Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/09/06. The contractual start date was in August 2016. The draft report began editorial review in December 2017 and was accepted for publication in July 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Luke Vale is a member of the National Institute for Health Research Health Technology Assessment Clinical Evaluation and Trials Board and co-ordinating editor of Cochrane Incontinence. Ash Monga was a paid speaker for Astellas Pharma (Tokyo, Japan), SEP Pharma Ltd (London, UK), Boston Scientific (Boston, MA, USA) and Atlantic Pharma Ltd (Bedford, UK). Phil Mackie is a member of the Scottish Independent Review of Transvaginal Mesh Implants.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Brazzelli et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of underlying health problem
Urinary incontinence (UI) is defined as an involuntary loss of urine. It is a common condition that is believed to affect millions of people. There are several types of UI; the focus of this research is stress urinary incontinence (SUI). SUI is the loss of urine when coughing, laughing, sneezing or exercising. It is a common and distressing condition, greatly affecting quality of life. The prevalence of SUI varies during life but is greater in women who have had children and in older women (20–50%). 1 The physical changes resulting from pregnancy, childbirth and menopause often contribute to SUI. For many women, SUI can worsen during the week before the menstrual period. Lower oestrogen levels can lead to lower muscular pressure around the urethra, which in turn increases the chances of leakage. Many women access conservative treatment with physiotherapy to deliver pelvic floor muscle training (PFMT) and bladder training initially but, if this fails, surgery is the mainstay of treatment. Data suggest that women have a 10% lifetime risk of having continence surgery. 1
The aim of surgery is to support or partially obstruct the bladder neck and/or urethra, thus blocking the leakage of urine on exertion or coughing. Women with mixed urinary incontinence (MUI) (a combination of SUI and urgency UI) may also be helped because they are better able to defer voiding and leakage. However, urinary urgency and urgency UI can be both caused by and made worse by SUI surgery. 1
Incontinence varies in degree of severity from several drops of urine to complete bladder emptying. It may occur daily, many times a day or only occasionally, perhaps once a month. It may be predictable or very unpredictable. These different factors – severity, frequency and predictability – all play a role in evaluating the impact of incontinence on behaviour, treatment choice, quality of life and economic burden. The precise economic burden has proved difficult to calculate. One published UK study suggests an estimated total figure for combined health, personal and societal expenditure of £818M for SUI at 1999/2000 prices (upwards of £1.1B at 2017 prices),2 whereas another study published in 2004 suggests a health-care cost to the UK NHS (SUI only) of £117M per year. 3
One of the main purposes of this research is to comparatively draw together all the relevant evidence from published randomised controlled trials (RCTs), accomplished through a network meta-analysis (NMA) and associated economic model. This allows all the available surgical treatments to be simultaneously compared with each other, for what we believe to be the first time, to determine which treatments should be offered in clinical practice on the basis of being the most clinically effective, safest and most cost-effective.
Description of current service provision
Women are likely to have tried many things prior to presenting to their general practitioner (GP), including lifestyle changes, PFMT and incontinence pants or pads. Embarrassment stops many seeking help from their GP until symptoms become unmanageable or begin to have a greater impact on everyday life. The treatment offered within primary care will depend on the type and severity of incontinence. Conservative treatments are usually tried first before moving on to medication. Conservative treatments can overlap with treatments tried by women prior to presenting and may include lifestyle changes (e.g. reduced caffeine intake, adjusted fluid intake, weight loss); PFMT, which can be aided by biofeedback, vaginal cones or electrical stimulation; and bladder training.
If these treatments are unsuccessful, medication is available. For SUI only one medication is available: duloxetine. The National Institute for Health and Care Excellence (NICE) recommends (as of September 2013) that duloxetine not be routinely offered as first-line treatment and that it be offered as second-line therapy only to women wishing to avoid other therapy (i.e. surgery). The guidelines further state that women should be counselled regarding the drug’s side effects. The evidence for duloxetine is uncertain. The drug failed to receive Food and Drug Administration (FDA) approval for SUI owing to concerns over liver toxicity and suicidal events. In the UK, as mentioned previously, it is currently recommended as an add-on medication for SUI instead of surgery. Its safety and utility for SUI have been evaluated in a number of meta-analyses, the latest of which, published in 2016 and based on clinical trial reports, found that, although effective for SUI, duloxetine’s associated harms were high and, when individual patient data were analysed, outweighed the benefits. 4
There are several surgical treatment options for the management of women who have failed first-line treatment for SUI. Furthermore, there are a number of variations on most techniques, but, essentially, they fall into nine distinct categories:
-
anterior vaginal repair (anterior colporrhaphy)
-
bladder neck needle suspension
-
open abdominal retropubic colposuspension
-
laparoscopic retropubic colposuspension
-
traditional suburethral retropubic sling procedures
-
mid-urethral sling (MUS) procedures
-
retropubic MUS
-
transobturator MUS
-
-
single-incision sling procedures (‘mini-slings’)
-
periurethral injection (injectable bulking agents).
One of the earliest operations described for SUI was anterior repair with urethral buttressing sutures (Kelly sutures). Although curing over half of women, the high failure rate (and that of another operation, bladder neck needle suspension) led to the development of colposuspension, which is an open abdominal method of elevating the bladder neck. The evidence base suggested that this was more effective but with greater morbidity and a longer recovery time than the previous options. Laparoscopic colposuspension, although a minimally invasive variation of colposuspension, was considered slightly less effective than open surgery. These issues led to the development of traditional suburethral sling procedures, in which a piece of material, which could be biological (such as a rectus sheath graft) or synthetic (such as a polypropylene mesh sling), is placed under the urethra and the free ends secured in one of a number of different ways. The advent of a new minimally invasive technique that enabled the sling to be placed without tension ushered in a new era of simpler, effective and cheaper treatment. This brief summary of the evidence concurs with the conclusions of the Cochrane reviews that have collated the relevant evidence for these types of procedures. 5–12
The number of women having surgery has been rising and the choice of operations has changed over the past decade. In 2013–14, Hospital Episode Statistics (HES) data for England show that around 12,000 women had a MUS operation, with around 500 having another type of continence procedure (colposuspension, ≈300; traditional slings, ≈200) and just over 700 having periurethral injections. In contrast, 10 years earlier just under 7000 women had a MUS operation, ≈1400 had a colposuspension and ≈250 had a traditional sling. There is no single database that records how many vaginal mesh implants are implanted or removed each year in women with SUI, making an assessment of trends difficult. However, it would appear that, until recently, there had been a shift towards minimally invasive MUS, with the majority of women choosing this procedure, which in turn led to a substantial increase in the total number of women having continence surgery. These trends are likely to have been driven, in part, by the perception of improved effectiveness and safety.
In 2014 the American Urogynecologic Society and Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction published a position statement: ‘The polypropylene mesh mid-urethral sling is the recognized worldwide standard of care for the surgical treatment of stress urinary incontinence. The procedure is safe, effective, and has improved the quality of life for millions of women’. 13 However, subsequent international media publicity regarding supposed long-term severe adverse effects from vaginal mesh procedures has caused anxiety in women, many of whom have decided, owing to high levels of uncertainty, to avoid any type of surgery involving synthetic material, including MUS, despite the lack of any robust new evidence to support this view.
Women’s concerns about the safety of vaginal mesh implants led to a patients’ campaign, which in turn led to an independent enquiry and the suspension of use of any vaginal mesh (including MUSs) in Scotland, UK parliamentary questions, a mandatory national audit and a national campaign, Hear Our Voice (www.scottishmeshsurvivors.com/). The debate encompasses the wider use of vaginal mesh in conditions not being considered in this report. There remains a lot of uncertainty surrounding the optimal choice of surgery, especially related to long-term safety, with recent news and media headlines adding to the ambiguity that clinicians and women face when making decisions regarding treatment options. It is likely that the trend in the use of minimally invasive MUSs has taken a downwards turn; however, what is currently unclear is the strength of evidence to support the choice of any one of the other surgery options.
Description of technologies under assessment
The technologies under assessment are the surgical techniques anterior vaginal repair (anterior colporrhaphy); bladder neck needle suspension; open abdominal retropubic colposuspension; laparoscopic retropubic colposuspension; traditional suburethral retropubic sling procedures; retropubic MUS; transobturator MUS; and single-incision sling procedures (mini-slings).
Decision problem
Currently there is no clear evidence to indicate which surgery is the best choice. It is unclear if the older operations that were previously available (such as anterior repair and colposuspension) really result in equivalent or better outcomes than the polypropylene MUS. However, the feeling of our clinical experts who used to offer colposuspension and traditional slings is that these techniques had more frequent and severe associated complications and returning to them may be detrimental to women. To enable women to make an evidence-based choice and inform practice guidelines, it is essential to collect reliable evidence in a transparent, concise manner to allow impartial counselling of women regarding the benefits and risks of the alternative surgical operations for the management of SUI.
The wide range of surgical operations available, the different techniques used to perform these operations and the lack of a consensus among surgeons make it challenging to establish which procedure is the most effective. The existing evidence base, including the Cochrane systematic reviews, has focused on discrete two-way comparisons, with no attempt being made to collate all of the evidence on the surgical options available and rank them in terms of clinical effectiveness, safety and cost-effectiveness. This has resulted in a piecemeal evidence base that is difficult for women and clinicians to interpret. This assessment includes an evidence synthesis of all available RCTs to determine the relative clinical effectiveness and safety of interventions, a discrete choice experiment (DCE) to explore women’s preferences, an economic decision model to determine the most cost-effective treatment and a value-of-information (VOI) analysis to help inform the focus of further research.
Aims and objectives of the research
The aim of this project was to evaluate the clinical effectiveness, safety and cost-effectiveness of surgical treatment for SUI and stress-predominant MUI in women.
The key objectives were to:
-
undertake an evidence synthesis using systematic review methods, including a NMA to estimate the relative clinical effectiveness of the different types of surgery and inform key clinical parameters for a decision model
-
undertake a review of safety/adverse effects associated with each type of surgical intervention
-
undertake a DCE to explore the preferences of women
-
develop a decision model to estimate the cost-effectiveness of surgical treatments for SUI and stress-predominant MUI
-
utilise the decision model to undertake a VOI analysis to assess the need for further primary research.
Chapter 2 Methods of clinical effectiveness review(s)
This chapter reports the methods used for conducting an objective synthesis of the current evidence for assessing the clinical effectiveness and safety of surgical interventions for the treatment of SUI or stress-predominant MUI in women. The evidence synthesis was carried out according to the general principles of the Centre for Reviews and Dissemination (CRD) guidance for undertaking reviews in health care,14 the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions15 and the NICE guide to the methods of technology appraisal16 and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 17 The methods were prespecified in a research protocol (PROSPERO database registration number CRD42016049339).
Search strategy
Literature searching was performed in two stages. First, relevant studies were identified from the existing relevant Cochrane systematic reviews published in the Cochrane Database of Systematic Reviews. Second, the Cochrane Incontinence Group Specialised Register was searched to identify new studies added since the publication of the Cochrane systematic reviews (henceforth ‘updated literature searches’).
The Cochrane Incontinence Group has published eight systematic reviews assessing nine distinct surgical procedures for the treatment of SUI in women. Two Cochrane systematic reviews that were obtained through personal communication and were in the process of being updated (review on traditional suburethral slings for UI in women: Dr Lucky Saraswat, Aberdeen Royal Infirmary, 2016; review on laparoscopic colposuspension for UI in women: Dr Muhammad Imran Omar, University of Aberdeen, 2016) were also used as source data. Both reviews have currently completed the peer-review process. On approval, the final versions of these systematic reviews are expected to be published in the Cochrane Database of Systematic Reviews.
We used these Cochrane systematic reviews to identify studies that met our prespecified inclusion criteria. To avoid duplicates, the studies were taken from the reviews in the following order:
-
Lapitan et al. 5 – open retropubic colposuspension for UI in women
-
Ford et al. 8 and Ogah et al. 18 – MUS operations for SUI in women
-
Nambiar et al. 9 – single-incision sling operations for UI in women
-
Saraswat et al. 7 and Rehman et al. 19 – traditional suburethral sling operations for UI in women
-
Freites et al. 6 and Dean et al. 20 – laparoscopic colposuspension for UI in women
-
Glazener and Cooper11 – bladder neck needle suspension for UI in women
-
Glazener and Cooper10 – anterior vaginal repair for UI in women
-
Kirchin et al. 12 – urethral injection therapy for UI in women.
There was a certain degree of overlap between systematic reviews, with some primary studies included in more than one review. The additional reports of primary studies included as second/multiple publications were checked across reviews.
The Cochrane Incontinence Group Specialised Trials Register was searched (date of last search: 8 June 2017) using the terms given in Appendix 1 to identify studies published since the conduct of the Cochrane systematic review. The Cochrane Incontinence Group Specialised Trials Register is updated regularly and contains studies from the following databases and other sources:
-
Cochrane Central Register of Controlled Trials (CENTRAL) [via Cochrane Register of Studies Online (CRSO)] (inception to 15 May 2017) (searched 15 May 2017)
-
MEDLINE (via OvidSP) (1946 to April week 3 2017)
-
MEDLINE In-Process & Other Non-Indexed Citations (via OvidSP) (covering 28 April 2017)
-
MEDLINE Epub Ahead of Print (via OvidSP) (covering 2 May 2017)
-
ClinicalTrials.gov via Cochrane Register of Studies (CRS) standalone
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP)
-
hand-searching of journals and conference proceedings.
EMBASE is not included in the above list because the Cochrane Centralised Search Service already searches EMBASE for identification of RCTs and adds them to CENTRAL. Details of the search methods used to build the Specialised Register are available from the group’s module in The Cochrane Library. 21
Inclusion and exclusion criteria
Types of studies
Randomised controlled trials or quasi-RCTs (using alternate allocation) were eligible for the assessment of clinical effectiveness. There was no restriction on the trials’ publication status (published or unpublished) or on the year or the language in which they were reported.
Population
The type of participants considered for this assessment were adult women with SUI or stress-predominant MUI. Either a clinical or a urodynamic diagnosis of SUI was considered suitable. We accepted the diagnoses as defined by the authors of the included trials. Women who underwent continence surgery as a primary or repeated procedure, women with SUI and concomitant prolapse and women who received concomitant prolapse surgery were deemed suitable for inclusion. Studies that did not specify the type of incontinence (stress, urge, mixed) or the predominant MUI symptoms (stress or urge) were excluded.
Interventions
The interventions detailed below were deemed suitable for inclusion. There are a number of variations on most surgical techniques, but, essentially, they fall into nine distinct categories, each of which has been previously evaluated in systematic reviews published in The Cochrane Library:
-
retropubic MUS operations
-
transobturator MUS operations
-
open retropubic colposuspension
-
laparoscopic colposuspension
-
traditional suburethral sling procedures
-
single-incision sling operations
-
anterior vaginal repair
-
bladder neck needle suspension
-
urethral injection therapy (periurethral injections/injectable bulking agents).
To be eligible for inclusion, studies had to compare two or more of the surgical interventions listed above. Studies that compared a surgical intervention with PFMT were also considered suitable for inclusion as they were useful for the development of a NMA treatment diagram for assessing direct and indirect treatment comparisons. For the purpose of this assessment, we considered eligible for inclusion PFMT programmes taught and monitored by health professionals, clinicians or instructors (defined as ‘supervised PFMT’). 22 PFMT programmes for which instructions were delivered using written material only (e.g. leaflets or flyers delivered to women), without any interaction or face-to-face contact with health-care professionals, were considered to be equivalent to no treatment and, therefore, excluded from this assessment.
We excluded, post hoc, studies that compared surgery with pharmacological treatments or no treatment, as they were not considered useful for the development of the treatment network diagram. We did not include studies comparing specific technical variations of the relevant surgical techniques (e.g. inside-out vs. outside-in transobturator MUS operations, or one injectable agent vs. another) as it was beyond the scope of this review to assess specific technical approaches within each surgical category.
Outcomes
The following outcome measures were considered.
Primary outcomes
-
Number of women cured (defined as resolution of clinical symptoms).
-
Number of women cured or improved (henceforth referred to as ‘improvement’).
Secondary outcomes
-
Long-term data:
-
number of women having repeated continence surgery.
-
-
Adverse events:
-
haemorrhage/major vascular complications, including haematoma
-
infection, including wound infection and urinary tract infection (UTI)
-
infection related to use of synthetic mesh
-
de novo symptoms of urgency or urgency incontinence
-
voiding difficulties including urinary retention
-
bladder or urethral perforation
-
tape/mesh/implant exposure
-
tape/mesh erosion or extrusion
-
persistent pain or discomfort, including osteitis, which is pertinent to the Marshall-Marchetti-Krantz procedure
-
dyspareunia (pain with intercourse)
-
death.
-
-
Resource use:
-
operating time
-
length of hospital stay.
-
We considered outcomes measured at 12 months or the nearest time point available as well as longer-term outcomes (e.g. at 2 years or 5 years). Studies with a time point of < 2 weeks were excluded.
The measurement of these outcomes was not used as an eligibility criterion for selecting studies for inclusion in this assessment.
Primary outcomes (cure and improvement) were defined in many different ways. For example, authors of individual studies defined cure as ‘no stress incontinence symptoms’, ‘negative testing’ or subjective reports of being ‘continent’, ‘dry’, ‘satisfied’ or ‘very much improved’. To have a more consistent definition of cure, we checked the original definitions used by the authors of each included study to ensure that ‘cure’ was used to refer to the resolution of SUI symptoms. We also accepted cases where authors reported resolution of ‘incontinence symptoms’ without specifying stress symptoms. Any indication of satisfactory improvement in SUI symptoms was defined as ‘improvement’.
A variety of measures could be used to define cure or improvement in SUI symptoms, including subjective (women-reported) measures such as women’s observations and objective measures such as quantification of symptoms (e.g. pad tests) and urodynamic tests. We chose to extract data based on a hierarchy of reported outcomes. For ‘cure’, women’s self-report of cure was given priority when available. When this measure was not available, a composite measure (a combination of women-reported and objective measures) was used instead. Pad test and urodynamic test results were considered only when the previous two outcome measures were not available. For ‘improvement’, the women’s self-report of improvement was preferred but if this was not available the women’s satisfaction rate was used as a proxy. If satisfaction rate was also not available, we considered improvement rates based on pad tests and then on urodynamic tests. Cough stress tests or diaries were considered less reliable measures for the assessment of cure and improvement.
Adverse event outcomes were extracted verbatim from the relevant Cochrane systematic reviews. The classification of secondary outcomes and time points of outcome measurements were only consistent within each Cochrane systematic review, but not necessarily across different Cochrane systematic reviews. For example, in certain reviews pain outcomes were classified by time (short term and long term) whereas in others this was by location (e.g. groin or abdominal). Haematoma was reported as either a distinct outcome (haematoma) or part of a group of outcomes (e.g. perioperative complications). Though some outcomes were redefined by Cochrane authors to facilitate meta-analysis, the definitions used were not always clearly reported. No attempt was made to standardise adverse event outcomes extracted from different Cochrane systematic reviews.
The GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach,23 which takes into account five criteria – study design (judged according to the Cochrane risk-of-bias tool), inconsistency, imprecision, indirectness and publication bias24 – was used for rating the quality of evidence of the two primary outcomes included in the NMA (cure and improvement). The following steps were taken: (1) assess the quality of evidence of direct treatment effect (head-to-head comparison), when available; (2) assess the quality of evidence of indirect treatment effect (i.e. two pairwise comparisons contributing to the first-order loop; the lower confidence rating of the two pairwise comparisons was used to indicate the overall quality of indirect treatment effect); (3) use the higher of the two quality ratings when both direct and indirect estimates of treatment effect are available; and (4) when only a direct or indirect estimate of treatment effect is available, base the network quality on that estimate. As GRADEpro GDT (McMaster University and Evidence Prime Inc, Hamilton, ON, Canada; https://gradepro.org) is a web-based tool that does not support assessment of the quality of evidence of network meta-analyses, we used Microsoft Excel® 2013 (Microsoft Corporation, Redmond, WA, USA). There are four levels of quality of evidence: high, moderate, low or very low. ‘High quality’ means that the authors have a lot of confidence that the true effect lies close to that of the estimated effect. ‘Moderate quality’ means that the authors believe that the true effect is probably close to the estimated effect but there is a possibility that it is substantially different. ‘Low quality’ means that the true effect might be markedly different from the estimated effect. ‘Very low quality’ means that the true effect is probably markedly different from the estimated effect.
Owing to the lack of suitable data and the fact that the risk-of-bias assessment in the relevant Cochrane systematic reviews was not always provided for individual outcomes, it proved unfeasible to use the GRADE approach for grading the quality of other outcomes.
Data collection
Selection of studies
The selection of studies included in the Cochrane systematic reviews was established by one reviewer (SW) and checked by a second reviewer (MI). Screening of the titles and abstracts of all citations identified by the updated literature searches was conducted by one reviewer (SW). Full text copies of all potentially relevant reports were retrieved by the same reviewer for eligibility and checked by a second reviewer (MI or MS) to ensure that they met the prespecified inclusion criteria.
Data extraction
Studies selected from Cochrane systematic reviews
The original data extraction performed by the authors of the individual Cochrane systematic reviews was used as a basis for the assessment of clinical effectiveness. The characteristics of included studies were extracted as reported in the relevant Cochrane systematic reviews. Outcome data presented in forest plots of each Cochrane systematic review were exported using RevMan version 5.3 (Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). Of these, data for primary outcomes (cure and improvement) were cross-checked against the original study reports and supplementary information (such as definitions and time points) was extracted to enable the performance of a NMA.
Cross-checking of secondary outcome data was performed only when there was inconsistency in the extracted data or when studies were originally included as abstracts in the Cochrane systematic reviews but subsequently published in full (eight studies). 25–32 In other cases, adverse event data were accepted as reported in the Cochrane reviews.
Some Cochrane systematic review authors attempted to contact the corresponding authors of included studies to obtain key missing data or have full-text copies of non-English-language translations. Any relevant information retrieved in such a manner was included in this assessment. In some cases, reports published in languages other than English were translated by the authors of the Cochrane reviews. When a translation could not be arranged, the information used in the Cochrane reviews was limited to the content of the English abstracts.
Studies identified by the updated literature searches
For new studies identified by the updated literature searches, data extraction was carried out by one reviewer and checked by a second reviewer (MI and MS) for errors or inconsistencies. Any disagreement was resolved through consensus or arbitration by a third party. A data extraction form was designed and piloted for the purpose of this assessment (see Appendix 2). Details related to study design, characteristics of participants, settings, characteristics of interventions and outcome measures were recorded. Outcome data were extracted as needed to allow calculation of summary statistics and measures of variance. Numbers of events and total number of participants in each treatment group were extracted for the assessment of dichotomous outcomes, and means and standard deviations (SDs) were extracted for the assessment of continuous outcomes. Missing data were not imputed and there was no attempt to contact study authors for missing data.
Risk-of-bias assessment of included studies
Studies selected from Cochrane systematic reviews
We relied on the original risk-of-bias assessments performed by the authors of the Cochrane systematic reviews. Assessment criteria varied across different Cochrane systematic reviews, which were accepted as reported. We updated the risk-of-bias assessments using the new criteria described below only for those studies that were initially included in the Cochrane systematic reviews as abstracts but subsequently published in full (eight studies). 25–32
Studies identified by the updated literature searches
For the studies identified by the updated literature searches, the Cochrane risk-of-bias assessment tool was used. 15 Critical judgments were made for the following domains: selection bias (random sequence generation, allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessor), attrition bias (incomplete outcome data), reporting bias (free of selective reporting) and other bias. Each included study was judged to be at ‘low risk of bias’, ‘high risk of bias’ or ‘unclear risk of bias’. The assessment was conducted by one reviewer (MI or MS) and checked by a second reviewer (MI or MS). Any disagreements were resolved by consensus or arbitration with a third reviewer (MB). Studies were not included or excluded on the basis of their methodological quality.
Data analysis
Network meta-analysis
Network meta-analysis aims to synthesise all of the available evidence within a distinct framework. It enables the integration of direct evidence with indirect evidence from a network of studies involving all possible intervention comparisons. Direct evidence is obtained from all possible head-to-head comparisons between the different interventions, whereas indirect evidence is obtained from comparisons of two or more interventions that share a common comparator. For example, direct evidence from comparing intervention A with B and B with C can be combined to provide indirect evidence for intervention A versus C.
We conducted a NMA to assess the effects of the surgical interventions for SUI in terms of the number of women who were cured or experienced an improvement in their incontinence symptoms (primary outcomes). Studies that reported 100% events in all arms (all participants were cured or improved) were excluded from the analysis as they provide no evidence for the analysis. The NMA included outcomes measured at 12 months or at a time point closest to 12 months (studies with a time point of < 2 weeks or > 36 months were excluded).
Convergence was assessed using Brooks–Gelman–Rubin plots, trace plots and autocorrelation plots. The NMA analysis was undertaken within a Bayesian framework, using WinBUGS 1.4.3 (MRC Biostatistics Unit, Cambridge, UK)33 and using code provided by Dias et al. 34 (see Appendix 3). The analysis used vague uniform prior and adjusted for multi-arm trials using conditional distributions. Consistency, which is where direct and indirect evidence are in agreement, was assessed by comparing the individual data point’s posterior mean deviance contributions for the consistency and inconsistency model and node splitting analysis35 using R 3.4.1 (R Foundation, Vienna, Austria).
In the results section, network diagrams are presented for each outcome and effect sizes are reported as posterior median odds ratios (ORs) and 95% credible intervals (Crls). We also present rankograms for all surgical interventions, which gives probabilities of an intervention being ranked 1 (the highest) to 9 (the lowest) as well as reporting the surface under the cumulative ranking curve (SUCRA), which is a numerical presentation of the overall ranking and presents a single number associated with each intervention. SUCRA values range from 0% to 100%. The closer to 100% the SUCRA value, the more likely that an intervention is in the top rank or one of the top ranks; the closer to 0 the SUCRA value, the more likely that an intervention is in the bottom rank or one of the bottom ranks. 36
Direct pairwise (head-to-head) meta-analyses
Adverse event outcomes as well as cure and improvement were summarised as direct head-to-head comparisons using a random effects model. Effect sizes are reported as ORs with 95% confidence intervals (CIs) for dichotomous outcomes and as mean differences with 95% CI for continuous outcomes. When data were available, meta-analyses assessing adverse events were performed at different time points (e.g. 6 months, 12 months, 24 months). Heterogeneity was assessed using the I2 statistic. Analyses were performed using Stata version 14 (StataCorp LP, College Station, TX, USA).
Subgroup analysis
We planned to undertake subgroup analyses for the following groups: women with stress-predominant MUI versus women with SUI alone; repeated surgery (after failed previous continence surgery) versus primary procedures; women with and without coexisting vaginal prolapse/having concomitant prolapse surgery. However, these were not performed owing to the lack of available data. For example, lack of clarity in some trial reports made it difficult to decipher whether study participants had SUI, MUI or both. Moreover, outcome data for each patient subgroup were not reported separately in all trials. Owing to such inconsistencies and limited reporting of suitable data in the included studies, we were unable to perform these analyses.
Chapter 3 Results of clinical effectiveness review(s)
Number of studies identified
Studies identified from Cochrane systematic reviews
From the eight published Cochrane systematic reviews that provided data suitable for this assessment, a total of 166 studies (in 443 reports) were initially selected as potentially relevant. Of these, 147 studies (in 406 reports) were included as they met the prespecified inclusion criteria for this assessment, 17 studies were excluded and one was merged with another study. 37 The number of included studies from each Cochrane systematic review is shown in Table 1.
| Source of studies | Number of studies selected |
|---|---|
| (a) Selected from published Cochrane systematic reviews | |
| Lapitan et al.:5 open retropubic colposuspension for UI in women | 47 |
| Ford et al.8 and Ogah et al.:18 MUS operations for SUI in women | 68 |
| Nambiar et al.:9 single-incision sling operations for UI in women | 24 |
| Saraswat et al.7 and Rehman et al.:19 traditional suburethral sling operations for UI in women | 6 |
| Freites et al.6 and Dean et al.:20 laparoscopic colposuspension for UI in women | 1 |
| Glazener and Cooper:11 bladder neck needle suspension for UI in women | 1 |
| Glazener and Cooper:10 anterior vaginal repair for UI in women | 0 |
| Kirchin et al.:12 urethral injection therapy for UI in women | 0 |
| Subtotal | 147 |
| (b) Identified via updated literature searches | |
| Subtotal | 28 |
| Total number of included studies (a + b) | 175 |
Studies identified from updated literature searches
The updated literature searches identified 591 potentially relevant titles and abstracts from which 216 reports were selected for full-text evaluation. Of these, 65 reports (describing 28 new studies) were considered suitable for inclusion. In addition, 100 reports were identified as additional references of studies already included in the relevant Cochrane systematic reviews and two reports were additional references of studies originally included in the Cochrane systematic reviews but subsequently excluded from the effectiveness and cost-effectiveness of surgical treatments for women with stress urinary incontinence (ESTER) report. A total of 26 reports of 23 ongoing trials were also identified and two further reports were included as ‘awaiting assessment’ and 21 reports were excluded.
In total, 175 studies were included in the assessment of clinical effectiveness. Of these, 43 studies were available only as conference abstracts. 38–80 A PRISMA flow chart summarising the study selection process is provided in Appendix 4. The list of included studies and associated references is reported in Appendix 5. Reasons for exclusion for a sample of excluded studies are described in Appendix 6. The list of ongoing trials is provided in Appendix 7.
Characteristics of included studies
The characteristics of the included studies are detailed in Appendix 8. The included studies involved a total of 21,598 women, with a median follow-up of 12 months, ranging from 1 month80 to 126 months. 81 Sample size ranged from 1570 to 65582 participants, with a median of 91 participants per study. There were 25 studies with a sample size of ≥ 200 participants. 28,37,61,65,72,82–101 The largest study assessed 655 women treated with either open colposuspension or traditional slings. 82 The mean or median age of women ranged from 34.338 to 65.0102 years.
There were 10 quasi-randomised trials (out of 175 included studies; 6%) considered to be at high risk of selection bias, as participants were allocated to treatment by alternation,103–110 date of birth111 or medical history numbers. 112
The primary references of the included studies (either the first publication or the first full-text publication) were published between 1978105 and 2016. 65,91,113–115 Around 10% (17 out of 175) of the included studies were published before 2000, 81 (46%) were published between 2000 and 2009 and 77 (44%) were published in 2010 or thereafter. All of those published before 2000 compared open colposuspension with other surgical procedures, whereas those published from 2000 onwards tended to include MUSs (retropubic or transobturator route) or single-incision slings as one of the study arms.
The number and type of intervention comparisons are shown in Table 2. Altogether, the included studies reported 21 treatment comparisons. The majority of included studies involved MUSs (retropubic or transobturator route) as part of their interventions. The most common intervention comparisons were between retropubic MUSs and transobturator MUSs (58 studies) and between transobturator MUS and single-incision slings (39 studies). The latter comparisons included 17 new studies, nearly two-thirds of the 28 new studies identified by the updated literature searches (17 out of 28; 61%). Another common comparison was between open colposuspension and other surgery (46 studies), followed by laparoscopic colposuspension (21 studies) and traditional slings (20 studies). Few studies were available for most other comparisons.
| Intervention | Number randomised | Number of studies | Number of new studies | References | |
|---|---|---|---|---|---|
| 1 (control) | 2 (experiment) | ||||
| Retro-MUS | Transob-MUS | 8876 | 58 | 4 | Darabi Mahboub et al.,26 Tarcan et al.,31 Wang,37 Cervigni et al.,41 Choe et al.,42 de Oliveira et al.,44 Diab et al.,45 El-Hefnawy et al.,48 Elshawaf and Al bahaie,49 Hammoud et al.,56 Kamel,58 Leanza et al.,61 Mansoor et al.,64 Palomba and Zullo,70 Riva et al.,71 Rudnicki et al.,72 Salem et al.,73 Aigmüller et al.,83 Aniuliene,84 Araco et al.,86 Chen et al.,90 Krofta et al.,94 Laurikainen et al.,96 Meschia et al.,97 Rechberger et al.,98 Richter et al.,99 Enzelsberger et al.,104 Lee et al.,107 Nerli et al.,110 Wang et al.,116 Andonian et al.,117 Chen et al.,118 Scheiner et al.,119 Alkady and Eid,120 Aniuliene et al.,121 Barber et al.,122 Barry et al.,123 David-Montefiore et al.,124 deTayrac et al.,125 Deffieux et al.,126 El-Hefnawy et al.,127 Freeman et al.,128 Jakimiuk et al.,129 Karateke et al.,130 Kiliç et al.,131 Kim et al.,132 Liapis et al.,133 Mehdiyev et al.,134 Nyyssönen et al.,135 Porena et al.,136 Ross et al.,137 Schierlitz et al.,138 Tanuri et al.,139 Teo et al.,140 Wang et al.,141 Wang et al.,142 Zhang and Zhu143 and Zullo et al.144 |
| Retro-MUS | Open colpo | 1240 | 13 | 0 | Trabuco et al.,32 Drahoradova et al.,46 Elshawaf and Al bahaie49 Halaska et al.,55 Han,57 Koelbl et al.,60 O’Sullivan et al.,69 Ward et al.,100 Liapis et al.,108 Bai et al.,145 Foote et al.146 and Paraiso et al.147 |
| Retro-MUS | Lap colpo | 651 | 8 | 0 | Adile et al.,39 Maher et al.,63 Mirosh and Epp,67 Foote et al.,146 Paraiso et al.,147 Persson et al.,148 Ustün et al.149 and Valpas et al.150 |
| Retro-MUS | Trad sling | 868 | 9 | 0 | Abouhashem et al.,38 Sharifiaghdas and Mortazavi,81 Guerrero et al.,92 Kondo et al.,106 Bai et al.,145 Amaro et al.,151 Arunkalaivanan and Barrington,152 Basok et al.153 and Song et al.154 |
| Retro-MUS | Single incision | 1092 | 9 | 3 | Lee et al.,62 Rudnicki et al.,72 Barber et al.,87 Wang et al.,116 Abdelwahab et al.,155 Andrada Hamer et al.,156 Basu and Duckett,157 Gopinath et al.158 and Ross et al.159 |
| Retro-MUS | Ant repair | 53 | 1 | 0 | Wadie et al.160 |
| Transob-MUS | Open colpo | 272 | 4 | 0 | El-Din Shawki et al.,47 Elshawaf and Al bahaie,49 Bandarian et al.161 and Sivaslioglu et al.162 |
| Transob-MUS | Lap colpo | 35 | 1 | 0 | Samiee et al.163 |
| Transob-MUS | Trad sling | 141 | 3 | 1 | Al-Azzawi,164 Silva-Filho et al.165 and Tcherniakovsky et al.166 |
| Transob-MUS | Single incision | 4612 | 39 | 17 | Bianchi et al.,25 Djehdian et al.,27 Lee et al.,28 Schweitzer et al.,29 Smith et al.,30 Dati et al.,43 Enzelsberger et al.,50 Fernandez et al.,52 Friedman,54 Kim et al.,59 Melendez Munoz et al.,65 Merali et al.,66 Rudnicki et al.,72 Seo et al.,74 Shawky et al.,75 Van Rensburg et al.,79 Yoon et al.,80 Gaber et al.,91 Masata et al.,101 Amat I Tardiu et al.,112 Jurakova et al.,113 Pastore et al.,114 Xin et al.,115 Wang et al.,116 Masata et al.,167 Oliveira et al.,168 Sottner et al.,169 Enzelsberger et al.,170 Foote,171 Hinoul et al.,172 Hota et al.,173 Mackintosh,174 Maslow et al.,175 Campos et al.,176 Schellart and Roovers,177 Sivaslioglu et al.,178 Tang et al.179 and Tommaselli et al.180 |
| Transob-MUS | Ant repair | 120 | 2 | 1 | El-Din Shawki et al.47 and Salari and Sohbati181 |
| Transob-MUS | PFMT | 460 | 1 | 1 | Labrie et al.95 |
| Open colpo | Lap colpo | 1402 | 12 | N/A | Burton et al.,40 Fatthy et al.,51 Morris et al.,68 Stangel-Wojcikiewicz,76 Summitt et al.,77 Ankardal et al.,85 Carey et al.,89 Kitchener et al.,93 Mak et al.,182 Su et al.,183 Tuygun et al.184 and Ustün et al.185 |
| Open colpo | Trad sling | 922 | 7 | N/A | Fischer et al.,53 Albo et al.,82 Demirci and Yucel,103 Henriksson and Ulmsten,105 Bai et al.,145 Enzelsberger et al.186 and Sand et al.187 |
| Open colpo | Bladder neck needle | 639 | 7 | N/A | Bergman et al.,88 Mundy,109 Athanassopoulos and Barbalias,111 Bergman et al.,188 Gilja et al.,189 German et al.190 and Palma et al.191 |
| Open colpo | Ant repair | 690 | 8 | N/A | El-Din Shawki et al.,47 Bergman et al.,88,188 Berglund and Lalos,192 Colombo et al.,193 Holmes et al.,194 Kammerer-Doak et al.195 and Liapis et al.196 |
| Open colpo | PFMT | 45 | 1 | N/A | Tapp et al.78 |
| Trad sling | Single incision | 72 | 1 | 1 | Sharifiaghdas et al.197 |
| Trad sling | Injectable | 45 | 1 | N/A | Maher et al.102 |
| Trad sling | Bladder neck needle | 20 | 1 | N/A | Hilton198 |
| Bladder neck needle | Ant repair | 346 | 3 | N/A | Bergman et al.88,188 and Di Palumbo199 |
Six trials were based on a three-arm design. 47,49,88,116,145,188 One four-arm trial was also converted to a three-arm trial because two of the four arms compared two variations of the same treatment and were therefore combined [i.e. tension-free vaginal tape-obturator (TVT-O) and transobturator tape (TOT) were combined as transobturator MUS]. 72
Some of the three-arm trials were converted into two-arm trials because either two of the three treatment arms compared two variations of the same surgical operation,91,92,117–119,167–169,189,200 or one of the three arms assessed a treatment that did not meet our inclusion criteria [e.g. de Olivera et al. 44 included pre-pubic tension-free vaginal tape (TVT) and Tapp et al. 78 included PFMT plus electrical stimulation].
The characteristics of the participants enrolled in the included studies are summarised in Table 3. The majority of studies (91 out of 175; 52%) included women with urodynamically confirmed SUI. 25,30,31,37,39,40,43,49,51,53–55,57,58,60,61,67–69,76–78,81,83,85,87–93,97,100–103,106,107,109,111,113,115,118,122–131,138,140–142,145–152,155,160–162,166,167,171,173,178,180,182,183,185,187–190,193–196,198,201–203 Eight studies included women with a clinical diagnosis based on either urodynamic tests or symptoms of SUI27,28,120,157,165,168,172,191 and the remaining studies appeared to use a diagnosis based on symptoms of SUI.
| UI diagnosis | Number of studies |
|---|---|
| Urodynamically confirmed stress incontinence | 91 |
| Symptom diagnosis of stress incontinence | 76 |
| Either urodynamic or symptom diagnosis of stress incontinence | 8 |
| MUI | |
| SUI/USI only, no MUI | 23 |
| SUI/USI or MUI | 53 |
| SUI/USI, unclear if MUI is included or excluded | 99 |
| Previous UI surgery | |
| Excluded | 81 |
| Excluded specific surgery only | 16 |
| Included | 31 |
| Not reported | 47 |
| Co-existing prolapse at recruitment | |
| Excluded | 11 |
| Excluded ≥ 2 degree only | 28 |
| Excluded ≥ 3 degree only | 28 |
| Excluded ‘major’ or ‘significant’ prolapse only | 11 |
| Included | 36 |
| Not reported | 61 |
| Concomitant prolapse surgery performed | |
| No | 39 |
| Yes | 35 |
| Yes (hysterectomy) | 6 |
| Not reported | 95 |
In general, it was difficult to determine from the relevant Cochrane systematic reviews whether or not the patient populations had other specified characteristics (e.g. mixed incontinence or mixed symptoms, previous incontinence surgery, co-existing prolapse) as information on participants’ characteristics was not reported consistently across reviews.
It was ascertained that, based on the reported information, 23 studies included women with SUI alone37,60,67,78,90,91,94,104,105,108,114,118,129,139,142,143,161,162,178,179,181,192,201 as they specifically mentioned exclusion of urgency UI or MUI. A total of 53 studies included women with SUI as well as some with MUI. 26,30–32,48,52,56,72,79,81,82,85,87,89,99,101,106,107,110,112,113,115–117,119,120,122,124–128,135,136,148,153,154,156,159,160,164,167–169,173,174,176,180,187,194,198,199
The majority of studies excluded women with any previous UI surgery (81 out of 175 studies)29–31,38,39,43,52,58,67,69–72,78,85,86,88,89,91,92,94–97,100,101,103,104,108,113–116,118,120,126,128–130,133,136,137,140,141,143,144,147,148,155–157,159–163,165,167,168,170,172,174–178,180–185,188,192–194,196,201–204 or certain types of incontinence surgery (16 out of 175 studies). 28,65,77,83,87,93,102,119,121,122,127,135,146,150,171,173 A total of 31 studies (out of 175; 18%) included women presenting with recurrent incontinence after failed surgery. 25,27,32,37,51,56,63,79,82,84,99,106,107,109,117,123–125,138,139,142,151,152,166,186,187,190,191,195,197,198 Of these, one study included only recurrent cases. 186 The remaining studies (47 out of 175) did not indicate whether study participants had primary or recurrent incontinence, or both.
In 45% of the studies (78 out of 175) women presenting with coexisting prolapse were excluded either completely (11 studies)60,63,86,104,105,107,113,125,129,149,203 or if they presented with moderate to severe prolapse (67 studies). Six studies included exclusively women with coexisting prolapse. 32,70,88,181,193,199 A total of 30 studies included a proportion of women with prolapse of varying degrees28,30,37,41,48,52,61,64,79,82,87,90,91,99,108,111,112,117,119,122,123,142,154,166,173,176,184,192,194,195 and the remaining 61 studies did not specify whether women with prolapse were included or excluded.
A total of 39 studies did not allow concomitant prolapse surgery to be performed. 39,50,60,63,67,77,81,83,85,86,93,94,100–102,104,105,107,113,116,125,126,129,133,135,137,146,148–150,156,159,167,171,174,179,186,188,203 Three studies reported that prolapse surgery was performed in all included women32,41,88 and 32 studies reported that some women received prolapse surgery. 28,30,31,37,43,48,52–54,61,79,82,87,89,99,106,112,117,119,120,122,123,127,138,160,173,176,185,187,193,195,196 Six studies explicitly reported that hysterectomy was performed. 103,147,182,183,194,199 The remaining 95 studies did not indicate whether or not concomitant prolapse surgery was performed.
The source of funding and the setting of included studies were not consistently reported in the relevant Cochrane systematic reviews. Out of the 36 studies with available information (28 studies identified by the updated searches and eight studies identified from the Cochrane systematic reviews), five studies appeared to be funded by industry28,29,159,176,177 and seven studies were conducted in more than one clinical centre. 28,72,79,95,159,176,177
The clinical experience of the surgeon performing the procedures was not consistently reported in the Cochrane systematic reviews. Among the 36 studies providing this information, the surgeon’s clinical experience varied from ‘having inserted a minimum of one sling prior to the study’29 to ‘having performed 200 surgical procedures’. 115 Five studies reported that surgeons tended to be less experienced in performing sling procedures than the comparator surgical intervention. 25,101,113,159
Risk-of-bias assessment of included studies
There is wide variation across Cochrane systematic reviews in the number and types of criteria (domains) used to assess risk of bias. For example, the number of risk-of-bias domains was four,7,11 five,8,9,18 six5 or seven6 across reviews. The 28 new studies identified by the updated literature searches, and the eight studies originally included as abstracts in the Cochrane systematic reviews and subsequently updated based on new full-text reports, were assessed using the current version of the Cochrane risk-of-bias tool, which involved a total of nine domains. An overall assessment of risk of bias is presented in Table 4 below. Appendix 9 provides the risk-of-bias results for all individual studies included in this assessment.
| Items | Risk, n (%) | Number of studies assessed | ||
|---|---|---|---|---|
| Low | Unclear | High | ||
| 1. Random sequence generation (selection bias) | 85 (49) | 80 (46) | 10 (6) | 175 |
| 2. Allocation concealment (selection bias) | 49 (28) | 116 (66) | 10 (6) | 175 |
| 3. Blinding of participants and personnel (performance bias) | 8 (5) | 123 (73) | 37 (22) | 168 |
| 4a. Blinding of outcome assessment (detection bias): all outcomes | 20 (15) | 107 (81) | 5 (4) | 132 |
| 4b. Blinding of outcome assessment (detection bias): patient reported outcomes | 4 (11) | 17 (47) | 15 (42) | 36 |
| 4c. Blinding of outcome assessment (detection bias): clinician-measured outcomes | 8 (22) | 20 (56) | 8 (22) | 36 |
| 5. Blinding (performance bias and detection bias) | 1 (14) | 6 (86) | 0 (0) | 7 |
| 6a. Incomplete outcome data (attrition bias): all outcomes | 54 (39) | 76 (55) | 9 (6) | 139 |
| 6b. Incomplete outcome data (attrition bias): patient-reported outcomes | 18 (50) | 16 (44) | 2 (6) | 36 |
| 6c. Incomplete outcome data (attrition bias): clinician-measured outcomes | 21 (58) | 13 (36) | 2 (6) | 36 |
| 7. Selective reporting (reporting bias) | 24 (65) | 7 (19) | 6 (16) | 37 |
| 8. Other bias | 0 (0) | 82 (100) | 0 (0) | 82 |
Selection bias (adequate sequence generation/allocation concealment)
For all 175 included studies, risk of selection bias was assessed in two domains: random sequence generation and allocation concealment. A total of 43 studies (out of 175; 25%) reporting both adequate sequence generation and adequate allocation concealment were considered to have an overall low risk of selection bias. 25,27–29,32,51,63,64,83,86,87,92,93,96,97,100,101,116,120,122,124–126,128,135–137,140,144,147,148,150,157,159,160,167,174–176,182,183,185 A further six studies (out of 175; 3%) reported adequate allocation concealment but they did not describe the method used for random sequence generation. 77,85,127,156,173,199 A total of 40 studies (out of 175; 23%) reported adequate sequence generation but did not provide information on allocation concealment. 26,30,31,37,41,52,60,65,72,79,82,88,89,91,94,99,101,114,119,129,130,138,141,143,146,162,164,172,178,180,181,186–189,194–196,198,203 Two studies (out of 175; 1%) with adequate random sequence generation specifically mentioned that the treatment allocations were not concealed. 95,193
There were eight quasi-randomised trials (out of 175 included studies; 5%) in which treatment allocation was based on a method of alternation103–107,109,110 or on date of birth. 111 These were considered to be at high risk of selection bias in terms of both allocation sequence generation and concealment of allocation. Two further studies (out of 175; 1%) allocated participants by alternation108 or by medical history numbers112 and were considered to be at high risk of selection bias, although allocation concealment was considered to be at unclear (rather than high) risk of bias by the authors of the Cochrane systematic reviews. 5,9 The remaining studies (74 out of 175; 42%) did not provide this information.
Performance and detection bias (blinding)
Blinding of patients and personnel provides a safeguard against performance bias and blinding of outcome assessors protects against detection bias. It is worth noting that, owing to the nature of the interventions, blinding of participants and personnel, especially the surgeon performing the operation, is not possible. Blinding of outcome assessment for patient-reported outcomes would similarly be difficult in this clinical context (with unblinded patients being the assessors), although it should be possible to blind health-care professionals who assess clinical outcomes.
In seven studies identified from the Cochrane systematic reviews assessing traditional slings7 and bladder neck needle suspension,11 risk of performance bias and detection bias was assessed using a single criterion (whether or not a lack of blinding could introduce performance and detection bias). One study (out of 7; 14%) was judged to be at low risk of bias92 and the other six studies (86%) at high or unclear risk of bias. 38,81,102,166,198,199
Risk of performance and detection bias was assessed separately in the 168 included studies identified from sources other than the two Cochrane reviews mentioned above. With respect to the assessment of whether or not lack of blinding of patients and personnel could introduce performance bias, eight studies (out of 168; 5%) were judged to be at low risk of bias87,89,117,128,129,151,157,191 and the other 160 studies (95%) were judged to be at high or unclear risk of bias. 25–32,37,39–80,82–86,88,90,91,93–101,103–114,116,118–127,130–150,152–156,158–165,167–190,192–197,201–203
Risk of detection bias in the 132 studies identified from Cochrane systematic reviews on MUS,8,18 open colposuspension,5 laparoscopic colposuspension6 and single-incision slings9 was assessed in terms of whether or not lack of blinding of outcome assessors could affect results. A total of 20 studies (out of 132; 15%) were judged to be at low risk of bias37,86,87,89,94,117,122,125,127,130,136,141,142,144,148,156,174,178,191,204 and the remaining 112 studies (85%) were judged to be at high or unclear risk of bias. 39–42,44–47,49,51,53–61,63,64,67–71,73,74,76–78,80,82–85,88,90,93,96–100,103–112,116,118–120,123,124,126,128,129,131–135,137–140,145–147,149–155,157,160–163,165,167–170,172,173,180,182–190,192–196,201–203
Detection bias in the 36 studies identified from other sources (e.g. new studies from the update literature searches) was assessed on a per outcome basis in terms of whether or not lack of blinding of outcome assessors could affect effect estimates of patient-reported outcomes such as subjective perception of cure of UI (where outcomes are assessed directly by women) and of clinician-measured outcomes such as urodynamic tests (where outcomes are assessed by care providers). One study (out of 36; 3%) was judged to be at low risk for patient-reported outcomes,159 five studies (14%) at low risk for clinician-measured outcomes,25,115,143,175,181 and three studies (8%) at low risk for both patient-reported and clinician-measured outcomes. 29,32,91 The remaining 27 studies (75%) were judged to be at high or unclear risk for either outcome. 26–28,30,31,43,48,50,52,62,65,66,72,75,79,95,101,113,114,121,158,164,171,176,177,179,197
Attrition bias (incomplete outcome data)
In 139 studies included in the relevant Cochrane systematic reviews, risk of bias was assessed for all outcomes concerned. A total of 54 were judged to be at low risk of attrition bias, with missing data either balanced between treatment groups or imputed using appropriate methods, or with no missing data;37,40,41,54,67,81–84,88,92–94,96–98,100,102,106,116,119,120,122,123,126–128,130,133,135–137,139,141,142,144,147–150,155,157,160,162,166,168,170,174,178,184,185,193,198,199 nine were judged to be at high risk of bias;86,87,112,140,156,172,173,180,189 and 76 were judged to be at unclear risk of bias. 38,39,42,44–47,49,51,53,55–61,63,64,68–71,73,74,76–78,80,85,89,90,99,103–105,107–111,116–118,124,125,129,131,132,134,138,145,146,151–154,161,163,165,167,169,182,183,186–188,190–192,194–196,201–203
In 36 studies identified from other sources (e.g. new studies from the updated literature searches), risk of attrition bias was assessed on a per outcome basis in terms of patient-reported outcomes and clinician-measured outcomes. Of these, 18 studies were judged to be at low risk for both patient-reported and clinician-measured outcomes,25,27,30,52,91,95,101,113,114,121,143,159,164,171,176,177,179,181 three studies were judged to be at low risk for clinician-measured outcomes but unclear for patient-reported outcomes,66,72,75 two studies were judged to be at high risk for both patient-reported and clinician-measured outcomes29,175 and the remaining 13 studies were judged to be at unclear risk of bias for both outcomes. 26,28,31,32,43,48,50,62,65,79,115,158,197
Reporting bias (free of selective reporting)
Few of the relevant Cochrane systematic reviews assessed the risk of reporting bias. Information was available from one study identified from the Cochrane systematic review assessing laparoscopic colposuspension6 and from 36 further studies (28 new studies and the eight studies originally included as abstracts in the Cochrane systematic reviews and subsequently published in full). Of these, 24 studies (out of 37; 65%) were judged to be at low risk of reporting bias on the basis that all outcomes specified in the methods section were reported in the results section of the study report,25,27–32,52,62,65,79,95,101,113–115,143,159,171,175,177,179,181,197 six studies (16%) were judged to be at high risk of bias on the basis that they did not report the results for all the outcomes specified in the method section of the study report,26,43,72,75,91,176 and the remaining seven studies (19%) did not provide sufficient information to formulate a judgement. 48,50,66,121,158,163,164
Other sources of bias
Information on which to assess ‘other sources of bias’ was available for 82 of the included studies. In these studies, there was no clear evidence that other sources of bias were present. 25–32,40,43,46–53,55,57,60,62,65,66,68,69,72,75–79,82,85,88,89,91,93,95,100,101,103,105,108,109,111,113–115,121,143,145,158,159,161–164,171,175,177,179,181–195,197,200–203
Assessment of clinical effectiveness
Network meta-analysis of primary outcomes: number of women cured and number of women who experienced an improvement in their incontinence symptoms
Technical information about the model
The NMA included eight surgical procedures for SUI:
-
retropubic MUS operations
-
transobturator MUS operations
-
open colposuspension
-
laparoscopic colposuspension
-
traditional sling operations
-
single-incision sling operations
-
bladder neck needle suspension
-
anterior vaginal repair.
The ninth procedure, urethral injection therapy, did not add any information to the network and was excluded from analysis (for the cure outcome analysis, urethral injection therapy was only connected to one intervention). Separate models were developed for the two primary outcomes: the number of women cured (defined as resolution of symptoms) and the number of women improved (defined as women experiencing an improvement in their incontinence symptoms, including cure). Figure 1 shows the network diagrams for the number of women cured and improved, respectively. The size of the circles reflects the number of participants and the line width reflects the number of direct comparisons. Figure 1 also includes the total number of women for each surgical intervention included in the NMA.
FIGURE 1.
Network plot for (a) the number of women cured; and (b) the number of women improved. Note: circle size reflects the number of participants; line width reflects the number of direct comparisons. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle suspension; open colpo, open colposuspension; lap colpo, laparoscopic colposuspension; retro-MUS, retropubic MUS; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator MUS.
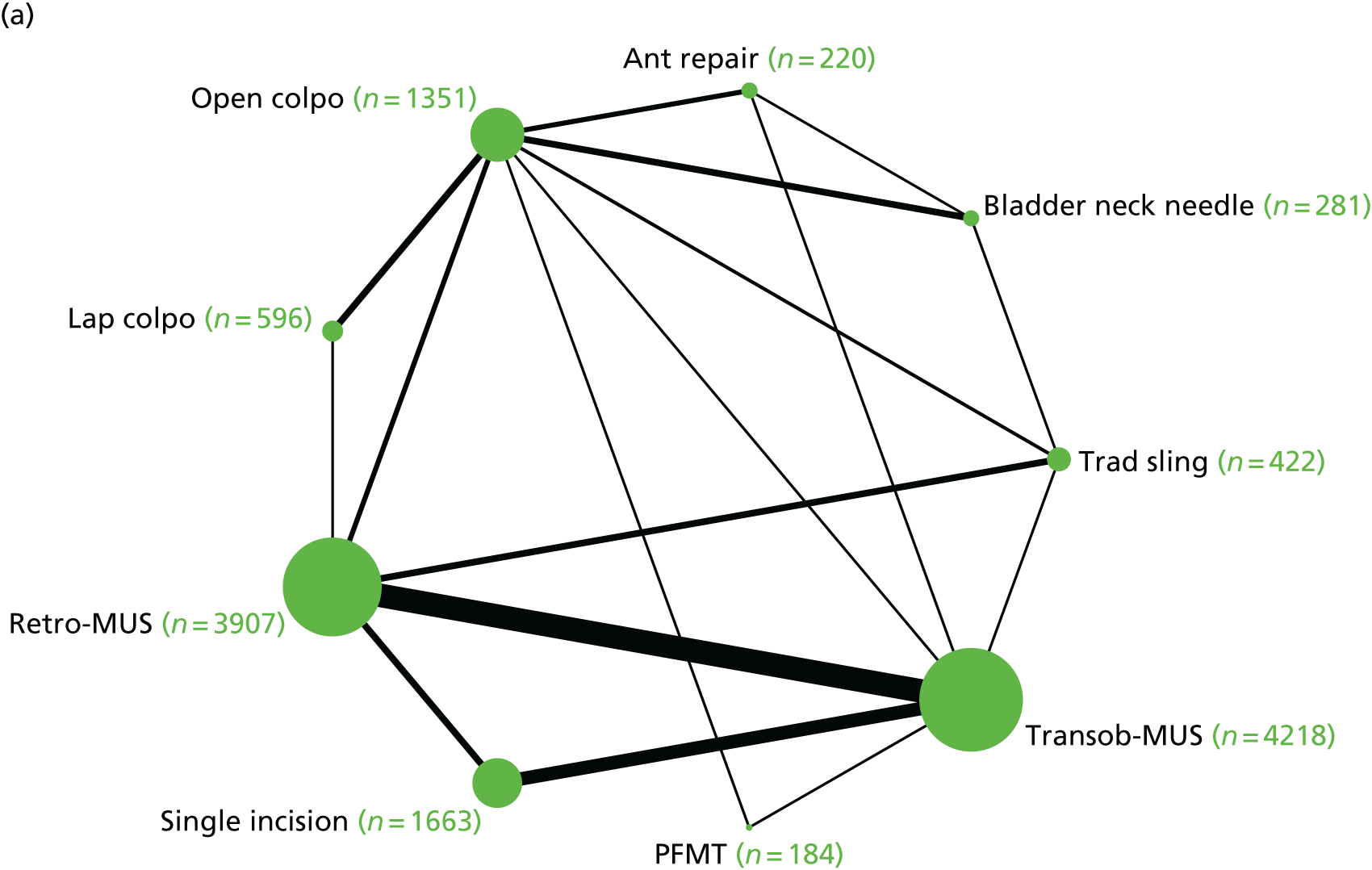
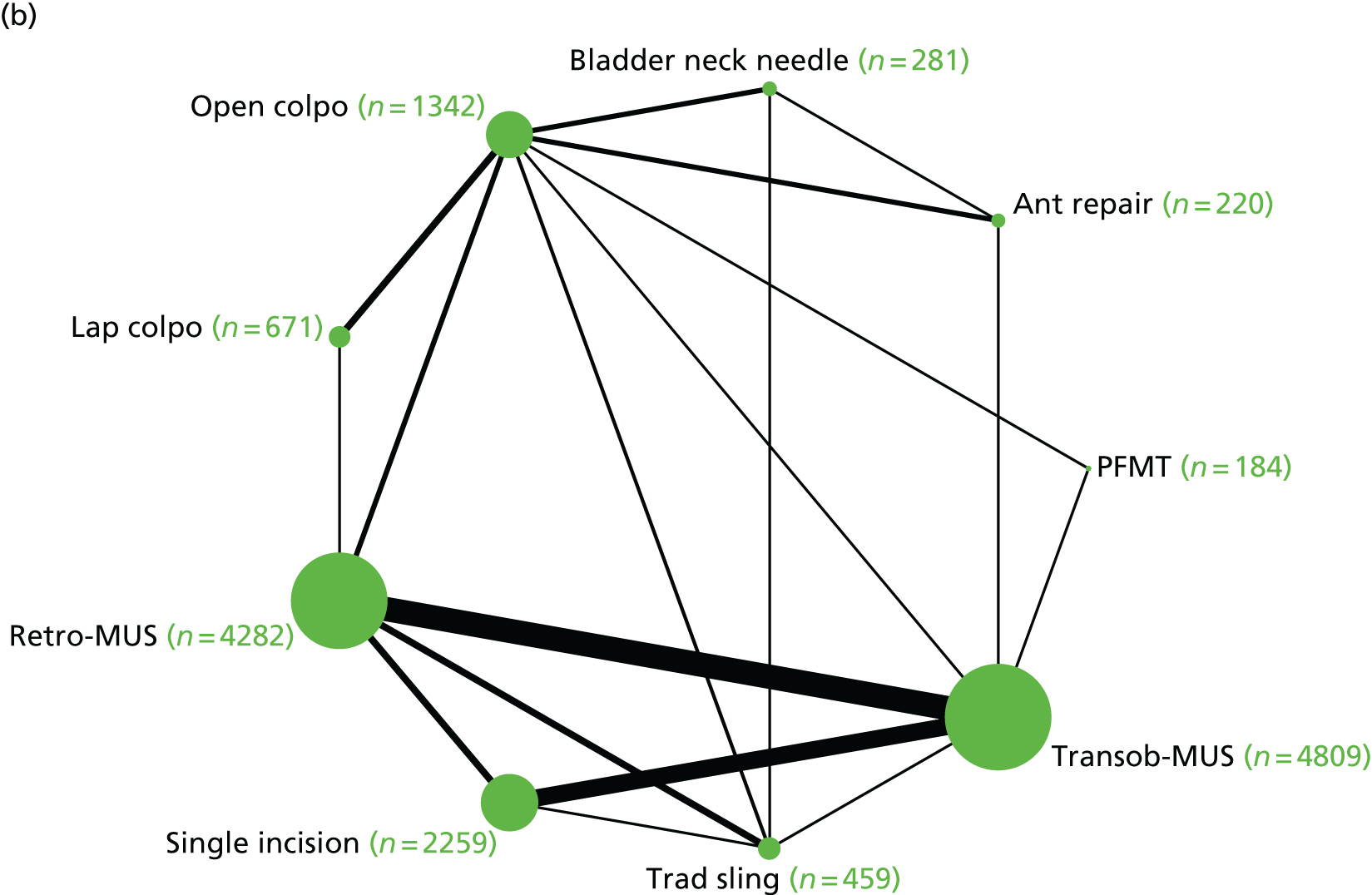
Cure or improvement of incontinence symptoms was assessed subjectively (by the woman), objectively (by a clinician) or by a combination of subjective and objective measures (composite measure). When more than one of these outcome measures were reported within a study, only one measure was included in the NMA. This measure was selected in the following order: women’s self-report assessment was given priority and, if this was unavailable, the composite outcome measure followed by the objective outcome measure were chosen as a proxy. The NMA included outcomes measured at 12 months or at a time point closest to 12 months.
The number of studies providing direct head-to-head (pairwise) evidence for each intervention that contributed data to the NMA is shown in Tables 5 and 6. The searches identified 125 trials that reported cure or improvement, or both. Three trials67,76,105 were excluded from the cure data set and four trials67,76,105,124 from the improvement dataset because they reported ‘100% events’ in all treatment arms (i.e. all participants in the study were cured or improved), providing no information for the NMA. Thus, 105 trials contributed to the NMA for assessing the number of women cured, and 120 trials were included in the analysis assessing the number of women improved. For ‘cure’, the analysis included four three-arm trials and 101 two-arm trials and generated a total of 17 direct comparisons, whereas for ‘improvement’ the analysis included five three-arm trials and 115 two-arm trials and generated a total of 18 direct comparisons. Appendix 10 shows the total number of trials for each treatment comparison for the assessment of both primary outcomes.
| Treatment | Direct evidence | NMA | GRADE | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | Number of trials | ORa | 95% CI | ORa | 95% CrI | |
| Transob-MUS | Retro-MUS | 36b | 0.83 | 0.71 to 0.97 | 0.74 | 0.59 to 0.92 | Moderate |
| Open colpo | Retro-MUS | 6b | 0.95 | 0.68 to 1.32 | 0.85 | 0.54 to 1.33 | Low |
| Lap colpo | Retro-MUS | 2 | 0.40 | 0.11 to 1.45 | 0.58 | 0.31 to 1.05 | Low |
| Trad sling | Retro-MUS | 6b | 0.87 | 0.58 to 1.29 | 1.06 | 0.62 to 1.85 | Very low |
| Single incision | Retro-MUS | 6b | 0.42 | 0.20 to 0.87 | 0.50 | 0.36 to 0.70 | Low |
| Bladder neck needle | Retro-MUS | N/A | N/A | N/A | 0.34 | 0.15 to 0.75 | Low |
| Ant repair | Retro-MUS | N/A | N/A | N/A | 0.22 | 0.10 to 0.45 | Very low |
| PFMT | Retro-MUS | N/A | N/A | N/A | 0.12 | 0.04 to 0.32 | Low |
| Open colpo | Transob-MUS | 1 | 0.90 | 0.30 to 2.69 | 1.16 | 0.72 to 1.86 | Low |
| Lap colpo | Transob-MUS | N/A | N/A | N/A | 0.79 | 0.42 to 1.46 | Low |
| Trad sling | Transob-MUS | 1 | 2.00 | 0.17 to 23.96 | 1.44 | 0.81 to 2.62 | Very low |
| Single incision | Transob-MUS | 21b | 0.74 | 0.54 to 1.00 | 0.68 | 0.51 to 0.91 | Low |
| Bladder neck needle | Transob-MUS | N/A | N/A | N/A | 0.46 | 0.21 to 1.02 | Very low |
| Ant repair | Transob-MUS | 1 | 0.50 | 0.15 to 1.62 | 0.30 | 0.14 to 0.62 | Very low |
| PFMT | Transob-MUS | 1 | 0.20 | 0.12 to 0.33 | 0.16 | 0.06 to 0.43 | Low |
| Lap colpo | Open colpo | 9 | 0.74 | 0.43 to 1.30 | 0.68 | 0.42 to 1.08 | Low |
| Trad sling | Open colpo | 3b | 2.47 | 0.73 to 8.40 | 1.24 | 0.66 to 2.45 | Very low |
| Single incision | Open colpo | N/A | N/A | N/A | 0.59 | 0.34 to 1.01 | Low |
| Bladder neck needle | Open colpo | 3b | 0.41 | 0.25 to 0.68 | 0.40 | 0.20 to 0.78 | Low |
| Ant repair | Open colpo | 3b | 0.20 | 0.07 to 0.60 | 0.26 | 0.14 to 0.48 | Very low |
| PFMT | Open colpo | 1 | 0.08 | 0.01 to 0.51 | 0.14 | 0.05 to 0.39 | Low |
| Trad sling | Lap colpo | N/A | N/A | N/A | 1.83 | 0.86 to 4.04 | Very low |
| Single incision | Lap colpo | N/A | N/A | N/A | 0.87 | 0.44 to 1.70 | Low |
| Bladder neck needle | Lap colpo | N/A | N/A | N/A | 0.59 | 0.26 to 1.33 | Very low |
| Ant repair | Lap colpo | N/A | N/A | N/A | 0.38 | 0.18 to 0.82 | Very low |
| PFMT | Lap colpo | N/A | N/A | N/A | 0.21 | 0.07 to 0.63 | N/A |
| Single incision | Trad sling | N/A | N/A | N/A | 0.47 | 0.25 to 0.88 | Very low |
| Bladder neck needle | Trad sling | 1 | 1.00 | 0.05 to 18.57 | 0.32 | 0.13 to 0.79 | Very low |
| Ant repair | Trad sling | N/A | N/A | N/A | 0.21 | 0.09 to 0.49 | Very low |
| PFMT | Trad sling | N/A | N/A | N/A | 0.11 | 0.04 to 0.34 | Very low |
| Bladder neck needle | Single incision | N/A | N/A | N/A | 0.67 | 0.29 to 1.56 | N/A |
| Ant repair | Single incision | N/A | N/A | N/A | 0.44 | 0.20 to 0.96 | Very low |
| PFMT | Single incision | N/A | N/A | N/A | 0.24 | 0.08 to 0.65 | Low |
| Ant repair | Bladder neck needle | 1b | 0.92 | 0.55 to 1.55 | 0.65 | 0.30 to 1.36 | Very low |
| PFMT | Bladder neck needle | N/A | N/A | N/A | 0.35 | 0.10 to 1.17 | Low |
| PFMT | Ant repair | N/A | N/A | N/A | 0.55 | 0.17 to 1.77 | Very low |
| Treatment | Direct evidence | NMA | GRADE | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | Number of trials | ORa | 95% CI | ORa | 95% CrI | |
| Transob-MUS | Retro-MUS | 40b | 0.86 | 0.70 to 1.06 | 0.76 | 0.59 to 0.98 | Moderate |
| Open colpo | Retro-MUS | 6b | 0.83 | 0.55 to 1.24 | 0.65 | 0.41 to 1.02 | Low |
| Lap colpo | Retro-MUS | 4 | 0.49 | 0.18 to 1.35 | 0.52 | 0.29 to 0.91 | Low |
| Trad sling | Retro-MUS | 6b | 0.62 | 0.38 to 1.02 | 0.69 | 0.39 to 1.26 | Low |
| Single incision | Retro-MUS | 6b | 0.42 | 0.20 to 0.89 | 0.50 | 0.35 to 0.71 | Moderate |
| Bladder neck needle | Retro-MUS | N/A | N/A | N/A | 0.25 | 0.11 to 0.58 | Low |
| Ant repair | Retro-MUS | N/A | N/A | N/A | 0.18 | 0.08 to 0.39 | Very low |
| PFMT | Retro-MUS | N/A | N/A | N/A | 0.43 | 0.14 to 1.37 | Low |
| Open colpo | Transob-MUS | 1 | 0.90 | 0.30 to 2.69 | 0.85 | 0.52 to 1.41 | Low |
| Lap colpo | Transob-MUS | N/A | N/A | N/A | 0.69 | 0.37 to 1.26 | Low |
| Trad sling | Transob-MUS | 1 | 2.00 | 0.17 to 23.96 | 0.91 | 0.49 to 1.72 | Very low |
| Single incision | Transob-MUS | 28b | 0.74 | 0.57 to 0.96 | 0.66 | 0.49 to 0.89 | Moderate |
| Bladder neck needle | Transob-MUS | N/A | N/A | N/A | 0.33 | 0.14 to 0.79 | Very low |
| Ant repair | Transob-MUS | 1 | 1.00 | 0.26 to 3.89 | 0.24 | 0.10 to 0.53 | Very low |
| PFMT | Transob-MUS | 1 | 0.18 | 0.10 to 0.33 | 0.56 | 0.19 to 1.78 | Low |
| Lap colpo | Open colpo | 9 | 0.93 | 0.58 to 1.48 | 0.81 | 0.49 to 1.31 | Low |
| Trad sling | Open colpo | 3b | 2.47 | 0.73 to 8.40 | 1.07 | 0.54 to 2.15 | Low |
| Single incision | Open colpo | N/A | N/A | N/A | 0.78 | 0.44 to 1.36 | Low |
| Bladder neck needle | Open colpo | 3b | 0.38 | 0.22 to 0.63 | 0.38 | 0.18 to 0.81 | Low |
| Ant repair | Open colpo | 3b | 0.20 | 0.07 to 0.60 | 0.28 | 0.14 to 0.55 | Very low |
| PFMT | Open colpo | 1 | 8.87 | 1.66 to 47.25 | 0.66 | 0.21 to 2.16 | Low |
| Trad sling | Lap colpo | N/A | N/A | N/A | 1.32 | 0.62 to 2.98 | Low |
| Single incision | Lap colpo | N/A | N/A | N/A | 0.97 | 0.50 to 1.87 | Low |
| Bladder neck needle | Lap colpo | N/A | N/A | N/A | 0.47 | 0.20 to 1.17 | Very low |
| Ant repair | Lap colpo | N/A | N/A | N/A | 0.34 | 0.15 to 0.79 | Very low |
| PFMT | Lap colpo | N/A | N/A | N/A | 0.82 | 0.25 to 2.88 | Very low |
| Single incision | Trad sling | 1 | 1.92 | 0.65 to 5.64 | 0.73 | 0.37 to 1.39 | Low |
| Bladder neck needle | Trad sling | 1 | 1.00 | 0.05 to 18.57 | 0.36 | 0.13 to 0.95 | Very low |
| Ant repair | Trad sling | N/A | N/A | N/A | 0.26 | 0.10 to 0.65 | Very low |
| PFMT | Trad sling | N/A | N/A | N/A | 0.62 | 0.18 to 2.18 | Very low |
| Bladder neck needle | Single incision | N/A | N/A | N/A | 0.49 | 0.20 to 1.24 | Very low |
| Ant repair | Single incision | N/A | N/A | N/A | 0.36 | 0.15 to 0.82 | Very low |
| PFMT | Single incision | N/A | N/A | N/A | 0.84 | 0.28 to 2.78 | Low |
| Ant repair | Bladder neck needle | 1b | 0.92 | 0.55 to 1.55 | 0.72 | 0.31 to 1.63 | Very low |
| PFMT | Bladder neck needle | N/A | N/A | N/A | 1.72 | 0.45 to 6.89 | Low |
| PFMT | Ant repair | N/A | N/A | N/A | 2.38 | 0.65 to 9.30 | Very low |
The direct pairwise analyses showed some heterogeneity in four direct comparisons for the number of women cured (single-incision sling vs. retropubic MUS; single-incision sling vs. transobturator MUS; laparoscopic colposuspension vs. open colposuspension; and anterior vaginal repair vs. open colposuspension) and one comparison for the number of women improved (laparoscopic colposuspension vs. retropubic MUS) (see Appendices 10 and 11).
Number of women cured
Table 5 shows the estimates of treatment effect from the direct pairwise meta-analyses and the NMA for the number of women cured (the direct meta-analysis results for all the included studies are presented in Appendix 11). The NMA showed that, on average, women who underwent a traditional sling or retropubic MUS operation were more likely to be cured compared with those who had other surgical procedures. Some of the comparisons had a limited number of studies and there is considerable uncertainty around the estimates of effect, for example for the comparison between retropubic MUS and traditional sling [OR 1.06, 95% CrI 0.62 to 1.85 (quality of evidence: very low)], between retropubic MUS and open colposuspension [OR 0.85, 95% CrI 0.54 to 1.33 (quality of evidence: very low)] and between retropubic MUS and laparoscopic colposuspension [OR 0.58, 95% CrI 0.31 to 1.05 (quality of evidence: very low)].
Number of women who experienced an improvement in their incontinence symptoms
Table 6 shows the estimates of treatment effect from the NMA and the overall estimates from the direct pairwise meta-analyses for the number of women with improvement in incontinence symptoms (the full set of direct meta-analyses results is presented in Appendix 12). The NMA showed that women who had retropubic MUS or transobturator MUS were more likely to experience an improvement in their incontinence symptoms. However, there is some uncertainty around the estimates of effect for some of the comparisons, for example the comparisons between retropubic MUS and open colposuspension [OR 0.65, 95% CrI 0.41 to 1.02 (quality of evidence: low)] and between retropubic MUS and traditional sling [OR 0.69, 95% CrI 0.39 to 1.26 (quality of evidence: low)].
Ranking of treatment effectiveness
Figure 2 shows the SUCRA values for all surgical interventions. The rankograms are reported in Appendix 13.
FIGURE 2.
Surface under the cumulative ranking curve values for (a) the number of women cured; and (b) the number of women improved. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle suspension; open colpo, open colposuspension; lap colpo, laparoscopic colposuspension; retro-MUS, retropubic MUS; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator MUS.
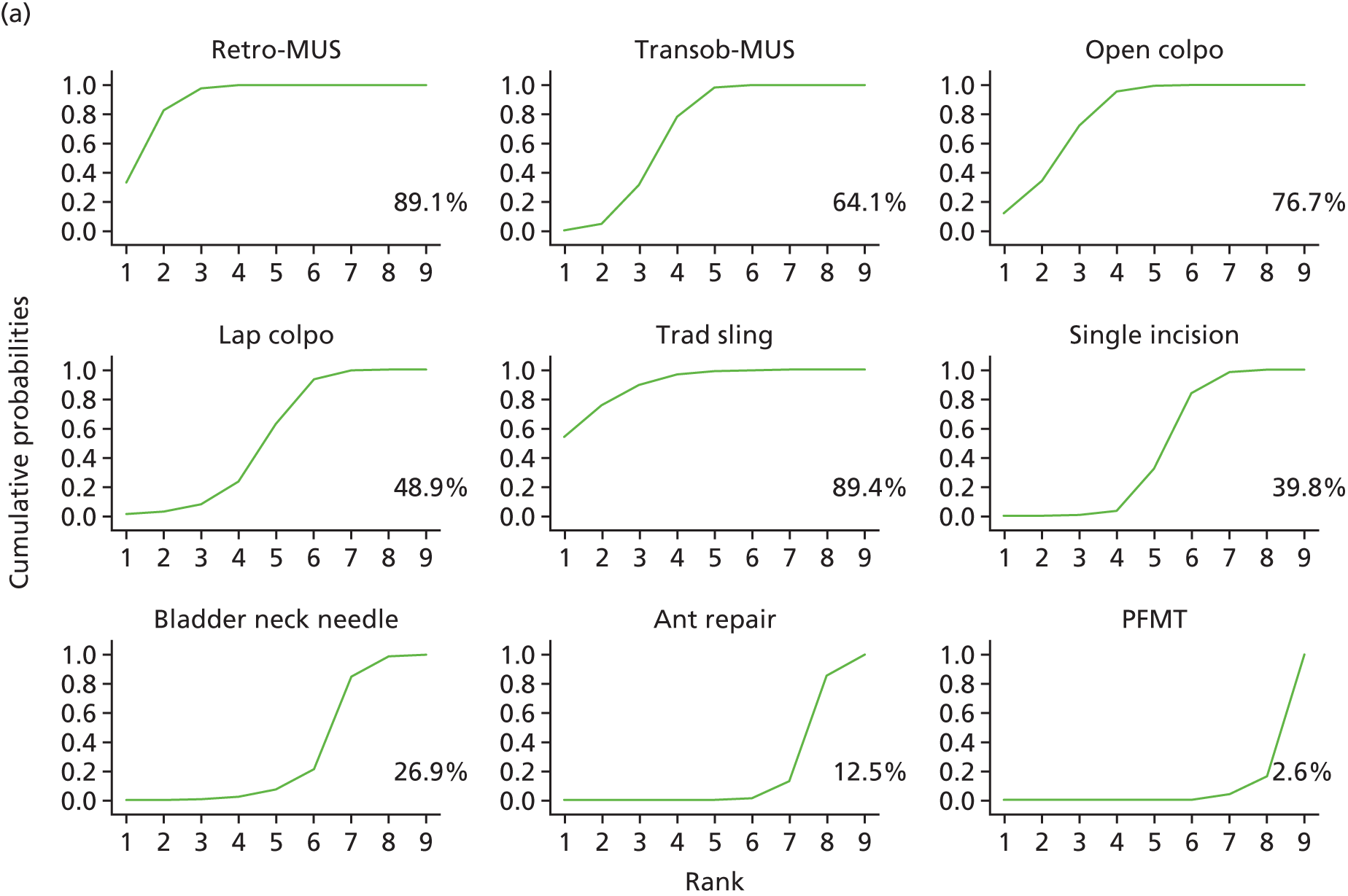
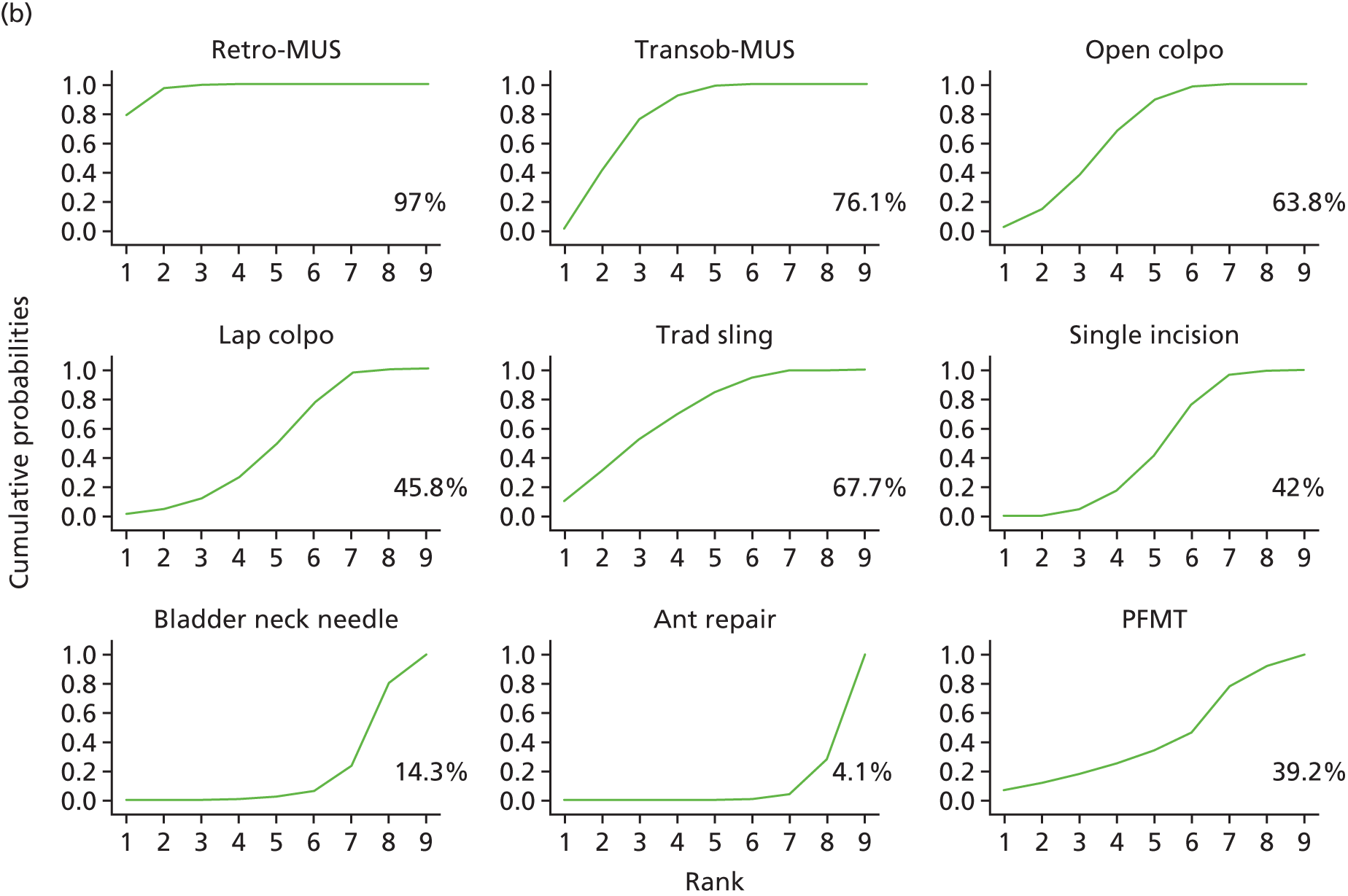
Traditional sling and retropubic MUS (see Figure 2a) are the treatments most likely to result in the highest proportion of women cured (89.4% and 89.1%, respectively), followed by open colposuspension (76.7%), transobturator MUS (64.1%), laparoscopic colposuspension (48.9%), single-incision sling (39.8%), bladder neck needle suspension (26.9%), anterior vaginal repair (12.5%) and PFMT (2.6%). On the other hand, retropubic MUS (97.0%) and transobturator MUS (76.1%) are the most likely treatments to result in the highest proportion of women with an improvement in their incontinence symptoms (see Figure 2b), followed by traditional sling (67.7%), open colposuspension (63.8%), laparoscopic colposuspension (45.8%), single-incision sling (42.0%), PFMT (39.2%), bladder neck needle suspension (14.3%) and anterior repair (4.1%).
Consistency between direct and indirect evidence
In the NMA there was no evidence of inconsistency for the cure outcome (see Appendix 14, Figure 45 and Table 33 for full details) and some evidence of inconsistency for the improvement outcome (see Appendix 14, Figure 46 and Appendix 14, Table 34). Consistency assessed using the node-splitting method (see Appendix 14, Table 34) showed inconsistencies for PFMT compared with transobturator MUS and for traditional sling and PFMT compared with open colposuspension. However, caution is required here, as the node splitting method can have low statistical power to detect inconsistency.
Adverse events: direct pairwise comparisons
The adverse event results are shown in Appendix 15. Full meta-analyses results for all included studies are available in Report Supplementary Material 1.
Overall, few studies reported adverse events. Numbers of events included in the analyses were generally small and, therefore, CIs were wide. It is worth noting that many of the adverse events meta-analyses were based on < 5 studies. This is mainly owing to the dearth of available data but also to the inconsistencies with regard to the type and definition of adverse events as well as to the time points at which these were measured across individual trials and across Cochrane systematic reviews. In particular, the lack of common definitions made it difficult to combine results and to incorporate data extracted from newly identified studies into the pool of data extracted from the relevant Cochrane reviews. For some of the included studies, follow-up time was unknown, as it could not be extracted from the relevant Cochrane systematic reviews. Below we summarise the most relevant meta-analyses results, focusing on comparisons for which most data were available (in terms of the number of studies and number of participants).
Repeat continence surgery
Appendix 15, Figure 47 shows a summary of the meta-analyses results (overall ORs and the 95% CI) for different treatment comparisons for repeat continence surgery based on the 30 studies that reported this outcome. The majority of studies compared retropubic MUS or transobturator MUS with other surgical procedures at different time points. In general, fewer repeat surgeries were observed after retropubic MUS compared with other interventions. However, the number of studies was generally small and CIs were wide.
For the comparison of transobturator MUS and retropubic MUS (seven studies, assessments conducted 12 months post surgery), the number of women requiring further surgery was 21 (out of 585; 3.6%) and 14 (out of 641; 2.2%), respectively. Pooled analysis of these studies showed wide CIs and considerable uncertainly around the estimated OR (seven studies, 12-month post-surgery: OR 1.37, 95% CI 0.55 to 3.46). At 12 to 60 months after the procedure, rates of repeat continence surgery were considerably higher in women undergoing transobturator MUS (32 out of 175; 18.3%) compared with retropubic MUS (1 out of 180; 0.5%), although only two studies were available for the analysis (OR 24.57, 95% CI 4.67 to 129.35). A similar trend was observed in studies with a longer follow-up period (i.e. > 60 months) but the pooled analysis of these studies showed wide CIs [five studies: 40 out of 422 (9.4%) vs. 7 out of 438 (1.5%); OR 4.06, 95% CI 0.80 to 20.74].
For the comparison of single-incision sling versus transobturator MUS (10 studies, assessments conducted 12 months post surgery), single-incision sling was associated with more repeat surgeries compared with transobturator MUS [35 out of 685 (5.1%) vs. 18 out of 614 (2.9%), respectively], but the pooled analyses showed some uncertainty around the estimated OR (OR 1.57, 95% CI 0.83 to 2.95). At > 36 months after the procedure, there were 19 (out of 185; 10.3%) versus 14 (out of 185; 7.6%) repeat surgery events, respectively (three studies: OR 1.42, 95% CI 0.68 to 2.97).
Open colposuspension was associated with fewer repeat surgeries than anterior vaginal repair, although only two studies were available for this analysis [assessments conducted 24 months post surgery: 22 out of 74 (29.7%) vs. 3 out of 129 (2.3%); OR 13.95, 95% CI 4.22 to 46.09].
Haemorrhage and major vascular complications including haematoma
Appendix 15, Figures 48–50 show a summary of the meta-analyses results for different treatment comparisons for haemorrhage, haematoma and other major vascular complications. The majority of the treatment comparisons compared retropubic MUS or transobturator MUS with other surgical interventions. Outcomes were reported using different definitions and assessed at different time points. For the comparison of transobturator MUS with retropubic MUS, the pooled analysis of 22 studies showed that major vascular complications were less likely to occur after transobturator MUS than after retropubic MUS [see Appendix 15, Figure 49; 10 out of 2008 (0.5%) vs. 47 out of 1966 (2.4%); OR 0.36, 95% CI 0.21 to 0.64]. Other comparisons were based on a smaller number of studies as well as a smaller number of events and were therefore insufficient to draw any meaningful conclusion.
De novo symptoms of urgency or urgency incontinence
Appendix 15, Figures 51 and 52 show the meta-analyses results for different treatment comparisons for de novo symptoms of urgency or UI and ‘detrusor instability’ (detrusor overactivity). The comparisons with the largest number of studies compared transobturator MUS with retropubic MUS within 12 months [see Appendix 15, Figure 51; 28 studies, within 12 months post surgery: 172 out of 2264 (7.6%) vs. 183 out of 2321 (9.5%); OR 0.93, 95% CI 0.74 to 1.17] and single-incision sling with transobturator MUS at 12 months [13 studies, 12 months post surgery: 63 out of 665 (9.5%) vs. 55 out of 597 (9.2%); OR 0.98, 95% CI 0.66 to 1.46]. The summary estimates did not favour one intervention over another. The comparison of single-incision sling with transobturator MUS at 6 months favoured transobturator MUS, even though there was considerable uncertainty around the estimate of effect [see Appendix 15, Figure 51; three studies, 6 months post surgery: 14 out of 118 (11.9%) vs. 4 out of 117 (3.4%); OR 3.33, CrI 1.08 to 10.23]. None of the other comparisons assessing de novo symptoms showed evidence of a difference between interventions. The incidence of detrusor instability appeared to be similar between interventions (see Appendix 15, Figure 52).
Voiding difficulties including urinary retention
Appendix 15, Figure 53 shows a summary of the meta-analysis for different treatment comparisons for voiding difficulties. The summary estimate of 36 studies comparing transobturator MUS with retropubic MUS favoured transobturator MUS [36 studies: 116 out of 3110 (3.7%) vs. 234 out of 3109 (7.5%); OR 0.51, 95% CI 0.40 to 0.64]. Fewer women treated with single-incision sling than women treated with transobturator MUS reported voiding difficulties during the perioperative period [23 out of 835 (2.8%) vs. 31 out of 689 (4.5%); OR 0.60, 95% 0.33 to 1.08] and at 12 months [43 out of 899 (4.8%) vs. 45 out of 802 (5.6%); OR 0.74, 95% CI 0.45 to 1.21]. Voiding difficulties appeared to be more common after laparoscopic colposuspension [12 out of 161 (7.5%) vs. 9 out of 177 (5.1%); OR 1.34, 95% CI 0.54 to 3.34] and traditional sling [40 out of 259 (15.4%) vs. 26 out of 255 (10.2%); OR 1.46, 95% CI 0.84 to 2.53] than after retropubic MUS. However, the summary estimates of these comparisons showed wide CIs indicating a certain degree of uncertainty. There was no evidence of a difference for the comparison assessing open colposuspension versus retropubic MUS [29 out of 374 (7.8%) vs. 31 out of 413 (7.5%); OR 0.87, 95% CI 0.41 to 1.82].
Bladder or urethral perforation
Appendix 15, Figure 54 shows a summary of the meta-analyses results for different treatment comparisons for bladder or urethral perforation. Compared with other surgical interventions, retropubic MUS was generally associated with a higher incidence of bladder or urethral perforation. In particular, there were more cases of bladder or urethral perforation after retropubic MUS than after transobturator MUS [38 studies: 5 out of 3161 (0.2%) vs. 157 out of 3171 (5.0%); OR 0.15, 95% CI 0.09 to 0.24], open colposuspension [six studies: 5 out of 338 (1.5%) vs. 28 out of 362 (7.7%); OR 0.23, 95% CI 0.10 to 0.55] and traditional sling [six studies: 16 out of 305 (5.2%) vs. 28 out of 276 (10.1%); OR 0.50, 95% CI 0.28 to 0.98]. Compared with open colposuspension, the rate of bladder or urethral perforation was higher for laparoscopic colposuspension [10 out of 267 (3.7%) vs. 2 out of 284 (0.7%); OR 4.65, 95% CI 1.15 to 18.75] but lower for traditional sling [2 out of 326 (0.6%) vs. 10 out of 329 (3.0%); OR 0.20, 95% CI 0.04 to 0.91].
Tape/mesh extrusion or exposure
Appendix 15, Figures 55 and 56 show a summary of the meta-analyses results for the different treatment comparisons for tape or mesh erosion or extrusion and tape or mesh exposure. It was not clear whether or not the terms ‘erosion’, ‘extrusion’ and ‘exposure’ were used consistently across individual studies and across Cochrane systematic reviews. The majority of the comparisons compared surgical interventions with either retropubic or transobturator MUS.
The meta-analysis results for the comparison between transobturator MUS and retropubic MUS showed similar rates of tape/mesh erosion or extrusion between the two surgical procedures [see Appendix 15, Figure 55; 27 studies: 53 out of 2225 (2.4%) vs. 48 out of 2298 (2.1%); OR 1.10, 95% CI 0.70 to 1.70]. The exact time points at which measurements occurred could not be derived from the Cochrane systematic reviews but most studies were reported to have a short follow-up period (≤ 12 months), with only a few studies having a follow-up period of ≥ 2 years.
The meta-analysis results for the comparison between single-incision sling and transobturator MUS (see Appendix 15, Figure 55; seven studies, 12-month post-surgery assessment) showed similar rates of mesh erosion or extrusion between interventions [19 out of 399 (4.8%) vs. 13 out of 354 (3.7%), respectively; OR 1.23, 95% CI 0.57 to 2.68]. Incidence of tape/mesh erosion or extrusion was lower for open colposuspension than for retropubic MUS [see Appendix 15, Figure 55; three studies: 0 out of 230 (0%) vs. 9 out of 273 (3.3%); OR 0.20, 95% CI 0.03 to 1.19].
Fewer data were available for the assessment of tape or mesh exposure. This may be owing to unclear distinction between the terms (‘extrusion’ and ‘exposure’) in the studies that assessed these outcomes. Rate of tape or mesh exposure was higher after transobturator MUS than after retropubic MUS [2 studies, 60–95 months post-surgery assessment: 12 out of 140 (8.6%) vs. 4 out of 145 (2.8%); OR 3.25, 95% CI 1.02 to 10.36]. Similarly, more women treated with transobturator MUS experienced tape or mesh exposure than those treated with single-incision sling, but CIs around the summary estimate were wide [see Appendix 15, Figure 56; seven studies, 12 months post surgery: 25 out of 494 (5.1%) vs. 11 out of 463 (2.4%); OR 1.74, 95% CI 0.59 to 5.07].
Pain
Appendix 15, Figures 57–59 show a summary of the meta-analyses results for different treatment comparisons for outcomes related to pain. It is worth pointing out that pain was defined and measured in many different ways across individual trials and across Cochrane systematic reviews. Some pain outcomes were categorised by location (e.g. suprapubic) or time (e.g. short or long term). These discrepancies made it difficult to combine data from different studies. Data were available mainly for the comparison between retropubic MUS and transobturator MUS and other surgical procedures.
Transobturator MUS was associated with a higher rate of groin pain than retropubic MUS [see Appendix 15, Figure 57; 22 studies: 116 out of 1833 (6.3%) vs. 24 out of 1798 (1.3%); OR 3.80, 95% CI 2.45 to 5.89] but with a lower rate of suprapubic pain [see Appendix 15, Figure 58; eight studies: 8 out of 687 (1.2%) vs. 27 out of 681 (4.0%); OR 0.37, 95% CI 0.17 to 0.84]. The time points at which measurements occurred could not be derived from the Cochrane systematic reviews, but most studies were reported to have a short follow-up period (≤ 12 months), with only a few studies having a follow-up of ≥ 2 years.
Rate of ‘post-operative pain’ was higher after retropubic MUS (176 out of 916, 19.2%) than after single-incision sling (64 out of 946; 6.8%) (see Appendix 15, Figure 59; 14 studies; OR 0.21, 95% CI 0.12 to 0.39). Rate of unspecified pain was higher after transobturator MUS than after single-incision sling both at 12 months [six studies; 4 out of 412 (1.0%) vs. 17 out of 328 (5.2%)] and at 24 months [two studies; 2 out of 138 (1.4%) vs. 13 out of 125 (10.4%)] (see Appendix 15, Figure 59; OR 0.24, 95% CI 0.06 to 0.92, and OR 0.16, 95% CI 0.04 to 0.62, respectively).
Dyspareunia
Limited evidence was available for the assessment of dyspareunia (see Appendix 15, Figure 60). In general, the number of studies included in the meta-analyses for the different treatment comparisons was small and CIs were wide.
Infection (including urinary tract infection, wound infection and infection related to mesh) and other complications
The number of available studies for the assessment of infection (see Appendix 15, Figures 61–63) was limited. Our meta-analyses results indicate that the rate of UTI was similar between single-incision sling and transobturator MUS [see Appendix 15, Figure 61; seven studies, 12 months post surgery: 36 out of 544 (6.6%) vs. 26 out of 447 (5.8%); OR 1.11, 95% CI 0.63 to 1.96]. For the other treatment comparisons the number of studies was small and CIs were wide.
Appendix 15, Figure 63 shows the summary estimate for the different treatment comparisons for the assessment of ‘complications’ as defined by the authors of the individual trials and of the Cochrane systematic reviewers. It is worth pointing out that perioperative complications may include outcomes such as haemorrhage, haematoma, cardiovascular events and pain as well as other unspecified outcomes. Transobturator MUS and retropubic MUS showed similar rates of perioperative complications [see Appendix 15, Figure 63; 15 studies: 127 out of 1084 (11.7%) vs. 150 out of 1153 (13.0%); OR 0.81, 95% CI 0.55 to 1.19].
Death
No deaths (related to surgery) were reported in any of the included studies.
Resource utilisation: pairwise comparison
Appendix 15, Figure 64 reports the meta-analyses results for the different treatment comparisons for the assessment of resource utilisation. For some comparisons only a limited number of studies were available and no firm conclusions can be drawn.
Length of hospital stay
Length of hospital stay after transobturator MUS was shorter than after retropubic MUS [17 studies: transobturator MUS vs. retropubic MUS, standardised mean difference (SMD) –0.38, 95% CI –0.70 to –0.06], open colposuspension (two studies: open colposuspension vs. transobturator MUS; SMD 1.83, 95% CI 1.36 to 2.30) and traditional sling (two studies: traditional sling vs. transobturator MUS; SMD 1.71, 95% CI 1.25 to 2.17).
Length of hospital stay after colposuspension was longer than after retropubic MUS (four studies: open colposuspension vs. retropubic MUS, SMD 2.26, 95% CI 1.98 to 2.55) or laparoscopic colposuspension (seven studies: laparoscopic colposuspension vs. open colposuspension; SMD –1.64, 95% CI –2.45 to –0.84) but shorter than after anterior repair (one study: anterior repair vs. open colposuspension; SMD 0.90, 95% CI 0.37 to 1.43).
Operation time
Operation time for transobturator MUS was shorter than that for retropubic MUS (32 studies: SMD –0.12, 95% CI –1.29 to –0.74) but longer than that for single-incision sling (18 studies: single-incision sling vs. transobturator MUS; SMD –0.53, 95% CI –0.86 to –0.19).
Summary of clinical effectiveness assessment
The systematic review of clinical effectiveness was based on data from 175 studies (21,598 women in total) comparing one surgical procedure with another for the treatment of SUI in women. The number of included studies identified from the eight published Cochrane systematic reviews was 147 (84%). A further 28 studies (16%) were identified through an updated literature search conducted in May 2017. This updated search used the same search strategy and eligibility criteria as those used for the included Cochrane systematic reviews.
A further, more recent, updated search was conducted in October 2017 and identified an additional 10 articles that appeared to meet our inclusion criteria. These studies have not been incorporated into the current assessment, but are listed, for information, in Appendix 16.
The majority of included studies had a high or unclear risk of bias across all risk-of-bias parameters but most notably for allocation concealment (selection bias). As blinding of participants and personnel is not feasible in trials assessing surgical interventions, protection against performance bias and detection bias was likely to be compromised in the included studies. This is a general issue with all surgical trials.
The assessment of effectiveness focused on two primary outcomes: the number of women cured from incontinence and the number of women who experienced an improvement in their incontinence symptoms. The NMA, which combined evidence from direct head-to-head comparisons and indirect comparisons, included 120 studies that reported data on cure or improvement. The NMA results indicate that retropubic MUS, transobturator MUS and traditional sling are more effective than other surgical procedures for both primary outcomes. Open colposuspension appears to be relatively effective for both outcomes (see the SUCRA ranking in Figure 2). For both primary outcomes, cure and improvement, the overall quality of evidence was low. As we were unable to extract study characteristics, we were unable to check the transitivity assumption (studies are similar with regard to important characteristics).
Assessment of adverse events was hampered by the dearth of available data. Direct head-to-head meta-analyses were available mainly for treatment comparisons involving retropubic MUS, transobturator MUS or single-incision sling. Follow-up time was generally short, with a median of 12 months.
Compared with retropubic MUS, transobturator MUS was associated with lower rates of major vascular complications and voiding difficulties but higher rates of repeat surgery.
For other intervention comparisons, the number of studies was generally small and the CIs wide. However, there was some evidence to suggest that bladder perforation was more likely to occur after retropubic MUS than after transobturator MUS, open colposuspension or traditional sling. Rate of tape or mesh erosion or extrusion was similar between transobturator MUS and retropubic MUS (27 studies with a total of 4523 women).
Transobturator MUS was associated with a higher rate of groin pain but a lower rate of suprapubic pain than retropubic MUS. Retropubic MUS had a higher rate of post-operative pain than single-incision sling and transobturator MUS had a higher rate of unspecified pain than single-incision sling. Studies that assessed pain had usually short follow-up periods (i.e. ≤ 12 months).
The main area of uncertainty for all surgical interventions relates to the lack of long-term data for the assessment of their safety.
Chapter 4 Discrete choice experiment
Introduction
To estimate women’s preferences for key aspects of surgical interventions being evaluated in this research we designed and conducted a DCE. DCEs describe an intervention or service in terms of a number of characteristics or attributes (e.g. post-operative complications, post-operative pain). The extent to which an individual values an intervention is expected to depend upon the level these characteristics take (e.g. whether or not patients could experience chronic post-operative pain). In other words, DCEs explore relative preferences for treatments with differing attributes,205 which allows an exploration of the relative importance of each attribute of a surgical treatment that may influence a patient’s decision for or against surgery.
Discrete choice experiments are used regularly in health economics to elicit preferences over health-care products and programmes and in the valuation of preference for health states206–208 and they offer an additional approach to investigate acceptability of different surgical treatments among patients. Several reviews have been conducted to compile the evidence of the use of DCEs in the health-care setting. 209–212 DCEs usually involve three inter-related components: (1) an experimental design used to implement a survey that aims to assess individual choices and generate choice data, (2) a quantitative analysis to estimate preferences from choice data and (3) the use of the estimated preferences to either derive welfare measures or construct other policy analyses. 205
A DCE was conducted to explore women’s preferences for surgical treatment options for SUI assessing differing attributes. Data were collected by means of a self-completed online survey. Best practice guidance for DCEs were followed throughout. 205,211 The DCE results provide policy-relevant information on average preferences for treatments and outcomes for women with SUI.
Aims
The DCE will answer the following research questions:
-
What are the key attributes of surgical treatments for SUI as expressed by female patients?
-
What are the relative preferences for different levels of these attributes among women and, more specifically, female patients?
-
What trade-offs are women/female patients willing to make between the different attributes?
Methods
The methods that were employed in the DCE study were informed by the Lancsar and Louviere205 and Ryan and Gerard211 reviews of the applications of DCEs in health care, considered to provide best practice guidance for DCEs. The methods can be broken down into four key steps: step 1 – identification of attributes and levels; step 2 – experimental design; step 3 – data collection; and step 4 – data analysis and interpretation. Details of the four steps, with regard to the current study, are provided below.
Step 1: identification of attributes and levels
The findings from the clinical effectiveness review (section 3) were consolidated to facilitate the creation of key attributes and associated levels related to women’s preferences for the different surgical treatment options. The chosen attributes and levels were plausible in both clinical and policy terms. 205 Once the attributes and levels were finalised a DCE design was generated (see Step 2: experimental design).
It is recognised that a reasonable number of attributes to be included within a DCE is around six, as more than this might lead to an unmanageable number of options to be meaningfully considered by the respondent. 213 The more attributes that are included in a DCE, the less likely respondents are to fully consider the pros and cons of different choices as described by differences in the attribute levels. Therefore, it may prove more difficult to identify trade-offs between attribute levels that a respondent is willing to make during the decision-making process, which is crucial when estimating marginal rates of substitution (MRS) (an estimation of the ratio between values that individuals place on different attributes, quantifying the trade-off a respondent is willing to make between two attributes). Probabilities for all adverse events included in the choice tasks were assumed to be similar and were therefore considered constant for all scenarios.
The final list of attributes and corresponding levels is reported in Table 7.
| Characteristic | Available options | Comments |
|---|---|---|
| Adverse events | New urinary symptoms (including UUI)a | Need to understand women’s preferences for certain types of adverse events and which adverse events are least preferred |
| Infections (post-operative or urinary tract) | ||
| Damage to organs/nerves | ||
| Pain during intercourse (dyspareunia) | ||
| Voiding difficulties | ||
| Chronic pain | Noa | Need to understand women’s preferences for being pain free after the operation. By definition, chronic pain refers to pain lasting for > 6 months |
| Mild | ||
| Moderate | ||
| Severe | ||
| Length of hospital stay (days) | 1 | The average duration for a hospital stay in the UK is ≈2.5 days.214 We are interested if women may trade off a longer hospital stay for an improvement in other attributes, so also include longer durations |
| 2 | ||
| 3 | ||
| 4 | ||
| 5 | ||
| 6 | ||
| Time to return to normal activities (weeks) | 2 | We are interested in identifying women’s preferences for recovery time and if they might be willing to trade off a longer duration for an improvement in other attributes |
| 4 | ||
| 6 | ||
| 8 | ||
| 10 | ||
| 12 | ||
| Risk of recurrence during 12 months after surgery (%) | 0 | We are interested in identifying women’s preferences for the recurrence risk and if they might be willing to trade off a higher risk for an improvement in other attributes |
| 10 | ||
| 20 | ||
| 30 | ||
| 40 | ||
| 50 |
Step 2: experimental design
The DCE survey consisted of a number of possible clinical scenarios based on the attributes and levels identified in step 1. Each scenario was made up of all five attributes and the associated levels contained in each attribute. The combination of attributes and levels presented in Table 7 would generate > 4000 possible scenarios [4320 (5 × 4 × 6 × 6 × 6)]. We reduced the number of scenarios to a manageable number by using a measure known as D-efficiency, which provides an efficient choice design by minimising the overlap in attribute levels between scenarios. The D-efficient design was used to reduce the number of scenarios to the minimum required to estimate all main effects and higher order interactions while still providing sufficient data to estimate preferences from responses. 205,209 We applied one restriction that implied that an adverse event of infection could only occur with a hospital stay of ≥ 2 days to mirror clinical practice in which post-operative infections extend the hospital stay.
The design for the DCE was generated using Ngene 1.1 (ChoiceMetrics, Sydney, NSW, Australia). The best design generated by Ngene was chosen with the aim of minimising standard errors. The reliability of the model parameters to be estimated can be quantified in terms of the asymptotic standard errors and covariances; thus, improvements in reliability indicate a reduction in the asymptotic standard errors (i.e. variance around preference estimates). 215 A blocked design of DCE choice sets was used to ensure greater variance in the data. We used three blocks of 12 questions to minimise respondents’ burden, randomly allocating respondents to a block of DCE choices. Based on a pilot run of the DCE, we updated the design to improve the validity of the results.
An example of a pairwise choice set is shown in Table 8. Respondents were asked to choose their preferred scenario from each pairwise choice set. An opt-out option was given, which in this instance was defined as the choice of no treatment (i.e. ‘I would choose not to undergo surgery’).
| Attribute | Option | ||
|---|---|---|---|
| Scenario A | Scenario B | Neither – I would choose not to undergo surgery | |
| Adverse event | Infections (post-operative or urinary tract) | New urinary symptoms | |
| Chronic pain | No | Moderate | |
| Length of hospital stay (days) | 5 | 3 | |
| Time until return to normal activities (weeks) | 4 | 6 | |
| Risk of recurrence during 12 months after surgery (%) | 10 | 20 | |
The DCE survey was part of a full questionnaire that included (1) questions on basic sociodemographics (including age, ethnicity and employment status), (2) questions on potential incontinence history, (3) an introductory text explaining the DCE task and (4) the main DCE survey.
Step 3: pretesting and data collection
Pretesting
Pretesting of the DCE component of the questionnaire was conducted to (1) test the wording used to describe attributes and levels, (2) assess ease of use and (3) identify missing attributes and levels. Members of the general public (n = 5) and the Cochrane Consumer Network (n = 5) were consulted to pretest and refine the draft questionnaire using cognitive interviewing and semistructured ‘think-aloud’ interviews. 216
Data collection
Data were collected via the online platform Qualtrics (Qualtrics, Provo, UT, USA), which is a standard provider of data collection and analysis products for academic research. The main data collection took place via an online survey and was conducted by a market research company (Research Now, Plano, TX, USA) between August and September 2017. Ethics approval for all aspects of the DCE study was granted from Newcastle University Ethics Committee (reference 11664/2016).
Participants
All participants were aged ≥ 18 years, resident in the UK and members of Research Now’s online panel. As part of the data collection process (and in accordance with Research Now’s procedure), participants received a small financial incentive (in the form of a voucher) to take part. Quota sampling was used to guarantee the representativeness of participants according to the age distribution of incontinence patients.
Sample size
Lancsar and Louviere205 highlight the complexities and problems of performing sample size calculations for DCEs and stress the need for further research in this area. Based on findings from previous health-related DCEs, where robust models have been estimated from samples sizes of 50 respondents,217 we aimed to collect data from 800 participants, which – following a rule of thumb of a minimum of 10 observations per parameter plus 50 – provided a more than sufficient sample size and allowed for some subgroup analyses.
Piloting the full questionnaire
The full questionnaire was piloted in a subset of the target population. The pilot sample size was big enough (n = 61) to conduct preliminary regression analyses, allowing for detection of potential inconsistencies (e.g. positive relations where negative ones were anticipated) and adjusting of the DCE design accordingly. The pilot sample was part of the main survey sample.
Step 4: data analysis and interpretation
Data were returned to the research team in an anonymised format. The research team did not receive contact details or any personal identifier information from survey participants.
Data were analysed using a random utility model framework and appropriate logistic regression techniques to estimate the mean change in utility that women place on different attribute levels compared with the reference level. This assumes that respondents choose the alternative in a choice set that gives them greatest utility out of the available options218 and that therefore the choices individuals make in a DCE reveal the utility they place on the alternatives presented.
Analyses were undertaken on the full study sample of the general population and separately for subgroups of women with and women without any type of UI.
Analysis methods
The sociodemographic profile and characteristics of respondents in the full sample and the subgroups were calculated in the univariate descriptive analyses in which means (and SDs) and number of observations (and proportions) were calculated for continuous and categorical variables, respectively.
Using bivariate analyses, we assessed whether or not preferences were influenced by characteristics of respondents (e.g. experience of previous treatments, socioeconomic factors). The standard approach to elicit responses and analyse data from choice sets with more than two options are conditional probit or logit models. Therefore, data were analysed using a random utility model framework and conditional and mixed logistic regressions to estimate mean change in utility placed on an attribute level compared with the reference level. The initial analysis employing a conditional logit model219 may have violated the assumption of independence compared with irrelevant alternatives assumption (IIA). This assumption requires the ratio of probabilities for any two alternatives to be independent of the attribute levels in a third alternative. To overcome this potential problem, we used a mixed logit (MXL) model that accounted for preference heterogeneity within the specified random variable. It allowed investigation of unobserved preference heterogeneity, that is, identifying if preferences for a specific attribute vary across respondents. If preference heterogeneity was present, the final coefficient for the specific attribute may have disguised the variation in preferences between respondents. The MXL model is a more general approach to a subgroup analysis because no assumptions are required regarding how individual characteristics may influence individual preferences. The alternative specific constant (ASC) variable was considered to be the random, normally distributed parameter and all other model parameters remained fixed. We used 100 Halton draws for the simulation of maximum likelihood.
Main effects parameters were estimated from the utility function (µ) (equation 1). The functional form incorporated 22 dummy attribute-level coefficients (see Table 7) so that:
where µ is the indirect utility function of individual q for alternative j, α is the ASC term, λ′Xqj is the vector of attribute levels included in the DCE survey and ϵqj is the random element that is added to reflect the unobservable factors affecting the estimation of the indirect utility function.
Different regression models were employed to analyse the effect of attribute levels on individual preferences for different characteristics of surgical treatments. Interaction terms were included to identify if and how individual characteristics mediated choices. The chosen interaction terms were used to explore whether or not preferences differed (e.g. between women with and without UI). For those without UI, the effect of knowing someone close with UI on overall preferences was also investigated. Given the sufficiently large sample size, subgroup analyses were run to identify potential differences in preferences between the total sample and subgroups of women with any type of UI and those women who did not have UI.
An ASC for options A or B was included in the regression model to account for any latent or unobserved factors that may have been associated with choosing an alternative of surgical treatment (option A or B) compared with no treatment (opt-out option). Dummy coding was used for the attributes adverse events and chronic pain and all other attributes (length of hospital stay, time until return to normal activities, risk of recurrence) were considered continuous variables and assumed to be linear. Reference levels for the DCE attributes used in the regression models were new urinary symptoms, including urge urinary incontinence (UUI), and no pain. Length of hospital stay, time until return to normal activities and risk of recurrence were included as continuous (linear) variables.
Model goodness of fit was assessed using the likelihood ratio (LR) test statistic.
Marginal rates of substitution were calculated for all attributes included in the DCE based on average willingness to wait for a return to normal activities (i.e. how much longer an individual would be willing to wait, on average, for a change in the utility of another attribute).
This analysis enables the estimation of the trade-offs between attribute levels and the magnitude of the coefficient in the regression models to be interpreted (i.e. the willingness to wait values can be directly compared in order to determine relative strength of preference across the remaining attributes).
Predictive uptake rates were also calculated based on the best-case scenario (as observed in the DCE) versus no surgery and worst case scenario versus no surgery. The statistics are presented as percentages and compare the variation in uptake rates associated with different configurations/outcomes of surgery.
Both MRS and predictive uptake rates were based on results from the MXL model (see Table 10).
Results
Descriptive analysis
A total of 789 women completed the DCE. Each of the respondents provided responses for 12 choices, resulting in a total of 9468 choices that were included in the analysis. Table 9 describes the sample population. The number of missing data for some of the characteristics describing the women responding to the survey was ≲ 1%.
| Characteristic | Respondents, n (%) | ||
|---|---|---|---|
| All (N = 789) | With UI (N = 353; 44.7%) | Without UI (N = 436; 55.3%) | |
| Age (years), mean (SD) | 53.1 (12.3) | 51.5 (12.1) | 54.4 (12.3) |
| Declared, n (%) | 786 (99.6) | 352 (99.7) | 434 (99.5) |
| Missing, n (%) | 3 (0.4) | 1 (0.3) | 2 (0.5) |
| Country | |||
| England | 632 (80.1) | 280 (79.3) | 352 (80.7) |
| Northern Ireland | 18 (2.3) | 9 (2.5) | 9 (2.1) |
| Scotland | 92 (11.7) | 42 (11.9) | 50 (11.5) |
| Wales | 47 (6.0) | 22 (6.2) | 25 (5.7) |
| Children | |||
| Yes | 559 (70.8) | 285 (80.7) | 274 (62.8) |
| No | 223 (28.3) | 66 (18.7) | 157 (36.0) |
| Prefer not to say | 5 (0.6) | 2 (0.6) | 3 (0.7) |
| Missing | 2 (< 1.0) | 0 (0.0) | 2 (< 1.0) |
| Marital status | |||
| Single | 126 (16.0) | 47 (13.3) | 79 (18.1) |
| Cohabiting/married/civil partnership | 537 (68.1) | 251 (71.1) | 286 (65.6) |
| Separated/divorced | 93 (11.8) | 41 (11.6) | 52 (11.9) |
| Widowed | 24 (3.0) | 11 (3.1) | 13 (3.0) |
| Other | 1 (0.1) | 1 (0.3) | 0 (0.0) |
| Prefer not to say | 5 (0.6) | 1 (0.3) | 4 (0.9) |
| Missing | 3 (< 1.0) | 1 (< 1.0) | 2 (< 1.0) |
| Employment status | |||
| Yes (full-/part-time) | 394 (49.9) | 186 (52.7) | 208 (47.7) |
| Self-employed | 41 (5.2) | 9 (2.5) | 32 (7.3) |
| Retired | 206 (26.1) | 75 (21.2) | 131 (30.0) |
| Unemployed | 74 (9.4) | 35 (9.9) | 39 (8.9) |
| Looking after children | 27 (3.4) | 16 (4.5) | 11 (2.5) |
| Other | 43 (5.4) | 30 (8.5) | 13 (3.0) |
| Prefer not to say | 4 (0.5) | 2 (0.6) | 2 (0.5) |
| Annual household income (£) | |||
| < 15,000 | 125 (15.8) | 64 (18.1) | 61 (14.0) |
| 15,000–25,999 | 170 (21.5) | 79 (22.4) | 91 (20.9) |
| 26,000–34,999 | 127 (16.1) | 53 (15.0) | 74 (17.0) |
| 35,000–49,999 | 147 (18.6) | 60 (17.0) | 87 (20.0) |
| 50,000–69,999 | 65 (8.2) | 25 (7.1) | 40 (9.2) |
| ≥ 70,000 | 85 (10.8) | 46 (13.0) | 39 (8.9) |
| Prefer not to say | 58 (7.4) | 17 (4.8) | 41 (9.4) |
| Do not know | 9 (1.1) | 7 (2.0) | 2 (0.5) |
| Missing | 3 (< 1) | 2 (< 1) | 1 (< 1) |
| Highest level of education | |||
| None | 14 (1.8) | 2 (0.6) | 12 (2.8) |
| Secondary school | 244 (30.9) | 104 (29.5) | 140 (32.1) |
| College | 206 (26.1) | 92 (26.1) | 114 (26.1) |
| University | 295 (37.4) | 143 (40.5) | 152 (34.9) |
| Other | 27 (3.4) | 11 (3.1) | 16 (3.7) |
| Prefer not to say | 1 (0.1) | 0 (0.0) | 0 (0.0) |
| Missing | 2 (< 1.0) | 1 (< 1.0) | 1 (< 1.0) |
| Ethnicity | |||
| White | 735 (93.2) | 331 (93.8) | 404 (92.7) |
| Other | 54 (6.8) | 22 (6.2) | 32 (7.3) |
| Health status | |||
| Excellent | 95 (12.0) | 33 (9.3) | 62 (14.2) |
| Good | 354 (44.9) | 121 (34.3) | 233 (53.4) |
| Fair | 219 (27.8) | 112 (31.7) | 107 (24.5) |
| Poor | 93 (11.8) | 64 (18.1) | 29 (6.7) |
| Very poor | 28 (3.5) | 23 (6.5) | 5 (1.1) |
| Type of UI | |||
| Stress | 128 (36.3) | ||
| Urge | 90 (25.5) | ||
| Both | 116 (32.9) | ||
| Do not know | 5 (1.4) | ||
| Other | 12 (3.4) | ||
| Missing | 2 (< 1.0) | ||
| UI limiting daily activities | |||
| Extremely | 34 (9.6) | ||
| Moderately | 102 (28.9) | ||
| Slightly | 168 (47.6) | ||
| Not at all | 45 (12.7) | ||
| Missing | 4 (1.1) | ||
| UI treatment history | |||
| Yes | 151 (42.8) | ||
| No | 202 (57.2) | ||
| Type of previous UI treatment | |||
| Surgical | 32 (9.1) | ||
| Non-surgical | 94 (26.6) | ||
| Both | 19 (5.4) | ||
| Do not know | 5 (1.4) | ||
| Missing | 1 (< 1.0) | ||
| SUI treatment scheduled | |||
| Yes | 51 (14.4) | ||
| No | 297 (84.1) | ||
| Missing | 5 (1.4) | ||
| Member of incontinence support group | |||
| Yes | 25 (7.1) | ||
| No | 328 (92.9) | ||
| Know someone close with UI (if not UI patient themselves) | |||
| Yes | 123 (28.2) | ||
| No | 307 (70.4) | ||
| Missing | 6 (1.4) | ||
| DCE responses (n) | 9468 | 4236 | 5232 |
| Option A (%) | 34.4 | 35.5 | 33.5 |
| Option B (%) | 31.9 | 31.5 | 32.1 |
| Opt-out option (no treatment) (%) | 33.7 | 33.0 | 34.4 |
The average age was 53 years and significantly lower in the patients group than in the non-patients group. The majority of respondents lived in England (80%), followed by Scotland (12%), Wales (6%) and Northern Ireland (2%). The percentage of women with children differed significantly between both groups: 81% of women with UI reported having children, whereas only 63% of women without UI reported having children. This is intuitively sensible, as having had children is a risk factor for developing some forms of incontinence. The majority of respondents in both groups lived with their partner (with UI, 71%; without UI, 66%) and around half were in full- or part-time employment (with UI, 53%; without UI, 48%), 21–30% were retired and 3–7% were self-employed. Most respondents in either group had an annual household income of £15,000–25,999 and between 15–20% reported an annual household income of ≤ £15,000 or £26,000–34,999 and £35,000–49,999, respectively. The distribution of educational attainments was relatively even between both groups, although a higher proportion of patients had a university degree (with UI, 41%; without UI, 35%). The majority of respondents (92–93%) had a white ethnic background. Health status varied significantly between both groups. On average, women with UI reported poorer health than those without UI and around two-thirds of non-patients described their general health to be ‘excellent’ or ‘good’.
Among women with UI, the most common type of UI was SUI (36%), followed by MUI (33%) and UUI (26%). The majority of women with UI found their incontinence to be not or only slightly limiting in their daily activities (13% and 48%, respectively), 29% reported it to be moderately limiting and 10% reported it to be extremely limiting. Around 43% had received treatment previously. However, the majority of previous treatment took the form of management of incontinence (i.e. non-surgical treatment). Out of the 128 patients with SUI, nearly half reported to have treatment scheduled and 7% reported to be a member of an incontinence support group.
Among women without UI, 28% knew someone close to them with UI.
Statistical analyses
Two-thirds of women were prepared to make a choice between surgical options and one-third of women declared that they would rather choose no surgery. Responses to the three choices were evenly split: around one-third of all responses was allocated to each of the options (A, B and the opt-out option), indicating that the majority of respondents would choose surgery (options A and B) over no surgical treatment (opt-out option).
Table 10 reports the marginal effects of each attribute on utility for the conditional models (1–7) and the MXL model (8). Conditional logistic regressions were run for all respondents (models 1–2), women with UI (models 3–6) and women without UI (model 7). Marginal utility values indicate relative preferences for levels within an attribute (for example, relative preferences against mild/moderate/severe pain compared with no pain). Positive marginal utility values indicate an attribute level is preferred to the reference level and negative marginal utility values indicate that the attribute level is valued less than the reference level. For the MXL model, means and SDs are reported for the random parameter. The sign of SDs is irrelevant; significant SDs imply preference heterogeneity among respondents for that specific attribute, suggesting that the reported coefficient may disguise differences in the underlying preferences. To identify which differences are statistically significant, p-values are included.
| Variable | Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Conditional logit | MXL | |||||||
| 1 (all) | 2 (all) | 3 (patients) | 4 (patients) | 5 (patients) | 6 (patients) | 7 (non-patients) | 8 (all) | |
| ASC (option A or B) | ||||||||
| Mean | 0.100 | 0.071 | –0.087 | 0.394*** | 0.274*** | –0.362** | 0.075 | 1.361*** |
| SD | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 4.029*** |
| Adverse event | ||||||||
| New urinary symptomsa | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Infections | 0.231*** | 0.231*** | 0.244*** | 0.245*** | 0.247*** | 0.248*** | 0.213*** | 0.280*** |
| Damage to organs/nerves | –0.107** | –0.106** | –0.127* | –0.151** | –0.136* | –0.140* | –0.084 | –0.088* |
| Pain during intercourse | 0.107** | 0.107** | 0.123* | 0.142** | 0.131* | 0.142** | 0.090 | 0.135*** |
| Voiding difficulties | –0.274*** | –0.274*** | –0.218*** | –0.217*** | –0.223*** | –0.219*** | –0.325*** | –0.278*** |
| Chronic pain | ||||||||
| Noa | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Mild | –0.036 | –0.036 | 0.034 | 0.044 | 0.037 | 0.036 | –0.099* | –0.053 |
| Moderate | –0.171*** | –0.171*** | –0.073 | –0.061 | –0.071 | –0.057 | –0.245*** | –0.185*** |
| Severe | –0.204*** | –0.204*** | –0.112* | –0.119** | –0.107* | –0.110* | –0.279*** | –0.204*** |
| Length of hospital stay | –0.031*** | –0.031*** | –0.030** | –0.030** | –0.028** | –0.032** | –0.032*** | –0.030*** |
| Time until return to normal activities | 0.021*** | 0.021*** | 0.022*** | 0.022*** | 0.022*** | 0.022*** | 0.023*** | 0.023*** |
| Risk of recurrence during 12 months after surgery | –0.002* | –0.002** | –0.001 | –0.001 | –0.001 | –0.001 | –0.003** | –0.002*** |
| Interactions and additional variables | ||||||||
| ASC × UI patient | ||||||||
| Patient | N/A | 0.063 | N/A | N/A | N/A | N/A | N/A | N/A |
| ASC × UI type (reference category: mixed) | ||||||||
| SUI | N/A | N/A | 0.348*** | N/A | N/A | 0.686*** | N/A | N/A |
| UUI | N/A | N/A | 0.123 | N/A | N/A | 0.221** | N/A | N/A |
| Other | N/A | N/A | 0.752*** | N/A | N/A | 0.569*** | N/A | N/A |
| ASC × limiting UI (reference category: extremely) | ||||||||
| Moderately | N/A | N/A | N/A | 0.150 | N/A | 0.339** | N/A | N/A |
| Slightly | N/A | N/A | N/A | 0.437*** | N/A | –0.158 | N/A | N/A |
| Not | N/A | N/A | N/A | 1.303*** | N/A | 1.079*** | N/A | N/A |
| ASC × treatment history | ||||||||
| Previous treatment | N/A | N/A | N/A | N/A | 0.754*** | 0.690*** | N/A | N/A |
| ASC × knowing someone with UI | N/A | N/A | N/A | N/A | N/A | N/A | 0.272 | N/A |
| Log (pseudo)likelihood | –10293.3 | –10292.2 | –4557.8 | –4462.4 | –4550.5 | –4359.2 | –5587.6 | –7838.0 |
The results were found to be very similar across all models, except for the marginal effect of the ASC capturing a preference for or against surgical treatment in general. Preferences for surgical treatment varied significantly in both the significance and direction of the effect depending on model specifications. The coefficient for the ASC was only significant in some of the models for women with UI (model 4–6) and the mixed-effects model (model 8), whereas the estimations for the full sample and women without UI suggest no significant result (i.e. no preference for or against surgical treatment in general). Significant coefficients for both the mean and SD from the mixed-effects model suggest that preference heterogeneity is present among respondents.
Preferences for the different types of adverse events were relatively robust to varying model specifications. Infections and pain during intercourse were found to be associated with a utility gain and, therefore, not disliked as much as the reference category of new urinary symptoms, and damage to organs or nerves and voiding difficulties were less preferred.
The results for different levels of chronic pain were in line with expectations, describing a gradient of increasingly negative preferences with higher levels of pain. Compared with the reference level of no pain, mild chronic pain was not found to affect utility significantly across most models, whereas moderate and severe pain were associated with a greater negative preference. However, the results were mediated in models for women with UI that included interactions between the ASC and how limiting the type of UI was perceived with regard to daily activities (models 4 and 6) and between the ASC and a positive treatment history (models 5 and 6). In these models, the negative gradient could still be observed but was no longer statistically significant. Instead, if respondents had had treatment before, and the more limiting their UI, the more likely they were to choose surgery.
As expected, women would prefer not to experience longer hospital stays or a higher risk of recurrence. However, the negative preference for a higher risk of recurrence was not significant in models for women with UI (models 3–6) in which interaction terms between the ASC (and, therefore, the overall preference for surgery) and different characteristics capturing patient experiences may have dominated the impact of different levels of pain. The sample of women without UI showed the strongest gradient of negative preferences for higher levels of pain. A longer time to return to normal activities was associated with a utility gain and, therefore, described a positive preference.
Adding interactions between ASCs and additional variables improved the goodness of fit for all patient models, and model 6 was found to be the best-fitted model. Compared with patients with a mixed form of UI, those suffering from SUI were more likely to choose surgery. Similarly, patients with a positive treatment history and a more limiting form of UI gained more utility from choosing surgical treatment options.
Comparing the log LRs between model 1 (conditional logit) and model 8 (MXL) that used the same variables and same study populations showed that the MXL model provided better model estimates when accounting for preference heterogeneity around the ASC. In the non-patient model 7, knowing someone close with UI did not significantly increase the preference for surgical treatment.
Marginal rates of substitution were calculated for all attributes included in the DCE based on average willingness to wait for a return to normal activities (i.e. how much longer an individual would be willing to wait, on average, for a change in the utility of another attribute). In comparison with new urinary symptoms, individuals would, on average, be willing to wait an additional 3.8 weeks to return to normal activities to avoid damage to their nerves or organs and up to an additional 12 weeks, on average, to avoid voiding difficulties. Individuals were not willing to wait any additional time to avoid infections or pain during intercourse in comparison with new urinary symptoms.
To avoid chronic pain, individuals would, on average, be willing to wait an additional 2.3 weeks to avoid mild pain compared with no pain. Individuals would be willing to wait an additional 8 and 9 weeks, on average, to avoid moderate and severe pain, respectively.
For a one-night reduction in their hospital stay an individual would, on average, be willing to wait 1 additional week to return to normal activities. To reduce the risk of recurrence by 1%, an individual would on average be willing to wait an additional 15 hours.
Predicted uptake rates, based on a hypothetical best-case surgery (adverse event of infection, no pain, a length of stay of 2 days, 12 weeks to return to normal activities and 0% risk of recurrence) versus a no surgery option were calculated. Given this option, it is predicted that 62% of respondents would choose the surgical option over no surgery. Similarly, for the hypothetical worst-case surgery (voiding difficulties, severe pain, length of stay of 6 days, 2 weeks to return to normal activities and 50% risk of recurrence) versus the no surgery option, the predicted uptake rates were estimated as 33% for the worst-case scenario. In this case, 67% of respondents would, on average, choose no surgery.
Discussion
Summary of results
To our knowledge, this is the first DCE to investigate differential characteristics of surgical treatment options for UI and their potential impact on women’s decisions to undergo surgery. Analysis of choice set data from the DCE revealed that around two-thirds of respondents chose a treatment option over no surgery. However, we found evidence that preferences around the choice of surgical treatment may vary across individuals.
In terms of types of adverse event associated with surgical treatment, infections and pain during intercourse were preferred to the reference category of new urinary symptoms, whereas damage to organs or nerves and voiding difficulties were less preferred. These preferences were relatively robust across all models, but the results, although confirming the same trend in preferences, were not statistically significant for damage to organs or nerves and pain during intercourse in non-patient respondents. Respondents associated increasing levels of disutility (i.e. negative preference) with higher levels of chronic pain, longer durations of hospital stay and higher risk of recurrence. We also found evidence that longer durations to return to normal activities after the surgery was associated with a statistically significant, positive preference.
Interpretation of results
The heterogeneity around a general preference for or against surgical treatment may be explained by the range of surgical treatments available, their level of invasiveness and, therefore, their varying impact on some of the attributes included in the DCE. The different subgroups in our sample may have contributed to the heterogeneity around the preference for surgical treatment in general. Comparing results across all models suggests that general preferences concerning surgical treatment vary not only between patients and non-patients but also within the patient subgroup, as implied by the change in sign of the ASC coefficient between model 4 and models 5 and 6. Although the results for the full sample suggest a preference for surgery, this finding may have been driven by the majority of non-patients within the sample. We found some evidence that patients in general may associate a negative preference with surgery for UI. However, those patients with SUI, who reported their UI to be extremely limiting with regard to daily activities and who had undergone surgical treatment before were more likely to choose surgery again. This may indicate that patients who have never undergone surgery fear the surgical procedure and are more reluctant to choose surgical treatment. One reason for this finding may be that patients are more used to managing their UI and may consider non-surgical treatment as long as their condition is not experienced as limiting their daily activities too much. Interviews conducted with patients during the pretesting stage of the DCE provided further support for this finding.
Preferences around different types of adverse event following surgery were captured compared with the reference of new urinary symptoms. Our findings suggest that infections and pain during intercourse are considered to be more acceptable adverse events, whereas damage to organs or nerves and voiding difficulties were less acceptable and reduced the likelihood of respondents choosing a surgical treatment option. This is also confirmed by the MRS analysis, which showed that individuals were willing to wait longer to recover to avoid damage to organs or nerves and to avoid voiding difficulties but were not willing to wait to avoid infections or pain during intercourse.
As expected, we found evidence for higher levels of chronic pain and increased risk of recurrence to be associated with negative preferences. However, although the same trend could be observed in all models, the statistical significance varied, which may indicate the difference in importance of these attributes for patients and non-patients. When accounting for patient characteristics around their type of UI, the degree to which it was limiting them in daily activities and their treatment history, preferences for chronic pain and risk of recurrence were less significant. Patients with SUI or UUI, extremely or moderately limiting UI and a treatment history had a stronger preference for surgery regardless of the associated level of pain or risk of recurrence.
There was a strong preference for shorter hospital stays, suggesting that the less invasive may be the preferred treatment options, with reduced risk of infections that may increase the length of hospital stay following surgery.
Other than expected, we found evidence for a preference for longer durations to return to normal activities, although the pilot data had suggested a negative preference for this attribute. A reason for this finding may be that respondents may have interpreted ‘return to normal activities’ as ‘return to work’ (assumes that they would not lose any wages). Alternatively, and especially for those who had never experienced any surgical treatment, respondents may have found the attribute levels to be unrealistic, expecting the recovery after surgery to be longer than the stated maximum of 12 weeks.
Strengths and weaknesses
A major strength of our study, which elicited preferences for different characteristics of surgical treatment options of UI is the use of a DCE in combination with an online panel. It allowed us to use a relatively large sample size and control for differences in respondent characteristics accordingly. The anonymity of the online setting may have allowed the responding UI patients to be more honest and report their problems in greater detail than they may feel comfortable to report in a health-care setting. The advantage of using a DCE for preference elicitation is that it allows consideration of real-life choice situations in which multiple factors may influence the decision-making process. The combined influence of those factors and potential trade-offs between their varying levels cannot be readily elucidated or quantified by other methods.
However, DCEs have been criticised as difficult for participants to understand. We aimed to minimise this risk by following best practice guidelines for the design and development of DCEs205,211 and engaged members of the general public and patients in the development process to maximise internal and external validity.
We acknowledge that the sample recruited by the research company is a convenience (i.e. non-random) sample that may not be representative of the target population and did not allow us to determine response rates to the survey. Some of our analyses were aimed at identifying differences in preferences between subgroups of patients and non-patients; however, the characteristics of those subgroups may have differed by definition (e.g. see the lower average health status and higher proportion of respondents with children in the patient subgroup). Alternative methods of recruitment and data collection in the context of DCEs, such as postal or telephone surveys, have been found to achieve very low response rates, thereby potentially reducing the representativeness and validity of results. 220
Implications of findings for research
To our knowledge, this research provides the first insights into what women (with and without) UI want their treatment options to be like and which fundamental surgical treatment characteristics they prefer. More than half of respondents had UI or knew someone close with UI. However, given the wide range of surgical treatments and significant differences between them, capturing specific influences on and preferences for or against certain treatment characteristics is a complex process. Our patient subsample was not large enough to capture sufficient variation beyond the interaction effects for patient experience already included in our analyses. More research is needed to distinguish trade-offs between different characteristics of surgical treatment options. One study found that women suffering from UI would choose the treatment with the lowest risk of recurrence. 221 Our results provide further support but suggest that this preference may be mediated by other factors such as previous treatment experience and that this finding cannot necessarily be generalised without further research.
Although UI can have a substantial impact on a woman’s daily activities and quality of life, previous research suggests that women under-report their condition and manage their incontinence before seeking treatment. 222 Barriers to seeking professional help may be imposed by a lack of awareness of treatment options, by the perception that these symptoms are normal after childbirth or in older age, or by feelings of shame or embarrassment. 223,224 Considering women’s preferences and trying to reduce those barriers may help to reduce the levels of unmet need for incontinence services and to improve the organisation of surgical services.
Conclusion
To our knowledge, this is the first DCE to investigate differential characteristics of surgical treatment options for UI and their potential impact on women’s decisions to undergo surgery. We found that women are less likely to choose surgical treatments that are associated with longer hospital stays, higher risks of recurrence and increased levels of chronic pain. However, although women with a treatment history had a negative preference for surgical treatments, those with forms of UI that were reported to be extremely or moderately limiting in daily activities preferred the surgical treatment option to no surgery. Further research investigating a woman’s choice for or against surgery needs to investigate treatment history in greater detail and consider more individual characteristics including personal beliefs and perceptions that may act as a barrier to seeking professional advice.
Chapter 5 Review of cost-effectiveness evidence
Methods
In addition to the review of the clinical effectiveness of surgical treatments for SUI, a review of full model-based economic evaluations was conducted. The purpose of the review of model-based evaluations was to identify robust models and inputs to inform the economic modelling in this study. Specifically, the objective was to perform a critique of existing economic models to identify a model suitable for augmentation or to justify the development of a new economic model. Additionally, the review would be used to identify clinical and health economic data that were used in the identified models that could also be used in a new economic model. Trial-based economic evaluations were not included in the review to minimise the time commitment required for this aspect of the work. The review work was conducted in accordance with the Centre for Reviews and Dissemination’s guidance for undertaking reviews in health care. 14
Search strategy
The search strategy is outlined in Appendix 17.
Data sources
The following databases were searched during the review process:
-
MEDLINE (via Ovid)
-
MEDLINE In-Process & Other Non-Indexed Citations (via Ovid)
-
Excerpta Medica Database (EMBASE) (via Ovid)
-
NHS Economic Evaluation Database (NHS EED) (via Ovid)
-
Health Management Information Consortium (via Ovid)
-
Cost-effectiveness Analysis (CEA) Registry.
All databases were searched using the Ovid interface, except for the CEA Registry, which was searched through the CEA Registry website (https://cevr.tuftsmedicalcenter.org/databases/cea-registry).
Study selection
Two researchers undertook the screening of titles and abstracts obtained through the search using EndNote® X7 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] reference management software. Prior to initial screening, deduplication of records was undertaken. After initial screening, all potentially relevant articles were obtained for further scrutiny against the full selection criteria, with any disagreements resolved by discussion. The inclusion criteria were as follows:
-
Study design: full economic evaluations involving a decision model-based analysis. A full economic evaluation can be defined as a comparative study including both costs and effects.
-
Population: women with SUI and stress-predominant MUI (adult women of any ethnic background).
-
Intervention: any of the surgical treatments for UI being evaluated in our own study (as either a primary or a repeat surgery).
-
Comparator: alternative treatment (surgical and non-surgical) or no treatment for UI.
-
Outcome: cost-effectiveness, cost estimates, utilisation estimates and quality-of-life estimates.
-
Language: studies with full text in English.
No restrictions were placed on the publication time frame or the study country. Modelling studies where data were imputed from multiple sources, without specific reference to the age and ethnic background of women, were included in the review. Studies comparing diagnostic/screening techniques or other non-surgical procedures without considering surgical interventions in the model pathway were excluded.
Data extraction
Relevant data were extracted into an Excel spreadsheet. Data on the following, where available, were extracted from included studies by one reviewer and checked by another:
-
study characteristics, such as study question, form of economic analysis, population, interventions, comparators, perspective, time horizon and form of modelling
-
clinical effectiveness and cost parameters, such as effectiveness data, health-state valuations (utilities), resource use data, unit cost data, cost year, discounting and key assumptions
-
results and sensitivity analyses.
Findings
A total of 821 titles and abstracts were identified from the original search, with 732 remaining after deduplication. Following title and abstract screening, 30 studies remained. Full-text copies of these 30 studies were obtained for scrutiny against the full selection criteria and 13 were excluded. Therefore, 17 studies were included in the final review. A flow diagram presenting the process of selecting studies can be found in Figure 3.
FIGURE 3.
Flow diagram showing study selection for the economic evaluations review.
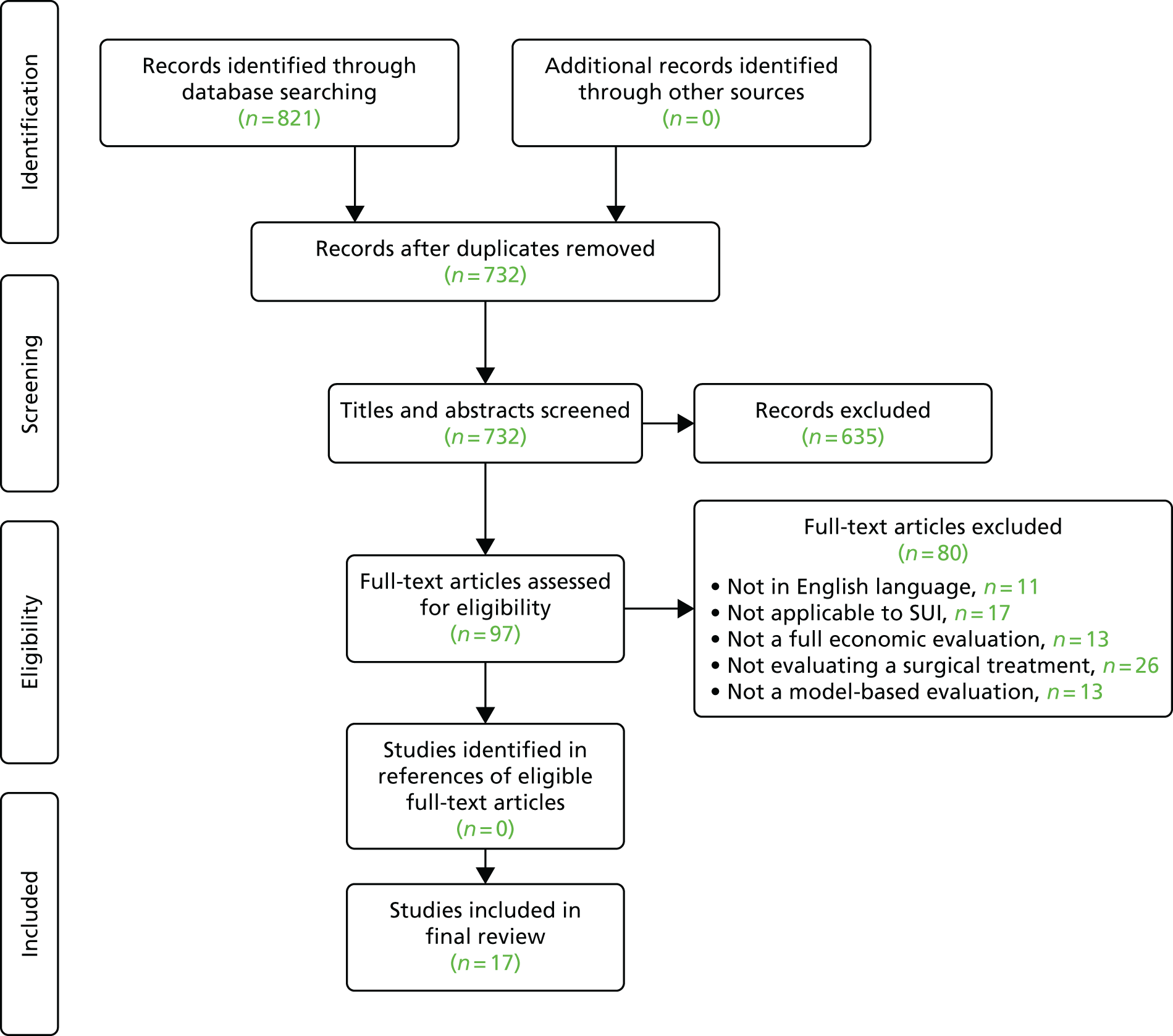
Summary of review data from included model-based economic evaluations
A total of 17 studies were included in the final review. An overview of the key data extracted from these studies is presented in Table 11. In the section that follows, a more comprehensive description of the data extracted from the included studies is presented. Finally, a descriptive quality assessment of the included studies is presented, based on the criteria defined in the Drummond checklist for economic evaluations. 242
| Number | Study | Population | Analysis type | Intervention | Comparator | Model type | Perspective | Time horizon | Time cycle | QoL measure | CE measure | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Kunkle et al.225 | SUI | CUA | MUS | Urethral BA | Decision tree | Health-care system | 1 year | N/A | NR | Cost/QALY | MUS compared with BA leads to an ICER of US$70,400 per utility gained |
| 2 | Von Bargen et al.226 | SUI | CUA | MUS |
|
Markov model | Societal | Lifetime | 1 year | NR | Cost/QALY |
Incontinence pessary was the more cost-effective option with US$11,411 cost/QALY With a WTP of US$60,000, MUS would be the most cost-effective option |
| 3 | Das Gupta et al.227 | SUI | CUA | Duloxetine |
|
Markov model | NR | 2–5 years | 3 months | NR | Cost/QALY |
First-line use of duloxetine alone and in combination with PFMT is more cost-effective than standard treatment, with ICERs of £8730 and £5854, respectively Second-line use of duloxetine alone and in combination with PFMT is less costly and more effective than standard treatment |
| 4 | Jacklin et al.228 | SUI | CUA | TVT | Duloxetine | Markov model | Health-care system | 10 years | 1 day | NR | Cost/QALY | TVT had an ICER of £7710 (US$12,651) at 10 years |
| 5 | Kilonzo et al.229 | SUI | CUA | TVT |
|
Markov model | Health-care system | 10 years | 1 year | EQ-5D | Cost/QALY | TVT dominates open colposuspension (lower cost and same QALYs) within 5 years after surgery |
| 6 | Laudano et al.230 | SUI | CUA | TVT | Open Burch colposuspension | Markov model | NR | 10 years | NR | NR | Cost/QALY | At 10-year follow-up, TVT was more cost-effective (CE, US$1495/QALY) than BC (CE, US$1824/QALY) |
| 7 | Oremus et al.231 | SUI | CEA | Collagen |
|
Decision tree | Health-care system | 1 year | N/A | N/A | Cost/treated woman |
Retropubic suspension vs. collagen ICER: CA$1824 Transvaginal suspension vs. collagen ICER: CA$5151 Sling procedure vs. collagen ICER: CA$6814 |
| 8 | Oremus and Tarride232 | SUI | CEA | Collagen |
|
Decision tree | Health-care system | 1 year | N/A | N/A | Cost/treated woman | ICER is CA$341.35 for Québec |
| 9 | Richardson and Sokol233 | SUI | CUA | MUS |
|
Decision tree | Third-party payer | 1 year | N/A | HUI | Cost/QALY | MUS was the more cost-effective strategy with an ICER of US$32,132/QALY |
| 10 | Sand et al.234 | SUI | CEA | Transurethral radiofrequency micro-modelling |
|
Markov model | Health-care system | 3 years | 3 months | N/A | Cost | Procedure costs for RF-SUI were less than half of the cost of sling treatments and were one-fifth of the cost of Burch surgery |
| 11 | Seklehner et al.235 | SUI | CUA | Retropubic MUS | Transobturator MUS | Markov model | Health-care system | 10 years | NR | NR | Cost/QALY | Transobturator MUS was more cost-effective than retropubic MUS with an ICER of US$177,027/QALY |
| 12 | Weber and Walters236 | SUI | CCA | Burch colposuspension | Sling procedure | Decision tree | NR | 10 years | N/A | N/A | Costs and clinical outcomes | N/A |
| 13 | Wu et al.237 | SUI | CUA | Burch colposuspension | TVT | Markov model | Health-care system | 10 years | 1 year | NR | Cost/QALY | The ICER was US$98,755 per QALY |
| 14 | Holtzer-Goor et al.238 | UI | CUA | Global optimum continence service specification | Current care pathway for UI in the Netherlands | Markov model | Societal | 3 years | 3 months | EQ-5D | Cost/QALY | The PSA results show that, with 95% certainty, the new care intervention dominates current care (i.e. it is more effective and cost-saving) |
| 15 | Weber and Walters239 | Symptomatic pelvic organ prolapse and SUI | CEA | Office evaluation and no further testing | Office evaluation and subsequent testing | Decision tree | Societal | 1 year | N/A | N/A | Cost/additional cure | In the base case, the strategy of basic office evaluation was more cost-effective than the strategy of urodynamic testing. In the short model the incremental cost-effectiveness (cost per additional cure of UI) was US$55,495 for urodynamic testing relative to basic office evaluation. In the full model a single additional cure of UI was achieved by urodynamic testing at a cost of US$328,601 relative to basic office evaluation |
| 16 | Weber et al.240 | SUI | CEA | Office evaluation and no further testing | Office evaluation and subsequent testing | Decision tree | Societal | 1 year | N/A | N/A | Cost/additional cure | In the base case, the strategy of basic office evaluation was more cost-effective than the strategy of urodynamic testing. In the short model the incremental cost-effectiveness (cost per additional cure of UI) was US$55,495 for urodynamic testing relative to basic office evaluation. In the full model a single additional cure of UI was achieved by urodynamic testing at a cost of US$328,601 relative to basic office evaluation |
| 17 | Imamura et al.241 | SUI | CUA | Treatment sequence 1 | Treatment sequence 2–8 | Markov model | Health-care system | 40 years | 3 months | EQ-5D | Cost/QALY | The strategy employing lifestyle changes and PFMT with extra sessions followed by TVT surgery has a > 70% probability of being considered cost-effective for all threshold values for WTP for a QALY presented. The other five strategies each have a probability of < 20% of being considered cost-effective |
Comprehensive overview of data extracted from included model-based economic evaluations
Country
Nine studies were based in the USA,225,226,230,233,235–237,239,240 four in the UK,227–229,241 three in Canada231,232,234 and one in the Netherlands. 238
Cost year
The cost year of four studies was 2012,226,233–235 of one study was 2007,228 of one study was 2001,229 of four studies was 1998,231,236,239,240 of one study was 2005,237 of one study was 2010,232 of two studies was 2013,225,238 of one study was 2008241 and of two studies was not reported. 227,230
Study population
All studies were conducted among a population of women with UI, SUI or MUI. 225–241
Population age
Three studies reported a population age of 45 years, based on the age of peak incidence of SUI. 226,229,241 One study reported a population aged ≤ 65 years. 240 One study reported a population aged > 65 years, chosen because elderly patients are likely to have a greater unmet need. 238 In all other studies, population age was not reported. 225,227–237,239,241
Analysis type
A total of 11 studies were cost–utility analyses,225–230,233,235,237,238,241 five were cost-effectiveness analyses231,232,234,236,240 and one was a cost–consequences analysis. 239
Perspective
Four studies reported a societal perspective,226,236,238,240 nine studies reported a health service perspective,225,228,229,231,232,234,235,237,241 one study reported a third-party payer perspective233 and three studies did not report a perspective. 227,230,239 However, on the basis of the costs included the perspective was interpreted as the health-care system for two of these studies230,239 and societal for the third. 227
Model structure and comparators
Model type
A total of 10 studies used a Markov model. 226–230,234,235,237,238,241 The remaining seven studies used a decision tree. 225,231–233,236,239,240
Time horizon
One study reported a lifetime time horizon,226 five studies reported a 10-year time horizon,228–230,235,237 seven studies reported a 1-year time horizon,225,231–233,236,239,240 two studies reported a 3-year time horizon,234,238 one study reported a 2- to 5-year time horizon227 and one study reported a 40-year time horizon. 241
Cycle length
Three studies used a 1-year cycle length,226,229,237 one study used a 1-day cycle length,228 four studies used a 3-month cycle length,227,234,238,241 two studies did not report cycle length230,235 and for seven studies cycle length was not applicable as they adopted a decision-tree approach. 225,231–233,236,239,240
Intervention
Three studies looked at MUS,225,226,233 three studies looked at TVT,228–230 one study looked at transurethral radiofrequency micro-remodelling,234 one study looked at retropubic MUS,235 two studies looked at Burch colposuspension,237,239 two studies looked at collagen injection,231,232 one study looked at duloxetine,227 one study looked at global optimum continence service specification,238 two studies looked at office evaluation and no further testing236,240 and one study looked at initial treatment with conservative therapies. 241
Comparator
One study compared the intervention with expectant management, PFMT, PFMT with electrical stimulation, vaginal cone or biofeedback and incontinence pessary,226 one study compared the intervention with duloxetine,228 one study compared the intervention with open colposuspension, laparoscopic colposuspension, traditional suburethral sling procedures and periurethral injectables,229 one study compared the intervention with open Burch colposuspension,230 one study compared the intervention with continence pessary and PFMT,233 one study compared the intervention with TVT, retropubic mid-urethral synthetic sling procedures, TOT, transobturator mid-urethral synthetic sling procedures, Burch colposuspension surgery and traditional bladder-neck autologous sling procedures,234 one study compared the intervention with transobturator MUS,235 one study compared the intervention with sling procedures,239 one study compared the intervention with TVT,237 one study compared the intervention with bladder neck needle suspension and Burch slings,231 one study compared the intervention with retropubic suspension, transvaginal suspension and sling procedures,231 one study compared the intervention with urethral bulking agents,225 one study compared the intervention with PFMT and surgery, colposuspension and traditional slings,227 one study compared the intervention with the current care pathway for UI in the Netherlands,238 two studies compared the intervention with office evaluation and subsequent urodynamic testing236,240 and one study compared the intervention with initial treatment with MUS. 241
Model inputs and analysis
Discounting
Three studies applied a 3.5% discount rate,227,228,241 two of which228,241 justified this rate on the basis of it being the discount rate recommended for the reference case in the NICE technical manual. 243 Two studies applied a 3% discount rate but did not justify this choice of rate. 226,237 One study applied a 4.54% discount rate based on the 10-year AAA corporate bond yield for that year. 230 One study applied a 5% discount rate but did not justify this choice of rate. 234 One study applied a 2.26% discount rate based on the 10-year AAA corporate bond yield for that year. 235 One study applied a 6% discount rate for costs and a 1.5% discount rate for quality-adjusted life years (QALYs);229 however, these rates were not justified in the text. For six studies, a discount rate was not applicable as the time horizon of the included model was only 1 year,225,231–233,236,240 and for two studies discounting was applicable but a discount rate was not reported. 238,239
Clinical effectiveness measure(s)
Eight studies used cure rate (objective or subjective) only,226,229,231,232,236,237,239,240 three studies used improvement rate (objective or subjective) only,233–235 one study used both cure rate and improvement rate,241 one study used the percentage of women continent,238 one study used probability of cure, probability of retreatment and probability of cure after retreatment,230 one study used success rate (defined as dry, which is resolution of symptoms),225 one study used reduction in incontinence episode frequency227 and one study used a change in incontinence episode frequency as the measure of clinical effectiveness. 228
Quality of life measure(s)
Three studies used EuroQol-5 Dimensions (EQ-5D),229,238,241 with one of those229 using data derived from Manca et al. 244 One238 used data derived from a cross-sectional study of quality of life in a general female population in the Netherlands aged 45–85 years, whereas another241 used data derived from Manca et al. 244 and Haywood et al. 245 Eight studies that used quality of life estimates in their analysis did not report a quality of life measure in their study225–228,230,233,235,237 and for six studies a quality of life measure was not applicable as they were conducted as either a CEA or a cost–consequences analysis (CCA), for which a quality of life measure is not required. 231,232,234,236,239,240
Cost-effectiveness measure
A total of 11 studies used cost per QALY,225–230,233,235,237,238,241 two studies reported costs and clinical outcomes in a disaggregated manner,234,239 two studies reported cost per increased probability of successful treatment231,232 and two studies reported cost per additional cure. 236,240
Complications/adverse events
One study reported UTI, voiding dysfunction, mesh erosion and intra-/post-operative adverse events;226 one study reported haematoma, urinary retention, detrusor overactivity, UTI, abscess, mesh or suture erosion, recurrent stress incontinence, pelvic organ prolapse, incisional hernia, bladder perforation and revision;230 one study reported voiding dysfunction, wound complication, mesh exposure or erosion and recurrent cystitis;234 one study reported mesh erosion/exposure, urinary retention, lower urinary tract symptoms, bladder perforation, infection, bleeding, neurological symptoms, catheterisation, anticholinergics, antibiotics, blood transfusion and drainage of haematoma;235 one study reported recurrent incontinence, detrusor instability and urinary retention;239 one study reported UTIs, fractures and skin breakdown;238 one study reported adverse events related to drugs only;241 one study reported mesh erosion;237 one study reported retention, voiding, infection and haematuria;231 one study reported immediate haemorrhage, immediate bladder injury, short-term urinary retention, short-term pain, short-term haematuria, long-term persistent urinary retention, long-term UTI, long-term mesh complication and long-term recurrent SUI; and seven studies did not report complications/adverse events. 227–229,231,233,236,240
Mortality modelling
Two studies incorporated all-cause mortality,226,237 one study incorporated all-cause mortality and surgery-specific mortality,241 three studies did not incorporate all-cause mortality,228–230 seven studies did not include mortality in their economic model,227,234–236,238–240 and for four studies mortality was not applicable owing to the short time horizon of their model. 225,231–233
Sensitivity analysis
One study conducted multivariable sensitivity analysis (SA),226 seven studies conducted deterministic SA only,228,230,231,233,234,237,239 seven studies conducted deterministic SA and probabilistic sensitivity analysis (PSA)225,227,229,231,235,238,241 and two studies conducted deterministic SA and a threshold analysis. 236,240
Resource use costs
Two studies used Medicare reimbursement codes to derive cost of treatment;226,233 one study239 collected costs using codes from Medicare diagnostic-related groups and the International Classification of Diseases, Ninth Edition (ICD-9); one study used a combination of literature (routine UK sources) and assumption;228 and two studies used a combination of relevant literature, such as reports from manufacturers, and advice from experts in the field. 229,241 One study derived costs from 2003 Medicare reimbursement data and diagnosis-related group codes,237 one study used only the Medicare fee schedule,225 two studies used the Medicare resource-based relative value scale,230,235 one study used a combination of Medicare and expert opinion,234 one study used previous economic evaluations to derive cost information,231 one study used a combination of hospital records and expert opinion,232 one study used a combination of HES, assumptions and literature227 and two studies236,240 used an issue of the Federal Register. One study used a combination of expert opinion, reimbursement prices and previous literature. 238
Data source for clinical effectiveness
Twelve studies used literature as a source,225–230,234,235,237–239,241 one study used data from the ATLAS (Ambulatory Treatments for Leakage Associated with Stress Incontinence) trial,233 one study used data from a RCT,231 one study used data from clinical guidelines231 and two studies used data from a combination of literature and consensus from the study team. 239,240
Quality assessment
The completed Drummond checklist for each of the included studies is presented in Appendix 18. In this section, a descriptive summary of the quality assessment of all included studies is presented.
1. Was a well-defined question posed in answerable form?
All of the included studies had a well-defined question posed in an answerable form and examined both the costs and the effects of the alternative options. 225–241 Only three of the included studies did not state a viewpoint for the analysis or place the study in any particular decision-making context. 225,230,239
2. Was a comprehensive description of the competing alternatives given (i.e. can you tell who did what to whom, where, and how often)?
Only three of the included studies did not provide a comprehensive description of the competing alternatives or provided only a comprehensive description of the intervention without focusing sufficiently on the comparator(s). 230,232,235 Only one study did not omit important alternatives from the analysis. 241 None of the studies included a do-nothing alternative in their comparison.
3. Was the effectiveness of the programme or services established?
All of the included studies established the effectiveness of the programme or services included in the model. 225–241 Of the studies that did establish effectiveness, three determined effectiveness through a clinical RCT. 227,232,233 A total of 13 studies established effectiveness through an overview of clinical studies. 226,228–231,233–237,239–241 Five studies used observational data or assumptions to establish effectiveness. 225,227,233,237,238
4. Were all the important and relevant costs and consequences for each alternative identified?
All of the included studies identified the important and relevant costs and consequences for the alternatives being compared. 225–241 The range of relevant costs and consequences was wide enough for the research question at hand in all studies other than in four, in which the range was unclear. 225,226,228,238 In one study it was determined that the range was not wide enough for the research question at hand. 231 Costs and consequences were covered from all relevant viewpoints (community or social viewpoint and those of patients and third-party payers) in only five studies. 226,236,238–240 In one study, the perspective was not clear. 230 In all remaining studies, at least one perspective (primarily patient perspective) was not considered. 225,227–235,237,241 Capital costs were included in eight studies;226–228,236,238–241 in the other nine studies, capital costs were not included. 225,229–235,237
5. Were costs and consequences measured accurately in appropriate physical units?
All of the included studies measured costs and consequences accurately in appropriate physical units. 225–241 None of the studies omitted identified items from its analysis. Only two of the included studies encountered circumstances (joint use of resources) that made measurement of costs and consequences difficult. 225,231 These circumstances were handled appropriately in the studies.
6. Were the costs and consequences valued credibly?
All of the included studies valued costs and consequences credibly and clearly identified the sources of all values. 225–241 Only one of these studies did not clearly identify the sources of all values. 231 In only four of the included studies was the valuation of consequences not appropriate for the question posed. 231,234,236,240
7. Were costs and consequences adjusted for differential timing?
In nine of the included studies, costs and consequences were adjusted for differential timing (and discounted). 226–230,234,235,237,241 In six studies, this was not applicable. 225,231–233,236,240 In two studies, this was not reported. 238,239 Of the studies that applied discounting, only four did not provide any justification for the discount rate used. 226,227,229,234
8. Was an incremental analysis of costs and consequences of alternatives performed?
Only two of the included studies did not conduct an incremental analysis of the costs and consequences of alternatives. 234,236 Only one of these studies did not compare the additional costs generated by one alternative over another with the additional effects, benefits or utilities generated. 236
9. Was allowance made for uncertainty in the estimates of costs and consequences?
Only four of the included studies did not make any allowance for uncertainty in the estimates of costs and consequences. 228,231,236,240 Eight of the included studies performed appropriate statistical analysis on stochastic data, meaning that the data incorporated in the model had a random probability distribution and an appropriate PSA was conducted. 225,227,229,230,232,235,238,241 Five studies did not perform appropriate statistical analysis on stochastic data. 228,231,233,236,240 In three studies this was not applicable as probabilistic distributions were not assigned to the model data. 234,237,239 Rather, these studies included a deterministic SA only. In one study, this was not clear. 226 Twelve studies provided justification for the range of values used in SA. 225–227,232–234,236–241 Five studies did not provide justification. 228–231,234 In 13 studies, the study results were sensitive to the change in values. 225,227–230,232,233,235–237,239–241 In three studies, study results were not sensitive to the change in values231,234,238 and in one study this was unclear. 226
10. Did the presentation and discussion of study results include all issues of concern to users?
Only in one of the included studies did the presentation and discussion of study results not include all issues of concern to users. 238 In 15 of the studies, the conclusions of the analysis were based on some overall index or ratio of costs to consequences. 225–233,235–238,240,241 In one study, an overall index was not presented239 and in one study this was not applicable. 234 Only one of the included studies did not compare their results with those of others who have investigated the same question. 233 Eight studies discussed the generalisability of the results to other settings and patient/client groups. 226,231–235,237,239 In the other nine studies, the authors did not discuss the generalisability of the results. 225,227–230,236,238,240,241 Only one of the included studies alluded to, or took account of, other important factors in the choice or decision under consideration. 241 Finally, none of the included studies discussed issues of implementation, such as the feasibility of adopting the ‘preferred’ programme given existing financial or other constraints, or whether or not any freed resources could be redeployed to other worthwhile programmes.
Limitations of identified model-based economic evaluations in informing economic analysis
A total of 17 model-based economic evaluations were identified through the systematic review. All studies were conducted among women with SUI or stress-predominant MUI and included at least one of the surgical treatments for UI being evaluated in this study (as either a primary or a repeat surgery). However, none of the models was sufficient for the analysis required for our own study.
First, the time horizons of the models identified were generally of insufficient length, with only one of the included studies assessing costs and consequences over a lifetime time horizon. 226 One study did report a 40-year time horizon, but even this would not be of sufficient length to capture the entire lifetime of all patients being modelled in our own analysis (patient starting age, 45–55 years). The majority of studies extended to a maximum time horizon of 10 years.
Second, only 11 of the identified studies were conducted as pure cost–utility analyses. 225–230,233,235,237,238,241 Of these, only three used EQ-5D as a quality of life measure in their analysis (the measure proposed for our own analysis). 229,238,241 The other eight studies that conducted a cost–utility analysis did not report a quality of life measure and this was noted as a generally poorly reported feature among the studies identified. 225–228,230,233,235,237
Furthermore, very few studies had used appropriate utility weights estimated using tools like EQ-5D and the Health Utilities Index227,229,233,235,241 for cured and incontinence health states in the economic models. 227,235 Because the intended outcome of the surgical treatments is increased quality of life, estimating effectiveness using an appropriate tool is essential for the estimation of actual treatment outcomes. Moreover, not all of the studies had included complications in the models. Complication after surgical treatment is another important factor that affects women’s quality of life, which highlights the importance of including major complications in the calculations.
Finally, only one of the identified models did not omit important alternatives from their analysis. 241 As highlighted during the quality assessment, all other studies failed to include at least one important alternative. 225–240
Given these limitations, and the information presented in this chapter, it was decided that a new economic model needed to be developed to estimate the relative cost-effectiveness of the nine surgical interventions.
Summary
A systematic review of economic studies modelling the management of women with UI was conducted. Specifically, the focus was on studies that included surgical treatments for SUI and stress-predominant MUI. In total, 17 studies were included in the final review. All data of interest were extracted from these studies, and studies were quality assessed using the Drummond checklist for economic evaluations. 242 None of the identified studies was considered suitable for use in the economic evaluation component of this study.
Chapter 6 Development of a new cost-effectiveness model
This chapter provides a detailed description of the modelling approach, the estimation of input parameters used to populate the model and the key assumptions underpinning the cost-effectiveness results. The results from the economic model are presented in two sections. In the first section, the results of the economic model are presented. In the second section, results from a VOI analysis, which can be used to aid decisions about the direction of further research, are presented (see Chapter 5, Summary). The chapter concludes with a summary of the results for all comparators and of the factors deemed to be most critical in affecting the cost-effectiveness of different surgical treatments for SUI and stress-predominant MUI.
Model overview
As seen in the review of model-based economic evaluations, no existing research has compared all the relevant comparators. Therefore, a decision-analytic model was developed to evaluate the cost-effectiveness of nine different surgical interventions for the treatment of women with SUI or stress-predominant MUI:
-
retropubic MUS
-
anterior vaginal repair
-
bladder neck needle suspension
-
open abdominal retropubic colposuspension (open colposuspension)
-
laparoscopic retropubic colposuspension (laparoscopic colposuspension)
-
traditional suburethral retropubic sling (traditional sling)
-
transobturator MUS
-
single-incision sling
-
periurethral bulking agents (urethral injection therapy).
The model is based on a hypothetical cohort of women (age range, 45–55 years) with either SUI (52%) or stress-predominant MUI (48%). 246 Health outcomes from the model were expressed in terms of QALYs, the year of the cost data is 2016 and the currency is pound sterling (GBP). The costs were estimated from a NHS and Personal Social Services (PSS) perspective. Both costs and QALYs were evaluated over 1-year, 10-year and lifetime time horizons and discounted using a 3.5% annual discount rate. 16 The expected cost and QALYs for each of the strategies were estimated and compared using incremental cost-effectiveness ratios (ICERs) where appropriate. The ICER represents the incremental cost per additional QALY associated with a more costly and effective strategy. The ICER can be compared with thresholds used by NICE to establish value for money in the NHS (i.e. £20,000–30,000 per additional QALY gained). These thresholds can be used to identify the optimal strategy in terms of cost-effectiveness considerations, based on existing evidence.
The model is probabilistic, meaning that most of the input parameters were entered into the model as probability distributions to reflect parameter uncertainty (i.e. uncertainty in the mean estimates). Monte Carlo simulation was used to address the uncertainty in input parameters in such a way that the results of the analysis can also be presented with their associated uncertainty.
Model structure
A Markov microsimulation (MM) model was developed to estimate the relative cost-effectiveness of the nine surgical interventions. The MM model is a computer modelling technique that simulates an individual’s life course from initial surgical treatment until death. Within the model, each person is represented by a record containing a unique identifier and a set of associated attributes (e.g. age, disease condition). A set of rules (transition probabilities) and state rewards (cost and health state utility) are then applied based on these characteristics. These rules may be deterministic or stochastic. The model applies all defined parameters and rules to simulate the passage of an individual through the model. This is then repeated for each individual in the cohort, thereby generating individual life histories for a specific population of women. The main reason that a microsimulation model was used as opposed to a cohort-based Markov model was to overcome the memorylessness of cohort-based Markov models. Building the MM model in TreeAge Pro® (TreeAge Software, Inc., Williamstown, MA, USA) enabled us to keep track of simulated patients about their treatment history and time since last treatment. Unfortunately, individual-level data were not available; therefore, we assumed a uniform distribution for age groups (45–55 years) and women were randomly selected and simulated within the model. In the model, 52% of the randomly selected women have SUI only, and are modelled as receiving treatments for SUI only. However, some women with SUI may experience UUI as a result of complications of surgical treatments for SUI, and these women receive UUI treatment as well. In 48% of random draws, women have MUI (SUI and UUI). Therefore, after receiving surgical treatments for SUI they would receive three lines of treatment for UUI, which could be successful or unsuccessful.
The structure of the model is shown in Figure 4. We assumed a 3-month cycle length. The reason for this assumption is that it will take between 3 and 6 months to determine if a procedure has worked and to decide if further treatment if required.
FIGURE 4.
Markov model structure. Tx, treatment.
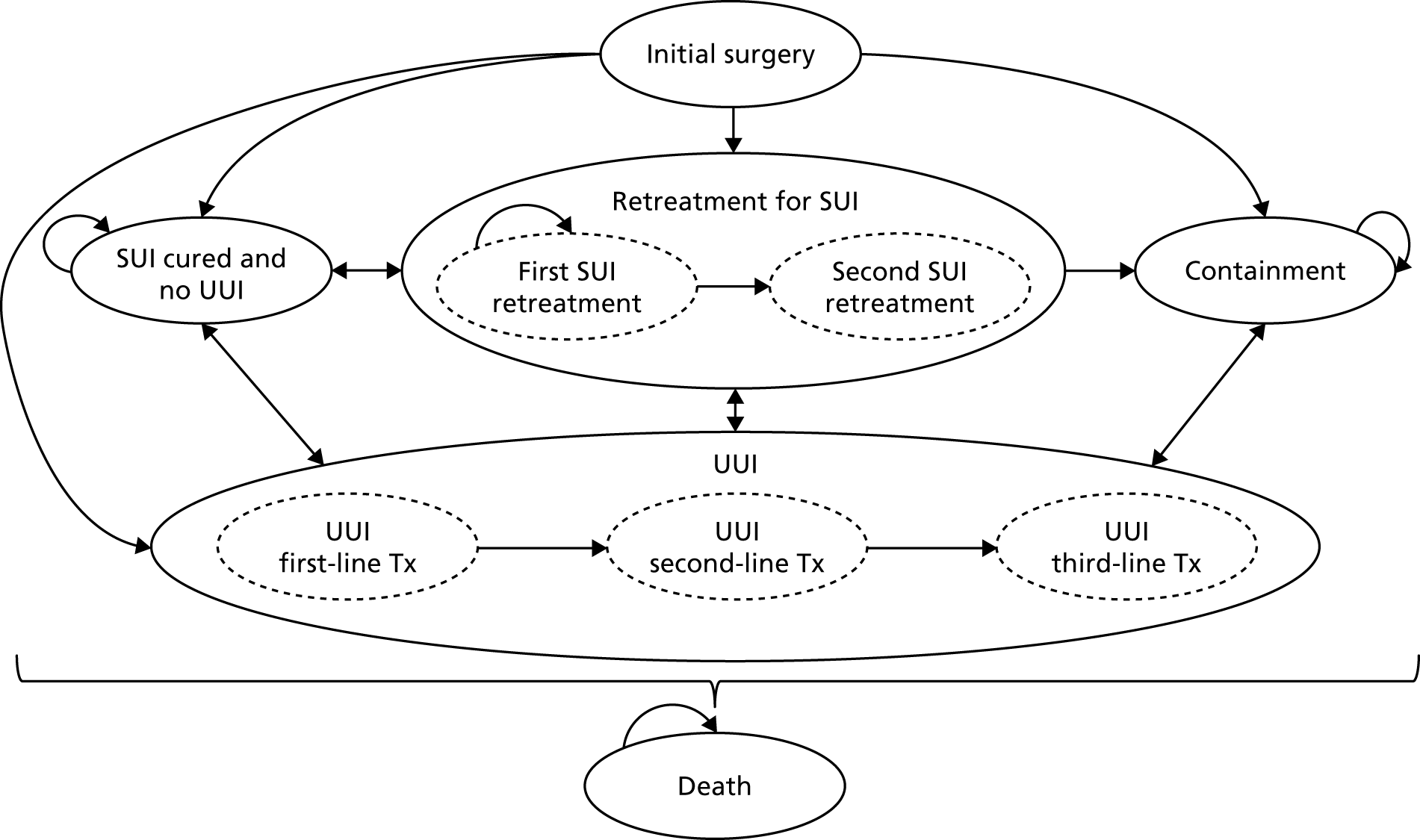
The MM model incorporates both the temporal and the logical sequences of treatment, including the events and complications that may happen after each procedure (e.g. pain), and the outcomes for the woman associated with each possible scenario. Hypothetical individual women pass through the model one at a time and are followed up until death. Treatment history for both SUI/stress-predominant MUI and UUI was recorded for each simulated woman and used to define the woman’s transition to different health states and treatment types. For example, if a woman with MUI is being simulated and she has already received a first repeat surgery for SUI and second-line treatment for UUI, then in the event of a recurrence of SUI or UUI she may only be given second repeat surgery for SUI or third-line treatment for UUI, respectively. The model was developed in TreeAge Pro.
On entry into the model, a woman can have either SUI or MUI (based on the specified proportion of women with SUI or MUI). Both groups of women will initially have one of the nine surgical treatments. The surgical treatment is for SUI, but a woman may still need further treatment for symptoms of UUI, which is a component of MUI, or develop UUI as a side effect of surgical treatment of SUI or the SUI component of MUI. After initial surgery, a woman can move into one of the following five health states:
-
cured and no UUI (continent) by subjective measures
-
cured from SUI but UUI exists (UUI caused as a side effect of the initial surgery or because the woman has MUI)
-
surgery fails to resolve the SUI but the woman proceeds to retreatment (as women can be offered a second or third surgery if initial surgery fails)
-
permanent state of incontinence (containment) (e.g. resorting to containment management of their incontinence by using pads)
-
death due to all-cause mortality or operation-related mortality, which can occur when a woman is exposed to the risks of open surgery such as colposuspension or traditional sling procedures (see Figure 4 and the detailed model structure in Appendix 19).
The model assumes that women can receive a maximum of three surgical treatments for treatment of SUI/MUI, which includes the initial surgery and two subsequent retreatments. If all three surgeries fail then the woman has to manage her symptoms using containment products. The model allows for individuals to elect to move to containment treatments at any point after initial failure. Women with MUI who still have UUI after successful treatment of SUI, or those who develop UUI owing to surgery, will receive three lines of treatment including first-line (bladder training), second-line (drug, i.e. oxybutynin hydrochloride) and third-line treatment (botulinum toxin type A).
Model inputs
In this section, the data required to populate the model are presented. Initially, clinical data are detailed. The main clinical data required for the model were the success rates of the different interventions (i.e. subjective cure rate), rates of retreatment and complications/adverse events and mortality rates, which were mainly sourced from the review of clinical effectiveness (see Chapter 3) and supplemented with UK data on mortality rates. Following on from this, information on resource use and unit costs utilised in the model are presented. These data were primarily sourced from the review of previous economic evaluation, supplemented by further information from the literature and UK databases. Finally, the utility data included in the model are presented. All the utility values were sourced from the review of economic evaluations.
Relative effectiveness of surgical treatments
The relative effectiveness of surgical treatments, in terms of subjective cure rates, were based on the results of the NMA reported in Chapter 3. Table 12 describes the mean and median ORs for different surgical treatments versus retropubic MUS, which was taken to be the reference treatment. The reported values for mean and median ORs were used to define log-normal distributions in the model.
| Treatment | OR | 95% CrI | |
|---|---|---|---|
| Mean | Median | ||
| Transobturator MUS vs. retropubic MUS | 0.742 | 0.738 | 0.588 to 0.923 |
| Open colposuspension vs. retropubic MUS | 0.874 | 0.853 | 0.544 to 1.325 |
| Laparoscopic colposuspension vs. retropubic MUS | 0.605 | 0.580 | 0.315 to 1.046 |
| Traditional sling vs. retropubic MUS | 1.106 | 1.061 | 0.623 to 1.846 |
| Single-incision sling vs. retropubic MUS | 0.511 | 0.504 | 0.360 to 0.699 |
| Bladder neck needle suspension vs. retropubic MUS | 0.368 | 0.340 | 0.154 to 0.745 |
| Anterior vaginal repair vs. retropubic MUS | 0.235 | 0.220 | 0.105 to 0.452 |
Estimation of absolute cure rates
The absolute cure rates were calculated in the model by combining the information on relative cure rates described in Table 13 with the absolute cure rates for retropubic MUS. The absolute cure rates at 1 year for retropubic MUS were estimated to be 84%, based on a meta-analysis of retropubic MUS trials (44 studies were included).
| Time (months) | Median | 95% CrI | Number of | |
|---|---|---|---|---|
| Studies | Participants | |||
| 6 | 0.776 | 0.175 to 0.983 | 17 | 908 |
| 12 | 0.841 | 0.214 to 0.990 | 44 | 2882 |
| 24 | 0.784 | 0.454 to 0.941 | 6 | 315 |
| 36 | 0.341 | 0.001 to 0.995 | 5 | 205 |
| 60 | 0.329 | 0.005 to 0.979 | 3 | 377 |
To calculate the absolute probability of success for each surgical treatment, the OR of a given intervention compared with the baseline treatment (retropubic MUS) was derived from the NMA. This figure was then converted into a relative risk (RR) using the following formula:
where:
The RR for each treatment was then applied to the baseline risk247 to estimate the absolute probability of success for each surgical treatment.
Transition probabilities
Because the comparative effectiveness of surgical treatments may wane/decline over time, an additional search was conducted to identify studies on the long-term effectiveness (> 1 year) of the baseline intervention. After extensive searching, very few data were identified on the long-term effectiveness of the baseline intervention. Therefore, estimates used in the model were based on extrapolation of the available data.
Results from the review of clinical effectiveness data showed that there were six trials that had reported cure rates at 2 years after retropubic MUS and three studies that had reported cure rates at 5 years. A meta-analysis was conducted on each set of studies. Table 13 shows the absolute probabilities for retropubic MUS at different time points along with the number of studies and participants. The probability that participants are cured at 6, 12, 24, 36 and 60 months are 78%, 84%, 78%, 87% and 68%, respectively. For 24, 36 and 60 months, there are considerably fewer studies and participants than for the other time points.
The long-term recurrence rates after retropubic MUS were used to estimate long-term recurrence rates for surgical treatments using a parametric survival model from the data reported in Table 14. Parametric methods are commonly used to extrapolate survival times beyond the duration of the studies. These methods assume that recurrence rates for women follow a given theoretical distribution, such as Weibull, exponential and log-normal.
| Scenario | Time (years) | Cure rate (%) | Source | Parameter | |
|---|---|---|---|---|---|
| Scale (λ) | Shape (γ) | ||||
| Base-case analysis | 1 | 84.0 | Meta-analysis | 0.08799444 | 0.4932644 |
| 2 | 78.4 | ||||
| Ward et al.248 | 1 | 85.0 | Ward et al.248 | 0.1969761 | 0.12368398 |
| 5 | 80.0 | ||||
| Song et al.249 | 1 | 78.0 | Ward et al.248 | 0.19391258 | 0.1788069 |
| 13 | 67.5 | ||||
Scale and shape parameters were estimated for a Weibull distribution using the reported cure rates. This distribution was chosen because it was felt to provide a reasonable representation of the estimated long-term recurrence rates and has been used in a previous study. 241 The scale parameter (λ) describes the probability that the woman becomes incontinent during the next cycle of the model, given that she is continent during the current time period. The shape parameter (γ) describes the hazard function of the Weibull function for the survival time. The hazard function for Weibull survival time could be increasing or decreasing with time, depending on the value of the parameter. If the shape parameter is < 1, the hazard decreases with time, and if the value is > 1, the hazard rate increases with time. If the shape parameter is equal to 1, the Weibull distribution is equivalent to an exponential distribution.
To estimate alternative values to explore in SA, the long-term recurrence rates of retropubic MUS were derived using the long-term cure rates of a trial conducted in the UK comparing TVT with Burch colposuspension,248 which provides an optimistic estimate of cure rates after retropubic MUS and has been used in a previous study, which included an economic evaluation of non-surgical and surgical treatments for SUI in the UK. 241 In the trial, the data from reported cure rates for ≤ 5 years were used to estimate longer-term recurrence rates using a Weibull survival model. In addition, we derived data from the study with the longest follow-up, which was conducted by Song et al,249 in which the reported cure rates at 1 year and 13 years were 78% and 67.5%, respectively, to estimate long-term cure rates after retropubic MUS.
The following survival hazard formula was used:
where S(t) is the probability of cure, t is time (measured in terms of the number of cycles, where each cycle is equivalent to 3 months), λ is the scale parameter (which describes the probability that the woman becomes incontinent during the next time period, given that she is continent during the current time period) and γ is the shape parameter (which describes the hazard function of the Weibull function for the survival time).
It was assumed that proportional hazards stand; therefore, the transition probabilities for other surgical treatments were estimated by combining the respective RR and long-term probabilities for retropubic MUS (Figure 5).
FIGURE 5.
Extrapolated long-term cure rates after retropubic MUS surgery. Note that each cycle is 3 months long.
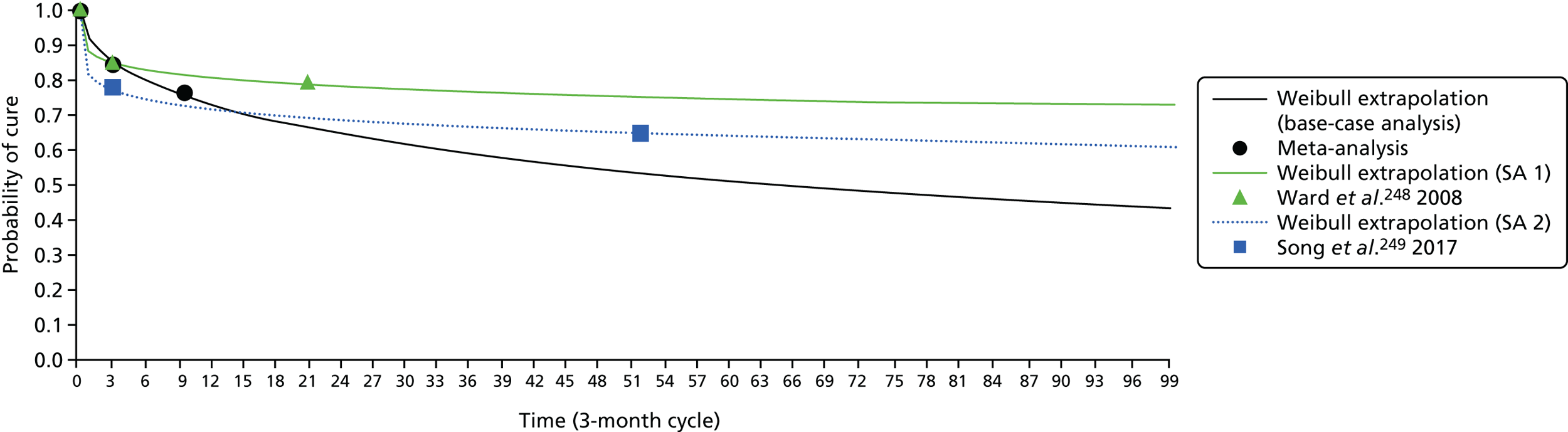
Because urethral injection therapy was not included in the NMA, the estimated short-term and long-term cure rates were obtained from a study by Ghoniem and Miller. 250 They performed a systematic review and meta-analysis to investigate the safety and effectiveness of silicon particles (Macroplastique®; Cogentix Medical, Inc, Orangeburg, NY, USA) for women with SUI (958 women from 23 cohorts were analysed). The cure rates were 43% (95% CI 33 to 54) in the short-term (< 6 months), 37% (95% CI 28 to 46) in the mid-term (6–18 months) and 36% (95% CI 27 to 46) in the long-term (> 18 months). Their meta-analysis suggested that long-term therapeutic benefit was frequently maintained. Cure rates in the short- and long-term were used to estimate longer-term success rates using Weibull survival models. 102 The parameters for the Weibull hazard functions for the cure rates are presented in Table 15 and cure rates are presented in Figure 6.
| Weibull parameters | Cure rate | ||
|---|---|---|---|
| Lower limit | Mean | Upper limit | |
| Lambda | 1.020173 | 0.767078 | 0.548895 |
| Gamma | 0.120006 | 0.137820 | 0.166837 |
FIGURE 6.
Extrapolated long-term cure rates after urethral injection therapy. Note that each cycle is 3 months long. LL, lower limit; UL, upper limit.
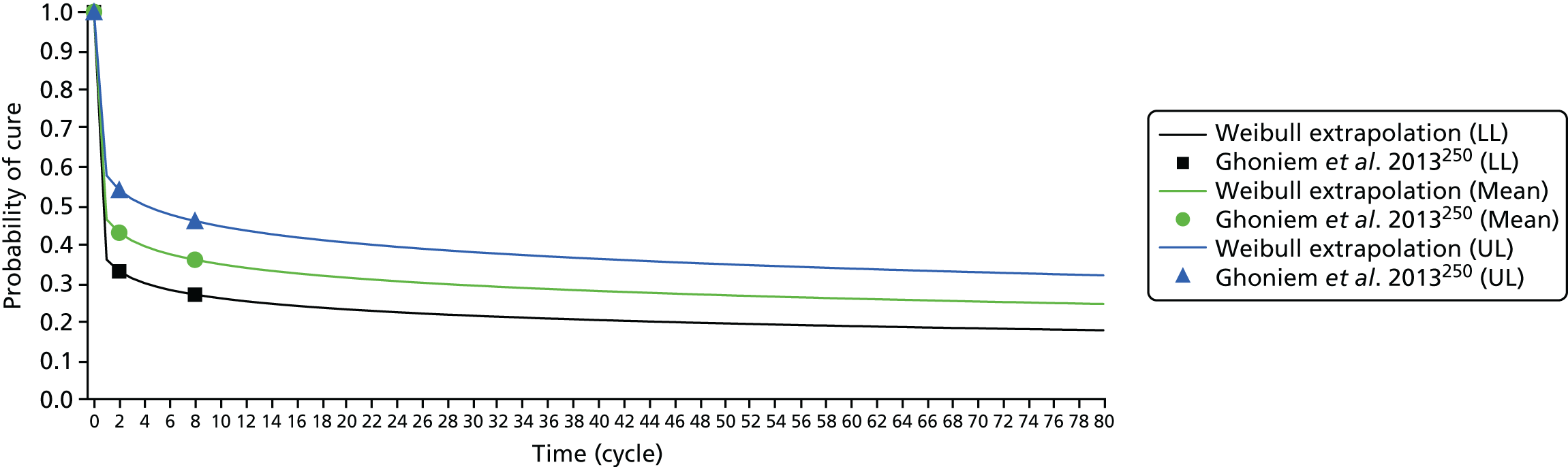
Repeat surgery
Because data from HES for England in 2013–14 and data for hospital discharge in Scotland in 1996–2014 show that around 91% to 96% of SUI surgeries were for MUS (retropubic, 55%; transobturator, 45%), and given that, from a clinical point of view, MUS (either retropubic or transobturator) can be offered after all types of surgery, it was assumed that all subsequent surgeries were either retropubic MUS (55%) or transobturator MUS (45%). 251 Owing to data limitations, subgroup analysis was not conducted to explore success rates after repeat surgery (after failed previous continence surgery) versus primary procedures. Therefore, it was assumed in the model that repeated MUS surgeries after failed primary surgeries are almost as effective as primary MUS surgeries, based on the finding from Kociszewski et al. 252 Kociszewski et al. 252 showed that 96% of women after primary sling implantation, and 88.46% of women after repeated sling, were dry at 6 months. The difference in percentage of negative pad test after primary and repeated procedure was not statistically significant. However, some previous studies show a lower success rate for retreatment with the same procedure. For example, Black and Downs253 showed that retreatment colposuspension was 78.4% less effective on average than primary colposuspension. Therefore, we tested two scenarios: in the first scenario it was assumed that subsequent surgeries (retropubic and transobturator MUS) are 90% as effective as they would have been as a primary surgery, and in the second scenario it was assumed that the subsequent surgeries are 75% as effective as primary retropubic and transobturator MUS.
Long-term repeat surgery rates estimation
To estimate the rate at which women choose to remain incontinent rather than seek retreatment in the model, individual-level data from a previous study was obtained. 254 In brief, the study used data from Aberdeen Maternity and Neonatal Databank (AMND) to estimate the lifetime risk of undergoing pelvic floor surgery in a cohort of UK parous women. The AMND stores linked information on all obstetric-related events occurring in women living in Aberdeen city and district since 1950 and currently contains data for approximately 200,000 women. Within the cohort of women, 762 (2.2%) had an operation for UI. We utilised this subset of data to estimate the risk of reoperation over time after different types of SUI surgeries. We excluded 11 women who had urogenital fistula repair surgery as it is not a SUI procedure. We analysed 751 cases that had SUI surgery. The number of women with one, two, three and four surgeries for each type of surgery are reported in Appendix 20. As some of the surgical treatments are no longer popular, this dataset was used because it contains data for those surgical treatments.
These data were analysed to estimate the rate at which women chose to remain incontinent rather than seek retreatment in the model. Parametric methods were used to extrapolate survival times beyond the follow-up duration in the data. We analysed the data using graphical exploration and statistical criteria of goodness of fit. First, Kaplan–Meier curves and survival, hazard and other related functions were examined graphically. The exponential, Gompertz, log-logistic, Weibull and log-normal distributions were fitted to the data and their fit was assessed visually and compared using statistical criteria based on log-likelihood, the Akaike information criterion (AIC) and the Bayesian information criterion (BIC); the model with the lowest AIC and BIC is preferred. 255 A log-normal distribution was applied to estimate the long-term rates of repeat surgery based on the AIC and BIC criteria. All fitted and observed survival data for different types of SUI surgeries are presented in Appendix 20.
Finally, the rate at which women choose to remain incontinent rather than seek retreatment was estimated based on the estimated cure rates and estimated repeat surgery rates at each time point. For example, if 1-year cure and repeat surgery rates after a particular surgery were 80% and 10%, respectively, the following formula was used to estimate the proportion of women who seek a second treatment following failure of the first treatment:
where Prt is the probability of having repeat surgery after a given surgery at time t and pcure is the probability of a surgery still being successful at time t.
The observed repeat surgery rates were compared with data from the included RCTs and pairwise meta-analysis results for repeat surgery rates after different surgical treatments. We felt that the observed repeat surgery rates were underestimating the actual rates. For example, results from the analysis show that the rate of repeat surgery after anterior vaginal repair (colporrhaphy) in 2 years is about 3%, whereas data from two trials show that the rate is ranging from 26.0% to 37.5%. 194,196 Therefore, in the base-case analysis it was assumed that (based on the data from previous assessment of surgical treatments for SUI) 75% of women whose first treatment was not successful would seek retreatment and 30% of women whose first retreatment failed would seek second retreatment in the base-case analysis. 256 We used the results from the analysis of AMND data in the SA to inform the model in terms of the proportion of women who will seek retreatment after failure of first surgery.
Complication rates after surgical treatments
There are different types of complications that can happen after each surgical treatment. The model incorporates only severe complications/adverse events that are important in terms of their effect on women’s quality of life, the cost and duration of treatments and data availability. To estimate complication incidence rates, random-effect meta-analysis models were fitted using WinBUGS software. 33 A Bayesian approach was used to combine existing knowledge with prior information based on established rules of probability. We checked the convergence of the model in different number of iterations; 50,000 Markov chain Monte Carlo iterations after a burn-in period of 20,000 iterations was chosen to get posterior distributions. The convergence was checked graphically using trace and autocorrelation plots. All the complications included in the model, and estimated incidence rates, are presented in Table 16. The estimated incidence rates were defined as distributions in the economic model (beta distribution). Lastly, the rates were used to estimate health-care costs and utility decrements associated with each treatment (see Resource use and unit costs and Health utility for more details).
| Surgery | Complication (%), mean (SD) | ||||||
|---|---|---|---|---|---|---|---|
| Infection | De novo symptoms of urgency or UI | Voiding difficulties including urinary retention | Bladder or urethral perforation | Tape/mesh erosion/extrusion/exposure | Short-term pain | Persistent pain or discomfort | |
| Anterior vaginal repair | NA | 15.84 (11.83) | 0.01 (0.15) | NA | NA | NA | NA |
| Bladder neck needle suspension | NA | 8.14 (4.87) | 1.67 (2.61) | NA | NA | 57.64 (30.08) | NA |
| Open colposuspension | 24.33 (21.82) | 5.78 (1.15) | 3.00 (1.04) | 1.02 (0.50) | 0.0 (NA) | 20.94 (25.65) | 0.15 (2.58) |
| Laparoscopic colposuspension | NA | 8.38 (3.98) | 6.32 (2.35) | 2.10 (1.22) | 0.0 (NA) | NA | NA |
| Traditional sling | 14.85 (12.49) | 7.85 (3.23) | 11.63 (3.60) | 1.82 (1.11) | 0.17 (0.34) | 28.99 (28.12) | 7.00 (8.98) |
| Retropubic MUS | 3.91 (4.72) | 4.30 (0.66) | 6.75 (0.95) | 4.89 (0.50) | 1.40 (0.31) | 4.36 (1.14) | 5.09 (2.37) |
| Transobturator MUS | 2.84 (1.03) | 5.31 (0.51) | 2.88 (0.44) | 5.13 (0.50) | 2.08 (0.26) | 7.04 (2.08) | 4.93 (1.22) |
| Single-incision sling | 3.22 (1.20) | 6.47 (0.81) | 2.15 (0.45) | 0.37 (0.18) | 2.38 (0.55) | 4.54 (3.21) | 1.28 (1.39) |
| Urethral injection therapy | 17.94 (24.59) | 17.94 (24.59) | 11.47 (20.70) | NA | NA | NA | NA |
All-cause mortality rates
In the model, women were at risk of death (from any cause) during any given cycle period. The cycle-specific risk of mortality was dependent on the simulated woman’s age. The risk of mortality will therefore increase with each cycle period (the ‘all-cause ageing effect’). Age-specific all-cause mortality rates were derived from general population mortality statistics reported in national life tables (Office for National Statistics). 232 The model incorporated the risk of operation-related death also. A rate of 0.0005 has been applied for open surgeries in previous studies241,256 based on the results from a report by Leach et al. 257 In addition, a recent study showed that urethral injection therapy had a higher mortality rate than open colposuspension [adjusted incidence rate ratio (IRR) 1.98, 95% CI 1.36 to 2.91]. They also showed retropubic MUS had a lower mortality rate than open colposuspension251 (adjusted IRR 0.65, 95% CI 0.44 to 0.96).
Clinical inputs for effectiveness of urge incontinence treatments
For those women with MUI who have UUI following surgery for SUI, or those SUI women who develop de novo UUI after surgery for SUI, three lines of treatment were assumed. Although it is possible to get more than three types of treatment for UUI, to simplify the model only three types of treatment were incorporated:
-
first-line treatment: bladder training
-
second-line treatment: anticholinergics drugs (oxybutynin hydrochloride)
-
third-line treatment: botulinum toxin type A.
The results from a systematic review undertaken by Lee et al. 258 showed that the efficacy of bladder training on symptoms of urgency ranges from 12% to 90%. In the base-case analysis, a 32% cure rate after bladder training was assumed.
The results from another NMA, which was conducted recently, showed that the absolute probability of being continent at 12 weeks after oxybutynin hydrochloride treatment is 21%. 259 Oxybutynin hydrochloride (5 mg twice daily) was used as an index second-line treatment. After 3 months, probabilities were assumed to be constant, which is consistent with the evidence from a long-term study suggesting that the treatment effect of antimuscarinic therapy at 4 months is maintained to 24 months. 260 Failure rates after botulinum toxin type A treatment at different time points were obtained from a previous economic evaluation that was conducted within the development of clinical guidelines for UI. 259 It was assumed that the cure rate at 6 months using botulinum toxin type A is 36%. 259
Resource use and unit costs
As mentioned in Model overview, the analysis was undertaken from a NHS and PSS perspective. Information on the precise description of resources required for each individual surgical treatment was based partially on data derived from the review of economic modelling studies, augmented where necessary by clinical experts in the study group and published economic literature. Unit costs were taken from appropriate routine sources, such as NHS Reference Costs,261 the Personal Social Services Research Unit (PSSRU)262 and the most recent British National Formulary (BNF)263 for medication.
Surgery costs
Surgeries for SUI and stress-predominant MUI vary in terms of the complexity of the procedure and the setting in which surgery would be conducted. For women undergoing anterior vaginal repair, bladder neck needle suspension, open colposuspension, laparoscopic colposuspension and traditional sling procedures, surgery would typically be conducted in an inpatient setting, based on expert clinical input. Women undergoing retropubic MUS and transobturator MUS procedures would typically be treated in a day case setting, based on expert clinical input. Costs for each of these individual surgeries were derived from NHS Reference Costs 2015/16. 261 Finally, both single-incision sling procedures and urethral injection therapy would be conducted in a day case setting, on the basis of clinical advice. No appropriate NHS reference costs were identified for these procedures and, therefore, costs for both of these surgeries were derived from previous literature, with costs inflated to a 2015/16 price year using the hospital and community health services (HCHS) index listed in the Unit Costs of Health and Social Care 2016. 262 The cost of each surgery is presented in Table 17.
| Resources | Cost (£) | Source | HRG code |
|---|---|---|---|
| Type of surgery | |||
| Anterior vaginal repair | 2236.50 | NHS Reference Costs 2015/16 261 | MA04C/D: intermediate open lower genital tract procedures – elective inpatient |
| Bladder neck needle suspension | 1819.72 | NHS Reference Costs 2015/16 261 | LB26A/B: intermediate endoscopic, prostate or bladder neck procedures – elective inpatient |
| Open colposuspension | 3909.55 | NHS Reference Costs 2015/16 261 | LB59Z: major, open or laparoscopic bladder neck procedures – elective inpatient |
| Laparoscopic colposuspension | 3909.55 | NHS Reference Costs 2015/16 261 | LB59Z: major, open or laparoscopic bladder neck procedures – elective inpatient |
| Traditional sling | 1924.32 | NHS Reference Costs 2015/16 261 | LB51A/B: vaginal tape operations for UI – elective inpatient |
| Retropubic MUS | 1351.10 | NHS Reference Costs 2015/16 261 | LB51A/B: vaginal tape operations for UI – day case |
| Transobturator MUS | 1351.10 | NHS Reference Costs 2015/16 261 | LB51A/B: vaginal tape operations for UI – day case |
| Single-incision sling | 1040.54 | Boyers et al.264 | N/A |
| Urethral injection therapy | 1820.29 | Kilonzo et al.229 | N/A |
| Additional resource use associated with surgery | |||
| Incontinence pads | 106.20 (3-month cost estimate) | NICE guidance document214 | N/A |
| Urodynamic test | 155.00 | NHS Reference Costs 2015/16 261 | N/A |
| Consultation pre surgery (20-minute consultation with surgical consultant) | 46.00 | PSSRU’s Unit Costs of Health and Social Care, 2016262 | N/A |
| Urine dipstick analysis | 3.94 | NICE clinical guidelines214 | N/A |
| Full blood count | 6.31 | NICE clinical guidelines214 | N/A |
| Diagnostic flexible cystoscopy | 152.00 | NHS Reference Costs 2015/16 261 | LB72A: diagnostic flexible cystoscopy |
| 500 mg of paracetamol (AAH Pharmaceuticals Ltd) × 32 | 0.16 (daily cost based on a recommended dose of 4 g a day) | BNF, 2016263 | N/A |
| 10g/15 ml of lactulose (AAH Pharmaceuticals Ltd) × 10 sachets | 0.50 (daily cost based on a recommended dose of 15 ml twice a day) | BNF, 2016263 | N/A |
| Urge incontinence treatment | |||
| Bladder training | 97.81 (3-month cost estimate) | Appendices of NICE guidelines214 | N/A |
| Band 6 hospital-based physiotherapist consultation (1-hour consultation) | 45.00 | PSSRU 2016262 | N/A |
| 5 mg of oxybutynin hydrochloride (AAH Pharmaceuticals Ltd) × 56 | 0.05 (daily cost based on a recommended dose of 5 mg twice a day) | BNF 2016263 | N/A |
| Consultant-led non-admitted follow-up face-to-face attendance in urology | 100.00 | NHS Reference Costs 2015/16 261 | N/A |
| Intermediate endoscopic bladder procedure (day case) | 971.00 | NHS Reference Costs 2015/16 261 | N/A |
| Botulinum toxin type A 100-unit powder for solution for injection vials (Allergan Ltd) | 138.20 | BNF 2016263 | N/A |
| Adverse event treatment | |||
| 250/125 mg of co-amoxiclav (AAH Pharmaceuticals Ltd) × 21 | 0.27 (daily cost based on a recommended dose of 250/125 mg every 8 hours) | BNF 2016263 | N/A |
| Attention to bladder catheter (outpatient, urology) | 123.00 | NHS Reference Costs 2015/16 261 | N/A |
| Self-catheterisation | 6.20 (daily cost based on 4 catheters required per day) | NICE guidance document214 | N/A |
| Mesh excision or repair | 1316.85 | NHS Reference Costs 2015/16 261 | MA04: intermediate open lower genital tract procedures – day case |
| 300 mg of aspirin (AAH Pharmaceuticals Ltd) × 28 | 0.40 (daily cost based on a recommended dose of 300 mg every 6 hours) | BNF 2016263 | N/A |
Additional costs associated with surgery
In addition to the cost of individual surgeries, costs associated with complementary tests, treatments and consultations that would typically be carried out in advance of, and following, each surgery were also considered. Clinical experts advised that women undergoing surgery for SUI and stress-predominant MUI would typically use incontinence pads until their condition had been resolved. The weekly cost of pads was estimated from a NICE guidance document214 with costs based on a guidance development group opinion on estimated pad usage per week. Costs reported were inflated to the current price year and converted to a 3-monthly cost to fit the model time cycle. Clinical experts advised that a urodynamic test would be conducted in a separate consultation before each surgery, and that the woman would also have a separate 20-minute consultation before undergoing surgery with the clinician carrying out the surgery. Costs for test and consultation were derived from NHS Reference Costs 2015/16261 and PSSRU 2016262 respectively.
Clinical experts involved in the study advised that a urine dipstick analysis and full blood count would need to be taken prior to each surgery, excluding injectable agent procedures, for which only a urine dipstick analysis would be required. Costs for both were obtained from NICE clinical guidelines for routine pre-operative tests for elective surgery. 214 In addition, it was advised that a cystoscopy on the day of the procedure would be mandatory for women undergoing a retropubic MUS or transobturator MUS procedure. The cost of a diagnostic flexible cystoscopy in an outpatient setting was obtained from NHS Reference Costs 2015/16. 261 Finally, the cost of medication needed for pain relief post surgery (paracetamol) was considered, with the duration of pain relief required greater for inpatient procedures (7 days) than for the less invasive day case procedures (3 days). It was also advised that lactulose would be taken as pain relief for 1 day following anterior vaginal repair only. Costs of medication were obtained from the BNF 2016. 263 All additional costs are reported in Table 17. Omitting the cost of incontinence pads, which are used by all women with incontinence regardless of the type of initial surgery, the total additional costs associated with anterior vaginal repair, bladder neck needle suspension, open colposuspension, laparoscopic colposuspension, traditional sling, retropubic MUS, transobturator MUS, single-incision sling and urethral injection therapy were £212.87, £212.37, £212.37, £212.37, £212.37, £363.73, £363.73, £211.73 and £205.42, respectively.
Urge urinary incontinence costs
As well as the cost of surgical treatments for SUI and stress-predominant MUI, the costs associated with treatment for UUI were also considered. The NICE clinical guidelines on the management of urge incontinence recommend three broad lines of treatment for women with this type of incontinence:214
-
conservative measures such as bladder training
-
antimuscarinic drugs, most typically oxybutynin hydrochloride
-
invasive therapy such as botulinum toxin type A.
This treatment pathway was confirmed by clinical experts in the study team. The cost of bladder training was obtained from the appendices of a NICE draft for consultation on guidelines for UI in women. 214 Costs reported in this document were based on women being seen 5 times over a 4-month period (i.e. initial consultation and once in each of the 4 months). To estimate 3-monthly bladder training costs to fit the model time cycle, it was assumed that the woman would have an initial consultation with a band 6 hospital-based physiotherapist and would be seen for training once in each of the 3 months. The cost of a consultation was based on data obtained from PSSRU 2016. 262 The cost of consumables required during training were obtained directly from the guidelines214 and were also included in the estimate. These costs were inflated to the current price year using the HCHS index listed in PSSRU 2016. 262
Antimuscarinic medication taken was assumed to be oxybutynin hydrochloride, on the basis of recommendations from the clinical guidelines214 and expert clinical advice. Appropriate costs were obtained from the BNF 2016. 263 Additionally, it was assumed that the woman would require a consultation with a specialist before beginning medication, and this cost was based on the average unit cost of a consultant-led non-admitted face-to-face follow-up attendance in urology, obtained from NHS Reference Costs 2015/16. 261 Cost of medication was estimated for 3 months. Finally, the cost of a botulinum toxin type A procedures was based on micro-costing details presented in a NICE draft for consultation on guidelines for UI in women. 214 Included in this overall procedure cost was the cost of an intermediate endoscopic bladder procedure (day case) and the cost of botulinum toxin type A 100-unit powder for solution for injection vials. These costs were obtained from NHS Reference Costs 2015/16261 and the BNF 2016,263 respectively. Additionally, it was assumed that the woman would require a consultation with a specialist before undergoing a botulinum toxin type A procedure, and this cost was based on the average unit cost of a consultant-led non-admitted face-to-face follow-up attendance in urology, obtained from NHS Reference Costs 2015/16. 261 Costs of urge incontinence treatments are reported in Table 17.
Adverse events treatment costs
The cost of treating complications associated with surgical treatments was also considered in the model. Typical treatments were informed by expert clinical advice and costs were obtained through routine sources. The cost of treating an infection was based on the cost (obtained from the BNF 2016263) of co-amoxiclav antibiotic medication over a 2-week period (advised duration of infection). It was advised that women experiencing voiding difficulties (including urinary retention), or bladder or urethral perforation, would require catheterisation. This cost was based on the cost, obtained from NHS Reference Costs 2015/16,261 of a bladder catheter procedure in an out-patient setting. As voiding difficulties may impact the woman for up to 3 months, the cost of self-catheterisation over this period was also estimated. For a bladder injury the cost of a suprapubic bladder catheter procedure in an out-patient setting was applied, as well as the cost of self-catheterisation over a 12-day period (based on expert clinical advice). The cost of a single catheter was obtained from the NICE draft for consultation on guidelines for UI in women214 and inflated to the 2016 price. It was assumed that the woman would require four catheters per day, based on data presented in the NICE guidelines. 214
The cost of a mesh excision or repair to treat mesh erosion was based on the cost of a partial removal of TVT [HRG (Healthcare Resource Group) code MA04: intermediate open lower genital tract procedures – day case], obtained from NHS Reference Costs 2015/16. 261 Based on the reference cost schedule, a relatively small percentage (16%) of these procedures will be major procedures. The intermediate option was chosen, reflecting that the greatest percentage of procedures are intermediate. The cost difference between the major and intermediate procedure is in the region of £200. This was assumed to be a one-off cost. It was advised that persistent pain would typically be treated through the use of non-steroidal anti-inflammatory drugs. For the purpose of this costing, medication taken for pain was assumed to be aspirin (based on expert clinical advice) and relevant costs were obtained from the BNF 2016. 263 The estimated incidence rates for each complication were used to estimate cost associated with complications after each surgical treatment by multiplying respective incidence rates by the cost of each complication. All costs associated with treating adverse events are reported in Table 17.
Health utility
The identified papers from the review of economic evaluation studies were screened specifically for utility estimates for women with SUI, stress-predominant MUI and UUI. The focus of the screening was to identify studies (economic evaluations or otherwise) that included populations of these women and were conducted in the UK (or elsewhere but included a UK-based subpopulation or population that was generalisable to a UK population). The baseline value for pretreatment SUI was derived from a previous UK-based economic evaluation comparing two types of surgical intervention for this condition. 244 The utility value for a successful treatment was derived from a UK-based study exploring health outcomes in women with UI. 245 This study was also used to estimate the utility values for health states following failed surgical treatment (Table 18). The same data were used to inform the utility weights in two previous studies of surgical and non-surgical treatment of SUI in the UK. 85,241
| EQ-5D | Utility value | Source | Duration |
|---|---|---|---|
| SUI pretreatment | 0.78 | Manca et al.244 | Variable |
| Mixed pretreatment | 0.78 | Manca et al.244 | Variable |
| Cured from SUI and no urge UI | 0.85 | Haywood et al.245 | Variable |
| UUI | 0.74 | Haywood et al.245 | Variable |
| Pure SUI retreatment | 0.74 | Haywood et al.245 | Variable |
| Mixed retreatment | 0.74 | Haywood et al.245 | Variable |
| SUI failure of treatment (containment) | 0.74 | Haywood et al.245 | Variable |
| Mixed failure of treatment (containment) | 0.74 | Haywood et al.245 | Variable |
| Adverse event | Utility decrement | Source | Duration |
| Infection | –0.19 | Shepherd et al.265 | 2 weeks |
| Voiding difficulties (long term) | –0.23 | Shepherd et al.265 | 3 months |
| Bladder/urethral perforation | –0.08 | Shepherd et al.265 | 2 weeks |
| Tape/mesh exposure/erosion | –0.25 | Shepherd et al.265 | 3 months |
| Short-term pain | –0.25 | Shepherd et al.265 | 2 weeks |
| Persistent pain | –0.25 | Shepherd et al.265 | 6 months |
The availability of utility values for outcomes and complications of surgical treatment for SUI, stress-predominant MUI and UUI were sparse. Only one study identified through the review of economic evaluation studies had reported appropriate utility data related to adverse events, conducted by Shepherd et al. 265 Owing to the unavailability of utility values for complications related to surgery, values in Shepherd et al. ’s study were assigned by an expert panel of six urogynecologists by matching complications included in the model to published data on similar conditions in different groups of women. This study was used to derive utility values for all adverse events included in the model. Utility decrements for all adverse events included in the model, as well as their duration in the economic model, are presented in Table 18. In the model, utility decrements were assigned only to the proportion of the woman population experiencing that complication for the duration each complication was expected to last.
Main modelling assumptions
-
As data from HES for England in 2013–14, and data for hospital discharge in Scotland in 1996–2014, showed that around 91% and 96% of SUI surgeries were MUS procedures (retropubic MUS, 55%; transobturator MUS, 45%), and given that, from a clinical point of view, MUS can be offered after all types of surgeries, it was assumed that all subsequent surgeries are either retropubic MUS or transobturator MUS.
-
No further conservative (i.e. PFMT, medication or lifestyle change) management of SUI were considered as a comparator, or within the treatment pathway, after surgery.
-
It was assumed that all women in containment, retreatment and urge incontinence states will use containment products.
-
For women with MUI, and those who develop UUI after surgical treatments for SUI, first-line treatment of UUI (bladder training) will be offered, and if the first line treatment fails they will be offered second-line treatment (drug, i.e. oxybutynin hydrochloride). In the event that second-line treatment fails, they will be offered third-line treatment (botulinum toxin type A) for UUI. We appreciate that there are multiple options for treating UUI, but for reasons of simplification we have used the most common treatments for UUI.
-
SUI and UUI are modelled independently, meaning that any treatment that has been received for SUI will not affect the effectiveness of UUI treatment and vice versa.
-
It was assumed that the time interval between initial surgery and any subsequent surgery for SUI is 1 year. The reason behind this assumption is that it will take up to 1 year to find out about results from surgical treatments and to decide if further surgery is required.
-
It was assumed that the time interval between first-line treatment for UUI and any subsequent treatment is 3 months.
-
The model assumes that women can receive a total of three treatments, which includes the initial surgery plus two subsequent repeat surgeries, if required.
-
Utility decrements associated with complications were incorporated based on their duration, utility decrement weights and respective incidence rates.
Incremental cost-effectiveness analysis
The joint estimates of costs and effects were combined in an incremental analysis, and presented in terms of the mean ICER for each comparator. The ICERs were calculated as the difference in costs divided by the difference in effects (QALYs) between treatment options. The ICERs were calculated for each successive alternative, from the least to the most costly. To help identify the optimal approach, the net monetary benefit (NMB) framework was used, where the NMB for a given strategy is equal to the accrued QALYs multiplied by the ceiling ratio (CR) of willingness to pay (WTP) per QALY, minus the strategy costs:
The value of £20,000, which is typically used by NICE as a threshold to inform judgements on cost-effectiveness, was placed on the CR. 16 The threshold means NICE is prepared to pay £20,000 for each extra QALY gained through different interventions. Measures of variance for the joint incremental costs and effects were obtained using Monte Carlo simulation within the PSA and presented graphically using cost-effectiveness planes and cost-effectiveness acceptability curves (CEACs).
Sensitivity analyses
Both deterministic SA and, as noted above, PSA were used to explore parameter and other forms of uncertainty surrounding estimates of cost-effectiveness. Deterministic sensitivity analyses were performed to determine the impact of changing key parameters on the model results. Therefore, many of the model parameters were subject to one- and two-way sensitivity analyses, using hypothetical increases or decreases, to determine the key drivers of the model results. Deterministic sensitivity analyses were also carried out to test for the effect of assumptions and variability. These analyses are described in this section.
When available, data were also entered into the model as distributions to fully incorporate the uncertainty around parameter values so that a PSA could be undertaken. In decision modelling, many of the parameter values are often estimated with a degree of uncertainty. The probabilistic distribution for each parameter was defined by considering the mean, standard error and anticipated shape of the distribution. The PSA was run with 10,000 simulations for each woman, and CEACs were produced to identify the probability of the different surgeries being cost-effective across a range of WTP thresholds. Estimation of costs and QALYs were calculated as the expectation over the joint distribution of the parameters. This quantification of decision uncertainty also provided the starting point for assessing the value of additional research.
This section details the technical specification of the sensitivity analyses conducted.
Applying higher incidence rates of mesh complications after mid-urethral sling procedures
As mentioned in the methods section, data from the trials were used to estimate the complications incidence rates after each surgical treatment. As some of the complications may happen over the longer term, and given that the trials are short in terms of the follow-up time, results from a very recent study on MUS were used to estimate the mesh complication incidence rates after retropubic MUS and transobturator MUS in the model. Keltie et al. 266 conducted a study to investigate the rate of adverse events after MUS procedures using data from the HES database. The mean follow-up time was 4.2 years (unconfounded cohort). They showed that the readmissions for further surgery after initial retropubic MUS and transobturator MUS were 3.7% [removal (2.7%), repair (1%), renewal (0%)] and 2.8% [removal (1.9%), repair (0.9%), renewal (0%)], respectively. These values were used within the SA for retropubic MUS and transobturator MUS. In addition, we explored the effect of assuming both a 10% and a 20% incidence rate of mesh complications both after retropubic MUS and after transobturator MUS on the results.
Incorporating longer duration for persistent pain complication
In the base-case analysis, it was assumed that persistent pain complication will last for, on average, 6 months. In this SA, the effect of longer-term suffering from persistent pain was explored: we tested scenarios in which women suffer for 3 years and women suffer for 5 years.
Applying higher incidence rates of persistent pain after mid-urethral sling procedures
In the base-case analysis, it was assumed that the incidence rate for persistent pain complication after retropubic MUS and transobturator MUS are 5.09% and 4.93%, respectively, based on the results from meta-analysis. In these sensitivity analyses, the effect of higher incidence rates of persistent pain (10% and 20%) after MUS procedures was explored.
Applying higher incidence rates and longer duration for persistent pain after mid-urethral sling procedures
A scenario analysis was also conducted by incorporating higher incidence rates of persistent pain after MUS procedures and longer duration. It was assumed that the incidence rates for persistent pain complication after retropubic MUS and transobturator MUS are 20% and that, on average, women with persistent pain will suffer for 5 years.
Assuming that all the women in the model have stress urinary incontinence
A SA was performed to investigate the disease type of women in the model. Owing to data limitations, it was not possible to do a full subgroup analysis and estimate different success rates for two subpopulations (i.e. women with SUI and women with MUI). In this SA it was assumed that all the women in the model have SUI and the success rates are the same as the base-case analysis.
Assuming alternative values for the proportion of women who will seek retreatment after failure of each surgical treatment
In the base-case analysis, it was assumed that 75% of women whose first treatment was not successful would seek retreatment and 30% of women whose first retreatment failed would seek second retreatment. This SA was conducted to explore results using data from the linked database (AMND) to estimate the proportion of women who will seek retreatment after failure of each surgical treatment.
As mentioned in the methods section, primary data from linked databases were analysed to estimate repeat surgery incidence rates over time and were then used to estimate the proportion of women who will seek retreatment after failure of the previous surgery. Because the linked database may not be complete, the health economists felt that the rates of repeat surgery were underestimated. In this SA, the method described in Repeat surgery was used to estimate the proportion of women who will seek retreatment. In addition, in this SA lower probabilities of repeat surgeries (50% and 10% for first retreatment and 20% and 0% for second retreatment) were explored.
Applying different values for short- and long-term success rates after retropubic mid-urethral sling
As indicated in the estimation of model probabilities, the short-term and long-term cure rates after retropubic MUS were estimated using a random-effects meta-analysis. There are some uncertainties associated with these estimates and it is probable that these values are either an overestimate or an underestimate because of small sample size. We have explored the effect of using two different sources of data (Ward et al. 248 and Song et al. 249) for extrapolation of long-term success rate after retropubic MUS in this SA. The short- and long-term cure rates were used to estimate an appropriate shape and scale parameter for a Weibull hazard function, and these parameters were used to estimate failure rates at each time point after retropubic MUS, as described in Transition probabilities.
Applying lower success rates when repeating same surgeries
This SA was conducted to explore the effect of assuming lower cure rates when the same surgeries are being conducted for a second or third time. In the base-case analysis it was assumed that all surgical treatments have the same effectiveness as a primary procedure, whereas in this SA the subsequent treatments are assumed to have less effectiveness: 90% and 75%, respectively.
Incorporating different health utility values and effect of natural decline in health utility over time
As mentioned in Health utility, the same values were used for SUI and MUI women using data from Manca et al. 244 and Haywood et al. 245 in the base-case analysis. Tincello et al. 267 showed that MUI (EQ-5D 0.75) may have a greater impact on the EQ-5D score than SUI (EQ-5D 0.85). SA was performed by adjusting the EQ-5D scores used in the base-case analysis with lower values applied to MUI health states. EQ-5D scores used for the MUI pretreatment and MUI after failure of first/second treatment states were 0.69 and 0.65, respectively. The impact of the natural decline in health utility over time was also considered in further SA. The values for the age-related reduction were derived based on published values for age-related health utility. 268
Results
Monte Carlo simulation was performed to obtain probabilistic estimates of the cost-effectiveness of retropubic MUS compared with all other surgical treatments. The results, in terms of total and incremental costs and effectiveness, and incremental cost per QALY, are presented in Table 19, and in the form of a CEAC in Figure 7. Table 19 reports strategies from least to most costly; the last column reports the ICERs. Over a lifetime time horizon, retropubic MUS is on average the least costly (£8099) and the most effective (24.22 QALYs) surgical treatment. All other surgical treatments are dominated as they are more costly and less effective than retropubic MUS except for traditional sling. Over a shorter time horizon (10 years), retropubic MUS remains the dominant strategy. However, over a 1-year time horizon single-incision sling is dominant compared with all other strategies except for open colposuspension. Figure 7 shows that over a lifetime time horizon retropubic MUS has a > 26% probability of being cost-effective at a WTP threshold value of £20,000. Given the number of comparators, if the interventions were comparable we would expect an 11% chance of being cost-effective. The only other strategies with reasonably sized probabilities of being cost-effective are traditional sling (≈27% across all WTP values presented, suggesting not much difference between retropubic MUS and traditional sling) and open colposuspension (≈14–16% across all WTP thresholds > £10,000). All other strategies have a < 10.5% probability of being cost-effective across all WTP values presented.
| Time horizon | Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective (%) at WTP threshold (£) | |
|---|---|---|---|---|---|---|---|---|
| 20,000 | 30,000 | |||||||
| 1 year | Single-incision sling | 1953 | 0.76 | 96.6 | 92.3 | |||
| Retropubic MUS | 2310 | 357 | 0.75 | –0.01 | Dominated | 2.9 | 5.6 | |
| Transobturator MUS | 2352 | 399 | 0.75 | –0.01 | Dominated | 0.5 | 1.4 | |
| Bladder neck needle suspension | 2756 | 803 | 0.75 | –0.01 | Dominated | 0.1 | 0.5 | |
| Traditional sling | 2772 | 819 | 0.72 | –0.04 | Dominated | 0.0 | 0.0 | |
| Urethral injection therapy | 2848 | 895 | 0.74 | –0.02 | Dominated | 0.0 | 0.1 | |
| Anterior vaginal repair | 3249 | 1296 | 0.76 | 0.00 | Dominated | 0.0 | 0.2 | |
| Open colposuspension | 4710 | 2757 | 0.77 | 0.01 | 233,209 | 0.0 | 0.0 | |
| Laparoscopic colposuspension | 4804 | 95 | 0.76 | –0.01 | Dominated | 0.0 | 0.0 | |
| 10 years | Retropubic MUS | 4649 | 7.33 | 51.0 | 44.9 | |||
| Traditional sling | 5235 | 585 | 7.28 | –0.05 | Dominated | 20.4 | 20.5 | |
| Single-incision sling | 5274 | 625 | 7.14 | –0.19 | Dominated | 3.7 | 3.5 | |
| Transobturator MUS | 5414 | 765 | 7.20 | –0.13 | Dominated | 4.3 | 4.4 | |
| Urethral injection therapy | 5676 | 1027 | 7.19 | –0.14 | Dominated | 8.8 | 9.5 | |
| Bladder neck needle suspension | 5958 | 1309 | 7.14 | –0.19 | Dominated | 4.0 | 4.3 | |
| Anterior vaginal repair | 6655 | 2006 | 7.11 | –0.22 | Dominated | 1.8 | 2.4 | |
| Open colposuspension | 7375 | 2725 | 7.29 | –0.04 | Dominated | 4.7 | 8.1 | |
| Laparoscopic colposuspension | 7818 | 3169 | 7.20 | –0.13 | Dominated | 1.3 | 2.5 | |
| Lifetime | Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 | |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 | |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 | |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 | |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 | |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 | |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 | |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 | |
FIGURE 7.
Cost-effectiveness acceptability curves for the nine surgical treatments. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle suspension; lap colpo, laparoscopic retropubic colposuspension; open colpo, open abdominal retropubic colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; transob-MUS, transobturator mid-urethral sling; trad sling, traditional suburethral retropubic sling.
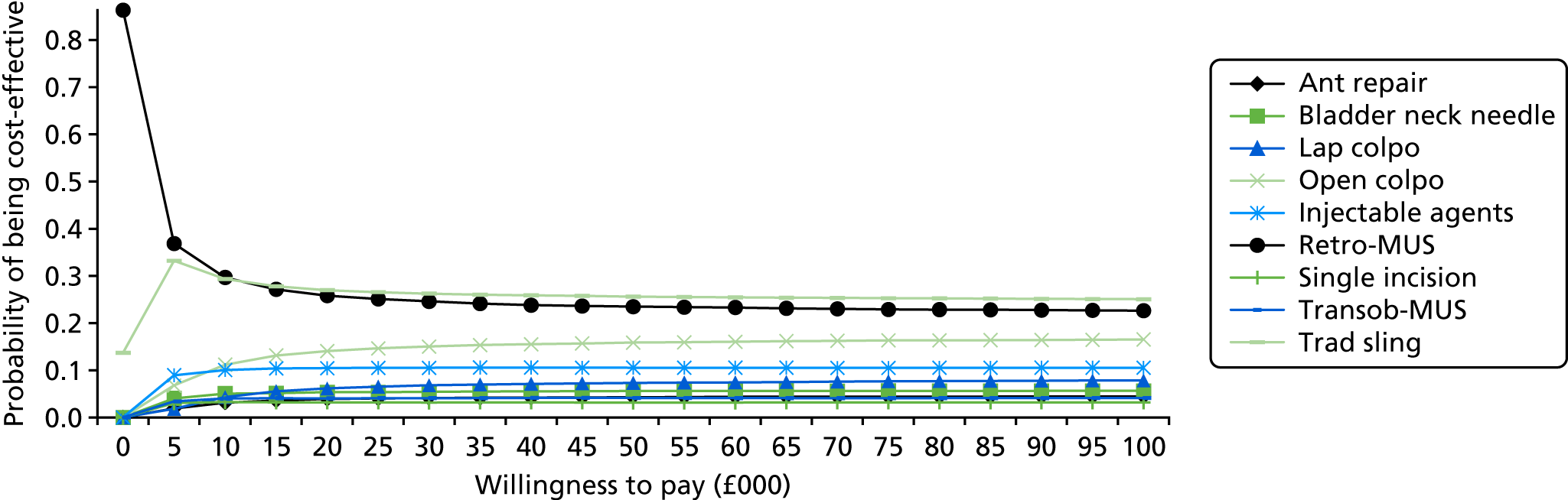
Deterministic sensitivity analyses
Applying higher incidence rates for mesh complications after mid-urethral sling procedures
In this SA, results from the study by Keltie et al. 266 were used to inform the mesh complication incidence rate after retropubic MUS and transobturator MUS. The results from this SA show that retropubic MUS remains the least costly strategy compared with the alternative surgical interventions and is the most cost-effective option, at a WTP threshold value of £20,000 (Table 20). However, when 10% and 20% incidence rates are used, traditional sling is the most cost-effective option, with an ICER of < £20,000 per each QALY gained.
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective (%) at WTP threshold (£) | |
|---|---|---|---|---|---|---|---|
| 20,000 | 30,000 | ||||||
| Base-case analysis estimating the incidence rate of mesh complications after MUS procedures based on the data from trials | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA estimating the incidence rate of mesh complications for retropubic MUS (3.7%) and transobturator MUS (2.8%) based on the data from Keltie et al.266 | |||||||
| Retropubic MUS | 8138 | 24.20 | 24.5 | 23.5 | |||
| Traditional sling | 8530 | 392 | 24.22 | 0.01 | 26,311 | 27.8 | 26.8 |
| Urethral injection therapy | 9560 | 1030 | 23.85 | –0.37 | Dominated | 10.7 | 10.7 |
| Single-incision sling | 9656 | 1125 | 23.58 | –0.63 | Dominated | 3.3 | 3.2 |
| Transobturator MUS | 9683 | 1153 | 23.69 | –0.53 | Dominated | 4.1 | 4.0 |
| Bladder neck needle suspension | 10,131 | 1601 | 23.67 | –0.55 | Dominated | 5.9 | 6.0 |
| Open colposuspension | 10,978 | 2448 | 24.09 | –0.13 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,073 | 2543 | 23.53 | –0.69 | Dominated | 3.9 | 4.2 |
| Laparoscopic colposuspension | 11,805 | 3275 | 23.81 | –0.41 | Dominated | 5.9 | 6.7 |
| SA assuming 10% incidence rate of mesh complications after retropubic MUS and transobturator MUS | |||||||
| Retropubic MUS | 8238 | 24.19 | 23.9 | 22.5 | |||
| Traditional sling | 8550 | 312 | 24.24 | 0.05 | 6631 | 29.1 | 28.1 |
| Urethral injection therapy | 9596 | 1045 | 23.86 | –0.37 | Dominated | 11.2 | 11.2 |
| Single-incision sling | 9705 | 1155 | 23.58 | –0.65 | Dominated | 3.2 | 3.1 |
| Transobturator MUS | 9817 | 1267 | 23.69 | –0.55 | Dominated | 4.0 | 4.2 |
| Bladder neck needle suspension | 10,180 | 1629 | 23.69 | –0.55 | Dominated | 5.8 | 5.9 |
| Open colposuspension | 11,010 | 2460 | 24.08 | –0.16 | Dominated | 13.1 | 14.2 |
| Anterior vaginal repair | 11,120 | 2570 | 23.54 | –0.70 | Dominated | 3.7 | 4.1 |
| Laparoscopic colposuspension | 11,843 | 3292 | 23.84 | –0.40 | Dominated | 6.0 | 6.8 |
| SA assuming 20% incidence rate of mesh complications after retropubic MUS and transobturator MUS | |||||||
| Retropubic MUS | 8381 | 24.17 | 0.00 | 23.6 | 22.4 | ||
| Traditional sling | 8579 | 198 | 24.21 | 0.04 | 4558 | 28.6 | 27.6 |
| Urethral injection therapy | 9644 | 1064 | 23.86 | –0.35 | Dominated | 10.7 | 10.8 |
| Single-incision sling | 9766 | 1186 | 23.58 | –0.64 | Dominated | 3.4 | 3.3 |
| Transobturator MUS | 9987 | 1407 | 23.66 | –0.56 | Dominated | 3.7 | 3.8 |
| Bladder neck needle suspension | 10,237 | 1657 | 23.67 | –0.54 | Dominated | 5.6 | 5.8 |
| Open colposuspension | 11,048 | 2469 | 24.07 | –0.14 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,185 | 2606 | 23.52 | –0.69 | Dominated | 3.6 | 3.8 |
| Laparoscopic colposuspension | 11,892 | 3312 | 23.82 | –0.39 | Dominated | 6.7 | 7.5 |
Incorporating longer duration for persistent pain complication
In the base-case analysis, it was assumed that persistent pain complication will last for, on average, 6 months. In these sensitivity analyses, the effect of longer-term suffering from persistent pain was explored and it was assumed that, on average, women with persistent pain will suffer for 3 and 5 years. The results from these sensitivity analyses show that with longer duration of persistent pain, the probability of retropubic MUS being the most cost-effective option decreases and the respective probability for open colposuspension increases (Table 21).
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective (%) at WTP threshold (£) | |
|---|---|---|---|---|---|---|---|
| 20,000 | 30,000 | ||||||
| Base-case analysis assuming that persistent pain complication will last on average for 6 months | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA assuming that persistent pain complication will last on average for 36 months | |||||||
| Retropubic MUS | 8097 | 24.02 | 22.3 | 20.9 | |||
| Traditional sling | 8523 | 426 | 24.01 | –0.01 | Dominated | 23.7 | 22.8 |
| Urethral injection therapy | 9547 | 1450 | 23.78 | –0.24 | Dominated | 12.7 | 12.6 |
| Single-incision sling | 9646 | 1549 | 23.45 | –0.56 | Dominated | 3.4 | 3.3 |
| Transobturator MUS | 9665 | 1567 | 23.50 | –0.52 | Dominated | 3.2 | 3.3 |
| Bladder neck needle suspension | 10,126 | 2029 | 23.59 | –0.43 | Dominated | 6.6 | 6.7 |
| Open colposuspension | 10,970 | 2872 | 24.02 | 0.00 | 1,134,541 | 17.1 | 18.2 |
| Anterior vaginal repair | 11,060 | 90 | 23.43 | –0.59 | Dominated | 4.0 | 4.1 |
| Laparoscopic colposuspension | 11,791 | 821 | 23.75 | –0.27 | Dominated | 7.1 | 8.1 |
| SA assuming that persistent pain complication will last on average for 60 months | |||||||
| Retropubic MUS | 8103 | 23.90 | 20.8 | 19.3 | |||
| Traditional sling | 8524 | 421 | 23.87 | –0.03 | Dominated | 20.7 | 19.9 |
| Urethral injection therapy | 9550 | 1447 | 23.74 | –0.17 | Dominated | 13.8 | 13.7 |
| Single-incision sling | 9648 | 1545 | 23.38 | –0.52 | Dominated | 3.3 | 3.2 |
| Transobturator MUS | 9666 | 1563 | 23.35 | –0.56 | Dominated | 2.5 | 2.6 |
| Bladder neck needle suspension | 10,127 | 2024 | 23.54 | –0.36 | Dominated | 7.1 | 7.3 |
| Open colposuspension | 10,976 | 2872 | 23.99 | 0.09 | 33,380 | 19.4 | 20.5 |
| Anterior vaginal repair | 11,059 | 83 | 23.38 | –0.61 | Dominated | 4.1 | 4.4 |
| Laparoscopic colposuspension | 11,793 | 818 | 23.71 | –0.28 | Dominated | 8.3 | 9.3 |
Applying higher incidence rates of persistent pain after mid-urethral sling procedures
Results from these sensitivity analyses show that when a higher incidence rate (10% and 20%) of persistent pain after retropubic MUS and transobturator MUS was assumed, the probability of retropubic MUS being the most cost-effective option decreases and the respective probability for traditional sling increases (Table 22). The probability of retropubic MUS and traditional sling being the most cost-effective are 23–24% and 28–29%, respectively.
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective (%) at WTP threshold (£) | |
|---|---|---|---|---|---|---|---|
| 20,000 | 30,000 | ||||||
| Base-case analysis assuming that incidence rate of persistent pain after retropubic MUS and transobturator MUS are 5.09% and 4.93%, respectively | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA assuming that incidence rate of persistent pain after retropubic MUS and transobturator MUS is 10% | |||||||
| Retropubic MUS | 8104 | 24.18 | 24.2 | 23.0 | |||
| Traditional sling | 8523 | 419 | 24.20 | 0.03 | 15,067 | 28.4 | 27.6 |
| Urethral injection therapy | 9557 | 1034 | 23.84 | –0.37 | Dominated | 11.1 | 11.1 |
| Single-incision sling | 9649 | 1126 | 23.57 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9672 | 1148 | 23.67 | –0.54 | Dominated | 3.8 | 3.8 |
| Bladder neck needle suspension | 10,128 | 1605 | 23.66 | –0.54 | Dominated | 5.7 | 5.8 |
| Open colposuspension | 10,977 | 2454 | 24.07 | –0.13 | Dominated | 13.8 | 14.8 |
| Anterior vaginal repair | 11,063 | 2540 | 23.51 | –0.69 | Dominated | 3.7 | 3.9 |
| Laparoscopic colposuspension | 11,799 | 3275 | 23.81 | –0.39 | Dominated | 6.2 | 7.0 |
| SA assuming that incidence rate of persistent pain after retropubic MUS and transobturator MUS is 20% | |||||||
| Retropubic MUS | 8109 | 24.13 | 23.3 | 22.1 | |||
| Traditional sling | 8520 | 410 | 24.19 | 0.06 | 6593 | 28.6 | 27.5 |
| Urethral injection therapy | 9557 | 1037 | 23.83 | –0.36 | Dominated | 10.8 | 10.9 |
| Single-incision sling | 9645 | 1125 | 23.56 | –0.63 | Dominated | 3.5 | 3.5 |
| Transobturator MUS | 9677 | 1158 | 23.61 | –0.58 | Dominated | 3.8 | 3.8 |
| Bladder neck needle suspension | 10,131 | 1612 | 23.65 | –0.54 | Dominated | 6.2 | 6.3 |
| Open colposuspension | 10,975 | 2455 | 24.07 | –0.12 | Dominated | 14.0 | 15.1 |
| Anterior vaginal repair | 11,063 | 2543 | 23.49 | –0.70 | Dominated | 3.5 | 3.8 |
| Laparoscopic colposuspension | 11,796 | 3277 | 23.80 | –0.39 | Dominated | 6.3 | 7.1 |
Applying higher incidence rates and longer duration for persistent pain after mid-urethral sling procedures
In this scenario analysis, the impact of incorporating higher incidence rates of persistent pain after MUS procedures and longer mean duration for persistent pain was tested on the base-case results. As would be expected, the probability of retropubic MUS being the most cost-effective with a £20,000 WTP decreases from 26% to 4.2% and the corresponding probability for traditional sling increases from 27% to 30.8%. The estimated ICER for traditional sling is £619 per QALY gained. Open colposuspension is not a dominated strategy and has a 25.8% probability of being cost-effective (Table 23).
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective (%) at WTP threshold (£) | |
|---|---|---|---|---|---|---|---|
| 20,000 | 30,000 | ||||||
| Base-case analysis assuming that incidence rate of persistent pain after retropubic MUS and transobturator MUS are 5.09% and 4.93%, respectively, and average duration of persistent pain is 6 months | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA assuming that incidence rate of persistent pain after retropubic MUS and transobturator MUS are 20% and average duration of persistent pain is 60 months | |||||||
| Retropubic MUS | 8118 | 22.97 | 4.2 | 3.8 | |||
| Traditional sling | 8527 | 409 | 23.63 | 0.66 | 619 | 30.8 | 29.5 |
| Urethral injection therapy | 9560 | 1033 | 23.37 | –0.26 | Dominated | 17.0 | 16.6 |
| Single-incision sling | 9652 | 1125 | 22.90 | –0.72 | Dominated | 2.8 | 2.7 |
| Transobturator MUS | 9683 | 1156 | 22.25 | –1.38 | Dominated | 0.1 | 0.1 |
| Bladder neck needle suspension | 10,130 | 1604 | 23.11 | –0.52 | Dominated | 7.0 | 7.0 |
| Open colposuspension | 10,978 | 2451 | 23.68 | 0.05 | 46,732 | 25.8 | 27.0 |
| Anterior vaginal repair | 11,064 | 86 | 22.89 | –0.79 | Dominated | 3.4 | 3.5 |
| Laparoscopic colposuspension | 11,797 | 819 | 23.32 | –0.36 | Dominated | 9.0 | 9.9 |
Applying different values for short- and long-term cure rates after retropubic mid-urethral sling
When data on long-term cure rates derived from the UK trial248 comparing TVT with Burch colposuspension were applied, the results show that the effectiveness of most of the strategies increased, as women spend more time continent over the modelling time horizon and have lower costs. The probability of retropubic MUS being cost-effective also increased, compared with the base-case analysis. When the data from Song et al. 249 were applied, the findings are broadly similar (Table 24).
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective (%) at WTP threshold (£) | |
|---|---|---|---|---|---|---|---|
| 20,000 | 30,000 | ||||||
| Base-case analysis applying estimated mean values from the meta-analysis for short- and long-term cure rates after retropubic MUS | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA applying values from Ward et al.248 for short- and long-term cure rates after retropubic MUS | |||||||
| Retropubic MUS | 7163 | 24.55 | 45.7 | 43.3 | |||
| Traditional sling | 8493 | 1330 | 24.22 | –0.33 | Dominated | 16.6 | 16.7 |
| Urethral injection therapy | 9418 | 2255 | 23.89 | –0.66 | Dominated | 8.3 | 8.5 |
| Transobturator MUS | 9422 | 2260 | 23.77 | –0.77 | Dominated | 4.2 | 4.3 |
| Single-incision sling | 9429 | 2267 | 23.65 | –0.90 | Dominated | 3.3 | 3.2 |
| Bladder neck needle suspension | 9944 | 2782 | 23.72 | –0.82 | Dominated | 4.6 | 4.9 |
| Anterior vaginal repair | 10,855 | 3692 | 23.58 | –0.97 | Dominated | 3.5 | 3.8 |
| Open colposuspension | 10,878 | 3715 | 24.11 | –0.44 | Dominated | 9.0 | 9.9 |
| Laparoscopic colposuspension | 11,653 | 4490 | 23.86 | –0.69 | Dominated | 4.9 | 5.6 |
| SA applying data from Song et al.249 for short- and long-term cure rates after retropubic MUS | |||||||
| Retropubic MUS | 7394 | 24.49 | 42.1 | 39.9 | |||
| Traditional sling | 8522 | 1128 | 24.22 | –0.27 | Dominated | 19.3 | 19.0 |
| Urethral injection therapy | 9437 | 2043 | 23.90 | –0.59 | Dominated | 8.1 | 8.3 |
| Single-incision sling | 9464 | 2070 | 23.64 | –0.85 | Dominated | 3.1 | 3.2 |
| Transobturator MUS | 9475 | 2080 | 23.77 | –0.72 | Dominated | 4.1 | 4.2 |
| Bladder neck needle suspension | 9979 | 2585 | 23.73 | –0.76 | Dominated | 5.3 | 5.4 |
| Anterior vaginal repair | 10,881 | 3486 | 23.59 | –0.90 | Dominated | 3.6 | 3.9 |
| Open colposuspension | 10,916 | 3522 | 24.11 | –0.38 | Dominated | 9.8 | 10.7 |
| Laparoscopic colposuspension | 11,680 | 4286 | 23.85 | –0.64 | Dominated | 4.6 | 5.3 |
Detailed results from the following sensitivity analyses are reported in Appendix 21, assuming that all of the women in the model have SUI; alternative values for the proportion of women who will seek retreatment after failure of each surgical treatment; applying lower success rate for repeating same surgeries; and incorporating different health utility values and effect of natural decline in health utility over time.
Value-of-information analysis
In addition to assessing the relative effectiveness and cost-effectiveness of the alternative surgical treatments, the economic model was used to quantify the main uncertainties facing decision-makers and to help inform decisions about the direction of future research. This was explored through variants of VOI analysis: expected value of perfect information (EVPI) and expected value of partial perfect information (EVPPI) analysis.
Expected value of perfect information
Decision-makers are interested in understanding the amount of uncertainty associated with a decision and this can be quantified directly from the PSA results. An assessment of the significance of this uncertainty also requires consideration of the consequences associated with uncertainty, in terms of the costs or equivalent health forgone if an incorrect decision is made. The scale and magnitude of these consequences needs to be reflected in the entire population who stand to be affected by a particular decision.
Value-of-information analysis can quantify the expected gain in net benefit from obtaining further information to inform a decision. Quantifying the value of an incorrect decision, alongside the probability of making an incorrect decision, allows us to estimate EVPI. The maximum amount that policy-makers should be willing to invest to reduce uncertainty in the decision can be informed by the EVPI. If the EVPI for a decision problem exceeds the cost of future research, additional investigation may be worthwhile.
As well as determining EVPI around the decision as a whole, VOI approaches can also be used for particular elements of the decision with the purpose of focusing research in areas where the elimination of uncertainty might have the most value. Partial EVPI, or EVPPI, analysis can be used to estimate the expected value of removing uncertainty surrounding specific parameters or groups of parameters to identify where future research should focus on identifying more precise and reliable estimates of specific pieces of information, e.g. relative effectiveness, costs or utilities. EVPI places an upper value on conducting further research overall, whereas EVPPI places an upper value on conducting further research on a specific area of information. On the basis of EVPI and EVPPI calculations, the potential value of a future trial, or other research designs, can be evaluated.
Population EVPI is calculated by multiplying the individual EVPI estimate by the expected number of people who would be affected by the information over the anticipated lifetime of the technology. Population size was calculated based on previous studies. HES data for England show that in 2013–14 around 12,000 women had a MUS operation, with around 500 having another type of continence procedure (colposuspension ≈300, traditional slings ≈200), and just over 700 having periurethral injections (13,200 in total). In Scotland, the total number of surgical procedure for treatment of SUI in the same period was 929. 251 In total, it was assumed that in the UK there are 15,000 surgical treatments conducted annually for the treatment of SUI. Two-level simulations were conducted to estimate the EVPI and EVPPI. The first level occurred within the microsimulation by randomly selecting women aged 45–55 years. Each selected woman was simulated 10,000 times (PSA) and values for the parameters were selected from the prespecified distributions. Results from the PSA were exported to Excel files and then SAVI 2.1.2 (University of Sheffield, Sheffield, UK; http://savi.shef.ac.uk/SAVI/) was used to estimate the EVPI and EVPPI.
The EVPI estimates in Table 25 quantify the expected value to decision-makers in the UK of removing all current decision uncertainty at a threshold of £20,000 per QALY gained. This will enable a comparison to be made with previous analyses, providing an idea of the scale of decision uncertainty in this topic compared with other previous decisions. If the number of people affected by the decision per year is 15,000, then the overall EVPI per year is £167.7M for the UK.
| The expected value of removing all current decision uncertainty | Overall EVPI | |
|---|---|---|
| £ | QALY | |
| Per person affected by the decision | 11,180 | 0.56 |
| Per year in UK assuming 15,000 persons affected per year | 167,700,000 | 8385 |
| > 5 years | 838,500,000 | 41,930 |
| > 10 years | 1,677,000,000 | 83,850 |
| > 15 years | 2,516,000,000 | 125,800 |
| > 20 years | 3,354,000,000 | 167,700 |
When thinking about the overall expected value of removing decision uncertainty, one needs to consider how long the current comparison will remain relevant. If the relevant time horizon is 20 years for the decision, then the overall expected value of removing decision uncertainty for the UK would be £3.345B.
Expected value of partial perfect information results
As mentioned earlier, the value of reducing uncertainty surrounding particular input parameters in the model can also be established by estimating EVPPI. The EVPPI could be used to calculate the maximum value of reducing uncertainty around particular parameters (or groups of parameters), allowing future research to be more specifically targeted at the parameters for which more precise estimates would be most valuable. There are four groups of uncertain parameters considered in the EVPPI analysis. These relate to:
-
health utility values
-
relative treatment effectiveness (cure rates)
-
operation-related mortality rates
-
combinations of parameters associated with all the complications
-
combinations of parameters associated with short-term and persistent pain
-
combinations of parameters associated with short-term and persistent pain and mesh erosion/removal.
Table 26 reports the EVPPI for a number of groups of parameters that were considered to represent groupings that were relevant to both broader policy questions and the actual design of further research. The EVPPI associated with all the complications incidence rates, relative treatment effectiveness, short-term and persistent pain, and health utility values consistently emerge as having significant influence on overall decision uncertainty, having the highest estimate across the different groups of parameters.
| Parameters | Per-person EVPPI per year (£) | EVPPI for UK (£) | |
|---|---|---|---|
| Per year | Over 20 years | ||
| Health utility values | 158 | 2,362,774 | 47,255,488 |
| Operation related mortality rates | 57 | 855,159 | 17,103,176 |
| Relative treatment effectiveness | 1315 | 19,717,921 | 394,358,420 |
| Combinations of parameters associated with all the complications | 3746 | 56,195,710 | 1,123,914,202 |
| Combinations of parameters associated with short-term and persistent pain | 405 | 6,068,657 | 121,373,135 |
| Combinations of parameters associated with short-term and persistent pain and mesh erosion/removal | 1766 | 26,488,639 | 529,772,777 |
Summary of cost-effectiveness and value-of-information analysis
The economic model presented in this report compared nine different strategical treatments for treatment of SUI and stress-predominant MUI. Data from network meta-analyses and standard databases were used to populate the economic model. The model compared cumulative costs and QALYs for a 1-year, 10-year and lifetime time horizon. The results suggest that retropubic MUS is less costly and more effective than all other surgical interventions over a lifetime time horizon; therefore, it is a dominant strategy. The probabilistic results show that retropubic MUS and traditional sling have the highest probabilities of being cost-effective across all WTP thresholds over a lifetime time horizon. Retropubic MUS remains dominant over a 10-year time horizon in the cure model. The only major deviation from these findings is when the time horizon is reduced to 1 year. In this scenario, the most cost-effective surgical intervention is single-incision sling.
Retropubic MUS was the least costly and a cost saving option owing in part to its lower initial cost. This is primarily because this procedure is conducted in a day case setting, and there is less chance of having retropubic MUS after repeat surgery owing to its higher cure rate than all other surgical treatments (except for traditional sling in the cure model). Results also showed that there were relatively small differences between retropubic MUS and traditional sling, in terms of total QALYs, in the cure model. Although the incremental cost-effectiveness estimates showed that retropubic MUS is less costly (£423 less than traditional sling), the probability of being cost-effective with a £20,000 WTP were 25.8% and 27.0% for retropubic MUS and traditional sling, respectively.
A total of 17 individual sensitivity/scenario analyses were carried out on the base-case model results. Traditional sling was a cost-effective option when the following scenarios were explored: assuming that all of the women in the model have SUI; using a linked database to estimate the proportion of women who will seek retreatment after failure of each surgical treatment; assuming lower cure rates when the same surgeries are being conducted for a second or third time; assuming a 10% and 20% incidence rate for mesh complications after retropubic MUS and transobturator MUS; assuming a 10% and 20% incidence rate for persistent pain complication after retropubic MUS and transobturator MUS; assuming lower health utility value for MUI health states; and assuming that the incidence rate of persistent pain after retropubic MUS and transobturator MUS is 20% and that the average duration of persistent pain is 60 months.
Value-of-information analyses were also carried out on the base-case probabilistic results. The EVPI per woman is £11,180. The population EVPI was also estimated based on an assumed 15,000 surgical interventions for SUI in the UK each year. Therefore, the population EVPI for 1 year is £167.7M. This figure increases as the time horizon (or period of time over which the information would be useful) is increased. The cost of future research to remove uncertainty around all model parameters would need to be less than these presented amounts, otherwise it would not be considered an efficient use of resources. EVPPI analyses were also conducted to estimate the value of removing uncertainty around particular parameters/groups of parameters. The largest value appears to be in removing uncertainty around the complications incidence rates, relative treatment effectiveness and health utility values.
Chapter 7 Discussion
Stress urinary incontinence is a common condition that may cause substantial disability and reduce women’s quality of life. 269 The insertion of synthetic mesh tapes has become the most common surgical procedure worldwide for the treatment of SUI in women. 266,270 Mesh tape procedures were initially adopted using a retropubic approach. A transobturator approach has been developed more recently with the aim of reducing the likelihood of damaging the bladder during the operation. A number of RCTs have assessed the use of mesh for the treatment of SUI in women. Recent trials have compared the retropubic approach with the transobturator approach to assess clinical effectiveness and complications. However, long-term data are scarce. In particular, the growing patient-led concern about the safety profile of these procedures has culminated in an international debate with a number of legal cases raised against the companies that manufacture the mesh tapes. The patients’ initial campaign has led to further national campaigns against the use of mesh [e.g. the Scottish Mesh Survivors’ campaign Hear Our Voice (www.scottishmeshsurvivors.com)], recent independent inquiries and an updating of existing clinical guidelines.
An independent review commissioned by the Scottish Government, which considered and analysed administrative data (routinely reported Scottish hospital inpatient data), reported that immediate complications were experienced by 3.7% of women after retropubic mesh procedures, 2.5% of women after transobturator mesh procedures, 7.1% of women after unspecified mesh procedures and 7.8% of women after open colposuspension (non-mesh open surgery). 271 Moreover, mesh procedures were reported to carry a similar risk of being readmitted for repeat surgery or for later complications compared with open colposuspension. The independent review concluded that the management of women with SUI should take place in the context of a multidisciplinary team supported by a quality assurance framework. Women must receive adequate information on all appropriate treatments (mesh and non-mesh) to make informed choices. When surgery involving the use of a synthetic mesh tape is considered, a retropubic approach should be recommended. 271 The findings of the Scottish Independent Review are in line with those of a large Scottish study published in 2017, which assessed a cohort of 13,133 women, identified in the same way as the Independent Review (i.e. from a national hospital admission database). 272 The cohort comprised women who underwent a first single incontinence surgical procedure between April 1997 and March 2016. This cohort study found that, compared with colposuspension, mesh procedures had a lower risk of immediate complications and subsequent prolapse surgery and a similar risk of further incontinence surgery and later complications. 272 The authors concluded that mesh procedures for SUI should be considered among possible surgical options and that further research on longer-term outcomes would be beneficial. Another large study of surgical mesh procedures for SUI (92,244 procedures, including 68,002 unconfounded procedures) published in 2017 investigated the rate of adverse events in NHS England over 8 years. 266 Cases were identified from the HES database. The study reported that 9.8% of women who underwent a surgical mesh procedure for SUI experienced a post-operative complication within 30 days or within 5 years. Perioperative complications and 30-day complications occurred in 2.4% and 1.7% of women, respectively. The proportion of women who required readmission for further mesh surgery within 5 years of the index procedure was 5.9%. The risk of readmission was higher during the first 2 years.
It is worth noting that the results of the two large cohort studies and the Scottish Independent Review mentioned above were all based on administrative data: routinely reported hospital inpatient data. 266,271,272 However, the rate of complications managed in outpatient or primary care settings were not captured by these reports. Moreover, the accuracy of the coding system for national databases and hospital records is known to be less than optimal owing to the lack of specific codes to identify particular complications of interest and the lag (sometimes of a few years) between the introduction of new surgical procedures (e.g. retropubic and TOT procedures) and the introduction of specific codes to identify these procedures.
The NHS England Mesh Oversight Group Report published in July 2017273 concluded that mesh procedures for the treatment of women with SUI are a safe option, though a number of recommendations need to be implemented to ensure better quality of care. These recommendations included improvements to surgical practice and training, updating of clinical guidance and standards, raising awareness of possible post-operative complications among GPs and offering quicker and improved access to clinical expertise for women with post-operative complications. 273 In particular, the Mesh Oversight Group Report stressed the importance of better reporting of adverse events and better HES coding procedures to gain a more complete picture of the level and seriousness of complications after SUI surgery. 273
The recent Consensus Statement of the European Urology Association and the European Urogynaecological Association on the Use of Implanted Materials for Treating Pelvic Organ Prolapse and Stress Urinary Incontinence274 indicates that the use of synthetic MUS procedures for the surgical treatment of SUI has good efficacy and acceptable morbidity. Patients should be adequately informed regarding the potential success rates and the mesh-related adverse events compared with non-mesh procedures and should be engaged in the decision-making process. 274
In general, recent cohort studies, consensus statements from clinical associations, and national inquiries seem to be in agreement that mesh procedures may be effective in the treatment of SUI, but there is uncertainty about long-term outcomes. Post-operative complications, as well as repeat SUI surgery, need to be carefully considered when weighing the benefits and risks of these interventions. In particular, it is worth mentioning that mesh implants with their anchoring system are intended to be permanent; therefore, their removal, if something goes wrong, can be extremely challenging if not impossible.
The NICE guidance on the safety of single-incision short sling mesh insertion for SUI published in October 2016275 maintains that complications including pain, discomfort and failure of the mesh procedure are infrequent but serious. The guidance recommends that patient selection should be performed by a multidisciplinary team with experience in the management of women with SUI and the surgical insertion performed by clinicians with specific training in mesh techniques. Moreover, the NICE clinical guidance on the management of SUI (CG171, updated Nov 2015)276 points out that ‘surgery for UI should be undertaken only by surgeons who have received appropriate training in the management of UI and associated disorders or who work within a multidisciplinary team with this training, and who regularly carry out surgery for UI in women’, and again that ‘when recommending optimal management the multidisciplinary team should take into account women’s preference, past management, comorbidities and treatment options’. NICE is currently updating its clinical guidance on the management of SUI. The new guidance is expected to be released in early 2019.
To our knowledge, the current evidence synthesis, discrete choice experiment and economic evaluation is the most comprehensive assessment of published evidence for the treatment of SUI (a total of 175 studies were included in the effectiveness evidence synthesis). The risk of bias was high or unclear across all risk-of-bias domains in the majority of included studies. The NMA, which combined evidence from direct and indirect comparisons, included 120 studies that reported data on the two primary outcomes: the number of women ‘cured’ from SUI and the number of women who experienced an ‘improvement’ in their SUI symptoms. The NMA results suggest that retropubic MUS, transobturator MUS and traditional sling are more effective than other surgical procedures for both primary outcomes. Open colposuspension also appears relatively effective in terms of cure and improvement rates compared with other surgical procedures. Results for other surgical interventions were variable.
An adequate assessment of adverse events was hampered by the dearth of suitable data and by the inconsistency in the way adverse events were defined and reported in individual studies. Direct head-to-head meta-analyses were available mainly for the comparisons involving retropubic MUS, transobturator MUS or single-incision sling. Follow-up time was generally short (median of 12 months). Transobturator MUS had a higher rate of further SUI procedures than retropubic MUS but a lower rate than single-incision sling.
The rate of tape and mesh exposure was higher after transobturator MUS than after retropubic MUS or single-incision sling, whereas it was similar between transobturator MUS and retropubic MUS. Retropubic MUS had a higher rate of major vascular complications, voiding difficulties and bladder or urethral perforation than transobturator MUS but a lower rate of groin pain. The rate of post-operative pain was higher after retropubic than single-incision sling and the rate of unspecified pain was higher after transobturator MUS than single-incision sling. The rate of infection (including UTI, wound infection and infection related to mesh) was similar between single-incision sling and transobturator MUS.
Our economic model used data from the systematic review and other published sources but was also limited by the lack of availability of robust evidence. The model results suggest that retropubic MUS is the least costly and the most effective option. However, the results from the PSA suggest that the retropubic MUS and traditional sling have comparable probabilities of being cost-effective (26% and 27%, respectively, using a £20,000 threshold). The findings from the model are in general agreement with other published cost-effectiveness findings.
One of the strengths of our economic model is the evaluation of nine different surgical treatments in one analysis, informed by data from a network meta-analyses in which all the direct and indirect evidence (120 trials) was used to estimate the relative effectiveness of different surgical treatments in terms of cure rates. Very few studies have included complications within the cost-effectiveness analyses, despite the fact that the incidence of each complication can have an impact on women’s quality of life and incur costs for the health system. Therefore, in the present study the impact of incident complications, such as infection, de novo symptoms of urgency incontinence, voiding difficulties, bladder or urethral perforation, tape/mesh erosion/extrusion/exposure, short-term pain and persistent pain, on cost and effect have been incorporated into the model and explored in SA. As about 50% of women who have SUI246 are also suffering from UUI symptoms, and given that UUI affects women’s quality of life potentially more than SUI,267 we have incorporated treatment pathways for SUI and UUI at the same time in the model to estimate absolute QALYs more accurately. Finally, the analysis was conducted using best practice methods277 and used a comprehensive range of sensitivity analyses to account for uncertainty. Our conclusions were broadly robust to the range of sensitivity analyses undertaken and comparable to the findings of other published evaluations.
There are a number of published cost-effectiveness analyses evaluating some of the surgeries that we have assessed, the general findings of which are presented to allow comparison. Two studies compared the single-incision sling versus MUS procedures over a 1-year time horizon, concluding that single-incision sling was less costly and of similar effectiveness. 264,278 Another compared the cost-effectiveness of TVT versus vaginoplasty, finding that TVT was a cost-effective option compared with vaginoplasty. 173 A UK study compared the cost-effectiveness of TVT versus open colposuspension, laparoscopic colposuspension, traditional sling and injectable agents, concluding that TVT dominated open colposuspension using a 5-year time horizon. 229 A US study compared the cost-effectiveness of TVT versus open Burch colposuspension, finding over a 10-year horizon that TVT was more cost-effective than open Burch colposuspension. 230 A cost–utility analysis in the UK to assess the cost-effectiveness of TVT compared with open Burch colposuspension found that TVT was less costly and more effective than open Burch colposuspension. 244 A further study to assess cost-effectiveness of TVT versus laparoscopic mesh colposuspension concluded that TVT was more cost-effective than laparoscopic mesh colposuspension over a 1-year time horizon. 279 A study based on US-based parameters compared TVT versus Burch colposuspension, finding that Burch colposuspension was more expensive than TVT but that the resulting ICER (US$98,755 per QALY gained) was above any WTP threshold used in the UK, making TVT the more cost-effective option. 237 Further analysis to assess the cost-effectiveness of collagen versus retropubic suspension, transvaginal suspension and sling procedure found that retropubic suspension was the most cost-effective option (ICER US$1824). 231 Although there are limitations with many of these studies and heterogeneity in methods, the results from all the above studies are largely in agreement with findings from our economic model, generally supporting the finding that retropubic MUS is likely to be the most cost-effective option when compared with the other types of surgeries for treatment of SUI.
However, there are some conflicting findings. Another study to evaluate the cost-effectiveness of MUS (either retropubic or transobturator) versus urethral bulking agents concluded that bulking agents are more cost-effective than MUS over a 1-year time horizon (this was in a population of SUI patients without urethral hypermobility). 225 Another examined the cost-effectiveness of retropubic MUS versus transobturator MUS over a 10-year time horizon and concluded that transobturator MUS is the cost-effective option compared with retropubic MUS. 235 A Canadian study examined the cost-effectiveness of transobturator MUS versus TVT over a 5-year time horizon, with results suggesting that transobturator MUS was more cost-effective than TVT. 137 The results from our model show that retropubic MUS has a slightly lower cost and higher effectiveness than transobturator MUS.
Three separate studies280–282 have investigated the cost-effectiveness of laparoscopic Burch colposuspension versus open Burch colposuspension with a relatively short-term time horizon. Two of these studies280,282 concluded that laparoscopic Burch colposuspension may be more cost-effective than open Burch colposuspension, whereas the third281 showed that laparoscopic colposuspension is not cost-effective when compared with open colposuspension during the first 6 months following surgery, but it may be cost-effective over 24 months.
The results from our study show that open colposuspension is associated with a slightly lower cost and higher effectiveness than is laparoscopic colposuspension. The findings from the model are in general agreement with other published cost-effectiveness findings.
Uncertainty about the assessment
The majority of the evidence for the assessment of the clinical effectiveness came from trials evaluating the effects of retropubic MUS or transobturator MUS. More than half of the included studies compared transobturator MUS with retropubic MUS (58 studies), or transobturator MUS with single-incision sling (39 studies). The majority of trials identified by the updated literature searches seem to focus on transobturator MUS, which is a more recent surgical procedure than retropubic MUS, or single-incision sling. However, few studies were available for other treatment comparisons, particularly mesh versus non-mesh procedures.
The definitions and measurements of cure and improvement were not consistent across included studies. We considered women-reported outcomes to be the best outcomes on which to judge the effectiveness of surgical treatments. However, patient-reported measures were not always available. We therefore opted for proxy measures based on the quantification of symptoms derived from pad or urodynamic tests. This decision was based on the assumption that subjective and objective measures correlate sufficiently, although this assumption could not be empirically tested within the current assessment.
The NMA assessed the primary outcomes of cure and improvement at 12 months or at a time point closest to 12 months. The availability of long-term data beyond 12 months was limited.
Assessment of adverse events was hampered by the lack of suitable data and, in particular, of long-term data. The median follow-up time for all included studies was 12 months.
A further challenge was the lack of consistency in the way adverse events were defined and reported in the published Cochrane systematic reviews. 5–12,18–20 Some of these outcomes were recategorised by Cochrane authors to conduct meta-analyses but outcome definitions and exact time points at which these outcomes were measured were often not explicitly reported. Most studies were reported to have a short follow-up period (up to 12 months), with only a few studies having a follow-up of ≥ 2 years. Inconsistent time points and outcome categories became problematic when we had to analyse and summarise a large number of studies across different Cochrane systematic reviews.
As a result of resource constraints and the inconsistency of reporting across studies, we graded the level of evidence for the two primary outcomes, but not for adverse events.
We focused on the main mesh surgical procedures for the treatment of SUI and did not consider procedure subtypes (e.g. up-down vs. down-up retropubic mesh insertion or inside-out vs. outside-in transobturator mesh insertion). There is a large volume of published literature comparing the different techniques that are available for one type of surgery; however, this was beyond the remit of the question that our work was addressing. It should be noted, however, that there remains uncertainty about the relative effectiveness and cost-effectiveness of these subtypes. In addition, there is likely to be a lack of consistency in their use within the NHS. This decision uncertainty still needs to be addressed through robust evidence collection and analysis.
The professional experience of the surgeons performing the operations was not consistently reported in the included studies and relevant Cochrane systematic reviews. Among studies that provided this information, the surgeon’s clinical experience varied from ‘having inserted a minimum of one sling prior to the study’29 to ‘having performed 200 surgical procedures’. 115 A few studies reported that surgeons tended to be less experienced in performing sling procedures than the comparator surgical intervention. The current NICE guideline on the management of SUI (CG171, updated November 2015)276 states that ‘an annual workload of at least 20 cases of each primary procedure for stress UI is recommended. Surgeons undertaking fewer than 5 cases of any procedure annually should do so only with the support of their clinical governance committee’. However, from current published studies it seems that, at present, there is considerable variation in clinical practice and it is unclear whether or not (and how) the surgeons must demonstrate their ability in performing these operations.
As with all modelling studies, several limitations exist within our study that should be considered when interpreting the results. One of the main limitations of the current study is the lack of long-term data, which necessitated the extrapolation of relatively short-term data to 10 years and over the lifetime of women included in the analyses. The results achieved would only apply in a situation where relative differences in effectiveness of retropubic MUS compared with the comparators do not change with longer follow-up. The long-term incidence of complications after the surgical treatments are currently not reliably known. Therefore, all the estimated incidence rates for complications after each surgical treatment were based on the data from trials with relatively short-term follow-up times. Nevertheless, we tested the impact of possible higher incidence rates of some of the complications on the results. It should be mentioned that a clinical trial is currently being conducted to estimate the 3-year outcome after standard tension-free MUS and single-incision mini-sling procedures. 283 Another limitation of our study is that urethral injection therapy was not included in the NMA; therefore, the short-term and long-term cure rates after urethral injection therapy were obtained from a meta-analysis that reported effectiveness of silicon particles (Macroplastique) for women with SUI (958 women from 23 cohorts were included in the analysis). 250 Furthermore, the economic model has focused on costs to the NHS. It has been assumed that certain costs, such as those for containment products, may be incurred by the NHS. In practice, women may also buy different products and may well incur the costs of containment management themselves. Other costs that may be incurred by women have not been included. These include the other costs of managing symptoms, such as laundry costs, and the time and travel costs related to receiving the treatments. It might be expected that the more effective treatments would reduce the costs of managing symptoms borne by the women and their families. Therefore, we expect that including those costs would probably improve the cost-effectiveness of retropubic MUS. Finally, we had intended to use results from the DCE to inform the economic model. One potential way to have done this would have been to have included cost as an attribute in the DCE, which would have enabled a cost–benefit/net benefit analysis to have been undertaken. However, it was decided at an early stage in the DCE design process that cost would not be an appropriate attribute for inclusion given the hypothetical nature of the DCE and that we were not asking women to choose between different surgical options but rather asking for their preferences regarding outcomes of surgery.
Chapter 8 Conclusions
The following implications for practice and research are based on the results of our evidence synthesis and economic evaluation, the information collected through our DCE and the findings of recent national inquiries, reviews and consensus statements from relevant clinical associations.
Implications for practice
-
The results of this evidence synthesis, although associated with some uncertainty and a lack of long-term data, indicated that cure and improvement rates were generally better for retropubic MUS, transobturator MUS and traditional sling compared with other surgical procedures. Open colposuspension appeared relatively effective in terms of cure and improvement rates compared with other interventions.
-
The current evidence base on long-term safety of mesh and non-mesh procedures is inadequate in quantity and quality.
-
Women should receive adequate information on the benefits and risks associated with the different types of surgical procedures for the treatment of SUI. In particular, women should be aware that mesh implants are intended to be permanent and their removal could be challenging, if not impossible.
Implications for research
-
The main uncertainty relates to the long-term assessment of surgical procedures for SUI. In particular, further evidence is required on long-term adverse effects and quality of life. The long-term assessment of complications and subsequent surgery after mesh and non-mesh procedures would require a large multicentre trial with an extended follow-up period (many years). More realistic would be to promote awareness, as well as adequate reporting and monitoring, of complications among surgeons and health professionals.
-
Studies of quality of life need to address the relationship between different levels of severity of SUI, quality of life and the average duration of each complication’s effects, as well as investigate the multiplicative effect of different complications on quality of life.
-
Further research investigating a woman’s choice regarding surgery as a treatment option needs to explore treatment history in greater detail while considering more individual characteristics, including personal beliefs and perceptions that may act as a barrier to seeking professional advice.
-
Although there is significant uncertainty in many of the parameters informing the modelling, the results from the VOI analysis indicate that further research should focus on adverse events that, although not very frequent, may have devastating effects on women’s quality of life when they do occur (e.g. tape extrusion/exposure). In particular, information on the incidence of complications in both primary and secondary care as well as accurate measures of the spectrum of possible complications and their impact on women’s quality of life would be useful.
-
Future research would be of greater value if investigators could improve the quality of their study reports and agree on common definitions of outcomes and measures for recording outcomes, in accordance with the COMET (Core Outcome Measures in Effectiveness Trials) Initiative (www.comet-initiative.org).
Acknowledgement
The authors are grateful to Lara Kemp and Janice Legge for their secretarial support and patience.
Contributions of authors
Miriam Brazzelli contributed to the co-ordination of all aspects of this assessment, interpreted data, drafted the discussion and conclusions sections and took overall responsibility for the clinical sections of the report.
Mehdi Javanbakht led the review of economic evaluations and the model development, contributed to the interpretation of data and the DCE, undertook the cost-effectiveness and VOI analyses and was responsible for drafting the economic sections of the report.
Mari Imamura led the day-to-day running of the clinical effectiveness review; contributed to protocol development; performed study selection, data extraction, risk-of-bias assessment and synthesis of included studies; provided supervision to junior members of the review team; and was responsible for drafting the clinical effectiveness sections of the report.
Jemma Hudson contributed to data extraction and interpretation of results, conducted all statistical analyses and drafted the methods and results sections of the clinical effectiveness sections of the report.
Eoin Moloney undertook the review of economic evaluations and model development, cost-effectiveness and VOI analysis and contributed to drafting the economic sections of the report.
Frauke Becker led the DCE, undertook the development of the survey and the analysis of the data and was responsible for drafting the DCE section of the report.
Sheila Wallace was responsible for providing further information and details on the existing Cochrane reviews, conducted the updated literature searches, led initial study screening and selection, provided reference management for the clinical effectiveness sections of the report and drafted sections of the report related to search strategies and search results.
Muhammad Imran Omar applied the GRADE approach for evaluating the quality of evidence of the primary outcomes assessed in the NMA and drafted the relevant part of the clinical effectiveness methods section of the report.
Michael Shimonovich contributed to study selection, risk-of-bias assessment and data extraction and to drafting parts of the clinical effectiveness sections of the report.
Graeme MacLennan provided statistical support and double checked all clinical effectiveness results and statistical analyses.
Laura Ternent contributed to the development of the DCE.
Luke Vale provided advice and guidance throughout the project.
Isobel Montgomery contributed a lay perspective to all aspects of the work from proposal to final report and drafted the Plain English summary.
Phil Mackie provided advice and guidance throughout the project.
Lucky Saraswat provided advice and guidance throughout the project.
Ash Monga provided advice and guidance throughout the project.
Dawn Craig was the principal investigator and took overall responsibility for the project, undertook an advisory role in all aspects of the work and contributed to the writing of all sections of the report.
All authors provided comments on draft versions of the report and approved its final version.
Data-sharing statement
Most technical data are included in the report in the appendices or as supplementary material. All additional data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Abrams P, Cardozo L, Khoury S, Wein A. Incontinence: 5th International Conference on Incontinence, Paris February, 2012. Arnhem: International Consultation on Urological Diseases, European Association of Urology; 2013.
- Turner DA, Shaw C, McGrother CW, Dallosso HM, Cooper NJ. MRC Incontinence Team . The cost of clinically significant urinary storage symptoms for community dwelling adults in the UK. BJU Int 2004;93:1246-52. https://doi.org/10.1111/j.1464-410x.2004.04806.x.
- Papanicolaou S, Pons ME, Hampel C, Monz B, Quail D, Schulenburg MGvd, et al. Medical resource utilisation and cost of care for women seeking treatment for urinary incontinence in an outpatient setting. Maturitas 2005;52:S35-47. https://doi.org/10.1016/j.maturitas.2005.09.004.
- Maund E, Guski LS, Gøtzsche PC. Considering benefits and harms of duloxetine for treatment of stress urinary incontinence: a meta-analysis of clinical study reports. CMAJ 2017;189:E194-E203. https://doi.org/10.1503/cmaj.151104.
- Lapitan MCM, Cody JD, Mashayekhi A. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database Syst Rev 2016;2. https://doi.org/10.1002/14651858.CD002912.pub6.
- Freites J, Agur WI, Stewart F, Omar MI. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database Syst Rev 2019.
- Saraswat L, Rehman H, Omar MI, Cody JD, Glazener CMA. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst Rev 2019.
- Ford AA, Rogerson L, Cody JD, Ogah J. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2015;7. https://doi.org/10.1002/14651858.CD006375.pub3.
- Nambiar A, Cody JD, Jeffery ST. Single-incision sling operations for urinary incontinence in women. Cochrane Database Syst Rev 2014;6. https://doi.org/10.1002/14651858.CD008709.pub2.
- Glazener CM, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database Syst Rev 2001;1. https://doi.org/10.1002/14651858.CD001755.
- Glazener CM, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database Syst Rev 2014;12. https://doi.org/10.1002/14651858.CD003636.pub3.
- Kirchin V, Page T, Keegan PE, Atiemo K, Cody JD, McClinton S. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev 2012;2. https://doi.org/10.1002/14651858.CD003881.pub3.
- AUGS-SUFU Joint Position Statement: Mesh Midurethral Slings for Stress Urinary Incontinence. Silver Spring, MD: American Urogynecologic Society; 2014.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Healthcare. York: Centre for Reviews and Dissemination, University of York; 2009.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. London: The Cochrane Collaboration; 2011.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. https://doi.org/10.1016/j.jclinepi.2009.06.005.
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.CD006375.pub2.
- Rehman H, Bezerra CC, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst Rev 2011;1. https://doi.org/10.1002/14651858.CD001754.pub3.
- Dean NM, Ellis G, Wilson PD, Herbison GP. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database Syst Rev 2006;3. https://doi.org/10.1002/14651858.CD002239.pub2.
- Cochrane Incontinence Group . Specialised Register 2018. https://incontinence.cochrane.org/resources/specialised-register (accessed November 2018).
- Bo K, Frawley H, Haylen B, Abramov Y, Almeida F, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and non-pharmacological management of female pelvic floor dysfunction. Neurourol Urodyn 2017;36:221-44. https://doi.org/10.1002/nau.23107.
- Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014;349. https://doi.org/10.1136/bmj.g5630.
- Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach. Updated October 2013. Hamilton, ON: The GRADE working group; 2013.
- Bianchi AH, Jarmy-Di-Bella ZI, Castro RA, Sartori MG, Girao MJ. Randomised trial of TVT-O™ and TVT-S™ for the treatment of stress urinary incontinence. Int Urogynecol J 2012;23:S216-7.
- Darabi Mahboub MR, Keshvari M, Sheikhi Z. Evaluation Study Between Tension-Free Vaginal Tape (TVT) and Transobturator Tape (TOT) in Treatment Stress Incontinence in Female n.d.
- Djehdian L, Araujo M, Takano C, Del Roy C, Castro R, Sartori MGF, et al. Randomised Trial of Ophira Mini-Sling System and Unitape for the Treatment of Stress Incontinence in Women. First Experiences After a Follow-up of 6 Months n.d.
- Lee J, Rosamilia A, Dwyer P, Lim YN, Thomas E, Murray C, et al. Miniarc and Monarc suburethral sling in women with stress urinary incontinence – a randomised controlled trial. Int Urogynecol J 2012;23:S142-4.
- Schweitzer KJ, Cromheecke GJ, Milani AL, van Eijndhoven HW, Gietelink D, Hallenleben E, et al. A randomised controlled trial comparing the TVT-O™ with the Ajust™ as primary surgical treatment of female stress urinary incontinence. Int Urogynecol J 2012;23:S77-8.
- Smith AL, Castillo P, Karp D, Gross C, Davila G, Aguilar VC. Transobturator versus single incision slings in women with stress urinary incontinence: a prospective randomised controlled trial. Int Urogynecol J 2011;22:S54-5.
- Tarcan T, Mangir N, Tanidir Y, Top T, Ilker Y. A Randomised Study Comparing Transvaginal and Transobturator Mid-Urethral Sling Surgeries in Women With STRESS Urinary Incontinence n.d.
- Trabuco E, Klingele C, Blandon R, Occhino J, McGree M, Weaver A, et al. A randomized comparison of incontinence procedures performed concomitantly with abdominal sacrocolpopexy: the Burch versus mid-urethral sling trial. Neurourol Urodyn 2014;33.
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS – a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 2000;10:325-37. https://doi.org/10.1023/A:1008929526011.
- Dias S, Welton NJ, Sutton AJ, Ades AE. NICE DSU Technical Support Document 2: A Generalised Linear Modelling Framework for Pairwise and Network Meta-Analysis of Randomised Controlled Trials. Sheffield: NICE Decision Support Unit; 2016.
- Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. NICE DSU Technical Support Document 4: Inconsistency in Networks of Evidence Based on Randomised Controlled Trials. Sheffield: NICE Decision Support Unit; 2014.
- Mbuagbaw L, Rochwerg B, Jaeschke R, Heels-Andsell D, Alhazzani W, Thabane L, et al. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0473-z.
- Wang W, Zhu L, Lang J. Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. Int J Gynaecol Obstet 2009;104:113-16. https://doi.org/10.1016/j.ijgo.2008.09.013.
- Abouhashem S, Mostafa M, Elbrombely W. Five-years follow-up of tension-free vaginal tape (TVT) versus rectus sheath sling for surgical treatment of female stress urinary incontinence. J Urol 2014;191. https://doi.org/10.1016/j.juro.2014.02.965.
- Adile B, Granese R, Lo Bue A, Gugliotta G, Cardella AM, Adile C. A Prospective Randomized Study Comparing Laparoscopic Burch Versus TVT. Short and Long Term Follow-up n.d.
- Burton G. A randomised comparison of laparoscopic and open colposuspension. Neurourol Urodyn 1994;13:497-8.
- Cervigni M, Natale F, La Penna C, Agostini M, Antomarchi F, Lo Voi R, et al. Surgical correction of stress urinary incontinence associated with pelvic organ prolapse: trans-obturator approach (MONARC) versus retropubic approach (TVT). Neurourol Urodyn 2006;25.
- Choe JH, Lee HD, Park SH, Jo DG, Lee HS, Lee JS, et al. Comparison of postoperative pain after transobturator or retropubic suburethral sling for female stress urinary incontinence: a prospective randomized study. J Endourol 2013;27.
- Dati S, Rombola P, Cappello S, Piccione E. Single-incision minisling (AJUST) vs obturator tension-free vaginal shortened tape (TVT-ABBREVO) in surgical management of female stress urinary incontinence. Int J Gynecol Obstet 2012;119. https://doi.org/10.1016/S0020-7292(12)61622-1.
- de Oliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM, Prior EL. Comparison of retro pubic TVT, pre pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence. Int Urogynecol J 2006;17.
- Diab DE, Zayed AM, Allam MN, Maroof AM, Ibraheem E, El-Sayed DE. A prospective randomized study comparing the safety and efficacy of transobturator tape (TOT) versus tension free vaginal tape (TVT) in treatment of female stress urinary incontinence. Eur Urol Suppl 2012;11. https://doi.org/10.1016/S1569-9056(12)60175-4.
- Drahoradova P, Masata J, Martan A, Svabik K. Comparative Development of Quality of Life Between TVT and Burch Colposuspension n.d.
- El-Din Shawki H, Kamel HH, El-Moghazy DA, El-Adawy AR, Mohammed HF. The role of transobturator vaginal tape (TVT-O) and some traditional surgical interventions in the management of female genuine stress urinary incontinence – randomized controlled trial. Int J Gynecol Obstet 2012;119. https://doi.org/10.1016/S0020-7292(12)60647-X.
- El-Hefnawy A, Abed A, Wadie B. TVT versus TOT: a single-center, prospective randomized study. Urol 2012;80:S142-3.
- Elshawaf H, Al bahaie Y. Randomized Prospective Trial Comparing Burch Colposuspension to Tension Free Vaginal Tape and Transobturator Suburethral Tape Procedures in Treating Female Genuine Stress Urinary Incontinence n.d.
- Enzelsberger H, Cemer I, Kostersitz E, Enzelsberger S. Ophira (Minisling) versus Monarc (TOT) – a prospective randomized study for the treatment of female stress urinary incontinence at a follow-up of 20 months. Int Urogynecol J Pelvic Floor Dysfunct 2011;22:S1835-6.
- Fatthy H, El Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. J Am Assoc Gynecol Laparosc 2001;8:99-106. https://doi.org/10.1016/S1074-3804(05)60557-9.
- Fernandez S, Martinez-Franco E, Lin X, Amat TL. Contasure-needleless compared with Monarc for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2015;26:S84-5.
- Fischer JR, Hale DS, McClellan E, Benson JT. The use of urethral electrodiagnosis to select the method of surgery in women with intrinsic sphincter deficiency. Int Urogynecol J 2001;12.
- Friedman M. TVT-O vs TVT-S: first randomized, prospective, comparative study of intraoperative complications, perioperative morbidity and one year postoperative results. J Pelvic Med Surg 2009;15.
- Halaska M, Kolbl H, Petri E, Danes L, Voigt R, Otcenasek M, et al. Preliminary results of a prospective randomized study comparing Burch colposuspension and tension-free vaginal tape – urodynamic and sexuological aspects. Neurourol Urodyn 2001;20:421-2.
- Hammoud K, Elsheikh M, Haitham M, Fayad A, Ghamrawy H, Aboumohamed A. Tension-free vaginal tape versus transobturator vaginal tape in management of female stress urinary incontinence. Long-term follow-up: which to choose?. Urol 2011;78:S209-10. https://doi.org/10.1016/j.urology.2011.07.627.
- Han WHC. Burch colposuspension or tension-free vaginal tape for female stress urinary incontinence?. Int Urogynecol J 2001;12.
- Kamel A. A Comparison Between TVT &Amp; TVTO As Regards Safety. An African Experience n.d.
- Kim Y, Jung W, Jo SW, Kim WT, Yun SJ, Lee S, et al. Prospective Comparative Study Between the TVT-Secur and TOT Procedures for Treatment of Stress Urinary Incontinence Patients n.d.
- Koelbl H, Halaska M, Ostermann S, Lautenschlaeger C. Burch colposuspension and TVT – perioperative results of a prospective randomized trial in patients with genuine stress incontinence. Neurourol Urodyn 2002;21.
- Leanza V, Dati S, Gasbarro N. A multicenter randomized trial of prepubic and retropubic Leanza-Gasbarro-Caschetto tension-free procedures. Int Urogynecol J 2009;20.
- Lee SH, Kim H, Choo MS, Park CM. Single Incision Mid-Urethral Sling and Tension-Free Vaginal Tape Procedure for the Treatment of Stress Urinary Incontinence: A 12-Month Follow-up Randomized Study n.d.
- Maher C, Qatawneh A, Baessler K, Cropper M, Schluter P. Laparoscopic colposuspension or tension-free vaginal tape for recurrent stress urinary incontinence and/or intrinsic sphincter deficiency – a randomised controlled trial. Neurourol Urodyn 2004;23:433-4.
- Mansoor A, Vedrine N, Darcq C. Surgery of female urinary incontinence using transobturator tape (TOT): a prospective randomised comparative study with TVT. Neurourol Urodyn 2003;22:488-9.
- Melendez Munoz J, Braverman M, Rosamilia A, Young NR, Leitch A, Lee J. TVT Abbrevo and MiniArc suburethral sling in women with stress urinary incontinence-a randomised controlled trial. 6 months results. Int Urogynecol J Pelvic Floor Dysfunct 2016;27:S75-6.
- Merali S, Dolhaniuk C, Unger T. Stress incontinence in women; a pilot study comparing the Miniarc single incision sling system to the Monarc transobturator sling system. J Minim Invasive Gynecol 2012;19:S33-4. https://doi.org/10.1016/j.jmig.2012.08.104.
- Mirosh M, Epp A. TVT Vs Laparoscopic Burch Colposuspension for the Treatment of Stress Urinary Incontinence n.d.
- Morris AR, Reilly ETC, Hassan A, Ramsay IN, Hawthorn RJS. 5-7 year follow-up of a randomised trial comparing laparoscopic colposuspension (LC) and open colposuspension (OC) in the treatment of genuine stress incontinence. Int Urogynecol J 2001;12.
- O’Sullivan S, Avery N, Bailey A, Keane D. The effect of surgery on the collagen metabolism of paraurethral tissue in women with genuine stress incontinence. Int Urogynecol J 2000;11.
- Palomba S, Zullo F. A Comparison in Terms of Efficacy and Safety Between Transobturator and Transvaginal Tape Performed at the Same Time of Anterior Defect Correction With Mesh 2008. http://clinicaltrials.gov/show/NCT00743535 (accessed 22 August 2017).
- Riva D, Sacca V, Tonta A, Casolati E, Luerti M, Banfi G, et al. TVT versus TOT a randomised study at 1-year follow-up. Int Urogynecol J 2006;17.
- Rudnicki M, Jakobsson U, Teleman P, Group SA. One-Year Comparison of an Single Incision Mini Sling and Conventional Midurethral Slings. A Randomized Controlled Study n.d.
- Salem H, Mostafa M, Diab DE, Abdulla A, Nageeb M, Hashem SA. A prospective randomized study comparing the safety and efficacy of transobturator tape (TOT) versus tension free vaginal tape (TVT) in treatment of female stress urinary incontinence. J Urol 2014;191. https://doi.org/10.1016/j.juro.2014.02.964.
- Seo JH, Kim GN, Kim JY, Seo HJ, Lee JW, Lee WG, et al. Comparison between transobturator vaginal tape inside out and single incision sling system in the treatment of female stress urinary incontinence: prospective randomized study. Neurourol Urodyn 2011;30.
- Shawky H, Mahmoud M, Mohammed H, Khalifa E, Mahran A. TVT-secur versus TVT-obturator: A randomized trial of suburethral sling operative procedures for stress urinary incontinence, el Minia experience. Int J Gynecol Obstet 2015;131.
- Stangel-Wojcikiewicz K. Laparoscopic burch colposuspension compared to laparotomy for treatment urinary stress incontinence. Neurourol Urodyn 2008;27.
- Summitt RL, Lucente V, Karram MM, Shull BL, Bent AE. Randomized comparison of laparoscopic and transabdominal burch urethropexy for the treatment of genuine stress incontinence. Obstet Gynecol 2000;95. https://doi.org/10.1016/S0029-7844(00)00572-X.
- Tapp AJS, Hills B, Cardozo L. Randomised study comparing pelvic floor physiotherapy with the Burch colposuspension. Neurourol Urodyn 1989;8:356-7.
- Van Rensburg JA, Jeffery ST, Sand Enbergh HA, Juul L, Steyn DW. Single incision-needleless and inside out TVT-O: a multicentre clinical equivalent randomised trial with preliminary 6 months and one year outcome for stress urine continence. Int Urogynecol J Pelvic Floor Dysfunct 2015;26:S136-7.
- Yoon H, Lee DH, Kim YJ. Early Results of Comparison of Contasure-Needleless® and TOT Outside-In Midurethral Slings n.d.
- Sharifiaghdas F, Mortazavi N. Tension-free vaginal tape and autologous rectus fascia pubovaginal sling for the treatment of urinary stress incontinence: a medium-term follow-up. Med Princ Pract 2008;17:209-14. https://doi.org/10.1159/000117794.
- Albo ME, Richter HE, Brubaker L, Norton P, Kraus SR, Zimmern PE, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med 2007;356:2143-55. https://doi.org/10.1056/NEJMoa070416.
- Aigmüller T, Tammaa A, Tamussino K, Hanzal E, Umek W, Kölle D, et al. Retropubic vs. transobturator tension-free vaginal tape for female stress urinary incontinence: 3-month results of a randomized controlled trial. Int Urogynecol J 2014;25:1023-30. https://doi.org/10.1007/s00192-014-2384-z.
- Aniuliene R. Tension-free vaginal tape versus tension-free vaginal tape obturator (inside-outside) in the surgical treatment of female stress urinary incontinence. Medicina 2009;45:639-43. https://doi.org/10.3390/medicina45080083.
- Ankardal M, Crafoord K, Ekerydh A, Ellstrom M, Franzen K, Olsson JH, et al. Burch Colposuspension by Laparoscopic or Abdominal Approach: Report from a Randomised Study n.d.
- Araco F, Gravante G, Sorge R, Overton J, De Vita D, Sesti F, et al. TVT-O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:917-26. https://doi.org/10.1007/s00192-007-0554-y.
- Barber MD, Weidner AC, Sokol AI, Amundsen CL, Jelovsek JE, Karram MM, et al. Single-incision mini-sling compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol 2012;119:328-37. https://doi.org/10.1097/AOG.0b013e318242a849.
- Bergman A, Ballard CA, Koonings PP. Comparison of three different surgical procedures for genuine stress incontinence: prospective randomized study. Am Jo Obstet Gynecol 1989;160:1102-6. https://doi.org/10.1016/0002-9378(89)90169-5.
- Carey M, Rosamilia A, Dwyer P, Cornish A, Murray C, Ugoni A, et al. Laparoscopic versus open colposuspension: a prospective multicentre randomised single-blind comparison. Neurourol Urodyn 2000;19:389-91.
- Chen HX, Lv JW, Leng J, Li JY, Bo JJ, Huang YR. Efficacy and complications of TVT procedure and TVT-O procedure in treatment of female stress urinary incontinence. [Chinese]. J Shanghai Jiaotong Univ (Med Sci) 2012;32:412-5.
- Gaber ME, Borg T, Samour H, Nawara M, Reda A. Two new mini-slings compared with transobturator tension-free vaginal tape for treatment of stress urinary incontinence: a 1-year follow-up randomized controlled trial. J Obstet Gynaecol Res 2016;42:1773-81. https://doi.org/10.1111/jog.13143.
- Guerrero K, Whareham K, Watkins A, Ismail S, Lucas M, Emery S. A randomised control trial comparing TVT, pelvicol and autologous fascial slings for the management of stress urinary incontinence in women. Neurourol Urodyn 2008;27.
- Kitchener HC, Dunn G, Lawton V, Reid F, Nelson L, Smith AR. COLPO Study Group . Laparoscopic versus open colposuspension – results of a prospective randomised controlled trial. BJOG 2006;113:1007-13. https://doi.org/10.1111/j.1471-0528.2006.01035.x.
- Krofta L, Feyereisl J, Otcenásek M, Velebil P, Kasíková E, Krcmár M. TVT and TVT-O for surgical treatment of primary stress urinary incontinence: prospective randomized trial. Int Urogynecol J 2010;21:141-8. https://doi.org/10.1007/s00192-009-1027-2.
- Labrie J, Berghmans L, Fischer K, Lagro-Janssen A, van der Vaart C. Long-term results of pelvic floor muscle training or midurethral sling surgery for female moderate to severe predominant stress urinary incontinence: a randomised controlled trial. Int Urogynecol J 2012;23:S139-40.
- Laurikainen E, Valpas A, Kivelä A, Kalliola T, Rinne K, Takala T, et al. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol 2007;109:4-11. https://doi.org/10.1097/01.AOG.0000249607.82768.a1.
- Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, et al. Peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:1257-61. https://doi.org/10.1007/s00192-007-0334-8.
- Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Skorupski P. The clinical effectiveness of retropubic (IVS-02) and transobturator (IVS-04) midurethral slings: randomized trial. Eur Urol 2009;56:24-30. https://doi.org/10.1016/j.eururo.2009.02.038.
- Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 2010;362:2066-76. https://doi.org/10.1056/NEJMoa0912658.
- Ward K, Hilton P. United Kingdom and Ireland Tension-free Vaginal Tape Trial Group . Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7355.67.
- Masata J, Svabik K, Hubka P, El Haddad R, Martan A. Randomized trial comparing the safety and peri-operative complications of transobturator introduced tension-free vaginal tape (TVT-O) and single-incision tape with adjustable length and anchoring mechanism (Ajust): three months results. Neurourol Urodyn 2013;32.
- Maher CF, O’Reilly BA, Dwyer PL, Carey MP, Cornish A, Schluter P. Pubovaginal sling versus transurethral Macroplastique for stress urinary incontinence and intrinsic sphincter deficiency: a prospective randomised controlled trial. BJOG 2005;112:797-801. https://doi.org/10.1111/j.1471-0528.2005.00547.x.
- Demirci F, Yucel O. Comparison of pubovaginal sling and burch colposuspension procedures in type I/II genuine stress incontinence. Arch Gynecol Obstet 2001;265:190-4. https://doi.org/10.1007/s004040000159.
- Enzelsberger H, Schalupny J, Heider R, Mayer G. TVT versus TOT – a prospective randomized study for the treatment of female stress urinary incontinence at a follow-up of 1 year [German]. Geburtshilfe Frauenheilkd 2005;65:506-11. https://doi.org/10.1055/s-2005-837654.
- Henriksson L, Ulmsten U. A urodynamic evaluation of the effects of abdominal urethrocystopexy and vaginal sling urethroplasty in women with stress incontinence. Am J Obstet Gynecol 1978;131:77-82. https://doi.org/10.1016/0002-9378(78)90478-7.
- Kondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O, Gotoh M, et al. Efficacy, safety and hospital costs of tension-free vaginal tape and pubovaginal sling in the surgical treatment of stress incontinence. J Obstet Gynaecol Res 2006;32:539-44. https://doi.org/10.1111/j.1447-0756.2006.00469.x.
- Lee KS, Han DH, Choi YS, Yum SH, Song SH, Doo CK, et al. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: 1-year followup. J Urol 2007;177:214-18. https://doi.org/10.1016/j.juro.2006.08.063.
- Liapis A, Bakas P, Creatsas G. Burch colposuspension and tension-free vaginal tape in the management of stress urinary incontinence in women. Eur Urol 2002;41:469-73. https://doi.org/10.1016/S0302-2838(02)00033-7.
- Mundy AR. A trial comparing the Stamey bladder neck suspension procedure with colposuspension for the treatment of stress incontinence. Br J Urol 1983;55:687-90. https://doi.org/10.1111/j.1464-410X.1983.tb03405.x.
- Nerli RB, Kumar AG, Koura A, Prabha V, Alur SB. Transobturator vaginal tape in comparison to tension-free vaginal tape: a prospective trial with a minimum 12 months follow-up. Indian J Urol 2009;25:321-5. https://doi.org/10.4103/0970-1591.56183.
- Athanassopoulos A, Barbalias G. Burch colposuspension versus stamey endoscopic bladder neck suspension: a urodynamic appraisal. Urol Int 1996;56:23-7. https://doi.org/10.1159/000282803.
- Amat I, Tardiu L, Martínez Franco E, Laïlla Vicens JM. Contasure-needleless compared with transobturator-TVT for the treatment of stress urinary incontinence. Int Urogynecol J 2011;22:827-33. https://doi.org/10.1007/s00192-011-1380-9.
- Jurakova M, Huser M, Belkov I, Janku P, Hudecek R, Stourac P, et al. Prospective randomized comparison of the transobturator mid-urethral sling with the single-incision sling among women with stress urinary incontinence: 1-year follow-up study. Int Urogynecol J 2016;27:791-6. https://doi.org/10.1007/s00192-015-2895-2.
- Pastore AL, Palleschi G, Al Salhi Y, Riganelli L, Fuschi A, Autieri D, et al. Evaluation of sexual function and quality of life in women treated for stress urinary incontinence: tension-free transobturator suburethral tape versus single-incision sling. J Womens Health 2016;25:355-9. https://doi.org/10.1089/jwh.2015.5416.
- Xin X, Song Y, Xia Z. A comparison between adjustable single-incision sling and tension-free vaginal tape-obturator in treating stress urinary incontinence. Arch Gynecol Obstet 2016;293:457-63. https://doi.org/10.1007/s00404-015-3949-x.
- Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH. Comparison of three mid-urethral tension-free tapes (TVT, TVT-O, and TVT-Secur) in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J 2011;22:1369-74. https://doi.org/10.1007/s00192-011-1445-9.
- Andonian S, St-Denis B, Lemieux MC, Corcos J. Prospective clinical trial comparing Obtape and DUPS to TVT: one-year safety and efficacy results. Eur Urol 2007;52:245-51. https://doi.org/10.1016/j.eururo.2006.12.035.
- Chen Z, Chen Y, Du GH, Yuan XY, Wu J, Zeng XY, et al. Comparison of three kinds of mid-urethral slings for surgical treatment of female stress urinary incontinence. Urologia 2010;77:37-42. https://doi.org/10.1177/039156031007700106.
- Scheiner DA, Betschart C, Wiederkehr S, Seifert B, Fink D, Perucchini D. Twelve months effect on voiding function of retropubic compared with outside-in and inside-out transobturator midurethral slings. Int Urogynecol J 2012;23:197-206. https://doi.org/10.1007/s00192-011-1543-8.
- Alkady HM, Eid A. Tension-free vaginal tape versus transobturator vaginal tape inside-out for the treatment of female stress urinary incontinence. Med J Cairo Univ 2009;77:317-26.
- Aniuliene R, Aniulis P, Skaudickas D. TVT-Exact and midurethral sling (SLING-IUFT) operative procedures: a randomized study. Open Med 2015;10:311-17. https://doi.org/10.1515/med-2015-0046.
- Barber MD, Kleeman S, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol 2008;111:611-21. https://doi.org/10.1097/AOG.0b013e318162f22e.
- Barry C, Lim YN, Muller R, Hitchins S, Corstiaans A, Foote A, et al. A multi-centre, randomised clinical control trial comparing the retropubic (RP) approach versus the transobturator approach (TO) for tension-free, suburethral sling treatment of urodynamic stress incontinence: the TORP study. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:171-8. https://doi.org/10.1007/s00192-007-0412-y.
- David-Montefiore E, Frobert JL, Grisard-Anaf M, Lienhart J, Bonnet K, Poncelet C, et al. Peri-operative complications and pain after the suburethral sling procedure for urinary stress incontinence: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. Eur Urol 2006;49:133-8. https://doi.org/10.1016/j.eururo.2005.09.019.
- deTayrac R, Deffieux X, Droupy S, Chauveaud-Lambling A, Calvanèse-Benamour L, Fernandez H. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol 2004;190:602-8. https://doi.org/10.1016/j.ajog.2003.09.070.
- Deffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H. Transobturator TVT-O versus retropubic TVT: results of a multicenter randomized controlled trial at 24 months follow-up. Int Urogynecol J 2010;21:1337-45. https://doi.org/10.1007/s00192-010-1196-z.
- El-Hefnawy AS, Wadie BS, El Mekresh M, Nabeeh A, Bazeed MA. TOT for treatment of stress urinary incontinence: how should we assess its equivalence with TVT?. Int Urogynecol J 2010;21:947-53. https://doi.org/10.1007/s00192-010-1138-9.
- Freeman R, Holmes D, Hillard T, Smith P, James M, Sultan A, et al. What patients think: patient-reported outcomes of retropubic versus trans-obturator mid-urethral slings for urodynamic stress incontinence – a multi-centre randomised controlled trial. Int Urogynecol J 2011;22:279-86. https://doi.org/10.1007/s00192-010-1343-6.
- Jakimiuk AJ, Issat T, Fritz-Rdzanek A, Maciejewski T, Rogowski A, Baranowski W. Is there any difference? A prospective, multicenter, randomized, single blinded clinical trial, comparing TVT with TVT-O (POLTOS study) in management of stress urinary incontinence. Short-term outcomes. Pelviperineology 2012;31:5-9.
- Karateke A, Haliloglu B, Cam C, Sakalli M. Comparison of TVT and TVT-O in patients with stress urinary incontinence: short-term cure rates and factors influencing the outcome. A prospective randomised study. Aust N Z J Obstet Gynaecol 2009;49:99-105. https://doi.org/10.1111/j.1479-828X.2009.00957.x.
- Kiliç G, Olgun G, Bilen MA, Orhan A, Dunn B. The comparison of TVT (tension free vaginal tape) and TOT (trans-obturator vaginal tape) in the treatment of the urinary incontinence and literature search. Jinekoloji Ve Obstetrik Dergisi 2007;21:26-31.
- Kim YW, Na YG, Sul CK. Randomized prospective study between pubovaginal sling using SPARC sling system and MONARC sling system for the treatment of female stress urinary incontinence: short term results. Korean J Urol 2005;46:1078-82.
- Liapis A, Bakas P, Giner M, Creatsas G. Tension-free vaginal tape versus tension-free vaginal tape obturator in women with stress urinary incontinence. Gynecol Obstet Invest 2006;62:160-4. https://doi.org/10.1159/000093320.
- Mehdiyev M, Itil IM, Sendag F, Akdemir A, Askar N. Comparing the transvaginal tape (TVT) and transobturator tape (TOT) in stress urinary incontinence for their efficiency and their effects on quality of life. [Turkish]. Turk Jinekoloji Ve Obstetrik Dernegi Dergisi 2010;7:117-24.
- Nyyssönen V, Talvensaari-Mattila A, Santala M. A prospective randomized trial comparing tension-free vaginal tape versus transobturator tape in patients with stress or mixed urinary incontinence: subjective cure rate and satisfaction in median follow-up of 46 months. Scand J Urol 2014;48:309-15. https://doi.org/10.3109/21681805.2013.863802.
- Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol 2007;52:1481-90. https://doi.org/10.1016/j.eururo.2007.04.059.
- Ross S, Robert M, Swaby C, Dederer L, Lier D, Tang S, et al. Transobturator tape compared with tension-free vaginal tape for stress incontinence: a randomized controlled trial. Obstet Gynecol 2009;114:1287-94. https://doi.org/10.1097/AOG.0b013e3181c2a151.
- Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol 2008;112:1253-61. https://doi.org/10.1097/AOG.0b013e31818db391.
- Tanuri AL, Feldner PC, Bella ZI, Castro RA, Sartori MG, Girão MJ. Retropubic and transobturator sling in treatment of stress urinary incontinence. Rev Assoc Med Bras 2010;56:348-54. https://doi.org/10.1590/S0104-42302010000300022.
- Teo R, Moran P, Mayne C, Tincello D. Randomized trial of tension-free vaginal tape and tension-free vaginal tape-obturator for urodynamic stress incontinence in women. J Urol 2011;185:1350-5. https://doi.org/10.1016/j.juro.2010.11.064.
- Wang AC, Lin YH, Tseng LH, Chih SY, Lee CJ. Prospective randomized comparison of transobturator suburethral sling (Monarc) vs suprapubic arc (Sparc) sling procedures for female urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2006;17:439-43. https://doi.org/10.1007/s00192-005-0035-0.
- Wang F, Song Y, Huang H. Prospective randomized trial of TVT and TOT as primary treatment for female stress urinary incontinence with or without pelvic organ prolapse in Southeast China. Arch Gynecol Obstet 2010;281:279-86. https://doi.org/10.1007/s00404-009-1098-9.
- Zhang Z, Zhu L. A Long Term Comparative Study on Efficacy, Quality of Life and Sexual Function Between TVT and TVT-O in Patients of Hypermobility Stress Urinary Incontinence: Prospective Randomized Comparative Trial 2014. www.chictr.org.cn/showproj.aspx?proj=5199 (accessed 22 August 2017).
- Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, et al. One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol 2007;51:1376-82. https://doi.org/10.1016/j.eururo.2006.10.066.
- Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK. Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension-free vaginal tape for stress urinary incontinence. Int J Gynaecol Obstet 2005;91:246-51. https://doi.org/10.1016/j.ijgo.2005.08.023.
- Foote AJ, Maughan V, Carne C. Laparoscopic colposuspension versus vaginal suburethral slingplasty: a randomised prospective trial. Aust N Z J Obstet Gynaecol 2006;46:517-20. https://doi.org/10.1111/j.1479-828X.2006.00652.x.
- Paraiso MF, Walters MD, Karram MM, Barber MD. Laparoscopic Burch colposuspension versus tension-free vaginal tape: a randomized trial. Obstet Gynecol 2004;104:1249-58. https://doi.org/10.1097/01.AOG.0000146290.10472.b3.
- Persson J, Teleman P, Eten-Bergquist C, Wolner-Hanssen P. Cost-analyses based on a prospective, randomised study comparing laparoscopic colposuspension with tension-free vaginal tape procedure. Acta Obstetricia Et Gynecologica Scandinavica 2002;81:1066-73. https://doi.org/10.1034/j.1600-0412.2002.811112.x.
- Ustün Y, Engin-Ustün Y, Güngör M, Tezcan S. Tension-free vaginal tape compared with laparoscopic Burch urethropexy. J Am Assoc Gynecol Laparosc 2003;10:386-9. https://doi.org/10.1016/S1074-3804(05)60268-X.
- Valpas A, Ala-Nissilä S, Tomas E, Nilsson CG. TVT versus laparoscopic mesh colposuspension: 5-year follow-up results of a randomized clinical trial. Int Urogynecol J 2015;26:57-63. https://doi.org/10.1007/s00192-014-2454-2.
- Amaro JL, Yamamoto HA, Kawano PR, Fugita O, Gameiro MOO, Barros G, et al. A prospective randomized trial of autologous fascial sling (AFS) versus tension-free vaginal tape (TVT) for treatment of stress urinary incontinence (SUI). J Urol 2007;177. https://doi.org/10.1016/S0022-5347(18)31661-6.
- Arunkalaivanan AS, Barrington JW. Randomized trial of porcine dermal sling (Pelvicol implant) vs. tension-free vaginal tape (TVT) in the surgical treatment of stress incontinence: a questionnaire-based study. Int Urogynecol J Pelvic Floor Dysfunct 2003;14:17-23. https://doi.org/10.1007/s00192-002-1000-9.
- Basok EK, Yildirim A, Atsu N, Basaran A, Tokuc R. Cadaveric fascia lata versus intravaginal slingplasty for the pubovaginal sling: surgical outcome, overall success and patient satisfaction rates. Urol Int 2008;80:46-51. https://doi.org/10.1159/000111729.
- Song YF, Huang HJ, Xu B, Hao L. Comparative study of tension-free vaginal tape and fascia lata for stress urinary incontinence. Zhonghua Fu Chan Ke Za Zhi 2004;39:658-61.
- Abdelwahab O, Shedid I, Al-Adl AM. Tension-free vaginal tape versus secure tension-free vaginal tape in treatment of female stress urinary incontinence. Current Urol 2010;4:93-8. https://doi.org/10.1159/000253420.
- Andrada Hamer M, Larsson PG, Teleman P, Etén-Bergqvist C, Persson J. Short-term results of a prospective randomized evaluator blinded multicenter study comparing TVT and TVT-Secur. Int Urogynecol J 2011;22:781-7. https://doi.org/10.1007/s00192-011-1381-8.
- Basu M, Duckett J. A randomised trial of a retropubic tension-free vaginal tape versus a mini-sling for stress incontinence. BJOG 2010;117:730-5. https://doi.org/10.1111/j.1471-0528.2010.02513.x.
- Gopinath D, Smith AR, Holland C, Reid FM. Why don’t women participate? A qualitative study on non-participation in a surgical randomised controlled trial. Int Urogynecol J 2013;24:969-75. https://doi.org/10.1007/s00192-012-1967-9.
- Ross S, Tang S, Schulz J, Murphy M, Goncalves J, Kaye S, et al. Single incision device (TVT Secur) versus retropubic tension-free vaginal tape device (TVT) for the management of stress urinary incontinence in women: a randomized clinical trial. BMC Res Notes 2014;7. https://doi.org/10.1186/1756-0500-7-941.
- Wadie BS, Edwan A, Nabeeh AM. Autologous fascial sling vs polypropylene tape at short-term followup: a prospective randomized study. J Urol 2005;174:990-3. https://doi.org/10.1097/01.ju.0000169492.96167.fe.
- Bandarian M, Ghanbari Z, Asgari A. Comparison of transobturator tape (TOT) vs Burch method in treatment of stress urinary incontinence. J Obstet Gynaecol 2011;31:518-20. https://doi.org/10.3109/01443615.2011.578776.
- Sivaslioglu AA, Caliskan E, Dolen I, Haberal A. A randomized comparison of transobturator tape and Burch colposuspension in the treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:1015-19. https://doi.org/10.1007/s00192-006-0279-3.
- Samiee H, Tavoli Z, Ghanbari Z, Poormand GH, Taslimi SH, Eslami B, et al. Treatment of urinary stress incontinence: laparoscopic Burch colposuspension versus transobturator tape procedure. Tehran Univ Med J 2009;67:629-36.
- Al-Azzawi IS. The first Iraqi experience with the rectus fascia sling and transobturator tape for female stress incontinence: a randomised trial. Arab J Urol 2014;12:204-8. https://doi.org/10.1016/j.aju.2014.04.004.
- Silva-Filho AL, Cândido EB, Noronha A, Triginelli SA. Comparative study of autologous pubovaginal sling and synthetic transobturator (TOT) SAFYRE sling in the treatment of stress urinary incontinence. Arch Gynecol Obstet 2006;273:288-92. https://doi.org/10.1007/s00404-005-0083-1.
- Tcherniakovsky M, Fernandes CE, Bezerra CA, Del Roy CA, Wroclawski ER. Comparative results of two techniques to treat stress urinary incontinence: synthetic transobturator and aponeurotic slings. Int Urogynecol J Pelvic Floor Dysfunct 2009;20:961-6. https://doi.org/10.1007/s00192-009-0880-3.
- Masata J, Svabik K, Zvara K, Drahoradova P, El Haddad R, Hubka P, et al. Randomized trial of a comparison of the efficacy of TVT-O and single-incision tape TVT SECUR systems in the treatment of stress urinary incontinent women – 2-year follow-up. Int Urogynecol J 2012;23:1403-12. https://doi.org/10.1007/s00192-012-1662-x.
- Oliveira R, Botelho F, Silva P, Resende A, Silva C, Dinis P, et al. Exploratory study assessing efficacy and complications of TVT-O, TVT-Secur, and Mini-Arc: results at 12-month follow-up. Eur Urol 2011;59:940-4. https://doi.org/10.1016/j.eururo.2011.01.018.
- Sottner O, Halaška M, Vláčil J, Maxová K, Malá I, Krombholz R, et al. A comparison of different types of suburethral slings in the treatment of urinary incontinence in geriatric patients. Ceska Gynekol 2012;77:403-7.
- Enzelsberger H, Cemer I, Enzelsberger S, Schalupny J. MiniArc versus Monarc a prospective randomized study of the treatment of female stress urinary incontinence with a follow-up of 2 years. Geburtshilfe Frauenheilkd 2010;70:499-502. https://doi.org/10.1055/s-0030-1249952.
- Foote A. Randomized prospective study comparing Monarc and Miniarc suburethral slings. J Obstet Gynaecol Res 2015;41:127-31. https://doi.org/10.1111/jog.12493.
- Hinoul P, Vervest HA, den Boon J, Venema PL, Lakeman MM, Milani AL, et al. A randomized, controlled trial comparing an innovative single incision sling with an established transobturator sling to treat female stress urinary incontinence. J Urol 2011;185:1356-62. https://doi.org/10.1016/j.juro.2010.11.083.
- Hota LS, Hanaway K, Hacker MR, Disciullo A, Elkadry E, Dramitinos P, et al. TVT-Secur (Hammock) versus TVT-Obturator: a randomized trial of suburethral sling operative procedures. Female Pelvic Med Reconstr Surg 2012;18:41-5. https://doi.org/10.1097/SPV.0b013e31823bdbcf.
- Mackintosh A. A Pilot, Randomised, Prospective Study of Transobturator Tape Versus Single Incision Sub-Urethral Tape in the Management of Female, Urodynamic Stress Incontinence 2010.
- Maslow K, Gupta C, Klippenstein P, Girouard L. Randomized clinical trial comparing TVT Secur system and trans vaginal obturator tape for the surgical management of stress urinary incontinence. Int Urogynecol J 2014;25:909-14. https://doi.org/10.1007/s00192-013-2312-7.
- Campos M, Palau-Jane M, Castaneda E, Poza JL, Montero F, . Multicentric Comparative Randomized Study of the Single-Incision Sling Ajust© Versus Suburethral Transobturator Slings 2013. http://clinicaltrials.gov/show/NCT01699425 (accessed 22 August 2017).
- Schellart RP, Roovers JPWR. A Prospective Multi-National Randomized Comparison of the Effectiveness and Safety of MiniArc© and Monarc© – MiniMo 2013. www.trialregister.nl/trialreg/admin/rctview.asp?TC=3783 (accessed 22 August 2017).
- Sivaslioglu AA, Unlubilgin E, Aydogmus S, Celen E, Dolen I. A prospective randomized comparison of transobturator tape and tissue fixation system minisling in 80 patient with stress urinary incontinence – 5 year results. J Urol 2012;188:194-9. https://doi.org/10.1016/j.juro.2012.02.2564.
- Tang X, Zhu L, Liang S, Lang J. Outcome and sexual function after transobturator tape procedure versus tension-free vaginal tape SECUR: a randomized controlled trial. Menopause 2014;21:641-5. https://doi.org/10.1097/GME.0000000000000119.
- Tommaselli GA, Di Carlo C, Gargano V, Formisano C, Scala M, Nappi C. Efficacy and safety of TVT-O and TVT-Secur in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J 2010;21:1211-17. https://doi.org/10.1007/s00192-010-1181-6.
- Salari Z, Sohbati S. Comparison Between Result of Trans-Obturator Tape Method and Anterior Vaginal Colporrhaphy in Treatment of Stress Urinary Incontinency 2010. www.irct.ir/searchresult.php?id=9433&number=1 (accessed 22 August 2017).
- Mak JHL, Cheon CW, Liu JYS, Lee TK, Tong WM, Wong THK. Prospective Randomized Controlled Trial Comparing Laparoscopic and Open Colposuspension n.d.
- Su TH, Wang KG, Hsu CY, Wei HJ, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress incontinence. Acta Obstet Gynecol Scand 1997;76:576-82. https://doi.org/10.3109/00016349709024588.
- Tuygun C, Bakirtas H, Eroglu M, Alisir I, Zengin K, Imamoglu A. Comparison of two different surgical approaches in the treatment of stress urinary incontinence: Open and laparoscopic burch colposuspension. Turk Uroloji Dergisi 2006;32:248-53.
- Ustün Y, Engin-Ustün Y, Güngör M, Tezcan S. Randomized comparison of Burch urethropexy procedures concomitant with gynecologic operations. Gynecol Obstet Invest 2005;59:19-23. https://doi.org/10.1159/000080619.
- Enzelsberger H, Helmer H, Schatten C. Comparison of Burch and lyodura sling procedures for repair of unsuccessful incontinence surgery. Obstet Gynecol 1996;88:251-6. https://doi.org/10.1016/0029-7844(96)00193-7.
- Sand PK, Winkler H, Blackhurst DW, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling for treatment of genuine stress incontinence with low-pressure urethra. Am J Obstet Gynecol 2000;182:30-4. https://doi.org/10.1016/S0002-9378(00)70487-X.
- Bergman A, Koonings PP, Ballard CA. Primary stress urinary incontinence and pelvic relaxation: prospective randomized comparison of three different operations. Am J Obstet Gynecol 1989;161:97-101. https://doi.org/10.1016/0002-9378(89)90242-1.
- Gilja I, Puskar D, Mazuran B, Radej M. Comparative analysis of bladder neck suspension using Raz, Burch and transvaginal Burch procedures. A 3-year randomized prospective study. Eur Urol 1998;33:298-302. https://doi.org/10.1159/000019563.
- German KA, Kynaston H, Weight S, Stephenson TP. A prospective randomized trial comparing a modified needle suspension procedure with the vagina/obturator shelf procedure for genuine stress incontinence. Br J Urol 1994;74:188-90. https://doi.org/10.1111/j.1464-410X.1994.tb16584.x.
- Palma PC, Soffiatti SA, Almeida SC, Pinotti JA. Stress urinary incontinence: a comparative study of surgical treatment by the Marshall-Marchetti-Krantz technique with endoscopic suspension of the bladder neck. Second report. Asia Oceania J Obstet Gynaecol 1988;14:31-6. https://doi.org/10.1111/j.1447-0756.1988.tb00069.x.
- Berglund AL, Lalos O. The pre- and postsurgical nursing of women with stress incontinence. J Adv Nurs 1996;23:502-11. https://doi.org/10.1111/j.1365-2648.1996.tb00012.x.
- Colombo M, Vitobello D, Proietti F, Milani R. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. BJOG 2000;107:544-51. https://doi.org/10.1111/j.1471-0528.2000.tb13276.x.
- Holmes DM, Stanton SL, Chamberlain GVP. Randomised trial to compare the colposuspension with the anterior repair in the management of genuine stress incontinence. London: St George’s Hospital; 1985.
- Kammerer-Doak DN, Dorin MH, Rogers RG, Cousin MO. A randomized trial of burch retropubic urethropexy and anterior colporrhaphy for stress urinary incontinence. Obstet Gynecol 1999;93:75-8.
- Liapis A, Pyrgiotis E, Kontoravdis A, Louridas C, Zourlas PA. Genuine stress incontinence: prospective randomized comparison of two operative methods. Eur J Obstet Gynecol Reprod Biol 1996;64:69-72. https://doi.org/10.1016/0301-2115(95)02247-3.
- Sharifiaghdas F, Nasiri M, Mirzaei M, Narouie B. Mini sling (Ophira) versus pubovaginal sling for treatment of stress urinary incontinence: a medium-term follow-up. Prague Med Rep 2015;116:210-18. https://doi.org/10.14712/23362936.2015.60.
- Hilton P. A clinical and urodynamic study comparing the Stamey bladder neck suspension and suburethral sling procedures in the treatment of genuine stress incontinence. Br J Obstet Gynaecol 1989;96:213-20. https://doi.org/10.1111/j.1471-0528.1989.tb01665.x.
- Di Palumbo VS. Four-corner bladder and urethral retropubic suspension versus anterior colporrhaphy in the correction of stress urinary incontinence with urethrocystocele 3-4. Randomized clinical trial. Urogynaecologia Int J 2003;17:57-68. https://doi.org/10.4081/uij.2003.57.
- Liapis AE, Asimiadis V, Loghis CD, Pyrgiotis E, Zourlas PA. A randomized prospective study of three operative methods for genuine stress incontinence. J Gynecol Surg 1996;12:7-14. https://doi.org/10.1089/gyn.1996.12.7.
- El-Barky E, El-Shazly A, El-Wahab OA, Kehinde EO, Al-Hunayan A, Al-Awadi KA. Tension free vaginal tape versus Burch colposuspension for treatment of female stress urinary incontinence. Int Urol Nephrol 2005;37:277-81. https://doi.org/10.1007/s11255-004-6101-6.
- Téllez Martínez-Fornés M, Fernández Pérez C, Fouz López C, Fernández Lucas C, Borrego Hernando J. A three year follow-up of a prospective open randomized trial to compare tension-free vaginal tape with Burch colposuspension for treatment of female stress urinary incontinence. Actas Urol Esp 2009;33:1088-96.
- Wang AC, Chen MC. Comparison of tension-free vaginal taping versus modified Burch colposuspension on urethral obstruction: a randomized controlled trial. Neurourol Urodyn 2003;22:185-90. https://doi.org/10.1002/nau.10092.
- Mostafa A, Agur W, Abdel-All M, Guerrero K, Lim C, Allam M, et al. A multicentre prospective randomised study of single-incision mini-sling (Ajust®) versus tension-free vaginal tape-obturator (TVT-O™) in the management of female stress urinary incontinence: pain profile and short-term outcomes. Eur J Obstet Gynecol Reprod Biol 2012;165:115-21. https://doi.org/10.1016/j.ejogrb.2012.06.022.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. PharmacoEconomics 2008;26:661-77. https://doi.org/10.2165/00019053-200826080-00004.
- Coast J, Flynn TN, Natarajan L, Sproston K, Lewis J, Louviere JJ, et al. Valuing the ICECAP capability index for older people. Soc Sci Med 2008;67:874-82. https://doi.org/10.1016/j.socscimed.2008.05.015.
- Flynn TN, Louviere JJ, Marley AA, Coast J, Peters TJ. Rescaling quality of life values from discrete choice experiments for use as QALYs: a cautionary tale. Popul Health Metr 2008;6. https://doi.org/10.1186/1478-7954-6-6.
- Ryan M, Netten A, Skåtun D, Smith P. Using discrete choice experiments to estimate a preference-based measure of outcome – an application to social care for older people. J Health Econ 2006;25:927-44. https://doi.org/10.1016/j.jhealeco.2006.01.001.
- de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ 2012;21:145-72. https://doi.org/10.1002/hec.1697.
- Ryan M, Bate A, Eastmond CJ, Ludbrook A. Use of discrete choice experiments to elicit preferences. Qual Health Care 2001;10:i55-60. https://doi.org/10.1136/qhc.0100055.
- Ryan M, Gerard K. Using Choice Experiments to Value Health Care Programmes: Current Practice and Future Challenges n.d.
- Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al. Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol Assess 2001;5. https://doi.org/10.3310/hta5050.
- Falagas ME, Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Curr Med Res Opin 2008;24:1719-41. https://doi.org/10.1185/03007990802085692.
- Urinary Incontinence in Women: Management. London: NICE; 2015.
- Rose JM, Bliemer MCJ, Hensher DA, Collins AT. Designing efficient stated choice experiments in the presence of reference alternatives. Transport Res B-Meth 2008;42:395-406. https://doi.org/10.1016/j.trb.2007.09.002.
- Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA/London: Sage; 2005.
- Dwight-Johnson M, Lagomasino IT, Aisenberg E, Hay J. Using conjoint analysis to assess depression treatment preferences among low-income Latinos. Psychiatr Serv 2004;55:934-6. https://doi.org/10.1176/appi.ps.55.8.934.
- Lancsar E, Savage E. Deriving welfare measures from discrete choice experiments: inconsistency between current methods and random utility and welfare theory. Health Econ 2004;13:901-7. https://doi.org/10.1002/hec.870.
- McFadden D. The measurement of urban travel demand. J Pub Econ 1974;3:303-28. https://doi.org/10.1016/0047-2727(74)90003-6.
- Watson V, Porteous T, Ryan M. Survey Mode Effects When Eliciting Public Preferences for Health Care: A Pilot Discrete Choice Experiment Study n.d.
- Basu M, Wise B, Duckett J. A qualitative study of women’s preferences for treatment of pelvic floor disorders. BJOG 2011;118:338-44. https://doi.org/10.1111/j.1471-0528.2010.02786.x.
- Hägglund D, Walker-Engström ML, Larsson G, Leppert J. Reasons why women with long-term urinary incontinence do not seek professional help: a cross-sectional population-based cohort study. Int Urogynecol J Pelvic Floor Dysfunct 2003;14:296-304. https://doi.org/10.1007/s00192-003-1077-9.
- Shaw C, Tansey R, Jackson C, Hyde C, Allan R. Barriers to help seeking in people with urinary symptoms. Fam Pract 2001;18:48-52. https://doi.org/10.1093/fampra/18.1.48.
- Strickland R. Reasons for not seeking care for urinary incontinence in older community-dwelling women: a contemporary review. Urologic Nursing 2014;34. https://doi.org/10.7257/1053-816X.2014.34.2.63.
- Kunkle CM, Hallock JL, Hu X, Blomquist J, Thung SF, Werner EF. Cost utility analysis of urethral bulking agents versus midurethral sling in stress urinary incontinence. Female Pelvic Med Reconstr Surg 2015;21:154-9. https://doi.org/10.1097/SPV.0000000000000173.
- Von Bargen E, Patterson D. Cost utility of the treatment of stress urinary incontinence. Female Pelvic Med Reconstr Surg 2015;21:150-3. https://doi.org/10.1097/SPV.0000000000000159.
- Das Gupta R, Caiado M, Bamber L. An evaluation of the cost-effectiveness of duloxetine as a treatment for women with moderate-to-severe stress urinary incontinence. J Med Econ 2006;9:1-25. https://doi.org/10.3111/200609001025.
- Jacklin P, Duckett J, Renganathan A. Analytic model comparing the cost utility of TVT versus duloxetine in women with urinary stress incontinence. Int Urogynecol J 2010;21:977-84. https://doi.org/10.1007/s00192-010-1132-2.
- Kilonzo M, Vale L, Stearns SC, Grant A, Cody J, Glazener CM, et al. Cost effectiveness of tension-free vaginal tape for the surgical management of female stress incontinence. Int J Technol Assess Health Care 2004;20:455-63. https://doi.org/10.1017/S0266462304001357.
- Laudano MA, Seklehner S, Chughtai B, Lee U, Tyagi R, Kavaler E, et al. Cost-effectiveness analysis of tension-free vaginal tape vs burch colposuspension for female stress urinary incontinence in the USA. BJU Int 2013;112:E151-8. https://doi.org/10.1111/bju.12180.
- Oremus M, Collet JP, Shapiro SH, Penrod J, Corcos J. Surgery versus collagen for female stress urinary incontinence: economic assessment in Ontario and Québec. Can J Urol 2003;10:1934-44.
- Oremus M, Tarride JE. An economic evaluation of surgery versus collagen injection for the treatment of female stress urinary incontinence. Can J Urol 2010;17:5087-93.
- Richardson ML, Sokol ER. A cost-effectiveness analysis of conservative versus surgical management for the initial treatment of stress urinary incontinence. Am J Obstet Gynecol 2014;211. https://doi.org/10.1016/j.ajog.2014.07.006.
- Sand PK, Owens GM, Black EJ, Anderson LH, Martinson MS. Cost effectiveness of radiofrequency microremodeling for stress urinary incontinence. Int Urogynecol J 2014;25:517-23. https://doi.org/10.1007/s00192-013-2230-8.
- Seklehner S, Laudano MA, Te AE, Kaplan SA, Chughtai B, Lee RK. A cost-effectiveness analysis of retropubic midurethral sling versus transobturator midurethral sling for female stress urinary incontinence. Neurourol Urodyn 2014;33:1186-92. https://doi.org/10.1002/nau.22483.
- Weber AM, Walters MD. Burch procedure compared with sling for stress urinary incontinence: a decision analysis. Obstet Gynecol 2000;96:867-73. https://doi.org/10.1097/00006250-200012000-00001.
- Wu JM, Visco AG, Weidner AC, Myers ER. Is Burch colposuspension ever cost-effective compared with tension-free vaginal tape for stress incontinence?. Am J Obst Gynecol 2007;197. https://doi.org/10.1016/j.ajog.2007.02.039.
- Holtzer-Goor KM, Gaultney JG, van Houten P, Wagg AS, Huygens SA, Nielen MM, et al. Cost-effectiveness of including a nurse specialist in the treatment of urinary incontinence in primary care in the Netherlands. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0138225.
- Weber AM, Walters MD. Cost-effectiveness of urodynamic testing before surgery for women with pelvic organ prolapse and stress urinary incontinence. Am J Obstet Gynecol 2000;183:1338-46. https://doi.org/10.1067/mob.2000.111251.
- Weber AM, Taylor RJ, Wei JT, Lemack G, Piedmonte MR, Walters MD. The cost-effectiveness of preoperative testing (basic office assessment vs. urodynamics) for stress urinary incontinence in women. BJU Int 2002;89:356-63. https://doi.org/10.1046/j.1464-4096.2001.01687.x.
- Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J, et al. Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14400.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275-83. https://doi.org/10.1136/bmj.313.7052.275.
- Guide to the methods of technology appraisal 2013 (PMG9). London: NICE; 2013.
- Manca A, Sculpher MJ, Ward K, Hilton P. A cost-utility analysis of tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence. BJOG 2003;110:255-62.
- Haywood KL, Garratt AM, Lall R, Smith JF, Lamb SE. EuroQol EQ-5D and condition-specific measures of health outcome in women with urinary incontinence: reliability, validity and responsiveness. Qual Life Res 2008;17:475-83. https://doi.org/10.1007/s11136-008-9311-z.
- Hunskaar S, Lose G, Sykes D, Voss S. The prevalence of urinary incontinence in women in four European countries. BJU Int 2004;93:324-30. https://doi.org/10.1111/j.1464-410X.2003.04609.x.
- Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ 2014;348. https://doi.org/10.1136/bmj.f7450.
- Ward KL, Hilton P. UK and Ireland TVT Trial Group . Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG 2008;115:226-33. https://doi.org/10.1111/j.1471-0528.2007.01548.x.
- Song PH, Kwon DH, Ko YH, Jung HC. The long-term outcomes of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence: data from minimum 13 years of follow-up. Low Urin Tract Symptoms 2017;9:10-4. https://doi.org/10.1111/luts.12099.
- Ghoniem GM, Miller CJ. A systematic review and meta-analysis of Macroplastique for treating female stress urinary incontinence. Int Urogynecol J 2013;24:27-36. https://doi.org/10.1007/s00192-012-1825-9.
- Morling J, Wood R. Using Routinely Available Health Data to Examine the Provision Of, and Outcomes Following, Surgery for SUI and POP in Scotland: Technical Report n.d. www.gov.scot/Publications/2015/10/8485/downloads (accessed November 2017).
- Kociszewski J, Majkusiak W, Pomian A, Tomasik P, Horosz E, Kuszka A, et al. The outcome of repeated mid urethral sling in SUI treatment after vaginal excisions of primary failed sling: preliminary study. Biomed Res Int 2016;2016. https://doi.org/10.1155/2016/1242061.
- Black NA, Downs SH. The effectiveness of surgery for stress incontinence in women: a systematic review. Br J Urol 1996;78:497-510. https://doi.org/10.1046/j.1464-410X.1996.01422.x.
- Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open 2011;1. https://doi.org/10.1136/bmjopen-2011-000206.
- Latimer NR. Survival analysis for economic evaluations alongside clinical trials – extrapolation with patient-level data: inconsistencies, limitations, and a practical guide. Med Decis Making 2013;33:743-54. https://doi.org/10.1177/0272989X12472398.
- Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al. Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence. Health Technol Assess 2003;7. https://doi.org/10.3310/hta7210.
- Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, et al. Female stress urinary incontinence clinical guidelines panel summary report on surgical management of female stress urinary incontinence. The American Urological Association. J Urol 1997;158:875-80. https://doi.org/10.1016/S0022-5347(01)64346-5.
- Lee H-E, Oh S-J. The effectiveness of bladder training in overactive bladder. Curr Bladder Dysfunct Rep 2014;9:63-70. https://doi.org/10.1007/s11884-013-0217-4.
- Urinary Incontinence in Women: The Management of Urinary Incontinence in Women. London: Royal College of Obstetricians and Gynaecologists; 2013.
- Sand PK, Heesakkers J, Kraus SR, Carlsson M, Guan Z, Berriman S. Long-term safety, tolerability and efficacy of fesoterodine in subjects with overactive bladder symptoms stratified by age: pooled analysis of two open-label extension studies. Drugs Aging 2012;29:119-31. https://doi.org/10.2165/11597970-000000000-00000.
- Reference Costs 2015–2016. London: DHSC; 2016.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: PSSRU, University of Kent; 2016.
- Medicines Complete . British National Formulary n.d. https://about.medicinescomplete.com (accessed May 2017).
- Boyers D, Kilonzo M, Mostafa A, Abdel-Fattah M. Comparison of an adjustable anchored single-incision mini-sling, Ajust®, with a standard mid-urethral sling, TVT-O(TM): a health economic evaluation. BJU Int 2013;112:1169-77. https://doi.org/10.1111/bju.12388.
- Shepherd JP, Lowder JL, Jones KA, Smith KJ. Retropubic and transobturator midurethral slings: a decision analysis to compare outcomes including efficacy and complications. Int Urogynecol J 2010;21:787-93. https://doi.org/10.1007/s00192-010-1121-5.
- Keltie K, Elneil S, Monga A, Patrick H, Powell J, Campbell B, et al. Complications following vaginal mesh procedures for stress urinary incontinence: an 8 year study of 92,246 women. Sci Rep 2017;7. https://doi.org/10.1038/s41598-017-11821-w.
- Tincello D, Sculpher M, Tunn R, Quail D, van der Vaart H, Falconer C, et al. Patient characteristics impacting health state index scores, measured by the EQ-5D of females with stress urinary incontinence symptoms. Value Health 2010;13:112-18. https://doi.org/10.1111/j.1524-4733.2009.00599.x.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: University of York, Centre for Health Economics; 1999.
- Norton P, Brubaker L. Urinary incontinence in women. Lancet 2006;367:57-6. https://doi.org/10.1016/S0140-6736(06)67925-7.
- Gibson W, Wagg A. Are older women more likely to receive surgical treatment for stress urinary incontinence since the introduction of the mid-urethral sling? An examination of Hospital Episode Statistics data. BJOG 2016;123:1386-92. https://doi.org/10.1111/1471-0528.13338.
- Scottish Independent Review of the Use, Safety and Efficacy of Transvaginal Mesh Implants in the Treatment of Stress Urinary Incontinence and Pelvic Organ Prolapse in Women: Final Report, March 2017. Edinburgh: Scottish Government; 2017.
- Morling JR, McAllister DA, Agur W, Fischbacher CM, Glazener CM, Guerrero K, et al. Adverse events after first, single, mesh and non-mesh surgical procedures for stress urinary incontinence and pelvic organ prolapse in Scotland, 1997–2016: a population-based cohort study. Lancet 2017;389:629-40. https://doi.org/10.1016/S0140-6736(16)32572-7.
- Mesh Oversight Group Report. Leeds: NHS England; 2017.
- Chapple CR, Cruz F, Deffieux X, Milani AL, Arlandis S, Artibani W, et al. Consensus statement of the European Urology Association and the European Urogynaecological Association on the use of implanted materials for treating pelvic organ prolapse and stress urinary incontinence. Eur Urol 2017;72:424-31. https://doi.org/10.1016/j.eururo.2017.03.048.
- Single-incision Short Sling Mesh Insertion for Stress Urinary Incontinence in Women. Interventional Procedures Guidance [IPG566]. London: NICE; 2016.
- Urinary Incontinence in Women: Management. London: NICE; 2013.
- Caro JJ, Briggs AH, Siebert U, Kuntz KM. ISPOR-SMDM Modeling Good Research Practices Task Force . Modeling good research practices – overview: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force – 1. Value Health 2012;15:796-803. https://doi.org/10.1016/j.jval.2012.06.012.
- Costantini E, Lazzeri M, Bini V, Zucchi A, Scarponi E, Porena M. Managing female urinary incontinence: a regional prospective analysis of cost-utility ratios (curs) and effectiveness. Arch Ital Urol Androl 2014;86:112-17. https://doi.org/10.4081/aiua.2014.2.112.
- Valpas A, Rissanen P, Kujansuu E, Nilsson CG. A cost-effectiveness analysis of tension-free vaginal tape versus laparoscopic mesh colposuspension for primary female stress incontinence. Acta Obstet Gynecol Scand 2006;85:1485-90. https://doi.org/10.1080/00016340601033584.
- Loveridge K, Malouf A, Kennedy C, Edgington A, Lam A. Laparoscopic colposuspension. Surg Endosc 1997;11:762-5. https://doi.org/10.1007/s004649900445.
- Dumville JC, Manca A, Kitchener HC, Smith AR, Nelson L, Torgerson DJ. COLPO Study Group . Cost-effectiveness analysis of open colposuspension versus laparoscopic colposuspension in the treatment of urodynamic stress incontinence. BJOG 2006;113:1014-22. https://doi.org/10.1111/j.1471-0528.2006.01036.x.
- Kung RC, Lie K, Lee P, Drutz HP. The cost-effectiveness of laparoscopic versus abdominal Burch procedures in women with urinary stress incontinence. J Am Assoc Gynecol Laparosc 1996;3:537-44. https://doi.org/10.1016/S1074-3804(05)80164-1.
- Abdel-Fattah M, MacLennan G, Kilonzo M, Assassa RP, McCormick K, Davidson T, et al. The SIMS trial: adjustable anchored single-incision mini-slings versus standard tension-free midurethral slings in the surgical management of female stress urinary incontinence. A study protocol for a pragmatic, multicentre, non-inferiority randomised controlled trial. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015111.
- Helmy H, El-Gamal S. Three-Year Continence Rates, Satisfaction and Adverse Events of Burch Urethropexy and Fascial Sling Surgery for Urinary Incontinence n.d.
- Wang WY, Zhu L, Lang JH, Sun ZJ, Hai N. [Clinical study on tension-free vaginal tape and tension-free vaginal tape obturator for surgical treatment of severe stress urinary incontinence] [Chinese]. Chin J Obstet Gynecol 2008;43:180-4.
- Pushkar DI, Kasian GR, Gvozdev MI, Lynova IL, Kupriianov IA. [Mini-invasive operations for correction of urinary incontinence in females] [Russian]. Urologiia n.d.:16-20.
- Karmakar D, Mostafa A, Abdel-Fattah M. A new validated score for detecting patient-reported success on postoperative ICIQ-SF: a novel two-stage analysis from two large RCT cohorts. Int Urogynecol J 2017;28:95-100. https://doi.org/10.1007/s00192-016-3070-0.
- Borstad E, Abdelnoor M, Mogimi K, Sandved M, Majida M, Western K, et al. Surgery for concomitant pelvic organ prolapse and urinary stress incontinence. A multicenter prospective randomized trial to compare the results of an incontinence procedure performed at the time of prolapse repair or 3 months after. Neurourol Urodyn 2008;27.
- Colombo M, Maggioni A, Scalambrino S, Vitobello D, Milani R. Surgery for genitourinary prolapse and stress incontinence: a randomized trial of posterior pubourethral ligament plication and Pereyra suspension. Am J Obstet Gynecol 1997;176:337-43. https://doi.org/10.1016/S0002-9378(97)70495-2.
- Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, et al. Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 2005;65:898-904. https://doi.org/10.1016/j.urology.2004.11.054.
- Kim J, Baek U, Kwon S, Jung H, Moon K, Park T, et al. The Efficacy of Iris Procedure in Stress Urinary Incontinence: Comparison With TVT and SPARC n.d.
- Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Okholm B, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence. Urol Int 1986;41:129-32. https://doi.org/10.1159/000281181.
- Lee PE, Kung RC, Drutz HP. Periurethral autologous fat injection as treatment for female stress urinary incontinence: a randomized double-blind controlled trial. J Urol 2001;165:153-8. https://doi.org/10.1097/00005392-200101000-00037.
- Miranda V, Alarab M, Murphy K, Pineda R, Drutz H, Lovatsis D. Randomized controlled trial of cystocele plication risks: a pilot study. J Obstet Gynaecol Can 2011;33:1146-9.
- Okulu E, Kayigil O, Aldemir M, Onen E. Use of three types of synthetic mesh material in sling surgery: a prospective randomized clinical trial evaluating effectiveness and complications. Scand J Urol 2013;47:217-24. https://doi.org/10.3109/00365599.2012.733962.
- Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU Int 2003;92:964-8. https://doi.org/10.1111/j.1464-410X.2003.04519.x.
- Quadri G, Scalambrino S, Boisio N, Marchesin R, Milani R. Randomized surgery for incontinence and prolapse: retropubic colposuspension versus anterior repair. Arch Gynecol 1985;237.
- Teixeira M, Pinto AR, Montalvao M, Candoso B. Systemic and Local Inflammatory Response in Collagen Versus Polypropylene Tapes for Stress Urinary Incontinence: Is There Any Difference? n.d.
- Teleb M, Salem EA, Naguib M, Kamel M, Hasan U, Elfayoumi AR, et al. Evaluation of transvaginal slings using different materials in the management of female stress urinary incontinence. Arab J Urol 2011;9:283-7. https://doi.org/10.1016/j.aju.2011.10.011.
- ter Meulen PH, Berghmans LC, Nieman FH, van Kerrebroeck PE. Effects of Macroplastique® Implantation System for stress urinary incontinence and urethral hypermobility in women. Int Urogynecol J 2009;20:177-83. https://doi.org/10.1007/s00192-008-0741-5.
- Tincello DG, Mayne CJ, Toozs-Hobson P, Slack M. Randomised Controlled Trial of Colposuspension Versus Anterior Repair Plus TVT for Urodynamic Stress Incontinence With Anterior Vaginal Prolapse: Proposal (Abstract) n.d.
- van der Ploeg JM, van der Steen A, Oude Rengerink K, van der Vaart CH, Roovers J. Multicentre randomised trial of vaginal prolapse repair versus vaginal prolapse repair with a midurethral sling in patients with pelvic organ prolapse and co-existing stress urinary incontinence. Neurourol Urodyn 2013;32.
- van Leijsen SA, Kluivers KB, Mol BW, Hout Ji, Milani AL, Roovers JP, et al. Value of urodynamics before stress urinary incontinence surgery: a randomized controlled trial. Obstet Gynecol 2013;121:999-1008. https://doi.org/10.1097/AOG.0b013e31828c68e3.
- Zargham M, Alizadeh F, Tadayyon F, Khorrami M-H, Nouri-Mahdavi K, Gharaati MR, et al. Concomitant surgical correction of severe stress urinary incontinence and anterior vaginal wall prolapse by anterior vaginal wall wrap: 18-month outcomes. J Res Med Sci 2013;18:588-93.
- Campeau L, Tu LM, Lemieux M, Naud A, Karsenty G, Schick E, et al. A multicenter, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn 2007;26:990-4. https://doi.org/10.1002/nau.20440.
- Caremel R, Tu LM, Baker K, Adli OEY, Loutochin O, Corcos J. A multicentric randomized controlled study comparing surgical and pharmacological therapy to treat mixed urinary incontinence. J Urol 2013;189. https://doi.org/10.1016/j.juro.2013.02.2271.
- Choi SJ, Kim YH, Choi SH, Ki WS, Kim SA, Jung H. A prospective study of transobturator tension free tape (TOT) and laparoscopic Burch operation for stress urinary incontinence. Int Urogynecol J 2006;17.
- Grigoriadis C, Bakas P, Derpapas A, Creatsa M, Liapis A. Tension-free vaginal tape obturator versus Ajust adjustable single incision sling procedure in women with urodynamic stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol 2013;170:563-6. https://doi.org/10.1016/j.ejogrb.2013.07.041.
- Larsson P, Tegerstedt G. Bulkamid Treatment of Stress Incontinence in Women With Urinary Stress Incontinence and Not Suitable to TVT-Procedure. A Prospective Randomized Study n.d.
- Nikas I, Koundouri MRA, Gavriil I, Kilbasanis I. Management of cystocele with associated urine incontinence in menopausal women. Maturitas 2012;71. https://doi.org/10.1016/S0378-5122(12)70307-9.
- Rose A, Ju M, Rehme C, Rubben H. Skeletal Muscle-Derived Cell Implantation in Female Patients With Stress Urinary Incontinence: A Multicenter, Randomized, Parallel-Group, Placebo-Controlled Clinical Study n.d.
- Sung VW, Wallace D. Effects of Surgical Treatment Enhanced With Exercise for Mixed Urinary Incontinence (ESTEEM) 2013. http://clinicaltrials.gov/show/NCT01959347 (accessed 20 August 2017).
- Tuncer M, Tarhan F, Kafkasli A, Demir K, Yucetas U, Faydaci G, et al. The effects of stress incontinence surgery on sexual function and life quality of women. Arch Ital Urol Androl 2016;88:106-10. https://doi.org/10.4081/aiua.2016.2.106.
- Wadie B, Taha D, Elhefnawy A, Gaballah M. Combined MUS and Anterior Colporrhaphy Versus MUS Alone in the Treatment of SUI, Randomized Controlled Trial n.d.
- Abdel-Fattah M. Adjustable Anchored Single-Incision Mini-Slings Versus Standard Tension-Free Mid-Urethral Slings in the Surgical Management of Female Stress Urinary Incontinence: A Pragmatic Multicentre Non-Inferiority Randomised Controlled Trial 2014. http://isrctn.org/ISRCTN93264234 (accessed 20 August 2017).
- Boyd K. Laparoscopic Treatment for Female Urinary Incontinence 2004. http://isrctn.org/ISRCTN44339585 (accessed 9 June 2004).
- Cardozo L, Rufford J. Comparative Study of the Efficacy, Acceptability, Morbidity and Cost-Effectiveness of the ’Tension Free Vaginal Tape’ and the Periurethral Injection of Collagen in the Management of Recurrent Stress Incontinence 2002.
- Carr LK, De Ridder D, Magali R, Carlson K, Quinlan D, Steele SS, et al. A Double-Blind, Randomized, Placebo-Controlled Study Evaluating the Safety and Effectiveness of Cook MyoSite Incorporated AMDC in Female Patients With Stress Urinary Incontinence 2011. http://clinicaltrials.gov/show/NCT01382602 (accessed 20 August 2017).
- Cavkaytar S, Aksakal SO, Kokanali MK, Topcu HO, Doganay M. Prospective Randomized Study Comparing TVT and TOT in Female Stress Urinary Incontinence With No Intrinsic Sphincter Deficiency 2013. http://clinicaltrials.gov/show/NCT01903590 (accessed 20 August 2017).
- Courtney-Watson C. Comparison of Two Surgical Methods for Curing Stress Incontinence (Recurrent) 2002.
- Ding J, Zhu L. Explore the Efficacy and Safety of Single-Center Randomized Controlled Polypropylene Mesh Auxiliary Plus Adipose-Derived Mesenchymal Stem Cells in the Treatment of Pelvic Organ Prolapse 2015. www.chictr.org.cn/showproj.aspx?proj=10516 (accessed 20 August 2017).
- Elsokkary M. Modified Needleless Single-Incision Mini-Sling Compared to Standard Trans-Obturator Mid-Urethral Sling in the Surgical Management of Female Stress Urinary Incontinence 2016. www.pactr.org/ATMWeb/appmanager/atm/atmregistry?dar=true&tNo=PACTR201607001696163 (accessed 20 August 2017).
- Fu Q, Lv J. Prospective Randomized Comparison of the Transobturator Mid-Urethral Sling With the Single-Incision Sling (Needleless) Among Women With Stress Urinary Incontinence: 1-Year Follow-up Study 2016. www.chictr.org.cn/showproj.aspx?proj=13532 (accessed 20 August 2017).
- Hilton P. A Prospective Randomised Comparative Trial of a Tension-Free Vaginal Tape (TVT) and Fascial Sling Procedure for ‘Secondary’ Genuine Stress Incontinence 2002.
- Innovation (Innovacell Biotechnologie AG) . A Multicenter, Randomized, Double-Blinded, Parallel-Group, Placebo Controlled Study to Assess the Efficacy and Safety of Skeletal Muscle-Derived Cell Implantation in Female Patients With Stress Urinary Incontinence 2010. www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2010-021871-10 (accessed 20 August 2017).
- Itkonen A-M. TVT Versus Bulkamid®-Injections in Treatment of Stress Urinary Incontinence – Patient Satisfaction and Complications of the Treatment 2015. https://clinicaltrials.gov/show/NCT02538991 (accessed 20 August 2017).
- Kaufman M. A Double-Blind, Randomized, Controlled Trial Comparing the Safety and Efficacy of AMDC-USR With Placebo in Female Subjects With Stress Urinary Incontinence 2013. http://clinicaltrials.gov/show/NCT01893138 (accessed 20 August 2017).
- Leitch A, Ow LL, Rosamilia A. Objective Cure Rate of Mini Sling or Retropubic Sling in Women With Intrinsic Sphincter Deficiency – A RCT Study (Mini RISD) 2016. www.anzctr.org.au/ACTRN12616000328471.aspx (accessed 20 August 2017).
- Maslow KD. Randomized Clinical Trial Comparing Mini-Arc Precise Pro and the Trans Vaginal Obturator Tape for Surgical Management of Stress Urinary Incontinence 2013. http://clinicaltrials.gov/show/NCT01799122 (accessed 20 August 2017).
- Oliveira E. Transobturator Sling Compared With Single-Incision Mini-Sling for the Treatment of Stress Urinary Incontinence: A Randomized Controlled Trial 2013. https://clinicaltrials.gov/show/NCT02540525 (accessed 20 August 2017).
- Reda A, Gomaa I. Retropubic Single Incision Minisling Versus Tension Free Vaginal Tape for Management of Stress Urinary Incontinence 2014. http://clinicaltrials.gov/show/NCT02263534 (accessed 20 August 2017).
- Saaid HA. Surgical Management of Mixed Urinary Incontinence 2008. https://clinicaltrials.gov/show/NCT03085979 (accessed 20 August 2017).
- Shen W, Fu J. Single-Incision Mini-Slings Versus Standard Midurethral Slings in Surgical Management of Female Stress Urinary Incontinence: A Prospective Randomized Controlled Trial to Evaluate the Efficacy and Safety 2015. www.chictr.org.cn/showproj.aspx?proj=10638 (accessed 20 August 2017).
- SUITE (Innovacell Biotechnologie AG) . Skeletal Muscle-Derived Cell Implantation in Female Patients With Stress Urinary Incontinence: A Multicenter, Randomized, Parallel-Group, Placebo-Controlled Clinical Study – SUITE Study 2009. www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2009-011797-15 (accessed 15 March 2017).
- Sweed MS. Trans-Obturator Tape, Tension-Free Vaginal Tape and Burch Colposuspension for Treatment of Female Mixed Urinary Incontinence: A Randomized Clinical Trial 2016. https://clinicaltrials.gov/show/NCT02775526 (accessed 20 August 2017).
- Zhu L, Tian Q. A Multi-Center, Randomized, Controlled Clinical Trial of the Safety and Efficacy of Regen Sling Treatment for Female Patients With Stress Urinary Incontinence 2014. http://clinicaltrials.gov/show/NCT02106299 (accessed 20 August 2017).
- Zhu L, Sun Z-J. A RCT of TVT-O and TVT-S in the Treatment of Stress Urinary Incontinence 2015. www.chictr.org.cn/showproj.aspx?proj=11725 (accessed 20 August 2017).
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 1997.
Appendix 1 Literature search strategies
To bring the searches for all reviews up to date, a search of the Cochrane Incontinence Group Specialised Trials Register was performed (date of last search: 8 June 2017) containing trials identified, at that time, from:
-
CENTRAL (via CRSO) (searched 15 May 2017)
-
MEDLINE (via OvidSP) (1946 to April Week 3 2017) (searched 1 May 2017)
-
MEDLINE In-Process & Other Non-Indexed Citations (via OvidSP) covering 28 April 2017 (searched 1 May 2017)
-
MEDLINE Epub Ahead of Print (via OvidSP) (covering 2 May 2017) (searched 3 May 2017)
-
ClinicalTrials.gov via CRS standalone (searched 29 May 2017)
-
WHO ICTRP (searched 6 June 2017).
Trials were identified by searching the Cochrane Incontinence Group Specialised Register using the terms given below. For each review, searches were tailored to bring the searching up to date, that is, searching was designed to retrieve any potentially relevant reports of studies added to the register since the date of the last search for each Cochrane review.
-
Lapitan et al. 5 – open retropubic colposuspension for UI in women
-
Ford et al. 8 and Ogah et al. 18 – MUS operations for SUI in women
-
Nambiar et al. 9 – single-incision sling operations for UI in women
-
Saraswat et al. 7 and Rehman et al. 19 – traditional suburethral sling operations for UI in women
-
Freites et al. 6 and Dean et al. 20 – laparoscopic colposuspension for UI in women
-
Glazener and Cooper11 – bladder neck needle suspension for UI in women
-
Glazener and Cooper10 – anterior vaginal repair for UI in women
-
Kirchin et al. 12 – urethral injection therapy for UI in women.
Search terms used for each review
All searches were of the keyword field in Reference Manager Professional Edition Version 12 (Thomson ResearchSoft, San Francisco, CA, USA) using the Cochrane Incontinence Group’s own keywords.
Lapitan et al.:5 open retropubic colposuspension for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND ({intvent.surg.abdo.} OR {intvent.surg.abdo.burch.} OR {intvent.surg.abdo.colposusp.} OR {intvent.surg.abdo.mmk.} OR {intvent.surg.burch.} OR {intvent.surg.colpo*} OR {intvent.surg.endopelvicFasciaPlication.})
Freites et al.6 and Dean et al.:20 laparoscopic colposuspension for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND39
Ford et al.8 and Ogah et al.:18 mid-urethral sling operations for stress urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND {INTVENT.SURG.SLIN*} OR {INTVENT.SURG.SUBURETHRAL SLING.} OR {INTVENT.SURG.ABDO.SLING.}
Saraswat et al.7 and Rehman et al.:19 traditional suburethral sling operations for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND ({INTVENT.SURG.SLIN*} OR {INTVENT.SURG.SUBURETHRAL SLING.} OR {INTVENT.SURG.ABDO.SLING.})
Glazener and Cooper:11 bladder neck needle suspension for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND ({intvent.surg.bladnecsusp.*} OR {intvent.surg.needle.*})
Nambiar et al.:9 single-incision sling operations for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND {INTVENT.SURG.SLINGS.MINISLING*}
Glazener and Cooper:10 anterior vaginal repair for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND ({INTVENT.SURG.} OR {INTVENT.SURG.ABDO.*} OR {INTVENT.SURG.ASSESS.} OR {INTVENT.SURG.colpofixation.staple.} OR {INTVENT.SURG.COLPORRHAPHY.ANTERIOR.} OR {INTVENT.SURG.CYSTOPLASTY.} OR {INTVENT.SURG.DIATHERMY.} OR {intvent.surg.endopelvicFasciaPlication.} OR {INTVENT.SURG.KELLY.} OR {INTVENT.SURG.PARVAGINALdefectrepair.} OR {INTVENT.SURG.PELVICFLOORREPAIR.} OR {INTVENT.SURG.PEREYRA*} OR {INTVENT.SURG.PERINEAL*} OR {INTVENT.SURG.RAMIREZ.} OR {INTVENT.SURG.RAZ.} OR {INTVENT.SURG.STAPLING.} OR {INTVENT.SURG.SUSPENSION.URETHRAL.} OR {INTVENT.SURG.URETHROCYSTOPEXY.ABDO.} OR {INTVENT.SURG.URETHROPEXY.MODPEREYRA.} OR {INTVENT.SURG.VAGINAL/PERINEAL.} OR {INTVENT.SURG.VAGINAL/PERINEAL.ANTERIOR REPAIR} OR {INTVENT.SURG.VAGINAL/PERINEAL.COLPORRHAPHY} OR {INTVENT.SURG.VAGINAL/PERINEAL.MICROWAVE})
Kirchin et al.:12 urethral injection therapy for urinary incontinence in women
Search terms used
topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND (INTVENT.SURG.INJECTIONS*)
Appendix 2 Data extraction forms
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| ID | |||
| Source Cochrane Review | |||
| Study name | |||
| Abstract or full-text publication | |||
| Study setting | |||
| Recruitment period | |||
| Follow-up (months) | |||
| Funding source | |||
| Intervention category (e.g. retropubic MUS) | |||
| Name of surgical procedure (e.g. tension-free vaginal tape) | |||
| Note | |||
| Number randomised | |||
| Number analysed | |||
| Number and reasons for loss to follow-up | |||
| Note | |||
| Number of surgeons involved | |||
| Surgeon experience | |||
| Inclusion criteria | |||
| Exclusion criteria | |||
| Type of stress incontinence diagnosis (e.g. symptom based or urodynamics) | |||
| UI status (e.g. stress-predominant MUI) | |||
| % MUI | |||
| Note | |||
| Age (mean, SD) | |||
| % women with previous UI surgery | |||
| % women with existing POP | |||
| % women with concurrent POP surgery | |||
| For ongoing trials only | |||
| Trial registration number | |||
| Trial start date | |||
| Trial end date | |||
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| ID | |||
| Study name | |||
| Intervention category | |||
| Outcome | |||
| Description (e.g. definition, how measured) | |||
| Time (months) | |||
| Event n | |||
| Total n | |||
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| ID | |||
| Study name | |||
| Intervention category | |||
| Outcome | |||
| Description (e.g. definition, how measured) | |||
| Time (months) | |||
| Event n | |||
| Mean | |||
| SD | |||
| Total n | |||
| ID | Judgement (low, high, unclear risk) | Support for judgement |
|---|---|---|
| Study name | ||
| Random sequence generation (selection bias) | ||
| Allocation concealment (selection bias) | ||
| Blinding of participants and personnel (performance bias) | ||
| Blinding of outcome assessor (detection bias) (patient-reported outcomes) | ||
| Blinding of outcome assessor (detection bias) (clinician-assessed outcomes) | ||
| Incomplete outcome data (attrition bias) (patient-reported outcomes) | ||
| Incomplete outcome data (attrition bias) (clinician-assessed outcomes) | ||
| Selective outcome reporting (reporting bias) | ||
| Other bias |
Appendix 3 WinBUGS code for network meta-analysis
Appendix 4 The PRISMA diagram for the clinical effectiveness assessment
Appendix 5 References to studies included in the clinical effectiveness review
This appendix includes two lists of included studies:
-
Included studies identified from the eight Cochrane systematic reviews of surgery for UI. Listed by Cochrane review in which they first appear (following the following hierarchy to avoid duplicates).
-
– Lapitan et al. 5 – open retropubic colposuspension for UI in women
-
– Ford et al. 8 and Ogah et al. 18 – MUS operations for SUI in women
-
– Nambiar et al. 9 – single-incision sling operations for UI in women
-
– Saraswat et al. 7 and Rehman et al. 19 – traditional suburethral sling operations for UI in women
-
– Freites et al. 6 and Dean et al. 20 – laparoscopic colposuspension for UI in women
-
– Glazener and Cooper11 – bladder neck needle suspension for UI in women
-
– Glazener and Cooper10 – anterior vaginal repair for UI in women
-
– Kirchin et al. 12 – urethral injection therapy for UI in women.
-
-
New studies from the updated searches of the Cochrane Incontinence Group Specialised Register.
a Primary reference where more than one report of a study was available; this is the name given to the study as it appears in the main text of the ESTER report.
b Report from a more recent update of another of the Cochrane surgery for UI reviews.
c New further report of study found in updated search.
NoteAny relevant study and reference identifiers (IDs) are included in square brackets following each citation, e.g. [database: identifier].
Identifiers containing ‘sr-incont’ relate to the Cochrane Incontinence Specialised Register; ‘CRSREF’ identifiers refer to the Cochrane Register of Studies Web version (CRS-Web); ‘other’ is used to refer to either the study acronym or the trial registration number from a number of trial registries; ‘Ref ID’ identifiers relate to those records being processed for inclusion in the Cochrane Incontinence Specialised Register.
1. Studies identified from the eight Cochrane systematic reviews of surgery for urinary incontinence
(i) Cochrane review: Lapitan et al.5 – open retropubic colposuspension for UI in women
Albo 200782
Albo M, Wruck L, Baker J, Brubaker L, Chai T, Dandreo KJ, et al. , for the Urinary Incontinence Treatment Network. The relationships among measures of incontinence severity in women undergoing surgery for stress urinary incontinence. J Urol 2007;177:1810–14. [Other: sr-incont23120]
aAlbo ME, Richter HE, Brubaker L, Norton P, Kraus SR, Zimmern PE, et al. , for the Urinary Incontinence Treatment Network. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med 2007;356:2143–55. [Other: sr-incont23077]
Brubaker L, Barber MD, Nygaard I, Nager CW, Varner E, Schaffer J, et al. Quantification of vaginal support: are continuous summary scores better than POPQ stage? Am J Obstet Gynecol 2010;203:512–16. [Other: NCT00065845; other: sr-incont40592]
bBrubaker L, Chiang S, Zyczynski H, Norton P, Kalinoski DL, Stoddard A, et al. The impact of stress incontinence surgery on female sexual function. Am J Obstet Gynecol 2009;200:562.e1-7. [CRSREF: 2843674; other: sr-incont31130]
Brubaker L, Richter HE, Norton PA, Albo M, Zyczynski HM, Chai TC, et al. 5-year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence. J Urol 2012;187:1324–30. [Other: NCT00064662; other: TrialID.SISTEr.; other: sr-incont44723]
bBrubaker L, Rickey L, Xu Y, Markland A, Lemack G, Ghetti C, et al. Symptoms of combined prolapse and urinary incontinence in large surgical cohorts. Obstet Gynecol 2010;115:310–16. [CRSREF: 2843676; other: sr-incont39373]
bBrubaker L, Stoddard A, Richter H, Zimmern P, Moalli P, Kraus SR, et al. Mixed incontinence: comparing definitions in women having stress incontinence surgery. Neurourol Urodyn 2009;28:268–73. [CRSREF: 2843677; other: 31415]
Brubaker L. Five year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence. Eur Urol Suppl 2012;11:e172. [Other: NCT00064662; other: TrialID.SISTEr.; other: sr-incont62253]
Bump RC, Brubaker LT, Fine PL, Norton PA, Chancellor MB, Zyczynski H, et al. Randomised clinical trial of Burch vs. sling procedure for stress urinary incontinence (known as SISTEr trial). CRISP database 2002. [Other: sr-incont17205]
Burgio KL, Brubaker L, Richter HE, Wai CY, Litman HJ, France DB, et al. Patient satisfaction with stress incontinence surgery. Neurourol Urodyn 2010;29:1403–9. [Other: sr-incont40322]
Chai T, Albo M, Richter H, Norton P, Dandreo K, Kenton K, et al. Adverse Events from a Randomized Trial for the Surgical Treatment of Stress Urinary Incontinence. Proceedings of the International Continence Society (ICS), 37th Annual Meeting, Rotterdam, 20–24 August 2007, abstract no. 512. [Other: sr-incont23535]
Chai TC, Albo ME, Richter HE, Norton PA, Dandreo KJ, Kenton K, et al. Complications in women undergoing Burch colposuspension versus autologous rectus fascial sling for stress urinary incontinence. J Urol 2009;181:2192–7. [Other: sr-incont31150]
Diokno AC, Richter HE, Kenton K, Norton P, Albo M, Kraus S, et al. Risk factors associated with failure of surgical treatment for stress urinary incontinence at 24 months follow-up. Neurourol Urodyn 2007;26:745. [Other: sr-incont23533]
FitzGerald MP, Burgio KL, Borello-France DF, Menefee SA, Schaffer J, Kraus S, et al. Pelvic-floor strength in women with incontinence as assessed by the Brink scale. Phys Ther 2007;87:1316–24. [Other: sr-incont23825]
Kenton K, Tennstedt S, Litman H, Zimmern P, Getti C, Kusek JW, et al. Improvement in Quality of life in Women at Two Years after Undergoing the Burch Colposuspension or Fascial Sling Procedure. Proceedings of the International Continence Society (ICS), 38th Annual Meeting, Cairo, 20–24 October 2008, abstract no. 206. [Other: sr-incont31863]
bKirby AC, Nager CW, Litman HJ, FitzGerald MP, Kraus S, Norton P, et al. Preoperative voiding detrusor pressures and stress incontinence surgery outcomes. Neurourol Urodyn 2010;29:860–2. [Other: sr-incont40122]
bKirby AC, Nager CW, Litman HJ, FitzGerald MP, Kraus S, Norton P, et al. Preoperative voiding detrusor pressures do not predict stress incontinence surgery outcomes. Int Urogynecol J 2011;22:657–63. [CRSREF: 2843685; other: sr-incont41732]
Kraus SR, Lemack GE, Sirls LT, Chai TC, Brubaker L, Albo M, et al. Urodynamic changes associated with successful stress urinary incontinence surgery: is a little tension a good thing? Urology 2011;78:1257–62. [Other: sr-incont42989]
Kraus SR, Markland A, Chai TC, Stoddard A, FitzGerald MP, Leng W, et al. Race and ethnicity do not contribute to differences in preoperative urinary incontinence severity or symptom bother in women who undergo stress incontinence surgery. Am J Obstet Gynecol 2007;197:92–6. [Other: sr-incont23802]
Lemack G, Krauss S, Litman H, FitzGerald M, Chai T, Nager C, et al. Preoperative urodynamic testing does not predict postoperative voiding dysfunction among women undergoing surgery for SUI: results from a prospective randomized trial comparing Burch versus pubovaginal sling. Neurourol Urodyn 2008;27:123. [Other: sr-incont26919]
bLemack G, Litman H, Nager C, Brubaker L, Lowder J, Norton P, et al. Pre-operative clinical, demographic and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence. Neurourol Urodyn 2012;31:215. [CRSREF: 2843689; other: sr-incont62279]
bLemack GE, Krauss S, Litman H, FitzGerald MP, Chai T, Nager C, et al. Normal preoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. J Urol 2008;180:2076–80. [CRSREF: 2843690; other: sr-incont27705]
bLemack GE, Litman HJ, Nager C, Brubaker L, Lowder J, Norton P, et al. Preoperative clinical, demographic, and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence. Int Urogynecol J 2013;24:269–74. [CRSREF: 2843691; other: sr-incont47045]
Lemack GE, Xu Y, Brubaker L, Nager C, Chai T, Moalli P, et al, for the Urinary Incontinence Treatment Network. Clinical and demographic factors associated with valsalva leak point pressure among women undergoing Burch bladder neck suspension or autologous rectus fascial sling procedures. Neurourol Urodyn 2007;26:392–6. [Other: sr-incont23233]
bMallett VT, Brubaker L, Stoddard AM, Borello-France D, Tennstedt S, Hall L, et al. The expectations of patients who undergo surgery for stress incontinence. Am J Obstet Gynecol 2008;198:308.e1-6. [CRSREF: 2843693; other:sr-incont27182]
Markland AD, Kraus SR, Richter HE, Nager CW, Kenton K, Kerr L, et al. Prevalence and risk factors of fecal incontinence in women undergoing stress incontinence surgery. Am J Obstet Gynecol 2007;197:662–7. [Other: sr-incont26334]
Nager C, Chai T, FitzGerald M, Lemack G, Kraus S, Sirls L, et al. , for the Urinary Incontinence Treatment Network. Valsalva leak point pressure and detrusor overactivity do not predict, but urodynamic stress incontinence does predict continence outcomes after Burch or pubovaginal sling procedures. Neurourol Urodyn 2007;26:709–11. [Other: sr-incont23532]
bNager C, Kraus S, Zyczynski H, Chai T, Lloyd K, FitzGerald M, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in women. J Pelvic Med Surg 2007;13:230–3. [CRSREF: 2843696; other: sr-incont34198]
bNager CW, Albo ME, FitzGerald MP, McDermott S, Wruck L, Kraus S, et al. Reference urodynamic values for stress incontinent women. Neurourol Urodyn 2007;26:333–40. [CRSREF: 2843697; other: sr-incont23232]
bNager CW, Albo ME, FitzGerald MP, McDermott SM, Kraus S, Richter HE, et al. Process for development of multicenter urodynamic studies. Urology 2007;69:63–7; discussion 67–8. [CRSREF: 2843698; other: sr-incont23195]
bNager CW, FitzGerald M, Kraus SR, Chai TC, Zyczynski H, Sirls L, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in selected women. J Urol 2008;179:1470–4. [CRSREF: 2843699; other: sr-incont27210]
Nygaard I, Brubaker L, Chai TC, Markland AD, Menefee SA, Sirls L, et al. Risk factors for urinary tract infection following incontinence surgery. Int Urogynecol J 2011;22:1255–65. [Other: sr-incont42698]
bRichter H, Goode P, Brubaker L, Zyczynski H, Stoddard A, Dandreo K, et al. Two-year outcomes after surgery for stress urinary incontinence in older versus younger women. Neurourol Urodyn 2008;27:682–3. [CRSREF: 2843701; other: sr-incont31854]
Richter HE, Brubaker L, Stoddard AM, Xu Y, Zyczynski HM, Norton P, et al. Patient related factors associated with long-term urinary continence after Burch colposuspension and pubovaginal fascial sling surgeries. J Urol 2012;188:485–9. [Other: NCT00064662; other: sr-incont45162]
Richter HE, Burgio KL, Brubaker L, Moalli PA, Markland AD, Mallet V, et al. , Urinary Inc. Factors associated with incontinence frequency in a surgical cohort of stress incontinent women. Am J Obstet Gynecol 2005;193:2088–93. [Other: sr-incont21231]
Richter HE, Diokno A, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. J Urol 2008;179:1024–30. [Other: sr-incont27213]
bRichter HE, Diokno AC, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. J Pelvic Med Surg 2007;13:227–8. [CRSREF: 2843705; other: sr-incont34197]
bRichter HE, Goode PS, Brubaker L, Zyczynski H, Stoddard AM, Dandreo KJ, et al. Two-year outcomes after surgery for stress urinary incontinence in older compared with younger women. Obstet Gynecol 2008;112:621–9. [CRSREF: 2843706; other: sr-incont29193]
Richter HE, Kenton K, Huang L, Nygaard I, Kraus S, Whitcomb E, et al. The impact of obesity on urinary incontinence symptoms, severity, urodynamic characteristics and quality of life. J Urol 2010;183:622–8. [Other: NCT00064662; other: NCT00325039; other: sr-incont49290]
bRickey LM, Huang L, Rahn DD, Hsu Y, Litman HJ, Mueller ER. Risk factors for urgency incontinence in women undergoing stress urinary incontinence surgery. Adv Urol 2013;2013:567375. [CRSREF: 2843708; other: sr-incont50474]
Steers WD. Randomized Clinical Trial of the Burch Modified Tanagho and Autologous Fascia Sling Procedures for Women with Predominantly Stress Urinary Incontinence. 2002. Trial registration number: NCT00064662. URL: http://clinicaltrials.gov/show/NCT00064662 (accessed 20 August 2017). [Other: NCT00064662; other: sr-incont49815]
Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstet Gynecol 2008;111:899–907. [Other: sr-incont27122]
Subak LL, Goode PS, Brubaker L, Kusek JW, Schembri M, Lukacz ES, et al. Urinary incontinence management costs are reduced following Burch or sling surgery for stress incontinence. Am J Obstet Gynecol 2014;211:171–7. [Other: NCT00064662; other: sr-incont62600]
Tennstedt S, Borello-France D, FitzGerlad MP, Goode P, Kraus S, Kusek J, et al. Identification of Factors Related to Health-related Quality of Life in women with stress urinary incontinence that may improve with surgical treatment. Proceedings of the International Continence Society (ICS), 35th Annual Meeting, Montreal, QC, 28 August to 2 September 2005, abstract no. 321. [Other: sr-incont21098]
Tennstedt S, for the Urinary Incontinence Treatment Network. Design of the Stress Incontinence Surgical Treatment Efficacy Trial (SISTEr). Urology 2005;66:1213–17. [Other: sr-incont21530]
bTennstedt SL, FitzGerald MP, Nager CW, Xu Y, Zimmern P, Kraus S, et al. Quality of life in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:543–9. [CRSREF: 2843714; other: sr-incont30914]
bTennstedt SL, Litman HJ, Zimmern P, Ghetti C, Kusek JW, Nager CW, et al. Quality of life after surgery for stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:1631–8. [CRSREF: 2843715; other: sr-incont31221]
Walsh LP, Zimmern PE, Pope N, Shariat SF, Urinary Incontinence Treatment Network. Comparison of the Q-tip test and voiding cystourethrogram to assess urethral hypermobility among women enrolled in a randomized clinical trial of surgery for stress urinary incontinence. J Urol 2006;176:646–9, discussion 650. [Other: sr-incont22387]
Zimmern P, for the Urinary Incontinence Treatment Network. Design of the SISTEr (Stress Incontinence Surgical Treatment Efficacy Trial) Study: A randomized surgical trial comparing Burch colposuspension and the autologous rectus fascia sling. A clinical trial of the NIH/NIDDK Urinary Incontinence Treatment Network (UITN). Prog Urol 2004;14(Suppl. 3):26. [Other: sr-incont19780]
Zimmern P, Nager CW, Albo M, FitzGerald MP, McDermott S, for the Urinary Incontinence Treatment Network (UITN). Interrater reliability of filling cystometrogram interpretation in a multicenter study. J Urol 2006;175:2174–7. [Other: sr-incont22424]
bZimmern P, Tennstedt S, Dickinson T, Dandreo K. Lessons learned from a patient burden survey following a large randomized controlled trial for the surgical management of stress urinary incontinence in women. Neurourol Urodyn 2009;28:770–1. [CRSREF: 2843718; other: 20805; other: sr-incont39356]
bZimmern PE, Dandreo KJ, Sirls L, Howell A, Hall L, Gruss J, et al. Lessons from a patient experience survey in a randomized surgical trial of treatment of stress urinary incontinence in women. Int Urogynecol J 2011;22:1273–8. [CRSREF: 2843720; other: sr-incont42697]
cBrubaker L, Litman HJ, Kim HY, Zimmern P, Dyer K, Kusek JW, et al. Missing data frequency and correlates in two randomized surgical trials for urinary incontinence in women. Int Urogynecol J 2015;26:1155–9. [Ref ID: 68159]
cKirby AC, Nager CW, Litman HJ, FitzGerlad MP, Kraus S, Norton P, et al. Perineal surface electromyography to measure urethral and pelvic floor activity does not typically demonstrate expected relaxation during normal voiding. J Pelvic Med Surg 2010;16(Suppl. 2):S80–S81. [Ref ID: 63670]
cLitman H, Kraus S, Lemack G, Chai T, Sirls L, Lloyd K, et al. Use of propensity scores to combine data from two similar clinical trials in the urinary incontinence treatment network. Clin Trials 2013;10(Suppl. 1):S54. [Other: sr-incont62162]
cZimmern P, Litman HJ, Nager CW, Lemack GE, Richter HE, Sirls L, et al. Effect of aging on storage and voiding function in women with stress predominant urinary incontinence. J Urol 2014;192:464–8. [Ref ID: 62543]
cZimmern PE, Gormley EA, Stoddard AM, Lukacz ES, Sirls L, Brubaker L, et al. Management of recurrent stress urinary incontinence after burch and sling procedures. [Review]. Neurourol Urodyn 2016;35:344–8. [Ref ID: 74150]
cZyczynski HM, Albo ME, Goldman HB, Wai CY, Sirls LT, Brubaker L, et al. Change in overactive bladder symptoms after surgery for stress urinary incontinence in women. Obstet Gynecol 2015;126:423–30. [Ref ID: 70333]
cZyczynski HM, Sirls LT, Greer WJ, Rahn DD, Casiano E, Norton P, et al. Findings of universal cystoscopy at incontinence surgery and their sequelae. Am J Obstet Gynecol 2014;210:480–8. [Ref ID: 62040]
Ankardal 200185
aAnkardal M, Crafoord K, Ekerydh A, Ellstrom M, Franzen K, Olsson J-H, et al. Burch Colposuspension by Laparoscopic or Abdominal Approach: Report from a Randomised Study. Proceedings of the International Continence Society (ICS), 31st Annual Meeting, Seoul, 18–21 September 2001, abstract no. 302. [Other: sr-incont14383]
Ankardal M, Ekerydh A, Crafoord K, Milsom I, Stjerndahl JH, Engh ME. A randomised trial comparing open Burch colposuspension using sutures with laparoscopic colposuspension using mesh and staples in women with stress urinary incontinence. BJOG 2004;111:974–81. [Other: sr-incont17915]
Ankardal M, Jarbrink K, Milsom I, Heiwall B, Lausten-Thomsen N, Ellstrom-Engh M. Comparison of health care costs for open Burch colposuspension, laparoscopic colposuspension and tension-free vaginal tape in the treatment of female urinary incontinence. Neurourol Urodyn 2007;26:761–6. [Other: sr-incont23845]
Ankardal M, Milsom I, Stjerndahl JH, Engh ME. A three-armed randomized trial comparing open Burch colposuspension using sutures with laparoscopic colposuspension using sutures and laparoscopic colposuspension using mesh and staples in women with stress urinary incontinence. Acta Obstet Gynecol Scand 2005;84:773–9. [Other: sr-incont20624]
cAnkardal M. Evaluation of Surgical Methods for Treatment of Female Stress Urinary Incontinence. PhD thesis. Gothenburg: University of Gothenburg; 2005. [Ref ID: 73958]
Athanassopoulos 1996111
Athanasopoulos A, Liatsikos EN, Perimenis P, Barbalias GA. Female stress urinary incontinence: predictive factors for the operative correction. Int Urogynecol J Pelvic Floor Dysfunct 1999;10(Suppl. 1):S140. [Other: sr-incont9840]
aAthanassopoulos A, Barbalias G. Burch colposuspension versus Stamey endoscopic bladder neck suspension: a urodynamic appraisal. Urol Int 1996;56:23–7. [Other: sr-incont4816]
Bai 2005145
Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK. Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension-free vaginal tape for stress urinary incontinence. Int J Gynaecol Obstet 2005;91:246–51. [Other: sr-incont21260]
Bandarian 2011161
Bandarian M, Ghanbari Z, Asgari A. Comparison of transobturator tape (TOT) versus Burch method in treatment of stress urinary incontinence. J Obstet Gynaecol 2011;31:518–20. [Other: sr-incont41697]
Berglund 1996192
Berglund AL, Eisemann M, Lalos A, Lalos O. Predictive factors of the outcome of primary surgical treatment of stress incontinence in women. Scand J Urol Nephrol 1997;31:49–55. [Other: sr-incont5650]
aBerglund AL, Lalos O. The pre- and postsurgical nursing of women with stress incontinence. J Adv Nurs 1996;23:502–11. [Other: sr-incont2794]
Lalos O, Berglund AL, Bjerle P. The long-term outcome of retropubic urethrocystopexy (sutures and fibrin sealant) and pubococcygeal repair. Acta Obstet Gynecol Scand 2000;79:135–9. [Other: sr-incont12900]
Lalos O, Bergmund AL, Bjerle P. Urodynamics in women with stress incontinence before and after surgery. Eur J Obstet Gynecol Reprod Biol 1993;48:197–205. [Other: sr-incont4948]
Bergman 1989a88
Bergman A, Ballard CA, Koonings PP. Primary stress urinary incontinence and pelvic relaxation: prospective randomized comparison of 3 different operations. Neurourol Urodyn 1989;8:334–5. [Other: sr-incont4512]
aBergman A, Koonings PP, Ballard CA. Primary stress urinary incontinence and pelvic relaxation: prospective randomized comparison of three different operations. Am J Obstet Gynecol 1989;161:97–101. [Other: sr-incont444]
Klutke JJ, Klutke CG, Bergman J, Elia G. Urodynamic changes in voiding after anti-incontinence surgery: an insight into the mechanism of cure. Urology 1999;54:1003–7. [Other: sr-incont9121]
Bergman 1989b188
aBergman A, Ballard CA, Koonings PP. Comparison of three different surgical procedures for genuine stress incontinence: prospective randomized study. Am J Obstet Gynecol 1989;160:1102–6. [Other: sr-incont450]
Bergman A, Elia G. Three surgical procedures for genuine stress incontinence: five-year follow-up of a prospective randomized study. Am J Obstet Gynecol 1995;173:66–71. [Other: sr-incont2962]
Elia G, Bergman A. Prospective randomized comparison of 3 surgical procedures for stress urinary incontinence: five-year follow-up. Neurourol Urodyn 1994;13:498–500. [Other: sr-incont2685]
Burton 199440
Burton G. A five year prospective randomised urodynamic study comparing open and laparoscopic colposuspension (Abstract). Int Urogynecol J Pelvic Floor Dysfunct 1999;10(Suppl. 1):S44–5. [Other: sr-incont9841]
Burton G. A five year prospective randomised urodynamic study comparing open and laparoscopic colposuspension (Abstract). Neurourol Urodyn 1999;18:295–6. [Other: sr-incont9875]
aBurton G. A randomised comparison of laparoscopic and open colposuspension. Neurourol Urodyn 1994;13:497–8. [Other: sr-incont2684]
Burton G. A three year prospective randomised urodynamic study comparing open and laparoscopic colposuspension. Neurourol Urodyn 1997;16:353–4. [Other: sr-incont5836]
Carey 200089
Carey M, Maher C, Rosamilia A, Cornish A, Ugoni A. Open or Laparoscopic Colposuspension – A Prospective Single Blinded Randomised Control Trial. Proceedings of the Royal Australian and New Zealand College of Obstetrics and Gynaecology (RANZCOG), Annual Meeting, Cairns, QLD, July 2000, abstract. [Other: sr-incont12089]
aCarey M, Rosamilia A, Maher C, Cornish A, Murray C, Ugoni A, et al. Laparoscopic versus open colposuspension: a prospective multi-centre randomised single-blind comparison. Neurourol Urodyn 2000;19:389–91. [Other: sr-incont9868]
Carey MP, Goh JT, Rosamilia A, Cornish A, Gordon I, Hawthorne G, et al. Laparoscopic versus open Burch colposuspension: a randomised controlled trial. BJOG 2006;113:999–1006. [Other: sr-incont22334]
Carey MP, Maher CF, Rosamilia A, Cornish A, Murray C, Moran P, et al. Laparoscopic versus Open Colposuspension: Early Results of a Single Blind Prospective Randomized Control Trial. Proceedings of the International Continence Society (ICS), 29th Annual Meeting, Denver, CO, 23–29 August 1999, abstract no. 532. [Other: sr-incont8023]
Carey MP, Rosamilia A, Maher C, Tsaltas J. Laparoscopic versus Open Colposuspension – Results of a Single Blind Prospective Randomized Control Trial. Proceedings of the Australian Gynaecological Endoscopic Society, IX Annual Scientific Meeting, Adelaide, SA, 1999, p. 51. [Other: sr-incont18194]
Cornish A, Carey M. Laparoscopic versus Open Colposuspension for Women with Stress Urinary Incontinence: A Prospective Multicentre Randomised Single Blind Comparison of Urodynamic Cure of Stress Urinary Incontinence at 6 months Following Surgery. 2005. URL: www.anzctr.org.au/ACTRN12605000439640.aspx (accessed 5 May 2015). [Other: ACTRN12605000439640; other: sr-incont64630]
Colombo 2000193
Colombo M, Vitobello D, Proietti F, Milani R. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. BJOG 2000;107:544–51. [Other: sr-incont8978]
Demirci 2001103
Demirci F, Yucel O. Comparison of free rectus fascial sling and Burch colposuspension procedures in type I and type II genuine stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2000;11(Suppl. 1):S48. [Other: sr-incont13419]
aDemirci F, Yucel O. Comparison of pubovaginal sling and Burch colposuspension procedures in type I/II genuine stress incontinence. Arch Gynecol Obstet 2001;265:190–4. [Other: sr-incont13079]
Drahoradova 200446
Drahoradova P, Masata J, Martan A, Svabik K. Comparative Development of Quality of Life Between TVT and Burch Colposuspension. Proceedings of the International Continence Society, 34th Annual Meeting, and jointly with the International Urogynecological Association, Paris, 23–27 August 2004, abstract no. 278. [Other: sr-incont19049]
El-Barky 2005201
El-Barky E, El-Shazly A, El-Wahab OA, Kehinde EO, Al-Hunayan A, Al-Awadi KA. Tension free vaginal tape versus Burch colposuspension for treatment of female stress urinary incontinence. Int Urol Nephrol 2005;37:277–81. [Other: sr-incont20774]
El-Din Shawki 201247
El-Din Shawki H, Kamel HH, El-Moghazy DA, El-Adawy AR, Mohammed HF. The role of transobturator vaginal tape (TVT-O) and some traditional surgical interventions in the management of female genuine stress urinary incontinence – randomized controlled trial. Int J Gynaecol Obstet 2012;119(Suppl. 3):S337. [Other: sr-incont62241]
Elshawaf 200949
Elshawaf H, Al bahaie Y. Randomized Prospective Trial Comparing Burch Colposuspension to Tension Free Vaginal Tape and Transobturator Suburethral Tape Procedures in Treating Female Genuine Stress Urinary Incontinence. Proceedings of the International Continence Society (ICS), 39th Annual Meeting, San Francisco, CA, 29 September to 3 October 2009, abstract no. 857. [Other: sr-incont35631]
Enzelsberger 1996186
aEnzelsberger H, Helmer H, Schatten C. Comparison of Burch and lyodura sling procedures for repair of unsuccessful incontinence surgery. Obstet Gynecol 1996;88:251–6. [Other: sr-incont2759]
Enzelsberger H, Kurz C, Seifert M, Raimann H, Schatten C. Surgical treatment of recurrent stress incontinence: Burch versus lyodura sling operation – a prospective study [Zur operativen Behandlung der Rezidivstre Binkontinenz: Burch versus Lyoduraschlingeoperation – eine prospektive studie]. Geburtshilfe Frauenheilkd 1993;53:467–71. [Other: sr-incont100]
Fatthy 200151
Fatthy H, El Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. J Am Assoc Gynecol Laparosc 2001;8:99–106. [Other: sr-incont11967]
Fischer 200153
Fischer JR, Hale DS, McClellan E, Benson JT. The use of urethral electrodiagnosis to select the method of surgery in women with intrinsic sphincter deficiency. Int Urogynecol J Pelvic Floor Dysfunct 2001;12(Suppl. 1):S33. [Other: sr-incont12008]
German 1994190
German K, Goodman C, Haynes R, Stephenson TP. A Randomised Trial Comparing a Modified Needle Suspension Procedure with the Vagina/Obturator Shelf Procedure for Genuine Stress Incontinence. Proceedings of the International Continence Society (ICS), 22nd Annual Meeting, Halifax, 1–4 September 1992, abstract no. 256. [Other: sr-incont12071]
aGerman KA, Kynaston H, Weight S, Stephenson TP. A prospective randomized trial comparing a modified needle suspension procedure with the vagina/obturator shelf procedure for genuine stress incontinence. Br J Urol 1994;74:188–90. [Other: sr-incont2104]
Gilja 1998189
Gilja I, Puskar D, Mazuran B, Radej M. Comparative analysis of bladder neck suspension using Raz, Burch and transvaginal Burch procedures. A 3-year randomized prospective study. Eur Urol 1998;33:298–302. [Other: sr-incont5872]
Halaska 200155
Halaska M, Kolbl H, Petri E, Danes L, Voigt R, Otcenasek M, et al. Preliminary results of a prospective randomized study comparing Burch colposuspension and tension-free vaginal tape – urodynamic and sexuological aspects. Neurourol Urodyn 2001;20:421–2. [Other: sr-incont12128]
Han 200169
Han WHC. Burch colposuspension or tension-free vaginal tape for female stress urinary incontinence? Int Urogynecol J Pelvic Floor Dysfunct 2001;12(Suppl. 3):S23. [Other: sr-incont12580]
Henriksson 1978105
Henriksson L, Asmussen M, Löfgren O, Ulmsten U. A urodynamic comparison between abdominal urethrocystopexy and vaginal sling plasty in female stress incontinence. Urol Int 1978;33:111–6. [Other: sr-incont5152]
aHenriksson L, Ulmsten U. A urodynamic evaluation of the effects of abdominal urethrocystopexy and vaginal sling urethroplasty in women with stress incontinence. Am J Obstet Gynecol 1978;131:77–82. [Other: sr-incont2670]
Holmes 1985194
aHolmes D, Stanton S, Chamberlain GVP. Randomised trial to compare the colposuspension with the anterior repair in the management of genuine stress incontinence. Personal communication, 1985. [Other: sr-incont9859]
Stanton SL, Chamberlain G, Holmes DM. The Anterior Repair or Colposuspension for the Cure of Stress Incontinence due to Urethral Sphincter Incompetence. A Randomised Study. Proceedings of the British Congress of Obstetrics and Gynaecology, 24th Congress, 1986, abstract no. 156. [Other: sr-incont8016]
Stanton SL, Chamberlain GVP, Holmes DM. Randomised Study of the Anterior Repair and Colposuspension Operation in the Control of Genuine Stress Incontinence. Proceedings of the International Continence Society (ICS),15th Annual Meeting, London, 3–6 September 1985, pp. 236–7. [Other: sr-incont5145]
Stanton SL, Chamberlain GVP, Holmes DM. The control of stress incontinence: comparison of anterior colporrhaphy and colposuspension. Arch Gynecol 1985;237(Suppl. 1):401–2. [Other: sr-incont9858]
Kammerer-Doak 1999195
Kammerer-Doak DN, Dorin MH, Rogers RG, Cousin MO. A randomized trial of Burch retropubic urethropexy and anterior colporrhaphy for stress urinary incontinence. Obstet Gynecol 1999;93:75–8. [Other: sr-incont8256]
Kitchener 200693
Dumville JC, Manca A, Kitchener HC, Smith AR, Nelson L, Torgerson DJ, COLPO Study Group. Cost-effectiveness analysis of open colposuspension versus laparoscopic colposuspension in the treatment of urodynamic stress incontinence. BJOG 2006;113:1014–22. [Other: sr-incont22332]
aKitchener HC, Dunn G, Lawton V, Reid F, Nelson L, Smith AR, COLPO Study Group. Laparoscopic versus open colposuspension – results of a prospective randomised controlled trial. BJOG 2006;113:1007–13. [Other: sr-incont22333]
Kitchener HC. A Randomised Trial of Open versus Laparoscopic Colposuspension for Genuine Stress Incontinence (MRC COLPO Trial). 2000. Trial registration number: ISRCTN14969683. URL: http://isrctn.org/ISRCTN14969683 (accessed 5 May 2015). [Other: sr-incont16345]
Smith A, Kitchener H, Dunne G, Torgerson D, Lawton V, Reid F, Ali N. A prospective randomised controlled trial of open and laparoscopic colposuspension. Neurourol Urodyn 2005;24:422–3. [Other: sr-incont20986]
Koelbl 200260
Koelbl H, Halaska M, Ostermann S, Lautenschlaeger C. Burch colposuspension and TVT – perioperative results of a prospective randomized trial in patients with genuine stress incontinence. Neurourol Urodyn 2002;21:327. [Other: sr-incont14541]
Liapis 1996200
aLiapis A, Pyrgiotis E, Kontoravdis A, Louridas C, Zourlas PA. Genuine stress incontinence: prospective randomized comparison of two operative methods. Eur J Obstet Gynecol Reprod Biol 1996;64:69–72. [Other: sr-incont2723]
Liapis AE, Asimiadis V, Loghis CD, Pyrgiotis E, Zourlas PA. A randomized prospective study of three operative methods for genuine stress incontinence. J Gynecol Surg 1996;12:7–14. [Other: sr-incont4537]
Liapis 2002108
aLiapis A, Bakas P, Creatsas G. Burch colposuspension and tension-free vaginal tape in the management of stress urinary incontinence in women. Eur Urol 2002;41:469–73. [Other: sr-incont14229]
Liapis A, Bakas P, Creatsas G. Comparison of open retropubic colposuspension with tension-free vaginal tape for the treatment of genuine stress incontinence in women. Neurourol Urodyn 2000;19:385–6. [Other: sr-incont9872]
Mak 2000182
Cheon WC, Mak JH, Liu JY. Prospective randomised controlled trial comparing laparoscopic and open colposuspension. Hong Kong Med J 2003;9:10–14. [Other: sr-incont15758]
aMak JHL, Cheon CW, Liu JYS, Lee TK, Tong WM, Wong THK. Prospective Randomized Controlled Trial Comparing Laparoscopic and Open Colposuspension. Proceedings of the Asian Society for Female Urology, 2nd Scientific Meeting, Hong Kong, 26–27 August 2000. pp. 59–61. [Other: sr-incont12120]
Morris 200168
Morris AR, Reilly ETC, Hassan A, Ramsay IN, Hawthorn RJS. 5–7 year follow-up of a randomised trial comparing laparoscopic colposuspension (LC) and open colposuspension (OC) in the treatment of genuine stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2001;12(Suppl. 3):S6. [Other: sr-incont12582]
Mundy 1983109
Mundy AR. A trial comparing the Stamey bladder neck suspension procedure with colposuspension for the treatment of stress incontinence. Br J Urol 1983;55:687–90. [Other: sr-incont672]
O’Sullivan 200069
O’Sullivan S, Avery N, Balley A, Keane D. The effect of surgery on the collagen metabolism of paraurethral tissue in women with genuine stress incontinence. Int Urogynecol J 2000;11(Suppl. 1):S5. [Other: sr-incont11903]
Palma 1985191
Palma P, David S, Pinotti JA. Comparative study between the Marshall–Marchetti–Krantz operation and the endoscopic suspension of the bladder neck for surgical correction of stress urinary incontinence. Arch Gynecol 1985;237(Suppl.1):402. [Other: sr-incont9864]
aPalma PC, Soffiatti SA, Almeida SC, Pinotti JA. Stress urinary incontinence: a comparative study of surgical treatment by the Marshall–Marchetti–Krantz technique with endoscopic suspension of the bladder neck. Second report. Asia Oceania J Obstet Gynaecol 1988;14:31–6. [Other: sr-incont15461]
Palma PCR, Suely A, Soffiatti D, Pinotti JA. Stress urinary incontinence: a comparative study of the surgical treatment by the Marshall–Marchetti–Krantz technique with endoscopic suspension of the bladder neck. Second report. Ginecol Obstet (Lima) 1986;30:15–19. [Other: sr-incont15464]
Sand 2000187
Culligan PJ, Goldberg RP, Sand PK. A randomized controlled trial comparing a modified Burch procedure and a suburethral sling: long-term follow-up. Int Urogynecol J 2003;14:229–33. [Other: sr-incont16706]
Culligan PJ, Winkler HA, Blackhurst DW, Sand PK. A Prospective Randomized Study of Modified Burch Retropubic Urethropexy and Suburethral Sling for Genuine Stress Incontinence and Low Pressure Urethra. Proceedings of the International Continence Society (ICS), 28th Annual Meeting, Jerusalem, 14–17 September 1998. p. 133. [Other: sr-incont5689]
Goldberg RP, Culligan PJ, Koduri S, Sand PK. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling: long term follow-up. Int Urogynecol J 2000;11(Suppl. 1):S8. [Other: sr-incont11904]
Goldberg RP, Sand PK, Koduri S, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling: long term follow-up. Int Urogynecol J Pelvic Floor Dysfunct 2001;12(Suppl. 1):S6. [Other: sr-incont12004]
aSand PK, Winkler H, Blackhurst DW, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling for treatment of genuine stress incontinence with low-pressure urethra. Am J Obstet Gynecol 2000;182:30–4. [Other: sr-incont9013]
Sivaslioglu 2007162
Sivaslioglu AA, Caliskan E, Dolen I, Haberal A. A randomized comparison of transobturator tape and Burch colposuspension in the treatment of female stress urinary incontinence. Int Urogynecol J 2007;18:1015–19. [Other: sr-incont23854]
Stangel-Wojcikiewicz 200876
Stangel-Wojcikiewicz K. Laparoscopic Burch colposuspension compared to laparotomy for treatment urinary stress incontinence. Neurourol Urodyn 2008;27:714. [Other: sr-incont31857]
Su 1997183
Su TH, Wang KG, Hsu CY, Wei HJ, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress incontinence. Acta Obstet Gynecol Scand 1997;76:576–82. [Other: sr-incont5558]
Summitt 200077
Summitt RL, Lucente V, Karram MM, Shull BL, Bent AE. Randomized comparison of laparoscopic and transabdominal Burch urethropexy for the treatment of genuine stress incontinence. Obstet Gynecol 2000;95:S2. [Other: sr-incont11862]
Tapp 198978
aTapp AJS, Hills B, Cardozo L, Tapp AJ. Randomised study comparing pelvic floor physiotherapy with the Burch colposuspension. Neurourol Urodyn 1989;8:356–7. [CRSREF: 3218505; other: sr-incont4515]
Tapp AJS, Hills B, Cardozo L. Pelvic Floor Physiotherapy Compared with the Burch Colposuspension in the Treatment of Genuine Stress Incontinence. Proceedings of the Silver Jubilee British Congress of Obstetrics and Gynaecology, London, 4–7 July 1989. p. 65. [CRSREF: 3218506; Other: sr-incont8015]
Téllez Martínez-Fornés 2009202
aTéllez Martínez-Fornés M, Fernandez Perez C, Fouz Lopez C, Fernandez Lucas C, Borrego Hernando J. A three year follow-up of a prospective open randomized trial to compare tension-free vaginal tape with Burch colposuspension for treatment of female stress urinary incontinence. Actas Urol Esp 2009;33:1088–96. [Other: sr-incont39608]
Téllez Martínez-Fornés M. A Three Year Follow-up Prospective Open Randomized Trial of Tension-free Vaginal Tape and Colposuspension for Primary Urodynamic Stress Incontinence. 2001. Trial registration number: NCT00782990. URL: http://clinicaltrials.gov/show/NCT00782990 (accessed 5 May 2015). [Other: sr-incont62910]
Trabuco 201432
aTrabuco E, Klingele C, Blandon R, Occhino J, McGree M, Weaver A, et al. A randomized comparison of incontinence procedures performed concomitantly with abdominal sacrocolpopexy: the Burch versus mid-urethral sling trial. Neurourol Urodyn 2014;33:1005. [Other: NCT00934999; other: sr-incont64705]
cTrabuco EC, Klingele CJ, Blandon R, Occhino JA, McGree ME, Weaver AL, et al. A randomized comparison of incontinence procedures performed concomitantly with abdominal sacral colpopexy: the Burch versus mid-urethral sling trial. Int Urogynecol J Pelvic Floor Dysfunct 2014;25(Suppl. 1):S1–S2. [Ref ID: 67464]
cTrabuco EC, Klingele CJ, Blandon RE, Occhino JA, Weaver AL, McGree ME, et al. Burch retropubic urethropexy compared with midurethral sling with concurrent sacrocolpopexy: a randomized controlled trial. Obstet Gynecol 2016;128:828–35. [Ref ID: 73496]
cTrabuco EC, Klingele CJ, Occhino J, Blandon RE, McGree ME, Weaver A, et al. Treatment success of burch and midurethral sling 2 years following combined procedure with sacrocolpopexy. Int Urogynecol J Pelvic Floor Dysfunct 2016;27(Suppl. 1):S46. [Ref ID: 73436]
cNCT00934999, Trabuco EC. A Randomized Comparison of Concomitant Incontinence Procedures Performed with Abdominal Sacral Colpopexy: The Burch versus Mid-urethral Sling Trial. 2009. Trial registration number: NCT00934999. URL: http://clinicaltrials.gov/show/NCT00934999 (accessed 20 August 2017). [Ref ID: 62908]
cSingh R, Blandon R, McGree M, Weaver A, Occhino JA, Klingele C, et al. Predictors of resolution of urgency urinary incontinence (UUI) after anti-incontinence procedures performed for mixed urinary incontinence. J Minim Invasive Gynecol 2015;22(Suppl. 1):S45. [Ref ID: 75731]
Tuygun 2006184
Tuygun C, Bakirtas H, Eroglu M, Alisir I, Zengin K, Imamoglu A. Comparison of two different surgical approaches in the treatment of stress urinary incontinence: open and laparoscopic Burch colposuspension. Turk Uroloji Dergisi 2006;32:248–53. [Other: sr-incont26724]
Ustün 2005185
Ustün Y, Engin-Ustün Y, Güngör M, Tezcan S. Randomized comparison of Burch urethropexy procedures concomitant with gynecologic operations. Gynecol Obstet Invest 2005;59:19–23. [Other: sr-incont20187]
Wang 2003203
aWang AC, Chen MC. Comparison of tension-free vaginal taping versus modified Burch colposuspension on urethral obstruction: a randomized controlled trial. Neurourol Urodyn 2003;22:185–90. [Other: sr-incont16021]
Wang AC, Liang CC, Lo TS, Tseng LH. Does tension-free vaginal tape procedure really exert no tension on the urethra? A randomized controlled study using the voiding mechanism. Int Urogynecol J 2001;12(Suppl. 3):S111. [Other: sr-incont15459]
Ward 2002100
Abrams P, Martin K, Bulmer P, Donovan J, Hilton P. Responsiveness of the Bristol Female Lower Urinary Tract Symptoms Questionnaire (BFLUTS-Q) to Surgical Intervention in a Randomised Controlled Trial. Proceedings of the International Continence Society (ICS), 30th Annual Meeting, Tampere, 28–31 August 2000:A173. [Other: sr-incont9954]
Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol 2004;191:73–82. [Other: sr-incont19277]
Manca A, Sculpher MJ, Ward K, Hilton P. A cost-utility analysis of tension-free vaginal tape (TVT) versus colposuspension for primary genuine stress incontinence (unpublished material). Personal communication, 2002. [Other: sr-incont12892]
Manca A, Sculpher MJ, Ward K, Hilton P. A cost-utility analysis of tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence. BJOG 2003;110:255–62. [Other: sr-incont14361]
Sculpher MJ, Ward KL, Hilton P. A Comparison of the Hospital Cost of Tension-free Vaginal Tape and Colposuspension. Proceedings of the International Continence Society (ICS), 30th Annual Meeting, Tampere, 28–31 August 2000:333–4. [Other: sr-incont9871]
aWard K, Hilton P on behalf of the United Kingdom and Ireland Tension-Free Vaginal Tape Trial Group. Prospective multicentre randomised trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ 2002;325:67–73. [Other: sr-incont14365]
Ward K, Hilton P, on behalf of the UK and Ireland TVT trial group. A randomised trial of colposuspension and ’TVT’ TM for primary genuine stress incontinence – 2 year follow-up. Personal communication, 2001. [Other: sr-incont12573]
Ward K, Hilton P, on behalf of the UK and Ireland TVT trial group. A randomised trial of colposuspension and tension-free vaginal tape (TVT) for primary genuine stress incontinence – 2 yr follow-up. Int Urogynecol J Pelvic Floor Dysfunct 2001;12(Suppl. 3):S7. [Other: sr-incont12574]
Ward K, Hilton P, on behalf of the UK and Ireland TVT trial group. A randomised trial of tension-free vaginal tape (TVT) and colposuspension for primary genuine stress incontinence [unpublished material]. Royal Victoria Infirmary, 2002, personal communication. [Other: sr-incont12891]
Ward K, Hilton P. Multicentre randomised trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: five year follow up. Neurourol Urodyn 2006;25:568–9. [Other: 23328]
Ward KL, Hilton P, Browning J, on behalf of the UK and Ireland TVT Trial group. A randomized trial of colposuspension and tension-free vaginal tape for primary genuine stress incontinence. Neurourol Urodyn 2000;19:386–8. [Other: sr-incont9869]
Ward KL, Hilton P, Browning J, on behalf of the UK and Ireland TVT Trial Group. Changes in Quality of Life Following Surgery with Tension Free Vaginal Tape (TVT) or Colposuspension for Primary Genuine Stress Incontinence. Proceedings of the International Continence Society (ICS), 30th Annual Meeting, Tampere, 28–31 August 2000. p. 314. [Other: sr-incont14348]
Ward KL, Hilton P, Browning J. Urodynamic variables in a randomized comparison of colposuspension and tension-free vaginal tape for primary genuine stress incontinence. Neurourol Urodyn 2000;19:388–9. [Other: sr-incont9870]
Ward KL, Hilton P, on behalf of the UK and Ireland TVT Trial Group. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 2004;190(2):324–31. [Other: sr-incont17301]
Ward KL, Hilton P, on behalf of the UK and Ireland TVT Trial Group. Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG 2008;115:226–33. [Other: sr-incont26268]
(ii) Cochrane review: Ford et al.8 and Ogah et al.18 – MUS operations for SUI in women
Aigmüller 201483
aAigmüller T, Tammaa A, Tamussino K, Hanzal E, Umek W, Kolle D, et al. Retropubic vs. transobturator tension-free vaginal tape for female stress urinary incontinence: 3-month results of a randomized controlled trial. Int Urogynecol J 2014;25:1023–30. [Other: NCT00441454; other: sr-incont62534; PubMed: 24819327]
Bjelic Radisic V, Trutnovsky G, Tammaa A , Hanzal E, Umek W, Koelle D, et al. Quality of life in patients with stress incontinence: results of a randomized trial comparing retropubic and transobturator tension-free vaginal tape. Int Urogynecol J 2013;24(Suppl. 1):S36–S37. [Other: sr-incont62184]
Tammaa A, Aigmueller T, Umek W, Hanzal E, Kropshofer S, Lang P, et al. Retropubic versus transobturator TVT: five-year results of the Austrian trial. J Minim Invasive Gynecol 2014;21(Suppl. 1):S21. [Other: sr-incont62148]
Tamussino K, Tammaa A, Hanzal E, Umek W, Bjelic V, Koelle D. TVT vs. TVT-O for primary stress incontinence: a randomized clinical trial. Int Urogynecol J 2008;19(Suppl. 1):S20–S21. [Other: sr-incont26969]
Alkady 2009120
Alkady HM, Eid A. Tension-free vaginal tape versus transobturator vaginal tape inside-out for the treatment of female stress urinary incontinence. Med J Cairo Univ 2009;77:317–26. [Other: sr-incont50307]
Andonian 2007117
Andonian S, St-Denis B, Lemieux MC, Corcos J. Prospective clinical trial comparing Obtape and DUPS to TVT: one-year safety and efficacy results. Eur Urol 2007;52:245–2. [Other: sr-incont23793]
Aniuliene 200984
Aniuliene R. Tension-free vaginal tape versus tension-free vaginal tape obturator (inside-outside) in the surgical treatment of female stress urinary incontinence. Medicina (Kaunas) 2009;45:639–43. [Other: sr-incont34372]
Araco 200886
aAraco F, Gravante G, Sorge R, Overton J, De Vita D, Sesti F, et al. TVT-O vs. TVT: a randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J 2008;19:917–26. [Other: sr-incont 27794]
Araco F, Gravante G, Sorge R, Piccione E. TVT-O vs. TVT: reply to comments by Burton et al. [letter]. Int Urogynecol J 2009;20:371–2. [Other: sr-incont27794]
Burton C, Latthe P, Toozs-Hobson P. Comments on Araco et al. TVT-O vs. TVT: a randomized trial in patients with different degrees of urinary stress incontinence [comment] [letter]. Int Urogynecol J 2009;20:369. [Other: sr-incont27794; other: srincont31410]
Barber 2008122
Barber M, Kleeman S, Karram M, Paraiso MF, Walters M, Vasavada S, et al. A multi-center randomized trial comparing the transobturator tape with tension-free vaginal tape for the surgical treatment of stress urinary incontinence. Neurourol Urodyn 2007;26:742–3. [Other: sr-incont23758]
Barber MD, Kleeman S, Karram MM, Paraiso MF, Ellerkmann M, Vasavada S, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol 2008;199:666.e1–7. [Other: NCT00475839; other: srincont29239]
aBarber MD, Kleeman S, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al. Transobturator tape compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol 2008;111:611–21. [Other: NCT00475839; other: srincont26837]
Barber MD, Kleeman SD, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al. A multi-center randomized trial comparing the transobturator tape with tension-free vaginal tape for the surgical treatment of stress urinary incontinence. J Pelvic Med Surg 2007;13:234–5. [Other: srincont34199]
Chen CC, Rooney CM, Paraiso MF, Kleeman SD, Walters MD, Karram MM, et al. Leak point pressure does not correlate with incontinence severity or bother in women undergoing surgery for urodynamic stress incontinence. Int Urogynecol J 2008;19:1193–8. [Other: srincont27712]
Frick AC, Ridgeway B, Ellerkmann M, Karram MM, Paraiso MF, Walters MD, et al. Comparison of responsiveness of validated outcome measures after surgery for stress urinary incontinence. J Urol 2010;184:2013–7. [Other: srincont40342]
Barry 2008123
aBarry C, Lim YN, Muller R, Hitchins S, Corstiaans A, Foote A, et al. A multi-centre, randomised clinical control trial comparing the retropubic (RP) approach versus the transobturator approach (TO) for tension-free, suburethral sling treatment of urodynamic stress incontinence: the TORP study. Int Urogynecol J 2008;19:171–8. [Other: sr-incont26462]
Barry CL, Lim Y, Muller R, Greenland H, Hitchens S, Corstiaans A, et al. A multi-centre, prospective, randomised trial comparing the retropubic (RP-SUS) approach versus the transobturator approach (TO-SUS) for tension free, suburethral sling treatment of urodynamic stress incontinence – the TORP study. Neurourol Urodyn 2006;25:572–3. [Other: sr-incont23754]
Cervigni 200641
Cervigni M, Natale F, La Penna C, Agostini M, Antomarchi F, Lo Voi R, et al. Surgical correction of stress urinary incontinence associated with pelvic organ prolapse: trans-obturator approach (MONARC) versus retropubic approach (TVT). Int Urogynecol J 2006;17(Suppl. 2):S215. [Other: srincont29660]
aCervigni M, Natale F, La Penna C, Agostini M, Antomarchi F, Lo Voi R, et al. Surgical correction of stress urinary incontinence associated with pelvic organ prolapse: trans-obturator approach (MONARC) versus retropubic approach (TVT). Neurourol Urodyn 2006;25:552. [Other: sr-incont23756]
Chen 2010118
Chen Z, Chen Y, Du GH, Yuan XY, Wu J, Zeng XY, et al. Comparison of three kinds of mid-urethral slings for surgical treatment of female stress urinary incontinence. Urologia 2010;77:37–42. [Other: srincont40354]
Chen 201290
Chen H-X, Lv J-W, Leng J, Li J-Y, Bo J-J, Huang Y-R. Efficacy and complications of TVT procedure and TVT-O procedure in treatment of female stress urinary incontinence [Chinese]. J Shanghai Jiaotong Univ (Med Sci) 2012;32:412–15. [Other: srincont59712]
Choe 201342
Choe JH, Lee HD, Park SH, Jo DG, Lee HS, Lee JS, et al. Comparison of postoperative pain after transobturator or retropubic suburethral sling for female stress urinary incontinence: a prospective randomized study. J Endourol 2013;27:A263. [Other: srincont62161]
Darabi Mahboub 201226
Darabi MR, Keshvari M, Sheikhi Z. Evaluation study between tension-free vaginal tape (TVT) and transobturator tape (TOT) in treatment stress incontinence in female. European Urology Supplements 2013;12:e1196. [Other: sr-incont62158]
aDarabi Mahboub MR, Keshvari M, Sheikhi Z. Evaluation Study Between Tension-free Vaginal Tape (TVT) and Transobturator Tape (TOT) in Treatment Stress Incontinence in Female. Proceedings of the International Continence (ICS), 42nd Annual Meeting, Beijing, 15–19 October 2012, abstract no. 788. [Other: srincont48402]
Mahbob MRD. Evaluation Study Between Tension-free Vaginal Tape and Transobturator Tape in Treatment Stress Incontinence in Women. 2009. Trial registration number: IRCT201112148228N4. URL: www.irct.ir/searchresult.php?id=8228&number=4 (accessed 18 August 2017). [Other: sr-incont 62304]
Mahboub MRD, Keshvari M, Sheikhi Z. Evaluation study between tension free vaginal tape and transobturator tape in treatment stress incontinence in female. J Endourol 2011;25(Suppl. 1):A12. [Other: srincont62292]
cShirvan MK, Rahimi HR, Darabi Mahboub MR, Sheikhi Z. Tension-free vaginal tape versus transobturator tape for treatment of stress urinary incontinence: a comparative randomized clinical trial study. Urol Sci 2014;25:54–7. [Ref ID: 62870]
cMahboub MRD, Keshvari M, Sheikhi Z, Ghoreifi A. Evaluation study between tension – free vaginal tape (TVT) and transobturator tape (TOT) in treatment stress incontinence in female. J Endourol 2012;26(Suppl. 1):A60. [Ref ID: 62244]
David-Montefiore 2006124
Ballester M, Bui C, Frobert JL, Grisard-Anaf M, Lienhart J, Fernandez H, et al. Four-year functional results of the suburethral sling procedure for stress urinary incontinence: a French prospective randomized multicentre study comparing the retropubic and transobturator routes. World J Urol 2012;30:117–22. [Other: srincont44520]
Darai E, Frobert JL, Grisard-Anaf M, Lienhart J, Fernandez H, Dubernard G, et al. Functional results after the suburethral sling procedure for urinary stress incontinence: a prospective randomized multicentre study comparing the retropubic and transobturator routes. Eur Urol 2007;51:795–802. [Other: srincont22550]
David-Montefiore E, Frobert JL, Grisard-Anaf M, Liehart J, Fernandez H, Dubernard G, et al. Functional results after suburethral sling procedure for urinary stress incontinence at 1 year: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. Int Urogynecol J 2006;17(Suppl. 2):S95. [Other: sr-incont49146]
aDavid-Montefiore E, Frobert JL, Grisard-Anaf M, Lienhart J, Bonnet K, Poncelet C, et al. Peri-operative complications and pain after the suburethral sling procedure for urinary stress incontinence: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. Eur Urol 2006;49:133–8. [Other: srincont21623]
de Oliveira 200644
Oliveira L, Sartori M, Castro R, Fonseca E, Rodrigues A, Girao M. A prospective randomized study to compare TVT, TVT-O and pre-pubic TVT for the treatment of women with stress urinary incontinence, with or without intrinsic sphincter deficiency. Int Urogynecol J 2008;19(Suppl. 2):S173–S174. [Other: srincont31051]
aOliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM, Prior EL. Comparison of retro pubic TVT, pre pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence. Int Urogynecol J 2006;17(Suppl. 2):S253. [Other: srincont27309]
Oliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM. Comparison of retro-pubic TVT, pre-pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence. Int Urogynecol J 2005;16(Suppl. 2):S80. [Other: srincont27307]
de Oliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM. Comparison of retro-pubic TVT, pre-pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence. Int Urogynecol J 2007;18(Suppl. 1):S180. [Other: srincont27310]
de Tayrac 2004125
ade Tayrac R, Deffieux X, Droupy S, Chauveaud-Lambling A, Calvanese-Benamour L, Fernandez H. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol 2004;190:602–8. [Other: sr-incont17259]
de Tayrac R, Droupy S, Calvanese L, Fernandez H. A Prospective Randomized Study Comparing TVT and Transobturator Suburethral Tape (T.O.T.) for the Surgical Treatment of Stress Incontinence. Proceedings of the International Continence Society (ICS), 33rd Annual Meeting, Florence, 5–9 October 2003. pp. 266–7. [Other: sr-incont17153]
Deffieux 2010126
Deffieux X, Daher N, Mansoor A, Debodinance P, Deval B, Salet-Lizee D, et al. Tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a multicenter randomised controlled trial. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S19–S20. [Other: NCT00135616; other: srincont27322]
aDeffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H. Transobturator TVT-O versus retropubic TVT: results of a multicenter randomized controlled trial at 24 months follow-up. Int Urogynecol J 2010;21:1337–45. [Other: NCT00135616; other: srincont40895; PubMed: 20552165]
Deffieux X, Fernandez H. Female sexual function following trans-obturator suburethral tape from inside to outside (TVT-O) and tension-free vaginal tape (TVT): a randomized controlled trial. J Minim Invasive Gynecol 2009;16:S22. [Other: NCT00135616; other: srincont40862]
Trichot C, Salet-Lizee D, Descamps P, Deval B, Hocke C, Fatton B, et al. [Functional results following transobturator and retropubic mid-urethral sling] [French]. J Gynecol Obstet Biol Reprod (Paris) 2010;39:614–23. [Other: NCT00135616; other: srincont41067]
cThubert T, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H, et al. Outpatient or inpatient: is there an impact on the functional results, complication of midurethral sling surgery for stress urinary incontinence? Neurourol Urodyn 2014;33:1013–14. [Ref ID: 64704]
cThubert T, Daher N, Mansoor A, Debodinance P, Fernandez H, Deffieux X. Outcomes associated with the use of midurethral slings for stress incontinence surgery according to the type of hospitalization. Int J Gynaecol Obstet 2015 May;129:123–7. [Ref ID: 66958; other: NCT00135616]
Diab 201245
Diab DE, Zayed AM, Allam MN, Maroof AM, Ibraheem E, El-Sayed DE. A prospective randomized study comparing the safety and efficacy of transobturator tape (TOT) versus tension free vaginal tape (TVT) in treatment of female stress urinary incontinence. Eur Urol Suppl 2012;11:e177. [Other: srincont62249]
El-Hefnawy 2010127
aEl-Hefnawy AS, Wadie BS, El Mekresh M, Nabeeh A, Bazeed MA. TOT for treatment of stress urinary incontinence: how should we assess its equivalence with TVT? Int Urogynecol J 2010;21:947–53. [Other: srincont40077]
Wadie BS, Elhefnawy AS. TVT versus TOT, 2-year prospective randomized study. World J Urol 2013;31:645–9. [Other: srincont48133]
Enzelsberger 2005104
Enzelsberger H, Schalupny J, Heider R, Mayer G. TVT versus TOT – a prospective randomized study for the treatment of female stress urinary incontinence at a follow-up of 1 year [German]. Geburtshilfe Frauenheilkd 2005;65:506–11. [Other: srincont21007]
Freeman 2011128
aFreeman R, Holmes D, Hillard T, Smith P, James M, Sultan A, et al. What patients think: patient-reported outcomes of retropubic versus trans-obturator mid-urethral slings for urodynamic stress incontinence – a multi-centre randomised controlled trial. Int Urogynecol J 2011;22:279–86. [Other: srincont41009]
Freeman R, Holmes D, Smith P, Hillard T, Yang Q, Agur W, et al. Is trans-obturator tape (TOT) as effective as tension-free vaginal tape (TVT) in the treatment of women with urodynamic stress incontinence? Results of a multicentre RCT. Neurourol Urodyn 2008;27:573–4. [Other: srincont31849]
Hammoud 201156
aHammoud K, Elsheikh M, Haitham M, Fayad A, Ghamrawy H, Aboumohamed A. Tension-free vaginal tape versus transobturator vaginal tape in management of female stress urinary incontinence. Long-term follow-up: which to choose. Urology 2011;78(Suppl. 1):S209–S210. [Other: srincont62233]
Hammoud KM, El Sheikh MG, Haitham M, Fayad AS, El Ghamrawy HK, Mohamed AARA. Tension-free vaginal tape versus trans-obturator vaginal tape in the management of female stress urinary incontinence long term follow-up: which to choose. J Endourol 2012;26(Suppl. 1):A59. [Other: srincont62245]
Jakimiuk 2012129
aJakimiuk AJ, Issat T, Fritz-Rdzanek A, Maciejewski T, Rogowski A, Baranowski W. Is there any difference? A prospective, multicenter, randomized, single blinded clinical trial, comparing TVT with TVT-O (POLTOS study) in management of stress urinary incontinence. Short-term outcomes. Pelviperineology 2012;31:5–9. [Other: sr-incont50305]
Jakimiuk AJJ, Maciejewski TM, Fritz AF, Baranowski WB, Wladysiuk-Blicharz MWB. Single-blind randomized clinical trial comparing efficacy and safety of TVT (tension free vaginal tape) vs TVT-O (tension free vaginal tape obturator system) in treatment of stress urinary incontinence (POLTOS) preliminary report. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S189. [Other: srincont27324]
Kamel 200958
Kamel A. A Comparison Between TVT and TVTO as Regards Safety. An African Experience. Proceedings of the International Continence Society (ICS), 39th Annual Meeting, San Francisco, CA, 29 September to 3 October 2009, abstract no. 830. [Other: srincont35630]
Karateke 2009130
Karateke A, Haliloglu B, Cam C, Sakalli M. Comparison of TVT and TVT-O in patients with stress urinary incontinence: short-term cure rates and factors influencing the outcome. A prospective randomised study. Aust N Z J Obstet Gynaecol 2009;49:99–105. [Other: srincont31429]
Kiliç 2007131
Kiliç G, Olgun G, Bilen MA, Orhan A, Dunn B. [The comparison of TVT (tension free vaginal tape) and TOT (trans-obturator vaginal tape) in the treatment of the urinary incontinence and literature search] [Turkish]. Jinekoloji ve Obstetrik Dergisi 2007;21:26–31. [Other: srincont28036]
Kim 2005132
aKim Y-W, Na Y-G, Sul C-K. [Randomized prospective study between pubovaginal sling using SPARC sling system and MONARC sling system for the treatment of female stress urinary incontinence: short term results] [Korean]. Korean J Urol 2005;46:1078–82. [Other: srincont22116]
Na YG, Rob AS, Youk SM, Kim YW, Kim HS, Sul CK, et al. A prospective multicentre randomized study comparing transvaginal tapes (SPARC sling system) and transobturator suburethral tapes (Monarc sling system) for the surgical treatment of stress urinary incontinence. Eur Urolog Suppl 2005;4:15. [Other: srincont26609]
Krofta 201094
Krofta L, Feyereisl J, Otcenasek M, Kasikova E, Pan M. [Tension free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence] [Czech]. Ceska Gynekol 2008;73:231–9. [Other: sr-incont27504]
aKrofta L, Feyereisl J, Otcenasek M, Velebil P, Kasikova E, Krcmar M. TVT and TVT-O for surgical treatment of primary stress urinary incontinence: prospective randomized trial. Int Urogynecol J 2010;21:141–8. [Other: sr-incont39511]
Laurikainen 200796
Brubaker L, Brincat C, Mueller E. Are we satisfied? Perspective on five-year outcomes of midurethral slings [editorial]. Eur Urol 2014;65:1115–16. [Other: sr-incont67651; PubMed: 24568893]
Laurikainen E, Takala T, Aukee P, Kivela A, Rinne K, Valpas A, et al. Retropubic TVT compared with transobturator TVT (TVT-O) in treatment of stress urinary incontinence: five-year results of a randomized trial. Neurourol Urodyn 2011;30:803–5. [Other: NCT00379314; other: srincont42162]
Laurikainen E, Valpas A, Aukee P, Kivela A, Rinne K, Takala T, et al. Five-year results of a randomized trial comparing retropubic and transobturator midurethral slings for stress incontinence. Eur Urol 2014;65:1109–14. [Other: sr-incont60594; PubMed: 24508070]
Laurikainen E, Valpas A, Kiilholma P, Takala T, Kivela A, Aukee P, et al. A prospective randomised trial comparing TVT and TVT-O procedures for the treatment of SUI: immediate outcome and complications. Int Urogynecol J 2006;17(Suppl. 2):S104–S105. [Other: sr-incont49149]
aLaurikainen E, Valpas A, Kivela A, Kalliola T, Rinne K, Takala T, et al. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol 2007;109:4–11. [Other: sr-incont22553]
Nilsson CG. A Randomized, Prospective, Multicenter Trial Comparing TVT with TVT-O Procedures in Treatment of Female Primary Urinary Stress Incontinence. 2004. Trial registration number: NCT00379314. URL: http://clinicaltrials.gov/show/NCT00379314 (accessed 18 August 2017). [Other: NCT00379314; other: srincont49342]
Palva K, Nilsson CG. Prevalence of urinary urgency symptoms decreases by mid-urethral sling procedures for treatment of stress incontinence. Int Urogynecol J 2011;22:1241–7. [Other: NCT00379314; other: srincont42695]
Palva K, Rinne K, Aukee P, Kivela A, Laurikainen E, Takala T, et al. A randomized trial comparing tension-free vaginal tape with tension-free vaginal tape-obturator: 36-month results. Int Urogynecol J 2010;21:1049–55. [Other: NCT00379314; other: srincont40052]
Rinne K, Aukee P, Heikkinen AM, Kalliola T, Kiilholma P, Kivela A, et al. A randomized clinical trial comparing TVT with TVT-O for treatment of stress urinary incontinence: 12 months results. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S28–S29. [Other: srincont27323]
Rinne K, Laurikainen E, Kivela A, Aukee P, Takala T, Valpas A, et al. A randomized trial comparing TVT with TVT-O: 12-month results. Int Urogynecol J 2008;19:1049–54. [Other: NCT000379314; other: srincont31311]
Rinne K. Comparison of Two Mid-urethral Sling Operations and Their Effect on Urethral Mobility Assessed by Dynamic Magnetic Resonance Imaging. Dissertations in Health Sciences, no. 33. PhD thesis. Kuopio: University of Eastern Finland; 2010. [Other: ISBN: 978-952-61-0236-8 (pdf); other: ISSN:1798-5714 (pdf); other: NCT00379314; other: srincont 60054]
Leanza 200961
Leanza V, Dati S, Gasbarro N, Leanza G. Retropubic versus transobturator tension free procedures: a comparative study. Neurourol Urodyn 2011;30:6–7. [Other: sr-incont50306]
aLeanza V, Dati S, Gasbarro N. A multicenter randomized trial of prepubic and retropubic Leanza–Gasbarro–Caschetto tension-free procedures. Int Urogynecol J 2009;20(Suppl. 2):S73. [Other: srincont39881]
Lee 2007107
aLee KS, Han DH, Choi YS, Yum SH, Song SH, Doo CK, et al. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: 1-year follow up. J Urol 2007;177:214–18. [Other: sr-incont28039]
Ryu KH, Shin JS, Du JK, Choo MS, Lee KS. Randomized trial of tension-free vaginal tape (TVT) vs. tension-free vaginal tape obturator (TVT-O) in the surgical treatment of stress urinary incontinence: comparison of operation related morbidity. Eur Urol Suppl 2005;4:15. [Other: srincont26610]
Choi YS , Park SY, Yum SH, Kim JB, Song SH, Doo CK, et al. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: one-year follow up. J Korean Continence Soc 2005;9:108–14. [Ref ID: 71471]
Liapis 2006200
Liapis A, Bakas P, Giner M, Creatsas G. Tension-free vaginal tape versus tension-free vaginal tape obturator in women with stress urinary incontinence. Gynecol Obstet Invest 2006;62:160–4. [Other: srincont22245]
Mansoor 200364
Mansoor A, Vedrine N, Darcq C. Surgery of female urinary incontinence using transobturator tape (TOT): a prospective randomised comparative study with TVT. Neurourol Urodyn 2003;22:488–9. [Other: sr-incont17107]
Mehdiyev 2010134
Mehdiyev M, Itil IM, Sendag F, Akdemir A, Askar N. Comparing the transvaginal tape (TVT) and transobturator tape (TOT) in stress urinary incontinence for their efficiency and their effects on quality of life. Turk Jinekoloji ve Obstetrik Dernegi Dergisi 2010;7:117–24. [Other: srincont62297]
Meschia 200797
aMeschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, et al. Peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O. Int Urogynecol J 2007;18:1257–61. [Other: srincont23958]
Meschia M, Pifarotti P, Baccichet R, Bernasconi F, Cortese P, Magatti F, et al. A multicenter randomized comparison of tension-free vaginal tape (TVT) and trans-obturator in-out technique (TVT-O) for the treatment of stress urinary incontinence: one year results. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S2. [Other: srincont27318]
Meschia M, Pifarotti P, Bernasconi F, Baccichet R, Magatti F, Cortese P, et al. A multicentre randomised comparison of tension free vaginal tape (TVT) and transobturator in-out technique (TVT-O) for the treatment of stress urinary incontinence. Int Urogynecol J 2006;17(Suppl. 2):S92–S93. [Other: sr-incont49147]
Minassian VA, Parekh M, Langroudi MH. Comment on Meschia et al: peri-operative morbidity and early results of a randomised trial comparing TVT and TVT-O [comment]. Int Urogynecol J 2008;19:1725. [Other: srincont31222]
Nerli 2009110
Nerli RB, Kumar AG, Koura A, Prabha V, Alur SB. Transobturator vaginal tape in comparison to tension-free vaginal tape: a prospective trial with a minimum 12 months follow-up. Indian J Urol 2009;25:321–5. [Other: srincont40242]
Nyyssonen 2014135
Nyyssonen V, Talvensaari-Mattila A, Santala M. A prospective randomized trial comparing tension-free vaginal tape versus transobturator tape in patients with stress or mixed urinary incontinence: subjective cure rate and satisfaction in median follow-up of 46 months. Scand J Urol 2014;48:309–15. [Other: sr-incont62072; PubMed: 24286482]
Palomba 200870
Palomba S, Zullo F. A Comparison in Terms of Efficacy and Safety Between Transobturator and Transvaginal Tape Performed at the Same Time of Anterior Defect Correction with Mesh. 2008. Trial registration number: NCT00743535. URL: http://clinicaltrials.gov/show/NCT00743535 (accessed 18 August 2017). [Other: srincont49348]
Porena 2007136
Costantini E, Kocjancic E, Saccomanni M, Giannantoni A, Porena M, Frea B. Tension free vaginal tape vs. trans obturator tape as surgery for stress urinary incontinence: results of a multicenter randomised trial. Neurourol Urodyn 2006;25:573–5. [Other: sr-incont23753]
Costantini E, Lazzeri M, Giannantoni A, Bini V, Kocjancic E, Porena M, et al. Retropubic versus transobturator mid-urethral slings: in a randomised controlled trial preoperative VLPP may not predict mid-term outcome. Neurourol Urodyn 2007;26:741–2. [Other: sr-incont23757]
Costantini E, Lazzeri M, Giannantoni A, Bini V, Vianello A, Kocjancic E, et al. Preoperative Valsava leak point pressure may not predict outcome of mid-urethral slings. Analysis from a randomized controlled trial of retropubic versus transobturator mid-urethral slings. Int Braz J Urol 2008;34:73–81; discussion 81–3. [Other: srincont27817]
Costantini E, Lazzeri M, Kocjancic E, Di Biase M, Salvini E, Porena M. Prolonged follow-up shows continence deterioration after trans-obturator tape: results from a randomised controlled study. Neurourol Urodyn 2013;32:525–6. [Other: sr-incont49187]
Costantini E, Lazzeri M, Zucchi A, Bruno R, Salvini E, Pietropaolo A, et al. Deterioration of continence after TOT when the follow-up is extended: results from a randomised controlled study. Eur Urol Suppl 2013;12:e729. [Other: sr-incont62144]
Costantini E, Lazzeri M, Zucchi A, Di Biase M, Porena M. Long-term efficacy of the transobturator and retropubic midurethral slings for stress urinary incontinence: single-center update from a randomized controlled trial. Eur Urol 2014;66:599–603. [Other: sr-incont64001; PubMed: 24768493]
Kocjancic E, Constantini E, Crivellaro S, Tosco L, Grossetti B, Frea B, et al. Mixed incontinence: The Best Solution for a Difficult Task. Proceedings of the International Continence Society (ICS), 38th Annual Meeting, Cairo, 20–24 October 2008, abstract no. 485. [Other: srincont31875]
Kocjancic E, Costantini E, Giannantoni A, Crivellaro S, Mearini L, Frea B, et al. Tension Free Vaginal Tape (TVT) and Trans Obturator Suburethral Tape (TOT) A Prospective Randomized Study. Proceedings of the American Urological Association (AUA), Annual Meeting, Anaheim, CA, 19–24 May 2007, poster abstract no. 1462. [Other: sr-incont23765]
aPorena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol 2007;52:1481–91. [Other: srincont23832]
Porena M, Kocjancic E, Costantini E, Cecchetti G, Bini V, Crivellaro S, et al. Tension free vaginal tape vs trans obturator tape as surgery for stress urinary incontinence: results of a multicenter randomised trial. Neurourol Urodyn 2005;24:416–18. [Other: sr-incont20982]
cCostantini E, Kocjancic E, Lazzeri M, Giannantoni A, Zucchi A, Carbone A, et al. Long-term efficacy of the trans-obturator and retropubic mid-urethral slings for stress urinary incontinence: update from a randomized clinical trial. World J Urol 2016;34:585–93. [Ref ID: 72105]
cCostantini E, Lazzeri M, Zucchi A, Bruno R, Salvini E, Pietropaolo A, et al. Deterioration of continence after TOT when the follow-up is extended: Results from a randomised controlled study. J Urol 2013;189(Suppl. 1):e555–e556. [Ref ID: 62195]
cCostantini E , Salvini E, Pietropaolo A, Quadrini F, Di BM, Bini V, et al. Sonography tape characteristic and incontinence outcome after trans-obturator tape (TOT) surgery. Eur Urol Suppl 2014;13:e383. [Ref ID: 62132]
Rechberger 200998
Rechberger T, Adamiak A, Jankiewicz K, Futyma K, Skorupski P. The comparison of clinical effectiveness of retropubic (IVS 02) and transobturator (IVS 04) midurethral slings. Int Urogynecol J 2006;17(Suppl. 2):S104. [Other: sr-incont49148]
Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Skorupski P. Body mass index does not influence the outcome of anti-incontinence surgery among women whereas menopausal status and ageing do: a randomised trial. Int Urogynecol J 2010;21:801–6. [Other: srincont40095]
aRechberger T, Futyma K, Jankiewicz K, Adamiak A, Skorupski P. The clinical effectiveness of retropubic (IVS-02) and transobturator (IVS-04) midurethral slings: randomized trial. Eur Urol 2009;56:24–30. [Other: srincont35437]
Rechberger T, Jankiewicz K, Futyma K, Adamiak A, Skorupski P. Clinical Effectiveness of Retropubic (IVS-02) and Transobturator (IVS-04) Slings in the Treatment of Female Stress Urinary Incontinence – A Semi-randomized Trial on 398 Patients. Proceedings of the International Continence Society (ICS), 38th Annual Meeting, 20–24 October 2008, Cairo, Egypt, abstract no. 515. [Other: srincont31877]
Rechberger T, Jankiewicz K, Skorupski P, Adamiak A, Futyma K, Gogacz M, et al. Transobturator vs. retropubic vaginal tape for female stress urinary incontinence: one year follow-up in 296 patients. Proceedings of the International Continence Society (ICS), 37th Annual Meeting, 20–24 August 2007, Rotterdam, The Netherlands, abstract no. 288. [Other: sr-incont23763]
Richter 201099
Brubaker L, Norton PA, Albo ME, Chai TC, Dandreo KJ, Lloyd KL, et al. Adverse events over two years after retropubic or transobturator midurethral sling surgery: findings from the Trial of Midurethral Slings (TOMUS) study. Am J Obstet Gynecol 2011;205:498.e1-6. [Other: NCT00325039; other: TOMUS; other: srincont43397]
Brubaker L, Rickey L, Stoddard A, Lemack G, Xu Y, Ghetti C, et al. Symptoms of combined prolapse and urinary incontinence in large surgical cohorts. Int Urogynecol J 2009;20(Suppl. 2):S96–7. [Other: NCT00064662; other: srincont39882]
Chai TC, Huang L, Kenton K, Richter HE, Baker J, Kraus S, et al. Association of baseline urodynamic measures of urethral function with clinical, demographic, and other urodynamic variables in women prior to undergoing midurethral sling surgery. Neurourol Urodyn 2012;31:496–501. [Other: NCT00325039; other: TOMUS; other: srincont49292]
Chai TC, Kenton K, Xu Y, Sirls L, Zyczynski H, Wilson TS, et al. Effects of concomitant surgeries during midurethral slings (MUS) on postoperative complications, voiding dysfunction, continence outcomes, and urodynamic variables. Urology 2012;79:1256–61. [Other: NCT00325039; other: srincont44637]
Gormley A. TOMUS-trial of Mid-urethral Slings [Results Posted Online]. Trials registration number: NCT00325039.URL: http://clinicaltrials.gov/show/NCT00325039 (accessed 18 August 2017). [Other: TOMUS; other: srincont49293]
Kenton K, Stoddard A, Zyczynski H, Rickey L, Wai C, Albo M, et al. 5-year outcomes after retropubic and transobturator midurethral sling. J Urol 2014;191(Suppl. 1):e493. [Other: sr-incont62138]
Kenton K, Stoddard AM, Zyczynski H, Albo M, Rickey L, Norton P, et al. 5-year longitudinal followup after retropubic and transobturator mid urethral slings. J Urol 2014;193:203–10. [Other: sr-incont64661; PubMed: 25158274]
Kraus S, Lemack G, Chai T, Leng W, Albo M, Mueller E, et al. Urodynamic changes 12 months after retropubic and transobturator midurethral slings. Neurourol Urodyn 2011;30:819–20. [Other: NCT00325039; other: TOMUS; other: sr-incont42167]
Kraus S, Lemack G, Chai T, Leng W, Albo M, Mueller E, et al. Urodynamic changes 12 months after retropubic and transobturator midurethral slings. Neurourol Urodyn 2011;30:210. [Other: NCT00325039; other: TOMUS; other: srincont41349]
Lemack GE, Litman HJ, Nager C, Brubaker L, Lowder J, Norton P, et al. Preoperative clinical, demographic, and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence. Int Urogynecol J 2013;24:269–74. [Other: NCT00064662; other: NCT00325039; other: SISTEr; other: TOMUS; other: srincont47045]
Norton PA, Nager CW, Chai TC, Mueller E, Stoddard A, Lowder J, et al. Risk factors for incomplete bladder emptying after midurethral sling. Urology 2013;82:1038–41. [Other: NCT00325039; other: srincont50470]
Nygaard I, Brubaker L, Chai TC, Markland AD, Menefee SA, Sirls L, et al. Risk factors for urinary tract infection following incontinence surgery. Int Urogynecol J 2011;22:1255–65. [Other: NCT00064662; other: NCT00325039; other: SISTEr; other: TOMUS; other: srincont42698]
aRichter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 2010;362:2066–76. [Other: NCT00325039; other: TOMUS; other: srincont39867]
Richter HE, Litman HJ, Lukacz ES, Sirls LT, Rickey L, Norton P, et al. Demographic and clinical predictors of treatment failure one year after midurethral sling surgery. Obstet Gynecol 2011;117:913–21. [Other: NCT00325039; other: TOMUS; other: srincont41490]
Rickey LM, Huang L, Rahn DD, Hsu Y, Litman HJ, Mueller ER. Risk factors for urgency incontinence in women undergoing stress urinary incontinence surgery. Adv Urol 2013;2013:567375. [Other: NCT00064662; other: NCT00325039; other: srincont50474]
Sirls LT, Tennstedt S, Albo M, Chai T, Kenton K, Huang L, et al. Factors associated with quality of life in women undergoing surgery for stress urinary incontinence. J Urol 2010;184:2411–5. [Other: NCT00325039; other: srincont49291]
Sirls LT, Tennstedt S, Lukacz E, Rickey L, Kraus SR, Markland AD, et al. Condition-specific quality of life 24 months after retropubic and transobturator sling surgery for stress urinary incontinence. Female Pelvic Med Reconstr Surg 2012;18:291–5. [Other: NCT00325039; other: srincont45799]
Urinary Incontinence Treatment Network. The trial of mid-urethral slings (TOMUS): design and methodology. J Appl Res 2008;8:1–13. [Other: NCT00325039; other: srincont27938]
Wai CY, Curto TM, Zyczynski HM, Stoddard AM, Burgio KL, Brubaker L, et al. Patient satisfaction after midurethral sling surgery for stress urinary incontinence. Obstet Gynecol 2013;121:1009–16. [Other: NCT00325039; other: srincont49289]
Zyczynski HM, Brubaker L. Sexual activity and function in women for two years after midurethral slings. Eur Urol Suppl 2012;11:e176. [Other: sr-incont62250]
Zyczynski HM, Rickey L, Dyer KY, Wilson T, Stoddard AM, Gormley EA, et al. Sexual activity and function in women more than 2 years after midurethral sling placement. Am J Obstet Gynecol 2012;207:421–6. [Other: NCT00325039; other: TOMUS; other: srincont45909]
cAlbo M, Litman H, Lemack G, Richter H, Chai T, Kenton K, et al. Twenty-four-month outcomes of randomized equivalence trial of retropubic and transobturator midurethral slings (TOMUS). J Urol 2011;185(Suppl. 1):e467. [Ref ID: 63660]
cAlbo ME, Litman HJ, Lemack GE, Richter HE, Chai TC, Kenton K, et al. Twenty-four month outcomes of randomized equivalence trial of retropubic and transobturator midurethral slings (TOMUS). Eur Urol Suppl 2012;11:e171-1a. [Ref ID: 62254]
cBrubaker L, Litman HJ, Kim HY, Zimmern P, Dyer K, Kusek JW, et al. Missing data frequency and correlates in two randomized surgical trials for urinary incontinence in women. Int Urogynecol J 2015 Aug;26:1155–9. [Ref ID: 68159]
cChai T, Kenton K, Gormley EA, Zyczynski H, Sirls L, Wilson T, et al. Effects of concomitant surgeries during mid-urethral slings (MUS) on post-operative complications, voiding dysfunction, continence outcomes, and urodynamic variables. J Urol 2011;185(Suppl. 1):e685. [Ref ID: 63658]
cFerrante K , Kim H-Y, Brubaker L, Wai C, Kraus S, Norton P, et al. Repeat post-op voiding trials: an inconvenient correlate with success. J Urol 2013;189(Suppl. 1):e230. [Ref ID: 62197]
cFerrante KL , Kim H, Brubaker L, Wai C, Kraus S, Norton P, et al. Repeat post-op voiding trials: an inconvenient correlate with success. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S110–11. [Ref ID: 62180]
cFerrante KL, Kim HY, Brubaker L, Wai CY, Norton PA, Kraus SR, et al. Repeat post-op voiding trials: an inconvenient correlate with success. Neurourol Urodyn 2014;33:1225–8. [Ref ID: 63987]
cLitman H, Kraus S, Lemack G, Chai T, Sirls L, Lloyd K, et al. Use of propensity scores to combine data from two similar clinical trials in the urinary incontinence treatment network. Clin Trials 2013;10(Suppl. 1):S54. [Other: sr-incont62162]
cLitman HJ , Albo ME, Lemack GE, Richter HE, Chai TC, Kenton K, et al. Twenty four month outcomes of randomized equivalence trial of two surgical techniques for women with stress urinary incontinence: retropubic and transobturator midurethral slings (TOMUS). Clin Trials 2011;8:508–9. [Ref ID: 62163]
cNorton P , Brubaker L, Nager C, Stoddard A, Sirls L, Lemack G, et al. Pelvic organ prolapse in a cohort of women treated for stress urinary incontinence. J Minim Invasive Gynecol 2014;21(Suppl. 1):S1. [Ref ID: 62149]
cNorton P, Brubaker L, Nager CW, Lemack GE, Zyczynski HM, Sirls L, et al. Pelvic organ prolapse in a cohort of women treated for stress urinary incontinence. Am J Obstet Gynecol 2014;211:550–5. [Ref ID: 64889]
cNorton P, Nager C, Chai T, Lemack G, Varner E, Lowder J, et al. Risk factors for incomplete bladder emptying after midurethral sling. Neurourol Urodyn 2011;30:818–19. [Ref ID: 63345]
cNorton P, Nager C, Varner RE, Chai TC, Lowder JL, Lemack G, et al. Risk factors for incomplete bladder emptying after midurethral sling. Female Pelvic Med Reconstr Surg 2011;17(Suppl. 1):S60. [Ref ID: 71508]
cSiff LN, Jelovsek JE, Barber MD. The effect of major depression on quality of life after surgery for stress urinary incontinence: a secondary analysis of the Trial of Midurethral Slings. Am J Obstet Gynecol 2016;215:455.e1–9. [Ref ID: 73091]
cSirls L, Tennstedt S, Richter H, Brubaker L, Kim H, Nygaard I, et al. The minimum clinically important difference for the International Consultation on Incontinence Questionnaire (ICIQ) in women with stress urinary incontinence. Neurourol Urodyn 2013;32:547–9. [Ref ID: 62172]
cSirls LT, Tennstedt S, Lukacz E, Rickey L, Kraus SR, Markland A, et al. Condition specific quality of life 24 months after retropubic and transobturator sling surgery for stress urinary incontinence. Eur Urol Suppl 2012;11:e174–e174a. [Ref ID: 62251]
cSirls LT, Tennstedt S, Brubaker L, Kim HY, Nygaard I, Rahn DD, et al. The minimum important difference for the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form in women with stress urinary incontinence. Neurourol Urodyn 2015;34:183–7. [Ref ID: 68072]
cWai CY , Brubaker L, Curto TM, Rickey LM, Stoddard A, Zyczynski HM, et al. Comparison of patient satisfaction between retropubic and transobturator midurethral sling at one year. Female Pelvic Med Reconstr Surg 2012;18(Suppl. 1):S9–S10. [Ref ID: 70946]
cZimmern P, Litman HJ, Nager CW, Lemack GE, Richter HE, Sirls L, et al. Effect of aging on storage and voiding function in women with stress predominant urinary incontinence. J Urol 2014;192:464–8. [Ref ID: 62543]
cZimmern PE, Gormley EA, Stoddard AM, Lukacz ES, Sirls L, Brubaker L, et al. Management of recurrent stress urinary incontinence after burch and sling procedures. [Review]. Neurourol Urodyn 2016;35:344–8. [Ref ID: 74150]
cZyczynski HM, Albo ME, Goldman HB, Wai CY, Sirls LT, Brubaker L, et al. Change in overactive bladder symptoms after surgery for stress urinary incontinence in women. Obstet Gynecol 2015;126:423–30. [Ref ID: 70333]
cZyczynski HM, Brubaker L, Gormley EA, Rickey LM, Wilson T, Dyer K, et al. Sexual activity and function in women for two years after retropubic and transobturator midurethral slings. Female Pelvic Med Reconstr Surg 2012;18(Suppl. 1):S13. [Ref ID: 71504]
cZyczynski HM, Sirls LT, Greer WJ, Rahn DD, Casiano E, Norton P, et al. Findings of universal cystoscopy at incontinence surgery and their sequelae. Am J Obstet Gynecol 2014;210:480–8. [Ref ID: 62040]
Riva 200671
Riva D, Sacca V, Tonta A, Casolati E, Luerti M, Banfi G, et al. TVT versus TOT a randomised study at 1 year follow up. Int Urogynecol J 2006;17(Suppl. 2):S93. [Other: sr-incont49150]
Ross 2009137
Lier D, Ross S, Tang S, Robert M, Jacobs P, Calgary Women’s Pelvic Health Research Group. Trans-obturator tape compared with tension-free vaginal tape in the surgical treatment of stress urinary incontinence: a cost utility analysis. BJOG 2011;118:550–6. [Other: NCT00234754; other: srincont41520]
Robert M, Birch C, Cenailo D, Murphy M, Carlson K, Baverstock R, et al. Patient expectations, subjective improvement and objective cure: is there a difference between the transobturator tape and the tension free vaginal tape procedure? Neurourol Urodyn 2009;28:846. [Other: NCT00234754; other: srincont39355]
Robert M, Lier D, Tang S, Jacobs P, Ross S. A Cost Utility Analysis of Trans-obturator Tape Compared with Tension-free Vaginal Tape in the Surgical Treatment of Stress Urinary Incontinence. Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, Toronto, ON, 23–27 August 2010, abstract no. 739. [Other: NCT00234754; other: srincont40198]
Ross S, Robert M, Lier D, Eliasziw M, Jacobs P. Surgical management of stress urinary incontinence in women: safety, effectiveness and cost-utility of trans-obturator tape (TOT) versus tension-free vaginal tape (TVT) five years after a randomized surgical trial. BMC Womens Health 2011;11:34. [Other: NCT00234754; other: srincont42691]
aRoss S, Robert M, Swaby C, Dederer L, Lier D, Tang S, et al. Transobturator tape compared with tension-free vaginal tape for stress incontinence: a randomized controlled trial. Obstet Gynecol 2009;114:1287–94. [Other: NCT00234754; other: srincont35356]
cBrennand EA, Tang S, Ross S, Birch C, Murphy M, Robert M. Impact of body mass index on one year outcomes after midurethral slings. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S117–S118. [Ref ID: 62176]
cBrennand EA , Tang S, Williamson T, Birch C, Murphy M, Robert M, et al. Twelve-month outcomes following midurethral sling procedures for stress incontinence: impact of obesity. BJOG 2015;122:1705–12. [Ref ID: 69234; other: NCT00234754]
cBrennand EA, Tang S, Birch C, Murphy M, Ross S, Robert M, et al. Five years after midurethral sling surgery for stress incontinence: obesity continues to have an impact on outcomes. Int Urogynecol J 2017;28:621–8. [Ref ID: 74265]
cLier D, Robert M, Tang S, Ross S. Surgical treatment of stress urinary incontinence-trans-obturator tape compared with tension-free vaginal tape-5-year follow up: an economic evaluation. BJOG 2017;124:1431–9. [Ref ID: 73040; other: NCT00234754]
cRoss S, Tang S, Eliasziw M, Lier D, Girard I, Brennand E, et al. Transobturator tape versus retropubic tension-free vaginal tape for stress urinary incontinence: 5-year safety and effectiveness outcomes following a randomised trial. Int Urogynecol J 2016;27:879–86. [Ref ID: 72243]
Salem 201473
Salem H, Mostafa M, Diab DE, Abdulla A, Nageeb M, Hashem SA. A prospective randomized study comparing the safety and efficacy of transobturator tape (TOT) versus tension free vaginal tape (TVT) in treatment of female stress urinary incontinence. J Urol 2014;191(Suppl. 1):e342–3. [Other: srincont62143]
Scheiner 2012119
Scheiner D, Betschart C, Kollbrunner S, Werder H, Fink D, Perucchini D. Retropubic or Transobturator Out-in or In-out Sling? A Prospective Randomized Study. Proceedings of the International Continence Society (ICS), 38th Annual Meeting, Cairo, 20–24 October 2008, abstract no. 484. [Other: NCT00642109; other: srincont31874]
Scheiner D, Betschart C, Werder H, Fink D, Perucchini D. Retropubic TVT vs transobturator outside-in TOT and inside-out TVT-O one-year results from our prospective randomized study. Neurourol Urodyn 2009;28:585–6. [Other: NCT00642109; other: srincont34588]
aScheiner DA, Betschart C, Wiederkehr S, Seifert B, Fink D, Perucchini D. Twelve months effect on voiding function of retropubic compared with outside-in and inside-out transobturator midurethral slings. Int Urogynecol J 2012;23:197–206. [Other: srincont44532]
cScheiner D, Betschart C, Wiederkehr S, Fink D, Perucchini D. Tension-free vaginal tape TVT compared with outside-in TOT and inside-out TVT-O transobturator tapes: a randomized controlled trial. Arch Gynecol Obstet 2010;282(Suppl. 1):S26. [Ref ID: 63371]
Schierlitz 2008138
De Souza A, Dwyer PL, Rosamilia A, Hiscock R, Lim YN, Murray C, et al. Sexual function following retropubic TVT and transobturator Monarc sling in women with intrinsic sphincter deficiency: a multicentre prospective study. Int Urogynecol J 2012;23:153–8. [Other: srincont44534]
De Souza A, Schierlitz L, Rosamilia A, Dwyer P, Murray C, Thomas E, et al. Sexual function following retropubic TVT and transobturator Monarc sling in women with intrinsic sphincter deficiency. ANZCJ 2008;14:104. [Other: srincont29144]
Murray C, Schierlitz L, Dwyer PL, Rosamilia A, Hiscock R, De Souza A, et al. Overactive bladder (OAB) symptoms following retropubic TVT and Monarc TOT in women with intrinsic sphincter deficiency (ISD) and stress incontinence. ANZCJ 2008;14:102. [Other: srincont29145]
Plotti F, Calcagno M, Sansone M, Panici PB. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial [comment] [letter]. Obstet Gynecol 2009;113:1368; author reply 1368–9. [Other: srincont31355]
Schierlitz L, Dwyer P, Rosamilia A, Murray C, Thomas E, Fitzgerald E, et al. A randomized controlled study to compare tension free vaginal tape (TVT) and Monarc trans-obturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD): the three-year follow-up. Neurourol Urodyn 2010;29:805–6. [Other: srincont40112]
Schierlitz L, Dwyer PL, Rosamilia A, Hiscock R, De Souza A, Lim YN, et al. A randomised controlled study to compare tension-free vaginal tape (TVT) and Monarc transobturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD): the three-year follow-up. ANZCJ 2010;16:120–2. [Other: srincont40800]
aSchierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol 2008;112:1253–61. [Other: ACTRN12608000093381; other: srincont28699]
Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Three-year follow-up of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstet Gynecol 2012;119:321–7. [Other: ACTRN12608000093381; other: srincont43343]
Schierlitz LHE, Dwyer PL, Rosamilia A, Murray C, Thomas E, Taylor N, et al. A randomized controlled study to compare tension free vaginal tape (TVT) and Monarc trans-obturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD). Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S19. [Other: srincont27321]
cAlvarez J, Dwyer P, Kaplan F, Schierlitz L, De SA, Cvach K. Why is the success rate higher with retropubic slings compared to transobturator slings in women with stress urinary incontinence and intrinsic sphincter deficiency: an analysis from an urodynamic point of view. Int Urogynecol J Pelvic Floor Dysfunct 2012;23(Suppl. 1):S73. [Ref ID: 67499]
cAlvarez J, Schierlitz L, Dwyer P, Rosamilia A, Murray C, Lee J. A randomized control study comparing tension free vaginal tape (TVT) and Monarc trans-obturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD) with a mean follow up of 60 months. Int Urogynecol J Pelvic Floor Dysfunct 2014;25(Suppl. 1):S7–S8. [Ref ID: 63846]
cSchierlitz L, Murray C, Thomas E, Taylor N, Hiscock R, Lim Y, et al. A randomised controlled study to compare tension free vaginal tape (TVT) and MONARC trans-obturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD).16th National Conference on Incontinence, Gold Coast, QLD, 2007. ANZCJ 2007;13:123–4. [Ref ID: 70180]
Tanuri 2010139
Tanuri AL, Feldner PC Jr, Bella ZI, Castro RA, Sartori MG, Girao MJ. [Retropubic and transobturator sling in treatment of stress urinary incontinence.] [Portuguese]. Rev Assoc Med Bras 2010;56:348–54. [Other: srincont40054]
Tarcan 201131
aTarcan T, Mangir N, Tanidir Y, Top T, IIker Y. A Randomised Study Comparing Transvaginal and Transobturator Mid-urethral Sling Surgeries in Women with Stress Urinary Incontinence. Proceedings of the International Continence Society (ICS), 41st Annual Meeting, Glasgow, 29 August to 2 September 2011, abstract no. 845. [Other: srincont42237]
Tarcan T, Sahan A, Sulukaya M, Mangir N, Ilker Y. 2-year Results of a Randomized Study Comparing Retropubic and Transobturator Mid-urethral Slings in the Treatment of Urodynamic Female Stress Urinary Incontinence. Proceedings of the International Continence Society (ICS), 43rd Annual Meeting, Barcelona, 26–30 August 2013, abstract no. 448. [Other: srincont60034]
cTarcan T, Mangir N, Sahan A, Tanidir Y, Sulukaya M, Ilker Y. Safety and efficacy of retropubic or transobturator midurethral slings in a randomized cohort of Turkish women. Urol Int 2014;93:449–53. [Ref ID: 64827]
Teo 2011140
aMayne C. Randomised Trial of Tension-free Vaginal Tape and Transobturator Tape as Treatment for Urinary Stress Incontinence in Women. 2004. Trial registration number: ISRCTN34377436. URL: http://isrctn.org/ISRCTN34377436 (accessed 19 August 2017). [Other: sr-incont62313]
Teo R, Moran P, Mayne C, Tincello D. Randomised trial of TVT and TVT-O for the treatment of urodynamic stress incontinence in women. Neurourol Urodyn 2008;27:572–3. [Other: srincont31848]
Teo R, Moran P, Mayne C, Tincello D. Randomised Trial of Tension-free Vaginal Tape and Transobturator Tape for the Treatment of Urodynamic Stress Incontinence in Women. Proceedings of the International Continence Society (ICS), 37th Annual Meeting, Rotterdam, 20–24 August 2007, abstract no. 283. [Other: srincont23761]
aTeo R, Moran P, Mayne C, Tincello D. Randomized trial of tension-free vaginal tape and tension-free vaginal tape-obturator for urodynamic stress incontinence in women. J Urol 2011;185:1350–5. [Other: srincont41497]
Wang 2006141
Wang AC, Lin YH, Tseng LH, Chih SY, Lee CJ. Prospective randomized comparison of transobturator suburethral sling (Monarc) vs suprapubic arc (Sparc) sling procedures for female urodynamic stress incontinence. Int Urogynecol J 2006;17:439–43. [Other: srincont22217]
Wang 200937
Wang WY, Zhu L, Lang JH, Sun ZJ, Hai N. [Clinical study on tension-free vaginal tape and tension-free vaginal tape obturator for surgical treatment of severe stress urinary incontinence] [Chinese]. Chin J Obstet Gynecol 2008;43:180–4. [Other: srincont27746] [Please note this was previously part of the study with study ID Wang 2008]
aWang W, Zhu L, Lang J. Transobturator tape procedure versus tension-free vaginal tape for treatment of stress urinary incontinence. Int J Gynaecol Obstet 2009;104:113–16. [Other: srincont29200]
Wang WY, Zhu L, Lang JH, Li B. [A prospective randomized trial of comparing the clinical outcome of tension-free vaginal tape and transobturator tape for stress urinary incontinence] [Chinese]. Chin Med J 2011;91(13):898–901. [Other: srincont41799]
Zhu I, Lang J, Chen R, Hai N, Wong F. Comparing TVT and TVT-O sub urethral tape for treatment patients with mild and moderate stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S198. [Other: srincont27325]
Zhu I, Lang J. A prospective randomised trial comparing tension free vaginal tape and transobturator suburethral tape for surgical treatment of slight and moderate stress urinary incontinence. Int Urogynecol J 2006;17(Suppl. 2):S307. [Other: sr-incont49151]
Zhu L, Lang J, Hai N, Wong F. Comparing vaginal tape and transobturator tape for the treatment of mild and moderate stress incontinence. Int J Gynaecol Obstet 2007;99:14–7. [Other: srincont23870]
Wang 2010142
Wang F, Song Y, Huang H. Prospective randomized trial of TVT and TOT as primary treatment for female stress urinary incontinence with or without pelvic organ prolapse in Southeast China. Arch Gynecol Obstet 2010;281:279–86. [Other: srincont35408]
Wang 2011116
Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH. Comparison of three mid-urethral tension-free tapes (TVT, TVT-O, and TVT-Secur) in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J 2011;22:1369–74. [Other: srincont42639]
Zullo 2007144
Angioli R, Plotti F, Muzii L, Montera R, Panici PB, Zullo MA. Tension-free vaginal tape versus transobturator suburethral tape: five-year follow-up results of a prospective, randomised trial. Eur Urol 2010;58:671–7. [Other: srincont41500]
aZullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, et al. One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol 2007;51:1376–82; discussion 1383–4. [Other: srincont23246]
(iii) Cochrane review: Nambiar et al.9 – single-incision sling operations for UI in women
Abdelwahab 2010155
Abdelwahab O, Shedid I, Al-Adl AM. Tension-free vaginal tape versus secure tension-free vaginal tape in treatment of female stress urinary incontinence. Curr Urol 2010;4:93–8. [CRSREF: 3347916; other: 42740]
Amat 2011112
aAmat L, Franco E, Vicens JM. Contasure-Needleless compared with transobturator-TVT for the treatment of stress urinary incontinence. Int Urogynecol J 2011;22:827–33. [CRSREF: 3347918; other: 42952]
Amat LL, Franco EM, Saavedra AH, Martinez AV. Needleless (R): a new technique for correction of urinary incontinence. Randomized controlled trial compared with TVT-O (R). Preliminary results. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S128. [CRSREF: 3347919; other: 27329]
cMartinez Franco E , Amat Tardiu L. Contasure-Needleless single incision sling compared with transobturator TVT-O for the treatment of stress urinary incontinence: long-term results. Int Urogynecol J 2015;26:213–8. [Ref ID: 66436]
Andrada Hamer 2011156
Andrada Hamer M, Larsson PG, Teleman P, Eten-Bergquist C, Persson J. One year results of a prospective randomized evaluator blinded multicenter study comparing TVT and TVT-Secur. Neurourol Urodyn 2012;31:728–9. [CRSREF: 3347921; other: 45455]
aAndrada Hamer M, Larsson PG, Teleman P, Eten-Bergqvist C, Persson J. Short-term results of a prospective randomized evaluator blinded multicenter study comparing TVT and TVT-Secur. Int Urogynecol J 2011;22:781–7. [CRSREF: 3347922; other: 41716]
cAndrada Hamer M, Larsson PG, Teleman P, Bergqvist CE, Persson J. One-year results of a prospective randomized, evaluator-blinded, multicenter study comparing TVT and TVT Secur. Int Urogynecol J 2013;24:223–9. [Ref ID: 46785]
Barber 201287
aBarber MD, Weidner AC, Sokol AI, Amundsen CL, Jelovsek JE, Karram MM, et al. Single-incision mini-sling compared with tension-free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol 2012;119:328–37. [CRSREF: 3347924; other: 43342]
cBarber MD, Weidner AC, Sokol AI, Amundsen C, Jelovsek JE, Karram MM, et al. A blinded multi-center randomized trial comparing TVT-SECUR “U” to the tension-free vaginal tape (TVT) for the surgical treatment of stress urinary incontinence. Female Pelvic Med Reconstr Surg 2011;17(Suppl. 1):S52–S53. [Ref ID: 71510]
cBarber MD. A blinded multi-center randomized trial comparing TVT-SECUR “U” to the tension-free vaginal tape (TVT) for the surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 1):S2–S3. [Ref ID: 62270; other: NCT00534365]
Basu 2010157
aBasu M, Duckett J. A randomised trial of a retropubic tension-free vaginal tape versus a mini-sling for stress incontinence. BJOG 2010;117:730–5. [CRSREF: 3347926; other: 39624]
Basu M, Duckett J. A randomised trial of the Miniarc single incision sling versus a retropubic TVT in the management of women with stress urinary incontinence – three year follow up. Int Urogynecol J 2012;23(Suppl. 2):S141–S142. [CRSREF: 3347927; other: 45466]
cNCT00843908, Duckett J. A randomized study of the treatment of urodynamic stress incontinence: the Tension Free Vaginal Tape (TVT) Versus the Miniarc Sling. 2008. Trial registration number: NCT00843908. URL: http://clinicaltrials.gov/show/NCT00843908 (accessed 19 August 2017). [Ref ID: 62914]
cBasu M, Duckett J. Three-year results from a randomised trial of a retropubic mid-urethral sling versus the Miniarc single incision sling for stress urinary incontinence. Int Urogynecol J 2013;24:2059–64. [Ref ID: 49467]
Bianchi 201225
aBianchi AH, Jarmy-Di-Bella ZI, Castro RA, Sartori MG, Girao MJ. Randomised trial of TVT-O™ and TVT-S™ for the treatment of stress urinary incontinence. Int Urogynecol J 2012;23(Suppl. 2):S216–S217. [CRSREF: 3347929; other: 45465]
Bianchi AM, Jarmy-Di Bella Z, Castro R, Sartori M, Girao M. Randomised trial of TVTO™ and TVTS™ for the treatment of stress urinary incontinence. Preliminary study. Neurourol Urodyn 2010;29:1025–6. [CRSREF: 3347930; other: 40147]
cBianchi-Ferraro AM, Jarmy-DiBella ZI, de Aquino CR, Bortolini MA, Sartori MG, Girao MJ. Randomized controlled trial comparing TVT-O and TVT-S for the treatment of stress urinary incontinence: 2-year results. Int Urogynecol J 2014;25:1343–8. [Ref ID: 63944]
cBianchi AH, Jarmy-Di Bella ZI, Castro RA, Sartori MG, Girao MJ. Randomised trial of TVT-O and TVT-S for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 1):S62. [Ref ID: 62265]
cBianchi-Ferraro AM, Jarmy-Di Bella ZI, Castro RA, Bortolini MA, Sartori MG, Girao MJ. Single-incision sling compared with transobturator sling for treating stress urinary incontinence: a randomized controlled trial. Int Urogynecol J 2013;24:1459–65. [Ref ID: 48452; other: NCT01095159]
cBianchi-Ferraro AH, Jarmy-Di Bella ZI, Bortolini MT, Castro RA, Sartori MG, Girao MJ. Randomised trial of transobturator and mini sling for treatment of stress urinary incontinence 30-months follow-up. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S116. [Ref ID: 62177; other: NCT01095159]
Djehdian 201027
Djehdian L, Araujo M, Takano C, Del Roy C, Castro R, Sartori MGF, et al. Randomised Trial of Ophira Mini-sling System and Unitape for the Treatment of Stress Incontinence in Women. First Experiences After a Follow-up of 6 Months. Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, Toronto, ON, 23–27 August 2010, abstract no. 768. [CRSREF: 3347932; other: 40201]
cNCT01094353, Djehdian LM. Randomised Trial of Ophira™ (Minisling System and Unitape™ for the Treatment of Stress Urinary Incontinence in Women. 2008. Trial registration number: NCT01094353. URL: http://clinicaltrials.gov/show/NCT01094353 (accessed 19 August 2017). [Ref ID: 62913]
cDjehdian LM, Araujo MP, Takano CC, Del-Roy CA, Sartori MG, Girao MJ, et al. Transobturator sling compared with single-incision mini-sling for the treatment of stress urinary incontinence: a randomized controlled trial. Obstet Gynecol 2014;123:553–61. [Ref ID: 60507]
cPascom AL, Castro RA, Bortolini MA, Sartori MM, Girao MB, Jarmy-DiBella ZI. Randomized controlled trial comparing Ophira® and Unitape T Plus® for the treatment of stress urinary incontinence: 3-year results. Int Urogynecol J Pelvic Floor Dysfunct 2016;27( Suppl. 1):S74–5. [Ref ID: 73435]
cDjehdian LM, Araujo M, Takano C, Del RC, Sartori M, Girao M, et al. Randomised trial of Ophira mini-sling system and Unitape transobturator suburethral sling for the treatment of stress urinary incontinence in women. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 3):S1814–16. [Ref ID: 62230; other: NCT01094353]
Enzelsberger 2010170
Enzelsberger H, Cemer I, Enzelsberger S, Schalupny J. [MiniArc versus Monarc a prospective randomized study of the treatment of female stress urinary incontinence with a follow-up of 2 years] [German]. Geburtshilfe Frauenheilkd 2010;70:499–502. [CRSREF: 3347934; other: 42521]
Friedman 200954
aFriedman M. TVT-O vs TVT-S: first randomized, prospective, comparative study of intraoperative complications, perioperative morbidity and one year postoperative results. J Pelvic Med Surg 2009;15:48. [CRSREF: 3347936; other: SR-INCONT42743]
Friedman M. TVT-S versus TVT-O: randomized, prospective comparative study of intraoperative complications, perioperative morbidity and short-term postoperative results. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S204. [CRSREF: 3347937; other: 27328]
Hinoul 2011172
aHinoul P, Vervest HA, den Boon J, Venema PL, Lakeman MM, Milani AL, et al. A randomized, controlled trial comparing an innovative single incision sling with an established transobturator sling to treat female stress urinary incontinence. J Urol 2011;185:1356–62. [CRSREF: 3347939; other: 41495]
Hinoul P. A Multi-centre Randomised Comparison of the Effectiveness and Safety of TVT-O and TVT-S. 2008. Trial registration number: NTR1141. URL: www.trialregister.nl/trialreg/admin/rctview.asp?TC=1141 (accessed 20 September 2012). [CRSREF: 3347940; other: 45470]
Page AS, Page GH. Re: A randomized, controlled trial comparing an innovative single incision sling with an established transobturator sling to treat female stress urinary incontinence: Hinoul P, Vervest HA, den Boon J, Venema PL, Lakeman MM, Milani AL, et al. J Urol 2011;185:1356–62 [letter]. J Urol 2012;187:357–8. [CRSREF: 3347941; other: 43003]
Hota 2012173
Hota LS, Hanaway K, Hacker MR, Disciullo A, Elkadry E, Dramitinos P, et al. TVT-Secur (Hammock) versus TVT-obturator: a randomized trial of suburethral sling operative procedures. Female Pelvic Med Reconstr Surg 2012;18:41–5. [CRSREF: 3347943; other: 44507]
Kim 201059
Kim Y, Jung W, Jo SW, Kim WT, Yun SJ, Lee S, et al. Prospective Comparative Study Between the TVT-Secur and TOT Procedures for Treatment of Stress Urinary Incontinence Patients. Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, Toronto, ON, 23–27 August 2010, abstract no. 1182. [CRSREF: 3347945; other: 40209]
Lee 201228
Dwyer PL, Rosamilia A, Lim YN, Lee J, Thomas E. MiniArc and Monarc Suburethral Sling in Women with Stress Urinary Incontinence – A Randomised Controlled Trial. 2012. Trial registration number: ACTRN12608000624381. URL: www.anzctr.org.au/ACTRN12608000624381.aspx (accessed 17 January 2012). [CRSREF: 3347955; other: SR-INCONT43058]
aLee J, Rosamilia A, Dwyer P, Lim YN, Thomas E, Murray C, et al. MiniArc and Monarc suburethral sling in women with stress urinary incontinence: a randomised controlled trial. Int Urogynecol J 2012;23(Suppl. 2):S142–S144. [CRSREF: 3347956; other: 45459]
cLee J, Rosamilia A, Dwyer P, Lim Y, Thomas E, Murray C, et al. MiniArc Monarc suburethral sling in women with stress urinary incontinence – an RCT. BJU Int 2013;111(Suppl. 1):15–17. [Ref ID: 63630]
cLee J, Rosamilia A, Dwyer P, Lim YN, Ulrich D. Miniarc monarc suburethral sling in women with stress urinary incontinence – an RCT-24 month follow up. Int Urogynecol J Pelvic Floor Dysfunct 2014;25(Suppl. 1):S3–S5. [Ref ID: 63603]
cLee JK, Rosamilia A, Dwyer PL, Lim YN, Muller R. Randomized trial of a single incision versus an outside-in transobturator midurethral sling in women with stress urinary incontinence: 12 month results. Am J Obstet Gynecol 2015;213:35.e1-9. [Ref ID: 68221; other: ACTRN12608000624381]
cLee J, Rosamilia A, Dwyer PL, Lim YN, Muller R, Thomas EA, et al. Miniarc Monarc suburethral sling in women with stress urinary incontinence – an RCT-36-month follow up. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S82–3S8. [Ref ID: 69561; other: ACTRN12608000624381]
cLee J, Rosamilia A, Lim YN, Thomas E, Murray C, Fitzgerald E, et al. Miniarc Monarc suburethral sling in women with stress urinary incontinence – an RCT – 12-month follow up. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S108–S109. [Ref ID: 62182; other: ACTRN12608000624381]
cLee J, Rosamilia A, Dwyer PL, Lim YN, Young NR, Thomas EA, et al. Miniarc monarc suburethral sling in women with stress urinary incontinence – an RCT-48-month follow up. Int Urogynecol J Pelvic Floor Dysfunct 2016;27(Suppl. 1):S46–S47. [Ref ID: 75446]
cYoung N, Lee J, Rosamilia A. Outcomes of patients who declined randomization to MiniMo trial. Eur J Obstet Gynecol Reprod Biol 2015;195:117–21. [Ref ID: 74175]
cYoung N, Rosamilia A, Lee J. Outcomes of patients who declined randomisation to Miniarc versus Monarc: a retrospective study. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S115–S116. [Ref ID: 62178]
Mackintosh 2010174
Mackintosh A. A Pilot, Randomised, Prospective Study of Transobturator Tape Versus Single Incision Sub-Urethral Tape in The Management of Female, Urodynamic Stress Incontinence. PhD thesis. Aberdeen: University of Aberdeen; 2010. [CRSREF: 3347960; other: 41122]
Masata 2012167
Masata J, Svabik K, Drahoradova P, Hubka P, Zvara K, El-Haddad R, et al. Randomized prospective trial of a comparison of the efficacy of TVT-O and TVT Secur system in the treatment of stress urinary incontinent women comparison of the long- and short-term results. Neurourol Urodyn 2011;30:805–6. [CRSREF: 3347966; other: 42163]
Masata J, Svabik K, Hubka P, Elhaddad R, Drahoradova P, Martan A. What happens with single incision tape (TVT-S) after surgery, in comparison with TVT-O? An ultrasound study results from a randomized trial. Int Urogynecol J 2012;23(Suppl. 2):S69–S71. [CRSREF: 3347967; other: 45468]
Masata J, Svabik K, Hubka P, Zvara K, El Haddad R, Drahoradova P, et al. Is the fixation of single incision tape (TVT-S) as good as a transobturator tape (TVT-O)? An ultrasound study, results from randomized trial. Neurourol Urodyn 2012;31:731–3. [CRSREF: 3347968; other: 45456]
Masata J, Svabik K, Zvara K, Drahodradova P, Hubka P, Elhaddad R, et al. [Comparison of short term results of TVT-O and TVT-S in the surgical treatment of stress urinary incontinence]. [Czech]. Ceska Gynekol 2012;77:350–7. [CRSREF: 3347969; other: 45851]
aMasata J, Svabik K, Zvara K, Drahoradova P, El Haddad R, Hubka P, et al. Randomized trial of a comparison of the efficacy of TVT-O and single-incision tape TVT SECUR systems in the treatment of stress urinary incontinent women – 2-year follow-up. Int Urogynecol J 2012;23:1403–12. [CRSREF: 3347970; other: 45853]
cMasata J, Svabik K, Hubka P, Martan A. Randomized prospective trial of a comparison of the efficacy of TVT-O and TVT SECUR system in the treatment of stress urinary incontinent women – long-term results with a minimum of five-years follow-up. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S137–S138. [Ref ID: 69596]
cMasata J , Martan A, Hubka P, Svabik K. Long-term Follow-up (with a Minimum of Five Years) Comparing the Efficacy of TVT-O and TVT SECUR System in the Treatment of Stress Urinary Incontinent Women – Randomized Trial. Proceedings of the International Continence Society (ICS), Annual Meeting, Tokyo, 13–16 September 2016, abstract no. 752. [Ref ID: 73459]
cMasata J, Svabik K, Elhaddad R, Hubka P, Drahoradova P, Martan A. Randomized prospective trial of a comparison of the efficacy of TVT-O and TVT SECUR system in the treatment of stress urinary incontinent women – long-term results. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 1):S3–S4. [Ref ID: 62269]
Mostafa 2012204
Boyers D, Kilonzo M, Mostafa A, Abdel-Fattah M. Single incision mini-slings versus standard mid-urethral slings in surgical management of female stress urinary incontinence: a cost-effectiveness analysis alongside a randomised controlled trial. Neurourol Urodyn 2012;31:726–7. [CRSREF: 3347972; other: 45457]
Mostafa A, Agur W, Abdel-All M, Guerrero K, Allam M, Lim C, et al. A multicentre randomised trial of single-incision mini-sling (AJUSTc) and tension-free vaginal tape-obturator (TVT-O™) in management of female stress urinary incontinence. Neurourol Urodyn 2011;30:806–8. [CRSREF: 3347973; other: 42164]
aMostafa A, Agur W, Abdel-All M, Guerrero K, Lim C, Allam M, et al. A multicentre prospective randomised study of single-incision mini-sling (Ajust®) versus tension-free vaginal tape-obturator (TVT-O™) in the management of female stress urinary incontinence: pain profile and short-term outcomes. Eur J Obstet Gynecol Reprod Biol 2012;165:115–21. [CRSREF: 3347974; other: 45867]
Mostafa A, Agur W, Abdel-All M, Guerrero K, Lim C, Allam M, et al. Multicentre prospective randomised study of single-incision midurethral sling (SIMS-Ajust™) versus tension-free vaginal tape-obturator (TVT-O™) in management of female stress urinary incontinence (SUI): a minimum of one year follow-up. Neurourol Urodyn 2012;31:724–5. [CRSREF: 3347975; other: 45454]
Mostafa A, Swami S, Fielding S, N’Dow J, Abdel-Fattah M. Exploring Factors Affecting Women’s Decision to Participate in Randomised Controlled Trials Assessing Surgical Treatment for Stress Urinary Incontinence. Proceedings of the International Continence Society (ICS), 41st Annual Meeting, Glasgow, 29 August to 2 September 2011, abstract no. 359. [CRSREF: 3347976; other: 42217; other: NCT01230450]
cBoyers D, Kilonzo M, Mostafa A, Abdel-Fattah M. Comparison of an adjustable anchored single-incision mini-sling, Ajust™, with a standard mid-urethral sling, TVT-O™: a health economic evaluation. BJU Int 2013;112:1169–77. [Ref ID: 49458; other: NCT01230450]
cMostafa A, Agur W, Abdel-All M, Yousef M, Allam M, Guerrero K, et al. A multicentre randomised trial comparing single-incision mini-sling (Ajust™) and tension-free vaginal tape-obturator (TVT-O) in management of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 1):S5–S7. [Ref ID: 47315]
cMostafa A, Agur W, Abdel-All M, Guerrero K, Lim C, Allam M, et al. Multicenter prospective randomized study of single-incision mini-sling vs tension-free vaginal tape-obturator in management of female stress urinary incontinence: a minimum of 1-year follow-up. Urology 2013;82:552–9. [Ref ID: 48534; other: NCT01230450]
cMostafa A, N’Dow J, Abdel-Fattah M. Factors influencing women’s decision to participate or not in a surgical randomised controlled trial for surgical treatment of female stress urinary incontinence. Biomed Res Int 2013;2013:139813. [Ref ID: 49436; other: NCT01230450]
cNCT01230450, Abdel-Fattah M. Feasibility of Comparing Two Surgical Treatment of Female Urodynamic Stress Incontinence (SITOT). 2009. Trial registration number: NCT01230450. URL: http://clinicaltrials.gov/show/NCT01230450 (accessed 19 August 2017). [Ref ID: 60004]
Oliveira 2011168
aOliveira R, Botelho F, Silva P, Resende A, Silva C, Dinis P, et al. Exploratory study assessing efficacy and complications of TVT-O, TVT-Secur, and Mini-Arc: results at 12-month follow-up. Eur Urol 2011;59:940–4. [CRSREF: 3347978; other: 41493]
Santos Oliveira R, Botelho F, Silva P, Silva CMPM, Dinis P, Cruz FJMR. Randomized clinical trial comparing TVT-O™, TVT-Secur™ and Mini-Arc™. Outcome at 12-months follow-up. Eur Urol Suppl 2010;9:145. [CRSREF: 3347979; other: 41579]
cLopes T, Resende A, Oliveira R, Pinto R, Botelho F, Tomada N, et al. Sexual function impact of stress urinary incontinence surgical treatment: comparison between midurethral and single-incision slings. J Sex Med 2011;8(Suppl. s5):390. [Ref ID: 62291]
cResende A, Oliveira R, Botelho F, Silva C, Dinis P, Cruz F. Randomized trial comparing a conventional mid-urethral sling and two single-incision slings: mid-term evaluation. Urology 2011;78(Suppl. 1):S211. [Ref ID: 62232]
Schweitzer 201229
aSchweitzer KJ, Cromheecke GJ, Milani AL, van Eijndhoven HW, Gietelink D, Hallenleben E, et al. A randomised controlled trial comparing the TVT-O® with the Ajust® as primary surgical treatment of female stress urinary incontinence. Int Urogynecol J 2012;23(Suppl. 2):S77–S78. [CRSREF: 3347985; other: 45467; other: NTR2558]
cSchweitzer KJ, Milani AL, van Eijndhoven HW, Gietelink DA, Hallensleben E, Cromheecke GJ, et al. Postoperative pain after adjustable single-incision or transobturator sling for incontinence: a randomized controlled trial. Obstet Gynecol 2015;125:27–34. [Ref ID: 66395; other: NTR2558]
Seo 201174
aSeo JH, Kim GN, Kim JY, Seo HJ, Lee JW, Lee WG, et al. Comparison between transobturator vaginal tape inside out and single incision sling system in the treatment of female stress urinary incontinence: prospective randomized study. Neurourol Urodyn 2011;30:832. [CRSREF: 3347987; other: 42169]
cLee WK, Kwon JB, Seo JH, Seo HJ, Kim JY, Lee JW, et al. A prospective randomized comparative study between tension free vaginal tape inside-out and suburethral single incision sling for the treatment of female stress urinary incontinence; 24-month follow-up. Eur Urol Suppl 2012;11:e173–3a. [Ref ID: 62252]
Sivaslioglu 2012178
aSivaslioglu AA, Unlubilgin E, Aydogmus S, Celen E, Dolen I. A prospective randomized comparison of transobturator tape and tissue fixation system minisling in 80 patients with stress urinary incontinence – 5-year results. J Urol 2012;188:194–9. [CRSREF: 3347989; other: 43318]
Sivaslioglu AA, Unlubilgin E, Aydogmus S, Celen E, Dolen I. A prospective randomized comparison of transobturator tape and tissue fixation system minisling in 80 patient with stress urinary incontinence – 3-year results. Pelviperineology 2010;29:56–9. [CRSREF: 3347990; other: 43317]
Sivaslioglu AA, Unlubilgin E, Dolen I, Kaplan M. The comparison of tissue fixation (TFS) system with transobturator tape (TOT) in the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(Suppl. 1):S36–7. [CRSREF: 3347991; other: 27327]
Smith 201130
aSmith AL, Castillo P, Karp D, Gross C, Davila G, Aguilar VC. Transobturator versus single incision slings in women with stress urinary incontinence: a prospective randomised controlled trial. Int Urogynecol J 2011;22(Suppl. 1):S54–5. [CRSREF: 3347993; other: 45303]
cNCT02599051, Davila GW. Transobturator Versus Single Incision Slings: 1-Year Results of a Randomized Control Trial. 2008. Trial registration number: NCT02599051. URL: https://clinicaltrials.gov/show/NCT02599051 (accessed 19 August 2017). [Ref ID: 69679]
cSmith AL, Castillo P, Karp D, Davila GW, Aguilar V. Transobturator vs. single incision sling in women with stress urinary incontinence: a prospective randomized controlled trial. Female Pelvic Med Reconstr Surg 2011;17(Suppl. 1):S170–1. [Ref ID: 71152]
cTieu AL, Hegde A, Castillo PA, Davila G, Aguilar V. Transobturator versus single incision slings in women with stress urinary incontinence: 1-year results of a randomized controlled trial. Female Pelvic Med Reconstr Surg 2013;19(Suppl. 1):S158–S159. [Ref ID: 72781]
cTieu AL, Hegde A, Castillo PA, Davila GW, Aguilar VC. Transobturator versus single incision slings in women with stress urinary incontinence: 1-year results of a randomized controlled trial. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S109–10. [Ref ID: 62181]
cTieu AL, Hegde A, Castillo PA, Davila GW, Aguilar VC. Transobturator versus single incision slings: 1-year results of a randomized controlled trial. Int Urogynecol J 2017;28:461–7. [Ref ID: 74312]
Sottner 2012169
aSottner O, Halaska M, Vlacil J, Maxova K, Mala I, Krombholz R, et al. [A comparison of different types of suburethral slings in the treatment of urinary incontinence in geriatric patients]. [Czech]. Ceska Gynekol 2012;77:403–7. [CRSREF: 3347995; other: 45893]
cSottner O, Halaska M, Maxova K, Vlacil J, Kolarik D, Hurt K, et al. Comparison of Three Different Midurethral Slings in the Treatment of Female Urinary Incontinence in Institutionalized Elderly Patients. Proceedings of the International Continence Society (ICS), 43rd Annual Meeting, Barcelona, 26–30 August 2013, abstract no. 859. [Ref ID: 60037]
Tommaselli 2010180
aTommaselli GA, Di Carlo C, Gargano V, Formisano C, Scala M, Nappi C. Efficacy and safety of TVT-O and TVT-Secur in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J 2010;21:1211–17. [CRSREF: 3347997; other: 40921]
cTommaselli GA, D’Afiero A, Formisano C, Fabozzi A, Di CC, Nappi C. Efficacy and safety of TVT-O and TVT-Secur in the treatment of female stress urinary incontinence: three years’ follow-up. Int J Gynaecol Obstet 2012;119(Suppl. 3):S503–S504. [Ref ID: 62239]
cTommaselli GA, D’Afiero A, Formisano C, Fabozzi A, Di Carlo C, Nappi C. Ultrasonographic evaluation of the positioning of TVT-O vs. TVT-Secur and their effect on the urethra: an ancillary analysis of a 36-months follow-up randomized study. Neurourol Urodyn 2013;32:781–2. [Ref ID: 49204]
cTommaselli GA, D’Afiero A, Di CC, Formisano C, Fabozzi A, Nappi C. Tension-free vaginal tape-O and -Secur for the treatment of stress urinary incontinence: a thirty-six-month follow-up single-blind, double-arm, randomized study. J Minim Invasive Gynecol 2013;20:198–204. [Ref ID: 47549]
cTommaselli GA, D’Afiero A, Di CC, Formisano C, Fabozzi A, Nappi C. Tension-free vaginal tape-obturator and tension-free vaginal tape-Secur for the treatment of stress urinary incontinence: a 5-year follow-up randomized study. Eur J Obstet Gynecol Reprod Biol 2015;185:151–5. [Ref ID: 66448]
Yoon 201180
Yoon H, Lee DH, Kim YJ. Early Results of Comparison of Contasure-needleless™ and TOT Outside-in midurethral Slings. Proceedings of the International Continence Society (ICS), 41st Annual Meeting, Glasgow, 29 August to 2 September 2011, abstract no. 852. [CRSREF: 3348001; other: 42238]
(iv) Cochrane review: Saraswat et al.7 and Rehman et al.19 – traditional suburethral sling operations for UI in women
Abouhashem 201438
Abouhashem S, Mostafa M, Elbrombely W. Five-years follow-up of tension-free vaginal tape (TVT) versus rectus sheath sling for surgical treatment of female stress urinary incontinence. J Urol 2014;191(Suppl. 1):e343. [CRSREF: 2843670; other: sr-incont62142]
Amaro 2007151
Amaro JL, Yamamoto H, Kawano PR, Barros G, Gameiro MO, Agostinho AD. Clinical and quality-of-life outcomes after autologous fascial sling and tension-free vaginal tape: a prospective randomized trial. Int Braz J Urol 2009;35:60–66; discussion 66–7. [CRSREF: 2843722; other: sr-incont31437]
aAmaro JL, Yamamoto HA, Kawano PR, Fugita O, Gameiro MOO, Barros G, et al. A prospective randomized trial of autologous fascial sling (AFS) versus tension-free vaginal tape (TVT) for treatment of stress urinary incontinence (SUI). J Urol 2007;177(Suppl. 4):482. [CRSREF: 2843723; other: sr-incont23764]
NCT00565838, Amaro JL. Clinical and Quality-of-life Outcomes after Autologous Fascial Sling and Tension-free Vaginal Tape: a Prospective Randomized Trial. 2001. Trial registration number: NCT00565838. URL: http://clinicaltrials.gov/show/NCT00565838 (accessed 19 August 2017). [CRSREF: 2843724; other: sr-incont59990]
Arunkalaivanan 2003152
Abdel-Fattah M, Arunkalaivanan AS, Barrington JW. Pelvicol™ Implant v TVT™: An Update. Proceedings of the International Urogynecological Association, 27th Annual Meeting, Prague, 21–24 August 2002, abstract. [CRSREF: 2843726; other: sr-incont22144]
Abdel-Fattah M, Barrington JW, Arunkalaivanan AS. Pelvicol pubovaginal sling versus tension-free vaginal tape for treatment of urodynamic stress incontinence: a prospective randomized three-year follow-up study. Eur Urol 2004;46:629–35. [CRSREF: 2843727; other: sr-incont19434]
aArunkalaivan AS, Barrington JW. Randomized trial of porcine dermal sling (Pelvicol™ implant) vs. tension-free vaginal tape (TVT) in the surgical treatment of stress incontinence: a questionnaire-based study. Int Urogynecol J 2003;14:17–23. [CRSREF: 2843728; other: sr-incont16033]
Arunkalaivanan AS, Barrington JW. Comparison of porcine pubo vaginal sling (Pelvicol) vs tension free vaginal tape (TVT) in the surgical management of stress incontinence. Int Urogynecol J 2001;12(Suppl. 3):S21. [CRSREF: 2843729; other: sr-incont16333]
Basok 2008153
Basok EK, Yildirim A, Atsu N, Basaran A, Tokuc R. Cadaveric fascia lata versus intravaginal slingplasty for the pubovaginal sling: surgical outcome, overall success and patient satisfaction rates. Urol Int 2008;80:46–51. [CRSREF: 2843735; other: sr-incont26435]
Guerrero 200892
aGuerrero K, Whareham K, Watkins A, Ismail S, Lucas M, Emery S. A randomised control trial comparing TVT, pelvicol and autologous fascial slings for the management of stress urinary incontinence in women. Neurourol Urodyn 2008;27:571. [CRSREF: 2843748; other: sr-incont31847]
Guerrero KL, Emery SJ, Wareham K, Ismail S, Watkins A, Lucas MG. A randomised controlled trial comparing TVT, Pelvicol and autologous fascial slings for the treatment of stress urinary incontinence in women. BJOG 2010;117:1493–502. [CRSREF: 2843749; other: sr-incont40338]
Khan Z, Nambiar A, Emery S, Lucas M. Long-term follow-up of a multicentre randomised controlled trial comparing TVT, Pelvicol™ and autologous fascial slings for the treatment of stress urinary incontinence in women. Neurourol Urodyn 2014;33:937–8. [CRSREF: 2843750; other: NCT01057550; other: sr-incont64340]
Lucas M, Emery S, Alan W, Kathy W. Failure of Porcine Xenograft Sling in a Randomised Controlled Trial of Three Sling Materials in Surgery for Stress Incontinence. Proceedings of the International Continence Society, 34th Annual Meeting, and the International Urogynecological Association, Paris, 23–27 August 2004, abstract no. 309. [CRSREF: 2843751; other: sr-incont19056]
Lucas M. Sling Operation for Stress Urinary Incontinence: Randomized Trial of Three Operative Procedures. 2001. UK National Research Register. [CRSREF: 2843752; other: sr-incont16379]
Lucas MG, Guerrero K. A Randomised Controlled Trial Comparing TVT, Pelvicol and Autologous Fascial Slings for the Treatment of Stress Urinary Incontinence in Women. 2001. Trial registration number: NCT01057550. URL: http://clinicaltrials.gov/show/NCT01057550 (accessed 19 August 2017). [CRSREF: 2843753; other: sr-incont59998]
Nambiar AK, Khan ZA, Morley R, Chapple CR, Emery SJ, Lucas MG. Long term follow-up of a multicentre randomised controlled trial comparing TVT, Pelvicol™ and autologous fascial slings for the treatment of stress urinary incontinence in women. BJU Int 2014;113(Suppl. S5):50–1. [CRSREF: 2843754; other: sr-incont64349]
cKhan ZA, Nambiar A, Morley R, Chapple CR, Emery SJ, Lucas MG. Long-term follow-up of a multicentre randomised controlled trial comparing tension-free vaginal tape, xenograft and autologous fascial slings for the treatment of stress urinary incontinence in women. BJU Int 2015;115:968–77. [Ref ID: 68156; other: NCT01057550]
Hilton 1989198
Hilton P. A clinical and urodynamic study comparing the Stamey bladder neck suspension and suburethral sling procedures in the treatment of genuine stress incontinence. Br J Obstet Gynaecol 1989;96:213–20. [CRSREF: 2843761; other: sr-incont453]
Kondo 2006106
aKondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O, Gotoh M, et al. Efficacy, safety and hospital costs of tension-free vaginal tape and pubovaginal sling in the surgical treatment of stress incontinence. J Obstet Gynaecol Res 2006;32:539–44. [CRSREF: 2843763; other: sr-incont22233]
Kondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O. A Randomized Control Trial of Tension-free Vaginal Tape vs Pubovaginal Sling: Cure Rates and QOL Improvement. Proceedings of the International Continence Society (ICS), 35th Annual Meeting, Montreal, QC, 28 August to 2 September 2005, abstract no. 629. [CRSREF: 2843764; other: sr-incont21077]
Kondo A, Kimura K, Isobe Y, Kamihira O, Matsuura O. A randomised control trial of tension-free vaginal tape in comparison with pubovaginal sling in the treatment of stress incontinence. Neurourol Urodyn 2003;22:485–7. [CRSREF: 2843765; other: sr-incont17109]
Maher 2005102
Maher CF, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Pubovaginal sling or transurethral macroplastique for genuine stress incontinence and intrinsic sphincter deficiency: a prospective randomised trial. Int Urogynecol J 2001;12(Suppl. 3):S9. [CRSREF: 2843771; other: sr-incont14360]
aMaher CF, O’Reilly BA, Dwyer PL, Carey MP, Cornish A, Schluter P. Pubovaginal sling versus transurethral Macroplastique for stress urinary incontinence and intrinsic sphincter deficiency: a prospective randomised controlled trial. BJOG 2005;112:797–801. [CRSREF: 2843772; other: sr-incont20579]
Sharifiaghdas 200881
aSharifiaghdas F, Mortazavi N. Tension-free vaginal tape and autologous rectus fascia pubovaginal sling for the treatment of urinary stress incontinence: a medium-term follow-up. Med Princ Pract 2008;17:209–14. [CRSREF: 2843788; other:31878; other: sr-incont27098]
cSharifiaghdas F, Mirzaei M, Daneshpajooh A, Narouie B. Long-term results of tension-free vaginal tape and pubovaginal sling in the treatment of stress urinary incontinence in female patients. Clin Exp Obstet Gynecol 2017;44:44–7. [Ref ID: 75581]
Silva-Filho 2006165
Silva-Filho AL, Candido EB, Noronha A, Triginelli SA. Comparative study of autologous pubovaginal sling and synthetic transobturator (TOT) SAFYRE sling in the treatment of stress urinary incontinence. Arch Gynecol Obstet 2006;273:288–92. [CRSREF: 2843792; other: sr-incont21600]
Song 2004154
Song YF, Huang HJ, Xu B, Hao L. [Comparative study of tension-free vaginal tape and fascia lata for stress urinary incontinence]. [Chinese]. Chin J ObstGynecol 2004;39:658–61. [CRSREF: 2843794; other: sr-incont20768]
Tcherniakovsky 2009166
Tcherniakovsky M, Fernandes CE, Bezerra CA, Del Roy CA, Wroclawski ER. Comparative results of two techniques to treat stress urinary incontinence: synthetic transobturator and aponeurotic slings. Int Urogynecol J 2009;20:961–6. [CRSREF: 2843796; other: sr-incont32120]
Wadie 2005160
Wadie B, Henawy A. Does Urethral Pressure Measurement Correlate to the Outcome of Incontinence Surgery? Proceedings of the ICS, 37th Annual Meeting, Rotterdam, 20–24 August 2007, abstract no. 546. [CRSREF: 2843804; other: sr-incont26689]
Wadie BS, Edwan A, Nabeeh A. Autologous Fascial Sling versus Polypropylene Tape at Short-term Follow-up, a Prospective Randomized Study. Proceedings of the International Continence Society (ICS), 35th Annual Meeting, Montreal, QC, 28 August to 2 September 2005, abstract no. 636. [CRSREF: 2843805; other: sr-incont21100]
aWadie BS, Edwan A, Nabeeh AM. Autologous fascial sling vs polypropylene tape at short-term followup: a prospective randomized study. J Urol 2005;174:990–3. [CRSREF: 2843806; other: sr-incont20796]
Wadie BS, El Hefnawy AS. Urethral pressure measurement in stress incontinence: does it help? Int Urol Nephrol 2009;41:491–5. [CRSREF: 2843807; other: sr-incont32131]
Wadie BS, Mansour A, El-Hefnawy AS, Nabeeh A, Khair AA. Minimum 2-year follow-up of mid-urethral slings, effect on quality of life, incontinence impact and sexual function. Int Urogynecol J 2010;21:1485–90. [CRSREF: 2843808; other: sr-incont41437]
(v) Cochrane review: Freites et al.6 and Dean et al.20 – laparoscopic colposuspension for UI in women
Adile 200339
Adile B, Cucinella G, Gugliotta G, Lo BA, Grifo S, Caputo A. A prospective randomised study of Burch laparoscopy versus tension-free vaginal tape: 2-year follow-up [Italian]. Urogynaecologia Int J 2001;15(Suppl. 1):121–2. [CRSREF: 2978577; other: sri-incont13093]
aAdile B, Granese R, Lo Bue A, Gugliotta G, Cardella AM, Adile C. A Prospective Randomized Study Comparing Laparoscopic Burch versus TVT. Short- and Long-Term Follow-up. Proceedings of the International Continence Society (ICS), 33rd Annual Meeting; Florence, 5–9 October 2003. p. 563. [CRSREF: 2978578; other: sr-incont17164]
Cucinella G, Adile B, Gugliotta G, Lo Bue A, Grifo S, Caputo A. A prospective randomized study comparing laparoscopic Burch versus TVT. Two years’ follow-up. Int Urogynecol J 2001;12(Suppl. 3):107. [CRSREF: 2978579; other: sr-incont14358]
Foote 2006146
Foote A, Carne C, Lowndes C. Laparoscopic colposuspension versus vaginal mesh sling: a randomised prospective trial. Neurourol Urodyn 2004;23:434–5. [CRSREF: 2978607; other: sr-incont19006]
aFoote AJ, Maughan V, Carne C. Laparoscopic colposuspension versus vaginal suburethral slingplasty: a randomised prospective trial. Aust N Z J Obstet Gynaecol 2006;46:517–20. [CRSREF: 2978608; other: sr-incont22592]
Maher 200463
Maher C, Qatawneh A, Baessler K, Cropper M, Schluter P. Laparoscopic colposuspension or tension-free vaginal tape for recurrent stress urinary incontinence and/or intrinsic sphincter deficiency – a randomised controlled trial. Neurourol Urodyn 2004;23:433–4. [CRSREF: 2978616; other: sr-incont19005]
Mirosh 200567
Mirosh M, Epp A. TVT vs Laparoscopic Burch Colposuspension for the Treatment of Stress Urinary Incontinence. Proceedings of the International Incontinence Society (ICS), 35th Annual Meeting, Montreal, QC, 28 August to 2 September 2005, abstract no. 640. [CRSREF: 2978618; other: sr-incont20990]
Paraiso 2004147
Jelovsek JE, Barber MD, Karram MM, Walters MD, Paraiso MF. Randomised trial of laparoscopic Burch colposuspension versus tension-free vaginal tape: long-term follow up. BJOG 2008;115:219–225, discussion 225. [CRSREF: 2978622; other: sr-incont26265]
Paraiso MF, Walters M, Karram M, Barber M. Laparoscopic Burch colposuspension versus the tension-free vaginal tape procedure: a randomized clinical trial. Neurourol Urodyn 2003;22:487–8. [CRSREF: 2978623; other: sr-incont17108]
aParaiso MF, Walters MD, Karram MM, Barber MD. Laparoscopic burch colposuspension versus tension-free vaginal tape: a randomized trial. Obstet Gynecol 2004;104:1249–58. [CRSREF: 2978624; other: sr-incont19401]
Persson 2002148
aPersson J, Teleman P, Eten-Bergquist C, Wolner-Hanssen P. Cost-analyses based on a prospective, randomised study comparing laparoscopic colposuspension with tension-free vaginal tape procedure. Acta Obstet Gynecol Scand 2002;81:1066–73. [CRSREF: 2978628; other: sr-incont14362]
Persson J. Stress Urinary Incontinence Among Women: Aspects of Risk Factors, Evaluation and Surgical Treatment. PhD thesis. Lund: Lund University; 2001. [CRSREF: 2978629; other: sr-incont16386]
Samiee 2009163
Samiee H, Tavoli Z, Ghanbari Z, Poormand GH, Taslimi SH, Eslami B, et al. [Treatment of urinary stress incontinence: laparoscopic burch colposuspension versus transobturator tape procedure]. Tehran Univ Med J 2009;67:629–36. [CRSREF: 2978633; other: sr-incont43325]
Ustün 2003149
Ustün Y, Engin-Ustün Y, Güngör M, Tezcan S. Tension-free vaginal tape compared with laparoscopic burch urethropexy. J Am Assoc Gynecol Laparosc 2003;10:386–9. [CRSREF: 2978641; other: sr-incont16694]
Valpas 2004150
aValpas A, Ala-Nissila S, Tomas E, Nilsson CG. TVT versus laparoscopic mesh colposuspension: 5-year follow-up results of a randomized clinical trial. Int Urogynecol J 2015;26:57–63. [CRSREF: 2978645; other: sr-incont64697]
Valpas A, Kivela A, Penttinen J, Kauko M, Kujansuu E, Tomas E, et al. Comparison of TVT and Laparoscopic Colposuspension in the Treatment of Stress Urinary Incontinence. Proceedings of the Nordic Federation of Societies of Obstetricians and Gynecologists (NFOG), XXXIII Congress, Umea, 1–4 June 2002. [CRSREF: 2978646; other: sr-incont14356]
Valpas A, Kivela A, Penttinen J, Kauko M, Kujansuu E, Tomas E, et al. Tension-free vaginal tape and laparoscopic mesh colposuspension in the treatment of stress urinary incontinence: immediate outcome and complications – a randomized clinical trial. Acta Obstet Gynecol Scand 2003;82:665–71. [CRSREF: 2978647; other: sr-incont16587]
Valpas A, Kivela A, Penttinen J, Kauko M, Kujansuu E, Tomas E, Haarala M, Meltomaa S, Nilsson CG. Intra-operative and Immediate Post-operative Results Comparing Tension-free Vaginal Tape (TVT) and Laparoscopic Colposuspension (LC) in the Treatment of Female Stress Urinary Incontinence (SUI) – A Randomized Clinical Trial (Preliminary Results). Proceedings of the European Society for Gynaecological Endoscopy, 10th Congress, Lisbon, 21–24 November 2001. pp. 355–8. [CRSREF: 2978648; other: sr-incont13460]
Valpas A, Kivela A, Penttinen J, Kujansuu E, Haarala M, Nilsson CG. Tension-free vaginal tape and laparoscopic mesh colposuspension for stress urinary incontinence. Obstet Gynecol 2004;104:42–9. [CRSREF: 2978649; other: sr-incont19322]
Valpas A, Rissanen P, Kujansuu E, Nilsson C. A cost-effectiveness analysis of tension-free vaginal tape procedure vs. laparoscopic mesh colposuspension for primary female stress incontinence – a randomised clinical trial. Neurourol Urodyn 2005;24:418–19. [CRSREF: 2978650; other: sr-incont20987]
Valpas A, Rissanen P, Kujansuu E, Nilsson CG. A cost-effectiveness analysis of tension-free vaginal tape versus laparoscopic mesh colposuspension for primary female stress incontinence. Acta Obstet Gynecol Scand 2006;85:1485–90. [CRSREF: 2978651; other: sr-incont22539]
Valpas AK, Rissanen P, Kujansuu E, Nilsson CG. In a randomised clinical trial tension-free vaginal tape is more cost-effective than laparoscopic colposuspension. Int Urogynecol J 2005;16(Suppl. 2):S58–9. [CRSREF: 2978652; other: sr-incont29162]
(vi) Cochrane review: Glazener and Cooper11 – bladder neck needle suspension for UI in women
Di Palumbo 2003199
Di Palumbo VS. Four-corner bladder and urethral retropubic suspension versus anterior colporrhaphy in the correction of stress urinary incontinence with urethrocystocele 3-4. Randomized clinical trial. Urogynaecol Int J 2003;17:57–68. Sr-incont21004
2. New studies from the updated searches of the Cochrane Incontinence Group Specialised Register
Al-Azzawi 2014164
Al-Azzawi IS. The first Iraqi experience with the rectus fascia sling and transobturator tape for female stress incontinence: a randomised trial. Arab J Urol 2014;12:204–8. [Ref ID: 68245]
Aniuliene 2015121
Aniuliene R, Aniulis P, Skaudickas D. TVT-Exact and midurethral sling (SLING-IUFT) operative procedures: a randomized study. Open Med 2015;10:311–17. [Ref ID: 74253]
Campos 2013176
aNCT01699425, Campos M, Palau-Jane M, Castaneda E, Poza JL, Montero F, et al. Multicentric Comparative Randomized Study of the Single-incision Sling Ajust® Versus Suburethral Transobturator Slings. 2013. Trial registration number: NCT01699425. URL: http://clinicaltrials.gov/show/NCT01699425 (accessed 19 August 2017). [Ref ID: 62924]
Sabadell J, Palau-Gene M, Huguet E, Montero-Armengol A, Salicru S, Poza JL. Multicentre randomized trial of the Ajust™ single-incision sling compared to the Align™ transobturator tape sling. Int Urogynecol J 2017;28:1041–7. [Ref ID: 75475]
Dati 201243
Dati S, Rombola P, Cappello S, Piccione E. Single-incision minisling (AJUST) vs obturator tension-free vaginal shortened tape (TVT-ABBREVO) in surgical management of female stress urinary incontinence. Int J Gynaecol Obstet 2012;119(Suppl. 3):S670. [Ref ID: 62238]
El-Hefnawy 2012127
El-Hefnawy A, Abed A, Wadie B. TVT versus TOT: a single-center, prospective randomized study. Urology 2012;80(Suppl. 1):S142–3. [Ref ID: 65378]
Enzelsberger 201150
Enzelsberger H, Cemer I, Kostersitz E, Enzelsberger S. Ophira (Minisling) versus Monarc (TOT) – a prospective randomized study for the treatment of female stress urinary incontinence at a follow-up of 20 months. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 3):S1835–S1836. [Ref ID: 62229]
Fernandez 201552
aFernandez S , Martinez-Franco E, Lin X, Amat TL. Contasure-needleless compared with Monarc for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S84–S85. [Ref ID: 69517]
Fernandez-Gonzalez S, Martinez FE, Lin M, X, Amat TL. Contasure-needleless compared with Monarc for the treatment of stress urinary incontinence. Int Urogynecol J 2016;28:1077–84. [Ref ID: 75229]
Foote 2015171
aFoote A. Randomized prospective study comparing Monarc and Miniarc suburethral slings. J Obstet Gynaecol Res 2015;41:127–31. [Ref ID: 67401; other: ACTRN12612000314820]
Foote A. A Randomised Trial Comparing Two Vaginal Prolene Sling Surgeries for Female Urinary Incontinence. 2012. Trial registration number: ACTRN12612000314820. URL: www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=362208 (accessed 1 March 2013). [CRSREF: 3348019; other: 45458]
Gaber 201691
Gaber ME, Borg T, Samour H, Nawara M, Reda A. Two new mini-slings compared with transobturator tension-free vaginal tape for treatment of stress urinary incontinence: a 1-year follow-up randomized controlled trial. J Obstet Gynaecol Res 2016;42:1773–81. [Ref ID: 74183]
Gopinath 2013158
Gopinath D, Smith AR, Holland C, Reid FM. Why don’t women participate? A qualitative study on non-participation in a surgical randomised controlled trial. Int Urogynecol J 2013;24:969–75. [Ref ID: 48114]
Jurakova 2016113
Huser M, Belkov I, Janku P, Texl J, Jarkovsky J, Ventruba P. Prospective randomized comparison of the trans-obturator mid-urethral sling and the single-incision sling in women with stress urinary incontinence: one-year follow-up study. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S135–S136. [Ref ID: 68573]
aJurakova M, Huser M, Belkov I, Janku P, Hudecek R, Stourac P, et al. Prospective randomized comparison of the transobturator mid-urethral sling with the single-incision sling among women with stress urinary incontinence: 1-year follow-up study. Int Urogynecol J 2016;27:791–6. [Ref ID: 72046; other: NCT02506309]
NCT02506309, Huser M. Prospective Randomized Comparison of the Trans-obturator Mid-urethral Sling and the Single-incision Sling in Women with Stress Urinary Incontinence. 2012. Trial registration number: NCT02506309. URL: https://clinicaltrials.gov/show/NCT02506309 (accessed 19 August 2017). [Ref ID: 68782]
Labrie 201295
Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, et al. Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med 2013;369:1124–33. [Ref ID: 48476]
aLabrie J, Berghmans L, Fischer K, Lagro-Janssen A, van der Vaart C. Long-term results of pelvic floor muscle training or midurethral sling surgery for female moderate to severe predominant stress urinary incontinence: a randomised controlled trial. Int Urogynecol J 2012;23(Suppl. 2):S139–S140. [Ref ID: 62385]
Labrie J, Lagro-Janssen AL, Fischer K, Berghmans LC, van der Vaart CH, the Portret Study Group. Who will undergo midurethral sling surgery after initial pelvic floor muscle training for moderate to severe predominant stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2012;23(Suppl. 1):S140–S141. [Ref ID: 64416]
Labrie J, Lagro-Janssen AL, Fischer K, Berghmans LC, van der Vaart CH. Predicting who will undergo surgery after physiotherapy for female stress urinary incontinence. Int Urogynecol J 2015;26:329–34. [Ref ID: 66416; other: TrialID.PORTRET.; other: NTR1248]
van der Vaart CH. A Randomised Controlled Trial Comparing the Cost-effectiveness of Pelvic Floor Muscle Exercise versus the TVT (O)™ Procedure for Female Moderate to Severe Stress Urinary Incontinence. 2008. Trial registration number: NTR1248. URL: www.trialregister.nl/trialreg/admin/rctview.asp?TC=1248 (accessed 19 August 2017). [Ref ID: 23746]
Lee 201562
Lee SH, Kim H, Choo MS, Park CM. Single Incision Mid-urethral Sling and Tension-free Vaginal Tape Procedure for the Treatment of Stress Urinary Incontinence: A 12-month Follow-up Randomized Study. Proceedings of the International Continence Society (ICS), 45th Annual Meeting, Montreal, QC, 6–9 October 2015, abstract no. 350. [Ref ID: 68815]
Masata 2013101
Farhat F, Svabik K, Hubka P, Martan A, Masata J. [Ultrasound comparison of adjustable single-incision (Ajust) and transobturator tapes to assess post-operative fixation and function and clinical efficacy]. [Czech]. Ceska Gynekol 2016;81:324–35. [Ref ID: 74412]
Masata J, Svabik K, Zvara K, Hubka P, Toman A, Martan A. Comparison of the efficacy of tension-free vaginal tape obturator (TVT-O) and single-incision tension-free vaginal tape (Ajust™) in the treatment of female stress urinary incontinence: a 1-year follow-up randomized trial. Int Urogynecol J 2016;27:1497–505. [Ref ID: 73121]
aMasata J, Svabik K, Hubka P, Elhaddad R, Martan A. Comparison of the safety and peri-operative complications of transobturator introduced tension-free vaginal tape (TVT-O) and single-incision tape with adjustable length and anchoring mechanism (Ajust) in a randomized trial: short term results. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S114–15. [Ref ID: 62179]
Masata J, Martan A, Svabik K, Hubka P, El Haddad R. Randomized trial of a comparison of the efficacy of TVT-O and single incision tape ajust in the treatment of stress urinary incontinent women – one-year follow up. Int Urogynecol J Pelvic Floor Dysfunct 2014;25(Suppl. 1):S9–10. [Ref ID: 67462]
Masata J, Svabik K, Hubka P, El HR, Martan A. Randomized trial comparing the safety and peri-operative complications of transobturator introduced tension-free vaginal tape (TVT-O) and single-incision tape with adjustable length and anchoring mechanism (Ajust): three months results. Neurourol Urodyn 2013;32:783. [Ref ID: 49203]
Masata J, Svabik K, Hubka P, Martan A. Randomized trial to compare the efficacy of TVT-O and single incision tape Ajust in the treatment of stress urinary incontinent women-two year follow-up. Neurourol Urodyn 2015;34:S418–20. [Ref ID: 68736]
Smazinka M, Svabik K, Hubka P, Haddad ER, Masata J. [Comparison of quality of life of patients treated for SUI by surgical approaches AJUST and TVT-O – 3-month results from randomized trial]. [Czech]. Ceska Gynekol 2015;80:196–203. [Ref ID: 68235]
Maslow 2014175
aMaslow K, Gupta C, Klippenstein P, Girouard L. Randomized clinical trial comparing TVT Secur system and trans vaginal obturator tape for the surgical management of stress urinary incontinence. Int Urogynecol J 2014;25:909–14. [Ref ID: 62080; other: NCT00527696]
Maslow KD. Trial Comparing TVT SECUR System and Transvaginal Obturator Tape for Surgical Management of Stress Urinary Incontinence. 2011. Trial registration number: NCT00527696. URL: https://clinicaltrials.gov/ct2/show/NCT00527696 (accessed 1 March 2013). [CRSREF: 3348021; other: SR-INCONT42750]
Melendez Munoz 201665
aMelendez Munoz J, Braverman M, Rosamilia A, Young NR, Leitch A, Lee J. TVT Abbrevo and MiniArc suburethral sling in women with stress urinary incontinence – a randomised controlled trial. 6 months results. Int Urogynecol J Pelvic Floor Dysfunct 2016;27(Suppl. 1):S75–S76. [Ref ID: 73434]
Rosamilia A, Lee J, Leitch A. Tension Free Vaginal Tape (TVT) Abbrevo and Miniarc Suburethral Sling in Women with Stress Urinary Incontinence – A Randomised Controlled Trial. Trials registration number: ACTRN12611001151921. URL: www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=347618 (accessed 1 March 2013). [CRSREF: 3348025; other: SR-INCONT43056]
Merali 201266
Merali S, Dolhaniuk C, Unger T. Stress incontinence in women; a pilot study comparing the Miniarc single incision sling system to the Monarc transobturator sling system. J Minim Invasive Gynecol 2012;19(Suppl. 1):S33–S34. [Ref ID: 62237]
Pastore 2016114
aPastore AL , Palleschi G, Al Salhi Y, Riganelli L, Fuschi A, Autieri D, et al. Evaluation of sexual function and quality of life in women treated for stress urinary incontinence: tension-free transobturator suburethral tape versus single-incision sling. J Womens Health 2016;25:355–9. [Ref ID: 72067]
Al Salhi,Y, Pastore AL, Palleschi G, Riganelli L, Autieri D, Fuschi A, et al. Evaluation of sexual function and quality of life in women treated for stress urinary incontinence: tension-free transobturator suburethral tape vs. single incision sling. Neurourol Urodyn 2016;35:S49. [Ref ID: 75564]
Ross 2014159
aRoss S, Tang S, Schulz J, Murphy M, Goncalves J, Kaye S, et al. Single incision device (TVT Secur) versus retropubic tension-free vaginal tape device (TVT) for the management of stress urinary incontinence in women: a randomized clinical trial. BMC Res Notes 2014;7:941. [Ref ID: 66440; other: NCT00685217]
Robert M, Ross S, Schulz J. Transvaginal Tape (TVT) Secur versus TVT Randomised Controlled Trial (RCT). 2012. Trial registration number: NCT00685217. URL: https://clinicaltrials.gov/ct2/show/NCT00685217 (accessed 1 March 2013). [CRSREF: 3348023; other: SR-INCONT43064]
Rudnicki 201672
Arenholt LT, Glavind K, Rudnicki M, Teleman P. Monarc and Ajust for treatment of urinary stress incontinence-ultrasonic evaluation and subjective cure. Female Pelvic Med Reconstr Surg 2014;20:S350. [Ref ID: 72527]
NCT01754558, Rudnicki M, Hviid U, Svendsen S. One Year Outcome Using the Ajust System for Treatment of Urinary Stress Incontinence. 2012. Trial registration number: NCT01754558. URL: http://clinicaltrials.gov/show/NCT01754558 (accessed 19 August 2017). [Ref ID: 62918]
aRudnicki M, Jakobsson U, Teleman P, Group SA. One-year Comparison of a Single Incision Mini Sling and Conventional Midurethral Slings. A Randomized Controlled Study. Proceedings of the International Continence Society (ICS), Annual Meeting, Tokyo, 13–16 September 2016, abstract no. 520. [Ref ID: 73456; other: NCT01754558]
Salari 2010127
aSalari Z, Sohbati S. Comparison between result of trans-obturator tape method and anterior vaginal colporrhaphy in treatment of stress urinary incontinency. 2010. Trial registration number: IRCT201204109433N1. URL: www.irct.ir/searchresult.php?id=9433&number=1 (accessed 19 August 2017). [Other: sr-incont62302]
Sohbati S, Salari Z, Eftekhari N. Comparison between the transobturator tape procedure and anterior colporrhaphy with the Kelly’s plication in the treatment of stress urinary incontinence: a randomized clinical trial. Nephrourology Monthly 2015;7:e32046. [Ref ID: 70600]
Schellart 2013177
Roovers J, Schellart R, Van der Aa F. A randomized comparison of single incision mid-urethral sling (MINIARCTM) and transobturator mid-urethral sling (MONARC™) for treatment of stress urinary incontinence: 2-year clinical outcomes. J Minim Invasive Gynecol 2015;22(Suppl. 1):S2. [Ref ID: 75734]
Roovers J-P, Schellart RP, Kimpe B, Lucot J-P, De RD, Rengerink KO. A randomized comparison of single incision midurethral sling (Miniarc™) and transobturator midurethral sling (Monarc) for treatment of stress urinary incontinence: 2-year clinical outcomes. Neurourol Urodyn 2015;34(Suppl. 1):S95. [Ref ID: 68569; other: NTR3783]
Chellart RP, Casteleijn FM, Dijkgraaf MG, Tutolo M, Roovers JW. Are patients willing to trade cure rate against less pain? Patients’ preferences for single incision midurethral sling or transobturator standard midurethral sling. Neurourol Urodyn 2016;36:1187–93. [Ref ID: 73603]
aSchellart RP, De Ridder D, Kimpe B, Lucot JP, Van der Aa F, Ruiter L, et al. A randomized comparison of single incision midurethral sling (Miniarc) and transobturator mid-urethral sling (Monarc) in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S107–8. [Ref ID: 62183; other: NTR3783]
Schellart RP, Dijkgraaf MG, Van der Aa F, Lucot J, Kimpe B, De RD, et al. A randomized comparison of single incision mid-urethral sling (MiniArc) and transobturator mid-urethral sling (Monarc) for treatment of stress urinary incontinence: 2-year clinical outcomes. Int Urogynecol J Pelvic Floor Dysfunct 2014;25(Suppl. 1):S158–9. [Ref ID: 64337]
Schellart RP, Oude RK, De RD, Kimpe B, Lucot JP, Van der Aa F, et al. A randomized comparison of single incision midurethral sling (MiniArc) and standard midurethral sling (Monarc) in women with stress urinary incontinence: Results at 36-months follow-up. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S76–7. [Ref ID: 68576; other: NTR3783]
Schellart RP, Oude RK, Van der Aa F, Lucot JP, Kimpe B, De Ridder DJ, et al. A randomized comparison of a single-incision midurethral sling and a transobturator midurethral sling in women with stress urinary incontinence: results of 12-mo follow-up. Eur Urol 2014;66:1179–85. [Ref ID: 64888; other: NTR3783]
Schellart RP, Oude RK, Van der Aa F, Lucot JP, Kimpe B, Dijkgraaf MG, et al. A randomised comparison of single-incision versus traditional transobturator midurethral sling in women with stress urinary incontinence: results of a 24-month follow-up. Int Urogynecol J 2016;27:871–7. [Ref ID: 73016]
Schellart RP, Roovers JPWR. A Prospective Multi-national Randomized Comparison of the Effectiveness and Safety of MiniArc® and Monarc® – MiniM. 2013. Trial registration number: NTR3783. URL: www.trialregister.nl/trialreg/admin/rctview.asp?TC=3783 (accessed 20 August 2017). [Ref ID: 64542]
Sharifiaghdas 201581
Sharifiaghdas F, Nasiri M, Mirzaei M, Narouie B. Mini sling (Ophira) versus pubovaginal sling for treatment of stress urinary incontinence: a medium-term follow-up. Prague Med Rep 2015;116:210–8. [Ref ID: 69267]
Shawky 201575
Shawky H, Mahmoud M, Mohammed H, Khalifa E, Mahran A. TVT-Secur versus TVT-Obturator: a randomized trial of suburethral sling operative procedures for stress urinary incontinence, el Minia experience. Int J Gynaecol Obstet 2015;131(Suppl. 5):E597. [Ref ID: 72571]
Tang 2014179
aTang X, Zhu L, Liang S, Lang J. Outcome and sexual function after transobturator tape procedure versus tension-free vaginal tape SECUR: a randomized controlled trial. Menopause 2014;21:641–5. [Ref ID: 62113]
Zhu L, Tang X, Liang S. Coital incontinence in urogynecologic patients: Incidence and risk factors. Female Pelvic Med Reconstr Surg 2014;20(Suppl. 1):S296–7. [Ref ID: 75022]
Van Rensburg 201579
Van Rensburg JA, Jeffery ST, Sand Enbergh HA, Juul L, Steyn DW. Single incision-needleless and inside out TVT-O: a multicentre clinical equivalent randomised trial with preliminary 6 months and one year outcome for stress urine continence. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S136–7. [Ref ID: 69597]
Xin 2016115
Xin X, Song Y, Xia Z. A comparison between adjustable single-incision sling and tension-free vaginal tape-obturator in treating stress urinary incontinence. Arch Gynecol Obstet 2016;293:457–63. [Ref ID: 70513]
Zhang 2014143
Zhang Z , Zhu L, Xu T. Retropubic tension-free vaginal tape and inside-out transobturator tape: a long-term randomized trial. Int J Gynaecol Obstet 2015;131(Suppl. 5):E309. [Ref ID: 71498; other: ChiCTR-TRC-14004371]
Zhang Z, Zhu L, Xu T, Lang J. Retropubic tension-free vaginal tape and inside-out transobturator tape: a long-term randomized trial. Int Urogynecol J 2016;27:103–11. [Ref ID: 70497; other: ChiCTR-TRC-14004371]
aZhang Z, Zhu L. A Long Term Comparative Study on Efficacy, Quality of Life and Sexual Function Between TVT and TVT-O in Patients of Hypermobility Stress Urinary Incontinence: Prospective Randomized Comparative Trial. 2014. Trial registration number: ChiCTR-TRC-14004371. URL: www.chictr.org.cn/showproj.aspx?proj=5199 (accessed 20 August 2017). [Ref ID: 64515]
Zhu L, Zhang Z. Retropubic tension-free vaginaltape and inside-out transobturator tape: a longterm randomized trial. Int Urogynecol J Pelvic Floor Dysfunct 2015;26(Suppl. 1):S79–81. [Ref ID: 71174; other: ChiCTR-TRC-14004371]
Zhu L, Zhang Z, Xu T, Lang J. A long-term RCT on the efficacy and the impact on quality of life of TVT and TVT-O in SUI patients. J Minim Invasive Gynecol 2014;21(Suppl. 1):S215. [Ref ID: 67286]
Zhu L, Zhang Z, Xu T, Lang J. Long-term complications and efficacy after retropubic tension-free vaginal tape and inside-out obturator tape: a prospective randomized trial. J Minim Invasive Gynecol 2015;22(Suppl. 1):S83. [Ref ID: 75285]
Zhu L, Zhang Z. A long term comparative study on efficacy and quality of life between TVT and TVT-O in patients of hypermobility stress urinary incontinence: prospective randomized comparative trial. Female Pelvic Med Reconstr Surg 2014;20:S338. [Ref ID: 71488; other: ChiCTR-TRC-14004371]
Appendix 6 Sample of excluded studies with reasons for exclusion
a Primary reference where more than one report of a study was available; this is the name given to the study as it appears in the main text of the ESTER report.
b New further report of study found in updated search.
NoteAny relevant study and reference identifiers (IDs) are included in square brackets following each citation, e.g. [database: identifier].
Identifiers containing ‘sr-incont’ relate to the Cochrane Incontinence Specialised Register; ‘CRSREF’ identifiers refer to the Cochrane Register of Studies Web version (CRS-Web); ‘other’ is used to refer to either the study acronym or the trial registration number from a number of trial registries; ‘Ref ID’ identifiers relate to those records being processed for inclusion in the Cochrane Incontinence Specialised Register.
| Study ID | Reason for exclusion |
|---|---|
| Studies selected from Cochrane reviews but excluded on further assessment | |
| Borstad 2010288 | Not relevant comparison. TVT + concomitant prolapse surgery vs. TVT 3 months after prolapse repair |
| Colombo 1997289 | Not relevant population. Includes women with severe prolapse with clinical stress UI or ‘potential’ stress UI |
| Corcos 2005290 | Not relevant study design. Randomisation to surgery and injectable. Which type of surgery to have was decided based on surgeon’s preference |
| Kim 2004291 | Not relevant comparison. One type of retropubic MUS vs. another type of retropubic MUS vs. IRIS procedure (not relevant intervention) |
| Klarskov 1986292 | Not relevant study design. Randomisation to surgery and PFMT. Which type of surgery to have was decided based on VCUG and anatomy |
| Lee 2001293 | Not relevant comparison. Injectables vs. no treatment (placebo) |
| Miranda 2011294 | Not relevant population. Study participants do not have stress UI |
| Okulu 2013295 | Not relevant comparison. One type of retropubic MUS vs. another |
| Osman 2003296 | Not relevant study design. Randomisation to surgery and pharmacological treatment. Which type of surgery to have was dictated by VLPP |
| Quadri 1985297 | Not relevant population. Includes incontinent women with severe prolapse. Unclear if UI is predominantly stress. Available as abstracts only with insufficient details |
| Teixeira 2008298 | Not relevant comparison. One type of transobturator MUS vs. another |
| Teleb 2011299 | Not relevant comparison. One type of traditional sling vs. another |
| ter Meulen 2009300 | Not relevant comparison. Injectable vs. no treatment. Unsupervised PFMT (written instruction only) considered equivalent to no active treatment |
| Tincello 2004301 (CARPET study) | Not relevant study design. 31 women included, of whom 4 were allocated by randomisation and 27 by preference |
| van der Ploeg 2013302 | Not relevant intervention. VPR + MUS vs. VPR alone |
| van Leijsen 2013303 | Not relevant study design. Diagnostic cohort study with an embedded non-inferiority RCT. Data pertinent to RCT not available |
| Wang 2008285 | Duplicate. Included as part of the study with study ID Wang 200937 |
| Zargham 2013304 | Not relevant intervention. Anterior vaginal wall sling vs. retropubic MUS. Anterior vaginal wall sling not a relevant intervention |
| New studies from update search | |
| Campeau 2007305 | Not relevant comparison. Retropubic MUS (TVT) vs. no treatment |
| Caremel 2013306 | Not relevant comparison. Transobturator MUS vs. pharmacological treatment (anticholinergics). Participants had MUI. Anticholinergics is generally for treatment of urgency UI |
| Choi 2006307 | Not relevant study design. No clear evidence of randomisation. Available as abstract |
| Grigoriadis 2013308 | Not relevant study design. No clear evidence of randomisation |
| Larsson 2014309 | Not relevant population. Participants are patients not suitable for TVT operations. Injectable vs. no treatment |
| Nikas 2012310 | Not relevant comparison. Anterior repair vs. pharmacological treatment |
| Rose 2012311 | Not relevant comparison. Injectables vs. pharmacological treatment vs. no treatment |
| Sung 2013312 | Not relevant population. Ongoing trial with women with MUI. Not predominantly stress UI |
| Tuncer 2016313 | Not relevant study design. Not RCT |
| Wadie 2016314 | Not relevant comparison. Combined MUS and anterior repair vs. MUS alone |
| Awaiting assessment | |
| Helmy 2012284 | Awaiting classification in the open colposuspension Cochrane review.5 Unclear if this is related to the study with study ID Albo 2007 (included study).82 Awaiting author response |
| Karmakar 2017287 | Awaiting assessment. Secondary analysis. Unclear if data are related to SIMS (single-incision mini-slings) trial (Mostafa 2013; included study)204 or pilot of SIMS174 |
| Pushkar 2011286 | Awaiting classification in the single-incision sling Cochrane review.9 In Russian with English abstract. Study design unclear. Single-incision (TVT-S) vs. transobturator MUS (TVT-O) |
References for excluded studies
(i) Studies included in Cochrane reviews but excluded from ESTER, as they did not meet the ESTER inclusion criteria
Borstad 2010288
Borstad E, Abdelnoor M, Mogimi K, Sandved M, Majida M, Western K, et al. Surgery for concomitant pelvic organ prolapse and urinary stress incontinence. A multicenter prospective randomized trial to compare the results of an incontinence procedure performed at the time of prolapse repair or 3 months after. Neurourol Urodyn 2008;27:713. [Other: NCT00308009; other: sr-incont29653]
aBorstad E, Abdelnoor M, Staff AC, Kulseng-Hanssen S. Surgical strategies for women with pelvic organ prolapse and urinary stress incontinence. Int Urogynecol J 2010;21:179–86. [Other: NCT00308009; other: sr-incont39362]
Colombo 1997289
Colombo M, Maggioni A, Scalambrino S, Vitobello D, Milani R. Surgery for genitourinary prolapse and stress incontinence: a randomized trial of posterior pubourethral ligament plication and Pereyra suspension. Am J Obstet Gynecol 1997;176:337–43. [Other: sr-incont4762]
Corcos 2005290
aCorcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, et al. Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 2005;65:898–904. [Other: sr-incont20346]
Corcos J, Collet JP, Shapiro S, Schick E, Macramallah E, Tessier J, et al. Surgery vs collagen for the treatment of female stress urinary incontinence (SUI): results of a multicentric randomized trial. J Urol 2001;165(Suppl. 1):198. [Other: sr-incont12912]
Oremus M, Tarride JE. An economic evaluation of surgery versus collagen injection for the treatment of female stress urinary incontinence. Can J Urol 2010;17:5087–93. [Other: sr-incont39605]
Helmy 2012284
Helmy H, El-Gamal S. Three-year Continence Rates, Satisfaction and Adverse Events of Burch Urethropexy and Fascial Sling Surgery for Urinary Incontinence. Proceedings of the International Continence (ICS), 42nd Annual Meeting, Beijing, 15–19 October 2012, abstract no. 589. [CRSREF: 2843756; other: sr-incont45471]
Kim 2004291
Kim J, Baek U, Kwon S, Jung H, Moon K, Park T, et al. The Efficacy of Iris Procedure in Stress Urinary Incontinence: Comparison with TVT and SPARC. Proceedings of the International Continence Society (ICS), 34th Annual Meeting, and the International Urogynecological Association, Joint Meeting, Paris, 23–27 August 2004, abstract no. 313. [Other: srincont19058]
Klarskov 1986292
Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Hald T, et al. Pelvic Floor Exercise versus Surgery for Female Urinary Stress Incontinence: Preliminary Results. Proceedings of the International Continence Society (ICS), 14th Annual Meeting, Innsbruck, September 1984. p. 159. [CRSREF: 3218453; other: sr-incont9874]
aKlarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Okholm B, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence. Urol Int 1986;41:129–32. [CRSREF: 3218454; other: sr-incont592]
Klarskov P, Kroyer K, Kromann B, Maegaard E. Long-term results of pelvic floor training and surgery for female genuine stress incontinence. Neurourol Urodyn 1989;8:357–9. [CRSREF: 3218455; other: sr-incont4516]
Klarskov P, Nielson KK, Kromann-Andersen B, Maegaard E. Long-term results of pelvic floor training and surgery to female genuine stress incontinence. Int Urogynecol J 1991;2:132–5. [CRSREF: 3218456; other: sr-incont6655]
Klarskov P, Vedel Jepsen P, Dorph S. Reliability of voiding colpocystourethrography in female urinary stress incontinence before and after treatment. Acta Radiologica 1988;29:685–8. [CRSREF: 3218457; other: sr-incont469]
Lee 2001293
Lee P. Periurethral Autologous Fat Injection as a Treatment for Female Stress Urinary Incontinence. Proceedings of the FIGO World Congress of Obstetrics and Gynaecology, XVI Meeting, Washington, DC, 3–8 September 2000. Book 4. p. 46. [Other: sr-incont12087]
aLee PE, Kung RC, Drutz HP. Periurethral autologous fat injection as treatment for female stress urinary incontinence: a randomized double-blind controlled trial. J Urol 2001;165:153–8. Sr-incont11797
Miranda 2011294
Miranda V, Alarab M, Murphy K, Pineda R, Drutz H, Lovatsis D. Randomized controlled trial of cystocele plication risks: a pilot study. J Obstet Gynaecol Can 2011;33:1146–9. [Other: sr-incont42731]
Okulu 2013295
aOkulu E, Kayigil O, Aldemir M, Onen E. Use of three types of synthetic mesh material in sling surgery: a prospective randomized clinical trial evaluating effectiveness and complications. Scand J Urol 2013;47:217–24. [Other: sr-incont48505; PubMed: 23095128]
Okulu E. Synthetic Mesh Materials in Sling Surgery. 2011. Trial registration number: NCT01348334. URL: http://clinicaltrials.gov/show/NCT01348334 (accessed 19 December 2011). [Other: srincont42756]
bOkulu E, Kayigil O, Aldemir M, Onen E. The use of three types of synthetic mesh materials in the surgery for stress incontinence: the clinical results. Int Urogynecol J Pelvic Floor Dysfunct 2011;22(Suppl. 2):S1024–S1025. [Ref ID: 62216]
Osman 2003296
Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU Int 2003;92:964–8. [CRSREF: 3218478; other: sr-incont16660]
Quadri 1985297
Colombo M, Scalambrino S, Gallazzi S, Milani R. Burch Colposuspension versus Anterior Repair in Severe Genital Prolapse with Stress Incontinence: Long Term Follow-up. Proceedings of the International Continence Society, 23rd Annual Meeting, Rome, 8–11 September 1993, abstract no. 174. pp. 440–2. [Other: sr-incont12045]
Milani R, Scalambrino S, Vicandone G, Sirtori P, Spazzini D. Complementary Drug Therapy Improving Results of Surgery for Incontinence and Prolapse into Two Randomized Procedures: Vaginal versus Suprapubic Operation. Proceedings of the International Continence Society (ICS), 14th Annual Meeting, Innsbruck, September 1984. pp. 440–1. [Other: sr-incont9867]
aQuadri G, Scalambrino S, Boisio N, Marchesin R, Milani R. Randomized surgery for incontinence and prolapse: retropubic colposuspension versus anterior repair. Arch Gynecol 1985;237(Suppl.):402. [Other: sr-incont8019]
Scalambrino S, Biosio N, Marchesin R, Quadri G, Alegri M, Milani R. Clinical and Urodynamic Results in a Surgical Trial for Incontinence and Prolapse. Proceedings of the International Continence Society (ICS), 15th Annual Meeting, London, 3–6 September 1985. pp. 484–5. [Other: sr-incont9865]
Teixeira 2008298
Teixeira M, Pinto AR, Montalvao M, Candoso B. Systemic and Local Inflammatory Response in Collagen versus Polypropylene Tapes for Stress Urinary Incontinence: Is There Any Difference? Proceedings of the International Continence Society (ICS), 38th Annual Meeting, Cairo, 20–24 October 2008, abstract no. 527. [CRSREF: 2843798; other: sr-incont31878]
Teleb 2011299
Teleb M, Salem EA, Naguib M, Kamel M, Hasan U, Elfayoumi AR, et al. Evaluation of transvaginal slings using different materials in the management of female stress urinary incontinence. Arab J Urol 2011;9:283–7. [CRSREF: 2843800; other: sr-incont59731]
ter Meulen 2009300
ater Meulen PH, Berghmans LC, Nieman FH, van Kerrebroeck PE. Effects of Macroplastique® Implantation System for stress urinary incontinence and urethral hypermobility in women. Int Urogynecol J 2009;20:177–83. [Other: Sr-incont29204]
ter Meulen PH, Berghmans LCM, Nieman FHM, Dormans-Linssen M, van Kerrebroeck PE. Macroplastique® Implantation System for the Treatment of Urodynamic Stress Urinary Incontinence Caused by Urethral Hypermobility in Adult Women after Non-successful Conservative Treatment: a Randomized Clinical Trial. Proceedings of the International Continence Society (ICS), 38th Annual Meeting, Cairo, 20–24 October 2008, abstract no. 499. [Other: Sr-incont31836]
Tincello 2004301
Tincello DG, Kenyon S, Slack M, Toozs-Hobson P, Mayne C, Jones D, et al. Colposuspension or TVT with anterior repair for urinary incontinence and prolapse: results of and lessons from a pilot randomised patient-preference study (CARPET 1). BJOG 2009;116:1809–14. [Other: ISRCTN34759911; other: sr-incont34323]
aTincello DG, Mayne CJ, Toozs-Hobson P, Slack M. Randomised Controlled Trial of Colposuspension versus Anterior Repair plus TVT for Urodynamic Stress Incontinence with Anterior Vaginal Prolapse: Proposal (Abstract). Proceedings of the United Kingdom Continence Society (UKCS), 11th Annual Scientific Meeting, Bournemouth, 18–19 March 2004. p. 46. [Other: sr-incont17170]
van der Ploeg 2013302
van der Ploeg JM, van der Steen A, Oude Rengerink K, van der Vaart CH, Roovers J. Multicentre randomised trial of vaginal prolapse repair versus vaginal prolapse repair with a midurethral sling in patients with pelvic organ prolapse and co-existing stress urinary incontinence. Neurourol Urodyn 2013;32:814. [Other: sr-incont49198]
van Leijsen 2013303
Mengerink BB. The impact of midurethral sling operation on sexual function in women with stress urinary incontinence, a multicenter prospective study. Int Urogynecol J Pelvic Floor Dysfunct 2013;24(Suppl. 1):S147. [Other: sr-incont62175]
avan Leijsen SA, Kluivers KB, Mol BW, Hout Ji, Milani AL, Roovers JP, et al. Value of urodynamics before stress urinary incontinence surgery: a randomized controlled trial. Obstet Gynecol 2013;121:999–1008. [Other: sr-incont47434; PubMed: 23635736]
van Leijsen SA, Kluivers KB, Mol BWJ, Broekhuis SR, Milani FL, van der Vaart CH van D, et al. Protocol for the value of urodynamics prior to stress incontinence surgery (VUSIS) study: a multicenter randomized controlled trial to assess the cost effectiveness of urodynamics in women with symptoms of stress urinary incontinence in whom surgical treatment is considered. BMC Womens Health 2009;9:22. [Other: sr-incont32078; PubMed: 19622153]
bvan Leijsen S, Vierhout M, Heesakkers J, Kluivers K, Mol BW. A Multicentered Randomised Controlled Trial to Test the Cost Effectiveness of Urodynamics in Women with Symptoms of Stress Urinary Incontinence in whom Surgical Treatment is Considered. 2008. Trial registration number: NCT00814749. URL: http://clinicaltrials.gov/show/NCT00814749 (accessed 20 August 2017). [Ref ID: 64469]
Wang 2008285
(Merged with the included study: Wang 200937)
Wang WY, Zhu L, Lang JH, Sun ZJ, Hai N. [Clinical study on tension-free vaginal tape and tension-free vaginal tape obturator for surgical treatment of severe stress urinary incontinence] [Chinese]. Chin J Obstet Gynecol 2008;43:180–4.
Zargham 2013304
Zargham M, Alizadeh F, Tadayyon F, Khorrami M-H, Nouri-Mahdavi K, Gharaati MR, et al. Concomitant surgical correction of severe stress urinary incontinence and anterior vaginal wall prolapse by anterior vaginal wall wrap: 18-month outcomes. J Res Med Sci 2013;18:588–93. [CRSREF: 2843810; other: sr-incont59874]
(ii) New studies from the updated searches, excluded from ESTER
Campeau 2007305
aCampeau L, Tu LM, Lemieux M, Naud A, Karsenty G, Schick E, et al. A multicenter, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn 2007;26:990–4. [Ref ID: 23914]
Campeau L, Tu LM, Lemieux M, Naud A, Karsenty G, Shrier I, et al. A multicenter prospective randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Int Urogynecol J 2006;17(Suppl. 2):S94. [Ref ID: 49144]
Campeau L, Tu LM, Lemieux M, Naud A, Karsenty G, Shrier I, et al. A multicenter prospective randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn 2006;25:571–2. [Ref ID: 23755]
Campeau L, Tu LM, Lemieux MC, Naud A, Karsenty G, Corcos J. A multicentric, prospective, randomized clinical trial comparing tension-free vaginal tape surgery and no treatment for the management of stress urinary incontinence in elderly women. Neurourol Urodyn 2007;26(Suppl. 1):1065. [Ref ID: 26691]
Caremel 2013306
aCaremel R, Tu LM, Baker K, Adli OEY, Loutochin O, Corcos J. A multicentric randomized controlled study comparing surgical and pharmacological therapy to treat mixed urinary incontinence. J Urol 2013;189(Suppl. 1):e760. [Ref ID: 64308]
Caremel R, Tu LM, Baker K, El Yazami AO, Loutochin O, Corcos J. A multi-centre randomized controlled study comparing surgical and pharmacological therapy to treat mixed urinary incontinence. Eur Urol Suppl 2013;12:e785. [Ref ID: 64358]
Caremel R, Tu LM, Baker K, El Yazami AO, Loutochin O, Corcos J. A multicentred randomized controlled study comparing surgical and pharmacological therapy to treat mixed urinary incontinence. Neurourol Urodyn 2013;32:188–9. [Ref ID: 65233]
Choi 2006307
Choi SJ, Kim YH, Choi SH, Ki WS, Kim SA, Jung H. A prospective study of transobturator tension free tape (TOT) and laparoscopic Burch operation for stress urinary incontinence. Int Urogynecol J 2006;17(Suppl. 2):S307. [Ref ID: 64442]
Grigoriadis 2013308
Grigoriadis C, Bakas P, Derpapas A, Creatsa M, Liapis A. Tension-free vaginal tape obturator versus Ajust adjustable single incision sling procedure in women with urodynamic stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol 2013;170:563–6. [Ref ID: 59816]
Karmakar 2017287
Karmakar D, Mostafa A, Abdel-Fattah M. A new validated score for detecting patient-reported success on postoperative ICIQ-SF: a novel two-stage analysis from two large RCT cohorts. Int Urogynecol J 2017;28:95–100.
Larsson 2014309
aLarsson P, Tegerstedt G. Bulkamid Treatment of Stress Incontinence in Women with Urinary Stress Incontinence and Not Suitable to TVT-procedure. A Prospective Randomized Study. Proceedings of the International Continence Society (ICS), 44th Annual Meeting, Rio de Janeiro, 20–24 October 2014, abstract no. 790. [Ref ID: 64743; other: NCT00984958]
Larsson P-G, Pedroletti C, Tegerstedt G, Olsson I. Bulkamid Treatment of Stress Incontinence in Women with Urinary Stress Incontinence and Not Suitable to TVT-procedure Because of Suspected ISD: a Prospective Randomized Study. 2009. Trial registration number: NCT00984958. URL: http://clinicaltrials.gov/show/NCT00984958 (accessed 20 August 2017). [Ref ID: 63739]
Nikas 2012310
Nikas I, Koundouri MRA, Gavriil I, Kilbasanis I. Management of cystocele with associated urine incontinence in menopausal women. Maturitas 2012;71(Suppl. 1):S74. [Other: sr-incont47266]
Pushkar 2011286
Pushkar DI, Kasian GR, Gvozdev MI, Lynova IL, Kupriianov IA. [Mini-invasive operations for correction of urinary incontinence in females] [Russian]. Urologiia 2011:16–20. [CRSREF: 3348017; other: SR-INCONT43390]
Rose 2012311
aRose A, Ju M, Rehme C, Rubben H. Skeletal Muscle-derived Cell Implantation in Female Patients with Stress Urinary Incontinence: a Multicenter, Randomized, Parallel-group, Placebo-controlled Clinical Study. Proceedings of the International Continence (ICS), 42nd Annual Meeting, Beijing, 15–19 October 2012, abstract no. 549. [Ref ID: 46738; other: EUCT2010-021867-34]
Rose A, Ju M, Rehme C, Rubben H. Dose independent effect of intrasphincteric implantation of autologous myoblasts for the treatment of stress urinary incontinence in women. Int Urogynecol J Pelvic Floor Dysfunct 2012;23(Suppl. 1):S144–5. [Ref ID: 67238]
Sung 2013312
Komesu YM, Richter HE, Dinwiddie DL, Siddiqui NY, Sung VW, Lukacz ES, et al. Methodology for a vaginal and urinary microbiome study in women with mixed urinary incontinence. Int Urogynecol J 2017;28:711–20. [Ref ID: 74215]
Newman DK, Borello-France D, Sung VW. Structured behavioral treatment research protocol for women with mixed urinary incontinence and overactive bladder symptoms. Neurourol Urodyn 2018;37:14–26. [Ref ID: 74912]
Sung VW, Borello-France D, Dunivan G, Gantz M, Lukacz ES, Moalli P, et al. Methods for a multicenter randomized trial for mixed urinary incontinence: rationale and patient-centeredness of the ESTEEM trial. Int Urogynecol J 2016;27:1479–90. [Ref ID: 73960]
aSung VW, Wallace D. Effects of Surgical Treatment Enhanced with Exercise for Mixed Urinary Incontinence (ESTEEM). 2013. Trial registration number: NCT01959347. URL: http://clinicaltrials.gov/show/NCT01959347 (accessed 20 August 2017). [Other: ESTEEM; other: srincont49234]
Tuncer 2016313
Tuncer M, Tarhan F, Kafkasli A, Demir K, Yucetas U, Faydaci G, et al. The effects of stress incontinence surgery on sexual function and life quality of women. Arch Ital Urol Androl 2016;88:106–10. [Ref ID: 74137]
Wadie 2016314
aWadie B, Taha D, Elhefnawy A, Gaballah M. Combined MUS and Anterior Colporrhaphy vs. MUS Alone in the Treatment of SUI, Randomized Controlled Trial. Proceedings of the International Continence Society (ICS), Annual Meeting, Tokyo, 13–16 September 2016, abstract no. 329. [Ref ID: 73378]
Wadie B, Ramadan DE, Elhefnawy A, Gaballah M. Combined MUS and Anterior Colporrhaphy vs. MUS Alone in the Treatment of SUI with Low Grade Anterior POP, a Randomized Controlled Trial. Proceedings of the International Continence Society (ICS), 45th Annual Meeting, Montreal, QC, 6–9 October 2015, abstract no. 558. [Ref ID: 68813]
Appendix 7 Ongoing trials
a Primary reference where more than one report of a study was available; this is the name given to the study as it appears in the main text of the ESTER report.
NoteAny relevant study and reference identifiers (IDs) are included in square brackets following each citation, e.g. [database: identifier].
Identifiers containing ‘sr-incont’ relate to the Cochrane Incontinence Specialised Register; ‘CRSREF’ identifiers refer to the Cochrane Register of Studies Web version (CRS-Web); ‘other’ is used to refer to either the study acronym or the trial registration number from a number of trial registries; ‘Ref ID’ identifiers relate to those records being processed for inclusion in the Cochrane Incontinence Specialised Register.
| Study ID | Interventions | Start date | End date | Trial registration number |
|---|---|---|---|---|
| Abdel-Fattah 2014315 | RP-TVT vs. transobturator MUS (TO-TVT) vs. SIMS | 1 December 2013 | 31 May 2019 | 3/069/13 |
| Boyd 1996316 | Open colposuspension vs. laparoscopic colposuspension | 1 March 1994 | 28 February 1996 | ISRCTN44339585 |
| Cardozo 2002317 | Retropubic MUS (TVT) vs. periurethral injection of collagen | 1 March 2000 | 1 March 2002 | N0116091776 |
| Carr 2011318 | Injectable (autologous muscle-derived cells) vs. control | December 2011 | February 2016 | NCT01382602 |
| Cavkaytar 2013319 | Retropubic MUS (TVT) vs. transobturator MUS (TOT) | 1 June 2013 | 1 June 2014 | NCT01903590 |
| Courtney-Watson 2002320 | Retropubic MUS (TVT) vs. injectable (Macroplastique) | 1 May 1999 | 1 January 2002 | N0280055971 |
| Ding 2015321 | Transobturator MUS (TVT-O) vs. TVT-O plus injectable (adipose-derived mesenchymal stem cells) | NR | NR | ChiCTR-ICR-15006045 |
| Elsokkary 2016322 | Transobturator MUS (TOT) vs. modified needleless SIMS | 1 February 2013 | 2 December 2015 | PACTR201607001696163 |
| Fu 2016323 | Transobturator MUS (inside-out TOT) vs. innovative single-incision sling (needleless) | NR | NR | ChiCTR-INR-16008068 |
| Hilton 2002324 | Retropubic MUS (TVT) vs. traditional sling (fascial sling) | 1 June 1998 | 1 November 1999 | N0503016202 |
| Innovation 2010325 | Injectable (autologous muscle-derived cells) (ICES13; Innovacell Biotechnologie, Innsbruck, Austria) vs. placebo | 18 April 2012 | NR | 2010–021871–10 |
| Itkonen 2015326 | Retropubic MUS (TVT) vs. Bulkamid® (Contura International A/S, Soeborg, Denmark) injection | 1 September 2015 | 1 December 2022 | NCT02538991 |
| Kaufman 2013327 | Injectable (autologous muscle-derived cells for USR) vs. placebo | 1 October 2013 | 1 December 2018 | NCT01893138 |
| Leitch 2016328 | Retropubic MUS vs. SIMS | 21 April 2016 | 31 December 2017 | ACTRN12616000328471 |
| Maslow 2013329 | Transobturator MUS (TVT-O) vs. single-incision sling (MiniArc® Precise Pro; American Medical Systems Inc., Minnetonka, MN, USA) | NR | NR | NCT01799122 |
| Oliveira 2013330 | Transobturator MUS vs. Ophira® (Promedon, Córdoba, Argentina) SIMS | 1 January 2013 | 1 July 2014 | NCT02540525 |
| Reda 2014331 | Retropubic MUS (TVT) vs. SIMS | 1 November 2014 | 1 June 2016 | NCT02263534 |
| Saaid 2008332 | Retropubic MUS (TVT) vs. transobturator MUS (TOT) vs. Burch colposuspension | 1 October 2008 | 1 May 2015 | NCT03085979 |
| Shen 2015333 | Transobturator MUS (modified TVT-O) vs. SIMS ‘TVT-Adjust’ [sic] | 16 March 2015 | 16 September 2016 | ChiCTR-IOR-15006140 |
| SUITE 2009334 | Injection (skeletal muscle-derived cells) vs. SNRI (duloxetine) vs. placebo | 18 December 2009 | NR | 2009–011797–15 |
| Sweed 2016335 | Retropubic MUS (TVT) vs. transobturator MUS (TOT) vs. Burch colposuspension | 1 May 2016 | 1 December 2018 | NCT02775526 |
| Zhu 2014336 | Transobturator MUS (TVT-O) vs. Regen Sling® (Medprin Regenerative Medical Technologies Co., Ltd., Guangzhou, China) | 1 January 2014 | 1 December 2015 | NCT02106299 |
| Zhu 2015337 | Transobturator MUS (TVT-O) vs. single-incision sling (TVT-S) | NR | NR | ChiCTR-IPR-15006967 |
References for ongoing trials
Abdel-Fattah 2014315
aAbdel-Fattah M. Adjustable Anchored Single-incision Mini-Slings versus Standard Tension-free Mid-urethral Slings in the Surgical Management of Female Stress Urinary Incontinence: a Pragmatic Multicentre Non-inferiority Randomised Controlled Trial. 2014. Trial registration number: ISRCTN93264234. URL: http://isrctn.org/ISRCTN93264234 (accessed 20 August 2017). [Ref ID: 64517]
Davidson T, McDonald A, McPherson G, Norrie J. A comparison of an objective and subjective test of stress urinary incontinence (SUI) and their acceptability to participants. Trials 2015;16(Suppl. 2):P58. [Ref ID: 75102]
Davidson T, McDonald A, McPherson G, Norrie J. Evaluating the use of real-time data collection using SMS texts in the SIMS study. Trials 2015;16(Suppl. 2):O65. [Ref ID: 75610]
Boyd 1996316
Boyd K. Laparoscopic Treatment for Female Urinary Incontinence. 2004. Trial registration number: ISRCTN44339585. URL: http://isrctn.org/ISRCTN44339585 (accessed 9 June 2004). [Other: sr-incont17206]
Cardozo 2002317
Cardozo L, Rufford J. Comparative Study of the Efficacy, Acceptability, Morbidity and Cost-effectiveness of the ’Tension Free Vaginal Tape’ and the Periurethral Injection of Collagen in the Management of Recurrent Stress Incontinence. 2002. Trial registration number: N0116091776. [CRSREF: 3254222; other: sr-incont16380]
Carr 2011318
Carr LK , De Ridder D, Magali R, Carlson K, Quinlan D, Steele SS, et al. A Double-blind, Randomized, Placebo-controlled Study Evaluating the Safety and Effectiveness of Cook MyoSite Incorporated AMDC in Female Patients with Stress Urinary Incontinence. 2011. Trial registration number: NCT01382602. URL: http://clinicaltrials.gov/show/NCT01382602 (accessed 20 August 2017). [Ref ID: 49828]
Cavkaytar 2013319
Cavkaytar S, Aksakal SO, Kokanali MK, Topcu HO, Doganay M. Prospective Randomized Study Comparing TVT and TOT in Female Stress Urinary Incontinence with No Intrinsic Sphincter Deficiency. 2013. Trial registration number: NCT01903590. URL: http://clinicaltrials.gov/show/NCT01903590 (accessed 20 August 2017). [Other: srincont49363]
Courtney-Watson 2002320
Courtney-Watson C. Comparison of Two Surgical Methods for Curing Stress Incontinence (Recurrent). 2002. Trial registration number: N0280055971. [CRSREF: 3254224; other: sr-incont16382]
Ding 2015321
Ding J, Zhu L. Explore the Efficacy and Safety of Single-center Randomized Controlled Polypropylene Mesh Auxiliary plus Adipose-derived Mesenchymal Stem Cells in the Treatment of Pelvic Organ Prolapse. 2015. Trial registration number: ChiCTR-ICR-15006045. URL: www.chictr.org.cn/showproj.aspx?proj=10516 (accessed 20 August 2017). [Ref ID: 67577]
Elsokkary 2016322
Elsokkary M. Modified Needleless Single-incision Mini-sling Compared to Standard Trans-obturator Mid-urethral Sling in the Surgical Management of Female Stress Urinary Incontinence. 2016. Trial registration number: PACTR201607001696163. www.pactr.org/ATMWeb/appmanager/atm/atmregistry?dar=true&tNo=PACTR201607001696163 (accessed 20 August 2017). [Ref ID: 73367]
Fu 2016323
Fu Q, Lv J. Prospective Randomized Comparison of the Transobturator Mid-urethral Sling with the Single-incision Sling (Needleless) Among Women with Stress Urinary Incontinence: 1-year Follow-up Study. 2016. Trial registration number: ChiCTR-INR-16008068. URL: www.chictr.org.cn/showproj.aspx?proj=13532 (accessed 20 August 2017). [Ref ID: 71377]
Hilton 2002324
Hilton P. A Prospective Randomised Comparative Trial of a Tension-free Vaginal Tape (TVT) and Fascial Sling Procedure for ‘Secondary’ Genuine Stress Incontinence. 2002. Trial registration number: N0503016202. [CRSREF: 2843900; other: sr-incont16383]
Innovation 2010325
Innovation (Innovacell Biotechnologie AG). A Multicenter, Randomized, Double-blinded, Parallel-group, Placebo Controlled Study to Assess the Efficacy and Safety of Skeletal Muscle-derived Cell Implantation in Female Patients with Stress Urinary Incontinence. 2010. Trial registration number: EUCTR2010-021871-10-DE. URL: www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2010-021871-10 (accessed 20 August 2017). [Ref ID: 64562]
Itkonen 2015326
Itkonen A-M. TVT versus Bulkamid®-Injections in Treatment of Stress Urinary Incontinence – Patient Satisfaction and Complications of the Treatment. 2015. Trial registration number: NCT02538991/ URL: https://clinicaltrials.gov/show/NCT02538991 (accessed 20 August 2017). [Ref ID: 68788]
Kaufman 2013327
NCT01893138, Kaufman M. A Double-blind, Randomized, Controlled Trial Comparing the Safety and Efficacy of AMDC-USR with Placebo in Female Subjects with Stress Urinary Incontinence. 2013. Trial registration number: NCT01893138. URL: http://clinicaltrials.gov/show/NCT01893138 (accessed 20 August 2017). [Ref ID: 61589]
Leitch 2016328
Leitch A, Ow LL, Rosamilia A. Objective Cure Rate of Mini Sling or Retropubic Sling in Women with Intrinsic Sphincter Deficiency – A RCT Study (Mini RISD). 2016. Trial registration number: ACTRN12616000328471. URL: www.anzctr.org.au/ACTRN12616000328471.aspx (accessed 20 August 2017). [Ref ID: 71376]
Maslow 2013329
Maslow KD. Randomized Clinical Trial Comparing Mini-Arc Precise Pro and the Trans Vaginal Obturator Tape for Surgical Management of Stress Urinary Incontinence. 2013. Trial registration number: NCT01799122. URL: http://clinicaltrials.gov/show/NCT01799122 (accessed 20 August 2017). [Ref ID: 62915]
Oliveira 2013330
Oliveira E. Transobturator Sling Compared with Single-incision Mini-sling for the Treatment of Stress Urinary Incontinence: a Randomized Controlled Trial. 2013. Trial registration number: NCT02540525. URL: https://clinicaltrials.gov/show/NCT02540525 (accessed 20 August 2017). [Ref ID: 68787]
Reda 2014331
Reda A, Gomaa I. Retropubic Single Incision Minisling versus Tension Free Vaginal Tape for Management of Stress Urinary Incontinence. 2014. Trial registration number: NCT02263534. URL: http://clinicaltrials.gov/show/NCT02263534 (accessed 20 August 2017). [Ref ID: 64746]
Saaid 2008332
Saaid HA. Surgical Management of Mixed Urinary Incontinence. 2008. Trial registration number: NCT03085979. URL: https://clinicaltrials.gov/show/NCT03085979 (accessed 20 August 2017). [Ref ID: 76076]
Shen 2015333
Shen W, Fu J. Single-incision Mini-slings versus Standard Midurethral Slings in Surgical Management of Female Stress Urinary Incontinence: a Prospective Randomized Controlled Trial to Evaluate the Efficacy and Safety. 2015. Trial registration number: ChiCTR-IOR-15006140. URL: www.chictr.org.cn/showproj.aspx?proj=10638 (accessed 20 August 2017). [Ref ID: 67571]
SUITE 2009334
aSUITE (Innovacell Biotechnologie AG). Skeletal Muscle-derived Cell Implantation in Female Patients with Stress Urinary Incontinence: a Multicenter, Randomized, Parallel-group, Placebo-controlled Clinical Study – SUITE Study. 2009. Trial registration number: EUCTR 2009-011797-15-DE. URL: www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2009-011797-15 (accessed 20 August 2017). [Ref ID: 64582]
SUITE (Innovacell Biotechnologie AG). Skeletal Muscle-derived Cell Implantation in Female Patients with Stress Urinary Incontinence: a Multinational and Multicenter Open Follow-up Study. 2009. Trial registration number: EUCTR 2009-016597-32. URL: www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2009-016597-32 (accessed 20 August 2017). [Ref ID: 64576]
Sweed 2016335
Sweed MS. Trans-obturator Tape, Tension-free Vaginal Tape and Burch Colposuspension for Treatment of Female Mixed Urinary Incontinence: a Randomized Clinical Trial. 2016. Trial registration number: NCT02775526. URL: https://clinicaltrials.gov/show/NCT02775526 (accessed 20 August 2017). [Ref ID: 73339]
Zhu 2014336
Zhu L, Tian Q. A Multi-center, Randomized, Controlled Clinical Trial of the Safety and Efficacy of Regen Sling Treatment for Female Patients with Stress Urinary Incontinence. 2014. Trial registration number: NCT02106299. URL: http://clinicaltrials.gov/show/NCT02106299 (accessed 20 August 2017). [CRSREF: 2843902; other: sr-incont61984]
Zhu 2015337
Zhu L, Sun Z-J. A RCT of TVT-O and TVT-S in the Treatment of Stress Urinary Incontinence. 2015. Trial registration number: ChiCTR-IPR-15006967. URL: www.chictr.org.cn/showproj.aspx?proj=11725 (accessed 20 August 2017). [Ref ID: 68802]
Appendix 8 Characteristics of included studies
| Study ID (first author and year) | Source reviewa | Length of FU or last FU (months) | Intervention | N randomised | Age (mean or median) | UI diagnosis | Previous UI surgery in some or all participants | Co-existing POP in some or all participants | Concomitant POP surgery in some or all participants |
|---|---|---|---|---|---|---|---|---|---|
| Abdelwahab 2010155 | Nambiar | 9 |
I. Retro-MUS II. Single incision |
I. 30 II. 30 |
I. 39.2 II. 40.2 |
USI (DO excluded) | No | Yes (> 2 POP-Q excluded) | NR |
| bAbouhashem 201438 | Saraswat | 60 |
I. Retro-MUS II. Trad sling |
Total 56 | 34.3 | SUI | No | NR | NR |
| bAdile 200339 | Ford | 36 |
I. Retro-MUS II. Lap colpo |
I. 67 II. 66 |
51 | USI | No | NR | No |
| Aigmüller 201483 | Ford | 3 |
I. Retro-MUS II. Transob-MUS |
I. 285 II. 269 |
I. 59.7 II. 58.6 |
USI (DO or predominant OAB excluded) | No except for previous anterior repair | NR | No |
| Al-Azzawi 2014164 | New | 12 |
I. Transob-MUS II. Trad sling |
I. 40 II. 40 |
I. 42.8 II. 39.2 |
SUI, predominant SUI | NR | Yes (> 1 grade cystocele excluded) | NR |
| Albo 200782 | Lapitan | 60 |
I. Open colpo II. Trad sling |
I. 329 II. 326 |
I. 52.2 II. 51.6 |
SUI, predominant SUI | Yes | Yes | Yes |
| Alkady 2009120 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 15 II. 15 |
I. 48 II. 50 |
USI, SUI, MUI (DO excluded) | No | Yes (≥ 4 stage excluded) | Yes |
| Amaro 2007151 | Ford | 36 |
I. Retro-MUS II. Trad sling |
I. 20 II. 21 |
I. 52 II. 49 |
USI (DI excluded) | Yes | NR | NR |
| Amat 2011112 | Nambiar | 54 |
I. Transob-MUS II. Single incision |
I. 71 II. 87 |
I. 60.6 II. 59.9 |
SUI, MUI | NR | Yes | Yes |
| Andonian 2007117 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 112 II. 78 |
I. 57–61 II. 56.2 |
SUI, MUI | Yes | Yes | Yes |
| Andrada Hamer 2011156 | Nambiar | 12 |
I. Retro-MUS II. Single incision |
I. 69 II. 64 |
I. 48 II. 47 |
SUI, predominant SUI | No | NR | No |
| Aniuliene 200984 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 114 II. 150 |
I. 51 II. 49 |
SUI (OAB excluded) | Yes | Yes (> 2 stage excluded) | NR |
| Aniuliene 2015121 | New | 12 |
I. Retro-MUS II. Transob-MUS |
I. 78 II. 76 |
I. 50 II. 67 |
SUI (predominant OAB excluded) | No previous suburethral sling | Yes (> 2 POP-Q excluded) | NR |
| Ankardal 200185 | Lapitan | 12 |
I. Open colpo II. Lap colpo |
I. 120 II. 120 |
I. 42.6 II. 40.9 |
USI, predominant SUI | No | NR | No |
| Araco 200886 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 120 II. 120 |
54 | SUI (OAB excluded) | No | No | NA |
| Arunkalaivanan 2003152 | Ford | 36 |
I. Retro-MUS II. Trad sling |
I. 68 II. 74 |
I. 54 II. 53 |
USI (DO excluded) | Yes | NR | NR |
| Athanassopoulos 1996111 | Lapitan | 8–27 |
I. Open colpo II. Bladder neck needle |
I. 27 II. 24 |
50 | USI | NR | Yes | NR |
| Bai 2005145 | Lapitan | 12 |
I. Retro-MUS II. Open colpo III. Trad sling |
I. 31 II. 33 III. 28 |
I. 58.2 II. 56.5 III. 56.3 |
USI (DO excluded) | NR | Yes (> 2 grade excluded) | NR |
| Bandarian 2011161 | Lapitan | 22 |
I. Transob-MUS II. Open colpo |
I. 31 II. 31 |
I. 49.4 II. 46.9 |
USI only (no MUI) | No | Yes (> 1 POP-Q stage excluded) | NR |
| Barber 2008122 | Ford | 24 |
I. Retro-MUS II. Transob-MUS |
I. 88 II. 82 |
I. 52 II. 53 |
USI, MUI (DO excluded) | No previous sling surgery | Yes | Yes |
| Barber 201287 | Nambiar | 24 |
I. Retro-MUS II. Single incision |
I. 127 II. 136 |
I. 54.6 II. 54.6 |
USI, MUI | No previous sling surgery | Yes | Yes |
| Barry 2008123 | Ford | 3 |
I. Retro-MUS II. Transob-MUS |
I. 107 II. 80 |
I. 53.6 II. 54.2 |
USI (some had OAB) | Yes | Yes | Yes |
| Basok 2008153 | Ford | 12 |
I. Retro-MUS II. Trad sling |
I. 72 II. 67 |
I. 50.3 II. 47.4 |
SUI, MUI | NR | Yes (excluded uterine prolapse, rectocele, enterocoele, grade III or IV cystocoele) | NR |
| Basu 2010157 | Nambiar | 36 |
I. Retro-MUS I. Single incision |
I. 33 II. 38 |
I. 48.2 II. 49.7 |
USI, SUI (some had DO) | No | Yes (> 2 POP-Q excluded) | NR |
| Berglund 1996192 | Lapitan | 60–84 |
I. Open colpo II. Ant repair |
I. 30 II. 15 |
50 | SUI only (no UUI) | No | Yes (included cystocele but excluded other gynaecological disease requiring surgery) | NR |
| Bergman 1989a88 | Lapitan | 12 |
I. Open colpo II. Bladder neck needle III. Ant repair |
I. 101c II. 98c III. 99c 339 randomised |
57 | USI (DI excluded) | No | Yes (all) | Yes (all) |
| Bergman 1989b188 | Lapitan | 60 |
I. Open colpo II. Bladder neck needle III. Ant repair |
I. 38c II. 34c III. 35c 127 randomised |
55 | USI | No | NR (excludes other gynaecological disease needing surgery) | No |
| Bianchi 201225 | Nambiar | 24 |
I. Transob-MUS II. Single incision |
I. 56 II. 66 |
I. 52.1 II. 54.1 |
USI (DO excluded; some had urgency) | Yes | Yes (> 2 POP-Q excluded) | NR |
| bBurton 199440 | Lapitan | 60 |
I. Open colpo II. Lap colpo |
I. 30 II. 30 |
NR | USI | NR | NR | NR |
| Campos 2013176 | New | 12 |
I. Transob-MUS II. Single incision |
I. 28 II. 30 |
I. 59.1 II. 60.8 |
SUI, predominant SUI | No | Yes | Yes |
| Carey 200089 | Lapitan | 60 |
I. Open colpo II. Lap colpo |
I. 104 II. 96 |
I. 52.3 II. 50.7 |
USI, MUI | No | Yes (but excluded major degrees of POP requiring surgery other than a simple rectocele repair) | Yes |
| bCervigni 200641 | Ford | NR (in-hospital stay only?) |
I. Retro-MUS II. Transob-MUS |
Total 118 | 57.4 | SUI | NR | Yes (include ≥ 2 stage) | Yes (all) |
| Chen 2010118 | Ford | NR |
I. Retro-MUS II. Transob-MUS |
I. 77 II. 110 |
I. 52.2 II. 47–52 |
USI only (no MUI) | No | Yes (> 2 grade cystocele excluded) | NR |
| Chen 201290 | Ford | 24 |
I. Retro-MUS II. Transob-MUS |
I. 102 II. 103 |
NR | USI only (no MUI) | NR | Yes | NR |
| bChoe 201342 | Ford | NR (in-hospital stay only?) |
I. Retro-MUS II. Transob-MUS |
Total 41 |
I. 55.6 II. 53.7 |
SUI | NR | NR | NR |
| Colombo 2000193 | Lapitan | 96–204 |
I. Open colpo II. Ant repair |
I. 37 II. 34 |
I. 54.9 II. 55.7 |
USI (DI excluded) | No | Yes (all had grade 2 or 3 cystocele) | Yes |
| Darabi Mahboub 201226 | Ford | 30 |
I. Retro-MUS II. Transob-MUS |
I. 50 II. 50 |
I. 52.0 II. 52.3 |
Predominant SUI | NR | Yes (> 2 grade excluded) | NR |
| bDati 201243 | New | 6 |
I. Transob-MUS II. Single incision |
I. 58 II. 57 |
NR | USI | No | Yes (> 3 stage POP excluded) | Yes |
| David-Montefiore 2006124 | Ford | 48 |
I. Retro-MUS II. Transob-MUS |
I. 42 II. 46 |
I. 56.8 II. 53.4 |
USI, MUI | Yes | NR | NR |
| bde Oliveira 200644 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 41d II. 42d |
52.6 | SUI | NR | Yes (≥ 2 stage excluded) | NR |
| de Tayrac 2004125 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 31 II. 30 |
I. 53.6 II. 54.7 |
USI, predominant SUI | Yes | No | NA |
| Deffieux 2010126 | Ford | 24 |
I. Retro-MUS II. Transob-MUS |
I. 75 II. 74 |
I. 54.6 II. 52.8 |
USI, MUI | No | Yes (> 1 stage POP-Q excluded) | No |
| Demirci 2001103 | Lapitan | 12 |
I. Open colpo II. Trad sling |
I. 23 II. 23 |
I. 48.1 II. 48.9 |
USI (some had UUI but not DI) | No | Yes (severe POP excluded) | Yes? (hysterectomy) |
| Di Palumbo 2003199 | Glazner 2014 | 48 |
I. Bladder neck needle II. Ant repair |
I. 28 II. 52 |
I. 60.6 II. 59.8 |
SUI, MUI, UUI, urge-predominant MUI (% not reported) | NR | Yes [all women had urethrocystocele (anterior prolapse) grade 3 or 4] | Yes? (hysterectomy) |
| bDiab 201245 | Ford | 26 |
I. Retro-MUS II. Transob-MUS |
I. 32 II. 31 |
NR | SUI | NR | NR | NR |
| Djehdian 201027 | Nambiar | 36 |
I. Transob-MUS II. Single incision |
I. 61 II. 69 |
I. 51.9 II. 54.2 |
USI, SUI (DO excluded; some had urgency) | Yes | Yes (> 1 grade excluded) | NR |
| bDrahoradova 200446 | Lapitan | 12 |
I. Retro-MUS II. Open colpo |
I. 79 II. 60 |
59 | SUI | NR | NR | NR |
| El-Barky 2005201 | Lapitan | 24 |
I. Retro-MUS II. Open colpo |
I. 25 II. 25 |
I. 50 II. 50 |
USI only (no MUI) | No | Yes (> 1 grade cystocele excluded) | NR |
| bEl-Din Shawki 201247 | Lapitan | 3 |
I. Transob-MUS II. Open colpo III. Ant repair |
Total 60 | NR | SUI | NR | NR | NR |
| El-Hefnawy 2010127 | Ford | 24 |
I. Retro-MUS II. Transob-MUS |
I. 45 II. 42 |
I. 47 II. 45 |
USI, predominant SUI | No pelvic or vaginal surgery within the preceding 6 months | Yes (> 2 stage excluded) | Yes |
| bEl-Hefnawy 2012127 | New | 12 |
I. Retro-MUS II. Transob-MUS |
Total 75 |
I. 47 II. 45 |
SUI, predominant SUI | NR | Yes | Yes (‘grade II cystocele or rectocele were only concomitant procedure allowed per protocol’) |
| bElshawaf 200949 | Lapitan | 6 |
I. Retro-MUS II. Transob-MUS |
I. 25 II. 25 III. 25 |
NR | USI | NR | NR | NR |
| Enzelsberger 1996186 | Lapitan | 48 |
I. Open colpo II. Trad sling |
I. 36 II. 36 |
I. 59.8 II. 56.3 |
SUI | Yes (all recurrent case) | Yes (grade 3 cysto- or rectocele excluded) | No |
| Enzelsberger 2005104 | Ford | 15 |
I. Retro-MUS II. Transob-MUS |
I. 52 II. 53 |
51 | SUI only (no MUI) | No | No | NA |
| Enzelsberger 2010170 | Nambiar | 24 |
I. Transob-MUS II. Single incision |
I. 45 II. 45 |
I. 54 II. 53 |
SUI | No | NR | NR |
| bEnzelsberger 201150 | New | 20 |
I. Transob-MUS II. Single incision |
I. 25 I. 25 |
NR | SUI | NR | NR | No |
| bFatthy 200151 | Lapitan | 18 |
I. Open colpo II. Lap colpo |
I. 40 II. 34 |
I. 42.9 II. 40.3 |
USI (DI excluded) | Yes | Yes (stage 3–4 excluded) | NR |
| bFernandez 201552 | New | 27 |
I. Transob-MUS II. Single incision |
I. 98 II. 89 |
I. 57.8 II. 57.6 |
SUI, predominant SUI | No | Yes | Yes |
| bFischer 200153 | Lapitan | 6 |
I. Open colpo II. Trad sling |
I. 11 II. 11 |
NR | USI | NR | NR | Yes |
| Foote 2006146 | Ford | 28.8 |
I. Retro-MUS II. Lap colpo |
I. 49 II. 48 |
I. 52.4 II. 51.2 |
USI (DO excluded) | No previous retropubic surgery excluded | Yes (‘significant’ POP excluded) | No |
| Foote 2015171 | New | 6 |
I. Transob-MUS II. Single incision |
I. 25 II. 25 |
I. 46.2 II. 49.6 |
USI | No previous retropubic UI surgery | NR | No? (‘other vaginal surgical procedures being performed concurrently’ excluded) |
| Freeman 2011128 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 92 II. 100 |
I. 50 II. 54 |
USI, predominant SUI | No | Yes (POP extending beyond the hymen excluded) | NR |
| bFriedman 200954 | Nambiar | 12 |
I. Transob-MUS II. Single incision |
I. 42 II. 42 |
NR | USI | NR | NR | Yes |
| Gaber 201691 | New | 12 |
I. Transob-MUS II. Single incision |
I. 70 II. 140 |
I. 44.1 II. 43–44 |
USI only (no MUI) | No | Yes | NR |
| German 1994190 | Lapitan | 24 |
I. Open colpo II. Bladder neck needle |
I. 24 II. 26 |
I. 50 II. 53 |
USI | Yes | NR | NR |
| Gilja 1998189 | Lapitan | 36 |
I. Open colpo II. Bladder neck needle |
I. 56 II. 90 |
36 | USI | NR | NR | NR |
|
Gopinath 2013158 [Pilot RCT was mentioned in a qualitative research paper; no further detail provided on the RCT] |
New | NR |
I. Retro-MUS II. Single incision |
NR | NR | NR | NR | NR | NR |
| Guerrero 200892 | Saraswat | 120 |
I. Retro-MUS II. Trad sling |
I. 72 II. 129 |
I. 54.3 II. 52 |
USI (DO excluded) | No | Yes (> 2 POP-Q excluded) | NR |
| bHalaska 200155 | Lapitan | 6 |
I. Retro-MUS II. Open colpo |
I. 15 II. 11 |
I. 58.3 II. 53.4 |
USI | NR | NR | NR |
| bHammoud 201156 | Ford | NR |
I. Retro-MUS II. Transob-MUS |
I. 60 II. 50 |
I. 43 II. 42 |
SUI, MUI | Yes | Yes (included cystocele grade 1–2) | NR |
| bHan 200169 | Lapitan | 6 |
I. Retro-MUS II. Open colpo |
I. 25 II. 25 |
NR | USI | NR | NR | NR |
| Henriksson 1978105 | Lapitan | 3 |
I. Open colpo II. Trad sling |
I. 15 II. 15 |
I. 56 II. 50 |
SUI only (no UUI) | NR | No | NA |
| Hilton 1989198 | Saraswat | 24 |
I. Trad sling II. Bladder neck needle |
I. 10 II. 10 |
I. 53.7 II. 57.1 |
USI, MUI | Yes | NR | NR |
| Hinoul 2011172 | Nambiar | 12 |
I. Transob-MUS II. Single incision |
I. 98 II. 96 |
I. 53.2 II. 52.3 |
USI, SUI (some had OAB) | No | Yes (≥ 2 stage excluded) | NR |
| Holmes 1985194 | Lapitan | 24 |
I. Open colpo II. Ant repair |
I. 26 II. 25 |
I. 44.3 II. 47.1 |
USI, MUI | No | Yes | Yes? (hysterectomy) |
| Hota 2012173 | Nambiar | 12 |
I. Transob-MUS II. Single incision |
I. 44 II. 43 |
I. 50.5 II. 52 |
USI, predominant SUI | No previous suburethral sling | Yes | Yes |
| Jakimiuk 2012129 | Ford | 6 |
I. Retro-MUS II. Transob-MUS |
I. 19 II. 16 |
NR | USI only (no MUI) | No | No | NA |
| Jurakova 2016113 | New | 13 |
I. Transob-MUS II. Single incision |
I. 48 II. 45 |
I. 64.3 II. 62.3 |
USI, predominant SUI | No | No | NA |
| bKamel 200958 | Ford | NR |
I. Retro-MUS II. Transob-MUS |
I. 60 II. 60 |
NR | USI | No | NR | NR |
| Kammerer-Doak 1999195 | Lapitan | 12 |
I. Open colpo II. Ant repair |
I. 19 II. 16 |
I. 44.5 II. 53 |
USI (DI excluded) | Yes | Yes | Yes |
| Karateke 2009130 | Ford | NR |
I. Retro-MUS II. Transob-MUS |
I. 83 II. 84 |
I. 49.3 II. 49.1 |
USI (DO/OAB excluded) | No | Yes (> 1 stage POP-Q excluded) | NR |
| Kiliç 2007131 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 10 II. 10 |
I. 55.8 II. 60.2 |
USI | NR | NR | NR |
| Kim 2005132 | Ford | 3 |
I. Retro-MUS II. Transob-MUS |
I. 65 II. 65 |
I. 45.4 II. 45.7 |
SUI | NR | NR | NR |
| bKim 201059 | Nambiar | NR |
I. Transob-MUS II. Single incision |
I. 20 II. 20 |
I. 50.7 II. 49.6 |
SUI | NR | NR | NR |
| Kitchener 200693 | Lapitan | 24 |
I. Open colpo II. Lap colpo |
I. 147 II. 144 |
I. 50.0 II. 50.5 |
USI (DO excluded) | No previous retropubic surgery but allowed for other previous UI surgery | NR | No |
| bKoelbl 200260 | Lapitan | NR (in-hospital stay only?) |
I. Retro-MUS II. Open colpo |
I. 83 II. 83 |
59.5 | USI only (no MUI) | NR | No | NA |
| Kondo 2006106 | Ford | 24 |
I. Retro-MUS II. Trad sling |
I. 32 II. 31 |
I. 59.1 II. 54.0 |
USI, MUI | Yes | NR | Yes |
| Krofta 201094 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 149 II. 151 |
I. 57.2 II. 57.8 |
SUI only (no UUI) | No | Yes (≥ 2 stage POP-Q excluded) | No |
| Labrie 201295 | New | 12 |
I. Transob-MUS II. PFMT |
I. 230 II. 230 |
I. 50.2 II. 50.0 |
SUI (some had OAB) | No | Yes (≥ 2 POP-Q excluded) | NR |
| Laurikainen 200796 | Ford | 60 |
I. Retro-MUS II. Transob-MUS |
I. 136c II. 132c 273 randomised |
I. 53 II. 54 |
SUI | No | Yes [> 2 degree (Baden-Walker) excluded] | NR |
| bLeanza 200961 | Ford | 45 |
I. Retro-MUS II. Transob-MUS |
I. 229 II. 211 |
NR | USI | NR | Yes | Yes? (‘other pelvic defects were solved during the same operation for a complete repair of pelvic floor’) |
| Lee 2007107 | Ford | 13 |
I. Retro-MUS II. Transob-MUS |
I. 60 II. 60 |
I. 54.4 II. 51.1 |
USI, predominant SUI | Yes | No | NA |
| Lee 201228 | Nambiar | 36 |
I. Transob-MUS II. Single incision |
I. 118 II. 117 |
I. 51 II. 52.2 |
USI, SUI (some had DO) | No previous MUS | Yes | Yes |
| bLee 201562 | New | 12 |
I. Retro-MUS II. Single incision |
Total 187 | NR | SUI | NR | NR | NR |
| Liapis 1996200 | Lapitan | 60 |
I. Open colpo II. Ant repair |
I. 105c II. 50c 170 randomised |
50.6 | USI (DI excluded) | No | NR | Yes |
| Liapis 2002108 | Lapitan | 24 |
I. Retro-MUS II. Open colpo |
I. 36 II. 35 |
I. 46.5 II. 48.4 |
SUI only (no UUI) | No | Yes (included ≤ stage 1 cystocele) | NR |
| Liapis 2006133 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 46 II. 43 |
I. 53 II. 52 |
SUI (OAB/DO excluded) | No | NR | No |
| Mackintosh 2010174 | Nambiar | 3 |
I. Transob-MUS II. Single incision |
I. 15 I. 14 |
I. 47.7 II. 50.6 |
SUI, predominant SUI | No | NR | No |
| bMaher 200463 | Ford | 6 |
I. Retro-MUS II. Lap colpo |
I. 40 II. 42 |
NR | SUI | Yes | No | NA |
| Maher 2005102 | Saraswat | 12 |
I. Trad sling II. Injectable |
I. 22 II. 23 |
I. 63 II. 65 |
USI (some had DI) | No previous sling surgery but allowed for other surgery | NR | No |
| Mak 2000182 | Lapitan | 12 |
I. Open colpo II. Lap colpo |
I. 43 II. 47 |
I. 50.4 II. 51.1 |
USI | No | NR | Yes? (hysterectomy) |
| bMansoor 200364 | Ford | 6 |
I. Retro-MUS II. Transob-MUS |
I. 54 II. 48 |
NR | SUI | NR | Yes | NR |
| Masata 2012167 | Nambiar | 60 |
I. Transob-MUS II. Single incision |
I. 68 II. 129 |
I. 56.6 II. 55–58 |
USI, predominant SUI | No | Yes (≥ 2 stage excluded) | No |
| Masata 2013101 | New | 24 |
I. Transob-MUS II. Single incision |
I. 50 II. 50 |
I. 58.9 II. 55.8 |
USI, predominant SUI | No | Yes (POP > 3 excluded) | No |
| Maslow 2014175 | New | 12 |
I. Transob-MUS II. Single incision |
I. 50 II. 56 |
I. 48.7 II. 48.8 |
SUI (predominant OAB excluded) | No | Yes (> 1 stage POP excluded) | NR |
| Mehdiyev 2010134 | Ford | NR |
I. Retro-MUS II. Transob-MUS |
I. 15 II. 17 |
NR | SUI | NR | NR | NR |
| bMelendez Munoz 201665 | New | 6 |
I. Transob-MUS II. Single incision |
I. 113 II. 111 |
NR | SUI (some had OAB) | No previous failed suburethral tapes | NR | NR |
| bMerali 201266 | New | 12 |
I. Transob-MUS II. Single incision |
I. 19 II. 18 |
NR | SUI | NR | NR | NR |
| Meschia 200797 | Ford | 6 |
I. Retro-MUS II. Transob-MUS |
I. 114 II. 117 |
I. 56 II. 58 |
USI (DO excluded) | No | Yes? (POP requiring treatment excluded) | NR |
| bMirosh 200567 | Ford | 12 |
I. Retro-MUS II. Lap colpo |
I. 16 II. 14 |
NR | USI only (no MUI) | No | Yes (POP-Q > 2 excluded) | No |
| bMorris 200168 | Lapitan | 72 |
I. Open colpo II. Lap colpo |
I. 35 II. 38 |
NR | USI | NR | NR | NR |
| Mostafa 2012204 | Nambiar | NR |
I. Transob-MUS II. Single incision |
I. 68 II. 69 |
I. 49.4 II. 52.6 |
SUI, predominant SUI | No | NR | NR |
| Mundy 1983109 | Lapitan | 12 |
I. Open colpo II. Bladder neck needle |
I. 26 II. 25 |
48 | USI (no DI) | Yes | NR | NR |
| Nerli 2009110 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 18 II. 18 |
I. 39.5 II. 50.2 |
SUI, predominant SUI | NR | Yes (stage 3–4 excluded) | NR |
| Nyyssonen 2014135 | Ford | 46 |
I. Retro-MUS II. Transob-MUS |
I. 50 II. 50 |
I. 51 II. 54 |
SUI, predominant SUI | No previous mini-invasive operation for SUI | NR | No |
| Oliveira 2011168 | Nambiar | 24 |
I. Transob-MUS II. Single incision |
I. 30 II. 60 |
I. 52 II. 52.7 |
USI, SUI, predominant SUI | No | Yes (≥ 2 POP-Q excluded) | NR |
| bO’Sullivan 200069 | Lapitan | 6 |
I. Retro-MUS II. Open colpo |
I. 11 II. 9 |
NR | USI | No | Yes (‘clinically significant’ POP excluded) | NR |
| Palma 1985191 | Lapitan | 21 |
I. Open colpo II. Bladder neck needle |
I. 30 II. 40 |
I. 46 II. 44 |
USI, SUI | Yes | NR | NR |
|
Palomba 200870 (Trial terminated owing to poor recruitment. No results published) |
Ford | NR |
I. Retro-MUS II. Transob-MUS |
Total 15 | NR | SUI (DI excluded) | No | Yes (all had cystocele) | NR |
| Paraiso 2004147 | Ford | 65 |
I. Retro-MUS II. Lap colpo |
I. 36 II. 36 |
I. 53.3 II. 54.8 |
USI (DO excluded) | No | Yes (POP-Q > 1 excluded) | Yes? (hysterectomy and adhesiolysis) |
| Pastore 2016114 | New | 12 |
I. Transob-MUS II. Single incision |
I. 24 II. 24 |
I. 49.8 II. 50.2 |
SUI only (no UUI) | No | NR | NR |
| Persson 2002148 | Ford | 12 |
I. Retro-MUS II. Lap colpo |
I. 38e II. 32e 79 randomised |
I. 48 II. 51 |
USI, predominant SUI | No | Yes (POP-Q > 1 excluded) | No |
| Porena 2007136 | Ford | 99 |
I. Retro-MUS II. Transob-MUS |
I. 73 II. 75 |
I. 61.8 II. 60.6 |
SUI, predominant SUI | No | Yes (> 1 stage excluded) | NR |
| Rechberger 200998 | Ford | 18 |
I. Retro-MUS II. Transob-MUS |
I. 269 II. 268 |
I. 55.6 II. 55.8 |
SUI | NR | Yes (> 1 grade POP-Q excluded) | NR |
| Richter 201099 | Ford | 60 |
I. Retro-MUS II. Transob-MUS |
I. 298 II. 299 |
I. 52.7 II. 53.1 |
SUI, predominant SUI | Yes | Yes | Yes |
| bRiva 200671 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 66 II. 65 |
NR | SUI | No | Yes (urethro-cystocele of grade 0–2) | NR |
| Ross 2009137 | Ford | 60 |
I. Retro-MUS II. Transob-MUS |
I. 105 II. 94 |
I. 51.8 II. 50.1 |
SUI (UUI included; OAB excluded) | No | NR | No |
| Ross 2014159 | New | 12 |
I. Retro-MUS II. Single incision |
I. 40 II. 34 |
I. 47.2 II. 52.4 |
SUI, MUI | No | NR | No |
| bRudnicki 201672 | New | 12 |
I. Retro-MUS II. Transob-MUS III. Single incision |
I. 83 II. 67 III. 155 |
NR | SUI, predominant SUI | No | Yes (> 2 POP-Q excluded) | NR |
| Salari 2010127 | New | 12 |
I. Transob-MUS II. Ant repair |
I. 30 II. 30 |
I. 44.1 II. 37.8 |
SUI only (no UUI) | No | Yes (all had stage 1 or 2 cystocele) | NR |
| bSalem 201473 | Ford | 60 |
I. Retro-MUS II. Transob-MUS |
I. 39 II. 37 |
35.3 | SUI | NR | NR | NR |
| Samiee 2009163 | Freites | NR |
I. Transob-MUS II. Lap colpo |
I. 19 II. 16 |
NR | SUI (DO excluded) | No | Yes (excluded severe anterior vaginal prolapse and uterine prolapse) | NR |
| Sand 2000187 | Lapitan | 72 |
I. Open colpo II. Trad sling |
I. 19 II. 17 |
I. 61.3 II. 60.4 |
USI, MUI | Yes | Yes (significant pelvic support defects excluded) | Yes |
| Scheiner 2012119 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 80 II. 80 |
I. 57.8 II. 57–5 |
SUI, predominant SUI | No previous sling surgery | Yes (a symptomatic cystocele stage 2 or higher according to the POP-Q system was corrected first. Participants with concomitant sling insertion to repair prolapse were included) | Yes |
| Schellart 2013177 | New | 36 |
I. Transob-MUS II. Single incision |
I. 96 II. 97 |
I. 53 II. 53 |
SUI | No | Yes (≥ 2 stage POP excluded) | NR |
| Schierlitz 2008138 | Ford | 63 |
I. Retro-MUS II. Transob-MUS |
I. 82 II. 82 |
I. 60 II. 6 |
USI | Yes | NR | Yes |
| Schweitzer 201229 | Nambiar | 12 |
I. Transob-MUS II. Single incision |
I. 56 II. 100 |
I. 48.3 II. 50.8 |
SUI | No | Yes (> 1 POP-Q excluded) | NR |
| bSeo 201174 | Nambiar | 24 |
I. Transob-MUS II. Single incision |
I. 39 II. 41 |
I. 46.5 II. 46.9 |
SUI | NR | NR | NR |
| Sharifiaghdas 200881 | Saraswat | 126 |
I. Retro-MUS II. Trad sling |
I. 48 II. 52 |
I. 49.1 II. 55.0 |
USI, MUI | NR | Yes (> 1 POP-Q excluded) | No? (gynaecological problems which need simultaneous repairs such as high-grade prolapse excluded) |
| Sharifiaghdas 2015197 | New | 13.8 |
I. Trad sling II. Single incision |
Total 72 |
I. 52.2 II. 55.6 |
SUI | Yes | Yes (≥ 3 grade cystocele excluded) | NR |
| bShawky 201575 | New | 12 |
I. Transob-MUS II. Single incision |
I. 28 II. 30 |
NR | SUI | NR | NR | NR |
| Silva-Filho 2006165 | Ford | 6 |
I. Transob-MUS II. Trad sling |
I. 10 II. 10 |
I. 55.2 II. 49.8 |
USI, SUI (DO excluded) | No | NR | NR |
| Sivaslioglu 2007162 | Lapitan | 24 |
I. Transob-MUS II. Open colpo |
I. 49 II. 51 |
I. 45.4 II. 46.1 |
USI only (no UUI) | No | Yes (> 1 POPQ stage excluded) | NR |
| Sivaslioglu 2012178 | Nambiar | 60 |
I. Transob-MUS II. Single incision |
I. 40 II. 40 |
I. 51.5 II. 54.0 |
USI only (no UUI/MUI) | No | NR | NR |
| Smith 201130 | Nambiar | 15.3 |
I. Transob-MUS II. Single incision |
I. 49 II. 49 |
I. 48.9 II. 52.9 |
USI, predominant SUI | No | Yes (median stage 3) | Yes |
| Song 2004154 | Ford | 20–37 |
I. Retro-MUS II. Trad sling |
I. 48 II. 19 |
I. 53 II. 71 |
SUI, MUI | NR | Yes | NR |
| Sottner 2012169 | Nambiar | NR |
I. Transob-MUS II. Single incision |
I. 12 II. 31 |
NR | Predominant SUI | NR | NR | NR |
| bStangel-Wojcikiewicz 200876 | Lapitan | 18 |
I. Open colpo II. Lap colpo |
I. 57 II. 51 |
NR | USI (OAB excluded) | NR | Yes (> 2 POPQ grade excluded) | NR |
| Su 1997183 | Lapitan | 6 |
I. Open colpo II. Lap colpo |
I. 46 II. 46 |
I. 44.3 II. 42.4 |
USI (DO excluded) | No | Yes (> 1 degree cystocele excluded) | Yes? (hysterectomy) |
| bSummitt 200077 | Lapitan | 12 |
I. Open colpo II. Lap colpo |
I. 28d II. 34d |
NR | USI (DO excluded) | No previous retropubic urethropexy, needle suspension or suburethral sling | NR | No |
| Tang 2014179 | New | 24 |
I. Transob-MUS II. Single incision |
I. 48 II. 46 |
I. 51.3 II. 49.8 |
SUI only (no UUI) | NR | Yes (POP requiring extensive surgery excluded) | No |
| Tanuri 2010139 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 10 II. 20 |
NR | SUI only | Yes | Yes (> 2 stage excluded) | NR |
| bTapp 198978 | Lapitan | 6 |
I. Open colpo II. PFMT |
I. 24 II. 21 |
NR | USI only (no MUI) | No | NR | NR |
| Tarcan 201131 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
Total 54 | 54 | USI, predominant SUI | No | Yes (≥ 3 stage excluded) | Yes |
| Tcherniakovsky 2009166 | Saraswat | 12 |
I. Transob-MUS II. Trad sling |
I. 21 II. 20 |
I. 46.5 II. 52.1 |
USI | Yes | Yes | NR |
| Téllez Martínez-Fornés 2009202 | Lapitan | 36 |
I. Retro-MUS II. Open colpo |
I. 24 II. 25 |
I. 47.13 II. 50 |
USI (OAB excluded) | No | Yes (> I grade cystocele excluded) | NR |
| Teo 2011140 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 66 II. 61 |
I. 52.4 II. 50.9 |
USI (DO excluded) | No | Yes (> 1 stage excluded) | NR |
| Tommaselli 2010180 | Nambiar | 63 |
I. Transob-MUS II. Single incision |
I. 42 II. 42 |
I. 58.2 II. 57.8 |
USI, predominant SUI | No | Yes (≥ 2 POP-Q excluded) | NR |
| Trabuco 201432 | Lapitan | 6 |
I. Retro-MUS II. Open colpo |
I. 57 II. 56 |
I. 56 II. 56 |
SUI, predominant SUI | Yes | Yes (all; > 90% had POP-Q ≥ 2) | Yes (all) |
| Tuygun 2006184 | Lapitan | 38.7 |
I. Open colpo II. Lap colpo |
I. 33 II. 27 |
I. 53 II. 52 |
SUI | No | Yes | NR |
| Ustün 2003149 | Ford | 18 |
I. Retro-MUS II. Lap colpo |
I. 23 II. 23 |
I. 45.6 II. 45 |
USI | NR | No | NA |
| Ustün 2005185 | Lapitan | 14.2 |
I. Open colpo II. Lap colpo |
I. 26 II. 26 |
I. 42.3 II. 43.6 |
USI (DI excluded) | No | NR | Yes |
| Valpas 2004150 | Ford | 60 |
I. Retro-MUS II. Lap colpo |
I. 70 II. 51 |
I. 50 II. 48 |
USI | No but allowed for previous anterior repair | NR | No |
| bVan Rensburg 201579 | New | 12 |
I. Transob-MUS II. Single incision |
I. 41c II. 51c |
I. 55.7 II. 54.4 |
SUI, MUI | Yes | Yes | Yes |
| Wadie 2005160 | Ford | 54 |
I. Retro-MUS II. Ant repair |
I. 28 II. 25 |
I. 44.9 II. 45.3 |
USI, predominant SUI | No | Yes (> 2 grade excluded) | Yes |
| Wang 2003203 | Lapitan | 22 |
I. Retro-MUS II. Open colpo |
I. 49 II. 49 |
51.6 | USI | No | No | NA |
| Wang 2006141 | Ford | 9 |
I. Retro-MUS II. Transob-MUS |
I. 29 II. 31 |
I. 51.4 II. 50.5 |
USI | No | Yes (> 2 stage POP excluded) | NR |
| Wang 200937 | Ford | 20 |
I. Retro-MUS II. Transob-MUS |
I. 160 II. 155 |
I. 55 II. 54.8 |
USI only (no UUI) | Yes | Yes | Yes |
| Wang 2010142 | Ford | 12 |
I. Retro-MUS II. Transob-MUS |
I. 70 II. 70 |
I. 60 II. 58 |
USI only (no UUI) | Yes | Yes | NR |
| Wang 2011116 | Ford and Nambiar | 12 |
I. Retro-MUS II. Transob-MUS III. Single incision |
I. 32d II. 36d III. 34d 108 randomised |
I. 56.6 II. 56.0 III. 57.3 |
SUI, predominant SUI | No | NR | No |
| Ward 2002100 | Lapitan | 60 |
I. Retro-MUS II. Open colpo |
I. 175 II. 169 |
NR | USI (DO excluded) | No | Yes (vaginal prolapse requiring treatment excluded) | No |
| Xin 2016115 | New | 12 |
I. Transob-MUS II. Single incision |
I. 184 II. 184 |
I. 56.5 II. 57.6 |
USI, predominant SUI | No | Yes (≥ 2 POP-Q excluded) | NR |
| bYoon 201180 | Nambiar | 1 |
I. Transob-MUS II. Single incision |
I. 51 II. 52 |
I. 57.0 II. 52.9 |
SUI | NR | NR | NR |
| Zhang 2014143 | New | 95 |
I. Retro-MUS II. Transob-MUS |
I. 70 II. 70 |
I. 55 II. 51 |
SUI only (no MUI) | No | Yes (> 1 stage POP excluded) | NR |
| Zullo 2007144 | Ford | 60 |
I. Retro-MUS II. Transob-MUS |
I. 35 II. 37 |
I. 52.8 II. 53.4 |
SUI (DO/OAB excluded) | No | Yes (> 1 stage excluded) | NR |
Appendix 9 Risk-of-bias assessment of 175 included studies
| Source reviewa | Study ID (first author and year) | Interventionb | Risk-of-bias assessment criterionb | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | 4a | 4b | 4c | 5 | 6a | 6b | 6c | 7 | 8 | ||
| Ford | Aigmüller 201483 | Retro-MUS | Trans-MUS | L | L | H | H | L | ||||||||
| Ford | Alkady 2009120 | Retro-MUS | Trans-MUS | L | L | U | U | L | ||||||||
| Ford | Andonian 2007117 | Retro-MUS | Trans-MUS | U | U | L | L | U | ||||||||
| Ford | Aniuliene 200984 | Retro-MUS | Trans-MUS | U | U | U | U | L | ||||||||
| New | Aniuliene 2015121 | Retro-MUS | Trans-MUS | U | U | H | H | H | L | L | U | U | ||||
| Ford | Araco 200886 | Retro-MUS | Trans-MUS | L | L | U | L | H | ||||||||
| Ford | Barber 2008122 | Retro-MUS | Trans-MUS | L | L | U | L | L | ||||||||
| Ford | Barry 2008123 | Retro-MUS | Trans-MUS | U | U | U | U | L | ||||||||
| Ford | cCervigni 200641 | Retro-MUS | Trans-MUS | L | U | U | U | L | ||||||||
| Ford | Chen 2010118 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Chen 201290 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | cChoe 201342 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | dDarabi Mahboub 201226 | Retro-MUS | Trans-MUS | L | U | U | U | U | U | U | H | U | ||||
| Ford | David-Montefiore 2006124 | Retro-MUS | Trans-MUS | L | L | U | U | U | ||||||||
| Ford | cde Oliveira 200644 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | de Tayrac 2004125 | Retro-MUS | Trans-MUS | L | L | U | L | U | ||||||||
| Ford | Deffieux 2010126 | Retro-MUS | Trans-MUS | L | L | H | U | L | ||||||||
| Ford | cDiab 201245 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | El-Hefnawy 2010127 | Retro-MUS | Trans-MUS | U | L | U | L | L | ||||||||
| New | cEl-Hefnawy 201248 | Retro-MUS | Trans-MUS | U | U | U | U | U | U | U | U | U | ||||
| Lapitan | cElshawaf 200949 | Retro-MUS | Trans-MUS | Open colpo | U | U | U | U | U | U | ||||||
| Ford | Enzelsberger 2005104 | Retro-MUS | Trans-MUS | H | H | U | U | U | ||||||||
| Ford | Freeman 2011128 | Retro-MUS | Trans-MUS | L | L | L | U | L | ||||||||
| Ford | cHammoud 201156 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Jakimiuk 2012129 | Retro-MUS | Trans-MUS | L | U | L | U | U | ||||||||
| Ford | cKamel 200958 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Karateke 2009130 | Retro-MUS | Trans-MUS | L | U | U | L | L | ||||||||
| Ford | Kiliç 2007131 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Kim 2005132 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Krofta 201094 | Retro-MUS | Trans-MUS | L | U | H | L | L | ||||||||
| Ford | Laurikainen 200796 | Retro-MUS | Trans-MUS | L | L | U | U | L | ||||||||
| Ford | cLeanza 200961 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Lee 2007107 | Retro-MUS | Trans-MUS | H | H | U | U | U | ||||||||
| Ford | Liapis 2006133 | Retro-MUS | Trans-MUS | U | U | U | U | L | ||||||||
| Ford | cMansoor 200364 | Retro-MUS | Trans-MUS | L | L | U | U | U | ||||||||
| Ford | Mehdiyev 2010134 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Meschia 200797 | Retro-MUS | Trans-MUS | L | L | U | U | L | ||||||||
| Ford | Nerli 2009110 | Retro-MUS | Trans-MUS | H | H | U | U | U | ||||||||
| Ford | Nyyssonen 2014135 | Retro-MUS | Trans-MUS | L | L | U | U | L | ||||||||
| Ford | cPalomba 200870 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Porena 2007136 | Retro-MUS | Trans-MUS | L | L | U | L | L | ||||||||
| Ford | Rechberger 200998 | Retro-MUS | Trans-MUS | U | U | U | U | L | ||||||||
| Ford | Richter 201099 | Retro-MUS | Trans-MUS | L | U | U | U | U | ||||||||
| Ford | cRiva 200671 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Ross 2009137 | Retro-MUS | Trans-MUS | L | L | U | U | L | ||||||||
| New | cRudnicki 201672 | Retro-MUS | Trans-MUS | Single incision | L | U | U | U | U | U | L | H | U | |||
| Ford | cSalem 201473 | Retro-MUS | Trans-MUS | U | U | U | U | U | ||||||||
| Ford | Scheiner 2012119 | Retro-MUS | Trans-MUS | L | U | U | U | L | ||||||||
| Ford | Schierlitz 2008138 | Retro-MUS | Trans-MUS | L | U | U | U | U | ||||||||
| Ford | Tanuri 2010139 | Retro-MUS | Trans-MUS | U | U | U | U | L | ||||||||
| Ford | dTarcan 201131 | Retro-MUS | Trans-MUS | L | U | U | U | U | U | U | L | U | ||||
| Ford | Teo 2011140 | Retro-MUS | Trans-MUS | L | L | H | H | H | ||||||||
| Ford | Wang 2006141 | Retro-MUS | Trans-MUS | L | U | U | L | L | ||||||||
| Ford | Wang 200937 | Retro-MUS | Trans-MUS | L | U | U | L | L | ||||||||
| Ford | Wang 2010142 | Retro-MUS | Trans-MUS | U | U | H | L | L | ||||||||
| Ford | Wang 2011116 | Retro-MUS | Trans-MUS | Single incision | L | L | U | U | L | |||||||
| New | Zhang 2014143 | Retro-MUS | Trans-MUS | L | U | H | H | L | L | L | L | U | ||||
| Ford | Zullo 2007144 | Retro-MUS | Trans-MUS | L | L | U | L | L | ||||||||
| Lapitan | Bai 2005145 | Retro-MUS | Open colpo | Trad sling | U | U | U | U | U | U | ||||||
| Lapitan | cDrahoradova 200446 | Retro-MUS | Open colpo | U | U | U | H | U | U | |||||||
| Lapitan | El-Barky 2005201 | Retro-MUS | Open colpo | U | U | U | U | U | U | |||||||
| Lapitan | cHalaska 200155 | Retro-MUS | Open colpo | U | U | U | U | U | U | |||||||
| Lapitan | cHan 200157 | Retro-MUS | Open colpo | U | U | U | U | U | U | |||||||
| Lapitan | cKoelbl 200260 | Retro-MUS | Open colpo | L | U | U | U | U | U | |||||||
| Lapitan | Liapis 2002108 | Retro-MUS | Open colpo | H | U | U | U | U | U | |||||||
| Lapitan | cO’Sullivan 200069 | Retro-MUS | Open colpo | U | U | U | U | U | U | |||||||
| Lapitan | Téllez Martínez-Fornés 2009202 | Retro-MUS | Open colpo | U | U | H | U | U | U | |||||||
| Lapitan | dTrabuco 201432 | Retro-MUS | Open colpo | L | L | H | L | L | U | U | L | U | ||||
| Lapitan | Wang 2003203 | Retro-MUS | Open colpo | L | U | U | U | U | U | |||||||
| Lapitan | Ward 2002100 | Retro-MUS | Open colpo | L | L | H | U | L | U | |||||||
| Ford | cAdile 200339 | Retro-MUS | Lap colpo | U | U | U | U | U | ||||||||
| Ford | Foote 2006146 | Retro-MUS | Lap colpo | L | U | U | U | U | ||||||||
| Ford | cMaher 200463 | Retro-MUS | Lap colpo | L | L | U | U | U | ||||||||
| Ford | cMirosh 200567 | Retro-MUS | Lap colpo | U | U | U | U | L | ||||||||
| Ford | Paraiso 2004147 | Retro-MUS | Lap colpo | L | L | U | U | L | ||||||||
| Ford | Persson 2002148 | Retro-MUS | Lap colpo | L | L | U | L | L | ||||||||
| Ford | Ustün 2003149 | Retro-MUS | Lap colpo | U | U | U | U | L | ||||||||
| Ford | Valpas 2004150 | Retro-MUS | Lap colpo | L | L | U | U | L | ||||||||
| Saraswat | cAbouhashem 201438 | Retro-MUS | Trad sling | U | U | U | U | |||||||||
| Ford | Amaro 2007151 | Retro-MUS | Trad sling | U | U | L | U | U | ||||||||
| Ford | Arunkalaivanan 2003152 | Retro-MUS | Trad sling | U | U | U | U | U | ||||||||
| Ford | Basok 2008153 | Retro-MUS | Trad sling | U | U | U | U | U | ||||||||
| Saraswat | Guerrero 200892 | Retro-MUS | Trad sling | L | L | L | L | |||||||||
| Ford | Kondo 2006106 | Retro-MUS | Trad sling | H | H | U | U | L | ||||||||
| Saraswat | Sharifiaghdas 200881 | Retro-MUS | Trad sling | U | U | U | L | |||||||||
| Ford | Song 2004154 | Retro-MUS | Trad sling | U | U | U | U | U | ||||||||
| Nambiar | Abdelwahab 2010155 | Retro-MUS | Single incision | U | U | U | U | L | ||||||||
| Nambiar | Andrada Hamer 2011156 | Retro-MUS | Single incision | U | L | H | L | H | ||||||||
| Nambiar | Barber 201287 | Retro-MUS | Single incision | L | L | L | L | H | ||||||||
| Nambiar | Basu 2010157 | Retro-MUS | Single incision | L | L | L | U | L | ||||||||
| New | Gopinath 2013158 | Retro-MUS | Single incision | U | U | U | U | U | U | U | U | U | ||||
| New | cLee 201562 | Retro-MUS | Single incision | U | U | U | U | U | U | U | L | U | ||||
| New | Ross 2014159 | Retro-MUS | Single incision | L | L | H | L | H | L | L | L | U | ||||
| Ford | Wadie 2005160 | Retro-MUS | Ant repair | L | L | U | U | L | ||||||||
| Lapitan | Bandarian 2011161 | Trans-MUS | Open colpo | U | U | U | U | U | U | |||||||
| Lapitan | cEl-Din Shawki 201247 | Trans-MUS | Open colpo | Ant repair | U | U | U | U | U | U | ||||||
| Lapitan | Sivaslioglu 2007162 | Trans-MUS | Open colpo | L | U | H | U | L | U | |||||||
| Freites | Samiee 2009163 | Trans-MUS | Lap colpo | U | U | U | U | U | U | U | ||||||
| New | Al-Azzawi 2014164 | Trans-MUS | Trad sling | L | U | H | H | U | L | L | U | U | ||||
| Ford | Silva-Filho 2006165 | Trans-MUS | Trad sling | U | U | U | U | U | ||||||||
| Saraswat | Tcherniakovsky 2009166 | Trans-MUS | Trad sling | U | U | U | L | |||||||||
| Nambiar | Amat 2011112 | Trans-MUS | Single incision | H | U | H | U | H | ||||||||
| Nambiar | dBianchi 201225 | Trans-MUS | Single incision | L | L | U | U | L | L | L | L | U | ||||
| New | Campos 2013176 | Trans-MUS | Single incision | L | L | H | H | U | L | L | H | U | ||||
| New | cDati 201243 | Trans-MUS | Single incision | U | U | U | U | U | U | U | H | U | ||||
| Nambiar | dDjehdian 201027 | Trans-MUS | Single incision | L | L | H | H | U | L | L | L | U | ||||
| Nambiar | Enzelsberger 2010170 | Trans-MUS | Single incision | U | U | U | U | L | ||||||||
| New | cEnzelsberger 201150 | Trans-MUS | Single incision | U | U | U | U | U | U | U | U | U | ||||
| New | cFernandez 201552 | Trans-MUS | Single incision | L | U | U | H | H | L | L | L | U | ||||
| New | Foote 2015171 | Trans-MUS | Single incision | U | U | U | U | H | L | L | L | U | ||||
| Nambiar | cFriedman 200954 | Trans-MUS | Single incision | U | U | U | U | L | ||||||||
| New | Gaber 201691 | Trans-MUS | Single incision | L | U | H | L | L | L | L | H | U | ||||
| Nambiar | Hinoul 2011172 | Trans-MUS | Single incision | L | U | H | U | H | ||||||||
| Nambiar | Hota 2012173 | Trans-MUS | Single incision | U | L | H | U | H | ||||||||
| New | Jurakova 2016113 | Trans-MUS | Single incision | U | U | H | H | H | L | L | L | U | ||||
| Nambiar | cKim 201059 | Trans-MUS | Single incision | U | U | U | U | U | ||||||||
| Nambiar | dLee 201228 | Trans-MUS | Single incision | L | L | H | H | U | U | U | L | U | ||||
| Nambiar | Mackintosh 2010174 | Trans-MUS | Single incision | L | L | H | L | L | ||||||||
| Nambiar | Masata 2012167 | Trans-MUS | Single incision | L | L | H | U | U | ||||||||
| New | Masata 2013101 | Trans-MUS | Single incision | L | L | H | H | U | L | L | L | U | ||||
| New | Maslow 2014175 | Trans-MUS | Single incision | L | L | H | U | L | H | H | L | U | ||||
| New | cMelendez Munoz 201665 | Trans-MUS | Single incision | L | U | H | H | U | U | U | L | U | ||||
| New | cMerali 201266 | Trans-MUS | Single incision | U | U | U | U | U | U | L | U | U | ||||
| Nambiar | Mostafa 2012204 | Trans-MUS | Single incision | L | L | H | L | U | ||||||||
| Nambiar | Oliveira 2011168 | Trans-MUS | Single incision | U | U | U | U | L | ||||||||
| New | Pastore 2016114 | Trans-MUS | Single incision | L | U | U | U | U | L | L | L | U | ||||
| New | Schellart 2013177 | Trans-MUS | Single incision | U | U | H | H | H | L | L | L | U | ||||
| Nambiar | dSchweitzer 201229 | Trans-MUS | Single incision | L | L | H | L | L | H | H | L | U | ||||
| Nambiar | cSeo 201174 | Trans-MUS | Single incision | U | U | U | U | U | ||||||||
| New | cShawky 201575 | Trans-MUS | Single incision | U | U | U | U | U | U | L | H | U | ||||
| Nambiar | Sivaslioglu 2012178 | Trans-MUS | Single incision | L | U | U | L | L | ||||||||
| Nambiar | dSmith 201130 | Trans-MUS | Single incision | L | U | H | H | H | L | L | L | U | ||||
| Nambiar | Sottner 2012169 | Trans-MUS | Single incision | U | U | U | U | U | ||||||||
| New | Tang 2014179 | Trans-MUS | Single incision | U | U | H | H | H | L | L | L | U | ||||
| Nambiar | Tommaselli 2010180 | Trans-MUS | Single incision | L | U | H | U | H | ||||||||
| New | cVan Rensburg 201579 | Trans-MUS | Single incision | L | U | H | H | U | U | U | L | U | ||||
| New | Xin 2016115 | Trans-MUS | Single incision | L | U | U | U | L | U | U | L | U | ||||
| Nambiar | cYoon 201180 | Trans-MUS | Single incision | U | U | U | U | U | ||||||||
| New | Salari 2010127 | Trans-MUS | Ant repair | L | U | U | U | L | L | L | L | U | ||||
| New | Labrie 201295 | Trans-MUS | PFMT | L | H | H | H | U | L | L | L | U | ||||
| Lapitan | Ankardal 200185 | Open colpo | Lap colpo | U | L | U | U | U | U | |||||||
| Lapitan | Burton 199440 | Open colpo | Lap colpo | U | U | U | U | L | U | |||||||
| Lapitan | Carey 200089 | Open colpo | Lap colpo | L | U | L | L | U | U | |||||||
| Lapitan | cFatthy 200151 | Open colpo | Lap colpo | L | L | U | U | U | U | |||||||
| Lapitan | Kitchener 200693 | Open colpo | Lap colpo | L | L | H | H | L | U | |||||||
| Lapitan | Mak 2000182 | Open colpo | Lap colpo | L | L | U | U | U | U | |||||||
| Lapitan | cMorris 200168 | Open colpo | Lap colpo | U | U | U | U | U | U | |||||||
| Lapitan | cStangel-Wojcikiewicz 200876 | Open colpo | Lap colpo | U | U | U | U | U | U | |||||||
| Lapitan | Su 1997183 | Open colpo | Lap colpo | L | L | U | U | U | U | |||||||
| Lapitan | cSummitt 200077 | Open colpo | Lap colpo | U | L | U | U | U | U | |||||||
| Lapitan | Tuygun 2006184 | Open colpo | Lap colpo | U | U | U | U | L | U | |||||||
| Lapitan | Ustün 2005185 | Open colpo | Lap colpo | L | L | U | U | L | U | |||||||
| Lapitan | Albo 200782 | Open colpo | Trad sling | L | U | H | H | L | U | |||||||
| Lapitan | Demirci 2001103 | Open colpo | Trad sling | H | H | U | U | U | U | |||||||
| Lapitan | Enzelsberger 1996186 | Open colpo | Trad sling | L | U | U | U | U | U | |||||||
| Lapitan | cFischer 200153 | Open colpo | Trad sling | U | U | U | U | U | U | |||||||
| Lapitan | Henriksson 1978105 | Open colpo | Trad sling | H | H | U | U | U | U | |||||||
| Lapitan | Sand 2000187 | Open colpo | Trad sling | L | U | U | U | U | U | |||||||
| Lapitan | Athanassopoulos 1996111 | Open colpo | Bladder neck needle | H | H | U | U | U | U | |||||||
| Lapitan | Bergman 1989a88 | Open colpo | Bladder neck needle | Ant repair | L | U | U | U | L | U | ||||||
| Lapitan | Bergman 1989b188 | Open colpo | Bladder neck needle | Ant repair | L | U | U | U | U | U | ||||||
| Lapitan | German 1994190 | Open colpo | Bladder neck needle | U | U | U | U | U | U | |||||||
| Lapitan | Gilja 1998189 | Open colpo | Bladder neck needle | L | U | U | U | H | U | |||||||
| Lapitan | Mundy 1983109 | Open colpo | Bladder neck needle | H | H | U | U | U | U | |||||||
| Lapitan | Palma 1985191 | Open colpo | Bladder neck needle | U | U | L | L | U | U | |||||||
| Lapitan | Berglund 1996192 | Open colpo | Ant repair | U | U | U | U | U | U | |||||||
| Lapitan | Colombo 2000193 | Open colpo | Ant repair | L | H | U | U | L | U | |||||||
| Lapitan | Holmes 1985194 | Open colpo | Ant repair | L | U | U | U | U | U | |||||||
| Lapitan | Kammerer-Doak 1999195 | Open colpo | Ant repair | L | U | U | U | U | U | |||||||
| Lapitan | Liapis 1996200 | Open colpo | Ant repair | L | U | U | U | U | U | |||||||
| Lapitan | cTapp 198978 | Open colpo | PFMT | U | U | U | U | U | U | |||||||
| New | Sharifiaghdas 2015197 | Trad sling | Single incision | U | U | U | U | U | U | U | L | U | ||||
| Saraswat | Maher 2005102 | Trad sling | Injectable | U | U | U | L | |||||||||
| Saraswat | Hilton 1989198 | Trad sling | Bladder neck needle | L | U | U | L | |||||||||
| Glazener | Di Palumbo 2003199 | Bladder neck needle | Ant repair | U | L | U | L | |||||||||
| Risk | 1 | 2 | 3 | 4a | 4b | 4c | 5 | 6a | 6b | 6c | 7 | 8 | ||||
| Low, n (%) | 85 (49) | 49 (28) | 8 (5) | 20 (15) | 4 (11) | 8 (22) | 1 (14) | 54 (39) | 18 (50) | 21 (58) | 24 (65) | 0 (0) | ||||
| Unclear risk, n (%) | 80 (46) | 116 (66) | 123 (73) | 107 (81) | 17 (47) | 20 (56) | 6 (86) | 76 (55) | 16 (44) | 13 (36) | 7 (19) | 82 (100) | ||||
| High risk, n (%) | 10 (6) | 10 (6) | 37 (22) | 5 (4) | 15 (42) | 8 (22) | 0 (0) | 9 (6) | 2 (6) | 2 (6) | 6 (16) | 0 (0) | ||||
| Total, n | 175 | 175 | 168 | 132 | 36 | 36 | 7 | 139 | 36 | 36 | 37 | 82 | ||||
Appendix 10 Network meta-analysis: total number of trials included in each treatment comparison for the number of women cured or improved
| Intervention comparison | Cure, n (%) (N = 105) | Improvement, n (%) (N = 120) |
|---|---|---|
| Transob-MUS vs. retro-MUS | 36 (34.3) | 40 (33.3) |
| Open colpo vs. retro-MUS | 6 (5.7) | 6 (5.0) |
| Lap colpo vs. retro-MUS | 2 (1.9) | 4 (3.3) |
| Trad sling vs. retro-MUS | 6 (5.7) | 6 (5.0) |
| Single incision vs. retro-MUS | 6 (5.7) | 6 (5.0) |
| Open colpo vs. transob-MUS | 1 (1.0) | 1 (0.8) |
| Trad sling vs. transob-MUS | 1 (1.0) | 1 (0.8) |
| Single incision vs. transob-MUS | 21 (20.0) | 28 (23.3) |
| Ant repair vs. transob-MUS | 1 (1.0) | 1 (0.8) |
| PFMT vs. transob-MUS | 1 (1.0) | 1 (0.8) |
| Lap colpo vs. open colpo | 9 (8.6) | 9 (7.5) |
| Trad sling vs. open colpo | 3 (2.9) | 3 (2.5) |
| Bladder neck needle vs. open colpo | 3 (2.9) | 3 (2.5) |
| Anterior repair vs. open colpo | 3 (2.9) | 3 (2.5) |
| PFMT vs. open colpo | 1 (1.0) | 1 (0.8) |
| Single incision vs. trad sling | 0 (0) | 1 (0.8) |
| Bladder neck needle vs. trad sling | 1 (1.0) | 1 (0.8) |
| Transob-MUS vs. single-incision vs. retro-MUS | 1 (1.0) | 2 (1.7) |
| Open colpo vs. trad sling vs. retro-MUS | 1 (1.0) | 1 (0.8) |
| Bladder neck needle vs. anterior repair vs. open colpo | 2 (1.9) | 2 (1.7) |
Appendix 11 Meta-analyses results: number of women cured
FIGURE 8.
Transobturator MUS vs. retropubic MUS: cure.
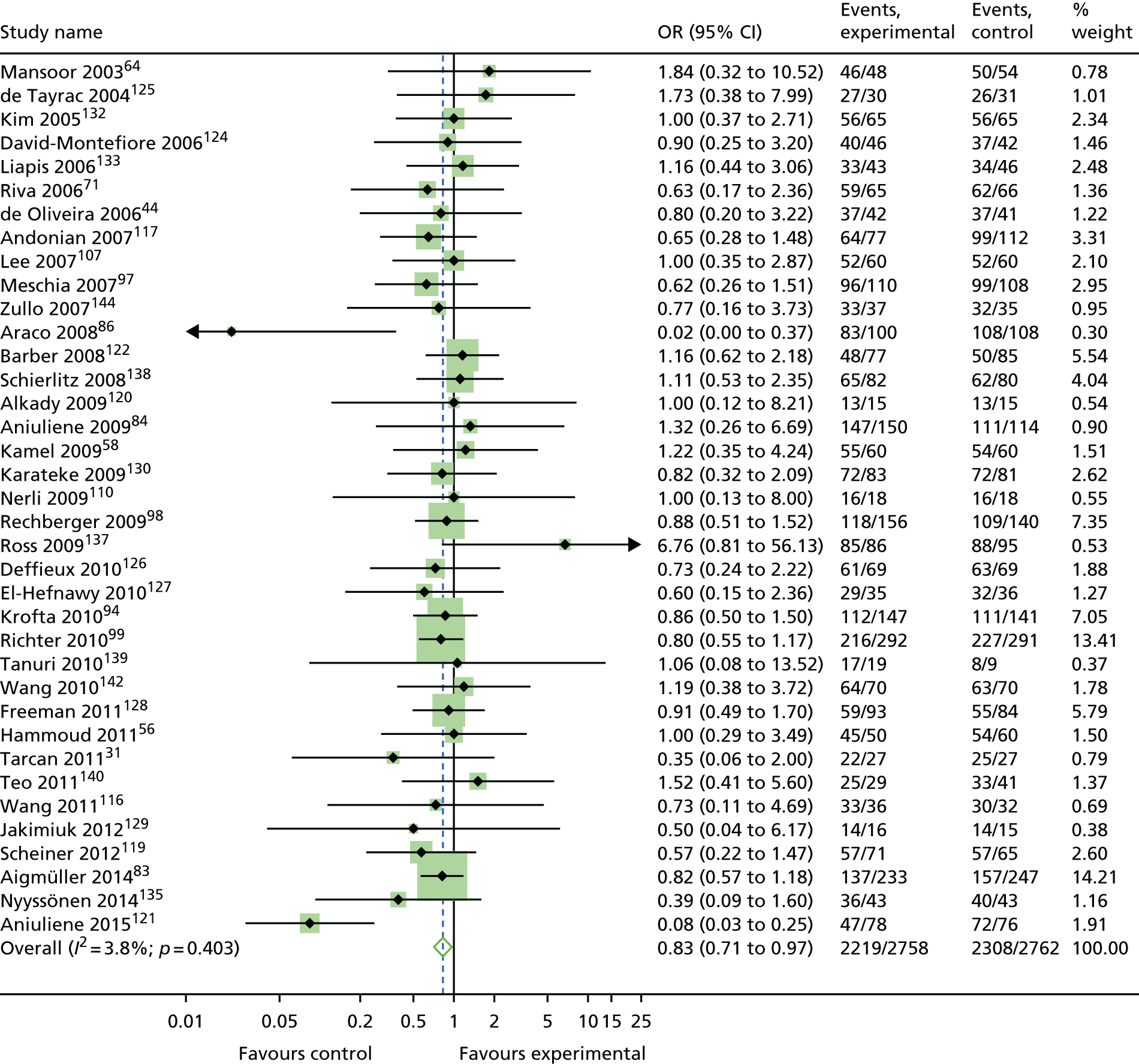
FIGURE 9.
Open colposuspension vs. retropubic MUS: cure.
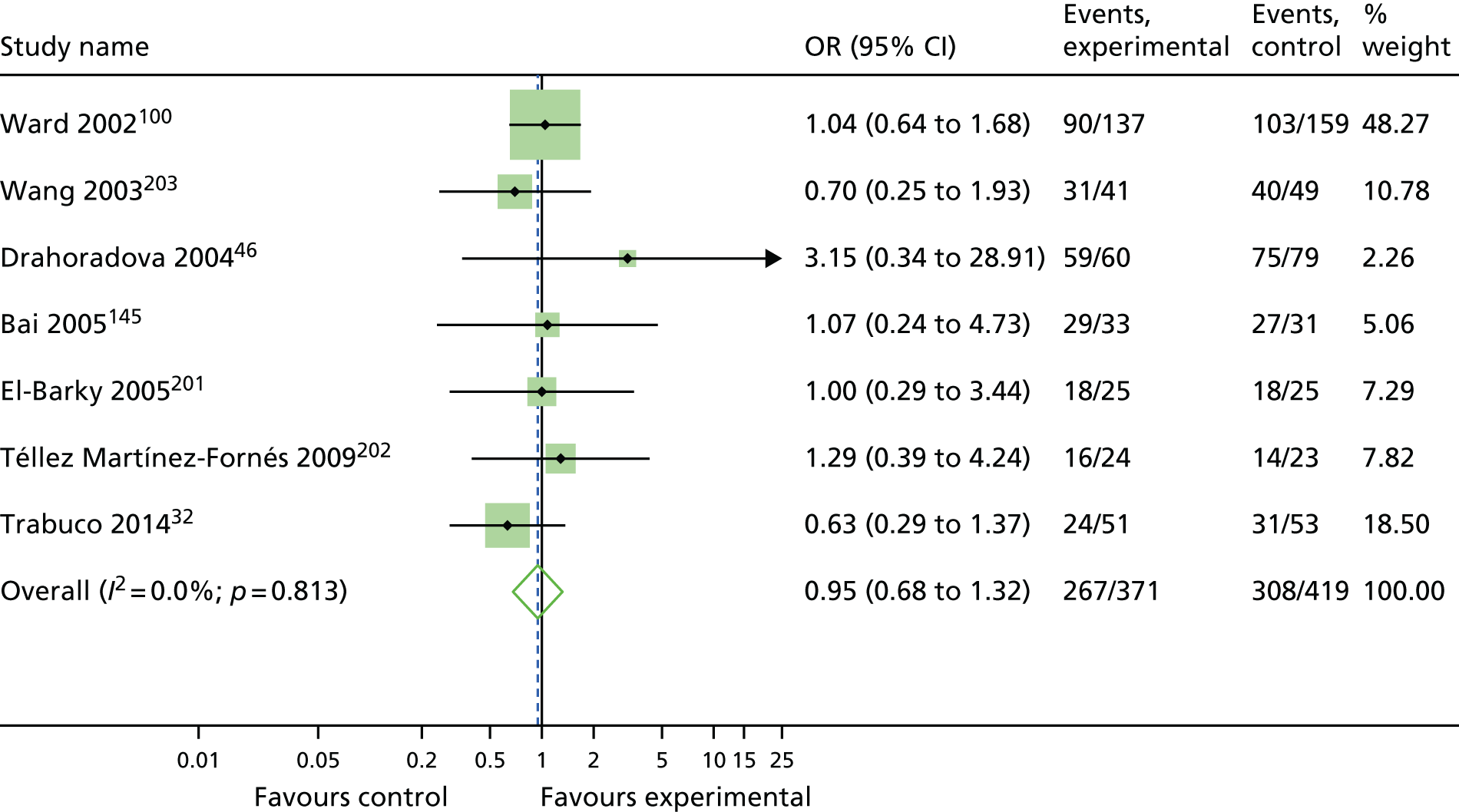
FIGURE 10.
Laparoscopic colposuspension vs. retropubic MUS: cure.
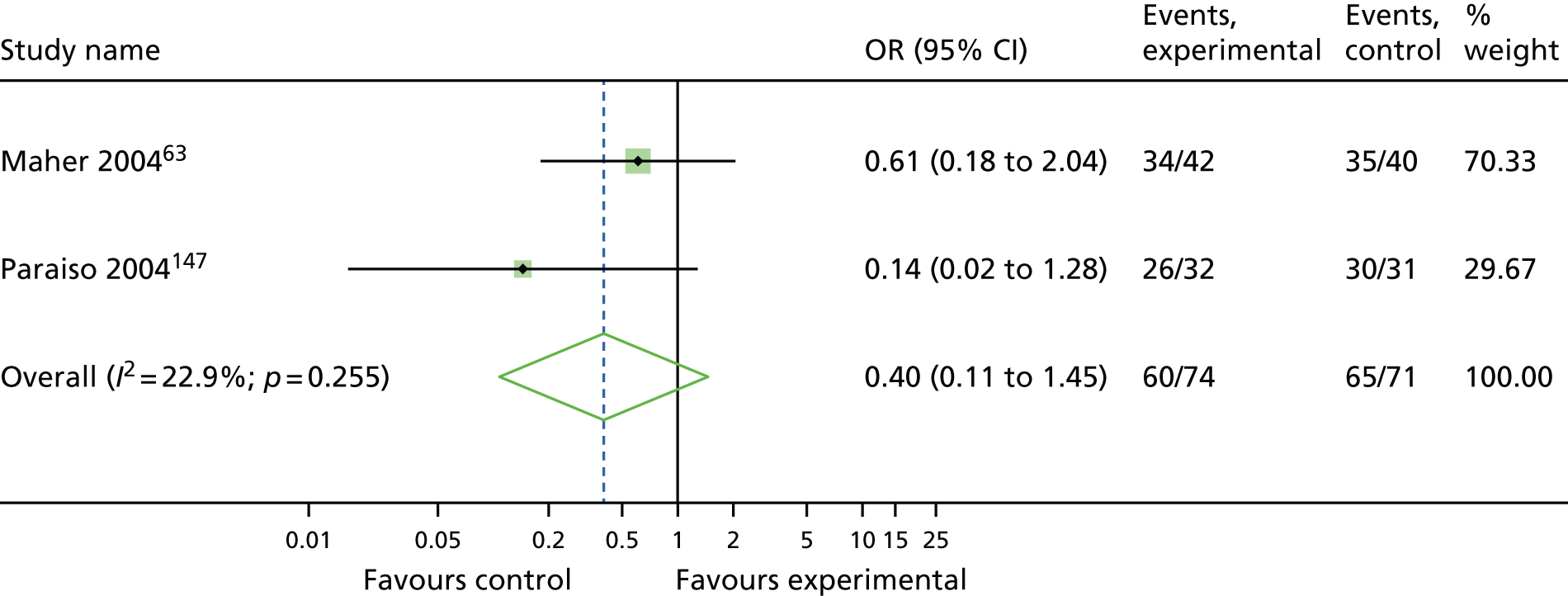
FIGURE 11.
Traditional sling vs. retropubic MUS: cure.
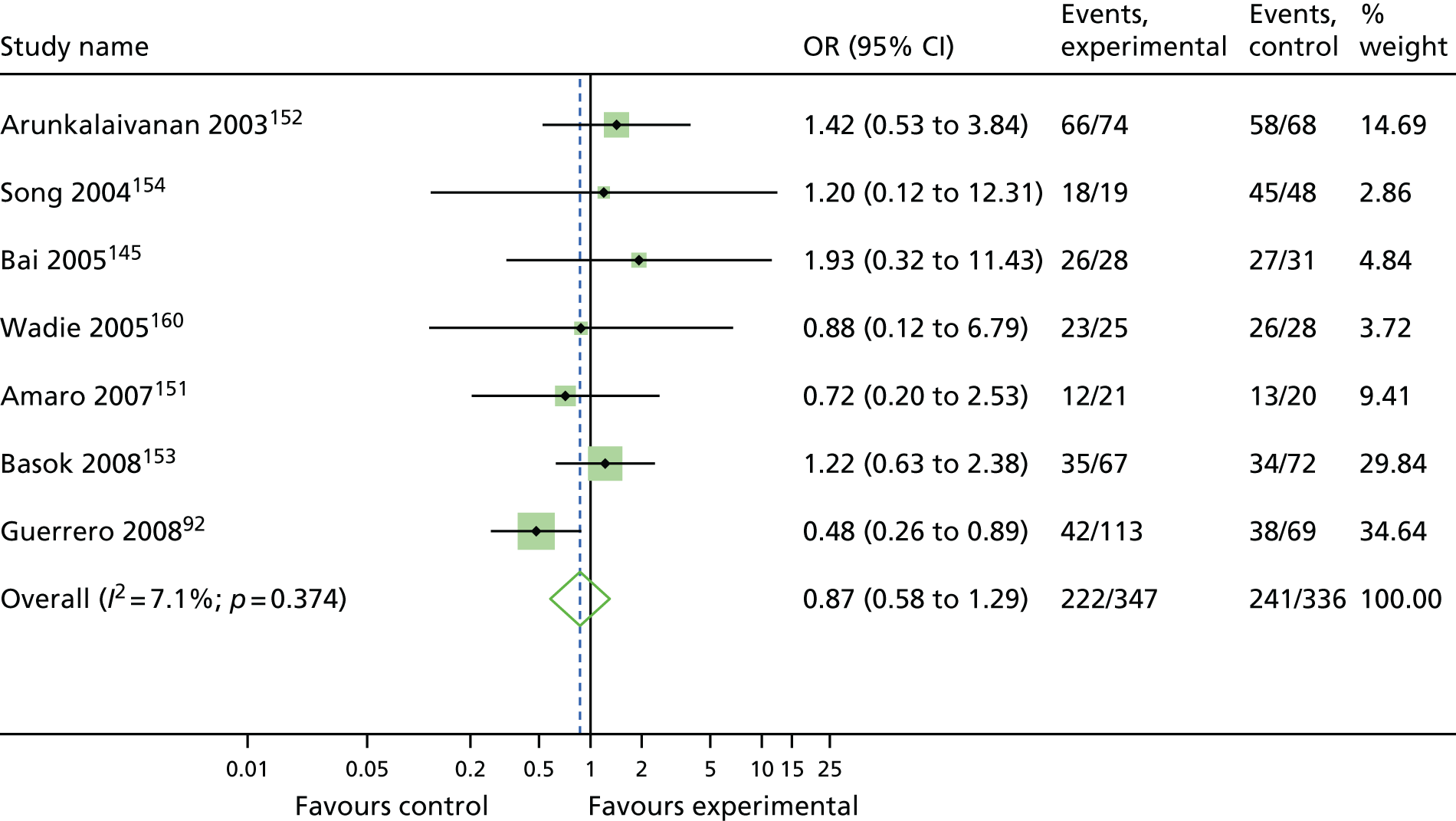
FIGURE 12.
Single incision vs. retropubic MUS: cure.
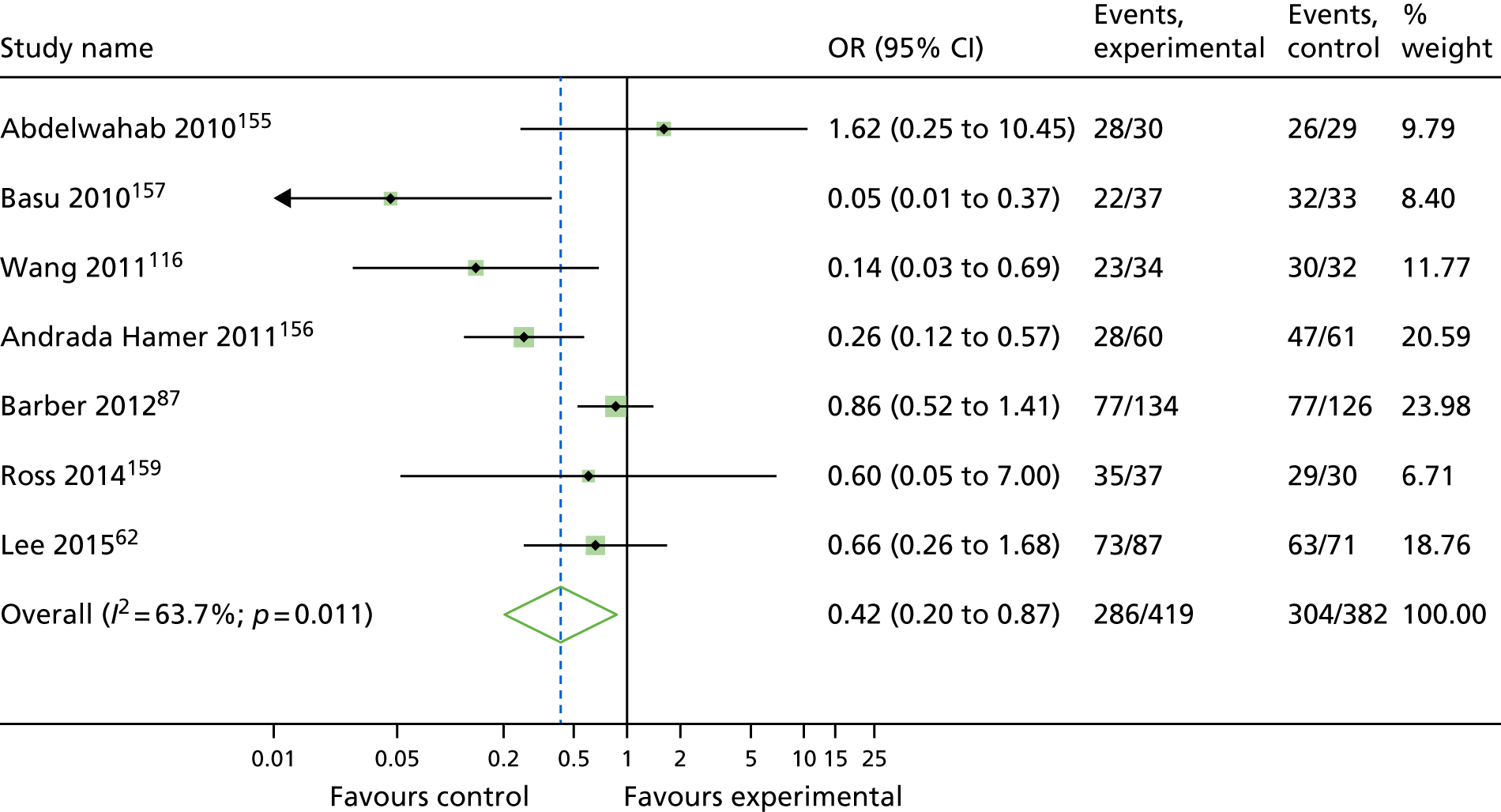
FIGURE 13.
Open colposuspension vs. transobturator MUS: cure.
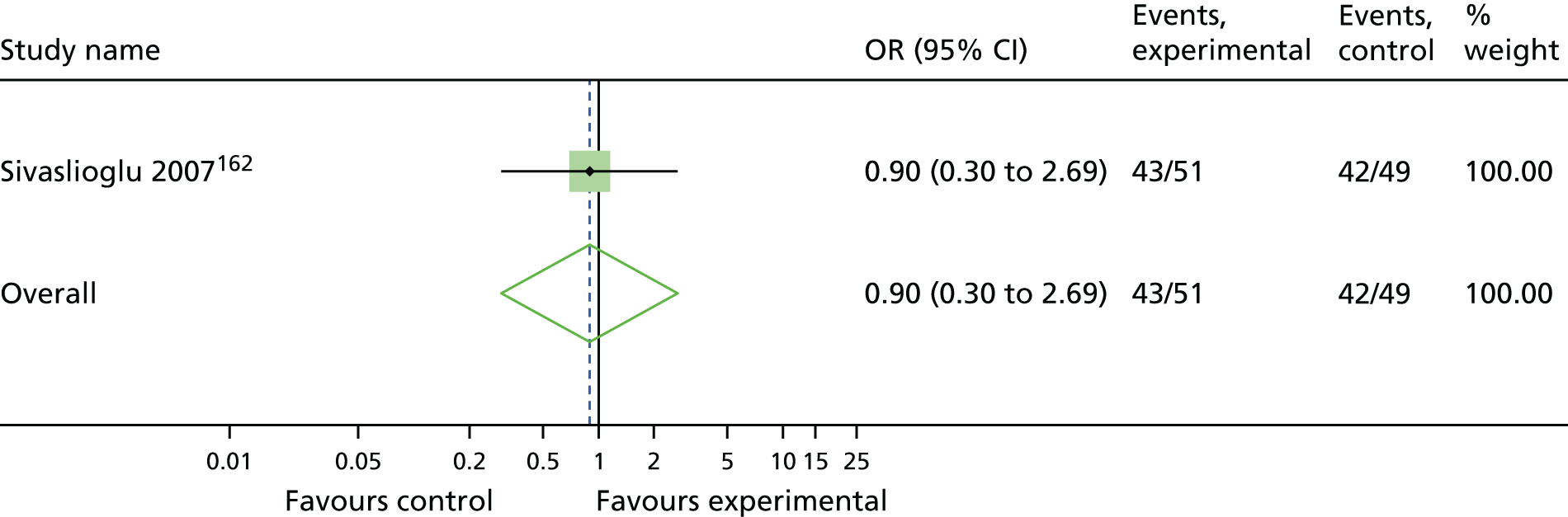
FIGURE 14.
Traditional sling vs. transobturator MUS: cure.
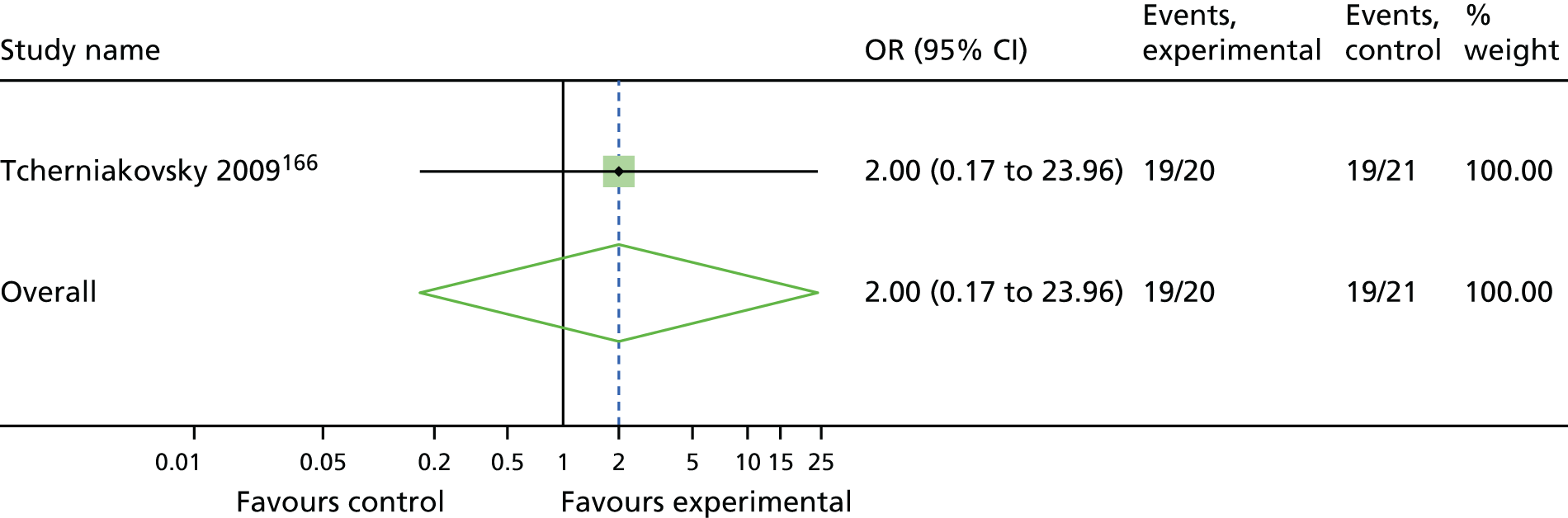
FIGURE 15.
Single incision vs. transobturator MUS: cure.
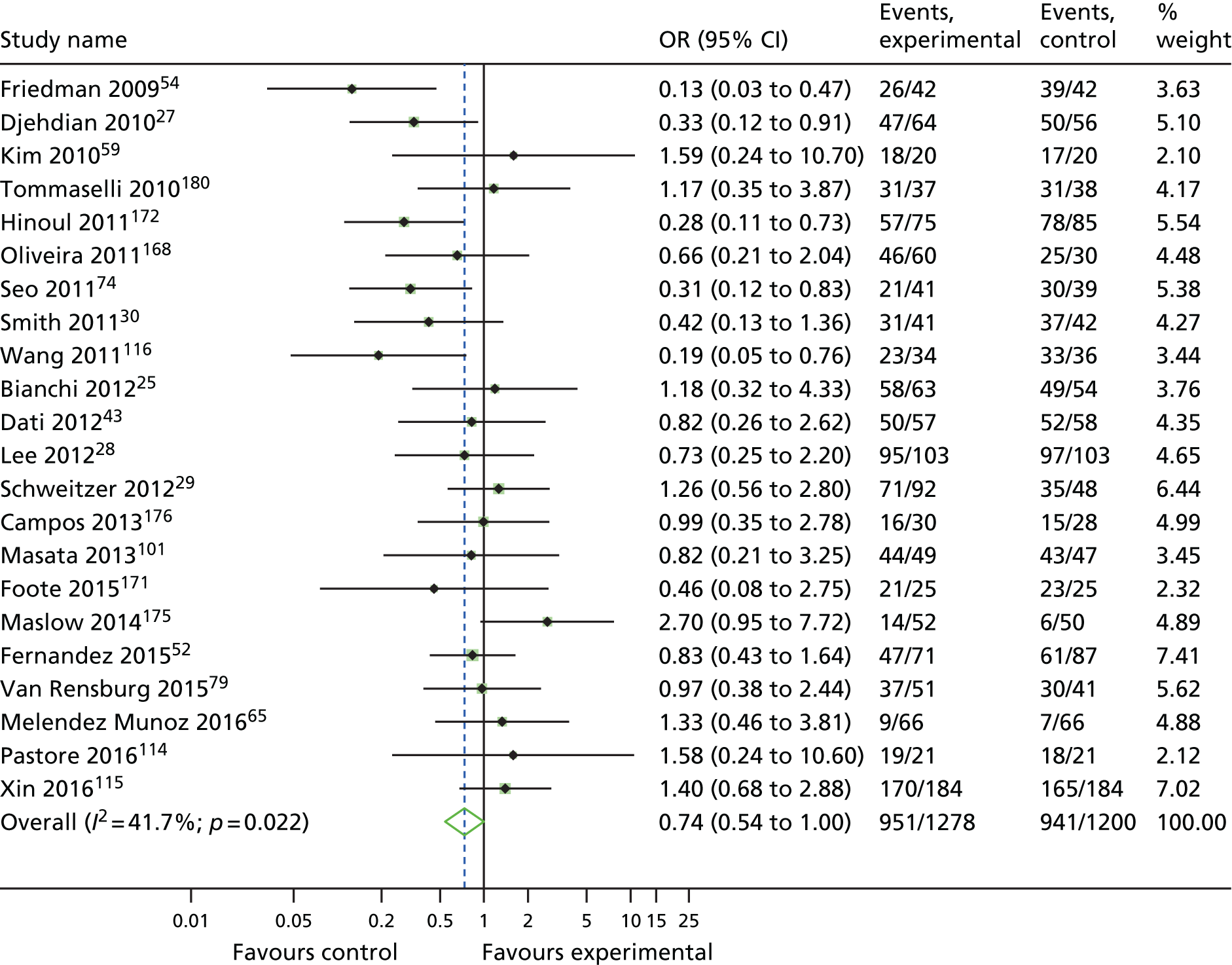
FIGURE 16.
Anterior vaginal repair vs. transobturator MUS: cure.
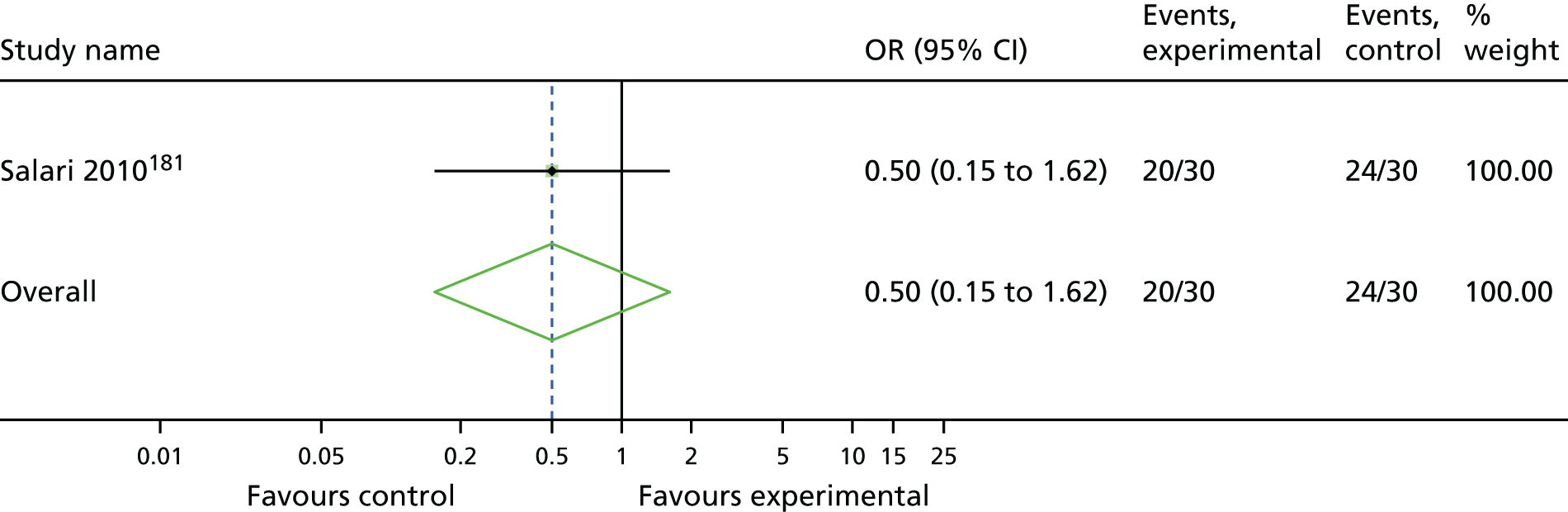
FIGURE 17.
Pelvic floor muscle training vs. transobturator MUS: cure.
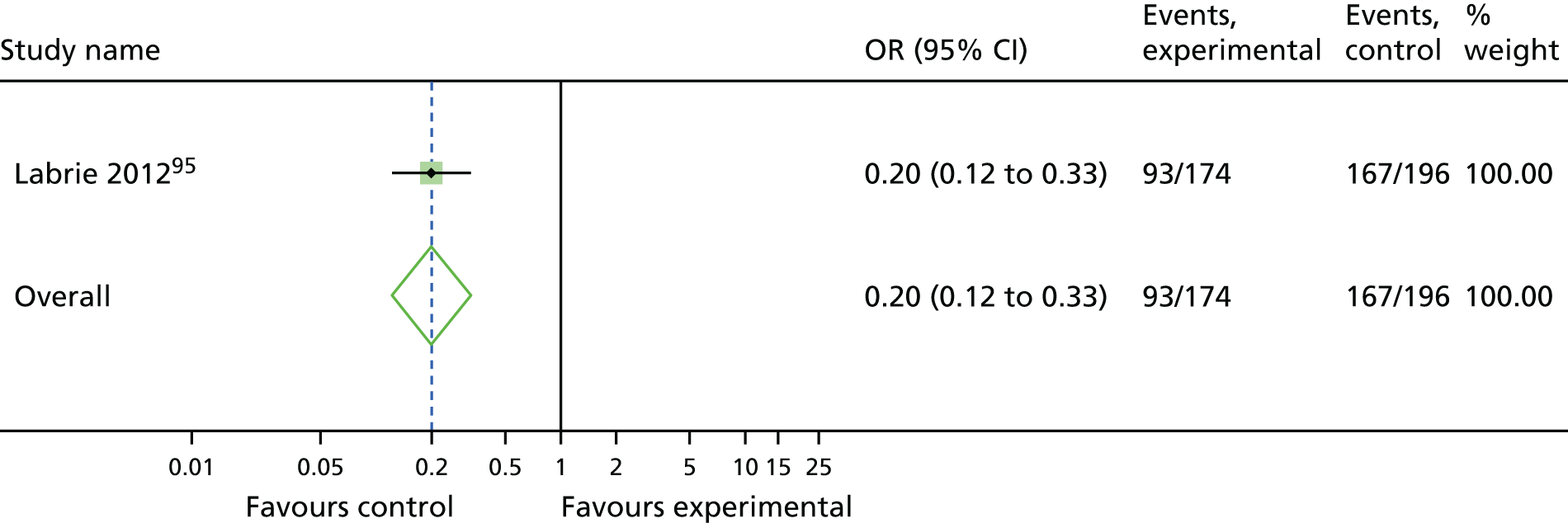
FIGURE 18.
Laparoscopic colposuspension vs. open colposuspension: cure.
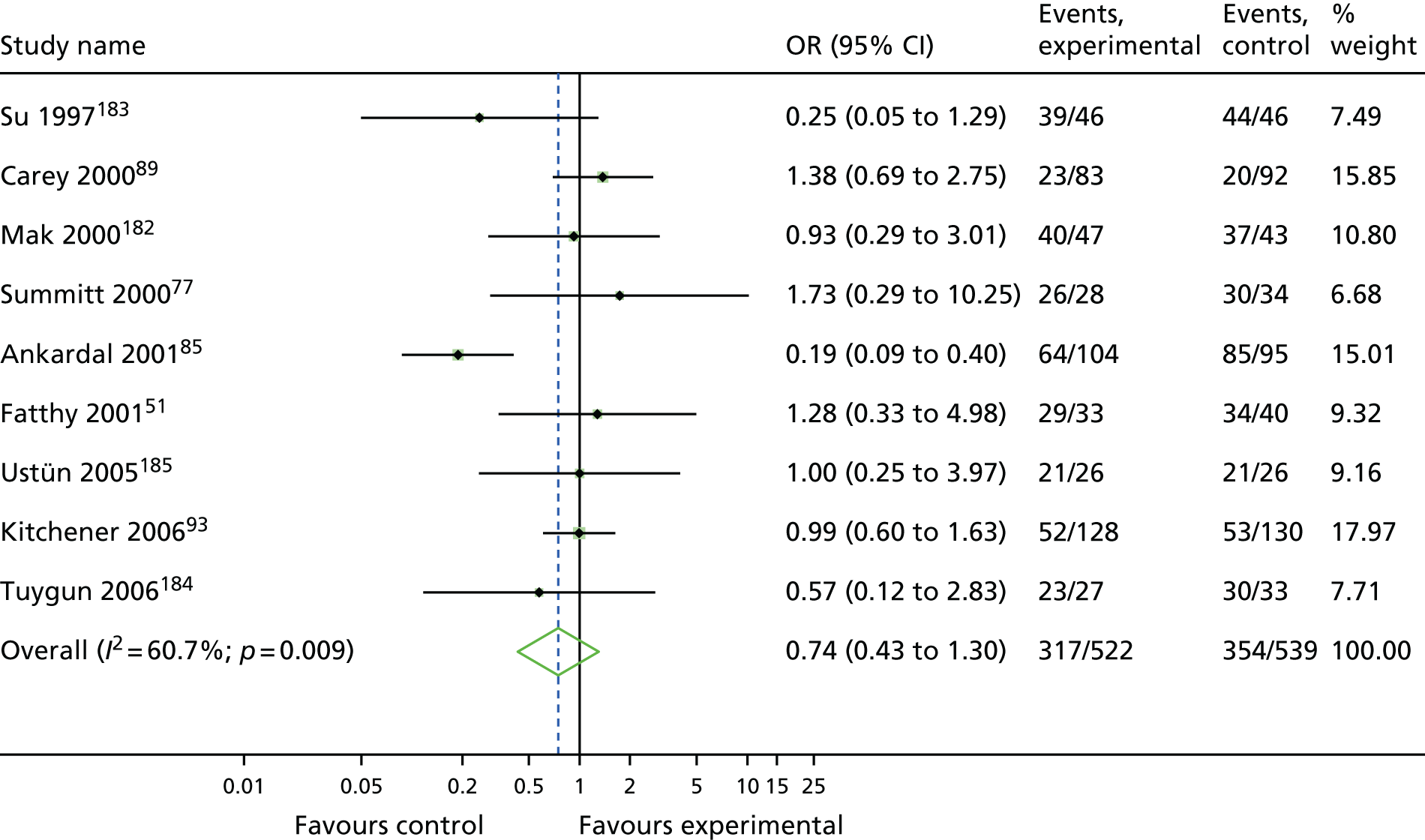
FIGURE 19.
Traditional sling vs. open colposuspension: cure.
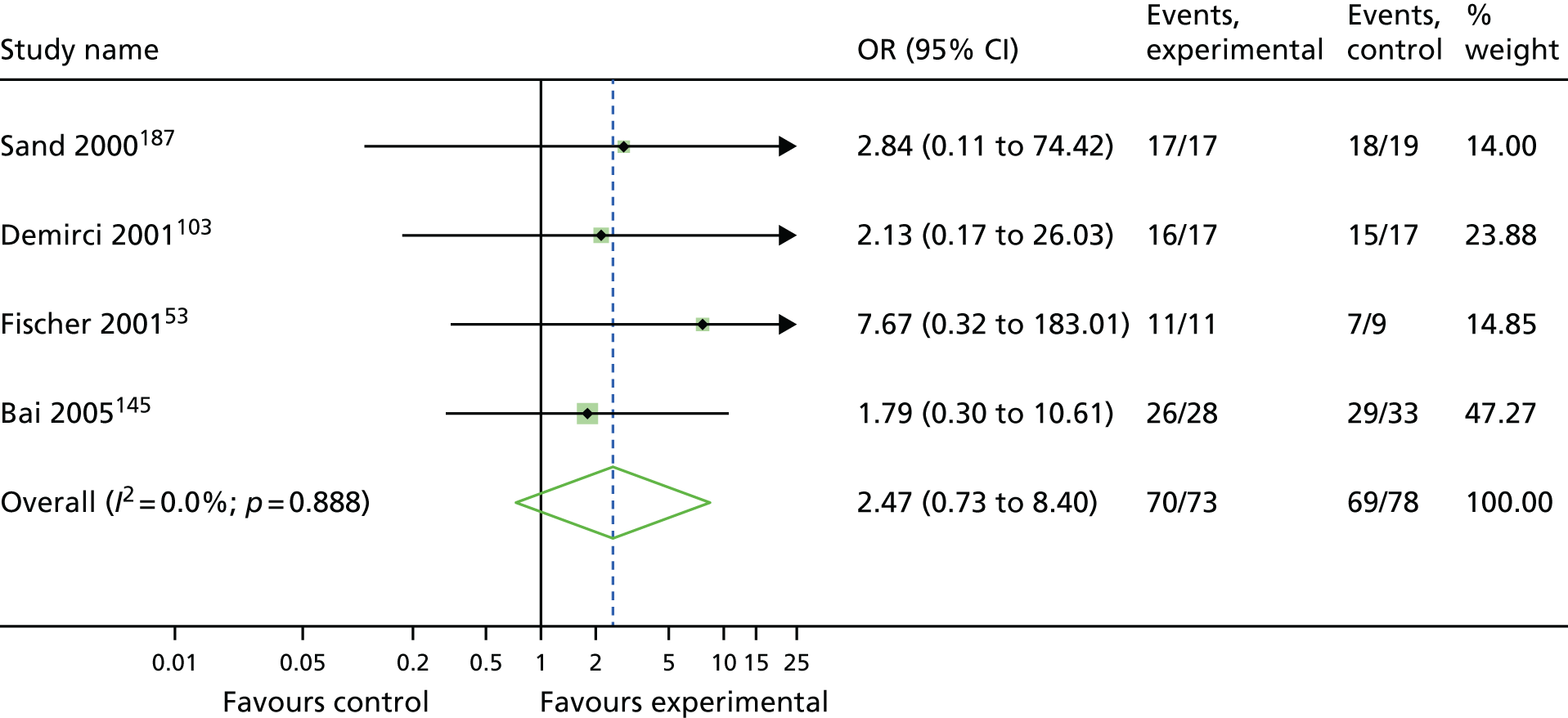
FIGURE 20.
Bladder neck needle suspension vs. open colposuspension: cure.
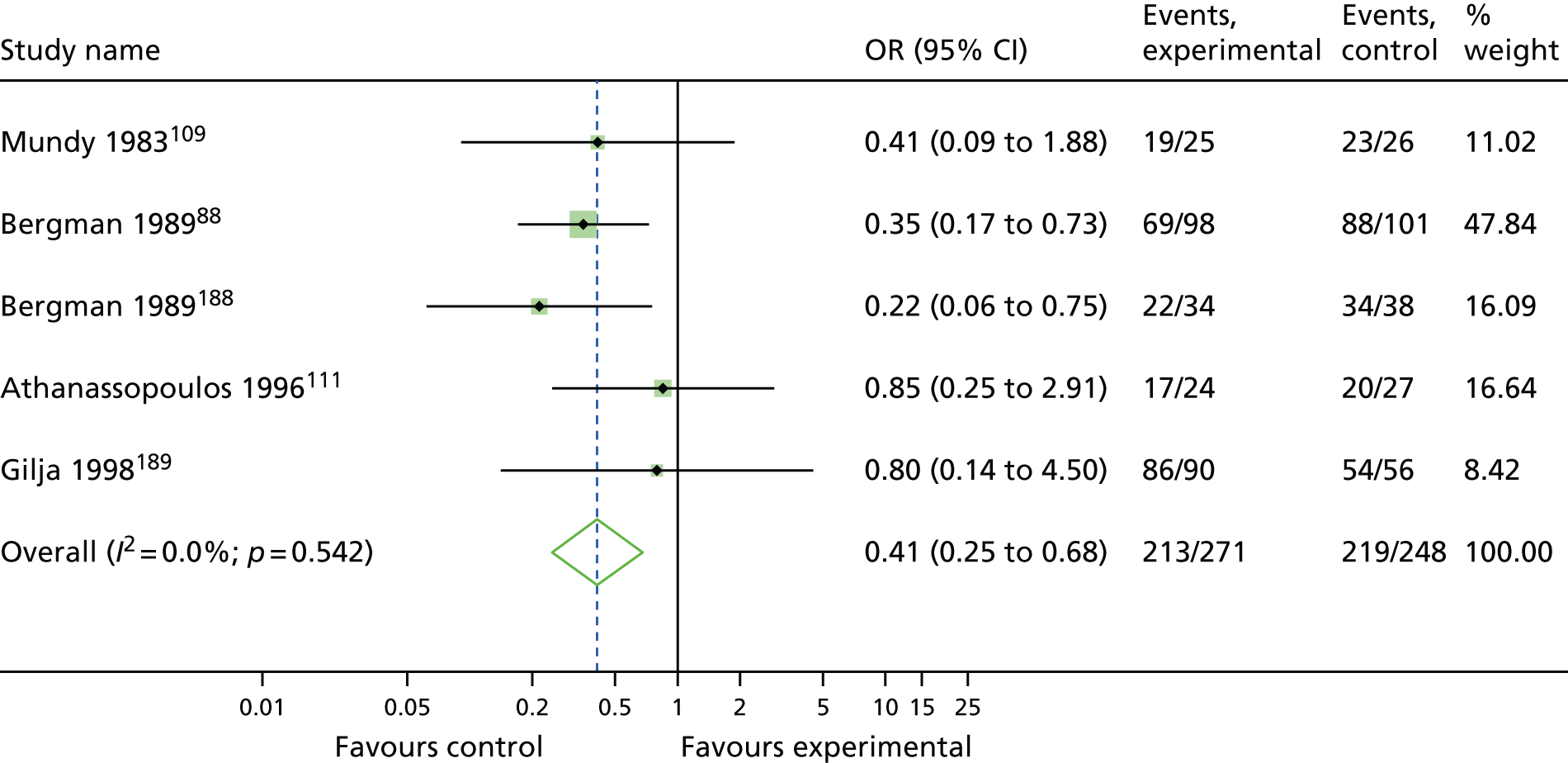
FIGURE 21.
Anterior vaginal repair vs. open colposuspension: cure.
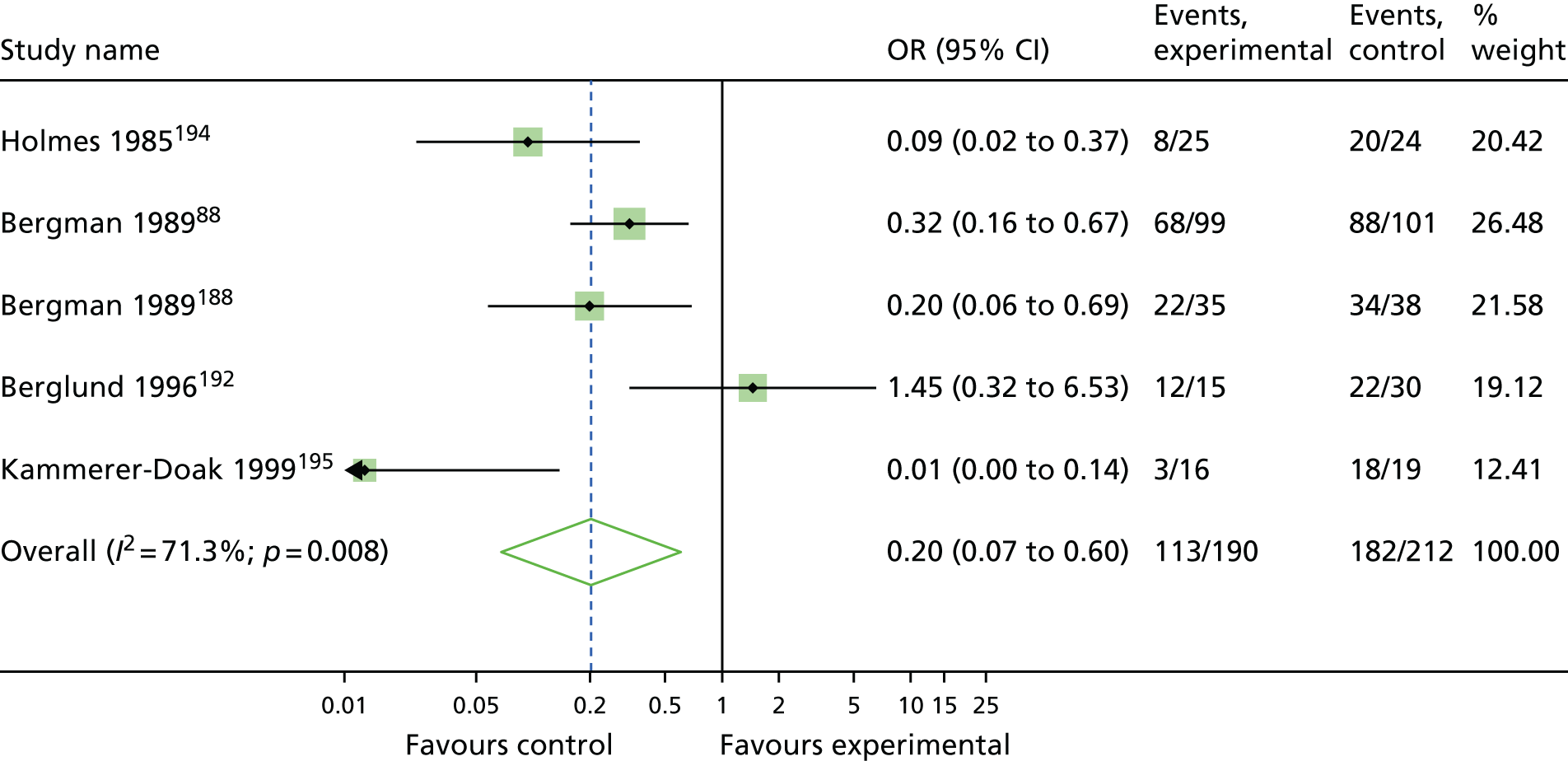
FIGURE 22.
Pelvic floor muscle training vs. open colposuspension: cure.
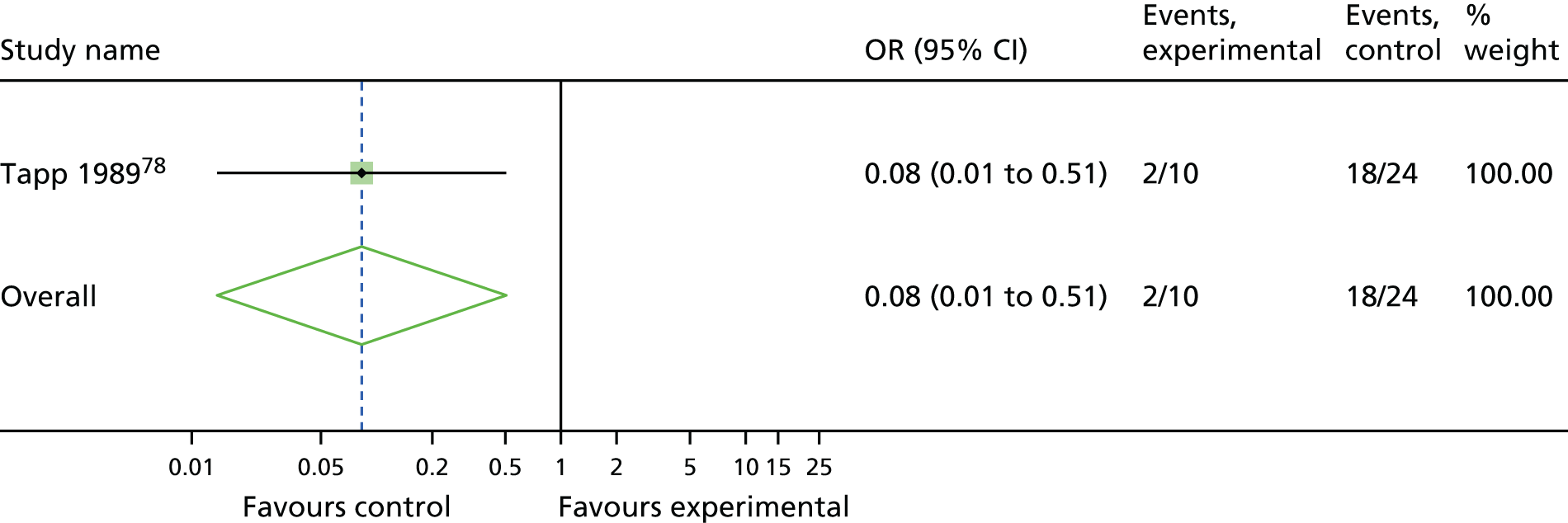
FIGURE 23.
Bladder neck needle suspension vs. traditional sling: cure.
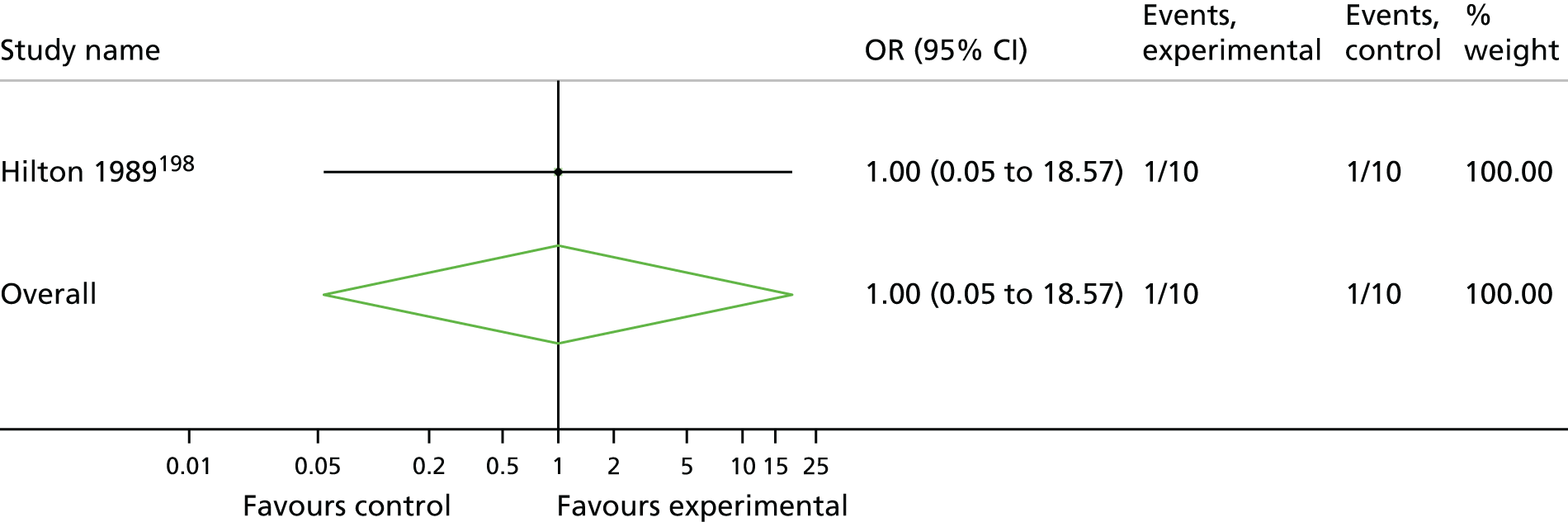
FIGURE 24.
Anterior vaginal repair vs. bladder neck needle suspension: cure.
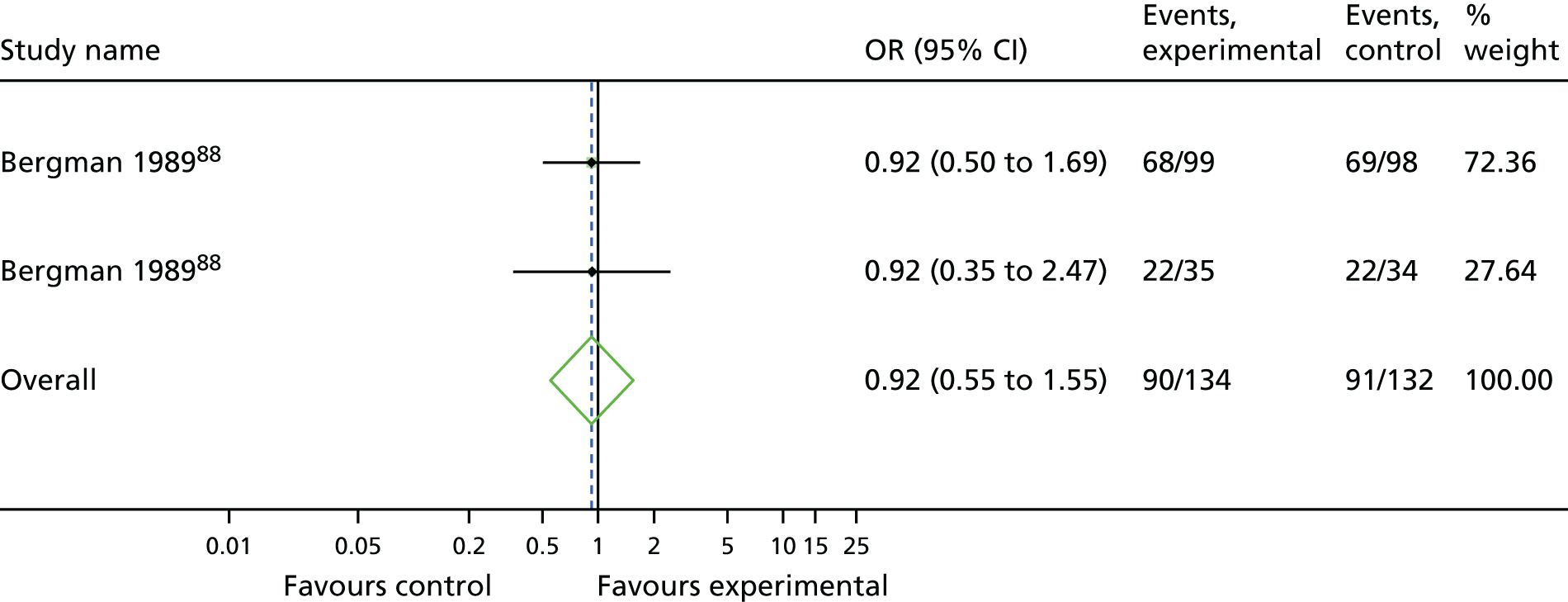
Appendix 12 Meta-analyses results: number of women improved
FIGURE 25.
Transobturator MUS vs. retropubic MUS: improvement.
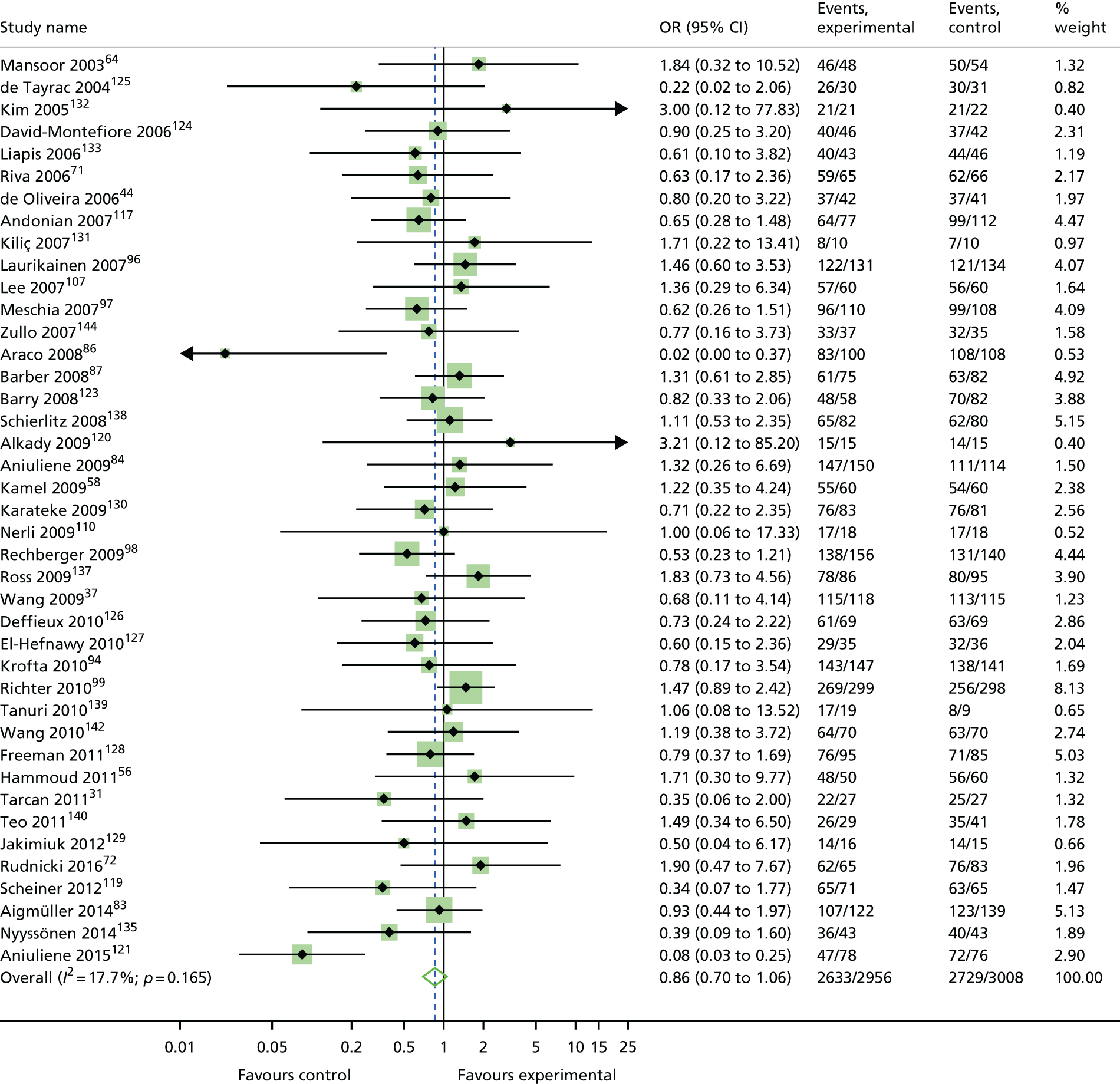
FIGURE 26.
Open colposuspension vs. retropubic MUS: improvement.

FIGURE 27.
Laparoscopic colposuspension vs. retropubic MUS: improvement.
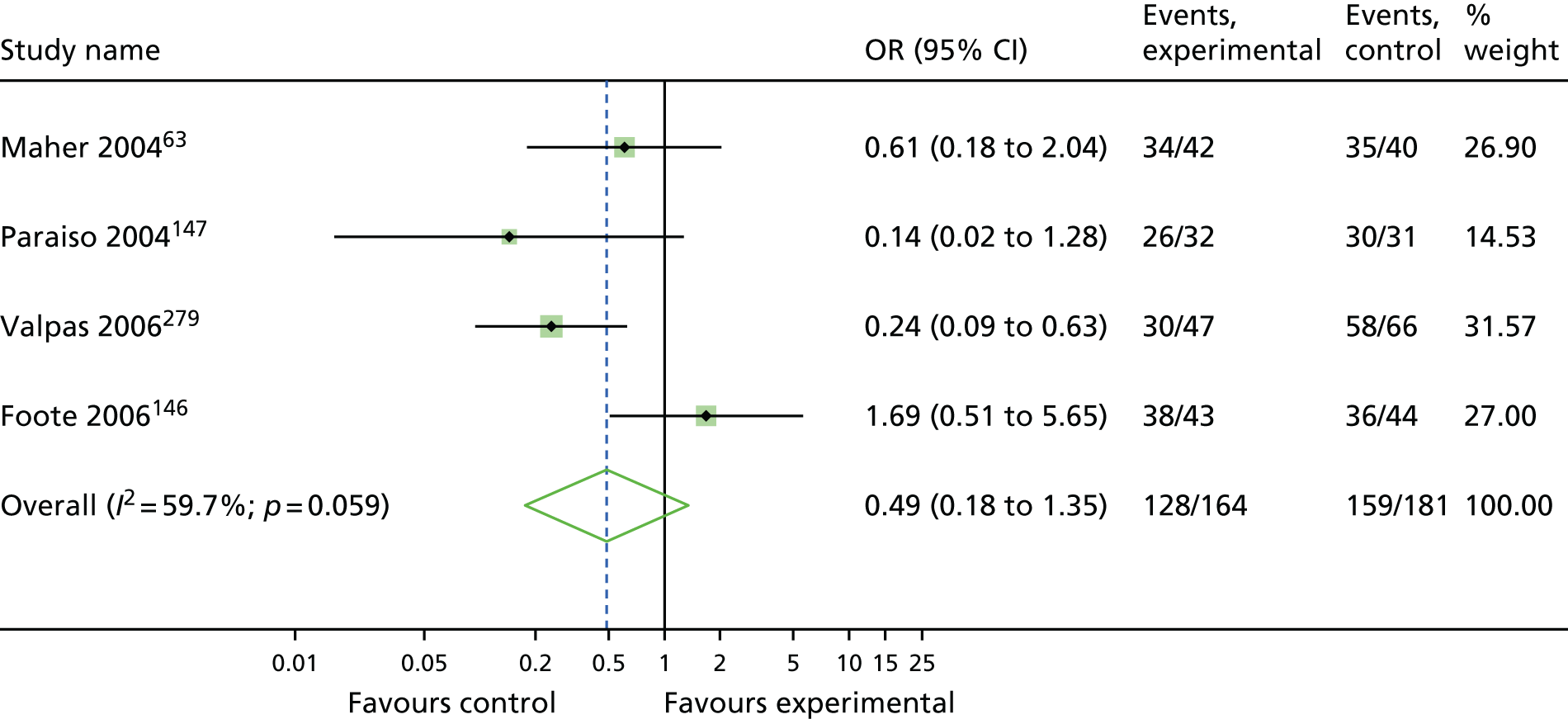
FIGURE 28.
Traditional sling vs. retropubic MUS: improvement.
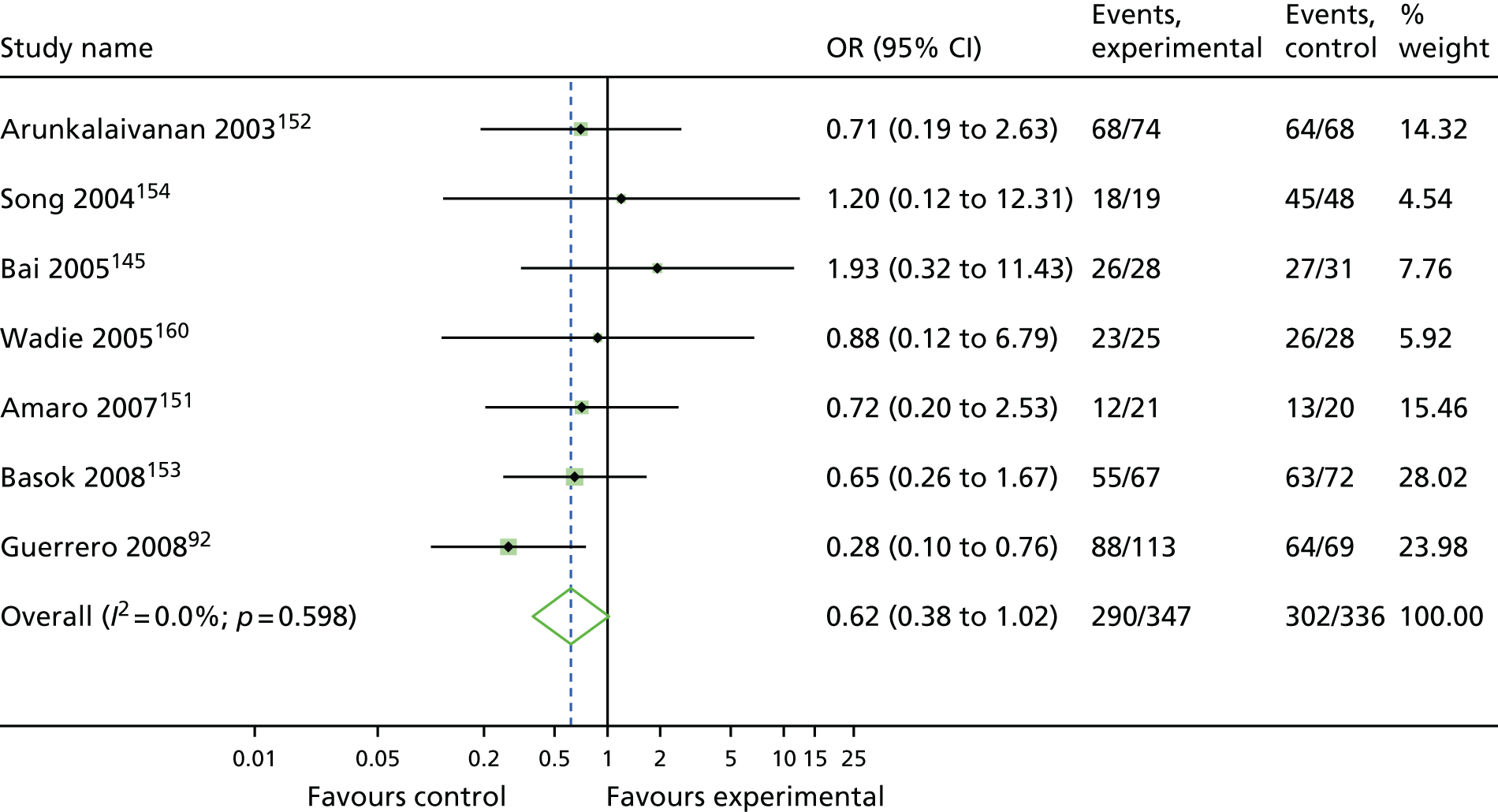
FIGURE 29.
Single-incision sling vs. retropubic MUS: improvement.
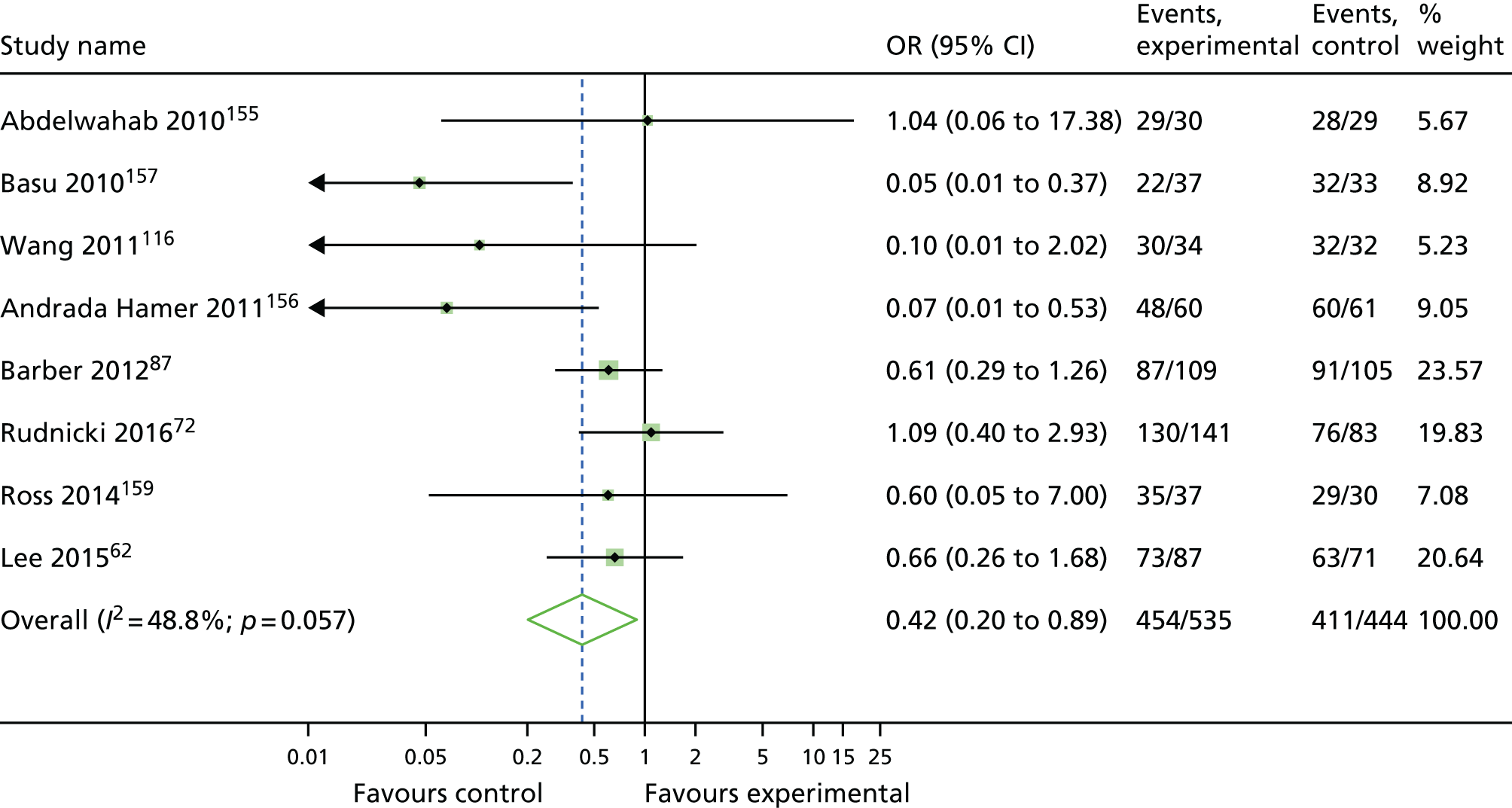
FIGURE 30.
Open colposuspension vs. transobturator MUS: improvement.
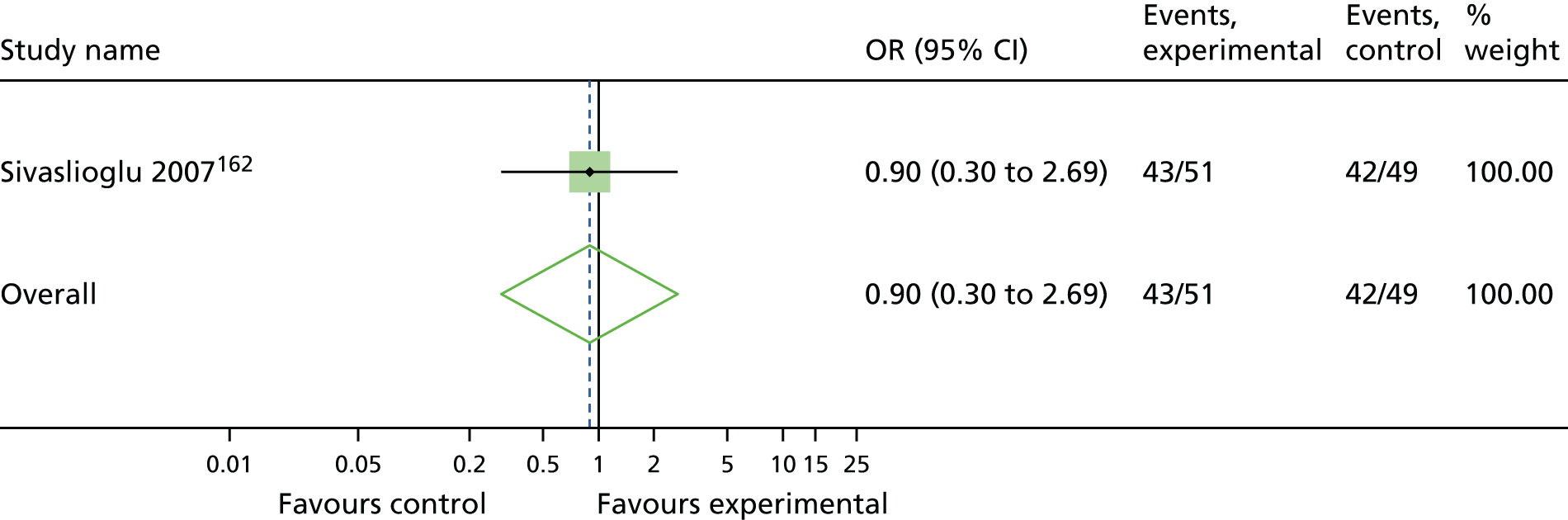
FIGURE 31.
Traditional sling vs. transobturator MUS: improvement.
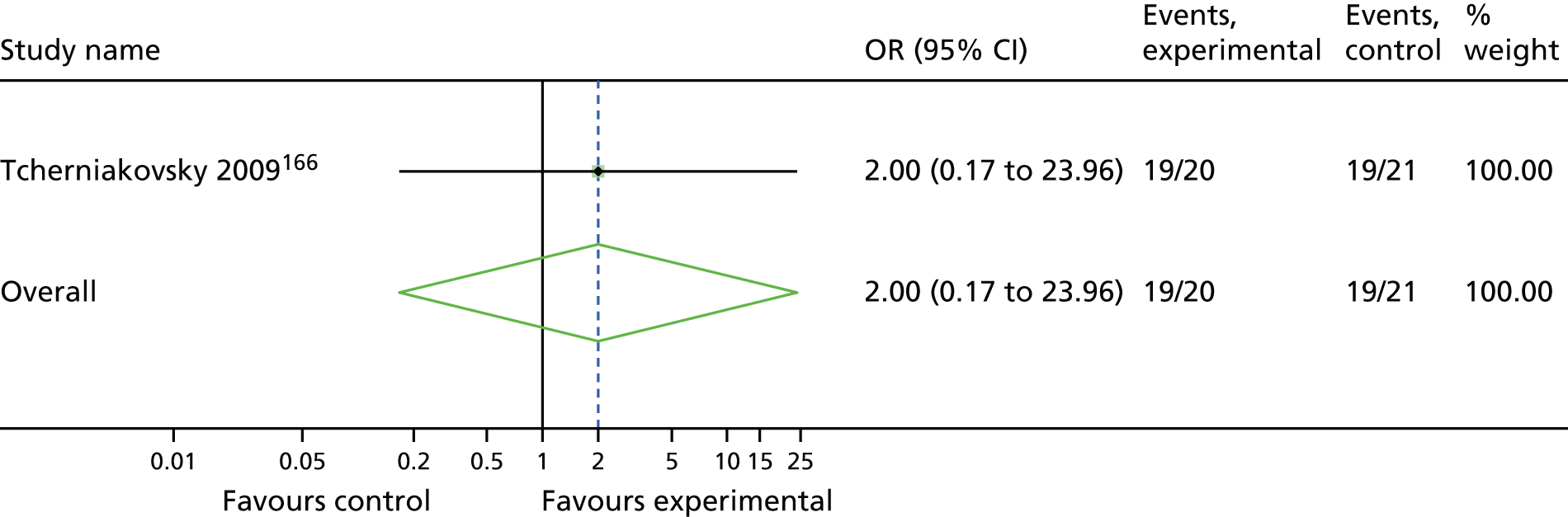
FIGURE 32.
Single-incision sling vs. transobturator MUS: improvement.
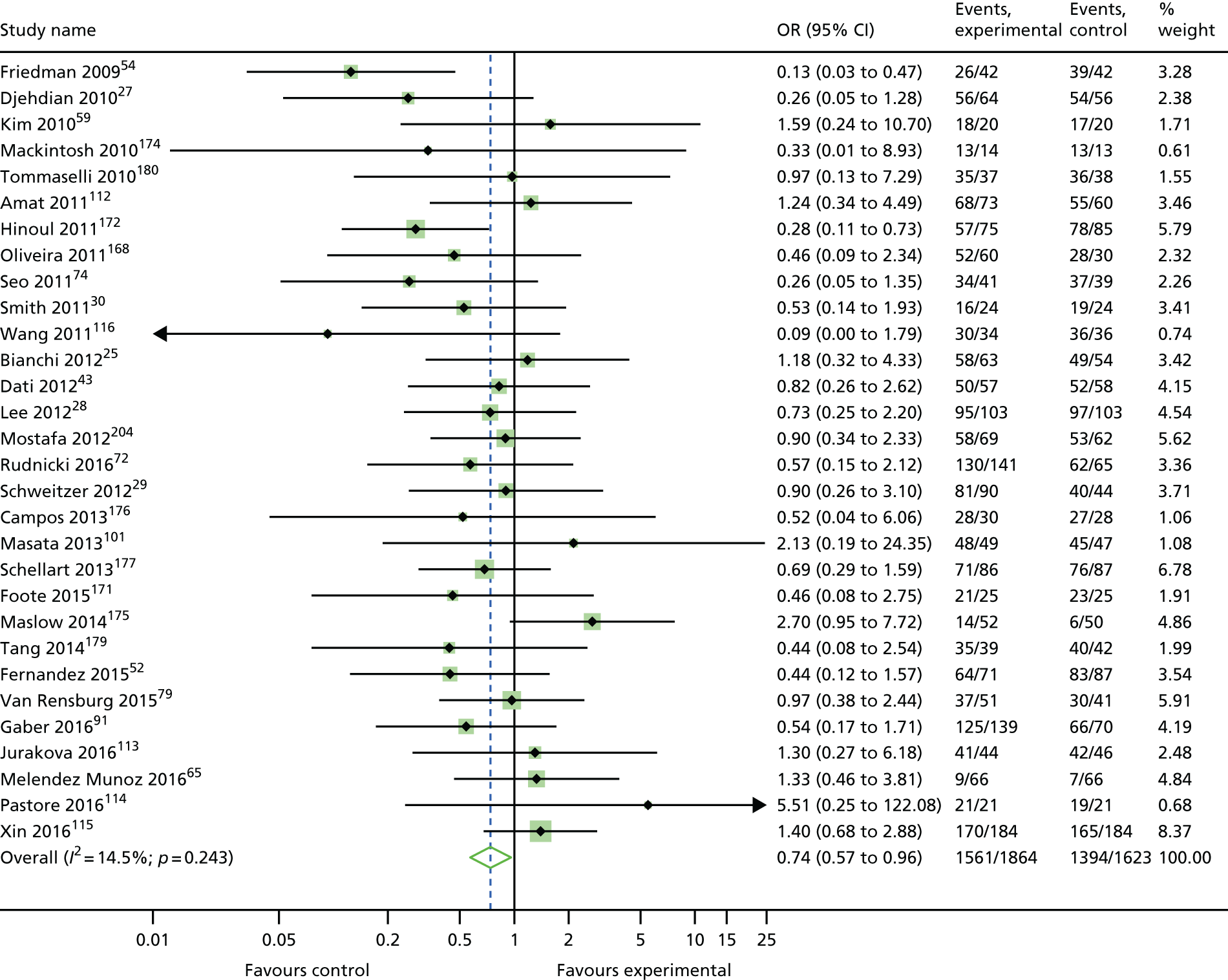
FIGURE 33.
Anterior vaginal repair vs. transobturator MUS: improvement.
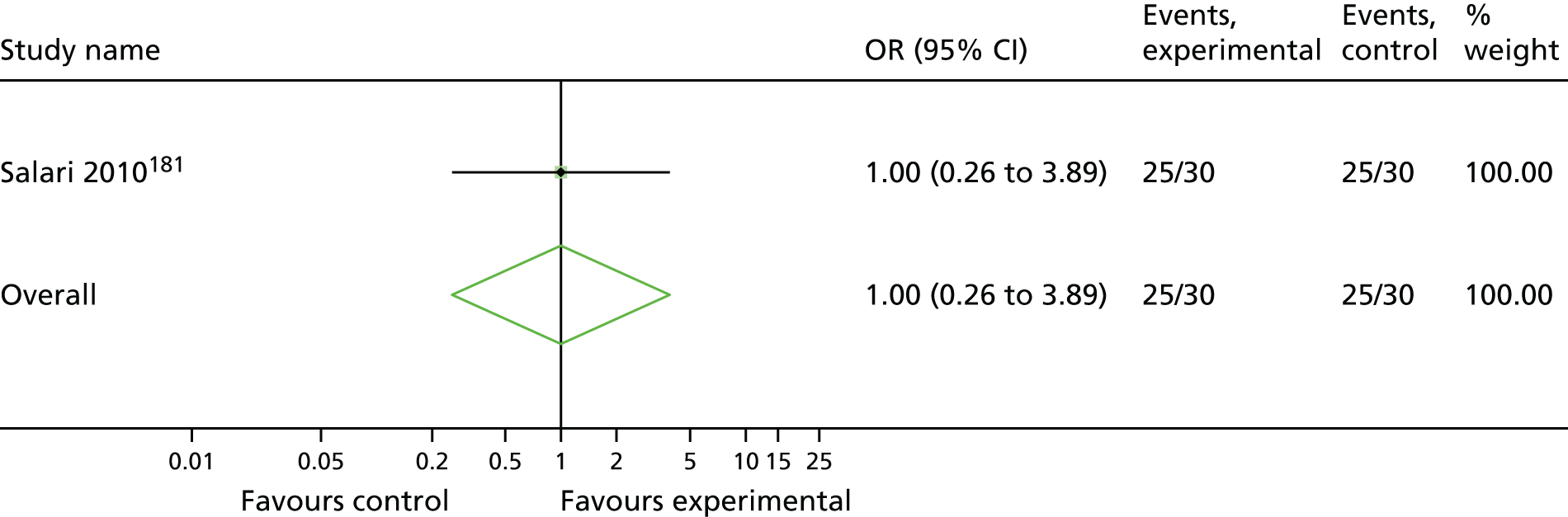
FIGURE 34.
Pelvic floor muscle training vs. transobturator MUS: improvement.
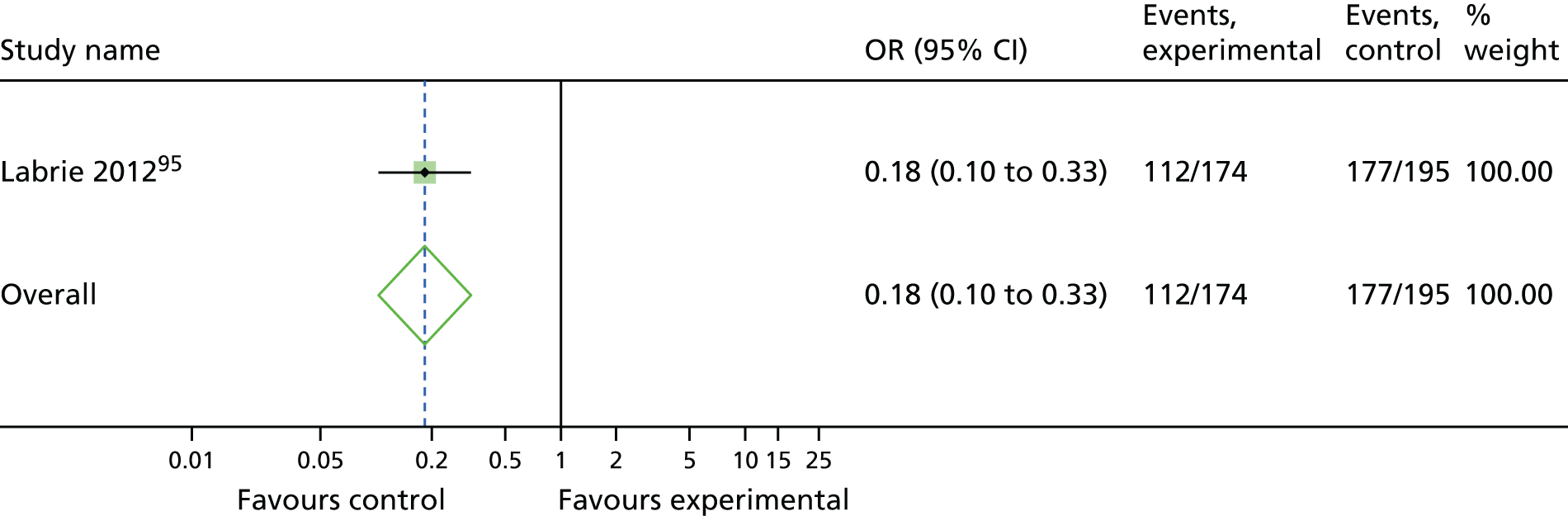
FIGURE 35.
Laparoscopic colposuspension vs. open colposuspension: improvement.
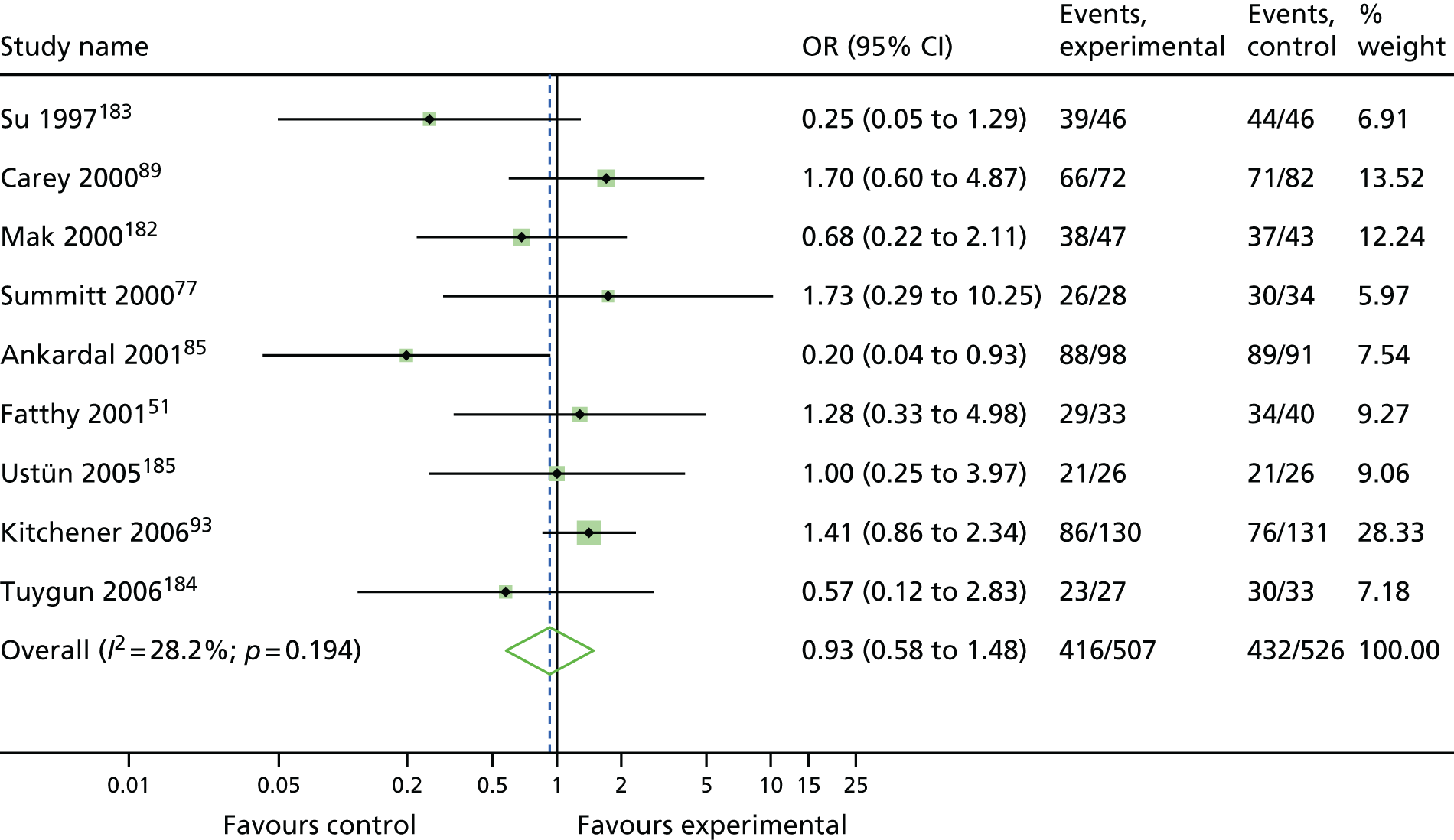
FIGURE 36.
Traditional sling vs. open colposuspension: improvement.
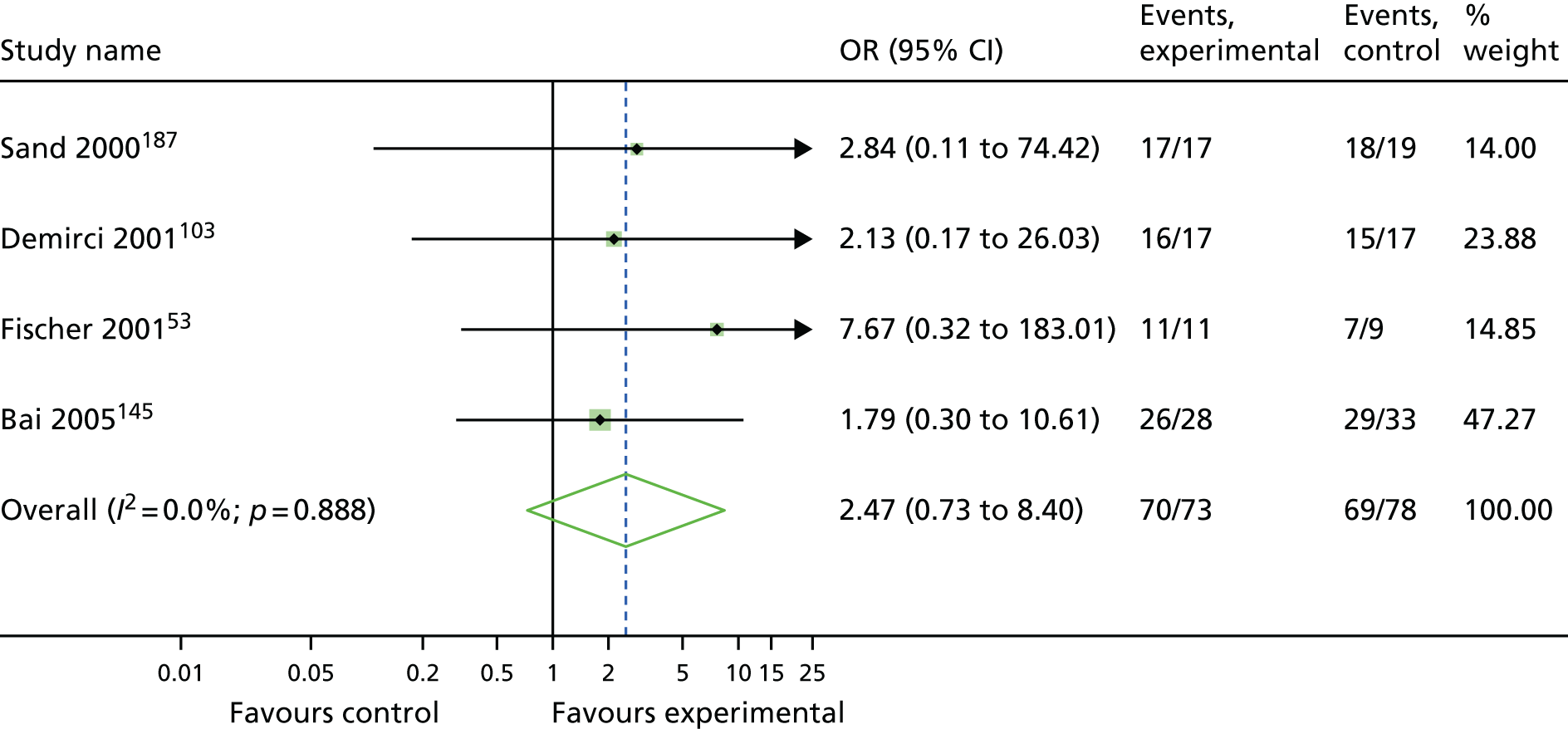
FIGURE 37.
Bladder neck needle suspension vs. open colposuspension: improvement.
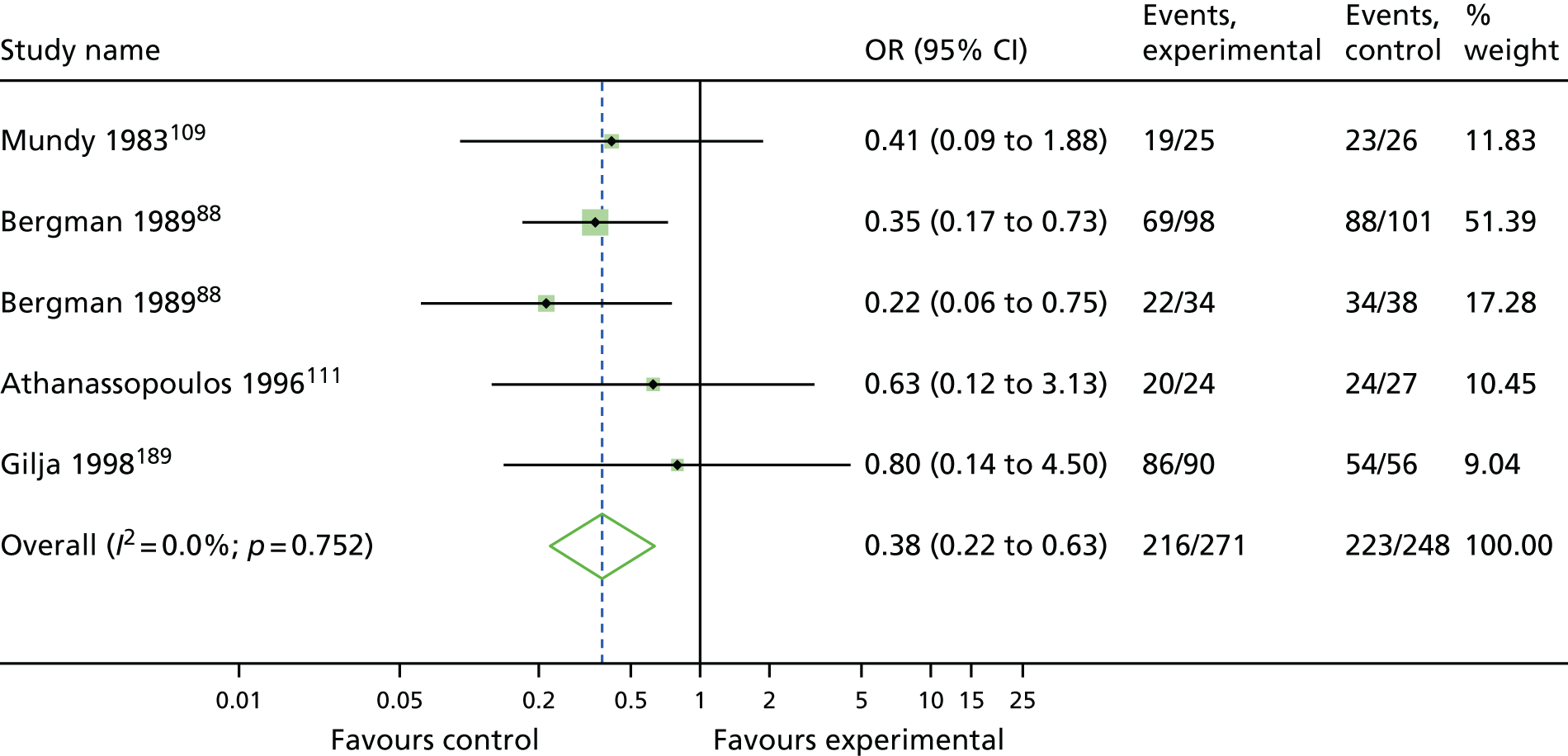
FIGURE 38.
Anterior vaginal repair vs. open colposuspension: improvement.
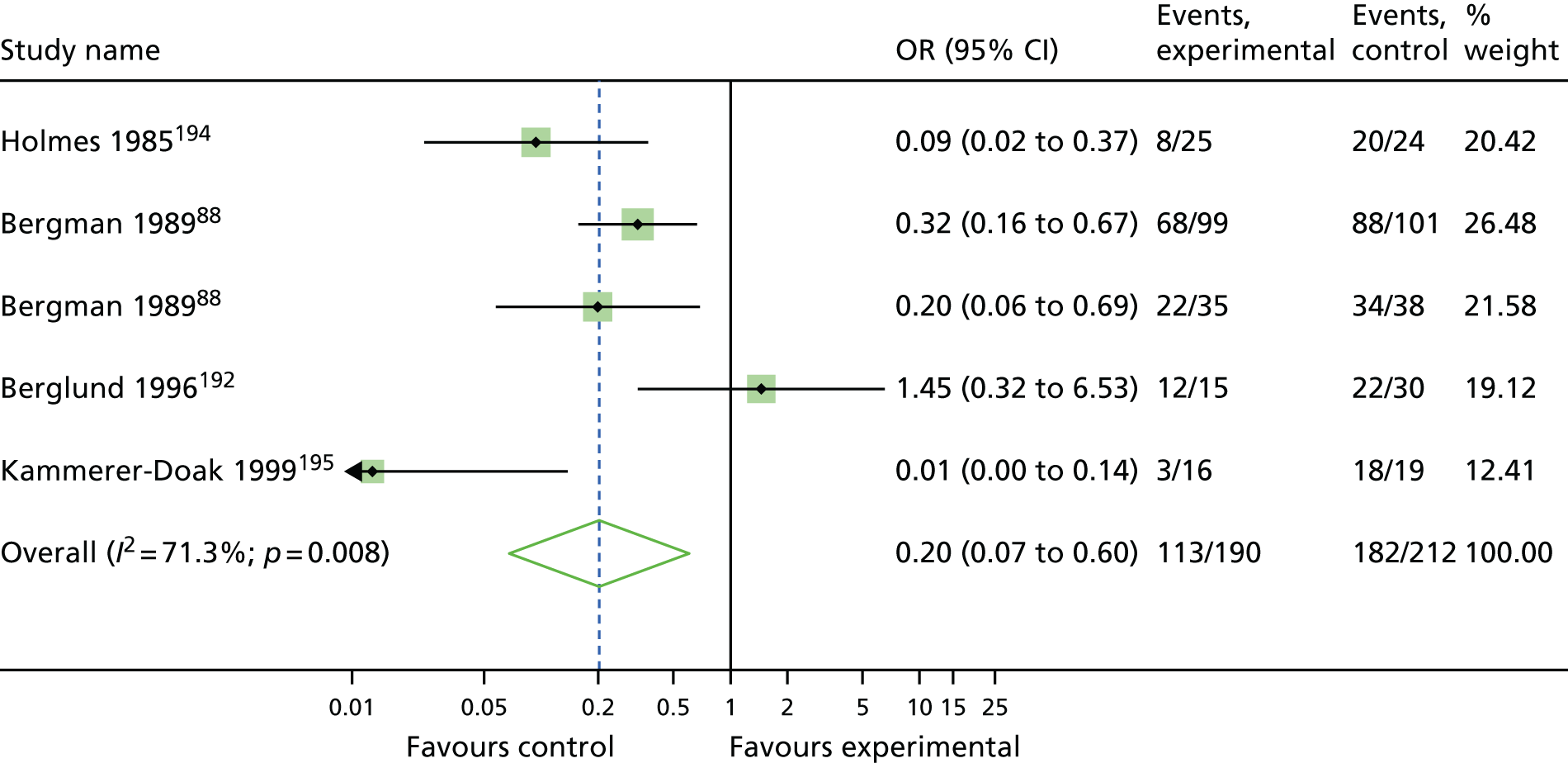
FIGURE 39.
Pelvic floor muscle training vs. open colposuspension: improvement.
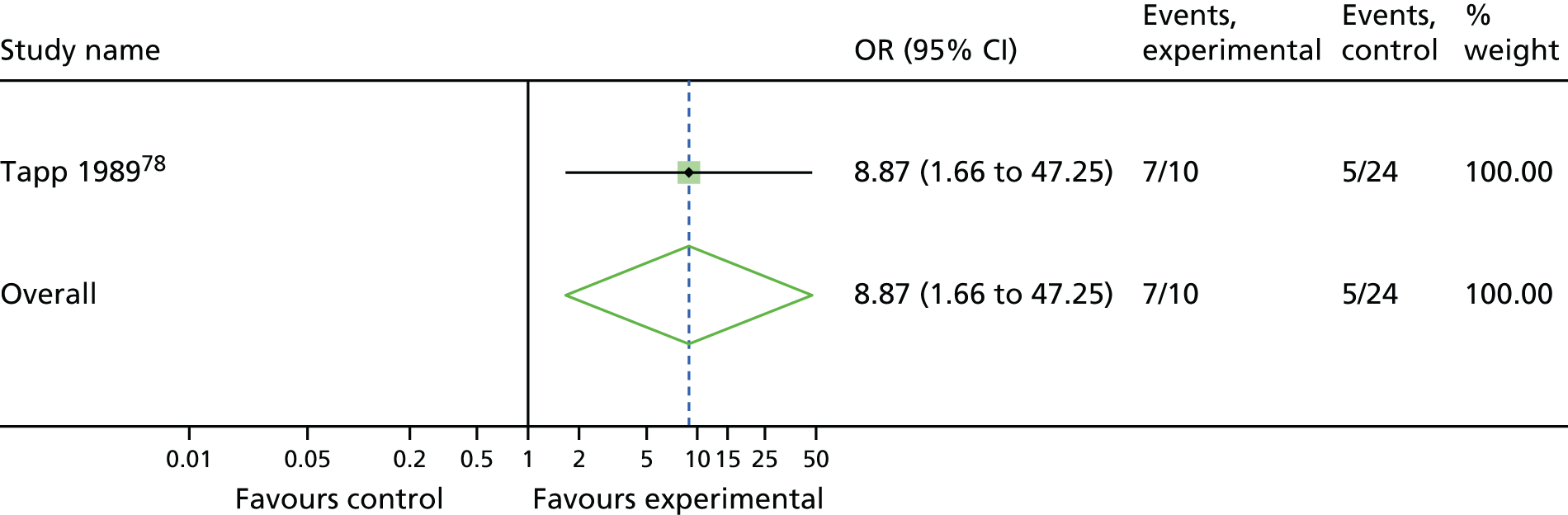
FIGURE 40.
Single-incision sling vs. traditional sling: improvement.
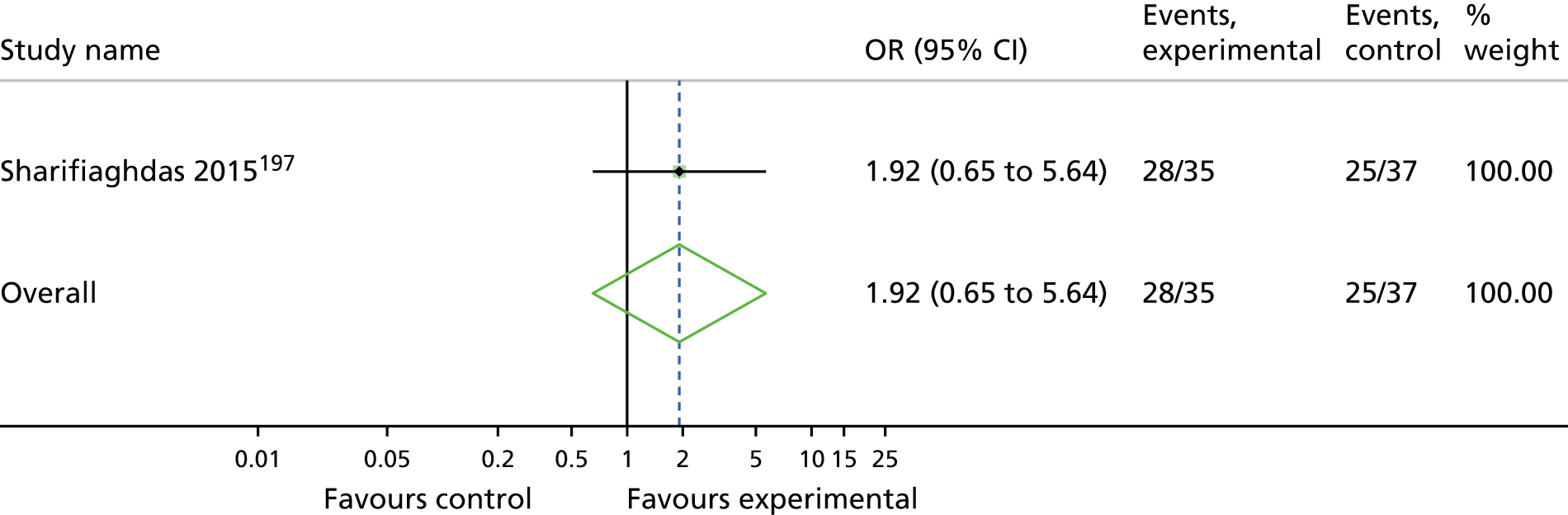
FIGURE 41.
Bladder neck needle suspension vs. traditional sling: improvement.
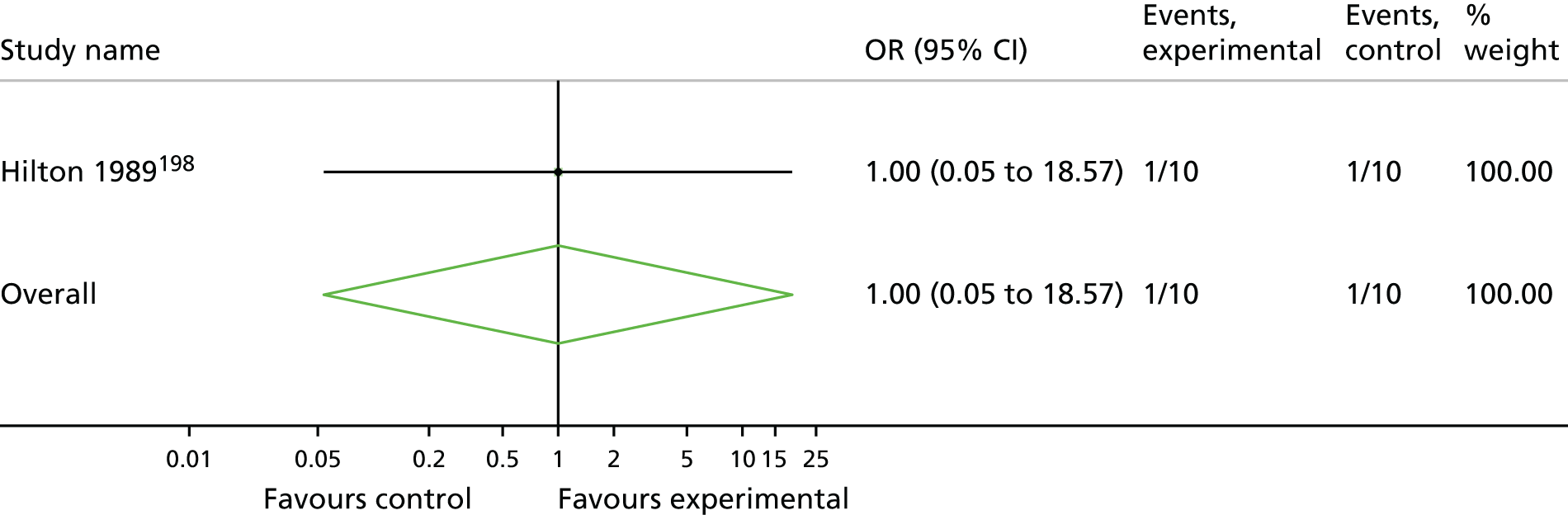
FIGURE 42.
Anterior vaginal repair vs. bladder neck needle suspension: improvement.
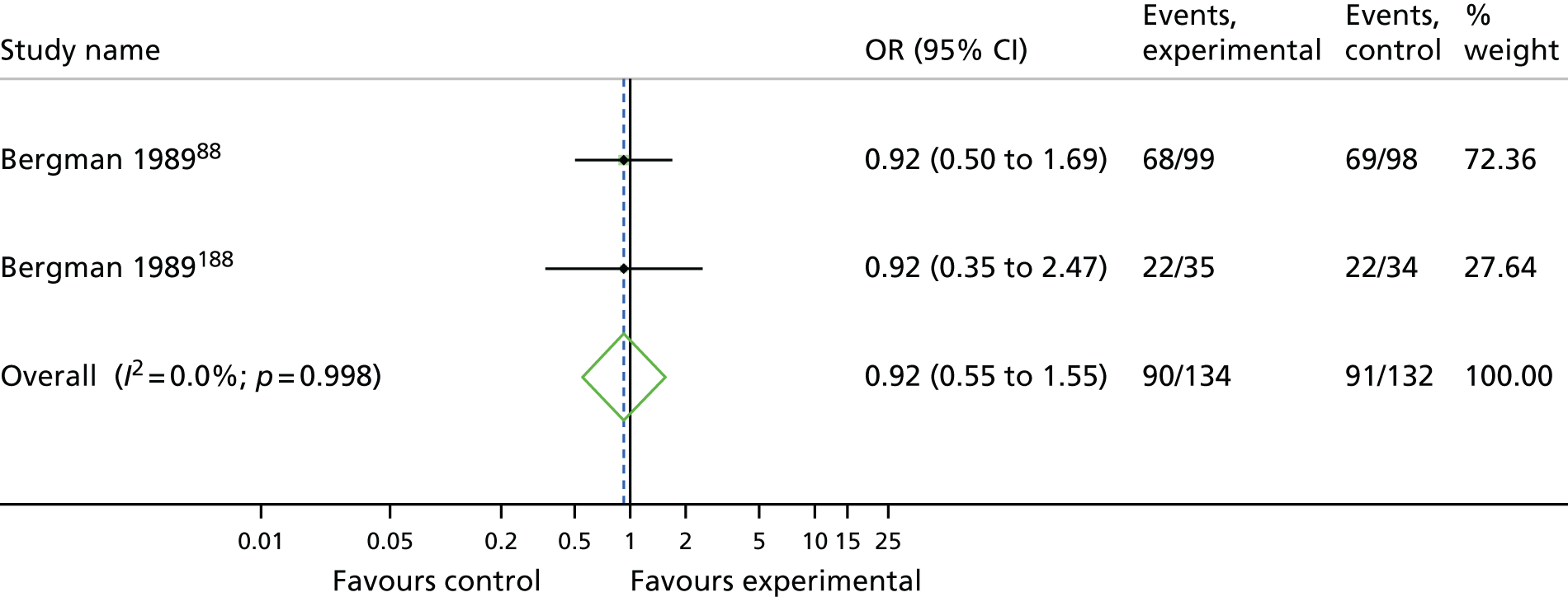
Appendix 13 Network meta-analysis: rankogram for each intervention for the number of women cured or improved
FIGURE 43.
Rankograms for each intervention for number of women cured. (a) Retropubic mid-urethral sling; (b) transobturator mid-urethral sling; (c) open colposuspension; (d) laparoscopic colposuspension; (e) traditional sling; (f) single-incision sling; (g) bladder neck needle suspension; (h) anterior vaginal repair; and (i) PFMT.
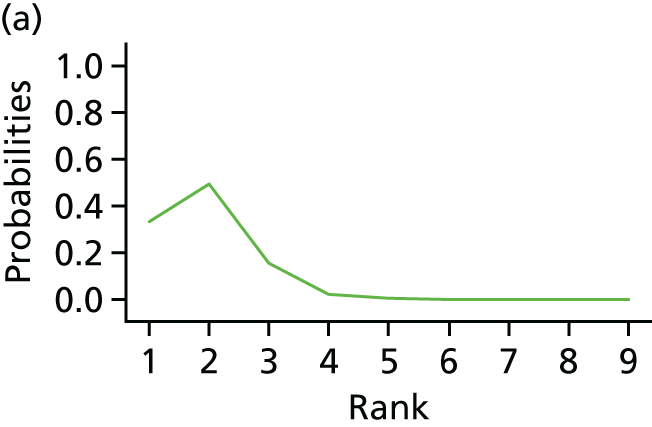
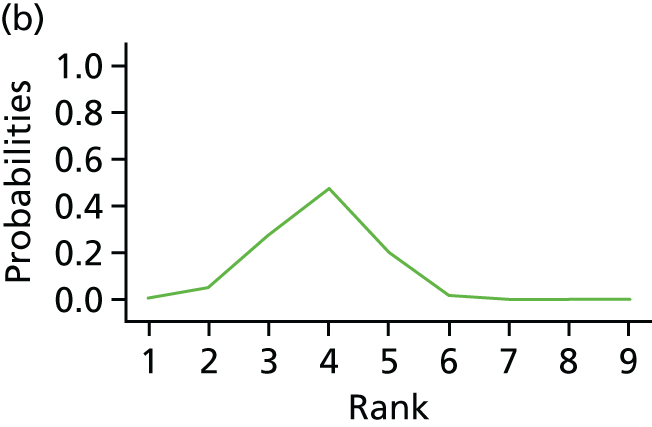
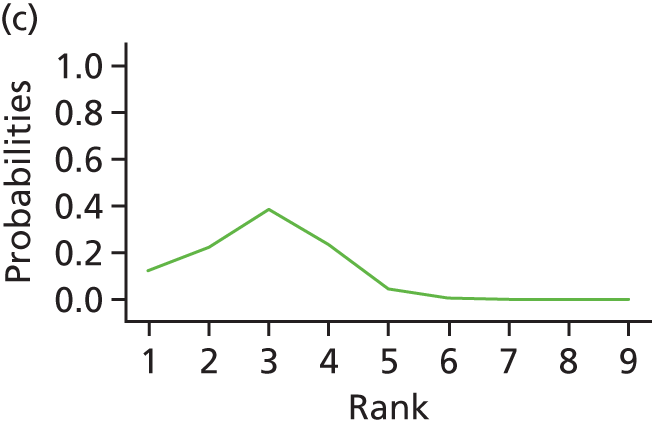
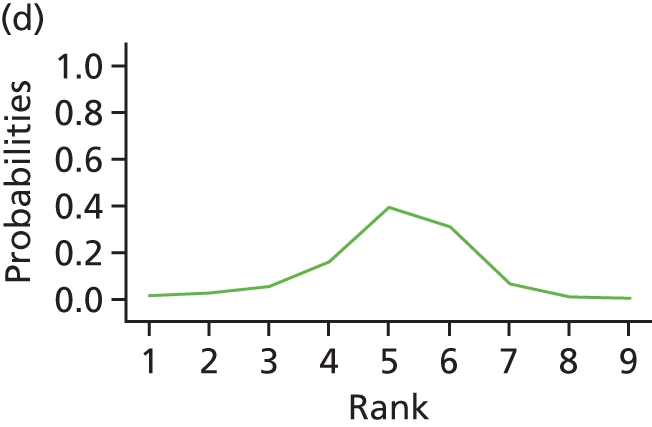
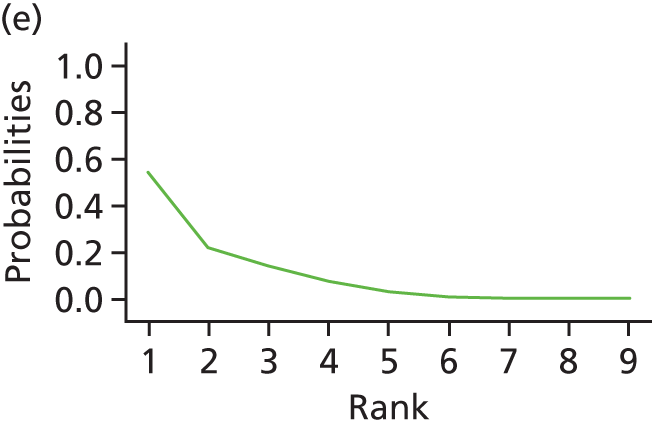
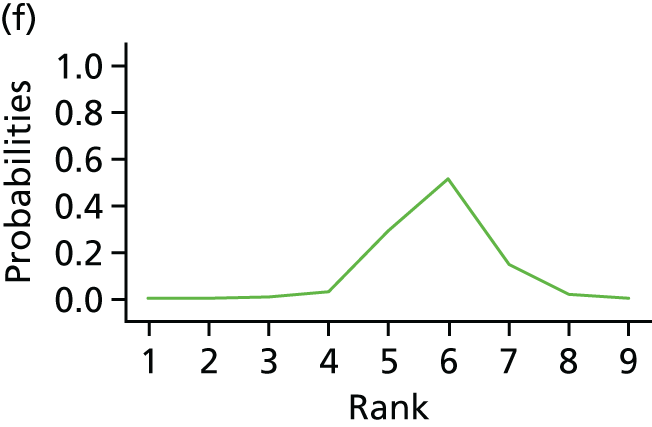
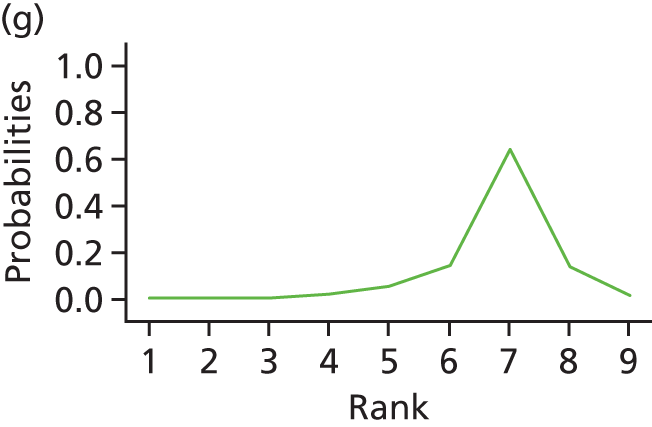
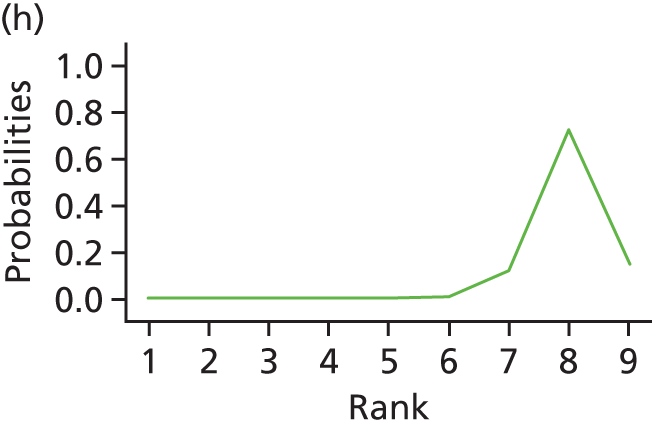
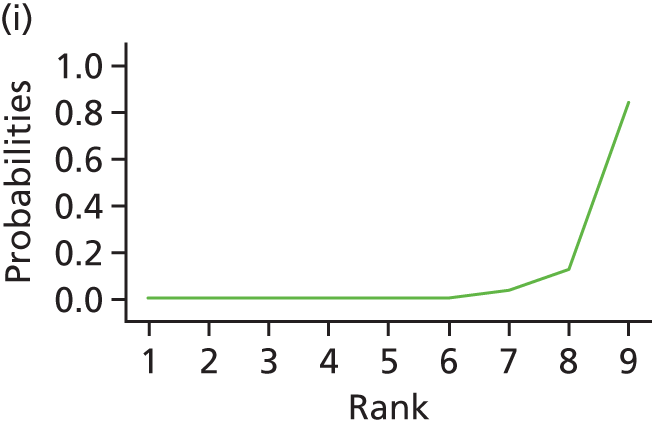
FIGURE 44.
Rankograms for each intervention for number of women improved. (a) Retropubic mid-urethral sling; (b) transobturator mid-urethral sling; (c) open colposuspension; (d) laparoscopic colposuspension; (e) traditional sling; (f) single-incision sling; (g) bladder neck needle suspension; (h) anterior vaginal repair; and (i) PFMT.
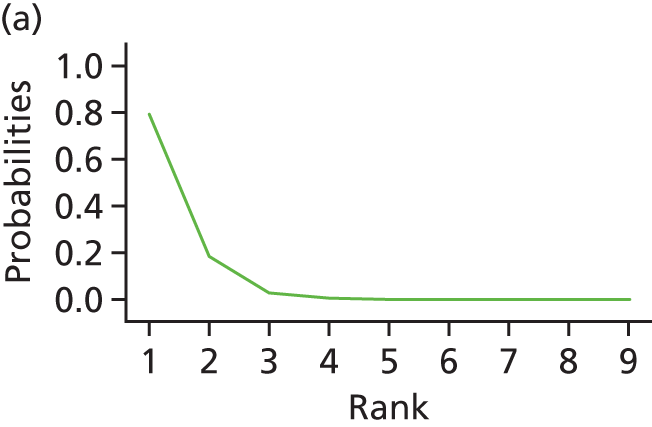
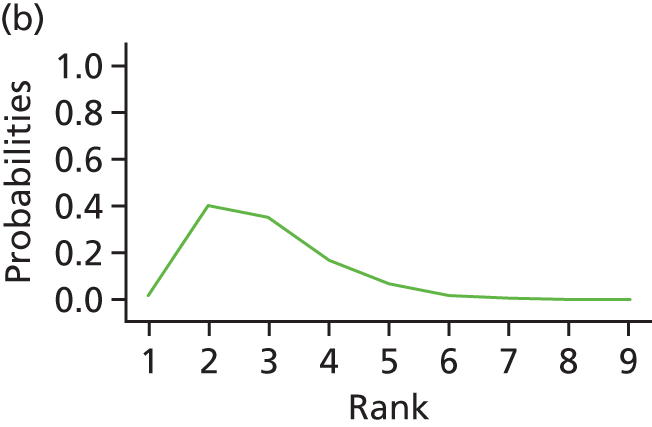
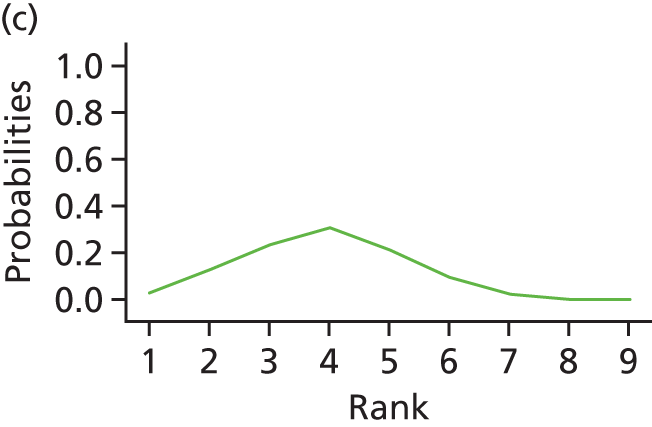
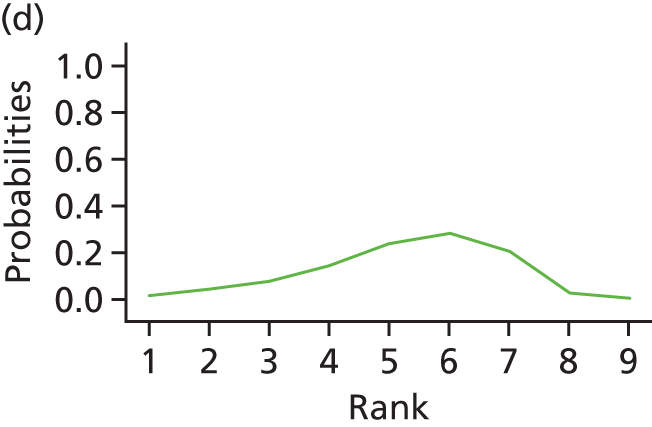
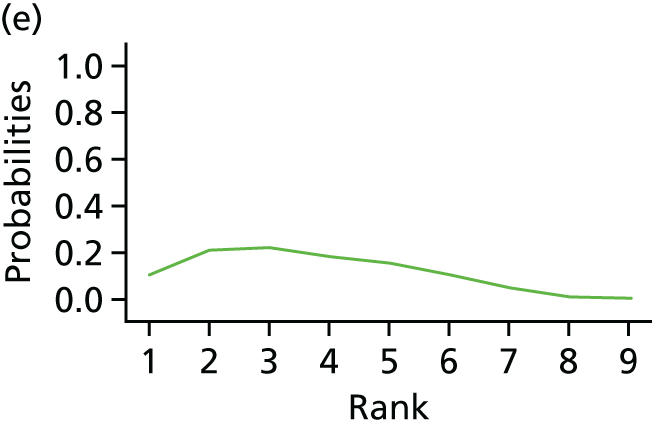
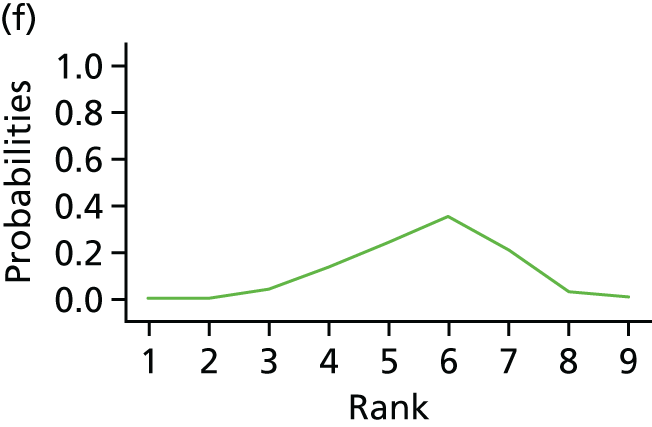
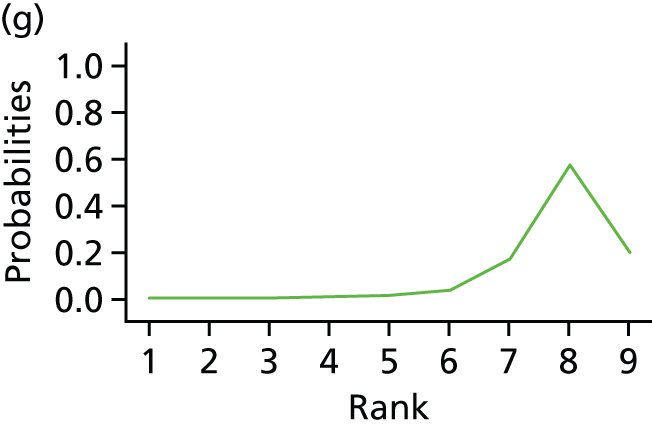
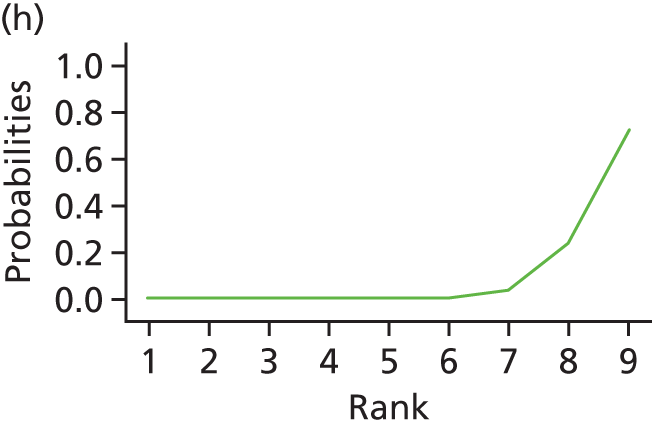
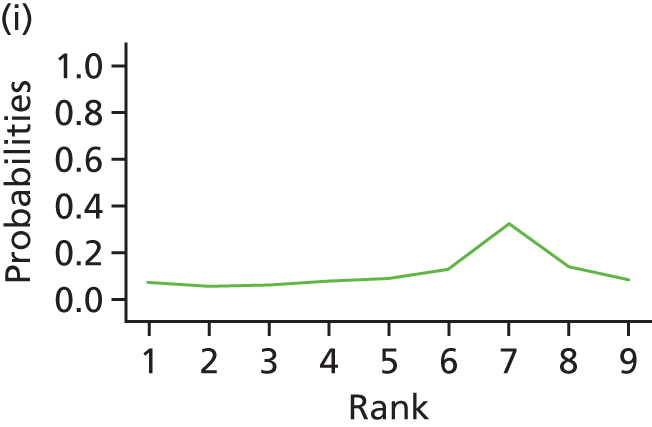
Appendix 14 Network meta-analysis: inconsistency analysis and node-splitting analysis for total number of women cured or improved
FIGURE 45.
Plot of the individual data points’ posterior mean deviance contributions for the consistency and inconsistency model along with the line of equality for the number of women cured.
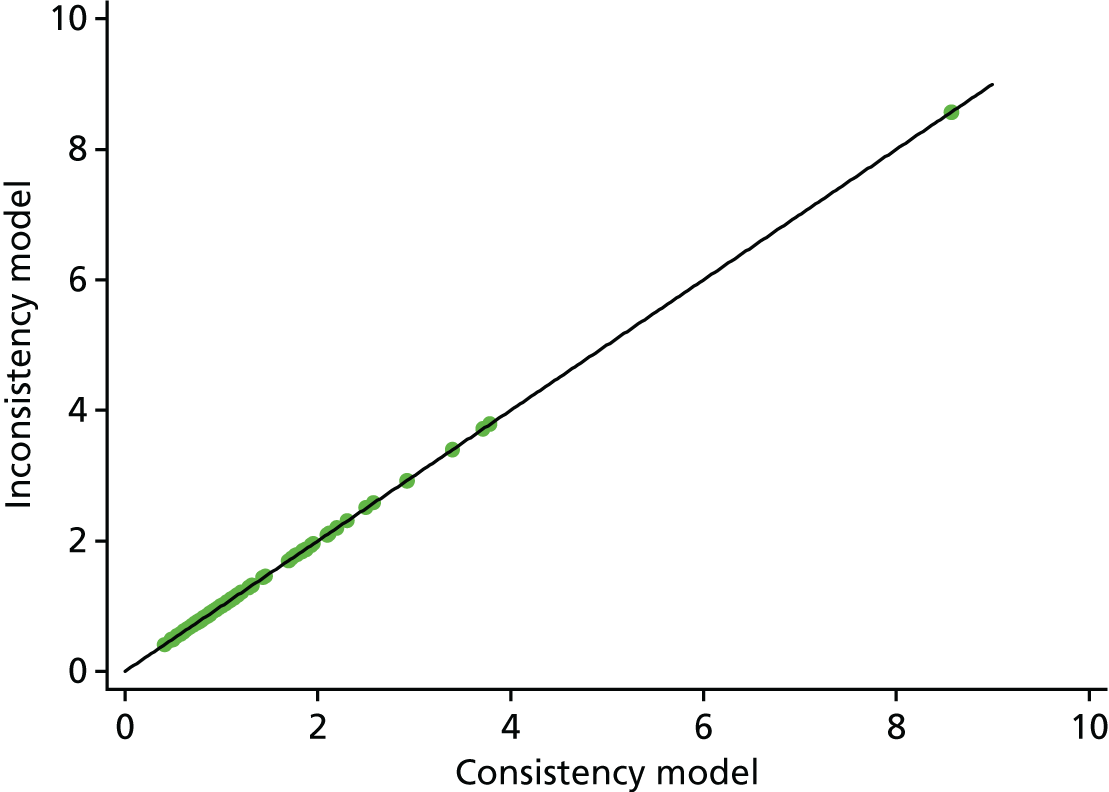
| Intervention comparison | Analysis, median (95% CI) | Bayesian p-value | |||
|---|---|---|---|---|---|
| NMA | Direct | Indirect | Inconsistency estimate | ||
| Transob-MUS vs. retro-MUS | –0.304 (–0.532 to –0.080) | –0.240 (–0.485 to 0.006) | –0.658 (–1.224 to –0.102) | 0.417 (–0.182 to 1.035) | 0.170 |
| Open colpo vs. retro-MUS | –0.159 (–0.609 to 0.281) | –0.036 (–0.586 to 0.522) | –0.370 (–1.134 to 0.382) | 0.335 (–0.593 to 1.270) | 0.476 |
| Lap colpo vs. retro-MUS | –0.545 (–1.157 to 0.045) | –1.057 (–2.406 to 0.182) | –0.409 (–1.088 to 0.274) | –0.652 (–2.171 to 0.780) | 0.370 |
| Trad sling vs. retro-MUS | 0.059 (–0.473 to 0.613) | –0.061 (–0.638 to 0.531) | 0.945 (–0.574 to 2.696) | –1.007 (–2.823 to 0.630) | 0.230 |
| Single incision vs. retro-MUS | –0.686 (–1.022 to –0.358) | –0.948 (–1.534 to –0.383) | –0.543 (–0.954 to –0.145) | –0.406 (–1.109 to 0.294) | 0.250 |
| Open colpo vs. transob-MUS | 0.145 (–0.332 to 0.619) | –0.127 (–1.658 to 1.371) | 0.174 (–0.330 to 0.679) | –0.300 (–1.914 to 1.284) | 0.708 |
| Trad sling vs. transob-MUS | 0.363 (–0.206 to 0.962) | 0.901 (–1.913 to 4.506) | 0.353 (–0.238 to 0.964) | 0.547 (–2.333 to 4.198) | 0.720 |
| Single incision vs. transob-MUS | –0.380 (–0.672 to –0.098) | –0.343 (–0.666 to –0.023) | –0.513 (–1.191 to 0.148) | 0.170 (–0.559 to 0.915) | 0.652 |
| Ant repair vs. transob-MUS | –0.775 (–1.580 to 0.023) | –0.723 (–2.313 to 0.825) | –1.359 (–2.202 to –0.531) | 0.634 (–1.162 to 2.412) | 0.482 |
| PFMT vs. transob-MUS | –1.211 (–1.953 to –0.473) | –1.623 (–2.756 to –0.496) | –2.610 (–5.073 to –0.546) | 1.000 (–1.358 to 3.685) | 0.420 |
| Lap colpo vs. open colpo | –1.813 (–2.817 to –0.847) | –0.315 (–0.811 to 0.185) | –0.952 (–2.358 to 0.378) | 0.640 (–0.779 to 2.125) | 0.380 |
| Trad sling vs. open colpo | –0.388 (–0.857 to 0.077) | 1.320 (–0.088 to 2.986) | –0.060 (–0.786 to 0.665) | 1.388 (–0.199 to 3.180) | 0.088 |
| Bladder neck needle vs. open colpo | 0.218 (–0.420 to 0.895 | –0.909 (–1.619 to –0.208) | 0.264 (–3.859 to 4.079) | –1.171 (–5.064 to 3.008) | 0.530 |
| Ant repair vs. open colpo | –1.356 (–1.983 to –0.739) | –1.531 (–2.245 to –0.850) | –0.815 (–2.497 to 0.820) | –0.716 (–2.487 to 1.096) | 0.424 |
| PFMT vs. open colpo | –1.957 (–3.018 to –0.940) | –2.697 (–5.173 to –0.661) | –1.734 (–2.977 to –0.499) | –0.979 (–3.699 to 1.425) | 0.434 |
| Bladder neck needle vs. trad sling | –1.141 (–2.067 to –0.237) | 0.008 (–3.834 to 3.861) | –1.239 (–2.205 to –0.316) | 1.247 (–2.678 to 5.221) | 0.506 |
| Ant repair vs. bladder neck needle | –0.437 (–1.190 to 0.304) | –0.162 (–1.060 to 0.737) | –0.784 (–1.900 to 0.313) | 0.621 (–0.729 to 1.992) | 0.368 |
FIGURE 46.
Plot of the individual data points’ posterior mean deviance contributions for the consistency and inconsistency model along with the line of equality for the number of women improved.
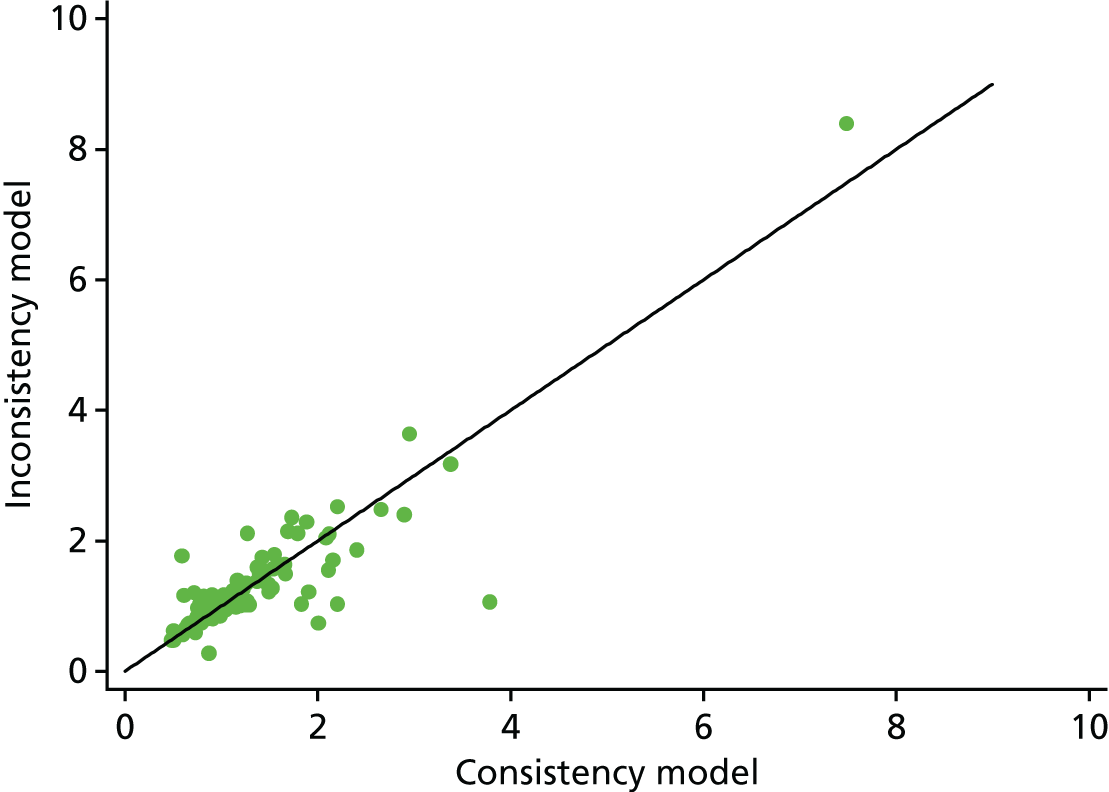
| Intervention comparison | Analysis, median (95% CrI) | Median | |||
|---|---|---|---|---|---|
| NMA | Direct | Indirect | Inconsistency estimate | ||
| Transob-MUS vs. retro-MUS | –0.279 (–0.532 to –0.023) | –0.236 (–0.513 to 0.043) | –0.460 (1.070 to 0.134) | 0.223 (–0.426 to 0.888) | 0.498 |
| Open colpo vs. retro-MUS | –0.436 (–0.894 to 0.021) | –0.152 (–0.750 to 0.464) | –0.806 (–1.536 to –0.104) | 0.655 (–0.265 to 1.611) | 0.160 |
| Lap colpo vs. retro-MUS | –0.653 (–1.230 to –0.092) | –0.761 (–1.633 to 0.093) | –0.575 (–1.349 to 0.201) | –0.187 (–1.350 to 0.974) | 0.750 |
| Trad sling vs. retro-MUS | –0.372 (–0.947 to 0.230) | –0.405 (–1.101 to 0.297) | –0.265 (–1.345 to 0.867) | –0.141 (–1.466 to 1.151) | 0.828 |
| Single incision vs. retro-MUS | –0.688 (–1.050 to –0.340) | –1.118 (–1.806 to –0.456) | –0.498 (–0.921 to –0.076) | –0.618 (–1.419 to 0.155) | 0.116 |
| Open colpo vs. transob-MUS | –0.158 (–0.662 to 0.347) | –0.113 (–1.785 to 1.524) | –0.160 (–0.683 to 0.372) | 0.043 (–1.697 to 1.762) | 0.960 |
| Trad sling vs. transob-MUS | –0.094 (–0.707 to 0.540) | 0.924 (–2.022 to 4.706) | –0.134 (–0.761 to 0.512) | 1.057 (–1.947 to 4.900) | 0.498 |
| Single incision vs. transob-MUS | –0.410 (–0.712 to –0.115) | –0.366 (–0.704 to –0.040) | –0.657 (–1.408 to 0.081) | 0.290 (–0.526 to 1.101) | 0.478 |
| Ant repair vs. transob-MUS | –1.442 (–2.253 to –0.641) | –0.013 (–1.842 to 1.825) | –1.775 (–2.662 to –0.902) | 1.762 (–0.283 to 3.806) | 0.088 |
| PFMT vs. transob-MUS | –0.580 (–1.662 to 0.575) | –1.712 (–2.925 to –0.506) | 2.346 (0.321 to 4.583) | –4.060 (–6.629 to –1.701) | 0.002 |
| Lap colpo vs. open colpo | –0.217 (–0.722 to 0.271) | –0.174 (–0.747 to 0.392) | –0.379 (–1.391 to 0.624) | 0.203 (–0.946 to 1.357) | 0.728 |
| Trad sling vs. open colpo | 0.063 (–0.614 to 0.767) | 1.383 (–0.094 to 3.158) | –0.318 (–1.093 to 0.455) | 1.709 (0.047 to 3.611) | 0.044 |
| Bladder neck needle vs. open colpo | –0.962 (–1.697 to –0.216) | –0.971 (–1.774 to –0.190) | 0.105 (–3.731 to 4.202) | –1.078 (–5.268 to 2.843) | 0.566 |
| Ant repair vs. open colpo | –1.286 (–1.976 to –0.607) | –1.571 (–2.336 to –0.841) | 0.268 (–1.636 to 2.208) | –1.846 (–3.921 to 0.196) | 0.076 |
| PFMT vs. open colpo | –0.419 (–1.545 to 0.772) | 2.342 (0.376 to 4.511) | –1.723 (–3.036 to –0.430) | 4.080 (1.679 to 6.591) | < 0.001 |
| Single incision vs. trad sling | –0.317 (–0.986 to 0.327) | 0.676 (–0.911 to 2.298) | –0.518 (–1.247 to 0.196) | 1.192 (–0.552 to 3.004) | 0.178 |
| Bladder neck needle vs. trad sling | –1.026 (–2.019 to –0.056) | –0.007 (–3.975 to 3.989) | –1.117 (–2.145 to –0.098) | 1.106 (–2.974 to 5.199) | 0.558 |
| Ant repair vs. bladder neck needle | –0.322 (–1.168 to 0.489) | –0.141 (–1.156 to 0.882) | –0.482 (–1.712 to 0.736) | 0.340 (–1.177 to 1.881) | 0.654 |
Appendix 15 Summary of meta-analyses of direct head-to-head comparisons for adverse events and resource use
FIGURE 47.
Repeat continence surgery. Ant repair, anterior vaginal repair; ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
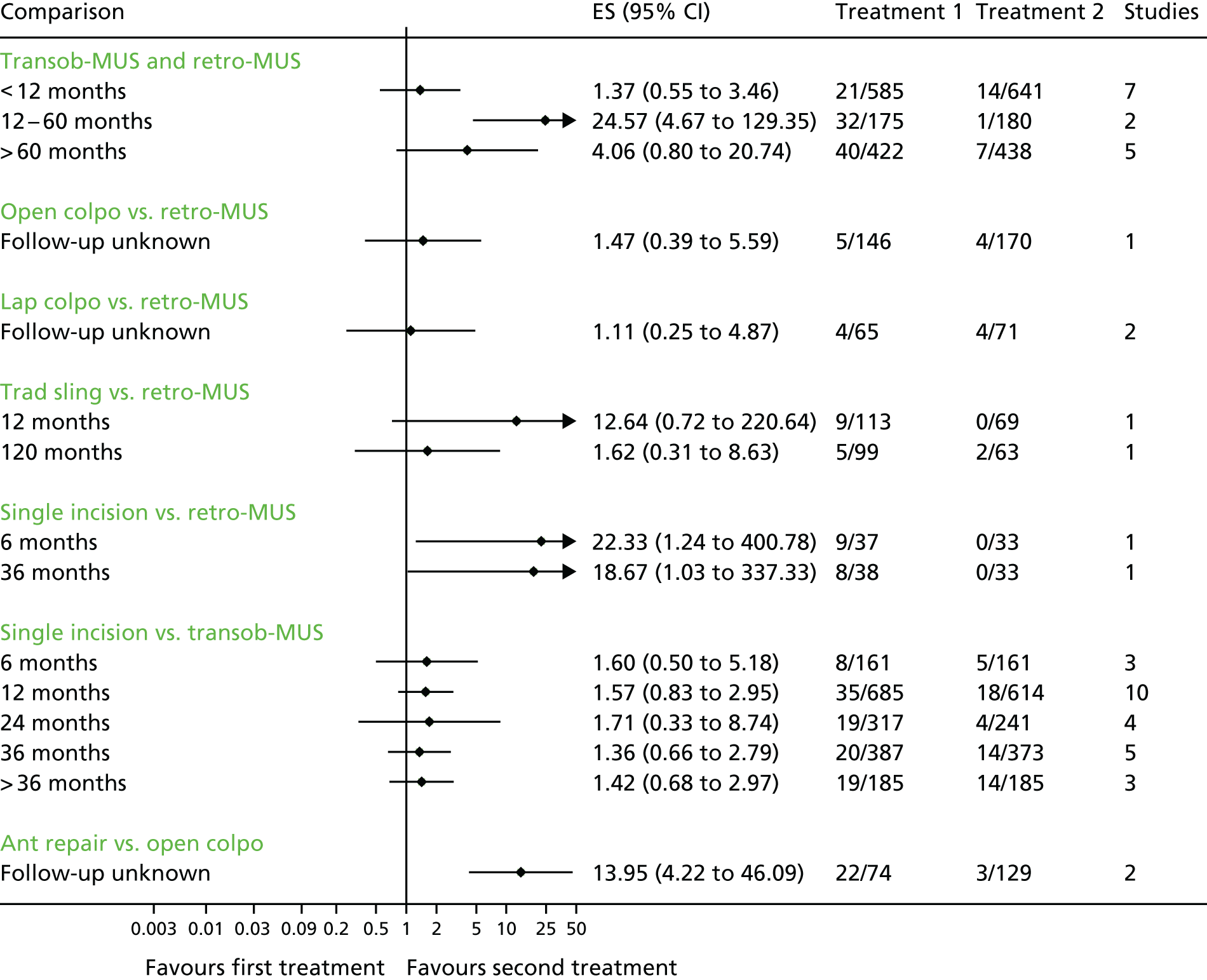
FIGURE 48.
Haemorrhage. ES, effect estimate (OR); single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
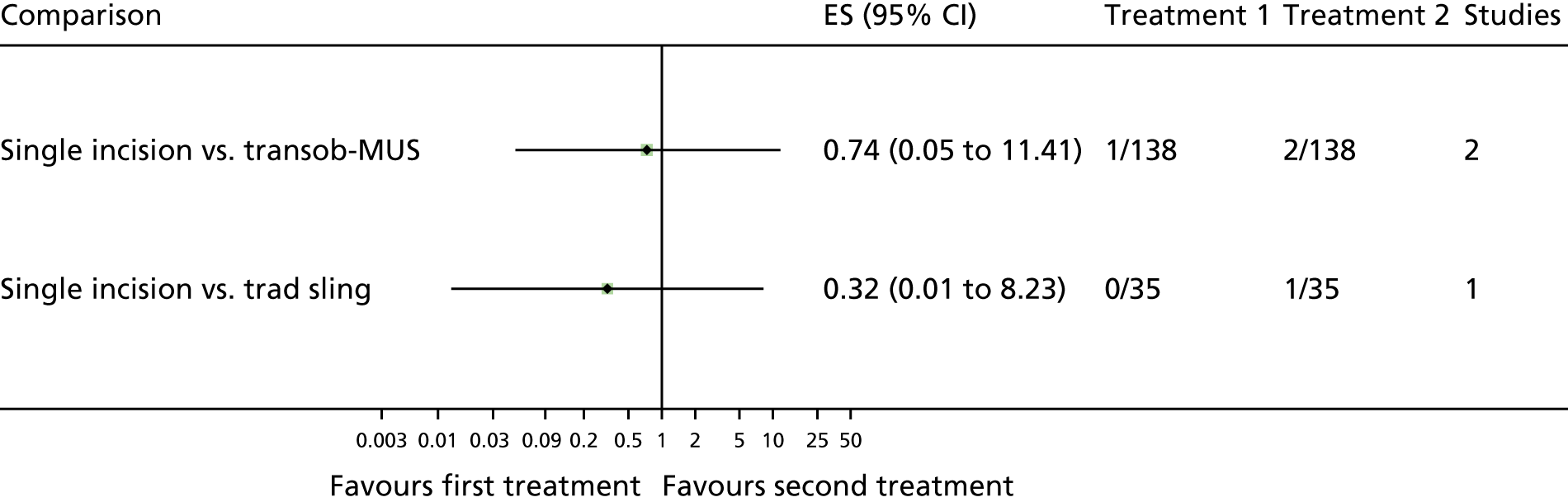
FIGURE 49.
Haematoma, major vascular complications and myocardial infarction. ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
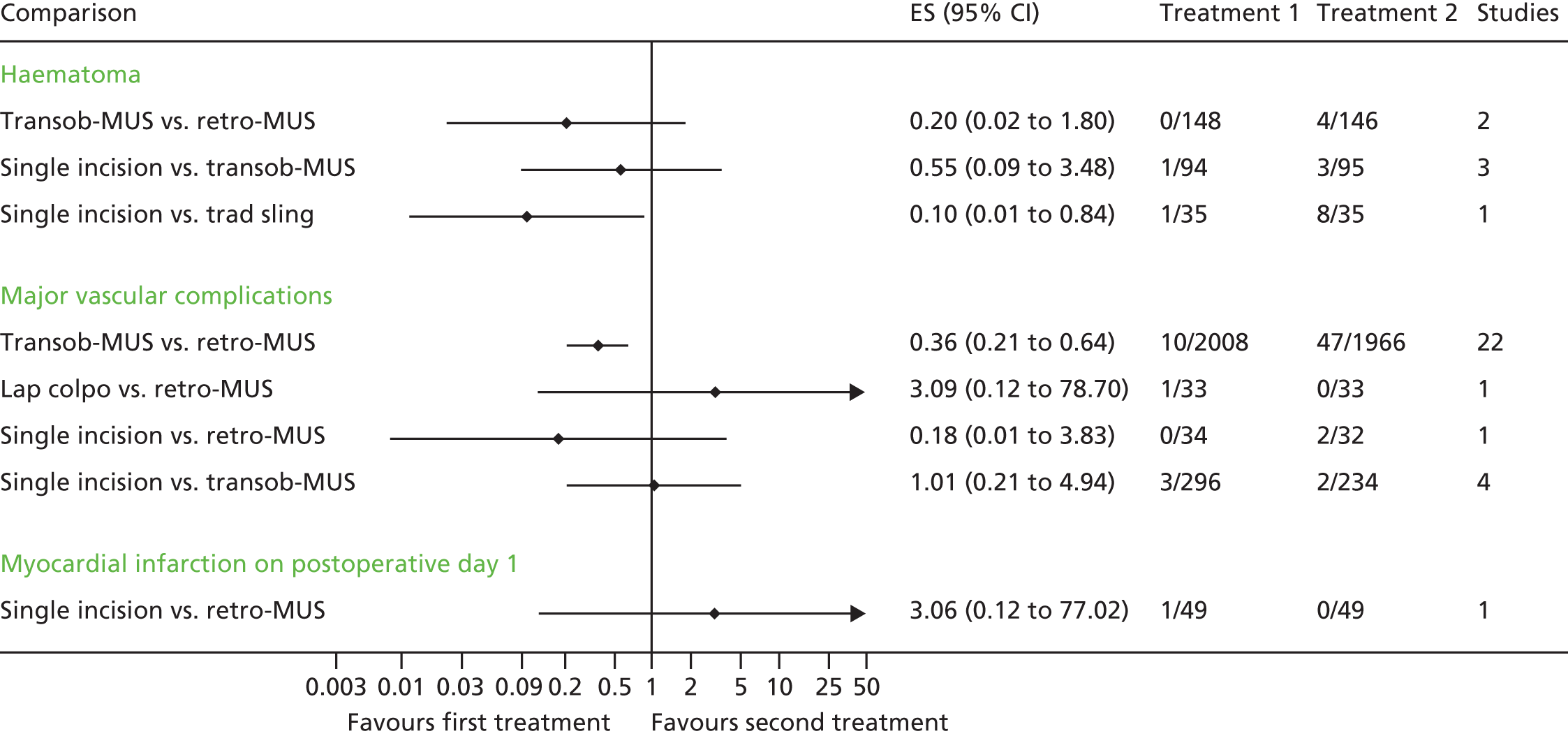
FIGURE 50.
Bleeding. ES, effect estimate (OR); retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; transob-MUS, transobturator mid-urethral sling.
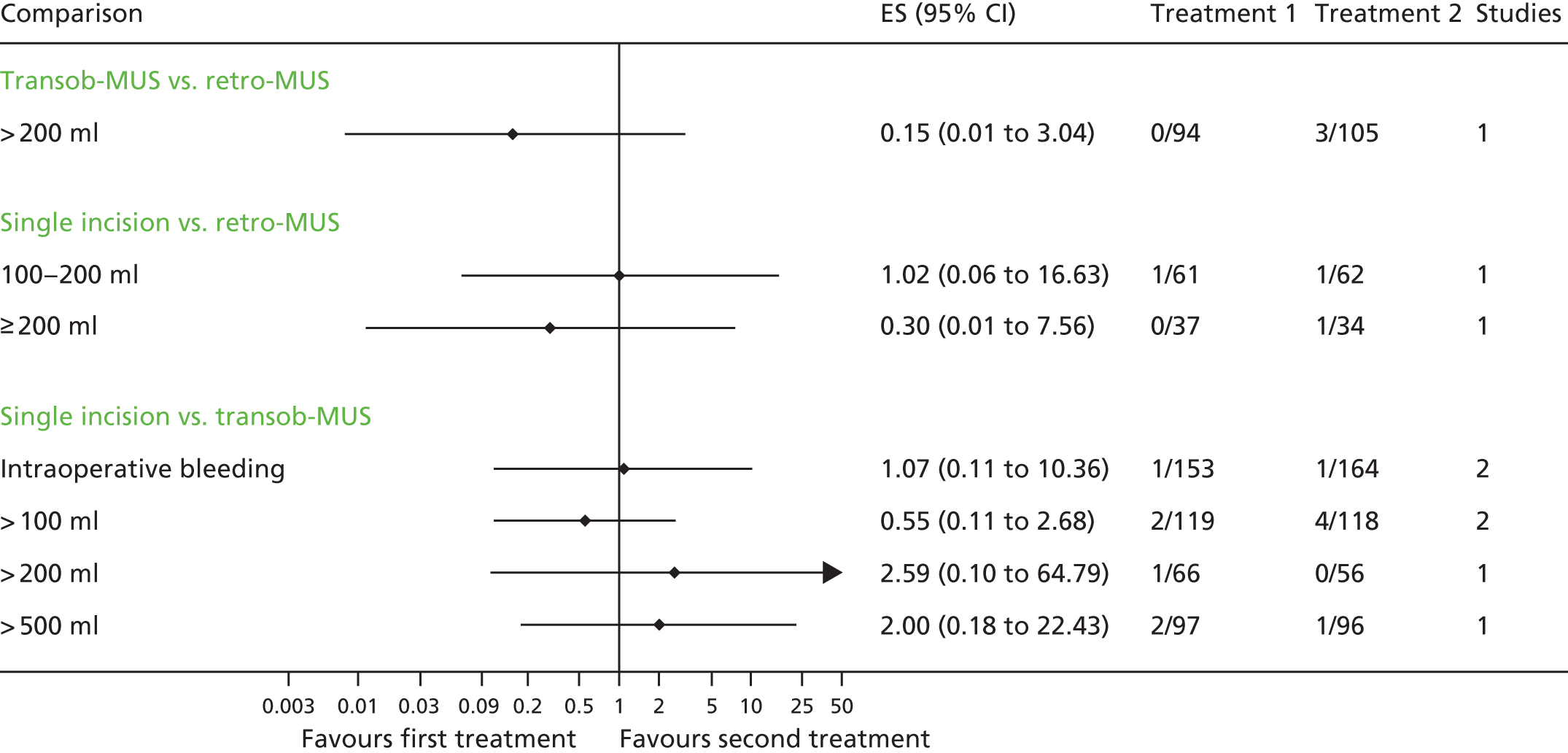
FIGURE 51.
De novo symptoms of urgency or urgency incontinence. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle colposuspension; ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
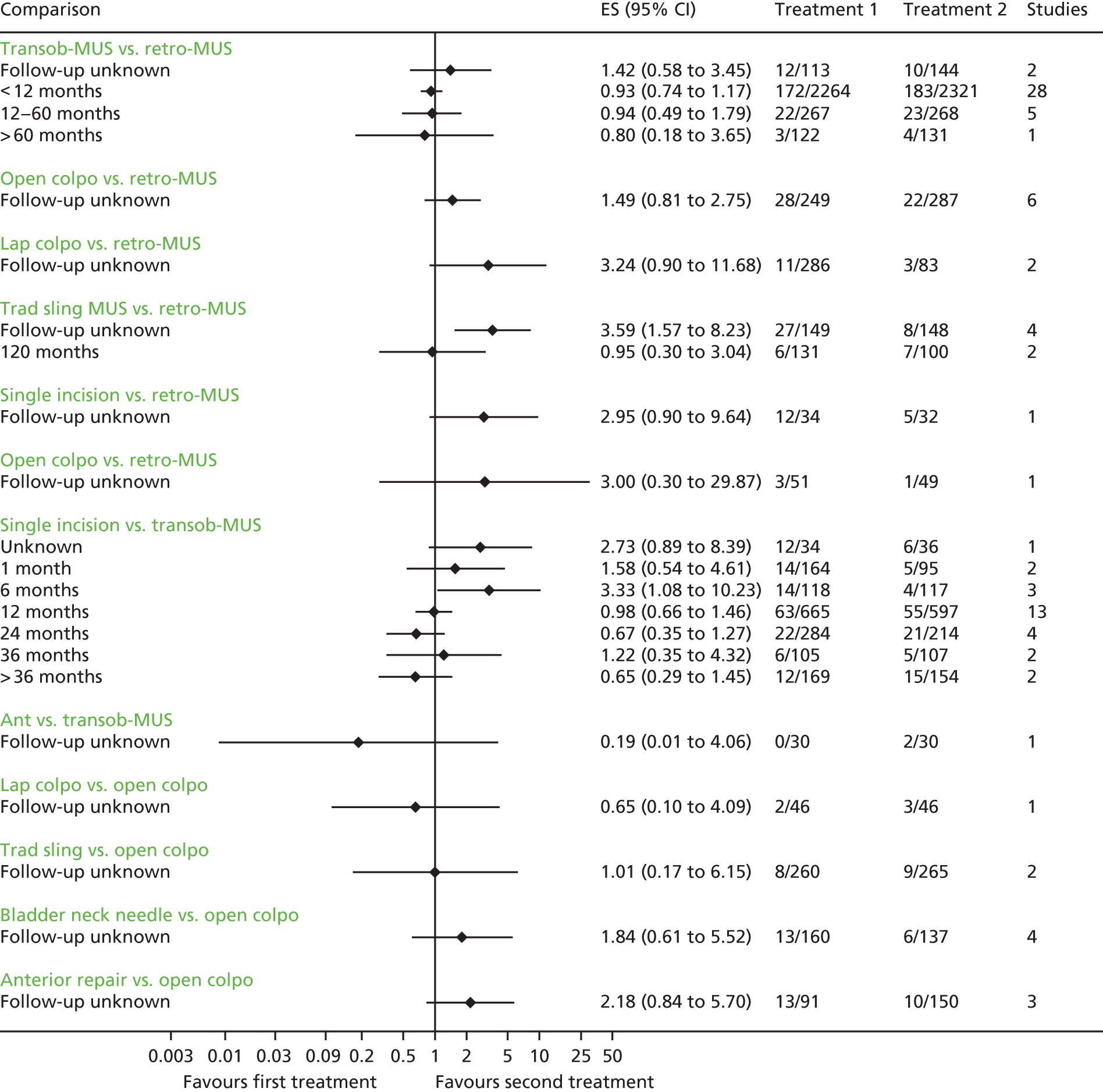
FIGURE 52.
Detrusor instability. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle colposuspension; ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
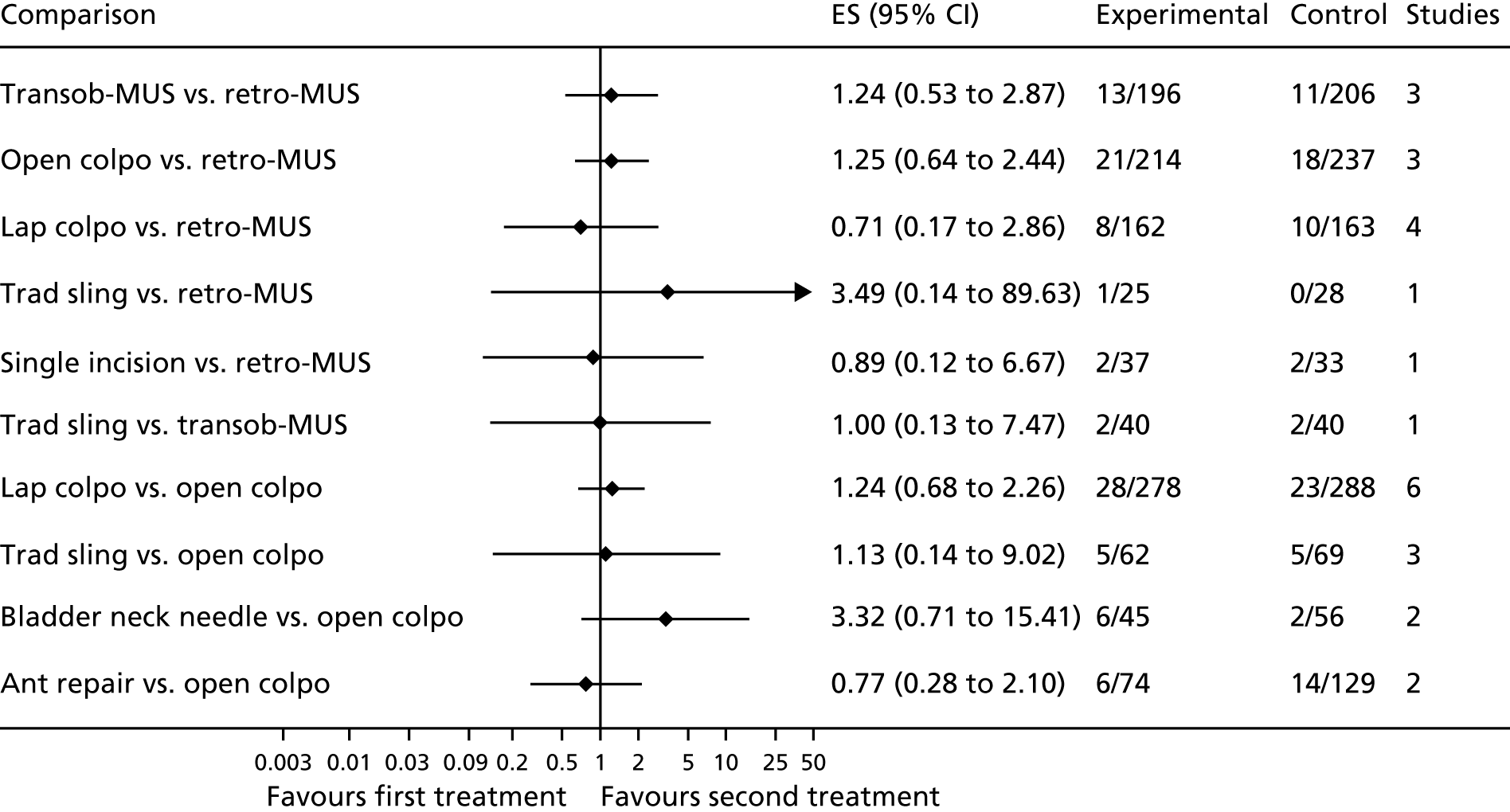
FIGURE 53.
Voiding difficulty. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle colposuspension; ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
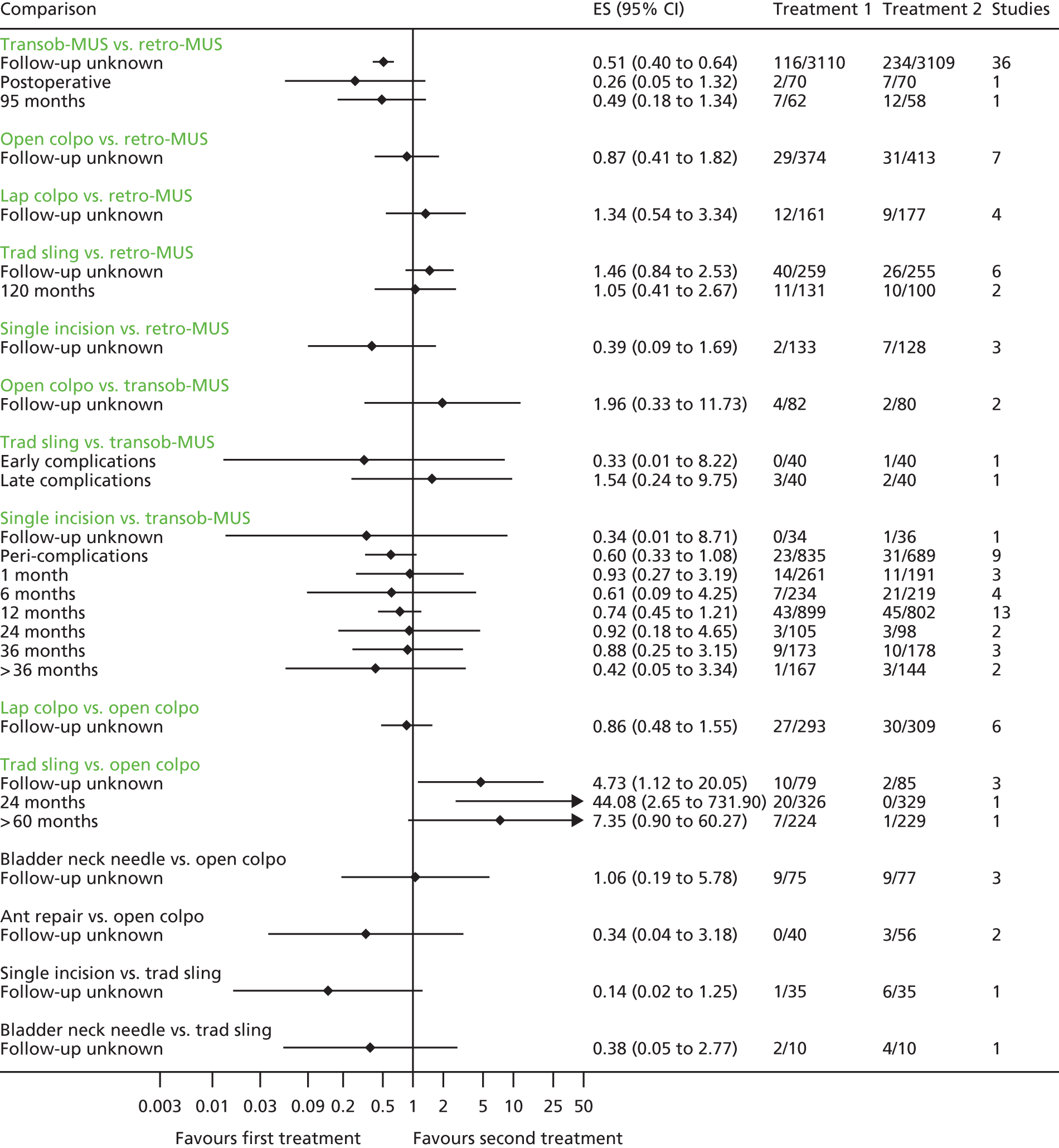
FIGURE 54.
Bladder or urethral perforation. ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
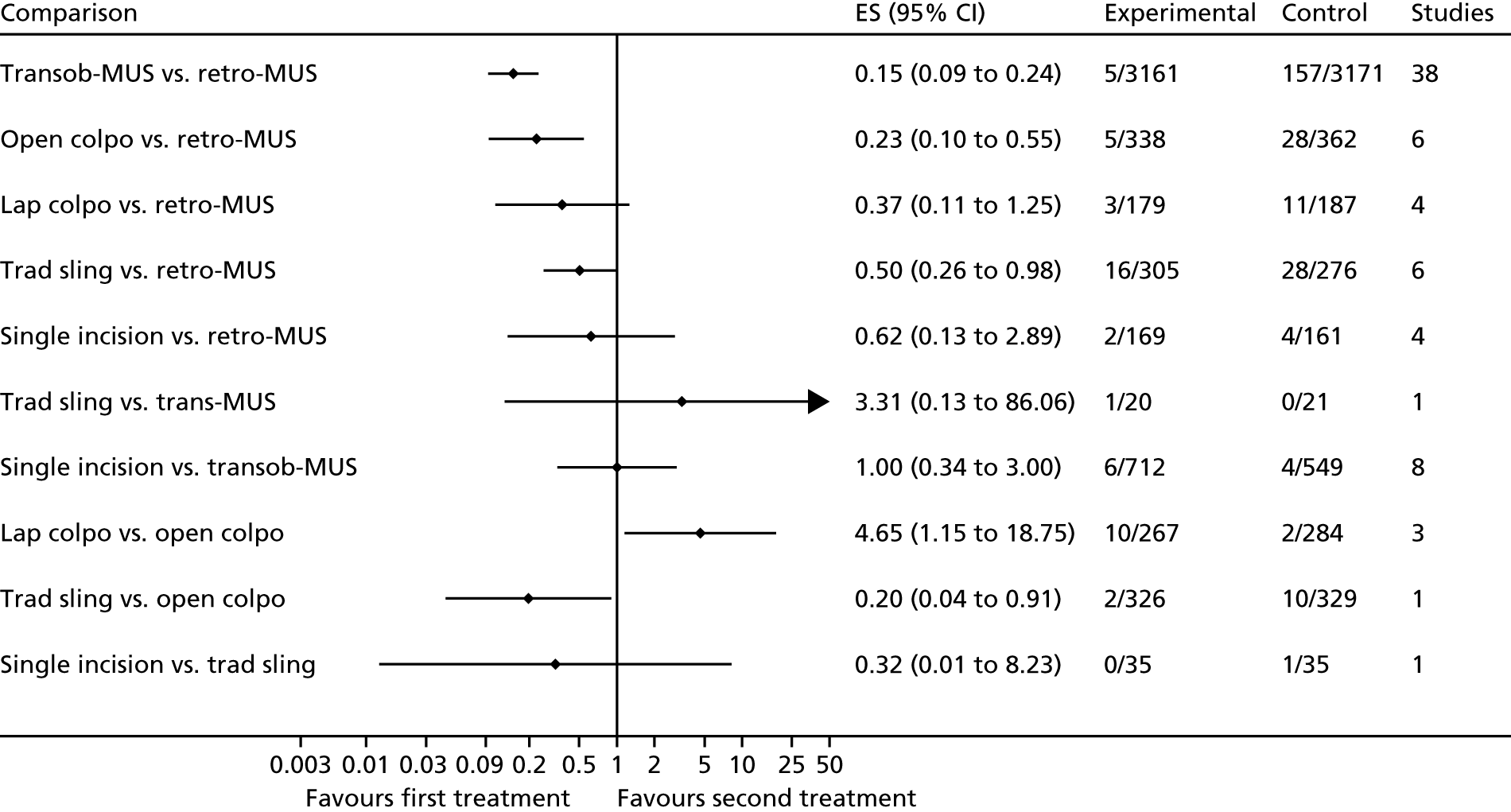
FIGURE 55.
Tape/mesh erosion or extrusion. ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
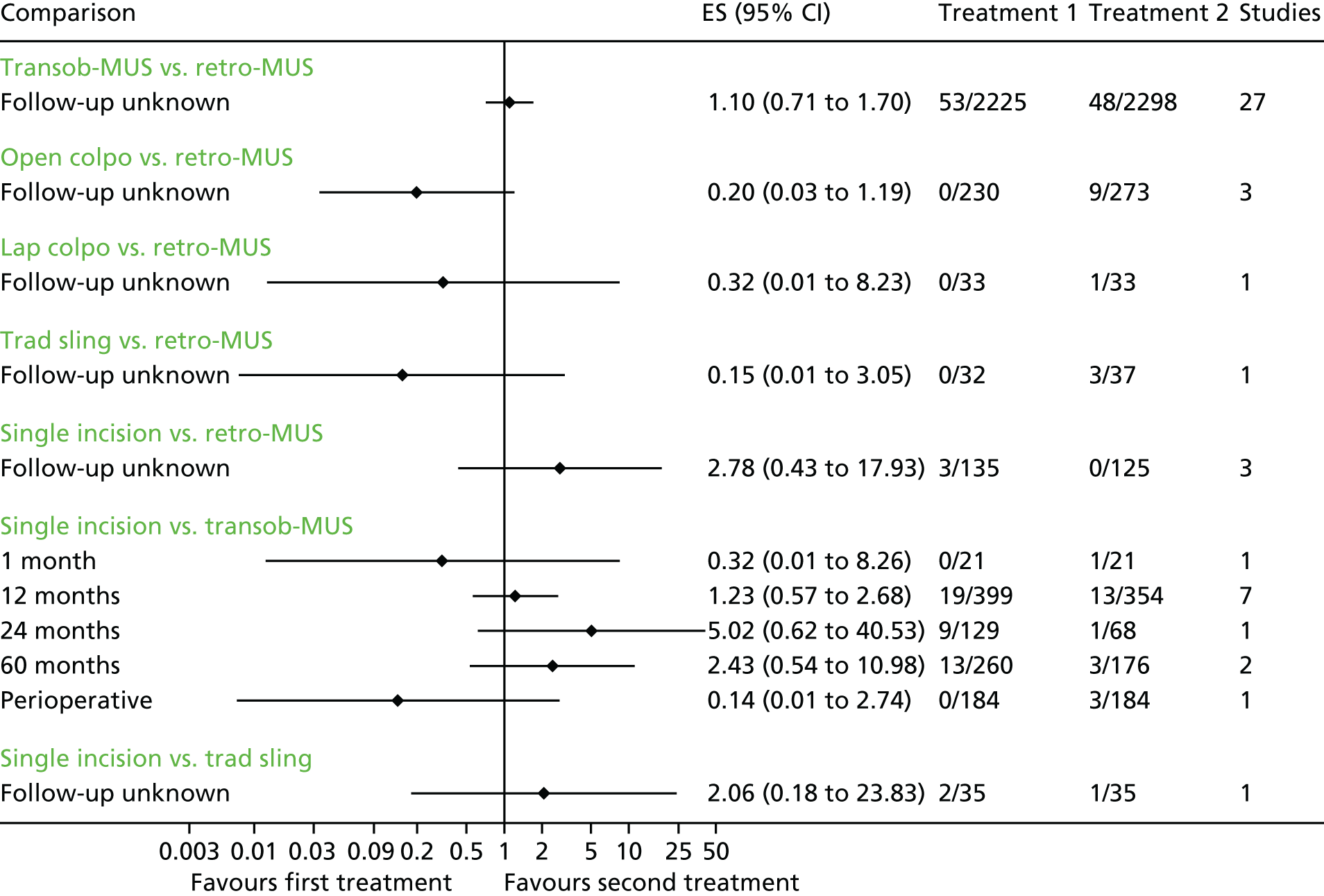
FIGURE 56.
Tape/mesh/implant exposure. ES, effect estimate (OR); retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
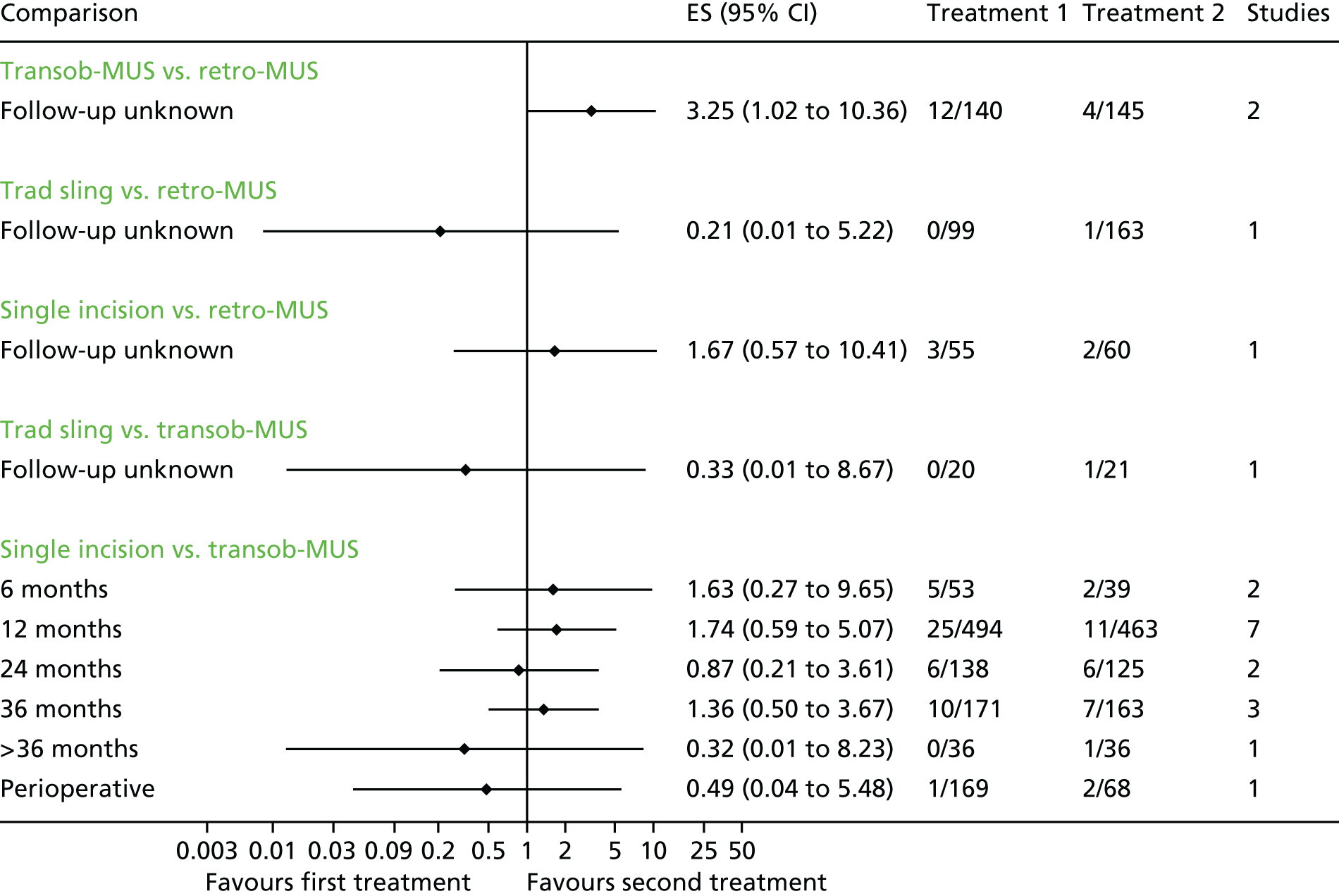
FIGURE 57.
Groin pain. ES, effect estimate (OR); open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
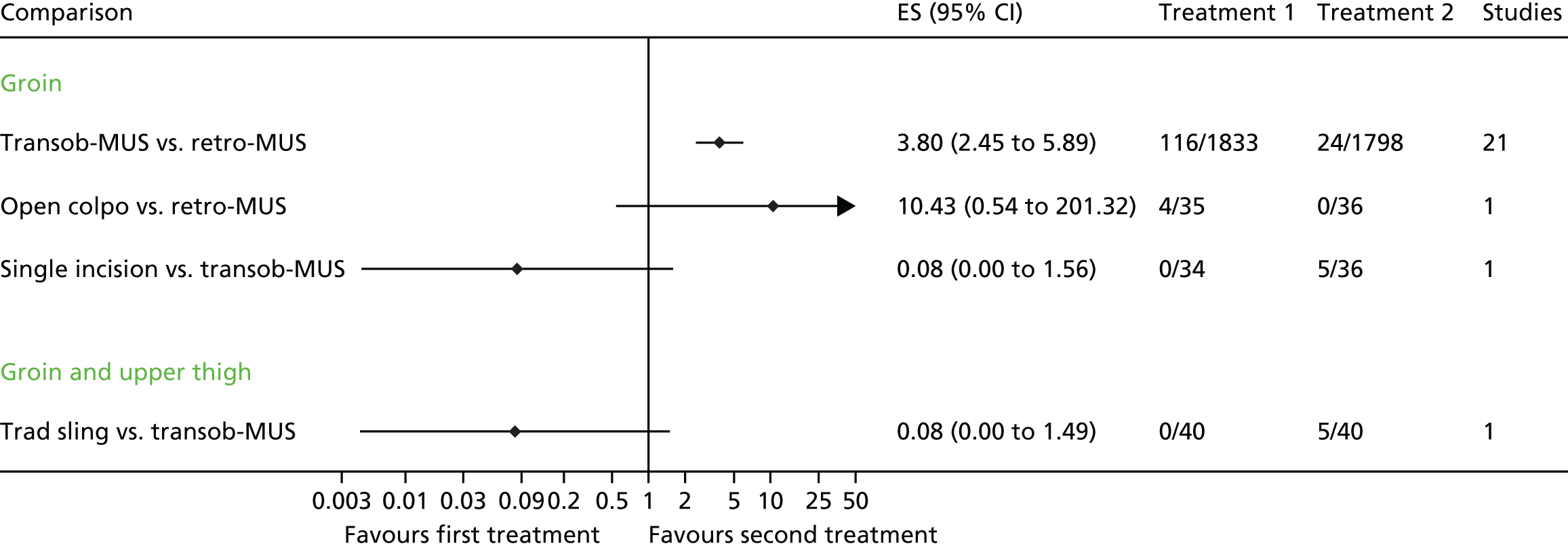
FIGURE 58.
Suprapubic pain. ES, effect estimate (OR); open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
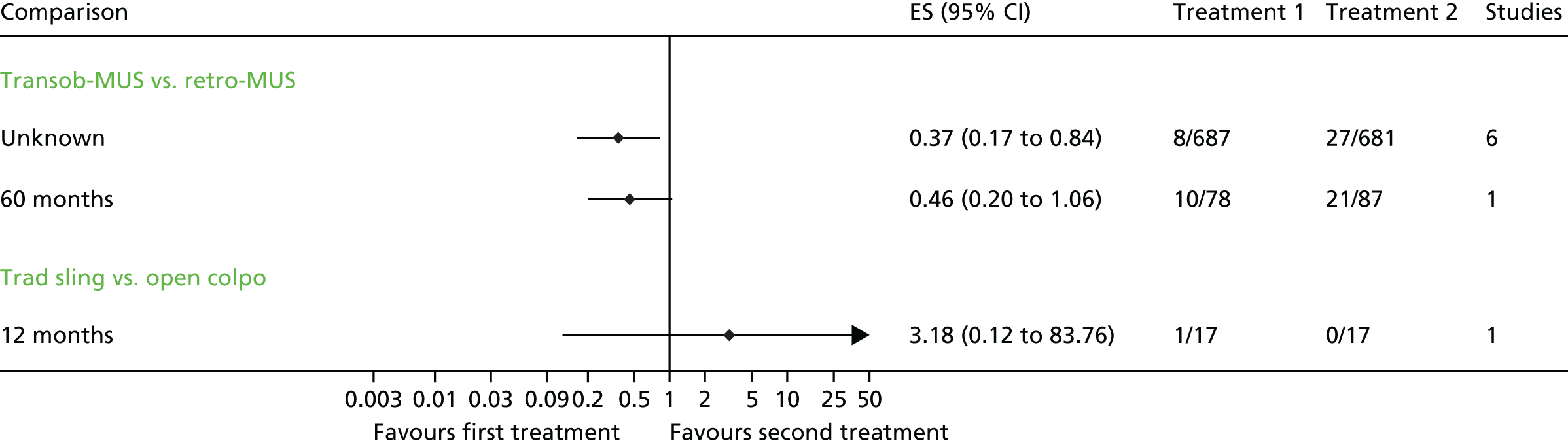
FIGURE 59.
Pain. ES, effect estimate (OR); retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; transob-MUS, transobturator mid-urethral sling.
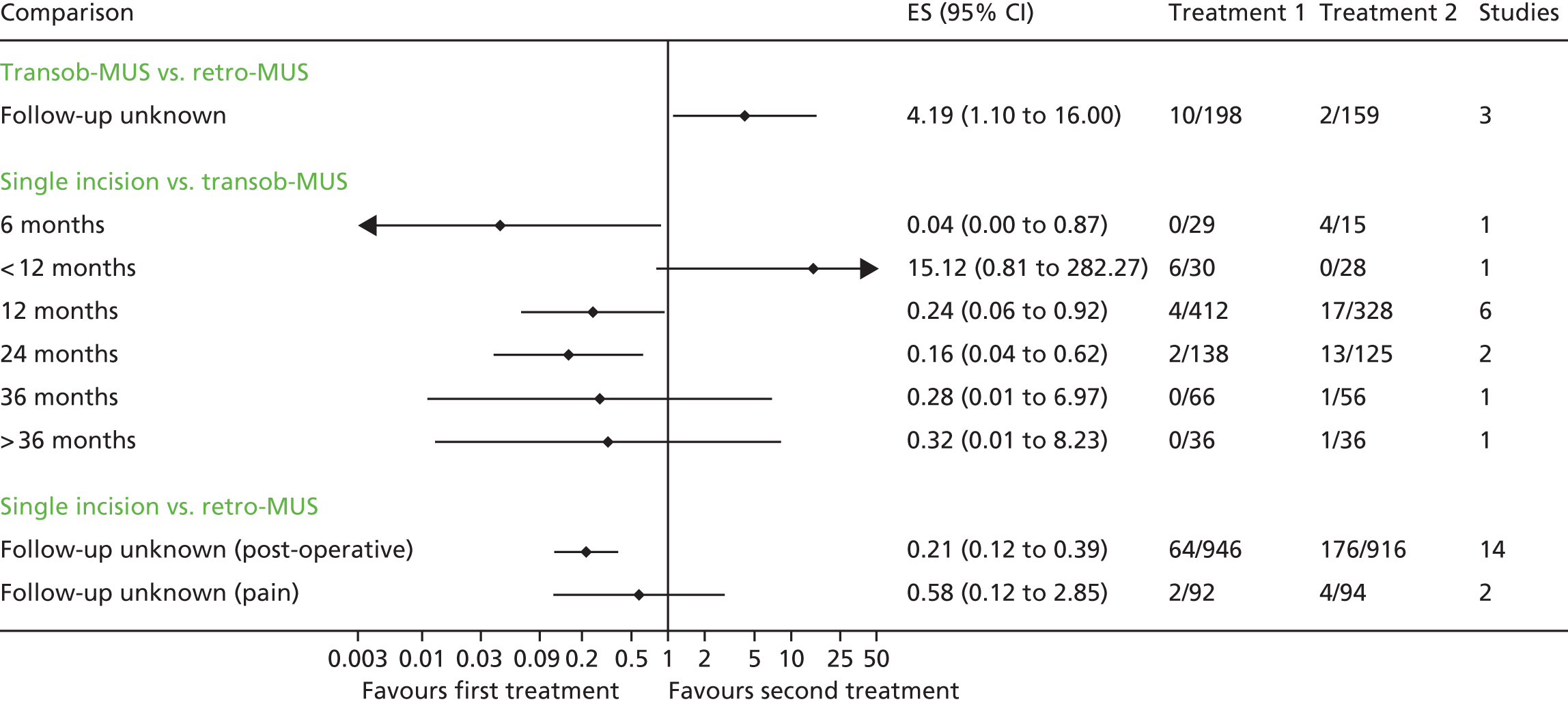
FIGURE 60.
Dyspareunia. Ant repair, anterior vaginal repair; ES, effect estimate (OR); open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
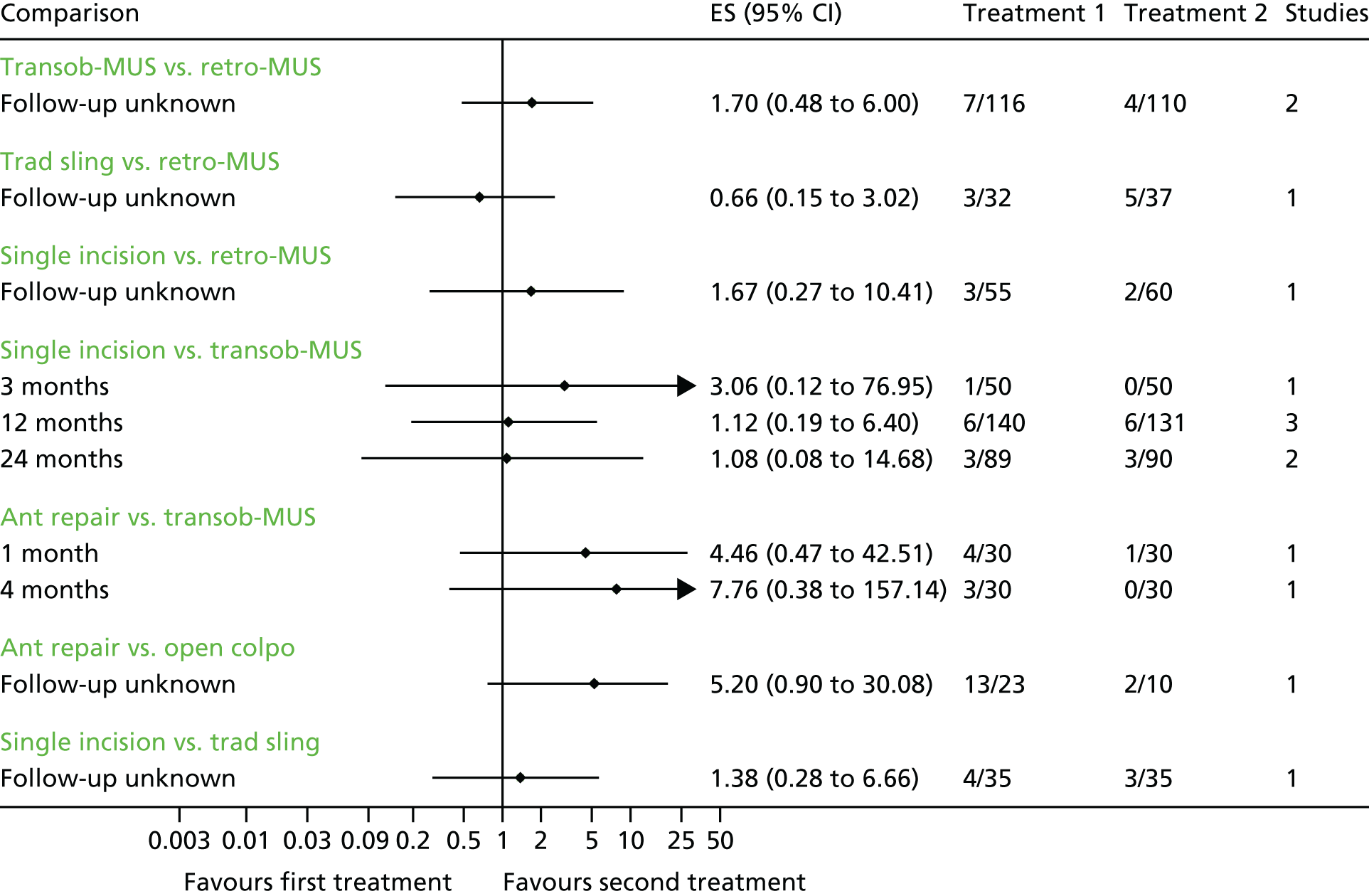
FIGURE 61.
Urinary tract infection. ES, effect estimate (OR); open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
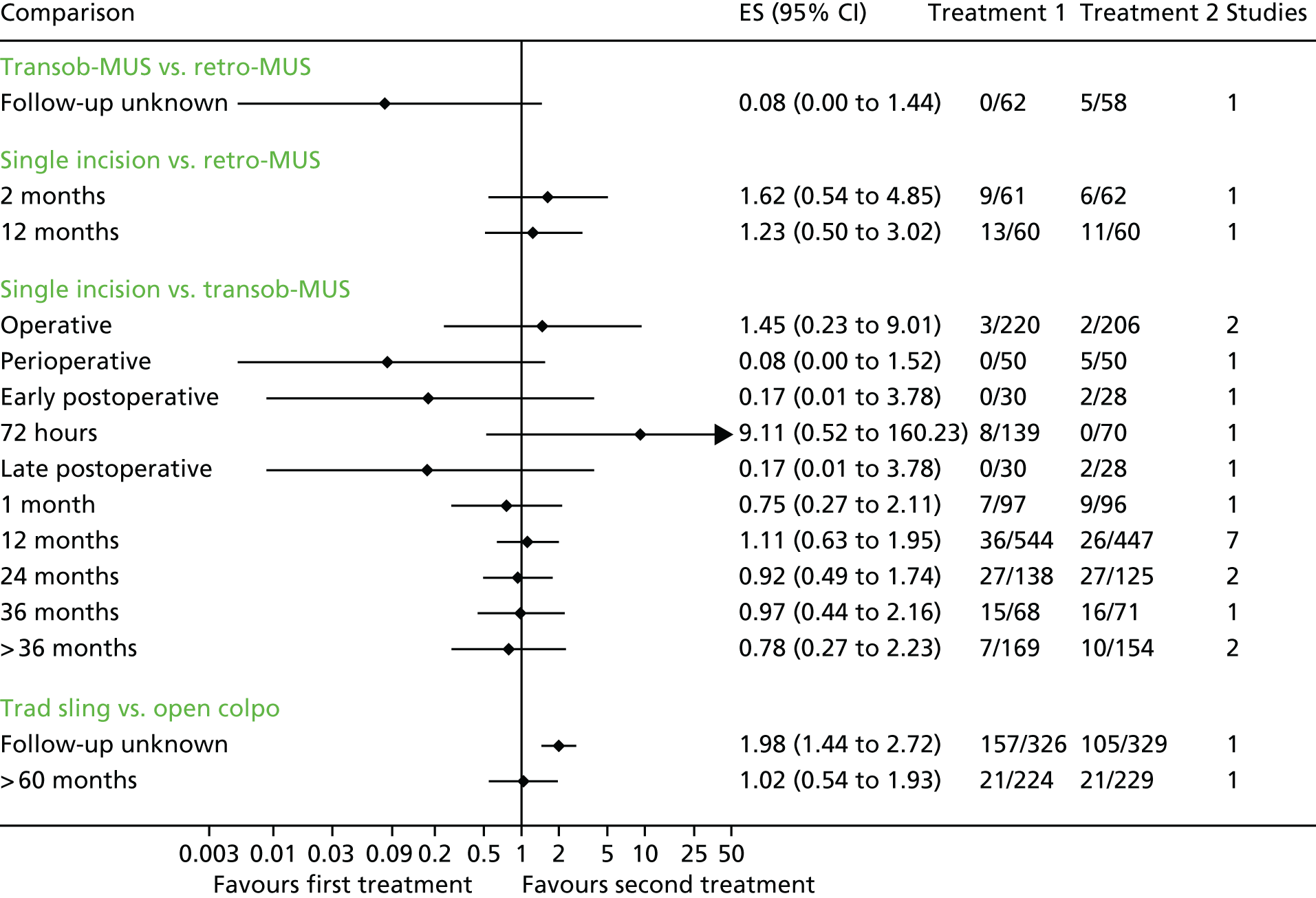
FIGURE 62.
Wound infection and infection related to use of synthetic mesh. ES, effect estimate (OR); retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; transob-MUS, transobturator mid-urethral sling.
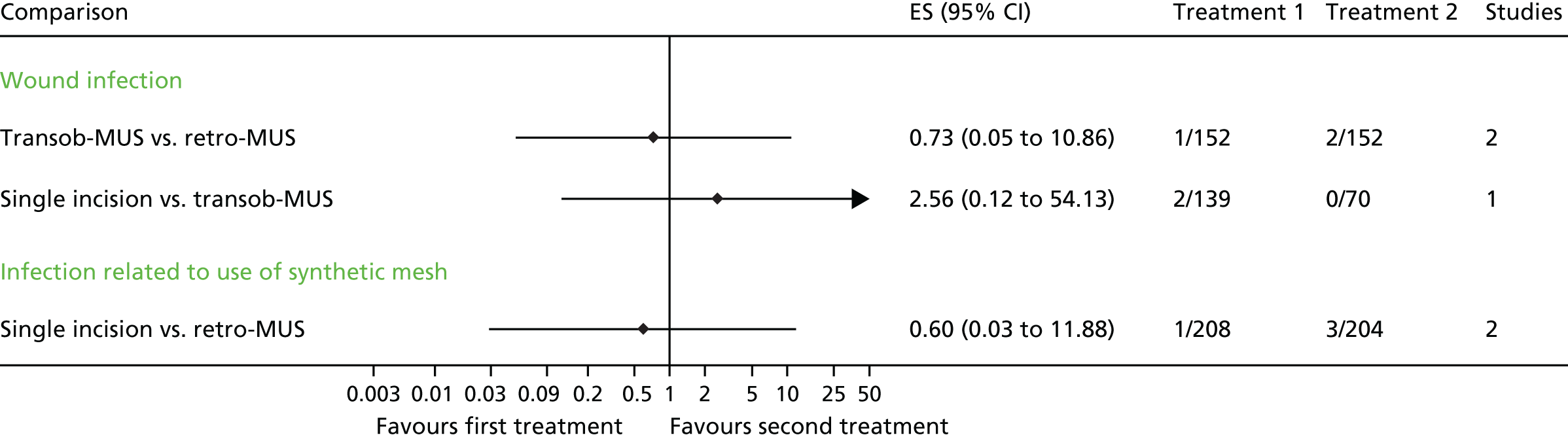
FIGURE 63.
Complications. Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle colposuspension; ES, effect estimate (OR); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
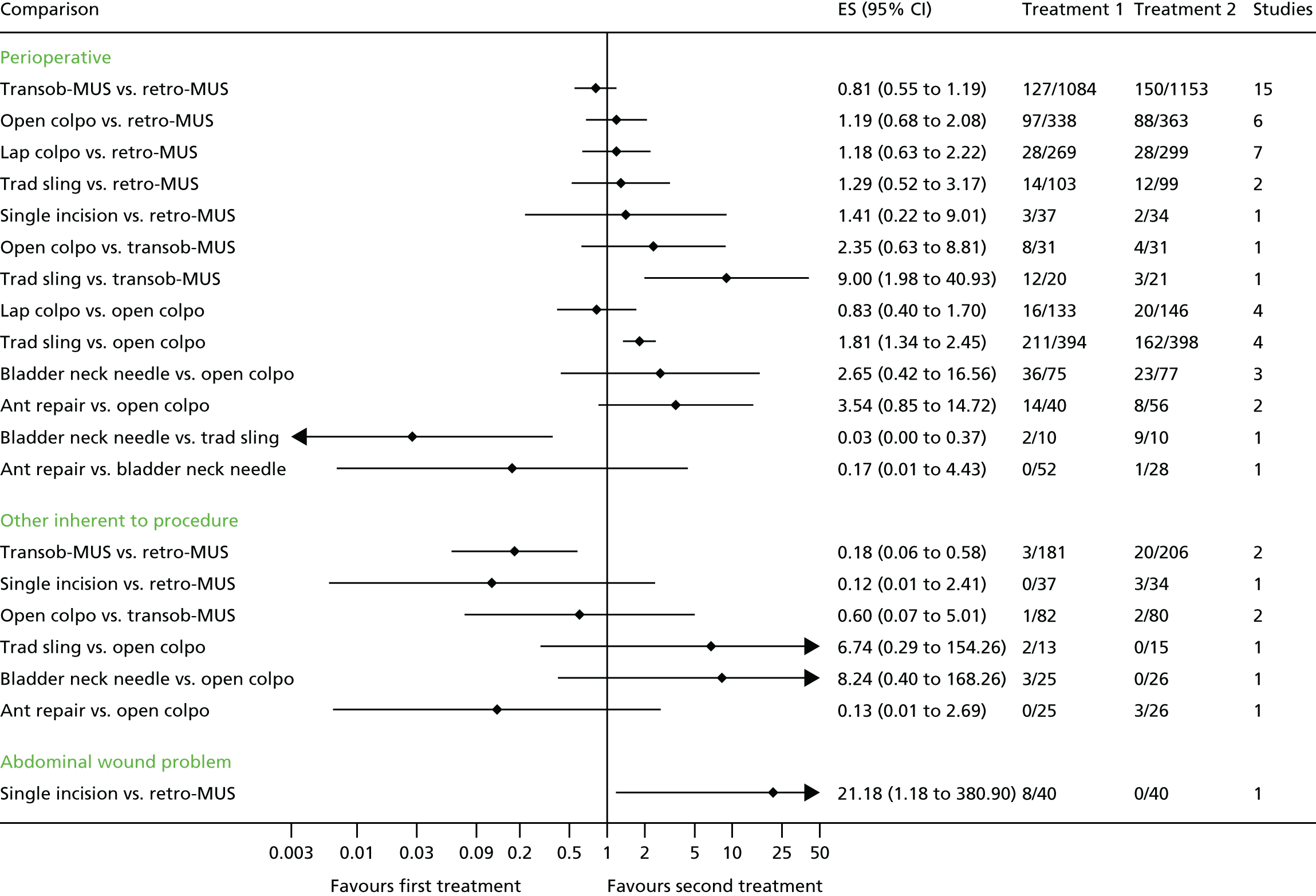
FIGURE 64.
Resource utilisation (hospital stay and operation time). Ant repair, anterior vaginal repair; bladder neck needle, bladder neck needle colposuspension; ES, effect estimate (standardised mean difference); lap colpo, laparoscopic colposuspension; open colpo, open colposuspension; retro-MUS, retropubic mid-urethral sling; single incision, single-incision sling; trad sling, traditional sling; transob-MUS, transobturator mid-urethral sling.
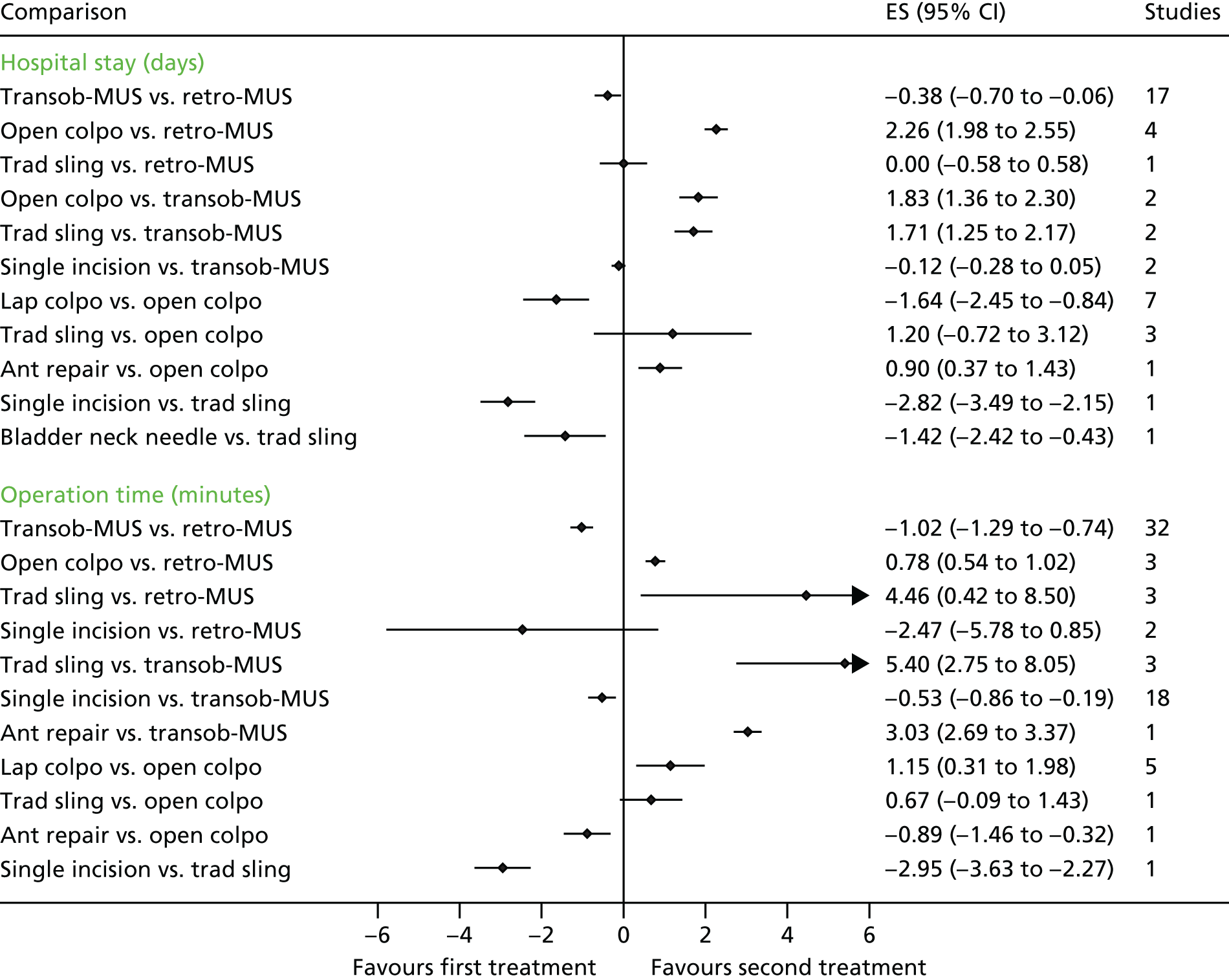
Appendix 16 Additional reports of trials identified by an updated search of the Cochrane Incontinence Group Specialised Register on 9 October 2017
| Citation for newly identified trial report | Sample size | Intervention | Notes |
|---|---|---|---|
| Extra reports of already included studies | |||
| Richter 201099 | |||
| Chai TC, Moalli PA, Richter HE, Lake AG, Kim H-Y, Nager CW, et al. Preoperative urodynamic parameters (Valsalva leak point pressure and maximum urethral closure pressure), urinary collagen and plasma vitamin D levels as predictors of mid urethral sling surgery outcome. J Urol 2016;196:819–23. [Ref ID: 77662] | This study report not relevant to ESTER | Retro-MUS vs. transob-MUS |
Extra report of the already included study: Richter 2010 [TOMUS (Trial of Midurethral Slings)] Design: RCT Trial registration number: NCT00325039 (Not directly relevant to the ESTER project) |
| Thomas TN, Siff LN, Jelovsek JE, Barber M. Surgical pain after transobturator and retropubic midurethral sling placement. Obstet Gynecol 2017;130:118–25. [Ref ID: 76639] | Pain at up to 24 months. Not clear how many participants in each arm contributed data at 24 months. At 6 months: transob-MUS, n = 276; retropubic-MUS, n = 274 | Retro-MUS vs. transob-MUS |
Extra report of the already included study: Richter 2010 (TOMUS) Design: RCT Trial registration number: NCT00325039 ‘At 24 months, seven participants in the transobturator group and four participants in the retropubic group reported any pain related to the incontinence operation’ Some labels missing from some of the tables, so not clear what some of the information is |
| Rudnicki 201672 | |||
| Rudnicki M, von Bothmer-Ostling K, Holstad A, Magnusson C, Majida M, Merkel C, et al. Adjustable mini-sling compared with conventional mid-urethral slings in women with urinary incontinence. A randomised controlled trial. Acta Obstet Gynecol Scand 2017;96:1347–56. [Ref ID: 76834] | At 12 months: single incision, n = 135; MUS, n = 129 | Single incision vs. MUS (either retro-MUS or transob-MUS) |
Full report of the already included study: Rudnicki 2016 (previously only two conference abstracts and a ClinicalTrials.gov registration were available) Design: RCT Trial registration number: NCT01754558 Intervention: single incision (Ajust) vs. MUS [either retro-MUS (TVT) or transob-MUS (TVT-O or Monarc)] Length of follow-up: 12 months |
| Aigmüller 201483 | |||
| Tammaa A, Aigmüller T, Hanzal E, Umek W, Kropshofer S, Lang PFJ, et al. Retropubic versus transobturator tension-free vaginal tape (TVT vs. TVT-O): five-year results of the Austrian randomized trial. Neurourol Urodyn 2018;37:331–8. [Ref ID: 76933] | Overall, 331 (58%) of operated patients were available for follow-up at 5 years (331 completed questionnaires, 277 were also examined clinically) | Retro-MUS (TVT) vs. transob-MUS (TVT-O) |
Extra report of the already included study: Aigmüller 2014 (full-text report of the 5-year follow-up; previously only available as a conference abstract) Design: RCT Trial registration number: NCT00441454 |
| Melendez Munoz 201665 | |||
| Melendez MJ, Braverman M, Rosamilia A, Young N, Leitch A, Lee J. Miniarc vs. TVT abbrevo midurethral sling in women with stress urinary incontinence – an RCT-6 and 12-month follow-up. Neurourol Urodyn 2017;36(Suppl. S3):S517–S519. [Ref ID: 77508] | At 12 months: single incision, n = 88; transob-MUS, n = 82 | Single incision (MiniArc) vs. transob-MUS (TVT Abbrevo) |
Extra conference abstract report of the already included new study: Melendez Munoz 2016 (only conference abstract available for inclusion) includes 6- and 12-month follow-up Design: RCT Trial registration number: ACTRN12611001151921 |
| Schellart 2013177 | |||
| Schellart RP, Zwolsman SE, Lucot JP, De Ridder DJMK, Dijkgraaf MGW, Roovers JWR. A randomized, nonblinded extension study of single-incision versus transobturator midurethral sling in women with stress urinary incontinence. Int Urogynecol J 2018;29:37–44. [Ref ID: 76921] | 71 patients (73%) in the MiniArc group and 74 patients (77%) in the Monarc group could be analyzed for subjective cure, and 75 (77%) and 75 (78%), respectively, for objective cure at 36 months | Single incision (MiniArc) vs. transob-MUS (Monarc) |
Extra report of the already included Schellart 2013 (full-text report of 36 months; previously only available as a conference abstract) Design: RCT Trial registration number: NTR3783 |
| Extra reports of studies listed in main report as ongoing | |||
| Abdel-Fattah 2014 | |||
| Abdel-Fattah M, MacLennan G, Kilonzo M, Assassa RP, McCormick K, Davidson T, et al. The SIMS trial: adjustable anchored single-incision mini-slings versus standard tension-free midurethral slings in the surgical management of female stress urinary incontinence. A study protocol for a pragmatic, multicentre, non-inferiority randomised controlled trial. BMJ Open 2017;7:e015111. [Ref ID: 76746] | Target, n = 650 (325 in each arm) | Single incision vs. MUS (retro-MUS or transob-MUS) |
Protocol for a study listed as ongoing study in the main ESTER report: Abdel-Fattah 2014 Design: RCT Trial registration number: ISRCTN93264234 Ages: ≥ 18 years Condition: ‘urodynamic stress incontinence or urodynamic MUI with predominant SUI bothering symptoms’ Recruitment start date: 4 February 2014 Follow-up end date: February 2020 Place: UK, 20 research centres Funding: Health Technology Assessment (HTA) Programme |
| Fu 2016 | |||
| Fu Q, Lv J, Fang W, Jiang C, Gu Y, Leng J, et al. The clinical efficacy of needleless sling technique and TOT in the treatment of female stress urinary incontinence: a prospective randomized controlled trial. Int J Clin Exp Med 2017;10:7084–90. [Ref ID: 77232] | At 12 months, data available: single incision, n = 78; transob-MUS, n = 86 | Single incision (needleless) vs. transob-MUS |
Full text report for the study listed as ongoing in the main ESTER report: Fu 2016 Design: RCT Trial registration number: ChiCTR-INR-16008068 Diagnosis: USI Ages: 35–70 years Place: Shanghai, China Funding: ‘SHDC1201591’ |
| New ongoing studies | |||
| Leitch A, Ow LL. Efficacy of mini sling versus retropubic sling in women with stress urinary incontinence – a RCT study (Mini Retro). 2017. Trial registration number: ACTRN12617000167369. URL: www.anzctr.org.au/ACTRN12617000167369.aspx (accessed 27 November 2017). [Ref ID: 76200] | Target sample size, n = 176 | Single incision (Altis) vs. retro-MUS (TVT) |
Design: RCT Trial registration number: ACTRN12617000167369 Recruitment start date: April 2017 Recruitment end date: April 2019 Diagnosis: USI Ages: 18–80 years Place: Monash Medical Centre, Australia Funding: Coloplast Corp. |
| Luo D, Shen H. Comparison of the efficacy and safety of TVT-EXACT vs. TVT-ABBREVO in the treatment of female stress urinary incontinence. 2017. Trial registration number: ChiCTR-IOR-17011788. URL: www.chictr.org.cn/showproj.aspx?proj = 20086 (accessed 27 November 2017). [Ref ID: 76204] | Target, n = 150 (75 each arm) | Retro-MUS (TVT-Exact) vs. transob-MUS (TVT-Abbrevo) |
Design: RCT Trial registration number: ChiCTR-IOR-17011788 Recruitment start date: 1 April 2015 Recruitment end date: 31 October 2018 Ages: 40–75 years Place: Chengdu, China Funding: National Nature Science Foundation of China |
Appendix 17 Economic search strategy
| Number | Search term | Facet | Results |
|---|---|---|---|
| MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations | |||
| 1 | exp models, economic/ | Economic evaluations | 12,189 |
| 2 | *models, theoretical/ | 50,817 | |
| 3 | *models, organizational/ | 5483 | |
| 4 | Markov chains/ | 11,679 | |
| 5 | monte carlo method/ | 23,376 | |
| 6 | exp decision theory/ | 10,620 | |
| 7 | (Markov* or monte carlo).ti,ab. | 49,644 | |
| 8 | econom* model*.ti,ab. | 2789 | |
| 9 | (decision* adj2 (tree* or analy* or model*)).ti,ab. | 16,267 | |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 | 145,603 | |
| 11 | URINARY INCONTINENCE/ | Disease | 19,864 |
| 12 | URINARY INCONTINENCE, STRESS/ | 10,063 | |
| 13 | ((stress$or mix$or urg$or urin$) adj3 incontinen$).tw. | 25,719 | |
| 14 | colporrhaphy.tw. | 519 | |
| 15 | colpoperineoplast$.tw. | 28 | |
| 16 | Sling procedure$.tw. | 898 | |
| 17 | Sling$procedure$.tw. | 905 | |
| 18 | Bladder neck needle suspensions suspension$.tw. | 7 | |
| 19 | Anterior vaginal repair$.tw. | 45 | |
| 20 | 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 | 37,510 | |
| 21 | 10 and 20 | Final numbers | 139 |
| EMBASE | |||
| 1 | URINE INCONTINENCE/ | Disease | 41,326 |
| 2 | STRESS INCONTINENCE/ | 19,497 | |
| 3 | URGE INCONTINENCE/ | 6053 | |
| 4 | MIXED INCONTINENCE/ | 1624 | |
| 5 | ((stress$or mix$or urg$or urin$) adj3 incontinen$).tw. | 39,155 | |
| 6 | URINARY URGENCY/ | 5368 | |
| 7 | URINARY FREQUENCY/ | 6154 | |
| 8 | ((urgency adj frequency) or (frequency adj urgency)).tw. | 1930 | |
| 9 | ((urinary adj frequency) or (urinary adj urgency)).tw. | 3722 | |
| 10 | colporrhaphy.tw. | 948 | |
| 11 | colposuspension$.tw. | 1337 | |
| 12 | Sling procedure$.tw. | 1554 | |
| 13 | Sling$procedure$.tw. | 1572 | |
| 14 | Bladder neck needle suspensions suspension$.tw. | 7 | |
| 15 | Anterior vaginal repair$.tw. | 83 | |
| 16 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 | 69,648 | |
| 17 | statistical model/ | Economic evaluations | 149,789 |
| 18 | exp economic aspect/ | 1,386,763 | |
| 19 | 17 and 18 | 21,900 | |
| 20 | *theoretical model/ | 27,446 | |
| 21 | *nonbiological model/ | 4142 | |
| 22 | stochastic model/ | 9838 | |
| 23 | decision theory/ | 2696 | |
| 24 | decision tree/ | 9013 | |
| 25 | monte carlo method/ | 30,151 | |
| 26 | (Markov* or monte carlo).ti,ab. | 52,002 | |
| 27 | econom* model*.ti,ab. | 4018 | |
| 28 | (decision* adj2 (tree* or analy* or model*)).ti,ab. | 22,474 | |
| 29 | 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 | 144,098 | |
| 30 | 16 and 29 | Final numbers | 269 |
| NHS Economic Evaluation | |||
| 1 | URINARY INCONTINENCE/ | Disease | 31 |
| 2 | URINARY INCONTINENCE, STRESS/ | 34 | |
| 3 | ((stress$or mix$or urg$or urin$) adj3 incontinen$).tw. | 97 | |
| 4 | colporrhaphy.tw. | 3 | |
| 5 | colpoperineoplast$.tw. | 0 | |
| 6 | sling procedure$.tw. | 4 | |
| 7 | sling$procedure$.tw. | 4 | |
| 8 | Bladder neck needle suspensions suspension$.tw. | 0 | |
| 9 | anterior vaginal repair$.tw. | 0 | |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 | Final numbers | 100 |
| Health Management Information Consortium | |||
| 1 | URINARY INCONTINENCE/ | Disease | 110 |
| 2 | URINARY INCONTINENCE, STRESS/ | 0 | |
| 3 | ((stress$or mix$or urg$or urin$) adj3 incontinen$).tw. | 174 | |
| 4 | colporrhaphy.tw. | 0 | |
| 5 | colpoperineoplast$.tw. | 0 | |
| 6 | Sling procedure$.tw. | 0 | |
| 7 | Sling$procedure$.tw. | 0 | |
| 8 | Bladder neck needle suspensions suspension$.tw. | 0 | |
| 9 | Anterior vaginal repair$.tw. | 0 | |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 | Final numbers | 220 |
| Cost-effectiveness Analysis Registry | |||
| 1 | URINARY INCONTINENCE | Disease | 32 |
| 2 | STRESS URINARY INCONTINENCE | 14 | |
| 3 | Mixed incontinence | 1 | |
| 4 | URINARY | 72 | |
| 5 | Incontinent | 3 | |
| 6 | colporrhaphy | 0 | |
| 7 | olposuspension | 6 | |
| 8 | sling procedure | 1 | |
| 9 | Bladder neck needle suspensions suspension | 0 | |
| 10 | anterior vaginal repair | 0 | |
| 11 | Sling | 14 | |
| 12 | Incontinence | 50 | |
| 13 | or/1–12 | Final numbers | 93 |
| Database | Numbers retrieved |
|---|---|
| MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations | 139 |
| EMBASE | 269 |
| NHS Economic Evaluation Database | 100 |
| Health Management Information Consortium | 220 |
| Cost-effectiveness Analysis Registry | 93 |
| Total | 821 |
Appendix 18 Quality assessment of economic studies
Quality assessment of the economic studies evaluating surgical treatments for SUI using the Drummond checklist. 338
| Item | Study | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Von Bargen 2015226 | Jacklin 2010228 | Kilonzo 2004229 | Laudano 2013230 | Richardson 2014233 | Sand 2014234 | Seklehner 2014235 | Weber 2000236 | Wu 2007237 | Oremus 2010232 | Oremus 2003231 | Kunkle 2015225 | Das Gupta 2006227 | Holtzer-Goor 2015238 | Weber 2000239 | Weber 2002240 | Imamura 2010241 | |
| 1. Was a well-defined question posed in answerable form? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 1.1. Did the study examine both costs and effects of the service(s) or programme(s)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 1.2. Did the study involve a comparison of alternatives? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 1.3. Was a viewpoint for the analysis stated and was the study placed in any particular decision-making context? | Yes | Yes | Yes | No | Yes | Yes | Yes | NC | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No |
| 2. Was a comprehensive description of the competing alternatives given (i.e. can you tell who did what to whom, where and how often)? | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2.1. Were there any important alternatives omitted? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 2.2. Was (should) a do-nothing alternative be considered? | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| 3. Was the effectiveness of the programme or services established? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3.1. Was this done through a randomised controlled clinical trial? If so, did the trial protocol reflect what would happen in regular practice? | No | No | No | No | Yes | No | No | No | No | Yes | No | No | Yes | No | No | No | No |
| 3.2. Was effectiveness established through an overview of clinical studies? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes |
| 3.3. Were observational data or assumptions used to establish effectiveness? If so, what are the potential biases in results? | No | No | No | No | Yes | No | No | No | Yes | No | No | Yes | Yes | Yes | No | No | No |
| 4. Were all the important and relevant costs and consequences for each alternative identified? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4.1. Was the range wide enough for the research question at hand? | NC | NC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | NC | Yes | NC | Yes | Yes | Yes |
| 4.2. Did it cover all relevant viewpoints? (Possible viewpoints include the community or social viewpoint, and those of patients and third-party payers. Other viewpoints may also be relevant depending on the particular analysis.) | Yes | No | No | NC | No | No | No | Yes | No | No | No | No | No | Yes | Yes | Yes | No |
| 4.3. Were the capital costs, as well as operating costs, included? | Yes | Yes | No | No | No | No | No | Yes | No | No | No | No | Yes | Yes | Yes | Yes | Yes |
| 5. Were costs and consequences measured accurately in appropriate physical units (e.g. hours of nursing time, number of physician visits, lost work-days, gained life-years)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 5.1. Were any of the identified items omitted from measurement? If so, does this mean that they carried no weight in the subsequent analysis? | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| 5.2. Were there any special circumstances (e.g. joint use of resources) that made measurement difficult? Were these circumstances handled appropriately? | No | No | No | No | No | No | No | No | No | No | Yes | Yes | No | No | No | No | No |
| 6. Were the cost and consequences valued credibly? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6.1. Were the sources of all values clearly identified? (Possible sources include market values, patient or client preferences and views, policy-makers’ views and health professionals’ judgements.) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 6.2. Were market values employed for changes involving resources gained or depleted? | N/A | N/A | No | Yes | N/A | No | Yes | Yes | Yes | Yes | No | No | No | Yes | N/A | N/A | N/A |
| 6.3. Where market values were absent (e.g. volunteer labour), or market values did not reflect actual values (such as clinic space donated at a reduced rate), were adjustments made to approximate market values? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 6.4. Was the valuation of consequences appropriate for the question posed (i.e. has the appropriate type or types of analysis – cost-effectiveness, cost–benefit, cost–utility – been selected)? | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | No | Yes |
| 7. Were costs and consequences adjusted for differential timing? | Yes | Yes | Yes | Yes | N/A | Yes | Yes | NC | Yes | N/A | N/A | N/A | Yes | NC | N/A | N/A | Yes |
| 7.1. Were costs and consequences that occur in the future ‘discounted’ to their present values? | Yes | Yes | Yes | Yes | N/A | Yes | Yes | NC | Yes | N/A | N/A | N/A | Yes | NC | N/A | N/A | Yes |
| 7.2. Was there any justification given for the discount rate used? | No | Yes | No | Yes | N/A | No | Yes | N/A | Yes | N/A | N/A | N/A | No | No | N/A | N/A | Yes |
| 8. Was an incremental analysis of costs and consequences of alternatives performed? | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8.1. Were the additional (incremental) costs generated by one alternative over another compared with the additional effects, benefits or utilities generated? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Was allowance made for uncertainty in the estimates of costs and consequences? | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | No | Yes |
| 9.1. If data on costs and consequences were stochastic (randomly determined sequence of observations), were appropriate statistical analyses performed? | NC | No | Yes | Yes | No | N/A | Yes | N/A | N/A | Yes | No | Yes | Yes | Yes | No | No | Yes |
| 9.2. If a sensitivity analysis was employed, was justification provided for the range of values (or for key study parameters)? | Yes | No | No | No | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 9.3. Were the study results sensitive to changes in the values (within the assumed range for sensitivity analysis, or within the confidence interval around the ratio of costs to consequences)? | NC | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes |
| 10. Did the presentation and discussion of study results include all issues of concern to users? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| 10.1. Were the conclusions of the analysis based on some overall index or ratio of costs to consequences (e.g. cost-effectiveness ratio)? If so, was the index interpreted intelligently or in a mechanistic fashion? | Yes | Yes | Yes | Yes | Yes | N/A | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10.2. Were the results compared with those of others who have investigated the same question? If so, were allowances made for potential differences in study methodology? | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10.3. Did the study discuss the generalisability of the results to other settings and patient/client groups? | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | No |
| 10.4. Did the study allude to, or take account of, other important factors in the choice or decision under consideration (e.g. distribution of costs and consequences, or relevant ethics issues)? | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | Yes |
| 10.5. Did the study discuss issues of implementation, such as the feasibility of adopting the ‘preferred’ programme given existing financial or other constraints, and whether or not any freed resources could be redeployed to other worthwhile programmes? | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
Appendix 19 Economic model structure
FIGURE 65.
Economic model structure. AVR, anterior vaginal repair (anterior colporrhaphy); BNNS, bladder neck needle suspension; LRC, laparoscopic retropubic colposuspension; MUS, mid-urethral sling; OARC, open abdominal retropubic colposuspension; PUI, periurethral injection (injectable bulking agents); RMUS, retropubic mid-urethral sling; TMUS, transobturator mid-urethral sling; TSRS, traditional suburethral retropubic sling procedures; SISP, single-incision sling procedure.
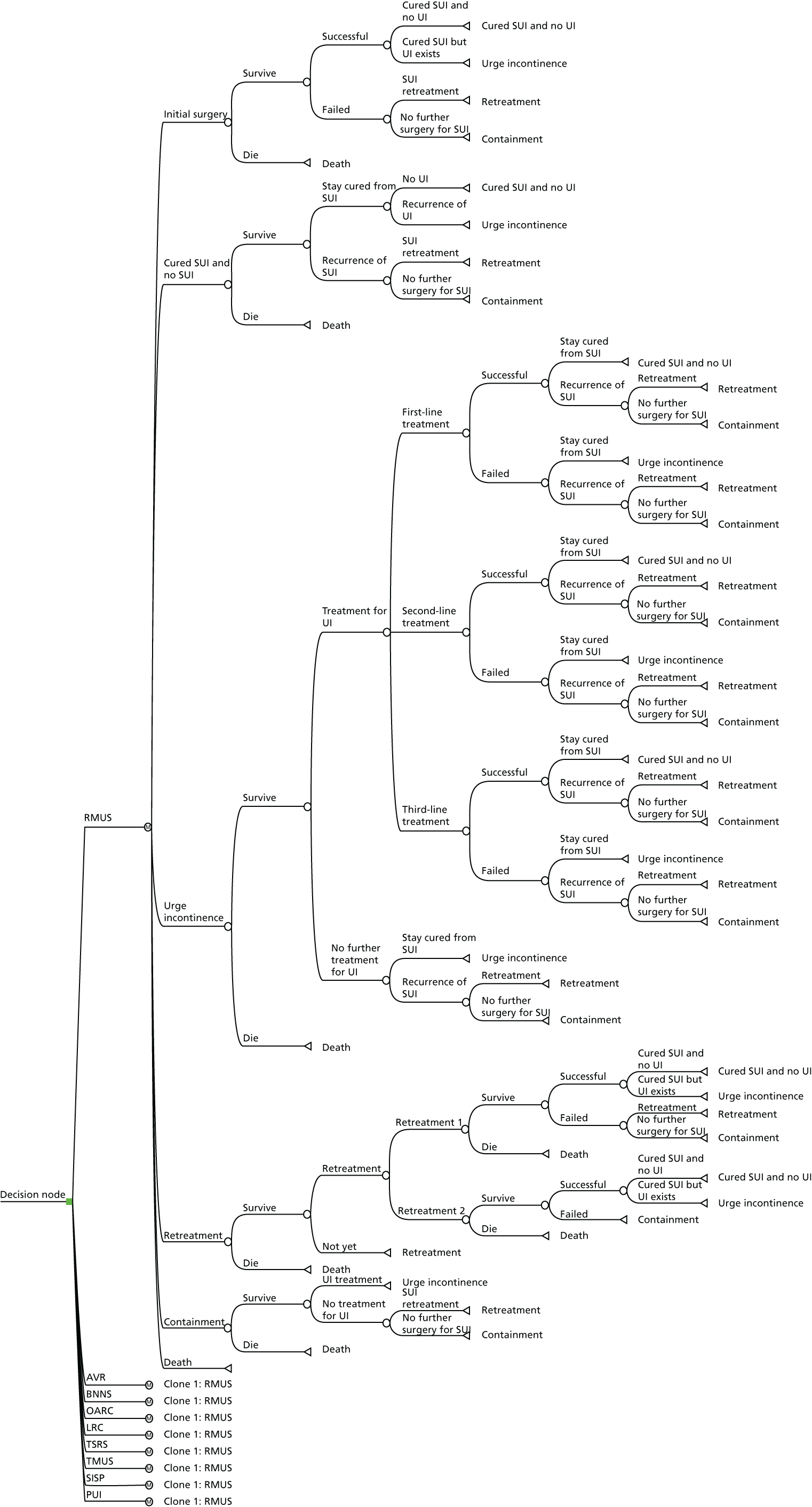
Appendix 20 Results of database analysis
Tables 36 and 37 and Figure 66 provide the results from analysing data from AMND.
| SUI operation | Number of SUI surgery | Total | |||
|---|---|---|---|---|---|
| One (%) | Two (%) | Three (%) | Four (%) | ||
| Abdominal retropubic procedure | 285 (89.0) | 28 (9.0) | 5 (2.0) | 1 (0.3) | 319 |
| MUS | 331 (97.0) | 10 (3.0) | 1 (0.3) | 0 (0.0) | 342 |
| Colporrhaphy | 66 (83.0) | 13 (16.0) | 1 (1.0) | 0 (0.0) | 80 |
| Urethral injection therapy | 5 (5.0) | 2 (20.0) | 2 (20.0) | 1 (10.0) | 10 |
| Total | 687 | 53 | 9 | 2 | 751 |
| Model | Obs | ll (null) | ll (model) | df | AIC | BIC |
|---|---|---|---|---|---|---|
| Exponential | 750 | –302.621 | –291.366 | 4 | 590.7 | 609.2 |
| Gompertz | 750 | –298.106 | –286.081 | 5 | 582.2 | 605.3 |
| Log-logistic | 750 | –297.233 | –285.114 | 5 | 580.2 | 603.3 |
| Log-normal | 750 | –295.889 | –284.734 | 5 | 579.5 | 602.6 |
| Weibull | 750 | –297.391 | –286.166 | 5 | 582.3 | 605.4 |
FIGURE 66.
Fitted vs. observed survival in data from AMND. K–M, Kaplan–Meier.
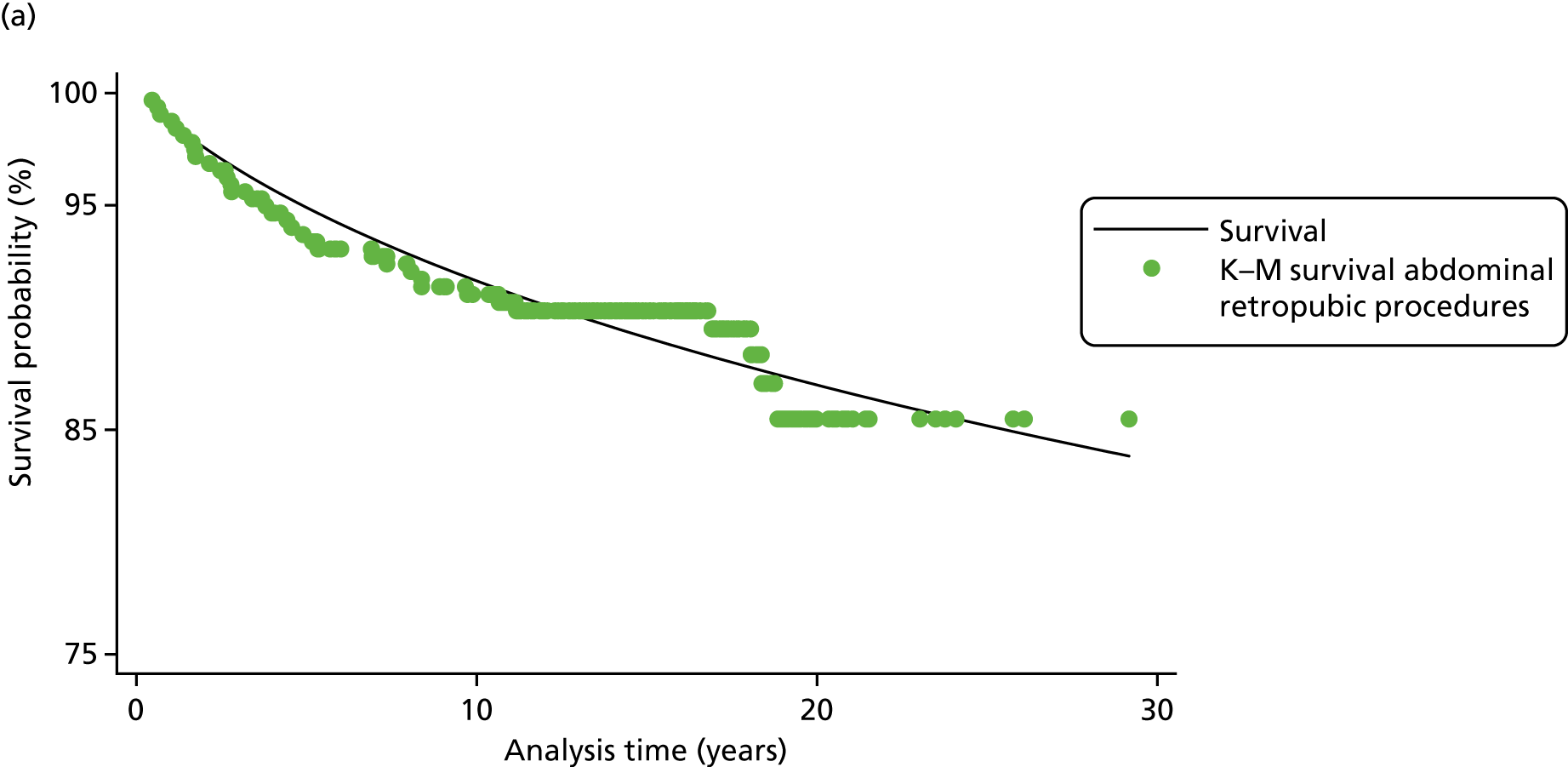
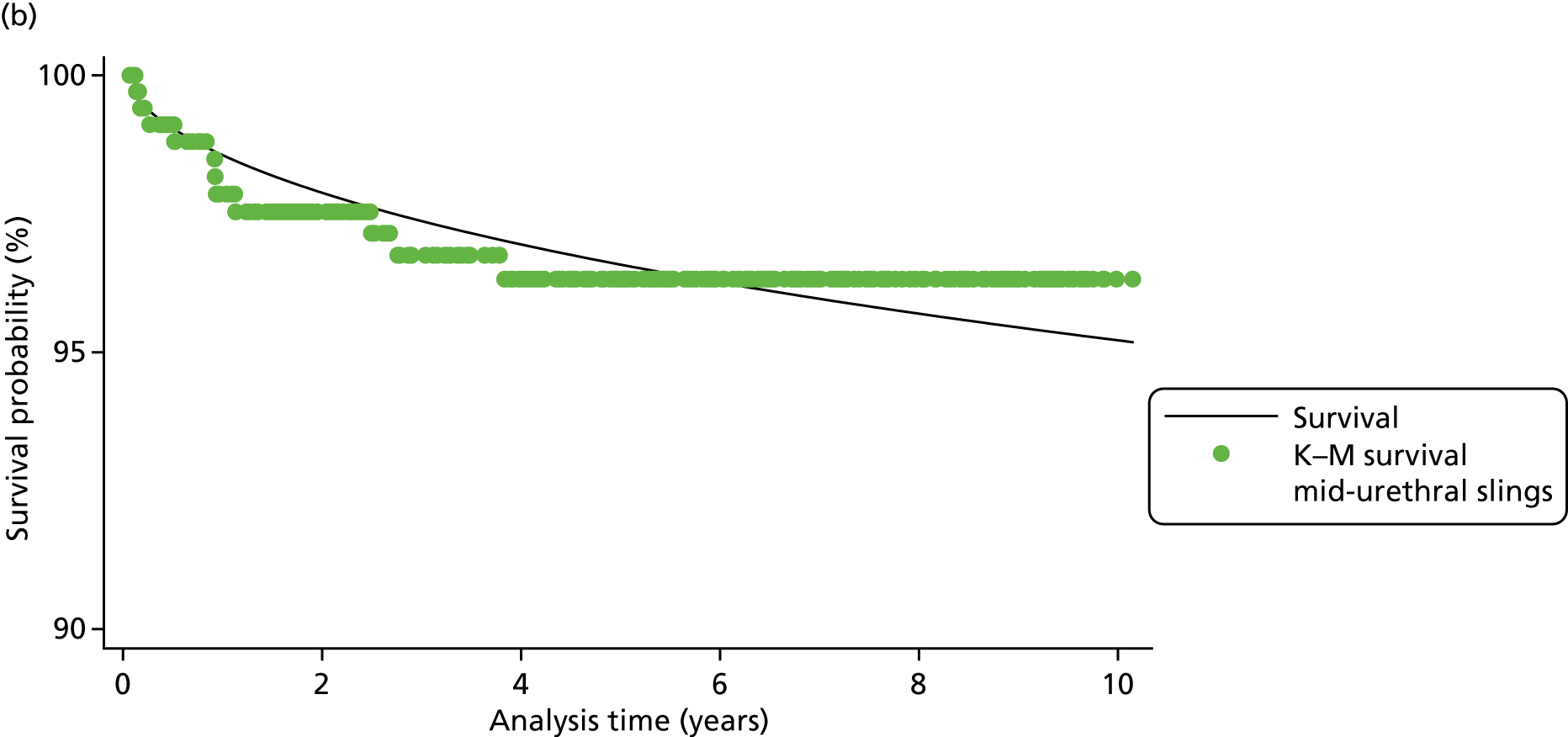
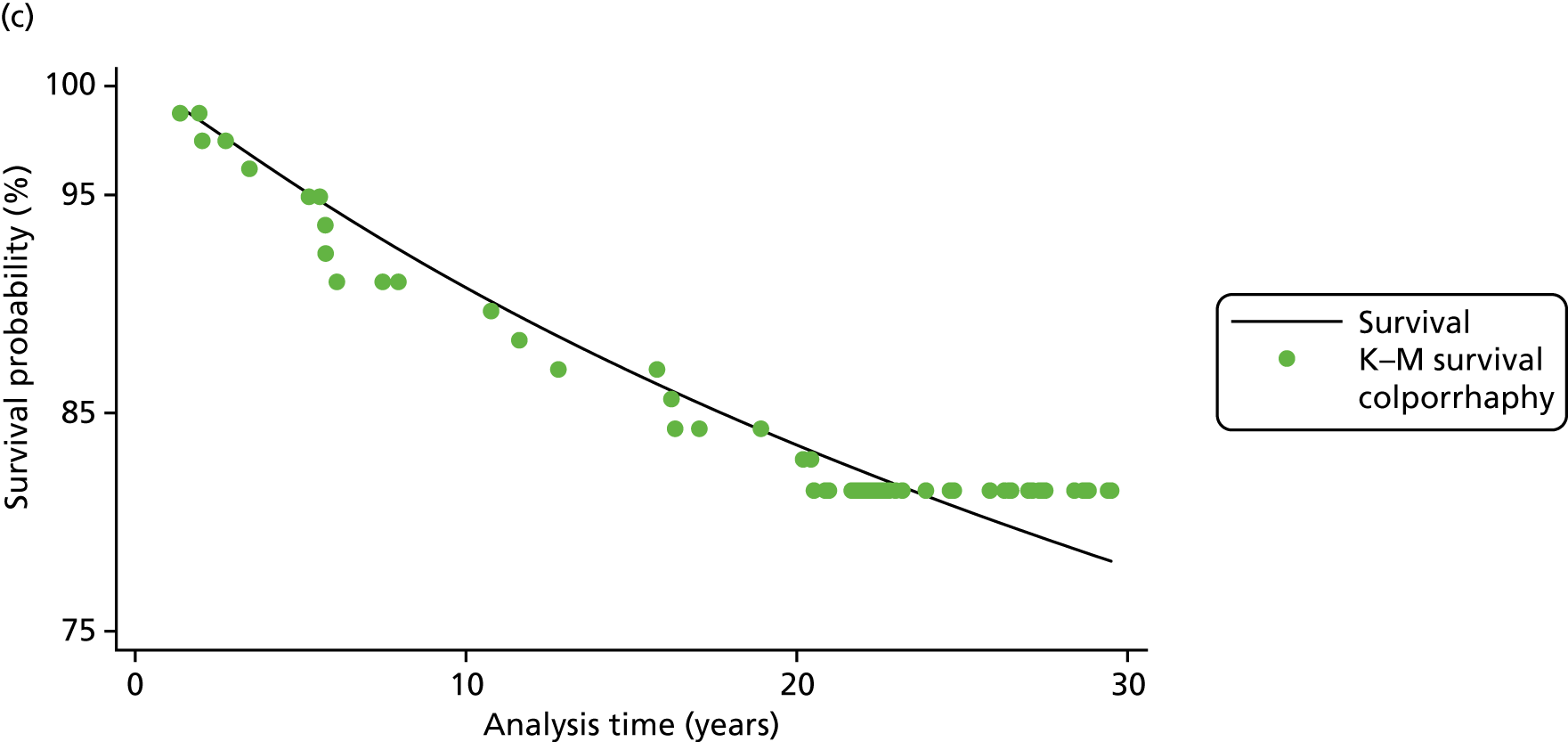
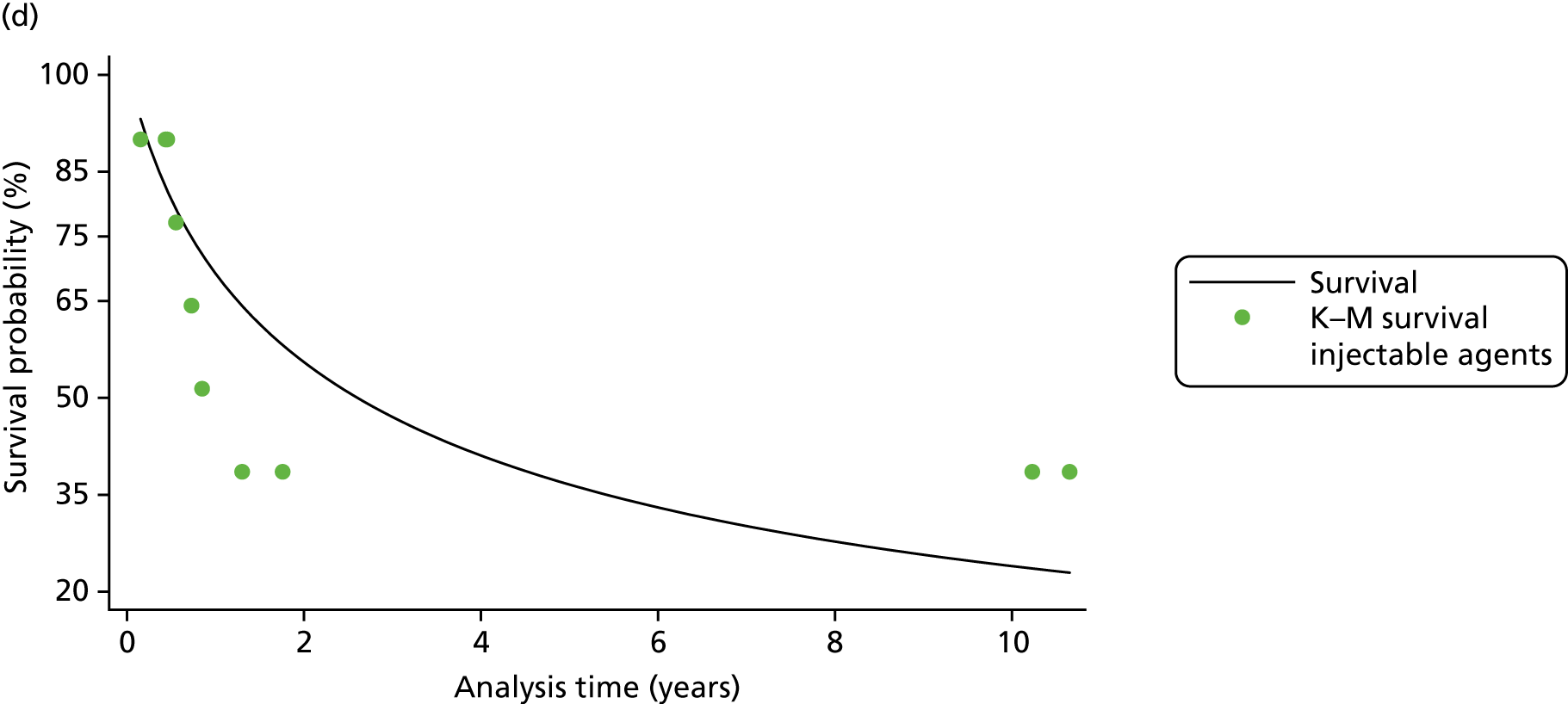
Appendix 21 Deterministic sensitivity analyses
Assuming that all women in the model have stress urinary incontinence
The results from this SA, in which it is assumed that all women in the model have SUI, show that, compared with the base-case analysis, all strategies have a lower total cost and greater effectiveness (Table 39). Retropubic MUS remains the least costly strategy compared with the alternative surgical interventions but traditional sling is the most cost-effective option with an ICER of £8024 per QALY gained. Table 40 shows that the probability of being cost-effective with a £20,000 WTP was 25.5% and 31.0% for retropubic MUS and traditional sling, respectively.
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective for different threshold (%) | |
|---|---|---|---|---|---|---|---|
| £20,000 | £30,000 | ||||||
| Base-case analysis: 52% of the women in the model have SUI and 48% have MUI | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA assuming all women in the model have SUI | |||||||
| Retropubic MUS | 5282 | 25.11 | 32.1 | 30.5 | |||
| Traditional sling | 5668 | 385 | 25.16 | 0.05 | 8024 | 36.9 | 36.2 |
| Transobturator MUS | 7820 | 2153 | 24.22 | –0.94 | Dominated | 1.9 | 1.9 |
| Urethral injection therapy | 7947 | 2280 | 24.34 | –0.81 | Dominated | 5.8 | 6.1 |
| Single-incision sling | 8220 | 2553 | 23.94 | –1.22 | Dominated | 1.0 | 1.1 |
| Open colposuspension | 8498 | 2831 | 24.87 | –0.29 | Dominated | 14.9 | 16.0 |
| Bladder neck needle suspension | 8648 | 2980 | 24.09 | –1.06 | Dominated | 2.6 | 2.7 |
| Laparoscopic colposuspension | 9877 | 4209 | 24.39 | –0.77 | Dominated | 3.9 | 4.4 |
| Anterior vaginal repair | 9971 | 4303 | 23.80 | –1.36 | Dominated | 1.0 | 1.2 |
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective for different threshold (%) | |
|---|---|---|---|---|---|---|---|
| £20,000 | £30,000 | ||||||
| Base-case analysis: 75% of women whose first treatment was not successful would seek retreatment and 30% of women whose first retreatment failed would seek second retreatment | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA using data from the linked database analysis to estimate proportion of the women who will seek retreatment after failure of each surgical treatment | |||||||
| Retropubic MUS | 8067 | 24.03 | 25.5 | 24.2 | |||
| Traditional sling | 8477 | 410 | 24.08 | 0.05 | 8114 | 31.0 | 30.0 |
| Transobturator MUS | 9472 | 995 | 23.48 | –0.60 | Dominated | 3.9 | 4.0 |
| Single-incision sling | 9587 | 1110 | 23.28 | –0.81 | Dominated | 1.9 | 1.9 |
| Urethral injection therapy | 9602 | 1125 | 23.74 | –0.35 | Dominated | 14.4 | 14.7 |
| Bladder neck needle suspension | 10,134 | 1657 | 23.35 | –0.73 | Dominated | 3.1 | 3.2 |
| Open colposuspension | 10,937 | 2460 | 23.89 | –0.19 | Dominated | 13.7 | 14.8 |
| Anterior vaginal repair | 11,045 | 2568 | 23.18 | –0.90 | Dominated | 1.4 | 1.6 |
| Laparoscopic colposuspension | 11,752 | 3275 | 23.56 | –0.52 | Dominated | 5.0 | 5.6 |
| SA assuming 50% of women whose first treatment was not successful would seek retreatment and 20% of women whose first retreatment failed would seek second retreatment | |||||||
| Retropubic MUS | 8061 | 24.14 | 27.0 | 25.6 | |||
| Traditional sling | 8479 | 418 | 24.15 | 0.01 | 35,896 | 29.0 | 28.3 |
| Transobturator MUS | 9551 | 1072 | 23.59 | –0.57 | Dominated | 4.2 | 4.1 |
| Urethral injection therapy | 9579 | 1100 | 23.72 | –0.43 | Dominated | 9.1 | 9.1 |
| Single-incision sling | 9584 | 1106 | 23.44 | –0.71 | Dominated | 2.8 | 2.7 |
| Bladder neck needle suspension | 10,090 | 1611 | 23.54 | –0.61 | Dominated | 4.8 | 4.9 |
| Open colposuspension | 10,930 | 2451 | 24.01 | –0.15 | Dominated | 14.6 | 15.7 |
| Anterior vaginal repair | 11,003 | 2525 | 23.38 | –0.78 | Dominated | 2.4 | 2.7 |
| Laparoscopic colposuspension | 11,739 | 3261 | 23.71 | –0.44 | Dominated | 6.3 | 6.9 |
| SA assuming 10% of women whose first treatment was not successful would seek retreatment and 0% of women whose first retreatment failed would seek second retreatment | |||||||
| Retropubic MUS | 8069 | 24.00 | 29.2 | 27.9 | |||
| Traditional sling | 8482 | 413 | 24.03 | 0.03 | 14,748 | 33.4 | 32.4 |
| Transobturator MUS | 9493 | 1011 | 23.42 | –0.61 | Dominated | 3.8 | 3.7 |
| Single-incision sling | 9608 | 1126 | 23.22 | –0.81 | Dominated | 1.8 | 1.7 |
| Urethral injection therapy | 9693 | 1211 | 23.50 | –0.53 | Dominated | 6.0 | 6.2 |
| Bladder neck needle suspension | 10,141 | 1659 | 23.32 | –0.71 | Dominated | 3.5 | 3.7 |
| Open colposuspension | 10,937 | 2455 | 23.85 | –0.18 | Dominated | 15.4 | 16.6 |
| Anterior vaginal repair | 11,041 | 2559 | 23.14 | –0.89 | Dominated | 1.4 | 1.6 |
| Laparoscopic colposuspension | 11,752 | 3270 | 23.53 | –0.50 | Dominated | 5.5 | 6.2 |
Assuming alternative values for the proportion of women who will seek retreatment after failure of each surgical treatment
In this SA, in which data from the linked database were applied, results show that the effectiveness of all surgical interventions is reduced slightly compared with the base-case analysis, and traditional sling, with an ICER of £8114 per QALY gained, is the most cost-effective option compared with the other surgical treatments. In the additional SA, in which it was assumed that 50% of women whose first treatment was not successful would seek retreatment and 20% of women whose first retreatment failed would seek second retreatment, total costs and effectiveness are reduced for most of the surgical interventions compared with the base-case analysis. Results from this SA show that retropubic MUS remains the least costly strategy compared with the alternative surgical interventions and is the most cost-effective option. When 10% and 0% were assumed for the rates of first and second treatments, traditional sling procedure was a cost-effective option with an ICER of £14,748, which is lower than £20,000 (Table 40).
Applying lower success rate for repeating same surgeries
In this SA, the effect of assuming lower cure rates (90% and 75%, respectively) when the same surgeries are being conducted for a second or third time was explored. As would be expected, the results of these sensitivity analyses show that all strategies have a higher cost and lower effectiveness. However, traditional sling is the most cost-effective option compared with other surgical treatments at a WTP threshold value of £20,000 (Table 41).
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective for different WTP thresholds (%) | |
|---|---|---|---|---|---|---|---|
| £20,000 | £30,000 | ||||||
| Base-case analysis: assuming same cure rates when the same surgeries are being conducted for a second or third time | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA assuming lower cure rates (90%) when the same surgeries are being conducted for a second or third time | |||||||
| Retropubic MUS | 8703 | 24.07 | 27.6 | 26.3 | |||
| Traditional sling | 9079 | 377 | 24.10 | 0.03 | 12,623 | 31.5 | 30.5 |
| Transobturator MUS | 10,554 | 1475 | 23.53 | –0.58 | Dominated | 4.3 | 4.4 |
| Urethral injection therapy | 10,586 | 1507 | 23.61 | –0.49 | Dominated | 7.4 | 7.6 |
| Single-incision sling | 10,809 | 1730 | 23.34 | –0.76 | Dominated | 2.3 | 2.3 |
| Bladder neck needle suspension | 11,252 | 2172 | 23.43 | –0.67 | Dominated | 4.4 | 4.5 |
| Open colposuspension | 11,689 | 2610 | 23.95 | –0.15 | Dominated | 15.2 | 16.3 |
| Anterior vaginal repair | 12,309 | 3229 | 23.27 | –0.84 | Dominated | 2.0 | 2.2 |
| Laparoscopic colposuspension | 12,735 | 3656 | 23.63 | –0.47 | Dominated | 5.4 | 6.0 |
| SA assuming lower cure rates (75%) when the same surgeries are being conducted for a second or third time | |||||||
| Retropubic MUS | 8889 | 24.04 | 27.9 | 26.3 | |||
| Traditional sling | 9239 | 349 | 24.07 | 0.03 | 12,036 | 32.6 | 31.7 |
| Transobturator MUS | 10,846 | 1607 | 23.45 | –0.61 | Dominated | 4.0 | 4.1 |
| Urethral injection therapy | 10,907 | 1668 | 23.53 | –0.53 | Dominated | 6.6 | 6.8 |
| Single-incision sling | 11,160 | 1921 | 23.26 | –0.81 | Dominated | 2.5 | 2.5 |
| Bladder neck needle suspension | 11,586 | 2347 | 23.36 | –0.71 | Dominated | 3.8 | 4.0 |
| Open colposuspension | 11,912 | 2673 | 23.88 | –0.19 | Dominated | 14.8 | 15.9 |
| Anterior vaginal repair | 12,685 | 3447 | 23.17 | –0.89 | Dominated | 2.0 | 2.2 |
| Laparoscopic colposuspension | 13,023 | 3784 | 23.56 | –0.51 | Dominated | 5.9 | 6.6 |
Incorporating different health utility values and effect of natural decline in health utility over time
In this SA, EQ-5D scores were adjusted and lower values were used for MUI health states compared with women with only SUI. The results from this SA show that traditional sling is the most cost-effective option (with an ICER of £7183 per QALY gained) compared with other surgical treatments. The impact of the natural decline in health utility over time was also considered in further SA. Results from this SA show that retropubic MUS remains the least costly strategy compared with the alternative surgical interventions and is the most cost-effective option (Table 42).
| Strategy | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£) (ΔCost/ΔQALY) | Probability cost-effective for different WTP thresholds (%) | |
|---|---|---|---|---|---|---|---|
| £20,000 | £30,000 | ||||||
| Base-case analysis assuming health states values are the same for women with SUI and MUI and fixed utility values over time | |||||||
| Retropubic MUS | 8099 | 24.22 | 25.8 | 24.6 | |||
| Traditional sling | 8522 | 423 | 24.22 | 0.01 | 60,863 | 27.0 | 26.2 |
| Urethral injection therapy | 9554 | 1032 | 23.86 | –0.36 | Dominated | 10.5 | 10.5 |
| Single-incision sling | 9649 | 1127 | 23.59 | –0.63 | Dominated | 3.2 | 3.2 |
| Transobturator MUS | 9665 | 1142 | 23.71 | –0.51 | Dominated | 4.1 | 4.1 |
| Bladder neck needle suspension | 10,125 | 1603 | 23.69 | –0.53 | Dominated | 5.4 | 5.4 |
| Open colposuspension | 10,977 | 2455 | 24.10 | –0.12 | Dominated | 14.1 | 15.0 |
| Anterior vaginal repair | 11,057 | 2535 | 23.54 | –0.69 | Dominated | 3.9 | 4.1 |
| Laparoscopic colposuspension | 11,797 | 3274 | 23.83 | –0.40 | Dominated | 6.2 | 6.8 |
| SA assuming lower health utility value for MUI health states | |||||||
| Retropubic MUS | 8104 | 23.70 | 30.4 | 29.1 | |||
| Traditional sling | 8526 | 423 | 23.75 | 0.06 | 7183 | 37.4 | 36.4 |
| Urethral injection therapy | 9551 | 1025 | 23.09 | –0.67 | Dominated | 6.9 | 7.0 |
| Single-incision sling | 9648 | 1122 | 22.63 | –1.13 | Dominated | 1.1 | 1.1 |
| Transobturator MUS | 9668 | 1142 | 22.86 | –0.89 | Dominated | 1.9 | 2.0 |
| Bladder neck needle suspension | 10,125 | 1599 | 22.78 | –0.98 | Dominated | 2.8 | 3.0 |
| Open colposuspension | 1097 | 2452 | 23.49 | –0.26 | Dominated | 14.5 | 15.7 |
| Anterior vaginal repair | 11,057 | 2531 | 22.53 | –1.23 | Dominated | 1.3 | 1.3 |
| Laparoscopic colposuspension | 11,797 | 3271 | 23.04 | –0.71 | Dominated | 3.9 | 4.6 |
| SA incorporating the impact of the natural decline in health utility over time | |||||||
| Retropubic MUS | 8096 | 21.81 | 26.9 | 25.4 | |||
| Traditional sling | 8523 | 427 | 21.79 | –0.01 | Dominated | 27.6 | 26.8 |
| Urethral injection therapy | 9552 | 1456 | 21.48 | –0.33 | Dominated | 10.6 | 10.6 |
| Single-incision sling | 9647 | 1552 | 21.24 | –0.56 | Dominated | 3.5 | 3.4 |
| Transobturator MUS | 9666 | 1570 | 21.36 | –0.45 | Dominated | 4.3 | 4.4 |
| Bladder neck needle suspension | 10,124 | 2028 | 21.33 | –0.48 | Dominated | 5.8 | 6.1 |
| Open colposuspension | 10,978 | 2882 | 21.68 | –0.12 | Dominated | 12.5 | 13.5 |
| Anterior vaginal repair | 11,063 | 2967 | 21.20 | –0.61 | Dominated | 3.4 | 3.6 |
| Laparoscopic colposuspension | 11,798 | 3702 | 21.46 | –0.35 | Dominated | 5.5 | 6.3 |
Glossary
- Anterior vaginal repair
- A surgical treatment used to treat stress urinary incontinence by lifting and supporting the bladder. One or more placating sutures are used to secure the fascia, which elevates the bladder neck and urethra.
- Bladder neck needle suspension
- A procedure usually performed on women for whom colposuspension is considered challenging, including women with limited vaginal mobility. The bladder neck is elevated with a long needle that threads sutures from the vagina to the anterior abdominal fascia.
- Laparoscopic colposuspension
- A relatively minimally invasive surgery that requires one or more small incisions through the lower abdomen. The aim is also to lift the junction between the urethra and the bladder.
- Open retropubic colposuspension
- A procedure during which a large incision is made in the lower abdomen to lift and stitch up the tissues near the bladder neck and urethra.
- Retropubic mid-urethral sling operation
- Mid-urethral sling surgery during which a tape or sling is placed underneath the urethra. The surgery is retropubic as the sling incision is made through the vagina with two other incisions made through the lower abdomen.
- Single-incision sling operation
- An operation similar to a mid-urethral sling procedure in that it supports the urethra through the use of a sling. There is a single access made through the vagina and the sling is shorter than that used in mid-urethral sling procedures, making it a less invasive procedure than other slings.
- Traditional suburethral sling procedure
- A procedure that improves urethral support by lifting the urethra–vesical junction and supporting it with autologous or synthetic material.
- Transobturator mid-urethral sling operation
- Mid-urethral sling surgery that is considered to be transobturator if one incision is made through the vagina and an incision is made on either inner thigh.
- Urethral injection therapy (periurethral injections or injectable bulking agents)
- A procedure in which high-pressure devices are required to advance the agents through the bladder neck. Once this is done, the bulking agents are intended to create cushions within the urethral submucosa.
List of abbreviations
- AIC
- Akaike information criterion
- AMND
- Aberdeen Maternity and Neonatal Databank
- ASC
- alternative specific constant
- BIC
- Bayesian information criterion
- BNF
- British National Formulary
- CCA
- cost–consequences analysis
- CEA
- cost-effectiveness analysis
- CEAC
- cost-effectiveness acceptability curve
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CI
- confidence interval
- CR
- ceiling ratio
- CRD
- Centre for Reviews and Dissemination
- CrI
- credible interval
- CRS
- Cochrane Register of Studies
- CRSO
- Cochrane Register of Studies Online
- DCE
- discrete choice experiment
- EQ-5D
- EuroQol-5 Dimensions
- EVPI
- expected value of perfect information
- EVPPI
- expected value of partial perfect information
- GP
- general practitioner
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HCHS
- hospital and community health services
- HES
- Hospital Episode Statistics
- ICER
- incremental cost-effectiveness ratio
- ICTRP
- International Clinical Trials Registry Platform
- ID
- identifier
- IIA
- irrelevant alternatives assumption
- IRR
- incidence rate ratio
- LR
- likelihood ratio
- MCMC
- Markov chain Monte Carlo
- MM
- Markov microsimulation
- MRS
- marginal rates of substitution
- MUI
- mixed urinary incontinence
- MUS
- mid-urethral sling
- MXL
- mixed logit
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NMA
- network meta-analysis
- NMB
- net monetary benefit
- OR
- odds ratio
- PFMT
- pelvic floor muscle training
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSA
- probabilistic sensitivity analysis
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RR
- relative risk
- SA
- sensitivity analysis
- SD
- standard deviation
- SMD
- standardised mean difference
- SUCRA
- surface under the cumulative ranking curve
- SUI
- stress urinary incontinence
- TOT
- transobturator tape
- TVT
- tension-free vaginal tape
- TVT-O
- tension-free vaginal tape-obturator
- UI
- urinary incontinence
- UTI
- urinary tract infection
- UUI
- urge urinary incontinence
- VOI
- value of information
- WHO
- World Health Organization
- WTP
- willingness to pay
