Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/161/05. The contractual start date was in May 2017. The draft report began editorial review in December 2019 and was accepted for publication in August 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© 2021 Gould et al. This work was produced by Gould et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Gould et al.
Chapter 1 Introduction
Background
What is generalised anxiety disorder?
Generalised anxiety disorder (GAD) is the most common anxiety disorder among older people, with estimated prevalence rates ranging from 1.2% to 11.2%. 1,2 The main symptoms that characterise GAD are excessive anxiety and worry, which the person experiences as difficult to control, as well as feelings of fear, dread and uneasiness that have occurred on more days than not for at least 6 months. Other symptoms include restlessness or feeling ‘on edge’, tiredness, irritability, muscle tension, difficulties with concentrating, difficulties with sleeping, shortness of breath, fast heartbeat, sweating and dizziness. 3 It is a condition that may persist for decades, with a mean symptom duration of 20–30 years, in older people across community, medical and mental health samples in multiple countries. 4,5
Generalised anxiety disorder in older people is associated with poorer health-related quality of life, increased disability, greater health-care utilisation, increased medication intake and functional limitations in comparison with non-anxious older people. 6–8 Comorbidity with other anxiety, mood and personality disorders is common and is associated with poorer outcomes. 6,9–12 For example, comorbid anxiety and depression is associated with more severe somatic symptoms, poorer social functioning, greater suicidal ideation and a higher likelihood of prescription of benzodiazepines, as well as poorer treatment response. 13,14 Several factors are associated with treatment-resistant anxiety, including comorbid physical and mental health conditions, noncompliance and environmental stressors. 13
How is generalised anxiety disorder currently managed in the NHS?
National Institute for Health and Care Excellence (NICE) guidelines currently recommend a stepped care approach to the management of GAD. 15 Step 1 comprises identification and assessment, followed by education and active monitoring within primary care. If symptoms have not improved, then in step 2 one or more low-intensity psychological interventions, such as guided self-help based on cognitive behavioural therapy (CBT) and psychoeducational groups, are offered, again within primary care. Should symptoms persist, or if there is marked functional impairment, then pharmacotherapy [(e.g. selective serotonin reuptake inhibitors) and/or high-intensity, individual psychotherapy (either CBT or applied relaxation)] are offered (step 3). Following this, if symptoms still persist, a referral to specialist mental health services (usually located within secondary care) for assessment and treatment is recommended as step 4. Suggested treatment options in step 4 include offering interventions from steps 1–3 that have been previously declined and offering combination therapy (e.g. pharmacological plus psychological therapy).
What is the evidence for the management of generalised anxiety disorder in older people?
With respect to psychological interventions, the majority of studies have examined the efficacy of CBT for GAD in older people. 8,16–26 Only a few have examined other psychological interventions such as acceptance and commitment therapy (ACT) and mindfulness-based stress reduction. 27,28 Pooled odds ratios in favour of these interventions when compared with waiting list or usual care controls have been reported, but not when compared with active controls or other forms of psychotherapy. 29
Furthermore, there is evidence of smaller treatment effect sizes among older people than among working age adults, as well as higher drop-out rates. 30–32 For example, a recent meta-analysis of CBT for GAD reported an overall effect size that was nearly double that achieved in younger people than in older people {g = 0.94 [95% confidence interval (CI) 0.52 to 1.36] in working-age adults vs. g = 0.55 (95% CI 0.22 to 0.88) in older people}. 33 As the authors of this meta-analysis noted, there is clearly room for improvement in the provision of effective psychological interventions for GAD in older people.
‘Treatment-resistant’ older people, that is, older people who fail to respond adequately to first-line pharmacological and psychological interventions, are by definition less likely to respond to treatment. Although there is no agreed definition of treatment-resistant generalised anxiety disorder (TR-GAD),34 when a person with GAD fails to respond to treatment after completing the first three steps of the stepped care approach,15 GAD can be considered to be resistant to treatment. A previous systematic review35 was unable to identify any randomised controlled trial (RCT) or prospective comparative study of either pharmacological or psychological interventions for treatment-resistant anxiety in older people. Given that the older adult population is projected to increase rapidly in the next 40 years,36 and hence more people will present with TR-GAD to older adult services, identifying effective interventions for this population is clearly a priority.
One possible intervention for managing TR-GAD in older people is CBT. However, as noted above, evidence of lower efficacy of CBT for GAD in older people than in working-age adults suggests that an alternative form of psychological intervention may be required. ACT could be a particularly promising candidate for this age group, given that older people with chronic pain respond better to ACT than to CBT, whereas younger people respond better to CBT than to ACT. 37 Consequently, the present study sought to investigate whether or not ACT is an acceptable and feasible approach for potentially managing TR-GAD in older people.
What is acceptance and commitment therapy?
Acceptance and commitment therapy is an acceptance-based behaviour therapy38 with a strong evidence base for improving outcomes (such as functioning, quality of life and mood) in chronic pain39 and a growing evidence base in chronic disease40 and mental health contexts. 41 It aims to (1) teach people new skills for managing thoughts, feelings and sensations; (2) help them to clarify what they value and what is important and meaningful to them in their lives; and (3) identify ways in which they can best live their lives in accordance with these values alongside the thoughts, feelings and sensations they may be experiencing. It achieves this through a variety of ‘core’ acceptance, mindfulness, commitment and behaviour change processes (as shown in Table 1), with the ultimate aim of increasing ‘psychological flexibility’. Psychological flexibility is defined as ‘the ability to contact the present moment more fully as a conscious human being and to either change behaviour or persist, when doing so serves valued ends’. 42 Research has supported the applicability of these core ACT processes in a variety of clinical populations, including in older people. 43
| PIP | Description | PFP | Description |
|---|---|---|---|
| Experiential avoidance | Trying to avoid, get rid of or change the frequency or form of internal experiences (e.g. thoughts, emotions, sensations) | Acceptance | Reducing avoidance of or opening up to internal experiences (when this might be a barrier to life-enriching activity) so that one can do what matters to oneself |
| Cognitive fusion | Getting hooked by or fused with thoughts, images or memories, or acting as if they are literally true | Defusion | Reducing the degree to which one is caught up in thoughts, images or memories by stepping back from them and seeing thoughts as just thoughts |
| Dominance of past and future | Being stuck in one’s head, ruminating about the past or worrying about the future | Contact with the present moment | Reducing the amount of time one is stuck in one’s head by increasing awareness of the present moment |
| Self-as-content | Being attached to the stories that one tells about oneself, or seeing oneself as the content of one’s internal experiences | Self-as-context | Seeing oneself as distinct from the content of one’s internal experiences (e.g. thoughts, emotions, sensations) |
| Lack of clarity or loss of contact with values | Losing connection with or not knowing what really matters to oneself | Values | Knowing what really matters to oneself in one’s life (i.e. what is important and meaningful) |
| Inaction, impulsivity or avoidant persistence | Failing to act in accordance with what really matters to oneself through avoidance or inaction | Committed action | Committing to doing what really matters (i.e. engaging in personally meaningful activities that support what one values) |
Acceptance and commitment therapy can be seen as a novel alternative to traditional forms of psychotherapy such as conventional CBT. The focus of conventional CBT is on alleviating distress or symptoms by changing how one thinks and behaves in emotional situations (e.g. by challenging the validity of negative thoughts or solving problems). The phrase ‘catch it, check it, change it’, in relation to negative thoughts, captures the essence of conventional CBT. By contrast, ACT is focused on increasing personally meaningful behaviour in the presence of distress and symptoms (although distress or symptoms may improve as a by-product of therapy). The phrase ‘Accept your experiences and be present, Choose a meaningful direction for your life, and Take action’ sums up ACT. 44
What is the rationale for acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder?
There are several reasons why ACT may be a beneficial intervention for older people with TR-GAD. First, a preliminary RCT of ACT versus CBT for GAD in older people reported improvements in worry/anxiety and depression with both interventions and higher treatment completion rates with ACT than with CBT. 27 Although these results are promising, this study was limited by its small sample size (n = 7 in the ACT condition and n = 9 in the CBT condition) and limited applicability to older people with TR-GAD in the UK (as the study did not exclusively recruit those with TR-GAD and was conducted in the USA).
Second, the approach taken to managing unwanted thoughts, emotions and sensations in ACT may be a better fit for older people with TR-GAD than the approach taken in conventional CBT. ACT aims to reduce attempts to control, eliminate or avoid unwanted thoughts, emotions and sensations and to improve function through increased engagement in valued, meaningful activities. Conventional CBT, on the other hand, aims to change or suppress emotional experiences, for example by challenging the validity of unwanted thoughts or trying to eliminate or solve problems. Such approaches may not work well with older people with TR-GAD given that multiple, comorbid chronic physical and mental health conditions and multiple losses (e.g. to one’s health, family, social network, role/identity and financial status) are common in this population. This is because issues such as these may not be amenable to being solved or eliminated, and thoughts about them may be entirely valid. Furthermore, challenging the validity of worries about future losses may be perceived negatively by older people with TR-GAD because, although excessive and unhelpful, they may have an obvious basis in reality.
Third, there is evidence that control-orientated strategies, such as trying to eliminate problems that cannot be solved, are actually detrimental to older people’s well-being. 45 This may partly explain two related findings: first, why smaller effect sizes in favour of CBT for GAD, as well as higher drop-out rates, have been reported among older people than among younger people;30,32,33 and, second, why older people with chronic pain were more likely to clinically respond to ACT than CBT, whereas younger people were more likely to respond to CBT than ACT. 37 ACT, with its focus on increasing adaptive functioning and how best to live with such difficulties and worries (as opposed to challenging, changing or trying to eliminate them), may be more appropriate in this population. Supporting this, ACT has been shown to better fit the needs of people with disabling long-term conditions46 and may be particularly helpful when distress is associated with realistic or valid thoughts. 47
Finally, ACT has been found to be as effective as CBT and applied relaxation in the treatment of GAD in working-age adults. 48–51 Furthermore, greater recovery rates and lower drop-out rates have been reported with ACT than with CBT in the management of treatment-resistant mental health problems in working-age adults. 52 Whether or not ACT is similarly effective in older people with TR-GAD is clearly worthy of further investigation.
What is the evidence for acceptance and commitment therapy in older people with treatment-resistant generalised anxiety disorder?
Although ACT has been applied to a wide range of mental and physical health conditions including anxiety, depression and chronic pain,53,54 very few studies of ACT have been conducted with older people. The majority of studies have examined ACT for chronic pain,55–58 with only a few other studies focusing on GAD,27 veterans aged ≥ 65 years with depression59 and those living in long-term care facilities. 60 Beneficial effects on symptoms of depression, anxiety and functional measures have been reported in these studies, along with high rates of attendance. For example, 100% session attendance was reported in 7 out of 7 (100%) older people with GAD27 and in 59 out of 76 (78%) older people with depression. 59 However, to our knowledge, no studies to date have examined ACT specifically for older people with TR-GAD.
Research question
At present, there is a lack of evidence to guide the management of TR-GAD in older people and indeed in working-age people. There are several compelling justifications for an alternative form of psychological intervention that sufficiently meets the needs of older people with TR-GAD. ACT shows great promise as this alternative form, but has not yet been applied to this target population. Consequently, we examined the feasibility of this approach in the current study. Specifically, we aimed to address the following research question: how feasible is a study to examine the clinical effectiveness and cost-effectiveness of ACT for TR-GAD in older people?
Aims and objectives
Aims
The aim of the current study was to develop an intervention based on ACT specifically for older people with TR-GAD, and to examine the feasibility and acceptability of its delivery in the NHS.
Objectives
The objectives of the current study were to:
-
develop and refine a manualised intervention in accordance with Medical Research Council (MRC) guidelines for developing and evaluating complex interventions61 and using qualitative methodological approaches
-
use qualitative interviews to explore the intervention’s acceptability and feasibility to older people with TR-GAD
-
use a nationwide survey to clarify usual care for older people with TR-GAD (information that could be used for a future substantive trial)
-
obtain quantitative and qualitative estimates of the acceptability and feasibility of the intervention and study methods in an open, uncontrolled, feasibility study
-
clarify key study design parameters for a future substantive trial of clinical effectiveness and cost-effectiveness (e.g. the choice of comparator and outcome measures, and the number of recruitment sites based on referral/recruitment/attrition rates in the uncontrolled feasibility study).
Chapter 2 Intervention development
Parts of this chapter have been reproduced from Lawrence et al. 62 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
As noted in Chapter 1, guidance on managing TR-GAD in older people (and indeed in working-age people) is lacking. Developing treatment strategies that are acceptable and effective for older people with TR-GAD is therefore a high public and mental health priority, particularly in the context of population ageing. 7,35 ACT may be particularly suitable for older people with TR-GAD, who often experience comorbid chronic physical and mental health conditions and multiple losses, and for whom conventional ‘change strategies’ (e.g. changing the content of thoughts or trying to solve problems) might not be as effective.
In a small preliminary study, ACT was reported to be feasible for use with older people with GAD, as well as being effective at reducing worry. 27 However, the effects observed were substantially smaller than those reported in younger people with GAD. The authors concluded that ACT requires adaptation to ensure its relevance and acceptability to older people.
Consequently, the first phase of the current study used qualitative methods to optimise the relevance, acceptability and feasibility of ACT for older people with TR-GAD, in accordance with MRC guidelines. 61 This has been reported in Lawrence et al. 62 The objectives were to use:
-
qualitative methodological approaches to develop and refine a manualised intervention in accordance with MRC guidelines for developing and evaluating complex interventions
-
qualitative interviews to explore the intervention’s acceptability and feasibility to older people with TR-GAD.
Methods
Design
A person-centred approach was used to ground the development of the intervention in the perspectives and lives of the older people for whom it was intended. 63 Systematic, qualitative methods were used alongside patient and public involvement (PPI) to build on an ACT protocol previously piloted with a small number of older people with GAD (n = 7), but not specifically those with TR-GAD. 27 Stage 1 (intervention planning) investigated intervention preferences and priorities, relevant experiences, and barriers to and facilitators of engaging with talking therapy. Stage 2 (intervention design and development) involved formulating design objectives, and intervention features relevant to each objective, for the ACT intervention. Table 2 shows a summary of the person-based activities involved in each stage of intervention development.
| Stage of intervention development and evaluation | Person-based intervention development activities | Objective of person-based intervention development activities |
|---|---|---|
| Stage 1: intervention planning |
|
Qualitative interviews to elicit views on intervention preferences and priorities (including relevant previous experience and barriers to and facilitators of engaging with talking therapy in general) |
| Stage 2: intervention design, development and optimisation |
|
Consultation to agree guiding principles, comprising:
|
Participants
Older people with TR-GAD were eligible to participate in the study if they met the following eligibility criteria.
Inclusion criteria
-
Aged ≥ 65 years with a primary diagnosis of GAD as determined by the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), Axis I Disorders64 and Structured Clinical Interview for DSM-IV Axis II Disorders. 65
-
Failed to respond to treatment in steps 1–3 of the stepped care approach for GAD.
-
Living in the community.
-
Able to provide informed, written consent.
-
Sufficient understanding of English to enable engagement in the study.
Exclusion criteria
-
Diagnosis of dementia.
-
A Standardised Mini-Mental State Examination (SMMSE)66 total score of < 25 points.
-
Other medical or psychosocial factors that could compromise full study participation, such as imminently life-limiting illness or severe sensory deficits (e.g. blindness).
Recruitment procedures
Stage 1: intervention planning
We recruited older people with TR-GAD via primary care services [i.e. general practice surgeries and Improving Access to Psychological Therapies (IAPT) services], secondary care services [i.e. Community Mental Health Teams (CMHTs)] and self-referrals following the distribution of study posters and leaflets to local day centres and activity groups for older people. Recruitment was purposive to include older people with different living situations and lengths and severities of illness, of different sexes, across a range of age groups and from both inner-city (London) and rural (Oxfordshire) settings in order to provide access to a range of perspectives. Clinicians from primary and secondary care services identified and approached potentially eligible participants and sought verbal consent for researchers to contact them. A researcher (KK) contacted prospective participants to discuss the patient information sheet, answer questions about the study and schedule a written consent and screening appointment.
We recruited health-care professionals in primary and secondary care, including general practitioners (GPs), psychologists, psychiatrists, community psychiatric nurses and occupational therapists, via online forums and secondary care services for older people. This was to ensure that a range of experiences of working with older people with GAD who do not seem to respond adequately to treatment was obtained. We invited interested participants who had contacted the research team to participate in a 30- to 40-minute telephone interview. In addition, we approached academic clinicians from the Mental Health of Older People research group at University College London and invited them to participate in a 1-hour focus group.
Stage 2: intervention design and development
We invited the same older people with TR-GAD who completed interviews in stage 1 to participate in semistructured face-to-face interviews in stage 2. In addition, we invited older people with lived experience of TR-GAD who were part of the study’s Service User Advisory Group, and academic clinicians who were involved in the study as co-applicants/collaborators, to participate in discussions about the intervention. Finally, the academic clinicians and therapists who would be involved in delivering the intervention provided further feedback on the developed intervention.
Procedure
Stage 1: intervention planning
We conducted semistructured face-to-face interviews between July and September 2017 with 15 older people with TR-GAD who had previously been offered other psychotherapies. A sample size of 15 participants was consistent with the sample size recommended for qualitative interviews. 67 Stage 1 interviews used a topic guide flexibly to identify relevant issues specific to this population that the intervention would need to consider, including individuals’ attitudes towards their condition, its perceived impact on their lives, their experiences of medication and psychological therapies and their views on which elements of ACT interventions might be suitable or relevant for older people (see Report Supplementary Material 1). We revised the guide iteratively to allow exploration of the main concerns of participants. We conducted face-to-face interviews in participants’ homes (n = 9), the care setting in which they were recruited (n = 4) or at the lead university (n = 2) in accordance with participant preference. Interviews were recorded and transcribed verbatim with contextual notes and reflections documented in an analytical diary.
We also conducted semistructured telephone interviews during this same period with 31 health-care professionals. In addition, a 1-hour focus group was conducted with five academic clinicians from the Mental Health of Older People research group at University College London. Again, interviews used a topic guide flexibly to explore the challenges of supporting older people with GAD and how an intervention could be more attractive, persuasive and feasible to implement (see Report Supplementary Material 1). Interviews continued until we achieved theoretical saturation of data. We recorded views and recommendations in detailed research notes.
Stage 2: intervention design and development
We developed themes relating to the specific needs, issues and challenges of people with GAD into recommendations for optimising an ACT intervention and presented these to the study’s Service User Advisory Group, which comprised five older people with lived experience of TR-GAD, for discussion. Views on the salience and feasibility of the proposed intervention components, together with discussions with eight academic clinicians involved as co-applicants/collaborators in the research, informed the guiding principles and design of the ACT intervention manual.
We conducted further semistructured face-to-face interviews with the 15 older people with TR-GAD who completed interviews in stage 1 using ‘think aloud’ techniques. 68 This is when researchers observe people using an intervention while saying their thoughts out loud. We used a topic guide flexibly to explore opinions about the developed intervention (see Report Supplementary Material 1). We mailed out a written summary of the key features of the manualised intervention to participants in advance of the interview to help elicit their views. We also asked participants to voice their thoughts during and after a sample of intervention exercises. We iteratively modified the features in the ACT intervention to improve acceptability. This was then subject to further feedback from eight academic clinicians involved in the management of the study and 15 therapists involved in the provision of ACT for the study.
Data analyses
We used the framework approach69 to facilitate analysis within and between individual cases and groups of participants. One author (KK) conducted the interviews and focus group with academic clinicians, listened to all recordings and repeatedly read the transcripts and research notes to familiarise herself with the data. We noted key issues, recurrent themes and interpretations, and discussed these in supervision and at research team meetings. Two additional authors (VL and RG), who had not analysed the other transcripts, reviewed three transcripts to help identify alternative viewpoints. We developed a descriptive theoretical framework of key beliefs about GAD, coping strategies and therapy specific to this group and considered relevant to the intervention by consensus and used this to index subsequent transcripts. Data were then charted into matrices to help map and interpret the data set as a whole; comparisons were made across themes and participants to help synthesise the findings.
Ethics
Ethics approval was granted by the London–Camberwell St Giles Research Ethics Committee (REC) on 9 May 2017 and Health Research Authority approval was granted on 12 May 2017 [Integrated Research Approval System (IRAS) identifier (ID) 214775, REC reference 17/LO/0704; see Report Supplementary Material 2].
Results
Participants
As shown in Table 3, the majority of older people with TR-GAD were recruited from secondary care services (n = 8, 53%) and self-identified as female (n = 11, 73%), were in their 70s (n = 8, 53%), were married (n = 7, 47%) and were educated to at least degree level (n = 8, 53%). All self-identified as white/white British (n = 15, 100%). The majority of health-care professionals and academic clinicians self-identified as female (n = 27, 75%) and were most commonly clinical or counselling psychologists (n = 13, 36%) or psychiatrists (n = 10, 28%) working in secondary care settings (n = 25, 84%).
| Variable | N (missing n, %) | n (%) |
|---|---|---|
| Older people with TR-GAD (n = 15) | ||
| Sex | 15 (0, 0) | |
| Female | 11 (73) | |
| Male | 4 (27) | |
| Age (years) | 15 (0, 0) | |
| 60–69 | 5 (33) | |
| 70–79 | 8 (53) | |
| 80–89 | 2 (13) | |
| Ethnicity | 15 (0, 0) | |
| White/white British | 15 (100) | |
| Marital status | 15 (0, 0) | |
| Married | 7 (47) | |
| Divorced | 2 (13) | |
| Single | 1 (7) | |
| Co-habiting | 1 (7) | |
| Widowed | 4 (27) | |
| Education | 15 (0, 0) | |
| No qualifications | 2 (13) | |
| O level/GCE/GCSE | 3 (20) | |
| A level | 2 (13) | |
| Undergraduate degree and higher | 8 (53) | |
| Recruitment setting | 15 (0, 0) | |
| Primary care | 2 (13) | |
| Secondary care | 8 (53) | |
| Self-referral | 5 (33) | |
| Health-care professionals (n = 31) and academic clinicians (n = 5) | ||
| Sex | 36 (0, 0) | |
| Female | 27 (75) | |
| Male | 9 (25) | |
| Profession | 36 (0, 0) | |
| Clinical or counselling psychologist | 13 (36) | |
| CBT therapist | 1 (3) | |
| Occupational therapist | 4 (11) | |
| GP | 4 (11) | |
| Psychiatrist | 10 (28) | |
| Nurse | 4 (11) | |
| Service level | 35 (1, 3) | |
| Primary care | 5 (14) | |
| Secondary care | 29 (83) | |
| Tertiary care | 1 (3) | |
Key themes in stage 1
Interviews with older people and health-care professionals identified key issues, needs and challenges that would need consideration when developing the intervention. These were categorised into four key themes: (1) ‘expert in one’s own condition’, (2) ‘deep-seated coping strategies’, (3) ‘expert in therapy’ and (4) ‘support with implementation’. Subthemes within each key theme were also identified. We present data across the participant groups, with similarities and discrepancies highlighted where relevant. Sample quotations are presented in Appendix 1.
Theme 1: expert in one’s own condition
The majority of older people with GAD presented themselves as experts in their own condition, recounting deep-seated views of self, contributing factors, circumstances that triggered their anxiety and the futility of this response (see theme 1 in Appendix 1, Table 51). Many described themselves as having a propensity to worry, with anxiety being an inherent part of who they are. Worry was often intertwined with negative aspects of ageing, including pain, lack of mobility, poor health and bereavement. There was consensus among health-care professionals that physical health problems contributed to GAD, were difficult to resolve and limited older peoples’ ability to attend and concentrate in therapy sessions. Yet a large proportion of professionals were also critical of what they viewed as ‘entrenched negativity’, whereby identifying worrying as part of one’s sense of self could prevent individuals from taking ownership of their condition or assuming a role in effecting change. They suggested that this led to an over-reliance on services and, subsequently, a need to socialise older people to a therapeutic model that is fully collaborative and directed towards change. Nevertheless, health-care professionals recognised that older people had unrivalled knowledge of their condition, which was further evidenced by the detailed accounts that individuals gave of the circumstances and thoughts that triggered their anxiety, such as the health and well-being of their children, social interaction, travelling and finances. Many older people recognised that worrying was to a large extent unnecessary and, to an even greater degree, futile, yet some health-care professionals felt that older people with TR-GAD required a deeper understanding of just how unproductive these existing thinking patterns could be.
Theme 2: deep-seated coping strategies
Older people had often established deep-seated coping strategies over the course of their illness (see theme 2 in Appendix 1, Table 51). Almost all commented, often with regret, that they had come to avoid most social contact and activities, as these were a major cause of anxiety. Those who continued to meet with friends described how they circumvented particularly uncomfortable aspects of the social situation (e.g. by getting a taxi to a friend’s house to avoid public transport) or concealed their anxiety. Putting on a ‘brave face’ was a source of both pride and pain. Another common strategy was to plan for the worst by anticipating all eventualities. Two older women reflected that these efforts to exercise control over the events and people in their lives had been detrimental to their relationships. Health-care professionals acknowledged the challenge of addressing these entrenched behaviours, which were widely recognised, suggesting that they necessitated longer and more ‘intensive’ therapy.
Theme 3: expert in therapy
Participants had accumulated considerable personal experience of talking therapies, most often CBT (see theme 3 in Appendix 1, Table 51). Therapies were criticised for being ‘too academic’ and for relying on short-term courses and inexperienced therapists who lacked the life experience to truly understand their problems. One woman indicated her discomfort at reflecting on her behaviour during therapy; another reported that she found it difficult to change how she thinks at this stage in her life.
There was evident frustration among health-care professionals in primary and secondary care as they described the difficulty of engaging these older people in thinking about their anxieties. One GP suggested that years of medication had created a distance between older people with GAD and their distress, and eroded individuals’ awareness of their internal states. Older people were ambivalent about medication: most felt it had the potential to ameliorate anxiety in some cases but had side-effects and, like talking therapy, did not eliminate underlying problems. A handful of participants articulated a desire for a ‘magic pill’ that would remove their distress. Health-care professionals saw this wish for a cure as further evidence of older people’s unwillingness to assume responsibility for change themselves, leading to an over-reliance on services and an expectation that therapists should provide treatment without recognising the need for active participation on the older person’s part. Health-care professionals stressed the importance of reaching realistic, shared goals for therapy and of adopting a collaborative approach. It was striking that almost all older people highlighted the qualities of the therapist as the most important aspect of therapy. Participants indicated that empathy was a prerequisite for any therapeutic alliance, with value placed on therapists who did not make judgements but listened carefully to understand their experience.
Theme 4: support with intervention
It was widely recognised among older people that implementing relaxation techniques in their lives required practice and commitment (see theme 4 in Appendix 1, Table 51). Most were receptive to this in principle, but felt they lacked sufficient discipline in practice. Many were sceptical of the ability of talking therapies to produce a sustained benefit, but nonetheless were forthcoming in contributing suggestions to achieve this. For example, it was thought that meditation could be supported using audio tapes, videos and telephone reminders. However, input from others via weekly groups, brief follow-up contact with health-care professionals and family encouragement were considered necessary to embed this practice in their lives. Health-care professionals routinely advocated using handouts and engaging family members so that they could fully understand and support this work. There was a consensus among professionals that interventions needed to be flexible, offering a range of activities that could be practised at home with the support of handouts and, some suggested, occasional home visits.
Guiding principles in stage 2
Themes identified in stage 1 were developed into guiding principles for therapy (Table 4), in consultation with the Service User Advisory Group, and modified in response to follow-up interviews with older people with TR-GAD and via further discussion with experts (clinical academics and therapists involved in the study). Some of the key features for optimising an ACT intervention for older people with TR-GAD are described in this section. The final outputs from the process of intervention design, development and optimisation have been presented rather than incremental changes being itemised.
| Key issue | Design objectives that address each key issue | Key intervention features relevant to each design objective |
|---|---|---|
| Expert in one’s own condition |
|
|
|
|
|
|
|
|
| Deep-seated coping strategies |
|
|
|
|
|
| Expert in therapy |
|
|
|
|
|
|
|
|
| Support with implementation |
|
|
Theme 1: expert in one’s own condition
Examine beliefs around ‘self as worrier’
Older people acknowledged that exploring beliefs around the view of the self as a worrier may be of benefit, including evaluating how this might help or hinder individuals from living the life they want. Clinical academics felt that the perceived inevitability of worrying in the context of age, pain, lack of mobility, poor health and bereavement should be discussed, as this could develop into a negative self-stereotype and deter individuals from attempting to change their behaviour. Similarly, older people could be helped to understand that worrying not only is futile but could also limit their activities beyond those imposed by any chronic illness or functional impairment.
Listening and respecting values and enduring concerns
Older people were unequivocal in their view that therapy must respect their lifelong knowledge and experience. All stakeholders agreed that this information can be used to personalise activities and to support therapists in using metaphors and exercises, as is typical in ACT, that are relevant and meaningful to individual service users.
Theme 2: deep-seated coping strategies
Evaluate the costs of deep-seated coping strategies
Although not raised in interviews with older people, members of the Service User Advisory Group agreed that therapy should examine the consequences of the coping behaviours that older people have developed over many years to help them control their worrying. This should include raising awareness of the costs of trying to control their worries (e.g. through avoidance behaviour), including the emotional toll of concealing anxiety and of trying to control situations, people and events. Experts felt that therapy should consider the extent to which curtailing social contact and activities had caused individuals to lose contact with the things that gave meaning to their life (i.e. their values).
Consider any useful functions of avoidance behaviour
Older people felt that it should not be assumed that all control and avoidance behaviour is problematic; older people are experts in living with their own condition and certain behaviours may serve a useful function. Clinicians subsequently supported this point.
Theme 3: expert in therapy
Communicate the goal of acceptance and commitment therapy
Older people liked the fact that ACT does not involve challenging thoughts around losses that may be realistic, and all saw the benefit of focusing on remaining resources and living life in accordance with deeply held values. Members of the Service User Advisory Group stressed that the aim of ACT should be clearly communicated and differentiated from the aim of CBT, with which older people may be more familiar; it should be stressed that the purpose of ACT is not to fix problems or change thoughts and feelings.
Helping older people to recognise and discuss thoughts and feelings
Regular mindfulness exercises were suggested by academic clinicians and endorsed by older people as a way to develop skills in recognising and describing their thoughts and their feelings. They thought that the use of concrete metaphors and experiential exercises (i.e. those using visual or physical props) could make concepts easier to understand for some, but not others, with some older people expressing a preference for ‘speaking plainly’ without the use of metaphors or props.
Working in collaboration
There was consensus among older people and clinicians that therapy should be a collaborative partnership between the therapist and the older person. Older people continued to prioritise an empathic approach and therapists expressed confidence in validating individuals’ experiences and emotions. However, members of the Service User Advisory Group acknowledged that therapists should not be expected to ‘fix’ the individual or provide solutions. Rather, individuals must be active in pursuing value-based goals.
Theme 4: support with implementation
Provide strategies and materials to support implementation
All agreed that multiple strategies should be used to help older people apply therapeutic principles in their lives. As it is common that older people experience mild age-related cognitive changes, adaptations should be made to accommodate for potential changes in memory, attention and processing speed. Older people responded positively to the following practices and suggestions: repetition of key ACT phases throughout the intervention, working at a slower pace when necessary, providing a summary of the sessions as a reminder of what has been discussed and asking the service user to discuss their understanding of weekly practice tasks in their own words, to check that what has been set by the therapist has been understood.
Work with close family and friends
Older people thought that the aim of ACT should be clearly communicated to all those involved in the health and welfare of the client at the start of therapy. Partners, family members or close friends could contribute to the account of an individual’s difficulties and help them to work through potential barriers to behavioural change. However, members of the Service User Advisory Group cautioned that many would not want to burden their children by involving them in this way.
Discussion
The findings suggest that ACT psychopathological processes can be identified in people with TR-GAD, underlining the potential suitability of using an ACT approach with this population. For example, participants appeared to have difficulty in separating themselves from the literal meaning of their thoughts (cognitive fusion), frequently telling themselves that they are worriers (self-as-content) and placing limits on their behaviour (lack of committed action). They described avoided situations that make them feel uncomfortable and attempts to try to control their thoughts and emotions (experiential avoidance). These approaches have been associated with distress in older people,70 and participants confirmed that they exert an emotional burden. As posited elsewhere,43 the goal of ACT to live life in accordance with deeply held values, despite the many challenges that may be experienced, seemed to resonate with this group; group members had experienced little success with control-orientated treatment strategies such as CBT in the past.
The findings also highlight the unique experience of older people with TR-GAD and important implications for how talking therapies and, more specifically, ACT are applied with this group. Some generic implications included ensuring that attention is given to validating and accommodating the individual’s knowledge and experience in therapy, and that therapeutic strategies are used to compensate for age-related cognitive changes. Implications specific to ACT included differentiating the aims of ACT from those of CBT and using mindfulness to support discussion of thoughts and feelings. Notably, not all older people responded positively to the use of metaphors and experiential exercises, key tools in ACT for communicating abstract concepts. This reinforces previous suggestions that these techniques must be used thoughtfully and tailored to the client’s language and life experience. 71 Participants also cautioned against assuming that all efforts to control unwanted thoughts and experiences are unhelpful. Brock et al. 71 elaborate on this point, suggesting that there may be times when avoiding certain emotional experiences is the functional thing to do and therapists should identify the role that avoidance plays in the client’s day-to-day life. The concept of workability, that is, how well a strategy is helping a person to live their life in accordance with their values, is key here.
There was a large overlap in the views of older people and health-care professionals. Notably, despite expressing optimism around the principles of ACT, both groups described feelings of hopelessness with respect to change. One of the strongest themes to emerge in the data was the idea of ‘entrenched negativity’, requiring an early focus on cognitive fusion in relation to negative attitudes about ageing and the individual’s sense of self. However, health-care professionals felt that this also necessitated a change in how older people with TR-GAD approach therapy. Positioning ACT as a collaborative partnership between clients and therapists and exploring older people’ expectations around therapy should support this. It has previously been noted that there is a risk that therapists delivering ACT will be drawn into the content of their clients’ experiences and develop a wish to eliminate clients’ suffering (Mark A Serfaty, Division of Psychiatry, University College London, 2017, personal communication). Therapists are advised to validate the experience, not the content, and to help clients reflect on how the situation could be changed (Mark A Serfaty, personal communication). The client–therapist relationship in ACT has been described as ‘strong, open, accepting, mutual, respectful and loving’,72 which is accordant with the emphasis that older people placed on therapists who are interested in understanding their experiences. It is notable that, although older people valued empathy, their comments suggested a desire for more than ‘just’ a passive listener. Finally, health-care professionals may also need to examine their own beliefs around working with older people with TR-GAD that might impede therapeutic progress. Acquiring experience of an intervention that works with older people with TR-GAD is likely to inculcate therapeutic optimism in service users and clinicians alike.
How acceptance and commitment therapy was adapted for older people with treatment-resistant generalised anxiety disorder
A description of the specific adaptations made to the ACT intervention for older people with TR-GAD is presented below. This takes into account the guiding principles identified in Table 4, as well as previous recommendations with respect to using ACT with older people. 43
Acceptance and commitment therapy assessment
Several key areas were assessed during the initial session and throughout the intervention with respect to their contribution to the development and maintenance of TR-GAD, as it is important to understand the biopsychosocial context in which a person’s difficulties are occurring. These key areas included:
-
biological factors (e.g. comorbid physical health difficulties and mild age-related cognitive difficulties)
-
psychological factors (e.g. unwanted internal experiences, loss, psychiatric comorbidity, core ACT processes)
-
sociocultural factors (e.g. financial, social, cultural and environmental factors)
-
suicidal ideation and risk of harm to self
-
substance misuse (including alcohol and illicit and prescribed drugs).
Therapists were encouraged to develop an idiosyncratic ACT case conceptualisation for each participant in sessions 1–5 so that the order in which ACT processes were chosen to be targeted was hypothesis driven in sessions 6–15.
Introduction to acceptance and commitment therapy
An introduction to ACT was provided in the first session, which included (1) what ACT is and a rationale for it, (2) the aim of ACT and its focus on change (i.e. ‘living better’ rather than ‘feeling better’), (3) an emphasis on active participation in therapy (i.e. a ‘doing therapy’ rather than a ‘talking therapy’), (4) an explanation of the importance of skills practice between sessions and (5) an emphasis on working collaboratively together ‘as a team’, highlighting willingness as a choice (i.e. the participant always gets to choose whether or not they are willing to take part in experiential exercises).
Early focus on values and committed action
Previous research with older people with GAD has suggested that it may be beneficial to adapt ACT so that there is an early focus on values and committed action. 27 Consequently, a focus on values and committed action was introduced early into the intervention (after the initial assessment) and repeatedly revisited throughout the intervention.
Focus on workability
The desire to get rid of anxiety or feel better (i.e. attachment to the emotional control agenda in ACT terms) is more likely in those with treatment-resistant anxiety disorders, particularly those who have a lifelong history of GAD and have been struggling with their symptoms for years. Therefore, there was a greater focus on workability in the intervention than may ordinarily be used to target entrenched or narrowed behavioural repertoires. This involved exploring (1) what strategies a person had been using to try and get rid of anxiety (e.g. avoidance behaviour); (2) how these had been working in the short and long term (i.e. the costs and benefits of these strategies), both in terms of anxiety and quality of life; and (3) the degree to which they were helping the person to live a rich, full and meaningful life (i.e. doing what is most important to them and being who they most want to be). This also involved validating and normalising the desire to want to get rid of anxiety or feel better, as well as the desire for a ‘magic pill’. In addition, it involved exploring the alternative to emotional control (i.e. trying to get rid of anxiety) by encouraging a willingness to experience uncomfortable thoughts and feelings to help people move towards the things that are important and matter to them. (In ACT terms, the process of discovering how control is often the problem is called ‘creative hopelessness’ or ‘workability’.)
Use of concrete metaphors and experiential exercises
Some older people may struggle to understand abstract concepts, particularly those with age-related cognitive difficulties. Consequently, care was taken to ensure that as many metaphors and experiential exercises used visual and/or physical props or physical demonstrations as possible. Examples of these are as follows:
-
acceptance – ‘tug of war’ metaphor with a rope; ‘Chinese finger trap’ metaphor with a Chinese finger trap; sticky notes exercise with sticky notes; acting out the ‘pushing paper’ exercise; cactus metaphor with a spiky ball; ‘holding a book’ metaphor with a book; acting out ‘passengers on the bus’ metaphor
-
defusion – ‘milk, milk, milk’ exercise; sing the thought/say it in a silly voice/say it very slowly and very quickly; ‘I’m noticing I’m having the thought that . . .’ exercise; write the thought in different colours, different styles and reverse order; sticky notes exercise with sticky notes; acting out ‘passengers on the bus’ metaphor; ‘take your mind for a walk’ exercise
-
contact with the present moment – mindful eating, drinking, stretching, walking, etc.; daily mindfulness (e.g. mindful showering, mindful shopping)
-
self-as-context – ‘cup and contents’ exercise with a paper cup and sachets of coffee, milk and sugar; labels exercise with actual luggage labels and stickers; house and furniture exercise with a visual handout
-
values – lifetime achievement award with the client listening to the recorded speech.
Whenever possible, therapists were encouraged to customise metaphors and experiential exercises to participants’ struggles, needs, history, own language and preferences, as suggested by others. 73
Focus on mindfulness
As we previously noted,43 some older people may experience difficulties in recognising, describing, observing or being aware of their internal states. Therefore, we introduced a mindfulness exercise at the beginning of each session, in addition to sessions dedicated to developing mindful awareness, to develop and increase skills in awareness of internal states.
Focus on cognitive fusion and self-as-content (or attachment to the conceptualised self)
Older people with TR-GAD who report lifelong issues with worrying may be strongly fused with a conceptualised sense of themselves as having ‘always been a worrier’ or of worrying as being a part of who they are (and therefore not knowing who they are without worrying). They may also demonstrate strong fusion with a conceptualised future self (e.g. ‘my health is only going to get worse and there’ll be nobody to look after me’), which, although based in reality, may interfere with value-driven behaviours. In addition, cognitive fusion with negative attitudes about ageing (e.g. ‘I am too old to exercise’, ‘feeling depressed is a normal part of ageing’) and chronic ill health or physical/cognitive impairment (e.g. ‘I can’t do anything more’, ‘I’m not the person I used to be’) may be apparent, and may also serve as an internal barrier to behavioural change. Thus, therapists helped participants to explore the workability of holding onto such self-beliefs (i.e. how well they were helping them to live a life in service of their values rather than in service of avoiding difficult thoughts, feelings, sensations). In addition, therapists helped participants to develop skills for stepping back from thoughts and for holding views about themselves lightly so that they could move towards the things that are important and matter to them and be who they want to be.
Laidlaw and Kishita’s CBT conceptual framework74 advises that cohort beliefs, and beliefs in relation to transitions in role investments (e.g. due to retirement, caring for another person or bereavement) and intergenerational linkages, should be considered when working with older people. Examples of shared generational cohort beliefs include ‘always keep a stiff upper lip’, ‘you can’t teach an old dog new tricks’ and ‘needing help is a sign of weakness’. Examples of beliefs in relation to transitions in role investments and intergenerational linkages include ‘I’m a nobody now’, ‘I’m no longer needed’ and ‘I’m a burden on my family’. Therapists were similarly advised to consider cognitive fusion with such beliefs when using ACT with older people with TR-GAD because these may pose a further internal barrier to behavioural change. In addition, therapists were advised to explore cognitive fusion in relation to seeking help, because discussing shame in seeking help has been suggested to be helpful when working psychotherapeutically with older people. 75
Use of principles of selective optimisation with compensation
Principles of selective optimisation with compensation were originally developed to aid adaptation to the challenges of ageing and have since been successfully used in ACT for chronic pain. 55,76 They involve strategies for helping people to choose the best functional domains in which to focus their resources, engage in tasks that they perform best and find ways of compensating for losses. They can be similarly applied to older people with TR-GAD to help them to participate as fully as possible in their lives in ways that are meaningful to them and to help them achieve valued goals despite the challenges of ageing. Consequently, the use of principles of selective optimisation with compensation was specifically incorporated into sessions focusing on committed action.
Examples of using principles of selective optimisation with compensation in ACT include:
-
selecting or limiting goals to those that are in service of the person’s most important values
-
selecting or limiting goals to those that are in the best domains of functioning for the person
-
adapting goals or focusing on specific aspects of a goal so that they can be more realistically achieved
-
replacing goals that are no longer achievable by identifying what it is that a person liked about the original goal
-
optimising engagement in goal-related activities (e.g. by practising or learning new skills and capitalising on a person’s strengths)
-
utilising additional resources so that goals can be achieved (e.g. asking others for help)
-
using alternative strategies, aids or tools to compensate for losses in function due to mental or physical health-related difficulties to achieve valued goals (such as memory aids and walking aids).
Compensating for age-related cognitive changes
It is important to compensate for mild age-related cognitive changes in working memory, attention and processing speed when working with older people with GAD because these have been associated with a reduced response to CBT in this population. 77 We incorporated standard therapeutic strategies that can compensate for age-related cognitive changes in the intervention, as suggested by others. 43,78 These included:
-
providing modifiable worksheets (so that they can be adapted for visual impairment) and session summaries as a reminder of the content of the sessions
-
repeating key concepts and skills in and between sessions (e.g. recapping on the previous session at the beginning of the next session)
-
asking participants to repeat home practice assignments in their own words to check their understanding of the assignments or working through an example before the session ends
-
having the flexibility to work at a slower pace when necessary
-
providing appointment reminders by automated text message reminder systems, with consent from participants.
Working with comorbidities
Physical and mental health comorbidity (e.g. depression, other anxiety disorders, personality disorders, mild cognitive deficits, physical ill-health, pain) is common in TR-GAD and is associated with poor treatment response. 13 It was emphasised to therapists that, as ACT is a transdiagnostic form of psychological therapy, comorbidities can be dealt with in the same way as TR-GAD: by targeting the ACT processes that are hypothesised to be responsible for the narrowing of the person’s behavioural repertoires.
Working with substance misuse
Substance misuse, including excessive use of prescription medication (e.g. benzodiazepines and other hypnotic drugs), over-the-counter medication (e.g. sedative antihistamines), alcohol and illicit substances (e.g. cannabis), is common in GAD. Engagement in substance misuse is typically formulated in the ACT model as a means of reducing or avoiding unwanted internal experiences (e.g. anxiety symptoms). This may interfere with therapy because a person may not be able to fully benefit from exercises aimed at helping them to increase their willingness to have anxiety symptoms (in order to do the things that are important and matter to them and be the type of person they want to be). Therefore, an ‘optional session’ was included in the intervention in which psychoeducation about substance misuse, the risks and benefits of this, and ways of reducing this during the provision of ACT (e.g. via supervised gradual withdrawal)79 could be addressed, if necessary.
Working with skills deficits
Standard CBT manuals for GAD in older people typically include sessions on problem-solving and sleep hygiene in recognition of the fact that some older people with GAD may have poor problem-solving skills, or poor sleeping habits. 21,24,80 Thus, an ‘optional session’ on problem-solving for external problems and sleep hygiene was also included in the intervention, which therapists could introduce if necessary. It was emphasised to therapists that these were ACT consistent so long as the following provisos were met: (1) problem-solving was used to address external problems but not internal problems (e.g. thoughts, feelings, sensations) and (2) sleep hygiene was focused on improving sleep habits and not reducing associated distress.
Working with families and health-care professionals
With participants’ consent, we invited partners, family members or close friends to attend the first therapy session to communicate the aim of ACT and its therapeutic stance to all involved given that it is not focused on reducing distress. They were also invited to attend sessions focused on committed action, as this can be helpful in working through potential barriers to behavioural change and helping participants to implement action plans.
One of the most challenging behavioural repertoires in GAD for partners, families, friends and health-care professionals is reassurance seeking. Repetitive questioning and requests for reassurance may take the form of repeated conversations with partners, telephone calls to family members, visits to the GP and accident and emergency (A&E) or telephone calls to emergency services. It was emphasised to therapists that this can be addressed, as with other behaviours, by examining the function of the behaviour (e.g. whether or not the function of reassurance seeking is to reduce anxiety) and its workability. Therapists were encouraged to discuss an ACT-consistent strategy for dealing with repeated reassurance seeking with all parties involved, in conjunction with the participant (and with their consent).
Use of terminology in acceptance and commitment therapy
Throughout the intervention, we emphasised to therapists the importance of ‘speaking plainly’ (i.e. using jargon-free language), using terms that participants understood and establishing participants’ preferred terms for things such as anxiety, GAD and homework.
Limitations
It is important to note that the sample of older people with TR-GAD involved in the study reported high levels of academic achievement, few would be categorised as ‘older old’ (i.e. in their 80s) and all identified themselves as white British. Health-care professionals, Service User Advisory Group members and academic clinicians were encouraged to reflect on experiences across cultural and socioeconomic groups, but it cannot be assumed that the findings of the current study apply to this broader population. Furthermore, health-care professionals and some older people advocated engaging family members so that they could fully understand and support therapy. We cannot comment on family carers' attitudes towards this because they were not included in the qualitative interviews. Telephone conversations with health-care professionals were not audio-recorded (instead, comprehensive notes were taken with key quotations recorded verbatim). However, this can be balanced against the insights gained from the large sample size and the resultant opportunities to verify and amend interpretations of the data. This study was committed to understanding and interweaving the experiences of service users and staff, consistent with experience-based co-design. 81 However, additional benefit may have been gained by bringing stakeholders together to jointly reflect on their shared experiences.
Conclusions
The aim of this study was twofold. First, the study aimed to demonstrate the value of adopting an iterative, person-centred approach to developing an intervention that is fit for purpose. We used rigorous methods, triangulating the perspectives of older people and health-care professionals and examining alternative explanations using analytical diaries, multiple coding exercises, supervision and discussions with service users and experts. Second, in describing the decisions and processes involved in developing ACT for older people with TR-GAD, the study aimed to lay the foundations for a therapeutic intervention that can be built on and replicated in future research. This was an important step forward designed to maximise the likelihood of a successful outcome if the intervention is subsequently evaluated for clinical effectiveness and cost-effectiveness in a future substantive trial.
Chapter 3 Survey
Introduction
Little is known about the usual care that is typically offered to and received by older people with TR-GAD. Such information would be useful in clarifying the best comparator for a future substantive trial of ACT for older people with TR-GAD. Consequently, we invited older people with TR-GAD and health-care professionals to take part in a brief online survey of what constitutes ‘usual care’ in this population in phase 1 of the FACTOID (a Feasibility study of Acceptance and Commitment Therapy for Older people with treatment-resistant generalised anxiety Disorder) study. Although it may have been possible to gather this information from the open uncontrolled feasibility study conducted in phase 2, this information would have been relevant only to those living in London. We anticipated that there might be regional variations in usual care for TR-GAD in older people, for example because psychological therapies are easier to access in urban than rural settings. Therefore, we judged that a brief online survey would more accurately clarify what constitutes usual care in this population.
In addition to clarifying usual care, we explored the perceived helpfulness of psychological therapy and/or pharmacotherapy for TR-GAD in service users and health-care professionals. Although the very definition of TR-GAD suggests that, overall, treatments would be perceived to be helpful to a degree at best, little is actually known about this in older people with TR-GAD. Knowing what forms of treatment are perceived to be the most helpful (either previously or currently) could inform the choice of comparison condition in a future substantive trial. For example, it might suggest what form of treatment could be used as a comparison condition in a non-inferiority or superiority trial. It could also suggest what form of treatment might optimise recruitment rates in a future substantive trial.
Methods
Design
This was a cross-sectional study.
Participants
Participants were:
-
Older people aged ≥ 60 years who were experiencing or had experienced difficulties with GAD or worrying. All older people who self-identified as experiencing difficulties with worrying were invited to complete the survey, as opposed to just those who were experiencing TR-GAD, because it was thought that participants might find it difficult to identify whether or not they qualified as ‘treatment resistant’ (i.e. failed to respond after completion of steps 1–3 of the stepped-care approach for GAD).
-
Health-care professionals who work with this population of older people in primary and secondary care settings (including GPs, psychiatrists, clinical psychologists, community psychiatric nurses, occupational therapists and social workers).
Settings
Older people were recruited from the community via convenience sampling through GP practices (via local Clinical Research Networks across the UK), primary and secondary care services (IAPT services and CMHTs for older people), a mental health charity [Mind, URL: www.mind.org.uk (accessed 2 February 2021)], local community groups [University of the Third Age (U3A) groups], a service user research forum [INVOLVE, URL: www.invo.org.uk/communities/information-for-members-of-the-public/ (accessed 2 February 2021)], and online forums for older people [Fifty Plus Forum, URL: www.fiftyplusforum.co.uk (accessed 2 February 2021); Pensioners Forum, URL: www.pensionersforum.co.uk/ (accessed 2 February 2021); Senior Forums, URL: www.seniorforums.com (accessed 2 February 2021); Buzz 50, URL: www.buzz50.com (accessed 2 February 2021); Senior Chatters, URL: https://seniorchatters.co.uk (accessed 2 February 2021)]. Several other online forums for older people were approached to assist with advertising the survey but declined involvement or did not permit this [Age UK, URL: www.ageuk.org.uk/get-involved/social-groups/older-peoples-forums/ (accessed 2 February 2021); Gransnet, URL: www.gransnet.com/forums (accessed 2 February 2021); Silver Surfers, URL: www.silversurfers.com/silversurfers-forum/ (accessed 2 February 2021)].
Health-care professionals were identified through GP practices (via local Clinical Research Networks across the UK), online forums associated with occupation-specific organisations (Royal College of Psychiatrists, Royal College of Nursing, The British Psychological Society) and an online forum for those working in health and social care [Contact, Help, Advice and Information Network (CHAIN), URL: www.chain-network.org.uk (accessed 2 February 2021)]. The Royal College of Occupational Therapists was approached to assist with advertising the survey but declined involvement.
Survey
The brief online survey comprised a series of multiple-choice questions with free-text boxes that enabled provision of further information if desired. There were two versions of the survey – one for service users and one for health-care professionals – because the content of questions and terminology differed for the two groups of respondents. The survey was kept as brief as possible to maximise completion rates and took approximately 5–10 minutes to complete.
Service user version
The service user version comprised 15 questions about demographic information (e.g. age, sex, ethnicity, education), clinical information (e.g. diagnosis, duration of worrying), treatments offered previously or currently, whether or not these treatments were taken up and perceptions of the helpfulness of these treatments on a 5-point Likert scale [from 1 (not at all helpful) to 5 (extremely helpful)]. It also included a brief screening tool, the Generalised Anxiety Disorder-7 (GAD-7),82 which is routinely used in IAPT services and GP surgeries, to ascertain the severity of current difficulties with GAD. A copy of the service user survey is available as Report Supplementary Material 3.
Clinician version
As shown in Report Supplementary Material 4, the clinician version comprised 19 questions about demographic information (e.g. age, sex, ethnicity), professional information (e.g. profession, years since qualification), clinical information (e.g. the percentage of older people seen per month, the proportion of these with GAD), treatments typically offered when an older person has completed steps 1–3 of the stepped-care approach for GAD and how often, why treatments might not be offered and perceptions of the helpfulness of these treatments rated on a 5-point Likert scale [from 1 (not at all helpful) to 5 (extremely helpful)].
Procedure
We contacted a range of organisations across the UK and asked them to advertise the survey (see Settings). The survey used a web-based survey tool, Opinio, version 7 (2017) (ObjectPlanet, Inc., Oslo, Norway). A paper-based version of the survey was available on request but was not routinely distributed as originally hoped owing to resource limitations (both finances and time). A participant information sheet was provided at the beginning of the survey; if participants proceeded to complete the survey, it was assumed that they were providing their consent to participate. The survey was open for data collection from September 2017 to December 2017. The survey was piloted with our PPI group prior to data collection. All responses were anonymous.
Rural Urban Classification83 was used to categorise participants’ geographical area of residence (based on postcode or closest city/town). Areas with a population > 10,000 were categorised as urban and those with a population ≤ 10,000 were categorised as rural.
Data analyses
Responses were excluded if participants indicated that they were aged < 60 years or had ‘never experienced difficulties with long-term worrying or their nerves’. Those with current symptoms of GAD and a treatment history suggestive of TR-GAD were identified in post hoc analyses so that what constitutes usual care in this specific group of respondents could be clarified. Current symptoms of GAD were defined as a score of > 5 points on the GAD-7 and a treatment history suggestive of TR-GAD was defined as either having received at least two types of treatment (pharmacotherapy and/or psychological therapy) for worrying or having been offered at least two types of treatment (pharmacotherapy and/or psychological therapy) for worrying and having refused.
Data relating to demographic and clinical characteristics of service users and demographic and professional characteristics of health-care professionals were summarised using frequencies and percentages, and means and standard deviations (SDs) or medians and interquartile ranges (IQRs) for very skewed distributions (i.e. skewness values < –2 or > 2). 84 Perceived helpfulness of treatments was rated on a 5-point Likert scale from 1 (not at all helpful) to 5 (extremely helpful) and was summarised using medians and IQRs.
Parametric rather than non-parametric tests were chosen to analyse Likert scale responses, as previously recommended. 85,86 Data pertaining to the perceived helpfulness of treatments in service users and health-care professionals were analysed as follows. The perceived helpfulness of treatments in service users was examined by submitting data to an exploratory two-way (treatment × time) within-subjects analysis of variance (ANOVA), with type of treatment (pharmacotherapy vs. psychological therapy vs. a combination of pharmacotherapy and psychological therapy) and time (current vs. past) as within-subjects variables. The perceived helpfulness of treatments in health-care professionals was examined by submitting data to a one-way within-subjects ANOVA, with type of treatment as a within-subjects variable. Post hoc Bonferroni-adjusted pairwise comparisons were used to examine differences between conditions, where appropriate.
Ethics
Ethics approval was granted by the London–Camberwell St Giles Research Ethics Committee on 9 May 2017, with Health Research Authority approval granted on 12 May 2017 (IRAS ID 214775; REC reference 17/LO/0704).
Results
Service users
A total of 136 service users completed the online survey. Responses were excluded for three service users (2%) who were aged < 60 years and for 11 service users (8%) who had ‘never experienced difficulties with long-term worrying or their nerves’. Therefore, we analysed data from 122 service users (90%). Post hoc analyses identified 58 service users (48%) who were considered to have current symptoms of GAD and a treatment history suggestive of TR-GAD. We report data for all service users in Appendix 2.
As shown in Table 5, the majority of service users were aged 65–74 years (n = 33, 57%). Most self-identified as female (n = 55, 95%) and white/white British (n = 54, 93%) and resided in urban areas (n = 50, 86%), mainly in the London region (n = 34, 59%). Just under half of service users had a degree or postgraduate qualification (n = 28, 48%), with only five service users (9%) reporting no educational qualifications.
| Variable | N (missing n, %) | n (%) |
|---|---|---|
| Age (years) | 58 (0, 0) | |
| 60–64 | 13 (22) | |
| 65–74 | 33 (57) | |
| 75–84 | 11 (19) | |
| 85–94 | 1 (2) | |
| ≥ 95 | 0 (0) | |
| Prefer not to say | 0 (0) | |
| Sex | 58 (0, 0) | |
| Male | 3 (5) | |
| Female | 55 (95) | |
| Prefer not to say | 0 (0) | |
| Ethnicity | 58 (0, 0) | |
| Asian/Asian British | 1 (2) | |
| Black/black British | 0 (0) | |
| Mixed | 1 (2) | |
| White/white British | 54 (93) | |
| Other | 2 (3) | |
| Prefer not to say | 0 (0) | |
| Age (years) left school/education | 58 (0, 0) | |
| 14–16 | 22 (38) | |
| 17–19 | 32 (55) | |
| 20–22 | 0 (0) | |
| 23–25 | 3 (5) | |
| ≥ 26 | 1 (2) | |
| Highest educational qualification | 58 (0, 0) | |
| School Leaving Certificate | 0 (0) | |
| O level/GCSE | 9 (16) | |
| Diploma | 9 (16) | |
| A level | 3 (5) | |
| Undergraduate degree | 18 (31) | |
| Master’s degree | 9 (16) | |
| PhD | 1 (2) | |
| No educational qualifications | 5 (9) | |
| Other | 4 (7) | |
| Prefer not to say | 0 (0) | |
| Geographical area | 58 (0, 0) | |
| Urban | 50 (86) | |
| Rural | 2 (3) | |
| Prefer not to say/no response | 6 (10) | |
| Region of the UK | 58 (0, 0) | |
| Englanda | 49 (84) | |
| East Midlands | 4 (7) | |
| East of England | 0 (0) | |
| London | 34 (59) | |
| North East | 0 (0) | |
| North West | 0 (0) | |
| South East | 6 (10) | |
| South West | 2 (3) | |
| West Midlands | 2 (3) | |
| Yorkshire and the Humber | 1 (2) | |
| Northern Ireland | 1 (2) | |
| Scotland | 1 (2) | |
| Wales | 1 (2) | |
| Prefer not to say/no response | 6 (10) |
With respect to clinical characteristics displayed in Table 6, there was a wide variation in the reported number of years experiencing difficulties with long-term worrying, with ≥ 30 years (n = 25, 43%) being the most common. The overall mean total score on the GAD-7 was in the moderate range (14.0 points, SD 4.3 points), and 75% of service users scored in the moderate to severe range. The mean number of comorbid mental health complaints was 4.1 (SD 1.9): comorbid symptoms of depression (n = 53, 91%), panic (n = 40, 69%), post-traumatic stress disorder (PTSD) (n = 36, 62%), social phobia (n = 35, 60%) and agoraphobia (n = 30, 52%) were the most commonly reported.
| Variable | N (missing n, %) | n (%) | Mean (SD) |
|---|---|---|---|
| Number of years experiencing difficulties with long-term worrying | 58 (0, 0) | ||
| < 1 | 0 (0) | ||
| 1–5 | 10 (17) | ||
| 6–10 | 13 (22) | ||
| 11–20 | 5 (9) | ||
| 21–30 | 4 (7) | ||
| > 30 | 26 (45) | ||
| GAD-7 total score, points (possible range 0–21 points) | 57 (1, 2) | 14.0 (4.3) | |
| GAD-7 total score (points) severity | 57 (1, 2) | ||
| None (0–5) | N/Aa | ||
| Mild (6–10) | 14 (25) | ||
| Moderate (11–15) | 19 (33) | ||
| Severe (16–21) | 24 (42) | ||
| Comorbid mental health complaints | |||
| Depressive symptoms | 58 (0, 0) | ||
| Yes | 53 (91) | ||
| No | 5 (9) | ||
| Prefer not to say | 0 (0) | ||
| Panic symptoms | 58 (0, 0) | ||
| Yes | 40 (69) | ||
| No | 16 (28) | ||
| Prefer not to say | 2 (3) | ||
| Agoraphobia symptoms | 58 (0, 0) | ||
| Yes | 30 (52) | ||
| No | 28 (48) | ||
| Prefer not to say | 0 (0) | ||
| Social phobia symptoms | 58 (0, 0) | ||
| Yes | 35 (60) | ||
| No | 23 (40) | ||
| Prefer not to say | 0 (0) | ||
| Specific phobia symptoms | 58 (0, 0) | ||
| Yes | 19 (33) | ||
| No | 38 (66) | ||
| Prefer not to say | 1 (2) | ||
| PTSD symptoms | 58 (0, 0) | ||
| Yes | 36 (62) | ||
| No | 22 (38) | ||
| Prefer not to say | 0 (0) | ||
| OCD symptoms | 58 (0, 0) | ||
| Yes | 12 (21) | ||
| No | 45 (78) | ||
| Prefer not to say | 1 (2) | ||
| Other symptoms | 14 (44, 76) | ||
| Yes | 10 (71) | ||
| No | 4 (29) | ||
| Prefer not to say | 0 (0) | ||
| Number of comorbid mental health complaints (possible range 0–8) | 58 (0, 0) | 4.1 (1.9) | |
In terms of reported treatments for worrying in the past or currently (either received or refused), just under half of service users were currently receiving pharmacotherapy (n = 28, 48%), with antidepressants being the most commonly reported medication (n = 28, 62%; Table 7). In contrast, only one-quarter of service users (n = 13, 24%) were currently receiving psychological therapy, with counselling being most commonly reported (n = 4, 44%). Most service users had tried some form of pharmacotherapy or psychological therapy in the past (n = 42, 72%, and n = 45, 83%, respectively). One-quarter of participants (n = 14, 26%) reported trying at least three different types of pharmacotherapy in the past, and just under half reported trying at least two different types of psychological therapy in the past (n = 26, 48%). The most common forms of pharmacotherapy tried in the past were antidepressants (n = 24, 45%) and sedatives (n = 19, 36%), whereas the most common forms of psychological therapy were CBT (n = 20, 40%) and counselling (n = 9, 18%). Approximately one-third of service users reported refusing pharmacotherapy in the past (n = 17, 30%), whereas the number of service users who reported refusing psychological therapy in the past was small (n = 4, 8%). Forty-two per cent of service users reported not receiving any form of current pharmacotherapy or psychological therapy, despite the mean GAD-7 total score being in the moderate range (13.3 points, SD 4.0 points) for this subsample, with five service users scoring in the mild range, 10 scoring in the moderate range and eight scoring in the severe range.
| Variable | N (missing n, %) | n (%) |
|---|---|---|
| Pharmacotherapy for worry | ||
| Currently | 58 (0, 0) | |
| Yes | 28 (48) | |
| No | 30 (52) | |
| In the past | 58 (0, 0) | |
| Yes | 42 (72) | |
| No | 16 (28) | |
| Offered in the past but declined | 56 (2, 3) | |
| Yes | 17 (30) | |
| No | 39 (70) | |
| Self-reported type of current pharmacotherapy for worrya | 25 (3, 11) | |
| Antidepressants | 28 | |
| Anxiolytics (e.g. buspirone) | 0 | |
| Sedatives (e.g. benzodiazepines) | 5 | |
| Hypnotics (e.g. Z drugs) | 0 | |
| Antihypertensives (e.g. propranolol) | 4 | |
| Anti-epileptics (e.g. pregabalin) | 3 | |
| Antipsychotics (e.g. olanzapine) | 2 | |
| Antihistamines (e.g. hydroxyzine) | 0 | |
| Other | 3 | |
| Self-reported type of past pharmacotherapy for worrya | 18 (24, 57) | |
| Antidepressants | 24 | |
| Anxiolytics (e.g. buspirone) | 0 | |
| Sedatives (e.g. benzodiazepines) | 19 | |
| Hypnotics (e.g. Z drugs) | 2 | |
| Antihypertensives (e.g. propranolol) | 2 | |
| Anti-epileptics (e.g. pregabalin) | 1 | |
| Antipsychotics (e.g. olanzapine) | 2 | |
| Antihistamines (e.g. hydroxyzine) | 0 | |
| Other | 3 | |
| Number of different types of medication for worry tried in the past | 54 (4, 7) | |
| 1–2 | 31 (57) | |
| 3–4 | 8 (15) | |
| ≥ 5 | 6 (11) | |
| Cannot remember | 3 (6) | |
| Other | 6 (11) | |
| Psychological therapy for worry | ||
| Currently | 54 (4, 7) | |
| Yes | 13 (24) | |
| No | 41 (76) | |
| In the past | 54 (4, 7) | |
| Yes | 45 (83) | |
| No | 9 (17) | |
| Offered in the past but declined | 52 (6, 10) | |
| Yes | 4 (8) | |
| No | 48 (92) | |
| Self-reported type of current psychological therapy for worrya | 9 (4, 31) | |
| CBT | 2 | |
| Relaxation therapy | 0 | |
| Mindfulness-based therapy | 0 | |
| ACT | 0 | |
| Psychodynamic psychotherapy | 1 | |
| Counselling | 4 | |
| Other | 0 | |
| Unclear | 2 | |
| Self-reported type of past psychological therapy for worrya | 36 (9, 20) | |
| CBT | 20 | |
| Relaxation therapy | 0 | |
| Mindfulness-based therapy | 2 | |
| ACT | 1 | |
| Psychodynamic psychotherapy | 1 | |
| Counselling | 9 | |
| Other | 6 | |
| Unclear | 11 | |
| Number of different types of psychological therapy for worry tried in the past | 54 (4, 7) | |
| 1 | 20 (37) | |
| 2 | 11 (20) | |
| ≥ 3 | 15 (28) | |
| Cannot remember | 3 (6) | |
| Other | 5 (9) | |
| No current pharmacotherapy or psychological therapy for worry | 55 (3, 5) | 23 (42) |
Service users rated the perceived helpfulness of current and past treatments for worrying on a scale from 1 (not at all helpful) to 5 (extremely helpful). As shown in Table 8, there was little variation in the median ratings across current and past treatments, although an inspection of the data suggested that there was a possible trend for medication alone to be perceived as less helpful than other forms of treatment.
| Perceived helpfulnessa | N (missing n, %) [N/A n, %] | Median (IQR) |
|---|---|---|
| Current medication | 30 (3, 5) [25, 43] | 2.5 (2.0–3.0) |
| Current psychological therapy | 22 (3, 5) [33, 57] | 3.0 (2.0–4.0) |
| Current combination of medication and psychological therapy | 14 (3, 5) [41, 71] | 3.0 (1.8–4.0) |
| Past medication | 43 (2, 3) [13, 22] | 2.0 (2.0–4.0) |
| Past psychological therapy | 47 (2, 3) [9, 16] | 3.0 (2.0–4.0) |
| Past combination of medication and psychological therapy | 27 (2, 3) [29, 50] | 3.0 (2.0–4.0) |
Data were submitted to ANOVAs to compare ratings across different types of treatment. Unfortunately, it was not possible to conduct a two-way ANOVA with time (current vs. past) and treatment (pharmacotherapy vs. psychological therapy vs. a combination of pharmacotherapy and psychological therapy) as within-subjects variables because data were available for only 11 service users owing to missing data or no ratings being given (i.e. a ‘not applicable’ response). Consequently, separate one-way ANOVAs for current and past treatment were conducted, with treatment (pharmacotherapy vs. psychological therapy vs. a combination of pharmacotherapy and psychological therapy) as a within-subjects variable. The main effect of current treatment [F(2,20) = 1.14, mean squared error (MSE) = 0.27, p = 0.340, ηp2 = 0.102] and the main effect of past treatment [F(2,52) = 1.57, MSE = 0.78, p = 0.218, ηp2 = 0.057] were non-significant. There were no statistically significant differences in perceived helpfulness across different types of treatment, either currently or in the past (Table 9).
| Perceived helpfulnessa | n | Mean (SE) |
|---|---|---|
| Current medication | 11 | 2.64 (0.31) |
| Current psychological therapy | 11 | 2.91 (0.29) |
| Current combination of medication and psychological therapy | 11 | 2.91 (0.34) |
| Past medication | 27 | 2.89 (0.22) |
| Past psychological therapy | 27 | 3.22 (0.23) |
| Past combination of medication and psychological therapy | 27 | 3.11 (0.23) |
Health-care professionals
Data from 86 health-care professionals who completed the online survey were analysed. As shown in Table 10, approximately two-thirds of health-care professionals were in their 40s or 50s (n = 59, 69%). The majority self-identified as female (n = 65, 76%) and white/white British (n = 74, 86%) and worked in urban areas (n = 76, 89%), primarily in the South West, South East and London regions of England (n = 64, 74%). The most common clinical professions were psychology (n = 27, 32%) and psychiatry (n = 24, 28%), and medicine for older people; social work and occupational therapy were the least represented professions (total n = 4, 5%). There was wide variation in the level of profession, although 60% of health-care professionals (n = 49) were in senior positions (e.g. GP, consultant, grade 8). Correspondingly, 51% of health-care professionals (n = 43) had been qualified for ≥ 16 years. The majority worked in secondary care (n = 58, 70%) and in the NHS (n = 76, 91%).
| Variable | N (missing n, %) | n (%) |
|---|---|---|
| Age (years) | 86 (0, 0) | |
| < 20 | 0 (0) | |
| 20–29 | 7 (8) | |
| 30–39 | 20 (23) | |
| 40–49 | 31 (36) | |
| 50–59 | 28 (33) | |
| 60–69 | 0 (0) | |
| ≥ 70 | 0 (0) | |
| Prefer not to say | 0 (0) | |
| Sex | 86 (0, 0) | |
| Male | 20 (23) | |
| Female | 65 (76) | |
| Prefer not to say | 1 (1) | |
| Ethnicity | 86 (0, 0) | |
| Asian/Asian British | 6 (7) | |
| Black/black British | 0 (0) | |
| Mixed | 4 (5) | |
| White/white British | 74 (86) | |
| Other | 1 (1) | |
| Prefer not to say | 1 (1) | |
| Geographical area | 86 (0, 0) | |
| Urban | 76 (89) | |
| Rural | 1 (1) | |
| Prefer not to say/no response | 9 (11) | |
| Region of the UK | 86 (0, 0) | |
| Englanda | 74 (86) | |
| East Midlands | 2 (2) | |
| East of England | 2 (2) | |
| London | 11 (13) | |
| North East | 0 (0) | |
| North West | 3 (4) | |
| South East | 19 (22) | |
| South West | 34 (40) | |
| West Midlands | 2 (2) | |
| Yorkshire and the Humber | 1 (1) | |
| Northern Ireland | 1 (1) | |
| Scotland | 1 (1) | |
| Wales | 1 (1) | |
| Prefer not to say/no response | 9 (11) | |
| Clinical profession | 85 (1, 1) | |
| General practice | 13 (15) | |
| Medicine for older people | 1 (1) | |
| Nursing | 12 (14) | |
| Psychiatry | 24 (28) | |
| Psychology | 27 (32) | |
| Occupational therapy | 2 (2) | |
| Social work | 1 (1) | |
| Other | 5 (6) | |
| Level of profession | 82 (4, 5) | |
| Bands 2–5 | 6 (7) | |
| Band 6 | 9 (11) | |
| Band 7 | 12 (15) | |
| Band 8 | 18 (22) | |
| GP | 13 (16) | |
| Consultant | 18 (22) | |
| Other | 6 (7) | |
| Years since qualifying as a health-care professional | 84 (2, 2) | |
| < 1 | 2 (2) | |
| 1–5 | 9 (11) | |
| 6–10 | 9 (11) | |
| 11–15 | 21 (25) | |
| 16–20 | 16 (19) | |
| ≥ 21 | 27 (32) | |
| Health-care setting | ||
| Type | 84 (2, 2) | |
| NHS | 76 (91) | |
| Private | 6 (7) | |
| Other | 2 (2) | |
| Level | 83 (3, 3) | |
| Primary care | 22 (27) | |
| Secondary care | 58 (70) | |
| Tertiary care | 3 (4) | |
| Other | 0 (0) | |
Table 11 presents data on the reported treatment of older people with TR-GAD. Health-care professionals estimated that, as a percentage of all people seen per month, an average of just over three-quarters (78.7, SD 29.1) were aged ≥ 65. However, among these, health-care professionals estimated that only one-fifth had TR-GAD or clinically significant chronic anxiety (20.6, SD 20.1). In terms of the types of treatment typically offered or referred for in this population, the most common types of pharmacotherapy were antidepressants (n = 55, 64%) and anti-epileptics (n = 26, 30%), with CBT (n = 66, 77%), mindfulness-based therapy (n = 46, 54%) and relaxation therapy (n = 42, 49%) being the most common types of psychological therapy. Just over half of health-care professionals reported typically offering or referring for pharmacotherapy ‘a lot of the time’ or ‘always’ (n = 40, 52%), which rose to 65% (n = 50) for psychological therapy. The most commonly endorsed reasons for not offering or referring for pharmacotherapy were patient preference (n = 53, 62%), side effects (n = 40, 47%) and comorbid health problems (n = 39, 45%). Patient preference was the most common reason for not offering or referring for psychological therapy (n = 52, 61%), followed by a lack of availability of this type of treatment (n = 30, 35%).
| Variable | N (missing n, %) | n (%) | Mean (SD) |
|---|---|---|---|
| Percentage of all people seen per month who are aged ≥ 65 years | 81 (5, 6) | 78.7 (29.1) | |
| Percentage of all people seen per month who are aged ≥ 65 years with TR-GAD | 73 (13, 15) | 20.6 (20.1) | |
| Type of treatment typically offered or referred for | 86 (0, 0) | ||
| Antidepressants | 55 (64) | ||
| Anxiolytics (e.g. buspirone) | 9 (11) | ||
| Sedatives (e.g. benzodiazepines) | 19 (22) | ||
| Hypnotics (e.g. Z drugs) | 14 (16) | ||
| Anti-epileptics (e.g. pregabalin) | 26 (30) | ||
| Antipsychotics (e.g. olanzapine) | 19 (22) | ||
| Antihistamines (e.g. hydroxyzine) | 0 (0) | ||
| CBT | 66 (77) | ||
| Relaxation therapy | 42 (49) | ||
| Mindfulness-based therapy | 46 (54) | ||
| Psychodynamic psychotherapy | 17 (20) | ||
| Counselling | 27 (31) | ||
| Signpost to other services | 40 (47) | ||
| Other | 17 (20) | ||
| Typical frequency of offers (or referrals) for pharmacotherapy | 77 (9, 11) | ||
| Always | 11 (14) | ||
| A lot of the time | 29 (38) | ||
| About half of the time | 5 (7) | ||
| Some of the time | 16 (21) | ||
| Never | 3 (4) | ||
| Not applicable for my clinical profession | 13 (17) | ||
| Other | 0 (0) | ||
| Typical frequency of offers (or referrals) for psychological therapy | 77 (9, 11) | ||
| Always | 20 (26) | ||
| A lot of the time | 30 (39) | ||
| About half of the time | 8 (10) | ||
| Some of the time | 16 (21) | ||
| Never | 1 (1) | ||
| Not applicable for my clinical profession | 2 (3) | ||
| Other | 0 (0) | ||
| Factors that typically stop offers (or referrals) for pharmacotherapy | 86 (0, 0) | ||
| Comorbid health problems | 39 (45) | ||
| Side effects | 40 (47) | ||
| Patient preference | 53 (62) | ||
| Personal clinical experience | 12 (14) | ||
| I do not think it would work | 12 (14) | ||
| Not applicable for my clinical profession | 16 (19) | ||
| Other | 4 (5) | ||
| Factors that typically stop offers (or referrals) for psychotherapy | 86 (0, 0) | ||
| Comorbid health problems | 8 (9) | ||
| Patient preference | 52 (61) | ||
| Personal clinical experience | 9 (11) | ||
| Lack of availability of psychological therapy | 30 (35) | ||
| I do not think it would work | 4 (5) | ||
| Not applicable for my clinical profession | 2 (2) | ||
| Other | 9 (11) |
Ratings of the perceived helpfulness of treatments for older people with TR-GAD or clinically significant chronic anxiety by health-care professionals are shown in Table 12. There was some variation in the median ratings across pharmacotherapy and psychological therapy, with a possible trend for the majority of pharmacotherapy to be perceived as less helpful than psychological therapy. Data were submitted to a one-way ANOVA, with type of treatment as a within-subjects variable, to statistically compare ratings across different types of treatment.
| Perceived helpfulnessa | N (missing n, %) [‘I have no opinion’ n, %] | Median (IQR) |
|---|---|---|
| Pharmacotherapy | ||
| Antidepressants | 65 (11, 13) [10, 12] | 3.0 (2.0–3.0) |
| Anti-epileptics (e.g. pregabalin) | 49 (11, 13) [26, 30] | 2.0 (1.0–3.0) |
| Anxiolytics (e.g. buspirone) | 56 (11, 13) [19, 22] | 2.0 (2.0–3.0) |
| Antipsychotics (e.g. olanzapine) | 53 (11, 13) [22, 26] | 2.0 (1.0–3.0) |
| Sedatives (e.g. benzodiazepines) | 63 (11, 13) [12, 14] | 2.0 (2.0–2.0) |
| Hypnotics (e.g. Z drugs) | 59 (11, 13) [16, 19] | 2.0 (1.0–2.0) |
| Antihistamines (e.g. hydroxyzine) | 44 (11, 13) [31, 36] | 1.0 (1.0–2.0) |
| Psychological therapy | ||
| CBT | 73 (11, 13) [2, 2] | 4.0 (3.0–4.0) |
| Mindfulness-based therapy | 65 (11, 13) [10, 12] | 3.0 (3.0–4.0) |
| Relaxation therapy | 69 (11, 13) [6, 7] | 3.0 (2.5–4.0) |
| Psychodynamic psychotherapy | 51 (11, 13) [24, 28] | 3.0 (2.0–4.0) |
| Counselling | 65 (11, 13) [10, 12] | 3.0 (2.0–3.0) |
It was possible to include data from only 27 health-care professionals owing to missing data or no ratings being given (i.e. an ‘I have no opinion’ response). Mauchly’s test of sphericity was significant (p < 0.05) and, therefore, Greenhouse–Geiser-corrected degrees of freedom and p-values are reported. There was a statistically significant main effect of the type of treatment [F(5.6,146.4) = 22.39, MSE = 23.73, p < 0.0005, ηp2 = 0.46]. Post hoc Bonferroni-adjusted pairwise comparisons showed that CBT, mindfulness-based therapy and relaxation therapy were rated as more helpful than all medications excluding antidepressants (Table 13). In addition, CBT was rated as more helpful than counselling. Antidepressants were rated as more helpful than all other medications excluding anxiolytics. Medications with potentially sedative effects (sedatives, hypnotics and antihistamines) were rated the least helpful of all treatments.
| Perceived helpfulnessa | Mean (SE) | Bonferroni-adjusted pairwise comparisonsb |
|---|---|---|
| 1. CBT | 3.56 (0.15) | 1 > 6, 7, 8, 9, 10, 11, 12 |
| 2. Mindfulness-based therapy | 3.52 (0.15) | 2 > 7, 8, 9, 10, 11, 12 |
| 3. Relaxation therapy | 3.19 (0.13) | 3 > 7, 8, 9, 10, 11, 12 |
| 4. Psychodynamic psychotherapy | 2.96 (0.18) | 4 > 11, 12 |
| 5. Antidepressants | 2.93 (0.15) | 5 > 7, 9, 10, 11, 12 |
| 6. Counselling | 2.85 (0.15) | 6 > 11, 12 and 6 < 1 |
| 7. Anti-epileptics (e.g. pregabalin) | 2.30 (0.22) | 7 > 12 and 7 < 1, 2, 3, 5 |
| 8. Anxiolytics (e.g. buspirone) | 2.30 (0.18) | 8 > 12 and 8 < 1, 2, 3 |
| 9. Antipsychotics (e.g. olanzapine) | 2.19 (0.21) | 9 > 12 and 9 < 1, 2, 3, 5 |
| 10. Sedatives (e.g. benzodiazepines) | 2.11 (0.19) | 10 < 1, 2, 3, 5 |
| 11. Hypnotics (e.g. Z drugs) | 1.82 (0.14) | 11 < 1, 2, 3, 4, 5, 6 |
| 12. Antihistamines (e.g. hydroxyzine) | 1.44 (0.11) | 12 < 1, 2, 3, 4, 5, 6, 7, 8, 9 |
Discussion
The aim of this study was to examine usual care that is offered to and received by older people with TR-GAD in order to assist in clarifying the content of a best comparator for a future substantive trial.
Main findings with respect to usual care
Approximately half of service users (n = 28, 48%) reported currently receiving pharmacotherapy, with antidepressants being the most commonly reported (n = 28). By contrast, only one-quarter of service users (n = 13, 24%) reported currently receiving psychological therapy, with counselling being most commonly reported (n = 4, 31%). A substantial proportion of service users (n = 23, 42%) reported not receiving any form of current pharmacotherapy or psychological therapy, despite the mean GAD-7 total score being in the moderate range (13.3 points, SD 4.0 points) for this subsample.
To be included in these analyses, service users had to have received or been offered at least two types of treatment (pharmacotherapy and/or psychological therapy) for worrying in the past. Again, the most common types of pharmacotherapy were antidepressants (n = 24) and sedatives (e.g. benzodiazepines, n = 19), whereas the most common forms of psychological therapy were CBT (n = 20) and counselling (n = 9). Approximately one-third of service users reported refusing pharmacotherapy in the past (n = 17, 30%), whereas the number of service users who reported refusing psychological therapy in the past was small (n = 4, 8%).
Health-care professionals estimated that, on average, only one-fifth of older service users (i.e. those aged ≥ 65 years) whom they saw each month were experiencing TR-GAD or clinically significant chronic anxiety. They reported that the most common types of pharmacotherapy they offered or referred for were antidepressants (n = 55, 64%) and anti-epileptics (n = 26, 30%). CBT, mindfulness-based therapy and relaxation therapy were the most common types of psychological therapy that they offered or referred for (n = 66, 77%; n = 46, 54%; and n = 42, 49%, respectively). Patient preference was the most common reason for not offering or referring for pharmacotherapy or psychological therapy (n = 53, 62%; and n = 52, 61%, respectively).
Service users rated different types of pharmacotherapy and psychological therapy as equally helpful, both currently and in the past, with mean ratings in the slightly to moderately helpful range. By contrast, health-care professionals rated CBT, mindfulness-based therapy and relaxation therapy as more helpful than all medications excluding antidepressants, with mean ratings in the moderately helpful range for these forms of psychotherapy. This is consistent with the types of treatment that health-care professionals reported most frequently offering or referring for. Medications with potentially sedative effects (i.e. sedatives, hypnotics and antihistamines) were rated the least helpful of all treatments, with mean scores in the not at all helpful to slightly helpful range.
Research implications
There are a number of implications with respect to study design that arise from the survey findings. The first relates to the choice of comparator group for a future substantive trial of ACT. There are three types of comparators that could be used in such a trial: a non-active control arm (such as treatment as usual), an active control arm (such as a supportive talking control) or an alternative treatment. Non-active controls do not control for non-specific factors, such as therapist time and social attention, whereas active controls do. However, active controls do not permit comparisons with what the NHS is currently offering, given that active controls are not usually part of treatment as usual.
If a non-active control (such as treatment as usual) was used then it might be expected that one-quarter of participants in the treatment-as-usual arm would receive psychological therapy, which might dilute any treatment effect. On the plus side, the results of the survey suggest that very few would be offered or referred for ACT. However, the fact that treatment as usual does not typically include access to psychological therapy might lead to higher withdrawal rates in a non-active control arm owing to resentful demoralisation (i.e. participants dropping out because they wanted to be allocated to the intervention arm). One way of overcoming this might be to offer access to study materials after a final follow-up outcome assessment. Possibly in opposition to the notion of resentful demoralisation is the observation that some participants in our survey reported refusing pharmacotherapy or psychological therapy in the past (n = 17, 30%; and n = 4, 8%, respectively). Participants such as these may actually prefer to be in a non-active control arm, although whether or not they would even agree to be involved in a treatment trial in the first place is, of course, debatable.
On the other hand, if an active control (such as a supportive talking control) was used then this not only might serve as an incentive to participate in the trial but might also reduce the chances of withdrawal due to resentful demoralisation. Supporting this, no differences in drop-out rate were found between CBT and talking–treatment control arms in a RCT of CBT for older people with depression. 87 An additional bonus of this would be the increased scientific rigour that comes with controlling for non-specific factors such as therapist time and social attention. However, research costs would be increased because provision of a supportive talking control would constitute a research activity rather than an excess treatment cost. Furthermore, a larger sample size would be required to detect a treatment effect, and such a trial would not be able to answer the question of whether or not the intervention was better than treatment as usual.
Of course, one way of overcoming these issues might be to include both a non-active control (such as treatment as usual) and an active control (such as a supportive talking control) in a future substantive trial of ACT. This study design was used in a RCT of CBT for older people with depression. 87 However, this would further increase research costs, and necessitate an even larger sample size to randomly allocate a sufficient number of participants to each arm. An alternative to this would be to conduct a non-inferiority RCT in which the equivalence of ACT to current front-line treatment would be investigated. The feasibility of such an approach has been demonstrated in a non-inferiority RCT of ACT compared with CBT in working-age people with mixed anxiety disorders. 88 The results of our survey with respect to perceived helpfulness of treatments suggest that an appropriate comparison condition would be psychological therapy (such as CBT) rather than pharmacotherapy.
The second implication of the survey findings relates to possible inclusion criteria in a future substantive trial. The necessity of a medication dose stabilisation period (e.g. 4 weeks) is highlighted by the fact that approximately half of service users in this study were currently receiving pharmacotherapy. Furthermore, the fact that only one-quarter of service users reported currently receiving psychological therapy suggests that the standard procedure of asking participants to refrain from receiving other concurrent formal psychological therapy during the receipt of ACT would not be problematic in this population. However, it should be noted that these findings may be unrepresentative and may simply reflect the type of participants who completed this online survey (e.g. those who are interested in actively pursuing treatment for TR-GAD).
The third implication of the survey findings relates to recruitment rates. Health-care professionals estimated that, on average, only one-fifth of older service users (i.e. aged ≥ 65 years) who they saw each month were experiencing TR-GAD or clinically significant chronic anxiety. Health-care professionals reported working in a range of services in primary and secondary care settings, with the majority working in secondary care (n = 58, 70%). It might be expected that those working in secondary care would tend to see more older people with TR-GAD or clinically significant chronic anxiety than those in other settings. However, even in this subgroup of health-care professionals, 48% estimated that they were seeing only 0–10% of older service users with TR-GAD or clinically significant chronic anxiety each month, with 36% estimating this to be 11–30%. Such low identification rates may be expected given that GAD is a frequently undiagnosed condition in clinical practice, often being misdiagnosed as major depressive disorder with comorbid anxiety or ‘mixed anxiety and depression’ rather than GAD. 2,89 This suggests that referring clinicians in a future RCT may need additional support to help identify potential participants with TR-GAD on their caseloads.
Finally, the fact that the survey was not able to examine usual care for older people with TR-GAD across the UK as well as we had hoped suggests that an online survey might be useful in the site identification/set-up process of a future substantive trial. This could be used to (1) ascertain whether or not usual care provision differs across Clinical Commissioning Groups, (2) assess the degree to which access to ACT is routinely available at specific sites and (3) explore whether or not any routinely available services might conflict with eligibility criteria.
Strengths and limitations
This is the first study, to our knowledge, to explore the usual care that is offered to and received by older people with current symptoms of GAD and a treatment history suggestive of TR-GAD in the UK. It would appear that usual care is quite limited, focusing mainly on pharmacotherapy, and, on average, is perceived as being only slightly to moderately helpful. Therefore, it provides some indication of what usual care might look like in a larger-scale RCT of ACT for older people with TR-GAD. Furthermore, care was taken to ensure that the survey used terminology that older people with TR-GAD could understand and identify with. For example, the term ‘difficulties with long-term worrying or your nerves’ was used rather than ‘generalised anxiety disorder’. This was deemed necessary given that GAD is a frequently undiagnosed condition in clinical practice, as noted in Research implications, and many may not have identified with the formal diagnostic label.
However, there are a number of limitations in the current study, which mean that findings should be interpreted with caution. First, the majority of service users self-identified as female (n = 55, 95%) and white/white British (n = 54, 93%) and resided in urban areas (n = 50, 86%) in England, primarily London (n = 34, 59%). Being female is one of the known risk factors for anxiety disorders in older people90 and, therefore, a higher proportion of female service users is to be expected. Similarly, a higher proportion of people living in urban locations is to be expected given that 83% of the UK population live in urban locations. 91 However, it does mean that findings cannot be generalised to men, those from ethnic minorities or those living in rural locations or geographical locations other than London. Furthermore, it may not be possible to generalise findings to service users who do not have access to the internet or a personal computer (PC) given that data were collected via an online survey. Finally, as noted in Research implications, these findings may be representative of the type of participants who completed this online survey (e.g. those who are interested in actively pursuing treatment for TR-GAD). This suggests that a larger-scale investigation of usual care in men, those living in rural settings, those living in geographical locations other than London, those from ethnic minorities and those without access to the internet or a PC is warranted. A similar issue with representativeness was seen with health-care professionals, with the majority self-identifying as female (n = 65, 76%) and white/white British (n = 74, 86%), in their 40s and 50s (n = 59, 69%) and working in urban areas (n = 76, 89%) in southern regions of England (n = 64, 74%). This supports the notion that a larger-scale investigation of usual care offered by health-care professionals and received by service users in more diverse populations is warranted.
Second, the sample size with respect to those with current symptoms of GAD and a treatment history suggestive of TR-GAD (n = 58, 48% of the total data set) and health-care professionals (n = 86) was relatively small, which may have increased the likelihood of a type II error (i.e. reporting a false-negative finding). Appropriately resourcing the study to enable recruitment via GP surgeries and CMHTs across the UK and to enable the provision of a postal survey may have increased recruitment rates. Contacting Clinical Commissioning Groups across the UK may have also increased recruitment rates of health-care professionals.
Third, it was not possible to conduct a formal assessment of GAD, nor was it possible to verify the accuracy of self-reported information with respect to treatment history, etc. Furthermore, single-item screening questions were used to assess the presence of comorbid mental health conditions. Thus, some service users may not have actually been experiencing TR-GAD and some information may have been inaccurate, which may have contaminated the findings. Some confidence that service users were experiencing TR-GAD can be gained from the fact that nearly half of service users (43%) reported difficulties with long-term worrying for ≥ 30 years, 75% of service users scored in the moderate to severe range on the GAD-7 and the mean number of comorbid mental health complaints was 4.1, with symptoms of depression being the most common (91%). This fits what is known about the clinical picture of GAD in older people. For example, psychiatric comorbidity is known to be common in GAD,2 and the co-occurrence of depression and GAD is associated with greater chronicity92 as well as poorer treatment responsiveness and higher severity of GAD among older people. 93
Finally, the use of subjective rather than objective ratings of the helpfulness of treatments for worrying may have introduced a degree of variability in responses from both service users and health-care professionals. This is because subjective interpretations of ‘helpfulness’ may differ across individuals. Defining what was meant by ‘helpfulness’ may have helped to reduce variability in responses.
Conclusions
This was a small-scale survey of service users’ and health-care professionals’ views and experiences of what constitutes usual care for TR-GAD in older people. Pharmacotherapy, most commonly in the form of antidepressants, was reported by approximately half of service users, whereas psychotherapy was reported by only one-quarter of them. By contrast, 42% of service users reported not receiving any form of current pharmacotherapy or psychological therapy. The fact that service users and health-care professionals rated the majority of treatments as being in the slightly helpful to moderately helpful range, on average, suggests that there is room for improving the perceived helpfulness of treatments offered to older people with TR-GAD.
Chapter 4 Uncontrolled feasibility study: quantitative data
Parts of this chapter have been reported in Gould et al. 94 This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
Introduction
Chapter 2 described the development of an ACT intervention (comprising a therapist manual, accompanying client workbook and training package) specifically for older people with TR-GAD. We assessed the acceptability and feasibility of this newly developed intervention in an uncontrolled feasibility study in phase 2 of the FACTOID study. The objectives were to:
-
obtain quantitative estimates of the acceptability and feasibility of the newly developed intervention and study methods in an open, uncontrolled feasibility study
-
clarify key study design parameters for a future substantive trial of clinical effectiveness (e.g. the choice of comparator and outcome measures, and the number of recruitment sites based on referral/recruitment/attrition rates).
Methods
All reporting is in accordance with the Consolidated Standards of Reporting Trials (CONSORT) extension for randomised pilot and feasibility trials,95 where possible, as this was not a randomised trial, and the Template for Intervention Description and Replication (TIDieR) guidelines. 96 CONSORT and TIDieR checklists are provided in Appendices 3 and 4.
Design
This was an open, uncontrolled feasibility study that employed both quantitative and qualitative methodological approaches.
Participants
Participants were included in the study if:
-
They were aged ≥ 65 years with a primary diagnosis of GAD as determined by the Mini-International Neuropsychiatric Interview (MINI)97 and the Structured Clinical Interview for DSM-IV Axis II Disorders. 65
-
They had failed to respond to treatment in steps 1–3 of the stepped-care approach for GAD (i.e. 6 weeks of an age-appropriate dose of antidepressant medication or a course of individual psychotherapy), failed to tolerate this treatment or had previously refused this treatment and were still symptomatic. When determining whether or not a person had failed to respond to treatment for GAD, if they had remitted and then relapsed in relation to GAD then treatment received prior to remission was not considered when deciding whether or not they currently met criteria for treatment resistance.
-
They were living in the community.
-
They were able to provide informed, written consent.
-
They had sufficient understanding of English to enable them to engage in ACT and complete patient-reported outcome measures.
-
They had not participated in phase 1 of the study (i.e. qualitative interviews focused on development of the intervention).
-
There was a minimum of a 1-month interval between previous psychotherapy and engagement in ACT.
Participants were not able to participate in the study if:
-
they had a diagnosis of dementia
-
they had a total score of < 25 points on the SMMSE66
-
they were currently receiving ongoing psychotherapy or were unwilling to refrain from engaging in other forms of psychotherapy during the receipt of ACT
-
they were expressing suicidal ideation with active intent (because an inpatient admission would have been more appropriate management)
-
there were other medical or psychosocial factors that could compromise full study participation, such as imminently life-limiting illness or severe sensory deficits (e.g. blindness)
-
they were diagnosed with intellectual disabilities.
It is common to specify a psychotropic drug stabilisation period (e.g. a stable dose for at least 2 months) as one of the inclusion criteria in psychotherapy studies to control for the potential confound of pharmacotherapy on mental well-being. However, this was not included in the current study as it was thought that this would have a significantly negative impact on recruitment, as many potential participants would be either ineligible or unwilling to wait for drug stabilisation to occur before receiving psychotherapy. Service users are frequently referred to CMHTs for medication reviews, which usually entails switching to another psychotropic drug, augmenting current treatment with another psychotropic drug or changing psychotropic drug dosages, and so it can take a number of months before a stable dose is achieved. Instead of including a psychotropic drug stabilisation period, all drug use was monitored during the course of therapy and accounted for in subsequent data analyses, where necessary.
Setting
Potential participants were recruited from a number of sources:
-
referrals from organisations within primary care settings, including GP surgeries in the North Thames Clinical Research Network, South London Clinical Research Network and IAPTs
-
referrals from secondary care settings, including CMHTs for older people in Camden and Islington NHS Foundation Trust; South London and Maudsley NHS Foundation Trust; Barnet, Enfield and Haringey Mental Health NHS Trust; and North East London NHS Foundation Trust
-
self-referral from the community.
Recruitment procedures
Potentially eligible participants from primary and secondary care settings were identified and approached about the study in one of four ways. First, clinicians from GP surgeries, IAPTs and CMHTs identified and approached potentially eligible participants and sought verbal consent for members of the research team to contact them. Older people who meet diagnostic criteria for GAD are frequently referred to IAPTs and CMHTs with a diagnosis of major depression and comorbid anxiety rather than GAD. Consequently, clinicians in these services were asked to screen service users who were referred with a diagnosis of major depression and comorbid anxiety for GAD using the GAD-7. 82 For any service user scoring ≥ 11 on this scale (corresponding to moderate or severe GAD), clinicians asked the service user which symptoms were most distressing, severe or of most concern to them. If symptoms of GAD were most distressing, most severe or of most concern to them, or if symptoms of GAD and depression were equally problematic, then the clinician discussed the study with them and sought verbal consent for members of the research team to contact them. If symptoms of depression were most distressing, most severe or of most concern to them then the clinician referred them for appropriate treatment.
Second, potentially eligible participants were identified and approached through local ‘consent for research contact’ procedures. Any potentially eligible participants who had previously agreed to being contacted about research were identified by clinicians and then contacted by band 5 clinicians.
Third, nurses or GPs in participating GP practices (i.e. those who had expressed an interest in participating in research through primary care research networks and local contacts) conducted searches of their electronic medical records to identify those with diagnoses of GAD and other chronic anxiety states using a broad list of Read codes, a hierarchical coding system used to record clinical information such as diagnoses. 98 Once potentially eligible participants were identified through electronic medical record searches, nurses or GPs in participating GP practices approached them and sought verbal consent for members of the research team to contact them.
Finally, leaflets and advertisements were distributed in GP surgeries and other community settings, such as luncheon clubs and activity groups for older people, to facilitate self-referral. Leaflets included the GAD-7,82 a brief seven-item screening tool, and potential participants were invited to contact the research team if they scored ≥ 11 points on this scale (corresponding to moderate or severe GAD and above). In addition, the study was promoted through presentations at local community groups (e.g. luncheon clubs and activity groups) and team meetings in IAPTs and CMHTs.
Once potentially eligible participants were identified and verbal consent for contact was obtained, eligible participants were contacted by telephone by a member of the research team. The study was described to them and any questions or concerns about it were discussed. If they expressed an interest in participating in the study then, with their verbal consent, they were sent an information sheet and invitation letter. They were then contacted a minimum of 48 hours later by a member of the research team to determine whether or not they were still interested in participating in the study. If they were, then an appointment for a screening interview (lasting 1.5 hours) was arranged with a member of the research team. Written informed consent was sought from potentially eligible participants by a band 5 clinician, research nurse or research assistant during this screening interview, after which eligibility for inclusion in the study was determined.
Intervention
The intervention comprised up to 16 individual (i.e. one-to-one) sessions of ACT, delivered in person, with each session lasting up to 1 hour. This was consistent with previous recommendations of 12–16 sessions of ACT for older people,43,59 as well as with step 3 of the stepped-care approach for GAD. 15 Step 3 states that CBT or applied relaxation should usually consist of 12–15 sessions, with more sessions being offered if clinically required. The provision of 16 sessions allowed therapists to work at a slower pace, which is a recommended compensatory strategy for age-related cognitive changes in memory, attention and processing speed when working with older people. 78 There was a phased ending to the sessions, such that they were weekly for the first 14 sessions and then fortnightly thereafter, as some older people experience difficulties when therapy ends abruptly. An individual, rather than group, therapy approach was used because of the anticipated complexity of each individual’s presenting problems. The intervention was designed so that it could be delivered in the GP surgery, outpatient clinic or service user’s home (for those who were unable to travel because of physical and/or mental health issues). The location of the intervention delivery depended on participant preference and service restrictions. The intervention was tailored to the needs of older people with TR-GAD following the findings of qualitative interviews outlined in Chapter 2, as well as previous suggestions. 43 Table 14 and Figure 1, and Table 15 and Figure 2, list the outline of sessions, together with accompanying home practice tasks. A therapist manual and accompanying client workbook were developed to support the delivery of the intervention (available on request from the corresponding author).
| Session(s) | Focus of the session |
|---|---|
| 1 | Assessment of current issues and aims of therapy; introduction to ACT; psychoeducation about GAD |
| 2 | Identifying values (lifetime achievement award, values list or values questions) |
| 3 | Exploring how you would like your life to be (pieces of the pie or life compass) |
| 4 | Exploring workability (what strategies have been tried; how each of the strategies has worked in the short and long term; the costs of control) |
| 5 | Control is the problem (chocolate cake exercise; polygraph machine or what are the numbers?; Chinese finger trap exercise) |
| 6–15a | See Figure 1 |
| 16 | Review skills and concepts, and ways of handling symptoms in the future |
FIGURE 1.
An outline of sessions 6–15, together with associated ACT metaphors and exercises. CWTPM, contact with the present moment.
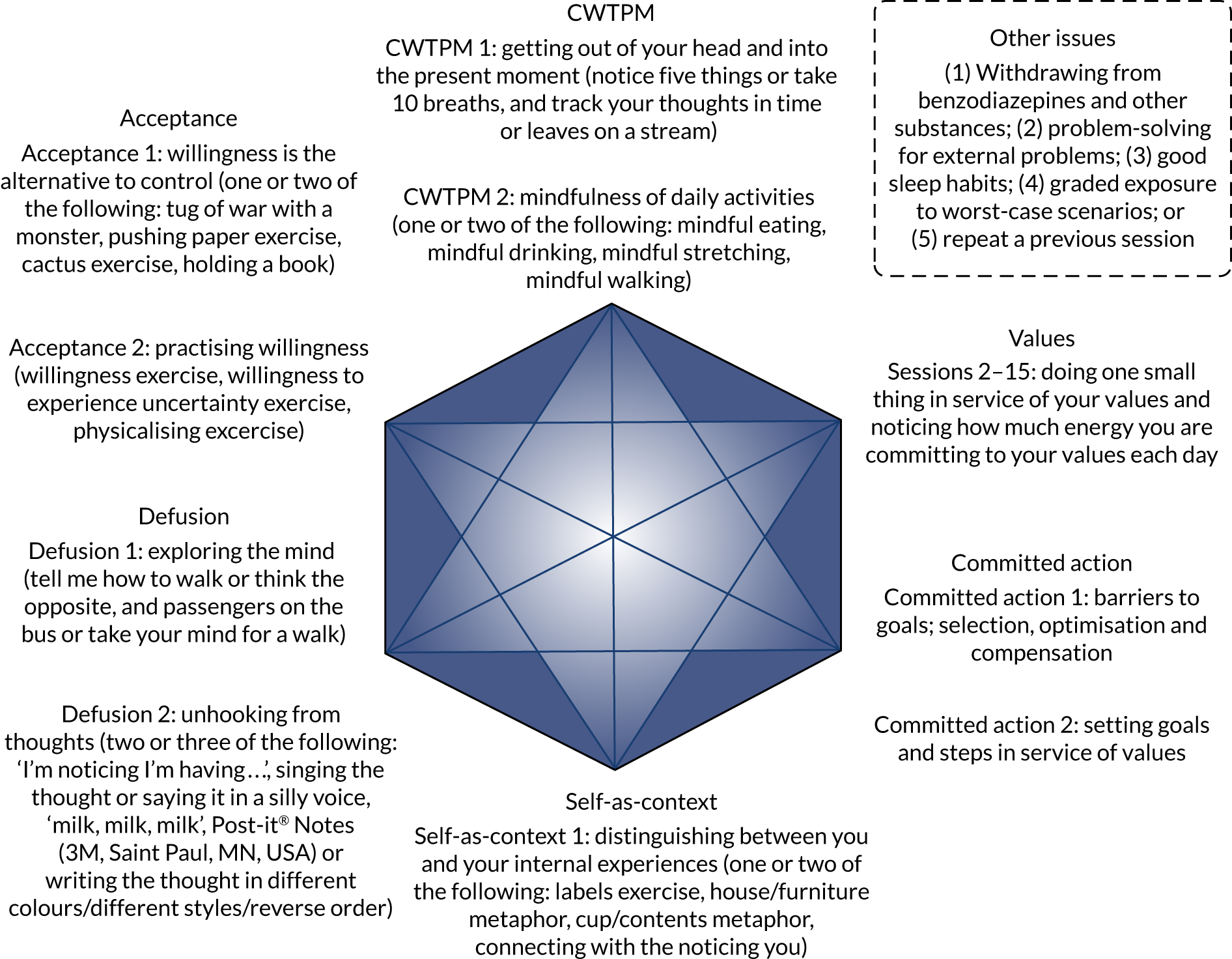
| Session(s) | Home practice |
|---|---|
| 1 | Read a leaflet about chronic worry; notice the things that you are doing to try to deal with the worry and anxiety over the next week |
| 2a | Notice how you are acting in line with your values, notice how much energy you are committing to your values each day, and notice how much energy you are committing to your worry and anxiety each day |
| 3a | Notice how you are acting in line with your values, notice how much energy you are committing to your values each day, and notice how much energy you are committing to your worry and anxiety each day |
| 4a | Notice the things that you are doing to try to avoid, get rid of, control, change or reduce the worry and anxiety over the next week, and whether or not they take you towards or away from your values |
| 5a | Notice the painful or unwanted thoughts, feelings and sensations that you have been struggling with and how well they have worked for you, and whether or not they take you towards or away from your values |
| 6–15a,b | See Figure 2 |
| 16 | N/A |
FIGURE 2.
An outline of the home practice for sessions 6–15, together with associated ACT metaphors and exercises. CWTPM, contact with the present moment.
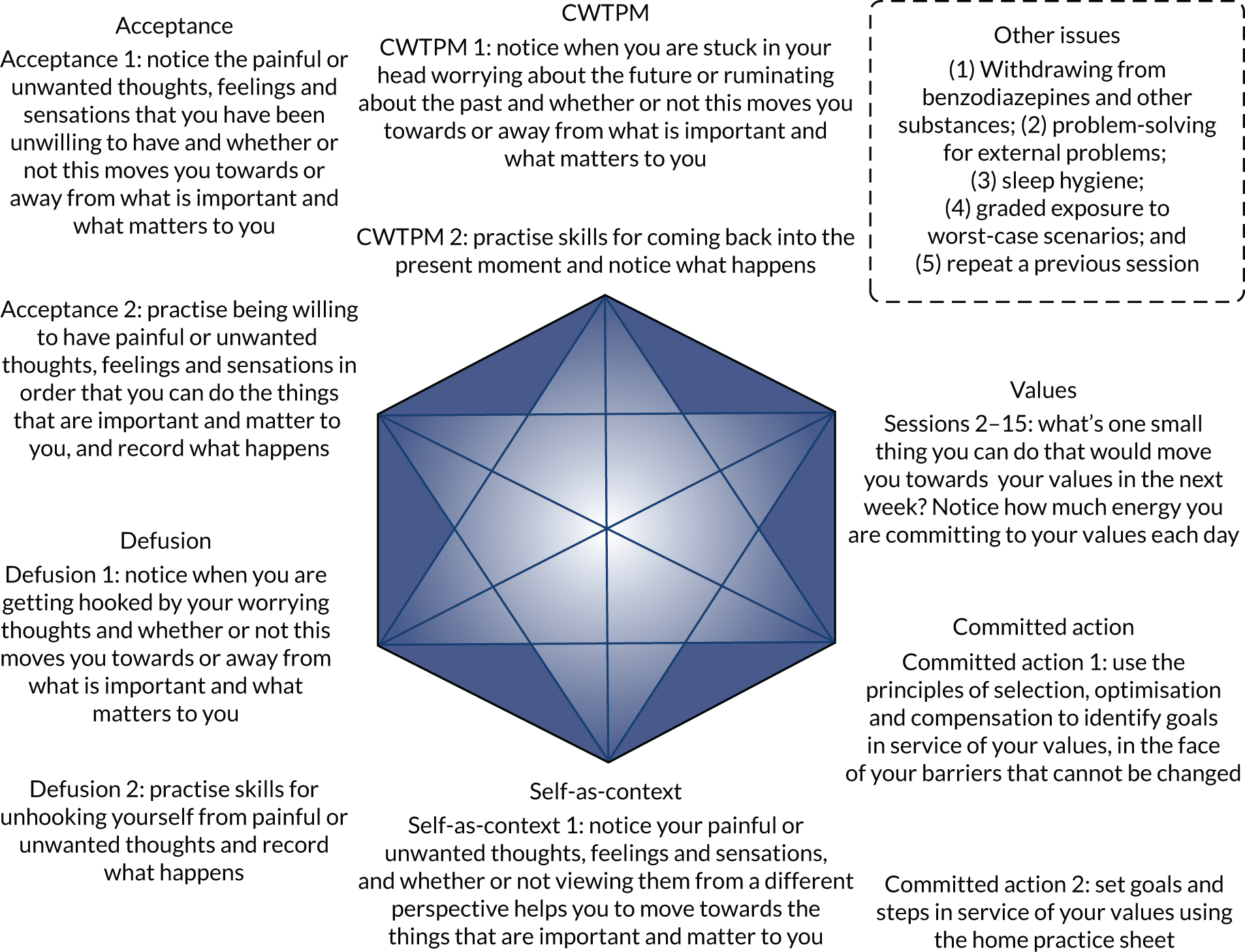
As can be seen in Table 14, the intervention addressed the six core ACT processes, in addition to exploring the workability of current strategies used to avoid, change or get rid of anxiety and worry. Each session was associated with a specific set of skills, metaphors, experiential exercises and home practice tasks designed to increase psychological flexibility. All sessions, bar the first and last sessions, followed the same structure. Sessions commenced with a short mindfulness exercise that was designed to increase awareness of the present moment, because some older people may experience difficulties in recognising, describing, observing or being aware of their internal states. 43 This was followed by brief ratings of worry, the struggle with worry and the degree to which the participant had been living a rich, full and meaningful life in the past week to help monitor progress. The presence of suicidal ideation (as well as any plans, intent and protective factors, if necessary) was also assessed at this point. Following this, there was a recap of the concepts and issues discussed in the previous session, as well as a discussion of the participant’s experience of the home practice. The rest of the session was spent addressing the target ACT process for that week’s session. The session ended with a summary of what had been discussed in the session, as well as a discussion of that week’s home practice.
The intervention was manualised, with the order and content being pre-determined for sessions 1–5 and the content alone being pre-determined for sessions 6–16. Consistent with the emphasis on psychological flexibility in ACT interventions, therapists had flexibility in deciding the order of delivery of sessions 6–16. In addition, they had a choice about which and how many metaphors and experiential exercises would be delivered in each session. For example, therapists may have been given the choice of three experiential exercises in a session, and may have been asked to deliver one or two of them. This meant that the pace of the sessions could be modified, depending on the needs and abilities of the individual client. Therapists also had flexibility in deciding the content of the ‘Other issues’ session, depending on the client’s needs and goals. The focus of this session could be on (1) withdrawing from prescribed or illicit substances (e.g. benzodiazepines); (2) problem-solving for external problems (as opposed to internal problems such as difficult thoughts, feelings and sensations); (3) establishing good sleep habits; (4) graded exposure; or (5) repeating a previous session (e.g. a session from which it was felt that the client would benefit from further practice). Overall, having some aspects of the sessions that were predetermined and others that were not gave therapists sufficient room to respond flexibly to clients’ idiosyncratic presentations while helping them to feel sufficiently supported to deliver the intervention. Feeling sufficiently supported was particularly important as the majority of therapists were new to ACT, as detailed below.
Training
Therapists initially attended a 4-day experientially based ACT training workshop, which was developed and delivered by members of the research team with training and experience in delivering ACT (MS and RG). There is no formal training pathway for ACT in the UK, so ACT is typically learnt through attendance at training workshops delivered by experts in the field and supervision of practice. Marc A Serfaty is a consultant psychiatrist and British Association for Behavioural and Cognitive Psychotherapies-accredited CBT therapist (1994) and fellow (2016). He had attended 12 days of ACT training workshops and had > 12 years’ experience in weekly ACT supervision by the time of training. In addition, he had 2 years’ experience of co-ordinating weekly ACT peer group workshops, as well as previous experience conducting a RCT of ACT for advanced cancer. Rebecca L Gould is a clinical psychologist with 9 years’ post-qualification experience of delivering psychotherapy interventions. She had attended 10 days of ACT training workshops and had 3 years’ experience in delivering ACT by the time of training. In addition, she had completed level 1 mindfulness teacher training through Bangor University, which shares some features with ACT.
The initial ACT training workshop (days 1–4) occurred while the manualised intervention was being developed. Details of the training workshop are listed in Table 16 (materials are available on request from the corresponding author). Each session comprised a combination of didactic learning through teaching and demonstrations, experiential learning through the personal experience of ACT metaphors and exercises, and practical learning through role plays with other therapists (observed by RG and MS). Following the development of the intervention, therapists attended a 1-day experientially based training workshop on the specific application of ACT to older people with TR-GAD (day 5).
| Day | Content |
|---|---|
| 1 |
|
| 2 |
|
|
|
| 3 |
|
| 4 |
|
| 5 |
|
Supervision
Following initial training, therapists were asked to practise delivering ACT to any two service users on their caseload. Fortnightly group supervision and consultation on these cases was provided by telephone by members of the research team (MS and JW) and an independent ACT therapist (Chris Graham). Supervisors were band 8 equivalent or higher clinical psychologists or psychotherapists with a minimum of 5 years’ experience in delivering ACT, as well as experience in supervising ACT. Marc A Serfaty and Julie Loebach Wetherell also had experience of supervising therapists to deliver ACT as part of RCTs. Supervisors observed some of each others’ sessions to ensure that a consistent approach was used with therapists.
After completion of the training workshop, fortnightly group supervision and consultation by telephone was provided by Marc A Serfaty, Julie Loebach Wetherell and Chris Graham for the remainder of the feasibility study. Anonymised supervision notes were taken by the research assistant in each session and made available to therapists and supervisors. The mean number of sessions attended by therapists was 19.1 (SD 9.8), ranging from three sessions (for one therapist who joined the study at a late stage) to 37 sessions.
Therapists
Seventeen therapists received training in ACT, 12 of whom actually delivered the intervention to participants in the study (Table 17). Five therapists dropped out of the study, four without seeing any participants in the study: three because of leaving their job to take up a position elsewhere, one because of retiring and one because of ill health. Therapists were band 7 or 8 clinical psychologists, accredited CBT therapists or counselling psychologists with a minimum of 1 year’s experience in delivering psychotherapy interventions. The majority were based in secondary care in CMHTs for older people (n = 14, 82%), with only three therapists (18%) based in primary care in IAPT services.
| Site | Number of therapists who received ACT training | Number of therapists who dropped out of the study | Number of therapists who dropped out before seeing any participants |
|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 7 | 3 | 2 |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 5 | 1 | 1 |
| Camden and Islington NHS Foundation Trust | 1 | 0 | 0 |
| Whittington Health NHS Trust | 2 | 1 | 1 |
| North East London NHS Foundation Trust | 2 | 0 | 0 |
| Total | 17 | 5 | 4 |
Treatment fidelity
All therapy sessions were recorded using encrypted digital voice recorders to monitor adherence to the treatment manual. Ten per cent of sessions were randomly selected and assessed for treatment fidelity by one of two independent ACT therapists with training and experience in delivering ACT using an adapted form of the ACT Treatment Integrity Coding Manual. 99 This is a well-established tool for assessing treatment fidelity in ACT interventions that assesses fidelity in four areas: (1) ACT (six items: deliteralisation/defusion, willingness/acceptance, creative hopelessness/workability, values and goals, committed action, and ACT therapeutic relationship); (2) other (one item: general assessment); (3) anti-ACT (five items: challenging cognitions, using experiential avoidant change strategies, providing a cognitive therapy rationale, implying that thoughts and feelings cause action, and using in-session exposure as a means of decreasing anxiety); and (4) global ratings of adherence (two items: overall adherence to the FACTOID intervention and overall competence of the therapist). All items are rated on a scale of 1 (not at all) to 5 (extensively) with respect to frequency and/or depth of coverage in the session. The mean scores were calculated for each item.
Assessment of treatment fidelity occurred on an ongoing basis throughout the delivery of the intervention. Independent ACT raters were blind to the identity of therapists, and vice versa. Therapists received written feedback from the independent ACT raters as soon as treatment fidelity had been assessed, as well as periodic feedback from Rebecca L Gould with respect to common issues that ACT raters were observing. The random selection of sessions was stratified according to therapist, phase of the intervention (early, middle or late) and phase of study recruitment (early, middle or late), as recommended in psychosocial interventions. 100
In addition to the ACT Treatment Integrity Coding Manual, therapists completed a checklist of ACT components, ACT techniques and themes discussed in each session, together with any ACT-inconsistent deviations from the manual, to facilitate monitoring of treatment adherence.
Usual care
In addition to receiving ACT, all participants received usual care, which was monitored using a modified version of the Client Service Receipt Inventory (CSRI) adapted for use in older people. 87,101 It was anticipated that usual care would comprise GP care with or without multidisciplinary team interventions, including assessment, medication review and management, psychotherapy, occupational therapy and case management. As noted in the eligibility criteria, participants were required to refrain from engaging in other forms of psychotherapy during the receipt of ACT.
Data collection
Data collection was conducted face to face at screening and 0 weeks (baseline) and face to face or by telephone at 20 weeks (follow-up). Data were collected in the participant’s home or at the clinic, depending on patient preference. The following sociodemographic and clinical data were recorded at screening or baseline:
-
age, sex, ethnicity, marital status, years of education, highest level of educational qualification, current occupation and highest level of occupational attainment
-
psychiatric diagnoses using the MINI97 and the Structured Clinical Interview for DSM-IV Axis II Disorders65
-
previous and current treatment for GAD, ongoing medication use including prescribed or illicit substances (dose and frequency) and length of current episode
-
GAD using the GAD-782
-
global cognition using the SMMSE66
-
suicidal ideation, intent and plans
-
physical illness and disability using the Cumulative Illness Rating Scale for Geriatrics. 102
Baseline assessments were completed within 2 weeks of starting therapy to account for the fact that all sites refused to fast track study participants to receive therapy because they felt that this would give study participants an unfair advantage over other patients on their therapy waiting lists.
Outcome measures
Primary outcome measures
The co-primary outcome measures were:
-
Acceptability –
-
Participants attending ≥ 60% sessions (i.e. ≥ 10 sessions).
-
‘Satisfactory’ ratings of therapy using the Satisfaction with Therapy and Therapist Scale-Revised,103 a self-report measure of satisfaction with therapy (6-item subscale) and satisfaction with the therapist (6-item subscale), with each item being rated on a 5-point scale of 1 (strongly disagree) to 5 (strongly agree). Scores range from 6 to 30 points for each subscale, with higher scores indicating greater satisfaction with therapy or the therapist. The questionnaire also includes a single item measuring perception of global improvement, which is rated on a scale of 1 (made things a lot better) to 5 (made things a lot worse), with lower scores indicating greater self-reported global improvement. There is no set definition of what constitutes ‘satisfactory’ and so this was defined as a total score of ≥ 21 out of 30 points on the Satisfaction with Therapy subscale. As a reference point, a participant who rated all items as ‘neutral’ (i.e. neither satisfied nor dissatisfied) would score 18 out of 30 points.
-
-
Feasibility –
-
recruitment of ≥ 80% of the target sample size (n = 40) in a 10-month recruitment period
-
retention rate of ≥ 60% as measured by attendance at the final follow-up assessment.
-
Three out of four of these a priori indicators of success needed to be met to demonstrate success (i.e. feasibility of the study).
Secondary outcome measures
The secondary outcome measures were:
-
Acceptability –
-
Failures to recruit due to lack of acceptability of the intervention.
-
Participants dropped out owing to lack of acceptability of the intervention.
-
Credibility/Expectancy Questionnaire after the first session of the intervention. 104 It is important to evaluate treatment credibility and expectancy when developing a new intervention as this can have a significant impact on uptake and drop-out rates. The Credibility/Expectancy Questionnaire is a 6-item self-report measure that assesses the credibility of the rationale for therapy and treatment expectancy, which was adapted for GAD and measured immediately after the first therapy session. Four items are rated on a 9-point scale from 1 to 9 (lower scores are worse) and two items are scored on an 11-point scale from 0% to 100%. Because the measure includes items rated on two scales, the items rated on a percentage scale were subjected to a linear transformation, with a minimum of 1 and a maximum of 9, to produce rating scales similar to the other items. Credibility and expectancy scores were calculated as the total scores of the relevant items, with a possible range of 3 to 27 points on each subscale.
-
-
Feasibility –
-
Eligible referrals overall and in each referral subgroup (self-referral, GPs, GP list searches, IAPT services and CMHTs).
-
Eligible participants recruited.
-
Failures to recruit for reasons other than dissatisfaction with therapy (together with reasons for this).
-
Participants who dropped out for reasons other than dissatisfaction with therapy (together with reasons for this).
-
Scores on the ACT Treatment Integrity Coding Manual,99 a coding system that has been developed to assess treatment integrity in ACT interventions and has been used in previous RCTs of ACT. 105 In this coding system, the frequency and depth of coverage of major components of ACT (defusion, willingness/acceptance, creative hopelessness/workability, values and goals, committed action, general assessment of goals for treatment, symptoms and general functioning), together with overall adherence and overall therapist competence, are rated on a 5-point scale from 1 (not at all) to 5 (extensively). Coding was completed by an independent ACT therapist who was blind with respect to who the therapist was.
-
ACT-inconsistent deviations from the manual using the adherence checklist, a checklist of ACT components, ACT techniques and themes discussed in each session, together with any ACT-inconsistent deviations from the manual, which was adapted from the CanACT (Acceptance and commitment therapy for adults with advanced cancer) trial. 106 The outcome was ACT-inconsistent deviations from the manual.
-
-
Patient-reported outcome measures at 0 weeks (baseline) and 20 weeks (follow-up):
-
Geriatric Anxiety Inventory107 – a 20-item ‘agree/disagree’ self-report measure of anxiety developed specifically for older people so that it minimises somatic symptoms because these frequently overlap with physical health conditions commonly found in older people.
-
Penn State Worry Questionnaire108 – a 16-item self-report measure of worry severity widely used in GAD, rated on a 5-point scale of 0 (not at all typical of me) to 5 (very typical of me).
-
Geriatric Depression Scale-15109 – a 15-item ‘yes/no’ self-report measure of depression developed specifically for use with older people for reasons noted above, necessary as GAD is most frequently comorbid with depression.
-
EuroQol-5 Dimensions, five-level version (EQ-5D-5L), including the EuroQol Visual Analogue Scale (EQ-VAS)110,111 – the EQ-5D-5L is a 5-item self-report measure of health-related quality of life, used to calculate utility scores for quality-adjusted life-years (QALYs), rated on a 5-point scale from no problems to extreme problems (discussed in Chapter 5).
-
A modified version of the CSRI87,101 – a measure of service utilisation used to calculate QALYs (discussed in Chapter 5);
-
Acceptance and Action Questionnaire-II112 – a seven-item process measure of experiential avoidance or psychological inflexibility commonly used in ACT.
-
Measures of bias
Because a drug stabilisation period was not included in the feasibility study, the name, dose and frequency of all psychotropic medication prescribed, and any changes to this, were recorded during the course of the study. This information was extracted from GP medical records, with participants’ consent. This was then included as a covariate in statistical analyses, where necessary. Participants were asked to refrain from engaging in other forms of psychotherapy during the delivery of the intervention because engaging in two types of psychotherapy concurrently may lead to conflicts in therapeutic approaches and goals. Other psychological or psychosocial interventions that participants engaged in during the course of the study were recorded, along with any interventions that participants were referred for after receiving the intervention. Evidence of any adverse effects from the intervention was also monitored and recorded throughout the feasibility study.
Data analyses
Primary outcome analysis
In accordance with current recommendations of good clinical practice in the analysis of feasibility studies,113,114 quantitative analyses were descriptive. Binary and other categorical measures were summarised using frequencies and percentages, and continuous measures using means and SDs or medians and IQRs for very skewed distributions (i.e. skewness values < –2 or > 2). 84
Secondary outcome analysis
Binary and other categorical measures were summarised using frequencies and percentages, and continuous measures using means and SDs or medians and IQRs for very skewed distributions (i.e. skewness values < –2 or > 2). 84 Changes in scores on patient-reported outcome measures between 0 and 20 weeks were estimated by calculating a change score for each individual who had observations at both time points and then estimating the average change across individuals, as well as the accompanying 95% confidence interval (CI). Change between 0 and 20 weeks was also estimated using a linear mixed model with a random effect of participant to account for repeated measures from the same individual at the two time points. This model analysed all available data, including from participants with missing data at either 0 or 20 weeks. A further linear mixed model with a random effect of participant was fitted to adjust for symptom severity (measured using the GAD-7), cognitive function (measured using the SMMSE), number of comorbid mental health disorders and use of psychotropic medication at baseline. Cognitive function, psychiatric comorbidity and symptom severity were selected as covariates as they have been associated with poor treatment response in older people with GAD. 1,22,77
Clustering by therapist was assessed by fitting models with a random effect of both therapist and participant and comparing these with models with a random effect of participant only. Likelihood ratio tests comparing these nested models did not provide any evidence of clustering within therapist. Therefore, we report results from the simpler models with just a random effect of participant.
Sensitivity and other planned analyses
Some missing data were anticipated at the 20-week follow-up. The number of missing values for each of the outcome measures was summarised and reported. Multilevel models for longitudinal data account for missing data under the missing-at-random assumption (i.e. that missingness is conditional on other observed measures included in the analysis). Power analyses were conducted to calculate the sample size necessary to detect an effect of the intervention in a future substantive trial.
Reliable change and clinically significant change
Reliable Change Index (RCI) and clinically significant change (CSC) scores were calculated using the Leeds Reliable Change Indicator calculator. 115 This was used to calculate whether or not any changes in patient-reported outcome measures from 0 to 20 weeks were reliable (i.e. greater in magnitude than could be explained by measurement error or artefacts of repeated measurement) and whether or not any reliable changes were clinically significant (i.e. indicating clinical ‘recovery’). 116 This analysis was restricted to patient-reported outcome measures in which statistical evidence of pre–post changes were identified in linear mixed models. For each identified measure, established norms for clinical and non-clinical populations (means and SDs) and an estimate of reliability (Cronbach’s alpha) were used to calculate RCI and CSC scores. Where possible, established norms were selected from older populations with and without anxiety/mood disorders to increase applicability and relevance to participants in the current study. Established cut-off scores were used to determine clinically significant reliable changes. Five types of change were possible:
-
clinically significant improvement – improvement from pretreatment that meets both RCI and CSC criteria (i.e. a reliable change that is also clinically significant)
-
reliable improvement – improvement from pretreatment that meets RCI but not CSC criteria (i.e. a reliable change that is not clinically significant)
-
no reliable change – the magnitude of any change following treatment is within the expected range due to measurement error
-
reliable deterioration – deterioration from pretreatment that meets RCI but not CSC criteria (i.e. a reliable change that is not clinically significant)
-
clinically significant deterioration – deterioration from pretreatment that meets both RCI and CSC criteria (i.e. a reliable change that is also clinically significant).
Sample size calculation
A sample size of 40 was chosen for a number of reasons. A sample size of 35 is generally recommended for feasibility studies to provide sufficient data and precision of means and variances. 117 Forty participants allows for a 12.5% loss to follow-up based on a preliminary study of ACT in older people with GAD. 27 With respect to session attendance, making the conservative assumption that 80% of participants in the feasibility study will attend ≥ 60% of sessions (i.e. ≥ 10 sessions), a sample size of 35 (after loss to follow-up) would give a 95% CI of 0.63 to 0.92, indicating that we could be 95% certain that at least 63% of the target population would attend ≥ 60% of sessions. Although 100% attendance at ACT sessions was reported in 100% of older people with GAD27 and 78% of older people with depression,59 a conservative estimate was chosen, given the target population (older people with TR-GAD). With respect to recruitment, making a conservative estimate that 60 participants would be eligible to participate in the feasibility study but only 40 would consent to participate, a sample size of 40 would give a 95% CI of 0.53 to 0.78.
Ethics
Ethics approval was granted by the London–Camberwell St Giles Research Ethics Committee on 29 August 2017, with Health Research Authority approval being given on 4 September 2017 (IRAS ID 224111; REC reference 17/LO/1314; see Report Supplementary Material 5).
Results
Findings are reported in accordance with CONSORT reporting guidelines for pilot and feasibility studies. 95
Participant recruitment and flow
Overall participant recruitment and flow
The flow of participants is shown in Figure 3, and the recruitment rate per month is shown in Appendix 5. The study was due to open for recruitment in November 2017, but this was delayed by 2 months because of delays in NHS recruiting sites providing their confirmation of capacity and capability. A total of 81 potential participants were referred from 2 January 2018 to 31 October 2018, and the 20-week follow-ups occurred between 8 June 2018 and 24 April 2019. On average, 8.1 referrals per month were received. Among the 53 potential participants assessed for eligibility, 11 (21%) were not eligible after pre-screening with the GAD-7 and five others (9%) were excluded for other reasons. A total of 37 of the 42 (88%) eligible participants consented to participate in the study, seven (19%) of whom were lost to follow-up and two (5%) of whom withdrew from the intervention alone. The most common reasons for loss to follow-up or withdrawing from the intervention alone were dissatisfaction with the intervention (n = 4, 44%) and deterioration in physical health (n = 2, 22%). Among the participants who were dissatisfied with the intervention, three stated a preference for a more counselling-type approach in which they could ‘just talk’ and one thought that ACT was not a good fit for them. Among the participants who were dissatisfied with the intervention, two withdrew from both the intervention and the study and two withdrew from the intervention alone (i.e. they completed follow-up outcome measures). Twenty-two participants (59%) attended all 16 sessions, with 27 (73%) attending at least eight sessions.
FIGURE 3.
The CONSORT flow diagram: summary of recruitment and follow-up of participants in the study. This figure has been reported in Gould et al. 94 This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited. The figure below includes minor additions and formatting changes to the original figure.
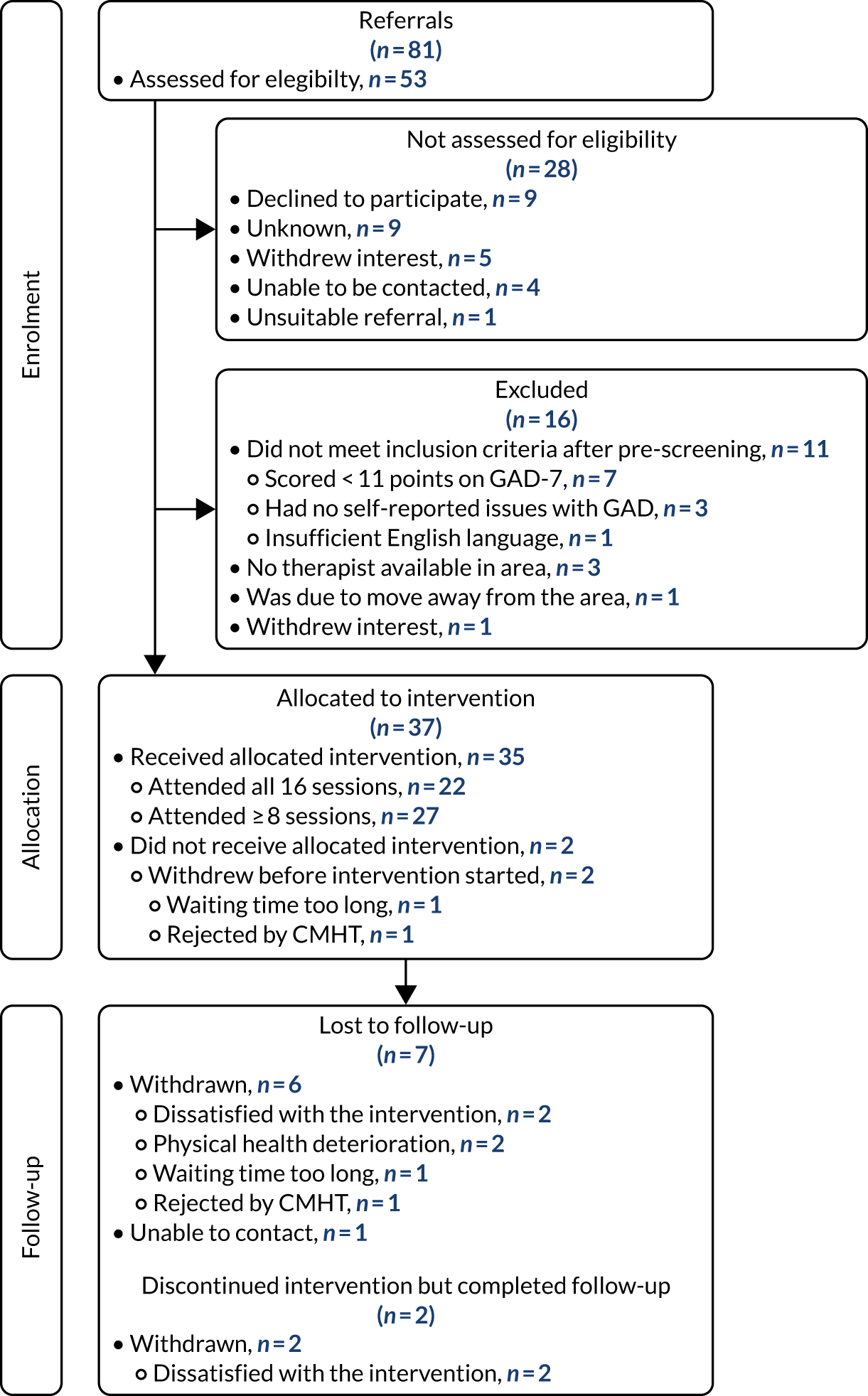
Participant recruitment and flow per site
Recruitment of participants per site is shown in Table 18. Four out of five sites (South London and Maudsley NHS Foundation Trust; Barnet, Enfield and Haringey Mental Health NHS Trust; Camden and Islington NHS Foundation Trust; and Whittington Health NHS Trust) opened for recruitment on 2 January 2018, with a fifth site (North East London NHS Foundation Trust) opening on 25 July 2018. Two-thirds of the referrals (n = 54, 67%) came from just two sites: Barnet, Enfield and Haringey Mental Health NHS Trust, and South London and Maudsley NHS Foundation Trust. The procedure of using the GAD-7 to pre-screen potential participants was a very effective way of ensuring that time and resources were not wasted completing screening interviews. Following the 38 screening interviews completed, all participants were eligible to take part in the study, but one person was not able to proceed any further because no study therapists were located in their local geographical area. The most common sources of referrals for those who completed screening interviews were CMHTs (n = 23) and IAPTs (n = 9), whereas relatively few referrals were obtained via GPs and self-referrals (n = 3 and n = 2, respectively, with n = 1 missing data).
| Site | Total number of referrals | Number not assessed for eligibility | Number not eligible after pre-screening or excluded for other reasons | Number completed screening interview | Number who met eligibility criteria and were able to participate |
|---|---|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 25 | 9 | 2 | 14 | 14 |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 29 | 9 | 7 | 13 | 13 |
| Camden and Islington NHS Foundation Trust | 18 | 6 | 6 | 6a | 5 |
| Whittington Health NHS Trust | 4 | 0 | 0 | 4 | 4 |
| North East London NHS Foundation Trust | 5 | 4 | 0 | 1 | 1 |
| Total | 81 | 28 | 15 | 38 | 37 |
As shown in Table 19, only a small proportion of participants (n = 2, 5%) did not receive the allocated intervention. The largest numbers of participants lost to follow-up were seen in South London and Maudsley NHS Foundation Trust (4/14) and Barnet, Enfield and Haringey Mental Health NHS Trust (2/13). This is unsurprising given that 73% of participants (27/37) were recruited from these sites.
| Site | Number recruited | Number received allocated intervention | Number lost to follow-up | Number withdrawn from intervention alone |
|---|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 14 | 13 | 4a | 1 |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 13 | 13 | 2 | 1 |
| Camden and Islington NHS Foundation Trust | 5 | 4 | 1a | 0 |
| Whittington Health NHS Trust | 4 | 4 | 0 | 0 |
| North East London NHS Foundation Trust | 1 | 1 | 0 | 0 |
| Total | 37 | 35 | 7 | 2 |
Session attendance
Overall session attendance
A total of 438 hours of therapy sessions were attended (Figure 4). Twenty-two participants (59%) attended all 16 sessions, with 26 (70%) attending ≥ 10 sessions.
FIGURE 4.
Number of sessions attended by participants.
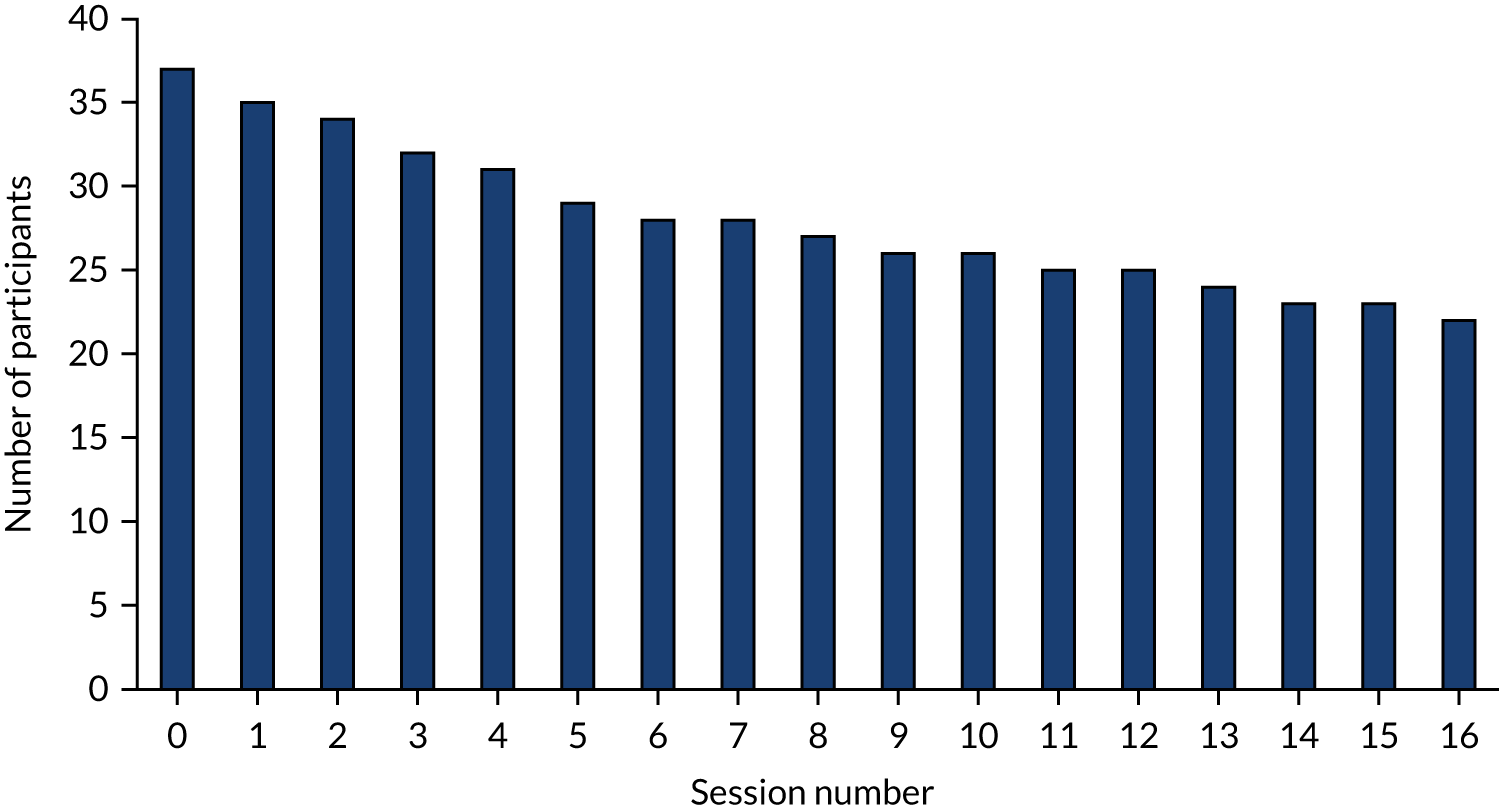
Session attendance per site
As shown in Table 20, the lowest session attendance rates were seen in Camden and Islington NHS Foundation Trust and South London and Maudsley NHS Foundation Trust, with 40% and 43% of their participants receiving all 16 sessions, respectively.
| Site | Number of participants | Number of participants who completed at least one session | Number of participants who attended ≥ 10 sessions | Number of participants who attended all 16 sessions | Mean (SD) number of sessions completed,a n (SD) |
|---|---|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 14 | 13 | 9 | 6 | 10.2 (6.6) |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 13 | 13 | 9 | 9 | 12.5 (5.5) |
| Camden and Islington NHS Foundation Trust | 5 | 4 | 3 | 2 | 10.4 (6.9) |
| Whittington Health NHS Trust | 4 | 4 | 4 | 4 | 16.0 (0.0) |
| North East London NHS Foundation Trust | 1 | 1 | 1 | 1 | 16.0 (–) |
| Total | 37 | 35 | 26 | 22 | 11.84 (5.9) |
Waiting time for therapy
The mean waiting time for therapy was 10.2 weeks (SD 8.8 weeks), though there was some variation across sites, with waiting times being the longest for South London and Maudsley NHS Foundation Trust and Camden and Islington NHS Foundation Trust (Table 21). Waiting times were slightly longer for those who were lost to follow-up or withdrew from the intervention.
| Site | Number of participants | Mean waiting time (weeks) for therapy for all participants (N = 37), n (SD) | Mean waiting time (weeks) for therapy for those lost to follow-up or withdrawn from the intervention (N = 9), n (SD) | Mean waiting time (weeks) for therapy for participants who completed the study (N = 28) (SD), n (SD) |
|---|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 14 | 17.5 (10.4) | 20.5 (12.8) | 16.2 (9.8) |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 13 | 4.7 (2.7) | 4.3 (2.1) | 4.8 (2.9) |
| Camden and Islington NHS Foundation Trust | 5 | 9.8 (3.2) | N/Aa | 9.8 (3.2) |
| Whittington Health NHS Trust | 4 | 6.3 (3.2) | N/Ab | 6.3 (3.2) |
| North East London NHS Foundation Trust | 1 | 4.0 (–) | N/Ab | 4.0 (N/A)c |
| Total | 37 | 10.2 (8.8) | 13.6 (12.6) | 9.4 (7.7) |
Demographic and clinical characteristics
All participants
As shown in Table 22, the majority of participants self-identified as white/white British (n = 32, 86%) women (n = 30, 81%) who were retired (n = 28, 76%) and not in a marital or co-habiting relationship (n = 22, 59%). The age of participants ranged from 65 to 89 years, with a mean age of 74.8 years (SD 6.3 years). Most participants reported having no educational qualifications (n = 15, 41%) and only a small proportion reported qualifications at Advanced level (A level) and above (n = 10, 27%).
| Demographic variables | N (missing n, %) | n (%) | Mean (SD) |
|---|---|---|---|
| Mean age (years) | 37 (0, 0) | 74.8 (6.3) | |
| Age (years) | 37 (0, 0) | ||
| 65–69 | 9 (24) | ||
| 70–79 | 20 (54) | ||
| 80–89 | 8 (22) | ||
| 90–99 | 0 (0) | ||
| ≥ 100 | 0 (0) | ||
| Sex | 37 (0, 0) | ||
| Female | 30 (81) | ||
| Male | 7 (19) | ||
| Ethnicity | 37 (0, 0) | ||
| Asian/Asian British | 1 (3) | ||
| Black/black British | 1 (3) | ||
| Mixed | 1 (3) | ||
| White/white British | 32 (86) | ||
| Other | 2 (5) | ||
| Marital status | 37 (0, 0) | ||
| Married | 14 (38) | ||
| Divorced | 8 (22) | ||
| Single | 3 (8) | ||
| Co-habiting | 1 (3) | ||
| Widowed | 8 (22) | ||
| Separated | 3 (8) | ||
| Years of education | 37 (0, 0) | 10.2 (2.9) | |
| Highest educational qualification | 37 (0, 0) | ||
| Master’s degree | 1 (3) | ||
| Undergraduate degree | 5 (14) | ||
| A level/baccalaureate | 4 (11) | ||
| O level/GCE/GCSE | 3 (8) | ||
| School Leaving Certificate | 3 (8) | ||
| No qualifications | 15 (41) | ||
| Unclear | 6 (16) | ||
| Employment status | 37 (0, 0) | ||
| Paid work | 2 (5) | ||
| Voluntary work | 6 (16) | ||
| Retired | 28 (76) | ||
| Other | 1 (3) |
With respect to clinical characteristics displayed in Table 23, the overall mean total score on the GAD-7 was at the upper end of the moderate range (15.2 points, SD 2.7 points), with scores ranging from 11 to 21 points (none scored < 11 points because of pre-screening with the GAD-7). There was wide variation in the reported number of years experiencing difficulties with worrying, with 1–5 years (n = 13, 35%) and ≥ 30 years (n = 13, 35%) being the most common. The most common comorbid psychiatric disorders were major depressive episode with and without melancholic features (n = 21, 57%) followed by social phobia (n = 8, 22%), panic disorder with and without agoraphobia (n = 7, 19%) and agoraphobia (n = 7, 19%). Although half of the participants reported current alcohol or drug use, this was occurring at levels higher than recommended in national guidelines in only a very small percentage of participants (n = 3, 8%). Reports of current suicidal ideation were common (n = 27, 73%), but a previous history of suicide attempt or self-harm was not (n = 11, 30%). Few participants were identified as having a possible personality disorder on the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) Axis II Disorders screening questionnaire (n = 6, 16%). The majority of participants reported currently taking psychotropic medication (n = 27, 73%), with the most common type being antidepressants (n = 24, 69%). Only a small proportion of participants (n = 5, 14%) reported changes to psychotropic medication within 2 months of the assessment. The majority of participants reported receiving pharmacotherapy (n = 29, 78%) and psychological therapy (n = 31, 84%) in the past. Many participants reported physical health problems (n = 35, 95%), although the mean total score on the Cumulative Illness Rating Scale for Geriatrics was relatively low. Severe problems were reported in at least one category on the Cumulative Illness Rating Scale for Geriatrics by 78% of participants (n = 29), and 19% (n = 7) reported extremely severe problems in at least one category.
| Clinical variable | N (missing n, %) | n (%) | Mean (SD) | Median (IQR) |
|---|---|---|---|---|
| GAD-7 total score, points (possible range 11–21 points because of pre-screening)a | 37 (0, 0) | 15.2 (2.7) | ||
| GAD-7 severity classification, pointsb | 37 (0, 0) | |||
| Moderate (possible range 11–15 points) | 22 (60) | |||
| Severe (possible range 16–21 points) | 15 (41) | |||
| Duration (years) of current difficulties with worrying | 37 (0, 0) | |||
| < 1 | 3 (8) | |||
| 1–5 | 13 (35) | |||
| 6–10 | 3 (8) | |||
| 11–20 | 4 (11) | |||
| 21–30 | 1 (3) | |||
| > 30 | 13 (35) | |||
| Number of participants meeting MINI diagnostic criteria | 37 (0, 0) | |||
| GAD | 37 (100) | |||
| Major depressive episode without melancholic features | 8 (22) | |||
| Major depressive episode with melancholic features | 13 (35) | |||
| Mood disorder with psychotic features | 2 (5) | |||
| Panic disorder | 3 (8) | |||
| Panic with agoraphobia | 4 (11) | |||
| Agoraphobia | 7 (19) | |||
| Social phobia | 8 (22) | |||
| Dysthymia | 3 (8) | |||
| OCD | 3 (8) | |||
| PTSD | 4 (11) | |||
| Psychotic disorders | 0 (0) | |||
| Manic episode | 0 (0) | |||
| Alcohol dependence | 1 (3) | |||
| Substance abuse | 0 (0) | |||
| Number of mental health comorbidities on the MINI | 37 (0, 0) | 1.5 (1.1) | ||
| Current alcohol or drug use | 37 (0, 0) | |||
| Yes | 19 (51) | |||
| No | 18 (49) | |||
| More than 14 units of alcohol per week | ||||
| Yes | 3 (8) | |||
| No | 31 (84) | |||
| Unclear | 3 (8) | |||
| Current suicidal ideation | 37 (0, 0) | |||
| Yes | 27 (73) | |||
| No | 10 (27) | |||
| History of suicide attempt or self-harm | 37 (0, 0) | |||
| Yes | 11 (30) | |||
| No | 26 (70) | |||
| Possible personality disorder identified by the Structured Clinical Interview for DSM-V Axis II Disorders | 37 (0, 0) | |||
| Yes | 6 (16) | |||
| No | 31 (84) | |||
| Number of participants meeting screening criteria for DSM-V Axis II Disorders | 37 (0, 0) | |||
| Avoidant personality disorder | 3 (8) | |||
| Obsessive–compulsive personality disorder | 3 (8) | |||
| Borderline personality disorder | 2 (5) | |||
| Dependent personality disorder | 1 (3) | |||
| Current psychotropic medication | 37 (0, 0) | |||
| Yes | 27 (73) | |||
| No | 10 (27) | |||
| Mean number of psychotropic medications at assessment | 37 (0, 0) | 1.4 (1.2) | ||
| Number of participants with changes to psychotropic medication within 2 months of assessment | 37 (0, 0) | 5 (14) | ||
| Current psychotropic medication | 37 (0, 0) | |||
| Antidepressantsc | 24 (69) | |||
| Anxiolytics (e.g. buspirone) | 0 (0) | |||
| Sedatives (e.g. benzodiazepines) | 8 (23) | |||
| Hypnotics (e.g. Z drugs) | 4 (11) | |||
| Anti-epileptics (e.g. pregabalin) | 8 (23) | |||
| Antipsychotics (e.g. olanzapine) | 2 (6) | |||
| Antihistamines (e.g. hydroxyzine) | 0 (0) | |||
| Previous pharmacotherapy | 37 (0, 0) | |||
| Yes | 29 (78) | |||
| No | 8 (22) | |||
| Number of different types or episodes of previous pharmacotherapy (tried or declined) | 37 (0, 0) | 1.0 (1.0–2.0) | ||
| Previous psychological therapy | 37 (0, 0) | |||
| Yes | 31 (84) | |||
| No | 6 (16) | |||
| Number of different types or episodes of previous psychological therapy (tried or declined) | 37 (0, 0) | 1.7 (1.2) | ||
| SMMSE total score, points (possible range 0–30 points)d,e | 37 (0, 0) | 28.4 (1.5) | ||
| SMMSE total score range, points (possible range 0–30 points)e | 37 (0, 0) | 25–30f | ||
| Self-reported physical health problems | 37 (0, 0) | |||
| Yes | 35 (95) | |||
| No | 2 (5) | |||
| Cumulative Illness Rating Scale for Geriatricse | 37 (0, 0) | |||
| Total number of endorsed categories (possible range 0–14)e | 4.7 (2.1) | |||
| Total score, points (possible range 0–56 points)g | 10.4 (5.0) | |||
| Severity Index (total score/total number of endorsed categories) | 2.1 (0.7) | |||
| Number of categories at level 3 severityh (possible range 0–14) | 1.7 (1.3) | |||
| Number of categories at level 4 severityi (possible range 0–14) | 0.2 (0.4) |
Further information about current psychotropic medication is presented in Table 24. The most common types of psychotropic medication were venlafaxine (n = 8), mirtazapine (n = 8), pregabalin (n = 8) and diazepam (n = 6). There was a wide variation in the length of time that participants self-reported taking psychotropic medication. Excluding single cases, the longest times were reported for diazepam (mean 211.5 months, SD 264.5 months), venlafaxine (mean 34.6 months, SD 31.6 months), mirtazapine (mean 34.2 months, SD 27.4 months) and pregabalin (mean 21.4 months, SD 18.5 months), consistent with the most common types of psychotropic medication.
| Psychotropic medication | N (missing n, %) | Mean (SD) |
|---|---|---|
| Dosage (mg) of current psychotropic medication | ||
| Antidepressantsa | ||
| SSRIs | ||
| Sertraline | 5 (0, 0) | 90.0 (41.8) |
| Citalopram | 2 (0, 0) | 20.0 (0.0) |
| Fluoxetine | 1 (0, 0) | 40.0 (N/A)b |
| Paroxetine | 1 (0, 0) | 30.0 (N/A)b |
| SNRIs | ||
| Venlafaxine | 8 (0, 0) | 126.6 (69.3) |
| Duloxetine | 1 (0, 0) | 60.0 (N/A)b |
| Tetracyclic | ||
| Mirtazapine | 8 (0, 0) | 35.0 (14.9) |
| Tricyclic | ||
| Amitriptyline | 4 (0, 0) | 23.8 (14.9) |
| Sedatives | ||
| Diazepam | 6 (1, 17) | 2.3 (1.6) |
| Oxazepam | 1 (0, 0) | 10.0 (N/A)b |
| Lorazepam | 1 (0, 0) | 1.0 (N/A)b |
| Hypnotics | ||
| Zopiclone | 4 (0, 0) | 5.6 (2.2) |
| Anti-epileptics | ||
| Pregabalin | 8 (0, 0) | 190.6 (124.6) |
| Antipsychotics | ||
| Olanzapine | 2 (0, 0) | 7.5 (3.5) |
| Length of time (months) taking current psychotropic medication | ||
| Antidepressants | ||
| SSRIs | ||
| Sertraline | 3 (2, 40) | 32.3 (45.1) |
| Citalopram | 2 (0, 0) | 13.0 (1.4) |
| Fluoxetine | 1 (0, 0) | 72.0 (N/A)b |
| Paroxetine | 1 (0, 0) | 144.0 (N/A)b |
| SNRIs | ||
| Venlafaxine | 8 (0, 0) | 34.6 (31.6) |
| Duloxetine | 1 (0, 0) | 1.0 (N/A)b |
| Tetracyclic | ||
| Mirtazapine | 6 (2, 25) | 34.2 (27.4) |
| Tricyclic | ||
| Amitriptyline | 1 (3, 75) | 36.0 (N/A)b |
| Sedatives | ||
| Diazepam | 4 (2, 33) | 211.5 (264.5) |
| Oxazepam | 1 (0, 0) | 1.0 (N/A)b |
| Lorazepam | 1 (0, 0) | 5.0 (N/A)b |
| Hypnotics | ||
| Zopiclone | 4 (0, 0) | 14.0 (15.3) |
| Anti-epileptics | ||
| Pregabalin | 7 (1, 13) | 21.4 (18.5) |
| Antipsychotics | ||
| Olanzapine | 2 (0, 0) | 10.0 (2.8) |
Participants who remained in the intervention and study versus those who were lost to follow-up or withdrew from the intervention
Tables 25–27 present demographic, clinical and pharmacological data for participants who remained in the intervention and study (n = 28) compared with those who were lost to follow-up or withdrew from the intervention (n = 9). No formal statistical analyses were conducted because of the small number who were lost to follow-up or withdrew from the intervention. However, the data suggest that participants who were lost to follow-up or withdrew from the intervention were possibly less likely to be married and more likely to have no qualifications, report current suicidal ideation and have a history of suicide attempt or self-harm.
| Demographic characteristic | Participants who remained in the intervention and study | Participants who were lost to follow-up or withdrew from the intervention | ||||
|---|---|---|---|---|---|---|
| N (missing n, %) | n (%) | Mean (SD) | N (missing n, %) | n (%) | Mean (SD) | |
| Mean age (years) | 28 (0, 0) | 74.0 (6.2) | 9 (0, 0) | 77.2 (6.6) | ||
| Age (years) | 28 (0, 0) | 9 (0, 0) | ||||
| 65–69 | 7 (25) | 2 (22) | ||||
| 70–79 | 16 (57) | 4 (44) | ||||
| 80–89 | 5 (18) | 3 (33) | ||||
| 90–99 | 0 (0) | 0 (0) | ||||
| ≥ 100 | 0 (0) | 0 (0) | ||||
| Sex | 28 (0, 0) | 9 (0, 0) | ||||
| Female | 23 (82) | 7 (78) | ||||
| Male | 5 (18) | 2 (22) | ||||
| Ethnicity | 28 (0, 0) | 9 (0, 0) | ||||
| Asian/Asian British | 1 (4) | 0 (0) | ||||
| Black/black British | 0 (0) | 1 (11) | ||||
| Mixed | 1 (4) | 0 (0) | ||||
| White/white British | 24 (86) | 8 (89) | ||||
| Other | 2 (7) | 0 (0) | ||||
| Marital status | 28 (0, 0) | 9 (0, 0) | ||||
| Married | 13 (46) | 1 (11) | ||||
| Divorced | 5 (18) | 3 (33) | ||||
| Single | 3 (11) | 0 (0) | ||||
| Co-habiting | 0 (0) | 1 (11) | ||||
| Widowed | 5 (18) | 3 (33) | ||||
| Separated | 2 (7) | 1 (11) | ||||
| Years of education | 28 (0, 0) | 10.6 (3.2) | 9 (0, 0) | 9.0 (1.3) | ||
| Highest educational qualification | 28 (0, 0) | 9 (0, 0) | ||||
| Master’s degree | 1 (4) | 0 (0) | ||||
| Undergraduate degree | 4 (14) | 1 (11) | ||||
| A level/baccalaureate | 3 (11) | 1 (11) | ||||
| O level/GCE/GCSE | 2 (7) | 1 (11) | ||||
| School Leaving Certificate | 3 (11) | 0 (0) | ||||
| No qualifications | 9 (32) | 6 (67) | ||||
| Unclear | 6 (21) | 0 (0) | ||||
| Employment status | 28 (0, 0) | 9 (0, 0) | ||||
| Paid work | 1 (4) | 1 (11) | ||||
| Voluntary work | 6 (21) | 0 (0) | ||||
| Retired | 20 (72) | 8 (89) | ||||
| Other | 1 (4) | 0 (0) | ||||
| Clinical characteristic | Participants who remained in the intervention and study | Participants who were lost to follow-up or withdrew from the intervention | |||||
|---|---|---|---|---|---|---|---|
| N (missing n, %) | n (%) | Mean (SD) | Median (IQR) | N (missing n, %) | n (%) | Mean (SD) | |
| GAD-7 total score, points (possible range 11–21 points because of pre-screening)a | 28 (0, 0) | 15.3 (2.6) | 9 (0) | 15.2 (3.3) | |||
| GAD-7 total score range, points (possible range 0–21 points)b | 28 (0, 0) | 11–21c | 9 (0) | 11–21c | |||
| GAD-7 severity classificationb | 28 (0, 0) | 9 (0) | |||||
| Moderate (possible range 11–15 points) | 17 (61) | 5 (56) | |||||
| Severe (possible range 16–21 points) | 11 (39) | 4 (44) | |||||
| Duration (years) of current difficulties with worrying | 28 (0, 0) | 9 (0) | |||||
| < 1 | 2 (7) | 1 (11) | |||||
| 1–5 | 10 (36) | 3 (33) | |||||
| 6–10 | 3 (11) | 0 (0) | |||||
| 11–20 | 2 (7) | 2 (22) | |||||
| 21–30 | 0 (0) | 1 (11) | |||||
| > 30 | 11 (39) | 2 (22) | |||||
| Number of participants meeting MINI diagnostic criteria | 28 (0, 0) | 9 (0) | |||||
| GAD | 28 (100) | 9 (100) | |||||
| Major depressive episode | 5 (18) | 3 (33) | |||||
| Major depressive episode with melancholic features | 10 (36) | 3 (33) | |||||
| Mood disorder with psychotic features | 2 (7) | 0 (0) | |||||
| Panic disorder | 2 (7) | 1 (11) | |||||
| Panic with agoraphobia | 4 (14) | 0 (0) | |||||
| Agoraphobia | 5 (18) | 2 (22) | |||||
| Social phobia | 6 (21) | 2 (22) | |||||
| Dysthymia | 3 (11) | 0 (0) | |||||
| OCD | 2 (7) | 1 (11) | |||||
| PTSD | 4 (14) | 0 (0) | |||||
| Psychotic disorders | 0 (0) | 0 (0) | |||||
| Manic episode | 0 (0) | 0 (0) | |||||
| Alcohol dependence | 1 (4) | 0 (0) | |||||
| Substance abuse | 0 (0) | 0 (0) | |||||
| Number of mental health comorbidities on the MINI | 28 (0, 0) | 1.6 (1.2) | 9 (0) | 1.3 (0.9) | |||
| Current alcohol or drug use | 28 (0, 0) | 9 (0) | |||||
| Yes | 16 (57) | 3 (33) | |||||
| No | 12 (43) | 6 (67) | |||||
| More than 14 units of alcohol per week | 28 (0, 0) | 9 (0) | |||||
| Yes | 1 (4) | 2 (22) | |||||
| No | 24 (86) | 7 (78) | |||||
| Unclear | 3 (11) | 0 (0) | |||||
| Current suicidal ideation | 28 (0, 0) | 9 (0) | |||||
| Yes | 19 (68) | 8 (89) | |||||
| No | 9 (32) | 1 (11) | |||||
| History of suicide attempt or self-harm | 28 (0, 0) | 9 (0) | |||||
| Yes | 6 (21) | 5 (56) | |||||
| No | 22 (79) | 4 (44) | |||||
| Possible personality disorder identified on Structured Clinical Interview for DSM-V Axis II Disorders | 28 (0) | 9 (0) | |||||
| Yes | 5 (18) | 1 (11) | |||||
| No | 23 (82) | 8 (89) | |||||
| Number of participants meeting screening criteria for DSM-V Axis II Disorders | 28 (0, 0) | 9 (0) | |||||
| Avoidant personality disorder | 3 (11) | 0 (0) | |||||
| Obsessive–compulsive personality disorder | 2 (7) | 1 (11) | |||||
| Borderline personality disorder | 1 (4) | 1 (11) | |||||
| Dependent personality disorder | 1 (4) | 0 (0) | |||||
| Current psychotropic medication | 28 (0, 0) | 9 (0) | |||||
| Yes | 20 (71) | 7 (78) | |||||
| No | 8 (29) | 2 (22) | |||||
| Mean number of psychotropic medications at assessment (SD, range) | 28 (0, 0) | 1.3 (1.2, 0–4) | 9 (0) | 1.8 (1.4, 0–4) | |||
| Number of participants with changes to psychotropic medication within 2 months of assessment | 28 (0, 0) | 4 (15) | 9 (0) | 1 (11) | |||
| Types of current psychotropic medication | 28 (0, 0) | 9 (0) | |||||
| Antidepressantsd | 18 (69) | 6 (67) | |||||
| Anxiolytics (e.g. buspirone) | 0 (0) | 0 (0) | |||||
| Sedatives (e.g. benzodiazepines) | 5 (19) | 3 (33) | |||||
| Hypnotics (e.g. Z drugs) | 3 (12) | 1 (11) | |||||
| Anti-epileptics (e.g. pregabalin) | 6 (23) | 2 (22) | |||||
| Antipsychotics (e.g. olanzapine) | 1 (4) | 1 (11) | |||||
| Antihistamines (e.g. hydroxyzine) | 0 (0) | 0 (0) | |||||
| Previous pharmacotherapy | 28 (0, 0) | 9 (0) | |||||
| Yes | 24 (86) | 5 (56) | |||||
| No | 4 (14) | 4 (44) | |||||
| Number of different types or episodes of previous pharmacotherapy (tried or declined) | 28 (0, 0) | 1.0 (1.0–2.0) | 9 (0) | 1.8 (2.2) | |||
| Previous psychological therapy | 28 (0, 0) | 9 (0) | |||||
| Yes | 24 (86) | 7 (78) | |||||
| No | 4 (14) | 2 (22) | |||||
| Number of different types or episodes of previous psychological therapy (tried or declined) | 28 (0, 0) | 1.9 (1.2) | 9 (0) | 1.0 (0.7) | |||
| SMMSE total score, points (possible range 0–30 points)b,e | 28 (0, 0) | 28.5 (1.5) | 9 (0) | 28.2 (1.6) | |||
| SMMSE total score range, points (possible range 0–30 points)b | 28 (0, 0) | 25–30f | 9 (0) | 26–30f | |||
| Self-reported physical health problems | 28 (0, 0) | 9 (0) | |||||
| Yes | 26 (93) | 9 (100) | |||||
| No | 2 (7) | 0 (0) | |||||
| Cumulative Illness Rating Scale for Geriatricsb | 28 (0, 0) | 9 (0) | |||||
| Total number of endorsed categories (possible range 0–14)g | 4.5 (2.1) | 5.2 (2.0) | |||||
| Total score, points (possible range 0–56 points)g | 9.8 (5.1) | 12.2 (4.4) | |||||
| Severity Index (total score/total number of endorsed categories) | 2.0 (0.7) | 2.4 (0.4) | |||||
| Number of categories at level 3 severityh (possible range 0–14) | 1.8 (1.2) | 1.4 (1.3) | |||||
| Number of categories at level 4 severityi (possible range 0–14) | 0.0 (0.0–0.0) | 0.6 (0.5) | |||||
| Variable | Participants who remained in the intervention and study | Participants who were lost to follow-up or withdrew from the intervention | |||
|---|---|---|---|---|---|
| N (missing n, %) | Mean (SD) | Median (IQR) | N (missing n, %) | Mean (SD) | |
| Dosage (mg) of current psychotropic medication | |||||
| Antidepressants | |||||
| SSRIs | |||||
| Sertraline | 2 (0, 0) | 75.0 (35.4) | 3 (0, 0) | 100.0 (50.0) | |
| Citalopram | 2 (0, 0) | 20.0 (0.0) | 0 (0, 0) | N/A | |
| Fluoxetine | 1 (0, 0) | 40.0 (N/A)a | 0 (0, 0) | N/A | |
| Paroxetine | 1 (0, 0) | 30.0 (N/A)a | 0 (0, 0) | N/A | |
| SNRIs | |||||
| Venlafaxine | 7 (0, 0) | 123.2 (74.1) | 1 (0, 0) | 150.0 (N/A)a | |
| Duloxetine | 1 (0, 0) | 60.0 (N/A)a | 0 (0, 0) | N/A | |
| Tetracyclic | |||||
| Mirtazapine | 4 (0, 0) | 45.0 (0.0) | 4 (0, 0) | 25.0 (15.8) | |
| Tricyclic | |||||
| Amitriptyline | 3 (0, 0) | 16.7 (5.8) | 1 (0, 0) | 45.0 (N/A)a | |
| Sedatives | |||||
| Diazepam | 4 (0, 0) | 2.0 (2.0–4.3) | 2 (1, 50) | 0.5 (N/A)a | |
| Oxazepam | 1 (0, 0) | 10.0 (N/A)a | 0 (0, 0) | N/A | |
| Lorazepam | 0 (0, 0) | N/A | 1 (0, 0) | 1.0 (N/A)a | |
| Hypnotics | |||||
| Zopiclone | 3 (0, 0) | 6.3 (2.2) | 1 (0, 0) | 3.75 (N/A)a | |
| Anti-epileptics | |||||
| Pregabalin | 6 (0, 0) | 216.7 (124.2) | 2 (0, 0) | 112.5 (123.7) | |
| Antipsychotics | |||||
| Olanzapine | 1 (0, 0) | 10.0 (N/A)a | 1 (0, 0) | 5.0 (N/A)a | |
| Length of time (months) taking current psychotropic medication | |||||
| Antidepressants | |||||
| SSRIs | |||||
| Sertraline | 1 (1, 50) | 12.0 (N/A)a | 2 (1, 33) | 42.5 (58.7) | |
| Citalopram | 2 (0, 0) | 13.0 (1.4) | 0 (0, 0) | N/A | |
| Fluoxetine | 1 (0, 0) | 72.0 (N/A)a | 0 (0, 0) | N/A | |
| Paroxetine | 1 (0, 0) | 144.0 (N/A)a | 0 (0, 0) | N/A | |
| SNRIs | |||||
| Venlafaxine | 7 (0, 0) | 27.6 (26.4) | 1 (0, 0) | 150.0 (N/A)a | |
| Duloxetine | 1 (0, 0) | 1.0 (N/A)a | 0 (0, 0) | N/A | |
| Tetracyclic | |||||
| Mirtazapine | 4 (0, 0) | 28.0 (12.6) | 2 (2, 50) | 46.5 (53.0) | |
| Tricyclic | |||||
| Amitriptyline | 1 (2, 67) | 36.0 (N/A)a | 0 (1, 100) | N/A | |
| Sedatives | |||||
| Diazepam | 2 (2, 50) | 360.0 (339.4) | 2 (0, 0) | 63.0 (80.6) | |
| Oxazepam | 1 (0, 0) | 1.0 (N/A)a | 0 (0, 0) | N/A | |
| Lorazepam | 0 (0, 0) | N/A | 1 (0, 0) | 5.0 (N/A)a | |
| Hypnotics | |||||
| Zopiclone | 3 (0, 0) | 16.3 (17.9) | 1 (0, 0) | 7.0 (N/A)a | |
| Anti-epileptics | |||||
| Pregabalin | 6 (0, 0) | 24.3 (18.5) | 1 (1, 50) | 4.0 (N/A)a | |
| Antipsychotics | |||||
| Olanzapine | 1 (0, 0) | 12.0 (N/A)a | 1 (0, 0) | 8.0 (N/A)a | |
Data collection
Participants initially completed a screening assessment in which key demographic and clinical data were collected to determine eligibility for inclusion in the study. Outcome assessments were conducted at 0 weeks (within 2 weeks prior to starting therapy) and 20 weeks. Two participants were withdrawn from the study before completing baseline outcome measures and one participant refused to complete these measures at baseline because of stress. In addition, seven participants were lost to follow-up at 20 weeks. Hence, data collection occurred for 92% (n = 34) of participants at 0 weeks and 81% (n = 30) of participants at 20 weeks. As noted in Waiting time for therapy and Table 21, the mean waiting time for therapy was 10.2 weeks (SD 8.8 weeks), though there was variability across sites. Consequently, the mean number of therapy sessions completed by the 20-week follow-up was 12.1 sessions (SD 3.6 sessions) out of a possible 16 sessions (Table 28).
| Site | Number of participants who completed assessment at 0 weeks | Number of participants who completed assessment at 20 weeks | Mean number of therapy sessions completed at 20 weeks,a n (SD) |
|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 13 | 10 | 10.8 (4.4) |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 12 | 11 | 12.4 (3.4) |
| Camden and Islington NHS Foundation Trust | 4 | 4 | 12.0 (3.5) |
| Whittington Health NHS Trust | 4 | 4 | 14.3 (1.0) |
| North East London NHS Foundation Trust | 1 | 1 | 14.0 (N/A)b |
| Total | 34c | 30d | 12.1 (3.6) |
Examining completion rates further in participants who completed the outcome assessment at 0 and 20 weeks (n = 34 and n = 30, respectively), excellent completion rates were obtained for all questionnaires with the exception of the Credibility/Expectancy Questionnaire (Table 29). The main reason that rates were lower for the Credibility/Expectancy Questionnaire was that some participants reported struggling with estimating responses to the questions and/or did not like having to ‘guess’ responses to the questions.
| Questionnaire | 0 weeks (n = 37)a | 20 weeks (n = 37)b | Number in analysis of change (n = 37)c | Number in linear mixed model (n = 37) |
|---|---|---|---|---|
| Geriatric Anxiety Inventory | 34 | 30 | 29 | 35 |
| Penn State Worry Questionnaire | 34 | 29 | 28 | 35 |
| Geriatric Depression Scale-15 item | 34 | 30 | 29 | 35 |
| Acceptance and Action Questionnaire II | 34 | 30 | 29 | 35 |
| STTS-R Satisfaction with Therapy subscale | N/A | 30 | N/A | N/A |
| STTS-R Satisfaction with Therapist subscale | N/A | 30 | N/A | N/A |
| STTS-R Global Improvement subscale | N/A | 30 | N/A | N/A |
| CEQ Credibility subscale | 26 | N/A | N/A | N/A |
| CEQ Expectancy subscale | 26 | N/A | N/A | N/A |
| ACT Treatment Integrity Coding Manuald | N/A | N/A | N/A | N/A |
| ACT-inconsistent deviations from the manual using the adherence checklistd | N/A | N/A | N/A | N/A |
Primary outcomes
There were four co-primary outcomes: two focusing on feasibility and two focusing on acceptability. Excellent feasibility was demonstrated by a recruitment rate of 93% and a retention rate of 81%, both of which exceeded the targets (Table 30). A high level of acceptability was found with respect to session attendance, as demonstrated by 70% of participants attending ≥ 10 sessions. Rates of satisfaction with therapy were adequate, with 60% of participants scoring ≥ 21 out of 30 on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised. However, it should be noted that the median number of sessions completed at 20 weeks was 13.0 sessions (IQR 4.5–14.0 sessions), and 80% (24/30) participants were still undergoing the intervention at the time of the 20-week follow-up assessment. Rates of satisfaction with therapy may have been higher had participants finished receiving their sessions by the time of the 20-week follow-up assessment.
| Co-primary outcome | n/N (%) |
|---|---|
| Feasibility | |
| ≥ 80% target sample recruited in 10 months (i.e. ≥ 32) | 37/40 (93) |
| Retention rate ≥ 60% | 30/37 (81) |
| Acceptability | |
| Participants attending ≥ 60% sessions (i.e. ≥ 10 sessions) | 26/37 (70) |
| ‘Satisfactory’ rating of therapy on the STTS-R Satisfaction with Therapy subscalea | |
| Score of ≥ 21/30 points on STTS-R Satisfaction with Therapy subscale | 18/30 (60) |
Secondary outcomes
Acceptability
A high level of acceptability was further demonstrated by:
-
A low rate of attrition (i.e. loss to follow-up) and a low rate of withdrawal from the intervention alone due to dissatisfaction with the intervention (only four participants withdrew for this reason: two withdrew from both the intervention and the study and two withdrew from the intervention alone).
-
Zero reports of eligible participants not being recruited because of dissatisfaction with the intervention being offered (n = 0, 0%).
-
Adequate mean ratings of credibility (16.5, SD 5.0) and expectancy (14.5, SD 5.0) on the Credibility/Expectancy Questionnaire (no norms are available). The possible range on each subscale is 3–27 points; higher scores indicate greater credibility and greater expectation that the intervention will help.
-
A low rate of adverse or serious adverse events, with none deemed to be related to the intervention (Table 31).
| Type of event and category | Number of events | Related to intervention |
|---|---|---|
| Adverse event | ||
| Physical health | ||
| Participant had a fall | 2 | Unlikely |
| Mental health | ||
| Participant referred to Home Treatment Team | 1 | Unlikely |
| New reports of suicidal ideation without intent | 1 | Unlikelya |
| Serious adverse event | ||
| Physical health | ||
| Unplanned hospital admission | ||
| Participant had a fall | 2 | Unlikely |
| Mental health | ||
| New reports of suicidal ideation with intent or self-harm | ||
| Attempted overdose with hospital admission | 1 | Unlikelya |
Feasibility
As shown in Table 32, the overall rate of conversion of referrals to eligible participants was 47%, although rates varied across sites. The majority of eligible participants came from CMHTs (n = 23, 61%), followed by IAPT services (n = 9, 24%). There was only one case of an eligible participant not being recruited for reasons other than lack of acceptability of the intervention. In this case, therapists were no longer available in the eligible participant’s geographical area and so they were not able to participate in the study. There was a relatively low rate of attrition and eligible participants not being recruited for feasibility-related reasons (i.e. not dissatisfaction with the intervention; n = 5, 14%). The logistical issue of delivering therapy emerged as the most common feasibility-related reason (total n = 3, 8%). Overall, results further support the feasibility of the intervention and study delivery.
| Secondary feasibility variables | n/N (%) |
|---|---|
| Rate of conversion of referrals to eligible participants across sites | 38/81 (47) |
| South London and Maudsley NHS Foundation Trust | 14/25 (56) |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 13/29 (45) |
| Camden and Islington NHS Foundation Trust | 6/18 (33) |
| Whittington Health NHS Trust | 4/4 (100) |
| North East London NHS Foundation Trust | 1/5 (20) |
| Source of eligible participants | 38 |
| CMHTs | 23 (61) |
| IAPT services | 9 (24) |
| GPs/GP list searches | 3 (8) |
| Self-referral | 2 (5) |
| Missing source | 1 (3) |
| Eligible participants recruited | 37/38 (97) |
| Failures to recruit eligible participants for reasons other than lack of acceptability of therapy | |
| Therapists were no longer available in the local area | 1/38 (3) |
| Attrition (i.e. lost to follow-up) for reasons other than dissatisfaction with therapy | 5 (14) |
| Physical health deterioration | 2 (5) |
| Logistical issues of delivering therapy (e.g. waiting time too long, rejected by CMHT) | 2 (5) |
| Unknown | 1 (3) |
An additional secondary outcome in relation to feasibility was the degree to which the intervention was delivered by therapists as intended. This was rated using the ACT Treatment Integrity Coding Manual. As shown in Table 33, 9% (n = 39) of sessions were rated by an independent ACT therapist throughout the duration of the intervention period. The mean ratings for ACT items show that each of the ACT items were discussed, on average, several times and/or in a moderately in-depth manner per session. Furthermore, the overall mean number of ACT items discussed per session (i.e. with a rating of ≥ 2 per session) was high (5.2/6, SD 0.8), consistent with a core ACT skill of moving flexibly between ACT processes within sessions (so-called ‘dancing around the hexaflex’). Crucially, there was no evidence of anti-ACT items in the rated sessions. In addition, high rates of overall adherence to the manual and overall ACT competence of therapists were observed. This demonstrates that novice ACT therapists could be trained to successfully deliver the intervention.
| Variable | Site | Total | ||||
|---|---|---|---|---|---|---|
| SLAM | BEH | C&I | WH | NELFT | ||
| Sessions rated,a n/N (%) | 14/143 (10) | 13/163 (8) | 4/52 (8) | 6/64 (9) | 2/16 (13) | 39/438 (9) |
| ACT items,b mean (SD) | ||||||
| Deliteralisation/defusion | 2.6 (1.3) | 3.8 (1.1) | 4.0 (1.0) | 3.3 (0.8) | 2.5 (0.7) | 3.2 (1.2) |
| Willingness/acceptance | 3.6 (1.2) | 4.3 (1.0) | 3.3 (1.3) | 3.5 (1.0) | 3.0 (0.0) | 3.8 (1.1) |
| Creative hopelessness/workability | 3.2 (1.5) | 3.0 (0.9) | 3.0 (1.2) | 3.3 (1.0) | 2.0 (1.4) | 3.1 (1.2) |
| Values and goals | 3.4 (1.3) | 4.2 (0.8) | 3.5 (1.3) | 3.3 (1.0) | 2.0 (0.0) | 3.6 (1.1) |
| Committed action | 2.9 (1.2) | 3.8 (0.8) | 2.5 (1.7) | 2.8 (0.8) | 2.0 (0.0) | 3.1 (1.2) |
| ACT therapeutic relationship | 1.4 (0.6) | 1.5 (0.8) | 3.0 (1.4) | 2.0 (1.4) | 1.0 (0.0) | 1.7 (1.0) |
| No. of ACT items with a rating of ≥ 2 per session | 4.9 (1.0) | 5.3 (0.6) | 5.8 (0.5) | 5.7 (0.5) | 4.5 (0.7) | 5.2 (0.8) |
| General assessmentb | 2.5 (0.7) | 2.5 (2.1) | 4.0 (N/A) | N/A (N/A) | N/A (N/A) | 2.8 (1.3) |
| Anti-ACT items,b mean (SD) | ||||||
| Challenging cognitions | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) |
| Experiential avoidant change strategies | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) |
| Cognitive therapy rationale | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) |
| Thoughts and feelings cause action | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) |
| In-session exposure (to reduce anxiety) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) |
| No. of anti-ACT items with a rating of ≥ 2 per session | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| Global ratings of adherence,b mean (SD) | ||||||
| Overall adherence to intervention | 4.1 (0.9) | 4.5 (0.5) | 4.3 (0.5) | 4.3 (0.8) | 2.5 (0.7) | 4.2 (0.8) |
| Overall competence of therapist | 4.1 (0.9) | 4.4 (0.7) | 4.5 (0.6) | 3.8 (0.8) | 2.5 (0.7) | 4.1 (0.8) |
Treatment integrity in the form of ACT-inconsistent deviations from the manual was further assessed using the adherence checklist. This was a measure developed for the purposes of this study, which was completed by therapists after each session. It comprised a checklist of ACT components, ACT techniques and themes discussed in each session, together with any ACT-inconsistent deviations from the manual. Overall, adherence checklists were completed for 79% of sessions (n = 348), as illustrated in Table 34. No ACT-inconsistent deviations from the manual were self-reported by therapists. This is consistent with the high rate of overall adherence to the ACT model and manual found with the ACT Treatment Integrity Coding Manual.
| Site | Number of participants for whom the adherence checklist could be completed | Number of adherence checklists completed, n/N (%) | Number of ACT-inconsistent deviations |
|---|---|---|---|
| South London and Maudsley NHS Foundation Trust | 13a | 98/143 (69) | 0 |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 13 | 137/163 (84) | 0 |
| Camden and Islington NHS Foundation Trust | 4a | 40/52 (77) | 0 |
| Whittington Health NHS Trust | 4 | 60/64 (94) | 0 |
| North East London NHS Foundation Trust | 1 | 13/16 (81) | 0 |
| Total | 35 | 348/438 (79) | 0 |
Patient-reported outcomes measures
There was evidence of a 2-point reduction between 0 and 20 weeks’ follow-up for both anxiety (Geriatric Anxiety Inventory score –2.30 points, 95% CI –3.83 to –0.76 points) and depression (Geriatric Depression Scale-15 score –2.04 points, 95% CI –3.31 to –0.77 points) in the unadjusted linear mixed model analysis (Table 35). There was also evidence of a 3-point reduction in psychological inflexibility (Acceptance and Action Questionnaire-II score –3.93 points, 95% CI –7.16 to –0.70 points). Improvements of similar magnitude were observed after adjusting for GAD severity, global cognition, number of comorbid psychiatric conditions and use of psychotropic medication at baseline. Estimated changes in other outcome measures were in the direction consistent with a reduction in worry.
| Outcome measure | 0 weeks (N = 34), mean (SD) | 20 weeks (N = 30), mean (SD) | Unadjusted analysis of change, estimated change (95% CI) | Unadjusted linear mixed model, estimated change (95% CI) | Adjusted linear mixed model,a estimated change (95% CI) |
|---|---|---|---|---|---|
| GAI (possible range 0–20)b | 15.8 (4.1) | 13.8 (5.1) | –2.62 (–4.28 to –0.96) | –2.30 (–3.83 to –0.76) | –2.30 (–3.83 to –0.77) |
| PSWQ (possible range 16–80)c | 64.4 (10.6) | 61.9 (11.5) | –4.64 (–9.72 to 0.43) | –3.05 (–7.73 to 1.63) | –3.11 (–7.76 to 1.54) |
| GDS-15 (possible range 0–15)d | 9.82 (3.21) | 7.83 (4.04) | –2.10 (–3.49 to –0.72) | –2.04 (–3.31 to –0.77) | –2.06 (–3.32 to –0.81) |
| AAQ-II (possible range 7–49)e | 34.4 (8.0) | 30.6 (10.3) | –4.07 (–7.63 to –0.51) | –3.93 (–7.16 to –0.70) | –4.09 (–7.31 to –0.87) |
Power calculations
Power analyses were conducted to calculate the sample size necessary to detect an effect of the intervention in a future substantive trial. A total of 368 older people with TR-GAD (184 per arm) will allow for detection of an effect size of 0.4 SDs, with a two-sided alpha of 5% and 90% power. This assumes 20% loss to follow-up at 26 weeks (based on 18.9% attrition at 20 weeks in the feasibility study), 30 therapists (two therapists per site at 15 sites) and an intraclass correlation coefficient of 0.01 among therapists (as used in other psychotherapy trials118). To our knowledge, there are no published data with respect to what a clinically important difference is on the Geriatric Anxiety Inventory questionnaire in older people with GAD. Therefore, our sample size is based on a clinically meaningful pooled effect size of 0.4 SDs reported in a meta-analysis of 39 RCTs of ACT for mental and physical health conditions compared with controls. 41
Reliable Change Index
Three patient-reported outcome measures identified from linear mixed-model analyses (Geriatric Anxiety Inventory, Geriatric Depression Scale-15 and Action and Acceptance Questionnaire-II) were analysed using the RCI and CSC analyses. Data used to calculate RCI and CSC scores for each of these measures are outlined in Table 36.
| Outcome measure | Geriatric Anxiety Inventory | Geriatric Depression Scale-15 | Action and Acceptance Questionnaire-II |
|---|---|---|---|
| Source | Johnco et al.119 | Snyder et al.120 | Bond et al.112 |
| Population | Older people aged ≥ 60 years with and without comorbid anxiety and mood disorder | Older people aged ≥ 60 years with GAD with and without a comorbid depressive disorder | University students, people in the community and people seeking outpatient psychological treatment |
| Cronbach’s alpha | 0.93 | 0.73 | 0.84 |
| Clinical norms | |||
| Mean | 11.08 | 7.40 | 28.30 |
| SD | 4.86 | 3.20 | 9.90 |
| Non-clinical norms | |||
| Mean | 0.58 | N/A | 18.51 |
| SD | 1.32 | N/A | 7.05 |
| Cut-off score (points) used for determining CSC | 11a | 5b | 24c |
Among the 29 participants with scores at 0 and 20 weeks, 13 (45%) showed a reliable improvement in scores on the Geriatric Anxiety Inventory at 20 weeks’ follow-up (Figure 5), with six (21%) of these also meeting the criterion for CSC (i.e. scored below the clinical cut-off point). Just over half of participants (n = 15, 52%) showed no reliable change, and only one participant (3%) showed a reliable deterioration in their scores, but this was not clinically significant.
FIGURE 5.
Symptoms of anxiety at 0 and 20 weeks as measured by the Geriatric Anxiety Inventory (n = 29). Participants with the same scores at 0 and 20 weeks share the same marker on the graph. Orange lines indicate the RCI. Further details about the cut-off score for CSC are provided in Table 36.
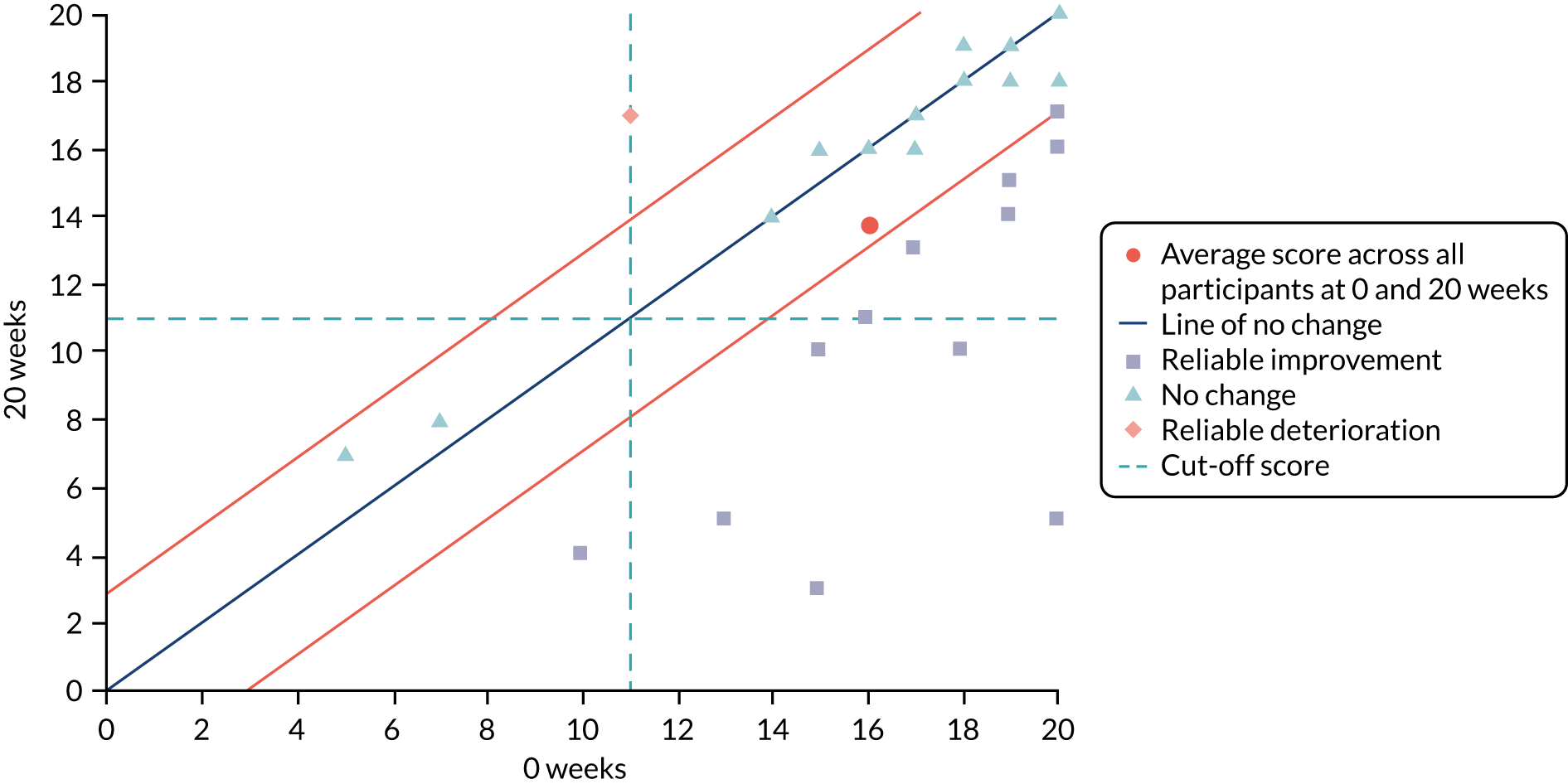
For the Geriatric Depression Scale-15, just under one-quarter of participants (n = 7, 24%) showed a reliable improvement in scores at the 20-week follow-up, with five (17%) of these also meeting the criterion for CSC (i.e. scored below the clinical cut-off point; Figure 6). Three-quarters of participants (n = 22, 76%) showed no reliable change, and no participants showed a reliable deterioration in their scores.
FIGURE 6.
Symptoms of depression at 0 and 20 weeks as measured by the Geriatric Depression Scale-15 (n = 29). Participants with the same scores at 0 and 20 weeks share the same marker on the graph. Orange lines indicate the RCI. Further details about the cut-off score for CSC are provided in Table 36.
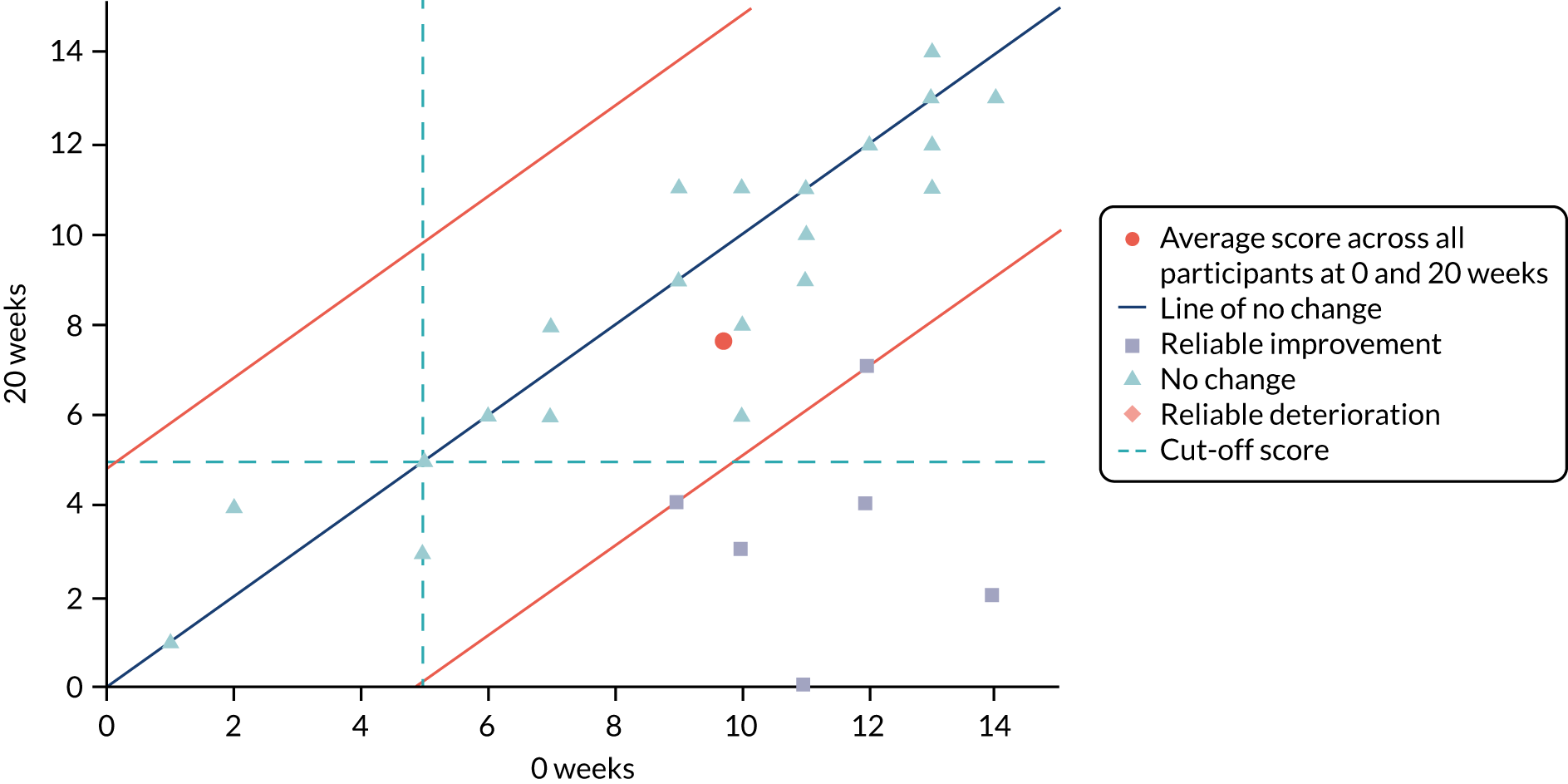
As illustrated in Figure 7, just under one-quarter of participants (n = 7, 24%) showed a reliable improvement in scores on the Action and Acceptance Questionnaire-II at the 20-week follow-up, with four (14%) of these also meeting the criterion for CSC (i.e. scored below the clinical cut-off point). Two-thirds of participants (n = 19, 66%) showed no reliable change, and three participants (n = 10%) showed a reliable deterioration in their scores, but none of these met the criterion for clinically significant change.
FIGURE 7.
Psychological flexibility at 0 and 20 weeks as measured by the Action and Acceptance Questionnaire-II (n = 29). Participants with the same scores at 0 and 20 weeks share the same marker on the graph. Orange lines indicate the RCI. Further details about the cut-off score for CSC are provided in Table 36.
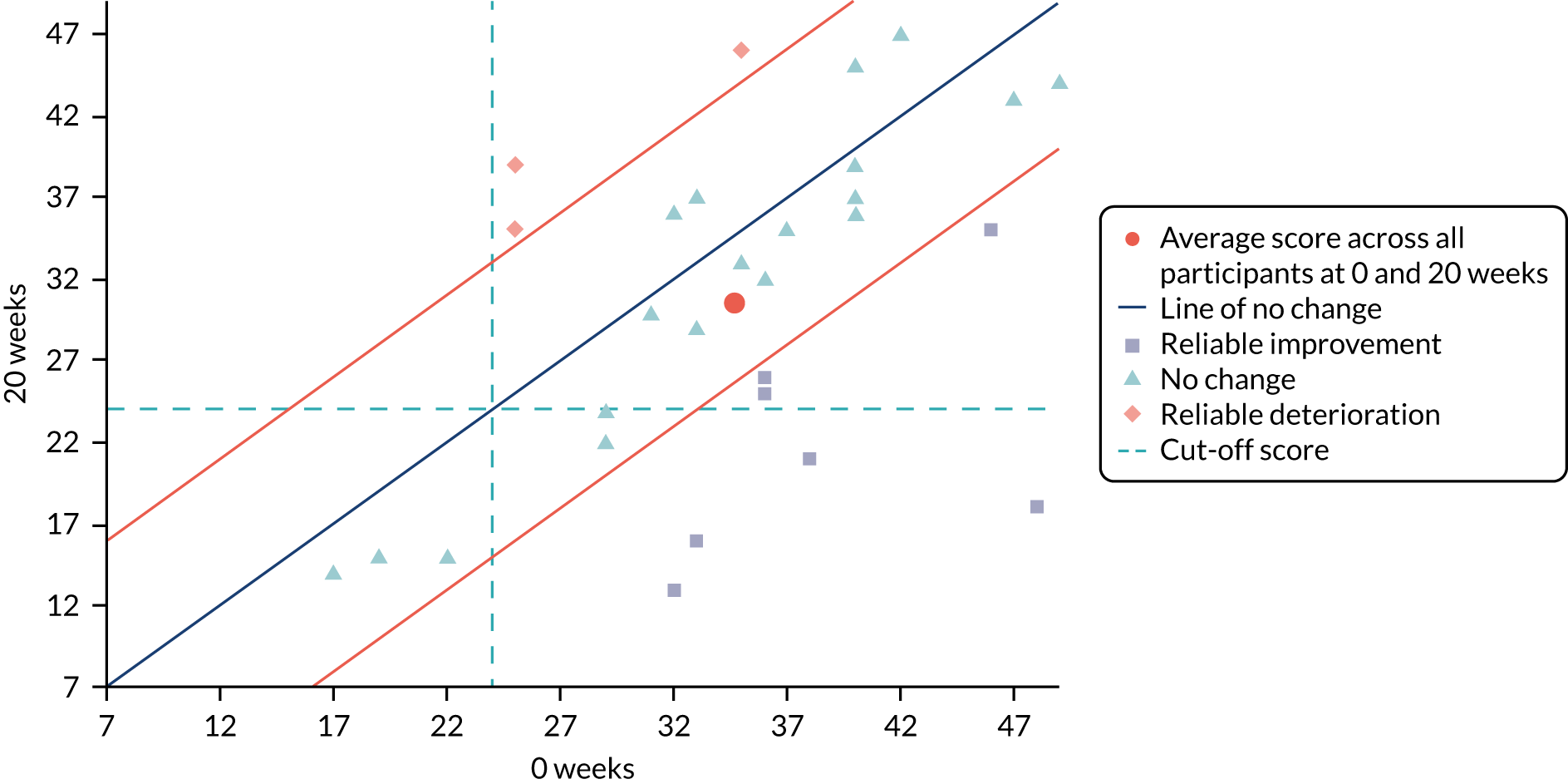
Discussion
Summary of the main findings
The main purpose of this uncontrolled feasibility study was to assess the acceptability and feasibility of our newly developed ACT intervention for older people with TR-GAD within the NHS. In summary, a high level of feasibility was demonstrated by a recruitment rate of 93% and a retention rate of 81%, both of which exceeded the targets (≥ 80% and ≥ 60%, respectively). A high level of acceptability was found with respect to session attendance, as demonstrated by 70% of participants attending ≥ 60% sessions (i.e. ≥ 10 sessions). Rates of satisfaction with therapy were adequate, with 60% of participants scoring ≥ 21 out of 30 on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised, although 80% of participants had not finished receiving their therapy sessions at the time of rating them. Secondary outcome measures further supported the feasibility and acceptability of the ACT intervention for older people with TR-GAD.
Even though the study was not powered to examine clinical effectiveness, there was indicative evidence of improvements in scores on the Geriatric Anxiety Inventory (–2.30 points, 95% CI –3.83 to –0.76 points), Geriatric Depression Scale-15 (–2.04 points, 95% CI –3.31 to –0.77 points) and Acceptance and Action Questionnaire-II (–3.93 points, 95% CI –7.16 to –0.70 points) from the 0 to the 20-week follow-up. Reliable improvements in scores were found in 45% of participants on the Geriatric Anxiety Inventory and in 24% of participants on both the Geriatric Depression Scale-15 and the Acceptance and Action Questionnaire-II. These results were particularly impressive given that all participants had failed to respond to prior pharmacological and/or psychological therapy for GAD. Furthermore, there was indicative evidence of improvement in scores on the Geriatric Depression Scale-15, even though participants were selected on the basis of GAD and not depressive symptoms.
These improvements are partially consistent with the results of a very small study of ACT for older people with GAD in which participants showed significant pre–post improvements in worry and depressive symptoms but not in anxiety. 27 The small discrepancy in findings might be explained by a number of issues in the previous study: (1) the Hamilton Anxiety Rating Scale was used to assess anxiety rather than a measure designed specifically for older people, such as the Geriatric Anxiety Inventory, (2) older people were not specifically included on the basis of TR-GAD and (3) the sample size was very small (n = 7). The improvements reported here are also partially consistent with the results of a small RCT of ACT compared with a waiting list control for older people with symptoms of depression and/or anxiety who were living in long-term care facilities. 60 This study reported significant between-group differences in depression but not anxiety, which the authors suggested was due to mean scores for anxiety being below clinical cut-offs at baseline.
A number of key issues should be highlighted when considering these results. First, this small, uncontrolled feasibility study cannot answer questions concerning the efficacy or clinical effectiveness of the ACT intervention. Nevertheless, these results suggest that the intervention may have the potential to reduce anxiety and depression and to increase psychological flexibility in older people with TR-GAD.
Second, symptomatic reductions in anxiety and depression were observed, even though this is not the main focus of ACT. The focus in ACT is on ‘living better’ rather than ‘feeling better’, and any symptomatic reductions are generally seen as a by-product of therapy. A measure that tapped into ‘living better’ may have demonstrated even larger improvements in scores.
Third, evidence of improvements in scores were found on the Acceptance and Action Questionnaire-II. This is a measure of psychological flexibility that primarily examines the degree to which a person is engaging in experiential avoidance. It does not measure other ACT processes and, therefore, it does not provide a comprehensive assessment of change in ACT processes. It may be that greater changes in ACT processes would have been observed with a broader measure such as the Comprehensive Assessment of Acceptance and Commitment Therapy Processes (CompACT) questionnaire. 122 This is a 23-item measure that examines (1) willingness to experience thoughts, feelings, sensations, etc., without trying to control, avoid or get rid of them; (2) mindful attention to current behaviour or actions; and (3) engagement in meaningful activity or valued actions.
Fourth, rates of satisfaction with therapy were found to be adequate on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised, with 60% of participants scoring ≥ 21 out of 30 points. As previously noted in Outcome measures, Primary outcome measures, there is no set definition of what constitutes ‘satisfactory’ and so this was arbitrarily defined as a total score of ≥ 21 out of 30 points on this subscale. If, however, a total score of ≥ 18 out of 30 points had been chosen (which corresponds to a ‘neutral’ rating on all items, i.e. the lower limit of acceptability), then 70% of participants would have rated the therapy as ‘satisfactory’. There are a number of reasons why rates of satisfaction with therapy may have been lower than expected. It may be that the intervention requires further refinement to make it acceptable to a larger proportion of older people with TR-GAD. This is explored in Chapter 6. It may also have been due to the fact that 80% of participants had not finished receiving their therapy sessions by the 20-week follow-up assessment. Finally, it may have been a result of the type of questionnaire chosen to assess satisfaction with therapy. The Satisfaction with Therapy and Therapist Questionnaire-Revised was developed for ‘fix it’ therapies (i.e. those that are focused on getting rid of problematic thoughts, feelings and situations) and, hence, it is less suitable for therapies that are focused on ‘living better’ rather than ‘feeling better’. Higher rates of satisfaction with therapy may have been found with a questionnaire focused on changes in life satisfaction rather than symptomatic change.
Finally, this study demonstrated not only the acceptability and feasibility of the intervention and study but also that it is possible to train novice ACT therapists to deliver this intervention to older people with TR-GAD within the NHS. This is consistent with previous findings. 27,123 No other studies have examined pharmacological or psychological treatments for older people with TR-GAD.
Research implications
This study examined whether or not it was feasible to deliver an ACT-based intervention to older people with TR-GAD within the NHS, and it explored the acceptability of this intervention. Although it was not powered to demonstrate clinical effectiveness, results indicated that reliable changes in key patient-reported outcome measures were observed in some participants. Most notably, reliable improvement in scores on the Geriatric Anxiety Inventory was observed in 45% of participants at the 20-week follow-up. This suggests that there is potential for clinical effectiveness in this population, which should be tested in a future substantive trial.
A wide variation in the reported number of years experiencing difficulties with worrying was observed in the current study: just over one-third of participants (n = 13, 35%) reported experiencing difficulties for the past 1–5 years, and just over one-third (n = 13, 35%) reported experiencing difficulties for > 30 years. A bimodal distribution of age at onset has been found in other studies of GAD in working age adults and older people. 124–126 This suggests that there may be two different subpopulations here: (1) a subpopulation in which GAD is lifelong and (2) a subpopulation in which GAD is more recent, because excessive worry and anxiety are required to be present only for at least 6 months to meet International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10),127 and DSM-V,128 diagnostic criteria (along with the presence of other symptoms). Alternatively, it may be that some people in the latter subpopulation also experience lifelong GAD but are able to use coping strategies to ‘mask’ GAD symptoms during their working life (e.g. overengagement in activity or work as a means of distracting themselves from worries). When these coping strategies are no longer available owing to age-related factors (such as retirement or physical health problems that do not permit overengagement in activity), then GAD symptoms are ‘unmasked’, giving the appearance of a recent onset. Whether or not there are qualitative differences between these subpopulations with respect to demographic, clinical and personality characteristics, as well as treatment response, should be explored further in a larger study. Furthermore, subgroup analyses that account for the age at onset of GAD should be included in any future RCT examining the clinical effectiveness of ACT for TR-GAD, given that higher rates of psychiatric comorbidity, psychotropic medication use and severe worry have been reported in older people with an earlier rather than a later onset (i.e. before vs. after the age of 50 years). 124
Following on from this, it has been argued that ‘the letters GAD would better stand for godawful diagnosis’129 and that this diagnostic category should be abandoned. Three possible diagnostic replacements have been suggested for GAD: (1) a diagnosis of mixed anxiety–depression due to the fact that these symptoms commonly occur together, so-called cothymia;130 (2) a diagnosis of ‘general neurotic syndrome’ or ‘general nervous syndrome’ due to the overlap between personality status and GAD; and (3) an adjustment disorder due to experiencing a major life event (i.e. life event-precipitated GAD).
Data reported here suggest that none of these possible diagnostic replacements applies to all of the participants in the current study, and many participants would fit more than one category. Sixty-two per cent (n = 23) of participants met MINI diagnostic criteria for GAD plus major depressive episode with or without melancholic features or mood disorder with psychotic features. Only a small proportion of participants (n = 6, 16%) met screening criteria on the Structured Clinical Interview for DSM-IV Axis II Disorders, with only two people reporting a comorbid diagnosis of personality disorder. However, a larger proportion of participants (n = 12, 32%) were unable to report a period of time in their life during which they experienced no difficulties with excessive worrying (suggestive of a recurrent, life-long condition that Tyrer129 would describe as ‘general neurotic syndrome’ or ‘general nervous syndrome’). Just over one-third of participants (n = 13, 35%) reported that a major or stressful life event had preceded excessive worrying and anxiety. It is possible that the response to pharmacological and/or psychological treatment and, hence, management of excessive worry and anxiety, may differ across these possible subpopulations. However, the fact that 43% (n = 16) of participants fit more than one category may blur any such distinctions. Thus, again, an examination of demographic, clinical and personality characteristics, as well as treatment response, should be explored further in a larger study.
Strengths of the study
To our knowledge, this is the first study to report the acceptability and feasibility of a psychological intervention that was developed specifically for older people with TR-GAD for delivery within the NHS. Other strengths of the study include the following:
-
We were able to demonstrate that it is feasible to successfully recruit participants whom many clinicians find challenging to work with owing to chronicity and resistance to treatment of GAD symptoms.
-
Engagement was high and drop-out was relatively low given that participants were experiencing difficult to treat symptoms by definition.
-
We demonstrated strong evidence of feasibility and acceptability for the majority of primary and secondary outcomes.
-
Given the chronicity and resistance to treatment of GAD symptoms, the fact that reliable improvements in scores on the Geriatric Anxiety Inventory were found in almost half of older people with TR-GAD was impressive.
-
We were able to train therapists who are new to the ACT model to deliver the intervention within the NHS, with excellent levels of adherence and competence.
-
We established a therapist supervision model that helped therapists to feel supported in the delivery of the intervention, which could be easily adopted in a future substantive trial.
Limitations of the study
There are a number of limitations of the current study. First, there was no control condition; therefore, it is uncertain whether or not any changes in outcome measures were related to the intervention or were a product of other non-specific therapeutic factors such as social support or spontaneous recovery. Three participants reported withdrawing from the intervention as they would have preferred a more counselling-type of approach in which they could ‘just talk’. This suggests that an appropriate comparison could have been a talking control condition in which participants were allowed to ‘just talk’. It has previously been shown that it is not only feasible to deliver such a talking control condition to older people with depression but also acceptable to them. 131 There would be a number of advantages of including a talking control condition in a future RCT of ACT for older people with TR-GAD. This would not only control for non-specific therapeutic factors such as social support but could also reduce attrition due to resentful demoralisation, which can occur when participants are allocated to a non-active control condition such as treatment as usual. An additional benefit is that it may be easier to recruit participants with TR-GAD into a RCT of ACT if it is compared with a talking control condition. The very nature of GAD means that potential participants may worry about which arm they would be randomly allocated to in a RCT. Consequently, they may decline to participate because they want to avoid this uncertainty. Including a talking control condition rather than a non-active control such as treatment as usual may remove some of this uncertainty.
Another limitation is that the majority of participants were white/white British women who would be categorised as ‘younger old’ (i.e. in their 60s and 70s). Although just over half of participants were in their 70s, we recruited as many participants in their 80s as those in their 60s, which is acceptable for late-life mental health studies. Furthermore, although the number of participants from ethnic minorities was small and clearly under-representative, we demonstrated that we were able to recruit from these populations. In addition, although the majority of participants were women, this is unsurprising given that being female is one of the known risk factors for anxiety disorders in older people,90 and the older that people are, the more likely they are to be female. However, these sampling issues do mean that the results cannot be generalised to a broader population, particularly ‘older old’ (i.e. in their 80s or older) men from ethnic minorities. Recruiting ‘harder to reach’ older people is a common problem in research trials in general, and identifying successful strategies for recruiting from these populations would be important in any future study. Such strategies may include those recommended by the TIBaR model for recruiting ‘hard-to-reach’ older people: (1) build up Trust, (2) offer Incentives, (3) identify individual Barriers and (4) be Responsive. 132 They may also include strategies identified from RCTs of different recruitment approaches. For example, a previous study of physical activity in older people found that an invitation letter plus a patient information sheet that was followed up by up to four attempts at telephone contact was the most effective recruitment strategy. 133
A further limitation is the fact that participants were recruited only from urban and suburban areas in the London region, because this was a feasibility study, thus limiting external validity. Clearly, recruiting participants from multiple sites across the UK, including those in rural regions, would enhance the representativeness of findings in a future substantive trial.
The fact that outcome measures were assessed at only 0 and 20 weeks is an additional limitation of the current study. Some participants had not finished their ACT sessions by 20 weeks owing to the long waiting list for therapy at some sites, which may have negatively affected change scores. Furthermore, no follow-up after 20 weeks was conducted and, therefore, it is uncertain whether or not any gains were maintained beyond 20 weeks. It is also not clear whether or not a follow-up after 20 weeks would be feasible in a future substantive trial. Clearly, including an additional follow-up assessment in a future substantive trial would help to clarify these uncertainties.
Another limitation is that the sample size was relatively small, although this was consistent with previous recommendations of 24–35 participants for pilot and feasibility studies to provide sufficient data and precision of means and variances. 117,134,135 Consequently, conclusions should be drawn with caution, particularly those relating to patient-reported outcomes.
A final limitation relates to the assessment of treatment fidelity in the delivery of training and intervention sessions. We did not conduct any direct visual observation of intervention sessions to assess treatment fidelity for pragmatic reasons (including the desire to avoid anxiety-provoking study procedures in an already anxious group and to reduce potential demand characteristics). 136 Instead, an independent ACT therapist assessed treatment fidelity through audio-recordings of sessions – a standard approach that has been used in previous RCTs. 87 Although the training sessions were developed by members of the research team with knowledge and experience in delivering ACT and training therapists to deliver ACT, we did not directly assess the fidelity of the training sessions. Therefore, the degree of adherence to the ACT model could not be ascertained.
Conclusions
In conclusion, we found good evidence of feasibility (as demonstrated by a recruitment rate of 93% and a retention rate of 81%), and good evidence of acceptability (as demonstrated by 70% of participants attending ≥ 10 sessions). Secondary outcome measures further supported the feasibility and acceptability of our newly developed ACT intervention for older people with TR-GAD. However, the fact that 60% of participants scored ≥ 21 out of 30 points on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised suggests that further refinement of the intervention is necessary, as described in Chapter 5. Furthermore, even though the study was not powered to examine clinical effectiveness, there was evidence of improvements in scores on the Geriatric Anxiety Inventory, Geriatric Depression Scale-15 and Acceptance and Action Questionnaire-II from 0 to 20 weeks. Reliable improvements in scores were found in 45% of participants on the Geriatric Anxiety Inventory and in 24% of participants on the Geriatric Depression Scale-15 and Acceptance and Action Questionnaire-II. Although this small uncontrolled feasibility study cannot answer questions concerning the clinical effectiveness of our ACT intervention, these results suggest that it may have the potential to reduce anxiety and depression and increase psychological flexibility in older people with TR-GAD. Recommended changes with respect to the design and delivery of a future substantive trial of the clinical effectiveness of ACT for older people with TR-GAD that emerge from the current findings are discussed in Chapter 7.
Chapter 5 Uncontrolled feasibility study: health economic data
Introduction
In Chapter 4 we reported on quantitative estimates of the acceptability and feasibility of the newly developed ACT intervention and study methods in an uncontrolled feasibility study. The feasibility of undertaking an economic evaluation of ACT for TR-GAD in older people, in addition to key study design parameters for a future substantive trial of cost-effectiveness, are considered in this chapter. The objectives were to:
-
obtain estimates of the costs associated with implementing the intervention (and hence indicative costs in a future trial)
-
clarify key study design parameters for a future substantive trial of cost-effectiveness (e.g. the choice of outcome measures).
Methods
Outcome measures
All reporting is in accordance with the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist, where possible, because this was neither a randomised trial nor a full economic evaluation and did not include a cost-effectiveness analysis (see Appendix 6).
Intervention costs
Nationally published costs137 were used to calculate the costs of intervention delivery (with and without overheads) based on the number of sessions attended per participant, session duration, therapist pay grade, therapist training and supervision. The intervention and therapist training are described in Chapter 4.
Quality-adjusted life-years
Quality-adjusted life-years were calculated from utility scores collected with the EQ-5D-5L using the area under the curve method adjusting for baseline utility. 138 The EQ-5D-5L is a 5-item self-report measure of health-related quality of life, used to calculate utility scores for QALYs, rated on a 5-point scale from no problems to extreme problems. It also includes the EQ-VAS: a single-item self-report measure of health-related quality of life rated on a vertical visual analogue scale from 0 (worst health you can imagine) to 100 (best health you can imagine). The EQ-5D-5L is preferred to the EuroQol-5 Dimensions, three-level version (EQ-5D-3L), as the latter suffers from ceiling effects. 139 The EQ-5D-5L was collected at 0 weeks (baseline) and 20 weeks (follow-up).
Resource use
Costs were collected from a health and social care perspective only. A modified version of the CSRI was used to collect information on health and social care resource use in the preceding 3 months at 0 weeks (baseline) and 20 weeks (follow-up). This included use of inpatient services, outpatient services, day care services, community services, any other community services and medication.
Data analysis
Intervention costs
The overall mean cost of the intervention (including costs of intervention delivery, training and supervision) was calculated by participant, with and without overheads. To calculate costs for intervention delivery, information on the number and duration of sessions attended by each participant, as well as therapists’ pay grades, was collected. Therapists were employed on NHS Agenda for Change bands 7–8c and were costed using 2018/19 Personal Social Services Research Unit calculations of mean salary and costs. 137 Calculations included the cost of travel for therapists to deliver the intervention to participants in their own home, where necessary, as well as the cost of therapists’ time spent travelling. Travel time was assumed to be an average of 1 hour per therapist per session, and the cost of travelling to each session was assumed to be equivalent to a 1-day any-time travelcard for zones 1–6. 140
Costs for training and supervision (described in Chapter 4) were calculated by collecting information on the number of training and supervision sessions delivered/attended and therapists’ and supervisors’ pay grades. Training and supervision were delivered by clinical psychologists (band 8b/8c equivalent) and a consultant psychiatrist (threshold 6) and were costed at an hourly rate for the hours spent delivering this. Training and supervision costs for therapists included the cost of therapists’ time to attend training and supervision and the cost of travelling to University College London for the training days. Travel time was assumed to be an average of 2 hours per therapist per training day, and the cost of travelling to each training day was assumed to be equivalent to a 1-day any-time travelcard for zones 1–6. 140
Additional costs included the cost of printing materials (at a rate of £0.05 per sheet), refreshments provided during training (at a rate of £15 per day) and teleconference services for therapists’ group supervision (assuming an average of £25 per session).
Quality of life
The mean and SDs for utility scores were calculated based on responses to the EQ-5D-5L. The current EQ-5D-5L value set available for England141 is not recommended for use by the NICE as there are concerns about the quality and reliability of the data that were used in the development of the value set. 142 Therefore, the NICE recommends using a ‘crosswalk’ model to map the EQ-5D-5L onto the EQ-5D-3L. 143 However, there is uncertainty about whether or not a mapping algorithm can accurately reflect what individuals would have answered if they had been presented with three levels in the first place. Therefore, for completeness, we have calculated utility scores and accompanying QALYs using both methods. The analysis of change in utility scores between 0 and 20 weeks follows the same method as for other patient-reported outcomes described in Chapter 4.
Resource use
The percentage of patients and data completeness for each type of service use were reported. These were costed using Unit Costs of Health and Social Care 2019137 and NHS reference costs 2018–19. 144 Medication use was costed using the British National Formulary. 145 All costs are in 2018/19 Great British pounds (GBP). The overall mean cost per participant (with 95% CIs) was calculated at 20 weeks, adjusting for baseline service use. A full cost-effectiveness analysis was not conducted because this was an uncontrolled feasibility study with no comparator.
Results
Missing data
Data were collected from 34 participants at 0 weeks and 30 participants at 20 weeks. As shown in Table 37, there were low rates of missing data for the EQ-5D-5L and the modified CSRI. Some participants reported finding it difficult to estimate their health using a visual analogue scale in the EQ-5D-5L.
Intervention costs
A detailed breakdown of the costs associated with the delivery of the intervention, including training and supervision of therapists, is presented in Table 38. The highest costs were for training (£31,802.34 without overheads and £53,235.50 with overheads) and the lowest costs were for supervision (£15,403.22 without overheads and £25,062.00 with overheads). With overheads, the estimated total cost was £112,866.75, equating to a mean cost of £3050.45 per participant. Without overheads, the estimated total cost was £68,200.41, equating to a mean cost of £1843.25 per participant.
| Item | Unit cost (£) | Number of units | Total cost (£) with overheads | Total cost (£) without overheads | Details |
|---|---|---|---|---|---|
| Training | |||||
| Therapists’ time to attend traininga | Hourly rate with/without overheads:
|
10 band 7, four band 8a and three band 8c therapists at 35 hours each | 37,450.00 | 21,895.86 | 7 hours per day for 5 days |
| Travel for therapists attending training | 90.50 | 17 | 1538.50 | 1538.50 | Assumes a cost of 1-day any-time travelcard for zones 1–6 (£18.10) for 5 days of training |
| Therapists’ time to travel to attend traininga | Hourly rate with/without overheads:
|
10 band 7, four band 8a and three band 8c therapists at 10 hours each | 10,700.00 | 6255.96 | Assumes an average of 2 hours travelling per day for 5 days |
| Refreshments | 15.00 | 5 | 75.00 | 75.00 | Assumes an average of £15 per day for 5 days |
| Trainers’ time to deliver traininga | Hourly rate with/without overheads:
|
42 hours | 3472.00 | 2037.02 | 7 hours per day for 5 days for one trainer; 7 hours for 1 day for one trainer; no costs of travel as training was delivered at the place of employment |
| Subtotal | 53,235.50 | 31,802.34 | |||
| Intervention delivery | |||||
| Therapists’ time to deliver the interventiona | Hourly rate with/without overheads:
|
Seven band 7, four band 8a and one band 8c therapists; 438 hours of therapy | 27,085.00 | 15,805.08 | 1 hour per session |
| Travel for therapists delivering the intervention to participants in their own home | 18.10 | 96 sessions | 1737.60 | 1737.60 | Assumes cost of 1-day any-time travelcard for zones 1–6 (£18.10) per session |
| Therapists’ time to travel to deliver the intervention to participants in their own homea | Hourly rate with/without overheads:
|
Three band 7 and two band 8a therapists; 96 hours of travelling | 5492.00 | 3197.52 | Assumes an average of 1 hour travelling per session |
| Subtotal | 34,314.60 | 20,740.20 | |||
| Supervision | |||||
| Therapists’ time to attend supervision before and during intervention delivery perioda | Hourly rate with/without overheads:
|
10 band 7, four band 8a and three band 8c therapists; 266 hours of supervision | 16,771.00 | 9790.74 | 1 hour per session |
| Supervisors’ time to provide supervisiona | Hourly rate with/without overheads:
|
Two band 8b equivalents, one band 8c equivalent and one consultant threshold 6; 72 hours of supervision | 6491.00 | 3812.49 | 1 hour per session |
| Teleconference service for supervision | 25.00 per session | 72 sessions | 1800.00 | 1800.00 | Assumes an average of £25 per session |
| Subtotal | 25,062.00 | 15,403.22 | |||
| Other | |||||
| Printing materials | 0.05 per sheet | 71 | 254.65 | 254.65 | 17 training packs, 17 manuals and 37 client workbooks |
| Subtotal | 254.65 | 254.65 | |||
| Overall cost (£) | 112,866.75 | 68,200.41 | |||
| Overall cost (£) per participant | 3050.45 | 1843.25 | Based on 37 participants | ||
Quality of life
EuroQol-5 Dimensions, five-level version, dimensions
Table 39 provides a breakdown of the number and proportion of participants reporting at each of the levels within the EQ-5D-5L dimensions, as previously recommended. 146 The dimension with the least number of self-reported problems was self-care (with n = 4 reporting at least moderate problems at baseline), and the dimension with the most self-reported problems was anxiety/depression (with n = 31 reporting at least moderate problems at baseline). Somewhat surprisingly, three participants reported slight or no problems with anxiety/depression at 0 weeks. These outliers are at odds with the fact that participants had to score in at least the moderate range on the GAD-7 to be invited to attend a screening interview. A closer examination of individual data revealed clear discrepancies between scores on this dimension and scores on the Geriatric Anxiety Inventory and Geriatric Depression Scale for two out of three of these participants.
| Level (severity of problem) | Dimension, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain or discomfort | Anxiety or depression | ||||||
| 0 weeks (N = 34) | 20 weeks (N = 30) | 0 weeks (N = 34) | 20 weeks (N = 30) | 0 weeks (N = 34) | 20 weeks (N = 30) | 0 weeks (N = 34) | 20 weeks (N = 30) | 0 weeks (N = 34) | 20 weeks (N = 30) | |
| 1 (no problems) | 7 (21) | 7 (23) | 24 (71) | 22 (73) | 12 (35) | 11 (37) | 5 (15) | 4 (13) | 1 (3) | 2 (7) |
| 2 (slight) | 7 (21) | 8 (27) | 6 (18) | 4 (13) | 3 (9) | 7 (23) | 7 (21) | 6 (20) | 2 (6) | 3 (10) |
| 3 (moderate) | 11 (32) | 6 (20) | 4 (12) | 3 (10) | 14 (41) | 5 (17) | 13 (38) | 12 (40) | 13 (38) | 15 (50) |
| 4 (severe) | 9 (26) | 9 (30) | 0 (0) | 1 (3) | 5 (15) | 7 (23) | 5 (15) | 7 (23) | 13 (38) | 6 (20) |
| 5 (unable/extreme) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 4 (12) | 1 (3) | 5 (15) | 4 (13) |
| Reporting at least moderate problems | 20 (59) | 15 (50) | 4 (12) | 4 (13) | 19 (56) | 12 (40) | 22 (65) | 20 (67) | 31 (91) | 25 (83) |
EuroQol-5 Dimensions, five-level version, utility scores and QALYs
As noted in Methods, Data analysis, Quality of life, two methods were used to calculate utility scores from the EQ-5D-5L: the EQ-5D-5L value set and the mapping algorithm. Both methods and accompanying QALYs (unadjusted and adjusted for baseline utility) are reported in Table 40.
| Outcome measure | Time point | |
|---|---|---|
| 0 weeks (n = 34) | 20 weeks (n = 30) | |
| EQ-5D-5L value set score, points (SD) | 0.52 (0.25) | 0.55 (0.28) |
| QALYs (95% CI) | – | 0.212 (0.180 to 0.244) |
| Adjusted QALYs (95% CI) | – | 0.208 (0.190 to 0.226) |
| EQ-5D-5L mapping algorithm score, points (SD) | 0.42 (0.27) | 0.49 (0.27) |
| QALYs (95% CI) | – | 0.181 (0.149 to 0.214) |
| Adjusted QALYs (95% CI) | – | 0.178 (0.160 to 0.197) |
Table 41 reports estimated changes in utility scores from 0 to 20 weeks. Estimated changes were in a direction consistent with an improvement in health-related quality of life. The mapping algorithm consistently assigned lower utility scores to individuals than the value set, but appeared to be more sensitive to changes in health-related quality of life.
| Outcome measure | Time point, mean (SD) | Estimated change (95% CI) | |||
|---|---|---|---|---|---|
| 0 weeks (N = 34) | 20 weeks (N = 30) | Unadjusted analysis of change | Unadjusted linear mixed model | Adjusted linear mixed modela | |
| EQ-5D-5L value set (possible range 0–1) | 0.52 (0.25) | 0.55 (0.28) | 0.041 (–0.066 to 0.149) | 0.037 (–0.063 to 0.137) | 0.049 (–0.054 to 0.152) |
| EQ-5D-5L mapping algorithm (possible range 0–1) | 0.42 (0.27) | 0.49 (0.27) | 0.071 (–0.047 to 0.190) | 0.068 (–0.040 to 0.176) | 0.085 (–0.027 to 0.197) |
Health and social care resource use
Low rates of service use were reported at both time points (Table 42), with very little service use being self-reported at 20 weeks. The most common types of services used were outpatient services (n = 11, 33%), with psychiatric outpatient services being the most frequently reported (n = 8, 24%). Community mental health centre was the only category endorsed in day activity services. Community care services mostly featured those focused on mental health [e.g. Care Programme Approach (CPA) key worker, community psychiatric nurse]. No use of criminal justice services was reported at 0 or 20 weeks.
| Service receipt | N (missing n, %) | Number of participants at 0 weeks, n (%) | N (missing n, %) | Number of participants at 20 weeks, n (%) |
|---|---|---|---|---|
| Inpatient services | 33 (4, 11) | 0 (0) | 29 (8, 22) | 0 (0) |
| Outpatient services | 33 (4, 11) | 11 (33) | 29 (8, 22) | 1 (3) |
| Psychiatric | 8 (24) | 1 (3) | ||
| Special unit | 2 (6) | 0 (0) | ||
| Other | 1 (3) | 0 (0) | ||
| Day activity services | 33 (4, 11) | 3 (9) | 29 (8, 22) | 0 (0) |
| Community mental health centre | 3 (9) | 0 (0) | ||
| Community care services | 33 (4, 11) | 2 (6) | 29 (8, 22) | 2 (6) |
| CPA key worker | 1 (3) | 1 (3) | ||
| Older persons community team member | 1 (3) | 0 (0) | ||
| Home treatment team | 0 (0) | 1 (3) | ||
| Other community care services | 33 (4, 11) | 4 (12) | 29 (8, 22) | 1 (3) |
| Psychologist | 1 (3) | 0 (0) | ||
| Community psychiatric nurse | 1 (3) | 0 (0) | ||
| Chiropodist | 1 (3) | 0 (0) | ||
| GP | 1 (3) | 1 (3) | ||
| Criminal justice service | 33 (4, 11) | 0 (0) | 29 (8, 22) | 0 (0) |
| Psychotropic medication use | 33 (4, 11) | 25 (76) | 29 (8, 22) | 23 (74) |
The total cost of service use per participant is reported in Table 43, broken down into community care, secondary care and medication costs. Costs appear to be lower at the 20-week follow-up than at baseline. The higher costs at baseline are driven by a couple of individuals with very high costs across all types of services, including multiple psychiatric outpatient appointments and many contacts with a CMHT and CPA key worker, as well as the prescription of various medications. Without a control group and given the small sample size and skewed nature of the costs, the reduction in costs between 0 and 20 weeks cannot be conclusively attributed to the intervention.
| Type of service | Time point, cost (£) | |
|---|---|---|
| 0 weeks (n = 33) | 20 weeks (n = 29) | |
| Community care, mean (SD) | 162.54 (559.47) | 10.10 (38.95) |
| Secondary care, mean (SD) | 67.21 (126.96) | 3.83 (20.61) |
| Medication, mean (SD) | 43.46 (88.66) | 48.89 (100.75) |
| Total cost, mean (SD) | 280.39 (681.30) | 63.32 (127.49) |
| Baseline-adjusted cost, mean (95% CI) | – | 71.30 (41.86 to 100.74) |
Discussion
The feasibility of collecting data on resource use, intervention costs and quality of life was examined in this small uncontrolled feasibility study. The findings highlighted a number of issues that would need to be considered in a future substantive trial of the cost-effectiveness of ACT for older people with TR-GAD, as follows.
Main findings and associated factors that would need to be considered in a future substantive trial
Excellent completion rates were obtained for the EQ-5D-5L and the modified CSRI, indicating their feasibility for use in a future substantive trial. In support of this, these instruments have been successfully applied in previous studies of cost-effectiveness in older people. 87,147 Furthermore, a systematic review of instruments for measuring quality of life outcomes for economic evaluations recommended the EQ-5D-5L for use with older populations. 148
Calculation of intervention costs
A detailed breakdown of the costs associated with training, intervention delivery and supervision showed that therapist training made the greatest contribution to costs (47% of the total costs). Additional costs not relevant to a feasibility study but that would need to be considered in a future substantive trial include higher costs of travel for therapists from different UK sites to attend training at a central site and 1-day top-up training for therapists (e.g. 12 months after initial training).
Cost collection instruments
Although excellent completion rates were obtained for the modified CSRI, rates of reported resource use were low, which may have been due to the use of self-reporting. This may have resulted in inaccurate recall and under-reporting of service use, an observation that has been reported in other studies. For example, patients with chronic diseases were found to self-report less health-care utilisation than recorded in computerised provider records. 149 Consequently, a future trial could ensure that data are extracted from GP medical records, with participants’ consent. This could not only improve the accuracy of data collection, as it would not rely on patient recall of service use, but also reduce burden on participants. However, the additional financial and researcher time costs would need to be factored into a future trial.
If the modified CSRI is chosen for use in a future substantive trial, findings from this study suggest that a number of changes could be made to improve data collection. Memory clinic services and audiology services could be added as specific appointment categories within outpatient services to more accurately capture data in relation to service use. Other categories aside from community mental health centre and criminal justice services could be removed to shorten the questionnaire and improve response rate due to low reported service use in these areas. Finally, yes/no tick boxes could be included to help differentiate between missing data and ‘0’ contacts.
Health-related quality of life instruments
Although the current study was not designed to examine clinical effectiveness owing to the lack of a comparator group, estimated changes over time in utility scores on the EQ-5D-5L were in a direction consistent with improvements in health-related quality of life. Larger improvements in health-related quality of life may not have been observed in the current study for a couple of reasons. First, a systematic review of the responsiveness of the EuroQol-5 Dimensions (EQ-5D) in people with depression or anxiety suggested that it may lack responsiveness in older people. 150 This was based on the findings of a RCT of CBT compared with treatment as usual for older people with depression, in which CBT was found to be superior to treatment as usual on a measure of depression, but not on the EQ-5D. 87 Second, the majority of EQ-5D-5L dimensions are focused on improvement of symptoms such as anxiety/depression, pain/discomfort and mobility, which is not consistent with the aim of ACT: to help people to ‘live better’ rather than ‘feel better’. A dimension of the EQ-5D-5L that is potentially more consistent with ACT’s aim of helping people to ‘live better’ is ‘usual activities’, which is the dimension that appeared to show the biggest changes at 20 weeks in the current study.
There were clear discrepancies between scores on the anxiety/depression dimension of the EQ-5D-5L and scores on the Geriatric Anxiety Inventory and Geriatric Depression Scale in two out of three participants who reported slight or no problems with anxiety/depression at 0 weeks. This may have been due to the fact that these participants did not recognise themselves as being anxious or depressed on the EQ-5D-5L but did so on the Geriatric Anxiety Inventory and Geriatric Depression Scale. This, in turn, may have been due to the use of different terminology in the questionnaires. For example, the EQ-5D-5L asks a person to indicate the degree to which they are ‘anxious’ or ‘depressed’, whereas ‘anxious’ is used only once in 20 statements in the Geriatric Anxiety Inventory, and ‘depressed’ is never used in the Geriatric Depression Scale. A previous study has shown that older people may use different terminology to describe anxiety symptoms than younger people; for example, older people tend to use terms such as ‘fret’ or ‘concern’ rather than ‘anxiety’. 151 This suggests that, if the EQ-5D-5L is chosen for use in a future trial, it would be beneficial to check for potential discrepancies such as these.
Calculation of utility scores from the EuroQol-5 Dimensions, five-level version
Two methods were used to calculate utilities from the EQ-5D-5L: (1) a method using the EQ-5D-5L value set for England141 and (2) a method that maps the EQ-5D-5L onto the EQ-5D-3L using a crosswalk model. 143 Two methods were used because there is debate as to which method is the most appropriate. The EQ-5D-5L is believed to broaden the measurement spectrum and be more sensitive to clinical changes than the EQ-5D-3L. 152 However, the mapping algorithm introduces artificial floor effects that negate this and may result in utilities that do not accurately reflect responses to the EQ-5D-5L. 143 On the other hand, the NICE recommends using the mapping algorithm because there have been some concerns over the quality and reliability of the data used in the development of the EQ-5D-5L value set for England. 142,153 Thus, in a future substantive trial it would seem appropriate to use the method recommended by the NICE as we would hope the results of the study would inform the NICE guidance with respect to the management of TR-GAD in older people.
Strengths and limitations
No evidence currently exists with respect to the cost-effectiveness of psychological or pharmacological interventions for older people with TR-GAD. This study represents the first steps to addressing this. However, there are a number of limitations of the study, as outlined in Chapter 4 and in this section.
First, we were unable to perform a cost-effectiveness analysis because of the lack of a control group. Consequently, this would need to be performed alongside a future substantive RCT.
Second, although health-related quality of life was measured using the EQ-5D-5L in the current study, no other measure of quality of life was included. Ideally, a measure that focused more on psychological health as opposed to physical health should have been included, in addition to the EQ-5D-5L, because it would not have been overly influenced by physical health problems that are common in this population. Such an example is the McGill Quality of Life Questionnaire-Revised,154 which is a global measure of quality of life that has satisfactory psychometric properties. This questionnaire places relatively less emphasis on physical well-being than other measures of quality of life, which means that scores would not be overly influenced by physical health problems. Furthermore, this measure includes items that are consistent with the treatment goals of ACT: assessing participants’ ability to undertake personally meaningful and purposeful activities and to achieve life goals in the presence of TR-GAD. However, this questionnaire cannot be used to calculate QALYs and so could not contribute to a cost–utility analysis alongside the EQ-5D-5L.
Other quality of life measures that could be used in addition to the EQ-5D-5L (or an equivalent instrument) to assess the psychological component of quality of life and contribute to a cost–utility analysis include the Short Form questionnaire-36 items (SF-36) and the ICEpop CAPability measure for Older people (ICECAP-O). 155,156 The SF-36 can be used to calculate QALYs whereas the ICECAP-O can be used to calculate capability-adjusted life-years and aims to capture well-being broader than just health. The ICECAP-O would be preferred over the SF-36 because the mental health component of the SF-36 focuses more on symptoms of psychological distress (e.g. feeling nervous or downhearted and ‘blue’) than the ICECAP-O. This may be more appropriate for ‘fix it’ therapeutic approaches that are aimed at helping people to feel better (e.g. CBT) rather than therapeutic approaches that are aimed at helping people to live better alongside their difficulties (e.g. ACT). By contrast, the ICECAP-O focuses on love and friendship, the ability to think about the future without concern, the ability to do things that make a person feel valued, enjoyment and pleasure, and independence. Some of these items fit better with the aims of ACT and, therefore, may be more sensitive to change than the SF-36.
Finally, one of the limitations noted in Chapter 4 was the fact that the majority of participants were in their 60s or 70s, which meant that the results cannot be generalised to those in their 80s or older. The small number of participants reporting at least moderate problems with self-care on the EQ-5D-5L at 0 and 20 weeks (n = 4) further suggests that results may not be representative of frailer older people living in the community.
Conclusions
Overall, the findings of this small uncontrolled feasibility study suggest that a future substantive trial of the cost-effectiveness of ACT for older people with TR-GAD would be feasible. Recommended changes with respect to the design and delivery of such a trial are discussed in Chapter 7.
Chapter 6 Uncontrolled feasibility study: qualitative data
Introduction
Chapter 4 reports on quantitative estimates of the acceptability and feasibility of the newly developed ACT intervention and study methods in an uncontrolled feasibility study. Qualitative data on the perceived acceptability and feasibility of the newly developed ACT intervention were gathered through individual qualitative interviews with a sample of older people with TR-GAD who had participated in the uncontrolled feasibility study, and with therapists who had delivered ACT in the study.
Methods
Design
The study used an explorative, flexible, qualitative research design to gather in-depth data. 157
Participants and recruitment procedures
Older people with TR-GAD who had participated in the uncontrolled feasibility study and therapists who had delivered ACT in the study were invited to participate in individual qualitative interviews. Purposive sampling was conducted on the basis of sex, ethnicity, recruitment source and session attendance to explore a range of perspectives. Participants who withdrew from the intervention or study were invited to participate in qualitative interviews; all declined. All therapists were invited to participate in individual qualitative interviews to examine how the intervention was delivered in practice.
Procedure
Semistructured interviews were conducted with 18 older people with TR-GAD and 11 therapists until data saturation was reached. The topic guide for older people with TR-GAD was used flexibly to explore participants’ experiences of receiving ACT, how helpful they found it, how easy it was to understand, the degree to which it met their needs, any difficulties experienced, any facilitators of and barriers to engaging in ACT, and any recommendations for revising the intervention (see Report Supplementary Material 6). The topic guide also explored any changes that people had experienced in their lives as a result of receiving ACT, as well as opinions in relation to the design of a future substantive trial.
The topic guide for therapists was used flexibly to examine therapists’ experiences of delivering ACT, how easy it was to deliver ACT to older people with TR-GAD, how understandable and how suitable it was for older people with TR-GAD, any difficulties experienced, any facilitators of and barriers to engaging in ACT, and any recommendations for revising the intervention. The topic guide also explored any changes that they had noticed in participants as a result of receiving ACT, as well as in their own professional practice, and opinions about the design of a future substantive trial.
Interviews with older people with TR-GAD were completed after the participant had finished receiving their therapy sessions. Interviews with therapists were completed once they had finished delivering all of their therapy sessions to study participants. All interviews were conducted by one researcher (KK) and were audio-recorded and transcribed verbatim. All participants consented to participate in semistructured interviews.
Data analyses
Thematic analysis was used to analyse qualitative data. This method of analysis was chosen as it allows accessibility and flexibility in its approach. 158 Thematic analysis can be used to identify and report patterns in the data and to interpret various aspects of a research topic. 159 One researcher (KK) listened to all audio-recordings and repeatedly read the transcripts and research notes to familiarise herself with the data. Key issues, recurrent themes and interpretations were noted and discussed in supervision.
Ethics
Ethics approval was granted by the London–Camberwell St Giles Research Ethics Committee on 29 August 2017 and Health Research Authority approval granted on 4 September 2017 (IRAS ID 224111, REC reference 17/LO/1314; see Report Supplementary Material 5).
Results
Older people with treatment-resistant generalised anxiety disorder
Demographic and clinical characteristics
The mean number of sessions completed by older people with TR-GAD who participated in semistructured interviews was 14.6 sessions (SD 2.5 sessions). As shown in Table 44, the majority of participants self-identified as white/white British (n = 14, 78%) women (n = 15, 83%) who were retired (n = 12, 67%) and married (n = 9, 50%). The age of participants ranged from 65 to 89 years, with a mean age of 75.9 years (SD 6.6 years). There was a wide range in educational qualifications, with 39% (n = 7) of participants reporting a school leaving certificate or no qualifications and 28% (n = 5) reporting a qualification equivalent to or higher than A level.
| Demographic characteristic | N (missing n, %) | n (%) | Mean (SD) |
|---|---|---|---|
| Area | 18 (0, 0) | ||
| South London and Maudsley NHS Foundation Trust | 5 (28) | ||
| Barnet, Enfield and Haringey Mental Health NHS Trust | 5 (28) | ||
| Camden and Islington NHS Foundation Trust | 3 (17) | ||
| Whittington Health NHS Trust | 4 (22) | ||
| North East London NHS Foundation Trust | 1 (6) | ||
| Age (years) | 18 (0, 0) | 75.9 (6.6) | |
| Age (years) | 18 (0, 0) | ||
| 60–69 | 2 (11) | ||
| 70–79 | 11 (61) | ||
| 80–89 | 5 (28) | ||
| 90–99 | 0 (0) | ||
| ≥ 100 | 0 (0) | ||
| Sex | 18 (0, 0) | ||
| Female | 15 (83) | ||
| Male | 3 (17) | ||
| Ethnicity | 18 (0, 0) | ||
| Asian/Asian British | 1 (6) | ||
| Black/black British | 0 (0) | ||
| Mixed | 1 (6) | ||
| White/white British | 14 (78) | ||
| Other | 2 (11) | ||
| Marital status | 18 (0, 0) | ||
| Married | 9 (50) | ||
| Divorced | 2 (11) | ||
| Single | 2 (11) | ||
| Co-habiting | 0 (0) | ||
| Widowed | 5 (28) | ||
| Separated | 0 (0) | ||
| Mean number of years of education | 18 (0, 0) | 10.6 (3.3) | |
| Highest educational qualification | 18 (0, 0) | ||
| Master’s degree | 1 (6) | ||
| Undergraduate degree | 2 (11) | ||
| A level/baccalaureate | 2 (11) | ||
| O level/GCE/GCSE | 2 (11) | ||
| School Leaving Certificate | 3 (17) | ||
| No qualifications | 4 (22) | ||
| Unclear | 4 (22) | ||
| Employment status | 18 (0, 0) | ||
| Paid work | 1 (6) | ||
| Voluntary work | 4 (22) | ||
| Retired | 12 (67) | ||
| Other | 1 (6) |
With respect to clinical characteristics displayed in Table 45, the overall mean total score on the GAD-7 was at the upper end of the moderate range (14.7 points, SD 2.3 points), with scores ranging from 11 to 19 points (none scored < 11 points owing to pre-screening with the GAD-7). There was a wide variation in the reported number of years experiencing difficulties with worrying, with ≥ 30 years (n = 7, 39%) and 1–5 years (n = 6, 33%) being the most common. The most common comorbid psychiatric disorders were major depressive episode with and without melancholic features (n = 8, 44%), social phobia (n = 5, 28%) and panic disorder with and without agoraphobia (n = 4, 22%). Although two-thirds of the participants reported current alcohol or drug use, this was occurring at levels higher than recommended in national guidelines in only one person (6%). Reports of current suicidal ideation were fairly common (n = 11, 61%), but a previous history of suicide attempt or self-harm was not (n = 3, 17%). Only one person was identified as having a possible personality disorder on the Structured Clinical Interview for DSM-V Axis II Disorders screening questionnaire (6%). The majority of participants reported currently taking psychotropic medication (n = 27, 73%), with the most common type being antidepressants (n = 12, 71%). Only a small proportion of participants (n = 3, 18%) reported changes to psychotropic medication within 2 months of the assessment. The majority of participants reported receiving pharmacotherapy (n = 15, 83%) and psychological therapy (n = 15, 83%) in the past. Many participants reported physical health problems (n = 16, 89%): severe problems were reported in at least one category on the Cumulative Illness Rating Scale for Geriatrics by 78% of participants (n = 14) and 6% of participants (n = 1) reported extremely severe problems in at least one category.
| Clinical characteristic | N (missing n, %) | n (%) | Mean (SD) | Median (IQR) |
|---|---|---|---|---|
| GAD-7 total score, points (possible range 11–21 points owing to pre-screening)a | 18 (0, 0) | 14.7 (2.3) | ||
| GAD-7 severity classification | 18 (0, 0) | |||
| Moderate (possible range 11–15 points)b | 13 (72) | |||
| Severe (possible range 16–21 points)b | 5 (28) | |||
| Duration (years) of current difficulties with worrying | 18 (0, 0) | |||
| < 1 | 2 (11) | |||
| 1–5 | 6 (33) | |||
| 6–10 | 2 (11) | |||
| 11–20 | 1 (6) | |||
| 21–30 | 0 (0) | |||
| > 30 | 7 (39) | |||
| Number of participants meeting MINI diagnostic criteria | 18 (0, 0) | |||
| GAD | 18 (100) | |||
| Major depressive episode | 1 (6) | |||
| Major depressive episode with melancholic features | 7 (39) | |||
| Mood disorder with psychotic features | 1 (6) | |||
| Panic disorder | 1 (6) | |||
| Panic with agoraphobia | 3 (17) | |||
| Agoraphobia | 1 (6) | |||
| Social phobia | 5 (28) | |||
| Dysthymia | 3 (17) | |||
| OCD | 1 (6) | |||
| PTSD | 3 (17) | |||
| Psychotic disorders | 0 (0) | |||
| Manic episode | 0 (0) | |||
| Alcohol dependence | 0 (0) | |||
| Substance abuse | 0 (0) | |||
| Number of mental health comorbidities on the MINI | 18 (0, 0) | 1.4 (1.1) | ||
| Current alcohol or drug use | ||||
| Yes | 12 (67) | |||
| No | 6 (33) | |||
| > 14 units of alcohol per week | 18 (0, 0) | |||
| Yes | 1 (6) | |||
| No | 15 (83) | |||
| Unclear | 2 (11) | |||
| Current suicidal ideation | 18 (0, 0) | |||
| Yes | 11 (61) | |||
| No | 7 (39) | |||
| History of suicide attempt or self-harm | 18 (0, 0) | |||
| Yes | 3 (17) | |||
| No | 15 (83) | |||
| Possible PD identified on Structured Clinical Interview for DSM-V Axis II Disorders | 18 (0, 0) | |||
| Yes | 1 (6) | |||
| No | 17 (94) | |||
| Number of participants meeting screening criteria for DSM-V Axis II Disorders | 18 (0, 0) | |||
| Avoidant personality disorder | 1 (6) | |||
| Obsessive compulsive personality disorder | 0 (0) | |||
| Borderline personality disorder | 1 (6) | |||
| Dependent personality disorder | 0 (0) | |||
| Current psychotropic medication | 18 (0, 0) | |||
| Yes | 13 (72) | |||
| No | 5 (28) | |||
| Mean number of psychotropic medications at assessment | 18 (0, 0) | 1.3 (1.2) | ||
| Number of participants with changes to psychotropic medication within 2 months of assessment | 17 (1, 6) | 3 (18) | ||
| Current psychotropic medication | 17 (1, 6) | |||
| Antidepressantsc | 12 (71) | |||
| Anxiolytics | 0 (0) | |||
| Sedatives | 4 (24) | |||
| Hypnotics | 2 (12) | |||
| Anti-epileptics | 4 (24) | |||
| Antipsychotics | 0 (0) | |||
| Antihistamines | 0 (0) | |||
| Previous pharmacotherapy | 18 (0, 0) | |||
| Yes | 15 (83) | |||
| No | 3 (17) | |||
| Number of different types or episodes of previous pharmacotherapy (tried or declined) | 18 (0, 0) | 1.0 (1.0–2.0) | ||
| Previous psychological therapy | 18 (0, 0) | |||
| Yes | 15 (83) | |||
| No | 3 (17) | |||
| Number of different types or episodes of previous psychological therapy (tried or declined) | 18 (0, 0) | 1.9 (1.2) | ||
| SMMSE total score, points (possible range 0–30 points)d | 18 (0, 0) | 28.5 (1.4) | ||
| SMMSE total score range, points (possible range 0–30 points)b | 18 (0, 0) | 26–30e | ||
| Self-reported physical health problems | 18 (0, 0) | |||
| Yes | 16 (89) | |||
| No | 2 (11) | |||
| Cumulative Illness Rating Scale for Geriatricsb | 18 (0, 0) | |||
| Total number of endorsed categories (possible range 0–14)f | 4.0 (2.3) | |||
| Total score, points (possible range 0–56 points)f | 9.1 (5.7) | |||
| Severity Index (total score/total number of endorsed categories) | 2.0 (0.8) | |||
| Number of categories at level 3 severity (possible range 0–14)g | 1.8 (1.3) | |||
| Number of categories at level 4 severity (possible range 0–14)h | 0.0 (0.0–0.0) |
Qualitative themes
Four key themes were identified in qualitative interviews with older people with TR-GAD: (1) acceptability of ACT, (2) experience of ACT, (3) feasibility of ACT and (4) engaging in research. Subthemes within each key theme were also identified. Implications of the key themes and subthemes with respect to refining the intervention are discussed in Table 46.
| Theme/subtheme | Supporting quotations | Suggested revisions to the intervention |
|---|---|---|
| 1. Acceptability of ACT | ||
| Understanding ACT | I understand the principle, and I think it’s quite easy to understandP15I could see what she was saying to me, what to do, but doing it is hardP22 |
|
| Barriers to engaging in ACT | No. Because now I’m older and that . . . I always say, ‘Once a worrier, always a worrier’P01You don’t have that long future to look forward to, you don’t have the knowledge that you could still change your life, that things could improve, you could go into a new job or you could have a new relationship or whatever. Pretty much wherever you are when you get to my age is pretty much where you areP23I think that where I had to push myself sometimes, was when I didn’t feel very well, or where the side effects of the medications that I was taking was being difficult [tiredness], and I had to get myself through that. That, in itself, can actually prevent people from participatingP24 |
|
| Motivation to change | But I closed my mind to the fact that, you know, why I was thinking this. And, because I thought, well, it’s got to do some good, and it didP08Well, in my case having tried CBT and medication, I wanted it explained to me what it was. I said, well, thank god that there’s somebody doing something on this front, so I was very pleased to be accepted into the programme . . .P20 |
|
| Self-reported improvements to the intervention | ACT therapy . . . acceptance and commitment. I suppose the commitment word . . . I mean, acceptance I was told meant accepting where you are in life at this stage. Commitment [unclear] . . . I suppose maybe it could do with more clarificationP06Not just for older people, but for people who weren’t accustomed to using theoretical language at all. It was alienatingP24 |
|
| 2. Experience of ACT | ||
| Behaviour changes | I think, probably, I think people have noticed, and particularly the family, but I’m more relaxed, and if those step out of line, they know itP06I think dealing with my anxious thoughts was probably the main benefit, that’s helping me, and trying to live in the present moment. So that’s come out; I knew about that before in theory but having gone through this programme I think I’m using itP20Well now, I seem to be managing it. I seem to be . . . like, you know, some mornings I wake really, oh I don’t want to get up, and then I sort of, say to myself, you know, I’ve got to get up. I’ve got to get up and get myself dressed and then go up to my friend’sP04 |
|
| Relationship with therapist | The therapist was very accepting. She’s firm in her own way that sometimes I do get out of the equation and talk about something else. And she brings me back to it. And she tries to accept whatever I’m saying and sometimes makes me aware of what I’m sayingP34I just wonder, and you might not like this comment, if somebody as young as her could understand my woes. Whether it would be better if there were more mature therapists dealing with somebody of nearly 80 who’s lived a lifeP27 |
|
| Expectations of ACT | Well, I say at the beginning, I suppose I entered into it expecting miracles and bit by bit I began to realise it wasn’t quite like that. Accepting the human condition and so forth . . .P20I’ll be honest. You always want more, don’t you? So, if I’m honest, it didn’t achieve what I was hoping it would do, but I have moved on a bit. If I was a four, I’ve moved on to about eightP29I didn’t really have any expectations but I was very pleased with the resultP07 |
|
| Positive and negative experiences | I find that, quite frankly, not for me. I’m much better at talking about something, rather than fiddling around with stuffP06At first, I couldn’t relate to that at all. It wasn’t so much as putting your worries aside, and then move away. But it was just the involvement of the visual experience of the floating stream. And I think that made me realise that the things that I found most helpfulP24 |
|
| 3. Feasibility of ACT | ||
| Home practice | What I couldn’t get my head around, and I’ll be honest, is the homework. Because I’m not a, how can I say? Like they said when you think of something write it down. I’m not that sort of a person. I’m not a big writer anyway, but at the same time I’ll say, I’ll do that later, but then I thought, hold on, what was I thinking at the time? So, I wasn’t the bestP29 |
|
| Number and duration of sessions | I’d say an hour was just about right, yes. I’d say that was just about right. I had normally had . . . It went at a nice paceP20I think I felt that probably 12 weeks would have been enoughP23I would like to go with 16P01 |
|
| Location | But, yes, therapy at home is just wonderful. Well, it cuts out, even though you may have a car, you’ve got to find somewhere to park, it just alleviated a massive part of the process, quite frankly. For me and for my husband, it was greatP06 |
|
| 4. Engaging in research | ||
| Being a research participant | I think I find questionnaires when you’re talking about emotions or feelings quite frustrating in a way, but probably a lot of people do, because you’re being asked to give a number or say a lot or not at all on a continuum, and sometimes it’s hardP23I did think at one point, why are they asking me about how I felt when I was, what, 5 years old, 10 years old? I don’t know. I’m 70 years old. I cannot remember back that far. I thought, well, that’s a bit silly. I don’t know how I felt thenP27I’m glad that, you know, this is being done and I hope it succeeds and goes forward and I’m glad, you know, to have taken partP07 |
|
| Engagement in a future RCT | I see what you mean. I don’t know whether I couldn’t cope with being put back into CBT. I think the answer would be definitely notP23Oh no, I wouldn’t do anything without knowing all about itP27I would like to do something more, you know?P08 |
|
1. Acceptability of acceptance and commitment therapy
This theme reflected factors that affected participants’ understanding of ACT concepts, their engagement in the intervention, their motivation to change and their views as to how the intervention could be made more acceptable. Some participants felt that clearer explanations of ACT concepts could have been given. Others reflected on the difference between intellectually understanding concepts such as ‘willingness’ versus the challenge of putting them into practice. Continued fusion with beliefs about the ability to change (e.g. due to age), as well as attachment to the self as conceptualised by one’s mind (e.g. ‘always a worrier’), acted as barriers to engaging in ACT. Other barriers included a dislike of being asked to complete written exercises, in-session dwelling on worrying thoughts and side effects of medication (e.g. tiredness). With respect to motivation to change, some participants reported that they were more motivated to participate in the intervention as previous experiences of therapy had not been successful for them (i.e. had not got rid of the anxiety). Others reported an anticipation that the very act of doing something would help with their anxiety. A number of improvements to the intervention were suggested by participants, including simplifying the terminology used, reducing the number of written exercises, follow-up of participants by therapists a few months after the end of the intervention, and scheduling more time between sessions. Although most improvements could be accommodated in a revision of the intervention, spacing out sessions more would not be recommended because it is difficult to maintain the flow of sessions when there are large gaps between them.
2. Experience of acceptance and commitment therapy
On this theme, participants reported on their overall experiences of ACT, providing a more in-depth understanding of changes in themselves and in their behaviour during and after therapy, their relationship with their therapist and their experiences of particular ACT exercises. This theme also highlighted the expectations that some participants had prior to commencing therapy, which were key in understanding what contributed to positive or negative experiences of the intervention. Participants had varied expectations of ACT prior to commencing therapy: some reported expectations that their anxiety would be gone by the end of the intervention (leading to disappointment) and others reported few expectations of the intervention (leading to a positive surprise). The majority of participants reported changes in themselves and in their behaviour as a consequence of engaging in the intervention. Most notably, participants were not necessarily reporting that their anxiety had gone but that they were now able to live alongside their anxiety, in line with the aim of ACT. Some participants did not appear to be aware of the changes that had occurred until they were given the opportunity to reflect on this in the qualitative interviews. Specific behavioural changes are explored more in Behavioural changes. Participants reflected on what they found important in their relationship with their therapists. Commonly reported therapist attributes were patience, being able to develop good rapport with participants and being clear about what the therapy consisted of. A few participants commented on the age of therapists and expressed a preference for older therapists because they questioned if younger therapists could understand their difficulties. Participants reflected on their experiences of specific ACT exercises: responses were mixed for many of the exercises, with the most popular exercises being the ‘leaves on a stream’ exercise, ‘labels’ exercise and ‘centring’ exercise.
3. Feasibility of acceptance and commitment therapy
A number of subthemes emerged in relation to the feasibility of the intervention: (1) home practice, (2) number and duration of sessions and (3) location. Some participants reported difficulties in completing home practice, particularly in relation to written exercises and feeling that they were ‘back at school’. Others reflected that they lacked the commitment and motivation needed to ‘make time’ for home practice. However, there was enthusiasm for the use of aids such as audio tapes, videos and telephone reminders to help individuals embed meditation in their lives beyond the study. Participants reported preferences for between 12 and 16 sessions. Home visits were welcomed as an option, and those who were given this option preferred this and saw it as an important factor in maintaining engagement.
4. Engaging in research
Reflections on being ‘research participants’ were highlighted for this theme, along with opinions about engaging in a future RCT. The main issue identified with participating in research was the completion of outcome measures. Although many participants were happy to complete outcome measures, a few participants felt that this was an added burden. With respect to engaging in a future RCT, some participants explicitly stated that they would not want to receive CBT again (should CBT be used a comparison condition), whereas others reported that they would be open to being in either condition. As an illustration of how GAD can interfere with engagement in RCTs, some participants noted that they would not be keen to engage if they did not know beforehand which treatment arm they were going to be randomised into.
Behavioural changes
One of the subthemes that emerged in qualitative interviews with older people with TR-GAD was behavioural changes (under the theme ‘experience of ACT’). As shown in Table 47, when asked, the majority of participants reported making behavioural changes in their lives as a result of participating in the intervention (n = 15/18). Although the majority of behaviours appear to be ACT consistent, some are potentially less so (e.g. ‘tries to push away bad thoughts more’, ‘used ideas from the sessions to keep busy’, ‘can now distract herself’). It is difficult to know whether or not these behavioural changes are (1) ACT consistent and this is just an issue of the language being used, (2) ACT consistent because the behaviour is actually in service of the participant’s values (i.e. the behaviour is helping the participant to move towards the things that are important and matter to them) or (3) whether or not the behaviour resembles yet another ‘feel better’ strategy (i.e. a strategy aimed at getting rid of anxiety). Clearly, it would be important to clarify the function of behaviours if monitoring behavioural change in a future RCT.
| ID | Self-reported behavioural change(s) |
|---|---|
| P01 | No changes reported |
| P04 | Able to get out of bed; makes herself go out even if she does not ‘feel’ like it; sees friends more; able to leave the house more by herself without needing someone around; has reduced checking behaviours in the house; has reduced engaging in anxious thoughts about the washing machine; tries to push away bad thoughts more |
| P06 | Does not berate herself any more; more relaxed; can accept anxious thoughts and does not react to them any more; listening to more music (previous hobby); pacing herself a bit more |
| P07 | More accepting of anxious thoughts; has less anxiety about housing issues and does not react as much; was able to use a wheelchair to attend an arts gallery (was previously too anxious to do this) |
| P08 | Feels a lot calmer; less angry about everything; has played in a jazz concert since having ACT; addresses anxious thoughts more and does not engage with them |
| P09 | Focuses on values more; has seen more positive changes in relationships since receiving ACT; feels more relaxed and is less anxious in completing tasks; can now slow her pace and relax if she needs to |
| P10 | Has joined a college course; wants to practise going out more; more willingness to be in the community; engaged in making more creative cards; thinks more clearly |
| P15 | No changes reported |
| P20 | Avoids spending time ruminating; living in the present moment; using mindfulness to confront obsessional thinking |
| P22 | Has used ideas from the sessions to keep busy; planning to start walking more as she has been avoiding this prior to ACT sessions |
| P23 | ‘Unhooking from thoughts’ helped her view anxiety differently; does not feel as anxious any more |
| P24 | Has become more aware of the effects of anxiety on relationships around her; can now distract herself and do more practical things such as knitting |
| P26 | Completes tasks more slowly instead of rushing around |
| P27 | No changes reported |
| P29 | Does not focus on tightness in his back; forces himself to do more despite feeling anxious; spending more time with family; less annoyed by wife’s health appointments |
| P33 | Feeling more courageous generally; changed friendship groups so that there is less negativity around her |
| P34 | More accepting of anxiety; sees situations differently (more positive); has become busier; feels a lot better |
| P35 | Has been more accepting of anxiety and able to leave the house more even though they have still felt very anxious |
Therapists
Demographic and professional characteristics
As shown in Table 48, all therapists self-identified as female (n = 11, 100%), with the majority being white/white British (n = 6, 60%) and aged 25–54 years (n = 8, 73%). The majority of therapists were clinical psychologists (n = 7, 64%), with just over half having been qualified for ≤ 10 years (n = 6, 55%) and most working in secondary care settings (n = 9, 82%).
| Demographic characteristic | N (missing n, %) | n (%) |
|---|---|---|
| Area | 11 (0, 0) | |
| South London and Maudsley NHS Foundation Trust | 4 (36) | |
| Barnet, Enfield and Haringey Mental Health NHS Trust | 4 (36) | |
| Camden and Islington NHS Foundation Trust | 1 (9) | |
| Whittington Health NHS Trust | 1 (9) | |
| North East London NHS Foundation Trust | 1 (9) | |
| Age (years) | 10 (1, 9) | |
| 25–34 | 3 (30) | |
| 35–44 | 2 (20) | |
| 45–54 | 3 (30) | |
| 55–64 | 1 (10) | |
| 65–74 | 1 (10) | |
| Sex | 11 (0, 0) | |
| Female | 11 (100) | |
| Male | 0 (0) | |
| Ethnicity | 10 (1, 9) | |
| Asian/Asian British | 2 (20) | |
| Black/black British | 0 (0) | |
| Mixed | 1 (10) | |
| White/white British | 6 (60) | |
| Other | 1 (10) | |
| Profession | 11 (0, 0) | |
| Clinical psychologist | 7 (64) | |
| Counselling psychologist | 2 (18) | |
| CBT psychotherapist | 2 (18) | |
| Professional qualifications | 11 (0, 0) | |
| Doctorate in clinical psychology | 6 (55) | |
| Doctorate in counselling psychology | 2 (18) | |
| MSc in clinical psychology | 1 (9) | |
| Postgraduate diploma/certificate | 3 (27) | |
| Educational qualifications (degree and above) | 11 (0, 0) | |
| PhD | 2 (18) | |
| Master’s degree | 6 (55) | |
| Undergraduate degree | 12 (109)a | |
| Number of years since qualifying | 11 (0, 0) | |
| 0–5 | 5 (45) | |
| 6–10 | 1 (9) | |
| 11–20 | 3 (27) | |
| 21–30 | 2 (18) | |
| Service level | 11 (0, 0) | |
| Primary care | 2 (18) | |
| Secondary care | 9 (82) |
Qualitative themes
Five key themes were identified in qualitative interviews with therapists: (1) delivering the intervention, (2) personal experiences as therapists, (3) working with TR-GAD, (4) feasibility of ACT and (5) future research. Subthemes within each key theme were also identified. Implications of the key themes and subthemes with respect to refining the intervention are discussed in Table 49.
| Theme/subtheme | Supporting quotations | Suggested revision(s) to the intervention |
|---|---|---|
| 1. Delivering the intervention | ||
| Support for therapists | Everything about the process was very thorough. I thought the training was really high quality. I felt really supported as a therapist. If I had any queries, [KK] or the PI were always available to answer themTherapist 3, secondary careAfter a particular supervision, I just thought to myself, all these things that we’re discussing and I kind of think I know nothing about, I actually know like that back of my hand almostTherapist 12, secondary careIt was good having other people in the service doing it. So, I would speak to the other therapist who works here quite a bit actually and then we could kind of just say, you know, where we were at with it or just how you’re feeling with it or what would you do, you know. So a bit of peer supervision. So that was helpful to have, to be honestTherapist 8, secondary care |
|
| Using a manual | As I said I’m quite eclectic, so I would always tailor any intervention to a client. I think the manual was good because within each session there was a choice of exercises, and so I would always make sure I selected something which I thought would be most suitable. So there was some flexibility built in thereTherapist 9, secondary careNo, I think the manual was OK. I think there were certain weeks when it didn’t work. It kind of fell flat because we had a few weeks where we had to follow a set topic and I guess sometimes that didn’t resonate with the person as much as other weeks. Largely I think it was OK because it was quite flexible with the others, with what we could do. I didn’t find it too rigidTherapist 11, secondary careYes, so that was really good. I suppose there’s just things that I got and didn’t get in the manual. Stuff about holding a book, an exercise about holding a book and never really went with that. So, it then makes it really difficult for me to help somebody else to make use of that exercise. So, if I don’t really see it myself, it’s more difficult to use it. Not impossible, but more difficultTherapist 1, primary care |
|
| Home practice | Pen and paper tasks, yes, they did find it difficult, I have to say, most of them. I find it difficult, too, to explain to them. I think the first four sessions, those homework, the wordings are quite difficultTherapist 7, secondary care |
|
| 2. Personal experiences as therapists | ||
| Anxieties | I would be sitting there thinking, when somebody says something, oh my gosh, what is an ACT-consistent response or question? There’s always this, what’s ACT consistent, and sort of thinking, right, don’t wear my CBT hat or any other hat. That was quite difficultTherapist 4, secondary careI’m not very good with recording things or hearing myself or the thought of it being listened to and being judged and all thatTherapist 8, secondary careSo, I found that there were some difficulties and there were some anxieties. I would say the one of the difficulties that were more of a practical thing was just having a handle on all the paperworkTherapist 1, secondary care |
|
| Personal growth | I really noticed that throughout the whole of this, the great thing was I wasn’t getting caught up as well. That’s the one thing I really noticed. Because normally, if a patient comes in and they’re kind of feeling completely overwhelmed . . .Therapist 12, secondary careFor me, I think it was a privilege to have the opportunity. I really loved the idea of learning one model and having the opportunity to work in a very model specific way, because I haven’t really had that before. And I suppose my mind was always telling me things like, you need to do this, so I really loved the opportunity to do that and to have the on-model supervision and all of that. And to really get a chance to get my teeth stuck into it and to see my confidence grow, and my flexibility growTherapist 10, secondary care |
|
| 3. Working with TR-GAD | ||
| ‘Fix it’ agenda | Oh, we discussed it. Yes, we talked about it and, you know, sort of, avoiding or avoiding situations that make you anxious, constantly trying to avoid it or control it. How’s that worked for you so far? It hasn’t. OK, let’s do something different. NoTherapist 4, secondary careAgain, I think it still comes back to the fix-it agenda. I think because there still was a thing that, well, it’s not making me feel better, and sort of not getting that sometimes you’re doing something even if it’s not making you feel betterTherapist 9, secondary careAnd so they were already a bit on board with the idea of acceptance and those kinds of things. I think ACT provided another nice reinforcer of those kinds of ideas that they had been picking upTherapist 10, secondary careI think it is a really nice model to understand and I feel like it was well received. I feel like maybe one of the points that we revisited more often was the idea of not feeling better, being willing to not feel good all the time. Because that kept creeping in all the time, how important it is to be happy and to not feel badTherapist 6, secondary care |
|
| Behaviour changes | I think the main change, which I’m very pleased, and I really hope to get them to, is the willingness to accept. It’s a choice, it’s your openness that makes all the difference because it’s still under your control. So that bit, I feel, is actually very powerfulTherapist 7, secondary careThe lady who had a lot of checking behaviours and reassurance seeking, she made huge amounts of progress and, in fact, she said to me in our first session, there’s no way I’m going to be able to do X, as in, let’s not even set that as something to aim for because there’s no way I’m going to be able to do it. And by the tenth session, she was doing it and a whole range of other things as wellTherapist 3, secondary careShe was definitely doing more of the mindfulness activities, like mindful breathing, mindful walking and trying to be more present, more aware of what it was that she needed, values wise and possibly getting to the point of realising that she is anxious but she can still do thingsTherapist 11, secondary care |
|
| Challenges | Obviously his mobility and his functionality, what he’s able to do, got in the way. There were real hurdles to find ways around. And obviously his anxiety would make the Parkinson’s [disease] worse . . . and vice versaTherapist 8, secondary careThe second person, definitely much more about the cognitive abilityTherapist 9, secondary care |
|
| 4. Feasibility of ACT | ||
| Number of sessions | Yes, it was feasible. It’s definitely longer than anything else I’ve been doing before. But I think because it’s a new thing and perhaps there is a bit of repetition and drawing themes throughout and jumping around, and different examples which may be proving the same point in different directionsTherapist 6, secondary careIt’s just about giving the skills and then they need to go out and practise it. So yes, I think it is the right amount, and maybe a few more at the end if it’s . . . If he needs to cover a bit more as well, because it did feel quite rushed, didn’t it, in that 16. Not quite good enoughTherapist 8, secondary care |
|
| Frequency of sessions | No, I think weekly is good. You can really lose the momentum if you meet less frequently than weekly, due to various practical issues and patient engagement and so on. Often there was fortnightly gaps between sessions and it’s always a bit more difficult to build momentum and to help the patient stick to what we’re trying to do hereTherapist 1, primary careI would spread them out though. You know, if I’m sort of, coming up to the end, and we’re talking about discharge, I’d do it alternate weeks, then maybe every three, then every four, you knowTherapist 4, secondary care |
|
| 5. Future research | ||
| Maximising engagement | Maybe checking in and seeing if they need any support, to think about more practice, etc. But you need to have enough trust and faith in your clients that they will take up what they feel is useful. We’re not in school, we’re not checking up on themTherapist 10, secondary careI’m not sure, if I’m honest. I don’t know because they were quite anti-homework anyway. Maybe that would have taken the pressure off me, if there was someone else encouraging practice, as wellTherapist 11, secondary careBut I still feel that weekly sessions, an hour, they have paper to take home, those have things, would be enough. They need to help themselves as well. I don’t particularly feel that I would want to suggest you give them even more support during the week. I don’t think soTherapist 7, primary care |
|
| Comparison group in a future RCT | Either guided self-help or a full course of CBT, depending on where we thought we needed to make the intervention, low intensity or high intensityTherapist 1, primary careI suppose . . . no treatment at all, because there’s passing of time. Treatment as usual. Another therapy. A supportive conversation with an interested personTherapist 10, secondary care |
|
| Participation in research | I think people would be . . . I would guess that they would be quite open to it, because on the whole people seem to be quite glad for what they’re offeredTherapist 1, primary careIf you’re feeling absolutely wretched, and there’s this kind of possibility dangled in front of you and you don’t then get it, or you’re told, well, you might get it [or] you’re on the waiting list, you might get it in 6 months’ time . . .Therapist 4, secondary care |
|
1. Delivering the intervention
The support that therapists received when delivering the intervention, their experiences of working with a manualised intervention and experiences of home practice were highlighted in this theme. ACT training, peer support and weekly consultation calls were highlighted as important sources of support for therapists. However, some therapists noted the difficulty of attending weekly supervision sessions, even though these were deemed to be useful. Therapists tended to make positive comments about the flexibility of session delivery in the manual, although it was felt that some ‘fixed’ sessions did not fit with participants’ individual needs as well as others. Some therapists reported on how they felt pressured to complete all tasks in the manual. Others commented on the challenges that participants experience with completing written tasks.
2. Personal experiences as therapists
On this theme, therapists reported on what they found personally challenging in delivering the intervention, as well as any personal growth they observed. A number of anxieties were described with respect to the desire to be adherent to the ACT model, to appear competent on audio-recordings to external raters and to correctly complete study paperwork. Some therapists reported experiences of personal growth, including not getting caught up in participants’ ‘emotional content’ and observing the growth of one’s confidence and psychological flexibility within the ACT model, and others reported how their work with participants was affected by feelings of doubt or incompetence.
3. Working with treatment-resistant generalised anxiety disorder
The perceived ‘fix it’ agenda of older people, behavioural changes and challenges were prominent subthemes when considering therapists’ experiences of working with the ACT model with older people with TR-GAD. With respect to the ‘fix it’ agenda, therapists discussed how some participants were on board with the aims of ACT (e.g. ‘living better’ rather than ‘feeling better’) whereas others were not. Even in those who were on board with the aims of ACT, the importance of repeatedly coming back to these aims was stressed, given how easily emotional control could creep back onto the agenda. Therapists reported a number of behavioural changes that they observed in participants during the course of the intervention: (1) willingness to accept anxiety rather than trying to change it, (2) increased functioning in daily activities and doing more activities in service of values rather than avoidance, (3) increased openness with immediate family about their difficulties and (4) increased awareness of anxiety and associated behaviours. A number of challenges were reported with respect to working with older people with TR-GAD. These included participants appearing confused by some of the ACT concepts; some participants finding it difficult to engage with written tasks; worrying habits being difficult to overcome; suspected cognitive impairments that interfered with therapy, which may have developed over the course of the therapy; and physical mobility and other complex health issues.
4. Feasibility of acceptance and commitment therapy
A couple of subthemes emerged in relation to the feasibility of the intervention: number of sessions and frequency of sessions. Therapists reported differing opinions with regard to how many sessions should be offered, with answers ranging from 10 to more than 16 sessions. A number of therapists reflected on the benefits of delivering 16 sessions, such as providing multiple opportunities to illustrate and practise skills. Some therapists preferred weekly sessions and others preferred more spaced out sessions. Overall, therapists reported that the intervention was feasible to deliver within their services.
5. Future research
On this theme, therapists suggested ways of maximising engagement and gave their opinions on the best comparison condition in a future RCT and whether or not older people with TR-GAD would participate in such an RCT. Most therapists reported that enough support was being provided with respect to home practice tasks and weekly sessions. Some therapists felt that some participants might benefit from extra support over the telephone to encourage completion of home practice tasks. Numerous suggestions were given with respect to a suitable comparison condition in a future RCT, including CBT and supportive therapy. Some therapists thought that older people with TR-GAD might hesitate about participating if they did not know what treatment they would be offered.
Discussion
Summary of the main findings
Qualitative data support quantitative data in showing that there is sufficient evidence of acceptability and feasibility. However, a number of suggested revisions to the intervention should be considered to improve acceptability and feasibility. Overall, most participants reported positive behavioural changes, consistent with ACT principles, as a result of engaging in the intervention. In addition, therapists reported enjoying the experience of taking part in the study and applying ACT to older people with TR-GAD. Furthermore, the majority of older people with TR-GAD were positive about engaging in a future RCT.
There were similarities and differences in opinion between older people with TR-GAD and therapists. Both older people with TR-GAD and therapists were in agreement that there were issues with completing written tasks. The optional requirement of writing down observations should be emphasised in a future RCT. Older people with TR-GAD and therapists were also in agreement that language should be simplified with respect to ACT concepts. In addition, they were in agreement that older people with TR-GAD might hesitate in participating in a future RCT if they did not know what treatment they would be offered (e.g. ACT vs. treatment as usual). By contrast, therapists’ views differed to those of older people with TR-GAD in suggesting CBT as a potential comparison group in a future RCT. Some older participants explicitly stated that they would not engage in CBT again. This suggests that a future RCT comparing ACT with a supportive talking control (i.e. a design in which all participants get some form of ‘treatment’) might be most beneficial where recruitment is concerned.
Strengths and limitations
To our knowledge, this is the first study to report a qualitative evaluation of the acceptability and feasibility of a psychological intervention for older people with TR-GAD. However, there are a number of limitations of the current study. Similar limitations to those noted in Chapter 4 are relevant here. Most notably, caution is required when applying the findings to broader populations given the limited demographic characteristics of older people with TR-GAD and therapists, and the fact that the intervention was developed with an exclusively white/white British sample. Further refinement of the intervention is needed to ensure that it meets the cultural needs of older people from black, Asian and minority ethnic populations.
In addition, even though participants who withdrew from the intervention were invited to participate in qualitative interviews, all declined to take part in these. Consequently, it cannot be assumed that the qualitative findings reported here reflect the views of all participants in the study.
Another limitation was that qualitative interviews were conducted only with older people with TR-GAD and therapists. Further insights into the acceptability and feasibility of the intervention might have been gained from conducting interviews with close family members or friends. On the plus side, an advantage of prior knowledge is that it would have enhanced the researcher’s sensitivity to the data.
Finally, although the sample size of 18 older people with TR-GAD was sufficient, the sample size of 11 therapists was smaller than is recommended for qualitative interviews to achieve data saturation (n = 15). 67 As noted in Chapter 4, Methods, Therapists, although 17 therapists were initially trained to deliver the intervention, only 12 actually delivered the intervention to participants in the study. One of these therapists left the study because they took up a position elsewhere, so only 11 therapists could be interviewed.
Conclusion
In conclusion, qualitative results support quantitative findings in suggesting that an ACT intervention adapted specifically for older people with TR-GAD is acceptable and feasible to deliver to this population within the NHS.
Chapter 7 Overall conclusions
Summary of key findings
-
The indicators of success in the feasibility study were in relation to session attendance, satisfaction with therapy, recruitment and retention. Three out of four of these indicators of success needed to be met to demonstrate success (i.e. feasibility of the study), which is what was found. This suggests that it would be feasible to examine the clinical effectiveness of ACT for TR-GAD in older people, and that a larger-scale RCT is warranted.
-
Although a high level of acceptability of the intervention was demonstrated with respect to session attendance, satisfaction with therapy ratings were lower than anticipated (although 80% of participants had not finished receiving their therapy sessions at the time of rating them). This suggests that further refinement of the intervention is necessary to improve its acceptability to older people with TR-GAD, as discussed in Chapter 6.
-
Indicative evidence of improvements in anxiety, depression and psychological flexibility were observed in the feasibility study, even though it was not powered to examine clinical effectiveness. Furthermore, reliable improvements in scores were found in 45% of participants for anxiety and in 24% of participants for depression and psychological flexibility. This was particularly noteworthy given that all participants had failed to respond to prior pharmacological and/or psychological treatment for GAD.
-
Findings from the feasibility study suggest that it would be feasible to examine the cost-effectiveness of ACT for TR-GAD in older people in a future substantive trial. However, findings also highlighted a number of issues that would need to be considered to maximise the chances of successful outcomes in such a study.
Recommendations for a future randomised controlled trial
Recommended changes with respect to refinement of the intervention are discussed in Chapter 6 and are not repeated here for the sake of brevity. A number of recommended changes with respect to the design and delivery of a future substantive trial of ACT for older people with TR-GAD emerge from the current findings, as shown in Table 50.
| Observation | Recommended change(s) |
|---|---|
| Timescales | |
| There was a delay of 2 months in obtaining confirmation of capacity and capability from recruitment sites in the feasibility study | Factor in more time for confirmation of capacity and capability from recruitment sites |
| Recruitment and retention | |
|
Use key figures to inform recruitment and estimate the sample size for a future substantive trial |
| 86% of eligible referrals came from CMHTs and IAPT services | Focus recruitment on CMHTs and IAPT services, with a lesser focus on GP practices |
| The majority of participants were white/white British women who would be categorised as ‘younger old’ (i.e. in their 60s or 70s) | Identify strategies for recruiting men, the ‘older old’ (i.e. participants in their 80s and older) and participants from ethnic minorities that have been successful in other research studies. This may include reaching out more to churches, luncheon clubs, men’s clubs, etc. |
| Participants were recruited only from urban and suburban areas in the London region | Include recruitment sites across the UK |
| The logistical issue of delivering therapy emerged as the most common feasibility-related reason for attrition and eligible participants not being recruited | Potentially include research costs for additional therapists who can be brought in to deliver ACT sessions if therapists are no longer available in an area (e.g. owing to drop-out) or if CMHTs reject eligible participants (e.g. because their level of complexity is not high enough for the services) |
| Eligibility criteria | |
| 13 out of 58 (22%) older people with TR-GAD who completed the online survey were aged 60–64 years | Lower the age limit to ≥ 60 years to maximise recruitment |
| Three participants (8%) reported drinking > 14 units of alcohol per week. One participant (3%) met criteria for alcohol dependence on the MINI | Exclude those who meet criteria for alcohol dependence or substance abuse on the MINI as this may affect engagement with the intervention and confound results. For those who report drinking > 14 units of alcohol per week, ask them to agree to drink 14 units of alcohol or less per week in case there is under-reporting of alcohol use |
| Intervention and control arms | |
| Three participants (8%) dropped out of the intervention or study stating a preference for a more counselling-type approach in which they could ‘just talk’ as opposed to making behavioural changes in their lives | Include a talking control condition to optimise recruitment as some participants wanted to ‘just talk’ and to reduce resentful demoralisation (due to being allocated to treatment as usual). Alternatively, consider a non-inferiority trial comparing ACT with CBT so that all participants receive some form of treatment. Emphasise the aims of ACT in the participant information sheet and highlight that ACT is not just about talking or getting rid of anxiety |
| The median waiting time for therapy was 7 weeks, though this ranged from 2 to 33 weeks | Potentially include research costs for additional therapists who can be brought in to deliver ACT sessions if the waiting list is too long at a site (as all sites refused to fast-track participants to receive therapy because it was felt that this would give participants an unfair advantage over other referrals on waiting lists). Alternatively, factor in waiting time for therapy into the study design |
| Seventeen therapists received training in ACT, 12 of whom actually delivered the intervention to participants in the study | Potentially account for a 29% drop-out rate of therapists when identifying and training therapists. Ensure that at least two therapists are trained per site to ensure continued delivery of the intervention |
| Outcome measures and measures of bias | |
| Completion rates were lower for the Credibility/Expectancy Questionnaire | Do not include this measure in a future substantive trial. Expectancy could be assessed using a simple Likert scale in response to ‘How much do you expect . . . ?’ |
| Symptomatic reductions in anxiety and depression were observed, with the largest being found for the Geriatric Anxiety Inventory. This is despite the fact that ACT is not focused on reducing symptoms and any such reductions are generally seen as a by-product of therapy | Ideally, include a measure of psychological well-being such as the McGill Quality of Life Questionnaire-Revised as the primary outcome measure because of ACT’s focus on ‘living better’ rather than ‘feeling better’. Alternatively, include the Geriatric Anxiety Inventory as the primary outcome measure because the McGill Quality of Life Questionnaire-Revised was not included in the feasibility study |
| The Satisfaction with Therapy and Therapist Questionnaire-Revised was developed for ‘fix it’ therapies (i.e. those that are focused on getting rid of problematic thoughts, feelings and situations) and is less suitable for therapies that are focused on ‘living better’ rather than ‘feeling better’ | Identify a satisfaction with therapy questionnaire that is focused on changes in life satisfaction rather than symptomatic change. Such a questionnaire might ask ‘How much has your life improved since receiving this therapy?’ rather than ‘How much have your symptoms improved since receiving this therapy?’ |
| The Acceptance and Action Questionnaire-II is a measure of psychological flexibility that primarily examines the degree to which a person is engaging in experiential avoidance. It does not measure other ACT processes and therefore does not provide a comprehensive assessment of change in ACT processes | Include the Comprehensive Assessment of Acceptance and Commitment Therapy processes questionnaire122 as a measure of psychological flexibility rather than the Acceptance and Action Questionnaire-II |
| Health economics | |
| Rates of service use as measured by the modified CSRI were lower than expected, most likely because data were self-reported rather than being extracted from medical records, etc. | Where consent is provided, ensure that data are extracted from GP medical records on GP/nurse consultations, prescribing and referrals in the specified months before and after the baseline assessment |
| In the modified CSRI, memory clinic services were categorised under psychiatric outpatient services, whereas audiology services were categorised under ‘other’ outpatient services. Various categories were not endorsed | Include memory clinic and audiology services as specific appointment categories in outpatient services. Shorten the modified CSRI by removing all except community mental health centre services from day activity services and by removing criminal justice services. Include yes/no tick boxes to help differentiate between missing data and 0 contacts |
| Clear discrepancies between scores on the anxiety/depression dimension of the EQ-5D-5L and scores on the Geriatric Anxiety Inventory and Geriatric Depression Scale were evident in two out of three participants who reported slight or no problems with anxiety/depression at 0 weeks. This may have been because these people did not see themselves as anxious or depressed | Check for potential discrepancies between the anxiety/depression dimension of the EQ-5D-5L and scores on the Geriatric Anxiety Inventory and Geriatric Depression Scale, if these measures are used |
| Two methods were used to calculate utility scores from the EQ-5D-5L | Use the mapping algorithm to calculate utility scores from the EQ-5D-5L so that the results of the study could inform the NICE guidance with respect to the management of TR-GAD in older people |
| A measure that focused more on the psychological component of quality of life should have been included in addition to the EQ-5D-5L so that it would not have been overly influenced by physical health problems that are common in this population | Include a quality of life measure such as the ICECAP-O,156 in addition to the EQ-5D-5L, to better assess the psychological component of quality of life and contribute to a cost–utility analysis |
| The costing of training, intervention delivery and supervision was relevant only to a feasibility study | Consider additional costs relevant to a future substantive trial (e.g. higher costs of travel for therapists from different UK sites to attend training, and 1-day top-up training for therapists at 12 months after initial training) |
| Assessment time points | |
| The median waiting time for therapy across all sites was 7 weeks, though this ranged from 2 to 33 weeks. The median number of therapy sessions completed by the 20-week follow-up was 13 sessions; thus, some participants had not finished their ACT sessions by the time of the follow-up assessment. No follow-up after 20 weeks was conducted | Factor in waiting time for therapy by specifying a primary end point at 6 months. Include an outcome assessment at 9 or 12 months to assess whether or not any gains are maintained beyond the primary end point. Include an exclusion criterion with respect to planned breaks of > 6 weeks (i.e. exclude participants who are planning to go away for > 6 weeks in the next 6 months and ensure that they are re-referred when they return to the UK). Potentially complete the baseline assessment and randomisation only when a therapist becomes available |
| Statistical analyses | |
| There was a wide variation in the reported number of years experiencing difficulties with worrying, with 1–5 years (n = 13, 35%) and ≥ 30 years (n = 13, 35%) being the most common. This suggests that there are two groups of service users: one in which GAD is lifelong and one in which it is more recent | Consider exploring subgroup analyses with respect to (1) those with and without lifelong GAD, (2) those with and without comorbid depression (i.e. cothymia), (3) those meeting and not meeting screening criteria for a personality disorder and (4) those with and without a major life event that precipitated GAD |
| Treatment fidelity | |
| Few ACT-inconsistent deviations from the FACTOID manual were observed with the adherence checklist, consistent with the ACT Treatment Integrity Coding Manual | Do not include both the adherence checklist and the ACT Treatment Integrity Coding Manual. The ACT Treatment Integrity Coding Manual should be favoured as it minimises workload on therapists |
| No over-riding framework was used to guide the assessment of treatment fidelity | Use the National Institutes of Health Behavioural Change Consortium’s treatment fidelity framework to guide assessment in five domains: study design, provider training, treatment delivery, treatment receipt and treatment enactment136 |
| An assessment of the fidelity of training was not conducted | Assess the fidelity of training through observations of training workshops by an independent ACT therapist |
| There were no visual observations of intervention sessions to assess delivery/receipt of the intervention | Possibly consider conducting visual observations of intervention sessions to assess treatment fidelity, keeping in mind that this anxiety-provoking procedure may interfere with the therapeutic process |
| A limited number of participants per therapist (ranging from one to four participants) meant that learning curves with respect to intervention delivery could not be meaningfully examined | Address learning curves in a number of ways:
|
| Adaptations for future waves of the COVID-19 pandemic | |
| Pandemic-related restrictions may preclude in-person study procedures | Adapt study procedures so that they can all be conducted remotely (e.g. by video call, by telephone, online and by post) |
| Pandemic-related restrictions may preclude in-person therapy sessions | Adapt the intervention (including training and the manual) so that it can be delivered remotely by video call and/or telephone |
Acknowledgements
We would like to thank all of the participants (older people with GAD, health-care professionals, academic clinicians and therapists) who took part in phases 1 and 2 of the FACTOID study and the clinicians who made referrals to the study.
We would also like to thank our PPI collaborator (DH) and members of our Service User Advisory Group (SB, Michael Belcher, Susan Boyle, Sheila Dainow and Jackie Persoff), who attended meetings, provided invaluable advice and guidance about key issues such as recruitment from a service user perspective, reviewed themes in qualitative data analyses, contributed to the development and revision of the intervention manual and provided feedback on study materials and the final study results.
We would like to thank the following therapists for participating in training and for subsequently delivering the intervention (denoted by *): Janet Balabanovic, Julia Brownlie, Charlotte Gardner,* Danielle Gaynor,* Rachel Holliss, Debbie Hunt,* Joana Johnson,* Stephanie Jones, Gemma Knight,* Victoria Lawson,* Ruth Lukeman,* Monique Maroney,* Meenaxi Patel,* Catherine Simpson,* Nicola Stanhope,* Debbie Walker and Grace Wong.* We would also like to thank Professor Julie Wetherell, Dr Marc Serfaty and Dr Chris Graham for providing fortnightly supervision of and consultation with therapists. In addition, we would like to thank Steve Boddington, Janet Wingrove, Debbie Walker, Julia Brownlie, Ruth Lukeman, Rachel Butterfield, Alison Milton, Eleanor Martin, Harry O’Hayon and Georgina Charlesworth, who facilitated the involvement of therapists in the study.
We would also like to thank the following members of the Study Steering Committee, who provided invaluable advice and guidance: Dr Iracema Leroi (Independent Chairperson, Old Age Psychiatrist), Dr Robert Barber (Independent Member, Old Age Psychiatrist), Ms Ellen Lee (Independent Member, Statistician), Dr Jo Cook (Independent Member, Clinical Psychologist) and Ms Aska Matsunaga (Independent Observer, National Institute for Health Research Clinical Research Network).
In addition, we would like to thank Ms Dhriti Ratra, Ms Maitri Khurana and Ms Lisa Carmody, who assisted with data entry and part of the qualitative analyses. We would also like to thank Dr Caroline Clarke, who provided comments on Chapter 5.
Finally, we would like to thank the North Thames Clinical Research Network and the South London Clinical Research Network for their support in conducting the study. In particular, we would like to thank Ms Eva Klamerus and Ms Lisa Carmody for providing support with screening, consenting and recruiting participants and outcome assessments.
Funding acknowledgements
We would like to thank the National Institute for Health Research (NIHR) Health Technology Assessment Programme for funding this study. We would also like to thank the following NHS trusts for providing funding for excess treatment costs to cover therapist training, supervision and intervention delivery: South London and Maudsley NHS Foundation Trust; Barnet, Enfield and Haringey Mental Health NHS Trust; Camden and Islington NHS Foundation Trust; Whittington Health NHS Trust; and North East London NHS Foundation Trust. This research was supported by the NIHR Biomedical Research Centre at University College London and King’s College London.
Contributions of authors
Rebecca L Gould (https://orcid.org/0000-0001-9283-1626) (Associate Professor and Honorary Clinical Psychologist) acted as chief investigator; wrote the grant application; contributed to the conception and design of the study; wrote the protocol; wrote and submitted the ethics applications; submitted the study for Health Research Authority approval; submitted the trial registration; identified sites and therapists at each site; liaised with research and development, Local Clinical Research Networks and the sponsor for site setup; developed the case report forms; developed and revised the intervention manual (based on Julie Loebach Wetherell’s original manual); developed and delivered therapist training; devised the qualitative interviews and the online survey; analysed some quantitative and qualitative data; supported day-to-day management of the study; wrote the report; and is guarantor.
Julie Loebach Wetherell (https://orcid.org/0000-0002-7402-3331) (Professor in Residence) contributed to the conception and design of the study, wrote the original manual on which the intervention was based, contributed to the development and revision of the intervention manual, provided fortnightly consultation to therapists and contributed to the development of the qualitative interviews and the online survey.
Marc A Serfaty (https://orcid.org/0000-0001-8388-0776) (Professor of Psychotherapy) contributed to the conception and design of the study, contributed to the development and revision of the intervention manual, provided fortnightly supervision of therapists, contributed to the development of the qualitative interviews and the online survey and mentored Rebecca L Gould.
Kate Kimona (https://orcid.org/0000-0003-0548-3737) (FACTOID Research Assistant) screened participants for eligibility, consented participants, conducted outcome assessments at 0 and 20 weeks, conducted qualitative interviews, analysed all qualitative data, developed the trial master file, prepared site information packs, set up databases, supported therapists with research-related tasks, contributed to the development and revision of the intervention manual, set up the online survey in Opinio and supported day-to-day management of the study.
Vanessa Lawrence (https://orcid.org/0000-0001-7852-2018) (Senior Lecturer) contributed to the conception and design of the study, analysed some qualitative data, supervised the qualitative analysis, contributed to the development and revision of the intervention manual and contributed to the development of the qualitative interviews and the online survey.
Rebecca Jones (https://orcid.org/0000-0001-6924-0924) (Principal Research Fellow) contributed to the conception and design of the study, analysed quantitative data and wrote part of the report.
Gill Livingston (https://orcid.org/0000-0001-6741-5516) (Professor of Psychiatry of Older People) contributed to the conception and design of the study, contributed to the development and revision of the intervention manual and contributed to the development of the qualitative interviews and the online survey.
Philip Wilkinson (https://orcid.org/0000-0003-2642-0604) (Honorary Senior Clinical Lecturer) contributed to the conception and design of the study, the development and revision of the intervention manual and the development of the qualitative interviews and online survey.
Kate Walters (https://orcid.org/0000-0003-2173-2430) (Professor of Primary Care and Epidemiology) contributed to the conception and design of the study, the development and revision of the intervention manual and the development of the qualitative interviews and online survey.
Marie Le Novere (https://orcid.org/0000-0002-9479-8599) (Research Fellow) analysed the health economic data and contributed to the report.
Robert J Howard (https://orcid.org/0000-0002-3071-2338) (Professor of Old Age Psychiatry) contributed to the conception and design of the study, contributed to the development and revision of the intervention manual, contributed to the development of the qualitative interviews and online survey and mentored Rebecca Gould.
Publications
Lawrence V, Kimona K, Howard RJ, Serfaty MA, Loebach Wetherell J, Livingston G, et al. Optimising the acceptability and feasibility of Acceptance and Commitment Therapy for treatment-resistant generalised anxiety disorder in older adults. Age Ageing 2019;48:735–44.
Gould RL, Wetherell JL, Kimona K, Serfaty MA, Jones R, Graham CD, et al. Acceptance and commitment therapy for late-life treatment-resistant generalised anxiety disorder: a feasibility study. Age Aging 2021;afab059.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Wetherell JL, Lenze EJ, Stanley MA. Evidence-based treatment of geriatric anxiety disorders. Psychiatr Clin North Am 2005;28:871-96. https://doi.org/10.1016/j.psc.2005.09.006.
- Wolitzky-Taylor KB, Castriotta N, Lenze EJ, Stanley MA, Craske MG. Anxiety disorders in older adults: a comprehensive review. Depress Anxiety 2010;27:190-211. https://doi.org/10.1002/da.20653.
- American Psychiatric Association (APA) . Diagnostic and Statistical Manual of Mental Disorders 2000.
- Lenze EJ, Mulsant BH, Mohlman J, Shear MK, Dew MA, Schulz R, et al. Generalized anxiety disorder in late life: lifetime course and comorbidity with major depressive disorder. Am J Geriatr Psychiatry 2005;13:77-80. https://doi.org/10.1097/00019442-200501000-00011.
- Rubio G, López-Ibor JJ. Generalized anxiety disorder: a 40-year follow-up study. Acta Psychiatr Scand 2007;115:372-9. https://doi.org/10.1111/j.1600-0447.2006.00896.x.
- Gonçalves DC, Pachana NA, Byrne GJ. Prevalence and correlates of generalized anxiety disorder among older adults in the Australian National Survey of Mental Health and Well-Being. J Affect Disord 2011;132:223-30. https://doi.org/10.1016/j.jad.2011.02.023.
- Porensky EK, Dew MA, Karp JF, Skidmore E, Rollman BL, Shear MK, et al. The burden of late-life generalized anxiety disorder: effects on disability, health-related quality of life, and healthcare utilization. Am J Geriatr Psychiatry 2009;17:473-82. https://doi.org/10.1097/JGP.0b013e31819b87b2.
- Wetherell JL, Thorp SR, Patterson TL, Golshan S, Jeste DV, Gatz M. Quality of life in geriatric generalized anxiety disorder: a preliminary investigation. J Psychiatr Res 2004;38:305-12. https://doi.org/10.1016/j.jpsychires.2003.09.003.
- Beekman AT, de Beurs E, van Balkom AJ, Deeg DJ, van Dyck R, van Tilburg W. Anxiety and depression in later life: co-occurrence and communality of risk factors. Am J Psychiatry 2000;157:89-95. https://doi.org/10.1176/ajp.157.1.89.
- Cairney J, Corna LM, Veldhuizen S, Herrmann N, Streiner DL. Comorbid depression and anxiety in later life: patterns of association, subjective well-being, and impairment. Am J Geriatr Psychiatry 2008;16:201-8. https://doi.org/10.1097/JGP.0b013e3181602a4a.
- Schaub RT, Linden M. Anxiety and anxiety disorders in the old and very old – results from the Berlin Aging Study (BASE). Compr Psychiatry 2000;41:48-54. https://doi.org/10.1016/S0010-440X(00)80008-5.
- van Balkom AJ, Beekman AT, de Beurs E, Deeg DJ, van Dyck R, van Tilburg W. Comorbidity of the anxiety disorders in a community-based older population in The Netherlands. Acta Psychiatr Scand 2000;101:37-45. https://doi.org/10.1034/j.1600-0447.2000.101001037.x.
- Bystritsky A. Treatment-resistant anxiety disorders. Mol Psychiatry 2006;11:805-14. https://doi.org/10.1038/sj.mp.4001852.
- Lenze EJ, Mulsant BH, Shear MK, Alexopoulos GS, Frank E, Reynolds CF. Comorbidity of depression and anxiety disorders in later life. Depress Anxiety 2001;14:86-93. https://doi.org/10.1002/da.1050.
- National Institute for Health and Care Excellence (NICE) . Generalised Anxiety Disorder and Panic Disorder in Adults: Management. Clinical Guideline [CG113] 2011. www.nice.org.uk/guidance/cg113 (accessed 20 August 2020).
- Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Telephone-delivered cognitive behavioral therapy and telephone-delivered nondirective supportive therapy for rural older adults with generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry 2015;72:1012-20. https://doi.org/10.1001/jamapsychiatry.2015.1154.
- Jones SL, Hadjistavropoulos HD, Soucy JN. A randomized controlled trial of guided internet-delivered cognitive behaviour therapy for older adults with generalized anxiety. J Anxiety Disord 2016;37:1-9. https://doi.org/10.1016/j.janxdis.2015.10.006.
- Mohlman J, Gorman JM. The role of executive functioning in CBT: a pilot study with anxious older adults. Behav Res Ther 2005;43:447-65. https://doi.org/10.1016/j.brat.2004.03.007.
- Mohlman J, Gorenstein EE, Kleber M, de Jesus M, Gorman JM, Papp LA. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: two pilot investigations. Am J Geriatr Psychiatry 2003;11:24-32. https://doi.org/10.1097/00019442-200301000-00005.
- Stanley MA, Beck JG, Glassco JD. Treatment of generalized anxiety in older adults: a preliminary comparison of cognitive-behavioral and supportive approaches. Behav Ther 1996;27:565-81. https://doi.org/10.1016/S0005-7894(96)80044-X.
- Stanley MA, Beck JG, Novy DM, Averill PM, Swann AC, Diefenbach GJ, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol 2003;71:309-19. https://doi.org/10.1037/0022-006x.71.2.309.
- Stanley MA, Wilson NL, Novy DM, Rhoades HM, Wagener PD, Greisinger AJ, et al. Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial. JAMA 2009;301:1460-7. https://doi.org/10.1001/jama.2009.458.
- Stanley MA, Wilson NL, Amspoker AB, Kraus-Schuman C, Wagener PD, Calleo JS, et al. Lay providers can deliver effective cognitive behavior therapy for older adults with generalized anxiety disorder: a randomized trial. Depress Anxiety 2014;31:391-40. https://doi.org/10.1002/da.22239.
- Wetherell JL, Ayers CR, Sorrell JT, Thorp SR, Nuevo R, Belding W, et al. Modular psychotherapy for anxiety in older primary care patients. Am J Geriatr Psychiatry 2009;17:483-92. https://doi.org/10.1097/JGP.0b013e3181a31fb5.
- Wetherell JL, Stoddard JA, White KS, Kornblith S, Nguyen H, Andreescu C, et al. Augmenting antidepressant medication with modular CBT for geriatric generalized anxiety disorder: a pilot study. Int J Geriatr Psychiatry 2011;26:869-75. https://doi.org/10.1002/gps.2619.
- Wetherell JL, Petkus AJ, White KS, Nguyen H, Kornblith S, Andreescu C, et al. Antidepressant medication augmented with cognitive-behavioral therapy for generalized anxiety disorder in older adults. Am J Psychiatry 2013;170:782-9. https://doi.org/10.1176/appi.ajp.2013.12081104.
- Wetherell JL, Afari N, Ayers CR, Stoddard JA, Ruberg J, Sorrell JT, et al. Acceptance and commitment therapy for generalized anxiety disorder in older adults: a preliminary report. Behav Ther 2011;42:127-34. https://doi.org/10.1016/j.beth.2010.07.002.
- Lenze EJ, Hickman S, Hershey T, Wendleton L, Ly K, Dixon D, et al. Mindfulness-based stress reduction for older adults with worry symptoms and co-occurring cognitive dysfunction. Int J Geriatr Psychiatry 2014;29:991-1000. https://doi.org/10.1002/gps.4086.
- Gonçalves DC, Byrne GJ. Interventions for generalized anxiety disorder in older adults: systematic review and meta-analysis. J Anxiety Disord 2012;26:1-11. https://doi.org/10.1016/j.janxdis.2011.08.010.
- Covin R, Ouimet AJ, Seeds PM, Dozois DJ. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord 2008;22:108-16. https://doi.org/10.1016/j.janxdis.2007.01.002.
- Gould RL, Coulson MC, Howard RJ. Efficacy of cognitive behavioral therapy for anxiety disorders in older people: a meta-analysis and meta-regression of randomized controlled trials. J Am Geriatr Soc 2012;60:218-29. https://doi.org/10.1111/j.1532-5415.2011.03824.x.
- Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev 2007;1. https://doi.org/10.1002/14651858.CD001848.pub4.
- Kishita N, Laidlaw K. Cognitive behaviour therapy for generalized anxiety disorder: is CBT equally efficacious in adults of working age and older adults?. Clin Psychol Rev 2017;52:124-36. https://doi.org/10.1016/j.cpr.2017.01.003.
- Lanouette NM, Stein MB. Advances in the management of treatment-resistant anxiety disorders. FOCUS 2010;8:501-24. https://doi.org/10.1176/foc.8.4.foc501.
- Barton S, Karner C, Salih F, Baldwin DS, Edwards SJ. Clinical effectiveness of interventions for treatment-resistant anxiety in older people: a systematic review. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18500.
- United Nations . World Population Ageing 2017. www.un.org/en/development/desa/population/theme/ageing/WPA2017.asp (accessed 19 August 2020).
- Wetherell JL, Petkus AJ, Alonso-Fernandez M, Bower ES, Steiner AR, Afari N. Age moderates response to acceptance and commitment therapy vs. cognitive behavioral therapy for chronic pain. Int J Geriatr Psychiatry 2016;31:302-8. https://doi.org/10.1002/gps.4330.
- Hayes S, Strosahl K, Wilson K. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. New York, NY: The Guilford Press; 1999.
- Hann KEJ, McCracken LM. A systematic review of randomized controlled trials of Acceptance and Commitment Therapy for adults with chronic pain: outcome domains, design quality, and efficacy. J Context Behav Sci 2014;3:217-27. https://doi.org/10.1016/j.jcbs.2014.10.001.
- Graham CD, Gouick J, Krahé C, Gillanders D. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev 2016;46:46-58. https://doi.org/10.1016/j.cpr.2016.04.009.
- A-Tjak JG, Davis ML, Morina N, Powers MB, Smits JA, Emmelkamp PM. A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychother Psychosom 2015;84:30-6. https://doi.org/10.1159/000365764.
- Wilson K, Murrell A, Hayes S, Follette V, Linehan M. Mindfulness and Acceptance: Expanding the Cognitive–Behavioral Tradition. New York, NY: Guilford Press; 2004.
- Petkus AJ M.A, Wetherell JL. Acceptance and commitment therapy with older adults: rationale and considerations. Cogn Behav Pract 2013;20:47-56. https://doi.org/10.1016/j.cbpra.2011.07.004.
- Harris R. Getting Unstuck in ACT: A Clinician’s Guide to Overcoming Common Obstacles in Acceptance and Commitment Therapy. Oakland, CA: New Harbinger Publications; 2013.
- Isaacowitz DM, Seligman ME. Cognitive style predictors of affect change in older adults. Int J Aging Hum Dev 2002;54:233-53. https://doi.org/10.2190/J6E5-NP5K-2UC4-2F8B.
- Kangas M, McDonald S. Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychol Rehabil 2011;21:250-76. https://doi.org/10.1080/09602011.2010.540920.
- Jourdain RL, Dulin PL. ‘Giving it space’: a case study examining acceptance and commitment therapy for health anxiety in an older male previously exposed to nuclear testing. Clin Case Stud 2009;8:210-25. https://doi.org/10.1177/1534650109334631.
- Avdagic E, Morrissey SA, Boschen MJ. A randomised controlled trial of acceptance and commitment therapy and cognitive-behaviour therapy for generalised anxiety disorder. Behav Change 2014;31:110-30. https://doi.org/10.1017/bec.2014.5.
- Hayes-Skelton SA, Roemer L, Orsillo SM. A randomized clinical trial comparing an acceptance-based behavior therapy to applied relaxation for generalized anxiety disorder. J Consult Clin Psychol 2013;81:761-73. https://doi.org/10.1037/a0032871.
- Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. J Consult Clin Psychol 2008;76:1083-9. https://doi.org/10.1037/a0012720.
- Zargar F, Asgharnejad Farid AA, Atef-Vahid MK, Afshar H, Maroofi M, Omranifard V. Effect of acceptance-based behavior therapy on severity of symptoms, worry and quality of life in women with generalized anxiety disorder. Iran J Psychiatry Behav Sci 2012;6:23-32.
- Clarke S, Kingston J, James K, Bolderston H, Remington B. Acceptance and commitment therapy group for treatment-resistant participants: a randomized controlled trial. J Context Behav Sci 2014;3:179-88. https://doi.org/10.1016/j.jcbs.2014.04.005.
- Sharp K. A review of acceptance and commitment therapy with anxiety disorders. Int J Psychol 2012.
- Smout MF, Hayes L, Atkins PWB, Klausen J, Duguid JE. The empirically supported status of acceptance and commitment therapy: an update. Clin Psychol 2012;16:97-109. https://doi.org/10.1111/j.1742-9552.2012.00051.x.
- Alonso MA, López A, Losada A, González JL. Acceptance and commitment therapy and selective optimization with compensation for older people with chronic pain: a pilot study. Behav Psychol Psicol Conduct 2013;21:59-7.
- Alonso-Fernández M, López-López A, Losada A, González JL, Wetherell JL. Acceptance and commitment therapy and selective optimization with compensation for institutionalized older people with chronic pain. Pain Med 2016;17:264-77. https://doi.org/10.1111/pme.12885.
- McCracken LM, Jones R. Treatment for chronic pain for adults in the seventh and eighth decades of life: a preliminary study of Acceptance and Commitment Therapy (ACT). Pain Med 2012;13:860-7. https://doi.org/10.1111/j.1526-4637.2012.01407.x.
- Wetherell JL, Afari N, Rutledge T, Sorrell JT, Stoddard JA, Petkus AJ, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011;152:2098-107. https://doi.org/10.1016/j.pain.2011.05.016.
- Karlin BE, Walser RD, Yesavage J, Zhang A, Trockel M, Taylor CB. Effectiveness of acceptance and commitment therapy for depression: comparison among older and younger veterans. Aging Ment Health 2013;17:555-63. https://doi.org/10.1080/13607863.2013.789002.
- Davison TE, Eppingstall B, Runci S, O’Connor DW. A pilot trial of acceptance and commitment therapy for symptoms of depression and anxiety in older adults residing in long-term care facilities. Aging Ment Health 2017;21:766-73. https://doi.org/10.1080/13607863.2016.1156051.
- Medical Research Council (MRC) . Developing and Evaluating Complex Interventions 2008.
- Lawrence V, Kimona K, Howard RJ, Serfaty MA, Wetherell JL, Livingston G, et al. Optimising the acceptability and feasibility of acceptance and commitment therapy for treatment-resistant generalised anxiety disorder in older adults. Age Ageing 2019;48:741-50. https://doi.org/10.1093/ageing/afz082.
- Yardley L, Ainsworth B, Arden-Close E, Muller I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud 2015;1. https://doi.org/10.1186/s40814-015-0033-z.
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-IP). New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002.
- First M, Gibbon M, Spitzer R, Williams J, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, DC: American Psychiatric Press; 1997.
- Molloy DW, Alemayehu E, Roberts R. Reliability of a Standardized Mini-Mental State Examination compared with the traditional Mini-Mental State Examination. Am J Psychiatry 1991;148:102-5. https://doi.org/10.1176/ajp.148.1.102.
- Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods 2006;18:59-82. https://doi.org/10.1177/1525822X05279903.
- Haak MJVD, Jong MDTD, Schellens PJ. Evaluation of an informational web site: three variants of the think-aloud method compared. Tech Commun 2007;54:58-71.
- Ritchie J, Spencer L. Qualitative Data Analysis for Applied Policy Research. London: Routledge; 1994.
- Krause N. Thought suppression and meaning in life: a longitudinal investigation. Int J Aging Hum Dev 2007;64:67-82. https://doi.org/10.2190/2044-390U-7106-5610.
- Brock MJ, Batten SV, Walser RD, Robb HB. Recognizing common clinical mistakes in ACT: a quick analysis and call to awareness. J Context Behav Sci 2015;4:139-43. https://doi.org/10.1016/j.jcbs.2014.11.003.
- Hayes S, Strosahl K, Wilson K. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. New York, NY: Guilford Press; 2012.
- Stoddard J, Afari N. The Big Book of ACT Metaphors: A Practitioner’s Guide to Experiential Exercises and Metaphors in Acceptance and Commitment Therapy. Oakland, CA: New Harbinger Publications; 2014.
- Laidlaw K, Kishita N. Age-appropriate augmented cognitive behavior therapy to enhance treatment outcome for late-life depression and anxiety disorders. GeroPsych 2015;28:57-66. https://doi.org/10.1024/1662-9647/a000128.
- Dakin EK, Areán P. Patient perspectives on the benefits of psychotherapy for late-life depression. Am J Geriatr Psychiatry 2013;21:155-63. https://doi.org/10.1016/j.jagp.2012.10.016.
- Baltes PB, Baltes MM, Baltes PB, Baltes MM. Successful Aging: Perspectives from the Behavioral Sciences. New York, NY: Cambridge University Press; 1990.
- Caudle DD, Senior AC, Wetherell JL, Rhoades HM, Beck JG, Kunik ME, et al. Cognitive errors, symptom severity, and response to cognitive behavior therapy in older adults with generalized anxiety disorder. Am J Geriatr Psychiatry 2007;15:680-9. https://doi.org/10.1097/JGP.0b013e31803c550d.
- Boddington S, Whittington A, Grey N. How to Become a More Effective CBT Therapist: Mastering Metacompetence in Clinical Practice. Chichester: John Wiley & Sons, Inc.; 2014.
- Gould RL, Coulson MC, Patel N, Highton-Williamson E, Howard RJ. Interventions for reducing benzodiazepine use in older people: meta-analysis of randomised controlled trials. Br J Psychiatry 2014;204:98-107. https://doi.org/10.1192/bjp.bp.113.126003.
- Gorenstein E, Papp L, Kleber M. Cognitive behavioral treatment of anxiety in later life. Cog Behav Pract 1999;6:305-20. https://doi.org/10.1016/S1077-7229(99)80050-9.
- Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ 2015;350. https://doi.org/10.1136/bmj.g7714.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- Department for Environment, Food and Rural Affairs . Rural Urban Classification 2016. www.gov.uk/government/collections/rural-urban-classification (accessed 19 August 2020).
- George D, Mallery M. SPSS for Windows Step by Step: A Simple Guide and Reference, 17.0 Update. Boston, MA: Allyn & Bacon; 2010.
- Norman G. Likert scales, levels of measurement and the ‘laws’ of statistics. Adv Health Sci Educ Theory Pract 2010;15:625-32. https://doi.org/10.1007/s10459-010-9222-y.
- Sullivan GM, Artino AR. Analyzing and interpreting data from likert-type scales. J Grad Med Educ 2013;5:541-2. https://doi.org/10.4300/JGME-5-4-18.
- Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry 2009;66:1332-40. https://doi.org/10.1001/archgenpsychiatry.2009.165.
- Arch JJ, Eifert GH, Davies C, Plumb Vilardaga JC, Rose RD, Craske MG. Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. J Consult Clin Psychol 2012;80:750-65. https://doi.org/10.1037/a0028310.
- Koychev I, Ebmeier KP. Anxiety in older adults often goes undiagnosed. Practitioner 2016;260:17-20.
- Beekman AT, Bremmer MA, Deeg DJ, van Balkom AJ, Smit JH, de Beurs E, et al. Anxiety disorders in later life: a report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry 1998;13:717-26. https://doi.org/10.1002/(SICI)1099-1166(1998100)13:10<717::AID-GPS857>3.0.CO;2-M.
- Trading Economics . Urban Population: Percent of Total 2016. https://tradingeconomics.com/united-kingdom/urban-population-percent-of-total-wb-data.html (accessed 19 August 2020).
- Schoevers RA, Deeg DJ, van Tilburg W, Beekman AT. Depression and generalized anxiety disorder: co-occurrence and longitudinal patterns in elderly patients. Am J Geriatr Psychiatry 2005;13:31-9. https://doi.org/10.1097/00019442-200501000-00006.
- Hopko DR, Bourland SL, Stanley MA, Beck JG, Novy DM, Averill PM, et al. Generalized anxiety disorder in older adults: examining the relation between clinician severity ratings and patient self-report measures. Depress Anxiety 2000;12:217-25. https://doi.org/10.1002/1520-6394(2000)12:4<217::AID-DA5>3.0.CO;2-6.
- Gould RL, Wetherell JL, Kimona K, Serfaty MA, Jones R, Graham CD, et al. Acceptance and commitment therapy for late-life treatment-resistant generalised anxiety disorder: a feasibility study. Age Ageing 2021. https://doi.org/10.1093/ageing/afab059.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22-33.
- Walters K, Rait G, Griffin M, Buszewicz M, Nazareth I. Recent trends in the incidence of anxiety diagnoses and symptoms in primary care. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0041670.
- Plumb JC, Vilardaga R. Assessing treatment integrity in acceptance and commitment therapy: strategies and suggestions. Int J Behav Consult Ther 2010;6:263-95. https://doi.org/10.1037/h0100912.
- Nezu A, Nezu C. Evidence-based Outcome Research: A Practical Guide to Conducting Randomized Controlled Trials for Psychosocial Interventions. New York, NY: Oxford University Press; 2008.
- Beecham J, Knapp M, Thornicroft G, Brewin C, Wing J. Measuring Mental Health Needs. London: Gaskell; 2001.
- Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res 1992;41:237-48. https://doi.org/10.1016/0165-1781(92)90005-N.
- Oei TPS, Green AL. The Satisfaction With Therapy and Therapist Scale-Revised (STTS-R) for group psychotherapy: psychometric properties and confirmatory factor analysis. Prof Psychol Res Pract 2008;39:435-42. https://doi.org/10.1037/0735-7028.39.4.435.
- Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 2000;31:73-86. https://doi.org/10.1016/S0005-7916(00)00012-4.
- Twohig MP, Hayes SC, Plumb JC, Pruitt LD, Collins AB, Hazlett-Stevens H, et al. A randomized clinical trial of acceptance and commitment therapy versus progressive relaxation training for obsessive-compulsive disorder. J Consult Clin Psychol 2010;78:705-16. https://doi.org/10.1037/a0020508.
- Serfaty M, Armstrong M, Vickerstaff V, Davis S, Gola A, McNamee P, et al. Acceptance and commitment therapy for adults with advanced cancer (CanACT): A feasibility randomised controlled trial. Psycho-Oncology 2019;28:488-96. https://doi.org/10.1002/pon.4960.
- Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E. Development and validation of the Geriatric Anxiety Inventory. Int Psychogeriatr 2007;19:103-14. https://doi.org/10.1017/S1041610206003504.
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990;28:487-95. https://doi.org/10.1016/0005-7967(90)90135-6.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982;17:37-49. https://doi.org/10.1016/0022-3956(82)90033-4.
- EuroQol Group . EuroQol: a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther 2011;42:676-88. https://doi.org/10.1016/j.beth.2011.03.007.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. https://doi.org/10.1111/j.2002.384.doc.x.
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol 2010;10. https://doi.org/10.1186/1471-2288-10-1.
- Morley S, Dowzer C. The Leeds Reliable Change Indicator. Leeds: University of Leeds; 2014.
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991;59:12-9. https://doi.org/10.1037//0022-006x.59.1.12.
- Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-264.
- Kuyken W, Byford S, Byng R, Dalgleish T, Lewis G, Taylor R, et al. Study protocol for a randomized controlled trial comparing mindfulness-based cognitive therapy with maintenance anti-depressant treatment in the prevention of depressive relapse/recurrence: the PREVENT trial. Trials 2010;11. https://doi.org/10.1186/1745-6215-11-99.
- Johnco C, Knight A, Tadic D, Wuthrich VM. Psychometric properties of the Geriatric Anxiety Inventory (GAI) and its short-form (GAI-SF) in a clinical and non-clinical sample of older adults. Int Psychogeriatr 2015;27:1089-97. https://doi.org/10.1017/S1041610214001586.
- Snyder AG, Stanley MA, Novy DM, Averill PM, Beck JG. Measures of depression in older adults with generalized anxiety disorder: a psychometric evaluation. Depress Anxiety 2000;11:114-20. https://doi.org/10.1002/(SICI)1520-6394(2000)11:3<114::AID-DA5>3.0.CO;2-C.
- Almeida OP, Almeida SA. Short versions of the geriatric depression scale: a study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int J Geriatr Psychiatry 1999;14:858-65. https://doi.org/10.1002/(SICI)1099-1166(199910)14:10<858::AID-GPS35>3.0.CO;2-8.
- Francis AW, Dawson DL, Golijani-Moghaddam N. The development and validation of the Comprehensive assessment of Acceptance and Commitment Therapy processes (CompACT). J Context Behav Sci 2016;5:134-45. https://doi.org/10.1016/j.jcbs.2016.05.003.
- Lappalainen R, Lehtonen T, Skarp E, Taubert E, Ojanen M, Hayes SC. The impact of CBT and ACT models using psychology trainee therapists: a preliminary controlled effectiveness trial. Behav Modif 2007;31:488-511. https://doi.org/10.1177/0145445506298436.
- Le Roux H, Gatz M, Wetherell JL. Age at onset of generalized anxiety disorder in older adults. Am J Geriatr Psychiatry 2005;13:23-30. https://doi.org/10.1097/00019442-200501000-00005.
- Rhebergen D, Aderka IM, van der Steenstraten IM, van Balkom AJLM, van Oppen P, Stek ML, et al. Admixture analysis of age of onset in generalized anxiety disorder. J Anxiety Disord 2017;50:47-51. https://doi.org/10.1016/j.janxdis.2017.05.003.
- Chou KL. Age at onset of generalized anxiety disorder in older adults. Am J Geriatr Psychiatry 2009;17:455-64. https://doi.org/10.1097/JGP.0b013e31818f3a93.
- World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines 1992.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Tyrer P. Against the stream: generalised anxiety disorder (GAD) – a redundant diagnosis. BJPsych Bull 2018;42:69-71. https://doi.org/10.1192/bjb.2017.12.
- Tyrer P. The case for cothymia: mixed anxiety and depression as a single diagnosis. Br J Psychiatry 2001;179:191-3. https://doi.org/10.1192/bjp.179.3.191.
- Serfaty M, Csipke E, Haworth D, Murad S, King M. A talking control for use in evaluating the effectiveness of cognitive-behavioral therapy. Behav Res Ther 2011;49:433-40. https://doi.org/10.1016/j.brat.2011.05.005.
- Kammerer K, Falk K, Herzog A, Fuchs J. How to Reach ‘Hard-to-Reach’ Older People for Research: The TIBaR Model of Recruitment 2019. https://surveyinsights.org/?p=11822 (accessed 19 August 2020).
- Harris TJ, Carey IM, Victor CR, Adams R, Cook DG. Optimising recruitment into a study of physical activity in older people: a randomised controlled trial of different approaches. Age Ageing 2008;37:659-65. https://doi.org/10.1093/ageing/afn159.
- Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287-91. https://doi.org/10.1002/pst.185.
- Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res 2016;25:1057-73. https://doi.org/10.1177/0962280215588241.
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent 2011;71:S52-S63. https://doi.org/10.1111/j.1752-7325.2011.00233.x.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: Personal Social Services Research Unit, University of Kent; 2019.
- Hunter RM, Baio G, Butt T, Morris S, Round J, Freemantle N. An educational review of the statistical issues in analysing utility data for cost-utility analysis. PharmacoEconomics 2015;33:355-66. https://doi.org/10.1007/s40273-014-0247-6.
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717-27. https://doi.org/10.1007/s11136-012-0322-4.
- Transport for London . Caps and Travelcard Prices 2020. https://tfl.gov.uk/fares/find-fares/tube-and-rail-fares/caps-and-travelcard-prices (accessed 19 August 2020).
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- National Institute for Health and Care Excellence (NICE) . Position Statement on Use of the EQ-5D-5L Value Set for England (Updated October 2019) 2019. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 19 August 2020).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- National Cost Collection for the NHS 2020. https://improvement.nhs.uk/resources/national-cost-collection/ (accessed 19 August 2020).
- Joint Formulary Committee . British National Formulary (online) n.d. www.medicinescomplete.com (accessed 19 August 2020).
- Devlin N. 5 Things You Should Do With EQ-5D Data 2016. www.ohe.org/news/5-things-you-should-do-eq-5d-data (accessed 19 August 2020).
- Sandberg M, Jakobsson U, Midlöv P, Kristensson J. Cost-utility analysis of case management for frail older people: effects of a randomised controlled trial. Health Econ Rev 2015;5. https://doi.org/10.1186/s13561-015-0051-9.
- Bulamu NB, Kaambwa B, Ratcliffe J. A systematic review of instruments for measuring outcomes in economic evaluation within aged care. Health Qual Life Outcomes 2015;13. https://doi.org/10.1186/s12955-015-0372-8.
- Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. J Clin Epidemiol 2001;54:136-41. https://doi.org/10.1016/S0895-4356(00)00261-4.
- Peasgood T, Brazier J, Papaioannou D. A Systematic Review of the Validity and Responsiveness of EQ-5D and SF-6D for Depression and Anxiety. HEDS Discussion Paper 12/15. Sheffield: University of Sheffield; 2012.
- Stanley MA, Novy DM. Cognitive-behavior therapy for generalized anxiety in late life: an evaluative overview. J Anxiety Disord 2000;14:191-207. https://doi.org/10.1016/S0887-6185(99)00048-1.
- Janssen MF, Birnie E, Bonsel GJ. Quantification of the level descriptors for the standard EQ-5D three-level system and a five-level version according to two methods. Qual Life Res 2008;17:463-73. https://doi.org/10.1007/s11136-008-9318-5.
- Hernandez Alava M, Wailoo A, Grimm S, Pudney S, Gomes M, Sadique Z, et al. EQ-5D-5L versus EQ-5D-3L: the impact on cost effectiveness in the United Kingdom. Value Health 2018;21:49-56. https://doi.org/10.1016/j.jval.2017.09.004.
- Cohen SR, Sawatzky R, Russell LB, Shahidi J, Heyland DK, Gadermann AM. Measuring the quality of life of people at the end of life: the McGill Quality of Life Questionnaire-Revised. Palliat Med 2017;31:120-9. https://doi.org/10.1177/0269216316659603.
- Ware JJ, Kosinski M, Bjorner J, Turner-Bowker D, Gandek B, Meruish M. User’s Manual for the SF-36v2 Health Survey. Lincoln: QualityMetric Incorporated; 2007.
- Coast J, Flynn TN, Natarajan L, Sproston K, Lewis J, Louviere JJ, et al. Valuing the ICECAP capability index for older people. Soc Sci Med 2008;67:874-82. https://doi.org/10.1016/j.socscimed.2008.05.015.
- Robson C, McCartan K. Real World Research. Chichester: John Wiley & Sons, Inc.; 2016.
- Ritchie J, Lewis J, McNaughton NC, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publishing Ltd; 2013.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
Appendix 1 Key themes and subthemes identified in stage 1
Key themes and subthemes identified in stage 1 are listed in Table 51.
| Theme | Views of older people with TR-GAD | Views of health-care professionals |
|---|---|---|
| 1. Expert in one’s own condition | ||
| Deep-seated view of self | Worrying as a part of oneself:I’ve always had the potential for a worrying mindP110, female, 79 | Identifying worrying as a part of oneself can prevent change:It’s just part of their personality; they say they can’t help itOccupational therapist, secondary careThey’ve been a worrier all their life so found it harder to engage with the cognitive side of CBTCommunity psychiatric nurse, secondary care |
| Life events and co-morbidity | Worry intertwined with poor health and negative aspects of ageing:The anxiety is really tied up with being on my own, I thinkP07, male, 72I get very concerned about, very often health but it can be other things, I don’t like uncertainty, I find that they recur and I’m going round and round in circlesP115Awareness of triggers and concerns:I worry about my daughter a lot. And I worry about my other daughter I don’t see too much . . . just all stupid things all the time. What if the lights go off? What if this, what if that? And by the time I finish all of those worries I feel so alone and frightenedP114, female, 87 | Life events and comorbidity contribute to GAD and are difficult to resolve:There are life issues that can’t be solvedClinical psychologist, secondary careTablets won’t work if the problem is still socialGP, primary careThere are lots of life changes, adjustment and I find making changes harder in this client groupClinical psychologist, secondary careCognitive and physical health problems as barriers to engagementBack pain interfered in sessionsClinical psychologist, secondary careCBT didn’t help as she didn’t engage due to physical mobilityClinical psychologist, secondary care |
| Futility of worrying | Recognition of futility of worrying:I’ve spent a lot of time worrying disproportionally about things that aren’t worth worrying about or may never happenP101, male, 72 | Need to promote understanding of unproductive thinking patterns:Explain how unproductive their thinking patterns have been, add this to the psycho-education sectionOccupational therapist, secondary care |
| 2. Deep-seated coping strategies | ||
| Established coping strategies including concealing anxieties, avoidance and controlling behaviour | Brave face:I don’t like it to show so I’ve always tried to hide it. Always, since I was smallP106, female, 67No, I’m able to cover it up . . . I don’t think anybody else except my wife knew about itP115, male, 82Avoid activities/social situations:I think I’m pretty good, actually, at avoiding the things that cause me anxiety. And, yes, I think I am . . . I can get taxis if I need. And I avoid being involved with things that are difficult journeys and where the only way I could get there is driving. Yes, so I suppose avoidance is my primary, you know, what’s the word? StrategyP110, female, 79Efforts to exert control:I was more controlling than I needed to be, with children, again, because of worrying about what might happenP110, female, 79 | Entrenched behaviours present challenges to therapy:A [learnt] helplessness – people not having an ownership of their illness and therefore their role (in bringing about change)Psychiatrist, secondary careRequires more intense therapy:6–8 or 8–12 [sessions] probably longer term needed with older people to shift patterns and allow for practice and set new habitsOccupational therapist, secondary careThey need individual plans and longer than 6 weeks of treatmentCounselling psychologist, secondary care |
| 3. Expert in therapy | ||
| Talking therapy ineffective | CBT inadequate:I think it [CBT] probably is for people with problems that, fresh problems or younger mind. You know, people that didn’t, they are not so intenseP103, Female, 73 | Failure to engage with therapy:This man was reluctant to engage with psychological therapy. He attended but he never brought any ideas, he never did the homeworkClinical psychologist, secondary careA lot of medication over the years that has created distance between them and their distress – so hard to engagePsychiatrist, secondary care[Clients] being too quick to judge therapy and giving upPsychiatrist, secondary care |
| Search for a magic pill | Desire for a cure:I find it very difficult in any therapy to accept what’s going on in my life. That would be very hard to accept. It would have to be some kind of marvellous therapy that you could say I’m going to accept all of these things and get on with it . . .P114, Female, 87 | Importance of shared, realistic goals and transparency:Tell them the truth that there is no ‘magic pill’GP, primary careGiving a clear message in the beginning of therapy about the potential of changeClinical psychologist, primary careUnwillingness to change behaviour:There was an unwillingness to change his behaviour or bring any ideas about how to change his behaviourPsychiatrist, secondary care |
| Desire for an empathic listener | Therapy requires an empathic listener:I think it’s by far the most important thing, the therapist, far, far away it’s an order of magnitude different to anything else . . . The person is sympathetic but not sympathetic in a sickly sweet sympathetic but is, you know, doing their honest best to understand your problems and to help you face themP101, male, 72Somebody you can trust, somebody that doesn’t judge you, they understand you, they are there to help you and give you advice, you know, even if they don’t give you direct advice, they give in a way that you understand what to doP103, female, 73 | Collaborative approach involving active participation of therapist and older person:I try to work with them and understand and think about all the aspects. What medication would be best? It’s important to think about the range of things available and explain that all these things are treatment not just the tabletPsychiatrist, secondary careYou need to see them a minimum of once a week to help build up therapeutic relationship and to build routine structure and expectations about their role and mineClinical psychologist, secondary care |
| 4. Support with implementation | ||
| Support to practice skills | Tools to support implementation:It requires . . . you’ll say right I’ve got to do this, I’m going to do this and then so, you know, for a few days you do it. And then, you know, you have a bad day and lots of things going wrong and you’re dealing with phone calls and then it all slips away again . . . I think regular practice is good and anything which encourages regular practice is good . . . When I try and do this meditation I use CDs [compact discs] that I got as part of the course and I think that’s goodP101, male, 72 | Tools to support implementation:Giving handouts can help. The lady I spoke about was still reading the information. Giving a folder can helpPsychiatrist, secondary care[For] loss of sight, big-lettered documents, bright colours, ask which they can’t see wellNurse, secondary care |
| Family and group support | Peer support:If you’ve got a group and more people it would be better because you commit [to therapy]. As far as I am concerned, I wouldn’t like to let the people down, so if I said this group of people meet to do this, you’ve got to come. I will do it because I wouldn’t like the people let downP103, female, 73Family involvement:Somebody would have to remind me to do it if I had a problem, or, you know, set an alarm clock on your phone, or whatever, or a partner saying, isn’t it time you sat down and did your practise?P104, female, 65 | Peer support:Group sessions that illustrates that it’s worked – so others can see the effect, so have patients help each otherCounselling psychologist, primary careFamily involvement:Having family there in consultationsClinical psychologist, secondary care |
Appendix 2 Data for all service users in the online survey
A total of 136 service users completed the online survey. Responses were excluded for three participants (2%) who indicated that they were aged < 60 years and 11 participants (8%) who had ‘never experienced difficulties with long-term worrying or their nerves’. Therefore, data from 122 service users (90%) were analysed. As shown in Table 52, the majority of service users were aged 65–74 years (n = 72, 59%). Most self-identified as white/white British (n = 114, 93%) women (n = 113, 93%) and resided in urban areas (n = 98, 91%). Just under half of service users had a degree or postgraduate qualification (n = 56, 46%), with only 13 (11%) reporting no educational qualifications.
| Variable | N (missing n, %) | n (%) |
|---|---|---|
| Age (years) | 122 (0, 0) | |
| 60–64 | 20 (16) | |
| 65–74 | 72 (59) | |
| 75–84 | 28 (23) | |
| 85–94 | 2 (2) | |
| ≥ 95 | 0 (0) | |
| Prefer not to say | 0 (0) | |
| Sex | 122 (0, 0) | |
| Male | 9 (7) | |
| Female | 113 (93) | |
| Prefer not to say | 0 (0) | |
| Ethnicity | 122 (0, 0) | |
| Asian/Asian British | 1 (1) | |
| Black/black British | 0 (0) | |
| Mixed | 1 (1) | |
| White/white British | 114 (93) | |
| Other | 3 (3) | |
| Prefer not to say | 3 (3) | |
| Age left school in years | 122 (0, 0) | |
| 14–16 | 47 (39) | |
| 17–19 | 67 (55) | |
| 20–22 | 3 (3) | |
| 23–25 | 4 (3) | |
| ≥ 26 | 1 (1) | |
| Highest educational qualification | 122 (0, 0) | |
| School Leaving Certificate | 2 (2) | |
| O level/GCSE | 21 (17) | |
| Diploma | 18 (15) | |
| A level | 7 (6) | |
| Undergraduate degree | 39 (32) | |
| Master’s degree | 16 (13) | |
| PhD | 1 (1) | |
| No educational qualifications | 13 (11) | |
| Other | 4 (3) | |
| Prefer not to say | 1 (1) | |
| Geographical area | 108 (14, 11) | |
| Urban | 98 (91) | |
| Rural | 10 (9) |
With respect to the clinical characteristics displayed in Table 53, there was a wide variation in the reported number of years experiencing difficulties with long-term worrying, with ≥ 30 years (n = 42, 36%) being the most common. In addition, there was a fairly even distribution of GAD-7 total scores across the severity categories, with the overall mean total score falling in the mild range. The mean number of comorbid mental health complaints was 3.0 (SD 2.1): comorbid symptoms of depression (n = 83, 68%), panic (n = 61, 50%) social phobia (n = 58, 48%) and PTSD (n = 54, 44%) were the most commonly reported.
| Variable | N (missing n, %) | n (%) | Mean (SD) |
|---|---|---|---|
| Number of years experiencing difficulties with long-term worrying | 116 (6, 5) | ||
| < 1 | 6 (5) | ||
| 1–5 | 19 (16) | ||
| 6–10 | 23 (20) | ||
| 11–20 | 17 (15) | ||
| 21–30 | 6 (5) | ||
| ≥ 30 | 42 (36) | ||
| Other | 3 (3) | ||
| GAD-7 total score, points (possible range 0–21 points) | 117 (5, 4) | 10.1 (6.0) | |
| GAD-7 total score (points) severity | 117 (5, 4) | ||
| None (0–5) | 32 (27) | ||
| Mild (6–10) | 31 (26) | ||
| Moderate (11–15) | 24 (21) | ||
| Severe (16–21) | 30 (26) | ||
| Comorbid mental health complaints | |||
| Depressive symptoms | 122 (0, 0) | ||
| Yes | 83 (68) | ||
| No | 36 (30) | ||
| Prefer not to say | 3 (3) | ||
| Panic symptoms | 122 (0, 0) | ||
| Yes | 61 (50) | ||
| No | 58 (48) | ||
| Prefer not to say | 3 (3) | ||
| Agoraphobia symptoms | 122 (0, 0) | ||
| Yes | 40 (33) | ||
| No | 81 (66) | ||
| Prefer not to say | 1 (1) | ||
| Social phobia symptoms | 122 (0, 0) | ||
| Yes | 58 (48) | ||
| No | 61 (50) | ||
| Prefer not to say | 3 (3) | ||
| Specific phobia symptoms | 122 (0, 0) | ||
| Yes | 37 (30) | ||
| No | 82 (67) | ||
| Prefer not to say | 3 (3) | ||
| PTSD symptoms | 122 (0, 0) | ||
| Yes | 54 (44) | ||
| No | 63 (52) | ||
| Prefer not to say | 5 (4) | ||
| OCD symptoms | 122 (0, 0) | ||
| Yes | 20 (16) | ||
| No | 98 (80) | ||
| Prefer not to say | 4 (3) | ||
| Other symptoms | 24 (98, 80) | ||
| Yes | 15 (63) | ||
| No | 9 (38) | ||
| Prefer not to say | 0 (0) | ||
| Number of comorbid mental health complaints (possible range 0–8) | 122 (0, 0) | 3.0 (2.1) | |
In terms of reported treatments for worrying in the past or currently (either received or refused), the majority of service users were not currently taking pharmacotherapy (n = 67, 62%) or receiving psychological therapy (n = 83, 86%; Table 54). However, the majority had received pharmacotherapy (n = 58, 54%) or psychological therapy (n = 63, 64%) in the past, with one or two different types of pharmacotherapy and one type of psychological therapy being most commonly reported. No medication or psychological therapy was reported currently or in the past (either received or refused) by 20 service users, 12 (60%) of whom reported current symptoms of GAD on the GAD-7 (eight in the mild range, two in the moderate range and two in the severe range).
| Variable | N (missing n, %) | n (%) |
|---|---|---|
| Pharmacotherapy for worry | ||
| Currently | 108 (14, 11) | |
| Yes | 41 (38) | |
| No | 67 (62) | |
| In the past | 108 (14, 11) | |
| Yes | 58 (54) | |
| No | 50 (46) | |
| Offered in the past but declined | 106 (16, 13) | |
| Yes | 20 (19) | |
| No | 86 (81) | |
| Psychological therapy for worry | ||
| Currently | 97 (25, 21) | |
| Yes | 14 (14) | |
| No | 83 (86) | |
| In the past | 98 (24, 20) | |
| Yes | 63 (64) | |
| No | 35 (36) | |
| Offered in the past but declined | 95 (27, 22) | |
| Yes | 6 (6) | |
| No | 89 (94) | |
| Number of different types of medication for worry tried in the past | 100 (22, 18) | |
| 1–2 | 42 (42) | |
| 3–4 | 11 (11) | |
| ≥ 5 | 7 (7) | |
| Cannot remember | 8 (8) | |
| Other | 32 (32) | |
| Number of different types of psychological therapy tried in the past | 97 (25, 21) | |
| 1 | 32 (33) | |
| 2 | 17 (18) | |
| ≥ 3 | 16 (16) | |
| Cannot remember | 6 (6) | |
| Other | 26 (27) | |
| No treatment received currently or in the past or refused | 104 (18, 15) | |
| Yes | 20 (19) | |
| No | 84 (81) | |
Participants rated the helpfulness of current and past treatments for worrying on a scale from 1 (not at all helpful) to 5 (extremely helpful), as shown in Table 55. There was little variation in the mean ratings across current and past treatments, with the mean rating ranging from 2.7 to 3.2. On average, current and past treatments were rated as being slightly to moderately helpful, with little difference between medication and psychological therapy.
| Perceived helpfulness rated on a scale from 1 (not at all helpful), through 3 (moderately helpful), to 5 (extremely helpful) | N (missing n, %) [N/A n, %] | Mean (SD) |
|---|---|---|
| Current medication | 42 (24, 20) [56, 46] | 2.9 (1.2) |
| Current psychological therapy | 28 (24, 20) [70, 57] | 2.9 (1.2) |
| Current combination of medication and psychological therapy | 18 (24, 20) [80, 66] | 2.7 (1.1) |
| Past medication | 59 (23, 19) [40, 33] | 2.8 (1.2) |
| Past psychological therapy | 65 (23, 19) [34, 28] | 3.2 (1.3) |
| Past combination of medication and psychological therapy | 38 (23, 19) [61, 50] | 3.2 (1.3) |
Appendix 3 The Consolidated Standards of Reporting Trials checklist (extension for randomised pilot or feasibility trials) and Consolidated Standards of Reporting Trials for Abstracts checklist
The CONSORT checklist (extension for randomised pilot or feasibility trials) and the CONSORT for Abstracts checklist are presented as Tables 56 and 57.
| Section/topic | Item number | CONSORT checklist item | Where located |
|---|---|---|---|
| Title and abstract | |||
| 1a | Identification as a pilot or feasibility randomised trial in the title | Title page | |
| 1b | Structured summary of pilot trial design, methods, results, and conclusions (for specific guidance see CONSORT abstract extension for pilot trials) | Scientific summary | |
| Introduction | |||
| Background and objectives | 2a | Scientific background and explanation of rationale for future definitive trial, and reasons for randomised pilot trial | Chapter 1, Background |
| 2b | Specific objectives or research questions for pilot trial | Chapter 1, Research question and Chapter 1, Aims and objectives | |
| Methods | |||
| Trial design | 3a | Description of pilot trial design (such as parallel, factorial) including allocation ratio | Chapter 4, Methods, Design |
| 3b | Important changes to methods after pilot trial commencement (such as eligibility criteria), with reasons | N/A | |
| Participants | 4a | Eligibility criteria for participants | Chapter 4, Methods, Participants |
| 4b | Settings and locations where the data were collected | Chapter 4, Methods, Setting | |
| 4c | How participants were identified and consented | Chapter 4, Methods, Recruitment procedures | |
| Interventions | 5 | The interventions for each group with sufficient details to allow replication, including how and when they were actually administered | Chapter 4, Methods, Intervention, Training, Supervision, Therapists |
| Outcomes | 6a | Completely defined prespecified assessments or measurements to address each pilot trial objective specified in 2b, including how and when they were assessed | Chapter 4, Methods, Data collection, Outcome measures |
| 6b | Any changes to pilot trial assessments or measurements after the pilot trial commenced, with reasons | N/A | |
| 6c | If applicable, prespecified criteria used to judge whether, or how, to proceed with future definitive trial | Chapter 4, Methods, Outcome measures | |
| Sample size | 7a | Rationale for numbers in the pilot trial | Chapter 4, Methods, Sample size calculation |
| 7b | When applicable, explanation of any interim analyses and stopping guidelines | N/A | |
| Randomisation | |||
| Sequence generation | 8a | Method used to generate the random allocation sequence | N/A |
| 8b | Type of randomisation(s); details of any restriction (such as blocking and block size) | N/A | |
| Allocation concealment mechanism | 9 | Mechanism used to implement the random allocation sequence (such as sequentially numbered containers), describing any steps taken to conceal the sequence until interventions were assigned | N/A |
| Implementation | 10 | Who generated the random allocation sequence, who enrolled participants and who assigned participants to interventions | N/A |
| Blinding | 11a | If done, who was blinded after assignment to interventions (for example, participants, care providers, those assessing outcomes) and how | N/A |
| 11b | If relevant, description of the similarity of interventions | N/A | |
| Statistical methods | 12 | Methods used to address each pilot trial objective whether qualitative or quantitative | Chapter 4, Methods, Data analyses |
| Results | |||
| Participant flow | 13a | For each group, the numbers of participants who were approached and/or assessed for eligibility, randomly assigned, received intended treatment and were assessed for each objective | Chapter 4, Results, Participant recruitment and flow |
| 13b | For each group, losses and exclusions after randomisation, together with reasons | Chapter 4, Results, Participant recruitment and flow | |
| Recruitment | 14a | Dates defining the periods of recruitment and follow-up | Chapter 4, Results, Participant recruitment and flow |
| 14b | Why the pilot trial ended or was stopped | N/A | |
| Baseline data | 15 | A table showing baseline demographic and clinical characteristics for each group | Chapter 4, Results, Demographic and clinical characteristics |
| Numbers analysed | 16 | For each objective, number of participants (denominator) included in each analysis. If relevant, these numbers should be by randomised group | Chapter 4, Results, Data collection |
| Outcomes and estimation | 17 | For each objective, results including expressions of uncertainty (such as 95% CI) for any estimates. If relevant, these results should be by randomised group | Chapter 4, Results, Primary outcomes and Chapter 4, Results, Secondary outcomes |
| Ancillary analyses | 18 | Results of any other analyses performed that could be used to inform the future definitive trial | Chapter 4, Results, Primary outcomes and Chapter 4, Results, Secondary outcomes |
| Harms | 19 | All important harms or unintended effects in each group (for specific guidance see CONSORT for harms) | Chapter 4, Results, Primary outcomes and Chapter 4, Results, Secondary outcomes |
| 19a | If relevant, other important unintended consequences | N/A | |
| Discussion | |||
| Limitations | 20 | Pilot trial limitations, addressing sources of potential bias and remaining uncertainty about feasibility | Chapter 4, Discussion, Limitations of the study |
| Generalisability | 21 | Generalisability (applicability) of pilot trial methods and findings to future definitive trial and other studies | Chapter 4, Discussion, Limitations of the study |
| Interpretation | 22 | Interpretation consistent with pilot trial objectives and findings, balancing potential benefits and harms, and considering other relevant evidence | Chapter 4, Discussion, Conclusions |
| 22a | Implications for progression from pilot to future definitive trial, including any proposed amendments | Chapter 7, Overall conclusions | |
| Other information | |||
| Registration | 23 | Registration number for pilot trial and name of trial registry | Scientific summary, Trial registration |
| Protocol | 24 | Where the pilot trial protocol can be accessed, if available | https://www.fundingawards.nihr.ac.uk/award/15/161/05 |
| Funding | 25 | Sources of funding and other support (such as supply of drugs), role of funders | Scientific summary, Funding and Acknowledgements, Funding acknowledgements |
| 26 | Ethics approval or approval by research review committee, confirmed with reference number | Report Supplementary Material 2 and 5 | |
| Item | Description | Where located |
|---|---|---|
| Title | Identification of the study as randomised | N/A |
| Authorsa | Contact details for the corresponding author | Title page |
| Trial design | Description of the trial design (e.g. parallel, cluster, non-inferiority) | Scientific summary, Phase 2, Design |
| Methods | ||
| Participants | Eligibility criteria for participants and the settings where the data were collected | Scientific summary, Phase 2, Setting, Participants |
| Interventions | Interventions intended for each group | Scientific summary, Phase 2, Intervention, Usual care |
| Objective | Specific objective or hypothesis | Scientific summary, Phase 2, Main objectives |
| Outcomes | Clearly defined primary outcome for this report | Scientific summary, Phase 2, Primary outcome measure |
| Randomisation | How participants were allocated to interventions | N/A |
| Blinding (masking) | Whether or not participants, care givers, and those assessing the outcomes were blinded to group assignment | N/A |
| Results | ||
| Number randomised | Number of participants randomised to each group | Scientific summary, Phase 2, Results |
| Recruitment | Trial status | Scientific summary, Phase 2, Results |
| Number analysed | Number of participants analysed in each group | Scientific summary, Phase 2, Results |
| Outcome | For the primary outcome, a result for each group and the estimated effect size and its precision | Scientific summary, Phase 2, Results |
| Harms | Important adverse events or side effects | N/A |
| Conclusions | General interpretation of the results | Scientific summary, Conclusions |
| Trial registration | Registration number and name of trial register | Scientific summary, Trial registration |
| Funding | Source of funding | Scientific summary, Funding |
Appendix 4 The Template for Intervention Description and Replication checklist
The TIDieR checklist is presented as Table 58.
| Item number | Item | Where located | |
|---|---|---|---|
| Section | Other (details) | ||
| BRIEF NAME | |||
| 1. | Provide the name or a phrase that describes the intervention | Chapter 1, Background | |
| WHY | |||
| 2. | Describe any rationale, theory, or goal of the elements essential to the intervention | Chapter 1, Background | |
| WHAT | |||
| 3. | Materials: describe any physical or informational materials used in the intervention, including those provided to participants or used in intervention delivery or in training of intervention providers. Provide information on where the materials can be accessed (e.g. online appendix, URL) | Chapter 4, Intervention, Training | |
| 4. | Procedures: describe each of the procedures, activities, and/or processes used in the intervention, including any enabling or support activities | Chapter 4, Intervention, Training, Supervision | |
| WHO PROVIDED | |||
| 5. | For each category of intervention provider (e.g. psychologist, nursing assistant), describe their expertise, background and any specific training given | Chapter 4, Therapists, Supervision | |
| HOW | |||
| 6. | Describe the modes of delivery (e.g. face to face or by some other mechanism, such as internet or telephone) of the intervention and whether it was provided individually or in a group | Chapter 4, Intervention | |
| WHERE | |||
| 7. | Describe the type(s) of location(s) where the intervention occurred, including any necessary infrastructure or relevant features | Chapter 4, Intervention | |
| WHEN and HOW MUCH | |||
| 8. | Describe the number of times the intervention was delivered and over what period of time including the number of sessions, their schedule, and their duration, intensity or dose | Chapter 4, Intervention | |
| TAILORING | |||
| 9. | If the intervention was planned to be personalised, titrated or adapted, then describe what, why, when, and how | Chapter 2, Discussion | |
| MODIFICATIONS | |||
| 10. | If the intervention was modified during the course of the study, describe the changes (what, why, when, and how) | N/A | |
| HOW WELL | |||
| 11. | Planned: if intervention adherence or fidelity was assessed, describe how and by whom, and if any strategies were used to maintain or improve fidelity, describe them | Chapter 4, Treatment fidelity | |
| 12. | Actual: if intervention adherence or fidelity was assessed, describe the extent to which the intervention was delivered as planned | Chapter 4, Results, Secondary outcomes | |
Appendix 5 Recruitment graph
The uncontrolled feasibility study opened for recruitment on 2 January 2018 and closed for referrals on 31 October 2018. As shown in Figure 8, the recruitment rate from March to November 2018 appears to reflect the ‘true’ recruitment rate.
FIGURE 8.
Rate of recruitment to the uncontrolled feasibility study.
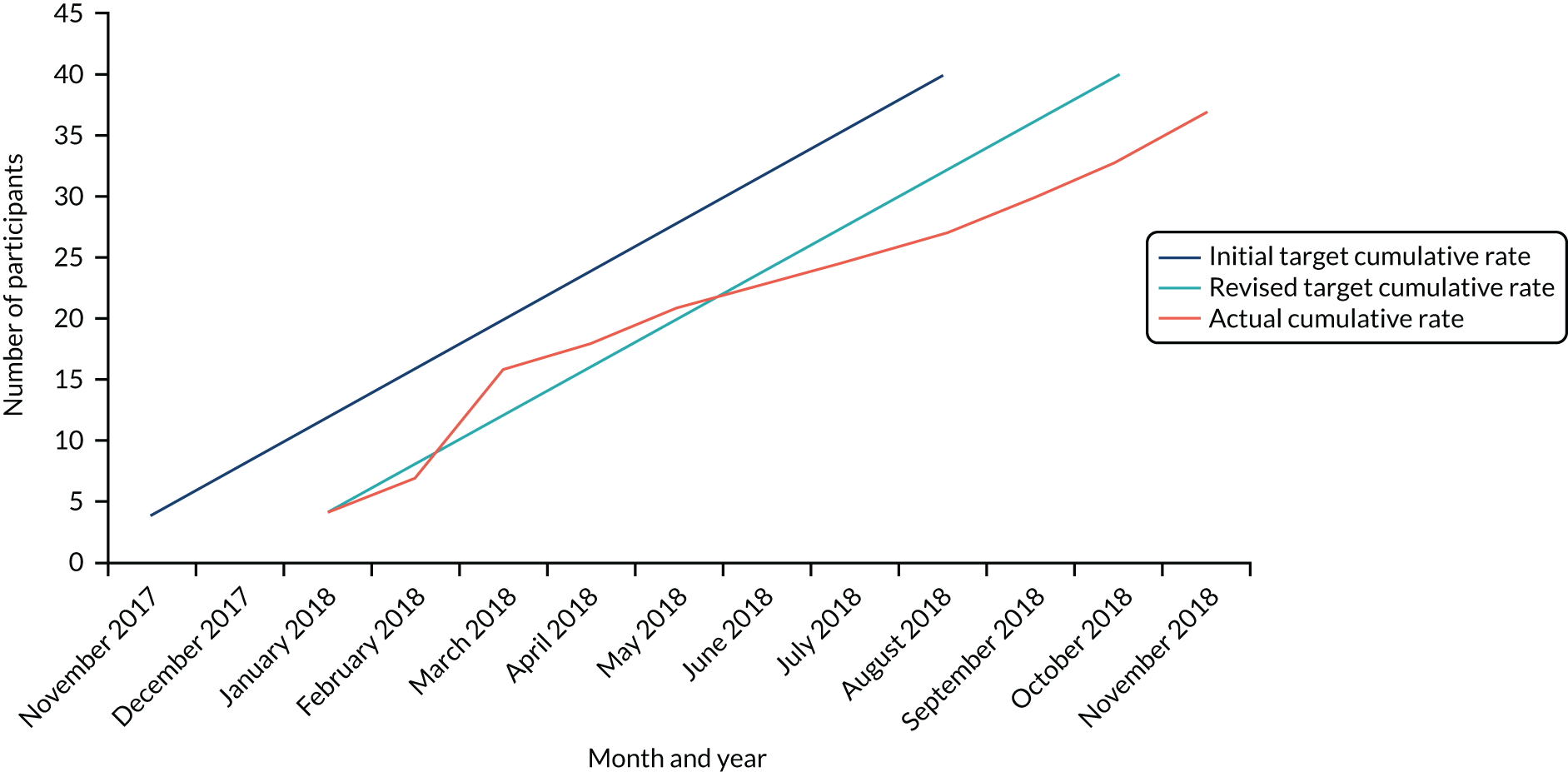
Appendix 6 The Consolidated Health Economic Evaluation Reporting Standards checklist
The CHEERS checklist is listed in Table 59.
| Section/item | Item number | Recommendation | Where located |
|---|---|---|---|
| Title and abstract | |||
| Title | 1 | Identify the study as an economic evaluation or use more specific terms such as ‘cost-effectiveness analysis’, and describe the interventions compared | N/A |
| Abstract | 2 | Provide a structured summary of objectives, perspective, setting, methods (including study design and inputs), results (including base-case and uncertainty analyses) and conclusions | Scientific summary, Main objectives; Scientific summary, Phase 2 and Scientific summary, Results |
| Introduction | |||
| Background and objectives | 3a | Provide an explicit statement of the broader context for the study | Chapter 5, Introduction |
| 3b | Present the study question and its relevance for health policy or practice decisions | Chapter 5, Introduction | |
| Methods | |||
| Target population and subgroups | 4 | Describe characteristics of the base-case population and subgroups analysed including why they were chosen | Chapter 4, Methods, Participants |
| Setting and location | 5 | State relevant aspects of the system(s) in which the decision(s) need(s) to be made | Chapter 4, Methods, Setting |
| Study perspective | 6 | Describe the perspective of the study and relate this to the costs being evaluated | Chapter 5, Introduction |
| Comparators | 7 | Describe the interventions or strategies being compared and state why they were chosen | N/A |
| Time horizon | 8 | State the time horizon(s) over which costs and consequences are being evaluated and say why appropriate | Chapter 5, Methods |
| Discount rate | 9 | Report the choice of discount rate(s) used for costs and outcomes and say why appropriate | N/A |
| Choice of health outcomes | 10 | Describe what outcomes were used as the measure(s) of benefit in the evaluation and their relevance for the type of analysis performed | Chapter 5, Methods |
| Measurement of effectiveness | 11a | Single study-based estimates: describe fully the design features of the single effectiveness study and why the single study was a sufficient source of clinical effectiveness data | N/A |
| 11b | Synthesis-based estimates: describe fully the methods used for the identification of included studies and synthesis of clinical effectiveness data | N/A | |
| Measurement and valuation of preference based outcomes | 12 | If applicable, describe the population and methods used to elicit preferences for outcomes | N/A |
| Estimating resources and costs | 13a | Single study-based economic evaluation: describe approaches used to estimate resource use associated with the alternative interventions. Describe primary or secondary research methods for valuing each resource item in terms of its unit cost. Describe any adjustments made to approximate to opportunity costs | Chapter 5, Methods |
| 13b | Model-based economic evaluation: describe approaches and data sources used to estimate resource use associated with model health states. Describe primary or secondary research methods for valuing each resource item in terms of its unit cost. Describe any adjustments made to approximate to opportunity cost | N/A | |
| Currency, price date, and conversion | 14 | Report the dates of the estimated resource quantities and unit costs. Describe methods for adjusting estimated unit costs to the year of reported costs if necessary. Describe methods for converting costs into a common currency base and the exchange rate | Chapter 5, Methods |
| Choice of model | 15 | Describe and give reasons for the specific type of decision-analytic model used. Providing a figure to show model structure is strongly recommended | N/A |
| Assumptions | 16 | Describe all structural or other assumptions underpinning the decision-analytic model | N/A |
| Analytical methods | 17 | Describe all analytic methods supporting the evaluation. This could include methods for dealing with skewed, missing or censored data; extrapolation methods; methods for pooling data; approaches to validate or make adjustments (e.g. half-cycle corrections) to a model; and methods for handling population heterogeneity and uncertainty | N/A |
| Results | |||
| Study parameters | 18 | Report the values, ranges, references and, if used, probability distributions for all parameters. Report reasons or sources for distributions used to represent uncertainty where appropriate. Providing a table to show the input values is strongly recommended | Chapter 5, Results |
| Incremental costs and outcomes | 19 | For each intervention, report mean values for the main categories of estimated costs and outcomes of interest, as well as mean differences between the comparator groups. If applicable, report incremental cost-effectiveness ratios | Chapter 5, Results |
| Characterising uncertainty | 20a | Single study-based economic evaluation: describe the effects of sampling uncertainty for estimated incremental cost, incremental effectiveness, and incremental cost-effectiveness, together with the impact of methodological assumptions (such as discount rate, study perspective) | N/A |
| 20b | Model-based economic evaluation: describe the effects on the results of uncertainty for all input parameters, and uncertainty related to the structure of the model and assumptions | N/A | |
| Characterising heterogeneity | 21 | If applicable, report differences in costs, outcomes or cost-effectiveness that can be explained by variations between subgroups of patients with different baseline characteristics or other observed variability in effects that are not reducible by more information | N/A |
| Discussion | |||
| Study findings, limitations, generalisability, and current knowledge | 22 | Summarise key study findings and describe how they support the conclusions reached. Discuss limitations and the generalisability of the findings and how the findings fit with current knowledge | Chapter 5, Discussion and Chapter 7, Overall conclusions |
| Other | |||
| Source of funding | 23 | Describe how the study was funded and the role of the funder in the identification, design, conduct and reporting of the analysis. Describe other nonmonetary sources of support | Acknowledgements |
| Conflicts of interest | 24 | Describe any potential for conflict of interest among study contributors in accordance with journal policy | Title page |
Glossary
- Acceptance and commitment therapy
- A novel form of talking therapy that uses acceptance- and mindfulness-based techniques to help someone to accept their emotional experiences and things outside their control and to commit to changing their behaviour in ways that help them to achieve a full and meaningful life. The acronym ‘Accept your experiences and be present, Choose a meaningful direction for your life, and Take action’ (Harris R. ACT Made Simple: An Easy-to-Read Primer on Acceptance and Commitment Therapy. Oakland, CA: New Harbinger Publications; 2009) sums up acceptance and commitment therapy.
- Cognitive behavioural therapy
- A form of talking therapy that is conventionally offered for generalised anxiety disorder, along with applied relaxation, following National Institute for Health and Care Excellence guidelines, which involves changing how one thinks and behaves in emotional situations. The ‘3Cs’ phrase ‘catch it, check it, change it’ in relation to negative thoughts captures the essence of cognitive behavioural therapy.
- Community Mental Health Team
- A mental health service based in secondary care, typically comprising a team of health-care professionals including psychiatrists, clinical psychologists, community psychiatric nurses and occupational therapists.
- Generalised anxiety disorder
- An anxiety disorder characterised by chronic worry about a variety of everyday problems.
- Improving Access to Psychological Therapies service
- A talking-therapy service based in primary care.
- Treatment-resistant generalised anxiety disorder
- A failure to respond after completion of steps 1–3 of the stepped-care approach for generalised anxiety disorder. Step 1 comprises identification, assessment, education and active monitoring. Step 2 includes low-intensity psychological interventions such as guided self-help based on cognitive behavioural therapy. Step 3 consists of pharmacotherapy and/or high-intensity, individual psychotherapy (either cognitive behavioural therapy or applied relaxation). Steps 1–3 typically occur in primary care (general practices and Improving Access to Psychological Therapies services), whereas step 4 occurs in specialist mental health services (Community Mental Health Teams).
List of abbreviations
- A level
- Advanced level
- ACT
- acceptance and commitment therapy
- ANOVA
- analysis of variance
- CBT
- cognitive behavioural therapy
- CHEERS
- Consolidated Health Economic Evaluation Reporting Standards
- CI
- confidence interval
- CMHT
- Community Mental Health Team
- CONSORT
- Consolidated Standards of Reporting Trials
- CPA
- Care Programme Approach
- CSC
- clinically significant change
- CSRI
- Client Service Receipt Inventory
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- DSM-V
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-VAS
- EuroQol Visual Analogue Scale
- FACTOID
- a Feasibility study of Acceptance and Commitment Therapy for Older people with treatment-resistant generalised anxiety Disorder
- GAD
- generalised anxiety disorder
- GAD-7
- Generalised Anxiety Disorder-7
- GP
- general practitioner
- IAPT
- Improving Access to Psychological Therapies
- ICECAP-O
- ICEpop CAPability measure for Older people
- ID
- identifier
- IQR
- interquartile range
- IRAS
- Integrated Research Application System
- MINI
- Mini-International Neuropsychiatric Interview
- MRC
- Medical Research Council
- MSE
- mean squared error
- NICE
- National Institute for Health and Care Excellence
- PC
- personal computer
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- QALY
- quality-adjusted life-year
- RCI
- Reliable Change Index
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- SMMSE
- Standardised Mini-Mental State Examination
- TIDieR
- Template for Intervention Description and Replication
- TR-GAD
- treatment-resistant generalised anxiety disorder
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hta25540).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
