Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 14/183/02. The contractual start date was in September 2016. The final report began editorial review in September 2021 and was accepted for publication in April 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Coulton et al. This work was produced by Coulton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Coulton et al.
Chapter 1 Structure of the report and background to the research
Structure of the report
The study assessed the clinical effectiveness and cost-effectiveness of a multicomponent psychosocial intervention [i.e. the RISKIT-Criminal Justice System (RISKIT-CJS) intervention], compared with treatment as usual (TAU), in reducing substance use for adolescent substance users who were involved in the criminal justice system (CJS). The trial protocol has been published previously. 1 The RISKIT-CJS randomised controlled trial (RCT) was a two-armed, mixed-methods, prospective, pragmatic, individually RCT in young people aged 13–17 years (inclusive). The trial was carried out across four geographical areas of England (i.e. North East, North West, South East and London) and involved a baseline assessment and follow-ups at months 6 and 12, with month 12 designated as the primary outcome point. The study included an integrated qualitative component that evaluated young people’s and stakeholders’ views on the acceptability and suitability of the intervention, in addition to exploring the process of change associated with the intervention. All participants were eligible to receive any TAU available in their area. Participants in the intervention group received a multicomponent intervention that comprised a single one-to-one motivational interview, followed by two half-day group sessions and a final one-to-one motivational session. Interventions were provided by specifically trained youth workers with experience of working with young people with substance misuse issues.
Research questions
The study built on the Medical Research Council guidelines Developing and Evaluating Complex Interventions. 2 We conducted research to explore the theoretical validity of the intervention and synthesised this theoretical approach with the current evidence base and with the views of potential participants to model an appropriate intervention approach. We tested the feasibility of implementing the intervention in the target population and refined the intervention and its delivery as a result of that feasibility study. We conducted an appropriately designed pilot study to explore potential effectiveness on the key parameters and from this found evidence of potential effect in reducing substance use and risk-taking behaviour, as well as high levels of satisfaction and engagement. The next step was to conduct a rigorous evaluation to address key outcomes in a way that provides valid scientifically rigorous evidence and is useful to those engaged with this population and commissioners of services. To this end, we have conducted a full multicentre RCT of the RISKIT-CJS intervention compared with TAU, with an embedded qualitative component, to explore the effectiveness of the intervention in reducing substance use and improving mental well-being. The RCT is acceptable to participants and is economically viable to deliver.
Chapters of the report
This report is structured as seven chapters that detail the design, management and outcomes of the main trial. The report starts by providing an overview of the existing evidence and outlines the key literature that informed the design of the trial. Following this, a chapter is dedicated to each core component of the trial. Chapter 2 addresses the design of the intervention and the outcomes used to assess clinical effectiveness and cost-effectiveness. Chapter 3 reports the results of the statistical analysis, presenting the findings of the primary and secondary outcomes and exploring baseline and process factors that may have an impact on the outcomes observed. Chapter 4 details the design, methods and results of the economic aspects of the study. Chapter 5 provides the design and outcomes of the integrated qualitative aspects of the study. Chapter 6 provides a discussion on the results and, finally, Chapter 7 provides the key conclusions of the study and recommendations for future research.
Research ethics
The study was granted ethics approval by the University of Kent Social Research Ethics Committee (reference SRCEA169) in December 2016. The University of Kent acted as sponsor of the research and the trial was registered as ISRCTN77037777.
Changes to the original study protocol
The original protocol was published in 20171 and the current protocol is revision 4. Since the application, a number of modifications were made with the agreement of the Trial Steering Committee (TSC) and the funder. First, our original target population was adolescents aged 13–17 years (inclusive) who were actively managed by a youth offending team (YOT) and who scored ≥ 2 on the ASSET tool3 for substance use, indicating that substance use was associated with their criminal activity. Since the original application was submitted, the Youth Justice Board (YJB) has implemented a number of strategies to reduce the number of young people engaged with the CJS. These strategies have included taking a youth-first approach to offending, diverting out of the CJS for early offenders and focusing on education rather than punishment. These strategies have resulted in a large reduction in the number of young people managed by YOTs. Consequently, we sought, and received, permission to extend our recruitment to include young people who had been diverted from the CJS, that is, young people who had committed an offence involving substance use and had been referred for assessment by a substance misuse team (SMT) and young people educated in pupil referral units (PRUs) who had been involved with the CJS and actively used substances.
Second, in our original sample size calculation, we aimed to detect an effect size of 0.3, with 80% power and an alpha of 0.05, using a two-sided test and allowing for a 30% attrition at month 12. We expected there to be sufficient consenting participants in each YOT to allow allocation to be conducted in the ratio of 2 : 1, control to RISKIT-CJS intervention, respectively. This would maximise the cost-efficiency of the trial. However, as the study progressed, it became apparent that the numbers recruited per YOT were not sufficient to create appropriate-sized groups for the RISKIT-CJS intervention and permission was sought, and received, from the TSC to switch from a 2 : 1 allocation ratio to a 1 : 1 allocation ratio. This reduced the overall sample required from 567 to 502. To adjust any analysis by the impact of this change, an outcome identifying whether a participant was recruited under the 2 : 1 or 1 : 1 scenario was included as a secondary analysis.
Third, to reduce participant burden and to employ the most scientifically rigorous outcome assessment, we made some changes to the outcome measures collected between the original application and the latest version of the protocol. In our original application, we proposed to assess emotional regulation and behaviour using the Strengths and Difficulties Questionnaire. 4 Recent research suggests5 a high level of correlation between the Strengths and Difficulties Questionnaire and our proposed measure of well-being, that is, the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS). 6 As WEMWBS has more established psychometric properties, particularly sensitivity to change, we reduced participant burden by assessing only WEMWBS. In our original application, we planned on assessing motivational stage of change using the Readiness to Change Questionnaire – Treatment Version. 7 During the implementation stage of the study, concerns were raised about the validity of this instrument for adolescents and for substances other than alcohol. As a consequence we replaced the Readiness to Change Questionnaire – Treatment Version with a brief assessment of motivation to change designed for multiple substances and validated in an adolescent population [i.e. the Stages Of Change Readiness And Treatment Eagerness Scale – 7 Dimensions (SOCRATES-7DS)8,9]. All changes were discussed with, and approved by, the TSC.
Fourth, in our original application, we aimed to collect and analyse criminal justice outcomes, including arrests, charges and convictions in the 12 months prior to and 12 months after randomisation. We planned on deriving these outcomes from the Police National Computer at the end of the final follow-up period. Initial approaches to the Home Office were denied because of a major information technology infrastructure upgrade, and approaches to the Criminal Records Office were denied because the research was considered beyond its scope. We finally had agreement to source the data through the Ministry of Justice and we sought ethics approval in September 2019. Unfortunately, as the COVID-19 pandemic progressed, all non-essential access to data and data safe havens was denied and access to these data has not been possible at the time of submission. Consequently, we have not included analysis addressing recidivism and we have excluded criminal involvement from our wider public sector economic analysis.
Research management
The Trial Management Group (TMG) was responsible for ensuring the appropriate, effective and timely implementation of the trial. The TMG usually met once per month, depending on the needs of the trial, and comprised the chief investigator, trial co-ordinator, researchers working on the trial, co-applicants and representatives of the service delivering the intervention. A TSC was appointed to provide an independent overview of the trial conduct and represent the interests of the funders. The TSC subsumed the role of Data Monitoring and Ethics Committee. The TSC met annually throughout the study and its remit included measuring progress against agreed milestones in terms of recruitment and retention, adherence to the protocol, participant safety and reviewing of adverse events, and considering emerging evidence pertinent to the key research questions. Written terms of reference were agreed and used by the TMG and TSC (see Report Supplementary Material 1).
Research governance
The study complied with the requirements of the General Data Protection Regulations 201610 and the Freedom of Information Act 2000. 11 The trial was managed and conducted in accordance with the Medical Research Council’s guidelines on good clinical practice in clinical trials,12 which includes national and international regulations on the ethics involvement of participants in clinical research (including the Declaration of Helsinki 2013). All data were encrypted at the point of collection and held in a secure environment, with participants’ information identified using a unique identification number. Any personally identifiable information was stored separate from outcome and process data and was accessible only to those who needed to access the information. All research staff were employed by academic institutions and had enhanced Disclosure and Barring Service clearance. In addition, all research staff were governed by the conditions of service of the employing institution.
Background
Adolescence as a critical developmental stage
Adolescence is a critical developmental stage when young people make behavioural and lifestyle choices that have the potential to affect their health and well-being into adulthood. Although risk-taking is important for healthy psychological development for many, inappropriate risk-taking is significantly associated with health and social harms during adolescence, and these harms can persist well into adulthood. 13 Young people are much more vulnerable than adults to the adverse effects of substance use because of a range of physical and psychological factors that often interact and because of the differential impact of substances on the developing brain. 14–16 In addition to an increased risk of accidents and injury,17 substance use in adolescence is also associated with poor educational performance and exclusion from education. Over the academic year 2015–16, almost 10% of permanent school exclusions in state secondary schools were because of alcohol and substance use. 18 In the longer term, substance use is also associated with an increased prevalence of non-communicable diseases, such as cancer, cardiovascular disease and gastrointestinal disorders. 19,20
Prevalence of substance use among young people in the UK
The number of young people who consume alcohol is declining, although those who do drink tend to drink more. In 2018, 54% of youths aged 14 years and 69% of youths aged 15 years consumed alcohol, with 23% having consumed alcohol in the past week. 21 The mean weekly alcohol consumption for males at age 14 years was 5 units and for those aged 15 it was 7 units, where one unit equals 10 ml or 8 g of pure ethanol. For females, the mean weekly alcohol consumption was 5.5 units and 5 units, respectively. Six per cent of youths aged 14 years and 11% of youths aged 15 years reported having used cannabis in last month. In addition, 2% of 14-year-olds and 4% of 15-year-olds reported having used a class A substance at least once. 21
Young people in the criminal justice system
Although the relationship between criminal activity and substance use is complex, there is clear evidence that the prevalence of substance use is far higher in the youth offending population than in the general youth population. Data derived from the YOT AssetPlus3 indicate that most (76%) young people in the CJS use substances and 72% have a mental health need.
Data from the Juvenile Cohort Study22 show that 32% of young offenders score ≥ 2 on the ASSET tool for substance use, indicating that substance use is at least, in part, a reason for them associating in criminal activity, and 12% of young offenders score ≥ 3. Substance use is defined as the use of alcohol, traditional illicit substances or legal highs, as well as inappropriate use of prescribed medication. Although the relationship between substance use and criminal activity is complex, it is clearly a major issue in the youth offending population.
In the CJS, substance use and offending are related to other forms of disinhibitory behaviour, such as aggression and risk-taking. Young people involved in the CJS are a particularly vulnerable group, with a greater propensity to take risks that are likely to have a long-term impact on their future health and well-being. This is because young offenders often lead chaotic lives and face complex problems, including substance use, unsuitable accommodation and emotional or mental health issues. 23 Literacy levels among young people involved in the CJS are unacceptably low, and the vast majority of young people involved in the CJS have, in the past, been excluded from school. 24 As a result of the above risk factors, the list of negative consequences that result from substance use by young people is extensive and includes physical, psychological and social problems in both the short and the long term. In 2020, the number of young people receiving education in a PRU was just over 15,000,25 of whom 10% had been excluded from mainstream education because of substance use. Being excluded from school and educated in a PRU increases the propensity for young people to engage in criminal activity and 23% of new entrants to the CJS are educated in a PRU. 26
Young people who offend often experience a range of complex multiple risks and vulnerabilities, including neglect and abuse,27 substance use and related problems,28 and exclusion from school. 29 Research has shown that young people who offend are more likely to experience a range of inequalities in later life, for example worse physical health,28 early pregnancy in females,30 and higher rates of tobacco use and drug and alcohol dependence,29,31,32 reduced employment opportunities and economic hardship. 33 Indeed, there is widespread agreement that young people who offend are at an increased risk of health and social problems, making them one of the most vulnerable populations in the UK. 34 Furthermore, the UK has one of the highest youth custody populations in western Europe. 35 Epidemiological studies have shown that, in common with other vulnerable groups of young people, such as the homeless and those in care, young offenders are a hard-to-reach group from a health needs perspective, accessing physical and mental health services only in times of crisis, and that accessing these services is often associated with involvement with other agencies. 32,36,37
The Youth Justice System in England and Wales works to prevent offending and re-offending by those aged < 18 years. The latest available data indicate that there were 19,000 arrests of young people in 2019, which is an 82% drop from 2009. 38 Boys accounted for 83% of these arrests, and the average age of offenders was 15.3 years. Over the same period, there were 11,000 first-time entrants, that is, those receiving first reprimand or warning of community conviction, to the Youth Justice System, which is a reduction of 84% since 2009. 38 It is estimated that 38.5% of new offenders go on to re-offend after serving their initial sentence. 38
The ASSET tool is a standardised assessment tool that was developed within the CJS in England and Wales. The ASSET tool aims to identify the underlying causes of a young person’s offending behaviour to plan appropriate interventions. 3 The ASSET tool is often used on multiple occasions to help measure change in young offenders’ health and social needs and the risk of re-offending over time, and has been used with all young offenders in England and Wales since 2000. The ASSET tool examines 12 dynamic risk factors: (1) living arrangements, (2) family and personal relationships, (3) education, (4) neighbourhood, (5) lifestyle, (6) substance use, (7) physical health, (8) emotional health, (9) perception of self and others, (10) thinking and behaviour, (11) attitudes to offending and (12) motivation to change. The severity of each domain is rated on a scale of 0–4, with 0 being the least severe and 4 being the most severe, and a score of ≥ 2 is indicative that the domain contributes to the individual’s offending behaviour. 3
Previous research
To date, systematic reviews of interventions for substance-using offenders in CJS environments have not identified a clear evidence-based intervention strategy,39–41 but they have highlighted the paucity of good-quality research in the area and a lack of UK-based studies, with no scientifically rigorous studies focusing on young offenders. A recent meta-analysis of 22 studies42 synthesised the evidence regarding the use of motivational interventions for adolescents (aged 12–20 years) who engage in substance use. The results showed that, compared with TAU, the use of motivational interventions reduces the number of heavy alcohol use days by 0.7 days per month [95% confidence interval (CI) –1.6 to –0.02 days], substance use days by 1.1 days per month (95% CI –2.2 to –0.3 days), and overall substance-related problems by a standardised net mean difference of 0.5 (95% CI –1.0 to 0).
Developing and evaluating the RISKIT multicomponent intervention
The development of the RISKIT multicomponent intervention43 was based on two streams of work: (1) a participatory consultation with young people and (2) a review of the current research evidence. The theoretical perspective was informed by the social development model. 44–46 This approach suggests that the distal influences of socioeconomic status, biology, normative regulation and discipline are mediated through proximal influences on behaviour, which are identified as perceived opportunities for poor antisocial behaviour and perceived rewards for this behaviour. The social development model marries the ecological context of young people’s behaviour to an explanation of how this ecology influences their behaviour. It suggests that, even in the absence of a structural change to their health ecology, the provision of socioemotional and cognitive skills can help young people prevent or reduce risk-taking behaviour and suggests that the building of bonds with organisations promoting prosocial learning and opportunities is important in the reduction of risk-taking. The model provides a coherent and empirically validated approach that suggests that intervention approaches should be multicomponent and encompass knowledge and education, cognitive and learning skills, self-efficacy and motivation.
The participatory consultation was adapted from participatory action research47,48 and was carried out with a number of groups of young people. The aim of the exercise was to establish, with young people, what they perceived as risk-taking behaviour, why they took risks, the consequences of taking risks and how they perceived the problems could be addressed. The main themes in terms of risk-taking behaviour centred around criminal activity, substance use and sexual activity, and these activities were considered as being linked. The participants thought that prevention programmes that focused on the negative outcomes of risk failed to appreciate that risk-taking can be positive and can lead to positive outcomes, an issue highlighted by other research exploring the processes associated with risk-taking. 45,49 The young people identified the need for education regarding risks and consequences, but particularly highlighted the preference for interventions that provided skills and strategies to manage risk and the opportunity to discuss these skills with peers and to learn how to implement them. Interestingly, parental influences were not considered critical to any intervention, and many young people considered parental involvement to be inappropriate and unacceptable. The primary focus for the young people was not on eradication of risk-taking, but rather a focus on how risk could be reduced and how the negative consequences could be minimised.
Our second stream of work focused on the current evidence base that could inform the development of a multicomponent intervention. We consulted a number of existing reviews and research studies50–55 and found that, although there is a growing body of research in the field, there is a paucity of rigorously evaluated interventions, with the majority of research arising from the USA, with limited applicability to the UK. Of importance was what has been proven not to work, and this includes focusing on negative aspects of risk and abstinence from risk-taking behaviours. Promising intervention approaches include motivational interviewing and cognitive and socioemotional life skills training. In addition, there is emerging recognition of the importance of providing interventions in a structured manner and, with the young people’s preference for peer group interventions, the importance of managing the potentially negative effects of labelling and peer influence.
A synthesis of the participatory group views, the theoretical underpinnings and a review of the evidence was undertaken, and the RISKIT intervention model was developed as an approach that focuses on those who are vulnerable to the negative consequences of their risk-taking behaviour. The RISKIT intervention combines individual motivational interviewing sessions to target motivation and behaviour change with eight group-orientated life skills sessions that cover a variety of areas, including identifying and managing risk, communication skills, assertiveness training, anger management, preparing for behaviour change and sexual health. In addition, the group sessions focus on identifying resources within the community that could be of benefit for the young people and provide opportunities to access these resources.
An initial feasibility study was undertaken followed by a larger quasi-experimental study43 in which the RISKIT intervention was delivered across schools in Kent to 226 adolescents who were identified as engaging in excessive risk behaviour. Consent rates in the eligible population were high (80%), with almost all adolescents attending at least part of the intervention and 74% of adolescents attending all the intervention sessions. Follow-up rates were high, with 82% of adolescents being followed up at 6 months. At this point, 32% of the intervention group had reduced their risk-taking behaviour to a point where it was of no further concern and significant improvements were observed in terms of number of days abstinent from alcohol and other substances, indicating a positive effect on this domain. Participant views were positive, with high levels of engagement and satisfaction, and a general view that the intervention had been useful in developing new skills, was informative and could lead to changes in behaviour. Delivery of the model was sustainable, but required the input of specialist, rather than generic, staff, and a full economic evaluation of cost-effectiveness was not undertaken. The most recent outcomes for the RISKIT intervention, delivered in school settings over 2014 and 2015, indicated a 92.9% completion rate for those youths identified as being eligible, a 37.8% reduction in any alcohol consumption, a 24.6% reduction in using other substances and, for those who continued using illicit drugs, a reduction of 27.2% in drug-using days. In addition, improvements were observed in terms of mental health and well-being. Further to our pilot study, the RISKIT intervention was tested for feasibility in both custodial and community CJSs, with high levels of satisfaction on the part of the participants. A recent study in the community setting,56 commissioned by Kent Police as an element of their diversionary strategy, targeting young offenders committing a drug-related offence (n = 175), suggested that consent and engagement was high, with 90% of young offenders consenting, 100% of young offenders attending at least one session and 95% of young offenders attending all sessions. Further analysis at 6 months post intervention indicated a 50% reduction in re-offending rates, that is, a significantly greater reduction than that observed in a similar population who received youth justice interventions only. As part of this work, we adapted the intervention in terms of delivery by providing it over two half-day sessions over consecutive weeks on weekends, rather than the 8-weekly 1-hour sessions provided in the school-based study. 1
Aims
Our aim was to evaluate the clinical effectiveness and cost-effectiveness of the RISKIT-CJS intervention, compared with TAU, in reducing substance use for adolescents engaged with the CJS.
Primary objective
-
To conduct a prospective pragmatic RCT to evaluate the effectiveness of the RISKIT-CJS intervention, compared with TAU, for substance-using adolescents involved in the CJS.
Secondary objectives
-
To evaluate the cost-effectiveness of the intervention compared with TAU.
-
To explore participants’ and criminal justice staff’s experience of the intervention and the acceptability of the methods employed.
-
To assess the fidelity with which the intervention was conducted and to explore the role of fidelity, therapeutic alliance and baseline psychological factors on the outcomes observed.
-
If the intervention was shown to be effective within the parameters set, to develop a protocol for dissemination and integration of the intervention in current practice.
Outcomes and measurements
Validated and reliable tools were used to capture the primary and secondary outcomes.
Primary outcome
Our primary outcome measure was per cent days abstinent (PDA) from substance use in the 28 days prior to the 12-month follow-up and this was measured using the Timeline Followback 28 (TLFB28),57 which is a valid and reliable tool for assessing the quantity and frequency of substance use over time periods ranging from 1 to 365 days. The outcome has been validated for use in adolescent populations58 and recent pilot work has indicated high levels of agreement between the shorter, 28-day, and longer, 90-day, reference period.
Secondary outcomes
In addition to PDA, the TLFB28 allows for the derivation of a number of secondary outcomes over the period, including quantity and type of substances consumed. The TLFB28 is completed by a trained member of research staff and takes approximately 20 minutes. The outcome was measured at baseline and at 6 and 12 months. Mental health and well-being was assessed using the WEMWBS. The WEMWBS is a 14-item self-completed scale that addresses different aspects of eudemonic and hedonic mental health and well-being. The scale has established valid reliable psychometric properties in adolescent populations5 and is sensitive to change. 59 The WEMWBS instrument is highly correlated with other measures of psychological health and well-being, including the Strengths and Difficulties Questionnaire and the General Health Questionnaire. The WEMWBS was administered at baseline and then again at 6 and 12 months.
Motivational state and readiness to change substance use behaviour was measured using SOCRATES-7DS. The using SOCRATES-7DS contains 20 items and has four items for each stage of precontemplation, contemplation, preparation, action and maintenance. When an individual item is missing, then this results in a missing score for the relevant domain of behaviour change.
The Brief Situational Confidence Questionnaire (BSCQ) was used to assess self-efficacy. 60 The BSCQ comprises eight visual analogue scales to record confidence (on a scale of 0–100) in resisting the temptation to use drugs in a variety of situations.
Health-related quality of life was measured using the KIDSCREEN-10 Index. 61 This unidimensional measure represents a global score incorporating elements of physical and psychological well-being, autonomy and parent relations, peer and social support, and school environment. The KIDSCREEN-10 Index comprises 10 items rated on a Likert scale from 1 to 5, which are summed to give a total score. In addition, the KIDSCREEN-10 Index includes an overall self-reported assessment of general health (i.e. poor, fair, good, very good or excellent). The total score for the 10 items is calculated when there are no missing values for any individual item.
Process outcomes
Therapeutic alliance was measured at the end of the intervention using the Therapeutic Alliance Scale for Children: Youth version (TASC-r). 62 The TASC-r distinguishes between the affective bond and client–therapist collaboration. Items are rated on a scale from 1 (not true) to 4 (very much true) and are summed to give a total score. When fewer than four items are missing, the total is estimated using mean substitution for missing values.
All individual motivational interventions were recorded and a random sample of 20% (stratified by region, age and therapist) were selected and assessed by independent raters using the Behaviour Change Counselling Index (BECCI)63 to assess fidelity and quality. Overall scores were calculated by summing the checklist item scores and by dividing by the number of items to give a mean score. Mean substitution was used when an item on the checklist was not applicable.
Attendance at each of steps 1 to 4 of the intervention was recorded for each participant. Each interventionist delivering the RISKIT-CJS intervention was assigned a unique identifier and this was recorded for each step of the intervention for each individual.
Economic outcomes
The economic outcome measures addressed the costs of delivering the interventions, changes in health utility in the 12 months after randomisation and the costs associated with participants in the 12 months after randomisation. Costs associated with delivering the intervention were derived using a micro-costing approach, accounting for the actual costs, including associated training, facilities and overheads, and management costs. Health utility was assessed using the self-completed EuroQol-5 Dimensions, five-level version (EQ-5D-5L), and the Child Health Utility – 9 dimensions (CHU-9D),64 which were assessed at baseline and at 6 and 12 months. Service utilisation on the part of the participant was assessed using a specifically designed Client Receipt Service Inventory65 previously used with the adolescent population. Service use was assessed from a wide public sector perspective, encompassing health and social care, criminal justice, education and employment service utilisation.
Qualitative outcomes
Twelve RISKIT-CJS groups were purposefully selected according to geographical region and group dynamics, and a group discussion was conducted at the end of step 3 of the intervention, that is, the last group session attended. The group discussions were facilitated by experienced qualitative researchers, trained in both qualitative methods and the participatory rapid appraisal approach. 66 The researchers had experience of the RISKIT-CJS intervention but had not been part of the session delivery, enabling young people a space to share both positive and negative responses. Two researchers joined the selected groups at the close of the last group session and this created a distinction between the role of the researchers and interventionists. The approach employed was a participatory rapid appraisal66 to elicit in-depth exploration of the acceptability and perceived effectiveness of the programme and of the different elements within it.
To explore the RISKIT-CJS intervention from the perspective of the practitioners, 23 semistructured telephone interviews were conducted 2 weeks after the final motivational interviewing intervention. The semistructured interviews and field notes maintained by interventionists were used to explore a number of key objectives, feasibility, acceptability and perceived effectiveness of the programme.
Telephone interviews were carried out with a purposively selected sample of practitioners, including staff working in YOTs, PRUs and SMTs, who were involved with RISKIT-CJS programme and were chosen according to their profession and region. The aim was to explore the impact of the RISKIT-CJS intervention from the perspective of the YOT staff who worked with the target population. It was proposed that there would be 24 semistructured telephone interviews with staff across the participating teams and that these should be conducted 4 weeks after the final step 4 of the motivational interviewing intervention.
Chapter 2 Trial process and delivery of the intervention
Introduction
All young people recruited into the trial, regardless of the arm they were allocated to, continued to receive TAU, as was delivered in the setting and location they were recruited from.
Patient and participant involvement
Young people played a critical role in the co-production of the RISKIT intervention. The trial processes and materials were reviewed by a young person’s advisory group. A young person was invited to attend the TMG and trial TSC meetings and provide input on the ongoing trial progress. As part of the qualitative work, we asked young people for their views on the interpretation of the trial results.
Describing treatment as usual
During the study, it was apparent that TAU varied across settings and locations and, bearing in mind that youths with severe substance use or youths subject to an order related to their substance use were excluded from participation, in many centres no intervention was offered specifically to address substance use. In the YOT setting, some participants were able to access structured psychoeducation, delivered either individually by a youth worker or as part of a small group. The general topics included exploring peer pressure, consequential thinking and making choices, victim awareness, alcohol awareness, substance use and the law, and substance use and health. In addition, some YOTs used community resolution and community payback to enable offenders to reflect on the impact of their offences on others. In general, it was observed that participants tended not to engage with psychoeducation or community interventions unless they had been dictated by a court order. In the PRU settings, all schools provided personal, social, health and economic (PSHE) education and although there are no prescriptive guidelines of what constitutes PSHE it usually covers alcohol and substance use. Although PSHE varies from school to school, it tends to cover risks associated with substance use, provision of information leaflets and videos, advice delivered by teachers and external speakers, and information for parents. In addition to PSHE, PRUs offered a number of different approaches for social, emotional and behavioural support, sometimes in response to a specific recommendation in an education health and care plan and sometimes across the whole school. Often these approaches were evidence informed rather than evidence based, and included Lego® (The Lego Group, Billund, Denmark) therapy, gardening, equine therapy, positive mentoring and mindfulness.
Those participants recruited from SMTs received the most standardised form of TAU, and this involved a medical assessment to identify any additional clinical needs, single-session brief interventions based on a motivational interviewing approach and individual sessions addressing anxiety management and behavioural triggers for substance use.
As the TAU varied by setting, we adjusted our analysis to take account of these variations.
Trial processes
Study setting and population
Young people aged 13–17 years (inclusive) were targeted. Young people were recruited from a mixture of YOTs, PRUs and SMTs between September 2017 and June 2020. Recruitment was conducted in four geographical areas of England (i.e. North East, South East, London and North West).
In the YOTs, all young people are routinely screened using the ASSET tool, and research staff approached any young person who scored ≥ 2 on the substance use domain, indicating a relationship between criminal behaviour and substance use. In PRUs, school staff identified potential participants who were subsequently assessed by research staff to ensure that they had been involved with CJS and were engaged in substance use. The SMT cohort included young people who had recently come to the attention of the police for being involved in criminal activity and who were also found to be in possession of illegal substances. As part of a scheme to divert these young people from criminal justice services, they were referred to a young person’s SMT for assessment and, when necessary, intervention.
Eligibility checks were conducted by a researcher trained in the process and who had previously worked with adolescent populations. Young people who were eligible were provided with detailed trial information (see Report Supplementary Material 2) both verbally and in writing and were asked to consider participating. It was made clear that a participant could withdraw from the intervention or the trial completely at any stage and withdrawing would have no effect on any intervention they would receive as TAU. All young people, irrespective of eligibility and consent, were recompensed for their time with a £10 voucher. If a participant was willing to consent, then the researcher decided whether or not the young person aged ≥ 16 years met the criteria for being Gillick competent and, if they were, then consent was taken. For young people aged < 16 years and young people aged ≥ 16 years and considered not to be Gillick competent, assent was taken from the young person and formal consent taken by contacting the primary caregiver, who was provided with a copy of the trial information sheet. The young person was asked to consent both to the trial and for access to offence records held on the Police National Computer. After consent had been taken, the researcher conducted the TLFB28 on paper. The young person completed the rest of the baseline assessment on a tablet device using specifically designed software. The researcher was available to aid any young person who had difficulty in understanding the questions. After the completion of the baseline assessment, randomisation was conducted automatically through the tablet device and the young person was informed of their allocation. Once sufficient numbers of young people had been allocated to the intervention to form a group, usually six or more, but not exceeding eight, then the list of group members was reviewed by staff within centres to identify any potential risks, such as a lone female in a dominant male group, group members known to be engaged in violent conflict or associated with different gangs and very vulnerable participants. If any risks did arise, then the young person was considered for another group at the same setting. If no other group was available, then the young person received the individual components of the intervention. Follow-up was conducted as close to the 6- and 12-month follow-up as possible. Young people had a choice in how they were followed up: in person with a researcher, by telephone with a researcher or by completing a paper-based questionnaire by e-mail or post. Once follow-up was completed at 6 and 12 months, participants were recompensed for their time with a £10 voucher at both time points. This both recognised the contribution the participant made to the research and was designed to reduce attrition over time. 67
Inclusion and exclusion criteria
To maximise the generalisability of the trial population, inclusion and exclusion criteria were kept to a minimum. Participants were included if they were aged 13–17 years (inclusive), if they had recently engaged in substance use and had been involved in the CJS, and if they were engaged in a participating YOT, PRU or SMT.
Participants were excluded if the severity of their substance use was such that a referral to specialist services for detoxification was required, if the severity of criminal involvement was such that the young person was likely to be incarcerated during the intervention or follow-up period, or if the young person was currently on a court-mandated order with alcohol or substance use abstinence as a prerequisite.
Randomisation
Randomisation was conducted at the level of the participant by an independent secure randomisation service, using random permuted blocks of random length. Strings developed independently were encrypted and stored, with the tablet devices and allocation revealed only when a participant had been judged eligible, provided written consent and completed the baseline assessment. Copies of the strings for audit and quality assurance purposes were held in an encrypted database by an organisation not associated with the research. Randomisation was stratified by site, sex and age group [i.e. 13–15 years (inclusive) vs. 16–17 years (inclusive)].
Staff identified to deliver the RISKIT-CJS intervention
We worked in collaboration with youth substance misuse services provided by Addaction, now renamed We Are With You (London, UK). Staff delivering the interventions were paid, experienced youth workers and youth substance misuse workers who had been trained and accredited, and had experience of delivering motivational interviewing. Many of the staff had experience of delivering the schools version of the RISKIT intervention, which is similar to the RISKIT-CJS intervention but is delivered for 1 hour per week over an 8-week period.
RISKIT-CJS intervention training and support
Staff were invited to participate in a 2-day training course as part of their continuous professional development. In addition to providing an overview of their roles and responsibilities relating to the trial, the 2-day course explored the theoretical underpinning of the RISKIT-CJS intervention, detailing delivery of each programme element, including managing group dynamics, managing ambivalence, identifying risks and safeguarding. Staff engaged in written coursework and role play, and had an opportunity to conduct motivational interviews and manage groups while being observed by an experienced senior practitioner. Only when a staff member had been deemed competent by the senior practitioner were they allowed to deliver the RISKIT-CJS intervention. Intervention delivery was monitored on an ongoing basis by senior staff who observed practice in individual and group sessions, providing ongoing guidance and supervision.
The RISKIT-CJS intervention
The RISKIT-CJS intervention was based on a similar individual and group intervention developed in collaboration with young people and delivered in school settings. 43 The intervention delivered in the trial consisted of four distinct steps. The first step, delivered immediately after randomisation, was an individual face-to-face session with a trained interventionist, lasting approximately 40 minutes. This session used techniques associated with motivational interviewing to discuss substance use, to explore the role substance use plays in risk-taking behaviour or emotional dysregulation, to explore and support behaviour change, and to enhance motivation to engage with the intervention. Step 2 was a group session delivered about 1 week after step 1. The group session, delivered over half a day at a convenient location for the participants, employed a group cognitive–behavioural therapy approach, employing group discussion and interactive whiteboards. The aim of the session was to provide both psychoeducation and skills development, encompassing understanding substance use and associated harms, understanding triggers to substance use, developing strategies for harm minimisation and reducing consequential risks, exploring techniques to divert or distract from substance use, and exploring substance use and sexual health risks. The actual topics and depth covered were decided at the beginning of the session to meet the needs of the group. Step 3 occurred usually 1 week after step 2 and took a similar group approach, but with a greater emphasis on skill development. Topics included communication strategies and assertiveness training, managing anger and anxiety, mindfulness and planning for the future. Two interventionists covered each group, with one interventionist delivering the content and the other encouraging engagement within the group. Step 4 was conducted about 1 week after step 3 and comprised a 40-minute face-to-face session conducted in a mutually convenient location. This session, using a similar motivational interviewing approach as step 1, explored outstanding barriers to change, managing expectancy and enhancing self-efficacy. In addition, each step 4 intervention was tailored individually to consolidate what had been learned from the group sessions and to explore opportunities to engage in local services and provision to encourage pro-social behaviour. Participants were not paid to attend any of the sessions, although they were reimbursed for any travel expenses and provided with refreshments.
Assessing intervention fidelity
Intervention fidelity relates to the extent to which an intervention is true to the underlying therapeutic theory. Researchers need to be able to determine whether or not the intervention is delivered as intended and, although complete manualisation of an intervention goes against many therapeutic principles, it is important to be able to assess the content of an intervention. High-fidelity delivery of an intervention makes it more appropriate to draw causal conclusions regarding any intervention and effect observed; it also makes any intervention easier to replicate in practice. In addition to keeping a log of what subjects were covered in the group sessions, interventionists sought the consent of young people to audio-record their individual sessions. From the sessions recorded, a 20% random sample was drawn, stratified by sessions (1 or 4), interventionist and site. These sessions were listened to by two independent raters. The raters scored the sessions using BECCI,68 that is, a tool specifically designed to measure the micro-skills of behaviour change counselling and motivational interviewing.
The BECCI focusses on the interventionist’s consulting behaviour and attitude rather than a self-report. Scores are provided on a scale of 0–4 (where 0 = not at all, 1 = minimally, 2 = to some extent, 3 = a good deal and 4 = a great extent). Ratings consider 15 domains of practitioner skill and are completed in accordance with the rater manual. Two raters considered each recording and made decisions regarding the overall score. When significant deviation regarding the allocated rating occurred, the two raters listened to the recording together and came to a consensus on the score. Ratings were incorporated into the assessment of fidelity reported in Chapter 3.
Chapter 3 Trial methods and results
Trial summary
The RISKIT-CJS RCT was a mixed-methods, prospective, pragmatic RCT with individual allocation, combining both quantitative and qualitative evidence. The trial was conducted across four geographical areas in England (i.e. South East, South London, North East and North West), covering a diverse socioeconomic and ethnic population. The study evaluated the clinical effectiveness and cost-effectiveness of the RISKIT-CJS intervention in addition to TAU, compared with TAU only, on substance use 12 months after randomisation.
Inclusion criteria
Young people were included if they were aged 13–17 years (inclusive), if they had recently engaged in substance use and had been involved in the CJS, and if they were engaged in a participating YOT, PRU or SMT. In addition, young people had to be willing and able to provide consent.
Exclusion criteria
Young people were excluded if the severity of their substance use was such that a referral to specialist services for detoxification was required, if the severity of their criminal involvement was such that the young person was likely to be incarcerated during the intervention or follow-up period or if the young person was currently on a court-mandated order with alcohol or substance use abstinence as a prerequisite.
Sample size and power calculation
We aimed to recruit 500 participants over a 19-month period, with the aim of assessing at least 350 of these participants at the 12-month assessment point. We estimated a loss to follow-up at the primary end point (i.e. 12 months post randomisation) of 30%. Our sample was designed to identify a clinically important effect size difference of 0.3 in the primary outcome measure (i.e. PDA from all substances), with an alpha of 0.05 and power at 80%, using a two-sided test.
Primary and secondary outcomes
The primary outcome measure was PDA from all illicit substances (including alcohol) in the 28 days prior to the 12-month follow-up, and this was derived using TLFB28 method.
Secondary outcomes derived from TLFB28 were PDA for all illicit substances excluding alcohol and PDA for 11 types of illicit substance use: (1) alcohol, (2) cannabinoids/marijuana, (3) cocaine/crack, (4) amphetamine-type stimulants, (5) opiates, (6) prescribed opioid substitution, (7) MDMA (3,4-methylenedioxy-methamphetamine)/ecstasy, (8) prescription medication, (9) inhalants, (10) hallucinogens and (11) novel psychoactive substances.
Mental health and well-being was measured using the WEMWBS. The WEMWBS total score was derived by summing the individual items score. When more than three individual item scores were missing, the total score was assumed to be missing. When fewer than three items were missing, the total score was estimated using mean substitution for missing values.
Readiness to change was measured using SOCRATES-7DS. The SOCRATES-7DS contains 20 items, with four items for each stage of precontemplation, contemplation, preparation, action and maintenance. When an individual item was missing, then this resulted in a missing score for the relevant domain of behaviour change.
The BSCQ was used to assess self-efficacy. The BSCQ comprises eight visual analogue scales to record confidence (on a scale of 0–100) in resisting the temptation to use drugs in a variety of situations.
Health-related quality of life was measured using the KIDSCREEN-10 Index. This unidimensional measure presents a global score incorporating elements of physical and psychological well-being, autonomy and parent relations, peer and social support, and school environment. The KIDSCREEN-10 Index comprises 10 items rated on a Likert scale from 1 to 5, which are summed to give a total score. The KIDSCREEN-10 Index also includes an overall self-reported assessment of general health (i.e. poor, fair, good, very good or excellent). The total score of the 10 items was calculated when there were no missing values for individual items.
Primary and secondary outcomes were measured at baseline and at 6 and 12 months.
Therapeutic alliance was measured at the end of the intervention using the TASC-r. The TASC-r distinguishes between the affective bond (i.e. the extent to which the therapist is an ally) and client–therapist collaboration on therapeutic tasks and goals (i.e. the extent to which it is difficult to work with the therapist on solving problems). Twelve items are rated on a Likert scale from 1 (not true) to 4 (very much true) and summed to give a total score. When more than three individual item scores were missing, then the total score was assumed to be missing. When fewer than three items were missing, then the total score was estimated using mean substitution for missing values.
All individual motivational interventions were recorded when consent to record had been granted. A random sample of 20% of recordings (stratified by region, age and therapist) was selected and assessed by independent raters using BECCI63 to assess fidelity and quality. Overall scores were calculated by summing the checklist item scores and by dividing by the number of items to give a mean score. Mean substitution was used when an item on the checklist was not applicable.
To assess how well the blind was maintained, researchers conducting follow-up assessments completed a five-point scale to record their confidence in treatment allocation.
Attendance at each of steps 1–4 of the intervention was recorded for each participant. Each interventionist delivering the RISKIT-CJS intervention was assigned a unique identifier, and this was recorded for each step of the intervention for each individual.
Statistical analysis plan
Two data sets were created for the statistical analysis. The primary analysis was based on the analysis by treatment allocated (ATA) data set. The secondary analyses examined treatment effects under different scenarios for compliance with allocation/treatment, including complier-average causal effect (CACE) and per protocol (PP). The definition of compliance with allocation for this trial was (1) participants attending at least one individual session and at least one group session are considered ‘compliers’ in the active treatment group (Table 1, cell A) and (2) participants in the control group who did not receive any intervention (see Table 1, cell D). All non-compliers in the treatment group were regarded as being ‘contaminated’ because they received the control condition. For the control group, there is no option for control participants to access the intervention and so there cannot be non-compliance (see Table 1, cell C).
| Treatment allocated | Treatment received | |
|---|---|---|
| RISKIT-CJS intervention | Control | |
| RISKIT-CJS intervention | A. Treatment complier: one individual session and one group session | B. Treatment non-complier: only individual or group attended; no sessions attended |
| Control | C. Control non-complier: n/a | D. Control complier: control group participant |
Analysis by treatment allocated
The data set contains all available data for participants who were randomised, regardless of whether or not they complied with allocation. This includes participants who were withdrawn from the trial post randomisation. These analyses are a lower-bound estimate of treatment effects, as they represent the effect of offering a programme, rather than the effect of actually receiving that programme.
Complier-average causal effect
We assessed treatment effects in the presence of non-compliance, with compliance measured at the individual level and including all those allocated as part of the trial. Our approach for assessing treatment effects under non-compliance was to use the instrumental variables framework. 69 The benefit of using an instrumental variables approach is that randomisation is maintained in the analysis, which is crucial for estimating unbiased treatment effects. 70 CACE weights the ATA treatment effect by the proportion of compliers:
If the proportion compliant is 1.0 (i.e. perfect compliance), then the CACE estimate is the same as the ATA estimate, but otherwise the impact of this approach is to increase the magnitude of the treatment effect.
Complier-average causal effect uses a two-stage least squares approach. The stage 1 model uses treatment received (T) as the outcome, with random allocation (Z) as the independent variable:
Based on the stage 1 model, we then calculate predicted values of treatment received (T^) for use in stage 2. The stage 2 model predicts the substantive outcome (Y, e.g. days abstinent) using the predicted values of treatment received (T^) based on the stage 1 model:
The CACE analysis was conducted using a two-stage least squares estimation with the ivregress command in Stata® version 16.1 (StataCorp LP, College Station, TX, USA). A linear regression modelling approach was used for PDA and WEMWBS score.
Per-protocol data set
The PP data set contains all data for participants who complete the trial as planned without any major protocol violations or exclusions. PP analyses essentially drop those individuals who have not strictly complied with their allocated treatment, that is, both those who only partially complied with their allocated treatment and those who did not receive their allocated treatment. This means that PP represents a likely ‘best case scenario’ for treatment effect estimation.
Missing data
The proportion of missing data and patterns of missingness were examined for the primary and secondary outcomes. Levels of missing data are reported along with any systematic occurrences of missing data observed in the data sets. When outcomes were derived scores, individual item scores were checked for systematic missingness by comparing the proportion of missing values by age (< 16 years or ≥ 16 years), sex, service type (i.e. YOT, PRU or SMT) and allocated group.
To avoid loss of efficiency, it was planned to impute missing outcome values (both primary and secondary WEMWBS score) using multiple imputation, if the proportion of missing data was > 5% and < 40%. 71 Multiple imputation methods perform less well when the number of missing data is substantial (i.e. if > 40% of the primary outcome data are missing in the primary analysis, then the assumptions are less plausible).
For PDA all substances and WEMWBS score, the percentage of data missing at 12 months was 45% and 55%, respectively, and, consequently, multiple imputation was performed as a sensitivity analysis only and not as part of the main analysis.
We explored the mechanism of missing data to establish whether the data could be considered missing completely at random or missing at random (MAR). For each allocated arm, and overall, participants were grouped based on the time they were lost to follow-up or withdrew, and means/medians at baseline and each time point were examined to assess whether there were systematic differences between those who dropped out at specific time points and those who remained in the study.
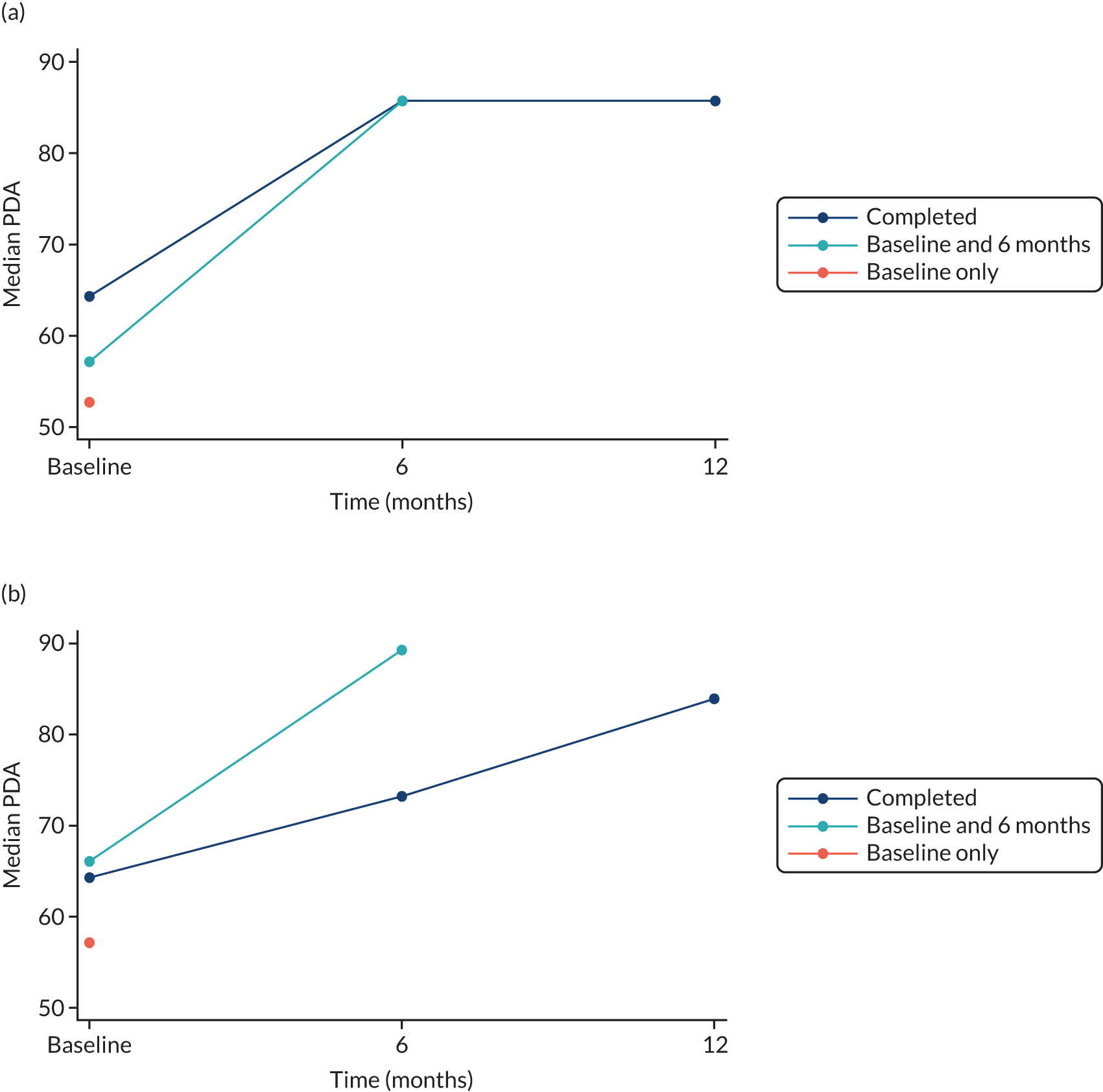
Figure 1 shows that the median PDA at baseline was lower for participants with only baseline data than for participants who remained in the study, and this was the same in both arms. Compared with participants with complete data at 12 months, participants with only baseline and 6-month data had a greater increase in median PDA at 6 months in both arms, although the number of participants in this group was smaller. These data suggest that the assumption of MAR may not be plausible.
FIGURE 1.
Median PDA all substances by allocated arm. (a) RISKIT-CJS intervention; and (b) control.
A sensitivity analysis was performed using a pattern mixture approach and multiple imputation to compare the sensitivity of conclusions with varying assumptions about the missing value mechanism. It is possible that participants who failed to attend their follow-ups differed from those who did attend (e.g. had fewer days abstinent and, therefore, would have lower PDA than if they had attended the follow-up, or vice versa). This would mean that the data were missing not at random (MNAR) and would represent a departure from the MAR assumption. The sensitivity of the primary analysis results to departures from the MAR assumption were explored using a pattern mixture model, implemented using the rctmiss command in Stata. 72,73
Deviation from the statistical analysis plan
Plots of the primary outcome, by dropout time, to assess the missing value mechanism suggested that missing values are not MAR. In addition, the planned analysis to compare the sensitivity of conclusions with varying assumptions about the missing data uses multiple imputation, which is less tenable given the high proportion of missing values. These analyses were completed as a sensitivity analysis, and two additional approaches were used and reported as secondary analyses. The first approach used last observation carried forward (LOCF) for each individual to estimate the 12-month data value when data at 6 months were measured. The second approach, when the 6-month data were missing, used a combination of LOCF and baseline observation carried forward (BOCF), and this method assumes that individuals remain at the same level as their last measurement after they are lost to follow-up or leave the study.
Pearson’s correlation coefficient was calculated for the primary outcome to estimate the strength of association between time points (i.e. baseline, 6 months and 12 months) and scatterplots were also produced.
Methods
Analysis and results are presented in accordance with CONSORT (Consolidated Standards of Reporting Trials) guidelines. All statistical analysis was conducted using Stata/IC.
The primary analysis was based on the ATA data set, which contains all available data for participants who were randomised, regardless of whether or not they complied with allocation.
Diagnostic tests and plots to assess the assumptions of normality for PDA were performed prior to analysis. There were significant departures from normality and an alternative model was implemented, as specified in the statistical analysis plan, to allow for the fractional nature of the primary outcome response. A fractional linear logistic model74 was fitted, assuming that the variance in response was proportional to a binomial distribution and using the logit link function to maintain bounds between 0 and 1. Fixed effects were included for allocated arm, service type (i.e. YOT, PRU and SMT), age (< 16 years and ≥ 16 years) and sex. The outcome was adjusted for baseline by including the baseline measure as a covariate. Results are presented as odds ratios (ORs) between the RISKIT-CJS intervention and control group, with accompanying 95% CIs.
The secondary outcome of WEMWBS score was analysed using analysis of covariance to compare the mean response across treatment arms, with fixed effects for treatment arm, service type (i.e. YOT, PRU and SMT), age (< 16 years and ≥ 16 years) and sex. The outcome was adjusted for baseline by including the baseline measure as a covariate. Results are presented as mean differences between the RISKIT-CJS intervention and control group, with accompanying 95% CIs.
Secondary analysis was performed for the PP data set and using the CACE approach for the primary outcome and WEMWBS score. The primary outcome and WEMWBS score at the 6-month follow-up were also analysed.
Stepwise regression analysis was performed to model the relationship between pre-randomisation factors and observed outcomes at 12 months, separately for the primary outcome and WEMWBS score. Interaction terms with treatment arm were included in the analysis, and a significance level of 0.1 was used to determine which factors were added and removed from the regression model. Pre-randomisation factors included in this analysis included demographic data (i.e. sex and social class measured using the Index of Multiple Deprivation by postcode), readiness to change (i.e. the SOCRATES-7DS) and self-efficacy measures (i.e. the BSCQ). This analysis was augmented by an additional analysis that included participants in the RISKIT-CJS intervention arm only, for the primary outcome and WEMWBS score and using the same pre-randomisation factors, but also including process measures of adherence, therapeutic alliance (i.e. the TASC-r) and interventionist.
Other secondary outcomes and outcomes derived from TLFB28 and demographic data were summarised to compare allocated arms. Means and standard deviations (SDs) were calculated for continuous normally distributed variables, medians and interquartile ranges (IQRs) for non-normally distributed variables, and frequencies and percentages for categorical variables.
A description of TAU at each site was collected and is presented as part of the analysis.
Change in allocation ratio
At the start of the trial, the randomisation allocation ratio was 2 : 1, with one-third of participants receiving the RISKIT-CJS intervention. During the trial, it was agreed to change the allocation ratio to 1 : 1. However, for an interim period, the allocation ratio was 1 : 2, with twice as many participants receiving the RISKIT-CJS intervention as the control, until there was an equal number of participants in the control and intervention groups, when the allocation ratio was switched to 1 : 1 for the remainder of the trial.
An additional analysis was performed for the primary outcome and WEMWBS score to take account of any bias incurred from the change in allocation ratio during the trial. 75 An individual patient data meta-analysis approach was taken to analyse the data, using the one-stage approach. 76 The data were analysed using the statistical model specified previously for the main analysis. A fixed effect for allocation ratio group was added to the model, with interactions of allocation ratio group with treatment group and covariates. This one-stage individual patient data model was used to estimate differences between treatment groups and 95% CIs for each allocation ratio group and overall.
Sensitivity analyses
Sensitivity analyses were performed using a pattern mixture approach and multiple imputation to compare the sensitivity of conclusions with varying assumptions about the missing value mechanism. The pattern mixture model works by including a sensitivity parameter, quantifying the departure from the MAR assumption. For example, if it is expected that participants who were lost to follow-up after the baseline visit, on average, have a difference of 20% in PDA at 12 months compared with participants who remained in the study, then the sensitivity parameter would be equal to 20.
The pattern mixture model is used to obtain an estimate of the treatment effect given this level of departure from the MAR assumption. Graphs of the adjusted mean difference in PDA and WEMWBS score between treatment groups for varying values of the sensitivity parameter are reported. Analysis was performed assuming that the value of the sensitivity parameter was equal in both groups (i.e. missing data were equally informative in both groups).
Safety data
Serious adverse events and partial compliance because of safeguarding concerns are summarised by type and treatment arm. Safeguarding concerns occur when a young person is withdrawn from a group session, but not an individual session, because there are concerns of iatrogenic effects of participation.
Results
Box and whisker plots and summary statistics are reported in Report Supplementary Material 3, Figures 1–26, for all the primary and secondary outcomes.
Of those participants allocated to the intervention, 214 (87%) received the initial motivational interview, 98 (40%) attended the first group session and 74 (30%) attended the second group session and the second motivational interview. Table 2 provides an overview of these figures.
| Intervention step | RISKIT-CJS intervention (N = 246), n (%) |
|---|---|
| Motivational interviewing session 1 | 214 (87) |
| Group session 1 | 98 (40) |
| Group session 2 | 74 (30) |
| Motivational interviewing session 2 | 74 (30) |
| Compliera | 104 (42) |
| PPb | 47 (19) |
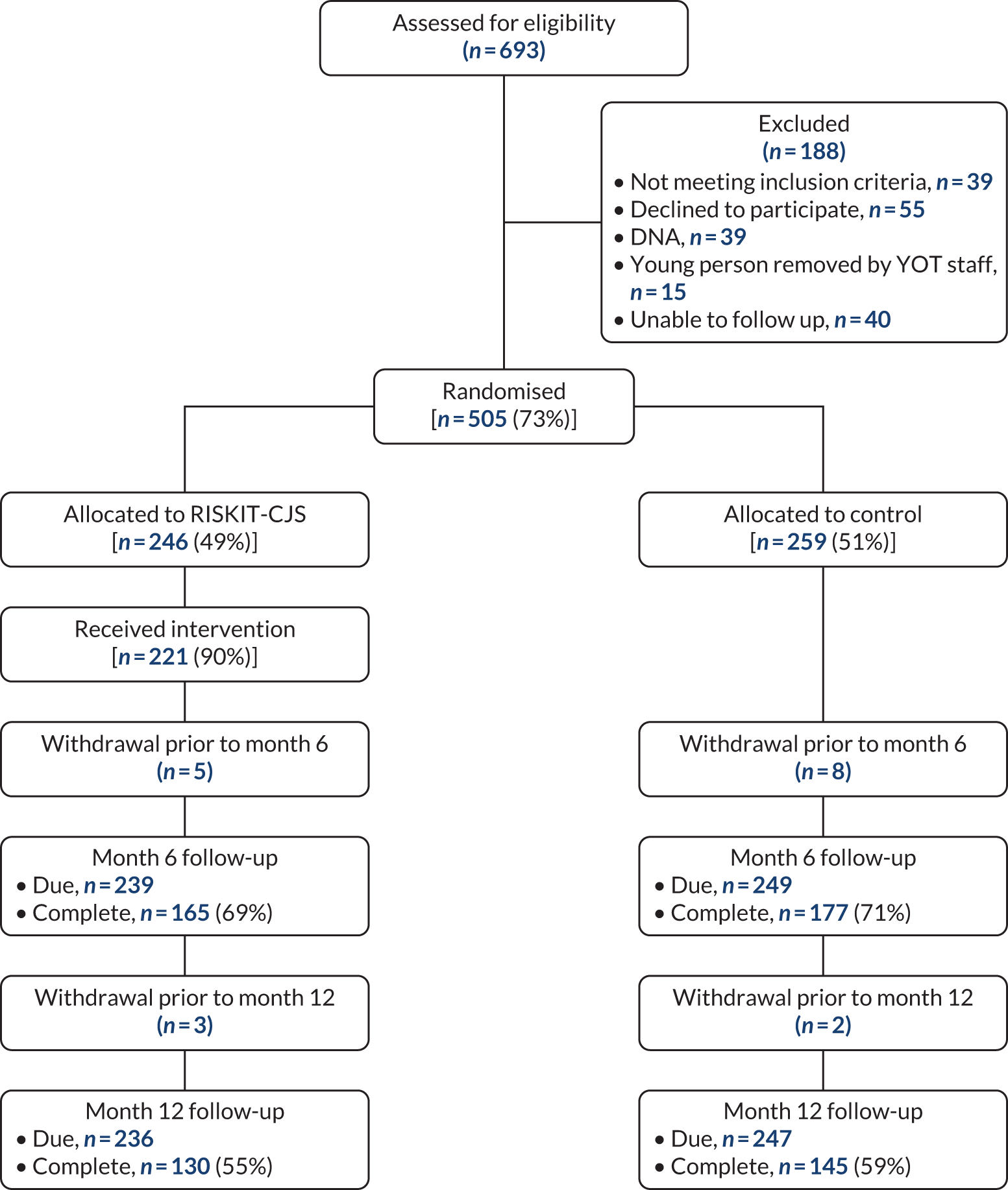
A full CONSORT diagram is provided in Figure 2. There were 505 participants at baseline, with 191 (37.8%) participants recruited from YOTs, 262 (51.9%) participants recruited from PRUs and 52 (10.3%) participants recruited from SMTs. The mean age of participants was similar for both arms (15.2 years vs. 15.3 years for the RISKIT-CJS intervention and the control, respectively) and the proportion of participants younger than 16 years overall was 58.8%. There were fewer female participants than male participants, with 24.6% female participants overall. Table 3 contains a summary of demographic variables at baseline and Table 4 contains details on the main substances consumed.
FIGURE 2.
The RISKIT-CJS CONSORT diagram. DNA, did not attend.
| Demographic information | Treatment group | |
|---|---|---|
| RISKIT-CJS intervention (n = 246, 48.7%) | Control (n = 259, 51.3%) | |
| Age (years), mean (SD) | 15.2 (1.13) | 15.3 (1.15) |
| Aged < 16 years, n (%) | 149 (60.6) | 148 (57.1) |
| Male, n (%) | 181 (73.6) | 200 (77.2) |
| Service type, n (%) | ||
| YOT | 83 (33.7) | 108 (41.7) |
| PRU | 135 (54.9) | 127 (49.0) |
| SMT | 28 (11.4) | 24 (9.3) |
| Main substance consumed | Treatment group | |
|---|---|---|
| RISKIT-CJS intervention (N = 243), n (%) | Control (N = 256), n (%) | |
| Alcohol | 143 (58.8) | 160 (62.5) |
| Cannabinoids/marijuana | 185 (76.1) | 196 (76.6) |
| Cocaine/crack | 19 (7.8) | 19 (7.4) |
| Amphetamine-type stimulants | 4 (1.6) | 3 (1.2) |
| Opioid analgesics | 6 (2.5) | 2 (0.8) |
| Prescribed OST | 0 | 0 |
| MDMA/ecstasy | 24 (9.9) | 25 (9.8) |
| Prescription medication | 7 (2.9) | 3 (1.2) |
| Inhalants | 5 (2.0) | 5 (2.0) |
| Hallucinogens | 3 (1.2) | 1 (0.4) |
| Novel psychoactive | 1 (0.4) | 0 |
The proportion of missing data and patterns of missingness were examined for the primary and secondary outcomes. The majority of participants who were lost to follow-up or withdrew from the study dropped out after the baseline visit and before 6 months, and this was the same for both treatment arms. The proportion of missing data for the primary outcome at 12 months was similar for both treatment arms (47.6% and 43.6% for the RISKIT-CJS intervention and the control, respectively) (Tables 5 and 6).
| Loss and withdrawal by time point | Treatment group | Overall | |
|---|---|---|---|
| RISKIT-CJS intervention | Control | ||
| Lost to follow-up, n | |||
| 6 months | 74 | 72 | 146 |
| 12 months | 32 | 30 | 62 |
| Withdrew, n | |||
| 6 months | 5 | 8 | 13 |
| 12 months | 3 | 2 | 5 |
| Dropouts, n | 114 | 112 | 226 |
| Allocated, n | 246 | 259 | 505 |
| Dropout rate, % | 46.3 | 43.2 | 44.8 |
| Outcome | Number (%) of missing values | ||
|---|---|---|---|
| Baseline | 6 months | 12 months | |
| PDA all substances | |||
| RISKIT-CJS intervention (n = 246) | 3 (1.22) | 115 (46.7) | 117 (47.6) |
| Control (n = 259) | 3 (1.16) | 125 (48.3) | 113 (43.6) |
| Overall (n = 505) | 6 (1.19) | 240 (47.5) | 230 (45.5) |
| WEMWBS | |||
| RISKIT-CJS intervention (n = 246) | 0 (0) | 151 (61.4) | 140 (56.9) |
| Control (n = 259) | 2 (0.772) | 158 (61.0) | 139 (53.7) |
| Overall (n = 505) | 2 (0.396) | 309 (61.2) | 279 (55.2) |
A greater proportion of males than females dropped out of the study, and primary outcome data at 12 months were recorded for 66.1% of female participants, but only 50.7% of male participants. There were more participants lost to follow-up from YOTs and SMTs than from PRUs. Primary outcome data at 12 months were available for 47.6% of participants from YOTs and 26.9% of participants from SMTs compared with 64.9% of participants from PRUs. Similar patterns were observed for WEMWBS score.
Tables 7 and 8 summarise baseline data by arm. There is no evidence of differences at baseline between treatments, supporting balance between the treatment arms and successful implementation of the randomisation procedure.
| Outcome | RISKIT-CJS intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| Median | 25% percentile | 75% percentile | n | Median | 25% percentile | 75% percentile | n | |
| PDA | ||||||||
| All substances | 60.7 | 7.14 | 89.3 | 243 | 61.8 | 3.57 | 85.7 | 256 |
| Substances alone | 64.3 | 7.14 | 96.4 | 243 | 64.3 | 3.57 | 96.4 | 256 |
| Alcohol alone | 96.4 | 89.3 | 100 | 243 | 96.4 | 89.3 | 100 | 256 |
| Cannabinoids/marijuana | 67.9 | 10.7 | 96.4 | 243 | 67.9 | 7.14 | 96.4 | 256 |
| Cocaine/crack | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Amphetamine-type stimulants | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Opioid analgesics | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Prescribed OST | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| MDMA/ecstasy | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Prescription medication | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Inhalants | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Hallucinogens | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| Novel psychoactives | 100 | 100 | 100 | 243 | 100 | 100 | 100 | 256 |
| BSCQ | ||||||||
| Unpleasant emotions | 30.5 | 1 | 70 | 246 | 49 | 10 | 93 | 259 |
| Physical discomfort | 50 | 10 | 100 | 246 | 50 | 3 | 100 | 259 |
| Pleasant emotions | 46.5 | 2 | 75 | 246 | 32 | 0 | 70 | 259 |
| Testing control over alcohol/drugs | 50 | 0 | 100 | 246 | 50 | 0 | 100 | 259 |
| Urges and temptations | 48 | 0 | 83 | 246 | 48 | 0 | 90 | 259 |
| Conflict with others | 50 | 10 | 100 | 246 | 50 | 3 | 100 | 259 |
| Social pressure to use | 51.5 | 11 | 100 | 246 | 55 | 6 | 100 | 259 |
| Pleasant time with others | 23.5 | 0 | 60 | 246 | 26 | 0 | 70 | 259 |
| Outcome | RISKIT-CJS intervention | Control | ||||
|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | |
| WEMWBS | 48.3 | 9.67 | 246 | 48.4 | 8.80 | 257 |
| SOCRATES-7DS | ||||||
| Pre contemplation | 13.1 | 2.67 | 243 | 14.0 | 2.61 | 254 |
| Contemplation | 9.64 | 3.70 | 243 | 9.16 | 3.53 | 254 |
| Preparation | 8.29 | 3.47 | 243 | 7.74 | 3.29 | 254 |
| Action | 12.4 | 4.26 | 241 | 11.5 | 4.53 | 253 |
| Maintenance | 11.1 | 3.99 | 241 | 10.6 | 4.23 | 252 |
| KIDSCREEN-10 Index | 31.7 | 5.30 | 237 | 31.5 | 5.25 | 248 |
Figure 3 shows the median and IQR over time by treatment arm for the primary outcome PDA all substances. For both treatment groups, the PDA increases at 6 months compared with baseline values, and median values at 6 and 12 months appear to be similar. Figure 4 shows the mean and SD of WEMWBS over time by treatment arm, and there are no obvious differences between the RISKIT-CJS intervention and control or between times.
FIGURE 3.
Median and IQR for PDA all substances by time and allocated arm.
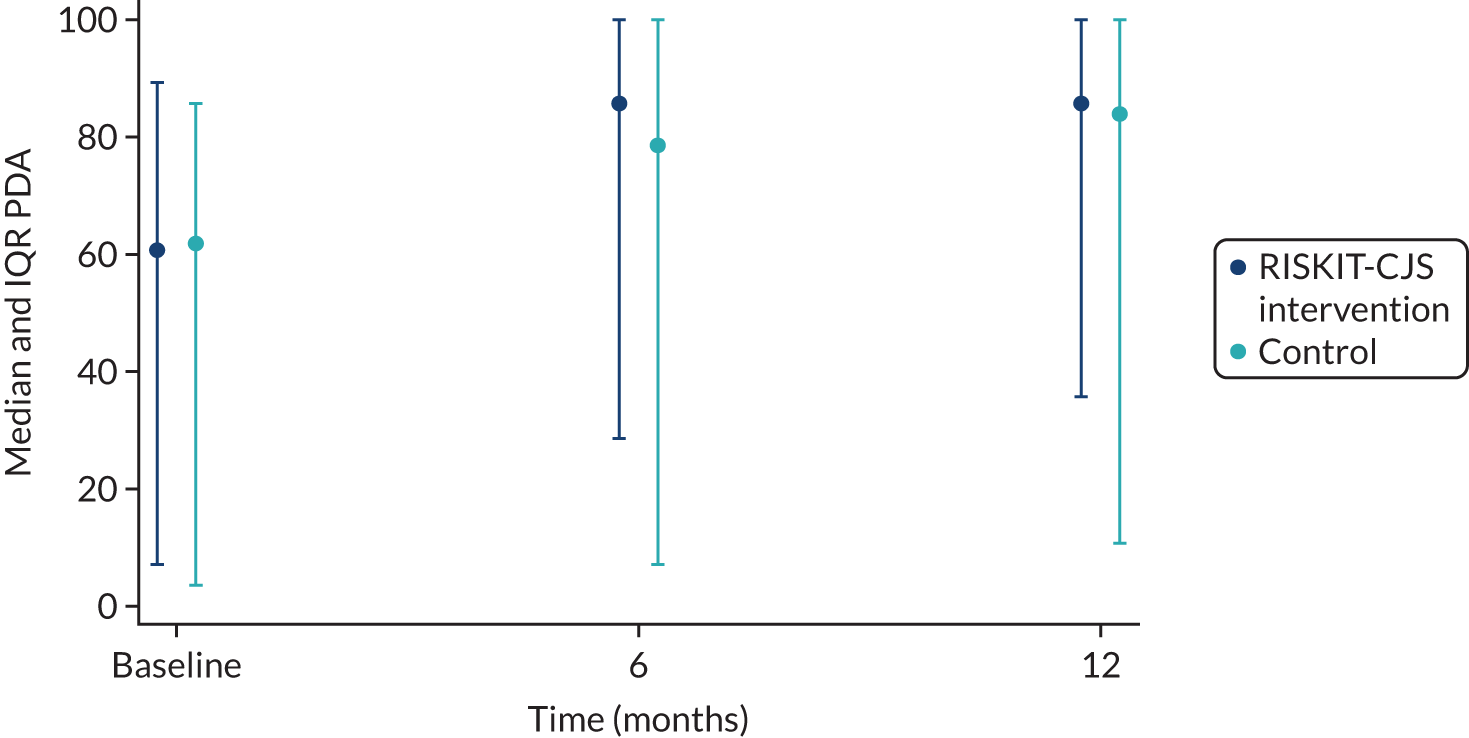
FIGURE 4.
Mean and SD for WEMWBS by time and allocated arm.
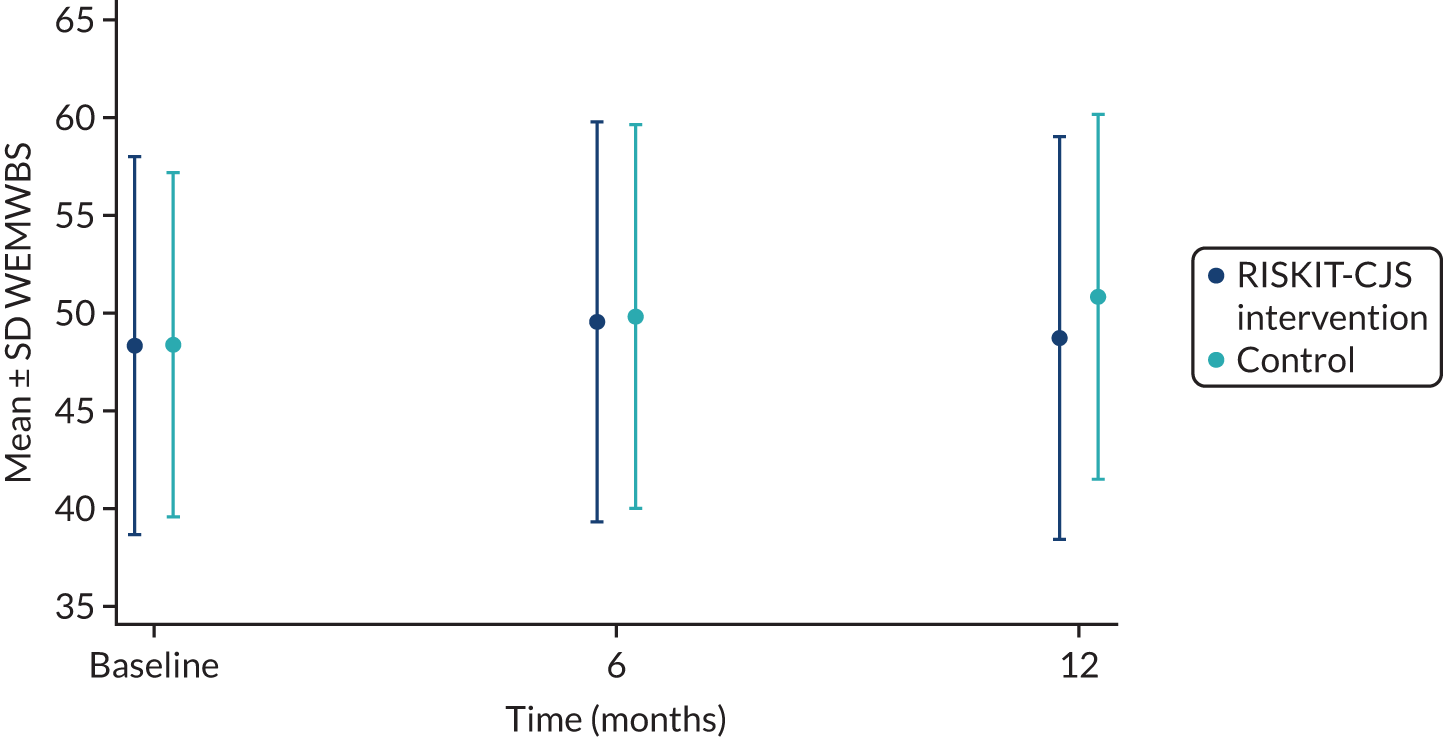
Tables 9 and 10 show the results from the statistical analysis of primary and secondary outcomes at 6 months and 12 months. There were no statistically significant differences between allocated arms for the primary outcome, PDA all substances, or for the secondary outcome, WEMWBS score.
| Outcome | RISKIT-CJS intervention, median | Control, median | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| PDA all substances | 85.7 | 83.9 | 1.14 | 0.743 to 1.76 | 0.542 |
| PDA all substances (PP) | 82.1 | 83.9 | 0.827 | 0.434 to 1.58 | 0.565 |
| PDA substances alone | 100 | 96.4 | 1.21 | 0.742 to 2.23 | |
| PDA alcohol alone | 96.4 | 100 | 1.01 | 0.625 to 1.64 | |
| PDA cannabinoids | 100 | 94.6 | 1.53 | 0.778 to 3.02 | |
| RISKIT-CJS intervention, meana | Control, meana | Treatment difference | |||
| WEMWBS | 49.3 | 50.4 | –1.10 | –3.45 to 1.25 | 0.357 |
| WEMWBS (PP) | 49.3 | 50.7 | –1.37 | –5.13 to 2.40 | 0.474 |
| KIDSCREEN-10 Index | 32.0 | 32.1 | –0.0821 | –1.60 to 1.44 |
| Outcome | RISKIT-CJS intervention, median | Control, median | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| PDA all substances | 85.7 | 78.6 | 1.39 | 0.900 to 2.15 | 0.137 |
| PDA all substances (PP) | 92.9 | 78.6 | 1.69 | 0.793 to 3.59 | 0.174 |
| PDA substances alone | 89.3 | 96.4 | 1.29 | 0.768 to 2.17 | |
| PDA alcohol alone | 100 | 100 | 1.31 | 0.687 to 2.50 | |
| PDA cannabinoids/marijuana | 87.5 | 96.4 | 1.27 | 0.729 to 2.20 | |
| RISKIT-CJS intervention, meana | Control, meana | Treatment difference | |||
| WEMWBS | 49.7 | 49.6 | 0.101 | –2.19 to 2.39 | 0.931 |
| WEMWBS (PP) | 51.3 | 49.8 | 1.51 | –2.21 to 5.22 | 0.424 |
| KIDSCREEN-10 Index | 31.7 | 32.3 | –0.685 | –2.20 to 0.831 |
There was a statistically significant difference between the sexes for WEMWBS score at 12 months (p < 0.01), with lower WEMWBS scores for female participants than for male participants (mean difference –4.20, 95% CI –6.79 to –1.61), but no evidence of an interaction with treatment.
Of the 246 participants in the intervention group, 47 participants completed all four steps of the intervention and were included in the PP analysis. The results from the PP analysis support those of the primary analysis.
Complier-average causal effect results
Based on the predefined compliance criteria, 104 participants in the intervention group were considered compliant with the intervention. The results presented in Table 11 show that there were no statistically significant differences between treatments for the primary outcome, PDA all substances, or for the secondary outcome, WEMWBS score, after accounting for non-compliance. The results from the CACE analysis support those from the primary analysis.
| Outcome | Analysis | Treatment difference (RISKIT-CJS intervention – control) | 95% CI | p-value |
|---|---|---|---|---|
| 12 months | ||||
| PDA all substances | ATA | 2.78 | –6.17 to 11.7 | 0.541 |
| CACE | 5.46 | –11.9 to 22.8 | 0.538 | |
| WEMWBS | ATA | –1.10 | –3.45 to 1.25 | 0.357 |
| CACE | –2.05 | –6.36 to 2.26 | 0.351 | |
| 6 months | ||||
| PDA all substances | ATA | 6.89 | –2.36 to 16.1 | 0.144 |
| CACE | 13.2 | –4.41 to 30.7 | 0.183 | |
| WEMWBS | ATA | 0.101 | –2.19 to 2.39 | 0.931 |
| CACE | 0.183 | –3.87 to 4.24 | 0.930 | |
Missing value substitution using last observation carried forward and last observation carried forward/baseline observation carried forward
The Pearson correlation coefficient between the 6- and 12-month data for the primary outcome showed a medium to strong association (correlation 0.562). Similarly, the correlation between the WEMWBS score at 6 and 12 months was 0.579 (Table 12 and Figure 5).
| Outcome | Pearson’s correlation coefficient | ||
|---|---|---|---|
| Baseline | 6 months | 12 months | |
| PDA all substances | |||
| Baseline | 1.00 | ||
| 6 months | 0.362 | 1.00 | |
| 12 months | 0.402 | 0.562 | 1.00 |
| WEMWBS | |||
| Baseline | 1.00 | ||
| 6 months | 0.570 | 1.00 | |
| 12 months | 0.423 | 0.579 | 1.00 |
FIGURE 5.
Scatterplot of PDA all substances and WEMWBS at 6 and 12 months. (a) PDA all substances; and (b) WEMWBS.
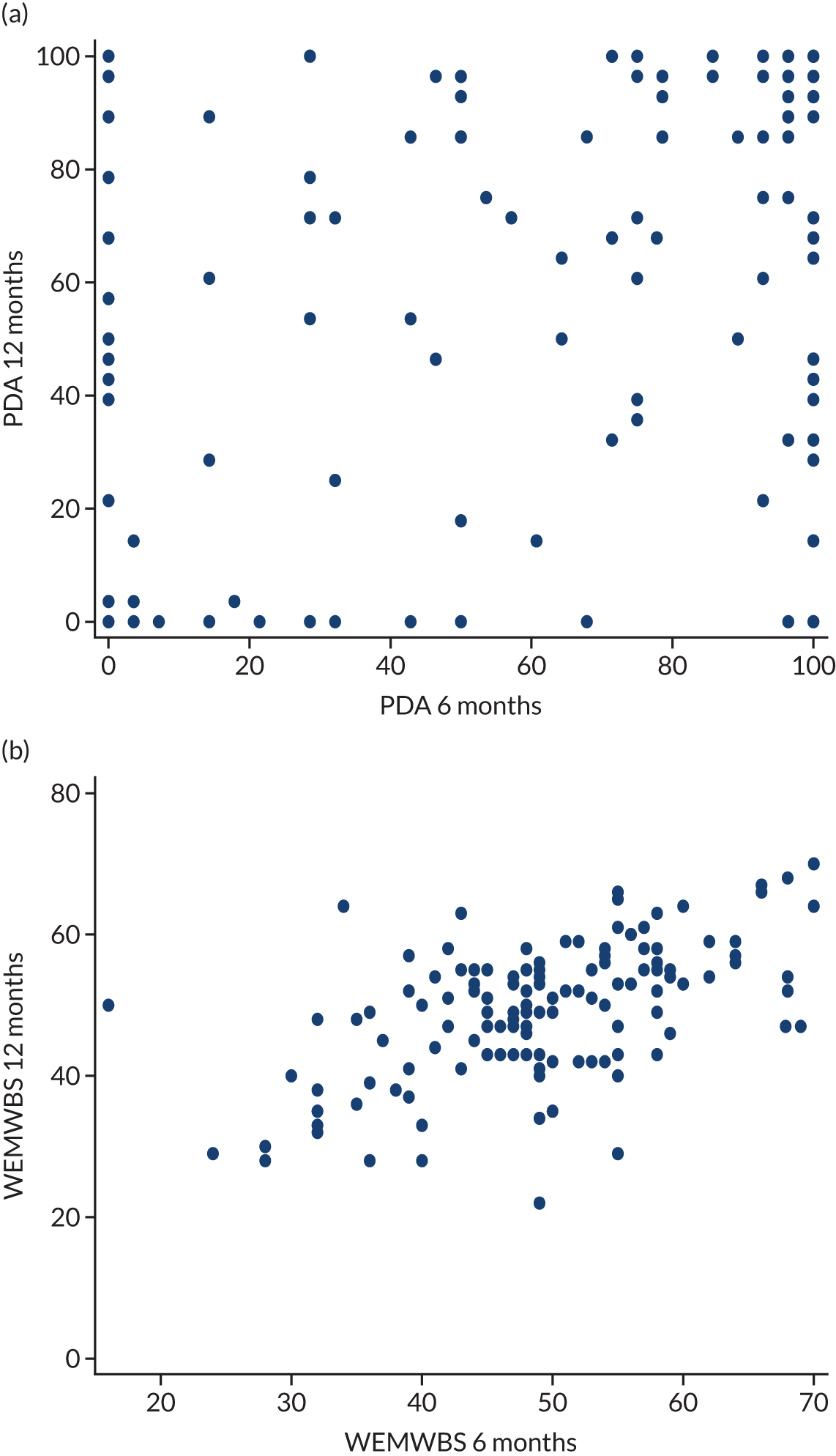
The findings from the analysis using LOCF and a combination of LOCF/BOCF to estimate missing values are presented in Tables 13 and 14. The results support those of the main analysis.
| Outcome | RISKIT-CJS intervention, median | Control, median | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| PDA all substances | 85.7 | 85.7 | 0.903 | 0.618 to 1.32 | 0.600 |
| RISKIT-CJS intervention, meana | Control, meana | Treatment difference | |||
| WEMWBS | 49.7 | 50.2 | 0.572 | –1.40 to 2.54 | 0.568 |
| Outcome | RISKIT-CJS intervention, median | Control, median | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| PDA all substances | |||||
| 12 months | 73.2 | 75.0 | 0.959 | 0.705 to 1.31 | 0.790 |
| 6 months | 74.5 | 64.3 | 0.786 | 0.576 to 1.07 | 0.129 |
| RISKIT-CJS intervention, meana | Control, meana | Treatment difference | |||
| 12 months | 49.5 | 49.7 | 0.198 | –1.01 to 1.41 | 0.749 |
| 6 months | 49.1 | 49.0 | –0.0106 | –0.974 to 0.953 | 0.983 |
Sensitivity analysis
The sensitivity analysis to explore departures from MAR for PDA and WEMWBS at 12 months shows that, even with large differences from the MAR assumption, the impact on the treatment effect is small (Figures 6 and 7).
FIGURE 6.
Impact of departures from MAR for PDA all substances at 12 months.
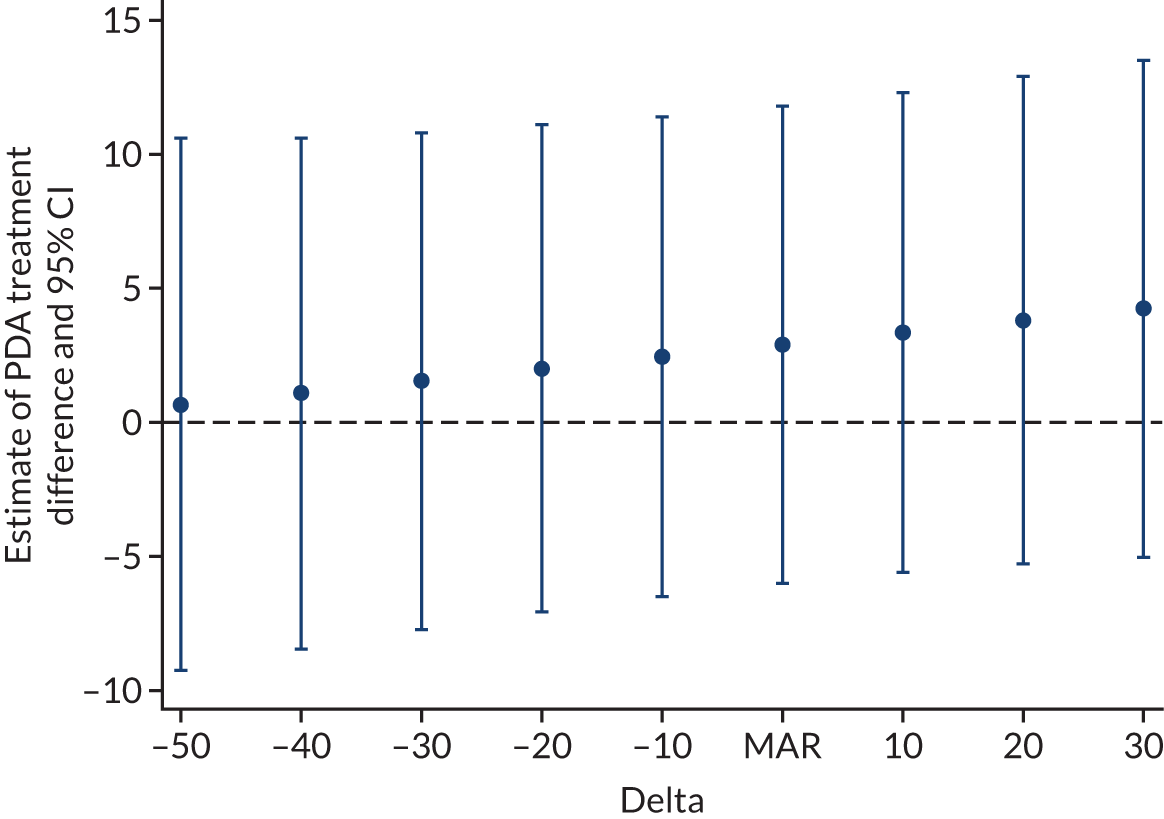
FIGURE 7.
Impact of departures from MAR for WEMWBS at 12 months.

Pre-randomisation factors
The exploratory analysis of the relationship between PDA all substances at 12 months and pre-randomisation factors showed statistical significance (p < 0.001) for the SOCRATES-7DS preparation stage, BSCQ question 1 (unpleasant emotions) and BSCQ question 2 (physical discomfort). Higher scores in SOCRATES-7DS preparation were related to fewer days abstinent at 12 months. Higher scores of confidence in BSCQ questions 1 and 2 were related to more days abstinent. There were no significant interactions with treatment group (see Report Supplementary Material 4, Table 1, for details).
The exploratory analysis of PDA for the intervention group only, which included process measures of adherence, therapeutic alliance and interventionist, showed statistical significance (p < 0.001) for the SOCRATES-7DS precontemplation stage, BSCQ question 1 (unpleasant emotions) and interventionist. Higher scores in both SOCRATES-7DS precontemplation and confidence in BSCQ question 1 were related to more days abstinent. Participants for one interventionist (n = 30) had significantly more days abstinent at 12 months compared with the other therapists, which may warrant further exploration. The therapist effect was still evident after adjusting for baseline PDA (see Report Supplementary Material 4, Table 2, for details).
The exploratory analysis of the relationship between WEMWBS score at 12 months and pre-randomisation factors showed statistical significance (p < 0.001) for the SOCRATES-7DS preparation stage and BSCQ question 7 (social pressure to use). Higher scores in SOCRATES-7DS preparation were related to lower well-being at 12 months and higher scores of confidence in BSCQ question 7 were related to greater well-being. There were no significant interactions with treatment group (see Report Supplementary Material 4, Table 3, for details).
The exploratory analysis of WEMWBS scores in the intervention group only, which included process measures of adherence, therapeutic alliance and interventionist, showed statistical significance (p < 0.001) for the Index of Multiple Deprivation, SOCRATES-7DS preparation stage, BSCQ question 3 (pleasant emotions) and BSCQ question 7 (social pressure to use). Higher scores in the SOCRATES-7DS preparation stage and the Index of Multiple Deprivation decile were related to lower well-being at 12 months, and higher scores of confidence in BSCQ questions 3 and 7 were related to greater well-being at 12 months (see Report Supplementary Material 4, Table 4, for details).
Change in allocation ratio
Analyses to account for the changes in the treatment allocation ratio during the study showed no evidence of a difference between allocation ratio groups for PDA all substances or WEMWBS score at 12 months. There were no significant interactions with treatment group.
Safety data
Two participants in the intervention group were excluded from group sessions because staff had concerns of a heightened risk to other participants. No participants were excluded in the control arm of the study.
Chapter 4 Health economic methods and results
Overview of methods
The primary economic analysis tested the null hypotheses that the RISKIT-CJS intervention in addition to TAU is no more cost-effective than TAU for adolescents involved in the CJS at the two National Institute for Health and Care Excellence (NICE)-recommended willingness-to-pay (WTP) thresholds of £20,000 (cost-effective) and £30,000 (borderline cost-effective). This was followed by an exploration of uncertainty, the results of which are presented graphically as cost-effectiveness planes (CEPs) and cost-effectiveness acceptability curves (CEACs).
Within-trial cost–utility analysis
The primary health economic analysis was a within-trial cost–utility analysis. The cost–utility analysis is a variation of the cost-effectiveness analysis when the outcome is measured in quality-adjusted life-years (QALYs). The incremental cost-effectiveness ratio (ICER) compares the treatment group with the control group77 and is the estimate of the additional cost associated with gaining an additional QALY. The perspective for the analysis was health and social care:
ΔC represents the incremental total cost of the treatment per participant and will consist of the total cost of running the intervention, ΔINT, and the incremental difference in service use cost between the treated and control population, ΔServiceUse. The CIs are calculated using the Fieller method. 78
The estimation of QALYs either gained or lost relies on the participant valuing their health state, with a score of 1 assigned to perfect health and a score of 0 assigned to being dead. This valuation was assessed using a generic health-related quality-of-life instrument, that is, the EQ-5D-5L. The EQ-5D-5L is a tool aimed at the general population and comprises five questions, each with five response levels. The EQ-5D-5L represents an improvement on the properties of the EuroQol-5 Dimensions, three-level version, as it allows for greater responsiveness, addressing known issues associated with ceiling and floor effects. 79,80 We rely on the crosswalk value sets for the UK, which are available from the EuroQoL Group [URL: https://euroqol.org (accessed 20 May 2022)], to convert responses to QALYs.
The estimation of costs between the RISKIT-CJS intervention and control was based on the additional costs of delivering the intervention, including costs associated with training, premises and overheads. As the RISKIT-CJS intervention and control arms both received TAU, we did not cost this element of treatment because costs would cancel out across arms of the study. We assessed the cost of participants’ use of resources [e.g. general practitioner (GP) appointments, inpatient and outpatient appointments, accident and emergency visits, mental health and social care appointments] at baseline and again at 6 and 12 months using a client service receipt approach. As the time horizon was 12 months, no discounting was applied.
Cost–consequence analysis
The cost–consequence analysis presents the costs and effects data of the RISJKIT-CJS intervention as a balance sheet. A series of comparisons of cost and effects by allocated group are presented without any formal attempt to combine effects and costs. This approach has the potential to capture wider effects and allows the commissioner to make decisions based on their own priorities.
Changes to the original protocol
As discussed in Chapter 1, data on the criminal justice activity of participants had not been made available to the research team, and this meant that the economic analysis could not be conducted from the public sector and societal perspective and, therefore, analysis conducted from the health and social care perspective is presented.
Measures
Quality of life
The primary outcome measure in the economic evaluation is QALYs derived from the EQ-5D-5L. The descriptive system, which comprises five dimensions81 (i.e. mobility, self-care, usual activities, pain/discomfort and anxiety/depression) was converted into utility scores at baseline and at the 6- and 12-month follow-up interviews, using the EQ-5D-5L value set developed for the general UK population. 82,83 Assuming that health status changes gradually over time between the follow-up points, QALYs were calculated from the utility scores using the area under the curve method. 84
Costs of using health and social care
The services used by participants were informed by other studies with similar populations. 85,86 Each participant was asked, at baseline and at 6 and 12 months, to indicate how often they had used services in the 6-month period prior. Each contact with services was allocated a unit cost. All costs were measured in 2019–20 prices either by directly relying on unit costs measures in the NHS reference costs or via established sources of unit costs of health and social care87,88 and, when necessary, including appropriate adjustment for inflation. Table 15 shows the costs associated with each resource item, and Table 5 in Report Supplementary Material 5 provides corresponding references and explanations for these costs. The cost of service per participant was calculated as the product of units used and cost per unit, and this cost was summed across all service categories.
| Resource item | Setting | Cost (£) | Unit |
|---|---|---|---|
| Health care | |||
| Hospital nights | Secondary care admitted | 375 | Per night |
| A&E visits | A&E | 190 | Per attendance |
| Walk-in clinic | A&E | 46 | Per attendance |
| Minor injury unit | A&E | 74 | Per attendance |
| Outpatient | Secondary care not admitted | 127 | Per attendance |
| Day hospital | Secondary care admitted | 341 | Per attendance |
| GP | Primary care | 39 | Per contact |
| Practice nurse | Primary care | 42 | Per hour |
| Health visitor | Primary care | 81 | Per hour |
| Optician | Primary care | 80 | Per hour |
| Family therapist | Family support services | 58 | Per hour |
| Individual therapist | Family support services | 58 | Per hour |
| Psychiatrist | Secondary care not admitted | 230 | Per hour |
| Sexual health clinic | Community health | 90 | Per attendance |
| Other health visit | Primary care | 38 | Per hour |
| Community and social care | |||
| Social worker | Social care | 52 | Per hour |
| Other social care | Social care | 25 | Per hour |
| Foster care | Social care | 622 | Per week |
| Residential care | Social care | 712 | Per day |
| Supported living | Social care | 1711 | Per week |
| After school club | Community | 63 | Per week |
Cost of the intervention
The resources assessed for the delivery of the intervention included those costs that would be incurred if the intervention was delivered in practice. Therefore, the resources associated with the scientific evaluation were excluded. In a similar manner, resources that were common across both arms of the study (i.e. TAU) were also excluded.
The costs of the RISKIT-CJS intervention have been calculated based on the actual resource use and the corresponding national unit costs for individuals with qualifications required to deliver the intervention (e.g. substance misuse/youth workers). These workers were invited to training sessions to obtain the necessary skills to deliver the intervention. The cost of the training component involved the opportunity costs of time devoted to the training by all the participants, trainers and the venue hire costs. It was calculated based on the actual costs that were incurred and then divided over the number of participants allocated to the RISKIT-CJS intervention arm at the start of the trial.
The intervention took place over 2 consecutive weeks and included the four steps described in detail in Chapter 2, Trial processes, that is, (1) an individual face-to-face 40-minute session with the interventionist; (2) a group session over half a day (4 hours) at a convenient location (by two interventionists); (3) a group session over half a day (4 hours) conducted a week after step 2, with the same participants, same staff and at the same location; and (4) a concluding individual face-to-face 40-minute session with an interventionist.
Total cost
The total cost for each participant in the RISKIT-CJS intervention arm was estimated as the cost of delivering the intervention, including costs allocated for training and supervision, divided by the number of participants receiving it and the individual-level resource use costs at follow-up across health and social care. In the control arm, the costs were estimated as individual-level resource use costs at follow-up across health and social care.
Secondary effectiveness measures from the trial
The secondary outcome measures analysed for the cost-effectiveness and cost–consequence analyses included the CHU-9D (i.e. a child-specific generic quality-of-life instrument), the number of days using substances in the past 28 days at month 12 (assessed using the TLFB28) and well-being (assessed using the WEWBMS). The recorded sociodemographic characteristics of participants included sex, age and geographical location (i.e. South East, North East, London or North West).
Data
Data included in the analysis relied on responses from participants who were eligible and consented to participate in the trial. Primary analysis was conducted using a per allocation approach, with participants’ outcomes analysed according to the group they were allocated to rather than the treatment they received.
For the incremental cost-effectiveness analysis, the differential in the arithmetic means of individual annual costs89 and the differential in the adjusted means of annual cost have been estimated using the multiple regression analysis, controlling for sex, site and baseline costs, and this concurs with the approach taken for the clinical analysis described.
Managing uncertainty
As the costs and outcomes data are usually not normally distributed, we employed a non-parametric bootstrap to determine the level of sampling uncertainty in incremental costs and benefits and, hence, cost-effectiveness/cost–utility. 90 Non-parametric bootstrapping is a sampling approach that generates multiple replications of ICERs by sampling with replacement data from the original data set. The bootstrap method is preferable for the skewed distributions, as it does not rely on the parametric assumptions about the underlying data. 89 One thousand bootstrap replications91 produced ICERs for the CEP and CEAC to explore the uncertainty. 92 The latter allowed the graphical representation of the probability that the RISKIT-CJS intervention is preferred to TAU at different values of WTP. 93
Sensitivity analysis and missing data
The cost-effectiveness analysis could be sensitive to the quality of data, predominantly when the distribution of the cost data is affected by outliers, various assumptions that are necessary to construct the measure of the total cost and the measures from which the QALYs are derived. Therefore, the primary analysis will be subject to sensitivity checks along several dimensions, including (1) exclusion of outliers in terms of costs; (2) replacement of individually varying intervention costs with fixed costs based on the total cost of intervention spread across all of the participants in the treated group; and (3) replacement of actual training costs incurred within the trial, with the training costs spread over a larger number of participants and assuming that, in real life, one trained interventionist would be able to deliver the intervention to six cohorts of participants on average. Each of these checks has been undertaken as a one-way analysis, followed by the corresponding analysis taking into account sampling uncertainty.
The clinical analysis showed a significant proportion of missing data for the primary and secondary outcomes. For the PDA from all substances and WEMWBS score, the percentage of data missing at 12 months was 45% and 55%, respectively, and, consequently, the multiple imputations were not performed. The situation is even more problematic with the EQ-5D-5L combined with the cost measures, as only 70 (27%) individuals in the control group and 62 (25%) individuals in the treatment group provided all of the data needed for the cost-effectiveness analysis. As a result, the primary economic analysis is based on complete cases without imputations. However, multiple imputations have been performed for costs and outcomes (following Faria et al. 94) and within the scope of the sensitivity analysis of uncertainty. Eight scenarios are explored,95 with the health-related quality of life and the total costs being 10% lower or higher in one or both arms as compared with the MAR setting.
Results of the primary economic analysis
Out of the 505 participants recruited at baseline, 495 provided baseline information but only about one-quarter provided information at the follow-ups, which was needed for the health economic analysis. Given the significant proportion of missing data, the primary economic analysis is based on 132 participants (RISKIT-CJS intervention group, n = 62; TAU group, n = 70), with both cost and outcomes information provided at three points in time (i.e. baseline, 6 months and 12 months).
Costs
Table 16 summarises the intervention costs. As the screening and recruitment costs and the TAU costs were the same for both the intervention and the control groups, they are omitted from the incremental cost-effectiveness analysis.
| Source of cost | RISKIT-CJS intervention | Comment |
|---|---|---|
| Intervention cost (£) (SD) per participant | 267.28 (162.37) | The variation in RISKIT-CJS intervention costs derives from the actual participation in individual sessions and the varying cost of group sessions, depending on the number of attendees |
| Training cost (£) per participant | 42.94 | Based on the 1-day training session with two trainers (band 7 youth worker £58/hour) and opportunity cost for 24 interventionists (£49/hour), including venue costs88 |
| Cost (£) of individual MI sessions per participant | 65.34 | Two 40-minute sessions with a substance misuse worker (£49/hour)88 |
| Number (SD) of individual sessions attended | 1.37 (0.55) | Based on actual attendance data |
| Group costs (£) per session | 428 | Half-day session (4 hours) based on two interventionists (band 7 youth worker £58/hour and substance misuse worker £49/hour)88 |
| Number (SD) of group sessions attended | 0.98 (0.89) | Based on actual attendance data |
The RISKIT-CJS intervention consisted of two individual sessions, which each lasted 40 minutes each and cost £32.67 per participant, and two group sessions, each lasting for 4 hours and costing £428 per session. The number of participants in the group sessions varied from one to nine, with an average of 4.64 (SD 2.29) for the first group session and an average of 4.16 (SD 2.28) for the second group session. The training cost was divided by the total number of participants allocated to the RISKIT-CJS intervention, and this was £49.24 per participant. Therefore, the overall cost of delivering the RISKIT-CJS intervention amounts to £267.28 (SD £162.37) per participant.
Service use from the health and social care perspective, at baseline and at 6 and 12 months by allocated group, is presented in Table 17. Respondents did not report any family and individual therapist visits and so these categories are excluded.
| Service use | Baseline | Month 6 | Month 12 | |||
|---|---|---|---|---|---|---|
| Control | RISKIT-CJS intervention | Control | RISKIT-CJS intervention | Control | RISKIT-CJS intervention | |
| Number of observations | 70 | 62 | 70 | 62 | 70 | 62 |
| Hospital nights | 0.13 (0.48) | 0.42 (2.11) | 0.03* (0.17) | 0.20* (0.80) | 0.09 (0.45) | 0.11 (0.37) |
| A&E | 0.07 (0.40) | 0.22 (1.11) | 0.01 (0.12) | 0.05 (0.30) | 0.07 (0.31) | 0.05 (0.22) |
| Walk-in clinic | 0.02 (0.12) | 0.36 (2.02) | 0 | 0 | 0.02 (0.12) | 0.02 (0.13) |
| Minor injury | 0 | 0 | 0 | 0 | 0 | 0.04 (0.26) |
| Outpatient | 0 | 0.02 (0.13) | 0 | 0.09 (0.67) | 0 | 0.09 (0.66) |
| Other hospital | 0 | 0.04 (0.26) | 0 | 0 | 0 | 0 |
| GP | 0.19 (1.44) | 0.32 (1.50) | 0.09 (0.73) | 0.03 (0.26) | 0.06 (0.34) | 0.21 (0.83) |
| Practice nurse | 0 | 0.08 (0.64) | 0 | 0 | 0 | 0.08 (0.45) |
| Optician | 0.01 (0.12) | 0.02 (0.13) | 0 | 0 | 0 | 0 |
| Psychiatrist | 0.41 (2.89) | 0 | 0 | 0 | 0 | 0 |
| Sexual health | 0.01 (0.12) | 0.03 (0.25) | 0 | 0.02 (0.13) | 0 | 0.03 (0.25) |
| Social worker | 0.67 (3.25) | 0.90 (3.81) | 0.04 (0.36) | 0.17 (1.05) | 0.65 (4.21) | 0.08 (0.42) |
| Other social service | 0 | 0 | 0 | 0 | 0 | 0.03 (0.25) |
| Foster care (days) | 1.36 (11.08) | 0.25 (1.87) | 1.97 (15.36) | 0 | 0 | 1.67 (12.25) |
| Supported living (days) | 0 | 0 | 3.44 (26.89) | 0 | 1.50 (11.26) | 0 |
| Other living (days)a | 7.61 (43.80) | 4.95 (25.76) | 3.97 (17.10) | 1.32 (5.70) | 3.57 (20.49) | 4.19 (19.24) |
| Education absence (days) | 3.47 (6.44) | 4.42 (6.90) | 3.79 (6.46) | 4.03 (7.24) | 3.98 (7.13) | 4.14 (9.05) |
| Education exclusions | 2.91 (3.57) | 4.52 (7.64) | 2.50 (3.06) | 2.00 (1.30) | 2.38 (1.67) | 3.86 (4.41) |
| Working hours per week | 10.19 (4.28) | 8.17 (2.56) | 12.15 (11.49)* | 25.27 (14.23)* | 22.14 (17.60) | 21.19 (15.06) |
| Working absence (days) | 3.70 (9.50) | 1.17 (2.40) | 0.71 (1.26) | 0.36 (0.81) | 1.27 (3.63) | 0.29 (0.61) |
Among participants in education, 33% in the control group compared with 16% in the RISKIT-CJS intervention received at least one exclusion, with the difference being statistically significant at a 5% level. Furthermore, at the 6-month follow-up, participants in the RISKIT-CJS intervention group who were working reported more working hours than participants in the control group [25.27 (SD 14.23) hours vs. 12.15 (SD 11.49) hours, respectively], with the difference being statistically significant at the 5% level.
The costs of health and social care service use were estimated as the products of each resource use category in Table 17 and the corresponding unit costs reported in Table 15. These costs were then added to the cost of intervention from Table 16 to obtain the total cost for each participant in both the treatment group and the control group over the year (Table 18). These calculations show that the resources used in the health and social care sectors are the most significant contributor to the total cost. The mean health and social care cost for the RISKIT-CJS intervention group over the first 6 months was £91.96 (SD £332.25), compared with the £901.32 (SD £6246.40) in the control group, resulting in a difference of –£809.36 (95% CI –£2381.45 to £762.73). At the 12-month follow-up, the health and social care cost was £201.12 (SD £1034.58) for the RISKIT-CJS intervention group and £394.69 (SD £2643.03) for the control group, a difference of –£193.56 (95% CI –£901.50 to £514.37). Therefore, the total cost over the 12 months was £560.36 (SD £140.26) for the RISKIT-CJS intervention group and £1296 (SD £1055.95) for the control group. The residual 12-month costs after adjustment for the RISKIT-CJS intervention group were £279.11 (SD £266.38) and £848.47 (SD £993.36) for the control group, resulting in a difference favouring the RISKIT-CJS intervention of –£569.37 (95% CI –£2716.48 to £1577.74). This difference indicates that the RISKIT-CJS intervention resulted in cost savings from the health and social care perspective, compared with the TAU. However, the CI is wide and includes zero, and so the difference is not statistically significant at the 5% level.
| Time point | Mean (SD) cost (£) | Mean difference (95% CI) (£) | |
|---|---|---|---|
| RISKIT-CJS intervention (n = 62) | Control (n = 70) | ||
| Baselinea | 258.56 (1081.50) | 308.61 (1248.39) | –50.05 (–454.78 to 354.68) |
| Month 6a | 91.96 (332.25) | 901.32 (6246.40) | –809.36 (–2381.45 to 762.73) |
| Month 12a | 201.12 (1034.58) | 394.69 (2643.03) | –193.56 (–901.50 to 514.37) |
| Intervention cost | 267.28 (162.37) | n/a | 267.28 (n/a) |
| Unadjusted cost over 12 months | 560.36 (1104.40) | 1296.00 (8834.69) | –735.64 (–2971.66 to 1500.38) |
| Residual cost over 12 months after adjustmentb | 279.11 (2097.49) | 848.47 (8311.03) | –569.37 (–2716.48 to 1577.74) |
Outcomes
Table 19 shows the differences in the EQ-5D-5L-based utility scores at baseline and at 6 and 12 months between the RISKIT-CJS intervention group and the control group, as well as the calculated QALYs. The utility scores at the three time periods are used to calculate the QALYs using the area under the curve method. The residual mean changes in QALYs after adjustment were 0.3756 (SD 0.0949) and 0.3842 (SD 0.0928) for the RISKIT-CJS intervention group and the control group, respectively. The resulting incremental changes in QALYs between the RISKIT-CJS intervention group and the control group were –0.0427 (95% CI –0.0958 to 0.0105) without adjustment and –0.0086 (95% CI –0.0409 to 0.0238) after adjustment.
| Time point | Mean (SD) | Mean difference (95% CI) | |
|---|---|---|---|
| RISKIT-CJS intervention (n = 62) | Control (n = 70) | ||
| EQ-5D-5L | |||
| Baseline | 0.8519 (0.2300) | 0.8905 (0.1254) | –0.0386 (–0.1014 to 0.0242) |
| Month 6 | 0.8977 (0.1812) | 0.8599 (0.1944) | 0.0377 (–0.0273 to 0.1027) |
| Month 12 | 0.8353 (0.2071) | 0.8819 (0.2071) | –0.0467 (–0.1181 to 0.0248) |
| Unadjusted QALYs over 12 months | 0.8435 (0.1777) | 0.8862 (0.1298) | –0.0427 (–0.0958 to 0.0105) |
| Residual QALYs over 12 months after adjustmenta | 0.3756 (0.0949) | 0.3842 (0.0928) | –0.0086 (–0.0409 to 0.0238) |
Results of the cost-effectiveness analysis
Table 20 brings together the incremental changes in QALYs with the incremental changes in costs to produce the ICERs. In both cases, within and without adjustment, both mean costs and mean QALY gains were smaller in the RISKIT-CJS intervention group than in the control group. However, the Fieller 95% CIs are wide, meaning that we cannot be 95% confident that the two approaches (i.e. the RISKIT-CJS intervention and control) differ in value.
| Analysis | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| RISKIT-CJS intervention (n = 62) | Control (n = 70) | RISKIT-CJS intervention (n = 62) | Control (n = 70) | |
| Total cost (SD) (£) | 560.36 (1104.40) | 1296 (8834.69) | 279.10 (2079.49) | 848.47 (8311.03) |
| QALYs (SD) | 0.8435 (0.1777) | 0.8862 (0.1525) | 0.3756 (0.0949) | 0.3842 (0.0928) |
| ICER (£) (95% Fieller’s CI) | 15,644 (–35,404 to 186,798) | 67,000 (cannot compute) | ||
We used a bootstrap resampling method, consisting of 1000 replications, to assess the uncertainty surrounding the cost-effectiveness estimates to construct the CEP and the CEAC. 96 The adjusted CEAC is presented in Figure 8.
FIGURE 8.
(a) Cost-effectiveness plane; and (b) CEAC, adjusted for baseline utility and costs, age, sex and site at 12 months (completed cases).
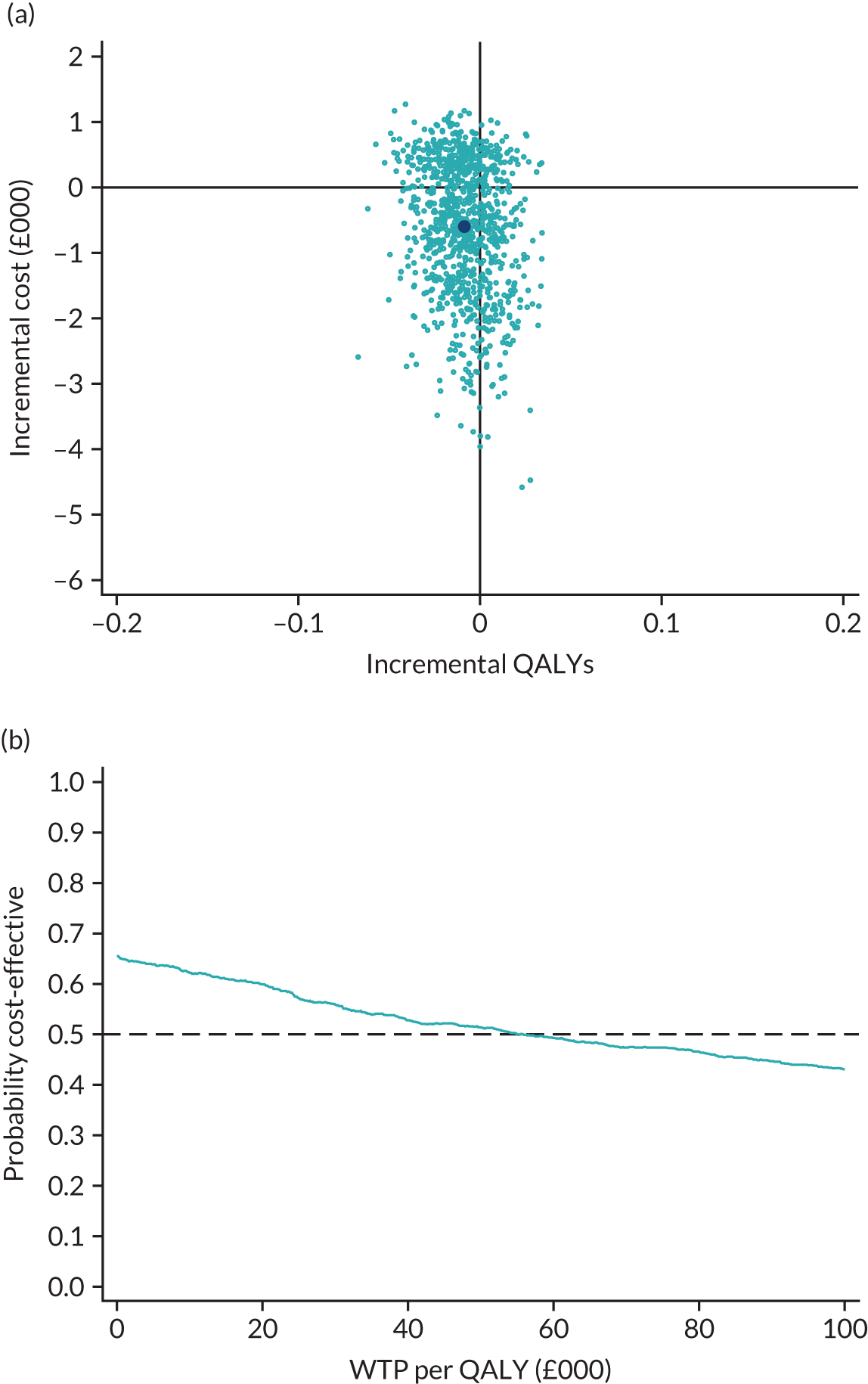
The CEP is divided into four quadrants and allows us to visualise the variation within the resulting bootstrapped sample of ICERs. The horizontal axis represents incremental effects with positive ones, indicating that the RISKIT-CJS intervention is more clinically effective than the control. The adjusted mean effect becomes smaller in absolute value, with the combinations of incremental costs and effects distributed across all four quadrants and the majority in the south-west and south-east quadrants, suggesting cost saving with no effect on QALYs. The CEAC shows a 69% probability that the RISKIT-CJS intervention is cost saving when the WTP is equal to zero. At the NICE-recommended thresholds, the probability that the RISKIT-CJS intervention is more cost-effective than control is 60–63%.
Sensitivity analysis
Sensitivity analyses were conducted to evaluate the robustness of the findings in the primary analysis.
Table 6 in Report Supplementary Material 5 provides the results of the incremental cost-effectiveness analyses for all three sensitivity tests.
Sensitivity test 1
Excluding cost outliers leads to a considerable change in mean costs for the control group, regardless of adjustment [the difference in total costs is £338.33 (95% CI £168.51 to £508.15) and the difference in adjusted costs is £301.03 (95% CI £142.29 to £459.79), with little change in terms of QALYs]. Therefore, in the case with no adjustment, the Fieller’s CI suggests that for a WTP greater than £22,389 (i.e. within the £20,000–30,000 NICE-recommended interval) the RISKIT-CJS intervention and control do not differ in value. However, at WTP lower than £22,389, the control represents good value compared with the RISKIT-CJS intervention. Moreover, as Figure 27 in Report Supplementary Material 6 illustrates, this change led to a shift of the mass of incremental cost–incremental effects pairs almost entirely to the north-west quadrant without adjustment, with an almost equal distribution between the north-west and north-east quadrants after adjustment. Furthermore, the CEACs for both cases show a low probability of the RISKIT-CJS intervention being cost-effective compared with control within the NICE-recommended interval of WTP. Therefore, the exclusion of outliers does not produce more conclusive evidence on whether the RISKIT-CJS intervention is dominating or dominated by the control in terms of cost-effectiveness.
Sensitivity test 2
Using the intervention costs fixed across all participants led to minimal changes in the mean total cost for the treatment group, which decreased from £560.35 to £550.32 in the case with no adjustment and increased slightly for both the RISKIT-CJS intervention group and the control group after adjustment. However, the results based on Fieller’s CI are very similar to the primary analysis results. Likewise, the CEPs and CEACs in Report Supplementary Material 6, Figure 28, show uncertainty similar to the primary analysis.
Sensitivity test 3
To bring the estimates of the training costs closer to the real-life situation, the analysis was repeated with the training costs spread across six cohorts of participants. This resulted in the training cost becoming six times smaller (£8.21 vs. £49.24 in the primary analysis). The results are very similar to the primary analysis, in terms of both the conclusions from the Fieller’s CI consideration and the CEPs and CEACs depicted in Report Supplementary Material 6, Figure 29 (as there is no WTP at which the two approaches would differ in value with 95% confidence level).
Results of the secondary economic analysis
The secondary economic analysis involves two modifications. The first modification is related to the compliance of the participants in the treated group with the treatment indicated in the research protocol. The second modification is related to the construction of the QALY gain based on the CHU-9D measure rather than the EQ-5D-5L. The results are summarised in Report Supplementary Material 5, Table 7, with the graphical representation of the CEPs and CEACs in Report Supplementary Material 6, Figure 30.
Modification 1
Exclusion of non-compliers (PP analysis) leads to a situation in which the differences in mean costs are very similar to those in the primary economic analysis [i.e. unadjusted: –£749.81 (95% CI –£3563.68 to £2064.06); adjusted: –£525.09 (95% CI –£3216.74 to £2166.55)], but there is a completely different picture for the mean outcomes [i.e. unadjusted: –0.0301 (95% CI –0.0904 to 0.0302); adjusted: –0.0069 (95% CI –0.0426 to 0.0288)]. Nevertheless, the conclusion remains the same as in the primary analysis, that is, the two approaches (RISKIT-CJS intervention and control) do not differ from each other in value (see Report Supplementary Material 5, Table 7, and Report Supplementary Material 6, Figure 31). Sensitivity analysis on the PP sample was repeated excluding the outliers and the results were similar to the primary analysis excluding the outliers.
Modification 2
Replacing the QALY measure based on the EQ-5D-5L instrument with the QALY measure based on the CHU-9D instrument shows some difference from the primary analysis in the case of adjusted costs and effects in terms of point estimates, as well as in the shape and position of the CEP and the CEAC. However, similarly to the primary analysis, there is no WTP for which the two approaches would differ in value at the 5% level of significance.
Additional health economic analyses
Cost–consequence analysis
As the completed cases for the cost data are available for only 132 participants, the estimation of the effect of the intervention on outcomes is repeated for the sample with cost data to enable meaningful comparison between the costs and consequences. However, complete cost data for the primary and secondary clinical outcomes were available for only 128 participants. Table 21 presents the total costs and the primary and secondary clinical outcomes for the RISKIT-CJS intervention group and the control group, as well as the difference between them.
| Outcome | RISKIT-CJS intervention, median | Control, median | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| PDA all substances | 85.7 | 67.9 | 1.17 | 0.63 to 2.17 | 0.614 |
| RISKIT-CJS intervention, meana | Control, meana | Treatment difference | |||
| WEMWBS | 48.98 | 49.76 | –1.37 | –4.45 to 1.71 | 0.379 |
| Total cost (£) | 601.40 | 1278.36 | –628.25 | –2911.91 to 1655.40 | 0.587 |
Cost-effectiveness analysis for other outcomes
Incremental cost-effectiveness ratios were estimated for the primary outcome of PDA from substances in the last 28 days at the 12-month follow-up and the secondary outcome of WEMWBS score for 128 complete cases, after adjusting for a set of covariates (i.e. sex, age, site, and baseline cost and outcome). Table 22 shows ICERs and Fieller’s 95% CIs. As can be seen, the latter are unbounded from the right and, therefore, for the PDA all substances, for WTP > £971, there is no 95% CI for the RISKIT-CJS intervention and TAU to differ in cost-effectiveness. Similarly, for the WEMWBS score, for WTP > £80, the two interventions do not differ in cost-effectiveness. It is not common in the literature to construct CEPs and CEACs for outcomes other than health economic ones. In addition, these measures do not have recommended WTP thresholds. However, exploration of these outcomes, given their clinical importance, may present additional evidence to the primary health economic analysis findings.
| Outcome | ICER | Fieller’s 95% CI |
|---|---|---|
| PDA all substances | 3508 | 971 to ∞ |
| WEMWBS | 1.161e+ 09 | 80 to ∞ |
Handling missing data
Given the proportion of missing data and the low likelihood that data are MAR, a decision was made to build the primary economic analysis on the available data, limiting it to those participants who responded to all the questions needed to construct cost and outcome variables. Unfortunately, it cannot be considered an intention-to-treat analysis because randomised patients with follow-up data were excluded if they did not provide information at any one time point. 97 However, as a very high proportion of the data needed for the cost-effectiveness analysis in the RISKIT-CJS trial were missing, it is very difficult to rely confidently on imputation methods. Therefore, imputations are employed in the sensitivity analysis only. Furthermore, multiple imputations have been chosen over single imputation with mean values because the former underestimate the uncertainty. 94
Baseline values were available for 495 participants and were not imputed for this analysis.
Multiple imputations by chained equations were performed for QALYs and health and social care costs at the 6- and 12-month follow-ups, using predictive means matching and baseline variables of sex, age, type of service, utility score and primary outcome at baseline. The number of imputations was set to 50, stratified by arm. Using imputed variables, the QALY gains were calculated using the area under the curve, and the total costs were calculated as the sums of the health and social care costs over the previous 6 months (reported at the 6- and 12-month follow-ups).
Figure 9 offers CEPs (see Figures 9a–h) and CEACs (see Figure 9i) for eight scenarios, each of which is described by the multiplicative factor (i.e. QALYTAU, QALYRISKIT, CostTAU, CostRISKIT). Therefore, the first scenario (see Figure 9a) is the base-case scenario with imputations performed under the MAR assumption. The rest of the scenarios represent various combinations to reflect possible patterns of MNAR. For example, scenario 5 differs from scenario 1 (MAR) only in terms of the QALYs for the treated group, assuming that those of the treated participants who are missing have 10% lower QALY gain over the year, as compared with the MAR assumption. Scenario 6 represents the reverse situation: participants in the control group for whom the information is missing have a 10% lower QALY gain. The CEACs and CEPs are constructed from a bootstrapped data with 1000 replications.
FIGURE 9.
Cost-effectiveness planes and CEACs, all adjusted for baseline utility and costs, at 12 months, MAR multiple imputations (scenario 1) and sensitivity for MNAR (scenarios 2–7). MNAR scenarios are defined by the four parameters, which represent multiplicative factors to change the imputed parameter to reflect MNAR possibility. The outcomes in the order of appearance are QALYs for the control group, QALYs for the treatment group, total cost for the control group and total cost for the treatment group. (a) CEP, scenario 1; (b) CEP, scenario 2; (c) CEP, scenario 3; (d) CEP, scenario 4; (e) CEP, scenario 5; (f) CEP, scenario 6; (g) CEP, scenario 7; (h) CEP, scenario 8; and (i) CEACs.
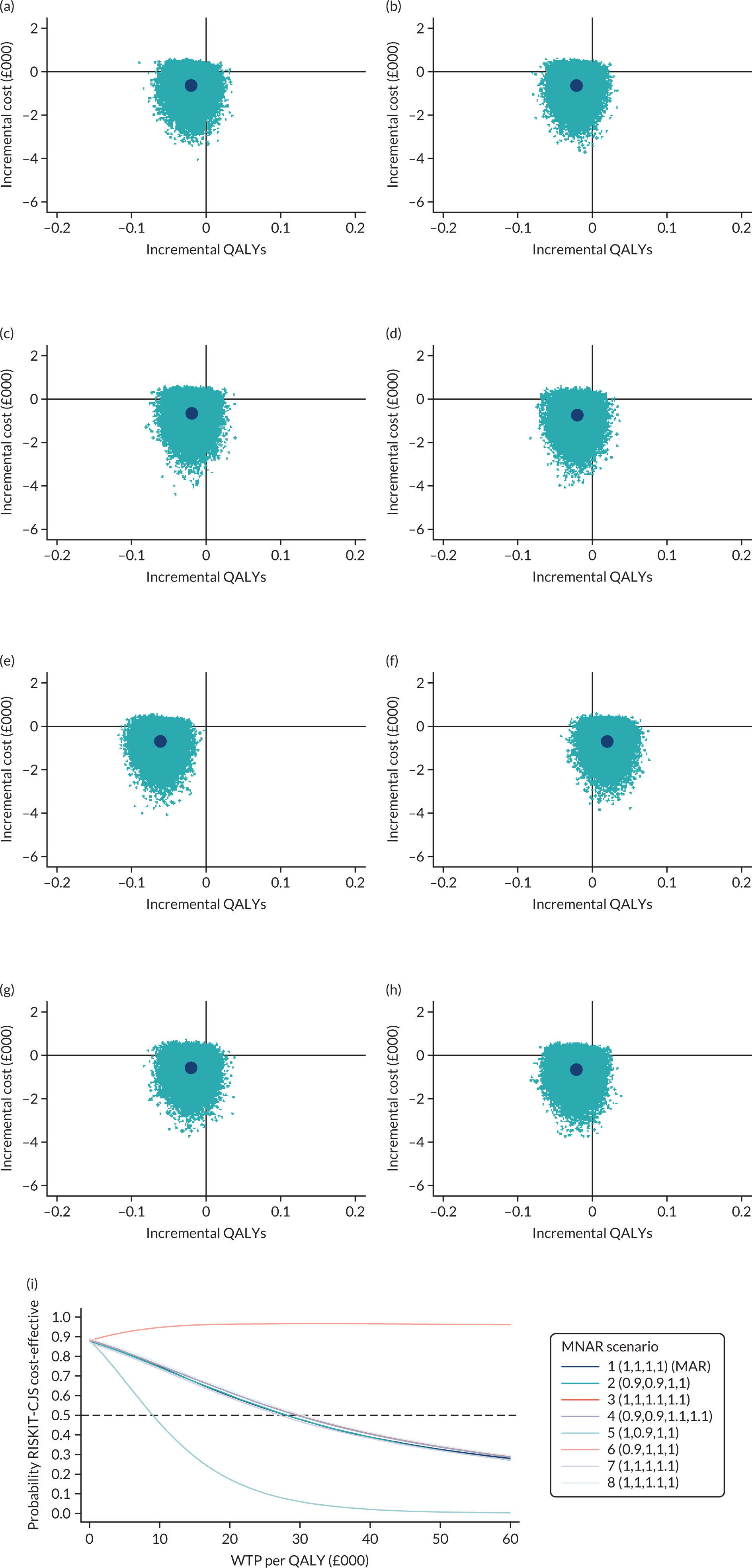
Figures 9a–h shows the CEPs for all eight scenarios. At first glance, it seems that the CEP based on the MAR imputation (see Figure 9a) provides similar evidence to the primary analysis based on the complete cases shown in Figure 8. However, the corresponding CEAC (see Figure 9i) shows a different picture, with a much higher probability of the RISKIT-CJS intervention being more cost-effective than TAU within the NICE-recommended threshold range of £20,000–30,000, although still not statistically significant. However, the value of the MNAR analysis lies in the comparison between the scenarios. Note that six out of eight scenarios produce a very similar result.
Nevertheless, two of the scenarios stand out, both of which refer to the pattern in the missing outcome measure. First, if participants who dropped out from the treatment group or chose not to answer EQ-5D-5L questions had, on average, a 10% lower QALY gain over 1 year (see Figure 9e), then the RISKIT-CJS intervention has a very low probability of being cost-effective. However, with the same costs, if the participants in the control group who dropped out or chose not to answer the EQ-5D-5L questions had, on average, a 10% lower QALY gain over 1 year (see Figure 9f), then the RISKIT-CJS intervention would have been cost-effective.
As the results are sensitive to the exclusion of outliers, the exploration of uncertainty was also performed for the sample without the outliers. The results for this analysis are presented in Report Supplementary Material 6, Figure 32. For all the scenarios but one, the majority of the incremental costs–incremental outcome pairs are located in the north-west quadrant, which means that the RISKIT-CJS intervention is associated with a lower effect at an increased cost. The CEACs show close to zero probability of the RISKTIT-CJS intervention being cost-effective. Only scenario 6 (see Figure 9f), leads to a probability of 50–70% that the intervention is cost-effective within the NICE-recommended threshold range.
Conclusions of the economic analysis
The primary economic analysis has been performed from the health and social care perspective and tested the null hypothesis that the RISKIT-CJS intervention in addition to TAU was no more cost-effective than TAU for adolescents involved in the CJS. Given the significant proportion of missing data on service use and health economic outcomes, the analysis has been limited to complete cases, with the imputations used for the sensitivity analysis.
From the health and social care perspective, the results of the economic analysis suggest that the RISKIT-CJS intervention is no more cost-effective than TAU. However, the sensitivity analysis with the MNAR scenarios indicates that, had participants from the control group dropped out because of worse outcomes, the RISKIT-CJS intervention would have been cost-effective. Moreover, lack of data from the CJS means that we could not carry out the economic analysis from the public sector perspective, as well as the societal perspective, which might have resulted in a considerable change in the incremental cost-effectiveness of the considered intervention.
Chapter 5 Qualitative methods and results
Qualitative summary
In this chapter we present the qualitative methods and analyses for the study. The purpose of the qualitative data collection was to inform decisions on if and how to implement the RISKIT-CJS programme, and to enable judgements to be made on the configurations of contexts, mechanisms and outcomes (CMOs) through which the programme worked. With this in mind, the qualitative analysis answers the following three questions:
-
What are the perceived strengths and weaknesses of the programme with respect to what seems to work and what does not work?
-
What are the perceived usefulness and acceptability of the intervention?
-
What is the potential for implementing the intervention in routine practice?
Qualitative analysis plan
Data sources
The qualitative study used four core data sources: (1) records of meetings with a purposive sample of participants, (2) focus groups with participants, (3) interviews with practitioners and (4) field notes taken by interventionists. Table 23 shows the sources of qualitative data by type and site.
| Source of qualitative data | Setting, n | Site, n | Total, n | |||
|---|---|---|---|---|---|---|
| PRU | YOT | London | South East | North East | ||
| Participant interview notes | 43 | 16 | 18 | 23 | 18 | 59 |
| Participant focus group | 10 | 4 | 3 | 5 | 6 | 14 (40 young people) |
| Interviews with professional interviews | 7 | 6 | 5 | 8 | 10 | 23 |
| Researcher field notes | 8 | 9 | 10 | 7 | 1 | 18 |
The first data source was notes taken in meetings between the practitioner and young person at baseline and at each follow-up point. These notes recorded the participant’s attitudes towards, and views of, the RISKIT-CJS programme. We purposively sampled the notes to achieve data saturation for each of the following criteria: setting, site and sex. The number of participants sampled was 59 (PRUs, n = 43; YOTs, n = 16), mean age was 15 years (range 13–17 years) and 32% of participants identified as female.
The second data source was participatory research focus groups that ran at the end of the second group session. We employed participatory rapid appraisal tools. 98 Across the sites, 14 focus groups were conducted, involving 40 young people. Three groups were conducted in London, five in the South East and six in the North East, with 10 focus groups taking place in a PRU and four within a YOT.
The data were collected through verbal group discussions, while being aided and recorded using written materials, such as flip charts and Post-it® Notes (3M, Bracknell, UK). The data included short comments about the ‘good’ and ‘bad’ bits of the programme; ranking the programme elements using different coloured dots on a flip chart; rating programme elements as a timeline, with participants drawing a line across a flip chart on which a horizontal axis was pre-drawn (their line showed how their experience of the programme in terms of how useful or not it was over time); and review of risks using a ‘ladder of risk’ of young people’s behaviour (arrow-shaped Post-it Notes were placed on the ladder to show the extent to which the programme had, in the young people's view, influenced their risk behaviours). To address potential literacy issues within the groups, research staff provided support to enable all participants to take part in the discussion; this included taking notes of comments and verbally reading the comments to the group.
A third source of data was face-to-face or telephone interviews with practitioners. These semistructured interviews were conducted with purposively selected informants from the CJS, YOTs, PRUs and early help, as well as interventionists, headteachers, administrative staff and social workers. All of these informants worked with young people within the participating settings and played a role in referring or facilitating the RISKIT-CJS programme in their setting. Overall, 23 interviews were conducted: 10 with interventionists, seven in PRUs and six in YOTs. Each interview was recorded and lasted between 45 minutes and 1 hour.
The fourth source of data was field notes taken by research staff. These included observations made while facilitating the focus groups (e.g. elaborating on brainstorming and discussions of the strengths and weaknesses of the programme elements, and the association with risk behaviour). Field notes were also taken on contextual issues at the intervention sites that were observed in setting up and implementing the project. In total, 18 such field notes were compiled and analysed. All data collected were anonymised, transcribed verbatim or photographed and stored in NVivo (QSR International, Warrington, UK) for analysis.
Data analysis
To analyse the data, we used the approach of ‘adaptive coding’. 99 NVivo11 software acted as a data management tool, which enabled us to analyse various types of data in one place. Four researchers completed the coding of all the data. The perceived contexts and mechanism of action were explored by starting with a list of provisional orienting codes, which were developed before data coding began. Our approach of ‘adaptive coding’ was based on both our pre-existing understanding of the underlying theory, that is, the social development model,43,45 which informed the three qualitative research questions, and researchers’ experience of being involved in the implementation and the delivery of the programme. We also identified new ‘grounded’ codes based on relevant items found in the data that were not included in the provisional codes.
In answering the third research question on implementation, we combined our adaptive coding of the data with normalisation process theory (NPT)100 as a sensitising tool to consider issues of translation of the RISKIT-CJS intervention into routine practice. NPT is an implementation theory, developed within the context of health-care innovations, which largely focuses on understanding the implementation, embedding and integration of new technologies and organisational innovations. 101 In this context, it was used to provide a theoretical basis for exploring the implementation of the RISKIT-CJS intervention into routine practice in a YOT or PRU setting, and this demonstrated the adaptability of NPT for use in different settings.
Using the RISKIT-CJS theoretical model in conjunction with the NPT framework enables analysis of how the likely presence of CMO configurations could either facilitate or hinder implementation into routine practice. NPT challenges researchers to consider how their intervention might become normalised in routine practice (Table 24). 102
| Construct | Description |
|---|---|
| Coherence | ‘Sense-making’: how is the intervention understood by participants? How do participants compare it with other practices? |
| Cognitive participation | How do participants come to take part in a practice? What keeps participants motivated to continue taking part? |
| Collective action | How do participants make it work? How are participant’s activities organised and structured? |
| Reflexive monitoring | How do participants evaluate a practice? How does this change over time and what are its effects? |
Results
Question 1: what are the perceived strengths and weaknesses of the programme with respect to what seems to work and what does not work?
Positive outcomes and perceived strengths
Many participants and practitioners reported achieving positive outcomes for the young people who took part in the RISKIT-CJS programme. For example, some participants reported that they had become abstinent from all substances, although it was more common for them to continue to use alcohol and to stop other substance use. Several participants reported changing their patterns of drug use in ways that would reduce their risk; an example of this was when one participant talked about moving from smoking cannabis every day ‘from my eyes opening in the morning, through the day to the evening’ to using it only a few times a week, or only at weekends (PRU 6). For participants, and the people who worked with them, it appeared to be more important that young people were reducing risks and associated harms, rather than being completely abstinent, and such reduction is an important goal in youth substance use prevention. 103,104
Alongside these observed reductions in substance use, some other improvements in health behaviours were observed, including participants reporting that they had changed the group of people they associated with to avoid drug use and ‘getting into trouble’ (PRU48) and, therefore, reducing impulsivity. An example of this was observed in some of the participant focus groups, in which several young people reported that ‘I will think before I act’ (PRU64) or that the programme had ‘helped me think about consequences’ (PRU65 and PRU68).
Some participants also reported reductions in their offending. There were many participants who reported at both the 6- and 12-month follow-ups that they had stopped engaging in criminal and/or antisocial behaviour. One young male, for example, had been charged with grievous bodily harm in the run-up to starting the RISKIT-CJS programme. At a follow-up meeting, the young male reported that things had ‘calmed down’ (PRU65). During a motivational interview, another participant reported appreciating the programme because it meant that he was no longer getting into trouble with the police. In one focus group, a participant reported ‘changing actions when getting angry, take a second before I hit someone, walk away’ (PRU4).
Within the context of the post-intervention interviews, several PRU staff reported an increase in school attendance among some young people, whereas others observed noticeable improvements in young people’s educational engagement and attainment. A direct example of this was that one interviewee was able to recount their experience of a young person who had significantly improved their outcomes after completing the programme:
I know they were a heavy user, especially of like weed. I spoke to them, and they have basically cut down like completely . . . They’ve even sort of disassociated themselves from certain friends . . . this was someone who we thought we were going to have withdraw from exams but ended up coming and sitting every one of their GCSEs [General Certificate of Secondary Education] . . . Obviously I think there were other factors that have gone on in their life, you know, outside of school as well, but I think perhaps through the programme there must have been skills, there must have been conversations or something that has I guess planted a seed or something in their head for it to be able to transform like that so quickly.
PRU6
What makes it work?
The RISKIT-CJS programme contained a wide range of intervention styles and settings, including assessment, individual motivational interviewing, learning and discussing (using standard learning materials) in a small interactive group, with individual follow-up. Both participants and practitioners from YOTs and PRUs mentioned that the different components of the programme were helpful for the range of needs of the participants. Some practitioners mentioned that the process of assessment could help by enabling the participant to reflect on their level of substance use, and whether or not they wanted to continue it. Some participants appreciated the information provided on the physical and legal consequences of illicit substance use, whereas other participants appreciated the opportunities to discuss more personal issues in meetings with the practitioners. Therefore, we suggest that a strength of the RISKIT-CJS programme is its variety of components that can meet a wide range of needs of young people by using different interaction styles that suit them. As one practitioner put it, the programme ‘sparks little bits of information that they are carrying around’ (YOT5). The combination of providing some ‘basic’ information (e.g. on drug effects and laws) and the opportunity to reflect on it with both peers and skilled workers seemed to work for some young people for whom the simple provision of information had not previously influenced their behaviour. In one follow-up interview, a participant said ‘I did actually learn a couple of things’ (PRU 68).
Some participants already had a high degree of involvement in risk behaviours, but their knowledge of these risks could be improved by the programme. At least one practitioner noted ‘alarming’ levels of misinformation on sexual risk behaviours among male participants, which they challenged. Several participants also reported the benefit of learning consequences of risk behaviours. This observation emerged both from the motivational interviewing and from reflection on the substance use participants reported when completing the TLFB28 form at intake. It was also an explicit aim of the ‘drugs grid’ and ‘ladder of risk’ group activities to encourage discussion and reflection among peers on harmful consequences of risk behaviours, and subsequently on how to avoid or mitigate these risks. One practitioner observed:
I think it’s about having a safe, confidential space . . . young people got an opportunity to explore areas of risk which they probably don’t get to experience anywhere else with an adult and I think that’s the key for me. Is that there’s a place where they can have a sensible, informed conversation around risk-taking behaviour which is not led by ‘why did you do that?’ or ‘what have you done that for?’.
INT4
This provision, by the RISKIT-CJS programme, of multiple paths towards a more reflective and informed relationship with risk was in keeping with the original design of the programme.
Negative outcomes and perceived weaknesses
Two main issues were identified as being associated with negative outcomes of engagement with the programme. One issue was whether or not the programme content was appropriate for the 13–17 years age range and the other issue related to the times that sessions were delivered (explored in more detail in Acceptability to young people).
A negative aspect of the group sessions was that disruptive behaviour could be problematic, with some participants taking these group sessions as an opportunity to boast about their risk-taking rather than to reflect on issues. Likewise, some participants exemplified these risk behaviours by being under the influence of substances or displaying aggressive behaviour during group sessions. Some negative interpersonal dynamics were also observed between some participants, such as belittling or dismissal.
Some interventionists pointed out that, although the programme covered both male and female issues, the larger number of males in the groups meant that the intervention delivery often lacked a ‘girls aspect’. When discussing sexual health and the different connotations for males and females, one interventionist recalled their experience:
I don’t really recall much of a conversation around pregnancy, STIs [sexually transmitted infections] from the female perspective or even sexual coercion. Yes, it was mentioned but mentioned broadly because there really isn’t the space for a young girl in a group of boys, even if there’s two of them which there often is, the space is quite a male-dominated space. It’s quite an emotive subject to talk about and I do feel it came from the right line, yeah just with a male undertone to it.
INT3
Quite often in a male space, the conversations were directed towards consent, coercion and the law, whereas conversations relating to pregnancy, sexually transmitted infections and what constitutes a healthy relationship were absent.
Question 2: what is the perceived usefulness and acceptability of the intervention?
Usefulness to young people
For many participants, it was important for them to feel listened to and have their voices heard. Having a confidential and ‘non-judgemental’ space where the participants could speak freely with the interventionists, and reflect on experiences among peers, was highlighted as particularly useful for some of the young people. For others, the group intervention proved to be less useful, with a small number of young people feeling that they would have benefited more if the intervention had been a one-to-one experience [e.g. ‘you would have got more information’ (PRU11)].
The intervention was often perceived by practitioners and site staff as more useful for participants at the younger end of the targeted age range (i.e. participants aged 13 or 14 years) than for older participants (i.e. participants aged 16 or 17 years). One interviewee described how age could affect participant receptivity to the intervention:
You could tell that in certain young people, when they got to a certain age, they were less responsive to what you’re delivering for them, and it was kind of just water off a duck’s back with some of those guys, whereas the younger ones seemed to take it on more on board.
INT2
Some staff commented that young people are using substances at an early age, from age 11 years and sometimes younger, and suggested that the age limit could be lowered to include these young people: ‘I know there are kids who are younger that are involved in that, doing drugs and so forth, so I think definitely if it could have been opened up to a few younger years’ (PRU6).
Although many participants found some parts of the programme useful, others found the session content hard to understand and sometimes ‘difficult to put into practice’ (PRU54). A small number of participants said that they found little value in the programme and felt that they ‘learned nothing’ (PRU11) and ‘won’t change anything’ (PRU11).
Acceptability to young people
In the PRU setting, participants frequently reported finding the programme sessions ‘better than school’ (PRU11, PRU12 and PRU54), as they were more engaging and took them out of their ‘normal lessons’ during the school day. In YOTs, participants were generally required to attend programme sessions outside school or college hours and this posed a particular challenge for attendance, as demonstrated by the large number of missed appointments. As one worker explained, ‘it’s difficult to get them to engage on a programme in youth justice as it is because they don’t want to be on that programme, let alone do additional stuff’ (YOT6).
Participants who took part in the group sessions often found them to be ‘better than expected’ (PRU64, PRU68 and PRU12), although feedback from the focus groups suggested a perceived level of mistrust at the first one-to-one session, which tended to ease after the first group session. It was also common for participants’ level of enjoyment to grow each successive week throughout the intervention. Some of the participants expressed a preference for smaller groups, of two to five participants, rather than larger groups, which were seen as being more chaotic.
Participants often reported that they enjoyed the intervention. Intervention staff were seen as ‘friendly’ (PRU69) and ‘funny’ (PRU54 and PRU69) and some participants found it ‘easy to be open and honest’ (PRU69) with them. However, the experience of the sessions was not consistent across all sites, as staff changed depending on location. Participants in a small number of groups rated the sessions ‘poorly’ (PRU18).
For some, the group work was ‘boring’ (PRU11, PRU18, PRU64 and PRU69) and not engaging, and a small number of individuals left early. Others thought that the group sessions (which lasted 3–4 hours) were ‘too long’ (PRU18, PRU68 and PRU69) or that the sessions contained ‘too much information’ (PRU11 and PRU65). Participants who found the sessions too long expressed a preference for shorter group sessions, and more of them, to allow for deeper exploration of the session content. Conversely, there were some participants who found the length of the sessions to be manageable.
Site and programme staff also highlighted the length of the group sessions as challenging, particularly for some of the young people involved. Attention issues among participants were observed by programme staff who delivered the intervention. One interviewee explained that ‘. . . given the learning styles and often the diagnosed or undiagnosed behaviours of the young people we’re working with . . . it was sometimes a big ask . . . and it was a long time to be delivering to them’ (INT4).
Staff frequently suggested that the programme would be more appropriate for the target population if it involved ‘shorter sessions and more of them’ (INT3, INT8 and YOT5). The original RISKIT programme43 was delivered in school over eight 1-hour weekly sessions. The compression of the programme into fewer and longer sessions to make it more feasible to deliver in YOTs and PRUs may have made it less enjoyable for and less acceptable to young people.
Some participants found participating in the programme uncomfortable because of having to share personal information or being in a group with peers. Despite reassurance from staff, participants were often hesitant about disclosing information relating to their substance use and other activities, as they were concerned about the information being shared with parents/guardians, teachers, case managers or police. In several cases, most at the same site, misinformation (e.g. rumours that staff were undercover police or social workers) caused young people to decline to take part. For instance, interventionists had arrived at a PRU to hear of a rumour that had been circulated that morning that they were in fact ‘the feds’ (i.e. police) and not researchers, and this led to several young people refusing to participate over the day. One young person was also advised by her mother to not share any information, as she was under the impression that the interventionists would pass on information to the police, and, despite assurances, the young person declined to take part.
A small number of data items referred to the possibility of ‘treatment fatigue’. This group of young people are often required or invited to take part in a wide range of activities that are intended to change their feelings and behaviours, and, for some participants, the programme could be seen as just another activity. One practitioner thought that this could have reduced young people’s willingness to take part in the intervention:
They feel they already have a lot of input for substance misuse from us as a provision, so for some of them it felt like it was another thing, ‘why do I have to do it again?’ Even though it was a completely different programme, they didn’t see it that way.
PRU1
Some young people were also involved with multiple agencies and often had ‘too many people working with them’ (PRU4). Several site staff suggested that this was a barrier to some young people engaging with the programme staff: ‘. . . it’s like another professional they have to work with and a new face they have to meet and someone else who might now need to or want to know their story’ (YOT3).
Usefulness to organisations
Several practitioners reported observing positive outcomes for participants. However, some staff at intervention sites, particularly YOTs, felt that the intervention was less useful for their organisation, as they did not observe positive outcomes or noticeable changes in behaviour. One interviewee suggested that ‘although it opened a dialogue and it enabled young people to talk more openly about it initially, it didn’t have an actual impact on them wanting to reduce their risk-taking behaviour’ (PRU1). A small number of practitioners felt that the programme was not beneficial for their population of young people, suggesting that earlier intervention was needed.
At several YOT sites, the group aspect of the intervention was not overly useful. It was often difficult in YOTs to gather the numbers of young people needed for group sessions, as more young people are now diverted away from the CJS. One interviewee explained that ‘we don’t actually get the same numbers through that we have in the past so it’s really difficult to get bigger numbers to actually run proper group work’ (YOT2). For others, group work was often deemed unviable because of risk issues: ‘. . . there’s certain people you can’t put together. . . the whole kind of street gang stuff and drug dealing . . . that is what makes group work almost unviable nowadays’ (YOT2).
Acceptability to organisations
From the outset, PRU staff were generally positive about the intervention and perceived it to be beneficial for their organisation and cohort of young people: ‘. . . any kind of input to our young people to keep them safe is absolutely invaluable’ (PRU2).
At YOT sites, the process of delivering the intervention was generally more complex. The initial ‘buy-in’ from management did not always translate to front-line staff and, although the intervention provided the opportunity for staff and young people to use statutory hours, uptake tended to be low. Case managers often had limited knowledge and understanding of the programme and they commonly reported a lack of communication and information from managers.
Where the intervention was successful, set-up and delivery were frequently viewed by host organisations as ‘really well organised’ (PRU1) and ‘very professional’ (PRU12). Host organisations generally reported a better experience when the RISKIT-CJS intervention staff managed the process, as it required less input from site staff. One interviewee described their experience: ‘. . . it was really easy. The RISKIT staff were fantastic. They literally did everything themselves. They just set up a date, a time and were very, very easy to accommodate’ (PRU1).
Programme staff were often seen as ‘flexible’ and responsive to the organisation’s needs: ‘. . . they were very flexible, very in tune with, you know, if something was going on here and we just needed to have 5 minutes to get on with that. Yeah, they left us to it’ (INT1).
Pupil referral unit staff generally found that the intervention fitted within the school day, as ‘everything went in within the timetable and there were no overruns’ (PRU4). Programme sessions were usually scheduled for mid-morning, which often suited the PRU: ‘. . . for us it was better that the sessions weren’t first thing in the morning because students are often late to school’ (PRU1).
Some of the organisations experienced a range of other issues that made hosting the intervention more challenging. Smaller sites typically had a lack of space, with limited room capacity and availability, which made accommodating the intervention more difficult: ‘. . . the only difficulty we had was finding rooms where people wouldn’t be disturbed and sometimes the rooms weren’t available’ (PRU6).
Lack of staff and high workloads were also identified as key factors that made hosting the intervention more burdensome for some organisations. At the YOT sites, programme staff observed ‘a resistance according to workload’, with some staff appearing ‘overstretched’, with high caseloads and a lack of capacity to take on any additional work. One interviewee described the ‘reality’ for practitioners: ‘. . . we’re all always busy, we never want additional work and that’s just a reality really of the challenges that you’re facing’ (YOT2).
A small number of PRU sites also found hosting the programme ‘a lot of work’ (YOT1, YOT2 and YOT4) on top of existing demands. One interviewee suggested that ‘getting all the consent and the sign-ups and the agreement and then getting the appointments, booking rooms, you know, at a time when everybody can make’ (YOT1) was a lot of ‘extra work’.
A number of organisations experienced difficulties getting young people to attend the programme sessions. Getting young people to attend was most challenging for YOT sites in rural areas, where participants were required to travel greater distances for the intervention. In one site, staff had the resources to overcome this obstacle by driving participants to and from the group sessions: ‘. . . we’ve got a people carrier so we could go round and pick them all up’ (YOT5).
However, this was not common practice. Several case managers reported sending text reminders to young people to encourage them to attend. Despite this, programme sessions in the YOT setting were often poorly attended.
Question 3: what is the potential for implementing the intervention in routine practice?
Coherence: meaning and sense-making by participants
The RISKIT-CJS intervention was distinct from the standard practice of host sites. The context meant that it was delivered and evaluated under trial conditions. Site staff generally agreed that the programme did fit well with the aims of both YOTs and PRUs. It was seen as bolstering their work around substance use. One PRU head teacher said that ‘it fits well within our ethos’ (PRU3).
Staff across all sites facilitated the screening process. Eligibility criteria were provided to enable the identification of potential participants and this process was described by staff at nearly all sites as simple and easy to understand: ‘[t]he screening process was quick, it was straightforward . . . the kids engaged with the process. No problems at all’ (PRU2).
One head teacher explained how their relationships with the young people also aided the screening process:
It was easy to identify the young people to put forward because we know them so well, so we knew which ones were absolutely involved in substance misuse, and they’re very open with us so for us, it was a very easy process to do.
PRU1
However, some practitioners noted that PRU staff sometimes overlooked potential participants on the basis that they did not think that they were engaged with substance use or criminal activity. Therefore, programme staff conducted a second screening process, which was simply an informal chat with the potential participant. Interviewees who were involved in delivering the RISKIT-CJS intervention noted that participants would often share information on their substance use and criminal activity that had not been shared with PRU staff (INT5).
The screening process was less likely to overlook eligible participants in a YOT setting because of the information held on a young person on a YOT order. A list provided to programme staff showed young people whose substance use was linked to criminal activity. Staff were able to quickly assess which young people were eligible for referral to the RISKIT-CJS intervention. One member of programme staff notes the distinction between the differing sites:
The eligibility criteria were much clearer and much better executed in the YOTs than in the PRUs . . . in the PRUs there’s a grey area . . . assumptions staff make about certain types of people where they could miss the quieter ones who maybe didn’t display some of the behaviours that we were looking at.
INT5
Programme staff noted that some YOT staff had voiced concerns of a ‘threat to role’ (YOT3 and YOT13), both their own role and that of external intervention providers, seeing the RISKIT-CJS intervention as a replacement for their own work, rather than, as intended, an additional intervention to be provided alongside treatment as usual. One interviewee said that ‘people started to worry a little bit, they were thinking, “well I do that, I do group sessions, or I do drug treatment work or we do gangs, we have that organisation that comes in” ’ (INT5). Threat to role was not observed with site staff in the PRU settings.
Cognitive participation: commitment and engagement by participants
During early scoping meetings with senior YOT management, the RISKIT-CJS intervention was positively received, with agreements to facilitate the intervention in local teams. Management ‘buy-in’ was, in part, due to the element of research evaluation, which was perceived as being useful for local commissioning purposes.
Although the initial set-up at management level was positive, this enthusiasm did not naturally filter down to the staff working directly with the participants. Although YOT staff were not expected to deliver the intervention themselves, programme staff faced barriers when working with the teams in setting up referrals, as well as the individual and group sessions. Many YOT staff, when interviewed, mentioned the ‘additional’ (YOT1, YOT2, YOT4 and YOT11) work required of them to engage their young people with the programme. As one YOT staff member explained:
Ultimately, it’s the case managers who are going to be putting the work in to try and get the buy-in from the young people and if they weren’t really buying into it themselves, they’re not going to get young people to buy into it . . . Also, for us, it was all like had to happen really quickly, we had very little notice.
YOT2
Programme staff often experienced ‘resistance’ (INT3, INT4 and INT5) when trying to engage YOT caseworkers to refer participants. A number of programme staff noted that ‘misinformation’ (INT10, INT1, INT5) was often the reason they experienced barriers to implementation owing to a ‘terrible lack of cohesion with YOT staff and terrible communication’ (INT4). A senior caseworker told us that staff saw it as ‘extra hassle, when they are already burdened with a full workload’ (YOT16). Many YOT staff told us that managers did not do enough to stress the importance of the project; this suggests that senior management understood the point of the intervention, but a lack of translation hindered the implementation in YOTs.
In one YOT site and many PRU sites, programme staff noted that, when a staff member fully engaged and promoted the programme internally, others were actively motivated and delivery was smoother. These individuals were described as ‘champions’ and, when on site, programme staff felt that they were supported to deliver the intervention and that previously experienced barriers were removed. Subsequently, this translated to a higher retention rate for the group work despite the numbers involved being small: ‘. . . we found that when the staff were really on board with the programme and really sort of ‘championed’ the group sessions and we did get a good turnout’ (INT6).
Collective action: the work participants do to make the intervention function
The success of the intervention required the delivery of all four stages of the project to be accessible to participants and this required YOT and PRU staff engagement to facilitate both the one-to-one work and the group sessions. Participants also had to engage with the RISKIT-CJS intervention, and we found that this occurred more often when organisations were fully committed to the intervention. Delivery in what we coded as ‘resistant settings’ and ‘disorganised settings’ proved difficult.
Participant engagement was more effective in PRUs than in YOTs. Once PRUs had committed to facilitate the intervention, they appeared to adopt a collective commitment that transferred to staff and participants alike. One PRU staff member told us that ‘[w]e just said that we were taking part in a study, and they were all quite happy to engage really. It wasn’t really an issue, there wasn’t really any barriers’ (PRU7). Programme staff’s experience of the PRU was often positive: ‘[e]ngagement’s much better with staff in the PRUs’ (INT3).
Delivering group work was challenging in nearly all YOT settings. Observations revealed that the group work element was not compatible with existing YOT practices in many teams. Following participant allocation to the groups, YOT staff conducted risk assessments and placed restrictions on who could mix with whom. Assessments were based around vulnerability concerns and known safeguarding issues, with the concern that certain participants could be ‘compromised if encouraged to further spend time with the others who are much more criminally sophisticated offenders’ (YOT6). Staff facilitated the initial screening process and one-to-one sessions, but group work was nearly always problematic in YOTs. A senior case manager told us:
I think the main issue that we have in YOT teams is managing the risk when we run group work. There’re certain people you can’t put together . . . the whole kind of street gang stuff and drug dealing . . . that is what makes group work almost unviable nowadays which is why we don’t run very much of it. It’s horrendous . . .
YOT 2
In contrast, we found that the group element not only fitted well with normal practice in PRUs but also enhanced the work already being carried out by staff, particularly with interventions addressing well-being, substance use and risk reduction. The RISKIT-CJS intervention encompassed all these elements. It is also important to note that because of cuts in some local authorities’ drug and alcohol service funding, the RISKIT-CJS intervention filled a resource gap.
Reflective monitoring: participants reflect on or appraise the intervention
There was an overall sense that the intervention had been beneficial, but many site staff were unsure of how they could evaluate it for their own purposes, partly because trial conditions prevented them from observing RISKIT-CJS intervention group sessions. Some sites had groups in which the RISKIT-CJS intervention was provided and groups in which TAU was provided. Staff were provided with only general information about the intervention. Site staff were often ambivalent about whether or not they would use the RISKIT-CJS intervention in the future. Responses appeared to be based on observing young people’s responses to the programme. A typical comment was as follows:
It benefited our students in some way . . . it would be very difficult for me to say how because we weren’t allowed to be present for the content . . . there were definitely benefits otherwise our kids would have walked out of that room or refused to go in, but I couldn’t tell you what they were.
PRU54
However, most sites interviewed said that they would use the RISKIT-CJS intervention again, at least in some form. Having access to the final intervention evaluation was important to them for future implementation, with one PRU simply wanting to ‘. . . know what information was really useful? . . . for the school it would help to facilitate any changes . . . to help make some improvements’ (PRU54).
Some interviewees, including both YOT and PRU staff, said that they would implement the intervention once the trial outcomes were available.
Some interviewees said that they would not use the intervention, as they felt that it was not suitable for the young people they work with. One reason for this was, as previously mentioned, that they felt that the intervention came too late and at time when substance use was already entrenched. However, interviewees did feel that the intervention could benefit children of the same target age in mainstream school when risk-taking and substance use would probably be at an experimental stage. One head teacher said that they would not use the RISKIT-CJS intervention again, as their young people are:
. . . not at the beginning of substance misuse . . . if they were children that were considering it or had dabbled or tried it, but not children who were smoking three to five joints a day and it had become part of their lifestyle. I think for them, the intervention . . . didn’t have an impact. It did make them think and they did want to talk about it, so it opened a dialogue, but it didn’t change their behaviour.
PRU1
However, staff in PRUs felt that frequent substance use was a reason that the RISKIT-CJS was needed. Many staff observed that most of their young people used substances and so any intervention that may add to ongoing work in the area must surely be advantageous for target users.
Summation: a programme theory and logic model of how the RISKIT-CJS intervention worked in theory and practice
The advantage of using mixed methods in a RCT is that it enables analysis of how the intervention works and not just whether or not it works. 105 To understand these processes, we developed a theory of how the intervention operates. 106,107 Drawing on the approach of realist evaluation,108,109 we provide here a programme theory in the form of a diagrammatic logic model (Figure 10). The diagrammatic logic model identifies the possible CMO combinations through which the RISKIT-CJS programme operated for the individuals and sites that took part in this trial. The diagrammatic logic model includes the intended and revealed pathways towards positive outcomes for young people, as well as the potential pathways to more ambivalent or negative outcomes, otherwise known as ‘dark logic’. 110 In recognition of the complexity of delivering this complex intervention in varied settings, the model includes negative and positive moderators that affect the outcomes of contexts and mechanisms in practice.
FIGURE 10.
The RISKIT-CJS logic model: a multicomponent risk reduction programme for adolescents involved in the CJS. The logic model diagram is based on the template provided by the evidence-based practice unit. In addition to the CMOs of the realist evaluation framework, it includes a description of the programme’s targets, interventions and moderators, as observed in the operation of the programme (not just as described in the programme manual).
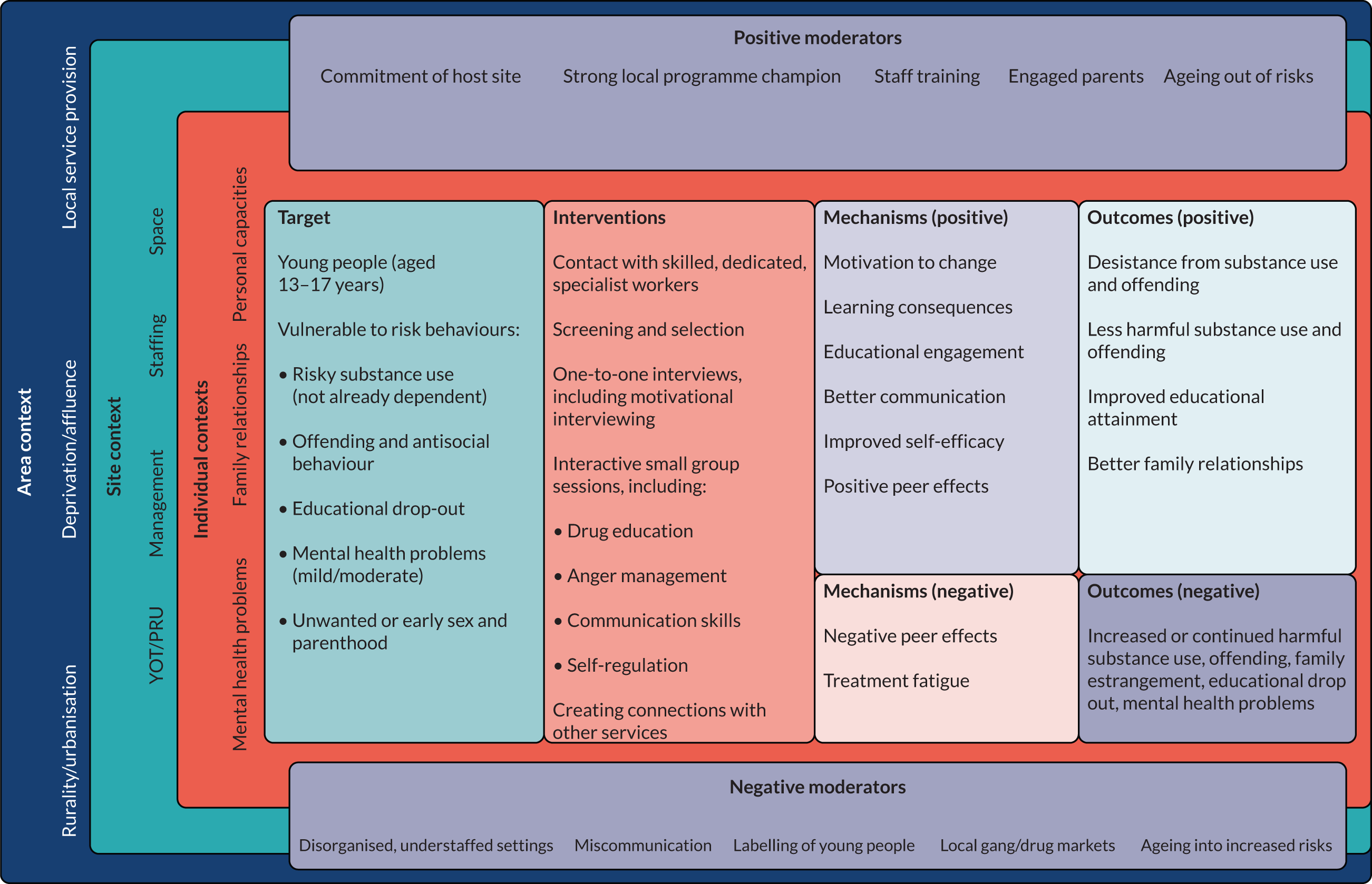
Contexts
In the data analysis, we identified relevant contexts at three levels: (1) area, (2) setting and (3) individual.
Area
Rurality/urbanisation of the area of implementation affected the operation of the programme by determining how easy it was to get participants to the places where the intervention was being delivered at the right time and how easy it was to connect them to other local services for additional support. In more rural areas, the greater distances between programme participants and services made both of these aspects of the programme more difficult.
The levels of deprivation or affluence of the areas in which the programme operated also affected how it worked. More affluent areas tended to offer more opportunities for support and onward progression for young people than did the more deprived areas, and this is partly because there were more employment opportunities for older programme participants in the more affluent areas. However, there has also been an effect of the politics of austerity in reducing funding for council services most severely in the most deprived communities,111 and this means that councils in the most deprived areas have been the least able to protect provision of non-statutory support services for the types of young people with complex needs who were engaged in the RISKIT-CJS programme. This is important for the operation of the RISKIT-CJS programme because it is a multicomponent, but relatively brief, programme and it partly relies on connecting participants to other services in the area. If these services are absent or underfunded, then this component of the programme is less able to succeed in supporting young people towards positive outcomes.
Setting
As the RISKIT-CJS programme evolved, it was implemented in different types of setting. We observed systematic differences between YOTs and PRUs that affected implementation. A combination of these features meant that the programme was generally easier to implement in PRUs than in YOTs. Three features of settings that were likely to affect implementation and outcomes were management, staffing and space. In general, it was easier to implement the programme where there was strong commitment to its implementation by senior management and where the host agency was well managed (i.e. where there were clear lines of responsibility and communication in the organisation). There were also problems in delivering the programme at sites that were short of staff or that did not have much space to use for private and confidential discussions or group work.
Individual
As discussed below, many of the participants in the programme had issues with mental health and family estrangement that both deepened their need for support and complicated the provision of such support. These are important contexts for the operation of the programme, as early problems in parental relationships and self-regulation have been identified as part of the ‘developmental cascade’ for early-onset and problematic substance use and other risk behaviours. 44,112,113
Target population
The age of the target population (i.e. 13–17 years) led to the inclusion of participants who displayed a range of complex needs, including early-onset and escalation of risky substance use, as well as offending and antisocial behaviour, educational drop-out or exclusion with high levels of truancy and poor attainment of key stage learning objectives, mental health problems (e.g. anxiety and depression), and exposure to early or unwanted sex and parenthood. In the data, we saw several examples of individuals having mild to moderate mental health problems (including previous diagnoses of depression and anxiety) and a few participants whose mental health problems were severe enough for them to be already engaged with child and adolescent mental health services.
Patterns of early illicit drug use tend to cluster with other risk factors, including risky sexual behaviours,114 poor educational attainment115 and mental health problems, both during adolescence and in early adulthood. 116 These associations heighten the need to work effectively with these young people, to counter the combined impact of the various risk factors they experience which increase their propensity for escalating and persistent negative behaviours and outcomes. Our data suggested that the programme was effective in initially reaching people who shared these vulnerabilities.
Intervention
The RISKIT-CJS intervention manual describes the components of the programme to be delivered to the recruited participants. In practice, programme staff had to be flexible in delivering these components, depending on the needs and resources of the host sites and the recruited participants.
Each component listed in the logic model was mentioned as being important by at least some staff and participants. There were some participants who did not value any aspect of the programme, as demonstrated by their unwillingness to engage and their early drop out. However, for other participants, the combination of individual and group support provided a range of opportunities that they experienced as helpful, and this points to the value of a multicomponent programme providing a range of different opportunities, but also to the danger of overloading some participants who are less willing or able to engage.
A potentially limiting feature was that we observed some problems in using group work with mixed sex groups, which tended to be dominated by male participants, as this tended to leave less space for female participants to discuss issues that were relevant to them, especially around sexual health.
Mechanisms
Positive mechanisms
Participants entered the programme with a range of types and levels of motivations, and this was an explicit aim of including motivational interviewing in the one-to-one aspects of the intervention, as this could work with ambivalence: ‘. . . some of them . . . wanted to change. They just didn’t know how, they didn’t know where to go’ (INT10).
The programme gave such participants a place and tools to use. For example, the enhanced motivation to change was combined, in some cases, with learning consequences of risk behaviours.
For some participants, the programme provided an opportunity to improve their educational engagement, as well as to have better communication with parents and teachers. Several participants reported that they found the programme sessions to be ‘better than school’ (PRU11, PRU12 and PRU54), as they were more active, relevant and engaging. Some participants increased their attendance and achievement in other educational provision. Communication is one of the life skills targeted by the programme.
We included improved self-efficacy in the logic model, as the term brings together various reports of participants’ improved ability to regulate their own behaviours, identify consequences and act towards desired goals. Self-efficacy would be expected to result from the intention of the programme to improve the information that participants have about risks, their skills in putting this information into practice and the opportunity to practise these skills in individual and group sessions.
Positive peer effects relate to the beneficial effects that some staff and young people reported from being able to share experiences with other young people who were experiencing similar trials and tribulations. Some of the group sessions worked as intended in enabling young people to share and reflect on experiences, as triggered by the planned elements of the group sessions and the skilled intervention of programme practitioners.
Negative mechanisms
Data analysis did reveal some mechanisms that would be expected to reduce or even counter the positive effects of the programme, including treatment fatigue and potential for negative peer effects.
Moderators
The data included information on moderators that could affect the pathway between contexts, intervention components, mechanisms and outcomes. These moderators can be seen as ways in which contexts and mechanisms of the programme interact.
Negative moderators
Labelling, otherwise known as ‘secondary deviance’,117 refers to the possibility that placing the label of ‘offender’ on a young person may have the effect of confirming for them that they are ‘deviant’ and so lead them to increase or prolong negative behaviours, as has been observed in longitudinal studies of young people who offend,118 and this was a possibility that was stated by managers of sites who were reluctant to take part in the programme. Others told us that their young people were already too entrenched in offending behaviour to make it worthwhile to trial the programme with them, and this could itself be seen as a form of labelling.
In some interviews, including follow-up interviews with participants, it was noted that participants lived in places with active drug markets and ‘gang’ or ‘on-road’ activity, which is particularly prevalent in deprived urban areas,119 and this provides opportunities and temptations for young people, which may reduce or overwhelm the prospects of the programme helping them towards reduced substance use and offending.
Some practitioners noted the wide range of age ranges targeted by the programme, which brackets the peak in the classical ‘age–crime curve’, which tends to occur in the mid-teens. 120 Substance use also tends to increase from childhood through adolescence. 121 Participants at the younger end of the targeted age range may have been recruited into the programme while they were on the ‘natural’ progression to more substance use and offending, that is, as they were ageing into increased risks.
Positive moderators
Practitioners involved in the programme observed and reported that it was more likely to succeed where there was strong commitment of host sites and strong local champions for the programme at these sites.
Staff training was identified as being crucial to the success of the programme. The RISKIT-CJS intervention manual describes the aims and framework of the programme, but it cannot, on its own, give staff the skills they need to provide a variety of programme components effectively with a group of young people who experience a range of risk factors and who often display behaviours that are difficult to manage.
In some cases, the presence of engaged parents was mentioned as being supportive of the programme’s effect in producing good outcomes for young people. When young people reported that their parents were active and supportive in discussing the problems they faced, they were more likely also to report engaging with the programme and achieving good outcomes.
For participants at the older end of the targeted age range, the downwards slope of the age–crime curve after the mid-teens may have helped them in using the programme to age out of risks, especially for those who entered employment or became a parent.
Conclusion
This pattern of mixed results is to be expected when working with a group of young people with complex lives and needs. As anticipated by the social development model, there are multiple pathways through which young people may move towards positive or negative outcomes. The young people targeted and reached by the RISKIT-CJS programme are among those who are most likely, according to this model, to move towards problematic patterns of substance use and offending as they grow up.
The extent to which the RISKIT-CJS programme had an impact on the life trajectory of these young people is addressed by the quantitative and randomised elements of this trial (see Chapter 3). The qualitative analysis and the logic model presented here provide a programme theory for explaining and interpreting how the RISKIT-CJS programme ‘worked’ and for whom. Broadly speaking, there were contexts at the level of areas, sites and individuals who took part in the programme that combined with programme interventions for the targeted group to trigger mechanisms, some of which were moderated by interactions with the contexts, to produce a range of outcomes for programme participants.
Chapter 6 Discussion
This mixed-methods multicentre RCT evaluated the clinical effectiveness and cost-effectiveness of a multicomponent psychosocial intervention (i.e. the RISKIT-CJS intervention) to reduce substance use among adolescents, aged 13–17 years, engaged with the CJS. The RISKIT-CJS trial built on pilot work of the same intervention delivered to school pupils who had been identified as engaging in risk-taking behaviour. The pilot work indicated that the intervention was associated with reductions in risk-taking and reductions in the quantity and frequency of alcohol and substance use. 43 We modified the intervention to allow the two group components to be delivered over 2 half-days on consecutive weeks, rather than hour-long sessions over 8 weeks. We recruited participants across diverse regions in England (i.e. South East, London, North East and North West). Our aim was to detect a small effect size difference of 0.3 in terms of PDA from substances 12 months after randomisation. In our original sample size calculation, in which we planned on allocating twice as many participants to control than the group intervention, we estimated, allowing for 30% attrition, that we would require 567 participants to be allocated. However, as the trial progressed it was clear that this differential allocation ratio was a hindrance and we sought, and were granted, permission to change the ratio to ensure that participants were allocated with equal probability to control or intervention. This reduced the required sample recruited from 567 to 502 participants. In our original application, we planned on recruiting a population of adolescent substance users who were engaged with the CJS. However, it became apparent during the recruitment phase that the YJB had implemented a number of critical changes regarding how young people are managed within the CJS and these changes had a significant impact on the number of young people potentially eligible in YOTs, which had seen a significant reduction in caseloads since 2014. Many young people who used substances were being diverted out of the CJS, particularly when these offences did not involve possession with an intent to supply. As there is a strong association between substance use, criminal activity and school exclusion, and to extend our recruitment, we extended our recruitment beyond YOTs to include those young people diverted out of the CJS, for example young people educated in PRUs.
Over the recruitment period, we assessed 693 potential participants, of whom 505 (73%) met the inclusion criteria and consented to participate. Of these, 262 (51.9%) were recruited in PRUs, 191 (37.8%) were recruited in YOTs and 52 (10.3%) were recruited in SMTs, after being diverted from the CJS. Many of the participants were polysubstance users; the most common substance used was cannabis [used by 381 (75%) participants], closely followed by alcohol [used by 303 (60%) participants]. Of the participants allocated, 246 (49%) were allocated to the RISKIT-CJS intervention and 259 (51%) were allocated to the control. They were no differences on key demographics or outcomes between the groups, and we are confident that the allocation worked as intended.
Overall, 214 (87%) participants allocated to the intervention received at least some intervention; however, attrition was noticeable over time, with only 74 (30%) participants attending the second motivational interview and only 47 (19%) participants attending all elements of the intervention. Attrition over time was also greater than anticipated for both groups, with 54%, rather than our anticipated 70%, of participants followed up at the primary 12-month end point, although this rate compares favourably with other studies of interventions to address substance use in CJS populations. 39
At both 6 and 12 months, the PDA from all substances had increased for both groups, indicating a decrease in the frequency of use. We did not observe any meaningful differences between the groups, and this finding was consistent for the ATA and PP populations, and robust when sensitivity analysis was applied. Similar findings were found for the secondary outcomes.
Our economic analysis was limited to a health and social care perspective. We had planned to collect data on CJS recidivism and extend our perspective to include public sector costs, but the onset of the COVID-19 pandemic significantly affected our access to the data. The results of the economic analysis indicated that RISKIT-CJS intervention was no more cost-effective than the control. The results would indicate that there is insufficient evidence to recommend the adoption of the RISKIT-CJS intervention for substance using adolescents engaged with the CJS. Overall, the quantitative results were consistent across all outcomes. The RISKIT-CJS intervention demonstrated no evidence of additional benefit over and above TAU.
The acceptability of the RISKIT-CJS intervention varied by setting. On the one hand, staff in PRU and SMT settings considered the intervention to be acceptable and, in several cases, enjoyable. On the other hand, staff in YOT settings saw the intervention as another demand on their time and were less willing to engage. This observation was mirrored among practitioners, with most staff within PRU and SMT settings reporting positive effects of the intervention and high levels of satisfaction, whereas those in YOTs felt that the intervention was too little, too late for their caseload, as young people’s substance use had become entrenched and was a key factor in their offending. Overall, staff in PRU settings were most positive about the intervention, reporting noticeable changes in behaviour, attendance and educational attainment. Staff in YOT settings, however, were less positive, in part because the young people in their caseload was more severe and more entrenched in both substance use and criminality. Staff in YOTs expressed a concern that group work was not widely used in their settings and had higher levels of potential risk. Notably, staff in PRUs indicated that they would be keen to implement the RISKIT-CJS intervention in some form in their setting, irrespective of the outcome of the trial.
Overall, although the quantitative clinical and economic analysis provide no clear evidence of benefit from implementing the RISKIT-CJS intervention, it is important to note that the elements of the RISKIT-CJS intervention are evidence informed. With regard to YOTs, it is clear that key organisational factors make the implementation of the RISKIT-CJS intervention more difficult, in addition to them constituting a more entrenched substance-using population. However, staff in SMTs and PRUs were far more positive about the intervention, as it was a better fit for the work they usually do with young people, and they reported a number of subtle but beneficial changes. It is also worth noting that bar one event, in which a participant was considered at potential risk and so was withdrawn from the intervention groups, no adverse effects of the intervention were reported. The RISKIT-CJS intervention is probably not suitable for implementation in YOTs, but delivering the RISKIT-CJS intervention, probably in its original form, that is, weekly over several weeks and for a younger population, is probably feasible and acceptable in SMTs and PRUs.
Strength and limitations
The trial employed scientifically rigorous methods to address key questions regarding clinical effectiveness and cost-effectiveness, using reliable and validated outcome measures. The trial employed a mixed-methods approach with a comprehensive qualitative component. We successfully recruited a sufficient number of staff to deliver the intervention across all participating sites, and each member of staff attended training and was assessed as competent prior to delivering the RISKIT-CJS intervention. We also recruited sufficient participants to meet our predetermined sample size calculation, but it was clear as the trial progressed that we were unlikely to recruit sufficient numbers from YOTs and so we extended the recruitment to SMTs and PRUs. Although there were no differences in the demographic profiles of those recruited in different locations, we cannot be sure that they did not differ in terms of their entrenched criminal involvement, something highlighted in the qualitative research. In our sample size calculation, we estimated that attrition at 12 months would not exceed 30%, and this was an underestimate. Prior to the COVID-19 pandemic, we were on target to achieve close to our follow-up target, but the pandemic had a significant impact on how we conducted follow-ups, as most organisations, including YOTs, PRUs and SMTs, moved to remote working. All face-to-face follow-up was suspended and the research team had to resort to alternative means, including post, e-mail and telephone. It was clear that a lack of face-to-face interaction resulted an increase in attrition. Allied to this, our plan to derive CJS outcomes from the YJB was significantly affected by the pandemic. Access to the required data is available only using a dedicated terminal located at the YJB office. However, as staff had moved to remote working, access to the computing system was limited to essential reporting activity and because the project was not considered essential we had no access to this data set for analysis.
Although we used validated and reliable tools to assess outcomes, our primary outcome relied on self-report, the use of which may have led to inaccurate reporting of substance use. However, adolescent self-report of substance use is generally considered to be reliable,122,123 and we used an established reliable and valid method to assess substance use,57 which has been validated for both self-completion and interviewer completion. Whenever possible, we attempted to conduct follow-up assessments blind to treatment allocation by using different researchers to conduct assessments, but we could not guarantee that this was always the case, and nor could we guarantee that young people did not reveal their allocation as part of the assessment process. The statistical analysis followed a predetermined statistical analysis plan, which was agreed in advance with the TSC, and analysis was conducted blind to allocation. There was evidence of a reduction in the frequency of substance use across both groups at month 12, and it may be suggested that this is a regression to the mean effect, although this is unlikely, as there was no threshold for inclusion over and above having used substances. The economic component of the study used internationally accepted methods of best practice and was based on a detailed and explicit analysis plan that was finalised prior to embarking on any analysis. In terms of methods, the intervention training and delivery was micro-costed, and rigorous methods were employed to ensure that all resource costs were captured and sensitivity analyses conducted to test the stability of the underlying assumptions. The study employed an internationally accepted instrument for assessing quality of life and generating QALYs, that is, the EQ-5D-5L. The results of the study suggest that short-term health impacts are, at best, very small, but the study aimed to present the results in terms of traditional cost-effectiveness and as cost–consequence. A limitation to the economic analysis was our inability to include CJS costs and explore cost-effectiveness from a wider public sector perspective.
A strength of the study is the deployment of mixed methods that yield a detailed understanding of how the RISKIT-CJS intervention works and whom it might work for and in what setting. The qualitative research concurred with the experience of the research team, who found working in YOT settings difficult and often unproductive. Staff in these settings often experienced systemic changes in working practices and seemed most remote from their senior management, with little culture of evaluation. In addition, the research project seemed a burden for many staff in YOTs who did not usually deliver group work and did not have the facilities to deliver it. In PRUs and SMTs, however, the RISKIT-CJS intervention integrated well with existing practices and addressed a need many in these settings had identified. Consequently, the reaction to the project was far more positive and staff were keen to facilitate the research.
A strength of the qualitative focus groups conducted with young people was feasibility of delivery, and this was owing to the group discussions being conducted immediately after the intervention delivery. A potential limitation was the possibility of biased responses from young people during the focus group sessions, which can affect the validity of findings. However, this limitation was acknowledged and reduced by having a clear separation between the interventionists’ and researchers’ roles. Researchers entered the room after the interventionists had finished the last programme session, introducing and welcoming the young people to the qualitative focus group. This set-up provided the young people a new ‘space’ to explore how they felt about the programme elements and make positive or negative observations without concern, thereby reducing the potential for biased responses. Some group sessions had particularly small numbers and, therefore, were unsuitable for a focus group; instead, young people provided some feedback, which was not included in the analysis of the focus groups. One limitation of the study relates to the fact that the co-production of the RISKIT intervention involved a population of school pupils who had less involvement with CJS than the RISKIT-CJS population. This may, in part, explain why adherence and outcomes were noticeably better in the feasibility work. On reflection, it may have been worth engaging in a second co-production process with a different population prior to embarking on the RISKIT-CJS trial.
Although not strictly a limitation, the study raised key issues about how research interventions are funded outside the NHS. The study team had significant difficulty is securing the intervention costs, and it was clear that, although there was a desire by all parties to ensure that intervention costs were provided to conduct research of this type, there was no clear mechanism for identifying the source or access to these costs.
The research has advanced our understanding of how to conduct research in this population and across a variety of settings. Although the study did not provide evidence of the clinical effectiveness or cost-effectiveness of the RISKIT-CJS intervention, it is an evidence-informed intervention, and many staff in PRU and SMT settings considered the intervention to have some beneficial effect and to have addressed a clear need that they had in these settings. As the study reported no adverse events, there is no reason why these settings should not deliver the intervention if they wish to do so. However, evidence from YOTs was less positive and implementation of the intervention in this setting is unlikely to be considered without a strong evidence base. It was also clear that the form of delivery should be more akin to the pilot work conducted in schools, where the group element is delivered once per week for 1 hour over several weeks, and perhaps at an earlier age, before substance misuse and criminal activity become entrenched.
Chapter 7 Conclusions
Implications for public health
This study does not provide evidence of clinical effectiveness and cost-effectiveness of the RISKIT-CJS programme for adolescents involved in the CJS and using substances. Evidence from the qualitative component of the study suggests that some young people and stakeholders found the intervention useful and acceptable, and associated it with changes in substance use and behaviour, but these findings were more likely to occur in PRU settings than in YOTs. The programme is based on evidence-informed practice and is more likely to be useful for a younger population with less severe and entrenched substance use. There was no evidence that the RISKIT-CJS programme incurred significantly greater costs than TAU, nor was there any evidence of it being associated with more adverse events or safeguarding incidents. The RISKIT-CJS programme is an additional resource that can be used by those working with young people who are concerned about their risk-taking behaviour and substance use.
Recommendations for future research
-
It was clear in conducting the research that some staff within the CJS were resistant to research being conducted in their services. Although there are efforts to embed a research culture in the CJS, more information is required on how this can be of benefit for these services to see the potential value of engaging in research.
-
It was clear from working with staff in PRUs that they felt that there was a paucity of research addressing the social, behavioural and mental health needs of young people in alternative education provision. We recommend that more research is conducted to establish an evidence base for effective approaches to manage social, educational, behavioural and mental health needs of young people in these settings.
-
Young people involved in criminal activity are increasingly being diverted from the CJS. Many of these young people are involved in diversionary schemes and are at an early stage in their substance use career. Considering the evidence from our pilot work in schools, an evaluation of the effectiveness of the RISKIT-CJS programme for those diverted from the CJS is warranted.
-
In a similar vein, evidence from the qualitative analysis suggested that stakeholders felt that a population younger than our target (i.e. 13–17 years) may benefit more, particularly if the intervention was delivered at an earlier stage in a young person’s risk-taking trajectory. Our previous pilot work in schools suggested a positive effect in terms of alcohol and substance use and risk-taking behaviour. This evidence was based on a quasi-experimental study design and we recommend that a formal multicentre RCT is conducted to evaluate the clinical effectiveness and cost-effectiveness of the RISKIT-CJS intervention delivered in schools.
-
Complete analysis of recidivism and changes to engagement in CJS was not possible because of restrictions implemented during the COVID-19 pandemic. When access to these data becomes available, we recommend that these elements of the quantitative and economic analysis are undertaken.
-
One finding of the prognostic analysis exploring the relationship between interventionist skill (assessed using the TASC-r) and outcome suggested a strong relationship between some therapists and increased PDA at 12 months. More research is recommended into exploring what key competencies and skills contribute to better therapeutic outcomes when working with young people.
-
Within the study, a great deal of qualitative data were collected from stakeholders, young people and researchers who wrote observational notes. We recommend that these data are further analysed to conduct a comparative analysis of the complex, potentially causal, effects of different patterns of characteristics of settings and individuals.
Acknowledgements
We would like to thank all the young people who took part in the study and the staff at the sites we worked with. We also acknowledge the important contribution of staff from Addaction who helped deliver the intervention, in particular Steve Butler, Nick Hickmott, Lynn Dougan and Leigh Fitzpatrick in the North East. We would like to thank the young people on the Addaction Young Person’s Advisory Panel who provided feedback to the TMG throughout the study.
Work of this kind is complex, and we would like to thank staff from within the wider research groups who helped with the project: Ms Anna Walker, Professor Jenny Billings, Dr Joanna Milward, Dr Sadie Boniface, Dr Andrew Divers, Ms Parisa Diba, Dr Alex Sutherland, Dr Ed Wilson, Ms Emma Cuthbertson, Dr Kelly Stockdale, Dr Grant McGeechan, Mr Simon Wood, Ms Racine Hope Tanner and Mr Rob Crow.
We would like to thank members of the TSC who have provided insightful and constructive advice throughout the study: Professor Ian Russell (Chairperson, Swansea University), Professor Jeremy Bray (Economics, University of North Carolina), Anna-Marie Jones (Statistics, Sussex Partnership Foundation Trust), Dr Abi Hamoodi (Public Health and the CJS, Public Health England) and Dr Jess Mookherjee (Public Health, Kent County Council).
Contributions of authors
Simon Coulton (https://orcid.org/0000-0002-7704-3274) (Professor of Health Research, University of Kent) was chief investigator for the study, took overall responsibility for the design and conduct of the study and writing of the report, and was a member of the TMG and TSC.
Olena Nizalova (https://orcid.org/0000-0002-1704-2632) (Senior Research Fellow in Health Economics, University of Kent) was responsible for analysing, interpreting and drafting the economic aspects of the report (see Chapter 4).
Tracy Pellatt-Higgins (https://orcid.org/0000-0002-2543-461X) (Senior Research Fellow in Health Statistics, University of Kent) was responsible for analysing, interpreting and drafting the statistical aspects of the report (see Chapter 3).
Alex Stevens (https://orcid.org/0000-0002-4878-3871) (Professor of Criminology, University of Kent) was a principal investigator with overall responsibility for qualitative aspects of the study, and was responsible for analysing, interpreting and drafting the qualitative aspects of the report (see Chapter 5).
Nadine Hendrie (https://orcid.org/0000-0001-6437-0826) (Research Associate, University of Kent) was the trial co-ordinator for the South East, and contributed to the analysis, interpretation and drafting of the qualitative aspects of the report (see Chapter 5).
Catherine Marchand (https://orcid.org/0000-0003-2092-9127) (Research Associate, University of Kent) was the trial manager for the study, and contributed to the analysis, interpretation and drafting of the qualitative aspects of the report (see Chapter 5).
Rosa Vass (https://orcid.org/0000-0002-1457-8896) (Research Associate, University of Kent) was the trial researcher for the South East, and contributed to the analysis, interpretation and drafting of the qualitative aspects of the report (see Chapter 5).
Paolo Deluca (https://orcid.org/0000-0002-9511-7230) (Reader in Addiction Research, King’s College London) was a principal investigator and trial co-ordinator for the London region, and contributed to the interpretation of data and drafting of the report.
Colin Drummond (https://orcid.org/0000-0001-9379-5452) (Professor of Addiction Psychiatry, King’s College London) was a principal investigator, and contributed to the interpretation of data and drafting of the report.
Jennifer Ferguson (https://orcid.org/0000-0002-1719-269X) (Research Associate, Teesside University) contributed to the drafting of the final report.
Gillian Waller (https://orcid.org/0000-0003-1873-3766) (Research Associate, Teesside University) was a trial co-ordinator for the North East and North West, and contributed to the drafting of the final report.
Dorothy Newbury-Birch (https://orcid.org/0000-0003-0065-8649) (Professor of Alcohol and Public Health Research, Teesside University) was a principal investigator, and contributed to the design and conduct of the study; to the collection, analysis and interpretation of data; and to drafting the final report.
Publication
Coulton S, Stockdale K, Marchand C, Hendrie N, Billings J, Boniface S, et al. Pragmatic randomised controlled trial to evaluate the effectiveness and cost effectiveness of a multi-component intervention to reduce substance use and risk-taking behaviour in adolescents involved in the criminal justice system: a trial protocol (RISKIT-CJS). BMC Public Health 2017;17:246.
Data-sharing statement
All data requests should be made direct to the corresponding author for consideration. Access to anomysed data may be made subject to review. Exclusive access will be retained by the research team until the publication of major outputs.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Coulton S, Stockdale K, Marchand C, Hendrie N, Billings J, Boniface S, et al. Pragmatic randomised controlled trial to evaluate the effectiveness and cost effectiveness of a multi-component intervention to reduce substance use and risk-taking behaviour in adolescents involved in the criminal justice system: a trial protocol (RISKIT-CJS). BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4170-6.
- Medical Research Council (MRC) . Developing and Evaluating Complex Interventions 2000.
- Youth Justice Board . Asset – Young Offender Assessment Profile 2006.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Clarke A, Friede T, Putz R, Ashdown J, Martin S, Blake A, et al. Warwick–Edinburgh Mental Well-being Scale (WEMWBS): validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-487.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Heather N, Luce A, Peck D, Dunbar B, James I. The development of a treatment version of the Readiness to Change Questionnaire. Addict Res 1999;7:63-8. https://doi.org/10.3109/16066359909004375.
- Maisto SA, Chung TA, Cornelius JR, Martin CS. Factor structure of the SOCRATES in a clinical sample of adolescents. Psychol Addict Behav 2003;17:98-107. https://doi.org/10.1037/0893-164x.17.2.98.
- Miller WR, Tonigan JS. Assessing the drinkers’ motivation for change: the Stages Of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychol Add Beh 1996;10:81-9. https://doi.org/10.1037/0893-164X.10.2.81.
- Great Britain . General Data Protection Regulations 2016 2016.
- Great Britain . Freedom of Information Act 2000 2000.
- Medical Research Council (MRC) . MRC Guideline for the Management of Global Health Trials v3.0 2019.
- Odgers CL, Caspi A, Nagin DS, Piquero AR, Slutske WS, Milne BJ, et al. Is it important to prevent early exposure to drugs and alcohol among adolescents?. Psychol Sci 2008;19:1037-44. https://doi.org/10.1111/j.1467-9280.2008.02196.x.
- Battistella G, Fornari E, Annoni JM, Chtioui H, Dao K, Fabritius M, et al. Long-term effects of cannabis on brain structure. Neuropsychopharmacology 2014;39:2041-8. https://doi.org/10.1038/npp.2014.67.
- Copeland WE, Adair CE, Smetanin P, Stiff D, Briante C, Colman I, et al. Diagnostic transitions from childhood to adolescence to early adulthood. J Child Psychol Psychiatry 2013;54:791-9. https://doi.org/10.1111/jcpp.12062.
- Parlar M, MacKillop E, Petker T, Murphy J, MacKillop J. Cannabis use, age of initiation, and neurocognitive performance: findings from a large sample of heavy drinking emerging adults. J Int Neuropsychol Soc 2021;27:533-45. https://doi.org/10.1017/S1355617721000618.
- NHS Digital . Smoking, Drinking and Drug Use Among Young People in England in 2016 2017.
- Department for Education . Permanent and Fixed-Period Exclusions in England: 2015 to 2016 2017.
- Aldington S, Harwood M, Cox B, Weatherall M, Beckert L, Hansell A, et al. Cannabis use and risk of lung cancer: a case–control study. Eur Respir J 2008;31:280-6. https://doi.org/10.1183/09031936.00065707.
- World Health Organization (WHO) . Global Status Report on Alcohol and Health, 2014 2014.
- NHS Digital . Smoking, Drinking and Drug Use Among Young People 2018.
- Wilson E. Youth Justice Interventions – Findings from the Juvenile Cohort Study (JCS). London: Ministry of Justice Analytical Series; 2013.
- Newbury-Birch D, Jackson K, Hodgson T, Gilvarry E, Cassidy P, Coulton S, et al. Alcohol-related risk and harm amongst young offenders aged 11–17. Int J Prison Health 2015;11:75-86. https://doi.org/10.1108/IJPH-08-2013-0041.
- Youth Justice Board/Ministry of Justice . Youth Justice Statistics 2013 14. England and Wales 2015.
- Department for Education . Permanent Exclusions and Suspensions in England 2021.
- Home Office . Serious Violence Strategy 2018.
- Social Exclusion Unit . Reducing Reoffending by Ex-Prisoners 2002.
- Coffey C, Veit F, Wolfe R, Cini E, Patton GC. Mortality in young offenders: retrospective cohort study. BMJ 2003;326. https://doi.org/10.1136/bmj.326.7398.1064.
- Galahad SMS Ltd . Substance Misuse and Juvenile Offenders 2004.
- Ritakallio M, Kaltiala-Heino R, Kivivuori J, Rimpelä M. Brief report: delinquent behaviour and depression in middle adolescence: a Finnish community sample. J Adolesc 2005;28:155-9. https://doi.org/10.1016/j.adolescence.2004.07.002.
- Galahad SMS Ltd . Evaluation of the Substance Misuse Project in the Young Person’s Secure Estate 2009.
- Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Adolesc Psychiatry 1998;37:594-601. https://doi.org/10.1097/00004583-199806000-00009.
- Willmott D, van Olphen J. Challenging the health impacts of incarceration: the role for community health workers. Calif J Health Promot 2005;3:38-4. https://doi.org/10.32398/cjhp.v3i2.1762.
- British Medical Association . Young Lives Behind Bars: The Health and Human Rights of Children and Young People Detained in the Criminal Justice System 2014.
- Khan L. Reaching Out, Reaching In: Promoting Mental Health and emotional Well-Being in Secure Settings. London: Centre for Mental Health; 2010.
- Anderson L, Vostanis P, Spencer N. Health needs of young offenders. J Child Health Care 2004;8:149-64. https://doi.org/10.1177/1367493504041873.
- Stallard P, Thomason J, Churchyard S. The mental health of young people attending a youth offending team: a descriptive study. J Adolesc 2003;26:33-4. https://doi.org/10.1016/S0140-1971(02)00117-3.
- Youth Justice Board/Ministry of Justice . Youth Justice Statistics 2019 20. England and Wales 2020. https://doi.org/10.1177/1473225420953057.
- Perry A, Coulton S, Glanville J, Godfrey C, Lunn J, McDougall C, et al. Interventions for drug-using offenders in the courts, secure establishments and the community. Cochrane Database Syst Rev 2006;3. https://doi.org/10.1002/14651858.CD005193.pub2.
- Henderson CE, Wevodau AL, Henderson SE, Colbourn SL, Gharagozloo L, North LW, et al. An independent replication of the adolescent–community reinforcement approach with justice-involved youth. Am J Addict 2016;25:233-40. https://doi.org/10.1111/ajad.12366.
- D’Amico EJ, Hunter SB, Miles JN, Ewing BA, Osilla KC. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. J Subst Abuse Treat 2013;45:400-8. https://doi.org/10.1016/j.jsat.2013.06.005.
- Steele DW, Becker SJ, Danko KJ, Balk EM, Adam GP, Saldanha IJ, et al. Brief behavioral interventions for substance use in adolescents: a meta-analysis. Pediatrics 2020;146. https://doi.org/10.1542/peds.2020-0351.
- Stevens A, Coulton S, O’ Brien K, Butler S, Gladstone B, Tonkin J. RISKIT: the participatory development and observational evaluation of a multi-component programme for adolescent risk-behaviour reduction. Drug Educ Prev Pol 2014;21:24-3. https://doi.org/10.3109/09687637.2013.787526.
- Catalano R, Oxford M, Harachi T, Abbott R, Haggerty K. A test of the social development model to predict problem behaviour during the elementary school period. Crim Beh Men Health 1999;9:39-56. https://doi.org/10.1002/cbm.290.
- Catalano R, Hawking J, Hawkings J. Delinquency and Crime: Current Theories. Cambridge: Cambridge University Press; 1996.
- Duerden MD, Gillard A. An approach to theory-based youth programming. New Dir Youth Dev 2011;2011:39-53. https://doi.org/10.1002/yd.418.
- Cahill C. Doing research with young people: participatory research and the rituals of collective work. Child Geogr 2007;5:297-312. https://doi.org/10.1080/14733280701445895.
- Cornwall A, Jewkes R. What is participatory research?. Soc Sci Med 1995;41:1667-76. https://doi.org/10.1016/0277-9536(95)00127-s.
- Fagan J, Piquero AR. Rational choice and developmental influences on recidivism among adolescent felony offenders. J Empir Leg Stud 2007;4. https://doi.org/10.1111/j.1740-1461.2007.00105.x.
- Buhler A, Kroger C. Prevention of Substance Misuse. EMCDDA Insights. Lisbon: EMCDDA; 2008.
- Foxcroft DR, Ireland D, Lister-Sharp DJ, Lowe G, Breen R. Primary prevention for alcohol misuse in young people. Cochrane Database Syst Rev 2002;3. https://doi.org/10.1002/14651858.CD003024.
- Grimshaw GM, Stanton A. Tobacco cessation interventions for young people. Cochrane Database Syst Rev 2006;4. https://doi.org/10.1002/14651858.CD003289.pub4.
- Kavanagh J, Trouton A, Oakley A, Powell C. A Systematic Review of the Evidence for Incentive Schemes to Encourage Positive Health and other Social Behaviours in Young People. London: Institute of Education; 2006.
- McGrath Y, Sumnall H, Edmonds K, McVeigh J, Bellis M. Review of the Grey Literature on Drug Prevention Among Young People. London: National Institute for Health and Care Excellence; 2006.
- National Institute for Health and Care Excellence (NICE) . Interventions to Reduce Substance Use Among Vulnerable Young People 2007.
- Kent Police . Evaluation of the Kent Youth Drug Intervention Scheme 2017.
- Sobell L, Sobell M. Alcohol Timeline Followback Users’ Manual. Toronto, ON: Addiction Research Foundation; 1995.
- Levy S, Sherritt L, Harris SK, Gates EC, Holder DW, Kulig JW, et al. Test–retest reliability of adolescents’ self-report of substance use. Alcohol Clin Exp Res 2004;28:1236-41. https://doi.org/10.1097/01.ALC.0000134216.22162.A5.
- Maheswaran H, Weich S, Powell J, Stewart-Brown S. Evaluating the responsiveness of the Warwick Edinburgh Mental Well-Being Scale (WEMWBS): group and individual level analysis. Health Qual Life Outcomes 2012;10. https://doi.org/10.1186/1477-7525-10-156.
- Breslin FC, Sobell LC, Sobell MB, Agrawal S. A comparison of a brief and long version of the Situational Confidence Questionnaire. Behav Res Ther 2000;38:1211-20. https://doi.org/10.1016/S0005-7967(99)00152-7.
- Müller M, Haenni Hoti A. Item analysis of the KIDSCREEN-10 using Rasch modelling. Health Qual Life Outcomes 2020;18. https://doi.org/10.1186/s12955-020-01596-6.
- Shirk S, Saiz C. Clinical, empirical and developmental; perspectives on the therapeutic relationship in child psychotherapy. Dev Psychopath 1992;4:713-21. https://doi.org/10.1017/S0954579400004946.
- Lane C. The Behaviour Change Counselling Index (BECCI) Manual for Coding Behaviour Change Counselling. Cardiff: University of Wales College of Medicine; 2002.
- Stevens K. Valuation of the Child Health Utility 9D Index. PharmacoEconomics 2012;30:729-47. https://doi.org/10.2165/11599120-000000000-00000.
- Deluca P, Coulton S, Alam MF, Cohen D, Donoghue K, Gilvarry E, et al. Linked randomised controlled trials of face-to-face and electronic brief intervention methods to prevent alcohol related harm in young people aged 14–17 years presenting to emergency departments (SIPS junior). BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1679-4.
- Beebe J. Basic concepts and techniques of rapid appraisal. Human Org 1995;54:42-51. https://doi.org/10.17730/humo.54.1.k84tv883mr2756l3.
- Willie N. Systematic Review of Strategies to Reduce Attrition in Randomised Controlled Trials n.d.
- Lane C, Huws-Thomas M, Hood K, Rollnick S, Edwards K, Robling M. Measuring adaptations of motivational interviewing: the development and validation of the behavior change counseling index (BECCI). Patient Educ Couns 2005;56:166-73. https://doi.org/10.1016/j.pec.2004.01.003.
- Sussman JB, Hayward RA. An IV for the RCT: using instrumental variables to adjust for treatment contamination in randomised controlled trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c2073.
- Ye C, Beyene J, Browne G, Thabane L. Estimating treatment effects in randomised controlled trials with non-compliance: a simulation study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005362.
- Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Med Res Methodol 2017;17. https://doi.org/10.1186/s12874-017-0442-1.
- White I. RCTMISS: Stata Module to Analyse a Randomised Controlled Trial (RCT) Allowing for Informatively Missing Outcome Data 2018. https://ideas.repec.org/c/boc/bocode/s458304.html (accessed June 2022).
- White IR, Kalaitzaki E, Thompson SG. Allowing for missing outcome data and incomplete uptake of randomised interventions, with application to an internet-based alcohol trial. Stat Med 2011;30:3192-207. https://doi.org/10.1002/sim.4360.
- Liu W, Xin J. Modelling Fractional Outcomes With SAS 2014. https://support.sas.com/resources/papers/proceedings14/1304-2014.pdf (accessed 18 May 2022).
- Altman DG. Avoiding bias in trials in which allocation ratio is varied. J R Soc Med 2018;111:143-4. https://doi.org/10.1177/0141076818764320.
- Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med 2017;36:855-75. https://doi.org/10.1002/sim.7141.
- Drummond MF, Sculper MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. New York, NY: Oxford University Press; 2005.
- Fieller E. Some problems in interval estimation. J R Stat Soc Ser B Methods 1954;16:175-85. https://doi.org/10.1111/j.2517-6161.1954.tb00159.x.
- Pickard AS, De Leon MC, Kohlmann T, Cella D, Rosenbloom S. Psychometric comparison of the standard EQ-5D to a 5 level version in cancer patients. Med Care 2007;45:259-63. https://doi.org/10.1097/01.mlr.0000254515.63841.81.
- Janssen MF, Birnie E, Haagsma JA, Bonsel GJ. Comparing the standard EQ-5D three-level system with a five-level version. Value Health 2008;11:275-84. https://doi.org/10.1111/j.1524-4733.2007.00230.x.
- Devlin N, Parkin D, Janssen B. Methods for Analysing and Reporting EQ-5D Data. Berlin: Springer; 2020.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for EuroQuol: Results from a UK Population Survey. York: Centre for Health Economics; 1995.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. https://doi.org/10.1002/hec.901.
- Deluca P, Coulton S, Alam MF, Boniface S, Donoghue K, Gilvarry E, et al. Screening and brief interventions for adolescent alcohol use disorders presenting through emergency departments: a research programme including two RCTs. Programme Grants Appl Res 2020;8. https://doi.org/10.3310/pgfar08020.
- Giles E, Coulton S, Deluca P, Drummond C, Howel D, Kaner E. Multicentre individual randomized controlled trial of screening and brief alcohol intervention to prevent risky drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012474.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2020. Canterbury: PSSRU, University of Kent; 2020.
- Glick H, Doshi J, Sonnad S, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- Pratt J, Raiffa H, Schlaifer R. Introduction to Statistical Decision Theory. Cambridge, MA: MIT Press; 1995.
- Elliot R, Payne K. Essentials of Economic Evaluation in Healthcare. London: PharmaPress; 2004.
- Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed?. BMJ 2000;320:1197-200. https://doi.org/10.1136/bmj.320.7243.1197.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. https://doi.org/10.1002/hec.635.
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/10.1007/s40273-014-0193-3.
- Leurent B, Gomes M, Carpenter J. Comment on: sensitivity analysis for not-at-random missing data in trial-based cost-effectiveness analysis: a tutorial. PharmacoEconomics 2018;36. https://doi.org/10.1007/s40273-018-0700-z.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. https://doi.org/10.1192/bjp.187.2.106.
- White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011;342. https://doi.org/10.1136/bmj.d40.
- Chambers R. The origins and practice of participatory rural appraisal. World Dev 1994;22:953-69. https://doi.org/10.1016/0305-750X(94)90141-4.
- Layder D. Sociological Practice: Linking Theory and Social Research. London: SAGE Publications Ltd; 1998.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Nam JM. Power and sample size for stratified prospective studies using the score method for testing relative risk. Biometrics 1998;54:331-6. https://doi.org/10.2307/2534020.
- May CR, Cummings A, Girling M, Bracher M, Mair FS, May CM, et al. Using normalization process theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0758-1.
- Advisory Council on the Misuse of Drugs . Prevention of Drug and Alcohol Dependence n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/406926/ACMD_RC_Prevention_briefing_250215.pdf (accessed 18 May 2022).
- Room R. Preventing youthful substance use and harm – between effectiveness and political wishfulness. Subst Use Misuse 2012;47:936-43. https://doi.org/10.3109/10826084.2012.663297.
- Morris S, Smith A, Fox C. Time to reset the clock on the design of impact evaluations in criminology: the case for multi-methodology designs. Br J Community Justice 2020:1-18.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Byrne D. Applying Social Science: The Role of Social Research in Politics, Policy and Practice. Bristol: Policy Press; 2011.
- Pawson R, Tilley N. Realistic Evaluation. Thousand Oaks, CA: SAGE Publications Ltd; 1998.
- Breuer E, Lee L, De Silva M, Lund C. Using theory of change to design and evaluate public health interventions: a systematic review. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0422-6.
- Bonnell C, Jamal F, Harden A, Wells H, Parry W, Fletcher A. Systematic review of the effects of schools and school environment interventions on health: evidence mapping and synthesis. Public Health Res 2013;1. https://doi.org/10.3310/phr01010.
- Hastings A, Bailey N, Bramley G, Gannon M, Watkins D. The Cost of the Cuts: The Impact on Local Government and Poorer Comunities. York: Joseph Rowntree Foundation; 2015.
- Otten R, Mun CJ, Shaw DS, Wilson MN, Dishion TJ. A developmental cascade model for early adolescent-onset substance use: the role of early childhood stress. Addiction 2019;114:326-34. https://doi.org/10.1111/add.14452.
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2017;2:e356-e366. https://doi.org/10.1016/S2468-2667(17)30118-4.
- Agrawal A, Few L, Nelson EC, Deutsch A, Grant JD, Bucholz KK, et al. Adolescent cannabis use and repeated voluntary unprotected sex in women. Addiction 2016;111:2012-20. https://doi.org/10.1111/add.13490.
- Silins E, Fergusson DM, Patton GC, Horwood LJ, Olsson CA, Hutchinson DM, et al. Adolescent substance use and educational attainment: an integrative data analysis comparing cannabis and alcohol from three Australasian cohorts. Drug Alcohol Depend 2015;156:90-6. https://doi.org/10.1016/j.drugalcdep.2015.08.034.
- Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood. JAMA Psychiatry 2019;76:426-34. https://doi.org/10.1001/jamapsychiatry.2018.4500.
- Lemert EM. Social Pathology: A Systematic Approach to the Theory or Sociopathic Behavior. New York, NY: McGraw-Hill Book Company; 1951.
- McAra L, McVie S. The usual suspects? Street-life, young people and the police. Crim Justice 2005;5:5-36. https://doi.org/10.1177/1466802505050977.
- Young T, FitzGerald M, Hallsworth S, Joseph I. Groups, Gangs and Weapons. London: Youth Justice Board for England and Wales; 2007.
- Hirschi T, Gottfredson M. Age and the explanation of crime. AJS 1983;89:552-84. https://doi.org/10.1086/227905.
- Jones HJ, Gage SH, Heron J, Hickman M, Lewis G, Munafó MR, et al. Association of combined patterns of tobacco and cannabis use in adolescence with psychotic experiences. JAMA Psychiatry 2018;75:240-6. https://doi.org/10.1001/jamapsychiatry.2017.4271.
- Shillington AM, Roesch SC, Reed MB, Clapp JD, Woodruff SI. Typologies of recanting of lifetime cigarette, alcohol and marijuana use during a six-year longitudinal panel study. Drug Alcohol Depend 2011;118:134-40. https://doi.org/10.1016/j.drugalcdep.2011.03.009.
- Percy A, McAlister S, Higgins K, McCrystal P, Thornton M. Response consistency in young adolescents’ drug use self-reports: a recanting rate analysis. Addiction 2005;100:189-96. https://doi.org/10.1111/j.1360-0443.2004.00943.x.
List of abbreviations
- ATA
- analysis by treatment allocated
- BECCI
- Behaviour Change Counselling Index
- BOCF
- baseline observation carried forward
- BSCQ
- Brief Situational Confidence Questionnaire
- CACE
- complier-average causal effect
- CEAC
- cost-effectiveness acceptability curve
- CEP
- cost-effectiveness plane
- CHU-9D
- Child Health Utility – 9 dimensions
- CI
- confidence interval
- CJS
- criminal justice system
- CMO
- context, mechanism and outcome
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- ICER
- incremental cost-effectiveness ratio
- IQR
- interquartile range
- LOCF
- last observation carried forward
- MAR
- missing at random
- MDMA
- 3,4-methylenedioxy-methamphetamine
- MNAR
- missing not at random
- NICE
- National Institute for Health and Care Excellence
- NPT
- normalisation process theory
- OR
- odds ratio
- PDA
- per cent days abstinent
- PP
- per protocol
- PRU
- pupil referral unit
- PSHE
- personal, social, health and economic
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RISKIT-CJS
- RISKIT-Criminal Justice System
- SD
- standard deviation
- SMT
- substance misuse team
- SOCRATES-7DS
- Stages Of Change Readiness And Treatment Eagerness Scale – 7 Dimensions
- TASC-r
- Therapeutic Alliance Scale for Children: Youth version
- TAU
- treatment as usual
- TLFB28
- Timeline Followback 28
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
- WTP
- willingness to pay
- YJB
- Youth Justice Board
- YOT
- youth offending team
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/FKPY6814).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
