Notes
Article history paragraph text
The research reported in this issue of the journal was funded by the HTA programme as project number 97/10/99. The contractual start date was in May 2007. The draft report began editorial review in October 2011 and was accepted for publication in July 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Adrian Grant has received salary support from the NIHR as director of the NIHR Programme Grants for Applied Research programme.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Grant et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Executive summary
Background
In the Health Technology Assessment (HTA)-commissioned REFLUX trial, laparoscopic fundoplication for people with chronic symptoms of gastro-oesophageal reflux disease (GORD) was shown to significantly improve reflux-specific and general health-related quality of life (HRQoL) at least up to 12 months after surgery. However, cost-effectiveness was uncertain without more reliable information about longer-term costs and benefits. Here, we report the findings from longer-term follow-up of the REFLUX trial.
Objective
To evaluate, at 5 years after surgery, the clinical effectiveness, cost-effectiveness and safety of a policy of relatively early laparoscopic surgery compared with continued medical management among people with GORD symptoms that are reasonably controlled by medication and who are judged suitable for both surgical and medical management.
Methods
Design
-
Long-term follow-up of a pragmatic randomised controlled trial (with parallel non-randomised preference groups) comparing a laparoscopic surgery-based policy with a continued medical management policy to assess relative clinical effectiveness.
-
An economic evaluation of laparoscopic surgery for GORD to compare the cost-effectiveness of the two management policies, based on a within-trial (5-year) economic analysis and exploration of the need for a longer-term model.
Setting
Participants had originally been recruited in 21 UK hospitals through local partnership between surgeon(s) and gastroenterologist(s) who shared the secondary care of patients with GORD. After operation (surgical groups) and after optimisation of anti-reflux therapy (medical groups), participants were returned to the care of their general practitioners (GPs). Follow-up was by annual postal questionnaire and selective case notes review when questionnaires indicated reflux-related health-care events.
Participants
Participants in this study were questionnaire responders among the 810 original participants. At trial entry, all had both documented evidence of GORD and symptoms for > 12 months. Annual questionnaire response rates (years 1–5) were 89.5%, 77.5%, 76.7%, 69.8% and 68.9%.
Intervention
Of the 810 participants, 357 were recruited to the randomised comparison (178 randomised to surgical management and 179 randomised to continued medical management) and 453 to the parallel non-randomised preference arm (261 surgical management and 192 medical management). The type of fundoplication was left to the discretion of the surgeon.
Main outcome measures
The principal outcome measure was a disease-specific instrument (the REFLUX questionnaire developed specifically for this study). Secondary measures were the Short Form questionnaire-36 items (SF-36), the European Quality of Life-5 Dimensions (EQ-5D), surgical events including complications, reflux medication use, GP visits, hospital outpatient consultations, day and overnight hospital admissions, and their costs.
Results
At entry to the original trial, participants had been taking GORD medication for a median of 32 months and had a mean age of 46 years, and 66% were men; the randomised groups had been well balanced. Responders at 5 years were older, had been on medication for a shorter time prior to trial entry and had higher baseline quality-of-life scores than non-responders; however, the randomised groups of responders were similar in baseline characteristics. Primary analyses were based on the ‘intention-to-treat’ (ITT) principle, with secondary per-protocol analyses based on those who, at 1 year, had received their allocated treatment.
By 5 years, 63% (n = 112) of the 178 randomised surgery participants and 13% (n = 24) of the 179 randomised medical management participants had actually received fundoplication (equivalent figures in the preference groups were 85% and 3%). There had been a mixture of clinical and personal reasons for those allocated surgery not receiving it, sometimes related to long waiting times. A total or partial wrap procedure had been performed depending on surgeon preference; perioperative complications had been uncommon with no deaths associated with surgery.
At each year, there were significant differences in the REFLUX score (a third of a SD; p < 0.01 at 5 years) favouring the randomised surgical group, reflecting differences in general discomfort (particularly), wind and frequency, nausea and vomiting, and activity limitation subscores. SF-36 and EQ-5D scores also favoured the randomised surgical group, especially SF-36 norm-based general health, but differences attenuated over time and were generally not statistically significant at 5 years [EQ-5D difference (ITT) 0.047, 95% confidence interval (CI) −0.013 to 0.108; p = 0.13]. The lower the REFLUX score and hence the worse the symptoms at trial entry, the larger the benefit observed after surgery. Post hoc exploratory analyses showed that those randomly allocated to medical management who subsequently had surgery had worse symptoms (lower baseline scores) than those who continued on medical management as allocated; following surgery, the scores of these patients markedly improved and this explains, at least in part, why differences in outcome between the randomised groups became less marked over time.
The preference surgical group also had low REFLUX scores at baseline. These scores improved substantially after surgery and at 5 years they were slightly better than those in the preference medical group.
Overall, 4% (n = 16) of the total 364 in the study who had fundoplication had a subsequent reflux-related operation, of whom two had a further (i.e. third) operation. Reoperation was most often conversion to a different type of wrap or a reconstruction of the same wrap. There were only two cases of reversal of the fundoplication and neither was in the randomised comparison. In total, 3% (n = 12) of those who had fundoplication required surgical treatment for a complication directly related to the original surgery, including oesophageal dilatation (n = 4) and repair of incisional hernia (n = 3). Patterns of ‘difficulty swallowing’, flatulence and ‘wanting to vomit but being physically unable to do so’ – all problems that have previously been associated with anti-reflux surgery – were similar in the two randomised groups.
Economic evaluation
Differences in mean costs and mean quality-adjusted life-years (QALYs) at 5 years were used to derive an estimate of the cost-effectiveness of laparoscopic fundoplication and continued medical management from the perspective of the NHS. Conventional decision rules were used to estimate incremental cost-effectiveness ratios (ICERs). Sensitivity analysis (including probabilistic sensitivity analysis) was used to explore and quantify uncertainty in the cost-effectiveness results.
Health-care resource-use data were collected prospectively as part of the clinical report forms and patient questionnaires at each follow-up point. The cost for each individual patient in the trial was calculated by multiplying their use of NHS resources by the associated unit costs (from published sources) and discounting at an annual rate of 3.5%. For the base-case analysis, total costs constituted the costs of surgery, complications due to surgery, reoperations, reflux-related prescribed medication, reflux-related visits to and from the GP and reflux-related hospital inpatient, outpatient and day visits. For the sensitivity analysis, all GP visits and all hospital admissions were included in the calculation of total costs. Health outcomes were expressed in terms of QALYs. HRQoL was assessed at each follow-up point using the EQ-5D. Incremental mean QALYs between randomised treatment groups were estimated with and without adjustment for baseline utility, using ordinary least squares regression.
The extent of missing data throughout the trial follow-up was significant; for this reason, the base case drew on the multiple imputed data set ITT analysis. A separate scenario – the complete-case analysis, in which only participants who returned all questionnaires and completed all EQ-5D profiles are included – was employed for both ITT and per-protocol analyses. Multiple imputation provides unbiased estimates of treatment effect if data are missing at random. Sensitivity analysis was used to test the impact on the cost-effectiveness results if data were missing not at random, that is, if patients with worse outcomes or greater costs were more likely to have missing data.
The results show that, for the base-case analysis (multiple imputed data set), the participants randomised to fundoplication accrued greater costs (incremental mean cost £1518; 95% CI £1006 to £2029) but also reported greater overall HRQoL (incremental mean QALYs 0.2160; 95% CI 0.0205 to 0.4115) than participants randomised to continued medical management. Laparoscopic fundoplication is a cost-effective strategy for GORD patients eligible for the REFLUX trial on the basis of the range of cost-effectiveness thresholds used by the National Institute for Health and Care Excellence (NICE) (£20,000–30,000 per additional QALY). The results for the complete-case analysis concurred with the multiple imputed data set: across analyses adjusted and unadjusted for baseline EQ-5D, ICERs ranged between £5468 and £8410, well below the NICE cost-effectiveness thresholds. For both data sets (multiple imputation and complete case), the probability of surgery being the more cost-effective intervention was > 0.82 for incremental analyses unadjusted for baseline EQ-5D and > 0.93 once incremental QALYs were adjusted for baseline EQ-5D.
A sensitivity analysis was carried out comparing the groups according to their ‘per-protocol’ status at 1 year. A per-protocol analysis compares the efficacy of the treatments received, whereas an ITT analysis compares the effectiveness of the strategies as offered to patients. The per-protocol analysis (in complete cases) suggested that surgery was more cost-effective than medical management. Other sensitivity analyses were carried out using a wider set of resource-use data. The results of the first alternative scenario, using the costs of primary care visits for any reason rather than only reflux-related reasons, increased the ICER slightly in relation to the base case. Nevertheless, the ICER remains well below conventional thresholds, and the probability of surgery being cost-effective was > 0.85 for both adjusted and unadjusted analyses. In the second alternative scenario, replacing reflux-related hospital costs by all hospital costs, medical management was ‘dominated’ by the surgical policy; the probability of surgery being cost-effective was > 0.90.
The base-case analysis imputes missing data. This assumes that missing data are missing at random, that is, their values can be predicted (with uncertainty) from observed data. This assumption is impossible to confirm or repute but its effect on the results can be tested in sensitivity analysis. The base-case analysis may be biased if the values of a missing variable are different from the observed values (for given values of other covariates). Sensitivity analysis using the multiple imputation data set showed that the cost-effectiveness of surgery was relatively insensitive to any increase in costs: cost-effectiveness changed little when costs were increased for patients with missing data in both treatment groups and when costs were increased just for patients randomly allocated surgery with missing data. A similar result was observed after reducing the total QALYs for all patients with missing data. In contrast, the cost-effectiveness of surgery was highly sensitive to the assumption that patients randomly allocated surgery with missing data experience lower HRQoL than patients with complete data. A 10% decrease in QALYs for patients randomised to surgery with missing data results in the cost-effectiveness increasing above £20,000 per QALY gained. This scenario shows that missing data can have an impact on the results. Nevertheless, although it is impossible to empirically confirm or refute this scenario from the data in the trial, it would seem improbable in practice that surgical patients with poor quality of life are less likely to respond to follow-up questionnaires than similar participants undergoing medical management.
Comparison with similar randomised trials
The findings of the REFLUX trial were considered in the context of the three other randomised trials that have compared laparoscopic surgery with medical management. In respect of benefits, the trials consistently show better relief of GORD symptoms following surgery, with parallel, though less marked, improvements in generic HRQoL. The four trials are also consistent in respect of complications of surgery, with small numbers having associated visceral injuries, postoperative problems and dilatation of the fundoplication wrap. The REFLUX trial suggests that 4.5% have a reoperation and the other trials are broadly consistent with this. Difficulty swallowing (dysphagia), flatulence and bloating have been linked with fundoplication in the other trials. In contrast, although a small number of REFLUX participants had a dilatation of the fundoplication wrap, responses to the questionnaires did not show a difference between those randomised to surgery and those randomised to medical management in these respects.
Conclusions
After 5 years' follow-up, a policy of relatively early laparoscopic fundoplication among patients for whom reasonable control of GORD symptoms requires long-term medication and for whom both surgery and medical management are suitable continues to provide better relief of GORD symptoms with associated better quality of life. Complications of surgery were rare. Despite being initially more costly, a surgical policy is likely to be more cost-effective for such patients suffering from GORD who were eligible for the REFLUX trial.
Implications for health care
Extending the use of laparoscopic fundoplication to people whose GORD symptoms require long-term medication for reasonable control and who would be suitable for surgery would provide health gains that extend over a number of years. The longer-term data reported here indicate that this would also be a cost-effective use of resources. The more troublesome the symptoms, the greater the potential benefit from surgery.
Recommendations for research
Most patients taking anti-reflux medication are managed in general practice. It is uncertain how many of these people might be suitable for surgery and hence what the most efficient provision of future care might be. Further research to explore the feasibility and resource impact of alternative policies for fundoplication within the NHS is therefore recommended.
Trial registration
This study is registered as ISRCTN15517081.
Funding
Funding for this study was provided by the Health Technology Assessment programme of the National Institute for Health Research.
Chapter 1 Introduction
This report describes the long-term follow-up of the REFLUX trial assessing the clinical effectiveness and cost-effectiveness of laparoscopic surgery compared with continued medical management for people with gastro-oesophageal reflux disease (GORD). This comparison was identified as a priority for research by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme, which funded the trial in two stages. The first stage, encompassing preliminary economic modelling, outcome development, trial recruitment, initial clinical management, follow-up to a time equivalent to 1 year after surgery and modelling of cost-effectiveness based on results available at that time, was reported in 2008. 1–5 The second stage, reported here, describes analyses based on further follow-up to 5 years after surgery.
Gastro-oesophageal reflux disease
The lower oesophagus, at its junction with the stomach, normally acts as a sphincter to prevent the contents of the stomach flowing back up the oesophagus. When the sphincter does not work adequately, the acid stomach contents leak, or ‘reflux’, into the oesophagus. The commonest symptom that this causes is heartburn, a burning sensation in the chest or throat. GORD has been defined through an international consensus process as ‘a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications’; in this consensus, symptoms were considered ‘troublesome’ ‘if they adversely affected a patient's well-being’. 6
Symptoms caused by gastro-oesophageal reflux are common: between 20% and 30% of a ‘Western’ adult population experience heartburn and/or reflux intermittently. 7–9
Treatment of GORD includes both medical and surgical management, the options depending on the severity of symptoms. The majority of people with reflux have only mild symptoms and require little, if any, medication. The simplest is self-administered antacids with advice to alter lifestyle factors such as dietary modification, smoking cessation and weight reduction. A minority have severe symptoms and develop overt complications, despite full medical therapy, and require surgical intervention. Among the remainder, control of symptoms requires regular or continuous acid-suppression therapy using either histamine receptor antagonists (H2RAs) or proton pump inhibitors (PPIs); initial high-dose therapy may be followed by maintenance treatment using these drugs either intermittently or continuously at a reduced dose sufficient to suppress symptoms. It is from this intermediate group of patients with significant disease requiring maintenance medical treatment that most of the treatment costs for the health service arise.
Laparoscopic fundoplication
Interest in surgery as an alternative to long-term medical therapy for GORD has been considerable since the introduction of the minimal access laparoscopic approach in the early 1990s. 10 Randomised trials conducted comparing laparoscopic with open surgery showed similar improvement in symptoms but with clear benefits of the laparoscopic approach in terms of recovery and fewer postsurgical complications.11 As a consequence, surgery was suggested as an alternative to long-term maintenance medical treatment with anti-reflux drugs.
The operative method, whether using an open or a laparoscopic approach, involves performing a fundoplication by wrapping the fundus of the stomach around the lower oesophagus to create a high-pressure zone, thus reducing gastro-oesophageal reflux. The wrap created can be either complete (360°) or partial. Many operative variants have been described. The commonest operation is a 1-cm complete wrap fashioned over a large bougie, the so-called ‘short-floppy Nissen’. 12,13 There has been debate about the use of a partial rather than a total fundoplication. The partial approach has a number of potential advantages (such as fewer postoperative complications) but several controlled studies have shown broad equivalence between the two approaches;14 for the purpose of this study they were therefore regarded as equivalent. Although fundoplication is reported to produce resolution of reflux symptoms in upwards of 90% of patients, like all surgery it carries risks and can have side effects. There is also uncertainty about the durability of benefit and frequency and severity of side effects following surgical therapy. Long-term follow-up to 12 years after open reflux surgery suggested attenuated but continuing better control of reflux symptoms; however, other symptoms such as difficulties swallowing (dysphagia), rectal flatulence and inability to belch or vomit were more common in surgical patients. 15 An important objective of this study was to determine if the long-term pattern of symptoms following laparoscopic surgery was similar.
Medical management
Proton pump inhibitors, sometimes supplemented with prokinetics or alginates, are the most effective medical treatment for moderate to severe GORD. Once started on PPIs, the majority of patients with significant GORD remain on long-term treatment. 16 It is estimated that around 1% or more of the UK adult population are prescribed PPI maintenance therapy. 17–19 The cost to the NHS of medical management of GORD is considerable. In England alone, the cost of PPIs is estimated to be £220M per year. 20 Of this budget, most of this prescribing occurs within the primary care setting. 21,22
Although PPIs are generally considered safe, there is increasing acknowledgement of their possible adverse effects. 23,24 Gastric acid suppression predisposes to enteric infections and the sustained hypergastrinaemia resulting from PPI use causes rebound acid hypersecretion and the development of acid-related symptoms if the drug is stopped. Acute severe hypomagnesaemia has been recognised relatively recently as a rare adverse reaction to PPIs; the mechanism underlying it is not known. The clinical significance of impaired vitamin B12 and iron absorption due to PPIs is uncertain; there is also controversy about the risk of fractures and pneumonia and about the occurrence and significance of gastric mucosal atrophy and intestinal metaplasia, which have been seen in Helicobacter pylori-positive patients taking PPIs. Drug–drug interactions have also been a cause for concern,25 although unequivocal evidence of their occurrence does not in itself establish clinical significance.
For the purpose of this study, medical therapy was taken to mean long-term therapy with PPIs (or H2RAs if intolerant to PPIs).
Rationale for the study design
The original study design was based on the belief that decisions about the management of GORD should be made using unbiased, statistically precise comparisons of alternative policies. At study entry all patients fulfilled three criteria: they were on long-term acid suppression with PPIs; they had symptoms that were thought to be adequately controlled; and they were suitable in terms of fitness and comorbidity for either surgical or continuing medical treatment for their GORD. At the time that the study was planned, the consensus opinion of clinicians was that these three criteria identified GORD patients for whom surgical and continuing medical treatment could be considered equally acceptable treatment options and that, consequently, the comparison should be undertaken in patients meeting these criteria.
The most likely sources of bias were in the ways in which the groups being compared were selected; how their outcomes were assessed; and how the management was actually delivered. This is the basis for using a pragmatic randomised controlled trial (RCT) design. Random allocation protected against selection bias. Confining the trial to those with no clear treatment preference limits biased patient-centred assessment of outcome, and pragmatic comparison of alternative policies [with intention-to-treat (ITT) analysis] avoids bias introduced by individual cases of non-compliance. This approach had limitations, however, and for this reason we chose to incorporate two parallel, non-randomised preference groups.
Including those with a clear preference for one policy or the other allows broader extrapolation and generalisability. Study of this group may give insights into the reasons for preference and hence give pointers to patient choices after the study. 26 Furthermore, preference may influence outcome and, if so, this may also help when making treatment decisions. 26,27 A third reason for the parallel, non-randomised preference groups28 was that the addition of data from the preference groups may reduce imprecision around the estimates from the randomised comparison and this may be particularly useful for rare events, such as complications that can be confidently ascribed to one or other treatment. (The limitation is that the preference groups are not derived by random allocation, and hence the comparisons are exposed to the biases of non-randomised studies.)
Reliable comparisons within and between randomised and preference groups require valid measurement of treatment outcome. Although there were a number of quality-of-life (QoL) tools available, none was sufficiently specific to assess the spectrum of gastrointestinal symptoms associated with the treatment of GORD, particularly those due to surgery. For this reason we developed and validated a new outcome measure (the REFLUX questionnaire). We have continued to use this as the primary outcome measure in the longer-term follow-up reported here. Details of the REFLUX questionnaire and its derivation have been described elsewhere. 1,4
Gastro-oesophageal reflux disease and its management represent a very significant call on NHS resources. Although clinical effectiveness, acceptability and safety will be important determinants of future policy, the issues of cost and resource use may be over-riding. This is the reason for the economic evaluation component of this study. Policy should be guided by both assessment of the relative cost-effectiveness of alternative policies and assessment of the impact that possible policy changes would have for the NHS and for patients with GORD.
The cost of laparoscopic fundoplication appears to be equivalent to the cost of 2–3 years of maintenance treatment with PPIs, although it is acknowledged that the costs of PPIs are falling. 29 The costs of surgery are related largely to two factors: the incidence of complications/length of hospital stay and the number of patients requiring long-term medical interventions after surgery.
We addressed cost-effectiveness in our report of the first phase of the REFLUX trial. 1 We reported both a within-trial cost-effectiveness analysis based on the results up to 12 months after surgery and an extended cost-effectiveness model that explored a number of scenarios beyond 12 months. The within-trial analysis related the extra mean costs associated with the surgical policy to the estimated increase in mean quality-adjusted life-years (QALYs) associated with surgery up to that time. The incremental cost-effectiveness ratio (ICER) was around £19,000 when the ITT analysis was used. Taking into account the uncertainties around the estimates of both costs and utilities, it was calculated that the chance that the surgical policy would be cost-effective at a threshold of £20,000 per QALY was 46%. This indicated considerable uncertainty at thresholds that are currently commonly applied to costs per QALY. The limitations of the within-trial analysis were discussed in detail in the earlier report, in particular that it ignored costs and benefits that accrued after 1 year.
The economic model was designed to address the limitations of the within-trial analysis. It explored a range of scenarios of varying lifetime benefits and costs, and analyses gave a wide range of incremental costs per QALY of £1000–44,000, again indicative of wide uncertainty. The factors contributing most to this uncertainty were the projected health-related quality-of-life (HRQoL) parameters and the long-term uptake of medication following surgery.
Thus, although data available up to a time equivalent to 1 year after surgery provided promising evidence that surgical management might well be cost-effective, there was too much uncertainty, especially about longer-term costs and benefits, to provide clear guidance for decision-makers. This was the justification for the longer-term follow-up to 5 years reported here.
Chapter 2 Methods
Original study design
The study had two complementary components:
-
a multicentre, pragmatic30 RCT (with parallel non-randomised preference groups) comparing a laparoscopic surgery-based policy with a continued medical management policy to assess their relative clinical effectiveness
-
an economic evaluation of laparoscopic surgery for GORD to compare the cost-effectiveness of the two management policies, identify the most efficient provision of future care and describe the resource impact that various policies for fundoplication would have on the NHS.
Eligible patients who consented to participate in the RCT were randomly allocated to either laparoscopic surgery or continued medical management. Those patients who had a strong preference for one or other of the two treatment options could be recruited to the preference study. Clinical history was recorded at study entry. Participants completed health status questionnaires at the time of recruitment to the study and then at specified times equivalent to 3 and 12 months and then 2, 3, 4 and 5 years after surgery.
Approval for this study was obtained from the Scottish Multicentre Research Ethics Committee and the appropriate Local Research Ethics Committees.
Clinical centres
Clinical centres were based on local partnerships between surgeons with experience of laparoscopic fundoplication and gastroenterologists, with whom they shared the secondary care of patients with GORD. Centres were eligible if they included:
-
a surgeon who had performed at least 50 laparoscopic fundoplication operations
-
one or more gastroenterologists who agreed to collaborate with the surgeon(s) in the trial.
Study population
Eligible patients were those for whom care had been provided by a participating clinician who was uncertain which management policy (surgical or medical) was better. In addition, patients had to have documented evidence of GORD (based on endoscopy and/or manometry/24-hour pH monitoring) as well as symptoms for >12 months requiring maintenance PPI therapy for reasonable symptom control. Patients who were intolerant to PPIs and therefore required H2RA therapy to control their symptoms were also eligible. Patients who were morbidly obese [body mass index (BMI) > 40 kg/m2] or who had Barrett's oesophagus of > 3 cm or evidence of dysplasia, a paraoesophageal hernia or an oesophageal stricture were all excluded.
Eligible patients who did not want to take part in the randomised trial because of a strong preference for one type of management or the other were invited to take part in the preference arm of the study. For logistical reasons and to maintain a balance between the sizes of the randomised and the preference groups, we aimed to cap the numbers of participants recruited to the preference arms to 20 per arm in each centre.
All participants gave their informed consent.
Health technology policies being compared
Laparoscopic surgery policy
For those participants allocated to the randomised surgical group or recruited to the preference surgical group of the trial, subsequent deferring or declining of surgery, by either the participant or the surgeon, was always an option (i.e. even after trial entry), particularly among those recruited by a gastroenterologist and referred to a surgeon for consideration of surgery within the trial. Participants who had not had manometry/pH studies underwent these tests before surgery to exclude achalasia.
The surgery was performed either by an experienced surgeon who had undertaken > 50 laparoscopic fundoplications or by a less experienced surgeon working under the supervision of an experienced surgeon. It was recommended that crural repair be routine and that non-absorbable synthetic sutures (not silk) be used for the repair. The type of fundoplication used was left to the discretion of the experienced surgeon. For the purposes of the main comparisons, the different surgical techniques for laparoscopic fundoplication were considered as part of a single policy. The study design, however, allowed for indirect comparisons between techniques.
Medical management policy
Those allocated to the medical management policy had their therapy reviewed and adjusted as necessary by the local gastroenterologist to be ‘best medical management’. It was recommended that management conformed to the principles of the Genval Workshop Report. 31 These include stepping down antisecretory medication in most patients to the lowest dose that maintained acceptable symptom control. Following the therapy review by the gastroenterologist, trial participants had their medication managed by their general practitioner (GP). Although, in general, trial participants allocated to medical management were managed in this way, the protocol did include the option of surgery if a clear indication for it subsequently developed.
Study registration (and treatment allocation when randomised)
The treatment allocation for participants in the randomised component of the trial was computer generated; it was stratified by centre, with balance in respect of other key prognostic variables – age (18–49 years or 50+ years), sex (male or female) and BMI (≤ 28 or > 29 kg/m2) – by a process of minimisation. Randomisation was organised centrally at the Health Services Research Unit, University of Aberdeen, and was independent of all clinical collaborators.
Clinical management
Participants who were allocated to surgical management were invited to a consultation with the collaborating surgeon. During this consultation, the surgeon confirmed that there was no contraindication to surgery and discussed the operation in more detail, before arranging an operation date. The surgeon recorded intraoperative details on specially designed study forms. All other in-hospital data collection was the responsibility of the local study nurse. In all respects, other than the trial interventions, clinical management was left to the discretion of the clinician responsible for care. This continued to be the case in the extended follow-up phase, which is the focus of this report, with GPs monitoring subsequent care needs throughout the follow-up period.
Data collection
Follow-up by postal questionnaire was first performed at 3 months after surgery, or at an equivalent time among those who did not have surgery, and then annually. The questionnaire used for the follow-up at 2–5 years was similar to the questionnaire that had been used in the earlier phase of the trial up to 12 months after surgery. Non-responders received up to two reminder telephone calls or letters to encourage return of their postal questionnaires. On occasion, and at the participants' convenience, a shortened version of the questionnaire was completed over the telephone.
From around half-way through the 5-year follow-up, participants were sent a £5 gift voucher with their final postal reminder to compensate for their time in completing the questionnaire. This decision was taken based on the findings of a systematic review of the effects of incentives on postal questionnaire return32 and specific randomised trials that evaluated the use of vouchers. 33–35
All data were sent to the trial office in Aberdeen for processing. A random 10% sample of all data was double-entered to check accuracy and no significant errors were identified. Extensive range and consistency checks further enhanced the quality of the data.
The principal study outcome measure
The primary outcomes for measuring the differences in effects between medical and surgical management were:
-
a ‘disease-specific’ measure incorporating assessment of reflux and other gastrointestinal symptoms and the side effects and complications of both therapies (the REFLUX questionnaire was developed specifically for this study4)
-
NHS costs including treatments, investigations, consultations and other contacts with the health service.
The secondary outcome measures were:
-
HRQoL – measured using the European Quality of Life-5 Dimensions (EQ-5D)36 and Short Form questionnaire-36 items (SF-36)37
-
patient costs, including loss of earnings, reduction in activities and the costs of prescriptions and travel to health care
-
other serious morbidity, such as operative complications
-
(further) anti-reflux surgery
-
mortality.
An example of the annual questionnaire used for collecting this information is provided in Appendix 1.
Sample size
The original aim was to recruit 600 participants to the randomised trial to give 80% power to identify a difference between the two groups of 0.25 of a standard deviation (SD) in respect of the disease-specific instrument and other continuous variables such as EQ-5D and SF-36, using a significance level of 5%. Based on the same arguments, it was planned that 300 people would be recruited to each arm of the preference study. The cost savings of a surgical policy largely depend on the number of patients managed surgically who no longer require PPI treatment, and a trial with 300 surgically managed patients would have estimated this proportion to within about 5% with 95% statistical confidence.
However, prompted by a lower rate of recruitment than expected, this target was revised in January 2003 in consultation with the Data Monitoring Committee (DMC) and representatives of the HTA programme. It was agreed that a larger benefit (0.3 of a SD) was clinically plausible based on improvements seen after surgery in the accruing literature among more severely affected people (who were not eligible for the trial). This was calculated to require 196 in each group to give 80% power (2p = 0.05).
Statistical considerations
This report describes analyses of annual questionnaire data up to 5 years after surgery (or an equivalent time if managed medically). As a general rule, in the tables and analyses presented in this report, the participants in the randomised groups are separate from those in the preference groups. A sizeable group of patients allocated to surgery did not receive surgery. Therefore, to investigate the potential influence of this non-compliance with allocation, summary statistics in the results tables are given for four main analysis populations (comprising eight groups of participants):
-
Randomised ITT population (groups that were randomised to either surgery or medical management).
-
Per-protocol (PP) population (groups that were either randomised to surgery and received surgery in the first year or randomised to medical management and did not receive surgery in the first year).
-
Preference ITT population (groups that preferred either surgery or medical management at recruitment).
-
Preference PP population (groups that either preferred surgery at recruitment and received surgery in the first year or preferred medical management and did not receive surgery in the first year).
The primary outcome measure (REFLUX QoL score) and secondary outcome measures (SF-36, EQ-5D, REFLUX symptom scores, anti-reflux surgery and use of reflux-related drugs) were analysed using general linear models. The analyses adjusted for the minimisation covariates (age, BMI and sex) and where appropriate (defined by significant at the 5% significance level) also adjusted for baseline measures and baseline measures by treatment interaction. A secondary, pre-stated subgroup analysis explored the differential effects of surgeon's preferred operative procedure on the primary outcome measure. All analyses were reported with 95% confidence intervals (CIs).
The primary analysis of the randomised groups was by ITT. The ITT approach sustains the integrity of the randomisation and gives the least biased estimate of effectiveness of the two forms of management. Given that a sizeable minority of the randomised surgical participants did not receive surgery, we were also interested in estimating the efficacy of the initial treatment received as a secondary comparison (i.e. commonly known as a PP analysis). In an open trial design a PP analysis can have substantial selection bias. To minimise the effects of selection bias we used the method of ‘adjusted treatment received’ as described by Nagelkerke et al. 38 and others. 39,40 The method used a two-stage least-squares approach whereby treatment randomised was regressed onto treatment received and the residuals from that model were used as an independent variable in a second model, together with the treatment received, to estimate the effects on the various primary and secondary outcome measures.
For the preference study, only the primary outcome was analysed statistically. The analysis compared the preference surgical group with the preference medical group and adjusted for the minimisation factors. As described above, for logistical reasons and to maintain balance between the randomised and preference groups, we capped the number of preference participants at 20 per group per centre. The study design was not therefore a true comprehensive cohort. We did consider modelling differences between the randomised and preference groups; however, it is not universally accepted that formal modelling is appropriate in this context. In this case we knew from the randomised arms that there was a strong interaction between treatment effects and baseline REFLUX QoL, and in addition we knew that there was a large difference in QoL between preference arms at baseline (and patient demographics such as age and sex). We therefore decided that formal modelling of the arms would add little to the comparison given the large confounding between preference groups.
Sensitivity analyses
The sensitivity of the primary outcome analysis result was investigated using two approaches – the effect of excluding a large centre and the effects of missing data. In the first approach the largest recruiting centre, Aberdeen, was excluded and the analysis as described above was rerun. Second, previous work demonstrated that the primary outcome was likely missing at random (MAR) or missing completely at random (MCAR) and that a repeated measures analysis (using all available data) was an appropriate statistical method for analysing data up to 12 months. 41 We therefore used a repeated measures analysis on the primary outcome across all of the follow-up data (12 months to 5 years) to investigate the effect of incorporating a profile of measures for each participant. No further imputation for missing values was necessary.
Data monitoring
During recruitment, an independent DMC met on three occasions and each time saw no reason to recommend any fundamental changes to the protocol. The committee did not meet after recruitment was completed.
Chapter 3 Trial results and clinical effectiveness
Recruitment to the trial
Participants were recruited in 21 clinical centres, all within the UK (their locations are listed on the left-hand side of Table 1). Recruitment to the trial was open from March 2001 until the end of June 2004, although not all centres enrolled over the total period because of the staggered introduction of centres and early closure for logistical reasons in a few places. 1
| Randomised participants, n (%) | Preference participants, n (%) | |||
|---|---|---|---|---|
| Surgical (n = 178) | Medical (n = 179) | Surgical (n = 261) | Medical (n = 192) | |
| Aberdeen: Aberdeen Royal Infirmary | 38 (21.3) | 40 (22.3) | 20 (7.7) | 21 (10.9) |
| Belfast: Royal Victoria Hospital | 15 (8.4) | 14 (7.8) | 4 (1.5) | 20 (10.4) |
| Bournemouth: Royal Bournemouth Hospital | 4 (2.2) | 3 (1.7) | 20 (7.7) | 3 (1.6) |
| Bristol: Bristol Royal Infirmary | 12 (6.7) | 11 (6.1) | 18 (6.9) | 20 (10.4) |
| Bromley: Princess Royal Infirmary | 3 (1.7) | 3 (1.7) | 20 (7.7) | 17 (8.9) |
| Edinburgh: Royal Infirmary of Edinburgh | 11 (6.2) | 11 (6.1) | 1 (0.4) | 15 (7.8) |
| Guildford: Royal Surrey County Hospital | 10 (5.6) | 10 (5.6) | 17 (6.5) | 10 (5.2) |
| Hull: Hull Royal Infirmary | 7 (3.9) | 7 (3.9) | 1 (0.4) | 2 (1.0) |
| Inverness: Raigmore Hospital | 7 (3.9) | 8 (4.5) | 2 (0.8) | 8 (4.2) |
| Leeds: Leeds General Infirmary | 1 (0.6) | 2 (1.1) | 10 (3.8) | 3 (1.6) |
| Leicester: Leicester Royal Infirmary | 0 (0.0) | 0 (0.0) | 3 (1.1) | 1 (0.5) |
| London: St Mary's Hospital | 8 (4.5) | 7 (3.9) | 4 (1.5) | 10 (5.2) |
| London: Whipps Cross Hospital | 4 (2.2) | 3 (1.7) | 16 (6.1) | 5 (2.6) |
| Poole: Poole Hospital | 10 (5.6) | 10 (5.6) | 25 (9.6) | 13 (6.8) |
| Portsmouth: Queen Alexandra Hospital | 10 (5.6) | 10 (5.6) | 15 (5.7) | 1 (0.5) |
| Salford: Hope Hospital | 0 (0.0) | 1 (0.6) | 6 (2.3) | 3 (1.6) |
| Stoke-on-Trent: North Staffordshire Hospital | 5 (2.8) | 6 (3.4) | 20 (7.7) | 9 (4.7) |
| Swansea: Morriston Hospital | 8 (4.5) | 8 (4.5) | 14 (5.4) | 9 (4.7) |
| Telford: Princess Royal Hospital | 11 (6.2) | 12 (6.7) | 24 (9.2) | 8 (4.2) |
| Yeovil: Yeovil District Hospital | 9 (5.1) | 8 (4.5) | 18 (6.9) | 8 (4.2) |
| York: York District Hospital | 5 (2.8) | 5 (2.8) | 3 (1.1) | 6 (3.1) |
| Total | 178 (100) | 179 (100) | 261 (100) | 192 (100) |
A total of 357 participants were recruited to the randomised component: 178 allocated to surgery and 179 allocated medical management. 453 participants agreed to join the preference component: 261 choosing surgery and 192 choosing medical management. Table 1 shows recruitment by centre. Around one-fifth of the randomised participants were enrolled in Aberdeen; no centre contributed > 10% of participants in the preference component.
Analysis populations
Throughout the analyses presented later in this chapter, the participants in the randomised component are kept separate from those in the preference component (other than for rare surgical events). The numbers of participants in each of the four main analysis populations are shown in Table 2. All 357 who joined the randomised component are in the randomised ITT population; only the 280 within this group who actually received their allocated management over the first year are in the randomised PP population. All 453 participants who joined the preference component are in the preference ITT population; the 407 of these who, by the end of the first year, were managed as originally chosen were in the preference PP population.
| Surgical, n (%) | Medical, n (%) | Total, n | |
|---|---|---|---|
| Randomised ITT | 178 (49.9) | 179 (50.1) | 357 |
| Randomised PP | 111 (39.6) | 169 (60.4) | 280 |
| Preference ITT | 261 (57.6) | 192 (42.4) | 453 |
| Preference PP | 218 (53.6) | 189 (46.4) | 407 |
Trial conduct
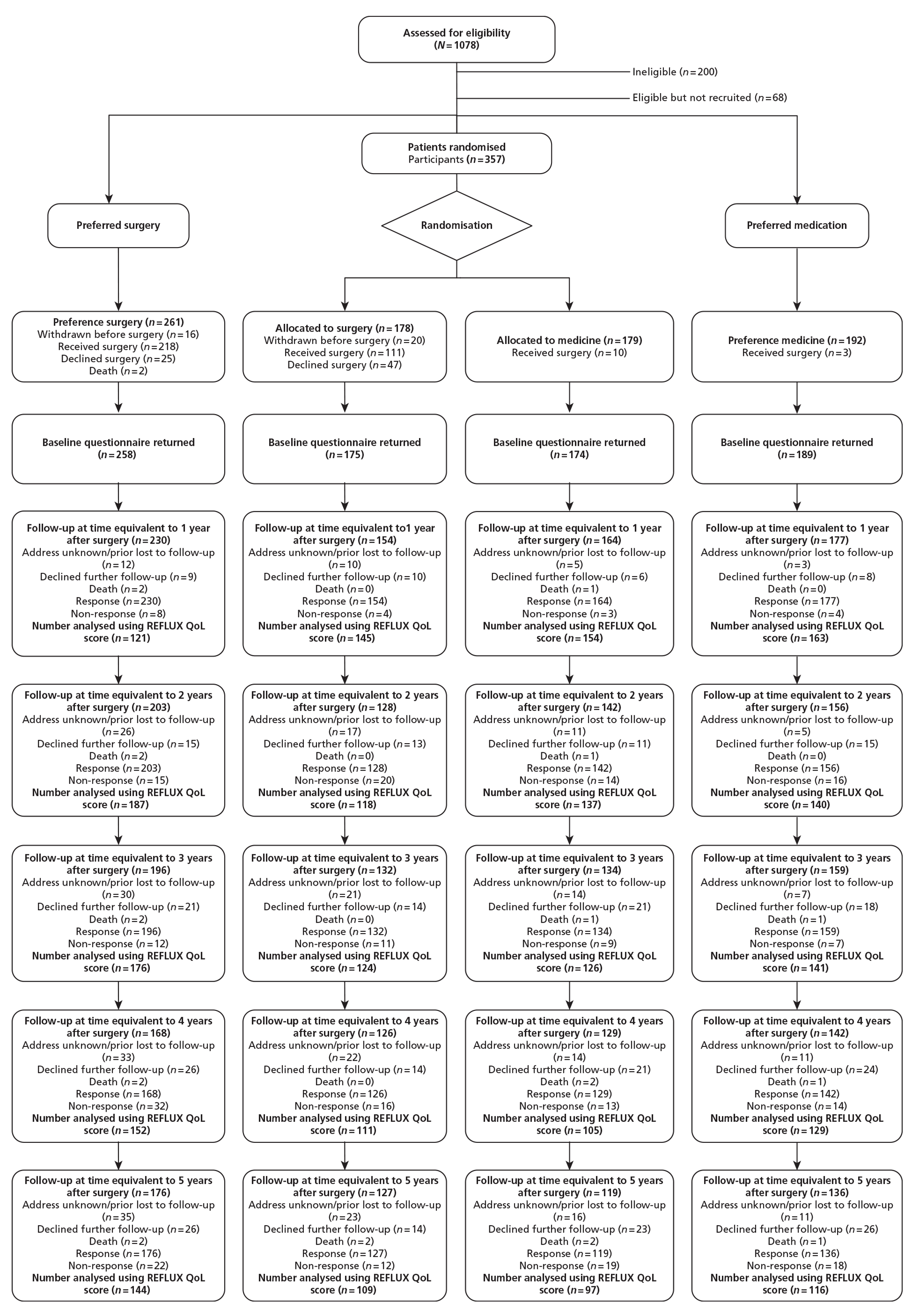
The derivation of the main study groups and their progress through the stages of follow-up in the trial are shown in Figure 1. This is in the form of a CONSORT (Consolidated Standards of Reporting Trials) flow diagram. In total, 1078 patients were considered for trial entry and 200 of these were found not to meet one or more of the eligibility criteria. Of the 68 patients eligible for the study but not recruited, 51 declined to participate, six were subsequently deemed inappropriate for the study by the surgeon responsible for care and the remaining 11 were missed.
FIGURE 1.
The CONSORT diagram.
Details of the clinical management actually received are described later in this chapter.
The mean (SD) time intervals in months between the receipt by the trial office of each subsequent annual postal questionnaire are shown in Table 3; all were near 12 months, as would be expected. There was, however, a difference between the randomised groups in the time interval between the 1-year and the 2-year questionnaires (mean 12.2 months surgical group vs 13.9 months medical group). In part, this was due to more late returns in the medical management group – the median intervals were closer: 12.00 and 13.00 months respectively. As described previously,1 early follow-up was adjusted to be at a time equivalent to 3 and 12 months after surgery. The adjustments in the medical group to match this could be only approximate and this is the explanation for the difference that remained between the randomised groups. An advantage of long-term follow-up to 5 years is that any difference in the timing of follow-up becomes proportionately smaller over time.
| Randomised participants | Preference participants | |||
|---|---|---|---|---|
| Surgical | Medical | Surgical | Medical | |
| ITT (n = 178) | ITT (n = 179) | ITT (n = 261) | ITT (n = 192) | |
| 1 year to 2 years | 12.2 (1.9) | 13.9 (3.1) | 12.4 (1.8) | 12.9 (4.6) |
| 2 years to 3 years | 11.8 (1.2) | 11.6 (1.2) | 11.6 (1.5) | 11.8 (1.2) |
| 3 years to 4 years | 12.0 (1.5) | 12.0 (1.4) | 12.1 (1.2) | 12.0 (1.1) |
| 4 years to 5 years | 11.8 (1.3) | 12.0 (1.3) | 12.1 (1.5) | 12.0 (1.3) |
More details of the response rates to the annual questionnaires are provided in Table 4. The overall rates of return of annual follow-up questionnaires (years 1–5) were 89.5%, 77.7%, 76.7%, 69.8% and 68.9% of the study participants. Seven participants are known to have died up to the end of the 5-year follow-up; equivalent response rates among those not known to have died are 89.8%, 77.9%, 77.0%, 70.2% and 69.5%. There were no substantive differences in response rates between the groups.
| Year | Category | Randomised participants, n (%) | Preference participants, n (%) | ||
|---|---|---|---|---|---|
| Surgical (n = 178) | Medical (n = 179) | Surgical (n = 261) | Medical (n = 192) | ||
| 1 | Responded | 154 (87) | 164 (92) | 230 (88) | 177 (92) |
| Declined further follow-up | 10 (6) | 6 (3) | 9 (3) | 8 (4) | |
| Deceased | 0 (0) | 1 (1) | 2 (1) | 0 (0) | |
| Address unknown/lost to follow-up | 10 (6) | 5 (3) | 12 (5) | 3 (2) | |
| Non-responder | 4 (2) | 3 (2) | 8 (3) | 4 (2) | |
| 2 | Responded | 128 (72) | 142 (79) | 203 (78) | 156 (81) |
| Declined further follow-up | 13 (7) | 11 (6) | 15 (6) | 15 (8) | |
| Deceased | 0 (0) | 1 (1) | 2 (1) | 0 (0) | |
| Address unknown/lost to follow-up | 17 (10) | 11 (6) | 26 (10) | 5 (3) | |
| Non-responder | 20 (11) | 14 (8) | 15 (6) | 16 (8) | |
| 3 | Responded | 132 (74) | 134 (75) | 196 (75) | 159 (83) |
| Declined further follow-up | 14 (8) | 21 (12) | 21 (8) | 18 (9) | |
| Deceased | 0 (0) | 1 (1) | 2 (1) | 1 (1) | |
| Address unknown/lost to follow-up | 21 (12) | 14 (8) | 30 (11) | 7 (4) | |
| Non-responder | 11 (6) | 9 (5) | 12 (5) | 7 (4) | |
| 4 | Responded | 126 (71) | 129 (72) | 168 (64) | 142 (74) |
| Declined further follow-up | 14 (8) | 21 (12) | 26 (10) | 24 (13) | |
| Deceased | 0 (0) | 2 (1) | 2 (1) | 1 (1) | |
| Address unknown/lost to follow-up | 22 (12) | 14 (8) | 33 (13) | 11 (6) | |
| Non-responder | 16 (9) | 13 (7) | 32 (12) | 14 (7) | |
| 5 | Responded | 127 (71) | 119 (66) | 176 (67) | 136 (71) |
| Declined further follow-up | 14 (8) | 23 (13) | 26 (10) | 26 (14) | |
| Deceased | 2 (1) | 2 (1) | 2 (1) | 1 (1) | |
| Address unknown/lost to follow-up | 23 (13) | 16 (9) | 35 (13) | 11 (6) | |
| Non-responder | 12 (7) | 19 (11) | 22 (8) | 18 (9) | |
Three participants died before the 1-year follow-up was reached: two in the preference surgery group and one in the randomised medical group. None of these participants actually had surgery. Four died subsequently; there is no evidence linking these deaths to trial participation.
Description of the groups at trial entry
Sociodemographic and clinical factors
Table 5 provides a description of the groups at trial entry. The main division within the table is between participants in the randomised component and those in the preference component. These two halves of the table are further divided according to the allocation of participants and then subdivided according to ITT or PP.
| Characteristic | Randomised participants | Preference participants | ||||||
|---|---|---|---|---|---|---|---|---|
| Surgical | Medical | Surgical | Medical | |||||
| ITT (n = 178) | PP (n = 111) | ITT (n = 179) | PP (n = 169) | ITT (n = 261) | PP (n = 218) | ITT (n = 192) | PP (n = 189) | |
| Baseline questionnaire returned, n (%) | 175 (98.3) | 111 (100.0) | 174 (97.2) | 165 (97.6) | 256 (98.1) | 216 (99.1) | 189 (98.4) | 186 (98.4) |
| Age (years), mean (SD) | 46.7 (10.3) | 46.3 (10.2) | 45.9 (11.9) | 45.9 (11.9) | 44.4 (12.0) | 44.5 (12.2) | 49.9 (11.8) | 50 (11.7) |
| Male, n (%) | 116 (65.2) | 68 (61.3) | 120 (67.0) | 115 (68.0) | 170 (65.1) | 139 (63.8) | 111 (57.8) | 110 (58.2) |
| BMI (kg/m2), mean (SD) | 28.5 (4.3) | 28.7 (4.1) | 28.4 (4.0) | 28.3 (4.0) | 27.7 (4.0) | 27.5 (3.7) | 27.4 (4.1) | 27.4 (4.1) |
| Duration of prescribed medication for GORD (months), median (IQR) | 33 (15–83) | 30 (16–76) | 31 (16–71) | 30 (15–71) | 35 (14–71) | 36 (14–65) | 27 (13–60) | 26.5 (13–60) |
| Employment status, n (%) | ||||||||
| Employed full-time | 116 (66.3) | 72 (65.5) | 110 (61.8) | 104 (61.9) | 168 (65.1) | 138 (64.2) | 100 (52.4) | 97 (51.6) |
| Employed part-time | 13 (7.4) | 12 (10.9) | 16 (9.0) | 15 (8.9) | 35 (13.6) | 29 (13.5) | 20 (10.5) | 20 (10.6) |
| Student | 5 (2.9) | 3 (2.7) | 3 (1.7) | 3 (1.8) | 2 (0.8) | 2 (0.9) | 3 (1.6) | 3 (1.6) |
| Retired | 12 (6.9) | 9 (8.2) | 22 (12.4) | 20 (11.9) | 18 (7.0) | 16 (7.4) | 35 (18.3) | 35 (18.6) |
| Housework | 11 (6.3) | 6 (5.5) | 10 (5.6) | 10 (6.0) | 17 (6.6) | 15 (7.0) | 15 (7.9) | 15 (8.0) |
| Seeking work | 6 (3.4) | 1 (0.9) | 3 (1.7) | 2 (1.2) | 5 (1.9) | 5 (2.3) | 2 (1.0) | 2 (1.1) |
| Other | 12 (6.9) | 7 (6.4) | 14 (7.9) | 14 (8.3) | 13 (5.0) | 10 (4.7) | 16 (8.4) | 16 (8.5) |
| Age (years) left full-time education, n (%) | ||||||||
| ≤ 16 | 110 (62.5) | 68 (62.4) | 108 (60.7) | 102 (60.7) | 151 (58.5) | 128 (59.3) | 105 (55.3) | 104 (55.6) |
| 17–19 | 38 (21.6) | 24 (22.0) | 40 (22.5) | 40 (23.8) | 63 (24.4) | 51 (23.6) | 45 (23.7) | 43 (23.0) |
| 20+ | 28 (15.9) | 17 (15.6) | 30 (16.9) | 26 (15.5) | 44 (17.1) | 37 (17.1) | 40 (21.1) | 40 (21.4) |
| Current smoker, n (%) | 46 (25.8) | 29 (26.1) | 40 (22.3) | 36 (21.3) | 71 (27.2) | 61 (28.0) | 39 (20.3) | 39 (20.6) |
| Erosive oesophagitis, n (%) | 85 (54.8) | 48 (50.0) | 97 (62.2) | 91 (62.3) | 104 (46.4) | 80 (43.2) | 87 (50.9) | 86 (51.2) |
| Comorbidity: Helicobacter pylori status, n (%) | ||||||||
| Positive (subsequently treated) | 12 (9.0) | 5 (6.1) | 14 (10.4) | 13 (10.3) | 18 (8.4) | 14 (7.9) | 15 (10.5) | 15 (10.7) |
| Positive (subsequently untreated) | 1 (0.8) | 0 (0.0) | 3 (2.2) | 3 (2.4) | 8 (3.7) | 8 (4.5) | 2 (1.4) | 2 (1.4) |
| Negative | 75 (56.4) | 48 (58.5) | 73 (54.1) | 67 (53.2) | 118 (54.9) | 101 (56.7) | 74 (51.7) | 72 (51.4) |
| Uncertain | 45 (33.8) | 29 (35.4) | 45 (33.3) | 43 (34.1) | 71 (33.0) | 55 (30.9) | 52 (36.4) | 51 (36.4) |
| Hiatus hernia present, n (%) | 94 (57.3) | 64 (61.0) | 102 (60.4) | 94 (59.1) | 168 (68.9) | 146 (71.2) | 101 (59.8) | 99 (59.6) |
| Asthma, n (%) | 21 (11.9) | 14 (12.7) | 21 (11.8) | 19 (11.3) | 30 (11.5) | 23 (10.6) | 36 (18.8) | 36 (19.0) |
Randomised arms
Within the randomised groups there were no apparent imbalances between the medical and surgical intervention arms. The patients were, on average, 46 years old, 66% were men, around two-thirds were in full employment and participants had been on GORD medication for a median of 32 months. The baseline characteristics in the randomised PP groups were similar.
Preference arms
The sociodemographic characteristics of the preference participants were broadly similar to those of the randomised participants. However, preference medical participants tended to be older (mean age 50 years) and were more likely to be female, fewer were in full-time employment and participants had been on GORD medication for a shorter period (approximately 6 months less than randomised participants).
Prescribed medications
The prescribed medications at the time of trial entry are shown in Table 6. There was a similar profile of prescribed medications across the randomised and preference groups. As would be expected, nearly all participants reported taking a reflux-related drug in the previous 2 weeks. Over 90% had taken a PPI, of which lansoprazole was the most common.
| Medication | Randomised participants | Preference participants | ||||||
|---|---|---|---|---|---|---|---|---|
| Surgical | Medical | Surgical | Medical | |||||
| ITT (n = 178) | PP (n = 111) | ITT (n = 179) | PP (n = 169) | ITT (n = 261) | PP (n = 218) | ITT (n = 192) | PP (n = 189) | |
| PPIs, n (%) | ||||||||
| Any PPI | 161 (92.0) | 105 (94.6) | 162 (93.1) | 153 (92.7) | 225 (87.9) | 191 (88.4) | 173 (91.5) | 170 (91.4) |
| Omeprazole | 46 (26.3) | 32 (28.8) | 46 (26.4) | 43 (26.1) | 49 (19.1) | 36 (16.7) | 61 (32.3) | 61 (32.8) |
| Lansoprazole | 77 (44.0) | 47 (42.3) | 72 (41.4) | 69 (41.8) | 100 (39.1) | 92 (42.6) | 69 (36.5) | 66 (35.5) |
| Pantoprazole | 6 (3.4) | 6 (5.4) | 11 (6.3) | 11 (6.7) | 21 (8.2) | 17 (7.9) | 11 (5.8) | 11 (5.9) |
| Rabeprazole | 12 (6.9) | 6 (5.4) | 13 (7.5) | 13 (7.9) | 21 (8.2) | 16 (7.4) | 14 (7.4) | 14 (7.5) |
| Esomeprazole | 20 (11.4) | 14 (12.6) | 20 (11.5) | 17 (10.3) | 37 (14.5) | 33 (15.3) | 18 (9.5) | 18 (9.7) |
| H2RAs, n (%) | ||||||||
| Any H2RA | 14 (8.0) | 6 (5.4) | 12 (6.9) | 9 (5.5) | 22 (8.6) | 16 (7.4) | 13 (6.9) | 13 (7.0) |
| Ranitidine | 13 (7.4) | 6 (5.4) | 8 (4.6) | 6 (3.6) | 11 (4.3) | 7 (3.2) | 11 (5.8) | 11 (5.9) |
| Famotidine | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.4) | 1 (0.5) | 1 (0.5) | 1 (0.5) |
| Cimetidine | 1 (0.6) | 0 (0.0) | 1 (0.6) | 0 (0.0) | 1 (0.4) | 1 (0.5) | 0 (0.0) | 0 (0.0) |
| Nizatidine | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (1.2) | 3 (1.4) | 0 (0.0) | 0 (0.0) |
| Over-the-counter H2RA | 0 (0.0) | 0 (0.0) | 4 (2.3) | 3 (1.8) | 7 (2.7) | 4 (1.9) | 2 (1.1) | 2 (1.1) |
| Prokinetics, n (%) | ||||||||
| Any prokinetics | 12 (6.9) | 7 (6.3) | 8 (4.6) | 6 (3.6) | 11 (4.3) | 10 (4.6) | 5 (2.6) | 4 (2.2) |
| Domperidone | 8 (4.6) | 5 (4.5) | 4 (2.3) | 3 (1.8) | 7 (2.7) | 6 (2.8) | 4 (2.1) | 3 (1.6) |
| Metoclopramide | 4 (2.3) | 2 (1.8) | 4 (2.3) | 3 (1.8) | 4 (1.6) | 4 (1.9) | 1 (0.5) | 1 (0.5) |
| Any reflux-related drug, n (%) | 170 (97.1) | 108 (97.3) | 169 (97.1) | 160 (97.0) | 235 (91.8) | 198 (91.7) | 184 (97.4) | 181 (97.3) |
| Other prescribed drugs, n (%)a | ||||||||
| Alginates | 22 | 12 | 21 | 18 | 37 | 33 | 14 | 13 |
| Antispasmodics (e.g. dicycloverine) | 0 | 0 | 2 | 2 | 3 | 3 | 0 | 0 |
| Chelates (e.g. sucralfate) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other ulcer-healing drugs | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| Mucogel® (Chemidex) | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| Asilone® (Thornton & Ross) | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| Non-gastrointestinal | 7 | 2 | 4 | 4 | 5 | 4 | 6 | 6 |
| Anti-nausea | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
Health status
Randomised arms
The HRQoL scores at study entry are displayed in Table 7. The scores were broadly similar in the randomised surgical and randomised medical groups, although they were slightly higher (better health) in the randomised medical group. When the DMC first met after the initial 143 participants had been recruited to the randomised component, the committee did ask us to change the enrolment procedure to ensure that baseline questionnaires were completed before formal entry and randomisation. We understand that this was because they were concerned about an apparent imbalance between the randomised groups in baseline health status at that time. After satisfying themselves that this was not due to a breakdown in the randomisation procedure, the DMC surmised that this might be due to prior knowledge of the treatment allocation affecting questionnaire responses (with those allocated surgery tending to project worse health status than those allocated medical management). Certainly, the groups based on the first 143 participants were well balanced in other respects, and there was subsequently good balance in health status as well. The apparent small imbalance between the randomised groups in health status measures is therefore likely to be a reflection of the imbalance in the first 143 participants.
| HRQoL instrument | Randomised participants | Preference participants | ||||||
|---|---|---|---|---|---|---|---|---|
| Surgical | Medical | Surgical | Medical | |||||
| ITT (n = 178) | PP (n = 111) | ITT (n = 179) | PP (n = 169) | ITT (n = 261) | PP (n = 218) | ITT (n = 192) | PP (n = 189) | |
| REFLUX QoL, mean (SD) | 63.6 (24.1) | 61.9 (24.5) | 66.8 (24.5) | 68.2 (24.2) | 55.8 (23.2) | 55.9 (23.2) | 77.5 (19.7) | 78.0 (19.1) |
| REFLUX symptom score, mean (SD) | ||||||||
| General discomfort symptom score | 58.5 (24.5) | 57.1 (25.1) | 61.3 (25.8) | 62.4 (25.7) | 49.1 (24.4) | 48.7 (25.2) | 73.1 (21.3) | 73.6 (20.9) |
| Wind and frequency symptom score | 48.1 (20.9) | 46.2 (20.9) | 49.3 (21.4) | 49.5 (21.7) | 47.1 (21.4) | 47.5 (21.2) | 59.6 (22.7) | 59.8 (22.7) |
| Nausea and vomiting symptom score | 81.5 (19.5) | 81.6 (18.8) | 80.7 (21.9) | 81.6 (21.7) | 76.9 (19.9) | 77.5 (19.5) | 89.7 (13.6) | 90.1 (12.9) |
| Activity limitation symptom score | 78.5 (16.9) | 77.6 (16.3) | 78.9 (17.3) | 79.5 (17.1) | 74.4 (16.1) | 73.9 (16.2) | 86.8 (13.0) | 87.0 (13.0) |
| Constipation and swallowing symptom score | 77.5 (19.9) | 77.3 (20.3) | 74.8 (21.0) | 75.6 (20.4) | 75.8 (22.0) | 74.8 (22.6) | 83.0 (17.7) | 83.3 (17.6) |
| SF-36 score, mean (SD) | ||||||||
| Norm-based physical functioning | 46.8 (10.2) | 46.1 (10.3) | 47.5 (10.5) | 47.7 (10.5) | 46.3 (9.4) | 46.1 (9.3) | 47.1 (10.8) | 47.0 (10.9) |
| Norm-based role physical | 46.9 (10.7) | 46.6 (10.8) | 46.8 (10.6) | 47.0 (10.4) | 44.7 (10.9) | 44.6 (10.7) | 46.7 (10.9) | 46.6 (10.9) |
| Norm-based bodily pain | 44.4 (10.1) | 44.1 (9.9) | 44.6 (10.4) | 44.9 (10.3) | 41.8 (9.5) | 41.9 (9.6) | 47.1 (9.8) | 47.2 (9.8) |
| Norm-based general health | 40.9 (9.9) | 40.2 (9.6) | 41.1 (10.6) | 41.4 (10.6) | 40.6 (10.2) | 40.8 (10.0) | 42.4 (10.0) | 42.4 (9.9) |
| Norm-based vitality | 43.5 (10.5) | 43.9 (10.3) | 44.0 (11.7) | 44.4 (11.4) | 42.8 (11.1) | 42.8 (11.3) | 45.5 (10.7) | 45.6 (10.7) |
| Norm-based social functioning | 44.4 (11.1) | 44.1 (10.6) | 44.7 (11.7) | 45.2 (11.5) | 42.2 (11.6) | 42.1 (11.5) | 46.8 (10.2) | 46.7 (10.2) |
| Norm-based role emotional | 46.6 (11.5) | 47.2 (11.5) | 45.8 (12.9) | 46.3 (12.6) | 45.9 (12.2) | 46.1 (12.1) | 46.9 (11.8) | 46.8 (11.8) |
| Norm-based mental health | 46.0 (11.6) | 46.9 (11.0) | 46.7 (11.6) | 47.1 (11.3) | 44.6 (11.4) | 44.6 (11.6) | 46.4 (10.7) | 46.3 (10.8) |
| EQ-5D, mean (SD) | 0.711 (0.258) | 0.718 (0.239) | 0.720 (0.255) | 0.732 (0.246) | 0.682 (0.259) | 0.679 (0.259) | 0.750 (0.223) | 0.752 (0.222) |
| EQ-5DVAS, mean (SD) | 68.6 (17.1) | 69.2 (15.9) | 70.5 (18.1) | 71.2 (17.6) | 67.2 (18.5) | 67.0 (18.5) | 71.3 (16.7) | 71.5 (16.6) |
The most prevalent reflux symptoms (those with lowest scores) were general discomfort and wind. The participants had lower SF-36 and EQ-5D scores than a normal UK population with the same average age and sex characteristics (SF-36 population norm approximately 50 for all domains; EQ-5D norm 0.88).
Preference arms
The preference for surgery participants reported worse REFLUX QoL scores and worse health in general than the preference for medicine participants. It can be seen from Table 7 that the randomised participants reported QoL measures in between these two extremes.
Baseline characteristics of groups compared at 5 years
There were differences in baseline characteristics between those who had completed a questionnaire at 5 years and those who had not (Table 8). For example, responders had a higher mean age (47.9 years vs 43.6 years), had been on prescribed medication for a shorter period at recruitment to the REFLUX trial (50.5 months vs 60.2 months) and had higher QoL scores at baseline (measured on the disease-specific REFLUX instrument, EQ-5D and SF-36).
| Characteristic | Responder (max. n = 558) | Non-responder (max. n = 252) | p-value (two- sided) |
|---|---|---|---|
| BMI (kg/m2), mean (SD), n | 27.9 (4.0), 557 | 28.2 (4.3), 252 | 0.37 |
| Age (years), mean (SD), n | 47.9 (11.2), 558 | 43.6 (12.2), 252 | < 0.01 |
| Sex, n/N (%) | |||
| Male | 343/558 (61) | 174/252 (69) | 0.04 |
| Female | 215/558 (39) | 78/252 (31) | – |
| Duration of prescribed medication (months), mean (SD), n | 50.5 (62.9), 544 | 60.2 (65.2), 250 | 0.05 |
| Erosive oesophagitis, n/N (%) | |||
| Yes | 262/493 (53) | 111/213 (52) | 0.78 |
| No | 231/493 (47) | 102/213 (48) | |
| Helicobacter pylori status, n/N (%) | |||
| Positive (subsequently treated) | 39/440 (9) | 20/186 (11) | 0.81 |
| Positive (subsequently untreated) | 9/440 (2) | 5/186 (3) | – |
| Negative | 238/440 (54) | 102/186 (55) | – |
| Uncertain | 154/440 (35) | 59/186 (32) | – |
| Hiatus hernia, n/N (%) | |||
| Yes | 330/524 (63) | 135/222 (61) | 0.58 |
| No | 194/524 (37) | 87/222 (39) | – |
| Age (years) left full-time education, n/N (%) | |||
| ≤ 16 | 304/552 (55) | 170/250 (68) | < 0.01 |
| 17–19 | 143/552 (26) | 43/250 (17) | – |
| 20+ | 105/552 (19) | 37/250 (15) | – |
| Employment status, n/N (%) | |||
| Full-time | 348/551 (63) | 146/251 (58) | 0.01 |
| Part-time | 65/551 (12) | 19/251 (8) | – |
| Student | 6/551 (1) | 7/251 (3) | – |
| Retired | 62/551 (11) | 25/251 (10) | – |
| Housework | 32/551 (6) | 21/251 (8) | – |
| Seeking work | 10/551 (2) | 6/251 (2) | – |
| Other | 28/551 (5) | 27/251 (11) | – |
| REFLUX QoL, mean (SD), n | 66.6 (24.2), 533 | 61.3 (24.1), 226 | < 0.01 |
| REFLUX symptom score, mean (SD), n | |||
| General discomfort symptom score | 61.1 (25.5), 544 | 55.4 (25.4), 231 | < 0.01 |
| Wind and frequency symptom score | 51.5 (21.7), 546 | 48.9 (23.0), 235 | 0.13 |
| Nausea and vomiting symptom score | 83.8 (18.3), 549 | 77.1 (21.5), 239 | < 0.01 |
| Activity limitation symptom score | 79.9 (16.1), 547 | 77.5 (17.4), 232 | 0.06 |
| Constipation and swallowing symptom score | 78.8 (20.0), 550 | 75.2 (21.7), 236 | 0.03 |
| EQ-5D, mean (SD), n | 0.735 (0.234), 544 | 0.662 (0.279), 239 | < 0.01 |
| SF-36 score, mean (SD), n | |||
| SF-36 physical | 45.2 (9.5), 530 | 44.0 (9.7), 232 | 0.10 |
| SF-36 mental | 46.3 (11.2), 530 | 42.7 (12.9), 232 | < 0.01 |
| Norm-based physical functioning | 47.2 (9.9), 545 | 46.1 (10.7), 239 | 0.15 |
| Norm-based role physical | 46.6 (10.7), 546 | 45.0 (11.0), 238 | 0.06 |
| Norm-based bodily pain | 45.1 (10.1), 546 | 42.3 (9.9), 236 | < 0.01 |
| Norm-based general health | 42.0 (9.8), 544 | 39.3 (10.7), 236 | < 0.01 |
| Norm-based vitality | 44.3 (10.8), 549 | 42.8 (11.4), 237 | 0.07 |
| Norm-based social functioning | 45.5 (10.8), 542 | 41.8 (12.0), 237 | < 0.01 |
| Norm-based role emotional | 47.0 (11.5), 543 | 44.5 (13.2), 239 | 0.01 |
| Norm-based mental health | 47.0 (10.6), 549 | 42.9 (12.4), 237 | < 0.01 |
| Any PPI, n/N (%) | 508/552 (92) | 213/242 (88) | 0.07 |
| Any reflux drug, n/N (%) | 530/552 (96) | 225/242 (93) | 0.07 |
However, the baseline characteristics of those in the randomised surgical and randomised medical groups who completed a questionnaire at 5 years were very similar, with the only notable difference being in BMI (Table 9). The mean baseline BMI among responders in the randomised surgical group was higher (29.0 kg/m2) than that for responders in the randomised medical management group (27.7 kg/m2). As described in Chapter 2, these results confirmed that a repeated measures analysis assuming no differential loss to follow-up could be considered.
| Characteristic | Surgical (max. n = 127) | Medical (max. n = 119) | p-value (two-sided) |
|---|---|---|---|
| BMI (kg/m2), mean (SD), n | 29.0 (4.3), 127 | 27.7 (3.8), 119 | 0.01 |
| Age (years), mean (SD), n | 48.5 (9.3), 127 | 46.4 (11.6), 119 | 0.12 |
| Sex, n/N (%) | |||
| Male | 79/127 (62) | 76/119 (64) | 0.79 |
| Female | 48/127 (38) | 43/119 (36) | – |
| Duration of prescribed medication (months), mean (SD), n | 57.2 (63.4), 124 | 46.3 (60.1), 117 | 0.17 |
| Erosive oesophagitis, n/N (%) | |||
| Yes | 63/111 (57) | 68/107 (64) | 0.35 |
| No | 48/111 (43) | 39/107 (36) | – |
| Helicobacter pylori status, n/N (%) | |||
| Positive (subsequently treated) | 6/96 (6) | 10/91 (11) | 0.52 |
| Positive (subsequently untreated) | 1/96 (1) | 2/91 (2) | – |
| Negative | 55/96 (57) | 45/91 (49) | – |
| Uncertain | 34/96 (35) | 34/91 (37) | – |
| Hiatus hernia, n/N (%) | |||
| Yes | 73/117 (62) | 71/114 (62) | 0.99 |
| No | 44/117 (38) | 43/114 (38) | – |
| Age (years) left full-time education, n/N (%) | |||
| ≤ 16 | 77/125 (62) | 70/119 (59) | 0.46 |
| 17–19 | 27/125 (22) | 31/119 (26) | – |
| 20+ | 21/125 (17) | 18/119 (15) | – |
| Employment status, n/N (%) | |||
| Full-time | 86/124 (69) | 76/118 (64) | 0.77 |
| Part time | 13/124 (10) | 10/118 (8) | – |
| Student | 2/124 (2) | 1/118 (1) | – |
| Retired | 9/124 (7) | 13/118 (11) | – |
| Housework | 4/124 (3) | 7/118 (6) | – |
| Seeking work | 4/124 (3) | 3/118 (3) | – |
| Other | 6/124 (5) | 8/118 (7) | – |
| REFLUX QoL, mean (SD), n | 65.9 (23.7), 121 | 68.6 (24.0), 110 | 0.38 |
| REFLUX symptom score, mean (SD), n | |||
| General discomfort symptom score | 60.1 (24.1), 123 | 63.9 (25.2), 115 | 0.23 |
| Wind and frequency symptom score | 48.0 (19.7), 125 | 48.7 (20.9), 117 | 0.78 |
| Nausea and vomiting symptom score | 82.9 (18.9), 125 | 84.7 (18.9), 117 | 0.46 |
| Activity limitation symptom score | 79.9 (15.2), 124 | 79.9 (16.8), 117 | 0.99 |
| Constipation and swallowing symptom score | 78.2 (19.2), 124 | 75.9 (20.0), 118 | 0.35 |
| EQ-5D, mean (SD), n | 0.736 (0.223), 122 | 0.755 (0.228), 118 | 0.51 |
| SF-36 score, mean (SD), n | |||
| SF-36 physical | 44.8 (10.0), 121 | 46.1 (9.1), 114 | 0.30 |
| SF-36 mental | 46.6 (11.0), 121 | 46.5 (11.1), 114 | 0.98 |
| Norm-based physical functioning | 46.8 (10.0), 123 | 48.4 (10.2), 117 | 0.22 |
| Norm-based role physical | 46.9 (10.8), 124 | 47.0 (10.8), 116 | 0.96 |
| Norm-based bodily pain | 44.6 (10.1), 123 | 45.7 (10.1), 117 | 0.39 |
| Norm-based general health | 41.4 (9.4), 124 | 42.4 (10.2), 116 | 0.41 |
| Norm-based vitality | 43.9 (10.4), 125 | 44.9 (11.2), 117 | 0.47 |
| Norm-based social functioning | 45.4 (10.5), 124 | 46.4 (10.8), 115 | 0.45 |
| Norm-based role emotional | 47.2 (11.4), 124 | 46.7 (12.1), 116 | 0.74 |
| Norm-based mental health | 47.3 (10.9), 125 | 48.0 (10.6), 117 | 0.60 |
| Any PPI, n/N (%) | 120/125 (96) | 109/118 (92) | 0.23 |
| Any reflux drug, n/N (%) | 124/125 (99) | 113/118 (96) | 0.08 |
Surgical management
Table 10 summarises the use of surgery in the four study groups over the full 5-year follow-up period. At the end of the first year, 111 participants (62.4%) randomised to surgery had actually undergone fundoplication. Over the next 4 years, one more member of this group had fundoplication, bringing the total to 112 (62.9%). In the randomised medical group, 10 participants (5.6%) had fundoplication in the first year, with a further 14 participants having fundoplication in subsequent years, bringing the total at 5 years to 24 (13.4%). In the preference surgical group, 218 participants (83.5%) had fundoplication in the first year, with four more in the period up to 5 years, taking the percentage to 85.1%. Surgical management applied to only three participants (1.6%) in the preference medical group in the first year, with a further three being operated on in the subsequent 4 years (total 3.1%).
| Surgery | Randomised participants | Preference participants | ||
|---|---|---|---|---|
| Surgical (n = 178) | Medical (n = 179) | Surgical (n = 261) | Medical (n = 192) | |
| First fundoplication in first year, n (%) | 111 (62.4) | 10 (5.6) | 218 (83.5) | 3 (1.6) |
| First fundoplication after first year, n | 1 | 14 | 4 | 3 |
| In second year | 0 | 1 | 2 | 0 |
| In third year | 0 | 7 | 1 | 2 |
| In fourth year | 1 | 4 | 1 | 1 |
| In fifth year | 0 | 2 | 0 | 0 |
| Fundoplication at any time during 5-year follow-up, n (%) | 112 (62.9) | 24 (13.4) | 222 (85.1) | 6 (3.1) |
Information about the reasons why participants allocated surgery did not receive it in the first year is available for 47. For 25 of these 47, this was a clinical decision, most commonly the surgeon deciding that surgery was not appropriate; most of the other 22 changed their minds about surgery for a variety of work- or home-related reasons. A further 20 withdrew for unknown reasons. There is no doubt, however, that a number of these participants suffered long delays before being formally offered surgery, and this was an important factor in their eventual decision to choose not to have surgery after all. The trial was conducted at a time when there was great pressure on surgical services in the NHS, with long delays for elective surgery for non-life-threatening benign conditions being common. Indeed, the average time between trial entry and surgery in the trial was 8–9 months. 1
Details of the surgery received by the 111 participants (62.4%) randomised to surgery and the 218 preference participants (83.5%) who actually received surgery in the first year, the perioperative complications that they experienced and their hospital stay have been reported previously but are summarised in Appendix 2 for completeness. There were no perioperative deaths.
Table 11 shows the numbers of those who had fundoplication who subsequently had a second reflux-related operation during the 5 years of follow-up. Overall, this applied to 16 participants (4.4%) among the 364 who had a first operation: five (4.5%) in the randomised surgery group; one (4.2%) in the randomised medical group; eight (3.6%) in the preference surgery group; and two (33.3%) in the preference medical group. In total, five of the 16 operations were reconstructions of the same wrap, three were repairs of hiatus hernia only, six were conversions to a different type of wrap and two were reversals of the fundoplication. Two of these 16 participants had a third reflux-related operation; both were in the preference surgery group – one a reconstruction of the same wrap and one a repair of hiatus hernia only.
| Surgery | Randomised participants | Preference participants | Total cohort | ||
|---|---|---|---|---|---|
| Surgical (n = 178) | Medical (n = 179) | Surgical (n = 261) | Medical (n = 192) | ||
| First fundoplication operation at any time, n | 112 | 24 | 222 | 6 | 364 |
| Second reflux-related reoperation, n (%) | 5 (4.5) | 1 (4.2) | 8 (3.6) | 2 (33.3) | 16 (4.4) |
| Reconstruction of same wrap | 2 | 1 | 1 | 1 | 5 |
| Repair of hiatus hernia only | 1 | 0 | 2 | 0 | 3 |
| Conversion of type of wrap | 2 | 0 | 4 | 0 | 6 |
| Reversal of fundoplication | 0 | 0 | 1 | 1 | 2 |
| Third reflux-related reoperation, n | |||||
| Reconstruction of same wrap | 0 | 0 | 1 | 0 | 1 |
| Repair of hiatus hernia only | 0 | 0 | 1 | 0 | 1 |
| Conversion of type of wrap | 0 | 0 | 0 | 0 | 0 |
| Reversal of fundoplication | 0 | 0 | 0 | 0 | 0 |
Late postoperative complications
Table 12 describes late postoperative complications among those participants who had surgery, in each of the study groups and overall. Of the total 364 who had fundoplication, 12 (3.3%) had a late complication: four (1.1%) were oesophageal dilatations/stricture dilatations; three (0.8%) were repairs of incisional hernias; and five (1.4%) were a heterogeneous group of other complications as detailed in the table.
| Complication | Randomised participants | Preference participants | Total cohort | ||
|---|---|---|---|---|---|
| Surgical (n = 178) | Medical (n = 179) | Surgical (n = 261) | Medical (n = 192) | ||
| First fundoplication operation at any time | 112 | 24 | 222 | 6 | 364 |
| Late postoperative complications (within first year of original operation), n | |||||
| Oesophageal dilatation/stricture dilatation | 0 | 0 | 3 | 0 | 3 |
| Repair of incisional hernia | 0 | 0 | 1 | 0 | 1 |
| Other (admission for deep-vein thrombosis/pulmonary embolism) | 0 | 0 | 1 | 0 | 1 |
| Late postoperative complications (within second year following operation), n | |||||
| Oesophageal dilatation/stricture dilatation | 1 | 0 | 0 | 0 | 1 |
| Repair of incisional hernia | 0 | 0 | 0 | 0 | 0 |
| Other (pain from operation; hole between stomach and liver) | 0 | 0 | 1 | 1 | 2 |
| Late postoperative complications (beyond second year), n | |||||
| Oesophageal dilatation/stricture dilatation | 0 | 0 | 0 | 0 | 0 |
| Repair of incisional hernia | 0 | 0 | 2 | 0 | 2 |
| Other (pain due to original wrap shifting; bleed in stomach/bowel) | 1 | 0 | 0 | 1 | 2 |
| Total late postoperative complications, n (%) | 2 (1.8) | 0 (0.0) | 8 (3.6) | 2 (33.3) | 12 (3.3) |
Medication
Figure 2 summarises reported use of any PPI medication in the previous 2 weeks across the follow-up time points of the trial. Full details are provided in the tables in Appendix 3. From the time of the first annual follow-up onwards, rates in both medical groups were consistently around 80%. The rates in the randomised surgical ITT group at the first, second and third annual follow-ups were approximately 36–38%, rising to 43% in the fifth year. The extent to which these rates reflected medication taking among those allocated to surgery and who had fundoplication (rather than those who did not have surgery) can be gauged from the randomised surgery PP group: 7.3% (3 months), 12.5% (1 year), 15.1% (2 years), 19.6% (3 years), 23.9% (4 years) and 25.6% (5 years).
FIGURE 2.
Use of PPI medication at baseline and at follow-up points up to 5 years.
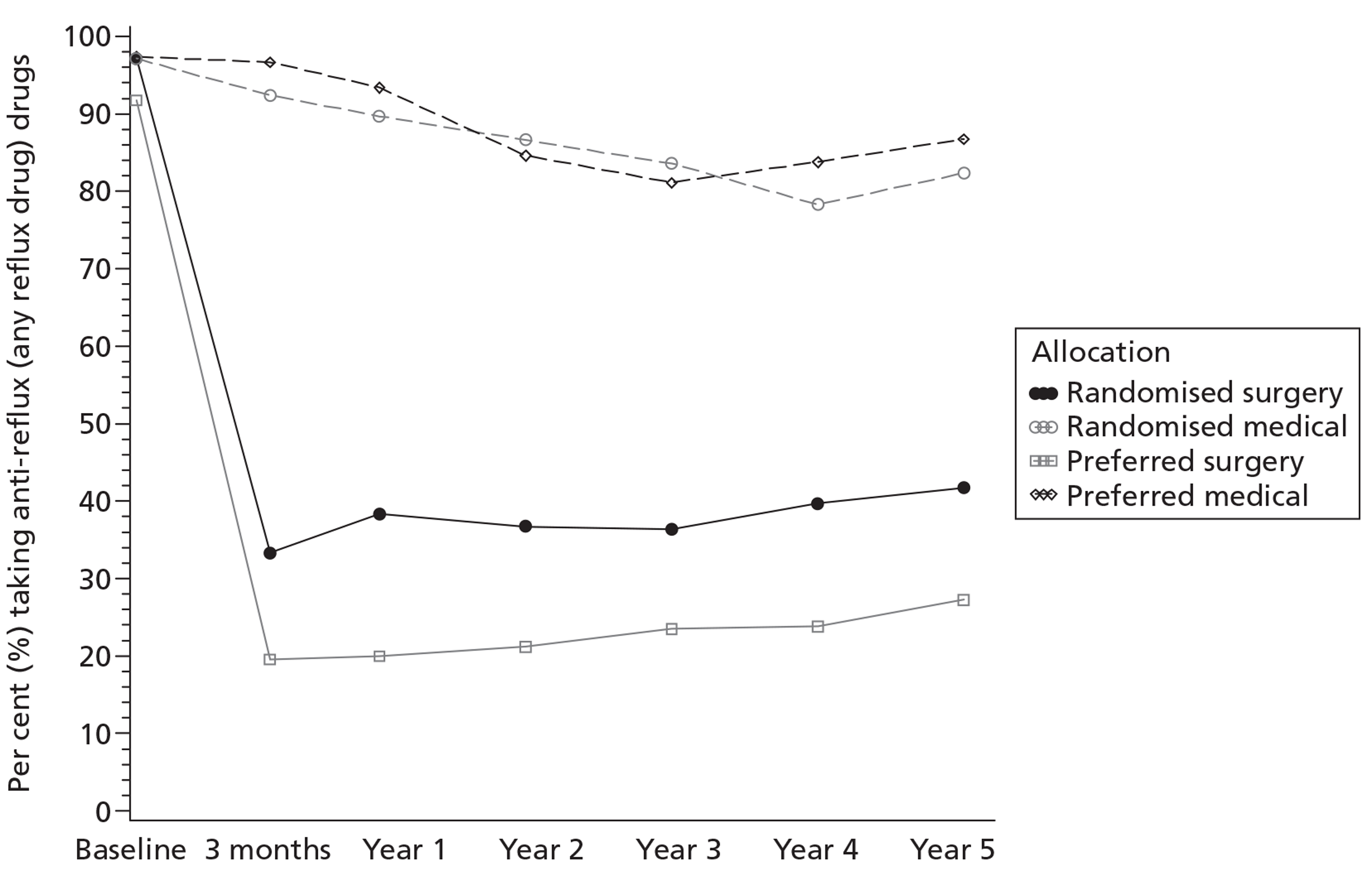
Table 13 allows further exploration of the reasons for the rise in medication use in the randomised surgery group. It distinguishes those reporting taking medication at the end of the first year of follow-up from those who indicated that they were not taking medication at that time. It shows that around 10–20% of those taking medication at the end of the first year did not report medication use at subsequent annual follow-up. Among those not taking medication at the first annual follow-up in the surgical groups, around 10% rising to around 20% reported medication use at subsequent annual follow-up. This contrasts with the rates in the medical groups, with around 50–60% of those not taking medication at the end of the first year reporting anti-reflux drug use in subsequent annual follow-up. The pattern of type of PPI used changed over the course of the study. Although lansoprazole had been the most commonly used PPI at trial entry, omeprazole use increased over time to become the predominant PPI.
| Randomised participants | Preference participants | |||||||
|---|---|---|---|---|---|---|---|---|
| Surgery | Medical | Surgery | Medical | |||||
| ITT | PP | ITT | PP | ITT | PP | ITT | PP | |
| Known whether or not taking medication at end of first year, n | 154 | 104 | 165 | 156 | 232 | 205 | 181 | 178 |
| Group taking anti-reflux drugs at end of the first year | ||||||||
| Taking anti-reflux drugs at end of the first year, n | 51 | 10 | 140 | 137 | 42 | 20 | 154 | 152 |
| Taking any anti-reflux drug at end of, n/N (%) | ||||||||
| Second year | 37/42 (88) | 7/8 (88) | 111/119 (93) | 110/116 (95) | 27/34 (79) | 14/17 (82) | 117/130 (90) | 116/128 (91) |
| Third year | 34/41 (83) | 8/9 (89) | 101/115 (88) | 101/114 (89) | 26/33 (79) | 12/14 (86) | 117/134 (87) | 116/132 (88) |
| Fourth year | 34/41 (83) | 7/9 (78) | 94/112 (84) | 93/110 (85) | 20/28 (71) | 9/13 (69) | 106/119 (89) | 105/117 (90) |
| Fifth year | 33/39 (85) | 8/9 (89) | 89/101 (88) | 88/99 (89) | 20/29 (69) | 10/12 (83) | 105/117 (90) | 103/115 (90) |
| Group not taking anti-reflux drugs at end of the first year | ||||||||
| Not taking anti-reflux drugs at end of first year, n | 103 | 94 | 25 | 19 | 190 | 185 | 27 | 26 |
| Taking any anti-reflux drug at end of, n/N (%) | ||||||||
| Second year | 10/86 (12) | 7/78 (9) | 12/23 (52) | 11/19 (58) | 16/169 (9) | 14/165 (8) | 15/26 (58) | 15/25 (60) |
| Third year | 14/91 (15) | 10/83 (12) | 11/19 (58) | 11/19 (58) | 20/163 (12) | 20/161 (12) | 12/25 (48) | 12/24 (50) |
| Fourth year | 16/85 (19) | 14/79 (18) | 7/17 (41) | 7/17 (41) | 20/140 (14) | 20/139 (14) | 13/23 (57) | 13/22 (59) |
| Fifth year | 20/88 (23) | 16/81 (20) | 9/18 (50) | 9/17 (53) | 28/147 (19) | 27/146 (18) | 13/19 (68) | 12/18 (67) |
Outcome
Health status
Full details of the health status and QoL measures at each time point of follow-up are in the tables in Appendix 4. Details of the statistical testing of the health status and QoL scores can be found in the next section of this chapter.
REFLUX score
Figure 3 summarises changes in the disease-specific REFLUX score over the follow-up period. From this it can be seen that the scores at all time points are highest (indicating fewest symptoms) in the randomised surgical and preference surgical groups. However, the differences between the surgical and medical groups narrow over time. This is due principally to the scores in the randomised medical group improving over the first 3 years and, to a lesser extent, those in the preference medical group improving over the latter end of the follow-up period. The scores for the five components of the measure are summarised graphically in Figures 4–8. These show that the overall difference between the groups is principally due to the ‘general discomfort’ component and, to a lesser extent, the ‘nausea and vomiting’ and ‘activity limitations’ components.
FIGURE 3.
Mean REFLUX QoL score at baseline and at follow-up points up to 5 years (score range 0–100; the higher the score, the better the patient felt).
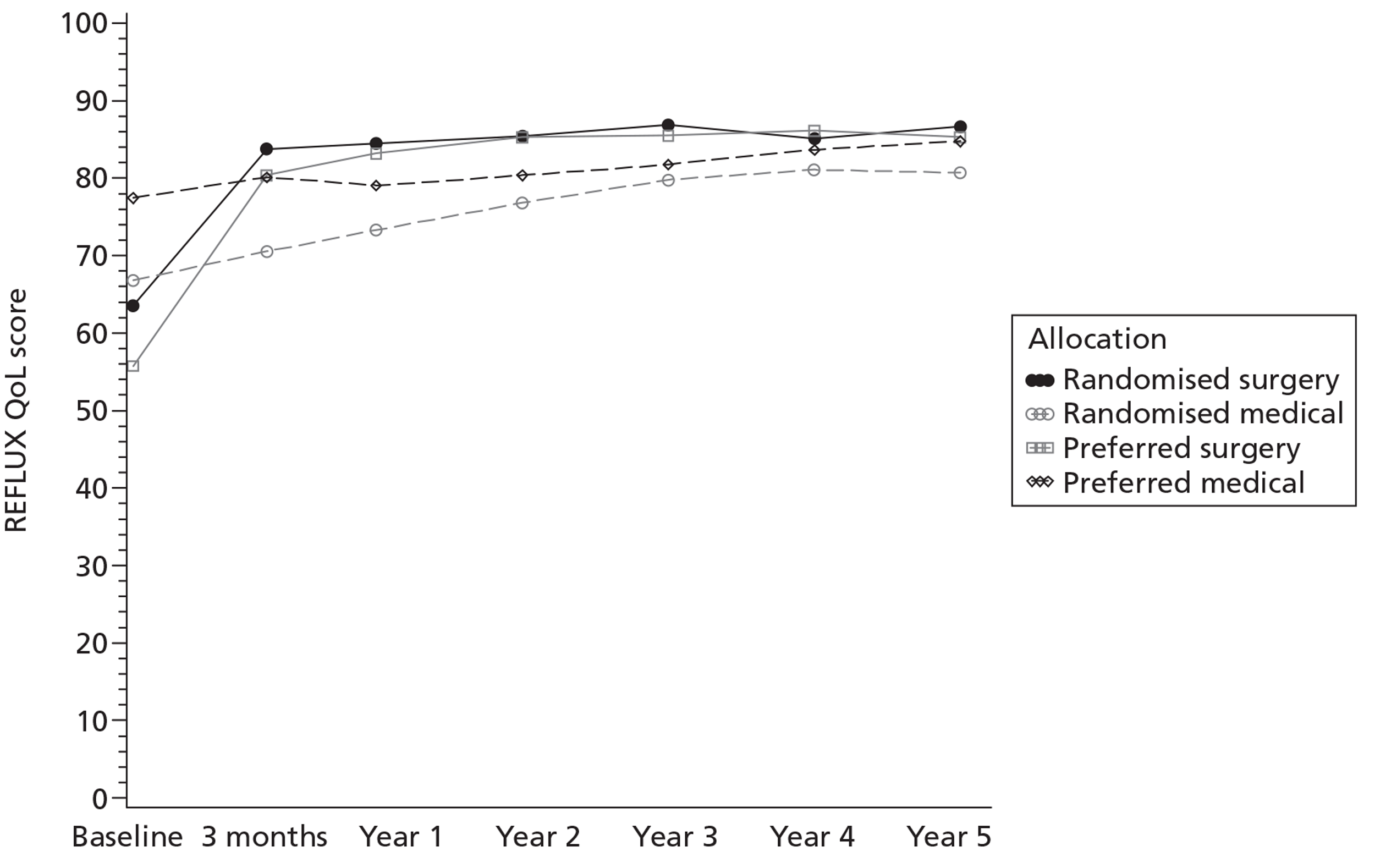
FIGURE 4.
Mean REFLUX QoL general discomfort symptom score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
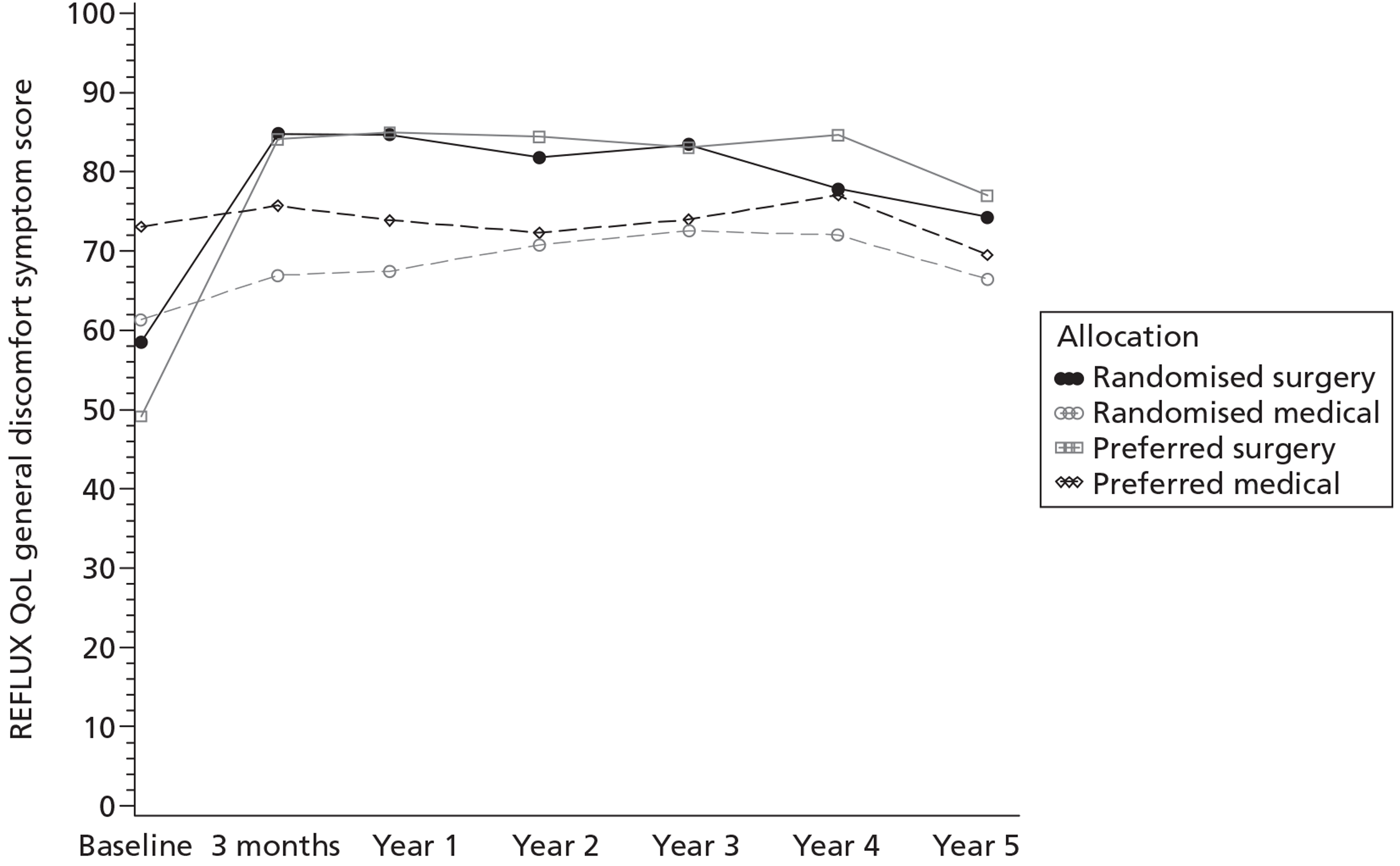
FIGURE 5.
Mean REFLUX QoL wind and frequency symptom score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
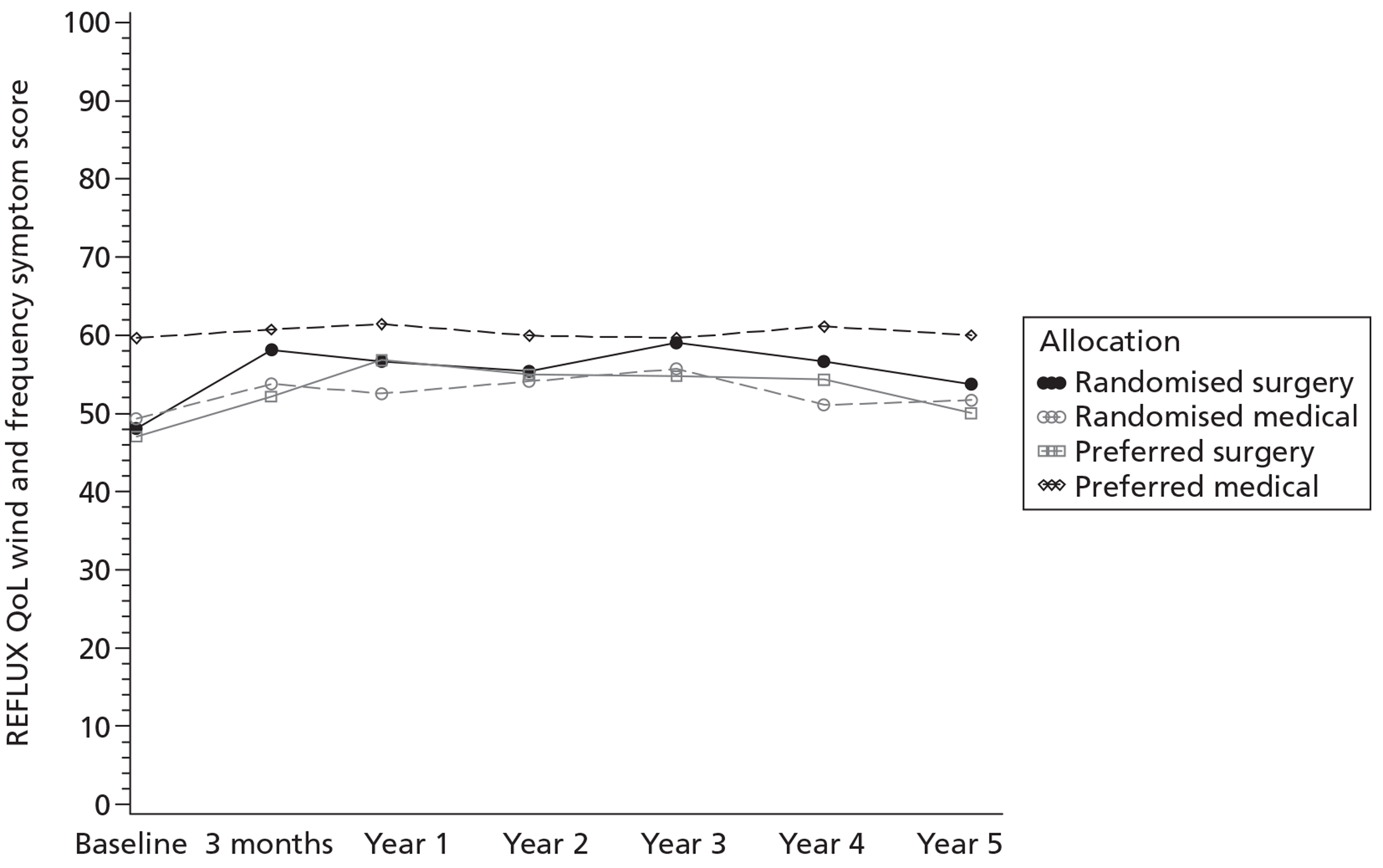
FIGURE 6.
Mean REFLUX QoL nausea and vomiting symptom score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
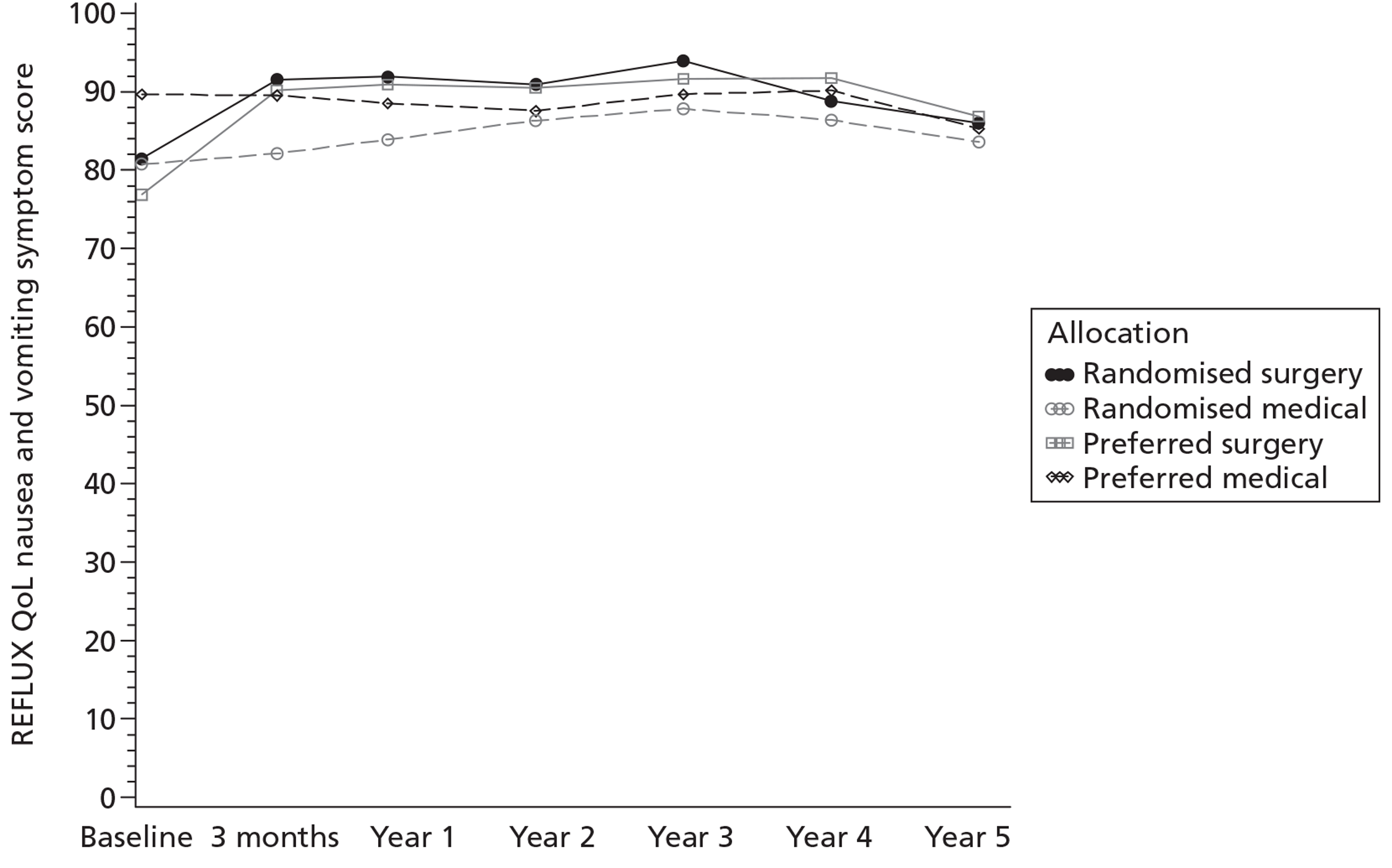
FIGURE 7.
Mean REFLUX QoL activity limitation symptom score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
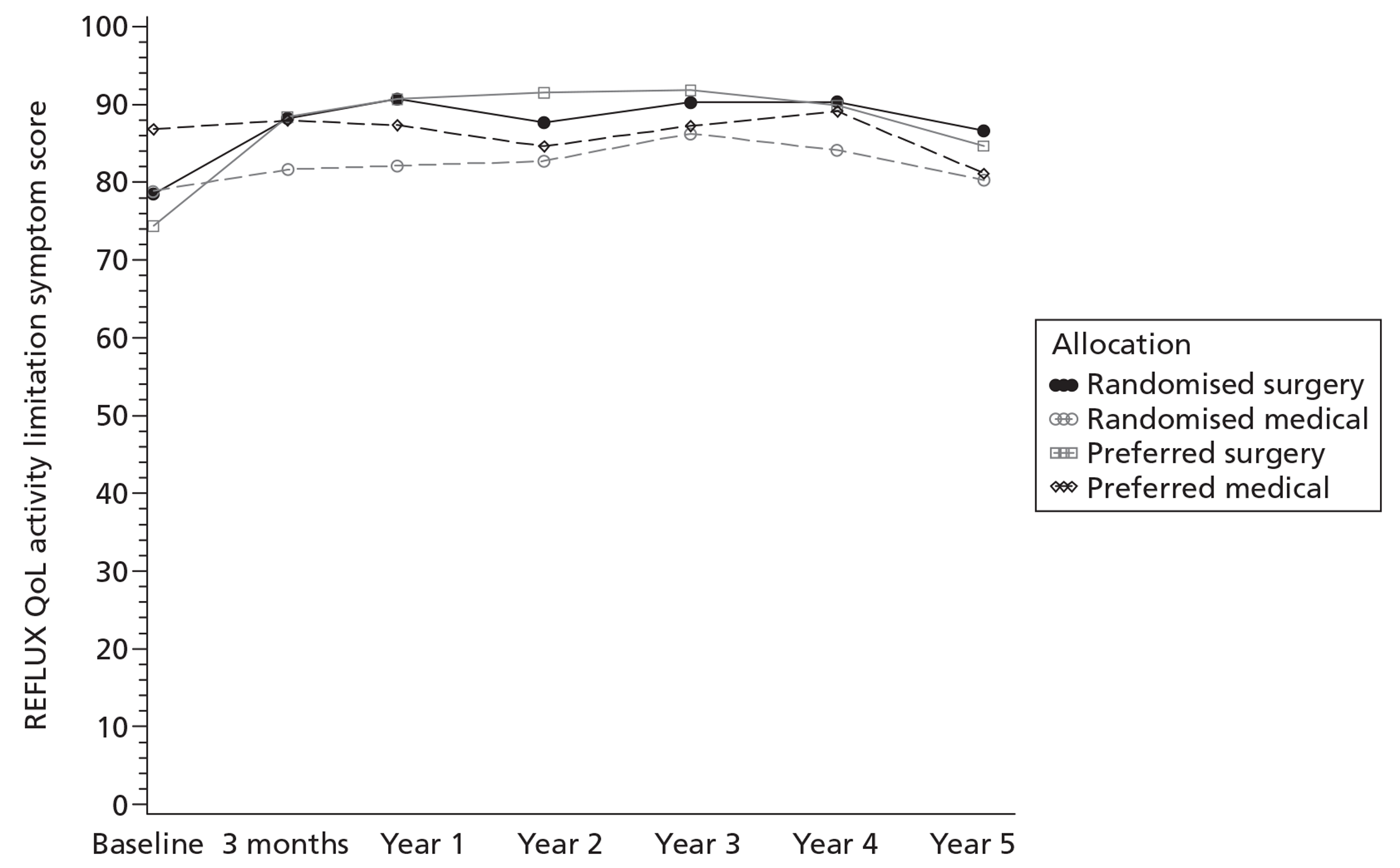
FIGURE 8.
Mean REFLUX QoL constipation and swallowing symptom score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
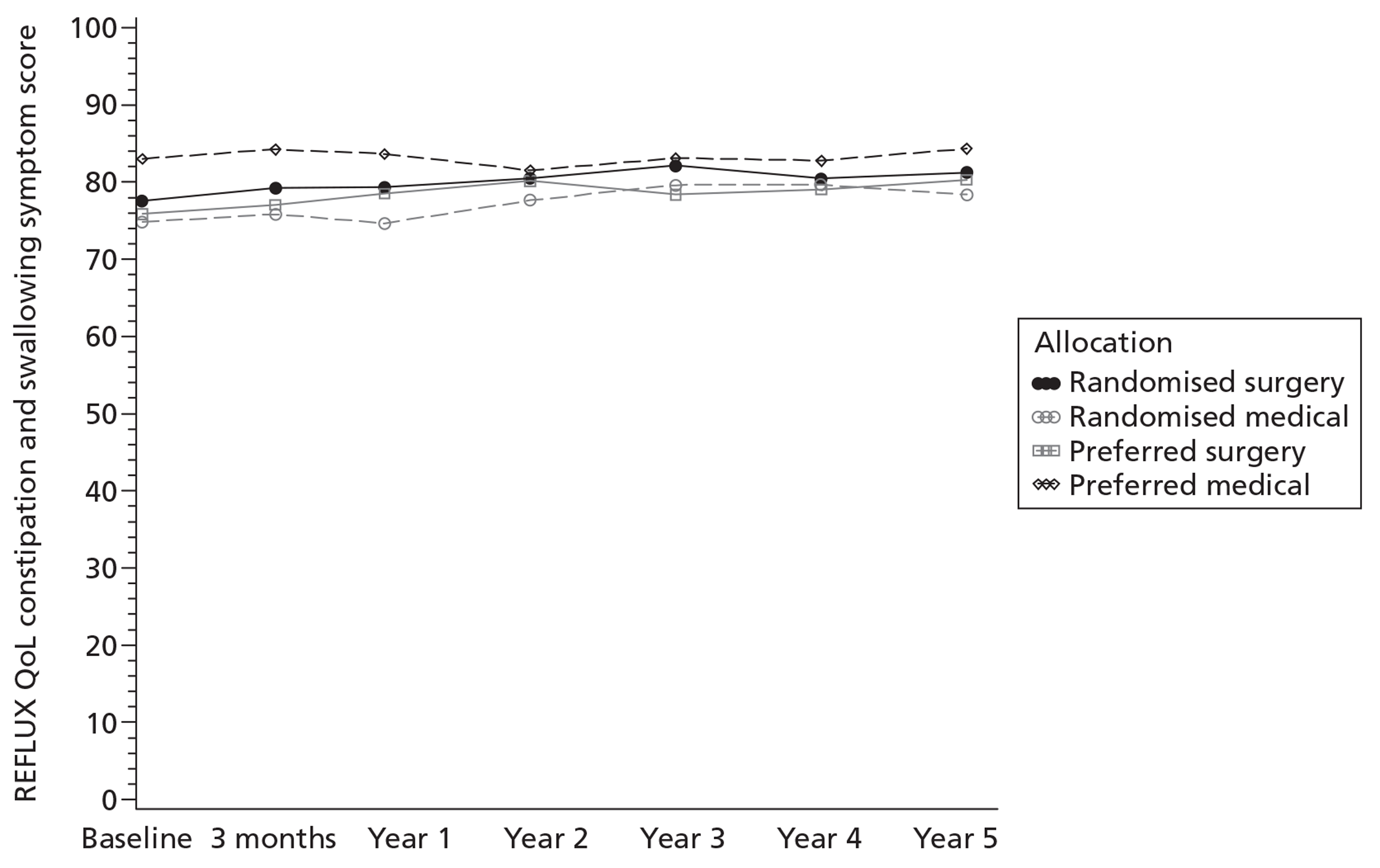
Short Form questionnaire-36 items
The pattern of SF-36 scores, both for the composite physical and mental scores and for the individual dimensions (Figures 9–16), was similar to that seen for the REFLUX score, although more compact. Differences narrowed over the 5 years of follow-up, with the ‘general health’ dimension showing the clearest differences between the surgery and the medical management groups.
FIGURE 9.
Mean SF-36 norm-based physical functioning score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
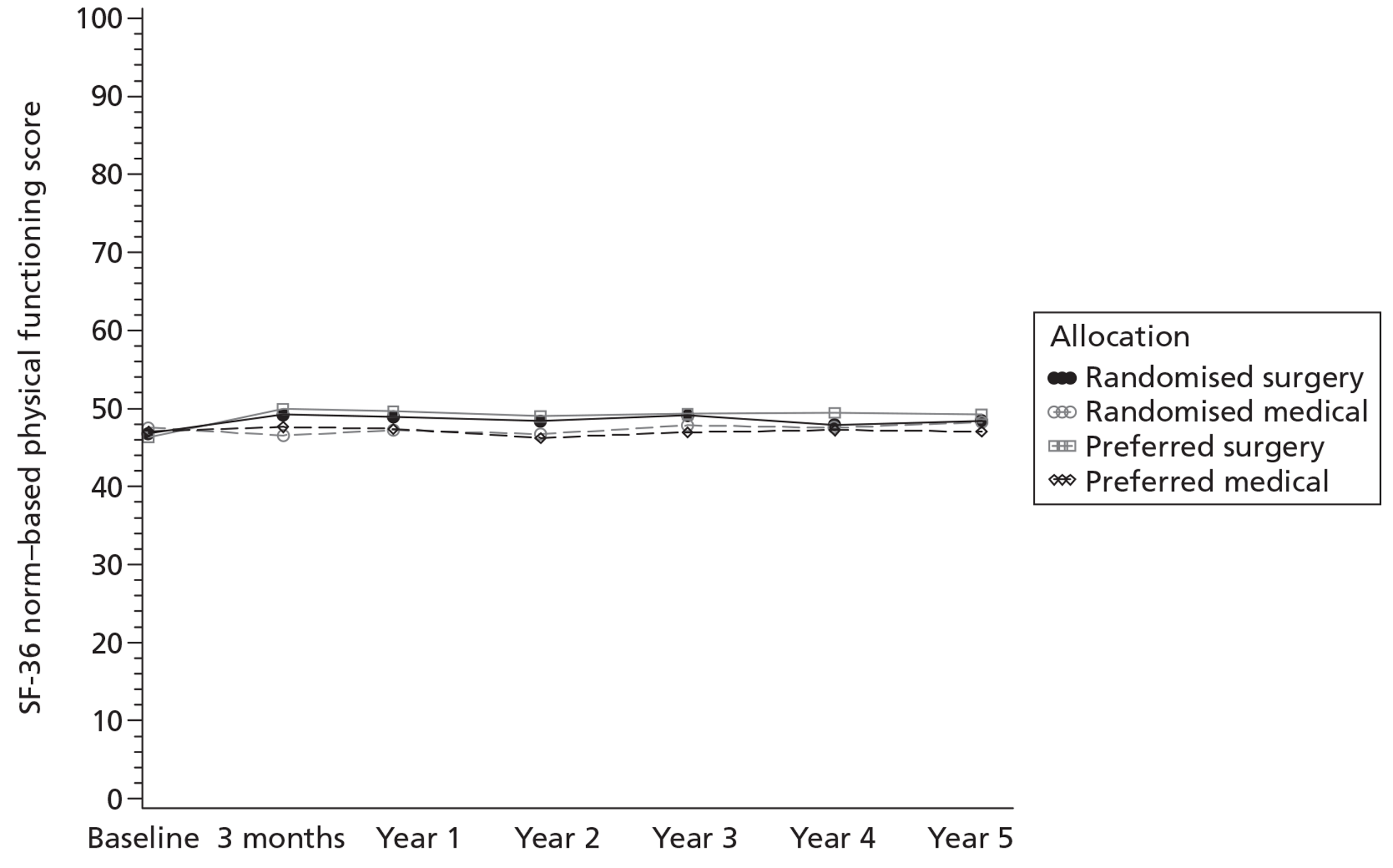
FIGURE 10.
Mean SF-36 norm-based role physical score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
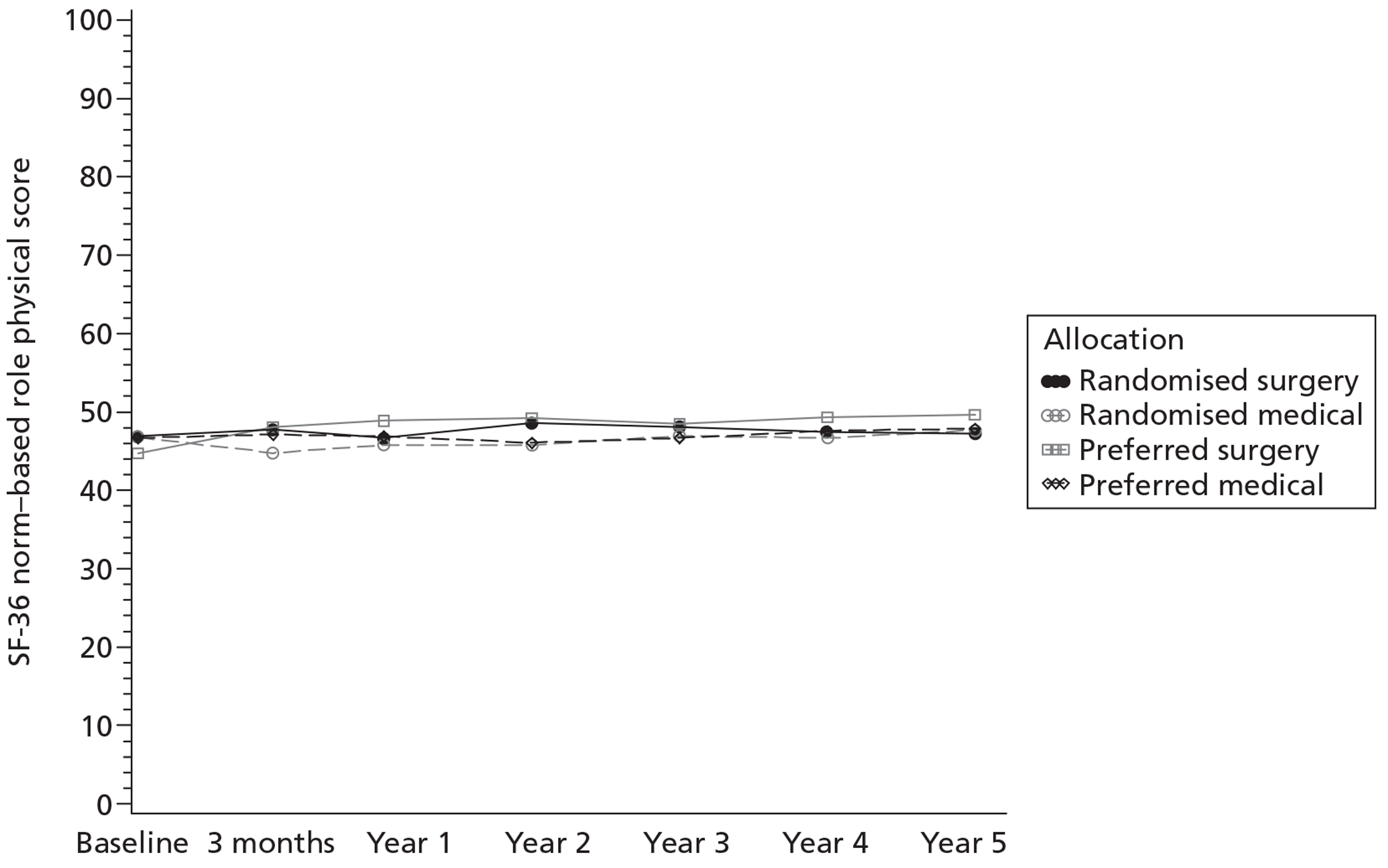
FIGURE 11.
Mean SF-36 norm-based bodily pain score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
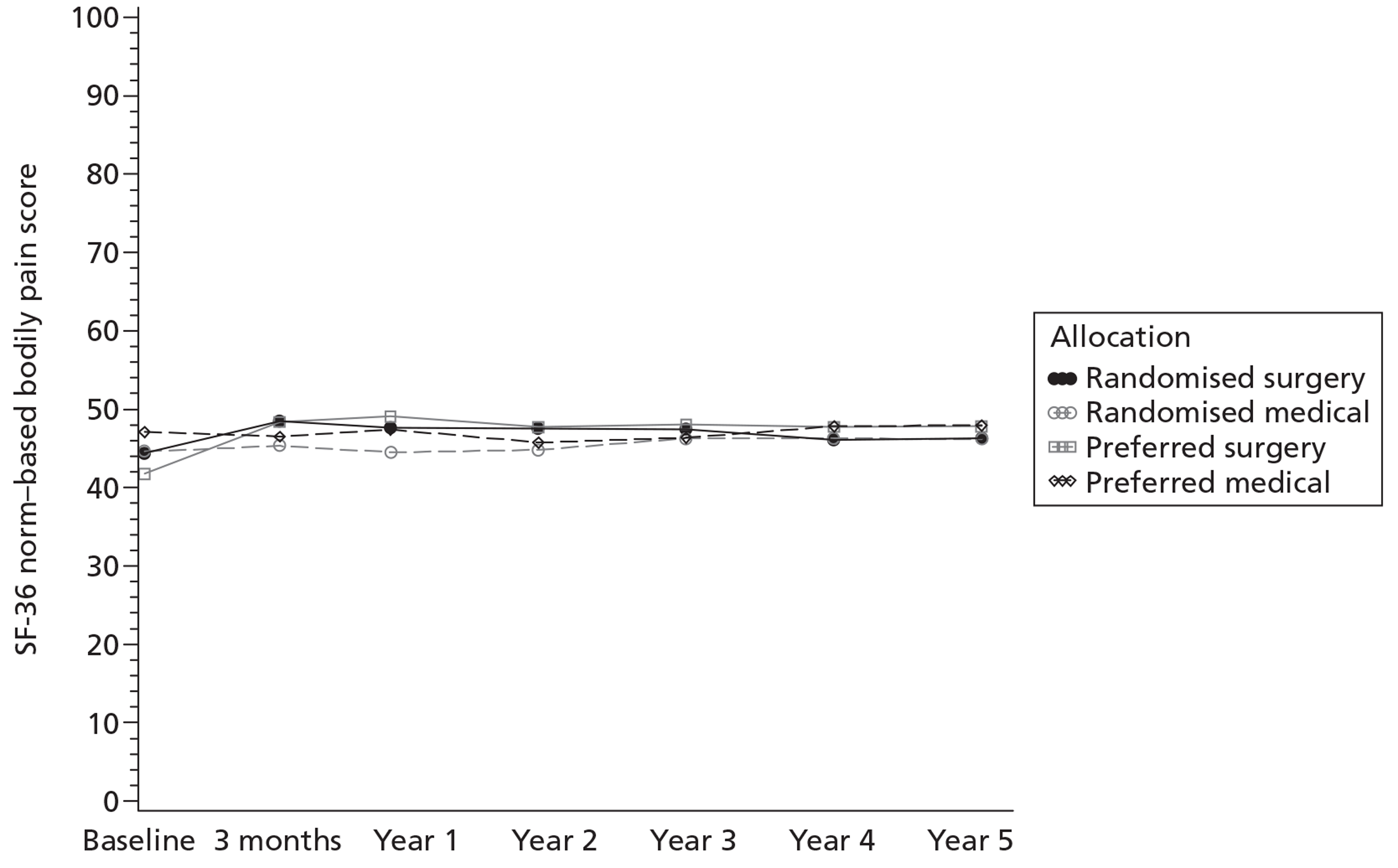
FIGURE 12.
Mean SF-36 norm-based general health score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
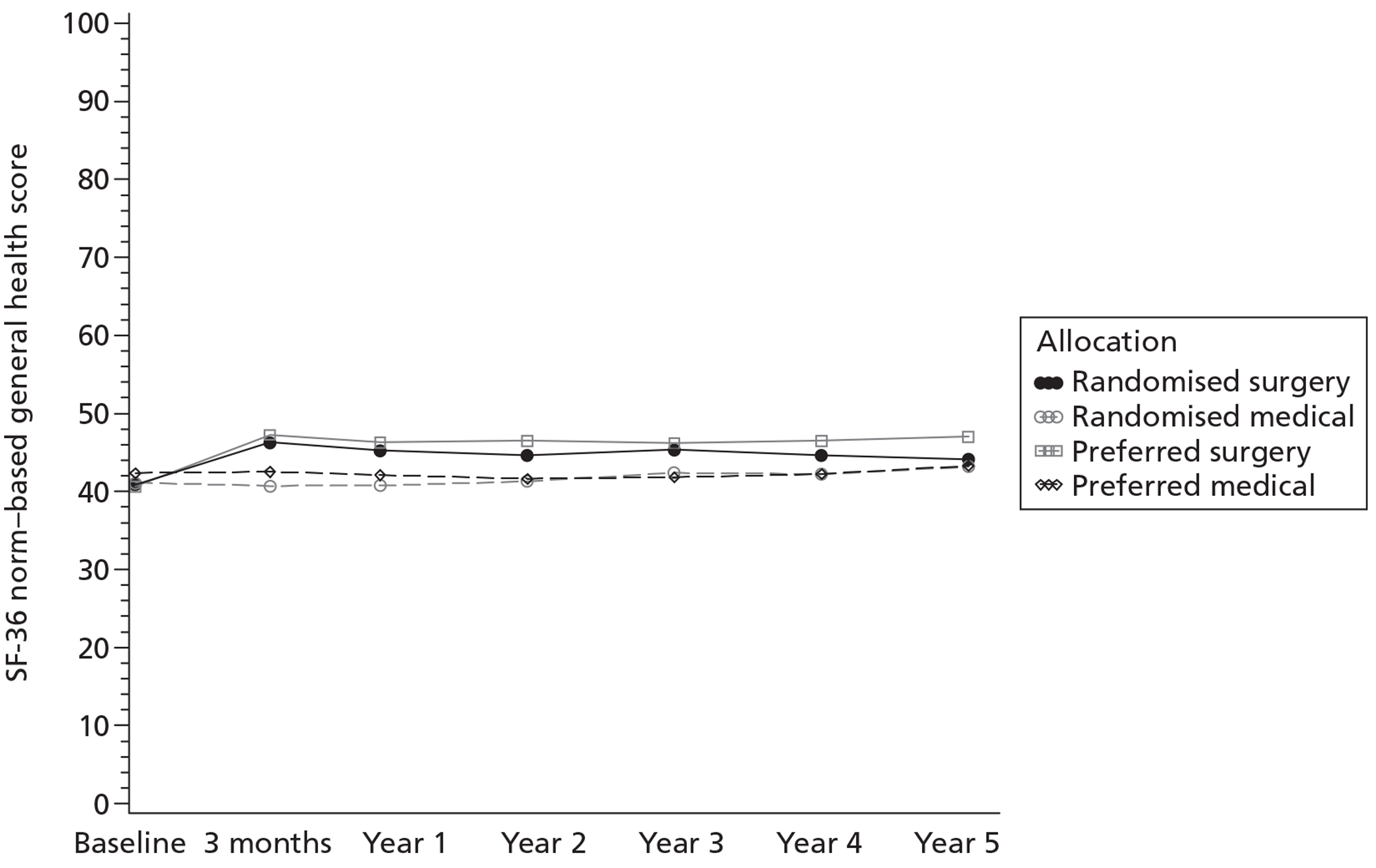
FIGURE 13.
Mean SF-36 norm-based vitality score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
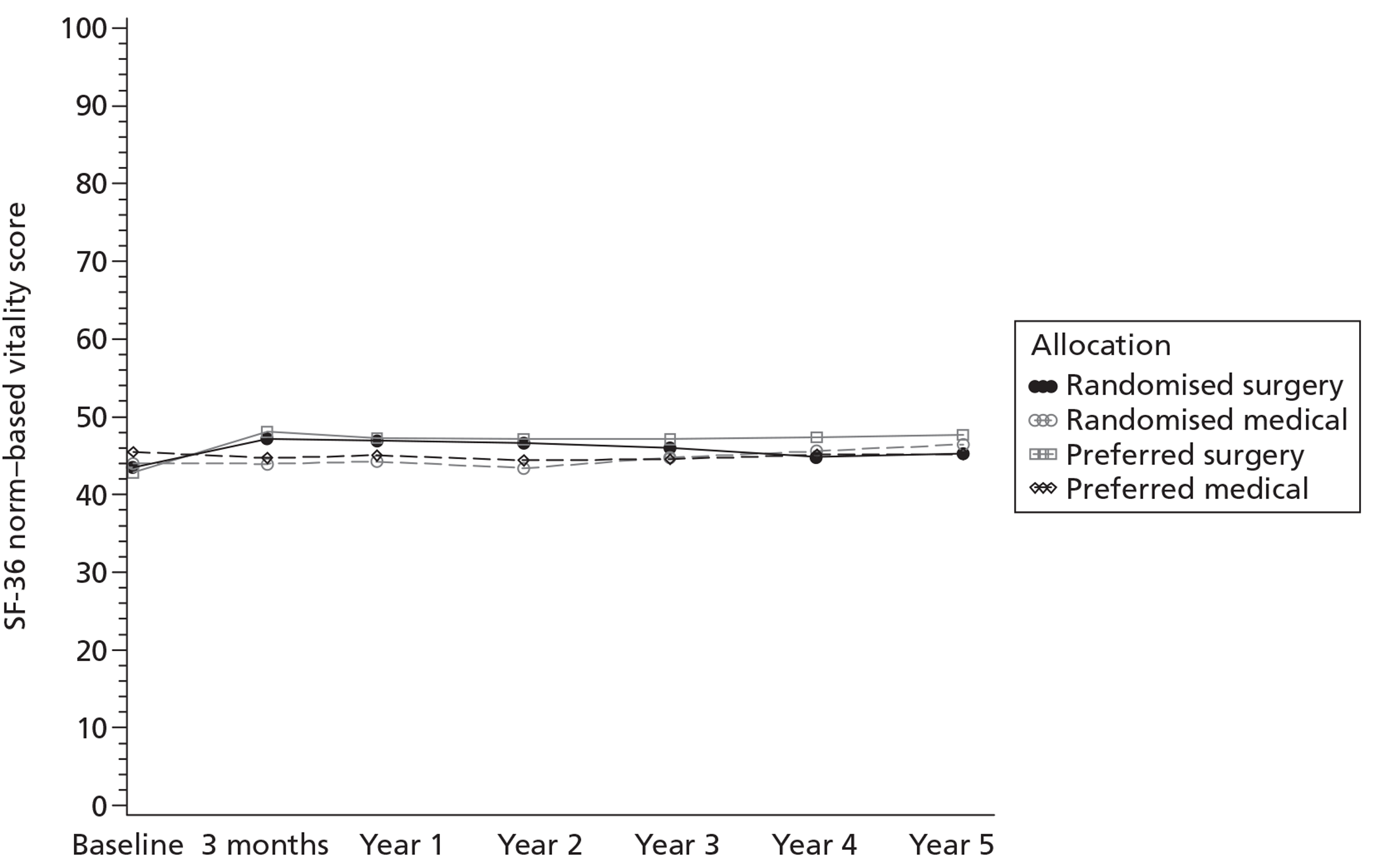
FIGURE 14.
Mean SF-36 norm-based social functioning score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
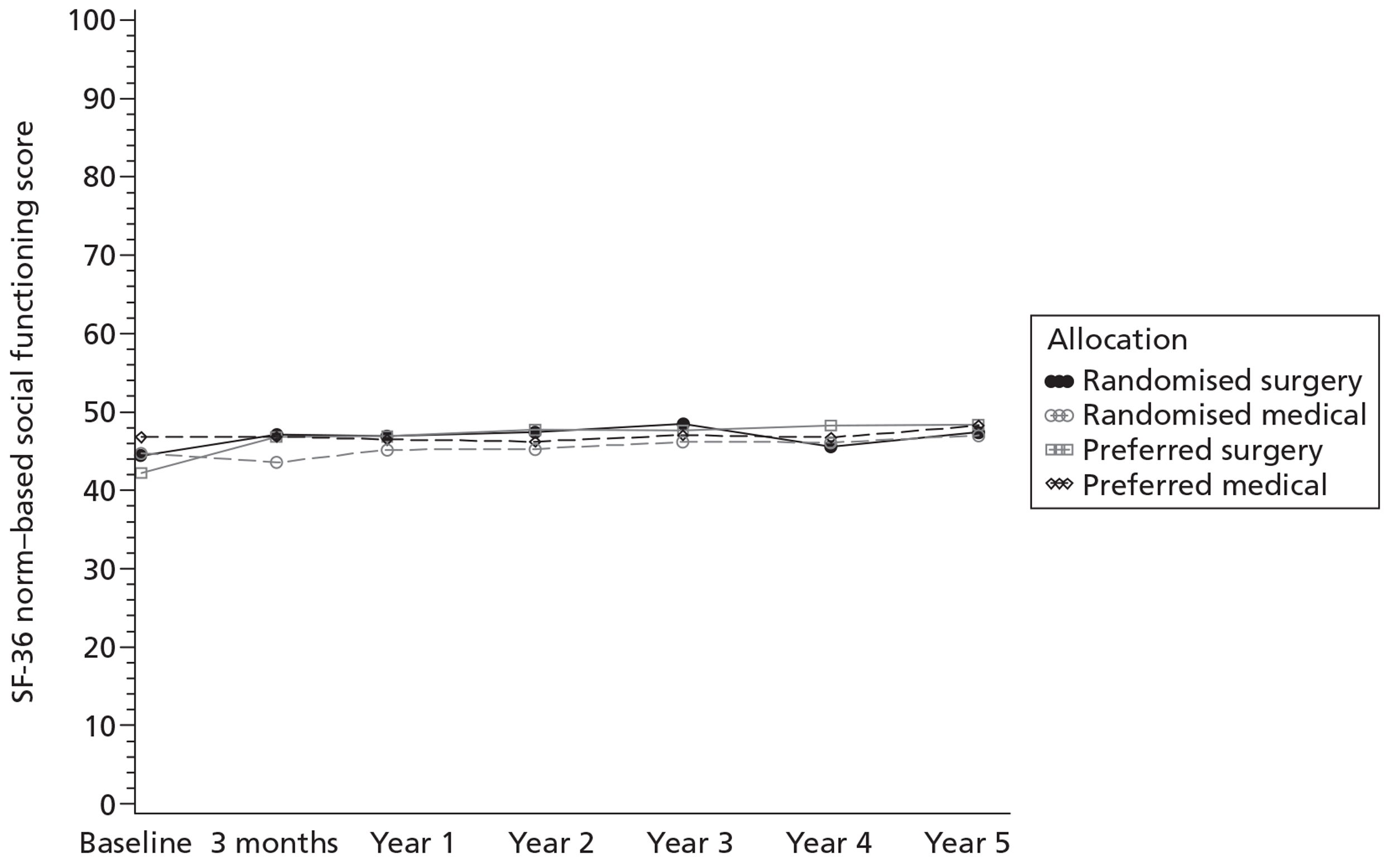
FIGURE 15.
Mean SF-36 norm-based role emotional score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
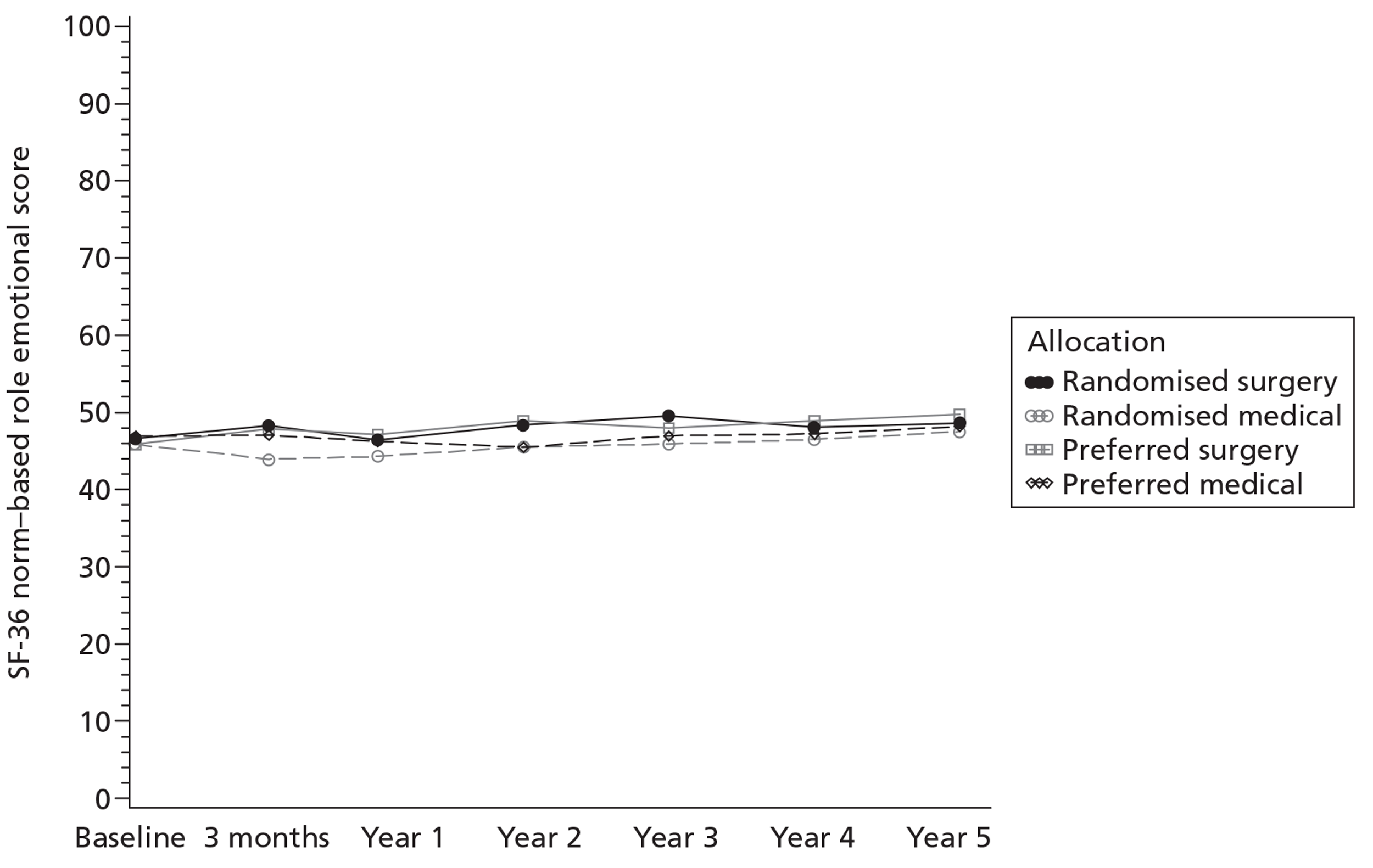
FIGURE 16.
SF-36 norm-based mental score at baseline and follow-up points to 5 years (score range 0–100; the higher the score, the better the patient felt).
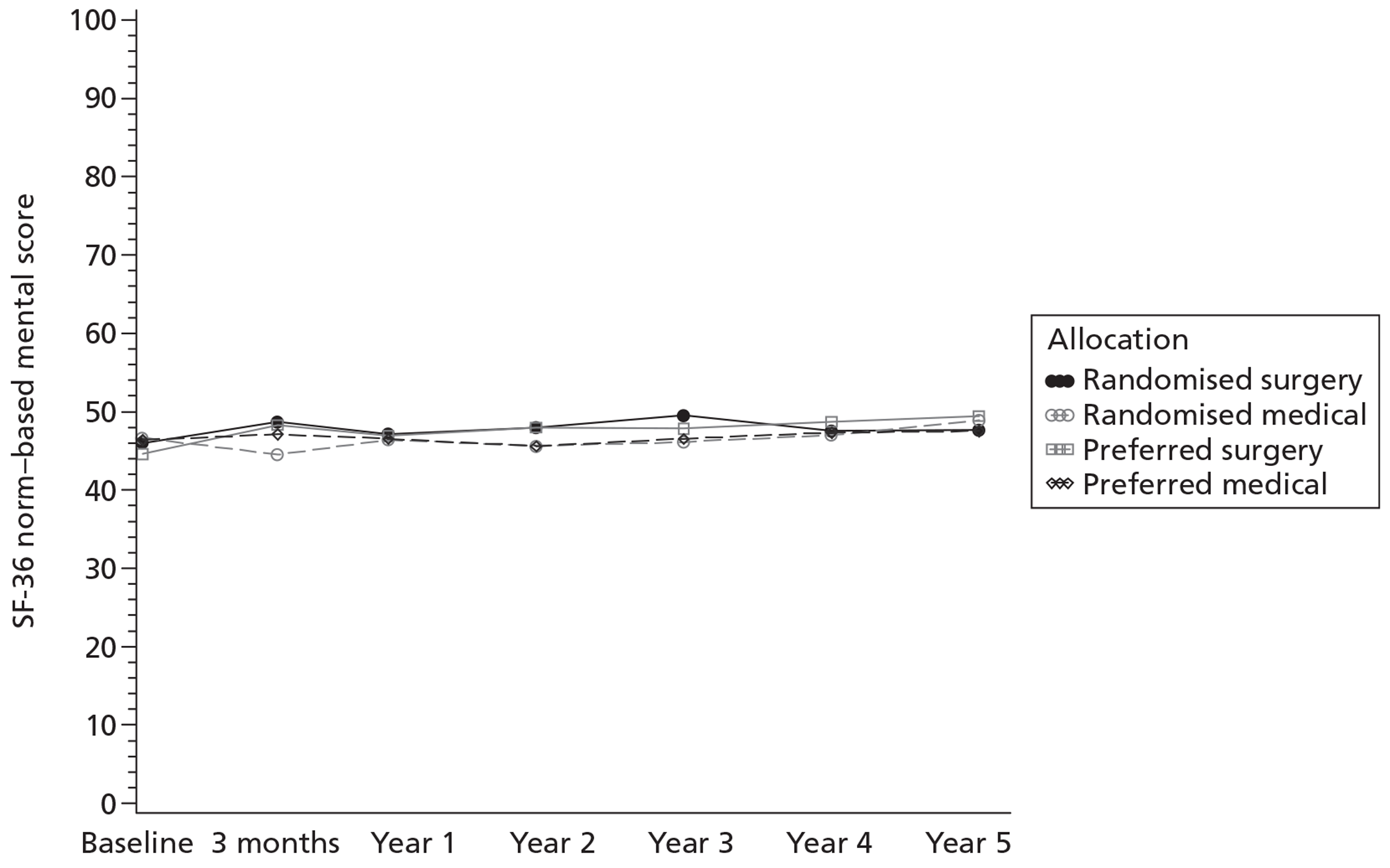
European Quality of Life-5 Dimensions
Figure 17 graphically displays the EQ-5D scores over the course of the follow-up period. The pattern is similar to that seen for the REFLUX score although differences are less marked and only clearly seen over the first 3 years.
FIGURE 17.
EQ-5D at baseline and follow-up points to 5 years.
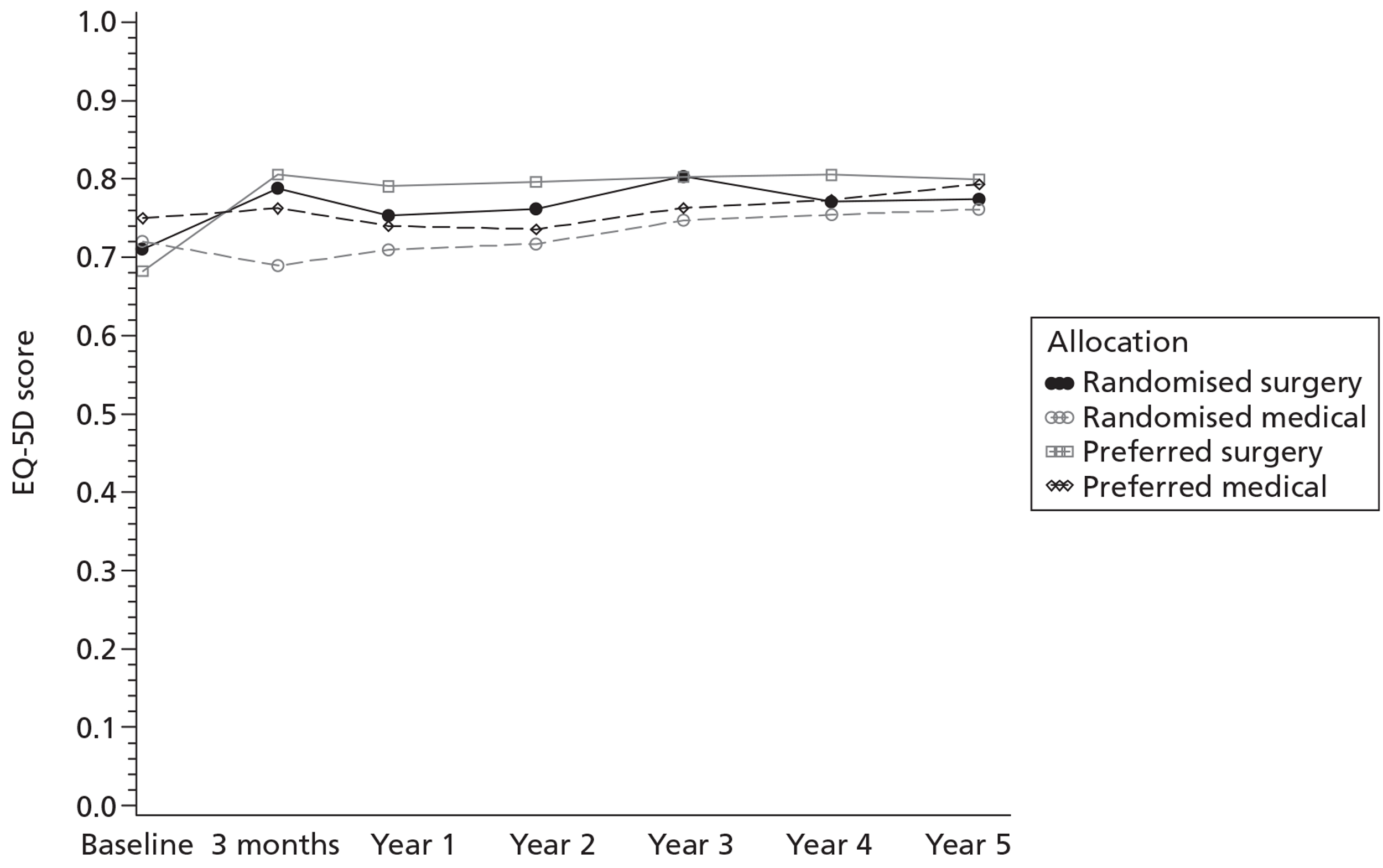
Use of health services
Table 14 shows use of health services for the randomised groups. The larger number of overnight hospital admissions in the medical group largely reflected admissions for surgery; as described above, 14 participants allocated to medical management had fundoplication after the first year. However, seven participants in the medical group compared with one in the surgical group had admissions for a non-surgery-related reason (data not shown).
| Use of health service | Year | Randomised surgical | Randomised medical |
|---|---|---|---|
| Overnight hospital admissions: reflux-related (and all reasons), n | 1 | 4 (8) | 2 (8) |
| 2 | 1 (8) | 2 (10) | |
| 3 | 2 (6) | 9 (10) | |
| 4 | 2 (2) | 9 (10) | |
| 5 | 0 (1) | 8 (11) | |
| Day hospital admissions: reflux related (and all reasons), n | 1 | 22 (40) | 24 (53) |
| 2 | 5 (23) | 4 (24) | |
| 3 | 4 (4) | 6 (10) | |
| 4 | 12 (13) | 9 (11) | |
| 5 | 4 (7) | 11 (14) | |
| Visits to and from the GP: reflux related (and all reasons), n | 1 | 110 (394) | 103 (376) |
| 2 | 34 (269) | 115 (373) | |
| 3 | 38 (381) | 99 (386) | |
| 4 | 55 (422) | 126 (469) | |
| 5 | 36 (404) | 119 (370) |
Numbers of day-case hospital admissions were similar in the two groups. The larger number of visits to or from a GP for a reflux-related reason in the randomised medical group reflected both more individuals attending their GPs and a higher frequency of visits for those who sought GP care.
Individual symptoms of gastro-oesophageal reflux disease or its treatment
Table 15 shows the frequency with which participants reported symptoms of GORD or its treatment at 3 and 5 years of follow-up for the randomised groups. At both 3 and 5 years, heartburn was reported by a higher proportion of participants in the randomised medical group than in the randomised surgical group. In addition, a higher proportion of participants in the randomised medical group reported more frequent heartburn than in the randomised surgical group. At both time points, a higher proportion of participants in the randomised medical management group also reported regurgitation symptoms and burping/belching than in the randomised surgical group. At both 3 and 5 years, the proportions who reported no difficulty swallowing and no wind from the lower bowel were similar between the randomised surgical and the randomised medical groups. There was also little difference between the groups at each time point in the proportion of participants who reported a feeling of wanting to be sick but being physically unable to do so.
| GORD symptom | 3 years | 5 years | ||
|---|---|---|---|---|
| Randomised surgery | Randomised medical | Randomised surgery | Randomised medical | |
| Frequency of heartburn, n (%) | ||||
| None at all | 77 (58.8) | 46 (34.8) | 65 (58.6) | 28 (26.4) |
| One to three times per week | 44 (33.6) | 64 (48.5) | 38 (34.2) | 64 (60.4) |
| More than three times per week | 10 (7.6) | 22 (16.7) | 8 (7.2) | 14 (13.2) |
| Frequency of regurgitation, n (%) | ||||
| None at all | 102 (77.3) | 83 (61.9) | 89 (75.4) | 71 (63.4) |
| One to three times per week | 27 (20.5) | 47 (35.1) | 26 (22.0) | 37 (33.0) |
| More than three times per week | 3 (2.3) | 4 (3.0) | 3 (2.5) | 4 (3.6) |
| Frequency of difficulty swallowing, n (%) | ||||
| None at all | 100 (75.8) | 102 (76.1) | 91 (77.1) | 82 (74.5) |
| One to three times per week | 30 (22.7) | 27 (20.1) | 25 (21.2) | 25 (22.7) |
| More than three times per week | 2 (1.5) | 5 (3.7) | 2 (1.7) | 3 (2.7) |
| Frequency of wind from the bowel, n (%) | ||||
| None at all | 19 (14.4) | 20 (15.0) | 14 (11.9) | 14 (12.7) |
| One to three times per week | 37 (28.0) | 35 (26.3) | 27 (22.9) | 30 (27.3) |
| More than three times per week | 76 (57.6) | 78 (58.6) | 77 (65.3) | 66 (60.0) |
| Frequency of burping/belching, n (%) | ||||
| None at all | 53 (40.2) | 33 (24.8) | 46 (39.3) | 27 (24.5) |
| One to three times per week | 39 (29.5) | 48 (36.1) | 40 (34.2) | 37 (33.6) |
| More than three times per week | 40 (30.3) | 52 (39.1) | 31 (26.5) | 46 (41.8) |
| Frequency of wanting to be sick but being physically unable to, n (%) | ||||
| None at all | 116 (87.9) | 110 (83.3) | 101 (85.6) | 92 (82.9) |
| One to three times per week | 15 (11.4) | 17 (12.9) | 15 (12.7) | 16 (14.4) |
| More than three times per week | 1 (0.8) | 5 (3.8) | 2 (1.7) | 3 (2.7) |
Statistical analyses
Primary outcome
The pre-chosen primary outcome was the REFLUX QoL score after 5 years of follow-up. The differences between groups with corresponding 95% CIs are shown in Table 16. Two types of analysis are presented for the randomised participants – ITT and adjusted treatment received. Table 16 also displays the impact of including adjustment for baseline score and randomised group* baseline score interaction terms.
| REFLUX QoL score | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Mean differencea | 95% CI | p-value | Mean differencea | 95% CI | p-value | |
| Adjusted for minimisation variables | 6.4 | 1.6 to 11.2 | 0.009 | 9.4 | 1.7 to 17.0 | 0.017 |
| Adjusted for minimisation variables and baseline REFLUX QoL score | 7.6 | 3.0 to 12.2 | 0.001 | 10.6 | 3.3 to 17.9 | 0.004 |
| Adjusted for minimisation variables, baseline score and treatment*baseline REFLUX QoL score interaction | 8.5 | 3.9 to 13.1 | < 0.001 | 11.5 | 4.2 to 18.7 | 0.002 |
Intention to treat
For the ITT analysis there was a mean difference of 6.4 between the groups in favour of surgery when only the minimisation variables were adjusted for (95% CI 1.6 to 11.2; p = 0.009). A repeated measures analysis across the 5 years gave a difference of 8.1 (95% CI 4.4 to 11.7). This was not the most parsimonious model – there was strong evidence of an interaction effect between randomised group and baseline REFLUX QoL score (interaction term was −0.23, 95% CI −0.43 to −0.03; p = 0.023). This implied that as baseline REFLUX QoL score increased the treatment effect decreased. Estimating the treatment difference at the trial baseline mean REFLUX QoL score of 65.2 resulted in a trial effect size of 8.5 (95% CI 3.9 to 13.1; p < 0.001). If the average patient had a lower mean REFLUX QoL score at baseline of 56.0, the effect size increased to 10.6 (95% CI 5.3 to 15.8). If the patient had a higher baseline score of 78.0, the treatment effect size decreased to 5.5 (95% CI 0.6 to 10.4). All results, however, showed strong evidence of increases in REFLUX QoL scores favouring surgery.
Adjusted treatment received
The adjusted treatment received analyses attempted to mitigate the effect of non-compliance with the allocated treatment and hence provide an estimate of ‘efficacy’. 40 As expected, this approach gave a larger difference, but with wider CIs (9.4, 95% CI 1.7 to 17.0; p = 0.017).
Preference groups
The preference for surgery participants reported considerably worse mean REFLUX QoL scores at baseline than the preference for medicine participants (55.8 vs 77.5) (see Table 7). Despite starting from a much lower baseline score, at follow-up, the REFLUX QoL score slightly favoured the surgical group using an ITT analysis (difference = 0.61; 95% CI −3.44 to 4.66; p = 0.767) and an adjusted treatment received analysis (difference = 0.10; 95% CI −4.77 to 4.97; p = 0.967). The differences were not, however, statistically significant.
Secondary outcomes
The secondary outcomes were the health status measures (EQ-5D, SF-36) and REFLUX symptom score at times equivalent to 3 months and then annual follow-up after surgery, and REFLUX QoL (at time points other than 5 years, when it was the primary end point). Analyses of these outcomes are shown in Tables 17–22.
| Secondary outcomes | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Differencea | 95% CI | p-value | Differencea | 95% CI | p-value | |
| REFLUX QoL | 15.0 | 10.5 to 19.4 | < 0.001 | 20.7 | 13.9 to 27.5 | < 0.001 |
| REFLUX symptom score | ||||||
| General discomfort symptom score | 19.2 | 14.9 to 23.6 | < 0.001 | 26.0 | 19.6 to 32.4 | < 0.001 |
| Wind and frequency symptom score | 4.6 | 0.5 to 8.6 | 0.027 | 5.1 | −1.0 to 11.3 | 0.101 |
| Nausea and vomiting symptom score | 8.8 | 5.8 to 11.9 | < 0.001 | 12.4 | 7.7 to 17.1 | < 0.001 |
| Activity limitation symptom score | 7.1 | 3.2 to 11.0 | < 0.001 | 9.1 | 3.2 to 15.1 | 0.003 |
| Constipation and swallowing symptom score | 2.0 | −1.9 to 6.0 | 0.318 | 2.1 | −3.9 to 8.2 | 0.486 |
| SF-36 score | ||||||
| Norm-based physical functioning | 3.1b | 1.3 to 4.9 | 0.001 | 4.4b | 1.5 to 7.2 | 0.003 |
| Norm-based role physical | 2.7 | 0.5 to 4.9 | 0.018 | 3.4 | −0.04 to 6.8 | 0.053 |
| Norm-based bodily pain | 3.2b | 1.1 to 5.3 | 0.003 | 4.1b | 0.9 to 7.2 | 0.012 |
| Norm-based general health | 5.8b | 3.8 to 7.8 | < 0.001 | 7.8b | 4.8 to 10.7 | < 0.001 |
| Norm-based vitality | 3.0 | 0.9 to 5.1 | 0.006 | 3.9 | 0.7 to 7.1 | 0.018 |
| Norm-based social functioning | 3.6 | 1.3 to 5.8 | 0.002 | 4.6 | 1.1 to 8.1 | 0.010 |
| Norm-based role emotional | 3.3 | 0.7 to 5.8 | 0.012 | 4.1 | 0.2 to 8.0 | 0.042 |
| Norm-based mental health | 4.2b | 2.1 to 6.2 | < 0.001 | 5.5b | 2.4 to 8.6 | 0.001 |
| EQ-5D, mean (SD) | 0.099b | 0.048 to 0.150 | < 0.001 | 0.129b | 0.051 to 0.207 | 0.001 |
| Secondary outcomes | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Differencea | 95% CI | p-value | Differencea | 95% CI | p-value | |
| REFLUX QoL | 14.0 | 9.6 to 18.4 | < 0.001 | 19.4 | 13.0 to 25.8 | < 0.001 |
| REFLUX symptom score | ||||||
| General discomfort symptom score | 18.3 | 13.8 to 22.9 | < 0.001 | 26.1 | 19.6 to 32.5 | < 0.001 |
| Wind and frequency symptom score | 4.9 | 0.8 to 9.1 | 0.019 | 6.7 | 0.6 to 12.8 | 0.033 |
| Nausea and vomiting symptom score | 7.8 | 4.6 to 10.9 | < 0.001 | 11.5 | 7.0 to 16.0 | < 0.001 |
| Activity limitation symptom score | 8.4 | 5.2 to 11.7 | < 0.001 | 12.0 | 7.3 to 16.7 | < 0.001 |
| Constipation and swallowing symptom score | 3.5 | −0.5 to 7.5 | 0.085 | 5.0 | −0.9 to 10.9 | 0.099 |
| SF-36 score | ||||||
| Norm-based physical functioning | 2.3b | 0.6 to 4.0 | 0.007 | 3.4b | 0.9 to 5.9 | 0.008 |
| Norm-based role physical | 0.9 | −1.1 to 3.0 | 0.383 | 1.2 | −1.8 to 4.3 | 0.434 |
| Norm-based bodily pain | 3.4b | 1.4 to 5.5 | 0.001 | 5.1b | 2.1 to 8.0 | 0.001 |
| Norm-based general health | 4.8b | 2.7 to 6.8 | < 0.001 | 7.0b | 4.0 to 10.0 | < 0.001 |
| Norm-based vitality | 2.5 | 0.4 to 4.6 | 0.018 | 3.7 | 0.6 to 6.8 | 0.019 |
| Norm-based social functioning | 2.3 | 0.1 to 4.5 | 0.040 | 3.3 | 0.04 to 6.6 | 0.047 |
| Norm-based role emotional | 1.8 | −0.8 to 4.4 | 0.177 | 2.7 | −1.1 to 6.5 | 0.168 |
| Norm-based mental health | 1.0b | −1.0 to 3.1 | 0.312 | 1.5b | −1.5 to 4.5 | 0.324 |
| EQ-5D | 0.047b | −0.004 to 0.097 | 0.07 | 0.068b | −0.006 to 0.142 | 0.072 |
| Secondary outcomes | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Differencea | 95% CI | p-value | Differencea | 95% CI | p-value | |
| REFLUX QoL | 11.4 | 6.8 to 16.0 | <0.001 | 15.7 | 8.5 to 22.9 | <0.001 |
| REFLUX symptom score | ||||||
| General discomfort symptom score | 13.08 | 7.99 to 18.17 | < 0.001 | 17.66 | 9.82 to 25.50 | < 0.001 |
| Wind and frequency symptom score | 3.74b | −1.06 to 8.53 | 0.126 | 5.67b | −2.05 to 13.38 | 0.149 |
| Nausea and vomiting symptom score | 6.34 | 2.85 to 9.83 | < 0.001 | 9.48 | 4.04 to 14.92 | 0.001 |
| Activity limitation symptom score | 7.02 | 3.38 to 10.65 | < 0.001 | 10.03 | 4.25 to 15.80 | 0.001 |
| Constipation and swallowing symptom score | 3.29b | −1.11 to 7.68 | 0.142 | 4.98b | −2.09 to 12.05 | 0.167 |
| SF-36 score | ||||||
| Norm-based physical functioning | 2.73 | 0.83 to 4.63 | 0.005 | 4.27 | 1.21 to 7.34 | 0.007 |
| Norm-based role physical | 3.11 | 0.99 to 5.22 | 0.004 | 4.69 | 1.27 to 8.10 | 0.007 |
| Norm-based bodily pain | 3.64 | 1.51 to 5.77 | 0.001 | 5.46 | 2.04 to 8.88 | 0.002 |
| Norm-based general health | 4.13 | 1.91 to 6.35 | < 0.001 | 5.96 | 2.39 to 9.54 | 0.001 |
| Norm-based vitality | 3.48 | 1.20 to 5.76 | 0.003 | 5.38 | 1.66 to 9.09 | 0.005 |
| Norm-based social functioning | 2.74 | 0.30 to 5.19 | 0.028 | 3.79b | −0.14 to 7.72 | 0.059 |
| Norm-based role emotional | 2.03b | −0.80 to 4.85 | 0.159 | 3.06b | −1.49 to 7.61 | 0.187 |
| Norm-based mental health | 2.33 | 0.08 to 4.59 | 0.043 | 3.86 | 0.22 to 7.49 | 0.038 |
| EQ-5D | 0.068b | 0.005 to 0.131 | 0.036 | 0.098b | −0.003 to 0.199 | 0.057 |
| Secondary outcomes | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Differencea | 95% CI | p-value | Differencea | 95% CI | p-value | |
| REFLUX QoL | 9.0 | 4.9 to 13.1 | < 0.001 | 12.9 | 6.3 to 19.5 | < 0.001 |
| REFLUX symptom score | ||||||
| General discomfort symptom score | 11.86 | 6.84 to 16.88 | < 0.001 | 16.25 | 8.37 to 24.14 | < 0.001 |
| Wind and frequency symptom score | 4.98b | −0.26 to 10.22 | 0.063 | 15.95b | 8.03 to 23.87 | < 0.001 |
| Nausea and vomiting symptom score | 6.69 | 3.65 to 9.73 | < 0.001 | 9.71 | 4.98 to 14.44 | < 0.001 |
| Activity limitation symptom score | 4.61 | 0.99 to 8.22 | 0.013 | 6.37 | 0.58 to 12.15 | 0.031 |
| Constipation and swallowing symptom score | 2.62b | −1.51 to 6.76 | 0.212 | 6.51b | 0.73 to 12.29 | 0.027 |
| SF-36 score | ||||||
| Norm-based physical functioning | 2.61 | 0.56 to 4.67 | 0.013 | 3.83 | 0.52 to 7.14 | 0.023 |
| Norm-based role physical | 1.82b | −0.43 to 4.07 | 0.113 | 3.82b | 0.52 to 7.12 | 0.024 |
| Norm-based bodily pain | 2.33 | 0.24 to 4.42 | 0.029 | 3.74 | 0.36 to 7.12 | 0.030 |
| Norm-based general health | 3.69 | 1.50 to 5.87 | 0.001 | 5.21 | 1.70 to 8.73 | 0.004 |
| Norm-based vitality | 2.29b | −0.23 to 4.81 | 0.075 | 5.29b | 1.77 to 8.81 | 0.003 |
| Norm-based social functioning | 3.27 | 0.87 to 5.68 | 0.008 | 4.81 | 0.93 to 8.69 | 0.015 |
| Norm-based role emotional | 4.03 | 1.50 to 6.57 | 0.002 | 6.89 | 2.77 to 11.01 | 0.001 |
| Norm-based mental health | 4.60 | 2.29 to 6.91 | < 0.001 | 7.39 | 3.65 to 11.14 | < 0.001 |
| EQ-5D, mean (SD) | 0.070b | 0.015 to 0.126 | 0.013 | 0.108 | 0.016 to 0.201 | 0.022 |
| Secondary outcomes | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Differencea | 95% CI | p-value | Differencea | 95% CI | p-value | |
| REFLUX QoL | 8.3 | 3.2 to 13.4 | 0.001 | 11.6 | 3.5 to 19.8 | 0.005 |
| REFLUX symptom score | ||||||
| General discomfort symptom score | 8.81 | 3.49 to 14.13 | 0.001 | 11.48 | 3.11 to 19.84 | 0.007 |
| Wind and frequency symptom score | 5.98 | 0.70 to 11.26 | 0.027 | 9.55 | 0.95 to 18.14 | 0.030 |
| Nausea and vomiting symptom score | 2.93b | −1.00 to 6.86 | 0.143 | 3.25b | −3.01 to 9.51 | 0.307 |
| Activity limitation symptom score | 4.38 | 0.64 to 8.12 | 0.022 | 5.95b | −0.03 to 11.93 | 0.051 |
| Constipation and swallowing symptom score | 0.26b | −4.21 to 4.74 | 0.908 | 0.54b | −6.72 to 7.80 | 0.884 |
| SF-36 score | ||||||
| Norm-based physical functioning | 2.14 | 0.00 to 4.28 | 0.050 | 3.10b | −0.36 to 6.55 | 0.079 |
| Norm-based role physical | 1.36b | −1.23 to 3.96 | 0.302 | 2.42b | −1.79 to 6.62 | 0.259 |
| Norm-based bodily pain | 1.72b | −0.57 to 4.02 | 0.140 | 2.59b | −1.13 to 6.31 | 0.172 |
| Norm-based general health | 4.02 | 1.61 to 6.44 | 0.001 | 5.74 | 1.84 to 9.63 | 0.004 |
| Norm-based vitality | 0.17b | −2.25 to 2.60 | 0.888 | 0.28b | −3.66 to 4.22 | 0.890 |
| Norm-based social functioning | 1.26b | −1.60 to 4.12 | 0.387 | 1.92b | −2.72 to 6.56 | 0.416 |
| Norm-based role emotional | 1.79b | −1.28 to 4.85 | 0.253 | 2.77b | −2.21 to 7.75 | 0.274 |
| Norm-based mental health | 1.55b | −1.03 to 4.12 | 0.238 | 1.85b | −2.31 to 6.00 | 0.382 |
| EQ-5D | 0.036b | −0.020 to 0.091 | 0.212 | 0.052b | −0.039 to 0.142 | 0.265 |
| Secondary outcomes | Randomised participants | |||||
|---|---|---|---|---|---|---|
| ITT | Adjusted treatment received | |||||
| Differencea | 95% CI | p-value | Differencea | 95% CI | p-value | |
| REFLUX symptom score | ||||||
| General discomfort symptom score | 11.82 | 6.50 to 17.14 | < 0.001 | 15.59 | 7.52 to 23.66 | < 0.001 |
| Wind and frequency symptom score | 3.34b | −1.98 to 8.66 | 0.218 | 5.12b | −3.50 to 13.73 | 0.243 |
| Nausea and vomiting symptom score | 4.97 | 1.53 to 8.41 | 0.005 | 7.32 | 2.04 to 12.60 | 0.007 |
| Activity limitation symptom score | 5.97 | 2.03 to 9.91 | 0.003 | 8.27 | 2.03 to 14.52 | 0.010 |
| Constipation and swallowing symptom score | 2.54b | −2.09 to 7.18 | 0.281 | 4.11b | −3.40 to 11.62 | 0.282 |
| SF-36 score | ||||||
| Norm-based physical functioning | 2.01b | −0.26 to 4.28 | 0.082 | 3.35b | −0.33 to 7.03 | 0.074 |
| Norm-based role physical | 0.57b | −2.10 to 3.24 | 0.674 | 1.14b | −3.20 to 5.47 | 0.606 |
| Norm-based bodily pain | 1.52b | −0.90 to 3.94 | 0.218 | 1.65b | −2.25 to 5.54 | 0.406 |
| Norm-based general health | 2.76 | 0.21 to 5.31 | 0.034 | 3.79b | −0.29 to 7.88 | 0.068 |
| Norm-based vitality | 0.37b | −2.23 to 2.98 | 0.777 | 0.19b | −4.03 to 4.41 | 0.928 |
| Norm-based social functioning | 1.72b | −1.05 to 4.49 | 0.221 | 2.36b | −2.13 to 6.84 | 0.301 |
| Norm-based role emotional | 2.67 | 0.07 to 5.27 | 0.044 | 4.56 | 0.34 to 8.79 | 0.034 |
| Norm-based mental health | 0.59b | −1.96 to 3.14 | 0.650 | 0.40b | −3.72 to 4.51 | 0.849 |
| EQ-5D | 0.047b | −0.013 to 0.108 | 0.126 | 0.069b | −0.029 to 0.167 | 0.168 |
REFLUX symptom score
There were statistically significantly higher REFLUX QoL scores at all time points, albeit with some diminution over time in the surgical group (see Figure 3). Although symptom category scores favoured surgery across all domains at all time points, the most marked and sustained difference was in ‘general discomfort’.
Short Form questionnaire-36 items
The SF-36 scores in all domains also favoured the surgical group at all time points. Differences decreased over time and this was reflected in most p-values being < 0.05 up to 3 years, whereas at year 5 this applied to only ‘norm-based general health’ and ‘norm-based role emotional’.
European Quality of Life-5 Dimensions
Differences in EQ-5D had a similar pattern to differences in REFLUX QoL and SF-36 scores – differences all favoured the surgical group but tended to narrow such that scores at years 2 and 3 were statistically significantly different, but at later time points they were not. Variability tended to increase over time. Despite the general narrowing of the EQ-5D difference over time, at year 5 it was actually the same as that at 12 months after surgery but with wider CIs.
Adjusted treatment received
As would be expected, all (with a small number of exceptions) the adjusted treatment received analyses had larger differences than the corresponding ITT analyses (around 25–50% higher), but with wider CIs.
Subgroup analyses
Removal of data from the single largest clinical centre (Aberdeen)
No formal exploration of centre effects was undertaken because of the small numbers of participants recruited in many of the clinical centres. However, a sensitivity analysis removing the data from the Aberdeen centre, the centre where the largest number of participants were recruited, did not significantly change the conclusions (adjusted difference in REFLUX score at 60 months = 5.43, 95% CI 0.96 to 9.90).
Partial compared with total wrap procedure
In an observational analysis, there was no evidence of a difference between a total wrap procedure and a partial wrap procedure. The difference in the REFLUX QoL score between these procedures at time equivalent to 5 years post surgery was −1.0 (95% CI −5.4 to 3.7; p = 0.649).
Discussion
Follow-up to 5 years after laparoscopic surgery described here provides clear evidence of sustained improvement in GORD symptoms, as judged by the REFLUX QoL scores. Differences between the groups as randomised did tend to diminish over the course of the study; nevertheless, the analyses at 5 years (the primary end point) showed highly statistically significant results with effect sizes of the order of 0.6 of a SD.
This report concentrates on the data collected annually at a time equivalent to between 2 and 5 years post surgery. Data were collected through self-complete postal questionnaires, backed up by postal and telephone reminders and occasional completion of the questionnaire over the telephone. The response rate did drop over time, from 90% at 1 year to around 70% at 5 years. The principal reason for not obtaining a follow-up questionnaire was a loss of contact, such as following a home move; the second most common reason was a decision by a participant to decline further follow-up. The category of ‘non-responder’ accounted for only around 8% of those without a follow-up questionnaire. Response analysis showed that responders at 5-year follow-up had a higher mean age, had been prescribed anti-reflux medication for a shorter period of time at recruitment and had higher QoL at baseline. However, the characteristics of responders and non-responders at 5 years were similar across the two randomised groups.
Randomised trials, such as the REFLUX trial, that compare surgery with medical management are challenging to mount because of the stark contrast between the treatments compared. As described in the previous report of this study, recruitment was not easy and it is to the credit of the many staff in the 21 centres involved in the trial that this was accomplished successfully. A second challenge was that, after randomisation, a sizable proportion of participants did not receive the treatment to which they had been allocated – again, reflecting the contrasts in the treatments. We explored the impact of this in a number of ways.
Figure 18 shows the results of a supplementary analysis of the group randomly allocated surgery stratified by whether or not they actually had surgery. It shows that those who had surgery started from a lower REFLUX QoL baseline score (had worse symptoms) than those who did not undergo surgery, and then had a sharp rise in score following the operation such that their scores were consistently higher than those who did not actually have fundoplication. To put this another way, the improvement seen among those who had surgery was greater than that in the randomised group overall.
FIGURE 18.
Mean REFLUX QoL scores for (a) all randomised to surgery, (b) those randomised to surgery who had fundoplication and (c) those randomised to surgery who did not have surgery.
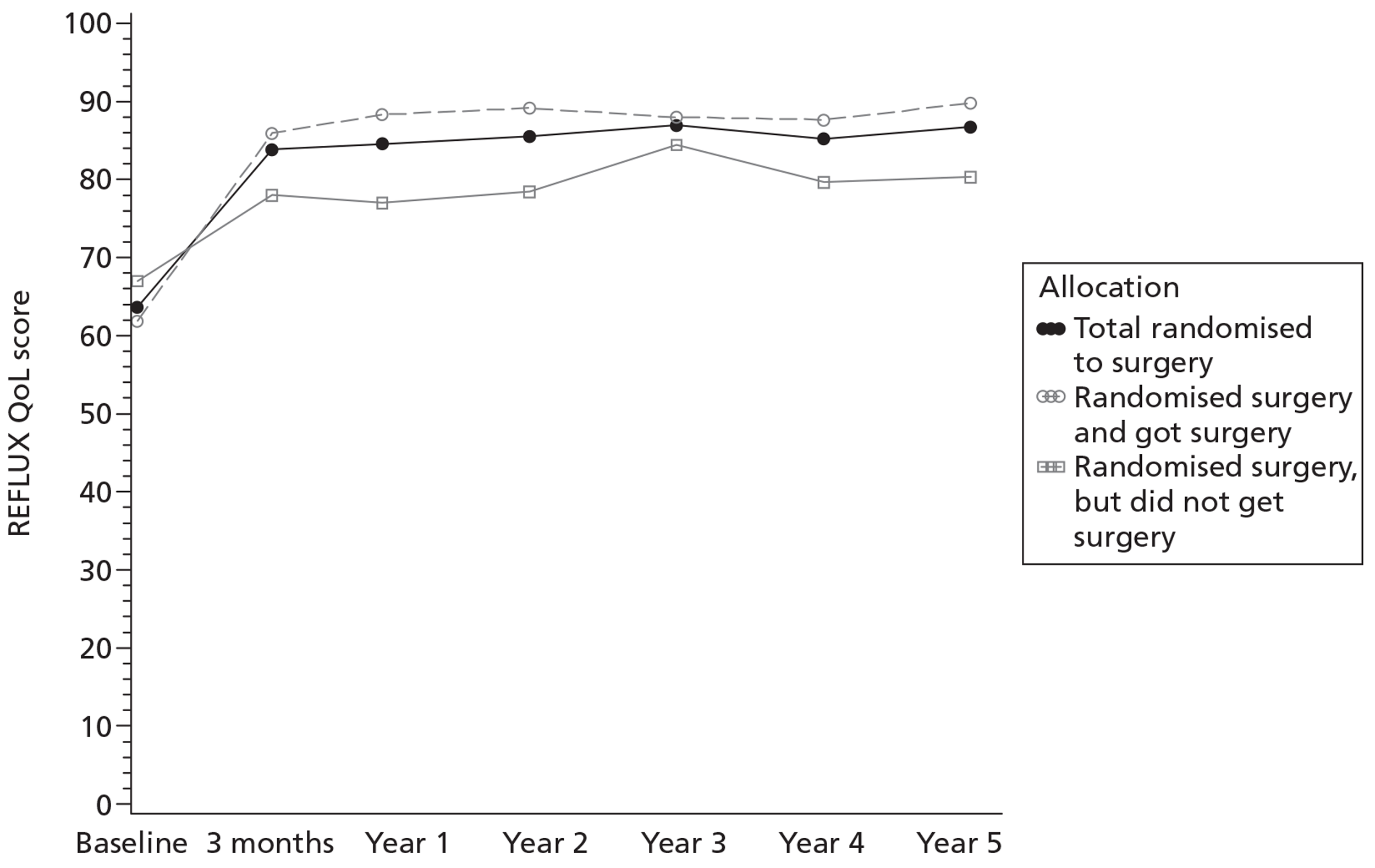
Figure 19 shows a similar supplementary analysis of the group allocated medical management stratified by whether or not they in fact had surgery in the first year. This shows that those who had fundoplication (the lowest line) had more severe symptoms of GORD (low REFLUX QoL scores) at the time of trial entry, worse even than the preference surgical group. In contrast, those solely managed medically had relatively high baseline scores. Scores among those randomised to medical management who had surgery improved markedly over the course of the follow-up, such that by years 4 and 5 the scores in the two strata were similar. This indicates that much of the narrowing of the scores in the ITT groups over the 5 years can be explained by surgery in the randomised medical group.
FIGURE 19.
Mean REFLUX QoL scores for (a) all randomised to medical management, (b) those randomised to medical management who did not have surgery and (c) those randomised to medical management who had fundoplication.
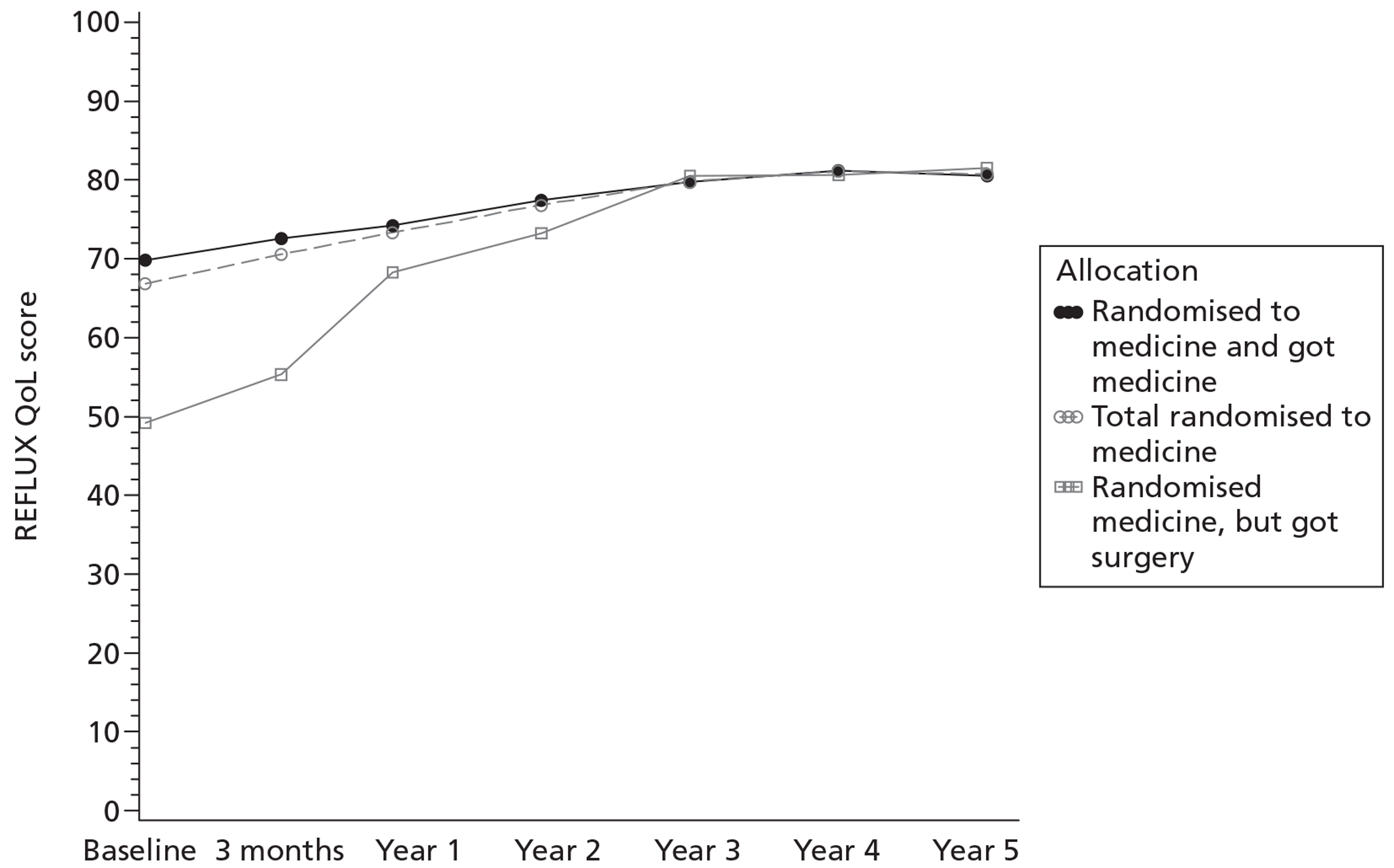
We assessed more formally the extent to which surgery in the randomised medical management group might have affected the results by undertaking adjusted treatment received analyses. We decided to base these on treatment status at the first year follow-up point. We chose this partly to be consistent with our previous report of the results up to 1 year and partly because we considered that those who had surgery after that time point were likely to be highly selected. To put this another way, we were concerned that a PP analysis up to 5 years would be particularly prone to bias. The adjusted treatment received analyses, as expected, indicated larger effects of surgery – with differences in score around 25–50% higher. As illustrated by the preference groups in this study, the proportion of those recommended surgery and willing to have it who subsequently go on to have fundoplication is likely to be higher in everyday practice. Hence, we would argue that the results of the adjusted treatment received analyses are likely to provide a better estimate of the benefits of a policy of laparoscopic fundoplication as would apply in the health service.
The principal concern about laparoscopic fundoplication is possible risks associated with the surgery. We described intra- and postoperative surgical outcomes in our previous report. 1 Among the 329 patients in the randomised surgical and preference surgical groups who had fundoplication in the first year, there were no major surgical complications. Two patients (0.6%; 95% CI 0.1% to 2.2%) required conversion to an open procedure; eight (2.4%; 95% CI 1.2% to 4.7%) had a visceral injury; and one (0.3%; 95% CI < 0.1% to 1.7%) had a blood transfusion. Three were admitted to a high-dependency unit, but none to an intensive care unit. The 5-year follow-up provides information about longer-term risks. We are aware of seven deaths among trial participants; however, none has an apparent link to the trial. Twelve (3.3%) of the total of 364 participants who had a fundoplication had a late complication: four were oesophageal dilatations/stricture dilatations, three had repairs of incisional hernias and five were a heterogeneous group of other complications (see Table 12). Sixteen (4.4%) of those who had fundoplication required further surgery (see Table 11): five reconstruction of the same wrap, six conversion to another type of wrap, three repair of hiatus hernia only and two reversal of fundoplication. These, albeit uncommon, complications need to be taken into account when surgery is being considered.
Proton pump inhibitor use in the randomised medical group was consistently around 80%, although these participants were not always the same people at each follow-up. In our questionnaire, we chose to ask about anti-reflux drug use over the preceding 2 weeks as we thought that a recollection over a longer period would be unreliable. Nevertheless, taking of PPIs seems to be dynamic (patients stopping and restarting) and rates of use at any time over a longer period would likely have been higher. We did observe more visits to GPs in the medical groups for reflux-related reasons during the 5 years of follow-up but are not able to say whether this was due to routine reassessments or because symptom control was less stable or inadequately controlled in the medical group.
The pattern of PPIs used did change over the course of the study. At baseline, the commonest PPI was lansoprazole, but omeprazole superseded this over the course of the trial. Much of this change occurred in the first year and hence could be a consequence of the review of medical management that was part of the trial management for those randomised to medical management.
The larger number of overnight hospital admissions in the randomised medical management group was largely, but not totally, explained by the minority who went on to have surgery; as discussed in Chapter 5 describing the economic evaluation, this was the principal driver of extra resource use by the medical group during the longer-term follow-up.
Despite the methodological challenges alluded to above, the study, through the data presented here, has successfully addressed the first of the objectives of this longer-term follow-up: to assess whether or not short-term clinical benefits, principally in terms of symptom control, are sustained – they are, albeit attenuated. In the next chapter we consider the REFLUX trial in the context of the three other randomised trials that have been conducted worldwide comparing laparoscopic fundoplication with medical management, and assess whether or not the results of the REFLUX trial are consistent with those of the other trials.
Chapter 4 Comparison of the REFLUX trial with other randomised trials of laparoscopic surgery compared with medical management for gastro-oesophageal reflux disease
Introduction
The REFLUX trial is one of four randomised trials that have compared laparoscopic surgery with medical management of GORD. Although the REFLUX trial has similarities to the other trials, its design is the most pragmatic42 and this is reflected in significant differences in comparison with the other trials. The characteristics of the four trials are summarised in some detail in Appendix 5; key similarities and differences in characteristics between the REFLUX trial and the other trials will be highlighted here. This overview draws heavily on the relevant Cochrane review,43 two of whose authors are authors of this report, but incorporates reports published since the Cochrane review, identified primarily through an updated search using a similar strategy to the one described in the Cochrane review.
The three comparable trials
The Anvari et al. trial44–46 is a publicly funded single-centre trial conducted in Canada, led by upper gastrointestinal surgeons. It is the smallest of the four trials (104 randomised). The two intervention policies were standardised and the surgery was undertaken by only four surgeons (Table 23). Reflecting this, nearly all participants – unlike in the REFLUX trial – were managed in the way allocated. Like the REFLUX trial, its primary outcome was a GORD-related QoL instrument (the GERSS or Gastro-Esophageal Reflux Symptom Score), and HRQoL was measured with the same instruments as in REFLUX (SF-36 and EQ-5D). The first report described the trial up to 12 months after surgery,44 and recent papers have reported 3-year results45 and an economic evaluation. 46 At 3 years, participants in the medical group were offered surgery and a large proportion (42%) accepted; hence, although further follow-up is reported to be ongoing, it will be of limited usefulness in comparing laparoscopic surgery with medical management.
| Trial | Surgeon experience | Crural repair | Gastric division | No. of surgeons participating |
|---|---|---|---|---|
| Anvari44–46 | > 50 procedures performed | Not reported | Short vessels divided | 4 |
| LOTUS47–50 | > 40 procedures performed and current workload ≥ 20 per annum | Protocol specified posterior repair | Protocol specified division | 40 trained |
| Mahon51–53 | ‘Experienced’ | Yes, all patients | Short vessels divided | 2 |
| REFLUX1–3 | > 50 procedures performed | Surgeon discretion | Surgeon discretion | Not reported |
The LOng-Term Usage of esomeprazole versus Surgery for treatment of chronic GERD (LOTUS) trial47–50 is the largest of the four trials (554 randomised). The study was funded by a pharmaceutical company, AstraZeneca, and the reports all include authors based in the company. The trial involved 39 centres in 11 European countries and was led by an upper gastrointestinal surgeon. The trial is described as ‘not designed as a superiority or equivalence trial but, rather, was an exploratory study to estimate the efficacy of laparoscopic anti-reflux surgery and PPI treatment in PPI responders’. Unlike in the REFLUX trial, all participants had shown response to PPI treatment in a run-in phase, and both clinical management policies were strictly standardised (see Table 23).
The method by which the total fundoplication approach was standardised has been described in detail. 50 In the medically managed group, the only PPI used was esomeprazole, initially at the standard dose of 20 mg. Both the surgical and medically treated patients were followed up by the investigators at 6-monthly intervals and symptoms were assessed using the Gastrointestinal Symptoms Rating Scale (GSRS) questionnaire. In the medically treated group, esomeprazole could be increased to 40 mg once a day and then to 20 mg twice a day if symptom control was insufficient. Another key difference from the REFLUX trial was that the primary outcome measure was ‘treatment failure’. A single definition of treatment failure could not be used for both trial groups; rather, this was specifically defined for each group (including in the medical group need for escalation of medication and in the surgical group, need for regular medication). The concern is that the thresholds for these may not reflect similar levels of GORD. A GORD-specific QoL instrument (Quality of Life in Reflux and Dyspepsia or QOLRAD54) was among the secondary outcomes but was given relatively little emphasis in the reporting of the trial. No HRQoL instruments were used and there was no economic evaluation. Although the main analysis was said to be carried out on an ITT basis, it seems that the 40 people allocated surgery who did not receive it were excluded from analyses. Results were first reported after 3 years' follow-up47 and recently 5-year data have been published. 48
The Mahon et al. trial51–53 was a two-centre UK trial led by and involving two upper gastrointestinal surgeons. It is not clear how the main trial was funded but supplementary funds were provided by Jansen Pharmaceuticals ‘for physiological studies’ and by Ethicon Endo-Surgery for the economic analysis. 52 In total, 217 people were randomised; the sequence was ‘computerised’ but the randomisation process and extent of concealment were not described. The two surgeons used a similar Nissen fundoplication method (see Table 23) and there was the option of four different PPI regimens depending on what PPI a participant had been taking prior to the trial. A range of outcome measures were reported and these included a gastrointestinal symptom score (GSRS) and a HRQoL measure [Psychological General Well-Being Index (PGWI)]. 55 All those allocated to medical management were offered surgery after 1 year (and apparently this was made clear to potential participants before trial entry) and the majority [54/94 (57%)] then had surgery. The 1-year follow-up was thus essentially the end of this randomised trial, even though a further follow-up has been reported. 53
Gastro-oesophageal reflux disease-related quality-of-life and symptom scores
Data available for each of the trials that describe GORD QoL or symptom scores at 1, 3 and 5 years' follow-up are summarised in Tables 24–26. Although it is not possible to combine data because different instruments (or subscales of instruments) were used in the trials, the results are consistent.
| Trial | Surgical | Medical | Mean difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Anvari44–46 | ||||||
| GERSS | 52 | 8.3 (8.4) | 52 | 13.6 (9.5) | −5.3 (−8.7 to −2.0) | 0.002 |
| LOTUS47–50 | ||||||
| QOLRAD | ||||||
| Vitality | 203 | 6.84 (0.52) | 220 | 6.42 (0.92) | 0.42 (0.28 to 0.56) | < 0.001 |
| Food and drink | 203 | 6.78 (0.60) | 220 | 6.34 (0.98) | 0.44 (0.28 to 0.60) | < 0.001 |
| Sleep | 203 | 6.87 (0.49) | 220 | 6.53 (0.76) | 0.34 (0.22 to 0.46) | < 0.001 |
| Physical/social | 203 | 6.93 (0.36) | 220 | 6.72 (0.52) | 0.21 (0.12 to 0.30) | < 0.001 |
| GSRS | ||||||
| REFLUX dimension | 248 | 1.18 (0.44) | 266 | 1.66 (0.88) | −0.48 (−0.60 to −0.36) | < 0.001 |
| Mahon51–53 | ||||||
| GSRS | 80 | 37.0 (5.4) | 86 | 35.0 (7.3) | 2.00 (0.003 to 3.94) | 0.003 |
| REFLUX1–3 | ||||||
| REFLUX QoL | 178 | 84.6 (17.9) | 179 | 73.4 (23.3) | 14.0 (9.6 to 18.4) | < 0.001 |
| Trial | Surgical | Medical | Mean difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Anvari44–46 | ||||||
| GERSS | 49 | 6.21 (8.66) | 44 | 9.05 (10.40) | −2.84 (−6.77 to 1.09) | 0.166 |
| LOTUS47–50 | ||||||
| QOLRAD | ||||||
| Vitality | 181 | 6.90 (0.31) | 189 | 6.53 (0.85) | 0.37 (0.24 to 0.50) | < 0.001 |
| Food and drink | 181 | 6.85 (0.40) | 189 | 6.38 (0.91) | 0.47 (0.33 to 0.61) | < 0.001 |
| Sleep | 181 | 6.92 (0.33) | 189 | 6.53 (0.82) | 0.39 (0.26 to 0.52) | < 0.001 |
| Physical/social | 181 | 6.94 (0.25) | 189 | 6.74 (0.58) | 0.20 (0.11 to 0.29) | < 0.001 |
| Mahon51–53 – trial terminated at 1 year | ||||||
| REFLUX1–3 | ||||||
| REFLUX QoL | 132 | 87.0 (15.0) | 134 | 79.7 (20.1) | 9.0 (4.9 to 13.1) | < 0.001 |
| Trial | Surgical | Medical | Difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Anvari44–46 – no data available | ||||||
| LOTUS47–50 | ||||||
| QOLRAD | ||||||
| Vitality | 160 | 6.86 (0.44) | 179 | 6.49 (0.99) | 0.37 (0.20 to 0.54) | < 0.001 |
| Food and drink | 160 | 6.80 (0.51) | 179 | 6.47 (0.80) | 0.33 (0.18 to 0.48) | < 0.001 |
| Sleep | 160 | 6.89 (0.47) | 179 | 6.61 (0.72) | 0.28 (0.15 to 0.41) | < 0.001 |
| Physical/social | 160 | 6.94 (0.23) | 179 | 6.75 (0.51) | 0.19 (0.10 to 0.28) | < 0.001 |
| Mahon51–53 – trial terminated at 1 year | ||||||
| REFLUX1–3 | ||||||
| REFLUX QoL | 127 | 86.7 (13.8) | 119 | 80.7 (20.3) | 6.42 (1.61 to 11.23) | 0.009 |
At 1 year there are eligible data from all four trials (see Table 24). In each case there are highly statistically significant differences all favouring the surgically managed groups. As mentioned above, the randomised element of the Mahon et al. trial51–53 ended at 1 year but data at 3 years are available for the other three trials (see Table 25). Again, all favour the surgical group and this was statistically significant in both the LOTUS47–50 and the REFLUX1–3 trials.
Only the LOTUS and (now) the REFLUX trial have reported 5-year follow-up. GORD-related QoL scores significantly favour the surgical groups in both trials (see Table 26).
Health-related quality of life
No general HRQoL measure has been reported for the LOTUS trial. 47–50 Data for the other three trials are shown in Tables 27–29. The SF-36 was used in the Anvari et al. trial44–46 as it was in the REFLUX trial. 1–3 Unfortunately, it is reported only as the two summary component scores, physical (PCS) and mental (MCS), plus the ‘general health’ domain score. For comparability, in Tables 27 and 28 the same score formats are shown for the REFLUX trial but it should be borne in mind that the eight domain scores shown in Chapter 3 for the REFLUX trial are more informative.
| Trial | Surgery | Medical | Difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Anvari44–46 | ||||||
| SF-36 | ||||||
| PCS | 52 | 46.4 (10.9) | 52 | 43.9 (10.3) | 3.15 (−0.94 to 7.23) | 0.13 |
| MCS | 52 | 52.7 (10.9) | 52 | 51.5 (9.1) | 0.98 (−2.8 to 4.76) | 0.61 |
| General health domain score | 52 | 75.4 (23.2) | 52 | 66.4 (23.6) | 12.3 (3.7 to 20.8) | 0.005 |
| LOTUS47–50 – not reported | ||||||
| Mahon51–53 | ||||||
| PGWB | 79 | 106.2 (16.3) | 86 | 100.4 (18.9) | 5.8 (0.43 to 11.17), adjusted 7.1 (2.5 to 11.7) | |
| REFLUX1–3 | ||||||
| SF-36 | ||||||
| PCS | 150 | 48.0 (10.2) | 161 | 45.1 (9.7) | 3.51 (1.77 to 5.25) | < 0.001 |
| MCS | 150 | 46.6 (12.8) | 161 | 45.1 (13.1) | 1.63 (−0.79 to 3.85) | 0.195 |
| General health domain score | 178 | 45.2 (11.1) | 179 | 40.7 (11.2) | 4.8 (2.7 to 6.8) | < 0.001 |
| EQ-5D | 178 | 0.75 (0.25) | 179 | 0.71 (0.27) | 0.047 (−0.004 to 0.097) | 0.07 |
| Trial | Surgery | Medical | Difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Anvari44–46 | ||||||
| SF-36 | ||||||
| PCS – not reported | ||||||
| MCS – not reported | ||||||
| General health domain score | 49 | 78.50 (19.76) | 44 | 71.41 (21.73) | 12.19a (2.65 to 21.72) | 0.0124 |
| LOTUS47–50 – not reported | ||||||
| Mahon51–53 – trial terminated at 1 year | ||||||
| REFLUX1–3 | ||||||
| SF-36 | ||||||
| PCS | 128 | 47.2 (9.9) | 127 | 46.6 (10.0) | 1.43 (−0.45 to 3.32) | 0.136 |
| MCS | 128 | 48.9 (10.6) | 127 | 45.6 (12.6) | 4.05 (1.57 to 6.52) | 0.001 |
| General health score | 132 | 45.3 (10.0) | 134 | 42.4 (11.8) | 3.69 (1.50 to 5.87) | 0.001 |
| EQ-5D | 132 | 0.803 (0.231) | 134 | 0.747 (0.262) | 0.070 (0.0015 to 0.126) | 0.013 |
| Trial | Surgery | Medical | Difference (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Anvari44–46 – no data available | ||||||
| LOTUS47–50 – not reported | ||||||
| Mahon51–53 – trial terminated at 1 year | ||||||
| REFLUX1–3 | ||||||
| SF-36 | ||||||
| PCS | 113 | 46.1 (9.9) | 109 | 46.1 (10.5) | 1.47 (−0.84 to 3.79) | 0.211 |
| MCS | 113 | 47.8 (11.7) | 109 | 47.9 (11.7) | 1.27 (−1.36 to 3.90) | 0.343 |
| General health domain score | 117 | 44.1 (10.3) | 111 | 43.2 (11.5) | 2.76 (0.21 to 5.31) | 0.034 |
| EQ-5D | 127 | 0.774 (0.259) | 119 | 0.761 (0.282) | 0.047 (−0.013 to 0.108) | 0.126 |
At 1 year, in both trials, the PCS and MCS favour the surgical group, although only the difference in the PCS in the REFLUX trial1–3 is statistically significant. Both trials showed marked differences in the ‘general health’ domain score. There was also a statistically significant difference favouring surgery in the Mahon et al. trial51–53 (based on the PGWI).
Although EQ-5D data were collected in the Anvari et al. trial,44–46 they were not reported in a way that allows interpretation. At baseline, scores were markedly lower in the surgery group [mean 0.68 (SD 0.28) vs 0.76 (SD 0.21)] and the reason for this imbalance is not clear. At 1 year the equivalent results were 0.79 (SD 0.23) compared with 0.81 (SD 0.19), that is, still lower in the surgery group. As shown in Table 27, in the REFLUX trial,1–3 the mean 1-year EQ-5D score was higher in the surgery group (p = 0.07).
At 3 years, the report of the Anvari et al. trial mentions collection of the SF-36 ‘every 3 months’ but the only data reported are for the ‘general health’ domain score. This, as in the REFLUX trial, significantly favours the surgical group (see Table 28). There is no mention of collection of EQ-5D data in the 3-year follow-up of the Anvari et al. trial. At 5 years, the only data describing generic HRQoL are from the REFLUX trial (as the LOTUS trial has not included a measure) (see Table 29).
Individual symptoms of gastro-oesophageal reflux disease or its management
Data describing individual symptoms are available for all trials, although only dysphagia was reported in the Mahon et al. trial. 51–53
Heartburn
As would be expected from the overall GORD-related QoL and symptom scores, all three trials providing data reported less heartburn in their surgical groups. At 1 year in the Anvari et al. trial,44–46 the GERSS heartburn subscore is lower in the surgical group (p < 0.001); in the LOTUS trial47–50 there is clearly less heartburn in the surgical group but data are presented only graphically; and in the REFLUX trial1–3 heartburn rates in the surgical group are around half those in the medical group. At 3 years, Anvari et al. 44–46 report significantly more heartburn-free days in the surgical group (p = 0.008); in the LOTUS trial,47–50 less heartburn in the surgical group is shown graphically and the p-value is reported as < 0.001; and in the REFLUX trial1–3 51% of the randomised surgical group compared with 75% of the randomised medical management group report any heartburn (see Table 15). At 5 years, data are available only from the LOTUS and REFLUX trials. In LOTUS,47–50 8% in the surgery group compared with 16% in the medical group are reported to have heartburn, ‘although there was no significant difference in the severity of heartburn (p = 0.14)’. In the REFLUX trial,1–3 41% in the surgery group compared with 74% in the medical group reported any heartburn (see Table 15).
Regurgitation
Again, as would be expected from the overall GORD-related QoL and symptom scores, all three trials providing data reported less regurgitation in the surgical groups. At 1 year in the Anvari et al. 44–46 trial, the GERSS regurgitation subscore is significantly lower in the surgical group (p = 0.002); in the LOTUS trial,47–50 graphical presentation clearly indicates less regurgitation in the surgical group, although no figures are reported; and in the REFLUX trial,1–3 regurgitation rates in the surgical group are half those in the medical group. At 3 years, information is available only for the LOTUS and REFLUX trials and both report lower rates in the surgical groups. At 5 years in the LOTUS trial, 2% in the surgical group compared with 13% in the medical group (p < 0.001) have regurgitation, and in the REFLUX trial 25% in the surgical group compared with 37% in the medical group report any regurgitation.
Dysphagia
As mentioned in Chapter 1, dysphagia following both open fundoplication and laparoscopic fundoplication has been reported. At 1 year, Anvari et al. 44–46 report a higher GERSS dysphagia subscore in the surgical group but this was not statistically significant (p = 0.8); in the LOTUS trial47–50 there were more reports of dysphagia in the surgical group but data were presented only graphically; in the Mahon et al. trial,51–53 dysphagia persisting beyond 3 months was reported in 5 out of 104 (4.8%) having surgery; and in the REFLUX trial,1–3 rates of ‘difficulty swallowing’ were the same in the two randomised groups. At 3 and 5 years, information is available only from the LOTUS and REFLUX trials. In the LOTUS trial there is more dysphagia in the surgical group (p < 0.001) at both time points: at 5 years 11% in the surgical group report dysphagia compared with 5% in the medical group. In the REFLUX trial, one further participant had undergone oesophageal dilatation (see Table 12), but the numbers reporting difficulty swallowing were the same in the two randomised groups (see Table 15, e.g. any difficulty swallowing 24.2% vs 23.9%).
Flatulence
Flatulence has also been reported as more common after both open and laparoscopic fundoplication. Information is available only from the LOTUS47–50 and REFLUX1–3 trials. In the LOTUS trial, flatulence was more common in the surgery group than in the medical management group at 1, 3 and 5 years. At 5 years, the rates are 57% in the surgical group and 40% in the medical group (p < 0.001). In the REFLUX trial, rates of ‘wind from the lower bowel’ are not statistically significantly different between the groups [more than three times per week: 65.0% in the randomised surgical group vs 59.4% in the randomised medical group at 1 year; 57.6% vs 58.5% at 3 years; and 65.3% vs 60.0% at 5 years (see Table 15 for more detail)].
Other symptoms
In the LOTUS trial,47–50 ‘bloating’ was reported more commonly in the surgical group (40% vs 28% at 5 years). In contrast, ‘bloating/trapped wind’ was reported less commonly in the surgical group in the REFLUX trial1–3 (at 1 year: 72.1% vs 82.4%). A particular concern following fundoplication is an inability to vomit despite wanting to. In the REFLUX trial we attempted to address this through a question on ‘frequency of wanting to be sick but being physically unable to’ and found no difference between the groups (see Table 15).
Surgical complications
Like all procedures involving surgery under general anaesthesia, laparoscopic fundoplication carries risks. Table 30 summarises intra and early postoperative complications reported in the four trials.
| Trial | n having operation | Conversion, n (%) | Intraoperative complications, n (%) | Postoperative complications, n (%) |
|---|---|---|---|---|
| Anvari44–46 | 51 | 0 (0.0) | 0 (0.0) | 7 (13.7) |
| LOTUS47–50 | 248 | 6 (2.4) | Unclear | 7 (2.8) |
| Mahon51–53 | 109 | 1 (0.9) | 4 (3.7) | 6 (5.5) |
| REFLUX1–3 | ||||
| Randomised | 111 | 2 (1.8) | 2 (1.8) | 1 (0.9) |
| Preference | 218 | 0 (0.0) | 4 (1.8) | 2 (0.9) |
Conversion to an open procedure
The decision to convert from a laparoscopic to an open approach is usually indicative of difficulties experienced during the procedure. Rates varied from 0% in the Anvari et al. trial44–46 to 2.4% in the LOTUS trial47–50 (see Table 30).
Intraoperative complications
In the Mahon et al. 51–53 and REFLUX1–3 trials combined, the 10 intraoperative complications reported (overall rate 2.3%) were injuries to the spleen (n = 3), liver (n = 3), pleura (n = 3) and oesophagus (n = 1). In the LOTUS trial47–50 it was unclear whether intraoperative complications occurred or whether they were incorporated within all postoperative complications; however, the report noted that 29 participants encountered a variety of operative difficulties that were described as ‘trivial’.
Early postoperative complications
In the Anvari et al. trial,44–46 seven (14%) participants had postprandial bloating, two of whom were treated with a single dilatation of the wrap. No details are given of the postoperative complications in the LOTUS trial. In the Mahon et al. trial51–53 there were three wrap migrations, two respiratory tract infections and one case of a sutured nasogastric tube. In the REFLUX trial,1–3 one participant in the randomised group and two in the preference group were admitted to a high-dependency unit immediately after the surgical procedure.
Reoperations
By the time of the 3-year follow-up in the Anvari et al. trial,44–46 4 of 51 (7.8%) participants had undergone a second fundoplication operation. Four (3.7%) in the Mahon et al. trial51–53 required reoperation within 3 months of their first fundoplication, one of whom had a gastric resection because of necrosis. It is not clear if anyone in the LOTUS trial47–50 had a reoperation. As shown in Table 11, in the REFLUX trial,1–3 5 of the 112 (4.5%) randomised to surgery who actually had a fundoplication had a second reflux-related operation, and this applied to 16 (4.4%) of the total 364 participants in the study who had a laparoscopic fundoplication.
Other late postoperative complications
Dilatation of the wrap was reported for two (3.9%) people in the Anvari et al. trial44–46 and four (3.7%) in the Mahon et al. trial. 51–53 It is not stated whether or not dilatation occurred in the LOTUS trial. 47–50 In the REFLUX trial,1–3 two (1.8%) participants in the randomised surgical group (plus two in the preference surgical group – giving an overall rate of 1.1%) had stricture dilatation or food disimpaction (see Table 12). There were three cases (0.8%) of repair of incisional hernia in the REFLUX trial – all in the preference group – but this complication was not mentioned in the other trials' reports. There were no deaths in any of the trials associated with surgical or medical management.
Surgery-related mortality
No perioperative deaths were reported among the 771 people in the four trials who had fundoplication surgery.
Discussion
Of the four trials, the REFLUX trial is the most pragmatic in design. It involved a large proportion of UK centres where laparoscopic anti-reflux surgery is undertaken and the surgery was undertaken by NHS upper gastrointestinal surgeons within these centres, all of whom had experience of carrying out the procedure. The exact method of fundoplication was left to the discretion of the surgeon, so he or she was comfortable with the approach. After surgery and, in the medically treated patients, after optimisation of their PPI medication, care of the participants was the responsibility of GPs. The principal measure of outcome was a patient-reported disease-specific QoL measure. Unlike the other trials, the REFLUX trial was coordinated from an accredited trials unit, local recruitment was led by gastroenterologist/gastrointestinal surgeon partnerships rather than by gastrointestinal surgeons alone, and the trial was publicly funded through the HTA programme rather than by industry.
In respect of potential benefits of surgery, the four trials appear to be consistent. All show significantly better relief of GORD symptoms for as long as the length of their current follow-up. (Surprisingly, the LOTUS trial report48 does not draw attention to this but, judged on data describing the QOLRAD reported in an e-table, there are significant differences between the groups in all dimensions of this instrument, favouring surgery.) Data available describing the principal symptoms of GORD (heartburn and regurgitation) show large differences, again favouring surgery. Only limited data are available from generic QoL measures, and much of this is from the REFLUX trial; although differences are less marked than for the GORD-related QoL instruments, they are consistent with benefit from surgery.
The four trials are broadly consistent in respect of intraoperative and early postoperative complications: a small number of operations are converted to an open procedure, a small number of laparoscopic procedures have associated visceral injuries, a small number of people have problems postoperatively and a small number require dilatation of the wrap. The REFLUX trial suggests that 4.5% have reoperations and the other trials are broadly consistent with this. None of the trials had a reported perioperative death. Data from the Finnish Registry56 suggest a mortality of 0.1%, but this is based on a single case among 1162 people who had laparoscopic fundoplication; furthermore, the registry included all cases of fundoplication and hence went beyond the sorts of patients recruited to the REFLUX trial.
The other trials, particularly the LOTUS trial, show higher rates of dysphagia and flatulence following laparoscopic fundoplication than in the medically managed group. As mentioned above, a small number of participants in the REFLUX trial did have a dilatation procedure, presumably because of difficulty swallowing, but this was not reflected in responses to the REFLUX questionnaire, suggesting that there were only a few isolated cases of dysphagia following surgery in this trial. Similarly, there were no significant differences in flatulence in the REFLUX trial.
Hence, taking all four trials together, it is now possible to give a clear picture of most of the potential benefits and risks of laparoscopic fundoplication, at least up to 5 years. There are, however, differing resource implications of surgery and medical management. In the next chapter we explore whether or not the benefits of surgery in patients with established GORD requiring long-term PPI therapy for reasonable control and suitable for either clinical policy (average age around 45 years) are sufficient to outweigh any differences in costs.
Chapter 5 Economic analysis
The economic evaluation aimed to determine the cost-effectiveness of laparoscopic fundoplication compared with continued medical management in patients with GORD symptoms that are reasonably controlled by medication and who are judged suitable for both surgical and medical management. The analysis entailed three components:
-
systematic review of existing cost-effectiveness evidence
-
within-trial (5-year) economic analysis
-
validation of within-trial analysis and exploration of the need for a longer-term model.
Systematic review of existing cost-effectiveness evidence
The aim of this systematic review is to identify any existing cost-effectiveness studies that compare laparoscopic fundoplication with medical management for GORD. A previous HTA report included a review of the evidence available from 1995 to December 2005 and identified three relevant studies (described below). 1 The updated search focuses on the period from December 2005 to April 2011. The methods used to identify studies and the results of the systematic search are discussed in the sections below.
Methods
The following data sets were searched to identify published evidence: MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (1948 to present), EMBASE (1996 to week 15, 2011), Cochrane Database of Systematic Reviews (CDSR) and the NHS Centre for Reviews and Dissemination databases [Database of Abstracts of Reviews of Effects (DARE), NHS Economic Evaluation Database (NHS EED), HTA]. The search strategy incorporated broad reflux-related search terms as used in a recent Cochrane Review. 57 The search also focused on identifying health-related and GORD-specific QoL evidence.
Studies were considered relevant for inclusion in the review if they were published in English and were full health economic evaluations (cost-effectiveness, cost-utility or cost–benefit analysis) comparing costs and outcomes associated with laparoscopic fundoplication and medical management. For the purpose of this study laparoscopic fundoplication includes both complete and partial wrap procedures. Publications outside the above criteria were excluded from this review. Details of the updated search strategy are presented in Appendix 6.
Results
A total of 3662 references were identified from the searches (MEDLINE: 1640, EMBASE: 1825, CDSR: 44, DARE: 56, NHS EED: 85, HTA: 12). Titles and/or abstracts were reviewed and studies that satisfied all inclusion criteria were included in the review. Papers describing five additional studies were obtained for inclusion. These were published between 2007 and 2011 and were related to the UK and Canadian settings. Of the total of eight studies, five are linked to three of the randomised trials described in Chapter 4: Anvari et al. ,44–46 Mahon et al. 51–53 and the REFLUX trial,1 the long-term follow-up of which is the topic of this report. There is no economic evaluation in the LOTUS trial. 48 Three of the studies were based on the REFLUX trial. These were published as part of the earlier HTA report1 and in two journal articles. 3,5 Summaries of the two within-trial economic evaluations are presented in Appendix 7. Below is a brief description of the eight reports – the five linked to the three randomised trials are considered first, followed by the three studies based on observational data.
Economic analyses based on clinical trials
Economic evaluation based on the Anvari et al. trial46
This was an economic evaluation conducted alongside the Anvari et al. trial described in Chapter 4. Laparoscopic fundoplication was compared with PPI for patients with chronic GORD. The follow-up period was 3 years and the analysis was conducted from a societal perspective. Cost-effectiveness was reported in terms of cost per QALY gained.
Three generic preference-based questionnaires were administered during the trial: Health Utilities Index Mark 3 (HUI3), EQ-5D and Short Form questionnaire-6 dimensions (SF-6D). Although these instruments have been valued by large general public samples, they differ in the attributes used for their descriptive system and the method of valuation applied. The EQ-5D has been valued using time trade-off whereas the SF-6D and HUI3 use the standard gamble. Utility scores showed an improvement in patients' HRQoL in both groups across the three utility instruments; however, the degree of improvement varied according to the utility instrument used. The base-case analysis (using the HUI3 instrument), after adjustment for baseline differences, indicated that, over the 3 years, laparoscopic fundoplication patients experienced a 0.109 gain in QALYs compared with PPI patients. The ICER for laparoscopic fundoplication patients was around C$29,400 (£19,000) per QALY gained. An increased ICER of C$76,300 (£49,300) was obtained using the EQ-5D as the HRQoL measure.
Economic evaluation based on the Mahon et al. trial52
This study looked at the cost-effectiveness of laparoscopic fundoplication compared with maintenance PPI medication for severe GORD based on the Mahon et al. randomised trial described in Chapter 4. Results based on the 12-month follow-up were extrapolated using other published data sets. Costs and outcomes for up to 12 months were obtained from a sample of patients in the trial (the first 100) and resource use was quantified using data from hospital records and GPs' notes. The incremental cost of laparoscopic fundoplication compared with PPI therapy per additional patient returned to a physiologically normal acid score (< 13.9) at 3 months was £5515 (95% CI £3655 to £13,400) and the incremental cost per point improvement in combined gastrointestinal and psychological well-being score at 12 months was £293 (90% CI £149 to £5250). The authors concluded that laparoscopic surgery would break even compared with medical management after 8 years and would be cost saving thereafter.
Economic evaluation based on the REFLUX trial1,3,5
Bojke et al. 5 present a preliminary cost-effectiveness analysis conducted before the availability of the 1-year REFLUX trial results. The analysis compared the cost-effectiveness of surgery (laparoscopic fundoplication) with long-term medical management (PPIs) for GORD disease in an average 45-year-old man. A lifetime (30 years) Markov model that adopted the perspective of the NHS was developed. Effectiveness data were obtained from a fixed-effect meta-analysis that synthesised data from multiple sources. QALYs were estimated using utility scores (measured by the EQ-5D instrument) derived from a subset of UK patients included in the REFLUX trial. Over a lifetime, expected costs associated with surgery (£5014) were higher than expected costs associated with PPI (£4890). Expected QALYs associated with surgery (13.04) were greater than QALYs associated with PPIs (12.36). The incremental cost per QALY gained (ICER) for surgery compared with medical care was £180. The estimated probability that surgery was cost-effective at the threshold of £30,000 per QALY was 0.639. The authors highlighted important areas for further research, such as the HRQoL of patients on PPIs or post surgery.
The within-trial cost-effectiveness analysis, comparing laparoscopic fundoplication with medical management 1 year post surgery, was described in full in the 2008 report of the REFLUX trial.1 The analysis was conducted on an ITT basis from a NHS perspective. HRQoL was assessed at baseline and at 3 and 12 months' follow-up using the EQ-5D. Cost-effectiveness was reported in terms of the difference in mean QALYs between the treatment groups. This difference was estimated using ordinary least squares (OLS) regression, adjusting for baseline differences in EQ-5D between individuals. The estimated difference in mean costs between the groups was £1280 (95% CI £1054 to £1468). The HRQoL of patients randomised to surgery tended to improve on average by 0.066 more QALYs (95% CI 0.023 to 0.107) than in the medical management group. The estimated mean ICER was around £19,000. At a threshold of £30,000 per QALY, the probability of surgery being cost-effective was 0.86.
Epstein et al. 3 developed a Markov model using 12-month data from the REFLUX trial and other sources in order to extrapolate the cost-effectiveness of laparoscopic fundoplication compared with medical management over the longer term (lifetime). Cost-effectiveness was reported in terms of the cost per QALY gained from surgery. The analysis was conducted from a NHS perspective. Under base-case assumptions, surgery had an additional mean cost of £847 and additional mean QALYs of 0.37 over the lifetime of the patients. The incremental cost per additional QALY gained was around £3000. At a threshold of £20,000 per QALY, the probability that surgery was cost-effective was around 0.74.
Economic analyses based on observational data
Economic evaluation based on Romagnuolo et al.58
This study is based on observational data and compares the cost-effectiveness of maintenance regimens of omeprazole and laparoscopic fundoplication within the Canadian medical system. The effectiveness, HRQoL and resource-use data were derived from studies published between 1985 and 2000. Outcomes were expressed as QALYs and costs were estimated from the perspective of a provincial health ministry. A two-stage Markov model (healing and maintenance phases) was used to estimate costs and utilities using a time horizon of 5 years. Laparoscopic fundoplication was the most cost-effective option at 3.3 years of follow-up and was cost saving at 5 years. These results were sensitive to the price of omeprazole. QALYs did not differ significantly between treatment groups.
Economic evaluation based on Arguedas et al.59
This study, also based on observational data, compared the cost-effectiveness of laparoscopic fundoplication and medical management in patients with severe reflux oesophagitis. Outcomes were quantified using QALYs with model inputs derived from the published literature. A Markov simulation model was used to extend a previous analysis to a 10-year time horizon. Procedure and hospitalisation costs were estimated using Medicare reimbursement rates from the authors' institution. Medical therapy was associated with a total cost of $8798 and 4.59 QALYs, whereas the surgery was more expensive ($10,475) and less effective (4.55 QALYs). The authors concluded that medical therapy dominated surgery.
Economic evaluation based on Comay et al.60
This is a cost-effectiveness analysis, based on observational data, principally concerned with assessing an endoscopic therapy (Stretta procedure) compared with PPIs and laparoscopic fundoplication in the management of GORD. The Strettra procedure is out of the scope of our analysis; however, the data on costs and QALYs provided by the authors allow us to better understand QoL related to these technologies and make comparisons with other authors' estimates. The authors constructed a Markov model that tracked patients over a period of 5 years. Analysis was undertaken from the Canadian Ministry of Health perspective. A literature review for published studies before 2004 was carried out to derive effectiveness and utility data. Symptom-free months and QALYs were used to measure benefit. PPI was the dominant strategy, producing more symptom-free months at lower costs than the other strategies. Laparoscopic fundoplication was associated with higher costs and generated more QALYs. The discounted mean QALYs over 5 years were 4.6487 for laparoscopic fundoplication and 4.6357 for PPI. The ICER for laparoscopic fundoplication compared with PPI was C$384,692 (£240,470). This is unlikely to be considered cost-effective.
Conclusions
The different outcomes used make it difficult to compare the results of the various studies analysed here. For those studies quantifying the benefits associated with the two treatments using QALYs, the results differ depending on the type of analysis conducted. Although the trial-based results suggest that there is good short- and medium-term evidence indicating that surgery may well represent a cost-effective alternative intervention, the model-based studies are not so optimistic.
The ICER for surgery ranged from £180 to £49,000 per QALY gained. However, the limitations of the studies included in this review suggest that we should be cautious when interpreting these results. The decision model developed as part of the REFLUX trial extrapolated from data at 12 months and was based on the assumption that the treatment effect of surgery (in terms of impact on HRQoL) remains constant over the lifetime of patients. However, as would be expected, the results of the sensitivity analysis suggested that surgery was less cost-effective when the beneficial effect of surgery was limited to 5 years (increasing the ICER to £11,300) and when HRQoL was worse in those for whom surgery failed (increasing the ICER to £11,310 when considering very high rates of surgical failure).
The value of conducting additional research to reduce any uncertainty in the REFLUX model was demonstrated. The expected value of perfect information (EVPI) is the maximum amount that a decision-maker should be willing to pay to eliminate all uncertainty that arises because of imprecision in the parameters of the model. The value of information analysis suggested that further research could be worthwhile. At a threshold of £30,000, the per-patient EVPI was £15,106.
Within-trial economic evaluation
Follow-up data from the REFLUX trial up to 5 years after surgery are now available. These economic data represent the longest follow-up of randomised patients currently available. These data can help to inform the question regarding the sustainability of initial improvement in HRQoL following surgery. This section describes the updating of the cost-effectiveness analysis using these data to reduce the level of uncertainty about the cost-effectiveness of surgery and thus its role in the NHS.
Overview
Differences in mean costs and QALYs at 5 years (based on data collected within the REFLUX trial) were used to derive an estimate of the cost-effectiveness of laparoscopic surgery (laparoscopic fundoplication) and continued medical management. The extent of missing data throughout the trial follow-up is significant; therefore, the base case consists of the multiple imputed data set following ITT analysis. A separate scenario – complete-case analysis, in which patients with any missing data are excluded – was employed for ITT and PP for 1-year analyses. Costs and QALYs were evaluated on the basis of costs falling on the NHS and Personal Social Services expressed in UK pounds sterling at a 2010 price base. All analysis and modelling were undertaken in Stata/SE 11.1 (StataCorp LP, College Station, TX, USA).
Methods
Patient population
As described in earlier chapters, the patient population in the REFLUX trial was patients with GORD whose symptoms required medication for reasonable control and for whom either surgery or continued medical management appeared to be an acceptable treatment option. A policy of offering relatively early laparoscopic fundoplication was compared with the alternative policy of continued medical management. The analysis used data only from the randomised trial component of the REFLUX trial (i.e. not from the preference groups). As described in Chapter 3, 357 patients were randomised to either surgical treatment (n = 178) or medical management (n = 179) and patients were followed for up to 5 years.
Health-care resource use
Health-care resource-use data were collected prospectively as part of the clinical report forms and patient questionnaires at 3 and 12 months and 2, 3, 4 and 5 years. Patient questionnaires at 3 and 12 months collected information for the previous 3 and 9 months respectively. In addition, a questionnaire at 12 months recorded resource use for the whole of the first year (see following section on costs). Patient questionnaires from the second year onwards collected information for the previous 12 months on hospital admissions (day and overnight admissions) and GP visits, and data on medication for the previous 2 weeks. Clinical report forms collected data on surgery and perioperative complications of surgery.
Costs
The cost for each individual patient in the trial was calculated by multiplying his or her use of health-care resources by the associated unit costs (Table 31). Discount was applied from year 2. Unit costs were all sourced from published data (see Table 31). Total costs include the costs of surgery, GP visits, hospital admissions and medication. Incremental costs (laparoscopic fundoplication vs medical management) for each year and per category of resource use, according to ITT allocation, were calculated using OLS regression.
| Health-care activity | Resource | Cost (£) | Source |
|---|---|---|---|
| Laparoscopic fundoplication surgery | Endoscopy | 218.52 | Grant et al.1 (inflated to 2009–10 prices using Curtis64) |
| pH test | 81.85 | ||
| Manometry | 76.94 | ||
| Operation cost per minute | 6.36 | ||
| Capital cost per surgery | 11.71 | ||
| Consumables | 1080.96 | ||
| High-dependency unit per night | 797.86 | ||
| General ward per nighta | 282.78 | NHS Reference Costs 2009–10 (excess bed stay)63 | |
| Hospital admissionsb | Overnight admission due to surgery | 2108.22 | Mean surgery cost |
| Overnight admission due to complicationsa | 1534.76 | NHS Reference Costs 2009–10 (elective inpatient)63 | |
| Day case | 559.00 | NHS Reference Costs 2009–10 (day case)63 | |
| Outpatient | 221.98 | NHS Reference Costs 2009–10 (outpatient)63 | |
| GP use | Visit from GP | 120.00 | Curtis64 |
| Visit to GP | 36.00 | ||
| Medication | |||
| PPI | Omeprazole 10 mg, 28 capsules | 1.92 | Drug Tariff December 201061 |
| Omeprazole 20 mg, 28 capsules | 1.81 | ||
| Omeprazole 40 mg, 7 capsules | 1.95 | ||
| Lansoprazole 15 mg, 28 capsules | 1.44 | ||
| Lansoprazole 30 mg, 28 capsules | 2.23 | ||
| Pantoprazole 20 mg, 28 tablets | 1.79 | ||
| Pantoprazole 40 mg, 28 tablets | 2.82 | ||
| Rabeprazole 10 mg, 28 tablets | 11.56 | ||
| Rabeprazole 20 mg, 28 tablets | 19.55 | ||
| Esomeprazole 20 mg, 28 tablets | 18.50 | ||
| Esomeprazole 40 mg, 28 tablets | 25.19 | ||
| H2RA | Ranitidine 150 mg, 60 tablets | 1.97 | |
| Ranitidine 300 mg, 30 tablets | 2.17 | ||
| Famotidine 20 mg, 28 tablets | 4.40 | ||
| Famotidine 40 mg, 28 tablets | 5.55 | ||
| Nizatidine 150 mg, 30 capsules | 12.04 | ||
| Nizatidine 300 mg, 30 capsules | 15.34 | ||
| Cimetidine 400 mg, 60 tablets | 7.61 | ||
| Cimetidine 800 mg, 30 tablets | 21.63 | ||
| Prokinetic | Domperidone 10-mg tabletsc | 1.53 | |
| Metoclopramide 10 mg, 28 tablets | 1.01 | ||
The questionnaires asked for details of anti-reflux medication taken in the previous 2 weeks: name, dose and number of tablets/capsules. The cost of anti-reflux medication during these 2 weeks was calculated by multiplying the prices published in the Drug Tariff for December 201061 for each medicine by the number of tablets taken. Yearly medication costs are calculated using the area under the curve method,62 which assumes linear interpolation between follow-up points. The costs of reflux-related inpatient, outpatient and day-case visits were derived from the NHS Reference Costs 2009–10,63 in which the relevant codes were weighted by activity level.
For the base-case analysis, total costs included the costs of surgery, complications due to surgery, reoperations, reflux-related prescribed medication, reflux-related visits to and from the GP and reflux-related hospital inpatient, outpatient and day visits. For the sensitivity analysis, all GP visits and all hospital admissions are included in the calculation of total costs (see Incremental analysis for more details on sensitivity analysis). Costs of hospital admissions and GP visits were obtained by multiplying the relevant unit costs by the numbers of admissions and visits reported by the patients respectively. Patients themselves classified how many visits and admissions were reflux related in relation to the total number of visits. There is a possibility that patients may not have fully understood the clinical consequences of GORD; hence, they may misclassify the reason for a consultation. If such misclassification is different across treatment groups, estimates of incremental costs may be biased.
For the first year of the trial, data on resource use were collected at 3 months and 12 months, and for the whole year using an additional questionnaire. To make the most efficient use of the data available for the first year of the trial, resource use at 1 year was estimated as the greater of the area under the curve between the first and second questionnaire and the 12-month health-care survey. This is in line with the procedure employed for the earlier publication evaluating the REFLUX trial. 1
The cost of surgery included the costs of (1) presurgical procedures (endoscopy, pH monitoring and manometry), (2) the surgery team, (3) operative complications, (4) hospital stay, (5) capital costs and overheads and (6) consumables. The cost of reoperations was assumed to be equivalent to the mean cost of the first surgery. The cost of reflux-related visits to and from the GP was assumed to be equivalent to the average cost of visits to and from the GP. 64
Quality-adjusted life-years
Health outcomes were expressed in terms of QALYs. HRQoL was assessed in the REFLUX trial at baseline and 3 months and then yearly until 5 years using the EQ-5D. 65,66 The EQ-5D is a standardised and validated generic instrument for the measurement of HRQoL. It has five dimensions: mobility, ability to self-care, ability to undertake usual activities, pain and discomfort, and anxiety and depression. Each dimension has three possible responses (no problems, moderate problems or severe problems), creating 245 mutually exclusive health states. Each of these health states has been valued in a large UK population study using the time trade-off method, in which 1 corresponds to perfect health (thus the maximum value possible) and 0 corresponds to death. 65,66
QALYs for each patient were calculated as the area under the curve following the trapezium rule,67 which assumes linear interpolation between follow-up points. Incremental mean QALYs between treatment groups were estimated with and without adjustment for baseline utility, using OLS regression.
Discounting
Costs and outcomes from year 2 were discounted using a 3.5% annual discount rate, in line with current guidelines. 65,68
Missing data and multiple imputation
Given the extent of missing data, the multiple imputed data set is presented as the base case. This was created using all available data and multiple imputation with chained equations. 69 Mean imputation was used to predict missing data at baseline,70 as randomisation should ensure equal distribution of potentially confounding variables. Complete-case analysis refers to only those patients who returned all questionnaires and completed all EQ-5D profiles.
Missing or inconsistent answers to questions on resource use were dealt with as follows. For medication use, patients were asked at each follow-up questionnaire whether or not they were using prescribed medication for reflux and, if so, to indicate the name, strength and the number of tablets taken in the past 2 weeks. It was evident from preliminary analyses that the answers to the first question were not necessarily consistent with the answers to the second question. Therefore, the following rule was applied for the costing of drugs: (1) if the patient provided the name, strength and number of tablets taken, he/she was assumed to be taking medication; (2) if the patient did not specify either a drug or the number of tablets taken, he/she was considered not to be taking medication; (3) if the patient specified a particular drug but no dosage, the missing data were imputed as the median of all other patients on that medication. Similarly, missing answers to the questions regarding GP visits and hospital admissions were assumed to indicate that no visits or admissions occurred. Because of the nature of the questionnaire, it is reasonable to assume that absence of an answer indicates no use of services.
Multiple imputation71 was the statistical technique chosen to deal with missing cost and HRQoL data because of non-returned questionnaires and incomplete EQ-5D profiles, using the user-defined programme ‘ice’ in Stata 11.1. Multiple imputation presents three major advantages over standard ad hoc methods for dealing with missing data (such as mean imputation and last value carried forward): (1) it makes full use of all of the available data, (2) it incorporates uncertainty associated with the missing data and (3) it ensures unbiased estimates and standard errors as long as data are MAR. 69 [Little and Rubin72 defined three missing data mechanisms: (1) MCAR if the probability of data being unobserved is independent of both observed and unobserved values; (2) MAR if the probability of data being unobserved is dependent on the observed values but independent of unobserved ones and (3) missing not at random (MNAR) if the probability of data being unobserved is dependent on unobserved values.]
Multiple imputation follows three steps. First, regression models are used to predict plausible values for the missing observations from the observed values. A random component is included to reflect the uncertainty around the predictions. These values are then used to fill in the gaps in the data set. This process is repeated m number of times (m being the number of imputations), creating m number of imputed data sets. Second, each data set is analysed independently using complete-case methods. Third, the estimates obtained from each imputed data set are combined to generate mean estimates of costs and QALYs, variances and CIs using Rubin's rules,73 in such a way that the uncertainty around the predicted values is fully taken into account. 69,74 Because the REFLUX trial has missing data for both costs and EQ-5D scores, multiple imputation using chained equations (MICE) was employed. For MICE, each variable is predicted with its own regression model. Each imputed data set is created by running the regression models over several cycles, in which each variable informs the prediction of the other variables. 69,74 To obtain overall estimates of mean and incremental costs and QALYs across all of the imputed data sets, the ‘mim’ command was used. 75 Semi-parametric bootstrapping in Stata 11.1 was employed to estimate the probability that surgery is cost-effective, while maintaining the correlation between costs and QALYs (see Incremental analysis for more details). 76
Plausible prediction of the missing data depends on the appropriate specification of the regression models used in MICE. 74 If a model is misspecified, the distribution of imputed values may not resemble that of the observed values, and thus the estimates of treatment effect may be biased. 69 The regression model specified will depend on the type and distribution of the variable to be predicted. 70 The variables required for the economic evaluation are costs for each year and EQ-5D scores at each time point. Both are continuous variables and neither is normally distributed; EQ-5D scores in the REFLUX trial are bounded between −0.594 and 1,66 and costs are bounded at zero and tend to present a positive skew. Two approaches to deal with non-normality with MICE have been suggested in the literature:69 (1) transformation towards normality and (2) predictive mean matching. [In predictive mean matching the missing observation is imputed with an observed value from an individual with a similar linear predictor. 70 Consequently, the distribution of imputed values tends to closely match the distribution of the observed values. 69] Using the REFLUX data set none of the transformation approaches (Box–Cox,77 log-transformation and log-transformation of non-zero values with generation of an indicator variable78) were successful in transforming the data distribution to normality. As a result, predictive mean matching was the strategy employed to ensure that the distribution of imputed values closely resembled the distribution of observed values. All known covariates thought to be associated with the missingness mechanism, costs and EQ-5D scores were included in the prediction equations: EQ-5D scores at each follow-up point, costs at each year, allocation, BMI, age and sex. A total of 100 imputations (m = 100) was used to ensure efficient and reproducible estimates. 69
Multiple imputation provides unbiased estimates of treatment effect if data are MAR. Whether or not data are MAR is an untestable assumption by definition, as unobserved values are unknown. Departure from the MAR assumption may have implications for decision-making if the results from the cost-effectiveness analysis differ from those of the base case. Sensitivity analysis was used to test the impact on the cost-effectiveness results if data were MNAR, that is, if patients with worst outcomes or greater costs were more likely to have missing data. 70,79 Four scenarios were tested. In scenario (1), all patients with missing data had their total QALYs reduced by 10%, 20%, 30%, 40% and 50%. Conversely, in scenario (2), for all patients with missing data costs were increased by the same proportions (10%, 20%, 30%, 40% and 50%). In scenario (3), only surgery patients with missing data had their QALYs reduced. In scenario (4), costs were increased only for patients undergoing surgery.
Incremental analysis
The cost-effectiveness of surgery was evaluated by comparing the costs and QALYs incurred in the surgery arm with the costs and QALYs in the medical management arm at 5 years of follow-up, using conventional decision rules and estimating ICERs as appropriate. 80 If one intervention is associated with greater mean QALYs and lower mean costs it is deemed cost-effective by dominance. The ICER is calculated if either treatment arm does not dominate. The ICER summarises the additional costs associated with one intervention over another and relates this to the additional benefits. This ICER is then compared with a threshold for the cost per QALY. The National Institute for Health and Care Excellence (NICE) uses a threshold cost per QALY of around £20,000–30,000 to determine whether or not an intervention represents good value for money in the NHS. 65 Consequently, if the ICER is < £20,000, laparoscopic fundoplication could be considered potentially cost-effective. ICERs between £20,000 and £30,000 per QALY are considered borderline and an ICER > £30,000 is not typically considered cost-effective.
The ICER can be re-expressed using the net monetary benefit (NMB). The NMB of an intervention is the value of the health benefits gained from a particular intervention compared with standard care in monetary terms, minus the incremental costs of the intervention. The translation of health benefits into the monetary scale was made using a cost-effectiveness threshold of £20,000. This is the threshold commonly use by NICE (this corresponds to 1 QALY being valued at £20,000). Therefore, the NMB provides a measure of the gain (or loss) in resources of investing in a particular intervention when those resources could have been used elsewhere. 81 The NMB of laparoscopic fundoplication and medical management were calculated and used to demonstrate the influence of trial duration on the estimates of cost-effectiveness of surgery.
As discussed previously, the multiple imputed data set was used as the base case for the cost-effectiveness analysis because of the large proportion of data lost for the complete-case analysis. Because total costs and total QALYs are cumulative quantities, any missing data at any of the follow-up points will result in that patient being dropped from a complete-case analysis. The cost-effectiveness results using the complete case are presented for comparison. Complete-case analysis will provide unbiased estimates only if the data are MCAR, that is, the probability of data being unobserved is independent of both observed and unobserved values. Multiple imputation ensures unbiased estimates if the data are MAR (the probability of data being unobserved is dependent on the observed values but independent of unobserved ones). Because unobserved values are unknown, the missing data mechanism and hence the validity of either assumption is untestable. Nevertheless, multiple imputation presents two advantages. First, it requires a less stringent assumption for ensuring unbiased estimates. Second, if data are MCAR, both complete-case and multiple imputation estimates will be unbiased whereas, if data are MAR, complete-case analysis will be biased.
Analysis of uncertainty for incremental analysis
Sensitivity analysis is used to explore and quantify any uncertainty in the cost-effectiveness results. Three types of sensitivity analysis were undertaken: structural, scenario and probabilistic sensitivity analysis. Structural and scenario sensitivity analyses were carried out on the complete-case data set. Probabilistic sensitivity analysis was carried out in both the complete case and the multiple imputation data set.
Structural sensitivity analysis consisted of a PP analysis that classified patients according to treatment compliance at 1 year of follow-up, that is, whose management at 1 year was consistent with their original random allocation. Consequently, the PP data set consisted of the patients randomised to surgery who actually had surgery, and of the patients randomised to medical management who did not undergo surgery at 1 year. Patients randomised to medical management who had surgery might differ from those randomised to medical management who were managed medically without surgery, for several reasons. A patient's condition might have worsened, prompting surgery, or patients might have changed their preferences and wish to be taken off medication. The latter implies that, had they been screened for the study at the point in time when they had surgery, they would not have been eligible for the study. These patients would have had a preference and would not have accepted randomisation. The condition itself is complex because of its recurrent and cyclical nature (patients suffering from reflux have punctual exacerbations, which can lead them to change their preferences and request surgery). Therefore, the reasons for not complying with randomisation are likely to be a combination of the two motives (worsening of condition and change in preference). PP was chosen because it was thought to be more similar to clinical practice, where patients can experience a wait for surgery and change their preferences during this period. Any switching of treatment after 1 year is assumed to be because of a change in clinical status, which would preclude inclusion in the clinical trial.
The base-case analysis included only the costs of reflux-related GP visits and hospitalisations. Two alternative costing scenarios were tested in sensitivity analysis: including either all GP visits or all hospital use, regardless of whether they had been classified as reflux or non-reflux related.
Probabilistic sensitivity analysis attempts to quantify the joint effect of uncertainty around the costs and QALYs. Semiparametric bootstrapping was used to estimate the probability that each intervention is cost-effective for a range of cost-effectiveness threshold values. In bootstrapping, the original data are sampled with replacement to create a new data set, in order to calculate estimates of treatment effect. Repeating this process a large number of times results in a vector of replicated statistics, which ultimately provide an empirical estimate of the CIs around mean incremental costs and QALYs. The probability of an intervention being the most cost-effective is the conventional method of presenting the uncertainty around the cost-effectiveness results. The CIs around the ICER are not presented because they are difficult to interpret and are not easy to use: a negative ICER can indicate that an intervention dominates (because it is associated with more benefits and lower costs than its comparator) or it is dominated (because it is associated with fewer benefits and higher costs). 76
Validation
Several procedures were used to ensure the validity of the analysis. First, two statistical analysis codes (written in Stata) were developed in parallel and their results compared. Second, the code was developed by one analyst and checked independently by another. Third, the results were cross-checked in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) for a sample of the data set. Lastly, selected results were represented graphically and examined for face validity. The validity of the imputation strategy was explored by (1) analysing the data for predictors of missingness,70 (2) comparing the distributions of the observed and imputed values graphically70 and (3) estimation of Monte Carlo errors. 69Appendix 8 describes the validation process in more detail.
Results
Patient population
Complete-case analysis consisted of the patients who returned all questionnaires and completed all EQ-5D profiles. Overall, there are 172 patients in the complete-case analysis (88 randomised to medical management and 84 randomised to surgery). Table 32 shows the numbers of questionnaires returned (includes those with some missing data) and the numbers of completed questionnaires returned for each year. As expected, the number of questionnaires returned in each year of follow-up decreases with time. The return of questionnaires does not follow a monotonic pattern, that is, patients who did not return the questionnaire for one particular year may have returned a questionnaire in subsequent years. Therefore, the number of patients in the complete-case analysis is lower than the number of completed questionnaires in year 5. The large number of patients not included in the complete-case analysis because of missing data strengthens the rationale for using the multiple imputation data sets in the base case.
| Year | Questionnaires returned, n (%) | Completed questionnaires,a n (%) | ||
|---|---|---|---|---|
| Surgery | Medical management | Surgery | Medical management | |
| 1 | 154 (87) | 164 (92) | 134 (75) | 147 (82) |
| 2 | 128 (72) | 142 (79) | 121 (68) | 134 (75) |
| 3 | 132 (74) | 134 (75) | 112 (63) | 119 (66) |
| 4 | 126 (71) | 129 (72) | 114 (64) | 118 (66) |
| 5 | 127 (71) | 119 (66) | 115 (65) | 113 (63) |
| Number of patients in complete-case analysis | 88 (49) | 84 (47) | ||
Health-care resource use
Table 33 summarises yearly health-care resource use in the two trial arms according to ITT analysis. During the first year of the trial, 111 patients randomised to surgery and 10 patients randomised to medical management underwent laparoscopic fundoplication. The 111 patients who were randomised to and received surgery constituted the surgery group in the PP analysis. The 169 patients who were randomised to medical management and did not undergo surgery during the first year of follow-up constituted the medical management group in the PP analysis. In the subsequent years of follow-up there were 15 patients who underwent surgery (one patient who had been randomised to surgery and 14 patients who had been randomised to medical management). These patients are included in the overnight hospital admissions category. Patients randomised to medical management reported more hospital and GP visits than the surgery patients over the 5 years of follow-up.
| Health-care resource | Year | Reflux-related reasons, n | All reasons, n | ||
|---|---|---|---|---|---|
| Surgery (n = 178) | Medical management (n = 179) | Surgery (n = 178) | Medical management (n = 179) | ||
| Laparoscopic fundoplication (first year) | 1 | 111 | 10 | N/A | N/A |
| Hospital overnight admissions (excluding surgery in the first year) | 1 | 4 | 2 | 8 | 8 |
| 2 | 1 | 2 | 8 | 10 | |
| 3 | 2 | 9 | 6 | 10 | |
| 4 | 2 | 9 | 2 | 10 | |
| 5 | 0 | 8 | 1 | 11 | |
| Total | 9 | 30 | 25 | 49 | |
| Hospital day admissions | 1 | 22 | 24 | 40 | 53 |
| 2 | 5 | 4 | 23 | 24 | |
| 3 | 4 | 6 | 4 | 10 | |
| 4 | 12 | 9 | 13 | 11 | |
| 5 | 4 | 11 | 7 | 14 | |
| Total | 47 | 54 | 87 | 112 | |
| Visits to and from GP | 1 | 110 | 103 | 394 | 376 |
| 2 | 34 | 115 | 269 | 373 | |
| 3 | 38 | 99 | 381 | 386 | |
| 4 | 55 | 126 | 422 | 469 | |
| 5 | 36 | 119 | 404 | 370 | |
| Total | 273 | 562 | 1870 | 1974 | |
| Number of patients on reflux-related medication | 1 | 58 | 148 | N/A | N/A |
| 2 | 48 | 124 | N/A | N/A | |
| 3 | 51 | 113 | N/A | N/A | |
| 4 | 51 | 106 | N/A | N/A | |
| 5 | 56 | 98 | N/A | N/A | |
Table 34 shows the costs associated with health-care use according to ITT analysis for all available cases (see Appendix 9 for corresponding table for PP). All available cases uses data from all questionnaires returned at each time point. Per annum costs and costs per category refer to all available data, that is, to all participants who returned the questionnaire for that particular year or for that particular category. Therefore, the sum of the costs per category is different from the sum of the costs per annum. Similarly, total costs for complete-case analysis do not correspond to the sum of the costs per category or to the sum of the costs per annum because complete case is a subset of all available data because of the non-monotone missing data pattern. Total costs for complete-case analysis refer to the patients who returned all questionnaires and completed all EQ-5D profiles (84 surgery patients and 88 medical management patients).
| Returned questionnaires in each year | Mean (SD) resource-use cost (£) | Incremental mean cost (cost surgery – cost medical management) (95% CIa) (£) | |||
|---|---|---|---|---|---|
| Surgery | Medical management | Year | Surgery | Medical management | |
| 154 | 164 | 1 | 2500.75 (1697.99) | 559.62 (1006.81) | 1941.13 (1621.43 to 2260.83) |
| 128 | 142 | 2 | 94.15 (317.63) | 150.96 (356.57) | −56.81 (−138.08 to 24.46) |
| 132 | 134 | 3 | 94.35 (340.33) | 276.41 (894.16) | −182.05 (−345.87 to −18.24) |
| 126 | 129 | 4 | 111.41 (394.00) | 303.50 (1337.26) | −192.09 (−436.56 to 52.28) |
| 127 | 119 | 5 | 58.38 (178.58) | 234.03 (629.33) | −175.65 (−290.26 to −61.03) |
| Cost category | |||||
| Surgery in year 1b | 1734.05 (1407.58) | 164.31 (644.63) | 1569.74 (1342.05 to 1797.42) | ||
| Reflux-related hospital night admissions | 343.82 (1176.05) | 302.34 (818.41) | 41.47 (−247.48 to 330.42) | ||
| Reflux-related hospital day admissions | 221.67 (633.61) | 250.35 (631.37) | −28.68 (−209.24 to 151.87) | ||
| Reflux-related GP visits | 127.18 (178.96) | 200.13 (462.53) | −72.95 (−173.26 to 27.35) | ||
| Medication | 121.34 (265.05) | 365.70 (517.05) | −244.35 (−361.82 to −126.89) | ||
Patients randomised to medical management accumulate lower costs than patients randomised to surgery. Table 34 indicates that surgery patients accrued a large proportion of the total costs in the first year, and accumulated lower costs during the remaining 4-year follow-up than the medical management group. In contrast, the costs accrued by medical management patients are evenly distributed across the duration of the trial. These results suggest that the cost trend in medical management patients is steeper than in surgery patients; hence, that cumulative costs in medical management patients tend to increase at a greater rate than in surgery patients. Costs associated with surgery were the major cost driver for the surgery group. Costs associated with reflux-related medication were significantly greater for the medical management group than for the surgery group. Costs associated with admissions to hospital and GP visits were not statistically significantly different between the two groups. Surgery during years 2–5 is accounted for in the overnight hospital admissions. There were a few crossovers from medical management to surgery from year 2; hence, the difference in costs associated with overnight hospital admissions between the two treatment groups is small. These results suggest that patients undergoing surgery in subsequent years are not a major cost driver in determining the cost-effectiveness of surgery.
Quality-adjusted life-years
Table 35 summarises the EQ-5D scores reported at each follow-up point for all available cases (see Appendix 9 for the corresponding table for PP). All available cases uses data from all questionnaires returned at each time point. The surgery group appears to have better HRQoL than the medical management group, despite starting from a lower baseline EQ-5D on average (0.7201 in the medical management group and 0.7107 in the surgery group). The difference in HRQoL between the two treatment groups decreased with time. This may be due to patients randomised to medical management undergoing surgery throughout the follow-up period and/or to diminishing treatment effect over time.
| Completed questionnaires returned at each time point | Follow-up | Mean (SD) EQ-5D | Difference in EQ-5D (surgery – medical management) (95% CI)b,c | ||
|---|---|---|---|---|---|
| Surgery (n = 178a) | Medical management (n = 179a) | Surgery | Medical management | ||
| 171 | 173 | Baseline | 0.7107 (0.2581) | 0.7201 (0.2545) | −0.0094 (−0.0638 to 0.0445) |
| 149 | 153 | 3 months | 0.7881 (0.2328) | 0.6894 (0.3012) | 0.0987 (0.0376 to 0.1597) |
| 152 | 164 | Year 1 | 0.7537 (0.2468) | 0.7097 (0.2715) | 0.0440 (−0.0136 to 0.1016) |
| 122 | 138 | Year 2 | 0.7619 (0.2718) | 0.7172 (0.3127) | 0.0447 (−0.0273 to 0.1167) |
| 129 | 132 | Year 3 | 0.8034 (0.2312) | 0.7474 (0.2621) | 0.0560 (−0.0043 to 0.1163) |
| 125 | 127 | Year 4 | 0.7713 (0.2438) | 0.7544 (0.2719) | 0.0169 (−0.0472 to 0.0810) |
| 124 | 117 | Year 5 | 0.7743 (0.2590) | 0.7612 (0.2815) | 0.0131 (−0.0555 to 0.0817) |
Comparison of costs and quality-adjusted life-years between multiple imputation and complete case
Table 36 shows the comparison of the total costs per year between the complete-case data set and the multiple imputation results. Complete case includes only those participants who returned all questionnaires and fully completed the EQ-5D questionnaires. The similarity of both the means and the CIs provides some reassurance of the validity of the multiple imputation model. The distribution of costs and EQ-5D scores in the imputed data sets matches reasonably well the distribution of the original data (see Appendix 8 for details). Furthermore, the Monte Carlo errors are < 15% of the coefficient and CI estimates, suggesting that 100 imputations are sufficient to ensure reproducibility and statistical efficiency. 69
| Year | Incremental mean cost (cost surgery - cost medical management) (95% CIa) (£) | Difference in mean EQ-5D (surgery - medical management) (95% CIa) | |||
|---|---|---|---|---|---|
| Complete case | Multiple imputation | Follow-up | Complete case | Multiple imputation | |
| N/A | N/A | N/A | Baseline | −0.0388 (−0.1083 to 0.0308) | −0.0091 (−0.0615 to 0.0433) |
| N/A | N/A | N/A | 3 months | 0.0848 (0.0122 to 0.1573) | 0.0825 (0.0232 to 0.0142) |
| 1 | 2197.14 (1779.67 to 2614.61) | 1958.46 (1617.31 to 2299.62) | Year 1 | 0.0519 (−0.0198 to 0.1237) | 0.0407 (−0.0150 to 0.0963) |
| 2 | −139.14 (−237.02 to −41.26) | −44.58 (−129.68 to 40.52) | Year 2 | 0.0467 (−0.0356 to 0.1289) | 0.0445 (−0.0218 to 0.1108) |
| 3 | −193.44 (−361.94 to −24.93) | −127.42 (−306.36 to 51.52) | Year 3 | 0.0508 (−0.0195 to 0.1211) | 0.0454 (−0.0150 to 0.1057) |
| 4 | −37.66 (−173.02 to 97.70) | −144.61 (−374.78 to 85.56) | Year 4 | 0.0324 (−0.0395 to 0.1044) | 0.0260 (−0.0356 to 0.0875) |
| 5 | −165.12 (−304.74 to −25.50) | −123.90 (−236.56 to −11.24) | Year 5 | −0.0095 (−0.0871 to 0.0680) | 0.0294 (−0.0358 to 0.0945) |
| Total cost | 1661.78 (1130.00 to 2193.55) | 1517.95 (1006.49 to 2029.41) | Total QALYs (unadjusted) | 0.1976 (−0.0857 to 0.4810) | 0.1948 (−0.0356 to 0.4251) |
| Monte Carlo errorb | 10.16 | Monte Carlo errorb | 0.0034 | ||
| Total QALYs (adjusted)c | 0.3039 (0.0928 to 0.5150) | 0.2160 (0.0205 to 0.4115) | |||
| Monte Carlo errorb | 0.0035 | ||||
For both the complete-case and multiple imputation data sets, the participants randomised to laparoscopic fundoplication accrued greater costs but also reported greater HRQoL than participants randomised to continued medical management. The 95% CI for mean incremental QALYs crosses zero for the unadjusted for baseline estimates, whereas it remains above zero for the adjusted values. This result reflects the baseline imbalance in mean utility between treatment groups. Therefore, these results strongly indicated that surgery is associated with a greater QALY improvement than medical management. The sum of the differences in EQ-5D for the ITT groups does not correspond to the incremental mean QALYs because of the effect of discounting.
Cost-effectiveness
The results of the incremental analysis suggest that laparoscopic fundoplication is a cost-effective strategy for GORD patients eligible for the REFLUX trial (Table 37). The results for the complete-case analysis concur with those for the multiple imputation data set; across adjusted and unadjusted ICER for baseline EQ-5D, ICERs range between £5468 and £8410, well below conventional cost-effectiveness thresholds of £20,000 and £30,000 per additional QALY. For both data sets (complete case and multiple imputation), the probability of surgery being the more cost-effective intervention is > 0.82 for incremental analysis unadjusted for baseline EQ-5D and > 0.93 once incremental QALYs are adjusted for baseline EQ-5D. In the ITT analysis the ICER is higher for the multiple imputed data than for the complete case if QALYs are adjusted for baseline EQ-5D, but lower if QALYs are unadjusted. This might reflect the effect of having baseline EQ-5D in the prediction model, which would preclude the need for adjustment.
| Data set | Adjustment for baseline EQ-5D? | Incremental mean costs (£) (95% CI) | Incremental mean QALYs (95% CI) | ICER (£) | Probability cost-effective at £20,000 per QALYa | Probability cost-effective at £30,000 per QALYa |
|---|---|---|---|---|---|---|
| Complete case | No – unadjusted QALYs | 1661.78 (1130.00 to 2193.55) | 0.1976 (−0.0857 to 0.4810) | 8409.82 | 0.828 | 0.866 |
| Yes – adjusted QALYs | 1661.78 (1130.00 to 2193.55) | 0.3039 (0.0928 to 0.5150) | 5468.36 | 0.989 | 0.996 | |
| Multiple Imputation | No – unadjusted QALYs | 1517.95 (1006.49 to 2029.41) | 0.1948 (−0.0356 to 0.4251) | 7792.35 | 0.861 | 0.906 |
| Yes – adjusted QALYs | 1517.95 (1006.49 to 2029.41) | 0.2160 (0.0205 to 0.4115) | 7027.55 | 0.932 | 0.962 |
Figure 20 shows how the NMB associated with laparoscopic fundoplication increases with the duration of the trial. This reflects the increase in costs associated with the medical group, which offsets the initial investment made in laparoscopic fundoplication in the surgery group.
FIGURE 20.
Net monetary benefit (incremental QALYs × £20,000 per QALY – incremental costs) over the duration of the REFLUX trial for the multiple imputation and complete-case data sets (QALYs adjusted by baseline EQ-5D).
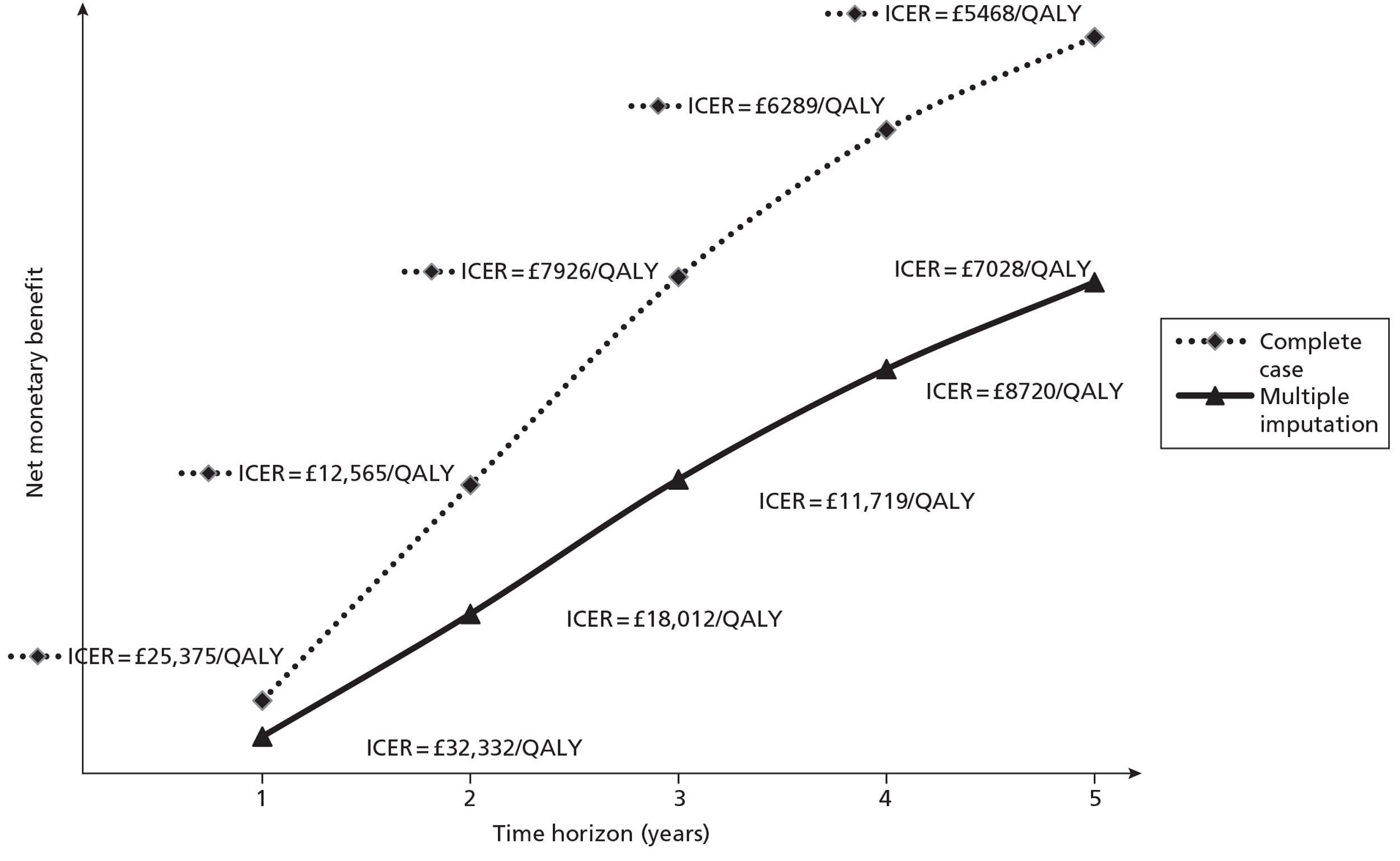
Structural sensitivity analysis: per-protocol status for the complete case
Structural sensitivity analysis consisted of PP status at 1 year for the complete case. In the PP analysis patients are classified according to the treatment actually received at 1 year of follow-up. The PP group consists of 111 patients who were randomised to surgery and who actually had surgery during the first year of the trial and 169 patients who were randomised to medical management and who did not undergo surgery during this time period. However, complete-case data exist only for 84 medical management patients and 66 laparoscopic fundoplication patients. Appendix 9 presents detailed results for costs and HRQoL according to PP analysis. As expected, patients who actually had surgery have higher costs than patients who did not undergo surgery, regardless of their randomisation. Table 38 summarises the incremental results of the PP analysis. Similar to the ITT analysis, the surgical policy is likely to be cost-effective at conventional (NICE) thresholds for cost-effectiveness. The incremental costs are higher and the incremental QALYs lower for the PP analysis (for surgery compared with medical management) than for the ITT analysis if no adjustment is made for baseline imbalances in EQ-5D. Therefore, the ICER is also greater (surgery is less cost-effective than suggested by the ITT analysis). Once total QALYs are adjusted for baseline EQ-5D, however, the incremental mean QALYs increase substantially and the ICER is reduced. Nevertheless, the adjusted ICER in the ITT analysis is lower than that in the PP analysis by around £2000.
| Adjustment for baseline EQ-5D | Incremental mean costs (95% CI) (£) | Incremental mean QALYs (95% CI) | ICER (£) | Probability cost-effective at £20,000 per QALYa | Probability cost-effective at £30,000 per QALYa |
|---|---|---|---|---|---|
| Unadjusted QALYs | 2323.77 (1799.90 to 2847.65) | 0.1782 (−0.1316 to 0.4879) | 13,043.90 | 0.672 | 0.747 |
| Adjusted QALYs | 2323.77 (1799.90 to 2847.65) | 0.3200 (0.0837 to 0.5562) | 7262.85 | 0.957 | 0.983 |
Scenario sensitivity analysis: all general practitioner and all hospital costs for complete case
The results of the scenario analyses strengthen the case for the surgical policy (Table 39). For scenario 1, replacing reflux-related GP costs by all GP costs, the ICER increased slightly in relation to the base case. Nevertheless, the ICER remains well below conventional thresholds and the probability of surgery being cost-effective is > 0.83, for both adjusted and unadjusted analyses. In scenario 2, replacing reflux-related hospital costs by all hospital costs, medical management was ‘dominated’ by the surgical policy because of this intervention being associated with greater benefits in terms of QALYs and lower costs. For this scenario the probability of surgery being cost-effective was > 0.93.
| Sensitivity analysis | Adjustment for baseline EQ-5D? | Incremental mean costs (95% CI) (£) | Incremental mean QALYs (95% CI) | ICER (£) | Probability cost-effective at £20,000 per QALYa | Probability cost-effective at £30,000 per QALYa |
|---|---|---|---|---|---|---|
| Scenario 1: all GP costs | No – unadjusted QALYs | 1685.60 (1103.97 to 2267.23) | 0.2125 (−0.0748 to 0.4998) | 7932.23 | 0.826 | 0.863 |
| Yes – adjusted QALYs | 1685.60 (1103.97 to 2267.23) | 0.3191 (0.1061 to 0.5321) | 5282.36 | 0.987 | 0.994 | |
| Scenario 2: all hospital costs | No – unadjusted QALYs | −262.72 (−860.08 to 334.65) | 0.2125 (−0.0748 to 0.4998) | Medical management dominated | 0.930 | 0.928 |
| Yes – adjusted QALYs | −£262.72 (−860.08 to 334.65) | 0.3191 (0.1061 to 0.5321) | Medical management dominated | 0.999 | 0.999 |
Sensitivity analysis for the multiple imputation model: departure from missing at random assumption
The multiple imputation procedure assumes that the individuals who completed and returned all questionnaires are similar to the individuals who did not, conditional on their observed characteristics (MAR assumption). 69,79 However, this may not be the case: patients who did not return a questionnaire may have experienced worse HRQoL and accrued higher health service costs, or vice versa. Sensitivity analysis on the multiple imputation model tested how sensitive the cost-effectiveness results are to the MAR assumption. Figure 21 represents the change in NMB adjusted for baseline EQ-5D as costs and QALYs are varied in patients with missing data. The origin, marked as ‘base case’, refers to the incremental results from the multiple imputed data set (ICER = £7028 per additional QALY). The right quadrant plots NMB after increasing the total costs in steps of 10% for patients for whom there was missing data, for both treatment groups and for surgery-allocated patients. The left quadrant plots NMB after decreasing total QALYs in similar fashion. Positive values for NMB indicate that surgery is cost-effective; negative values indicate that surgery is not cost-effective for a threshold of £20,000 per additional QALY.
FIGURE 21.
Net monetary benefit (incremental QALYs adjusted for baseline EQ-5D × £20,000 per QALY – incremental costs) over variation in total costs and total QALYs in the multiple imputed data set.
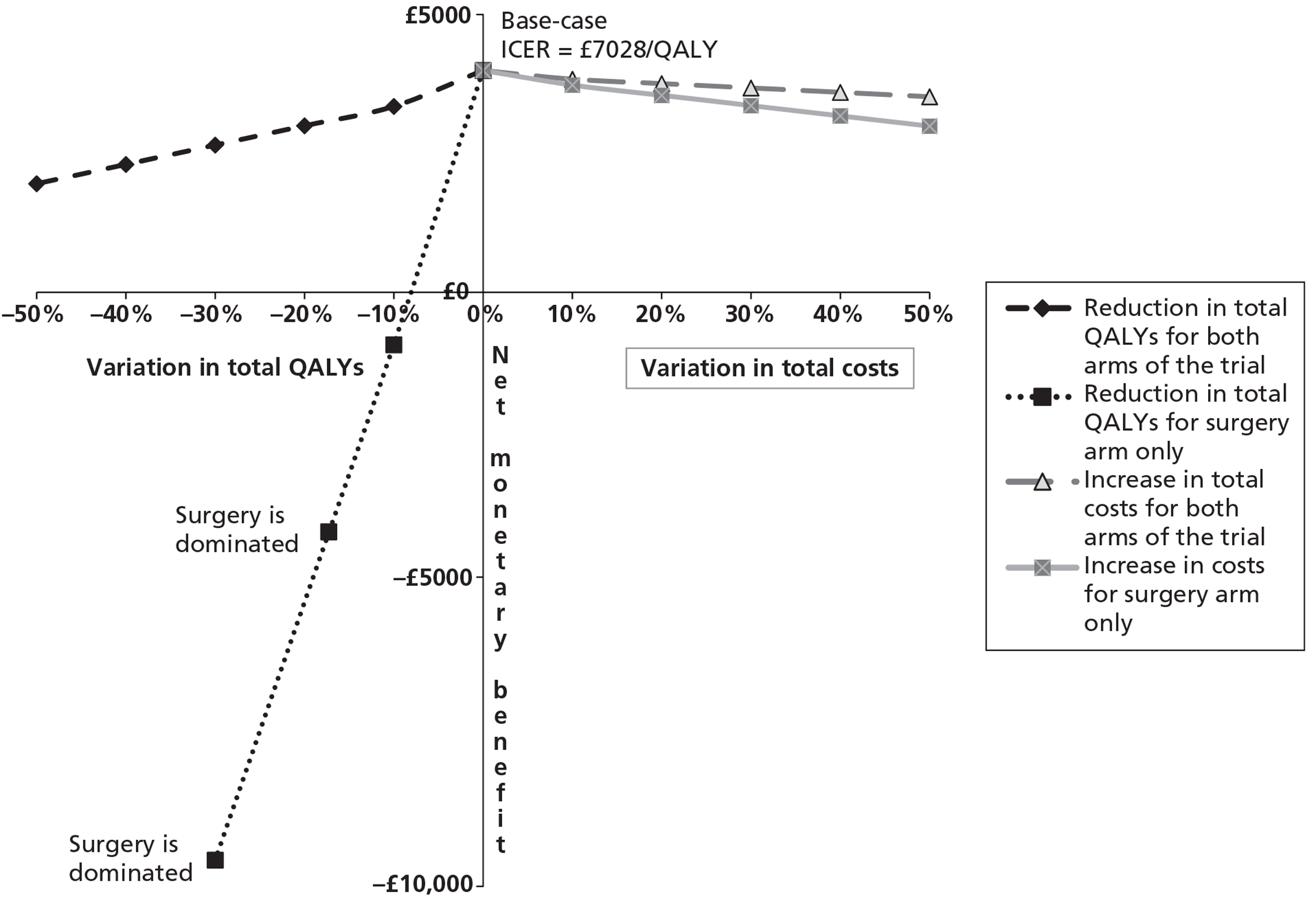
The cost-effectiveness of surgery is relatively insensitive to any increase in costs; the NMB changes little if costs are increased for patients with missing data in both treatment groups and if costs are increased just for surgery-allocated patients with missing data. A similar result is observed for the reduction in total QALYs for all patients with missing data. In contrast, the cost-effectiveness of surgery is highly sensitive if it is assumed that surgery-allocated patients with missing data experience lower HRQoL than patients with complete data. A 10% decrease in QALYs for patients randomised to surgery with missing data results in NMB decreasing to negative values. This scenario shows that missing data can have an impact on the results under certain conditions. It is impossible to empirically confirm or refute the scenario from the data in the trial, but it could be considered an extreme case. It seems improbable in practice that surgical patients with poor quality of life are less likely to respond to follow-up questionnaires than similar participants undergoing medical management.
Conclusion
The results of the within-trial economic analysis suggest that laparoscopic fundoplication is the more cost-effective option for the management of the sorts of patients suffering from GORD who were eligible for the REFLUX trial. The ICER for the ITT approach in the complete case was between £5468 and £8410 per additional QALY, and for the multiple imputed data set was between £7028 and £7792 per additional QALY, depending on whether QALYs are unadjusted or adjusted for baseline. Adjusted results are likely to be more reflective of the improvement in HRQoL associated with surgery. The probability of surgery being cost-effective was > 0.80 for all analyses. The results are robust to the scenario analyses testing assumptions regarding resource-use and missing data mechanism apart from when surgery-allocated patients with missing data were assumed to experience lower HRQoL than other patients. In all scenarios the ICERs were similar to the base case ICERs and well below NICE cost-effectiveness thresholds.
Validation of within-trial (5-year) analysis and exploration of the need for a long-term model
Introduction
The within-trial analysis found that surgery was cost-effective over a 5-year time horizon. A sufficient condition for surgery to be unambiguously cost-effective over a longer term is that, in each year after 5 years, HRQoL is lower and costs are the same or increasing faster in the medical group than in the surgical group. The results from both the multiple imputation and the complete-case analysis suggest that surgery is likely to be a cost-effective alternative over the longer term. Based on the ITT analyses undertaken so far, it is unlikely that mean HRQoL in patients who had surgery will become lower than that in patients on medical management after 5 years, and it is also very unlikely that mean annual costs incurred by surgery patients will exceed those incurred by medical management patients. If these results are robust, then there is no need to develop an economic model to extrapolate the 5-year results over a longer time horizon. Surgery would simply become more cost-effective over time.
This section develops a statistical model to investigate whether or not the results obtained in the within-trial economic analysis are robust to alternative assumptions and methods, and uses the results to consider whether or not the evidence supports this sufficient condition over the longer term.
Methods
Overview
The aim of this analysis was to estimate the difference in costs and the difference in HRQoL (measured with the EQ-5D) between the surgical and medical management randomised groups and describe how this difference evolves over time. A simple way of doing this would be to estimate the difference in costs and outcomes at each time point independently. The results of this analysis were shown in Table 34 (for costs) and Table 35 (for EQ-5D). These showed that costs were greater in the surgical group in the first year but greater in the medical group thereafter. EQ-5D tended to be higher in the surgical group in years 4 and 5 but the CIs crossed zero. There are two main limitations of this simple analysis:
-
The outcomes at each time point are unlikely to be independent. If the outcomes at one time point are correlated with those at other time points this analysis may lead to biased estimates of standard errors.
-
The analysis does not take account of missing data. If missing data are not MCAR then this analysis may lead to biased estimates of the mean of the coefficients.
The multiple imputation accounts for the correlation of responses from the same individuals and for the missing data (see Table 36). However, the validity of this analysis depends on the correct specification of the equations used to impute the missing data. Moreover, other regression-based methods are available for handling missing data in longitudinal studies, principally mixed models, and results may be sensitive to the methods used. This section uses a mixed model to handle the missing data and compares predicted outcomes with those using multiple imputation.
Mixed models
A mixed model is a regression-based method for handling continuous data that is measured at more than one time point during follow-up. It allows estimation of treatment effects under the assumption that the data are MAR, that is, dropout may depend on intermediate values. Analysing each time period separately assumes that dropouts are MCAR, a stronger assumption. A mixed model uses all of the observed data. Individuals who dropped out after providing intermediate data contribute to the estimation of the final outcomes. This analysis has the same aims as multiple imputation but uses a different method and with different assumptions. Therefore, it can also be viewed as a sensitivity analysis to test the robustness of the multiple imputation.
The mixed model can be written as:
Where for an individual i,
Yi = α +βRi+Xi+ ei, ei ∼ MVN(0,Σ)
Ri = randomised group
Yi = vector of all outcomes (at times 1…T)
Xi = vector of covariates
The variance-covariance matrix Σ is unstructured, that is, no prior assumptions are made about the values of the correlations. Separate models are fitted for costs and for EQ-5D. Baseline values of the EQ-5D are included as an ‘outcome’ (i.e. at t = 1). Dummies representing time points 1 to T were included as covariates Xi. Treatment effects are included as time* randomised group interactions although no treatment effect at baseline is allowed. No other covariates are included in the model.
Results
Costs
Figure 22 shows the difference in costs (excluding initial surgery) in years 1–5. Mean costs are greater in the medical management arm of the trial after the first year and the CIs only just cross zero. These results are very similar to those of Table 34.
FIGURE 22.
Difference in costs (£) excluding initial surgery (mean, 95% CI).
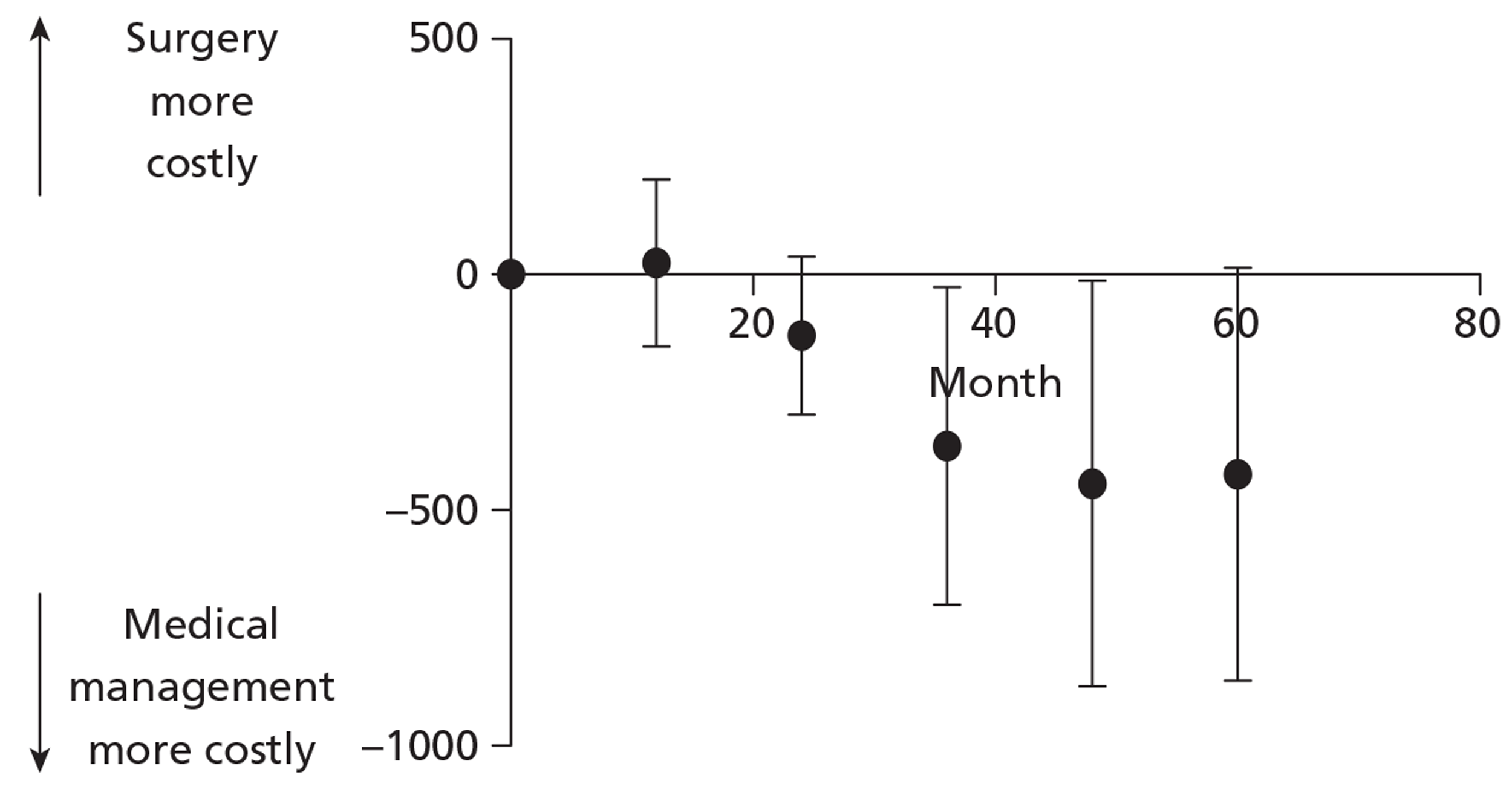
European Quality of Life-5 Dimensions
Figure 23 shows the difference in EQ-5D at 3 months and in years 1–5. Mean HRQoL tends to be greater in the surgical group during the trial, although the CIs cross zero in some periods. These results are very similar to those of Table 35.
FIGURE 23.
Difference in EQ-5D, adjusted for baseline (mean, 95% CI).
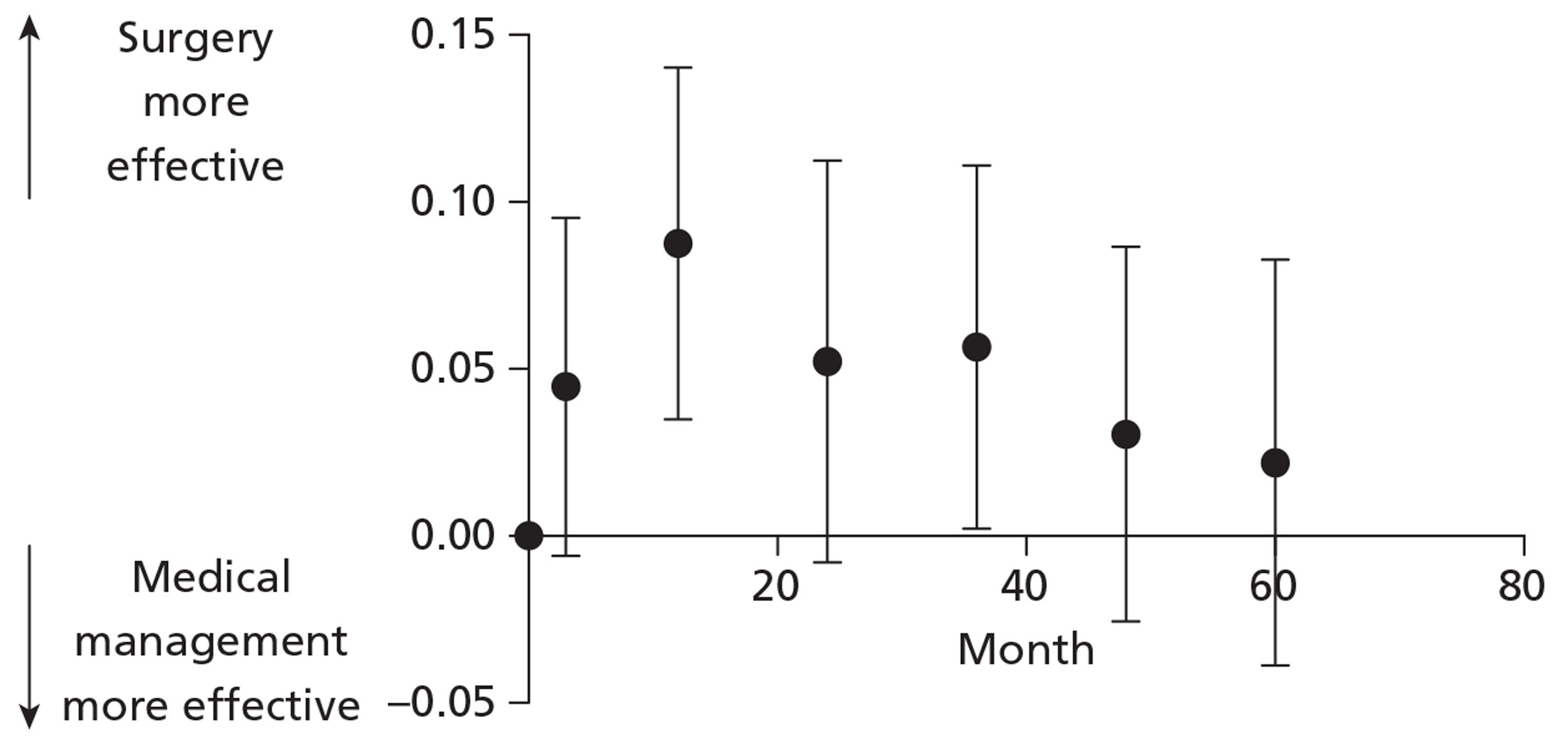
Conclusion
The results of the mixed model (taking account of correlations and missing data) are very similar to those of the complete-case analyses (which assumed that data at different time points were independent) and the multiple imputation (see Table 36). All of these analyses show that follow-up costs are significantly greater in the medical management arm of the trial (because of greater reflux-related hospital admissions, GP visits and use of medication). The analyses also show that surgery tends to be more effective, in terms of HRQoL, than medical management over the 5-year follow-up. Although this treatment difference appears to weaken over time, there is no reason to expect that surgery will become less effective with a longer follow-up. Consequently, the evidence suggests that the cost-effectiveness of laparoscopic fundoplication will not diminish if measured over a longer follow-up time. Nevertheless, there is uncertainty surrounding these conclusions because of the large proportion of missing data.
Discussion
The results of the cost-effectiveness analysis strongly suggest that a policy of offering laparoscopic fundoplication to people with GORD who require long-term PPI treatment for symptom control is more cost-effective than continuing to manage them with PPIs (with selective use of surgery if symptoms are poorly controlled), assuming that the cost-effectiveness thresholds used by NICE (£20,000–30,000 per QALY) are appropriate for the NHS. Surgery represents a greater initial investment and lower medium-term costs, whereas costs associated with medical management remain relatively constant or slightly increase over time. The difference in HRQoL achieved with surgery is sustained over 5 years, although the results indicate that mean EQ-5D scores for surgery and medical management tended to converge (as discussed in Chapter 3, in part this reflects later surgery in patients randomised to medical management). The ICER favours surgery when incremental QALYs are both adjusted and unadjusted for baseline EQ-5D. Nevertheless, adjusted incremental QALYs are likely to be a more reliable estimate of treatment effect as they account for differences in baseline utility. Patients randomised to medical management reported higher baseline utility than patients randomised to surgery. Failure to adjust for these baseline differences could result in a biased ICER, as discussed elsewhere.62 The results from the multiple imputed data set are likely to be more accurate than the results from the complete-case analysis because of the large number of patients with incomplete data (> 50%). Therefore, multiple imputation was chosen for the base case. Nevertheless, the results are similar across the data sets and laparoscopic surgery is the more cost-effective intervention for both.
There is little uncertainty regarding the cost-effectiveness results once adjustment for EQ-5D at baseline is performed. The probability of surgery being cost-effective ranged between 0.932 and 0.999 for the base case and across the scenarios tested. Furthermore, it is clear from the results of the scenario analysis that the base-case results are robust to alternative costing assumptions. The PP analysis is used to test whether or not the ITT analysis is potentially misleading because of the dilution of treatment effect (some patients randomised to surgery did not have surgery and some patients randomised to medical management actually had surgery). The PP analysis has the advantage of mimicking clinical practice and could be thought to be more relevant to decision-makers. However, the PP analysis is not without its limitations. First, and as with any PP analysis, it is sensitive to selection bias because of breaking randomisation. Second, the PP analysis may still underestimate the effect of surgery because patients having surgery between 2 and 5 years are counted as medical management. Third, the PP analysis is actually a subset of the ITT groups, which further reduces the data set. For these reasons, the ITT results are likely to be more reliable. It is important to characterise any uncertainty in the analysis as failure to do so can result in inaccurate estimates of cost-effectiveness, particularly when costs and benefits are highly skewed. 82 In addition, any analyses of uncertainty can help to illustrate where caution should be exercised when interpreting the results of a cost-effectiveness analysis. The results of the sensitivity analyses suggest that the uncertainty is likely to be driven by HRQoL. If QALYs for randomised surgery patients with missing data are reduced, surgery may no longer be cost-effective.
For the within-trial analysis no assumptions are needed about the longer-term effectiveness and costs associated with surgery and medical management. However, the within-trial analysis has some disadvantages. First, it does not account for any differences in costs and QALYs that may be expected over the longer term (> 5 years), which could be due to differences in recurrence/relapse, medication use, NHS service utilisation or HRQoL. Second, it uses data only from the REFLUX trial and does not consider other sources of evidence. Third, only a limited range of sensitivity analyses was possible. Finally, the large proportion of missing observations required an assumption regarding the mechanism of missing data, which may have some impact on the cost-effectiveness estimates. The exploration of the need for a longer-term model aimed to address the first limitation of the within-trial analysis. A mixed model was used to examine the trend in the difference in costs and the difference in QALYs between treatment groups over time.
No evidence was found to suggest that the cost-effectiveness of surgery diminishes over a longer follow-up time. Both multiple imputation and mixed models are commonly used methods to handle missing data. Multiple imputation was used in the previous section because, by imputing missing data, it naturally allows the estimation of the total cost and total QALYs for each patient in the trial. Furthermore, it can handle correlation between several outcomes (in this case costs and QALYs) as well as correlation between outcomes over time. Mixed models do not explicitly impute missing data but adjust the estimates of the differences between treatment groups at each discrete follow-up time to take account of the missing data. The approach therefore offers an alternative method to multiple imputation to examine trends in the difference in costs and the difference in QALYs between treatment groups over time. Because the analyses using multiple imputation and mixed models agree, we can have more confidence that the results are valid and that surgery is the most cost-effective intervention.
A number of other studies have quantified the cost-effectiveness of laparoscopic fundoplication and medical management. Not all of these, however, use a common metric (such as QALYs) to measure benefits. Of those studies quantifying the benefits associated with the two treatments using QALYs, the ICER for surgery ranged from £180 to £49,000. There are a number of key differences between the methodologies used in the studies, which limit the extent to which comparisons can be made between results. Importantly, not all of the studies are based on within-trial analysis; in fact, only two are: those by Grant et al. 1 and Goeree et al. 46 The remainder use modelling techniques to either extrapolate short-term trial results over the longer term or pool available evidence to generate estimates of costs and outcomes. Comparing the results from Grant et al. 1 with those from Goeree et al. 46 we can see that there are quite significant differences in the estimates of cost per QALY, from £19,000 in Grant et al. 1 to £49,000 in Goeree et al. 46 This difference is primarily driven by the difference in QALYs. In Goeree et al. 46 the EQ-5D score is actually lower in the surgical group than in the medical management group (this is unadjusted for baseline imbalances) whereas the HUI3 score is higher for the surgical group than the medical management group. The reason for the difference between the EQ-5D and the HUI3 scores is not discussed in the paper. The cost differences in the two studies were similar. Comparing the results from Goeree et al. 46 with those from the updated trial analysis we see even starker contrast between the ICERs produced (£7028 vs £49,000). Again, this is driven by the differences in EQ-5D scores observed throughout the trial period. The EQ-5D scores in the REFLUX 5-year analysis are consistently higher in the surgery group than in the medical management group, although there is a tendency for convergence towards the end of the follow-up period. Further research is required to look at why the trials produce such different results using the EQ-5D.
Other considerations
The generalisability of these findings to the GORD population in the UK is difficult to ascertain because the proportion of GORD patients meeting the entry criteria for this trial is uncertain. The surgeons participating in the trial may be more proficient in the procedure than those in actual practice. Furthermore, capacity constraints may limit the offer of the surgery policy to all potentially eligible patients.
Chapter 6 Conclusions
In the report of the first phase of the REFLUX trial1 we concluded that, among the sorts of patients recruited to the trial, laparoscopic fundoplication ‘significantly increases general and reflux related QoL measures, at least up to 12 months after surgery’. There was, however, considerable uncertainty about cost-effectiveness, largely because the follow-up period was so short. Varying plausible assumptions about the longer-term effects of surgery, particularly in terms of QALYs gained and costs of medication, led to markedly differing results. This was the basis for this second phase of the trial, in which follow-up has been extended out to a time equivalent to 5 years after surgery.
The trial has a pragmatic design and compared two policies for managing GORD, rather than directly comparing surgery with PPI therapy. This is the basis for the primary analyses being based on the ITT principle as this directly compares the policies. The first policy can be characterised as relatively early surgery for most eligible patients but with the option to take medication if considered helpful, irrespective of whether or not surgery had been performed. The second policy can be described as medical management as appropriate with ‘delayed’ surgery in selected cases. Hence, we have not made an assumption that those taking medication after surgery are ‘failures’. In our view, although surgery may have improved symptoms, the addition of PPIs may give further improvement and hence should be considered to be a component of both policies.
In contrast to the other large randomised trial (the LOTUS trial,48 discussed in Chapter 4), whose primary outcome was ‘treatment failure’, we chose patient-reported outcome measures as our primary and main secondary outcome measures. The advantage is that they provide a ‘common currency’ across the two trial policies and do not depend on clinical judgements (as ‘treatment failures’ do). There is, however, a concern that completion of the patient-reported outcome questionnaires may be influenced by the nature of the management received. We had a reminder of this in the early stages of our trial. The DMC noticed an imbalance in baseline scores of the first few patients randomised, but not in other descriptive characteristics. It seemed that this might have been due to completion of the form after the allocation was known (although it could still have been due to chance); once it was made a requirement that the form had to be filled in before the allocation was known, however, this discrepancy disappeared. We believe that a strength of the long-tem follow-up as reported here is that, as the time from the differentiating event (surgery or no surgery) gets increasingly long, the possibility of such reporting bias becomes remote. Protection was also provided by the partially randomised patient preference design: the randomised component was limited to patients who were uncertain which treatment to choose while those who had strong views were enrolled into the preference groups.
We designed the trial with the aim of making the management policies as similar as possible to normal NHS care. So, for example, a large number of centres were involved (both teaching and non-teaching hospitals); recruitment was based on gastroenterologist–upper gastrointestinal surgeon partnerships; surgeons chose the type of fundoplication and other aspects of the procedure; after optimisation of medical management in secondary care, all subsequent medical care was in general practice; there was no requirement for extra tests or hospital visits; and simple entry criteria identified people with chronic troublesome GORD symptoms that required anti-reflux medication for reasonable control suitable for either policy (average age 46 years). The results should, therefore, be easily generalisable to standard NHS care.
The one area in which we think the trial did not ‘mimic’ usual care is in the relatively low proportion of those allocated surgery who actually had surgery (62%; see Table 10). There are reasons for thinking that the unusual circumstances of a randomised trial comparing medical management with surgery were partly responsible for the large proportion who did not have surgery. We think the rate (84%) in the preference group is likely to be more indicative of ‘normal’ acceptance rates. For this reason we undertook secondary adjusted treatment received analyses aimed to compensate for this. These analyses are likely to give a better estimate of differential effects in usual care, but because they depart from the randomised groups and hence may be prone to bias they should be treated with appropriate caution. We also explored this issue through post hoc analyses stratified by whether or not those allocated surgery actually had fundoplication. This showed (see Figure 18) that those who had surgery had lower baseline REFLUX scores (worse symptoms) than those who did not have an operation, but that, following surgery, their scores were consistently higher that those who did not have surgery.
Despite our best attempts to retain the cohort of participants there has been some attrition over the course of the follow-up period. The response rate of 69% at 5 years can be considered satisfactory in a study of this type and is similar to the rate in the LOTUS trial (67%). 48 The rate in the REFLUX trial reflects the decision among some participants to withdraw, but with high levels of return among those remaining. Responders did differ from non-responders but we used analysis techniques to make the most of the available data (repeated measures and imputation), and the responders in the two randomised groups were generally reassuringly similar in respect of baseline characteristics.
The new results provide clear evidence of a sustained greater improvement in GORD-related QoL in the group randomised to surgery. The results also suggest sustained benefit in respect of generic health-related measures of QoL, although the differences attenuate over time and are not statistically significant at 5 years. In these respects the REFLUX trial is in line with the results of the other three randomised trials that have compared laparoscopic surgery with medical management. The worse the symptoms at entry (the lower the score at baseline), the greater are the benefits of surgery.
By 5 years, 24 (13%) of the participants randomly allocated to medical management had undergone anti-reflux surgery. Exploratory analyses (see Figure 19) showed that, as a group, these 24 had low REFLUX questionnaire scores (worse symptoms) at trial entry, which subsequently improved markedly after surgery. Hence, this group is at least a contributory factor to the narrowing of differences between the randomised groups over time (see, in particular, Figures 3 and 17) and a reason for thinking that the ITT-based analyses comparing the two management policies are likely to underestimate the effects of surgery.
The follow-up has clarified the rates of longer-term use of PPI medication in both policies. In the randomised medical group, 87% were taking medication at 1 year, falling gradually to 82% at 5 years (see Figure 2). The equivalent figures in the randomised surgery group were 36% at 1 year (15% among those who had surgery) and 41% (26%) at 5 years. This was in response to a question that, to avoid problems with recall, asked just about the preceding 2 weeks (rather than the full year), and we have assumed that the 2 weeks are typical of the previous year. We know, however, that medication use is sometimes dynamic – that patients stop and start. This is apparent in Table 13, for example: among those in the medical group who were not taking medication at the end of the first year, 13 (68%) of the 19 respondents reported that they were taking PPIs at 5 years.
Short-term complications of surgery were described in more detail in the first report of this trial. However, the REFLUX trial is consistent with the other three trials in this respect, with small numbers having associated visceral injuries, postoperative problems and dilatation of the wrap. The longer-term follow-up has now clarified the likelihood of further surgery following a fundoplication. Overall, 4% (n = 16) of the total 364 in the study who had fundoplication had a subsequent reflux-related operation, of whom two had a further (i.e. third) operation. Reoperation was most often conversion to a different type of wrap or a reconstruction of the same wrap. There were only two cases of reversal of the fundoplication and neither was in the randomised comparison. In total, 3% (n = 12) of those who had fundoplication required surgical treatment for a complication directly related to the original surgery, including oesophageal dilatation (n = 4) and repair of incisional hernia (n = 3). As described in Chapter 4, although it is not possible to extract exactly comparable data, these results are broadly in line with those of the other trials.
Where the REFLUX trial results do differ from the results of the other trials, especially the LOTUS trial, is in the likelihood and extent of adverse symptoms associated with fundoplication. Dysphagia, flatulence and bloating, and inability to vomit despite wanting to have all been reported to be problematical after fundoplication. However, in the REFLUX trial, the patterns of difficulty swallowing, flatulence and wanting to vomit but being physically unable to do so were similar in the two randomised groups (see Table 15), with no statistically significant differences.
The economic analysis of the 5-year data from the REFLUX trial had two phases. First, a within-trial 5-year cost-effectiveness analysis was undertaken; this was followed by an exploration of the need to develop a longer-term model. Differences in mean costs and mean QALYs at 5 years were used to derive an estimate of relative cost-effectiveness. The base-case approach used multiple imputation (principally because of the extent of missing data), an ITT analysis and adjustment for baseline QALYs. As described in Chapter 5, complete-case and PP analyses were also undertaken, as were a range of structural, scenario and probabilistic sensitivity analyses. Costs were estimated from a health-care perspective and consideration was limited to randomised trial participants. Costs for each participant were calculated by multiplying their use of health-care resources by associated unit costs and were discounted at an annual rate of 3.5%. HRQoL was calculated from serial EQ-5D measurements. The mean (SD) costs in the first year were £2501 (£1698) in the surgical group compared with £560 (£1007) in the medical group; in each subsequent year the mean costs were around £175 higher in the medical group. The estimated incremental mean cost of the surgical policy was £1518 (95% CI £1006 to £2029) with incremental mean QALYs of 0.2160 (95% CI 0.0205 to 0.4115), giving an ICER of £7028. The probability of the surgical policy being the more cost-effective was 0.93 at a threshold of £20,000 per QALY and 0.96 at a threshold of £30,000 per QALY. The complete-case analysis gave similar results and the conclusions were robust to plausible changes in assumptions, the only exception being when surgery-allocated patients with missing data were assumed to experience lower HRQoL than other patients. A regression-based mixed-model approach was then used to explore the robustness of the findings and to gauge the likelihood that the current strong evidence for cost-effectiveness might be reversed over subsequent years. The regression-based model gave very similar results to the base-case imputation approach. Given the trends in both costs and benefits, it was concluded that it was highly unlikely that the cost-effectiveness of surgery would be reversed when extrapolated beyond 5 years.
Thus, this second phase of the REFLUX trial has accomplished what it set out to do. After 5 years' follow-up, a policy of relatively early laparoscopic fundoplication among patients for whom reasonable control of GORD symptoms requires long-term medication and for whom both surgery and medical management are suitable continues to provide better relief of GORD symptoms with associated better QoL. Although surgery carries risks, complications were rare. And despite being initially more costly, a surgical policy was found to be highly likely to be cost-effective for such patients at conventional threshold costs per QALY.
Implications for health care
Extending the use of laparoscopic fundoplication to people whose GORD symptoms require long-term medication for reasonable control and who would be suitable for surgery would provide health gain that extends over a number of years. The longer-term data reported here indicate that this is highly likely to be a cost-effective use of resources. The more troublesome the symptoms, the greater the potential benefit from surgery.
Recommendations for research
The practical implications for health services of any extension of the use of laparoscopic fundoplication depend on how many patients might seek such surgery as a consequence. Most patients taking anti-reflux medication are managed in general practice. Currently, it is uncertain how many people require long-term medication for reasonable control of their GORD symptoms, how many of these would be suitable for surgery and how many would seek it; hence, it is not clear what the most efficient provision of future care might be. We therefore recommend further research to address these issues and explore the practical and resource implications of alternative policies for laparoscopic fundoplication, which include extending its use within the NHS to the sorts of patients enrolled in the REFLUX trial.
Acknowledgements
The authors wish to thank Janice Cruden and Pauline Garden for their secretarial support and data management; Samantha Wileman and Julie Bruce for invaluable help with the overview of trials; the following researchers for their assistance in nurse co-ordination, patient recruitment and follow-up: Maureen GC Gillan, Marie Cameron, Christiane Pflanz-Sinclair, Lynne Swan; Sharon McCann, who was involved in the piloting of the practical arrangements of this trial; and Allan Walker, Daniel Barnett and Gladys McPherson for database and programming support.
Members of the (1) Trial Steering Group and (2) Data Monitoring Committee who oversaw the first phase of this study were:
-
Wendy Atkin* (Independent chairperson), John Bancewicz, Garry Barton (1999–2002), Ara Darzi, Robert Heading, Janusz Jankowski,* Zygmunt Krukowski, Richard Lilford,* Iain Martin (1997–2000), Ashley Mowat, Ian Russell, Mark Sculpher and Mark Thursz.
-
Jon Nicholl,* Chris Hawkey* and Iain MacIntyre. *
* Independent of trial.
Members of the REFLUX trial group responsible for recruitment in the clinical centres were as follows:
| Aberdeen: Aberdeen Royal Infirmary | A Mowat, Z Krukowski, E El-Omar, P Phull and T Sinclair |
| Belfast: Royal Victoria Hospital | B Clements, J Collins, A Kennedy and H Lawther |
| Bournemouth: Royal Bournemouth Hospital | D Bennett, N Davies, S Toop and P Winwood |
| Bristol: Bristol Royal Infirmary | D Alderson, P Barham, K Green and R Mittal |
| Bromley: Princess Royal University Hospital | M Asante and S El Hasani |
| Edinburgh: Royal Infirmary of Edinburgh | A De Beaux, R Heading, L Meekison, S Paterson-Brown and H Barkell |
| Guildford: Royal Surrey County Hospital | G Ferns, M Bailey, N Karanjia, TA Rockall and L Skelly |
| Hull: Hull Royal Infirmary | M Dakkak, J King, C Royston and P Sedman |
| Inverness: Raigmore Hospital | K Gordon, LF Potts, C Smith, PL Zentler-Munro and A Munro |
| Leeds: Leeds General Infirmary | S Dexter and P Maoyeddi |
| Leicester: Leicester Royal Infirmary | DM Lloyd |
| London: St Mary's Hospital | V Loh, M Thursz and A Darzi |
| London: Whipps Cross Hospital | A Ahmed, R Greaves, A Sawyerr, J Wellwood and T Taylor |
| Poole: Poole Hospital | S Hosking, S Lowrey and J Snook |
| Portsmouth: Queen Alexandra Hospital | P Goggin, T Johns, A Quine, S Somers and S Toh |
| Salford: Hope Hospital | J Bancewicz, M Greenhalgh and W Rees |
| Stoke-on-Trent: North Staffordshire Hospital | CVN Cheruvu, M Deakin, S Evans, J Green and F Leslie |
| Swansea: Morriston Hospital | JN Baxter, P Duane, MM Rahman, M Thomas and J Williams |
| Telford: Princess Royal Hospital | D Maxton, A Sigurdsson, MSH Smith and G Townson |
| Yeovil: Yeovil District Hospital | S Gore, RH Kennedy, ZH Khan and J Knight |
| York: York District Hospital | D Alexander, G Miller, D Parker, A Turnbull and J Turvill |
The Health Services Research Unit is funded by the Chief Scientist Office of the Scottish Government Health Directorate.
Contribution of authors
Adrian Grant (Professor, Health Services Research Trialist) was the principal grant applicant and contributed to the development of the trial protocol and the preparation of the report and had overall responsibility for the conduct of the study.
Charles Boachie (Statistician, Health Statistics) conducted the statistical analysis.
Seonaidh Cotton (Trial Co-ordinator, Health Services Research Trialist) was responsible for the day-to-day management of the trial, monitored data collection and assisted in the preparation of the report.
Rita Faria (Research Fellow, Health Economics) was involved in the cost-effectiveness section, namely conducting the economic evaluation and writing the final report.
Laura Bojke (Senior Research Fellow, Health Economics) was responsible for the cost-effectiveness section – supervising the economic evaluation and the systematic review of existing economic evidence and writing the final report.
David Epstein (Honorary Research Fellow, Health Economics) was involved in the cost-effectiveness section – conducting and supervising the economic evaluation and writing the final report.
Craig Ramsay (Professor, Health Services Research Statistician/Trialist) contributed to the grant application and the trial design and conducted the statistical analysis.
Belen Corbacho (Research Fellow, Health Economics) was responsible for the systematic review of existing health economic evidence – study selection, data extraction, validity assessment and writing the final report.
Mark Sculpher (Professor of Health Economics, Health Economics) was responsible for the economic evaluation section of the grant application and overseeing the economic evaluation.
Zygmunt Krukowski (Surgeon, Gastroenterology) advised on clinical aspects of the trial and commented on the draft report.
Robert C Heading (Honorary Professor) advised on clinical aspects of the trial design and the conduct of the trial and commented on the draft report.
Marion Campbell (Director, Health Services Research Statistician/Trialist) contributed to the development of the trial design and all aspects of the conduct of the trial and commented on the draft report.
Publications
-
Grant AM, Cotton SC, Boachie C, Ramsay CR, Krukowski ZH, Heading RC, et al. Minimal access surgery compared with medical management for gastro-oesophageal reflux disease: five year follow-up of a randomised controlled trial (REFLUX) BMJ 2013;346:f1908. DOI: http://dx.doi.org/10.1136/bmj.f1908 (published online on 18 April 2013).
-
Faria R, Bojke L, Epstein D, Corbacho B, Sculpher M, on behalf of the REFLUX trial group. Cost-effectiveness of laparoscopic fundoplication versus continued medical management for the treatment of gastro-oesophageal reflux disease based on long-term follow-up of the REFLUX trial. Br J Surg 2013; in press. DOI: http://dx.doi.org/10.1002/bjs.9190.
Disclaimer
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al. The effectiveness and cost-effectiveness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The REFLUX trial. Health Technol Assess 2008;12.
- Grant AM, Wileman SM, Ramsay CR, Mowat NA, Krukowski ZH, Heading RC, et al. Minimal access surgery compared with medical management for chronic gastro-oesophageal reflux disease: UK collaborative randomised trial. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a2664.
- Epstein D, Bojke L, Sculpher MJ. REFLUX trial group . Laparoscopic fundoplication compared with medical management for gastro-oesophageal reflux disease: cost effectiveness study. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2576.
- Macran S, Wileman S, Barton G, Russell I. The development of a new measure of quality of life in the management of gastro-oesophageal reflux disease: the Reflux questionnaire. Qual Life Res 2007;16:331-43. http://dx.doi.org/10.1007/s11136-006-9005-3.
- Bojke L, Hornby E, Sculpher M. A comparison of the cost effectiveness of pharmacotherapy or surgery (laparoscopic fundoplication) in the treatment of GORD. Pharmacoeconomics 2007;25:829-41. http://dx.doi.org/10.2165/00019053-200725100-00003.
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group . The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006;101:1900-20. http://dx.doi.org/10.1111/j.1572-0241.2006.00630.x.
- Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 1997;112:1448-56. http://dx.doi.org/10.1016/S0016-5085(97)70025-8.
- Kennedy T, Jones R. The prevalence of gastro-oesophageal reflux symptoms in a UK population and the consultation behaviour of patients with these symptoms. Aliment Pharmacol Ther 2000;14:1589-94. http://dx.doi.org/10.1046/j.1365-2036.2000.00884.x.
- Heading RC. Prevalence of upper gastrointestinal symptoms in the general population: a systematic review. Scand J Gastroenterol 1999;34:3-8.
- Davis CS, Baldea A, Johns JR, Joehl RJ, Fisichella PM. The evolution and long-term results of laparoscopic antireflux surgery for the treatments of gastroesophageal reflux disease. JSLS 2010;13:332-41. http://dx.doi.org/10.4293/108680810X12924466007007.
- Peters MJ, Mukhtar A, Yunus RM, Khan S, Pappalardo J, Memon B, et al. Meta-analysis of randomized clinical trials comparing open and laparoscopic anti-reflux surgery. Am J Gastroenterol 2009;104:1548-61. http://dx.doi.org/10.1038/ajg.2009.176.
- Donahue PE, Larson GM, Stewardson RH, Bombeck CT. Floppy Nissen fundoplication. Rev Surg 1977;34:223-4.
- DeMeester TR, Bonavina L, Albertucci M. Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg 1986;204:9-19. http://dx.doi.org/10.1097/00000658-198607000-00002.
- Broeders JAJL, Mauritz FA, Ahmed Ali U, Draaisma WA, Ruurda JP, Gooszen HG, et al. Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg 2010;97:1318-30. http://dx.doi.org/10.1002/bjs.7174.
- Lundell L, Miettinen P, Myrvold HE, Hatlebakk JG, Wallin L, Engstrom C, et al. Comparison of outcomes twelve years after antireflux surgery or omeprazole maintenance therapy for reflux esophagitis. Clin Gastroenterol Hepatol 2009;7:1292-8. http://dx.doi.org/10.1016/j.cgh.2009.05.021.
- Chiba N, De Gara CJ, Wilkinson JM, Hunt RH. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta analysis. Gastroenterology 1997;112:1798-810. http://dx.doi.org/10.1053/gast.1997.v112.pm9178669.
- Boutet R, Wilcock M, Mackenzie I. Survey on repeat prescribing for acid suppression drugs in primary care in Cornwall and the Isles of Scilly. Aliment Pharmacol Ther 1999;13:813-17. http://dx.doi.org/10.1046/j.1365-2036.1999.00524.x.
- McCullagh M, Brown C, Bell D, Powell K. Long term acid suppressing treatment survey shows variation in practice. BMJ 1994;308. http://dx.doi.org/10.1136/bmj.308.6938.1238.
- Ryder SD, O’Reilly S, Miller RJ, Ross J, Jacyna MR, Levi AJ. Long term acid suppressing treatment in general practice. BMJ 1994;308:827-30. http://dx.doi.org/10.1136/bmj.308.6932.827.
- Dibley LB, Norton C, Jones R. Non-pharmacological intervention for gastro-oesophageal reflux disease in primary care. Br J Gen Pract 2010;60:e459-65. http://dx.doi.org/10.3399/bjgp10X544050.
- Roberts SJ, Bateman DN. Prescribing of antacids and ulcer-healing drugs in primary care in the north of England. Aliment Pharmacol Ther 1995;9:137-43. http://dx.doi.org/10.1111/j.1365-2036.1995.tb00362.x.
- Bashford JNR, Norwood J, Chapman SR. Why are patients prescribed proton pump inhibitors? Retrospective analysis of the link between morbidity and prescribing in the General Practice Research Database. BMJ 1998;317:452-6. http://dx.doi.org/10.1136/bmj.317.7156.452.
- Yang Y, Metz DC. Reviews in basic and clinical gastroenterology and hepatology safety of proton pump inhibitor exposure. Gastroenterology 2010;139:1115-27. http://dx.doi.org/10.1053/j.gastro.2010.08.023.
- Sheen E, Triadafilopoulos G. Adverse effects of long-term proton pump inhibitor therapy. Dig Dis Sci 2011;56:931-50. http://dx.doi.org/10.1007/s10620-010-1560-3.
- Ogawa R, Echizen H. Drug–drug interaction profiles of proton pump inhibitors. Clin Pharmacokinet 2010;49:509-33. http://dx.doi.org/10.2165/11531320-000000000-00000.
- Henshaw RC, Naji SA, Russell IT, Templeton AA. Comparison of medical abortion with surgical vacuum aspiration: women's preferences and acceptability of treatment. BMJ 1993;307:714-17. http://dx.doi.org/10.1136/bmj.307.6906.714.
- Cooper KG, Grant AM, Garratt AM. The impact of using a partially randomised patient preference design when evaluating alternative managements for heavy menstrual bleeding. Br J Obstet Gynaecol 1997;104:1367-73. http://dx.doi.org/10.1111/j.1471-0528.1997.tb11005.x.
- Brewin CR, Bradley C. Patient preferences and randomised clinical trials. BMJ 1989;299:313-15. http://dx.doi.org/10.1136/bmj.299.6694.313.
- British national formulary. London: BMA and RPS; 2006.
- Torgerson D, Sibbald B. Understanding controlled trials: what is a patient preference trial?. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7128.360.
- Dent J, Brun J, Fendrick AM, Fennerty MB, Janssens J, Kahrilas PJ, et al. An evidence-based appraisal of reflux disease management – the Genval Workshop Report. Gut 1999;44:S1-16.
- Edwards PJ, Roberts IG, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I, et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev 2007;2.
- Brealey S, Atwell C, Bryan S. Improving response rates using monetary incentives for patient completion of questionnaires: an observational study. BMC Med Res Methodol 2007;7. http://dx.doi.org/10.1186/1471-2288-7-12.
- Kenyon S, Pike K, Jones D, Taylor D, Salt A, Marlow N, et al. The effect of a monetary incentive on return of a postal health and development questionnaire: a randomised trial. BMC Health Serv Res 2007;5. http://dx.doi.org/10.1186/1472-6963-5-55.
- Dirmaier J, Harfst T, Koch U, Schulz H. Incentives increased return rates but did not influence partial nonresponse or treatment outcome in a randomized trial. J Clin Epidemiol 2007;60:1263-70. http://dx.doi.org/10.1016/j.jclinepi.2007.04.006.
- Brooks R. EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Jenkinson C, Layte R, Wright L, Coulter A. The UK SF-36: an analysis and interpretation manual. Oxford: Health Services Research Unit; 1996.
- Nagelkerke N, Fidler V, Bersen R, Borgdorff M. Estimating treatment effects in randomised clinical trials in the presence of non-compliance. Stat Med 2000;19:1849-64. http://dx.doi.org/10.1002/1097-0258(20000730)19:14⟨1849::AID-SIM506⟩3.0.CO;2-1.
- White IR. Uses and limitations of randomization-based efficacy estimators. Stat Methods Med Res 2005;14:327-47. http://dx.doi.org/10.1191/0962280205sm406oa.
- Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al. Contamination in trials of educational interventions. Health Technol Assess 2007;11.
- Fielding S, Fayers P, Ramsay CR. Investigating the missing data mechanism in quality of life outcomes: a comparison of approaches. Health Qual Life Outcomes 2009;7. http://dx.doi.org/10.1186/1477-7525-7-57.
- Roland M, Torgerson DJ. What are pragmatic trials?. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7127.285.
- Wileman SM, McCann S, Grant AM, Krukowski ZH, Bruce J. Medical versus surgical management for gastro-oesophageal reflux disease (GORD) in adults. Cochrane Database Syst Rev 2010;3.
- Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, et al. A randomized controlled trial of laparoscopic Nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: one-year follow-up. Surg Innov 2006;13:238-49. http://dx.doi.org/10.1177/1553350606296389.
- Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, et al. A randomized controlled trial of laparoscopic Nissen fundoplication versus proton pump inhibitors for the treatment of patients with chronic gastroesophageal reflux disease (GERD): 3-year outcomes. Surg Endosc 2011;25:2547-54. http://dx.doi.org/10.1007/s00464-011-1585-5.
- Goeree R, Hopkins R, Marshall JK, Armstrong D, Ungar WJ, Goldsmith C, et al. Cost-utility of laparoscopic Nissen fundoplication versus proton pump inhibitors for chronic and controlled gastroesophageal reflux disease: a 3-year prospective randomized controlled trial and economic evaluation. Value Health 2011;14:263-73. http://dx.doi.org/10.1016/j.jval.2010.09.004.
- Lundell L, Attwood S, Ell C, Fiocca R, Galmiche J, Hatlebakk J, et al. Comparing laparoscopic antireflux surgery with esomeprazole in the management of patients with chronic gastro-oesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut 2008;57:1207-13. http://dx.doi.org/10.1136/gut.2008.148833.
- Galmiche J, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD. The LOTUS randomized clinical trial. JAMA 2011;305:1969-77. http://dx.doi.org/10.1001/jama.2011.626.
- Attwood SE, Lundell L, Hatlebakk JG, Eklund S, Junghard O, Galmiche J, et al. Medical or surgical management of GERD patients with Barrett's esophagus: the LOTUS trial 3-year experience. J Gastrointest Surg 2008;12:1646-55. http://dx.doi.org/10.1007/s11605-008-0645-1.
- Attwood SEA, Lundell L, Ell C, Galmiche J, Hatlebakk J, Fiocca R, et al. Standardization of surgical technique in antireflux surgery: the LOTUS trial experience. World J Surg 2008;32:995-8. http://dx.doi.org/10.1007/s00268-007-9409-4.
- Mahon D, Rhodes M, Decadt B, Hindmarsh A, Lowndes R, Beckingham I, et al. Randomized clinical trial of laparoscopic Nissen fundoplication compared with proton-pump inhibitors for treatment of chronic gastro-oesophageal reflux. Br J Surg 2005;92:695-9. http://dx.doi.org/10.1002/bjs.4934.
- Cookson R, Flood C, Koo B, Mahon D, Rhodes M. Short-term cost effectiveness and long-term cost analysis comparing laparoscopic Nissen fundoplication with proton-pump inhibitor maintenance for gastro-oesophageal reflux disease. Br J Surg 2005;92:700-6. http://dx.doi.org/10.1002/bjs.4933.
- Mehta S, Bennett J, Mahon D, Rhodes M. Prospective trial of laparoscopic Nissen fundoplication versus proton pump inhibitor therapy for gastroesophageal reflux disease: seven-year follow-up. J Gastrointest Surg 2006;10:1312-17. http://dx.doi.org/10.1016/j.gassur.2006.07.010.
- Wiklund I, Bigard MA, Grace E, Talley NJ, Kamm M, Veldhuyzen van Zanten S, et al. Quality of life in reflux and dyspepsia patients. Psychometric documentation of a new disease-specific questionnaire (QOLRAD) 11. Eur J Surg 1998;164:41-9. http://dx.doi.org/10.1080/11024159850191238.
- Dimenas E. Methodological aspects of evaluation of quality of life in upper gastrointestinal diseases. Scand J Gastroenterol 1993;28:18-21. http://dx.doi.org/10.3109/00365529309098350.
- Rantanen TK, Salo JA, Sipponen JT. Fatal and life-threatening complications in antireflux surgery: analysis of 5502 operations. Br J Surg 1999;86:1573-7. http://dx.doi.org/10.1046/j.1365-2168.1999.01297.x.
- van Pinxteren B, Sigterman KE, Bonis P, Lau J, Numans ME. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev 2010;11.
- Romagnuolo J, Meier MA, Sadowski DC. Medical or surgical therapy for erosive reflux oesophagitis: cost–utility analysis using a Markov model. Ann Surg 2002;236:191-202. http://dx.doi.org/10.1097/00000658-200208000-00007.
- Arguedas MR, Heudebert GR, Klapow JC, Centor RM, Eloubeidi M, Wilcox CM. Re-examination of the cost-effectiveness of surgical versus medical therapy in patients with gastroesophageal reflux disease: the value of long-term data collection. Am J Gastroenterol 2004;99:1023-8. http://dx.doi.org/10.1111/j.1572-0241.2004.30891.x.
- Comay D, Adam V, da Silveira EB, Kennedy W, Mayrand S, Barkun AN. The Stretta procedure versus proton pump inhibitors and laparoscopic Nissen fundoplication in the management of gastroesophageal reflux disease: a cost-effectiveness analysis. Can J Gastroenterol 2008;22:552-8.
- HMSO Electronic Drug Tariff for the National Health Service of England and Wales. London: HMSO; 2010.
- Manca A, Hawkins N. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. http://dx.doi.org/10.1002/hec.944.
- NHS reference costs 2009–2010. London: DoH; 2010.
- Curtis L. Unit costs of health and social care. Canterbury: PSSRU, University of Kent; 2010.
- Guide to the methods of technology appraisal. London: NICE; 2008.
- Dolan P, Gudex C, Kind P, Williams A. Discussion paper 138. York: Centre for Health Economics, University of York; 1995.
- Billingham LJ, Abrams KR, Jones DR. Methods for the analysis of quality-of-life and survival data in health technology assessment. Health Technol Assess 1999;3.
- Green book: appraisal and evaluation in central government. London: The Stationery Office; 2003.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2010;30:377-99. http://dx.doi.org/10.1002/sim.4067.
- White IR, Mander A, Wason J, Bond S. n.d.
- Royston P. Multiple imputation by the MICe system of chained equations. Implementation in Stata. J Stat Softw 2011;45. www.jstatsoft.org (accessed 5 December 2012).
- Little RJA, Rubin DB. Statistical analysis with missing data. New York, NY: Wiley; 1987.
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987.
- Horton NJ, Kleinman KP. Much ado about nothing: a comparison of missing data methods and software to fit incomplete data regression models. Am Stat 2007;61:79-90. http://dx.doi.org/10.1198/000313007X172556.
- Galati JC, Carlin JB, Royston P. MIM: Stata Module to Analyse and Manipulate Multiply Imputed Datasets n.d. http://EconPapers.repec.org/RePEc:boc:bocode:s456825 (accessed 1 July 2011).
- Briggs AH, Gray A. Handling uncertainty when performing economic evaluation of healthcare interventions. Health Technol Assess 1999;3.
- Box GEP, Cox DR. An analysis of transformations. J R Stat Soc Series B 1964;2:211-43.
- Burton A, Billingham LJ, Bryan S. Cost-effectiveness in clinical trials: using multiple imputation to deal with incomplete cost data. Clin Trials 2007;4:154-61. http://dx.doi.org/10.1177/1740774507076914.
- White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011;342:910-12. http://dx.doi.org/10.1136/bmj.d40.
- Johannesson M, Weinstein S. On the decision rules of cost-effectiveness analysis. J Health Econ 1993;12:459-67. http://dx.doi.org/10.1016/0167-6296(93)90005-Y.
- Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18:S68-80. http://dx.doi.org/10.1177/0272989X9801800209.
- Claxton K. Exploring uncertainty in cost-effectiveness analysis. Pharmacoeconomics 2008;26:781-98. http://dx.doi.org/10.2165/00019053-200826090-00008.
Appendix 1 Annual questionnaire
Appendix 2 Intra- and postoperative surgical outcomes
Appendix 3 Tables showing medication use in preceding fortnight at each time point of follow-up
Tables showing medication use in preceding fortnight at each time point of follow-up (PDF download)
Appendix 4 Tables showing health status measures at each time point of follow-up
Tables showing health status measures at each time point of follow-up (PDF download)
Appendix 5 Characteristics of the four randomised controlled trials of laparoscopic fundoplication compared with medical management
Characteristics of the four randomised controlled trials of laparoscopic fundoplication compared with medical management (PDF download)
Appendix 6 Search strategies for economic evaluation review
Search strategies for economic evaluation review (PDF download)
Appendix 7 Within-trial cost-effectiveness analysis: health-related quality-of-life and cost-effectiveness results
Within-trial cost-effectiveness analysis: health-related quality-of-life and cost-effectiveness results (PDF download)
Appendix 8 Validation of the multiple imputation
Appendix 9 Costs and health-related quality of life for allocation according to per protocol at 1 year: structural sensitivity analysis
Costs and health-related quality of life for allocation according to per protocol at 1 year: structural sensitivity analysis (PDF download)
Appendix 10 Protocol
List of abbreviations
- BMI
- body mass index
- CDSR
- Cochrane Database of Systematic Reviews
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DARE
- Database of Abstracts of Reviews of Effects
- DMC
- Data Monitoring Committee
- EQ-5D
- European Quality of Life-5 Dimensions
- EVPI
- expected value of perfect information
- GERSS
- Gastro-Esophageal Reflux Symptom Score
- GORD
- gastro-oesophageal reflux disease
- GP
- general practitioner
- GSRS
- Gastrointestinal Symptoms Rating Scale
- H2RA
- histamine receptor antagonist
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- HUI3
- Health Utilities Index Mark 3
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- LOTUS
- LOng-Term Usage of esomeprazole versus Surgery for treatment of chronic GERD
- MAR
- missing at random
- MCAR
- missing completely at random
- MCS
- mental component score
- MICE
- multiple imputation using chained equations
- MNAR
- missing not at random
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NMB
- net monetary benefit
- OLS
- ordinary least squares
- PCS
- physical component score
- PGWI
- Psychological General Well-Being Index
- PP
- per protocol
- PPI
- proton pump inhibitor
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- QOLRAD
- Quality of Life in Reflux and Dyspepsia
- RCT
- randomised controlled trial
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- SF-6D
- Short Form questionnaire-6 dimensions
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or at the end of the table.