Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number NIHR127655. The contractual start date was in March 2019. The final report began editorial review in November 2020 and was accepted for publication in May 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Corrections
-
This article was corrected in March 2022. See Turner J, Knowles E, Simpson R, Sampson F, Dixon S, Long S, et al. Corrigendum: Impact of NHS 111 Online on the NHS 111 telephone service and urgent care system: a mixed-methods study. Health Serv Deliv Res 2022;9(21):148–149. https://doi.org/10.3310/hsdr09210-c202203
Permissions
Copyright statement
Copyright © 2021 Turner et al. This work was produced by Turner et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Turner et al.
Chapter 1 Background
Introduction
Demand for emergency and urgent care
Emergency and urgent care is provided by a range of services, including emergency services (999 ambulance service, emergency departments), urgent-care services [general practitioner (GP) out of hours, minor injury units, walk-in centres, urgent care treatment centres, NHS 111] and in-hours general practice (requests for same-day appointments and telephone advice). There is widespread concern about rising demand for urgent and emergency care services. In England, national statistics show that in March 2015 there were 1.76 million first attendances at emergency departments (including minor injury units and walk-in centres), 543,172 ambulance responses to 999 calls and 1.08 million calls answered by the NHS 111 telephone service. Four years later, in March 2019, these figures had risen to 2.17 million, 730,000 and 1.32 million, respectively,1 and NHS England estimates that each year there are 85 million same-day urgent care contacts with primary care. 2 These demand increases are not wholly explained by population increases or an ageing population. 3
With demand rising year on year and increasing difficulties in recruiting and retaining a sustainable workforce,4 it is questionable if emergency and urgent care services have the capacity to deal with future demand increases. There are also concerns that some of this demand is a result of clinically unnecessary service use, for example where people choose a higher-acuity service level than is clinically necessary5,6 and could be diverted to lower-level care. Developing and improving the delivery of emergency and urgent care has been a key policy issue for a number of years. In 2013, the NHS England Urgent and Emergency Care Review7 was published, which set out to address ongoing concerns about the increasing and potentially unsustainable pressure faced by emergency and urgent care services. Underpinning the review was the premise that care should be provided ‘as close to home’ as possible by helping people with urgent care needs to get the right advice, in the right place, first time. This emphasis has continued, with emergency and urgent care provision identified as one of the four areas for further development in the 2017 NHS Five Year Forward Plan. This includes an explicit commitment to the introduction of an online version of NHS 111 to help people navigate access to urgent care. 8
Developing remote access to emergency and urgent care
Over the last two decades, a number of different organisational interventions have been implemented in England to attempt to manage demand for emergency and urgent care services. A cornerstone has been the introduction of telephone advice and triage via NHS Direct, subsequently replaced by NHS 111. This is a telephone service to provide clinical assessment and direct people with non-urgent or low-acuity non-emergency health problems to the most appropriate service, or to provide self-care advice for their clinical need. Despite these services’ apparent success in terms of receiving large call volumes, they have had little impact on reducing the demand for emergency services. 9 NHS England data show that, in 2017/18, NHS 111 answered 14,995,168 calls, an average of 46,082 per day, and this is expected to continue increasing. The outcomes of these calls were that 21% had ambulances despatched or were recommended to attend an emergency department (ED), 60.7% were recommended to attend primary care, 4.6% were recommended to attend another service and 14% were given information or self-care advice. 1 The Five Year Forward View8 policy has prompted significant efforts to further enhance the NHS 111 service by increasing the clinical assessment capacity and supporting more integration with other services. It also highlighted the potential for some lower-urgency calls to be handled through online services, which may relieve some of the pressure on the telephone service by diverting some activity, make more efficient use of the workforce, support demand management and reduce costs. An online service also fits with the broader aspirations of exploiting technological innovations to improve health-care delivery and offer alternative access systems in a world where digital solutions have transformed the way people live. This has been done successfully with the introduction of smartphone application (app)-based services to help people manage specific conditions such as diabetes. 10 More broadly, with service provision, as it is currently delivered, reaching saturation, it has been suggested that strategies to reduce patient health-seeking behaviours and increase self-management should be a focus for the NHS. 11
In response to this policy, four pilot online NHS 111 services were introduced in different geographical areas across England in 2017. A useful description of these services is provided in a recent discussion,12 but, briefly, they comprise online and app-based platforms that provide symptom checkers and advice on what users should do next, either self-care or contact another service. Early results from the pilot study reported that NHS 111 Online uptake across all pilots varied between 2% and 15%, but on average was approximately 6%. However, it was hoped that uptake would increase over time to a similar level to that reached in a similar Australian service, where calls to the equivalent telephone triage service decreased by 33% 3 years after the service was introduced. 13
During 2018, the service rapidly expanded to cover the whole of England. In addition, a decision was taken to use only one of the original four platforms across the country. This is the online application developed from the NHS Pathways clinical assessment system used by the NHS 111 telephone service. The service can be accessed via a web-based application or the NHS app and allows users to work through a set of symptom-based questions. It then provides advice on what service to access themselves, options for further telephone assessment with NHS 111 clinicians, out-of-hours GP or other services, appointments with services or self-care advice.
Need for evaluation research
The principles behind introducing an online service as an access point to urgent care in the NHS are based on an expectation that it can make access easier, direct people to appropriate levels of care and divert some activity away from the NHS 111 telephone service and, hence, slow increases in demand for that service.
However, there is also a risk that this new system may increase overall demand, duplicate health-care contacts, change the pattern of service use through differences in triage outcomes, remove some of the ‘gatekeeping’ that the telephone service provides, or provide unsafe advice. The uptake of an online service may be influenced by a lack of consideration of the many and varied reasons why patients chose particular services, including access to primary care; perceived urgency, anxiety and the value of reassurance from emergency-based services; views of family, friends or health-care professionals; convenience; and the perceived need for ambulance or hospital care, treatment or investigations. 14
A recent systematic review of digital and online symptom checkers for urgent health problems undertaken by the University of Sheffield found little evidence to suggest that digital and online symptom checkers are harmful to patient safety, but this may be because this outcome was reported by small, short-term studies only. 15 Deficiencies have been reported in the diagnostic and triage capabilities of symptom checker algorithms that would potentially be used in a digital 111 platform. 16 The systematic review identified that research is needed to investigate the pathways followed by patients using a digital 111 service and to identify whether or not the overall number and level of contacts with the health system can be reduced without the quality and safety of patient care being affected. 15
This research has been designed to meet a clear need set out by NHS England to evaluate and establish the current and future potential impact of an online service on the existing NHS 111 telephone service and wider urgent care system. There is a commitment to providing a national NHS 111 Online service, but robust evidence is needed to inform future plans about what the online offering should look like, and the likely impact on service use and associated costs, and to identify any potential unintended consequences that need to be addressed as the service continues to develop.
Conceptual framework
To our knowledge, there is no established and agreed theoretical framework that underpins the delivery of urgent care, but we have used three conceptual approaches to guide and interpret this research:
-
Our recent extensive evidence review of models for delivering urgent care3 found a clear consensus that evaluation research concerned with the provision of urgent care services needs to take an emergency and urgent care system-wide perspective, rather than focus on a single service. This research uses an emergency and urgent care system model.
-
The provision of an online NHS 111 service is one element of the broader NHS England emergency and urgent care strategy set out in the 2013 Urgent and Emergency Care Review7 and is relevant to the principles set out in that review of providing access to care that is ‘right first time’, providing better support for people to self-care and providing more care closer to home in local communities. More specifically, enhancing the NHS 111 service by improving integration with other services to provide efficient patient care pathways, increasing clinical assessment and adding an online access gateway are critical to the concepts set out in the NHS England Next Steps on the Five Year Forward View8 to help manage demand for urgent care. A key objective to achieving this is the development of online triage services that enable patients with urgent health-care problems to enter their symptoms and receive tailored advice or a call back from a health-care professional. Conceptually, therefore, the population of potential users of NHS 111 Online is expected to be similar to that of those who currently use the NHS 111 telephone service. More broadly, the addition of an online NHS 111 service fits with the NHS Digital Technology strategy to harness the potential of digital technology in ways that can empower and support people to take control of their health and care. 8 The call for this research is embedded in a very clear policy need, and these underlying urgent care policy principles have been used to frame the questions and design of this study and will be used to support the interpretation of the findings.
-
NHS 111, whether a telephone or an online service, provides a point of access for people who have health problems that they perceive to be urgent. The operating model of using a symptom-based approach to assessment assumes an immediate need and uncertainty about what to do rather than simply seeking information about available services. This demand for and use of urgent care services is driven by the health-seeking behaviours of a population, but these have been poorly understood. This issue has been addressed in two recent National Institute for Health Research (NIHR)-funded studies on sense-making strategies and help-seeking behaviours associated with use of urgent care16 and a population study on the drivers of the demand for urgent care. 17 These studies were unpublished when this study was being designed but the researchers were available to help with the interpretation of this study’s findings.
Aims and objectives
The primary aim of this study is to evaluate the impact of providing an NHS 111 Online service to access urgent health-care advice and signposting to services on the telephone-based NHS 111 service. The secondary aim is to explore the potential effects on the wider urgent care system and the implications of providing a national NHS 111 Online service. The objectives are to:
-
update and summarise the evidence on digital and telephone-based services for accessing urgent care, building on existing systematic and rapid evidence reviews
-
measure the impact of the NHS 111 Online system on contacts with the NHS 111 telephone service, and estimate the effects on other services in the emergency and urgent care system and on NHS 111 services in the future
-
explore and compare in detail the characteristics of users of the NHS 111 Online service and the NHS 111 telephone service, service processes, patient care pathways and user experience and satisfaction
-
assess the practical issues associated with the implementation of the new service and the workforce implications of any changes to the overall NHS 111 telephone service and, specifically, the impact on clinical assessment teams
-
estimate the cost–consequences of implementing an NHS 111 Online service for the overall costs of the combined online and telephone 111 services and model the potential cost effects for the emergency and urgent care system.
Chapter 2 Overview of the study
Study design
The overall design is an observational mixed-methods study using a set of discrete but inter-related work packages (WPs) to address the broad range of issues identified in the objectives. The findings of the WPs were integrated during the study to provide information for the economic analysis and at the end of the study to provide a broad picture of the overall impact on services and the people who use them and to assess the potential implications for the future provision of NHS 111.
The five WPs and corresponding chapters are as follows:
-
WP1 – an update of two systematic reviews to assess the current evidence about telephone and digital access services to urgent care (see Chapter 3).
-
WP2 – the use of routine activity data to (1) explore the characteristics of people who use each type of service and whether this results in different types of advice or direction from other services, (2) measure if the introduction of an online service has diverted some activity in the telephone service and other urgent care services and (3) use the trends from this analysis to predict potential future use (see Chapters 4 and 5).
-
WP3 – a survey of telephone and online NHS 111 service users to establish what services people actually use, and compliance with advice and satisfaction, and patient interviews to look in more detail at whether people using the online service find it accessible, useable and valuable (see Chapters 6 and 7).
-
WP4 – interviews with a range of staff and other stakeholders to explore whether or not the online service has had any effect on the telephone service in terms of response to telephone calls, clinical assessment services and staff recruitment and retention (see Chapter 8).
-
WP5 – a cost–consequences analysis to measure the economic impact of introducing an online service on the telephone service and wider emergency and urgent care system (see Chapter 9).
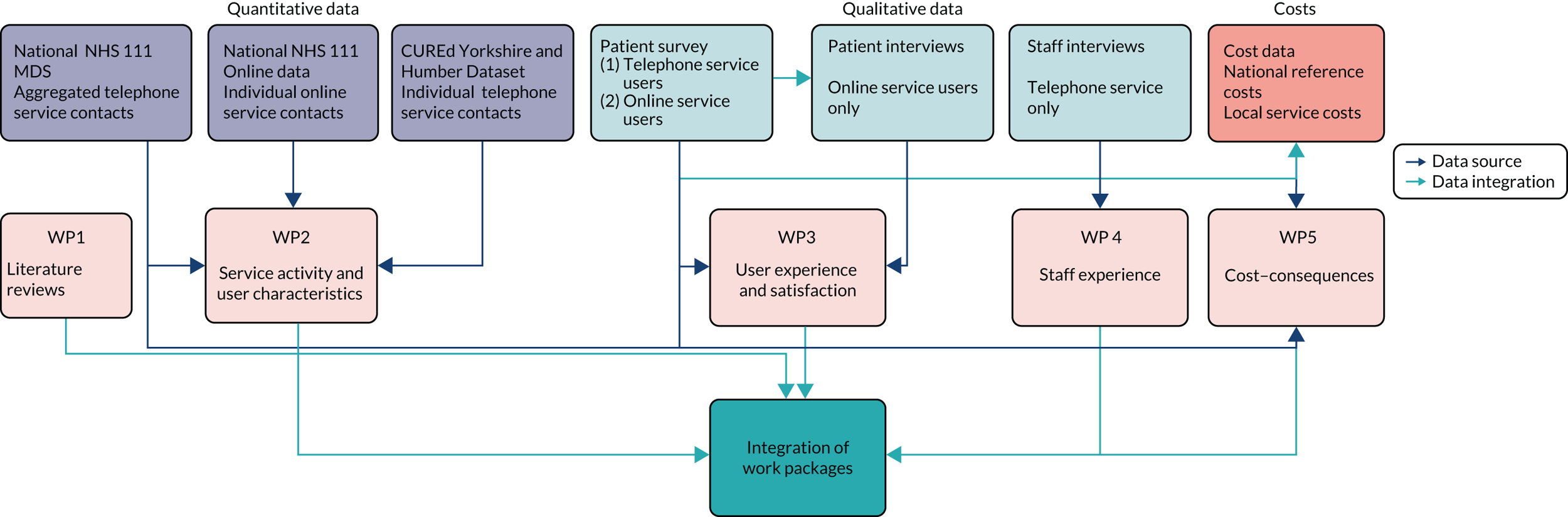
Unlike some mixed-methods studies, the short timescales of this project meant that the quantitative and qualitative components had to be conducted simultaneously. Most of the integration took place at the end of the study; however, there were two earlier integration points. First, in WP3, early interim results from the survey of NHS 111 Online users helped with framing the questions for the user interviews. Second, the results of the surveys of both NHS 111 telephone and online services were used to inform the cost–consequences analysis in WP5. Figure 1 provides an overview of the data sources used for each WP and where integration occurred.
FIGURE 1.
Overview of data sources and WPs. CUREd, Centre for Emergency & Urgent Care.
Changes from the original proposal
-
The introduction of an NHS 111 Online service is a significant policy issue, and there was a requirement for this research to be completed within a short time frame (16 months). In our proposal, we stressed that meeting this would be contingent on obtaining the routine, patient-level data collected by the NHS 111 telephone and online services that were needed to explore changes in activity and user characteristics early in the project. Data for the online service are collected centrally, as the online service is a single service. Data for the telephone service are collected both at the local service level and centrally by the NHS Pathways service. Our preference was to use the single source of NHS Pathways to avoid making multiple data requests of individual sites. Unfortunately, this proved difficult. Extensive discussions took place over several months about whether the anonymised data could be shared directly or whether these needed to be requested via the NHS Digital Data Access Request Service (DARS). This was eventually resolved for the online service, and patient-level data were supplied, but this was not the case for the telephone service data, which necessitated access via the DARS. However, NHS Pathways data are not a data asset held by the DARS, and so these data need to be migrated before an application can be made. At this point, we were already 9 months into the project. Data migration, the DARS application process and then a minimum wait of 3 months for supply would have added at least 6 months to the project. Given that this research was commissioned to address an urgent policy issue, we made a pragmatic decision not to pursue this further and instead used the publicly available data available from the NHS 111 minimum data set (MDS). This provided sufficient data on call volumes and dispositions to allow the time series analyses to be undertaken. However, these data are aggregated, not patient level, and, consequently, we were unable to complete some intended analyses. Principally, this meant we could not make the detailed comparisons of the characteristics of the NHS 111 telephone and online populations that we had planned. This was mitigated to some extent by using historical data we already hold, but it limited what we were able to explore. The MDS data are also collected by broad areas, so we had to change some of our intended study sites. The changes are described in Chapters 3 and 4.
-
In our proposal we intended to identify four of our study sites as case studies where we would combine the findings from the different WPs and compare different models of service delivery, for example by service provider type for the telephone service or by geographical type (urban vs. rural). However, we were able to recruit only two sites to undertake the user survey for the telephone service. This, combined with the changes to sites needed for the quantitative analyses described above, meant that we had insufficient complete sites to be able to use a case study approach.
-
The planned economic evaluation comprised two parts: a cost–consequences analysis and scenario analyses. The second item depended on the data mining of patient-level records, which was not possible for the telephone user population, and delays in obtaining data left minimal time for the economic work. We therefore focused on completing the cost–consequences analysis.
Public involvement
There was a very short time period during which we could consult the public about this research opportunity. However, we are fortunate that we have access to the Sheffield Emergency Care Forum (SECF), a public involvement group with whom we have a well-established and excellent working relationship. They identified a co-applicant for us (DF), who reviewed and commented on our proposal and helped to construct the lay summary. The research team also met with a small group of four SECF members to discuss the planned research and the relevance to the general public of a new access point for urgent care. This helped us focus our research questions and design.
Once the study started, we gave a presentation about the research to the full SECF group and provided them with a link to the online service so that they could try it themselves before the meeting. This provided valuable feedback about the usefulness of the service for different age groups and the issues we needed to consider when developing the questions for the user surveys and interviews, with a particular emphasis on the accessibility and usability of the online platforms.
Daniel Fall was a member of the project management group and had a liaison role with the SECF throughout the study to provide input into the development of topic guides for the qualitative research with service users and questions to be added to existing user surveys. He also contributed to writing the lay summary for the ethics application and the plain English summary for this report.
A member of a second public involvement group – the Deepend cluster, a public involvement group supporting GPs in the most deprived areas of Sheffield – was a member of the Study Steering Committee, providing feedback on emerging findings and contributing to writing the report’s plain English summary.
We will continue to work with the public involvement groups to develop our dissemination strategy and to consider how to disseminate the work to the general population, as well as to develop lay summaries for dissemination.
Patient involvement members were paid for their contribution to the project.
Ethics
Ethics approval for the interview-based work with service users and stakeholders was granted by North West Haydock Research Ethics Committee (reference 19.NW/0361). The University of Sheffield Research Ethics Committee granted ethics approval for the telephone and online NHS 111 user surveys (reference 030991) and the secondary use of routine data (reference 031640).
Study Steering Committee
A Study Steering Committee provided oversight of the research. The Study Steering Committee was chaired by Dr Alison Porter (Swansea University) and comprised members representing service providers, clinical commissioners, primary care, public health, NHS 111 Online development, NHS Digital and public involvement. NHS Digital provided additional technical input. The Study Steering Committee met three times during the study.
Study setting and intervention
The NHS 111 service
The NHS 111 service has been in operation since 2010, with the core function of providing a free-to-use telephone access service for people with urgent health-care problems that is available 24 hours per day, 365 days of the year. The service provides health information and an assessment service, which uses the NHS Pathways system to ask callers a series of questions about their problem and then direct them to an appropriate service using a local Directory of Services (DoS), provide telephone clinical advice or provide self-care advice. The initial assessment is conducted by a non-clinical call adviser and, where appropriate, the call can be passed on for further assessment by a clinician (usually a nurse).
As it has developed, the NHS 111 service has grown to include a secondary function of providing a single point of access for urgent care services, including out-of-hours services, to create a fully integrated urgent care access, clinical advice and treatment service. Integrated urgent care services have access to a wide range of general and specialist clinicians. They offer advice to health professionals in the community and to the ambulance service, manage patients over the telephone who have called NHS 111 and, in some cases, provide appointment booking services and face-to-face management of patients in treatment centres, the patient’s residence or another location, if required. Although a national service, NHS 111 is commissioned by Clinical Commissioning Groups (CCGs) using a variety of providers, including ambulance services, social enterprise organisations and commercial organisations. The geographical footprint of providers is very variable, ranging from large regional services covering multiple CCGs to small areas of two or three CCGs. The range and scope of integration with other services also varies by area and by commissioning arrangements.
The introduction of the NHS 111 Online service has essentially added another arm to the NHS 111 service by providing an alternative access point for people who need information and advice about what to do when they have an urgent health problem.
How does NHS 111 Online work?
The NHS 111 Online service has been designed so that people can get medical help or advice using a smartphone, laptop or other digital device. Users of the service can ask questions about their symptoms, get advice about what to do and where to go and, if needed, get further advice from a nurse, doctor or other trained health professional. The service can be accessed via a website (https://111.nhs.uk/) or the NHS App (https://digital.nhs.uk/services/nhs-app) for smartphones and tablet devices.
The online version of NHS 111 uses an adapted version of NHS Pathways to replicate the questions that are asked by the health advisers in the NHS 111 telephone service.
The implementation of the NHS 111 Online service has occurred in three phases:
-
Phase 1 – people accessing the service can answer questions about their health problem and the results direct them to the appropriate service using the local DoS.
-
Phase 2 – in addition to advice on appropriate service, users can, where needed, book a clinical call-back from the telephone NHS 111 service or integrated urgent care provider.
-
Phase 3 – in addition to 1 and 2 above, users can receive a call back from services such as out-of-hours GPs, dentists, urgent treatment centres and other services, where the technology links have been put in place to accept referrals from the online service.
There are some differences between the online process and the telephone process. These are described in Table 1.
| NHS 111 Online | NHS 111 telephone | Site differences |
|---|---|---|
| The home screen welcomes the user and asks them to enter their postcode |
After dialling 111, the caller is asked to press 9 to confirm that they wish to continue. When the service is busy, a recorded message informs the caller that the online service is available for people over the age of 17 years and asks whether they wish to be sent a link Otherwise, the caller is transferred to the local 111 service. Depending on area, an interactive voice response may allow them to select different options for particular problems, which direct them to specialist clinicians or external services. All other calls are connected to an NHS 111 health adviser |
Interactive voice response options differ by site. Can include:
|
|
The user is directed to the emergency rule-out page (module 0) and asked to confirm that they do not have any of six symptoms which could indicate a life-threatening condition. If they cannot rule out these six symptoms, the user is told to call 999 immediately and triage ends If continuing, the user is asked to enter their age and sex. If they are asking about a person under the age of 5 years, or if they cannot confirm the sex or that the person they are asking about has a gender identity other than male or female, they are told to call NHS 111 |
A health adviser asks the caller for some basic personal details and to confirm that they do not have any of six symptoms that could indicate a life-threatening condition. If they cannot rule out all of these symptoms, the call is transferred for a 999 ambulance response Callers in some areas are transferred to a clinical adviser at this point if they are calling about a person under 5 years or over a particular age |
|
| The user enters an initial symptom. They then work through the questions and can move backwards and forwards through the answers until they reach a disposition | The caller is asked about an initial symptom and the health adviser will work through questions until a disposition is reached | |
| For 999 dispositions, the user is asked to call 999 | For 999 dispositions, the call is transferred to 999 | Some 999 dispositions are assessed by a clinician (revalidation) before transfer |
| For ED or other urgent care treatment services dispositions, users are advised to attend and a list of available services in their area is provided | For ED or other urgent care treatment services dispositions, users are advised to attend and a list of available services in their area is provided | Some ED dispositions are assessed by a clinician (revalidation) before the caller is given this advice |
| If the disposition suggests that the user needs to speak to an NHS 111 clinical advisor, then they are offered a call back and are asked to enter their telephone number, and the date of birth, current location and home address of the person they are asking about. These details are transferred to the local NHS 111 telephone service and added to the clinical advisor call queue | If the disposition suggests that clinical advice in needed, the caller is transferred to a clinical adviser, or asked to wait for a call back | Availability of specialist clinical advisers differs between sites (e.g. mental health, dental, palliative care) |
| If the disposition suggests that the user needs to speak to primary care or other service, they are advised to contact primary care themselves. In some areas, a call back with a primary care clinician or other service can be offered | If the disposition suggests that the user needs to speak to primary care or other service, they are advised to contact primary care themselves. In some areas, a call back with a primary care clinician or other service can be offered | Availability of call-back booking with other services differ between sites |
| If the disposition suggests a service where direct booking is available, the user is asked to enter personal details so that the direct booking can be arranged | If the disposition suggests a service where direct booking is available, the call handler/clinician will arrange a direct booking | Services available for booking differ between sites |
| For other dispositions, users are advised to contact other services (dentist, pharmacy, optician). Where available, the contact details of local services are provided | For other dispositions, users are advised to contact other services (dentist, pharmacy, optician). Where available, the contact details of local services are provided | |
| If no service is needed, users are provided with self-care advice | If no service is needed, users are provided with self-care advice |
As with the telephone service, NHS 111 Online is a national service, but the outputs of a user’s interaction with the central NHS Pathways assessment system are customised and linked to the provider of the telephone and integrated urgent care service in their postcode area. So, for example, if a user is advised to go to an emergency department or other service, a list of local available services and opening hours is provided. If a call back with a clinician is booked, then this is passed to the NHS 111 service that covers their area.
Some early adopters of the NHS 111 Online service implemented the three phases sequentially, but areas that went live later implemented a full phase 3 service from the outset. The service was available nationally from December 2018. We spoke to nine NHS 111 provider sites, which identified the following main features of the set-up and implementation phases:
-
Setting up and testing technical links for Personal Demographics Service matching. When a user of the NHS 111 Online service enters their details (date of birth, full home address, home telephone and emergency telephone number) for a call back, a Personal Demographics Service look-up automatically identifies the patient’s GP practice and NHS number. If a full match is found, this populates a document that is sent into a call queue at the NHS 111 service so that the clinical adviser has access to the patient’s details. If a full match is not found, the patient is allocated an individual patient identification number for the NHS 111 call. When the clinical advisor calls back, they clarify personal details in order to find the full match. Rates of automatic Personal Demographics Service matching vary between sites.
-
DoS profiling so that the NHS Pathways disposition at the end of the NHS 111 triage session maps to the right service from which direct referrals (for call backs or appointments) can be made. The ability to make direct referrals to other services differs by site, depending on the local services available, but can include dental services, urgent treatment centres and GP out-of-hours services. The correct technical links (electronic transfer and e-mail requests) were also put in place. The range of services to which online users can be referred is likely to increase as the integrated urgent care hubs expand and incorporate more specialist services, such as mental health, end-of-life care and pharmacy.
-
The process of project set-up and commissioning of the online service appeared to be relatively straightforward, particularly for the later sites, which described how some of the teething problems had been resolved by earlier sites. Project set-up phases were short, with the most resource-intensive work reported to be developing, testing and re-testing the DoS to ensure that all pathways ended in the correct dispositions. The technical links for referrals were tested robustly to make sure that they worked correctly.
-
Sites reported having a clear plan of the actions required to set up the online service and clear instructions of responsibilities set out by NHS Digital. Discussions between providers and commissioners were uncomplicated, although some site leads reported that commissioners were concerned that the introduction of the online service may lead to increased demand. Site leads reported that detailed descriptions for dealing with clinical governance and clear guidance were provided by NHS England, which helped to oversee the robust testing phase.
-
The pilot phase and early roll-out of the NHS 111 Online service involved significant work in adapting and testing NHS Pathways questions to make them as user-friendly as possible. The tone and language of questions were adapted to maximise how easy these would be for the general public to understand. The question development process aimed to ensure that there was as accurate a match as possible between the wording of the online questions and the scripted questions read out by the call advisers on the telephone service.
-
The work required to implement the online NHS 111 service was absorbed into existing job roles and none of the site leads reported needing any additional resources or staffing to get the sites up and running. Some site leads expressed concerns about potential future cost implications if call volumes increase as use of the online service exapands due to the increased length of clinical adviser time for online NHS 111 users.
Study services
In our original plan, we identified nine NHS 111 provider sites to include in our study: four sites that had implemented early (from 2017) and five that had implemented later. The nine sites were chosen to represent a range of size of coverage, geographies (urban and rural areas) and provider types. As described earlier, the need to change one of our main data sources meant that we were unable to use this specific set of sites for the main time series analyses. We have still included some of these sites in other WPs, but these vary. The sites used are described in the methods section of each relevant chapter.
Chapter 3 Rapid update of the evidence base on telephone and online urgent care access services
Introduction
This section addresses objective 1. In recent years, this research team have conducted a number of related systematic and rapid evidence reviews in the topic areas. In 2012, as part of our earlier evaluation of NHS 111 telephone service pilot sites, we published a systematic review of the evidence on appropriateness of and compliance with telephone triage advice. 18 In 2015 the NIHR Rapid Evidence Review Centre based in ScHARR (School of Health and Related Research), University of Sheffield, published a review of models for urgent care. 3 This included a comprehensive analysis of the evidence on telephone triage services.
Most recently the NIHR Rapid Evidence Review Centre conducted a systematic review of digital and online symptom checkers and health assessment/triage services for urgent care. 15 We have therefore already synthesised the related evidence in detail. Given this is a time limited study we have updated these reviews utilising the existing search and review strategies (e.g. inclusion and exclusion criteria) used for these reviews to identify relevant new evidence from the cut-off point of the earlier studies. The purpose is not to create new reviews but to assess whether or not there is recent evidence that changes the overall findings and conclusions of the earlier reviews and which might influence the interpretation of this study.
Methods
Database search strategies
Telephone triage
For telephone triage, the 2012 and 2015 reviews used a similar search strategy but the 2012 version was broader, so, for completeness, we have replicated the search used for this review. The search used a combination of free-text and medical subject headings (MeSH), including telephone, triage or consultation, NHS Direct, telephone triage, call centre triage, advanced nursing, appropriate, under-referral, safe, decision-making, technology transfer, general practice, teleconsultation, telepathology, video conferencing, virtual reality, video consultation and epidemiology.
The following databases were searched: MEDLINE (via Ovid SP), EMBASE (via Ovid), the Cochrane Library (via Wiley Online Library), Web of Science (via the Web of Knowledge) and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (via EBSCOhost). Searches were limited by publication date from 1 July 2010 to 28 March 2019.
All search results were downloaded into EndNote X9 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA].
Inclusion criteria
-
Empirical data from patient-based studies.
-
Requests for emergency/urgent care.
-
Telephone triage/advice/consultations.
-
Report relevant outcomes: accuracy, compliance, appropriateness, safety, impact on other services, patient satisfaction.
-
Written in English.
Exclusion criteria
-
Descriptive studies with no assessment of outcome.
-
Telephone services for single conditions.
-
Telephone services for non-urgent advice.
-
Opinion pieces and editorials.
-
Non-English-language papers.
-
Conference abstracts.
Digital and online symptom checkers
The search strategy used in our recent systematic review15 was replicated. Search terms included symptom checker(s); self-diagnosis; self-triage; online, web based, electronic, digital, app; online diagnosis; web based triage; and electronic triage.
The following databases were searched: MEDLINE (via Ovid SP), EMBASE (via Ovid), the Cochrane Library (via Wiley Online Library), and CINAHL (via EBSCOhost). Searches were limited by publication date from 1 January 2018 to 22 May 2020.
Inclusion criteria
-
Systems providing information to address urgent health problems.
-
Any online digital service designed to assess symptoms, provide health advice and direct patients to appropriate services.
-
Report relevant outcomes: accuracy, compliance, appropriateness, safety, impact on other services, costs, patient satisfaction.
-
Written in English.
Exclusion criteria
-
Descriptive studies with no assessment of outcome.
-
Systems for single conditions or information only (no direction to care services).
-
Opinion pieces and editorials.
-
Non-English-language papers.
-
Studies from low-/middle-income countries.
Review process
The same process was used for both reviews. Titles and abstracts of references identified from database searches were scrutinised by one member of the research team and assessed for relevance using the inclusion and exclusion criteria. A randomly generated 10% sample of studies from the database searches was double sifted by another member of the study team. A single reviewer assessed full papers of potential inclusions, with a 10% random sample assessed by a second reviewer. Studies where there was uncertainty were agreed by consensus by the two reviewers.
Data extraction was carried out directly into summary tables, rather than using detailed data extraction forms. We used a simple broad template to summarise the key characteristics from each included paper, including the study design used; the population and setting; the main purpose and objectives, including the outcomes measured; and the key findings and conclusions. A formal quality assessment of inclusions was not carried out.
Findings were synthesised in a narrative summary that included commentary on the quality of the included studies. The main focus was on identifying any key new evidence that changed or strengthened the conclusions of the previous reviews.
Results
Telephone triage
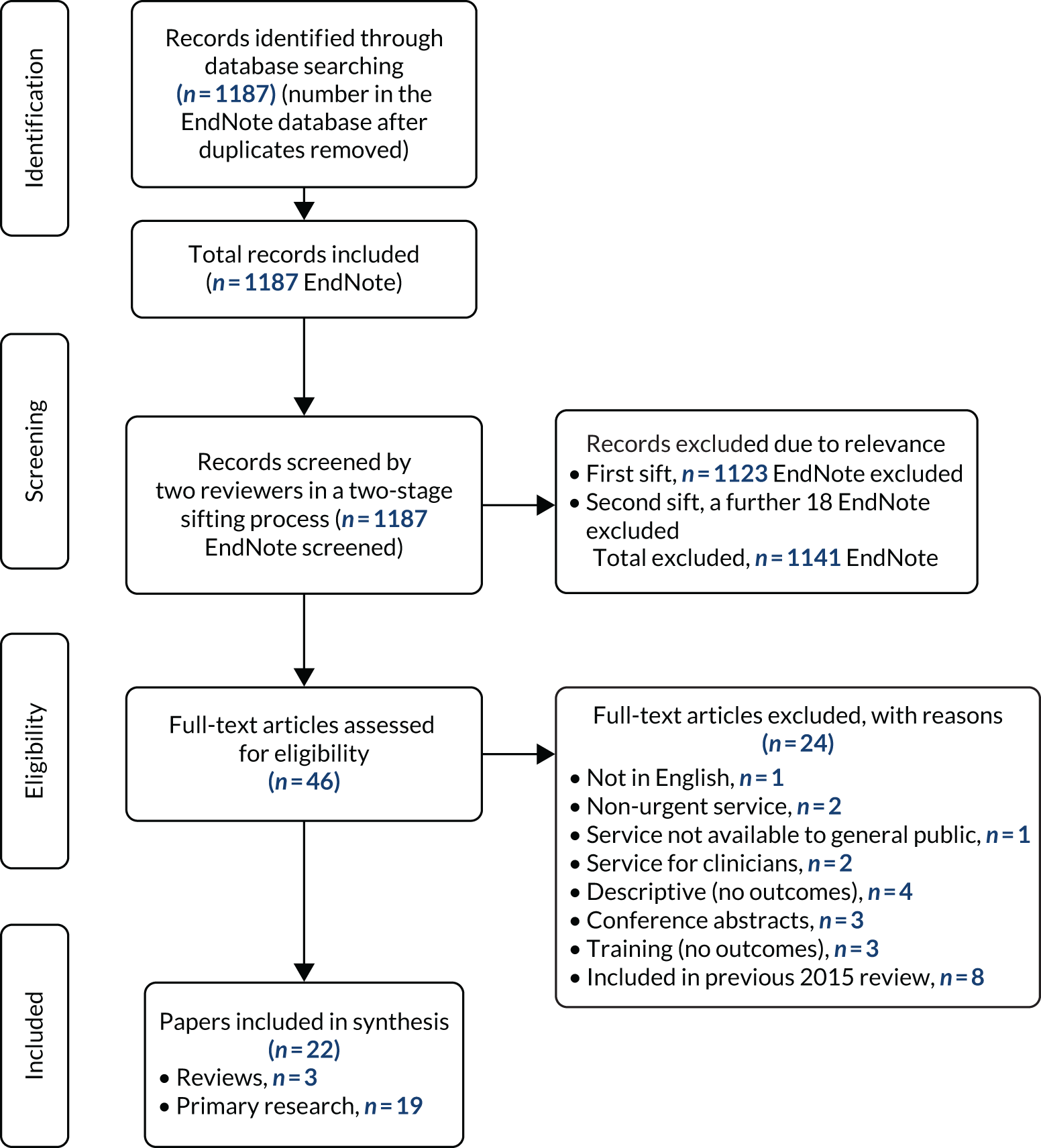
The results of the review sifting process are given in Figure 2. Among 46 full-text reviews, 22 papers were included for data extraction and narrative summary. Eight papers were duplicates included in our previous 2015 review and were not considered again. There were three review papers. Of the 19 inclusions presenting primary evidence, four (21%) each were from the UK and Australia, two (10.5%) were from the USA and nine (47.5%) were from the rest of Europe. By broad study design type, there were six (31.6%) observational studies, four (21%) mixed-methods studies, three (15.8%) survey studies, two (10.5%) each of cohort and qualitative studies and one (5.8%) each of modelling and uncontrolled before-and-after designs. The majority of studies were conducted in an urgent care setting (13/19, 68.4%), four (21%) were conducted in primary care and one each was conducted in an emergency department and an emergency medical services setting. A description of each of these 19 studies is provided in Appendix 1, Table 26.
FIGURE 2.
The PRISMA flow diagram for telephone triage.
Summary of findings
Of the three review articles identified, one19 was a review of 10 existing systematic reviews about telephone triage in urgent care settings. Seven of these systematic reviews were included in our own 2015 review. 3 As a result, the conclusions about the same broad themes concurred with our earlier work; that is, there is variation in the measured estimates of appropriateness of triage decisions depending on the definition used. Compliance with advice is variable and higher for emergency care (ED) or self-care than for primary care; patient satisfaction is generally high; overall decisions tend to be safe but higher risk for more serious conditions; and there is some evidence of impact on service utilisation, but this is mainly for primary care. Evidence is weak about the impact of telephone triage on access and costs, showing potential for only modest savings. One review20 focused specifically on telephone secondary triage of low-urgency ambulance (emergency medical services) emergency calls. Findings have been consistent that this process can divert suitable calls away from an ambulance response, although this rate varies from 52% to 83% depending on the setting and call type. The process has also been found to be safe, with very low reports of adverse events, high levels of patient satisfaction and the potential for cost savings through the reduction of unnecessary hospital admissions. The final review paper21 examined the evidence on the safety of triage decisions made by clinical and non-clinical assessors. It found that nurses had higher levels of appropriate referral rates (91%) than non-clinicians (82%) and were most likely to be cost-effective, although different triage systems were used. The authors compared nurses with non-clinical emergency medical dispatchers and concluded that the latter group were less effective clinical decision-makers, but the authors also acknowledged that this might not have been a useful comparison as the two groups perform different functions.
The 19 primary research studies identified addressed key outcomes relevant to telephone triage.
Compliance
Two papers from Australia22,23 examined compliance with nurse telephone triage decisions. One reported compliance rates of 68.6% for ED, 64.6% for clinician consultation and 77.5% for self-care22 and another reported a similar rate for ED (66.5%). 23 Both studies found similar rates of self-referral to ED against advice of 7%22 and 6.2%. 23 Another study24 found that 22% of callers who intended to go to ED did not follow GP telephone advice. One study25 of low-urgency emergency medical services calls found that patients were more likely to follow advice provided by telephone triage (95%) than that provided by a paramedic on-scene treat-and-refer scheme. Several papers examined caller characteristics and the relationship to compliance and found that calls made out of hours, from patients in disadvantaged areas, by another person on the patient’s behalf and by people with an intention to attend ED are associated with lower compliance. 22 Callers living in remote or rural areas are less likely to comply with advice to attend ED. 22,23 The level of care advised, the extent to which advice agreed with the caller’s prior intention, care option availability and perceptions of risk also have an effect, with compliance seven times higher if the highest level of care is advised. 26 One paper27 investigated the effect of English-language proficiency and found that those with limited proficiency were less likely (60.9%) to follow advice than those who were proficient (69.4%) and were more likely to have a higher level of care disposition.
Appropriateness
A UK study28 used GPs to review ED dispositions in a nurse-led telephone triage service and found 73% would have been given an alternative disposition to lower-level care. A Danish study29 in an out-of-hours primary care telephone triage service examined calls from people referred for a face-to-face consultation and estimated that 84% were relevant but 12% could have been managed over the telephone. Two papers30,31 explored the use of caller self-reported degree of worry to help in the decision-making process and found that a high degree of worry was associated with symptom duration of > 24 hours,30,31 more serious illness30 and an increased likelihood of needing a face-to-face disposition. 31
Safety
Only one paper32 explored safety and the rate of potential adverse events from undertriage by examining telephone triage cases which resulted in a subsequent emergency ambulance call and hospital admission, and found the rate to be small, at 0.04% of all calls. These calls resulted from inadequate communication and non-normative symptom description. One other paper33 compared nurse telephone triage, hospital clinicians and GP assessment of ED walk-in patients and found low congruence between the three types of assessment and a risk to health of 0.65%, although the sample size, of 208, was small. One interesting development is emerging research about the effects of the work environment and clinical and non-clinical call advisor performance. A study by Turnbull et al. 34 explored the management of risk by NHS 111 non-clinical call handlers and found that a substantial part of the handlers’ work involves the management of risk, in terms of both assessing patients safely and balancing this with allocating scare resources. The study highlighted that, although technologies have been introduced to support risk, risk has not been removed but has been redistributed to create a new task of ‘making technology work’. Another qualitative study35 of nurses from telephone triage call centres found that most found that the work was rewarding and enabled them to use their clinical skills. However, it was also cognitively demanding, and a lack of support from the workplace and other health-care professionals had a negative impact on the nurses’ ability to do their jobs effectively.
Patient satisfaction
Existing evidence has shown a consistently high rate of satisfaction among users of telephone triage services, and this persists in two papers25,36 that report ≥ 80% of patients being satisfied or very satisfied. More interesting is new evidence that examines reasons for variation in satisfaction with different patient characteristics or types of advice. One study in a primary care out-of-hours service found that satisfaction was significantly lower among patients who had received a treatment centre consultation than among those who had received a telephone consultation. Call answering delays, waiting for call backs and shorter consultations were also associated with lower satisfaction. 37 Two Swedish studies38,39 examined satisfaction with nurse telephone advice. One found that callers who expected a higher level of care and/or did not agree with the disposition were less satisfied than those who did agree. 38 The former were also more likely to self-refer to another service within 3 days. The other found that younger callers and those receiving a self-care disposition were significantly less satisfied than other callers and that reassurance had the most effect on increasing satisfaction. 39
Impact on other services
There is limited new evidence about the impact on other services. One study24 showed that telephone triage produced a small reduction (3.6%) in ED attendance compared with callers’ original intention. A comparison of two types of out-of-hours primary care telephone triage showed a reduction in utilisation of a GP emergency service of 17.8–58.3%, depending on the service configuration. 40 A modelling study using nurse telephone triage advice and patient self-reported subsequent service use concluded that, overall, a triage service reduced health-care utilisation, except where a patient’s original intended action had been to attend the ED and the nurse’s advice was self-care. 26 Only two studies considered costs. A Swedish study estimated an overall health service cost saving of 3.3% for actual action compared with intended action after telephone triage and 12.7% if all nurse advice dispositions were followed. 26 A smaller study28 of ED disposition review by GPs estimated a potential cost saving to EDs of £52,528 compared with GP employment costs of £41,416. However, the impact would be limited, as only 11% of telephone triage calls have an ED disposition.
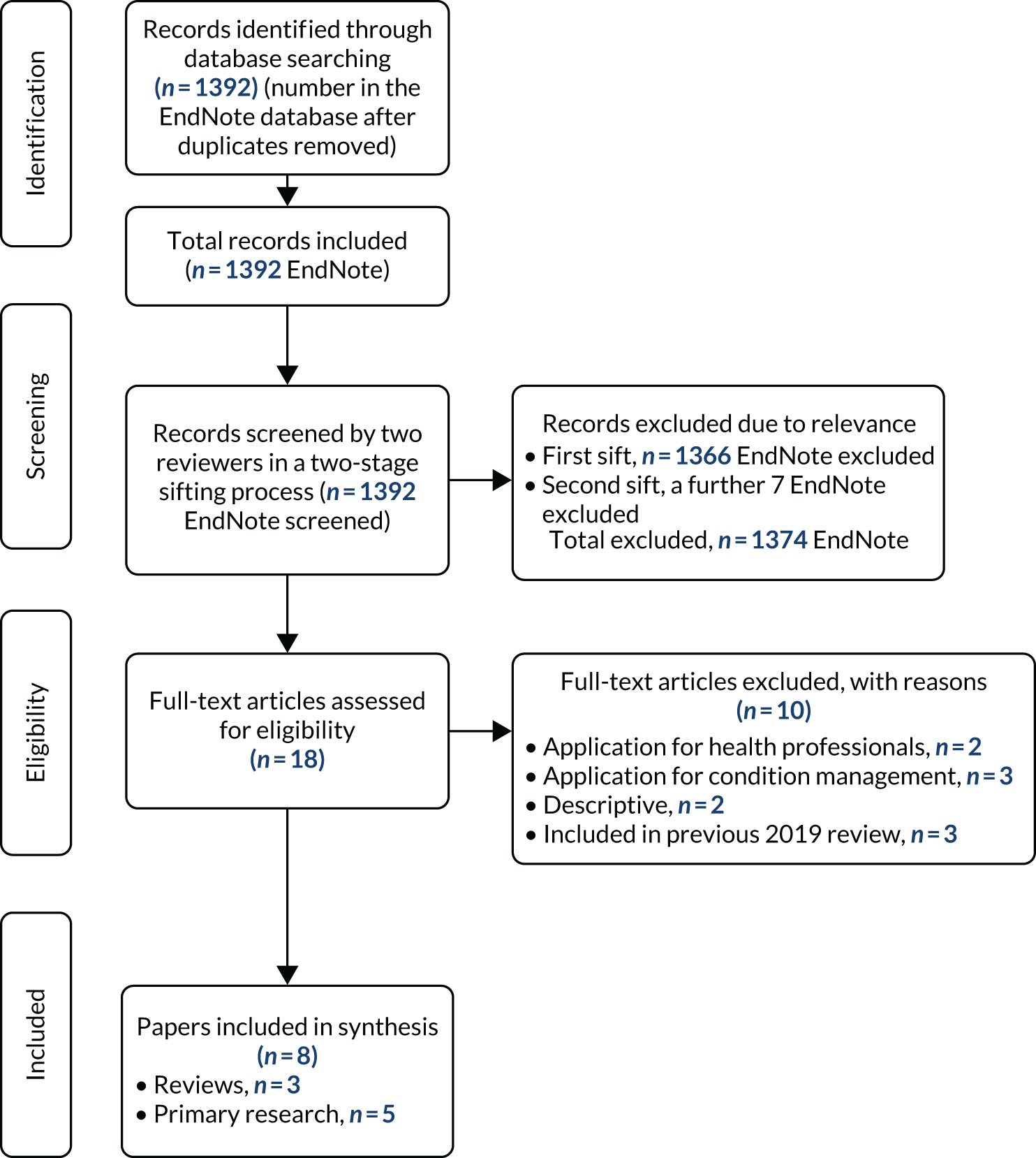
Digital and online symptom checkers
The results of the review sifting process are given in Figure 3. Among 18 full-text reviews, eight papers were included for data extraction and narrative summary. Three were review papers and five presented primary evidence: one each from Hong Kong and Australia and three from the USA. A description of each of these eight studies is provided in Appendix 2, Table 27.
FIGURE 3.
The PRISMA flow diagram for online and digital symptom checkers.
Of the three review papers, one was a systematic review of digital interventions for parents of ill children to enable decision-making for self-limiting infections. Three studies were included, with two triage services reporting sensitivity of 84% and 93% when compared with nurse triage decision for ED intervention and none of the studies demonstrating a reduction in the use of urgent care services. 41 A scoping review42 of self-diagnosing digital platforms synthesised 19 inclusions, although more than half were conceptual or opinion articles, with primary research representing specific conditions rather than urgent care. The authors identified significant research gaps in the use of digital interventions and the complexity in the number of applications and diseases considered, and that more research is needed to understand user experience. The third systematic review43 focused on digital triage for primary care problems and synthesised the same evidence included in our review,15 and concluded that evidence is limited, with more evaluation needed.
Three of the primary research papers were simulation studies using patient records to create vignettes to test symptom checker applications. One study tested five symptom checkers for hepatitis C and HIV (human immunodeficiency virus) infection and found that they had poor diagnostic accuracy; only 20% of infections were identified at the first diagnosis and 55% of the checkers did not identify either infection at all, with substantial variation between applications. A correct emergency care triage decision was more accurate for hepatitis C (59.7%) than for HIV (35.6%). 44 A study using case records of ED patients compared the accuracy of two symptom checkers with the ED triage category and found accuracy of 74% and 50%. Sensitivity for emergency cases was 70% and 45%, with low negative predictive values (43% and 24%), leading to the conclusion that the symptom checkers were not a suitable alternative to ED triage. 45 A study in Australia46 investigated the performance of 36 public access diagnostic and triage symptom checkers using medical condition vignettes. Diagnostic symptom checkers listed the correct diagnosis first in 36% of cases (range 12–61%) and in the top 10 in 58% of cases. Triage applications provided the correct advice for 49% of tests and were more accurate for emergency and urgent care advice (63% and 56%, respectively) than for non-urgent or self-care (30% and 40%, respectively). The authors concluded that the quality of symptom checkers was variable and that triage applications were generally risk averse, often recommending higher levels of care than were needed. 46
An experimental study47 comparing the accuracy of three symptom checkers for cough in an outpatient setting found that their diagnostic accuracy was poor when compared with physician assessment reference standard, with a 26.2% difference in correct diagnoses. A recent paper48 described the rapid introduction of a digital self-triage and scheduling tool for COVID-19 integrated into a primary care system. Users enter their information, and people who are asymptomatic receive information and advice is provided, whereas people who are symptomatic are triaged to four categories from emergency care to self-care and, where needed, directed to appointment scheduling or a telephone hotline. In the first 16 days of use, the tool’s sensitivity in detecting the need for emergency-level care was 87.5%, and there were early indications of reductions in unnecessary face-to-face visits, telephone calls and messages. 48
Summary
For telephone triage, there is a substantial existing body of evidence that has been synthesised in numerous systematic reviews. Most of the new evidence identified in this exercise has confirmed earlier findings; that is, that compliance and appropriateness are variable depending on service and setting, patient satisfaction tends to be high and little attention has been directed at issues around impact on access. A conclusion of our previous systematic review18 was that more investigation was needed into the association between appropriateness of a decision and subsequent compliance and satisfaction. The most valuable and relevant new evidence is from research that has started to investigate the more complex patient and system factors that can explain variation and behaviours. There is an emerging theme about the important relationships between caller expectations, intended action, attitudes to risk, agreement with triage decision and subsequent satisfaction and utilisation of services,26,27,38,39 together with environmental factors such as rurality and deprivation,22,23 all of which need to be considered as part of service design. There are interesting developments about how patient-reported characteristics, such as degree of worry, might be incorporated into triage questioning31,40 and about the effect of language proficiency. 27 There is also important new evidence that has started to consider workforce factors, such as managing risk and demand, and the subsequent impact on safety and performance for telephone triage services. 34. 35
For digital symptom checkers and triage tools, the updated evidence review has confirmed our own recent findings, which are that the evidence on patient safety is weak, diagnostic accuracy is variable between systems but generally low, and algorithm-based triage tends to be more risk averse than that of health professionals. There is also very limited evidence on patients’ compliance with online triage advice. The reporting of the rapid development of a digital self-triage tool for COVID-1948 illustrates how the advantages of digital development – speed, remote working, scale and reach – can be exploited in response to a health emergency and provides an example of how digital technologies can be used in the future.
Chapter 4 Time series analysis of NHS 111 telephone and online contact outcomes
Introduction
The introduction of NHS 111 Online has added a new access point for urgent care. One of the intended policy expectations is that the new service will divert some activity from the NHS 111 telephone service and direct more people with less urgent problems away from emergency care services. 2 This chapter addresses objective 2 of the evaluation. The aim of this work package was to use NHS 111 telephone call and online contact data to determine whether or not the NHS 111 Online service has had an effect on the number of calls to the NHS 111 telephone service and its impact on other emergency and urgent care services.
Methods
Data collection
Data on NHS 111 calls and online contacts were collected between October 2010 and December 2019 and between January 2018 and December 2019, respectively. The NHS 111 calls data were obtained from the NHS 111 Minimum Data Set, Time Series, to December 2019 and accessed online (URL: www.england.nhs.uk/statistics/statistical-work-areas/nhs-111-minimum-data-set/nhs-111-minimum-data-set-2019-20/) in January 2020. 49 The NHS 111 Online data were provided by NHS Digital. Call data provided monthly counts at the NHS 111 area code level, whereas online provided daily, individual-level data. As call data were at a summary level only, analyses of both data sets were conducted at this level. Both data sets provided variables for all calls and contacts; triaged calls and contacts; calls and contacts passed for clinical advice; and the final disposition for the call/contact as the advice about which service to contact or attend, or where no service was needed.
The call data were made up of 71 NHS 111 area codes and the online data were classified by both Sustainability and Transformation Partnership (STP) and CCG areas, which were mapped to 38 of the NHS 111 area codes. For historical call data, some of the older codes have been merged into newer area codes. These 38 area codes were the potential sites for our analysis. However, because of the way the NHS 111 telephone service is commissioned, geographical coverage of different service providers means that either the area codes can be made up of multiple STPs or some STPs can be split over two area codes. Because the NHS 111 Online service was introduced at STP level, this meant that not all online area codes could be included, as some STPs had different start dates. In addition, for the interrupted time series analysis, 1 full year of NHS 111 Online data were required; therefore, any area codes where the online service had not been operating for at least 1 year were removed. For consistency, the call data were capped at 2 years prior to the introduction of the NHS 111 Online service, so each area code had a minimum of 36 months of data. This meant that there were 18 area codes remaining for the analysis; however, these areas are spread across the country and represent a range of geographical, service size and provider types, so we are confident that they are a reasonable representation. It was unfortunate that the area where the NHS 111 Online service was first introduced (Yorkshire and the Humber) and, therefore, had the longest post-implementation time could not be used. This is because the NHS 111 telephone call data are reported for Yorkshire and the Humber as a single area, but there are 22 CCGs and the NHS 111 Online service became live at different times in these CCGs, meaning that we could not account for the time point of change in the interrupted time series models. A list of the 18 sites included is provided in Appendix 3, Table 28.
Outcomes measured
The primary outcome was the impact of introducing the NHS 111 Online service on the number of triaged calls to the original NHS 111 call service. Triaged calls are those where a call advisor assesses the call using NHS Pathways and excludes calls that, for example, just provide health information with no assessment.
The secondary outcomes were to explore the impact of NHS 111 Online on the total number of calls, the number of clinical call backs and the effect on the relative proportions of final dispositions and hence on other related services.
These primary and secondary outcomes can be split into those which affect the NHS 111 telephone service only and those that have an impact on the wider NHS system.
NHS 111 telephone service only:
-
triaged calls
-
total calls answered – including non-triaged calls for health information, and those where the caller terminates before triage
-
clinical call backs – calls referred to clinical advisors for further assessment.
Wider NHS system:
-
emergency ambulance referrals or advice to contact 999
-
advice to attend an emergency department or other urgent care treatment facility
-
advice to contact primary care
-
advice to contact with community service
-
advice to attend another service
-
no recommendations to attend any service and self-care advice.
For calls to the telephone service, there is a specific data variable recording the number of calls passed for and receiving a clinical assessment. This is less clear for the NHS 111 Online data, as clinical call-backs are managed outside the online platform. The online data provided two data variables, a clinical call back variable (offered and sent or offered and failed to send) and the final disposition (advice) code (DX code) at the end of the questioning. There were 11 DX codes for ‘speak to a clinician from our service immediately’ as the final disposition. If a patient had both a clinical call back variable and a relevant DX code, they were assigned as having a clinical call back. The online clinical call backs were added to the telephone call clinical call backs as the outcome for this analysis.
The secondary outcomes, which look at the impact on the wider NHS system, were created in a similar way to the clinical call back outcome. The outcome was made up of a combination of the dispositions (DX codes) from both the call and the online data. For example, the outcome of all ambulance referrals is made up of all the ambulance dispositions in the call data plus all the ambulance dispositions to call 999 in the online data.
Statistical analysis
All analysis was conducted using R, version 3.6.3 (R Core Team, 2020; The R Foundation for Statistical Computing, Vienna, Austria).
Interrupted time series
To model whether or not the introduction of the NHS 111 Online service has had an impact on the monthly number of calls, an interrupted time series was used. However, unlike with conventional interrupted time series, a dose–response model was used. This means that instead of the number of calls being modelled as a function of the time after the launch of the online service, it was modelled as a function of the number of online contacts that month. The dose–response model provides an estimate of the reduction or increase in the number of telephone calls per online contact. The model also included some systematic components: an underlying time trend, a step change for when NHS 111 Online was introduced and ‘fixed’ seasonal effects (four levels: December–February, March–May, June–August and September–November).
As each area code had different start dates for the introduction of NHS 111 Online, each was modelled separately and a meta-analysis was used to determine the overall effect (see Meta-analysis). Given that there were 18 different area codes and a range of outcomes to model, we decided to use the same model for each site and outcome, but different models were used as a sensitivity analysis.
To determine which model to use, four area codes were chosen independently by two statisticians (RS and RJ) to test the models. Both statisticians chose the same four sites (Hertfordshire, Milton Keynes, North East and Nottinghamshire) as these represented areas with large to small numbers of calls. The models tested were Poisson or negative binomial, and whether or not the model was autoregressive (AR) was also examined.
To determine whether an AR model was appropriate, the primary outcome was differenced to remove the general upwards trend (see Appendix 3, Figure 19) and the autocorrelation function and partial autocorrelation function plots were investigated. It was agreed for all four models that an AR model was not needed but there may be some seasonality. Seasonality would be accounted for with the season variable which was prespecified to be included in the model.
As the primary outcome variable was the number of triaged calls to 111 each month, these are count data, so either a Poisson or a negative binomial model was considered. After fitting both the Poisson and the negative binomial models, the model output for the Poisson model showed that the data were overdispersed. Given this, the negative binomial model was chosen over the Poisson model. The autocorrelation function and partial autocorrelation function plots were investigated again and it was confirmed that an AR model was not needed (see Appendix 3, Figures 20 and 21).
The final model used for the analysis was:
where the outcome is the number of calls to the NHS 111 telephone service each month, time is a linear variable 0, 1, 2, . . ., dose is the number of NHS 111 Online contacts for each month, step is a binary variable that is coded 0 before the introduction of NHS 111 Online and 1 afterwards, and season is a fixed variable that represents the four seasons in the year.
For sensitivity analyses, an AR(1) model and a non-linear model with a non-linear term for time were used.
Both of these sensitivity models were applied to all sites and outcomes. The Isle of Wight was one of the 18 area codes included in the analysis. Owing to the size of the Isle of Wight, with small call volumes and an atypical urgent care service configuration, we have included a further sensitivity analysis from which we have excluded the Isle of Wight.
All three of these models included a log-link function. For the linear and non-linear negative binomial model, the glm.nb function of the Modern Applied Statistics with S (MASS) package was used. 50 For the AR model the tsglm function of the tscount package was used. 51
Meta-analysis
For each of the outcomes, the dose from the individual area analyses were summarised using forest plots with estimates displayed as the incidence rate ratio per 1000 online contacts. The results from each area were combined to estimate the average effect of introducing the online service on each outcome using a random-effects meta-analysis. 52 The between-area variance, τ2, was estimated using the DerSimonian–Laird method53 and heterogeneity was evaluated using the I2-statistic. 54 The overall estimate for each outcome and a 95% confidence is reported along with a p-value. Meta-analysis was conducted using the metagen function of the meta library. 55
Meta-analysis was repeated for all sensitivity analyses and the overall estimate and 95% confidence interval (CI) for each model was displayed on a forest plot for comparison.
Results
Primary outcome (triaged calls)
The primary outcome for the analysis was the number of triaged NHS 111 calls. Triaged calls are all the calls that were triaged which excludes both calls which were abandoned and those not triaged. Figure 4 presents LOESS (locally estimated scatterplot smoothing) plots for the four area codes in which the model was chosen.
FIGURE 4.
The LOESS plots of the number of triaged calls and online contacts for the four test area codes. Blue, triaged NHS 111 calls; orange, online NHS 111 contacts. (a) Hertfordshire; (b) Milton Keynes; (c) North East; and (d) Nottinghamshire.
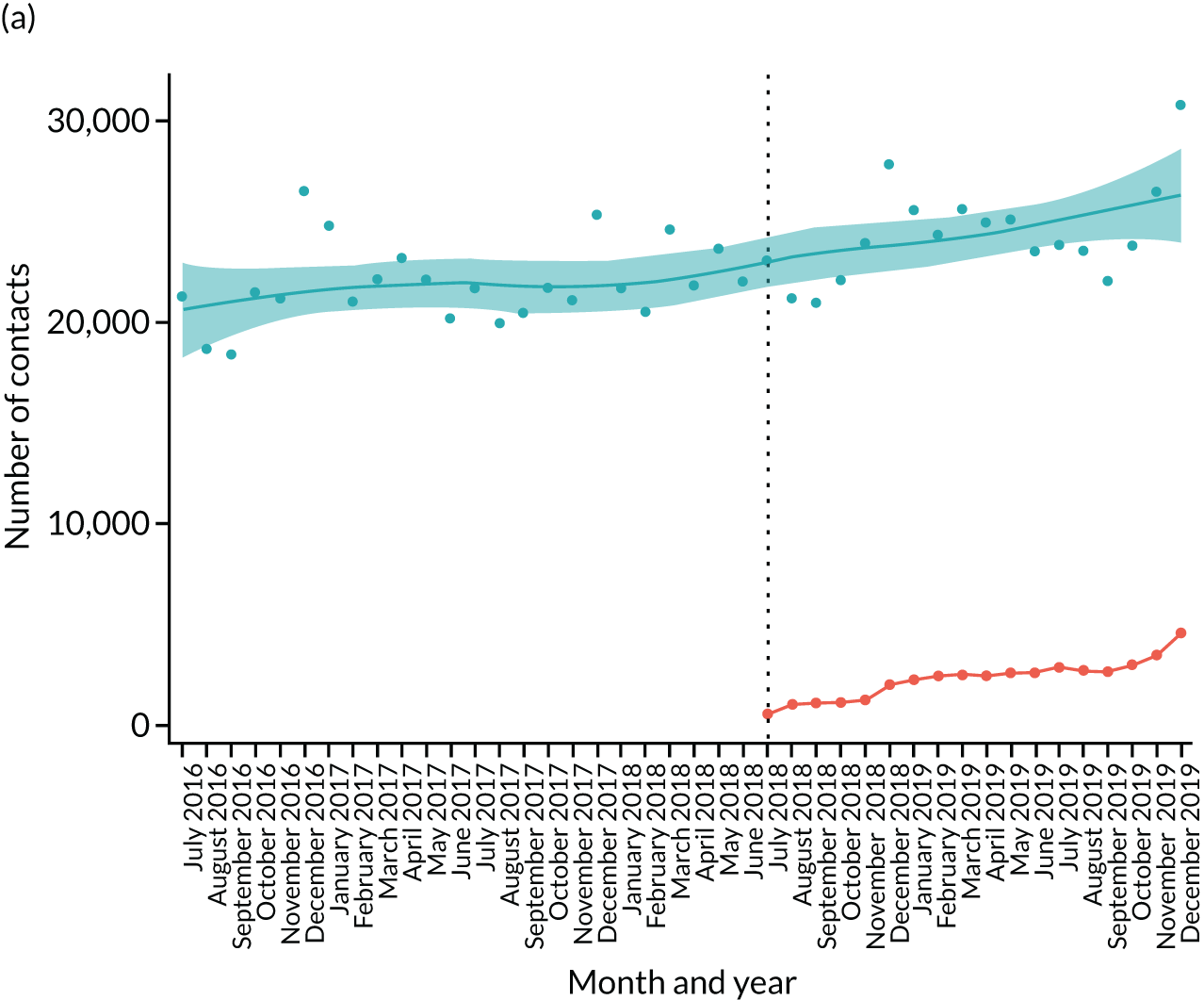
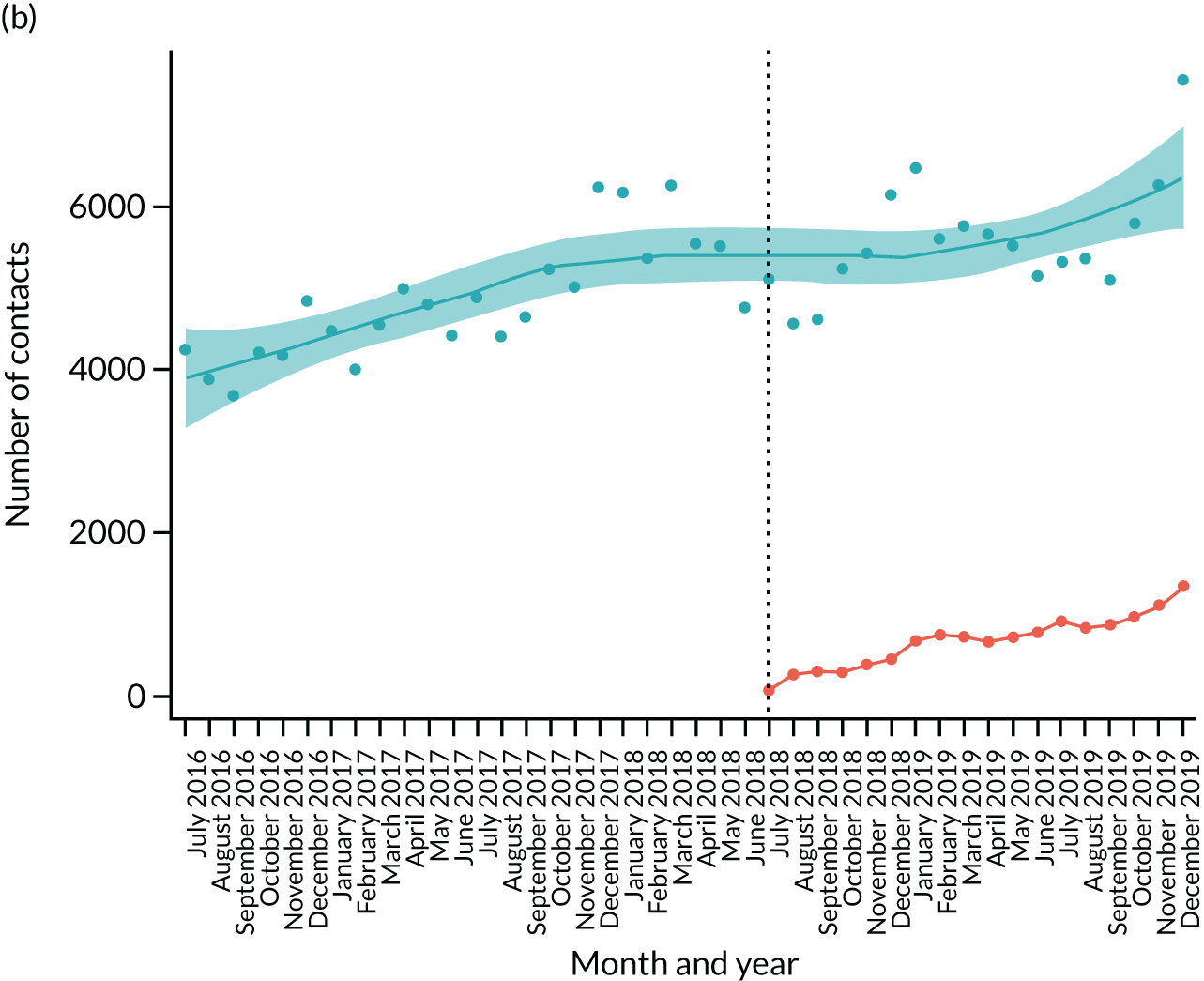
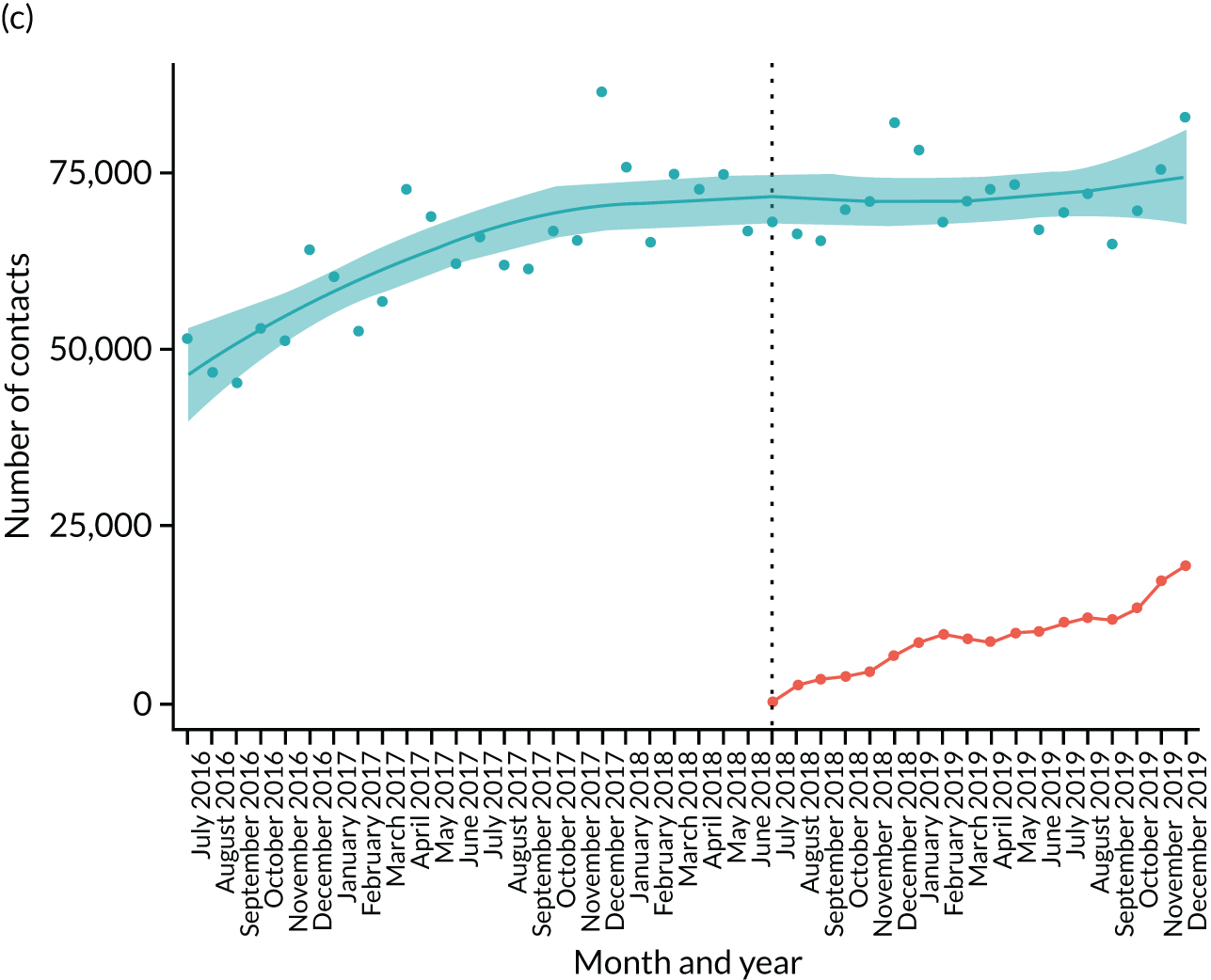
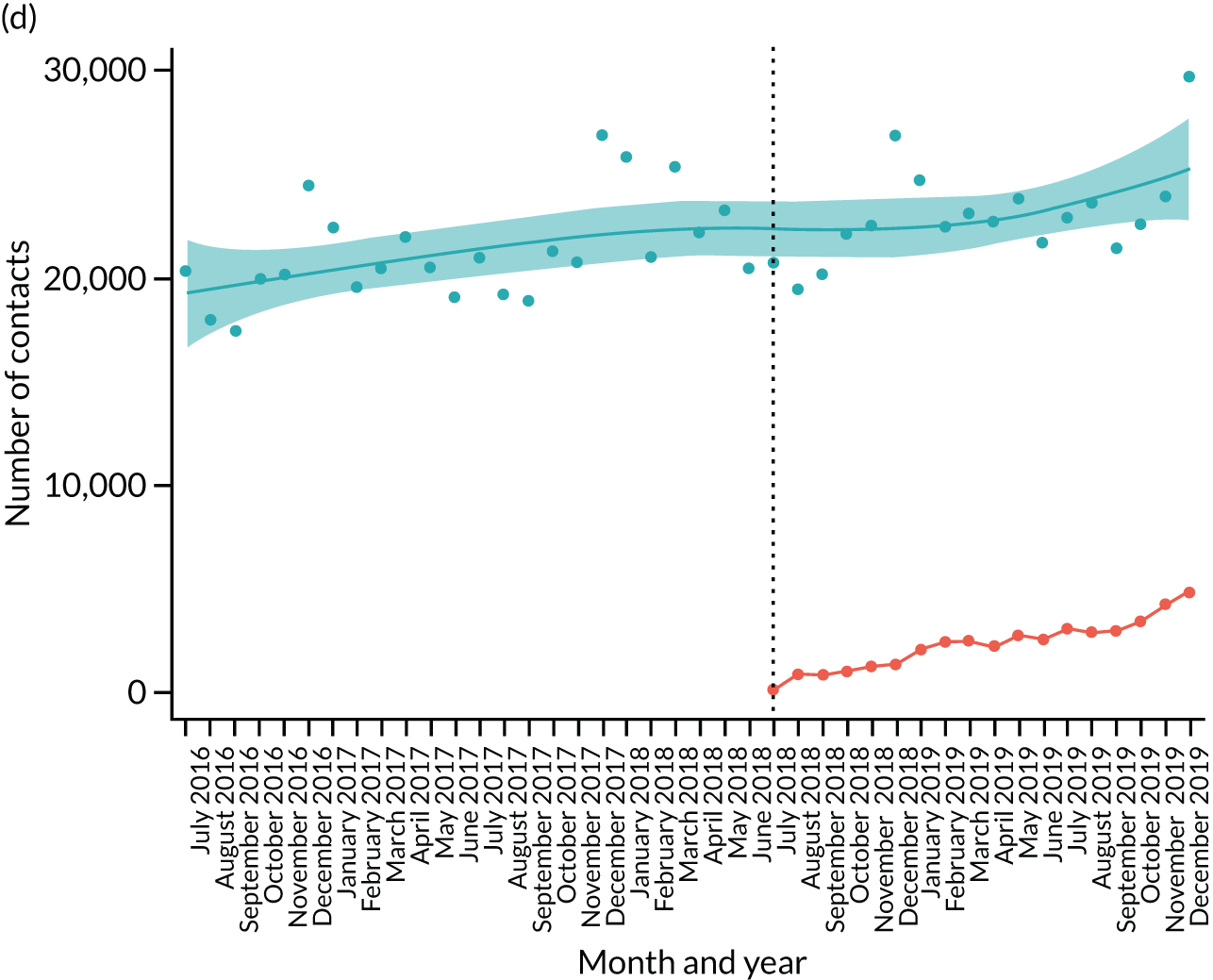
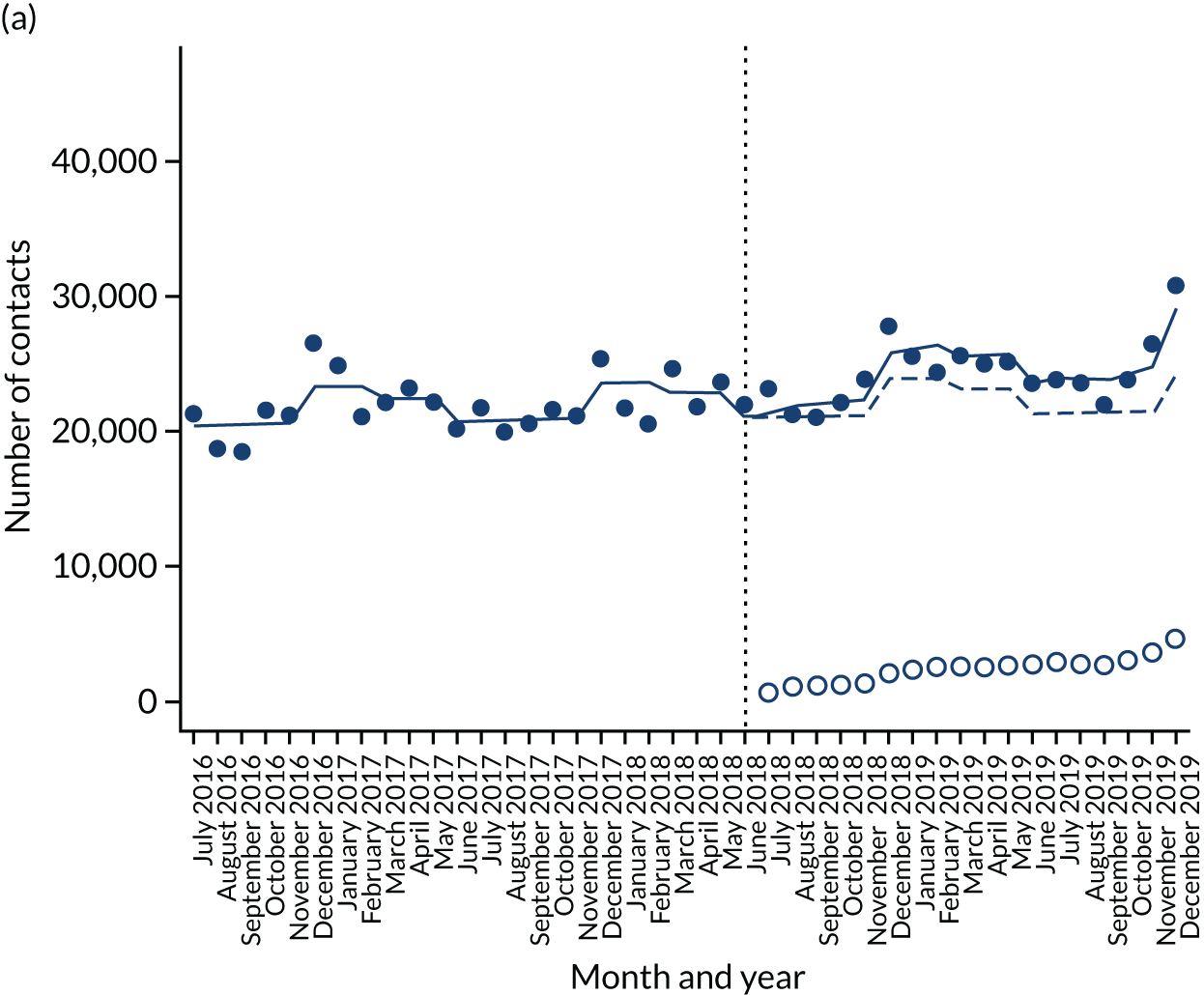
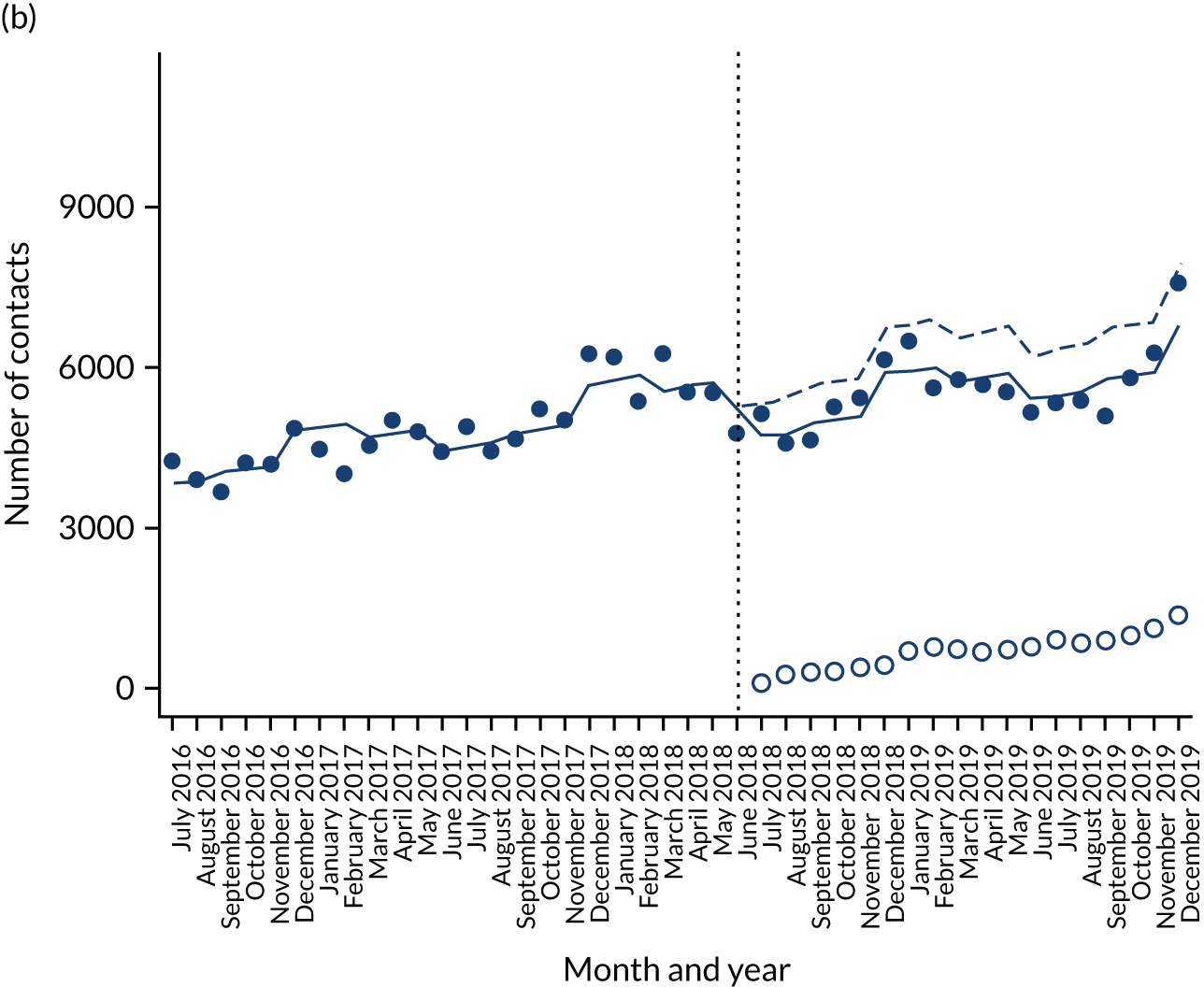
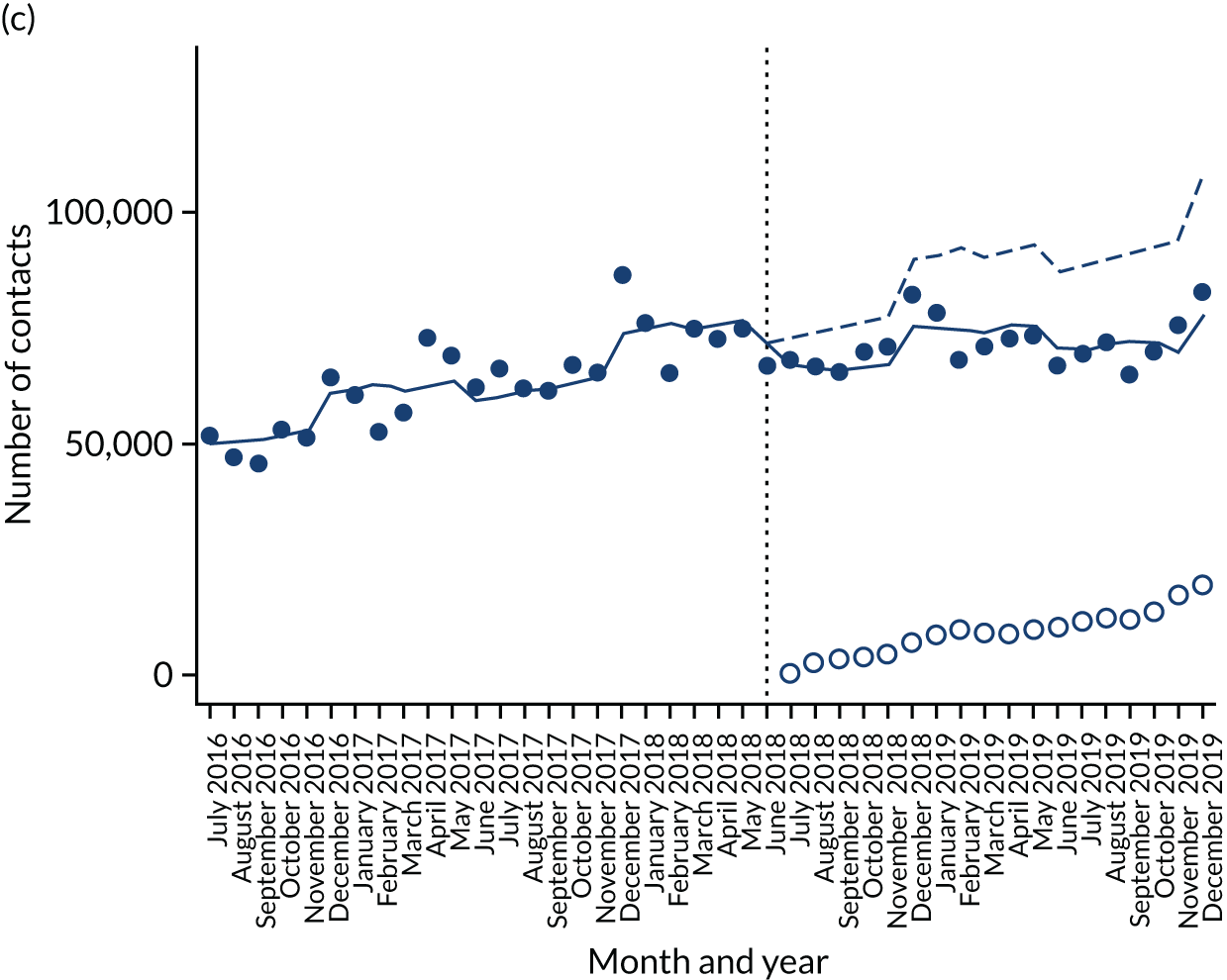
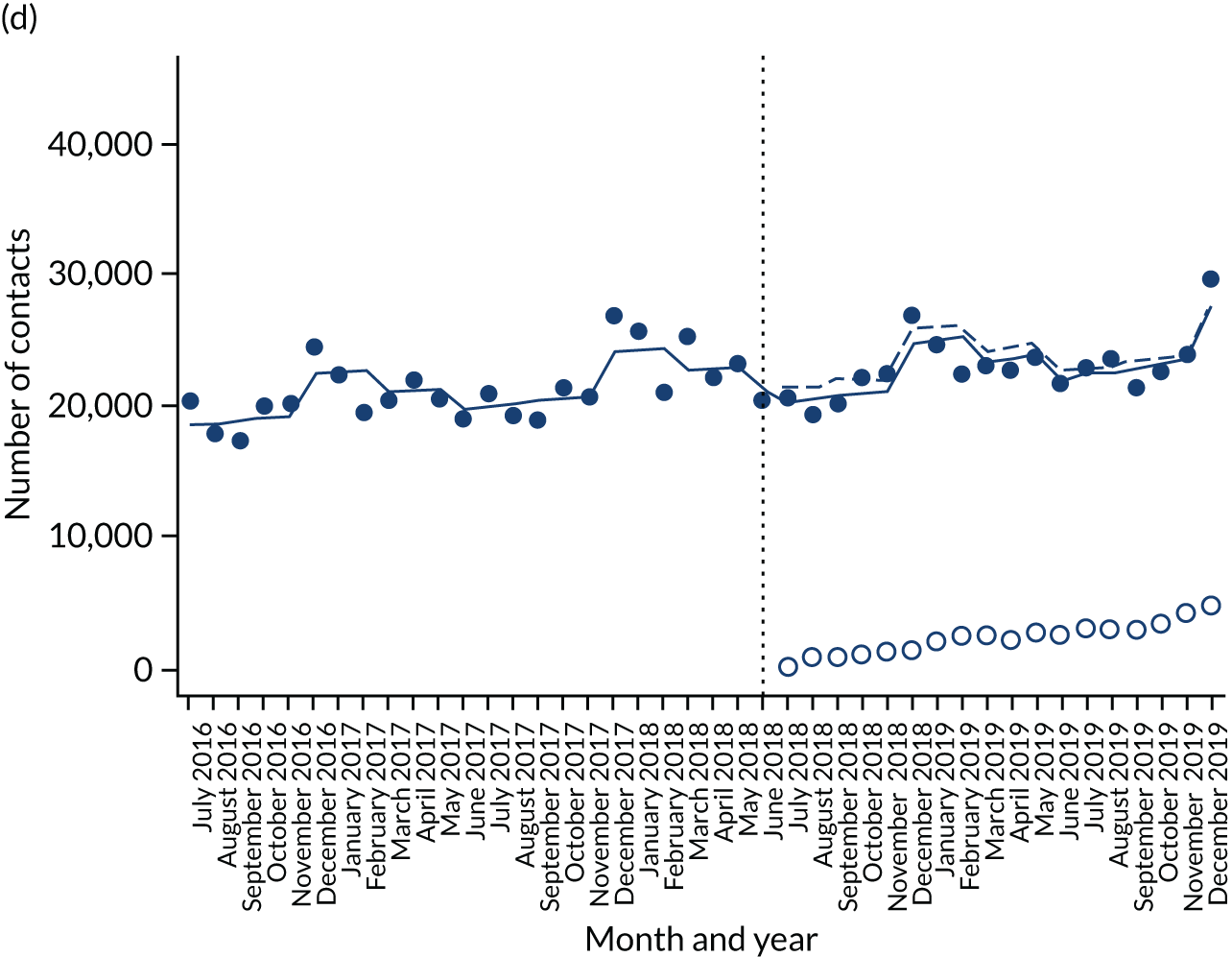
Figure 5 presents the interrupted time series model for the four area codes for the primary analysis method [linear negative binomial with no AR(1)].
FIGURE 5.
The interrupted time series plots for the four test sites. Solid blue line, interrupted time series model; dashed blue line, null model (no intervention); solid dots, triaged NHS 111 calls; hollow dots, online NHS 111 contacts. (a) Hertfordshire; (b) Milton Keynes; (c) North East; and (d) Nottinghamshire.
Meta-analysis
Below are the meta-analysis results of triaged 111 NHS calls for the primary analysis method for each site and then for each sensitivity analysis overall.
Negative binomial generalised linear model
Figure 6a shows the forest plot of results for the primary analysis. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.013 (95% CI 0.996 to 1.029; p = 0.127). This means that, on average, for every 1000 online contacts, the number of calls to the NHS 111 telephone service that are triaged has increased by 1.3% (95% CI –0.4% to 2.9%). However, this result is not statistically significant.
FIGURE 6.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of triaged calls to the NHS 111 telephone service. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 71.5% (95% CI 54.1% to 82.3%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
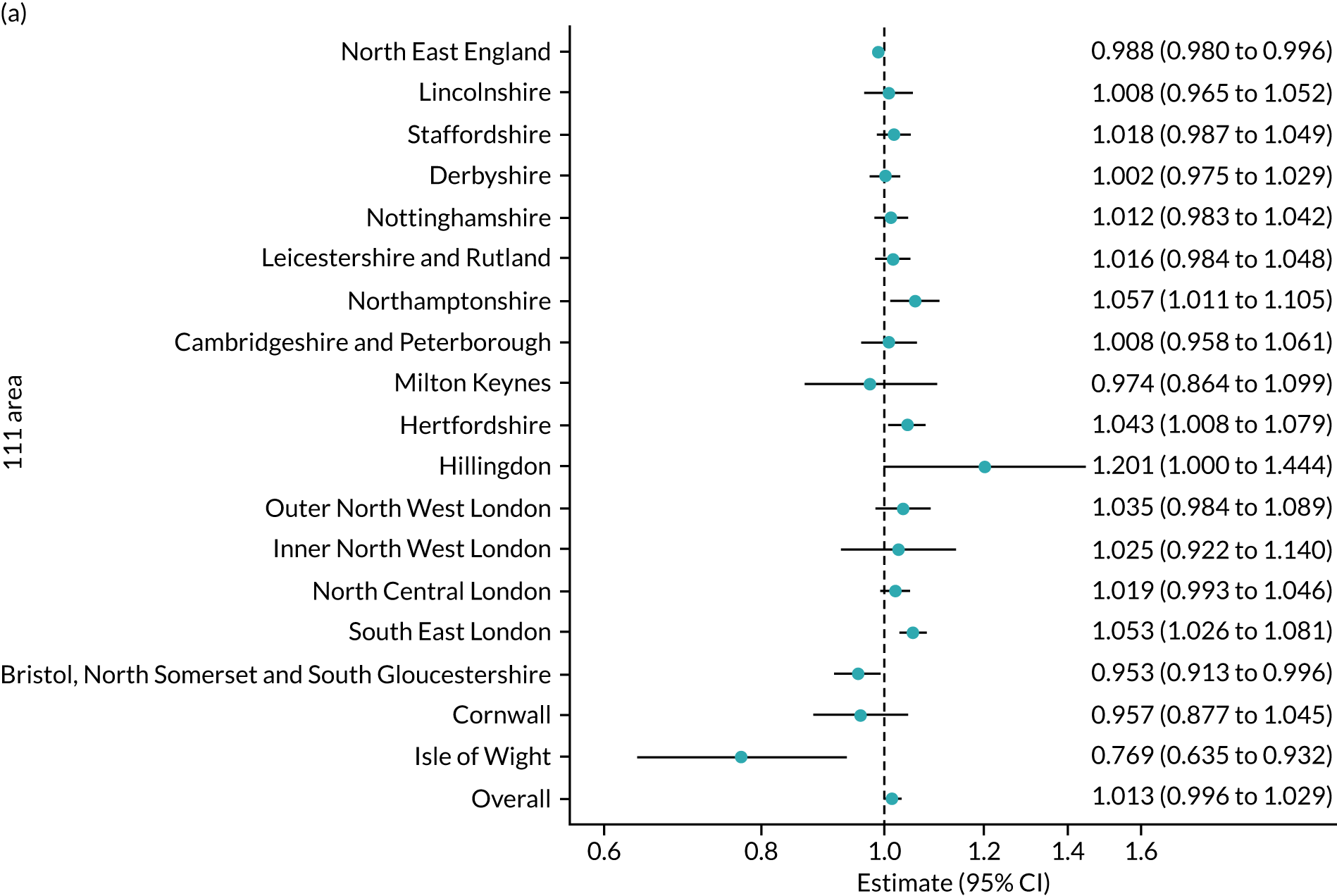
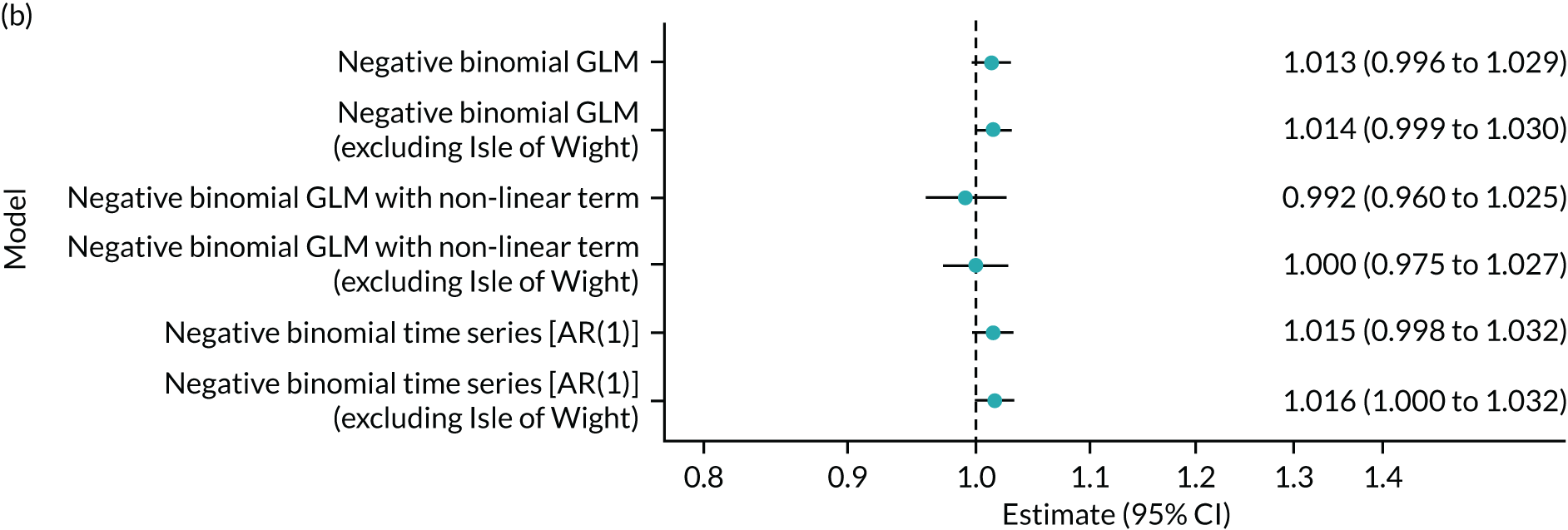
Figure 6b shows the forest plot of the main analysis method and various sensitivity analyses. Excluding the Isle of Wight has little effect on the estimate. Including a non-linear term for time increases the standard error and lowers the estimates, but the overall conclusion remains the same. The AR(1) model provides similar incidence rate estimates and CIs.
Secondary outcomes
Total calls
Total calls is all calls offered to NHS 111, reflecting how many people attempted to contact the service. Figure 7a shows the forest plot of total calls for all area codes for the primary analysis method. The x-axis is showing the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.008 (95% CI 0.992 to 1.025; p = 0.313). This means that, on average, for every 1000 online contacts, the number of calls to NHS 111 has increased by 0.8% (95% CI –0.8% to 2.5%). However, this result is not significant.
FIGURE 7.
Forest plots showing the effect of introducing the NHS 111 Online service on the total number of calls to the NHS 111 telephone service. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 68.0% (95% CI 47.7% to 80.4%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
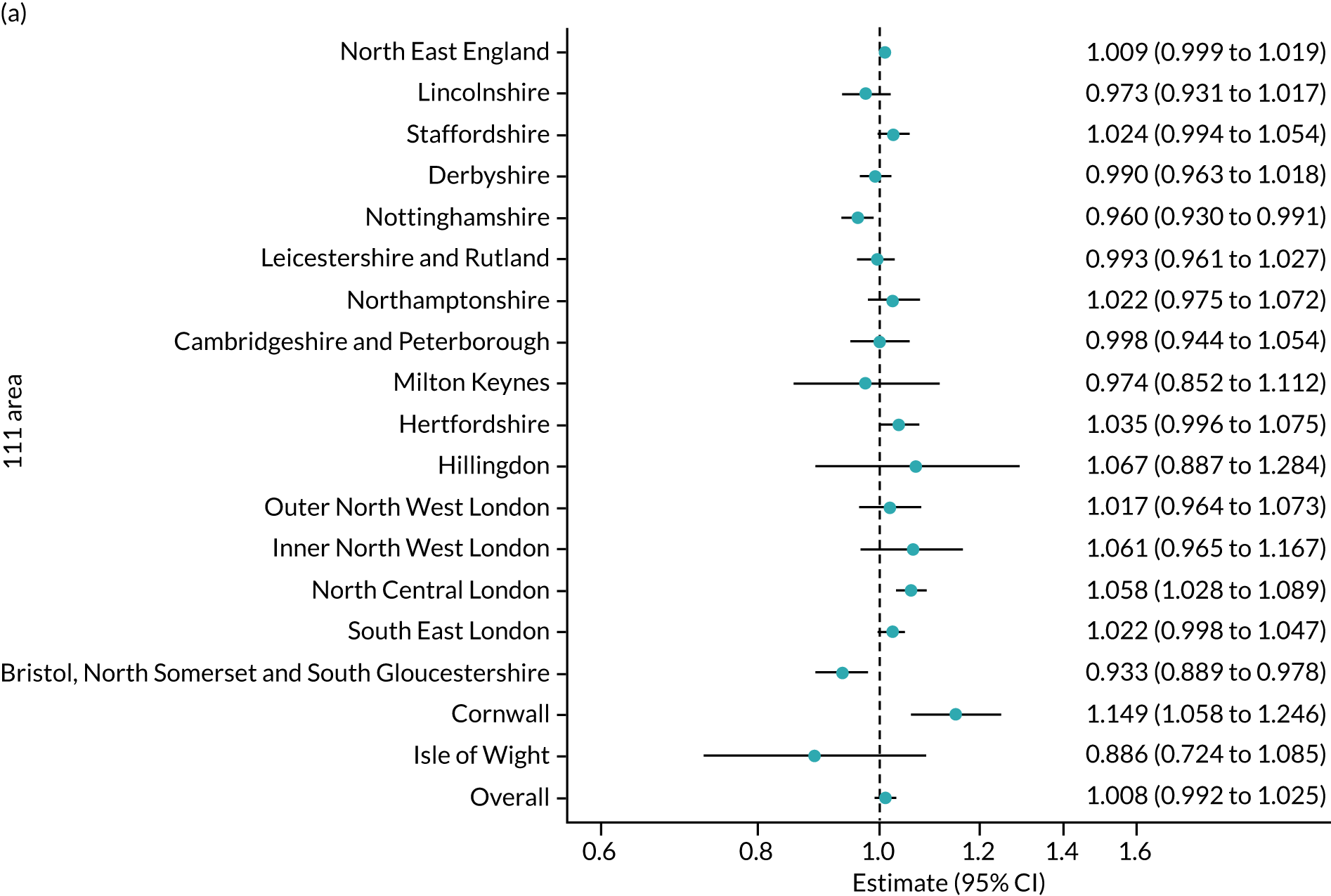
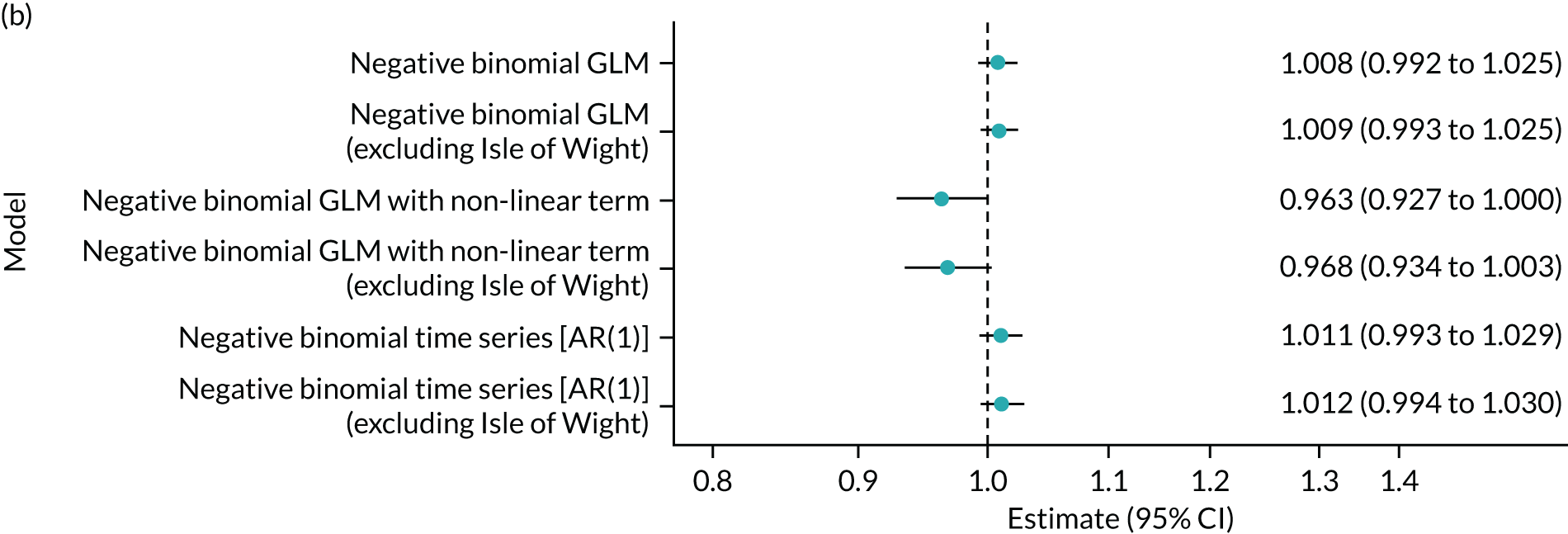
Figure 7b shows the forest plot of the main analysis method and various sensitivity analyses. Excluding the Isle of Wight has little effect on the estimate. Including a non-linear term for time increases the standard error and decreases the incidence rate ratio; there is now a 3–4% decrease in calls per 1000 online contacts, but the overall conclusion remains the same. The AR(1) model provides similar incidence rate estimates and CIs.
Clinical calls
Clinical calls are calls or online contacts that resulted in a disposition of call back from a clinical adviser. For the telephone data, the number of actual clinical assessments is recorded. For the online data, the disposition reflects a request for a call back but not whether or not this call back actually took place.
Figure 8a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 0.946 (95% CI 0.901 to 0.993; p = 0.025). This means that, on average, for every 1000 online contacts, the number of clinical call backs decreases by 5.4% (95% CI –9.9% to –0.7%). This result is considered a statistically significant effect, suggesting that, on average, the online 111 service has caused a reduction in the number of NHS 111 contacts (calls and online) that result in a clinical call back.
FIGURE 8.
Forest plots showing the effect of introducing the NHS 111 Online service on the total number of call backs or requests for call backs from a clinical advisor. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 94.5% (95% CI 92.7% to 95.9%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
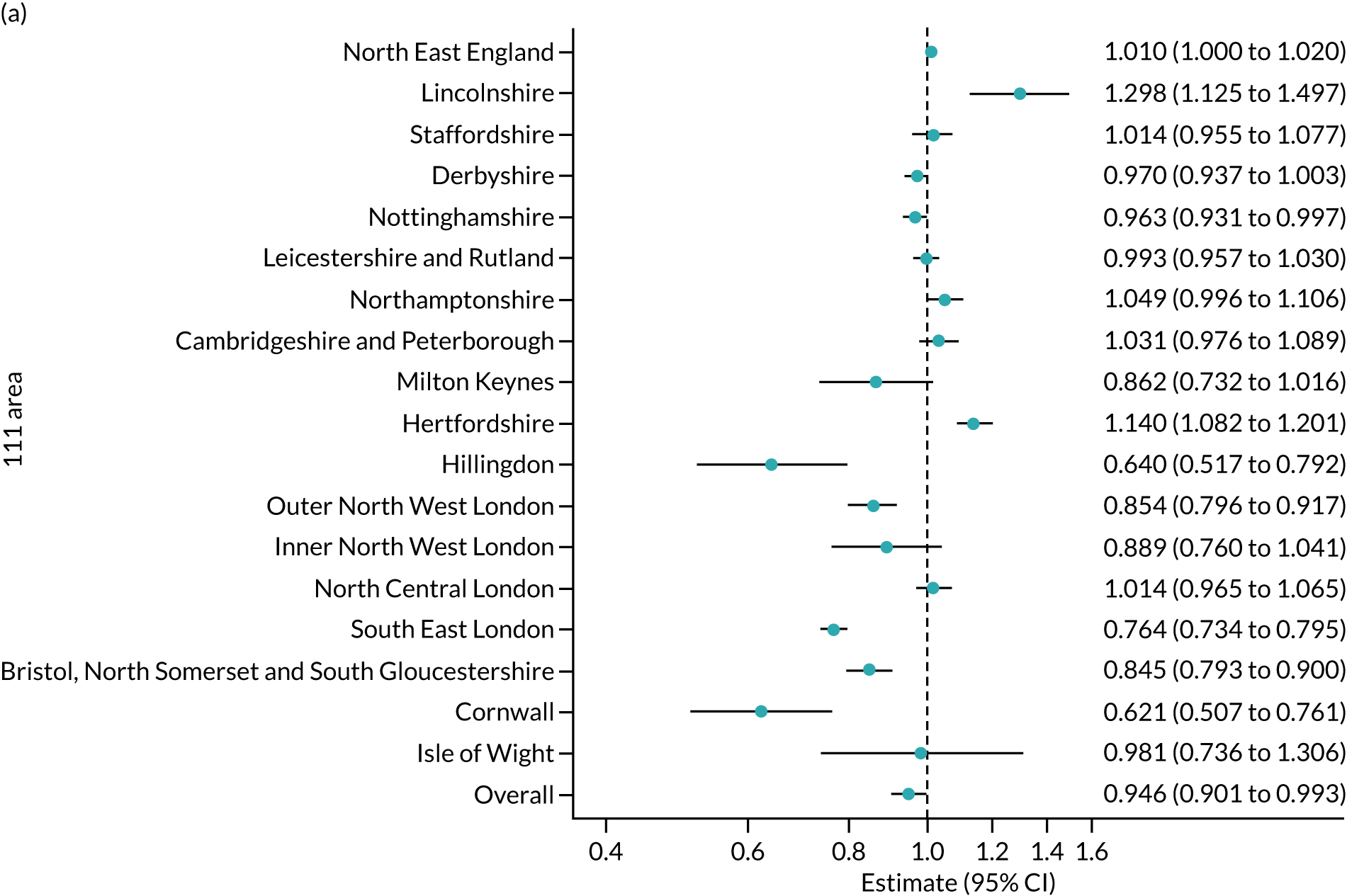
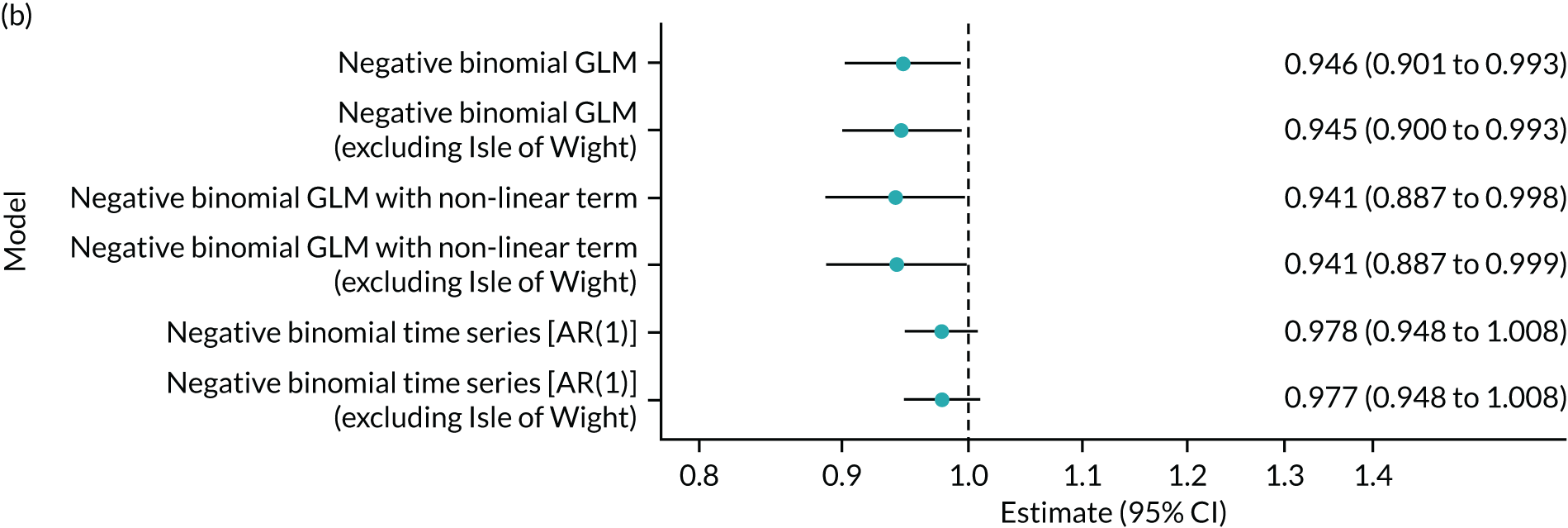
Figure 8b shows the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimate. The non-linear model also has little effect on the estimate and CIs. The AR(1) model provides slightly smaller incidence rate estimates but the result is no longer statistically significant (p = 0.148).
Ambulance dispositions
One disposition at the end of an NHS 111 contact is to recommend an emergency ambulance response. Within the telephone service, this is facilitated by NHS 111 sending the request directly to the local ambulance service. For NHS 111 Online contacts the disposition advice is to call 999. The outcome for this analysis is the number of ambulance dispositions for both NHS 111 calls and NHS 111 Online. Figure 9a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.067 (95% CI 1.035 to 1.100; p < 0.001). This means that, on average, for every 1000 online contacts, the number of ambulance dispatches potentially increases by 6.7% (95% CI 3.5% to 10.0%) if all online contacts follow this advice. This result is considered a statistically significant effect, suggesting that, on average, the online 111 service has the potential to result in an increase in the number of ambulance dispatches overall.
FIGURE 9.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of ambulance dispositions. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 89.8% (95% CI 85.4% to 92.8%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
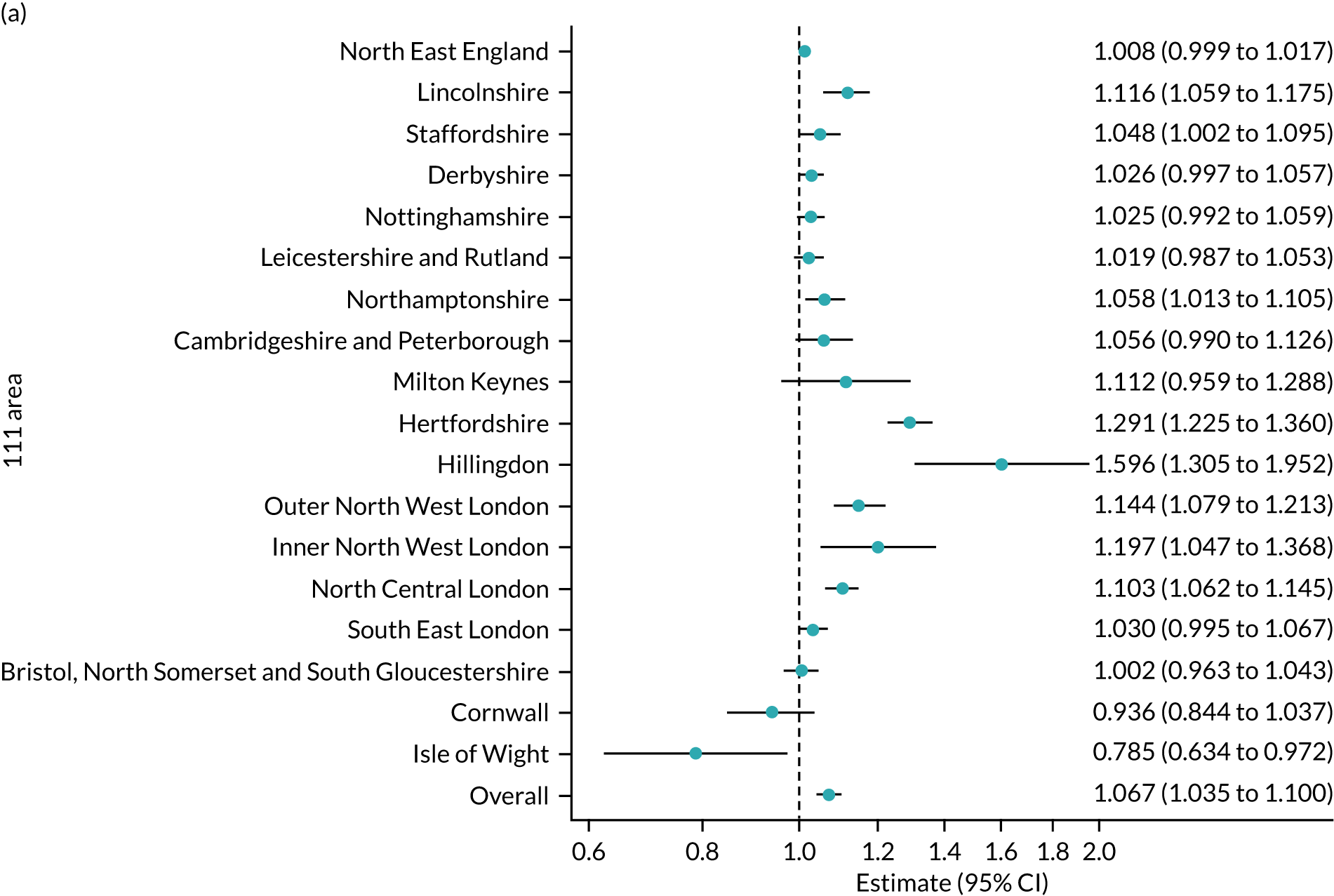
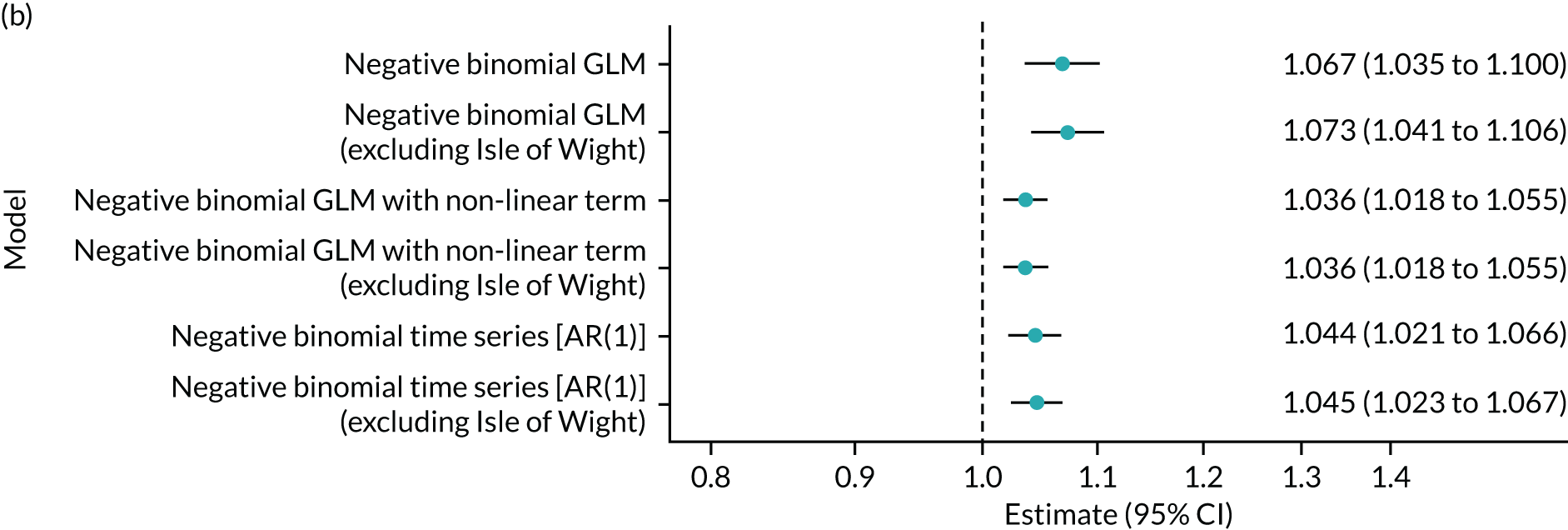
Figure 9b shows the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimate. The non-linear model also has little effect on the estimate and CIs; the estimates have decreased slightly, and this is similar for the AR(1) model.
Emergency department dispositions
The outcome of this analysis is the number of ED recommendations for both NHS 111 calls and NHS 111 Online. Figure 10a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.050 (95% CI 1.010 to 1.092; p = 0.014). This means that, on average, for every 1000 online contacts, the number of recommendations to attend has increased by 5% (95% CI 1.0% to 9.2%). This result is considered a statistically significant effect, suggesting that, on average, the NHS 111 Online service has caused an increase in the number ED recommendations overall.
FIGURE 10.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of recommendations to attend ED. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 94.4% (95% CI 92.4% to 95.8%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
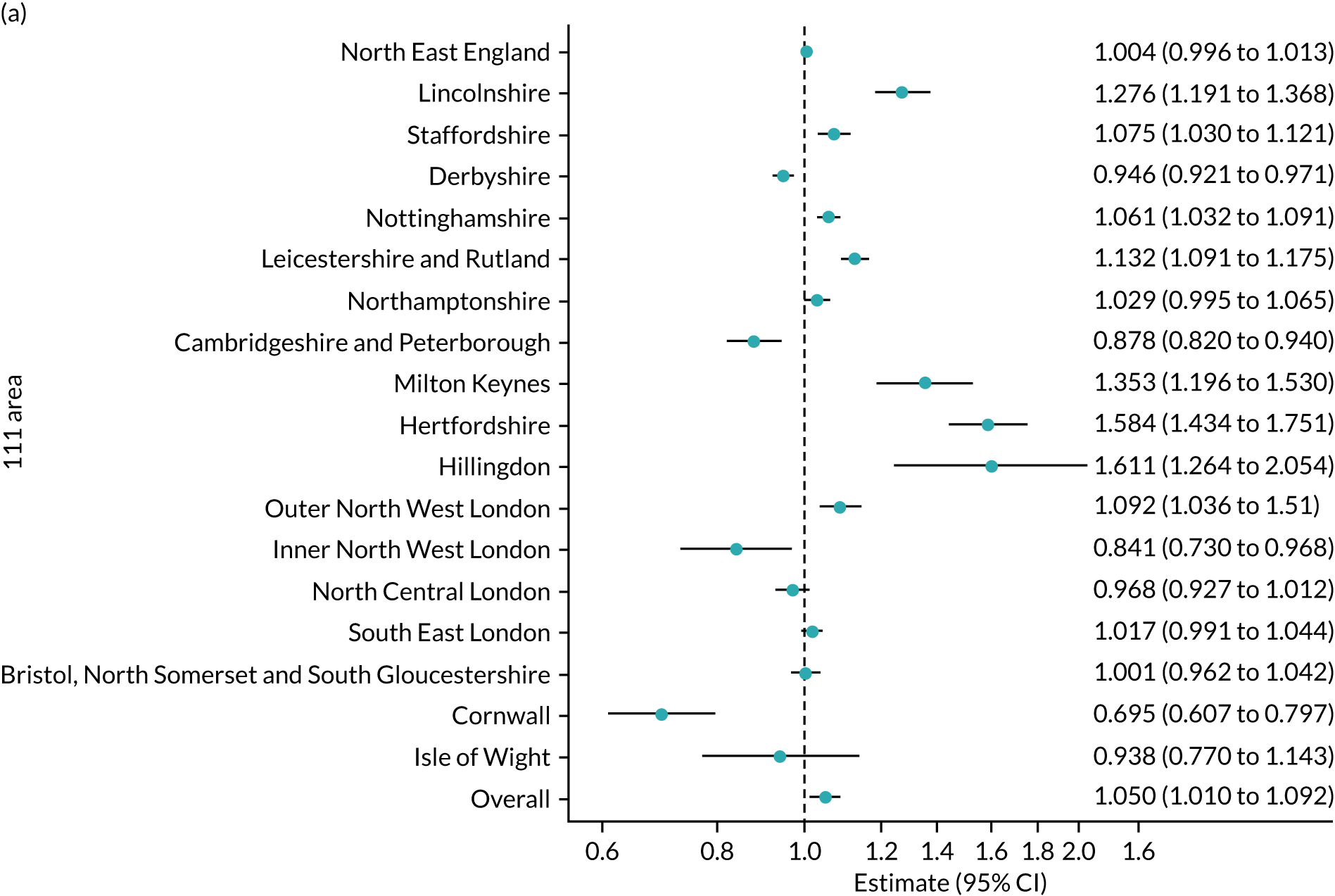
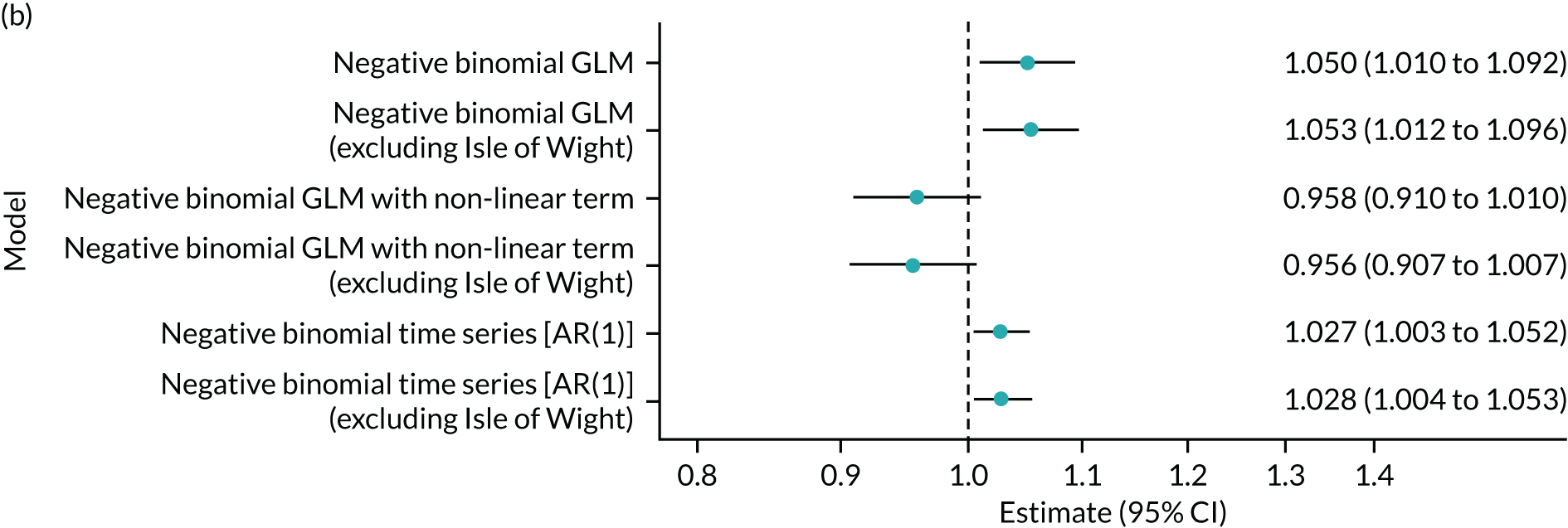
Figure 10b presents the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimate, and this is similar for the AR(1) model. The non-linear model changes the direction of the effect; however, this result is no longer significant (p = 0.110).
Contact with primary care
Being recommended to primary care can be a suggestion that a patient speak to or attend various different services. Patients can contact primary care (GP and related services) or they can be recommended to contact a pharmacy or dentist (community care). The analysis for this section looks at primary care and community care separately.
Primary care only
The outcome of this analysis focuses on the number of primary care recommendations for both NHS 111 calls and NHS 111 Online. Figure 11a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.051 (95% CI 1.027 to 1.076; p < 0.001). This means that, on average, for every 1000 online contacts, the number of primary care recommendations increases by 5.1% (95% CI 2.7% to 7.6%). This result is considered a statistically significant effect, suggesting that, on average, the NHS 111 Online service has potential to result in an increase in the number of primary care contacts overall.
FIGURE 11.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of recommendations to contact primary care. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 84.3% (95% CI 76.4% to 89.5%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
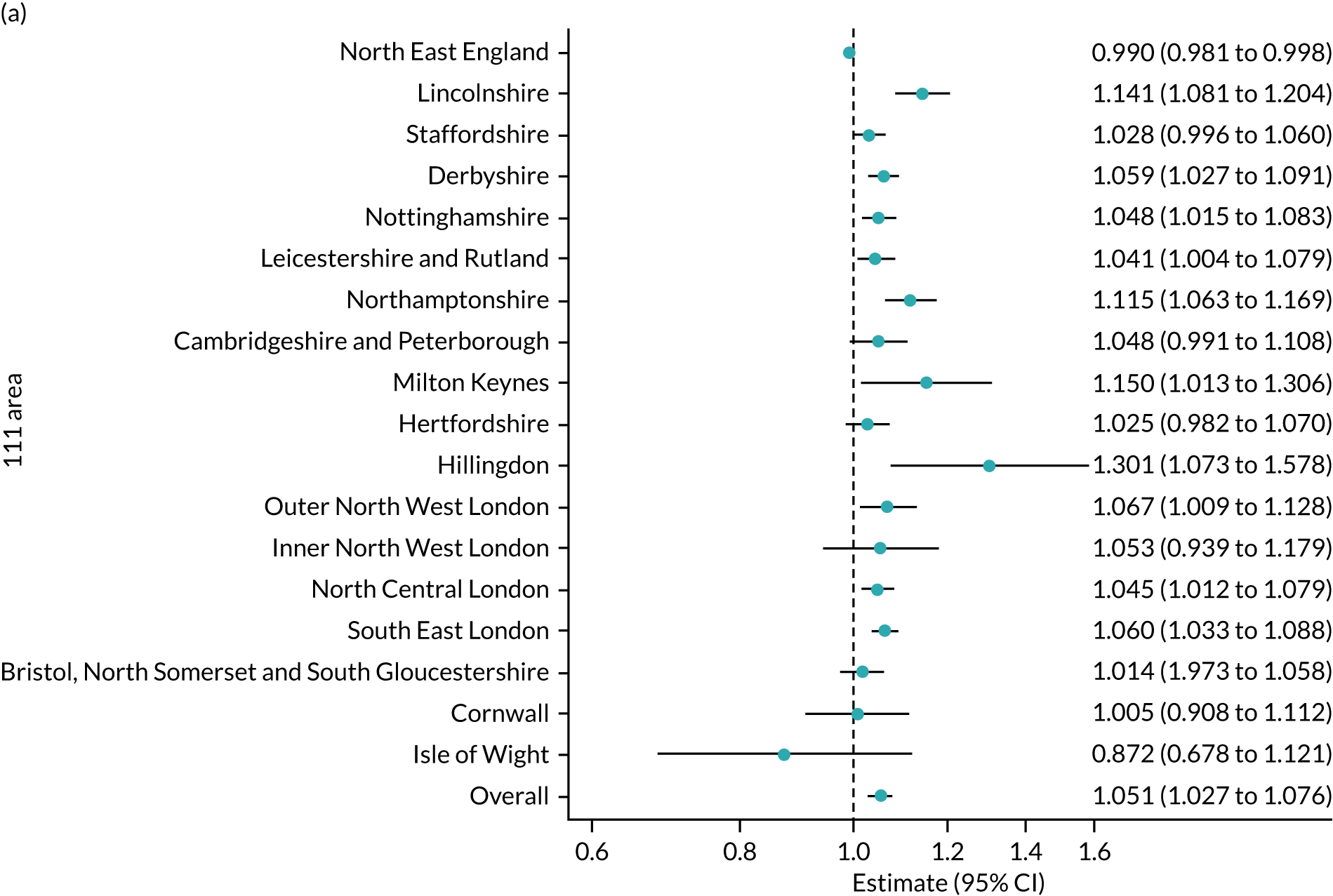
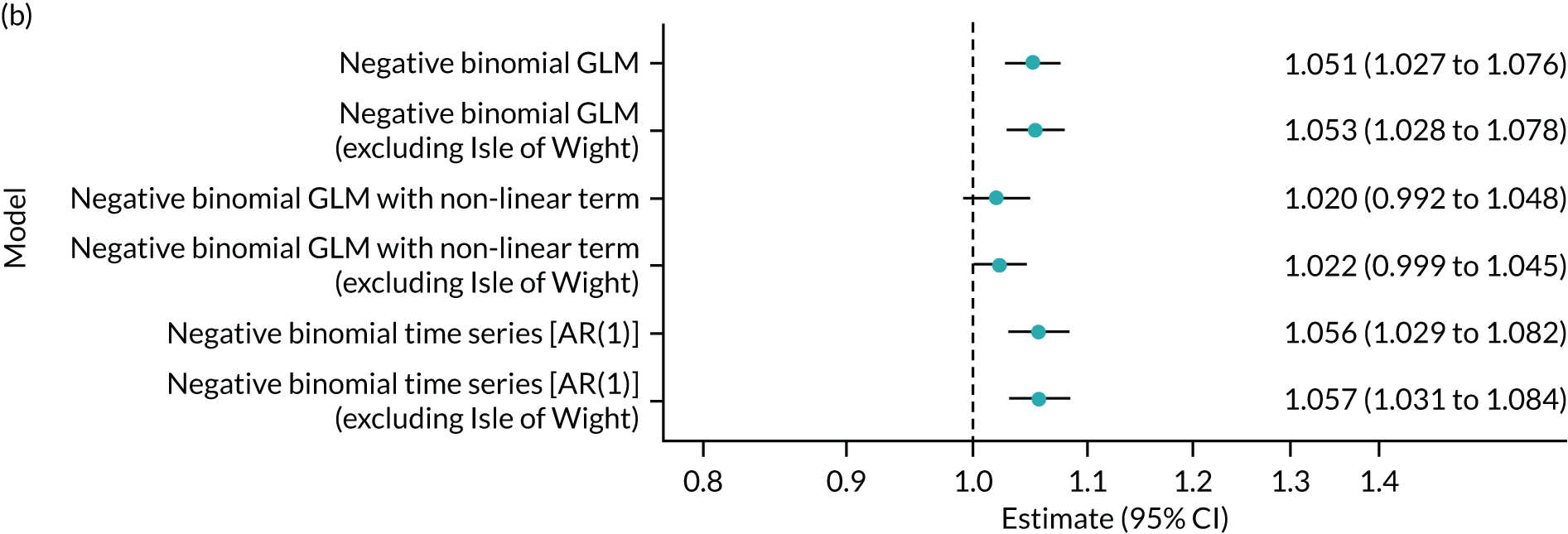
Figure 11b shows the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimate and similarly for the non-linear model and the AR(1) model. The non-linear model has slightly smaller estimates but is no longer statistically significant (p = 0.168).
Community care (dentist and pharmacy) only
The outcome of this analysis focuses on the number of dentist and pharmacy recommendations from both NHS 111 calls and NHS 111 Online. Figure 12a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.042 (95% CI 1.005 to 1.080; p = 0.027). This means that, on average, for every 1000 online contacts, the number of dentist and pharmacy recommendations increases by 4.2% (95% CI 0.5% to 8.0%). This result is considered a statistically significant effect, suggesting that, on average, the NHS 111 Online service has the potential to result in an increase in the number of dentist and pharmacy recommendations overall. This result is very similar to the primary care result.
FIGURE 12.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of recommendations to contact a dentist or pharmacy. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 86.5% (95% CI 80.2% to 90.9%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
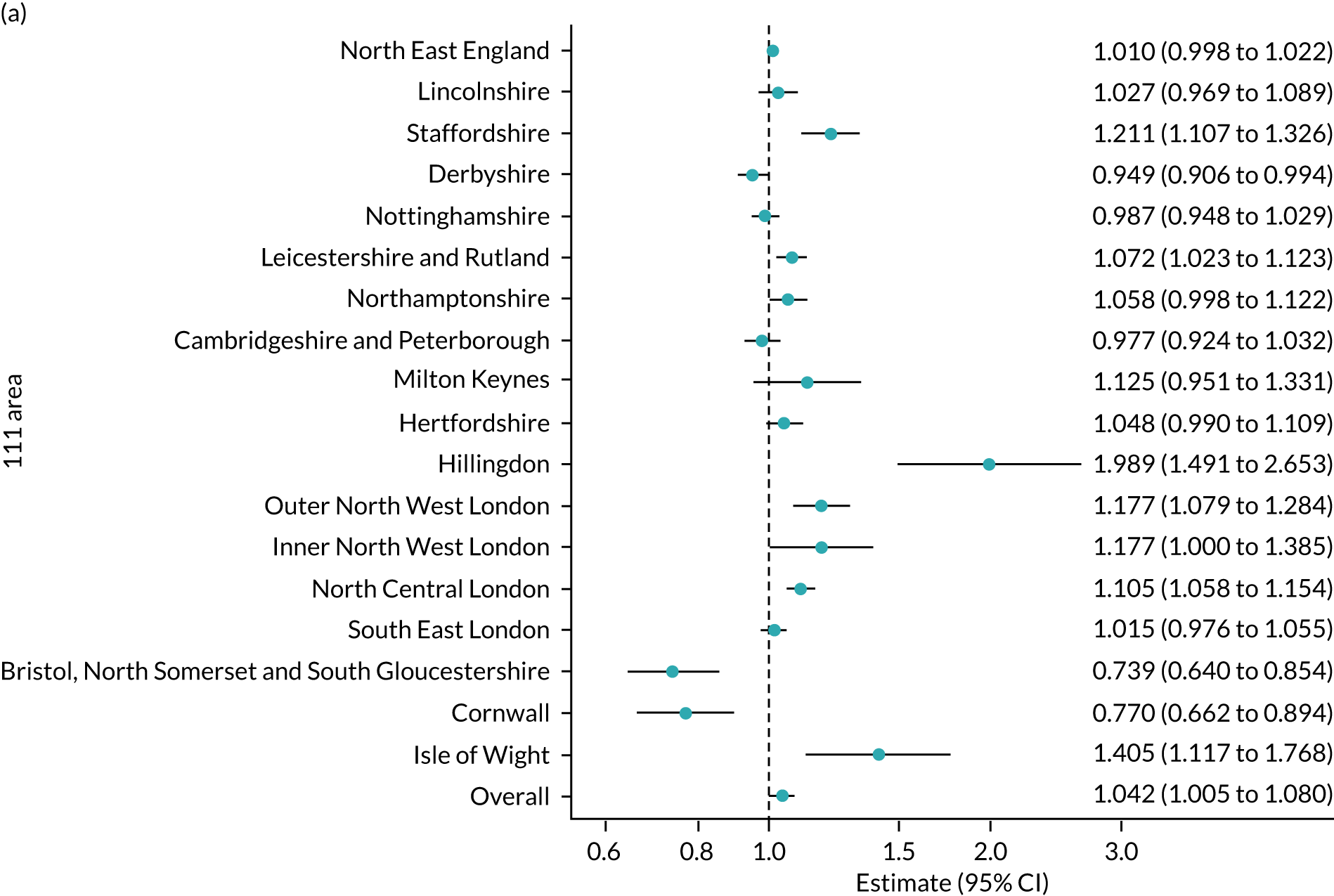
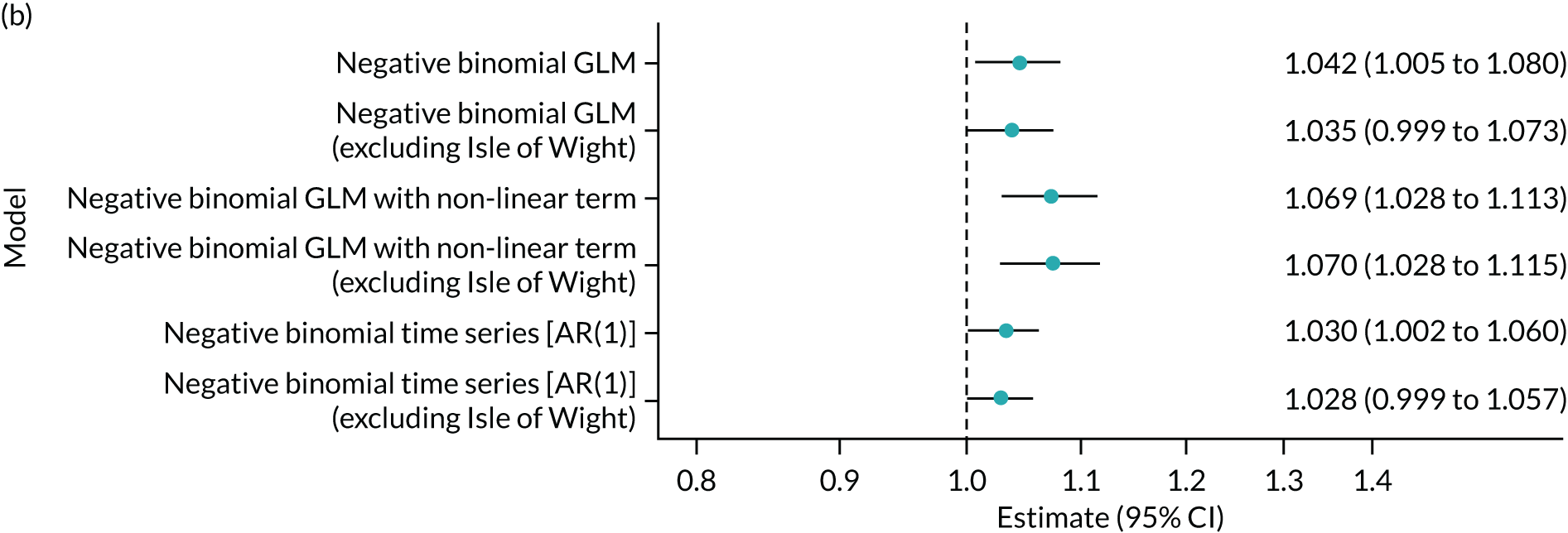
Figure 12b shows the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimates, and this is similar for the AR(1) model but the non-linear model has slightly larger estimates.
Attend another service
Another of the various dispositions at the end of a 111 contact is to be recommended to attend another service that is not ambulance, ED or primary/community care. The outcome of this analysis is the number of recommendations to attend another service for both NHS 111 calls and NHS 111 Online contacts. Figure 13a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.216 (95% CI 1.115 to 1.327; p < 0.001). This means that, on average, for every 1000 online contacts, the number of recommendations to attend another service increases by 21.6% (95% CI 11.5% to 32.7%). This result is considered a statistically significant effect, suggesting that, on average, the NHS 111 Online service has increased the number of recommendations to attend another service overall.
FIGURE 13.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of recommendations to attend or contact another service. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 94.9% (95% CI 93.2% to 96.2%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
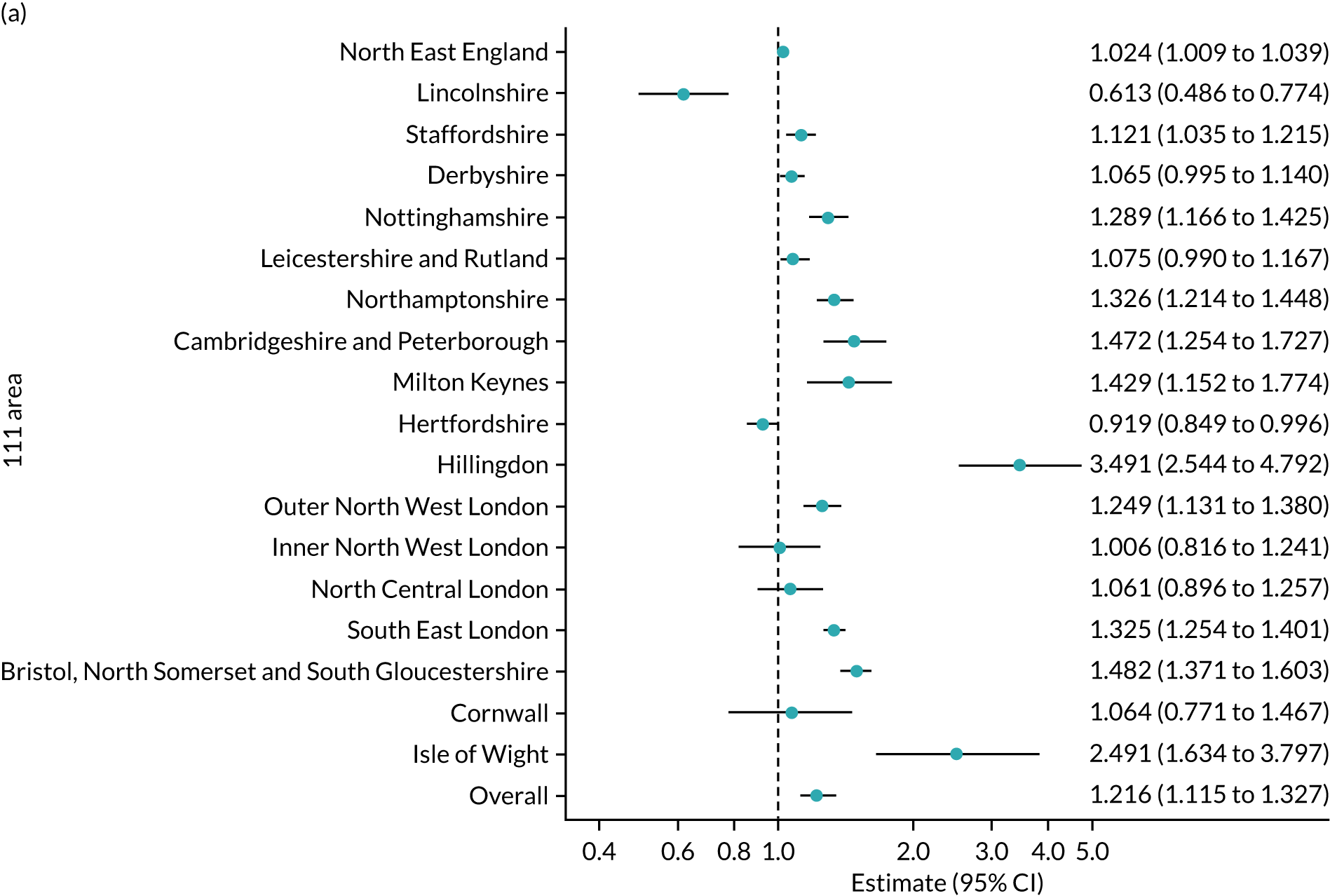
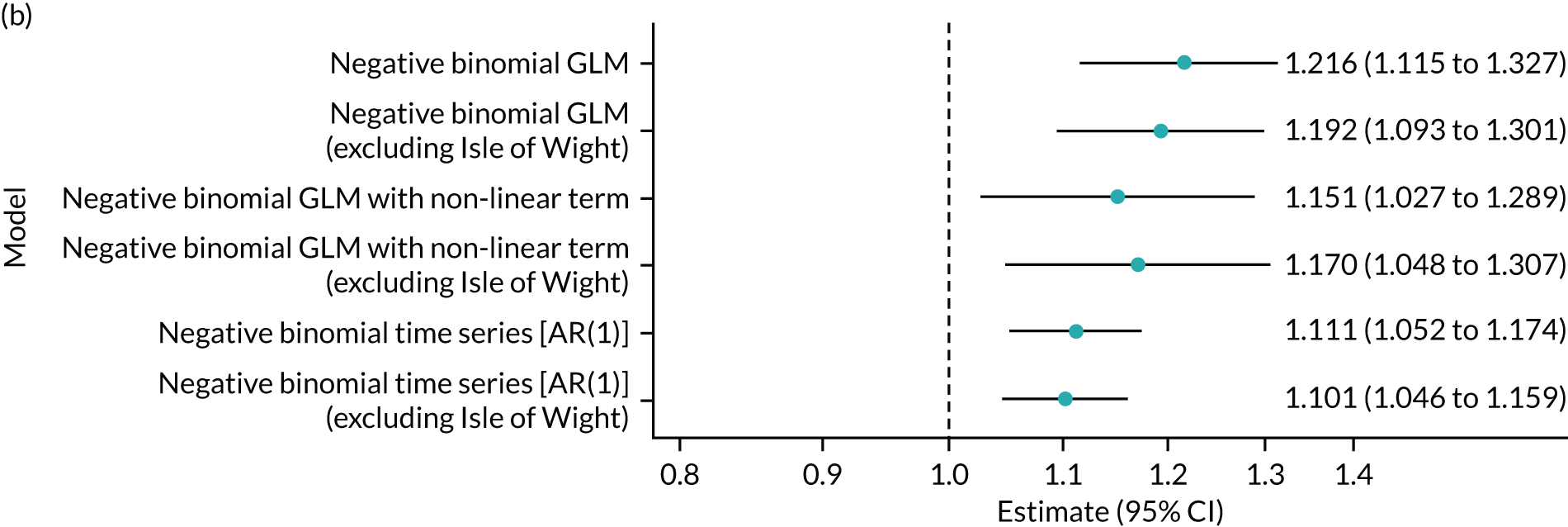
Figure 13b shows the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimate, and this is similar for the non-linear model and the AR(1) model. Both the non-linear model and the AR(1) model have smaller estimates but are still statistically significant.
Not recommended any service
The final of the various dispositions at the end of a 111 contact is to be recommended not to attend any service. The outcome of this analysis is the number of recommendations not to attend any service for both NHS 111 calls and online. Figure 14a shows the forest plot of clinical calls for all area codes for the primary analysis method. The x-axis shows the incidence rate ratio per 1000 online contacts. The overall incidence rate ratio per 1000 online contacts is 1.034 (95% CI 1.002 to 1.067; p = 0.035). This means that, on average, for every 1000 online contacts, the number of recommendations to not attend any service increases by 3.4% (95% CI 0.2% to 6.7%). This result is considered a statistically significant effect, suggesting that, on average, the NHS 111 Online service has the potential to increase the number of recommendations to not attend any service overall.
FIGURE 14.
Forest plots showing the effect of introducing the NHS 111 Online service on the number of recommendations to not attend any service. (a) Estimated effects for individual areas and the overall average effect from the primary analysis (negative binomial GLM), heterogeneity I2 = 87.1% (95% CI 81.1% to 91.2%); and (b) average effects from the primary analysis and sensitivity analyses. Estimates are incident rate ratios per 1000 online contacts. GLM, generalised linear model.
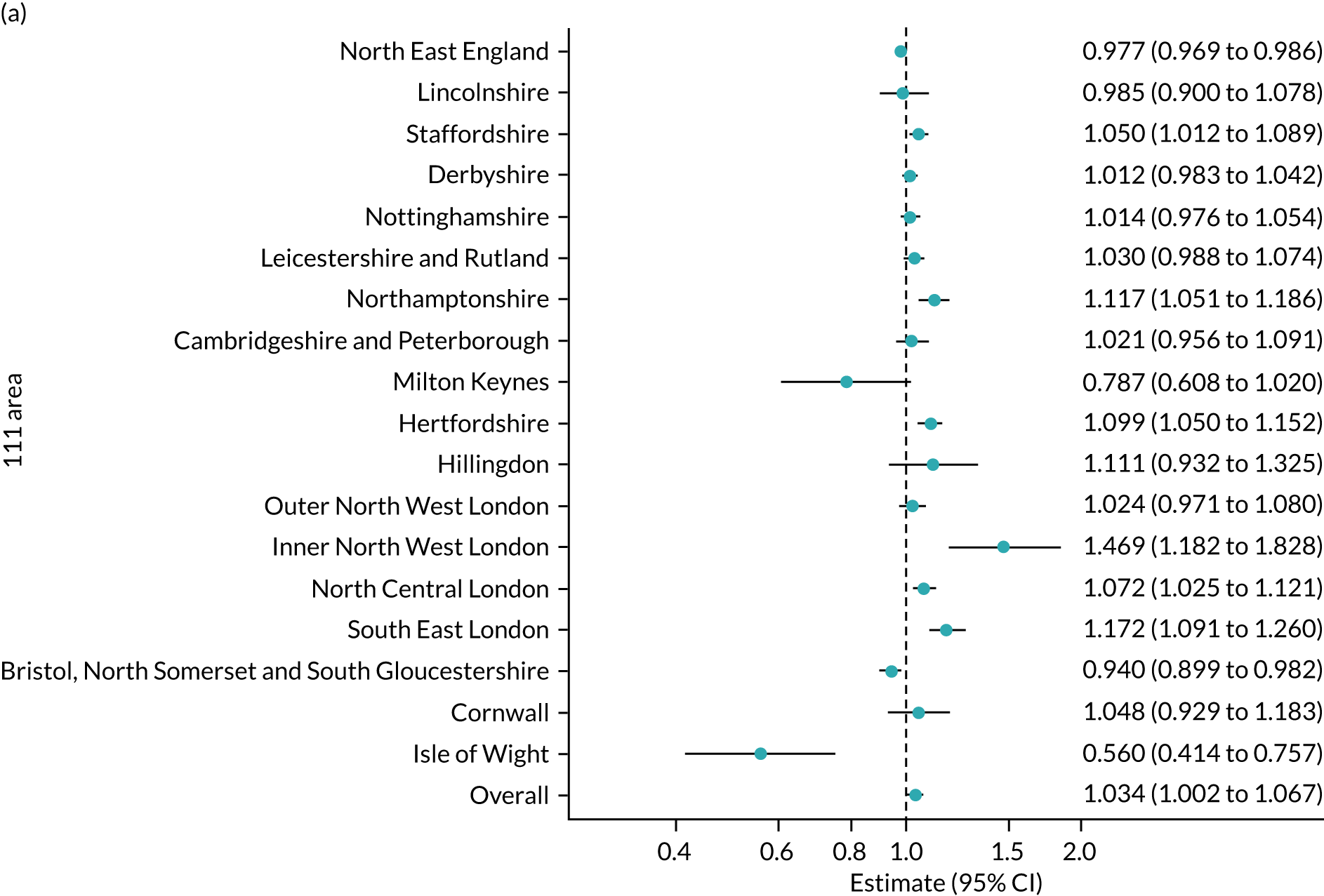
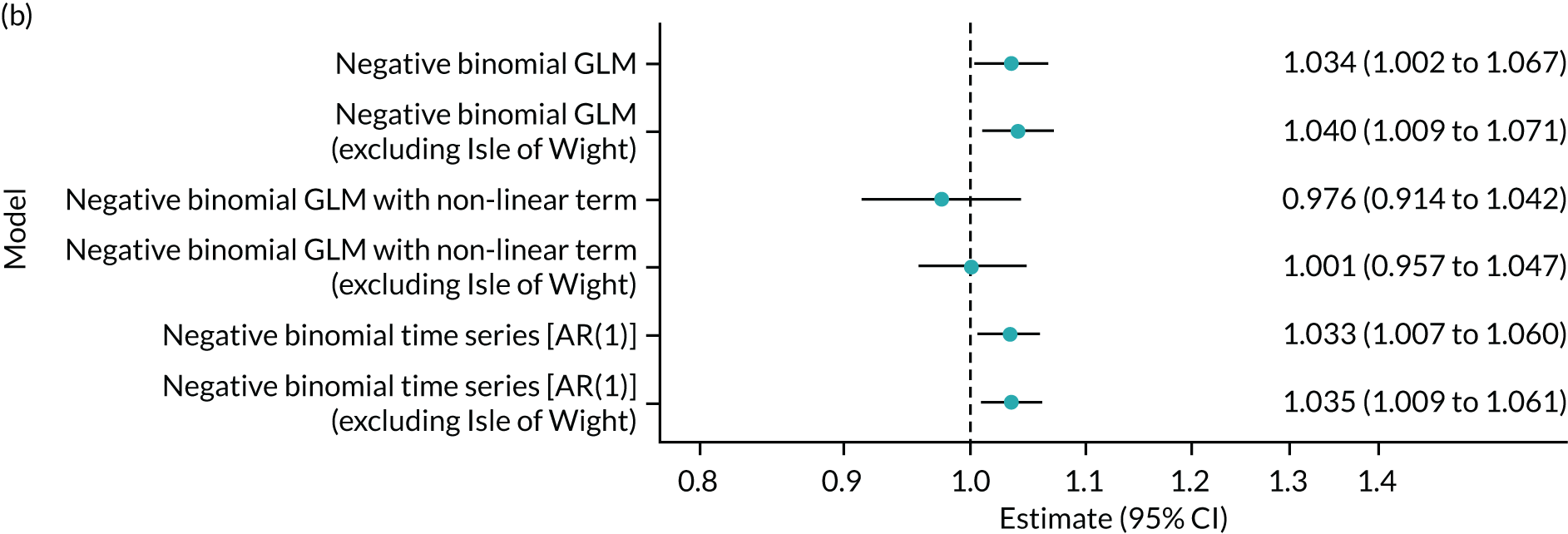
Figure 14b shows the forest plot of the main analysis method and various sensitivity analyses. Again, excluding the Isle of Wight has little effect on the estimate, and this is similar for the AR(1) model. The non-linear model has smaller estimates and the result is no longer statistically significant (p = 0.474).
Summary
The introduction of the NHS 111 Online service has added another access point for urgent and emergency care in the NHS. The online service operates as well as, not instead of, the existing telephone service, creating two sources of activity. Both services direct users to services in the emergency and urgent care system, unless the health problem is suitable for self-care. We have conducted an interrupted time series analysis to assess changes in activity following the introduction of NHS 111 Online using a dose–response model, where the ‘dose’ is the number of contacts with the NHS 111 Online service. The results for the primary and secondary outcomes assessed are summarised in Table 2.
| Outcome | Incidence rate ratio per 1000 online contacts (95% CI) | Activity change per 1000 NHS 111 Online contacts (%) |
|---|---|---|
| NHS 111 triaged calls | 1.013 (0.996 to 1.029; p = 0.127) | +1.3 |
| NHS 111 offered calls | 1.008 (0.992 to 1.025; p = 0.313) | +0.8 |
| Clinician calls | 0.946 (0.901 to 0.993; p = 0.025)a | –5.4 |
| Ambulance disposition | 1.067 (1.035 to 1.100; p < 0.001)a | +6.7 |
| ED disposition | 1.050 (1.010 to 1.092; p = 0.014)a | +5.0 |
| Primary care disposition | 1.051 (1.027 to 1.076; p < 0.001)a | +5.1 |
| Other community service disposition | 1.042 (1.005 to 1.080; p = 0.027)a | +4.2 |
| Other service disposition | 1.216 (1.115 to 1.327; p < 0.001)a | +21.6 |
| No service | 1.034 (1.002 to 1.067; p = 0.035)a | +3.4 |
The primary outcome was the impact on activity to the NHS 111 telephone service as the two are directly related. We found that the online service has little impact on the number of triaged and offered calls, so the workload for NHS 111 has neither increased nor decreased as a result of the introduction of NHS 111 Online, suggesting that there has been no substantial shift to using the online service instead of the telephone service. However, this was not a consistent finding, and four sites showed a reduction in triaged calls, indicating that it is possible that there has been a shift away from the telephone service to the online service.
The secondary outcome most directly related to the NHS 111 service is assessment by an NHS 111 clinician, as the online service has a facility for requesting a clinical call back from an NHS 111 clinician. We found that the number of clinical calls decreased, which was unexpected, as there is potential for additional activity to be generated by NHS 111 Online ‘speak to our clinician’ dispositions. This may be a genuine finding, that more people with less urgent problems may be using the online service and having their problem resolved without the need for a clinician assessment, diverting these people from the telephone service. However, it could also be a consequence of the way we have identified clinician call-backs in the NHS 111 Online data. We took a cautious approach and included contacts recorded as clinical call back offered and sent and with a final disposition (advice) code of ‘speak to our clinician’. It is possible that there were some relevant contacts where only one of these conditions was fulfilled and, as a consequence, the total number of clinical call backs has been undercounted.
For all other secondary outcomes, and hence for indirectly related services, the combined activity from the NHS 111 telephone service and the online service increased the overall number of recommendations to contact or attend those services following the introduction of the NHS 111 Online service. The biggest increase is for ‘other services’, which account for a relatively small proportion of NHS 111 telephone dispositions (6–7%). 49 This finding may reflect a lower urgency for online contacts that can be directed to services such as an optician. At face value, the results would suggest a net increase in the demand for emergency and urgent care services, and this would not be surprising. For the 18 sites in our analyses, there were almost 600,000 contacts with the NHS 111 Online service, with no apparent shift away from the telephone service, and, nationally, there were over 2 million contacts during 2019. Previous research has shown that the introduction of new services and access points for emergency and urgent care, including NHS Direct, NHS 111 and walk-in centres, has created an increase in, and therefore new demand for, services. 56–58 It is entirely plausible that this new online service could produce the same effect. However, the findings of the previous research were based on data of actual utilisation of other services in the emergency and urgent care system. For this analysis, we have been able to demonstrate only the recommendations about services to contact or attend and so potential increases in service utilisation. The potential service use increases estimated by our analyses would hold true only if every recommendation was acted on and if, by using NHS 111 Online, users subsequently accessed a service that they would not have used without a recommendation from the online service. The actual change in service utilisation is dependent on user behaviour: whether they choose to contact the recommended service, another service or no service or if they use the online service to confirm an action they would have carried out anyway (e.g. attend the ED or call their GP). We explore these factors in Chapters 6 and 7, in which we report the findings of the user survey and interviews, and we comment further in the discussion in Chapter 10.
It is also likely that any changes in demand may be influenced by other external factors. We have used a meta-analysis to produce an overall summary measure of effect from the 18 sites included in the analyses. However, the forest plot figures presented show considerable variation between different area codes, indicating that there may be local differences, for example in service availability and the amount of integration between services, and hence that the effect of introducing NHS 111 Online is unlikely to be consistent across different health economies.
Limitations
There are some limitations to these analyses. First, because of the rapid roll-out of NHS 111 Online as a national service, we were not able to use an experimental design with a control arm. This means that we cannot establish if the effects we have found are the direct result of the introduction of the new service or if they would have happened anyway because of other factors influencing both the NHS 111 telephone service and the wider emergency and urgent care system.
Second, the compromise of using the NHS 111 minimum data set aggregated data rather than patient-level data for the telephone service meant that we were able to successfully match only 18 of the 38 potential area codes to NHS 111 Online data, so we have not been able to establish a national estimate of impact. However, we are confident that the 18 sites included are representative of different geographical areas, activity volume and provider types across England to allow reasonable inferences.
Third, we evaluated the impact of the NHS 111 Online service during the early stage of its implementation, and at the sites we used it had been in operation for only 12–18 months. We have therefore estimated system impact based on the ‘dose’, in terms of contacts with the new service, present at that time. As the service becomes more widely understood by the public and as contacts increase, it is possible the impact may change and any subsequent assessment of impact would be more robust.
Finally, as discussed above, we have considered only recommendations for care, not actual care accessed, which might be quite different and will depend on how people use the service and their subsequent utilisation of other services: both those in the emergency and urgent care system and those in routine primary care. This makes it difficult to estimate how much new demand there may be. This is discussed further in Chapter 10.
Chapter 5 Characteristics of the NHS 111 Online and telephone populations
Introduction
The NHS 111 Online and telephone services both provide triage and advice about what services to contact for people with urgent health problems and offer different ways of accessing this advice. In this chapter, we describe and compare the characteristics and usage patterns of each service to see if there are differences between the online and telephone user populations (objective 3).
Methods
Data collection
Four data sets were used for this descriptive work.
NHS 111 telephone service
-
We used the same aggregated call data from the NHS 111 minimum data set described in Chapter 4. These data provided information on the total volumes of calls and disposition (service recommendations) as monthly counts. We used the same 18 sites described in Chapter 4.
-
To examine and compare demographic characteristics between the online and telephone service populations, patient-level data are required. We were unable to obtain contemporary patient-level data for the telephone service within the timescales for this study. Instead, we used an existing historical patient-level data set held by our institution. We created a data set extracted from the ‘Connected Health Cities: Data linkage of urgent care data’ study (known as the ‘CUREd research database’). Data relate to calls to the NHS 111 telephone service in the Yorkshire and the Humber region between January and December 2016. The CUREd database has permissions to receive and store health and social care data without patient consent for patients using emergency and urgent care services in Yorkshire and the Humber. Approvals are in place from an NHS Research and Ethics Committee and the NHS Health Research Authority. Robustly anonymised data from this data set can be provided to external organisations for research purposes on request, but, as the analyst for this project (RS) is also a member of the CUREd team, permission to extract data was not required. Data from individual call records were extracted, including age, sex, date of contact, time of contact, area and disposition.
NHS 111 Online service
NHS Digital provided data on individual contacts to the NHS 111 Online service. Variables included date, time, age, sex, area, number of triages, length of online session, main health problem, final health problem and disposition. NHS Digital provided two data sets:
-
For all contacts between January 2018 and December 2019 – this is the data set also used for the interrupted time series analyses.
-
Early in the study, before we had to make the decision to use the NHS 111 MDS for telephone call data, NHS Digital provided the same data set for the period January 2018 to July 2019 for the nine original intended study sites. Some descriptive analyses were conducted early in the study using this data set.
Descriptive statistics
The NHS 111 MDS provides aggregated data only, so the Yorkshire and the Humber CUREd data were used as the source of the characteristics of the telephone user population, which were compared with the characteristics of those who used the online service.
Descriptive analyses comparing the final dispositions of both online and call data could be compared within our data set alongside overall summaries of the characteristics of the online data population for the 18 area codes.
For the more detailed analysis of the NHS 111 Online population, including the reasons for contacts, univariate analysis was used to describe the frequencies and distributions of single variables. Bivariate and multivariate analyses were used to compare different variables.
Results
Demographics
Table 3 presents the demographic data for both the NHS 111 telephone call (January–December 2016) and 111 Online (January–December 2019) contacts for Yorkshire and the Humber. These data allow a comparison of the characteristics of those who choose to call 111 and those who use 111 Online.
| Yorkshire and the Humber | Online,a n (%) | Calls,b n (%) |
|---|---|---|
| N (%) | 275,538 (100) | 1,350,280 (100) |
| Sex | ||
| Female | 186,524 (67.7) | 762,741 (56.5) |
| Male | 89,014 (32.3) | 585,625 (43.4) |
| Not known | – | 587 (0.0) |
| Not specified | – | 1327 (0.1) |
| Total | 275,538 (100) | 1,350,280 (100) |
| Age group (years) | ||
| 0–1 | – | 138,969 (10.3) |
| 2–15 | 25,636 (9.3) | 188,414 (14.0) |
| 16–34 | 168,295 (61.1) | 421,536 (31.2) |
| 35–74 | 78,823 (28.6) | 415,247 (30.8) |
| ≥ 75 | 2771 (1) | 186,096 (13.8) |
| NA | 13 (0) | 18 (0.0) |
| Total | 275,538 (100) | 1,350,280 (100) |
| Time of day | ||
| Night | 95,224 (34.6) | 423,546 (31.4) |
| Day | 180,314 (65.4) | 926,734 (68.6) |
| Total | 275,538 (100) | 1,350,280 (100) |
| Weekend/week | ||
| Week | 184,712 (67) | 774,167 (57.3) |
| Weekend | 90,826 (33) | 576,113 (42.7) |
| Total | 275,538 (100) | 1,350,280 (100) |
| Disposition | ||
| 5.23 (ambulance) | 34,571 (12.5) | 135,999 (10.1) |
| 5.24 (A&E) | 22,678 (8.2) | 101,840 (7.5) |
| 5.25 (primary care) | – | 824,134 (61.0) |
| 5.25a (contact primary care) | 118,162 (42.9) | – |
| 5.25b (speak to primary care) | 19,427 (7.1) | – |
| 5.25c (dental and pharmacy) | – | – |
| 5.25d (dental) | 37,129 (13.5) | – |
| 5.25e (pharmacy) | 1492 (0.5) | – |
| 5.26 (other service) | 40,057 (14.5) | 55,511 (4.1) |
| 5.27 (no service) | – | 229,910 (17.0) |
| 5.27a (health information) | – | – |
| 5.27b (home care) | 1159 (0.4) | – |
| 5.27c (non-clinical) | – | – |
| NA | 863 (0.3) | 2886 (0.2) |
| Total | 275,538 (100) | 1,350,280 (100) |
For both calls and online, there were more female users; however, among online users this percentage is higher. The biggest difference was in age. Those who called NHS 111 tended to be older, whereas those in the 16–35 years age group used NHS 111 Online most often, at 61% of the population. A higher percentage use NHS 111 during the week than at the weekend for both calls and online, this percentage being higher for online. Online contacts had a higher percentage for all dispositions except for those recommended to not attend any service. However, this may be because of differences in how final disposition is recorded in each data set. Because of this, the number of callers offered clinician assessment cannot be included. In telephone data the disposition after clinician assessment is recorded, whereas in the online data this is an end disposition.
We have also compared the NHS 111 Online service dispositions with telephone call data for each of the 18 study sites used in the analyses in Chapter 4 (see Report Supplementary Material 1). Overall, the pattern of dispositions is the same, with ambulance, ED and contact primary care dispositions higher among the NHS 111 Online population. However, these comparisons should be treated with caution as the Yorkshire and the Humber data may not reflect individual site differences.
NHS 111 Online service only demographics by area code
Tables 4 and 5 present the characteristics of those who use NHS 111 Online in each area code. The percentages with each characteristic tended to be similar for each code, with almost 90% of online users overall in the 16–75 years age group. Less than 2% of contacts with the service were in the ≥ 75 years age group. Over 60% of contacts were made during daytime hours (08.00–20.00) and proportionally more were made during weekdays, although this is spread over 5 days rather than the 2 or 3 days for weekends and bank holidays.
| Site | N | Sex, n (%) | Age group (years), n (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Total | 2–16 | 16–35 | 35–75 | ≥ 75 | NA | Total | ||
| North East | 142,373 | 99,088 (69.6) | 43,285 (30.4) | 142,373 (100) | 15,834 (11.1) | 81,521 (57.3) | 43,239 (30.4) | 1775 (1.2) | 4 (0) | 142,373 (100) |
| Lincolnshire | 26,469 | 18,302 (69.1) | 8167 (30.9) | 26,469 (100) | 2730 (10.3) | 15,387 (58.1) | 7998 (30.2) | 354 (1.3) | – | 26,469 (99.9) |
| Nottinghamshire | 36,263 | 25,169 (69.4) | 11,094 (30.6) | 36,263 (100) | 3089 (8.5) | 23,047 (63.6) | 9761 (26.9) | 366 (1) | – | 36,263 (100) |
| Derbyshire | 39,085 | 27,356 (70) | 11,729 (30) | 39,085 (100) | 3770 (9.6) | 22,934 (58.7) | 11,947 (30.6) | 433 (1.1) | 1 (0) | 39,085 (100) |
| Isle of Wight | 4675 | 3088 (66.1) | 1587 (33.9) | 4675 (100) | 550 (11.8) | 2382 (51) | 1649 (35.3) | 92 (2) | 2 (0) | 4675 (100.1) |
| Inner North West London | 12,955 | 8247 (63.7) | 4708 (36.3) | 12,955 (100) | 524 (4) | 9084 (70.1) | 3255 (25.1) | 90 (0.7) | 2 (0) | 12,955 (99.9) |
| Hillingdon | 6498 | 4451 (68.5) | 2047 (31.5) | 6498 (100) | 567 (8.7) | 4020 (61.9) | 1848 (28.4) | 63 (1) | – | 6498 (100) |
| Hertfordshire | 34,320 | 23,531 (68.6) | 10,789 (31.4) | 34,320 (100) | 3607 (10.5) | 19,201 (55.9) | 11,091 (32.3) | 421 (1.2) | – | 34,320 (99.9) |
| Cambridgeshire and Peterborough | 30,132 | 20,268 (67.3) | 9864 (32.7) | 30,132 (100) | 3047 (10.1) | 17,378 (57.7) | 9362 (31.1) | 344 (1.1) | 1 (0) | 30,132 (100) |
| Northamptonshire | 26,765 | 18,398 (68.7) | 8367 (31.3) | 26,765 (100) | 2898 (10.8) | 15,259 (57) | 8275 (30.9) | 331 (1.2) | 2 (0) | 26,765 (99.9) |
| Milton Keynes | 10,368 | 7232 (69.8) | 3136 (30.2) | 10,368 (100) | 1065 (10.3) | 6014 (58) | 3201 (30.9) | 87 (0.8) | 1 (0) | 10,368 (100) |
| Leicestershire and Rutland | 38,235 | 26,230 (68.6) | 12,005 (31.4) | 38,235 (100) | 3740 (9.8) | 22,699 (59.4) | 11,356 (29.7) | 438 (1.1) | 2 (0) | 38,235 (100) |
| Outer North West London | 20,100 | 13,488 (67.1) | 6612 (32.9) | 20,100 (100) | 1651 (8.2) | 12,456 (62) | 5768 (28.7) | 224 (1.1) | 1 (0) | 20,100 (100) |
| North Central London | 30,083 | 20,103 (66.8) | 9980 (33.2) | 30,083 (100) | 1942 (6.5) | 19,623 (65.2) | 8197 (27.2) | 321 (1.1) | – | 30,083 (100) |
| South East London | 47,243 | 32,329 (68.4) | 14,914 (31.6) | 47,243 (100) | 3357 (7.1) | 30,346 (64.2) | 13,183 (27.9) | 353 (0.7) | 4 (0) | 47,243 (99.9) |
| Bristol, North Somerset and South Gloucestershire | 26,046 | 17,248 (66.2) | 8798 (33.8) | 26,046 (100) | 2054 (7.9) | 15,830 (60.8) | 7903 (30.3) | 258 (1) | 1 (0) | 26,046 (100) |
| Cornwall | 16,786 | 11,230 (66.9) | 5556 (33.1) | 16,786 (100) | 1916 (11.4) | 8772 (52.3) | 5790 (34.5) | 307 (1.8) | 1 (0) | 16,786 (100) |
| Staffordshire | 36,846 | 25,378 (68.9) | 11,468 (31.1) | 36,846 (100) | 4083 (11.1) | 21,114 (57.3) | 11,225 (30.5) | 424 (1.2) | – | 36,846 (100) |
| Total | 585,242 | 401,136 (68.5) | 184,106 (31.5) | 585,242 | 56,424 (9.6) | 347,067 (59.3) | 175,048 (29.9) | 6681 (1.14) | 22 (0.0) | 585,242 |
| Site | N | Time of day, n (%) | Weekend/weekday, n (%) | ||||
|---|---|---|---|---|---|---|---|
| Night | Day | Total | Weekday | Weekend | Total | ||
| North East | 142,373 | 45,105 (31.7) | 97,268 (68.3) | 142,373 (100) | 91,021 (63.9) | 51,352 (36.1) | 142,373 (100) |
| Lincolnshire | 26,469 | 9809 (37.1) | 16,660 (62.9) | 26,469 (100) | 16,979 (64.1) | 9490 (35.9) | 26,469 (100) |
| Nottinghamshire | 36,263 | 13,473 (37.2) | 22,790 (62.8) | 36,263 (100) | 24,143 (66.6) | 12,120 (33.4) | 36,263 (100) |
| Derbyshire | 39,085 | 14,519 (37.1) | 24,566 (62.9) | 39,085 (100) | 25,742 (65.9) | 13,343 (34.1) | 39,085 (100) |
| Isle of Wight | 4675 | 1662 (35.6) | 3013 (64.4) | 4675 (100) | 3231 (69.1) | 1444 (30.9) | 4675 (100) |
| Inner North West London | 12,955 | 4298 (33.2) | 8657 (66.8) | 12,955 (100) | 9514 (73.4) | 3441 (26.6) | 12,955 (100) |
| Hillingdon | 6498 | 2514 (38.7) | 3984 (61.3) | 6498 (100) | 4417 (68) | 2081 (32) | 6498 (100) |
| Hertfordshire | 34,320 | 12,617 (36.8) | 21,703 (63.2) | 34,320 (100) | 22,035 (64.2) | 12,285 (35.8) | 34,320 (100) |
| Cambridgeshire and Peterborough | 30,132 | 11,173 (37.1) | 18,959 (62.9) | 30,132 (100) | 19,249 (63.9) | 10,883 (36.1) | 30,132 (100) |
| Northamptonshire | 26,765 | 9793 (36.6) | 16,972 (63.4) | 26,765 (100) | 17,271 (64.5) | 9494 (35.5) | 26,765 (100) |
| Milton Keynes | 10,368 | 3707 (35.8) | 6661 (64.2) | 10,368 (100) | 7123 (68.7) | 3245 (31.3) | 10,368 (100) |
| Leicestershire and Rutland | 38,235 | 13,761 (36) | 24,474 (64) | 38,235 (100) | 25,118 (65.7) | 13,117 (34.3) | 38,235 (100) |
| Outer North West London | 20,100 | 7838 (39) | 12,262 (61) | 20,100 (100) | 13,634 (67.8) | 6466 (32.2) | 20,100 (100) |
| North Central London | 30,083 | 10,943 (36.4) | 19,140 (63.6) | 30,083 (100) | 20,957 (69.7) | 9126 (30.3) | 30,083 (100) |
| South East London | 47,243 | 18,118 (38.4) | 29,125 (61.6) | 47,243 (100) | 32,416 (68.6) | 14,827 (31.4) | 47,243 (100) |
| Bristol, North Somerset and South Gloucestershire | 26,046 | 9910 (38) | 16,136 (62) | 26,046 (100) | 17,298 (66.4) | 8748 (33.6) | 26,046 (100) |
| Cornwall | 16,786 | 6383 (38) | 10,403 (62) | 16,786 (100) | 10,551 (62.9) | 6235 (37.1) | 16,786 (100) |
| Staffordshire | 36,846 | 13,588 (36.9) | 23,258 (63.1) | 36,846 (100) | 24,189 (65.6) | 12,657 (34.4) | 36,846 (100) |
| Total | 585,242 | 209,211 (35.8) | 376,031 (64.3) | 585,242 | 384,888 (65.8) | 200,354 (34.2) | 585,242 |
NHS 111 Online contact characteristics
Triage completion and duration
These analyses were conducted using the early NHS 111 Online data set for January 2018–July 2019 (470,008 cases). We examined the method of contact and the completion rates of online triage sessions. The most common method of accessing the service was using a smartphone (77.8%). Less commonly, a desktop computer (15.3%) or a tablet (6.9%) was used. Figure 15 shows the rapid increase in service use during the first 18 months of the service and the mode of access.
FIGURE 15.
Monthly contacts to NHS 111 Online.
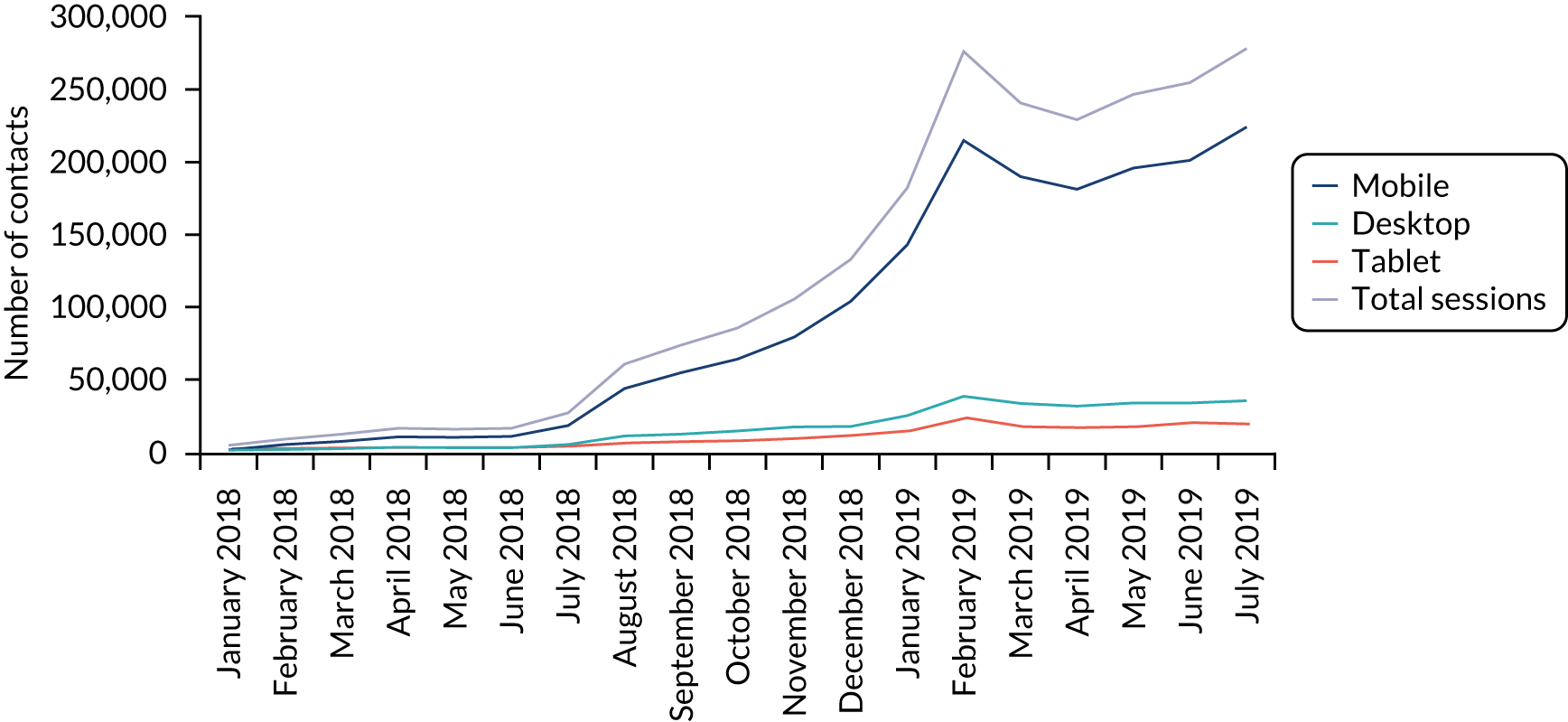
Table 6 shows the number and proportion of contacts where the triage was completed and session times.
| Number (%) | |
|---|---|
| Completion status | |
| Not completed | 25,807 (5.5) |
| Completed | 444,261 (94.5) |
| Call back | |
| No call back attempted | 419,224 (89.20) |
| Call back offered but failed to send | 657 (0.13) |
| Call back offered and sent | 50,187 (10.67) |
| Completed triages during session | |
| Not completed | 25,807 (5.4) |
| 1 | 394,292 (83.7) |
| 2 | 50,751 (8.6) |
| ≥ 3 | 9218 (2.3) |
Most contacts (83.7%) were completed in a single triage session. It is possible to reach a disposition and then go back through the questions, answer them again and arrive at a different disposition. Of those completing more than one session, 8.6% used two sessions and a small number (2.3%) used three or more sessions. Eleven per cent of contacts were offered a call back from a clinician. Figure 16 presents the distribution of triage and session times and shows that the majority of triages were completed within a much shorter time, with the majority completed within 6 minutes.
FIGURE 16.
Distribution of NHS 111 Online triage duration. Triage 1, triage completed in 1 session; triage 2, triage completed in two sessions; triage ≥ 3, triage completed in three or more sessions.
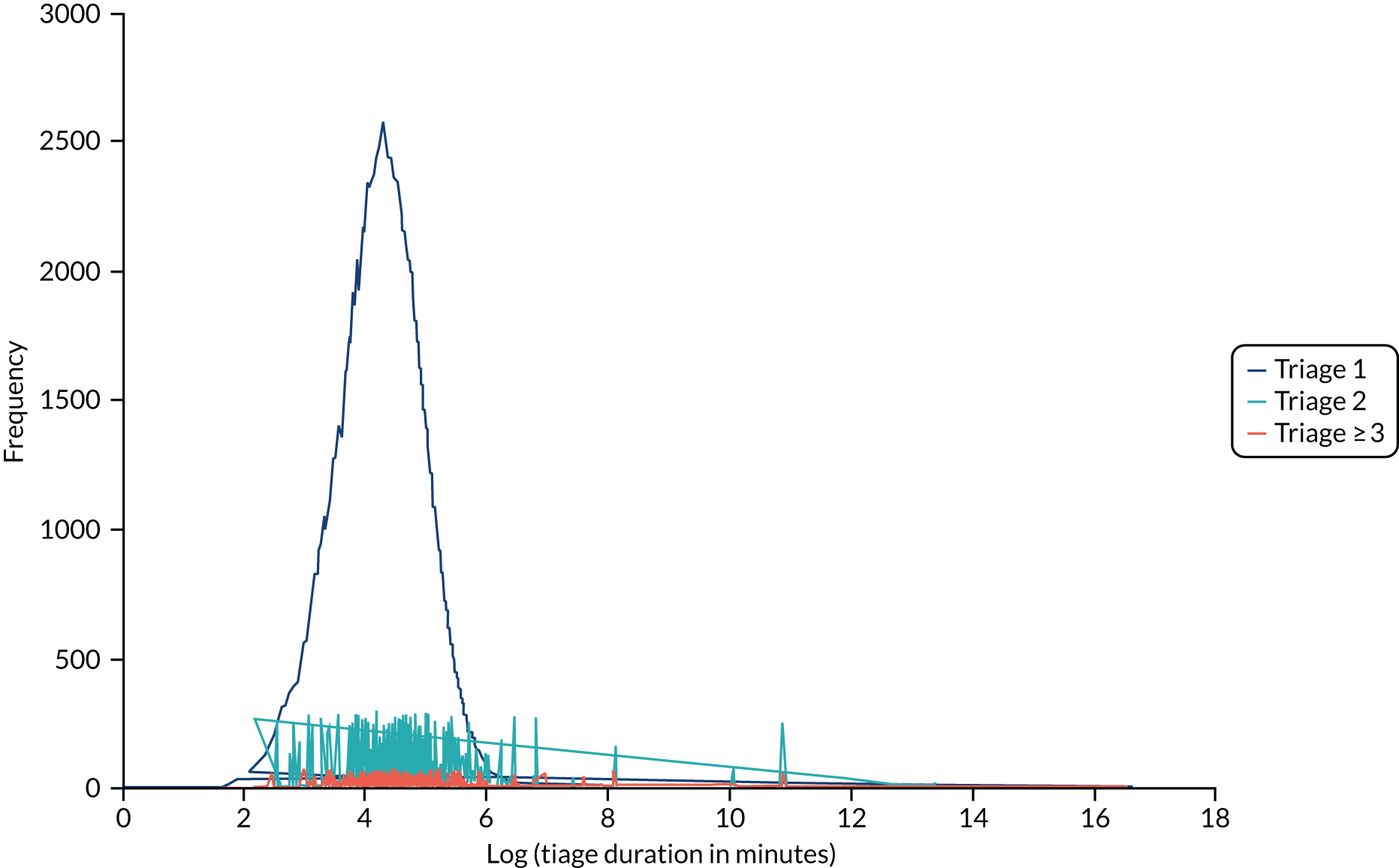
Figures 17 and 18 show the distribution of contacts by hour of day and day of week. There are two peaks of activity during the day, 9.00–10.00 and 18.00–19.00, which coincide with the working day. Although proportionally more of the total contacts occur on weekdays, the distribution shows there is more activity at weekends.
FIGURE 17.
Distribution of contacts by hour of day.
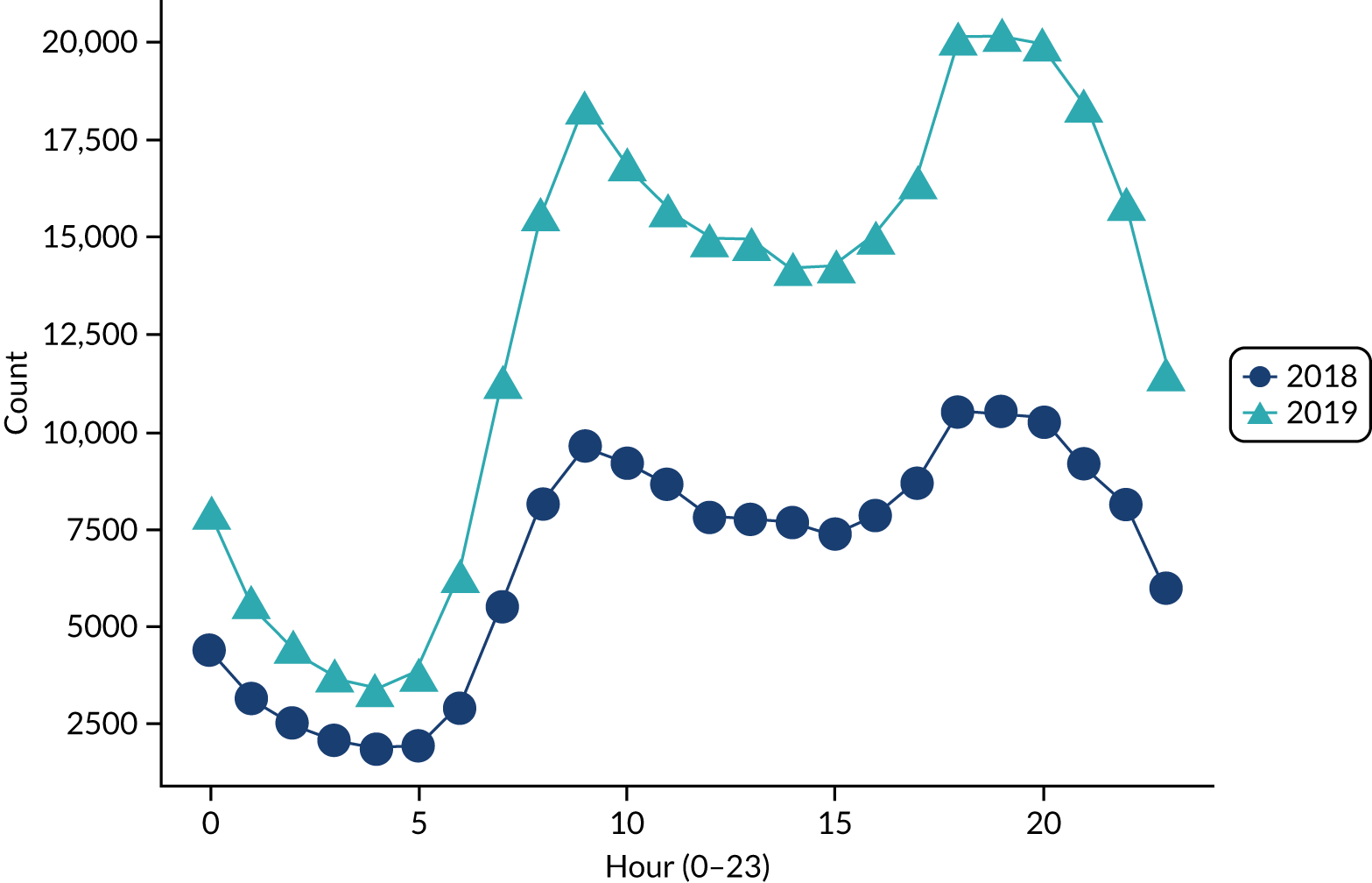
FIGURE 18.
Distribution of contacts by day of week. 1 = Monday.
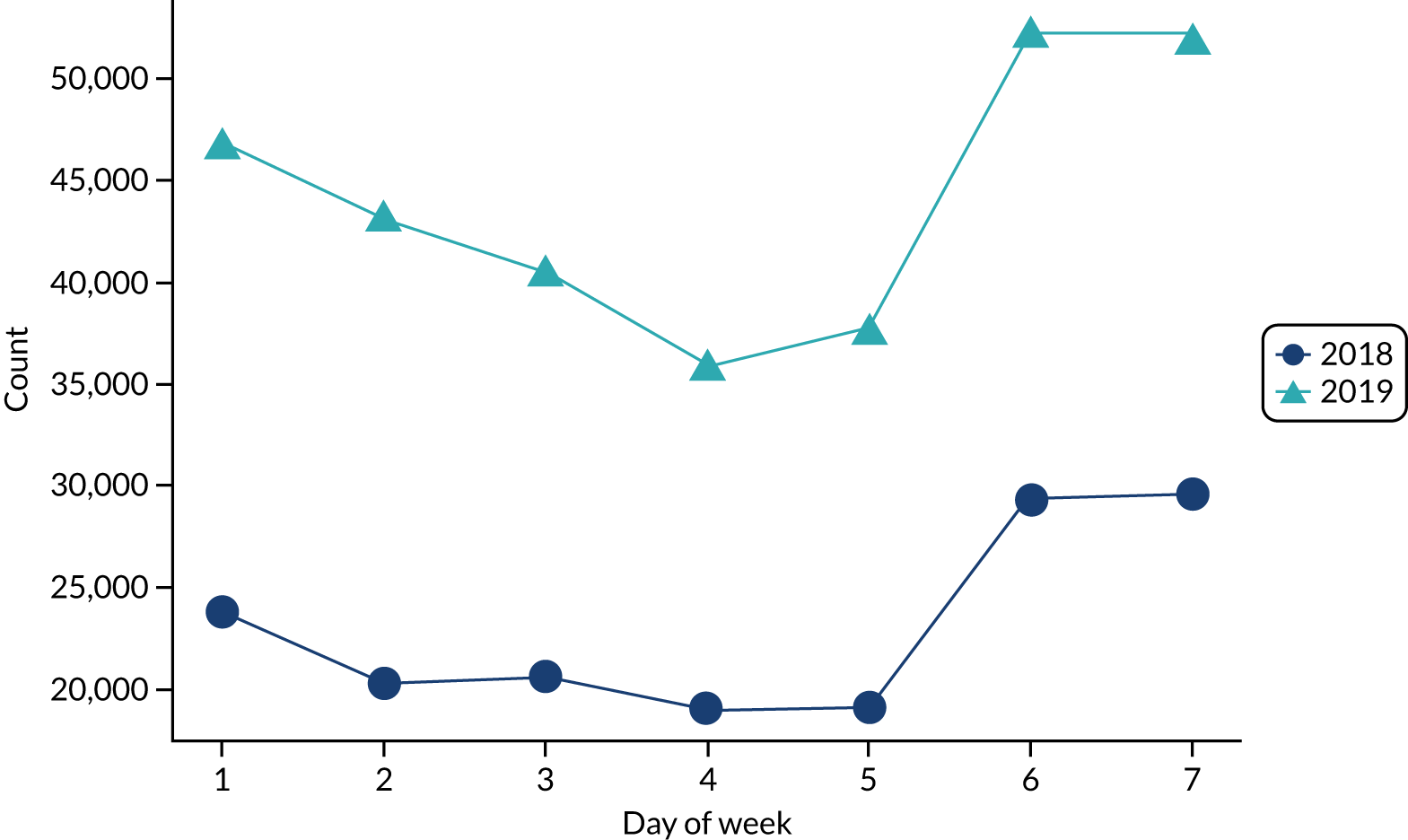
Final disposition
Table 7 provides a more detailed breakdown of the final disposition for NHS 111 Online contacts where a triage was completed. These are the DX codes generated by the NHS Pathways system by broad type. There are a large number of iterations for some types of disposition; so, for example, Primary Care can be speak to primary care or contact primary care and within these recommendations for time frames – for example immediately, within 4 hours, 12 hours, 24 hours. The user will receive additional information, for example the location of local services or the time frame for contacting a service. There are some contacts where, presumably as a result of insufficient information, a final DX code was not reached. Just over 70% of contacts were triaged to an emergency service (ambulance, ED) or primary care, including GP practice for a routine appointment. One-tenth were advised to contact dental services and a much smaller number were directed to a range of more specialist services. The distribution was similar across age groups, although there were more ambulance dispositions for the youngest (2–15 years) and oldest (≥ 75 years) age groups. There were also more speak to clinician from our service dispositions for the youngest age group.
| Final disposition category | All, N (%) | Age group (years), n (%) | |||
|---|---|---|---|---|---|
| 2–15 | 16–34 | 35–74 | ≥ 75 | ||
| Primary care service | 204,310 (43.5) | 20,697 (49.80) | 120,418 (45.33) | 60,333 (45.84) | 2862 (52.68) |
| Emergency ambulance | 58,199 (12.4) | 3918 (9.43) | 36,992 (13.93) | 16,425 (12.48) | 864 (15.90) |
| Clinician from our (111) service | 53,237 (11.3) | 6554 (15.77) | 30,713 (11.56) | 15,528 (11.80) | 442 (8.14) |
| Dental practice | 42,713 (9.1) | 2706 (6.51) | 25,045 (9.43) | 14,624 (11.11) | 338 (6.22) |
| Emergency treatment centre | 39,100 (8.3) | 4342 (10.45) | 22,973 (8.65) | 11,367 (8.64) | 418 (7.69) |
| GP practice | 32,682 (6.9) | 2089 (5.03) | 20,706 (7.79) | 9565 (7.27) | 322 (5.93) |
| Contact pharmacist | 2779 (0.6) | 341 (0.82) | 1555 (0.59) | 847 (0.64) | 36 (0.66) |
| No pathway found | 2681 (0.6) | 227 (0.55) | 1584 (0.60) | 795 (0.60) | 75 (1.38) |
| Mental health/crisis service | 2321 (0.5) | 91 (0.22) | 1721 (0.65) | 502 (0.38) | 7 (0.13) |
| Symptom management advice | 1595 (0.3) | 247 (0.59) | 910 (0.34) | 433 (0.33) | 5 (0.09) |
| Non-emergency ambulance | 1540 (0.3) | 205 (0.49) | 813 (0.31) | 491 (0.37) | 31 (0.57) |
| Speak to midwife | 991 (0.2) | 4 (0.01) | 917 (0.35) | 70 (0.05) | – |
| Contact genitourinary clinic | 741 (0.1) | 1 (0.00) | 635 (0.24) | 104 (0.08) | 1 (0.02) |
| Assistance needed | 467 (0.1) | 46 (0.11) | 179 (0.07) | 221 (0.17) | 21 (0.39) |
| Contact optician | 458 (0.1) | 55 (0.13) | 234 (0.09) | 164 (0.12) | 5 (0.09) |
| 999 for police | 198 (0.04) | 23 (0.06) | 121 (0.05) | 53 (0.04) | 1 (0.02) |
| Repeat prescription | 123 (0.02) | 8 (0.02) | 59 (0.02) | 52 (0.04) | 4 (0.07) |
| Emergency dental treatment | 114 (0.02) | 8 (0.02) | 67 (0.03) | 38 (0.03) | 1 (0.02) |
| No further action | 12 (0.002) | – | 5 (0.00) | 7 (0.01) | – |
Reasons for contact
We have examined the reasons for contacting the NHS 111 Online service using the starting pathway. This is a description of the main complaint pathway the NHS Pathways system uses to begin the triage process after the user has entered a text description of what their problem is. There are 130 starting pathways and the full list is provided in Report Supplementary Material 1, Table 2. Table 8 shows the 20 most common reasons for contacting the service. Dental problems constituted the highest proportion, followed by abdominal pain, with pain featuring in 7 out of 20 reasons. These 20 complaints account for 60% of the reasons for contacting the service. Table 9 shows the 10 most frequently used starting pathways by age group. There are some differences between the groups; for example, symptoms associated with infections are more common in the under 15 years group. Dental problems and abdominal pain are present across all groups and breathing problems are present in three of the four groups.
| Starting pathway | Number | Percentage |
|---|---|---|
| Dental problems | 50,317 | 10.7 |
| Abdominal pain | 34,320 | 7.3 |
| Skin problems | 17,501 | 3.7 |
| Flank or side pain | 15,953 | 3.4 |
| Chest and upper back pain | 14,567 | 3.1 |
| Lower limb pain or swelling | 12,853 | 2.7 |
| Headache | 12,812 | 2.7 |
| Sore throat or hoarse voice | 12,415 | 2.6 |
| Breathing problems, breathlessness or wheeze | 12,194 | 2.6 |
| Passing urine, associated pain, frequency or smell | 11,220 | 2.4 |
| Lower back pain | 10,830 | 2.3 |
| Vomiting and/or nausea | 10,283 | 2.2 |
| Vaginal bleeding | 9535 | 2.0 |
| Cold or flu (declared) | 9346 | 2.0 |
| Cough | 8839 | 1.9 |
| Earache | 8702 | 1.8 |
| Dizziness or vertigo | 8563 | 1.8 |
| Fever | 8472 | 1.8 |
| Mental health problems | 8223 | 1.7 |
| Other symptoms | 7750 | 1.6 |
| Starting pathway | Age group (years) | |||||||
|---|---|---|---|---|---|---|---|---|
| ≤ 15 | % of contacts | 16–34 | % of contacts | 35–74 | % of contacts | ≥ 75 | % of contacts | |
| 1 | Abdominal pain | 9.0 | Dental | 11.9 | Dental | 13.5 | Pain/swelling lower limb | 7.2 |
| 2 | Skin problems | 8.4 | Abdominal pain | 8.4 | Abdominal pain | 6.1 | Dental | 5.9 |
| 3 | Fever | 8.1 | Flank/side pain | 3.7 | Pain/swelling lower limb | 4.3 | Breathing problems | 5.0 |
| 4 | Dental | 6.1 | Skin problems | 3.6 | Flank/side pain | 4.0 | Passing urine, pain, frequency or smell | 4.8 |
| 5 | Sore throat | 4.4 | Chest pain | 3.5 | Chest pain | 3.7 | Other symptoms | 3.9 |
| 6 | Vomiting/nausea | 4.3 | Headache | 3.2 | Breathing problems | 3.1 | Abdominal pain | 3.8 |
| 7 | Earache | 4.1 | Sore throat | 3.0 | Lower back pain | 2.9 | Vomiting/nausea | 3.7 |
| 8 | Cough | 3.1 | Vaginal bleeding | 2.9 | Passing urine, pain, frequency or smell | 2.6 | Cough | 3.5 |
| 9 | Cold/flu | 3.0 | Passing urine, pain, frequency or smell | 2.6 | Headache | 2.3 | Skin problems | 3.5 |
| 10 | Breathing problems | 3.0 | Lower back pain | 2.5 | Cough | 2.3 | Dizziness | 3.3 |
Summary
We have undertaken a limited comparison of the demographic characteristics for NHS 111 Online and telephone service users. Users of the NHS 111 Online service are younger with over 60% in the 16–34 years age group. Less than 2% of people aged ≥ 75 years use the online service. Disposition rates for different services are broadly similar, although more people in the online group are advised to attend services other than primary care and dental services. For primary care dispositions, a larger proportion of online contacts than telephone contacts are advised to contact primary care rather than speak to primary care. This does not necessarily mean higher acuity, as a larger number may be advised to book a routine appointment with their GP. Ten per cent of those contacting the online service are offered a clinician call back. For the NHS 111 Online service there are clear patterns to when the service is accessed, with peak activity in the morning and late afternoon/early evening. There is also more activity at weekends, presumably because some services are closed or have limited access.
The completion rate is high, with 95% of contacts following the questioning to reach a disposition, usually in a single assessment. It has been suggested that people could ‘game’ the service and keep repeating the assessment process until they reach a disposition with which they agree. However, this does not appear to be the case, as only 2.3% of contacts complete more than two triage assessments. From a user perspective, the assessment process is rapid, with most contacts completed within 6 minutes.
The most common health problems for which the NHS 111 Online service is used are dental problems and abdominal pain. Pain in general features highly, as do general symptoms such as nausea and vomiting, coughs, respiratory problems and sore throat. Chest pain is the fifth most frequently used complaint in the 16–74 years age group.
Limitations
We have not been able to undertake the in-depth analyses of patient characteristics and case-mix differences that we had planned, as we were unable to obtain detailed patient-level data for the telephone population. In particular, we could not compare the reasons for contacting the services to determine if there were different levels of acuity. We did use our own existing data to enable some comparisons, but these data are older and for a single area and so are limited in terms of generalisability.
Chapter 6 Users’ experience of NHS 111 Online, and comparison with NHS 111 telephone users
Introduction
It is important to understand users’ experiences and views of new services. If users are not satisfied with a service, and they have access to alternative forms of care, they are less likely to use that service again in the future. Two specific issues could not be answered by routine data. These were (1) user views on their experience of and satisfaction with their encounter with the service, and (2) what actions were taken and what services were accessed by NHS 111 users after their encounter with the service.
The experiences and care pathways of recent service users were sought. This, in part, addresses objective 3. A survey was undertaken with users of the NHS 111 Online service and the NHS 111 telephone service to seek their perceptions of their experiences with the service, and their care pathways following the encounter. The survey also allowed us to explore preferences for using NHS 111 Online over the NHS 111 telephone service.
Methods
Settings
NHS 111 Online user experience survey data were obtained from NHS Digital. Data were collected for all users who accessed the service between September 2019 and May 2020. We did not place geographical exclusions on these data, collecting user data from across England.
NHS 111 telephone user experience data were obtained for two geographical areas, Yorkshire and the Humber, and Hampshire, which were provided by Yorkshire Ambulance Service and South Central Ambulance Service, respectively. Data were collected during the same time period in both areas (between October 2019 and February 2020).
The questionnaires
Providers of both the NHS 111 Online service (NHS Digital) and NHS 111 telephone services undertake regular monitoring of user experience using questionnaires. Individual service providers determine the content of these questionnaires, the methods of delivery and frequency of this monitoring. Data are collected using various survey methods, which include post, telephone, online and text message.
All NHS 111 providers are mandated to ask a series of five questions, with closed responses. These form part of the MDS. The MDS questions and response sets were lifted, verbatim, from a questionnaire developed by members of the research team in an earlier evaluation of the NHS 111 telephone service:59
-
How helpful was the advice given by the 111 service?
-
Did you follow the advice given by the 111 service?
-
Seven days after the call to the 111 service, how was the problem?
-
Overall, how satisfied or dissatisfied were you with the way the 111 service handled the whole process?
-
If the 111 service had not been available, would you have contacted another service about your health problem?
Respondents were asked to answer most of the questions using a closed response set. Some questions allowed for a free-text comment to allow respondents to elaborate on their closed response. For example, if a respondent indicated that they did not agree with the advice provided, they were asked to explain this further in a free-text box.
Additionally, we wanted to understand if, and why, some users were ‘channel shifting’, that is, using the online version of NHS 111 instead of the telephone service. We constructed a question in consultation with NHS Digital to be asked of online users. We adapted this question for use with telephone users to allow us to understand if there were instances when 111 users preferred telephone to online assessment (as well as vice versa).
Survey administration
Users of NHS 111 Online are invited to complete a questionnaire directly after their clinical assessment (the ‘live’ survey). Users completing the live survey are invited to input their e-mail address if they agree to receiving a second survey (the ‘follow up’ survey). The follow-up survey is administered approximately 2 weeks after their clinical assessment. In the study settings, telephone users received a postal questionnaire, which may have arrived a number of weeks after their contact with the service, which may have implications for recall among those users.
Questionnaire data were collected by each NHS 111 provider. An anonymised data extract was forwarded to the research team for analysis.
Analysis
We analysed the data in two ways:
-
NHS 111 Online users – descriptive statistics to report responses to questions, such as subsequent service use, overall levels of satisfaction and convergence with and divergence from advice given
-
comparison of NHS 111 Online and NHS 111 telephone users.
Data were analysed in IBM SPSS Statistics version 26 (IBM Corporation, Armonk, NY, USA). We compared differences between online and telephone users using the chi-squared test for proportions. Because levels of satisfaction may depend on users’ characteristics, we adjusted for any differences between users using binary logistic regression and multinomial logistic regression. We adjusted for age group (0–15, 16–44, 45–64, 65–74, ≥ 75 years), sex (male, female), ethnicity (white, ethnic minority group) and presence of a long-term condition (LTC) (LTC or no LTC), because these demographics can affect people’s satisfaction levels regardless of the quality of the service given.
NHS Digital anonymised some of the free-text comments provided by NHS 111 Online respondents before forwarding them to the research team. The anonymisation process was resource intensive. NHS Digital prioritised the anonymisation of free-text comments derived from residents of our initial case study areas (Bedfordshire and Luton, Derbyshire, Hampshire, South West London, and Yorkshire and the Humber). This generated a considerable number of data, which we grouped into themes (where possible).
Results
Survey data were collected during the sampling period for 3728 users of NHS 111 Online, compared with 795 telephone users (Table 10). The response rates to the postal surveys sent by Yorkshire and the Humber and Hampshire were 12% and 13%, respectively. This is the typical response rate for these surveys when reported to the national NHS 111 MDS. The ‘response rate’ for the NHS 111 Online user survey is more difficult to calculate, as, unlike the telephone surveys, which are of samples of callers who are contacted directly, there is an option at the end of every online contact to complete a survey. Without a personal approach, uptake tends to be much lower. In addition, we used the 2-week follow-up survey, which has a lower uptake than the first survey after a contact. During the study period (September 2019–May 2020), there were 4.85 million completed contacts, which would give a response rate of 0.07%. However, because of the COVID-19 pandemic, contacts with NHS 111 Online increased 10-fold from March onwards, which will have affected the response rate as a result of a much larger denominator. We estimate that, prior to the pandemic, the response rate to the follow-up survey was 0.7% of all contacts.
| Telephone (Hampshire) | Telephone (Yorkshire and the Humber) | Online | |
|---|---|---|---|
| Sampling period | October 2019–February 2020 | October 2019–February 2020 | September 2019–May 2020 |
| Questionnaire administration method | Postal | Postal | Online |
| Completed questionnaires returned (n) | 293 | 502 | 3728 |
Respondent demographics
The demographics of patients were collected consistently across all providers (Table 11). Telephone and online respondents differed in age group (p < 0.001), ethnicity (p < 0.001) and presence of a long-term condition (p < 0.001). There was less evidence of a difference between the groups with respect to sex (p = 0.009).
| Characteristic | Category | Telephone, % (n) | Online, % (n) | p-value |
|---|---|---|---|---|
| Age group (patient) (years) | 0–15 | 4 (28) | 5 (187) | < 0.001 |
| 16–24 | 7 (46) | 7 (238) | ||
| 25–34 | 6 (44) | 9 (330) | ||
| 35–44 | 8 (55) | 12 (442) | ||
| 45–54 | 9 (66) | 19 (675) | ||
| 55–64 | 15 (106) | 24 (884) | ||
| 65–74 | 21 (147) | 17 (632) | ||
| 75–84 | 20 (142) | 6 (199) | ||
| ≥ 85 | 10 (72) | 1 (44) | ||
| Sex (patient) | Female | 59 (437) | 64 (2308) | 0.009 |
| Male | 41 (306) | 36 (1305) | ||
| Ethnicity (patient) | White British | 94 (714) | 88 (3142) | < 0.001 |
| Other | 6 (45) | 13 (447) | ||
| LTC (patient) | LTC | 43 (298) | 51 (1747) | < 0.001 |
| No LTC | 57 (397) | 49 (1691) |
There were fewer older NHS 111 Online users (i.e. aged ≥ 75 years) among the respondents. Overall, the proportion of respondents identifying themselves as ‘white British’ was higher than the population estimate for the UK (82%; Census 201160). This was particularly evident in the telephone user group. Overall, around half of the survey respondents had a long-term condition. This proportion was higher for online users (51%) than for telephone users (43%).
Previous use of NHS 111
Respondents were asked about their previous use of the NHS 111 service that they had contacted (e.g. telephone users were asked about their previous use of the NHS 111 telephone service). Given that NHS 111 Online is a relatively new service, it was not surprising to find that 93% (n = 1897) of respondents reported using this service for the first time. Sixty per cent (n = 446) of telephone users reported using the NHS 111 telephone service for the first time.
Perceptions of intended behaviour
Stakeholders are often interested in what people say they would have done had a service not been in operation. We should be mindful that this is a hypothetical question and that a perception of intention may not reflect actual behaviour. Service users were asked if they would have contacted another service had NHS 111 not been available (Table 12). Owing to differences in the question wording, some users were asked to tick one option only, whereas some users ticked as many as applied to them. We analysed the responses of respondents who indicated that they would have contacted a single service, rather than multiple services.
| Response | Telephone, % (n) (N = 696) | Online, % (n) (N = 2037) | Unadjusted p-value | Adjusteda p-value, chi-squared, df |
|---|---|---|---|---|
| Called 999 ambulance | 20 (138) | 1 (16) | < 0.001 | < 0.001, 986.7, 6 |
| Visited emergency department | 26 (181) | 3 (64) | ||
| Contacted primary care (GP) | 29 (201) | 17 (341) | ||
| Contacted MIU/WIC/UCC | 18 (125) | 5 (100) | ||
| Telephoned 111 | – | 21 (427) | ||
| Would not have contacted a service | 5 (35) | 43 (874) | ||
| Something elseb | 2 (16) | 11 (215) |
A small proportion of NHS 111 Online users reported that they would have made contact with high-acuity services such as 999 ambulance (1%) or an ED (3%); 43% reported that they would not have contacted another service if NHS 111 Online had not been available.
When considering differences between telephone and online users, we found that respondents using the telephone service were more likely to report contacting a higher-acuity service (e.g. the 999 ambulance service, ED or general practice) than those using the online service. Users of the online service were more likely to report that they would not have contacted another service if NHS Online had not been available. These differences persisted even after adjusting for age, gender, ethnicity and long-term condition (p < 0.001).
Helpfulness of, and compliance with, advice
Respondents were asked how helpful they found the advice given by NHS 111 (Table 13). This question was not asked of users of the NHS 111 telephone service in Yorkshire and the Humber.
| Response | Telephone,a % (n) (N = 292) | Online, % (n) (N = 3515) | ‘Very helpful’ vs. ‘other’ | |
|---|---|---|---|---|
| Unadjusted p-value | Adjustedb p-value, odds ratio (95% CI) | |||
| Very helpful | 69 (202) | 43 (1495) | < 0.001 | < 0.001, 0.33 (0.24 to 0.44) |
| Quite helpful | 21 (61) | 32 (1138) | ||
| Not very helpful | 8 (22) | 15 (515) | ||
| Not helpful at all | 2 (7) | 10 (367) | ||
Three-quarters (75%) of online users felt that the advice given had been helpful.
When considering differences between telephone and online users, telephone users were more likely to report that they found the advice to be ‘very helpful’, even after adjusting for age, gender, ethnicity and long-term condition (p < 0.001).
Respondents were asked about whether or not they had followed the advice given by NHS 111 (Table 14). NHS 111 Online users were provided with a dichotomous response set: ‘complied’ or ‘did not comply’. Telephone users were given three response options: ‘full compliance’, ‘some compliance’ and ‘did not comply’. To enable binary logistic regression analysis, we compared those reporting ‘full compliance’ with those reporting that they ‘did not comply’ with the advice.
| Telephone, % (n) (N = 711) | Online, % (n) (N = 3599) | ‘Full compliance’ vs. ‘no compliance’ | ||
|---|---|---|---|---|
| Unadjusted p-value | Adjusteda p-value, odds ratio (95% CI) | |||
| Full compliance with advice | 88 (683) | 67.5 (2430) | < 0.001 | < 0.001, 0.07 (0.04 to 0.11) |
| Partial compliance with advice | 9 (63) | – | ||
| Did not comply with advice | 4 (28) | 32.5 (1169) | ||
Just over two-thirds (67.5%) of online users reported complying with the advice provided. When considering differences between telephone and online users, telephone users were more likely to report that they fully complied with the advice, even after adjusting for age, gender, ethnicity and long-term condition (p < 0.001).
Those using the online service were asked for the reasons why they had not followed the advice given. Respondents were asked to identify all of the reasons that applied to them (Table 15).
| Reason | Online, % (n) (N = 1169) |
|---|---|
| Wanted to wait and see if symptoms changed | 27 (313) |
| Did not want to waste anyone’s time | 26 (307) |
| Unable to follow | 24 (276) |
| Symptoms improved | 18 (209) |
| Did not agree | 15 (174) |
| Could not get an appointment | 8 (96) |
| Did not understand the advice | 4 (52) |
| Symptoms got worse | 3 (31) |
Around one-quarter (24%) of respondents reported that they had been unable to follow the advice. Similar proportions had wanted to wait and see if their symptoms changed, or had not wanted to waste the time of the service they were advised to contact. Around 1 in 10 of respondents could not get an appointment with the service they were advised to contact. A small number of respondents (4%) did not understand the advice.
Respondents who answered that they had been unable to follow the advice were invited to explain their answer further in a free-text comment; 55 responses were analysed. Over half of those who commented (n = 32) said that they could not access the service they had been advised to contact by NHS 111 Online. This was predominantly in relation to GP care, with a minority not able to access dental care. Some respondents said that they had been advised to contact a GP during the weekend, when their own GP surgery was closed. Four respondents had been unable to follow the advice given because of difficulties in arranging transport to get to the service advised by NHS 111 Online.
Satisfaction
Respondents were asked a number of questions that could indicate their satisfaction with NHS 111 (Table 16). Fifty per cent of NHS 111 Online users indicated that they were ‘very satisfied’ with the service; when considering differences between telephone and online users, telephone users were more likely to report that they were ‘very satisfied’, even after adjusting for age, gender, ethnicity and LTC (p < 0.001). Fifty-seven per cent of NHS 111 Online users reported that they were ‘very likely’ to recommend the NHS 111 Online service to family and friends; when considering differences between telephone and online users, telephone users were more likely to report that they were ‘very likely’ to recommend the NHS 111 service to family and friends, even after adjusting for age, gender, ethnicity and LTC (p < 0.001).
| Telephone, % (n) | Online, % (n) | Unadjusted p-value | Adjusteda p-value, odds ratio (95% CI) | |
|---|---|---|---|---|
| Overall, how satisfied or dissatisfied were you with the 111 service (‘very satisfied’)? | 71 (555) | 50 (1880) | < 0.001 | < 0.001, 0.40 (0.33 to 0.49) |
| How likely are you to recommend the NHS 111 service to friends and family (‘very likely’)? | 69 (543) | 57 (2083) | < 0.001 | < 0.001, 0.55 (0.46 to 0.67) |
| How likely are you to use NHS 111 Online again (‘very likely’)? | NA | 56 (2028) | NA | NA |
Just over half of NHS 111 Online users (56%) reported that they were ‘very likely’ to use the online service again. Telephone users were not asked this question. A total of 313 respondents (9%) indicated that they were ‘unlikely’ or ‘very unlikely’ to use NHS 111 Online again. Among these respondents, 60 free-text comments were analysed: 22 attributed their response to feeling dissatisfied with the information or advice offered by NHS 111 Online; eight respondents referred to a problem with the call back from NHS 111; and five respondents preferred the NHS 111 telephone service or another service where they could speak to someone.
NHS 111 Online users were asked if they had got everything that they wanted from the service. NHS 111 telephone users were not asked this question. Most respondents (84%, n = 3140) reported that they had received at least some of what they wanted from NHS 111 Online; 16% (n = 588) of NHS 111 Online users reported that they ‘got none of what I wanted’.
NHS 111 Online users were presented with a series of statements about the process of using NHS 111 and were asked whether they agreed with these statements (Table 17). We selected to dichotomise at ‘strongly agree’ versus all other options because research has shown that people who state that they are ‘satisfied’ (equivalent to, or similar to, ‘agree’ with positive statements) can identify some areas for improvement with the service, whereas those who state ‘very satisfied’ (equivalent to ‘strongly agree’) can see no room for improvement. 61
| Telephone, % (n = 283) | Online, % (n = 3170) | Unadjusted p-value | Adjusteda p-value, odds ratio (95% CI) | |
|---|---|---|---|---|
| The questions about the symptoms were relevant | 51 (145) | 39 (1250) | < 0.001 | < 0.001, 0.55 (0.41 to 0.73) |
| I understood how to answer the questions about the symptoms | – | 55 (1747) | – | – |
| The advice and information I was given was helpful | – | 37 (1158) | – | – |
| NHS 111 Online was easy to use | – | 55 (1742) | – | – |
NHS 111 Online users indicated that there was room for improvement across each of the statements but particularly with regard to the relevance of questions and the helpfulness of the advice and information given. Only one process question was asked of telephone users: relevance of questions. This question was included in the questionnaire administered to Hampshire users only, but worded slightly differently (‘The questions asked by the 111 service were relevant’). When considering differences between telephone and online users, telephone users were more likely to report that they felt that the questions were relevant, even after adjusting for age, gender, ethnicity and LTC (p < 0.001).
Seven-day health status and use of services
Respondents were asked about any improvement in their health 7 days after their contact with NHS 111 (Table 18). Around one-fifth of users reported that they felt ‘completely better’ 7 days after their contact with NHS 111. When considering differences between telephone and online users, telephone users were more likely to report that they felt that their health problem had improved or was completely better, even after adjusting for age, gender, ethnicity and LTC (p < 0.001).
| Telephone, % (n) (n = 757) | Online, % (n) (n = 3702) | ‘Completely better/improved’ vs. ‘the same/worse’ | ||
|---|---|---|---|---|
| Unadjusted p-value | Adjusteda p-value, odds ratio (95% CI) | |||
| Completely better | 22 (164) | 21 (788) | < 0.001 | < 0.001, 0.63 (0.51 to 0.79) |
| Improved | 56 (425) | 47 (1750) | ||
| The same | 16 (121) | 20 (749) | ||
| Worse | 6 (47) | 11 (415) | ||
Respondents were asked to identify the services that they had contacted in the 7 days after their contact with NHS 111 (Table 19). Data from telephone users in Hampshire were excluded because of differences in the phrasing of this question.
| Telephone, % (n = 478) | Online, % (n = 3256) | Unadjusted p-value | Adjusteda p-value, odds ratio (95% CI) | |
|---|---|---|---|---|
| 999 ambulance | 9 (41) | 1 (47) | < 0.001 | < 0.001, 0.17 (0.10 to 0.28) |
| Emergency department | 33 (157) | 7 (232) | < 0.001 | < 0.001, 0.14 (0.11 to 0.19) |
| Primary careb | 47 (225) | 43 (1411) | 0.124 | 0.081, 0.82 (0.65 to 1.03) |
| NHS 111 (telephone) | – | 11 (348) | – | – |
| NHS 111 (online) | 3 (16) | 7 (230) | 0.002 | 0.006, 2.63 (1.32 to 5.23) |
| Something else | 5 (25) | 20 (662) | < 0.001 | < 0.001, 5.55 (3.36 to 9.18) |
| No contact | 16 (74) | 31 (1014) | < 0.001 | < 0.001, 2.53 (1.87 to 3.52) |
One-third (31%) of NHS 111 Online users reported making no contact with a service in the 7 days after their contact with NHS 111. A small proportion (1%) of NHS 111 Online users made contact with the 999 ambulance service, and 7% reported visiting an ED.
In terms of differences between telephone and online users, NHS 111 Online users were less likely to report contacting the 999 ambulance service (p < 0.001), visit an ED (p < 0.001) or make any contact with a health service (p < 0.001) in the 7 days after contacting NHS 111. These differences remained even after adjustment for age, gender, ethnicity and LTC (p < 0.001).
Channel shift
We were interested to know why respondents had chosen to contact NHS 111 Online rather than the NHS 111 telephone service. A list of response options was provided. Respondents were asked to select one response (Table 20). NHS 111 Online users were given the opportunity to expand on their response by providing a free-text comment.
| Response set for NHS 111 telephone users | Telephone, % (n = 749) | Online, % (n = 3604) | Response set for NHS 111 Online users | Unadjusted p-value | Adjusteda p-value, chi-squared, df |
|---|---|---|---|---|---|
| I called NHS 111 without thinking about using NHS 111 Online | 40 (300) | 26 (926) | I used NHS 111 Online without thinking about phoning | < 0.001 | < 0.001, 563.5, 5 |
| I had already tried NHS 111 Online | 5 (40) | 3 (123) | I spoke to someone at NHS 111 before I used NHS 111 Online | ||
| I did not want to use NHS 111 Online | 15 (113) | 35 (1268) | I did not want to phone NHS 111 | ||
| I was using NHS 111 Online at the same time as calling NHS 111 | 2 (11) | 2 (68) | I spoke to NHS 111 and used NHS 111 Online at the same time | ||
| I did not know that NHS 111 Online existed | 27 (207) | 1 (47) | I did not know you could phone NHS 111 | ||
| Other | 9 (66) | 22 (789) | Other | ||
| 11 (383) | I phoned 111 but they took too long to answerb | ||||
| No access to a computer/online servicesb | (2) 12 | – |
Over one-third (35%) of those using NHS 111 Online reported that they did not want to use the telephone service; 1114 respondents expanded on their answer by providing a free-text comment. Reasons included that the problem did not feel urgent enough; they did not want to waste NHS resources; they had difficulty speaking or preferred not to speak to someone (owing to either the health problem or anxiety about using the telephone); or perceived that there would be a long wait to speak to someone on the NHS 111 telephone service.
One-quarter of NHS 111 Online users (26%) reported not thinking about using the telephone service. Around 1 in 10 online users (11%) had tried to access the telephone service but found that it had taken too long for their call to be answered and so they had used NHS 111 Online instead. A small proportion (3%) of NHS 111 Online users had already spoken to the telephone service. Free-text comments suggested that many had gone on to use NHS 111 Online because of an actual or a perceived lengthy wait for a call back. A similar proportion (2%) of NHS 111 Online users were using the telephone and online service simultaneously. Fifty-three respondents expanded their answer by providing a free-text comment. Comments focused on delays in getting through to the telephone service: respondents felt that they would get a quicker response using NHS 111 Online.
Just over one-quarter (27%) of respondents who used the NHS 111 telephone service had not been aware that NHS 111 Online existed.
There were apparent differences when comparing telephone and online users (p < 0.001). However, there are difficulties in interpreting these differences. Almost one-quarter of NHS 111 Online users reported an ‘other’ reason for using the online instead of the telephone service; 709 respondents expanded on their answer by providing a free-text comment. A wide range of reasons were reported in these comments. These included difficulties in communication (owing to either their health problem or an underlying anxiety about using the telephone); taking a personal decision not to ‘burden’ the NHS 111 telephone service (particularly during the COVID-19 pandemic); perceptions of long waiting times to access the telephone service; receiving a recorded message to use the online service after calling NHS 111; and perceptions that the problem was not urgent enough to warrant a telephone call to NHS 111. These comments were similar to those provided in response to ‘I didn’t want to phone NHS 111’, so it is probable that we have underestimated the proportion of NHS 111 Online users not wanting to telephone NHS 111.
Summary
Overall, respondents using NHS 111 Online were less satisfied than users of the NHS 111 telephone service. Satisfaction levels among NHS 111 Online users were also lower than they were among early users of the NHS 111 telephone service, where 73% of respondents reported that they were very satisfied with the ‘new’ service. 61
One-quarter of NHS 111 Online users reported that they did not find the advice helpful, and there were indications that some service users did not find the questions relevant or found them difficult to interpret. This was the first experience of using NHS 111 Online for over 90% of respondents. We did not explore expectations of what service users thought NHS 111 Online could provide. It is possible that there was a mismatch between the expectations of these first-time service users and what NHS 111 Online has been set up to provide. This might also explain the lower levels of satisfaction among NHS 111 Online users.
Some NHS 111 Online respondents used the service after the start of the COVID-19 pandemic. Public health campaigns and media reporting about the pressures on the NHS may have influenced their decision to use NHS 111 Online over the NHS 111 telephone service, or other health services. This may have had a negative impact on user satisfaction if usual care pathways were not accessible to respondents.
One-third of NHS 111 Online respondents did not follow the advice.
Despite sharing a common name (NHS 111), ‘NHS 111 Online’ and ‘NHS 111’ are different services, and it may not be helpful to draw comparisons between them. There appears to be a different case mix between the two services: NHS 111 telephone users were more likely to report using higher-acuity services if the service had not been available, and reported using higher-acuity services in the 7 days after their telephone call. Users of the online service were much more likely to not use any service after their contact. This suggests that users of the NHS 111 telephone service have more urgent health problems than those using NHS 111 Online and, hence, that there is not a simple, single population of NHS 111 users. There appear to be some subtle differences between the telephone and online populations in terms of clinical need and, hence, in the type of response needed in terms of both the subsequent service use and the extent to which an online or ‘human’-based assessment is of more benefit.
One-third (or more) of NHS 111 Online respondents used the service because they did not want to contact NHS 111. This suggests that there is potential for some of the population to use NHS 111 Online instead of the telephone service in the future (‘channel shifting’). In addition to using the online service for less urgent problems, the online service appears to meet a need for groups of the population who prefer services delivered online rather than over the telephone. Given that one-quarter of telephone users had not been not aware of the existence of NHS 111 Online, it is likely that demand for the online service will grow as awareness increases.
Limitations
The main limitation is the representativeness of the respondents, as white British people are over-represented when compared with population norms. There were also proportionally more respondents in the older age groups than in the user age profiles described in Chapter 5. This is particularly true of the NHS 111 Online respondents, as the largest proportion of its users are younger. It is possible that the user groups under-represented in the survey may have different views about the experience and might have made different choices about subsequent health contacts. The response rates to the surveys were low and therefore subject to responder bias, which means that the experiences of under-represented groups are not reflected in our findings.
The last 3 months of the survey period coincided with the beginning of the COVID-19 pandemic. NHS 111 rapidly adapted to provide triage and signposting for suspected COVID-19 symptoms, with information added to the NHS 111 Online website and an information message introduced for callers to the telephone service, including how to access the online service. This will have influenced some users’ reasons for contacting both services and created contacts from people who may not otherwise have used the service. Where possible, we have highlighted in the results findings that were specifically attributed to using the service for assessing COVID-19 symptoms, but it is possible that the experiences and responses reported may be different between users contacting the service about COVID-19 and those contacting for other urgent health problems.
Chapter 7 A qualitative interview study of NHS 111 Online user experience
Introduction
The aim of this study component was to explore user experience of the NHS 111 Online service in more depth (objective 3). Given that the service operates nationally, but was not yet widely used among the population at the time of this evaluation, we also wanted to understand factors that might be important in the future development of the service and explore any potential channel shift between the telephone and online services provided by NHS 111.
Methods
Design
We undertook a qualitative interview study with recent users of the NHS 111 Online service.
Patient recruitment
We undertook semistructured interviews with recent users of the NHS 111 Online service. Interview participants were recruited following the completion of two online user questionnaires administered by NHS Digital: one immediately after use of the service and one 2 weeks later. On the second of these questionnaires, a web link to our project web page was provided, which invited survey respondents to read about and consider taking part in the interview study. After reading this information, potential interview participants were invited to complete a short online form, registering their interest. The form asked for their name, their contact details (telephone/e-mail address) and the date of their NHS 111 assessment. A researcher contacted these individuals, by telephone, within 1 week of completing the form (where possible), with the intention of undertaking the interview shortly after. Therefore, interviews took place at least 2 weeks after the individual’s contact with NHS 111 Online. Potential participants were given the opportunity to ask any questions about the study prior to deciding whether or not to take part. Interviews were booked over the telephone. Written confirmation of the interview date and time, a copy of the patient information sheet, and the consent form were sent to the interview participant by e-mail or post.
Data collection
Interviews took place over the telephone between December 2019 and April 2020. Informed consent was recorded at the start of each interview. The topic guide was developed based on our research objectives and discussion at our project management group. The topic guide covered general use of online services and health services, previous use of NHS 111 (both telephone and online), their experience of using NHS 111 Online, any preferences for using the online service ahead of the telephone service (and vice versa), and the likelihood of them using the online service in the future (see Report Supplementary Material 2). One researcher (JL) undertook all of the interviews. Interviews were digitally recorded and lasted between 24 and 55 minutes. Participants were sent a £20 high-street shopping voucher on completion of an interview.
Sampling
We planned to undertake up to 40 interviews. At the start of recruitment, we took an unstratified approach to sampling, interviewing all service users who had expressed an interest in participating. This resulted in a predominantly female, middle-aged, ethnically white sample, who reported having received a call back from NHS 111 after their online assessment. After completing 20 interviews, we took a more selective approach to recruitment, targeting younger service users and those reporting that they had not received a call back from NHS 111.
Data analysis
We audio-recorded each interview and transcribed it verbatim. Transcripts were checked for accuracy. We uploaded the finalised transcripts and summaries into NVivo 12 (QSR International, Warrington, UK), which was used throughout to facilitate data management and retrieval.
We analysed all interviews using framework analysis. 62 First, we familiarised ourselves with the interviews by reading a sample of transcripts. Second, we developed a thematic framework based on our research questions, the topic guide and reading a sample of transcripts. The thematic framework consisted of descriptive themes, including positive and negative aspects of the experience of using NHS 111 Online, compliance with advice, propensity to use NHS 111 Online again, and recommended future development of the service. Third, we coded all of the transcripts to the framework, adding further emergent themes and subthemes throughout the process of coding transcripts. One researcher (JL) undertook the coding of transcripts.
We (JL and EK) read extracts of transcripts within a theme, considering connections between themes and refining the thematic framework.
Results
Fifty-five NHS 111 Online service users indicated an initial interest in participating by completing the online form. Twenty users were not invited to take part in an interview because they did not meet the demographic profile, two users could not be contacted by a researcher after three attempts to contact and one service user declined to take part.
We undertook 32 interviews with those who consented. All of these interviews were included in the analysis.
Demographics of interview participants
Data on the age groups of interview participants were collected. Around half (n = 15) of the participants reported being in the 45 and 64 age groups. Younger people aged under 35 years, whom we were particularly interested in recruiting, were represented in the sample by seven participants.
Two-thirds of interview participants were women (n = 22), and most interviewees reported their ethnicity as white (n = 28).
Most made contact with NHS 111 Online with regard to themselves (n = 30); one made contact in their capacity as a carer and one did so on behalf of a friend/family member.
Two-thirds of participants used the service during a weekend or weekday out-of-hours period (n = 21) and the remaining participants used the service during the day on a weekday (n = 11).
Participants described a range of health problems that were the focus of their contact with NHS 111 Online. A number of participants described symptoms that could be linked to COVID-19, with six contacting NHS 111 Online specifically because they felt that they were displaying signs of COVID-19. A further 12 participants described respiratory problems, such as breathing difficulties, cough, sore throat, and flu-type symptoms. Localised pain was described by a number of participants (n = 9), including dental, leg, kidney, groin and chest pain. The remaining four participants described health problems that were not shared by others: bleeding during pregnancy, skin problem, thumb problem and eye redness.
User experience and views
Prior use of NHS 111
For most participants this was their first experience of using NHS 111 Online (n = 26). Most participants appeared to have used the NHS 111 telephone service at some point. Just four participants had no recollection of previously using the NHS 111 telephone service.
Expectations of NHS 111 Online assessment
Participants were asked what they had hoped NHS 111 would provide, and they provided a range of responses. Many participants had been seeking clarification about the severity of their symptoms, or what course of action they should take, which are key functions of the NHS 111 Online service.
Four participants had made contact because they thought that NHS 111 could provide them with access to a health-care professional. Three of these participants wanted an emergency dental appointment.
Participants contacting 111 in relation to COVID-19 did so to check whether their symptoms indicated it, because they wanted to rule it out or because they were seeking information about what action to take with respect to their symptoms.
Process of using NHS 111 Online
We asked participants about the process of using NHS 111 Online, for example their experiences of locating the website, the ease of using the service and the questions that were asked during the assessment.
Thirty participants identified at least one positive aspect with respect to the process of using NHS 111 Online, while 22 reported some negative aspect of the process of using NHS 111 Online; as can be seen from these numbers, for most people the experience had both positive and negative aspects.
A large number of participants (n = 24) described the process of accessing and using the service as ‘straightforward’: access to the service was immediate, and available 24/7, the website was easy to find, the online interface was easy to navigate and the time spent completing the assessment was short. The length of time spent using NHS 111 Online was particularly identified as favourable in comparison with accessing the NHS 111 telephone service:
In some ways it’s [NHS 111 Online] better than the phone service, because you don’t have that waiting in a queue.
P10
It saves faffing about for half an hour on the phone, because sometimes it’s quite long-winded when you go to 111 on the phone. Yeah, speak to the triage, and then if they think it warrants speaking to the doctor then you’ve gotta wait for a call back and all this business. So, in one hit it [NHS 111 Online] was done and dusted.
P29
NHS 111 phone just so laborious and it’s just you seem to wade through mortar before you get anywhere. Erm for me it is purely just that, that [NHS 111 Online] provides a quicker response.
P16
Participants had mixed reactions to the questions asked during the NHS 111 Online assessment. Although many (n = 20) described the questions as relevant to their situation and felt that the online service used language that was easy to understand and did not provoke concern, there was also a considerable amount of criticism of questions (n = 19), with some describing them as ‘basic’, ‘generalised’, ‘simple’, ‘not relevant’ or poorly worded. This made participants question the professionalism of the service, and affected the value they placed on the advice given:
I found it was very basic and for me that meant that I would not have been completely reassured with any conclusive advice it would have given because it seemed very generic, you know? And it’s like those horoscopes that come through the e-mail. It just didn’t seem professional enough for me.
P20
They [the online question] said ‘is this a new cough’ you know, or is it the old cough come back, you know just a bland question ‘is this a new cough?’ just doesn’t hack it, you didn’t know how to answer it.
P25
It [the questions] was very black and white. There was nothing in the middle, it was very general-, it was almost like can you breathe or can’t you breathe. There was nothing in the middle. (. . .) specific enough, there weren’t enough options.
P2
Some participants (n = 4) felt that the questions did not allow complex problems to be dealt with, for example chronic conditions, or even problems with more than one symptom. One participant felt that the basic level of questioning did not allow NHS 111 Online to pick up on the severity of their particular situation. Participants noted that information about current medication regimens was not sought. There was also criticism that the online service was not set up to take account of underlying health conditions, which may have provided some context for the health problem about which they were seeking advice:
It was a bit limited with regards to COPD [chronic obstructive pulmonary disease]. The questions didn’t go anywhere and I suspect probably there was not enough depth for it to have been terribly useful. I was feeling I knew more than the 111.
P24
They did ask a general question ‘which is the symptom that most troubles you?’ as the opening symptom, now that seems to be a fairly critical question, so I started with fatigue and that was ok, but I thought if I have fatigue and breathlessness shouldn’t they be interested in that [the breathlessness] as well even though the fatigue is the worst of the two?
P25
I had a sore throat, but I had no option to say that I’m asthmatic as well, which was the reason why I am worried.
P20
Outcome of using NHS 111 Online
Participants were asked about their satisfaction with the outcome of their NHS 111 Online assessment.
Twenty-five participants identified a positive aspect with respect to the outcome of the online assessment, and 17 participants identified some negative aspect; as in the previous section, many reported a mixed experience.
Two-thirds of participants (n = 20) reported that NHS 111 Online provided appropriate advice about what action to take or reassurance that no action was needed. Not only was this information useful for this health episode, but participants described this as potentially useful in the future, for example providing previously unknown information about health services’ availability. For some participants, the advice provided by NHS 111 Online confirmed their own thoughts about appropriate action, and enabled them to feel confident that they were already ‘doing the right thing’:
It’s good for like getting advice and figuring out what to do next, like what steps to take and I suppose it’s good, it’s reassuring ‘cause it helps you figure out whether your problem is kinda serious or not so serious and that. So it’s just helpful to figure out what to do next and what steps you should take.
P18
I think it’s reassurance that you’re doing the right thing. That’s what it gave me.
P26
However, one-third of participants (n = 11) felt that the advice provided was too general, and was not specific to how to deal with the situation. Participants said that advice was focused on the appropriate service to contact, rather than informing them about what self-care they could undertake. Some participants felt that the advice could not be more specific because insufficient information had been sought during the questioning, thus linking to the negative aspects of the process identified above. It was clear that some were hoping for a diagnosis, or more information about what action they could take to relieve their symptoms while they linked to the next service:
The advice seems to be too generic rather than narrowing down to specifics . . . I do think it was a little bit lightweight.
P24
It would be more helpful if it would give some other bits of information, for example if I’m not allergic to any painkillers that I could take something to relieve the pain or . . . any other options to do.
P19
You just want something to take you to the in-between steps that’s all, intermediate steps, the steps from you getting here [NHS 111] to getting there [service advised]. If you’re not well, you’re ill, you’ve hurt yourself, you don’t wanna make things worse, but you don’t know how.
P14
Five participants felt that the advice was too risk-averse, identifying that this could lead to unnecessary use of NHS resources:
It flagged up you need to ring an ambulance, ring 999 now. And that was where I thought, I know, look, it isn’t that serious. I don’t need to ring 999.
P15
Four participants expressed dissatisfaction with their outcome after being given advice that they felt was impossible to follow, for example seeking GP care during the out-of-hours period, or advice that they had already tried prior to contacting NHS 111 Online:
I thought at the end of the day there’s gonna be an outcome, somebody’s gonna tell me to do something or whatever. And then I just got this box saying contact your GP. I thought ‘well what a waste of time that was! An hour out of my life that I can’t get back and they’re telling me to contact my GP, who told me in the first instance to contact 111!’
P30
Some participants who identified being unhappy with the advice given by NHS 111 Online wanted the option of being able to indicate this at the end of the assessment or to speak to someone at NHS 111 about it. They felt that if they had been able to provide more information during the assessment, or via a call back, then different advice might have been given:
It [online assessment] drove you down one straight route, you couldn’t necessarily pose questions, whereas with something like chat over the internet you can actually ask questions.
P24
I was hoping to actually get to where somebody would actually speak to me . . . I thought it would have maybe a section on where ‘do you require a call back?’ or ‘can we e-mail you?’ or something. But at the end it was dismissive. It was ‘Please contact your GP’.
P30
One participant, who had been advised that they would receive a call back from NHS 111, was disappointed in the delay in receiving it:
I found the online a bit misleading, because it did say a call back within 20 minutes, and it were nearly 2 hours. And when you’re in pain, that 2 hours seems forever.
P9
Four participants felt that using NHS 111 Online made it easier to access other sources of help, either by validating the need for a higher-acuity service, such as the 999 ambulance service, or by facilitating access to other services, such as GP appointments:
When I rang up [my GP] I actually said I’d been on the online 111 and it’d recommended I see somebody [GP] and they [GP receptionist] just got me an appointment there and then (. . .) I think I could’ve pushed it and I would’ve got an appointment anyway, but I didn’t have to push it. It was, I just said look I’ve done this and it said this and here I am and they just gave me an appointment.
P16
Adherence to advice
Eighteen participants said that they had not adhered to aspects of the advice given to them by NHS 111 Online. Among those not adhering, a range of advice was reported: four participants had been advised to call the 999 ambulance service, one to visit an ED, 10 to contact a GP, one to contact a dentist, one to arrange a call back and one to administer self-care.
In general, those advised to contact a higher-acuity service (999/ED) had not followed the advice because they did not agree with it, whereas those advised to contact a GP had agreed with the advice but had been unable to follow it.
All of those not following the advice to contact the ambulance service felt that their condition had not been serious enough to warrant calling 999. They described that advice as ‘wrong’, and felt that a call to the 999 service, followed by a possible transfer to the ED, would have been a waste of NHS resources. Two participants also said that ambulance crews had told them on previous occasions that NHS 111 Online was advising contact with the 999 ambulance service sometimes unnecessarily, which had reinforced their decision not to follow the advice. One participant described receiving the advice to contact the 999 ambulance service as worrying – ‘[it] really freaked me’ (P2) – and they thought that they may have mistakenly inputted an answer during their online assessment to trigger this advice. After some deliberation, this participant called NHS 111 to query the advice given by NHS 111 Online, who confirmed that an ambulance was not needed, and arranged an appointment at the GP out-of-hours centre instead. Again, this reinforced the participant’s view that contact with the ambulance service had not been necessary. One participant who did not follow the advice did use the ambulance service the following day, as advised by their GP.
The participant who was advised to contact the ED did not adhere to the advice due to repeated NHS 111 Online advice to contact the ED: ‘it’s always go to A&E’ (P14). In addition, this participant did not want to go to the ED because of a perception of long waiting times or parking difficulties at the hospital. Therefore, NHS 111 Online had not given them the advice that they wanted.
Those advised to contact a GP or dentist reported different time frames for following this advice: ‘within an hour’, ‘within 24 hours’ or ‘tomorrow’. Nine participants felt that they had been unable to follow the advice. Some participants had felt that they could not do so because of the time frames attached to the advice: because either GP services were not open or their personal circumstances prevented them from doing so, including being unable to contact a GP because of work commitments or feeling too ill to drive to the GP surgery. Participants described being told to seek ‘urgent’ or ‘same-day’ GP care during the evening or at the weekend, but did not follow this advice, probably because they had interpreted the advice in terms of contacting their ‘own GP’. One participant found that there was no availability when they tried to make a GP appointment, and another had assumed that it would be too late in the day (after 4 p.m.) to obtain the ‘same-day’ appointment advised by NHS 111 Online. Three participants did not follow the advice of NHS 111 Online because they had believed that it would be a waste of NHS resources.
Propensity to shift from the NHS 111 telephone service to NHS 111 Online
We explored whether or not participants were likely to use NHS 111 Online again, and, if so, if they would choose to contact the online service ahead of the telephone service.
Using the online service again
Most participants (n = 29) indicated that they would use NHS 111 Online again. They described their propensity to use the service again in various ways, ranging from it being their ‘first port of call’ to using it as a ‘last resort’. Despite some negative experiences of the service, the majority of participants identified that they would ‘definitely’ or ‘probably’ use it again.
Participants described being willing to use NHS 111 Online again for information or advice relating to what they perceived to be simple health problems (e.g. a ‘stomach bug’, ‘diarrhoea’, ‘high temperature’, ‘cold’, ‘sore throat’) or for identifying the location of an emergency dentist. Over one-third of participants (n = 12) identified that they were most likely to use NHS 111 Online service again during the out-of-hours period (evenings and weekends), or if they could not get hold of their GP.
Just over one-third of participants (n = 12) identified a propensity to use the NHS 111 Online again because it avoided using NHS resources inappropriately. They felt confident that using the service did not take up anyone’s time, and took pressure off other parts of the NHS.
Preferring NHS 111 Online to the NHS 111 telephone service
Just over half of the interview participants (n = 19) expressed a preference for using the online service over the telephone service. As highlighted earlier in this section, there was a perception that NHS 111 Online was quicker to use than the telephone service in terms of access, assessment and reaching an outcome.
Some participants said that NHS 111 Online allowed them to access health information or advice without ‘bothering anyone’. NHS 111 Online was described as using minimal NHS resources, in comparison with the telephone service. This benefit influenced participants’ willingness to use the online service again in the future. (It is worth noting that the advent of the COVID-19 pandemic and media coverage of the pressures on the NHS may have exacerbated participants’ concerns about not wanting to add additional burden on the NHS.) One participant described NHS 111 Online as a ‘lifeline’. They described having a number of health issues and felt that NHS 111 Online provided them with an opportunity to explore what action they should take without requiring them to make verbal contact with a health-care professional.
Two participants reported a preference for the online service over the telephone service because they felt anxious about talking over the telephone. Two further participants liked being able to move through the questions at their own pace. One participant described struggling to understand strong accents, and had concerns about keeping up with the pace of call handlers’ questions. NHS 111 Online allowed them to complete the questions in their own time, which eliminated the pressure they felt during telephone interactions. One participant reported that they liked the anonymity of the online service in terms of not having to disclose their name or address, which they perceived that they would have to do over the telephone:
I usually choose the online just cause it’s slightly easier because like I do have a bit of like anxiety issues, and like while I can talk on the phone and stuff, like a lot of the time it’s easier just to go online.
P18
If I don’t understand something then you know you never know how people explain things. Sometimes accents can be . . . like English accent . . . the pace someone is speaking [can be a problem] . . . factors like that are something that I would consider. So for me it’s only when I can have a think about or check the translation of some questions . . . it’s the time that I can take to do, to answer the questions. I feel, you know, on the phone, I would be stressed a bit just to answer as quickly as possible because there might be someone else waiting. So for me, the time I can do it and then having the option to go back to the questions.
P19
Let’s say I’m looking after my son or something else is going on in my life I get a phone call or something, I can stop [NHS 111 Online] at any time I want, I can restart it at any time I want so I like that kind of convenience.
P31
One participant said that they chose to use the online service instead of the telephone service as they perceived the telephone service to be risk averse and thought that it would always result in an ambulance being sent.
Instances where NHS 111 Online would not be used again
Around two-thirds of participants (n = 20) identified instances when they would not use the online service again, for example for health problems that were perceived to be ‘serious’ or ‘urgent’, for advice about specific health problems (e.g. asthma, rashes) or for advice regarding children. The reluctance to use the online service in these instances appeared to be related the need for reassurance (about the symptoms or the patient group, i.e. children). Participants reported that it was often easier to describe symptoms over the telephone, and that human interaction was reassuring if they were particularly worried about something. Speaking to someone over the telephone provided immediate reassurance. This was a strong theme running throughout the interviews:
More severe symptoms like with increased difficulty of breathing and stuff. I think I’d rather just talk to someone. It’s easier to explain over the phone what you’re experiencing.
P23
You’re talking to someone who’s trained and it’s not necessarily a computer-generated response. So, not bog-standard, well in theory shouldn’t be . . . I don’t know if it feels, perhaps, a bit more individual and a bit more sort of person-centred, because at least you had the conversation and that there is a person with skills and knowledge on the other end of the phone. Sort of making the decisions, or giving that advice, someone with experience, rather than sort of bog-standard information . . . I think, particularly in this situation, can be quite emotional and worrying and I don’t know, I think having that person’s contact . . . having more personalised care in, in a difficult situation probably makes you more at ease.
P28
Because you’re getting interaction straight away aren’t you? Somebody’s actually listening to what you’re telling them and you’re getting that reassurance straight back. Whereas you’re not typing it out and then sat stewing and waiting. I don’t think I’d be quite as patient if I’d got a grandchild with me that was ill.
P9
Just one participant said that they probably would not use the online service again. They expressed a number of reasons for this. They felt that the online service was no quicker to use than the telephone service, and it also did not allow them to explain or explore their symptoms in any depth. For example, they queried how NHS 111 Online could distinguish between different types of rash. This participant also felt that the online service sends people to ED unnecessarily. Another participant described using the online service again only as a ‘last resort’. It was clear that this person preferred human interaction, and felt that the questions asked during the online service assessment were generalised and not relevant to their individual problem:
Well, I always like to talk. Well, it’s always better ‘cos you can, you get a rapport with someone and usually it’s relevant questions . . . normally you can tell almost immediately whether they’re trained well enough to do the job or not . . . I have confidence in people . . . I suppose it’s because I prefer dealing with people than machines.
P22
Some users described using the online service and telephone service in combination
Some participants described using the online service while they were waiting in a queue for the telephone service. Others said that they would try the online service and then contact the telephone service if they were not comfortable with the advice provided by the online service, or would call 111 if the problem was not getting any better following online advice. One participant described how they had used the online service first, and then contacted the telephone service to check if this provided the same advice.
Recommendations for the future development of NHS 111 Online
As a relatively new service, participants offered suggestions as to how the NHS 111 Online service could develop in the future, and identified issues regarding current service delivery that might be changed.
Improving the question format used by NHS 111 Online
The most frequently cited criticism of the NHS 111 Online service was in relation to the questions posed during the assessment. Eighteen participants identified issues related to the questions, and suggested possible solutions.
Increasing the depth of online questions
As described earlier, many participants described the questions asked during the assessment as ‘broad’, ‘limited’, ‘vague’ and ‘basic’, and not able to deal with multiple symptoms or health problems. This led to a perception that NHS 111 Online could only deal with simple health problems and left participants querying how reliable the advice offered by NHS 111 Online could be if a problem was more complex. However, participants acknowledged that there was a fine balance between enabling the questions to be more ‘sophisticated’ and not making them difficult to answer.
Presenting information using images/diagrams/spoken word
Participants felt that some questions or information could be presented in picture rather than word format. For example, to explore the cause of a rash, NHS 111 Online could present a series of images of rashes that a user could select the one most closely resembling ‘their’ rash. Another participant reported being confused about the specific location of their ‘lower back’. They suggested that NHS 111 Online could show a diagram of the human body with arrows pointing to specific parts of the body.
Although none of our interviewees described having a visual impairment, one participant suggested that NHS 111 Online could provide the assessment using audio, with simple voice-activated responses, for those with visual impairment or reading difficulties.
Improving the interpretation of questions
Some participants found questions irrelevant or difficult to interpret. One participant described themselves as ‘second guessing’ the interpretation of some of the questions. During a verbal interaction interpretation can be checked, but NHS 111 Online did not allow users to do this. Participants provided examples, as described earlier in the chapter, when they had found it difficult to interpret a question. One participant suggested adding a ‘further information’ icon that users could click if they needed clarification of particular questions, such as those used by other online services such as banking or completing of tax returns.
Including a human interaction element to NHS 111 Online
A number of participants (n = 10) said that the problem with NHS 111 Online was that it did not provide human interaction during assessment, which meant that it did not allow users to check anything that was unclear, and could not ask probing questions in the way a human being can. NHS 111 Online was seen as ‘impersonal’ to some. Reassurance is particularly important with respect to health, and participants described uncertainty about the level of reassurance offered by NHS 111 Online. Participants offered some potential solutions.
Introducing a live chat facility
Providing a live keyboard ‘chat’ facility was suggested. Participants offered examples of this working well in other sectors (i.e. banking). In addition to offering reassurance, a live chat facility might help users when, for example, they are answering questions that they have difficulty interpreting.
Providing the option of a call back to all users
Some participants suggested offering users the option of an NHS 111 call back at the end of the NHS 111 Online assessment. The call back would allow users to clarify any advice given or provide the user with the opportunity to share important information that they felt had not been adequately captured during the online service assessment.
Improving the advice offered
Fifteen participants made suggestions for improving the advice offered.
Ensuring that advice can be followed
Some participants described being given advice that they could not follow and their frustration with this. Participants asked why, if a postcode had been submitted, NHS 111 Online could not link up with information about local services and offer advice only when it could be actioned within the specified timeframe.
Improving the communication of interim self-care advice
NHS 111 Online provides interim self-care advice; for example, if a user is advised to contact their GP in the next 48 hours, interim advice is also offered to help alleviate their symptoms. Despite this, it appeared that some service users felt that this interim advice had not been provided. One participant also wanted further advice about what to do if their symptoms worsened while they were waiting to follow the advice offered by NHS 111 Online. NHS 111 Online may need to consider how this information is communicated to service users.
Offering a diagnosis
Participants understood the difficulties of offering a diagnosis as part of an online assessment, but five participants described wanting more information about what their problem might be.
Ensuring that a 999 ambulance disposition does not create anxiety for the user
One participant described feeling anxious when NHS 111 Online advised that a 999 ambulance was required. The participant had not been expecting to be advised to call the 999 service. They had been alone at the time of the online assessment, and this created anxiety. A chat facility or an instant call back for those receiving a 999 ambulance disposition may reduce anxiety.
Managing perceptions that NHS 111 Online offers over cautious advice
Three participants described NHS 111 Online as overcautious in providing ED or 999 ambulance dispositions. They did not feel that their health problem had warranted this response and they did not follow the advice. If there is a widespread perception that NHS 111 Online is overcautious, then this could work in two ways: it could attract users who are seeking an ED/999 disposition in order to provide a justification for their action, or it could deter potential users who do not want to receive a higher-acuity disposition.
Providing information about locally available services
Two participants wanted NHS 111 Online to provide a list of locally available services. For example, at the end of the assessment they wanted to see a list of all services (which included opening hours and location), so that they could make a choice about how to manage their health problem themselves.
Suggestions to improve NHS 111 Online, in general
Improving awareness, and perceptions, of NHS 111 Online
Some of the interviews took place prior to the COVID-19 pandemic. Some participants said that they had not been aware of NHS 111 Online and had been directed to it from another service. Awareness campaigns encouraging the public to seek help from NHS 111 in relation to COVID-19 may have raised the profile of the service since our interviews were undertaken.
There were some misperceptions about NHS 111 Online. One participant perceived that NHS 111 Online can only offer an ED disposition, and others felt that the service triggers a more urgent response than is needed. Improving population understanding of the service offered by NHS 111 Online may be useful. Addressing misconceptions is important if the service is to be accessed by those who need it most.
There was an overwhelming perception that NHS 111 Online deals with relatively minor health problems only. This is a problem if the population is using higher-acuity services for problems that could be dealt with by NHS 111 Online but that they perceive to be outside the scope of the service.
Summary
Overall, participants shared mixed views about NHS 111 Online. Although the majority of interview participants expressed satisfaction with the ease and speed with which an NHS 111 Online assessment was obtained, there were elements of the service with which they were less satisfied. Dissatisfaction predominantly focused on a perception that the questions were simplistic and, for some, this led to a lack of confidence in the advice given.
Just over half of participants did not follow some aspect of the advice given by NHS 111 Online. Those advised to contact a higher-acuity service such as 999/ED did not follow the advice because they did not agree with it. Those advised to contact a GP agreed with the advice but felt that it was difficult to act on.
Almost all of the participants reported that they would use NHS 111 Online again, most likely for help with simple health problems or when it was difficult to access other forms of health care. More than half expressed a preference for using NHS 111 Online prior to accessing the NHS 111 telephone service, whereas others felt that the reassurance and greater depth offered by verbal interaction made the telephone service their first preference. A quickly accessible online format was preferable for some people, such as those with busy lives or with communication difficulties. NHS 111 Online was also seen as a service that used minimal NHS resources.
Limitations
The detailed interviews with service users provided a rich source of insights into how people experience this new service, but there are some limitations. As with the survey reported in Chapter 6, the most important limitation is about representativeness. Participants were predominantly older, female and of white ethnicity. Although we attempted more inclusive sampling, it was difficult to engage the interest of those from other ethnic groups and from younger people, who are much more frequent users of the online service than those represented in the interviews. As the participants were identified from users who had initially completed the NHS 111 Online user survey recruitment was influenced by any respondent bias present in this survey.
The latter stages of recruitment for the user interviews coincided with the early stages of the COVID-19 pandemic. Concerns about this new and very specific potential health problem are likely to have affected the reasons for contacting the online service and the responses to the questions. It also means that some users who may not have previously contacted the service chose to use it as a result of national publicity. Nevertheless, the questions about experience remained relevant to main objective of this work package and provided some useful insights. In particular, using the online service to minimise use of other NHS services at a time when they were becoming increasingly under pressure was an important consideration for some of these later participants.
Chapter 8 Staff and stakeholder views on NHS 111 Online
Introduction
The stakeholder interviews aimed to identify stakeholders’ perspectives on the challenges of and barriers to the implementation of NHS 111 Online and the workforce implications of the introduction of NHS 111 Online. This work package addresses objective 4. In particular, we aimed to understand areas of operation where refinement and development of the operational model were needed, and consequences that need to be considered for future service commissioning. Within the original proposal, we had intended to understand technological issues, criteria for choosing an online platform and implementation costs in order to help the future commissioning and rollout of services. However, as the rollout went ahead before the research started, we focused instead on trying to understand the impact of the online service on the NHS 111 telephone service, including issues around changes to case mix, workload and staff morale and retention.
Methods
Recruitment procedure
Participants were recruited via a key contact at the NHS 111 sites. We asked sites to circulate an invitation letter, together with the information sheet to participants who had the role of health advisers, senior health advisers, clinical advisers, senior floor walkers, specialist clinical advisers or other management, as well as those with any other roles that the sites felt would be relevant. Participants were asked to contact us (FS) directly if they wished to take part. Our purposive sampling strategy aimed to recruit staff in a mix of roles, at a mix of sites and with different lengths of experience.
Recruitment took place between November 2019 and June 2020. After a low initial response rate, we submitted an amendment to the study ethics committee to allow us to provide participants with a Love2Shop voucher as a thank-you for taking part. We then resubmitted the invitations in February 2020. Sites reported low recruitment as a result of significant pressures on the service. Owing to the procedure agreed with ethics and to GDPR (General Data Protection Regulation), we were reliant on site leads sending out the invitations.
Recruitment was low during January because of the pressures that the system was under, and recruitment started towards the end of January, but was then halted because of the COVID-19 pandemic. Sites reported that they could no longer take part in non-COVID-related research owing to the pressures on the system.
The implementation process was rapid, and rollout occurred before our research was undertaken. We were unable to obtain sufficient information about the implementation process to enable us to apply a generic implementation framework to our analysis.
Data analysis
Telephone interview schedules were developed initially following conversations with the project management group and were discussed with patient and public involvement representatives prior to submission for ethics approval. Some additional questions were added following discussions with site leads for the data gathering exercise to understand the models of service delivery.
Interviews were transcribed verbatim and entered into NVivo version 12. Data were analysed using thematic analysis according to the principles of Braun and Clarke. 63 Interviews were read and re-read by Fiona Sampson. A sample of transcripts were read by Emma Knowles and Jaqui Long and a coding framework was developed. Analysis was based on a number of a priori themes: impact on workload/resource implications, impact on wider services, challenges to implementation, perceptions of how people use NHS 111 Online, value of the service/role in the urgent and emergency care system, future development and refinement, and safety. We also developed themes around trustworthiness and belief, knowledge and awareness, and integration.
Results
A total of 33 NHS 111 staff who had been working at NHS 111 for over 1 year responded to the invitation. We sent consent forms to the remaining respondents and sent up to two reminder e-mails to set up the interviews. After non-responses and participants dropping out due to workload, we undertook 16 interviews. The characteristics of the participants are detailed in Table 21. Interviews lasted between 15 and 62 minutes.
| Participant ID | Date of interview | Length of interview | Site | Role | Length of experience | Male/female |
|---|---|---|---|---|---|---|
| SH01 | 9 November 2019 | 61 minutes 46 seconds | 1 | Clinical team manager | Female | |
| SH02 | 9 December 2019 | 35 minutes 53 seconds | 2 | GP background, clinical adviser in 111 triage and GP clinical adviser in CAS | 1 year in 111 and 8 months in CAS | Male |
| SH03 | 12 December 2019 | 33 minutes 33 seconds | 2 | Head of integrated urgent care | Female | |
| SH04 | 17 December 2019 | 36 minutes 31 seconds | 3 | Health adviser and dental | Male | |
| SH05 | 15 January 2020 | 54 minutes 3 seconds | 3 | Clinical home worker | Female | |
| SH06 | 28 January 2020 | 32 minutes 23 seconds | 4 | Clinical adviser, ED nurse | 11 months in 111 | Female |
| SH07 | 28 January 2020 | 23 minutes 17 seconds | 1 | Health adviser | 19 months | Female |
| SH08 | 28 January 2020 | 16 minutes 14 seconds | 1 | Health adviser | 5 years | Female |
| SH09 | 4 February 2020 | 15 minutes 41 seconds | 4 | Non-clinical team leader and licensed pathways trainer | 3 years | Male |
| SH10 | 6 February 2020 | 33 minutes 22 seconds | 4 | Health adviser | 6 years | Female |
| SH11 | 11 February 2020 | 32 minutes 6 seconds | 4 | Non-clinical team leader integrated urgent care | 7 years | Female |
| SH12 | 24 February 2020 | 21 minutes 49 seconds | 4 | Clinical dental adviser | 6 years | Female |
| SH13 | 26 February 2020 | 30 minutes 52 seconds | 3 | Clinical shift manager | 8 years | Female |
| SH14 | 12 March 2020 | 30 minutes 37 seconds | 4 | Commissioner | Male | |
| SH15 | 1 April 2020 | 18 minutes 42 seconds | 4 | Pharmacy adviser | 2 years | Female |
| SH16 | 19 June 2020 | 42 minutes 1 second | 1 | Commissioner | 5 years | Female |
Knowledge and awareness of NHS 111 Online
NHS 111 staff demonstrated a lack of awareness of, or misconceptions about, how NHS 111 Online worked. With the exception of those from commissioners or senior management, answers about the online service were often speculative and demonstrated low levels of understanding about, for example, how users receive call backs from the telephone service or how online referrals work. Staff spoke in uncertain terms when describing how the system works, using terms such as ‘I think’ or ‘I assume’. Even team leaders did not always fully understand how the online service worked and was integrated into the rest of the integrated urgent care system. For example, this clinical team manager describes how the system works, including their perception of how most online interactions are referred into the clinical queue:
Yeah, so if, if a, when they fill in the online form, I, I mean I’ve gotta say I’m not 100% about it, but, erm when they fill in the online form, if they need a, an appointment for a dentist, err they come through to us if it’s a small timeframe. If they need primary, primary care, they, they come through to us, pain management, not quite sure about pain management actually. Erm, no I don’t, know, I don’t think they come through to us. Any ambulance disposition they’ll get advice to call 999, but they also come through to us. Erm, any, you know, dispositions that are ‘speak to clinician’, from operator-generated ones, will come through to us. Erm, so, ya know, like you say the, the online will give its own information, but there’s very few, as far as I can tell, that don’t end up being safety-netted by ending up in the queue.
SH01 clinical team manager
Erm no, the NHS online is a lot shorter version than questions that we have to ask. We have to go through a full assessment, it’s not actually–, obviously because I’ve used it myself at one point, it’s not actually a full assessment of what we would normally ask in a telephone.
SH10 health adviser
We haven’t had a full briefing on what the system does or how close it is to pathways. It seems when I’ve done one example of something, it seemed to come out fairly similar to on [telephone] pathways.
SH04
Most of the interviewees had not received information from their managers about how the NHS 111 Online service worked. Many had found out about the service by chance, for example when a caller to the telephone service reported having used the service, when the online call back requests started ‘popping into’ their call queues, or when they received queries from other providers who had received a referral from an online user. Some participants reported that they had received an e-mail from their manager telling them that the online service was going live and to expect some referrals from this, but they had been given little detail about how this was to happen:
We actually, the first knowledge I had really was from a patient to say, you know, we’ve done this, we’ve done the online 111 service (OK). So I’ve not really had any background into it. And then I asked, obviously, because I thought, well, something I hadn’t actually heard of it.
SH08
No to be honest. I don’t know much and it’s not something that is spoken about, not even in the training I: [. . .] It’s not something oh by the way people can do their assessments online (OK). It’s not mentioned, not something that we talk about.
SH06
Engagement with NHS 111 Online was low; some participants had had a ‘play around’ with the online service to see how it worked and others had not looked at it at all. One participant reported having used it for a genuine problem because of the length of time that they had known they would have had to wait for the telephone service. This lack of knowledge about NHS 111 Online and how it worked may have had an impact on participants’ perceptions of the impact of the online service on their workload. Similarly, staff were unclear about the purpose and role of NHS 111 Online in the wider urgent and emergency care system. Whereas some referenced the online service as being intended to reduce demand for the telephone service, others talked about it as offering an additional, rather than a replacement, service:
So do you feel that the online service, from what you know, has worked as anticipated?
I never knew what the goals were. That’s what I’m saying. They never implemented it like they do others things and pathways.
SH05
Well I think from my perspective it hasn’t reduced the amount of activity going through, but we didn’t necessarily set out to reduce activity. What it has done, of course, is to have allowed certain individuals to, whoever wants to use the service, to possibly use it as a precursor to dialling 111 because people like to get the same info– like to be reassured by getting the same information or same answers from different sources (interviewer: right), whether it’s Google or anything else. So people do use the service before they dial 111.
SH14
Impact of the introduction of NHS 111 Online on the workload of NHS 111 staff
Overall, participants perceived a limited impact of the introduction of NHS 111 Online on their workload or job roles. This was attributed in part to the small numbers of patients being referred to the telephone service for call backs, with staff each seeing a handful of calls per shift. However, there were three ways in which the NHS 111 Online service was reported to have had an impact on the workload of the telephone service: (1) increasing clinician time required for online referrals; (2) increasing health adviser time when users of the online service called the telephone service to clarify advice given online and (3) responding to other services requesting information about an online referral.
Increased clinician time required for online referrals
Clinical advisers expressed frustration at the increased time required to undertake clinical call backs for online users. For patients who have had a telephone pathways assessment with a health adviser, the pathways information is available to the clinical adviser when they open the case from the clinical queue. The clinical adviser can then probe around particular questions and adjust or validate the answers provided if necessary. For the online call backs, the case information is accessed differently and there is no option to adjust existing answers. Instead, the clinical adviser has to copy the case information to their screen and run through the entire pathways triage again, which caused some frustration for staff:
I think it would be easier if the online, I mean, we’ve been online for a couple of years now, it’s about time they actually adapted the template that would go into it and sit on our queue and we’d just open it up like a normal one that’s been done by call handler. Really. And when you think about it we are IT driven it seems a shame that they haven’t! [laughs].
SH05
The initial health adviser telephone assessment was seen as important because of the need to probe and obtain the ‘softer’ information that may be missing from the online referrals. Participants talked about how the training and skill of the health advisers enabled them to probe for further information and would help to ensure that they were accessing the correct algorithm that would direct users to the most appropriate disposition. In particular, the initial ‘offload information’, where the user describes their presenting complaint, was seen as key to understanding how to select the most appropriate algorithm. Similarly, clinical advisers described how they would use their probing and prompting skills when re-triaging pathways for online users to revise previous answers that may not have been interpreted correctly, to ensure that the answers were correct:
I guess because they [clinical adviser] don’t have perhaps the same information they might have got through 111 pathways health advisor assessment you know you get some of the more softer details that a call handler will add in as notes as they put you through the assessment. I would say from that from their perspective calling back an online case takes a bit longer because they have to gather a bit more of the softer information that’s not available to them, because it’s come online, it’s just click, click, click, click, click; you don’t get to add in any real supporting information, if that’s the right phrase. So from a GP’s perspective and probably a clinical advisor as well the call back times are slightly elevated for an online case because of that reason.
SH03
Participants expressed frustration at this lengthier process, as well as concerns about the potential financial impact, particularly if clinical call back volumes were to increase. There was some evidence that this may lead to staff avoiding picking up online calls when there are pressures to meet targets, or that calls in the clinical queue would be passed on to the health advisers to be re-triaged at busy times:
What we’re doing at the moment is if we have call handlers available, erm and because the triage for the clinician is so long if there’s one of these online ones in the queue, quite often I have to ask the call handler to phone back and do the assessment because it sort of doubles the length of the call for a clinician and our clinicians are really, er, you know, there’s we’ve got big queues at the moment.
SH13
NHS 111 Online users call NHS 111 to clarify information provided by the online service
Participants also described how online NHS 111 users called NHS 111 to clarify information provided by the online service because of difficulties in interpreting questions in the online pathways, or because they did not agree with the disposition suggested. Patients were sometimes frustrated about having to repeat assessments and did not understand that NHS 111 staff were unaware of what users had input in their online assessment. Work to improve the wording of NHS Pathways questions had been undertaken during the initial set-up of NHS 111 Online to make the questions clearer and reduce any ambiguity. However, participants perceived there to be some areas where questions were still unclear and where probing or prompting from the health adviser was needed to ensure that the answers provided were accurate:
When we speak to someone I can, as a nurse, I can question that. How bad is your chest pain? ‘Oh it’s really bad’. But I say ‘I’m talking to you and I cannot feel that you’re struggling for a pain that is very, very bad. Your voice is, you know, fluent, you’re not struggling, you’re not gasping for air. So pain that’s really, really bad will not make you sound so well. So are you sure that you have understood this question?’
SHO6
And I also think going back to the timing, it lengthens so much of our clinician queue because again, because we get minimal information the clinicians don’t have all the information [. . .] they have to phone back or get one of us to phone back for an assessment because they’ve put like tummy pains or toothache or headache when they’ve not actually explained; have they got anything else like a fever? Have they been sick? Why do they think they’ve got these tummy pains? Have they eaten anything? Is it anything–, because obviously, like chest pain for example, some types of chest pain will lead from anxiety. But they’ve just put chest pain in it. So we have to probe around that normally. And then we can go on. If we don’t think the outcome that we’ve done is appropriate, we can go on to ask one of our head clinicians and they don’t have that.
SH10
Some participants felt that NHS online users were sometimes referred to clinical advisers inappropriately, when they would have not been referred by a telephone health adviser. Health advisers have knowledge of local services, and their ability to probe and prompt users for further information enables them to interpret information and deflect some of the work away from clinical advisers. One example of this that was reported in multiple interviews was the excessive referral of dental patients for clinical assessment because of concerns about toxic ingestion. Any NHS 111 Online user who responds that they have taken three or more types of painkillers will be automatically referred for clinical advice, whereas health advisers asking the question directly to telephone patients are able to ascertain whether there is a true risk of toxic ingestion, or if a different interpretation:
We were saying about the dental, and when they say oh they’ve err, they’ve exceeded the maximum amount of painkillers for example. [. . .] Erm, if someone has said I’ve exceeded because I’ve taken one extra ibuprofen, then that would be much less of a concern, than someone who’s taken a whole packet of paracetamol, you know, it’s, it, that would be quite helpful to know.
SH01
Additional work resulted from responding to other services requesting information about an online referral
NHS 111 staff described how they received calls from other services chasing up NHS 111 Online referrals or wanting to confirm telephone numbers for people who had been referred from NHS 111 Online. This was problematic for NHS 111 telephone staff who could not access the online records and did not have any details about the online users:
Yeah, or through, via the out of hours ringing up to say, ‘we’ve tried to ring the patient but we can’t get through’, so whether they put the mobile number in wrong which happens quite a bit! [Laugh].
SH11
Right, it’s, it’s quite minimal to be fair, impact for the staff, there’s not a lot of impact. The only real impact we see as team leaders is sometimes like, if we get asked to do a number check if like the, they can’t get hold of the patient or whatever then it’s quite difficult ‘cos we literally, we’ve only got the number that they’ve put in online.
SH09
Impact on wider services
We specifically asked about the potential impact on wider services, in part to understand whether we should speak to staff and stakeholders in those wider services. Interviewees did not perceive that stakeholders would have seen any impact of the introduction of NHS 111 on any wider services, or would be able to differentiate between whether people had used the NHS 111 telephone or NHS 111 Online services:
And the problem is this, it’s difficult to differentiate whether it’s online or [telephone] advice to be honest with you. I assume there’s probably an element of both. It’s just impossible unless we were to sit down and actually do survey of how many come through, it’s be impossible to know.
SH02
There were some speculative concerns that people would use NHS 111 Online as a shortcut to clinical advice, as they could manipulate the questions to get through to a clinician or to get an out-of-hours GP referral.
Perceptions of channel shift
Participants across all sites did not present any consistent perception of an increase or a decrease in demand for telephone service or evidence of channel shift from telephony to online, describing the overwhelming increase in call volumes and limited volume of online calls being too small to make any impact. Participants described how demand had increased significantly for the telephone service, in line with demand for face-to-face urgent and emergency care services, amid a significant ‘winter crisis’. This increase in demand meant that it was difficult to attribute any changes to the introduction of the online 111 service:
Well the workload, I mean, it’s hard to separate it out at the moment. Our workload at the moment is colossal. I remember seeing such an increase in calls coming through out of, through 111 we were up on average about 65% just in the last month. Because I haven’t checked the figures on 111 Online, it could be that that is increasing as well, my feeling is that it is, certainly in the last 12 months onwards in reviewing figures monthly, they are going up each month, the number of users online you know, like I say whether it’s a mix, it’s just so busy at the moment.
SH03
Well we have seen call volumes go up. So of course that’s very hard then to say well they’ve gone up because of online 111. Or they’ve gone up because they would have gone up, as a natural. I mean there may be some piece of work that will come through to us and let us know at some point. But at the moment we don’t understand it, the impact.
SH07
Some participants felt that the online service had the potential to reduce telephony demand, and used the fact that people were using NHS 111 Online (e.g. when receiving calls from out-of-hours providers chasing online referrals) as evidence of some channel shift. One user described evidence of increasing volumes as an indication of new activity:
So, you say the, it should have value in terms of taking pressure off call centres?
Yeah, definitely.
Do you see that happening at the moment?
Yeah, I mean it’s hard to tell because obviously the, our pressures go up and down so it’s hard to tell like an exact reduction but, there’s definitely people using the online service because the calls are coming on to our queue. So, even if it’s only a small reduction it’s definitely working it’s just scaling it up hopefully.
SH09
Some staff, particularly senior staff and commissioners who were involved at the implementation phase, reported that initial concerns about a potential increase in demand for the telephone service following the introduction of NHS 111 Online appeared unfounded. However, others expressed concern that the online service had induced demand, rather than shifting demand, evidenced by people using both the online and the telephone services:
I think the early aim was to try and get people to not have to phone through to us but also have more of an idea what’s happening, what NHS 111 does as well. I also think it was set up to help other health advisors to not have as much of an influx of calls, but I think that doubles that problem. I think they do use NHS 111 Online and then they call up say, ‘Well, NHS 111 Online told me this’ and we’ve told them something else. Then they’re wanting to either complain or to complain about 111 Online and it’s just a massive circle that wouldn’t need to be there if they just called 111 up, we just went through an assessment and then we would have got the appropriate care to them.
SH10
So we have an increase in volumes that are coming through to us that need clinical call backs, we did, hoped that we would see a sort of channel shift and that we would see a reduction in the number of cases coming through via the telephones. And potentially offset the costs associated with increased activity with our clinicians by reduced activity with the call handlers but we’ve not seen that, it’s just been new activity I think. In fact our, our telephony calls are going up and up and up. So yeah it has been impactful in terms of there’s extra stuff for people to do, I think previously, I think it’s just new medium. It’s a bit like when 111 was introduced you know, new people use it rather than old people changing their behaviours.
SH03
Again, perceptions of channel shift or changes in demand were based on personal experience rather than data, and many participants revealed a lack of information coming from management with regard to the volume of calls from online. Some expressed a desire for further information about online user volumes as well as telephony volumes and the interaction between the two services, as this could help them to understand demand and the role of the online service:
Well I, we haven’t had anything in our, like, higher management and we haven’t had any thing it’s not you know, you’re not in our like staff (yeah), we get like statistics like every week it’s never been put in there which I don’t know if they could do, it might work.
Yeah would you find that useful?
Yeah ‘cause then at least then we get to know like how many are still using the phone 111 service (yeah) and the online together (yeah), going to doctors and the out-of-hours service err just so we can get a guide of, I don’t know, just like good to know as well.
SH11
What, what we’ve seen is a growth in that activity anyway on the on– to, we’ve seen a growth in online and we’ve seen a growth in 111 usage anyway. And, but we’re not able to say there’s a– I don’t think we’ve got anything that tells us there’s a (pause) we haven’t got enough information or the right information to tell us how that, how the two things are, two elements of the service are interacting (Interviewer: right) at this point in time.
SH14
Role and value of NHS 111 Online
Participants viewed NHS 111 Online as a valuable adjunct, but not alternative, to NHS 111 telephone service
Despite some negativity relating to the NHS 111 Online service, participants almost universally felt that the NHS 111 Online service added value. The service was seen as useful, but with necessary limitations that would make it an adjunct to, rather than a replacement for, the telephone service:
OK so, do you feel that 111 Online has value?
Oh absolutely. Yes, yes definitely. I think it’s the future, I absolutely I do. I think it’s part of the integration of urgent care system, I think it’s essential, that it needs to be part of the bigger picture moving forward to try and empower patients to be able to make the right choice to have the right information, absolutely essential.
SH16
Staff perceived NHS 111 Online as offering an easy-to-use, risk-free alternative to the telephone service, or as an alternative to other online sources of health information (e.g. Google). The NHS 111 Online service was seen as a low-risk option for users who could undertake the online assessment, without the level of responsibility that is associated with a telephone call or a face-to-face interaction. The service was felt to be valuable to people who preferred the option of an online interaction to a telephone interaction, but also for people who wanted the reassurance of both services. Participants described how some people used the online service as a first step to considering whether they needed to seek help for their health concerns, or as a pre-screen to validate their need to make a telephone call. In particular, staff felt that people used NHS 111 Online to justify their decision to then use the NHS 111 telephone service:
They’ll go onto online 111 and put in whatever and this it comes out with ‘well, this is what you should do’. And then they’re calling into the service. [. . .] But now they’ve got a tool there and in a way it makes it more acceptable for them to ring in to the service because they’ve got the excuse.
SH07
What it has done, of course, is to have allowed certain individuals to, whoever wants to use the service, to possibly use it as a precursor to dialling 111 because people some– like to get the same info, like to be reassured by getting the same information or same answers from different sources, whether it’s Google or anything else. So people do use the service before they dial 111.
SH14
But, a lot of patients would still want the, the clarification from this service. So, they’ve done it online, then they’ll want the call back and then they’ll want the confirmation yes this is what you need to do. So, in a way, it’s like a belt and braces, it’s security for the patients that it is right what they’re doing.
SH12
NHS 111 Online is of value to particular groups
NHS 111 staff felt that NHS 111 Online offered value in particular for lower-acuity conditions (e.g. dental pain, minor injuries) but was less appropriate for high-acuity conditions. Staff felt that users chose the online service for a convenient, low-risk interaction, with some using the online system as back-up while waiting for their NHS 111 telephone consultation. The speed of the interaction and the ability to go through similar pathways at a quicker pace online than by telephone was seen as beneficial, and some participants stated that they would personally prefer to use the online service for this reason:
I mean if I was going to use, I would use the online [laugh], if I needed to; I would actually use the online rather than speaking because I know it can take a while, but that’s only ‘cos I work there but, erm I would actually use the online ‘cos I know it’d be quicker, and not because I know the questions but I just know, you know you can just get through it rather than having to wait on the phone.
SH11
Participants felt that, although it was used by a broad range of people, the service was of higher value to certain groups of patients who used online services as a lifestyle choice, notably younger patients who were more ‘computer-savvy’ (SH04) and used online services in other areas of their lives (e.g. students, ‘professional people’). The online service was also seen as adding value for people who did not like using or were unable to use the telephone, and particularly those who wanted to avoid human interaction, including people consulting about genitourinary or sexual health problems. The impersonal nature of online interaction was also felt to be useful for people who wanted to consult about mental health problems:
We get, we get erm, I suppose it’s surprising, for me alarming, erm, amount of people with mental health problems. Because that, in a way, it’s frightening because you don’t want them to just fill forms in, you want to be able to talk to them. But we do understand that, it might be a really good first step for seeing help. Because you don’t have to talk to somebody, you can just fill, fill those in, and then sort of cast it out and hope that someone can help you. Er, as opposed to ringing and having to, you know, say out loud how you feel.
SH01
NHS 111 telephone service is of greater value than NHS 111 Online
NHS 111 staff perceived the telephone service to offer further benefits beyond that offered by NHS 111 Online. The human aspect of the telephone service was seen as too valuable to be replaced by the online algorithms, which were open to interpretation and seen as difficult for patients to understand. The telephone service was also seen as important for people who wanted the social interaction of a telephone call, or for people who wanted the reassurance of human contact. Participants also described the importance of the physical presence of clinicians and supervisors alongside health advisers when providing 111 telephone advice, in terms of being able to answer queries and reassure them that they were giving users the correct advice:
Yeah I certainly think, that, if somebody wants to see a doctor or a nurse or out of hours they’ll use the telephony service, if they want information or to reassure themselves about their condition they’ll use the online.
SH16
Yes. They’ve put their, what they perceive to be their symptoms, their issues, into the online service, and then whatever the online service is then telling them to do, they’re phoning in to the service well it says I need to this, or it says I need to do that. So then they want, in my perception is, they then want the human contact. They want somebody to say yes that’s right, that’s what you need to be doing. Or well I’ll assess it and I’ll do this for you.
SH07
Importantly, staff appeared to have lower levels of trust and respect in the dispositions elicited by the online service than in those elecited by the telephone service. They contrasted the experience of talking to trained health advisers who could help users interpret questions correctly with the simple task of ‘filling a form in’:
You don’t want to be sitting there filling a form in and if you’re in situation which doesn’t require 999 but requires 111 such as severe nasty stomach cramps I suspect most people aren’t going to sit there and fiddle about with an online form, they’re going to pick up the phone because it’s a darn sight quicker and probably if you’re in that state you’re not quite compos mentis enough to fiddle around on a computer.
SH15
So, there’s, there’s a sort of, there’s just an element of, online ones, of the credibility of the, of the answers. Erm, until, until you get to talk to them, there’s often, you know, unsure answers and things like that.
SH01
Safety concerns
NHS 111 telephone service staff felt responsible for patients who were referred from NHS 111 Online
The ‘disposable’ nature of the online interaction caused some difficulties for NHS 111 telephone service staff when trying to contact users. Although the online service was associated with a low level of responsibility for users, telephone service staff had the same level of concern and responsibility for 111 Online users as they had for 111 telephone users and described difficulties if they could not contact the patient for a call back and were then unsure whether the user had fallen asleep or was seriously ill. Although they verified back-up contact details that they could use to ‘safety net’ the telephony patients, staff had no way of contacting patients who had provided the wrong telephone number:
So, the, the difference between the two, erm, for good or bad, is that we don’t have to act in the end when we, when we can’t contact people online. Erm, whereas when people call, if we can’t get in touch with them, we would then have to assess, what do we do next. Can, can this patient be safely left or, you know, do we have to allocate other services? Erm, so I think err, like a lot of services online, it’s very, it’s very easy, very disposable, with not a lot of responsibility attached.
SH01
Although staff reported that patients generally did not use NHS 111 Online for high-acuity conditions, they felt some anxiety when they were unable to contact a patient and had only the information that the user had input online, which might lack important details (e.g. medication). Staff described the anxieties they felt when following up patients who had completed the online assessment because they had less trust in the data that the user had entered:
But sometimes if I’m worried about somebody who called to say they had a chest pain, an elderly person, then it’s up to my judgement to say maybe I should send a welfare check or an ambulance to go. But with the assessment online we think I haven’t really spoken, and I don’t have all that information. What if they are not at that address I might be wasting, you know, resources, by chasing it.
SH06
So if somebody says I’ve taken three more types of pain relief, and they’re not answering, then I’m worried because I’m thinking how much pain relief have they been taken (yeah). And then if they’re not answering again I’m thinking am I safe to close this call or not?
SH06
Future development of NHS 111 Online
Participants felt that NHS 111 Online had an important and increasing role in future NHS services, with online health advice seen to be the ‘the way things are going’. Although there was no consensus about whether or not the increasing use of NHS 111 Online would reduce the workload of the telephone service, some participants felt that the online model was vital, particularly given difficulties of NHS 111 staff recruitment and retention:
It has to, well, the answer, the answer really is that it, it– given the challenges we have around workforce, then it has to feature very heavily going forward in an integrated service offering, alongside the telephone-based model, or even video-based model.
SH15
Participants felt that there was a need to improve public awareness of NHS 111 Online, particularly by using a realistic advertising campaign to show the public what online and telephone NHS 111 can and cannot do. In addition, further work and education to convince staff of the value to the online service to enable them to recommend the service to patients contacting the telephone service.
It needs more airplay. And we need more education at the coalface so that we can actually sell it with conviction to family and friends really. But certainly I can’t see the take-up in the role that I have and certainly I think my colleagues would agree. So when I say that I’m not saying it loosely (yeah), you know, I just think it should be, you know patients should be made more aware of it really. Like on the advert. Well, have you thought about instead of ringing us, why don’t you make your referral online? [. . .] And actually with the call volumes that we have, that would be something that’d really help. It would reduce our calls considerably.
SH05
I’ve not noticed any impact at all on the call volumes. To be honest, in my opinion, I don’t think it’s been advertised very much because most of the people that I talk to, like staff and public, don’t know about the online service. So, I don’t know whether or not that’s something that’ll come with time or, I suppose it’s similar to when we started, that hardly anyone knew and then word of mouth and that it gets round. But, I’d say most of the population don’t know that there’s an online version.
SH09
Participants also felt that it was important for staff to have an understanding of how NHS 111 worked so that they could understand the system and promote it to users. Improving the intelligence and data available to staff would also help them to understand demand and channel shift. There was also a suggestion that improved data on pathways of care would help staff understand how to improve the service and pathways of care:
So how about the NHS 111 Online, do you see that, how do you see that developing?
I don’t know. I can’t really offer anything on that because I don’t know enough about it. Having never used it and had no access and no training about it, I don’t know.
What training do you feel, if any, would be useful?
Well it would be useful if we’d all sat and perhaps had a dummy run on one. If they’d got a test server where we could all go on and see how it works, see the kind of information it’s asking. See how it relates to what we do (OK). I mean we spend a lot of time on our pathways training for running the assessment, does the online system kind of do the same? Is it asking those kind of questions? Does it have the same algorithm built into it? So if somebody was on the phone to me and at the same time doing the online service, would we be doing the same steps? (Yeah OK) That would be interesting to know (right). And now you’ve made me think about it so I’ll have to ask that question at work! [laughs]
SH07
But we’re not able, we haven’t got the analytical ability to be able to go back and actually go back and look and see whether that was the right, the right thing to do. So, in my view, we need more research about the pathways of care that people are on.
SH15
Other suggested improvements included continued refinements to Pathways to improve the online algorithms and improved direct booking of appointments (e.g. in-hours GP appointments, repeat prescriptions). Improved and transparent communication between NHS Digital and individual sites and commissioners was suggested as important to future service development and particularly in providing services to meet the needs of local populations:
I do think, I do think that it’s interesting that different areas work in different ways. Because of 111 Online being a national service and following all the national guidelines, NHS England guidelines, national disposition, it is challenging for, for me, as a co-ordinator in the [area], because we have lots of nuances, I have commissioners that want a different ring back time or they want somebody to go to this area rather than that area and that’s outside the standard. [. . .] Inner-city [area] is very different to rural [area] and the needs of the patients in those two different areas are very different, so commissioners want different things. And that’s not something online can really adapt to, it has to be the national guidelines and I understand that. But I do hear that as a frustration.
SH16
So I think the, so the, I think the challenge for us is– in a sense it’s been set up, that the, the computer algorithms will be amended by NHS Digital. Are NHS Digital involving commissioners in that? Not to, not to any great. So, and, though every impression that I get from those events I’ve been to with NHS Digital is that actually the patients are quite happy with the service, and as I’m sitting here today talking to you I’m not aware of any issues (I: right). I’m not certain that that’s the case.
(SH15)
Impact of COVID-19 on perceptions of NHS 111 Online
The majority of interviews took place prior to the COVID-19 pandemic, and the substantial role that NHS 111 played in managing demand for health care during the pandemic meant that we were unable to finish recruitment during this period of the study. We undertook two interviews after February 2020 in which participants suggested that the role of NHS 111 Online may have changed during the pandemic, in terms of both increased awareness of the online service and the value of the service. One participant suggested that the online service was more trusted after COVID-19, and that the demographic using the service had changed, perhaps because they saw the value of the service once they had understood how many cases were going through the online service, and also possibly because older people were now more familiar with technology:
I do see it continuing in the future because I think the culture of technology has changed for lots of different generations now because of Zooming and Microsoft Teaming, and people that were technophobes that feel more comfortable it, and accessing stuff online.
SH16
There were suggestions that the increased role of NHS 111 Online in managing demand during the COVID-19 pandemic may have increased the level of respect for the service:
So I think it’s different, I think in answer to your question, I think the perception of how it’s used is different, I think it’s more trusted. You know the advertising of the politician saying on national news, go on 111 Online trust it, use it, let be the guide that tells you what to do next if you’re concerned or needing more information.
SH16
Summary
NHS 111 telephone staff had limited awareness of the impact of the online service overall, partly because of the small numbers of users who were referred into the clinical queues, but also because of a lack of understanding of how NHS 111 Online operated. Overall, participants presented no evidence of channel shift from telephony to online, with many participants not aware of online user volumes. Significant increases in call volumes were noted (the interviews took place at a time of significant increased demand for urgent and emergency care services), but these were not necessarily attributed to the introduction of NHS 111 Online and staff were unable to discern whether or not NHS 111 Online had taken work away from the telephone service. There was evidence of some additional work required as a result of the increased time required to re-triage online referrals and respond to external queries about online referrals and also because of difficulties arising from self-direction of pathways. Overall, staff saw NHS 111 Online as a useful adjunct to the telephone service, particularly for lower-acuity conditions, but with limitations due to the important role that health advisers play in eliciting information.
Future development of NHS 111 Online should include improved information about how the online services work for users and staff at NHS 111 and other services. Other suggested refinements to the service include:
-
Streamline the process of triage for online referrals so that this is similar to telephone referrals (particularly if reimbursement and targets are involved), particularly if the longer call time may disincentivise staff.
-
Allow NHS 111 telephony to have access to online referral case notes.
-
Include local commissioners in the development of services.
Limitations
There were some limitations to this work. Despite sites writing to up to 200 staff at each site, we were unable to recruit sufficient staff to undertake the interviews. Recruitment of staff to studies has been recognised as increasingly problematic in recent years because of increasing pressure on the system. 64 In addition, the lack of awareness about the online 111 system may have acted as a barrier to staff participating in the interviews. The impact of COVID-19 on the NHS 111 service also limited staff’s ability to take part in research.
Chapter 9 Cost–consequences of introducing NHS 111 Online
Introduction
This work package addresses objective 5. The aim is to calculate the estimated cost per person associated with using the NHS 111 Online and NHS 111 telephone services. This will be scaled up to estimate the national costs associated with the use of NHS 111.
By itself, a cost analysis is not an economic evaluation; that is, it cannot be used to assess value for money. However, in tandem with the other components of the evaluation reported in the other chapters, an economic assessment is possible, albeit not based on a single, summary measure of cost-effectiveness; this is termed a ‘cost–consequences’ analysis.
The primary purpose of the analysis is to compare the costs of alternative NHS 111 service provision options: NHS 111 Online only, NHS 111 telephone only and the parallel running of both services. The analysis proceeds with the estimation of cost per case for the first two options, followed by a national policy analysis for all three options using the costs per case and national call volumes.
Methods
The evaluation takes the NHS perspective and has a time horizon limited to two further contacts with the NHS in relation to the initial contact. In practical terms, these subsequent contacts will take place within 7 days of the initial contact, and, therefore, they do not relate to the long-term care of health problems identified as a result of the initial contact. The costs calculated are based on the proportions of services used and the unit costs of each of those services.
Data
The proportions of each service used are taken from the analysis of user surveys in Chapter 6. The only additional service use data used in the model are the proportions of patients offered a clinical call back from the 111 service, which are 17% and 12% for the telephone and online services, respectively. The source of the call back data is the NHS 111 MDS, and our analysis is reported in Chapter 5.
The unit costs of each service were primarily taken from standard sources, using 2018/19 prices. The exceptions to this are the unit costs for NHS 111 telephone, NHS 111 Online and clinical call back, as there are no standard reference costs for these. The estimated costs of the online service were provided by NHS Digital. Costs of the telephone services are more complex as the services are commissioned locally through competitive tendering processes and the costs are commercially sensitive. Via our personal contacts we obtained the likely costs from two CCGs and from NHS England, which are confidential, and used these to provide an estimated cost (Table 22). The cost of ‘other service use’ was derived using proportions of different services indicated in survey responses (see Table 22).
| Costs | £ | Lower estimate (£) | Upper estimate (£) | Source |
|---|---|---|---|---|
| Cost of using NHS 111 Online | 1.00 | 0.50 | 1.50 | NHS Digital. Lower and upper estimate ± 50% |
| Cost of a call to NHS 111 by telephone | 11.40 | 7 | 13 | Confidential |
| Cost of clinical call back including clinical time | 14.10 | 7.05 | 21.15 | Confidential. Lower and upper estimate ± 50% |
| Cost of A&E attendance | 166.05 | 133 | 236 | All A&E attendances, NHS reference costs 2018–19.65 Lower estimate type 1, category 1 investigation, category 1–2 treatment, not admitted (£133); upper estimate median cost of all type 1 HRGs, admitted and not admitted (£236) |
| Cost of ambulance | 209.00 | 104.50 | 313.50 | See and treat or refer; NHS reference costs 2018–19.65 Lower and upper estimate ± 50% |
| Cost of ambulance | 257.00 | 128.50 | 385.50 | See and treat and convey; NHS reference costs 2018–19.65 Lower and upper estimate ± 50% |
| Cost of primary care | 39.00 | 10.85 | 93.70 | GP consultation, PSSRU Unit Costs of Health and Social Care staff 2018/19.66 Lower estimate, practice nurse (£10.85); upper estimate median walk-in centre and minor injury unit HRGs (£93.70) |
| Cost of other service | 21.86 | 10.70 | 32.00 | Calculated using 11.2% dentist, 32.1% pharmacist, 0.2% mental health, 28.3% practice nurse, 28.3% GP. Lower and upper estimate ± 50% |
| Cost of dentist contact | 21.60 | – | – | Band 1 dental appointment (examination, simple treatment or emergency treatment), PSSRU Unit Costs of Health and Social Care Staff 2018/2066 |
| Cost of pharmacist contact | 14.00 | – | – | Community pharmacist consultation, advanced service specification – NHS Community Pharmacist Consultation Service, NHS England and NHS Improvement, 2019 |
| Cost of practice nurse contact | 10.85 | – | – | Cost per hour, PSSRU Unit Costs of Health and Social Care staff (duration of 15.5 minutes from PSSRU 2014/1566) |
| Cost of mental health service | 155 | – | – | NHS Reference Costs 2018/19,65 other mental health specialist team, adult and elderly |
Analysis
The primary analysis is based on each of the two NHS 111 services running without the other in operation. In these circumstances, the access to the alternative NHS 111 service is not possible; that is, when NHS 111 telephone is operating in isolation, patients cannot access online 111, and vice versa. A scenario analysis is undertaken to generate costs for the two NHS 111 services if they were to run in parallel. In this scenario analysis, access to the alternative NHS 111 service is possible.
Sensitivity analysis
Sensitivity analysis is limited to deterministic one-way sensitivity analyses relating to unit costs. Where plausible alternative estimates of representative unit costs have been identified, an upper and a lower value are used in a sensitivity analysis. Where alternative estimates could not be sourced, the primary analysis estimate is reduced and increased by 50%. The estimates used in these sensitivity analyses are shown in Table 22.
National policy analysis
The primary analysis compares the cost per patient of the NHS 111 telephone service without the parallel running of NHS 111 Online with the cost of NHS 111 Online without the parallel running of the NHS 111 telephone service. However, we also undertake a policy analysis that incorporates two additional facets: first, a third-policy option of running parallel services, and, second, the national cost of the three policy options.
The costs per patient for NHS 111 telephone and NHS 111 Online described above represent the individual services. When the services are run in parallel, these costs need to be amended to allow for the possibility that NHS 111 telephone service patients also access NHS 111 Online for the same incident, and vice versa. Additional parameters required for the national costs are the numbers of calls to the services and the degree of substitution of NHS 111 Online for NHS 111 telephone (i.e. the degree to which NHS 111 Online reduces the demand for the NHS 111 telephone service).
The national costs are based on 13,765,413 triaged calls for the NHS 111 telephone service (NHS 111 MDS49), which are assumed to represent the calls for both the NHS 111 Online only service and the NHS 111 telephone-only service. For the parallel service, the same 13,765,413 triaged calls for the NHS 111 telephone service are used in addition to 1,985,387 NHS 111 Online user sessions (the total number of contacts for 2019 in the data supplied to us by NHS Digital). Different degrees of substitution between the two services are explored; with 0% substitution, NHS 111 telephone calls are assumed to be unaffected by the NHS 111 Online service, whereas with 100% substitution, NHS 111 telephone calls reduce by the number of NHS 111 Online user sessions (i.e. 1,985,387).
Results
Using our preferred parameters, the primary analysis shows that NHS 111 Online is £67.90 per person cheaper than the NHS 111 telephone service (£39 vs. £106.80), as shown in Table 23. The initial contact with the NHS 111 Online service is cheaper than the initial contact with the telephone service (£1 vs. £11.40), but the saving in NHS costs is predominantly a result of the use of a different mix of services that are less costly.
| Telephone (N = 478), n (%) | Online (N = 3256), n (%) | Unit cost (£) | Primary analysis | Scenario analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Telephone | Online | Difference | Telephone | Online | ||||
| Cost per call (£) | Cost per call (£) | |||||||
| Initial contact with NHS 111 | 478 (100) | 3256 (100) | 111 | 11.40 | 1.00 | –10.40 | 11.40 | 1.00 |
| Ambulance without conveyance | 30 (6) | 38 (1) | 209 | 13.10 | 2.40 | –10.70 | 13.10 | 2.40 |
| Ambulance with conveyance | 11 (2) | 9 (0) | 257 | 5.90 | 0.70 | –5.20 | 5.90 | 0.70 |
| ED | 157 (33) | 232 (7) | 166 | 54.50 | 11.80 | –42.70 | 54.50 | 11.80 |
| Primary care | 225 (47) | 1411 (43) | 39 | 18.40 | 16.90 | –1.50 | 18.40 | 16.90 |
| Call backs | 17% | 12% | 14 | 2.40 | 1.70 | –0.70 | 2.40 | 1.70 |
| Other | 25 (5) | 662 (20) | 21 | 1.10 | 4.30 | 3.20 | 1.10 | 4.30 |
| No contact | 74 (15) | 1014 (31) | 0 | 0.00 | 0.00 | 0.0 | 0.00 | 0.00 |
| NHS 111 telephone | 0 (0) | 348 (11) | 11 | 0.00 | 0.00 | 1.20 | ||
| NHS 111 Online | 16 (3) | 230 (7) | 1 | 0.10 | 0.00 | 0.10 | ||
| Total (including multiple contacts) | 538 | 3944 | 106.80 | 39.00 | –67.90 | 106.90 | 40.20 | |
The general magnitude of the cost difference between the two types of NHS 111 service is largely unaffected by changes in the cost parameters (Table 24). This is principally because any changes influence both services to some degree and, therefore, partly cancel out the changes. The biggest impact is the change in emergency department costs, which creates a cost difference of £59 or £86, depending on alternative estimates of the unit cost of an attendance.
| Cost component | Lower parameter estimate | Upper parameter estimate | ||||
|---|---|---|---|---|---|---|
| Telephone | Online | Difference | Telephone | Online | Difference | |
| Cost of using NHS 111 Online | 106.80 | 38.40 | –68.40 | 106.80 | 39.50 | –67.30 |
| Cost of a call to NHS 111 by telephone | 102.40 | 39.00 | –63.50 | 108.40 | 39.00 | –69.50 |
| Cost of clinical call back | 105.60 | 38.10 | –67.50 | 108.00 | 39.80 | –68.20 |
| Cost of A&E attendance | 96.00 | 36.60 | –59.40 | 129.80 | 44.00 | –85.90 |
| Cost of ambulance (see treat or refer) | 100.30 | 37.80 | –62.50 | 113.40 | 40.20 | –73.20 |
| Cost of ambulance (see treat and convey) | 103.90 | 38.60 | –65.30 | 109.80 | 39.30 | –70.50 |
| Primary care | 93.20 | 25.20 | –68.00 | 133.40 | 65.80 | –67.60 |
| Other service cost | 106.30 | 36.80 | –69.50 | 107.40 | 41.10 | –66.20 |
When national policy costs are examined, the NHS 111 Online service is associated with £537M of NHS services compared with £1471M for the NHS 111 telephone service. In a parallel service, with zero substitution between online and telephone, the costs are higher still, at £1551M (Table 25). However, if ≥ 38% of NHS 111 Online contacts result in a corresponding reduction in NHS 111 telephone calls, then the parallel service is cheaper than the NHS 111 telephone-only service. If all NHS 111 Online contacts result in a corresponding reduction in NHS 111 telephone calls, then the parallel service is associated with £1339M of NHS services (see Table 4).
| Policy scenario | Calls | Cost (£M) | |||||
|---|---|---|---|---|---|---|---|
| NHS 111 Online only | 13,765,413 | 536.6 | |||||
| NHS 111 telephone only | 13,765,413 | 1470.7 | |||||
| Proportion of NHS 111 Online calls that result in a reduction in NHS 111 telephone service | 0% | 20% | 40% | 60% | 80% | 100% | |
| Parallel telephone and online NHS 111 | 15,750,800a | 1551.0 | 1508.5 | 1466.1 | 1423.7 | 1381.2 | 1338.8 |
Summary
The analysis shows that although the costs per contact of the two NHS 111 services are similar (£1 vs. £11 for online and telephone, respectively), the subsequent use of services is considerably different, such that the overall cost to the NHS is £68 higher with the NHS 111 telephone service. If used in parallel, the two services can produce a saving in comparison with an NHS 111 telephone-only service if ≥ 38% of NHS 111 Online contacts offset NHS 111 telephone calls.
However, the analysis has several limitations. The most significant limitation is that the cost estimates are probably not directly comparable as they relate to different self-selected patient groups; it is likely that the patients using NHS 111 Online had less severe conditions than those contacting the NHS 111 telephone service. As a result, the higher cost of the telephone service reflects, in part, differences in patient characteristics rather than differences in service effects.
In addition, the analysis is based on relatively few surveys. These surveys were required because the routine data did not provide the necessary information on service use. The use of these survey data means that the results are associated with considerable sampling error, together with recall biases and respondent errors.
Given the likely self-selection bias underpinning the model results, a probabilistic sensitivity analysis was not undertaken as it was thought that probabilistic statements of uncertainty would be misleading because they would be based on biased estimates. A deterministic sensitivity analysis was undertaken as the results of this can be used to indicate which individual parameters have the greatest influence on the results and conclusions; this information is considered to be more useful than probabilistic statements.
When interpreting the costs of the NHS 111 telephone and online services, it should be recognised that, without these services, the costs to the NHS attributable to these patients are not zero. In the absence of these two services, it is likely that many of the patients would access NHS services in some other way, for example calling 999, attending the emergency department or contacting a GP for an urgent appointment.
We also noted earlier that the time horizon of the analysis is too short to capture any long-term effects of care initiated by the different NHS 111 services. So, for example, the greater proportion of patients going to the emergency department following contact with the telephone service could be associated with a more comprehensive patient assessment and lower subsequent costs.
In terms of the national policy analysis, this was limited to observed call/contact volumes in 2019. It is unclear to what extent these reflect future demand for the services, in any of the three policy options and in particular if usage behaviour with an online service would be the same as that with a telephone service. However, the methodology can be easily adapted to use alternative projections. Looking forward, it would be useful to explore the cost-effectiveness of encouraging more use of the online service by making the telephone service unavailable or less accessible by, for example, allowing longer waiting times for answering calls or providing clinical call backs.
Finally, the analysis in this chapter refers only to costs. Any differences in patient outcomes of patient experience need to be factored into any decision about the future of the two services. Although the NHS 111 telephone appears more expensive, if this is associated with better patient outcomes then this additional cost may be worthwhile.
Chapter 10 Discussion and conclusions
Introduction
The NHS 111 telephone service triages over 14 million calls per year from the general public to help them navigate what, if any, health care they need and advise them on what service to contact or attend. The service is also increasingly expanding its role as a single point of access for a range of other urgent health-care requests as part of the development of integrated urgent care systems. As such, in common with all emergency and urgent care services, it is under pressure from annual increases in demand. The NHS 111 Online service has been developed to provide an alternative way for people to access advice for an urgent health-care problem using the same triage system (NHS Pathways).
We have investigated the impact of the new NHS 111 Online service on services, patients and staff during its first full year of operation using a mixed-methods approach to take account of these different perspectives. To our knowledge, this is the first study to comprehensively evaluate the impact of a national digital triage service. The findings for each WP have been discussed in the relevant chapters. In this section, we discuss the integration of these findings to present an overall summary in relation to the original study objectives, the limitations of the research and implications for service delivery.
Integration
The integration of different WPs and methods is important to maximise the value of the data and ensure that ‘the whole is greater than the sum of its parts’. We had planned to undertake some work packages sequentially, which would have allowed earlier WPs to inform later ones. Owing to the difficulties in obtaining the routine data and the impact of the COVID-19 pandemic, with the resulting delays in data collection for some WPs, it was not always possible to do this. The exception is the economic evaluation, where the results of the user surveys provided critical information for estimating the cost–consequences of the new service. Despite this, we have been able to bring together findings from all of the WPs to help provide explanation and context for some findings and identify overall learning.
We used an adapted triangulation protocol67 to bring together the key findings from each of the WPs and allow us to identify the overarching conclusions of and recommendations from the whole study. 17 First, we identified key objectives of the study. Then, we presented findings related to the objective from each component on the same page and considered how the findings converged or disagreed or when there was no finding from a component. The triangulation grid is provided in Appendix 4, Table 29. We have used these findings to review the extent to which this research has been able to fulfil the five study objectives. Relevant evidence identified from WP1 (objective 1) has been used to aid interpretation of the findings for the four primary research WPs.
What has been the impact of the NHS 111 Online service on the NHS 111 telephone service and wider health-care system?
NHS 111
In the simplest terms, people with a health problem use an urgent care triage service because they have two questions: (1) what is wrong with me?; and (2) what do I need to do? There is now a choice of ways to access NHS 111. Some people who might have used the telephone service can now choose to use the online service instead (substitution); some may use both services, using one to confirm the decision received from the other (duplication); and some who would not have used the service at all might use the online service because it is quick, convenient and instant or because it provides a more accessible way to get help, for example where language is a barrier to using the telephone service (new demand).
We have taken the approach that NHS 111 is a single service that now has two points of entry and, hence, two streams of activity that can be pooled. The primary outcome was the impact on activity to the NHS 111 telephone service for every 1000 contacts with the online service, that is, whether or not the trend in demand for the telephone service changed following the introduction of the online service. Using pooled data from 18 sites, we found that the online service had little impact on the number of triaged and offered calls to the NHS 111 telephone service during the first year of operation, indicating that the workload for this service did not increase or decrease as a result of the introduction of NHS 111 Online. This suggests there has been no substantial shift to using the online service instead of the telephone service. There was variation between individual sites, indicating that in some areas activity for the telephone service has increased (duplication) but in others it has decreased (substitution). However, the changes were very small, indicating that the majority of contacts with the NHS 111 Online service are ‘new’ activity from the perspective of the total number of people accessing the NHS 111 service for advice. The interviews with staff suggested that there had been no obvious shift following the introduction of the online service, at least in terms of reducing call volumes; this varied between sites, but staff had experienced calls from people who had used the online service and then called the telephone service to confirm the advice given online (duplication). There was also some evidence of duplication in the survey of, and interviews with, service users.
Some contacts with NHS 111 result in a clinical assessment as a result of either the call being passed to an NHS 111 clinician as part of the telephone triage or a request for a clinician to call back (from an NHS telephone service clinician) an online contact. This creates the possibility of additional work for clinicians. Our analysis found an overall reduction in clinician contacts after the introduction of the online service. However, we are uncertain about whether this is a genuine effect, perhaps because users of the online service have lower-acuity problems, or because we have not accurately estimated the number of clinician call back requests from the online service data. The experiences of staff did not indicate any substantial increase in clinician workload, although staff cautioned that this may no longer be the case if the volumes of contacts with the online service continue to increase. Staff also reported that not all requests for a clinician call back take place, as patients do not always answer when they are called. NHS 111 staff also reported that clinician call backs took longer for online users than for telephone callers, but we were unable to test this using our data.
Emergency and urgent care system
Currently, NHS 111 is primarily a triage and signposting service and does not provide direct care, although it can facilitate care by, for example, arranging appointments. Of course, the integrated care hubs that are increasingly connected with the NHS 111 service do provide care, but, for the purpose of this evaluation, the signposting component is the focus. Each contact results in a disposition – a recommendation – about which service to contact or attend (unless no service is needed) and, hence, results in the potential use of an emergency or urgent care service. We assessed what effect the combined activity from the NHS 111 telephone service and online service has on the overall number of recommendations to contact or attend different services following the introduction of NHS 111 Online. We found that recommendations to attend one of the main emergency and urgent care services (emergency ambulance, ED, primary care and community services) increased by between 4.2% and 6.7% for every 1000 NHS 111 Online contacts. The biggest increase, of 21.6%, was for other services outside the usual emergency and urgent care system, such as opticians and sexual health clinics, but these accounted for a very small number of contacts. However, this does illustrate the increasing breadth of services that are becoming available as part of integrated urgent care systems. Overall, the findings suggest a potential net increase in demand for emergency and urgent care services, a finding that has been reported previously when new services have been implemented. 56–58 However, this analysis reflects recommendations for care. The extent to which this translates into actual utilisation of services depends on patient factors, including their original intentions about service access before they used NHS 111 and the actions they take afterwards. There are a number of possible scenarios, and the user surveys and interviews provide some insights into user intentions and actions:
-
Some people may not have considered using any service – 43% of NHS 111 Online users reported that they would not have contacted another service if NHS 111 Online had not been available, compared with 5% of telephone service users. This represents potential new demand, although some may have still chosen not to access a service. Some of this ‘new’ demand might also have been from people who had previously found it difficult to access services and for whom the online option provided a more accessible entry point. This is an important distinction in avoiding the interpretation that all ‘new’ demand is ‘unnecessary’ demand.
-
Some people may have intended to use a service but used NHS 111 Online to check and confirm this action. Any subsequent service contact would be not additional utilisation (although it might be for a different level of service) but an extra step added in their care pathway. Some may decide not to access a service, resulting in a potential saving. The survey did not ask this question directly, but 32.5% of NHS 111 Online users reported they did not comply with the advice given and half of these did not access any service. Interviewees who had used the service did describe using the service in this way.
-
Users who contact NHS 111 because they are uncertain about what to do can follow the advice and use the recommended service, decide to use a different service (which may be at a higher or lower level than recommended) or decide not to contact any service at all. Only 4% of telephone service users did not comply with advice, compared with 32.5% online users. In the 7 days after the contact, 31% of NHS 111 Online users used no service compared with 16% of telephone service users. There were some reports in the user interviews that recommendations for higher-level care, such as an emergency ambulance, were perceived as inappropriate and unnecessary.
It is entirely plausible that introducing this additional access point for emergency and urgent care will create some extra demand; an additional 2 million contacts were created during 2019. The integrated findings show that, although there is potential for demand to increase, it is unlikely to be of the scale suggested by the interrupted times series analyses, as a substantial proportion of the NHS 111 Online user population limit their use of services. One objective of the NHS 111 service from its inception has been to try to reduce some of the unnecessary demand on emergency (999 ambulance and ED) services,7 so additional demand would be counterproductive. The available data do not allow us to determine the clinical appropriateness of NHS 111 Online dispositions to emergency care. However, the evidence from this study suggests that only a small proportion of service users subsequently access emergency services. Previous research has also demonstrated a degree of risk averseness within the NHS Pathways assessment system, with GP review judging that 73% of ED dispositions are suitable for lower-level care. 28 It is, therefore, likely that potential increases in emergency service use are less concerning than they first appear. There is, however, a population of people now accessing services who would not have done so if the NHS 111 Online service was unavailable, representing potential new demand. The findings from the surveys and interviews also indicate that there may be a case-mix difference between the telephone and online populations, with overall lower acuity in the online population and the impact of new demand more skewed towards primary care and community-based services.
Who uses NHS 111 Online and what is their experience?
More women than men use the NHS 111 Online service compared with the telephone service, and substantially more young people use the online service, with more in the 16–35 years age group (61%) than in all other ages groups combined. The same pattern was found among respondents to the survey. Over 75% used a smartphone to access the online service and nearly all (95%) completed the triage process to arrive at a disposition. Dental problems were the most common reason for accessing NHS 111 Online, followed by abdominal pain. A similar proportion of NHS 111 Online and telephone contacts were recommended an emergency ambulance response or to attend ED, but the survey data suggest that this advice was not always followed. Information on user-reported actions showed that those accessing the online service were less likely to report using higher-acuity services if the service had not been available. Among online users there was less use of the emergency ambulance service or ED within 7 days of their contact, and more people chose not to access any service than among telephone service users, suggesting that online patients constitute a group with lower-acuity issues and more self-limiting problems. A common finding in previous research has been that digital symptom checkers designed to triage urgent health problems tend to be risk averse and direct some people to higher-level care than is needed. 15,45,46
One-quarter of NHS 111 Online users reported that they did not find the advice helpful, compared with 10% of those using the telephone service. They also reported lower satisfaction and were less likely to comply with advice. Satisfaction was lower than that reported for early users of the NHS 111 telephone service (50% vs. 73%). 61 Of course, this does mean that 75% of users of the online service did find the advice helpful, and over half reported that they would recommend the service to others and use it again themselves. For a variety of reasons, a substantial proportion of people (35%) used the online service who would not have used the telephone service, indicating that the provision of an online service has widened access for at least some people. Others found the online service more convenient and preferable to waiting in a queue for the telephone service.
Overall, there is a bigger proportion of people for whom the online service does not appear to provide what they need when compared with the early-implementation stage of the NHS 111 telephone service. NHS 111 Online is a new service and, although we did not explore expectations, it is possible that there is a mismatch between what service users thought NHS 111 Online could provide and what NHS 111 Online has been set up to provide. For example, some users indicated that they expected the service to provide a diagnosis rather than just a recommendation about who to contact, although the NHS Pathways system is not intended to provide a diagnosis. This might also explain the lower levels of satisfaction among NHS 111 Online users. Survey respondents and service user interviewees did provide some insights into why the service did not work satisfactorily for them, and a recurring theme was the questioning, which they found difficult to navigate, not always relevant and difficult to interpret. In addition, people did not always agree with the advice given, particularly those who were advised to contact a higher-acuity service such as the emergency ambulance service, and so they did not follow it. Those advised to contact a GP agreed with the advice, but felt that it was difficult to act on. This is consistent with findings from other studies that have explored patients’ decision-making when they need urgent care, in which difficulty, both real and perceived, in accessing GP or primary care has been identified as a barrier. 14,16,17
Towards the end of our study the COVID-19 pandemic began, and some survey respondents and interviewees had used the service since that time. Public health campaigns and media reporting about the pressures on the NHS may have influenced respondents’ decision to use NHS 111 Online instead of the NHS 111 telephone service or other health services. This may have had a negative impact on user satisfaction if usual care pathways were not accessible. On the other hand, respondents also expressed a view that they recognised these pressures and that the online service provided a way of assessing if they needed to access care without having to self-present or contact services first.
Has introducing NHS 111 Online had an impact on the NHS 111 telephone service workforce?
We experienced some difficulties recruiting staff to take part in the interviews for this WP but nevertheless gained some useful insights into their perceptions about the effects of the online service on the wider NHS 111 service. As NHS 11 Online was a new service, not all staff had a clear understanding of how it operated, which made it difficult for them to judge if there had been any impact. At the time of the interviews there were significant increases in call volumes, but these were not necessarily attributed to the introduction of NHS 111 Online and staff were unable to discern whether this was due to the online service, rather than usual fluctuations in demand, or whether the online service had diverted work from the telephone service. An important aspect was the extent to which offering a call back from a clinician as a disposition for the online service affected workload for NHS 111 telephone service clinicians. This did not appear to have created a significant issue as it was reported that relatively small numbers of people were being referred into clinical queues. The analyses of NHS 111 Online dispositions showed that 10% of users were offered a call back. However, there was evidence of some additional work required as a result of the increased time required to re-triage online referrals and respond to external queries about online referrals and owing to difficulties arising from self-direction of pathways. Staff had also encountered examples of callers using the online system before calling the telephone service, which concurs with the evidence from the surveys, although the number of people who reported using the service in this way was small. This reflects the concept of candidacy,68 that is, using the online service allowed them to feel validated in calling NHS 111 (and possibly attending other services) to demonstrate their ‘candidacy’ when subsequently calling the NHS 111 telephone service. The theoretical work on sense-making strategies used when accessing urgent care conducted by Turnbull et al. 16 identified legitimation and sanctions as one of the pillars of ‘work’ people engage in as part of decision-making. A digital entry point may provide patients with the means to navigate these issues with less fear of criticism or what they perceive as possibly wasting the time of staffed services.
Staff did see the potential advantages of providing an NHS 111 Online service but thought it most likely to be useful as an adjunct to the telephone service. It was suggested that the service may be most useful for people who have lower-acuity conditions that might be simpler to resolve using a digital, algorithm-based system that provides limited information. These views compare with previous research,69 which has highlighted the limitations of computerised algorithms and the importance of the human interaction between caller and health adviser or clinician in eliciting the information needed to help people reach appropriate decisions. The more recent evidence on digital and artificial intelligence-based symptom checkers that involve no clinician interaction also suggests that, in terms of urgent care, these may be better suited to simple, low-acuity problems. 46
We have evaluated the service in the early stages of implementation when contact volumes might not have been large enough to create a noticeable difference, but this may change as more people use the service.
What are the costs associated with providing the NHS 111 Online service?
We conducted a cost–consequences analysis to identify any differences in costs for the two services and to estimate the annual costs of providing the NHS 111 service in different scenarios. We used the results of the user surveys to provide a more representative assessment of service use than the service triage recommendations. The analysis shows that that the overall cost per contact is £68 higher for the telephone NHS 111 service, primarily because, as the survey showed, users of the online service accessed fewer emergency services and total services within 7 days of their contact. We estimated that the annual costs would be £537M for an online-only service and £1471M for telephone only. The higher costs of the telephone service most likely reflect not only differences in the cost of providing the NHS 111 service but also differences in case mix, with more users needing higher-level care. The online service was not intended to replace the telephone service, so the more realistic scenario is that both services run in parallel. If used in parallel and with no substitution of the online service for the telephone service, then the annual costs will be higher, at £1551M, but if ≥ 38% of telephone contacts moved to online contacts then there would be a saving in comparison with a telephone-only service. These costs represent the provision of an NHS 111 service and subsequent health service use. Without these services the NHS would still incur costs as patients would still access services directly.
Implications
The purpose of this evaluation changed during the time from the commissioning brief for the research to starting the study. During that time the NHS 111 Online service was implemented nationally so the value of the research is not to answer questions about if the NHS should provide this service. What it can do is identify issues that need to be considered as the service grows and matures and whether there are ways it could be improved to operate more effectively.
For context, it is worth revisiting where the NHS 111 Online service sits in the emergency and urgent care landscape. The service was developed for three main reasons: (1) to provide an alternative signposting service to relieve some pressure on the telephone equivalent, (2) to improve access and provide a simple and convenient system to help people choose what to do and, (3) where appropriate, direct people to lower-level care who might otherwise have chosen differently. 2 In theory, the online service could be viewed as a replacement for the telephone service, but this is not stated as a policy intention and we have taken the perspective of the two services running in parallel. So, how might the two services be best used to gain maximum benefit and value? One approach would be to view users of NHS 111 as a single population who could use either service to meet their needs and therefore create a straightforward substitute between services. Alternatively, there could be two populations, with some overlap, but also with distinct features that better suit one service or the other. Our findings suggest that the latter description is the more plausible, with some evidence of case-mix differences between the two. There is some evidence that there has been little substitution between services: some of the users of the online service are ‘new’ demand; some have lower-acuity problems, for which the service works more effectively; and people have personal preferences about how to communicate with services. These differences highlight the complexity of patients’ characteristics and decision-making behaviour when they need urgent care. More recent research has started to identify the more complex patient and system factors that can explain variation and behaviours. New evidence has shown the important relationships between caller expectations, intended action, attitudes to risk, agreement with triage decisions and subsequent satisfaction and utilisation of services,26,27,38,39 as well as the effect of language proficiency. 27 Call answering delays, waiting for call backs and shorter consultations have been associated with lower satisfaction,37 as have the expectation of a higher level of care and disagreement with a triage disposition. 38 These are all features present in our findings. The NIHR-funded Drivers of Demand for Emergency and Urgent Care (DEUCE) study explored the drivers that influence decision-making behaviour of people needing emergency or urgent care. The study found that three groups of factors were important: symptoms, and the effect that these have on functioning, causing anxiety and uncertainty about the seriousness of the problem and the need for relief from symptoms; patient, including coping capacity, fear of consequences (particularly when responsible for other people’s health, e.g. a child) and the influence of social networks; and health services, including previous experiences of services, lack of timely access to some services and compliance with health service staff’s advice. 17 Some of these features are apparent in the findings of this study. Both the DEUCE study and the work on sense-making strategies16 have also identified the complexity of the NHS urgent care system and how this makes it difficult for individuals to navigate accessing the right care. A recent study that asked urgent care service users about the features they would like to see in an ‘ideal’ system also highlighted complexity as a problem. Participants expressed the view that a simplified system with a single point of access would be preferable. 70 Much of the NHS urgent care policy agenda over recent years has been grounded in the approach of providing a simplified system that can deliver ‘right care, right place, first time’,7 but patient experiences seem to suggest that the urgent care system is not simple, and NHS 111 Online has added another entry point, potentially making it more complex.
So, taking the perspective that there are two services with some overlap, and that there are some differences between the NHS 111 Online and telephone populations, there are a number of implications for the future delivery of services.
Demand
Previous research has shown that the introduction of new services and access points for emergency and urgent care has created an increase in and, therefore, new demand for services, and it is likely that adding another new service has had the same effect. However, the findings of the previous research were based on data of actual utilisation of other services in the emergency and urgent care system. Our analyses were limited to estimating demand using service recommendations, and the survey results have shown a gap between recommended and subsequent service use. Better patient-level data that links NHS 111 service use to subsequent service utilisation is needed to properly estimate the impact of NHS 111 Online on the emergency and urgent care system. This would also allow a better understanding of the relationships between new demand, service substitution and service duplication. However, there is a barrier in that the current configuration of NHS 111 Online would not support this as, unless a user requests a clinical call back or is provided with an appointment, the only personal information collected is age and postcode, which would be insufficient to link to health records.
User characteristics
The lack of patient-level data prevented us from examining more closely the characteristics of the two NHS 111 populations. Understanding these characteristics, including the types of problems for which people contact each service, may provide better information for users when they have to choose whether to use NHS 111 Online or the NHS 111 telephone service.
Triage
The NHS Pathways system is well established and has been adapted to operate on a remote digital platform. There are clear advantages to having a single interoperable system across both NHS 111 services. Our research has shown that there is a gap between recommendations from the triage system and the action people subsequently take. For the online service, the proportion of contacts with a higher service level disposition of emergency ambulance or ED was similar to the telephone service, but uptake was much lower. Within the telephone service, calls with an initial disposition of ambulance or ED are reviewed by a clinician (revalidation) to reduce unnecessary ambulance dispatches and ED attendances. With the online service, this option is less straightforward. In some areas, assessments that arrive at a ‘call 999 ambulance’ disposition will offer a call back, but, at the time of our study, this was not in place in all sites. However, it is unclear if this is still recorded as an ambulance disposition in the online service data. The number of ambulance dispositions may reduce as there is further integration and clinician call backs increase. Nevertheless, it was clear from responses to the survey and interviews that some patients are themselves, to some extent, ‘revalidating’ these recommendations by choosing not to access these services. All triage systems where there is no face-to-face contact have a level of risk averseness, and this is certainly a feature of digital systems where there is no human interaction. 15 Further scrutiny of the online triage process to reduce overtriage would likely improve confidence in the service for users and reduce potential unnecessary demand on emergency services.
Clarity of purpose
Despite sharing a common name (NHS 111), ‘NHS 111 Online’ and ‘NHS 111’ are different services, and although some people may be able to use either service successfully others will have a preference for one or the other. Choosing the ‘wrong’ option increases the risk of duplication. There is a clear value to providing an online service; one-third of NHS 111 Online respondents used the service because they did not want to contact NHS 111, and it also met a need of groups of the population who prefer services delivered online rather than over the telephone. Users also appreciated the value of the online service during the COVID-19 pandemic as they did not want to make unnecessary contacts at a time when the NHS was under severe pressure. However, at the moment the online service does not seem to meet some users’ expectations. If a service meets expectations, then people are more likely to use it again and recommend it to others. If one objective is ‘channel shift’ – people using the online service instead of the telephone service – then it may be helpful to provide more explicit information to users about what the online service can provide and when to use it. To support more effective use of the service and improve user experience and satisfaction, some further development of the online service could result in more benefits, including cost savings, as we have shown that these can be realised only if there is substitution of services. Finally, the importance of an integrated urgent care system cannot be overemphasised. Some dissatisfaction arises from users being unable to action the recommendations of the online triage in terms of appropriate service access. If these do not match up, then people will continue to self-present to higher-level services, which they perceive to be always open, even if this level of care is not needed. 17 The NHS has committed to developing integrated urgent care services8 and has published a detailed service specification describing what this should look like. 71 Historically, NHS 111 has been a separately commissioned and delivered service that refers callers to other, external services, such as GP out of hours. Individual services have formed more integrated partnerships, but there is now a national ambition to develop the ‘provision of a functionally integrated, 24/7 urgent care access, clinical advice and treatment service’. 71 This will be staffed by multidisciplinary teams that include GP, pharmacy, mental health, dental and palliative care clinicians with NHS 111 (telephone and online) as part of the integrated urgent care service as the ‘front door’ to access. This means that users should expect their problem to be managed and resolved in a single encounter, described as a ‘consult and complete’ model of service delivery rather than ‘assess and refer’. The successful implementation of integrated urgent care services will be a central component of maximising the potential benefits of the NHS 111 Online service and improving efficiency and patient experience. Clarity about who should use each service given the possible differences between the telephone and online populations will improve efficiency and contribute to reducing the complexity of navigation that current users experience.
Potential improvements
Evidence from the user surveys and interviews and staff interviews provided some suggestions of factors that could improve the online digital process and management of contacts. These were:
-
Further refine the questioning. Some users found questions difficult to navigate, and the need to provide binary yes/no answers did not help them convey their problem. Where people had multiple symptoms this was difficult to manage as they had to choose one.
-
Provide images or diagrams to help better understand the questions (examples were pictures of rashes so the user could choose the nearest one to their problem, or a diagram of a body to indicate what is meant by ‘lower back’).
-
Provide more options for a ‘human’ interaction either through an online ‘chat’ function (which people are familiar with from other service industries) or the option for anyone to request a clinician call back (rather than the current system when this is offered only for some contacts where a ‘speak to clinician’ disposition is reached). This does have implications for clinician workload.
-
The starting point for this study is when a user has accessed the online service. However, there is a step before this, not within scope, which is how people navigate to find the NHS 111 Online service. This may be simple, such as putting ‘NHS 111’ into a search engine, or people may first access the NHS website or app and use this to navigate to the online service. Further exploration of this process would help better understand how easy, or how difficult, people find it to access the service.
-
Provide more information about locally available services and when they are open. This is already a feature of the NHS 111 Online service and depends on integration with the local DoS. It may be that some early survey responses reflected use before these were all fully integrated, but there may be other types of services of interest to users that are not currently included.
NHS 111 telephone service staff made some suggestions of improvements to make the process more efficient. These were:
-
Provide better information to the public about what the NHS 111 Online service can offer and when to use it.
-
Streamline the process of triage for online referrals so that they are similar to telephone referrals (particularly if reimbursement and targets are involved). This would reduce longer call times that may be a disincentive for staff.
-
Allow NHS 111 telephone service to have access to online referral case notes.
-
Include local commissioners more in the development of services.
Service expansion
This evaluation presents findings from the early-implementation stage of the NHS 111 Online service. There is a tension between the need to provide early evidence on the impact and effectiveness of a new service and the limitation that this may not reflect what happens when a service has developed and matured. Use of the NHS 111 Online service increased dramatically during this study. There were just over 2 million contacts during the first year of national provision (2019), the time frame for this work. NHS Digital data (not in the public domain) recorded 7.45 million contacts for the first 10 months (January–October) of 2020. Of course, this was in part fuelled by the COVID-19 pandemic. In response to this, the NHS 111 Online service was rapidly adapted to provide a digital symptom checker for coronavirus, and between March and November 2020 this was used over 3.5 million times. 72 It is a striking example of how digital technologies can be utilised to provide a functional, national service triage service capable of managing huge volumes of contacts in a short time in response to a public health crisis. It is impossible to estimate what the growth in use of the online service would have been without the pandemic, although use was clearly already increasing rapidly. The high profile of the COVID-19 symptom checker will undoubtedly have increased awareness of the NHS 111 Online service and have driven growth. It is also possible that some people who might not have considered using NHS 111 Online but used the symptom checker will now use the service again in the future. It was also clear from the surveys and the interviews that service users valued a digital alternative that could deflect some of the pressure from other NHS services. Both of these factors may influence future behaviour about choice and decision-making when accessing urgent care. This means that the combined populations of NHS 111 telephone and online users will be substantially greater in the future than the one we have examined and the impact may already be changing. It also has significant implications for the NHS and reinforces the need to take steps to try to maximise the channel shift from the telephone service to the online service and minimise duplication of service use and growth in new demand. This will become even more important if the NHS 111 First programme73 – in which people are encouraged to call NHS 111 before attending an ED– is expanded nationally. The combined NHS 111 telephone triage, NHS 111 Online and NHS 111 First populations will create a huge cohort of people with expectations of a rapid response to their urgent health problem.
Limitations
The limitations of this study have already been discussed in part throughout this chapter, but the most important ones are:
-
Because of the rapid roll-out of NHS 111 Online as a national service, we were not able to use an experimental design with a control arm. This means that we cannot establish if the effects we have found are the direct result of introducing the new service or if they would have happened anyway because of other factors influencing both the NHS 111 telephone service and the wider emergency and urgent care system.
-
The lack of patient-level data for the NHS 111 telephone service meant that we had to make some significant compromises to our original plans. The main ones were as follows. (1) We were able to include only 18 sites in the interrupted time series analysis and so have not been able to establish a national estimate of impact. However, we are confident that the 18 sites included are representative of different types of service provision to make reasonable inferences. (2) The comparison of the characteristics of the NHS 111 telephone and online populations was seriously limited, so we could not explore case-mix differences by health problem type and associated dispositions.
-
This evaluation of NHS 111 Online took place in the early stage of implementation during a period when use was growing and the service had been in operation for only 12–18 months. Estimated system impact is based on the ‘dose’, in terms of contacts with the new service, present at that time. As the service becomes more widely understood by the public, and as contacts increase, it is possible that the impact may change and any subsequent assessment of impact would be more robust.
-
The estimates of costs have considered the NHS 111 telephone and online users as equivalent groups, but they are probably not directly comparable as they relate to different self-selected patient groups. It is likely that the patients using NHS 111 Online had less severe conditions than those contacting the telephone service, so the higher cost of NHS 111 telephone reflects, in part, differences in patient characteristics rather than differences in service effects. In addition, the lack of patient-level data for telephone users or of any health service level utilisation data meant that we had to base the estimates on relatively small surveys, which introduces sampling and respondent errors. Using survey data did, however, provide a more accurate reflection of service use than triage service recommendations. For the national policy analysis, this was limited to the observed call/contact volumes in 2019, but these may not reflect future demand for the services.
Recommendations for research
We have evaluated the NHS 111 Online service in the early stages of implementation. Some related issues are already being investigated by a complementary NIHR-funded project on patient pathways and eHealth literacy. 74 This study is mapping pathways to urgent care and where NHS 111 fits in these. It comprises a survey to explore eHealth literacy and ability to use online services, observations of and and interviews with staff across the urgent care system to assess workforce implications and interviews with staff involved in the similar Health Direct service in Australia. 73 The findings of this study have identified areas of useful further research related to the effects of further expansion and service maturity and service development and improvement.
-
Re-evaluate the impact on the NHS 111 service and wider health system using linked data that provide a more robust and comprehensive assessment of the different types of demand (new, substitution, duplication) and subsequent service utilisation in a more mature online service environment. The addition of primary care data would further enhance this. This would also support a more robust evaluation of the cost–consequences of the two services.
-
Carry out further research with service users to explore expectations, reasons for using the service, improvements to the triage questioning process itself and interface with additional human communication. These would improve the information about what the service can provide and help increase the uptake of the service as an alternative to telephoning, confidence in the service decisions and satisfaction.
-
Conduct further, patient-level comparisons of the characteristics of the two NHS 111 populations and the relationships between characteristics. This would help identify which people are most likely to benefit from using the two types of service and provide information that would help patients choose which service to use.
-
An interesting group are people who choose not to follow the advice or recommendations for care. Further follow-up to assess health outcomes would provide important evidence about whether or not their decisions were correct, which in turn could help improve the triage process. This would also challenge some of the assumptions about compliance and how useful it is as a measure of urgent care triage effectiveness.
Conclusions
NHS 111 Online is a new service that allows people to access advice for urgent health problems using a digital triage system as an alternative to the established NHS 111 telephone service. So far, the new service appears to have had little impact on the number of calls to the telephone service, and there is a risk that new demand may be generated. Although users of the service report less compliance and satisfaction with the online service than users of the telephone service, there is a clear need for an alternative to the telephone as some people prefer the convenience and communication process of a digital service. Overall, the service was viewed positively, but there are a number of ways in which the service could be improved to make it more attractive to users, including improving the questioning and streamlining the links between the online and telephone service when people need a health-care professional to provide further advice or reassurance. For the online service to be effective and provide good value for money, more people need to use it instead of the telephone service. Future development should focus on refining the triage process so that more people are encouraged to make this change. Finally, the NHS 111 service is only one part of the emergency and urgent care system and does not operate in isolation. For it to be effective and trusted by the people who use it, they need to be able to action advice and recommendations about which service to access in a timely way. If they cannot, then they will continue to exercise their own judgement about service choice, which will perpetuate system inefficiencies.
Acknowledgements
We would like to thank the following organisations and individuals for their invaluable time and support during this study.
Yorkshire and the Humber, Surrey, Derbyshire, Mersey, SW London, Hampshire, Staffordshire, Bedfordshire & Luton, Cambridgeshire & Peterborough NHS 111 services for providing information on the structure and implementation of NHS 111 Online into their services.
Yorkshire and the Humber, Derbyshire, Hampshire and Bedfordshire & Luton NHS 111 services for facilitating recruitment for the staff and stakeholder interviews.
The NHS 111 Online team at NHS Digital: Debbie Floyd and Jeffery Miller for providing background information on the NHS 111 Online service, facilitating links to NHS services and managing the transfer of data.
Thanks also for allowing us to adapt the NHS 111 Online user experience questionnaire to meet the needs of the study, and facilitating access to these data. Particular thanks go to Jeanette Attan and Christine McKinney for their support during this process.
NHS 111 telephone providers for adapting their user experience questionnaires to meet the needs of the study: Yorkshire Ambulance Service (in particular Keeley Townend and Bob Sunley), and South Central Ambulance Service (in particular Helen Pocock, Amanda Painter and Sarah Taylor).
The Sheffield Emergency Care Forum for facilitating public involvement.
The members of the Study Steering Committee (Matt Widdows, John Harris, Richard Oliver, John Soady, Alastair Pickering, Deborah Floyd and Helen Rice) for their insightful observations.
Dr Jennifer Read, ScHARR, for help with the evidence review data extraction.
Mr Marc Chattle, ScHARR, for providing administrative support.
Contributions of authors
Janette Turner (https://orcid.org/0000-0003-3884-7875) (Reader in Emergency and Urgent Care Research) was the principal investigator and had oversight of the study. She designed the study, led the evidence reviews, wrote drafts of Chapters 1–3 and 10 and was responsible for oversight of the final report.
Emma Knowles (https://orcid.org/0000-0003-3372-1245) (Senior Research Fellow) designed and conducted the patient surveys and user interviews, analysed the survey and interview data and wrote the drafts of Chapters 6 and 7.
Rebecca Simpson (https://orcid.org/0000-0003-1677-5938) (Lecturer in Medical Statistics) designed and conducted the interrupted time series analysis and descriptive statistical analysis and wrote the draft of Chapter 4.
Fiona Sampson (https://orcid.org/0000-0003-2321-0302) (Senior Research Fellow) designed and conducted the staff and stakeholder user interviews, analysed the interview data and wrote the draft of Chapter 8.
Simon Dixon (https://orcid.org/0000-0001-7394-7009) (Professor of Health Economics) designed and conducted the cost–consequences analysis and wrote the draft of Chapter 9.
Jaqui Long (https://orcid.org/0000-0002-6889-6195) (Research Associate) conducted the interviews with service users and contributed to the analysis of data.
Helen Bell-Gorrod (https://orcid.org/0000-0001-8054-8073) (Research Associate, Health Economics) contributed to the cost–consequences analysis and the draft of Chapter 9.
Richard Jacques (https://orcid.org/0000-0001-6710-5403) (Senior Lecturer in Medical Statistics) contributed to the design of the statistical analysis plan and the draft of Chapter 4.
Joanne Coster (https://orcid.org/0000-0002-0599-4222) (Research Fellow) contributed to the sifting and data extraction for the evidence reviews and the draft of Chapter 3.
Hui Yang (https://orcid.org/0000-0002-3372-4801) (Analyst) conducted descriptive statistical analysis and contributed to the draft of Chapter 5.
Jon Nicholl (https://orcid.org/0000-0001-5436-1264) (Professor of Health Service Research) provided expert advice on the overall study design and statistical analysis and contributed to the draft of Chapter 4.
Peter Bath (https://orcid.org/0000-0002-6310-7396) (Professor of Health Informatics and Applied Data Analytics) provided expert advice on study design and contributed to the descriptive statistical analysis.
Daniel Fall (https://orcid.org/0000-0002-2330-2082) (Public Involvement Co-applicant) contributed to the study design, development of questions for the user surveys, interpretation of findings and production of the plain English summary.
Tony Stone (https://orcid.org/0000-0002-0167-3800) (Data Architect and Senior Data Manager) conducted the acquisition of the routinely recorded data, initial processing and interpretation of these data and contributed to the analysis of data.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- NHS England . Statistical Work Areas. n.d. www.england.nhs.uk/statistics/statistical-work-areas/ (accessed 19 March 2021).
- NHS England . The NHS Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 19 March 2021).
- Turner J, Coster J, Chambers D, Cantrell A, Phung VH, Knowles E, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03430.
- Nuffield Trust . The NHS Workforce in Numbers 2018. www.nuffieldtrust.org.uk/resource/the-nhs-workforce-in-numbers (accessed 19 March 2021).
- Becker J, Dell A, Jenkins L, Sayed R. Reasons why patients with primary health care problems access a secondary hospital emergency centre. S Afr Med J 2012;102:800-1. https://doi.org/10.7196/samj.6059.
- Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department?. Emerg Med J 2012;29:487-91. https://doi.org/10.1136/emj.2010.107276.
- NHS England . Transforming Urgent and Emergency Care Services in England. Urgent and Emergency Care Review End of Phase 1 Report 2013. www.nhs.uk/nhsengland/keogh-review/documents/uecr.ph1report.fv.pdf (accessed 19 March 2021).
- NHS England . Next Steps on the NHS Five Year Forward View 2017. www.england.nhs.uk/wp-content/uploads/2017/03/NEXT-STEPS-ON-THE-NHS-FIVE-YEAR-FORWARD-VIEW.pdf (accessed 19 March 2021).
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003451.
- Veazies S, Winchell K, Gilbert J, Paynter R, Ivlev I, Eden K, et al. Mobile Health Applications for Self Management of Diabetes. Rockville, MD: Agency for Healthcare and Research Quality; 2018.
- Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. National Institute for Health Research School for Primary Care Research . Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Armstrong S. The apps attempting to transfer NHS 111 Online. BMJ 2018;360. https://doi.org/10.1136/bmj.k156.
- NHS England . NHS111 Online Evaluation. 2017.
- Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 2017;24:1137-49. https://doi.org/10.1111/acem.13220.
- Chambers D, Cantrell A, Johnson M, Preston L, Baxter SK, Booth A, et al. Digital and online symptom checkers and assessment services for urgent care to inform a new digital platform: a systematic review. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07290.
- Turnbull J, McKenna G, Prichard J, Rogers A, Crouch R, Lennon A, et al. Sense-making strategies and help-seeking behaviours associated with urgent care services: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07260.
- O’Cathain A, Knowles E, Long J, Connell J, Bishop-Edwards L, Simpson R, et al. Drivers of ‘clinically unnecessary’ use of emergency and urgent care: the DEUCE mixed-methods study. Health Serv Deliv Res 2020;8. https://doi.org/10.3310/hsdr08150.
- Blank L, Coster J, O’Cathain A, Knowles E, Tosh J, Turner J, et al. The appropriateness of, and compliance with, telephone triage decisions: a systematic review and narrative synthesis. J Adv Nurs 2012;68:2610-21. https://doi.org/10.1111/j.1365-2648.2012.06052.x.
- Lake R, Georgiou A, Li J, Li L, Byrne M, Robinson M, et al. The quality, safety and governance of telephone triage and advice services – an overview of evidence from systematic reviews. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2564-x.
- Eastwood K, Morgans A, Smith K, Stoelwinder J. Secondary triage in prehospital emergency ambulance services: a systematic review. Emerg Med J 2015;32:486-92. https://doi.org/10.1136/emermed-2013-203120.
- Wheeler SQ, Greenberg ME, Mahlmeister L, Wolfe N. Safety of clinical and non-clinical decision makers in telephone triage: a narrative review. J Telemed Telecare 2015;21:305-22. https://doi.org/10.1177/1357633X15571650.
- Tran DT, Gibson A, Randall D, Havard A, Byrne M, Robinson M, et al. Compliance with telephone triage advice among adults aged 45 years and older: an Australian data linkage study. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2458-y.
- Gibson A, Randall D, Tran DT, Byrne M, Lawler A, Havard A, et al. Emergency department attendance after telephone triage: a population-based data linkage study. Health Serv Res 2018;53:1137-62. https://doi.org/10.1111/1475-6773.12692.
- McKenzie R, Dunt D, Yates A. Patient intention and self-reported compliance in relation to emergency department attendance after using an after hours GP helpline. Emerg Med Australas 2016;28:538-43. https://doi.org/10.1111/1742-6723.12619.
- Krumperman K, Weiss S, Fullerton L. Two types of prehospital systems interventions that triage low-acuity patients to alternative sites of care. South Med J 2015;108:381-6. https://doi.org/10.14423/SMJ.0000000000000303.
- Martinsson J, Gustafsson S. Modelling the effects of telephone nursing on healthcare utilization. Int J Med Inform 2018;113:98-105. https://doi.org/10.1016/j.ijmedinf.2018.02.004.
- Njeru JW, Damodaran S, North F, Jacobson DJ, Wilson PM, St Sauver JL, et al. Telephone triage utilization among patients with limited English proficiency. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2651-z.
- Anderson A, Roland M. Potential for advice from doctors to reduce the number of patients referred to emergency departments by NHS 111 call handlers: observational study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009444.
- Huibers L, Moth G, Carlsen AH, Christensen MB, Vedsted P. Telephone triage by GPs in out-of-hours primary care in Denmark: a prospective observational study of efficiency and relevance. Br J Gen Pract 2016;66:e667-73. https://doi.org/10.3399/bjgp16X686545.
- Thilsted SL, Egerod I, Lippert FK, Gamst-Jensen H. Relation between illness representation and self-reported degree-of-worry in patients calling out-of-hours services: a mixed-methods study in Copenhagen, Denmark. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020401.
- Gamst-Jensen H, Lippert FK, Egerod I. Under-triage in telephone consultation is related to non-normative symptom description and interpersonal communication: a mixed methods study. Scand J Trauma Resusc Emerg Med 2017;25. https://doi.org/10.1186/s13049-017-0390-0.
- Gamst-Jensen H, Frishknecht E, Lippert F, Folke F, Egerod I, Huibers L, et al. Self-rated worry predicts hospitalisation in out-of-hours services telephone triage. BMJ Open 2018;8:A25-6. https://doi.org/10.1136/bmjopen-2018-EMS.67.
- Meer A, Gwerder T, Duembgen L, Zumbrunnen N, Zimmermann H. Is computer-assisted telephone triage safe? A prospective surveillance study in walk-in patients with non-life-threatening medical conditions. Emerg Med J 2012;29:124-8. https://doi.org/10.1136/emj.2009.080614.
- Turnbull J, Prichard J, Pope C, Brook S, Rowsell A. Risk work in NHS 111: the everyday work of managing risk in telephone assessment using a computer decision support system. Health Risk Soc 2017;19:189-208. https://doi.org/10.1080/13698575.2017.1324946.
- Wahlberg AC, Bjorkman A. Expert in nursing care but sometimes disrespected – telenurses’ reflections on their work environment and nursing care. J Clin Nurs 2018;27:4203-11. https://doi.org/10.1111/jocn.14622.
- McAteer A, Hannaford PC, Heaney D, Ritchie LD, Elliott AM. Investigating the public’s use of Scotland’s primary care telephone advice service (NHS 24): a population-based cross-sectional study. Br J Gen Pract 2016;66:e337-46. https://doi.org/10.3399/bjgp16X684409.
- Kelly M, Egbunike JN, Kinnersley P, Hood K, Owen-Jones E, Button LA, et al. Delays in response and triage times reduce patient satisfaction and enablement after using out-of-hours services. Fam Pract 2010;27:652-63. https://doi.org/10.1093/fampra/cmq057.
- Rahmqvist M, Ernesäter A, Holmström I. Triage and patient satisfaction among callers in Swedish computer-supported telephone advice nursing. J Telemed Telecare 2011;17:397-402. https://doi.org/10.1258/jtt.2011.110213.
- Gustafsson S, Martinsson J, Wälivaara BM, Vikman I, Sävenstedt S. Influence of self-care advice on patient satisfaction and healthcare utilization. J Adv Nurs 2016;72:1789-99. https://doi.org/10.1111/jan.12950.
- Dunt D, Wilson R, Day SE, Kelaher M, Gurrin L. Impact of telephone triage on emergency after hours GP Medicare usage: a time-series analysis. Aust New Zealand Health Policy 2007;4. https://doi.org/10.1186/1743-8462-4-21.
- Donovan E, Wilcox CR, Patel S, Hay AD, Little P, Willcox ML. Digital interventions for parents of acutely ill children and their treatment-seeking behaviour: a systematic review. Br J Gen Pract 2020;70:e172-e178. https://doi.org/10.3399/bjgp20X708209.
- Aboueid S, Liu RH, Desta BN, Chaurasia A, Ebrahim S. The use of artificially intelligent self-diagnosing digital platforms by the general public: scoping review. JMIR Med Inform 2019;7. https://doi.org/10.2196/13445.
- Gottliebsen K, Petersson G. Limited evidence of benefits of patient operated intelligent primary care triage tools: findings of a literature review. BMJ Health Care Inform 2020;27. https://doi.org/10.1136/bmjhci-2019-100114.
- Berry AC, Cash BD, Wang B, Mulekar MS, Van Haneghan AB, Yuquimpo K, et al. Online symptom checker diagnostic and triage accuracy for HIV and hepatitis C. Epidemiol Infect 2019;147. https://doi.org/10.1017/S0950268819000268.
- Yu SWY, Ma A, Tsang VHM, Chung LSW, Leung SC, Leung LP. Triage accuracy of online symptom checkers for accident and emergency department patients. Hong Kong J Emerg Med 2019;27:217-22. https://doi.org/10.1177/1024907919842486.
- Hill MG, Sim M, Mills B. The quality of diagnosis and triage advice provided by free online symptom checkers and apps in Australia. Med J Aust 2020;212:514-19. https://doi.org/10.5694/mja2.50600.
- Berry AC, Berry NA, Wang B, Mulekar MS, Melvin A, Battiola RJ, et al. Symptom checkers versus doctors: a prospective, head-to-head comparison for cough. Clin Respir J 2020;14:413-15. https://doi.org/10.1111/crj.13135.
- Judson TJ, Odisho AY, Neinstein AB, Chao J, Williams A, Miller C, et al. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J Am Med Inform Assoc 2020;27:860-6. https://doi.org/10.1093/jamia/ocaa051.
- NHS England . NHS 111 Minimum Data Set 2018–19 n.d. www.england.nhs.uk/statistics/statistical-work-areas/nhs-111-minimum-data-set/statistical-work-areas-nhs-111-minimum-data-set-nhs-111-minimum-data-set-2018-19/ (accessed 17 March 2021).
- Venables WN, Ripley BD. Modern Applied Statistics with S. New York, NY: Springer; 2002.
- Liboschik T, Fokianos K, Fried R. tscount: an R package for analysis of count time series following generalized linear models. J Stat Software 2017;82:1-51. https://doi.org/10.18637/jss.v082.i05.
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342. https://doi.org/10.1136/bmj.d549.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. https://doi.org/10.1016/0197-2456(86)90046-2.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. https://doi.org/10.1002/sim.1186.
- Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019;22:153-60. https://doi.org/10.1136/ebmental-2019-300117.
- Munro J, Nicholl J, O’Cathain A, Knowles E. Impact of NHS direct on demand for immediate care: observational study. BMJ 2000;321:150-3. https://doi.org/10.1136/bmj.321.7254.150.
- Turner J, O’Cathain A, Knowles E, Nicholl J, Tosh J, Sampson F, et al. Evaluation of NHS 111 Pilot Sites. Final Report to the Department of Health 2012.
- Arain M, Campbell MJ, Nicholl JP. Impact of a GP-led walk-in centre on NHS emergency departments. Emerg Med J 2015;32:295-300. https://doi.org/10.1136/emermed-2013-202410.
- O’Cathain A, Knowles E, Turner J, Nicholl J. Acceptability of NHS 111 the telephone service for urgent health care: cross sectional postal survey of users’ views. Fam Pract 2014;31:193-200. https://doi.org/10.1093/fampra/cmt078.
- Office for National Statistics . Census Data 2011 n.d. www.ons.gov.uk/census/2011census/2011censusdata (accessed 19 March 2021).
- Collins K, O’Cathain A. The continuum of patient satisfaction – from satisfied to very satisfied. Soc Sci Med 2003;57:2465-70. https://doi.org/10.1016/S0277-9536(03)00098-4.
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. The Qualitative researcher’s Companion 2002;573:305-29.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Sheard L, Peacock R. Fiddling while Rome burns? Conducting research with healthcare staff when the NHS is in crisis. J Health Organ Manag 2020;34:77-84. https://doi.org/10.1108/JHOM-04-2019-0105.
- NHS England . National Schedule of NHS Costs 2018 19 n.d. www.england.nhs.uk/publication/2018-19-national-cost-collection-data-publication/ (accessed 20 September 2021).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: Personal Social Services Research Unit, University of Kent; 2019.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- Checkland K, Harrison S, Marshall M. Is the metaphor of ‘barriers to change’ useful in understanding implementation? Evidence from general medical practice. J Health Serv Res Policy 2007;12:95-100. https://doi.org/10.1258/135581907780279657.
- O’Cathain A, Sampson FC, Munro JF, Thomas KJ, Nicholl JP. Nurses’ views of using computerized decision support software in NHS Direct. J Adv Nurs 2004;45:280-6. https://doi.org/10.1046/j.1365-2648.2003.02894.x.
- NHS England . Integrated Urgent Care Service Specification 2017. www.england.nhs.uk/wp-content/uploads/2014/06/Integrated-Urgent-Care-Service-Specification.pdf (accessed 19 March 2021).
- Ablard S, Kuczawski M, Sampson FC, Mason S. What does the ideal urgent and emergency care system look like? A qualitative study of service user perspectives. Emerg Med J 2020;37:200-5. https://doi.org/10.1136/emermed-2019-208921.
- NHS Digital . NHS Pathways Coronavirus Data Dashboard n.d. https://digital.nhs.uk/coronavirus/nhs-111-online-coronavirus-services/potential-coronavirus-symptoms-reported-through-nhs-pathways-and-111-online#nhs-pathways-coronavirus-data-dashboard (accessed 19 March 2021).
- Department of Health and Social Care . New Measures to Improve Patient Care Ahead of Winter 2020. www.gov.uk/government/news/new-measures-to-improve-patient-care-ahead-of-winter (accessed 19 March 2021).
- Pope C, Prichard J, Turnbull J, Browne D, Chisambi M, Petter E, et al. Ethnographic study of patient pathways and workforce implications of NHS 111 Online. Health Serv Deliv Res 2021.
Appendix 1 Summary of references included in the telephone triage literature review
| First author, year, country | Study design | Population and setting | Triage and system information | Purpose of study | Main outcomes | Main findings |
|---|---|---|---|---|---|---|
| Lake, 2017, Australia19 | Literature review | Ten SRs from 2003 to 2013 included. TTAS | TTAS | Overview of SRs to determine the scope, consistency and generalisability of findings for governance, safety and quality of TTAS | TTAS performance reported across nine indicators: access, cost, appropriateness, compliance, patient satisfaction, safety, health service utilisation, physician workload and clinical outcomes |
TTAS performance reported across nine key indicators TTAS patient satisfaction was generally high. Some consistent evidence that TTAS can reduce clinical workload TTAS safety measures show that no major difference between TTAS and traditional care |
| Eastwood, 2015, Australia20 | Systematic review: qualitative synthesis |
ES telephone calls to ambulance service triaged as low priority Six articles and one report identified between 1981 and November 2012 |
Telephone secondary triage for low-priority ambulance service ES calls | SR of structure, safety and success of ES secondary telephone triage | Narrative themes |
Main themes: safety and accuracy of secondary telephone low priority triage; low incidence of adverse events; patient satisfaction – patients appeared satisfied with secondary triage ES service ED intervention should be used with caution when assessing triage systems |
| Wheeler, 2015, USA21 | Narrative review | PubMed and CINAHL; 19 papers published between 2002 and 2012 | Telephone triage by clinical and non-clinical (emergency medical dispatchers and clerical) staff | To examine telephone triage safety by clinical and non-clinical decision-makers |
System completeness = presence of a decision-maker, guidelines, documentation, training, standards Safety = appropriate referrals (measured by professional role and referral rates) |
Appropriate referral rates: nurses (91%), physicians (82%) Clerical staff had no system or perform telephone triage by standard definitions Nurses were felt to be the most cost-effective professional who can safely perform the task. Nurse decision-making safety could be enhanced by improving system quality (clinical training, practice and call centre standards) Non-clinicians are not safe decision-makers, even when adhering to expert software Physicians used only one system (documentation) and this was not done consistently |
| Tran, 2017, Australia22 | Observational follow-up study, using data linkage |
Australian telephone triage service callers aged ≥ 45 years to July 2008–December 2011 who had completed questionnaires from the 45 and Up Study; recorded ED/hospital presentations/medical consultation claims 8406 subjects resulting in 11,088 calls |
Telephone triage by nurse using decision support tool | To assess extent disposition compliance in callers aged ≥ 45 years and how sociodemographic, lifestyle and health characteristics and call features affect this |
Call disposition Disposition compliance Caller characteristics: age; sex; time of call; caller–patient relationship; pre-call caller original intent; triage protocol used |
Complied with advice (%): ED 68.6; doctor consult 64.6; self-care 77.5 Self-referral to ED against advice: 7.0% of calls Characteristics: disadvantaged areas; OOH calls; calls made by another person; caller intention was ‘to attend ED’ Reduced ED compliance: rural/remote locations; high/very high psychological distress levels Reduced ‘see doctor’ compliance: rural/remote areas; taking five or more medications Reduced self-care compliance: aged ≥ 65 years Self-referrals to ED: callers concerned with bleeding, cardiac, gastrointestinal, head and facial injury symptoms and given self-care advice |
| Gibson, 2018, Australia23 | Data linkage observational cohort study | 1.04 million calls to Australian telephone triage service between 2009 and 2012 | GP or nurse telephone triage using decision support tool 24 hours/7 days a week | Investigate compliance with disposition for ED and acuity of post-call ED attenders |
Compliance with ED disposition advice; ED presentations within 24 hours of a call Caller characteristics; disposition advice; medical condition |
66.5% callers compliant with ED dispositions; 6.2% low-urgency dispositions self-referred to ED in 24 hours Low rates of over-referral to ED suggested Other factors affecting self-referral to ED after call: living in remote area or having made many previous calls in last 6 months |
| McKenzie, 2016, Australia24 | Descriptive study using routinely collected data | 2783 Australian telephone triage/advice line callers between 2011 and 2012 | OOH nurse triage and telephone advice line or OOH PC helpline | To determine ED attendance and compliance with OOH telephone triage advice | ED attendance post call; disposition compliance |
Overall: small reduction (3.6%) in ED attendance compared with callers’ original intentions Pre-call intention: ED (29.7%); self-care (20.3%); primary care (27%); unsure (19.1%) Post-call actions: ED (30%); self-care (26%); primary care (44%) 22% of callers who intended to go to the ED did not follow GP’s advice |
| Krumperman, 2015, USA25 | Retrospective comparative study using self-reports |
Low-acuity emergency medical services callers Model A: 374 cases; model B: 216 cases Populations varied according to demographics and location (urban/rural) |
Compares two care models for 911 calls: A: paramedics treat, and refer (ETR) on scene; B: nurses telephone triage and refer (TTR) |
Comparison of percentage of patients adhering to disposition advice and patient satisfaction between two models | Adherence to disposition advice; satisfaction with call |
Self-reports suggest that ETR model has lower disposition adherence Satisfaction rates were equivalent for both care models |
| Martinsson, 2018, Sweden26 | Ordinal regression model development | Using validated questionnaire data from a cross-sectional 2014 study of all callers to Swedish telephone triage service (225/500 responders) | Nurse telephone triage with decision support tool. (NHS direct model 24-hour) | Regression model to estimate effects of telephone triage on patient behaviour, health-care utilisation and potential cost savings | Patient behaviour, health-care utilisation effects, potential cost savings |
Bayesian ordinal regression model that predicts 76.4% of patients’ health-care utilisation after using telephone triage service Model suggests that telephone triage reduces health-care utilisation; has potential to save costs Compliance depends on level of care advised; advice agreement with patient’s prior intention; care option availability, influenced by patients’ perceptions of risk (compliance seven times higher if highest level of care is advised) |
| Njeru, 2017, USA27 | Retrospective cohort study | USA PC network between 1 January 2012 and 30 June 2013 and previously consented data use | Computer-aided, nurse-led telephone triage service | Determine characteristics of LEP callers and compare with age-matched English proficient (EP) cohort | Call and caller characteristics; advised and actual actions post call |
LEP and EP cohort 587 patients each; no significant difference between call volumes Call length (minutes): LEP 13.9 vs. EP 12.2 (p = 0.0002) Surrogate caller: LEP 34.6% vs. 6.0% (p < 0.0001) Higher-acuity care recommendations: LEP 49.4% vs. EP 39.0% (p < 0.0004) Disagreement with advice: LEP 30.1% vs. EP 20.9% (p = 0.0004) Less likely to follow advice: LEP 60.9% vs. EP 69.4% (p = 0.0029) |
| Anderson, 2015, UK28 | Observational study | 24-hour NHS 111 call centre, ED dispositions (one region) over 4 months |
24-hour NHS 111 call centre using decision support software GPs placed in 111 call centres to review OOH calls with ED disposition |
What effect does using GPs to review 111 call handlers’ advice to attend ED have on the number of ED referrals? | Percentage of calls where the GP would not advise to attend ED |
73% of 1474 OOH ED referrals reviewed by GPs would have been given an alternative disposition 5.2% to minor injuries unit; 40% to OOH GP clinic; 27.8% self-care Potential cost saving to EDs of £52,528 vs. GP employment costs of £41,416. Impact could be limited as only 6% of A&E attendances are a result of 111 advice |
| Huibers, 2016, Denmark29 | Prospective observational study | Central Denmark region OOH PC telephone triage callers June 2010 to May 2011 | OOH PC telephone triage by GPs |
To describe telephone contacts triaged to face-to-face contacts Contact details from self-reported questionnaire from GP call handler GPs assessing face-to-face dispositions described efficiency and nature of triage decisions |
Relevance of face-to-face triage disposition GP reported caller characteristics, duration of health problem, problem severity and appropriateness of OOH call |
Face-to-face dispositions: 12% could have been telephone consults; 84% were relevant; 4–5% were not relevant to GP OOH service Irrelevant dispositions associated with > 24-hour problems; contacts on weekday nights; contacts < 2 hours before own GP opened Relevant dispositions associated with number of shifts per year of the triage GP; patient age; medical severity Telephone consult dispositions (60% calls) associated factors: younger patients; more short term; fewer potentially severe problems Face-to-face dispositions (40% calls) associated factors: aged > 40 years; persisting problem for 12–24 hours |
| Thilsted, 2018, Denmark30 | Convergent parallel mixed-methods design | Convenience sample of callers aged ≥ 15 years from 3 consecutive days in 2016 to a Danish OOH telephone triage service | Telephone OOH triage for acute, non-emergency medical calls by nurses/physicians | To examine relationship between patients’ illness representations and self-reported DOW |
Qualitative DOW themes Quantitative scale of DOW |
180 calls analysed Low DOW themes: strong illness identity; illness duration of < 24 hours; clear cause and solution High DOW: medium illness identity, illness duration of > 24 hours; high illness consequence |
| Gamst-Jensen, 2017, Denmark31 | Mixed-methods: descriptive statistics and thematic analysis | Adults in Copenhagen, Denmark; 180 OOH capital city telephone triage service callers over 3 days in 2016 | OOH telephone triage by nurse or physician with decision tool | Explored DOW (scale of 1–10) and associated factors and themes | DOW thematic content; DOW for each call; association of DOW and caller variables; effect of DOW on disposition |
94.4% participants rated DOW (median 3) High DOW associated with female sex (95% CI 1.13 to 3.45) Symptom duration of > 24 hours (95% CI 1.13 to 3.45) increases odds ratio of receiving face-to-face disposition Exploring caller’s DOW helps involvement in decision-making and information-sharing |
| Gamst-Jensen, 2018, Denmark32 | Simultaneous mixed methods: exploration of PUTC with descriptive statistics and thematic analysis of subset (n = 31) | 327 non-life-threatening calls PUTC to OOH (medical hotline) capital city OOH telephone triage service in 2014 | Non-emergency nurse or physician OOH telephone (plus decision tool) triage service using a GP OOH service or nurse-led medical helpline | To describe undertriage and identify communication patterns contributing to undertriage | PUTC; distribution of PUTC; themes of PUTC |
327 (0.04%) of all calls PUTC: digestive (24%); circulatory (19%); respiratory (15%); others (42%) PUTC resulted from inadequate communication and non-normative symptom description Systematic collaboration to identify problems and obtain non-normative symptom description suggested |
| Meer, 2012, Switzerland33 | Prospective observational study | 208 adults with non-life-threatening issues attending Swiss hospital ED 8 a.m.–8 p.m. (December 2005–March 2008) | Nurse telephone triage (with GP support if needed) and decision support tool | Investigation of computer-assisted telephone triage decision safety | Evaluation of safety of telephone triage advice | Computer-assisted nurse telephone triage undertaken by competent specialists found to be safe method of potential clinical risk |
| Turnbull, 2017, UK34 | Ethnographic study | Five NHS 111 call centre provider sites from August 2011 to March 2012 | Telephone triage by call handlers using computer decision support tools | Description and explanation of how risk work is configured across NHS 111 | Management of risk themes |
Substantial part of front-line staff’s everyday practice, experience and interaction concerned the management of risk Technologies have redistributed risk (while appearing to reduce or even remove risk) |
| Wahlberg, 2018, Sweden35 | Qualitative content analysis | 24 telephone advice nurses from six Swedish call centres varying in size and location | 24-hour Swedish telephone health care staffed by nurses | To describe telenurses’ views of work environment and impact on care | Themes regarding telehealth nurses’ working environments | Work was cognitively demanding. Caller appreciation and feeling able to provide qualified nursing care made work worthwhile |
| McAteer, 2016, UK36 | Population-based cross-sectional mixed methods | Adults registered with 14 Scottish GP practices between March and September 2013; 3515 questionnaires; response rate 34.1% (1190/3515) ; 30 telephone interviews | NHS 24 (nurse telephone advice and triage service) | Explore public’s beliefs about and use and understanding of service | Self-reported user/non-user characteristics; satisfaction with service and health-care utilisation post service use |
49.5% (n = 589) never used service Reasons for non-use: lack of need (79.4%); prefer face to face (23.5%); unaware of telephone number (15.8%) User characteristics: female, aged 25–34 years, had at least one child; 58.9% users accessed service more than once; 47.4% used it in the last year; 92.4% used it OOH; 54.6% used it on behalf of someone Reason for use: problem occurred OOH, 87.5%; too ill to leave home, 16.5%; unsure who else to contact, 8.9% Presenting symptoms: new, 69.0%; ongoing, 28.5%; general advice required, 2.5% Post-call action: contacted health professional, 38.6% (GP, 58.9%; ED or 999, 23.3%; and local OOH service, 11.4%) > 80% of users were satisfied or very satisfied NHS 24 viewed as an out OOH GP alternative; not appropriate for minor symptoms; deemed valuable for avoiding resource waste Service use encouraged by OOH availability and convenience |
| Kelly, 2010, UK37 | Cross-sectional study using survey data | Users of nine OOH PC telephone services 2007–8, 3 EDs and a Welsh national telephone advice service | OOH PC providers; the GP OOH services provide the option of telephone advice, treatment centre consultation and a home visit | Identify predictors of user satisfaction and enablement across unscheduled care in Wales |
Patient self-reported: service use; professional consulted; service experience; consultation Satisfaction |
26% response rate (855/3250) Treatment centre vs. telephone consultations: treatment centre consultations significantly associated with reduced satisfaction (odds ratio 0.58; p = 0.03) and reduced enablement Statistically significant reduced satisfaction associated with call-answering delays; triage call back; shorter consultations Satisfaction of home visit disposition vs. telephone advice not significantly different (p = 0.48) |
| Rahmqvist, 2011, Sweden38 | Before-and-after study using postal questionnaire data linked to health-care utilisation data | 273 completed postal questionnaires from randomly selected callers to Swedish Health care Direct in October 2008 | Health care Direct telenurses using decision support systems | Investigation of telenursing satisfaction and disposition of callers given less urgent disposition than expected | Caller characteristics; caller satisfaction; caller behaviour; nurse classification of emergency | If caller and the nurse disagree about recommendations, consequence can be dissatisfied caller and more unnecessary health-care visits |
| Gustafsson, 2016, Sweden39 | Cross-sectional study using a postal questionnaire | 500 randomly selected callers to Swedish Healthcare Direct (total of 1500) in March 2014 | 24-hour Swedish Healthcare Direct telephone nursing NHS Direct-type advice service | Explore influence of nurse-led self-care advice on health-care utilisation and patients’ satisfaction (compared with medical care advice) | Self-reported caller satisfaction; intended actions before consultation; disposition advice; actual disposition |
Young callers and those watchful waiting significantly less satisfied with call; reassurance influences satisfaction most Self-care advice reduced health-care utilisation in 66.1% of self-reported cases Self-care disposition rather than GP referral negatively influenced patient satisfaction |
| Dunt, 2007, Australia40 | Time series analysis | After-hours primary medical care trials centres. All primary care OOH service users | Two types of OOH telephone triage: standalone – OOH nurses responded to calls; embedded – GP or nurses providing OOH triage and advice | To determine if telephone triage reduced emergency GP after hours service utilisation | Emergency GP OOH service use (GP first call-out) |
Both systems identified reduced GP emergency OOH use Standalone system identified significant reductions in total monthly OOH utilisation rate in three out of four services Embedded system identified significant reductions in monthly OOH utilisation deputising centre, but no change in local triage centre |
Appendix 2 Summary of references included in the digital symptom checkers literature review
| First author year, country | Study design | Population and setting | Purpose of study | Main outcomes | Main findings |
|---|---|---|---|---|---|
| Donovan, 2020, UK41 | Systematic review | SR to assess digital interventions designed to help parents decide whether to seek treatment or self-care for children with acute illness | Whether or not digital interventions reduced urgent care service use | Three studies included. For self-triage interventions, sensitivity and specificity of one was 84% and 74% compared with nurse triage and sensitivity was 93.3% and specificity 13% for another when compared with need for ED intervention. No intervention reduced need for urgent care services | |
| Aboueid, 2019, Canada42 | Scoping review | General population. Digital platforms using artificial intelligence algorithms for self-diagnosis | To map the scope of digital platforms using artificial intelligence for diagnosis and identify knowledge gaps | Accuracy; regulation; sociological factors; user experience; privacy and security; ethics; design | 19 studies included. Accuracy varied substantially depending on disease and type of platform. Women and more highly educated more likely to choose correct diagnosis from potential options. More likely to be used by those with no access to health care or a stigmatising condition. Regulation lacking |
| Gottliebsen, 2020, Sweden43 | Systematic review | Primary care. Use of digital triage tools by patients accessing primary care | To explore the evidence on features and benefits of patient-operated primary care triage tools | Efficacy; tool type; factors associated with successful implementation; risk factors | 17 studies included. Limited evidence on actual benefits and performance of tools. Available symptom checkers seem to be risk averse and need more real-world testing. Risk of increased or redistribution of workloads. Evaluation guidelines and regulation need development |
| Berry, 2019, USA44 | Retrospective observational | Case records of 168 patients with HIV or hepatitis C attending ED | To test the diagnostic and triage accuracy of five symptom checkers for HIV/hepatitis C | Symptom checker diagnostic accuracy, differential diagnosis and triage advice compared with ED physician diagnosis | All symptom checkers had poor diagnostic accuracy for correct diagnosis listed in top 1, top 3, top 10 or any listing of differential diagnosis (< 20%, < 35%, < 40% and < 45%, respectively) with significant variation between tools. For triage, a significantly higher proportion of hepatitis C found with emergent criteria than HIV (59.7% vs. 35.6%). Symptom checker diagnostic capability inferior to physician diagnosis |
| Yu, 2019, Hong Kong45 | Retrospective observational | 100 random case records for patients attending ED | To test triage accuracy of two online SCs | Sensitivity, sensitivity for emergency cases and specificity of SC compared with ED nurse decision | One SC had overall better sensitivity than the other (74% vs. 50%); sensitivity for emergency conditions was poorer (70% vs. 45%), with low negative predictive value (43% vs. 24%). Current SCs are unsuitable alternatives to ED triage protocols |
| Hill, 2020, Australia46 | Experimental study | 48 medical condition vignettes used in 36 SC tools (1700 diagnosis tests, 688 triage tests) | To determine the quality of diagnostic and triage advice provided by digital SC | Accuracy of diagnosis and triage advice | For 27 diagnostic SCs, correct diagnosis listed first in 36% of tests, in the top three results in 52% and in the top 10 results in 58%. SCs using artificial intelligence algorithms listed the correct diagnosis first in 46% of tests compared with 32% for other types of SC. Rate of first correct result varied from 12% to 61%. 19 triage SCs provided correct advice for 49% of tests. Emergency care (63%; 95% CI 52% to 71%) and urgent care vignette tests provided more appropriate advice (63% and 56%) compared with advice for non-urgent and self care (30% and 40%). Quality of advice provided by SCs is variable; triage advice is risk averse and more likely to recommend higher-level care than needed |
| Berry, 2020, USA47 | Prospective observational | 116 patients attending outpatients clinic with cough | To test diagnostic accuracy of three SC | Diagnostic accuracy of SC alone compared with physician using SC information and three physicians using SC information and clinic notes | For SC only correct diagnosis identified first in list 34.5–16.4% and in top 3 71.6–31%. Mean correct diagnosis first in list 26.4% for SC only, 29.9% for physician using SC information only and 52.6% for physician using SC information and clinic notes. Variation in accuracy between physicians but overall diagnostic accuracy is superior with a combination of SC and physician review |
| Judson, 2020, USA48 | Prospective observational | 950 primary care patients (1159 contacts) in one university health system | To test a rapidly developed online self-triage and scheduling tool for patients with potential COVID-19 | Accuracy of triage; triage time; face-to-face contacts | For symptomatic patients, sensitivity and specificity of detecting need for emergency care was 87.5% and 76.2%, respectively. Sensitivity and specificity of detecting need for self-care was 53.7% and 89.5%, respectively; 61% of asymptomatic patients had no health service contacts within 48 hours. For clinician appointments, time was significantly shorter from start of self-triage to appointment using the online tool than calling a hotline (median 2 minutes vs. 2 hours 15 minutes). Self-triage tools have potential to improve triage efficiency and reduce unnecessary clinic visits |
Appendix 3 Interrupted time series additional information
| Code | CCG |
|---|---|
| North East-111AA1 | NHS Darlington CCG |
| NHS Durham Dales, Easington and Sedgefield CCG | |
| NHS Hartlepool and Stockton-on-Tees CCG | |
| NHS Newcastle Gateshead CCG | |
| NHS North Durham CCG | |
| NHS North Tyneside CCG | |
| NHS Northumberland CCG | |
| NHS South Tees CCG | |
| NHS South Tyneside CCG | |
| NHS Sunderland CCG | |
| Lincolnshire-111AA2 | NHS Lincolnshire East CCG |
| NHS Lincolnshire West CCG | |
| NHS South Lincolnshire CCG | |
| NHS South West Lincolnshire CCG | |
| Nottinghamshire-111AA4 | NHS Mansfield and Ashfield CCG |
| NHS Newark and Sherwood CCG | |
| NHS Nottingham City CCG | |
| NHS Nottingham North and East CCG | |
| NHS Nottingham West CCG | |
| NHS Rushcliffe CCG | |
| Derbyshire-111AA5 | NHS Derby and Derbyshire CCG |
| NHS Erewash CCG | |
| NHS Hardwick CCG | |
| NHS North Derbyshire CCG | |
| NHS Southern Derbyshire CCG | |
| Isle of Wight-111AA6 | NHS Isle of Wight CCG |
| Inner North West London–111AA7 | NHS Central London (Westminster) CCG |
| NHS Hammersmith and Fulham CCG | |
| NHS West London CCG | |
| Hillingdon-111AA9 | NHS Hillingdon CCG |
| Hertfordshire-111AB2 | NHS East and North Hertfordshire CCG |
| NHS Herts Valleys CCG | |
| Cambridgeshire and Peterborough-111AC5 | NHS Cambridgeshire and Peterborough CCG |
| Northamptonshire–111AC6 | NHS Corby CCG |
| NHS Nene CCG | |
| Milton Keynes-111AC7 | NHS Milton Keynes CCG |
| Leicestershire and Rutland-111AC8 | NHS East Leicestershire and Rutland CCG |
| NHS Leicester City CCG | |
| NHS West Leicestershire CCG | |
| Outer North West London–111AD4 | NHS Brent CCG |
| NHS Ealing CCG | |
| NHS Harrow CCG | |
| NHS Hounslow CCG | |
| North Central London–111AD5 | NHS Barnet CCG |
| NHS Camden CCG | |
| NHS Enfield CCG | |
| NHS Haringey CCG | |
| NHS Islington CCG | |
| South East London-111AD7 | NHS Bexley CCG |
| NHS Bromley CCG | |
| NHS Greenwich CCG | |
| NHS Lambeth CCG | |
| NHS Lewisham CCG | |
| NHS Southwark CCG | |
| Bristol, North Somerset & South Gloucestershire-111AE7 | NHS Bristol, North Somerset and South Gloucestershire CCG |
| Cornwall-111AF1 | NHS Kernow CCG |
| Staffordshire-111AF4 | NHS Cannock Chase CCG |
| NHS East Staffordshire CCG | |
| NHS North Staffordshire CCG | |
| NHS South East Staffordshire and Seisdon Peninsula CCG | |
| NHS Stafford and Surrounds CCG | |
| NHS Stoke on Trent CCG |
FIGURE 19.
Model fit: difference plot of four test sites: (a) Hertfordshire; (b) Milton Keynes; (c) North East; and (d) Nottingham.
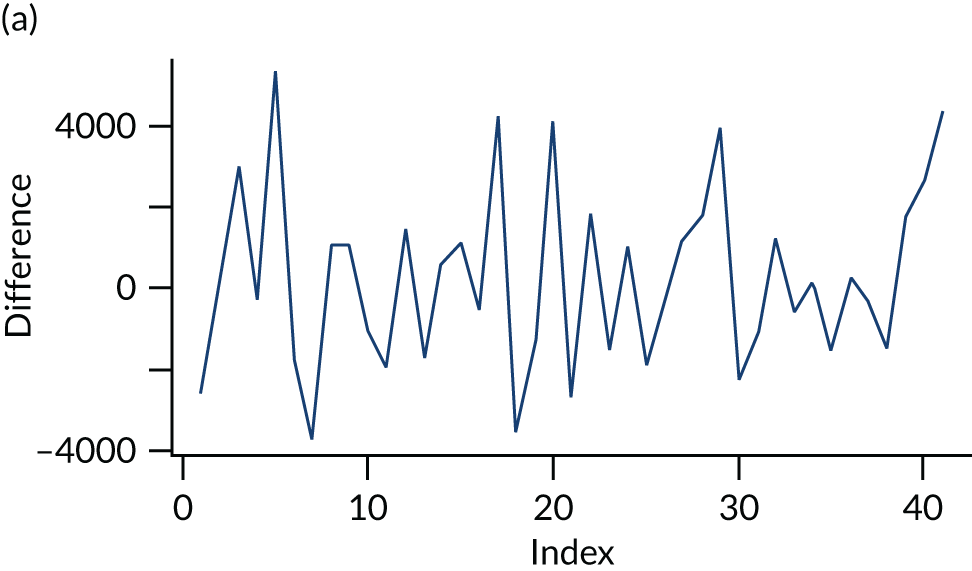
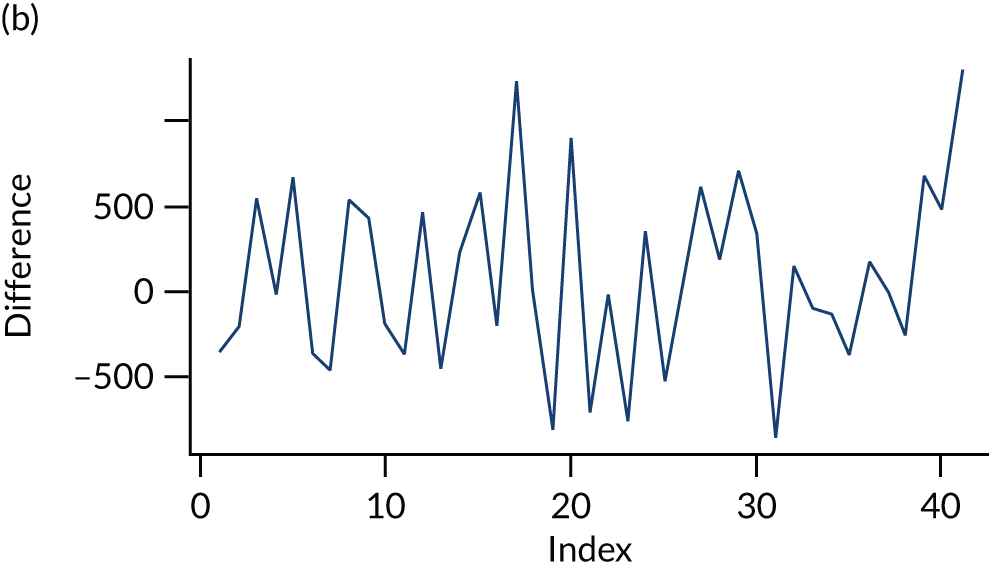
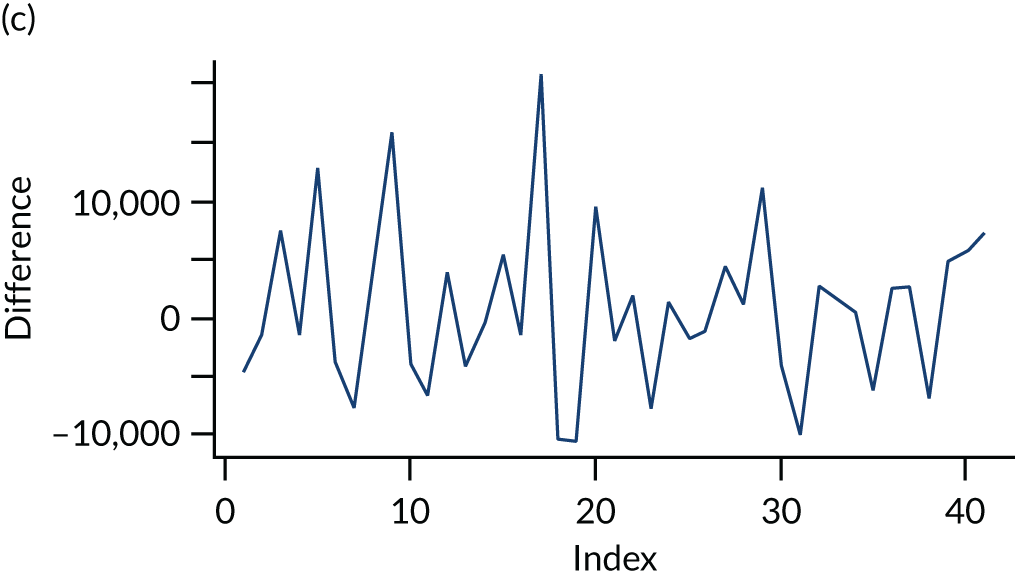
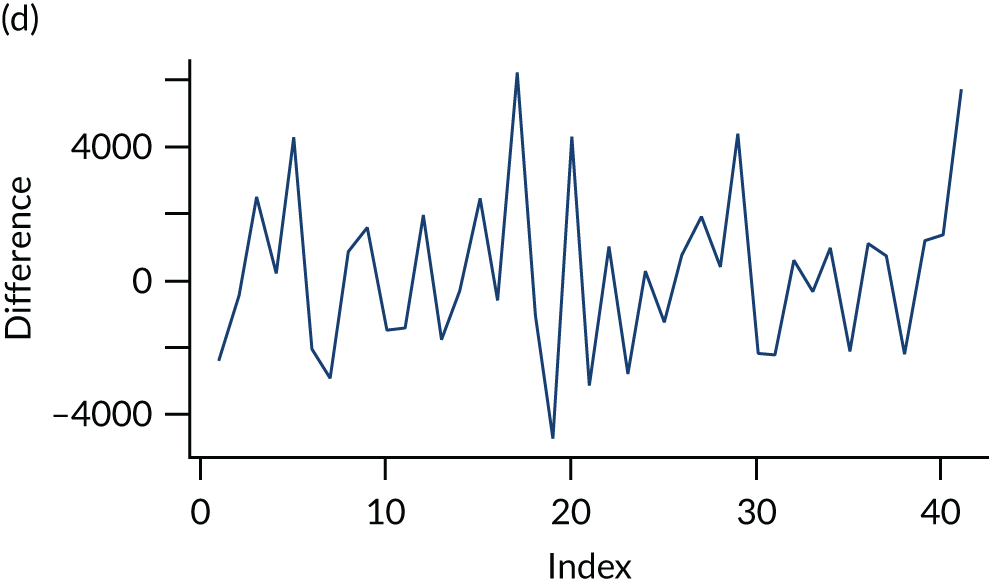
Model fit: autocorrelation function
FIGURE 20.
Autocorrelation function plots of the four test sites: (a) Hertfordshire; (b) Milton Keynes; (c) North East; and (d) Nottingham. ACF, autocorrelation function.
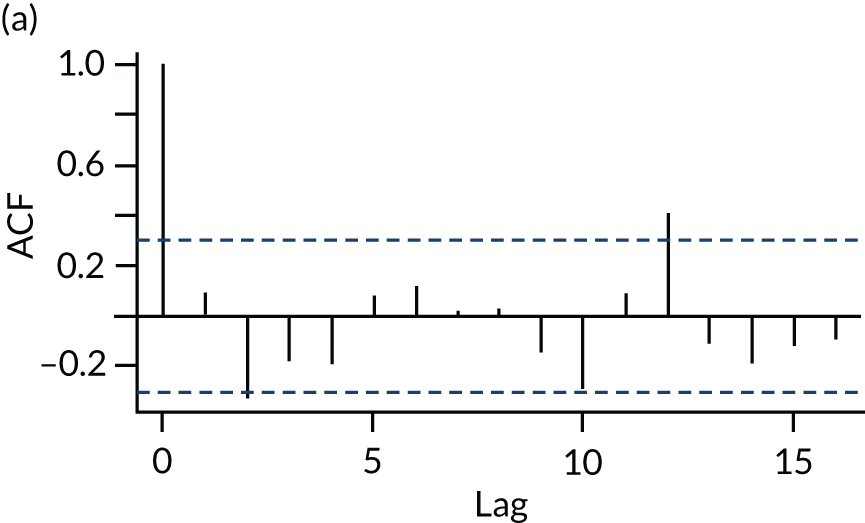
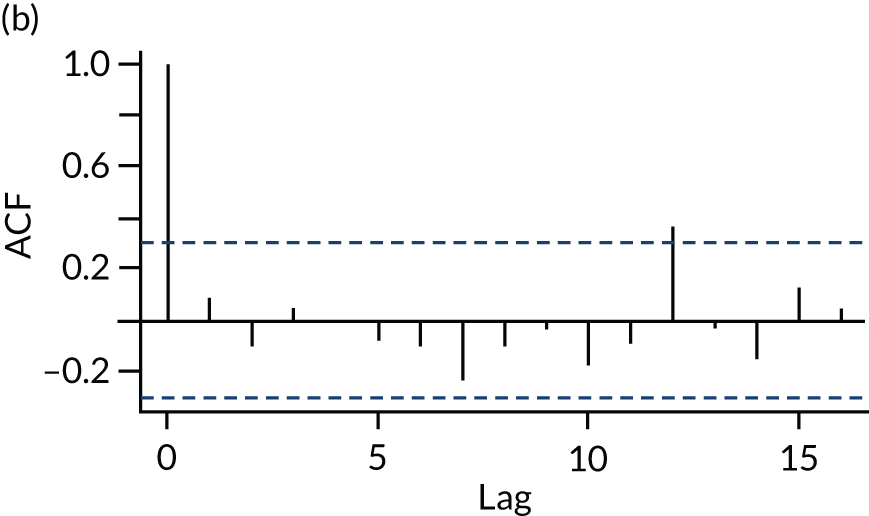
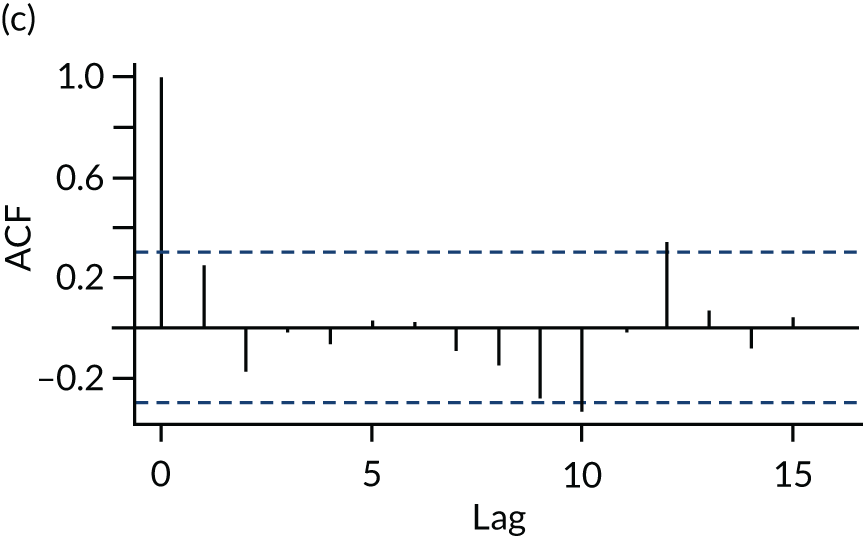
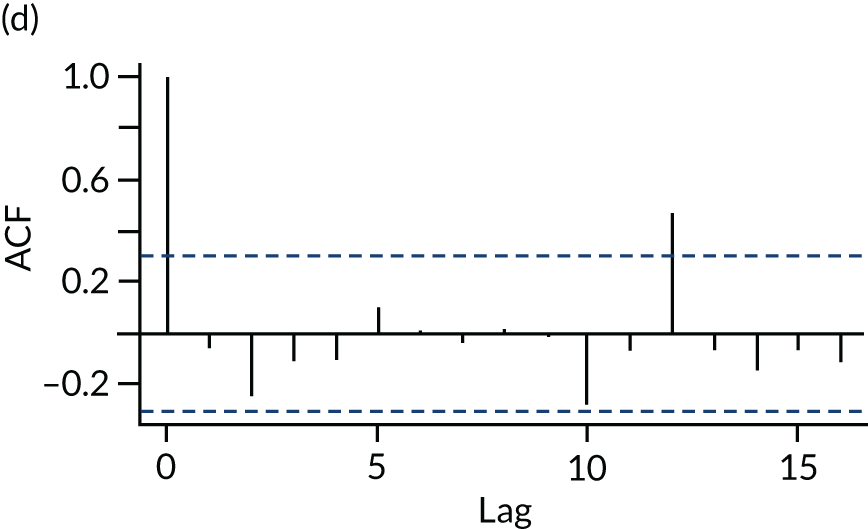
Model fit: partial autocorrelation function
FIGURE 21.
Partial autocorrelation function plots of the four test sites: (a) Hertfordshire; (b) Milton Keynes; (c) North East; and (d) Nottingham. ACF, autocorrelation function.
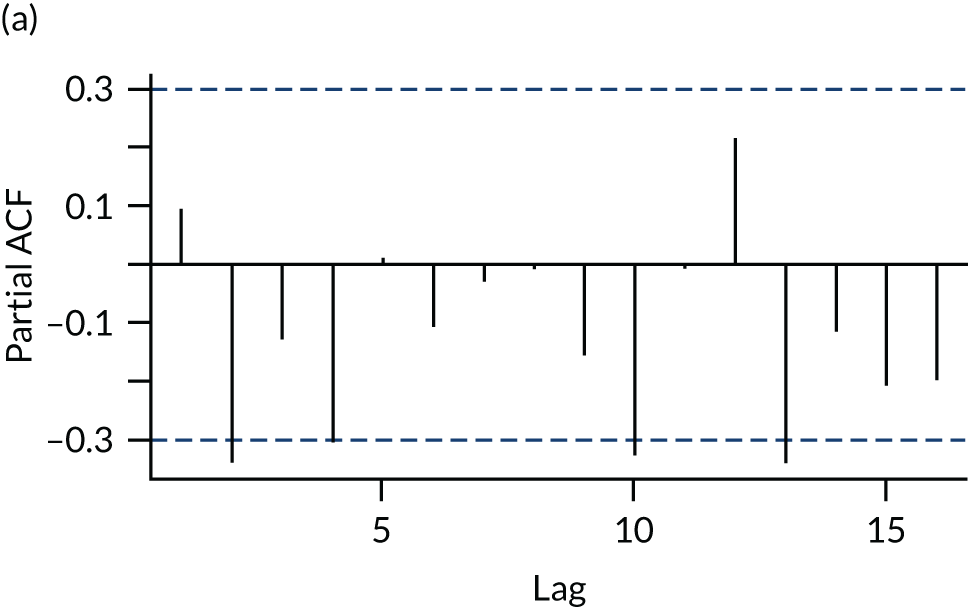
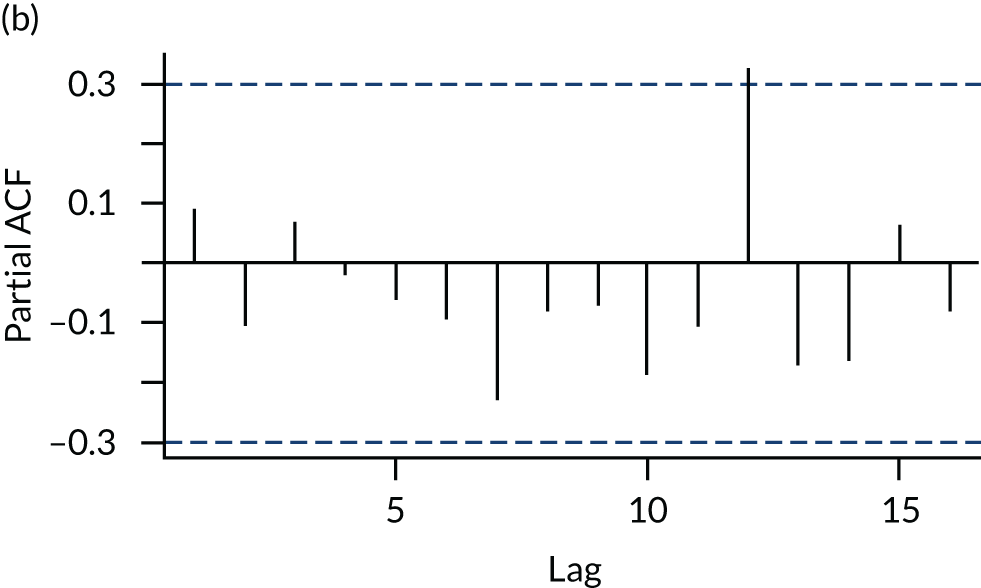
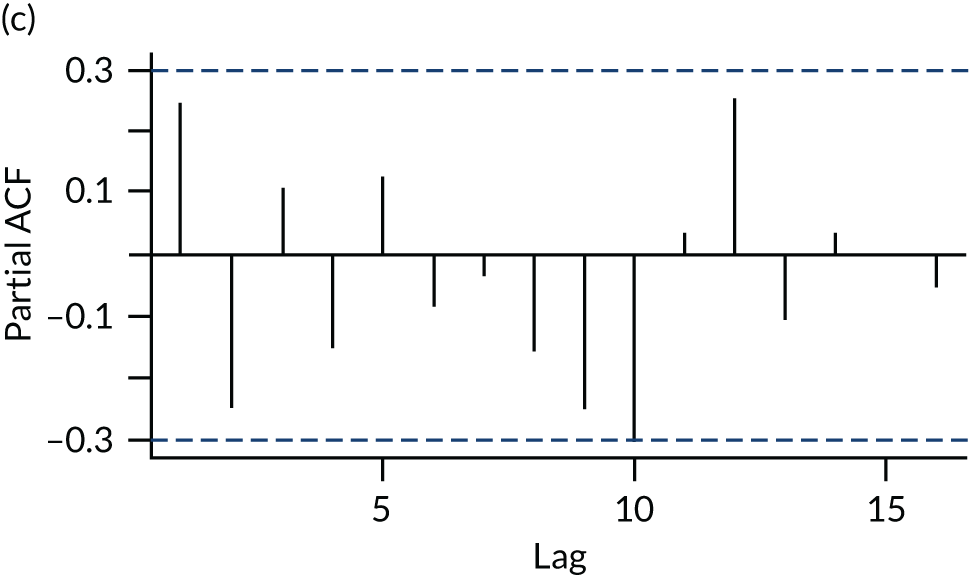
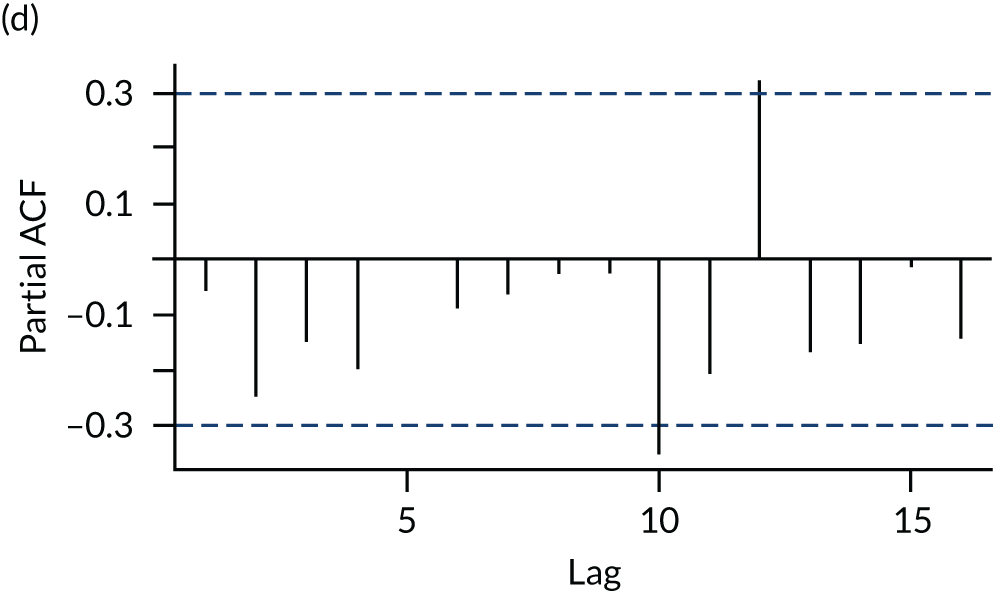
Appendix 4 Integration grid
| Objectives | WP1: rapid evidence review | WP2: routine data (impact on wider system) | WP3: routine data – population characteristics | WP3: user survey | WP3: user interviews | WP4: stakeholder interviews | WP5: economic evaluation | Convergence, divergence or silence |
|---|---|---|---|---|---|---|---|---|
| 1. Update and summarise the evidence on digital and telephone-based services for accessing urgent care building on existing systematic and rapid evidence reviews |
Telephone triage – emerging evidence about the important relationships between caller expectations, intended action, attitudes to risk, agreement with triage decision and subsequent satisfaction and utilisation of services Symptom checkers – evidence on patient safety, diagnostic accuracy and algorithm-based triage is weak |
NA | NA | NA | NA | NA | NA | NA |
| 2. Measure the impact of the NHS 111 Online system on contacts with the NHS 111 telephone service | NA |
There is variation in the impact of introducing the NHS 111 Online service on the NHS 111 telephone service between different NHS 111 areas The overall estimates of combining results from the different NHS 111 areas suggest that NHS 111 Online has little impact on the number of triaged and total calls to the NHS 111 telephone service but results in a decrease in the number of clinical calls |
NA | NA | NA |
NHS 111 staff did not perceive a significant impact on demand for NHS 111 telephony from the NHS 111 Online service at the time of the interviews, partly because of the low uptake of online NHS 111 at the time, but also because of rising demand for NHS 111 Some concern that online users may be referred to clinical advisers inappropriately as a result of risk-averse algorithms Clinical adviser spent longer on online referrals than telephone referrals because of the need to clarify information from the online assessment |
NA | Some convergence, but possibly too early in the delivery of NHS 111 Online to say with any conviction |
| Estimate the effects on other services in the emergency and urgent care system and NHS 111 services in the future | Some evidence for reducing OOH primary care | There was an overall increase in all dispositions (ambulance, recommend to attend ED, recommend to contact primary care, recommend to contact community care and recommend to contact another service) as a result of introducing the NHS 111 Online service | Higher proportion of contacts recommended no service for online than for telephone |
NHS 111 Online users were less likely than users of the telephone service to report that they would have used 999 ambulance/ED if NHS 111 Online had not been available NHS 111 Online users were more likely than users of the telephone service to report that they would not have contacted another service had NHS 111 Online not been available NHS 111 Online users were less likely to report complying with the advice given than users of the telephone service: 33% of NHS 111 Online users did not comply with advice – possible implications for subsequent service use NHS 111 Online users were less likely to report contact with 999/ED in the 7 days after the event than telephone users NHS 111 Online users were more likely to report making no contact with a service in the 7 days after the event than users of the telephone service |
NA Mixed views on compliance with advice. 18 of 32 participants reported not complying with some aspect of advice, although it is unclear if this was in respect to a suggested contact with another health service Participants not complying with advice to contact the 999 ambulance service felt that their condition was not serious enough to warrant a call to the ambulance service |
NA Staff felt that wider services would not be able to distinguish between referrals from NHS 111 Online and those from NHS 111 telephone calls |
The results of user surveys were used to assess the costs of the different 111 services on the emergency and urgent care system |
Divergence Not comparing same populations as people do not use online and telephone services for similar problems Possible higher proportion of people use online to check out minor problems Online disposition proportions similar to telephone but fewer people use services, suggesting lower acuity |
| 3. Explore and compare in detail the characteristics of users of the NHS 111 Online service and the NHS 111 telephone service | NA | NA |
More users of both calls and online are female; however, for online this percentage is higher The biggest difference was for age. People calling tend to be older and among those using the online service those in the age group 16–35 years use it the most 95% of contacts with the online service completed triage. Peak use in the morning, late afternoon and weekends |
NA | Some participants described NHS 111 Online as a valuable resource for those who were not comfortable using the telephone or had time pressures (i.e. looking after children). Participants described using NHS 111 Online for low-acuity conditions, or when access to other services was limited | Staff felt that NHS 111 Online was of particular value to younger people, people with time pressures and those who use online services in other areas of their lives. People used NHS 111 Online particularly for lower-acuity conditions, for dental health and to make contact for mental health problems | NA |
Convergence NHS 111 Online users tended to be (or were perceived to be) younger people, presenting with lower-acuity problems, or using NHS 111 Online when access to other services was limited |
| Explore and compare the service processes of the NHS 111 Online service and the NHS 111 telephone service | NA | NA | NA | NHS 111 Online users were less likely to report that the questions about their symptoms were relevant than users of the telephone service |
Most participants reported at least one positive aspect of using NHS 111 Online Positive views about the process of using NHS 111 Online: ‘straightforward’, ‘easy to access’ and ‘quick to use’ This compared favourably with the NHS 111 telephone service, for which lengthy waits were described Mixed views with respect to comprehension, and relevance of questions |
Staff reported that NHS 111 Online users subsequently called NHS 111 to clarify information received online. The importance of the health advisers in helping users assess the correct pathway was seen as a barrier to NHS 111 Online | NA |
Convergence There appeared to be issues with the questions, or the ability to understand the questions, posed by NHS 111 Online |
| Explore and compare patient care pathways of the NHS 111 Online service and the NHS 111 telephone service | Evidence shows that people are more likely to comply with advice for higher-level care and self care than for primary care. Compliance and satisfaction were associated with original intention of service choice | NA | NA |
NHS 111 Online users were less likely to report contact with 999/ED in the 7 days after the event than telephone users NHS 111 Online users were more likely to report making no contact with a service in the 7 days after the event than users of the telephone service |
NA | NA | NA |
Silence Insufficient patient-level data available to explore pathways and populations |
| Explore and compare user experience and satisfaction of the NHS 111 Online service and the NHS 111 telephone service | NA | NA | NA |
NHS 111 Online users were less likely than users of the telephone service to describe the advice received as helpful NHS 111 Online users were less likely than users of the telephone service to describe being satisfied with the service or to recommend it to family and friends |
Mixed views regarding satisfaction with advice Two-thirds of participants reported that NHS 111 Online provided reassurance and appropriate advice, but one-third felt that the advice was too generalised and did not provide specific information about how to deal with the situation Most participants indicated that they would use NHS 111 Online again. There was evidence that the telephone service would be used in favour of NHS 111 Online in some situations, such as for urgent problems, specific conditions (asthma, rashes) or problems relating to children |
NA | NA |
Possibly some convergence The survey indicated that users of NHS 111 Online appeared less satisfied than users of the telephone service and some interview participants identified aspects of the service with which they were dissatisfied |
| 4. Assess the practical issues associated with implementation of the new service, the workforce implications of any changes to the overall NHS 111 telephone service and specifically the impact on clinical assessment teams | Emerging evidence about the impact of risk management by workforce and demand stress on safety of decisions | NA | NA | NA | NA | Staff reported limited impact on their workload or workforce. None of the sites we spoke to had changed workforce as a result of the introduction of NHS 111 Online. Staff had limited awareness of the online service and how it had been implemented | NA | Silence |
| 5. Estimate the cost–consequences of implementing an NHS 111 Online service on the overall costs of the combined online and telephone 111 services and model the potential cost effects for the emergency and urgent care system | NA | NA | NA | The user survey provided the service use data for the economic evaluation | NA | NA |
The cost per person of the online service was £68 lower than that for telephone service If run in parallel, if ≥ 38% of online service contacts result in a corresponding reduction in telephone service calls, then the parallel service is cheaper than the telephone-only service |
Some convergence Costs for online service lower than telephone, mainly because online users utilise fewer services |
| Channel shift | No evidence of significant substitution of telephone service for online service | One-third of NHS 111 Online users did not want to use the telephone service and one-quarter did not think about telephoning 111. Some evidence that NHS 111 Online users were also making use of the telephone service during the same episode | 19 of 32 participants expressed a preference for using NHS 111 Online ahead of the NHS 111 telephone service | Staff had limited knowledge of online and telephone NHS 111 use. They did not perceive there to be any evidence of channel shift. NHS 111 Online was seen as a useful adjunct but not a replacement for the telephony service. People use the services for different purposes, and may use online NHS 111 prior to calling | N/A |
Convergence Evidence suggests that more potential new demand than service substitution, with some duplication |
Glossary
- Clinical Commissioning Group
- An organisation that has responsibility for identifying what health services are needed for a local community and agreeing (commissioning) which local organisations (hospitals, ambulance services, community services) will provide these services.
- Directory of Services
- A list of all urgent care services available in a local area, including when they are open. NHS 111 uses this directory to direct people to the right service for their problem.
- Emergency and urgent care system
- The collective term for all the different services in a geographical area that people can use to access care for an emergency or urgent health problem. It includes the 999 ambulance service, NHS 111, emergency departments (accident and emergency), minor injury units, urgent care centres, walk-in centres and general practitioner services (daytime and out of hours).
- Integrated urgent care
- Developing services that bring together the clinical assessment functions of NHS 111 with other services so that appointments or referrals can be made directly with, for example, urgent care centres, general practitioner out-of-hours services, emergency dental services and pharmacists.
- NHS 111
- A free-to-use telephone service that the public can use to get help for urgent health problems. Callers are asked a series of questions by a call advisor and directed to an appropriate service (e.g. ambulance, emergency department, general practitioner) or passed to a nurse for further assessment and advice on what to do.
- NHS 111 Online
- A web-based version of the NHS 111 telephone service. People can access the service via a website or a smartphone application (app) and answer a series of questions about their health problem. At the end of the assessment, a user is provided with information on what to do next – to attend or make an appointment with a specific service, to request a call back from an NHS 111 nurse or, where available, to receive a call back from an out-of-hours general practitioner or other service.
- NHS Digital
- The part of the NHS that has responsibility for the development and management of digital technology across the NHS. It also collects and keeps secure patient information and other information on the use of services.
- NHS Pathways
- The triage or assessment system used by NHS 111 to identify what the health problem is, how urgent it is and what service is needed.
- Telephony
- The telecommunications-based infrastructure that supports communication between NHS 111 and callers and the associated transfer of information.
List of abbreviations
- app
- smartphone application
- AR
- autoregressive
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- DARS
- Data Access Request Service
- DEUCE
- Drivers of Demand for Emergency and Urgent Care
- DX code
- disposition code
- DoS
- Directory of Services
- ED
- emergency department
- GP
- general practitioner
- LOESS
- locally estimated scatterplot smoothing
- LTC
- long-term condition
- MDS
- minimum data set
- NIHR
- National Institute for Health Research
- ScHARR
- School of Health and Related Research
- SECF
- Sheffield Emergency Care Forum
- STP
- Sustainability and Transformation Partnership
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09210).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
