and information extraction was more of an iterative than linear activity and these activities overlapped considerably in practice. To assist in determining if services were relevant for inclusion, a flow chart was created in consultation with the Project Advisory Group (see Appendix 2).
Once services were deemed to meet the inclusion criteria, detailed information was collected about their operation. This information was extracted either from materials available in the public domain such as service websites and promotional materials or by requesting the information via telephone, e-mail or by asking a service representative to complete an online form. All information extracted was inputted into a spreadsheet for each of the categories in Table 7.
Typology generation
The typology of early intervention mental health service/support for LGBTQ+ young people was developed by five members of the research team. Framework analysis was used to create the typology of services from the information extracted during the mapping process. 98,99 Framework analysis consists of five processes: familiarisation, identification of thematic framework, indexing, charting, followed by interpretation. 100
During the familiarisation process, the researchers highlighted themes and similarities between the services. These initial observations along with the findings of the MNR informed the creation of the thematic framework, which provided the basis of the indexing and charting. A matrix format was utilised for the indexing and charting processes to a group of services. 98 The grouping of services informed the development of the service typology. Finally, the research team along with the wider project advisory group discussed the criteria for the service typology and produced a simple typology that identified the type of service provision available in the UK.
Case study selection
Case study sites were selected from each category of the service typology. The case study selection criteria were developed by five members of the research team and are outlined in Table 8. The criteria were developed to reflect the capacity of the service to participate in the research and to include a diversity of service models in a range of settings at a variety of geographical sites. The CSS were determined in consultation with the project advisory group and LGBTQ+ young people. Twelve CSS were selected.
| Criteria | Criteria description |
|---|---|
| Type of service | There should be a case study site for each of the services in the typology |
| Theoretical approach/model | Case study sites should include a range of approaches/models of mental health support, for example, CBT, person-centred, affirmative, activist/advocacy, youth work, peer-led, pedagogical, empowerment, social model, clinical model |
| Geography | At least one site in the four nations – England, Scotland, Wales and NI |
| Capacity | Case study sites must be robust enough to undergo an evaluation and can demonstrate:
|
| Operation | Case study sites are operational for the 12 months of the data collection period |
| Urban/rural | Case study sites should include a mix of urban and rural provision |
| Age | The 12 case study sites include the full age range of the study (12–25 years old) |
| Trans/gender diversity | One to two of the case study sites should be trans/gender specific |
Stage 3: case study evaluation method
The third stage of the proposed study addressed research questions 3–5:
-
How, why and in what context do mental health early intervention and supported self-care work for LGBTQ+ young people?
-
In what ways do LGBTQ+ young people access and navigate formal and informal mental health early intervention services and self-care support?
-
How can LGBTQ+ young people be encouraged to access and engage with mental health early intervention services and self-care support?
And objectives 3–5:
-
To develop a programme theory of how, why and in what context mental health early intervention services and self-care support work for LGBTQ+ young people.
-
To increase understanding of LGBTQ+ young people’s access to and navigation of formal and informal mental health early intervention services and self-care support.
-
To generate commissioning guidance (including service costs) on mental health early intervention and supported self-care services for LGBTQ+ young people.
Methods overview
The third stage of the project comprised a collective case study evaluation of mental health early intervention and self-care support services for LGBTQ+ youth across 12 case studies. A case study is an empirical enquiry that focuses on a single phenomenon in its real-life context, especially useful (as in our circumstances) when a description or explanation is required. 101 Collective case studies are those in which multiple cases are studied simultaneously or sequentially in an attempt to generate a broad appreciation of a particular issue. 69 Yin62,101 defines a ‘case’ as a ‘bounded entity’, a broad and flexible definition that allows the case to be as varied as an event, an individual, a service or a policy. In this project, we have defined the case as ‘mental health early intervention and self-care support service for LGBTQ+ young people in the UK’.
The 12 case studies were purposively102 selected from services identified in stage 2 (service mapping) to reflect the different dimensions of the stage 2 service typology. We estimated that 12 would be an adequate number of cases to capture the range of services identified in stage 2. Data were collected from key stakeholders in each of the CSS (n = 12) to examine factors such as service acceptability, gaps in provision, barriers/facilitators to access, views on service improvement and encouraging access/engagement. At each case study site, data were collected via:
-
Online interviews with LGBTQ+ young people, family members and service staff (n = 10)
-
Documentary review
-
Non-participant observation
-
Data were collected on service cost.
Case study evaluation is a theory-driven evaluation methodology and therefore the data analysis strategy is theoretical using the ‘explanation-building’ (EB) analytical technique. 62 The findings from each case study site were used to gradually refine the theoretical model developed in stage 1 of the study to produce an overarching theoretical understanding of how, why and in what context mental health early intervention services and self-care support work for LGBTQ+ young people. 69
Sampling and recruitment
A purposive sampling strategy64 was used to select participants within the case study sites to ensure that a diverse range of appropriate stakeholders (LGBTQ+ youth, parents and carers, health, social care and education professionals, and volunteers) were invited to participate.
For service staff, the inclusion criteria were that they worked for the case study service and had experience supporting the mental health of LGBTQ+ young people. For parent/carers inclusion criteria were that they had experience caring for an LGBTQ+ young person with common mental health difficulties who had sought mental health support. For LGBTQ+ young people, the eligibility criteria were as follows:
-
12–25 years old
-
Identifies as LGBTQ+
-
Experience of seeking support for a common mental health difficulty
-
Currently engaged with the case study service
-
Not in crisis.
Recruitment of LGBTQ+ young people was via digital flyers and posters circulated by the service staff. In some cases, research staff went along to online youth group sessions to introduce Queer Futures 2 and invite participation. In other cases, support workers passed the digital flyers directly to individuals they thought may be interested and safe to take part. Individual LGBTQ+ young people were selected purposively to ensure we involved a diverse range of LGBTQ+ young people including in relation to gender and sexual identity, ethnicity, poverty and disability. Recruitment of service staff was also purposive to gain diverse insights into LGBTQ+ youth mental health support depending on job role. Parents/carers were recruited only where there was a specific parent/carer support group.
In total 93 participants took part in the study: 45 LGBTQ+ young people, 42 service staff, 6 parents/carers (see Table 9 for demographic characteristics of participants).
| Variable | Classification | Young people (n = 45) | Service staff/volunteers (n = 42) | Parents/carers (n = 6) |
|---|---|---|---|---|
| Age (years) | 12–16 | 11 | ||
| 17–20 | 23 | 2 | ||
| 21–25 | 11 | 4 | ||
| 26–35 | 16 | |||
| 36–45 | 12 | 1 | ||
| 46–55 | 6 | 5 | ||
| 56–65 | 2 | |||
| Gender | Man/boy | 18 | 13 | |
| Woman/girl | 8 | 23 | 6 | |
| Non-binary | 13 | 3 | ||
| Othera | 6 | 3 | ||
| Are you trans? | Yes | 32 | 7 | |
| No | 8 | 33 | 6 | |
| Unsure | 2 | 1 | ||
| Prefer not to say | 3 | 1 | ||
| Ethnicity | Black African | 1 | ||
| Black British | 1 | 1 | ||
| Black Caribbean | 1 | |||
| Chinese | 1 | |||
| Irish | 3 | |||
| Latino | 1 | |||
| Mixed ethnicity white/Asian | 2 | 2 | ||
| Mixed ethnicity white/Black Caribbean | 3 | |||
| Other | 1 | |||
| Other (mixed ethnicity)a | 2 | 2 | ||
| Pakistani | 1 | |||
| Prefer not to say | 1 | |||
| White (other) | 5 | 2 | 1 | |
| White English/Irish/Scottish/Welsh/British | 29 | 29 | 4 | |
| Sexual orientation | Asexual | 7 | ||
| Bisexual | 6 | 7 | 2 | |
| Gay | 8 | 9 | ||
| Heterosexual | 2 | 10 | 4 | |
| Lesbian | 2 | 6 | ||
| Pansexual | 4 | 1 | ||
| Queer | 9 | 7 | ||
| Questioning | 2 | 1 | ||
| Othera | 5 | 1 | ||
| Are you disabled? | Yes | 21 | 6 | |
| No | 20 | 35 | 6 | |
| Prefer not to say | 4 | 1 | ||
| Type of disability | Chronic illness | 2 | 2 | |
| Learning disability | 9 | 1 | ||
| Mental health condition | 27 | 4 | ||
| Mobility impairment | 4 | 1 | ||
| Neurodiversity | 12 | |||
| Othera | 1 | |||
| Prefer not to say | 1 | |||
| Sensory impairment | 4 | |||
| Undiagnosed mental health condition | 26 | |||
| Highest qualification | No qualifications | 6 | ||
| GCSE | 16 | |||
| AS levels | 1 | 1 | ||
| A levels | 15 | 2 | 2 | |
| HE diploma | 2 | 2 | 1 | |
| First degree | 2 | 20 | 1 | |
| Higher degree | 2 | 15 | 2 | |
| Trade apprenticeship | 1 | |||
| Prefer not to say | 2 | |||
| Employment | Student | 28 | 2 | |
| Unemployed | 9 | |||
| Full-time employment | 1 | 26 | 5 | |
| Part-time employment | 4 | 12 | 1 | |
| Other | 3 | 1 | ||
| Prefer not to say | 1 | |||
| Parent degree | Yes | 23 | ||
| No | 16 | |||
| Unsure | 6 | |||
| Free school meals | Yes | 18 | ||
| No | 19 | |||
| Unsure | 8 |
Data collection
Semistructured online interviews
We conducted semistructured qualitative interviews with three groups of participants:
-
Service staff using online video apps – Zoom or Microsoft Teams
-
Parent/carers using online video apps – Zoom or Microsoft Teams
-
LGBTQ+ young people via WhatsApp (text only).
The aim of the interviews was to generate in-depth, exploratory data from the perspectives of the participants. 103 The rationale for employing different modes of interviewing were the difficulties of researching a marginalised group, collecting data during the COVID-19 pandemic and the sensitivity of the topic. There are difficulties recruiting samples because participants may be unwilling to be open about their LGB or T and/or mental health status. Previous studies, including the lead author’s, have demonstrated that online interviews can be successfully used to examine LGBTQ+ youth’s mental health. 13,42,104 This is because a virtual interface provides unique access to LGBTQ+ youth who may not otherwise participate in research,105 and the internet is an important vehicle by which LGBTQ+ youth seek information and support regarding their sexual orientation, gender identity and mental health. 104,106
The decision to use WhatsApp as a method of interviewing LGBTQ+ young people was based on consultation with LGBTQ+ young people. While Instagram was popular too, WhatsApp offered superior data security via end-to-end encryption. WhatsApp also offered functionality for sending picture messages and links to, for example, the demographic survey and participant information video. Finally, the anonymity afforded to LGBTQ+ young people and the mode of answering questions, that is, via typing text, was desirable as it was likely that many would be taking part from their domestic environments during lockdown. WhatsApp offered privacy that was not otherwise available via video interviewing. Albeit limited, there was also some published evidence about the effectiveness of using WhatsApp for interviewing young people about mental health topics. 107,108
All topic guides for the individual interviews were informed by stage 1 (existing evidence review) and piloted with our PPI groups. Questions were standardised and made friendly and accessible for LGBTQ+ young people through the use of images (see Report Supplementary Material 1). Qualtrics was used to collect demographic information and service cost data (see Report Supplementary Material 2). The links to online forms for completion were forwarded through WhatsApp or e-mail (for staff/parents or carers) as part of the interviews.
The online video interviews were recorded and converted to audio only for transcription. The WhatsApp interviews were downloaded direct to Lancaster University’s secure encrypted cloud storage – Microsoft OneDrive. Non-professional participants (e.g. young people and parents/carers) were offered £20 in gift vouchers as a token of thanks for participation.
Non-participation observation
Most case study sites at the point of data collection were providing an online service. Data from these sites were collected via ‘netnographic’ non-participation observation. Netnography is a form of ethnography that has been used in the study of online health behaviour,109 and similar to ethnography, it is concerned with everyday routine behaviours in a natural setting. 110 This method is appropriate for the observation of services that may operate entirely online. All non-participant observation was recorded in a case study workbook template that was designed to standardise data collection across the sites. Data was collected, for example, on the manner in which the service was run, duration, timings, model of mental health provision, staff and volunteer organisation, partnerships and relationships.
Documentary review
Where available, relevant documentary evidence was collected from each site such as operational manuals, service evaluations, administrative service datasets, strategic plans, intervention protocols, information leaflets. This documentary evidence largely served to provide a contextual background to, and additional understanding of, the 12 case studies. All documentary data were recorded in a case study workbook template that was designed to standardise data collection across the sites.
Service cost data
Information on resource use was collected from individuals when interviewed via an online survey tool, shared via a weblink at the end of the interview (see Report Supplementary Material 2). This was done for the purpose of supporting the development of the NHS commissioning guidance only. The aim of the health economic analysis was to determine the pattern of service use by LGBTQ+ young people and generate average service costs per user. Utilising a combination of the findings of the stage 2 service mapping and feedback from PPI, participants were asked about their use of a wide range of healthcare and social services visits such as general practitioner (GP), nurse at GP surgery, psychiatrist, community mental health/psychiatrist nurse, other mental health services and other service use. Each participant was also asked about their use of services in the case study site including 1 : 1 sessions, peer support, activity sessions and other sessions. Participants self-reported their use of services using a survey developed for this study with a recall period of 4 weeks.
Costs were considered for health care provided in primary care, community mental health services, emergency services, social care services and other services. We also considered the care-provided case study sites. All costs are presented in pounds sterling using 2021 available costs.
Data analysis
First, the data sets – interview transcripts, non-participant observation and documentary evidence – from each individual case study site were imported into Atlas.ti.9 computer software designed to assist in the organisation and analysis of qualitative and multi-methods data (the service cost data were not included).
The resulting data set was extensive and diverse as is characteristic of case study research. This volume of data needs to be managed systematically62,101,111 with a clear analytical data strategy in place prior to data collection. 111 Case study evaluation is a theory-driven evaluation methodology, and therefore, we drew on Yin’s EB data analysis strategy that is designed for case studies with multiple case sites (like ours) and aims to build a general explanation that fits each individual case.
Yin111 (p. 142) states this is ‘analogous to creating overall explanation, in science, for findings from multiple experiments’. EB is used where ‘how’ and ‘why’ questions (i.e. causal questions) are regarding complex topics that are difficult to measure. The explanation is therefore narrative and more robust if there is a central theoretical proposition. The theoretical framework/model developed from stage 1 MNR provided this and a coherent orientation for our case study data analysis. Generally, this approach has been poorly operationalised and described by other studies and therefore we relied upon insights from Yin. 111 There are three fundamental aspects of case study data analysis that informed our strategy:
-
This is a deductive and inductive approach
Explanation building is partly deductive because we had a theoretical model from stage 1 that we proposed explains early intervention mental health support for LGBTQ+ youth. This model came from the literature/evidence, and we were ‘testing this’ with our 12 case study sites. EB is also partly inductive because we suspected the model was inadequate and we were using data from the case study sites to revise and improve the model.
-
Includes within-case analysis and cross-case synthesis
What is important to case study analysis is a whole-case approach. In a sense, the case study site is the unit of analysis. This means for each case study site we conducted a ‘within-case’ analysis, followed by cross-case synthesis comparing whole-case study sites. The aim was to retain the integrity of each entire case study site. In this way, the findings from each case study site data analysis were used to gradually refine the theoretical model developed in stage 1 to produce an overarching theoretical understanding of the mechanisms by which mental health early intervention services can support LGBTQ+ young people with common mental health problems.
-
Uses a series of iterations
The iterative nature of EB is central to the approach of a case study with multiple case study sites. Eventual explanation results from a series of iterations, and if done in relation to a theoretical proposition increases the trustworthiness of the findings. The findings from each case study site were examined and compared to the theoretical model from stage 1 which was then revised, and the evidence examined again. This iterative process was important to ensure other plausible explanations were considered in the process. 62
In this way, the findings from each case study site data analysis were used to gradually refine the theoretical model developed in stage 1 to produce an overarching theoretical understanding of the mechanisms by which mental health early intervention services and self-care can support LGBTQ+ young people with common mental health problems.
Operationalising EB data analysis in a case study evaluation with multiple case study sites is difficult because we had a large amount of complex data. Our analysis was conducted on each site only when all data had been collected for that individual case study site. The iterations of analysis were in four phases as follows:
-
Deductive within-case analysis Revision of model
-
Deductive/inductive cross-case analysis Revision of model
-
Inductive within-case analysis Revision of model
-
Inductive cross-case analysis Final revision of the model.
The four phases of the case study analysis process are represented in Figure 1.
FIGURE 1.
Four-phase case study analysis.
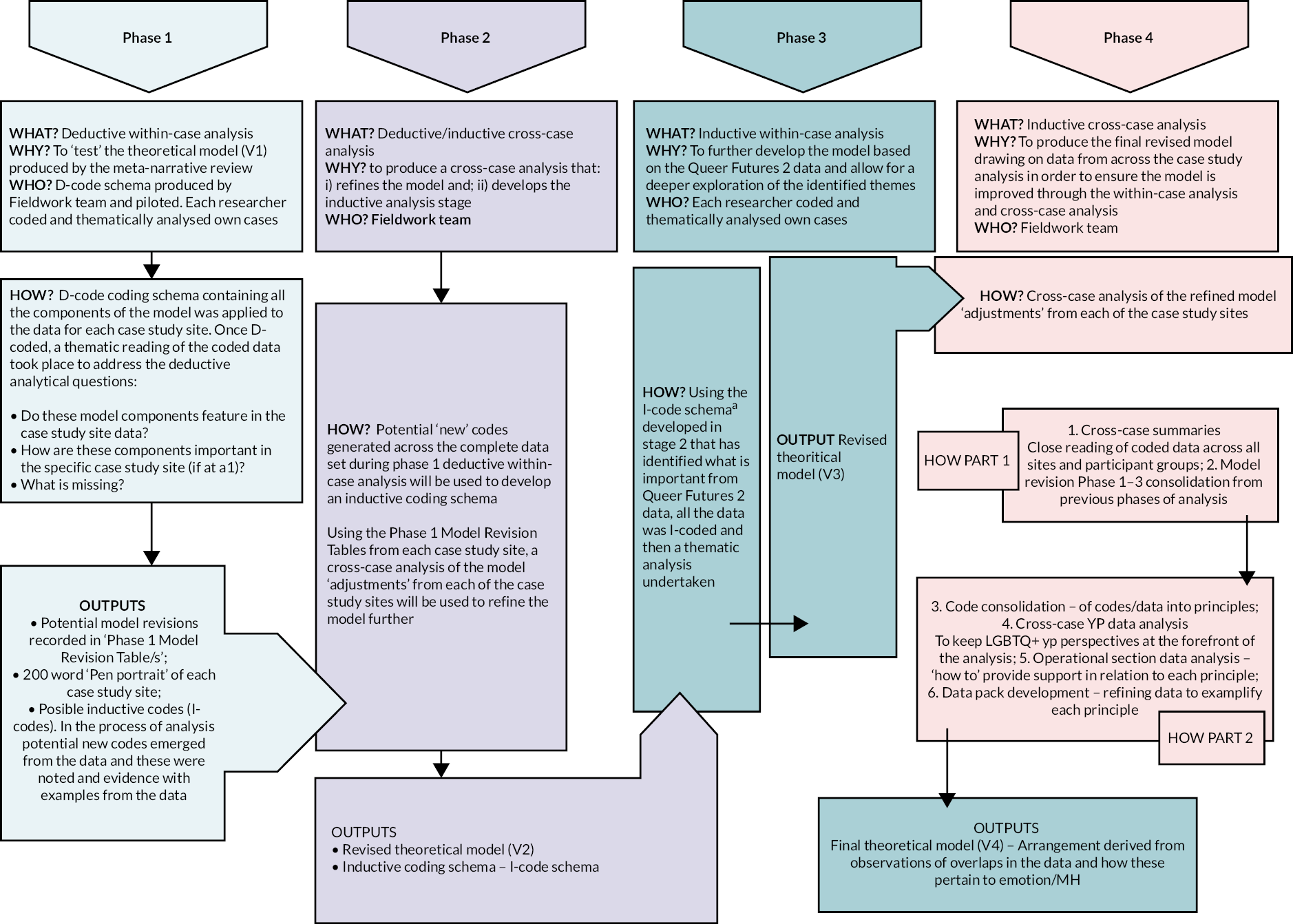
Intersectionality, including factors that were ‘missing’ or privileged, was held at the forefront of the analytical process throughout.
Coding took place in Phase 1 using a coding framework developed from the theoretical model from stage 1: MNR. As this coding was deductive, these were referred to as ‘D-codes’. Inductive codes (‘I-codes’) deduced from the data through this initial coding process were then applied in Phase 3 (see Appendix 3 for coding frameworks).
Service cost analysis
Following NICE guidance,112 the economic analysis was undertaken from an NHS and personal social services perspective. A top-down micro-costing approach113 was undertaken to value the services used. Total and average costs were calculated separately for each case study site based on the information regarding service use given by participants recruited.
Service use was costed by applying national average unit costs, obtained from unit costs of Health and Social Care 2021114 or other sources as appropriate. Unit costs used include overheads, capital, and infrastructure costs, allocated according to staff time. Information about inpatient admissions, A&E, clinical tests and use of medicines was not collected and therefore is not considered in the analysis. Travel expenses were not accounted for. In order to obtain the average costs, we multiplied the average use of services by the corresponding cost.
Validation
Key findings and the theoretical model devised from the process of analysis were subject to a process of validation by LGBTQ+ young people.
Research governance and ethics
This study was a low-risk study, as it did not recruit young people who are in mental health crises and focused on their views and experiences of mental health services and support, as opposed to the specifics of their mental health or sexuality. The team experience in consultation with the LGBTQ+ Youth Advisory Group indicated that LGBTQ+ young people are motivated to take part in research about mental health when given the opportunity and perceive the topic to be important and valuable. 13,40,42 The ethical considerations of the study are addressed in detail below.
Informed consent
For participants in online interviews, informed consent was gained through an electronic signature on a data-secure form before taking part in the interview. Informed consent is an ongoing process, with participants being reminded of their right to withdraw at intervals throughout the study. LGBTQ+ young people aged 12–15 years were afforded the right to give consent without the need to involve their parents/guardians. Requiring parental consent may have placed the young person at risk of hostility, abuse and rejection if their parents were previously unaware of their sexual orientation or gender diversity. 86 There is evidence that disclosure of LGBTQ+ identity to some parents and carers can have potentially harmful consequences and risks familial rejection, abuse, homelessness, and violence. 42,115–118
It is increasingly recognised that young people under 16 years of age are able, and should, give consent for taking part in research as long as they are judged as competent. 119–121 In the UK and globally it is recognised that children’s opinions should be considered in all matters that affect them, and this is ratified by the UN Convention on the Rights of the Child as a fundamental right. 122 It is now common practice for research studies examining LGBTQ+ young people and health to waive parental consent. 123–128 Studies suggest that the majority of parents agree that parental consent should not be required for LGBTQ+ young people to participate in research because of the risk of harm. 129 In addition, studies show that LGBTQ+ young people are less likely to participate in research if parental consent was required. 130 The LGBTQ+ Young People’s Advisory Group for this study confirmed that it was important that parental consent was waived to encourage young people to participate in research and contribute their views and experiences.
Research guidelines for recruiting and protecting LGBTQ+ young people suggest that waiving parental consent is warranted if the research involves only minimum risk, the rights and welfare of the participants will not be adversely affected and the research could not be conducted without a parental waiver. 131,132 The three main components of informed consent are as follows: the information is presented in an understandable way; consent is voluntary; and the participant has capacity to provide consent. 120 In Medical Research Council ethics guidance on research with children, competency is considered not to depend primarily on age, but rather on the ability to understand and weigh up options. 133 Competency can be influenced by the way information is presented and many young people will be competent if information is presented in an appropriate way and they are supported through the decision-making process. 133 We worked alongside the LGBTQ+ Young People’s Advisory Group to ensure the informed consent process was appropriate and the study took the following steps to obtain informed consent:
-
Informed consent was gained through a digital signature for all participants (young people, key/youth/education workers, parents/carers). Participation in the study was discussed with a study researcher who was independent and not involved in any services the young person was receiving, or staff were delivering. The project information sheet and consent form were available before an interview was conducted to ensure participants had time to consider the material, ask questions and seek any further information.
-
The study materials for LGBTQ+ young people were presented in an accessible way and in an age-appropriate format to help ensure those who may have literacy problems, are younger or have language barriers were able to provide informed consent. The participant information sheet (PIS) for young people was presented in three formats (see Report Supplementary Material 3): (1) accessible language written PIS; (2) visual infographic abbreviated PIS; and (3) PIS video with voiceover audio description. The PIS materials were co-produced in collaboration with the study LGBTQ+ Young People’s Advisory Group to ensure they used appropriate language, at an appropriate level of comprehension and address the correct issues and concerns that young people may have about participating in the study.
-
To facilitate the informed consent process, study materials were available on the study website (www.queerfutures2.co.uk). The Chief Investigator’s previous studies have shown that online content about the research study enables LGBTQ+ young people to learn more about the study, who is involved, why it is happening and what will actually happen if they participate in an interview. 42 Online content allows potential participants to read the information in their own time, in a format that is familiar. The project website had been designed in collaboration with the study’s LGBTQ+ Young People’s Advisory Group, in an accessible format with safety features such as a quick exit button to ensure they can leave the webpage quickly if necessary and maintain their privacy.
-
Participants were advised of their right to withdraw from the study at any stage and the right to request their data to be deleted from the study dataset.
-
Young people aged 12–15 years gave informed consent if they were deemed competent. For a young person to be deemed competent, they had to have study information presented in an understandable way; understand consent is voluntary; and have the capacity to provide consent. 134 In line with guidelines for researching children’s mental health,120 four criteria were used to assess capacity to consent:
-
Can the individual understand the information given to them?
-
Can the individual retain that information long enough to be able to make a decision?
-
Can the individual weigh up the information available to make a decision?
-
Can the individual communicate their decision to you?
-
Risks, burden and benefits
Risk of distress
There is potential for distress to be generated by discussing people’s experiences of seeking help for mental health problems. During interviews, the researchers were vigilant for signs of distress or discomfort in the text chat or online interviews. As a matter of course, all participants were asked how they were feeling at the start, during and at the end of the interview. Participants were informed that they could signal at any time if they need to take a short break, and they could end the interview at any point. When the interview was completed, the study researcher followed the ‘exit plan’ outlined at the end of the topic guide (see Report Supplementary Material 1).
Young people who participated in the research were made aware that any concern regarding the well-being of the participant and the participant’s support worker from the case study service would be informed. In addition, interviews with LGBTQ+ young people were all arranged with a check-in follow-up meeting with their support worker at the case study service immediately after the interview. This added an additional layer of care for the young person which was deemed appropriate during the context of the COVID-19 pandemic and lack of opportunity to meet in person. This strategy was agreed upon and devised between the research team and the case study services when we were making adaptations to the method design in response to COVID-19. In no cases did the support workers report any distress or adverse events for the LGBTQ+ young people as a result of taking part. Additional information about further support services was available through the Queer Futures 2 website and on the Participant Information Sheet (see Report Supplementary Material 3).
Benefits
Lesbian, gay, bisexual, trans, queer/questioning, plus young people are a marginalised group and may have very little opportunity to have their views and experiences heard. The Chief Investigator’s previous studies have shown that many LGBTQ+ young people benefit from participating in research because it is a form of social inclusion, a validation of their experiences and a meaningful way to help other young people. 42,104 This has been confirmed through our PPI activities undertaken with the LGBTQ+ Youth Advisory Group. LGBTQ+ young people stated they would be excited and interested in being involved in the current study because it gives LGBTQ+ young people a voice, allows them to improve current knowledge and gives them the chance to make a difference to existing mental health services in the UK. All LGBTQ+ young people were invited to receive a £20 voucher for Amazon or Love2Shop as a thank you for their time.
Confidentiality, data handling and record keeping
Key to ensuring that LGBTQ+ young people participated safely in the research was confidentiality and anonymity. The study was compliant with Lancaster University GDPR full policy. Data were handled and stored in three universities (Lancaster, Leeds and Brighton) during the active data collection phase. We took the following measures to protect participants’ confidentiality and secure the study data:
-
The three study researchers each maintained an electronic file of potential participants to be contacted to discuss the study and obtain informed consent. This file was a general record of the study recruitment process and will include names for the purpose of contacting potential participants to obtain consent and to arrange an interview and focus group date and location (where appropriate). Once the interview had taken place, these details were deleted from the register. The names and contact details of people who did not provide informed consent were deleted from the register, but a numeric count was kept to record the number of people who were unable to or unwilling to take part. Each University (Lancaster, Leeds, Brighton) stored its files on the Lancaster University secure encrypted cloud storage – OneDrive. Only the immediate research team undertaking fieldwork had access to this folder.
-
Online interviews were recorded direct using Teams or Zoom and immediately converted to audio-only files for transcription (to remove the video component to protect anonymity) and stored in OneDrive. WhatsApp interview chat was exported direct to OneDrive. Only the research team undertaking the fieldwork had access to the drive.
-
The signed participants’ consent sheets were completed online, and copies were exported and stored with other data in the secure OneDrive filestore.
-
Transcribers signed a confidentiality agreement when transcribing and accessed the recordings direct from OneDrive. A specific folder was set up to share with the transcribers, so they only had access to these files. Transcriber(s) were requested where possible to stream the audio direct (rather than download it to their own computer). Audio files were deleted immediately when the transcription was complete.
-
The complete anonymised study dataset was electronically stored in the encrypted Lancaster University OneDrive and accessible only to the Chief Investigator, two co-applicants and three study researchers.
-
Following the end of the study period (December 2021), all anonymised study data will be stored for 10 years in a secure network drive on the Lancaster University secure server and access restricted to the Chief Investigator. This is compliant with Lancaster University’s Research Ethics and Governance code of practice.
Reporting procedures for risk and adverse events
We employed a two-tier approach to responding and reporting concerns of risk or adverse events. If the participant became upset during the interview, it was planned to be addressed by taking a break or ending the interview if they become upset. All participants were provided with details of local support services and encouraged to seek support from their regular service provider. In addition, interviews with LGBTQ+ young people were all arranged with a check-in follow-up meeting with their support worker at the case study service immediately after the interview.
We obtained copies of each case study service’s safeguarding policy and in the event that a participant disclosed or presented with major concern or significant risk to themselves or others, we had an agreement with the case study service to follow this procedure. There were no reported risks or adverse events throughout the data collection period.
Patient and public involvement
Lesbian, gay, bisexual, trans, queer/questioning, plus young people, the public and service users were involved in the study with the aim of ensuring that we generated research that would be useful to a wide range of stakeholders. In our experience, it is not possible to produce high-quality research without the involvement of those it impacts upon. Being young, LGBTQ+, and having mental health problems remains stigmatising and isolating. As a consequence, some LGBTQ+ youth do not use mental health services and are reluctant to talk to adults in their lives. In order to identify and understand mental health early intervention services and self-care support for LGBTQ+ young people, we needed their active involvement to help us to ask the right questions, in the right way and to gain an in-depth rigorous understanding of their mental health support needs.
Our study involved service users and the public in three ways. A service user from OpenMinds, a LGBTQ+ mental health youth group, was part of the research team and attended research team management meetings. We provided training, support and payment for the service user to participate in these meetings. They had direct experience and knowledge of mental health services and the issues faced by LGBTQ+ young people.
The second way we involved the public and patients was through a LGBTQ+ Youth Advisory Group consisting of young people from three LGBTQ+ youth groups: The Proud Trust in Manchester, Darlington ARC and Allsorts in Brighton. This group ‘met’ virtually throughout the study using Facebook. This format was determined by the young people on the initial study training day. The lead author successfully used social media to involve LGBTQ+ young people in previous mental health research13 and the young people who were involved stated that using online media made it easier to take part. The LGBTQ+ young people’s advisory group also contributed to the development of study materials, participant recruitment, interpretation of findings and dissemination activities. The third strand of our PPI was the study’s Advisory Board which included a range of LGBTQ+ third-sector stakeholders working with young people, for example Gendered Intelligence, Albert Kennedy Trust.
Chapter 3 Stage 1 results: meta-narrative review
Sections of this chapter have been reproduced with permission from McDermott et al. 60 This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Our MNR on mental health early intervention support for LGBTQ+ youth aimed to develop a theoretical framework to explain effective mental health support. The specific review questions were:
-
What empirical studies have been undertaken on mental health early intervention services and self-care support for LGBTQ+ youth?
-
What are the theoretical propositions for how and why these services/support work?
Results
Search results
The search was conducted between March and June 2019. In total, 2951 titles and abstracts were screened, and 200 full papers reviewed. Eighty-one studies were excluded due to not meeting the inclusion criteria and 31 studies were excluded for quality reasons. Eighty-eight papers remained for inclusion in the final analysis (see Figure 2 for PRISMA flow chart).
FIGURE 2.
PRISMA flow chart.
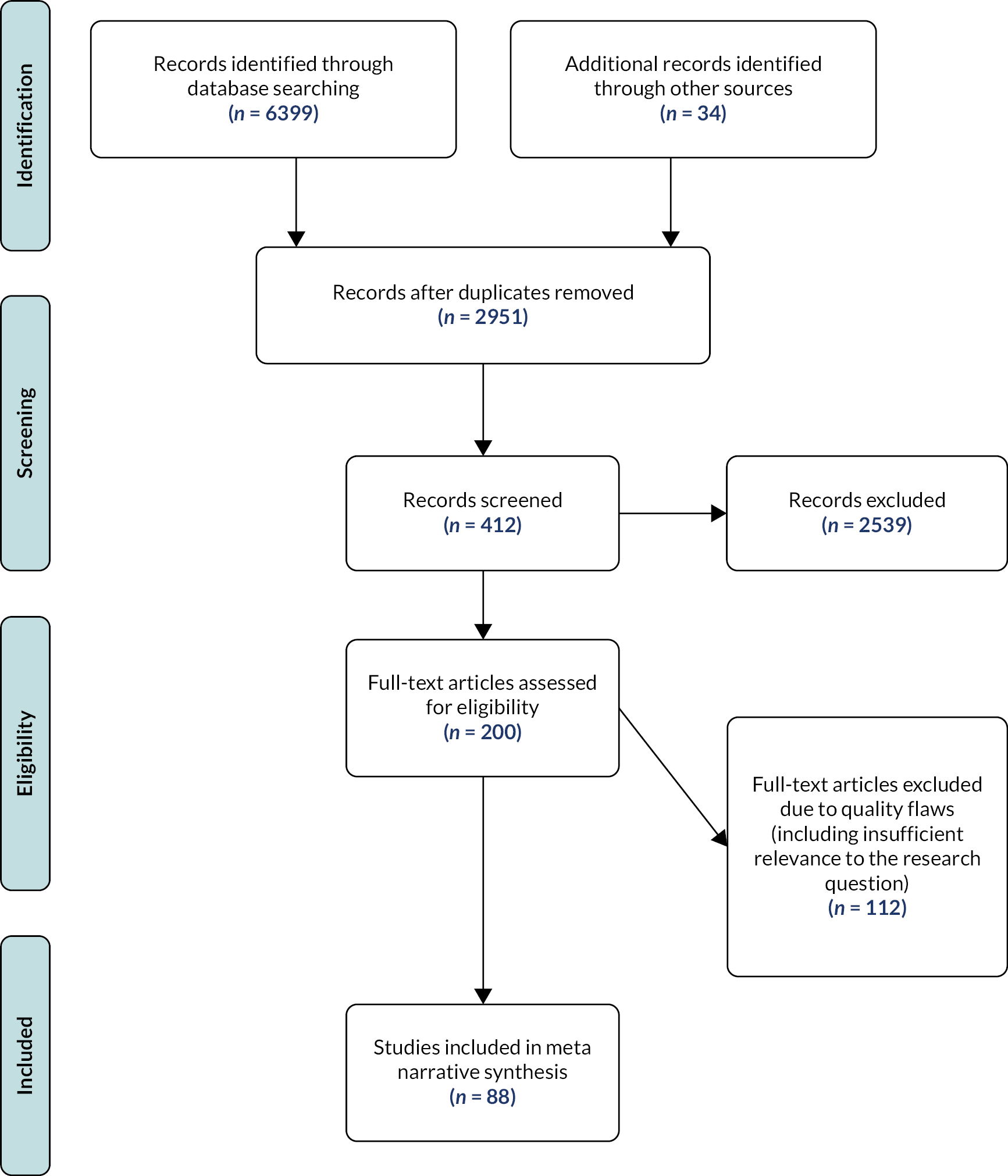
Stage 1. Synthesis: key research meta-narratives
We conceptualised the included literature into three meta-narratives: psychology, psychosocial, social/youth work (see Table 10 for included papers by paradigm). It is important to understand these are meta-narratives, that is, bodies of knowledge that have a shared approach to the topic. They do not refer to individual disciplines. We outline below the characteristics of these meta-narratives for each of the conceptual areas. There were often overlaps between the papers, and it was sometimes difficult to draw boundaries. For clarity, we grouped studies based on the underlying conceptualisation of mental health rather than the discipline of the author or journal.
| Psychological n = 28 | Psychosocial n = 27 | Social/youth work n = 33 |
|---|---|---|
| Abbott et al. 2014135 | Allen et al. 2012160 | Baker et al. 2016181 |
| Austin et al. 2018136 | Austin and Craig 2015161 | Bridget and Lucille 1996182 |
| Burns et al.137 | Bain et al. 2016162 | Chiang et al. 2018183 |
| Busa et al.138 | Chaudoir et al. 2017163 | aCover 201277 |
| Coulter et al. 2019139 | Chen-Hayes 2001164 | Craig et al. 201254 |
| Craig and Austin 2016140 | Cohler and Hammack 2007165 | Craig et al. 2017184 |
| Craig et al. 2013141 | Craig and Furman 2018166 | Davis et al. 2009185 |
| Craig et al. 2018142 | Gillig et al. 2019167 | Davis et al. 2010186 |
| Fleming et al. 2017143 | Heck et al. 2013168 | Erney and Weber 2018187 |
| aHatzenbuehler 2009144 | aJohnson 201471 | Fay 201743 |
| Hatzenbuehler and Pachankis 2016145 | McDermott 201541 | Ferguson and Macchio 2015188 |
| Heck 2015146 | aMcDermott and Roen 201613 | Gamarel et al. 2014189 |
| Hobaica et al. 2018147 | McDermott et al. 201642 | Hohnke and O’Brien 2008190 |
| Iacono 2018148 | McDonald 2018169 | Kwok 2018191 |
| Ioverno et al. 2016149 | McLaren et al. 2015170 | Kwok et al. 2012192 |
| Lucassen et al. 2013150 | Nodin et al. 2015171 | Lapointe and Crooks 2018193 |
| Lucassen et al. 2015151 | Oransky et al. 2018172 | Lapointe et al. 2018194 |
| Lucassen et al. 201845 | Proulx et al. 2019173 | LaFrançois 2013195 |
| McCallum and McLaren 2010152 | aRiggs et al. 2015174 | Medeiros et al. 2004196 |
| aMeyer 200372 | aRiggs and Treharne 201714 | MindOut 2016197 |
| Millar et al. 2016153 | Robinson 2010175 | O’Hara 2013198 |
| Pachankis and Goldfried 2010154 | Sandfort et al. 2010176 | Paceley 2016199 |
| Pepping et al. 2017155 | Tenenbaum 2012177 | Painter et al. 2018200 |
| Perry et al. 2017156 | Toomey et al. 20187 | Pallotta-Chiarolli and Martin 2009201 |
| Smith et al. 2017157 | Vincke and van Heeringen 2002178 | The Proud Trust 2016202 |
| Toomey et al. 2011158 | Vincke and van Heeringen 2004179 | Powell et al. 2016203 |
| Toomey et al. 2016159 | Zhang et al. 2018180 | Sadowski et al. 2009204 |
| Sansfaçon et al. 2018205 | ||
| Steinke et al. 2017206 | ||
| Wagaman et al. 2016207 | ||
| Wilkerson et al. 2017208 | ||
| Wilkerson et al. 2018209 | ||
| Wofford 2017210 |
Meta-narrative 1: psychology
The psychology meta-narrative focus is the brain and behaviour with the aim of understanding mental distress, rather than a mental disorder, and helping an individual to adjust to their circumstances. A high proportion of the publications within this paradigm were produced by psychologists and published in psychology journals. The dominant ontological and epistemological approach within the meta-narrative is positivist and, consequently, the research methods utilised are quantitative, typically using pre-test/post-test survey methods and standardised validated measures to undertake empirical trial research about interventions. The theoretical basis of these studies most often relied on Meyer’s72 Minority Stress Framework, in which LGBTQ+ identity is fixed and a discrete category. 72 For example, a paper may include measures of ‘distal stressors’ such as family homophobia and the impact on individual psychological functioning and identity development. In this meta-narrative, there was very little theorisation of youth, and the underpinning presumption was adolescent development.
In the psychology meta-narrative, the individual is the key object of study with the central aim to affect cognitive/behaviour change for individual LGBTQ+ youth. As a consequence, the paradigm concentrates on individual-level interventions such as cognitive–behavioural therapy (CBT), for example AFFIRM, an intervention aimed at trans youth and coping skills,140 and Rainbow SPARX, an online CBT programme aimed at sexual minority youth and depression. 151 Far less attention is paid to wider socio-cultural context of interventions.
Meta-narrative 2: psychosocial
The psychosocial meta-narrative considers the interplay of individual psychology and social contextual factors in mental health without conceptualising the two as discrete entities. This scholarship specifically aims to address the polarisation in debates between psychology and socio-historical perspectives of sexuality and gender. 13,71 The ontological and epistemological foundations of the papers within this meta-narrative were more varied (social constructionist, realist, positivist) and the generation of knowledge more interdisciplinary (and research teams multidisciplinary) and published across a wider range of journal types. Although quantitative methods remained the single most common approach, a broader range of methods was used here than in the psychology meta-narrative. However, mental health was frequently measured as per the psychological meta-narrative through standardised validated psychological measures.
As with the psychology meta-narrative, Meyer’s Minority Stress Theory72 was the dominant way in which LGBTQ+ youth mental health was conceptualised and the concept of youth was again under-theorised. There was also a significant use of queer theory and heteronormativity to critique normative adolescent development, mental health and minority stress theory. In addition, there is a more nuanced appreciation of the intersection of LGBTQ+ identity with other factors such as ethnicity and socioeconomic status. The support and interventions in this meta-narrative are more heterogeneous than those in the psychology meta-narrative. Individual support services/interventions are more likely to be multifaceted and include a social component (e.g. school belonging170) or delivery context (e.g. summer camp179) and be delivered in a community for example youth health centre172 or school setting, for example Gay-Straight Alliances. 168
Meta-narrative 3: social/youth work
This meta-narrative contains social/youth work scholarship or practice that considers individuals/youth in relation to their wider communities and resources. The ‘object of study’ for this meta-narrative is LGBTQ+ youth within their wider social context and much more attention is given to youth and their social world than in the other two meta-narratives. Mental health is usually loosely defined and untheorised. The dominant ontological and epistemological approach is social constructivist and interpretivist. Methodologically, this meta-narrative, congruent with the emphasis on youth participation, overwhelmingly uses a qualitative methodology frequently in collaboration with LGBTQ+ (youth) organisations. Youth is rarely theorised and the dominant conceptual framework regarding LGBTQ+ youth mental health is usually implicitly minority stress theory. Explicitly attending to cultural and ethnic diversity, this paradigm includes an intersectional perspective in theory and research practice, which means that compared to the psychological and psychosocial meta-narratives, there is a departure from considering LGBTQ+ youth as one homogeneous group.
The majority of the support/interventions discussed in this meta-narrative are social (rather than individual) and based in community (e.g. community support programme for Chinese trans youth191), school settings (e.g. mental health delivery in schools210) and (LGBTQ+) youth-specific organisations. 189 The interventions and recommendations for support from this meta-narrative were based on the experiences of LGBTQ+ youth as opposed to being ‘filtered’ through the perspectives of (adult) clinical or school perspectives.
Stage 2. Synthesis: developing a theoretical framework
The framework we have produced is ‘theoretical’ (Figure 3) and it is not a blueprint for a mental health support service. The framework contains the key dimensions, derived from the literature, of a service for successfully supporting, at an early stage, LGBTQ+ youth with common mental health problems. It draws on models found in the literature that attempt to capture the multilevel (macro, meso, micro) interacting complex factors required to support the mental health of LGBTQ+ youth. 172 Our framework has a critical approach to LGBTQ+ youth mental health support, paying attention to three key contestations across the meta-narratives: (1) the conceptualisation of adolescence/youth; (2) theorisations of mental health; and (3) the theoretical propositions for why LGBTQ+ populations have elevated rates of poor mental health.
FIGURE 3.
Theoretical non-pathologising framework for providing mental health support to LGBTQ+ young people.
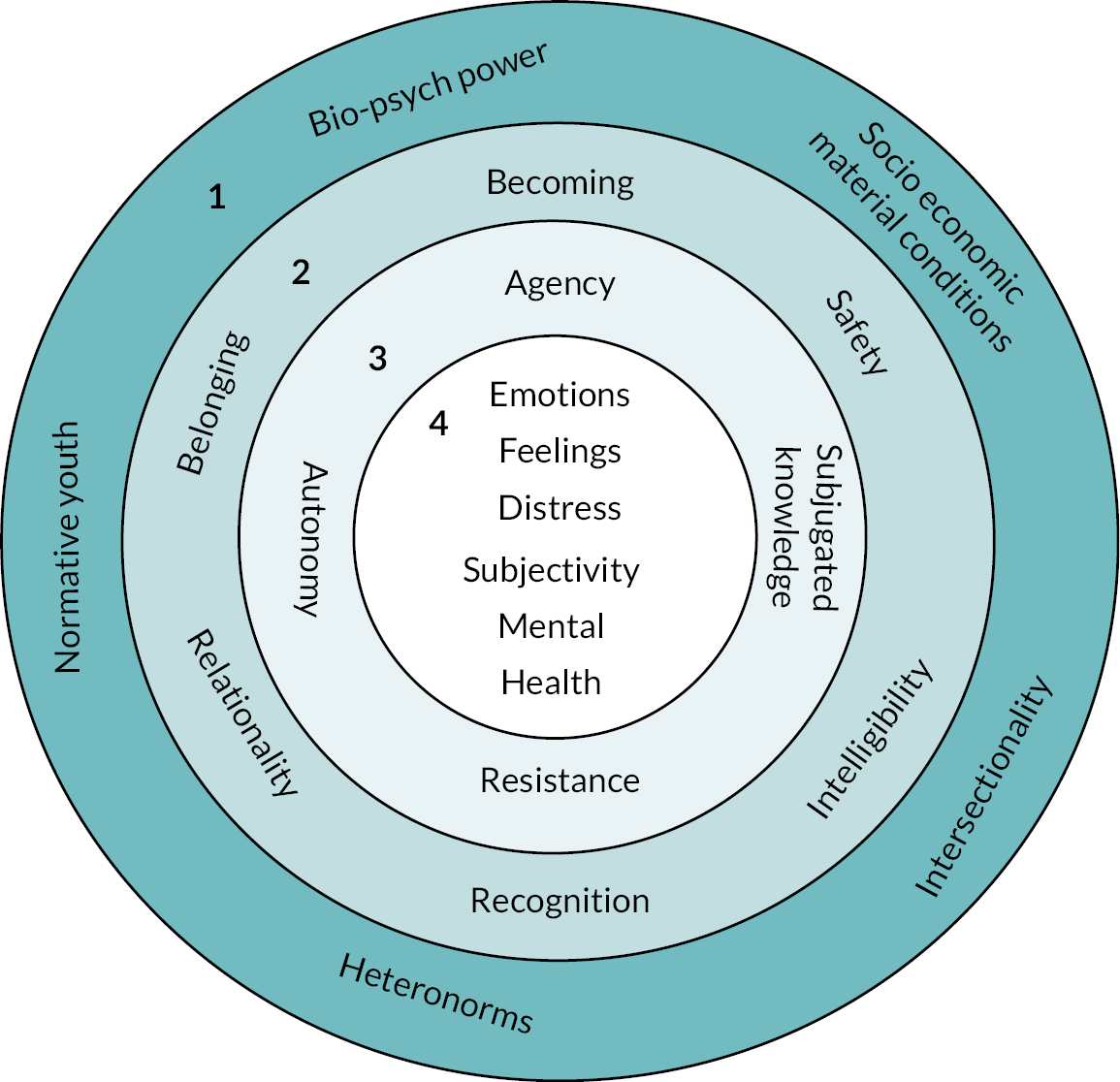
Explaining the theoretical framework
Macro outer ring 1
The outer ring represents the macro-level dimensions of power, norms and socioeconomic material conditions that are maintained through institutions, laws, discourses and people. These impact on how a LGBTQ+ young person may think about themselves, the actions they may take, their access to resources, how others may interact with them and their mental health.
At the macro level, the effects of Heteronorms (the dominance of cis-heterosexuality where gender identities and bodies align and everyone is assumed heterosexual) on LGBTQ+ youth mental health is of paramount importance. Heteronormativity is maintained through direct homo/bi/trans phobia and discrimination, in addition to marginalisation, silence, invisibility, misrepresentation and exclusion of LGBTQ+ sexualities and genders. Mental health support must have an anti-oppressive and social justice approach in which LGBTQ+ youth can learn to understand, cope with, and reject heteronormativity, for example, through CBT psychoeducation or peer-support groups.
Normative Youth refers to the social norm where youth are positioned as less than adults and they are configured as passive subjects ‘waiting’ for adulthood. In many cases, youth emotional distress is viewed as pathology, ignored and temporalised. To counter the disempowerment of youth and to diminish their distress, support services require an anti-paternalist, youth-centred approach enabled through advocacy and collaboration.
Bio-psych power refers to the pathologising impact of biomedicine and psychiatry on LGBTQ+ identities and youth mental health. Mental health support must hold the perspective that LGBTQ+ identity and difficult emotions are not a sign of psychological abnormality. Intersectionality means mental health support must acknowledge the multiple discriminations that arise as a result of multiple identity characteristics such as race, ethnicity, faith and disability. LGBTQ+ may not be the central facet of youth identity and experience.
Socioeconomic and Material Conditions refers to mental health support needing to understand the social and financial disadvantage experienced by youth. Most youth have limited access to resources and finances and are dependent on family or carers. Those without families, race and ethnicity, homeless, asylum seekers, refugees, and trans are especially precarious and vulnerable.
Meso inner ring 2
The meso-level components of the framework are important to the overarching provision of mental health support. Recognition refers to the need for mental health support to acknowledge through affirmation the plurality and fluidity of gender and sexual self-definition. This should foster a positive identity where the individual is valued, understood and accepted.
Relationality refers to the importance of connection to others as a way to support and improve mental health. Connections with peers and trusted adults may be more effective at reducing poor mental health where ‘mutual-care’ in addition to ‘self-care’ is operationalised. Belonging means LGBTQ+ youth should feel included, comfortable and like they ‘fit in’ the support service. Mental health support should be non-judgemental and inclusive, encouraging coping, trust and understanding.
Becoming means there is not a fixed pathway to a sexual or gendered identity or a final destination identity. Mental health support must prioritise gendered and sexual self-definition, space and flexibility for change and not make assumptions. The emotional, cultural, psychological and physical safety of youth should be paramount to mental health support. This must prioritise fostering trust, confidentiality, privacy through space and staff. Intelligibility is the capability of being understood, to be comprehended for different experiences connected to different and intersecting categorisations of identity.
Micro ring 3
The micro ring features are important to understand how the individual is regarded within the mental health support service. Agency means youth must be treated as acting, knowing subjects with support employing an advocacy, empowerment, collaboration and joint decision-making approach. Autonomy refers to youth self-determination and youth having an active voice in their care. Mental health support should promote self-efficacy, self-awareness and identifying personal strengths.
Subjugated knowledge indicates that valuing youth knowledge and experience is central to delivering appropriate support. Services should operate through a strength-based approach to youth competency. Resistance refers to support that enables youth to refuse to be diminished by their identity, age and mental health status. Positive mental health can be encouraged through developing coping strategies and building confidence, resilience, self-esteem and understanding through, for example, psychoeducation, activism, art, therapy, celebration, fun.
Centre ring 4
At the centre of the framework is Mental Health, which was conceptualised in a variety of ways in the three meta-narratives we identified. Our theoretical framework notes mental health can be a diagnostic category. It is also a complex phenomenon incorporating emotions, feelings, distress and subjectivity that are a natural part of human suffering and misery and not an indication of psychological abnormality. Early intervention mental health support must start with LGBTQ+ youth subjective assessment of their mental health needs rather than symptomology and diagnosis.
Discussion
This MNR aimed to assess the evidence on mental health early intervention services and support for LGBTQ+ youth. The theoretical framework we devised, based on an interpretative synthesis of the evidence, is aligned with the de-medicalisation of human misery and suffering because the pathologisation of emotional distress, difficult feelings/thoughts and behaviours has a stigmatising impact on individuals and societies. Our framework aimed at supporting youth with common mental health problems at an early point in their difficulties. It did not presume that psychiatry (which hardly featured in the literature we found) or individual psychology present the most effective ways of understanding how to intervene.
Our starting point was that LGBTQ+ youth do not need a mental health diagnosis before they could be supported to improve their mental health. A mental health diagnosis should not stop young people from accessing mental health support, and it is not always necessary that a young person’s mental health can be improved without a mental health diagnosis. Our framework suggested that early intervention must meet expectations in timely delivery, and that subjective assessment of mental health by a young person is sufficient to access support.
A further fundamental element of the framework to support LGBTQ+ youth mental health is to understand that they live in a heteronormative world that despite improvements continues to either explicitly denigrate LGBTQ+ identities or marginalise and silence those lives. This was acknowledged across all three meta-narratives and strongly suggests that youth must be supported to exist within/resist against these difficult normative environments.
We interpretively synthesised the literature to produce an individual and social theoretical framework for supporting LGBTQ+ youth mental health, understanding that LGBTQ+ youth mental health arises from intersectional and complex factors. This framework de-medicalised emotional distress and promoted youth-centred support that attends to the multifactored influences on mental health. Our framework suggested that those who provide support must understand individual lives, must connect with youth, must collaborate facilitating the young person’s autonomy and must encourage agency. The framework also aimed to have applicability across a variety of settings such as school, health care, online, community and youth work.
A central characteristic of the MNR method is premised upon Kuhn’s211 epistemological perspective that what we come to know about the world is not homogeneous and linear. Scientific knowledge progresses through paradigms that ebb and flow and develop in relation to each other and their ability to explain a particular phenomenon. The ‘story-lines’91 of the meta-narratives that contribute to the evidence base about LGBTQ+ mental health have been heavily shaped by legal, policy, biomedical, academic and public discourses/attitudes to sexual and gender diversity, and by the social movements that have aimed to gain equality for LGBTQ+ people. These have also been crucial to the development of research on LGBTQ+ youth mental health. As a result of this liberalisation, albeit uneven, we now know and acknowledge the prevalence of the problem. Stages 2 and 3 of this study contribute to the less developed areas of knowledge on how best to tackle mental health inequality.
Across the literature we reviewed, scholars worldwide were struggling with similar difficulties in trying to understand the problems and provide solutions. The background for each paper was the marginalisation and stigmatisation of young LGBTQ+ lives, the impact this had on their mental health, the dearth of appropriate mental health support and the need for research to support the development of effective mental health provision. The study of LGBTQ+ youth mental health has largely occurred across the disciplines of psychology, sociology, public health, social work and youth studies, which until now have operated independently of each other. Our interdisciplinary approach indicated that effective early intervention mental health support for LGBTQ+ youth must prioritise addressing normative environments that marginalises youth, LGBTQ+ identities and mental health problems. We appreciate that these macro-level changes may be difficult and take time. Perhaps indicative of this, we did not find any interventions that sought to change these normative environments beyond the community/school level.
Conclusions
The strength of this review was that it utilised a theory-led systematic review methodology to detail the underlying theory of effective mental health care. The review was of course limited by language and there may be important evidence written in countries that we were unable to include. In addition, we realise that the adaptation of the PICOS formula for selecting studies for MNR methodology is unwise. This is because the PICOS framework, although widely used within SR methodology, cannot be easily applied through an interpretive and iterative approach. This is the first, to our knowledge, theoretical framework to be produced for supporting LGBTQ+ youth mental health and represented the basis for the empirical testing conducted in stage 3 of the study to provide principles for appropriate LGBTQ+ youth mental health support.
Chapter 4 Stage 2 results: service mapping
Sections of this chapter have been reproduced with permission from Pattinson et al. 61 This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence (https://creativecommons.org/licenses/by-nc-nd/4.0/).
This chapter reports on stage 2 of the study that investigated and mapped current LGBTQ+ youth-specific mental health service provision across the UK.
Search results
The service mapping identified 111 services in the UK that offer early intervention mental health support for LGBTQ+ young people with common mental health problems (Figure 4). The majority (82%) of the services operated in England (n = 92), followed by Scotland (n = 7), NI (n = 5) and Wales (n = 4), and a small number of services operated UK-wide (n = 3). Services were predominantly based in urban settings (n = 84), focused around cities or towns, with only 13.5% providing for both urban and rural areas (n = 15), and 11% providing services in an exclusively rural area (n = 12).
FIGURE 4.
Mapping search results flow chart.
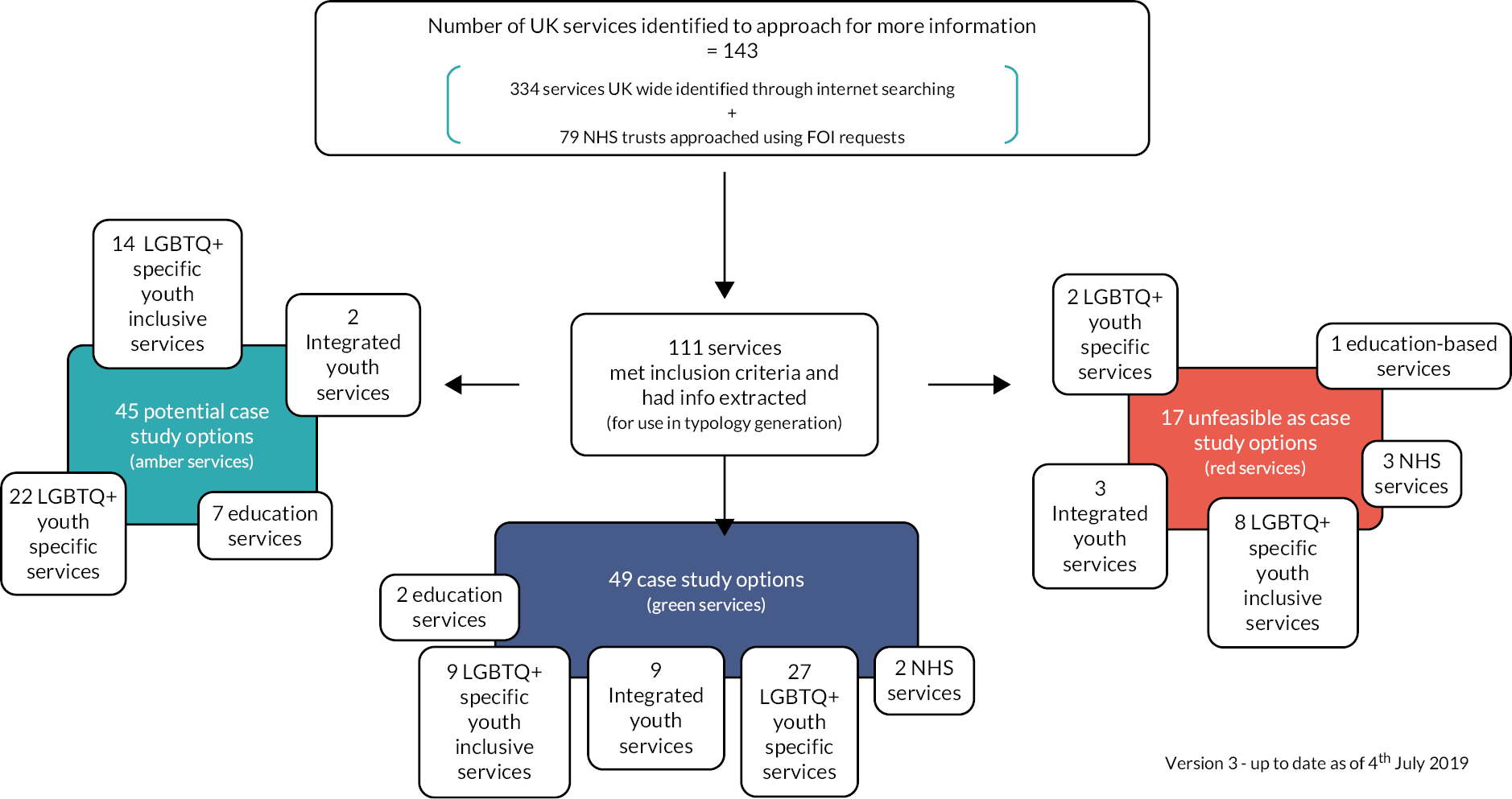
The main service provider of early intervention mental health services for LGBTQ+ young people were the community/voluntary sector (n = 81), followed by Local Authority services (n = 13), education/school-based services (n = 10), and a small number of services being provided directly by the NHS (n = 4) (Figure 5). Three services were provided by a voluntary sector service in partnership with the local CAMHS. There was a variety of age ranges targeted by the services, with the largest number (n = 40) aimed at young people ranging from under 16 years up to 25 years, 22.5% of services were aimed at under 16–19 years (n = 25) and 19.8% were aimed at all ages (n = 22). A smaller number of services had more specific age ranges such as under 16 years only (n = 5) and over 18 years only (n = 10).
FIGURE 5.
Service mapping by descriptive categories.
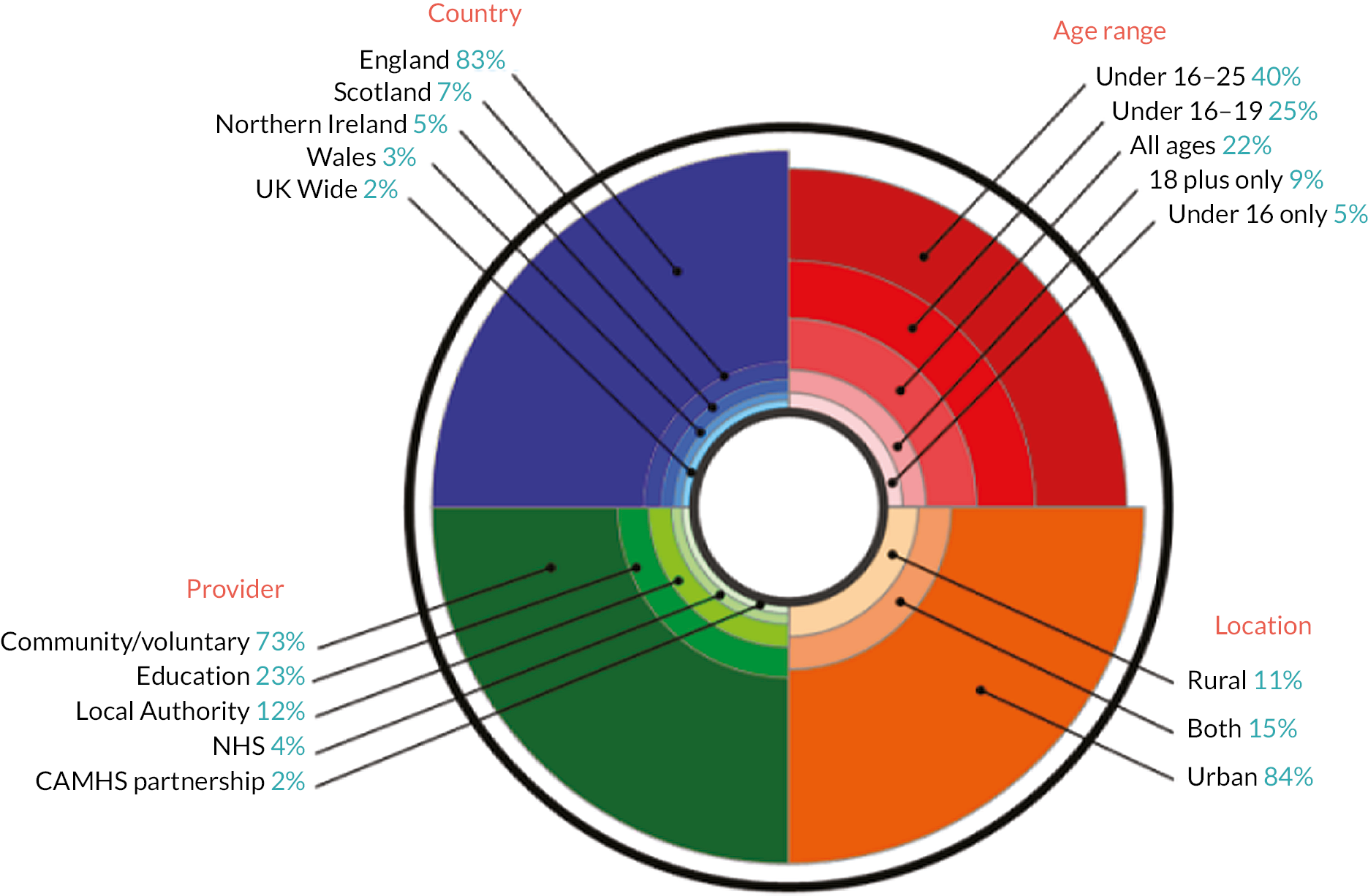
Service typology
The aim of developing a typology was to define groups of service models with a similar set of characteristics. The typologies identified were then used to inform the sampling of case studies in the Queer Futures 2 project to ensure that these represent the range of services across the UK. A simple typology of service provision was generated as there was very little LGBTQ+ youth mental health provision identified within the NHS, and services appeared to be located mainly in the community and voluntary sector in response to a demand for mental health support for LGBTQ+ young people. Third, although some of these services offered an online service component, we identified no exclusively online mental health support for LGBTQ+ young people (this however changed dramatically during the COVID-19 pandemic where most case study sites developed online provision). Finally, obtaining detailed information about LGBTQ+ mental health services within an educational setting proved especially difficult. The typology overview categories are presented in Table 11.
| Typology category | Definition | Number (n = 111) | |
|---|---|---|---|
| 1 | LGBTQ+ youth specific | Mental health provision provided by LGBTQ+ youth specific organisations (all service type providers) | 51 |
| 2 | LGBTQ+ specific youth inclusive | Mental health provision for all young people provided by LGBTQ+ organisations (all service type providers) | 31 |
| 3 | Integrated youth | Mental health provision provided for all young people with an LGBTQ+ specific component (all service type providers) | 14 |
| 4 | NHS | Any mental health service provided by NHS, for example CAMHS, sexual health providers | 5 |
| 5 | Education | Mental health services provided by schools, further and higher education | 10 |
Only 12.6% (n = 14) of the services identified in the mapping process were specifically targeted to give early intervention and prevention mental health support services for trans and gender-diverse young people. Overall, 98% of the services were offered primarily face-to-face services with two services offering a telephone-only service. A high number of the services offered one-to-one support (66%, n = 73) where a young person could talk in private to a staff member or youth worker, and peer support (77%, n = 86) which was primarily in the form of youth group activities. A smaller number of services focused on professional therapies (37%, n = 41) such as counselling or CBT; well-being activity sessions (47%, n = 52) which were usually one-to-one sessions rather than regular activities; and self-care resources (50%, n = 56) such as leaflets or online resources were offered by half of the services (Figure 6).
FIGURE 6.
Service mapping by support type.
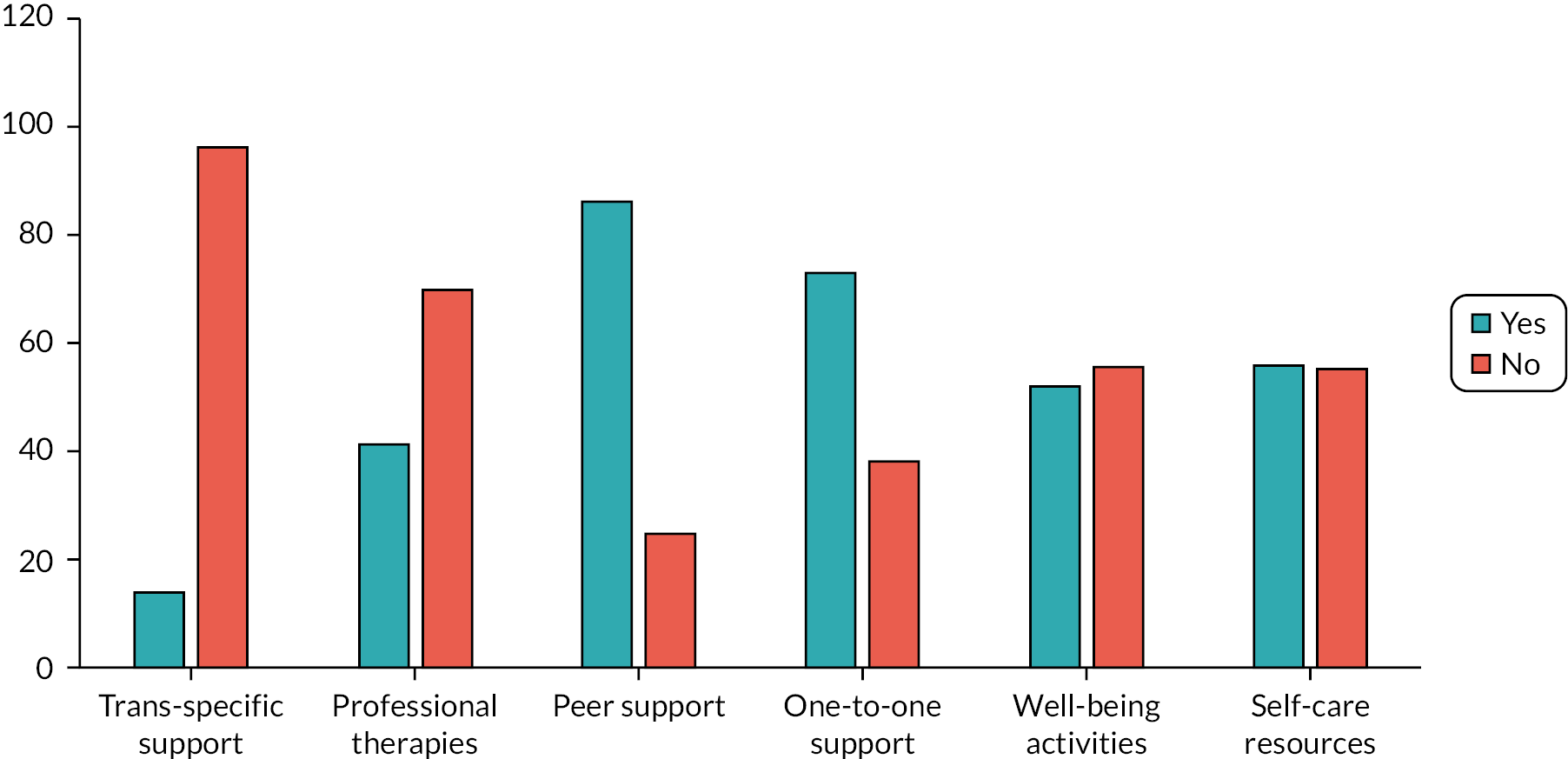
Case study sites
Twelve case study sites were selected from across the five categories of the service typology using the case study selection criteria (Table 12). These were the services that agreed to participate in the third, and final, stage of the study. As a consequence of the COVID-19 pandemic, there were some changes to the final 12 case study sites that participated in the study. Some services did not have the capacity to be involved in a study while continuing with the demands of service provision in extremely difficult circumstances.
| Typology category | Definition | Case study site (organisation) |
|---|---|---|
| LGBTQ+ youth specific | Mental health provision provided by LGBTQ+ youth specific organisations (all service type providers) | AllsortsGendered IntelligenceIntercom TrustLGBT+ NottsCara FriendProud TrustSAYiT |
| LGBTQ+ specific youth inclusive | Mental health provision for all young people provided by LGBTQ+ organisations (all service type providers) | 0 |
| Integrated youth | Mental health provision provided for all young people with an LGBTQ+ specific component (all service type providers) | Off the Record42nd StreetYPAS |
| NHS | Any mental health service provided by NHS, for example CAMHS, sexual health providers | Sandyford |
| Education | Mental health service provided by schools, further and higher education | Hugh Baird |
Discussion
This mapping stage of the study suggests three significant characteristics of current LGBTQ+ child and adolescent early intervention mental health provision in the UK. First, there is an absence of mainstream NHS support that specifically addresses the needs of LGBTQ+ young people. Second, the majority of LGBTQ+ youth mental health support in the UK is provided by voluntary/community organisations reliant on charity and non-statutory funding that is often precarious. Third, there is a rare model of service that is based on collaborative working between NHS trusts and community/voluntary organisations.
The dearth of mainstream NHS-specific mental health support for LGBTQ+ young people in the UK is a significant concern. Our view is that this is due, in part, to the lack of recognition of the necessity for adolescent mental health services to specifically address LGBTQ+ needs to tackle LGBTQ+ mental health inequality. Some NHS Trusts explicitly stated in their FOI responses that it was not necessary to offer LGBTQ+ specific mental health support, and this may even exclude young people. There were also examples of NHS Trusts conflating providing the ‘same’ service to everyone, as equitable service provision. This indicates a misunderstanding of (1) the heightened risk of poor mental health in this population group; (2) the reasons for this elevated psychiatric morbidity; (3) the underutilisation of mental health services by LGBTQ+ youth; and (4) LGBTQ+ youth poor experiences of mental health support. However, some NHS Trusts, despite not currently having a LGBTQ+ specific mental health service, reported their efforts towards developing inclusive support for LGBTQ+ young people. These service developments included, for example, funding and support for community/voluntary sector organisations to provide LGBTQ+ youth mental health support, collaborating with key stakeholders and LGBTQ+ young people to improve services, and LGBTQ+ visibility and staff training.
These developments in mainstream statutory services are to be welcomed but the majority of LGBTQ+ youth mental health support remains located within the charity and voluntary sector. These services were often developed in response to the absence of mainstream mental health services as attempts at meeting the demand from LGBTQ+ young people who often had poor experiences of NHS mental health support. 42 Our concern here is that the services in this sector are reliant on non-statutory and charity funding, which means the services are vulnerable to the instability of funding availability from a range of external sources. During the mapping exercise, there were instances where charity-provided services had to dramatically reduce their service provision or even close all together due to loss of funding especially during the COVID-19 pandemic. However, within the voluntary and community organisations was the expertise to provide appropriate and effective mental health support to LGBTQ+ young people. This was clearly orientated upon an understanding for services to generate an environment that affirmed marginalised sexual and gender identities (LGBTQ+) and were cognisant of the ways LGBTQ+ young people can encounter hostility, discrimination and victimisation, and feel like they do not ‘fit in’ within wider societal cis-heteronorms and how this may impact on adolescent mental health.
The example of collaborative working between mainstream statutory health services and voluntary organisations was an encouraging initiative. Three services highlighted a potential model for bridging the gap between the knowledge of the voluntary/community sector and the stability of the statutory sector, through a CAMHS partnership model. These services offered a collaborative approach that involved, for example, funding support and CAMHS practitioner support within charity/voluntary LGBTQ+ youth settings. This type of service encouraged knowledge sharing, facilitated safe and inclusive environments for LGBTQ+ young people, and began developing a ‘one-stop shop’ approach that addresses some of the barriers LGBTQ+ young people face when seeking mental health support.
Conclusions
The results of the mapping stage of this study highlighted promising pockets of service provision development in healthcare and education settings across the UK. This included expanding staff LGBTQ+ knowledge, addressing practical issues such as monitoring forms and gendered toilets, as well as including LGBTQ+ youth in the design and evaluation of new and existing service provision. However, provision remains limited mainly to non-statutory LGBTQ+ specific mental health services in urban settings which presents a clear barrier to access, suggesting those living in rural areas may have to travel sizeable distances to reach appropriate services. Similarly, the small number (12.6%) of services that offered trans or gender-diverse-specific mental health support illustrates the increased difficulty for trans and gender-diverse young people in accessing mental health services with appropriate training and knowledge.
Chapter 5 Stage 3 results: case study evaluation
An intersectional youth-rights approach to early intervention mental health support
Our analysis of the data from the case study evaluation suggests that an intersectional, youth-rights approach to early intervention mental health support for LGBTQ+ young people is the most appropriate way of supporting poor mental health in this population group. Youth rights should underpin the delivery of mental health support for LGBTQ+ young people to address the multiple marginalisation, isolation, and stigmatisation that they may experience. This approach should enable LGBTQ+ young people to make informed independent decisions about their own bodies and lives, and uphold the right to freedom of safe self-expression. These factors are paramount to appropriate mental health support.
An intersectional approach is crucial to this mental health support to ensure the upholding of the right to non-discrimination [article 2 United Nations Convention on the Rights of the Child (UNCRC)] on the basis of age, sexual orientation, gender identity and ethnicity, social class and disability. When thinking about the experience and impacts of oppression, identity categories are often conceived as ‘fixed’ and separate from each other. The centrality of race, including the privilege of whiteness, is frequently overlooked. LGBTQ+ identities are often represented in ways that do not recognise the many differences between LGBTQ+ experiences. LGBTQ+ young people should not be framed as an undifferentiated group whose experiences are the ‘same’ (and who are often assumed to be white, middle class, and non-disabled). Appropriate mental health support must be built on a foundation of recognising that LGBTQ+ young people may experience multiple marginalisation and discrimination.
The model of early intervention mental health support for LGBTQ+ young people that we have produced in Figure 7 contains 13 principles that are necessary to the provision of mental health support, and to improve access to, engagement with, and navigation of mental health services. Each principle is explained below but the model should be viewed with all component parts interacting. These principles of support are designed to guide mental health services in a variety of settings – education, clinical, community – and can be operationalised in a number of ways. There are further examples of the different ways these principles can be operationalised in the interactive digital version of the model (https://queerfutures2.co.uk/what-works/) and in the NHS commissioning guidance we have produced (https://queerfutures2.co.uk/resources/).
FIGURE 7.
Model for ‘What works’ in early intervention mental health support for LGBTQ+ young people.
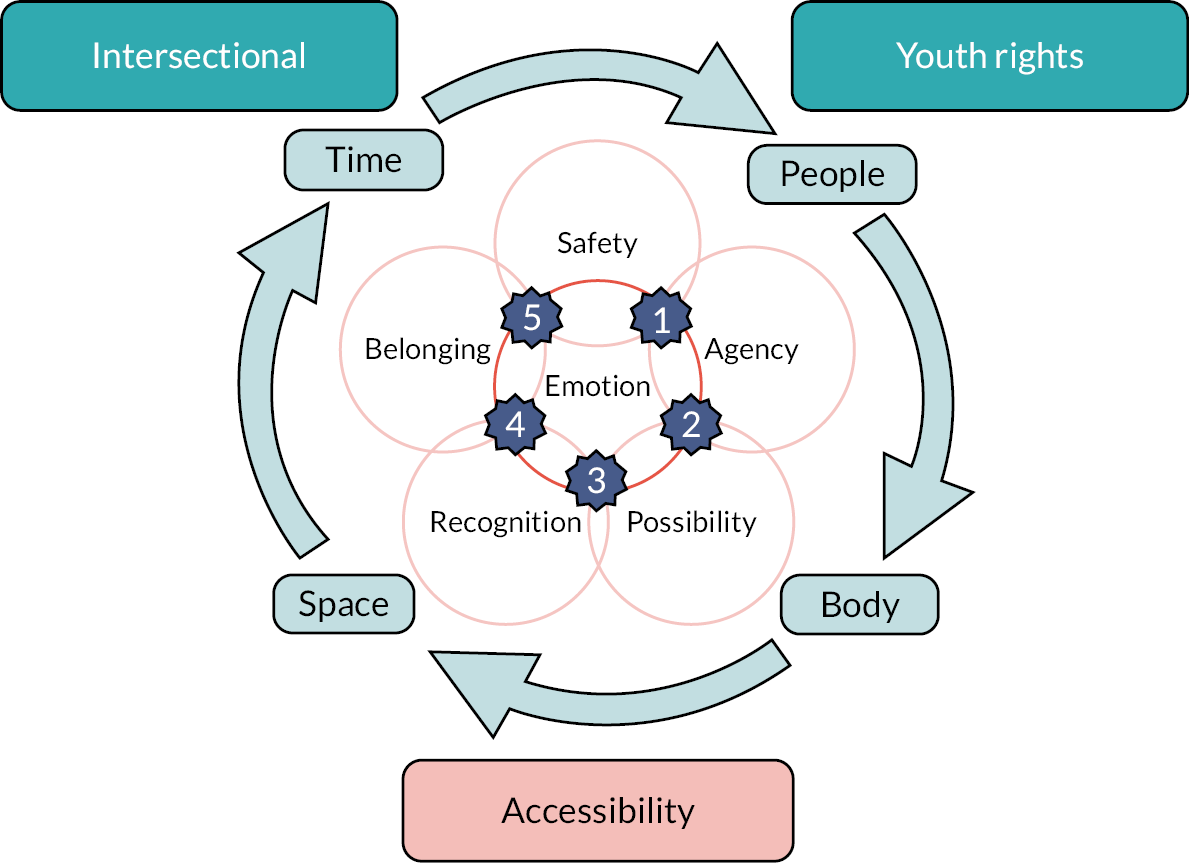
Principles of early intervention mental health support for LGBTQ+ young people
Youth rights
Our analysis suggests that youth rights should underpin the delivery of all early mental health support for LGBTQ+ young people. It is crucial that LGBTQ+ young people are enabled to make informed independent decisions about their own bodies and lives, and for the right to freedom of self-expression to be upheld so they can explore their LGBTQ+ identities safely. The UK is a signatory to the UNCRC which describes both youth rights and the right to good mental health but a rights-based approach to mental health service provision is not prominent or mainstream.
The ability of LGBTQ+ young people to make decisions about their mental health is often compromised by discrimination due to their LGBTQ+ identity and age often leaving them powerless compared to adults. This means they are less able to make decisions for themselves about their own lives and less able to be in control of the circumstances around them, for example what services they can access, opportunities to earn money, etc. 212 Where services enable LGBTQ+ youth rights, we found this had an impact on their mental health. Sandy, a staff member, stated:
I think confidence in being able to say: ‘actually, my rights are this, I can wear this uniform’ or ‘I can use the toilet that is assigned to my gender’ because that confusion, can create unease and anxiety. We’ve had young people who won’t use their school toilet for the whole day, all of these affect a young person’s mental health and wellbeing.
The analysis suggested that where typically the youth-rights discourse in the UK context is silent, in the services provided by the case study sites, there was frequently explicitly communicated commitment to upholding the rights of LGBTQ+ young people. This was especially apparent in relation to confidentiality and seeking healthcare services, for example for gender identity and transition support. When providing good mental health support, services made LGBTQ+ young people aware of safeguarding processes and the limits to their confidentiality in circumstances where there is a safeguarding concern.
Our findings indicate that the rights to non-discrimination are also key for LGBTQ+ young people who are at high risk for marginalisation, victimisation and harassment. LGBTQ+ young people must be supported in their right to safely explore and express their sexual and/or gender. UNCRC (1996) also highlights how LGBTQ+ young people have the right to know about rights. Being supported through advocacy and education to understand and express rights in different areas of life and feeling safe to express identity was imperative. In the case study sites, service staff were advocates for LGBTQ+ young people and they were helped to uphold their rights in health services and institutions such as schools, for example toilets and changing rooms and uniforms. Bryn, a service staff member, stated:
I think education of rights, psycho education, so LGBTQ+ people can understand that what they’re going through doesn’t mean that they’re crazy or insane or they should be judged or rejected or feel shame.
Case study example
The Young People’s Advisory Service (YPAS) is an integrated youth service with a specific LGBTQ+ strand of support and a skilled team of LGBTQ+ staff. The service offers mental health support such as counselling, as well as a LGBTQ+ group (GYRO) and a group for young people aged 12–18 who identify as trans or gender non-conforming [Trans Health Education (THE)]. YPAS offers information about rights and the UNCRC (1996) on all their forward-facing material, for example flyers for services and their website. This includes the flyers for LGBTQ+ services GYRO and THE (Trans Health Education project). Young people’s rights are made explicit whereby the rights ‘to be in a safe space, free from discrimination of any kind’ and to confidentiality are linked to being LGBTQ+:
The service we provide is confidential and we will respect your privacy. We will ask for your consent before we share information about you. We understand that you may not be “out” to anyone so we want to let you know that we will keep it that way until you feel ready to share. However, if we feel that you or someone else may be at risk, we may need to contact someone else. We would inform you of this first where possible.
Service document
Intersectionality
The experience and impacts of oppression and identity categories are often conceived as discrete from each other and static. LGBTQ+ identities are often represented in homogeneous ways, structured by homo- and trans norms that centre whiteness, heterosexuality, class privilege and being non-disabled in relation to the ‘right’ ways to be LGBTQ+. 79,80 These norms can and do assert themselves in LGBTQ+ spaces. 213,214 In our findings, the impact of services being structured around such norms is that LGBTQ+ young people feel the need to minimise or hide some parts of their experience, or to assume the burden of educating those providing them with support.
Yeah, being a trans person of colour is extra difficult and it’s another one of those things that you have to either censor yourself about or give people a crash course on racism and either try to convince them that the whole ‘I don’t see race’ thing is part of the problem or just give up and pretend they’ve got it. And aside from just skin colour there’s lots of cultural differences and challenges to navigate with parents from other cultures or who speak other languages etc that British people don’t understand.
Blue, young person
Doing intersectionality in mental health support services requires critical reflexive practice to support the identification of how to work in appropriate anti-oppressive ways, and the identification of intersections as they pertain to privilege. Intersectional mental health support needs to operate at multiple levels: interpersonal, disciplinary, cultural and structural. Services must consider the systems of operation; the culture and norms reproduced (or marginalised) by the service; and structural aspects such as location, opening times and financial support. Central in these considerations must be the questions of which LGBTQ+ young people are privileged and excluded, and how.
I think it’s about acknowledging the layers of stigma and prejudice that people carry and hold and the impact of all those are. I think we definitely need to have a [POC] LGBT+ worker, who personally understands that intersection because I think you can have all of the compassion in the world and the intent and the want to know and understand and that’s essential to being a good human, I think – but not understanding first hand is very different.
Alex, staff member
In practice, this means the service should ensure that ‘intersectionality’ is understood thoroughly, and that robust staff training is available to support understanding. Across our case studies, intersectional considerations related to age, different LGBTQ+ identities, chronic illness, disabilities, racism and colourism, neurodiversity, homelessness and poverty and experiences of the care system. Our analysis highlights the centrality of racism, colourism and white privilege in considerations around intersectional practice, and the need to shift positioning away from recognition of any ‘absence’ of LGBTQ+ young people of colour to the awareness that this represents dominance of whiteness in LGBTQ+ spaces. ‘Intersectionality’ does not only apply to marginalisation but also reflects intersections of privilege. Service providers and practitioners must be cognisant of power imbalances in relation to privilege and marginalisation and awareness that individuals can and do experience both.
Ensuring that practice is anti-oppressive and reflexive includes attending to the suitability of staff to deliver support for LGBTQ+ young people, by ensuring for example that targeted groups are run by adults who are also LGBTQ+ people of colour, or trans and non-binary people. Awareness of the benefits of lived experience of staff must be accompanied by adequate support for staff well-being, as multiply marginalised staff will also be managing the impact of experiences of racism, transphobia, classism, or ableism. Examples of practical support and inclusion for intersectional identities across the case studies included projects foregrounding specific experiences of marginalisation and offering support accordingly, such as groups for young LGBTQ+ people of colour, and the provision of time-out space(s) to support access related to neurodiversity.
Case study example
Allsorts runs a specific group for LGBTQ+ young people of colour, which is led by youth workers who are also people of colour. This group delivery is underpinned by long-term consultancy; the staff team includes an antiracist consultant whose role is to support young people attending Allsorts, assist youth workers, and create online resources celebrating the visibility of LGBTQ+ young people. An antiracism section on Allsorts’ website outlines the resources and support available, as well as directly addressing ongoing problems and work still to be done. Allsorts also offers emergency advocacy supporting LGBTQ+ young people to access support such as food parcels and financial aid, and it has resources to download for young LGBTQ+ people facing homelessness and young LGBTQ+ people of faith.
Time
Our analysis highlighted the importance of time in relation to young people’s access to and experience of mental health support. The analysis clearly indicated that time poverty impacted individuals and services. 215 Waiting times for accessing mental health support in the UK are well documented, as are the limitations in frequency and duration of mental health support provision through CAMHS and AMHS. 216,217 When the time to engage arrives it is often rushed and limited, with the duration of support being pre-defined and limited. Our analysis found that this had a damaging impact on LGBTQ+ young people:
Lack of time, access, trying to get an appointment. It’s really difficult for anyone but particularly for the young person if you’re holding stuff around identity and you really don’t want to discuss that with someone. So feelings around being rushed. Fears around being closed down.
Laurel, staff member
Time is crucial to support trusting relationships between support staff and LGBTQ+ young people. Having sufficient time to build trust with service practitioners made it easier for young people to open up about their feelings and experiences and reduced the risk of LGBTQ+ young people feeling frustrated and not cared for within support.
Having the ability to see the same staff member is very helpful as it gives a sense of continuation. You don’t have to explain yourself over and over again to a new person.
Jamie, young person
Our analysis also indicates that delivering support that works with the LGBTQ+ young people’s pace and direction will enable LGBTQ+ young people’s autonomy because they are afforded the time necessary to ensure that decisions they make about their care are fully informed, that is, time to ask questions, think and change their minds. In addition to the practical impact of waiting for support, our analysis demonstrated that services needed to understand that waiting resonates in specific ways within LGBTQ+ young people’s lives. Waiting to leave home or move away to be more ‘fully’ oneself, for example, is an experience many LGBTQ+ young people share. For trans and gender-diverse young people looking to transition, long waiting times to access Gender Identity Development Service (GIDS) or Gender Identity Clinic (GIC) care have a particularly burdensome impact. 218,219 Isla (staff member) highlighted the importance of offsetting the problem of waiting:
It’s more about the, yeah, the kind of social support, emotional support. Because I think that, yeah, I guess with medical transition there’s so much waiting that the social support really holds up your mental health throughout that time.
While time as a resource may be limited or constrained in ways that are beyond an individual services’ control, for example due to waiting lists for other services that young people may be referred to, our case studies highlighted that services can address and incorporate consideration of time. A rapid response to initial contact and ‘while you wait’ support reduced the possibility of LGBTQ+ young people falling through gaps in provision. In practice, this included ensuring that the service was available for some kind of engagement ‘any time’, for example, there being someone to talk to, or offering remote access via phone or Internet. ‘While you wait’ support included providing bridging support (e.g. online and face-face activities and ‘drop ins’) to ensure there are multiple pathways into support for LGBTQ+ young people.
Case study example
The Intercom Trust is a LGBTQ+-specific youth-inclusive service for LGBTQ+ and questioning adults and young people. The service offers youth groups for under-18s that LGBTQ+ young people can drop in for without needing to sign up, and one-to-one support with youth workers can be booked in with a lower waiting time than referrals to internal or external counselling services. The support provided by Intercom Trust explicitly addresses the difficulties young people experience while on CAMHS or GIDS/GIC waiting lists, and support workers are also able to offer advocacy, such as supporting a young person in accessing medical support.
People
Trusting relationships with adults can be complicated for LGBTQ+ young people due to fear and past prejudicial experiences from adults (e.g. teachers, parents and carers) about their sexual and gender identity, and LGBTQ+ young people often do not ask for help from adults even when they need it. 42 The analysis suggests that mental health support services should not presume that LGBTQ+ young people trust adults or have a trusted adult in their lives. Our research indicates that LGBTQ+ young people may feel unsafe in relationships with adults including authority figures and institutions such as social workers and the police. This distrust may be exacerbated due to multiple marginalisation and discrimination, for example institutional racism and how this intersects with being LGBTQ+ and navigating healthcare services. 220
We’re a mental health service, so we sometimes suffer from that lack of trust that young people might have in professionals, if they’ve been burnt before where someone has handled something in the wrong way, someone’s betrayed their trust, that’s quite a common problem.
Billie, staff member
Our findings demonstrate that important relationships for LGBTQ+ young people may include: support staff; peers; LGBTQ+ adults; family and school. Our analysis shows that services should actively seek to build trust between LGBTQ+ young people and adults in their lives. This is distinct from the presumption that their relationships are already (or should be) trusting ones. ‘Adult’ or cis/heteronormative assumptions about relationship hierarchies should also be avoided, for example parents and family as ‘most important’. For many, familial relationships could be the source of distress, harm or violence. Instead, the diversity of different relationships in an LGBTQ+ young person’s life should be celebrated and supported. Where relevant, supporting LGBTQ+ young people to navigate their relationships with their family/carers or teachers/school may be helpful. However, awareness that family and school relationships are important for some but may have little relevance for others, is imperative.
Being introduced to diverse LGBTQ+ adults is one way that trust in adults can be (re)built as this limits fear about being judged due to being LGBTQ+. Active facilitation of peer–peer relationship building through group work and sharing space, fun and activity is another important dimension that facilitates belonging. Relationships with support staff should have boundaries but also be reciprocal, for example listening and talking on both sides. This reciprocity helps address power imbalances inherent in this dynamic between an adult and a young person and fosters trust and security. In all instances, support to navigate relationships must prioritise the needs of the LGBTQ+ young person.
The service has helped me open up more although I do believe this is because of the human connection and experiences that my support practitioner has had, it makes me see the person as another human rather than well I guess a machine just doing their job if that makes sense, I’ve opened up due to that connection and the safety I feel.
Bea, young person
Case study example
Hugh Baird’s College’s ‘The POD’ is a ‘one-stop shop’ for the needs of students through financial, academic, well-being and mental health support within the college building. Although the service is not specifically designed for LGBTQ+ young people, the staff have received specific training and the service hosts LGBTQ+ specific events and workshops to meet the needs of LGBTQ+ students, such as pride and awareness activities, diversity events and specific support for trans students. The POD also uses the experiences and voices of students to provide appropriate training and information for staff and students to make the college a welcoming, safe place and support good relationships across the two.
Body
Physical health and well-being are interrelated with mental health outcomes; physical illness, activity levels, nutrition and sleep all impact on mental health. 221–224 The body is also a crucial site for self and gender expression, in terms of how people present and express themselves through appearance and comportment. Cis-heteronormative expectations around gender expression impact LGBTQ+ young people’s mental health, especially trans and gender-diverse young people. 225 In the case study sites we evaluated, LGBTQ+ young people reflected on experiences of inappropriate interest in and scrutiny of their bodies when accessing mental health support, as well as policing or invalidation of their gendered presentation and expression. Aspects of their distress that relate to the body were left unaddressed at best or exacerbated at worst.
[…] health services finding out I’m trans and ‘oh just out of personal curiosity’ a million inappropriate questions they didn’t need to ask me because ‘oo let’s ask the medical curiosity some stuff while they’re here’ attitude?
Kai, young person
Experiencing scrutiny, policing and the undermining of autonomous decisions in relation to the body not only detracts from the potential benefits of mental support for LGBTQ+ young people but actively contributes to distress. Isobel (young person) stated, ‘I had a counsellor that didn’t believe me being trans [...] like “I see a confused man in front of me who’s very lost with their identity” [...] it really doesn’t help especially when I’m feeling vulnerable’.
These experiences erode LGBTQ+ young people’s trust in services, contributing to their underuse of mental health services more broadly. Across the case study sites, we found that spaces and resources to explore self-expression were invaluable for the validation of LGBTQ+ identities and supporting mental health. Our analysis indicates that providing support around the body enables LGBTQ+ young people to build confidence in self-expression, attend to their physical health and well-being needs, and make informed decisions about their own bodies. Sophie (staff member) explained:
Offering the practical support alongside that emotional support is really important and being able to discuss topics or issues if there is something that maybe we don’t know, can say alright I’ll find that out for you; access to resources. […] the knowledge base is just the most important because if a young person wants to speak to us about binders for example, just the fact that we know about binders removes the barriers. And because […] it’s not a massive issue, and we understand and know about what binders are, check that they’re being safe with binders, and because I suppose we’ve got that knowledge base, it instantly removes barriers.
In practice, we found that services supported the body by upholding and advocating for the bodily autonomy of LGBTQ+ young people; providing practical, emotional and affirming support for gender exploration, expression and transition, including in relation to GIDS/GIC referrals; validating and including diverse trans and non-binary bodies through visibility and representation; and supporting LGBTQ+ young people’s physical health while avoiding reductive assumptions that exercise or weight loss represented ‘cures’ for mental health difficulties.
Case study example
Gendered Intelligence (GI) provides closed groups and popular annual residentials for trans, non-binary, gender-diverse and gender-questioning young people. At GI residentials, young people can build community, make friends, experience a trans-only space and have fun. The organisation’s youth group runs a separate annual residential specifically for trans, gender-variant and -questioning young people of colour. These spaces support the body by providing affirming environments away from cis-heteronormative pressures and expectations about how young people ‘should’ express or present themselves and facilitating access to activities such as trans-only sports sessions. Being in safer spaces such as these enables young people to understand their gender identity and build confidence in expressing themselves in the ways that feel best.
Space
The spaces in which mental health support is delivered are not benign for LGBTQ+ young people. The analysis of the case study data suggests that the space in which mental health support is provided needs to be (re)defined, owned, and occupied by LGBTQ+ young people and their needs. Our analysis found that LGBTQ+ young people felt that typically all spaces they inhabited were owned, controlled, surveilled and designed by adults. 212 As a consequence, they were contained and controlled by the demands of these adult and/or cis-heteronormative spaces. In our model ‘space’ is conceptualised as not only a physical factor but has emotional and social dimensions too.
I’ve written a lot about space in my practice, because it is something that is defined by other people and owned by other people and it’s problematic. People don’t give trans people any space without asking them to say why they’re taking it up.
Harper, staff member
Being comfortable and feeling powerful in the space is invaluable for LGBTQ+ young people’s mental health as this allows for freedom to explore and express LGBTQ+ identities. Services should prioritise building familiarity and ownership of space by LGBTQ+ young people including awareness that the space is not for parents/carers and uninvited adults. Meeting with other adults/professionals in spaces that are considered the ‘territory’ of LGBTQ+ young people can help address power imbalances between LGBTQ+ young people and adults. Laurel (staff member) elucidates:
We’ve set up an appointment to share with the psychiatrist, a community psychiatric nurse and the young person and that’s worked really well when we’ve been able to have that onsite that’s familiar to the young person. They’ve come in beforehand and we’ve laid out the chairs. It’s trying to think about their empowerment, to help them and to have their voice heard in a place where they feel that they’re already listened to, it’s not medical.
Our findings also demonstrated that orientation in the space can ensure services are navigable and not confusing or dis-orientating which can be intimidating and isolating. If possible, mental health services should ideally consult and co-design the space with LGBTQ+ young people to ensure it is safe on their own terms, for example time-out space or systems, trans and non-binary specific space.
Case study example
The Proud Trust and 42nd Street, both of which are based in and working across Greater Manchester, represent two examples of services whose buildings and support spaces have been co-designed with young people. The Proud Trust’s new centre, The Proud Place, which opened in 2022, was co-designed from start to finish with LGBTQ+ young people. 42nd Street, which is a therapeutic mental health service for young people, was also co-designed with young people to ensure the space does not feel clinical and is young person friendly. For example, there are no adults waiting at the reception desk and there is an entrance porch that provides some shelter and anonymity while waiting to access the service. LGBTQ+ identities are also very visible across the space with a range of LGBTQ+ flags and queer cultural resources present ‘all year round’ (i.e. not just Pride season).
Safety
Lesbian, gay, bisexual, trans, queer/questioning, plus young people often feel unsafe or insecure in areas of their lives such as with family, at school, or on the street due to bullying and harassment in relation to their gender or sexuality,37,226,227 and feelings of powerlessness due to their age. 13,212 The fear experienced as a result creates widespread uncertainty for LGBTQ+ young people about what may happen to them, including within mental health support services, with fears arising around the possibility of being judged or being outed to parents or carers by services. 42,51 In this context, safety does not only pertain to being safe from physical harm but also extends to emotional, social, and material safety. Where being LGBTQ+ places young people at risk of harassment and violence, this is exacerbated in the case of people who are multiply marginalised, such as LGBTQ+ young people who are black or people of colour, trans or gender diverse, or disabled. 37
They’re so scared that somebody will find out, and somebody will judge, and all that sort of thing. So when the young person comes to talk to us, we need to open up those layers that they find frightening.
Jasmine, staff member
Fostering safety in mental health support settings for LGBTQ+ young people involves active reassurance around confidentiality and anonymity. Our analysis demonstrated that services must ensure LGBTQ+ young people understand that nothing will happen ‘to them’ as a young person without either informed consent and agreement, or at least with knowledge about what is going to happen in the case of safeguarding interventions that necessitate confidence breaking. Transparent and honest communication between mental health support services and LGBTQ+ young people is essential to ensure young people feel trust and safety.
Experiencing emotions was beneficial, the service was just the only place where I felt safe to do so. So my sometimes having strong negative feelings in group was a result of me feeling safe.
Blue, young person
In practice, the service should understand that inadequate support services can be exclusionary and harmful, which can exacerbate mental health challenges. Our analysis highlights the importance of avoiding normative adult assumptions that the police and other authority figures represent safety for LGBTQ+ young people. In line with intersectional considerations, services must be aware that factors such as institutional racism increase the burden of risk and exclusion from mental health support services for LGBTQ+ young people of colour.
The young people were like: you should have warned us, you should have let us know they were going to be in our space, what are you thinking of bringing police here?
Leni, staff member
Some of the practicalities of creating safety for LGBTQ+ young people across the case study sites included the provision of all-gender toilets and using an online presence to manage expectations about ‘what will happen when you visit’ such as video service walk-throughs and offering ‘taster’ sessions. Service staff moderation of both in-person and online support was essential to ensure that support was welcoming and non-threatening. Across the case studies, safety was enacted via, for example, responding to and supporting those experiencing bullying, offering non ‘scene’ spaces away from alcohol and drugs, and sharing policy and practice to address bullying and victimisation.
Case study example
Off the Record (OTR) is an integrated mental health social movement by and for young people aged 11–25 years in Bristol, South Gloucestershire and Somerset. Freedom is the specific group within the service working with LGBTQ+ young people. OTR’s online sign-up form begins with a clear statement explaining confidentiality and privacy and links to further information about safeguarding are available as links on the website. The website’s resources section includes a downloadable rights information sheet covering young people’s rights around choice, confidentiality, consent and complaint. Through extensive NHS collaborations, OTR also supports LGBTQ+ young people’s safety in navigating wider services. Through the CAMHS Triage Assessment and Outreach Team, five Engagement Workers at OTR work alongside NHS clinicians to support young people who have been referred to CAMHS, and three Youth Transitions Workers for young people aged 16–25 years are also embedded in local community mental health teams to support young people moving from CAMHS into adult mental health services.
Agency
Due to legislative, policy and developmental norms, LGBTQ+ young people have limited autonomy and agency compared to their adult counterparts. 212 The conditions created in mainstream mental health support services frequently reinforce this disadvantage, for example when parent or carer consent is required for treatment decisions. 51,107 This ‘adult knows best’ standard frequently acts to minimise LGBTQ+ young people’s distress and experience.
I have only ever heard negative feedback, young people not feeling like they are being support or heard by CAMHS. Young people feel like their care plans aren’t being updated as they should, feel like they aren’t being listened to when suggesting what is not working for them or with regards to assessments/medications.
Service document
The analysis of the case study data demonstrated that to best support LGBTQ+ young people’s mental health, services need to facilitate and encourage autonomous decision-making and position LGBTQ+ young people as experts of their own experience. Supporting LGBTQ+ young people where they may be inexperienced due to, for example, their age requires a respectful option-based (not directive) approach which better enables LGBTQ+ young people to feel more powerful and confident in relation to their own lives and help-seeking.
They gave me a list of things and what those types of support would do and let me choose, they didn’t really keep anything from me or make me feel like I wasn’t in control of the decision but if I didn’t know what I needed they would advise me in what they think might be best but still let me choose.
Devon, young person
Our analysis highlights the importance of services integrating an awareness of the power imbalances between young people and adults into practice. The service should be young person-led wherever possible, through inclusive and accessible feedback mechanisms for example. In the case studies, support was delivered collaboratively with LGBTQ+ young people, to ensure that young people felt actively involved in provision and not as though things were being done to rather than with them. Services were transparent around confidentiality, privacy and safeguarding processes, and supported non-directive and options-based decision-making including the option for young people to say ‘no’. Ellie (young person) stated ‘[w]e were given a chance to explore ourselves and discover what we need. As well as being given the independence to make our own choices’.
Our findings suggest that upholding agency and autonomy requires taking seriously LGBTQ+ young people. Advocacy for LGBTQ+ young people should uphold their decisions where autonomous, agentic decision-making power may be limited due to multiple marginalisation on the basis of racism or ableism, for example.
Case study example
Young People’s Advisory Service LGBTQ+ workers are able to provide support to young people with issues such as how to come out at school, co-authoring GIDS or GIC referrals in some cases, or drawing on input from ‘GP Champs’. GP Champs operate at YPAS and provide professional advocacy for young people facing delays or obstruction from their own GPs, in order to support and uphold young people’s decisions around health care and transition.
Belonging
Social isolation and marginalisation are common for many LGBTQ+ young people and have a direct impact on mental health. 13,72 Socioeconomic and material limitations experienced due to being young, living in care and/or poverty exacerbate the situation, for example restricted funds or technology to access social spaces. 228 Furthermore, dominant cultural norms and assumptions related to LGBTQ+ young people as white, middle class etc. 79,229 mean that many may be excluded from ‘mainstream’ LGBTQ+ support. This is particularly the case for LGBTQ+ young people of colour, those living in poverty and trans or non-binary young people. 213,230
Being in the queer community and having mental health issues is one thing, but I feel being trans adds another layer. You can begin to feel ostracised and alone even in your own community (especially in the current political climate).
Harri, young person
Our analysis found that supporting LGBTQ+ young people’s mental health required services that foster belonging through active LGBTQ+ community building and group work to address social isolation while validating LGBTQ+ identity. If this is not available in a service signposting to trusted experienced providers of LGBTQ+ specific support should be available.
In practice, the case studies developed ‘community building’ in a multitude of ways that cultivated togetherness and unification through sharing, for example space, food, time, experience, identity characteristics and memories. This LGBTQ+ community building, our analysis suggests, nurtures individual relationships while raising awareness of the ‘wider world’ which unites LGBTQ+ young people through their shared experience of cis-heteronormativity. The case study site analysis indicated that there is no ‘one size fits all’ and that LGBTQ+ communities are multiple and diverse not homogeneous. Protected spaces to foster these communities, for example annual residentials or specific identity groups foster an understanding that everyone there ‘shares’ certain characteristics and experiences without that being the totality of their identity.
It enables trans youth to connect with each other which allows people to explore their identities more and just exist with other trans people. which I think in itself is very empowering and good for my mental health.
Sammy, young person
Our findings highlight how support should be offered in a way that promotes comfort and care for LGBTQ+ young people including in language (of care) and practices that actively support the young person to sustain a meaningful engagement with the service. These ‘care practices’ included helping a young person to ‘settle in’ to a group through checking in, reassurance, and buddying with another LGBTQ+ young person. The analysis also suggested that support can foster LGBTQ+ belonging in the service’s resources by presenting diverse LGBTQ+ identities in service promotion materials.
Case study example
The Proud Trust, based in Manchester and working across Greater Manchester boroughs, is an LGBTQ+ youth-specific service, one of the largest and longest running in the UK. The Proud Trust was founded by youth workers and operates upon youth work principles of voluntary participation, youth empowerment and youth leadership. The organisation runs groups and other activities designed to make young people feel good and make friends, rather than focusing directly on mental health topics. Staff that run groups make sure LGBTQ+ young people are as comfortable as possible and that the circumstances are fertile to foster new friendships. Identifying a ‘buddy’ for a new LGBTQ+ young person to connect with is one example. Celebrating wider queer culture through involvement in Pride or LGBTQ+ History month activities are other ways they bring people together.
Recognition
Our analysis demonstrated that, within mental health services, LGBTQ+ young people were often presumed to be cisgender and/or heterosexual and this can damage mental health. 13,231 A strong and consistent finding in the study showed that effective mental health support must actively recognise or affirm LGBTQ+ identities in the wider context that undermines them. Cal (staff member) described the importance of service affirmation of sexual and gender identity:
I may be the only adult in that young person’s life that celebrates their queer identity openly and unashamedly, unabashedly. Most of the stories they tell us, not all, but most of the stories they tell are of ignorant adults in their lives and I think it weighs on them.
Our analysis indicated that recognition of LGBTQ+ identity is concerned with the fundamental sense of being valued, respected and affirmed within a service. Our findings demonstrate that services should make it clear across in-service and promotional materials that diverse LGBTQ+ identities are respected, affirmed and valued. Across many case study sites, staff worked collaboratively with LGBTQ+ young people to ensure that the service was inclusive and safe for them.
This recognition and validation requires deep understanding and nuance. The findings suggested that a service needs to balance the ‘normalisation’ of LGBTQ+ identities that does not stray into the territory of fetishising or othering and an understanding that identities are fluid, not linear and becoming LGBTQ+ (or anything else) has no fixed destination. There is also the navigation of homo/trans-norms to consider whereby there exist assumptions and expectations about how LGBTQ+ young people become LGBTQ+ adults, for example medical transition pathways. Narrow conceptualisations of LGBTQ+ identities are problematic and understanding that one person’s (st)age does not map onto that of another is imperative. There is no singular version of an LGBTQ+ young person or who they will become, and early mental health support must be cognisant of this.
You don’t have to be a stereotypically masculine trans man or feminine trans woman, you can be whoever you are without judgement. You can use whatever name and pronouns. For many, it’s the only space they can use the name and pronouns they identify with.
Val, young person
Our findings show that affirming and validating LGBTQ+ identities can be facilitated through supporting access to LGBTQ+ affirmative resources (e.g. clothes, make-up, gender-neutral toilets) and opportunities including intergenerational relationships and queer cultural events that facilitate the validation and exploration of identity on their own terms. Pronoun sharing and re-checking as a standard is helpful but there should be no pressure to explain, disclose or ‘decide’ gender. Being ‘unsure’ is also a valid option and should be included in forms and conversations about LGBTQ+ identities.
I feel safe, welcomed, appreciated. The service is very inclusive. You don’t need to have anything figured out. They make sure they always include ‘unsure’ options. This is very welcoming and makes you feel like you can get support even if you don’t know.
Stevie, a young person
(Re)checking pronouns at each encounter respects fluidity of gender and upholds their safety, for example pronouns may be different with parent/carers. Staff should also share/display pronouns, for example on badges, online. Explicit and proactive validation of LGBTQ+ identities helps support inclusion and communication that ‘everyone is welcome’. Practical support and resources that are LGBTQ+ specific including gender-neutral toilets; LGBTQ+ sex education; binding and packing workshops; coming out support; transition support; safe space to explore and experiment with body, dress, pronouns also matter in terms of recognition and validation.
Case study example
Gendered Intelligence runs youth group sessions covering different age groups and provides specific groups for young trans people of colour – TPOCalypse – and trans feminine young people. TPOCalypse is designed to remove barriers to accessing support for young trans and non-binary people of colour by addressing the additional exclusions and stigma that they may be facing and is run by youth workers who are also people of colour. TPOCalypse consists of two groups, one for young people aged 13–17 years and a peer-led group for young people aged 18–30 years. GI’s Transfemme Group is dedicated to trans women, trans girls and young transfeminine people aged 13–25 years, with all youth workers, volunteers and visitors also identifying as transfeminine or as trans women. The provision of the Transfemme Group as a closed space addresses the specific ways in which misogyny and sexism intersect with trans experience and gender variance. This provision recognises goes some way to recognising the diversity of trans and non-binary identities and helps depart from any perceptions that there is one way to be a trans young person.
Possibility
The principle of possibility relates to LGBTQ+ young people’s ability to imagine happy and fulfilled futures for themselves on their own terms. This works to counteract the feeling of ‘failing’ to meet expectations around what or who they ‘should’ be (which they may face in other areas of their lives). Expectations and norms of becoming a future citizen make socially desirable a white, cis-heterosexual, educated future232–234 that LGBTQ+ are excluded from and can seem unattainable. 13,40,76 This contributes to a sense of hopelessness which itself is a risk factor for poor mental health.
I’d say hope and aspiration are key to LGBTQ+ mental health. A lot of young people feel that because you’re LGBT there’s a lot of limits put on you about goals and achievement and so on. It’s like, ‘oh, well you could go to university but you’re LGBT so that will be really hard for you’. You know it sort of labours that stuff.
Jem, staff member
Our findings suggest services can make sure LGBTQ+ young people can see their own experiences reflected in the adults providing support and enable LGBTQ+ young people to explore their passions and interests. (Psycho)education (including direct education about normative ideals and pressures, privilege, and power) to support LGBTQ+ young people’s understanding of these norms alongside support to act and resist is important to allow LGBTQ+ young people to build confidence and experience hope for their futures on their own terms.
As an LGBTQ person in a particularly homophobic school to be welcomed with such open arms was so good. I remember after my first session feeling like I could do anything I wanted to because I knew who I am isn’t a bad thing it’s something to be celebrated.
Tomi, a young person
Across our case study sites, services upheld possibility by nurturing and uplifting LGBTQ+ young people’s futures on their own terms and taking care not to assume or enforce ‘desirable’ social norms. In practice, this included facilitating access to training opportunities and support with education, fulfilling ambitions or goals, volunteering opportunities both inside and outside of services, and involving LGBTQ+ young people in producing content such as websites and podcasts. Services also supported community building and modelling of diverse LGBTQ+ futures through mixed age group work, employing diverse ‘out’ staff and hosting LGBTQ+ adult guests to talk about careers, family building, or other aspects of adult life.
Case study example
Manchester-based 42nd Street provides mental health support for young people and has an LGBTQ+ specific group called Q42. LGBTQ+ resources are also embedded throughout 42nd Street’s online presence, and the service staff includes many ‘out’ LGBTQ+ adults. The overall focus of Q42 is peer support, and Q42 also emphasises development and opportunities to build new skills; LGBTQ+ young people are involved in the creation of online resources such as a dedicated website and a podcast. Through Q42, LGBTQ+ young people are supported to go on trips and to events such as the annual Manchester Pride parade. Through the ‘Change Ambassadors’ scheme at 42nd Street, young people can also be supported to take on more active roles in advocacy and campaigning at local, regional and national levels, and have greater influence on the development of 42nd Street’s own services.
Emotion
Our findings indicate that mental health support must validate LGBTQ+ young people’s distress as a logical response to marginalisation and stigma; and support the development of emotional resilience. We found that the most effective mental health support centred on the young person’s emotions and moved away from the usual position of deficit in which something is ‘wrong’ with an LGBTQ+ young person, to focus instead on developing skills and trust in communicating about feelings.
Biomedical models of mental health support tend to be individualistic and pathologise human emotion as ‘irrational’ or ‘dysregulated’ when feelings are often reasonable reactions to life (dis)stress. 13,235 The pathologisation of feelings interplays with stereotypes of young people for whom normative discourses related to puberty and hormones also position them as inherently irrational and attention seeking. 107 Add to this the pejorative implications that LGBTQ+ identities are also ‘a phase’ that will be outlived236 and we have a set of norms that serve to diminish the distress of LGBTQ+ young people.
Rather than saying what’s wrong with the rest of the world, individual young people are deemed mad but the world is mad. If we had more capacity to do trans youth work and LGBT youth work, we wouldn’t see as much distress, and as much mental health conditions as we do see amongst our young people.
Harper, staff member
Our analysis identified that an asset-based emotion centred approach, which involves non-pathologising and usualising communication about feelings, is beneficial in validating the experience of LGBTQ+ young people. The feelings of LGBTQ+ young people must be taken seriously and responses or practices that may minimise their feelings need to be actively avoided. Conversely ‘good feelings’ can be boosted without any pressure to ‘be happy’, for example through relaxation, fun and activities that offer a ‘sense of purpose’.
The analysis suggested that explicit and open communication about feelings on young people’s terms using their own language (not necessarily verbal) can be facilitated by staff, for example actively reassuring around experiences that are likely to be difficult such as first meetings, wider world/media events. To be most effective, this can be done while tailoring reassurances to the needs of the person.
When things are happening with me, I don’t enjoy advice. I prefer comfort or a distraction. This is exactly what they would do. They’d take me into the kitchen or outside and just let me ramble, whether it’s about the issues I’m facing or my current hyperfix. They know what each individual needs and adapts to make sure that’s what they get.
Alix, a young person
The de-pathologisation of feelings and emotions, the findings indicate, includes ensuring a diagnosis is not a requirement to access the service and an understanding of the role of mental health diagnosis to young people. Maria (staff member) explains:
We’re conscious that young people often have a lot of diagnosis. For some that will have been a relief to have a diagnosis. And for some, it is not something they feel happy about and it feels that it was imposed on them. So diagnosis is important but more in terms of how that person views their own life choices.
Maria, staff member
Case study example
SAYiT currently defines themselves as ‘Emotional wellbeing support for LGBTQ+ young people in Sheffield’. Staff developed in-house and use a ‘rainbow assessment tool’ to support LGBTQ+ young people to set their own goals. The areas covered by the tool include well-being, relationships, community, identity, self-confidence and self-esteem, emotions, resilience and decisions. The rainbow assessment tool highlights how emotions are changeable and how they arise in relation to life’s complex difficulties and changes.
Emotion nexus points
In the model we have produced from the case study data analysis, we have drawn attention to key points where the principles of the model interconnect and are important to the provision of mental health support that works for LGBTQ+ young people. We outline these emotional nexus points below, but further explanation can be found on the digital interactive model housed on the study website https://queerfutures2.co.uk/what-works/:
-
(1 on Figure 7) A LGBTQ+ young person receiving mental health support should feel respected (not dismissed) where their agency and safety are upheld.
-
(2 on Figure 7) A LGBTQ+ young person receiving mental health support should feel in control (powerless) where their agency and possibility are upheld.
-
(3 on Figure 7) A LGBTQ+ young person receiving mental health support should feel hopeful (not despair) where their possibility and recognition are upheld.
-
(4 on Figure 7) A LGBTQ+ young person receiving mental health support should feel validated (marginalised) where their recognition and belonging are upheld.
-
(5 on Figure 7) A LGBTQ+ young person receiving mental health support should feel trusting (not vulnerable) where their belonging and safety are upheld.
Improving accessibility
We know LGBTQ+ youth may not access mental health services when they need support because their marginalised position makes access difficult compared to cis/heterosexual peers. The analysis from the case study evaluation is premised upon the idea that improving early intervention mental health support overall will also increase access to, navigation of, and engagement with those services. However, our findings indicate that there are some deep-seated multifactored complexities to LGBTQ+ young people seeking help and accessing appropriate mental health services.
Our analysis suggests that the navigation of mental health services, and access and engagement with these services are contingent upon the power differential between LGBTQ+ young people and the adults they seek help from. Key to our model is the understanding that being young is associated with a lack of power that can impact on the ability to access services. When LGBTQ+ youth feel more powerful and confident there is greater likelihood they will ask for help from mental health services and remain engaged to receive support. Utilising an intersectional approach our findings suggest that accessibility is improved through a combination of structural, cultural, disciplinary (systems) and interpersonal factors which we outline in greater detail below.
Structural
The findings suggest that improvement in accessibility structural factors is important. Services need to proactively demonstrate that they can support people to access them, for example hardship funds and transport costs, all-gender toilets and make this clear on the website or in information about the service. The service must be easy to locate and have an online presence – online material is very important for responding to searches for help and also for managing expectations and an online service can appeal to young people who are distant and cannot commit to regular attendance. Services should offer online as well as face-to-face support.
The analysis suggests the timing of services is crucial. Measures such as providing support after school, with regular drop-in hubs at different locations and times. Service locations and delivery (digital or in-person) are important, but our analysis indicates there is no ‘one size fits all’ and flexible hybrid structures offer the best chance of meeting most people’s needs, some of the time. Art (young person) said, ‘I haven’t actually taken part in the online sessions as I don’t find them very easy to access. I live with my family so don’t necessarily feel comfortable with the possibility of them overhearing me’.
Disciplinary (systems)
The findings suggest that the systems used to access services, for example referral forms, must not be too demanding, burdensome or exclude LGBTQ+ youth. For example, complicated referral forms, absence of LGBTQ+ identities within the service information, or pathologising LGBTQ+ identities in mental health assessment forms. Systems to access the service should also provide brief explanations of confidentiality, privacy and information sharing as part of sign-up forms and ensure that forms reflect the diversity of LGBTQ+ young people’s identities to encourage LGBTQ+ young people that the service is safe.
The fact it was made clear it was specifically for younger people made me feel comfortable about contacting them. [The referral form] was probably the most stressful part as I had no clue what to put for some of the answers since I was doing it for myself. But I e-mailed and they offered to call me and guide me through it which helped a lot.
Jack, a young person
Our analysis illuminated a power imbalance between different organisation types. Statutory services and NHS/clinicians have more authority than LGBTQ+ charity sector services despite the latter providing the majority of LGBTQ+ specific mental health support. This imbalance has implications for the robust, reliable networks of services that our findings demonstrated as necessary to ensure LGBTQ+ youth find suitable support. ‘Successful’ engagements of LGBTQ+ youth were often because wider institutions (e.g. schools) were aware of LGBTQ+ specialist services and were working effectively with them:
A support teacher at my school sat me down and we did the referral process together […] they told me about the support they have for LGBTQ+ teens […] Immediately I felt comfortable because I knew that I wouldn’t be judged.
Tomi, a young person
In 25% of our case study services, there were funded partnerships between statutory services/NHS and LGBTQ+ organisations. These funded partnerships provided appropriate support and resources while legitimating the role of non-statutory (LGBTQ+) service.
Cultural
Typically, we consider structural ‘barriers to access’ as factors such as service location, transport and opening hours. While important, this view of accessibility is limited and undermines the importance of myriad social and cultural factors. Our intersectional analysis found oppressive structures and associated discriminations are key barriers to access. Tackling these barriers from the ‘top down’, that is, having LGBTQ+ senior leadership, or grassroots responses to need, for example by Queer, Trans and Intersex Black people and People of Colour (QTIBPOC) for QTIBPOC, can facilitate access that is inclusive and operates against existing systems that marginalise LGBTQ+ youth.
Because it’s a trans only space, everything else about you is seen first or more importantly. So when you go as a trans person into a generic space or an LGBT space you’re seen as ‘the trans person’, right? But when you come into a trans only […] it’s the given and it’s the norm.
Harper, a young person
To be accessible, services must actively demonstrate an LGBTQ+ inclusive culture and ensure a multiplicity of LGBTQ+ identities is welcome, for example QTIBPOC, LGBTQ+ youth with disabilities. Inclusive resources co-designed with LGBTQ+ youth representing diverse identities can safeguard against exclusion. In addition, recruiting staff with diverse experiences and displaying LGBTQ+ inclusivity clearly in online and print resources can improve accessibility.
Interpersonal
Our model has emotions are the centre and the emotions of LGBTQ+ young people newly accessing services need to be intentionally and considerately managed in order to keep LGBTQ+ youth engaged with a service. The analysis suggests that LGBTQ+ young people need to feel ‘comfortable’ for service access and engagement to improve. Managing fear of the unknown, fear of being outed, fear of not being taken seriously means active efforts by services to ensure young people are reassured. Our analysis indicated measures such as featuring diverse service staff in online content, providing service walk-throughs online showing the service building and layout and offering buddy systems for first-time attendees were all effective ways of building the young person’s trust and confidence in the service.
We would meet them at our office, or at their home, or at school or in a café, wherever they felt most comfortable […] to reassure them or give them information about what to expect, what the groups are like […] to hopefully make them feel safer.
Ema, staff member
Case study example
Off the Record (OTR) is an integrated youth mental health service in Bristol defined as a mental health social movement for youth aged 14–25 years. LGBTQ+ inclusion is demonstrated across the service materials, and they run a specific LGBTQ+ project (Freedom). OTR operates at a range of locations and times through the week. Their different support strands are interlinked, for example Pride-themed video content produced by OTR features workers from Project Zazi (specifically for Youth of Colour). OTR’s website is young person friendly and easy to refer or sign up online. Their information-sharing policy is clear as a precursor to sign-up. Links to support are labelled clearly on the website landing page in a first-person non-pathologising way – ‘I’m thinking about my gender and/or sexuality’.
Service cost findings
The purpose of the service cost findings was to support the development of the NHS Commissioning Guidance at the end of the study. There was no specific health economics research question and this was partly because the aim of the study was to build a theoretical model of what works to support LGBTQ+ young people’s mental health, where there is very little evidence on the effectiveness or acceptability of services and interventions.
Use of care services
Our starting point was a crude analysis of the number of visits to and users of primary care, community health, community mental health services and other mental health as reported by the participants with a recall period of 4 weeks. We performed the same analysis for the services provided at each CSS (Table 13). There was a total of 486 contacts both with the NHS and CSS (280 contacts in CSS against 206 with NHS services) reported by 45 participants in a 4-week period with no missing values. The two least used services provided by the NHS were appointments with nurses at GP surgeries and GP appointments. On the opposite end, the two most used services were the ones provided by other mental health professionals (50 visits) and other services including helplines/online (56 visits). As for the CSS, activity sessions were the most frequent reason to visit (104 sessions) followed by peer support (78 contacts) and 1 : 1 sessions that motivated 76 visits.
| Case study site | No participants | Total contacts | NHS contacts | Case study site contacts | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP | Nurse | Psychiatrist | Community Mental Health (CMH) | Other MHV | Other service visits | Total | 1 : 1 visits | Peer support | Activity sessions | Other sessions | Total | |||
| CSS 1 | 5 | 65 | 5 | 7 | 8 | 6 | 8 | 8 | 42 | 8 | 0 | 7 | 8 | 23 |
| CSS 3 | 3 | 15 | 1 | 0 | 2 | 3 | 1 | 1 | 8 | 5 | 1 | 1 | 0 | 7 |
| CSS 4 | 3 | 45 | 1 | 0 | 1 | 1 | 0 | 0 | 3 | 0 | 21 | 21 | 0 | 42 |
| CSS 5 | 6 | 71 | 5 | 3 | 3 | 4 | 6 | 12 | 33 | 13 | 16 | 4 | 5 | 38 |
| CSS 6 | 2 | 20 | 0 | 0 | 0 | 1 | 6 | 1 | 8 | 0 | 6 | 6 | 0 | 12 |
| CSS 7 | 4 | 16 | 0 | 0 | 0 | 0 | 2 | 3 | 5 | 11 | 0 | 0 | 0 | 11 |
| CSS 9 | 4 | 23 | 0 | 1 | 0 | 5 | 6 | 1 | 13 | 3 | 6 | 1 | 0 | 10 |
| CSS 10 | 3 | 56 | 0 | 4 | 6 | 9 | 7 | 17 | 43 | 0 | 0 | 13 | 0 | 13 |
| CSS 11 | 1 | 3 | 0 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 1 |
| CSS 12 | 5 | 43 | 5 | 1 | 4 | 2 | 2 | 4 | 18 | 5 | 9 | 11 | 0 | 25 |
| CSS 13 | 4 | 81 | 2 | 0 | 0 | 0 | 7 | 9 | 18 | 19 | 14 | 30 | 0 | 63 |
| CSS 15 | 5 | 48 | 2 | 1 | 0 | 5 | 5 | 0 | 13 | 11 | 5 | 10 | 9 | 35 |
| Total | 45 | 486 | 21 | 18 | 25 | 36 | 50 | 56 | 206 | 76 | 78 | 104 | 22 | 280 |
We then calculated the mean frequency of use of all services for the same 4-week recall period (Table 15). Looking at the mean number of contacts reported by the patients, we observe that participants in CSS 13 had an average of 20.3 contacts in 4 weeks, followed by participants in CSS 10 reporting 18.7 on average for the same period. Participants in CSS 3, 7 and 9 had the lowest mean number of contacts across all the services available.
Overall use of health services was low, with a very small number of participants reporting high levels of service use. In CSS 6 and 7, participants have not reported any appointments with GP, nurses and psychiatrists. Participants in CSS 4 reported a low use of NHS services; however, the average use of services provided by this CSS was the second highest in our sample.
As the individuals using the NHS services and the CSS were the same, we computed a paired sample t-test to determine whether the difference between the mean use of NHS services (4.6) and the mean use of CSS (6.2) was statistically different from zero (Figure 8). A paired sample t-test is a statistical method used to compare the means of two related groups to determine if there is a significant difference between them in a given variable of interest; in this case, it was the mean use of services.
FIGURE 8.
Paired samples t-test.
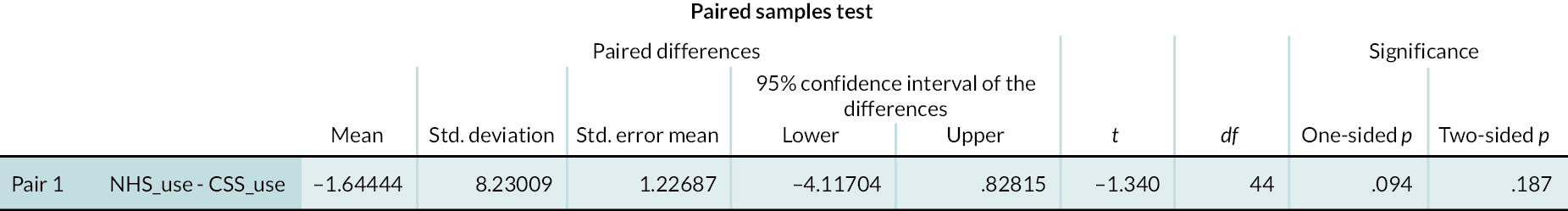
The results obtained for the differences between the values for the mean use of services in the NHS and in the CSS do not allow us to say that their average use by participants is not the same, as the confidence interval includes zero and the significance value is 0.187 (> 0.10) for a two-sided distribution, not allowing us to say that the differences observed have statistical significance.
Costs of services used
We applied the unit costs in Table 14 to the service use reported in Table 15 to calculate the cost of care services used presented in Table 16.
| Resource | Cost (£) | Unit | Source | |
|---|---|---|---|---|
| GP | 217.00 | Hour | Unit Costs of Health and Social Care 2021 (£33.19/9.22 million) | 10.3b GP – unit costs, p.111 |
| Nurse at GP practice | 42.00 | Hour | Unit Costs of Health and Social Care 2021 (£7/10 million) | 10.2b Nurse (GP practice) – unit costs, p.109 |
| Consultant: psychiatric | 123.00 | Hour | Unit Costs of Health and Social Care 2021 | 14. Hospital-based doctors |
| Community psychiatric nurse/community mental health nurse | 33.00 | Hour | Unit Costs of Health and Social Care 2021 | 10.1. Nurses, p.108 (band 4) |
| Other mental health professional (Counselling) | 51.00 | Hour | Unit Costs of Health and Social Care 2021 | 6.10 Counselling for children with mental or emotional difficulties – unit costs, p.80 |
| Other service use (helplines/online) | 25.00 | Hour | Unit Costs of Health and Social Care 2021 | 11.7 Support and outreach worker, p.128 |
| Case study site: 1 to 1 sessions | 51.00 | Hour | Unit Costs of Health and Social Care 2021 | 6.10 Counselling for children with mental or emotional difficulties – unit costs, p.80 |
| Case study site: Peer support (peer intern) | 26.00 | Hour | Unit Costs of Health and Social Care 2021 | 11.8 Peer intern, p.129 |
| Case study site: Activity session (support/outreach worker) | 25.00 | Hour | Unit Costs of Health and Social Care 2021 | 11.7 Support and outreach worker, p.128 |
| Case study site: Other sessions (support/outreach worker) | 25.00 | Hour | Unit Costs of Health and Social Care 2021 | 11.7 Support and outreach worker, p.128 |
| Case study site | Total contacts | NHS contacts | Case study site contacts | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP | Nurse | Psychiatrist | CMH | Other MHV | Other service visits | Total | 1 : 1 visits | Peer support | Activity sessions | Other sessions | Total | ||
| CSS 1 | 13.0 (10.77) | 1.0 (0.71) | 1.4 (1.14) | 1.6 (1.52) | 1.2 (2.17) | 1.6 (1.82) | 1.6 (3.58) | 8.4 (8.41) | 1.6 (3.58) | 1.4 (1.67) | 1.6 (3.58) | 4.6 (4.04) | |
| CSS 3 | 5.0 (5.00) | 0.3 (0.58) | 0.7 (1.15) | 1.0 (1.73) | 0.3 (0.58) | 0.3 (2.08) | 2.7 (3.79) | 1.7 (2.08) | 0.3 (0.58) | 0.3 (0.58) | 2.3 (2.08) | ||
| CSS 4 | 15.0 (6.08) | 0.3 (0.58) | 0.3 (0.58) | 0.3 (0.58) | 1.0 (1.73) | 7.0 (2.65) | 7.0 (2.65) | 14.0 (5.29) | |||||
| CSS 5 | 11.8 (10.70) | 0.8 (0.98) | 0.5 (0.55) | 0.5 (1.22) | 0.7 (1.63) | 1.0 (1.67) | 2.0 (2.45) | 5.5 (5.75) | 2.2 (3.43) | 2.7 (2.16) | 0.7 (1.21) | 0.8 (1.60) | 6.3 (5.39) |
| CSS 6 | 10.0 (1.41) | 0.5 (0.71) | 3.0 (4.24) | 0.5 (0.71) | 4.0 (5.66) | 3.0 (1.41) | 3.0 (2.83) | 6.0 (4.24) | |||||
| CSS 7 | 4.0 (4.32) | 0.5 (1.00) | 0.8 (0.96) | 1.3 (1.89) | 2.8 (2.50) | 2.8 (2.50) | |||||||
| CSS 9 | 5.8 (4.11) | 0.3 (0.50) | 1.3 (2.50) | 1.5 (1.73) | 0.3 (0.50) | 3.3 (3.59) | 0.8 (0.96) | 1.5 (3.00) | 0.3 (0.50) | 2.5 (2.65) | |||
| CSS 10 | 18.7 (17.21) | 1.3 (2.31) | 2.0 (2.65) | 3.0 (2.65) | 2.3 (3.21) | 5.7 (2.89) | 14.3 (12.86) | 4.3 (4.51) | 4.3 (4.51) | ||||
| CSS 11 | 3.0 | 1.0 | 1.0 | 2.0 | 1.0 | 1.0 | |||||||
| CSS 12 | 8.6 (6.43) | 1.0 (1.00) | 0.2 (0.45) | 0.8 (1.79) | 0.4 (0.89) | 0.4 (0.86) | 0.8 (0.84) | 3.6 (4.04) | 1.0 (1.73) | 1.8 (2.05) | 2.2 (1.79) | 5.0 (4.85) | |
| CSS 13 | 20.3 (9.11) | 0.5 (1.00) | 1.8 (2.22) | 2.3 (2.63) | 4.5 (5.45) | 4.8 (3.30) | 3.5 (3.87) | 7.5 (3.00) | 15.8 (8.30) | ||||
| CSS 15 | 9.6 (13.87) | 0.4 (0.55) | 0.2 (0.45) | 1.0 (1.41) | 1.0 (1.41) | 2.6 (2.79) | 2.2 (3.90) | 1.0 (2.24) | 2.0 (2.35) | 1.8 (4.02) | 7.0 (11.83) | ||
| Total | 10.8 (9.71) | 0.5 (0.73) | 0.4 (0.84) | 0.6 (1.22) | 0.8 (1.56) | 1.1 (1.72) | 1.2 (2.22) | 4.6 (5.99) | 1.7 (2.57) | 1.7 (2.61) | 2.3 (3.04) | 0.5 (1.85) | 6.2 (6.72) |
| Case study site | Total | NHS contacts | Case study site contacts | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP | Nurse | Psychiatrist | CMH | Other MHV | Other service visits | Total | 1 : 1 visits | Peer support | Activity sessions | Other sessions | Total | ||
| CSS 1 | 557.59 | 33.19 | 9.80 | 196.80 | 39.60 | 81.60 | 40.00 | 400.99 | 81.60 | 35.00 | 40.00 | 156.60 | |
| CSS 3 | 253.40 | 11.06 | 82.00 | 33.00 | 17.00 | 8.33 | 151.40 | 85.00 | 8.67 | 8.33 | 102.00 | ||
| CSS 4 | 420.06 | 11.06 | 41.00 | 11.00 | 63.06 | 0.00 | 182.00 | 175.00 | 357.00 | ||||
| CSS 5 | 432.99 | 27.66 | 3.50 | 61.50 | 22.00 | 51.00 | 50.00 | 215.66 | 110.50 | 69.33 | 16.67 | 20.83 | 217.33 |
| CSS 6 | 335.00 | 16.50 | 153.00 | 12.50 | 182.00 | 78.00 | 75.00 | 153.00 | |||||
| CSS 7 | 184.50 | 25.50 | 18.75 | 44.25 | 140.25 | 140.25 | |||||||
| CSS 9 | 209.25 | 1.75 | 41.25 | 76.50 | 6.25 | 125.75 | 38.25 | 39.00 | 6.25 | 83.50 | |||
| CSS 10 | 723.33 | 9.33 | 246.00 | 99.00 | 119.00 | 141.67 | 615.00 | 108.33 | 108.33 | ||||
| CSS 11 | 181.00 | 7.00 | 123.00 | 130.00 | 51.00 | 51.00 | |||||||
| CSS 12 | 339.39 | 33.19 | 1.40 | 98.40 | 13.20 | 20.40 | 20.00 | 186.59 | 51.00 | 46.80 | 55.00 | 152.80 | |
| CSS 13 | 682.85 | 16.60 | 89.25 | 56.25 | 162.10 | 242.25 | 91.00 | 187.50 | 520.75 | ||||
| CSS 15 | 331.88 | 13.28 | 1.40 | 33.00 | 51.00 | 98.68 | 112.20 | 26.00 | 50.00 | 45.00 | 233.20 | ||
| Total | 402.00 | 15.49 | 2.80 | 68.33 | 26.40 | 56.67 | 31.11 | 200.80 | 86.13 | 45.07 | 57.78 | 12.22 | 201.20 |
Overall costs are £402.00 per participant over 4 weeks. We have observed that the average use of services was higher in the CSS than in the healthcare services; however, costs are identical. The use of services provided by the CSS amounted to £201.20 and the use of services provided by the NHS was £200. The most meaningful costs are the 1 : 1 sessions (£86.13) followed by psychiatrist visits (£68.33) in the NHS. The mean costs of observed cases for nurse visits can be considered negligible (£2.80). The category with the lowest mean costs in the CSS was the one of other sessions (£12.22).
Our sample is too small to allow us to draw representative conclusions either at site level or at national level. Nevertheless, it is important to note the high use reported by the participants for a recall period of 4 weeks. In some CSS, participants had an average of 5 contacts per week. If we extrapolate our average 4 weeks costs to 52 weeks, each participant would have a cost around £5000. Overall use of health services in the NHS was low and skewed, with a small number of participants reporting very high levels of service use. In CSS around half of the participants reported no contacts in each category of services available.
Discussion
The model produced through the case study analysis was aimed at supporting LGBTQ+ youth with common mental health problems at an early point in their difficulties. The model also aimed to have applicability across a variety of settings such as school, health care, online, community and youth work. Our interdisciplinary approach indicated that effective early intervention mental health support for LGBTQ+ youth must prioritise addressing normative environments that marginalises youth, LGBTQ+ identities and mental health problems
Our case study analysis produced a theoretical model for supporting LGBTQ+ youth mental health, understanding that LGBTQ+ youth mental health arises from intersectional and complex factors. This model works with a de-medicalised concept of emotional distress and promotes youth-centred support that attends to the multifactored influences on LGBTQ+ youth mental health.
The model produced has 13 principles that interact to produce appropriate mental health support for LGBTQ+ young people. This early intervention model is premised primarily on addressing the social experiences of LGBTQ+ young people that marginalise, silence and denigrate those with diverse genders and sexualities. Developing an intersectional youth-rights mental health approach to mental health provision posits young people as rights holders and underlines the requirements of duty-bearers to meet these rights in line with international human rights instruments. A rights-based approach to LGBTQ+ youth early intervention mental health support must be premised upon the recognition and respect for the dignity and agency of young people; their empowerment and active participation in their own lives and mental health care; the promotion of positive mental health, well-being and development; and a commitment to the promotion, protection and fulfilment of their human rights, without discrimination.
At the centre of our youth-rights approach to mental health support is the recognition that ‘adolescence’ is an age category that disadvantages young people in terms of seeking mental health support and receiving effective mental health services. The model we have generated tackles directly the powerlessness of young people because they are considered as ‘adults in waiting’ and therefore, as ‘less than’ adults. Our model concurs with the UN’s analysis of the problem of ensuring adolescence rights are promoted and protected:
[...] the widespread negative characterization of adolescence leading to narrow problem-focused interventions and services, rather than a commitment to building optimum environments to guarantee the rights of adolescents and support the development of their physical, psychological, spiritual, social, emotional, cognitive, cultural and economic capacities. (3: 5)
Key to our approach is, as the UN emphasise, an understanding of and respect for the evolving capacities (UNCRC article 5) of young people. The UN defines evolving capacities as ‘an enabling principle that addresses the process of maturation and learning through which children progressively acquire competencies, understanding and increasing levels of agency to take responsibility and exercise their rights’ (3: 6). Young people as they develop move from a situation of depending on adults to developing greater autonomy. They need mental health support that can enable their right to exercise increasing levels of responsibility. This should not however remove the obligation to protect LGBTQ+ young people because their relative inexperience and lack of power can make them vulnerable to discrimination and violations of their rights and mental health.
This is why an intersectional approach, as advocated by the UN (3: 7), to mental health support, is crucial for LGBTQ+ young people because they commonly face difficulties because their age and identities expose them to discrimination, social exclusion, marginalisation, bullying, social injustice and non-inclusion in public spaces. This increases their vulnerability to poverty, homelessness, poor educational outcomes, high levels of detention in the criminal justice system and hence disproportionately high risk of poor mental health.
Conclusions
Our intersectional, youth-rights approach to early intervention mental health support for LGBTQ+ young people demonstrates that youth rights should underpin the delivery of mental health support for LGBTQ+ young people to address the multiple marginalisation, isolation and stigmatisation that LGBTQ+ young people may experience and to enable them to make informed independent decisions about their own bodies and lives, and for the right to freedom of safe self-expression to be upheld.
Chapter 6 Discussion
The model of what works to support LGBTQ+ young people’s mental health at an early point is the first evidence, nationally and internationally, to be produced. Currently, the evidence base on LGBTQ+ young people’s mental health is dominated by studies demonstrating prevalence and charting risk and resilience factors. Research investigating ways of addressing mental health problems in this population group is scarce. This study provides the first large-scale theory-led evaluation of early intervention mental health support for LGBTQ+ young people with common mental health problems. As a result, it directly provides the means to tackle the elevated prevalence of mental health problems in this group of young people. It provides evidence on ways of improving access to, navigation of, engagement with mental health support, to improve LGBTQ+ young people’s mental health.
Key findings and recommendations
Our analysis of the data from the case study evaluation suggests that an intersectional, youth-rights approach to early intervention mental health support for LGBTQ+ young people is the most appropriate way of supporting poor mental health in this population group. Youth rights should underpin the delivery of mental health support for LGBTQ+ young people to address the multiple marginalisation, isolation and stigmatisation that LGBTQ+ young people may experience and to enable them to make informed independent decisions about their own bodies and lives, and for the right to freedom of safe self-expression to be upheld. These are paramount to appropriate mental health support.
A fundamental element of the model to support LGBTQ+ youth mental health is to understand that they live in a cis-heteronormative world that despite improvements continues to either explicitly denigrate LGBTQ+ identities or marginalise and silence those lives. Our findings strongly demonstrate that youth must be supported to exist within/resist against these difficult normative environments. In the following sections, we outline how the findings of the study address three key problems and make recommendations for policy and practice:
-
LGBTQ+ young people have poor mental health outcomes.
-
LGBTQ+ young people underutilise mental health services.
-
LGBTQ+ young people have poor experiences of mental health services.
Key problem 1: LGBTQ+ young people have poor mental health outcomes
What’s the problem?
-
LGBTQ+ young people are more at risk of poor mental health and worse mental health outcomes than heterosexual peers. 5,6,8,59,237,238
-
These inequalities start as early as age 10, increasing throughout adolescence and peaking between the ages of 13 and 19. 6
-
Common mental health problems occur at higher rates for LGBTQ+ young people who are black or people of colour, trans or gender diverse, intersex or disabled. 37,239
The most prominent model in explaining these inequalities is ‘minority stress’12 whereby experiences of stigma, prejudice and discrimination create hostile environments, leading to mental health problems. Being LGBTQ+ means young people do not conform to expectations or ‘norms’, that is, that you are heterosexual and cisgender (non-transgender). LGBTQ+ young people are marginalised through lack of mainstream visibility, discrimination, (micro)aggression, bullying and victimisation they experience. 13,14 Even within LGBTQ+ communities, young people may also come up against assumptions and pressures about the ‘right’, ‘normal’ or ‘best’ ways to be LGBTQ+, such as stereotypes about ‘good’ or ‘bad’ bisexual people, or what it means to be ‘trans enough’.
Among peers and in places like school or college, stigma can result in social isolation; a quarter of the LGBTQ+ young people surveyed for Stonewall’s 2017 School Report experienced being ignored and isolated as a pattern of bullying. 28 Young people may also experience the erasure of their identities within service settings and in their interactions with adults, that is, where it is not considered that they could be LGBTQ+ and cis-heterosexuality is presumed.
Mental health inequalities faced by LGBTQ+ young people have been exacerbated by COVID-19 and the impact of national and regional lockdowns, with evidence emerging that lockdowns have led to high levels of stress and depressive symptoms reported by LGBTQ+ people, especially young people. 36,37 Among 1140 LGBTQ+ young people surveyed for research commissioned by the charity Just Like Us, 68% reported that their mental health worsened during the pandemic. Fifty-five per cent reported worrying daily about their mental health, rising to 65% for black LGBTQ+ young people, trans and gender diverse young people, and disabled LGBTQ+ young people. 37
What works to reduce poor mental health for LGBTQ+ young people?
Hopelessness and isolation are crucial components of poor mental health among LGBTQ+ young people. In the model of what works to support LGBTQ+ young people’s mental health at an early point the principles of Belonging, Possibility, Body were key. Feeling connected to a wider community enables LGBTQ+ young people to feel less alone and to experience a sense of collective care and respect. To uphold the principle of Belonging our findings suggest services can provide or facilitate access to LGBTQ+ youth groups across different age ranges and identities; connect LGBTQ+ young people with wider communities and community histories; help build bonds with peers, forming friendships.
The principle of Possibility relates to LGBTQ+ young people’s ability to imagine happy and fulfilled futures for themselves on their own terms. This works to counteract the feeling of ‘failing’ to meet expectations around what or who they ‘should’ be (which they may face in other areas of their lives). Our findings suggest services can make sure LGBTQ+ young people can see their own experiences reflected in the adults providing support and enable LGBTQ+ young people to explore their passions and interests. Support related to the Body centres LGBTQ+ young people’s bodily health and well-being, and their ability to express themselves, for example in dress, make-up, hairstyles, body hair and so on. Self-expression can support mental health. Our findings suggest services can facilitate access to LGBTQ+ specific sports or activities such as climbing or swimming (note: it is vitally important that young people are not pressured into these activities – implying that young people will feel better if they ‘go for a walk’ or lose weight can also be harmful) and provide safer spaces where LGBTQ+ young people can explore their self-expression and presentation. This may be facilitated through clothing swaps, and the provision of make-up, clothing or gender-affirming resources for young people to use.
Recommendations to improve LGBTQ+ young people’s mental health
Mental health services and policies need to:
-
Acknowledge isolation and hopelessness as major factors impacting LGBTQ+ young people’s mental health.
-
Develop support that supports connectedness, self-expression, and hope for the future on young people’s own terms.
-
Address isolation, for example:
-
Providing LGBTQ+ groups or signposting to trusted LGBTQ+ youth groups.
-
Connecting LGBTQ+ young people with wider communities in safe ways, such as hosting LGBTQ+ guest speakers or organising group attendance at Pride events.
-
-
Support self-expression, for example:
-
Providing resources for young people to dress and present themselves in ways they want to, and to be called by the names and pronouns that feel best.
-
Facilitating access to inclusive sports and activities and support around sleep, without framing exercise, weight loss or diet changes as ‘cures’ or obligations.
-
-
Address hopelessness, for example:
-
Modelling diverse LGBTQ+ lives and futures, whether directly (through visits or staff’s own lived experience) or indirectly (through partnership working with LGBTQ+ specific services or organisations).
-
Supporting LGBTQ+ young people’s skills and interests and providing or signposting to development opportunities.
-
Key problem 2: LGBTQ+ young people underutilise mental health services
What’s the problem?
Evidence shows that LGBTQ+ young people are reluctant to seek support, particularly from mainstream services or authority figures. Findings from a 2015 UK-based study indicated that in a sample of 789 LGBTQ+ young people, just over a fifth of the sample had not sought help at all when they were self-harming or feeling suicidal. 41 When they do seek support, LGBTQ+ young people tend to seek mental health help online and from peers40,41 and prefer accessing LGBTQ+ organisations for mental health support. 42,46 Experiences with ‘mainstream’ healthcare and mental health services are variable; helpfulness ratings for GPs and mental health services are low in comparison to friends, the Internet and LGBTQ+ youth groups. 42
Studies have found that LGBTQ+ young people are reluctant to access mental health support services because of:40,42–44,51
-
Actual or anticipated experiences of homophobia, biphobia and transphobia
-
Cisgender and heterosexual norms, including a fear that their sexual orientation and/or gender identity would be scrutinised or blamed for their mental health problems
-
Difficulties disclosing their sexual orientation and/or gender identity due to fear or lack of options for LGBTQ+ identities on forms
-
Fear of being misunderstood or judged by adults due to being young
-
Stigma related to having mental health problems
What works to increase LGBTQ+ young people’s use of mental health services?
A crucial starting point in establishing early intervention support pathways is ensuring LGBTQ+ young people do not need a mental health diagnosis before they can receive support for their mental health. Subjective assessment of mental health needs by an LGBTQ+ young person themselves should be sufficient to access support. Given the reluctance of LGBTQ+ young people to seek support from mainstream services or figures such as teachers, parents or school/college counsellors, access to care should not rely exclusively on referral pathways facilitated by adults. Referral can also be supported through the development of ‘one-stop-shop’ services based in the community, as advocated for by Future in Mind guidance. 240 Referral to services with waiting lists can be supported by complementary offers of group spaces and informal one-to-one support ‘while you wait’.
To increase access to, navigation of, and engagement with mental health services the model of what works to support LGBTQ+ young people’s mental health at an early point indicates the principles of Safety, Time, Recognition were key. To uphold the principle of Safety, our findings suggest services can implement clear and robust policies around discrimination and bullying; ensure that LGBTQ+ young people are able to see clearly that a service is safe for them to access and feel confident they will not face prejudice, discrimination, or stigma within it; ensure that it is clear in online information about a service that LGBTQ+ identities and experiences are affirmed and welcomed.
The way that Time is organised and structured within service delivery should centre LGBTQ+ young people’s lives and needs. It is crucial that young people not be left ignored and unheard while in distress. Our findings suggest services can ensure that there is always support and a response of some kind accessible. This could be supported online or via telephone, or through the provision of groups and non-clinical one-to-one support. In addition, services should ask for LGBTQ+ young people’s input on the frequency, pace, timing and duration of support. Recognition is concerned with the fundamental sense of being valued, respected and affirmed within a service. Our findings demonstrate that services should make it clear across in-service and promotional materials that diverse LGBTQ+ identities are respected, affirmed, and valued; work collaboratively with LGBTQ+ young people to ensure that the service is inclusive and safe for them; invest in staff knowledge and development to support LGBTQ+ young people.
Recommendations for increasing LGBTQ+ young people’s use of mental health services
Mental health services and policies need to:
-
Acknowledge that LGBTQ+ young people are more likely to access mental health support when they can see clearly that the service is safe, knowledgeable and affirming, and when the support offered fits into their lives.
-
Provide a safer service for example:
-
Transparent policy around confidentiality and safeguarding, communicated in young person-friendly ways, for example providing reassurance that no young person will be ‘outed’ without their consent.
-
Seek regular feedback from LGBTQ+ young people on the service’s safety.
-
-
Ensure that young people feel recognised, respected and affirmed, for example:
-
Service providers should have a demonstrable track record of working with and understanding LGBTQ+ young people’s identities and experiences.
-
Ensure facilities are accessible and inclusive, for example providing gender-neutral toilets.
-
-
Ensure that the service fits within LGBTQ+ young people’s lives, for example:
-
Provide rapid response to initial contact from LGBTQ+ young people, as well as ‘while you wait’ support.
-
Seek feedback from LGBTQ+ young people on the frequency, pace, timing and duration of support.
-
Provide drop-in as well as sign-up support sessions.
-
Key problem 3: LGBTQ+ young people have poor experiences of mental health services
What’s the problem?
For those LGBTQ+ young people who do access support services, research suggests an overall poor experience due to limited staff understanding of LGBTQ+ issues and minority stressors among service staff; fear of being ‘outed’ to parents/carers, other service providers, or other young people; and being excluded from decisions about their care. 38,40,241
A 2020 EU study found that barriers to health care for LGBTQ+ people are exacerbated by two related assumptions held by healthcare professionals. First, the assumption that patients are heterosexual and cisgender and, second, the assumption that LGBTQ+ people do not experience significant problems related to their LGBTQ+ identity, meaning that LGBTQ+ identity is viewed as incidental or irrelevant to the delivery of appropriate health care. 19
While it is unhelpful (and can be harmful) for the importance of the LGBTQ+ experience to be dismissed, it is also damaging for support practitioners to overemphasise LGBTQ+ identities in excessive or pathologising ways. When staff have limited understanding and awareness about LGBTQ+ identities this can manifest as the attribution of mental distress and poor mental health exclusively to a young person’s being LGBTQ+, particularly when the young person is trans or gender diverse. 13,49
What works to improve LGBTQ+ young people’s experiences of mental health services?
To improve LGBTQ+ young people’s experiences of mental health services, the model of what works to support LGBTQ+ young people’s mental health at an early point indicates the principles of Space, People, Agency and Emotion were key. LGBTQ+ young people usually navigate Space that is defined by adults and in which being cisgender or heterosexual is assumed. Having access to affirming spaces that centre LGBTQ+ young people is invaluable in supporting mental health and building LGBTQ+ young people’s confidence to explore the world around them beyond the service. Our findings suggest services should create LGBTQ+ only spaces that centre the experiences and needs of LGBTQ+ young people and seek LGBTQ+ young people’s input on the design, decoration, and layout of support spaces.
Trusting relationships with service staff, peers and other important People are crucial in supporting LGBTQ+ young people. Our findings demonstrate that services should pay attention to LGBTQ+ young people’s ability to form trusting connections both with other young people and with the adults providing them with support; recruit staff whose experiences LGBTQ+ young people can relate to (e.g. LGBTQ+ staff); facilitate LGBTQ+ groups to support friendship and peer connection.
The principle of Agency can be upheld when LGBTQ+ young people are actively involved in decisions about their own support. The idea that ‘adults know best’ means LGBTQ+ young people’s distress and experience may be minimised. To best support LGBTQ+ young people, our findings suggest services can facilitate and encourage independent decision-making; position young people as experts of their own experience; provide respectful options-based approaches to support LGBTQ+ young people where there may be gaps in their experience due to age. In addition, we found that mental health support approaches that centre Emotion and move away from the usual position of deficit in which something is ‘wrong’ with an LGBTQ+ young person, to focus instead on developing skills and trust in communicating about feelings. Our findings indicate that services should validate LGBTQ+ young people’s distress as a logical response to marginalisation and stigma and support the development of emotional resilience.
Youth work is unique in centring engagement with young people’s cultures and communities, and using asset-based philosophies to develop young people’s strengths and well-being. 242 Youth work frameworks are more likely to have anti-oppressive practice, non-pathologising and rights-oriented principles as foundations. These fundamental principles can counteract the kinds of exclusion and discrimination that may accompany experiences of mental distress,242 alongside the marginalisation that LGBTQ+ young people often face in relation to their sexuality and/or gender identity.
Recommendations for improving LGBTQ+ young people’s experiences of mental health services
Mental health services and policies need to:
-
Acknowledge that LGBTQ+ young people have better experiences of mental health services when they feel ownership of the support space and can build trust with the people providing support.
-
Ensure mental health provision supports LGBTQ+ young people’s informed independent decision-making.
-
Create spaces that centre LGBTQ+ young people, for example:
-
Services should have a demonstrable track record in offering LGBTQ+ focused spaces, or should be able to demonstrate robust signposting or referral pathways to LGBTQ+ specific spaces.
-
Detailed space planning and costs should demonstrate clear LGBTQ+ inclusion, for example through the provision of all-gender toilets.
-
-
Foster trusting relationships for example:
-
Advocacy support can help LGBTQ+ young people to navigate important relationships in their lives, for example at school or work, with family or caregivers, or with peers.
-
Ensure diverse LGBTQ+ identities and experiences among mental health service staff.
-
-
Develop agency and informed independent decision-making, for example:
-
Options-based support that upholds young people’s rights to be heard and to autonomy
-
Policy and service specification that prioritises LGBTQ+ young people and ensure that they will be included in decisions about their care.
-
-
Centre asset-based emotional support, for example:
-
Ensure that services have demonstrable expertise and understanding of LGBTQ+ young people’s emotions when seeking support, such as fears around being ‘outed’ to parents, carers, peers, or other services without their consent.
-
Include emotions and feelings words in service materials for example sadness, panic, fear, anger, hopelessness.
-
-
Incorporate youth work expertise and approaches in the development of mental health support services for LGBTQ+ young people, for example:
-
Include youth provision in mainstream NHS approaches to the commissioning of early intervention mental health services for this population.
-
-
Demonstrate long-term planning and development around how to ensure service/policy is reflective of diverse LGBTQ+ young people’s needs.
Implications for legislation, policy and practice
Centring human rights
The UN and the WHO identify the fundamental relationship between human rights and mental health. UNICEF (UK) argues that ‘it is key that local government, services and professionals frame good mental health as a basic human right, one all children and young people are entitled to’. 2 The UNCRC outlines the rights of children and young people to good mental health and mental health services (Article 24), alongside rights to non-discrimination (Article 2), and identity (Article 8). While the integration of youth rights into law, policy and practice worldwide has been slow and inconsistent,243 international human rights commitments for children and young people are emphasised in public facing and online presence of the children and young people’s commissioners for Scotland, Wales, and NI.
At the time of this report being written, LGBTQ+ young people are facing active legislative and policy attacks on their human rights; the UK was identified alongside Hungary and Poland in a 2021 Council of Europe report condemning attacks on LGBTQ+ human rights, particularly for trans people. 244 Legislative attacks have placed young people’s access to gender-affirming health care at risk,245,246 and trans and gender-diverse young people have been excluded from the development of legislation banning conversion practices. In addition to ongoing attacks on LGBTQ+ young people’s rights, the long-term legislative and policy implications of major political developments, such as Brexit on LGBTQ+ rights, remain uncertain. Within this uncertain landscape, it is more important than ever to centre and uphold children and young people’s human rights in service commissioning and delivery.
Under Section 149 of the Equality Act 2010, public sector services have duties to eliminate discrimination and advance equality of opportunity between groups who share a protected characteristic (including gender reassignment and sexual orientation) and those who do not share this characteristic. The Health and Care Act 2022 further emphasises Integrated Care Board responsibilities to address health inequalities across access to and outcomes from health services. 26
Between nations
While legislation such as the Equality Act 2020 applies to all four UK nations, there are also significant legislative and policy differences across NI, Scotland, Wales and England. The Scottish government is, at the time of writing, publicly affirming and taking steps towards a self-declaration legal model of gender recognition. Scotland has become the first country in the world to commit to embedding LGBTQ+ inclusive education across all schools. Access to gender-affirming health care is particularly difficult in NI, where young people must be referred to CAMHS before further referral can be made to the Knowing Our Identity service. Service backlogs and waiting lists are a major issue for young people trying to access gender-affirming health care across the UK, but due to this referral process, these difficulties are particularly acute in NI.
NHS England GIDS interim service specifications
Rapid and substantive changes to the landscape of care and rights for trans and gender-diverse young people in the UK make the creation of mental health services and policies challenging. At the time of writing, public consultation is ongoing regarding interim service specifications for two new GIDS regional centres. These specifications undermine the findings from this study with regard to LGBTQ+ young people’s mental health, particularly in the areas of framing transness and gender variance as a ‘phase’; discouraging social transition and implying that it is harmful to affirm young people as they develop understanding of their own gender; and implementing pre-referral gatekeeping processes that exclude young people from decisions about their care. It is likely that these specifications will make delivery of effective mental health support for trans and gender-diverse young people more difficult and underpins the urgent need for policy-makers, commissioners, and services to centre and uphold the human rights of trans and gender-diverse young people.
Methodological issues/limitations
Stage 1: limitations
The strength of the review was that it utilised a theory-led MNR methodology to detail the underlying theory of effective mental health care. This was the first, to our knowledge, theoretical framework to be produced for supporting LGBTQ+ youth mental health and was a significant advancement in developing effective services and interventions because eventually, after testing empirically, it was being used to provide the principles for appropriate LGBTQ+ youth mental health support. However, the review is of course limited by language and there may be important evidence written in countries that we were unable to include. In addition, we realise that the adaptation of the PICOS formula for selecting studies for MNR methodology is unwise. This is because the PICOS framework, although widely used within SR methodology, cannot be easily applied in interpretive and iterative approaches.
Stage 2: limitations
During the mapping exercise, there were instances where charity-provided services had to dramatically reduce their service provision or even close all together due to loss of funding especially during the COVID-19 pandemic. This meant we were not able to fully recruit sites across the four nations. We were unable to recruit any CSS in Wales and one site in Scotland was unable to participate in the study because they were over-burdened with providing support and services to LGBTQ+ young people. We did however have input in terms of Scotland through another CSS and through the Project Advisory Group.
Stage 3: limitations and the COVID-19 pandemic
Conducting a research study during the COVID-19 pandemic has been extremely demanding particularly given the focus was LGBTQ+ young people’s mental health. We had to revise the methodology which meant reconfiguring data collection tools and data security and consulting LGBTQ+ young people. We adjusted the research ethics protocol and experienced time delays while amendments had to be approved. These adjustments were instituted from 16 March 2020 and all data were collected exclusively online. This was only a partial deviation from the study protocol because online data collection was an integral component of the original stage 3 case study design. The Sponsor approved all three non-substantial changes to the ethics protocol. A summary of the revisions to the original protocol is given below:
-
Microsoft Teams/Zoom online interviews with staff only
-
WhatsApp text online interviews with LGBTQ+ young people only
-
Microsoft Teams/Zoom online carers and parent interviews only
-
The Research Team, Project Advisory Group and LGBTQ+ Youth Advisory group worked remotely and effectively.
Data collection during the pandemic and periods of lockdown and restrictions all impacted on fieldwork. This included:
-
Losing key CSS in Wales and Scotland and recruiting two new sites (in England).
-
Long delays with CSS due to service staffing problems, transferring services online, illness, etc.
-
Online communication fatigue from participants (staff and young people) and research staff slowed the recruitment process.
-
Data collection took much longer than usual.
-
We were unable to conduct the planned focus groups due to participant burden.
-
In order to ensure the adapted online methodology was ethically robust, we had to limit data collected to answer research question 4.
-
All the research staff have been affected by COVID-19, for example having COVID-19, child-care responsibilities, family caring commitments, death of close family/friends, accommodation difficulties, mental health problems, all of which have caused delays.
To compensate for some of these methodological issues, we conducted a number of verification activities. The aim of these activities was to substantiate the final data analysis in order to answer all the research questions and fulfil the remit of study in terms of Scotland and Wales. These activities focused on additional consultation with LGBTQ+ young people and interviews with key informants in Wales and Scotland.
WhatsApp was selected to use for interviews with LGBTQ+ young people based on feedback from LGBTQ+ young people and service staff. We acknowledge that digital technologies and the requirement to use a digital device to participate (e.g. smartphones or laptops) is exclusionary for some young people, for example due to digital poverty. To assist in this way, we offered vouchers to cover costs for data albeit this offer was not taken up by any LGBTQ+ young person. For some, we were aware that disabilities or living circumstances, for example being in care home settings, would limit participation remotely but in the context of COVID-19 national lockdowns we were unable to offer a face-to-face alternative. Overwhelmingly those who took part communicated directly that they appreciated the format as it offered them a chance to think about their responses and retain their privacy. We know that many LGBTQ+ young people prefer engaging online, so this method was facilitative to those who prefer this compared to face-to-face engagement.
Because we were unable to meet in person during the fieldwork, we were also unable to deliver our intended focus group activities with LGBTQ+ young people that were structured around a board game co-designed by LGBTQ+ young people.
The service cost analysis has some weaknesses. As is common practice, we relied on self-reported data on health service use. 247,248 This may have been subject to recall bias. In addition, the small sample size meant we were unable to draw any generalised conclusions from the study. The purpose of the service cost data was to inform the NHS commissioning guidance that was produced at the end of the study by key stakeholders in the NHS, local authorities NHS England etc. The guidance was cognisant of ‘best practice approaches’ to designing NHS commissioning guidance and the requirements of mental health services across a range of locations. It was decided that the service use costs did not fit into the priorities of the guidance which needs to be extremely succinct and practice orientated. Funding and costs are included within the guidance but as possible ways of funding a service. Please see: https://queerfutures2.co.uk/wp-content/uploads/2022/12/Queer-Futures-2-What-Works-NHS-Commissioning-Guidance.pdf.
Recommendations for future research
Further research on the implementation of an intersectional, youth-rights approach to early intervention mental health support for LGBTQ+ young people with mental health problems is required.
The study findings indicate that there is a gap in mental health provision for LGBTQ+ young people of colour. Few of the CSS had incorporated working practices that provided for this group of young people. Further research is required on why LGBTQ+ young people of colour have elevated rates of poor mental health, and how best to improve mental health in this population group.
Equality, diversity and inclusion
Equality, diversity and inclusion is at the centre of the study’s aims because it is focused on a group of young people who are marginalised and discriminated against on the basis of their gender diversity and/or sexual orientation. The study had an intersectional approach as a central theoretical tenet that prioritises the experiences of those LGBTQ+ young people who may be further excluded by virtue of their ethnicity, disability, gender, neurodiversity and socioeconomic status. We outline below key examples of how equality, diversity and inclusion has been pivotal to the study design.
Participant representation
The diversity of the participants recruited from the CSS was monitored to ensure the sample was diverse in terms of sexual orientation, gender identity, disability, ethnicity and socioeconomic status. To boost representation within the sample, we specifically targeted recruitment in terms of both ethnicity and gender. The ethnicity of the sample was increased through working with key CSS that either employed staff of colour or had a specific services provision for LGBTQ+ young people of colour. This strategy was successful in ensuring a third of the sample where from a range of ethnic backgrounds in comparison to two thirds who were White English/Irish/Scottish/British.
All the recruitment materials and outputs reflected the diversity of the LGBTQ+ young people. See for example the model of What works? housed on an interactive website https://queerfutures2.co.uk/what-works/.
The study findings indicated that there is a gap in mental health provision for LGBTQ+ young people of colour. Few of the CSS had incorporated working practices that provided for this group of young people. Further research is required on why LGBTQ+ young people of colour have elevated rates of poor mental health, and how best to improve mental health in this population group.
Reflections on research team and wider involvement
The research team included those from the LGBTQ+ population. To ensure diversity a researcher who was a LGBTQ+ person of colour and a researcher who was trans were recruited to the study. This ensured an inclusive approach to the research design.
The public were involved throughout the study but at key moments, we sought extra input from those working in the field especially LGBTQ+ staff of colour and gender diverse staff.
Patient and public involvement
The aim of our PPI strategy was to involve LGBTQ+ young people, the public, service providers and commissioners from the outset to help us to ask the right questions, in the right way and gain an in-depth rigorous understanding of the mental health support needs of LGBTQ+ young people. In our research PPI contributors were involved in three specific ways:
-
Charlie Tebrook is a member of our research team. Charlie is an LGBTQ+ young person with direct experience and knowledge of mental health services and the issues faced by LGBTQ+ young people.
-
LGBTQ+ young people, aged 12–25 years, from Allsorts, Brighton, The Proud Trust, Manchester, ARC Darlington, SAYiT and YPAS (Liverpool), contributed through face-to-face/online meetings with researchers and an online forum.
-
A project advisory group of a range of stakeholders with experience in service delivery that involves experts in CAMHS, mental health commissioning and charity sector LGBTQ+ support services. Meetings biannually.
Key activities our PPI contributors were involved with included:
-
Design of the website and research materials
-
Terminology, for example ‘LGBTQ+’ acronym
-
Inclusion criteria such as age range
-
Managing risk and taking care of participants
-
Identifying ways of describing the project in accessible formats to facilitate informed consent for participants
-
Development of fieldwork materials and reorientation of fieldwork approach due to COVID-19 disruptions. Materials included consent forms, demographic forms including options/language, project information (written and audio-described video material), interview resources (including picture prompts)
-
Design of a board game to collect data about how LGBTQ+ young people navigated mental health services
-
Trialling of WhatsApp chat methodology with Charlie Tebrook and online consultation with LGBTQ+ young people (age 15–18 years) to finalise data collection resources
-
Validation of research analysis and interpretations with LGBTQ+ young people through three group visits (SAYiT × 2, Gyro at YPAS) and consultation on outputs that would be useful to young people
-
Specific steering group devised for consultation on production of NHS commissioning guidelines
-
Young person researcher input into the design and presentation of resources aimed at young people
-
Social media and engagement activity throughout project life to enable digital interaction through the website and Twitter.
The impact of having a PPI strategy integrated throughout the study design meant that PPI activities were central to the research design and delivery. It shaped resources, methodological approach, validated findings and guided the way we have presented and disseminated outputs.
Lesbian, gay, bisexual, trans, queer/questioning, plus young people were pivotal in our research method approach when COVID-19 shifted all fieldwork online. Moving to data collection via WhatsApp was a completely new endeavour for the research team but young people helped design the approach and ensure that the research project stayed viable and relevant to young people’s mode of engagement.
Lesbian, gay, bisexual, trans, queer/questioning, plus young people reacted positively to the research findings with their input supporting our decisions about organising the study findings around key principles. These activities have also clarified priorities about the kinds of outputs young people want and would find useful, with a particularly strong emphasis on ‘know your rights’ resources for young people to help them navigating mental health care. This suite of videos made with our CSS explains their rights in relation to mental health support. This online resource was aimed at young people and was freely available via the study website.
We would advocate that all mental health research has an integrated PPI strategy and prioritises the importance of those with lived experience. Working with a number of LGBTQ+ community organisations has ensured young people’s engagement throughout the research. We have used a range of methods including face-to-face and online. The online platform was less successful, and it was difficult to maintain interest over a long project with intermittent opportunities to contribute and without a pre-established sense of community.
Conclusions
In the UK, a rights-based approach to mental health service provision is not prominent or mainstream. There is very little evidence that young people’s rights are of concern in the realm of mental health services. Research suggests that current practice in CAMHS in the UK highlights some disparities in services, which result in questions about human rights for young people. 40,195,249,250 For example, a children’s human rights-based approach was taken to examine the impact of the legislative and policy measures that were implemented in Scotland in response to the pandemic on children’s rights related to their mental health. The authors identified the problems of children’s rights to access mental health services, information, involvement in decision-making and discrimination of marginalised groups indicating that current practice approaches fall short of a rights-based framework. 250
In addition, at the time of this report being written, LGBTQ+ young people are facing active legislative and policy attacks on their human rights; the UK was identified alongside Hungary and Poland in a 2021 Council of Europe report condemning attacks on LGBTQ+ human rights, particularly for trans people. 244 Legislative attacks have placed young people’s access to gender-affirming health care at risk,245,246 and trans and gender-diverse young people have been excluded from the development of legislation banning conversion practices. Within this uncertain landscape, it is more important than ever to centre and uphold children and young people’s human rights in mental health services and support.
Our intersectional, youth-rights approach to early intervention mental health support for LGBTQ+ young people demonstrates that youth rights should underpin the delivery of mental health support for LGBTQ+ young people to address the multiple marginalisation, isolation and stigmatisation that LGBTQ+ young people may experience and to enable them to make informed independent decisions about their own bodies and lives, and for the right to freedom of safe self-expression to be upheld.
Impact
Throughout the study, we have worked with key stakeholders from the NHS, Public Health England, Local Authorities and third-sector organisations to ensure our research outputs are useful and will be adopted within the NHS and across wider services. There has been tremendous interest in the study especially the ‘What works?’ digital model of mental health early intervention support for LGBTQ+ young people, the NHS Mental Health Commissioning Guidance, mental health service checklist and slide pack, and the ‘Know your rights in mental health care?’ videos. These are all available freely on the website https://queerfutures2.co.uk/what-works/. The availability of resources, including recordings of the QF2 final webinar and slide-packs that can be accessed free of charge from the project website, has ensured a wide distribution and use. The website will be functioning until 2030.
Instead of a single knowledge mobilisation face-to-face conference, we organised a digital webinar series targeted at key stakeholders. We liaised with the Office for Health Improvement and Disparities, NHS England, NHS Mental Health Team, NHS Confederation, and mental health practitioners and commissioners to design and deliver these in September–November 2022. In total there were between 200 and 400 people participated in each of the six webinars.
During the project, there have been a number of ways in which the knowledge from the study has been utilised across the Office for Health Improvement and Disparities (OHID), the UK Government, NHS, Local authority, academy and Third sector. For example, through:
-
NHS LGBT Research and Evidence Roundtable
-
The Ireland, UK and Islands LGBT+ Youth Workers Conference 2020
-
Royal Society of Medicine LGBTQI+ Healthcare Digital webinar
-
The UK Government’s Children and Young People’s Mental Health Conference 2021
-
UK Government Suicide Prevention Strategy Meeting
-
IAYMH conference, Copenhagen.
Social media has been helpful to the project as a means of collecting an audience and securing engagement during the project, especially during the pandemic. The project has a Twitter handle and has gained over 500 followers over the last 4 years. We tweet regularly about our own activities and have found live tweeting during events we attend such as webinars and conferences helps to increase our followers and our online engagement, with our tweets being shared and retweeted, in some cases with over 2500 engagements per post (the number of times the tweet was seen by users on Twitter).
During the study, we used Twitter to recruit research staff and to promote events that project staff were attending or speaking at. We have also built a mailing list of over 100 names using posts encouraging sign-up on our website and Twitter and have successfully promoted our own webinar for research findings on the platform.
Additional information
Contributions of authors
Elizabeth McDermott (https://orcid.org/0000-0002-1960-9639) Professor of Mental Health and Society. Was the Principal Investigator and had overall responsibility for the project. She led on the design of the study and contributed to data collection, data analysis and interpretation, drafting of the final report and revision of the final report.
Rachael Eastham (https://orcid.org/0000-0001-6881-7875) Senior Research Associate, Health Research. Was involved in the design of the study, conducting the stage 1 review, conducting the stage 2 mapping study and conducting the stage 3 case study evaluation. She led on the analysis and interpretation of stage 3 case study evaluation data. She contributed to the writing and editing of the final report.
Elizabeth Hughes (https://orcid.org/0000-0002-4480-0806) Professor of Nursing. Was involved in designing the research project, contributing intellectual input throughout all three stages. She also contributed to editing of the final report.
Emily Pattison (https://orcid.org/0000-0003-0742-1943) Research Fellow. Was involved in conducting the stage 1 review, conducting the stage 2 mapping study, conducting stage 3 case study evaluation data collection and contributed to the editing of the final report.
Katherine Johnson (https://orcid.org/0000-0001-7092-4426) Professor of Psychology and Sexualities. Was involved in designing the research project, contributing intellectual input throughout all three stages. She contributed to the writing and editing of the final report.
Stephanie Davis (https://orcid.org/0000-0002-9296-8793) Research Officer. Was involved in conducting the stage 2 mapping study and conducting stage 3 case study evaluation data collection. She contributed to the editing of the final report.
Steven Pryjmachuk (https://orcid.org/0000-0002-6976-1727) Professor of Mental Health Nursing Education. Was involved collaboratively in the research project, contributing intellectual input throughout all three stages. He contributed to the editing of the final report.
Ceu Mateus (https://orcid.org/0000-0001-6219-219X) Professor of Health Economics. Led on analysis of cost survey data for the stage 3 case study evaluation. She contributed to the writing and editing of the final report.
Olu Jenzen (https://orcid.org/0000-0002-0792-6135) Director of the Centre for Transforming Sexuality and Gender. Was involved collaboratively in the research project, contributing intellectual input throughout all three stages. She contributed to the editing of the final report.
Felix McNulty (https://orcid.org/0000-0002-1179-5254) Research Associate. Was involved in writing up findings and outputs for the stage 3 case study evaluation and contributed to the writing and editing of the final report.
Acknowledgements
This study relied on the goodwill and efforts of many young people and organisations that have been working in the field of LGBTQ+ young people’s mental health. The project would not have been able to deliver the important outputs had these people and organisations not retained a sustained commitment to the aims of the research, in extremely difficult circumstances, throughout the COVID-19 pandemic. We are grateful for their willingness to be involved and their patience and understanding for the duration of the project.
We hope the outputs from the study will now be utilised by those who assisted us, and those working, wherever the location, to support and promote LGBTQ+ young people’s mental health and well-being.
Data-sharing statement
Due to the sensitivity of the data collected and ethical assurances to participants of confidentiality and anonymity, there are no data that can be shared. Any queries should be addressed to the corresponding author.
Ethics statement
This study received ethical approval from NHS North West – Greater Manchester Central Research Ethics Committee on 28 January 2020. REC reference: 19/NW/0642 Protocol number: HS&DR 17/09/04 IRAS project ID: 261446.
Information governance statement
The University of Birmingham is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation University of Birmingham is the Data Processor; and NIHR is the Data Controller, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here www.birmingham.ac.uk/university/leadership/governance/policies-regs/data-protection.aspx
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/KYWA6382.
Primary conflicts of interest: None.
Publications
McDermott E, Eastham R, Hughes E, Pattinson E, Johnson K, Davis S, et al. Explaining effective mental health support for LGBTQ+ youth: a meta-narrative review. SSM-Ment Health 2021;1:100004. https://doi.org/10.1016/j.ssmmh.2021.100004
Pattinson EM, McDermott E, Eastham R, Hughes E, Johnson K, Davis S, et al. Tackling LGBTQ+ youth mental health inequality: mapping mental health support across the UK. Br Stud Dr J 2021;5:20–9. https://doi.org/10.18573/bsdj.289
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- UNICEF . The State of the World’s Children 2021: On My Mind (Promoting, Protecting and Caring for Children’s Mental Health) 2021.
- UNICEF . Children’s Rights in the New Normal: Mental Health 2021.
- UNCRC . General Comment No. 20 (2016) on the Implementation of the Rights of the Child During Adolescence 2016.
- WHO . Comprehensive Mental Health Action Plan 2013–2030 2021.
- Amos R, Manalastas EJ, White R, Bos H, Patalay P. Mental health, social adversity, and health-related outcomes in sexual minority adolescents: a contemporary national cohort study. Lancet Child Adolesc Health 2020;4:36-45. https://doi.org/10.1016/S2352-4642(19)30339-6.
- Irish M, Solmi F, Mars B, King M, Lewis G, Pearson RM, et al. Depression and self-harm from adolescence to young adulthood in sexual minorities compared with heterosexuals in the UK: a population-based cohort study. Lancet Child Adolesc Health 2019;3:91-8. https://doi.org/10.1016/S2352-4642(18)30343-2.
- Toomey RB, Ryan C, Diaz RM, Russell ST. Coping with sexual orientation-related minority stress. J Homosex 2018;65:484-500. https://doi.org/10.1080/00918369.2017.1321888.
- Semlyen J, King M, Varney J, Hagger-Johnson G. Sexual orientation and symptoms of common mental disorder or low wellbeing: combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0767-z.
- King M, McKeown E, Warner J, Ramsay A, Johnson K, Cort C, et al. Mental health and quality of life of gay men and lesbians in England and Wales: controlled, cross-sectional study. Br J Psychiatry 2003;183:552-8. https://doi.org/10.1192/bjp.183.6.552.
- Rimes KA, Goodship N, Ussher G, Baker D, West E. Non-binary and binary transgender youth: comparison of mental health, self-harm, suicidality, substance use and victimization experiences. Int J Transgenderism 2019;20:230-40. https://doi.org/10.1080/15532739.2017.1370627.
- di Giancomo E, Krausz M, Colmegna F, Aspesi F, Clerici M. Estimating the risk of attempted suicide among sexual minority youth: a systematic review and meta-analysis. JAMA Pediatrics 2018;172:1145-52. https://doi.org/10.1001/jamapediatrics.2018.2731.
- Meyer IH. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol Sex Orientat Gend Divers 2015;2:209-13. https://doi.org/10.1037/sgd0000132.
- McDermott E, Roen K. Queer Youth, Suicide and Self-harm: Troubled Subjects, Troubling Norms. Houndsmills, Basingstoke, Hampshire; New York: Palgrave Macmillan; 2016.
- Riggs DW, Treharne GJ. Decompensation: a novel approach to accounting for stress arising from the effects of ideology and social norms. J Homosex 2017;64:592-605. https://doi.org/10.1080/00918369.2016.1194116.
- Smout SA, Benotsch EG. Experiences of discrimination, mental health, and substance use among bisexual young adults. J Bisex 2022;22:539-56. https://doi.org/10.1080/15299716.2022.2116514.
- Craney SR, Watson LB, Brownfield J, Flores MJ. Bisexual women’s discriminatory experiences and psychological distress: exploring the roles of coping and LGBTQ community connectedness. Psychol Sex Orientat Gend Divers 2018;5:324-37. https://doi.org/10.1037/sgd0000276.
- Parmenter JG, Galliher RV, Maughan ADA. LGBTQ+ emerging adults perceptions of discrimination and exclusion within the LGBTQ+ community. Psychol Sex 2021;12:289-304. https://doi.org/10.1080/19419899.2020.1716056.
- Jacobsen K, Devor A, Hodge E. Who counts as trans? A critical discourse analysis of trans tumblr posts. J Commun Inq 2021;46:60-81. https://doi.org/10.1177/01968599211040835.
- McGlynn N, Browne K, Sherriff N, Zeeman L, Mirandola M, Gios L, et al. Healthcare professionals’ assumptions as barriers to LGBTI healthcare. Cult Health Sex 2020;22:954-70. https://doi.org/10.1080/13691058.2019.1643499.
- Wilson C, Cariola LA. LGBTQI+ youth and mental health: a systematic review of qualitative research. Adolesc Res Rev 2020;5:187-211. https://doi.org/10.1007/s40894-019-00118-w.
- Hall WJ. Psychosocial risk and protective factors for depression among lesbian, gay, bisexual, and queer youth: a systematic review. J Homosex 2018;65:263-316. https://doi.org/10.1080/00918369.2017.1317467.
- Fulginiti A, Rhoades H, Mamey MR, Klemmer C, Srivastava A, Weskamp G, et al. Sexual minority stress, mental health symptoms, and suicidality among LGBTQ youth accessing crisis services. J Youth Adolesc 2021;50:893-905. https://doi.org/10.1007/s10964-020-01354-3.
- Rhoades H, Rusow JA, Bond D, Lanteigne A, Fulginiti A, Goldbach JT. Homelessness, mental health and suicidality among LGBTQ youth accessing crisis services. Child Psychiatry Hum Dev 2018;49:643-51. https://doi.org/10.1007/s10578-018-0780-1.
- Robinson BA. ‘They peed on my shoes’: Foregrounding intersectional minority stress in understanding LGBTQ youth homelessness. J LGBT Youth 2021;20:783-99. https://doi.org/10.1080/19361653.2021.1925196.
- Gattamorta KA, Salerno JP, Laporte RR. Family rejection during COVID-19: effects on sexual and gender minority stress and mental health among LGBTQ university students. LGBTQ+ Fam: Interdiscip J 2022;18:305-18. https://doi.org/10.1080/27703371.2022.2083041.
- Salerno JP, Gattamorta KA, Williams ND. Impact of family rejection and racism on sexual and gender minority stress among LGBTQ young people of color during COVID-19. Psychol Trauma: Theory Res Pract Policy 2022;15:637-47. https://doi.org/10.1037/tra0001254.
- Williams AJ, Jones C, Arcelus J, Townsend E, Lazaridou A, Michail M. A systematic review and meta-analysis of victimisation and mental health prevalence among LGBTQ+ young people with experiences of self-harm and suicide. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0245268.
- Bradlow J, Bartram F, Guasp A, Jadva V. School Report: The Experiences of Lesbian, Gay, Bi and Trans Young People in Britain’s Schools in 2017. London: Stonewall; 2017.
- Tankersley AP, Grafsky EL, Dike J, Jones RT. Risk and resilience factors for mental health among transgender and gender nonconforming (TGNC) youth: a systematic review. Clin Child Fam Psychol Rev 2021;24:183-206. https://doi.org/10.1007/s10567-021-00344-6.
- Hatchel T, Polanin JR, Espelage DL. Suicidal thoughts and behaviors among LGBTQ youth: meta-analyses and a systematic review. Arch Suicide Res 2021;25:1-37. https://doi.org/10.1080/13811118.2019.1663329.
- Ancheta AJ, Bruzzese J-M, Hughes TL. The impact of positive school climate on suicidality and mental health among LGBTQ adolescents: a systematic review. J Sch Nurs 2021;37:75-86. https://doi.org/10.1177/1059840520970847.
- Parmar DD, Tabler J, Okumura MJ, Nagata JM. Investigating protective factors associated with mental health outcomes in sexual minority youth. J Adolesc Health 2022;70:470-7. https://doi.org/10.1016/j.jadohealth.2021.10.004.
- Ceatha N, Koay ACC, Buggy C, James O, Tully L, Bustillo M, et al. Protective factors for LGBTI+ youth wellbeing: a scoping review underpinned by recognition theory. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph182111682.
- Postuvan V, Podlogar T, Sedivy NZ, De Leo D. Suicidal behaviour among sexual-minority youth: a review of the role of acceptance and support. Lancet Child Adolesc Health 2019;3:190-8. https://doi.org/10.1016/s2352-4642(18)30400-0.
- Burningham KL, Weiler LM. Natural mentoring and LGBTQ youth: a systematic review. Adolesc Res Rev 2021;6:391-407. https://doi.org/10.1007/s40894-020-00146-x.
- Kneale D, Bécares L. Discrimination as a predictor of poor mental health among LGBTQ+ people during the COVID-19 pandemic: cross-sectional analysis of the online Queerantine study. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-049405.
- Milsom R. Growing Up LGBT+: The Impact of School, Home and Coronavirus on LGBT+ Young People. London: Just Like Us; 2021.
- Williams KA, Chapman MV. Comparing health and mental health needs, service use, and barriers to services among sexual minority youths and their peers. Health Soc Work 2011;36:197-206. https://doi.org/10.1093/hsw/36.3.197.
- Williams KA, Chapman MV. Unmet health and mental health need among adolescents: the roles of sexual minority status and child–parent connectedness. Am J Orthopsychiatry 2012;82:473-81. https://doi.org/10.1111/j.1939-0025.2012.01182.x.
- McDermott E, Hughes E, Rawlings V. Norms and normalisation: understanding lesbian, gay, bisexual, transgender and queer youth suicidality and help-seeking. Cult Health Sex 2018;20:156-72. https://doi.org/10.1080/13691058.2017.1335435.
- McDermott E. Asking for help online: lesbian, gay, bisexual and trans youth, self-harm and articulating the ‘failed’ self. Health 2015;19:561-77. https://doi.org/10.1177/1363459314557967.
- McDermott E, Hughes E, Rawlings VE. Queer Futures Final Report: Understanding Lesbian, Gay, Bisexual and Trans (LGBT) Adolescents’ Suicide, Self-harm and Help-seeking Behaviour. UK: Lancaster University; 2016.
- Fay V. Getting It Right: What LGBT+ Young People Want and Need in Greater Manchester. Manchester: The Proud Trust; 2017.
- LaSala MC, Fedor JP. ‘A victim is a victim’: LGBT blindness among victim assistance workers. J Qualitative Crim Just Criminology 2020;9. https://doi.org/10.21428/88de04a1.76224421.
- Lucassen M, Samra R, Iacovides I, Fleming T, Shepherd M, Stasiak K, et al. How LGBT+ young people use the internet in relation to their mental health and envisage the use of e-therapy: exploratory study. JMIR Serious Games 2018;6. https://doi.org/10.2196/11249.
- Johnson K, Faulkner P, Jones H, Welsh E. Understanding Suicidal Distress and Promoting Survival in Lesbian, Gay, Bisexual and Transgender (LGBT) Communities. Brighton: University of Brighton; 2007.
- Acevedo-Polakovich I, Bell B, Gamache P, Christian AS. Service accessibility for lesbian, gay, bisexual, transgender, and questioning youth. Youth Soc 2013;45:75-97. https://doi.org/10.1177/0044118X11409067.
- Williams KA, Chapman MV. Mental health service use among youth with mental health need: do school-based services make a difference for sexual minority youth?. Sch Ment Health 2015;7:120-31. https://doi.org/10.1007/s12310-014-9132-x.
- Ellis SJ, Bailey L, McNeil J. Trans people’s experiences of mental health and gender identity services: a UK study. J Gay Lesbian Ment Health 2015;19:4-20. https://doi.org/10.1080/19359705.2014.960990.
- Turney C, Gardner P. Research Report: LGBTQ+ Youth & Mental Health in Cambridgeshire & Peterborough. Ely: The Kite Trust; 2022.
- Higgins A, Downes C, Murphy R, Sharek D, Begley T, McCann E, et al. LGBT+ young people’s perceptions of barriers to accessing mental health services in Ireland. J Nurs Manag 2021;29:58-67. https://doi.org/10.1111/jonm.13186.
- Newman CE, Prankumar SK, Cover R, Rasmussen ML, Marshall D, Aggleton P. Inclusive healthcare for LGBTQ+ youth: support, belonging, and inclusivity labour. Crit Public Health 2020;31:441-50. https://doi.org/10.1080/09581596.2020.1725443.
- Rossman K, Salamanca P, Macapagal K. A qualitative study examining young adults’ experiences of disclosure and nondisclosure of LGBTQ identity to health care providers. J Homosex 2017;64:1390-410. https://doi.org/10.1080/00918369.2017.1321379.
- Craig S, McInroy L, Austin A, Smith M, Engle B. Promoting self-efficacy and self-esteem for multiethnic sexual minority youth: An evidence-informed intervention. J Soc Serv Res 2012;38:688-98. https://doi.org/10.1080/01488376.2012.718194.
- EIF . Realising the Potential of Early Intervention 2018.
- HSCC (Health and Social Care Committee HoC) . Children and Young People’s Mental Health: Eighth Report of Session 2021–22 2021.
- EIF . Spending Review 2021: The Case for Early Intervention to Support Levelling Up and COVID Recovery 2021.
- Wilson H, Waddell S. COVID-19 and Early Intervention: Understanding the Impact, Preparing for Recovery. London: Early Intervention Foundation; 2020.
- Patalay P, Fitzsimmons E. Mental Ill-Health at Age 17 in the UK: Prevalence of and Inequalities in Psychological Distress, Self-harm and Attempted Suicide. London: Centre for Longitudinal Studies; 2020.
- McDermott E, Eastham R, Hughes E, Pattinson E, Johnson K, Davis S, et al. SSM Ment Health. 2021.
- Pattinson EM, McDermott E, Eastham R, Hughes E, Johnson K, Davis S, et al. Br Stud Dr J. 2021.
- Yin RK. Case Study Research Design and Methods. Thousand Oaks, CA: Sage; 2014.
- Coryn CLS, Noakes LA, Westine CD, Schröter DC. A systematic review of theory-driven evaluation practice from 1990 to 2009. Am J Eval 2011;32:199-226. https://doi.org/10.1177/1098214010389321.
- Parry GJ, Carson-Stevens A, Luff DF, McPherson M, Goldmann DA. Recommendations for evaluation of health care improvement initiatives. Acad Pediatr 2013;13:S23-30. https://doi.org/10.1016/j.acap.2013.04.007.
- Marchal B, van Belle S, van Olmen J, Hoerée T, Kegels G. Is realist evaluation keeping its promise? A review of published empirical studies in the field of health systems research. Eval 2012;18:192-21. https://doi.org/10.1177/1356389012442444.
- Raine R, Fitzpatrick R, Barratt HS, Bevan G, Black N, Boaden R, et al. Challenges, solutions and future directions in the evaluation of service innovations in health care and public health. NIHR: Health Serv Deliv Res 2016;4:1-136. https://doi.org/10.3310/hsdr04160-19.
- De Silva MJ, Breuer E, Lee L, Asher L, Chowdhary N, Lund C, et al. Theory of change: a theory-driven approach to enhance the Medical Research Council’s framework for complex interventions. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-267.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-100.
- Pawson R, Tilley N. Evaluation for the 21st Century: A Handbook. London, UK: Sage Publications; 1997.
- Johnson K. Sexuality: A Psychosocial Manifesto. Cambridge, UK: Policy Press; 2015.
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129:674-97. https://doi.org/10.1037/0033-2909.129.5.674.
- Clarke V, Ellis SJ, Peel E, Riggs DW. Lesbian, Gay, Bisexual, Trans & Queer Psychology: An Introduction. Cambridge, UK: Cambridge University Press; 2010.
- Diamond LM. What does sexual orientation orient? A biobehavioral model distinguishing romantic love and sexual desire. Psychol Rev 2003;110:173-92. https://doi.org/10.1037/0033-295x.110.1.173.
- Cass VC. Homosexual identity formation: testing a theoretical model. J Sex Res 1984;20:143-67. https://doi.org/10.1080/00224498409551214.
- McDermott E, Roen K, Scourfield J. Avoiding shame: young LGBT people, homophobia and self-destructive behaviours. Cult Health Sex 2008;10:815-29. https://doi.org/10.1080/13691050802380974.
- Cover R. Queer Youth Suicide, Culture & Identity: Unliveable Lives. London: Routledge; 2012.
- Collins PH. Intersectionality’s definitional dilemmas. Annu Rev Sociol 2015;41:1-20. https://doi.org/10.1146/annurev-soc-073014-112142.
- Archer M. Encyclopedia of Queer Studies in Education. Leiden, The Netherlands: Brill; 2021.
- Jackson R. Encyclopedia of Queer Studies in Education. Leiden, The Netherlands: Brill; 2021.
- Collins PH, Bilge S. Intersectionality. Cambridge, UK: Polity Press; 2020.
- Biddle L, Donovan J, Sharp D, Gunnell D. Explaining non-help-seeking amongst young adults with mental distress: a dynamic interpretive model of illness behaviour. Sociol Health Ill 2007;29:983-1002. https://doi.org/10.1111/j.1467-9566.2007.01030.x.
- Savin-Williams RC. A critique of research on sexual-minority youths. J Adolesc 2001;24:5-13. https://doi.org/10.1006/jado.2000.0369.
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0611-x.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Petticrew M. Time to rethink the systematic review catechism? Moving from ‘what works’ to ‘what happens’. Syst Rev 2015;4. https://doi.org/10.1186/s13643-015-0027-1.
- Gough D, Oliver S, Thomas J. An Introduction to Systematic Reviews. Los Angeles; London; New Delhi; Singapore; Washington, DC; Melbourne: SAGE Publications; 2017.
- Petticrew M, Roberts H. Systematic reviews – do they ‘work’ in informing decision-making around health inequalities?. Health Econ Policy Law 2008;3:197-211. https://doi.org/10.1017/S1744133108004453.
- Otte-Trojel T, Wong G. Going beyond systematic reviews: realist and meta-narrative reviews. Stud Health Technol Inform 2016;222:275-87. https://doi.org/10.3233/978-1-61499-635-4-275.
- EPPI . EPPI-Centre Methods for Conducting Systematic Reviews 2010.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med 2005;61:417-30. https://doi.org/10.1016/j.socscimed.2004.12.001.
- Greenhalgh T, Wong G, Westhorp G, Pawson R. Protocol – realist and meta-narrative evidence synthesis: evolving standards (RAMESES). BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-115.
- Greenhalgh T, Wong G. Training Materials for Meta-narrative Reviews. London: Queen Mary University of London; 2013.
- UNDESA . United Nations Youth: Definition of Youth 2013.
- Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Papers Educ 2007;22:213-28. https://doi.org/10.1080/02671520701296189.
- Jagosh J, Pluye P, Macauley AC, Salsberg J, Henderson J, Sirett E, et al. Assessing the outcomes of participatory research: protocol for identifying, selecting, appraising and synthesizing the literature for realist review. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-24.
- Greenhalgh T, Potts HWW, Wong G, Bark P, Swinglehurst D. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q 2009;87:729-88. https://doi.org/10.1111/j.1468-0009.2009.00578.x.
- Pryjmachuk S, Elvey R, Kirk S, Kendal S, Bower P, Catchpole R. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Health Serv Deliv Res 2014;2:1-212. https://doi.org/10.3310/hsdr02180.
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Evaluating Self-care Support for Children and Young People with Long-term Conditions. Southampton: National Institute for Health Research Service Delivery and Organisation Programme; 2010.
- Ritchie J, Spencer L. Analyzing Qualitative Data. London: Routledge; 1994.
- Yin RK. APA Handbook of Research Methods in Psychology, Vol 2 Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological. American Psychiatric Association; 2012.
- Patton MQ. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage; 1990.
- Braun V, Clarke V. Successful Qualitative Research: A Practical Guide for Beginners. Los Angeles; London; New Delhi; Singapore; Washington, DC: SAGE Publications; 2013.
- McDermott E, Roen K, Piela A. Hard-to-reach youth online: methodological advances in self-harm research. Sex Res Soc Policy 2013;10:125-34. https://doi.org/10.1007/s13178-012-0108-z.
- Hillier L, Rosenthal D. Special issue on gay, lesbian and bisexual youth. J Adolesc 2001;24:1-4. https://doi.org/10.1006/jado.2000.0368.
- Hillier L, Harrison L. Building realities less limited than their own: young people practising same-sex attraction on the internet. Sexualities 2007;10:82-100. https://doi.org/10.1177/1363460707072956.
- Gibson K. What Young People Want from Mental Health Services: A Youth Informed Approach for the Digital Age. London: Routledge; 2021.
- Gibson K. Bridging the digital divide: reflections on using WhatsApp instant messenger interviews in youth research. Qual Res Psychol 2022;19:611-31. https://doi.org/10.1080/14780887.2020.1751902.
- Liamputtong P. Focus Group Methodology: Principles and Practice. Los Angeles, CA: SAGE Publications; 2011.
- Kozinets RV. Netnography: Doing Ethnographic Research Online. Los Angeles, CA: SAGE Publications; 2010.
- Yin R. Case Study Research and Applications: Design and Methods. Thousand Oaks, CA; London, UK: SAGE Publications; 2018.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013 2013.
- Špacírová Z, Epstein D, García-Mochón L, Rovira J, Olry de Labry Lima A, Espín J. A general framework for classifying costing methods for economic evaluation of health care. Eur J Health Econ 2020;21:529-42. https://doi.org/10.1007/s10198-019-01157-9.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Riley E. Bullies, blades, and barricades: practical considerations for working with adolescents expressing concerns regarding gender and identity. Int J Transgend Health 2018;19:203-11. https://doi.org/10.1080/15532739.2017.1386150.
- D’Augelli AR, Hershberger SL, Pilkington NW. Lesbian, gay, and bisexual youth and their families: disclosure of sexual orientation and its consequences. Am J Orthopsychiatry 1998;68:361-71; discussion 372. https://doi.org/10.1037/h0080345.
- Durso LE, Gates GJ. Serving Our Youth: Findings from a National Survey of Services Providers Working with Lesbian, Gay, Bisexual and Transgender Youth Who Are Homeless or at Risk of Becoming Homeless. Los Angeles, CA: The Williams Institute, UCLA; 2012.
- Mills-Koonce WR, Rehder PD, McCurdy AL. The significance of parenting and parent–child relationships for sexual and gender minority adolescents. J Res Adolesc 2018;28:637-49. https://doi.org/10.1111/jora.12404.
- Alderson P, Morrow V. The Ethics of Research with Children and Young People: A Practical Handbook. London: SAGE Publications; 2011.
- O’Reilly M, Parker N. Doing Mental Health Research with Children and Adolescents: A Guide to Qualitative Methods. London: Sage; 2014.
- Morrow V, Richards M. The ethics of social research with children: an overview. Child Soc 1996;10:90-105. https://doi.org/10.1111/j.1099-0860.1996.tb00461.x.
- Assembly UGJUN, Treaty Series . Convention on the Rights of the Child 1989.
- Feinstein BA, Thomann M, Coventry R, Macapagal K, Mustanski B, Newcomb ME. Gay and bisexual adolescent boys’ perspectives on parent–adolescent relationships and parenting practices related to teen sex and dating. Arch Sex Behav 2018;47:1825-37. https://doi.org/10.1007/s10508-017-1057-7.
- Fortmann J, Fisher A, Hough R, Gregory A, Pugh G. Sleep quality, fatigue, and quality of life among teenage and young adult cancer survivors. J Adolesc Young Adult Oncol 2018;7:465-71. https://doi.org/10.1089/jayao.2018.0004.
- Flores D, Docherty SL, Relf MV, McKinney RE, Barroso JV. It’s almost like gay sex doesn’t exist’: parent–child sex communication according to gay, bisexual, and queer male adolescents. J Adolesc Res 2019;34:528-62. https://doi.org/10.1177/0743558418757464.
- Nathan S, Rawstorne P, Hayen A, Bryant J, Baldry E, Ferry M, et al. Examining the pathways for young people with drug and alcohol dependence: a mixed-method design to examine the role of a treatment programme. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010824.
- Porta CM, Corliss HL, Wolowic JM, Johnson AZ, Fogel KF, Gower AL, et al. Go-along interviewing with LGBTQ youth in Canada and the United States. J LGBT Youth 2017;14:1-15. https://doi.org/10.1080/19361653.2016.1256245.
- Ybarra ML, Rosario M, Saewyc EM, Goodenow C. Sexual behaviors and partner characteristics by sexual identity among adolescent girls. J Adolesc Health 2016;58:310-6. https://doi.org/10.1016/j.jadohealth.2015.11.001.
- Newcomb ME, Clifford A, Greene GJ, Mustanski B. Parent perspectives about sexual minority adolescent participation in research and requirements of parental permission. J Adolesc Health 2016;59:443-9. https://doi.org/10.1016/j.jadohealth.2016.05.014.
- Macapagal K, Coventry R, Arbeit MR, Fisher CB, Mustanski B. ‘I won’t out myself just to do a survey’: sexual and gender minority adolescents’ perspectives on the risks and benefits of sex research. Arch Sex Behav 2017;46:1393-409. https://doi.org/10.1007/s10508-016-0784-5.
- Elze DE. Handbook of Research with Lesbian, Gay, Bisexual, and Transgender Populations. New York: Routledge; 2008.
- Mustanski B. Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: a call to action for a scientifically informed approach. Arch Sex Behav 2011;40:673-86. https://doi.org/10.1007/s10508-011-9745-1.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Griffith R. What is Gillick competence?. Hum Vaccin Immunother 2016;12:244-7. https://doi.org/10.1080/21645515.2015.1091548.
- Abbott JAM, Klein B, McLaren S, Austin DW, Molloy M, Meyer D, et al. Out & online; effectiveness of a tailored online multi-symptom mental health and wellbeing program for same-sex attracted young adults: study protocol for a randomised controlled trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-504.
- Austin A, Craig SL, D’Souza SA. An AFFIRMative cognitive behavioral intervention for transgender youth: preliminary effectiveness. Prof Psychol Res Pr 2018;49:1-8. https://doi.org/10.1037/pro0000154.
- Burns MN, Montague E, Mohr D. Initial design of culturally informed behavioral intervention technologies: developing an mHealth intervention for young sexual minority men with generalized anxiety disorder and major depression. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2826.
- Busa S, Janssen A, Lakshman M. A review of evidence based treatments for transgender youth diagnosed with social anxiety disorder. Transgender Health 2018;3:27-33. https://doi.org/10.1089/trgh.2017.0037.
- Coulter RW, Sang JM, Louth-Marquez W, Henderson ER, Espelage D, Hunter SC, et al. Pilot testing the feasibility of a game intervention aimed at improving help seeking and coping among sexual and gender minority youth: protocol for a randomized controlled trial. JMIR Res Protoc 2019;8. https://doi.org/10.2196/12164.
- Craig SL, Austin A. The AFFIRM open pilot feasibility study: a brief affirmative cognitive behavioral coping skills group intervention for sexual and gender minority youth. Child Youth Serv Rev 2016;64:136-44. https://doi.org/10.1016/j.childyouth.2016.02.022.
- Craig S, Austin A, Alessi E. Gay affirmative cognitive behavioral therapy for sexual minority youth: a clinical adaptation. Clin Soc Work J 2013;41:258-66. https://doi.org/10.1007/s10615-012-0427-9.
- Craig SL, Austin A, Huang YT. Being humorous and seeking diversion: promoting healthy coping skills among LGBTQ+ youth. J Gay Lesbian Ment Health 2018;22:20-35. https://doi.org/10.1080/19359705.2017.1385559.
- Fleming JB, Hill YN, Burns MN. Usability of a culturally informed mHealth intervention for symptoms of anxiety and depression: feedback from young sexual minority men. JMIR Hum Factors 2017;4. https://doi.org/10.2196/humanfactors.7392.
- Hatzenbuehler ML. How does sexual minority stigma ‘get under the skin’? A psychological mediation framework. Psychol Bull 2009;135:707-30. https://doi.org/10.1037/a0016441.
- Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth research evidence and clinical implications. Pediatr Clin North Am 2016;63:985-97. https://doi.org/10.1016/j.pcl.2016.07.003.
- Heck NC. The potential to promote resilience: piloting a minority stress-informed, GSA-based, mental health promotion program for LGBTQ youth. Psychol Sex Orientat Gend Divers 2015;2:225-31. https://doi.org/10.1037/sgd0000110.
- Hobaica S, Alman A, Jackowich S, Kwon P. Empirically based psychological interventions with sexual minority youth: a systematic review. Psychol Sex Orientat Gend Divers 2018;5:313-23. https://doi.org/10.1037/sgd0000275.
- Iacono G. An affirmative mindfulness approach for lesbian, gay, bisexual, transgender, and queer youth mental health. Clin Soc Work J 2018;47:156-66. https://doi.org/10.1007/s10615-018-0656-7.
- Ioverno S, Belser AB, Baiocco R, Grossman AH, Russell ST. The protective role of gay-straight alliances for lesbian, gay, bisexual, and questioning students: a prospective analysis. Psychol Sex Orientat Gend Divers 2016;3:397-406. https://doi.org/10.1037/sgd0000193.
- Lucassen MFG, Hatcher S, Stasiak K, Fleming T, Shepherd M, Merry SN. The views of lesbian, gay and bisexual youth regarding computerized self-help for depression: an exploratory study. Adv Ment Health 2013;12:22-33. https://doi.org/10.5172/jamh.2013.12.1.22.
- Lucassen MFG, Hatcher S, Fleming TM, Stasiak K, Shepherd MJ, Merry SN. A qualitative study of sexual minority young people’s experiences of computerised therapy for depression. Australas Psychiatry 2015;23:268-73. https://doi.org/10.1177/1039856215579542.
- McCallum C, McLaren S. Sense of belonging and depressive symptoms among GLB adolescents. J Homosex 2010;58:83-96. https://doi.org/10.1080/00918369.2011.533629.
- Millar BM, Wang K, Pachankis JE. The moderating role of internalized homonegativity on the efficacy of LGB-affirmative psychotherapy: results from a randomized controlled trial with young adult gay and bisexual men. J Consult Clin Psychol 2016;84:565-70. https://doi.org/10.1037/ccp0000113.
- Pachankis JE, Goldfried MR. Expressive writing for gay-related stress: psychosocial benefits and mechanisms underlying improvement. J Consult Clin Psychol 2010;78:98-110. https://doi.org/10.1037/a0017580.
- Pepping CA, Lyons A, McNair R, Kirby JN, Petrocchi N, Gilbert P. A tailored compassion-focused therapy program for sexual minority young adults with depressive symptomatology: study protocol for a randomized controlled trial. BMC Psychol 2017;5. https://doi.org/10.1186/s40359-017-0175-2.
- Perry NS, Chaplo SD, Baucom KJW. The impact of cumulative minority stress on cognitive behavioral treatment with gender minority individuals: case study and clinical recommendations. Cogn Behav Pract 2017;24:472-82. https://doi.org/10.1016/j.cbpra.2016.12.004.
- Smith NG, Hart TA, Kidwai A, Vernon JRG, Blais M, Adam B. Results of a pilot study to ameliorate psychological and behavioral outcomes of minority stress among young gay and bisexual men. Behav Ther 2017;48:664-77. https://doi.org/10.1016/j.beth.2017.03.005.
- Toomey RB, Ryan C, Diaz RM, Russell ST. High school gay-straight alliances (GSAs) and young adult well-being: an examination of GSA presence, participation, and perceived effectiveness. Applied Developmental Science 2011;15:175-85. https://doi.org/10.1080/10888691.2011.607378.
- Toomey RB, Anhalt K. Mindfulness as a coping strategy for bias-based school victimization among Latina/o sexual minority youth. Psychol Sex Orientat Gend Divers 2016;3:432-41. https://doi.org/10.1037/sgd0000192.
- Allen KD, Hammack PL, Himes HL. Analysis of GLBTQ youth community-based programs in the United States. J Homosex 2012;59:1289-306. https://doi.org/10.1080/00918369.2012.720529.
- Austin A, Craig SL. Empirically supported interventions for sexual and gender minority youth. J Evid Inf Soc Work 2015;12:567-78. https://doi.org/10.1080/15433714.2014.884958.
- Bain CL, Grzanka PR, Crowe BJ. Toward a queer music therapy: the implications of queer theory for radically inclusive music therapy. Arts Psychotherapy 2016;50:22-33. https://doi.org/10.1016/j.aip.2016.03.004.
- Chaudoir SR, Wang K, Pachankis JE. What reduces sexual minority stress? A review of the intervention ‘toolkit’. J Soc Iss 2017;73:586-617. https://doi.org/10.1111/josi.12233.
- Chen-Hayes SF. Counseling and advocacy with transgendered and gender-variant persons in schools and families. J Humanist Couns Educ Dev 2001;40:34-49. https://doi.org/10.1002/j.2164-490X.2001.tb00100.x.
- Cohler BJ, Hammack PL. The psychological world of the gay teenager: social change, narrative, and ‘normality’. J Youth Adolesc 2007;36:47-59. https://doi.org/10.1007/s10964-006-9110-1.
- Craig SL, Furman E. Do marginalized youth experience strengths in strengths-based interventions? Unpacking program acceptability through two interventions for sexual and gender minority youth. J Soc Serv Res 2018;44:168-79. https://doi.org/10.1080/01488376.2018.1436631.
- Gillig TK, Miller LC, Cox CM. ‘She finally smiles. for real’: reducing depressive symptoms and bolstering resilience through a camp intervention for LGBTQ youth. J Homosex 2019;66:368-88. https://doi.org/10.1080/00918369.2017.1411693.
- Heck NC, Flentje A, Cochran BN. Offsetting risks: high school gay-straight alliances and lesbian, gay, bisexual, and transgender (LGBT) youth. Psychol Sex Orientat Gend Divers 2013;1:81-90. https://doi.org/10.1037/2329-0382.1.S.81.
- McDonald K. Social support and mental health in LGBTQ adolescents: a review of the literature. Issues Ment Health Nurs 2018;39:16-29. https://doi.org/10.1080/01612840.2017.1398283.
- McLaren S, Schurmann J, Jenkins M. The relationships between sense of belonging to a community GLB youth group; school, teacher, and peer connectedness; and depressive symptoms: testing of a path model. J Homosex 2015;62:1688-702. https://doi.org/10.1080/00918369.2015.1078207.
- Nodin N, Peel E, Tyler A, Rivers I. The RARE Research Report: LGB&T Mental Health-risk and Resilience Explored. London: PACE; 2015.
- Oransky M, Burke EZ, Steever J. An interdisciplinary model for meeting the mental health needs of transgender adolescents and young adults: the Mount Sinai adolescent mental health center approach. Cogn Behav Pract 2018;26:603-16. https://doi.org/10.1016/j.cbpra.2018.03.002.
- Proulx CN, Coulter RWS, Egan JE, Matthews DD, Mair C. Associations of lesbian, gay, bisexual, transgender, and questioning-inclusive sex education with mental health outcomes and school-based victimization in U.S. high school students. J Adolesc Health 2019;64:608-14. https://doi.org/10.1016/j.jadohealth.2018.11.012.
- Riggs DW, Ansara GY, Treharne GJ. An evidence-based model for understanding the mental health experiences of transgender Australians. Aust Psychol 2015;50:32-9. https://doi.org/10.1111/ap.12088.
- Robinson A. Living for the city: voices of black lesbian youth in Detroit. J Lesbian Stud 2010;14:61-70. https://doi.org/10.1080/10894160903058899.
- Sandfort TGM, Bos HMW, Collier KL, Metselaar M. School environment and the mental health of sexual minority youths: a study among Dutch young adolescents. Am J Public Health 2010;100:1696-700. https://doi.org/10.2105/ajph.2009.183095.
- Tenenbaum S. Tenoch’s gender journey: case study of a 13-year-old Mexican refugee with aboriginal ancestry – naming the gap between theory and practice. First Peoples Child Fam Rev 2012;7:27-33. https://doi.org/10.7202/1068838ar.
- Vincke J, Van Heeringen K. Confidant support and the mental wellbeing of lesbian and gay young adults: a longitudinal analysis. J Community Appl Soc Psychol 2002;12:181-93. https://doi.org/10.1002/casp.671.
- Vincke J, Van Heeringen K. Summer holiday camps for gay and lesbian young adults: an evaluation of their impact on social support and mental well-being. J Homosex 2004;47:33-46. https://doi.org/10.1300/J082v47n02_02.
- Zhang L, Finan LJ, Bersamin M, Fisher DA. Sexual orientation-based depression and suicidality health disparities: the protective role of school-based health centres. J Res Adolesc 2018;30:134-42. https://doi.org/10.1111/jora.12454.
- Baker D, Durr P, Scott P. Youth Chances Report. London: METRO; 2016.
- Bridget J, Lucille S. Lesbian youth support information service (LYSIS): developing a distance support agency for young lesbians. J Community Appl Soc Psychol 1996;6:355-64. https://doi.org/10.1002/(SICI)1099-1298(199612)6:5<355::AID-CASP386>3.0.CO;2-Y.
- Chiang SY, Fleming T, Lucassen MFG, Fouche C, Fenaughty J. From secrecy to discretion: the views of psychological therapists on supporting Chinese sexual and gender minority young people. Child Youth Serv Rev 2018;93:307-14. https://doi.org/10.1016/j.childyouth.2018.08.005.
- Craig SL, Austin A, Alessi EJ, McInroy L, Keane G. Minority stress and HERoic coping and ethnoracial sexual minority girls: intersections of resilience. J Adolesc Res 2017;32:614-41. https://doi.org/10.1177/0743558416653217.
- Davis TS, Saltzburg S, Locke CR. Supporting the emotional and psychological well being of sexual minority youth: youth ideas for action 2009;31:1030-41. https://doi.org/10.1016/j.childyouth.2009.05.003.
- Davis TS, Saltzburg S, Locke CR. Assessing communitiy needs of sexual minority youths: modeling concept mapping for service planning. J Gay Lesbian Soc Serv 2010;22:226-49. https://doi.org/10.1080/10538720903426354.
- Erney R, Weber K. Not all children are straight and white: strategies for serving youth of color in out-of-home care who identify as LGBTQ. Child Welfare 2018;96:151-77.
- Ferguson KM, Macchio EM. Promising programs for lesbian, gay, bisexual, transgender, and queer/questioning runaway and homeless youth. J Soc Serv Res 2015;41:659-83. https://doi.org/10.1080/01488376.2015.1058879.
- Gamarel KE, Walker JNJ, Rivera L, Golub SA. Identity safety and relational health in youth spaces: a needs assessment with LGBTQ youth of color. J LGBT Youth 2014;11:289-315. https://doi.org/10.1080/19361653.2013.879464.
- Hohnke M, O’Brien P. Discrimination against same sex attracted youth: the role of the school counsellor. Aust J Guid Couns 2008;18:67-75. https://doi.org/10.1375/ajgc.18.1.67.
- Kwok DK. Community support programme: support for Chinese trans* students experiencing genderism. Sex Educ: Sex Soc Lea 2018;18:406-19. https://doi.org/10.1080/14681811.2018.1428546.
- Kwok DK, Winter S, Yuen M. Heterosexism in school: the counselling experience of Chinese tongzhi students in Hong Kong. Br J Guid Couns 2012;40:561-75. https://doi.org/10.1080/03069885.2012.718735.
- Lapointe A, Crooks C. GSA members’ experiences with a structured program to promote well-being. J LGBT Youth 2018;15:300-18. https://doi.org/10.1080/19361653.2018.1479672.
- Lapointe A, Dunlop C, Crooks C. Feasibility and fit of a mental health promotion program for LGBTQ+ youth. J Youth Dev 2018;13:100-17. https://doi.org/10.5195/jyd.2018.585.
- LeFrancois BA. Queering child and adolescent mental health services: the subversion of heteronormativity in practice. Child Soc 2013;27:1-12. https://doi.org/10.1111/j.1099-0860.2011.00371.x.
- Medeiros DM, Seehaus M, Elliott J, Melaney A. Providing mental health services for LGBT teens in community adolescent health clinic. J Gay Lesbian Psychother 2004;8:83-95. https://doi.org/10.1080/19359705.2004.9962381.
- MindOut . Working With LGBTQ+ People Report 2016.
- O’Hara M. Through Our Minds: Exploring the Emotional Health and Wellbeing of Lesbian, Gay, Bisexual and Transgender People in Northern Ireland. Belfast, NI: The Rainbow Project; 2013.
- Paceley MS. Gender and sexual minority youth in nonmetropolitan communities: individual- and community-level needs for support. Fam Soc: J Contemp Soc Serv 2016;97:77-85. https://doi.org/10.1606/1044-3894.2016.97.11.
- Painter KR, Scannapieco M, Blau G, Andre A, Kohn K. Improving the mental health outcomes of LGBTQ youth and young adults: a longitudinal study. J Soc Serv Res 2018;44:223-35. https://doi.org/10.1080/01488376.2018.1441097.
- Pallotta-Chiarolli M, Martin E. ‘Which sexuality? Which service?’: bisexual young people’s experiences with youth, queer and mental health services in Australia. J LGBT Youth 2009;6:199-222. https://doi.org/10.1080/19361650902927719.
- TPT . LGBT Young People’s Health in the UK: A Literature Review With a Focus on Needs, Barriers and Practice 2016.
- Powell C, Ellasante I, Korchmaros JD, Haverly K, Stevens S. iTEAM: outcomes of an affirming systems of care serving LGBTQ youth experiencing homelessness. Fam Soc: J Contemp Soc Serv 2016;97:181-90. https://doi.org/10.1606/1044-3894.2016.97.24.
- Sadowski M, Chow S, Scanlon CP. Meeting the needs of LGBTQ youth: a ‘relational assets’ approach. J LGBT Youth 2009;6:174-98. https://doi.org/10.1080/19361650903013493.
- Sansfaçon AP, Hébert W, Lee EOJ, Faddoul M, Tourki D, Bellot C. Digging beneath the surface: results from stage one of a qualitative analysis of factors influencing the well-being of trans youth in Quebec. Int J Transgend 2018;19:184-202. https://doi.org/10.1080/15532739.2018.1446066.
- Steinke J, Root-Bowman M, Estabrook S, Levine DS, Kantor LM. Meeting the needs of sexual and gender minority youth: formative research on potential digital health interventions. J Adolesc Health 2017;60:541-8. https://doi.org/10.1016/j.jadohealth.2016.11.023.
- Wagaman MA, Keller MF, Cavaliere SJ. What does it mean to be a successful adult? Exploring perceptions of the transition into adulthood among LGBTQ emerging adults in a community-based service context. J Gay Lesbian Soc Serv 2016;28:140-58. https://doi.org/10.1080/10538720.2016.1155519.
- Wilkerson JM, Schick VR, Romijnders KA, Bauldry J, Butame SA, Montrose C. Social support, depression, self-esteem, and coping among LGBTQ adolescents participating in hatch youth. Health Promot Pract 2017;18:358-65. https://doi.org/10.1177/1524839916654461.
- Wilkerson JM, Lawler SM, Romijnders KA, Armstead AB, Bauldry J, Montrose C. Exploratory analyses of risk behaviors among GLBT youth attending a drop-in center. Health Educ Behav 2018;45:217-28. https://doi.org/10.1177/1090198117715668.
- Wofford NC. Mental health service delivery to sexual minority and gender non-conforming students in schools: a Winnicottian approach. Adolesc Res Rev 2017;34:467-78. https://doi.org/10.1007/s10560-016-0482-0.
- Kuhn TS. The Structure of Scientific Revolutions. Chicago: University of Chicago Press; 1962.
- Heath S, Brooks R, Cleaver E, Ireland E. Researching Young People’s Lives. London: Sage; 2009.
- Jones L. ‘If a Muslim says “homo”, nothing gets done’: racist discourse and in-group identity construction in an LGBT youth group. Lang Soc 2016;45:113-33. https://doi.org/10.1017/S0047404515000792.
- McCartan A. Glasgow’s contested LGBT pride spaces: examining dimensions of variegated homonormativities. Soc Cult Geogr 2022;25:68-86. https://doi.org/10.1080/14649365.2022.2121982.
- Giurge LM, Whillans AV, West C. Why time poverty matters for individuals, organisations and nations. Nat Hum Behav 2020;4:993-1003. https://doi.org/10.1038/s41562-020-0920-z.
- Appleton R, Gauly J, Mughal F, Singh SP, Tuomainen H. Perspectives of young people who access support for mental health in primary care: a systematic review of their experiences and needs. Br J Gen Pract 2022;72:e161-7. https://doi.org/10.3399/BJGP.2021.0335.
- Punton G, Dodd AL, McNeill A. ‘You’re on the waiting list’: an interpretive phenomenological analysis of young adults’ experiences of waiting lists within mental health services in the UK. PLOS ONE 2022;17. https://doi.org/10.1371/journal.pone.0265542.
- Carlile A. The experiences of transgender and non-binary children and young people and their parents in healthcare settings in England, UK: interviews with members of a family support group. Int J Transgend Health 2020;21:16-32. https://doi.org/10.1080/15532739.2019.1693472.
- Jones BA, Bowe M, McNamara N, Guerin E, Carter T. Exploring the mental health experiences of young trans and gender diverse people during the COVID-19 pandemic. Int J Transgend Health 2021;24:292-304. https://doi.org/10.1080/26895269.2021.1890301.
- Dawes HC, Williams DY, Klein LB, Forte AB, Gibbs DJ, McGarry B, et al. Experiences of queer people of color in mental health services and substance use treatment services: a systematic review. J Sociol Soc Work Res 2022;14:721-55. https://doi.org/10.1086/721454.
- Heinze K, Cumming J, Dosanjh A, Palin S, Poulton S, Bagshaw AP, et al. Neurobiological evidence of longer-term physical activity interventions on mental health outcomes and cognition in young people: a systematic review of randomised controlled trials. Neurosci Biobehav Rev 2021;120:431-41. https://doi.org/10.1016/j.neubiorev.2020.10.014.
- O’Neil A, Quirk SE, Housden S, Brennan SL, Williams LJ, Pasco JA, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health 2014;104:e31-42. https://doi.org/10.2105/AJPH.2014.302110.
- Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry 2014;75:964-74. https://doi.org/10.4088/JCP.13r08765.
- Sampasa-Kanyinga H, Colman I, Goldfield G, Janssen I, Wang J, Podinic I, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act 2020;17. https://doi.org/10.1186/s12966-020-00976-x.
- Morrison TG, Katz JW, Mirzaei Y, Zare S. The Oxford Handbook of Sexual and Gender Minority Mental Health. Oxford, New York: Oxford University Press; 2020.
- Bachmann CL, Gooch B. LGBT in Britain: Hate Crime and Discrimination. London: Stonewall; 2018.
- LGBTYS . Life in Scotland for LGBT Young People 2022.
- Bradlow J, Guasp A, Cooke V, Wicks H, Bush L, Douglas R, et al. Shut Out: The Experiences of LGBT Young People Not in Education, Training or Work. London: Stonewall; 2020.
- Johnson AH. Transnormativity: a new concept and its validation through documentary film about transgender men. Sociol Inq 2016;86:465-91. https://doi.org/10.1111/soin.12127.
- Davis S. Queer and Trans People of Colour in the UK: Possibilities for Intersectional Richness. London: Routledge; 2023.
- Meyer IH, Frost DM. Handbook of Psychology and Sexual Orientation. Oxford: Oxford University Press; 2013.
- Byrne B. Rethinking intersectionality and whiteness at the borders of citizenship. Sociol Res Online 2015;20:178-89. https://doi.org/10.5153/sro.3790.
- Johnson C. Heteronormative citizenship and the politics of passing. Sexualities 2002;5:317-6. https://doi.org/10.1177/1363460702005003004.
- Mavelli L. Neoliberal Citizenship: Sacred Markets, Sacrifical Lives. Oxford, England: Oxford University Press; 2022.
- McDermott E, Gabb J, Eastham R, Hanbury A. Family trouble: heteronormativity, emotion work and queer youth mental health. Health 2021;25:177-95. https://doi.org/10.1177/1363459319860572.
- Schwend AS. Trans health care from a depathologization and human rights perspective. Public Health Rev 2020;41. https://doi.org/10.1186/s40985-020-0118-y.
- Chakraborty A, McManus S, Brugha TS, Bebbington P, King M. Mental health of the non-heterosexual population of England. Br J Psychiatry 2011;198:143-8. https://doi.org/10.1192/bjp.bp.110.082271.
- Marshall MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: a meta-analytic review. J Adolesc Health 2011;49:115-23. https://doi.org/10.1016/j.jadohealth.2011.02.005.
- TTP . The Mental Health and Well-Being of LGBTQ Youth Who Are Intersex 2021.
- DoH . Future in Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing 2015.
- Brown A, Rice SM, Rickwood DJ, Parker AG. Systematic review of barriers and facilitators to accessing and engaging with mental health care among at risk young people. Asian Pacific Psychiatry 2016;8:3-22. https://doi.org/10.1111/appy.12199.
- NYA . A Guide to Commissioning Outcomes for Young People 2019.
- Lundy L, Kilkelly U, Byrne B, Kang J. The UN Convention on the Rights of the Child: A Study of Legal Implementation in 12 Countries. Belfast: Queen’s University Belfast; 2012.
- Ben Chikha F. Combating Rising Hate Against LGBTI People in Europe. Strasbourg: Council of Europe; 2021.
- Walsh RJ. A Blow to the Rights of Transgender Children. British Psychological Society (BPS) 2020. www.bps.org.uk/psychologist/blow-rights-transgender-children (accessed 23 August 2023).
- Siddique H. Appeal court overturns UK puberty blockers ruling for under-16s. The Guardian 2021. www.theguardian.com/society/2021/sep/17/appeal-court-overturns-uk-puberty-blockers-ruling-for-under-16s-tavistock-keira-bell (accessed 23 August 2023).
- Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev: MCRR 2006;63:217-35. https://doi.org/10.1177/1077558705285298.
- Petrou S, Murray L, Cooper P, Davidson LL. The accuracy of self-reported healthcare resource utilization in health economic studies. Int J Technol Assess Health Care 2002;18:705-10. https://doi.org/10.1017/s026646230200051x.
- Damodaran J, Sherlock C. Child rights and child and adolescent mental health services (CAMHS) in Ireland. Ir J Med Sci 2013;182:723-7. https://doi.org/10.1007/s11845-013-0940-z.
- McMellon C, MacLachlan A. Young people’s rights and mental health during a pandemic: an analysis of the impact of emergency legislation in Scotland. Young 2021;29:S11-34. https://doi.org/10.1177/11033088211032783.
Appendix 1 Search strategy from meta-narrative review protocol
| Electronic databases | Additional search strategies |
|---|---|
| CINAHL | Backwards and forwards citation tracking |
| PsycInfo | Expert informants |
| Academic Search Ultimate | Relevant journal searching |
| Web of Science | |
| British Education Index | |
| MEDLINE | |
| EMBASE | |
| SocINDEX with Full Text | |
| Child Development and Adolescent Studies | |
| ERIC | |
| Allied and Contemporary Medicine Database | |
| Campbell Collaboration | |
| Cochrane Library | |
| NHS evidence | |
| Social care online | |
| Gov.uk |
Appendix 2 Flow chart for decision-making in service mapping
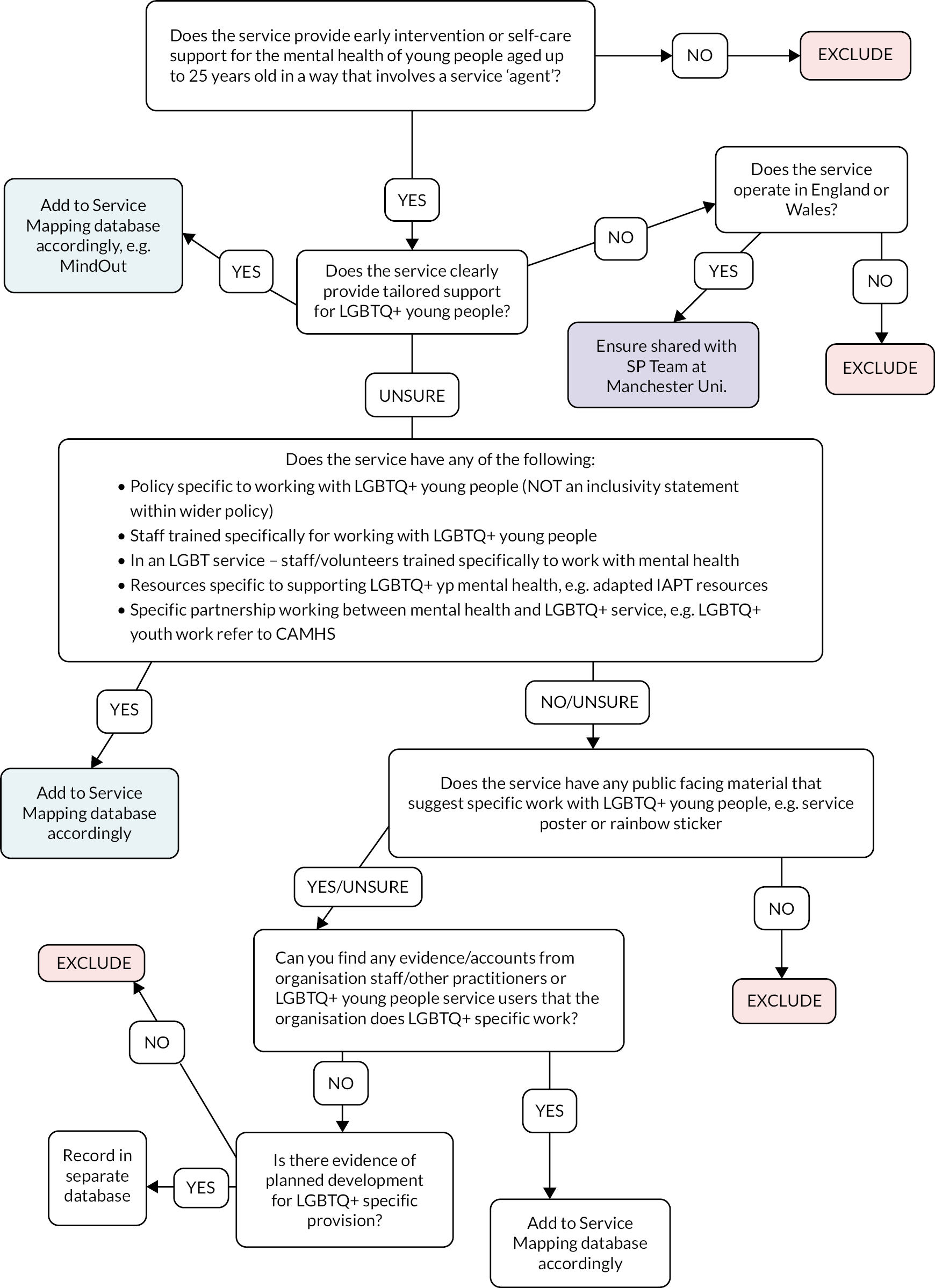
Appendix 3 Case study evaluation analysis D-code and I-code schemas
-
D-codes
| Code | Code definition |
|---|---|
| D-HeteroN | Heteronormativity – How heteronormativity is maintained through direct homo/bi phobia and discrimination, marginalisation, silence, invisibility, misrepresentation and exclusion; and the ways it is resisted |
| D-CisN | Cisnormativity – How cisnormativity is maintained through direct transphobia and discrimination, marginalisation, silence, invisibility, misrepresentation and exclusion; and the ways it is resisted |
| D-NYD | Normative Youth Development – Where youth are positioned as less than adult, assumes linear normative development. Youth emotional distress typically viewed as pathology, ignored, temporalised |
| D-BPP | Bio-psych power – The dominant biomedical systems and mental health institutions that govern mental health support including treatment approach and modes of service provision |
| D- Int-SEC | Socioeconomic material conditions (Int-Str) – The fundamental social structures, for example job markets, housing, education, and health that maintain youth (mental health) inequalities re: gender, sexuality, race, class and disability |
| D-Int Cult | Intersectionality: Cultural domain – The ideas and culture that perpetuate unequal power relations re: gender, sexuality, race, class and disability; and also those that affirm and redress power imbalance |
| D- Recog | Recognition – To be known, seen as LGBTQ+, to recognise the plurality and fluidity of a non-cis-heterosexual identity |
| D-Relat | Relationality – Connection to others, making ourselves in relation to others |
| D-Belong | Belonging – To be part of, to fit in, to be included, having a space to exist as ‘yourself’ |
| D-Becom | Becoming – The gendered and sexual self becomes possible over time and may changeThere is not a fixed pathway to LGBTQ+ identity, or a fixed destination/final identity |
| D-Safety | Safety – Emotional, cultural, psychological, physical safetyTo not feel under threat due to any aspect of identity |
| D-Int Disc | Intersectionality: Disciplinary domain – The rules/regulations/practices that are unfairly applied to people based on race, sexuality, class, gender and disability |
| D-Auton | Autonomy – Youth power to self-determine and control their bodies and selves |
| D-Agency | Agency – Young people as acting, knowing subjects |
| D-Resist | Resistance – Promoting the understanding of norms that diminish LGBTQ+, and ways of not accepting normative positioning |
| D- SubKnow | Subjugated Knowledges – Youth are experts in their own experience |
| D-Int Ind | Intersectionality: Interpersonal domain – How individuals experience the convergence of structural, cultural and disciplinary power |
| D-Emotion | Emotions and feelings – Recognition of emotions as part of being a human, and their impact on behaviour. This includes ‘distress’, that is feeling sad or worried |
| D-Subjectivity | Subjectivity – Emotional and affective aspects of identity/self |
| D-MH | Mental health – Young people’s experience of anxiety/depression (and other ‘diagnosable’) ‘symptomology’, they may or may not have a diagnosis |
-
I-Codes
| Code | Code definition |
|---|---|
| I-Family | How the support service navigates issues related to family and manages the impact of family relations on the young person. ‘What works?’ in this respect and conversely what are the challenges |
| I-School | How the support service navigates issues related to school and manages the impact of school on the young person. ‘What works?’ in this respect and conversely what are the challenges |
| I-Digital | Ways of supporting LGBTQ+ young people’s mental health online, for example messengers, zoom etc. |
| I-(St)age/I-Future | How being ‘(st)age appropriate’ and considering life/journey stage (rather than chronological age) manifests in the service and how support is provided in this way in relation to the needs of the individual young personPossibility and potential. Seeing and imagining one’s future self as they find desirable (not normative version) |
| I-Time | Time as it pertains to the individual LGBTQ+ young person and at service/organisational level; and the relationship between the two |
| I-Body | The importance and implications of the body for mental health |
| I-Space | Physical, safe environment to enact ‘becoming’, feel good and ‘take up’/be present in space. Respite from normative and/or disciplinary environments such as home, school, CAMHS etc. |
| I-Accessibility and engagement | Factors that facilitate and inhibit access and engagement |
| I-ProfRelWork | The intentional activities staff/services do to build relationships with and for LGBTQ+ young people |
| I-Reflex | Reflexivity. Critical evaluation of positionality, role, practices and wider circumstances in relation to the mental health of LGBTQ+ young people |
| I-NonPath | How mental health is actively de-pathologised and emotions/feelings are usualised by service support. |
| I-OrgSaf | Organisational Safety and Resilience |
| I-White priv/race/racism | How whiteness/white privilege is addressed at the site. How race, racism and it’s intersections are understood and addressed by the service. |
| I-Disabilities | How LGBTQ+ disabled young people, including those who are neurodiverse are supported by the site |
Glossary
Affirmed gender This term describes a person’s lived gender (e.g. after transition), rather than the gender assigned to them at birth.
Being ‘outed’ This refers to a person’s lesbian, gay, bisexual, trans, queer/questioning, plus identity or identities being disclosed without their consent. This disclosure could be to parents/carers or other family, to other services or practitioners, or to other young people. Consequences of ‘outing’ a person can include material impacts, for example a young person being made homeless, and psychological and emotional impacts for example loss of trust and fear of talking openly about lesbian, gay, bisexual, trans, queer/questioning, plus experiences in case these are shared again without consent in future.
Cisgender or cis This term describes people whose gender identity is the same or mostly the same as the gender assigned to them at birth, that is, non-transgender people.
Diagnosis This refers to clinically defined mental health problems, assessed according to standardised measures rather than subjective self-assessment. Diagnoses emphasise impairment in cognition, emotional regulation, or behaviour as these relate to a person’s day-to-day life.
Direct discrimination This describes discrimination whereby a person is treated less favourably than others on the basis of having a protected characteristic, including sexual orientation and gender reassignment. For example, staff in a service using lesbian, gay, bisexual, trans, queer/questioning, plus phobic slurs or making derogatory jokes about lesbian, gay, bisexual, trans, queer/questioning, plus people.
Distress This term describes intense feelings of anxiety, sadness, or emotional pain, which may be impacting upon a person’s day-to-day life. Queer Futures 2 uses this term as an alternative to diagnostic language; this aligns with an understanding of common mental health problems among lesbian, gay, bisexual, trans, queer/questioning, plus young people not as pathological, but as logical responses to experiences of marginalisation and discrimination.
Early intervention Queer Futures 2 uses ‘early intervention’ to refer to services that lesbian, gay, bisexual, trans, queer/questioning, plus young people can access to receive mental health support before reaching crisis point. While our focus is young people aged 12–25 years, early intervention more broadly covers all stages of a child’s development from birth onwards.
Gender-affirming health care Also referred to as medical transition or ‘gender reassignment’, gender-affirming health care refers to medical and/or surgical interventions that enable trans, non-binary and gender-variant people to feel safer and more comfortable in their bodies.
Gender reassignment (protected characteristic) Gender reassignment protection includes people who are gender fluid and non-binary and are not restricted to those who have undergone, are undergoing or plan to undergo medical transition, as established in the 2020 Taylor v Jaguar Land Rover case ruling.
Heterosexual/‘straight’ This term refers to men who have romantic or sexual attraction towards women or to women who have romantic or sexual attraction towards men.
Indirect discrimination Practices, policies or rules are applied to every person accessing a service but disadvantage some people.
Integrated Care Board Statutory National Health Service organisation replacing prior Clinical Commissioning Groups under the Health and Care Act (2022), responsible for planning to meet the health needs of Integrated Care Service area populations, managing National Health Service budget and commissioning health services in Integrated Care Service area.
Integrated Care Partnership Statutory committees formed between Integrated Care Boards and local authorities, responsible for producing integrated care strategy for meeting the health needs of the area population.
Integrated Care Service Under the Health and Care Act (2022), there are now 42 Integrated Care Services across England, representing partnerships of organisations to plan and deliver integrated health and care services.
LGBTQ+ Lesbian, gay, bisexual, trans and queer/questioning plus; ‘plus’ in this context indicates the multiplicity of identities and experiences falling under a lesbian, gay, bisexual, trans, queer/questioning, plus umbrella and the unfixed nature of individual terms. There are numerous different acronyms used to refer to sexual orientation and gender identity diversity. The acronym lesbian, gay, bisexual, trans, queer/questioning, plus was decided upon in consultation with young people, for whom this was the preferred term. For definitions of individual identities, please see Stonewall’s glossary of terms.
LGBTQ+ phobia An umbrella term for discrimination against, fear of, or dislike of lesbian, gay, bisexual, trans, queer/questioning, plus people (including those perceived to be lesbian, gay, bisexual, trans, queer/questioning, plus). Definitions of biphobia, homophobia, lesbophobia, transphobia and microaggressions are included in MindOut’s glossary of terms.
Marginalisation Encompassing social exclusion, this refers to the treatment of a person or group as insignificant and/or unimportant, with implications for how much influence and power that person or group can hold. This can manifest as barriers to accessing institutions, opportunities, and services, and gaps in service provision.
Minority stress Developed by Ilan H. Meyer, this explanatory framework argues that experiences of stigma, prejudice and discrimination create hostile environments, leading to mental health problems. Rather than seeing mental distress as inherent, minority stress highlights conditions producing common mental health problems that can be changed.
Multidisciplinary Team meetings Multidisciplinary Team meetings bring together healthcare practitioners and other professionals to assess, plan and manage an individual’s care; for example Multidisciplinary Teams may meet to assess safeguarding concerns and strategy for a young person.
Norm(s) We use this term throughout to refer collectively to the pressures, expectations and standards placed upon lesbian, gay, bisexual, trans, queer/questioning, plus young people about who or what they should be or achieve. These may relate to: sexuality or gender identity, that is, the assumption that people are cisgender and heterosexual; age, that is, assumptions about young people’s understanding of themselves and ideas that ‘adults know best’; and the future that is pressure to ‘perform well’ in narrow ways, such as through academic success.
Stigma This refers to negative perceptions or stereotypes about a characteristic or personal trait; for example stigma related to being lesbian, gay, bisexual, trans, queer/questioning, plus, or to having mental health problems.
Subjective self-assessment This refers to an individual’s own perception of their mental health and support needs.
Transition All processes or actions undertaken to enable an individual to feel safer and more affirmed in their gender. This can cover: social transition, that is, steps taken to be affirmed by others such as ‘coming out’ and using a different name and/or pronouns; legal transition, that is, steps taken to change legal and identifying documentation to reflect a person’s lived gender such as changing the gender marker on medical records or other documents; medical transition, that is, medical and/or surgical interventions undertaken to enable a person to feel safer and more comfortable in their body and to alleviate dysphoria. It is important to note that transition will look different for different people; for example some people will not ‘come out’ in the same way as others for their own safety, some do not desire or cannot access medical transition, and some do not desire or cannot access legal transition.
List of abbreviations
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive–behavioural therapy
- CSS
- case study site
- EB
- explanation building
- FOI
- Freedom of Information
- GI
- Gendered Intelligence
- GIC
- Gender Identity Clinic
- GIDS
- Gender Identity Development Service
- GP
- general practitioner
- LGBTQ+
- lesbian, gay, bisexual, trans, queer/questioning, plus
- MNR
- meta-narrative review
- NI
- Northern Ireland
- PICOS
- Population, Intervention, Comparison, Outcomes, Study
- PIS
- participant information sheet
- POC
- person of colour
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- QTIBPOC
- Queer, Trans and Intersex Black people and People of Colour
- UNCRC
- United Nations Convention on the Rights of the Child
Notes
-
Case study evaluation interview topic guides: LGBTQ+ young people; staff and volunteers; and parents/carers
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KYWA6382).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
