Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 11/3002/11. The contractual start date was in February 2014. The final report began editorial review in August 2019 and was accepted for publication in May 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Personal dedication
Our work aims to improve the life chances of babies. All babies are precious. Their wonderful potential, their joy and their sorrows can sometimes get lost when quantified statistically. It is often our personal knowledge that brings meaning to such numbers. I dedicate this report to my own grand-daughter, Luna Alice Atkins, who left us this year aged only three days old. She will forever remain precious to us and her life will always have meaning. Michael Robling, 2020
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Robling et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Parts of this chapter have been reproduced from the published protocol paper by Lugg-Widger et al. 1 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Summary
The Building Blocks: 2–6 years (BB:2–6) study has followed up the cohort of mothers originally recruited to the Building Blocks (BB) trial of the Family Nurse Partnership (FNP) in England, BB: 0–2 years (BB:0–2). Using routine data drawn from across public sector providers to augment trial data, the study offers a unique opportunity to evaluate the medium-term outcomes of the FNP as a preventative intervention to reduce child maltreatment in England. This chapter provides an introduction to the principal clinical domain addressed by the BB:2–6 study; presents previous research on the specialist home-visiting programme both in the UK and internationally; and provides a rationale and description for the current study aims and objectives.
Maltreatment
Maltreatment involves acts of omission (neglect) or commission (abuse), often by caregivers who either threaten to risk, risk or actually cause harm to a child. 2 Abuse may be physical, emotional or sexual. Neglect represents persistent failure to meet a child’s basic physical or psychological needs, often resulting in serious impairment of the child’s health or development. 2 Neglect may involve failing to do any of the following: protect a child from physical and emotional harm or danger, ensure adequate supervision or ensure access to appropriate medical care. In the financial year ending 31 March 2018 in England, there were 655,630 referrals to children’s social care (CSC) services (relating to 581,280 children, an average of 1.13 referrals per child), 406,770 children were starting an episode of need (an overall rate of 341.0 per 10,000) and 53,790 children became subject to a child protection plan. 3 A child protection plan is a plan drawn up by the local authority detailing how the child can be supported. The most common reason for a child to become subject to a child protection plan was neglect (48.0%), followed by emotional abuse (35.1%). 3
In the UK, preventing maltreatment is an important focus of government concern. The Children Act 19894 specifies agencies’ responsibilities to co-operate in the interests of vulnerable children, for children in need (section 17) and children suffering or likely to suffer from significant harm (section 47). A child in need (CIN) is defined as a child who is unlikely to achieve or maintain a reasonable level of health or development, a child whose health and development is likely to be significantly or further impaired without the provision of services, or a child who is disabled. 4 Local authority provisions may include supervision of activities; financial help; and/or provision of family accommodation, respite or home help, in addition to advice and guidance from social workers.
Specialist home visiting: the Family Nurse Partnership
There has been an increasing emphasis on the primary prevention of child maltreatment, including interventions directed at general populations and those targeting high-risk groups. The US Department of Health and Human Services’ Home Visiting Evidence and Effectiveness review5 maintains an ongoing assessment of evidence on home visiting as a preventative intervention. One such preventative home-visiting approach to reducing maltreatment is the FNP programme [developed in the USA as the Nurse–Family Partnership (NFP)], with three overarching goals: to improve birth outcomes; to improve child health and development, including reducing maltreatment; and to promote the economic self-sufficiency of mothers. 6 The programme aims to promote sensitive and competent caregiving and to reduce maltreatment through activities such as education about child development, modelling sensitive parent–child interaction, and guidance on accessing appropriate child care. The NFP is one of three preventative programmes shown to be effective in preventing maltreatment;7 in the USA, it is delivered in 42 states (plus the US Virgin Islands). 8 In three US trials (in Elmira, NY; Memphis, TN; and Denver, CO),9–11 the NFP has demonstrated improvements in prenatal health behaviours and birth outcomes; improvements in sensitive child care; reductions in child injuries, abuse and neglect; improvements in maternal life course (e.g. greater workforce participation); and improvements in child and adolescent functioning. The NFP has shown greatest impact on those at greater risk, and, although there is no net saving for married women or those of higher socioeconomic status, for low-income and unmarried mothers, the cost of the programme was recovered by a child’s fourth birthday.
In the first US trial,9 in the subgroup of poor unmarried teenage mothers, by the age of 2 years, there was verified abuse/neglect in 19% of control children, compared with 4% in the NFP group, and for the NFP group a 56% relative reduction in emergency department attendance for injuries and ingestions during the second year of life compared with the control group. Among the subgroup of children (56 families) with a state-verified report of maltreatment by age 4 years, the NFP group of children exhibited fewer risks for harm than the control group (e.g. fewer attendances for injuries/ingestions, safer home environment). 12 In the 15 years after birth, mothers as perpetrators of abuse were less common in the NFP arm than in the control arm (log incidence of 0.29 vs. 0.54, respectively; p < 0.001), an effect even greater for the most vulnerable subgroup: mothers of low socioeconomic status who were unmarried (log incidence of 0.11, compared with 0.53 for the control arm; p < 0.001). 13 Although the beneficial impact on state-verified first-time reports of maltreatment is generally experienced after age 5 years, the difference is seen earlier (age 3 years) for the most vulnerable subgroup of poor unmarried mothers of the NFP trials.
Common to other home-visiting programmes, the NFP aims to address several related child and maternal outcomes, and a key objective is to promote child development and school readiness. This can be supported by programme elements such as educating parents about child development, promoting positive parent–child interactions and linking families to additional specialist support. US trials of the NFP found improvements in mathematics (among mothers with low resource) and mental processing (whole sample and low resource) at age 6 years, and in reading and mathematics at ages 9 and 12 years. 14,15 Language skills were also improved at 34 and 48 months for children of mothers with low resource. 16,17
Family–Nurse Partnership and the Building Blocks trial
The NFP was adapted for the UK prior to implementation as the FNP and was introduced in England in 2007. Adaptations included rebranding professionals as family nurses, changing the programme name to the FNP, ‘anglicisation’ of programme surface structure (e.g. materials handed out to clients), and the addition of an eligibility criterion emphasising maternal age as a principal indicator of need. 18,19 An implementation evaluation reported progress in the delivery of the programme in 10 test sites. 20 The differing pattern of service provision and sociocultural context meant that the relative costs and benefits of the programme needed to be replicated in England before widespread implementation could be recommended. This was an explicit licensing requirement of the programme, and the stimulus for the BB:0–2 trial (ISRCTN23019866) of the FNP. We evaluated the short-term impact of the FNP (up to age 2 years) when added to usually available supportive services, compared with usual support alone. 21
Assessed against the FNP fidelity criteria, the programme was considered to have been adequately delivered in the trial and to have been delivered as would be expected when rolled out as an NHS service. 22 We found no differences in the two maternal primary outcomes: biomarker-calibrated self-reported tobacco use by the mother at late pregnancy and the proportion of women with a second pregnancy within 24 months post partum. Likewise, no differences were found in the two child primary outcomes: birthweight of the baby and emergency attendances and hospital admissions for the child within 24 months post partum. 22 We observed some differences in secondary child development outcomes, including maternally reported language development at age 2 years and the rate of safeguarding events reported in primary care records.
Despite the lack of benefit for some key outcomes that had been found in earlier trials of the programme and which had been prioritised by the original funding call, longer-term evaluation was considered essential for three reasons. First, previous evaluations had demonstrated benefit over the longer term (e.g. up to 15 years of age)23 for outcomes such as school readiness, attainment and antisocial behaviour. Second, for maltreatment outcomes, the pattern of benefit would be expected to become increasingly evident after age 4 years. 9 Third, the suggestion of benefit for clinically important child development outcomes, such as language, warranted tracking to determine if maternally reported differences at age 2 years would give rise to objective outcomes when children reach school.
Although the BB:0–2 trial commenced in 2008 at 18 sites and reported to the funder in 2015, the programme was concurrently rolled out across England. Up to 132 sites offered the programme, and by its 10th anniversary, in 2017, 30,000 babies had been born to families supported by the FNP, and 950 FNP nurses had been trained to deliver the programme. 24
Other evaluations of the Nurse–Family Partnership
In a Dutch trial of the NFP (the VoorZorg trial),25–27 the intervention was offered to women with multiple risk factors (e.g. psychological, health, economic, social). VoorZorg found that the NFP reduced rates of smoking in late pregnancy and increased rates of breastfeeding at 6 months post birth. 25,26 Programme impact on maltreatment was assessed at 3 years using Child Protective Services reports, with lower rates found for children in the intervention arm. 25 A trial assessing the effectiveness and cost-effectiveness of group FNP in England to reduce risk factors for maltreatment found no differences for child abuse potential and parent–infant interaction at 12 months. 20 Pro Kind is a German adaptation of the NFP; it was trialled between 2006 and 2012 with 755 first-time mothers. 28 A current study to evaluate the medium-term impact of Pro Kind (to age 7 years) will assess maltreatment by parental self-report and also assess child development and school achievement. 29 Another UK-based evaluation of the FNP in Scotland using routinely collected data will assess maltreatment and is due to report in 2021. 30 Appendix 1, Table 25, summarises the outcomes relevant to BB:2–6 that the NFP9–11 and VoorZorg25–27 trials evaluated.
Justification/rationale for the study
This study aimed to provide evidence for the medium-term effectiveness and costs of one of the most promising early-intervention programmes for reducing the risk of child maltreatment in a targeted vulnerable population. This would inform policy about whether or not to continue implementing a programme for which there is limited existing UK evidence for effectiveness. Although we generated evidence related to short-term effects in the BB:0–2 trial (i.e. up to the point when families graduate from the programme before or at their first child’s second birthday), the recognised potential programme benefits (in particular for child maltreatment) have largely been demonstrated only in the longer term. This study presented a unique opportunity to extend learning from the trial by using the existing outcome data in combination with newly arising routinely recorded data.
Research aims and objectives
Given the evidence from both US and Dutch trials of programme benefit for families arising in the 4-year period following the NFP graduation, we aimed to determine the medium-term impact of the FNP on child maltreatment outcomes and key indicators of neglect (e.g. injuries and ingestions), child development and educational outcomes, and other hypothesised programme impacts measurable through routine data.
Primary objective
The primary objective was to determine the effectiveness of the FNP programme in reducing objectively measured maltreatment outcomes when compared with usually provided health and social care alone. Using a multimethod multisource approach, main outcomes included CIN status, child protection registration and referral to social care.
Secondary objectives
The secondary objectives were to:
-
determine the effectiveness of the FNP programme in reducing maltreatment when assessed using associated measures of injuries and ingestions, hospital did-not-attend (DNA) rates and immunisation rates
-
determine the impact of the FNP programme on medium-term outcomes, most notably subsequent pregnancies, school readiness and educational outcomes
-
explore the impact of theoretical moderators of programme effect, including domestic abuse and baseline maternal characteristics
-
determine the costs and consequences of the FNP programme over the full period of available follow-up (i.e. data from the BB:0–2 trial22 and this follow-up study, BB:2–6).
This report continues with a description of the study methods. A substantive pilot phase was undertaken to establish the feasibility of the study design; this is reported in Chapter 3. Both the study protocol1 and the results of the feasibility study31 are already published, various material has been reproduced from these publications and are cited as appropriate for transparency and to provide some additional information. The original study title referred to ‘long-term’ follow-up. However, to reflect the extended duration of follow-up for the US trials of the NFP and contemporary evaluations of NFP-derived home visiting in Germany, we have updated this to reflect a medium-term follow-up. Study findings are then presented in Chapters 4–6, followed by a description of the public involvement activity that was undertaken in the course of delivering the study (see Chapter 7). Chapter 8 summarises our key findings, sets the work in broader research and policy context and provides recommendations for further work.
Chapter 2 Methods
Parts of this chapter have been reproduced from the published protocol paper by Lugg-Widger et al. 1 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/.
Research objectives
In the BB:2–6 study, we used existing trial cohort data linked to routinely collected national data sets to assess the medium-term impact of the FNP on objective measures and indicators of child maltreatment outcomes; child health, development and educational outcomes; and other programme-relevant outcomes.
Study design
The data-linkage study generated a linked anonymised database hosted by a data safe haven. We followed up participant mothers and children from BB:0–2 for a further 5 years using routine data only. Health, education and social care data from a range of routine public sector sources were retrieved and linked to existing trial cohort data on an individual level. This enabled children and mothers to be followed until the child reached Key Stage 1 (KS1), the 2 years of schooling when pupils are aged between 5 and 7 years. Participants were recruited to the BB:0–2 trial between June 2009 and July 2010; therefore, the follow-up for all participants was completed in May 2018, when the youngest children completed their KS1 assessment. A summary of the data sources is provided in Appendix 2, Table 26.
Study participants
In the BB:0–2 trial, we recruited nulliparous women aged ≤ 19 years, living in one of 18 local authority FNP catchment areas, who were at < 25 weeks’ gestation, who were able to provide consent and who could engage with the FNP in English. 21 Women expecting multiple births and those with a previous pregnancy ending in miscarriage, stillbirth or termination were eligible. Women planning to have their child adopted or to move outside the FNP catchment area for > 3 months were not eligible. Women and their first child (or twins, if relevant) who were not mandatorily withdrawn from the BB:0–2 trial (e.g. owing to miscarriage, stillbirth, infant death or adoption), or who did not electively withdraw (including their consent for use of their data) were eligible to be included in BB:2–6 study.
The BB:0–2 trial intervention
Experimental intervention
The FNP is an intensive programme of home visits for women expecting their first baby. In this trial, specially trained FNP nurses delivered the programme from early pregnancy until the child was 2 years old. It comprised a maximum of 64 scheduled visits (14 during pregnancy, 28 during infancy and 22 during toddlerhood), covering content domains of personal and environmental health, life course development, maternal role, family and friends, and access to health and social services. 32
Control
Although participants in both study arms received usually provided health and social care services for pregnancy and new mothers, participants in the control arm received these services alone. These services included maternity care and care provided by health visitors. 32
Outcomes
The study follows the multimethod multisource approach to maltreatment research, which considers an outcome continuum from child maltreatment to family wellness. 33,34 As we have access to routine data, which are a record of professionally determined outcomes, our data are primarily objective (in that we are not using parent-reported proxy outcomes). 35 Although professional decision-making will involve subjective assessment, our distinction is between assessments that are established by professionals and those directly involving parents. We have also distinguished between objective measures of maltreatment assessed in the CSC and associated measures of maltreatment assessed in health care. Although a primary outcome is identified, interpretation will collectively assess evidence for maltreatment.
Primary outcome
The primary outcome was CIN status recorded at any time during the follow-up period [sourced from the National Pupil Database (NPD)]. CIN status refers to a child who is unlikely to achieve or maintain a reasonable level of health or development, or a child whose health and development is likely to be significantly or further impaired without provision of services, or a child who is disabled. CIN is a legally defined and professionally determined measure of need, which is reported via the NPD. In most cases, children are assessed as in need because of maltreatment, followed by other reasons such as family dysfunction and acute family distress.
Secondary outcomes
The outcome domains and secondary outcomes are described here. A full listing is provided in Appendix 2, Table 27.
Objective measures of maltreatment
The objective measures of maltreatment used were referral to social services (overall, child protection referral, CIN referral), child protection registration, CIN categorisation, looked-after status (mother, child), all sourced from the NPD.
Associated measures of maltreatment
The associated measures of maltreatment used were recorded injuries and ingestions, and DNA rates for hospital appointments, both sourced from NHS Digital. We aimed to obtain General Practice Extraction Service data and examine immunisations rates, but these data were not available to researchers.
Maternal outcome
The maternal outcome measured was subsequent pregnancies (sourced from NHS Digital and abortions data).
Child health, developmental and educational outcomes
The child health, developmental and educational outcomes assessed were special educational needs (SEN), early educational and school attendance, and assessments [Early Years Foundation Stage (EYFS) and KS1], all sourced from the NPD. The data fields informing the disability outcome were not available from the NPD or NHS Digital for the years requested.
Costs
Health and social care resource use costs were calculated. The latter were to be sourced via education records, but were not available with sufficient detail for meaningful costings to be derived.
Data sets and data providers
The BB:0–2 trial
Data collected for the initial trial were used in the present study. 21,22 A baseline home assessment was conducted on trial entry using a computer-assisted personal interview. Follow-up was by a computer-assisted telephone interview at 34–36 weeks’ gestation and at 6, 12 and 18 months post natal. A final home-based personal interview was conducted at 2 years after birth. Several routinely collected data sets were accessed and data were obtained from the following sources: maternity records (medical and obstetric history items, antenatal attendances and maternal and neonatal outcomes), primary care notes for each mother-and-child dyad (consultations, immunisations, pregnancies, safeguarding), abortion data from the Department of Health and Social Care (DHSC) abortion statistics team and immunisation data via Cover of Vaccination Evaluated Rapidly programme contacts.
NHS Digital
The Hospital Episode Statistics (HES) data sets hold records on hospital admissions, outpatient and accident and emergency (A&E) episodes. Data can be requested from NHS Digital (formerly known as the Health and Social Care Information Centre),36 the executive non-departmental public body established under the Health and Social Care Act 2012. 37 These data were requested for mothers and children on recruitment to the BB:0–2 trial. A further request for data was made for the BB:2–6 study, in which mothers’ and children’s data were sought for follow-up. For the BB:2–6 study, all available records belonging to cohort members (mothers and children) were obtained from study entry of the mother, which occurred between June 2009 and July 2010, until the date the child turned 6 years of age. The data requested included diagnoses, procedures, duration of episode and external causes of injuries coded according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes. 38 NHS Digital has responsibility for collecting these data from across the health and social care system to allow NHS hospitals to be paid for the care they deliver. At the end of the financial year (March), a final data set is collated. This data set is cleaned and validated before being available for research at the end of each year (December). NHS Digital also provide access to data from the Personal Demographics Service (PDS), which is the national electronic database of NHS patient details. 39 This service can be used to update participant demographic details (e.g. name, NHS number, address, date of birth) when there is a legal basis to do so.
Office for National Statistics
The Office for National Statistics (ONS) collects information on cause of death from civil registration records. Mortality data can be accessed through NHS Digital and supplied as a linked file with the HES data. For registered deaths, the underlying cause of death is derived from the sequence of conditions leading directly to the death, and is recorded on the death certificate. Deaths are subsequently coded in line with the ICD-10. Maternal or child death was captured as an outcome. In December 2018, a lawful basis was established that enabled NHS Digital to collect mortality data directly from the ONS and release it as health data, in accordance with the Health and Social Care Act 2012. 36,37 At this point, ONS mortality data held by the study became civil registration mortality data (a data set controlled by NHS Digital). This report will continue to refer to mortality data as ONS data, as they were at the time of data receipt.
Department for Education
The Department for Education (DfE) holds information on pupils throughout the different phases of education. Records are sourced from publicly funded schools, local authorities and awarding bodies, and are held in the NPD, which is a collection of linked data sets. The data sets are available on various aspects of education (e.g. school census data, absence data and school attainment) and social care (e.g. the CIN census). 40 Data sets are collated throughout the year and are available at set time points annually; these time points differ across the data sets available to request.
Social care data
Social care data from local authorities are available through the NPD via two data sets: CIN and child looked after (CLA). The CIN census captures individual-level information on children referred to and assessed by CSC services within each 12-month period. CLA data are collected in the SSDA903 return: an annual statutory data collection for all local authorities. When a child is referred to English local authority children’s services, it is first recorded as a contact. Contacts are not submitted to the CIN census. If a case provisionally meets the threshold for support, it is passed on to the assessment team as a referral. All children who are referred to CSC for a social care assessment are in the CIN census, even if they are later assessed as ‘not in need’. The children in the CLA data set are, then, a subset of the children in the CIN census who are looked after by local authorities in England. Any child in the cohort who was in either of these data sets was identified, up to the age of 6 years. Mothers who were < 18 years at the time of participation in the BB:0–2 trial would also be identified in these data sets if present in any of the data sets requested. Children in medium-term foster placements or adopted within the 6-year study period could be linked up to the date of adoption. The primary outcome was sourced from the CIN data set.
The NPD carry out the matching to the CIN and CLA data sets by a two-step process. These data sets do not hold any identifiable data except for Unique Pupil Number (UPN). Therefore, to identify individuals in the CIN and CLA data sets, participants are first matched to the other NPD data sets. Their UPN is then identified and used to match again to the CIN and CLA data sets. This means that it was possible to identify records in the CLA and CIN data sets only once the children appeared in a school-level data set.
Education data
Education data are available through the NPD via a number of data sets, and contribute to the secondary outcomes for the BB:2–6 study.
The pupil-level annual school census (PLASC) and early years census (EYC) return data on maintained schools (funding and oversight is through the local authority), which represent the majority of schools, academies (funding and oversight is from the DfE), City Technology Colleges, maintained and non-maintained special schools, and hospital special schools. Schools that are entirely privately funded and home education are not included in the data; this represents 7% of English students,41 but is likely to include few/none of the trial participants. The data requested included the number of hours attended, early educational development, eligibility for free school meals and SEN provision type. All available records belonging to cohort members (children) were obtained until the date the child turned 6 years of age.
The EYFS is a statutory framework set by the DfE that sets the standards for the development, learning and care of children from birth to age 5 years. The EYFS profile assessment is carried out in the final term of the year in which a child reaches 5 years of age. It is based on ongoing observation and assessment in three prime areas of learning (communication and language; physical development; and personal, social and emotional development) and four specific areas of learning (literacy, mathematics, understanding the world, and creating and thinking critically). There are 17 early-learning goals linked to one of these areas of learning, and a child is judged on whether they are meeting the level of development expected at the end of the reception year (‘expected’), exceeding this level (‘exceeding’) or not yet reaching this level (‘emerging’). 42
Key Stage 1 is an assessment made by the teacher according to the national assessment framework for children aged 6 or 7 years in the May of that academic year. KS1 tests cover English reading, English grammar, punctuation and spelling (‘writing’), mathematics and science. Pupils are assessed against the standards provided in the framework. For reading, writing and mathematics, pupils can achieve one of three levels (1, lower than expected; 2, the expected level; and 3, greater depth of knowledge). For science, pupils can achieve either level 1 or level 2 only. Between the academic years 2016/17 and 2017/18, the Standards and Testing Agency introduced a revised teacher assessment framework in English writing. 43
Key Stage 1 data were received in two tranches from the NPD: first, for children assessed in the 2016/17 academic year (received in May 2018), and, second, for the younger children, who were assessed in 2017/18 (received May 2019). Reading, mathematics and science are examined for the whole cohort for children over both academic years.
Department of Health and Social Care
The DHSC is responsible for receiving and monitoring the returns of abortion notifications (HSA4 form) as required by the Abortion Act 1967. 44 Registered medical practitioners are legally required to notify the Chief Medical Officer of every abortion performed in England and Wales. With approval from the Chief Medical Officer, data can be accessed for scientific research. 45
Data for 1532 study participants were supplied to the DHSC with a unique participant identifier and their dates of birth and postcodes. Five were not submitted because they had no postcode. Matching was conducted on data for 2009–16, but data for 2012 were not available for matching because the date of birth was not stored (only age). Following the recommendations given by the DHSC, we used data on mothers for whom a match was found on exact date of birth and postcode (matching criterion 1). Matching criteria 2 and 3 [match found for exact date of birth and (1) postcode minus the last two letters and (2) postcode minus the last three digits, respectively] have an increased risk of false-positive matches, compared with criterion 1; therefore, matching criterion 1 is likely to be the most robust method for matching.
Dissent model
Recruitment/dissent
Participants previously consented to enter into the BB:0–2 trial and provided self-report and access to their routine records for the period up to 2 years post partum. To obtain an unbiased estimate of the effect of the FNP on medium-term objective and associated maltreatment outcomes, we sought section 251 support of the National Health Service Act 200646 approval from the Health Research Authority’s (HRA’s) Confidentiality Advisory Group (CAG) to pass identifiable participant data legally held by Cardiff University to the data providers to link to routine data. This did not require further consent from participants, but instead used an opt-out/dissent model.
Justification of dissent approach
Developing the opt-out approach was necessary because of (1) the child protection focus of the study and the consequent sensitivity and impracticality in asking directly for consent, (2) participant mobility and relative difficulty in maintaining ongoing direct access, (3) the likely introduction of non-ascertainment bias on sample representativeness – resulting in a non-random sample, and (4) the likely cost and logistical requirements of securing even modest levels of additional consent.
Methods of notifying participants
We discussed the issue of dissent and fair processing with the HRA CAG, and subsequently attempted to contact all mothers recruited to the original BB:0–2 trial to inform them that follow-up using anonymised records would be undertaken.
We updated details of participants’ residential addresses using the most recent address registered with their general practitioner (GP). When available, we used mobile phone numbers and e-mail addresses collected during the trial to send short message service (SMS) messages and e-mails to participants. We used all three modes of contact over a 2-day period and we provided participants with a 2-month window in which to contact the project team to discuss the project and opt out if they wished. We created a website with the same information where we encouraged participants to contact the project team if they wished.
We worked with a group of care-experienced young people (CASCADE Voices),47 who advised on the layout, wording and tone of a letter to be sent to all participants. A key consideration was to communicate the focus of this follow-on study in a sensitive manner. The final version of the letter was approved by both an NHS Research Ethics Committee (REC) and the CAG as part of overall governance approval for the study. The letter contained information about the trial and the follow-on study, and a flow chart for what to do if women wished to discuss the project and/or opt out (see Appendix 12).
We recorded women notifying us of their dissent as ‘opted out’ and removed them from all project data sets for this follow-up work and from identifiable data sets to be sent to data providers. They were not included in any of the data sets or analyses for this follow-on study.
Tracing
Two tracing exercises were undertaken to update the contact details of the mothers and children to ensure that (1) participants were contacted about the opportunity to opt out using their most recent address, (2) participants were not contacted if there had been a death (mother or child), (3) participants who had withdrawn prior to the birth of their child remained eligible (there had been a birth) and (4) the identifiers used provided the best opportunity for matching.
We used the NHS tracing system provided by NHS Shared Services Partnership to update the BB:0–2 trial cohorts’ contact details prior to contacting them to offer them the opportunity to opt out of becoming BB:2–6 study participants. On receipt of data from NHS Shared Services Partnership, there were a number of details that remained uncertain/in contradiction with what was previously held. These were then sent to the NHS Digital PDS for manual tracing. For example, differing NHS numbers or sex of a child were felt to be worth further investigation.
For the electively withdrawn trial participants, it was not always clear if the pregnancy had ended in a live birth or how many children had been born. Therefore, in an attempt to identify births including twins, the PDS investigated, via the mothers’ record, to identify presence and number of births at the time of the BB:0–2 trial. The REC and CAG provided approval for this via a substantial amendment.
Data access and storage
Data were requested in two stages: (1) for the pilot phase as part of the feasibility work and (2) the main data request. When the study started in 2014, the children were only 3 years of age, thus providing the opportunity for the pilot phase to ensure that we could access the data, link the records and address the primary and secondary outcomes using the data received. 31 Data were requested in autumn 2014 for data from NHS Digital and the NPD and then again in summer 2017 for the main extract. Data were requested from the Abortion Statistics Team in autumn 2017. The identifiers used to match the BB:2–6 study participants to each data provider are shown in Appendix 2, Table 28.
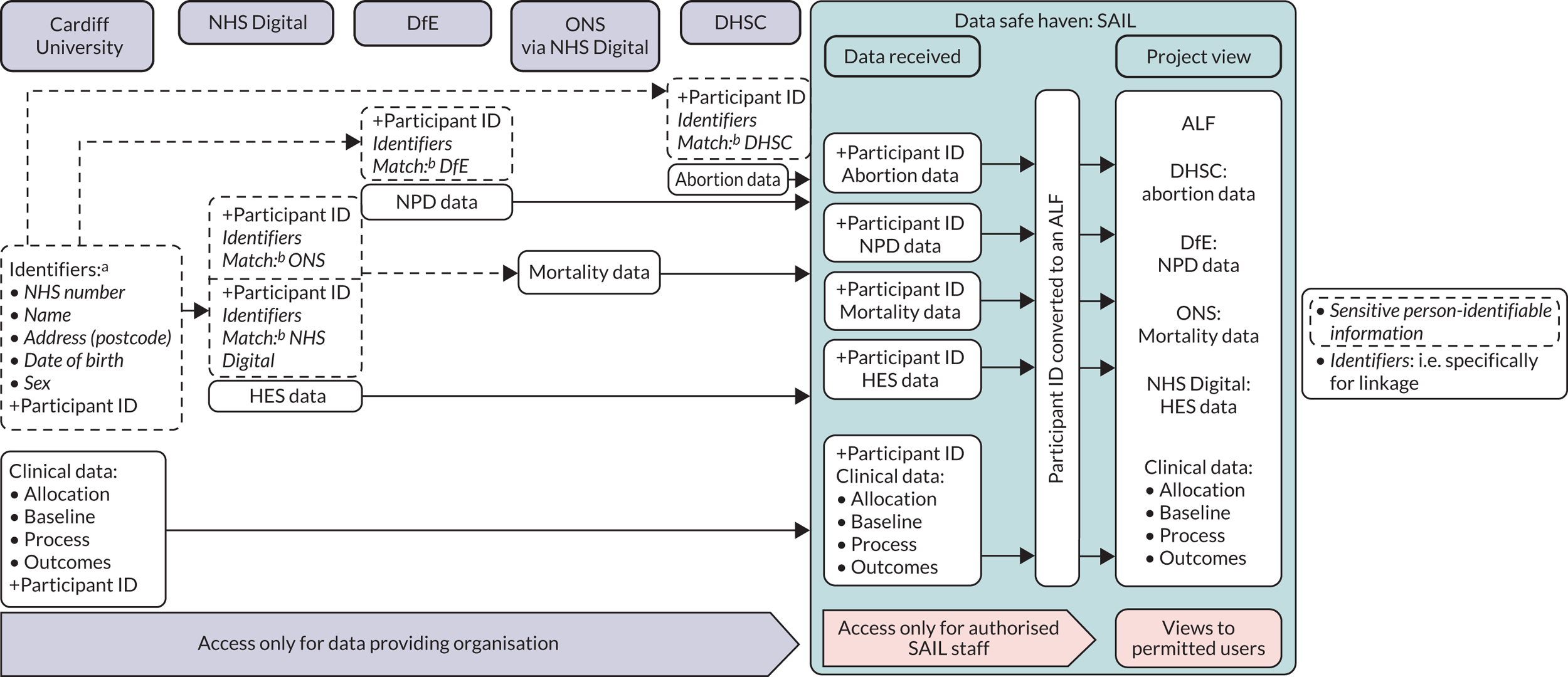
We used a data safe haven, the Secure Anonymised Information Linkage (SAIL) databank, to receive all data sent from data providers, replace the participant identifier with a new anonymous linking field (ALF) and store the corresponding identifier in a separate encrypted password-protected file. 48 All data held in SAIL must not be identifiable; therefore, the study team went through a de-identification and standardisation process to ensure that all variables (e.g. date of birth) were amended to be non-disclosive (e.g. week of birth) or removed from the data set prior to sending. Figure 1 depicts the data flow between data providers and the data safe haven. Participants are not identifiable to the study team, or to the SAIL analyst, but incoming data sets from all data providers could be linked at the individual level using the ALF. The study team have controlled remote access to these data, thus ensuring the security of the pseudonymised database. 49 All data cleaning and analyses were carried out via the remote portal by the study data manager(s), statistician and health economist.
FIGURE 1.
Final model of data flow, storage and access used in BB:2–6. a, De-identification and standardisation applied (e.g. date of birth to week of birth). b, Data providers confirm matching of BB/NHS Digital/ONS/DfE/DHSC IDs. ID, identifier.
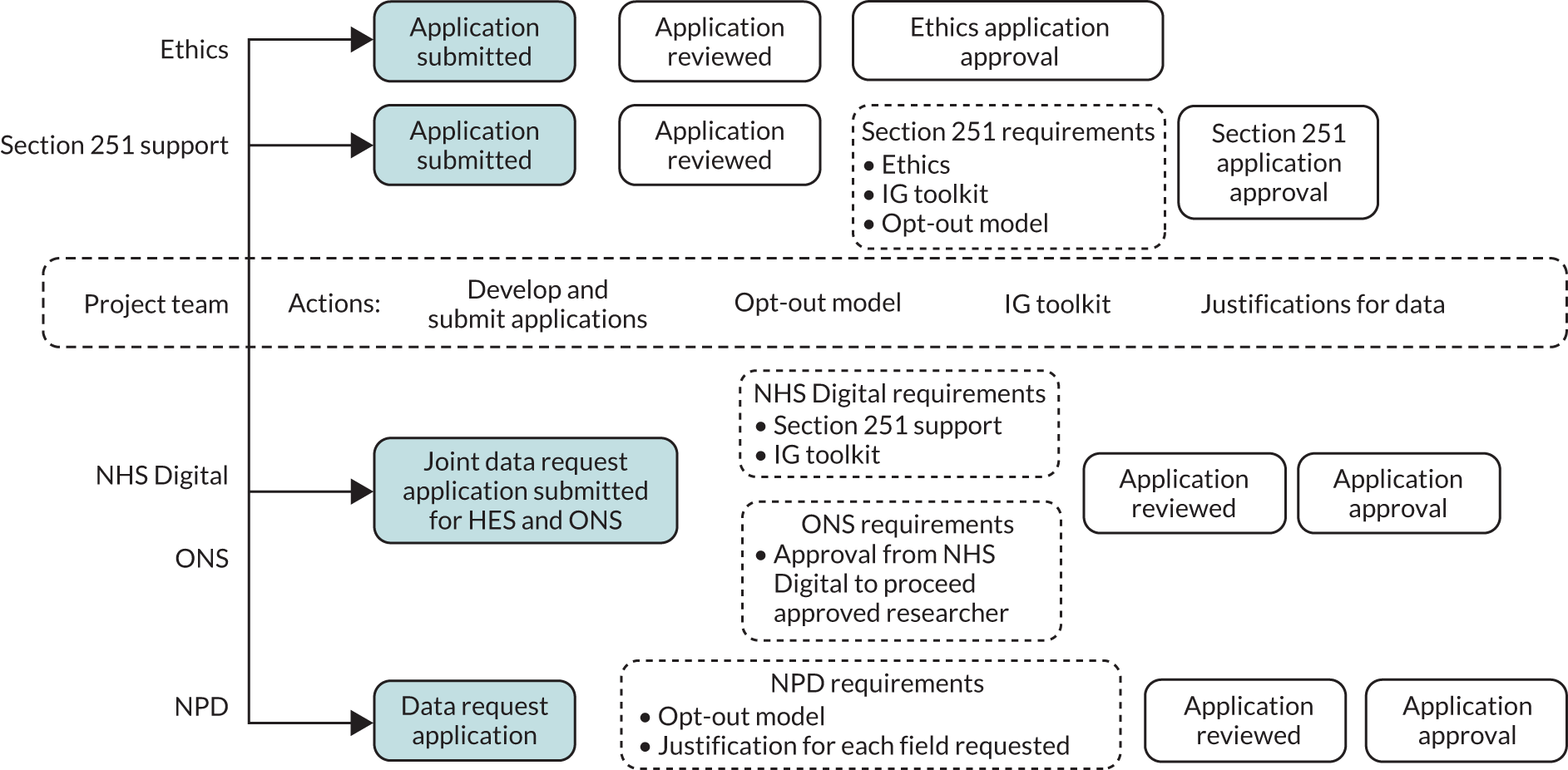
Governance
Following REC approval (reference number 14/WA10062) and section 251 support (CAG number 10-08(b)/2014), we could submit data request applications to the DfE, NHS Digital and the DHSC. To satisfy the requirements of the section 251 support and NHS Digital contract, the (then) information governance toolkit self-assessment50 (commissioned by the DHSC for NHS Digital to develop and maintain) was required. This is now known as the Data Security and Protection Toolkit. This organisation-level assessment provides reassurance of satisfactory information governance within the host research organisation. Both the section 251 support and the Data Security and Protection Toolkit are assessed and renewed on an annual basis. The opt-out model was also required to satisfy the section 251 support, as well as the DfE assessment of compliance with principle 1 of the Data Protection Act 1998. 51 Governance and data provider requirements prior to application approval are shown in Figure 2.
FIGURE 2.
Governance and data provider requirements prior to application approval. IG, information governance. The shading represents the starting point for each activity. The dotted-line boxes indicate the project team roles.
Statistical analysis
Sample size justification
The sample size was fixed according to the available trial cohort. Nevertheless, here we present the number of children required to observe clinically relevant differences and how that compares with the numbers we were able to link and follow up in the study.
Primary outcome (child-in-need status at any point between birth and 6 years of age)
For CIN status, available UK data on rates are not specific to the age range of interest, but the rate per 10,000 general population aged 5–9 years is 4.6% (calculated as an average rate of local authorities that the sites in the BB:0–2 trial covered). 52 The rate of CIN status would be expected to be greater in the specific study sample; therefore, we have assumed a rate of 8%. We hypothesised that the FNP would reduce the occurrence of CIN status in the first 6 years and assumed a difference of 4% as being important. To detect a difference of 4% (4% vs. 8%) we would require 602 children in each arm (1204 in total), using 80% power and a two-sided 5% alpha level. The BB:0–2 trial recruited 1645 women, with 1562 available for follow-up (i.e. excluding those subject to a mandatory withdrawal). Follow-up through medical records assuming 10% loss in tracking and linkage would result in 1405 participants, thus providing sufficient data to assess the primary outcome.
A key secondary maltreatment outcome is referral to CSC. Data from the FNP implementation evaluation (n = 1304 women) show an observed referral rate of children (in the period up to a child’s second birthday) of 8.2%. 53 A sample of 1319 for analysis will provide 90% power at the two-sided 2.5% alpha level to detect a difference between the two groups of 6.3% (14.5% to 8.2%) in the proportion having a referral to CSC. This represents a conservative estimate, as further referrals to CSC will be observed in the remaining 4-year period.
Randomisation
We had already randomised women in the BB:0–2 trial. In doing so, we applied individual minimisation using gestation at recruitment (< 16 weeks/≥ 16 weeks), smoking status at recruitment (smoker/non-smoker) and preferred language for data collection (English/non-English), and stratification by study site. We achieved balance across trial arms on these and other maternal characteristics. We acknowledge that there are possible threats to the balance of baseline characteristics and potential confounders by loss of participants through linkage to routine data in Chapter 4.
Participant population for analysis
We sent identifiers for the BB:2–6 trial cohort to the data providers. The population on which analysis was conducted were those participants whose identifiers could be sent, linked and data released by the data providers. This does not include participants whose individual data can be used but cannot be matched because of:
-
Incorrect linking fields.
-
Other exclusions from health or education, for example private or home schooling (would not appear in any NPD data sets).
-
Any national opt-outs. Patients in England are able to opt out of their personal confidential information being shared by NHS Digital for purposes other than their own direct care. National opt-outs apply to health data (NHS Digital) only and do not apply to that held by the NPD. They were previously referred to as type 2 opt-outs. 54
Therefore, the study populations for analysis (mother and child) depended on which data provider and outcome the data were coming from. For example, for the primary outcome of CIN status, the denominator would be all children who were matched to and appearing in any of the NPD data sets requested. We expected that all children by the age of 6 years would be registered with a primary school or alternative provision, so would be linked to the PLASC and alternative provision data sets. If they were not in PLASC/alternative provision data sets, but appeared in another data set (e.g. CIN), then we concluded that they were in the study population but, for some reason, were missing from the PLASC/alternative provision data set (e.g. home or privately schooled). Similarly for NHS Digital data, for any health data outcome, the denominator would be all participants who have their identifiers matched to any of the HES data sets (inpatients, outpatients, A&E). We expected each mother and child to have had at least one hospital admission event (birth of baby/being born, respectively), and so each participant should have appeared in the inpatient data.
For some outcomes, the maximum age of the child at assessment was strictly fixed by their chronological age (e.g. we included all health-care events such as inpatient and outpatient episodes for the child up to the day before their sixth birthday). For other outcomes, the maximum age varied according to the actual date of assessment within an annual cycle of assessment (e.g. EYFS profile and KS1), meaning that, at KS1, children could be either 6 or 7 years of age. Finally, maximum ages could be determined by data provider annual reporting census periods (e.g. formal reporting for CIN ran up to 31 March each year), which meant that, for the final year of data available to the study, the maximum age (of children) at which a child could have an event reported would depend on their date of birth (see Appendix 2, Table 29).
Missing data
Appendix 2, Table 29, shows each outcome and how we defined denominators, numerators and missing data considerations. Children who were not included in any of the NPD data sets were classed as missing. If a participant did not appear in an outcome data set (e.g. CLA or CIN data set), then we assumed that they did not have that event (rather than missing). We conducted all primary and secondary comparative analyses on an intention-to-treat (ITT) basis with complete-case population (those who have complete follow-up data). This modified ITT population consisted of all randomised participants in the groups they were randomised to in the BB:0–2 trial, regardless of the intervention they actually received.
We defined loss to follow-up in this study as a child death or an adoption, both of which we were able to determine. We excluded children from analyses of binary outcomes when a child had no event, and when follow-up was incomplete. With time-to-event analyses, children were censored at these loss to follow-up events.
Pooling of investigational sites
In the original BB:0–2 trial, randomisation was stratified by the 18 research sites and adjusted for in the analysis by including site as a random effect in all models.
Withdrawals
We excluded from all analyses individuals who had been mandatorily withdrawn from the BB:0–2 trial. We included participants who elected to withdraw from the BB:0–2 trial if they had not removed consent to further use of their data. During the first tracing exercise, we identified any mothers and/or children who had died between the trial ending and the point at which we updated their records. Mothers who had died (or whose child had died) were excluded. Any mothers who registered to opt out of the BB:2–6 study were removed along with their child(ren).
Small numbers
Small numbers were handled according to SAIL rules, whereby any cell counts of < 5 were suppressed and reported as < 5. We handled the presentation of abortion data in accordance with the data-sharing agreement with the DHSC, whereby counts of < 9 are suppressed (including 0).
Descriptive analysis
Baseline data
We quantified potential bias in the followed-up BB:0–2 trial sample by examining group differences (BB:0–2 vs. BB:2–6 participants) in baseline maternal, birth and baby demographics, and clinical and questionnaire data. For all BB:2–6 participants (mother and children) eligible and linked to data providers’ data, we used appropriate descriptive summaries of baseline maternal, birth and baby demographics, and clinical and questionnaire data, presented by trial arm. We used descriptive statistics [n (%), mean (standard deviation) and median (interquartile range)] to summarise baseline variables and identified any marked imbalance between the study arms. We did not formally test between-arm differences for any variables at baseline.
The participant population varied depending on which data provider was examined (NHS Digital/NPD), and so we examined baseline data for each population/data source combination. To assess potential bias, we compared those mothers and children who were successfully linked to NPD/NHS Digital data with the population of all participants in the BB:0-2 trial.
In addition, we assessed the characteristics of children not in any school data set, but who appeared in either health or social care data sets, to examine if they were different or at higher risk of adverse outcomes.
Main analytical approach
We conducted all analyses on a modified ITT basis and placed due emphasis on confidence intervals (CIs) for the between-arm comparisons. First, we examined binary outcomes in twins, to examine the correlation between them. If outcomes tended to always apply to both twins (e.g. in maltreatment data, we would expect both children to be under child protection), then we aimed to reduce the multilevel nature of the data (children within mother) to one child, as opposed to adjusting for twins. We used three-level multilevel modelling to allow for clustering of effect within a site and family nurse, whereby both were fitted as random effects. When there was little impact of clustering at the family nurse level, we aimed to present the results from the two-level model (site and participant). We used the Akaike information criterion to select the best-fitting model. We present all parameter estimates alongside a 95% CI and p-value. We adjusted for variables used in minimisations such as smoking status, gestational age and language.
Primary outcome
In the primary comparative analysis, we examined whether the firstborn (‘BB:0–2 child’) child had ever been referred to social services and classed as a CIN at any point between birth and 6 years of age. There is no flag in the data set to identify whether or not a child is in need after they have been referred to social services. Therefore, CIN was defined (as per DfE methodology)55 as all children referred to social services, excluding cases for which:
-
the referral is flagged as being a referral resulting in no further action
-
the only activity recorded is an assessment, and the case was closed after assessment with no further action.
As the outcome is binary (CIN or not), we used logistic multilevel modelling to investigate differences in the proportion defined as in need between the trial arms (FNP compared with usual care). We present the resulting estimate as an odds ratio (OR).
Secondary analyses of primary outcome
For children classed as in need, we calculated the interval between birth and the date (age) that the child was classed as in need for the first time (based on referral date). We examined group differences for this interval using Cox multilevel regression analysis to calculate hazard ratios for referral, together with 95% CIs. We censored those who were not ever classed as in need by 6 years of age; those who died in this period were censored at date of death.
We examined the number of distinct CIN referrals using multilevel Poisson regression modelling appropriate for count data. When distribution of events displayed signs of overdispersion (greater variance than might be expected in a Poisson distribution), then a negative binomial model was used (or a zero-inflated model if there was an excess of zero events). We present results as the (adjusted) incidence rate ratio (IRR) in the FNP arm, compared with the usual care arm.
Sensitivity analyses on primary outcome
The BB:0–2 trial sample is well characterised (in terms of demographic and clinical data recorded at baseline), and there are detailed records on programme fidelity. We explored:
-
Adjustment for any hypothesised confounders of outcomes at baseline.
-
How variation in adherence to programme fidelity (e.g. dosage) was associated with outcome variation. The efficacy of FNP visits on the primary outcome was estimated in a way that preserved randomisation using complier-average causal effect (CACE) modelling by fitting a structural mean model. As in the original BB:0–2 trial, we defined adherence as the total number of valid FNP visits that a woman received between programme enrolment and the child’s second birthday (covering pregnancy, infancy and toddlerhood). A valid visit was defined in the BB:0–2 trial (using FNP criteria) as the first visit on any calendar date of at least 15 minutes’ duration with the client present and recorded on the FNP information system form UK001 as having been completed.
-
The role of potential moderators and mediators of programme effect by extensions to the primary outcome model including predictive factors (main effects) and interaction terms. Pre-planned subgroup analysis is an investigation of whether or not any between-arm effects differ according to characteristics measured at baseline. Results are presented as the p-value for the interaction coefficients. We prioritised the following variables as a priori subgroup analyses on the primary outcome:
-
Maternal deprivation.
-
Not in employment, education or training (NEET) (applicable only to women aged > 16 years at baseline).
-
Maternal age at recruitment.
-
Sex of child as a possible effect moderator. This extends what was specified in the published protocol paper,1 but was included in the updated a priori statistical analysis plan.
-
We also explored the role of mothers’ care status (ever/never been placed in care) and the duration of maternal care as a potential moderator of programme effect. We also aimed to explore the role of potential mediators of programme effect, such as duration of maternal care and domestic abuse self-reported at 24 months. We conducted these subgroup analyses by the inclusion of appropriate interaction terms in the regression models. Results are presented as the p-value for the interaction coefficients. We also aimed to explore the role of potential moderators of programme effect, such as domestic violence self-reported at 24 months.
Secondary outcomes
Although the study was powered to examine a 4% difference in CIN status, we undertook secondary analyses to assess group differences in referral rates to social services and maltreatment profiles. We examined levels of concern by looking at the extent of action taken (e.g. category of abuse, subjected to a child protection conference and plan).
Objective measures of maltreatment
For binary outcomes [referral to social services, child protection plan (CPP), looked-after status of child] we used logistic multilevel modelling to investigate differences in proportions between the trial arms (FNP compared with usual care), with estimates presented as ORs. For categorical variables (CIN categorisation of primary need, CPP categorisation of abuse, legal status of child looked after), we examined group differences by multinomial regression and presented results as ORs. We also described the source of the referrals. The number of CIN referrals, the total period of care as a CIN (days) or a looked-after child (months) were examined using Poisson multilevel regression modelling appropriate for count data. When distribution of events displayed signs of overdispersion (greater variance than might be expected in a Poisson distribution), then a negative binomial model was used (or a zero-inflated model if there was an excess of zero events). Results are presented as IRRs in the FNP arm, compared with the usual care arm. Numbers and cause of death are descriptively presented when numbers are not disclosive.
Surveillance bias in detection of maltreatment during a child’s infancy and toddlerhood was assessed by examining subsequent reporting. The duration between birth and the date of first referral to social services was calculated and group differences examined using Cox regression analysis to calculate hazard ratios for referral, together with 95% CIs. Surveillance bias is most likely to occur during the intervention phase (i.e. FNP clients being in closer contact with health professionals up to the point of their graduation from the programme), although improved handover to other services at 2 years may lead to higher identification in the following year. Severity based on the primary need of the referral will also be compared between the two groups.
Associated measures of maltreatment
We examined the number of children who were not taken to at least one hospital outpatient appointment (DNAs) using a logistic regression model. We took a similar approach to analysis in the BB:0–2 trial: assessing injuries and ingestions occurring as emergency attendances in A&E, and admissions to hospital (see Appendix 2, Tables 30 and 31). We used logistic multilevel modelling to analyse the associated outcomes (e.g. proportion of children with at least one injury and ingestion by age 6 years); these events were grouped and described together and by data source. We analysed the number of admissions per child using Poisson or, when skewed, alternatives such as negative binomial or a zero-inflated model. Results are reported as IRRs. We also describe the length of hospital stay for children experiencing injuries and ingestions.
Maternal outcomes
We used a similar approach to the BB:0–2 trial by combining the following data sources: inpatients, outpatients, abortions (0–6 years post birth of the BB:0–2 child) to identify any pregnancy or related attendances/admissions that were not associated with the BB:0–2 trial. For outpatients, attendances of pregnancy were identified using codes for obstetric and midwifery as a main or treatment specialty. For the admissions data (inpatients), episodes of pregnancy, registrable births, abortions and miscarriage were identified using the coding list in Appendix 2, Table 32. For both these data sources, the same cut-off point of 100 days post birth of first baby to assume a new pregnancy was used, as in the BB:0–2 trial, but the admissions in the 29- to 100-day period were checked for abortions or miscarriages in the early pregnancy period. We assessed group differences in the proportion of women with at least one subsequent pregnancy recorded in inpatient/outpatient/abortion data using a logistic regression model. Results are reported as adjusted odds ratios (aORs) alongside 95% CIs. The number of births was described using a Poisson model, if suitable. If data were sparse, then a multinomial regression model was used and categories such as none, one, two and three-plus subsequent births were used. We examined the time to the first subsequent registered birth (interbirth interval) and analysed this data using a Cox regression model with hazard ratios alongside 95% CIs.
Child health, developmental and educational outcomes
Special educational needs (binary), early-education attendance (binary), type of day care [Office for Standards in Education, Children’s Services and Skills (Ofsted)-registered private, voluntary or independent (PVI) provider/pupils registered at school], early-years assessment (using the EYFS profile, an indicator of school readiness), school attendance and KS1 attainment were all sourced solely from the NPD. For binary outcomes (SEN, early-education attendance, school attendance and KS1 attainments), we used logistic multilevel modelling to investigate differences between trial arms in the proportion of children with or without these outcomes. Estimates were presented as aORs, alongside 95% CIs and p-values.
The early-years assessment (EYFS profile) was examined by the following outcomes: (1) the proportion of children achieving a good level of development (GLD) [i.e. achieving at least the expected level (2+)] in all five areas of learning, (2) the proportion of children achieving at least the expected level in all 17 early-learning goals (score of 2+) and (3) the average total point score (over all 17 early-learning goals) (scores can range from 17 to 51). For the early-years total point scores, a linear multilevel regression was run and residuals of the fitted model (kernel density, histograms, qnorm, pnorm) were examined to assess linearity. We examined differences in scores between trial arms, and estimates are presented using adjusted mean differences plus 95% CIs. School attendance was defined by overall absence rate (overall absence sessions/total number of sessions). When possible, these were broken down into unauthorised (e.g. holidays/arrived in school after registration closed) and authorised sessions (illness/medical or dental appointments).
Key Stage 1 attainment was examined using the proportion of children achieving at least the expected level (2+) in reading, writing, mathematics and overall science, and the proportion of children achieving lower than expected (level 1), the expected level (level 2) and a greater depth of knowledge (level 3) in reading, writing, mathematics and science.
Sensitivity analyses of secondary outcomes
We undertook sensitivity analyses (CACEs, imputation for missing subgroups) on the following secondary outcomes:
-
early-years assessment (EYFS profile total score)
-
KS1 assessment (achieving at least the expected level in each subject)
-
referral to social services.
Exploratory analysis
-
We included the following variables for subgroup examination in exploratory analyses: self-efficacy score,58 subjective (personal and family) social status,59 and social support and networks (i.e. the Medical Outcomes Study survey60). These data were sourced from the original BB:0–2 trial data set. A composite index of risk (based on these and other variables in the data set), which predicts subgroups that may particularly benefit from the FNP, was also constructed.
-
We planned to use a state-transition model using Markov chains to assess the probabilities of moving from one stage marker (state) to another. A Markov chain is an iterative process whereby subjects are assumed to stay in one cycle for a certain time and then make a transition to another cycle. The Markov chain contained the following states –
-
referred to social services
-
child identified as in need
-
CPP
-
CLA
-
placement.
The transition probabilities (the probability of the various state changes) in the model were derived from the data and compared between groups, if numbers allowed. The model also included children who leave and then re-enter the system, if numbers allowed.
-
-
Because a more robust measurement of mothers’ experiences in care was determined using the NPD data, this subgroup (of care-experienced women) was also to be examined for the BB:0–2 trial outcomes (i.e. smoking in pregnancy and birthweight). We also explored the BB:0–2 trial baseline characteristics to see which were associated with ever being in care.
Economic analysis
A health economics analysis was undertaken using the routinely collected data available from the BB:2–6 study.
The evaluation consisted of:
-
a description of the resource use and costs associated with the FNP during the BB:2–6 study
-
a cost–consequences analysis (CCA) of the FNP based on the outcomes reported in the BB:2–6 study
-
a summary of the total known health-care costs of the FNP over the full 6-year follow-up period, by summarising the costs associated with the FNP.
Summary of the BB:0–2 trial health economic evaluation
The BB:0–2 trial included a comprehensive economic evaluation, with a cost–utility analysis [incremental cost per maternal quality-adjusted life-year (QALY) gain] presented as the primary analysis, and a CCA presented as an alternative economic approach. 32,61 The analysis showed that there were marginal gains in maternal QALYs, but that these gains cost an extra £1992.89, on average, per person, and that there was a low probability of the FNP being cost-effective. The CCA reported that health-related costs were lower for women in the FNP arm, but non-health-related costs were higher.
Health economic methods in the BB:2–6 study
Prior to commencement of the analysis, a health economic analysis plan was produced, reviewed by the study team and incorporated into the statistical analysis plan. The analysis plan reflected several practical challenges in presenting a health economic analysis that could reflect the impact of the FNP over the full BB:0–2 and BB:2–6 time horizons. These challenges are summarised in the following paragraphs.
The BB:2–6 study captured secondary health-care data (A&E, hospital inpatient and hospital outpatient data) through HES, but not primary health-care/community resource use (e.g. visits to the GP, nurse, health visitor, counsellor), as captured in the BB:0–2 trial. In the BB:0–2 trial, additional consideration was given to non-health-care resource items such as social assistance, temporary education, educational attendance, child care and other services. In the BB:2–6 study data sets, the large variety of possible non-health-care resource interactions (e.g. who the child saw, how often they saw them, where the visits took place, how long for), and the limited data on such resources, meant that these could not be adequately translated into costs.
As a result, the perspective utilised in the BB:2–6 health economics analysis would be constrained to available costs from secondary health care.
In the BB:0–2 trial, resource use (health and non-health) and costs for each mother were included, alongside subsequent resource use and costs to their child, using published unit costs. In the BB:2–6 study, the available health-care costs to the mother were analysed and presented separately to those of the child.
Unlike the BB:0–2 trial, health-utility data (captured by measures such as the EuroQol-5 Dimensions) were not available; therefore, a cost–utility analysis for the BB:2–6 study could not be conducted.
It was recognised that the potential benefits of the FNP did not apply to only one system (i.e. health care), but cut across a range of public sector agencies (such as social care and education), and beyond to individuals, families and society. As a result, the outcomes of interest go beyond health outcomes – as reflected by the primary and secondary outcomes of interest in the BB:2–6 study.
A CCA was chosen as the most meaningful method to use, given the data available. This enabled the evaluation of available health-care resource use and cost data associated with the FNP over the follow-up period covered in the BB:2–6 study, and enabled comparison with the range of primary and secondary outcomes, in order to extend the original economic analysis reported in the BB:0–2 trial in a practical and informative way.
Perspective and time horizon of the BB:2–6 study
The costs of the FNP during the BB:2–6 study were considered from a secondary health-care provider (UK NHS) perspective. Costs were collected for mothers and children separately. The time horizon reflected the BB:2–6 study follow-up period (i.e. 4 years). The data used to inform the economic analysis were obtained from the linkage methods (see Data sets and data providers). The remainder of this chapter describes the additional steps for the economic analysis.
Resource use and costs included
Hospital Episode Statistics data sets
The HES data warehouse was used as the primary source of data comprising inpatient, outpatient and A&E attendance data sets. Similar principles to those used in the BB:0–2 trial were employed, when possible, to enable consistency in the costing methods between studies. Each data set was processed through the relevant section (Admitted Patient Care, Non-Admitted Consultations or Emergency Medicine) of the NHS Digital Reference Cost grouper to generate Healthcare Resource Group (HRG) codes for each activity record. The relevant annual grouper (e.g. 2009/10) was used, dependent on the discharge date of the activity record. Once the records were coded, they were then matched, using this HRG code, to the appropriate annual NHS Reference Costs. Inpatient data were costed split on whether patients underwent elective or emergency admissions, whereas A&E data were split on whether patients were discharged or admitted. Resource use was valued in Great British pounds at 2010 prices (baseline date).
The HES data-cleaning rules were used to check variables created by HES to identify possible errors. Several records, in each of the data sets, were unable to be coded, because either they did not have enough required data points or they had unrecognised codes. Once processed, if these data were uncoded, and therefore uncosted, average costs were imputed. Imputed costs used the average cost of all coded and costed attendances, of that particular type, for the year of that attendance. For example, an uncoded emergency hospital admission in the 2011/12 year would have had an average cost imputed from all of the coded and costed emergency hospital admissions for the year 2011/12. All data sets were checked to identify and remove duplicate records prior to analysis.
Outcomes
The primary and secondary outcomes reported (see Appendix 2, Table 27) were the same as the main study outcomes: CIN status, referral to social services, child protection registration, looked-after status, SEN, school attendance, early-years assessment, DNA rates for outpatient appointments, and recorded injuries and ingestions.
Cost–consequences analysis
A CCA was undertaken for the BB:2–6 study. A CCA is a form of economic evaluation in which the range of costs and outcomes (consequences) are reported without aggregation or weighting. 62 This allows the reader to assess the disaggregated costs and outcomes and to form their own opinion as to their relevance and importance to their own decision-making context. 63 The analysis follows a descriptive approach, which presents effectiveness results (primary and secondary outcomes) separately to that of the costs. The CCA approach is recommended for complex interventions that look to observe a broad range of effects, which are difficult to measure in a single common unit. 63,64 In essence, the reporting of a CCA takes the form of a balance sheet and helps to give a straightforward, but richer, set of information on costs and outcomes for decision-makers. 65
It should also be noted that there are limitations associated with CCAs that must be borne in mind when interpreting their results. They provide no guidance in relation to cost-effectiveness, they have limited generalisability and they are open to selective, non-transparent decision-making based on the results that best fit a decision-maker’s agenda. 63 Overall, a CCA allows for the consideration of a broader range of potential benefits when determining whether the FNP represents good value.
Analysis
Missing data
Data can be missing from routine health records. This occurs when individuals are missing a component of data. Theoretically, every study participant will have HES inpatient data from the birth; these might be missing in the data set or the individual may have a type 2 opt-out (see Participant population for analysis). It has been assumed that the absence of data for the inpatient, outpatient and A&E data sets means that no resource has been utilised.
Resource use and costs
A descriptive analysis of the resource use and costs associated with mother and child in the period covered by the BB:2–6 study was presented separately in the first instance, with means, medians and ranges presented for the FNP and usual-care arms.
Given that there was a focus on child maltreatment in the BB:2–6 study, health-care resource use for children was also separated by whether or not it was related to an injury or ingestion. Therefore, results were displayed in three categories: all resource use, all resource use excluding injuries and ingestions, and injuries and ingestions’ resource use.
Incremental mean differences in costs for each disaggregated cost category (e.g. secondary care admissions) were reported.
The costs across each disaggregated category were added to the relevant cost category in the BB:0–2 trial and a similar descriptive analysis was undertaken to present an illustration of the costs associated with the FNP, compared with usual care, across the full period of cohort follow-up (see Appendix 10).
Discounting
Health-care resource use occurred over multiple years. Therefore, once processed and costed, health-care costs were discounted back from the year of event to baseline (2009/10) on an annual basis at 3.5% to adjust for inflation.
Cost–consequences analysis
The costs and outcomes were summarised in a cost–consequences table(s) to report the disaggregated health-care resource costs for the FNP arm, compared with those for the usual-care arm, for mother and child over the BB:2–6 follow-up period and to report cumulative costs over the full period of cohort follow-up, tabulated against the outcomes.
Distributions of health-care resource use and cost were tested using the Kolmogorov–Smirnov test for normality. As all variables were skewed (i.e. not normally distributed), the non-parametric Mann–Whitney U-test was used to test the difference between the usual care and FNP arms.
Subgroup analysis
No subgroup analysis was undertaken.
Chapter 3 Pilot study
This chapter describes the work conducted in the pilot phase of the BB:2–6 study. The primary purpose of the pilot phase was to demonstrate the feasibility of using the routine data-linkage model to answer the research objectives and planned analysis. This phase, therefore, provided an opportunity to assess the model of data linkage being constructed, to provide reassurance that the final extract and analysis could progress effectively and as efficiently as possible and to make changes where required. Although not all data that we aimed to collect in the main study were being sought at this point, the study design was not expected to change significantly. Therefore, we regarded this phase as a pilot study (a small-scale version of a future study), rather than a more generic feasibility study. 66
Content in this chapter has been reproduced from the published feasibility study paper by Lugg-Widger et al. 31 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article). This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Aims/objectives
The aims of the pilot phase were (1) to establish and verify the governance, regulatory and logistical arrangements for linking data sets and (2) to prepare and assess the suitability of data for answering the research objectives and planned analysis.
Objectives
The key objectives of the pilot phase were to:
-
obtain data from the two primary data providers for the study
-
establish acceptable levels of record linkage
-
establish adequate data quality.
Methods
Obtaining data from data providers
We requested data from NHS Digital and the DfE (NPD) for a proportion of the BB:2–6 sample. For NHS Digital, this included data from trial entry of the first mother (June 2009) to 31 March 2015. Local authority safeguarding data, accessed via the modular NPD data sets, were requested to 31 March 2014, and education data were requested from the NPD to other end points in 2014. Appendix 3, Table 33, summarises the time periods requested for each data set. Data sets are released annually, but at different points throughout the year, by both NHS Digital and the NPD; therefore, the data were requested to allow the greatest number of years possible at the time of request.
We did not include participants electively withdrawn from the BB:0–2 trial in the pilot cohort sent for matching, as further tracing was ongoing at the time of data transfer. In addition, we did not send a small number of the main cohort for matching for the same reason (i.e. tracing indicated a different date of birth or sex, which needed further investigation). Figure 3 outlines participants’ progress through the trial processes, including the numbers of participants involved at each stage. It also includes the estimations of sample numbers at the time pending the tracing.
FIGURE 3.
Participant flow diagram showing numbers of mothers and children sent for matching and successfully linked in the pilot and main study phases. C, children; EW, elective withdrawals; M, mothers.
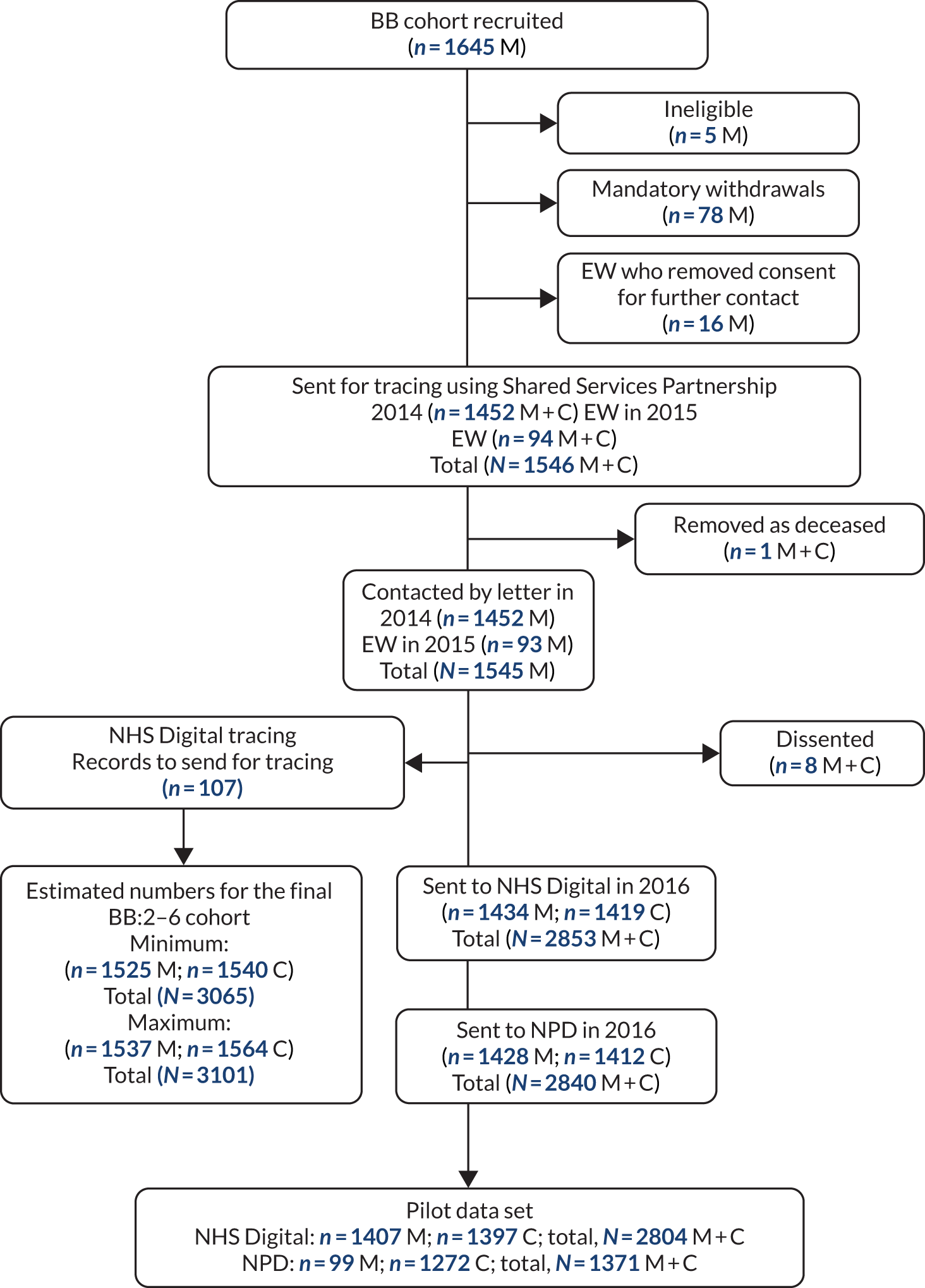
We used the participant identifier from the BB:0–2 trial to identify both mother and child. This was appended to all records sent to NHS Digital and the NPD for matching. We stated in the approved data access applications to both data providers that participant identifiers would be retained while stripping all other identifiable data from the records sent to SAIL (data safe haven) from the data provider. SAIL replaced the participant identifiers with ALFs to ensure that all records were anonymised and not identifiable to the study team by the participant identifiers. We checked that the numbers of records sent to each data provider, received by SAIL and then available to the study team were consistent and could be linked in the SAIL portal.
Establishing acceptable levels of record linkage
We assessed the number and proportion of participant identifiers matched to routine records by each data provider. For NHS Digital data, this also included an assessment of the match rate by each step in the matching algorithm (see Appendix 3, Table 34). For both data providers, matches would include both mothers and children. A match at step 1 meant that NHS Digital was able to exact match to all identifiers provided (i.e. NHS number, date of birth, sex and postcode); for records for which this was not possible, step 2 was attempted (matching on all identifiers except postcode). Partial match indicates when the date of birth partially matched the date of birth held by the data provider.
Establishing adequate data quality
We assessed data availability and completeness for all variables supplied from both data providers that would be required for primary and secondary analysis. Priority was placed on primary and key secondary outcomes. We reviewed numbers of available records, reasons for missingness and undertook a narrative assessment of potential impact to indicate the feasibility of the main study. For the data received from the NPD, we focused on the CIN and the CLA data sets, the latter a subset of the CIN data set, as the data in these data sets contributed to the primary outcome.
Results
Obtaining data from data providers
We submitted data applications in 2014 to both NHS Digital and the NPD. The NHS Digital application progressed slowly over an 18-month period owing to changes to their application process, changes to the assigned case officer and organisational requirements that the study team were required to action prior to application consideration. 31 Application submission to NHS Digital to data receipt in SAIL took 21 months.
The NPD application progressed more quickly, but was also delayed because of contractual problems. This resulted in a requirement for us to submit a second application for data, as too much time had passed since the original approval. The whole process to access data from the NPD took 17 months from first application submission to data receipt in SAIL.
Establishing acceptable record linkage
For NHS Digital, 1434 mothers’ and 1419 children’s unique records (mother/child) were sent, and 1407 mothers (98.1%) and 1397 children (98.4%) were matched. Of these, 99.9% of the records were matched at steps 1 or 2 (see Appendix 3, Table 34, for definition), indicating a greater reassurance of matching to the correct individual. There were 64 participants (31 mothers and 33 children) missing from the NHS inpatients data set where they would have been expected (i.e. as there should be at least a birth record) (see Appendix 3, Table 35). However, 15 of these were present in other NHS Digital data sets, indicating a successful match, but missing an inpatient record. Forty-nine participants did not appear in any data set, which is probably because of matching failure or national opt-out (whereby NHS patients in England electively opt out of their clinical data being used for purposes other than their own direct care). 54 In contrast, in the BB:0–2 trial, 17 participants did not appear in any data set and seven were missing an inpatient record. It is unclear why this discrepancy exists; it is probably due to matching errors. At the time of the trial, however, type 2 opt-outs (now national opt-outs, as of 25 May 2018) were not in place, and, indeed, would not have applied to the BB:0–2 trial cohort, as they had explicitly consented to the linkage. Based on the national average rate of type 2 opt-outs of 2.3%,67 we could expect to lose 65 participants; we have a lower rate in this pilot population.
For the NPD, 1428 mothers’ and 1412 children’s unique records were sent, 11 fewer than sent to NHS Digital because of the discrepancies in some of the identifiers being sent. (With NHS Digital we could exact match on NHS number if confident of that identifier; however, we could not do the same when sending to the NPD as it does not match on NHS number.)
Ninety-nine mothers (6.9%) and 1272 (90.0%) children were returned as matched from the NPD. All mothers would have been aged < 19 years at entry to the BB:0–2 trial (the youngest being aged 13 years) and, therefore, could have been present in the CIN and CLA data sets and/or in the school attainment data sets (see Appendix 3, Table 36). The denominator for planned study primary outcome analysis would be the 90.0% of children adequately matched.
Note that, in the UK, education is mandatory from the first school term after a child’s fifth birthday. Prior to this, some children may not have received formal early-years provision, and therefore may not appear in the data sets. A survey conducted in 2014–15,68 commissioned by the DfE, reported that, overall, 25% of children aged 0–4 years were not in receipt of any early-years provision. Older preschool children (aged 3 and 4 years), however, were far more likely to receive early-years provision (92%) than younger preschool children (aged 0–2 years) (61%). 68 We would therefore expect similar coverage rates for this study. Schools that are entirely privately funded and home education are not included in the data; this represents 7% of English students.
A small number of mothers were identified in the PLASC and pupil referral unit (PRU) census, which was expected. Fifty-four per cent of children were identified in the school census and 40% in the EYC. Summer 2014 was the last school census data set requested for this pilot phase; therefore, not all children would be expected to be in school (i.e. in March 2014, some children will have just turned 3 years of age). One data set requested, the EYFS, did not identify any participants; therefore, no records for this requested data set were returned. None of the children was at the required age (4 years) to be included in this data set for the requested years (2013 and 2014). The data set was requested because, at the time, it was unclear if some of the children may have completed the assessment in 2013/14.
Adequacy of data quality
Assessment of data quality included establishing that key outcomes could be adequately derived from supplied data. The primary study outcome is CIN status, to be derived from a combination of three NPD CIN data set fields (referral date, referral but no further action, reason for closure). For these and all fields retrieved, we undertook an impact assessment to clarify the field’s role in analysis, number of records retrieved, explanatory notes regarding missingness, and impact on planned analysis. A field’s purpose in analysis would include acting as primary or secondary outcome (either in combination or with other fields), for cross-checking/validation of other data, and for planned exploratory analysis. Impact was assessed as either no, low, medium, high or not required, with explanations when justified.
A summary version of the final assessment table is shown to demonstrate these key elements and how they informed the feasibility assessment for each variable (Table 1). As records for the primary outcome (CIN status) would appear in the data set only following a conditional event (i.e. a referral), it is not possible to assess absent valid cases, but it does indicate the potential number of cases for inclusion in the main analyses. Other secondary outcomes are similarly formed of several fields both for NPD data (e.g. child protection registration) and NHS Digital data (e.g. injuries and ingestions), and presence can be inferred by positive entries in one or more of the contributing fields. Levels of missingness in current pilot and original trial data matching are shown when relevant.
| Outcomes | Data source: native field name | Missing (n) | Commentary of findings | Impact |
|---|---|---|---|---|
| Primary | ||||
| CIN status as of 31 March each year | NPD > CIN: referral date | 1 | No data appear across one record – record to be excluded (this will apply to all fields in this table). Note: 34 records with dates prior to time point ranges (1997–2007). This is expected | None |
| NPD > CIN: referral – no further action | 42 | No data collected in 2008/9 time point (accounts for 38 records). Some blanks appear in 2009/10 time point; however, the referral date on these records is prior to 1 April of that data collection year. Assumption that time point cycle is April–March | Low: assumption that missing data indicate further action was required and that the child was in need | |
| NPD > CIN: reason for closure | 142 | No pattern – further investigation required | Low: as above | |
| Secondarya | ||||
| CIN categorisation | NPD > CIN: category of abuse | 329 | Only data from 2008/9 accessed in pilot. For main phase, data from 2012/3 will be accessed and also ‘NPD > CIN: latest category of abuse’ will be included, which may improve data quality | Still to be determined |
| CLA status | NPD > CLA: category of need; legal status; placement; REC | 0 | All records returned are complete | None |
| Child protection registration (plan) | NPD > CIN: child protection plan indicator | 195 | Expected – all missing cases from 2010/11 time point onwards. Data not collected during these years | Low: child protection plan flag can be determined from other fields |
| NPD > CIN: number of previous child protection plans | 320 | No pattern to missingness. Only 11 records have a value recorded; 9 of these are zero | Low: as above | |
| NPD > CIN: child protection plan start date | 320 | Expected – not all children will have had a child protection plan. Only 11 records have a date recorded; these correspond with data captured in the ‘number of previous child protection plans’ | Low: as above | |
| NPD > CIN: child protection plan end date | 327 | Expected – only four records have an end date recorded. Corresponds with those records for which a start date is recorded. Data check done – end dates are after the start date | Low: as above | |
| Exploratory Markov chain modellingb | NPD > CIN: date of initial child protection conference | 327 | Expected – not all children would have had a child protection conference. However, further checks required to confirm validity of data | Medium: low numbers may affect analysis |
| Injuries and ingestions | HES > A&E: A&E diagnosis (diag n) | 5981 | 45% missing (1650/6336 missing in BB:0–2 trial – 26% missing) | Medium: all diagnostic/treatment/investigation fields to be used in combination to define injuries and ingestionsc |
| HES > A&E: A&E diagnosis – 2 char (diag2 n D) | 3604 | 27% missing (1849/6336 missing in BB:0–2 trial – 29% missing) | Medium: as above | |
| HES > A&E: A&E investigation (invest n) | 1728 | 13% missing (1396/6336 missing in BB:0–2 trial – 22% missing) | Medium: as above | |
| HES > A&E: A&E investigation – 2 char (invest n D) | 1712 | 13% missing (1395/6336 missing in BB:0–2 trial – 22% missing) | Medium: as above | |
| HES > A&E: A&E treatment (treat n) | 2349 | 18% missing (1411/6336 missing in BB:0–2 trial – 22% missing) | Medium: as above | |
| HES > A&E: A&E treatment – 2 char (treat2 n D) | 2126 | 16% missing (1417/6336 missing in BB:0–2 trial – 22% missing) | Medium: as above | |
| HES > A&E: A&E diagnosis – anatomical area (diaga n D) | 9281 | 70% missing (4725/6336 missing in BB:0–2 trial – 74% missing) | ||
Some planned analyses were found to be potentially affected by the numbers of missing data (e.g. state-transition modelling) or small numbers (CLA status), which would either reduce the scope of the analysis or indicate a descriptive approach, respectively. However, as many of the fields in the HES data that show high numbers of missing data would be combined (e.g. diagnosis and treatment), when there is a value in one of these fields, it would be assumed that this was an event within the A&E data set. Missing data may also make some outcomes difficult to derive. In these cases, any assumptions made on the missing information would be stated and, if possible, varied (worst-/best-case scenario), and caveats made around results to aid interpretation. Despite this, it was felt that the primary and the secondary outcomes that were assessed were feasible.
Impact of the pilot study results on final study design
In this pilot work, we matched participant identifiers to a high proportion of routine records. The routine records included health data matched with a high level of precision using NHS Digital’s stepped algorithm process. Fields used in combination would form individual outcomes for the study, limiting the impact of some apparent missingness. Some variables had higher levels of missingness than observed for the same participants in the BB:0–2 trial; this may be because these variables are populated over time; therefore, later years have higher rates of missingness. Nevertheless, the primary outcome analysis was assessed as being feasible, as were analyses of most planned secondary outcomes. Low rates of some outcomes may indicate descriptive analysis only, and one of the planned analyses of state transition through phases of the child protection process would be limited by the reduced set of fields ultimately available via routine data.
The time taken to receive data from providers was considerable; therefore, steps were taken to communicate this risk to both the Study Steering Committee (SSC) and the funder. This risk remained for the main data extract. We did, as part of the pilot data request applications, build in reference to the main data request; therefore, all applications were approved on the understanding that a further request would be made. Both applications were therefore considered as ‘renewals with additional data’, rather than new data requests, which expedited the approvals somewhat.
Summary
Overall, we were satisfied that the main study objectives were achievable, although some secondary outcome and exploratory analyses may be restricted by missing data or small numbers. The data flows were acceptable to data providers; it was possible to access data from all providers requested and match rates were high. The time taken to receive data was identified as an ongoing risk; this reflected the timetable for submitting the renewal application to all data providers.
Chapter 4 Descriptive results
Study population
The study population following the BB:0–2 trial and the tracing and matching process is shown in Figure 4. Trial recruitment to the BB:0–2 trial started in June 2009 and ended in July 2010; 1645 women were recruited and randomised from 18 sites across England, and 1618 women completed a baseline interview and provided ongoing consent for data usage. Five women were ineligible and 78 were mandatory withdrawals, mainly due to fetal or infant death or adoption. Further details regarding mandatory withdrawals can be found in the trial report. 32 The 110 women who electively withdrew during the trial were given the opportunity to opt out from further data usage; 16 women removed consent for any further contact. Thus, 94 women who had electively withdrawn from the BB:0–2 trial were included and their details sent for tracing alongside the remaining 1452 mothers (a total of 1546 mother–child dyads) to update contact details to improve the matching process. One dyad was subsequently removed, and the remaining 1545 were contacted by letter, e-mail or text, of whom eight dissented from having their records linked. A total of 107 children had missing information that was needed to match to the NPD and NHS Digital data sets; they were manually traced by the NHS Digital tracing service to update one or more identifiers.
FIGURE 4.
Flow diagram of the tracing and matching process. C, child; EW, elective withdrawals; M, mother; MW, mandatory withdrawals.
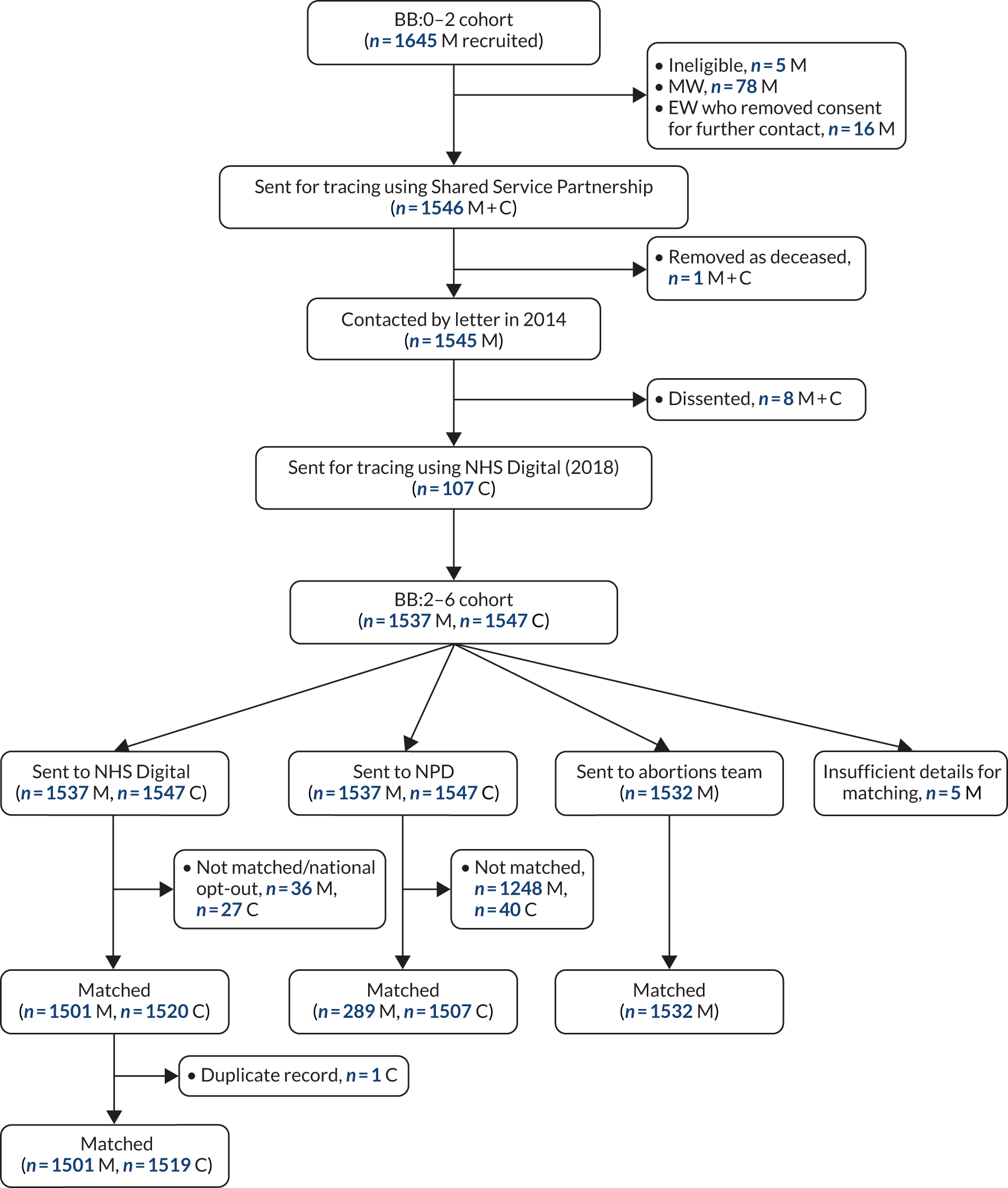
A total of 1537 mothers and 1547 children (1517 singletons and 15 sets of twins) were sent to the NPD and NHS Digital for matching. These formed the population for the BB:2–6 study. The numbers of mothers and children matched to and returned for analysis by data set are presented in Table 2. Owing to having discontinued their education, very few mothers, compared with children, were matched to any NPD data set (19% vs. 97%, respectively); these events were based mainly on the CIN data set. A high proportion of mothers and children were matched to the NHS Digital data set (> 97%). In addition, 1532 mothers’ records were supplied to and matched to abortions data by the DHSC; five mothers did not have a postcode and records were not supplied for matching. In the NHS Digital data sets, one set of twins was allocated the same HES identifier and all records relating to both were identical. One set of records was considered a duplicate and excluded from all analyses using NHS Digital data. This was not the case for NPD data sets, in which NHS numbers were not used in the matching, and we assume that records were unique to the child.
| Data set | Sent for matching to NPD and NHS Digital, n (%) | |
|---|---|---|
| Mothers (N = 1537) | Children (N = 1547) | |
| NPD | ||
| Not matched | 1248 (81.2) | 40 (2.6) |
| Match to any NPD data set | 289 (18.8) | 1507 (97.4) |
| PLASC | < 5 | 1498 (96.8) |
| CIN | 278 (18.1) | 414 (26.8) |
| CLA | 61 (4.0) | 52 (3.4) |
| EYFS profile | NA | 1476 (95.4) |
| KS1 | NA | 1472 (95.2) |
| EYC | NA | 642 (41.5) |
| PRU census | < 5 | 0 |
| Alternative provision | < 5 | < 5 |
| Absence | < 5 | 1494 (96.6) |
| NHS Digital | ||
| Not matched | 36 (2.3) | 27 (1.7) |
| Duplicate match | 0 | 1 (0.06) |
| Matched to any NHS Digital data set | 1501 (97.7) | 1519 (98.3) |
| A&E | 1360 (88.5) | 1392 (90.0) |
| Admitted Patient Care (inpatients) | 1498 (97.5) | 1507 (97.4) |
| Outpatient | 1495 (97.3) | 1189 (76.9) |
| Sent for matching to DHSC | N = 1532 | N = 0 |
| Abortions data set | 1532 (100) | NA |
Quality of matching
The quality of matching of mothers and children to the NHS Digital data set is presented in Table 3. Of the cohort, 98% had a match rank of 1 or 2 (highest matching). Equivalent data are not available for NPD data sets (which use a different matching process).
| Match rank | Mothers (n) | Children (n) |
|---|---|---|
| 1 – all fieldsa match exactly | 1344 | 1167 |
| 2 – all fields apart from postcode match exactly | 150 | 305 |
| 3 – all fields match exactly with partial match on date of birth | 0 | 1 |
| 5 – exact match on NHS number and postcode | 1 | 21 |
| 6 – exact match on all fields apart from NHS number | 6 | 0 |
| 8 – exact match on NHS number only | 0 | 25 |
| Total | 1501 | 1519 |
Quantifying bias in the BB:2–6 study sample
We could not assess potential bias in the BB:2–6 sample by describing mothers and children who were sent, but not linked, to NPD/NHS Digital data and then comparing with participants in the original BB:0–2 trial population. Any bias introduced through loss to follow-up was quantified in Table 4 by comparing maternal baseline characteristics of the full sample of mothers recruited to the BB:0–2 trial (n = 1618) with the sample retained in the BB:2–6 dataset (n = 1537). 32 Over all the selected baseline variables, the BB:2–6 study sample appears to be broadly representative of the original BB:0–2 trial cohort. The statistical analysis plan specified that baseline data for each population/data source combination would be examined, as the participant population would vary depending on which data provider was examined (NHS Digital/NPD). As the loss due to matching was very low, we would not expect this to attribute any additional bias in a sample.
| Characteristic | BB:0–2 trial sample (N = 1618) | BB:2–6 study sample (N = 1537) |
|---|---|---|
| Minimisation variables at randomisation | ||
| Gestational age at baseline, n (%) | ||
| ≥ 16 weeks | 658 (40.7) | 636 (41.4) |
| < 16 weeks | 959 (59.3) | 900 (58.6) |
| Smoking status, n (%) | ||
| No | 860 (53.2) | 822 (53.5) |
| Yes | 758 (46.8) | 715 (46.5) |
| Language, n (%) | ||
| English | 1611 (99.6) | 1530 (99.5) |
| Other | 6 (0.4) | 6 (0.4) |
| Missing | 1 (0.0) | 0 (0.0) |
| Trial and sociodemographic variables | ||
| Trial arm, n (%) | ||
| FNP | 808 (49.9) | 766 (49.8) |
| Usual care | 810 (50.1) | 771 (50.2) |
| Age at recruitment (years), median (25th to 75th centile) | 17.9 (16.9 to 18.8) | 17.9 (16.9 to 18.8) |
| Ethnicity, n (%) | ||
| White | 1425 (88.1) | 1355 (88.2) |
| Mixed | 89 (5.5) | 82 (5.3) |
| Asian (excluding Chinese) | 27 (1.7) | 25 (1.6) |
| Black | 71 (4.4) | 69 (4.5) |
| Chinese or other | 6 (0.4) | 6 (0.4) |
| Relationship status with baby’s father, n (%) | ||
| Married | 20 (1.2) | 16 (1.0) |
| Separated | 165 (10.2) | 150 (10.0) |
| Closely involved/boyfriend | 1222 (75.5) | 1168 (76.0) |
| Just friends | 211 (13.0) | 203 (13.2) |
| Live with father of baby n(%) | ||
| Yes | 368 (22.7) | 348 (22.6) |
| No | 1112 (68.7) | 1061 (69.0) |
| Missing | 138 (8.5) | 128 (8.3) |
| NEET status,a n (%) | ||
| Yes (i.e. NEET) | 663 (41.0) | 634 (41.2) |
| No (i.e. in EET) | 717 (44.3) | 678 (44.1) |
| Missing | 4 (0.2) | 4 (0.3) |
| Not applicable (aged ≤ 16 years) | 234 (14.5) | 221 (14.4) |
| Socioeconomic status: overall IMD score,b median (25th to 75th centile) | 38.2 (25.2 to 52.0); n = 1606 | 38.1 (25.0 to 52.1); n = 1525 |
| Maternal health and well-being | ||
| Generalised self-efficacy scale (score 10–40),c median (25th to 75th centile) | 30.0 (28.0 to 33.0); n = 1592 | 30.0 (28.0 to 33.0); n = 1533 |
| Adaptive functioning, n (%) | ||
| Difficulty in at least one basic skill | ||
| Yes | 430 (26.6) | 397 (25.8) |
| No | 1185 (73.2) | 1138 (74.0) |
| Missing | 3 (0.2) | 2 (0.1) |
| Had three or fewer life skills | ||
| Yes | 434 (26.8) | 403 (26.2) |
| No | 1178 (72.8) | 1129 (73.5) |
| Missing | 6 (0.4) | 5 (0.3) |
| At least one burden | ||
| Yes | 476 (29.4) | 451 (29.3) |
| No | 1131 (69.9) | 1075 (69.9) |
| Missing | 11 (0.7) | 11 (0.7) |
| Ever smoked (self-reported), n (%) | ||
| Yes | 1291 (79.8) | 1227 (79.8) |
| No | 327 (20.0) | 310 (20.2) |
| Missing | 0 (0) | 0 (0) |
In addition, we stated that we would assess the characteristics of children not in any school data set but appearing in either health or social care data sets to see if they were different on any measured baseline characteristic or at a higher risk of any adverse outcomes. Only 40 children were not matched to a school data set and also did not appear in any health or social care data sets; therefore, no further analysis was carried out.
Table 5 shows the characteristics for the children in both the BB:0–2 and BB:2–6 samples. Again, a representative sample of the children has been retained for the BB:2–6 study. However, as the BB:2–6 study contacted and included mothers who had electively withdrawn from the BB:0–2 trial, the study included a proportion of mothers who withdrew prior to giving birth. Therefore, the BB:2–6 study sample includes children who would not have formed part of the BB:0–2 trial sample (i.e. we are reporting on more children than were reported on in the BB:0–2 trial). This is reflected in the missing information for sex, birthweight and neonatal unit admissions.
| Characteristic | BB:0–2 trial sample (n = 1510) | BB:2–6 study sample (n = 1547) |
|---|---|---|
| Trial arm, n (%) | ||
| FNP | 742 (49.1) | 773 (50.0) |
| Usual care | 768 (50.9) | 774 (50.0) |
| Sex | ||
| Male, n (%) | 777 (51.5) | 787 (50.9) |
| Female, n (%) | 732 (48.5) | 758 (40.1) |
| Missing (n) | 1 | 72a |
| Birthweight (g), mean (SD) | 3207.3 (599.6) | 3219.6 (580.7) |
| Missinga (n) | 71 | |
| Neonatal unit admission | ||
| Yes, n (%) | 149 (10.0) | 142 (9.2) |
| Missing from data collection (n) | 13 | 11 |
| Missinga (n) | NA | 71 |
Descriptive analysis by trial arm
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Figure 5) shows the numbers in the BB:2–6 study by trial arm. For all participants (mothers and children) sent for matching, descriptive statistics are used to summarise the same baseline variables. No marked differences are observed between the trial arms in the characteristics identified in Table 6. Although the study populations will vary depending on which data provider is examined (NHS Digital or the NPD), because of the small number who are not matched to both data sources, there is a minimal risk of potential bias.
FIGURE 5.
The CONSORT flow diagram. C, child; EW, elective withdrawals; M, mother; MW, mandatory withdrawals.
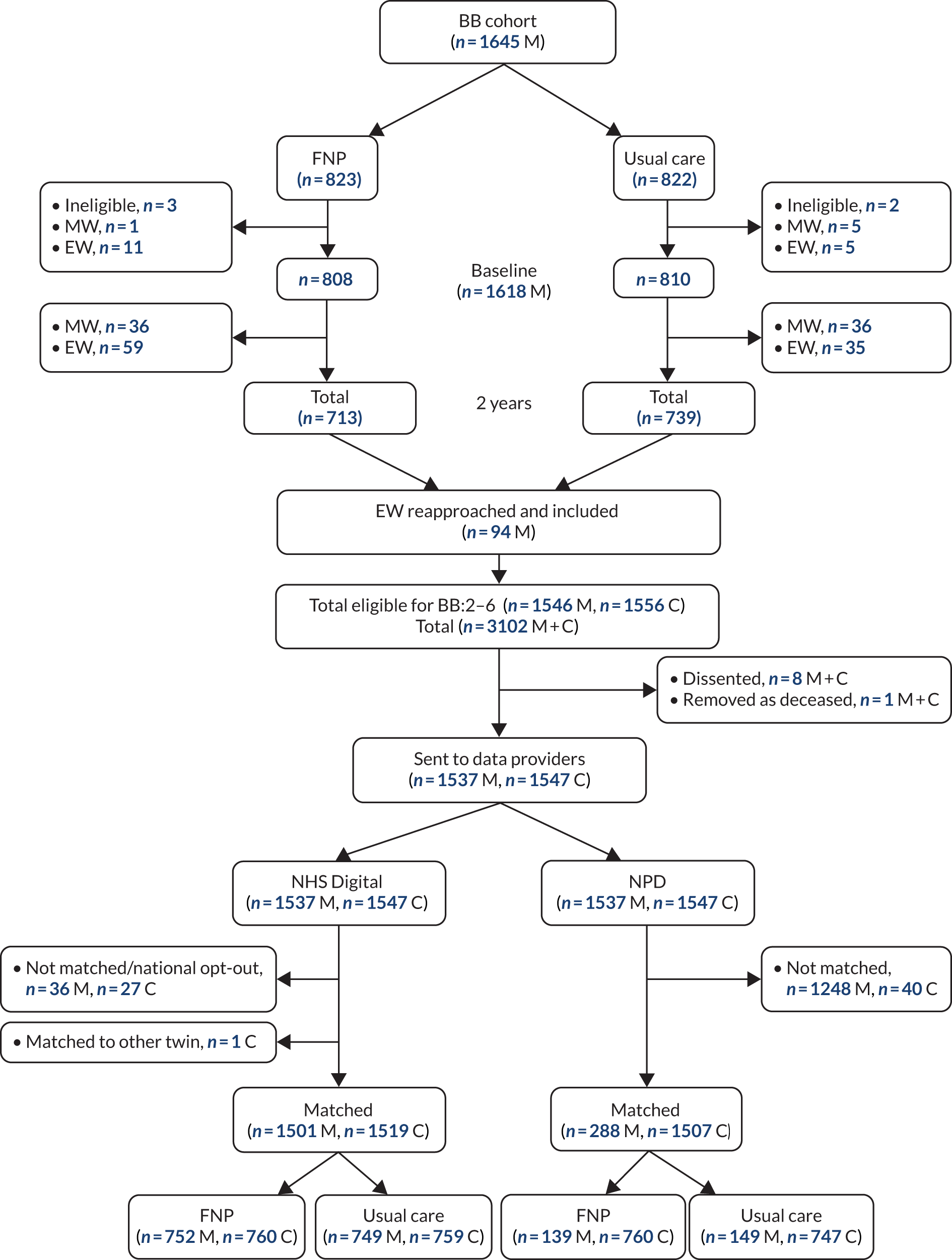
| Characteristic | Trial arm | |
|---|---|---|
| FNP | Usual care | |
| Mothers | N = 766 | N = 771 |
| Maternal age at recruitment (years), median (25th to 75th centile) | 17.9 (17.0 to 18.8) | 17.9 (16.9 to 18.8) |
| Ethnicity, n (%) | ||
| White | 675 (88.1) | 680 (88.2) |
| Mixed | 44 (5.7) | 38 (4.9) |
| Asian (excluding Chinese) | 15 (2.0) | 10 (1.3) |
| Black | 29 (3.8) | 40 (5.2) |
| Chinese or other | < 5 | < 5 |
| Relationship status with baby’s father, n (%) | ||
| Married | 6 (0.8) | 10 (1.3) |
| Separated | 72 (9.4) | 78 (10.1) |
| Closely involved/boyfriend | 582 (76.0) | 586 (76.0) |
| Just friends | 106 (13.8) | 97 (12.6) |
| NEET status,a n (%) | ||
| Yes (i.e. NEET) | 315 (41.1) | 319 (41.4) |
| No (i.e. in EET) | 345 (45.0) | 333 (43.2) |
| Participant academic age of < 16 years at interview | 104 (13.6) | 117 (15.2) |
| Missing | 2 (0.3) | 2 (0.3) |
| IMD overall score,b median (25th to 75th centile) | 38.1 (24.6 to 52.6); n = 760 | 38.1 (25.5 to 51.6); n = 765 |
| Generalised self-efficacy scale (score 10–40),c median (25th to 75th centile) | 30.0 (28.0 to 33.0); n = 764 | 30.0 (27.0 to 32.0); n = 769 |
| Adaptive functioning: difficulty in at least one basic skill, n (%) | ||
| Yes | 213 (27.8) | 184 (23.9) |
| No | 552 (72.2) | 586 (76.1) |
| Missing | 1 (0.1) | 1 (0.1) |
| Adaptive functioning: had three or fewer life skills (out of five), n (%) | ||
| Yes | 185 (24.2) | 218 (28.3) |
| No | 578 (75.8) | 551 (71.7) |
| Missing | 3 (0.4) | 2 (0.3) |
| Adaptive functioning: at least one burden, n (%) | ||
| Yes | 214 (28.2) | 237 (30.9) |
| No | 545 (71.8) | 530 (69.1) |
| Missing | 7 (0.9) | 4 (0.5) |
| Cigarette smoking, participant self-reported, n (%) | ||
| Ever smoked | ||
| Yes | 615 (80.3) | 612 (79.4) |
| No | 151 (19.7) | 159 (20.6) |
| Children | N = 773 | N = 774 |
| Sex | ||
| Male, n (%) | 381 (49.3) | 406 (52.5) |
| Female, n (%) | 392 (50.7) | 367 (47.5) |
| Missing (n) | 0 | 1 |
| Birthweight (g), mean (SD) | 3223.81 (606.0) | 3215.52 (555.56) |
| Missing (n) | 49 | 22 |
| Neonatal unit admission (direct or subsequent) | ||
| Yes, n (%) | 76 (10.6) | 66 (8.8) |
| No, n (%) | 640 (89.4) | 683 (91.2) |
| Missing (n) | 57 | 25 |
Number of valid Family Nurse Partnership visits received
Of the 766 women in the FNP arm in the BB:2–6 cohort, 69 did not enrol in the FNP. For the remaining 697 who were randomised and enrolled, 695 had received at least one valid visit and two did not receive any valid visits across the three phases (pregnancy, infancy and toddlerhood). The descriptives in Table 7 are based on the 697 women. More women received no visits during the infancy and toddlerhood phases [40 (5.7%) and 98 (14.1%) women, respectively] than during the pregnancy phase [6 (0.7%) women]. The results in Table 7 are similar to those reported for the BB:0–2 trial cohort, with comparable median valid visits, and proportions reaching the fidelity goals. 32
| Indicators of FNP client visit experience | Phase | ||
|---|---|---|---|
| Pregnancy | Infancy | Toddlerhood | |
| Women randomised to and enrolled in the FNP (n) | 697 | 697 | 697 |
| Women not receiving any valid visits, n (%) | 6 (0.7) | 40 (5.7) | 98 (14.1) |
| Women receiving at least one valid visit, n (%) | 691 (99.3) | 657 (94.3) | 599 (85.9) |
| Number of valid visits received | |||
| Median (25th to 75th centile) | 10 (8 to 12) | 19 (15 to 22) | 13 (10 to 16) |
| Mean (SD) | 9.74 (3.42) | 18.7 (5.97) | 13.28 (5.46) |
| Reaching fidelity goal of, n/N (%) | |||
| ≥ 80% | 401/697 (57.5) | – | – |
| ≥ 65% | – | 364/697 (52.2) | – |
| ≥ 60% | – | – | 297/697 (42.6) |
Chapter 5 Main results
Objective measures of maltreatment
This chapter describes the effectiveness of the FNP programme in reducing objectively measured medium-term maltreatment outcomes, when compared with usually provided health and social care alone, over the first 6 years of a child’s life. These outcomes of maltreatment are presented in sequential order, starting with the initial referral to CSC, CIN status (primary outcome), whether or not the child was subject to a CPP, and the looked-after status of the child. The denominator for all analyses is the 1507 children who were matched to any NPD data set (FNP, 760 children; usual care, 747 children). One child who died during follow-up was excluded from most analyses because of the incomplete follow-up period with no referrals to CSC services (we cannot conclude that, if we had observed complete follow-up until the age of 6 years, they would not have been referred).
Referral to children’s social care services
Over the 6 years’ follow-up, 414 (27.5%) children had at least one referral to CSC services; there was an absolute difference between arms of –0.8% (95% CI –5.3% to 3.7%), and no evidence of an intervention effect (Table 8). For these 414 children, 693 individual referrals to CSC services were made, with one to five separate referrals per child over the 6-year period (see Table 8). Although 9.9% more children in the FNP arm had only one referral made over the 6 years, marginally more children in the usual-care arm had more than one referral (descriptive analysis only). The majority of referrals came from school or the health service.
| Outcome | FNP arm (N = 760) | Usual-care arm (N = 746) | Adjusteda parameter estimate (95% CI) | p-value |
|---|---|---|---|---|
| Referred to CSC services, n (%) | ||||
| No | 554 (72.9) | 538 (72.1) | ||
| Yes | 206 (27.1) | 208 (27.9) | 0.97b (0.74 to 1.28) | 0.829 |
| Total referrals made (n) | 339 | 354 | ||
| Ratio of referrals to children | 1.65 | 1.70 | ||
| Referrals made per child, n (%) | ||||
| 1 | 159 (77.2) | 140 (67.3) | Not tested, descriptive only | |
| 2 | 34 (16.5) | 51 (24.5) | ||
| 3–5 | 13 (6.3) | 27 (8.2) | ||
| Age (days) at first referral, median (25th to 75th centiles) | 1541.5 (1272.75 to 1975.75) | 1631.0 (1190.50 to 1984.75) | 0.96c (0.79 to 1.17) | 0.694 |
| Unit of analysis = 1 referral | n = 339 | n = 354 | ||
| Source of referral | ||||
| Individual, n (%) | 29 (8.8) | 34 (10.0) | Not tested, descriptive only | |
| School/education, n (%) | 150 (45.7) | 136 (40.0) | ||
| Health services, n (%) | 114 (34.8) | 132 (38.8) | ||
| Local authority services, n (%) | 35 (10.7) | 38 (11.2) | ||
| Missing (n) | 11 | 14 | ||
| Primary need for referral | ||||
| Abuse or neglect, n (%) | 198 (58.9) | 205 (57.9) | Not tested, descriptive only | |
| Family dysfunction, n (%) | 72 (21.4) | 88 (24.9) | ||
| Family in acute stress, n (%) | 19 (5.7) | 21 (5.9) | ||
| Low income/absent parenting/socially unacceptable behaviour, n (%) | 11 (3.3) | 7 (2.0) | ||
| Parental/child’s disability illness, n (%) | 14 (4.2) | 11 (3.1) | ||
| Cases other than CIN, n (%) | 11 (2.3) | 12 (3.4) | ||
| Not stated, n (%) | 11 (3.3) | 9 (2.5) | ||
| Missing (n) | 3 | 1 | ||
Treatment efficacy on referrals to children’s social care services
Adjusting the analysis for receipt of full dosage of FNP visits made no difference to the conclusion of the main analysis for referral to social services (efficacy per visit OR 1.00, 95% CI 0.99 to 1.004; p = 0.613).
Subgroup analyses on referrals to children’s social care services
Appendix 4, Table 37, details the results of the subgroup analysis for the prespecified subgroups [maternal age, NEET status, Index of Multiple Deprivation (IMD) quintile, adaptive functioning and sex of child]. There was no evidence to suggest that any of the maternal and child baseline factors had any influence on the effect of the FNP on referrals to social services.
Surveillance bias in detection of maltreatment: timing and severity of the referral
Children in the FNP arm were referred to CSC services an average of 90 days earlier than children in the usual-care arm, but there was no statistical difference in age at first referral between arms to suggest a difference in detection of first referral (see Table 8). The primary needs identified from all referrals (indicating the severity of the referral) were mainly for abuse and neglect, followed by family dysfunction (descriptive analysis only) (see Table 8).
Primary outcome: child-in-need status
For the definition of a CIN, 277 referrals resulting in no further action (not classed as in need) were excluded and 634 referrals remained associated with a CIN status (Table 9). Overall, 323 (21.5%) of children in the BB:2–6 cohort had at least one referral to CSC, which resulted in them being classed as a CIN at any point between pregnancy (includes pre-birth CIN) and 6 years of age. There was no evidence of an intervention effect.
| Outcome | FNP arm (N = 760) | Usual-care arm (N = 746) | Adjusteda parameter estimate (95% CI) | p-value | Absolute risk difference (95% CI) |
|---|---|---|---|---|---|
| Child ever in need, n (%) | |||||
| No | 599 (78.8) | 584 (78.3) | |||
| Yes | 161 (21.2) | 162 (21.7) | 0.98b (0.74 to 1.31) | 0.902 | –0.53 (–0.47 to 0.36) |
| Age at first CIN referral, n (%) | |||||
| Pre birth | < 5 | < 5 | |||
| Birth to < 1 years | < 5 | < 5 | |||
| 1 to < 2 years, n (%) | 6 (3.7) | 6 (3.7) | |||
| 2 to < 3 years, n (%) | 15 (9.4) | 28 (17.3) | |||
| 3 to < 4 years, n (%) | 27 (16.9) | 23 (14.2) | |||
| 4 to < 5 years, n (%) | 47 (29.4) | 39 (24.1) | |||
| 5 to < 6 years, n (%) | 33 (20.6) | 41 (25.3) | |||
| 6 to < 7 years, n (%) | 20 (12.5) | 20 (12.3) | |||
| Missing (n) | 1 | 0 | |||
| Median (25th to 75th centile) | 1602.5 (1153 to 1978.75) | 1649.5 (1130.75 to 1980.25) | 0.98c (0.79 to 1.23) | 0.875 | |
| Uniqued CIN case per child | n = 161 | n = 162 | |||
| 1 case | 110 (68.3) | 110 (67.9) | |||
| 2 cases | 42 (26.1) | 42 (25.9) | |||
| ≥ 3 cases | 9 (5.5) | 10 (6.1) | |||
| Median (25th to 75th centiles) | 1 (1 to 2) | 1 (1 to 2) | 0.99e (0.82 to 1.19) | 0.890 | |
| CIN cases closed at 31 March 2017, n (%) | 116 (72.0) | 110 (67.9) | |||
| Duration of time in need (days), median (25th to 75th centile) | 210 (70.5 to 571.25) | 216 (72.75 to 503.25) | 1.20e (0.90 to 1.59) | 0.216 | |
| Primary need for first CIN case, n (%) | |||||
| Abuse or neglect | 92 (57.1) | 102 (63.0) | Reference | ||
| Family dysfunction | 29 (18.0) | 34 (21.0) | 0.95 (0.54 to 1.69)f | 0.868 | |
| Family in acute stress | 13 (8.1) | 10 (6.2) | 1.47 (0.61 to 3.54)f | 0.389 | |
| Low income, absent parenting, socially unacceptable behaviour, not stated | 13 (8.1) | 7 (3.7) | 2.38 (0.86 to 6.57)f | 0.093 | |
| Child/parent disability | 7 (4.3) | 5 (3.1) | 1.47 (0.45 to 4.84)f | 0.525 | |
| Cases other than CIN | 7 (4.3) | 5 (3.1) | 1.64 (0.50 to 5.37)f | 0.417 | |
Treatment efficacy on child-in-need status
Adjusting the analysis for receipt of the FNP made no difference to the conclusion of primary outcome (efficacy per visit OR 1.00, 95% CI 0.99 to 1.004; p = 0.613). Because only a small number [40 (2.7%)] of children were not linked to any NPD data set and not included in any of these analyses, no multiple imputations were carried out.
Subgroup analyses on child-in-need status
Appendix 5, Table 38, details the results of the subgroup analysis for the prespecified subgroups and shows no evidence to suggest that these had any influence on the treatment effect for CIN status.
Domestic abuse and child-in-need status
Domestic abuse was assessed using the Composite Abuse Scale (CAS) in the BB:0–2 trial at the 24-month follow-up (with a score of ≥ 1 indicating some sort of abuse). The CAS could be administered only if the interview was face to face (as opposed to by telephone) and only if the participant was alone (n = 607). In the BB:2–6 study sample, the CAS was administered to 595 participants (FNP, n = 322; usual care, n = 273); the proportion of participants experiencing some form of abuse was comparable to that found in the BB:0–2 trial [FNP, n = 122 (27.9%) vs. usual care, n = 113 (41.4%)]. There was also a relationship found between the CAS and CIN status, with 49 (20.9%) participants who experienced some abuse having a child being in need, versus 42 (11.8%) of those who did not experience abuse. Domestic abuse at 24 months was to be explored as a possible effect mediator, but, because of a lack of intervention effect in children’s CIN status, the need to examine the proportion of effect mediated by experience of domestic abuse at 24 months was redundant.
Secondary analysis: age of first child-in-need referral
For children classed as in need, the age at which the child was classed as in need for the first time (based on referral date) was calculated. Those who were never classed as in need were censored at 6 years (last date of follow-up), and those who died in this period were censored at date of death. Table 9 shows the distribution of the age at first referral. A total of six children had a date of referral before birth, all of which are feasible for the pre-birth period (around 6 months pre birth). One child had a referral after their seventh birthday and was excluded from this analysis. For the time-to-event analysis, all pre-births (i.e. children that are classed as in need before they are born) (negative days) are set to zero. There was an average of 47 days’ difference in age at first CIN referral between arms, but this was not statistically significant (see Table 9).
Secondary analysis: number of child-in-need referrals
The number of unique CIN referrals (defined by unique referral dates, as referrals can span several academic years) was examined using multilevel Poisson regression modelling appropriate for count data. Of the 323 children with at least one referral, the majority had one case only (67%). There was no evidence of an intervention effect in the number of CIN cases per child between arms (see Table 9).
Secondary outcomes relating to child in need
Total duration of child-in-need episodes
The duration of children’s time classed as in need was examined by using the start and closing date for a referral classed as in need, but can be assessed only for referrals that have closed. Table 9 shows that, for each arm, at least two-thirds of referrals had closed; the durations in days were comparable, being, on average, 6 days longer in the usual-care arm, with no evidence of a difference between the two arms.
Primary need of child
Overall, the majority of referrals for CIN were for abuse or neglect (60%), followed by family dysfunction (20%). There were no apparent differences between arms in the distribution of these categories (see Table 9).
Child protection registration
A total of 101 children were subjected to at least one child protection registration with evidence of a CPP (Table 10); there was no evidence of a difference in the rate of CPPs between trial arms.
| Outcome | FNP arm (N = 760) | Usual-care arm (N = 746) | Adjusteda parameter estimate (95% CI) | p-value | Absolute difference (95% CI) |
|---|---|---|---|---|---|
| CPP, n (%) | |||||
| No | 708 (93.2) | 697 (93.4) | |||
| Yes | 52 (6.8) | 49 (6.6) | 1.04b (0.69 to 1.57) | 0.846 | 0.27 (–0.23 to 0.28) |
| Initial category of abuse | n = 52 | n = 49 | |||
| Neglect, n (%) | 17 (32.7) | 22 (44.9) | Reference | ||
| Emotional, n (%) | 22 (42.3) | 12 (24.5) | 2.77c (1.02 to 7.56) | 0.046 | |
| Physical, n (%) | 6 (11.5) | 6 (12.2) | 1.25c (0.32 to 4.88) | 0.743 | |
| Sexual and multiple,d n (%) | 7 (13.5) | 9 (18.4) | 1.13c (0.33 to 3.86) | 0.848 | |
| CLA, n (%) | |||||
| No | 735 (96.7) | 719 (96.4) | |||
| Yes | 25 (3.3) | 27 (3.6) | 0.90b (0.52 to 1.57) | 0.712 | –0.3 (–0.2 to 0.2) |
| Total duration of care (months), values medians (25th to 75th centiles) | 10.0 (4.5 to 37.5) | 12.0 (6.0 to 33.0) | 0.75e (0.65 to 0.86) | < 0.001 | |
| Legal status of CLA | |||||
| Interim care order, n (%) | 6 (35.3) | 8 (34.8) | Not tested, descriptive only | ||
| Full care order, n (%) | 5 (29.4) | 6 (26.1) | |||
| Placement order granted | < 5 | < 5 | |||
| Single period of accommodation under section 20 | < 5 | < 5 | |||
| Death | < 10 (combining both arms) | Not tested, descriptive only | |||
At an initial child protection conference, a category of abuse will be agreed; however, this may be revised at any subsequent child protection conferences. This analysis looks only at the initial categories, which are listed in Table 10 by trial arm. Emotional abuse and neglect are the two over-riding reasons for child protection registration, with 73% of children in these categories of abuse. There is some evidence of a difference in the effect of the intervention on emotional abuse when compared with neglect (see Table 10). The relative risk of being in the emotional abuse category as an initial category of abuse was 2.77 times higher in the FNP arm in relation to the neglect category.
Looked-after status of child
A small number of children were ever ‘looked after’ within the 6-year follow-up period, with no evidence of a difference between trial arms (see Table 10). However, children in the usual-care arm spent, on average, 2 months longer in care than children in the FNP arm. The legal status of the most recent CLA episode is shown in Table 10 for 40 children; 12 children were missing a legal status. No formal testing was performed because of the small numbers involved; descriptive results only are shown.
Cause of death
The total number of child deaths across the full follow-up period was < 10; they were not further reported by study arm, in line with applicable non-disclosive data management policy.
Associated measures of maltreatment
Did-not-attend rates for hospital outpatient appointments
Of the 1546 children analysed with NHS digital data in the BB:2–6 cohort, 1157 (76.2%) had at least one outpatient appointment over the 6 years’ follow-up. Around 50% of children were not taken to at least one appointment, with no evidence of an intervention effect (Table 11).
| Outcome | FNP (N = 580) | Usual care (N = 577) | Adjusteda parameter estimate (95% CI) | Absolute risk difference (95% CI) |
|---|---|---|---|---|
| DNA, n (%) | ||||
| Attended all appointments | 290 (50.0) | 289 (50.1) | ||
| DNA at least once | 290 (50.0) | 288 (49.9) | 1.00b (0.79 to 1.26) | 0.09 (–5.6 to 5.8) |
| Injuries and ingestions | FNP (N = 760) | Usual care (N = 759) | ||
| Emergency attendancec | ||||
| None, n (%) | 317 (41.7) | 344 (45.3) | ||
| At least one, n (%) | 443 (58.3) | 415 (54.7) | 1.17a (0.95 to 1.45) | 3.6 (–1.4 to 8.6) |
| Number of attendances per child, median (25th to 75th centile) | 2 (1 to 2) | 2 (1 to 3) | 1.09d (0.93 to 1.28) | – |
| Admission to hospital | ||||
| None, n (%) | 671 (88.3) | 660 (87.0) | ||
| At least one, n (%) | 89 (11.7) | 99 (13.0) | 0.87b (0.63 to 1.20) | –1.3 (–4.7 to 2.0) |
| Unique admissions (n) | 109 | 119 | ||
| Ratio of admissions to children | 1.22 | 1.20 | ||
| Number of admissions per child, median (25th to 75th centile) | 1 (1 to 1) | 1 (1 to 1) | 0.93d (0.67 to 1.29) | – |
| Length of stay (days) | N = 106 | N = 119 | ||
| Median (25th to 75th centile) days | 0.5e (0.5 to 1.0) | 0.5 (0.5 to 1.0) | ||
| Hospital attendance and/or hospital admission n (%) | ||||
| None | 306 (40.3) | 324 (52.7) | Reference | |
| At least one | 454 (59.7) | 435 (57.3) | 1.11b (0.89 to 1.37) | 2.4 (–2.5 to 7.4) |
Recorded injuries and ingestions
Emergency attendances
A total of 7381 emergency attendances were recorded for 1377 children, of which 1792 (24.3%) (FNP, n = 911, vs. usual care, n = 881) were for an injury or an ingestion. The type of diagnosis by trial arm is listed in Appendix 6, Table 42. A total of 1937 (26%) attendances were missing a diagnosis, but received other investigations. More than 50% of children in both arms had attended an emergency establishment, with slightly higher rates of injuries and ingestions seen in the FNP arm, but there was no evidence of a difference between arms (see Table 11).
Admission to hospital
A total of 228 diagnoses were identified with an injury or an ingestion and are listed in Appendix 6, Table 43, based on all diagnoses in each position. There were no differences between the trial arms in the rate of admissions or the number of attendances per child (see Table 11). The median length of stay of hospital admissions were comparable between arms, with a median stay of 0.5 days (25th to 75th centile 0.5 to 1 day) (0.5 days is equivalent to same-day admission and discharge).
Emergency attendances or admissions to hospital
When these data sets were combined to identify children attending an emergency department or being admitted, there were no differences between the trial arms in the rate of admissions or the number of attendances (see Table 11).
Maternal outcomes
Subsequent pregnancies
All analyses for inpatient and outpatient were based on the 1501 mothers who were in NHS Digital data sources. When additional abortions data were available, these were also included as a subsequent pregnancy, but if there were no NHS Digital data or no abortion data, then these women were assumed as missing. Table 12 shows the rate of subsequent pregnancies since the birth of the BB:0–2 baby, by data source. These vary by source, with the lowest rate found in abortions (taking into account that 2012 data were not available) and the highest among inpatients. Overall, 78% of the cohort of mothers went on to have a subsequent pregnancy. There were no differences in subsequent pregnancy rates split by trial arm overall or by data source (Table 13).
| Subsequent pregnancy identified in each data set | Abortionsa | Inpatients | Outpatients | All sources (abortions, inpatients and outpatients) |
|---|---|---|---|---|
| No, n (%) | 1300 (84.9) | 40 (27.1) | 546 (36.4) | 326 (21.6) |
| Yes, n (%) | 232 (15.1) | 1094 (72.9) | 955 (63.6) | 1180 (78.4) |
| Total (n) | 1532 | 1501 | 1501 | 1506b |
| Outcome | FNP arm | Usual-care arm | Adjusteda OR (95% CI); p-value | Absolute risk difference (95% CI) |
|---|---|---|---|---|
| All sources | ||||
| No, n (%) | 163 (21.7) | 163 (21.7) | ||
| Yes, n (%) | 590 (78.4) | 590 (78.4) | 1.00 (0.79 to 1.28); 0.984 | 0.0 (–4.2 to 4.2) |
| Total (n) | 753 | 753 | ||
| Inpatients | ||||
| No, n (%) | 207 (27.5) | 200 (26.7) | ||
| Yes, n (%) | 545 (72.5) | 549 (73.3) | – | –0.8 (–5.3 to 3.7) |
| Total (n) | 752 | 749 | ||
| Outpatients | ||||
| No, n (%) | 280 (37.2) | 266 (35.5) | ||
| Yes, n (%) | 472 (62.8) | 483 (64.5) | – | –1.7 (–6.6 to 3.1) |
| Total (n) | 752 | 749 | ||
| Abortions | ||||
| No, n (%) | 653 (85.4) | 647 (84.4) | ||
| Yes, n (%) | 112 (14.6) | 120 (15.7) | – | –1.1 (–4.7 to 2.5) |
| Total (n) | 767 | 765 | ||
When registerable births were examined (using only admission data as a source), just over two-thirds of the cohort had at least one birth during the 6 years’ follow-up, with no difference between arms (Table 14). The number of births was also similar between arms, with no difference in the interbirth interval and no difference in time to subsequent birth (Figure 6).
| FNP arm (N = 752) | Usual-care arm (N = 749) | Adjusteda OR (95% CI); p-value | Absolute risk difference (95% CI) | |
|---|---|---|---|---|
| No subsequent birth, n (%) | 276 (36.7) | 266 (35.5) | ||
| Subsequent birth, n (%) | 476 (63.3) | 483 (64.5) | 0.95 (0.77 to 1.18); 0.662 | –1.2 (–6.0 to 3.7) |
| Of these, the number of births per mother over the 6-year follow-up period | ||||
| 1 | 326 (68.5) | 331 (68.5) | ||
| 2 | 124 (26.1) | 121 (25.1) | ||
| ≥ 3 | 26 (5.5) | 31 (6.4) | ||
| Number of subsequent births, n (%) | Adjusteda IRR (95% CI); p-value | |||
| No birth | 276 (36.7) | 266 (35.5) | Reference | |
| 1 | 326 (43.3) | 331 (44.2) | 0.95 (0.76 to 1.19); 0.655 | |
| 2 | 124 (16.5) | 121 (16.2) | 0.99 (0.73 to 1.34); 0.955 | |
| ≥ 3 | 26 (3.5) | 31 (4.1) | 0.80 (0.46 to 1.39); 0.435 | |
| Interbirth interval between first and second child (days) | Adjusteda HR (95% CI); p-value | |||
| Mean (SD) | 476 (1049.5) | 483 (1105.1) | 0.99 (0.88 to 1.13); 0.938 | |
| Median (25th to 75th centiles) | 1027 (590 to 1506.75) | 1065 (665 to 1538) | ||
FIGURE 6.
Time to subsequent birth (days) by trial arm.
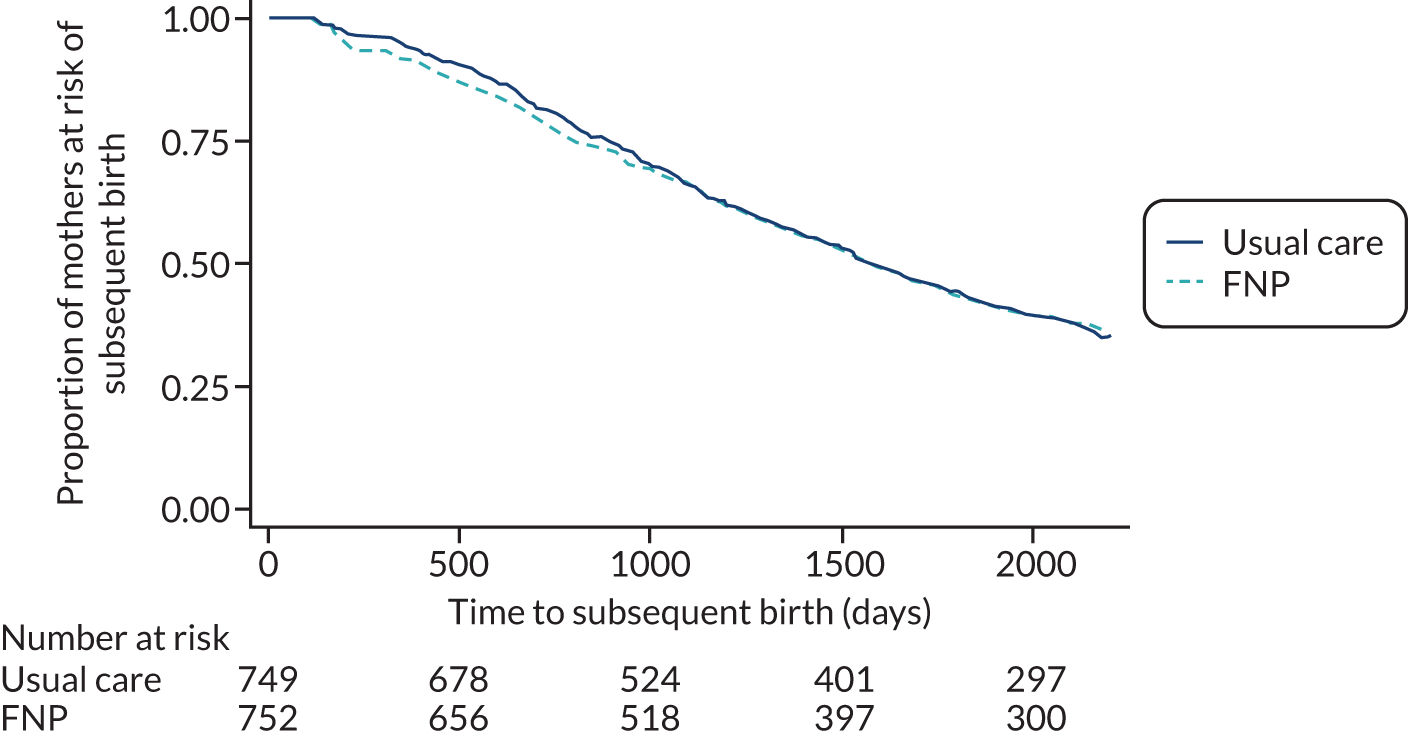
Child health, developmental and educational outcomes
Special educational needs
A child with SEN provision is recorded using the following codes: A = school action; P = school action plus; E = education, health and care plan; S = statement; and K = SEN support; the N code was used to indicate no SEN support in any of the following data sets between 2013 and 2017: PLASC (autumn, spring and summer terms), alternative provision, PRU census and EYC. If, for any of the years, no response was recorded, then the assumption was that the child was not included in the denominator as they were either not present on census day or not in school.
Forty children were not present in any of the data sources and were excluded from this analysis. Of the 1507 children included in the analysis, 1498 (99.5%) had complete census data (for all years and for all three terms) and eight did not (two had census data for autumn and spring only; six had no PLASC data, but were present in the EYC data set). A slightly higher proportion of children with SEN provision were found in the usual-care arm than in the FNP arm [245/747 (32.8%) vs. 219/759 (28.9%), respectively], with an absolute difference of –3.9 percentage points (95% CI –8.59 to 0.72 percentage points), and no evidence of a statistical difference (aOR 0.83, 95% CI 0.67 to 1.03; p-value = 0.097).
Early educational attendance
Early educational attendance takes place in a variety of settings, including state nursery schools, nursery classes and reception classes in primary schools, as well as settings outside the state sector, such as voluntary preschools, privately run nurseries or childminders. Two data sources capture this information for children aged 2–4 years: (1) EYC and (2) PLASC. Any PVI setting where children aged 2–4 years at 31 December were receiving early funded education is required to complete the EYC, whereas the PLASC includes registered pupils of local authority-maintained nursery or nursery classes in maintained schools and academies.
Among the 1507 children included in the analysis, the proportion of children attending early-years establishments (either an Ofsted-registered PVI establishment or school) by 4 years of age was similar in both arms, with > 99% of children attending (Table 15). Nearly all children were attending school by the age of 4 years, and comparable rates are observed between arms for the proportion of children attending school at the age of 2 and 3 years (not tested, descriptive only). A total of 642 children had attended at least one separate Ofsted-registered PVI establishment over the period of 2012–15, and rates were comparable by trial arm. The majority of children (490/642, 76.3%) attended one Ofsted-registered PVI establishment in one academic year; the remainder (23.7%) attended over several academic years. The type of establishment differed by arm, with more in the usual-care arm accessing private day care and more in the FNP arm attending local authority day nursery and other establishments (including registered independent school, childminding network and childminders).
| FNP arm (N = 760) | Usual-care arm (N = 747) | Adjusteda OR (95% CI); p-value | Absolute difference (95% CI) | |
|---|---|---|---|---|
| Children attending educationb up to the age of 4 years, n (%) | 758 (99.7) | 747 (100.0) | Not estimable | –0.26 (–0.95 to 0.28) |
| Children attending school up to the age of, n (%) | ||||
| 4 years | 753 (99.1) | 744 (99.6) | Not estimable | –0.52 (–1.52 to 0.39) |
| 3 years | 479 (63.0) | 482 (64.5) | Not tested, descriptive only | |
| 2 years | 137 (18.0) | 147 (19.7) | Not tested, descriptive only | |
| Attending an Ofsted-registered PVI establishment up to the age of 4 years, n (%) | 334 (43.9) | 308 (41.2) | 1.13 (0.91 to 1.40), 0.281 | 2.7 (–2.3 to 7.7) |
| Earliest type of day care, n (%) | N = 334 | N = 308 | ||
| Private | 217 (65.0) | 221 (71.8) | Not tested, descriptive only | |
| Voluntary | 52 (15.6) | 57 (18.5) | ||
| Local authority day nursery | 36 (10.8) | 22 (7.1) | ||
| Otherc | 29 (8.7) | 8 (2.6) | ||
Early-years assessment
Of the 1547 children in the cohort, 1476 (95.4%) were included in the EYFS profile data set, five of whom were marked as absent on the day or missing an assessment. These were excluded from the analysis, leaving 1471 children with an assessment remaining. The proportion of children achieving a GLD (a score of ≥ 2) in all five areas of learning and in all 17 early-learning goals was higher in the FNP arm than in the usual-care arm, with evidence of a significant between-arm difference (Table 16). This pattern was also observed for each of the five areas of learning, although it was not formally tested statistically. When the overall total point score was examined (ranging from 17 = score of 1 across all areas to 51 = score of 3 across all areas), the average scores were similar in each arm (see Table 16). Figure 7 shows the distribution of the total points score over all 17 areas. When the total score was categorised into scores equal to 34, scores < 34, and scores > 34, 34 points was the most common outcome (equivalent to a child achieving the expected level in every learning area), with 25% of children in both the FNP and usual-care arms achieving this score. The FNP arm had a higher proportion of children obtaining a score of > 34 than the usual-care arm.
| FNP arm (N = 743), n (%) | Usual-care arm (N = 728), n (%) | Total (N = 1471), n (%) | Adjusteda parameter estimate (95% CI) | p-value | Absolute differenceb (95% CI) | |
|---|---|---|---|---|---|---|
| Achieving a GLD | ||||||
| Achieving a GLD in all five areas of learningc | 431 (58.0) | 380 (52.2) | 811 (55.1) | 1.26d (1.03 to 1.55) | 0.026 | 5.8 (0.7 to 10.9) |
| Prime areas | ||||||
| Communication and language | 642 (86.4) | 613 (84.2) | 1255 (85.3) | Not tested, descriptive only | – | 2.2 (–1.4 to 5.8) |
| Physical development | 676 (91.0) | 643 (88.3) | 1319 (89.7) | Not tested, descriptive only | – | 2.7 (–0.5 to 5.8) |
| Personal, social and emotional development | 668 (89.9) | 634 (87.1) | 1302 (88.5) | Not tested, descriptive only | – | 2.8 (–0.4 to 6.1) |
| Specific areas | ||||||
| Literacy | 493 (66.4) | 458 (62.9) | 951 (64.6) | Not tested, descriptive only | – | 3.4 (–1.4 to 8.3) |
| Mathematics | 545 (73.4) | 516 (70.9) | 1061 (72.1) | Not tested, descriptive only | – | 2.5 (–2.1 to 7.0) |
| Achieving a GLD in all 17 early-learning goals | 412 (55.5) | 365 (50.1) | 777 (52.8) | 1.24 (1.01 to 1.52) | 0.043 | 5.3 (0.2 to 10.4) |
| Total point score | ||||||
| Mean (SD)e | 32.22 (7.25) | 31.59 (7.62) | 0.65f (–0.11 to 1.41) | 0.094 | – | |
| Score of < 34 | 325 (43.8) | 345 (47.4) | ||||
| Score = 34 | 187 (25.2) | 183 (25.1) | ||||
| Score of > 34 | 231 (31.1) | 200 (27.5) | ||||
FIGURE 7.
Distribution of the total point score over all 17 early-learning goals (range 17–51 points). (a) FNP; and (b) usual care. Source: NPD, DfE.
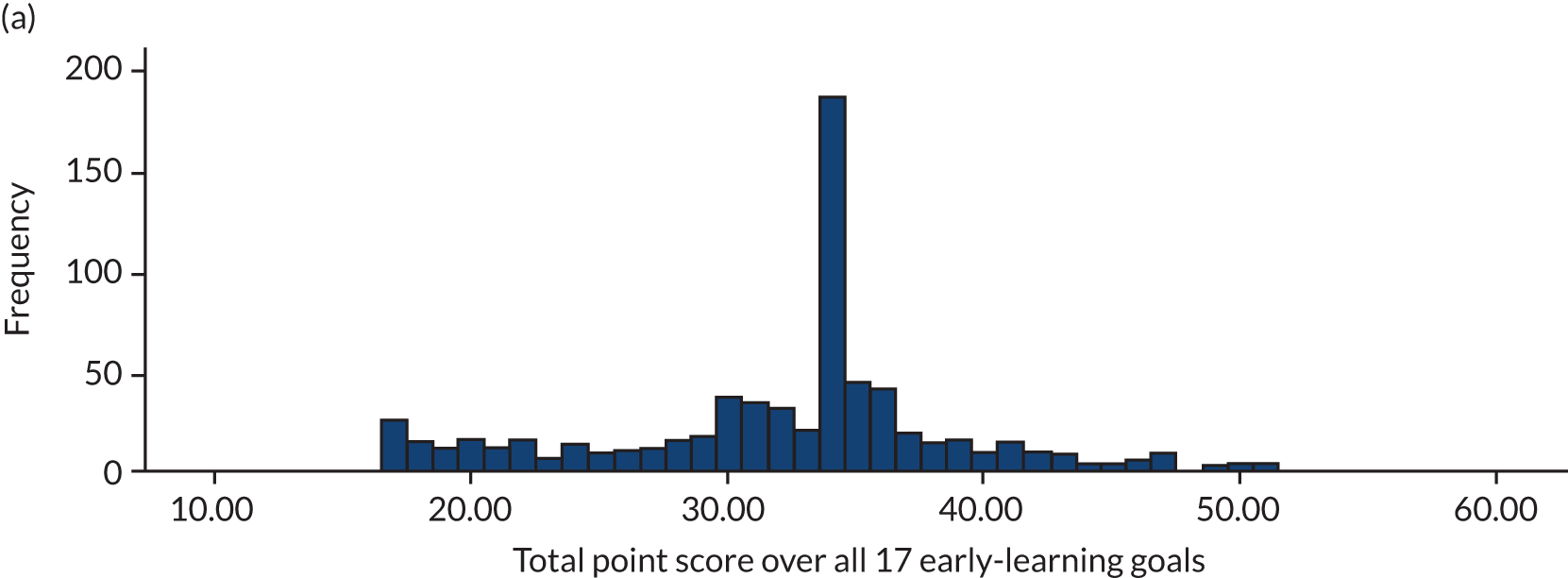
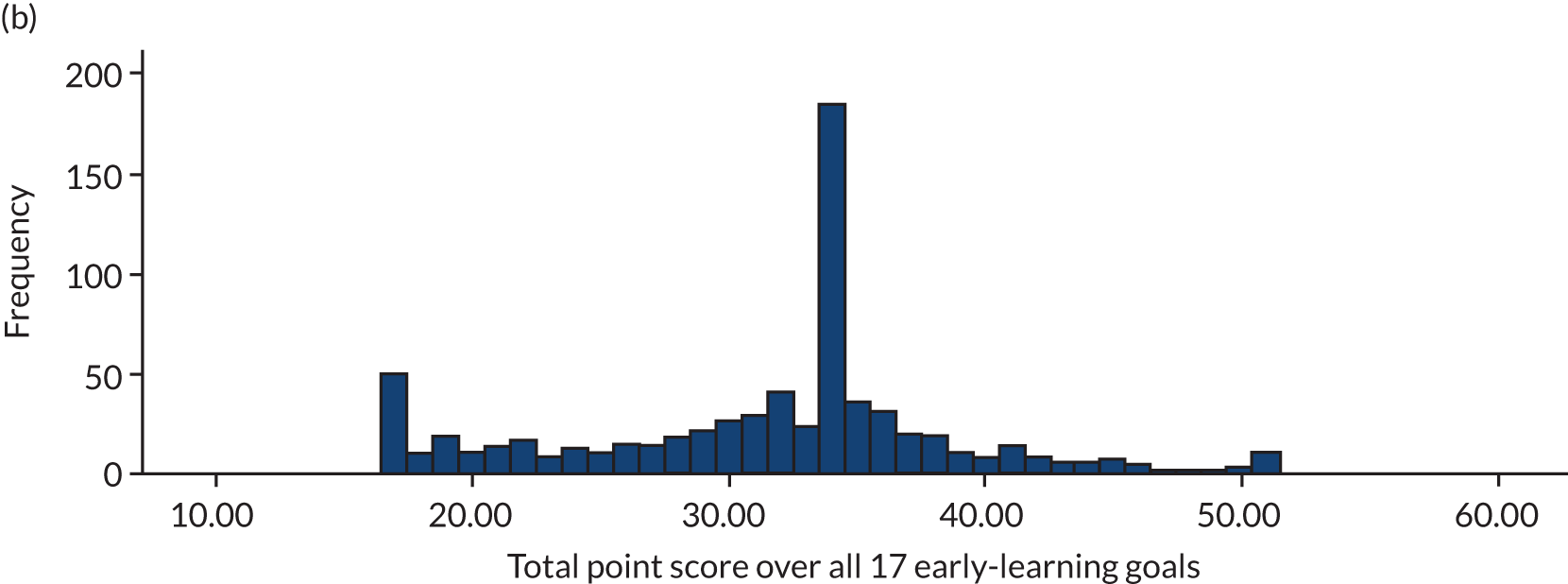
Treatment efficacy on the early-years assessment total point score
The primary analysis was re-run to investigate the effect of the FNP dosage (number of visits over all delivery phases) using complier-averaged causal effects modelling by fitting a structural mean model. Adjusting the analysis for receipt of FNP, we observe a 0.02 increase in point score in the between-arm mean difference in early-years total score (as the number of visits increase, so does the score); however, the CI around this estimate is wide (–0.004 to 0.040). The maximum number of visits over the whole period of the FNP is 64 (14 in the pregnancy phase, 28 in the infancy phase and 22 in the toddlerhood phase). The estimated treatment efficacy for participants receiving all 64 visits was 1.15 (95% CI –0.26 to 2.56; p = 0.106), showing no change to the overall conclusions, compared with the primary analysis.
Subgroup analyses on the early-years assessment total point score
Of the five prespecified subgroup analyses, the only subgroup that appeared to have a differential intervention effect was mothers aged < 16 years at recruitment, for which a 3.5-score difference was observed between arms (Figure 8) (see Appendix 7, Table 44).
FIGURE 8.
Forest plot of estimates from the subgroups for EYFS profile score. Vertical solid line represents no effect (mean difference = 0) vertical dashed line indicates the overall treatment effect for EYFS total score (adjusted mean difference = 0.65). EET, employment, education or training. Source: NPD, DfE.
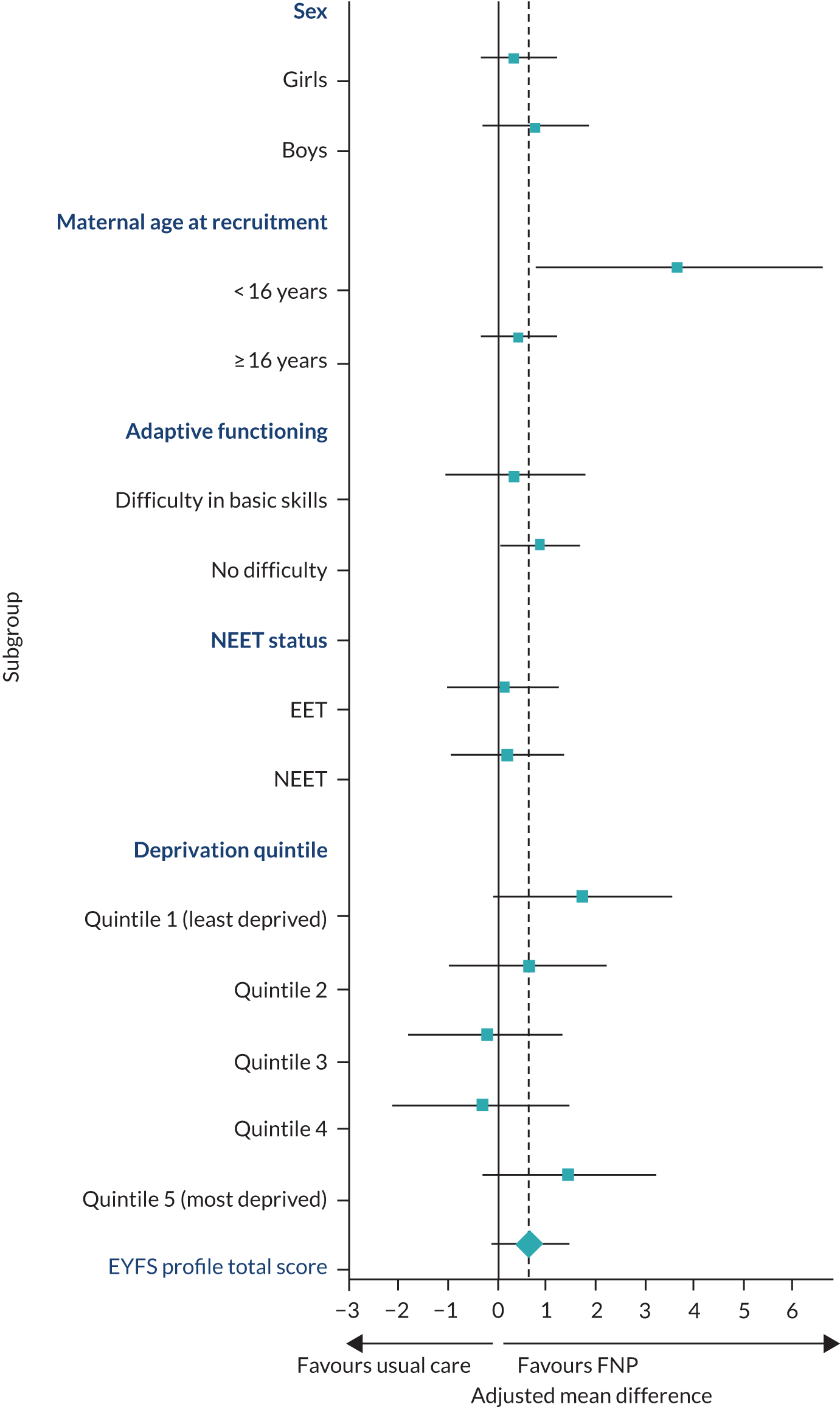
School absences
A total of 1494 children were included in the analysis (Table 17) for school absence. We define school attendance by examining the overall absence rate (overall absence sessions/total number of sessions) over the academic years available (2013 to spring 2017) and for all six terms per academic year. The majority of children had at least one absence; only 28 had full attendance. The distribution of the absence rate was skewed to the right, and the median overall absence rate was comparable between arms, at ≈5%. When this was dichotomised into children with no absence versus children with at least one absence, no difference was observed. When broken down into authorised and unauthorised absences, again, no evidence of a difference between arms existed.
| Outcome | FNP arm (N = 754) | Usual-care arm (N = 740) | Adjusteda OR (95% CI) | p-value |
|---|---|---|---|---|
| Number of sessions,b median (25th to 75th centiles) | 630 (264 to 638) | 630 (262 to 638) | ||
| Overall absence rate | ||||
| No absences, n (%) | 14 (1.9) | 14 (1.9) | Reference | |
| At least one absence, n (%) | 740 (98.1) | 726 (98.1) | 1.00 (0.47 to 2.12) | 0.998 |
| Absence rate, median (25th to 75th centiles) | 5.08 (2.69 to 8.73) | 5.19 (2.73 to 8.41) | ||
| Overall authorised absence | ||||
| No absences, n (%) | 26 (3.4) | 26 (3.5) | Reference | |
| At least one absence, n (%) | 728 (96.6) | 714 (96.5) | 1.01 (0.58 to 1.75) | 0.984 |
| Absence rate, median (25th to 75th centiles) | 3.50 (1.96 to 6.09) | 3.79 (2.02 to 6.11) | ||
| Overall unauthorised absence | ||||
| No absences, n (%) | 256 (34.0) | 245 (33.1) | Reference | |
| At least one absence, n (%) | 498 (66.0) | 495 (66.9) | 0.95 (0.76 to 1.18) | 0.620 |
| Absence rate, median (25th to 75th centiles) | 1.84 (0.76 to 4.34) | 1.57 (0.63 to 3.88) | ||
Key Stage 1 attainment
Key Stage 1 data were received in two tranches from the NPD: first, children assessed in the 2016/17 academic year (received in May 2018) and, second, the younger children who were assessed in 2017/18 (received May 2019). Reading, mathematics and science are examined for the whole cohort for children over both academic years. However, following changes made in the 2017/18 writing assessment (such that judgements in 2018 are not directly comparable with those made using the previous interim frameworks in 2016/17), writing was only statistically assessed using 2016/17 data, whereas the data from 2017/18 were described.
A total of 1472 children had KS1 data and were included in the analyses. A greater proportion of the sample was assessed in the 2016/17 academic year than in the 2017/18 academic year (985 vs. 487, respectively); there was good balance across arms (FNP arm: 50.5% in 2016/17 vs. 49.7% in 2017/18). For the reading, writing, mathematics and science assessments, there was no evidence of a difference between arms in the proportion of children reaching at least the expected standard, nor specifically in those working at the expected level or at a greater depth of knowledge (Table 18).
| KS1 assessment | FNP arm (N = 740) | Usual-care arm (N = 732) | Total (N = 1472) | Adjusteda parameter estimate (95% CI) | p-value | Absolute difference (95% CI) |
|---|---|---|---|---|---|---|
| Reading level, n (%) | ||||||
| Lower than expected | 257 (34.7) | 289 (39.5) | 546 (37.1) | Reference | ||
| Reaching at least the expected standardb | 483 (65.3) | 443 (60.5) | 926 (62.9) | 1.23 (0.99 to 1.53) | 0.051 | 4.8 (–0.2 to 9.7) |
| Expected standard | 371 (50.1) | 337 (46.0) | 708 (48.1) | 1.24 (0.99 to 1.56) | 0.056 | 4.1 (–1.0 to 9.2) |
| Higher standard | 112 (15.1) | 106 (14.5) | 218 (14.8) | 1.20 (0.88 to 1.65) | 0.250 | 0.7 (–3.0 to 4.3) |
| Mathematics level, n (%) | ||||||
| Lower than expected | 281 (38.0) | 283 (38.7) | 564 (383.) | Reference | ||
| Reaching at least the expected standardb | 459 (62.0) | 449 (61.3) | 908 (61.7) | 1.04 (0.84 to 1.28) | 0.731 | 0.7 (–4.3 to 5.6) |
| Expected standard | 392 (53.0) | 376 (51.4) | 768 (52.2) | 1.06 (0.85 to 1.32) | 0.611 | 1.6 (–3.5 to 6.7) |
| Higher standard | 67 (9.1) | 73 (10.0) | 140 (9.5) | 0.93 (0.64 to 1.35) | 0.711 | –0.9 (–3.9 to 2.1) |
| Science level, n (%) | ||||||
| Lower than expected | 203 (27.4) | 219 (29.9) | 422 (28.7) | Reference | ||
| Reaching at least the expected standardb | 537 (72.6) | 513 (70.1) | 1050 (71.3) | 1.14 (0.91 to 1.43) | 0.254 | 2.5 (–2.1 to 7.1) |
| Writing level, academic year 2016/17, n (%) | N = 498 | N = 487 | N = 985 | |||
| Lower than expected | 257 (51.6) | 278 (57.1) | 535 (54.3) | Reference | ||
| Reaching at least the expected standardc | 241 (48.4) | 209 (42.9) | 450 (45.7) | 1.24 (0.97 to 1.60) | 0.090 | 5.5 (–0.7 to 11.6) |
| Expected standard | 218 (43.8) | 182 (37.4) | 400 (40.6) | 1.29 (1.00 to 1.68) | 0.054 | 6.4 (0.3 to 12.5) |
| Higher standard | 23 (4.6) | 27 (5.5) | 50 (5.1) | 0.92 (0.51 to 1.64) | 0.769 | –0.9 (–3.8 to 1.9) |
| Writing level, academic year 2017/18, n (%) | N = 242 | N = 245 | N = 487 | |||
| Lower than expected | 82 (33.9) | 81 (33.1) | 163 (33.5) | |||
| Reaching at least the expected standardb | 160 (66.1) | 164 (66.9) | 324 (66.5) | Not tested, descriptive only | NT | –0.8 (–9.2 to 7.5) |
| Expected standard | 140 (57.9) | 132 (53.9) | 272 (55.8) | Not tested, descriptive only | NT | 4.0 (–4.8 to 12.7) |
| Higher standard | 20 (8.3) | 32 (13.1) | 52 (10.7) | Not tested, descriptive only | NT | –4.8 (–10.4 to 0.7) |
Additional adjustment for month of birth
What is observed from the writing assessment is the increase in the rates of children reaching at least the expected standard between the two academic years (overall, from 45.7% in 2016/17 to 66.5% in 2017/18). This is reflective of all assessments across the 2 academic years in each arm (Table 19). This is mainly explained by the distribution of births for the children for each academic year. Reflecting the recruitment period of the trial, children with KS1 results available in the academic year 2016/17 were born between October 2009 and August 2010, but the distribution of month of birth was skewed towards the summer months (42% were born between June and August 2010), whereas children appearing on the 2017/18 academic year were born between September 2010 and February 2011 (Figure 9).
| KS1 assessment | Trial arm | Academic year (%) | |
|---|---|---|---|
| 2016/17 | 2017/18 | ||
| Reading | FNP | 60.6 | 74.8 |
| Usual care | 54.0 | 73.5 | |
| Mathematics | FNP | 56.2 | 74.0 |
| Usual care | 54.0 | 75.9 | |
| Science | FNP | 68.5 | 81.0 |
| Usual care | 63.7 | 82.9 | |
FIGURE 9.
Distribution of children’s month of birth by trial arm. Source: NPD, DfE
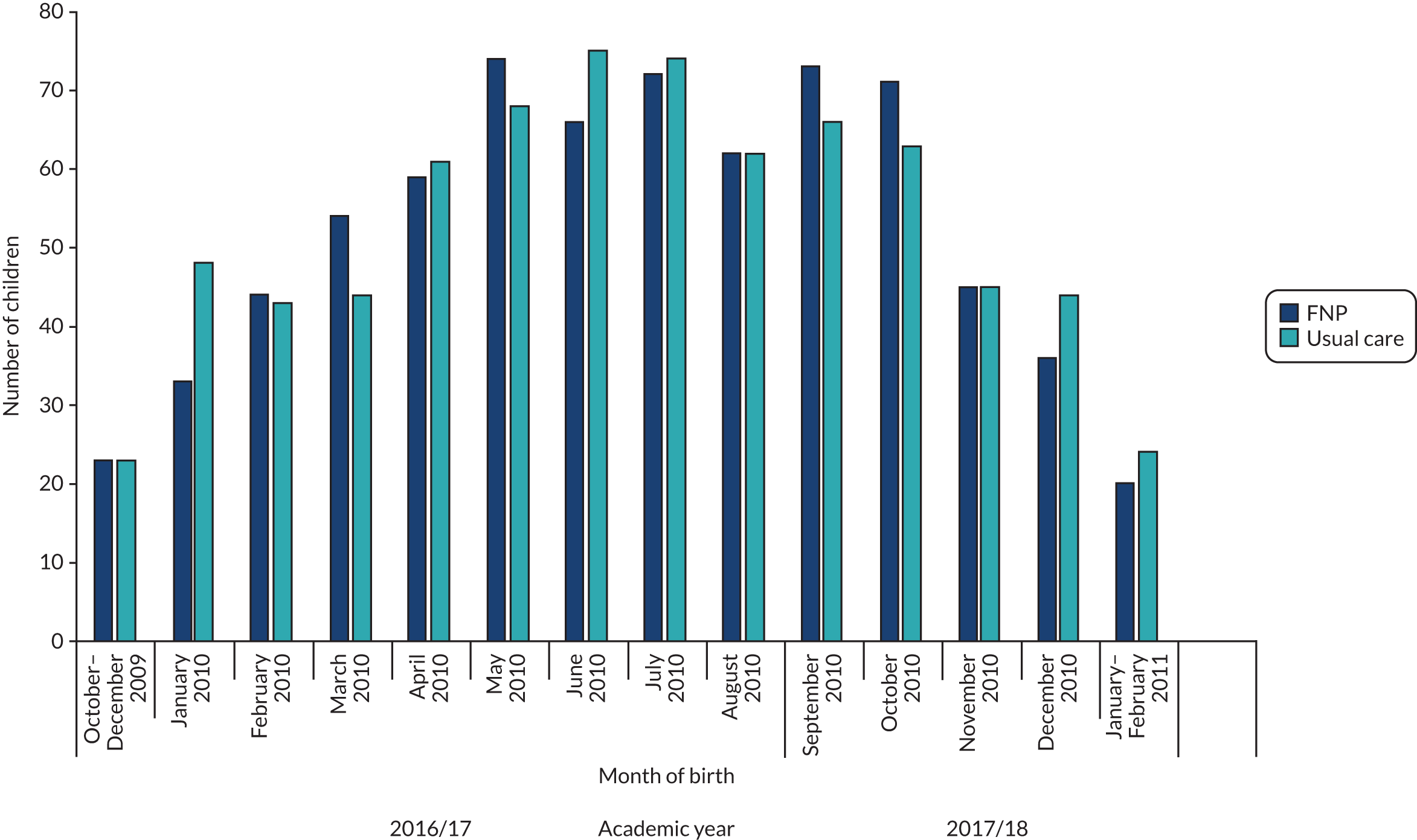
There is a nationally shown relationship between rates of children reaching the expected standard and month of birth, for example a 17% difference in reading level for children born in August and September. 70 Therefore, the 2017/18 cohort of children do not represent the whole academic year, but are biased towards those who are more likely to achieve the expected standard. This indicates that the rate of children reaching the expected standard varies by their month of birth, which is important as a moderator of programme effect. As a sensitivity analysis, the main analyses were adjusted for a child’s month of birth (categorised into quarter of birth); evidence of a between-arm difference was found in reading assessments (Table 20). In addition, the early-years assessments were also adjusted for a child’s month of birth (see Table 20), which strengthened the association found in Table 16.
| KS1 outcome | ORb (95% CI); p-value | |
|---|---|---|
| Adjusted for site and minimisation variablesc | Adjusted for site, minimisation variablesc and month of birth | |
| Reading level | ||
| Reaching at least the expected standard | 1.23 (0.99 to 1.53); 0.051 | 1.26 (1.02 to 1.57); 0.035 |
| Expected standard | 1.24 (0.99 to 1.56); 0.056 | 1.27 (1.01 to 1.59); 0.042 |
| Higher standard | 1.20 (0.88 to 1.65); 0.250 | 1.26 (0.91 to 1.75); 0.161 |
| Mathematics level | ||
| Reaching at least the expected standard | 1.04 (0.84 to 1.28); 0.731 | 1.06 (0.85 to 1.31); 0.613 |
| Expected standard | 1.06 (0.85 to 1.32); 0.611 | 1.07 (0.86 to 1.34); 0.527 |
| Higher standard | 0.93 (0.64 to 1.35); 0.711 | 0.93 (0.74 to 1.17); 0.522 |
| Science level | ||
| Reaching at least the expected standard | 1.14 (0.91 to 1.43); 0.254 | 1.16 (0.92 to 1.47); 0.197 |
| Writing level, academic year 2017/18 | ||
| Reaching at least the expected standard | 1.24 (0.97 to 1.60); 0.090 | 1.26 (0.98 to 1.62); 0.076 |
| Expected standard | 1.29 (1.00 to 1.68); 0.054 | 1.30 (1.00 to 1.69); 0.050 |
| Higher standard | 0.92 (0.51 to 1.64); 0.769 | 0.97 (0.54 to 1.75); 0.917 |
| Early-years assessment | ||
| Achieving a GLD in all five areas of learningd | 1.26 (1.03 to 1.55); 0.026 | 1.31 (1.05 to 1.62); 0.015 |
| Achieving a GLD in all 17 early-learning goals | 1.24 (1.01 to 1.52); 0.043 | 1.27 (1.03 to 1.58); 0.027 |
| Total point score | 0.65 (–0.11 to 1.41); 0.094 | 0.70 (–0.03 to 1.42); 0.060 |
Treatment efficacy on Key Stage 1 attainment
After adjusting for month of birth, we further explored treatment efficacy. Adjusting the analysis for FNP receipt, we observed an increase in the odds of an event occurring in the FNP arm, compared with the usual care arm, for every unit increase in FNP visits received. For all areas of learning (reading, writing, mathematics and science), adjusting the analysis for FNP receipt strengthens the effect of FNP. However, it is the reading and writing assessments for which, when the full dosage of 64 FNP visits is received, the odds reach statistical significance. For reading assessments, the odds of reaching the expected standard increase from 1.23 (95% CI 0.99 to 1.53; p = 0.051) in the main analysis to 1.38 (95% CI 1.07 to 1.77; p = 0.015). The efficacies per visit were as follows: reading, 1.005 (95% CI 1.001 to 1.009; p = 0.015); mathematics, 1.001 (95% CI 0.997 to 1.005; p = 0.535); science, 1.004 (95% CI 0.999 to 1.008; p = 0.112); and writing, 1.013 (95% CI 1.09 to 1.017; p = 0.001).
Subgroup analyses on Key Stage 1 attainment
The prespecified subgroup analyses (i.e. maternal age, NEET status, IMD quintile, adaptive functioning, and sex of child) are detailed in Appendix 8, Tables 46 and 47, for reading, mathematics and science and in Appendix 8, Table 48, for writing. They are also shown in Figures 10–13. There were no significant differences in the effect of the FNP between boys and girls [denoted by the p-value for comparison between two treatment effects (interaction only)], although the differences between boys and girls in the proportion of children reaching the expected level are large (and drive the significance of the overall interaction, including main effects). Effect differences for sex are seen for the writing assessment (which uses only data from academic year 2016/17). When examining how the intervention effects in each KS1 assessment differed for mothers aged < 16 years at recruitment, compared with mothers aged ≥ 16 years, differences were observed in mathematics and writing, with a larger effect seen in mothers aged < 16 years than for mothers aged ≥ 16 years at recruitment. None of these conclusions changed after adjusting for month of birth (post hoc analysis).
FIGURE 10.
Forest plot of estimates from the subgroups for reading. The vertical solid line represents no effect (OR 1), and the vertical dashed line indicates the overall treatment effect for the percentage reaching at least the expected standard in reading (aOR 1.26). EET, employment, education or training. Source: NPD, DfE.
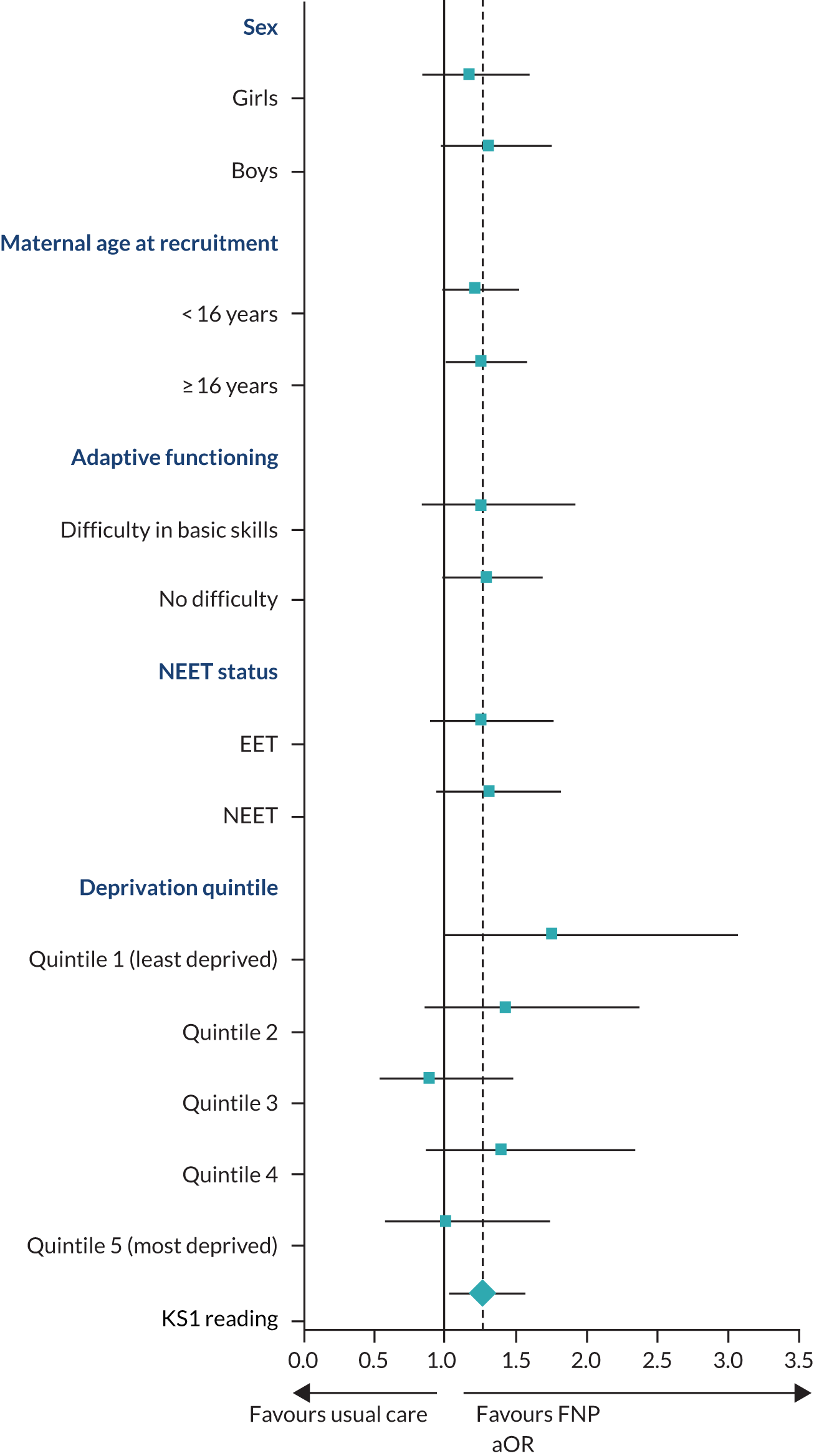
FIGURE 11.
Forest plot of estimates from the subgroups for mathematics. The vertical solid line represents no effect (OR 1), and the vertical dashed line indicates the overall treatment effect for the percentage reaching at least the expected standard in mathematics (aOR 1.06). EET, employment, education or training. Source: NPD, DfE.
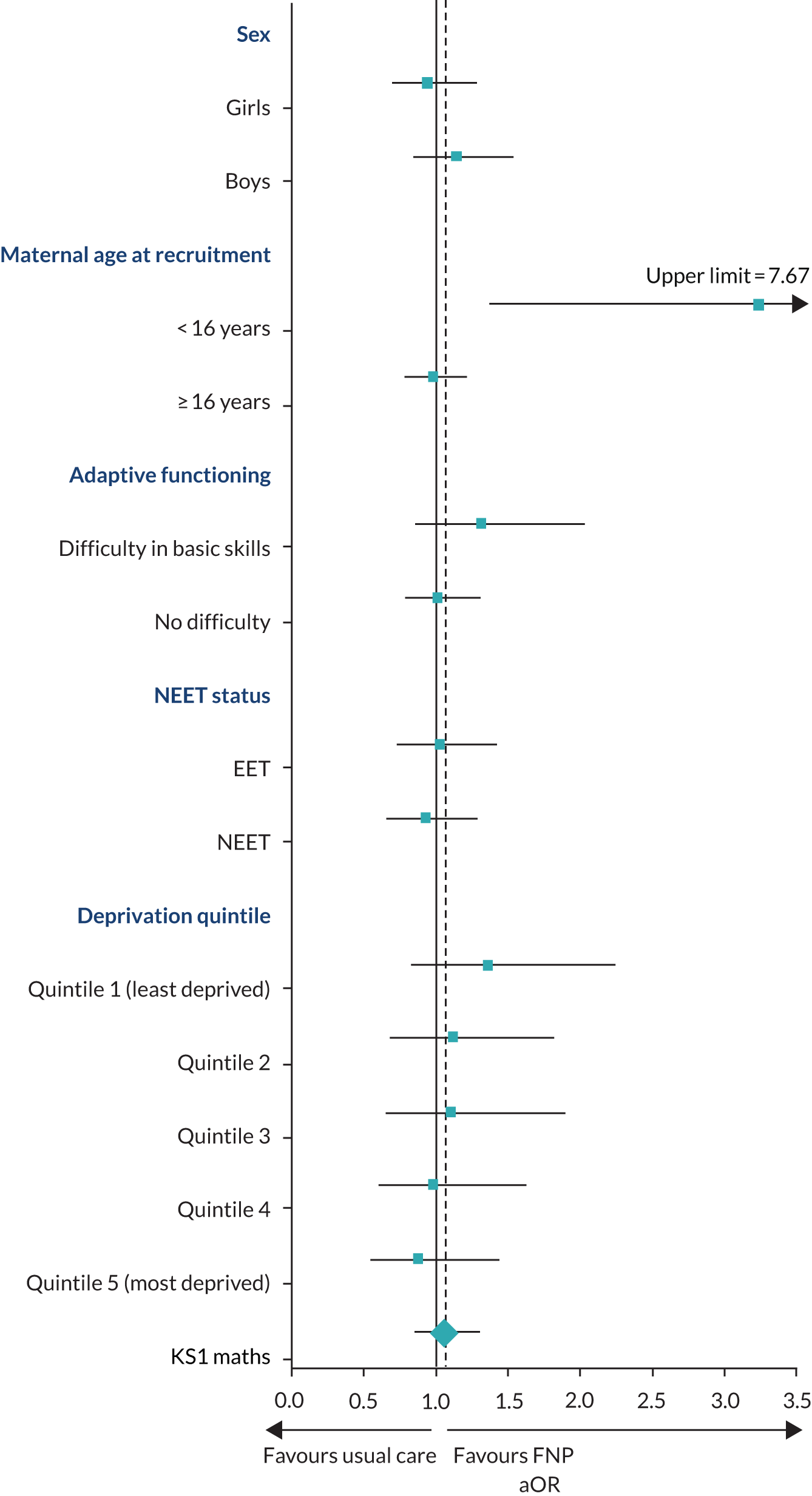
FIGURE 12.
Forest plot of estimates from the subgroups for science. The vertical solid line represents no effect (OR 1), and the vertical dashed line indicates the overall treatment effect for the percentage reaching at least the expected standard in science (aOR 1.16). EET, employment, education or training. Source: NPD, DfE.
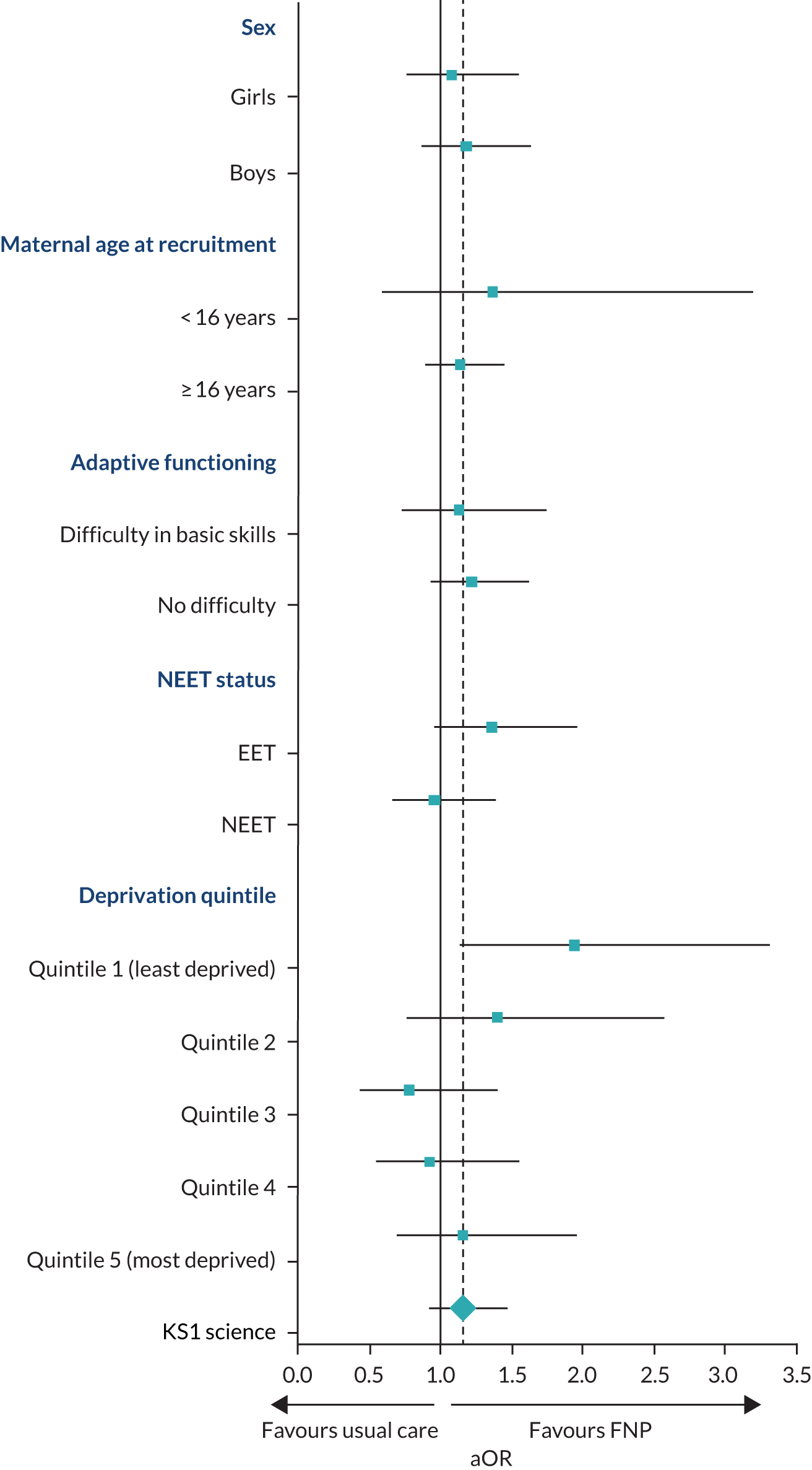
FIGURE 13.
Forest plot of estimates from the subgroups for writing. The vertical solid line represents no effect (OR 1), and the vertical dashed line indicates the overall treatment effect for the percentage reaching at least the expected standard in writing (aOR 1.26). EET, employment, education or training. Source: NPD, DfE.
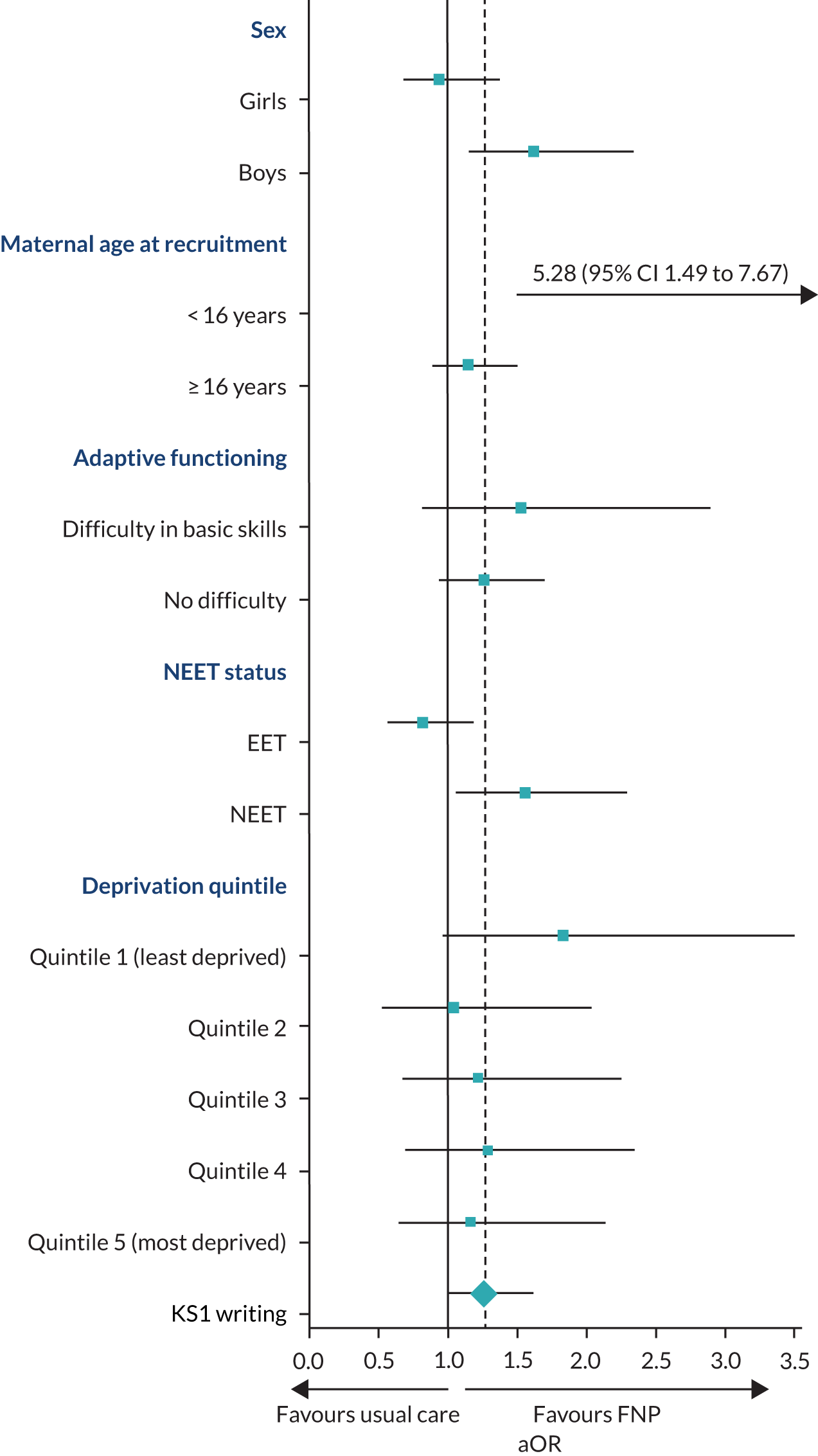
Exploratory analysis
Additional subgroup analyses
The role of potential moderators of programme effect on a child’s CIN status, early-years score, and KS1 outcomes were prespecified, including self-efficacy score, subjective social status score (personal and family) and social support score. No subgroup differences were found in intervention effect by any of these risk factors (see Appendix 5, Table 39; Appendix 7, Table 45; and Appendix 8, Table 49).
Composite index of risk
In addition, a composite index of risk based on baseline characteristics was created for CIN status and the proportion reaching the expected standard for reading at KS1. Models were developed using baseline maternal and child characteristics to predict CIN status to develop composite risk scores using the mother randomised to receive usual care (n = 774). For CIN status, 10 maternal risk factors were associated. Children were more likely to be defined as a CIN if their mothers had less than perfect health (EuroQol-5 Dimensions score), had difficulties in basic skills, were NEET, were younger, had less social support and fewer family resources, had ever been homeless, were more deprived and were a smoker. Apart from NEET, smoking and homelessness status, these all remained independently associated with CIN achievement (after being entered in a multivariable model) and were used to predict probabilities in both arms (see Appendix 5, Table 40, and Figure 18) (receiver operating characteristic = 0.68). Predicted probabilities are the probability of CIN status based on and calculated from the multivariable logistic regression model presented in Appendix 5, Table 40. These predicted probabilities were stratified into ‘low’ and ‘moderate to high’ risk of CIN status [predicted p < 0.5 (n = 1131) and predicted p ≥ 0.5 (n = 52), respectively]. Even though the moderate-/high-risk group had a higher proportion of children in need, no between-arm differences were found (see Appendix 5, Table 41).
For reading, three maternal factors were associated with reaching the expected standard at the univariable level: having no difficulty in basic skills, older maternal age and a higher personal social status. Two child factors were associated with reading achievement: being a girl and being born in the autumn/winter (vs. spring/summer). These all remained independently associated with reading achievement (after being entered in a multivariable model) and were used to predict probabilities in the intervention arm, as well as in the usual-care arm (see Appendix 8, Table 50 and Figure 19) (receiver operating characteristic = 0.68). These predicted probabilities were stratified into low risk and moderate to high risk of reaching the expected reading standard [predicted p < 0.7 (n = 1047) and predicted p ≥ 0.7 (n = 497), respectively]. These subgroups were then used to examine the intervention effect in each subgroup and were compared using an interaction term. No differential intervention effect was found between subgroups of risk (see Appendix 8, Table 51).
Care-experienced mothers
In addition, a subgroup analysis based on whether or not mothers were care-experienced at time of recruitment to the BB:0–2 trial was undertaken. This was defined from the CLA data set. Sixty-one mothers were identified as having experienced a period of care, four of whom were identified as care-experienced only after their BB:0–2 recruitment date. Duration of care was examined for 57 mothers, and the women randomised to receive the FNP experienced, on average, 9 months more care than women in the usual-care arm [FNP: median 40 months (25th to 75th centile 15.5 to 113.0 months); usual care: median 31 months (25th to 75th centile 7.0 to 69.5 months)]. After merging these care-experienced mothers with the children’s data set, 56 mothers remained; seven mothers were excluded from the subgroup analyses because their child did not have any NPD data. Children of these care-experienced mothers were at a higher risk of being defined as in need themselves, but no interaction was observed between trial arm and mothers’ care status (see Appendix 9, Table 52). The duration of the maternal care status as a possible mediator effect was also stated in the statistical analysis plan, but, similarly to domestic abuse, because of the lack of intervention effect in children’s CIN status, the need to examine the proportion of effect mediated by the duration of a mother’s care experience was redundant.
Predictors of care-experienced mothers
The main independent predictors of a mother ever having been in care at the time of recruitment in the BB:0–2 trial was age at recruitment (aOR 0.64, 95% CI 0.52 to 0.80; p < 0.001) and being homeless (aOR 2.2, 95% CI 1.16 to 4.17; p = 0.015), whereby being a younger mother and experiencing homelessness were associated with being in care at the time of recruitment (see Appendix 9, Table 53). Using the mothers’ care-experience status (in care or not) as a subgroup, the intervention effect was examined for two BB:0–2 trial outcomes: prenatal tobacco use (late pregnancy) and birthweight. There was no differential effect of the intervention in these two outcomes by maternal care status (see Appendix 9, Table 54).
State transitional model
State transition models using Markov chains were to be examined to assess the transition probabilities of moving from one state to another (i.e. subsequent to an initial social care referral), and to compare these between trial arms. Given the lack of evidence of a difference between arms in all of these states, no further analysis was required.
Chapter 6 Health economic results
This chapter presents the findings of the CCA conducted as part of the BB:2–6 study. Individual participant data were collected from available routine data sources for both study arms for the mother and child. Health-care resource use (Table 21) and associated costs (Tables 22 and 23) are described for both arms over the BB:2–6 study follow-up period. The incremental differences between the two arms are also reported (see Tables 22 and 23).
| Health-care resource | FNP arm | Usual-care arm | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n a | Mean | Median | Minimum | Maximum | n a | Mean | Median | Minimum | Maximum | |
| Mothers | N = 766 | N = 774 | ||||||||
| Resource use | ||||||||||
| Inpatient attendances | ||||||||||
| Overnight admissions (n) | 732 | 3.04 | 2 | 0 | 45 | 731 | 2.99 | 2 | 0 | 20 |
| Overnight length of stay (n nights) | 2329 | 2.32 | 1 | 1 | 170 | 2303 | 2.32 | 1 | 1 | 94 |
| Day admittances | 606 | 2.93 | 2 | 0 | 46 | 607 | 2.91 | 2 | 0 | 57 |
| All outpatient attendances | 746 | 23.29 | 19 | 0 | 184 | 740 | 22.61 | 19 | 0 | 175 |
| A&E visits (n) | 639 | 5.19 | 3 | 0 | 219 | 641 | 4.93 | 3 | 0 | 78 |
| Children | N = 773 | N = 774 | ||||||||
| Health-related resource use | ||||||||||
| Inpatient attendances: all | ||||||||||
| Overnight admissions (n) | 689 | 1.57 | 1 | 0 | 31 | 683 | 1.55 | 1 | 0 | 48 |
| Overnight length of stay (n nights) | 1214 | 3.57 | 2 | 1 | 248 | 1200 | 3.39 | 2 | 1 | 381 |
| Day admittances | 383 | 0.98 | 0 | 0 | 72 | 385 | 0.97 | 0 | 0 | 74 |
| Inpatient attendances: injuries and ingestions only | ||||||||||
| Overnight admissions (n) | 36 | 0.06 | 0 | 0 | 5 | 39 | 0.06 | 0 | 0 | 4 |
| Overnight length of stay (n nights) | 44 | 2.50 | 1 | 1 | 19 | 44 | 2.05 | 1 | 1 | 8 |
| Day admittances | 52 | 0.08 | 0 | 0 | 2 | 57 | 0.09 | 0 | 0 | 4 |
| Inpatient attendances: all, excluding injuries and ingestions | ||||||||||
| Overnight admissions (n) | 688 | 1.51 | 1 | 0 | 31 | 682 | 1.49 | 1 | 0 | 48 |
| Overnight length of stay (n nights) | 1170 | 3.61 | 1 | 1 | 248 | 1156 | 3.44 | 1 | 1 | 381 |
| Day admittances | 362 | 0.90 | 0 | 0 | 72 | 358 | 0.88 | 0 | 0 | 44 |
| All outpatient attendances | 581 | 6.89 | 3 | 0 | 124 | 577 | 7.44 | 3 | 0 | 240 |
| A&E | ||||||||||
| All A&E visits (n) | 691 | 4.93 | 3 | 0 | 50 | 686 | 4.62 | 3 | 0 | 39 |
| All A&E visits, excluding injuries and ingestions (n) | 633 | 3.80 | 1 | 0 | 46 | 619 | 3.52 | 0 | 0 | 35 |
| A&E visits, injuries and ingestions only (n) | 441 | 1.12 | 1 | 0 | 11 | 412 | 1.10 | 1 | 0 | 13 |
| Health-care resource | Mean resource use per participant | Mean cost per participant (£) | ||||
|---|---|---|---|---|---|---|
| FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | |
| Mothers | ||||||
| Health-related resource use | ||||||
| Inpatient attendances | ||||||
| Overnight admissions (n) | 3.04 | 2.99 | 0.05 | 2826.79 | 2844.58 | –17.79 |
| Overnight length of stay (n nights) | 2.32 | 2.32 | 0.00 | |||
| Day admittances | 2.93 | 2.91 | 0.02 | 1874.61 | 1890.11 | –15.50 |
| All outpatient attendances | 23.29 | 22.61 | 0.68 | 2244.62 | 2189.32 | 55.30 |
| A&E visits (n) | 5.19 | 4.93 | 0.26 | 411.34 | 392.03 | 19.31 |
| Total resource use | 7357.36 | 7316.04 | 41.32; p = 0.393 | |||
| Children | ||||||
| Health-related resource use | ||||||
| Inpatient attendances: all | ||||||
| Overnight admissions (n) | 1.57 | 1.55 | 0.02 | 1962.95 | 2033.71 | –70.76 |
| Overnight length of stay (n nights) | 3.57 | 3.39 | 0.18 | |||
| Day admittances | 0.98 | 0.97 | 0.01 | 744.94 | 724.90 | 20.04 |
| Inpatient attendances: all (excluding injuries and ingestions) | ||||||
| Overnight admissions (n) | 1.51 | 1.49 | 0.02 | 1883.44 | 1951.15 | –67.71 |
| Overnight length of stay (n nights) | 3.61 | 3.44 | 0.17 | |||
| Day admittances | 0.90 | 0.88 | 0.02 | 689.22 | 667.09 | 22.13 |
| Inpatient attendances: injuries and ingestions only | ||||||
| Overnight admissions (n) | 0.06 | 0.06 | 0.00 | 79.51 | 82.55 | –3.04 |
| Overnight length of stay (n nights) | 2.50 | 2.05 | 0.45 | |||
| Day admittances | 0.08 | 0.09 | –0.01 | 55.72 | 57.81 | –2.09 |
| All outpatient attendances | 6.89 | 7.44 | –0.55 | 673.24 | 727.79 | –54.55 |
| A&E | ||||||
| All A&E visits (n) | 4.93 | 4.62 | 0.31 | 395.73 | 366.83 | 28.90 |
| All A&E visits, excluding injuries and ingestions (n) | 3.80 | 3.52 | 0.28 | 305.12 | 280.20 | 24.92 |
| A&E visits, injuries and ingestions only (n) | 1.12 | 1.10 | 0.02 | 75.09 | 69.91 | 5.18 |
| Total resource use | 3778.13 | 3853.22 | –75.09; p = 0.865 | |||
| Consequence | OR (95% CI); p-value |
|---|---|
| CIN status recorded at any time during the follow-up period | 0.98 (0.74 to 1.31); 0.902 |
| Referral to social services | 0.97 (0.74 to 1.28); 0.829 |
| Child protection registration (CPP) | 1.04 (0.69 to 1.57); 0.846 |
| Details of a CPP | |
|
Reference |
|
2.77 (1.02 to 7.56); 0.046 |
|
1.25 (0.32 to 4.88); 0.743 |
|
1.13 (0.33 to 3.86); 0.848 |
| CIN categorisation | |
|
Reference |
|
0.95 (0.54 to 1.69); 0.868 |
|
1.47 (0.61 to 3.54); 0.389 |
|
2.38 (0.86 to 6.57); 0.093 |
|
1.47 (0.45 to 4.84); 0.525 |
| Looked-after status | 0.90 (0.52 to 1.57); 0.712 |
| Total length of care (in months) | 0.75 (0.65 to 0.86); < 0.001 |
| DNA appointments | |
|
1.00 (0.79 to 1.26); 0.997 |
| Injuries and ingestions | |
| Emergency attendance | |
|
Reference |
|
1.17 (0.95 to 1.45); 0.149 |
| Admission to hospital | |
|
Reference |
|
0.87 (0.63 to 1.20); 0.407 |
| Either hospital attendance and/or admission to hospital | |
|
Reference |
|
1.11 (0.89 to 1.37); 0.351 |
| SEN | 0.83 (0.67 to 1.03); 0.097 |
| Early-years assessment | |
|
1.26 (1.03 to 1.55); 0.026 |
|
1.24 (1.01 to 1.52); 0.043 |
| School attendance | |
| Overall absences | |
|
Reference |
|
1.00 (0.47 to 2.12); 0.998 |
| Overall unauthorised absences | |
|
Reference |
|
0.95 (0.76 to 1.18); 0.620 |
| Overall authorised absences | |
|
Reference |
|
1.01 (0.58 to 1.75); 0.984 |
| KS1 attainment | |
| Reading | |
|
Reference |
|
1.23 (0.99 to 1.53); 0.051 |
| Writing, academic year 2016/17 | |
|
Reference |
|
1.24 (0.97 to 1.60); 0.090 |
| Mathematics | |
|
Reference |
|
1.04 (0.84 to 1.28); 0.731 |
| Science | |
|
Reference |
|
1.14 (0.91 to 1.43); 0.254 |
In terms of consequences, the primary outcome (CIN status) of the BB:2–6 study and key secondary outcomes (objective and associated measures of maltreatment; and child health, developmental and education) are listed for both study arms (see Tables 22 and 23).
To envisage the full extent of the impact of the FNP on costs and consequences over the medium term, the benefits against the intervention costs for FNP and costs associated with health and non-health care resource use as reported in the BB:0–2 trial are also presented: these include the overall costs associated with the FNP, compared with usual care, for the full period of follow-up across both the BB:0–2 trial and the BB:2–6 study (see Appendix 10, Tables 55 and 56).
Analysis of health-care resource use and costs
The mean secondary health-care resource use for each participant (mother and child separately) between 2 and 6 years of follow-up is shown in Table 21. For both health-care resource use and associated costs, negligible incremental differences were observed across each resource type for both mothers and children. Resource use was generally slightly lower in the usual care arm than in the FNP arm across most categories, as detailed in Table 21.
Conversely, although small, the cost differences tended to be slightly lower for the FNP arm than for the usual-care arm. As resource data were costed individually, it is possible for costs to vary depending on what visits entailed (i.e. more complicated visits will incur a greater cost than less complicated visits of the same duration). Therefore, it is possible for one arm to have less, or equal, resource use than the other arm, but still incur a greater cost. This approach enables presentation of actual resource use and costs, based on recorded routine data for individual participants.
For mothers, the greatest mean resource use over the BB:2–6 study period was seen for outpatient attendances [23.29 (95% CI 21.83 to 24.75) for the FNP arm vs. 22.61 (95% CI 21.25 to 23.97) for the usual-care arm, mean difference 0.68; p = 0.356]. This was followed by A&E attendances [5.19 (95% CI 4.47 to 5.91) for the FNP arm vs. 4.93 (95% CI 4.42 to 5.44) for the usual-care arm, mean difference 0.26; p = 0.515], overnight admissions [3.04 (95% CI 2.83 to 3.25) for the FNP arm vs. 2.99 (95% CI 1.19 to 4.79) for the usual-care arm, mean difference 0.05; p = 0.500] and day admissions [2.93 (95% CI 2.68 to 3.18) for the FNP arm vs. 2.91 (95% CI 2.62 to 3.20) for the usual-care arm, mean difference 0.02; p = 0.589]. Similarly, for children, the greatest resource use was observed for outpatient attendances [6.89 (95% CI 6.02 to 7.76) for the FNP arm vs. 7.44 (95% CI 6.26 to 8.62) for the usual-care arm, mean difference –0.55; p = 0.821], followed by A&E visits [4.93 (95% CI 4.56 to 5.30) for the FNP arm vs. 4.62 (4.29 to 4.95) for the usual-care arm, mean difference 0.31; p = 0.292], overnight admissions (all cases) [1.57 (95% CI 1.43 to 1.71) for the FNP arm vs. 1.55 (95% CI 1.40 to 1.70) for the usual-care arm, mean difference 0.02; p = 0.882] and day admissions (all cases) [0.98 (95% CI 0.78 to 1.18) for the FNP arm vs. 0.97 (95% CI 0.76 to 1.18) for the usual-care arm, mean difference 0.01; p = 0.883].
Resource use and costs associated with the FNP arm, compared with the usual-care arm, are reported in the cost–consequences balance sheet (see Tables 22 and 23) for both mothers and children. For children, these were also stratified as all attendances, all attendances excluding injuries and ingestions, and injury and ingestion attendances only. Secondary care costs for all attendances were generally slightly lower for the FNP group than for the usual-care group. Overnight inpatient stays for both mother [£2827 (95% CI £2709 to £2944.19) for the FNP arm vs. £2845 (95% CI £2735 to £2954) for the usual-care arm, mean difference –£17.79; p = 0.521] and child [£1963 (95% CI £1669 to £2257) for the FNP arm vs. £2034 (95% CI £1638 to £2429) for the usual-care arm, mean difference –£70.76; p = 0.586] were the main drivers of costs; both were lower in the FNP arm than in the usual-care arm, but, again, the differences were negligible. The incremental differences in costs were small for mother and child over the BB:2–6 study period, but the FNP arm generally incurred slightly lower costs than the usual-care arm. The greatest incremental difference observed for mothers was in outpatient attendances (£55.30; p = 0.398), and favoured usual care over FNP. For children, the highest resource costs were associated with overnight admissions, followed by day admissions [£744.94 (95% CI £539.06 to £950.82) for the FNP arm vs. £724.90 (95% CI £550.38 to £899.42) for the usual-care arm, mean difference £20.04; p = 0.804], outpatient attendances [£673.24 (95% CI £586.49 to £759.99) for the FNP arm vs. £727.79 (95% CI £605.94 to £814.54) for the usual-care arm, mean difference –£54.55; p = 0.838], and A&E visits [£395.73 (95% CI £365.51 to £425.95) for the FNP arm vs. £366.83 (95% CI £340.45 to £393.21) for the usual-care arm, mean difference £28.90; p = 0.208].
When compared with the cost–consequences balance sheet from the BB:0–2 trial32 (costs are shown in Appendix 10), a similar pattern emerges for both studies, that is lower costs for inpatient stays and higher costs for outpatient attendances for FNP participants than for usual-care participants. However, unlike the BB:0–2 trial, the BB:2–6 study found higher A&E costs for FNP participants. Similar to the BB:0–2 trial, inpatient stays were the biggest driver of costs among mothers, but, unlike the BB:0–2 trial, they were not the greatest driver of cost difference; this was observed in outpatient attendances, and favoured the FNP over usual care. For children, however, inpatient stays were the biggest driver of both cost and incremental cost difference.
Sensitivity analysis
Each health-care resource analysed was coded and costed using the NHS Digital Reference Cost grouper,71 with each episode costed as it would have cost the NHS. This approach is more detailed and comprehensive than applying an average resource unit cost to each resource unit consumed and gives a more accurate picture of costs. 72 As costs were assigned based on the year that the resource use was consumed, it was possible that costs could be affected by inflation; therefore, sensitivity analyses were undertaken using different discount rates (1.5% and 3.5%). Using a discount rate of 1.5% instead of 3.5% showed no real difference in costs between FNP and usual care.
Analysis of costs and consequences
The CCA shows that there are no significant differences between the FNP and usual-care groups with respect to the primary study outcome of CIN status (OR 0.98, 95% CI 0.74 to 1.31; p = 0.902), balanced with little difference in secondary health-care costs over the medium term. In general, with respect to the secondary study outcomes (1) objective measures of maltreatment; (2) associated measures of maltreatment; and (3) child health, developmental and educational outcomes, no significant differences were observed between the trial arms, other than in the early-years assessment, for which, for both achieving a GLD in all five areas of learning (p = 0.026) and achieving a GLD in all 17 early-learning goals (p = 0.043), the results favoured FNP over usual care.
Summary
In summary, the BB:2–6 study shows minor differences in resource use and costs between the FNP and usual-care groups, for mother and child, over the BB:2–6 study follow-up period. This is mirrored in the consequences, for which analysis showed no benefit in the primary outcome, and with significant differences, favouring FNP, observed in only two of the secondary outcomes.
Chapter 7 Public involvement
Content in this chapter has been reproduced from the published feasibility study paper by Lugg-Widger et al. 31 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article). This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Aim
The aim of the public involvement activities was to involve and value lay input to optimise the quality of the research and its impact on policy and practice. We applied this aim to three main aspects of the study: data-linkage methods, study outcomes and dissemination of study findings. To meet the overall aim, the public involvement activity in the study had the following objectives:
-
To optimise the acceptability of the proposed models for dissent and data linkage in the BB:2–6 study to the study cohort.
-
To understand the acceptability of data linkage to members of the public. Acceptability here relates to the kinds of participant-level data collected, for example hospital attendance, child maltreatment, the linking of self-report and routine data, and how issues of consent or dissent are dealt with.
-
To ensure that communication with research participants explains issues relating to data linkage in a clear manner, including points relating to how their data are used, the security and de-identification processes employed, and participants’ rights in relation to consent/dissent.
-
To seek the views of members of the public on the importance of the study outcomes being measured and how best to present them in dissemination activities.
-
To consult on how to communicate the study’s findings to research participants (selection of dissemination methods, formatting of results presentation).
-
To assess how the public involvement methods used impact the quality and conduct of the research.
Thus, objectives 1–3 concerned data linkage, whereas objective 4 was related to the presentation of study outcomes, and which (if any) might be prioritised for inclusion in dissemination materials. Objective 5 covered the communication of study findings to participants, and objective 6 assessed the impact of the public involvement work and the extent to which we achieved our aim and objectives. Methods for and outcomes from work relating to objectives 1–5 are presented in this chapter. Objective 6 is addressed in Chapter 8, where we assess the extent to which the public involvement work addressed the aim and objectives.
Methods
The approach to public involvement
The activities involved four main groups: (1) CASCADE Voices, (2) Our Place, (3) FNP graduates and (4) The Advice Leading to Public Health Advancement (ALPHA) group. We worked with these four groups because they include representation of key demographic characteristics of the study participants (e.g. age, parenthood status) to a greater (FNP graduates, Our Place) or lesser extent (ALPHA group). We deliberately chose to involve members of the public who had been supported by the FNP, and individuals with experience of other similar interventions (e.g. those providing support to parents/carers), as these groups would have perspectives that were highly relevant to the focus of this study. We also anticipated that the insights from this study might have relevance for other evaluations of interventions that support parents/carers. Use of data linkage to complement and extend data collection by randomised controlled trials is now becoming more commonplace. Therefore, it is likely that the key insights from our work on the acceptability of, and communication of, data-linkage methods to research participants could be of direct relevance to other studies. We have also included both existing advisory groups (CASCADE Voices, ALPHA group), whose members have had some research training, and members of the public who have not previously undertaken such a role (e.g. FNP graduates) to provide contrasting perspectives. The three established groups (ALPHA group, Our Place, CASCADE Voices) have a scrolling membership that naturally changes over time.
Groups providing lay input to the study
CASCADE Voices
CASCADE Voices is a group of care-experienced young people who advise on research projects from design to dissemination. 47 The group was set up by Cardiff University in collaboration with Voices from Care Cymru. The group has received research methods training and typically provides input on participant information (primarily for children/young people), suggested methods for gathering data, ethics issues, setting research questions and developing dissemination materials (posters, videos, blogs). CASCADE Voices meets every 2 months; we requested on two occasions that the group review study documentation. This was facilitated by one of the original co-applicants (Sally Holland), who acted as the intermediary between the research team and CASCADE Voices.
Our Place
The Our Place group – funded by Children in Need and the Big Lottery – is a network of parents (mainly mothers) aged 16–24 years who have children aged 0–2 years. Our Place provides a programme of support for young parents through which they can build their emotional resilience to establish healthy, independent and happy lives. Its aims are to create an accessible, friendly meeting place for young mothers to increase their well-being and reduce their isolation; to give participants the opportunity to learn, question and examine choices, empowering them to make positive decisions; and to identify models in the programme that will effect change in lifestyles that will then be used to give young parents the voice to inform policy and influence policy-makers. The group meets weekly, and each session lasts approximately 3 hours. A different learning activity (lasting 1.5 hours) is included in each session, and the group has covered a broad range of topics including first aid, healthy relationships and personal finance. External visitors often talk to the group. A key aim of the Our Place group is to develop participants’ skills and build their self-confidence. Mothers and their children attend the sessions together (there is no child-care or crèche facility, but a child-care assistant is present to help mothers as necessary). Two members of staff are employed to support mothers during learning activities. The research team liaised with the Our Place co-ordinator to attend a number of their meetings throughout the project. The group has given advice on several research projects. Our Place also provided lay input during the BB:0–2 trial.
Family Nurse Partnership graduates and service users
Identification and recruitment of graduates of the FNP (i.e. former clients) involved liaising with FNP practitioners in Bath and Bristol (areas that were not involved in the BB:0–2 trial and, therefore, were not involved in the BB:2–6 study cohort). We also approached individuals who were currently receiving FNP support (again, via the FNP teams) and who were near the point of graduation (again, to be recruited through the FNP teams in those locations). Owing to recruitment difficulties experienced, we also contacted graduates in Wiltshire (although, for this location, we did not organise any group-based meetings; instead, we focused on one-to-one contact with graduates/FNP clients). Confirmation that we would include engagement with FNP graduates as part of our public involvement activities was a condition of approval from the HRA CAG when requesting section 251 support. We outlined our intention to work with members of the public in our application, but did not explicitly mention that this would include FNP graduates (although it was always our intention to involve them). The HRA CAG did not give a specific reason for seeking confirmation of involvement of FNP graduates (or link this to any concerns about our application). Nevertheless, we considered that FNP graduates could provide important insights.
In Bath and Bristol, we invited FNP graduates to attend meetings specially arranged by us, with the intention of holding group discussions. However, when difficulties were encountered with recruitment to these groups, we sought additional assistance from FNP teams to gather input from graduates (and clients approaching graduation) on a one-to-one basis or through informal groupings (e.g. one or two graduates who may be accompanied by friends).
The Advice Leading to Public Health Advancement group
The ALPHA group is the Centre for Development, Evaluation, Complexity and Implementation in Public Health Improvement (DECIPHer) research advisory group of young people aged 14–25 years. 73 The ALPHA group meets approximately monthly and provides input on studies across the DECIPHer research portfolio by discussing and debating its views on public health topics and research projects. A co-applicant part-based in DECIPHer enabled the research team to attend one of their meetings.
Involvement in committees and meetings
An independent lay representative was included on the SSC. This individual provided input on the dissent model undertaken during the first BB:2–6 SSC meeting. We considered that public involvement was best achieved by engaging with groups of members of the public, rather than including a lay representative on the Study Management Group (SMG). Accordingly, insights and feedback from the lay groups were fed back to the SMG and fed into the study decision-making processes. It should be noted that we also included professional representation (e.g. medical and social work academics) on the SSC, which ensured that such perspectives were also considered.
Roles of the research team in public involvement activities
Jeremy Segrott and Fiona Lugg-Widger led the public involvement activities. Working to the study’s public involvement protocol, they recruited organisations and public involvement participants, arranged meetings, and prepared and ran activities at these meetings. Additional team members also helped facilitate sessions with Our Place (LA and JK) and the ALPHA group (Peter Gee and LA). Fiona Lugg-Widger led all aspects of the design and development of an animation being developed to explain the use of routine data in research to members of the public. Members of the SMG (MR, JSa and GM) provided strategic input on the development of the public involvement objectives, implementation of activities, and evaluation of the extent to which objectives had been met.
A summary of the planned activities with each group, the objectives that they were designed to achieve, when they took place and the number of individuals involved is provided in Table 24.
| Group | Activity | When held | Purpose of activities | Meets objective (1–5) | Number of people attending |
|---|---|---|---|---|---|
| CASCADE Voices | Meeting 1 | May 2014 | Test acceptability and clarity of dissent documentation to be sent to study cohort | 1 | Not recorded |
| Meeting 2 | November 2014 | Test acceptability and clarity of dissent documentation to withdrawn participants of the study cohort | 1 | Not recorded | |
| Our Place | Meeting 1 | January 2017 | Discuss acceptability of data-linkage procedures, and how to explain these procedures to members of the public | 2, 3 | 20 mothers |
| Meeting 2 | September 2018 | Explore prioritisation and communication of key outcomes to members of the public; discuss dissemination modes/format | 4, 5 | 10 mothers | |
| Meeting 3 | September 2018 | Review animation script (describing routine data) | 3 | 4 mothers | |
| ALPHA | Meeting 1 | August 2018 |
|
3, 4, 5 | 6 (3 male, 3 female) |
| FNP graduates | Meeting 1 | Bristol, May 2018 | Explore prioritisation and communication of key outcomes to members of the public; discuss dissemination modes/format | 4, 5 | No participants attended (cancellations or no-shows) |
| Meeting 2 | Bath, June 2018 | Explore prioritisation and communication of key outcomes to members of the public; discuss dissemination modes/format | 4, 5 | No participants attended (cancellations or no-shows) | |
| Meeting 3 | Westbury, October 2019 | Explore prioritisation and communication of key outcomes to members of the public; discuss dissemination modes/format | 4, 5 | One (one-to-one meeting with FNP graduate) |
Planned activities
Public involvement work initially focused on objective 1 (communication with the BB:2–6 study cohort concerning data linkage). We worked with one of the groups with which we had an existing link (CASCADE Voices) and that had experience of providing input on research materials. For the remaining public involvement objectives (2–5) (covering data linkage, study outcomes and dissemination methods), we worked with Our Place (to capture the views of mothers with young children), ALPHA (to explore the views of young people more generally) and FNP graduates (who had direct experience of the intervention). For objectives 2–4, we worked with groups (e.g. ALPHA) on multiple aspects of the study, which necessitated a number of meetings to be organised. Difficulties in engaging with FNP graduates meant that we spent a significant amount of time developing and implementing recruitment strategies for this group.
Optimising the acceptability of data linkage in the BB:2–6 study to the study cohort (objective 1)
We asked members of CASCADE Voices to test the acceptability and clarity of the dissent documentation, including the letter that would be sent to the study cohort, as well as the planned dissent procedure (i.e. requiring participants to contact the research team to register their dissent). The focus here was on materials and processes to support the use of data linkage in the study, rather than the essential study design. Nevertheless, it was expected that the principle of routine data linkage would be discussed. The meeting with CASCADE Voices took place prior to us submitting documents to both the REC and the HRA CAG. Following a later decision to submit an amendment to enable the team to contact participants who had withdrawn from the BB:0–2 trial, a second letter for this subgroup was drafted. The CASCADE Voices group was asked to input on this letter. In particular, we aimed to ensure that wording clearly reflected that we knew that these mothers had withdrawn early from the BB:0–2 trial and were now being contacted about a follow-on study.
Meeting with Our Place to discuss data linkage (objectives 2 and 3)
The first session with Our Place in early 2017 aimed to provide an overview of the BB:2–6 study, and explored (1) the acceptability of the strategies being used by the BB:2–6 study to link self-report data with routinely collected health, education and social care data held by external organisations (and whether or not this depended on the nature of the information being collected) and (2) how best to explain the data-linkage processes being used in the BB:2–6 study to members of the public. Discussion covered arrangements for participant consent, the type of data to be collected, and how the data are used during the analysis and dissemination phases. Through these discussions, we also aimed to understand the views on the acceptability of data linkage in research studies more generally, so that lessons from the current study could be applied to future activity. For all activities, some didactic material/background was required (e.g. familiarisation with the study intervention and design), followed by discussions with the group members, and this approach was adopted for subsequent meetings with all the groups we worked with (adapted as necessary).
Animation development
Following suggestions from the first meeting held with Our Place, the development of an animation was considered to help explain the concepts of routinely collected data and data linkage. We intended to expand one of the dissemination sessions to incorporate the co-production of an animation with a graphic design company. This included developing a script and storyboard with the group and a representative from the animation company. Following the session, the animation company was able to develop a prototype animation about the nature, value and safeguards of using routinely collected health, social and other public sector data in research. This was then to be fed back at subsequent sessions and is an output of this public involvement work.
Activities to discuss presentation of study outcomes and dissemination methods (objectives 4 and 5)
Over the course of 2018, we planned four meetings: one with Our Place, one with the ALPHA group and two with FNP graduates. The aim was to co-produce a strategy and identify methods for disseminating the results to lay stakeholders.
The goals of these meeting were to (1) explore which key concepts need to be conveyed to lay stakeholders when disseminating study results (e.g. data linkage, maltreatment, understanding effect size, group differences, using evidence from research to influence policy); (2) assess the clarity and understanding of key terms used in planned dissemination materials; (3) consider participants’ views on which outcomes might be prioritised for inclusion in dissemination activities, and the rationale for this; (4) explore different modes of dissemination (e.g. paper-based, electronic, social media); and (5) explore different formats of presenting results (use of text, imagery, animations, etc.).
For the activities relating to study outcomes, we began by considering the study’s primary outcome before turning to the secondary outcomes. We then asked participants to give their views on the relative importance of the study’s secondary outcomes, and which outcomes might be prioritised for inclusion in dissemination. For the term maltreatment and the primary outcome of CIN status, we asked participants to consider (1) their initial understanding of both these terms (without elaboration or explanation from the research team) and (2) their thoughts on our own definitions (the extent to which they were clear and unambiguous, and the degree of alignment with their initial understandings).
Ethics issues
We were not asking members of the public involvement groups to talk directly about their own experience of topics the study is collecting data on (e.g. child maltreatment, parental well-being). However, we recognised that the discussions we held would cover sensitive topics that may have the potential to upset members of the groups (e.g. those who have experienced trauma such as domestic abuse), and that we might identify support needs or safeguarding issues. These issues were carefully considered in terms of the language we used, how we interacted with individuals and the provision of clear policies/procedures. This included making clear at the start of group discussions what information we would be collecting and how it would be used, ensuring that participants understood that we were not asking them to be research participants or to receive the intervention (FNP) being discussed and identifying a key contact in/linked to each group to whom we could signpost any individuals who became upset or expressed a support need.
We provided information to all potential members of the public involvement groups on what participation would involve via information sheets and by discussing these issues with the Our Place and ALPHA group leaders and the FNP practitioners who assisted us with recruitment. Audio-recording was planned for some of the sessions, for which verbal agreement was obtained.
Feedback and monitoring
For each of the groups that we worked with, we asked participants if they would be interested in receiving feedback on the ways in which we used their ideas and suggestions, and offered to do this either by a physical face-to-face meeting (e.g. attending Our Place) or through other means if they preferred.
Results
Optimising the acceptability of data linkage in the BB:2–6 study to the study cohort: dissent documentation (objective 1)
Members of CASCADE Voices provided input on the letter that we planned to send to the study cohort, and also the version of the same letter that would go out to withdrawn participants (from the BB:0–2 trial). Feedback covered both the process we were adopting (e.g. the dissent model) and the way in which this was presented in our draft letter to participants. The young people were concerned that people who had already expressed a wish to withdraw from the earlier study were now being contacted further. The group felt that a participant’s decision to withdraw was not being respected and stated that they would expect them to feel angry at being contacted again. The process for registering their dissent from the BB:2–6 study was seen as too difficult. The group felt that it would be more appropriate to ask people to opt in if they were happy for their data to be used, as opposed to having to text and engage in a further telephone call if they wanted to maintain their original decision to withdraw. The process to withdraw from the study was further criticised as it would incur a cost (text/call charge) to the participant. The young people felt that it was unclear what they should text, felt uneasy about having no named person to contact and were concerned about members of the study team having their mobile number. The group were also unclear about why it was necessary to have a further telephone call and expressed concern that they would be put under further pressure to participate. As an alternative, the group suggested sending the letter with an opt-in/-out slip using only the identifier number, together with a freepost envelope. The young people felt that it was not clear that the letter was directed at people who had left the BB:0–2 trial. The group expressed concern about the information sought by the study. Despite the bold wording emphasising anonymity, the group spoke at length about anxieties regarding the use of such personal information and what would be done with it. The reactions from the group suggested that those receiving the letter could feel concerned/upset by it. The young people stated that the letter should make clear who would have access to the information and why it was necessary. They indicated that this should make explicit the potential benefit/purpose of contacting people who had previously withdrawn.
Feedback from CASCADE Voices was used to modify the letters sent to the study cohort (both those participants who had not withdrawn from the BB:0–2 trial and those who had). Final versions are included in Appendix 12. To address the concerns and suggestions made by the group, the following changes were implemented:
-
Inclusion of additional headings and highlighting of text to emphasise key points that the young people felt needed to stand out more.
-
A clearer description of the rationale for a follow-on study to the BB:0–2 trial, particularly the importance of identifying whether or not longer-term impacts identified in previous (non-UK) studies of FNP were replicated in a UK setting.
-
Describing in more detail how the data being collected would be used, and who would have access to them (e.g. only the research team would be involved in analysis, and would not know the identity of any individual when doing so).
-
Providing multiple ways in which individuals could contact the research team (e-mail, text, telephone) and minimising the costs by offering to call participants back.
-
Providing clarity on what people would have to do if they wished to dissent (e.g. what they would need to say when contacting the research team). We provided additional explanation about the need to speak with participants by telephone (after their initial contact), so that we could confirm their identity and be certain that we knew which participant had made contact.
-
When possible, including named individuals as points of contact. This was not always feasible (e.g. when multiple staff members might answer telephone calls or be responsible for processing dissent requests).
-
The letter was revised to make clear that we were not conducting any further interviews/questionnaires with participants. This revision was designed to address concerns raised by CASCADE Voices that withdrawn participants might question why they were being asked to personally contribute additional information for the study in the form of direct contact with the research team.
Acceptability and communication of data-linkage methods (objectives 2 and 3)
Audio-recording of the discussion with Our Place mothers proved impracticable because of background noise; contemporaneous notes were taken instead. Twenty mothers (and their children) were in attendance at the meeting, so two groups with six and five mothers each spent time with the researchers separate to the main group to discuss data linkage and its use in more detail. Representing the data-linkage process using A3 sheets (for organisations) and A4 sheets (for data sets) and how anonymity was preserved when data were accessed by the research team appeared to be informative for participants. The group expressed preferences for a greater use of visual methods (e.g. pictures to represent organisations). The ease with which individuals could be identified through combining data across data sets arose as a question from the group. Members were content with the data-linkage procedure described and with reassurances about anonymity; nevertheless, concern was expressed about data being secured against hacking. The nature of the data being held (e.g. more sensitive data on maltreatment) did not affect the perceived acceptability of the linkage approach. One participant asked about the possibility of individuals requesting their own data, which may suggest that there remained some lack of clarity about the non-reversibility of anonymisation. One important area where some disagreement within the group arose was the use of the dissent model. The group appeared to be mostly supportive of this approach, given the original consent provided in the preceding trial, the efforts made by the researchers to contact women and the pseudonymisation of data involved. However, some participants preferred an opt-in approach as a general principle.
Animation development
Based on insights from the initial meeting with Our Place and drawing on our own reflections of communicating data linkage to the study cohort, key topics and messages for the animation were identified. Fiona Lugg-Widger prepared a draft script for the animation, which was discussed by the SMG. In the session with ALPHA, the group was split into pairs. Each pair was asked to read through the draft script and to suggest images that could be used to illustrate key points. During feedback from each pair, we were able to produce some potential visuals (Figures 14 and 15), and we also sought feedback from participants on any parts of the script that they felt were unclear or could be improved.
FIGURE 14.
Draft visuals from the ALPHA group session.
FIGURE 15.
The ALPHA group discussing the visuals for the animation.

Our Place
Seven mothers and their children attended the group on the day. Four participated in the session. The group was given a copy of the data-linkage script (which included the voice-over element only) and told that an animation was being developed that would clearly explain a research method we use, called ‘data linkage’. To test the current script, no further information was provided, as the animation itself needed to convey all the information. The voice-over element of the animation was read to the group and they were asked to identify any areas that were not clear, and to also provide suggestions on images/graphics that could accompany the voice-over.
Suggestions were made on minor changes to the script, but no major revisions were recommended and the group felt that, overall, it was easy to understand and follow. The group offered a number of ideas on possible dissemination channels for the film. As well as key social media sites [e.g. YouTube (YouTube, LLC, San Bruno, CA, USA)] and sites such as Mumsnet [www.mumsnet.com/ (accessed 29 September 2020)], they also suggested showing the animation in GP surgeries. It was noted, however, that GP surgeries often displayed films/animations without any volume, so our animation would not work in this context if it relied on a voice-over. Finally, the participants shared their thoughts on how to optimise public engagement with the animation. The group members were asked if they would be likely to click on (access) the animation if they came across it by chance. They said they would not be likely to click on the animation, and that, in general, they were unlikely to click on a link unless it was something that was clearly of relevance to them, a form of entertainment, or a site that had been recommended to them by someone they trusted. The group also made several suggestions concerning the kind of voice they would like to hear during the animation. There was a general preference for a voice that was conversational (i.e. friendly and not too formal in tone) and someone that they could relate to, and who was not too authoritative. The animation can be viewed at www.youtube.com/watch?v=4Ivio5XFgik (accessed 6 October 2020).
Value and presentation of study outcomes (objective 4)
Sessions held with the ALPHA group and Our Place focused on two broad issues: first, the meaning and clarity of key terms (particularly relating to outcomes), and, second, participants’ perspectives on the relative importance of the study’s secondary outcomes, and which of these might be prioritised for inclusion in dissemination.
Maltreatment
When asked to provide a definition of maltreatment (prior to being given the study’s definition), Our Place members put forward a number of suggestions. Most of these definitions were in line with that being employed by the study. Although some alternative terms were suggested by group members (e.g. ‘ill-treated’), there was no consensus on what these might be. The group could not identify a term that might be better than ‘maltreatment’, and noted that some of the potential alternatives (e.g. ill treatment) implied intent, which did not encompass neglect (which was included in our definition of maltreatment). The study definition of maltreatment included acts of omission (neglect) and commission (abuse), but did not define these or distinguish between them in terms of intention. However, group members perceived that some forms of neglect could be unintentional, contrasting with abuse, which was an inherently intentional behaviour.
Discussion with members of ALPHA focused on how the study should manage the sensitive nature of words such as maltreatment and mistreatment when presenting study results to research participants and members of the public. ALPHA members felt that the need to identify levels of maltreatment and other negative associated factors relating to a CIN status was important. However, they felt that, rather than say the study is looking at levels of maltreatment, it might state that it is looking into the quality of life or the development of the child. This was put forward as a way of managing the sensitive nature of maltreatment and of limiting its potential negative connotations.
Child in need
In the session held with ALPHA, members were asked to describe how they understood the term CIN. Their initial thoughts were related to their experience of the British Broadcasting Corporation (BBC) Children in Need charity night and its aims of improving the lives of children from around the world.
Having offered examples of what they thought might constitute a CIN, ALPHA members were provided with the legal definition (which was used by the study). ALPHA members compared their initial thoughts with the study definition to see if this needed to be reframed for members of the general public to understand. ALPHA members suggested that the definition of CIN status being used by the study was quite explanatory and that there was no need to include more information. However, they did suggest that it may be worthwhile to include a link to a CIN website or some more information that people would be able to access. They also suggested that it was important to mention that this study intervention would be addressing UK-based children in need.
In the Our Place session, participants’ initial definitions of the term CIN were also broadly aligned with the definition employed by the study. They felt that this term was clear and self-explanatory; they also felt that there was the possibility that members of the public might associate it with high-profile charity projects (e.g. BBC’s Children in Need), but that this was, to some extent, impossible to avoid.
Secondary outcomes
Each ALPHA member was asked to take one or two outcomes and consider their clarity of meaning (i.e. if more information was required to allow full understanding) and acceptability of phrasing. They were asked to do this without prior explanation from the researchers as to the rationale for the inclusion of outcomes, their exact meaning or how they would be interpreted (i.e. in which direction a favourable difference between intervention and control groups would be). For example, for length of time in care, we did not elaborate on whether or not we were assessing whether the FNP reduced or increased this. This approach was designed to help us understand how members of the public might interpret dissemination materials (whereby written/online information would need to be self-explanatory) and enable us to understand ALPHA members’ initial perceptions of what we were trying to measure and why. Each member discussed their outcomes with the group; this encouraged further feedback from those present.
Following this, the group was asked to discuss the relative importance of each outcome and to rank them accordingly (from least to most important). This was through informal discussion, rather than scoring each outcome. Appendix 11, Table 57, shows the agreed ranking and queries or suggestions regarding the presentation of each outcome.
For the session with Our Place, we knew that there might be greater limits on the amount of time we could work continuously with participants (e.g. because they were looking after young children); therefore, we modified the ranking exercise to take the form of two shorter activities. First, we asked participants to undertake a ranking exercise for the secondary outcomes relating specifically to maltreatment, and then repeated the same exercise for the remaining outcomes. As for the ALPHA members, we also asked participants to identify and discuss the meaning of each outcome and any that were unclear or problematic.
For maltreatment-related outcomes, Our Place participants ranked ‘injuries and ingestions’ and ‘Reasons why children are identified as being children in need’ as the two (joint) most important outcomes. The group suggested specifying the severity of the injury (i.e. major or minor). There was also concern regarding the reason for the injury. For example, a broken arm due to a ‘normal childhood accident’ (e.g. falling off their bike) would have a different meaning to ‘wilful’ abuse/neglect/ignorance. In relation to the second outcome (reasons why children are identified as being children in need), it was felt that ‘purposeful/wilful’ abuse or neglect was more important information to know, as this was very different from instances in which a child was disabled, or when a new mother might need extra support because of lack of knowledge.
Figure 16 and Appendix 11, Table 58, show the Our Place members’ ranking of the secondary outcomes relating to maltreatment, and their comments on each of the outcomes. Several outcomes were regarded as being of equal importance. Appendix 11, Table 59, shows the remaining outcomes and how they were ranked.
FIGURE 16.
Group activity to rank outcomes with Our Place members.
As can be seen, for some outcomes, the two groups (ALPHA and Our Place) were very similar in their rankings. For instance, ‘injuries and ingestions’ was given high importance by both groups. In other cases (even allowing for the slightly different methods used to rank the outcomes in the two groups), there were areas of divergence, such as the ranking of ‘cause of death’, which ALPHA placed greater emphasis on.
Both groups made similar points concerning the need to provide more specificity or detail on the meaning of certain outcomes. In ranking the secondary outcomes in terms of importance, Our Place participants reflected on the fact that how they ranked them was based, in part, on their own context (e.g. the age of their children) and that other members of the public reading the study findings may also identify what was important to know on this basis. For example, outcomes related to educational attainment might be more relevant (and, therefore, of more importance) to parents who had school-age children.
Our Place members made two other key points about the presentation and selection of outcomes. First, that each outcome should ideally be presented as a single concept, as this would make reading and comprehension easier. This applied to outcomes such as ‘injuries and ingestions’, for instance. Second, especially given the breadth of outcomes measured, they felt that it was important for the research team to make clear why they had chosen the selected outcomes. Thus, to some extent, they felt that the presentation of a clear rationale for why outcomes had been measured was as important as the ranking of the outcomes.
Dissemination methods (objective 5)
Written invitations to FNP graduates sent on our behalf by FNP teams inviting recipients to group-based discussions was one of the main recruitment strategies, but did not prove effective. We therefore revised the approach by asking FNP teams to identify clients/graduates with whom they could make face-to-face contact (e.g. by mentioning the study during routine home visits). The revised recruitment materials (and requests for FNP teams to help us) offered individuals a number of possible formats for meeting with us (e.g. one to one with a researcher, jointly with a friend/family members) and flexibility over timing and location (and not an invitation to a pre-planned group discussion on a specific date). At the time of writing (October 2020), one such meeting has now been held with a FNP graduate. Although this approach may not offer all of the advantages of a structured group discussion, it is hoped that it may increase levels of interest and engagement.
As outlined earlier, this work will focus on (1) the best methods to use for dissemination to research participants and members of the public (e.g. paper-based, websites, social media) and (2) how to format the presentation of results for the outcomes that are included in these dissemination materials. For instance, this might include text summaries, visualisations of key findings and various forms of graphs/bars/charts. Feedback from the FNP graduate who we have worked with has helped us to identify presentation formats that might be easier to navigate (e.g. bar charts rather than pie charts), and the potential value of written dissemination materials (if the reader is interrupted, written materials may be easier to pick up and re-engage with than some online media). We were also able to explore the prioritisation of outcomes for the dissemination activities. The discussion highlighted the potential importance of outcomes with immediate impacts on family well-being, in addition to the hypothesised long-term effects, for example prevention of child maltreatment. There were similarities between the key points made here and those that were highlighted during the work we did with Our Place members, and these merit further exploration with FNP graduates.
The work that we have completed (particularly with Our Place and ALPHA) has already helped us to develop key aspects of the approach to dissemination. For example, the groups we have worked with have helped us identify how complex aspects of the study (e.g. data-linkage methods) can be communicated in an accessible and clear manner through visualisations, and we will apply this learning to the framing of the key results. We have also strengthened our understanding of how to frame study outcomes in ways that make them more readily understandable by making the rationale for their inclusion explicit and presenting them as single concepts whenever possible. For example, in relation to children in care, Our Place members suggested separating ‘length of time in care’ and ‘legal status’ (we had presented them on a single card when we asked Our Place members to rank outcomes). More generally, we have developed our capacity to present key aspects of the study (rationale, methods, outcomes) to members of the public in a clear and accessible way, and this will feed directly into our approach to dissemination.
Discussion and conclusions
Public involvement has been important at many stages throughout the project. Involving the public has enabled us to bring new perspectives to our thinking and to reflect critically on the design and presentation of the research. We summarise the key contributions that the public involvement work has made to the quality and conduct of the study, mapped against the objectives that we set ourselves.
Optimising the acceptability of data linkage in the BB:2–6 study to the study cohort (objective 1)
Input from the CASCADE Voices group raised a number of issues, particularly regarding the information sent to withdrawn participants. When possible, we revised the framing of information included in the final version of the letter to optimise its acceptability. It was important to be able to demonstrate in our applications to the CAG, and for ethics approval, that we had involved members of the public in the drafting of our information for participants. The concerns raised by members of CASCADE Voices also enabled us to anticipate some of the questions that participants might raise during the opt-out process.
Acceptability and communication of data linkage (objectives 2 and 3)
Public involvement activities have enabled us to investigate how members of the public may understand the concepts and processes that comprise data linkage, their concerns about it and how best to address these concerns. In particular, through our work with Our Place members, we developed new ways of describing and visualising data linkage and used these insights to produce an animation that could be used in future studies. The animation has significant potential to enhance the explanation of data linkage in a clear and accessible manner during the recruitment process, and to help researchers seek consent from members of the public to access their routine data. We have subsequently obtained funding to further develop the animation and explore how it can be utilised (and, when necessary, adapted) for different population groups.
Meaning and presentation of study outcomes (objective 4)
Insights from ALPHA and Our Place members helped us to refine the content and framing of our dissemination activities, in particular how study findings would be communicated to members of the public. It was immensely valuable to be able to discuss with members of the public (including young people and mothers of a similar age to those participating in the study) how they understood key concepts (e.g. study outcomes) that we were seeking to describe, their perceptions of the importance of different outcomes and practical ways in which we could make our presentation of findings clearer and more meaningful.
Reflections/critical perspective
The importance of public involvement in research is now widely recognised. Recent methodological guidance, including the publication of national standards74 for public involvement by the Public Involvement Standards Development Partnership (a collaboration of national agencies and funders, including NIHR), has been designed to help research teams develop practices that will support and promote effective public involvement. The design of our public involvement activities did not draw on these standards (which were not published at the time), but they have informed our reflection on the successes, limitations and challenges of our public involvement work. The public involvement work that we have undertaken is strongly aligned with some of the key principles and actions recommended by the standards. 74 For example, we have sought to address barriers to involvement (a key focus of standard 174) and to build the skills and confidence of the members of the public that we have worked with (standard 374).
A key strength of our public involvement work is that we have sought to engage with multiple experiences and voices, including FNP graduates, other young mothers and young people from different backgrounds, for example those with experience of being looked after. By engaging with members of the public, both through group-based meetings and through our plans for one-to-one consultation, we have sought to ensure that adequate time has been provided for our discussions with the public, rather than limiting this to inclusion of a public representative in our SMG meetings. Whenever possible, we have met with members of the public in their own communities and provided as many options as possible regarding where and how they would like to meet. At each stage of our public involvement activities, we have sought to use accessible concepts and language, and to consider the skills and training needs of researchers and members of the public. Input from a specialist public involvement officer (Peter Gee) and regular team discussion after key activities has helped us to develop our skills in engaging with members of the public. Advice from Peter Gee and contacts in the organisations we have worked with has also been important in understanding what background information members of the public might need at the start of public involvement sessions, and how best to support those who might not be used to contributing to a group discussion. In terms of governance, public involvement has been a standing agenda item at our SMG meetings, which has helped embed it in the study and ensure that key insights have been shared with the broader research team. This approach is strongly aligned with the national standards for public involvement (standard 6),74 which emphasise the need for public involvement to be visible and accountable in research management structures and governance.
The work to develop an animation that explains key aspects of data linkage in research studies stemmed directly from the ideas generated by members of Our Place. We have subsequently worked with members of the group (and those in ALPHA) during its development, and sought input on content (e.g. the draft script), appearance (images, colours) and presentation (e.g. style of voice-over, appropriate length of the animation). In the field of public health, co-production of new interventions with members of the target population who will receive them has a number of important benefits, including optimising relevance, acceptability and credibility. 75 We have built co-production into the development of the animation, with the aim of realising these benefits.
During the public involvement work, a number of challenges were encountered. First, the session held with CASCADE Voices was run by a facilitator independent of the research team. Although this had many strengths as a way of working, it did mean that we were not able to discuss directly with the group which areas of feedback we were able to address, and those aspects of the study that, for various reasons, could not be modified. Although we provided information to the facilitator prior to the session concerning the reasons why we planned to contact withdrawn participants, it was not possible for us to pre-empt and therefore provide explanations in advance for all potential questions. Although some of the input from CASCADE Voices members focused on the letter, which we had drafted, some of it was concerned with the broad approach of opt-out versus consent, something we were unable to amend at that time. In subsequent activities with other groups, members of the research team led activities and engagement with participants (Our Place) or did so alongside the existing group facilitator (ALPHA). More direct involvement in the running of the meetings provided us with the opportunity to explain fully which aspects of the study we were seeking input on and to highlight those areas that had either already been finalised or that we were not able to modify. Our experience also suggests that, for a topic as complex as data linkage (and for which provision of some background information will often be needed), it may be helpful to hold more than one meeting with a group. As well as providing more time to focus on specific topics, this also has the advantage of building rapport and shared understanding between researchers and group members, and of providing time for all involved to reflect on learning, (mis)understandings and topics needing further discussion in the period between sessions.
Although we have identified the approach of working with members of the public in their own communities as a strength, this raised several practical challenges. Using mother and baby/toddler meetings (as we did with Our Place) was intended to provide a relaxed and comfortable environment for members of the public to talk with us. But, by virtue of their purpose, they could sometimes be noisy and chaotic environments in which mothers needed to ‘dip in and out’ of participation in discussions, where undertaking head counts of how many people had contributed to an activity was difficult, and where use of audio-recording was impracticable. We sought to address these issues by working with smaller groups of mothers in a separate room, but this was not always possible. These ‘breakout’ sessions were not recorded because of the level of background noise, but, on reflection, we might have sought to record at least part of the discussions, perhaps when we were asking for a summary of people’s thoughts, as this would have provided a more in-depth record. In later meetings with Our Place, we proactively designed activities to have more flexibility (e.g. having some activities that participants could easily join without having to be involved for the whole meeting).
The biggest challenge we faced has been in recruiting FNP graduates, particularly in relation to attending group meetings that we had organised. Whereas meetings with Our Place members took place with an existing group (and at a meeting that they were attending as part of this group), a different approach was required for organising activities with FNP graduates. They were not part of an existing social network or set of meetings that we could access, and they had received FNP on a one-to-one basis. We therefore organised bespoke events to bring FNP graduates together in their local community. The main method of contact was mail-outs that went via FNP staff already known to and trusted by the individuals concerned. We sought to reduce practical barriers to attendance, for example by choosing locations that we thought would be easily accessible by public transport, offering to reimburse travel costs on the day of the meeting and providing a crèche and free refreshments. Significant efforts were made to produce information promoting the events that was accessible and easy to understand. We offered incentives for attendance (lunch, retail vouchers) and also provided alternative ways for people to speak with us if they could not or did not wish to be part of a group discussion. FNP teams provided significant help at various points. They promoted the meetings on our behalf to individuals they thought might be interested, agreed to be present at the start of one of the meetings (so that participants would be greeted by a ‘familiar face’) and also provided feedback on the information we produced. They suggested that the information was approachable and clear and they did not recommend any major changes.
Despite all these efforts, few graduates agreed to take part, and nearly all those who did either cancelled prior to or on the day or did not attend as expected. It is difficult for us to ascertain the reasons why the meetings generated such low levels of interest. Nevertheless, based on our discussions as a research team and input from the FNP teams that helped us, a number of possible explanations have been identified.
Contact was made with FNP graduates via a mail-out that was distributed by FNP teams. We were not able to contact individual graduates directly because of data protection requirements. Therefore, the initial approach was less personalised than it would have otherwise been. FNP teams did not routinely use or update lists of graduates, as they were no longer working with these individuals. Feedback from FNP practitioners was that some contact details were, inevitably, out of date, and that some graduates (possibly a high proportion) may have moved home or even left the area. In Bath, the FNP team advised that, in general, it was extremely difficult to engage parents in group-based activities, and that some group-based meetings organised by local services in the city had ceased to exist partly as a result of this.
The FNP graduates had accessed the service on a one-to-one basis (i.e. one mother meeting with one FNP nurse). We sought to bring together groups of mothers, but, given the individual-level nature of the service, we were not tapping into an existing network or group of linked individuals. This may have made the proposed meetings less appealing, or more daunting for those uncomfortable with group settings, or may simply have meant that our invitation was not as relevant or meaningful to recipients as it might otherwise have been. In Wiltshire, some individuals indicated that they felt uncomfortable about meeting with a researcher whom they did not know. We responded by saying that we would be happy to meet graduates/clients with a family member/friend or FNP nurse present.
Finally, it is possible that, despite our best efforts, some practical barriers to attendance still existed. These may have included the need to use public transport to reach our venues (in Bath we knew that very few participants had access to private transport), work commitments (mentioned by one potential participant) and child-care commitments (e.g. picking up children from school). Despite these challenges, we have achieved the majority of our public involvement objectives. The activities undertaken have optimised the quality of our work and have built our capacity for and skills in undertaking effective public involvement. We are committed to using the valuable insights that this public involvement has generated to help maximise the impact of the study on policy and practice.
In summary, we have worked with different lay groups during the conduct of the study to address several objectives, which broadly relate to optimising study processes, better understanding lay views on the nature of the research and improving how we communicate with the public about it. Existing research and non-research organised groups of young people have added tangible benefits to the study, for example by improving participant-facing materials; by modifying study processes such as dissent registration; and by informing, in detail, an animation explaining routine data and their use in research. We had less success in engaging with individual graduates of the FNP programme, despite considerable thought and effort, and also support from FNP professionals. However, the breadth of input from other lay groups involved may have partially compensated for this. An interesting tension was found when exploring lay participant views on aspects of the study design such as reapproaching women who had withdrawn from the original BB:0–2 trial. Conflicting views arising within and between lay groups is perhaps inevitable in such involvement work, and acknowledging and respecting all perspectives is essential when making subsequent decisions about the study.
Chapter 8 Discussion
Principal findings
Maltreatment
A sizeable minority (27%) of all children followed up over the 6-year study period were referred at least once to children’s social services, but there was no difference in referral rates between study arms. Some children were referred on multiple occasions (up to five times). More children in the usual-care arm were referred on multiple occasions than children in the FNP arm, and children in the FNP arm were, on average, 90 days younger than children in the usual-care arm when referred. However, in both cases, the difference was not statistically significant.
A total of 323 referred children (21.5%) were assessed as in need at some point by age 6 years, but there was no difference in proportions between study arms (FNP, 21.1%; usual care, 21.7%), even when adjusting for number of FNP visits received. Similarly, there was no difference between study arms in the timing of the first referral for children subsequently assessed as in need. Adjusting for baseline maternal characteristics and child sex made no difference to the overall picture of CIN status. The duration for which children were assessed as in need was similar in the two study arms among those for whom the period of additional support had concluded. The proportion of all children in need with a primary need of abuse or neglect was similar across study arms (FNP, 57.1%; usual care, 63.0%).
The rates of children with a CPP (FNP, 6.8%; usual care, 6.6%) and who were looked after (FNP, 3.3%; usual care, 3.6%) were the same in both study arms. Of those with a CPP, a larger proportion of children in the FNP arm were assigned a primary code of emotional abuse and a smaller proportion were assigned a primary code of neglect than in the usual-care arm. There were similar proportions of children in care in both study arms, with children in the FNP arm spending, on average, 2 months less in care than children in the usual-care arm.
Children in the FNP arm were no less likely to miss a hospital outpatient appointment than children in the usual-care arm. Half of all children had attended an emergency department for an injury or ingestion. The slightly larger proportion of children in the FNP arm attending was not statistically significant. Similarly, the rates of children admitted and the duration of admission due to an injury or ingestion were similar between study arms.
Children of care-experienced mothers were more frequently defined as in need, but there was no difference in this rate found between the two study groups.
The treatment effects for referrals to social care and whether or not a child was ever classified as in need did not differ when explored by planned sample subgroups (i.e. child sex, and baseline maternal age, adaptive functioning, NEET status and deprivation). Further exploratory subgroup analysis (baseline levels of social support, self-efficacy and subjective social status – family and personal) found no differential programme effect.
The total number of child deaths was < 10, and therefore disclosive, so they cannot be reported.
Child development
The pattern of early educational attendance up to 4 years was equivalent across study arms. Fewer children in the FNP arm attended privately run day care and more attended local authority day nurseries or ‘other’ service providers than children in the usual-care arm. Rates of school attendance across all available academic years in follow-up were similar across study arms. Children in the FNP arm were more likely to reach a GLD across all five areas of learning by the end of the reception year (58.0%) than children in the usual-care arm (52.2%), and were also more likely to achieve a GLD in all 17 early-learning goals (FNP, 55.5%; usual care, 50.1%). In both cases, the effects were strengthened when adjusting for a child’s month of birth. The small advantage for children in the FNP arm was consistent across all five areas of learning, although we did not test each area of learning separately. In planned subgroup analysis, the beneficial impact of the FNP on total point score was mostly observed for younger (aged < 16 years) rather than older women at study entry, but no other differences by study subgroup were found. Variation in the observed number of visits from a family nurse made no difference to the size of the effect.
At KS1, 65.3% of children in the FNP arm reached the expected standard for reading, compared with 60.5% of children in the usual-care arm (aOR 1.23, 95% CI 0.99 to 1.53). The proportions of children reaching the expected standard for mathematics (FNP, 62.0%; usual care, 61.3%) and science (FNP, 72.6%; usual care, 71.0%) were similar across study arms. There was some difference across study arms for writing (FNP, 48.4%; usual care, 42.9%) when compared using data from the academic year 2016/17. However, none of the group differences for the KS1 outcomes was statistically significant.
As month of birth has a strong relationship with educational attainment in the general school population, we adjusted the main analyses for all KS1 outcomes to take birth month into account. Adjusting for month of birth, children in the FNP arm were more likely to reach the expected level for reading than children in the usual-care arm (aOR 1.26, 95% CI 1.02 to 1.57; p = 0.035). There were no group differences for other KS1 outcomes when making this adjustment.
For children whose families had more visits from a family nurse, the effect for reading was stronger (adjusted difference 1.38, 95% CI 1.07 to 1.77; p = 0.015, if families received all 64 visits). The increased efficacy per visit for writing was also statistically significant (aOR 1.005, 95% CI 1.09 to 1.017; p = 0.001), but there was no effect for either mathematics or science.
Overall, at KS1, sex differences were large, with girls outperforming boys in all four subject areas. The effect between study arms was greater for boys in the FNP arm than for girls, particularly for reading and writing (and strengthened after adjusting for month of birth); for writing, this reached statistical significance. Similarly, although children with younger mothers at recruitment were less likely to reach the expected standard overall, the differences between study arms in favour of children in the FNP arm were greater for younger women, for mathematics and for writing (academic year 2016/17), an effect that reached statistical significance. In addition, for writing (academic year 2016/17), a programme effect was observed for mothers NEET at the time of recruitment; the contrary was seen for mothers in employment, education or training (EET). When tested, no additional interaction effects were found at KS1.
The intervention effects for each of the main outcomes assessed are summarised in Figure 17, and demonstrate the differing pattern of impacts between maltreatment and child developmental outcomes.
FIGURE 17.
Forest plot of estimates from all main outcomes. Vertical solid line represents no effect (OR = 1). a, FNP compared with usual care. Analysis adjusted for stratification (site) and minimisation variables (gestational age, smoking status at recruitment, and first or preferred language). For Early Years and KS1 outcomes, additionally adjusted for month of birth. Source: NPD, DfE.
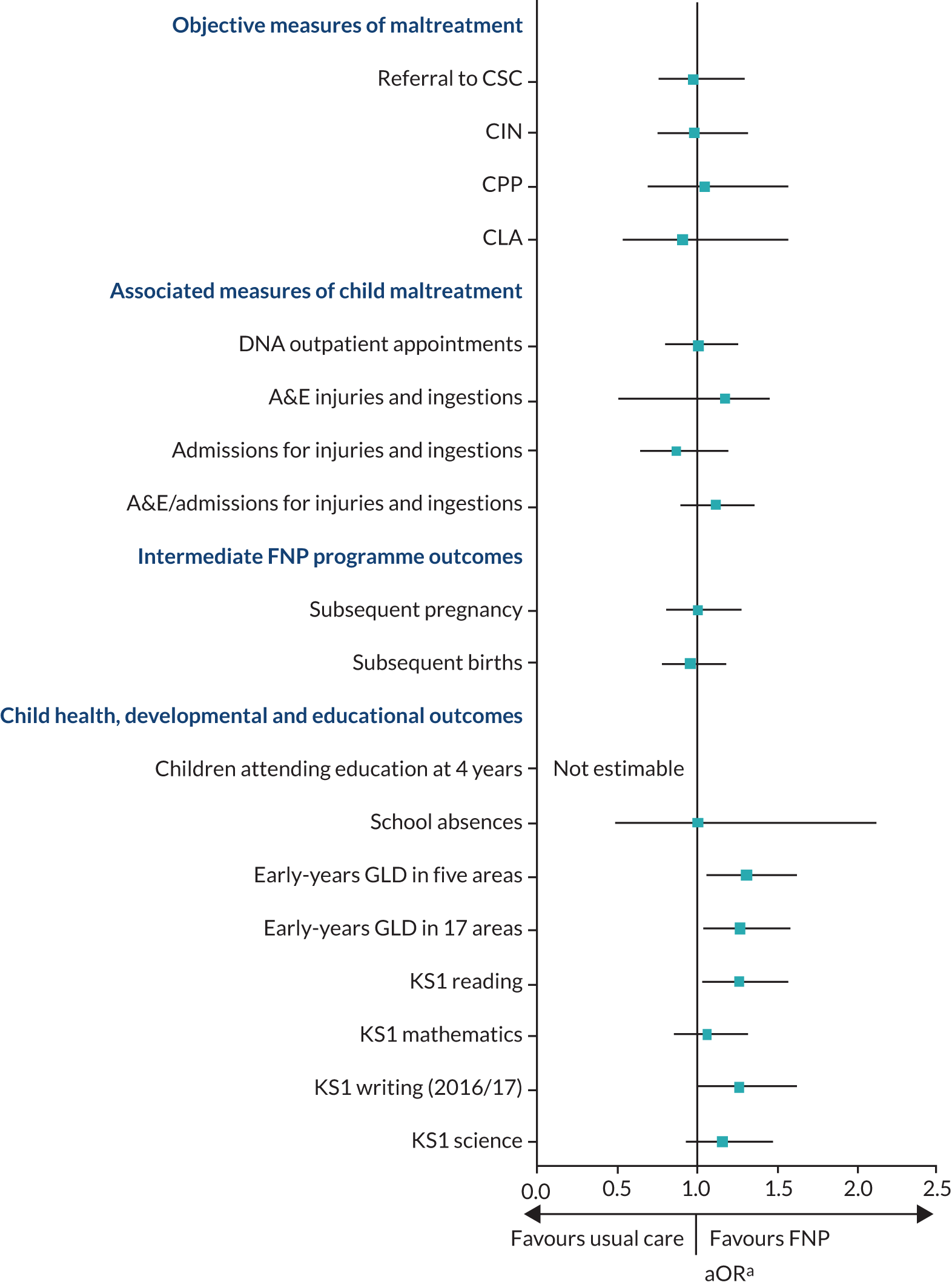
In an additional exploratory analysis, we developed two cumulative risk scores based on baseline predictors of CIN status and reading attainment at KS1 for children in the usual-care arm. Categorised into low and moderate/high risk, we explored programme subgroup effects, but found no additional benefit of the FNP for children with elevated baseline risk score.
Cost–consequences analysis
We examined the economic consequences of the FNP, compared with usual care, over the medium term for mother and child. This extends the short-term follow-up from the BB:0–2 trial,61 with particular focus on the costs, compared with potential benefits for the child. Over the medium term, there are no real differences in secondary care health resource use and costs for the FNP families, compared with usual-care families, balanced against the differences in outcomes described previously. The FNP could be considered cost-neutral compared with usual care over the medium term. Therefore, assessment should be based on the benefits associated with the primary and secondary outcomes, set against the original cost of programme delivery reported in the BB:0–2 trial.
Impact on inequalities
The FNP forms part of a progressive universal approach (i.e. universally accessible services with enhanced access for those requiring special or targeted support) of home visiting to support families at greater risk of adverse outcomes. Young maternal age was selected as a programme criterion, as it is associated with a wide range of adverse outcomes and is a proxy for socioeconomic disadvantage. 18 Although there is considerable complexity involved in potential causal mechanisms, poverty is strongly associated with the risk of a child suffering maltreatment. 76 The intervention, therefore, directly aims to address inequality. The results of the child development outcomes further indicate how the intervention may be especially important for children who may be at additional risk, for example those born to very young mothers, boys and those born in the later months of the school year. The feasibility of tailoring programme delivery (e.g. enrolment criteria, dosage) to intervene where the benefits may be most likely is beyond the scope of this study, but such adaptation is already part of the agenda for the FNP national unit delivering the programme in England. 77 In addition, the programme attempts to reduce inequality by supporting mothers to engage with education and employment, and thereby improve their life course and that of their children. In the current study, we have not been able to fully assess mothers’ economic circumstances because of the particular focus on maltreatment outcomes. The equivalent rates of second pregnancies that we observed provide no indication that the programme has modified one factor that may affect maternal life course. We have previously raised the broader question of how systemic differences between the USA and the UK may interact with the programme to support incremental benefit. 78 We consider that exploring such socioecological influences on programme implementation and outcome remains an important objective.
Interpretation
The FNP programme model aims to promote sensitive and competent parenting as a route to improved child health and development. Nurse-facilitated activities during regular home visits are intended to provide a stimulating and safe home environment, reducing maltreatment and improving language and executive functioning. In this study, we have found minimal evidence of programme impact on children’s likelihood of experiencing maltreatment, but we have found solid evidence of an advantage in early educational attainment.
The strongest evidence for the FNP’s impact on maltreatment comes from the original Elmira trial. 13,79 Olds et al. 13 found reduced substantiated reports of abuse and neglect in the first 15 years of a child’s life, an advantage that emerged only after age 4 years. The Dutch trial of VoorZorg25 similarly found reduced maltreatment reports to child protection services in the Netherlands within the first 3 years of a child’s life among mothers visited by a nurse.
Adapted versions of the NFP in Australia (Family Partnership Programme)80 and in Germany (Pro Kind)29 have also assessed programme impact on maltreatment. Segal et al. 80 reported reduced involvement with child protection and days in care for children in the Family Partnership Programme arm in a trial among indigenous Australian mothers. The German study of Pro Kind is yet to report on its longer-term evaluation, but has followed up children to a similar age as those in our study, using maternal self-report. A 2018 evaluation of the NFP in Pennsylvania, USA, used propensity score matching to compare NFP and control families in rates of use of hospital-based health care for injuries. 81 Although a higher rate of attendance was found among NFP families, these were mostly due to differences in minor injuries; no difference between groups for more serious injuries was observed. Matone et al. 81 point to the need for high-quality implementation to replicate beneficial trial findings. Olds’ original trial9 provides the most rigorous long-term evidence of programme impact when implemented as intended by the developer and when combining data sources to understand maltreatment outcomes. Although some differences were found in our study, for example length of time spent in care for care-experienced children, the numbers involved are small and the over-riding picture is of no overall group difference. The programme was also no more effective in tested subgroups. Although it is still possible that a benefit from the FNP may yet emerge as the children in our cohort get older, we have no evidence currently to suggest that this may be the case. It is also worth recognising differences in the population of clients in receipt of the programme across the different study populations, their social circumstances and how that may determine potential to benefit from the FNP. 78 Similarly, this study has not explored differences in social care systems across countries. Although conditions that may serve to vary the underlying risk of maltreatment, and its likelihood of being detected and then responded to, will differ across countries, our evidence is that the FNP makes no incremental difference in the English setting of our study.
The BB:0–2 trial found maternally reported benefits at age 2 years for children of nurse-visited mothers for both language and developmental outcomes. 22 This new study now provides objective medium-term evidence for programme impact on developmental outcomes at the end of the reception year and at the end of KS1, to build on that picture. The pattern of results shows broad positive impact on school readiness, one that is greatest for children born to the youngest mothers. Although there is overall programme benefit at KS1 when adjusting for birth month, there is also some particular benefit for children born to the youngest mothers (in mathematics and writing), however the small numbers for this group should also be noted.
Similar medium-term programme impact (to age 6 years) on developmental outcomes was reported by Olds et al. 82 in their Memphis trial. These included improvements in attendance at formal out-of-home care, and in intellectual functioning and receptive language scores. In Heckman et al. ’s83 reanalysis of the Memphis trial data, the cognitive benefits of the programme at age 6 years were attributed to both programme-induced improvements in maternal traits and family life investments at age 2 years. Looking forward, Heckman et al. 83 also found that the positive effects persisted through to age 12 years for boys, but not for girls. Although the positive difference found at KS1 for boys in the FNP group across each outcome did not reach statistical significance, it may be possible that the longer-term outlook, particularly for boys in our trial cohort, may be similarly beneficial.
A reduction in maltreatment and an improvement in school readiness and achievement are both predicted benefits of the FNP and are supported by existing US trial evidence. We identified a number of risk factors from the exploratory analyses that could influence both outcomes. These included both common factors (e.g. difficulties with basic skills, young maternal age) and non-common factors (e.g. smoking in pregnancy for children in need only). Further work is required to establish whether the differences in outcomes that we observed reflect theoretically different pathways to effect or, for example, differing contextual factors at operation in the different trial settings in England and the USA. Understanding why the programme may work for some outcomes and not for others in the UK may inform programme optimisation and lead to incremental benefit over usually provided services.
Two factors that we needed to consider further in our main and exploratory analysis, and in interpreting the results, were academic year of assessment and month of birth. School readiness as measured by a GLD in the EYFS has consistently improved in England in the years since children exited the trial at age 2 years. 84 Nationally, in 2014, 60.4% of all children met this threshold; by 2018, the figure was 71.5%. Girls consistently outperform boys, but the sex gap has narrowed during the same period of time (a 16.3-point difference in 2014 and a 13.5-point difference in 2018). In addition to sex, free school meal eligibility, month of birth and presence of SEN also contribute to variation in attainment of a GLD in the EYFS.
Key Stage 1 data are based on teacher assessments undertaken at the end of KS1 (Year 2), when a child is aged 6 or 7 years. Study data were sourced from two school years: 2016/17 and 2017/18. Nationally, girls outperform boys in all subjects, with the largest gap in writing. There are large differences in those reaching expected standards between students eligible for free school meals and by month of birth. In 2017, proportions of children reaching the expected standard increased for all subject areas (by between 1% and 3%), but remained lowest for writing (68%).
The birth dates for children in our study cohort resulted in an uneven spread of children born across calendar months in each year included. Although the individual-level trial randomisation retained a valid group comparison, we needed to further adjust for month of birth to extend generalisability. Doing so revealed the additional benefit the programme could have for those born in the summer months (who traditionally perform worse at KS1). Differences in attainment due to birth month can persist until General Certificate of Secondary Education (GCSE) stage; therefore, it is important to establish whether benefit attributable to the FNP at reception and KS1 is maintained in the long term or fades away. 85,86
In England, the FNP programme remains locally commissioned by a large number of local authorities. Since delivery of the programme to families in the BB:0–2 trial, and partly stimulated by the trial’s findings, the FNP national service unit has led a programme of universal improvements and local changes. These include clinical changes related to specific outcomes and system changes such as reviewing eligibility criteria and modifying visit dosage (both up and down). The subgroup differences that we report here may provide some support for such efforts to target the programme’s delivery. However, our exploratory work looking at benefits for those with multiple baseline risk factors was less informative, based on the data available to us.
Generalisability
The generalisability of the BB:0–2 trial cohort was established previously and found to be broadly representative of the population of women being offered the FNP. 22 With few women dissenting to follow-up in the current study, and with high rates of matching possible via NHS Digital and (for children) the NPD, there was little attrition in the sample up to age 6 years. When the original trial sample and the current study cohort are compared, there are no differences in baseline characteristics and no indication of bias having been introduced by the process of data linkage/dissenting.
The exploratory analysis adjusted for month of birth to determine programme effects when assuming an even distribution of births across the calendar (or academic) year. This was necessary as births to women in the original study were not balanced across months, and there are strong seasonal effects on KS1 scores. Adjusting for season of birth has allowed for a better generalisation of programme effect. Contemporary national data (England and Wales combined) showing month of birth for all women in the period 1995–2014 show a higher rate of births in the months of June to August, with a subsequent dip and then a higher peak of births in September. This is similar to the profile of month of births seen in our study, although there are relatively fewer births in the trial cohort for winter and spring months, compared with the general population. The distribution of months of birth for the study cohort reflects both the month of study recruitment for women and also their gestational age at recruitment. The former will have been driven by the staged opening of sites over a period of months and the total recruitment period (≈13 months). The latter will have been constrained by study eligibility criteria, but will have allowed some variation. However, in both cases, the individual randomisation will have ensured balance across study groups.
As the FNP is a preventative intervention for families at greater risk of adverse outcomes, we would expect families in our study’s usual-care arm to have poorer outcomes than those found in the general population. In comparable years, attainment at a national level was higher than for our usual-care arm for the EYFS profile assessment. In 2015, 66.3% of children achieved a GLD in all five areas of learning, and, in 2016, this rose to 69.3%. 84 This is compared with 52.2% in the study’s usual-care arm. Similarly, in 2015, 64.1% of children achieved the expected level in all 17 early-learning goals, compared with 50.1% in the study’s usual-care arm. At KS1, the pattern of difference is similar. In 2017, 76% of children nationally met at least the expected standard in reading; in 2018, this figure was 75%. 87 This is compared with 60.5% in the study’s usual-care arm.
In social care, the contrast between study participants and the general population of children in England is even more revealing, although published national figures are not summarised in a directly comparable manner to that used in the BB:2–6 study. In 2018, the national rate of children (aged < 18 years) in need at 31 March was 3.4%. 3 Of these, children aged 1–4 years accounted for 17.5% and those aged 5–9 years accounted for a further 24.1%. Although in our study we report a prevalence rate (i.e. of ever being in need up to age 6 years), the rate we found of 21.7% in the usual-care arm shows how vulnerable children in the study are, compared with the national population. In the BB:0–2 trial, we showed how vulnerable study families were based on baseline characteristics, compared with the broader population. In the BB:2–6 study, families not exposed to the intervention have much poorer outcomes than found for the general population. Despite important improvements for developmental benefits for children in the FNP arm, they are still much lower than the population average. Social care outcomes, in particular, remain poor for all families, compared with the broader population in England.
Strengths, weakness and ongoing challenges
The major strengths of the study are the high quality of data linkage achieved via NHS Digital using primarily NHS numbers and, overall, the high level of sample retention. This maintained the representativeness of the original trial and provided a large sample, and hence power, for the analyses. The lack of a similar unique linking field available to the study team for matching to NPD data resulted in a slightly smaller cohort of children available for analysis. Successful efforts to better link health and education identifiers at a national level would have benefits for research, but may also be challenging from a practical and ethics perspective. 88
In this study, we undertook a substantive pilot phase that addressed several objectives. 31 Although it was possible to identify, at the outset, a number of potential study challenges and mitigating strategies, the pilot phase enabled strategies to be optimised and evidenced, in addition to allowing unanticipated challenges to be addressed. The regulatory and governance context of the study, whereby we sought data from multiple providers with varying legal and ethics imperatives, was both complex and dynamic. Our approach had to accommodate multiple providers and be adapted over time (e.g. following the advent of General Data Protection Regulation). 89 The regulatory-compliant model of data linkage we have created has enabled greater understanding of the outcomes for families recruited to the original BB:0–2 trial. This may then inform further follow-up of the same cohort, as well as attempts by other researchers seeking to link data in this environment.
The current study benefits from the random allocation applied in the original trial and the further use of both outcome and descriptive data collected in that study. Although there are approaches that can be used to address the potential bias in observational studies of effectiveness, these were not required here. That, combined with the use of routine data collected wholly independently of the trial, provides substantial reassurance about potential biases. The reuse of trial data in tandem with use of routine service data is also consistent with policy imperatives for efficient study designs. 90,91 Although some costs involved in delivering this study were greater than anticipated for example, because of revisions in costing models used by NHS Digital, the total cost was substantially lower than would have been incurred if data were prospectively collected using maternal self-report.
Nevertheless, a study model reliant on routine data will have placed some limitations on the scope of what is achievable. This will be based both on what data are systematically collected by the services and the quality of data coding at source. For example, the available maltreatment data have provided an essential overview of the key outcomes for our study, but narrative data about individual cases may have added depth to our understanding. The inability to assess resource use, both within the primary care context and from women’s perspective, has placed some limitation on what we can conclude. Similarly, the lack of detailed social care resource data has limited the perspective of the CCA, which therefore primarily focuses on secondary health-care costs. Overall, accessing only routinely available data has enabled us to understand key programme and policy-relevant outcomes.
Using only routine data prescribes the outcomes available for analysis, some of which may lack the measurement properties that research instruments could offer. One such example is the EYFS measure of school readiness, which was a key secondary outcome in our study and which may be less sensitive to change than other instruments. 92 Nevertheless, it does allow ready comparison with both local and national populations. Furthermore, the fact that we were able to demonstrate a programme effect using this measure suggests that the underlying effect is probably even more substantial. Augmenting routine data with standardised research instruments would add value in a future longer-term evaluation.
We selected CIN status as a primary outcome because it was reliably available using routine data and follows a legally defined approach to safeguarding and promoting child welfare. Although its scope is broader than solely maltreatment, abuse and neglect form the majority of reasons why children are identified as in need. This then forms part of our overall assessment of programme impact, which incorporates other related measures such as CPPs, becoming looked after, and injuries and ingestions leading to emergency attendance and admission. We did not exclude as cases those with a primary reason of disability, but, as there were only 12 children in total (FNP, n = 7; usual care, n = 5), doing so would not alter the conclusions.
In the 15-year follow-up of the Elmira trial of the NFP, maternally reported incidents of domestic violence (the term used in the US trial) since birth of the study child were counted, with increased incidence associated with reduction in intervention effect for maltreatment. 93 The intervention itself was not found to alter levels of reported domestic violence, as was also the case in the BB:0–2 trial. Further exploration examined the possible mechanism of this effect and found that, among women experiencing low to moderate levels of domestic violence, programme impact on maltreatment outcomes was mediated through changes in maternal life course (reductions in number of subsequent children and use of public assistance). 94 In the BB:0–2 trial, just over half of all women (n = 607, 54.2%) completed the Composite Abuse Scale measure of intimate partner violence at 24 months (in part because of requirements for scale completion: a face-to-face assessment with no other person present). Small untested trial arm differences showed that non-completers were more likely to be separated at trial baseline, to not be in EET, to have higher deprivation scores based on postcode and to have more difficulties with adaptive functioning. Most completers (n = 362, 60.6%) reported no abuse (score of 0). In the BB:2–6 study, the lack of intervention effect for maltreatment outcomes, the shorter (than the Elmira trial) follow-up period and the availability of maternal-reported intimate partner violence only at 24 months limited our ability to explore any moderator or mediator effects. However, further exploratory work may yet be possible examining programme impact in the context of intimate partner violence.
Our approach to assessing maltreatment used multiple methods and sources of data, all of which were from service records (either social services or health services). This is similar to the method used by David Olds in his original Elmira trial,9 and contrasts with other approaches that have used maternal self-report, for example in the evaluation of the German Pro Kind intervention. 29 Although it has been suggested that surveillance bias is unlikely to be a serious problem when evaluating maltreatment using verified service data (i.e. unlikely to inflate numbers of children being reported when in receipt of home-visiting),25,95 others have found that this could be substantially higher when clients are actively engaged with services;96 therefore, the potential for such bias still needs to be acknowledged.
One other consideration when using routine data is that the method for assessing outcome can change independently of the evaluation. Changes in the 2017/18 Writing Teaching Assessment frameworks meant that the assessments in 2016 and 2017 are not directly comparable. 43 The changes made included a more flexible approach (i.e. greater discretion being applied by teachers to ensure that a particular weakness does not prevent an accurate judgement of overall attainment) and revised ‘pupil can’ statements (e.g. a greater emphasis on composition). This meant that we had to analyse the 2 years of data separately (and the later year only descriptively because of reduced numbers), although the trial’s individual randomisation still allowed for a valid comparison in both cases.
It is now standard practice to have active public involvement in clinical trials, but a less well-established practice in routine data studies. We considered that it was important to have strong involvement in this study because of the dissent model of linkage being used and the relative unfamiliarity among the general public of the use of routine data for research. 97 We extended a model of involvement used in our BB trial to include multiple lay stakeholder groups engaged at different touch points in the study (in part, this was led by requirements placed on us by the CAG review panel). The role of public stakeholders was synchronous with the study life cycle (e.g. from initial approvals through to dissemination) and helped shape different processes and materials, including the development of animations explaining what routine data are and how they are used in research. These will have benefits beyond the current study for researchers and members of the public alike. One group that we did have difficulty effectively engaging with were FNP graduates, despite substantial support from local FNP teams. It is possible, therefore, that unique perspectives of programme clients were not well represented in our planning, although the three other young people groups we did engage with are likely to have compensated for that to some extent.
We planned that all children would be followed up to KS1, representing the latest follow-up point for all children in the study. In practice, the annual release schedule of data from the NPD and the range of study children’s birth dates meant that the youngest children were not initially included in the main analysis for this outcome. We agreed with both the funder and the SSC that the remaining data should be added to enable a full data set, despite then delaying submission of the final report. By repeating the KS1 analysis on the now full data set, we identified discrepancies in rates of children reaching the expected standard, compared with the analysed partial data set. This informed additional post hoc analyses, which clarified the importance of month of birth (analysed by year quarter) as a moderator of programme effect. Adding month of birth was consistent with the original statistical analysis plan (i.e. as an additional subgroup) and has importantly augmented the final results, allowing a much more nuanced understanding of factors influencing educational outcome and how that interacts with the FNP.
A CCA provides a descriptive summary of the costs for decision-makers across a range of sectors. 63 It can examine whether or not investing resources earlier in the life course can generate benefits and potentially reduce costs over the longer term. 98 A CCA can capture a broad range of outcomes, not restricted to health outcomes, which may be especially meaningful for complex interventions generating multiple effects. It is also a pragmatic solution when health economic analyses such as a cost–utility or cost-effectiveness analysis is unfeasible. However, it is constrained by not providing definitive conclusions on value for money.
We aimed to replicate the CCA presented in the BB:0–2 trial, but there were differences in the populations of interest (e.g. the BB:0–2 trial focused on maternal costs), differences in data availability (e.g. no primary health-care data were available in the BB:2–6 study) and a lack of ‘rich’ data to accurately translate non-health-care items into costs. This lack of sufficiently detailed social care data in the routine data set meant that our original secondary objective to assess both health and social care resource use could not be fully achieved. The reported costs are limited to secondary health-care resource use against the primary and secondary outcomes. The current analysis shows costs to mother and child alongside child health and non-health outcomes, whereas the BB:0–2 trial focused on costs for the mother only, but consequences for both mother and child. In the BB:0–2 trial, only small differences in total health-related costs were seen in favour of the FNP, with the largest difference in secondary care resource use, particularly inpatient care. The BB:2–6 study findings are similar for the child, with the largest drivers of costs seen in hospital inpatient stays, but health-care costs showed only minor differences across both groups over the BB:2–6 study period.
The original BB:0–2 trial found that the FNP cost £1992.89 more per participant than usual care (when adjusted for baseline covariates, the difference was £1811, 95% CI –£2814 to £5547). 61 However, this did not take into account the total costs of delivering the FNP programme (i.e. time for family nurse visits and telephone calls were costed, but the involvement of other professionals in interacting with family nurses was not). This should be set against gains in benefits for children at 6 years of age, to determine whether or not the initial investment in the FNP is worthwhile.
The economic findings of this study are limited by the practical and analytical challenges of working with routine data, particularly with constraints in aligning resource use data other than HES in the BB:2–6 study to the BB:0–2 trial. These shortcomings affected the extent to which the full range of direct health-care costs could be reported, particularly primary care, and will be an underestimate of the full extent of costs over the medium term for both arms and, in particular, costs associated with social care and education.
Our cost-consequences approach has drawn on routine data (i.e. HES) to determine actual costs for each secondary care resource category and reported these against the range of consequences (outcomes), for the BB:2–6 study, across a range of sectors including social care and education. If suitably granular data were subsequently available, then further post hoc questions could be pursued to examine the relationship between costs and child maltreatment outcomes, especially with respect to non-health-care related resource use, for example social services interaction.
Our current analyses found differences in outcome linked to variation in visit dosage. We previously reported on visit frequency for women in receipt of the FNP during the original trial. 32 We compared these visit rates with those specified in programme fidelity targets, those observed in the implementation evaluation led by Birkbeck53 and those reported in the original US trials. 9–11 We concluded that visit completion in our trial exceeded that found in the implementation evaluation and the US trials, but fell short of programme fidelity targets. We also observed considerable between-site variation in the median number of visits received. However, recent developments in the FNP programme in England have addressed planned visit frequency, recognising that some women may benefit from more or less frequent visits. 77 Family nurses use a clinical tool (the New Mum Star) in combination with their clinical judgement to determine client need and adjust the frequency of home visits accordingly, including optimal timing for graduation. Although positively evaluated during the ADAPT programme,77 how this innovation is then linked to family outcomes will remain an important evaluation focus following commencement of its rollout to FNP sites in England from April 2020.
In this study, we identified a primary outcome and a cluster of related secondary outcomes relevant to the maltreatment focus of the commissioned call and predicted by the FNP logic model. In addition, we included secondary outcomes that were also predicted by the logic model. The planned analysis involved a large number of comparative tests, including for a priori subgroups. Therefore, we should be cautious, when interpreting the results, not to draw conclusions based on potentially spurious findings. However, there is a broadly consistent picture of findings across the maltreatment outcomes suggesting no effect. Similarly, there is a pattern of findings for educational attainment, which suggests an underlying beneficial effect. Although there are relatively few findings related to sample subgroups, those observed are similar to those observed in previous US trials. In each case, this provides confidence that the findings represent real programme effects.
A particular challenge for the original trial was evaluating an intervention for which there was a strong expectation of benefit from some policy and practice stakeholders and which was broadly implemented in England prior to trial results becoming available. We recognise that this was challenging not only for the research team but also for those delivering the programme. The evidence of only modest benefit from the trial generated debate about the selection of trial outcomes required by the funder and prioritised by the research team. The current evaluation was commissioned prior to the trial results becoming available and we have sought to include and report all potentially relevant outcomes available from routine record source. Some additional maternal-reported outcome data were included in our original funding request. However, although these were of programme relevance, they did not address the primary commissioning brief, which was focused on maltreatment, and we were unable to include them in our evaluation.
Although programme effects on developmental outcomes reached statistical significance, this does not necessarily indicate their clinical importance. For example, a public health perspective may value small effects for interventions being delivered at scale across a population. When effects are concentrated in population subgroups, the population likely to benefit most will be smaller. Therefore, the extent of ongoing FNP provision in England and the devolved UK nations will influence whether or not such levels of improvement are likely to be regarded as important. Other more focused educational interventions will also promote school readiness, reading and writing. The importance of such benefit from the FNP can be judged alongside such interventions. Particularly, this would be the case if the FNP programme effect was found to be restricted to just one (albeit important) domain. Much comparable evidence has been generated in North America; its relevance to the UK setting would need to be confirmed. For example, Chambers et al. ’s99 review of 32 studies of 22 early childhood programmes were all located in the USA, although all study populations were drawn from communities of high poverty. In Chambers et al. ’s99 review, average effect sizes for the most promising class of interventions were low to moderate (e.g. effect size of 0.15 for the effect of comprehensive programmes on literacy at the end of preschool). 100 Finally, complex home-visiting interventions such as the FNP aim to address a number of maternal and child domains over several years. This needs to be borne in mind when assessing the overall programme value.
Conclusions
There is little evidence of any important difference for a range of related maltreatment outcomes, even though children in the FNP arm who are assessed as in need are referred to social services sooner than children in the usual-care arm who are assessed as in need. These outcomes included designation as ever being a CIN, any referral to CSC, and injuries and ingestions resulting in emergency health-care attendance or admission. Similarly, rates of second pregnancies were equivalent across study groups, as were rates of child early educational attendance and provision of special educational support. Children in the FNP arm are more likely to exhibit a better all-round level of school readiness in their reception year. Adjusting for month of birth strengthens this effect. At KS1, more children in the FNP arm reach the expected standard for reading, an effect that is statistically significant when adjusting for month of birth. In planned subgroup analyses, programme effects at KS1 are larger for boys, but are statistically significant only for children of the youngest mothers (for mathematics and writing). Although the programme offers no apparent overall advantage for maltreatment prevention, it appears to provide support for child development, evident in reception and by the end of KS1. The use of objective routine data drawn together from a range of services has provided a clear picture of the medium-term impact of a specialist home-visiting service provided in England to teenage mothers expecting their first child.
Implications for practice
-
There are no evident benefits for maltreatment outcomes from FNP, but the programme generates higher rates of child attainment both at the end of the reception year and at KS1.
-
The FNP remains locally commissioned and delivered in England. Local needs and priorities may determine the weight attached to these different sets of outcomes.
-
Where local FNP resources are limited, study results may inform client prioritisation.
Recommendations for research
-
The programme benefits observed using routine educational data add to maternally reported developmental benefits from the original trial. The value of the programme will be more fully established by assessing longer-term impact on such developmental and educational outcomes. This should be informed by considerations of the continued availability of the programme, the cost of such an evaluation and intervening changes to the programme.
-
FNP modifications that personalise delivery based on client need and being introduced following the ADAPT programme may yet enhance outcomes. Adaptations such as varying visit dosage may be tentatively supported by our observations of dosage effects. The ability of this modified approach to deliver greater benefit than usually provided services will need to be further evaluated.
-
To capture the breadth of potential programme benefit and cost over a meaningful time frame, longer-term routine data from sources already used in this study should be gathered and supplemented by those from other sectors and also by prospectively collected data from families. Selection of outcomes for longer-term evaluation should be informed by the underlying programme theory, understanding of benefits observed in previous long-term evaluations of the programme and changes suggested in local evaluations such as the original FNP implementation evaluation.
Acknowledgements
The authors wish to acknowledge the contribution of a number of colleagues during the study. David Cohen, Christopher Butler, Alison Kemp, Kerina Jones and Sally Holland contributed to the original grant application. Rhys Williams-Thomas, Mark Odgers, Barry Lloyd and Dena Evans provided administrative support to the project. Mandy Lau provided statistical quality checks, Mirella Longo and Tom Winfield contributed to the health economic analysis plan, Kirsten McEwan was involved with initial data access and Gareth Watson provided data governance support throughout the project. We would also like to acknowledge Peter Gee who supported access to the ALPHA group and Mair Williams for access to Our Place. We would like to thank all members of CASCADE, ALPHA and Our Place for contributing to the study. Thanks are due to the FNP teams in Bristol, Bath and Wiltshire who helped us to make contact with FNP clients and graduates during our patient and public involvement work. We are especially grateful to Jacqueline Hewitt and colleagues in the Bath team for their support and advice. We thank all those not mentioned above who have contributed to the BB:2–6 study.
The Centre for Trials Research receives funding from Health and Care Research Wales and Cancer Research UK. The work was undertaken with the support of DECIPHer, a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. Joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UKCRC, is gratefully acknowledged. We would also like to acknowledge the contribution of members of the SSC.
Study Steering Committee membership
-
Ann Louise Kinmonth (Chairperson)
-
David Low
-
Gordon Taylor
-
Nina Biehal
-
Rachel Tonkin
-
Stavros Petrou
-
Silvia van den Heijkant
NHS Digital data re-use statement
Copyright © (2019), the Health and Social Care Information Centre. Re-used with the permission of the Health and Social Care Information Centre. All rights reserved.
Contributions of authors
Michael Robling (https://orcid.org/0000-0002-1004-036X) (Professor and Director of Population Health Trials) was the chief investigator with overall responsibility for the design, co-ordination and delivery of the study. With co-investigators, he conceived, designed and led the original grant application. He led on drafting report chapters and made substantial contributions to synthesis and write-up of chapters in the report, commented on drafts and outputs of the study and facilitated stakeholder activities.
Fiona Lugg-Widger (https://orcid.org/0000-0003-0029-9703) (Research Fellow: Routine Data) was responsible for data acquisition, co-ordination and team management; contributed to the public involvement activities; led on the drafting of Chapters 1–3; and collated, reviewed and commented on the final report.
Rebecca Cannings-John (https://orcid.org/0000-0001-5235-6517) (Senior Research Fellow) was responsible for conducting the statistical analysis, led on the drafting of Chapters 4 and 5 and reviewed and commented on the final report.
Julia Sanders (https://orcid.org/0000-0001-5712-9989) (Professor of Clinical Nursing and Midwifery) contributed to the original grant application; advised on the management of the study, data analysis and interpretation; and reviewed and commented on the final report.
Lianna Angel (https://orcid.org/0000-0003-3962-9773) (Research Associate) carried out data cleaning, contributed to the public involvement activities, co-led on drafting Chapter 2 and reviewed and commented on the final report.
Sue Channon (https://orcid.org/0000-0002-5394-1483) (Senior Research Fellow) contributed to the original grant application; advised on the management of the study, data analysis and interpretation; and reviewed and commented on the final report.
Deborah Fitzsimmons (https://orcid.org/0000-0002-7286-8410) (Professor and Director of Swansea Centre for Health Economics) provided senior oversight of the health economics analysis; advised on the management of the study, data analysis and interpretation; and reviewed and commented on the final report.
Kerenza Hood (https://orcid.org/0000-0002-5268-8631) (Director of the Centre for Trials Research) contributed to the original grant application; advised on the management of the study, data analysis and interpretation; and reviewed and commented on the final report.
Joyce Kenkre (https://orcid.org/0000-0002-2067-9001) (Professor of Primary Care) contributed to the original grant application and public involvement activities; advised on the management of the study, data analysis and interpretation; and reviewed and commented on the final report.
Gwenllian Moody (https://orcid.org/0000-0002-2000-4944) (Research Associate) carried out data cleaning and reviewed and commented on the final report.
Eleri Owen-Jones (https://orcid.org/0000-0003-0850-4724) (Research Associate) contributed to the original grant application; advised on the management of the study, data analysis and interpretation; and reviewed and commented on the final report.
Rhys Pockett (https://orcid.org/0000-0003-4135-7383) (Senior Lecturer) was responsible for conducting the health economics analysis, led on the drafting of Chapter 6 and reviewed and commented on the final report.
Jeremy Segrott (https://orcid.org/0000-0001-6215-0870) (Senior Lecturer) contributed to the original grant application; co-ordinated the public involvement activities; advised on the management of the study, data analysis and interpretation; led on the drafting of Chapter 7; and reviewed and commented on the final report.
Thomas Slater (https://orcid.org/0000-0003-3840-2454) (Lecturer) Advised on the management of the study, data analysis and interpretation, and reviewed and commented on the final report.
All authors contributed to the design of the final report and approved the final version.
Publications
Lugg-Widger F, Cannings-John R, Channon S, Fitzsimmons D, Hood K, Jones KH, et al. Assessing the medium-term impact of a home-visiting programme on child maltreatment in England: protocol for a routine data linkage study. BMJ Open 2017;7:e015728.
Lugg-Widger F, Cannings-John R, Angel L, Moody G, Segrott J, Kenkre J, Robling M. Assessing the impact of specialist home visiting upon maltreatment in England: a feasibility study of data linkage from a public health trial to routine health and social care data. Pilot Feasibility Stud 2018;4:98.
Lugg-Widger FV, Angel L, Cannings-John R, Hood K, Hughes K, Moody G, Robling M. Challenges in accessing routinely collected data from multiple providers in the UK for primary studies: managing the morass. Int J Popul Data Sci 2018;3:2.
Lugg-Widger F, Hood, K, Robling M. Written Evidence Submitted by Centre for Trials Research, Cardiff University (DIG0006). Science & Technology Commons Select Committee Digital Government inquiry; 2018. URL: http://data.parliament.uk/writtenevidence/committeeevidence.svc/evidencedocument/science-and-technology-committee/digital-government/written/90379.html (accessed 18 November 2020).
Data-sharing statement
All data requests should be submitted to opendata@cf.ac.uk for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Lugg-Widger FV, Cannings-John R, Channon S, Fitzsimmons D, Hood K, Jones KH, et al. Assessing the medium-term impact of a home-visiting programme on child maltreatment in England: protocol for a routine data linkage study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015728.
- Department for Children, Schools and Families . Working Together to Safeguard Children: A Guide to Inter-Agency Working to Safeguard and Promote the Welfare of Children n.d. www.education.gov.uk/publications/standard/publicationdetail/page1/dcsf-00305-2010 (accessed 5 December 2014).
- Department for Education . Characteristics of Children in Need: 2017 to 2018 n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/762527/Characteristics_of_children_in_need_2017-18.pdf (accessed 12 November 2019).
- Great Britain . Children Act 1989 1989.
- Home Visiting Evidence of Effectiveness (HomVEE) . Reductions in Child Maltreatment n.d. https://homvee.acf.hhs.gov/Outcome/2/Reductions-in-Child-Maltreatment/4/1 (accessed 12 November 2019).
- Olds DL, Hill PL, O’Brien R, Racine D, Moritz P. Taking preventive intervention to scale: the Nurse–Family Partnership. Cogn Behav Pract 2003;10:278-90. https://doi.org/10.1016/S1077-7229(03)80046-9.
- Levey EJ, Gelaye B, Bain P, Rondon MB, Borba CP, Henderson DC, et al. A systematic review of randomized controlled trials of interventions designed to decrease child abuse in high-risk families. Child Abuse Negl 2017;65:48-57. https://doi.org/10.1016/j.chiabu.2017.01.004.
- Nurse–Family Partnership . Annual Report 2017 n.d. www.nursefamilypartnership.org/wp-content/uploads/2018/04/2017AnnualReport_FINAL_INTERACTIVE.pdf (accessed 12 November 2019).
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78:65-78.
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA 1997;278:644-52. https://doi.org/10.1001/jama.1997.03550080054039.
- Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, Henderson CR, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics 2002;110:486-96. https://doi.org/10.1542/peds.110.3.486.
- Olds D, Henderson CR, Kitzman H, Cole R. Effects of prenatal and infancy nurse home visitation on surveillance of child maltreatment. Pediatrics 1995;95:365-72.
- Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA 1997;278:637-43. https://doi.org/10.1001/jama.1997.03550080047038.
- Kitzman HJ, Olds DL, Cole RE, Hanks CA, Anson EA, Arcoleo KJ, et al. Enduring effects of prenatal and infancy home visiting by nurses on children: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med 2010;164:412-18. https://doi.org/10.1001/archpediatrics.2010.76.
- Olds DL, Kitzman H, Hanks C, Cole R, Anson E, Sidora-Arcoleo K, et al. Effects of nurse home visiting on maternal and child functioning: age-9 follow-up of a randomized trial. Pediatrics 2007;120:e832-45. https://doi.org/10.1542/peds.2006-2111.
- Olds DL, Henderson CR, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life?. Pediatrics 1994;93:89-98.
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics 2004;114:1560-8. https://doi.org/10.1542/peds.2004-0961.
- Hall D, Hall S. The ‘Family–Nurse Partnership’: Developing an Instrument for Identification, Assessment and Recruitment of Clients. London: Department for Children, Schools and Families; 2007.
- Ball M, Barnes J, Meadows P. Issues Emerging from the First 10 Pilot Sites Implementing the Nurse–Family Partnership Home-visiting Programme in England. London: Department of Health and Social Care; 2012.
- Barnes J, Stuart J, Allen E, Petrou S, Sturgess J, Barlow J, et al. Randomized controlled trial and economic evaluation of nurse-led group support for young mothers during pregnancy and the first year postpartum versus usual care. Trials 2017;18. https://doi.org/10.1186/s13063-017-2259-y.
- Owen-Jones E, Bekkers MJ, Butler CC, Cannings-John R, Channon S, Hood K, et al. The effectiveness and cost-effectiveness of the Family Nurse Partnership home visiting programme for first time teenage mothers in England: a protocol for the Building Blocks randomised controlled trial. BMC Pediatr 2013;13. https://doi.org/10.1186/1471-2431-13-114.
- Robling M, Bekkers MJ, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55. https://doi.org/10.1016/S0140-6736(15)00392-X.
- Macmillan HL, Wathen CN, Barlow J, Fergusson DM, Leventhal JM, Taussig HN. Interventions to prevent child maltreatment and associated impairment. Lancet 2009;373:250-66. https://doi.org/10.1016/S0140-6736(08)61708-0.
- FNP National Unit . A Decade of FNP 2017. https://fnp.nhs.uk/about-us/a-decade-of-fnp/ (accessed 12 November 2019).
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Heymans MW, Crijnen A, Hirasing RA. The effect of VoorZorg, the Dutch nurse–family partnership, on child maltreatment and development: a randomized controlled trial. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0120182.
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Crone M, Crijnen A, HiraSing RA. Effects of nurse home visitation on cigarette smoking, pregnancy outcomes and breastfeeding: a randomized controlled trial. Midwifery 2014;30:688-95. https://doi.org/10.1016/j.midw.2013.08.006.
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Heymans MW, Hirasing RA, Crijnen AA. Effect of nurse home visits vs. usual care on reducing intimate partner violence in young high-risk pregnant women: a randomized controlled trial. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0078185.
- Sierau S, Dähne V, Brand T, Kurtz V, von Klitzing K, Jungmann T. Effects of home visitation on maternal competencies, family environment, and child development: a randomized controlled trial. Prev Sci 2016;17:40-51. https://doi.org/10.1007/s11121-015-0573-8.
- Kliem S, Sandner M, Lohmann A, Sierau S, Dähne V, Klein AM, et al. Follow-up study regarding the medium-term effectiveness of the home-visiting program ‘Pro Kind’ at age 7 years: study protocol for a randomized controlled trial. Trials 2018;19. https://doi.org/10.1186/s13063-018-2707-3.
- Lugg-Widger F, Robling M, Lau M, Paranjothy S, Pell J, Sanders J, et al. Evaluation of the effectiveness of the Family Nurse Partnership home visiting programme in first time young mothers in Scotland: a protocol for a natural experiment. Int J Popul Data Sci 2020;5. https://doi.org/10.23889/ijpds.v5i1.1154.
- Lugg-Widger F, Cannings-John R, Angel L, Moody G, Segrott J, Kenkre J, et al. Assessing the impact of specialist home visiting upon maltreatment in England: a feasibility study of data linkage from a public health trial to routine health and social care data. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0294-4.
- Robling M, Bekkers MJ, Bell K, Butler CC, Cannings-John R, Channon S, et al. The Building Blocks Trial 2014. www.cardiff.ac.uk/__data/assets/pdf_file/0009/504729/Building-Blocks-Full-Study-Report.pdf (accessed October 2020).
- Holmbeck GN, Li ST, Schurman JV, Friedman D, Coakley RM. Collecting and managing multisource and multimethod data in studies of pediatric populations. J Pediatr Psychol 2002;27:5-18. https://doi.org/10.1093/jpepsy/27.1.5.
- Sierau S, Brand T, Manly JT, Schlesier-Michel A, Klein AM, Andreas A, et al. A multisource approach to assessing child maltreatment from records, caregivers, and children. Child Maltreat 2017;22:45-57. https://doi.org/10.1177/1077559516675724.
- Barlow J, Johnston I, Kendrick D, Polnay L, Stewart-Brown S. Individual and group-based parenting programmes for the treatment of physical child abuse and neglect. Cochrane Database Syst Rev 2006;3. https://doi.org/10.1002/14651858.CD005463.pub2.
- NHS Digital . Data Access Request Service (DARS) n.d. https://digital.nhs.uk/services/data-access-request-service-dars (accessed 19 November 2020).
- Great Britain . Health and Social Care Act 2012 2012. https://doi.org/10.12968/eqhe.2012.1.7.5.
- World Health Organization . ICD-10: International Statistical Classification of Diseases and Related Health Problems 10th Revision. Vol. 2 2010.
- NHS Digital . Demographics n.d. https://digital.nhs.uk/services/demographics (accessed 27 June 2019).
- Department for Education . National Pupil Database: Apply for a Data Extract – GOV.UK n.d. www.gov.uk/guidance/national-pupil-database-apply-for-a-data-extract (accessed 14 November 2017).
- Gorard S, Smith E. Equity in Education: An International Comparison of Pupil Perspectives. Basingstoke: Palgrave Macmillan; 2010.
- Standards and Testing Agency . Early Years Foundation Stage Profile 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/301256/2014_EYFS_handbook.pdf (accessed 6 October 2020).
- Standards and Testing Agency . Teacher Assessment Frameworks at the End of Key Stage 1 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/738778/2017_Teacher_Assessment_Frameworks_at_the_end_of_key_stage_1_WEBHO.pdf (accessed 12 November 2019).
- Great Britain . Abortion Act 1967 1967.
- Department of Health and Social Care . Protocol for the Release of Confidential Abortions Data for Bona Fide Research Purposes n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/147131/dh_129928.pdf.pdf (accessed 24 September 2020).
- Great Britain . National Health Service Act 2006 2006.
- Cardiff University . CASCADE Voices – CASCADE: Children’s Social Care Research and Development Centre – Cardiff University n.d. http://sites.cardiff.ac.uk/cascade/people/young-peoples-advisory-group/ (accessed 13 November 2017).
- Lyons RA, Jones KH, John G, Brooks CJ, Verplancke JP, Ford DV, et al. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak 2009;9. https://doi.org/10.1186/1472-6947-9-3.
- Jones KH, Ford DV, Jones C, Dsilva R, Thompson S, Brooks CJ, et al. A case study of the Secure Anonymous Information Linkage (SAIL) Gateway: a privacy-protecting remote access system for health-related research and evaluation. J Biomed Inform 2014;50:196-204. https://doi.org/10.1016/j.jbi.2014.01.003.
- Department of Health and Social Care . Information Governance Toolkit n.d. www.igt.hscic.gov.uk/ (accessed 31 October 2017).
- Great Britain . Data Protection Act 1998 1998.
- Department for Education . Children In Need in England, Including Their Characteristics and Further Information on Children Who Were the Subject of a Child Protection Plan (2009–10 Children in Need Census – Final) Year Ending 31 March 2010 2010.
- Barnes J. Nurse–Family Partnership Programme. Second Year Pilot Sites Implementation in England: The Infancy Period 2009. https://webarchive.nationalarchives.gov.uk/20101009043641/http://www.education.gov.uk/research/data/uploadfiles/DCSF-RR166.pdf (accessed 19 November 2020).
- National Data Guardian for Health and Care, National Data Guardian for Health . Review of Data Security, Consent and Opt-Outs National Data Guardian 2016. www.gov.uk/government/uploads/system/uploads/attachment_data/file/535024/data-security-review.PDF (accessed 11 July 2017).
- Department for Education . Characteristics of Children in Need in England: 2014 to 2015 n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/469740/SFR41-2015_Methodology.pdf (accessed 12 November 2019).
- Booth CL, Mitchell SK, Barnard KE, Spieker SJ. Development of maternal social skills in multiproblem families: effects on the mother–child relationship. Dev Psychol 1989;25:403-12. https://doi.org/10.1037/0012-1649.25.3.403.
- Barnard K, Hilsinger G, Patteson D, Snyder C, Solchany J, Shangle M. Parent Protective Factors Project (1995–9), Final Report 1999.
- Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. Windsor: NFER-NELSON; 1995.
- Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics 2001;108. https://doi.org/10.1542/peds.108.2.e31.
- Hays R, Sherbourne C, Mazel R. User’s Manual for the Medical Outcomes Study (MOS) Core Measures of Health-related Quality of Life. Santa Monica, CA: The RAND Corporation; 1995.
- Corbacho B, Bell K, Stamuli E, Richardson G, Ronaldson S, Hood K, et al. Cost-effectiveness of the Family Nurse Partnership (FNP) programme in England: evidence from the building blocks trial. J Eval Clin Pract 2017;23:1367-74. https://doi.org/10.1111/jep.12799.
- National Institute for Health and Care Excellence . Developing NICE Guidelines: The Manual n.d. www.nice.org.uk/media/default/about/what-we-do/our-programmes/developing-nice-guidelines-the-manual.pdf (accessed 5 May 2017).
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Mauskopf JA, Paul JE, Grant DM, Stergachis A. The role of cost–consequence analysis in healthcare decision-making. PharmacoEconomics 1998;13:277-88. https://doi.org/10.2165/00019053-199813030-00002.
- Coast J. Is economic evaluation in touch with society’s health values?. BMJ 2004;329:1233-6. https://doi.org/10.1136/bmj.329.7476.1233.
- Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0150205.
- Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P. Data Resource Profile: Hospital Episode Statistics Admitted Patient Care (HES APC). Int J Epidemiol 2017;46:1093-1093i. https://doi.org/10.1093/ije/dyx015.
- Huskinson T, Hobden S, Oliver D, Keyes J, Littlewood M, Pye J, et al. Childcare and Early Years Survey of Parents 2014 to 2015 n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/516924/SFR09-2016_Childcare_and_Early_Years_Parents_Survey_2014-15_report.pdf.pdf (accessed 5 May 2017).
- Wilkinson DL, Sniehotta FF, Michie S. Targeting those in need: baseline data from the first English National Health Service (NHS) health trainer service. Psychol Health Med 2011;16:736-48. https://doi.org/10.1080/13548506.2011.564191.
- Department for Education . Phonics Screening Check and Key Stage 1 Assessments in England, 2016 (SFR 42 2016) 2016.
- NHS Digital . Downloads – Groupers and Tools n.d. https://digital.nhs.uk/services/national-casemix-office/downloads-groupers-and-tools (accessed 5 January 2021).
- Raftery J. Costing in economic evaluation. BMJ 2000;320. https://doi.org/10.1136/bmj.320.7249.1597.
- The ALPHA Group. ALPHA n.d. http://decipher.uk.net/public-involvement/young-people/ (accessed 6 December 2018).
- Public Involvement Standards Development Partnership . National Standards for Public Involvement in Research. 2018. www.invo.org.uk/wp-content/uploads/2014/11/Draft-Values-principles-and-standards-framework-071114.pdf (accessed 12 November 2019).
- Hawkins J, Madden K, Fletcher A, Midgley L, Grant A, Cox G, et al. Development of a framework for the co-production and prototyping of public health interventions. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4695-8.
- Bywaters P, Bunting L, Davidson G, Hanratty J, Mason W, McCartan C, et al. The Relationship Between Poverty, Child Abuse and Neglect: An Evidence Review. York: Joseph Rowntree Foundation; 2016.
- Dartington Service Design Lab, FNP National Unit . FNP ADAPT: Using Evidence, Pragmatism, and Collaboration to Change the FNP Programme in England n.d. www.fnp.nhs.uk/media/1359/fnp_adapt_report_web.pdf.
- Robling M, Cannings-John R, Channon S, Hood K, Moody G, Poole R, et al. What is usual care for teenagers expecting their first child in England? A process evaluation using key informant mapping and participant survey as part of the Building Blocks randomised controlled trial of specialist home visiting. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020152.
- Zielinski DS, Eckenrode J, Olds DL. Nurse home visitation and the prevention of child maltreatment: impact on the timing of official reports. Dev Psychopathol 2009;21:441-53. https://doi.org/10.1017/S0954579409000248.
- Segal L, Nguyen H, Gent D, Hampton C, Boffa J. Child protection outcomes of the Australian Nurse Family Partnership Program for Aboriginal infants and their mothers in Central Australia. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0208764.
- Matone M, Kellom K, Griffis H, Quarshie W, Faerber J, Gierlach P, et al. A mixed methods evaluation of early childhood abuse prevention within evidence-based home visiting programs. Matern Child Health J 2018;22:79-91. https://doi.org/10.1007/s10995-018-2530-1.
- Olds DL, Kitzman H, Cole R, Robinson J, Sidora K, Luckey DW, et al. Effects of nurse home-visiting on maternal life course and child development: age 6 follow-up results of a randomized trial. Pediatrics 2004;114:1550-9. https://doi.org/10.1542/peds.2004-0962.
- Heckman JJ, Holland ML, Makino KK, Pinto R, Rosales-Rueda M. An Analysis of the Memphis urse–Family Partnership Program n.d. www.nber.org/papers/w23610 (accessed 12 November 2019).
- Department for Education . Early Years Foundation Stage Profile Results in England, 2018 n.d. www.gov.uk/government/collections/statistics-early-years-foundation-stage-profile (accessed 26 April 2019).
- Sylva K, Melhuish E, Sammons P, Siraj I, Taggart B, Smees R, et al. Students’ Educational and Developmental Outcomes at Age 16. Effective Pre-School, Primary and Secondary Education (EPPSE 3-16) Project Research Report 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/351496/RR354_-_Students__educational_and_developmental_outcomes_at_age_16.pdf (accessed 6 October 2020).
- Crawford C, Dearden L, Meghir C. When You Are Born Matters: The Impact of Date of Birth on Child Cognitive Outcomes in England – Executive Summary. London: The Institute for Fiscal Studies; 2007.
- Department for Education . National Curriculum Assessments at Key Stage 1 and Phonics Screening Checks in England, 2018 2018.
- Valle I, La, Graham B, Payne L. A Consistent Identifier in Education and Children’s Services 2016. www.gov.uk/government/publications/using-a-consistent-identifier-education-and-childrens-services (accessed 6 October 2020).
- Lugg-Widger F, Angel L, Cannings-John R, Hood K, Hughes K, Moody G, et al. Challenges in accessing routinely collected data from multiple providers in the UK for primary studies: managing the morass. Int J Popul Data Sci 2018;3. https://doi.org/10.23889/ijpds.v3i3.432.
- Thabane L, Lancaster G. Improving the efficiency of trials using innovative pilot designs: the next phase in the conduct and reporting of pilot and feasibility studies. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-017-0159-2.
- Harron K, Gamble C, Gilbert R. E-health data to support and enhance randomised controlled trials in the United Kingdom. Clin Trials 2015;12:180-2. https://doi.org/10.1177/1740774514562030.
- Teager W, McBride T. An Initial Assessment of the 2-Year-Old Free Childcare Entitlement: Drivers of Take-up and Impact on Early Years Outcomes n.d. www.eif.org.uk/report/an-initial-assessment-of-the-2-year-old-free-childcare-entitlement (accessed 2 August 2019).
- Eckenrode J, Ganzel B, Henderson CR, Smith E, Olds DL, Powers J, et al. Preventing child abuse and neglect with a program of nurse home visitation: the limiting effects of domestic violence. JAMA 2000;284:1385-91. https://doi.org/10.1001/jama.284.11.1385.
- Eckenrode J, Campa MI, Morris PA, Henderson CR, Bolger KE, Kitzman H, et al. The prevention of child maltreatment through the nurse family partnership program: mediating effects in a long-term follow-up study. Child Maltreat 2017;22:92-9. https://doi.org/10.1177/1077559516685185.
- Drake B, Jonson-Reid M, Kim H. Surveillance bias in child maltreatment: a tempest in a teapot. Int J Environ Res Public Health 2017;14. https://doi.org/10.3390/ijerph14090971.
- Chaffin M, Bard D. Impact of intervention surveillance bias on analyses of child welfare report outcomes. Child Maltreat 2006;11:301-12. https://doi.org/10.1177/1077559506291261.
- Robling MR, Hood K, Houston H, Pill R, Fay J, Evans HM. Public attitudes towards the use of primary care patient record data in medical research without consent: a qualitative study. J Med Ethics 2004;30:104-9. https://doi.org/10.1136/jme.2003.005157.
- Tudor Edwards R, Bryning L, Lloyd-Williams H. Transforming Young Lives across Wales: The Economic Argument for Investing in Early Years. Bangor: Prifysgol Bangor University; 2016.
- Chambers B, Cheung ACK, Slavin RE. Literacy and language outcomes of comprehensive and developmental-constructivist approaches to early childhood education: a systematic review. Educ Res Rev 2016;18:88-111. https://doi.org/10.1016/j.edurev.2016.03.003.
- Education Endowment Foundation . Sutton Trust-EEF Teaching and Learning Toolkit &Amp; EEF Early Years Toolkit: Technical Appendix and Process Manual. Working Document v.01 2018. https://educationendowmentfoundation.org.uk/public/files/Toolkit/Toolkit_Manual_2018.pdf (accessed 12 Nov 2019).
Appendix 1 Summary findings of the Nurse–Family Partnership and VoorZorg trials
| Outcome | NFP trials | VoorZorg trial,25 n = 460 participants (recruitment 2007–9) | ||
|---|---|---|---|---|
| Elmira,9 n = 400 participants (recruitment 1978–80) | Memphis,10 n = 1139 participants (recruitment 1990–1) | Denver,11 n = 735 participants (recruitment 1994–5) | ||
| Maternal life course | ||||
| Number of subsequent pregnancies | ↓ Subsequent pregnancies at 15 years (1.5 vs. 2.2; p = 0.03)b | ↓ Subsequent pregnancies by: | Not significant at 48 months, 6 years or 9 years | |
| Maternal deaths | At 20 years, there were 5 vs. 22 deaths (not tested) | |||
| Child development | ||||
| Child attended head start, preschool, day care | ↑ Proportion attending at 72 months (82.0 vs. 74.9; p = 0.05)c | ↓ Attendance at 48 months (54.4% vs. 65.9%; p = 0.03)c | ||
| Total language score | ↑ Score at 48 months (91.39 vs. 86.73; p = 0.04)d | |||
| Arithmetic achievement standard score | ↑ At 72 months (88.61 vs. 85.42; p = 0.04)d | Not significant at 48 months, 6 years or 9 years | ||
| Reading achievement standard score | Not significant at 72 months | Not significant at 48 months, 6 years or 9 years | ||
| Special education or remedial services | Not significant at 48 months, 6 years or 9 years | |||
| Grade retention | Not significant at 48 months, 6 years or 9 years | |||
| Academically engaged | Not significant at 72 months | |||
| Classroom social skills | Not significant at 72 months | |||
| Mental processing composite | ↑ At 72 months (92.34 vs. 90.24; p = 0.03)c | |||
| GPA (reading and mathematics) | ↑ At 9 years (2.68 vs. 2.44; p = .016)c | |||
| ↑ At grades 1–6 at 12 years (2.46 vs. 2.27; p = 0.03)d | ||||
| ↑ At grades 4–6 at 12 years (2.27 vs. 2.08; p = 0.047)d | ||||
| Achievement tests (reading and mathematics) | ↑ At 9 years (44.89 vs. 35.72; p = 0.002)d | |||
| Any academic failures | Not significant at 9 years | |||
| Ever retained (child) | Not significant at 9 or 12 years | |||
| Ever placed in special education grades (child) | Not significant at 9 or 12 years | |||
| PIAT scores (reading and mathematics) | ↑ Score at 12 years (88.78 vs. 85.70; p = 0.009)d | |||
| Group achievement test scores (reading and mathematics) | ↑ Score at grades 1–6 at 12 years (40.52 vs. 34.85; p = 0.02).d Not significant at grades 4–6 at 12 years | |||
| Stimulation of language skills | ↑ Score at 34 months (6.14 vs. 5.12; p = 0.005); 46 months (6.71 vs. 6.03; p = 0.01)b | |||
| Child health and indicators of maltreatment | ||||
| Child foster care placements | Not significant at 0 to 12 years | |||
| Child deaths | At 20 years, there were 2 vs. 14 deaths (not tested)c | |||
| Rates of new cases of child abuse and neglect | ↓ Substantiated reports of child abuse and neglect (incidence log 0.11 vs. 0.53; p < 0.001) 15 yearsb,c | ↓ Number of CPS reports at 36 months (11% vs. 19%; p < 0.05)c | ||
| ↓ CPS reports involving mother as perpetrator at 15 years (0.32 vs. 0.65; p = 0.01)c | ||||
| ↓ CPS reports involving study child at 15 (0.44 vs. 0.73; p = 0.04).c Not significant from 25 to 48 months | ||||
| Injuries and ingestions in physician record | ↓ Number of injuries/ingestions (log incidence 1.09 vs. –0.59; p = 0.03)c | |||
| Emergency department visits | ↓ Number of visits (log incidence –0.10 vs. 0.42; p < 0.01)c | |||
| Emergency departmental visits for injuries and ingestions | Not significant from 25 to 50 months | |||
| Hospital admissions | Not significant from 25 to 50 months | |||
| Days hospitalised | ↑ Number of days (log incidence –0.8 vs. –1.46; p = 0.02)c | |||
Appendix 2 Additional tables to the methods
| BB:0–2 trial | BB:2–6 study | Provided by | Data set | Time perioda | Eligibility/coverage | Mother | Child | Indicative/key data items | |
|---|---|---|---|---|---|---|---|---|---|
| ✓ | Trial participants’ maternal self-reportb | Baseline | 2009–13 | Trial participants | Yes | No | Socioeconomic; maternal health and well-being; health behaviour; pregnancy complications, neonatal outcomes; feeding and development | ||
| ✓ | Late pregnancy | ||||||||
| ✓ | Post birth (months):
|
Yes | |||||||
| ✓ | |||||||||
| ✓ | |||||||||
| ✓ | |||||||||
| ✓ | Maternity records | Maternal outcomes | 2009–10 | UK | Yes | Yes | Maternal health and well-being, neonatal outcomes | ||
| ✓ | GP recordsb | GP consultations | 2009–13 | UK | Yes | Yes | Immunisations, safeguarding | ||
| ✓ | PCTsb | Immunisation | 2009–13 | England | No | Yes | Immunisations | ||
| ✓ | ✓ | DHSC | Abortions | 2009–13 | England and Wales: all abortions performed in the NHS or an approved independent sector | Yes | No | Abortions | |
| ✓ | ✓ | ONS | Mortality records | 2009–17 | UK | Yes | Yes | Mortality data | |
| ✓ | ✓ | NHS Digital/HES | Inpatient | 2009–17 | Any NHS hospital in England | Yes | Yes | Injuries and ingestions, subsequent pregnancies | |
| ✓ | ✓ | Outpatient | |||||||
| ✓ | ✓ | A&E | |||||||
| ✓ | DfE/NPD | CIN | 2009–17 | < 18 years. Registered with social services in England | Yes | Yes | CIN status and CLA status | ||
| ✓ | CLA | ||||||||
| ✓ | Alternative provision | Publicly funded tuition in non-maintained school | 2–19 years | Educational development and attainment, eligibility for free school meals | |||||
| ✓ | EYFS profile | 2013–17 | Public schools in England | 4 years | No | Yes | |||
| ✓ | Census | 2–19 years | |||||||
| ✓ | PRU | 2–19 years | |||||||
| ✓ | KS1 | 2016–18 | 5–7 years | No | Yes | ||||
| Domains | Outcomes | Maternal | Child | HES | ONS | NPD |
|---|---|---|---|---|---|---|
| Primary | ||||||
| CIN status recorded at any time during the follow-up period | CIN status as of 31 March each year | ✓ | ✓ | |||
| Secondary | ||||||
| Objective measures of maltreatment | Referral to social services | ✓ | ✓ | |||
| Child protection registration | ✓ | ✓ | ||||
| Category of child protection plan | ✓ | ✓ | ||||
| CIN categorisation | ✓ | ✓ | ||||
| CIN duration | ✓ | ✓ | ||||
| Looked-after status | ✓ | ✓ | ||||
| CLA period of care | ✓ | ✓ | ||||
| Legal status of CLA | ✓ | ✓ | ||||
| Cause of death | ✓ | ✓ | ||||
| Associated measures of maltreatment | DNA appointments | ✓ | ✓ | |||
| Injuries and ingestions | ✓ | ✓ | ||||
| Maternal outcomes | Subsequent pregnancies | ✓ | ✓ | |||
| Costs | Health and social care resource use | ✓ | ✓ | ✓ | ✓ | |
| Child health, developmental and educational outcomes | SEN | ✓ | ✓ | |||
| Disability | ✓ | ✓ | ✓ | |||
| Day-care attendance | ✓ | ✓ | ||||
| Early-years assessment | ✓ | ✓ | ||||
| School attendance | ✓ | ✓ | ||||
| KS1 attainment | ✓ | ✓ | ||||
| Variable name | NHS Digital | NPD | Abortions |
|---|---|---|---|
| BB participant identifier | ✓ | ✓ | ✓ |
| NHS number BB trial | ✓ | ||
| Other NHS number | ✓ | ||
| Date of birth | ✓ | ✓ | ✓ |
| Expected delivery date (if no date of birth) | ✓ | ||
| Flag showing if a baby was known to be born | ✓ | ||
| Age | ✓ | ||
| Flag showing if mother was aged < 18 years at recruitment | ✓ | ||
| Sex | ✓ | ✓ | |
| Forename(s) | ✓ | ✓ | |
| Surname(s) | ✓ | ✓ | |
| Previous surname | ✓ | ✓ | |
| Child’s surname for mother’s record | ✓ | ||
| Mother’s surname for child’s record | ✓ | ||
| Address | ✓ | ✓ | |
| Postcode | ✓ | ✓ | ✓ |
| Child’s postcode for mother’s record | ✓ | ||
| Mother’s postcode for child’s record | ✓ | ||
| Flag to depict if participant is mother, child A or child B | ✓ | ✓ | |
| Start date in BB trial | ✓ | ✓ | |
| End date in BB trial | ✓ | ✓ | |
| Flag to show if mother withdrew | ✓ |
| Outcomes | Population/denominator | Numerator source | Assumptions of missingness | Oldest age of child at follow-up |
|---|---|---|---|---|
| Primary | ||||
| CIN status recorded at any time during the follow-up period | All children linked with any NPD data sets | CIN: presence in/linked to CIN data set excluding children with no further action required | Absence of linkage to CIN indicates no CIN referral (i.e. rather than missing) | < 7 years |
| Secondary | ||||
| Referral to social services | All children linked with any NPD data sets | Any child appearing in the CIN data set | Absence of linkage to the CIN data set indicates no CIN referral and no CPP (i.e. rather than missing) | < 7 years |
| Child protection registration (CPP) | All children linked with any NPD data sets | CIN: child with a CPP flag | < 7 years | |
| Category of CPP | All children linked with any NPD data sets | CIN: CPP category | < 7 years | |
| CIN categorisation | All children linked with any NPD data sets | CIN: reason for CIN status | Absence of linkage to the CIN data set indicates no CIN referral (i.e. rather than missing) | < 7 years |
| CIN duration | All children linked with any NPD data sets | CIN: CIN start and end dates | < 7 years | |
| CLA status | All children linked with any NPD data sets | CLA: presence in/linked to CLA data set | Absence of linkage to the CLA data set indicates not looked after (i.e. rather than missing) | < 7 years |
| CLA period of care | All children linked with any NPD data sets | Child looked after: date episode starts and ends | < 7 years | |
| Legal status of CLA | All children linked with any NPD data sets | CLA: categorisation of CLA | < 7 years | |
| DNA appointments | All children linked with any HES data sets | Outpatients: flag for DNA | Absence of data indicates no outpatient appointments, but absence of a DNA code attached to an attendance does | < 6 years |
| Injuries and ingestions | All children linked with any HES data sets | Flag for injuries/ingestions | Absence of an injury or an ingestion indicates no event (i.e. rather than missing) | < 6 years |
| Subsequent pregnancies | All mothers linked with any HES data sets or abortions | Inpatient/outpatient/abortion: flag of a subsequent pregnancy | Absence of a pregnancy indicates no pregnancy (i.e. rather than missing) | < 6 years |
| SEN | All children linked with any NPD data sets | PLASC/PRU/alternative provision: presence of flag under ‘SENprovision’ | Absence of data ‘SENprovision’ indicates no SEN | < 7 years |
| Day-care attendance (funded early education [Ofsted-registered PVI providers/pupils registered at school (aged 2–4 years)] | All children linked with any NPD data sets | EYC/PLASC: presence in the EYC and/or PLASC | Absence in the EYC will indicate no day-care attendance | < 4 years |
| EYFS profile assessment (to be carried out in the final term of the year in which a child reaches the age of 5 years) | All children linked with any NPD data sets | EYFS: presence in the EYC with assessment scores | Absence of any assessment scores | 5 years at assessment |
| School attendance | All children linked with any NPD data sets | PLASC/alternative provision/PRU: presence in any of these three data sets | Absence in any of these three data sets will indicate no schooling (unless home or private) | < 4 years |
| KS1 attainment | All children linked with any NPD data sets | KS1 data | If the child is linked to PLASC, has not had a KS1 assessment | < 7 years 6 months at assessment |
Hospital Episode Statistics diagnoses codes
The codes in Tables 30–32 were used to select events from NHS Digital data sources for outcomes on injuries and ingestions and subsequent pregnancies.
| A&E code | Description |
|---|---|
| 01 | Laceration |
| 021 | Contusion |
| 022 | Abrasion |
| 03 | Soft-tissue inflammation |
| 041 | Concussion |
| 042 | Other head injury |
| 051 | Dislocation |
| 052 | Open fracture |
| 053 | Closed fracture |
| 054 | Joint injury |
| 055 | Amputation |
| 06 | Sprain/ligament injury |
| 07 | Muscle/tendon injury |
| 08 | Nerve injury |
| 09 | Vascular injury |
| 101 | Burns and scalds – electric |
| 102 | Burns and scalds – thermal |
| 103 | Burns and scalds – chemical |
| 104 | Burns and scalds – radiation |
| 11 | Electric shock |
| 12 | Foreign body |
| 13 | Bites/stings |
| 141 | Poisoning (including overdose) – prescriptive drugs |
| 142 | Poisoning (including overdose) – proprietary drugs |
| 143 | Poisoning (including overdose) – controlled drugs |
| 144 | Poisoning (including overdose) – other, including alcohol |
| 15 | Near drowning |
| 16 | Visceral injury |
| ICD-10 code | Description |
|---|---|
| S00–S09 | Injuries to the head (includes open wounds, fractures, crushing and dislocation) |
| S10–S19 | Injuries to the neck |
| S20–S29 | Injuries to the thorax |
| S30–S39 | Injuries to the abdomen, lower back, lumbar spine and pelvis |
| S40–S49 | Injuries to the shoulder and upper arm |
| S50–S59 | Injuries to the elbow and forearm |
| S60–S69 | Injuries to the wrist and hand |
| S70–S79 | Injuries to the hip and thigh |
| S80–S89 | Injuries to the knee and lower leg |
| S90–S99 | Injuries to the ankle and foot |
| T00–T07 | Injuries involving multiple body regions |
| T08–T14 | Injuries to unspecified part of trunk, limb or body region |
| T15–T19 | Effects of foreign body entering through natural orifice |
| T20–T32 | Burns and corrosions |
| T33–T35 | Frostbite |
| T36–T50 | Poisoning by drugs, medicaments and biological substances |
| T51–T65 | Toxic effects of substances chiefly non-medicinal as to source (sting, alcohol, solvents, etc.) |
| T66–T78 | Other and unspecified effects of external causes (effects of radiation, heat and light, hypothermia, electric shock, asphyxiation, food deprivation) |
| X40–X49 | Accidental poisoning by and exposure to noxious substances |
| ICD-10 code | Description |
|---|---|
| O00–O08 | Pregnancy with abortive outcome |
| O10–O16 | Oedema, proteinuria and hypertensive disorders in pregnancy, childbirth and the puerperium |
| O20–O29 | Other maternal disorders predominantly related to pregnancy |
| O30–O48 | Maternal care related to the foetus and amniotic cavity and possible delivery problems |
| O60–O75 | Complications of labour and delivery |
| O80–O84 | Delivery |
| O85–092 | Complications predominantly related to the puerperium |
| O94–O99 | Other obstetric conditions, not elsewhere classified |
| Z321 | Pregnancy confirmed |
| Z33 | Pregnant state, incidental |
| Z34 | Supervision of normal pregnancy |
| Z35 | Supervision of high-risk pregnancy |
| Z36 | Antenatal screening |
| Z37 | Outcome of delivery |
| Z38 | Live-born infants according to place of birth |
| Z39 | Post partum care and examination |
Appendix 3 Additional tables for the pilot study
| Provided by | Data set | Mother | Child | Requested for the pilot study |
|---|---|---|---|---|
| NHS Digital | Mortality records | ✓ | ✓ | Entry–31 March 2015 |
| Inpatient | ✓ | ✓ | Entry–31 March 2015 | |
| Outpatient | Entry–31 March 2015 | |||
| A&E | Entry–31 March 2015 | |||
| DfE | CIN | ✓ | ✓ | Entry–31 March 2014 |
| CLA | Entry–31 March 2014 | |||
| EYFS Profile | ✗ | ✓ | Assessment day July 2013 and July 2014 | |
| EYC | ✗ | ✓ | Census day January 2013 and January 2014 | |
| Alternative provision | ✓ | ✓ | Census day January 2013 and January 2014 | |
| PRU | ✓ | ✓ | Census day January 2014 | |
| School census | ✓ | ✓ | Winter term 2012–summer term 2014 | |
| KS1 | ✗ | ✓ | ✗ |
| Step (match rate)a | NHS number | Date of birth | Sex | Postcode |
|---|---|---|---|---|
| 1 | Exact | Exact | Exact | Exact |
| 2 | Exact | Exact | Exact | – |
| 3 | Exact | Partial | Exact | Exact |
| 4 | Exact | Partial | Exact | – |
| 5 | Exact | – | – | Exact |
| 6b | – | Exact | Exact | Exact |
| 7c | – | Exact | Exact | Exact |
| 8 | Exact | – | – | – |
| Data set name | Number in data set | Match step 1 and 2, n (%) (% based on n participants in data set) | Records in data set (multiple records per participant) (n) | ||
|---|---|---|---|---|---|
| Participants | Mothers | Children | |||
| A&E | 2451 | 1205 | 1246 | 2446 (99.8) | 13,211 |
| Outpatients | 2338 | 1398 | 940 | 2336 (99.9) | 39,067 |
| Inpatients | 2789 | 1403a | 1386b | 2786 (99.9) | 11,882 |
| Any NHS Digital data set | 2804 | 1407 | 1397 | 2801 (99.8) | |
| NPD data set name | Years provided | Number in data set | |||
|---|---|---|---|---|---|
| Records | Participants | Mothers | Children | ||
| PLASC | 2012/13, 2013/14 | 760 | 760 | 4 | 756 |
| PRU census | 2013/14 | 2 | 2 | 2 | 0 |
| Alternative provision | 2012/13, 2013/14 | 1 | 1 | 0 | 1 |
| EYC | 2012/13, 2013/14 | 581 | 565 | 0 | 565 |
| CLA | 2008/9–2013/14 | 23 | 23 | 10 | 13 |
| CIN | 2008/9–2013/14 | 331a | 169a | 98a | 71 |
| Any NPD data set | 99 | 1272 | |||
Appendix 4 Additional material for referrals to children’s social care services outcome
| Subgroup | Trial arm, n (%) referred | Adjusteda OR (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Child sex | ||||
| Boys | 99 (26.3) | 108 (27.7) | 0.93 (0.65 to 1.33); 0.69 | 0.78 |
| Girls | 107 (27.9) | 100 (28.1) | 1.01 (0.69 to 1.48); 0.94 | |
| Maternal age at recruitment | ||||
| < 16 years | 17 (34.7) | 19 (34.6) | 1.05 (0.44 to 2.46); 0.92 | 0.96 |
| ≥ 16 years | 189 (26.6) | 189 (27.4) | 0.96 (0.72 to 1.30); 0.81 | |
| Adaptive functioning | ||||
| No difficulty | 140 (25.4) | 149 (26.3) | 0.99 (0.71 to 1.38); 0.96 | 0.67 |
| Difficulty in basic skills | 66 (31.7) | 59 (33.0) | 0.81 (0.59 to 1.41); 0.67 | |
| NEET status | ||||
| In EET | 70 (20.3) | 75 (23.1) | 0.83 (0.54 to 1.29); 0.42 | 0.18 |
| NEET | 100 (32.5) | 89 (29.2) | 1.19 (0.80 to 1.78); 0.39 | |
| Deprivation quintile | ||||
| 1 – least deprived | 33 (20.4) | 34 (23.9) | 0.77 (0.44 to 1.36); 0.37 | 0.32 |
| 2 | 36 (23.8) | 30 (20.5) | 1.26 (0.61 to 2.60); 0.53 | |
| 3 | 42 (28.8) | 43 (27.9) | 0.96 (0.50 to 1.86); 0.91 | |
| 4 | 41 (31.1) | 39 (25.3) | 1.27 (0.69 to 2.31); 0.44 | |
| 5 – most deprived | 54 (33.3) | 61 (42.4) | 0.65 (0.35 to 1.22); 0.18 | |
Appendix 5 Additional materials for child-in-need outcome
| Subgroup | Trial arm, CIN, n (%) | Adjusteda OR (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Sex | ||||
| Boys | 80 (21.3) | 80 (20.5) | 1.05 (0.72 to 1.53); 0.81 | 0.56 |
| Girls | 81 (21.1) | 82 (23.0) | 0.91 (0.60 to 1.38); 0.65 | |
| Maternal age at recruitment | ||||
| < 16 years | 14 (28.6) | 16 (29.1) | 1.00 (0.41 to 2.43); 0.99 | 0.98 |
| ≥ 16 years | 147 (20.7) | 146 (21.1) | 0.98 (0.72 to 1.33); 0.88 | |
| Adaptive functioning | ||||
| No difficulty | 106 (19.2) | 113 (20.0) | 0.99 (0.70 to 1.42); 0.98 | 0.76 |
| Difficulty in basic skills | 55 (26.4) | 49 (27.4) | 0.93 (0.59 to 1.47); 0.76 | |
| NEET status | ||||
| In EET | 52 (16.0) | 52 (15.1) | 0.93 (0.57 to 1.53); 0.78 | 0.42 |
| NEET | 81 (26.3) | 72 (23.6) | 1.18 (0.77 to 1.77); 0.46 | |
| Deprivation quintile | ||||
| 1 – least deprived | 24 (14.8) | 22 (15.5) | 0.92 (0.49 to 1.73); 0.79 | 0.62 |
| 2 | 30 (19.9) | 22 (15.1) | 1.53 (0.68 to 3.47); 0.31 | |
| 3 | 32 (21.9) | 36 (23,4) | 0.89 (0.52 to 1.54); 0.68 | |
| 4 | 32 (24.2) | 34 (22.1) | 1.15 (0.64 to 2.06); 0.64 | |
| 5 – most deprived | 43 (26.5) | 48 (33.3) | 0.72 (0.38 to 1.38); 0.32 | |
| Subgroup | Trial arm, CIN, n (%) | Adjusteda OR (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Social supportb | ||||
| Less than adequate social support (score of < 100) | 132 (22.2) | 139 (23.6) | 0.92 (0.70 to 1.22); 0.58 | 0.38 |
| Maximum social support (score = 100) | 28 (17.8) | 23 (15.2) | 1.31 (0.70 to 2.45); 0.39 | |
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | |||
| Generalized Self-Efficacy Scale (score 10–40)c | 0.96 (0.92 to 1.00) | 0.98 (0.94 to 1.02) | 0.25 | |
| Subjective social status – family score | 0.96 (0.87 to 1.05) | 0.99 (0.89 to 1.09) | 0.22 | |
| Subjective social status –personal score | 0.93 (0.84 to 1.04) | 0.97 (0.8 to 1.08) | 0.97 | |
| Characteristics at recruitment | Crude OR (95% CI); p-value | Adjusteda OR (95% CI); p-value |
|---|---|---|
| Maternal characteristics | ||
| Self-efficacy score | 0.97 (0.94 to 1.01); 0.19 | – |
| EQ-5D | ||
| Perfect health | Reference | Reference |
| Less than perfect health | 2.17 (1.47 to 3.20); < 0.001 | 1.90 (1.23 to 2.95); 0.004 |
| Adaptive functioning | ||
| Life skill difficulty | 1.14 (0.77 to 1.68); 0.53 | – |
| Difficulty basic skill | 1.64 (1.09 to 2.47); 0.017 | 1.36 (0.96 to 2.16); 0.19 |
| Burden difficulty | 1.20 (0.82 to 1.78); 0.35 | – |
| NEET status | ||
| In EET | Reference | |
| NEET | 1.57 (1.04 to 2.36); 0.033 | – |
| Maternal age (years) | 0.74 (0.64 to 0.86); < 0.001 | 0.77 (0.66 to 0.91); 0.002 |
| Mental health score (Kessler Psychological Distress Scale) | 1.02 (0.99 to 1.05); 0.15 | – |
| Lives with father of baby | 1.04 (0.66 to 1.65); 0.86 | – |
| Cohabiting partner (father or other) | 0.92 (0.59 to 1.44); 0.71 | – |
| Social support (MOS scale) | 0.45 (0.27 to 0.76); 0.003 | 0.50 (0.28 to 0.90); 0.021 |
| Ever homeless | 0.59 (0.38 to 0.92); 0.021 | – |
| Family resources score | 0.93 (0.89 to 0.97); 0.002 | 0.94 (0.89 to 0.99); 0.014 |
| IMD quintiles | Reference (overall p = 0.035) | Reference (overall p = 0.061) |
| 1 – least deprived | Reference | Reference |
| 2 | 0.99 (0.51 to 1.93); 0.99 | 0.83 (0.39 to 1.74); 0.62 |
| 3 | 1.70 (0.92 to 3.16); 0.093 | 1.57 (0.80 to 3.10); 0.19 |
| 4 | 1.49 (7.9 to 2.81); 0.22 | 1.34 (0.66 to 2.73); 0.42 |
| 5 – most deprived | 2.32 (1.24 to 4.38); 0.009 | 2.15 (1.06 to 4.35); 0.033 |
| Family social status | 0.95 (0.86 to 1.06); 0.39 | – |
| Personal social status | 0.98 (0.88 to 1.08); 0.69 | – |
| Mother looked after | 6.11 (2.35 to 15.87); < 0.001 | 4.30 (1.47 to 13.51); 0.012 |
| Smoking status (cotinine based) | 1.42 (0.97 to 2.08); 0.072 | |
| Child characteristics | ||
| Sex | ||
| Male | Reference | |
| Female | 1.12 (0.78 to 1.61); 0.53 | – |
| Quarter of birth | Reference (overall p = 0.104) | |
| September–November | Reference | |
| December–February | 1.37 (0.79 to 2.40); 0.26 | – |
| March–May | 1.71 (1.01 to 2.89); 0.047 | – |
| June–August | 1.82 (1.09 to 3.04); 0.021 | – |
FIGURE 18.
Predicted probabilities of CIN status. Predicted probability is the probability of a child being registered as in need based on and calculated from the multivariable logistic regression model presented in Table 40.
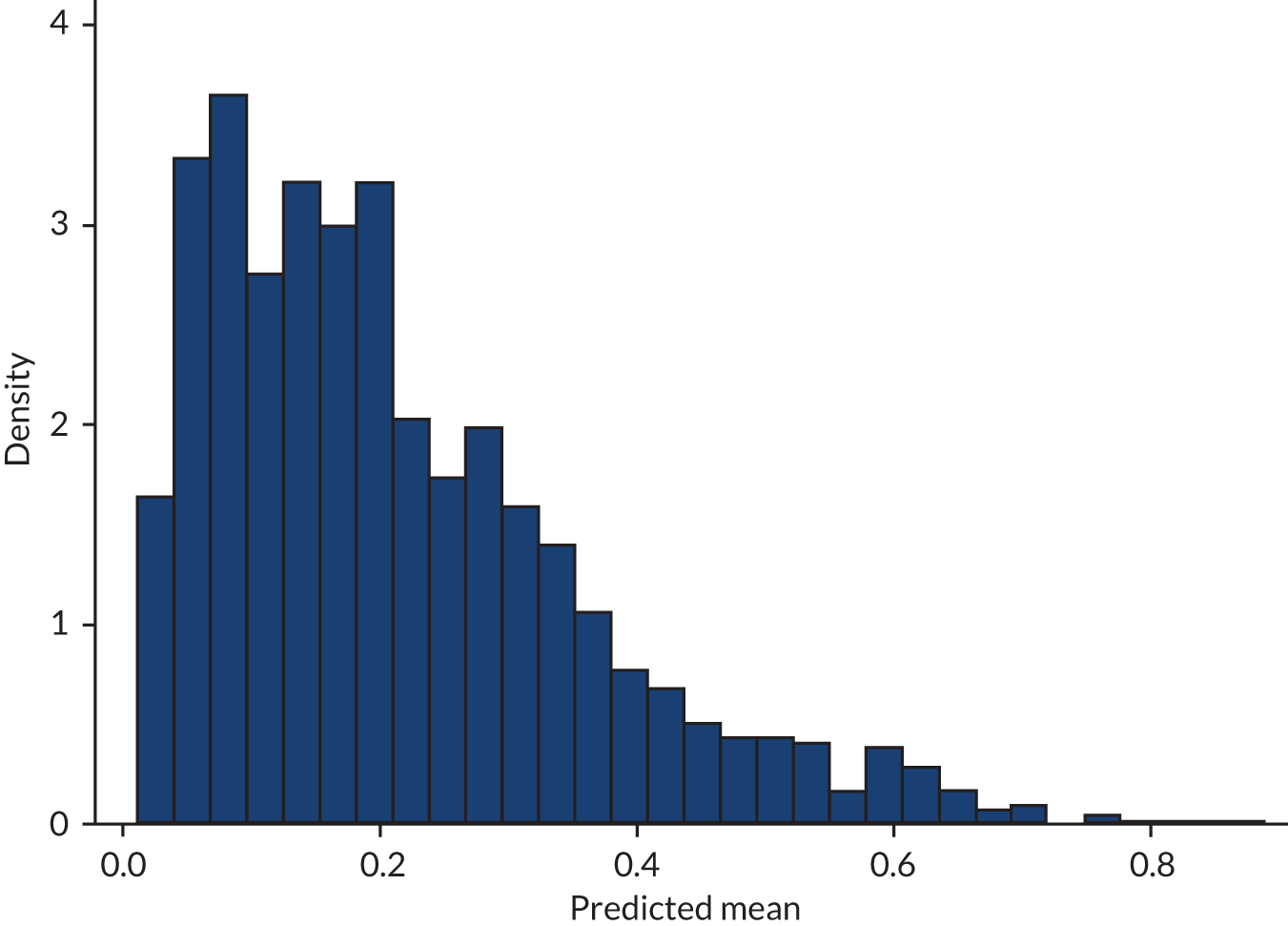
| Subgroup | Trial arm, CIN, n (%) | Adjusteda OR (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Low risk of CIN (n = 1337) | 135 (19.8) | 125 (18.9) | 1.06 (0.80 to 1.39); 0.70 | 0.30 |
| Moderate to high risk of CIN (n = 75) | 18 (51.4) | 26 (63.4) | 0.60 (0.23 to 1.54); 0.29 | |
Appendix 6 Additional materials for injuries and ingestions
| Injury/ingestion | Trial arm, n (%) | |
|---|---|---|
| FNP (N = 911) | Usual care (N = 881) | |
| Laceration | 136 (14.9) | 158 (17.9) |
| Contusion/abrasion | 90 (9.9) | 96 (10.9) |
| Soft-tissue inflammation | 63 (6.9) | 64 (7.3) |
| Head injury | 268 (29.4) | 249 (28.3) |
| Dislocation | 109 (12.0) | 84 (9.5) |
| Sprain/muscle/tendon injury | 35 (3.8) | 33 (3.8) |
| Nerve/vascular injury | 74 (8.1) | 60 (6.8) |
| Burns and scalds/electric shock | 48 (5.3) | 37 (4.2) |
| Foreign body | 40 (4.4) | 46 (5.2) |
| Bites and stings | 12 (1.3) | 20 (2.3) |
| Poisoning | 36 (4.0) | 34 (3.9) |
| Total | 911 | 881 |
| Diagnosis ICD-10 code | Trial arm, n (%) | |
|---|---|---|
| FNP (N = 109) | Usual care (N = 119) | |
| S00–S09 Injuries to the head | 52 (47.7) | 61 (51.3) |
| S20–S29 Injuries to the thorax | 9 (8.3) | 6 (5.0) |
| S30–S39 Injuries to the abdomen, lower back, lumbar spine and pelvis | ||
| S40–S49 Injuries to the shoulder and upper arm | ||
| S50–S59 Injuries to the elbow and forearm | ||
| S60–S69 Injuries to the wrist and hand | 8 (7.3) | 5 (4.2) |
| S70–S79 Injuries to the hip and thigh | 11 (10.1) | 11 (9.2) |
| S80–S89 Injuries to the knee and lower leg | ||
| S90–S99 Injuries to the ankle and foot | ||
| T00–T07 Injuries involving multiple body regions | 5 (4.6) | 10 (8.4) |
| T08–T14 Injuries to unspecified part of trunk, limb or body region | ||
| T20–T32 Burns and corrosions | ||
| T15–T19 Effects of foreign body entering through natural orifice | 5 (4.6) | 8 (6.7) |
| T36–T50 Poisoning by drugs, medicaments and biological substances | 11 (10.1) | 8 (6.7) |
| T51–T65 Toxic effects of substances chiefly non-medicinal as to source (sting, alcohol, solvents etc.) | 8 (7.3) | 10 (8.4) |
| T66–T78 Other and unspecified effects of external causes | ||
Appendix 7 Additional materials for Early Years Foundation Stage profile outcome
| Subgroup | Total point score by trial arm, mean (SD); n | Adjusteda mean difference (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Sex | ||||
| Boys | 30.57 (7.33); 369 | 29.84 (7.56); 383 | 0.75 (–0.31 to 1.82); 0.17 | 0.57 |
| Girls | 33.85 (6.79); 374 | 33.53 (7.22); 345 | 0.34 (–0.67 to 1.35); 0.51 | |
| Maternal age at recruitment | ||||
| < 16 years | 32.44 (6.71); 45 | 28.91 (7.70); 52 | 3.65 (0.76 to 6.55); 0.013 | 0.046 |
| ≥ 16 years | 32.21 (7.28); 698 | 31.80 (7.58); 676 | 0.42 (–0.36 to 1.21); 0.29 | |
| Adaptive functioning | ||||
| No difficulty | 32.99 (7.12); 540 | 32.11 (7.65); 552 | 0.88 (0.003 to 1.75); 0.049 | 0.50 |
| Difficulty in basic skills | 30.18 (7.20); 203 | 29.94 (7.33); 175 | 0.34 (–1.11 to 1.79); 0.65 | |
| NEET status | ||||
| In EET | 32.45 (7.12); 339 | 32.37 (7.68); 322 | 0.15 (–0.99 to 1.28); 0.80 | 0.95 |
| NEET | 31.72 (7.57); 304 | 31.50 (7.43); 299 | 0.19 (–1.00 to 1.38); 0.76 | |
| IMD quintiles | ||||
| 1 – least deprived | 33.16 (7.44); 159 | 31.53 (8.24); 139 | 1.72 (–0.07 to 3.50); 0.060 | ref |
| 2 | 32.16 (6.97); 148 | 31.59 (7.05); 144 | 0.65 (–0.96 to 2.27); 0.43 | 0.84 |
| 3 | 32.16 (6.79); 146 | 32.59 (7.27); 151 | –0.20 (–1.79 to 1.39); 0.80 | 0.21 |
| 4 | 30.95 (7.53); 128 | 31.11 (7.50); 148 | –0.31 (–2.11 to 1.48); 0.73 | 0.85 |
| 5 – most deprived | 32.41 (7.46); 156 | 31.03 (8.12); 140 | 1.45 (–0.33 to 3.22); 0.11 | 0.74 |
| Subgroup | Trial arm | Adjusteda mean difference (95% CI), p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Mean (SD) total point score | Mean (SD) total point score | |||
| Maximum social support (score = 100) | ||||
| No | 32.16 (7.36) | 31.54 (7.71) | 0.64 (–0.23 to 1.50); 0.15 | 0.94 |
| Yes (score = 100) | 32.44 (6.84) | 31.74 (7.42) | 0.70 (–0.91 to 2.31); 0.40 | |
| Adjusteda beta (95% CI) | Adjusteda beta (95% CI) | |||
| Self-efficacy score | 0.01 (–0.11 to 0.13) | 0.09 (–0.04 to 0.21) | 0.10 | |
| Subjective social status – family score | 0.03 (–0.28 to 0.35) | 0.02 (–0.31 to 0.35) | 0.11 | |
| Subjective social status – personal score | –0.04 (–0.32 to 0.23) | 0.41 (0.10 to 0.72) | 0.14 | |
Appendix 8 Additional materials for Key Stage 1 outcomes
| Outcomes | Reaching the expected standard | |||
|---|---|---|---|---|
| No | Yes | No | Yes | |
| Sex | Boys | Girls | ||
| Reading | ||||
| FNP, n (%) | 152 (41.8) | 212 (58.2) | 105 (27.9) | 271 (72.1) |
| Usual care, n (%) | 182 (47.3) | 203 (52.7) | 107 (30.8) | 240 (69.2) |
| Adjusteda OR (95% CI); p-value | 1.27 (0.95 to 1.69); 0.11 | 1.16 (0.84 to 1.59); 0.38 | ||
| Interaction p-value | 0.68 | |||
| Adjustedb OR (95% CI); p-value | 1.30 (0.96 to 1.75); 0.09 | 1.17 (0.84 to 1.62); 0.36 | ||
| Interaction p-value | 0.68 | |||
| Mathematics | ||||
| FNP, n (%) | 149 (40.9) | 215 (59.1) | 132 (35.1) | 244 (64.9) |
| Usual care, n (%) | 166 (43.1) | 219 (56.9) | 117 (33.7) | 230 (66.3) |
| Adjusteda OR (95% CI); p-value | 1.11 (0.83 to 1.49); 0.49 | 0.95 (0.69 to 1.29); 0.72 | ||
| Interaction p-value | 0.46 | |||
| Adjustedb OR (95% CI), p-value | 1.14 (0.84 to 1.54); 0.40 | 0.94 (0.69 to 1.29); 0.71 | ||
| Interaction p-value | 0.47 | |||
| Science | ||||
| FNP, n (%) | 120 (33.0) | 244 (67.0) | 83 (22.1) | 293 (77.9) |
| Usual care, n (%) | 138 (35.8) | 247 (64.2) | 81 (23.3) | 266 (76.7) |
| Adjusteda OR (95% CI); p-value | 1.16 (0.86 to 1.58); 0.34 | 1.08 (0.76 to 1.53); 0.68 | ||
| Interaction p-value | 0.77 | |||
| Adjustedb OR (95% CI); p-value | 1.18 (0.87 to 1.63); 0.28 | 1.08 (0.76 to 1.55); 0.66 | ||
| Interaction p-value | 0.72 | |||
| Maternal age at recruitment | < 16 years | ≥ 16 years | ||
| Reading | ||||
| FNP, n (%) | 21 (44.7) | 26 (55.3) | 236 (34.1) | 457 (65.9) |
| Usual care, n (%) | 29 (52.7) | 26 (47.3) | 260 (38.4) | 417 (61.6) |
| Adjusteda OR (95% CI); p-value | 1.21 (0.97 to 1.52); 0.09 | 1.49 (0.65 to 3.41); 0.34 | ||
| Interaction p-value | 0.66 | |||
| Adjustedb OR (95% CI); p-value | 1.50 (0.65 to 3.48); 0.34 | 1.25 (0.99 to 1.57); 0.07 | ||
| Interaction p-value | 0.62 | |||
| Mathematics | ||||
| FNP, n (%) | 16 (34.0) | 31 (66.0) | 265 (38.2) | 428 (61.8) |
| Usual care, n (%) | 32 (58.2) | 23 (41.8) | 251 (37.1) | 426 (62.9) |
| Adjusteda OR (95% CI); p-value | 3.15 (0.94 to 10.48); 0.06 | 0.96 (0.77 to 1.19); 0.69 | ||
| Interaction p-value | 0.011 | |||
| Adjustedb OR (95% CI); p-value | 3.23 (1.36 to 7.67); 0.008 | 0.98 (0.78 to 1.22); 0.83 | ||
| Interaction p-value | 0.014 | |||
| Science | ||||
| FNP, n (%) | 18 (38.3) | 29 (61.7) | 185 (26.7) | 508 (73.3) |
| Usual care, n (%) | 25 (45.4) | 30 (54.6) | 194 (28.7) | 483 (71.3) |
| Adjusteda OR (95% CI); p-value | 1.54 (0.53 to 4.47); 0.42 | 1.11 (0.88 to 1.41); 0.39 | ||
| Interaction p-value | 0.61 | |||
| Adjustedb OR (95% CI); p-value | 1.37 (0.59 to 3.19); 0.467 | 1.14 (0.89 to 1.45); 0.29 | ||
| Interaction p-value | 0.69 | |||
| Adaptive functioning | No difficulty with basic skills | Difficulty with basic skills | ||
| Reading | ||||
| FNP, n (%) | 152 (30.5) | 347 (69.5) | 87 (42.9) | 116 (57.1) |
| Usual care, n (%) | 188 (36.2) | 332 (63.8) | 84 (48.0) | 91 (52.0) |
| Adjusteda OR (95% CI); p-value | 1.29 (0.98 to 1.70); 0.07 | 1.23 (0.82 to 1.86); 0.32 | ||
| Interaction p-value | 0.61 | |||
| Adjustedb OR (95% CI); p-value | 1.29 (0.98 to 1.69); 0.07 | 1.25 (0.83 to 1.91); 0.29 | ||
| Interaction p-value | 0.95 | |||
| Mathematics | ||||
| FNP, n (%) | 186 (34.6) | 351 (65.4) | 95 (46.8) | 108 (53.2) |
| Usual care, n (%) | 192 (34.5) | 364 (65.5) | 91 (52.0) | 84 (48.0) |
| Adjusteda OR (95% CI); p-value | 1.01 (0.78 to 1.29); 0.97 | 1.27 (0.84 to 1.93); 0.26 | ||
| Interaction p-value | 0.38 | |||
| Adjustedb OR (95% CI); p-value | 1.01 (0.78 to 1.31); 0.93 | 1.32 (0.86 to 2.03); 0.20 | ||
| Interaction p-value | 0.28 | |||
| Science | ||||
| FNP, n (%) | 130 (24.2) | 407 (75.8) | 73 (36.0) | 130 (64.0) |
| Usual care, n (%) | 153 (27.5) | 403 (72.5) | 66 (37.7) | 109 (62.3) |
| Adjusteda OR (95% CI); p-value | 1.20 (0.92 to 1.58); 0.19 | 1.10 (0.71 to 1.69); 0.68 | ||
| Interaction p-value | 0.71 | |||
| Adjustedb OR (95% CI); p-value | 1.22 (0.93 to 1.62); 0.16 | 1.13 (0.73 to 1.74); 0.59 | ||
| Interaction p-value | 0.82 | |||
| NEET status | Not in EET | In EET | ||
| Reading | ||||
| FNP, n (%) | 105 (31.2) | 232 (68.8) | 109 (36.0) | 194 (64.0) |
| Usual care, n (%) | 115 (35.8) | 206 (64.2) | 121 (40.5) | 178 (59.5) |
| Adjusteda OR (95% CI); p-value | 1.26 (0.91 to 1.75); 0.17 | 1.21 (0.87 to 1.69); 0.26 | ||
| Interaction p-value | 0.86 | |||
| Adjustedb OR (95% CI); p-value | 1.31 (0.94 to 1.83); 0.17 | 1.25 (0.89 to 1.76); 0.19 | ||
| Interaction p-value | 0.83 | |||
| Mathematics | ||||
| FNP, n (%) | 122 (36.2) | 215 (63.8) | 122 (40.3) | 181 (59.7) |
| Usual care, n (%) | 107 (33.3) | 214 (66.7) | 120 (40.1) | 179 (59.9) |
| Adjusteda OR (95% CI); p-value | 0.89 (0.65 to 1.23); 0.48 | 0.99 (0.72 to 1.38); 0.97 | ||
| Interaction p-value | 0.64 | |||
| Adjustedb OR (95% CI); p-value | 0.93 (0.66 to 1.29); 0.65 | 1.03 (0.73 to 1.42); 0.90 | ||
| Interaction p-value | 0.68 | |||
| Science | ||||
| FNP, n (%) | 87 (25.8) | 250 (74.2) | 821 (27.1) | 221 (72.9) |
| Usual care, n (%) | 78 (24.3) | 243 (75.7) | 98 (32.8) | 201 (67.2) |
| Adjusteda OR (95% CI); p-value | 0.93 (0.65 to 1.33); 0.69 | 1.31 (0.92 to 1.87); 0.14 | ||
| Interaction p-value | 0.20 | |||
| Adjustedb OR (95% CI); p-value | 0.96 (0.67 to 1.39); 0.84 | 1.36 (0.95 to 1.95); 0.10 | ||
| Interaction p-value | 0.22 | |||
| KS1 assessment | Quartile | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 – least deprived | 2 | 3 | 4 | 5 – most deprived | ||||||
| Reaching the expected standard | ||||||||||
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| Reading | ||||||||||
| FNP, n (%) | 49 (30.3) | 113 (67.7) | 53 (36.3) | 93 (63.7) | 49 (33.6) | 97 (66.4) | 48 (37.2) | 81 (62.8) | 57 (37.8) | 94 (62.2) |
| Usual care, n (%) | 54 (38.9) | 85 (61.1) | 64 (44.1) | 81 (55.9) | 48 (31.8) | 103 (68.2) | 64 (43.0) | 85 (57.0) | 56 (39.4) | 86 (60.6) |
| Adjusteda OR (95% CI); p-value | 1.57 (0.88 to 2.77); 0.12 | 1.42 (0.88 to 2.29); 0.16 | 0.96 (0.59 to 1.57); 0.88 | 1.33 (0.81 to 2.18); 0.25 | 1.07 (0.60 to 1.89); 0.83 | |||||
| Adjustedb OR (95% CI); p-value | 1.75 (1.00 to 3.07); 0.05 | 1.42 (0.85 to 2.37); 0.18 | 0.89 (0.53 to 1.48); 0.64 | 1.41 (0.86 to 2.34); 0.18 | 1.00 (0.57 to 1.75); 0.99 | |||||
| Interaction p-value | 0.70 | |||||||||
| Interaction p-value | 0.37 | |||||||||
| Mathematics | ||||||||||
| FNP, n (%) | 56 (34.6) | 106 (65.4) | 57 (39.0) | 89 (61.0) | 50 (34.3) | 96 (65.7) | 55 (42.6) | 74 (57.4) | 62 (41.1) | 89 (58.9) |
| Usual care, n (%) | 52 (37.4) | 87 (62.6) | 60 (41.4) | 85 (58.6) | 56 (37.1) | 95 (62.9) | 60 (40.3) | 89 (59.7) | 54 (38.0) | 88 (62.0) |
| Adjusteda OR (95% CI); p-value | 1.15 (0.72 to 1.85); 0.56 | 1.12 (0.69 to 1.82); 0.65 | 1.17 (0.69 to 1.97); 0.56 | 0.93 (0.57 to 1.52); 0.77 | 0.91 (0.56 to 1.47); 0.69 | |||||
| Adjustedb OR (95% CI); p-value | 1.36 (0.82 to 2.24); 0.23 | 1.12 (0.68 to 1.82); 0.66 | 1.11 (0.65 to 1.90); 0.69 | 0.98 (0.60 to 1.62); 0.95 | 0.88 (0.54 to 1.44); 0.62 | |||||
| Interaction p-value | 0.91 | |||||||||
| Interaction p-value | 0.81 | |||||||||
| Science | ||||||||||
| FNP, n (%) | 37 (22.8) | 125 (77.2) | 36 (24.7) | 110 (75.3) | 40 (27.4) | 106 (72.6) | 45 (34.9) | 84 (65.1) | 44 (29.1) | 107 (70.9) |
| Usual care, n (%) | 45 (32.4) | 94 (67.6) | 45 (31.0) | 100 (69.0) | 35 (23.2) | 116 (76.8) | 47 (31.5) | 102 (68.5) | 46 (32.4) | 96 (67.6) |
| Adjusteda OR (95% CI); p-value | 1.68 (1.00 to 2.81); 0.048 | 1.39 (0.80 to 2.41); 0.25 | 0.82 (0.46 to 1.47); 0.51 | 0.89 (0.52 to 1.51); 0.65 | 1.24 (0.74 to 2.06); 0.42 | |||||
| Adjustedb OR (95% CI); p-value | 1.94 (1.13 to 3.30); 0.015 | 1.40 (0.76 to 2.57); 0.28 | 0.78 (0.43 to 1.40); 0.41 | 0.92 (0.55 to 1.55); 0.76 | 1.16 (0.69 to 1.96); 0.57 | |||||
| Interaction p-value | 0.25 | |||||||||
| Interaction p-value | 0.11 | |||||||||
| Subgroup | Trial arm, n (%) | Adjusteda OR (95% CI); p-value | Interaction p-value | Adjustedb OR (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|---|---|
| FNP | Usual care | |||||
| Sex | ||||||
| Boys | 109 (42.9) | 83 (31.8) | 1.61 (1.13 to 2.32); 0.009 | 0.034 | 1.62 (1.13 to 2.33), 0.009 | 0.039 |
| Girls | 132 (54.1) | 126 (55.8) | 1.03 (0.76 to 1.39); 0.87 | 0.94 (0.65 to 1.37), 0.76 | ||
| Maternal age at recruitment | ||||||
| < 16 years | 18 (54.6) | 9 (22.5) | 4.67 (1.47 to 14.84); 0.009 | 0.016 | 5.28 (1.49 to 18.73), 0.010 | 0.018 |
| ≥ 16 years | 223 (48.0) | 200 (44.7) | 1.13 (0.87 to 1.47); 0.35 | 1.15 (0.89 to 1.50), 0.29 | ||
| Adaptive functioning | ||||||
| No difficulty | 189 (52.5) | 174 (46.7) | 1.26 (0.93 to 1.70); 0.14 | 0.72 | 1.26 (0.93 to 1.70); 0.14 | 0.67 |
| Difficulty in basic skills | 52 (37.7) | 34 (30.1) | 1.41 (0.77 to 2.58); 0.26 | 1.53 (0.81 to 2.90); 0.19 | ||
| NEET | ||||||
| In EET | 109 (47.8) | 111 (52.9) | 0.82 (0.56 to 1.19); 0.29 | 0.019 | 0.82 (0.56 to 1.19); 0.29 | 0.028 |
| NEET | 105 (49.1) | 77 (38.3) | 1.56 (1.05 to 2.30); 0.027 | 1.56 (1.05 to 2.30); 0.027 | ||
| IMD quintile | ||||||
| 1 – least deprived | 63 (53.9) | 39 (42.9) | 1.65 (0.90 to 3.05); 0.11 | 0.89 | 1.83 (0.95 to 3.51); 0.07 | 0.86 |
| 2 | 48 (46.2) | 46 (44.7) | 1.00 (0.52 to 1.95); 0.99 | 1.04 (0.53 to 2.03); 0.92 | ||
| 3 | 46 (50.6) | 49 (46.7) | 1.20 (0.67 to 2.15); 0.53 | 1.22 (0.66 to 2.26); 0.53 | ||
| 4 | 40 (45.5) | 35 (38.5) | 1.28 (0.70 to 2.35); 0.42 | 1.28 (0.69 to 2.35); 0.43 | ||
| 5 – most deprived | 42 (44.2) | 39 (41.1) | 1.16 (0.64 to 2.08); 0.629 | 1.17 (0.64 to 2.14); 0.602 | ||
| Outcome | FNP | Usual care | Adjusteda OR (95% CI); p-value | Interaction p-value |
|---|---|---|---|---|
| Reading | ||||
| n (%) | n (%) | |||
| Maximum social support (score = 100) | ||||
| No | 374 (64.7) | 352 (60.9) | 1.19 (0.94 to 1.51); 0.16 | 0.52 |
| Yes (score = 100) | 103 (63.9) | 88 (59.1) | 1.40 (0.87 to 2.24); 0.16 | |
| Adjusteda OR (95% CI) | Adjusteda OR (95% CI) | |||
| Self-efficacy score | 1.03 (0.99 to 1.06) | 1.01 (0.98 to 1.05) | 0.55 | |
| Subjective social status – family score | 1.06 (0.96 to 1.16) | 0.97 (0.89 to 1.06) | 0.29 | |
| Subjective social status – personal score | 0.99 (0.92 to 1.08) | 1.08 (0.99 to 1.17) | 0.57 | |
| Writing, 2016/17 academic year | ||||
| n (%) | n (%) | |||
| Maximum social support (score = 100) | ||||
| No | 190 (48.6) | 174 (44.7) | 1.17 (0.88 to 1.54); 0.29 | 0.29 |
| Yes (score = 100) | 48 (47.5) | 33 (35.5) | 1.68 (0.91 to 3.11); 0.10 | |
| Adjusteda OR (95% CI) | Adjusteda OR (95% CI) | |||
| Self-efficacy score | 1.03 (0.99 to 1.07) | 1.00 (0.96 to 1.04) | 0.91 | |
| Subjective social status – family score | 1.04 (0.94 to 1.16) | 1.07 (0.96 to 1.20) | 0.16 | |
| Subjective social status – personal score | 0.98 (0.89 to 1.08) | 1.06 (0.96 to 1.17) | 0.88 | |
| Science | ||||
| n (%) | n (%) | |||
| Maximum social support (score = 100) | ||||
| No | 416 (72.0) | 400 (69.2) | 1.16 (0.90 to 1.49); 0.27 | 0.74 |
| Yes (score = 100) | 115 (74.7) | 110 (73.8) | 1.04 (0.62 to 1.75); 0.88 | |
| Adjusteda OR (95% CI) | Adjusteda OR (95% CI) | |||
| Self-efficacy score | 1.02 (0.98 to 1.06) | 1.04 (1.00 to 1.07) | 0.76 | |
| Subjective social status – family score | 1.00 (0.90 to 1.10) | 1.02 (0.93 to 1.12) | 0.26 | |
| Subjective social status – personal score | 0.99 (0.91 to 1.08) | 1.09 (1.00 to 1.20) | 0.45 | |
| Mathematics | ||||
| n (%) | n (%) | |||
| Maximum social support (score = 100) | ||||
| No | 356 (61.6) | 359 (62.1) | 0.99 (0.78 to 1.26); 0.93 | 0.50 |
| Yes (score = 100) | 97 (63.0) | 88 (59.1) | 1.18 (0.74 to 1.87); 0.49 | |
| Adjusteda OR (95% CI) | Adjusteda OR (95% CI) | |||
| Self-efficacy score | 1.01 (0.98 to 1.05) | 1.02 (0.98 to 1.05) | 0.35 | |
| Subjective social status – family score | 1.01 (0.92 to 1.10) | 0.96 (0.87 to 1.04) | 0.16 | |
| Subjective social status – personal score | 0.98 (0.90 to 1.06) | 1.05 (0.97 to 1.14) | 0.10 | |
| Variable | Crude OR (95% CI); p-value | Adjusteda OR (95% CI); p-value |
|---|---|---|
| Self-efficacy score | 1.01 (0.98 to 1.05); 0.41 | – |
| EQ-5D | ||
| Perfect health | Reference | |
| Less than perfect health | 0.80 (0.58 to 1.08); 0.15 | – |
| Adaptive functioning | ||
| Life skill difficulty | 0.90 (0.65 to 1.24); 0.51 | – |
| Difficulty basic skill | 0.63 (0.45 to 0.89); < 0.001 | 0.59 (0.41 to 0.85); 0.005 |
| Burden difficulty | 0.79 (0.57 to 1.09); 0.15 | – |
| NEET status | ||
| In EET | Reference | |
| NEET | 0.82 (0.59 to 1.14); 0.24 | – |
| Maternal age | 1.15 (1.02 to 1.29); 0.021 | 1.13 (1.00 to 1.28); 0.048 |
| Mental health score (Kessler Psychological Distress Scale) | 0.99 (0.97 to 1.02); 0.52 | – |
| Lives with father of baby | 1.05 (0.73 to 1.52); 0.78 | – |
| Cohabiting partner | 1.02 (0.72 to 1.46); 0.89 | – |
| Social support (MOS) | 0.93 (0.64 to 1.34); 0.68 | – |
| Ever homeless | 1.20 (0.83 to 1.73); 0.33 | – |
| Family resources score | 1.01 (0.98 to 1.05); 0.45 | – |
| IMD quintiles | ||
| 1 – least deprived | Reference overall = 0.22 | |
| 2 | 0.80 (0.50 to 1.29); 0.37 | – |
| 3 | 1.36 (0.84 to 2.21); 0.21 | – |
| 4 | 0.84 (0.53 to 1.35); 0.48 | – |
| 5 – most deprived | 0.98 (0.60 to 1.58); 0.92 | – |
| Family social status | 0.98 (0.89 to 1.07); 0.58 | – |
| Personal social status | 1.08 (1.00 to 1.18); 0.065 | – |
| Mother looked after | 0.64 (0.26 to 1.56); 0.33 | – |
| Smoking status (cotinine based) | 0.90 (0.66 to 1.23); 0.50 | – |
| Sex | ||
| Male | Reference | |
| Female | 2.01 (1.48 to 2.72); < 0.001 | 2.02 (1.47 to 2.76); < 0.001 |
| Quarter of birth | ||
| September–November | Reference overall p < 0.001 | Reference |
| December–February | 0.68 (0.43 to 1.09); 0.11 | 0.69 (0.43 to 1.11); 0.12 |
| March–May | 0.50 (0.32 to 0.77); 0.002 | 0.48 (0.31 to 0.74); 0.001 |
| June–August | 0.28 (0.18 to 0.43); < 0.001 | 0.28 (0.18 to 0.44); < 0.001 |
FIGURE 19.
Distribution of the predicted probabilities from the logistic model for reaching the expected standard in reading. Predicted probability is the probability of reaching the expected standard in reading based on and calculated from the multivariable logistic regression model presented in Table 49. Source: NPD, DfE.
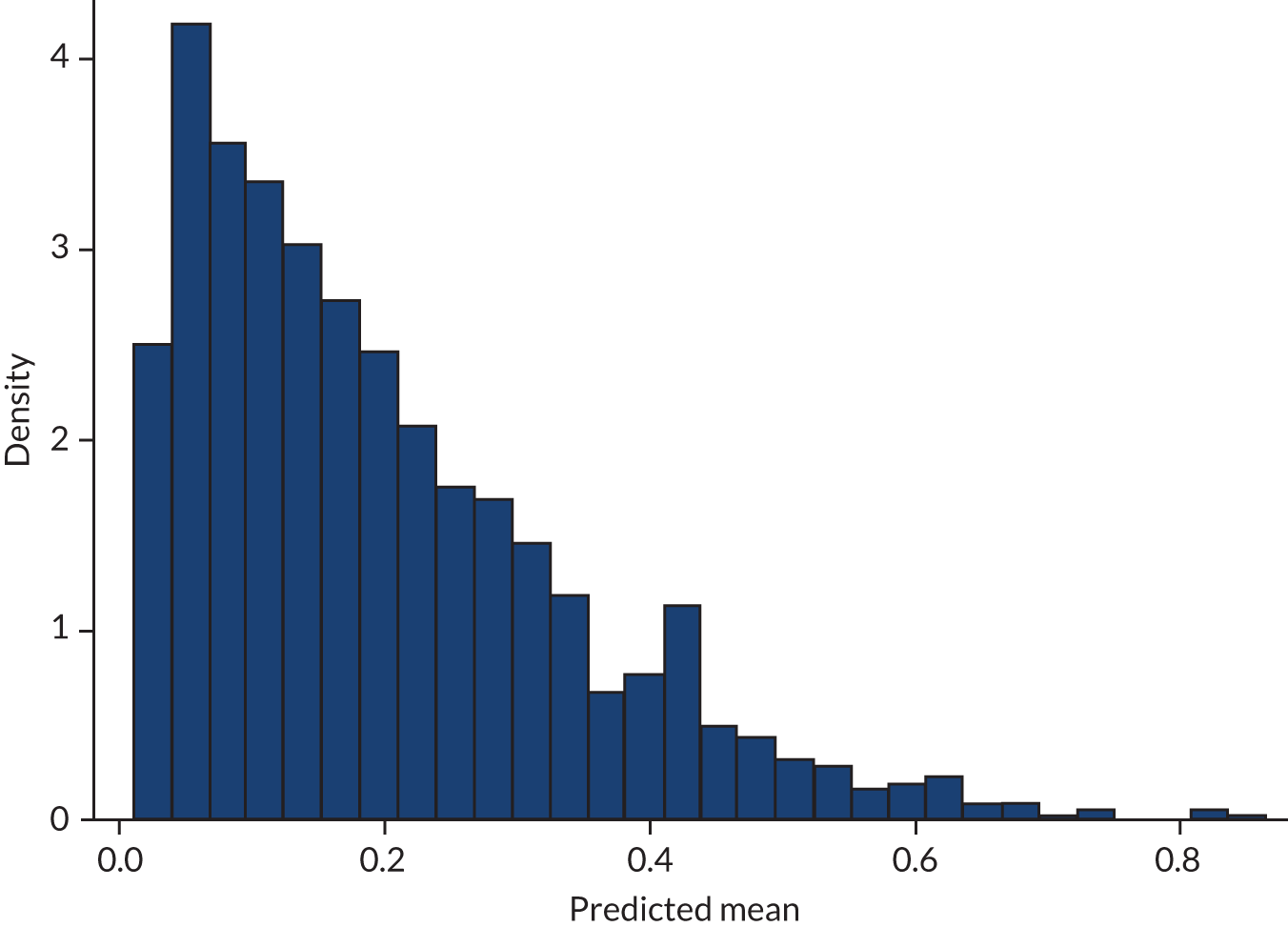
| Subgroup | Reaching the expected standard in reading, by trial arm, n (%) | Adjusteda OR (95% CI); p-value | Interaction p-value | |
|---|---|---|---|---|
| FNP | Usual care | |||
| Low risk (n = 1106) | 293 (57.9) | 257 (25.2) | 1.27 (0.98 to 1.63); 0.07 | 1.00 |
| Moderate to high risk (n = 46) | 190 (81.2) | 185 (77.4) | 1.26 (0.81 to 1.98); 0.31 | |
Appendix 9 Exploratory analyses
| CIN, by trial arm, n (%) | Adjusteda OR (95% CI); p-value | Interaction p-value | ||
|---|---|---|---|---|
| FNP | Usual care | |||
| Never been in care | 151 (20.6) | 150 (20.7) | 1.00 (0.77 to 1.30); 0.98 | |
| Ever been in care | 10 (35.7) | 12 (54.5) | 0.43 (0.13 to 1.37); 0.15 | 0.21 |
| Maternal characteristic at recruitment | Crude OR (95% CI); p-value | Adjusteda OR (95% CI); p-value |
|---|---|---|
| Self-efficacy score | 0.95 (0.90 to 1.01); 0.11 | – |
| EQ-5D | ||
| Perfect health | Reference | |
| Less than perfect health | 1.34 (0.76 to 2.37); 0.32 | – |
| Adaptive functioning | ||
| No difficulty | Reference | |
| Life skill difficulty | 1.04 (0.56 to 1.92); 0.91 | – |
| Difficulty basic skill | 1.27 (0.70 to 2.30); 0.44 | – |
| Burden difficulty | 1.49 (0.85 to 2.63); 0.17 | – |
| NEET status | ||
| In EET | Reference | |
| NEET | 0.87 (0.46 to 1.66); 0.68 | |
| Maternal age (years) | 0.68 (0.55 to 0.84); < 0.001 | 0.64 (0.52 to 0.80); < 0.001 |
| Mental health score | 1.02 (0.98 to 1.06); 0.35 | – |
| Lives with father of baby (reference = no) | 1.50 (0.77 to 2.91); 0.23 | – |
| Cohabiting partner (reference = no) | 1.18 (0.63 to 2.22); 0.61 | – |
| Social support (MOS) | 0.50 (0.21 to 1.19); 0.12 | – |
| Ever homeless (reference = no) | 1.69 (0.91 to 3.10); 0.09 | 2.20 (1.16 to 4.17); 0.015 |
| Family resources score | 1.03 (0.96 to 1.11); 0.44 | – |
| IMD quintile | ||
| 1 – least deprived | Reference (overall p = 0.23) | |
| 2 | 2.28 (0.91 to 5.71); 0.08 | – |
| 3 | 1.19 (0.43 to 3.30); 0.74 | – |
| 4 | 1.01 (0.36 to 2.83); 0.99 | – |
| 5 – most deprived | 1.23 (0.44 to 3.45); 0.69 | – |
| Family Social status | 0.97 (0.83 to 1.14); 0.71 | – |
| Personal Social status | 0.96 (0.83 to 1.11); 0.58 | – |
| Smoker (cotinine based) (reference = non-smoker) | 1.32 (0.72 to 2.42); 0.38 | – |
| Outcome | FNP | Usual care | Adjusteda mean difference (95% CI); p-value | Interaction p-value |
|---|---|---|---|---|
| Mean (SD) birthweight (g) | ||||
| Mother never been in care | 3226.3 (599.6); n = 697 | 3223.8 (549.8); n = 726 | 4.50 (–54.5 to 63.5); 0.88 | 0.33 |
| Mother ever been in care | 3160.7 (763.5); n = 27 | 2984.5 (670.4); n = 26 | 263.7 (–99.9 to 627.3); 0.16 | |
| Smoker in pregnancy, n (%) | Adjusteda OR (95% CI); p-value | |||
| Mother never been in care | 290 (55.8) | 294 (56.0) | 0.92 (0.68 to 1.26); 0.61 | 0.93 |
| Mother ever been in care | 10 (62.5) | 10 (62.5) | 0.94 (0.17 to 5.13); 0.94 | |
Appendix 10 Additional health economics tables
| Health-related resource use | BB:0–2 trial | BB:2–6 study | BB:0–6 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean resource use per participant (n) | Mean cost per participant (£) | Mean resource use per participant (n) | Mean cost per participant (£) | Mean resource use per participant (n) | Mean cost per participant (£) | |||||||||||||
| FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | |
| Inpatient attendances | ||||||||||||||||||
| Overnight admissions | 3.99 | 4.09 | –0.10 | 6354.58 | 6661.18 | –306.60 | 3.04 | 2.99 | 0.05 | 2826.79 | 2844.58 | –17.79 | 7.03 | 7.08 | –0.05 | 9181.37 | 9505.76 | –324.39 |
| Day admittances | 3.53 | 3.58 | –0.05 | 775.22 | 781.73 | –6.51 | 2.93 | 2.91 | 0.02 | 1874.61 | 1890.11 | –15.50 | 6.46 | 6.49 | –0.03 | 2649.83 | 2671.84 | –22.01 |
| Outpatient attendances | ||||||||||||||||||
| All outpatient attendances | 8.62 | 8.55 | 0.07 | 889.50 | 877.41 | 12.09 | 23.29 | 22.61 | 0.68 | 2244.62 | 2189.32 | 55.30 | 31.91 | 31.16 | 0.75 | 3134.12 | 3066.73 | 67.39 |
| Hospital-related resource use | ||||||||||||||||||
| A&E visits | 6.50 | 9.00 | –2.50 | 167.07 | 172.79 | –5.73 | 5.19 | 4.93 | 0.26 | 411.34 | 392.03 | 19.31 | 11.69 | 13.93 | –2.24 | 578.41 | 564.82 | 13.59 |
| Community-based resource use (number of clinic attendances/home visits) | ||||||||||||||||||
| Midwife/health visitor visits | 16.28 | 23.62 | –7.34 | 758.59 | 861.65 | –103.06 | Not available | Not available | Not available | Not available | ||||||||
| GP visitation (number of visits) | ||||||||||||||||||
| Surgery/home-based visits | 9.57 | 8.67 | 0.90 | 445.66 | 404.99 | 40.67 | Not available | Not available | Not available | Not available | ||||||||
| Nurse visitation (number of visits) | ||||||||||||||||||
| Surgery visits | 2.07 | 2.20 | –0.13 | 21.10 | 22.40 | –1.30 | Not available | Not available | Not available | Not available | ||||||||
| Total costs | 9411.72 | 9782.15 | –370.43 | 7357.36 | 7316.04 | 41.32 | 15,543.73 | 15,809.15 | –265.42 | |||||||||
| Health-related resource use | BB:0–2 trial | BB:2–6 study | BB:0–6 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean resource use per participant (n) | Mean cost per participant (£) | Mean resource use per participant (n) | Mean cost per participant (£) | Mean resource use per participant (n) | Mean cost per participant (£) | |||||||||||||
| FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | FNP | Usual care | Incremental (FNP – usual care) | |
| Inpatient attendances | ||||||||||||||||||
| Overnight admissions | 3.99 | 4.09 | –0.10 | 6354.58 | 6661.18 | –306.60 | 4.61 | 4.54 | 0.07 | 4789.74 | 4878.29 | –88.55 | 8.60 | 8.63 | –0.03 | 11,144.32 | 11,539.47 | –395.17 |
| Day admittances | 3.53 | 3.58 | –0.05 | 775.22 | 781.73 | –6.51 | 3.91 | 3.88 | 0.03 | 2619.55 | 2615.01 | 4.54 | 7.44 | 7.46 | –0.02 | 3394.77 | 3396.74 | –1.97 |
| Outpatient attendances | ||||||||||||||||||
| All outpatient attendances | 8.62 | 8.55 | 0.07 | 889.50 | 877.41 | 12.09 | 30.18 | 30.05 | 0.13 | 2917.86 | 2917.11 | 0.75 | 38.8 | 38.6 | 0.20 | 3807.36 | 3794.52 | 12.84 |
| Hospital-related resource use | ||||||||||||||||||
| A&E visits | 6.50 | 9.00 | –2.50 | 167.07 | 172.79 | –5.73 | 10.12 | 9.55 | 0.17 | 807.07 | 758.86 | 48.21 | 16.62 | 18.55 | –1.93 | 974.14 | 931.65 | 42.49 |
| Community-based resource use (number of clinic attendances/home visits) | ||||||||||||||||||
| Midwife/health visitor visits | 16.28 | 23.62 | –7.34 | 758.59 | 861.65 | –103.06 | Not available | Not available | Not available | Not available | ||||||||
| GP visitation (number of visits) | ||||||||||||||||||
| Surgery/home-based visits | 9.57 | 8.67 | 0.90 | 445.66 | 404.99 | 40.67 | Not available | Not available | Not available | Not available | ||||||||
| Nurse visitation (number of visits) | ||||||||||||||||||
| Surgery visits | 2.07 | 2.20 | –0.13 | 21.10 | 22.40 | –1.30 | Not available | Not available | Not available | Not available | ||||||||
| Total costs | 9411.72 | 9782.15 | –370.43 | 11,134.22 | 11,169.27 | –35.05 | 19,320.59 | 19,662.38 | –341.79 | |||||||||
Appendix 11 Additional public involvement tables
| Ranking (1 = most important) | Outcome | Suggestions on revisions |
|---|---|---|
| 1 | The cause of death for those children who have died in the study | |
| 2 | Injuries and ingestions that could have been avoided | |
| 3 | Disability | Be specific (i.e. what type and what level of disability) |
| 4 | Reasons why children are identified as being children in need | |
| 5 | Number of pregnancies | Be specific: pregnancy does not have to go to term |
| 6 | SEN | Include if they have a learning disability |
| 7 | Length of time children are identified as being a CIN | |
| 8 | School attendance | |
| 9 | Number of children who are on the child protection register | |
| 10 | The kind of CPP that children have | Provide options and what this means |
| 11 | Number of times people DNA a health/social care appointment | Define what health and social care appointments are |
| 12 | The cost of health and social care services used by families | |
| 13 | For children who are in care, how long are they in care for? What is their legal status? | Define ‘legal status’ and its meaning |
| 14 | Number of children who are looked after | (Who are in care) |
| 15 | Early-years assessment | Define what this is |
| 16 | Attainment at KS1 | Consider using a level or score |
| 17 | Day-care attendance | Define what this includes |
| Ranking (1 = most important) | Outcome | Comments (relating to rationale for ranking; meaning; acceptability) |
|---|---|---|
| 1a | Injuries and ingestions |
|
| 1b | Reasons why children are identified as being children in need | Rationale for ranking/meaning: it was felt that ‘purposeful/’wilful’ abuse or neglect is important information to know as this is very different from instances when a child is disabled, or when a new mother might need extra support because of lack of knowledge. ‘Blame’ and ‘responsibility’ were key points that arose during discussion |
| 2 | The kind of CPP that children have | Meaning: it was felt that it would be important to know whether or not CPPs were linked to wilful neglect/abuse on the part of parents/carers |
| 3 | Number of children who are on the child protection register | Acceptability: acceptable as is |
| 4a | Length of time that children are identified as being children in need | Rationale for ranking: the group mentioned the impact on the cost of services and the length of time a child is in danger |
| 4b | For children who are in care: how long they are in care for? What is their legal status? | Meaning: the group thought that how long a child is in care and their legal status were separate points and do not belong together. They also did not know what the term ‘legal status’ meant. Following discussion, they suggested changing the term to ‘legal guardian’ |
| 5 | Number of children who are ‘looked after’ (who are in care) | Meaning/rationale for ranking: the group found the term ‘looked after’ a little confusing. They thought that the term could be simplified (e.g. ‘in foster care’). They also thought that a child’s age may be important to know here. Being ‘in care’ may have a greater impact on a child’s development and self-esteem/self-confidence, dependant on their age |
| 6 | The cause of death for those children who have died | Acceptability: acceptable as is |
| Ranking (1 = most important) | Outcome | Comments (relating to rationale for ranking; meaning; acceptability) |
|---|---|---|
| 1 | Number of times people DNA a health/social care appointment (also being used in the study as an indicator of neglectful parenting) | Rationale for ranking: the cost associated with missed appointments was mentioned, and how this takes away from others who need the service |
| 2 | School attendance | Acceptability: acceptable as is |
| 3a | Disability | Meaning: specify severity and type of disability |
| 3b | SEN | Meaning: specify severity and type of need/cost |
| 4a | The cost of health and social care services used by families | Meaning: specify what that includes |
| 5 | Day-care attendance | Meaning: specify what that includes, special requirements, amount of time, funded or unfunded |
| 6 | Number of pregnancies | Meaning: specify that this does not need to go to term |
Appendix 12 Letters sent to participants
Glossary
- BB:0–2
- Building Blocks: 0–2 years, the original trial of Family Nurse Partnerships in England, which provides the study cohort for this follow-up study.
- BB:2–6
- Building Blocks: 2–6 years, follow-on study.
- Child looked after
- This is the official term used by the Department for Education/National Pupil Database, but we have also used the term ‘care experienced’ to reflect more contemporary language.
- Did not attend
- This reflects formal Hospital Episode Statistics coding and the original study protocol, but the term ‘taken to’ is also used to better reflect parental behaviour in attending health-care appointments.
- Family Nurse Partnership
- A specialist home-visiting programme delivered in England, based on the original US Nurse–Family Partnership model.
- Good level of development
- A threshold used in conjunction with the Early Years Foundation Stage profile to indicate school readiness.
List of abbreviations
- A&E
- accident and emergency
- ALF
- anonymous linking field
- ALPHA
- Advice Leading to Public Health Advancement
- aOR
- adjusted odds ratio
- BB
- Building Blocks
- BBC
- British Broadcasting Corporation
- CACE
- complier-average causal effect
- CAG
- Confidentiality Advisory Group
- CAS
- Composite Abuse Scale
- CCA
- cost–consequences analysis
- CI
- confidence interval
- CIN
- child in need
- CLA
- child looked after
- CPP
- child protection plan
- CSC
- children’s social care
- DECIPHer
- Development, Evaluation, Complexity and Implementation in Public Health Improvement
- DfE
- Department for Education
- DHSC
- Department of Health and Social Care
- DNA
- did not attend
- EET
- employment, education or training
- EYC
- early years census
- EYFS
- Early Years Foundation Stage
- FNP
- Family Nurse Partnership
- GLD
- good level of development
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HRA
- Health Research Authority
- HRG
- Healthcare Resource Group
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- IMD
- Index of Multiple Deprivation
- IRR
- incidence rate ratio
- ITT
- intention to treat
- KS1
- Key Stage 1
- NEET
- not in employment, education or training
- NFP
- Nurse–Family Partnership
- NPD
- National Pupil Database
- Ofsted
- Office for Standards in Education, Children’s Services and Skills
- ONS
- Office for National Statistics
- OR
- odds ratio
- PDS
- Personal Demographics Service
- PLASC
- pupil-level annual school census
- PRU
- pupil referral unit
- PVI
- private, voluntary or independent
- QALY
- quality-adjusted life-year
- REC
- Research Ethics Committee
- SAIL
- Secure Anonymised Information Linkage
- SEN
- special educational needs
- SMG
- Study Management Group
- SSC
- Study Steering Committee
- UKCRC
- UK Clinical Research Collaboration
