Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/114/95. The contractual start date was in January 2016. The final report began editorial review in May 2019 and was accepted for publication in December 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Glenn Robert reports that through The Point of Care Foundation in London he has previously provided advice on and training in experience-based co-design.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Jones et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Introduction and context
Stroke care in the UK has improved radically since the launch of the National Audit Programme in 19981 and the National Stroke Strategy in 2007. 2,3 Access to specialist services, reduced length of stay and community services such as early supported discharge are now accepted as standard. However, important efficiency and process improvements such as these have not always been matched by the experience of patients, especially those with moderate to severe disability, who can spend weeks and months on an inpatient stroke unit. Persistent concerns are raised about stroke unit environments that focus on organisational priorities, which provide minimal opportunities for patients’ social, cognitive or physical activity. 4,5 Results from observational studies on stroke units since the 1980s have consistently shown that, for most of the time (> 70%), patients are inactive and very often alone. 6–8
Currently, the focus in relation to activity levels is the provision of structured rehabilitation by therapists [physiotherapists (PTs), occupational therapists (OTs) and speech and language therapists], which is audited against a national guideline that recommends that every day each patient should receive at least 45 minutes of therapy, as appropriate. 9,10 However, audits and standards have not improved the experience of patients or increased activity opportunities outside these structured rehabilitation sessions with therapists. 11,12 This is critical as when patients are bored and inactive it can have an impact on aspects of their recovery and potentially foster a feeling that ‘nothing is being done’. 7
In a recent commentary on mainstream approaches to quality improvement and the potential role of co-production, Batalden13 highlighted how professionals and patients can become increasingly frustrated by product-dominant models, which focus solely on processes, actions and outputs, and that such approaches risk neglecting relationships and outcomes that are important to patients but are less easy to measure (such as patient preferences). However, improvement work to date in acute stroke care has been highly regulated and measured through national and local audits;3 there is an opportunity now for more creative responses to the persistent problem of very low activity levels in inpatient stroke units. Co-production uses the experiences and assets of patients with stroke and their families to work together with staff to address the problem. 14,15
We aimed to evaluate (1) whether or not co-production approaches can be used to improve the accessibility and quality of therapeutic activity in acute stroke care and (2) whether or not the co-produced solutions in one stroke unit are transferable to other similar acute inpatient services.
In this introductory chapter, we briefly describe stroke and stroke care and management, setting out the policy context before providing a brief summary of the persistent concerns about rehabilitation, inactivity and improving patient experience. We then describe experience-based co-design (EBCD), our chosen co-production method for quality improvement. Our rapid evidence synthesis, conducted during the set-up of the sites 1 and 2 and for the EBCD study, is mentioned here briefly. Chapter 2 provides a description of the methods and Chapter 3 provides the results. The paper was published in 2017. 16
Stroke: the state of play
Stroke statistics: organisational issues and impact
Stroke, known in recent public communications as a ‘brain attack’, can have a devastating impact on people’s lives and equally on the lives of those who live with and care for those people. 17 The effects of stroke are wide-ranging depending on the location and extent of the brain damage, but they can include paralysis and cognitive and communication difficulties among many other problems, such as difficulty with vision, continence and fatigue. 18 Stroke continues to be the largest cause of disability in the UK, and 84% of people leaving hospital will require help with activities of daily living. 17
Stroke incidence is high; 100,000 people will experience a stroke in the UK each year. 17 Although the numbers of first stroke have fallen significantly since 1990, by 2035 the rate of people over the age of 45 years having a stroke is expected to rise by 59% and the absolute number of people living with stroke will rise by 123%. 17 Population studies show that stroke incidence is not equal across different populations; people of black African, black Caribbean or South Asian ethnicity are more likely to have a stroke at a younger age. 19 In London, black people are twice as likely as white people to have a stroke. In addition, people from more socially deprived groups are likely to experience more strokes earlier in life. 20
These UK trends are also reflected in global studies that show that the absolute numbers of people who have a stroke every year, stroke survivors and related deaths, as well as the overall global burden of stroke, are great and increasing. 21 Estimates vary depending on the population sample and data sources, but it is suggested that in the UK there are 950,000 people aged ≥ 45 years. 22 This costs the UK economy approximately £8.9B per year (5% of the NHS budget), of which £4B is spent on treatment, including organised inpatient stroke unit care. 23 This figure is set to treble by 2035. 22
Recent decades have seen significant developments in the organisation and management of stroke, particularly following the implementation of the National Stroke Strategy by the Department of Health and Social Care in 2007. 24 The role of organised stroke care is well established in significantly improving outcomes after acute stroke. 25 Most people experiencing a stroke in the UK will get early access to care provided by stroke specialist staff. Large-scale service reconfigurations such as the London and Greater Manchester models have fundamentally changed care pathways, and the average length of stay on an inpatient stroke unit is likely to be around 17 days. 26,27 Large-scale reorganisation has also seen the case mix on stroke units change; patients with mild disability are discharged earlier as a result of the expansion of early supported discharge services, while critically ill patients with more complex and severe disability are likely to require a considerably longer inpatient stay. 1
Rehabilitation, recovery and persistent concerns
The component of acute stroke care consistently highlighted as likely to improve long-term outcome is rehabilitation. This assertion is informed by research showing that early activity post stroke not only improves overall prognosis but also can reduce disability. 28 This is reflected in the following statement from the Department of Health and Social Care’s National Stroke Strategy:
Rehabilitation after stroke works. Specialist co-ordinated rehabilitation, started early after stroke and provided with sufficient intensity, reduces mortality and long-term disability.
Rehabilitation is, therefore, a major part of stroke care. Multidisciplinary stroke teams typically include doctors, nurses, social workers, therapists, dietitians and psychologists, but OTs, PTs, and speech and language therapists are recognised as the central providers of rehabilitation who aim to maximise independence and prevent further complications after a stroke. 29
The fifth edition of the National Clinical Guideline for Stroke,9 published in 2016, includes a number of key recommendations that, if followed, would have the most impact on the quality of stroke care. One of these recommendations is about the intensity of rehabilitation, and states:
Patients with stroke should accumulate at least 45 minutes of each appropriate therapy every day, at a frequency that enables them to reach their rehabilitation goals, and for as long as they are willing and capable of participating and showing measurable benefit from treatment.
Reproduced with permission. Intercollegiate Stroke Working Party, page xiv9
Similar recommendations were published in the 2013 National Institute for Health and Care Excellence (NICE) guidelines for stroke rehabilitation30 and updated in more recent formulations of NICE stroke rehabilitation pathways:31
Offer initially at least 45 minutes of each relevant stroke rehabilitation therapy for a minimum of 5 days per week to people who have the ability to participate, and where functional goals can be achieved. If more rehabilitation is needed at a later stage, tailor the intensity to the person’s needs at that time.
Each of the recommendations is underpinned by high-quality evidence that increasing the frequency and intensity of rehabilitation improves recovery and clinical outcomes. 32,33 This has strongly influenced the design and implementation of organisational change interventions with a focus on achieving large doses of therapy and the belief that ‘more is better’. 18,34 However, this hypothesis is built on three assumptions: first, that national stroke guideline recommendations on rehabilitation intensity are interpreted and enacted consistently by therapists; second, that therapy is available over all 7 days of an inpatient week; and, third, that rehabilitation is the responsibility of therapists alone and not that of the whole multidisciplinary team.
Measuring the performance of stroke units against agreed standards is the responsibility of the Stroke Sentinel Stroke National Audit Programme (SSNAP). A minimum data set based on self-reported activity is collected continuously and reported quarterly, which includes performance against the rehabilitation intensity standard described above. Although the proportion of patients reported to require therapy remains constant (PT and OT, 80–85%; speech and language therapist, 50%), the median number of minutes received of the required intensity remains below the target of 45 minutes (PT and speech and language therapist, 30 minutes; OT, 40 minutes), with wide national and regional variation. Importantly, therapy is rarely a 7-day service; in 2016, SSNAP data showed that only 31% of stroke units had access to at least two types of therapy 7 days per week. 35
Several authors have stated concerns about the focus on a 45-minute therapy guideline:11,12 first, the accuracy of reporting and what is being counted and, second, that direct contact time with therapists could be considerably lower. Clarke et al. 11 carried out an ethnographic case study across eight stroke units comprising > 1000 hours of non-participant observations and 433 patient-specific therapy observations and found that a considerable amount of time was spent carrying out activities relating to information exchange rather than patient-focused therapy. In another ethnographic study across three stroke units, Taylor et al. 12 found that therapists wanted to provide more therapy and felt guilty for not doing so; there was also a lack of multidisciplinary rehabilitation. Both research teams found that rehabilitation was largely the responsibility of therapists, and patients were often observed as inactive outside their designated therapy sessions. Evidence from these studies and others shows that the issue of inactivity of stroke patients on stroke units persists. Studies consistently show that often the most disabled patients are likely to spend the majority of their time inactive and disengaged. 7,36
Some attempts have been made to address the enduring issue of inactivity, but with mixed results. A study in Australia37 concluded that dose-driven interventions, including circuit class therapy and 7-days-a-week therapy, increased the amounts of therapy provided but did not increase meaningful patient activity outside therapy sessions; the researchers called for greater understanding of the drivers of activity outside therapy sessions. Trammell et al. 38 found that a programme of physical activities ‘prescribed’ in addition to structured therapy on a stroke unit was feasible, but again this was overseen and graded by therapists. Although the research team found that staff and patients reported high satisfaction, levels of expectations about activity prior to implementation were not known and the activities consisted of repetitive exercises that required supervision.
We question whether current models of ‘therapist’-focused inpatient stroke rehabilitation and reliance on ‘waiting for therapy to be delivered’ may foster dependency and inactivity and are, therefore, at odds with promoting activity and self-management in hospital and after discharge. 39,40 The irony is that a highly medicalised stroke unit can meet national quality standards but is counterproductive to promoting patients’ independent activity. Overall, evidence suggests that acute health-care environments, staff, carers and patients could do more to enable an increase in activity, which could also have the potential to expedite discharge and decrease dependency on health and social care services in the longer term. 28,40,41 We have found that although studies have identified short-term methods to increase patients’ activity, these are often driven by the perspectives of professionals, with little evidence of patient and carer involvement in the development and implementation of interventions.
We subscribed to the ideal put forward by Sir Roger Boyle, previously the National Director for Heart Disease and Stroke, ‘to make rehabilitation the basis of the patient’s day’ (p. 4; contains public sector information licensed under the Open Government Licence v3.0). 42 We also recognise that there is an opportunity for patients with stroke, families and staff to work together to address the issue of inactivity. Studies thus far have emphasised the necessity to change but have not directly considered the ideas and experiences of the people that they seek to help.
Improving patient experience: acute health care
Improving patients’ experiences and putting patients at the centre of everything is a key aim of the NHS and is frequently reflected in health policy such as ‘putting patients first’, which highlighted citizen participation and empowerment as one of six characteristics of a high-quality, sustainable NHS. 43 The value of innovations, which build on patients’ rights to drive up quality of experience, is becoming more apparent. NHS England’s Five Year Forward View44 set out how the NHS must change, arguing for a more engaged relationship with patients and carers in order to promote well-being and prevent ill health. Frameworks are now available for organisations to carry out organisational assessments to evaluate how patient experience is embedded into culture and operational processes, with ‘good’ exemplified by evidence of staff and patients who have worked together to improve services. 45 To improve patients’ experiences, NHS policy-makers increasingly seek to encourage the development of new relationships between patients, carers and clinicians. These relationships are to be based on working together, in equal partnership, not only to make personal care decisions and agree care plans, but also to develop partnerships in which patients, carers and clinicians are involved in the co-design, co-commissioning and co-production of health-care services. 45,46
The NHS is a complex system, and to focus on patients’ experience when resources and workforce are under pressure is a fundamental and critical challenge. Some authors have raised concerns that ‘the picture [patient experience] is one of monitoring and compliance rather than ownership and motivation to improve this key aspect of quality’. 47 In addition, the empirical evidence for patient and public involvement is low and tends to be descriptive rather than evaluative. 48 Yet Berwick states that ‘workers and leaders can often find the best gaps that matter by listening very carefully to the people they serve’;49 similarly, Goodrich and Cornwell highlight that ‘patients’ stories and patients’ complaints remind us of the importance of seeing the person in the patient and bringing patients’ experience alive’ (© The King’s Fund; reproduced with permission under the CC BY-NC-ND 4.0 licence, see: https://creativecommons.org/licenses/by-nc-nd/4.0/). 50
Co-production
We believe that engaging patients and staff in service redesign of stroke units could provide solutions that address the lack of activity outside structured therapy. Co-production methods harness the power of patients, carers and staff to make changes they know and care most about. 46,51,52 In the broadest sense, co-production means delivering public services in an equal and reciprocal relationship between professionals and people using services and their families. 53 The central idea in co-production is that people who use services are hidden resources, not drains on the system, and that no service that ignores this resource can be efficient. Advocates of co-production see it as a different way of thinking about public services, with potentially transformational consequences, as people who use services take control of defining and managing their care:
The biggest untapped resources in the health system are not doctors but users. [. . .] We need systems that allow people and patients to be recognised as producers and participants, not just receivers of systems. [. . .] At the heart of [co-production], users will play a far larger role in helping to identify needs, propose solutions, test them out and implement them, together.
Cottam and Leadbeater, p. 16.
[. . .] assessing, and evaluating the relationships and actions that contribute to the health of individuals and populations. At its core [co-production] are the interactions of patients and professionals in different roles and degrees of shared work.
Batalden13
Batalden emphasises the value of health care as a co-produced service but that the essential aspects such as utilising all forms of knowledge are often neglected. The ambition of ‘shared work’ can be misinterpreted and the importance of trustworthiness between patients, carers and staff misunderstood.
Despite the increased focus on co-production in health-care policy and improvement, no studies have reported using a co-production approach or participatory methods to improve acute stroke care. However, there are examples from across other areas of acute health care. Our first research question was ‘What is known about the efficacy and effectiveness of co-production approaches in acute health care?’. A rapid evidence synthesis published in 2017 systematically reviewed the outcomes of studies that had developed and implemented co-produced interventions in acute health-care settings. 16 The review highlighted a lack of rigorous evaluation of the effectiveness and cost-effectiveness of co-produced interventions in acute health care (despite the increasing adoption of co-production as a form of intervention and one that typically drew on co-design approaches). Nonetheless, the impact of what might be perceived as ‘small, mundane things’ and the range and quality of patient-focused improvements seems to have a large impact on experience. As other authors have commented, an increasing focus on the attached meanings, rhythms and time frames in a health-care service – the degree and type of ‘the doing’ – can shape services in profound ways. 54
As interest in co-production within health-care improvement grows, so do the concerns that co-production may become misused or diluted from its original aim of enhancing collaborative work to produce public goods or services with citizens playing an active role. 16,55 Co-production originated through a recognition of the role that service users play in determining the effectiveness of public services, but several authors have highlighted issues with the false impression of equality or implicit professional dominance that can emerge as relationships between service users and providers are – supposedly – reconfigured. 55,56 Approaches that prioritise the narrative and lived experiences of those who use health-care services can have the power to captivate and engage staff, helping to create conditions necessary to enable shared improvement work.
Experience-based co-design
With increasing attention to the potential for co-production and applying design thinking as a means of improving health care, participatory approaches such as EBCD have become more widespread. The ‘co’ in ‘co-design’ refers specifically to partnership, equity and shared leadership in terms of face-to-face user and provider collaboration in the co-design of services. 47,51 EBCD originated in 2005 as a participatory action research approach that explicitly drew on design theory51 and was first piloted in a head and neck cancer service at Luton and Dunstable Hospital. 57 Through a structured six-stage process, EBCD entails staff, patients and carers sharing and reflecting on their experiences of a service, working together to identify improvement priorities, devising and implementing changes, and then jointly reflecting on their achievements. An important element of the approach is that patient experiences are gathered through filmed narrative interviews, and insights from these are shared with staff in an edited ‘trigger’ film. Several years ago, an international survey of completed, ongoing and planned EBCD projects in health-care services found that at least 59 EBCD projects had been implemented in at least six countries, with at least a further 27 projects in the planning stage. 58 The number of projects appears to be growing year on year, but, to our knowledge, EBCD has not been used in acute stroke services, despite the seemingly intractable issue of inactivity and boredom and an over-reliance on system- and (narrowly defined) outcome-focused improvement.
Full details of each of the six stages in EBCD can be found in The Point of Care Foundation’s free-to-access online toolkit, which also provides lessons and feedback from staff and patients, including details of an ‘accelerated’ form of the method, which was previously developed and evaluated with funding from the National Institute for Health Research (NIHR) Health Services and Delivery Research programme. 59,60 A general overview of the approach is provided in the study by Robert et al. 61
The EBCD cycle, which typically takes 9–12 months,51 is divided into six stages: (1) setting up the project; (2) gathering staff experiences through observational fieldwork and in-depth interviews; (3) gathering patient and carer experiences through observation and 12–15 filmed narrative-based interviews; (4) bringing staff, patients and carers together in a first co-design event to share – prompted by an edited 20- to 30-minute ‘trigger’ film of patient narratives – their experiences of a service and to identify priorities for change; (5) sustained co-design work in small groups (typically of four to six people) formed around those priorities; and (6) a celebration and review event. 47
One of the major barriers to the implementation of the approach is the time and costs involved. 16,60 Questioning whether it is always necessary – for the purposes of local quality improvement work – to generate local trigger films in the discovery phase, Locock et al. 60 tested an accelerated approach that used a national video and audio archive of films; they found that this method generated a comparable set of improvement activities. Building on this work, we first aimed to evaluate the feasibility of a full EBCD cycle and the impact of stroke patients, carers and staff co-designing and implementing interventions to increase activity in two stroke units. We then aimed to compare and contrast the impact of undertaking a full EBCD cycle in these two units with an ‘accelerated’ approach – which drew on the fieldwork and findings from the first two units – in two further units. We recognised that stroke projects addressing inactivity have focused mainly on physical activity, and for this project we used an umbrella term of ‘activity’ to be anything that patients do, however small, supervised or non-supervised, and encompassing physical, cognitive or social forms.
In summary, we believe that rehabilitation and the promotion of activity should be considered as a joint enterprise that draws continuously on both lay experience and professional expertise; this contrasts with the largely unsuccessful target- and audit-driven approaches employed to date. An EBCD cycle may provide a novel space and sufficiently flexible structure for staff, patients and families to think creatively about how post-stroke care in stroke units could be redesigned to increase activity. Central to the approach is the carefully considered development and implementation of workable solutions that can be applied and tested in routine practice through an iterative process of co-designing and prototyping. This extended type of engagement recognises the necessarily adaptive nature of stakeholder involvement, and of the gradual crafting, refinement and emergence of innovative interventions. Developing cultures of continuous rehabilitation is likely to require early and sustained involvement of the whole multidisciplinary team and some revision of their working practices, and the development of practical ways to engage and involve patients and their families.
This led us to formulate the following research questions to be explored through our empirical fieldwork in four acute stroke units in England:
-
How do patients and carers experience the use of a co-production approach and what impact does it have on the quality and intensity of independent and supervised therapeutic activity on a stroke unit?
-
How do staff from acute stroke units experience the use of a co-production approach and what improvements in independent and supervised therapeutic activities does the approach stimulate?
-
How feasible is it to adopt EBCD as a particular form of co-production for improving the quality and intensity of rehabilitation in acute stroke units?
-
What role can patients and carers have in improving implementation of National Clinical Guideline recommendations on the quality and intensity of rehabilitation in acute stroke units?
-
What are the factors and organisational processes that act as either barriers to or facilitators of successfully implementing, embedding and sustaining co-produced quality improvements in acute care settings, and how can these be addressed and enhanced?
Chapter 2 Methods: intervention development
This study involved two main aspects: (1) the ‘intervention’, consisting of ‘full and accelerated’ EBCD, to generate and implement a number of co-designed changes to increase supervised and independent activities within four stroke units, and (2) the evaluation, which was carried out pre and post implementation of the co-designed activities in each unit. For the purpose of the report, we first document the methods used in the intervention development and then present the evaluation components in Chapter 3.
Parts of this chapter are based on Clarke et al. 16 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
The intervention: full and accelerated experience-based co-design
Settings and sampling
We set out to recruit four stroke units: two in London and two in Yorkshire. We included stroke units that met the classification of a specialised stroke service defined as ‘capable of meeting the specific health, social and vocational needs of people with stroke of all ages’ set out in section 3.2 of the 2012 National Clinical Guideline for Stroke (reproduced with permission). 62 A stroke unit is classified as either a ‘routinely admitting stroke unit’ with hyperacute stroke units and acute stroke units or a ‘non-routinely admitting stroke unit’. 63 All stroke units provide acute and rehabilitation care, but only hyperacute units admit patients within the first 72 hours post stroke and return discharge data in SSNAP. 62 We also aimed to recruit stroke units with evidence of previous participation in research so that we could ensure that the units had an interest in delivering the research planned.
Stroke units were purposively selected following discussions held with senior staff and local stroke research networks. As advised by NIHR, we aimed to include not those stroke units that were based in large teaching hospitals and already taking part in clinical trials, but those that showed a willingness and commitment to take part in a study such as CREATE (Collaborative Rehabilitation in Acute Stroke) that comprised multiple stages over at least 12 months.
The two stroke units selected for the first stage and full EBCD were based in London and Yorkshire; we refer to these stroke units as sites 1 and 2. In the second stage, stroke units taking part in accelerated EBCD were also based in London and Yorkshire (sites 3 and 4). Each of the four sites was a non-routinely admitting unit that received patients only after they had been cared for in a hyperacute unit either in the same hospital (as at sites 2 and 4) or at a nearby major stoke centre (as at sites 1 and 3). More detail about each site is provided in Table 1.
| Characteristic | Site 1 | Site 2 | Site 3 | Site 4 |
|---|---|---|---|---|
| Number of stroke beds | 24 | 24 | 26 | 26 beds (14 and 12) |
| Hospital | District general hospital with 629 beds | District general hospital with 500 beds | City-centre teaching hospital with 700 beds | District general hospital with 600 beds |
| Layout | The stroke unit is on the third floor of the hospital. It has an L-shaped layout with five bays, each containing four beds, and four single rooms. The end of one corridor connects directly to another medical ward and the nursing desk is at the end of the other corridor. Visitor and staff catering services are on the ground floor of the hospital | The stroke unit is on the third floor of the hospital. It has an L-shaped layout, a long main corridor with five bays, each containing four beds, and three side rooms off this corridor. Day room and one-bed pre-discharge flat are in the smaller L-section. Visitor and staff catering services are on the ground floor of the hospital | The stroke unit is on the ground floor of the hospital. It has a central desk and one wide corridor with two male and two female bays, each with six beds, and two single rooms at the entrance to the ward. Visitor and staff catering services are on the ground and first floors of the hospital | The stroke unit is on the second floor of the hospital. It has a circular layout around four ‘pods’ that make up the stroke service. Three pods, 7a, 7b and 7d, are rehabilitation wards and 7c is the hyperacute ward. There is access by lift to outside spaces including a small therapy garden and walkways around the main hospital site. Visitor and staff catering services are on the ground floor of the hospital |
| Shared space | No day room; no outside access | Day room used by staff as a storage and meeting area at start of study. No outside access | Day room used also by staff; access to outside garden |
Day room on 7d in use as a chair store (32 chairs) at the start of the study Day room on 7b accessible but used frequently for staff meetings |
| Visiting hours | 14.00–20.00 | 11.00–20.00 | 14.00–17.00/18.00–20.00 | 11.00–20.00 |
| Meetings | Nursing handover between the day and night staff each morning. A brief morning multidisciplinary meeting, known as the ‘whiteboard meeting’, and weekly MDT meetings to review discharge plans. MDT meetings on Tuesdays | Nursing handover between the day and night staff each morning and at 12 o’clock for the late shift. Therapists and nurses meet each Monday morning. This ‘board round’ is at 09.00; MDT meeting every Wednesday | Nursing handovers every day at 08.00. and 20.00; MDT meetings on Friday afternoon | Nursing handover between the day and night staff each morning; therapist handovers follow this Monday to Friday |
| 7-day therapy service | No | An OT and a PT work on Saturday covering the acute and rehabilitation units. On Saturdays and Sundays one stroke rehabilitation assistant is on the unit | No | No |
| Performance in last Acute Organisation Report 201664 when units were graded against 10 key indicators (see Appendix 1, Table 15) | Achieved 7 of the 10 key indicators | Achieved 4 of the 10 key indicators | Achieved 8 of the 10 key indicators | Achieved 5 of the 10 key indicators |
Each of the four sites was included in the most recent biennial SSNAP Acute Organisational Audit report,64 published in 2016, which includes site-level and national performance against 10 key indicators (see Appendix 1, Table 15). The sites also return data continuously for the SSNAP Clinical Audit, which measures performance against standards for 10 key domains reflecting processes of care provided to patients. The clinical audit includes an overall performance score for 3 months, made up of a combined total indicator score derived from the average of patient- and team-centred key performance indicators, case ascertainment and audit compliance. Performance is graded A–E, with A indicating first-class service, B indicating good or excellent in many aspects, C indicating reasonable overall – some areas need improvement, D indicating several areas need improvement and E indicating substantial improvement required.
The SSNAP Acute Organisational Audit reports and the prospective clinical audit data provide an indicator of each site’s performance at a point in time, but reporting on these data carries several caveats. First, CREATE sites 1–4 did not treat patients within 72 hours (known as the hyperacute stage) following stroke and audit data also included results from these units providing hyperacute care. Second, Acute Organisational Audit data provide a snapshot of staffing at 10.00 and 22.00 and a whole-time equivalent at each grade against national indicators and the national medians on any given day, but this is likely to vary from day to day and does not include data about the severity of disability of the patients cared for. Appendix 1, Table 15, shows an overview of SSNAP Acute Organisational Audit site-level data and performance of all participating stroke units (1–4) against the 10 key indicators.
Project governance and management
The project needed Health Research Authority approval, including an independent ethics review. In each of the four sites, a senior clinician was identified who acted as principal investigator; they negotiated site access, supported local approvals and took day-to-day responsibility for the study, including identifying potential participants.
In addition to the senior clinician, each stroke unit nominated a group of core clinical staff, which included senior nurses, therapists, dietitians and psychologists. They played a key role in EBCD by helping facilitate introductions and communications with local stakeholders such as head of estates, volunteer co-ordinators, matrons, general operation managers, and communication leads for the trust. After receiving training from The Point of Care Foundation about the six stages of EBCD, the core groups assisted the research team with communications about the stages of co-design and explained to all staff how this might advance in their own stroke units. The Point of Care Foundation training was delivered by an independent facilitator who had experience in EBCD and it was carried out before EBCD commenced with teams from across the two stroke units in stage 1 and then later with the further two stroke units in stage 2. Training consisted of a full day for sites 1 and 2 but was reduced to a half-day for sites 3 and 4 following feedback from clinical teams. Further detail of training is in Report Supplementary Material 1.
In each stroke unit, the core staff and principal investigators helped researchers by identifying patients and family members who might want to engage with co-design and inviting them to do so. Following the guidance given in the EBCD toolkit,65 patients were recruited if they had been an inpatient on the unit in the previous 3–6 months and ranged in terms of ethnic group, gender and stroke severity. We set out to recruit patients with and patients without family members and a similar number of staff.
Steps of the process (full and accelerated experience-based co-design)
We followed all six stages of EBCD at sites 1 and 2, completing the full co-design process. This enabled staff, patients and families to reflect on their experiences of the acute stroke unit, work together to identify improvement priorities and devise and implement changes, and then jointly reflect on their achievements. At sites 3 and 4 we began an ‘accelerated’ process at the joint staff and patient event, using the composite films from sites 1 and 2 to trigger discussion about priorities for co-design. EBCD in CREATE was also embedded in our mixed-methods case evaluation and we undertook pre- and post-implementation data collection that is not part of a standard EBCD approach; this comprised extended ethnographic observations, behavioural mapping and patient-reported outcome measure (PROM)/patient-reported experience measure (PREM) questionnaires.
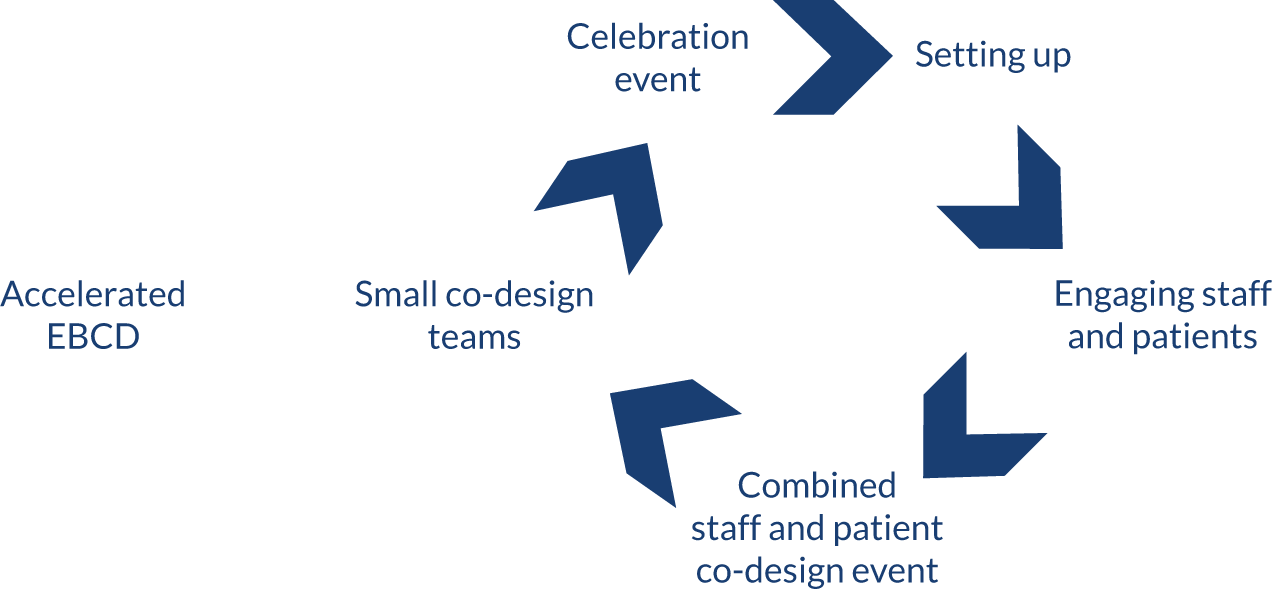
The six stages of the EBCD cycle are described as typically taking 9–12 months to complete. 51 The full EBCD cycle, contextualised to CREATE and used at sites 1 and 2, is shown in Figure 1 and described in more detail below.
FIGURE 1.
Full EBCD cycle used at sites 1 and 2.

Stage 1: setting up the project
Stage 1 involved a period of stakeholder mapping with the core staff team to identify key contacts and services and/or staff who could help champion the co-design process in the trust and expedite approvals required on each unit for changes in layout, décor, or activities. We formed study oversight groups with trust leads at sites 1 and 2, meeting in person and communicating by e-mail. Core staff, together with researchers, developed posters and flyers about the project and held briefings with larger staff groups at different times during the day, for example nursing handover, goal-setting meetings with therapists and weekly multidisciplinary team meetings.
Stage 2: gathering staff experiences through observational fieldwork and in-depth interviews
In stage 2, staff were interviewed to explore their experiences of working on the stroke unit, particularly with respect to routines, structures and interactions in the team and with patients (see Table 3 for numbers of staff interviews). We also explored how ‘activity’ was perceived and what staff felt were the barriers and limitations to activity that could be addressed through co-design. Researcher-led ethnographic observations, which contributed both to EBCD and to pre-implementation evaluation data collection, were carried out at each site. Observations were carried out over a 3-week period or less and included weekday and weekends between 07.30 and 12.30, between 08.30 and 13.30 or between 15.00 and 20.00. The purpose, described in more detail in the evaluation section of this chapter, was to develop an understanding of the social and organisational processes linked to activity and the regularities and irregularities of the organisation of work and of social interaction in order to enhance our understanding of how and why stroke patients may be active or inactive during the inpatient day.
Stage 3: gathering patient and carer experiences through observation and filmed narrative-based interviews
In stage 3, patients and families were observed as part of the researcher-led ethnographic observations and staff observations described above. Patients and families were recruited for filmed narrative interviews that were edited into one composite film specific to sites 1 and 2. Most patients were filmed in their homes, with one patient choosing to be interviewed in a university building. Interviews lasted between 1 and 2 hours, during which time their experiences of being a patient on the stroke unit were explored. Some patients chose to be interviewed with their family member or on occasion separately for practical reasons. Family members reflected on their experiences of visiting and supporting their relative during the admission. The interviews explored routines and structures that either helped or hindered activity; interviewers encouraged patients to reflect on their activity during a usual day and across the whole week, including weekends. The composite films were produced for sites 1 and 2 and comprised nine patients and three family members (site 1) and seven patients and four family members (site 2).
Stage 4: bringing staff, patients and carers together at separate and joint events
In stage 4, the interview and observational data from stages 2 and 3 were summarised to draw out key themes and help orientate discussions towards priorities for change. The composite films comprised a narrative of patients’ and family members’ reflections and experiences of being on the stroke unit and several touch points. The duration of the composite film was 20 minutes and 24 minutes for sites 1 and 2, respectively.
Patient events
Through a staged process of facilitation and discussion, following guidance and methods suggested by trainers from The Point of Care Foundation, patients and families viewed the composite film and explored their ideas for change. These methods included an icebreaker exercise and working in small groups to brainstorm ideas and emotions after viewing the film. Emotional mapping was used to rank and prioritise ideas for change from most to least important and to refine the final list to be shared with staff at the joint event.
Staff events
The staff events were structured in a similar way to the patient events but without the use of a composite trigger film. Discussion and ideas were generated following the research team’s presentation of observational data and staff interviews. Through a staged process of facilitation and emotional mapping exercises, they explored ideas about areas for change, and generated a list of ideas and priorities as a group to present to patients and families at the joint event.
Joint events
Patients and staff then came together for a joint event. The numbers of attendees at each event are shown in Table 2. Other stakeholders from the trust, including volunteer co-ordinators and senior nursing and therapy managers, also attended these events. Attendees watched the composite film, and the staff and patient/family groups then separately presented their list of priorities. Facilitated by the researchers alongside the core team members/champions, staff, patients and families worked in small groups through a staged process of sharing and discussing what they had heard, what resonated and what they perceived as the most important priorities for change. During several stages of discussion, each small group chose their joint priorities; through stages of voting and discussion, the wider group agreed a final list. Participants then indicated which priority areas they preferred to work on and signed up for one (or more if they wished) of the co-design groups at each site.
| Site | Co-design participants (n) | Number of co-design group meetings | ||
|---|---|---|---|---|
| Patients | Carers | Staff | ||
| Site 1 | 5 | 6 | 13 | 10 |
| Site 2 | 4 | 4 | 12 | 9 |
| Site 3 | 11 | 7 | 14 | 15 |
| Site 4 | 3 | 4 | 15 | 9 |
| Total | 23 | 21 | 54 | 43 |
Stage 5: sustained co-design work in small groups formed around priorities
In stage 5, co-design groups were held over 4–5 months, with groups meeting up to five times. Co-design groups were researcher supported and co-led with clinicians, and they typically lasted 1.5–2 hours. The groups were held in accessible spaces, usually on site at the hospitals, and timed for after the midday meal to gain maximum attendance from nursing staff. Refreshments and transport for patients and families were provided if required. Each group explored the ideas within their own priority area and developed action plans; researchers made notes and shared these with all participants after each group to confirm actions. Tasks such as contacting estates or local voluntary groups were delegated and shared among the group.
Stage 6: a celebration and review event
An important part of the EBCD process is the opportunity for staff, patients, carers and researchers to come together and celebrate their involvement in developing, implementing and sustaining the co-designed changes. 51,61 Celebration events were held in both sites 1 and 2 and were attended by approximately 60 patients, staff and families. The events included presentations and informal sharing of experiences by those staff and patients involved in the co-design process, reflecting on the changes that had occurred and the lessons learnt and summarising the post-implementation data from observations and staff and patient interviews. The research team gave an overview of the progress of the CREATE project across sites and the plans for the next stage. A number of additional events enabled further dissemination of the project, including a mayoral visit and an official launch of the changes in the stroke unit at site 1, as well as more detailed feedback of the results to small groups of staff and other stakeholders.
Break point
Our original proposal aimed to have a break point between phases 2 and 3 (full and accelerated EBCD) to review the results and evaluate changes in behavioural mapping data and experiences of implementing the co-produced interventions from qualitative findings. If a positive change was found in supervised and independent therapeutic patient activity following the implementation of co-produced interventions, evidenced in either behavioural mapping data or qualitative data from post-implementation interviews and feedback events, then we would proceed to test the interventions in two further stroke units in phase 3. Subsequently, ethics approvals (see Report Supplementary Material 3) stated that we would have to submit substantial amendments detailing the range of changes in phase 2 (sites 1 and 2) that might be expected, and this approval would need to be in place before recruiting and commencing at sites 3 and 4. We were able to demonstrate to the Study Steering Group that the qualitative data indicated positive change but changes in behavioural mapping data were inconsistent. Following guidance and discussion with our Study Steering Group and NIHR manager, we had agreement to proceed to phase 3. On reflection, the use of the break point should have been defined not as ‘potentially stopping’, but rather as using the findings from phase 2 (sites 1 and 2) to plan and inform the accelerated EBCD at sites 3 and 4.
‘Accelerated’ experience-based co-design sites 3 and 4
Our research questions asked how feasible it would be to adopt EBCD as a particular form of co-production for improving the quality and intensity of rehabilitation (activity) in acute stroke units. The full EBCD carried out at sites 1 and 2 took 9–10 months. Our methods for sites 3 and 4 were informed by Locock et al. ,60 who showed that it was possible to accelerate the process using a national video and audio archive. We were keen to use the stroke-specific trigger films developed at sites 1 and 2 and contextualised at two further sites using the methods outlined below. Consequently, at sites 3 and 4 we sought to reduce the length of the process by making two distinct changes from the methods of Locock et al. 60
First, we used the trigger films already generated by stroke participants at sites 1 and 2. Although staff and patients were still interviewed as part of our pre- and post-implementation data collection, we chose not to film the interviews or edit the narratives to produce a composite film; instead, we used the trigger films from sites 1 and 2.
Second, we progressed straight to a joint event after site set-up, interviews and observations without holding separate staff and patient events. This meant that staff, patients and carers saw the film together for the first time but the same methods were used in the joint event to explore ideas and priorities and to develop co-design groups. A total of 82 staff, patients and families attended the joint events at sites 3 and 4, and again co-design groups were formed around agreed priorities (Figure 2).
FIGURE 2.
Accelerated EBCD used at sites 3 and 4.
Celebratory events were held at sites 3 and 4 in a similar way as at sites 1 and 2. Staff, patient and family members gave presentations and shared experiences informally, and the research team gave a summary of the project and progress. Further dissemination and spread of project findings happened at sites 3 and 4, including a mayoral visit and official launch of the new common room at site 3, and an open day at site 4, as well as more detailed feedback of the results to small groups of staff and other stakeholders.
Chapter 3 Methods: the evaluation
Parts of this chapter are based on Clarke et al. 16 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Design and conceptual framework
Our evaluation used a mixed-methods, case comparison design. We conceptualised the development and implementation of the co-produced interventions as an organisational and social process involving interaction between the creators and the users of knowledge. Translating the knowledge arising from health services research into practice through the implementation of service innovations remains a key challenge in the drive to improve the quality of health care. Organisational and social processes will largely determine whether or not service improvements to patient, family and staff experiences are implemented in practice. Although frameworks have become increasingly sophisticated, the influence of context has not been fully accounted for in these models. 66
Our aim was to evaluate the feasibility and impact of patients, carers and clinicians co-producing and implementing interventions to increase supervised and independent therapeutic patient activity in acute stroke units. We were particularly interested in the processes by which co-designed improvements are implemented in particular contexts and settings, and whether or not this process could be enhanced. We aimed to study both the impact of the improvements designed to increase activity and the feasibility of using EBCD in stroke units for the first time and the experiences of staff, patients and families taking part. We used normalisation process theory (NPT) to study the implementation and assimilation of the co-produced interventions in the local context of our study settings. 67,68
The evaluation team consisted of researchers based at each site (FJ, KGW, DC and SH) who were supported by the wider project group (AM, GR, RH, CM and GC). The site researchers were responsible for all data collection. Analysis and interpretation were shared by the whole group. During phases 2 and 3, researchers were regularly present on the stroke units and attended staff meetings, handovers and training sessions to engage staff in the project and communicate with stroke unit-based clinical staff during pre and post data collection.
We used multiple data collection methods to generate quantitative and qualitative data to address the project’s research questions:
-
What is known about the efficacy and effectiveness of co-production approaches in acute health care?
-
How do patients and carers experience the use of a co-production approach and what impact does it have on quality and supervised and independent therapeutic activity on a stroke unit?
-
How do staff from acute stroke units experience the use of a co-production approach and what improvements in supervised and independent therapeutic activities does the approach stimulate?
-
How feasible is it to adopt EBCD as a particular form of co-production for improving the quality and intensity of rehabilitation in acute stroke units?
-
What role can patients and carers have in improving implementation of National Clinical Guideline recommendations on the quality and intensity of rehabilitation in acute stroke units?
-
What are the factors and organisational processes that act as either barriers to or facilitators of successfully implementing, embedding and sustaining co-produced quality improvements in acute care settings, and how can these be addressed and enhanced?
Question 1 was answered in a rapid evidence synthesis published in 2017. 16 We anticipated that the findings would inform intervention phases and highlight the gaps in existing studies that could be addressed through our project phases. The aim was to identify and appraise reported outcomes of co-production as an intervention to improve the quality of services in acute health-care settings.
There are no agreed international guidelines for designing and conducting a rapid evidence synthesis. However, there is overall agreement that the process should involve providing an overview of existing research on a defined topic area, together with a synthesis of the evidence provided by these studies to address specific review questions. Rapid evidence syntheses are typically completed in 2–6 months, which does not normally allow for all stages of traditional effectiveness reviews. The rapid evidence synthesis was conducted between January and June 2016. The search terms used were specific to the use of co-production in acute health-care settings (see Appendix 8). To keep the search focused on co-production approaches, we omitted broader search terms, including co-operative behaviour, patient participation, collaborative approach and service improvement.
Database searches were conducted for the period 1 January 2005 to 31 January 2016. Given that two more general reviews relating to co-production had been published previously,7,18 and given the CREATE study focus, we reviewed post-2005 evidence and only that reporting on studies in acute health-care settings. We completed citation tracking of five seminal papers; in addition, five experts in co-production were requested to nominate three to five seminal papers relevant to our review.
The databases searched and the inclusion and exclusion criteria are given in Appendix 8 and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram and checklist for the rapid evidence synthesis are in Report Supplementary Material 5.
Screening
Two reviewers independently read all titles and abstracts. Differences in retain or reject decisions were discussed by the two reviewers, with the involvement of a third reviewer when consensus could not be reached. Three reviewers independently read the included full-text papers; decisions to retain or reject were made independently based on the inclusion criteria. All three reviewers then reached a consensus on retain or reject recommendations. The same three reviewers completed data extraction. The quality appraisal checklists developed by NICE for quantitative and qualitative studies were used. These address 14 areas of study quality ranging from theoretical approach to study design, data collection and analysis methods and ethics review. Two reviewers undertook data extraction and quality appraisal independently for each study. We did not exclude studies on the basis of quality appraisal, including all studies in the synthesis to inform discussion of the evidence identified. A mixed research synthesis approach was used. Studies were grouped for synthesis not by methods (i.e. qualitative and quantitative) but by findings viewed as answering the same research questions, or addressing the same aspects of a target phenomenon.
Our main evaluation focused on research questions 2–6.
Prior considerations
During project set-up and commencement, we recognised that the term ‘rehabilitation’ as used in our original application can be misleading and is often interpreted by patients as treatment delivered by a therapist. In the CREATE study we focused on supervised or independent social, cognitive and physical activity undertaken by patients and occurring outside one-to-one therapy sessions. We used an umbrella term of ‘activity’ for anything that patients do with or without help, however small, outside an individual one-to-one scheduled session of therapy. This could also include ‘clinical’ or ‘daily living’ activities, such as walking assisted/unassisted to the bathroom or getting dressed, and talking to other patients or to staff.
Of note is that the ethnographic observations and semistructured interviews conducted with patients and carers and staff pre and post completion of the EBCD cycles were used both to inform the EBCD process and as part of our evaluation. Prior to the introduction of EBCD, data generated using these methods enabled the research team to develop an understanding of what was occurring at those points in time and what activity was wanted going forward, and of staff members’, patients’ and carers’ experiences in these stroke units. Post the EBCD cycles, these data enabled the research team to develop an understanding of staff members’, patients’ and carers’ experiences of the EBCD process and their perspectives on the changes designed and implemented to increase social, cognitive and physical activity opportunities in these four stroke units. An overview of our data collection methods and whether the methods were used for evaluation, EBCD or both is provided in Table 3.
| Site | Staff interviews: EBCD and evaluation | Patient interviews: EBCD and evaluation | Carer interviews: evaluation | PROMs/PREMs: evaluation | BM: number of participants | BM: number of observations | Observations: EBCD and evaluation |
|---|---|---|---|---|---|---|---|
| Site 1 pre | 13 | 9 | 4 | 22 | 9 | 702 | 50.2 hours |
| Site 1 post | 8 | 5 | 5 | 24 | 7 | 949 | 46.5 hours |
| Site 2 pre | 15 | 9 | 4 | 45 | 11 | 769 | 48 hours |
| Site 2 post | 7 | 6 | 2 | 26 | 10 | 528 | 44 hours |
| Site 3 pre | 6 | 9 | 3 | 28 | 12 | 945 | 49.2 hours |
| Site 3 post | 8 | 6 | 3 | 11 | 7 | 782 | 37 hours |
| Site 4 pre | 7 | 4 | 3 | 12 | 6 | 655 | 44 hours |
| Site 4 post | 12 | 5 | 3 | 11 | 6 | 701 | 46 hours |
| Total | 76 | 53 | 27 | 179 | 68 | 6031 | 364.9 hours |
Procedure and participants
The observations and the interviews were conducted with patients and carers and staff pre and post completion of the EBCD cycles. Behavioural mapping was carried out with patients who were present on the stroke unit and able to provide informed consent the day before data collection. Interviews with staff across all specialties and grades took place after observations had been completed (pre and post EBCD) in each site.
Patients’ interviews took place within 3–6 months of their discharge from the stroke unit, when enough time had passed for adaptation to life at home to have begun, but soon enough after their inpatient care episode to allow reasonably accurate recall. Family members were recruited at the same time as patients. PROMs and PREMs combined in a single questionnaire pack (see Table 3) were sent to all patients discharged from each stroke unit in the 6 months prior to data collection in the pre-EBCD period and all those cared for during the EBCD/intervention period at each site.
Sampling and recruitment
Recruitment
We aimed to recruit participants who reflected the population of stroke patients admitted and discharged from our sites, who would naturally include patients with different levels of stroke severity, gender, age and ethnicity. We also aimed to include participants who had communication and/or cognitive impairments in order to reflect the stroke population, and encouraged family members to provide support when patients were unable to complete the questionnaires or take part in interviews. Several strategies were used to estimate our target numbers for recruitment.
Based on stroke admission data across London and Yorkshire, we estimated that it would be possible to collect PROM/PREM data from an independent sample of 30 patients from each unit pre and post implementation of co-produced interventions.
Behavioural mapping data collection took place during non-consecutive days. We aimed to recruit a minimum of four and a maximum of eight patients who met the inclusion criteria and were able to provide consent on the day before the observation.
Pre implementation of EBCD cycles, we aimed to purposively recruit a sample of approximately 10–15 staff, stroke participants and family carer members (30–45 in total from each unit) to take part in interviews as part of the co-design process. Stroke participants and family members or friends (carers) were also recruited 3–6 months after discharge from the stroke unit to allow time for adaptation to life at home to begin, but sufficiently soon after their inpatient care episode to allow reasonably accurate recall.
Post implementation of EBCD cycles, we aimed to recruit a further sample of up to 10 members of staff/patients and carers in each of the four sites to participate in semistructured interviews to explore their experiences post implementation of co-designed interventions. We also aimed to carry out interviews with a sample of staff members, patients and families who took part in the co-design groups to explore their experiences of being part of the whole process. The size of the sample was also informed by reaching thematic saturation during data analysis.
Sampling technique
-
Convenience sampling was used to collect PROM/PREM data from consecutive patients and family/carer members discharged from participating stroke units over a 3- to 6-month period.
-
Purposive sampling was used for behavioural mapping to ensure that recruited participants included those with different levels of stroke severity and those with aphasia (who are often excluded from stroke research).
-
Purposive sampling was also used to recruit staff who worked on the participating stroke units. To ensure that a broad range of views were accommodated, we aimed to recruit staff from different grades and professional groups. In recruiting patients/families, we included those with experiences that varied according to the severity and range of impairment, as well as those stroke patients who may not have family members.
Data collection methods
Evaluation data collection took place pre and post implementation across all four sites. Table 3 shows the timings of data collection and the methods used:
-
Semistructured interviews with patients and carers were carried out to elicit their perceptions and recall of opportunities for and experiences of activity in the stroke units. Patients from each unit were interviewed post discharge, and (at sites 1 and 2) in the pre-implementation stage these interviews were filmed. Topic guides for all of the interviews are in Appendices 2–5.
-
Semistructured interviews with staff were carried out with staff with a range of stroke unit experience, from PTs, OTs and speech and language therapists, to nurses, doctors, psychologists, dietitians and support workers, at different grades, to elicit their perceptions of the stroke unit and the opportunities for and experiences of patient activity. In addition, staff perceptions of organisational processes that influenced activity with patients, carers and other members of the stroke team were explored, together with their views on areas in which additional supervised and independent therapeutic activity could be enhanced.
-
PROMs and PREMs were sent to more than 60 patients cared for in each unit in the 6 months pre and post implementation (and cared for during the EBCD period). These measures are postal self-completed measures previously developed, reviewed and agreed in consultation with experienced stroke clinicians in West Yorkshire as part of the Clinical Information Management System for Stroke study [a Collaboration for Leadership in Applied Health and Care (CLAHRC) project]. The measures allow a carer or a family member to record responses for a patient, if necessary, and were used successfully with patients after stroke in the Clinical Information Management System for Stroke study. The PROM incorporates validated measures including the Oxford Handicap Scale, the Subjective Index of Physical and Social Outcome and the EuroQol-5 Dimensions (EQ-5D). The PREM was developed by Kneebone et al. 69 and is a validated tool for patient-reported experience of neurological rehabilitation.
-
Non-participant observations (ethnographic fieldwork) in each stroke unit took place pre and post implementation. An observational framework developed for use in a previous process evaluation of caregiver training70 was used to record observations of the stroke unit contexts, organisational processes, staff and patient interactions and instances of planned and unplanned activity, including noting when timetabled therapy was occurring on a one-to-one or group basis (see Appendix 6). Observations, typically of 4–5 hours each, took place across 10 days at different times of the day, evenings and at weekends in order to develop understanding of how activity may vary across a range of times and days of the week.
-
Behavioural mapping was used to record any social, cognitive or physical activity. These data were generated to establish an indication of activity levels in each unit at a given time point before and after the EBCD cycle was implemented. The data were from separate groups of patients; thus, we did not seek to compare ‘before and after’ scores for individual patients but rather we used the behavioural mapping data as a broad indicator of activity level. The approach was adapted from that successfully employed in two earlier stroke studies concerned with increasing patient activity. 28,71 Patients on the stroke unit were screened 24 hours before to determine whether or not behavioural mapping would be feasible. We aimed to recruit a minimum of four and a maximum of 10 patients who met the inclusion criteria and were able to provide consent on the day before the observation. This number was achieved across all sites (see Table 3). The patients were observed at 10-minute intervals between 08.00 and 17.00 or between 13.00 and 20.00 on 3 separate days. This allowed for up to 60 observations of each patient per day. We varied the times and days of the week for behavioural mapping to allow for possible variation in activities by day of the week. During each 10-minute interval, the data for each patient were based on an observation made by the researcher over a period of no longer than 5 seconds. The researcher observed one participant and then progressed to the next participant. The researchers positioned themselves so that they could see the participants – at the same time taking steps to be inconspicuous – and noted where they were, what they were doing and who was present in the same location as the patient. Observations began at the commencement of each 10-minute interval (i.e. 08.00, 08.10, 08.20, 08.30, etc.). The behavioural mapping protocol and recording instrument are in Appendix 7.
In our initial proposal, we anticipated accessing the SSNAP data at an individual patient level to enable us to compare patient dependency during the periods of study, a factor that can influence the activity levels achieved. We had anticipated that we could collect these data on the ward before they were uploaded to SSNAP, but we were not able to gain permission for access.
We agreed that pursuing access to the anonymised SSNAP data would prove overly time-consuming and impossible within the project time scales. This change was discussed in full by the Study Steering Committee and approved by our Health Services and Delivery Research programme manager. An additional justification for this decision was that the national case-mix data are based on the patient cohort within the first 72 hours, that is while at the first routinely admitting stroke unit. Each of the CREATE sites was non-routinely admitting and received patients repatriated from the main routinely admitting hospital linked to their unit.
Data analysis
Qualitative data analysis
We first describe the processes used to analyse the qualitative data generated from non-participant observations of staff, pre EBCD training and activity, during EBCD (i.e. of the separate patient and carer, staff meetings, joint meetings and co-design meetings) and from interviews with patients, carers and staff pre and post EBCD. The integration of these data in the EBCD evaluation and also in the linked process evaluation involved an iterative approach to analysis that focused initially on the data generated at each site and then progressed, using team half-day analysis meetings, to a comparison between sites, as described below.
Interview data video files (patients and carers at sites 1 and 2) and audio files (staff all sites and patients and carers at sites 3 and 4) were transcribed verbatim. The research fellows and research lead for each site completed an initial thematic analysis of the data at each site (London and Yorkshire) and prepared summary memos identifying the main themes and summarising the key issues related to the presence or absence of activity outside therapy, the opportunities to make changes and the attitudes towards possible changes. These summary memos were then compared and reviewed iteratively in a series of half-day face-to-face meetings (held approximately every 3 months in London or Leeds) by all four researchers, before the summaries were presented to and discussed with Study Steering Committee members.
For observational data, field notes were prepared by each researcher conducting an observation and shared among the researchers for that site. On completion of the series of observations (pre and post implementation and during EBCD activities), summary memos were developed to identify recurring themes and to compare and contrast findings from pre- and post-EBCD activities within and then between sites in London and Yorkshire. Again, these were compared and reviewed iteratively by all four researchers in a series of half-day meetings (as described above) before being shared with Study Steering Committee members. The memos included references to contextual factors considered relevant to service delivery, and to patient experiences of the EBCD process in each site. These processes were used for sites 1 and 2 and then repeated for sites 3 and 4.
Following these half-day meetings and the discussions resulting from presentations of the ongoing data analysis, the core and cross-cutting themes reported in Chapter 5 were developed and agreed by the research leads for London and Yorkshire and shared with Study Steering Committee members.
Integration of data in the experience-based co-design evaluation and process evaluation
The data used in the process evaluation were not generated separately from those used in the main evaluation of the feasibility of using full and accelerated EBCD in the four sites; rather, the same data were critically examined using NPT’s four core constructs and associated components. A data collection plan linked to NPT’s four constructs was developed prior to data collection. The purpose of the plan was to engage with the NPT constructs as data were analysed at each time point, and to identify evidence of (in the summary memos described above) examples such as staff progression from coherence to cognitive participation. This might comprise staff making sense of the EBCD approach, then thinking about what introduction of and support for increased patient activity outside planned therapy would mean for them individually and for the routine service provision currently in place. Once the EBCD activities had ceased at sites 3 and 4, the summary memos and the researcher reflections were reviewed by the research lead for the process evaluation and a draft single integrated account was constructed. This was reviewed by the research team as a whole, and the final agreed account is presented in Chapter 5. Our approach comprised both an ongoing integrative analysis of these data focused on staff and patient engagement with the EBCD process and on designing and implementing changes to promote or directly support increased activity, and a post hoc review of the full integrative data set.
Confirmability of analysis was further enhanced through a process of independent, joint and team half-day analysis and review cycles, after which the emerging analysis was discussed with the Study Steering Committee members. Credibility and transferability of the analytical approach are evident in how we have used detailed data extracts and interview quotations to support plausible explanations of the observational and interview data in terms of participants’ engagement with EBCD and the facilitators of and barriers to its introduction and use in the four sites. We incorporated researcher reflection and reflexivity in the data collection process and used these insights in the team analysis of the data.
Quantitative data analysis
Behavioural mapping
We entered all data into a SPSS (Statistical Product and Service Solutions) (IBM Corporation, Armonk, NY, USA) file and described the frequency of activity occurrence for each participant during each data collection period. This approach, used by Askim et al. ,71 included additional categories in social and cognitive activity. These data were used to generate descriptive statistics to quantify the proportion of physical, social and cognitive activity occurring for each patient during the period of observation.
Patient-reported outcome measure and patient-reported experience measure data
These data were entered into a SPSS file and reported as descriptive statistics (or frequency counts) for each item. These data provide insight into patients’ perceived functioning post stroke (PROM) and their experiences on stroke units (PREM). Some of the PREM items sought responses directly related to opportunities and resources for activity.
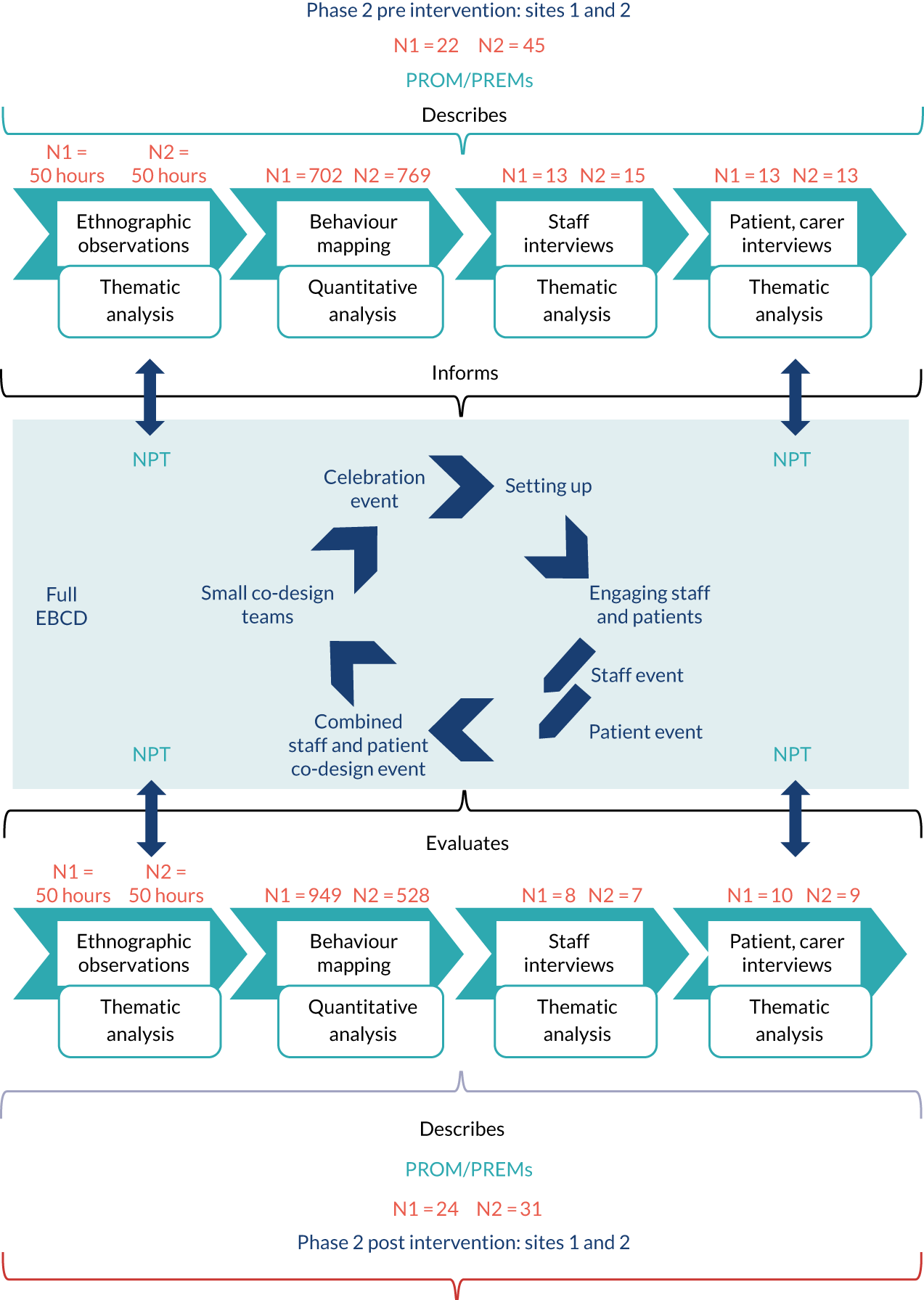
Figure 3 depicts our integrative approach to analysis across the whole data set (qualitative and quantitative) process evaluation.
FIGURE 3.
Data analysis for both the evaluation and the intervention (EBCD).
Process evaluation methods
A parallel process evaluation aimed to understand the functioning of the intervention (i.e. the co-design and generation of new activities in each stroke unit) by examining implementation, mechanisms of impact and contextual factors. Mechanisms of impact refer to the ways in which intervention activities and participants’ engagement with them trigger change in a given setting. Process evaluations contribute to understanding the impact and outcomes of complex interventions. We adopted primarily qualitative methods in the process evaluation (see below), which was informed by NPT. 72
Normalisation process theory is an established middle-range theory concerned with understanding how complex interventions are implemented and integrated into existing health-care systems. NPT is conceptualised through four main constructs (Table 4). These constructs or generative mechanisms can help explain how interventions are embedded and ‘normalised’ within routine care. In essence, the mechanisms represent what participants ‘do’ to get the required work done successfully. In general terms, the mechanisms can be understood as participants making sense of a new or different way of working, committing to working in that way, making the effort and working in that way and undertaking continuous evaluation and, if necessary, making adjustments to bring about a situation where what was once a new and complex intervention becomes a normal part of everyday practice. Clearly, not all interventions progress to successful implementation in this way; where this is the case, NPT can aid in understanding the factors that may explain this at both an organisational and an individual level. This focus on the work of implementation and the factors influencing this work was the reason for our use of NPT.
| NPT construct | Explanation |
|---|---|
| Coherence | The sense-making work that people do individually and collectively when faced with implementing changes to existing working practices. This would include differentiating new practices from existing work and thinking through not only the perceived value and benefits of desired/planned changes but also what work will be required of individual people in a setting to bring about these changes |
| Cognitive participation | The work that people need to do to engage with and commit to a new set of working practices. This often requires bringing together those who believe in and are committed to making changes happen. This also involves people working together to define ways to implement and sustain the new working practices |
| Collective action | The work that will be required of people to actually implement changes in practices, including preparation and/or training of staff. Often this entails rethinking how far existing work practices and the division of labour in a setting will have to be changed or adapted to implement the new practices. This requires consideration of not only who will do the work required, but also the skills and knowledge of people who will do the work and the availability of the resources they need to enact and sustain the new working practices |
| Reflexive monitoring | People’s individual and collective ongoing informal and formal appraisal of the usefulness or effectiveness of changes in working practices. This involves considering how the new practices affect the other work required of individuals and groups and whether or not the intended benefits of the new working practices are evident for the intended recipients and staff |
We used NPT to study the EBCD process and the implementation and assimilation of the co-produced interventions in the local context of our study settings. NPT was used in two main ways: first, to guide the generation of data at each site (Table 5) and, second, to inform our analysis of these data and drawing of conclusions related to the similarities and differences in implementing and integrating changes in each of the four study sites. In our analysis we used NPT as a sensitising device in our review of the data generated from observation, interviews and researcher process notes and reflections on EBCD activity. NPT’s constructs were used to identify and think through factors that may act as barriers to or facilitators of using EBCD and introducing change in the four sites. We also used NPT as a structuring device to progress the analysis from identifying barriers and facilitators to linking these, where appropriate, to NPT’s constructs and to develop an explanation of the work of implementation in the participating stroke units.
| Data source | Timing | Linked NPT construct |
|---|---|---|
| EBCD training events for local champions: researcher observations; participant evaluations | Prior to EBCD cycles commencing | Coherence |
| Non-participant observations of routine working practices, interactions between staff, patients and carers and between staff | Pre EBCD cycles commencing and post co-design group activity and implementation of ‘interventions’ and changes to working practices | Coherence, cognitive participation, collective action |
| Semistructured (audio-recorded) interviews with stroke service staff | Pre EBCD cycles commencing and post co-design group activity and implementation of ‘interventions’ and changes to working practices. Post co-design group activity and implementation interviews included volunteers, and staff working outside the stroke service who participated in EBCD elements | Coherence, cognitive participation, reflexive monitoring |
| Semistructured (video-recorded) interviews with former inpatient stroke survivors and carers | Pre EBCD cycles commencing | Coherence |
EBCD cycle elements:
|
Across ≈9 months at sites 1 and 2 Across ≈6 months at sites 3 and 4 |
Coherence, cognitive participation and collective action |
| Semistructured (audio-recorded) interviews with former inpatient stroke survivors and carers | Post co-design group activity and implementation of ‘interventions’ and changes to working practices in the stroke units. These interviews included EBCD participants and stroke survivors who had been inpatients during the EBCD activity and implementation phase | Coherence and reflexive monitoring |
| Study oversight groups’ meeting records and e-mail responses to researcher updates | Ongoing where these meetings could be established | Coherence and cognitive participation |
| Researcher reflections on facilitating unplanned elements in EBCD cycles, in recruitment activity and in generating data through observations and interviews | Ongoing | Informing evaluation and analysis of participants’ engagement with the EBCD process |
The CREATE process evaluation differs from some other evaluations of complex interventions in three ways. First, the EBCD approach uses a service improvement methodology in which locally designed changes to services are developed and implemented and therefore variation in the interventions evaluated is likely. Second, we evaluated the implementation and integration of interventions across a full EBCD cycle (approximately 9 months) in two sites and across an accelerated EBCD cycle and a reduced time period (approximately 6 months) in two further sites. Last, the researchers conducting the process evaluation were members of the core research team rather than independent of that team. These researchers were involved in data collection pre and post introduction of the EBCD approach; they also facilitated staff members’, former patients’ and carers’ work in co-design groups during the development and introduction of interventions in the four stroke units.
Data sources for process evaluation
The process evaluation draws on data generated to evaluate the impact of developing and implementing co-produced interventions on the quality and amount of independent and supervised activity occurring outside formal therapy in the four stroke units. Prior to initial data collection in the first two sites, a data collection plan linked to NPT’s four constructs was developed. This identified the kinds of data that would be generated through baseline and post-EBCD data collection at each site, and also participants’ engagement with and experience of each element of the planned EBCD cycle in each site. Process evaluation data collection also focused on additional opportunities presented by observations of training of staff in the EBCD approach, researchers’ reflections on their own involvement in facilitating each element of the EBCD cycles and researchers’ informal and formal engagement with participants in each site as part of recruitment activity and in generating data through observations and interviews.
Ethics and consent
Health Research Authority approval was gained before the project commenced and this included full ethics review by Brighton and Sussex Research Ethics Committee (reference number 16/LO/0212). Local Capacity and Capability assessment was undertaken in each study site and confirmation was gained from each hospital trust. The project was sponsored by St George’s, University of London. The approval letter can be found in Report Supplementary Material 3.
Consent issues were dealt with in several ways as data collection was varied and included data from patients, their family/friends and clinical staff. We gained overall site consent from the senior clinician (principal investigator) at each stroke unit; this enabled us to have a presence on the unit but not to collect data from individual patients or staff. We were aware of the need for sensitivity, especially during non-participant observations and behavioural mapping, and we used a pragmatic process approach to consent, regularly checking that both staff and patients agreed to being observed. Participants in behavioural mapping provided written informed consent. We developed an explanation of the project that was used on arrival and when moving to different parts of the ward; we also displayed a number of posters to describe the project as well as photographs of the research team. We gained individual informed consent for all interviews and behavioural mapping. Consent was implied by return of PROM/PREMs and, where local approvals allowed, some patients were asked for their permission to be contacted before they were discharged. See Report Supplementary Material 2 for examples of consent forms.
Project management and guidance
The project was led and managed jointly by Fiona Jones and David Clarke, with site management by Karolina Gombert-Waldron and Stephanie Honey. A project team of Fiona Jones, David Clarke, Stephanie Honey and Karolina Gombert-Waldron met monthly with co-applicants Glenn Robert, Alastair Macdonald, Ruth Harris and Chris McKevitt for the first 2 years, and every 3–4 months in the final year. Geoffrey Cloud moved to Melbourne, VIC, Australia, prior to the project starting but remained a supporter throughout the project, joining by Skype™ (Microsoft Corporation, Redmond, WA, USA) or in person when in the UK. The project team met in person every 9–12 months and members attended a proportion of staff, patient and joint events. Glenn Robert and Alastair Macdonald provided input into the EBCD and co-design activities; Geoffrey Cloud provided clinical advice from a local and national stroke perspective; Glenn Robert and Ruth Harris supported Fiona Jones and David Clarke with the rapid evidence synthesis; Chris McKevitt and the whole group contributed to analysis and interpretation of the empirical findings and report writing.
A Study Steering Committee including independent lay members, academics and senior clinicians met four times during the project and provided the project team with review and guidance.
Approach to public and patient involvement
Stroke survivors were involved in the initial development of our application, and plans were discussed at a Consumer Research Advisory Group that has links with the Cardiac and Stroke Network in Yorkshire, which includes stroke survivors and carers, some with national advisory roles. The outline was also presented in round-table discussions with stroke survivors and carers at the Yorkshire Stroke Research network consumer conference. Consumer Research Advisory Group members and conference participants strongly supported the proposed research. Most expressed a view that active inpatient rehabilitation was central to recovery after stroke but felt that they did not receive the amount of therapy identified in the national standard. Carers indicated that they wanted to help with rehabilitation but did not know how, and did not receive training from staff in this area. Two stroke survivors and one family member participated in research proposal writing groups, attending meetings in Leeds and London. Their comments helped the research team appreciate how the collaborative research process proposed may be viewed and engaged with by stroke survivors.
Patients’ and carers’ voices, experiences and ideas are a central tenet of EBCD. As such, active patient and carer involvement was a feature of every stage. Patients and carers took part in separate events and joint events with staff; they formed at least 50% of the membership of co-design groups and attended final events held at each site to share CREATE findings and discuss methods of dissemination. Overall, CREATE enabled patients and their carers to work in close partnership with front-line health-care professionals to develop, pilot and evaluate innovations in the delivery of rehabilitation therapy in acute settings.
In addition to patient and public involvement in intervention development, a stroke survivor and a carer were involved through their role on the CREATE Study Steering Committee. They participated in all aspects of the study, including a review of participant information sheets, discussion with researchers about conducting observations and interviews with patients and staff, and helped researchers shape the messaging in the EBCD feedback events.
Patients and carers have been updated about the findings at various stages of the project in various ways, including newsletters, individualised letters and e-mails, as well as from attending feedback events. For an example, see Report Supplementary Material 4.
Chapter 4 Results: rapid evidence synthesis and co-design – priorities for change
We first report on the findings of our rapid evidence synthesis (objective 1), which sought to identify and appraise reported outcomes of co-production as an intervention to improve the quality of services in acute health-care settings. The results, published in 2017,16 are reported briefly below.
Rapid evidence synthesis (objective 1)
A total of 712 titles and abstracts were identified for screening; of these, 24 papers went forward for full-text review. Eleven publications18,30–40 were included in the final evidence synthesis (see Report Supplementary Material 5 for the PRISMA flow diagram and checklist).
Included studies were conducted in five countries (Canada, England, New Zealand, Australia and the Netherlands) and published between 2008 and January 2016. Study settings included intensive care units (n = 1); inpatient and outpatient oncology services, including breast, lung, colorectal and haematology services (n = 5); mental health services (n = 1); emergency departments (n = 1); an outpatient clinic for people with multiple sclerosis (n = 1); and older people’s outpatient services (n = 1). A further study evaluated co-design projects in five Dutch hospitals; these were conducted in four oncology departments and one haematology department.
One study was a feasibility randomised controlled trial of a co-designed intervention. 73 Study design was stated in only one60 of the other 10 papers. The remaining studies utilised descriptive qualitative approaches to evaluate changes in services or to explore participants’ experiences or views, but these were not described in detail. Data collection methods included self-report postal questionnaires, ethnographic observations of patient journeys through services and of staff working practices, semistructured interviews with staff and patients (sometimes filmed), focus groups and emotional mapping exercises. Data analysis techniques were described in some detail in six18,31–34,36 of the 11 publications73–79 The focus of most papers was limited to processes to understand and co-design services rather than evaluation of outcomes of co-design or co-production activity; the exception was the feasibility randomised controlled trial. 73
Quality assessment ratings largely reflect the omission of detail on research methods, particularly in relation to stating research aims, questions and sampling decisions and discussing data analysis and findings. Four studies were rated ++ (i.e. good agreement with criteria) and the remaining seven were rated + (i.e. moderate agreement with criteria).
The aim of the rapid evidence synthesis was to identify and evaluate the reported outcomes of co-produced interventions designed to achieve patient-focused quality improvements in acute health-care settings. Methods used to understand participants’ experiences and views included observations, process mapping, interviews, focus groups and postal surveys. Overall, patients and staff reported positive experiences of participation similar to those reported in co-production studies in the public and health-care sector. 14,80–82 Co-production or co-design projects were effective in generating a wide range of ideas and specific suggestions for improving patients’ experiences across the different settings. However, in most of the studies, a lack of clarity about the implementation of improvements in services and/or evidence of resulting impacts on patient outcomes was a clear limitation. Reported service changes and quality improvements are summarised in our published table 3. 16 In the published report of the rapid evidence synthesis,16 we identified that reported ‘outcomes’ of the studies could be categorised in three main ways:
-
patient and staff involvement in the co-production or co-design process
-
ideas and suggestions for changes to processes, practices and clinical environments that have an impact on patients’ and/or carers’ experiences of a service (and often indirectly on staff members’ experiences)
-
tangible changes in services and their impact on patient or carer experiences.
Although the classification of approaches varied, a staged process of co-production was evident across all studies. The majority described patients, carers and staff reflecting on service experience and provision and then working together using participative methods in joint review and co-design activities focused on improving patient and/or carer experiences.
Level of participant engagement varied across the studies but there was overall satisfaction with the process. Use of co-production methods reportedly ensured that patients’ experiences, concerns and ideas for change were captured, presented to and discussed with service providers. Active engagement of patients in this way legitimated and gave urgency to service improvement plans;73,78 this was more evident where service managers participated in or actively supported co-production projects. Despite evidence of the contribution of co-production activities in generating ideas for patient-focused service improvements, in a number of projects participants expressed frustration at the lack of progression from problem and solution identification to actual quality improvements. 75–78
A commonly reported barrier to using co-production approaches in acute health-care settings was a lack of support, resources or managerial authority to bring about structural or environmental changes. 75–78,83 Practical or logistical problems were also identified, which included ensuring that frail elderly people could attend regular co-design meetings. 16,75 Recruiting and retaining patients and carers through the different stages of projects were highlighted as a challenge in several studies. 74,76–78,84 The findings from included studies highlighted the need to plan for and manage patients’ understanding of what may be a radically different form of engagement with hospital staff, often quite unlike that experienced previously by users of health services, and the need to support staff in this different form of engagement. 73–75 A factor linked to more successful co-production projects was the involvement of funded facilitators to manage or oversee projects. Where facilitators were involved it was more likely that projects (1) maintained momentum and were delivered as planned, (2) engaged and retained patients, carers and staff and (3) generated concrete examples of areas in which patients’ or carers’ experiences could be improved. 73,74,77,84
Changes in service organisation, care environments and in patient and carer experiences occurring either during or closely related to co-production activities were reported (see Table 3). However, none of the 11 studies formally evaluated whether co-production or co-design as a way of working had been sustained, or whether improvements made as a result of such approaches were sustained over any length of time. Last, no cost–benefit analyses were carried out related to the reported outcomes in any of the studies. Only one study reported a cost analysis of co-production methods by comparing the cost of an accelerated EBCD approach with that of standard EBCD. 74 The findings indicated a reduction in costs with the accelerated approach, which was linked to a reduction in the cost of producing the trigger film (a key stage of full EBCD). The cost of facilitating the EBCD process was quantified; in this study, over half of the costs incurred were the salaries of local facilitators.
The limitations of the rapid evidence synthesis were as follows:
-
We excluded broad search terms relating to patient participation, patient centredness, service improvement and clinical microsystems, including only search terms that we anticipated were likely to identify research studies reporting on the use of recognisable and structured co-production or co-design approaches. It is possible that the narrow focus of the search terms used in the rapid evidence synthesis meant that we did not identify research and evaluation of co-production projects in the health sector reported using some of the alternative terms described above. Such literature may have been consistent with or challenged our findings.
-
We concluded that the rapid evidence synthesis identified a lack of rigorous evaluation of effectiveness and cost-effectiveness of co-produced interventions in the acute health-care sector at both the service and the system level. Health services, whether public or private, operate within increasingly severe financial restraints where funding for quality improvement work is limited. Without robust critique, evaluation and evidence of the co-creation of value, there is a danger of co-production becoming another management fad or fashion,85 with the meaning of the term itself appropriated and co-opted but no longer ‘co-produced’. We recommended that future studies should evaluate clinical and service outcomes as well as the cost-effectiveness of co-production relative to other forms of quality improvement. Evaluation of potentially broader impacts on participants’ values and behaviours should also be considered.
Co-design: priorities for change
We set out to understand both the experience of taking part in EBCD (patients, staff and carers) and whether or not EBCD could be used successfully in both a full and an accelerated form. In this section we present the findings from qualitative data sources (fieldwork and interviews) about the priorities for change developed through EBCD. Where possible and relevant, we include photographic evidence of the issues that drove priorities and the areas in which changes were made.
In Chapter 5 we describe the impact on activity of implementing the new co-produced interventions/improvements and summarise the contextual data about activity and patient experience pre and post implementation with reference to quantitative data sources from behavioural mapping and PROM/PREMs. Finally, in Chapter 5 we present findings relating to the experiences of ‘implementation/engagement’ and our process evaluation informed by NPT.
There is inevitable overlap between the data collection methods we used (1) to underpin the EBCD process and (2) in the evaluation study. As a result, we have synthesised our findings across Chapters 4 and 5 to address all five of our evaluation research questions, and we conclude with a discursive commentary addressing each of the research questions in turn.
Figures 1–3 illustrated how the multiple data sources were utilised as well as the interaction between EBCD and the evaluation. The two stroke units taking part in the first stage and full EBCD are referred to as sites 1 and 2. The two stroke units taking part in the second stage and accelerated EBCD are referred to as sites 3 and 4.
We focused on supervised or independent social, cognitive and physical activity, and used an umbrella term of ‘activity’ for anything that patients do with or without help, however small, outside individual one-to-one scheduled therapy sessions.
Ideas that drove the changes
At sites 1 and 2, filmed patient interviews carried out pre implementation were synthesised to produce a composite film shown at all joint events. Staff interviews and ethnographic data were also analysed and contributed to the data corpus; these were presented at separate staff and patient events at sites 1 and 2. These data underpinned and drove the discussions, which led to the priority areas for co-design groups. The ideas generated were largely similar across all four sites and focused on space, activity and communication. With minimal local variation, ideas were revised or shaped at the joint meetings and then interpreted and adapted in co-design groups.
Space
I often thought, on the stroke unit, it would have been nice to have a little group where they all could be interactive with each other instead of sitting staring at the walls . . . make the day spread out a bit better . . . I was always sitting watching things and thinking they could have a little group in the corner where they could be doing little things.
Carer, site 2, pre
The above quotation illustrates the inter-relatedness of space (environment) and activity, which became increasingly clear during the EBCD process. The four sites differed in physical layout, colour scheme, room size and use, and available social and outdoor space. However, across the sites, staff members’, patients’ and family members’ suggestions to improve the environment were very similar. Site 1 had no shared space (day room) in which patients and visitors could meet, and visitors were cramped by the bedside. Site 2 had a day room but it was used mainly for staff meetings and equipment storage; this was replicated at site 3, which had a garden but it was accessible only through the day room, which patients did not use. At site 4, the day room had become a storage area for wheelchairs and specialist stroke chairs; another seating area was routinely used by staff for taking breaks and storing cleaning equipment. Our observations confirmed the restrictions posed by limited space and the impact on patient use; there was little or no space or opportunity to socialise in groups with peers or visitors. This issue was compounded by areas that could have been used by patients and visitors instead being used as storage for clinical items. Space and furnishings appeared to affect patient and carer morale; this issue was depicted in data from all four stroke units, although less so at site 3, but generally environments were felt to be uninspiring:
And it looks very much like a hospital environment, I think the colours are very hospital-y, I think the decor is a bit shabby and when you’re spending, when you spend, you know, you’re spending months in this hospital sometimes it just feels like there’s nothing that looks particularly homely.
Patient, site 1, pre
Restrictions on activity caused by the environment were also noted across all sites, as illustrated by how the way in which a ward is set up can limit communication between patients:
When she [the carer’s wife] first went in . . . a really elderly lady was in the next bed and she couldn’t communicate at all. If they could have rotated the beds round so that the ones who could talk to each other [were next to each other], rather than have to talk over them to another patient, that would have been better for them.
Carer, site 2, pre
Patients and staff felt that space could be repurposed to allow more opportunities to move about, play games and socialise. They suggested getting rid of clutter in therapy gyms, day rooms and corridors. The restrictions on activity caused by equipment storage was evidenced in observations (Figure 4):
The corridor is cluttered with table, trash bins etc. so we have to take turns [to pass] . . . The corridor is cluttered with a hoist, 3 wheelchairs, various trolleys and trash bins.
Field notes, site 1, pre
FIGURE 4.
Equipment storage in corridors at site 1. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.

In addition, the space around each bed was limited, and frequently tables were used for clinical equipment such as wipes or syringes, leaving little room for personal items (Figure 5). Frequently staff complained about the ward not being fit for purpose and restricting independent activity:
On the movable table next to his bed, I see a little jar with water and a cup half-filled with orange juice, tissues and a blue folder like the ones used for patients’ notes. On the bed side table there are two framed pictures – one is at the front and partially covers the other. The rest of the table is occupied by medical equipment.
Field notes, site 1, pre
I don’t think this ward is suitable for stroke rehab, we need a bigger ward definitely. We’re always falling over stuff. I think because, you know, a simple question of, ‘Can I go to the toilet?’ we’ve got to move everything . . . So the poor little patient’s waiting an extra 5, 10 minutes and they might have peed themselves so that’s not beneficial to them because that’s just promoting incontinence and, you know, they’re on a rehab ward.
Staff, site 4, pre
FIGURE 5.
Typical bed space and décor at site 1, described by patients and staff as cluttered and uninspiring. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.

The benefits of the bedside having a personal feel developed as a theme through our observations and interview data. We observed that when personal items were around the bedside, staff tended to interact in person-centred ways to a greater degree, asking the patient questions about a family member or a photograph:
I noted that the patient in bed 19 had a different bedside than other patients in the bay, as the family had brought in things that were important to her into the ward. She was keen to show me everything they had brought in, and felt it was immensely therapeutic to be able to look at pictures of family instead of the blank wall – she said she had spent time gazing at them and thinking about each of them.
Field notes, site 1, pre
Additionally, some carers had done their best to enhance and personalise the spaces around their relatives who were unable to get out of bed:
I took photographs and pictures and put them all on the wall to try and brighten it up, because it was just horrible, it was a horrible ward.
Carer, site 2, pre
The sense of being trapped in the ward and the lack of light seemed to add to the feeling of dreariness and loss of connection with the outside world:
[. . .] is sitting in bed. The lights are off and the blinds down. The room is quite dark. She is sitting in silence. The TV is still positioned in front of her but it’s off.
Field notes, site 1, pre
The necessity of having somewhere else to go apart from the bedside became a strong priority for change:
A table maybe in the middle of the ward to bring people together.
Carer, site 3, pre
It would have been good to mix with other people, so you can get to know them.
Patient, site 3, pre
One carer at site 4 mentioned that she struggled when using a wheelchair to take her husband to the hospital café, which was a considerable distance away, and that she would have preferred to have been able to go for a drink and change of scenery to a nearby day room. She also felt that being in the day room, rather than off the ward, would have made it less likely that her husband would miss therapy sessions. When space was available, it was often used only by staff, and the impact on activity was evidenced at sites 2, 3 and 4 (site 1 had no day room) (Figures 6 and 7):
I think the day room has, has been a bone of contention in terms of the nurses are upset they can’t use it as a restroom. The therapists and everybody else view, their view it’s not a restroom, it’s a day room, how do we try and accommodate everybody? It would be nice to have a bit more office space for everybody else, it would be nice to, you know, kit out the gym a little bit better so you could use it more. The garden I think, you know, we don’t use our garden space enough, yeah.
Doctor, site 3, pre
FIGURE 6.
Day rooms at sites 2 and 3, which tended to be used only as meeting rooms for staff. Reproduced with permission of Fiona Jones, University of London, and David Clarke, University of Leeds, personal communication, 2020.


FIGURE 7.
Day room at site 4, which was used for storing specialist chairs and wheelchairs. Reproduced with permission of David Clarke, University of Leeds, personal communication, 2020.

Activity
I think [being a patient in here] it must be incredibly and utterly boring, I think, I mean I think the odd occasional therapy session that they get from speech, OT and physio, I mean that would amount to maybe, what, two and a half hours, if that, maybe three.
Staff, site 2, pre
All of our data demonstrated limited activity opportunities beyond those provided in scheduled therapy sessions. During over 190 hours of pre-EBCD fieldwork across all sites, we saw very little evidence of patients independently practising activities (either games or prescribed exercises) and minimal or no involvement of other agencies such as volunteers or community groups:
Can you give me any examples of some activities that you saw other patients doing on their own?
Patient: No, nobody. I never see anybody doing anything on their own.
Patient, site 1, pre
Patients and staff highlighted the boredom and lack of stimulation, especially at weekends; this was corroborated by our fieldwork, which also took place at weekends. None of the units provided a 7-day therapy service, and interviewees felt that weekends were quieter, except at site 4; here, the patients interviewed suggested that there was little difference between weekdays and weekends, in that they found the days equally long with little to occupy their time except waiting for family and friends to visit. At this site, all patients interviewed complained of being bored in their free time between care tasks such as washing and dressing, and scheduled therapy sessions. Apart from visitors, the patients did not report much engagement with other people or much participation in physical or cognitive activities. At site 2, OTs and PTs worked on Saturdays but they spent the majority of their time assessing new patients on the adjacent hyperacute/acute unit. A stroke rehabilitation assistant worked on Saturdays and Sundays on the rehabilitation unit but focused attention on those who needed additional therapy and did not provide alternative social or cognitive activity opportunities:
‘Nothing happens’, says a Health Care Assistant [HCA]. ‘Weekends are long’, comments another HCA. ‘Weekdays are very busy – they [patients] have got everyone coming into their rooms. [At] weekends, they only see us. They get their care, obviously, but that’s it. It’s like – what happens now? Do I count down to Monday?’ she says looking down at her wrist.
Field notes, site 1, staff event
At all sites patients emphasised that they would have liked to have been more active and perhaps to be encouraged to play a game or sit with other patients in the bays or in a common area:
It would have been good to mix with other people, so you can get to know them.
Patient, site 3, pre
Observational data in particular highlighted to us how patients’ activity levels were influenced by staff members’ structures and routines. Inactivity was most marked between routines such as mealtimes, getting washed and dressed or receiving therapy. Patients tended to describe how their day was structured mainly around mealtimes:
I’d get up . . . they came round and they made the bed first . . . they gave us a cup of something or other to go with it and then they got on and did their own thing, other people, you know, and then hopefully [you were] one of the first ones, if not . . . 11.20 was the latest I ever got done [washed and dressed]. It should have been done before 9 o’clock you know . . . then they [the nurses] said ‘well, you know, basically you’ve got to get out the bed and sit at the side of it’ . . . Then we had breakfast, which we just got at the side of the bed. Then I tried to get some written work done [speech and language therapist exercises]. And then it’d be lunchtime and you all come round with the lunches and stuff and it’s fine, but then, then they just left you at the side of the bed and after lunch, you know. So there’s only speech therapy and physiotherapy . . . And then it was teatime and they put us all our stuff [food items] out.
Patient, site 4, pre
There was overwhelming agreement in staff interviews that patients had the potential to be more active than they were. Staff also acknowledged that this was hindered by their highly routinised work. Anything more than getting through a list of tasks was a bonus:
After so long then people [nurses] get to know, ‘This is the norm, this is the routine, this is what happens, you come to work, you do your jobs’. We’ve even got a list of jobs that you do, and not on any of that list is, not one that says, ‘Spend time with the patients to talk to them, or do games with them or anything,’ it’s all about getting things ticked in a box.
Staff, site 2, pre
The same staff member felt that as patients conformed to routines they became less likely to express their own views and ideas:
Hobbies and things, I think they probably don’t get the opportunity that often to do what they particularly like to do, we’ve got things that we can offer, like chess, draughts, puzzles, magazines, there’s the volunteers that come round with newspapers, but that’s sort of organisationally based as well, they don’t come at specific times. So, I think, to fit in something that, if they had a specific time to do it, if they said to us, ‘I’d like to do this at this particular time’, I think there are ways that we could try and accommodate it, but I think people come into hospital and think, they just conform to that routine of when the meal times are and that quite rigid set routine, and you find that they just seem to go along with it and don’t then tell you, ‘Well, actually, I prefer to do this at this time’, it’s almost like they seem to lose their voice.
Staff, site 2, pre
Promoting activity was not visible to any extent in many staff routines and structures. For example, as was observed, activities were not mentioned as part of the nursing handover:
All staff were following the handover of the night nurse. It wasn’t until the handover had happened did they look at the patient and have any interaction, asking questions like ‘did you sleep last night?’ It was often the lead nurse that did this, he went to the patient and shook their hand, smiled and said ‘hello’- most seemed to recognise who he was. Hardly anyone else interacted with the patient. I heard no hand over of information about what the patient could do for themselves, or any aspect of their recovery, or activity.
Field notes, site 1, pre
All staff members interviewed had concerns about patients being bored and not having enough stimulation. Some of the reasons cited here overlap with ‘space’ as a priority area but illustrate the restrictions given by staff as reasons:
There is nothing for them to do. [. . .] We need something in the way of entertainment for patients [. . .] they need something more.
Staff, site 3, pre
Exploring in staff and patient interviews what could be done to provide more activity opportunities generated many ideas:
I would just love us to have a bit of money to use at our own discretion . . . on therapeutic items. Because you can get lots of things that you can do, unilaterally, like one-arm technique to do like cross-stitch or something, like the stands and things that you can get and we don’t have anything like that. [. . .]. We’ve got very, very dated equipment.
Staff, site 2, pre
Staff also highlighted concerns about their unit, which was supposed to enable rehabilitation and recovery, and the negative impact of the structures, routines and atmosphere. This was compounded by an overall impression that staff were busy and had little time for anything other than clinical tasks. During observations, staff would frequently mention that they were busy, and during interviews members of staff reported that they were too busy to organise activities outside the normal therapy time:
Yes. Challengingly busy, but that’s inevitable. You know, obviously many of the patients are either lying or sitting in bed, not active. Once they’ve had their needs either addressed, or they’ve managed themselves, which is less common, they are spending a lot of time inactive. There’s, I guess, overall I find there’s very little social interaction with patients, very little chit chat, or chatter.
Staff, site 1, pre
Our observational data largely validated the perspectives of staff, patients and carers. In addition to the comments made in interviews, informal staff comments during observations indicated a shared perception that social, physical and cognitively stimulating activity outside therapy on stroke units had decreased over time rather than increased. Although there was a profound awareness that both scheduled and unscheduled activity needed to be increased and although there was a strong will for this to happen, there were some differences across sites in how some staff groups used their time. At site 1, all staff broadly acknowledged the impact of ‘downtimes’ such as weekends, but we saw little attention paid – or suggestions given – to patients regarding what they could do outside scheduled therapy. At site 2, although all staff routinely talked about how busy they were, there were late morning, post-lunch and post-evening meal ‘downtimes’ during which staff would congregate in a central area and chat. At sites 3 and 4, observations also indicated high nursing workloads and levels of patient dependency that left little time for staff to engage in activity with patients. However, when the units were fully staffed and less busy, the same behaviour was evident; there was a sense that when the routine care tasks were completed staff were entitled to stop and rest until the next set of tasks required completion. Although there were some exceptions at each site, promoting and supporting patient activity was not part of the ‘routines’ for most nursing staff.
Communication
The final issue was communication. There was an overall impression of missed opportunities to enable activity reflected in our ethnographic observations and the limitations of communication with staff was raised by patients and families. Each unit constituted a specific type of space where communications were structured around the tasks at hand, and outside this communications were related to information-giving (e.g. feedback on progress and prognosis), with very few ‘small-talk’ interactions. Unstructured phatic communication was not the norm. We saw very little evidence of personal and social interaction between staff and patients, or between patients; when this did happen, patients commented on how much it inspired or encouraged them to do more. Communication between staff and patients was again shaped by structures and routines, and the lack of interaction outside those times was noticeable. Patients also felt that communication could enable their activity and wanted more specific ideas from staff, and feedback on what they could do independently or with a carer. Patients and families had a shared perception that the staff group were very busy and had limited time. Our observational data largely supported these comments and we rarely saw anything other than task-orientated interactions. As noted in field notes, there was also a lack of ‘chatter’ between patients and members of staff, which created a rather quiet, uninteresting atmosphere:
Hardly anyone else interacted with the patient. I heard no hand over of information about what the patient could do for themselves, or any aspect of their recovery, or activity.
HCA [health-care assistant] walks in and push her trolley next to him. She records some routine observations of pulse and blood pressure. They don’t talk. He closes his eyes while she performs the procedure.
The group moved on without speaking to this patient. There was no other exchange of information other than about his PEG [percutaneous endoscopic gastrostomy] tube.
A nurse came in to attend to the patient in bed 21, the curtains were pulled but I heard no chatter.
Field notes, site 1, pre
It was not always what was said but what was not being said. One patient stressed the importance of ‘good morning welcomes’ (patient, pre, site 1) and others mentioned the importance of staff introducing themselves to patients:
I just found it horrible when no one even says a good morning, but they are discussing my condition . . . Even down to saying things like ‘I am waiting for a letter from the council’. It feels like your private life is not private at all . . . Because I have had a stroke you lose everything, dignity, the ability to talk and walk, it feels horrible.
Patient, site 3, pre
There were positive examples of communication. Those members of staff who spoke to the patients ‘as a person’ stood out during our ethnographic observations, and some of them were explicitly mentioned during the interviews:
She [health-care assistant] just made the unbearable bearable, she really did. We all hated the weekends when she wasn’t there, you’re just bored anyway and there was mostly agency staff at weekends and, you know, it was just, we just so missed having her around. She just, you know, she used to say to us like ‘we’ll laugh together and we’ll cry together’, you know, and she was just amazing.
Patient, site 3, post
Patients and families gave very few examples of knowing how to be more active; they could not remember being given advice and we rarely witnessed communication that would encourage activity:
It was only the second day, as soon as you got to the rehab ward you wanted your laptop, didn’t you, to check e-mails? [As] the relative, you think, ‘Oh, should I be doing that, will it harm him any more?’, so I went and asked the sister and she was very enthusiastic, ‘Oh yes, anything that will stimulate him, bring it in’, so she was really encouraging . . . You feel you need permission to do these things.
Carer, site 4, pre
Overall, our observations and experiences of communication varied, depending in part on how busy staff were or on the staff who were on the unit that day. However, patients felt that there was inconsistency in receiving information and in staff members’ understanding of their needs:
I mean the first day I got there [. . .], it’s just like, ‘this is your bed, get your clothes off and try and get into bed’. You’re not helped to even get in the bed and then I remember, I had to call, I went to call a nurse, one of them said ‘Why didn’t you call me by the bell?’ I said, ‘because all I was told was, we’re going to get weighed and straight into bed’, no one said a word to me, so I didn’t know anything, so you’re left in limbo. And you feel like a nuisance and don’t ask. And you shouldn’t have to be asking, you know. I remember that night crying and one of the nurses had to come and comfort me because I said I want to go home, I’d rather go home and not be able to do nothing, because that’s how I felt.
Patient, site 3, post
We found alignment between staff and patients/families on many issues relating to communication.
The sense that there was ‘no time for chat’ came through in many staff interviews, which resonated with patients’ and families’ interviews and our observations. Talking positively to patients and wanting to get to know them as a person was not necessarily considered part of the ‘work’. Staff reported that they felt limited by time and clinical priorities:
I just feel like there’s just limited time, like I’m sure everyone would love to sit down and have a conversation but they’ve got so much to do and I think that probably makes people feel more, more stressed and probably more afraid to get into like a conversation because then you have to be rude to get out of it, so maybe if you feel like you never get into it then you don’t have to be rude in that way.
Staff, site 1, pre
In addition to the lack of social communication, we observed, without exception and across all sites, that notices by patients’ beds described information for the purpose of conveying clinical information between staff and very little about personal needs, experiences or activity goals or plans. The sense of ‘the person’ was absent in this information (Figure 8).
FIGURE 8.
A typical method used at site 1 of conveying abbreviated clinical information written on whiteboards above beds. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.
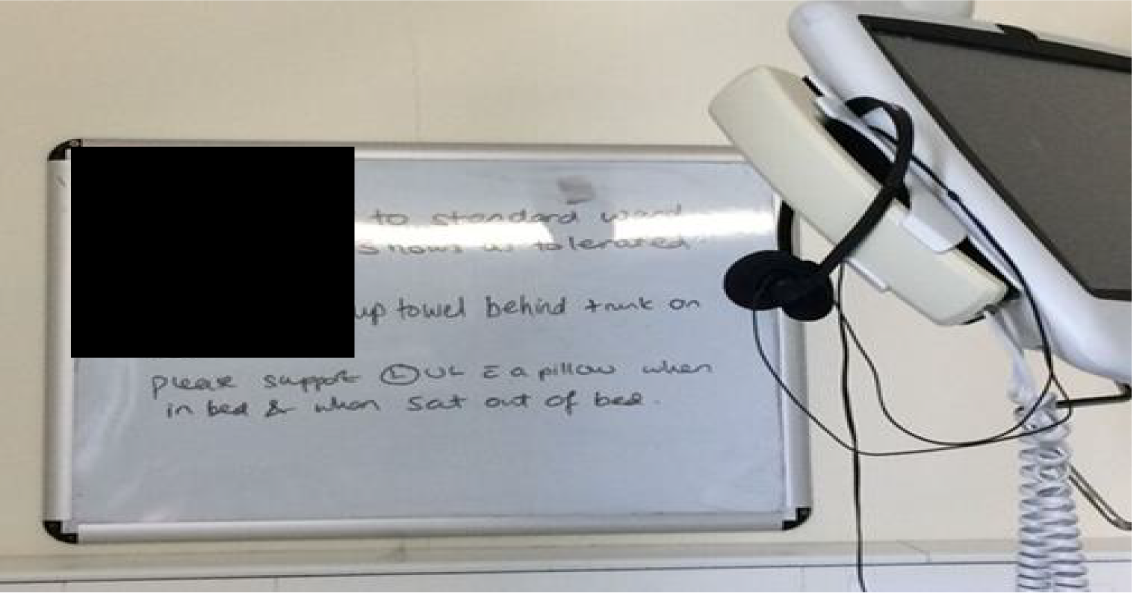
Staff cited many challenges with finding time in their existing schedules to prompt, set up and participate in activities with stroke survivors. These comments were mentioned by all staff groups but more commonly by nurses, who did not appear to see ‘increasing activity’ as a key nursing function. However, the challenges of doing anything other than routine tasks contrasted with the following comment from one staff member:
I do make a massive effort with everybody, I try to give them a bit of my time even if it’s me sitting down with them for 5 minutes, but I mean there’s no facilities to do much else with them than talk. Or if you do, you’ll probably told off for sitting down and talking to them. We [health-care support worker and a student nurse] were getting [patient name], up one morning, he’d just come onto the ward, anyway we were asking him about his life and, you know, joking with him because he had a really good sense of humour, he was only 42, 43 and he really enjoyed that, and we were getting him up, because he was like ‘I’ve been so bored since coming in here’ and he said ‘Thank you for you two coming in and cheering me up and making a difference’. And then one of the nurses popped their head in and was like ‘Less of this and more work’, and I was like ‘Have you actually listened to what he was actually saying to me? We were actually discussing his life with him’.
Staff, site 2, pre
In conclusion, although these units were delivering on national targets for therapy provision, the extent of patients’ inactivity outside scheduled treatment was concerning. This was compounded by spaces that limited activity opportunities and by staff routines that were structured to ensure that caseload was managed but not to promote activity. Communications between staff and patients were task oriented and not patient centred, so there were few instances of focusing on what patients would want to – and could – do on their own. There was a small number of instances of activity promotion (e.g. the art group at site 2), but in the main there was a clear mismatch between staff members’ understanding of the need for and benefits of increased activity and the current service provision in these stroke units. Participation in the EBCD process at all sites led to the identification of and agreement on priorities for improvements that it was considered would lead to increased activity. The impacts of some of these changes are summarised in Chapter 5.
Chapter 5 Results: impact of changes
Impact of changes: qualitative findings – staff, patients and families
In both forms (full and accelerated), the EBCD process facilitated some observable changes to the nature and use of communal spaces, to structured therapy-led group activity and to increasing activity opportunities at the individual and social group level. Whereas the impact of changes in activity by improving access to more groups or in space by having new or repurposed social areas was tangible and visible, less observable change was seen in communication, and this resonated with the findings of the pre-implementation analysis. This was despite several initiatives developed by the co-design groups, including new codes of conduct, changes to staff induction and renewed emphasis on communication in team meetings. Our data showed that interactions with most staff remained largely ‘task focused’. This raised our awareness of the numerous and sustained approaches needed to make changes in communication. The challenge of changing ‘how’ staff interacted in a prevailing culture of a highly medicalised clinically led environment remained and, findings from our post-implementation interviews and our observations substantiate this.
Beginning with space as the first priority area, we draw on multiple sources of qualitative data to explore the impact of changes. This section also includes an analysis of interviews with patients and carers who had not taken part in the co-design process but were patients on or visitors to the ward during or after the co-design. For greater insight we also explored whether or not these interviewees would report similar (perceived) changes to those reported by the patients, carers and staff who did take part in co-design.
Space
I mean the clock thing was something that really struck me. You know, you kind of assume that everyone has a watch or a phone or something so everyone knows the time but I guess, you know, people don’t and people of a different generation maybe don’t have a phone or whatever or you know.
Staff, site 1, post
Changes in the stroke unit ‘space’ included rethinking and repurposing existing spaces (all sites); repainting corridors and bays and creating and introducing artwork in the stroke unit (sites 1 and 3); reclaiming, repainting and equipping day rooms as spaces for activity and patient, family and volunteer use (sites 2, 3 and 4); personalising bed spaces (site 1); enabling greater access to kitchens and bathrooms; and introducing a tool to get to know patients as people: the ‘a little something about me’ board (site 2).
Different priorities did emerge. At site 1, for example, co-design groups prioritised creating the feel of ‘bringing the outside in’, and all of the bays were redecorated with a theme such as lavender or the seaside. Paintings or prints were put up; the walls were painted; digital clocks were put in each room visible to every patient; and hooks for visitors’ coats, photo-hangers and extra shelves to declutter patients’ bedside tables were added (Figure 9). Our interview and observation data support the positive impact that these changes had:
It is a picture of a beach and a cave, similar colours to the photograph from Cornwall that is on F’s wall. He [family member] also shows the photo to F and tells her this is very similar. She smiles.
Field notes, site 1, post
He also uses his photo-hanger. There are get well cards and photos.
Field notes, site 1, post
FIGURE 9.
One of the new colour schemes in a four-bedded bay at site 1. Clinical items were put on new shelves behind each bed, local art work was put on the wall, and a photo-hanger was put up beside each bed. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.

At site 2, the unit initially agreed that changes to the colour schemes and appearance of the unit should be made and worked with an artist to do this, but the changes were put on hold when estates raised concerns about costs, suitability and access. Corridors in the site remained dark and unwelcoming, in stark contrast to the bright, accessible and very well-used refurbished day room on this unit. Site 3 also worked with a local artist to redesign the colour scheme in the newly refurbished day room, and new communication about use of the space was developed. Site 4 already had light and bright corridors with some artwork in place, and the bedside curtains had local scenes and landmarks imprinted on the materials, so these areas were less of a priority for co-design groups.
All of the wards had emphasised creating a common space for patients and carers. Site 4 had a day room but it was used for wheelchair and seat storage. However, as the project began, the chairs were removed and the space become usable for individual and group activity. At site 4, a seating area (for four to six people) facing floor-to-ceiling windows looking out across the main car park and beyond to the hills surrounding the town was also repurposed. This area had previously been used mainly by staff taking their meal/rest breaks and for a display of Stroke Association materials. During the EBCD process, a magazine and newspaper stand was added, jigsaws were donated and several house plants were placed on an accessible window ledge. This space was used regularly by patients and carers both ad hoc or opportunistically and as part of planned therapy-linked activity, for example getting patients who liked gardening to play a part in watering and caring for the plants and encouraging patients with minor cognitive impairment to work on jigsaws with other patients (Figure 10):
We had a gentleman who was really disengaged, he wouldn’t really engage in therapy, but I gave him the job of watering the plants [in the window area] every day and he started doing that and apparently he did better in therapy after the engagement sessions. One of the physios said ‘I wasn’t up for this woolly hippy stuff [CREATE] that you lot are up to but, I could see how it worked, it worked really well’.
Staff, site 4, post
FIGURE 10.
New repurposed seating area at site 4. Reproduced with permission of David Clarke, University of Leeds, personal communication, 2020.

Another carer mentioned the value of having the window seating area as an alternative to the day room(s):
I think we did one or two [jigsaws] in there but people don’t all go in the dayroom you see, people tend to like the corners [the window seating area] there and people tend to join, you’ve got a nice view over the hills, you can look over the car park and you used to love sitting by the window and looking out and seeing what were going on.
Carer, site 4, post
The patients and carers at site 2 appreciated the newly refurbished day room. One patient, who had been on the unit before the room was available but had since seen it as part of a co-design group, felt that it would give patients a choice about what they could do and give them a change of scenery:
They [patients] can go there [to the day room] and there’s people there that will have had the same as they have had, and you can either talk to them or not talk to them . . . they can go to the dayroom and read a newspaper . . . or speak to somebody . . . but it’s just getting out of that bed space and moving. [Previously, when he was on the unit] we had a choice – sit in our bed space or walk to the end of the ward, or walk up and down and that was it.
Patient, site 2, post
The room was used for both scheduled and unscheduled activities. Staff reportedly encouraged patients to go in and participate in newly introduced groups. These groups included a regular Sunday lunch club run by volunteers and a breakfast club and a baking club run by the OTs. Other groups were also held there from time to time, such as music groups and bingo (Figure 11).
FIGURE 11.
New social space (day room) used for scheduled and unscheduled activities at site 2. Reproduced with permission of David Clarke, University of Leeds, personal communication, 2020.

At site 1, observations showed how patients used the new common area. This site previously had had no dedicated space for therapy-related independent practice or social interaction. Prompted by the co-design groups, the end of one corridor, which had been used to store equipment, was transformed into a new open seating area (Figures 12 and 13):
I moved through the ward to the new social corner where I met patient F. who was doing a puzzle. Someone had brought it in for him, it was not his own he told me. He told me he thought the ward had become more inclusive over the time he was there. And he said he liked the social space.
Field notes, site 1, post
FIGURE 12.
End of a corridor at site 1, previously used for storing chairs and hoists. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.
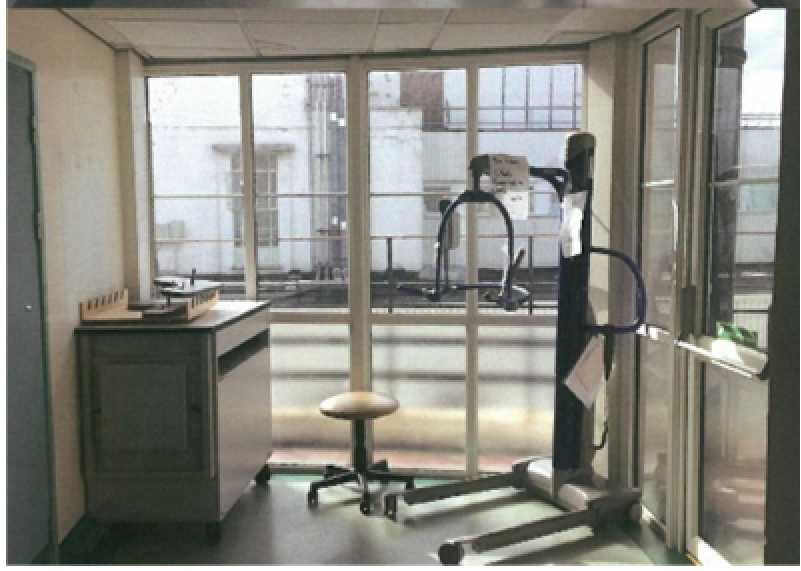
FIGURE 13.
New space at site 1, now an area for patients and families to meet and socialise. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.



Redesigning the space also involved taking stock of what was available to support increasing patient activity, and opening up areas previously inaccessible to patients and visitors:
Yeah because there’s patients’ relatives, instead of coming and ask you now, they go there, they make a cup of tea, they can make a cup of tea for their relative so there’s no point in going to the kitchen because they’re not even allowed, or sometimes we’re busy, you say oh I’m busy, but now they just walk straight and do, yeah, and do that which is good.
Staff, site 1, post
At all four sites, redecoration involved decluttering and rethinking how the space could be used. At site 3, funds were raised to redecorate the shared day room and add a new kitchen area for making drinks and snacks. A local artist painted the walls to make the space look less like a staff meeting room.
At site 4, the co-design groups explored a range of options for making iPads (Apple Inc., Cupertino, CA, USA) more accessible; towards the end of the project, purpose-built flexible stands on wheels were purchased, which meant that iPads were secure but could be used both in therapy sessions and independently (Figure 14):
I think it’s great. Those rooms, that [ward D day] room is particularly good because, you know, when it was full of chairs we couldn’t even go in there. Now it’s, now it’s a free resource we’re lucky to have it, you know, and anything is better, yeah, I think it’s great. I think those pagers are great, the iPads, you know, they’re great on the stands, wonderful.
Patient, site 4, post
FIGURE 14.
New mobile iPad stands used at the bedside at site 4. Reproduced with permission of David Clarke, University of Leeds, personal communication, 2020.

The changes to how the space was used also had an impact on communication. Having familiar home items in the space to make it more homely and placing a photo-hanger by patients’ bedsides contributed to conversations and to learning about the patient as a person:
I said that it is impressive as a fireman he must have saved many lives, and as an electrician bring light to people’s lives. Patient in bed 3 says ‘and electric shocks’ and he laughs. We talk about their photos in the photo hanger. Patient in bed 4 has a holiday photo from Germany, a river, in his photo hanger. It is black and white. He said he went with his wife and it was a long time ago. Patient in bed 4 is very good with names, I realised this before. He knew the names of members of staff when man in bed 4 didn’t. He asked him again about someone’s name and he knew it. I tell him he is very good with names, the man in bed 3 agrees, says yes, isn’t he. I spent about 20 minutes with them. The patient in bed 3 asks me to pass him his blanket, it is red and cosy. He says it is very nice, he is a bit cold. His granddaughter brought it for him. His grandson used to play rugby and they went to watch him on the weekends. He was very good he says. They say thank you and say it is very nice of me to put the programme on. They don’t want a newspaper to look at whilst waiting for the rugby to start.
Field notes, site 1, post
At site 2, a therapist commented on how the ‘a little something about me board’, which contained personal information about previous hobbies, activities or work that patients wanted to share with staff, had shaped the therapy activity she had decided to pursue with a patient:
I was planning some upper limb work with this chap but he was a little hard to motivate. I noticed that the board said was a keen domino player, so that’s what I suggested to him, we did the session focused around playing dominoes, something that he liked to do and we still did the upper limb work, so that’s something that’s happened because of the project for me.
Staff, site 2, post
The nature of the changes made to space meant that these were most visible and generated the majority of positive comments from patients and staff. We were also able observe the impact that the changes to spaces and the different ways space was being used had on patient activity. Staff members’ comments were orientated around the enabling impact of the changes, as well as the change in aesthetics, which gave a more homely, welcoming feel:
So I think the ward is different, I think definitely things look a lot better and a lot more inviting in the environment it’s engaging in, and I think that, that makes a difference in how we communicate on the ward and how we interact with that patient, because there’s stimulus to talk about, there’s pictures now on the wall to talk about and engage and help patients find their way in colours that help, signpost where they’re going and it’s something to talk about, a neutral that we can talk about that everyone has an opinion on and it doesn’t often require a lot of complex language as a speech therapist it’s nice to have something that people could gesture a thumbs up or a thumbs down, they can nod or shake their heads to say that they like a painting or a photograph. So in that respect I think that’s really helped how the ward, the ward interacts and changes.
Staff, site 1, post
Activities
Changes initiated by activity co-design groups included regular visits from therapy dogs (sites 1 and 2); new activity boxes for every bay (sites 1 and 3); increased structured group and individual therapeutic activities (all sites); and increased volunteer and external group supported activities (music, gardening, massage, pet therapy, art and crafts, social Sunday lunches) (all sites) (Figure 15):
We have huge gaps in the day where your patient’s doing nothing, they’re bored, they become institutionalised, so with these extras, like your volunteers coming in, you’ve got various groups, you’ve got your cooking group, your breakfast club, your lunch club, it just makes for a, well it’s a more positive experience isn’t it, well I feel it is.
Staff, site 2, post
FIGURE 15.
New activities (art groups and therapy dogs) available at site 1. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.

The co-design process often led to discussions about how to connect with community and voluntary groups to a greater extent. At site 1, for example, a family member of one of the patients worked as a local artist. Together with her colleagues, she applied for funding and organised art workshops on the ward at the weekends. At site 2, the patient experience office worked with the volunteer co-ordinator to train new volunteers to provide mealtime and social lunch support following discussion with the co-design group members. In addition, the local university’s music department was contacted, which led to two or three singers coming to the unit every 2 weeks to sing songs both they and the patients had chosen. At sites 3 and 4, co-design groups, aware of some of the activities that had been developed at sites 1 and 2, utilised this learning much earlier by connecting with community organisations, and at site 3 a programme of concerts by local choral and music groups was organised. Observations showed the impact of these activities:
One of the ladies told me she had to cry as she found it really moving and said in a good way. She also walked past the group again later and said that it was really nice and she smiled.
Field notes, site 3, post
Additionally at site 3, a retired PT and ex-patient had begun to hold fortnightly ‘exercise groups’. The feedback she had received was positive and our observations showed that the groups had almost got ‘too popular’. Many patients wanted to attend but there was limited space available, even in the repurposed day room. At site 4, a new breakfast group was set up and by the end of the co-design group activity it was running 7 days per week. This group was led by therapists and supported by nurses, who continued the activity at weekends when therapists were not present. The co-design group initiated other planned (arts and crafts groups) and ad hoc events (open afternoon, evening meal with other stroke survivors, a small group watching a favoured television programme) and some patients and families noticed the impact of these:
I do see evidence, psychological evidence [of being willing to engage in more activity] . . . and I also think patients are doing more now.
Patient and family members, site 4, post
Despite an increase in the opportunity to access activities, our observations showed that there were still long periods of time when patients were inactive. Opportunities to access activities were lost for patients who needed help to get out of bed:
I think certain members of staff are really great at getting patients out of bed and really proactive with that and will look at what patients are signed up to do, whether it be therapy sessions or whether it be something like the reading group which has gone on timetables. And then there are other members of staff who don’t look at the timetables at all.
Staff, site 3, post
Co-design groups wanted to focus attention on those patients who were unable to get out of bed and attend groups by designing and providing new activity boxes that could be brought to patients’ bedsides, but we rarely saw anyone using these:
Patient in bed 8 is alone. She is lying in bed. She is not very mobile, but there is nothing else e.g. radio, TV for her. She always smiles when she sees me walking past. The patient, gentleman, 92, is sitting alone. He is saying ‘no no no’ as he quite often does. The doctors are standing around the nurses’ station. 2 of them are looking on their phones, talking about something else, work unrelated.
Field notes, site 1, post
However, observations and interview data also supported the notion that a small number of patients did not necessarily want to engage even when increased activity opportunities were provided. Their pre-stroke behaviour, activity and leisure preferences were factors in their willingness to participate in what was offered:
There was various things going on that the volunteers organised. There was afternoon teas and stuff like that but you’d no desire to go had you?
Carer, site 4, post
Members of staff reported that they were more aware about the activities on the wards post implementation. This was also the case for members of staff who did not take part in the co-design groups:
There, everything, everything is there, everything is there, I’ll go there and give it to them if they are sitting down and there’s nothing to do, give them something to do, even if it is just to practice writing their name or practice signing, I’ll give them a piece of paper and pen so that they can practice and write. [. . .] Yeah, sometimes you think, you can see they want to write, do you want to write, you see them, sort of, practising, oh I don’t know how to write my name again, OK just practice, just keep like that. [. . .] Well before we, yeah now we are doing it but before, as I said, before we were not, no, we are not doing all these sort of things so, but now I don’t know because of the CREATE, the awareness, we’ve got the awareness now so we are trying to encourage them to do all these things.
Staff, site 1, post
In addition to being more aware of the need to promote activity, members of staff reported some examples of how their approach to activity had changed:
Well, we just, we’ve got to get the people out [of bed], washed and everything like that, and then we bring them, or they bring them in here [day room] and help with, anybody that’s available, really, help with breakfast . . . because we still do it on a weekend, even when therapy staff aren’t here, the nursing team still do it.
Staff, site 4, post
Communication
Co-design groups focused on a variety of ways to improve communication, and the changes had led to training for staff; redesigned ward information with emphasis on bringing items from home to personalise the wards; information on activities and how to access WiFi; common charters of communication agreed by staff – personal and social interaction (London sites); and a new website (London, site 3).
Sites 3 and 4 used many of the ideas developed sites 1 and 2, for example digital clocks, familiar home items list, and a list of activity-related apps that could be used on smartphones or tablets. At site 4 there was interest in adopting the ‘something about me’ board developed at site 2 and increasing volunteer activity. However, the board was not actually taken up by the co-design groups and volunteer activity could not be progressed as the volunteer co-ordinator on site would not engage with the groups. At this site increased volunteer support for and provision of activities occurred following personal contacts between individual members of staff and existing volunteers and volunteer groups. Many co-design groups prioritised updating and expanding the unit information leaflets to highlight how to access free WiFi on the unit and to highlight the activities now provided on and off the unit and how these could be accessed. At site 4, co-design groups also addressed a major concern for all stroke survivors that in leaving the ward for social activity that they may miss important therapy time. The groups sourced telephone ‘bleep’ devices no longer used by medical staff and gave these to patients and carers when leaving the unit so that they could be called back for therapy sessions if required.
Patients and families taking part in the co-design and those on the ward noted the improvements:
I think the information leaflet’s quite good because it says, it tells you things like where the day room is and that you can go into the garden and things like that. That new one, it’s also on the wall outside the ward isn’t it, the new one? Because I remember reading it there and I thought oh this is different from the one that used to be there when Mary was in.
Carer, site 4, post
One patient and their carer had been involved in the communication co-design group and were pleased that the ‘my journey’ communication sheets were being used on the ward at site 2. These sheets were for staff to write down information about the patient’s progress and for relatives to leave questions and comments for staff:
No, very happy [that the communication sheets were being used] because some days I’d try and ask [her husband] ‘oh what have you done today’? And sometimes he’d find it hard because when you went in later in the day they were tired and if they’ve had physio and everything else and half the time he’d just sleep, but whereas if you could pick something up and say ‘oh yeah, you did some therapy and how did that go today?’ . . . You can at least make conversation to him about it, without him saying ‘I can’t remember’ . . . Just nice to know he hasn’t just been lying in bed or sat in the chair and just ignored . . . at least if you could read it and say ‘that’s good well done’.
Carer, site 2, post
We also observed ways in which the changes to the space, such as the ‘a little something about me’ boards and the refurbished day room at site 2, had a positive impact on interaction and communication. Patients thought that the boards were useful and one patient remarked that they served to ‘break the ice’ with staff who did not know him. Relatives were observed helping staff fill the boards in or even filling them in themselves. Volunteers and other staff who were not based on the unit (e.g. phlebotomists) also appreciated the information provided on the boards and reported that it helped them find topics of conversation to bring up with patients. One phlebotomist said that it was helpful to know something about each patient and ‘see them more as individuals’. Sometimes the boards were not up to date because of bed moves. A health-care assistant reported that she and ‘a few others’ tried very hard to keep the boards up to date but that this could be difficult during busy periods. She also said that not everyone ‘bothers’ to do it, even if they had time.
At site 4, several changes were made to information for patients and visitors about how they could access different areas or be more engaged in their recovery. Staff felt that this was a tangible output that had made a big difference:
So you know the welcome to the ward sheets, we edited them so there’s one for every single ward now, and I know they get handed out at family meetings, I know on [site 4] they do that, the others need encouraging to do it, but there definitely are printed forms for every single ward. They had on what facilities were available, so we changed it to make it a bit more user friendly, it had like a spider diagram that said, there is WiFi, there is a garden, you can go to Costa, and it kind of touched on all the things that we spoke about [in the co-design group], so, actually, families can look at that straight away.
Staff, site 4, post
As part of the co-design process at site 3, information leaflets were produced for key workers to give to patients and family members, and the Stroke Association commenced monthly information drop-in sessions. Although those changes may well have facilitated the change in perception about feeling informed, it was difficult to keep track of and report the extent to which those changes were actually being implemented. As notes from an observation at site 3 show, even when new information leaflets and guidance about welcoming patients were put in place, not every patient was made aware of these:
One of the patients in particular is very interested in the project and wants to know more. He asks me to send him an email with some readings so I do. He has never seen any of the leaflets, Welcome to the Ward, Apps list etc. I give it to him. He later tells me he enjoyed seeing the Familiar home items list, but if it wasn’t for me he would have never seen any of it.
Field notes, site 3, post
Staff from across all sites felt that CREATE had raised awareness that activity was a priority and in some cases said that as a result they had made small changes in how they communicated or interacted with patients. This impression was given by both staff who did and staff who did not take part in the co-design groups:
I think staff are thinking more about how to involve patients and get them talking and for myself I always go in now and make sure that I say hello to everyone, regardless, or introduce myself even if I’m not seeing that particular patient.
Staff, site 1, post
One member of staff (site 3, nurse), who did not take part in the co-design groups, described how he now thought more about the patient as a person: ‘this is a person who needs to go out like myself’. He was more open with patients and involved family more, whereas before it had been ‘wash – dress – sit’. He shared an anecdote about two patients who did not like having the same breakfast every day and wanted to go to the canteen to get their own breakfast. Someone said he should take their orders and get it for them, but the patients wanted to go and choose for themselves. He then thought ‘yes, we keep them from making their own choices otherwise’. He took them to the canteen to get a breakfast takeaway, and they have done this every day since. He said that this had happened because of the CREATE study taking place on the unit, and now he would be thinking about alternatives.
Although staff often said that they were enabling in their interactions and communications, this was not always supported by our observations and was especially obvious between routine tasks as discussed previously:
The HCA [health-care assistant] comes back to the gentleman in bed 7. She talks to him. He says ‘sorry’, but I [observer] can’t understand what exactly he says. It seems to me he is apologising to her that she has to do certain things to help him. She goes back to bay 1-4 and talks to the patients in the room, she then grabs continence pads and tissues and goes back to patient in room 7. He says sorry again. She does her job, but doesn’t say anything like, its ok etc. She puts on apron and gloves. She goes in and closes the door.
Field notes, site 1, post
Although staff reported positive changes to their communication and interactions to promote activity, some supported our impressions that communication was ‘work in progress’:
I am not sure if we have achieved much in terms of the basic communication day to day between the carers of the ward. Not the carers, the staff caring for the patients, because I think that’s where we need an ongoing input. So, that’s I think a big part, that’s difficult to change and I’m not sure if it will change?
Staff, site 3, post
Impact of changes: quantitative findings (behavioural mapping and patient-reported outcome measures/patient-reported experience measures)
In this section, we present descriptive results from the quantitative data generated pre and post implementation of EBCD (the intervention): (1) behavioural mapping and (2) PREMs and PROMs. In addition, the results are compared within and between sites.
In summary, behavioural mapping results were inconsistent across sites and showed a mixed pattern of inactivity (social, cognitive and physical) pre and post implementation of co-designed changes. However, taking the broad measure of ‘any activity’, there was some improvement at sites 1 and 2 (full EBCD) but similar levels at both time points at sites 3 and 4 (accelerated EBCD). Our findings also demonstrate the discrepancies that arise when presenting overall activity/inactivity percentages, compared with the number of activities in the three domains (physical, cognitive and social).
Data analysis of PREMs/PROMs also showed a mixed picture across all sites. PREM data analysis showed inconsistencies across items and sites. Despite this, there were consistent changes in relation to item 5, which asked respondents whether ‘there were enough things to do in my free time’, which showed an improvement after the implementation of co-designed activities. No further firm conclusions from PREM data can be drawn. PROM data analysis confirmed that patients treated in the participating stroke units before and during EBCD implementation were not atypical and did not appear to be any more or less likely to be receptive to activity-based interventions than other groups of inpatient stroke survivors in other UK stroke units.
We make further commentary on our chosen quantitative measures, behavioural mapping and PREMs/PROMs, in our methodological consideration in Chapter 6.
Behavioural mapping
As outlined in Chapter 3, behavioural mapping was used to provide an indication of activity levels in each unit on 3 separate days at agreed time points before and after EBCD cycle implementation. The approach used in CREATE recorded episodes of social, cognitive or physical activity. These data were from separate groups of patients in each site; we did not seek to compare ‘before and after’ scores for individual patients but rather used the behavioural mapping data as a broad indicator of activity levels in each site. All patients recruited for behavioural mapping were observed at 10-minute intervals between 08.00 and 17.00 or between 13.00 and 20.00 on 3 separate days, including weekends. This allowed up to 60 observations of each patient per day. During each 10-minute interval, the data for each patient was based on an observation made by the researcher over a period no longer than 5 seconds (see Appendix 7 for the full behavioural mapping protocol).
Of note is that the percentages stated in tables relate to ‘inactivity’, so a reduction is a positive finding.
Within-site comparisons
Site 1 (pre, n = 9; post, n = 7)
Pre implementation, participants in the behavioural mapping at site 1 had a high level of physical inactivity, at 71%; levels of inactivity in the cognitive and the social domains were also high. However, level of inactivity reduced markedly in the physical domain between the two time points, from 71% to 42%; there was a more modest reduction in the level of social activity of 6% and a slight increase in cognitive inactivity of 4% (Table 6).
| Activity type | Pre intervention | Post intervention |
|---|---|---|
| No physical activity | 71% | 42% |
| No cognitive activity | 68% | 72% |
| No social activity | 58% | 52% |
The only physical activity recorded pre intervention for > 1% of the observations was engagement in activities of daily living (ADL) (which could include personal grooming, changing clothing, eating and drinking), at 7%. Changes were evident post intervention, with a 20% increase in engagement with ADLs and evidence of increases in the following activities: mobilising (7%), repositioning (5%), independent practice (usually of therapy-directed tasks) (4%) and transfers (2%). Although cognitive inactivity increased slightly overall, again, the post-implementation observations showed that some cognitive activities were now occurring, including writing and art activity, listening to music or audiobooks (5%) and reading (2%). There was a small reduction in social inactivity (6%), which seems to be accounted for by an increase in talking and communicating with other patients, relatives and staff.
Post intervention, overall level of any activity increased by 15.1% at site 1, despite inactivity being higher in the cognitive domain (Table 7).
| Overall (site 1) | Pre intervention | Post intervention |
|---|---|---|
| Activity | 62.1% | 77.2% |
| No activity | 37.9% | 22.9% |
Site 2 (pre, n = 10; post, n = 10)
As at site 1, levels of inactivity in all three domains at site 2 were disappointing, with only cognitive inactivity showing a reduction between the two time points (13%) and increases of 1–2% seen in levels of inactivity in the physical and social domains (Table 8).
| Activity type | Pre intervention | Post intervention |
|---|---|---|
| No physical activity | 65% | 66% |
| No cognitive activity | 64% | 51% |
| No social activity | 46% | 48% |
The most common activities recorded pre intervention were talking with other patients, relatives or staff (35%), engaging in ADL (which could include personal grooming, changing clothing, eating and drinking) (9%), watching television (8%) and reading (6%). Post intervention, some changes were evident, mainly in cognitive activity, with small increases in reading (14%), listening to music/using electronic devices (8%) and participating in group activities, including art and writing (6%). Despite the small decrease in social activity observed, there was in fact a small rise in the percentage of time spent talking/communicating among participants at this site (37% from 35%). When the overall levels of any activity and inactivity recorded are considered for this site, these data show a small increase in activity of 15.8% (Table 9).
| Overall (site 2) | Pre intervention | Post intervention |
|---|---|---|
| Activity | 72.7% | 88.5% |
| No activity | 27.3% | 11.5% |
Site 3 (pre, n = 12; post, n = 7)
Pre implementation, both physical and cognitive inactivity levels at site 3 were better than at sites 1 and 2 and similar to site 4. This site had lower levels of social inactivity than sites 1, 2 and 4. Between the two time points, levels of social activity remained the same, at just over one-third of the observed participant time. The level of cognitive inactivity fell by 5%, whereas the level of physical inactivity rose by 6% (Table 10).
| Activity type | Pre intervention | Post intervention |
|---|---|---|
| No physical activity | 50% | 56% |
| No cognitive activity | 49% | 44% |
| No social activity | 30% | 44% |
In common with sites 2 and 4, the most common activity at site 3 pre implementation was talking with other patients, relatives and staff (27%). Use of mobile phones accounted for 10% of observed participant time in social activity. Engaging with ADL accounted for 13% and mobility accounted for 3% of physical activity. Reading was the most common cognitive activity, at 10%, but patients also engaged with music or audiobooks 5% of the time, watched television 4% of the time and used electronic devices 3% of the time. Post-intervention talking with other patients, relatives and staff was unchanged (27%). There were small increases in using mobile phones (up 3%) and electronic devices (7% increase); participating in group activity was evident during 4% of observed time, as was mobilisation at 4%, and listening to music/audiobooks (up by 1%). Engaging with ADL fell slightly to 11% and reading fell to 9%, whereas watching television remained the same. At this site, overall activity levels changed very little (up 2.9%) but it had started with the highest baseline activity level of 82.4% (Table 11).
| Overall (site 3) | Pre intervention | Post intervention |
|---|---|---|
| Activity | 82.4% | 85.3% |
| No activity | 17.5% | 14.6% |
Site 4 (pre, n = 6; post, n = 6)
Here, too, the data show relatively high levels of inactivity in the three domains, with only social inactivity reducing by 10% between the two time points. As at site 2, post intervention there were small increases in inactivity in the physical domain and, at this site, also in the cognitive domain (Table 12).
| Activity type | Pre intervention | Post intervention |
|---|---|---|
| No physical activity | 61% | 65% |
| No cognitive activity | 46% | 45% |
| No social activity | 51% | 41% |
The most common activities engaged in pre intervention at site 4 were talking with other patients, relatives or staff (25%), watching television (22%), engaging in ADL (14%), using electronic devices (4%) and reading (3%). Post intervention, some changes were also evident at this site, most notably in talking with other patients/relatives or staff, which increased by 12%, and reading, which increased by 10%. There was a reduction in television viewing and in engaging with ADL. The trend evident at the other sites of changes in overall level of any activity was also seen at site 4, with an increase of 11.5% (Table 13).
| Overall (site 4) | Pre intervention | Post intervention |
|---|---|---|
| Activity | 80.6% | 92.1% |
| No activity | 19.4% | 7.9% |
Cross-site comparisons
Pre implementation, site 1 had the highest level of physical inactivity and site 3 had the lowest level of social inactivity. However, overall levels of inactivity across the three domains were broadly similar across the sites. The largest change in levels of inactivity occurred at site 1, where physical inactivity levels fell by 29%. At site 2, levels of cognitive inactivity fell by 13%, mostly accounted for by an increase in participants reading independently or with others. Social inactivity fell by 10% at site 4, accounted for by an increase in talking with other patients, relatives and staff. When comparing overall activity, site 1 had the lowest level pre implementation, at 62.1%, and levels at sites 2 and 4 were 72.7% and 80.6%, respectively, with site 3 having the highest overall level of activity, at 82.4%. Post implementation, all sites increased overall levels of activity, with sites 1 and 2 showing increases of 15%, site 4 showing an increase of 11% and site 3 showing an increase of 3% from its relatively high baseline level.
Summary
Although our behavioural mapping data are largely consistent with previously published work in terms of levels of inactivity, they do suggest that the overall time spent inactive on these stroke units was not as much as that seen in previous studies. 7,86 The behavioural mapping data, although from a small number of participants at each site, highlighted the differences in the provision of individually focused activity opportunities (which remained limited) and the changes we saw in the space/environment of the units, which led to an increase in structured group and informal social activities not easily captured by behavioural mapping. In addition, the behavioural mapping process highlighted the long periods of time that patients spent largely alone, despite the changes to space and activity opportunities, and was one of the main ways in which we observed the limited and task-oriented staff communication processes that largely did not change in the sites between the pre- and post-EBCD periods.
Overall, we question the relevance and validity of using behavioural mapping as a reporting tool in CREATE in relation to anomalies in reporting; the small number of patients who were able to consent the day before behavioural mapping took place; not including scheduled therapy as part of our reporting; and finally the impact of contextual issues such as staff shortages and the severity of disability of the inpatient caseload. These methodological considerations are discussed in more detail in Chapter 6.
Patient-reported experience measures and patient-reported outcome measures
Participants were sent a PROM/PREM pack containing a survey about their experiences as well as the impact of their stroke. Demographic details of all respondents can be found in Appendix 9.
We provide a summary of pre-implementation and post-implementation PREM and PROM data below and the full data set can be found in Appendices 10–12. First, we report on PREM items that scored particularly high or low, and on broad indicators of the quality of the patients’ experiences in these units. As these data are from different cohorts of stroke survivors at each time point and in each site, they provide an indication of patients’ overall experiences of these stroke services during their inpatient stay.
For reference, Box 1 shows the items referred to in the following commentary and Table 14 shows the PROM/PREM response rates.
-
When I arrived I was given information about the unit and what would happen during my stay.
-
The facilities on the unit were good.
-
There was somewhere secure to keep my belongings.
-
I was able to discuss personal matters in private.
-
There were enough things to do in my free time.
-
There was a friendly atmosphere in the unit.
-
I felt the staff really cared about me.
-
The staff worked well as a team.
-
I felt able to talk to the staff about any problems I had.
-
I was asked what I wanted to achieve during my stay.
-
I felt as though the staff and I were partners in the whole process of care.
-
The staff kept me informed every step of the way.
-
My family or carer was involved in discussions about my treatment if I wanted them to be.
-
I am happy about the amount of therapy I received for . . .
-
Swallowing problems
-
Speech and communication
-
Improving mobility
-
Independent living
-
Continence
-
Other
-
-
I received enough emotional support.
-
I felt well supported and prepared for my discharge.
-
I am satisfied with the progress I made during my stay.
-
Thinking about how you were treated during your therapy sessions, which of these statements would best describe how you felt: patronised, respected, offended, supported, ignored, listened to, frustrated, motivated?
| Site | Number sent out | Number returned | Response rate (%) |
|---|---|---|---|
| Pre implementation | |||
| 1 | 120 | 22 | 26 |
| 2 | 139 | 45 | 32 |
| 3 | 73 | 28 | 38 |
| 4 | 108 | 13 | 12 |
| Post implementation | |||
| 1 | 67 | 25 | 37 |
| 2 | 100 | 31 | 31 |
| 3 | 59 | 11 | 19 |
| 4 | 45 | 11 | 24 |
Pre-implementation patient-reported experience measure data: summary of findings
In terms of the specific focus on the CREATE study, responses to statement 5 were most relevant. Pre implementation, between 30% and 55% of respondents disagreed that there were enough things for them to do in their free time, with only 4% of respondents indicating agreement with the statement at site 1, 27% agreeing at sites 2 and 4 and 44% agreeing at site 3. By contrast, across all sites, ‘facilities’ were considered to be good, with between 74% and 82% agreeing with statement 2.
Across all units, some dissatisfaction was evident in areas of information provision, with < 50% agreement with statement 1 (range 36–48%). Similarly, there were low levels of agreement with statement 10 (range 27–48%), suggesting that limited attention was given to identifying personal goals for recovery. At the same time, these respondents had a higher frequency of agreement with statements 11–13, which focused on feeling as though they and the staff were partners in the process of care (statement 11: range 50–75%), that they had been kept informed during the care process (statement 12: range 41–61%) and that family or carer involvement in treatment discussions could occur if wanted (statement 13: range 67–82%).
There was strong agreement with the statements that there was a friendly atmosphere on the units (statement 6: range 82–91%) and that staff really cared about them (statement 7: range 68–87%), and there were similar levels of agreement that the staff worked well as teams (statement 8: range 67–85%). The respondents largely agreed with statement 9, that they felt that they could talk to staff if they had a problem (range 60–80%). Although the responses to statements 7–9 were positive, up to one-third of the participants disagreed with these, so experiences clearly varied within and across units.
The responses to statement 4 were more mixed, indicating some concerns related to feeling able to discuss personal matters in private (range 51–67%). This reflects to some extent the limited number of private rooms/spaces on the stroke units and echoes concerns raised by former patients in the filmed interviews at sites 1 and 2. At site 3, only 4% of respondents agreed that they received enough emotional support (statement 15), with 33% disagreeing. However, 59% of the respondents at this site indicated that this issue was not applicable to them; allowing for this, the responses still indicated a low level of agreement that enough emotional support was received. At site 1 only 35% agreed with this statement, whereas at sites 2 and 4 more than two-thirds of participants indicated that they had received enough emotional support (statement 15: both 67%).
In terms of respondents feeling happy with the amount of therapy or treatment received in relation to the five areas listed in statement 14, the main area of concern across sites was linked to problems related to continence. Here, agreement levels ranged from 26% at site 3 (although 41% indicated that this was not applicable to them) to 42% at site 2, 42% at site 4 and 57% at site 1. Site 3 had lower levels of agreement for swallowing, speech and mobility, at 33%, 48% and 52%, respectively. These differ quite markedly from those at sites 2 and 4, where levels of agreement relating to swallowing, speech and mobility ranged between 85% and 95%. At site 1, the levels of agreement ranged from 61% for therapy or treatment for swallowing to 80% for both speech and mobility. In respect of treatment or therapy to prepare people for independent living, levels of agreement ranged from 44% at site 3 to 56% at site 1 and 82% at sites 2 and 4, where, with the exception of continence, higher levels of satisfaction were also evident with other areas of therapy or treatment.
Post-implementation patient-reported experience measure data: summary of findings
The post-implementation response rates at sites 1 and 2 were higher than those at sites 3 and 4; the reasons for this were unclear, but the timing of the survey could be one factor, at sites 3 and 4 it was distributed close to the Christmas period. The response rates are detailed in Table 14; in all sites and at each time point when these were distributed, the response rate was < 40%.
We report here on the differences in scoring of PREM items between pre and post intervention. We cannot attribute these differences in responses directly to changes occurring in the stroke units during the EBCD process, but we report on the responses as broad indicators of the quality of the patients’ experiences in these units. The full data set can be found in Appendices 8 and 9.
Among the post-intervention responses, agreement with statement 5 increased at three sites; this was most marked at sites 1 and 2, where the proportion agreeing increased from 4% to 40% at site 1 and from 27% to 50% at site 2. At site 4, the increase was more modest, to 36% from 27%, and, despite these increases, the scores still indicate relatively low levels of opportunity to be independently active. However, the level of agreement with statement 5 at site 3 actually fell quite substantially, from 44% to 9%. These responses are not easy to explain and differ quite substantially from the qualitative data, which record that a range of increased activity opportunities were made available and occurred at this site.
As with the pre-implementation responses to statement 2, there were still quite high levels of agreement that the facilities on the sites were good, but, again, it is interesting to note that although the proportion agreeing with this statement increased at sites 2 and 3 by 4% and 8%, respectively, the level of agreement at sites 1 and 4 fell by 10% and 12%, respectively. In terms of information provision, an area of concern in the pre-implementation period, responses to statement 1 also varied post intervention, with sites 2 and 3 showing a reduction in agreement with this statement of 8% and 10%, respectively, and sites 1 and 4 showing no change.
Co-design groups at all sites had identified communication with patients and families (rather than information provision specifically) as an area for improvement. The post-implementation responses show that providing information early in the inpatient stay remains an area of concern for patients. At sites 3 and 4 the changes introduced (new unit information leaflets) came towards the end of the co-design period and may have occurred too late to be captured in these questionnaires, but at sites 1 and 2 communication-focused changes had been implemented for longer periods of time. At the same time, another statement related to information provision (12: ‘the staff kept me informed every step of the way’) showed improved levels of agreement at each site (range 56–64%, up from 41–61%).
Responses to statement 10 indicated higher levels of agreement at three out of the four sites (i.e. sites 1, 2 and 4) (range 40–64%, up from 27–48%), most notably showing a substantial increase at site 4, from 27% to 64%. At site 3, the level of agreement fell by 8%, from 48% to 40%. So, while acknowledging the lower overall response rates post implementation, some improvement was evident, but responses to these items in the PREM indicate that progression to a more patient-centred approach remains an issue for these sites.
Responses to statement 4 show higher levels of agreement in three out of the four sites (i.e. sites 2–4), with percentage increases of between 4% and 12% (range 55–73%). Site 1 had a 7% reduction to 60% agreement from 67%, so finding somewhere private to discuss personal matters was a concern for some patients. Statement 9 addresses broadly the same area of patients being able to talk to staff about any problems; agreement with this statement fell in three sites out of four from the relatively high pre-implementation levels, which ranged from 62% to 80% to 52% to 76% post implementation, a reduction of between 4% and 10%. Responses to statement 15, which explores receipt of emotional support, showed an increase in agreement in three out of the four sites (i.e. sites 1–3) (range 44–67%), with a substantial improvement at site 3 (up from 4% to 44% and with only 8% indicating that this was not applicable post implementation at this site, down from 59% pre implementation). At the same time as highlighting these areas where services still had room for improvement in communication and support, respondents indicated high levels of agreement with statement 6 (range 80–100% agreement), that there was a friendly atmosphere on the unit, statement 7, that patients felt that staff really cared about them (range 76–93%), and statement 8, that the staff worked well as a team (range 80–97%). Statement 17, relating to patients being satisfied with their progress during the inpatient stay, had higher levels of agreement at all four sites (range 76–86%). Statement 16, addressing patients feeling supported and prepared for discharge, showed small increases in agreement at sites 1 and 2 (to 56% from 54% and to 86% from 81%), whereas site 3 showed a small reduction, from 59% to 56%. The reduction in levels of agreement with statement 16 at site 4 is more marked, with this down 17% from 81% to 61%.
Responses to the five areas listed in statement 14 (respondents feeling happy with the amount of therapy or treatment received) present a mixed picture, as in the pre-implementation period. These post-implementation responses are from a smaller number of patients at all but site 1 and will reflect to some degree the individual post-stroke disabilities and impairments experienced by these respondents. At site 1 there were lower levels of satisfaction with therapy for swallowing problems (20% vs. 67%), but 64% of respondents indicated that this issue was not applicable to them and a further 22% indicated that they were unsure. A similar substantial reduction is seen in responses to the speech and communication statement at site 1 (36% vs. 80%) but again 48% indicated that this issue was not applicable. In addition, quite a large reduction in satisfaction is seen for continence (57% to 28%), but 52% indicated that this was not applicable, and the level of disagreement with this statement among patients at this site fell from 36% pre implementation to 12% post implementation. Improving mobility also showed a reduction but to a lesser extent (68% vs. 80%).
The overall PREM data analysis presented above shows a mixed picture across all sites, with inconsistencies across items and sites. Response rate fell significantly at site 3, which might have been related to the timing of data collection, either side of the Christmas period. Other than the changes in relation to item 5, which we would have expected following the implementation of co-designed activities, it is difficult to draw any firm conclusions from this relatively small sample. We make further commentary on our chosen PREM in our methodological consideration in Chapter 6.
Patient-reported outcome measures
The PROM questionnaire comprised the Subjective Index of Physical and Social Outcome, the EQ-5D and the Oxford Handicap Scale. We did not intend the PROM to be used to derive scores for each of the three subcomponents, but rather to review and describe participants’ perceived levels of disability and adjustment to life after stroke. As previously indicated, these self-completion questionnaires were distributed to two different cohorts of stroke patients, and returned by post. Those who returned questionnaires may not be representative of the stroke patients who received care in the participating stroke units during the time periods identified. Nonetheless, these data provide some insight into the post-stroke characteristics of patients who returned the questionnaires. Below, we describe the broad issues emerging from these data.
Questions 1–10 were from the Subjective Index of Physical and Social Outcome and were about physical functioning/mobility. All respondents had similar difficulties with dressing in the pre- and post-EBCD intervention cohorts; most reported some difficulty with dressing themselves, and on average 17% of respondents could not dress themselves fully post stroke. Across sites, up to 25% of respondents reported either a lot of difficulty with moving around their homes or not being able to move around their homes independently at all. Among the post-EBCD intervention cohorts, respondents at sites 1, 2 and 4 felt marginally more satisfied overall with their ability to perform daily activities around the home than did those at site 3.
With the exception of site 1, where rates were higher in the pre-intervention cohort, those participants responding in the post-EBCD periods reported that they had a lot of difficulty or could not shop for or carry a few items for themselves, indicating relatively high levels of dependency in this area. For question 5, those indicating they were completely dependent or needed assistance most of the time increased in the post-EBCD cohorts at sites 2, 3 and 4, but fell at site 1 from 58% to 32%.
Questions 6–10 related to social/emotional functioning. Except at site 2, where the percentage fell by 9%, response rates indicated that more people in the post-EBCD cohorts were never bored. In all but site 4, there was a small increase in the numbers of respondents reporting a good deal or quite a lot of communication with friends or associates. At site 4 there was a reduction of 30% in the response rate for these two options in the post-EBCD cohort. Again, in relation to levels of satisfaction with activities and interests, respondents were completely or mostly satisfied, whereas respondents at site 4 reported lower levels of satisfaction with responses to these two options in the post-EBCD cohort (down by 30%). There were no differences in response rates to the item relating to visiting friends in either the pre- or post-EBCD cohort.
Our data showed that, across sites, between one-third and half of respondents felt self-conscious to some degree about their appearance, with up to 11% reporting that they tried to avoid going out in public, which is a significant proportion. At the same time, between 45% and 60% of the remaining respondents indicated that they were perfectly happy with their appearance when out in public. There were no major differences in responses between sites in the pre- or post-EBCD cohort.
Questions 11–15 are from the EQ-5D. In this PROM we did not ask participants to rate their perceived level of severity in each of the five domains and so standard scoring is not applicable. We describe below the overall levels of agreement with the statements.
In all sites, > 46% of respondents reported some problems with walking, and between 5% and 18% reported being confined to bed. A similar pattern was evident for washing and dressing, with between 40% and 73% of respondents in the pre-intervention cohort at sites 1–3 reporting having some problems with washing and dressing or being unable to wash or dress themselves. In addition, a high proportion of respondents across all sites reported some problems performing usual activities or being unable to perform usual activities (range 55–84%), with some variation between sites. More than one-third of respondents experienced moderate pain or discomfort, with between 5% and 22% reporting extreme pain or discomfort. Responses also showed that 31% and 46% reported being moderately anxious or depressed. Rates differed slightly between the pre- and post-EBCD cohorts across sites, with a reduction in respondents selecting this response at site 1, no change at site 2 and increases of 5% and 13% at sites 3 and 4, respectively. Rates of those not reporting being anxious or depressed varied by site from 36% to 62%, but there was no consistent pattern between pre- and post-EBCD response rates.
Questions 16–21 are from the Oxford Handicap Scale. The first three items identified little or no impact of disability and impairment on everyday life and the remaining three items indicated moderate to severe impact on everyday life.
Overall, the responses indicate that between 55% and 89% of the respondents had no symptoms, symptoms that did not interfere with everyday life or symptoms that had caused some changes in the respondents’ lives but the respondent was still able to look after themselves. This level of response was largely similar in the pre- and post-EBCD cohorts at sites 1–3 but increased from 77% to 89% at site 4. However, responses to the remaining three items in this section of the questionnaire (questions 19–21) indicated that between 9% (site 3 pre- and site 4 post-EBCD cohorts) and 45% (site 2 pre-EBCD cohort) had moderate to severe symptoms that significantly changed their lives and resulted in their needing help to care for themselves. At the most dependent end of this spectrum, between 3% (site 2) and 27% (site 3) of participants in the post-EBCD cohorts at these sites reported needing constant attention day and night.
Commentary on patient-reported outcome measures
Acknowledging the limitations of the sample size and response rates across sites, these self-report data are largely consistent with the levels of mood disturbance reported in systematic reviews,21,75 and disability and impairment reported by the Stroke Association in the UK and in stroke data internationally. 17 There does not appear to be any great difference in levels of disability and impairment between sites and between the pre- and post-EBCD cohorts. There is, however, some indication that respondents in the post-EBCD cohort at site 3 reported higher levels of post-stroke impairment and disability than at other sites; however, the response rate is < 20% for this cohort. Similarly, any signals that respondents in the pre- and post-EBCD cohorts at site 4 reported less impairment and disability and lower levels of mood disturbance have to be viewed in the light of the very low response rate of only 12%. Overall, these data indicate that stroke patients treated in the participating stroke units before and during implementation of the EBCD intervention were not atypical and do not appear to be any more or less likely to have been receptive to activity-based interventions than other groups of inpatient stroke survivors in other UK stroke units.
Our target recruitment number was based on the anticipated numbers of patients likely to be cared for and discharged from the stroke unit in the 3 months prior to the commencement of the EBCD process and then cared for and discharged in the 3-month period during which EBCD activity took place in each unit. We recognised that this number was no more than a crude estimation influenced by external factors such as caseload factors and admission rate. As it quickly became apparent that response rates were low in almost all sites, we extended the period of time for distributing pre and post questionnaires to 6 months. The differences in the numbers of patients sent questionnaires reflects the number discharged from the units during each time point and known to be alive at that time. This partly reflects length of stay, which was often closely linked to stroke severity.
We had no direct contact with these potential participants, but at site 2 (Yorkshire) the consultant physicians encouraged their patients to complete PROM/PREM questionnaires at their 6-week follow-up appointment, which may have increased the pre-EBCD response rate at that site. We did not send repeat questionnaires at this site as the response rates were good; however, the consultants changed at that site so no similar process was in place for post-EBCD questionnaires. We requested that principal investigators use this method of completion at follow-up clinics at site 1 but they did not do so because of concern about participant burden. At site 3 there were no 6-week follow-up appointments and so, if no response had been received to the questionnaire, second copies were sent out 4 weeks later (after checking whether non-respondents were still alive). We judge that the difficulties with recruitment to and completion of the measures, as outlined above, influenced the validity and the contribution of the PROM/PREM data to our overall findings.
Implementation and engagement
The following section describes the experiences of staff, patients and families who took part in the co-design, and synthesises findings from across all post-implementation interviews. For the most part, taking part was viewed positively, even though patients and families had been approached about taking part at a time of great personal disruption in their lives and staff had little or no additional time to dedicate to the process:
I think CREATE has been an absolute breath of fresh air for the stroke unit and I think all the challenges that we still continue to face on the ward have been bearable because of CREATE and the positive influences that they have had, so . . .
OT, site 1, post
The ‘experience’ of taking part (staff, patients and families)
The themes below demonstrate our understanding of some of the more nuanced reasons why participants wanted to take part and found the whole experience positive. The themes demonstrate why they wanted to be involved and the benefits to individuals, as well as the perceptions of the advantages of working together in a group and seeing through the changes.
The added value of giving something back
Family members and patients appeared to be driven to be involved because of their desire to help others if possible, whether because of positive or negative reasons:
Well it was, it seemed good and it seemed hopefully helpful in understanding my experience, so no I’m pleased to be able to give something back more generally across the whole process. I feel I had very good care there, obviously you can always find little things that, and it’s good to have that patient, carer feedback is built in and I’m very happy to contribute to that.
Patient, site 4, post
For others, the sense of ‘giving back’ was an incentive to make the experience better for other patients in the future:
Because we had enough sort of concerns and situations she was in, so that’s why we decided to do it, and hopefully, [. . .], the little bit, the contribution we’ve made will help other people who are coming to that situation afterwards. So that was the reasoning out of it.
Carer, site 3, post
Patients and families felt that they had been taken seriously at the joint events, noting how members of staff came together and took time out of their working day to discuss how the stroke unit could improve. They felt that the groups provided an authentic way to share ideas and to give time to digest and discuss issues of importance:
Somebody said something about ‘well that’s all well and good, you know, but you have to bear in mind the schedule of the nurses’ or, and I thought ‘oh OK, this is like a real thing, this is not just like, or we could put up some new curtains in the wards, this is like people arguing about stuff’, and I thought ‘OK, cool, I’ll get stuck in, I’ll do my bit’, so yeah, I’ve enjoyed the process, it’s been very good.
Patient, site 3, post
The added value of seeing previous patients was highlighted by staff, who rarely had a chance to see those for whom they had previously cared. They viewed the experience as positive as a result of the learning they could gain from hearing the patients’ experiences:
So it’s actually nice to see them come back and see how they’re getting on, and actually not only see how they’ve improved in terms of their cognitive functioning, or their speech, or their mobility and stuff like that, but seeing them using their experience to then make a difference for others in a similar situation.
Staff, site 1, post
Similarly, staff felt that they had learned something from working together with the patients that would be of benefit to them in their professions:
I think I’ve learnt that when people sit together from different areas or different groups or different levels, it’s very powerful, very, very powerful because it’s so much easier to resolve a problem. And I think just to persist, just that just to continue by today, even sometimes when you like really you feel like I can’t go on anymore, just to continue, continue, continue, eventually it will happen.
Staff, site 1, post
The group dynamics
There is an ongoing debate about equity and power-sharing in co-design/co-production and we were concerned about the impact that aspects such as the setting (the ward), the members of the group (staff in uniform) and the facilitator (which in CREATE was the researcher) might have on equity. However, participants generally felt that they were regarded as valued members of the group and able to express their opinions to staff, and referred to examples of everyone contributing:
I think that worked well and there wasn’t a hierarchy, do you know, it wasn’t just a case . . . there wasn’t really a sort of an us and them sort of attitude, and I think that, you know, the staff that attended, and the support people, and the HCA [health-care assistant] people, they were very interactive, and I think that was good as well, because I don’t think anybody felt that they couldn’t say what they thought, which is important, yeah.
Patient, site 3, post
I thought once we’d got over the sort of initial, you know, start-up of it and everything, because you’re always a bit ‘what’s going on here’, but I think, yeah, we felt able to say what we wanted to say and what we wanted to say has turned out to have a valuable effect, so, that’s, yeah, very happy to say that we didn’t feel intimidated in any way.
Carer, site 4, post
With regard to staff being naturally more dominant, we anticipated that because the co-designed changes were to happen in the hospital it would be the staff who had the authority and power to change, and so they would take on the tasks. This would put them in a somewhat more ‘powerful’ position. Again, from the interviews, the patients did not comment negatively on this apparent power shift towards staff during the co-design process. In fact, at site 4, for example, one of the carers commented on the necessity of staff taking on those tasks and sustaining them:
I said at the first meeting, the staff were going to have to take the brunt of whatever the changes were, and could they fit it in? And that’s, the only thing I can say about going forward, it’s got to be kept, the momentum’s got to be kept up by the staff and that’s the only people you can ask to do it.
Carer, site 4, post
Staff members repeatedly stated that they viewed patients as equal members of the co-design groups and found their contributions invaluable. However, there was an ongoing balance to be struck between being creative with the changes and doing something plausible within the time frame:
I mean what is difficult with the nature of, and I think of the design where you had the patients and the staff within the co-design group is, the patients have fantastic ideas and really great ideas that we would be very keen to see, but almost, from sitting on a staff perspective, when these ideas are being suggested we straightaway know what’s plausible and what’s not plausible within economic constraints or within space constraints, or within the general sort of health-care system, and sometimes that can be quite a challenge in terms of relaying that back to the relatives or the patients in the group to say, actually it’s a great idea but it’s not going to be possible for X, Y and Z. So then it’s really up to us to then try and find a happy medium almost and try and suggest something that would be plausible within resources that we have.
Staff, site 1, post
The value of being part of a group
Being part of the group itself and not just seeing the changes take place was invaluable for some of the patients. They felt part of something that helped them to ‘forget’ about the stroke for a short time, while at the same time being able to process what had happened together with people who had had similar experiences:
It’s [CREATE] helped me through me life because the experiences I’ve gained from it, you know, not just talking about strokes, but actually being part of a group, I think that helps one heck of a . . . [. . .] forgetting all that, at the end of the day it’s just nice to be with a group of people that you can talk to, and without realising it, [. . .] they’ve had the same problem as me and we’re all talking about what we’ve had, [. . .] I know that it could happen, there’s no point in thinking negative [. . .] But the one good thing I know now, and that is, if I do have another stroke I know a few people at [site 1] that can help me through it, you know what I mean, so . . .
Patient, site 1, post
Hearing everybody else’s part of what they had gone through . . . it’s been really good, it opened my eyes quite a lot, because you sit there [on the unit] and you see things going on, so yes I enjoyed being part of making something better.
Carer, site 2, post
One member of staff who had not taken part in the initial events said that morale was higher on the ward now and that there were always new milestones to focus on and look forward to, as things were still being put in place. Before, she had thought that ‘things will never happen’, but after CREATE she knew that actions could actually occur as she was surprised at how quickly things had changed. In addition, in terms of teamwork, CREATE had had a positive impact:
I take from the process that getting people to work together can get a lot more done than one person trying to fight alone, which is sometimes the way it feels, so being able to quite easily get these things together, and also I’m not the only one that has ownership of it, [. . .], but there’s a whole team of us that sort of have ownership a bit of this, I think we’re all equal, so I think if, if something like doesn’t happen I can at least try and speak to those other people and see their thoughts, so I still feel that we’re a team even though we’re not meeting, we might not see each very often, but that, that team’s still there for, for future ways to work.
Staff, site 3, post
Staff in particular noted the way in which the project had enriched working life and given them a new purpose and meaning. Some felt that taking part in EBCD had helped staff morale through bonding and orientating around a common purpose:
Staff seemed to be enthusiastic. It felt like it had knitted them together, perhaps more than just ordinary work does.
Staff, site 1, post
Another member of staff said that everyone should feel part of it: ‘we are all in it’. This member of staff had not taken part in the co-design groups but also said that EBCD was for the staff as well as the patients. Members of staff commented that the ward was also now a nicer working environment for them. Staff also felt that they had personally learned from CREATE for their own practice and were more aware of how to improve activities, space and communication:
It’s really nice to get a perspective from them [stroke survivors and caregivers] as well, because I think they brought a few different things to the table, from an outside perspective of how relatives want to be involved and the things that they missed and the things they didn’t know about, because, again, you totally take for granted what we know because you’re doing it every day.
Staff, interview, post, site 4
Although interviews generated a lot of positive feedback about the experiences of taking part in the co-design groups, staff highlighted several caveats relating to the resulting additional workload, concerns about sustainability beyond the project and the need for buy-in and support from all staff, especially senior management:
I would, maybe like I say, just get more staff involved which is hard, or the staff that are involved to communicate with the other staff to tell them to pass that on so that things, some people didn’t know about the volunteers but . . . I think we should have more staff meetings within our groups just to say, especially after what’s happened on the wards ‘oh this and this and that’.
Staff, interview, post, site 2
The recognition senior leadership teams gave was inconsistent at some sites and the following quotation illustrates how some managers did not prioritise CREATE:
It’s not the first time they’ve disappointed me but that’s disappointing, because, you know, a lot of work was done, I mean I invited my boss, I did invite him quite last minute to be fair but, you know, they didn’t go, you know, ‘oh no, we’ve got other things on’, but they’re always saying ‘oh we’ll come and support you at things’ and then when you want them, they’re not there.
Staff, interview, post, site 3
For context and richness to further interpret the use of EBCD in these stroke units, we now describe our process evaluation.
Process evaluation
The process evaluation was informed by NPT. We draw on data generated on the impact of developing and implementing co-produced interventions on the quality and amount of independent and supervised activity (social, cognitive and physical activity) occurring outside formal therapy on the four stroke units. Table 5 shows the range of data sources used for analysis and interpretation.
Normalisation process theory is a middle-range theory concerned with understanding how complex interventions are implemented in and integrated into existing health-care systems. 72 As outlined in Chapter 3, NPT proposes four constructs that represent different kinds of work that people do around implementing a new practice: coherence, cognitive participation, collective action and reflexive monitoring (see Table 4). In our analysis we used NPT in two ways. First, we used it as a sensitising device in our review of the qualitative data generated through observation, interviews and researcher process notes and reflections on EBCD activity. NPT’s constructs were useful in identifying and thinking through factors that emerged as barriers to and facilitators of using EBCD and to introducing change at the four sites. This was particularly the case in relation to exploring what occurred at different stages of the implementation process within and across the participating sites. Second, we used NPT as a structuring device as we progressed in the analysis from identifying barriers to and facilitators of linking these, where appropriate, to NPT’s constructs. We used the constructs as part of interpreting how being part of the study and using EBCD had an impact on the day-to-day work of staff on the stroke units and, over time, how changes to spaces and to the availability of activity opportunities appeared to have an impact on stroke patients’ experiences.
To examine the factors and organisational processes acting as barriers to or facilitators of successfully implementing, embedding and sustaining co-produced quality improvements in these settings, we identified and considered the ways in which study participants engaged with the EBCD approach, and the CREATE researchers’ roles in supporting the participants at each site. We sought to understand how staff, former patients and carers participated in the process of identifying and agreeing priorities for change, designing solutions to realise changes and finding ways to introduce these changes into existing working practices in the stroke units. We return briefly to the use of NPT in Chapters 5 and 6.
Making sense of CREATE and the experience-based co-design process (coherence and cognitive participation over time)
Four members of each stroke unit team were invited to attend CREATE and EBCD training in London. Sites nominated staff; our only stipulations were that those attending should include both therapists and nurses, and that these staff should be aware they would be taking a lead role in the EBCD process at their site. During the full-day training for staff from sites 1 and 2, participants met with researchers and heard about the aims and design of the CREATE study. They also heard directly from one of the originators of the EBCD approach (GR) as well as from an experienced clinician who had led an early EBCD project. We involved a designer (AM) in this training. The day addressed the theory of (a.m.) and practical applications of EBCD (p.m.). Feedback suggested that participants found the day to be lengthy and that the more theoretical overview of the methods was less engaging and less useful than the practical applied material. Based on this, we reduced the training time for staff from sites 3 and 4 to a half-day; we retained the input from the experienced former clinician and focused on practical applications of EBCD by reporting how sites 1 and 2 had worked with the EBCD process and the changes they were putting in place.
Accepting the comments regarding the preference for the more applied approach to training, most participants evaluated the training sessions positively. Staff from sites 3 and 4 heard first-hand accounts of how those at sites 1 and 2 were working to increase activity and discussed examples of changes already made by these teams. The groups also generated a series of practical implementation questions that were discussed during the training session (Figure 16).
FIGURE 16.
The EBCD training event for staff from sites 3 and 4. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.

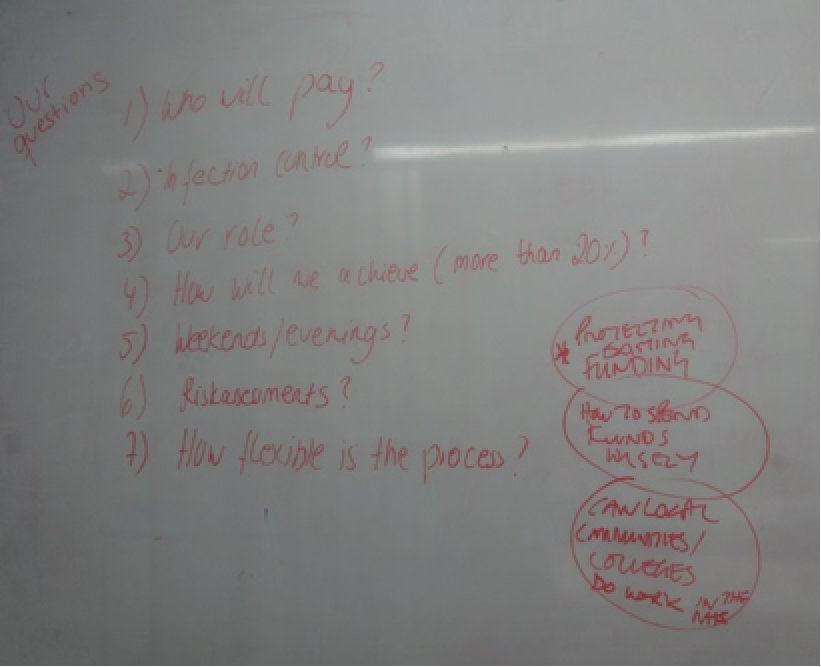
It was helpful meeting other people involved in the study on their wards. What they did and how it involved patients.
EBCD training feedback, sites 3 and 4
From researchers’ reflections on participating in the training sessions and from informal contacts with staff attending both sets of training, enthusiasm levels varied even at this early stage of the study. In both training sessions, staff from one site were much more engaged than staff from the other. In session 1, staff from site 2 (Yorkshire) were more engaged, whereas in session 2 staff from site 3 were more engaged (London). We explored whether this variation could be explained by whether staff had chosen to attend the training or had been selected; however, this was evident for nursing staff in one site only (who had been selected).
Attending training afforded these core staff groups the opportunity to start making sense of the EBCD approach and to think both individually and collectively about how to share this knowledge and understanding with their stroke unit colleagues, about what changes could occur in these settings and what such changes would entail practically for their day-to-day work and that of their colleagues. The training also challenged these staff to think about how working with patients and carers as part of the participatory EBCD approach would differ from their experience of using mainly written feedback on patients’ and carers’ experiences of the stroke units (e.g. through the Friends and Family Test and through surveys).
Making sense of the study and experience-based co-design in the wider stroke team (coherence and cognitive participation over time)
Stroke units are staffed by large teams of therapists and nurses, two or three physicians and support staff. Ensuring that all staff working in the study sites had an understanding of the study and of the EBCD approach remained challenging; one factor influencing this was the time between researchers introducing the study at sites and the data collection and EBCD activity commencing. At sites 1 and 2, major changes to the Health Research Authority and Research Ethics Committee approvals process, which occurred soon after approval for the study was sought, introduced a delay of almost 4 months between training the core groups and data generation and EBCD activity getting under way. Information about the study and the EBCD approach was disseminated through study posters and newsletters and by researchers explaining them at multidisciplinary team meetings and staff handovers at each site. However, the lengthy delay meant that early interest in the study shared by EBCD-trained core groups members quickly dissipated and the spread of understanding of what the study and the EBCD approach would mean for these units was minimal. We had anticipated that, after the training, the time before any study activity took place would have allowed core staff to make their own observations of patient activity/inactivity in their units and to identify and consider opportunities for increasing activity. However, as changes to working practices were not yet required and researchers’ access to sites was limited to planning meetings, only core team members at site 1 did this. The delay meant that in both sites the core staff and wider teams focused on routine work demands; the CREATE study and the EBCD process were not really ‘visible’ and, prior to data generation through observations and behavioural mapping, did not make demands on any staff group at this time.
Once the study was under way at sites, maintaining awareness of EBCD activity remained a challenge as, after the initial enthusiasm generated by the joint meetings dissipated, often some weeks would pass before the actions planned by co-design groups came to fruition and the changes became visible. Early ‘wins’ such as reclaiming the day room at site 4 and opening the new ‘Social Corner’ at site 1 ensured that participants and wider staff and inpatient groups became aware that change was happening. Researchers circulated newsletters on several occasions in each site to raise awareness among staff who were not directly involved in co-design group activity (see Report Supplementary Material 4).
Infection control restrictions on what materials could be displayed in public and staff circulation areas in some sites sometimes negated this strategy, and it was not uncommon in post-intervention interviews to hear some staff say that they had never read a newsletter and that they did not know what was happening in the study. Therapists at sites 2 and 4 reported routinely sharing information about the EBCD-driven changes during their daily handovers or weekly team meetings, so lack of awareness in these smaller therapy teams was not reported:
Because there’s been a couple of therapy staff involved from physiotherapy and occupational therapy mainly, we meet in a morning for a board meeting and we’ve handed over what the progressions have been from the CREATE study, so if they see anything on the wards this is what it is. So say for example we’re telling them about the updating of the garden and if we need to take anybody to the garden.
Staff, site 4, post
Nursing work patterns on stroke units are different from those of therapists, with larger numbers of nurses and health-care support workers in each team. Communication across nursing teams working early, late and at weekends, and on extended day and night duty, is more difficult to achieve, but it was notable that CREATE information was not included routinely in nursing handovers at any of the sites.
However, a factor that increased staff awareness at all sites was researchers commencing data generation; once this occurred, staff interest gradually increased. Some awareness of the study’s purpose also became evident among the patients being cared for on the units at that time through informal conversations and patient/carer questions during the ethnographic observations and through patients’ willingness to participate in behavioural mapping.
Raising awareness and engaging staff, patients and carers through researcher presence on units (coherence and cognitive participation)
At sites 3 and 4 there was no delay between training core staff groups and regular researcher presence on the units as data generation got under way. In all sites this regular researcher presence during the pre-EBCD observation and interview periods was a factor in enabling a wider group of staff to start to make sense of the study. Staff were curious about behavioural mapping and general observational processes, and researchers used this opportunity to provide brief verbal explanations of the study and EBCD to staff and patients on every occasion on which they were generating data. For staff, researchers supplemented verbal explanations with written study summaries, posters and newsletters indicating that the study was under way and explaining how it would proceed. In some units the presence of the researcher prompted staff trained in EBCD to discuss the study during routine team meetings, and this, in turn, reportedly encouraged team members to generate ideas for changes to increase activity. When researchers were conducting observations and behavioural mapping, staff commonly expressed their views about the low levels of current patient activity outside therapy and who could do what differently. Informal comments were very similar to those expressed in the semistructured interviews conducted after the observations:
The presence of researchers on the ward during ethnographic observations seems to have led to staff discussing the CREATE project and the subject of patient activity on the ward. Informally staff tell me they are aware that patients can become very bored and experience low mood if they do not engage in any activity for long periods. This, they report is especially true for patients who are on the ward for a long time; most staff say they know the worst times for inactivity were weekends and evenings. They comment [registered nurses, health-care support workers and therapists] that the study is necessary and that they hope that the situation can be improved. Some staff expressed an interest in being involved in the planned EBCD activities. There were different thoughts about whether this was something HCSWs [health-care support workers] would have more time to do or whether this should be something all staff contributed to. It’s possible that this increased awareness of inactivity led to the observed small number of efforts to increase activity on the ward during the weeks of formal observation.
Field notes, site 2
Although the initial researcher presence was helpful in raising awareness of the issue of inactivity and prompting wider staff groups to think about what would need to happen to change this, informal and pre-EBCD interview comments suggested that some staff were sceptical because they had experiences of good ideas for change being identified but not progressing. It was also difficult for most staff at this stage, namely prior to any EBCD activity, to envisage whether or not, or how, increasing patient activity may have an impact on their existing roles and working practices. Despite some enthusiasm for increasing activity levels, even at this early stage staff routinely expressed the view that their existing workloads and staffing levels, which were often below those recommended in the National Clinical Guideline for Stroke, would not allow them to spend time completing activities with patients. Nurses and health-care support workers most commonly expressed this view. In NPT terms, at this stage, for most staff, the ‘intervention’ was still undefined and not widely understood; commitment to change and comprehension of the possible benefits of changes were not widely evident. In turn, at all sites, there was no expectation or direction from senior therapists or ward managers at this stage that individual staff members or groups should review or change their working practices.
Patients and carers at each site also became aware of the study as a result of the observations and behavioural mapping and, as with staff, they sought information about the study and expressed their views on their current levels of activity outside therapy. This early contact and initial relationship with researchers appears to have influenced several inpatients later (after they had been discharged home) in consenting to participate in pre-EBCD interviews and, subsequently, in EBCD activities. In contrast to some EBCD studies identified in our rapid evidence synthesis, in which the recruitment and retention of service users was problematic, researcher presence proved beneficial in terms of both recruitment to these parts of our study and sustaining patient/carer involvement in EBCD activity throughout the study. 16
The influence of participation in experience-based co-design elements (coherence, cognitive participation and collective action)
At sites 1 and 2, the structured and facilitated approach of EBCD was a major factor in staff making sense of CREATE and the EBCD approach and progressing to a more engaged position, readier to commit to thinking about how change could happen in their site, to revised or new working practices and to thinking through who would need to be involved (cognitive participation). At these sites the initial (separate) staff meetings and then joint meetings enabled quite large groups of staff to experience participation in some of the EBCD cycle stages (see Table 2). They viewed edited trigger films, heard first-hand accounts of patients’ and carers’ experiences, and then jointly identified ‘touch points’, discussed experiences that patients said mattered most to them and considered some solutions to these issues. These were high-energy meetings at which there were strong levels of enthusiasm for change; they were a powerful catalyst for larger groups of staff beginning to share the view that changes to stroke unit environments, access to resources and routine working practices to increase patient activity were not only desirable but also possible (Figures 17 and 18):
It felt quite exciting – it will be interesting to see how it develops, keen to be involved and contribute.
Feedback after joint event, staff, site 3
FIGURE 17.
Staff event at site 2: thinking differently about activities for different patient groups and about how activity could occur in existing spaces. Reproduced with permission of David Clarke, University of Leeds, personal communication, 2020.
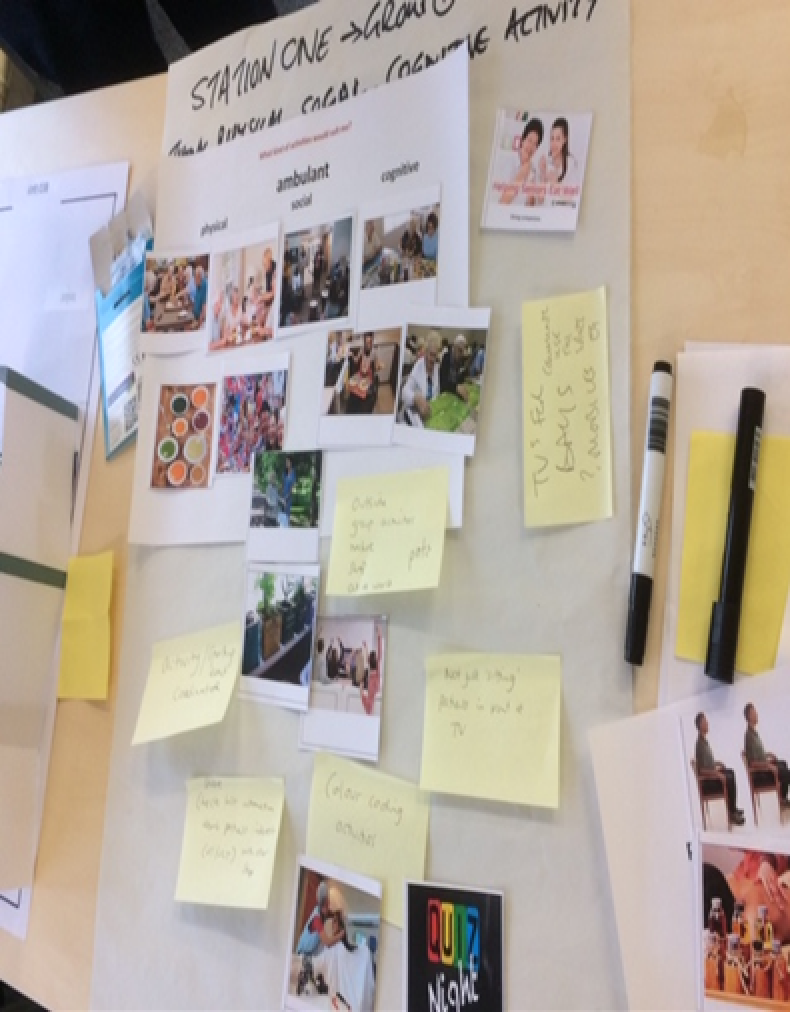
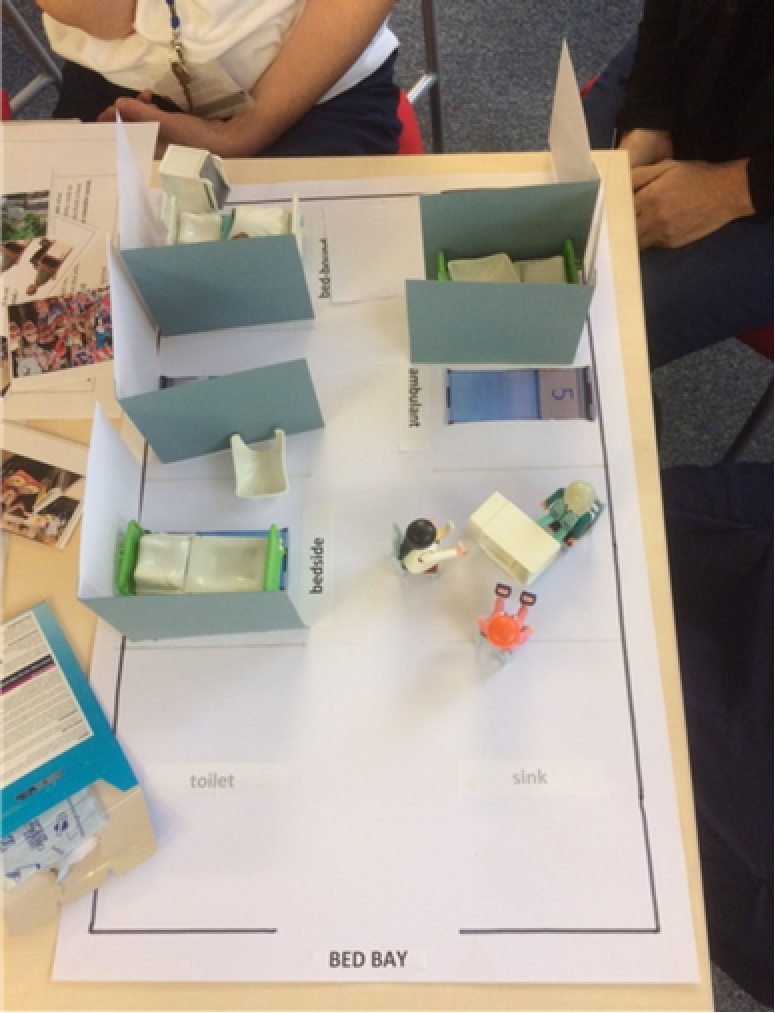
FIGURE 18.
Joint event at site 2. Reproduced with permission of David Clarke, University of Leeds, personal communication, 2020.

Other features of EBCD that facilitated the development and implementation of changes were the defined and time-limited nature of the EBCD process and its use as a previously tested patient-centred service improvement model. This seemed to legitimise the staff time and resource allocation committed to participation in the study and the associated intervention. Staff noted that the EBCD approach contrasted with previous attempts to introduce change in working practices, which were referred to as ‘poorly defined’ in terms of timescales, roles and responsibilities and as operating without additional resources. The patient-centred and participatory approach inherent in EBCD also appeared to have added a sense of responsibility for the core staff groups to deliver on agreed actions, and not to ‘let down’ the patients and carers with whom they worked in the co-design groups.
For patients and carers at sites 1 and 2, separate meetings provided the opportunity to explore their shared experience of stroke and stroke unit care. The trigger films demonstrated commonality of as well as differences in experiences, and watching the films began the process of identification by these former patients and their carers as a group of not only the shared experience of stroke, but also a shared belief in the importance of improving the experiences of patients and carers in their local stroke units. There were some differences in how the trigger films were received; at site 2 staff showed visible emotion at the experiences highlighted by patients, whereas at site 1 there was a mixed reaction:
During the film itself, there was intense attention among the participants and signs of recognition of what patients and family members were saying – for example I noticed some staff members nodding, laughter at some of the observations made by participants. I had expected the film to raise visible emotions but I didn’t see any [tears, sighs, shaking of heads]. There seemed to be recognition and some laughter. On the table of mostly staff where I was sitting there was quiet attention but no visible signs of emotion. I don’t know if on other tables there were more visibly emotional responses.
Researcher reflections, joint event, site 1
Former patients and carers at sites 3 and 4 did not have the trigger film participation in common but they recognised the issues described in the films by site 1 and 2 participants as similar to their own. It seemed that the shared experience of stroke and a desire to improve the experiences of others in these units were sufficient to form a common bond.
Researcher reflections on the joint meetings and co-design group meetings highlighted the importance of former patients articulating their stroke experience and the impact that their impairments had on their daily lives. This seemed to inform an ongoing consideration of why activity outside therapy mattered to patients and how, practically, it could be increased. This common sense of purpose and shared experience is often referred to in discussion of the concept of a ‘community of practice’. 77 A community of practice has been defined as: ‘a process of social learning that occurs when people who have a common interest in a subject or area collaborate over an extended period of time, sharing ideas and strategies, determine solutions, and build innovations’. 77 Although not ‘practitioners’ in the health-care sense, patients and carers participating in the EBCD activities in all of our sites shared a common experience not only with their peers, but also, to a greater or lesser extent in the different units, with the staff with whom they developed an ongoing relationship, shared ideas about activity post stroke and problem-solved in the co-design group meetings.
The structured approach of EBCD and the facilitated events and activities of the EBCD cycle provided former patients and carers with a way to express their experiences and involved them in a group where they worked as partners in bringing about improvements to the stroke units that would increase patient activity:
[. . .] I think, yeah, we felt able to say what we wanted to say and what we wanted to say has turned out to have a valuable effect, so, yeah, very happy to say that we didn’t feel intimidated in any way.
Carer, site 4, post
The same was true of participation by those who were ‘external’ to the day-to-day work of the stroke units. These opportunities contributed to participants’ progression in thinking from a shared understanding of the importance of change (coherence) to working together to define ways to implement, and ideas generated into existing working practices (cognitive participation). This progression includes thinking through how the changes designed to increase activity could be actioned, who would take responsibility for action and, in the longer term, who in everyday practice would deliver or support the actions. These mechanisms represent collective action in NPT terms, and, although the work of implementation on the stroke units commonly fell to staff, the findings section of this report identifies actions completed by carers and former patients to support change. These included designing and painting wall murals (sites 1 and 3) and redesigning patient- and carer-facing documentation (sites 2 and 4), actions designed to increase activity by providing stimulating spaces and ensuring that inpatients and their families were aware of spaces for and opportunities to undertake joint and independent activity.
The above may suggest that EBCD elements, including co-design group activity, progressed without incident. In terms of core group members and participation in co-design groups, this was not the case at most sites. At site 1, for various reasons, three of the four team members who received the EBCD training were not able to participate in the co-design work. However, other team members expressed an interest and volunteered to take on these roles, so staff commitment to the process evolved more naturally from the outset. At site 2, a core team member leading one of the co-design groups experienced problems with taking time away from their ward-based role and then had an extended period of sickness. This had an impact on and slowed the progress of this co-design group, but, as at site 1, other staff members, in this case supported by the ward manager and site researcher, maintained the activity and the agreed actions were progressed. Actions included securing funding for one of the health-care support workers to provide regular hairdressing and personal grooming sessions outside their normal ward role; this realised both person-centred and social activity goals.
At site 3, a champion emerged quickly who led the process at site level who encouraged staff to attend training and sign up for events and attended most if not all co-design groups. Site 3 had the most co-design groups and the most attendees, which we believe was largely because of the enthusiasm and persistence of the local champion (see Table 2). At site 4, two EBCD-trained core team members, both nurses, attended only the joint meeting and did not participate directly in any of the work of the co-design groups they had agreed to. Despite having support from their ward manager, both maintained that they could not take time out of their routine work to participate in the co-design meetings; other members of the co-design groups agreed to conduct the review of priorities and action-planning. Progress was slow in the three co-design groups and few actions were completed at this site until a combined meeting of the groups led to rapid realisation of several agreed activity support actions. The additional contribution of the site researchers as facilitators in supporting and sustaining co-design work is explored later. In our view, the development of communities of practice to a greater or lesser extent in the co-design groups at each site provided a support mechanism that sustained the work and progress of these groups when they were faced with the challenges outlined above.
Leadership, managerial authority and support (cognitive participation and collective action)
Previous EBCD studies have identified the central importance of senior staff support and leadership in service improvements generated through participation in EBCD cycles. Closely allied to this is the presence or absence of managerial authority, resource allocation and support for proposed changes. Based on our review of facilitators for co-production and EBCD-like projects, we aimed to set up project oversight groups with membership including directorate-level managers, senior nurses and those with cross-organisational roles. 16 At sites 1 and 2, we set up these groups, but the commitments of these often very senior managers meant that interaction was largely through e-mail updates or one-to-one meetings with researchers. We could not engage equivalent staff and establish an oversight group at site 3 or 4. The same processes of offering to meet with these staff individually and repeated invitations to attend EBCD activity were adopted, but these were largely not responded to or the promised attendance did not actually occur. One impact of the accelerated EBCD process was that researcher time at sites 3 and 4 was also reduced. Researchers enlisted the support of unit-based EBCD champions in seeking to involve more senior managers, but this did not lead to the involvement in oversight of the project that we sought. Although oversight group members at sites 1 and 2 were often not active participants, they were important in expressing their support for project activity, in helping to navigate often complex trust organisational structures and in specific situations for providing financial resources to enable co-design group ideas. For example, at site 3, staff raised £8000 from participating in a sponsored 10-km run. The chief executive at the site matched the sum raised and these funds were used to redecorate the day room and install a kitchenette. In our view, the oversight groups at sites 1 and 2 provided direct and indirect support for unit-based staff. Having defined senior managerial contacts in these organisations ensured that unit-based staff could activate these potential lines of support. This was not impossible to achieve, but it was made more difficult at sites 3 and 4, as only the chief executive and the therapy lead, respectively, engaged with the EBCD groups and the researchers.
In all sites, a range of staff working in the trust in roles including therapy service managers, matrons, patient experience managers, patient safety officers, volunteer co-ordination and estates management joined patients and carers in different co-design groups. Typically, these individuals were not involved in every co-design meeting held but their involvement was often significant (see below) and had an impact in terms of both cognitive participation and collective action. NHS staff are acutely aware of the resource constraints affecting their services, and often have experienced frustration at barriers they have encountered when seeking to improve or change services. These include infection control and patient safety requirements, lengthy delays or inaction when estates work is requested and lengthy and bureaucratic processes to work through when looking to include volunteers in unit-based activity. Collectively, we found that staff who were otherwise dynamic and enthusiastic advocates for increasing patient activity often shared the view that such barriers were fixed and would, inevitably, limit what could be achieved. The perceptions that ‘the trust’ would not ‘allow’, for example, murals to be painted on walls, shelving to be added in patient bays, hot drinks facilities to be added for patients and carers to use independently or volunteers supporting patients with social eating were pervasive and initially were shared by some of the clinical managers who attended joint meetings at site 1. These perceptions proved to be largely inaccurate.
The contributions of participants from the wider hospital, patient services and volunteer services were significant and these participants typically explained how changes could in fact be realised, and, importantly, provided examples of such changes already operating in the same trust. These participants were used to working with departments and services that were often criticised in the routine discourse of ‘infection control/estates will not allow it’ and understood what was required to introduce, generate support for and bring about changes involving these departments and services. Sometimes these participants undertook to make things happen themselves; for example, at site 2 the patient experience officer worked with the volunteer co-ordinator to identify new volunteers, develop a mealtime support training programme and follow this through to the provision of a regular volunteer-run social eating group on Sundays. At site 3, the volunteer co-ordinator attended the joint event and many of the co-design groups to provide a rapid link to possible volunteers for activities such as reading support and exercise groups. At site 4, the therapy services manager supported the idea of a breakfast club to increase social contact between patients and provide an opportunity for meaningful functional rehabilitation activity. This support was evidenced by changing the working times and early-morning responsibilities of two therapy assistants who were assigned to establish and run the breakfast group (collective action). Therapists and nurses supported the group, quickly establishing it as a 7-day-a-week activity. In this case the work of implementing change was consistent with staff members’ beliefs about the unit as a rehabilitation space, and the work required of the therapy assistants was defined as rehabilitation support integral to their job purpose and consistent with the kind of one-to-one kitchen activity interventions they already completed with patients prior to discharge (cognitive participation and collective action).
However, support from wider trust services was not always evident. At sites 1 and 4, volunteer co-ordinators either focused on the obstacles to volunteer involvement or ignored repeated requests to discuss routine volunteer involvement on the stroke unit. Co-design groups responded differently to such challenges; some decided not to pursue volunteer activity, whereas others, such as at site 4, made direct contact with existing volunteers to request support for arts and crafts sessions and contacted the volunteer programme of a local college, which already had permission to work in the trust, to set up their involvement in regular sessions of activity support on the unit.
At each site, unit-based leaders emerged; often, but not always, these were core group staff who had been through the EBCD training. They were not always the most senior or most experienced members of staff in the units. For example, at site 2, two members of the co-design groups who were particularly active in increasing patients’ social, cognitive and physical activity were a health-care support worker and a stroke rehabilitation assistant. A similar situation was apparent at site 4, where a therapy assistant worked across co-design groups and formed an alliance with the ward manager (who was not EBCD trained). Together, these two staff members drove the initial changes, which included reclaiming and equipping the day room, repurposing a large window seating area and encouraging therapists and nurses to use these. At site 1, one member of staff who had not been to the initial training emerged as the EBCD lead for the ward after the first joint meeting. A general manager and a hospital matron at site 1 also helped expedite changes such as new curtains, clocks and redecoration; their involvement was prompted entirely by a meeting at which unit staff presented the aspirations for the ward and asked them for help with the barriers being experienced. The meeting was organised by the lead facilitator (a dietitian) and the researcher for site 1. Direct actions related to the requests made by the EBCD champion suggested that these staff (a matron and a general manager) also developed some commitment to the project’s anticipated benefits, evidenced by their allocation of resources and continued involvement in seeing these planned changes through to completion. Although these staff were not necessarily part of the community of practice developed through the co-design groups, they made a defined contribution to the collective action needed to improve patients’ experiences at this site.
In terms of leadership style, perhaps the predominant approach evident across sites was an action-centred approach,78 with most staff (but, again, not all) leading co-design groups focusing on and reviewing progress against agreed tasks in each meeting but at the same time actively including, as far as they were able to, patients and carers as partners in the planning and decision-making of the groups. There were no instances in which patients or carers were invited to lead the co-design groups in any of the sites, although, as indicated above, their contributions were actively sought, and our findings confirm that these were influential in the changes that occurred across the four sites. Medical staff largely did not participate in the co-design meetings, but they continued to show interest in the EBCD approach and supported the work in practical ways. At site 4, the stroke consultant sourced and purchased secure, mobile iPad stands and accessed unused hospital bleepers. At site 1, the medical consultant helped facilitate and set up the staff and joint events and secured funds for equipment from his research budget. In recognition of this, the co-design groups chose to name the new social corner after him when he left the unit.
Experience-based co-design activity was welcomed but added to the workload of core group staff (cognitive participation, collective action and reflexive monitoring)
In common with findings from our rapid evidence synthesis of co-production and EBCD studies,55 core staff group members in the stroke units in CREATE were not expressly allocated any time out of their usual working day to participate in and action co-design activity. Instead, staff were encouraged to work flexibly, and their line managers largely encouraged and supported their staff to participate in the EBCD work. This was somewhat easier for therapists at each site than it was for nursing and health-care support workers, for whom taking time out to attend meetings in the course of a shift was often problematic. Ward managers at sites 2 and 4 tried increasing the number of nurses or health-care support workers on shift on days when EBCD meetings occurred but, on some occasions, the additional staff were moved to other wards perceived to be understaffed on those days, so this strategy was not repeated. These ward managers felt that this represented a lack of understanding in the wider organisation of the evidence about the staffing levels required to provide safe and effective care for stroke patients and was an understandable organisational response to recurring staff shortages in different areas of the trusts. However, the enthusiasm for the project at sites 2 and 3 was such that some staff came to the joint meeting on their days off. This kind of commitment was also evident later in the study at these sites, with staff coming in to work on their days off or before a shift commenced to participate in the co-design meetings. Core team members differed in the amount of time they were able to allocate to EBCD activity and progressing the actions agreed in co-design meetings, but most identified that they needed to complete some activities in their own time. These staff typically explained their willingness to undertake this extra work by referring to patient benefits, which were becoming more obvious as the co-design activity progressed in each site (collective action). Where the work of implementing increased patient activity was perceived to be enhancing the patient experience in ways consistent with staff members’ rehabilitation ethos, and where implementation was not requiring substantial change in staff members’ roles, core group members indicated that the extra effort was worthwhile (reflexive monitoring). Other, less involved, team members’ feedback on changes, and on how these were having a positive impact on patients being more independent, completing personal care tasks or engaging in therapy, increased the likelihood that the changes would be sustained:
No, I think it’s given me a massive workload, I think it’s doubled it . . . to be fair. But I was committed, I mean I took it on, I was committed, but I’ve enjoyed that, I’m glad for the changes. [. . .] it’s what I wanted for the ward, from the minute I got there I knew we needed changes, so I was happy to help bring the changes.
Staff, site 4, post
At each site there was some delay before the ideas and actions agreed in co-design meetings came to fruition. In most sites, changes began to happen, sometimes rapidly after the second co-design meetings and were then visible to the wider staff groups. Changes to the environment and use of space in each of the units were positively received. These spaces then began to be used for structured group activities. As these changes became visible to wider staff groups and involved more patients more regularly, these staff in turn appeared more receptive to further changes involving external partners or providers, for example complementary therapy from a local health network (site 1), singers from a local university (site 2) and young musicians from a community arts group (site 3). When changes became visible and change gained momentum across sites, this elicited both positive and negative responses. For example, at site 2 there were complaints that the ‘something about me board just appeared’, with no real consultation with the wider staff group about why it was needed or who would complete the information required. However, the same staff also said that they liked what the board was designed to do. Staff experiences and comments such as these highlight that it is difficult to secure cognitive participation and commitment to collective action from those stroke team members who have had limited engagement with the implementation of EBCD-driven co-designed interventions.
Overall, however, shifts in staff members’ perceptions and behaviours suggested that collective action and reflexive monitoring were becoming more widespread in most units as activity-focused space changes or opportunities became more evident. However, at sites 1 and 4, continuing the work to improve patients’ activity opportunities and engagement relied largely on core group members or those who had taken on these roles as other staff left or did not participate as expected in EBCD activity.
Researcher facilitation role
Our rapid evidence synthesis highlighted that the facilitator role in EBCD projects was an important factor influencing successful engagement in improvement work focused on service user experience. In CREATE, researcher presence on the units was less frequent than that reported for full- or part-time project facilitators in other EBCD projects, but it served a similar function in prompting, encouraging and supporting core team members to maintain their involvement in EBCD activities. 16,60 An important element of that was the role the site-based researchers played in getting the EBCD activity under way and in keeping the process moving at each site. Researchers agreed with core group members that they would organise the staff, patient and joint events in consultation with core team members, and researchers recruited former stroke patients and carers and took responsibility for ensuring that they could attend on the dates agreed. They booked accessible rooms for meetings and ensured that patients and carers were reimbursed for travel expenses or they arranged transport for former patients to get to and from meetings.
Researchers liaised with core team members to co-facilitate the staff and joint meetings, with staff presenting feedback on their agreed priorities and co-facilitating the small-group work at each of these meetings. This joint approach, although often initiated by researchers, helped to build the confidence of core team members, and at sites 1 and 2 it gradually increased the engagement of these key staff members in the EBCD activities, supporting cognitive participation and collective action. At sites 3 and 4, because the separate staff meetings did not occur, core team staff had less time and fewer opportunities to work with researchers before the joint meetings took place. At site 3 this appeared to have had little impact on the progression of the co-design meetings, whereas at site 4 core team members either were less confident in chairing and leading the co-design meetings or did not participate in these meetings, citing workload pressures. At this site, the researcher was asked to chair the co-design meetings and did so while ensuring that responsibility for action to bring about change was allocated to staff participants, sometimes in conjunction with former patients and carers, for example in redesigning the ward information leaflet and developing the WiFi access leaflet.
In common with reports from facilitators of other EBCD projects,79 researchers spent considerable time trying to make contact with core staff members and others participating in EBCD to set up meetings or to check on progress with agreed actions. Co-design meetings were commonly arranged to run late morning to early afternoon to maximise staff participation. Core staff were asked to record action plans for each meeting; this worked with some staff in some sites (most commonly when therapists or therapy assistants led the groups) but not in others. In consultation with the core team members, it was agreed that the researcher or one of the core team members would take responsibility for communicating a summary of the discussion and actions agreed at each meeting. The researchers prepared newsletters every 4–6 weeks to report on the work of the co-design group; these were circulated to wider staff and patient groups. Researchers at each site became aware of a degree of reliance on them to co-ordinate EBCD activities; this was more evident at sites 3 and 4, where researchers sometimes felt the need to go beyond their regular research role. For example, at site 3 they participated in a fundraising 10-km run, collected and transported paint supplies across the city so that a mural could be completed on the unit and attended a weekend music concert provided by children at Christmas. At site 4, the researchers attended and co-facilitated an open day set up by core group staff to showcase the work of the co-design groups.
This illustrates one of the main challenges faced by the researcher, and with the staff in the co-design groups in both phases was a practical and predicable response in that researchers agreed their role would include co-ordination of EBCD and co-design meetings. However, at sites 3 and 4, staff reliance sometimes went beyond researcher co-ordination to, on occasion, expecting that researchers would take on the responsibility for some of the actions agreed by the co-design group. It is possible that one reason for this in accelerated EBCD sites (i.e. sites 3 and 4) was that there was less time for staff members supporting the co-design groups to progress from cognitive participation, that is committing to a set of actions to bring about change, to a position of collective action and undertaking the work required to actually implement changes in practices. This may also be an unintended consequence of researchers’ regular presence on the units and their willingness to support staff in their EBCD-generated planning for change.
Increasing patient activity opportunities in routine work (cognitive participation, collective action and reflexive monitoring)
As the co-design groups completed their sets of three or four meetings and patient activity outside therapy was increasing, core staff group members in each site, particularly therapists, began to recognise that the changes to space and opportunity for activity could be incorporated into the daily routine of the unit. For most therapists and therapy assistants, the work of increasing activity was conceptualised not only as reducing boredom and occupying time for patients but also typically as a therapeutic opportunity. For example, in lunch and breakfast groups at sites 2 and 4, patients’ activity provided opportunities to work on therapy goals, including both cognitive challenge and functional task practice. These areas of work are consistent with the goals of rehabilitation and of therapists; they did not require therapists to work in particularly new or different ways and, as a result, were likely to be embraced and not resisted or rejected. Importantly, increasing patient activity did not mean that patients spent less time in formal therapy, which would have had a direct impact on the continuous SSNAP clinical audit of therapy provision. In some sites, staff reported that changes such as the ‘a little something about me’ board (site 2) or the ‘home in the ward’ personalisation of bed spaces (sites 1 and 3) could make therapy more interesting and relevant to patients if, during therapy sessions, staff were able to draw on patients’ personal information through these methods. In NPT terms, these staff had moved from committing to increasing activity (cognitive participation); they understood the work required to establish regular activities and they had identified staff who would lead on or routinely support activities (collective action). In these areas at sites 1 and 2, the work of implementation became more focused on embedding regularly occurring group or individually focused activity into the daily work patterns of therapists and therapy assistants (reflexive monitoring). Post-EBCD observations and interviews suggested that there was limited interprofessional consideration of activity promotion outside the initial joint and then regular co-design meetings. This was the case at all four sites, with dialogue about activity promotion being more likely to occur during uni-professional and non-professional contacts than in multi- or interdisciplinary forums, the latter tending to focus on discharge planning rather than on providing opportunities for reflexive monitoring of the changes brought about by EBCD activity.
Our observations suggested that nursing staff at each site had high workloads and were frequently affected by staff shortages. However, at all sites we also identified periods of up to 30 minutes every day and at the weekends when most health-care support workers would congregate at the shared workstation area. Observations indicated that conversations at these times were often, but not always, social rather than focused on patient planning or organisation. Registered nurses were more often engaged with activities that facilitated patient discharge or supported the organisational functions of the hospital, for example reporting bed status and ordering supplies. Nonetheless, there was limited evidence of registered nurses in charge of the ward encouraging or directing health-care support workers or other registered nurses to participate in patient-focused social or cognitive activity. This differed from some instances when we observed more senior therapists encouraging or directing stroke rehabilitation assistants or therapy assistants to prompt or support social and cognitive activities. In some cases, for example at sites 2 and 4, we observed health-care support workers trying to involve other nursing staff in activities they had set up with patients during these periods, but there were few observed instances when they were able to do so.
In our view, the observational and interview data suggested that, in NPT terms, many of the members of the nursing staff groups in each site did not develop an individual or a collective sense (coherence) of the CREATE project or the EBCD approach as something they needed to participate in (cognitive participation). Nursing staff typically expressed verbal support for the aims of the study and the intentions of the co-design groups when they became more aware of these, often after several co-design meetings had taken place and changes were more visible or evident, but they often did not seek to become part of these groups. Ward managers at sites 2 and 4 were very aware of the challenges that registered nurses face in taking time out of nursing care provision during typically very busy 8- or 12-hour shifts and were prepared to allocate time for the nurses to attend and participate in co-design meetings. Registered nurse and health-care support worker attendance occurred to some extent at site 2 but not at site 4. Although they did not obstruct or resist changes emerging from the co-design groups, nursing staff largely excluded themselves from this work. This suggested that, despite professing a commitment to facilitating rehabilitation and enabling stroke survivors to regain their independence, many members of the nursing teams in the participating sites did not appear to feel that increasing patients’ participation in social, cognitive and physical activity was consistent with their established view of what constituted legitimate and required nursing work in stroke units. There were some exceptions, particularly two registered nurses and a health-care support worker at site 2 who actively engaged in co-design work. Similarly, at site 4 the commitment of the nursing team, prompted by the ward manager, to the 7-day-a-week breakfast group was a specific example of nursing staff supporting a structured group activity. However, overall, across sites, nursing staff were less engaged than other staff groups and volunteers with increasing patients’ activity opportunities.
Did the reduced elements/accelerated approach impact on the implementation process (coherence, cognitive participation and collective action)?
In an earlier study of accelerated EBCD, Locock et al. 60 focused on the impact of using an edited film of patients’ experiences compiled from an existing national archive. In our study, at sites 3 and 4, we used existing films from our first two sites. However, we also removed the separate patient and staff meetings. As a result, all participants in these sites had less opportunity to explore experiences and to prioritise areas of change in working practices or resource availability. The other important impact of removing the separate staff meeting was that the opportunity for a larger group of staff members to discuss the project and gain insight into the EBCD process was lost. This appeared to have had an impact on the numbers of attendees at the joint meeting at site 4, which was much smaller than that at the meeting at site 2. The result was that the number of staff, particularly nursing staff, who knew of and sought to participate in study-related activities remained small. However, this was not the case at site 3, where the accelerated EBCD also occurred; here, staff participation was equal to that at site 1. In fact, members of staff asked for a separate staff meeting prior to the joint event so that they could brainstorm ideas for change beforehand, and thus somewhat initiated a replication of the staff event themselves, although this was much more brief. Their ideas were captured and formed a guide for their priorities at the joint event (Figure 19).
FIGURE 19.
Ideas captured at pre-meeting: staff at site 3. Reproduced with permission of Fiona Jones, University of London, personal communication, 2020.
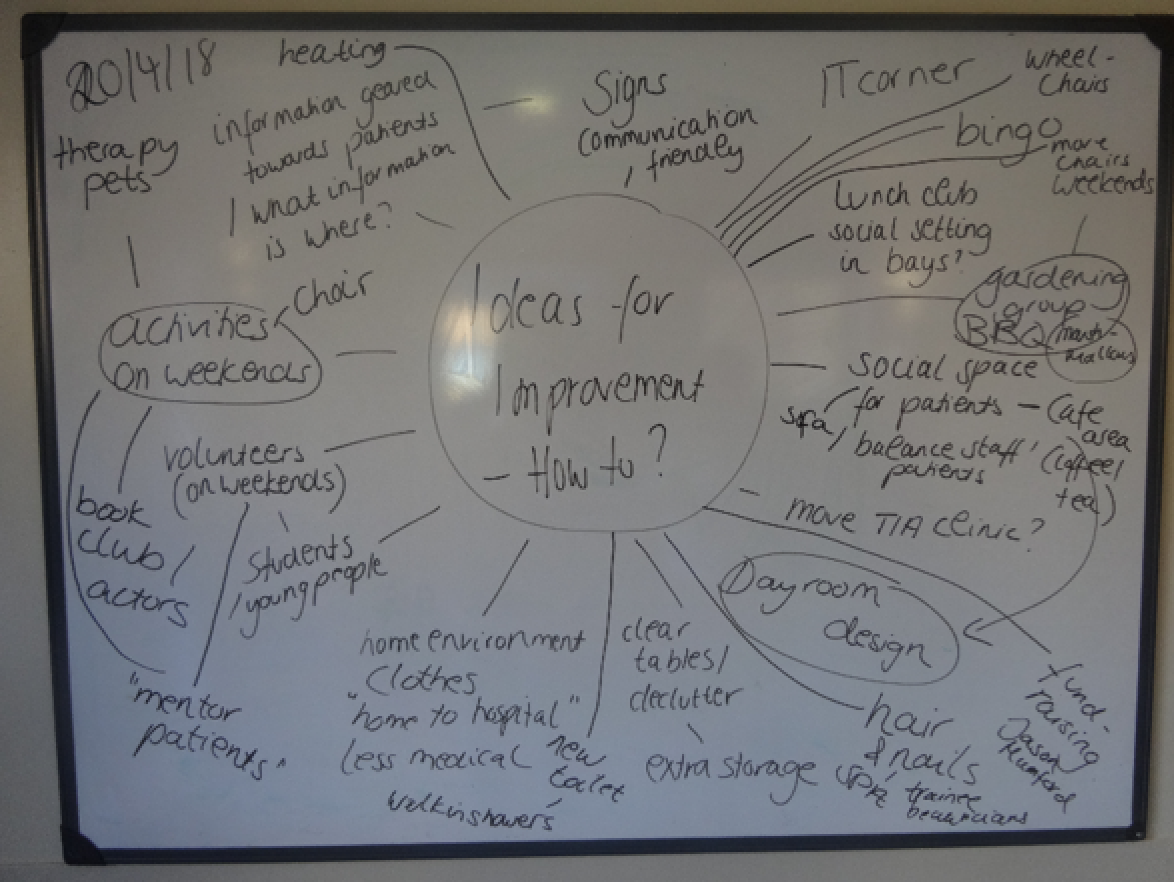
The absence of the edited film and separate patient meeting did not appear to have an impact on the commitment and engagement of former patients, carers and volunteers who participated in accelerated EBCD. Most of these participants had been recruited after being interviewed about their experiences in the stroke unit, so a basic relationship had been established with the researcher at that site. These former patients and carers participated in the majority of the EBCD activities and thus repeatedly engaged with dialogue about, action-planning for and, later, evaluation of changes to the environment and, to some extent, changes to the working practices of stroke unit staff.
Co-production approaches such as EBCD enable participants to focus on and make the changes they care most about in terms of their experience of a service;61 in the EBCD work in the CREATE study, former patients and carers spoke repeatedly of wanting to improve the experience of people who, like them, would need to spend an often extended period in a stroke unit. In this sense, the coherence and cognitive participation of stroke survivors, carers and volunteers was enabled by their continued participation in the work of co-design groups. Because former patients, carers and volunteers in each site were active contributors to designing changes, they played a key role in ensuring that EBCD champions and other staff involved in the work of the co-design groups maintained the momentum and that they saw through the work planned. Former patients and carers became an integral part of co-design groups in each site as they believed in and were committed to making changes happen. As indicated above, these participants were part of the communities of practice that developed following the joint events and through the regular co-design meetings. Opportunities for former patient and carer involvement in reflexive monitoring occurred to some extent as co-design meetings progressed. However, as these participants largely stopped being directly involved after the last co-design meeting, the celebration event was the main opportunity they had to engage with staff they worked with on the EBCD and to review what had been achieved and what was required to sustain these achievements.
Reviewing the qualitative data generated in our study using the lens of NPT ensured that we adopted a systematic approach to exploring the factors and organisational processes that acted as either barriers to or facilitators of successfully implementing, embedding and sustaining EBCD-driven co-produced quality improvement in the form of increases in social, cognitive and physical activity in these stroke units. NPT proved valuable for reviewing our interpretation of the findings from this large data set. In relation to barriers to and facilitators of using full or accelerated EBCD, and implementing complex interventions in health-care settings more generally, using NPT helped identify the challenge of ensuring not only that staff have the time and opportunity to comprehend the nature of the intended change in practice, but also that the mechanisms of change, in this case the facilitated, structured participatory co-production methods inherent in EBCD, are communicated to and involve as many staff in the change process as is feasible. The process evaluation highlighted that, despite its participatory approach, EBCD is subject to the same implementation challenges as other complex health-care interventions in terms of variable organisational buy-in, differences in the commitment of professional leaders, and differences in the engagement of staff whose primary concern is ensuring that their responsibility for care and treatment is discharged and for whom existing routine working practices are familiar and get the required work done.
However, moving beyond NPT’s focus on implementation and the work this brings, it has also been important to reflect on EBCD as a process and the ways in which many stroke unit staff engaged with this process. We found that, rather than being conceptualised by stroke unit staff as an additional burden to those already having an impact on their practice, such as the continuous clinical audit process of SSNAP and the continuing challenges associated with high workloads and staff shortages, the facilitated and structured approach inherent in EBCD provided a legitimate and, to some extent, protected space in which to jointly plan and co-design changes in unit spaces, unit processes and some staff practices. These changes were focused on issues that former stroke patients identified as important and that staff recognised and endorsed as areas that would improve patients’ levels of activity and overall experiences in stroke units. In the context of the CREATE study, although a significant number of changes became evident in all sites post EBCD, differences in enacting what was often referred to as the rehabilitation ethos in the participating stroke units also influenced the involvement of different staff members in promoting and facilitating increases in social, cognitive and physical activity. These, together with the cessation of the time-limited, facilitated and structured EBCD process and with the movement of staff, are factors that will influence the sustainability of the changes now evident in the participating units. Changes involving structured therapy-led activity, such as breakfast clubs and other group activities, are more likely to become embedded in staff members’ routine work and depend less on individual staff members. Activities that depend on volunteer and external group engagement are more at risk of cessation when key individuals move on. We have highlighted the challenge of sustaining changes that occur in co-production projects previously. 55
Chapter 6 Conclusions
In our results we have demonstrated that:
-
Despite increasing interest in and advocacy for co-production, there is a lack of rigorous evaluation of these approaches in acute health-care settings. In particular, there needs to be evaluation of clinical and service outcomes as well as cost-effectiveness of co-production approaches relative to other forms of quality improvement. The broader impacts on the values and behaviours of participants also merit evaluation (research question 1).
-
Completion of full and accelerated cycles of EBCD as a particular form of co-production in four stroke units was feasible. Both forms of the EBCD approach resulted in improvements in the quality of the stroke unit’s environment and increased activity opportunities for patients. Improvements were focused on issues that former patients and carers identified as part of the participatory EBCD approach. We found less evidence of positive change in enabling communication between staff and individual patients, which was more commonly task oriented than patient centred (research questions 2–4); these findings were evident in both the qualitative data and the responses to the PREMs in each site.
-
Qualitative evidence from different sources (interviews, ethnographic fieldwork) has shown that EBCD can lead to improvements in supervised and independent activity. This was achieved largely by increasing access to groups, both structured and staff-led groups and social groups facilitated by community volunteers, and by changing the use of existing ward spaces, which provided more opportunity for social interaction and informal group activity (research questions 2–4).
-
Changes in levels of social, cognitive and physical activity measured by behavioural mapping were inconsistent across sites and showed a mixed pattern of activity and inactivity in the small groups of patients observed pre or post implementation of co-designed changes (research questions 2–4). However, taking the broad measure of overall level of patient ‘activity or inactivity’, there was some improvement at sites 1 and 2 (full EBCD) but minimal changes at sites 3 and 4 (accelerated EBCD).
-
There were some signals in the post-EBCD cohorts’ responses to the PREM that at three out of the four sites there were more things for patients to do in their free time, and some indications that elements of patients’ experiences in the units had improved between the pre- and post-intervention data collection periods. However, these changes were not consistent across all sites and may reflect different patients completing the questionnaires at different time points rather than actual changes. PROM data indicated that the respondents were not atypical and had levels of physical impairment, dependency, emotional and social limitations congruent with national and international stroke statistics; however, rates of response to the PREM and PROM were low, varying from 12% to 38%.
-
Patients, family members and staff engaged well with both forms of EBCD and perceived that substantive changes had occurred. Co-design was a feasible method of stimulating new independent and therapeutic activities and prompted wider consideration of the influence of the stroke unit environment on patient activity in all sites (research questions 2 and 3).
-
Patients and carers played a significant role in highlighting priorities for improvement and sharing the work of co-design (research question 5).
-
There were no significant differences in experiences or outcomes between the full and the accelerated forms of EBCD. Accelerated EBCD contextualised to stroke units has the potential to spread across other stroke units and to other acute inpatient settings (research question 4).
-
Implementation of EBCD and of the co-designed changes was influenced by a number of factors and organisational processes, including established ward routines that were care and treatment focused rather than activity focused, and staff workload pressures. However, the structured and time-limited process of EBCD in both the full and the accelerated forms legitimised and supported participatory co-production activity. All participants recognised that increased activity needed to be embedded in everyday routines and work in stroke units. This aligned more easily with the existing working practices of therapists, but there were some indications that nursing work could also encompass prompting and supporting more social, cognitive and physical activity.
-
Communication between staff and patients which was patient-centred and supported activity was the most challenging to initiate and sustain (research question 6).
We now discuss how the CREATE findings compare with those from other research, and the strengths and weaknesses of the study. Finally, we discuss the implications for evaluating the implementation, spread and sustainability of EBCD and the overall impact on activity opportunities available for inpatient stroke patients.
Comparison with other research
Interventions to promote increased activity on stroke units
CREATE is similar to other studies that have set out to increase activity levels on stroke units, and we have shown mixed results. However, most previous research has focused on dose-driven interventions, including circuit class therapy and 7-day-a-week therapy. 37 These have increased the amounts of therapy provided but have not increased meaningful patient activity outside therapy sessions. A more general approach to the environmental enrichment of stroke units with attention given to cognitive and social activity as well as physical activity is now gaining interest. 2,87 The main studies,2,87 which have been conducted in Australia and have utilised controlled pre and post designs and are similar to CREATE, have evaluated the impact of a more stimulating environment on inpatient activity. The sample size was greater (n = 30) and the measures were focused largely on quantitative outcomes. Behaviour mapping results showed an increase in activity levels across all domains and sustained changes at 6 months post intervention. However, in these studies, the stimulating activities and changes made were driven by the perspectives of professionals, with no evidence of patient and carer involvement. The authors did highlight the benefit of using change management methods to address implementation, but, unlike in CREATE, they did not use a specified improvement approach.
Co-design approaches in acute health care
In accordance with the findings of our rapid evidence synthesis, we also found that co-design in acute health-care settings can be challenging and time-consuming to set up. Similar to other studies, engaging with co-design and implementing changes were viewed positively by patients, carers and staff. However, unlike many projects that have used EBCD, we incorporated more ‘designerly thinking’ into our project through the activities and support of our co-applicant Alastair Macdonald. We believe that this enabled greater creativity to emerge through the co-design groups and from the site champions.
We found no appreciable difference between the full EBCD cycle used at sites 1 and 2 and the accelerated form used at sites 3 and 4. This mirrors the finding of Locock et al. ,60 although, unlike in that study, we developed our trigger films locally in stroke units instead of using a national database.
Strengths and limitations
Strengths
We believe that the strengths of CREATE lie in the design and the multiple data sources used in our evaluation and intervention (EBCD), and include a considerable range of data from interviews with stroke patients, families and staff (n = 155) and ethnographic field work (365 hours). This has enabled us to reach a deep level of understanding of the experience for patients, families and staff taking part in co-design, and the staff groups who were less directly involved in co-design, as well as the priorities and impact of the improvements on patient activity. We believe that our staged and iterative approach to qualitative analyses has facilitated an understanding of both the similarities and the discrete differences between sites, which have informed our recommendations about the use of EBCD as an improvement approach in other stroke units.
Our process evaluation also drew on multiple data sources, including researcher reflections, which were kept by all members of the research team (FJ, DC, KG and SH) throughout the project. This collaborative approach to sharing experiences, insights and analysis has provided a new level of insight into ‘the work’ of co-design in acute health care and what it takes to succeed and to sustain change.
We believe the cyclical approach used through EBCD enabled a close relationship to be gained with the research teams based in each site. Although this could be viewed as a limitation, the strategies used, such as encouraging teams to seek ways to overcome barriers, involve local community groups to support their work and celebrate their achievements, all helped staff, patients and families to gain a sense of momentum and change.
Limitations
Inability to use patient-level Sentinel Stroke National Audit Programme data
In our protocol, we stated that we would access routinely collected data at ward level to summarise and compare demographic data, age, gender and stroke severity (National Institutes of Health Stroke Scale and modified Rankin Scale) from a cohort of 30 patients pre/post implementation in each unit. However, gaining access to these data proved difficult and the time required to do so did not fit into our project timeline and would have exceeded the data collection period for sites 1 and 2.
We were able to access SSNAP Acute Organisational Audit data for sites 1 and 2, but the repeat of that audit was delayed and had not been conducted before we submitted our final report. We were unable to access organisational audit data for sites 3 and 4 or to add anything on patient-level data on stroke severity/dependency.
Behaviour mapping
As part of our mixed-methods approach we used behavioural mapping, a validated approach developed primarily to observe level and type of physical activity but more recently also used to record social, cognitive and physical activity for individual patients at 10-minute intervals over 8-hour periods. Although the method was feasible to use in acute stroke units, we believe that our results should be interpreted with the following provisos.
Of concern were the anomalies that arise when reporting behavioural mapping findings. Principally it can be possible for physical activity to be recorded as less across the observation period (epoch) even though the patient may be more socially active; in addition, if a patient is sleeping, the response to ‘no activity’ would be ‘yes’. Thus, ‘no activity’ needs to be interpreted with the number of patients sleeping in mind, as this influences the overall ‘no activity’ percentage. Behavioural mapping is better utilised in studies where the impact of discrete intervention is measured in the same cohort of patients over short time periods. 28
Apart from the concerns about reporting outlined above, we believe that a number of other factors influenced the quality and relevance of behavioural mapping as a reporting method in CREATE. First, we consented patients the day before mapping took place, which led to restrictions in the numbers of possible participants. Numbers included ranged from 4 to 10, which meant that we were mapping the activity behaviour of only a small proportion of patients at any given time. Second, as our protocol determined, we did not include scheduled therapy sessions as part of recorded activity, and we also had a number of ‘unobserved’ recordings. For instance, if a patient was at an outside café or in the bathroom, they were not recorded as being active. Third, we believe that contextual issues such as staff shortages and the severity of disability of the inpatient caseload had a serious impact on the activity opportunities we could record. Nonetheless, the fact that we witnessed many instances of patients spending the majority of their time in bed or at the bedside with no interaction and nothing to do is a potent reminder that more work is needed to increase patient activity outside routine therapy in stroke units.
Low response rate to patient-reported outcome measures/patient-reported experience measures
We chose to use a validated PROM/PREM tool so that we could gain contextual data about the impact of stroke on patients post discharge and their experiences of being on a stroke unit. However, the return rate was low (< 40%) across sites, and in discussion with our NIHR manager and study steering group we used several strategies to increase this. We initially aimed to collect our pre-implementation PROM/PREM data retrospectively for 30 patients to coincide with SSNAP reporting periods (i.e. quarterly). We increased this to 6-monthly, which comprised two quarterly SSNAP periods, and we carried out repeat mailing and reminders. Overall, we believe that the post-implementation data collection period at sites 1 and 2, which was either side of Christmas, had a detrimental effect on the response rate, and, despite our efforts, we managed to reach our target of 30 returned questionnaires at site 2 only. Although the PROM/PREM has been validated for use with neurological inpatients, this is the first time, to our knowledge, that it has been used with stroke inpatients. In addition, the length of the questionnaire could have been a barrier and, overall, we believe that these surveys offered limited additional insight into the impact of CREATE beyond that gained through the semistructured interviews.
The challenge of the critical distance of the research team
We introduced a number of stages in our protocol to try to reduce researcher bias, such as using a standardised protocol and behavioural mapping tool for recording patient activity episodes and ensuring that recording sessions were spread across a 10- to 14-day period to allow maximum opportunity to account for variations in activity at different times of the day and on different days of the week/at weekends and the presence or absence of family members/visitors. Our behavioural mapping protocol also excluded individual therapy sessions to reduce the likelihood that increased activity levels would be captured later in the inpatient stay when individuals would be more active in therapy.
We were unable to use a purposive sampling approach as recruitment for behavioural mapping proved challenging at all four sites and, thus, given the convenience samples we worked with, we could not select patients at different points in their inpatient stay or with different levels of stroke severity.
However, our behavioural mapping results were clearly variable between the pre- and post-EBCD activity periods, indicating that, although patients, relatives and staff may have been more aware of the EBCD project and although opportunities for activity may have increased, this was not necessarily reflected in individual behavioural mapping profiles, which tended to indicate low levels of individually focused activity.
We were unsure whether there were any changes in staff behaviour as a result of researchers conducting behavioural mapping and observations/interviews. Our field notes and memos show that, across all sites, some early observations raised staff members’ awareness of the project and may have influenced some of their interactions with stroke survivors but, as in most observational studies, this effect quickly dissipated. As observations (pre and post) were extended over 10 sessions over 2–3 weeks and interspersed with behavioural mapping recording, staff became used to the researchers’ presence and we observed very little evidence of change in staff behaviour in favour of increased patient activity outside therapy during these (pre or post) periods of observation.
We do acknowledge the potential for the research fellows who were involved in supporting EBCD and facilitating co-design groups to develop a sense of ownership and investment in the project at each site but would point to the actual time spent at the sites being episodic, which meant that there was separation from the day-to-day work on the units. Overall, as a research team we had different roles and different levels of involvement. The research leads (FJ and DC) had considerably less time in the sites and less involvement in the co-design groups; however, they did conduct (pre and post) observations and interviews and added a different perspective on observed and reported activity from those of the researchers who routinely facilitated EBCD activities.
At sites 1 and 2, quite long periods of time separated the pre and post observations and interviews, and we sought different as well as similar interviewees (i.e. those directly involved and those not involved with EBCD). The process was broadly similar at sites 3 and 4 but, although the overall time was reduced, a gap of around 6–7 months remained. As a team, we were mindful of the need for objectivity in reporting on what was observed.
In our analysis meetings and in our integration of the data for the process evaluation, we had an opportunity to review field notes, summary memos and researcher reflections, which helped us identify factors that may have influenced the researchers’ perceptions and reporting of activity (or absence of activity) at sites; this included Study Steering Committee members robustly reviewing our presentation of the emerging and final data.
However, as stated in Chapter 5, one of the main challenges the researchers faced was that their role included both data collection and the co-ordination of EBCD and co-design meetings. Although there were examples of autonomous and proactive behaviours by staff, patients and family members, an unintended consequence of the researchers’ regular presence and willingness to facilitate improvement could have been a reduced commitment among staff to collective action and undertaking the work required to actually implement changes to practices. Paradoxically, the absence of researchers in future projects might facilitate greater commitment and engagement from clinical teams, notwithstanding the need for champions to emerge in each site to drive forward the improvement cycle.
Implications for health care
The added value of using co-design to initiate change
Traditional approaches to improving activity on stroke units have focused largely on setting national targets for therapy intensity. These have failed to have an impact on the stroke unit environment and the range and quality of activity opportunities outside formal therapy provision. We now question the narrow focus of this ‘top-down’ approach to therapy and its lack of consideration of the broader rehabilitation concern of increasing activity. Outside the narrow focus of clinical audit, action is required at both national (guideline recommendations) and local levels to increase therapeutic activity outside therapy. This needs to be based on a refocusing on rehabilitation post stroke, needs to be addressed at stroke unit team level (i.e. taking a multidisciplinary approach), and will benefit from the use of participatory service improvement methods such as EBCD.
The success of participatory approaches and EBCD used for the first time in acute stroke services lies in the knowledge that patients, families and staff decided and agreed on what mattered most to them as well as what could be achieved. We believe that the strength of EBCD in both its full and its accelerated form is the facilitated, structured, participatory and time-limited process. The nature of the ‘work’ in CREATE was fundamentally different from usual staff or externally driven quality improvement initiatives in stroke, and it prioritised the participation by stroke survivors and their families in more creative, tactile and relational interactions and outputs to improve opportunities for independent and supervised activity.
It was also evident that CREATE provided distinctly different experiences for staff who engaged in EBCD and that the changes agreed were driven not by external policy pressures or by local organisational demands, and not by external audit, but rather they were shaped very clearly by the experiences of patients and carers whom staff had recently cared for or treated, and were locally determined by small groups who took responsibility for bringing change about. This motivated groups to work together in co-design meetings to define ways to implement the new working practices, what Wenger refers to as ‘communities of practice’ in each site who were central to bringing about change. 88 The involvement of patients and carers increased the accountability of the staff who participated and made it more likely that the planned changes would proceed. Co-design also facilitated carers’ and volunteers’ continued involvement in activities and directly contributed to the sustainability of the changes made to the day-to-day working of these stroke units.
Co-design activities in CREATE also initiated new and ongoing engagement with local people and/or organisations for whom the hospital is a key part of their community. The positive aspect of greater community involvement was notable in one of the London sites threatened with closure at various times. As a result of increased engagement with art communities, CREATE was viewed locally as a ‘good news’ story in terms of providing examples of how co-produced changes improved inpatient services in the ‘local’ hospital. Figure 20 shows a mayoral visit that celebrated the opening of the new post-EBCD ward at site 1. We believe that acknowledgement and celebration of the efforts made by staff, patients and carers – the final part of the cycle of EBCD – is an important factor in raising awareness of change and sustaining achievements.
The ongoing challenge of (in)activity in stroke units
Culture change in any organisation is challenging, and in our project this was no different. The process evaluation highlighted the importance of organisational buy-in but also the challenges of achieving this at unit level and beyond. It was also clear that EBCD provided both a structure and a space for changes aimed at directly improving the experiences of stroke patients and their family carers. As a result of making these changes, the morale and commitment of staff also seemed to improve. Nonetheless, although improvements in activity opportunities were observed, the process evaluation also highlighted the challenge of involving and keeping engaged large groups of staff in the participatory change process. Similarly, differences in staff members’ perceptions of their role in rehabilitation and enacting this in day-to-day working practices highlighted that interdisciplinary rehabilitation and increased activity promotion across a whole stroke team would require more sustained intervention targeted at how teams work in this context, which was beyond the scope of CREATE. Although the tangible improvements to the space and activity opportunities was visible across all stroke units and validated by our qualitative findings, when behaviour mapping was used as an objective measurement tool no consistent change was found in the proportion of time on weekdays and weekend days that stroke patients in the participating units spent on physical, social and cognitive activities. The effectiveness and long-term impact of lengthy periods of co-design work (ranging from 4 to 9 months in this project) on the independent and supervised activity of stroke patients is still uncertain. Currently, work routines in participating units and day-to-day interactions between staff and patients are largely task driven, focusing on care needs and delivering scheduled therapy. Interactions that facilitate greater social exchange, cognitive activity or physical exercise are relatively uncommon, and we believe that to increase such activity opportunity requires a fundamentally different approach to how therapy and nursing contribution to rehabilitation is viewed and delivered so that stroke unit environments and work practices become more conducive to activity and so that activity is seen as a priority and part of the rehabilitation work of all staff, not only therapists.
At all CREATE sites we found concern that ‘something must be done’ and a willingness for staff, patients and families to work together to make improvements. We believe that, for this approach to be used across other stroke units, local facilitation needs to be provided by a member of staff who has protected time to be allocated to this work. Change required buy-in and commitment from multiple stakeholders including senior management to validate the shift from achieving national performance targets to a cultural recognition of the therapeutic value of a stroke unit. Change was facilitated when stroke unit staff worked with volunteers and people from the community. This will take time, but trigger films such as those developed in this project can help gain traction to make changes, some of which can be initiated quickly and relatively cheaply (e.g. photo-hangers by bedsides, and the ‘a little something about me’ board).
Costs and sustainability
It was not within the remit of CREATE to evaluate the cost of EBCD in its full or accelerated form, but we found no appreciable difference in the impact or extent of changes between the full and the accelerated EBCD cycles. We therefore conclude that accelerated EBCD is a feasible and efficient improvement method in stroke units and other acute care settings. However, we believe, based on our findings, that to streamline the processes further would be a risk to its success. Each of our sites has highlighted inherent contributors to effecting change in such a complex clinical environment, including having sufficient time to build a community of practice through the co-design work. Time is critical to the development of a sense of responsibility to the process (i.e. to deliver what was agreed), and to plan for and enact change, which often involved working with others to navigate bureaucracy and required the creativity and resourcefulness of co-design team members. This was seen at site 1, when the delay led a general manager and the head of nursing to expedite changes and seek solutions to funding issues, such as decorating the bays themselves. At site 3, the stroke team’s fundraising efforts were recognised by the trust chief executive, who agreed to match the amount raised. Finally, a stroke physician at site 4, frustrated by delays, brought about a solution to the lack of iPad stands by repurposing research and development funds. We believe that these actions would not have been possible within a shorter time frame.
Sustainability is also difficult to measure, and this too was influenced by operational and structural changes outside our control, such as hospital redesigns and staff shortages. Post completion, each site continued to make use of the activity improvements and some added further to these. For example, at site 1 the collaboration with local artists continued and a number of activities have been delivered for patients at weekends, culminating in a new mural and artwork in the ward space. At site 2, staff meetings that used to take pace in the reclaimed day room now take place in a shared therapy office between the rehabilitation room and the acute ward. At site 3, the new shared kitchen facility has been completed and this space is now accessed by staff, patients and families. At site 4, the day room previously used only for wheelchair storage has been maintained as a new activity space. The wheelchairs were moved to a room on the floor above and staff have to factor collecting and returning these wheelchairs into their working day; however, there have been no reports of this process eroding therapy time or inconveniencing staff. In addition, at site 4 there is continued use of the open window area that was previously used mainly for staff breaks, equipment storage and display of Stroke Association materials. Equipment is now stored in other areas close to the ward nurses’ station, and staff breaks are taken off ward or in the ward offices.
Implications for research
The cost-effectiveness of the methods used in CREATE are unknown, although quality improvement methods, such as the accelerated EBCD used at sites 3 and 4 could be highly cost-effective if improvements can reduce the inactivity of inpatient stroke patients, contribute to an increase in independence in activities of daily living and reduce length of stay. Equally, the participatory approaches used in EBCD can have a positive impact on the morale, meaning and purpose of staff in the face of increasing staff shortages and caseload pressures. Staff in our study felt that there was little time for any creative thought and relational work in their day-to-day practice, and the opportunity to take part in CREATE, to make a difference and to do something positive, was viewed as constructive across all stroke units.
We believe that CREATE has added to the knowledge about co-design in acute health care and that our methods could be applied and evaluated across other stroke units and other acute health-care environments. Our findings support Greenhalgh et al. ’s key principles for achieving impact in co-design, including the need ‘to frame this research as a creative enterprise with human experience at its core’80 and an emphasis on process, such as the nature of relationships, leadership style, governance and facilitation arrangements. Our rapid evidence synthesis highlighted common barriers encountered in co-production approaches and these barriers were similar in this study, which was similarly thwarted at times by a lack of resources or managerial authority to bring changes. 16 However, unlike other research projects, we had little difficulty recruiting patients and carers and retaining them in the project. This, we believe, was largely a result of the dedicated efforts of our local researchers and the willingness of staff in the co-design groups to both engage with and support stroke survivors and their families to participate in the EBCD process.
Any further research in this field requires early engagement and commitment from estates, general management, senior executives, and communications at the start of the project and to utilise methods to retain interest throughout and after completion. The stakeholder mapping exercise at the start of EBCD was critical.
Early consideration of community/voluntary sector engagement is also important and is a key learning point from sites 1 and 2, which used the full EBCD cycle. This enabled awareness-raising among and interest from a range of local community groups, which subsequently added to activity opportunities through art, exercise groups, reading and music.
Finally, several research questions have emerged from our study, which are as yet unexplored:
-
What are the additional steps that would be required to change the culture of activity on a stroke unit? In particular, what changes are required to achieve greater consistency in the use of enabling communication by all staff?
-
Can the CREATE accelerated EBCD approach using stroke-specific trigger films be used across other acute stroke units, and what would be the contextual adaptations required to enable similar levels of improvement?
-
What are the ‘costs’ of setting up accelerated EBCD in terms of time and people? How sustainable is the approach in a stroke unit and how frequently should an EBCD cycle run?
-
Are there transferable lessons outside a stroke unit environment (e.g. does it matter whether the ward is ‘specialist’, or for short, medium or long stay)?
-
What additional tools and methods are required to provide a more effective way of measuring any changes in activity, given our concerns about the sensitivity of behavioural mapping?
-
What additional approaches would be required to change the culture of activity on a stroke unit; how can ‘enabling activity’ be viewed as the work of all staff, including nursing staff?
-
To what extent can patients/families and local communities support sustained activity, providing greater opportunities for social, cognitive and physical activity outside scheduled therapy provision?
-
What is the longevity of the changes made, and will the CREATE stroke units continue to work with patient and carer groups to review these and make improvements?
-
What aspects of EBCD promote lasting change?
Chapter 7 Dissemination
Throughout the study, the project leads and the research team have disseminated the project and emergent findings in a varied range of conferences, seminars and journals.
Conferences and seminars include:
-
UK Stroke Forum 2016, 28–30 November 2016, Liverpool, UK
-
UK Stroke Forum 2017, 28–30 November 2016, Liverpool, UK
-
UK Stroke Forum 2018, 4–6 December 2018, Telford, UK
-
How2CoPro Event, 12 March 2019, St George’s, University of London, London, UK
-
King’s College London, Research Seminar, November 2017
-
South London Stroke Research Network Meeting, June 2017
-
European Stroke Organisation Conference (ESOC) 2017, 16–17 May 2017, Prague, Czech Republic
-
ESOC 2018, 16–May 2018, Gothenburg, Sweden
-
Health Services Research UK (HSR UK) Conference, 6–7 July 2017, Nottingham, UK
-
ESOC 2019, 22–24 May 2019, Milan, Italy
-
HSR UK, Conference, 2–3 July 2019, Manchester, UK.
The rapid evidence synthesis has been published:
-
Clarke D, Jones F, Harris R, Robert G, Collaborative Rehabilitation Environments in Acute Stroke (CREATE) team. What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open 2017;7:e014650.
Research teams have also held ‘feedback events’ at all sites to disseminate findings to all stakeholders.
At sites 1 and 3, local newspapers published articles about the project and the changes that occurred on the wards.
CREATE has gained followers on its Twitter account and we continue to update our followers about the project via our account @CREATE_project_.
In the longer term, our dissemination routes are to produce guidance for stroke units to use accelerated EBCD on their units to increase activity, and to run a training session at the UK Stroke Forum.
We will visit stroke units and spread this work through our national and international networks.
Acknowledgements
Contributions of authors
Fiona Jones (https://orcid.org/0000-0002-1452-3895) (Professor of Rehabilitation Research) was chief investigator. She co-designed and led the study, collected and analysed data, wrote the first draft of Chapters 1–3, and the summary sections in Chapters 4–7, and contributed to analysis and interpretation of the empirical findings and to report writing.
Karolina Gombert-Waldron (https://orcid.org/0000-0002-6573-0966) (Research Associate) was project manager for sites 1 and 3. She facilitated the co-design process, collected and analysed data and contributed to all sections of the report.
Stephanie Honey (https://orcid.org/0000-0002-2675-7824) (Research Associate) was project manager for sites 2 and 4. She facilitated the co-design process and collected and analysed data.
Geoffrey Cloud (https://orcid.org/0000-0002-8365-6907) (Consultant Stroke Physician) was a co-applicant. He provided clinical advice from a local and national stroke perspective, and contributed to analysis and interpretation of the empirical findings and to report writing.
Ruth Harris (https://orcid.org/0000-0002-4377-5063) (Professor of Health Care for Older Adults) was a co-applicant. She provided input into the EBCD and co-design activities, contributed to analysis and interpretation of the empirical findings and report writing, and supported the rapid review.
Alastair Macdonald (https://orcid.org/0000-0001-9282-6229) (Professor) was a co-applicant. He provided input into the EBCD and co-design activities, supported with visual illustration of material in the report, and contributed to analysis and interpretation of the empirical findings and to report writing.
Chris McKevitt (https://orcid.org/0000-0002-5290-4613) (Professor of Social Sciences & Health) was a co-applicant. He contributed to the analysis and interpretation of the empirical findings and to report writing.
Glenn Robert (https://orcid.org/0000-0001-8781-6675) (Professor) was a co-applicant. He provided input into the EBCD and co-design activities, contributed to analysis and interpretation of the empirical findings and to report writing, and supported the rapid review.
David Clarke (https://orcid.org/0000-0001-6279-1192) (Associate Professor, Stroke Care) co-designed and co-led the study. He facilitated the co-design process, was lead investigator for sites 2 and 4, collected and analysed data, wrote the first draft of the process evaluation, and contributed to analysis and interpretation of the empirical findings and to report writing.
Contributions of others
Research support
Tino Kulnik conducted pre-implementation interviews for site 1 and supported several co-design events and the input of behavioural mapping data.
Alessia Costa supported ethnographic fieldwork at site 1.
Louisa-Jane Burton and Sadia Ahmed supported the behavioural mapping and PROM/PREM analysis and interpretation.
Carole Pound supported co-design events at site 1.
Parminder Dhiman carried out data collection at site 1 (PROM/PREM and behavioural mapping).
Study Steering Committee
Dr Rebecca Palmer (chairperson)
Dr Gillian Cluckey
Amanda North
Pamela Beaumont
Jeanette Gledhill
Dr David Meads.
Site and support
Principal investigators at all sites: Dr Paul O’Mahoney and Dr Janet Putteril (site 1), Dr Liz Iveson (site 2), Dr Camille Julien and Dr Karen Kee (site 3), and Dr Anand Nair (site 4).
Participants and co-design groups at all collaborating sites – members of staff, patients and family members.
Community support
Hana Horack and Team Imagineers have applied for funding and run art workshops for the patients at weekends at our first site. Cherilyn Yeates from Croydon Arts and Music gave time to paint a mural at site 3.
Croydon Arts and Music give concerts at the weekends at site 3.
The Reader charity and the Stroke Association, in particular Jack Blaney, supported the co-design process at site 3. The UK Stroke Forum acknowledged CREATE through the Patient, Carer and Public Involvement Prize.
Publication
Clarke D, Jones F, Harris R, Robert G, Collaborative Rehabilitation Environments in Acute Stroke (CREATE) team. What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open 2017;7:e014650.
Data-sharing statement
All available data can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Cloud G, Hoffman A, Rudd A. Intercollegiate Stroke Working Party . National sentinel stroke audit 1998–2011. Clin Med 2013;13:444-8. https://doi.org/10.7861/clinmedicine.13-5-444.
- Department of Health and Social Care . National Stroke Strategy 2007.
- Rudd AG, Hoffman A, Paley L, Bray B. 20 years of researching stroke through audit. Clin Rehabil 2018;32:997-1006. https://doi.org/10.1177/0269215518784645.
- Rosbergen IC, Grimley RS, Hayward KS, Walker KC, Rowley D, Campbell AM, et al. Embedding an enriched environment in an acute stroke unit increases activity in people with stroke: a controlled before-after pilot study. Clin Rehabil 2017;31:1516-28. https://doi.org/10.1177/0269215517705181.
- Åstrand A, Saxin C, Sjöholm A, Skarin M, Linden T, Stoker A, et al. Poststroke physical activity levels no higher in rehabilitation than in the acute hospital. J Stroke Cerebrovasc Dis 2016;25:938-45. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.12.046.
- Kunkel D, Fitton C, Burnett M, Ashburn A. Physical inactivity post-stroke: a 3-year longitudinal study. Disabil Rehabil 2015;37:304-10. https://doi.org/10.3109/09638288.2014.918190.
- Bernhardt J, Dewey H, Thrift A, Donnan G. Inactive and alone. Stroke 2004;35:1005-9. https://doi.org/10.1161/01.STR.0000120727.40792.40.
- Esmonde T, McGinley J, Wittwer J, Goldie P, Martin C. Stroke rehabilitation: patient activity during non-therapy time. Aust J Physiother 1997;43:43-51. https://doi.org/10.1016/S0004-9514(14)60401-3.
- Intercollegiate Stroke Working Party . National Clinical Guideline for Stroke 2016.
- Taylor E, McKevitt C, Jones F. Factors shaping the delivery of acute inpatient stroke therapy: a narrative synthesis. J Rehabil Med 2015;47:107-19. https://doi.org/10.2340/16501977-1918.
- Clarke DJ, Burton L-J, Tyson SF, Rodgers H, Drummond A, Palmer R, et al. Why do stroke survivors not receive recommended amounts of active therapy? Findings from the ReAcT study, a mixed-methods case-study evaluation in eight stroke units. Clin Rehabil 2018;32:1119-32. https://doi.org/10.1177/0269215518765329.
- Taylor E, Jones F, McKevitt C. How is the audit of therapy intensity influencing rehabilitation in inpatient stroke units in the UK? An ethnographic study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-023676.
- Batalden P. Getting more health from healthcare: quality improvement must acknowledge patient coproduction – an essay by Paul Batalden. BMJ 2018;362. https://doi.org/10.1136/bmj.k3617.
- Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf 2016;25:509-17. https://doi.org/10.1136/bmjqs-2015-004315.
- Osborne SP, Radnor Z, Strokosch K. Co-production and the co-creation of value in public services: a suitable case for treatment?. Public Management Rev 2016;18:639-53. https://doi.org/10.1080/14719037.2015.1111927.
- Clarke D, Jones F, Harris R, Robert G. Collaborative Rehabilitation Environments in Acute Stroke (CREATE) team . What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014650.
- Stroke Association . State of the Nation Stroke Statistics 2018. www.stroke.org.uk/system/files/sotn_2018.pdf (accessed 14 April 2019).
- Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011;377:1693-702. https://doi.org/10.1016/S0140-6736(11)60325-5.
- Wang Y, Rudd AG, Wolfe CD. Age and ethnic disparities in incidence of stroke over time: the South London Stroke Register. Stroke 2013;44:3298-304. https://doi.org/10.1161/STROKEAHA.113.002604.
- Marshall IJ, Wang Y, Crichton S, McKevitt C, Rudd AG, Wolfe CD. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol 2015;14:1206-18. https://doi.org/10.1016/S1474-4422(15)00200-8.
- Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245-54. https://doi.org/10.1016/S0140-6736(13)61953-4.
- Patel A, Berdunov V, King D, Berdunov Z, Wittenberg R, Knapp M. Current, Future and Avoidable Costs of Stroke in the UK: Part 1. London: Centre for Primary Care & Public Health, Queen Mary University of London and the Personal Social Services Research Unit, London School of Economics and Political Science for the Stroke Association; n.d; n.d.
- Saka O, Serra V, Samyshkin Y, McGuire A, Wolfe CC. Cost-effectiveness of stroke unit care followed by early supported discharge. Stroke 2009;40:24-9. https://doi.org/10.1161/STROKEAHA.108.518043.
- Department of Health and Social Care . National Stroke Strategy 2007. https://webarchive.nationalarchives.gov.uk/20130104224925/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_081059.pdf (accessed 14 April 2019).
- Stroke Unit Trialists’ Collaboration . Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013;9.
- Fulop N, Boaden R, Hunter R, McKevitt C, Morris S, Pursani N, et al. Innovations in major system reconfiguration in England: a study of the effectiveness, acceptability and processes of implementation of two models of stroke care. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-5.
- Morris S, Ramsay AIG, Boaden RJ, Hunter RM, McKevitt C, Paley L, et al. Impact and sustainability of centralising acute stroke services in English metropolitan areas: retrospective analysis of hospital episode statistics and stroke national audit data. BMJ 2019;364. https://doi.org/10.1136/bmj.l1.
- Janssen H, Ada L, Bernhardt J, McElduff P, Pollack M, Nilsson M, et al. An enriched environment increases activity in stroke patients undergoing rehabilitation in a mixed rehabilitation unit: a pilot non-randomized controlled trial. Disabil Rehabil 2014;36:255-62. https://doi.org/10.3109/09638288.2013.788218.
- Dewey HM, Sherry LJ, Collier JM. Stroke rehabilitation 2007: what should it be?. Int J Stroke 2007;2:191-200. https://doi.org/10.1111/j.1747-4949.2007.00146.x.
- National Institute for Health and Care Excellence . Stroke Rehabilitation in Adults: Guidance 2013. www.nice.org.uk/guidance/CG162 (accessed 12 April 2020).
- National Institute for Health and Care Excellence . Stroke Overview – NICE Pathways 2020. https://pathways.nice.org.uk/pathways/stroke (accessed 13 April 2020).
- Schneider EJ, Lannin NA, Ada L, Schmidt J. Increasing the amount of usual rehabilitation improves activity after stroke: a systematic review. J Physiother 2016;62:182-7. https://doi.org/10.1016/j.jphys.2016.08.006.
- Lohse KR, Lang CE, Boyd LA. Is more better? Using meta-data to explore dose-response relationships in stroke rehabilitation. Stroke 2014;45:2053-8. https://doi.org/10.1161/STROKEAHA.114.004695.
- Kwakkel G, Wagenaar RC, Koelman TW, Lankhorst GJ, Koetsier JC. Effects of intensity of rehabilitation after stroke. Stroke 1997;28:1550-6. https://doi.org/10.1161/01.STR.28.8.1550.
- Royal College of Physicians, Clinical Effectiveness and Evaluation Unit on behalf of the Intercollegiate Stroke Working Party . Changes Over Time: 4 Years of Data April 2013 – March 2017: National Results Based on Stroke Patients Admitted to and Or Discharged from Hospital Between April 2013 – March 2017 2017.
- Huijben-Schoenmakers M, Rademaker A, van Rooden P, Scherder E. The effects of increased therapy time on cognition and mood in frail patients with a stroke who rehabilitate on rehabilitation units of nursing homes in the Netherlands: a protocol of a comparative study. BMC Geriatr 2014;14. https://doi.org/10.1186/1471-2318-14-68.
- English C, Bernhardt J, Hillier S. Circuit class therapy and 7-day-week therapy increase physiotherapy time, but not patient activity: early results from the CIRCIT trial. Stroke 2014;45:3002-7. https://doi.org/10.1161/STROKEAHA.114.006038.
- Trammell M, Kapoor P, Swank C, Driver S. Improving practice with integration of patient directed activity during inpatient rehabilitation. Clin Rehabil 2017;31:3-10. https://doi.org/10.1177/0269215515625100.
- Skarin M, Sjöholm A, Nilsson Å, Nilsson M, Bernhardt J, Lindén T. A mapping study on physical activity in stroke rehabilitation: establishing the baseline. J Rehabil Med 2013;45:997-1003. https://doi.org/10.2340/16501977-1214.
- Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med Rehabil 2011;92:1490-500. https://doi.org/10.1016/j.apmr.2011.04.005.
- Galvin R, Cusack T, O’Grady E, Murphy TB, Stokes E. Family-mediated exercise intervention (FAME): evaluation of a novel form of exercise delivery after stroke. Stroke 2011;42:681-6. https://doi.org/10.1161/STROKEAHA.110.594689.
- Lockhart J, James I, Linstead G. Mind the Gap. London: NHS Improvement; 2006.
- NHS England . Putting Patients First: The NHS England Business Plan for 2013 14–2015 16 n.d. www.england.nhs.uk/wp-content/uploads/2013/04/ppf-1314-1516.pdf (accessed 13 April 2020).
- NHS England . Five Year Forward View 2014 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 14 April 2019).
- NHS Improvement . Patient Experience Improvement Framework 2018. https://improvement.nhs.uk/documents/2885/Patient_experience_improvement_framework_full_publication.pdf (accessed 14 April 2019).
- Needham C, Carr S. Co-production: An Emerging Evidence Base for Adult Social Care Transformation. London: Queen Mary, University of London, and Social Care Institute for Excellence; 2009.
- Robert G, Cornwell J. Rethinking policy approaches to measuring and improving patient experience. J Health Serv Res Policy 2013;18:67-9. https://doi.org/10.1177/1355819612473583.
- Madden M, Speed E. Beware zombies and unicorns: toward critical patient and public involvement in health research in a neoliberal context. Front Sociol 2017;2. https://doi.org/10.3389/fsoc.2017.00007.
- Berwick DM. Improvement, trust, and the healthcare workforce. Qual Saf Health Care 2003;12:i2-6. https://doi.org/10.1136/qhc.12.suppl_1.i2.
- Goodrich J, Cornwell J. Seeing the Person in the Patient: The Point of Care Review Paper. London: The King’s Fund; 2008.
- Bate P, Robert G. Bringing User Experience to Healthcare Improvement: The Concepts, Methods and Practices of Experience-based Design. Abingdon: Radcliffe Publishing; 2007.
- Tsianakas V, Maben J, Wiseman T, Robert G, Richardson A, Madden P, et al. Using patients’ experiences to identify priorities for quality improvement in breast cancer care: patient narratives, surveys or both?. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-271.
- Cottam H, Leadbeater C. Red Paper 01 Health: Co-creating Services. London: Design Council; 2004.
- Baim-Lance A, Tietz D, Lever H, Swart M, Agins B. Everyday and unavoidable coproduction: exploring patient participation in the delivery of healthcare services. Sociol Health Illn 2019;41:128-42. https://doi.org/10.1111/1467-9566.12801.
- Farr M. Power dynamics and collaborative mechanisms in co-production and co-design processes. Crit Soc Policy 2018;38:623-44. https://doi.org/10.1177/0261018317747444.
- Filipe A, Renedo A, Marston C. The co-production of what? Knowledge, values, and social relations in health care. PLOS Biol 2017;15. https://doi.org/10.1371/journal.pbio.2001403.
- Bate P, Robert G. Toward more user-centric OD: lessons from the field of experience-based design and a case study. J Appl Behav Sci 2007;43:41-66. https://doi.org/10.1177/0021886306297014.
- Donetto S, Tsianakas V, Robert G. Using Experience-based Co-design to Improve the Quality of Healthcare: Mapping Where We Are Now and Establishing Future Directions. London: King’s College London; 2014.
- The Point of Care Foundation . What Is Experience-Based Co-Design n.d. www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit/step-by-step-guide/1-experience-based-co-design/ (accessed 9 April 2019).
- Locock L, Robert G, Boaz A, Vougioukalou S, Shuldham C, Fielden J, et al. Testing accelerated experience-based co-design: a qualitative study of using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02040.
- Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ 2015;350. https://doi.org/10.1136/bmj.g7714.
- Intercollegiate Working Party for Stroke . National Guidelines for Stroke 2012. www.strokeaudit.org/Guideline/Historical-Guideline/National-Clinical-Guidelines-for-Stroke-fourth-edi.aspx (accessed 14 April 2019).
- Sentinel Stroke National Audit Programme (SSNAP) . SSNAP Clinical Interactive Maps n.d. www.strokeaudit.org/results/Clinical-audit/Maps.aspx (accessed July 2020).
- Royal College of Physicians, Care Quality Improvement Department on behalf of the Intercollegiate Stroke Working Party . Sentinel Stroke National Audit Programme (SSNAP): Acute Organisational Report 2016. www.strokeaudit.org/Documents/National/AcuteOrg/2016/2016-AOANationalReport.aspx (accessed 13 April 2020).
- The Point of Care Foundation . EBCD: Experience-Based Co-Design Toolkit n.d. www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit/ (accessed 14 February 2019).
- Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1089-4.
- May CR, Finch T, Ballini L, MacFarlane A, Mair F, Murray E, et al. Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-245.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Kneebone II, Hull SL, McGurk R, Cropley M. Reliability and validity of the neurorehabilitation experience questionnaire for inpatients. Neurorehabil Neural Repair 2012;26:834-41. https://doi.org/10.1177/1545968311431962.
- Clarke DJ, Hawkins R, Sadler E, Harding G, McKevitt C, Godfrey M, et al. Introducing structured caregiver training in stroke care: findings from the TRACS process evaluation study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004473.
- Askim T, Bernhardt J, Salvesen O, Indredavik B. Physical activity early after stroke and its association to functional outcome 3 months later. J Stroke Cerebrovasc Dis 2014;23:e305-12. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.12.011.
- Normalization Process Theory . What Is NPT? n.d. www.normalizationprocess.org/what-is-npt/ (accessed 11 April 2019).
- Tsianakas V, Robert G, Maben J, Richardson A, Dale C, Griffin M, et al. Implementing patient-centred cancer care: using experience-based co-design to improve patient experience in breast and lung cancer services. Support Care Cancer 2012;20:2639-47. https://doi.org/10.1007/s00520-012-1470-3.
- Locock L, Robert G, Boaz A, Vougioukalou S, Shuldham C, Fielden J, et al. Using a national archive of patient experience narratives to promote local patient-centered quality improvement: an ethnographic process evaluation of ‘accelerated’ experience-based co-design. J Health Serv Res Policy 2014;19:200-7. https://doi.org/10.1177/1355819614531565.
- Bowen S, McSeveny K, Lockley E, Wolstenholme D, Cobb M, Dearden A. How was it for you? Experiences of participatory design in the UK health service. CoDesign 2013;9:230-46. https://doi.org/10.1080/15710882.2013.846384.
- Piper D, Iedema R, Gray J, Verma R, Holmes L, Manning N. Utilizing experience-based co-design to improve the experience of patients accessing emergency departments in New South Wales public hospitals: an evaluation study. Health Serv Manage Res 2012;25:162-72. https://doi.org/10.1177/0951484812474247.
- Larkin M, Boden ZV, Newton E. On the brink of genuinely collaborative care: experience-based co-design in mental health. Qual Health Res 2015;25:1463-76. https://doi.org/10.1177/1049732315576494.
- Vennik FD, van de Bovenkamp HM, Putters K, Grit KJ. Co-production in healthcare: rhetoric and practice. Int Rev Admin Sci 2016;82:150-68. https://doi.org/10.1177/0020852315570553.
- Thomson A, Rivas C, Giovannoni G. Multiple sclerosis outpatient future groups: improving the quality of participant interaction and ideation tools within service improvement activities. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0773-8.
- Greenhalgh T, Jackson C, Shaw S, Janamian T. Achieving research impact through co-creation in community-based health services: literature review and case study. Milbank Q 2016;94:392-429. https://doi.org/10.1111/1468-0009.12197.
- Bovaird T. Beyond engagement and participation: user and community coproduction of public services. Public Admin Rev 2007;67:846-60. https://doi.org/10.1111/j.1540-6210.2007.00773.x.
- Scottish Co-Production Network . Co-Production — How We Make a Difference Together 2016. www.scdc.org.uk/what/co-production-how-we-make-difference-together (accessed 20 September 2019).
- Boyd H, McKernon S, Mullin B, Old A. Improving healthcare through the use of co-design. N Z Med J 2012;125:76-87.
- Tollyfield R. Facilitating an accelerated experience-based co-design project. Br J Nurs 2014;23:136-41. https://doi.org/10.12968/bjon.2014.23.3.136.
- Walshe K. Pseudoinnovation: the development and spread of healthcare quality improvement methodologies. Int J Qual Health Care 2009;21:153-9. https://doi.org/10.1093/intqhc/mzp012.
- Keith RA, Cowell KS. Time use of stroke patients in three rehabilitation hospitals. Soc Sci Med 1987;24:529-33. https://doi.org/10.1016/0277-9536(87)90342-x.
- Rosbergen IC, Grimley RS, Hayward KS, Brauer SG. The impact of environmental enrichment in an acute stroke unit on how and when patients undertake activities. Clin Rehabil 2019;33:784-95. https://doi.org/10.1177/0269215518820087.
- Wenger E. Communities of Practice: Learning, Meaning, and Identity. Cambridge: Cambridge University Press; 1998.
- Palmer J. Stroke unit transformed at St Helier Hospital. Sutton &Amp; Croydon Guardian 2018. www.yourlocalguardian.co.uk/news/15921208.stroke-unit-transformed-at-st-helier-hospital/ (accessed 12 December 2019).
Appendix 1 Sentinel Stroke National Audit Programme key indicators and overview of Sentinel Stroke National Audit Programme organisational data
Key indicators
Performance-level indicators
-
Brain scanning.
-
Stroke unit.
-
Clot-busting treatment.
-
Specialist assessments.
-
Occupational therapy.
-
Physiotherapy.
-
Speech and language therapy.
-
Team working.
-
Standards met by discharge.
-
Discharge process.
| Performance-level indicator | April–July 2016 | December–March 2017 | January–March 2018 | October–December 2018 (not available at time of publication) | ||||
|---|---|---|---|---|---|---|---|---|
| Site 1 | Site 2 | Site 1 | Site 2 | Site 3 | Site 4 | Site 3 | Site 4 | |
| Brain scanning | B | C | B | C | B | C | ||
| Stroke unit | D | E | E↓ | D↑ | E | C | ||
| Clot-busting treatment | B | E | C↓ | C↑ | D | B | ||
| Specialist assessments | D | C | D | B↑ | D | C | ||
| Occupational therapy | A | B | A | B | A | A | ||
| Physiotherapy | B | B | A↑ | B | B | B | ||
| Speech and language therapy | A | E | A | C↑ | B | C | ||
| Team working | C | D | C | B↑ | C | C | ||
| Standards met by discharge | A | D | B↓ | B↑ | A | B | ||
| Discharge process | A | A | A | B↑ | A | A | ||
Appendix 2 Topic guide for patients and family members pre implementation
| Can you tell me about your experiences of being a patient on/or visiting a relative on the stroke unit? | What were some memorable experiences (positive or negative)? |
| Can you tell me something about a usual day? | What did/do you spend your time doing? |
| Patient: what opportunity was there for you to be active or do the things you want to do? | How much were you given the chance to have a go at things for yourself, and do the things you wanted to practice? |
| What opportunities are there for patients/families to be involved with their own activities? | Can you give me some examples of this, positive and negative? |
| Patient and staff: overall, what did you spend most of your time doing when on the stroke unit? | Not just during the day – what about in the evenings, weekends, or at other times? |
| What were your overall impressions of the ward and how it worked? | |
| How involved do you feel in your own therapy while a patient on the ward – what did you do outside your therapy sessions? | Before or after your physio/OT, speech and language therapy, what did you do? |
| Patient: what is the main reason for not practising or being active (in any way – this could mean doing a game, talking with others, not just physical activity)? | If there was something you wanted to do, what stopped you being able to do it? Were you encouraged by staff? |
|
Families: what impression did you have of the ward and how it worked? How much were you encouraged or did you become involved with helping your family member with their activities? |
|
| If you had to describe the experience of being on the stroke unit to anyone else, what would you say? |
Appendix 3 Topic guide for interviews with members of staff pre implementation
| Can you tell me about your experiences of working on the stroke unit? | What were some memorable experiences (positive or negative)? |
| Can you tell me something about a usual day? |
Can you take me step by step through what a usual day would look like, or was like? What did you do; if I was a fly on the wall what would I see you spending most of your time doing? |
| What opportunities are there for patients/families to be involved with their own activities? | Can you give me some examples of this, positive and negative? |
| Patient and staff: overall, what did you spend most of your time doing when on the stroke unit? | Not just during the day – what about in the evenings, weekends, or at other times? |
| What are your overall impressions of the ward and how it works? | |
| How much do patients do outside the scheduled therapy sessions? | How much unsupervised therapy do you see happening or encourage? |
| Staff: what is the main reason patients are not active outside scheduled therapy sessions? | If there was anything you would have liked to have provided for patients, what stopped you doing it? |
| Did you hear about the CREATE study? | How did you hear about CREATE? What are your thoughts on CREATE? |
| Is there anything else you would like to note about CREATE? | |
| If you had to describe the experience of working in the stroke unit to anyone else, what would you say? |
Appendix 4 Topic guide for patients and family members post implementation
-
Setting the scene: what co-design group were you part of? What did you do in your group? What was your contribution?
-
Feeling: what did you like/did not like? How did you like the experience-based co-design process (prompt – interview, film, feedback meetings)?
-
Group: how did you perceive your place in the co-design group? What did you think about the way in which group members worked with each other? What could have been improved?
-
Outcomes: are you happy with the changes made on the stoke unit? Did it meet your expectations? How could the outcomes be improved? Are some outcomes visible to you? If yes, how? If no, why do you think they are not being implemented? Are you satisfied with the outcomes? How could they be improved? What are things that help or hinder change from taking place? How do you think they can be sustainable?
-
Facilitation: what did you think about the help and support provided for the co-design groups? How could it have been better? Challenges?
-
The process: were there particular points in the process that you liked/did not like? How did you feel/what did you think at particular points in time?
-
For family members: what do you think the impact on your family member was? Positive/negative consequences of taking part in CREATE? Why?
-
Personal outcomes: what will you personally take away from participating in the study?
-
Any other thoughts?
Appendix 5 Topic guide for members of staff post implementation
-
Setting the scene: what group were you part of? What did you do in your group? What was your contribution?
-
Have you noticed anything being different in the unit? In terms of patient experience? In terms of activity?
-
Feeling: how did you like the process? What did you like/did not like?
-
Group: how did you perceive your place in the group? What did you think about the group dynamics? What did you like/not like? What could have been improved?
-
Outcomes: are you happy with the outcomes? Did it meet your expectations? How could the outcomes be improved? Are some outcomes visible to you? If yes, how? If no, why do you think they are not being implemented? Are you satisfied with the outcomes? How could they be improved?
-
What are barriers to/facilitators of introducing and embedding the interventions to the unit(s)?
-
Facilitation: what did you think about the overall process? Do you think working together with the patients and family members made a difference? How was CREATE different from other improvement projects you have been involved in? How could it have been better? Challenges?
-
The process: how did you perceive the process? Were there particular points in the process that you liked/did not like? How did you feel/what did you think at particular points in time? What had been the most important parts of the project? And why did you think they were important?
-
Work balance: in what ways has (or did) the EBCD process impact on or affect your working practice? Were there any challenges?
-
Long-term outcomes: what will you take away from the process?
-
Any other thoughts?
Appendix 6 Example ethnographic observations timetable
| Sunday 5 November | Monday 6 November | Tuesday 7 November | Wednesday 8 November | Thursday 9 November | Friday 10 November | Saturday 11 November |
|---|---|---|---|---|---|---|
| Late Ob KG | Early OB | Early ObIdentify 10 BM patients (need to be able to consent). Talk to them about the study. Leave PIS. Consent 10 BM patients. First check capacity. Fill out Pt reg. and Pt detail CRFS. Leave in site file | BM Early | Late Ob | Early Ob | |
| Sunday 12 November | Monday 13 November | Tuesday 14 November | Wednesday 15 November | Thursday 16 November | Friday 17 November | Saturday 18 November |
| Late Ob | Late Ob | Late ObIdentify 10 BM patients (need to be able to consent). Talk to them about the study. Leave PISConsent 10 BM patients. First check capacity. Fill out Pt reg. and Pt detail CRFS. Leave in site file | BM late | |||
| Sunday 19 November | Monday 20 November | Tuesday 21 November | Wednesday 22 November | Thursday 23 November | Friday 24 November | Saturday 25 November |
| Early ObIdentify 10 BM patients (need to be able to consent). Talk to them about the study. Leave PISConsent 10 BM patients. First check capacity. Fill out Pt reg. and Pt detail CRFS. Leave in site file | Late BM | Early Ob |
Appendix 7 Behavioural mapping protocol
CREATE (Collaborative rehabilitation in acute stroke) behavioural mapping protocol
Quick reference guidelines for completing observation day.
Aims
To estimate what proportion a weekday and weekend day, stroke survivors recovering on ward [. . .] spend in physical, social and cognitive activities.
The day before
Check with the staff which patients are suitable for observation (n = 10 are required).
The criteria for inclusion are:
-
Inpatient with a confirmed diagnosis of stroke.
-
Not being managed palliatively.
-
Able to understand English or have a family member who can act as an interpreter.
-
Able to give full informed consent on the day before the behavioural mapping.
-
Patient is happy to participate.
Check that the patients will consent to be observed.
You may want to explain to them about the research and tell them that you will be watching them every 10 minutes throughout the day to gather important information about their activity so that we may ultimately improve the care of people with stroke.
Tell staff which patients have consented to participate.
Confirm what bed the patients will be in the following day.
You will need to check this again in the morning as patient locations change. Also check that the patients are not going home that day. If there is a plan for the patient to be discharged in the morning then do not bother including them. If the patient may be discharged later that day, it is worth including them just in case.
Spreadsheets
Prepare the behavioural mapping spreadsheet so that no copying is required on the day of observations, including adding the date and time, in advance.
Procedure
The following procedure reflects what was performed as a part of the Enriched Environment Post Stroke Trial. We have adapted this protocol and the following procedures to meet the requirements of the CREATE study. Any modifications to the protocol must be agreed with Fiona Jones and David Clarke.
On the day
Observation time and breaks
Observations should be conducted between 08.00 and 17.30 (nine and a half hours) at 10-minute intervals. This will generate 48 observations per day (allowing for breaks).
Schedule four breaks of 15 minutes each throughout the day by picking a time out of a hat. Mark your break times on the sheet.
Standardised route
At the commencement of each 10-minute observation period, the researcher will begin observations from the same location, designated as the START LOCATION. The researcher will then proceed along a predetermined route, completing the standardised observational spreadsheet for each patient as they become visible. The researcher will then back track along this same route completing data for patients who may have not been observed during the initial walkthrough. Make sure you know where the quiet rooms, TV rooms and other common locations that patients may use are located. If they are adjacent to the ward, these should be visited.
Duration of each observation
During each 10-minute interval, the data for each patient will be based on an observation made by the researcher over a period no longer than 5 seconds. The researcher will position themselves so that the patient can be easily seen (but at the same time taking steps to be inconspicuous) and will then note where they are, who they are with and what they are doing. The patient can be recorded as performing more than one type of activity (i.e. physical, cognitive or social) at once. Once the researcher has noted all this information, data collection for this patient is complete and the researcher will move onto the next patient. Observations begin at the commencement of each 10-minute interval (i.e. 8.00 a.m., 8.10 a.m., 8.20 a.m., 8.30 a.m., etc.).
Unobserved epochs (10-minute period)
If the researcher is unable to either view or clearly view a patient during a 10-minute observation period, firstly, this observation should be clearly marked as unobserved. Then when clearly visible once more, the researcher is to either question the patient, staff or carer regarding where, who and what they themselves or the patient were doing. If activity is estimated via this process, this should be noted in the comments section as EST and the appropriate boxes completed. Activity estimates should err on the side of underestimating the activity. If this information is not easily or reliably able to be obtained, the patient should be marked as ‘unobserved’.
Explanation of terms used on spreadsheet
Location
Where in the hospital the patient is located (see list below). The patient can only ever be in one location.
Bedside: Within and around own room or bed.
In bed.
Therapy: Gym and all other allied health therapy/meeting rooms (includes OT kitchen).
Communal areas: Dining room/day room/reception area/nurses station/hallway.
Amenities: Toilet, shower or wash basin.
Offsite: Attending tests at another facility/home visit.
Outside: Cafe/walking or being wheeled in corridor/meeting room (i.e. relatives’ room).
People present
Who is with the patient?
More specifically, ‘people present’ is defined as any person in the near vicinity of the patient which is conducive to interaction. There is potential for more than one type of person to be with the patient.
Alone: No person/people in the near vicinity of the patient that is conducive to interaction.
Medical staff: Doctors.
Registered nurse.
Student nurse.
HCA: Health-care assistant.
PT: Physiotherapist.
OT: Occupational therapist.
ST: Speech and language therapist.
Therapy student.
Therapy assistant.
Ward orderly/kitchen staff/cleaner.
Patients: Patients within their own room or bay and patients visiting from elsewhere in the hospital.
Visitors: Including patient’s own and neighbouring patient’s family and friends.
Other: Contractors or those non-specified.
Interacting: State if patient is interacting with the person (people) present or not. Y for yes, N for no.
What patient is doing (type of activity)
Activity: a specific deed, action, function, or sphere of action.
Physical activity: everyday, personal, recreational or occupational activities that require physical skills and utilise strength, power, endurance, flexibility, range of motion or agility. Examples include: sitting unsupported, standing, walking, actively transferring with or without assistance, upper limb (UL) exercises, dressing, eating and grooming.
Repositioning in bed: State who is repositioning the patient. I for independent, N for nurse, T for therapist, C for carer.
Transfers: State who is transferring the patient. I for independent, N for nurse, T for therapist, C for carer.
Mobilising: State who is mobilising the patient. I for independent, N for nurse, T for therapist, C for carer.
ADLs (activities of daily living): Everyday activities generally involving functional mobility and personal care, such as bathing, brushing teeth, dressing, toileting and eating. (These activities are sometime referred to as PADLs – personal activities of daily living. For the purposes of this research we will use the term ADLs.)
DADLs (Domestic activities of daily living): These include household tasks such as shopping, cooking, laundry and cleaning.
Independent practice: Patient practising tasks or exercises prescribed by the therapists.
Cognitive activity: any non-physical leisure activity which involves the patient actively engaging in a mental task such as: reading a book, magazine or newspaper, listening to music or the radio, crosswords, puzzles, games, speech language exercises, OT cognitive exercises, video games, talking in a group situation, writing, computer use, playing a musical instrument, watching the television.
Social activity: any interaction which involves verbal communication with people present or through telecommunication devices, and other non-verbal interactions. These include: talking, laughing, crying, touching, kissing, holding, telephone, mobile phone, e-mail, group activities, internet forum use. For the purpose of analysis, social activity will be defined as those observations when the patient is interacting with the people present in the above outlined verbal and non-verbal ways. Additionally, observations made when the patient was communicating with others through the use of either a telephone or during online activities will also be included in the estimations of time spent in social activities.
Distinguishing between categories
Reading and writing: is to be categorised as a cognitive activity.
Group activities: if observed in group activities, there is the potential for the patient to be engaged in more than one type of activity. For example, talking while performing upper limb tasks in an upper limb group. If though, on observation the patient is in a position or situation conducive to interaction (as per the definition of ‘people present’), and no physical activity is observed, only social activity will be recorded.
Appendix 8 Rapid evidence synthesis
Search strategy (MEDLINE example)
Database: Ovid MEDLINE(R).
Date of search: February 2016.
Date range searched: 1996 to November week 3 2015.
-
co-produc*.tw. (1149)
-
coproduc*.tw. (620)
-
co design*.tw. (53)
-
codesign*.tw. (16)
-
co creat*.tw. (171)
-
cocreat*.tw. (52)
-
(co research and design).tw. (1)
-
experience based design*.tw. (7)
-
participatory design*.tw. (149)
-
(experience adj3 design).tw. (252)
-
(evidence* adj2 design*).tw. (550)
-
EBC?.tw. (1604)
-
collaborative design.tw. (44)
-
human centred design.tw. (10)
-
human centered design.tw. (38)
-
people centred design.tw. (0)
-
people centered design.tw. (0)
-
inclusive design.tw. (32)
-
practice led design.tw. (1)
-
practice based design.tw. (2)
-
interactive design.tw. (31)
-
open design.tw. (147)
-
user centred design.tw. (51)
-
user centered design.tw. (177)
-
or/1-24 [co-design] (5093)
-
(acute adj (setting* or hospital* or care or healthcare)).tw. (15,023)
-
((secondary or speciali?ed) adj care).tw. (4410)
-
hospital care.tw. (4817)
-
exp Hospitals/ (117,870)
-
Hospitalization/ (52,132)
-
(hospitali?ation* or hospitali?ed).tw. (119,506)
-
Inpatients/ (12,602)
-
inpatient*.tw. (52,413)
-
emergency medicine/ (8188)
-
Emergency treatment/ (8750)
-
emergency hospital admission*.tw. (240)
-
emergency hospitali#ation.tw. (116)
-
critical care/ (14,911)
-
ambulatory care/ (20,495)
-
urgent care.tw. (960)
-
or/26-40 [acute terms] (343,100)
-
Delivery of Health Care/ (45,257)
-
Efficiency, Organizational/ (17,793)
-
Efficiency/ (4714)
-
Health Services Research/ (23,584)
-
"Outcome Assessment (Health Care)"/ (50,681)
-
patient outcome assessment/ (1713)
-
exp Program Evaluation/ (54,529)
-
Quality Assurance, Health Care/ (38,609)
-
Quality Improvement/ (9440)
-
Quality Indicators, Health Care/ (11,744)
-
Quality of Health Care/ (43,880)
-
(bench mark* or benchmark*).tw,kf. (17,315)
-
(delivery adj2 health*).tw,kf. (12,585)
-
(efficien* adj2 (assess* or assurance* or evaluat* or improv* or indicat* or measur* or test*)).tw,kf. (23,714)
-
(performance adj2 (assess* or assurance* or evaluat* or improv* or indicat* or measur* or test*)).tw,kf. (74,378)
-
(outcome* adj2 (assess* or assurance* or evaluat* or improv* or indicat* or measur* or test*)).tw,kf. (256,084)
-
(program* adj2 (assess* or assurance* or evaluat* or improv* or indicat* or measur* or test*)).tw,kf. (27,836)
-
or/42-58 [outcome or evaluation terms] (611,767)
-
25 and 41 and 59 [co-design and acute care and outcome or evaluation terms] (45)
-
exp animals/not humans.sh. (2,031,513)
-
60 not 61 [human only studies] (45)
-
limit 62 to (english language and yr="2005 - 2015") (40).
Inclusion criteria
Reports research using a co-creation or co-production, or co-design or experience-based co-design approach in an acute health-care setting.
Reports patient or staff or organisational outcomes resulting from research using a co-creation, co-production, co-design, experience-based co-design approach in an acute health-care setting.
Outcomes of interest include:
-
any measure of the outcome of co-produced interventions on patient focused quality improvements in acute health-care settings as reported by patients or families or caregivers, or health service providers
-
including patient-reported outcome measures and patient- or staff-reported experience measures
-
using qualitative or quantitative data.
Acute health-care settings include:
-
emergency departments/accident and emergency departments
-
adult inpatient facilities, including acute medical or surgical admission units (often termed MAUs or SAUs), acute medical or surgical units, acute trauma units, acute neurological units, intensive or critical care units, acute care of the elderly or geriatric units, medical oncology or cancer services
-
adult outpatient facilities including medical, surgical, trauma, neurology, care of the elderly or geriatrics, medical oncology or cancer services.
Appendix 9 Demographic information
| Characteristic | Site 1 pre, n (%) | Site 2 pre, n (%) | Site 3 pre, n (%) | Site 4 pre, n (%) | Site 1 post, n (%) | Site 2 post, n (%) | Site 3 post, n (%) | Site 4 post, n (%) |
|---|---|---|---|---|---|---|---|---|
| Ethnicity | ||||||||
| White | 19 (86) | 45 (100) | 17 (63) | 12 (92) | 21 (84) | 30 (97) | 8 (73) | 11 (100) |
| Asian/Asian British | 2 (9) | 0 (0) | 5 (19) | 1 (8) | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
| Black/black British | 1 (5) | 0 (0) | 3 (11) | 0 (0) | 0 (0) | 0 (0) | 2 (18) | 0 (0) |
| Mixed | 0 (0) | 0 (0) | 1 (4) | 0 (0) | 0 (0) | 0 (0) | 1 (9) | 0 (0) |
| Chinese | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
| Other | 0 (0) | 0 (0) | 0 (0) | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 0 (0) | 1 (4) | 0 (0) | 2 (8) | 1 (3) | 2 (18) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 14 (100) | 25 (100) | 31 (100) | 13 (100) | 11 (100) |
| Sex | ||||||||
| Male | 10 (46) | 26 (58) | 15 (56) | 3 (23) | 11 (44) | 9 (29) | 3 (27) | 7 (64) |
| Female | 12 (55) | 19 (42) | 11 (41) | 10 (77) | 12 (48) | 21 (68) | 8 (73) | 4 (36) |
| Missing | 0 (0) | 0 (0) | 1 (4) | 0 (0) | 2 (8) | 1 (3) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| Age range (years) | ||||||||
| 30–39 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4) | 1 (3) | 0 (0) | 0 (0) |
| 40–49 | 2 (9) | 1 (2) | 0 (0) | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| 50–59 | 5 (23) | 1 (2) | 1 (4) | 0 (0) | 2 (8) | 2 (7) | 0 (0) | 0 (0) |
| 60–69 | 0 (0) | 8 (18) | 8 (30) | 8 (62) | 4 (16) | 2 (7) | 1 (9) | 2 (18) |
| ≥ 70 | 15 (68) | 35 (78) | 17 (63) | 5 (39) | 16 (64) | 24 (77) | 10 (91) | 9 (82) |
| Missing | 0 (0) | 0 (0) | 1 (4) | 0 (0) | 2 (8) | 1 (3) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| Marital status | ||||||||
| Single | 2 (9) | 1 (2) | 16 (59) | 1 (8) | 5 (20) | 2 (7) | 0 (0) | 1 (9) |
| Married | 14 (64) | 30 (67) | 1 (4) | 8 (62) | 8 (32) | 11 (36) | 6 (55) | 6 (55) |
| Remarried | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (9) |
| Separated | 1 (5) | 1 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Widowed | 4 (18) | 11 (24) | 5 (19) | 2 (15) | 7 (28) | 16 (2) | 4 (36) | 0 (0) |
| Divorced | 1 (5) | 2 (4) | 2 (7) | 2 (15) | 2 (8) | 1 (3) | 1 (9) | 3 (27) |
| Missing | 0 (0) | 0 (0) | 1 (4) | 0 (0) | 3 (12) | 1 (3) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| Highest level of education | ||||||||
| No qualifications | 12 (54) | 23 (51) | 5 (19) | 2 (15) | 10 (40) | 15 (48) | 4 (36) | 6 (55) |
| O level/CSE/GCSE | 3 (14) | 7 (16) | 7 (26) | 4 (31) | 4 (16) | 9 (29) | 2 (18) | 0 (0) |
| A/AS level | 2 (9) | 2 (4) | 3 (11) | 2 (15) | 1 (4) | 1 (3) | 1 (9) | 2 (18) |
| First degree | 0 (0) | 5 (11) | 0 (0) | 1 (8) | 0 (0) | 2 (7) | 0 (0) | 0 (0) |
| Higher degree | 2 (9) | 2 (4) | 1 (4) | 2 (15) | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
| NVQ/HNC/HND | 1 (5) | 2 (4) | 2 (7) | 0 (0) | 1 (4) | 0 (0) | 0 (0) | 1 (9) |
| Other | 1 (5) | 4 (9) | 6 (22) | 1 (8) | 2 (8) | 3 (10) | 1 (9) | 2 (18) |
| Missing | 1 (5) | 0 (0) | 3 (11) | 1 (8) | 6 (24) | 1 (3) | 3 (27) | 0 (0) |
| Total | 21 (96) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| First stay on unit? | ||||||||
| No | 1 (5) | 6 (13) | 1 (4) | 0 (0) | 0 (0) | 4 (13) | 4 (36) | 8 (82) |
| Yes | 21 (96) | 38 (84) | 25 (93) | 13 (100) | 23 (92) | 25 (81) | 7 (64) | 3 (18) |
| Missing | 0 (0) | 1 (2) | 1 (4) | 0 (0) | 2 (8) | 2 (7) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| Length of stay | ||||||||
| < 1 month | 10 (46) | 31 (69) | 17 (63) | 11 (85) | 15 (60) | 18 (58) | 8 (73) | 6 (55) |
| 1–3 months | 11 (50) | 10 (22) | 8 (30) | 2 (15) | 8 (32) | 9 (29) | 3 (27) | 5 (45) |
| 4–6 months | 1 (5) | 3 (7) | 1 (4) | 0 (0) | 0 (0) | 3 (10) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (2) | 1 (4) | 0 (0) | 2 (8) | 1 (3) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| Discharge destination | ||||||||
| Home | 21 (96) | 42 (93) | 23 (85) | 11 (85) | 22 (88) | 28 (90) | 11 (100) | 9 (82) |
| To supported accommodation | 0 (0) | 1 (2) | 0 (0) | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| To stay with friends or relatives | 0 (0) | 1 (2) | 0 (0) | 1 (8) | 0 (0) | 1 (3) | 0 (0) | 1 (9) |
| To a nursing home | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (9) |
| Other | 1 (5) | 0 (0) | 3 (11) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (2) | 1 (4) | 1 (8) | 3 (12) | 1 (3) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
| Who completed the questionnaire? | ||||||||
| The person who was the patient in the hospital | 15 (68) | 18 (40) | 14 (52) | 9 (69) | 14 (56) | 23 (74) | 3 (27) | 5 (46) |
| A friend or relative of the patient | 3 (14) | 5 (11) | 5 (19) | 3 (23) | 6 (24) | 3 (10) | 3 (27) | 1 (9) |
| Both the patient and a friend or relative together | 4 (18) | 18 (40) | 6 (22) | 1 (8) | 3 (12) | 3 (10) | 5 (46) | 5 (46) |
| The patient with the help of a health professional | 0 (0) | 2 (4) | 1 (4) | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 2 (4) | 1 (4) | 0 (0) | 2 (8) | 1 (3) | 0 (0) | 0 (0) |
| Total | 22 (100) | 45 (100) | 27 (100) | 13 (100) | 25 (100) | 31 (100) | 11 (100) | 11 (100) |
Appendix 10 Patient-reported outcome measure data
| Outcome | Site 1 pre (autumn 2016) | Site 1 post (October 2017) | Site 2 pre (September 2016) | Site 2 post (October 2017) | Site 3 pre (October 2018) | Site 3 post (October 2018) | Site 4 pre (February 2018) | Site 4 post (October 2018) |
|---|---|---|---|---|---|---|---|---|
| Since your stroke, how much difficulty do you have dressing yourself fully? (%) | ||||||||
| No difficulty at all | 32 | 40 | 37 | 32 | 30 | 18 | 54 | 40 |
| Slight difficulty | 26 | 28 | 17 | 26 | 7 | 27 | 23 | 30 |
| Some difficulty | 11 | 20 | 32 | 26 | 30 | 9 | 8 | 20 |
| A lot of difficulty | 0 | 11 | 8 | 2 | 10 | 4 | 0 | 0 |
| I cannot dress myself fully | 21 | 4 | 12 | 3 | 26 | 46 | 15 | 10 |
| Since your stroke, how much difficulty do you have moving around all areas? (%) | ||||||||
| No difficulty at all | 26 | 28 | 29 | 29 | 26 | 9 | 46 | 27 |
| Slight difficulty | 21 | 28 | 24 | 29 | 19 | 27 | 15 | 36 |
| Some difficulty | 37 | 32 | 34 | 16.10 | 19 | 18.00 | 23 | 18 |
| A lot of difficulty | 5 | 4 | 12 | 16.10 | 7 | 9.00 | ||
| I cannot move around all areas of my home | 11 | 8 | 0 | 6.5 | 26 | 36.0 | 15 | 9 |
| Since your stroke, how satisfied are you with your overall ability to perform daily activities in and around the home? (%) | ||||||||
| Completely satisfied | 11 | 28 | 17 | 22.60 | 22 | 9.00 | 31 | 20 |
| Mostly satisfied | 16 | 12 | 27 | 29 | 30 | 18 | 39 | 50 |
| Fairly satisfied | 47 | 40 | 32 | 16.10 | 15 | 18.00 | 23 | 20 |
| Not very satisfied | 16 | 12 | 22 | 22.60 | 11 | 18.00 | ||
| Completely dissatisfied | 11 | 8 | 2 | 6.50 | 15 | 36.00 | 8 | 10 |
| Since your stroke, how much difficulty do you have shopping for or carrying a few items when at the shops? (%) | ||||||||
| No difficulty at all | 16 | 24 | 28 | 16 | 19 | 9 | 39 | 10 |
| Slight difficulty | 11 | 12 | 8 | 23 | 11 | 18 | 23 | 30 |
| Some difficulty | 11 | 24 | 18 | 7 | 7 | 9 | 15 | 30 |
| A lot of difficulty | 11 | 4 | 5 | 7 | 11 | 9 | 8 | 20 |
| I cannot shop for and carry a few items | 53 | 32 | 41 | 45 | 48 | 46 | 8 | 10 |
| Since your stroke, how independent are you in your ability to move around your local neighbourhood? (%) | ||||||||
| I am completely independent | 16 | 28 | 24 | 26 | 19 | 9 | 39 | 20 |
| I prefer to have someone else with me | 11 | 8 | 20 | 10 | 22 | 18 | 31 | 50 |
| I need occasional assistance from someone | 16 | 32 | 22 | 19 | 11 | 9 | 8 | |
| I need assistance much of the time | 21 | 12 | 15 | 16 | 11 | 8 | ||
| I am completely dependent on others | 37 | 20 | 20 | 26 | 33 | 64 | 15 | 30 |
| Since your stroke, how often do you feel bored with your free time at home? (%) | ||||||||
| I am never bored with my free time | 21 | 32 | 46 | 37 | 37 | 55 | 31 | 40 |
| A little of my free time | 11 | 28 | 15 | 23 | 11 | 9 | 23 | 10 |
| Some of my free time | 47 | 20 | 32 | 23 | 19 | 18 | 31 | 40 |
| Most of my free time | 21 | 16 | 5 | 10 | 19 | 8 | ||
| All of my free time | 2 | 3 | 11 | 18 | 8 | 10 | ||
| Since your stroke, how would you describe the amount of communication between you and your friends/associates? (%) | ||||||||
| A great deal | 26 | 28 | 15 | 19 | 19 | 27 | 39 | 20 |
| Quite a lot | 36 | 36 | 32 | 32 | 22 | 27 | 31 | 20 |
| Some | 27 | 20 | 34 | 10 | 19 | 36 | 23 | 30 |
| A little bit | 8 | 15 | 26 | 26 | 8 | 30 | ||
| None | 5 | 10 | 11 | 9 | ||||
| Since your stroke, how satisfied are you with the level of interests and activities you share with your friends/associates? (%) | ||||||||
| Completely satisfied | 16 | 20 | 17 | 32 | 15 | 27 | 31 | 10 |
| Mostly satisfied | 37 | 16 | 29 | 13 | 30 | 36 | 39 | 30 |
| Fairly satisfied | 11 | 32 | 27 | 23 | 19 | 18 | 15 | 40 |
| Not very satisfied | 37 | 20 | 22 | 23 | 19 | 9 | 8 | 10 |
| Completely dissatisfied | 8 | 5 | 7 | 15 | 9 | 8 | 10 | |
| Since your stroke, how often do you visit friends/others? (%) | ||||||||
| Most days | 11 | 16 | 20 | 13 | 4 | 9 | 39 | |
| At least once a week | 42 | 32 | 27 | 26 | 30 | 27 | 31 | 22 |
| At least once a fortnight | 11 | 12 | 13 | 4 | 9 | 23 | 44 | |
| Once a month or less | 21 | 20 | 17 | 19 | 19 | 9 | 22 | |
| Never | 16 | 24 | 24 | 26 | 37 | 46 | 8 | 11 |
| Since your stroke, how do you feel about your appearance when out in public? (%) | ||||||||
| Perfectly happy | 47 | 52 | 60 | 58 | 44 | 46 | 54 | 56 |
| Slightly self-conscious | 26 | 24 | 21 | 13 | 19 | 27 | 23 | 33 |
| Fairly self-conscious | 16 | 8 | 7 | 7 | 11 | 18 | 8 | |
| Very self-conscious | 5 | 7 | 13 | 11 | 8 | |||
| I try to avoid going out in public | 5 | 4 | 5 | 7 | 11 | 9 | 8 | 11 |
| Mobility (%) | ||||||||
| No problems walking about | 42 | 28 | 33 | 30 | 33 | 27 | 31 | 33 |
| Some problems in walking about | 53 | 68 | 67 | 67 | 48 | 46 | 54 | 56 |
| Confined to bed | 5 | 4 | 3 | 15 | 18 | 15 | 11 | |
| Self-care (%) | ||||||||
| No problems with self-care | 42 | 60 | 52 | 55 | 37 | 27 | 77 | 78 |
| Some problems washing or dressing | 47 | 36 | 43 | 36 | 41 | 27 | 15 | 11 |
| Unable to wash or dress self | 11 | 4 | 5 | 10 | 19 | 46 | 8 | 11 |
| Usual activities (%) | ||||||||
| No problems performing usual activities | 16 | 28 | 24 | 36 | 26 | 18 | 23 | 44 |
| Some problems performing usual activities | 47 | 48 | 49 | 45 | 37 | 46 | 62 | 33 |
| Unable to perform usual activities | 37 | 24 | 27 | 19 | 33 | 36 | 15 | 22 |
| Pain/discomfort (%) | ||||||||
| No pain or discomfort | 37 | 64 | 55 | 45 | 37 | 36 | 46 | 44 |
| Moderate pain or discomfort | 58 | 32 | 45 | 52 | 37 | 64 | 46 | 44 |
| Extreme pain or discomfort | 5 | 4 | 3 | 22 | 8 | 11 | ||
| Anxiety/depression (%) | ||||||||
| Not anxious or depressed | 50 | 48 | 48 | 48 | 44 | 36 | 62 | 44 |
| Moderately anxious or depressed | 50 | 36 | 45 | 45 | 41 | 46 | 31 | 44 |
| Extremely anxious or depressed | 16 | 7 | 7 | 11 | 9 | 8 | 11 | |
| Symptoms (%) | ||||||||
| No symptoms at all | 16 | 20 | 10 | 10 | 15 | 10 | 15 | |
| I have a few symptoms but these do not interfere with my daily life | 21 | 8 | 19 | 26 | 15 | 31 | 22 | |
| I have symptoms which have caused some changes in my life but I am still able to look after myself | 26 | 32 | 26 | 23 | 26 | 46 | 31 | 67 |
| I have symptoms which have significantly changed my life and I need some help in looking after myself | 21 | 16 | 26 | 26 | 15 | |||
| I have quite severe symptoms which mean I need to have help from other people but I am not so bad | 16 | 14 | 13 | |||||
| I have major symptoms which severely handicap me and I need constant attention day and night | 16 | 5 | 3 | 9 | 27 | 8 | 9 | |
Appendix 11 Patient-reported experience measure data
| Site | Response (%) | ||||
|---|---|---|---|---|---|
| Mostly agree | Mostly disagree | Not sure | Not applicable | ||
| When I arrived, I was given information about the unit and what would happen during my stay | |||||
| Site 1 pre | 36 | 32 | 32 | ||
| Site 2 pre | 48 | 18 | 30 | ||
| Site 3 pre | 37 | 22 | 37 | ||
| Site 4 pre | 46 | 8 | 46 | ||
| Site 1 post | 36 | 28 | 28 | 4 | |
| Site 2 post | 40 | 13 | 43 | 3 | |
| Site 3 post | 27 | 36 | 36 | ||
| Site 4 post | 46 | 27 | 27 | ||
| The facilities on the unit were good | |||||
| Site 1 pre | 82 | 9 | 9 | ||
| Site 2 pre | 82 | 14 | 5 | ||
| Site 3 pre | 82 | 9 | 9 | ||
| Site 4 pre | 85 | 8 | 8 | ||
| Site 1 post | 72 | 8 | 12 | 4 | |
| Site 2 post | 86 | 10 | 3 | ||
| Site 3 post | 82 | 9 | 9 | ||
| Site 4 post | 73 | 27 | |||
| There was somewhere secure to keep my belongings | |||||
| Site 1 pre | 54 | 41 | 4 | ||
| Site 2 pre | 68 | 16 | 16 | ||
| Site 3 pre | 64 | 9 | 23 | ||
| Site 4 pre | 62 | 23 | 15 | ||
| Site 1 post | 60 | 8 | 24 | 4 | |
| Site 2 post | 77 | 10 | 10 | ||
| Site 3 post | 64 | 9 | 23 | ||
| Site 4 post | 82 | 9 | 9 | ||
| I was able to discuss personal matters in private | |||||
| Site 1 pre | 67 | 29 | 5 | ||
| Site 2 pre | 51 | 29 | 13 | ||
| Site 3 pre | 73 | 9 | 18 | ||
| Site 4 pre | 46 | 31 | 23 | ||
| Site 1 post | 56 | 12 | 20 | 8 | |
| Site 2 post | 62 | 17 | 14 | 7 | |
| Site 3 post | 73 | 9 | 18 | ||
| Site 4 post | 55 | 27 | 18 | ||
| There were enough things to do in my free time | |||||
| Site 1 pre | 4 | 36 | 59 | ||
| Site 2 pre | 27 | 55 | 18 | ||
| Site 3 pre | 9 | 46 | 36 | 9 | |
| Site 4 pre | 69 | 23 | 8 | ||
| Site 1 post | 40 | 24 | 24 | 8 | |
| Site 2 post | 50 | 23 | 20 | ||
| Site 3 post | 9 | 46 | 36 | 9 | |
| Site 4 post | 36 | 18 | 36 | 9 | |
| There was a friendly atmosphere on the unit | |||||
| Site 1 pre | 91 | 4 | 4 | ||
| Site 2 pre | 86 | 9 | 5 | ||
| Site 3 pre | 100 | ||||
| Site 4 pre | 77 | 15 | 8 | ||
| Site 1 post | 80 | 12 | 4 | 4 | |
| Site 2 post | 86 | 3 | 10 | ||
| Site 3 post | 100 | ||||
| Site 4 post | 91 | 9 | |||
| I felt the staff really cared about me | |||||
| Site 1 pre | 68 | 14 | 18 | ||
| Site 2 pre | 87 | 7 | 5 | ||
| Site 3 pre | 82 | 9 | 9 | ||
| Site 4 pre | 77 | 15 | 8 | ||
| Site 1 post | 76 | 12 | 8 | 4 | |
| Site 2 post | 93 | 3 | 3 | ||
| Site 3 post | 82 | 9 | 9 | ||
| Site 4 post | 91 | 9 | |||
| The staff worked well as a team | |||||
| Site 1 pre | 67 | 10 | 24 | ||
| Site 2 pre | 84 | 14 | 2 | ||
| Site 3 pre | 82 | 18 | |||
| Site 4 pre | 85 | 8 | 8 | ||
| Site 1 post | 80 | 8 | 8 | 4 | |
| Site 2 post | 97 | 0 | 3 | ||
| Site 3 post | 82 | 18 | |||
| Site 4 post | 91 | 9 | |||
| I felt able to talk to the staff about any problems I had | |||||
| Site 1 pre | 62 | 14 | 24 | ||
| Site 2 pre | 80 | 16 | 5 | ||
| Site 3 pre | 64 | 9 | 27 | ||
| Site 4 pre | 77 | 15 | 8 | ||
| Site 1 post | 52 | 24 | 16 | 4 | |
| Site 2 post | 76 | 7 | 10 | ||
| Site 3 post | 64 | 9 | 27 | ||
| Site 4 post | 70 | 30 | |||
| I was asked what I wanted to achieve during my stay | |||||
| Site 1 pre | 36 | 32 | 27 | 4 | |
| Site 2 pre | 27 | 32 | 39 | ||
| Site 3 pre | 46 | 18 | 36 | ||
| Site 4 pre | 42 | 25 | 25 | 8 | |
| Site 1 post | 40 | 28 | 20 | 8 | 4 |
| Site 2 post | 44 | 15 | 33 | 7 | |
| Site 3 post | 40 | 28 | 20 | 8 | 4 |
| Site 4 post | 64 | 9 | 27 | ||
| I felt as though the staff and I were partners in the whole process of care | |||||
| Site 1 pre | 50 | 36 | 14 | ||
| Site 2 pre | 75 | 9 | 16 | ||
| Site 3 pre | 64 | 18 | 18 | ||
| Site 4 pre | 77 | 8 | 8 | 8 | |
| Site 1 post | 52 | 24 | 12 | 8 | |
| Site 2 post | 75 | 7 | 14 | ||
| Site 3 post | 52 | 24 | 12 | 8 | |
| Site 4 post | 73 | 9 | 18 | ||
| The staff kept me informed every step of the way | |||||
| Site 1 pre | 41 | 46 | 14 | ||
| Site 2 pre | 61 | 21 | 18 | ||
| Site 3 pre | 73 | 9 | 18 | ||
| Site 4 pre | 69 | 23 | 8 | ||
| Site 1 post | 56 | 32 | 8 | ||
| Site 2 post | 63 | 22 | 15 | ||
| Site 3 post | 56 | 32 | 8 | ||
| Site 4 post | 64 | 18 | 18 | ||
| My family or carer was involved in discussions about my treatment if I wanted them to be | |||||
| Site 1 pre | 73 | 18 | 4 | 4 | |
| Site 2 pre | 82 | 11 | 2 | ||
| Site 3 pre | 100 | ||||
| Site 4 pre | 68 | 15 | 8 | 8 | |
| Site 1 post | 72 | 12 | 8 | 4 | |
| Site 2 post | 82 | 7 | 0 | 11 | |
| Site 3 post | 72 | 12 | 8 | 4 | |
| Site 4 post | 73 | 27 | 0 | ||
| I am happy with the amount of therapy or treatment I received for (where applicable) | |||||
| Swallowing problems | |||||
| Site 1 pre | 67 | 11 | 22 | ||
| Site 2 pre | 85 | 0 | 15 | ||
| Site 3 pre | 27 | 9 | 9 | 45 | |
| Site 4 pre | 100 | ||||
| Site 1 post | 20 | 8 | 22 | 64 | |
| Site 2 post | 73 | 18 | 9 | ||
| Site 3 post | 20 | 8 | 22 | 64 | |
| Site 4 post | 71 | 14 | 14 | ||
| Speech and communication | |||||
| Site 1 pre | 80 | 13 | 7 | ||
| Site 2 pre | 95 | 0 | 5 | ||
| Site 3 pre | 46 | 9 | 9 | 36 | |
| Site 4 pre | 100 | ||||
| Site 1 post | 36 | 8 | 4 | 48 | |
| Site 2 post | 95 | 5 | 0 | ||
| Site 3 post | 36 | 8 | 4 | 48 | |
| Site 4 post | 63 | 13 | 25 | ||
| Improving mobility | |||||
| Site 1 pre | 80 | 10 | 10 | ||
| Site 2 pre | 83 | 14 | 3 | ||
| Site 3 pre | 9 | 82 | 9 | ||
| Site 4 pre | 90 | 10 | |||
| Site 1 post | 68 | 12 | 16 | ||
| Site 2 post | 95 | 5 | 0 | ||
| Site 3 post | 68 | 12 | 16 | ||
| Site 4 post | 91 | 9 | |||
| Independent living | |||||
| Site 1 pre | 56 | 39 | 6 | ||
| Site 2 pre | 82 | 11 | 8 | ||
| Site 3 pre | 36 | 55 | 9 | ||
| Site 4 pre | 78 | 11 | 11 | ||
| Site 1 post | 56 | 8 | 4 | 28 | |
| Site 2 post | 91 | 9 | 0 | ||
| Site 3 post | 56 | 8 | 4 | 28 | |
| Site 4 post | 91 | 9 | |||
| Continence | |||||
| Site 1 pre | 57 | 36 | 7 | ||
| Site 2 pre | 42 | 33 | 25 | ||
| Site 3 pre | 27 | 64 | 9 | ||
| Site 4 pre | 75 | 25 | |||
| Site 1 post | 28 | 12 | 4 | 52 | |
| Site 2 post | 93 | 7 | 0 | ||
| Site 3 post | 28 | 12 | 4 | 52 | |
| Site 4 post | 50 | 50 | |||
| I received enough emotional support | |||||
| Site 1 pre | 35 | 30 | 25 | 10 | |
| Site 2 pre | 67 | 19 | 7 | ||
| Site 3 pre | 9 | 46 | 46 | ||
| Site 4 pre | 62 | 15 | 15 | 8 | |
| Site 1 post | 44 | 24 | 20 | 8 | |
| Site 2 post | 64 | 11 | 18 | ||
| Site 3 post | 44 | 24 | 20 | 8 | |
| Site 4 post | 46 | 9 | 46 | ||
| I felt well-supported and prepared for my discharge | |||||
| Site 1 pre | 54 | 32 | 14 | ||
| Site 2 pre | 81 | 16 | 2 | ||
| Site 3 pre | 73 | 18 | 9 | ||
| Site 4 pre | 77 | 8 | 8 | 8 | |
| Site 1 post | 56 | 20 | 12 | 8 | |
| Site 2 post | 86 | 7 | 4 | ||
| Site 3 post | 56 | 20 | 12 | 8 | |
| Site 4 post | 64 | 27 | 9 | ||
| I am satisfied with progress made during my stay | |||||
| Site 1 pre | 73 | 14 | 14 | ||
| Site 2 pre | 81 | 12 | 7 | ||
| Site 3 pre | 73 | 9 | 18 | ||
| Site 4 pre | 85 | 8 | 8 | ||
| Site 1 post | 76 | 16 | 4 | ||
| Site 2 post | 86 | 4 | 11 | ||
| Site 3 post | 76 | 16 | 4 | ||
| Site 4 post | 82 | 18 | |||
Appendix 12 Patient-reported experience measure data: feelings
| Feeling | Site 1 pre | Site 1 post | Site 2 pre | Site 2 post | Site 3 pre | Site 3 post | Site 4 pre | Site 4 post |
|---|---|---|---|---|---|---|---|---|
| Patronised | 9.1% | 8% | 4% | 0% | 11.1% | 0% | 8% | 0% |
| Respected | 54.5% | 60% | 62% | 65% | 70.4% | 70% | 69% | 64% |
| Offended | 4.5% | 4% | 2% | 3% | 0% | 0% | 8% | 0% |
| Supported | 81.8% | 64% | 78% | 65% | 70.4% | 80% | 85% | 64% |
| Ignored | 4.5% | 16% | 2% | 0% | 11.1% | 10% | 8% | 9% |
| Listened to | 40.9% | 40% | 40% | 36% | 59.3% | 50% | 62% | 64% |
| Frustrated | 4.5% | 12% | 22% | 3% | 25.9% | 10% | 8% | 9% |
| Motivated | 27.3% | 36% | 29% | 42% | 40.7% | 40% | 54% | 55% |
List of abbreviations
- ADL
- activities of daily living
- CREATE
- Collaborative Rehabilitation in Acute Stroke
- EBCD
- experience-based co-design
- EQ-5D
- EuroQol-5 Dimensions
- ESOC
- European Stroke Organisation
- HSRUK
- Health Services Research UK
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- OT
- occupational therapist
- PREM
- patient-reported experience measure
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROM
- patient-reported outcome measure
- PT
- physiotherapist
- SSNAP
- Sentinel Stroke National Audit Programme
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08350).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.

