Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 17/148/11. The contractual start date was in February 2019. The draft report began editorial review in August 2020 and was accepted for publication in January 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Drahota et al. This work was produced by Drahota et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Drahota et al.
Chapter 1 Introduction
Parts of this report have been reproduced with permission from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Description of the health condition
Falls, commonly defined as ‘an unexpected event in which the participants come to rest on the ground, floor, or lower level’,2 are a serious and growing threat to global trends in healthy life expectancy. 3 They have significant morbidity, mortality and economic impacts, particularly for older adults who are more at risk of both falls and fall-related injuries. 4,5 Falls constitute the most commonly reported safety incident in hospitals,5 with prevalence rates estimated to be two to three times higher in care settings (hospitals and care homes) than in the community. 6 Inpatient falls account for approximately one-quarter of the £2.3B cost of falls to the NHS each year,5,7 with falls in care homes contributing considerably to this cost.
The causes of falls are complex and multifaceted, and may stem from a combination of intrinsic risk factors related to the person (e.g. eyesight, mobility, cognition, comorbidities), extrinsic risk factors associated with the environment (e.g. trip/slip hazards, footwear, clothing, medication, disorientating environment, staffing), and the activity of the individual (e.g. mobilising from bed, going to the toilet). 8–10 Similarly, fall-related injuries are a product of an individual’s susceptibility to injury (e.g. as a result of bone strength, physical and cognitive impairments), the environment in which they fall (e.g. the surfaces they come into contact with, the presence of others) and the dynamics of the fall itself. 11,12
Fall-related injuries can vary from pain and bruising to lacerations, sprains, head injuries and fractures. Approximately 72% of inpatient falls may result in no visible harm;5 it is still vital to prevent these falls whenever possible because of their impact on the subsequent falls risk, behaviour and psychology of the individual. 13,14 Injurious falls have additional consequences, for example affecting independence and ongoing care needs. 15,16 In 2018 in the NHS, 2439 hip fractures occurred in inpatient settings, constituting 3.8% of all hip fractures in England and Wales. 17 In addition to having a higher 30-day mortality risk,17 those sustaining an inpatient hip fracture are at increased risk of moving into nursing homes or residential care to meet their ongoing care needs, and can experience a substantial loss of healthy life-years. 18 Although it is recognised that there is no single solution to prevent all falls, increasingly there is an emphasis placed on finding ways to reduce the number of severe falls.
Description of flooring interventions
Owing to the complex nature of falls, a wide range of interventions exists to try and prevent them. For example, in hospitals and care homes, there is low-quality evidence with uncertain conclusions to support the use of exercise, physiotherapy, sensor alarms and multifactorial interventions tailored to individuals’ risk factors. 19 Shock-absorbing flooring is an additional potential intervention for the prevention of injurious falls; however, although the evidence-base for flooring interventions has been mapped in a scoping review,20 it has not yet been systematically reviewed. By decreasing the stiffness of the ground surface, shock-absorbing (or compliant) flooring aims to reduce the impact forces of falls to lower the risk of injury. In the care sector, commonly used flooring materials may vary in stiffness; for example, some carpets may offer someone who falls a softer landing than a thin vinyl, and wooden subfloors may be less severe to land on than concrete subfloors. Yet the health and care sector is beginning to think beyond these standard flooring types, turning to the sports sector. A multitude of sports floors exists, designed to offer shock-absorbency for the protection and comfort of players in sports halls, which could be repurposed for use in hospitals and care homes. In addition, some specialist flooring manufacturers have recognised the gap in the market for purposefully designed shock-absorbing ‘health’ floors and novel flooring interventions are now available that have been designed with fall-related injury prevention in mind.
‘Shock-absorbing’ floors, therefore, can differ with regard to their intended purpose, thickness, material choice and composition, and will vary with regard to the level of shock-absorbency they offer. Some manufacturers offer shock-absorbing underlays, which are designed to be used in conjunction with a regular overlay material (such as a standard vinyl), and other manufacturers provide a complete flooring system that can be laid on a concrete or wooden subfloor.
Why it is important to do this review
Using the floor as an intervention to prevent injurious falls in care homes and hospitals has certain appeals, as, unlike other injury prevention interventions (such as hip protectors or helmets), it has the potential to ‘treat’ all those that come into contact with it (and whichever body part may come into contact with it), without necessarily requiring any active engagement or compliance from the user (patients/residents or staff). Once installed, a floor may be expected to last up to 20 years, which, if effective at reducing hip fractures and other injuries, offers the potential for a significant return on investment. 21–24 Yet the decision to implement a shock-absorbing floor is not a straightforward one. Softer floors can create greater rolling resistance for wheeled objects, making it harder to initiate and sustain movement when pushing or pulling furniture like beds, trolleys, hoists, etc. 25,26 Considerably greater forces and awkward work positions have been reported for pushing and/or pulling wheeled equipment on soft surfaces like carpet, compared with hard surfaces like linoleum,27,28 and the performance of pushing and pulling activities is strongly associated with the prevalence of musculoskeletal injuries in the health-care sector. 29,30 In this respect, there is a risk that staff may experience more adverse events when working on shock-absorbing floors.
Furthermore, although a potential benefit with regard to reducing musculoskeletal symptoms where workers must stand or walk for long periods has been reported,31 concerns exist as to whether or not a more compliant surface underfoot would introduce more instability in people who are already at higher risk of falling. Thus, in an attempt to decrease the proportion of falls resulting in injury, the implementation of a shock-absorbing floor may inadvertently increase the overall number of falls experienced. In laboratory-based research, a debate is ongoing as to whether or not the gait of older adults (particularly those individuals with complex health needs) may be adversely affected by softer floors,32–43 and yet evidence also suggests that older adults would benefit most from falling on softer floors. 33,44–48 The potential benefits and risks of shock-absorbing floors may differ depending on the individuals using them; however, clinical evidence is required to better inform our understanding of this issue.
A scoping review identified all of the published evidence on shock-absorbing flooring up until May 201620 and since then further studies have emerged. 49–54 We have undertaken this systematic review because, to our knowledge, the growing body of evidence has not yet been critically appraised or synthesised, with an exploration of different care settings and flooring types, to help resolve the current uncertainties, to better inform NHS investment decisions and to clearly identify the next steps for research activity.
Aims and objectives of the research
In this mixed-methods review (including randomised, non-randomised, qualitative and economic studies), we aimed to systematically review the evidence on shock-absorbing flooring use in care settings (hospitals and care homes) for fall-related injury prevention in older adults. The objectives were to:
-
assess the potential benefits (fall-related injury prevention) and risks (falls, staff injuries) of different flooring systems in care settings
-
assess the extent to which these potential benefits and risks may be modified by different studies/settings, intervention and participant characteristics
-
critically appraise and summarise current evidence on the resource use, costs and cost-effectiveness of shock-absorbing flooring in care settings for older adults, compared with standard flooring
-
summarise findings on the implementation of flooring interventions in the included studies
-
summarise the views and experiences of shock-absorbing flooring use from staff, patients’, residents’ and visitors’ perspectives
-
identify gaps in existing evidence.
Chapter 2 Review methods and results of the search
This systematic review explores what is known about the clinical effectiveness, cost-effectiveness and qualitative experiences of shock-absorbing flooring systems for fall-related injury prevention in care settings. For assessing the quantitative evidence, we have followed the general approach set out in the Cochrane Handbook for Systematic Reviews of Interventions Version 6.0,55 and for qualitative evidence we have used the Joanna Briggs Institute (JBI) handbook. 56 We have followed the guidance set out in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement,57 the Meta-analysis Of Observational Studies in Epidemiology statement,58 the Methodological Expectations of Cochrane Intervention Reviews standards59 and the JBI guidance for mixed-methods reviews60 in the reporting and conduct of this review. In this chapter, we detail the methods used for each component of the review and present the results of the study selection process.
Eligibility criteria
Types of studies
This systematic review set out to incorporate primary research that used experimental, quasi-experimental, observational and qualitative designs. Our broad inclusion criteria for quantitative evidence is justified because, although randomised trials of flooring interventions are feasible (given appropriate resources), the nature and logistics of the intervention make observational and opportunistic quasi-experimental designs far more practical; we know from our scoping review that randomised trials in the field are sparse. 20 Therefore, we have included non-randomised studies with the view to systematically report their findings and limitations to better inform practice. Qualitative evidence is most appropriate to understanding the views and experiences of shock-absorbing flooring interventions. As the different types of evidence set out to address different components of our research question, we have summarised the findings from each type of evidence separately (quantitative, see Chapter 3; qualitative, see Chapter 4; and economic, see Chapter 5), before drawing the evidence together in our discussion and conclusions (see Chapter 6).
To overcome variations in terminology, regardless of how study authors have labelled their study designs, we have classified included quantitative studies by their component design features. 61 The following study types were eligible:
-
Randomised controlled trials (RCTs). These may have been randomised at the individual or cluster level (e.g. with the unit of allocation by room/area/facility). Non-random methods of allocation (quasi-experimental studies, as per further examples later in this list) were also eligible.
-
Interrupted times series (e.g. evaluating a change in trend in outcome measures before and after shock-absorbing flooring installation).
-
Controlled before-and-after studies (e.g. non-randomised allocation to shock-absorbing flooring or control, whereby outcomes are measured concurrently in groups of participants residing in areas with different floors, before and after a change in floor in at least one group).
-
Cohort studies (e.g. prospectively or retrospectively observing groups of patients residing in areas with or without shock-absorbing flooring).
-
Case–control studies (e.g. retrospectively evaluating where patients with various classifications of fall-related injuries fell to see the effect of flooring type on outcome).
-
Partial and full economic evaluations based on a single study or model.
-
Qualitative studies involving interviews, focus groups, questionnaires or surveys, which explore experiences, attitudes and perceptions towards flooring interventions.
Simple before-and-after studies measuring quantitative outcomes, with no evaluation of time trends (i.e. a series of at least three observations prior and three observations post intervention), or concurrent control, were ineligible. Laboratory-based/biomechanical studies were excluded. We have not applied a threshold for risk of bias as part of the study design inclusion criteria; rather, the potential influence of risk of bias is addressed in the analyses and interpretation of the findings.
Population
The target population for this review is, broadly, older adults in hospitals and care homes. Notably, the adverse effects may be witnessed in staff who are occupying the same environment because of the potential need for increased effort to undertake tasks (e.g. moving wheeled equipment, such as beds, trolleys and hoists). Staff and visitors, along with patients/residents, may also offer useful qualitative insights into flooring use.
To be included, studies must have focused on adult populations in care settings; studies that were focused solely on paediatric care settings were ineligible. We took a pragmatic approach and were open to different definitions of ‘older adults’ (e.g. studies may have been conducted in settings with differing admissions criteria or employed various inclusion criteria of their own). We did not have a set cut-off criterion for age, as it is acknowledged that chronological age may not be a good indicator of frailty,62,63 and, owing to the nature and purpose of the intervention, we anticipated that studies would largely be conducted in high-risk environments where older adults were the predominant population and falls were more likely.
Settings
Studies must have been conducted in a care setting to be included in this review; this included hospitals (acute, sub-acute) and intermediate and long-term care settings (nursing and care homes). Studies conducted in people’s own homes or other settings (e.g. playgrounds, sporting venues) were excluded.
Care settings were broadly defined as:64
-
Care home environment – a facility that meets the following criteria: provides communal living facilities for long-term care; provides overnight accommodation; provides nursing or personal care; and provides for people with illness, disability or dependence.
-
Hospital environment – a facility that meets the following criteria: provides communal care whereby there is an expectation that this care is time limited, provides overnight accommodation, provides nursing and personal care, and provides for people with illness and disability.
Interventions
Eligible studies must have compared different types of flooring, with at least one intervention classifiable as a ‘shock-absorbing’ floor, as per the subsequent definition. Studies that included flooring as one component of a package of multiple interventions, in which the effects of the floor could not be discerned from other concurrent interventions, were ineligible.
‘Shock-absorbing flooring systems’ include floor coverings, underlays and subfloors considered to reduce the impact forces of falls. Alternative terminology may include variations on the terms: compliant flooring, safety flooring, soft flooring, impact-absorbing flooring, energy-absorbing flooring, low-impact flooring, dual-stiffness flooring, low-stiffness flooring, absorptive surfaces, cushioned flooring, rubber flooring, acoustic flooring and carpet. Interventions may include flooring systems that have been purposely designed to prevent fall-related injuries {e.g. SmartCells® [Seamless Attenuating Technologies (SATECH), Inc., Chehalis, WA, USA], SorbaSHOCK™ (SorbaShock LLC, Fort Wayne, IN, USA), Kradal™ (Charles Parsons Private Ltd, Sydney, Australia)}, thick vinyl [> 5 mm thick; e.g. repurposed sports floors, such as Tarkett Omnisports Excel (Tarkett S.A., La Défense, France)], carpet with or without underlay, and other combination flooring systems (e.g. vinyl overlays with padded underlays, such as foam or rubber, or wooden subfloors).
Fall mats were considered ineligible as they are not permanently affixed to the floor and do not provide universal coverage or protection. We excluded studies reporting exclusively on fall mats. Studies that compared different types of shock-absorbing flooring systems or that compared one or more shock-absorbing flooring system with a standard ‘rigid’ floor (e.g. concrete, ≤ 2 mm of vinyl/resilient sheeting) were eligible.
Outcomes
Although we expected quantitative studies to report on outcomes related to falls and fall-related injuries as a minimum, the reporting of specific outcomes did not form part of the inclusion criteria for this review. Rather, we considered the reporting of outcomes as part of our risk-of-bias assessments and assessment of reporting/publication bias.
Theoretical framework
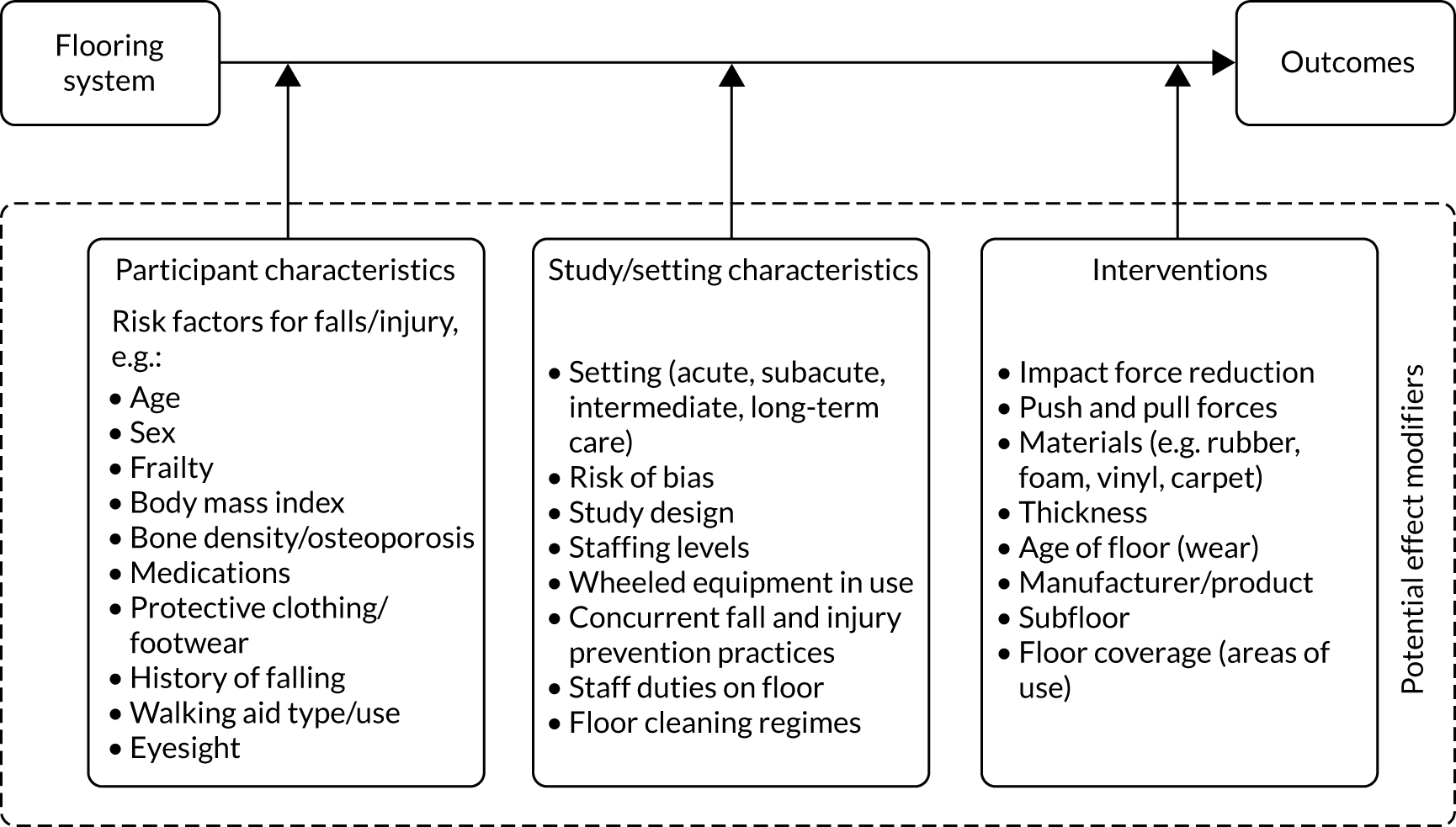
Figure 1 conceptualises the causal pathway between shock-absorbing floor systems and their outcomes (falls, fall-related injuries, adverse events – staff injuries), and potential (often related) moderators of that relationship (effect modifiers). We developed this framework during the initial stages of the review in consultation with our public involvement members. The purpose of this framework was to help direct the review process by informing data collection, risk-of-bias assessment (particularly in relation to confounding), exploration of heterogeneity and analysis of the data.
FIGURE 1.
Theoretical framework of potential effect modifiers.
Outcomes and prioritisation
There is no core outcome set specifically for shock-absorbing flooring interventions. A common outcome data set for fall injury prevention trials has been developed; however, it focuses on community-dwelling populations. 2 In addition, an international consensus statement for trials on hip protectors has also been developed. 65 In developing our outcomes, we considered these related core outcome sets (and their differences in foci with the current review), discussions with our public involvement group, wider stakeholder engagement activities66 and the peer review comments we received on our protocol. 67 Following these considerations, we opted to focus on the following outcome measures, in the following order of priority:
-
primary outcomes –
-
injurious falls rate per 1000 person-days
-
falls rate per 1000 person-days
-
-
secondary outcomes –
-
number of falls resulting in injuries (e.g. none, minor, moderate, severe, death)
-
number of fractures
-
number of hip fractures
-
number of fallers
-
number of adverse events (staff injuries)
-
number of head injuries
-
fractures per 1000 person-days
-
hip fractures per 1000 person-days
-
qualitative outcomes (e.g. staff’s, patients’/residents’ and visitors’ attitudes, views and experiences)
-
economic outcomes [to include assessments of quality-adjusted life-years (QALYs)]
-
process outcomes (e.g. ease of or problems with flooring installation).
-
The primary outcomes (1 and 2) were selected to assess the potential benefits and harms of flooring interventions for patients/residents, accounting for occupancy levels and follow-up time; the injurious falls rate additionally accounts for variations in the underlying falls rate as a pragmatic measure of effectiveness. For example, if shock-absorbing floors do reduce the proportion of falls resulting in injury, but inadvertently increase the number of falls, then the rate of injurious falls would provide a better reflection in real terms of how many injurious falls are occurring in practice. Rate measures are also considered most suitable when dealing with count data types.
The first seven prioritised outcomes have been incorporated into our summary of findings tables (which headline the findings for each comparison; see Chapter 3), and these outcomes formed the basis of our risk-of-bias and Grading of Recommendations Assessment, Development and Evaluation (GRADE) assessments. The quantitative outcomes (1–10) are reported in Chapter 3, qualitative outcomes (11) are reported in Chapter 4 and economic outcomes (12) are reported in Chapter 5. Process outcomes (13) are reported when available as part of the studies included in Chapters 3 and 4.
Search methods
The search of this systematic review built on a comprehensive search already conducted in a scoping review. 20 The scoping review identified literature relating to shock-absorbing flooring published up to and including 20 May 2016. The clinical effectiveness (n = 20), cost-effectiveness (n = 12), and qualitative (n = 2) records identified by the scoping review were all assessed for eligibility in this systematic review. The search strategy of the scoping review was updated and refined in scope (by AD) to focus on identifying studies of clinical effectiveness, cost-effectiveness and qualitative experiences. We searched the following electronic databases: AgeLine, Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE, Scopus, Web of Science and the NHS Economic Evaluation Database (NHS EED) (see Appendix 1, Table 22, for search strategies). The MEDLINE search strategy was adapted for the remaining databases by one review author (LMF) and checked by another (AD). With the exception of AgeLine (searched by DCM), all database searches were run by Lambert M Felix, who compiled the search ‘hits’ ready for screening in duplicate. We conducted forward and backward citation searches on included studies, and a hand-search of the journal Age and Ageing. The grey literature search included a review of clinical trial registries, ProQuest Dissertations & Theses, conference proceedings and relevant websites (Table 1). No language restrictions were placed on the search.
| Sources of literature | Date range searched |
|---|---|
| Previous searches | |
| Scoping review20 | Inception to May 2016 |
| Academic databases | |
| AgeLine (EBSCOhost; Simon Fraser University, Canada) | 1 May 2016–23 November 2019 |
| CINAHL (EBSCOhost; University of Portsmouth, UK) | 1 May 2016–29 September 2019 |
| MEDLINE (EBSCOhost; University of Portsmouth, UK) | 1 May 2016–29 September 2019 |
| Web of Science (Thomson Reuters; University of Portsmouth, UK) | 1 May 2016–29 September 2019 |
| Scopus (Elsevier; University of Portsmouth, UK) | 1 May 2016–29 September 2019 |
| NHS EED (Centre for Reviews and Dissemination, University of York, UK) [archived resource 2014] | Inception to 11 November 2019 |
| Grey literature | |
| WHO International Clinical Trials Registry Platform | 1 May 2016–3 October 2019 |
| ClinicalTrials.gov | 1 May 2016–1 April 2020 |
| ProQuest Dissertations & Theses | 1 May 2016–3 October 2019 |
| OpenGrey | Inception to 1 April 2020 |
| Biennial Conference of the Australian and New Zealand Falls Prevention Society | 2016 and 2018 |
| International Society for Posture and Gait Research World Congress | 2017 and 2019 |
| Canadian Association on Gerontology Annual Scientific and Educational Meeting | 2016, 2018 and 2019 |
| Gerontological Society of America’s Annual Scientific Meeting | 2019 |
| World Conference of Gerontechnology | 2017 |
| World Congress of the International Association of Gerontology and Geriatrics | 2017 |
| Agency for Healthcare Research and Quality | Last search: 22 April 2020 |
| Canadian Agency for Drugs and Technologies in Health | Last search: 22 April 2020 |
| Parachute Canada | Last search: 22 April 2020 |
| The National Institute for Occupational Safety and Health | 1 May 2016–22 April 2020 |
| US Center for Health Design | 2016–1 May 2019 |
| Hand-searches, backward and forward citation searches | |
| Reference lists of included studies published since 1 May 2019 | All |
| Tables of contents of the journal Age and Ageing | 1 May 2019–2 October 2019 |
| Forward citation searches of included studies [Web of Science (Thomson Reuters; University of Portsmouth, UK)] | Last search: 1 April 2020 |
Data collection
Data management
All references were imported into the reference management software EndNote online [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] and duplicates were removed. We managed the review strategy with the screening and data extraction software Covidence [Covidence systematic review software, Veritas Health Innovation, Melbourne, VIC, Australia, URL: www.covidence.org (accessed 26 February 2021)], which supported linking of related records, the screening, and elements of our data collection [other elements of data collection were conducted using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA)], to enable tasks to be done independently in duplicate, and to facilitate the identification and resolution of differences of opinions. Data were analysed in RevMan, version 5.3 (The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark), and summary of findings tables were created with the support of GRADEpro GDT (McMaster University and Evidence Prime Inc., Hamilton, ON, Canada).
Study selection
Titles, abstracts and full reports were screened independently by two reviewers using an eligibility checklist (based on the inclusion/exclusion criteria). One review author (LMF) screened all records and the duplicate screening was shared by other team members (AD, BEK, CCL and OO). All records included in the clinical effectiveness and cost-effectiveness sections of the scoping review were assessed at the full-report stage. Initial searches involved screening titles and abstracts, with potentially relevant records reviewed in full. Disagreements were resolved through a third independent arbitrator and discussion.
Data extraction
Data extraction of quantitative studies
Our approach to data collection was underpinned by our theoretical framework of potential effect modifiers (see Figure 1). We developed a data collection form, which was piloted on two included studies49,52 and amended as required. A data collection manual was developed to support the process across multiple review authors working independently in different locations. Data on study characteristics were collected in the software Covidence, and risk-of-bias assessments and outcome data were collected in Microsoft Excel.
Data collection included the following key components of information:
-
study identification (and linked publications)
-
funding sources
-
time/duration and geographical place of conduct
-
participant characteristics
-
intervention(s)
-
control(s)
-
outcome data acquisition – falls reporting (e.g. retrospective database review, prospective daily checks of patient notes, staff recall, triangulation of sources), classification system of injuries, identification of fractures (confirmation of diagnosis/type of fractures included), identification of adverse effects
-
setting
-
study design characteristics
-
risk-of-bias assessments, including assessments of confounding
-
outcomes and analyses (we extracted summary effect estimates when possible and raw data to enable our own calculations when appropriate)
-
patient and public involvement in the research
-
follow-up questions for study authors (missing and unclear information was flagged).
Data extraction of qualitative studies
Data extraction was conducted independently in duplicate, with one review author (CM) collecting data on all qualitative studies and two review authors supporting the duplicate data collection (AD, KFS). Data collection was undertaken in a predesigned Microsoft Excel workbook, with built-in instructions. We collected data on the following study characteristics: sponsor, country, setting, aims/objectives, authors’ conclusions, conflicts of interest, funding source, linked studies, patient and public involvement, methodology, methods, phenomena of interest, types of flooring discussed, data analysis, inclusion/exclusion criteria, number of participants, type of participants, age and sex.
Extraction of the study findings also formed the first stage of the qualitative synthesis (as per the JBI approach to meta-aggregation). 56 We defined a finding as ‘a verbatim extract of the authors’ analytic interpretation accompanied by either a participant voice, or fieldwork observations or other data’. 56 We extracted each finding alongside an illustration of that finding from the publication (e.g. a participant quotation, fieldwork observation or other supporting data) and made a judgement as to the credibility of the evidence (unequivocal, credible, not supported) according to the following criteria:56
-
unequivocal – findings accompanied by an illustration that is beyond reasonable doubt and, therefore, not open to challenge
-
credible – findings accompanied by an illustration lacking clear association with it and, therefore, open to challenge
-
not supported – findings are not supported by the data.
Although each paper was read in full, all of the findings were identified from the themes and metaphors presented in the results sections, and only those findings that were judged to be unequivocal or credible were taken forward to the analysis. Disagreements were resolved through discussion. One study focused on the environment more broadly; for this study, we extracted the findings relevant to flooring only. 68 Review authors who had authored one of the primary qualitative studies were not involved in the data collection or the assessment of credibility of their own studies.
Data extraction of economic studies
The main review method used for economic studies was iterative interrogation of the studies to review them against the basic elements of good-practice guidelines,69–71 specifically addressing a well-defined research question, using an appropriate type of study, with full description of options, a rationale for structure, relevant outcomes, and with an appropriate perspective, time frame, costs, assumption and methods. Data were extracted on each of these topics, with estimates made for key data when possible by James Raftery and checked by Amy Drahota.
Risk-of-bias assessment
Risk-of-bias assessments were undertaken at the outcome level, using the Cochrane Risk of Bias tool version 2.0 (RoB 2.0) for randomised trials,72 the Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) tool for non-randomised studies73 and the JBI critical appraisal checklist for qualitative studies. 56 The quantitative studies were all assessed by the same review author (LMF) and assessed independently in duplicate by one of the other team members (AD, CCL, BEK or OO). The qualitative studies were all assessed by the same review author (CM) and independently in duplicate by one other team member (AD or KFS). Disagreements were resolved through discussion (through e-mail and teleconference) and involvement of a third independent review author as necessary. Review authors were not blinded during risk-of-bias assessments; however, care was taken to ensure that no review authors assessed studies that they were involved in (i.e. as a co-author). We sought further information from study authors if there was inadequate information to form a risk-of-bias judgement; we approached study authors with open-ended questions asking them to describe the relevant study processes in more detail to avoid biased answers.
The public involvement members (Margaret Bell, Liz Burden and Joleen Tobias) supported the risk-of-bias assessments through group meetings and electronic liaison, in which they commented on the clarity and transparency of the reporting of our judgements. Feedback from our public involvement members influenced the style and wording of the supporting statements incorporated into the risk-of-bias tables (see Appendix 2).
Data analysis (quantitative studies)
Measures of treatment effect
We have used rate ratios (RaRs) with 95% confidence intervals (CIs) to summarise injurious falls rates per 1000 person-days, falls rates per 1000 person-days, fractures per 1000 person-days and hip fractures per 1000 person-days. We present risk ratios (RRs) with 95% CIs for number of falls resulting in injuries, number of fallers and number of head injuries, and we use odds ratios (ORs) with 95% CIs when outcomes were rare (number of fractures and number of hip fractures). Adverse events (staff injuries) and process outcomes (e.g. ease of installation) have been summarised descriptively in the text owing to the nature of the data reported. For all estimates of treatment effects, we used the reported estimates and 95% CIs when available, or calculated them using the raw data if feasible and appropriate.
Primary outcomes
Injurious falls rate per 1000 person-days
We defined the rate of injurious falls as the total number of falls sustaining any injury (minor, moderate or severe) per 1000 person-days of monitoring. The RaR compares the injurious falls rate in the intervention group with the injurious falls rate in the control group. When appropriate and feasible, we calculated the RaR per 1000 person-days using Equation 1:
To analyse these data using the generic inverse variance method in RevMan version 5.3; we also calculated the standard error of the log (RaR), as per Equation 2:
Falls rate per 1000 person-days
We defined the falls rate as the total number of fall events per 1000 person-days of monitoring. We followed the same approach as described previously for the injurious falls rate for handling and summarising these data.
Secondary outcomes
Number of falls resulting in injuries (e.g. none, minor, moderate, severe, death)
We explored the number of falls resulting in injuries using RRs and 95% CIs, using Equation 3 to calculate the RR when required:
This outcome was commonly presented as a primary outcome in observational studies, in which comparison groups were formed based on the number of falls documented on different types of flooring (i.e. the main unit of analysis was ‘falls’ rather than ‘participants’). This approach was in contrast to RCTs, which tended to follow up individuals who had been allocated to rooms with or rooms without shock-absorbing flooring. This outcome does not account for recurrent fallers (i.e. the same person may have contributed to multiple falls, so the denominator ‘falls’ does not retain the assumption of independence), and, in the observational studies, it is possible that the same people may have been analysed in one or both groups, depending on where they fell. There is no way for us to assess the impact of these unknown factors on the results; therefore, we have treated this outcome more cautiously in our interpretation and have considered all of the contributing data (even from RCTs) to be observational.
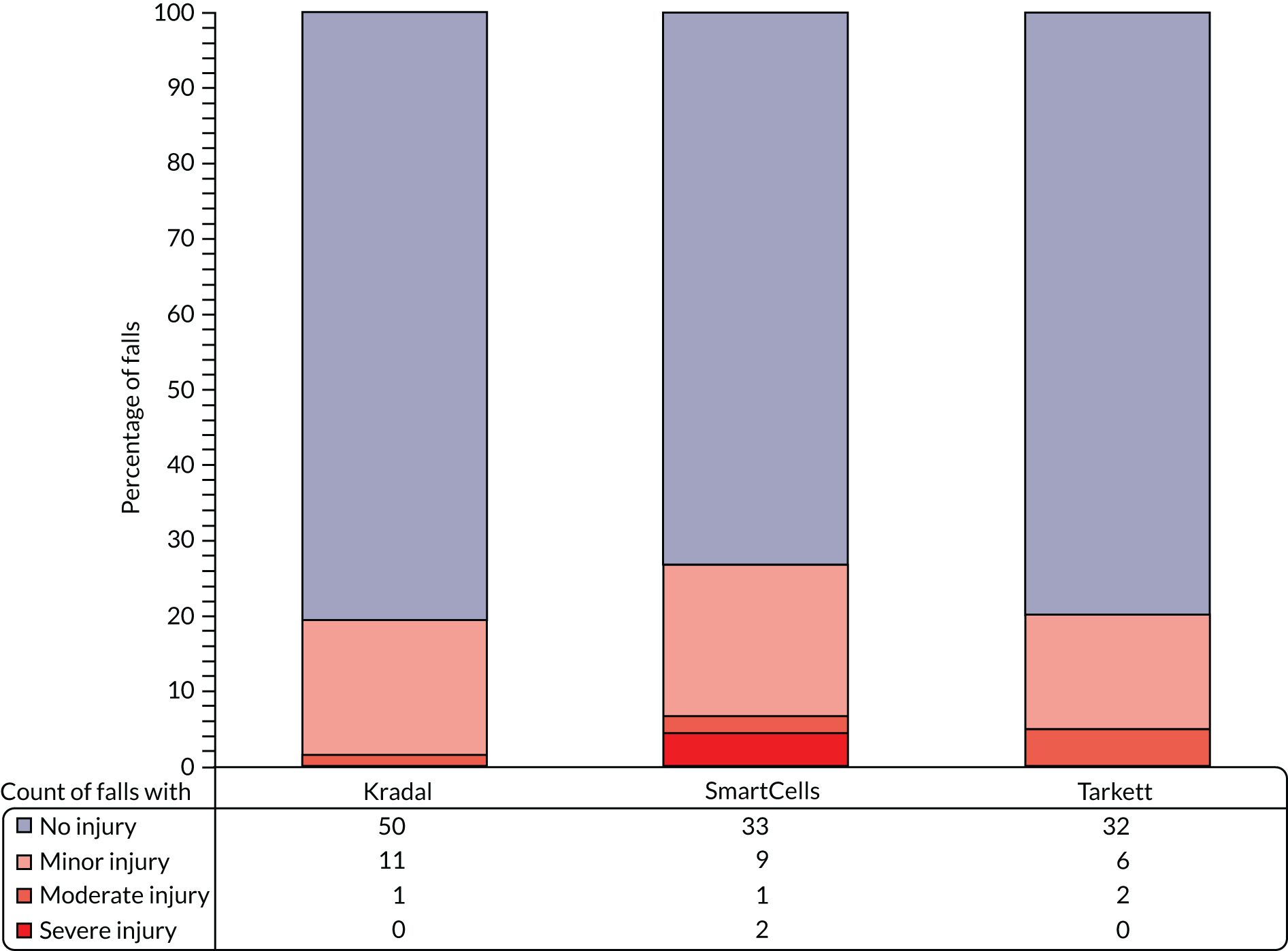
When studies presented a breakdown of the severity of injuries (as ordinal outcome data, e.g. none, mild, moderate, severe), we presented these descriptively as counts (n) and proportions (%), and displayed each study’s data using a stacked bar graph.
Number of fractures
We collected information on how the data for fractures were acquired in individual studies (e.g. whether or not they were radiologically diagnosed). Radiographic imaging has an estimated sensitivity of 90–98% (for hip fractures)74 and is an essential diagnostic tool providing orthopaedic surgeons with vital information to enable them to plan appropriate fracture management. Although clinicians have relatively good judgement at identifying fractures through clinical examination, not all clinically suspected fractures produce positive radiographs, even after occult fractures are followed up through further imaging techniques. 74,75 It is therefore recommended that fracture outcomes are radiologically confirmed for research purposes to provide more robust and reliable results. 2 We collected data on the number of participants with fractures (of any bone), whether or not it was clear if the fracture was a result of the documented fall. Some fragility fractures can occur spontaneously prior to a fall and not be the result of an impact with the floor, and sometimes it may not be clear from a scan whether the fracture is old or new. 12 We summarised the number of fractures using ORs [owing to the sparsity of these data, we used different analyses methods for pooling the data (see Data synthesis); however, in the situation of having few events to analyse, the odds produce very similar estimates to risks]. The odds of fracture in each group were primarily summarised using ‘number of participants with one or more fractures (of any bone)’ in the numerator and ‘number of participants without a fracture’ in the denominator.
We also re-expressed the odds of fracture using the ‘number of falls resulting in one or more fractures’ in the numerator and ‘number of falls without a fracture’ in the denominator to include all available data (including from an observational study). We handled these data more cautiously in our interpretation as ‘falls’ are non-independent count data (e.g. a particularly robust individual may have contributed recurrent falls to the denominator in one group, diluting the overall observed odds).
Number of hip fractures
Fractures were included in this outcome if they were described as a ‘hip fracture’ or ‘fractured neck of femur’ in the study report; we included all hip fractures whether or not it was clear that they were a result of the documented fall. We summarised the data using ORs with 95% CIs. As with the outcome ‘number of fractures’, we primarily calculated the odds for each group at the participant level and then re-expressed the odds at the falls level so as to include all available data (including from observational studies).
Number of fallers
We defined the number of fallers as the number of people who fell once or more. We summarised the outcome using RRs and 95% CIs, which compares the risk of being a faller in each study group. The risk of falling for each study group was calculated using the ‘number of participants who fell once or more’ as the numerator and the ‘number of participants’ as the denominator.
Number of adverse events (staff injuries)
Had data been available on either the number of staff-days observed or the total number of staff in each group, we would have reported these outcomes as RaRs and 95% CIs, or RRs and 95% CIs, respectively. As it was not possible to calculate these data (as the denominators were unknown), we simply reported the data as described in the papers, that is as the number of adverse events over the period of follow-up. We have noted that it would probably have been difficult for studies to collect and report this information on denominators because of study designs that mean that the same staff may variably work across study groups, and, in hospital settings, some reported adverse outcomes were related to staff who were visiting the ward from another department (e.g. radiographers).
Number of head injuries
We included all reported head injuries of any classified severity, and regardless of whether they were attributable to contact with the floor or another surface. We summarised head injuries using RRs and 95% CIs.
Fractures per 1000 person-days
We defined the fracture rate as the total number of fracture events per 1000 person-days of monitoring. We followed the same approach as described previously for the injurious falls rate for handling and summarising these data.
Hip fractures per 1000 person-days
Fractures were included in this outcome if they were described as a ‘hip fracture’ or ‘fractured neck of femur’ in the study report; we included all hip fractures, whether or not it was clear that they were a result of the documented fall. We followed the same approach as described previously for the injurious falls rate for handling and summarising these data.
Unit-of-analysis issues
We have included an observational study using a 2 × 2 factorial design (‘carpeted’ vs. ‘uncarpeted’, ‘wooden subfloor’ vs. ‘concrete subfloor’)76 and an observational study with parallel arms, in which the intervention group was composed of multiple shock-absorbing flooring types. 49 To avoid unit-of-analysis issues, we ensured that we did not double-count the same individuals (or falls) twice in any one analysis.
For the 2 × 2 factorial study,76 we analysed the data for ‘carpeted versus uncarpeted’ and ‘wooden subfloor versus concrete subfloor’ in separate subgroups, which we did not combine, to ensure that the data were not double-counted. The corresponding author of the study with parallel arms49 provided us with the segregated data for the different flooring types assessed in the intervention group so that we could perform subgroup analyses on different flooring types. For these subgroup analyses, we split the data in the control group between the pairwise comparisons so as not to overinflate the weight of the study in any pooled effect estimate. In the main analyses, we used the reported study data, in which the data for the different shock-absorbing flooring interventions were combined into one study group.
For the primary outcomes, we did not encounter any unit-of-analysis issues related to cluster randomised trials where clustering had not been taken into account. There was one included cluster randomised trial (a pilot study) that presented descriptive data pertaining to the secondary outcomes. 77 For each secondary outcome to which this study contributed, we approximated the correct analysis by adjusting the extracted data by the ‘design effect’ (DE), using the average cluster size (M = 71) and a ‘borrowed’ intracluster correlation coefficient (ICC), as per Equation 4:
With regard to identifying appropriate ICCs to incorporate in the analyses, we first attempted to identify ICCs for each relevant outcome, reported in other hospital-based cluster RCTs, that aligned with the trial for which we were adjusting. When this was not possible, we based our ICC estimates on what is known about the relationship between the ICC and the prevalence of outcomes. 78 Table 2 presents a summary of the estimates and subsequently we provide our justification for the selection of these figures.
| Outcome | ICC (ρ) | DE | Sensitivity analyses (DE)a |
|---|---|---|---|
| Number of falls resulting in injuries | 0.046 | 4.22 | 2.61 and 7.44 |
| Number of fractures | 0.013 | 1.91 | 1.46 and 2.82 |
| Number of hip fractures | 0.002 | 1.14 | 1.07 and 1.28 |
| Number of fallers | 0.020 | 2.40 | 1.70 and 3.80 |
| Fractures per 1000 person-day | 0.002 | 1.14 | 1.07 and 1.28 |
| Hip fractures per 1000 person-day | 0.002 | 1.14 | 1.07 and 1.28 |
Although the reporting of ICCs for the primary outcomes is relatively common, ICCs for the secondary outcomes in hospital settings were harder to identify. In the included cluster RCT,77 the number of falls resulting in injury had a prevalence of 42.4% in the control group, and, because prevalence of an outcome has been shown to correlate with the ICC, we made an informed assumption that the predicted ICC would be 0.046 for this outcome. 78 Similarly, for risk of fracture (control group prevalence 6%)77 and hip fracture (control group prevalence 3%),77 we opted for ICCs (0.013 and 0.002, respectively) which are estimated to be more suited to lower prevalence rates in the order of 10% and 1% (also see Sensitivity analyses). 78
We based our estimate for risk of one or more falls (number of fallers) on a cluster trial in rehabilitation wards, which reported an ICC of 0.02 (95% CI 0.00 to 0.04);79 this study had a similar prevalence of fallers (intervention, 8.38%; control, 12.51%) to that reported in the included cluster RCT (intervention, 13.78%; control, 9.87%). 77
With regard to ICCs for rate outcomes, a relatively small ICC of 0.002 (95% CI 0.001 to 0.004) has been specified for the primary outcome, rate of injurious falls,80 and this corroborates the analyses made in the included cluster RCT. 77 Because rarer outcomes are likely to have even smaller ICCs,78 we opted to take a conservative approach and use the same ICC for rates of fractures and hip fractures. An ICC of 0.002 has been shown to align with outcomes that have a prevalence in the order of 1%, and the prevalences of fractures and hip fractures in the included study were 0.43% and 0.22%, respectively. 77
To adjust for clustering in the analyses of the cluster RCT,77 for each relevant outcome in which the generic inverse variance method was used, we multiplied the standard error of the effect estimate (from an analysis that did not account for clustering) by the square root of the design effect. In analyses that were calculated from the raw data (fractures and hip fractures), we divided the number of events and totals in each group by the design effect and rounded each number to the nearest integer. These adjustments provide a more conservative estimate than would be given by ignoring clustering.
Dealing with missing data
One review author (LMF) approached seven corresponding authors of included studies by e-mail to obtain or clarify data when they were missing or unclear in the study reports. In some cases, unpublished data were obtained from personal communications; we have highlighted this in the footnotes of the relevant figures and tables.
When summary effect estimates (RaRs or RRs) were not reported, we calculated these, when feasible, using the raw data, as described previously. When data were missing or incomplete from individual participants, we conducted the analyses based on the available data and included an assessment of the problem as part of the risk-of-bias judgements.
Assessment of reporting bias
There was an insufficient number of studies that could be combined to assess for potential reporting biases using a test of funnel plot asymmetry. We aimed to reduce the risk of publication bias affecting our results by conducting a thorough search and by communicating with researchers in the field. During data extraction, we assessed the potential for each study to contribute to each outcome, and, when data were not reported or could not easily be derived, one review author (LMF) followed up with the corresponding authors in an attempt to obtain the relevant data. If we determined that any of the key outcomes were potentially affected by an included study not reporting (or only partially reporting) the outcome (if we felt that it would have been feasible for them to report the outcome in full), then we downgraded the evidence as part of our GRADE assessments.
Data synthesis
Studies were synthesised in RevMan (version 5.3). In cases where evidence exists from randomised and non-randomised studies, we have reported the randomised study data separately. When appropriate, we combined studies using the generic inverse variance method with a DerSimonian and Laird random-effects model, assuming that intervention effects are likely to vary across studies (informed by our scoping review20 and based on our theoretical framework of potential effect modifiers; see Figure 1). When feasible and considered appropriate, we supplemented the RCT evidence with the combined data from RCTs and observational studies to provide an overall summary effect estimate of all available evidence. If adjusted and unadjusted rates were presented in randomised trials, we used the unadjusted figures, unless the adjustment was for clustering. For non-randomised studies, we recorded the unadjusted and adjusted estimates and noted the factors for which they were adjusted. When multiple adjusted estimates were presented, we extracted the estimate highlighted as the primary model by the authors, or, if this was unclear, we used the model that had adjusted for the most covariates (see Sensitivity analyses).
We did not attempt to pool the data on different severities of injury, as different studies used different classification systems to distinguish between injury types and we had determined at the protocol stage that proportional ORs would be less useful for end users of the review.
Some of our outcomes were relatively rare events (i.e. fractures and hip fractures), with some studies having zero event counts in one or both study arms. The generic inverse variance method with random-effects model is not considered effective in these situations, and, in RevMan, continuity corrections are automatically applied when one study arm has an event count of zero, which should be avoided in the analysis of rare events. 81 We therefore opted to present the findings from Mantel–Haenszel analyses (fixed effect) as the main results for these outcomes and to run sensitivity analyses on the choice of analysis method.
Subgroup analysis and assessment of heterogeneity
When feasible, we plotted data onto forest plots, using the generic inverse variance data type in RevMan, and explored the heterogeneity. We explored heterogeneity irrespective of whether or not we decided to pool studies in a meta-analysis. Heterogeneity was assessed through a combination of visual inspection of the forest plots, along with consideration of tests for homogeneity (χ2 with statistical significance set at p < 0.10), and measures for inconsistency (I2) and heterogeneity (τ2).
The following study and intervention characteristics were explored in subgroups, when feasible:
-
study design (RCTs, prospective cohort studies, retrospective cohort studies)
-
study setting (hospitals, care homes)
-
flooring type (novel shock-absorbing flooring, sports flooring, carpet, wooden subfloors).
We had initially planned to explore acuity of care; however, this was not feasible with the available studies (see Changes from the protocol). We did not explore patient-level characteristics in subgroups as this level of data is more suited to individual-patient data meta-analyses, which was beyond the scope of this review. However, we anticipated that study-level characteristics relating to setting and the acuity of care provided would overlap with differences in patient-level factors, which we assessed and commented on narratively.
Sensitivity analyses
Sensitivity analyses were undertaken to determine the influence of the following:
-
Risk of bias (removing studies deemed to be at high/serious risk of bias).
-
Choice of effect estimates (e.g. when multiple adjusted estimates are presented).
-
Adjustment for clustering. We re-ran the analyses in which we had approximated the ICC for the cluster trial with a more and a less conservative estimate of the design effect. For this, we divided and multiplied each ICC by a factor of two before re-analysing the data. These figures were chosen based on the typical width of 95% CIs reported for known ICCs in the field. 79,80
-
Reported and unreported data. We based our main analyses on the data reported in the published reports of studies; however, through our liaison with authors, we also obtained revised figures for some of our outcomes, so we ran a check to see if the revised figures made a difference to the bottom-line findings of the analyses.
-
Choice of analysis method for rare events. The data did not always fit the assumptions of the Peto OR method as, although the event counts were low, the Peto method works best with event rates of < 1%, whereas the rates in the data were more in the order of 0.9–5.8% for fractures (and rarer for hip fractures) and some studies had imbalances between groups. The Mantel–Haenszel fixed-effects method is considered preferable to Peto in such situations. 81 We therefore assessed the influence of using fixed-effects methods, including both Peto and Mantel–Haenszel. Further sensitivity analyses were conducted over the influence of the selected ICC in these analyses.
One of the included economic studies (Lange82) reported some observational cohort data (falls and fractures), which appeared to be based in the same care home as another observational study (Gustavsson et al. 52). Although the studies were conducted independently, the data collection periods partially overlapped (7 out of 13 months’ data collection in Lange82 overlapped with Gustavsson et al. 52), and the quality of reporting in Lange82 was so poor that we could not determine, for example, if the study was retrospective or prospective, population characteristics, data collection methods, confounding or definitions of outcomes. Gustavsson et al. 52 did not separately report fracture data, although we obtained these data via personal communication (Johanna Gustavsson, Karlstad University, 2019). We therefore separately assessed the influence of including the Lange82 and Gustavsson et al. 52 fracture data in sensitivity analyses (our main analyses did not include either study). We did not assess the influence of the Lange82 data on falls outcomes owing to the risk of double-counting the same participants and events as reported by Gustavsson et al. ,52 which could have given inappropriate weight to data likely to be at serious risk of bias.
In addition, we had not planned how to handle the data from a 2 × 2 factorial design exploring combinations of different overlays and subfloors on hip fractures. 76 This study was complicated in that the groups were unbalanced and the findings were heterogeneous, which presented pros and cons for different approaches to presenting the data. We therefore opted to run a sensitivity analysis, in which the data for each pairwise comparison (‘carpeted vs. uncarpeted’ and ‘wooden subfloor vs. concrete subfloor’) were presented as whole (incorporating the heterogeneity from the additional factor in the study), as an alternative to stratifying the study data by the additional factor (to display the heterogeneity caused by the additional factor). So, for example, for the pairwise comparison of ‘carpeted versus uncarpeted’, we have presented the stratified data for the groups of ‘carpeted on wood versus uncarpeted on wood’ and ‘carpeted on concrete versus uncarpeted on concrete’, and also run a sensitivity analysis to report ‘carpeted (on wood or concrete) versus uncarpeted (on wood or concrete)’.
Synthesis of qualitative studies
We used the JBI approach to meta-aggregation of qualitative studies,56 with the support of NVivo software, version 12 (QSR International, Warrington, UK). The analysis followed a three-stage process:
-
The agreed findings from the data collection phase were identified and coded in the study reports using NVivo. Findings were assigned short names (usually the title of the subtheme to which they related), and accompanying illustrations (i.e. participant quotations) and other contextual information (i.e. the authors’ analytical descriptions) from the study reports were coded under each respective finding.
-
One review author (AD) organised the findings into categories (each containing at least two findings). This stage was achieved through reading and re-reading the findings to identify conceptual similarities across the data. Amy Drahota drafted a description for each category, and these were reviewed by other team members. The names for the categories were agreed through discussion between Amy Drahota and Chris Markham.
-
The categories were subsequently combined into a set of synthesised findings (each containing at least two categories), with accompanying descriptions. Amy Drahota created the initial synthesis and this was finalised through discussion with Chris Markham. The aim of this third stage was to develop a comprehensive set of statements (synthesised findings) that are representative of the collated categories and individual findings, and that can be used to inform evidence-based decision-making.
Synthesis of economic evidence
We have tabulated and summarised the results of included economic evaluations narratively in the text. We adjusted all costs to 2019 Great British pounds (GBP) values using gross domestic product (GDP) deflators83 and used relevant exchange rates for international comparisons.
Confidence in cumulative evidence
Confidence in quantitative evidence
We assessed the quality of evidence across the included studies at outcome level for each comparison using GRADE,84 and incorporated these assessments into ‘evidence profile’ and summary of findings tables using the GRADEpro software. The main comparison is ‘shock-absorbing flooring (all types) versus rigid flooring’; we have included separate summary of findings tables for hospitals and care homes. Supplementary summary of findings tables were developed for different types of shock-absorbing flooring (e.g. novel floors, sports floors, carpet, wooden subfloors) versus rigid flooring, and for head-to-head comparisons of different shock-absorbing flooring interventions. We included our top seven prioritised outcomes in these tables: (1) injurious falls rate per 1000 person-days, (2) falls rate per 1000 person-days, (3) number of falls resulting in injuries, (4) number of fractures, (5) number of hip fractures, (6) number of fallers and (7) number of adverse events.
The GRADE system provides a grade of the overall quality of the evidence for each outcome on one of four levels: high, moderate, low and very low. We used the following five GRADE criteria to assess the quality of the evidence: risk of bias, indirectness of evidence, inconsistency of effect (heterogeneity), imprecision of the effect estimates, and risk of publication bias. Two review authors (LMF and AD) independently assessed the GRADE criteria for all of these outcomes in a purposefully designed form in which we justified each grading decision. The final GRADE assessments were then agreed through discussion. One review author (LMF) transferred the agreed data to the GRADEpro table, using the GRADEpro GDT software, to create the summary of findings tables, the final content of which was checked and agreed through discussion (LMF and AD).
The summary of findings tables provide an absolute and relative measure of effect for each of the key outcomes. The relative measures of effect (taken from the meta-analyses) were re-expressed to provide an estimate of the absolute magnitude of effect based on a typical burden of the outcomes that might be expected when using a standard ‘rigid’ floor. For the hospital and care home summary of findings tables (see Tables 7 and 8), an illustrative risk was selected based on the data derived from the control groups of the RCT77 included in the review in hospitals and the RCT50 included in the review in care homes, respectively. We used the comments section of the summary of findings tables to support the interpretation of the findings; for example, we have explained the magnitude of effect in words to help end users of the review interpret the clinical significance of the finding, when it is indicated to be statistically significant.
For each outcome, we have summarised the number of studies addressing the outcome, along with an indication of the number of data contributing to the denominator of the outcome (e.g. as relevant: total number of participants, total number of person-days, total number of falls). The overall GRADE assessments are presented in the summary of findings tables; an explanation to support the downgrading decisions (note that we did not upgrade any evidence) and a further breakdown of these are given in the evidence profile tables (see Appendices 3–5). We reviewed the evidence profile tables in a meeting with the public involvement members (Margaret Bell, Liz Burden and Joleen Tobias), in which we discussed how we could improve the clarity and transparency of presentation.
Confidence in qualitative evidence
We used the GRADE–Confidence in the Evidence from Reviews of Qualitative research (CERQual) approach to summarise our confidence in the findings from the qualitative synthesis. 85 Each review finding was assessed across four domains: (1) the methodological limitations of the contributing studies,86 (2) the relevance of the contributing studies to the review question,87 (3) the coherence between the synthesised finding and the data presented in the contributing studies88 and (4) the adequacy of the data supporting the synthesised finding. 89 Judgements were made to classify each synthesised finding as having ‘no or minor concerns’, ‘minor concerns’, ‘moderate concerns’ or ‘substantial concerns’ (with reasons given) for each of the four domains. An overall judgement was then formulated by evaluating the level of concerns across each of the domains to provide an assessment of confidence in each finding, rated as high, moderate, low or very low. The final set of judgements (for individual domains and overall confidence in the findings) were agreed through discussion between two review authors (AD and CM).
Triangulation of methods
The review incorporates quantitative, qualitative and economic evidence, with each type of evidence contributing complementary information to our understanding of the use of shock-absorbing flooring in hospitals and care homes. Each type of evidence has its strengths in addressing different dimensions of the research question: clinical effectiveness (quantitative), views and experiences (qualitative), and cost-effectiveness (economic). Therefore, we opted to analyse each type of evidence separately prior to configuring the results in our overall discussion (see Chapter 5), in what is referred to as a convergent segregated approach to mixed-methods syntheses. 60,90 In configuring the findings, we employed a constant comparison approach to determine whether the findings from each type of evidence were supportive or contradictory, what each type of evidence adds (in terms of understanding and explanation), and what the different types of evidence contributed that was missing from the other studies.
Changes from the protocol
We were unable to search the World Health Organization (WHO) Health Evidence Network as planned because of a technical error with the server. We originally planned to conduct all of the data collection in Covidence; however, at the time of conducting this element of the review, we found that the software did not readily support a mixed-methods review, the various risk-of-bias assessment tools we were using or the outcome measures we were collecting. Therefore, we ended up using a mixture of Covidence and Microsoft Excel to undertake data collection, while maintaining the plan to conduct all of the review processes independently in duplicate. During the review process, in consultation with the advisory board members, we agreed on some of the potential confounding variables that then informed our assessment of the ‘confounding’ domain in the ROBINS-I tool. 73
We initially planned to undertake a subgroup analysis to explore the influence of acuity of care (acute, sub-acute, intermediate, long-term care); however, owing to the nature of the evidence included in the review, it was not logical to conduct this analysis. Instead, we analysed the studies according to whether they were based in hospitals or care homes. Some of the sensitivity analyses were not specified in the protocol, as we had not anticipated how to handle a 2 × 2 factorial observational study in the analysis or deal with personally communicated data that differed from the published report. We had also not specified the sensitivity analyses around rarer outcomes (fractures and hip fractures); however, our rationale for these alternative analyses is underpinned by methodological research, which highlights that our main approach to analysis (DerSimonian and Laird random-effects method) can provide biased estimates in the situation of rare events. 81 For the fracture data, the Mantel–Haenszel method had minimal impact and did not influence the review conclusions, compared with the DerSimonian and Laird method; however, we opted to report the Mantel–Haenszel figures as we considered this approach to be the most methodologically sound.
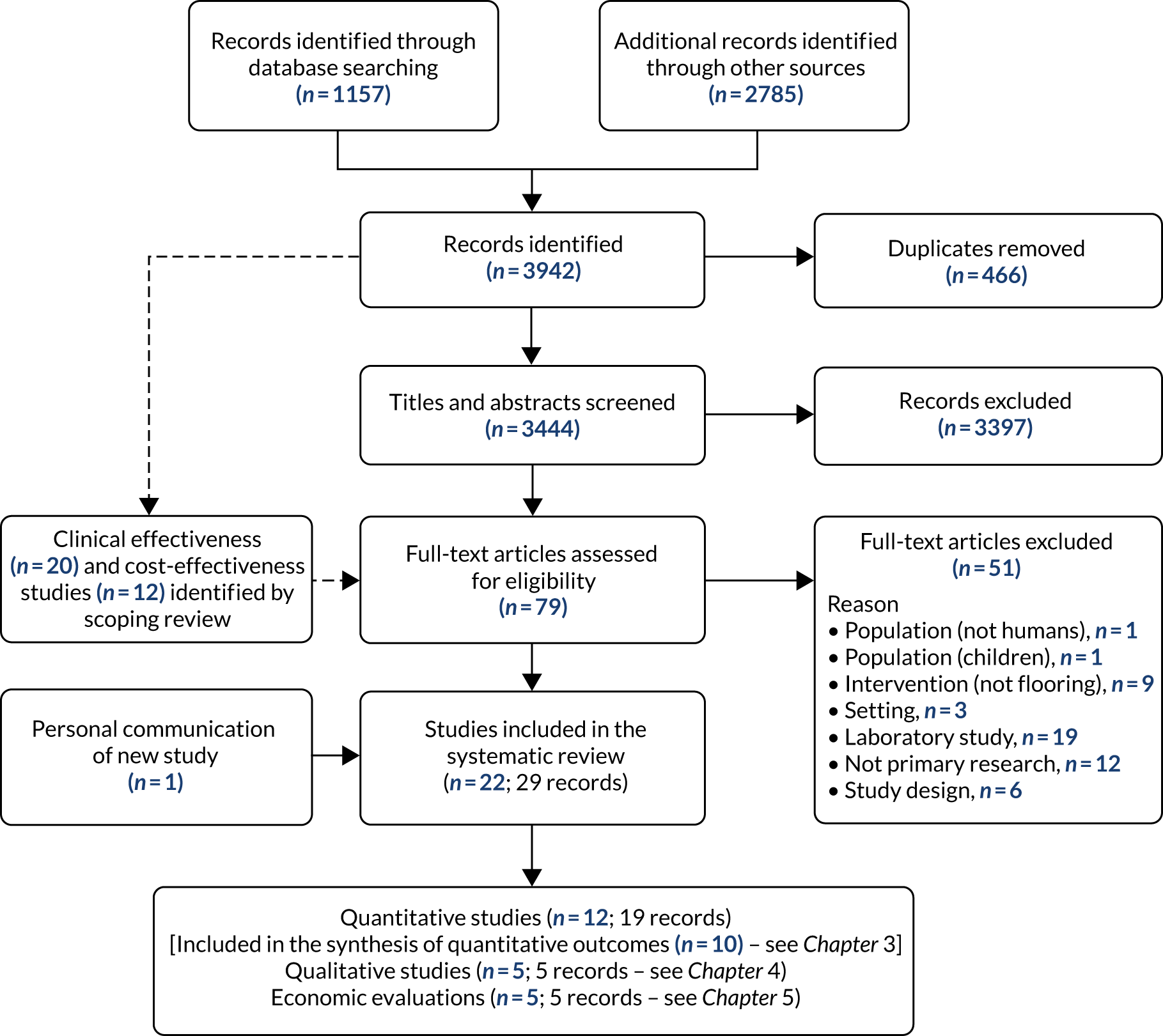
Results of the search
The majority of electronic databases were last searched on 29 September 2019 (see Table 1). The search results are summarised in the PRISMA flow diagram (Figure 2). One hundred records were identified through MEDLINE, 23 through CINAHL and 18 through AgeLine (all searched through EBSCOhost). We also searched Scopus (172 records identified), Web of Science (192 records identified), ProQuest Dissertations & Theses (two records identified), NHS EED (six records identified) and OpenGrey (four records identified). We searched trial registries: 14 records were identified through the WHO’s International Clinical Trials Registry Platform and 626 records were identified through ClinicalTrials.gov. Hand-searching, backwards and forwards citation searching, and review of conference proceedings and websites retrieved a further 2785 records for screening.
FIGURE 2.
The PRISMA flow diagram. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Characteristics of excluded studies
We excluded 51 studies that did not meet at least one of the inclusion criteria related to population (n = 2), intervention (n = 9), setting (n = 3) and study type (n = 37). See Report Supplementary Material 1 for the table of excluded studies. Of the two studies excluded primarily because of the population group, one study did not involve human participants (it was a sample of floor coverings)91 and the other study included children only. 92 Studies that were excluded on the grounds of setting took place in community-based settings (e.g. participants’ own homes). 93–95 Of the 37 reports excluded because of study type, the majority were laboratory-type experiments (n = 19) or different article types, such as reviews (n = 12). Six primary research studies were excluded because they did not have a contemporaneous control (n = 2)96,97 or were a type of case study (n = 2),98,99 cross-sectional survey (n = 1),100 or a knowledge-transfer workshop that included researchers and industry among the participants (n = 1). 66
Chapter 3 Results of clinical effectiveness evidence
In this chapter, we focus on the quantitative studies assessing the clinical effectiveness of shock-absorbing flooring.
Description of studies
Characteristics of included quantitative studies
We identified 12 studies that met the inclusion criteria;31,49,50,52,76,77,101–106 however, two of these did not report any of our prespecified outcomes. 31,104 Harris104 observed that patients assigned to carpeted rooms were less likely to be judged by health-care professionals as being at risk of falling than those being cared for in rooms with vinyl flooring; however, the study is unable to demonstrate cause and effect, and actual fall events were not measured. Wahlström et al. 31 measured pain ratings in specific body locations, at specific time points, among nursing assistants. This controlled before-and-after study aimed to explore musculoskeletal symptoms in the lower extremities that were hypothesised to be associated with working on a harder floor (2-mm vinyl). The study was not designed to explore potential adverse events that may be associated with pushing wheeled equipment on softer floors (e.g. other body areas that may be associated with push and pull injuries, such as the neck and shoulders, were not measured). Wahlström et al. 31 concluded that 4-mm vinyl is associated with reduced foot pain and similar pain in the hips, knees and lower back, compared with 2-mm vinyl. 31
Table 3 provides an overview of the characteristics of included studies. In the remainder of this section, we focus our descriptions on the 10 included studies to which our reported outcomes relate. The flooring industry funded the costs of flooring materials and installation in three of these studies,49,50,106 but had no further involvement in the conduct, and an additional study received a grant from the flooring manufacturer. 102 We have described the studies separately, according to whether they were conducted in hospital settings (six studies)49,77,101,103,105,106 or care home settings (four studies). 50,52,76,102
| Study | Design; setting; funding | Inclusion criteria (main) | Population | Intervention | Control | Quantitative outcomes |
|---|---|---|---|---|---|---|
| RCTs | ||||||
| Donald et al. 2000105 | RCT; hospital (sub-acute), UK; Gloucestershire Health Authority | Admitted for rehabilitation |
|
Hospital-duty Flotex® 200 carpet (Forbo Flooring Systems, Assendelft, the Netherlands); subfloor NR | Latex vinyl square tile; subfloor NR | Incidence of falls, injuries partially reported, satisfaction of cleaning |
| Drahota et al. 201377,107,108 | Cluster RCT; eight hospitals (acute, sub-acute), UK; Dunhill Medical Trust/National Osteoporosis Society | NHS patients in geriatric wards; floors with a slip-resistance rating of R9 |
|
Sports floor (8.3-mm Tarkett Omnisports Excel); concrete subfloors | 2-mm vinyl (three sites); 2-mm thermoplastic tiles (one site); concrete subfloors | Injurious falls rate, injury severity, falls rate, adverse events, numbers of fallers and falls |
| Mackey et al. 201950,109 | RCT; care home, Canada; Canadian Institutes of Health Research/SATECH Inc. provided flooring materials and installation | Residents living in study rooms of a long-term care facility |
|
Novel shock-absorbing floor (2.54-cm SmartCells) with 2-mm hospital-grade vinyl; concrete subfloor | 2.54-cm plywood with 2-mm hospital-grade vinyl; concrete subfloor | Serious fall-related injury, minor fall-related injury, any fall-related injury, falls, fractures |
| Observational studies | ||||||
| Gustavsson et al. 201852,110–112 | Prospective cohort; care home, Sweden; Karlstad Municipality/Swedish Civil Contingencies Agency | All residents of the residential care facility for older adults |
|
Novel shock-absorbing floor (12-mm Kradal); Concrete subfloor | Standard vinyl/linoleum/ceramic; concrete subfloor | Injury rate per fall, falls per 1000 person-days, number of falls resulting in injury, injury severity |
| Hanger et al. 201741,49 | Prospective cohort; hospital (sub-acute), NZ; flooring materials and installation provided by Acma Industries Ltd (Wellington, NZ), Jacobsens Creative Surfaces Ltd (Auckland, NZ) and Inzide Commercial Ltd (Auckland, NZ) | All admitted patients in the geriatric ward with a focus on medical and rehabilitation needs |
|
Novel shock-absorbing floors (12 mm Kradal and 25-mm SmartCells), and a sports floor (8-mm Tarkett Omnisport Excel); concrete subfloor | 3- to 4-mm vinyl; concrete subfloor | Falls rate per 1000 person-days, fall-related injury rate per 1000 person-days, injury severity, injury type |
| Hanger et al. 2020106 | Controlled cohort study; four older persons’ wards, NZ; flooring materials and installation provided as per Hanger49 | Any staff injury occurring on a study ward where mechanism of injury might be related to flooring |
|
Novel shock-absorbing floors (12-mm Kradal and 25-mm SmartCells), and a sports floor (8-mm Tarkett Omnisport Excel); concrete subfloor | Standard vinyl; concrete subfloor | Staff injuries |
| Harris 2017104 | Prospective cohort; hospital (sub-acute), country not clear; funding not described | Assigned to one of the six rooms in a telemetry unit for heart patients; other criteria unclear |
|
Carpet tile (tufted loop with thermoplastic composite polymer backing); subfloor NR | Vinyl composition tile; subfloor NR | Preferences/satisfaction, ‘risk of falling’ assessment ratings, behavioural mapping |
| Healey 1994103 | Retrospective cohort; hospital (sub-acute), UK; funding not described | Random sample of 225 accident forms from a care of the elderly unit over a 4-year period |
|
Carpet (varied but all single fibres rather than looped, with thin underlay); subfloor NR | Vinyl; subfloor NR | Fall-related injury |
| Knoefel et al. 2013102 | Retrospective/prospective cohort; care home, USA; grant from SATECH Inc./Care of the Elderly Physicians’ Association | All documented falls on novel flooring and every third fall on regular flooring |
|
Novel shock-absorbing flooring (SmartCells); subfloor NR | ‘Regular floor’; subfloor NR | Number of falls resulting in injury, type of injury, number of fractures |
| Simpson et al. 200476 | Prospective cohort; 34 care homes, UK; Research into Ageing/Royal College of Surgeons of England | Residents living in 34 participating care homes for older adults |
|
Carpet (with concrete or wooden subfloor); wooden subfloor (with or without carpet) | Uncarpeted (with concrete or wooden subfloor); concrete subfloor (with or without carpet) | Number of falls per room, fractures per 100 falls, number of hip fractures |
| Wahlström et al. 201231 | Controlled before-and-after study; two geriatric care centres, Sweden; Municipality of Sundsvall | All nursing assistants; male assistants excluded post hoc because of low response rate |
|
1.5-mm homogeneous polyvinyl chloride covering with 2.5-mm foam backing (total 4 mm) | 2-mm homogeneous polyvinyl chloride covering; concurrent control: 2.5-mm linoleum | Pain ratings in lower back, hips, knees and feet at 6 weeks, 1 year and 2 years. Adverse events not measured |
| Warren and Hanger 2013101 | Interrupted time series; hospital (sub-acute), NZ; research received no specific funding | All admitted patients in the geriatric ward |
|
5-mm carpet (tiles with loop pile); concrete subfloor | 5-mm vinyl; concrete subfloor | Falls rate per 1000 person-days, fall-related injuries, number of fractures |
Methods
We coded the included studies according to their study design characteristics (Table 4). Three studies were randomised;50,77,105 of the observational studies, three were prospective with contemporaneous controls,49,52,76 three were predominantly retrospective with contemporaneous controls,102,103,106 and one we have included because it presents graphical data depicting time trends, although the data were analysed as if they were from a simple before-and-after study. 101 This study did not have a concurrent control arm (some data are stratified by ward type) and it was predominantly retrospective. 101 Although this final study could be construed as an interrupted times series, we have reported on the findings separately in the text and have not attempted to include the study in any meta-analyses.
| Study | Study design | Allocation | Comparison | Group allocation | Prospective aspects | Comparability of variables | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Between groups | Within group | Randomisation | Quasi-randomisation | Other action of researchers | Time differences | Location differences | Treatment decisions | Participants’ preferences | On the basis of outcome | Policy/public health decisions | Cluster preference | Identification of participants/clusters | Assessment of baseline and allocation to intervention | Assessment of outcomes | Generation of hypothesis | Potential confounders | Baseline assessment of outcome variables | |||
| Randomised studies | ||||||||||||||||||||
| Donald et al. 2000105 | RCT | Individual | Yes | No | Yes | No | No | No | No | No | No | No | NA | NA | Yes | Yes | Yes | Yes | Yes | Yes |
| Drahota et al. 201377 | Cluster RCT | Group | Yes | No | Yes | No | No | No | No | NA | NA | NA | NA | NA | Yes | Yes | Yes | Yes | Yes | Yes |
| Mackey et al. 201950 | RCT | Individual | Yes | No | Yes | Yesa | No | No | No | No | No | No | NA | NA | Yes | Yes | Yes | Yes | Yes | Yes |
| Observational studies | ||||||||||||||||||||
| Gustavsson et al. 201852 | Prospective cohort study | Individual | Yes | No | No | No | Yes | No | Yes | Yes | Yes | No | NA | NA | Yes | Yes | Yes | Yes | Yes | No |
| Hanger 201749 | Prospective cohort study | Individual | Yes | No | No | No | No | Yesb | Yes | Yes | No | No | NA | NA | Yes | Yes | Yes | Yes | Yes | No |
| Hanger and Wilkinson 2020106 | Retrospective controlled cohort studyc | Group | Yes | Yes | No | No | No | Yes | Yes | NA | NA | NA | Yes | No | No | No | No | Yes | No | No |
| Healey 1994103 | Retrospective cohort study | Individual | Yes | No | No | No | No | No | Yes | No | No | No | NA | NA | No | No | No | Yes | No | No |
| Knoefel et al. 2013102 | Retrospective cohort studyd | Individual | Yes | No | No | No | No | No | Yes | P | P | No | NA | NA | No | No | No | Yes | Yes | No |
| Simpson et al. 200476 | Prospective cohort study | Individual | Yes | No | No | No | No | No | Yes | P | P | No | NA | NA | Yes | Yes | Yes | Yes | No | No |
| Warren and Hanger 2012101 | Interrupted times seriese | Group | No | Yes | No | No | No | Yes | No | NA | NA | NA | Yes | No | No | No | Nof | Yes | Yes | Yes |
Group allocation within the cohort-type designs (with concurrent controls) was largely based on location differences (i.e. intervention floors were laid in certain areas of the hospital/care home and not others). 49,52,76,102,103,106 Although it was not always explicit in the reports, we have considered that allocation may also have been influenced by treatment decisions (i.e. where care professionals decided the individual would be best placed during the stay),49,52,76,102 and participant preferences (i.e. where individuals decided they would most like to spend their time). 52,76,102 These underpinning influences of group allocation may not necessarily have been driven by the type of flooring, but they may have been related to participant characteristics. For example, care professionals may have opted to allocate certain high-risk individuals to rooms that provided them with greater opportunity for observation (e.g. closer to the nursing station), placing these individuals in a location with a different floor covering. 49 Participants who were more mobile may have opted to spend more time outside their bedrooms, walking along corridors and visiting communal areas that happened to have alternative floor coverings to their bedroom. 103 This issue becomes more pertinent in studies (or analyses) for which only fallers (or falls) were included, and individuals were allocated to groups based on where they fell. 49,52,76,102,103 We have analysed these issues in more depth in our assessments of risk of bias (and, in particular, in the domain for confounding).
Hospitals
Of the six hospital-based studies, one was an individually randomised 2 × 2 factorial trial,105 in which participants were randomised to flooring type (carpet or vinyl) and a physiotherapy group (conventional or additional exercise); for the purposes of this review, we have focused on the comparison of flooring types and treated the study as a simple parallel-group design. Drahota et al. 77 was a cluster randomised parallel-group trial. The remaining four studies used observational designs, comprising a prospective cohort study,49 retrospective cohort study,103 an interrupted times series-type design101 and a staff-focused study with group (ward-level) allocation using a mixture of between-group (contemporaneous) and within-group (time) controls. 106 Studies were conducted in the UK77,103,105 and New Zealand. 49,101,106 The median follow-up period for the intervention floors (or the period over which sampling was conducted) was 21.5 months (range 8–48 months). Only two out of the six studies reported total person-days: 9085 person-days77 and 16,903 person-days. 49
Care homes
Of the four care home-based studies, the Mackey et al. 50 study was an individually (resident room) randomised parallel-group trial conducted in Canada. The remaining studies were prospective cohort study designs conducted in Sweden,52 the USA102 and the UK. 76 The median follow-up/sampling period for the intervention floors was 39 months (range 24–68 months). Two studies provided total person-days: 95,036 person-days52 and 213,854 person-days. 50
Participants
Nine of the studies predominantly focused on patients/residents, whereas Hanger and Wilkinson106 report solely on staff outcomes (adverse events). The populations differed across studies concerning the sampling units: some studies drew their samples from all patients/residents in the setting (data from five studies related to 5560 patient/residents),50,52,77,101,105 Hanger49 sampled only those who fell during the study period (five studies reported a combined total of 551 fallers49,50,52,77,105) and three samples were drawn solely from the fall reports (nine studies accrued 11,857 falls49,50,52,76,77,101–103,105) or staff injury reports (Hanger and Wilkinson106 is based on 163 injuries). The majority of falls-level data were from care homes (9566 falls). Aside from age and sex, reporting on sample characteristics was generally poor (Table 5). Care home and hospital samples were similar in terms of average age (82 years; not reported in Simpson et al. 76) and sex distribution (median proportion of females: 60%; not reported in Simpson et al. 76). However, when data were reported on other characteristics, they were indicative of a higher level of use of ambulatory aids and diuretics among hospital patients, and more diagnoses of cognitive impairment (including dementia and severe confusion) and use of psychotropic/psychoactive drugs (including hypnotics and sedatives) among care home residents (see Table 5). Although it makes intuitive sense that hospital patients and care home residents will differ, not least because hospital patients will be more likely to be undergoing an acute illness episode, the reliability of the indications in Table 5 should be questioned because of the large number of missing data and different definitions used.
| Characteristic | Hospitals (five studies)a | Care homes (four studies)b | Total (nine studies) | |||
|---|---|---|---|---|---|---|
| Study-level data | Missing studies (n) | Study-level data | Missing studies (n) | Study-level data | Missing studies (n) | |
| Number of patients/residents, total (range) | 5143 (54–4641) | 2 | 471 (114–357) | 2 | 5560 (54–4641) | 4 |
| Number of fallers, total (range) | 239 (8–178) | 2 | 320 (75–245) | 2 | 551 (8–245) | 4 |
| Number of falls, total (range) | 2302 (11–1732) | 0 | 9566 (167–6641) | 0 | 11,857 (11–6641) | 0 |
| Females (%), total (range) | 59.5 (47.9–81.5) | 0 | 60.8 (47.0–70.2) | 1 | 59.7 (47.0–81.5) | 1 |
| Average age (years), median (range) | 82.8 (80.8–85.7) | 0 | 81.7 (74.2–84.9) | 1 | 82.3 (74.2–85.7) | 1 |
| Mean body mass index (kg/m2), median (range) | Not reported | 5 | 25.3 (24.7–25.9) | 2 | 25.3 (24.7–25.9) | 7 |
| Mobility (%),c median (range) | ||||||
| Ambulatory aids/‘unsafe walker’ | 63.6 (55.1–72.1) | 3 | 42.7 (40.6–44.7) | 2 | 49.9 (40.6–72.1) | 5 |
| Immobility/immobile without help | 25.7 (17.4–33.9) | 3 | 21.1 (21.0–21.1) | 2 | 21.1 (17.4–33.9) | 5 |
| Falls historyc (%) | ||||||
| History of falls | 64.5 | 4 | Not reported | 4 | 64.5 | 8 |
| Fall in previous 180 days | Not reported | 5 | 21.0 | 3 | 21.0 | 8 |
| Fall on admission | 18.5 | 4 | Not reported | 4 | 18.5 | 8 |
| Comorbidities (%),c median (range) if > 1 study | ||||||
| Dementia/cognitive impairment/severe confusion | 17.3 (16.7–17.9) | 3 | 52.5 (50.0–54.9) | 2 | 34.0 (16.7–54.9) | 5 |
| Osteoporosis | 15.2 | 4 | 12.3 | 3 | 13.8 (12.3–15.2) | 7 |
| Parkinson’s disease | 4.5 | 4 | 4.5 | 3 | 4.5 (4.5–4.5) | 7 |
| Stroke | 14.7 | 4 | 9.0 | 3 | 11.9 (9.0–14.7) | 7 |
| Medications (%),c median (range) if > 1 study | ||||||
| Antidiabetic | 15.2 | 4 | Not reported | 4 | 15.2 | 8 |
| Anticonvulsants/hypnotics/tranquilisers/sedatives | 15.6 | 4 | 34.0 (24.1–43.9) | 2 | 24.1 (15.6–43.9) | 6 |
| Antipsychotic | Not reported | 5 | 37.3 | 3 | 37.3 | 8 |
| Antianxiety | Not reported | 5 | 16.3 | 3 | 16.3 | 8 |
| Antidepressant | Not reported | 5 | 43.8 (43.0–44.5) | 2 | 43.8 (43.0–44.5) | 7 |
| Other psychotropic/psychoactive drugs | 11.2 | 4 | Not reported | 4 | 11.2 | 8 |
| Diuretics | 54.5 | 4 | 22.4 | 3 | 38.5 (22.4–54.5) | 7 |
| Cardiac glycoside (digoxin, etc.) | 54.7 | 4 | Not reported | 4 | 54.7 | 8 |
| Polypharmacy | 65.4 | 4 | Not reported | 4 | 65.4 | 8 |
| Average number of medications, median (range) | Not reported | 5 | 9.1 (8.1–10) | 2 | 9.1 (8.1–10) | 7 |
| Urinary incontinence (%) | 43.3 | 4 | Not reported | 4 | 43.3 | 8 |
| Visual impairment (%), median (range) | Not reported | 5 | 38.1 (29.7–46.5) | 2 | 38.1 (29.7–46.5) | 7 |
Comparability of baseline characteristics between study groups
As mentioned previously, the majority of studies did not provide a comprehensive description of population characteristics; therefore, there were minimal assessments made as to the comparability of the intervention and control groups. Baseline characteristics compared between study arms varied considerably across the studies (median 6 variables, range 0–38 variables, per study). Two studies did not report any characteristics by study arm;76,106 one study mentioned the comparability of baseline characteristics, but did not report the data. 102 Statistical testing for differences between groups in baseline characteristics is not recommended. 113,114 Of the eight studies reporting on baseline characteristics, four provided a descriptive assessment of comparability50,77,103,105 and four undertook statistical tests. 49,52,101,102 Two studies performed analyses to adjust outcomes for baseline characteristics;50,52 one purported to, but did not report the data;102 and one adjusted for clustering only. 77
Age and sex were the most frequent characteristics considered at baseline. Seven out of the eight reporting studies had comparable ages between groups;49,50,52,77,101,103,105 Knoefel et al. 102 reported that there were significantly younger residents in the intervention group (data not reported). Studies exploring carpet had a median of 13 percentage points more female participants in the carpet groups (4–24 percentage points more; Simpson et al. 76 did not report sex). 101,103,105 Drahota et al. 77 (sports flooring) had a higher proportion of female participants in the control group (22.6 percentage points more). Some other group differences were observed in individual studies (naturally more so in the studies that observed more variables), but there is wide variation in which variables were measured. 50,52,77,102 These included fewer medications,102 more antianxiety medication,50 less analgesic medication,50 more diagnoses of dementia,50 depression,50 history of falls,50 inability to stand independently,50 use of ambulatory aids,77 fewer ceiling lifts and fall mats,50 more internal transfers77 and shorter lengths of stay101 in various intervention groups. There were more diagnoses of diabetes,77 dizziness,77 falls/fractures/injuries,77 incontinence,77 prolonged immobility77 and reduced mobility/gait,77 and more fallers with unknown activity at the time of fall52 in certain control groups. In addition, Gustavsson et al. 52 highlighted that there were no falls in bathrooms in the intervention group (because intervention floors were not installed in these locations). Study groups were comparable in numerous other ways, when reported.
Interventions
Hospitals
Hanger49 and Hanger and Wilkinson106 explored three different types of shock-absorbing flooring versus standard control flooring; the remaining studies involved a single intervention floor versus a standard control floor. 77,101,103,105 The intervention floors comprised novel flooring (12-mm Kradal, 25-mm SmartCells underlay),49,106 sports flooring (8-mm Tarkett Omnisports Excel),49,77,106 and various types of carpet: hospital duty Flotex 200,105 various single-fibre carpets with a thin underlay,103 and 5-mm thick loop pile. 101 Control floors were typically vinyl (Drahota et al. 77 also included a site with 2-mm thermoplastic tiles), which varied in reported thicknesses from 2 mm to 5 mm (thickness not reported in three studies). 49,77,101,103,105,106 Four studies specified that they had concrete subfloors;49,77,101,106 in two studies, the type of subfloor was not reported. 103,105 Intervention and control floors were laid in comparable areas in four studies, either limited to the bedded areas49,77,105,106 or in all patient areas. 101 In Hanger and Wilkinson,106 the intervention ward had partial intervention coverage (12/20 bed spaces), which was compared with wards with control flooring throughout. Healey103 compared carpet laid in an acute admissions ward and the sitting rooms of five rehabilitation wards with vinyl laid in a couple of single bedrooms and all of the toilets in the acute admission ward, and the majority of the five rehabilitation wards. The majority of studies did not report how the thresholds between intervention and standard floors were managed; however, in Drahota et al. ,77 thresholds were managed using either a transition strip or a gradual ‘seamless’ gradient.
Care homes
Three care home studies compared a single novel intervention floor with control floors. 50,52,102 Simpson et al. 76 compared different combinations of overlays (carpeted/uncarpeted) and subfloors (wood/concrete). The novel intervention floors studied were 25.4-mm SmartsCells underlay (with 2-mm vinyl in Mackey et al. ;50 the overlay was not specified in Knoefel et al. 102) and 12-mm Kradal. 52 Simpson et al. 76 did not specify the type of carpets. Control floors varied in descriptions: (1) a 25.4-mm plywood underlay and 2-mm vinyl overlay;50 (2) vinyl, linoleum and ceramic tiles of unspecified thicknesses;52 (3) ‘regular’ flooring;102 and (4) ‘uncarpeted’. 76 Simpson et al. 76 compared subfloors, whereas Knoefel et al. 102 did not specify a subfloor, and the other two studies were conducted solely on concrete subfloors. 50,52
There was some variability in the types of areas observed as part of the studies, both within and across studies. Studies using SmartCells laid the intervention floor in the bedded areas and bathrooms; Mackey et al. 50 used comparable control areas, whereas Knoefel et al. 102 did not specify which areas of the facility were used as a control. The Gustavsson et al. 52 study of Kradal laid the intervention floor in the bedrooms and communal areas, with control areas being similar, but also including bathrooms. Simpson et al. 76 did not specify exactly where the floors were laid; however, they discussed that 65% of the bathrooms and toilets were uncarpeted with concrete subfloors; < 6% of other room types were uncarpeted with concrete subfloors; and carpeted areas included corridors, lounges and dining rooms. 76 Because the control and intervention floors were of the same thickness in Mackey et al. ,50 only thresholds between the renovated study areas and non-study areas needed to be managed; this was undertaken using 4-foot long transition ramps. Flooring transitions were not described in the other care home studies.
Definition and acquisition of outcomes
Injuries
Of the six studies that reported on injuries, three reported injuries on a four-point ordinal severity scale (none, minor, moderate, major/severe/serious),49,52,77 one used a three-point ordinal scale (none, minor, serious),50 one reported all injuries together as ‘any injury’103 and one reported on injury types alone (redness, bruise, abrasion, cut, two or more injuries, fracture, other). 102 An additional study indicated that minor injuries had been measured, but did not fully report on the outcome or provide a definition. 105 No two studies used the same definitions to classify injuries into their respective categories of severity. The care home studies defined severity according to whether or not access to health care was required, as well as the types of injuries and treatments received;50,52 one hospital-based study defined severity according to the type of treatment required,77 whereas another hospital-based study used a mixture of injury type and treatment to classify injury severity. 49
Of those that classified injury severity, some differences are evident. For example, injuries that require suturing by a health-care professional would have been classified as serious in one study50 and as moderate in three others. 49,52,77 Bruising may have been classified as serious in Mackey et al. 50 if it was accompanied by a diagnostic evaluation; moderate in Gustavsson et al. 52 under the same circumstances; minor or moderate in Drahota et al. ,77 depending on the treatment received; and minor or moderate in Hanger,49 depending on the perceived extent of bruising. Similarly, it is perceivable that the severity of head injuries may have been classified differently across studies. Complaint of pain was included in the definition of minor/any injury in four studies,49,50,77,103 and would have been considered a minor injury in one study if accompanied by a reduction in physical function,52 but it is ambiguous as to whether or not it would have fit the definition of an injurious fall in the Knoefel et al. 102 study.
Injury data were obtained prospectively in four studies,49,50,52,77 and retrospectively in two. 102,103 Three relied solely on the standard institutional incident reporting system,49,102,103 one supplemented this with an additional form52 and two utilised research assistants/nurses to complete standardised forms from a range of sources (e.g. incident forms, patient notes, hospital records) to ascertain the data. 50,77 Injuries were excluded in two studies if it was deemed clear that they were a result of something other than the flooring. 52,103
Falls
Of the six studies reporting falls outcomes, one did not provide a definition of a fall. 102 There were slight nuances in the definitions of the remaining five studies. 49,50,52,77,105 They all referred to falls as being accidental, unexpected or unintentional, and, although one referred just to the ground,105 others also referred to coming to rest/landing on the floor or lower level,49,50,52,77 object or other surface. 49 Donald et al. 105 defined falls as a ‘collapse’, as opposed to an unexpected event50,52,77 or change in position,49 which better encapsulate slips and trips. Part of Donald et al. ’s105 definition also specified that the falls were those that ‘led to the completion of an accident report form by the nursing staff’, hinting at the potential reporting issues within institutional settings and potential issues of relying solely on the standard incident reporting system. 115 Location was part of the outcome definition in two studies: being in a bedroom49 or study room. 50
Falls data were ascertained prospectively in five studies,49,50,52,77,105 and retrospectively and prospectively in one study,101 using the standard incident reporting system in all studies, with additional sources of verification in one study. 77
Fractures
Of the seven studies that reported on fractures (any type), four did not provide a definition,77,101,102,105 two specified radiologically/X-ray confirmed fractures (that were due to a fall in a study room)49,50 [one of these studies49 also reported clinical fractures (those that had been suspected but not seen on radiograph), but we did not use these in the review analysis] and one defined fractures as ‘medically recorded’. 52 Of those without a definition, one had zero events105 and another provided details to demonstrate that the reported outcomes had been follow-up using a radiograph. 77 Hip fractures were not defined in one study, which had zero events;105 were radiologically confirmed in three studies;49,50,77 and were ‘medically recorded’ in one. 52
Head injuries
We obtained head injury data from three studies (one via personal communication). 49,50,52 One care home-based study50 reported serious fall-related injuries to the head/skull, and one hospital-based study49 reported serious or moderate head injuries. A moderate head injury in Hanger49 was one that would have required a radiograph but for which no further injury was noted; this would have met the definition of serious in Mackey et al. 50 (those that resulted in an emergency department or hospital admission, and a treatment procedure or diagnostic evaluation performed). The data we received via personal communication (which related to Gustavsson et al. 52; Johanna Gustavsson, personal communication) related to injuries to the head of any severity.
Adverse events
We have obtained adverse events data associated with three studies (one via personal communication). 50,77,106 Hanger and Wilkinson106 provided the most comprehensive definition, focusing on staff injuries whereby the mechanism of injury might be caused by a change in flooring, such as falls, trips and slips; caught feet; patient handling/transferring; twists/muscle strains; back pain; and lifting objects. All injuries occurring on the included study wards were noted, regardless of whether or not the injured person normally worked on the ward. Similarly, Drahota et al. 77 considered adverse events to be any that were potentially related to the floor, for example falls or injury related to the physical condition of the flooring, or any problems or damage associated with the flooring itself. For the purposes of this review, we have considered problems and damage associated with the flooring under process outcomes, and focused on staff injuries for adverse events. Adverse events in Drahota et al. 77 may have related to any person accessing the study area. The adverse events measured in relation to Mackey et al. 50 were work-related musculoskeletal injuries sustained by staff.
Hanger and Wilkinson106 utilised the hospital’s routine event reporting system, in which staff self-reported injuries, and a senior manager was then responsible for confirming the report and investigating further when necessary. Similarly, Mackey et al. 50 used data routinely collected by the long-term care site (as described in the protocol109). Drahota et al. 77 relied on standardised forms being completed when events occurred in line with the trial’s standard operating procedures, which were overseen by a principal investigator and research nurses at each site.
Risk-of-bias assessment of included studies
Studies contributing data to the seven prioritised outcomes were assessed for risk of bias using one of three complementary tools, depending on whether the study was randomised at the individual level (RoB 2.0),72 cluster level (RoB 2.0 extension for cluster trials),116 or not at all (ROBINS-I tool). 73 A summary of the assessments is presented in Table 6 and a more detailed breakdown of the rationales underpinning the decisions is provided in Appendix 2, Tables 23–32. An overview of key methodological limitations is discussed here.
| Outcome | Study | Risk of bias | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Randomisation process | Recruitment of participants | Confounding | Selection of participants | Classification of intervention | Deviations from intervention | Missing data | Measurement of outcomes | Selective reporting | Overall | ||
| Injurious falls rate per 1000 person-days | |||||||||||
| RCTs | Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low |
| Mackey 201950 | Low | NA | NA | NA | NA | Low | Low | Low | Low | Low | |
| Observational | Hanger 201749 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious |
| Falls rate per 1000 person-days | |||||||||||
| RCTs | Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low |
| Mackey 201950 | Low | NA | NA | NA | NA | Low | Low | Low | Low | Low | |
| Observational | Gustavsson 201852 | NA | NA | Serious | Low | Low | Low | Low | Moderate | Moderate | Serious |
| Hanger 201749 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious | |
| Warren 2012101 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious | |
| Number of falls with injuries | |||||||||||
| RCTs | Donald 2000105 | Some concerns | NA | NA | NA | NA | Low | No information | High | High | High |
| Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low | |
| Mackey 201950 | Low | NA | NA | NA | NA | Low | Low | Low | Low | Low | |
| Observational | Gustavsson 201852 | NA | NA | Serious | Low | Low | Low | Low | Moderate | Moderate | Serious |
| Hanger 201749 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious | |
| Healy 1994103 | NA | NA | Serious | Low | Low | No information | Low | Serious | Moderate | Serious | |
| Knoefel 2013102 | NA | NA | Serious | Serious | Low | No information | No information | Serious | Serious | Serious | |
| Number of fractures | |||||||||||
| RCTs | Donald 2000105 | Some concerns | NA | NA | NA | NA | Low | Low | Some concerns | Some concerns | Some concerns |
| Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low | |
| Mackey 201950 | Low | NA | NA | NA | NA | Low | Low | Low | Low | Low | |
| Observational | Gustavsson 201852 | NA | NA | Serious | Low | Low | Low | Low | Low | Serious | Serious |
| Hanger 201749 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious | |
| Knoefel 2013102 | NA | NA | Serious | Serious | Low | No information | No information | Moderate | Serious | Serious | |
| Warren 2012101 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious | |
| Number of hip fractures | |||||||||||
| RCTs | Donald 2000105 | Some concerns | NA | NA | NA | NA | Low | Low | Some concerns | Some concerns | Some concerns |
| Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low | |
| Mackey 201950 | Low | NA | NA | NA | NA | Low | Low | Low | Low | Low | |
| Observational | Gustavsson 201852 | NA | NA | Serious | Low | Low | Low | Low | Low | Serious | Serious |
| Hanger 201749 | NA | NA | Serious | Low | Low | No information | Low | Low | Moderate | Serious | |
| Simpson 200476 | NA | NA | Serious | Low | Serious | Serious | Low | Low | Serious | Serious | |
| Number of fallers | |||||||||||
| RCTs | Donald 2000105 | Some concerns | NA | NA | NA | NA | Low | Low | High | Some concerns | High |
| Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low | |
| Mackey 201950 | Low | NA | NA | NA | NA | Low | Low | Low | Low | Low | |
| Adverse events (staff) | |||||||||||
| RCTs | Drahota 201377 | Low | Low | NA | NA | NA | Low | Low | Low | Low | Low |
| Hanger 2020106 | NA | NA | Serious | Low | Low | Low | Low | Moderate | Moderate | Serious | |
| Mackey 201950 | NA | NA | No information | No information | No information | No information | No information | No information | No information | No information | |
Of the three randomised trials assessed, we considered two to be at low risk of bias for the outcomes assessed. 50,77 Some concerns were raised with Donald et al. ,105 primarily because of a lack of information around allocation concealment, but injuries were also poorly defined and not fully reported (raising the risk of bias to high for the number of falls resulting in injuries), and the lack of blinding was also considered a risk for the measurement of fallers and injuries (see Appendix 2, Table 23). Drahota et al. 77 also lacked blinding; however, the procedures in place to ensure quality of outcome measurement were considered to mitigate against this risk (see Appendix 2, Table 24). All three randomised studies showed baseline imbalances between the groups for at least one of the participant characteristics, although these were judged to be more compatible with chance, rather than from issues with the selection process (see Appendix 2, Tables 23, 24 and 30).
We judged all of the non-randomised studies to have a serious risk of bias across all outcomes, with all having problems of confounding; none was judged to be at critical risk of bias. Gustavsson et al. 52 accounted for most of the important factors in their multivariate analyses; however, they did not consider factors such as history of falls and urinary incontinence, and the control areas were slightly different (including bathrooms) from the intervention areas (see Appendix 2, Table 25). The remaining six non-randomised studies that were assessed did not make any attempts to control for confounding in the analyses, and many potential confounders or co-interventions were not measured or assessed (see Appendix 2, Tables 26–29, 31 and 32). No protocols were available for any of the non-randomised studies, which presented moderate concerns for selective outcome reporting; we raised these concerns to serious risk of bias when there were inconsistencies between the stated methods and reported results, or when outcomes were only partially reported (see Appendix 2, Tables 25, 29 and 31).
Individual studies presented additional limitations. Knoefel et al. 102 selected every third fall in the control arm for inclusion in the analysis (see Appendix 2, Table 29). Without blinding, we cannot rule out the possibility that outcomes may have influenced the selection process (e.g. from which point researchers decided to start and stop selecting data). Healey103 included ‘complaint of pain’ as part of the definition of injury, but indicated that more people in the carpet group had dementia, meaning that this outcome may have been harder to ascertain for this group. In addition, the researchers were required to retrospectively judge (based on the fall report) whether or not the injury was a result of an impact with the floor, although it is likely that they were aware of the intervention received (see Appendix 2, Table 28). Simpson et al. 76 described a risk that staff were more vigilant during falls in the ‘uncarpeted concrete’ group (e.g. bathrooms), potentially reporting milder or less complete falls than for comparison groups, and a common definition of falls did not appear to be used (see Appendix 2, Table 31).
Assessment of clinical effectiveness
Any shock-absorbing flooring versus standard flooring
Three randomised trials (two hospital based, one long-term care based) and seven observational studies (four hospital based, three long-term care based) compared one or more types of shock-absorbing flooring with ‘standard/rigid flooring’. Table 7 presents a summary of findings for hospital settings, and Table 8 presents for a summary of findings for care home settings. We have summarised the studies for care homes and hospitals separately because of heterogeneity between these settings and populations. Data for different flooring types (novel flooring, sports flooring, carpet and wooden subfloors) are also detailed separately in a subgroup analysis within each outcome, and summarised in Table 9.
| Outcomes | Anticipated absolute effectsa (95% CI) | Relative effect (95% CI) | Total sample size (n studies) | Quality of the evidence (GRADE)b | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/rigid flooring | Risk with shock-absorbing flooring | |||||
| Injurious falls rate per 1000 person-days | ||||||
| RCTs | 3 per 1000 | 2 per 1000 (1 to 6) | RaR 0.58 (0.18 to 1.91) | 9085 person-days (1 RCT) |
⊕⊕◯◯ Low |
These data (on sports flooring) are too imprecise to offer any certainty for this outcome |
| All studies | 3 per 1000 | 2 per 1000 (1 to 3) | RaR 0.55 (0.36 to 0.84) | 25,989 person-days (2 studies) |
⊕◯◯◯ Very low |
If three injurious falls per day occur among 1000 inpatients on a standard floor, then very low-quality evidence suggests that there would be one fewer (95% CI two fewer to about the same number) injurious fall per day on a shock-absorbing floor |
| Falls rate per 1000 person-days | ||||||
| RCTs | 7 per 1000 | 8 per 1000 (5 to 13) | RaR 1.07 (0.64 to 1.81) | 9085 person-days (1 RCT) |
⊕⊕◯◯ Low |
These data (on sports flooring) are too imprecise to offer any certainty for this outcome |
| All studies | 7 per 1000 | 6 per 1000 (5 to 8) | RaR 0.88 (0.71 to 1.09) | 25,989 person-days (2 studies) |
⊕◯◯◯ Very low |
If seven falls per day occur among 1000 inpatients on a standard floor, then very low-quality evidence suggests that between two fewer falls and one more fall would occur per day on a shock-absorbing floor (there may be no difference) |
| Number of falls resulting in injury | ||||||
| All studiesc | 424 per 1000 | 165 per 1000 (64 to 433) | RR 0.39 (0.15 to 1.02) | 559 falls (3 studies) |
⊕◯◯◯ Very low |
If 424 out of 1000 inpatient falls resulted in an injury on a standard floor, then very low-quality evidence suggests that 259 fewer (95% CI 360 fewer to 9 more) injurious falls would occur on a shock-absorbing floor. A sensitivity analysis removing a study on carpets judged to be at high risk of bias removes the heterogeneity and increases the precision of the effect for novel/sports floors (RR 0.64, 95% CI 0.44 to 0.93) |
| Number of fractures | ||||||
| RCTs | 9 per 1000 | 3 per 1000 (0 to 69) | OR 0.33 (0.01 to 8.13) | 448 participants (1 RCT) |
⊕⊕◯◯ Low |
These data (on sports flooring) are too imprecise to offer any certainty for this outcome |
| All studies | 9 per 1000 | 3 per 1000 (0 to 16) | OR 0.28 (0.04 to 1.77) | 626 participants (2 studies) |
⊕◯◯◯ Very low |
These data (on sports and novel flooring) are too imprecise to offer any certainty for this outcome |
| Number of hip fractures | ||||||
| RCTs | 4 per 1000 | 1 per 1000 (0 to 32) | OR 0.33 (0.01 to 8.15) | 448 participants (1 RCT) |
⊕⊕◯◯ Low |
These data (on sports flooring) are too imprecise to offer any certainty for this outcome |
| All studies | 4 per 1000 | 4 per 1000 (1 to 25) | OR 0.88 (0.12 to 6.47) | 626 participants (2 studies) |
⊕◯◯◯ Very low |
These data (on sports and novel flooring) are too imprecise to offer any certainty |
| Number of fallers | ||||||
| RCTs | 99 per 1000 | 223 per 1000 (56 to 895) | RR 2.25 (0.56 to 9.04) | 502 participants (2 RCTs) |
⊕◯◯◯ Very low |
These data (on sports flooring and carpet) are too imprecise to offer any certainty. Only RCTs contributed data to this outcome |
| Adverse events | ||||||
| RCTs | Staff raised concerns about moving wheeled equipment on sports floors, and one staff member sustained a pulled lower back on the intervention floor over 12 months’ follow-up | Not reported (1 study) |
⊕◯◯◯ Very low |
See Chapter 4 for further descriptions of push and pull challenges | ||
| Observational studies | No evidence to suggest greater risk of injury on intervention flooring (28 injuries in 30 months), compared with three concurrent control wards (30 injuries per ward) or a post-intervention control site (45 injuries in 30 months) | Not reported (1 study) |
⊕◯◯◯ Very low |
|||
| Outcomes | Anticipated absolute effectsa (95% CI) | Relative effect (95% CI) | Total sample size (n studies) | Quality of the evidence (GRADE)b | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/rigid flooring | Risk with shock-absorbing flooring | |||||
| Injurious falls rate per 1000 person-days | ||||||
| RCTs | 3 per 1000 | 3 per 1000 (2 to 4) | RaR 0.91 (0.62 to 1.32) | 213,854 person-days (1 RCT) |
⊕⊕⊕⊕ High |
This study compared a novel underlay with vinyl overlay and concrete subfloor, with a plywood underlay with vinyl overlay and concrete subfloor |
| All studies | 3 per 1000 | 3 per 1000 (2 to 4) | RaR 0.91 (0.62 to 1.32) | 308,981 person-day (2 studies) |
⊕◯◯◯ Very low |
Data are missing from one observational study (novel vs. standard floors), rated as having a high risk of bias, that did not report on this outcome |
| Falls rate per 1000 person-days | ||||||
| RCTs | 8 per 1000 | 10 per 1000 (7 to 14) | RaR 1.21 (0.87 to 1.68) | 213,854 person-days (1 RCT) |
⊕⊕⊕◯ Moderate |
This study compared a novel underlay with vinyl overlay and concrete subfloor, with vinyl with a plywood underlay and concrete subfloor |
| All studies | 8 per 1000 | 7 per 1000 (4 to 13) | RaR 0.87 (0.47 to 1.62) | 308,981 person-days (2 studies) |
⊕◯◯◯ Very low |
|
| Number of falls resulting in injury | ||||||
| All studiesc | 330 per 1000 | 264 per 1000 (231 to 300) | RR 0.80 (0.70 to 0.91) | 2800 falls (3 studies) |
⊕◯◯◯ Very low |
If 330 out of 1000 resident falls resulted in injuries on a rigid floor, then very low-quality evidence suggests that 66 fewer (95% CI 99 fewer to 30 fewer) injurious falls would occur on a shock-absorbing floor |
| Number of fractures | ||||||
| RCTs | 58 per 1000 | 44 per 1000 (18 to 106) | OR 0.74 (0.29 to 1.92) | 357 participants (1 RCT) |
⊕⊕◯◯ Low |
These data (on novel flooring vs. vinyl on plywood underlay) are too imprecise to offer any certainty for this outcome |
| All studiesc | 11 per 1000 | 7 per 1000 (3 to 16) | OR 0.61 (0.26 to 1.48) | 2074 falls (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of hip fractures | ||||||
| RCTs | 12 per 1000 | 11 per 1000 (2 to 76) | OR 0.94 (0.13 to 6.74) | 357 participants (1 RCT) |
⊕⊕◯◯ Low |
These data (on novel flooring vs. vinyl on plywood underlay) are too imprecise to offer any certainty for this outcome |
| All studiesc | 2 per 1000 | 3 per 1000 (2 to 4) | OR 1.17 (0.77 to 1.80) | 8548 falls (2 studies) |
⊕◯◯◯ Very low |
These data are too heterogeneous to offer any certainty for this outcome |
| Number of fallers | ||||||
| RCTs | 676 per 1000 | 697 per 1000 (602 to 798) | RR 1.03 (0.89 to 1.18) | 357 participants (1 RCT) |
⊕⊕⊕⊕ High |
This study compared a novel underlay with vinyl overlay and concrete subfloor, with vinyl with a plywood underlay and concrete subfloor. Only this RCT contributed data to this outcome |
| Adverse events | ||||||
| All studies | There was no evidence to suggest an increase in force-induced musculoskeletal injuries in care home staff | Not reported (1 study) |
⊕◯◯◯ Very low |
Personal communication (Dawn C Mackey, Simon Fraser University, 2020). Nested pre–post design in RCT study | ||
| Outcomes | Anticipated absolute effectsa (95% CI) | Relative effect (95% CI) | Total sample size (n studies) | Quality of the evidence (GRADE)b | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/rigid flooring | Risk with shock-absorbing flooring | |||||
| Injurious falls rate per 1000 person-days | ||||||
| Novel floors | 3 per 1000 | 2 per 1000 (2 to 3) | RaR 0.80 (0.59 to 1.09) | 225,124 person-days (2 studies) |
⊕◯◯◯ Very low |
One RCT rated as being at low risk of bias produced a RaR of 0.91 (95% CI 0.62 to 1.32) |
| Sports floors | 3 per 1000 | 1 per 1000 (1 to 3) | RaR 0.46 (0.23 to 0.92) | 14,720 person-days (2 studies) |
⊕◯◯◯ Very low |
If three injurious falls per day occur among 1000 inpatients on a standard floor, then very low-quality evidence suggests that two fewer (95% CI two fewer to about the same) injurious falls per day would occur on a sports floor |
| Falls rate per 1000 person-days | ||||||
| Novel floors | 7 per 1000 | 6 per 1000 (5 to 9) | RaR 0.89 (0.65 to 1.24) | 320,251 person-days (3 studies) |
⊕◯◯◯ Very low |
These studies are too heterogeneous to offer any certainty for this outcome. One RCT rated as being at low risk of bias produced a RaR of 1.21 (95% CI 0.87 to 1.68) |
| Sports floors | 7 per 1000 | 6 per 1000 (4 to 9) | RaR 0.85 (0.56 to 1.28) | 14,720 person-days (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of falls resulting in injuryc | ||||||
| Novel floors | 424 per 1000 | 335 per 1000 (297 to 373) | RR 0.79 (0.70 to 0.88) | 2871 falls (3 studies) |
⊕◯◯◯ Very low |
If 424 out of 1000 falls resulted in injury on a rigid floor, then very low-quality evidence suggests that 89 fewer (95% CI 127 fewer to 51 fewer) injurious falls would occur on a novel floor |
| Sports floors | 424 per 1000 | 246 per 1000 (127 to 475) | RR 0.58 (0.30 to 1.12) | 152 falls (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Carpet | 424 per 1000 | 68 per 1000 (30 to 170) | RR 0.16 (0.07 to 0.40) | 213 falls (1 study) |
⊕◯◯◯ Very low |
If 424 out of 1000 falls resulted in injury on a vinyl floor, then very low-quality evidence suggests that 356 fewer (95% CI 394 fewer to 254 fewer) injurious falls would occur on carpeted floors |
| Number of fractures | ||||||
| Novel floors | 9 per 1000 | 6 per 1000 (3 to 13) | OR 0.67 (0.28 to 1.59) | 482 participants (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Sports floors | 9 per 1000 | 3 per 1000 (0 to 25) | OR 0.31 (0.03 to 3.07) | 289 participants (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Carpet | Not estimable; see comments | 54 participants (1 study) |
⊕◯◯◯ Very low |
One small study did not observe any fractures | ||
| Number of hip fractures | ||||||
| Novel floors | 4 per 1000 | 6 per 1000 (1 to 28) | OR 1.25 (0.24 to 6.47) | 482 participants (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Sports floors | 4 per 1000 | 1 per 1000 (0 to 35) | OR 0.33 (0.01 to 8.15) | 447 participants (2 studies) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Carpetc | 30 per 1000 | 36 per 1000 (23 to 54) | OR 1.19 (0.77 to 1.84) | 6641 falls (1 study) |
⊕◯◯◯ Very low |
|
| Wooden subfloorc | 30 per 1000 | 18 per 1000 (14 to 24) | OR 0.59 (0.45 to 0.78) | 6641 falls (1 study) |
⊕◯◯◯ Very low |
If 30 out of 1000 falls result in hip fracture on concrete subfloors, then very low-quality evidence suggests that 12 fewer (95% CI 16 fewer to 6 fewer) hip fractures would occur on wooden subfloors |
| Number of fallers | ||||||
| Novel floors | 99 per 1000 | 102 per 1000 (88 to 116) | RR 1.03 (0.89 to 1.18) | 357 participants (1 RCT) |
⊕⊕⊕⊕ High |
|
| Sports floors | 99 per 1000 | 138 per 1000 (62 to 306) | RR 1.40 (0.63 to 3.10) | 448 participants (1 RCT) |
⊕⊕⊕◯ Moderate |
These data are too imprecise to offer any certainty for this outcome |
| Carpet | 99 per 1000 | 641 per 1000 (85 to 1000) | RR 6.50 (0.86 to 49.30) | 54 participants (1 RCT) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Adverse events | ||||||
| Novel floors | No evidence to suggest an increase in force-induced musculoskeletal injuries in care home staff | Not reported (1 study) |
⊕◯◯◯ Very low |
Personal communication (Dawn C Mackey). Nested pre–post design in RCT study | ||
| Sports floors | Staff raised concerns about moving wheeled equipment on sports floor. One staff member pulled lower back on sports floor during 12-month follow-up | Not reported (1 study) |
⊕◯◯◯ Very low |
See Chapter 4 for further descriptions on push and pull challenges | ||
Primary outcomes
Injurious falls rate per 1000 person-days
Two randomised trials rated as being at low risk of bias (one hospital-based pilot study and one care home-based trial) and one observational study rated as having serious concerns for risk of bias (based in a hospital) contributed data to this outcome. 49,50,77 The pooled effect from two RCTs (Figure 3) provides no clear evidence to support shock-absorbing flooring use for reducing the injurious falls rate (RaR 0.87, 95% CI 0.61 to 1.25; p = 0.46; two studies; I2 = 0%). 50,77 There was no evidence of a differential effect by settings based on the RCT data [test for subgroup differences: χ2 = 0.50, degrees of freedom (df) = 1; p = 0.48; I2 = 0%; see Appendix 6, Table 36]; however, the hospital-based study was very imprecise. The observational study reported a non-parametric test because the data were not normally distributed. 49 This study reported ‘a non-significant trend’ of lower injury rates in the shock-absorbing flooring cohort than among the control cohort [p = 0.059; intervention: median of three injurious falls per 1000 person-days (interquartile range 0–6); control: median of five injurious falls per 1000 person-days (interquartile range 0–8)]. 49
FIGURE 3.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: injurious falls rate per 1000 person-days. a, Number of person bed-days (total) in each group provided by the study author; b, data derived from unpublished data. Published analysis reports a non-significant result (p = 0.059). IV, inverse variance; SE, standard error. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
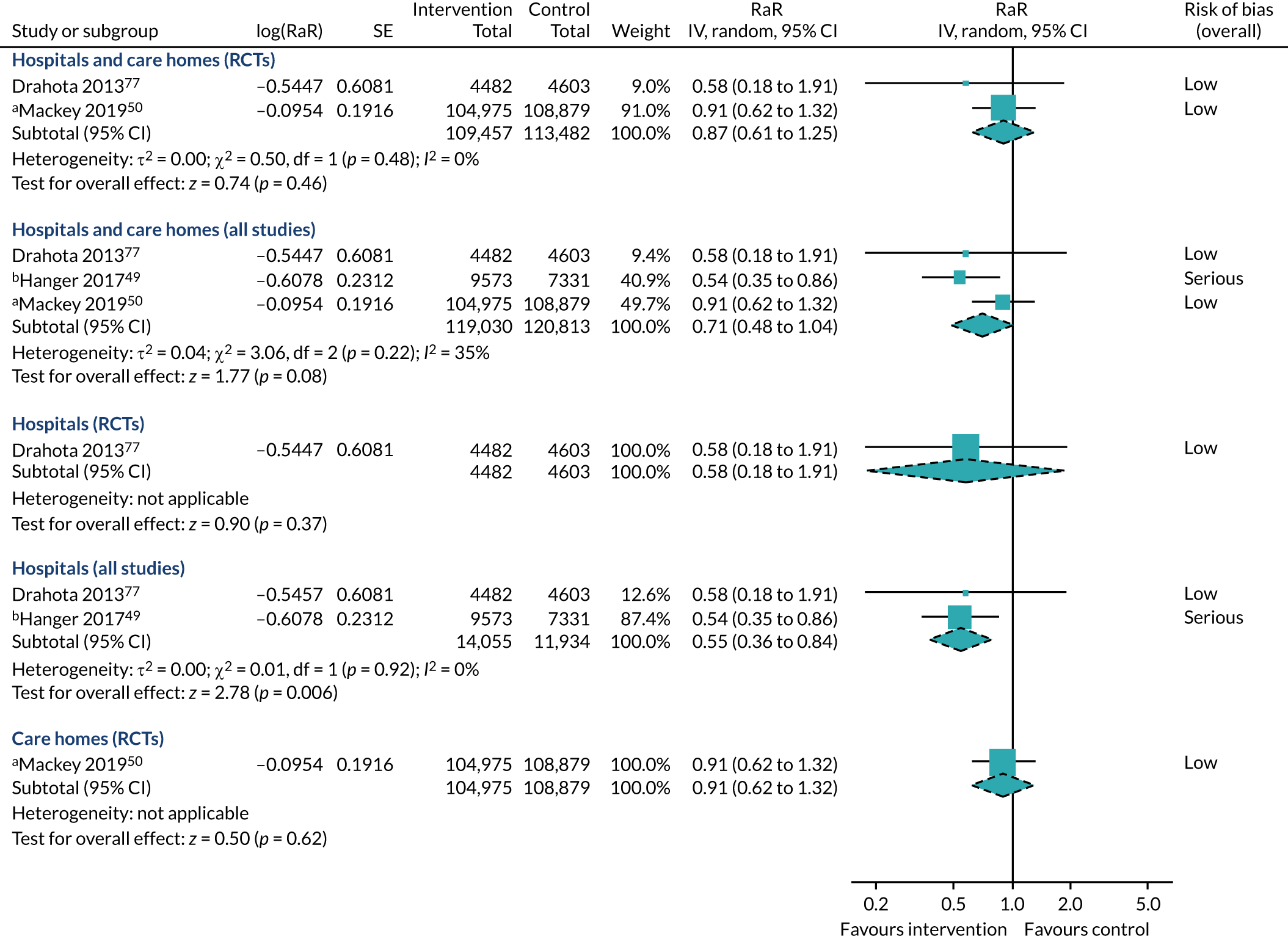
Unpublished data, supplied by the contact author of the observational study, enabled data to be derived for pooling. These data should be interpreted with extreme caution, especially as it is noted that the derived analysis provides a more positive effect estimate for the study. 49 Incorporating evidence from the observational study maintains a reasonable level of statistical homogeneity (τ2 = 0.04, χ2 = 3.06, df = 2; p = 0.22; I2 = 35%), but decreases the effect estimate more in favour of shock-absorbing flooring, still incorporating the potential for no effect (RaR 0.71, 95% CI 0.48 to 1.04; p = 0.08; three studies; see Figure 3). Tests for subgroup differences were non-significant when exploring both setting type (χ2 = 3.05, df = 1; p = 0.08; I2 = 67.2%; see Appendix 6, Table 36) and study design (χ2 = 2.56, df = 1; p = 0.11; I2 = 61.0%; see Appendix 6, Table 36).
One RCT conducted in hospital settings was too imprecise to determine the effect of shock-absorbing flooring on injurious falls rate, as the 95% CI incorporates the potential for no effect, for benefit and for harm (RaR 0.58, 95% CI 0.18 to 1.91; p = 0.37; see Figure 3). 77 However, incorporating the derived data, with caution, from an observational study (which has published data indicative of a non-significant effect; p = 0.059),49 suggests that shock-absorbing flooring may reduce the injurious falls rate in hospital settings (RaR 0.55, 95% CI 0.36 to 0.84; p = 0.006; two studies; I2 = 0%; very low-quality evidence; see Figure 3). There was no evidence of a differential effect by study design in the data for hospital settings (χ2 = 0.01, df = 1; p = 0.92; I2 = 0%; see Appendix 6, Table 36).
A single RCT conducted in a care home setting found an injurious falls rate on a novel underlay covered in vinyl with a concrete subfloor that was similar to that of a comparison group of vinyl on a plywood underlay with a concrete subfloor (RaR 0.91, 95% CI 0.62 to 1.32; p = 0.62; see Figure 3). 50 Observational studies from care homes did not contribute any data to this outcome.
A subgroup analysis limited to RCTs exploring flooring types only (sports flooring and novel shock-absorbing flooring) produces the same analysis as for the subgroup on settings of care (χ2 = 0.50, df = 1; p = 0.48; I2 = 0%; see Appendix 6, Table 36), providing no evidence to support a difference in treatment effects between flooring types.
A subgroup analysis by flooring type that also incorporates the unpublished and derived data from an observational study deemed to have serious concerns for risk of bias49 showed no evidence of a difference in treatment effects between flooring types for rate of injurious falls (χ2 = 2.01, df = 1; p = 0.16; I2 = 50.2%; Figure 4). The data on sports flooring were also hospital based and were indicative of positive treatment effects, with large uncertainty around the size of those effects (RaR 0.46, 95% CI 0.23 to 0.92; p = 0.03; I2 = 0%; very low-quality evidence). The data for novel shock-absorbing flooring (which were obtained from a hospital and a care home) incorporated the potential of ‘no effect’, as well as of potential benefit (RaR 0.80, 95% CI 0.59 to 1.09; p = 0.15; I2 = 0%; very low-quality evidence).
FIGURE 4.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: injurious falls rate per 1000 person-days. a, Data for Hanger49 are derived and unpublished; control group data are shared between comparisons; b, number of person bed-days (total) in each group provided by the study author. IV, inverse variance; SE, standard error.

Analyses removing studies judged to be at serious risk of bias produce the same results as detailed previously for RCT evidence only. The care home-based RCT also reported a multivariable model that adjusted for age, dementia, falls history, anti-anxiety medication and analgesic medication (RaR 1.09, 95% CI 0.75 to 1.58). 50 Incorporating these data into the analyses does not alter the bottom-line conclusions of the analyses (see Appendix 7, Table 37). However, the data do provide more conservative estimates for RCT-based evidence (RaR 1.03, 95% CI 0.72 to 1.47; p = 0.87; I2 = 0%) and novel shock-absorbing floors (RaR 0.84, 95% CI 0.55 to 1.27; p = 0.40; I2 = 33%), and introduces more statistical heterogeneity into the analysis of all studies combined (RaR 0.75, 95% CI 0.43 to 1.29; p = 0.30; heterogeneity: τ2 = 0.14; χ2 = 5.67, df = 2; p = 0.06; I2 = 65%).
Falls rate per 1000 person-days
Five studies contributed data to this outcome (two RCTs and three observational studies). 49,50,52,77,101 Only four studies provided data suitable for use in a meta-analysis,49,50,52,77 with data from one of these studies obtained via personal communication. 49
The CI of the pooled effect estimate from two RCTs judged to be at low risk of bias (one care home based, one hospital based) incorporates the possibilities that shock-absorbing flooring may increase the rate of falls or make little to no difference (RaR 1.17, 95% CI 0.89 to 1.54; p = 0.27; two studies; I2 = 0%; Figure 5). There was no evidence of a differential effect by setting (χ2 = 0.14, df = 1; p = 0.71; I2 = 0%; see Appendix 6, Table 36).
FIGURE 5.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: falls rate per 1000 person-days. a, Gustavsson et al. 52 is adjusted for age, sex, cognitive ability, walking ability, medications (antidepressants and sedatives) and visual impairment; b, Hanger49 data are derived and obtained via personal communication (Dr Carl Hanger, Burwood and The Princess Margaret Hospitals, Christchurch, New Zealand, 2020). IV, inverse variance; SE, standard error. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
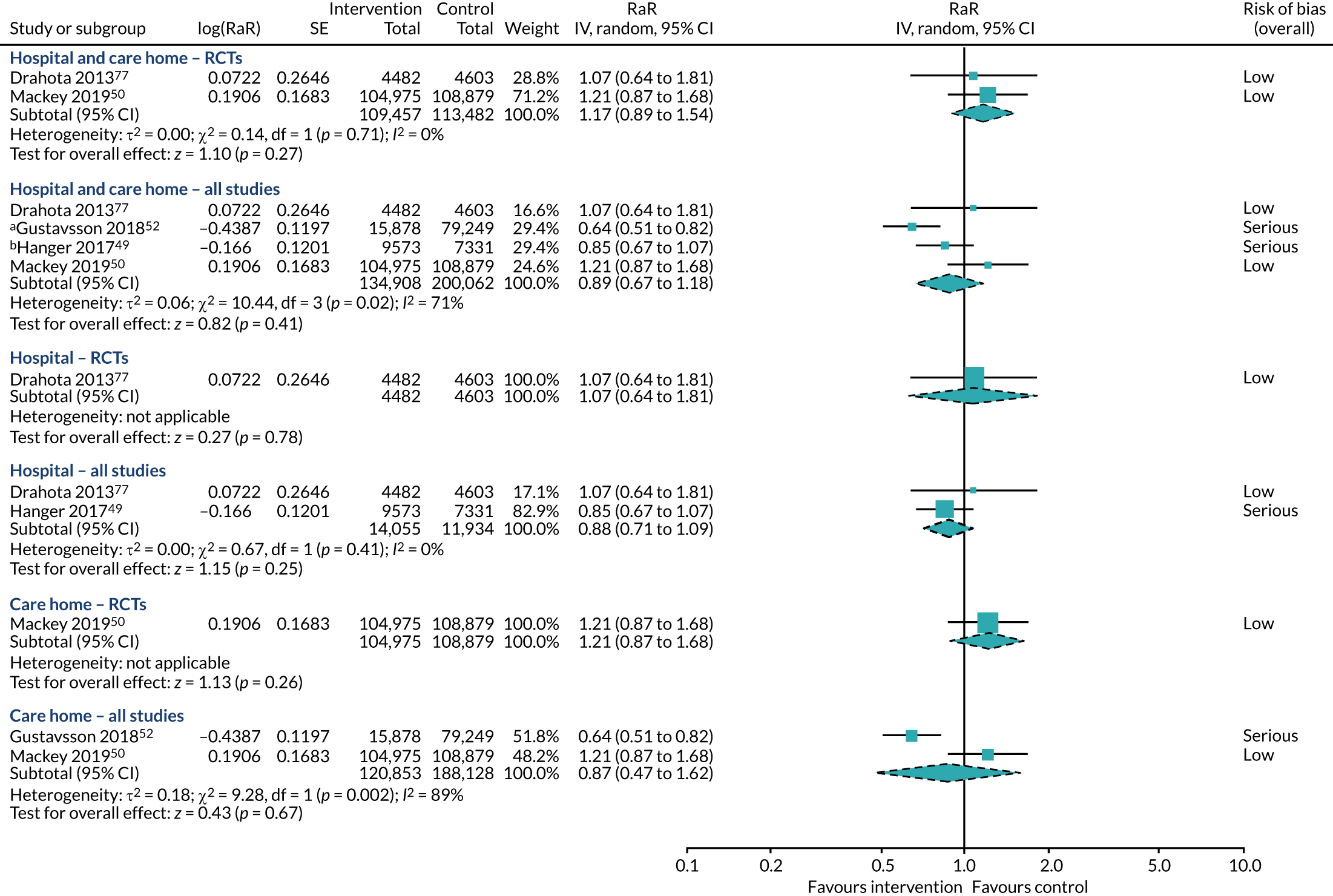
Two hospital-based observational studies (exploring novel flooring, sports flooring and carpet) also reported non-significant differences in falls rates from analyses unsuitable for meta-analysis. 49,101 We obtained personally communicated and derived data from one of these studies (on novel and sports flooring),49 and, alongside a third observational study of novel flooring in a care home setting,52 we were able to assess the suitability of incorporating observational data into the meta-analysis.
Incorporating the two observational studies into the meta-analysis increases the heterogeneity (τ2 = 0.06; χ2 = 10.44, df = 3; p = 0.02; I2 = 71%); although pooling these studies is, therefore, questionable, the probability that any observed effects are due to chance is maintained (RaR 0.89, 95% CI 0.67 to 1.18; p = 0.41; four studies; see Figure 5). The heterogeneity can be somewhat explained by study design (χ2 = 5.44, df = 1; p = 0.02; I2 = 81.6%; see Appendix 6, Table 36), with the pooled effect of prospective cohort studies deemed to be at serious risk of bias positively favouring the intervention (RaR 0.74, 95% CI 0.57 to 0.97; p = 0.03; two studies; I2 = 61%), counter to the RCT evidence that was judged to be at low risk of bias. There is no evidence to suggest a differential effect by settings (χ2 = 0.00, df = 1; p = 0.98; I2 = 0%; see Appendix 6, Table 36).
One small cluster randomised trial judged to be at low risk of bias was too imprecise to determine the influence of shock-absorbing flooring on falls rate. 77 The CI incorporates the possibility that shock-absorbing floors may increase the risk of falls; however it also suggests that any observed differences may be due to chance alone (RaR 1.07, 95% CI 0.64 to 1.81; p = 0.78; low-quality evidence; see Figure 5). Including data from an observational study judged to have serious concerns for risk of bias improves precision and maintains the possibility that the range of possible intervention effects on falls rates includes no difference (RaR 0.88, 95% CI 0.71 to 1.09; p = 0.25; two studies; I2 = 0%; very low-quality evidence; see Figure 5). There was no evidence of a differential effect by study design in the hospital evidence (χ2 = 0.67; p = 0.41; I2 = 0%; see Appendix 6, Table 36). Not included in this analysis are data from an observational study,101 judged to be at serious risk of bias, comparing carpet with vinyl through an observation of time trends; this study also found no evidence to support an effect on falls rate per 1000 person-days. 101
One trial (on SmartCells flooring) deemed to be at low risk of bias incorporated the probability that shock-absorbing flooring may make no difference to falls rates. 50 However, the 95% CI also incorporated the possibility of harm (RaR 1.21, 95% CI 0.87 to 1.68; p = 0.26; one study; see Figure 5). Including data from an observational study (on Kradal flooring)52 deemed to be at serious risk of bias introduced substantial heterogeneity (τ2 = 0.18, χ2 = 9.28, df = 1; p = 0.002; I2 = 89%), with the two studies demonstrating opposite effects (test for subgroup differences: χ2 = 9.28, df = 1; p = 0.002; I2 = 89.2%; see Appendix 6, Table 36).
A subgroup analysis limited to RCTs only, exploring flooring types (sports flooring and novel shock-absorbing flooring), produces the same results as for the subgroup analysis on settings of care (χ2 = 0.14, df = 1; p = 0.71; I2 = 0%; see Appendix 6, Table 36), providing no evidence to support a difference in falls rates between flooring types.
Exploring the heterogeneous evidence from all studies by flooring type does not resolve the heterogeneity, with the data for novel shock-absorbing floors still providing mixed effects (τ2 = 0.08; χ2 = 11.38, df = 3; p = 0.010; I2 = 74%), and displaying similar combined results to those of sports flooring (χ2 = 0.04, df = 1; p = 0.84; I2 = 0%; Figure 6). These findings are also compatible with the non-significant observational study comparing carpet with vinyl,101 providing no evidence to suggest that different flooring types affect falls rates differentially.
FIGURE 6.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: falls rate per 1000 person-days. a, Gustavsson et al. 52 is adjusted for age, sex, cognitive ability, walking ability, medications (antidepressants and sedatives) and visual impairment; b, Hanger49 data are derived (unpublished); the control arm has been split between comparisons. IV, inverse variance; SE, standard error.
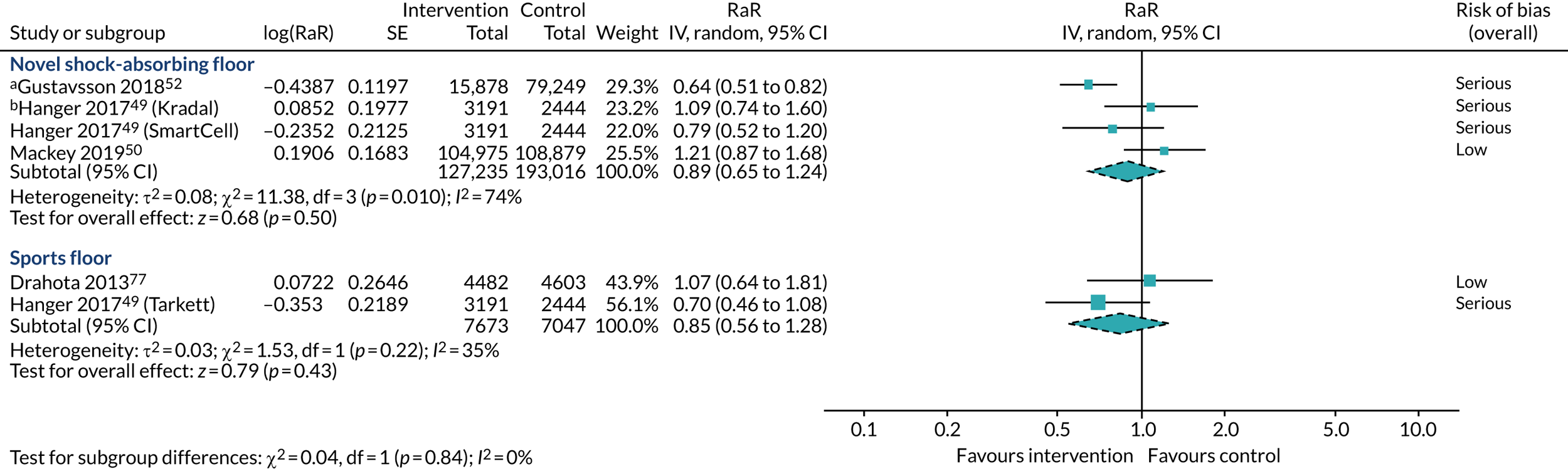
A sensitivity analysis removing studies judged be at serious risk of bias is identical to the RCT evidence presented previously. One RCT presented a multivariate model for falls rates adjusted for age, falls history, dementia, anti-anxiety medication and analgesic medication (RaR 1.32, 95% CI 0.94 to 1.84). 50 Incorporating these data into the analyses instead of the unadjusted estimates did not alter the overall conclusions (see Appendix 7, Table 37).
Through our personal communications with the study authors of two of the observational studies, potential errors in the published data were revealed. The contact author of the care home study supplied us with new data suggestive of an even more beneficial effect in the shock-absorbing flooring group (RaR 0.60, 95% CI 0.48 to 0.74); however, there was uncertainty around the accuracy of these data, as some of the numbers did not add up as expected. 52 These revised data served to increase the heterogeneity in the review findings only and did not change the over-riding conclusions (see Appendix 7, Table 37). The contact author of the hospital-based observational study identified a coding error for one fall attributed to the wrong group;49 the impact of this was negligible (revised RaR 0.86, 95% CI 0.68 to 1.09 vs. RaR 0.85, 95% CI 0.67 to 1.07) and did not seriously alter the bottom-line results of the analyses (see Appendix 7, Table 37).
Secondary outcomes
Number of falls resulting in injury
Six studies (three hospital based, three in care homes) provided data for this outcome. 49,50,52,77,102,103 We believe that these data are not as robust as the data contributing to the primary outcome of injurious falls rates for a number of reasons and should therefore be interpreted with extreme caution:
-
The samples are not independent (i.e. the same individuals may contribute more than once to the risk in each group and, in some cases, may contribute to both groups).
-
There is no adjustment for exposure time or ‘at-risk time’.
-
For this outcome, we are treating the RCT data as if they are observational data and not reporting them with elevated prominence, as the outcome denominator is based on the observed number of falls and not the number of people randomised to each group.
-
Not all of the data have been adjusted for covariates and many of the studies are subject to confounding, thereby putting the data at high risk of bias.
More studies are able to contribute data to this outcome, however, as the outcome lends itself to observational study designs, which take the falls data recorded in the study setting as the starting point for generating the intervention and control groups, and these study types often report this as the primary outcome.
Figure 7 summarises the descriptive data for injurious falls by severity. Heterogeneity exists in the classification systems used for injury severity types, along with the types of floors, settings and study designs employed. Donald et al. 105 did not provide sufficient information to be incorporated into our synthesis, as data were not provided at a group level (one-third of falls resulted in minor injuries; there were no fractures, but there was only a single fall on vinyl).
FIGURE 7.
Studies comparing shock-absorbing flooring with rigid flooring; outcome: proportion of falls resulting in injuries of different severities. a, Fracture data have been inserted for Knoefel et al. 102 under severe injury.

The descriptive data indicate that a smaller proportion of falls resulted in injury in the intervention arms and that (when measured) the injuries that did occur tended to be less severe, more noticeably so in hospital environments (see Figure 7). Healey103 is a clear outlier, with a very high proportion of falls classified as injurious in the control arm. The proportion of falls resulting in injury was also high in Knoefel et al. 102 and neither of these studies classified the injuries by severity. Knoefel et al. 102 did consider various injury types (redness, bruise, abrasion, cut, two or more injuries, fracture, other), some of which were termed ‘significant injuries’; however, the presentation of the data precludes an assessment of severity breakdown, as the independence of data between categories is unclear.
We have cautiously summarised the data according to risk of falls resulting in any injury (Figure 8). The findings of all studies combined, although in favour of shock-absorbing flooring (RR 0.69, 95% CI 0.52 to 0.90; p = 0.006), are heterogeneous (τ2 = 0.06, χ2 = 14.71, df = 5; p = 0.01; I2 = 66%). This heterogeneity appears to be largely explained by Healey’s103 highly positive study exploring carpet versus vinyl (see the subsequent section, Subgroup analyses by flooring type). The pooled point estimate for RCTs (RR 0.77, 95% CI 0.67 to 0.88) was more conservative and precise than those of prospective cohort studies (RR 0.68, 95% CI 0.51 to 0.89) and retrospective cohort studies (RR 0.41, 95% CI 0.07 to 2.35); however, there was no evidence to suggest a differential effect according to study design (χ2 = 1.10, df = 2; p = 0.58; I2 = 0%; see Appendix 6, Table 36) and, as highlighted previously, the RCT evidence for this outcome should be considered less robust than that of our primary outcome. Similarly, although there was some heterogeneity between the subgroups of hospitals (RR 0.39, 95% CI 0.15 to 1.02; see Figure 8) and care homes (RR 0.80, 95% CI 0.70 to 0.91; see Figure 8), the test for subgroup differences was not significant (χ2 = 2.08, df = 1; p = 0.15; I2 = 51.9%; see Appendix 6, Table 36).
FIGURE 8.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: number of falls resulting in injury. a, Data have been adjusted for clustering (ICC = 0.046); b, data adjusted for age, sex, body mass index, visual and cognitive impairments, walking ability, hip protectors, fall location (room type), activity when falling and time of day. IV, inverse variance; SE, standard error. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
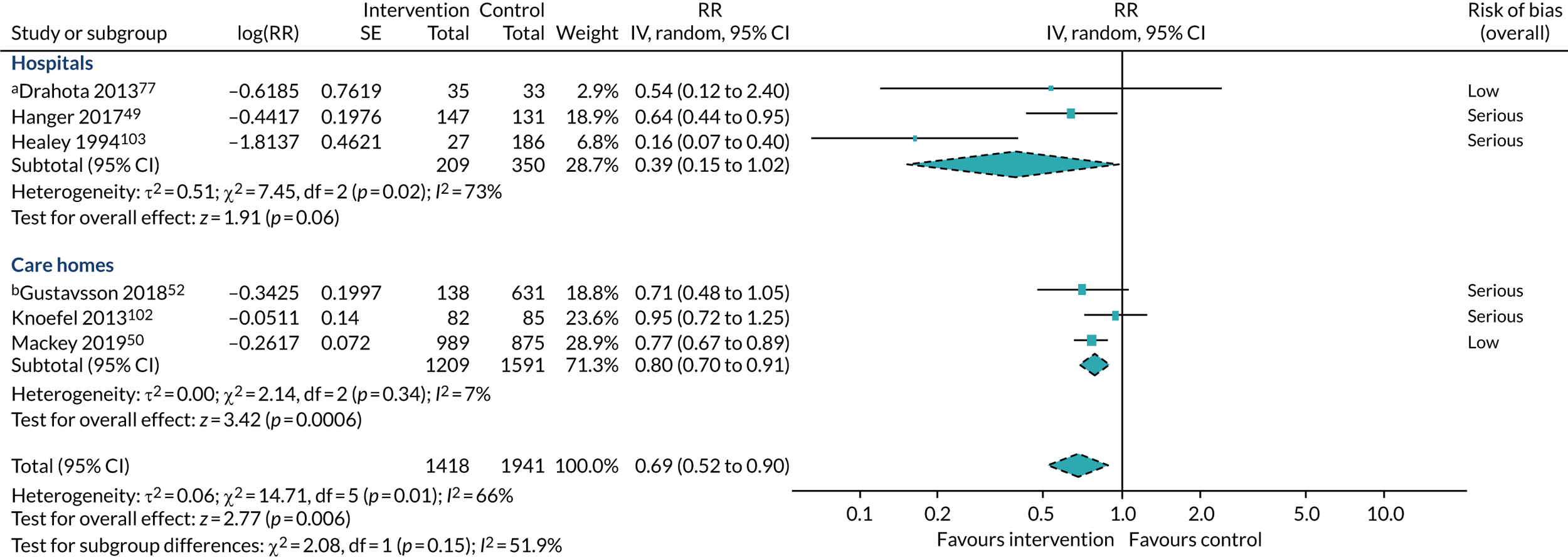
A subgroup analysis including all studies exploring the number of falls resulting in injury suggests that the type of flooring makes a difference to the outcome (χ2 = 12.09, df = 2; p = 0.002; I2 = 83.5%; Figure 9). However, this result is largely down to the findings for carpet versus vinyl, which, counterintuitively, are much more favourable than the findings for both novel and sports floors versus vinyl. The single study contributing to this subgroup was a retrospective cohort study judged to be at serious risk of bias and with large imbalances between study arms. 103 Removing this subgroup from the analysis indicates that the findings for novel floors and sports floors are similar (χ2 = 0.81, df = 1; p = 0.37; I2 = 0%). The data for sports floors are very imprecise and indicate a range of possible effects, from improved outcomes with the intervention to no difference (RR 0.58, 95% CI 0.30 to 1.12; p = 0.11; I2 = 0%; see Figure 9). The data for novel floors are more precise and are positively in favour of the intervention (RR 0.79, 95% CI 0.70 to 0.88; p < 0.0001; I2 = 0%; see Figure 9).
FIGURE 9.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: number of falls resulting in injury. a, Data adjusted for age, sex, body mass index, visual and cognitive impairments, walking ability, hip protectors, fall location (room type), activity when falling and time of day; b, Hanger49 data were obtained via personal communication (Dr Carl Hanger); the control arm has been split between comparisons; c, data have been adjusted for clustering (ICC = 0.046). IV, inverse variance; SE, standard error.
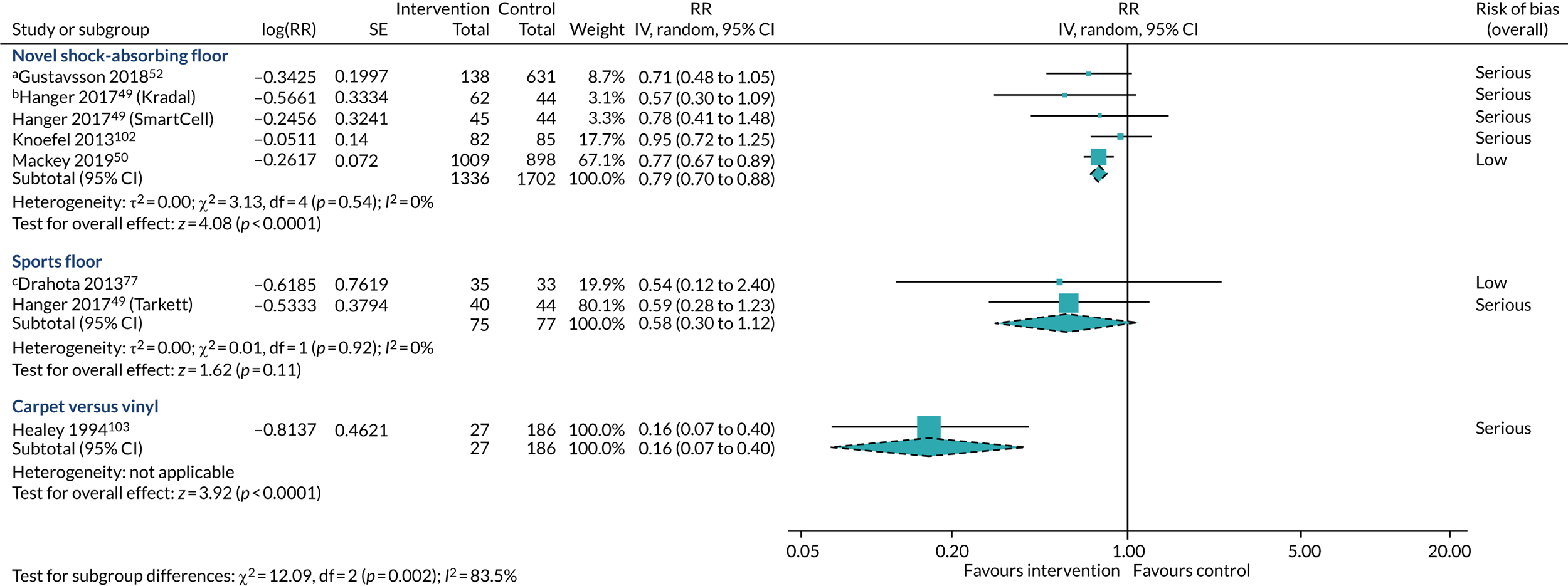
The subgroup of hospital studies was sensitive to the estimated ICC in Drahota et al. ,77 with a smaller ICC (0.023) resulting in CIs that no longer cross the line of no effect (RR 0.40, 95% CI 0.16 to 0.97; p = 0.04; I2 = 73%). Removing the controversial carpet study from this subgroup (while keeping the original, more conservative, ICC) also resolves the heterogeneity and positions the effect estimate more precisely in favour of the intervention (RR 0.64, 95% CI 0.44 to 0.93; p = 0.02; I2 = 0%). Other adjustments to the ICC did not make any material difference to the findings (see Appendix 7, Table 37).
We assessed the influence of some slightly revised data received via personal communication on Hanger (with Dr Carl Hanger);49 however, this made a negligible difference to the overall results (see Appendix 7, Table 37). A sensitivity analysis based on risk of bias provides the same results as the RCT evidence covered previously.
Number of fractures
Five studies (three RCTs and two observational studies) reported on the outcome of number of fractures. 49,50,77,102,105 Four studies reported on the number of participants who sustained a fracture (three RCTs and one observational study),49,50,77,105 and another retrospective cohort study observed the number of falls that resulted in fracture (data that are also derivable from the first four studies). 102 The number of fracture events in the majority of the studies were very few, resulting in imprecise estimates; three studies had zero events in one or both arms. 77,102,105 One small RCT with zero events in both arms was unable to contribute any information to the analyses. 105 We have analysed the number of fractures as a function of the number of participants and the number of falls to incorporate all of the evidence. Caution needs to be exercised when interpreting data from the latter method because the same individuals may contribute one or more falls to the study groups [and, in one study, it is possible that the same individual(s) contributed to falls counts in both groups]. 102 Therefore, the data are not independent and it is impossible to gauge how much overall influence this has on the findings. However it can be seen that the RCT evidence is biased slightly more in favour of the intervention when using number of falls as the denominator (Figure 10).
FIGURE 10.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: number of fractures. a, Study displayed for information purposes; it was not included in analyses as it had zero events; b, data adjusted for clustering (ICC = 0.013). M–H, Mantel–Haenszel. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
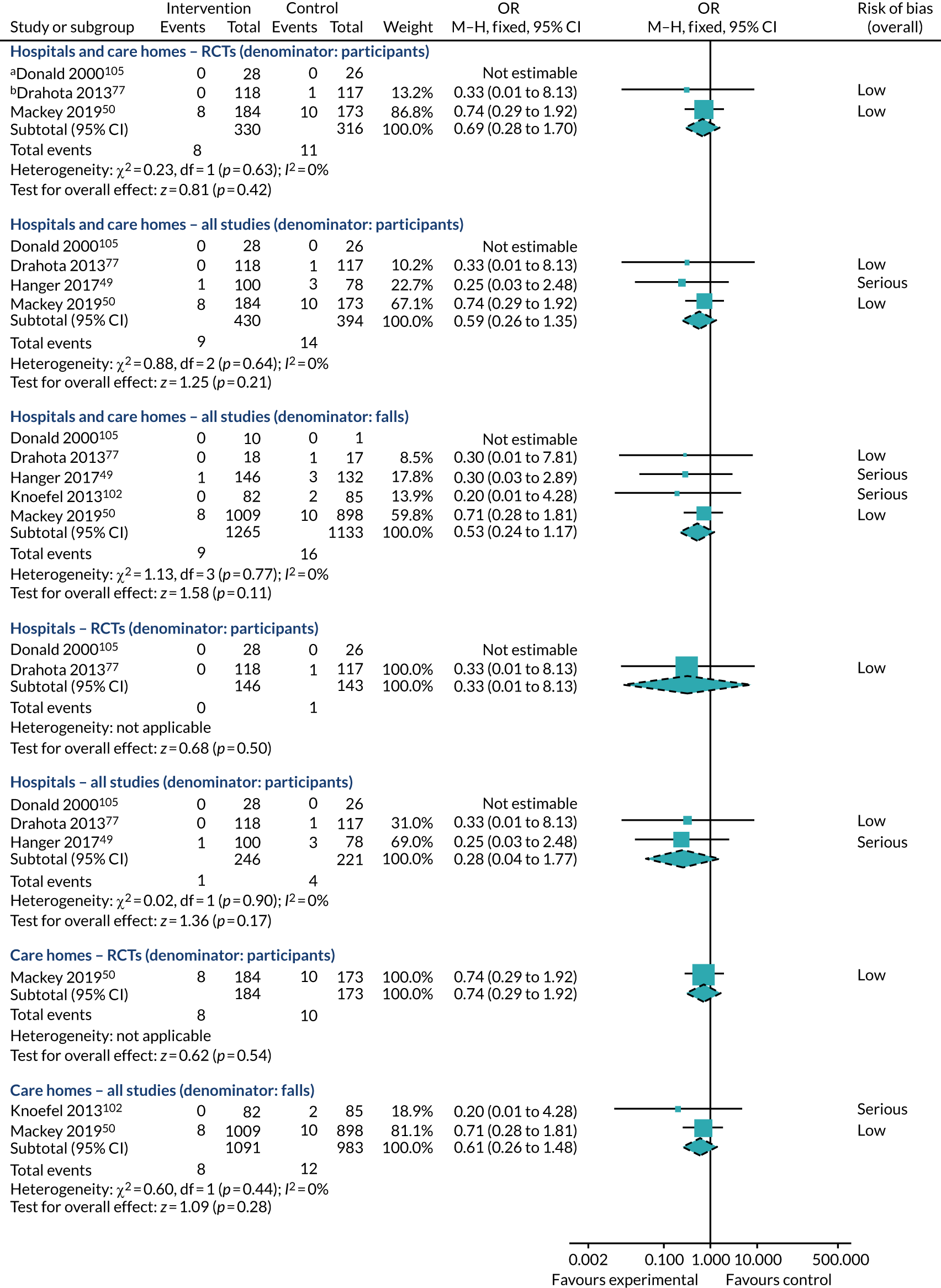
The pooled effect estimate from the two RCTs that contributed data was imprecise; the 95% CI included the potential for substantial benefit, no effect or possible harm (OR 0.69, 95% CI 0.28 to 1.70; p = 0.42; two studies; I2 = 0%; see Figure 10). Incorporating the observational evidence into the pooled effect estimates increases the precision somewhat, without contributing to increased statistical heterogeneity, when participants are the denominator (OR 0.59, 95% CI 0.26 to 1.35; p = 0.21; three studies; I2 = 0%; see Figure 10) and when falls are the denominator (OR 0.53, 95% CI 0.24 to 1.17; p = 0.11; four studies; I2 = 0%; see Figure 10). However, although the point estimates are in favour of the intervention, the wide CIs mean that there is insufficient information to detect a signal.
With low precision and statistically homogeneous findings, we found no evidence to suggest a differential effect by settings when focusing on the RCT evidence alone (χ2 = 0.23, df = 1; p = 0.63; I2 = 0%; see Appendix 6, Table 36) or all evidence combined (by participants: χ2 = 0.86, df = 1; p = 0.35; I2 = 0%; by falls: χ2 = 0.48, df = 1; p = 0.49; I2 = 0%). There was no indication of a differential effect by study design in these data (χ2 = 0.85, df = 2; p = 0.65; I2 = 0%; see Appendix 6, Table 36). We have subgrouped the data for hospitals alone and care homes alone in Figure 10; the data are too imprecise to determine whether or not shock-absorbing flooring is beneficial for reducing fractures in either setting.
Owing to the levels of uncertainty in the data, there was no evidence that the type of shock-absorbing flooring had a differential effect on the number of fractures when looking at RCTs alone (χ2 = 0.23, df = 1; p = 0.63; I2 = 0%; see Appendix 6, Table 36), or all available evidence analysed at the participant level (χ2 = 0.37, df = 1; p = 0.54; I2 = 0%; see Appendix 6, Table 36) or the falls level (χ2 = 0.23, df = 1; p = 0.63; I2 = 0%; see Appendix 6, Table 36). Although data in each subgroup showed minimal statistical heterogeneity, the studies were too imprecise to detect a signal for this outcome (Figure 11).
FIGURE 11.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: number of fractures. a, Unreported data; data for the control arm have been split between the three comparisons; b, study displayed for information; this study contributed no data to the analyses. M–H, Mantel–Haenszel.
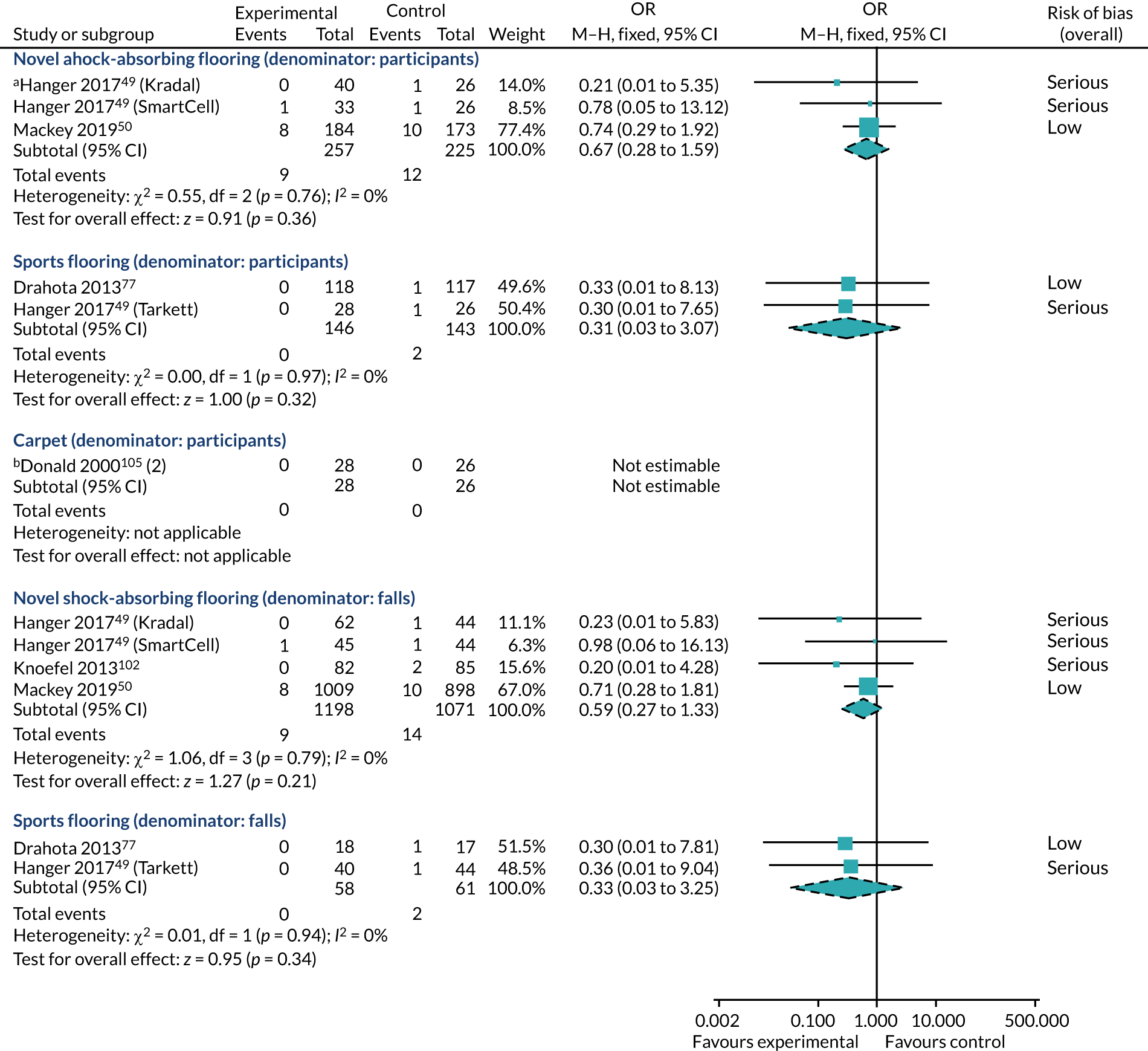
We ran sensitivity analyses on the choice of analysis method, using Peto ORs instead, with negligible impact on the findings (see Appendix 7, Table 37). Our choice of ICC for the cluster RCT also did not alter the overall effect estimates77 and some slightly revised unpublished figures received from Hanger49 were inconsequential to the review findings. Gustavsson et al. 52 provided us with some unpublished data (all of the serious falls in this observational study resulted in one or more fractures) (Johanna Gustavsson, personal communication); including these (unadjusted) data in the analyses did not alter the overall conclusions (see Appendix 7, Table 37). We ran a sensitivity analysis to include the observational data reported in Lange;82 however, this made no material difference to the findings. We did not run any sensitivity analyses on risk of bias, as these would have produced the same findings as looking at RCT evidence alone.
Number of hip fractures
Five studies (three RCTs and two observational studies) reported the number of hip fractures. 49,50,76,77,105 Four studies reported the number of participants who sustained a hip fracture (three RCTs and one observational study)49,50,77,105 and Simpson et al. 76 observed the number of falls that resulted in hip fracture (data that are also derivable from the other four studies). The Simpson et al. 76 study was a factorial study, exploring carpeted and uncarpeted floors, and if the subfloors were wooden or concrete. In Figure 12, we have focused the comparisons on overlay and underlay materials (for Simpson et al. 76 this is carpeted vs. uncarpeted floors), and subsequently, in the assessment of different flooring types, we have also segregated the evidence for wooden versus concrete subfloors. The number of events in the majority of studies was very small, resulting in imprecise estimates; three studies had zero events in one or both arms,49,77,105 with Donald et al. 105 not contributing any information to the analyses.
FIGURE 12.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: number of hip fractures. a, Donald et al. 105 displayed for information purposes; it was not included in analyses as it had zero events; b, Drahota et al. 77 data are adjusted for clustering (ICC = 0.002); c, Mackey et al. 50 events data were obtained via personal communication; d, Simpson et al. 76 data compare carpeted with uncarpeted floors on different subfloors. M–H, Mantel–Haenszel.
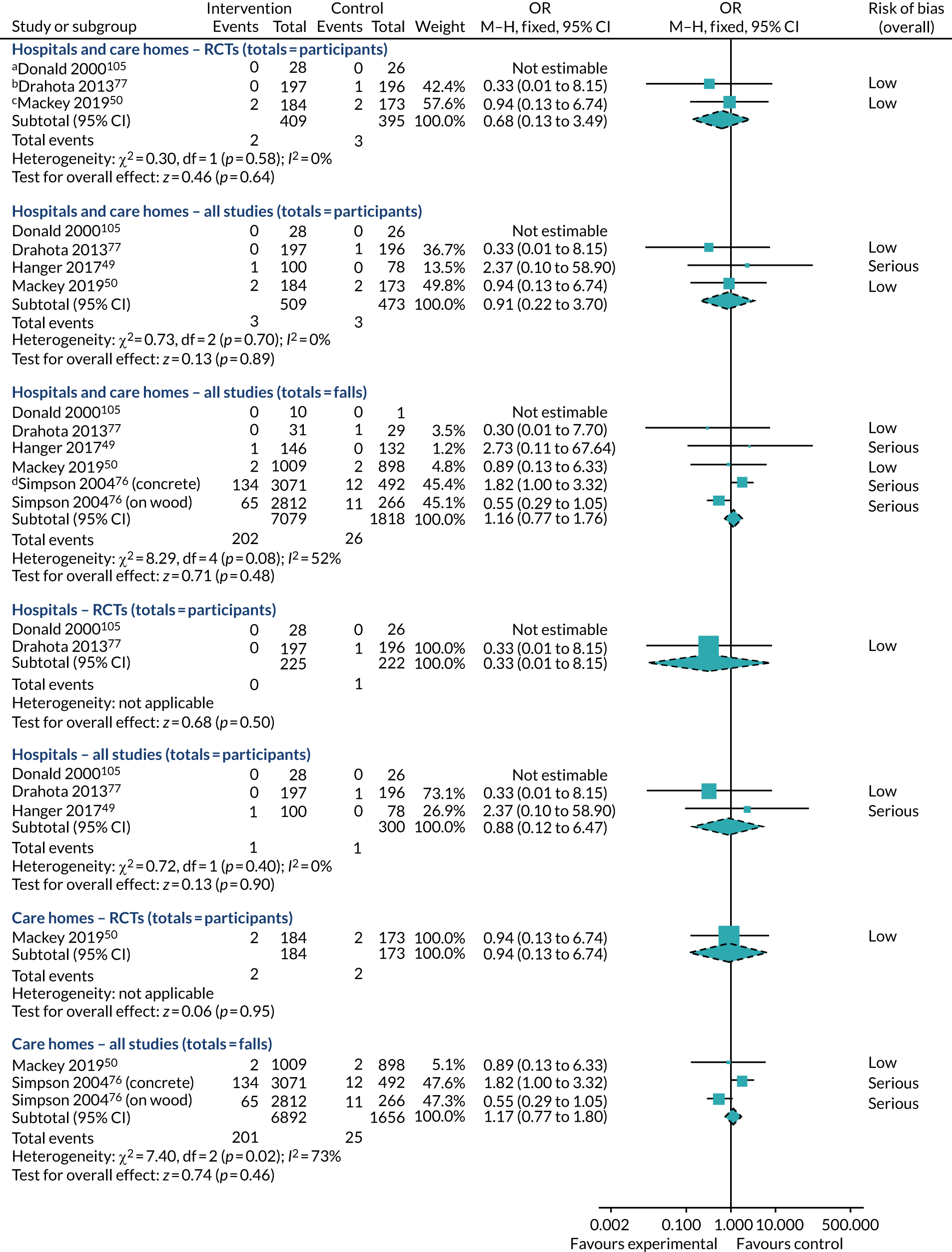
For the outcome ‘any fracture’, we have summarised the data with participants as the unit of analysis, and, secondary to this, with falls as the unit of analysis to incorporate the additional observational study. Studies have slightly inflated point estimates when analysed by the number of falls (for RCTs this bias is more in favour of the intervention, for Hanger49 it is more in favour of control). However, owing to the imprecision in the data, none of the analyses is able to detect whether or not shock-absorbing flooring can help reduce the number of hip fractures (see Figure 12).
The Simpson et al. 76 study contributes heterogeneity to the analyses when the data are stratified by subfloor type, as we have presented in Figure 12, although see Sensitivity analyses; the other studies are largely homogeneous. The Simpson et al. 76 data are at serious risk of bias due to confounding. The unbalanced groups in this study are an artefact of the smaller number of falls occurring on uncarpeted floors (likely, in part, due to less exposure to these surfaces). The counterintuitive finding that fewer fractures occurred on uncarpeted concrete floors (the hardest of all surfaces to land on) was deemed by the study authors to be associated with such areas being bathrooms, which may be subject to increased staff vigilance, or more handrails and other items to help break the fall. 76
There is no evidence to suggest a differential effect by setting type (RCT evidence: χ2 = 0.30, df = 1; p = 0.59; I2 = 0%; all studies’ participant-level data: χ2 = 0.00, df = 1; p = 0.96; I2 = 0%; all studies’ falls-level data: χ2 = 0.06, df = 1; p = 0.81; I2 = 0%; see Appendix 6, Table 36) or study design (participant-level data: χ2 = 0.46, df = 1; p = 0.50; I2 = 0%; falls-level data: χ2 = 0.30, df = 1; p = 0.59; I2 = 0%; see Appendix 6, Table 36).
The data on novel shock-absorbing flooring (OR 1.25, 95% CI 0.24 to 6.47; p = 0.79; two studies; I2 = 0%) and sports flooring (OR 0.33, 95% CI 0.01 to 8.15; p = 0.50) were too sparse to detect whether or not these floors are effective at reducing hip fractures (Figure 13). Although Simpson et al. 76 found no evidence to suggest that carpeted floors were more effective than uncarpeted floors (OR 1.19, 95% CI 0.77 to 1.84; p = 0.44), the data for wooden versus concrete subfloors, overall, was indicative of a beneficial effect in favour of wooden subfloors (OR 0.59, 95% CI 0.45 to 0.78; p = 0.008; serious risk of bias). Uncarpeted floors contributed heterogeneity to this study’s findings (χ2 = 7.09, df = 1; p = 0.008; I2 = 86%), and the data were also confounded by room type (e.g. uncarpeted areas were typically bathrooms, toilets and utility areas). Assuming that four out of 100 falls result in a hip fracture (based on the control arm of Simpson et al. 76), the effect estimate can be re-expressed to suggest that one fewer person will fracture their hip for every 63 falls (95% CI 47 to 118 falls) that occur on wooden, as opposed to concrete, subfloors (very low-quality evidence). Or, if 40 out of 1000 falls result in hip fracture on a concrete subfloor, then 16 (95% CI 9 to 22) fewer falls out of 1000 will result in hip fracture on wooden subfloors (see Table 9 for an alternative re-expression based on a lower assumed risk).
FIGURE 13.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: number of hip fractures. a, Hanger49 are unpublished data; data for the control arm have been split between the three comparisons; b, Mackey et al. 50 events data were obtained via personal communication; c, Drahota et al. 77 data are adjusted for clustering (ICC = 0.002); d, Donald et al. 105 is displayed for information; it contributed no data to the analyses. M–H, Mantel–Haenszel. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
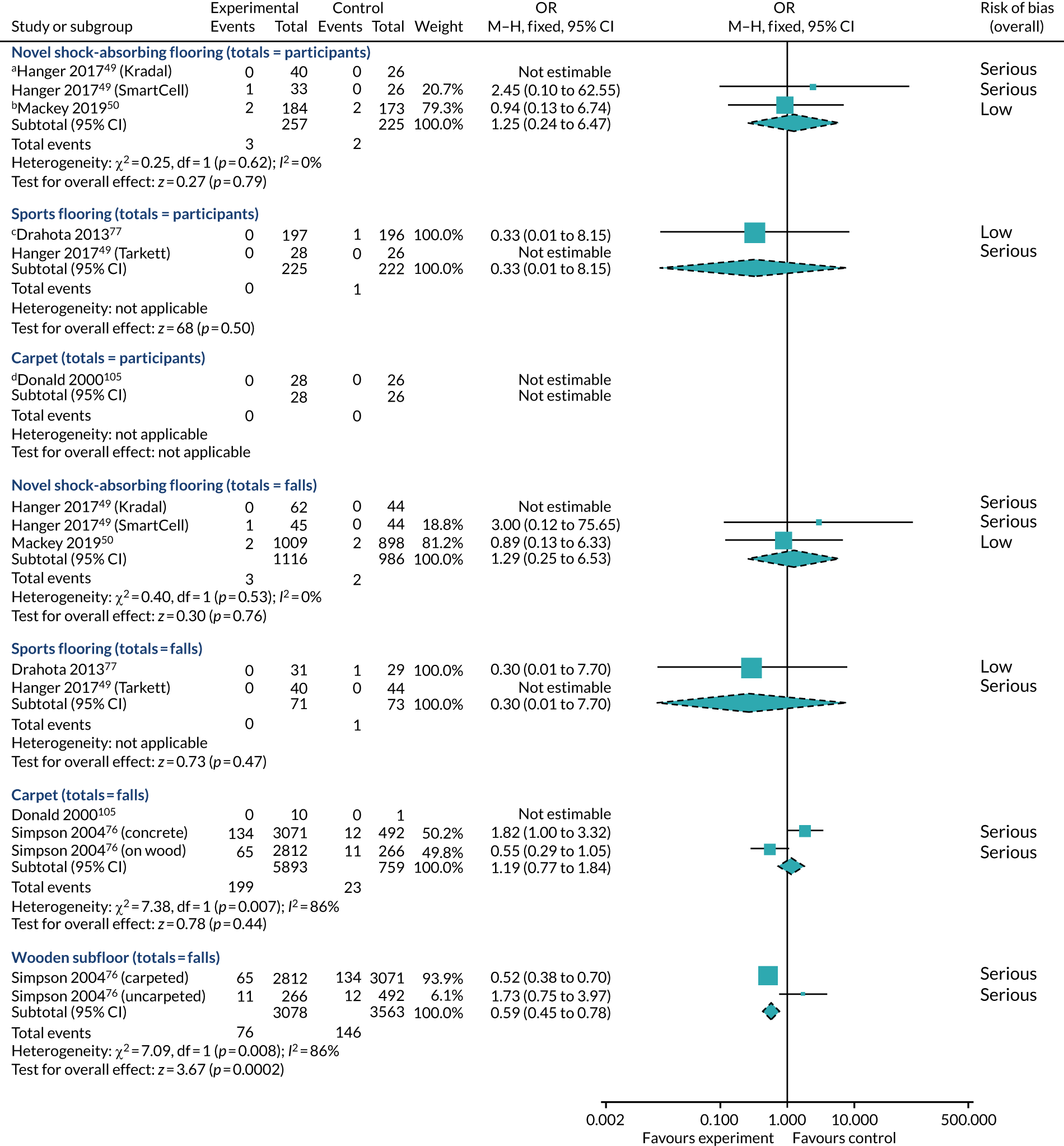
Owing to the imprecision in the majority of the data, there was no indication of a differential effect by flooring types (see Appendix 6, Table 36). This was the case when focusing on the participant-level data (χ2 = 0.53, df = 1; p = 0.47; I2 = 0%); falls-level data comparing novel, sports and carpeted floors (χ2 = 0.69, df = 2; p = 0.71; I2 = 0%); and falls-level data comparing novel floors, sports floors and wooden subfloors (χ2 = 1.03, df = 2; p = 0.60; I2 = 0%). We have not run the test for subgroup differences between all four flooring types in one analysis because the Simpson et al. 76 data contribute to two of the subgroups.
The choice of analysis method (Peto vs. Mantel–Haenszel) did not affect the findings, nor did the choice of ICC for Drahota et al. 77 or adjusting Hanger49 for slightly revised figures that were personally communicated to us (see Appendix 7, Table 37). Reanalysing the data without stratifying Simpson et al. 76 did not alter the bottom-line findings in any of the analyses (see Appendix 7, Table 37). This was the case for carpeted versus uncarpeted floors (stratified: OR 1.19, 95% CI 0.77 to 1.84; combined raw data: OR 1.12, 95% CI 0.72 to 1.73) and for wooden versus concrete subfloors (stratified: OR 0.59, 95% CI 0.45 to 0.78; combined raw data: OR 0.59, 95% CI 0.45 to 0.79). When Simpson et al. 76 was not stratified by the other factor explored in the study, the statistical heterogeneity was removed from all of the analyses. For example, in the analysis of care home studies, for any type of shock-absorbing floor versus control (see Figure 12), the statistical heterogeneity went from being substantial (χ2 = 7.40, df = 2; p = 0.02; I2 = 73%) to unnoteworthy (χ2 = 0.05, df = 1; p = 0.82; I2 = 0%). We received some unpublished data from Gustavsson et al. 52 on the number of hip fractures observed (Johanna Gustavsson, personal communication); however, including these data did not alter the bottom-line conclusions (see Appendix 7, Table 37).
Number of fallers
Three RCTs contributed data to the outcome of number of fallers. 50,77,105 Although the point estimate is in favour of control floors, the CI for the pooled studies incorporates the possibility that shock-absorbing flooring may make no difference to the risk of being a faller (RR 1.28, 95% CI 0.73 to 2.25; p = 0.40; I2 = 46%; Figure 14). Although there was no evidence of a differential effect by setting type (χ2 = 1.20, df = 1; p = 0.27; I2 = 16.4%), it should be noted that the underlying event rates were much higher in the care home study, in which participants had longer exposure to the floors under investigation (68% of the control arm fell in Mackey et al. ,50 compared with 10% in Drahota et al. 77 and 4% in Donald et al. 105). The hospital studies are, therefore, subject to greater imprecision and it is possible that further evidence may change the findings of this analysis.
FIGURE 14.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: number of fallers. a, Drahota et al. 77 has been adjusted for clustering (assumed ICC = 0.02). IV, inverse variance; SE, standard error. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
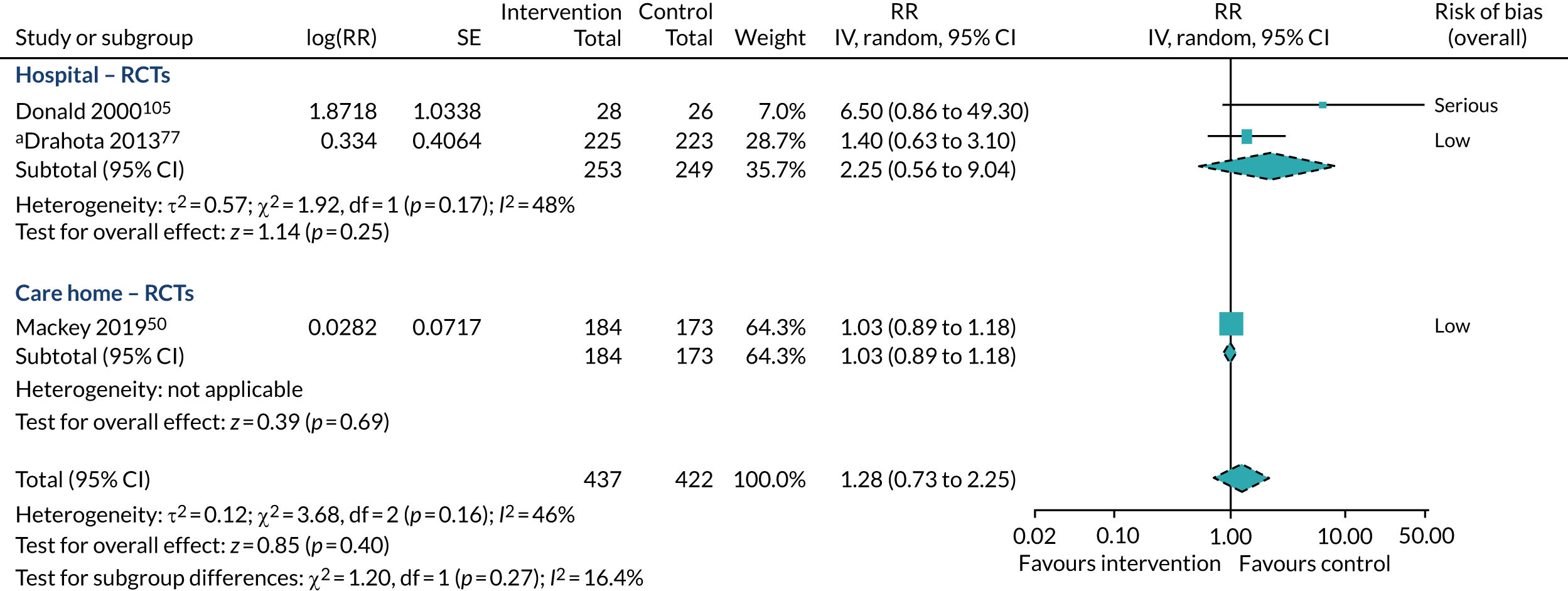
Pooled data from two imprecise trials49,77 offer inconclusive evidence on the influence of shock-absorbing flooring on falling risk in hospitals (RR 2.25, 95% CI 0.56 to 9.04; two studies; I2 = 48%; very low-quality evidence; see Figure 14). Although the CIs overlap, there is some variation between the two studies (τ2 = 0.57), and these studies were quite different with regard to the flooring type under investigation (carpet and sports flooring); Donald et al. 105 was even more prone to random error, as the study was so small, and was also considered to be at higher risk of bias.
Evidence from a single trial suggests that vinyl with a novel shock-absorbing underlay has little or no effect on the risk of being a faller in care homes, when compared with a vinyl floor covering with plywood underlay (RR 1.03, 95% CI 0.89 to 1.18; one trial; high-quality evidence; see Figure 14). 50
The evidence is too sparse to determine if there is a differential effect by flooring type, although none is indicated (χ2 = 3.68, df = 2; p = 0.16; I2 = 45.7%; Figure 15); with only one study per subgroup, this analysis is somewhat problematic and should be interpreted with caution.
FIGURE 15.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: number of fallers. a, Drahota et al. 77 has been adjusted for clustering (assumed ICC = 0.02). IV, inverse variance; SE, standard error.

Sensitivity analyses exploring the influence of the ICC adjustment in Drahota et al. 77 did not change the conclusions for this outcome (see Appendix 7, Table 37). Limiting the analysis to the two studies deemed to be at low risk of bias removes the heterogeneity (τ2 = 0.00, χ2 = 0.55, df = 1; p = 0.46; I2 = 0%) and the pooled effect estimate remains centred around the line of no effect (RR 1.04, 95% CI 0.90 to 1.19; p = 0.60; two studies). 50,77
Adverse events (staff injuries)
Two RCTs collected data on staff injuries;50,77 however, because the unit of allocation in Mackey et al. 50 was the resident room, the data pertaining to staff injuries from working in the care home are more akin to a pre–post design and have not been published. The unit of allocation in Drahota et al. 77 was at the facility level, so staff were randomised in clusters to a ward with or without an intervention flooring bay. One further observational study associated with Hanger49 has since been published in 2020. 106 This study compared injury data over 30 months from the intervention ward with those of three concurrent control wards (no baseline period), and also with a 30-month post-intervention period when the ward was moved to a new site without the intervention flooring (no concurrent control). Hanger and Wilkinson106 is analysed using non-parametric tests, with no adjustments for potential confounding, and time-series data are presented in charts.
Neither of the two hospital-based studies were able to determine a denominator population. In both studies, adverse events occurring in the participating wards were reported, and could have related to staff based both internally and externally to the wards, meaning robust data on the number of staff members and exposure time were not obtained. Hanger and Wilkinson106 obtained staff injury data from the electronic Quality Improvement Event Reporting system, whereas Drahota et al. 77 relied on sites completing adverse events forms as part of the study’s standard operating procedures.
Drahota et al. 77 reported one pulled lower back in the intervention group (8.3-mm sports floor) during the 12-month follow-up period, which occurred while moving a patient on a trolley and did not require medical attention. Staff across the intervention sites raised concerns about moving wheeled equipment on the intervention floor, captured in the qualitative interviews (see Chapter 4), and five additional adverse events forms were submitted to raise concerns (received from two of the four intervention sites), but these did not pertain to specific events/injuries; no adverse events were reported by the control group. 77 Over a 30-month follow-up period, Hanger and Wilkinson106 found no evidence to suggest that there was a higher risk of staff injuries on intervention flooring; if anything, the risk appeared to be lower on the intervention flooring (however, this could have been confounded by improved reporting on control floors).
The care home-based study collected data on staff musculoskeletal injuries from routinely completed staff incident reports for 2 years pre intervention and 1 year post intervention. 109 Data were collected for three groups of staff: (1) all staff (food services, housekeeping, laundry, maintenance, resident care, therapies, administration, housing or other), (2) resident care staff and (3) resident care staff who specifically worked in the four units/villages where the trial was occurring. Overall, the analyses suggested that the intervention flooring (a 25.4-mm novel underlay covered with vinyl) did not increase the risk of force-induced musculoskeletal injuries among long-term care staff, or among resident care staff specifically (unpublished data, Dawn C Mackey, 2020, personal communication).
Overall, the data suggest that, although initial concerns of working on a shock-absorbing floor may be raised, there is very low-quality evidence to suggest that, over longer periods of follow-up, there may be no difference in staff injuries (Table 10).
| Study | Main findings | Comments | Risk of bias |
|---|---|---|---|
| Drahota et al. 201377 | Concerns raised and one pulled lower back in intervention arm. No adverse events reported in control arm (12-month follow-up) | See Chapter 4, Category 4: push and pull challenges | Low |
| Hanger and Wilkinson 2020106 | There were no statistically significant differences in staff injuries between intervention (28 injuries in 30 months) and concurrent control wards (average 30 injuries per ward), or the post-intervention control ward (45 injuries in 30 months) | Quality of reporting improved post intervention | Serious |
| Mackey et al. 201950 | The intervention did not increase force-induced musculoskeletal injuries (24-month follow-up) | Unpublished data. Based on pre–post nested design | Not assessed |
Head injuries
Two studies reported the number of head injuries49,50 and we also obtained personally communicated data pertaining to Gustavsson et al. 52 (Johanna Gustavsson, personal communication) (see Sensitivity analyses). We have analysed the data with both the number of participants and number of falls as the unit of analysis, as it is not clear whether the number of events are independent or could possibly relate to recurrent fallers; this makes a negligible difference to the findings (Figure 16). Although the CIs include the possibility that shock-absorbing flooring may help to reduce the number of head injuries, the data were too imprecise to know this with any certainty and the possibility remains that shock-absorbing flooring makes no meaningful difference when focusing on the RCT data alone (RR 0.60, 95% CI 0.24 to 1.51; p = 0.28) or both studies combined (RR 0.52, 95% CI 0.24 to 1.12; p = 0.10; I2 = 0%). The two studies were statistically similar, although they were conducted in different settings and used different study designs (test for subgroup differences: χ2 = 0.26, df = 1; p = 0.61; I2 = 0%).
FIGURE 16.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: unit of analysis; outcome: number of head injuries. a, Events based on location of serious fall-related injuries (head/skull). IV, inverse variance; SE, standard error. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
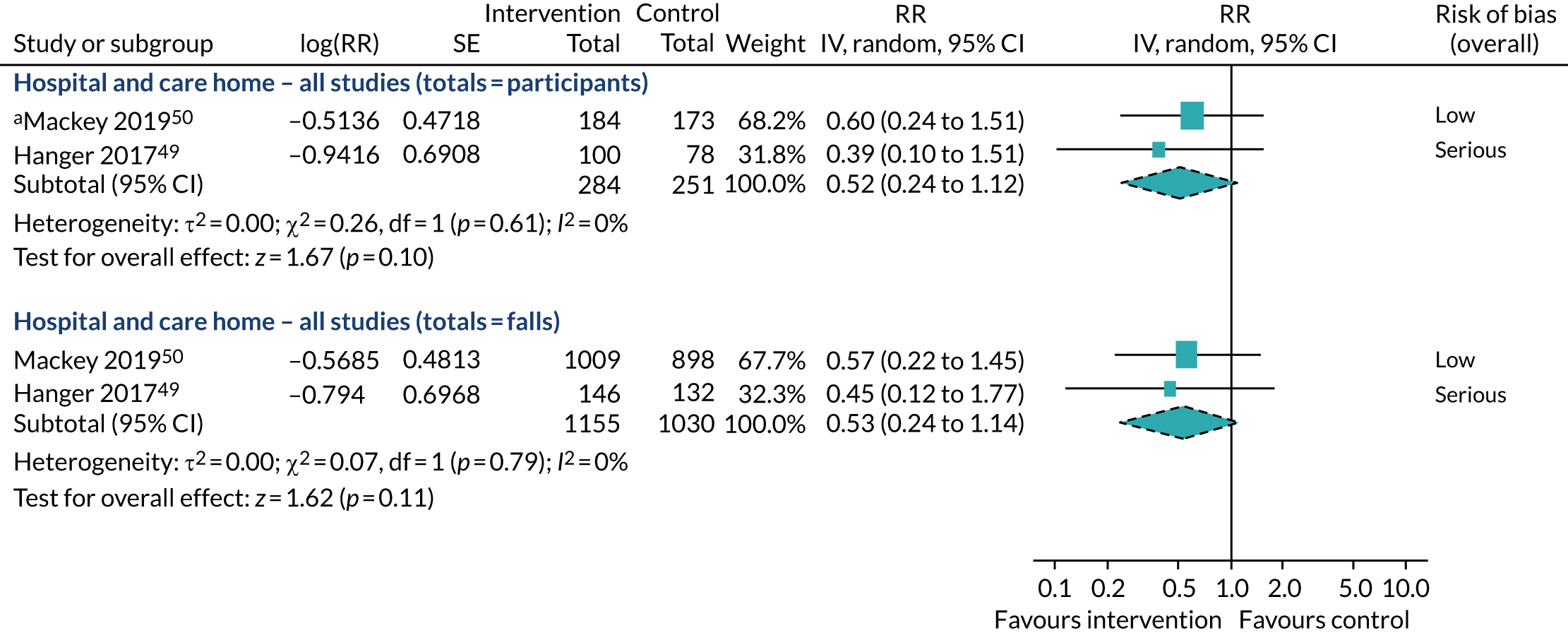
Segregating the data according to flooring type does not reveal any noteworthy differences between novel and sports floors (Figure 17), as the data remain too imprecise to detect any effects (test for subgroup differences at the participant level: χ2 = 0.53, df = 1; p = 0.47; I2 = 0%).
FIGURE 17.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: flooring type; outcome: number of head injuries. a, Hanger49 data unpublished; control group has been split between the three comparisons; b, events based on location of serious fall-related injuries (head/skull). IV, inverse variance; SE, standard error.

We received unreported data from Hanger49 that were slightly different to those published, and data for Gustavsson et al. 52 that had not been previously published (Johanna Gustavsson, personal communication). The Hanger49 data made no material difference to the findings (see Appendix 7, Table 37). The inclusion of Gustavsson et al. 52 improved the precision of the effect estimate to indicate that shock-absorbing flooring may reduce the number of head injuries (all studies combined), when analysed with falls as the unit of analysis (RR 0.55, 95% CI 0.31 to 0.97; p = 0.04; three studies; I2 = 0%). The Gustavsson et al. 52 data also improved the precision of the effect estimate, but not the overall conclusions, when exploring care home findings (RR 0.57, 95% CI 0.31 to 1.07; p = 0.08; two studies; I2 = 0%) and data for novel shock-absorbing floors (RR 0.59, 95% CI 0.33 to 1.04; p = 0.07; three studies; I2 = 0%). The head injury data personally communicated to us from the Gustavsson et al. 52 study included head injuries of any severity, and should be interpreted with some caution as they are from an observational study and have not been adjusted for confounding (see Appendix 7, Table 37).
Fractures per 1000 person-days
It was possible to derive fracture rates for three of the included quantitative studies (none of these analyses have previously been reported). 49,50,77 Mackey et al. 50 opted not to fit regression models for fractures because of the low event rates and data for the other studies were even fewer. 49,77 These data do not provide any further information above and beyond the analyses we have already presented for the number of fractures. The data were too imprecise to detect whether or not shock-absorbing flooring makes a difference to fracture rates when focusing on RCTs alone (RaR 0.75, 95% CI 0.31 to 1.82; p = 0.52; two studies; I2 = 0%; low risk of bias) or all studies (RaR 0.65, 95% CI 0.28 to 1.48; p = 0.30; three studies; I2 = 0%; Figure 18), and there were no indications of any differences by setting type (χ2 = 1.39, df = 1; p = 0.24; I2 = 28.2%; see Figure 18) or study design (χ2 = 0.75, df = 1; p = 0.39; I2 = 0%; see Appendix 6, Table 36). We opted not to run subgroup analyses for flooring type because of the number of continuity corrections required when using this analysis method; instead, we refer readers to the outcome of number of fractures for this exploration.
FIGURE 18.
Forest plot of comparison: any shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: fracture rate per 1000 person-days. a, Adjusted for clustering (assumed ICC = 0.002); continuity correction of 0.5 added to event counts because there were zero events in the intervention arm; b, number of person-days obtained via personal communication. IV, inverse variance; SE, standard error.
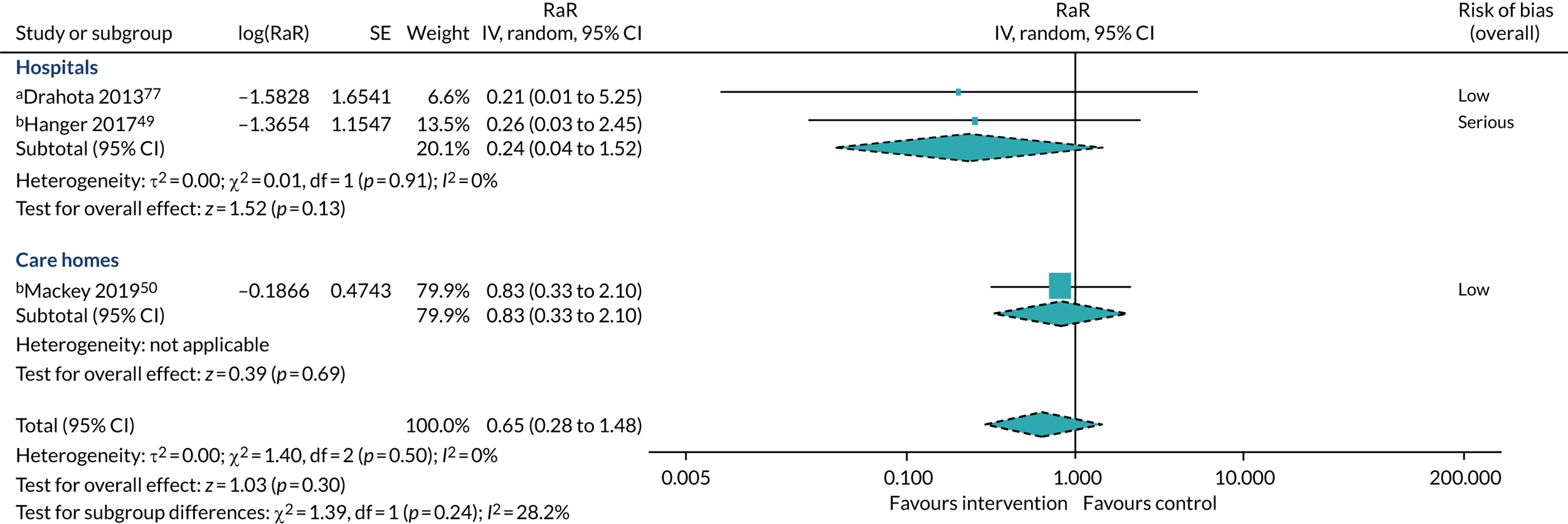
Selecting more or less conservative ICCs for Drahota et al. 77 did not affect the overall conclusions (see Appendix 7, Table 37). We ran a sensitivity analysis to include the data cited in the economic study by Lange;82 however, this only marginally improved the precision, without affecting the overall conclusions (see Appendix 7, Table 37).
Hip fractures per 1000 person-days
Derived hip fracture rates were obtainable from three studies (Figure 19). 49,50,77 The data were sparse and the imprecision means that there is insufficient information to determine whether or not shock-absorbing flooring can influence hip fracture rates (RCTs deemed to be at low risk of bias: RaR 0.73, 95% CI 0.13 to 4.01; p = 0.72; all studies: RaR 0.94, 95% CI 0.21 to 4.23; p = 0.94). There was no evidence to indicate any difference by setting (χ2 = 0.02, df = 1; p = 0.88; I2 = 0%; see Figure 19) or study design (χ2 = 0.38, df = 1; p = 0.54; I2 = 0%; see Appendix 6, Table 36). We opted not to run subgroup analyses for flooring type because of the number of continuity corrections required when using this analysis method and splitting Hanger49 down into even smaller pairwise comparisons; we refer readers to the outcome of ‘number of hip fractures’ for this exploration.
FIGURE 19.
Forest plot of comparison: shock-absorbing flooring vs. rigid flooring; subgroups: settings; outcome: hip fractures per 1000 person-days. a, Adjusted for clustering (assumed ICC = 0.002); continuity correction of 0.5 added to event counts because there were zero events in the intervention arm; b, number of person-days obtained via personal communication; continuity correction of 0.5 added to event counts because there were zero events in the control arm; c, number of events and person-days obtained via personal communication. IV, inverse variance; SE, standard error.

Selecting more or less conservative ICCs for Drahota et al. 77 did not affect the overall conclusions (see Appendix 7, Table 37).
Process outcomes
We did not identify any published process evaluations associated with the included studies; however, installation and maintenance were discussed as part of the qualitative outcomes, as well as rich data on the practical issues of using the floor (see Chapter 4). In addition, two hospital-based quantitative studies reported on practicality issues associated with shock-absorbing flooring, summarised in the following section. 49,77
The initial phase of Hanger49 was to determine the practicality issues associated with shock-absorbing flooring; additional costs of shock-absorbing flooring were identified as being one of the factors that influenced decision-making not to invest further in the products. No further details were provided of what these costs were and no mention was made of any issues related to installation. 49 Drahota et al. 77 described how the installation process was managed, with hospital wards planning for a 1-week installation in which intervention bays were gradually ‘run down’ by not admitting new patients or by transferring patients to vacant beds elsewhere in the ward or hospital. The installation process was planned directly between each hospital estate and facilities department and the prime contractors installing the floor. Thresholds between the intervention floors and standard floors in adjoining areas were managed using a transition strip or gradual ‘seamless’ gradient. The installation processes took place in accordance with the study schedule. One out of four of the intervention sites in Drahota et al. 77 reported a 20- to 30-cm split seam in the new floor, attributed to the welding at installation, which was subsequently repaired.
One of the potential advantages of shock-absorbing floors is that they require no adherence, as such, on the part of patients/residents and staff. However, an overview of the evidence reveals that they are not a panacea in this regard, as not all flooring types are deemed suitable for all areas of an institution and falls do not always occur in the areas in which the shock-absorbing flooring maybe implemented. Table 11 reports data for studies in which we can assess the implementation areas for intervention and control groups. The hospital studies were similar in that they targeted the bedded areas, which are where most falls occurred (weighted average 84%; two studies). 49,77 The care home studies investigated different floor types, which were selected for use in different areas; notably, the SmartCells floor50 is a shock-absorbing underlay, which can be combined with vinyl coverings suitable for use in wet areas (the percentage of falls protected against was not given). Gustavsson et al. 52 included the communal areas alongside resident rooms (excluding bathrooms in the intervention group); 91% of falls occurred on one of the surfaces being compared in this study [note that the majority of the falls excluded (7.6%) occurred on mattresses and fall mats]. However, approximately 118 of the falls in the control group of Gustavsson et al. 52 were in bathrooms (not an area covered by the intervention floor), which, if accounted for, bring the proportion of falls occurring on target areas down to 78% in this study.
| Study | Intervention | Areas covered by intervention flooring | Total number of falls | Percentage of falls on target areas |
|---|---|---|---|---|
| Hospitals | ||||
| Drahota et al. 201377 | Tarkett Omnisports Excel | Hospital bays (bedded areas excluding bathrooms and corridors) | 68 | 75 |
| Hanger 201749 | Tarkett Omnisports Excel, Kradal and SmartCells | Hospital bays (bedded areas excluding bathrooms and corridors) | 323 | 86 |
| Care homes | ||||
| Mackey et al. 201950 | SmartCells | Resident rooms (living, bathroom and closet areas) excluding common areas (dining rooms, hallways, lounges, outside areas) | Not described; only bedroom falls reported | |
| Gustavsson et al. 201852 | Kradal | Resident apartments, communal dining room, corridor (excluding bathrooms and outdoor areas) | 851 | 78 |
Both Hanger49 and Drahota et al. 77 referred to issues associated with the increased effort required to move wheeled equipment across the intervention floors. Information documented in the 2011 full report of Drahota et al. 118 highlighted that one of the four intervention sites increased staffing (raised from six staff at baseline to seven staff during follow-up covering the 07.00–15.00 shift), which was reportedly to assist with the manual handling of equipment during the busy morning periods. Another intervention site in the same study altered the shift patterns of staff (maintaining the overall staffing levels), moving one staff member from the morning shift to increase the cover on the night shift. This alteration coincided with a patient group change (from a general care of the elderly to a care of the elderly with fractured neck of femur), but it was reported verbally to the researchers that the change was in response to concerns regarding moving equipment on the intervention floor during the night.
Head-to-head comparisons
Hanger49 was the only study that was able to provide (unpublished) data to support the direct comparison of different types of shock-absorbing floors. In this observational, hospital-based study, the published data from the different intervention floors were pooled into one intervention group to improve the power of the analyses; therefore, the analyses we present here are subject to large degrees of imprecision. The data have not been adjusted for confounding and the outcomes are at serious risk of bias. For these reasons, the quality of the evidence for all head-to-head comparisons has been graded as very low (Tables 12–14).
| Outcomes | Anticipated absolute effectsa (95% CI) | Relative effect (95% CI) | Total sample size (n studies) | Quality of the evidence (GRADE)b | Comments | |
|---|---|---|---|---|---|---|
| Risk with SmartCells | Risk with Kradal | |||||
| Injurious falls rate per 1000 person-days | ||||||
| Observational studies | 2 per 1000 | 2 per 1000 (1 to 5) | RaR 1.00 (0.45 to 2.23) | 6382 person-days (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Falls rate per 1000 person-day | ||||||
| Observational studies | 9 per 1000 | 13 per 1000 (9 to 19) | RaR 1.38 (0.94 to 2.02) | 6382 person-days (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of falls resulting in injury | ||||||
| Observational studiesc | 254 per 1000 | 185 per 1000 (91 to 370) | RR 0.73 (0.36 to 1.46) | 107 falls (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of fractures | ||||||
| Observational studies | 43 per 1000 | 12 per 1000 (0 to 236) | OR 0.27 (0.01 to 6.79) | 73 participants (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of hip fractures | ||||||
| Observational studies | 11 per 1000 | 3 per 1000 (0 to 69) | OR 0.27 (0.01 to 6.79) | 73 participants (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of fallers | ||||||
| Observational studies | No data available | |||||
| Adverse events | ||||||
| Observational studies | No data available | |||||
| Outcomes | Anticipated absolute effectsa (95% CI) | Relative effect (95% CI) | Total sample size (n studies) | Quality of the evidence (GRADE)b | Comments | |
|---|---|---|---|---|---|---|
| Risk with Tarkett Omnisports Excel | Risk with Kradal | |||||
| Injurious falls rate per 1000 person-days | ||||||
| Observational studies | 2 per 1000 | 3 per 1000 (1 to 7) | RaR 1.50 (0.61 to 3.67) | 6382 person-days (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Falls rate per 1000 person-days | ||||||
| Observational studies | 8 per 1000 | 12 per 1000 (8 to 18) | RaR 1.55 1.04 to 2.31) | 6382 person-days (1 study) |
⊕◯◯◯ Very low |
If eight falls occur per day among 1000 inpatients on Tarkett Omnisports Excel (sports flooring), then very low-quality evidence suggests that four more (95% CI 0 to 10 more) falls per day may occur on Kradal (novel flooring) |
| Number of falls resulting in injury | ||||||
| Observational studiesc | 229 per 1000 | 222 per 1000 (98 to 494) | RR 0.97 (0.43 to 2.16) | 102 falls (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of fractures | ||||||
| Observational studies | Not estimable, as there were zero events in both groups | 68 participants (1 study) |
⊕◯◯◯ Very low |
There were zero events in both groups | ||
| Number of hip fractures | ||||||
| Observational studies | Not estimable. See comments | 68 participants (1 study) |
⊕◯◯◯ Very low |
There were zero events in both groups | ||
| Number of fallers | ||||||
| Observational studies | No data available | |||||
| Adverse events | ||||||
| Observational studies | No data available | |||||
| Outcomes | Anticipated absolute effectsa (95% CI) | Relative effect (95% CI) | Total sample size (n studies) | Quality of the evidence (GRADE)b | Comments | |
|---|---|---|---|---|---|---|
| Risk with Tarkett Omnisports Excel | Risk with SmartCells | |||||
| Injurious falls rate per 1000 person-days | ||||||
| Observational studies | 2 per 1000 | 3 per 1000 (1 to 7) | RaR 1.50 (0.61 to 3.67) | 6382 person-days (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Falls rate per 1000 person-days | ||||||
| Observational studies | 8 per 1000 | 9 per 1000 (6 to 13) | RaR 1.13 (0.73 to 1.72) | 6382 person-days (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of falls resulting in injury | ||||||
| Observational studiesc | 229 per 1000 | 304 per 1000 (139 to 670) | RR 1.33 (0.61 to 2.93) | 85 falls (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome |
| Number of fractures | ||||||
| Observational studies | Not estimable. The risk with Tarkett is currently unknown because there are few data | OR 2.63 (0.10 to 67.17) | 61 participants (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome | |
| Number of hip fractures | ||||||
| Observational studies | Not estimable. The risk with Tarkett is currently unknown because there are few data | OR 2.63 (0.10 to 67.17) | 61 participants (1 study) |
⊕◯◯◯ Very low |
These data are too imprecise to offer any certainty for this outcome | |
| Number of fallers | ||||||
| Observational studies | No data available | |||||
| Adverse events | ||||||
| Observational studies | No data available | |||||
Three different shock-absorbing floors were incorporated into the study: two novel floors specifically designed for fall-related injury prevention among older adults (Kradal and SmartCells), and one originally designed as a sports floor (Tarkett Omnisports Excel).
Primary outcomes
Injurious falls rate per 1000 person-days
For this analysis, the number of person-days in each group was approximated based on the total number of bed-days estimated in the intervention arm of the published study (3191 person-days for each floor type). There were 12 injurious falls on SmartCells flooring and Kradal flooring, and eight injurious falls on Tarkett; the data were too imprecise to detect if any flooring may be superior to another at preventing injurious falls (Figure 20).
FIGURE 20.
Forest plot of head-to-head comparisons; outcome: injurious falls rate per 1000 person-days. a, Data obtained via personal communication for Hanger (with Dr Carl Hanger). 49 IV, inverse variance; SE, standard error.
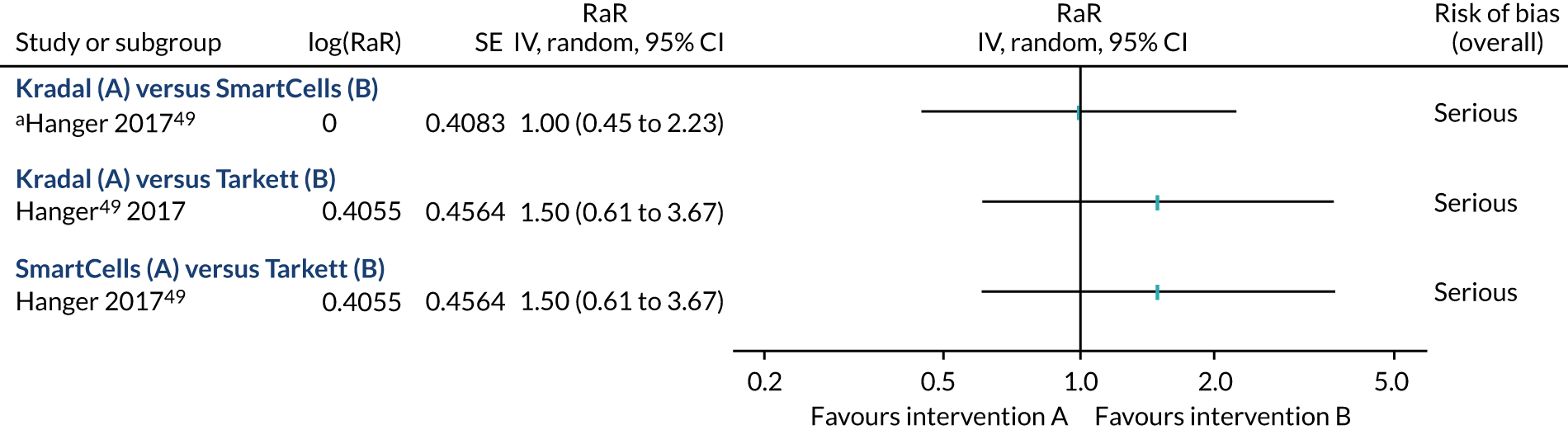
Falls rate per 1000 person-days
As with the injurious falls rate, the number of bed-days in each group of this analysis were approximated to equal 3191. Fewer falls were experienced on Tarkett flooring (40 events) than on Kradal flooring (62 events), indicative of a positive effect, with uncertain clinical significance due to large imprecision (RaR 1.55, 95% CI 1.04 to 2.31; p = 0.03). These data should be interpreted with caution because any observed difference may be due to confounding. A similar number of falls (n = 45) were experienced on SmartCells as on Tarkett and, owing to the imprecision, it is not clear whether SmartCells may be any better or worse than the other floors (Figure 21).
FIGURE 21.
Forest plot of head-to-head comparisons; outcome: falls rate per 1000 person-days. a, Data obtained via personal communication for Hanger (with Dr Carl Hanger). 49 IV, inverse variance; SE, standard error.
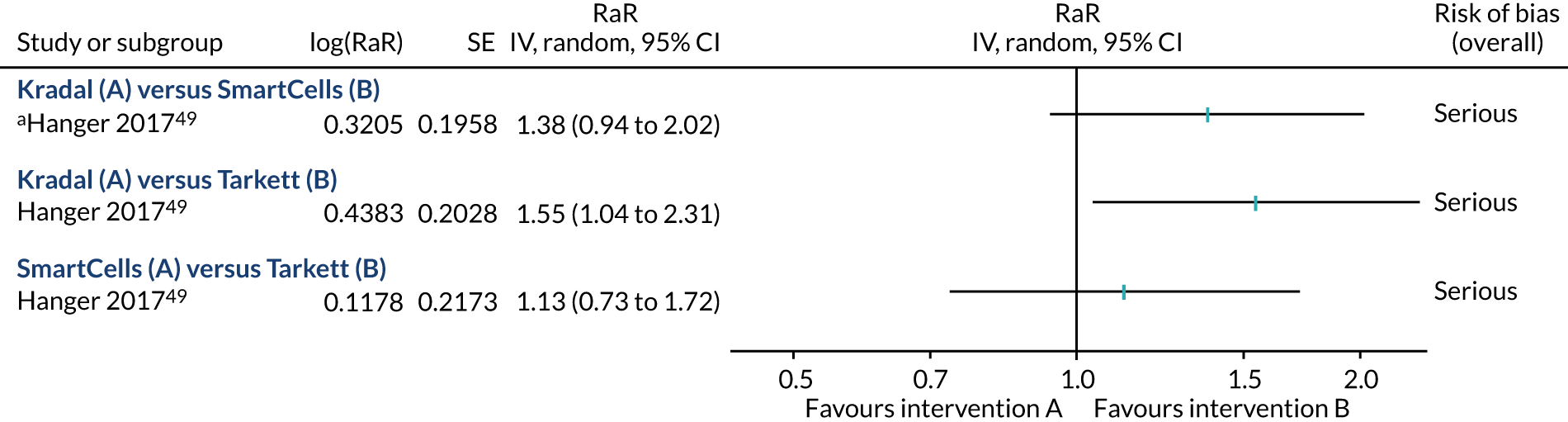
Secondary outcomes
Number of falls resulting in injury
The two serious injuries that occurred in the intervention group in Hanger49 both occurred in a bedroom with the SmartCells flooring (one hip fracture and one head injury with a major laceration, which was caused by hitting the door surrounds rather than the floor). Patients experienced a similar proportion of minor and moderate injuries across the various shock-absorbing flooring types in Hanger49 (Figure 22).
When exploring the number of falls that result in any type of injury, the data are too imprecise to determine any meaningful differences (Figure 23); it is possible that there are no differences between the shock-absorbing flooring types observed, but we cannot conclude this with any certainty.
FIGURE 23.
Forest plot of head-to-head comparisons; outcome: number of falls resulting in injury. a, Data obtained via personal communication for Hanger (with Dr Carl Hanger). 49 IV, inverse variance; SE, standard error.
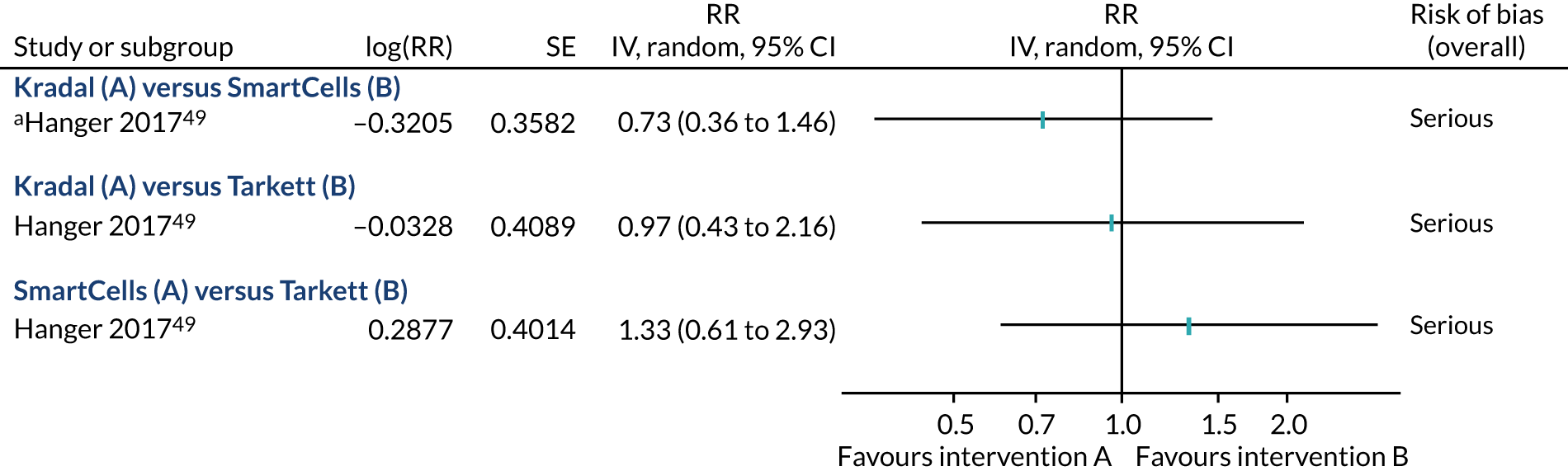
Number of fractures
Only one fracture occurred on shock-absorbing flooring (SmartCells) in Hanger49 out of the 33 people who fell on the SmartCells flooring. Forty people fell on Tarkett flooring and 28 people fell on Kradal flooring, without fractures. 49 There are too few data to detect any suggestion of a difference between shock-absorbing flooring types.
Number of hip fractures
The single fracture that occurred on SmartCells in Hanger49 was to the hip; however, as stated previously, the data are too few to draw any meaningful conclusions as to whether or not certain shock-absorbing floor types may be more successful than others at reducing the risk of hip fracture.
Number of fallers
No data are available on the risk of being a faller from Hanger;49 this is because the data collected in the study were on those who fell only and not the entire patient population.
Number of head injuries
Data on the number of head injuries were also few in Hanger;49 in Figure 24, we present the comparisons using the Mantel–Haenszel method of analysis with ORs; however, the conclusions remain the same if using RRs. Although no head injuries were reported from falls on the Tarkett flooring, one of the head injuries in the SmartCells group was a result of an impact with the door surrounds, rather than the flooring, and only two further moderate head injuries were documented (one in each of the SmartsCells group and the Kradal group). With these data, we cannot conclude if any particular intervention floor is more favourable or confidently state if they have similar effects on head injuries.
FIGURE 24.
Forest plot of head-to-head comparisons; outcome: number of head injuries. a, Data obtained via personal communication for Hanger (with Dr Carl Hanger). 49 M–H, Mantel–Haenszel.
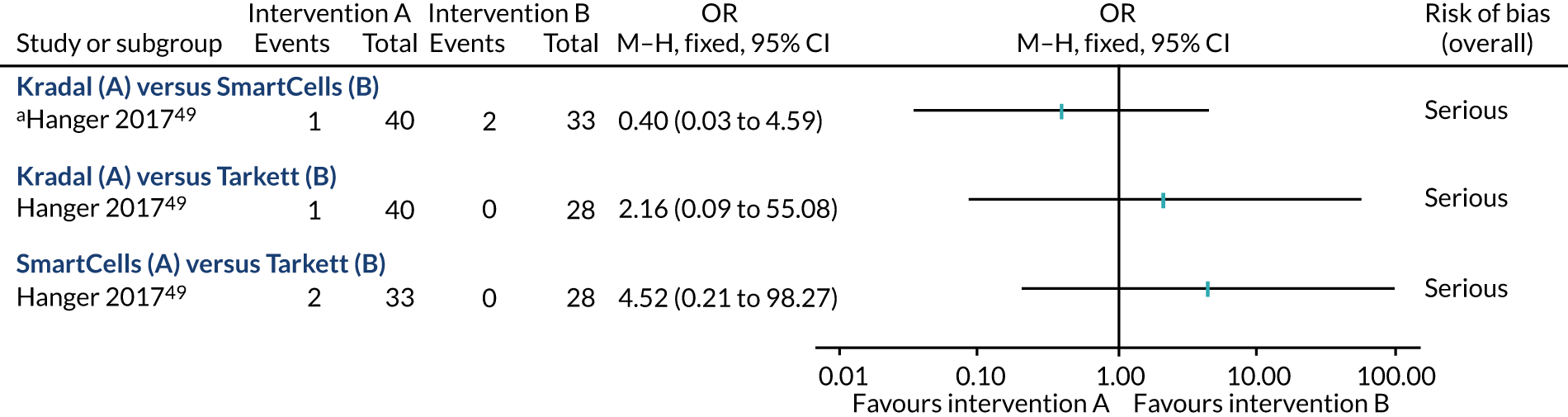
Rate of fractures and hip fractures
Given the sparsity of fractures (one fracture in the SmartCells group only) in Hanger,49 we have not attempted to derive fracture rates to make head-to-head comparisons for this one study.
Process outcomes
We do not have any data from direct comparisons of different shock-absorbing floor types pertaining to process outcomes.
Conclusions
We included 12 quantitative studies; however, only 10 of these contributed data to our prespecified outcomes, ranging from three to seven studies for any one outcome. We identified two well-conducted RCTs from different settings (one being very imprecise),50,77 and another small RCT with concerns around risk of bias;105 each of the RCTs investigated a different floor type. Potential confounding alongside other risks of bias afflicts the observational evidence. The studies were heterogeneous concerning the comparisons explored, settings and areas studied, population sampling, and definition of outcomes.
With these caveats in mind, there is very low-quality hospital-based evidence to suggest that certain types of shock-absorbing flooring may reduce injuries without increasing the rate of falls. The hospital-based data for risk of falling, fracture and head injury are too imprecise to determine effectiveness. The care home-based evidence suggests that novel shock-absorbing flooring (specifically SmartCells underlay with vinyl overlay and concrete subfloor) does not reduce the number of injuries (high-quality evidence), nor increase the number of falls (moderate-quality evidence) or fallers (high-quality evidence), when compared with a vinyl overlay with plywood underlay and concrete subfloor. 50 Incorporating the observational data on care homes suggests that shock-absorbing flooring may reduce the number of falls resulting in injury (very low-quality evidence). The fracture and head injury data in care homes are too imprecise to determine effectiveness.
The data for different types of floor coverings were often imprecise, with few studies in each subgroup. There were also some overlaps between setting type and flooring type, meaning that it is difficult to attribute any signals in the data to one particular factor. Novel floors, sports floors and carpet all demonstrated a reduction in injuries (very low-quality evidence) depending on how the data were analysed (i.e. as a rate or risk), while retaining the probability that they may not increase the risk of falls or of being a faller. The data on fractures were generally too imprecise to be conclusive; however, one observational study judged to be at high risk of bias, which compared wooden with concrete subfloors, indicated that fewer hip fractures were likely to occur on wooden subfloors. 76 The head-to-head comparisons for different flooring types were all personally communicated from the same observational study (unadjusted for confounding), and subject to large imprecision. Only one of the comparisons for one outcome (falls rate) was indicative of a potential difference, with Tarkett sports flooring outperforming Kradal novel flooring (very low-quality evidence); however, owing to the large imprecision and risk of bias for all of the head-to-head comparisons, the evidence remains uncertain.
The data for adverse events suggest that, although initial concerns of staff working on a shock-absorbing floor may be raised, there may be no difference in staff injuries over longer periods of follow-up; this evidence is of very low quality. Process outcomes indicate that shock-absorbing flooring affects the work environment, resulting in adaptations to staffing levels and schedules to accommodate the increased effort required to move wheeled objects on the intervention flooring. Some shock-absorbing floors have limitations as to where they can be laid (e.g. they are not all suitable for wet areas) and other objects can break a fall causing further injury (e.g. doorways and furniture). Therefore, the implementation of shock-absorbing floor coverings will not successfully protect 100% of fallers (even if they offer suitable shock absorbency); however, covering at least the bedded areas captured upwards of 75% of falls in these studies.
In summary, the high-quality quantitative evidence does not support the use of shock-absorbing flooring; however, this relates to a specific comparison (vinyl with novel underlay and concrete subfloor vs. vinyl with plywood underlay and concrete subfloor) in care homes. It is possible that a control group of vinyl on a concrete subfloor and/or a hospital setting with a higher turnover of (acutely unwell) patients would have produced a more pronounced effect. There is very low-quality evidence that shock-absorbing flooring may be beneficial; however, any estimate of effect is very uncertain.
Chapter 4 Findings from qualitative evidence
Description of studies
Characteristics of included studies
We have included five qualitative studies (Table 15): one study was conducted in elderly care wards across eight hospitals in the UK,118 three studies were conducted with individuals from 18 nursing homes (Sweden, two studies;51,53 Canada, one study54), and one was conducted with staff from seven inpatient hospices and nine care homes in England and Australia. 68 The data represent the views and experiences of 147 people, including the perspectives of hospital patients (n = 12), hospital visitors (n = 8), hospital/hospice staff (n = 84) across a range of roles (managerial, doctors, nurses, allied health professions, domestic staff), residents (n = 8), long-term care enrolled nurses (n = 8) and senior managers of nursing homes (n = 27).
| Study | Setting | Population | Inclusion criteria (main) | Phenomena of interest | Flooring discussed | Approach | Public involvement | Conflict of interest | Analysis categoriesa |
|---|---|---|---|---|---|---|---|---|---|
| Drahota et al. 2011118 | 8 elderly care hospital wards, UK | 12 patients (11 female), 8 visitors, 77 hospital staffb (67 female) | Patients/visitors in the ‘study area’, orientated to person/time/place. Staff with experience of working in the study area | User views and perceptions on the intervention flooring and existing flooring | Tarkett Omnisports Excel (8.3-mm sports floor); vinyl | Exploring perceptions through semistructured face-to-face interviews; thematic content analysis | Yesc | No | 1–9 |
| Gustavsson et al. 201751 | 1 nursing home, Sweden | 8 enrolled nurses; aged 40–60 years; male = 0; female = 8 | Enrolled nurses with 12 months’ experience of impact-absorbent flooring | Experiences of impact-absorbing flooring | Kradal (12-mm closed cell tiles) | Exploratory study of shared experiences; two focus groups; qualitative content analysis | None described | No | 1–4, 7–8 |
| Gustavsson et al. 201853 | 2 nursing homes, Sweden | 8 residents; aged 74–94 years; male = 2; female = 6 | Sufficient cognitive ability to participate in an interview. Lived in residential care with compliant flooring for ≥ 3 months | Experience of falls, risk of fall injury, prevention in general and specifically compliant flooring | Kradal (12-mm closed cell tiles) | Grounded theory study using in-depth semistructured individual interviews | None described | No | 1–2 |
| Lachance et al. 201854 | 16 nursing homes, Canada | 18 senior managers; aged 37–66 years; male = 3; female = 15 | In a senior management role at a long-term care site in the locality; involved in clinical and operational aspects, including implementing fall injury prevention interventions | Perspectives of barriers to and enablers of adoption of compliant flooring to prevent falls in long-term care homes | Purpose-designed compliant flooring (a padded layer, generally found beneath vinyl or carpet) | Exploring perceptions through in-depth, semistructured face-to-face interviews, analysed using a thematic framework method | None described | No | 2–10 |
| Rigby and O’Connor 201268 | 7 hospices and 9 care homes, England and Australia | Hosts: 14 nurse managers or ward sisters; 1 palliative care specialist nurse; 1 medical consultant. Plus other ‘interested staff’. Host staff all ‘older’ females | Staff at participating institutions. Host staff provided a guided tour; other ‘interested staff’ also joined in discussions. No exclusion criteria described | Experiences of working in care home/hospice buildings | Carpets and vinyl | Exploring experiences through guided tours and conversations lasting 1–6 hours at each site. Extensive note-taking post visit of observations and conversations. Analysis method not described | None described | No | 4, 8 |
One study discussed the built environment more broadly, within which the topic of carpets was raised (in this study, we extracted only the findings relevant to our research question). 68 All four remaining studies included individuals who had direct experience of novel/sports shock-absorbing flooring (n = 84, range 7–61). Three studies explored the views and experiences of specific flooring systems (Tarkett Omnisports Excel, one study;118 Kradal, two studies51,53), and one explored perspectives towards the adoption of ‘purpose-designed compliant’ flooring more generally. 54 Studies used face-to-face semistructured interviews (n = 3), focus groups (n = 1) and ‘mini-ethnographic’ guided tours and discussions (n = 1), with a variety of approaches to analysis (thematic content analysis, grounded theory, thematic framework method). The hospital-based study presented two thematic analyses: one for patients and visitors, and another for staff. The two analyses resulted in some overlapping themes, but they were not identical; for the purposes of this synthesis, the findings have been extracted from each analysis separately. 118
Patient and public involvement in the studies was typically not described; however, the UK-based study did incorporate public involvement into the development and oversight of the project. 118 All of the studies appear free of any potential conflicts of interest and did not involve any industry funding. The majority of studies were conducted as part of programmes of research involving the same research teams as those of studies presented in Chapters 3 and 5. 50,52,77,119
Quality assessment of included studies
None of the studies provided a detailed description of the underpinning philosophical perspective (ontology or epistemology), and Drahota et al. 118 lacked a clear description of the researchers’ cultural or theoretical positions, and how these may have influenced the findings. Rigby and O’Connor68 lacked a clear description of the analysis method, and, owing to the nature of data collection, the researchers relied on personal recall to make extensive notes of observations and conversations immediately after site visits, meaning that the report relies on the researchers’ interpretations and lacks representation of the participant voices. However, all other quality markers according to the JBI critical appraisal tool56 were adequately addressed across all of the studies (Table 16).
| Quality assessment criteria | Drahota et al.118 2011 | Gustavsson et al.51 2017 | Gustavsson et al.53 2018 | Lachance et al.54 2018 | Rigby and O’Connor68 2012 |
|---|---|---|---|---|---|
| 1. Is there congruity between the stated philosophical perspective and the research methodology? | Unclear | Unclear | Unclear | Unclear | Unclear |
| 2. Is there congruity between the research methodology and the research question or objectives? | Yes | Yes | Yes | Yes | Yes |
| 3. Is there congruity between the research methodology and the methods used to collect data? | Yes | Yes | Yes | Yes | Yes |
| 4. Is there congruity between the research methodology and the representation and analysis of data? | Yes | Yes | Yes | Yes | Unclear |
| 5. Is there congruity between the research methodology and the interpretation of results? | Yes | Yes | Yes | Yes | Yes |
| 6. Is there a statement locating the researcher culturally or theoretically? | No | Yes | Yes | Yes | Yes |
| 7. Is the influence of the researcher on the research, and vice versa, addressed? | No | Yes | Yes | Yes | Yes |
| 8. Are participants, and their voices, adequately represented? | Yes | Yes | Yes | Yes | No |
| 9. Is there evidence of ethics approval by an appropriate body? | Yes | Yes | Yes | Yes | Yes |
| 10. Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data? | Yes | Yes | Yes | Yes | Yes |
Qualitative results
The five included qualitative studies yielded 69 findings, of which 61 were considered ‘unequivocal’ and eight were judged to be open to challenge, and therefore rated as ‘credible’. These findings were aggregated into 10 categories representing similar concepts (see Report Supplementary Material 2), which were subsequently grouped into three synthesised findings (Figure 25). We have numbered the 69 study findings according to their category (i.e. finding 1.1 is the first finding in category 1; 1.2 is the second finding in category 1, etc.), and tabulated them with illustrative quotations in Report Supplementary Material 2. Six findings contributed to two categories each owing to their breadth in scope; the remaining 63 findings contributed to one category each.
FIGURE 25.
Qualitative synthesis overview flow chart. Reproduced from Drahota et al. 1 © The Author(s) 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
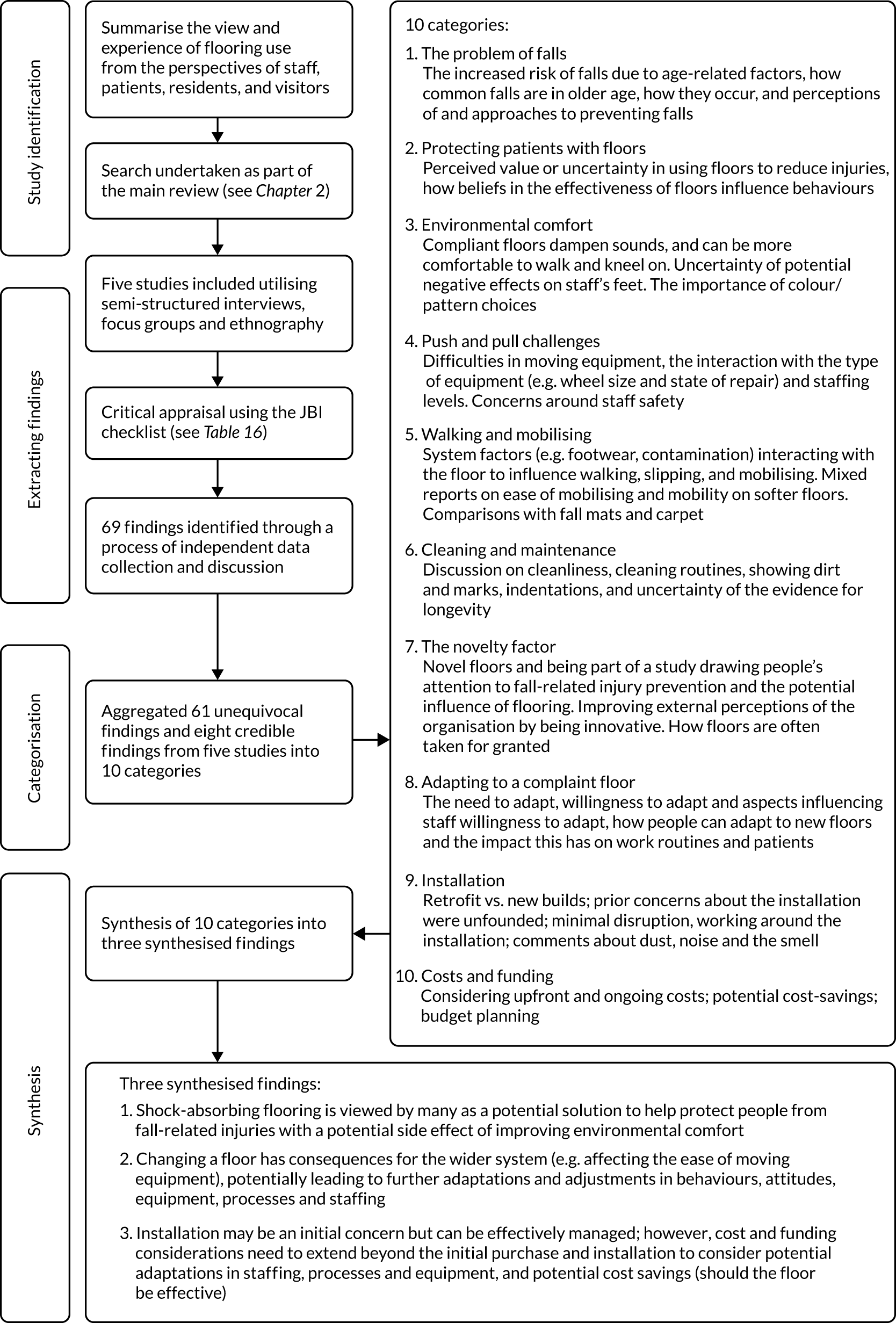
The three synthesised findings were graded according to an assessment of confidence in the evidence, using the CERQual approach (Table 17). 85 We have moderate confidence in the evidence supporting the first and third synthesised findings, and high confidence in the second synthesised finding; a breakdown of our assessments can be viewed in the evidence profile table (see Appendix 9, Table 39). The findings should be read together to obtain the most coherent understanding of the evidence. The first finding relates largely to positive perspectives towards shock-absorbing flooring and the second finding captures more of the negative consequences of shock-absorbing flooring; the third finding has a smaller number of supporting data, but its congruence with the other findings strengthens its case.
| Review finding | CERQual assessment of confidence in the evidence | Explanation of CERQual assessment | Studies contributing to the review finding |
|---|---|---|---|
| Shock-absorbing flooring is viewed by many as a potential solution to help protect people from fall-related injuries, with a potential side effect of improving environmental comfort |
⊕⊕⊕◯ Moderate confidence |
This finding should be read alongside the second synthesised finding. This finding was graded as moderate confidence because of moderate concerns regarding coherence, as, if read in isolation, it does not provide a complete picture of the review findings | Four studies51,53,54,118 |
| Changing a floor has consequences for the wider system (e.g. affecting the ease of moving equipment), potentially leading to further adaptations and adjustments in behaviours, attitudes, equipment, processes and staffing |
⊕⊕⊕⊕ High confidence |
Four studies51,54,68,118 | |
| Installation may be an initial concern, but can be effectively managed; however, cost and funding considerations need to extend beyond the initial purchase and installation to consider potential adaptations in staffing/processes/equipment, and potential cost savings from fall-related injury prevention (should the floor be effective) |
⊕⊕⊕◯ Moderate confidence |
This finding was graded as moderate confidence because of moderate concerns regarding the number of data contributing to the finding (only two studies with data from two settings: hospitals in UK installing sports flooring and care homes in Canada) | Two studies54,118 |
Synthesised finding 1
Shock-absorbing flooring is viewed by many as a potential solution to help protect people from fall-related injuries, with a potential side effect of improving environmental comfort (moderate confidence in the evidence).
Hospital and care home staff and residents acknowledged that falls and related injuries were a common problem in older age. There was discussion of how not all falls are preventable and the wide range of contributing factors that lead to falls (category 1: the problem of falls). Against this backdrop, shock-absorbing floors were seen as a potentially useful solution to help prevent fall-related injuries (category 2: protecting older adults with floors). Participants (particularly senior managers) expressed some uncertainty around the effectiveness of floors and the need to see more evidence; however, there were also staff who held strong beliefs about the value of floors for preventing fall-related injuries. These beliefs led to changes in where staff placed patients and the reduced use of other injury prevention interventions, and provided staff with reassurance that there was a ‘safety net’ in place should their attention be focused elsewhere.
Participants discussed the benefits to staff in terms of improved morale (that they are better able to prevent fall-related injuries), and some conflicted findings on improved comfort when walking and kneeling (category 3: environmental comfort). Shock-absorbing floors were also discussed in relation to their noise-reduction properties, and, where people had witnessed a change in flooring, there were mixed views expressed around colour and pattern choices, and their influence on the ambient environment, emphasising the need to consider the overall environmental design when changing a floor. We grouped 28 study findings into the three categories that make up this first synthesised finding [two study findings ‘2.3/3.7’ and ‘2.9/3.10’ (i.e. category 2, finding 3; category 3, finding 7; etc.; see Qualitative results) were grouped into two categories].
Category 1: the problem of falls
This category describes people’s perceptions and experiences surrounding the increased risk of falls owing to a variety of age-related factors. Participants expressed how common (or normal) falls are in older age, the reasons they believed falls occur, whether or not falls are perceived to be preventable, and the ways in which people attempt to prevent them. Eleven findings (nine unequivocal, two credible) from three studies contributed to this category.
Enrolled nurses in care homes acknowledged the problem of falls and discussed the ways in which falls come about, such as through misjudging distances (finding 1.1, unequivocal evidence). 51 Although the interviews with hospital staff were focused on the topic of flooring, they discussed how the floor is part of a wider system of factors influencing fall outcomes, such as a patient’s condition (finding 1.2, unequivocal evidence),118 clutter (finding 1.3, unequivocal evidence)118 and being in an unfamiliar environment (finding 1.4, unequivocal evidence):118
Obviously it depends on the patient, it’s very patient based . . . so if we’ve got somebody who backward leans quite a lot then you’re gonna get that movement anyway of feet sliding along the floor, so we would automatically block somebody’s feet anyway.
Staff member, hospital. 118
At home they’re more likely to fall on a carpet or they know which piece of furniture to reach for because they’re in their own environment, but in hospital if they’re the slightest bit confused and you’ve put them into a strange environment [. . .] they’re more likely to fall.
Staff member, hospital. 118
Care home residents trivialised falls as ‘these little things’ (finding 1.5, unequivocal evidence)53 and considered them a normal part of life (finding 1.6, unequivocal evidence). 53 Despite this, residents expressed worries and fears about falling and the subsequent consequences (finding 1.7, unequivocal evidence):53
I was in another care home and I fell. I hit my head badly and was bleeding, but that’s common.
Resident, care home53
The fall can be the end of me. I once saw someone fall by the toilet door and they never recovered. It makes you think about the consequences of a fall.
Resident, care home53
Care home residents discussed how fear of falls can affect their lives, with demanding situations (such as new environments and social events) giving rise to insecurities about falling (finding 1.8, credible evidence),53 and a feeling of having a body that lets you down and cannot be trusted (finding 1.9, credible evidence). 53 Residents accepted falls as inevitable events that you cannot prepare for (finding 1.10, unequivocal evidence),53 with their ideas for preventing falls often being vague or about trying to be careful (finding 1.11, unequivocal evidence):53
You can’t prepare for them [the falls], it never happens at the same time. When it happens it happens. It’s simply a surprise.
Resident, care home53
I think you have to be very careful. When I’m going to sit here on this chair, I’ll take small steps and turn around. I’m very, very careful of course.
Resident, care home53
Category 2: protecting older adults with floors
This category brings together nine findings (eight unequivocal, one credible) from four studies, which discuss the perceived value that participants placed in the shock-absorbing floors under evaluation. A number (but not all) of the participants had formulated strong belief systems as to the effectiveness of shock-absorbing flooring based on their experiences of using it. Senior managers (not all of whom had personal experience of using shock-absorbing flooring in their own care homes) expressed more uncertainty in using floors to reduce injuries and expressed a desire to see further research evidence. Those staff who believed in the effectiveness of the shock-absorbing floors they had in situ also talked about changes in their attitudes and behaviours as a result of having the floor.
Enrolled nurses in care homes (finding 2.1, unequivocal evidence),51 senior care home managers (finding 2.2, unequivocal evidence),54 hospital patients and visitors (finding 2.3, unequivocal evidence)118 and hospital staff (finding 2.4, unequivocal evidence)118 all expressed their beliefs in the ability of shock-absorbing floors to protect people from fall-related injuries. Care home residents were also considered to have embraced the idea of flooring as an injury prevention measure; however, there were some dissenting views on this (finding 2.5, credible evidence):53
I think we all experience that there’s no harm done, they just softly sit down [on the impact-absorbing flooring].
Enrolled nurse, care home51
This [shock-absorbing] floor is a safer option [. . .] it would cushion any fall [. . .] it makes it less hard underfoot and also I suppose for patients . . . if they did fall or fell out of bed [. . .] the impact is less and that potential damage is much less.
Visitor, hospital. 118
People who have slipped, fallen in that room [with shock-absorbing flooring], it’s, yeah, it has made a difference to injuries or potential injuries that people can sustain from sliding or falling, um, so in that way it’s saved lives, I think . . . A recent one [example] for me was last week, quite a big guy, little bit wobbly on his feet . . . considering how big he was and his risk of internal bleeding because of his disease um, luckily after his fall . . . there wasn’t even any bruising where he could’ve, you know, there could have been serious consequences had he fallen on to hard flooring like in here.
Staff member, hospital. 118
One interviewee [care home resident] felt that she had been forced to move in to residential care and had no opinion of the special flooring, except that she had little faith in its protective capabilities.
Gustavsson et al. 53
Senior care home managers also expressed uncertainties over the clinical effectiveness (finding 2.6, unequivocal evidence),54 and wanted to see more research evidence to support the idea of shock-absorbing flooring and assess the applicability of this evidence to their own context (finding 2.7, unequivocal evidence):54
I would need to know more about how it’s going – like, even this one site, what is the population like? [. . .] do they have the complex residents that we have? So [. . .] I would want to see at another site before I felt comfortable.
Senior manager, care home54
The findings also revealed that, as a consequence of believing in the floor’s capabilities, hospital staff felt reassured (finding 2.4, unequivocal evidence)118 and care home managers also spoke of the potential benefits that better injury prevention could bring to long-term care staff who are emotionally affected by witnessing the consequences of resident falls (finding 2.8, unequivocal evidence). 54 The beliefs that hospital staff held about the flooring’s effectiveness also led them to consider where best to place patients, thereby affecting the ward routines (finding 2.9, unequivocal evidence):118
If for any reason we are engaged somewhere else, like we were with the emergency the other night, and there was no staffing near that bay at the time because of the priority and that patient fell, having at the back of my mind on a day to day basis that that flooring is in there, to save lives and injury, is a comfort.
Staff member, hospital. 118
. . . from a staff perspective watching staff when somebody has fallen and seeing their faces [. . .] it affects people, especially, you know, if you see a rotated hip and the legs rotated and all of that. So it’s just – anything we can do to reduce that [. . .] is a fantastic.
Senior manager, care home54
Because we’ve got that floor we know it’s a special floor and we, and we put our vulnerable patients in that bay because we know if they fall and they fall on that floor then they’re gonna be protected more than they would if they fell in another bay.
Staff member, hospital. 118
Category 3: environmental comfort
This category summarised 10 findings (nine unequivocal, one credible) from three studies, around how shock-absorbing floors can influence feeling comfort for the ears, eyes and body. Some enrolled nurses questioned whether or not the floor used in their care home (12-mm Kradal tiles) might have initially contributed to muscle soreness, whereas hospital staff commented more positively about the comforting effects of the flooring to which they were exposed (8.3-mm Tarkett Omnisports Excel). Findings on visual attractiveness are also included in this category, which would be a consideration of any new floor regardless of its shock-absorbing properties.
Senior care home managers (finding 3.1, unequivocal evidence),54 care home staff (finding 3.2, unequivocal evidence), 51 hospital patients and visitors (finding 3.3, unequivocal evidence)118 and hospital staff (finding 3.4, unequivocal evidence)118 all spoke of improvements to the acoustic environment that shock-absorbing flooring can bring:
It’s a very, I don’t know, nice sound. There’s never that echoing, just a very dampened and good sound.
Enrolled nurse, care home51
It’s quieter, if something falls, it tends to give ‘dunk’ instead of ‘clatter-clunk’ [laughs] . . . I think to the patient it would make a big difference because when you’re ill you know, noises can be quite toxic to your recovery . . . so I think that way it’s definitely more therapeutic.
Staff member, hospital. 118
In discussing the visual attributes of floors (findings 3.5 and 3.6, unequivocal evidence), topics were raised by hospital patients, visitors and staff around homeliness, brightening up the room and considering how appearance is important for patients with visual impairments or particular diseases that can affect their perceptions:
You just want a plain surface really for walking . . . which is what you need in a hospital, you don’t want anything too overpowering with patients with impairments.
Staff member, hospital. 118
It’s [the shock-absorbing floor] more attractive than the others, it’s more homely. My mother says it looks more homely in here. I think that’s why . . . my mother thought it looked beautiful.
Visitor, hospital. 118
Hospital staff (finding 3.7, unequivocal evidence),118 and patients and visitors (finding 3.8, unequivocal evidence)118 discussed how they found the new sports flooring to provide more comfort underfoot; this contrasted to a debateable finding from care home staff that the novel flooring was demanding to walk on, initially provoking some muscle soreness, which subsided over time (finding 3.9, credible evidence). 51 For hospital staff, they felt that this additional comfort affected their daily routines, making tasks that involve kneeling (such as changing dressings) and lots of walking more pleasurable (finding 3.10, unequivocal evidence):118
It was very conscious, when you walked on it [the shock-absorbing floor]; it was so different from the ward hallway, extremely conscious . . . It was more comfortable to walk on; definitely . . . just surprised it was very nice.
Visitor, hospital. 118
I had terrible pain in my feet but I don’t think it was because of the [novel] floor because it went away, I mean there’s a difference between different types of pain.
Enrolled nurse, care home51
I wish the rest of the ward was fitted with it [shock-absorbing sports floor] . . . Because it’s nice on your feet, it doesn’t, you know, as nurses we’re pounding the corridors non-stop so it’s really quite a comfort thing and um it’s nice to walk on, I feel quite confident and comfortable on it.
Staff member, hospital. 118
Synthesised finding 2
Changing a floor has consequences for the wider system (e.g. affecting the ease of moving equipment), potentially leading to further adaptations and adjustments in behaviours, attitudes, equipment, processes and staffing (high confidence in the evidence).
This finding synthesised five categories, composed of 36 findings, from four studies [one study finding labelled ‘4.5’ and ‘8.8’ contributed to two categories within this synthesised finding; see Report Supplementary Material 2]. It draws together the potential consequences (whether actual or perceived) that implementing a new shock-absorbing floor can have, namely in push and pull challenges (category 4), walking and mobilising (category 5), cleaning and maintenance (category 6), and the introduction of a ‘novelty factor’ (category 7) into the environment. Some of these categories (e.g. categories 5 and 6) demonstrated that different people held different perceptions regarding the consequences of the shock-absorbing floors, and it should be recognised that these qualitative studies were measuring perceptions and people’s interpretations of their experiences of using the floors, rather than physical observations. Regardless of whether these consequences were actual or perceived, they contributed to adaptations in people’s behaviours and attitudes, and, with particular reference to push and pull challenges (category 4), led people to consider adaptations to the wider system with regard to processes, staffing and equipment (category 8: adapting to a compliant floor).
Category 4: push and pull challenges
This category brought together one credible and nine unequivocal findings from four studies, representing the views of hospital staff, patients, visitors and care home staff. The findings in these studies consistently emphasised the difficulties experienced by staff in moving equipment, how these difficulties may interact with the type of equipment (e.g. wheel size and state of repair) and staffing levels, and people’s concerns around staff safety.
Hospital staff emphasised how they found it ‘really, really difficult’ to move equipment such as beds, hoists, drugs trolleys or bedside tables on shock-absorbing flooring, compared with the regular hospital floors (finding 4.1, unequivocal evidence),118 and the difficulties that staff experienced were recognised by patients too (finding 4.2, unequivocal evidence). 118 Hospital staff explained how the intervention floors influenced their routines when it came to moving equipment, with quotations relating to a back injury, a hurt neck and having the sensation that the equipment breaks had been left on. One such routine that staff were concerned about was the need to move a bed away from the wall quickly in an emergency situation to gain access to a patient’s head (finding 4.3, unequivocal evidence):118
I’ve actually hurt my neck today transferring a patient using a turntable um, the patient was stood on the turntable and when I went to turn it, it wouldn’t turn at all um, and that’s not usual for a turntable and it wasn’t anything that the patient or myself or my assistant were doing, it was the floor that was stopping the turntable moving . . . I actually hurt my neck on it because the patient didn’t move and I did move.
Staff member, hospital. 118
Two of them [hospital staff] were moving a bed round one day and one of them said to the other ‘This blooming floor’ . . . they were definitely grumbling about it.
Patient, hospital. 118
Care home staff additionally recognised the added difficulties of pushing and pulling equipment on novel flooring (finding 4.4, unequivocal evidence)51 and carpet (finding 4.5, credible evidence). 68 Senior care home managers were concerned about staff safety (finding 4.6, unequivocal evidence)54 and were uncertain of the floors’ effects on staff safety (finding 4.7, unequivocal evidence). 54
It’s like they [the larger wheelchairs] kind of sink down a bit. They just get stuck.
Enrolled nurse, care home51
Four of the units [. . .] were fully carpeted, which was intended to provide a homely environment for the occupants but caused difficulties for staff when moving beds, hoists, and similar items.
Rigby and O’Connor68
Well, the big, big concern for me is that, you know, the lifts. Pushing. Because I don’t really—I’m fan of not injuring anybody’s self. Like, my main staff is supposed to be all the time safe.
Senior manager, care home54
The additional effort required to move wheeled equipment on shock-absorbing flooring was recognised as compounded by the condition of the equipment (finding 4.8, unequivocal evidence);118 the weight of patients and equipment (finding 4.9, unequivocal evidence);118 and the size of the wheels, with smaller castor wheels that change direction thought to be more problematic (finding 4.10, unequivocal evidence):118
I think the main thing is just pushing with the trolleys but I think it could be because of old trolleys as well, wheels don’t work as well and . . . It could be the equipment needs changing as well.
Staff member, hospital. 118
Category 5: walking and mobilising
This category brings together nine unequivocal findings from two studies (covering the perspectives of hospital patients and staff, and care home senior managers) relating to the perceived influence of flooring on walking and mobility, and the influence of these perceptions on staff routines.
The findings highlighted how wider system factors (such as footwear, contamination and the condition of the patient) can interact with the floor (or contribute more than the floor does) to walking and mobilising issues (findings 5.1 and 5.2, unequivocal evidence):118
It’s not the floor’s fault, it’s my legs.
Patient, hospital. 118
There were mixed perceptions regarding the contribution of shock-absorbing flooring to walking and mobilising; on the topic of slipperiness, hospital staff (findings 5.3 and 5.4, unequivocal evidence)118 and patients (finding 5.5, unequivocal evidence)118 offered mixed opinions as to whether the shock-absorbing floors they were exposed to were deemed more or less slippery than regular vinyl. Regardless of who was correct, it was evident that beliefs about slipperiness potentially influenced staff behaviours, as highlighted in the following quotation in which the staff member did not feel the same sense of urgency to clean up a potential slip hazard:
I don’t think the slipperiness is an issue, I think if anything it’s not so slippery . . . Well, because of the resistance when you’re doing anything and certainly, you know, when sometimes if talcum powder gets spilt on the floor on the normal floor, [. . .] you have to stop yourself from falling, but on there I don’t notice that. So I thought that was quite good, because you know sometimes I’m kind of powdering patients and some gets on the floor and you think, ‘oh I’d better mop that up quick’, but no, it’s not an issue there.
Staff member, hospital. 118
Views were similarly divergent on the use of shock-absorbing sports flooring during the rehabilitation process and its interaction with walking aids. For example, some staff felt that the sports flooring provided a poor reflection of how patients were managing and so they did their mobilising work away from the shock-absorbing flooring; an opposing view was that it better replicated carpet, which was considered better for patients to practise on in preparation for returning home (finding 5.6, unequivocal evidence). 118 With regard to staff members’ own sensations of stability on the more shock-absorbing surface, again, there were mixed reports, with some people being more sensitive to the change than others and needing to adjust (finding 5.7, unequivocal evidence):118
The patients don’t find it a problem generally with their frames . . . they find it goes slower, so the run of it is slower than it is on the ordinary lino[leum] floors, they have to put in more effort but that probably replicates a carpet better and most of our patients have carpets at home.
Staff member, hospital. 118
Senior care home managers expressed that the influence of shock-absorbing flooring on resident mobility was something they would like to learn more about (finding 5.8, unequivocal evidence). 54 Comparisons were also made as to how shock-absorbing floors would be better than an alternative intervention of fall mats in terms of increasing resident mobility (finding 5.9, unequivocal evidence):54
We were talking about fall mats, I think, and – ’cause there’s always a tripping hazard with fall mats. So just having everything that’s on one surface, be so much better.
Senior manager, care home54
Category 6: cleaning and maintenance
This category brought together six unequivocal findings from two studies, related to cleanliness, cleaning routines, showing up dirt and marks, indentations, and uncertainty surrounding the longevity of flooring performance. The findings on cleaning were typically related to the properties of the floor surface (i.e. colour, finish, pattern, texture), how it shows dirt or dust (whether this is a good or bad thing), and how easily marks mop off (finding 6.1, unequivocal evidence). 118 In addition, a novel floor was considered better than carpet for improved cleaning capabilities (finding 6.2, unequivocal evidence). 54 A number of the quotations demonstrated a divergence of perceptions among participants, highlighting the subjectivity of the appraisals being made regarding floor cleanliness (finding 6.3, unequivocal evidence). 118 In addition, the influence of these perceptions on cleaning processes was highlighted. These issues would be a consideration for any new flooring system (regardless of its shock-absorbing properties), and were explained to affect the amount of time spent cleaning and how reassured individuals were that the floor was clean. Hospital staff also highlighted the cleanliness of floors and cleaning products to be important features of the wider safety system tackling falls prevention (finding 6.4, unequivocal evidence):118
If there’s talc[um powder] or anything like that it’s really slippery . . . Yeah, it’s really slippery with talcum powder, I’ve noticed . . . I have noticed that it’s slippery if you bath somebody or wash somebody in the chair or if there’s any talc[um powder] on the floor you can tell it’s there.
Staff member, hospital. 118
Findings related to maintenance more closely concerned the shock-absorbing qualities of the floors, with uncertainties as to how it would perform over the longer term (finding 6.5, unequivocal evidence)54 and a desire for more research evidence on longevity (finding 6.6, unequivocal finding). 54 Staff discussed temporary indentations in relation to the perceived appearance of the sports flooring (finding 6.3, unequivocal evidence), which were thought to rectify after about half an hour and were not highlighted as a major concern:118
I’d be interesting to know if, over the long term, the product breaks down or becomes less effective over time.
Senior manager, care home54
Well, my immediate concern I think was um, it being punctured . . . so that was a concern thinking you know all this money, will it be worth it if it’s punctured somehow or split, but I haven’t noticed anything like that.
Staff member, hospital. 118
Category 7: the novelty factor
This category brought together six unequivocal findings from three studies, representing the views of hospital patients, visitors and staff, enrolled nurses in care homes, and senior managers in care homes. The findings highlighted that flooring can be considered quite a mundane concept of ‘just a floor’ (findings 7.1 and 7.2, unequivocal evidence)118 that may be taken for granted and not be at the forefront of people’s minds. Despite this, the process of implementing a new floor and undertaking a study on it can draw people’s attention to fall-related injury prevention and the potential influence of flooring (finding 7.3, unequivocal evidence) on improving the safety culture within the organisation (finding 7.4, unequivocal evidence):54
It’s just a floor, as far as I’m concerned, a floor’s a floor’s a floor . . . I’m just lucky that I can put one foot before the other at the moment.
Patient, hospital. 118
Yeah, I think by having – just by having it, you up the discussions about it, and it becomes more out there. So you’ve got this flooring in your building. People talk about it. So I think your safety awareness goes up, and your prevention goes up.
Senior manager, care home54
Some findings discussed how implementing a novel floor may affect external perceptions of the organisation, with it being viewed as more innovative (finding 7.5, unequivocal evidence). 51 There were unknowns surrounding the potential of marketing compliant flooring to recruit care home residents, and this was considered likely to be influenced by the type of organisation and how it was funded (finding 7.6, unequivocal evidence):54
So you wouldn’t necessarily entice people to come to your care home ’cause they don’t really have the option.
No, we have a huge long wait list. [. . .] If we were, like, a private – people have to pay privately, perhaps that might be an enticing feature.
Lachance et al. 54
Category 8: adapting to a compliant floor
This category brought together six findings (four unequivocal, two credible) from four studies, representing the views of senior managers and other care home staff, and staff in hospitals. The findings discussed the need for staff to adapt, willingness to adapt, aspects that influence staff willingness to adapt, the types of adaptations that can be made, and the impact of these on staff and patients/residents.
There was a sense from care home nurses (finding 8.1, unequivocal evidence)51 and senior managers (finding 8.2, unequivocal evidence)54 that long-term care staff were open to making changes to the workplace to accommodate shock-absorbing flooring. This was especially the case if staff have a sense that the overall outcome will benefit the residents, as well as providing other potential benefits to staff (e.g. environmental comfort). Some uncertainties over openness to change were expressed (finding 8.3, credible evidence),54 with the view that there may be initial resistance, but that gradual implementation (e.g. an area at a time) with information and feedback would enable the changes to gain traction:
A very general statement about our staff culture is, they generally get on board with things they see are good for the residents. And I think it would be pretty hard – I just can’t see them not being on board with compliant flooring that may help reduce injuries.
Senior manager, care home54
Adapting equipment to accommodate the push and pull challenges of a shock-absorbing floor may pose subsequent challenges for promoting resident mobility (finding 8.4, unequivocal evidence). 54 From this perspective, it was explained that ceiling-based lifts can decondition residents, who would otherwise be encouraged to weight-bear with a floor-based lift, to maintaining some independence. Further ways to adapt to the push and pull challenges were staffing related, from asking for additional help when moving heavy equipment to rotating where staff are placed on the ward to give people a break from the shock-absorbing floor and assigning more staff on certain shifts to support manual handling activities. Staff also discussed how they were slowing down and focusing more on proper manual handling techniques (finding 8.5, unequivocal evidence). 118 In the hospital environment, there were some different opinions as to the necessity of various adaptations (such as increasing the number of people it takes to move equipment, or the staffing levels on the ward); this could be related to the usual routines and staffing in the respective hospital environments that were included in the study:
At the moment we’re having to have an extra staff on night times because of the floor, um, to help in there on a night because if the nurses are doing tablets for instance it would be my job or my colleague’s job to be in there on my own and you know if I had to get on with stuff and I couldn’t get anybody else so they’d give me an extra person for that room which isn’t brilliant really, financially anyway.
Staff member, hospital. 118
I wouldn’t say we’re using more staff to be able to use the hoist . . . it’s not using any more staff, it’s just a bit more manual handling if you like to try and get it into position.
Staff member, hospital. 118
If it’s somebody who’s been off with back pain I’ll maybe put them down the other end of the ward . . . which is not what I want to do, I’d rather have the continuity of the same staff looking after the same patients, but we do, we’re swapping round more to give people a break from it.
Staff member, hospital. 118
Staff also discussed conducting certain activities away from the shock-absorbing flooring, such as leaving the medicine trolley outside the bay when doing the drugs round (which then takes longer). 118 Similarly, in the study that discussed the push and pull challenges on carpet, an example was provided of how all residents who required a hoist to use the toilet were being taken to a communal bathroom to avoid using the en-suite facilities in their own carpeted rooms (finding 8.6, credible evidence). 68 More patient-centred changes were also discussed, such as supporting injury prevention by admitting higher-risk patients to the area with the shock-absorbing flooring and supporting mobility by undertaking rehabilitation on a different flooring area (finding 8.5, unequivocal evidence):118
Only the fact of when we’re admitting patients I’m more aware of saying ‘are they high risk of falls?’ because then I can make sure I’ve got a bed space in that bay, um and that’s probably something we will work towards . . . just obviously about the admitting, that’s the only thing that’s changed really.
Staff member, hospital. 118
We’re having to take the patient out of that environment and put them, like we’ll do therapy with them in that ward and we’re like, oh they need two people coz they struggle to move the frame, we take them out of that environment . . . we don’t tend to do as much mobility practise [sic] on there now to what we would in the other bays.
Staff member, hospital. 118
Synthesised finding 3
Installation may be an initial concern, but this can be effectively managed; however, cost and funding considerations need to extend beyond the initial purchase and installation to consider potential adaptations in staffing, processes, equipment and potential cost-savings (should the floor be effective) (moderate confidence in the evidence).
This finding synthesised evidence from two categories comprising eight findings from two studies, representing the views of hospital staff and senior managers from care homes.
Category 9: installation
This category brought together three unequivocal findings from two studies that discuss the installation process, the suitability of installing compliant flooring as a retrofit, and dealing with thresholds. Senior managers of care homes highlighted their concerns about installation, particularly when it is undertaken as a retrofit rather than as part of a new build (finding 9.1, unequivocal evidence). 54 Similarly, hospital staff who had experienced the installation of a shock-absorbing sports floor highlighted their initial concerns, but went on to describe how the process was effectively managed (finding 9.2, unequivocal evidence). 118 Staff described the minimal disruption and being able to work around the installation, and some commented about dust, noise and the smell of glue. In the hospital study, only one bay in each ward had the shock-absorbing flooring installed, so staff described how the individual bay was sealed off and how some staff were re-allocated to work on a different ward during the installation. 118 There were some installation challenges described in the care home evidence, with thresholds between different floor types with different thicknesses highlighted as an issue that needs to be managed (finding 9.3, unequivocal evidence). 54 The findings in this category come from studies describing the installation of different flooring types (sports flooring and novel flooring) and settings (hospital and care home), and it is likely that each flooring type and the environment within which it is being installed will present a different blend of challenges:
Very effective actually, I thought that they did a marvellous job, I was kind of, I envisaged you know a huge amount of dust, a lot of disruption and I was very impressed . . . There was some [dust], there was a tiny amount but you know they sealed everything up very well and then the deep clean happened so it was really good . . . I just thought, ‘well I’m sure they know what they’re doing’ [laughs] and left them to it.
Staff member, hospital. 118
A challenge because this facility was not built to have those kind of flooring. So when that was put in, the outside hall and the room, there is a little bit of an elevated surface. So then it’s a tripping hazard for the staff.
Senior manager, care home54
Category 10: costs and funding
This category brought together five findings (three unequivocal, two credible) from one care home study54 in which senior managers considered the upfront and ongoing costs of shock-absorbing flooring, potential cost savings and budget planning. Senior managers of care homes were concerned about the availability of funding and cost of implementing shock-absorbing flooring (finding 10.1, unequivocal evidence). Many of the interviewees stated, when prompted, that they would want to install shock-absorbing flooring if they had access to the material and installation costs (finding 10.2, credible evidence). The mechanisms of securing funding for a new-build installation in Canada (finding 10.3, credible evidence) or of planning the costs into the following year’s budget (finding 10.4, unequivocal evidence) were described as facilitators of obtaining the additional upfront costs. Aside from the initial costs of purchase and installation, senior managers were additionally cognisant of extra costs associated with obtaining suitable equipment for use on the floor, and staff training (finding 10.5, unequivocal evidence). Participants described the potential cost savings as well, for example through potentially negating the need for fall mats, and savings for the health authority because of reduced injuries, resulting in fewer hospitalisations, treatments and procedures:
You’d have to look at the flooring [. . .] at where it’s going and then if you have to look at the motorized lifts and [. . .] different equipment to accommodate the flooring. [. . .] And training for the staff on proper body mechanics. [. . .] it’s not just how much the flooring costs.
Senior manager, care home54
Conclusions
Five qualitative studies of reasonable quality contributed to this synthesis, resulting in three synthesised findings:
-
Shock-absorbing flooring is viewed by many as a potential solution to help protect people from fall-related injuries, with a potential side effect of improving environmental comfort (moderate confidence in evidence.)
-
Changing a floor has consequences for the wider system (e.g. affecting the ease of moving equipment), potentially leading to further adaptations and adjustments in behaviours, attitudes, equipment, processes and staffing (high confidence in evidence).
-
Installation may be an initial concern, but it can be effectively managed; however, cost and funding considerations need to extend beyond the initial purchase and installation to consider potential adaptations in staffing/processes/equipment and potential cost savings from fall-related injury prevention (should the floor be effective) (moderate confidence in the evidence).
The studies predominantly focused on novel and sports floors; however, one study on carpet contributed credible evidence on issues of push and pull tasks. A broad range of views were represented from patients, residents, visitors and different staff roles. Although there may be divergent views on the effects of shock-absorbing flooring on slips, trips and falls risks; mobility; cleanliness; and how demanding it is to walk on, the findings highlighted that beliefs and attitudes towards the flooring are important as they can affect behaviours, routines and experiences. Views were convergent when it came to the increased effort required to push and pull equipment, and it would make sense for organisations to consider the adaptations required for this if they were considering implementing a shock-absorbing floor. Alongside the divergent views were findings expressing the desire for further evidence to support implementation decisions, not least around clinical effectiveness, giving rise to future research directions on the longevity of shock-absorbing floors, cost-effectiveness evidence that incorporates the costs of wider adaptations, effects on staff health and well-being, and the influence of shock-absorbing flooring on patient/resident mobility.
Chapter 5 Review of cost-effectiveness evidence
Five relevant studies for consideration were identified in the literature search, each exploring the cost effectiveness of shock-absorbing flooring. 82,119–122 All five studies can be classified as models, that is they made quantitative estimates based on a variety of sources. They are reviewed here against the basic elements of good-practice guidelines,69–71 specifically the following: addressing a well-defined research question; using an appropriate type of study design, with a full description of options; providing a rationale for the structure; and having relevant outcomes, with appropriate perspective, time frame, costs, assumptions and methods.
The main review method used was iterative interrogation of the studies on each of these topics, with estimates made for key data when possible (undertaken by JR and checked by AD). In brief, the studies were disparate because of differences in settings, interventions and methods. Three studies reported that the intervention floors increased benefits and reduced costs. 120–122 Lange82 found increases in both benefits and costs. Only Latimer et al. 119 found reductions in both costs and QALYs.
The studies
Five economic studies were included in this review. 82,119–122 Two studies were based in Sweden,82,121 one in New Zealand,122 one in the UK119 and one in the USA. 120 Four studies were in care homes, one was in hospitals (Table 18). We have assessed the studies against the 24-item Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist to summarise the quality of reporting (see Report Supplementary Material 3). We have rated the reporting quality as poor (< 50% of items addressed), moderate (50–75% of items addressed) or high (> 75% of items addressed) according to how many items on the CHEERS checklist were addressed (see Table 18).
| Study | Evaluation details | Population and setting | Methods | Outcomes and analysis | Funding, CoI, reporting quality |
|---|---|---|---|---|---|
| Zacker and Shea 1998120 | Cost-effectiveness and cost-benefit analysis of > 25-mm dual stiffness underlay vs. standard concrete floor | Simulated high-risk care home residents, USA |
|
|
|
| Lange 201282 | Cost–utility analysis of Kradal vs. linoleum | 59 nursing home residents, Sweden |
|
Costs: purchase, installation, medical costs associated with hip fracture and death, health-care consumption; QALY loss due to hip fracture/death. ICER |
|
| Ryen and Svensson 2015121 | Cost–utility analysis of Kradal vs. ‘standard’ floor | Simulated care home residents, Sweden |
|
Costs: installation, hip fracture (inpatient, outpatient and general practitioner costs; rehabilitation/physical therapy; transport), added life-years. QALY weights for healthy and hip fracture states. ICER |
|
| Njogu and Brown 2008122 | Cost–utility analysis of Kradala vs. traditional floor | Simulated care home residents, NZ |
|
Costs: additional purchase costs (not installation), hip fracture (inpatient and rehabilitation costs), cost of head injury and other fracture reported but not used in analysis. QALY loss due to hip fracture. ICER |
|
| Latimer et al. 2013119 | Cost–utility analysis of 8.3-mm Tarkett Omnisports Excel vs. 2-mm vinyl/2-mm thermoplastic tiles on concrete | 452 older adult hospital inpatients, UK |
|
Costs: installation, hospitalisation, falls of different severities, 3-month post-discharge resource use (hospital admissions, outpatient/health-care visits, place of residence), mortality. QALYs associated with different types of falls. ICER |
|
Research questions, interventions and settings
The shared, general research question was whether or not, and to what extent, absorbent floors were cost-effective in comparison with standard floors. However, the precise meaning of the question depended on the details of the alternatives compared and the assumptions made, both of which are discussed below.
Rationale
In principle, the processes by which more absorbent floors were expected to bring about benefits would be through reducing the impact forces experienced by the faller when contacting the floor, leading to fewer injuries and/or hip fractures. Only Latimer et al. 119 distinguished between types of falls and the injury caused. All studies but Latimer et al. 119 focused on hip fracture, with one121 including the costs, but not the disbenefits of other injuries. Latimer et al. 119 included the costs of treating all injuries resulting from falls.
Interventions
All interventions were alternative floorings, of which one seems to have been at an early stage of development (Zacker and Shea120),47,48 and three were Kradal, a commercial floor covering. 82,121,122 Latimer et al. 119 compared a sports floor (8.3-mm vinyl over fibreglass mat with polyvinyl chloride foam backing – Tarkett Omnisports Excel – laid on concrete) with standard flooring in hospital wards for older adults (described more fully in the trial report77). None of the interventions was fully described in the economic papers, but this may be offset by most of the interventions being commercially available. Kradal flooring has been more fully described elsewhere. 52
More importantly, perhaps, the alternatives were also not fully described. Linoleum was the control in Lange;82 however, it was unclear what subfloor was used. Zacker and Shea,120 Ryen and Svensson121 and Njogu and Brown122 used a ‘standard floor’ as control (Zacker and Shea120 indicated a concrete subfloor, but the overlay material was unclear). Given that floors, particularly in care homes, might be wooden or concrete, knowing which alternatives are being assessed matters. 76 In Latimer et al. ,119 the control floors were concrete subfloors with 2-mm vinyl (about 5 years old) in three sites, and 2-mm thermoplastic tiles (> 30 years old) in one site (see the trial report77). The failure in most studies to fully specify the control floor is a weakness in the study reports.
Methods
Four studies used decision trees (of which three82,119,122 were explicit and one120 implicit) and one121 used a Markov model. The Markov model considers the risks and effects of recurrent events using time-dependent transition probabilities. Decision trees show pathways, generally for one-off events, within limited time frames. Longer time frames and the possibility of recurrence would seem desirable, particularly when modelling the effects of floors with long life expectancies in residential care homes. The studies, however, were limited by the data available.
The data used to populate the models varied widely. Only one study, Latimer et al. 119 (associated with Drahota et al. 77), used new data from a randomised comparison; however, when there were very few data, assumptions were based on the literature. 119 Another study82 used data from a small non-randomised experiment (not referenced but based on observing the effects in an extension to an existing care home), but supplemented by best estimates from the literature, which was made necessary by the small size of that study. The other three were desktop exercises using available estimates mainly from the published literature. 120–122 Although questions might be asked about the inclusion of these three studies,120–122 they are included here for completeness.
Outcomes and rationale
Four studies aimed to estimate a cost per QALY and hence can be classified as cost–utility exercises. 82,119,121,122 Zacker and Shea120 reported results of both cost-effectiveness and cost–benefit analyses (benefits measured in money based on best estimates of willingness to pay). Ryen and Svensson121 alone estimated the cost per hip fracture averted. Only one study119 distinguished between severity of fall (none, minor, moderate, major injury). Only that same study119 used data collected directly on the utility differences between the alternatives compared.
The reductions in hip fractures or injuries varied by study (Table 19). Only Latimer et al. 119 explored the influence of a relative difference in the number of falls between intervention and control groups (an increase in the intervention group). All five studies reported a reduction in injuries and linked costs due to falls. These were mainly hip fractures, but, in Latimer et al. ,119 included all costs of fall-related injuries. The reductions in injuries varied from 42%119 to 90%. 82
| Study | Reduction (%) | Key outcome | Comments |
|---|---|---|---|
| Zacker and Shea 1998120 | –50 | Hip fractures | Assumed |
| Lange 201282 | –90 | Hip fractures | Assumed |
| Ryen and Svensson 2015121 | –60 | Hip fractures | Assumed |
| Njogu and Brown 2008122 | –63 | Hip fractures | Assumed |
| Latimer et al. 2013119 | –42 | Injurious falls | Observed |
These approaches led to differences in the utility decrement as a result of a fall. These were generally large; only one study119 showed absorbent floors decreasing utility (0.006 QALY loss). The others assumed large gains in utility as a result of an avoided hip fracture:
Mortality in terms of increased risk due to hip fracture or related injuries was included in all studies except Njogu and Brown. 122 A 25% reduction was assumed by Zacker and Shea,120 30% in Ryen and Svensson,121 and 35% in Lange. 82 Latimer et al. 119 extrapolated differences in life expectancy from the trial, which amounted to a 53% extension for those who did not fall (from 0.81 to 1.24 years).
Perspective and time frame
The studies varied in perspective. A societal perspective was claimed in three studies, but was limited. Both Swedish studies82,121 included costs due to increased life-years, an aspect that is not included in the methods used by the National Institute for Health and Care Excellence. Zacker and Shea120 took a societal perspective, but included little beyond health-care costs and estimates of societal willingness to pay for avoiding hip fracture and death. The perspective was not stated in Njogu and Brown,122 and a health service and personal social services perspective was taken by Latimer. 119
The relevant time frame for a fixed investment in flooring is not obvious because of the likely mismatch between the period over which benefits might accrue for patients and the time before the flooring might need to be replaced. The life expectancy of the new floor was assumed to be 40 years in Njogu and Brown;122 20 years in Lange,82 Ryen and Svensson,121 and Zacker and Shea;120 and 15 years in Latimer et al. 119 In all studies, the cost of the new floor was expressed as an annual net present value using a variety of discount rates from 3%82,121 to 5%. 120
Costs
The cost of the intervention needs to be distinguished from the total cost effects measured for the alternatives compared.
As the unit cost attributed to the novel flooring intervention varied widely (by floor area, currency and year), these must be put in a standard form. A further complication was the number of beds per area. Studies varied widely in what they reported (Table 20).
| Cost year | Gross cost (£) | Net cost (£) | |||||
|---|---|---|---|---|---|---|---|
| Zacker and Shea120 | Lange82 | Ryen and Svensson121 | Njogu and Brown122 | Latimer et al.119 | Zacker and Shea120 | Lange82 | |
| 1995 | 26 | 24 | |||||
| 2006 | 54 | ||||||
| 2009 | 164 | ||||||
| 2011 | 138 | 138 | 104 | ||||
| Updated to 2019 prices using GDP deflator83 | |||||||
| 2019 | 41 | 159 | 159 | 69 | 195 | 38 | 119 |
All of the studies set in care homes used a different standard room size; Ryen and Svensson121 used 30 m2, Lange82 used 25 m2, Njogu and Brown122 used 20 m2, and Zacker and Shea120 used 11.6 m2 (based on four beds per intervention bay). This poses obvious problems for given differences in care homes. Latimer et al. 119 took the unit as hospital ward bays, averaging 10.45 m2 per bed. This also implies that the cost of the intervention depends on the assumed area covered.
The currency and the year also varied: US dollars,120 Swedish krona,82,121 New Zealand dollars122 and GBP119 were used. To convert these to a common currency, such as GBP, the year needs to be stated unambiguously. This was unclear in two studies121,122 and only explicit in Latimer et al. ,119 Lange,82 and Zacker and Shea. 120 Njogu and Brown122 was assumed to be in 2006 prices, and Ryen and Svensson121 was assumed to be in 2011 prices, based on cost-related references cited by each study. When put in GBP and updated using the GDP deflator83 (see Table 20), the cost of the flooring varied from £41 to £195 per m2.
The total cost difference used in the cost-effectiveness studies also varied widely, with reductions from £52 to £4952, and the increase at £1443 per patient (Table 21). Given the differences in floor area and type in each study discussed, these differences are unsurprising.
| Cost year | Dual stiffness underlay | Kradal | Tarkett | ||
|---|---|---|---|---|---|
| Zacker and Shea120 | Lange82 | Ryen and Svensson121 | Njogu and Brown122 | Latimer et al.119 | |
| 1995 | –3118 | ||||
| 2006 | –41 | ||||
| 2009 | –843 | ||||
| 2011 | 1223 | –2786 | |||
| Updated to 2019 prices using GDP deflator83 | |||||
| 2019 | –4952 | 1443 | –3200 | –52 | –1003 |
Another way of considering the differences in total cost is as a proportion of the total cost in the control arm. This was possible for only three studies. In Lange82 the cost increase was 3.5%; in Njogu and Brown122 it was –8.8%; and in Latimer et al. 119 it was –2.2%.
Uncertainty
The uncertainty in cost-effectiveness estimates is usually explored in sensitivity analyses, which all five studies undertook: Zacker and Shea120 and Njogu and Brown122 used a simple one-way sensitivity analysis, Latimer et al. 119 tested seven scenarios, Ryen and Svensson121 used a cost-effectiveness acceptability curve121 and Lange82 used a scatter diagram. Given the differences in approaches outlined previously, no further analyses of uncertainty were deemed worthwhile.
Results and discussion
Three studies found that absorbent floors dominated standard floors, that is costs were lower and outcomes were better. 120–122 Only Lange82 and Latimer et al. 119 disagreed. Lange82 estimated that the new floors had increased both cost and QALYs, but at a cost per increased QALY well above the accepted threshold level. Only Latimer et al. 119 found reduced QALYs, albeit with reduced costs, which, despite a favourable incremental cost-effectiveness ratio (ICER), was considered a result unlikely to lead to implementation.
What is more striking is the differences in relation to benefits. All of the studies but Latimer et al. 119 showed an increase in benefits. The QALY gains in the relevant studies were a direct result of assuming relatively large QALY losses due to hip fracture. Only Latimer et al. 119 collected data on quality of life.
The quality-of-life difference in Latimer et al. 119 was small, at 0.006 QALYs, well below estimates of the minimally important difference, which is put at around 0.4. Furthermore, the QALY loss was very sensitive to the overall risk of falling. In a sensitivity analysis in which the number of fallers was equalised, but the lower proportion of severe falls in the intervention group maintained, the flooring intervention would become dominant. 119
Overall conclusions on the studies
Overall, the quality of the studies was poor, with Latimer et al. 119 being the only exception. What is striking is that the best study found much less benefit than any of the other studies. 119 Although there was heterogeneity between the floors, settings and population groups assessed, it seems reasonable to conclude that the assumptions made in the other studies were unduly optimistic. Yet, in Latimer et al. ,119 both the cost and QALY differences were very small; neither was statistically significant. Given the differences discussed previously, it is clear that each study attempted to answer different research questions to do with particular comparisons and costs, and with very different assumptions.
Research recommendations for any future study might include: (1) improved specification of the alternatives evaluated; (2) distinguishing falls by severity; (3) specifying the processes by which reductions in type of falls were expected to lead to improved health; (4) using appropriate time frames, particularly when mortality was included; and (5) providing greater details (perhaps in an impact inventory) to enable different definitions of costs to be used in estimated ICERs.
Chapter 6 Discussion
Here we set out the main findings in relation to each of the review objectives, prior to discussing how the quantitative, qualitative and economic data complement each other, to consider the gaps and directions for future research.
Summary of main results
The potential benefits and risks of different flooring systems in care settings
There is high-quality evidence that a vinyl overlay with novel shock-absorbing underlay and concrete subfloor produces similar injury and falls rates per 1000 person-days to those produced with a vinyl overlay with plywood underlay and concrete subfloor in care homes. We found very low-quality evidence that shock-absorbing flooring may reduce the number of falls resulting in injury in care homes. There is very low-quality evidence that shock-absorbing flooring use in hospitals may reduce injuries without increasing the rate of falls. Data on fractures and head injuries were generally too imprecise to determine effectiveness in care homes and hospitals; however, one observational study at high risk of bias indicated that fewer hip fractures were likely to occur on wooden subfloors than on concrete subfloors in care homes. Including unadjusted, unpublished observational data on head injuries indicated that shock-absorbing flooring may reduce head injuries; however, these data are of very low quality. Although some adverse events were described, there is very low-quality evidence that novel and sports floors do not result in more staff injuries in up to 2 years’ follow-up.
The extent to which potential benefits and risks may be modifiable
Novel floors, sports floors and carpet all demonstrated a reduction in injuries (very low-quality evidence) depending on how the data were analysed (i.e. as a rate or risk), while retaining the probability that the different floor types assessed may not increase the rate of falls or of being a faller. Head-to-head comparisons of different shock-absorbing flooring types were all based on one study, which was subject to large imprecision, and the evidence remains uncertain.
Prespecified subgroup analyses were unable to detect any differential effects by setting, flooring type or study design for the majority of outcomes. Only one subgroup analysis, exploring the effect of flooring type on the number of falls resulting in injury, indicated a quantitative interaction of different degrees of benefit across subgroups; however, this counterintuitive finding (placing carpets as the most effective) was due to a highly problematic study on carpet that had unbalanced groups and was deemed to be at high risk of bias for confounding. Removing this study from the subgroup analyses indicated similar effects between novel floors and sports floors. The subgroup analyses need to be interpreted with caution because they typically related to few data, with few studies contributing to each subgroup, and there were issues with confounding; for example, sports floors were investigated only in hospitals.
We were unable to explore the level of acuity of study settings because of the nature of the included studies. Participant characteristics were poorly described in the majority of studies and were not a factor that we attempted to explore statistically, as we had not planned to undertake individual patient data meta-analyses. The descriptive data indicated that care home and hospital participants were of similar age and sex profiles, but may have differed in other characteristics, such as use of ambulatory aids, diagnoses of dementia and medications. The data on fallers highlighted that the underlying risk of being a faller was much higher in care homes, where residents had longer exposure to the floors. Future research should consider exploring time to first fall as a potential safety indicator to evaluate whether or not there is an increased risk of falling when first exposed to a shock-absorbing floor, which, if present, would prove more problematic in hospital settings where the turnover of patients is higher. Although this was not an outcome we analysed in the present review, only one included study evaluated this (care home data), finding no difference between groups. 50
The current economic evidence on shock-absorbing flooring
Five studies contributed economic data, four of which were of very low quality. Although there was heterogeneity between the floors, settings and population groups assessed, the assumptions made in the poorer-quality studies may have been unduly optimistic. Three of these found that shock-absorbent floors dominated standard floors, that is costs were lower and outcomes better, and one estimated that shock-absorbing floors increased both cost and QALYs, but at a cost per increased QALY well above the accepted threshold level. The QALY gains in these studies were a result of assuming relatively large QALY losses due to hip fracture. Only the higher-quality study collected data on quality of life. This study found reduced QALYs, albeit with reduced costs, which, despite a favourable ICER, was noted to be unlikely to lead to implementation. The reduced QALYs in this study were based on the assumption that shock-absorbing flooring increases falls risk; a sensitivity analysis demonstrated that, if shock-absorbing flooring does not increase the number of fallers, but reduces the number of injurious falls, the intervention floor would become dominant.
The implementation of flooring interventions
Shock-absorbing floors affected the work environment, resulting in adaptations to staffing levels and schedules to accommodate the increased effort required to move wheeled objects. Implementing shock-absorbing flooring will not successfully protect all falls; however, covering at least the areas with beds captured upwards of 75% of falls in the studies we assessed. Details on the implementation of floors in the included studies were sparse; however, no major issues with installation were reported. One site reported a split seam, which was thought to have resulted from the installation process, and this was rectified by the installation company. Sites found ways to manage the transition between different flooring materials of different thicknesses by way of transition strips or applying a gradual gradient. Further details on flooring implementation were captured by the qualitative findings, summarised below.
The views and experiences of shock-absorbing flooring use
Based on the qualitative evidence, we have moderate confidence that shock-absorbing flooring is viewed by many as a potential solution to help protect people from fall-related injuries, with a potential side effect of improving environmental comfort. We have a high level of confidence that changing a floor has consequences for the wider system (e.g. affecting the ease of moving equipment), potentially leading to further adaptations and adjustments in behaviours, attitudes, equipment, processes and staffing. We have moderate confidence that installation may be an initial concern, but this can be effectively managed; however, cost and funding considerations need to extend beyond the initial purchase and installation to consider potential adaptations in staffing/processes/equipment and potential cost savings from fall-related injury prevention (should the floor be effective).
Triangulation and identifying gaps in existing evidence
The different types of evidence in this review were largely complementary of each other, exploring different elements of the research question; however, there were some exceptions. Qualitative evidence indicated that many people (including patients, residents, visitors and staff) view shock-absorbing flooring as a potential solution for preventing injurious falls. Although the more robust quantitative evidence did not confirm this to be true, very low-quality quantitative evidence was indicative of a positive effect. This poses a quandary, as it cannot be discerned whether the personal belief systems held about the effectiveness of shock-absorbing flooring are contributing to the bias in the low-quality evidence (leading to overly beneficial estimates) or if the qualitative evidence is merely reflecting what the low-quality quantitative evidence has found to be true. It may also be the case, as has been highlighted by senior care home managers54 and wider stakeholder groups,66 that individuals, such as senior managers, hold more guarded views: that they are open to shock-absorbing flooring as a potential intervention if it is first shown to be effective. The qualitative data were not directly linked to the specific comparison assessed in the non-significant trial contributing to the more robust quantitative evidence,50 which may further explain this contradiction. More robust quantitative evidence is required to resolve this impasse, as the current high-quality quantitative evidence relates to only one trial of a specific comparison (i.e. SmartCells underlay vs. plywood underlay, both with vinyl overlays and concrete subfloors) in care homes. 50
The qualitative and quantitative data were aligned in their conclusions that staff found manoeuvring equipment on shock-absorbing floors harder, and this can lead to adaptations being made in the workplace. The very low-quality quantitative data indicated that there were no more staff injuries on shock-absorbing floors than on rigid floors; however, it could not be discerned whether this was because of adaptations made to accommodate increased push and pull forces on the softer floors (e.g. increasing the number of staff involved in manoeuvring wheeled equipment), or despite any adaptations that may have been made. The numbers of adverse events reported in the trial data were much fewer than those from the observational research, despite employing similar definitions. This may be a product of the data collection mechanisms employed by the different types of research (spontaneous report monitoring vs. surveillance systems), in which the trial may have been more likely to capture only those events with higher perceived causality linked to the floor. 77 The observational data, on the other hand, may have been better at ascertaining all events that were possibly linked to the floor, but not necessarily caused by it. 106 The qualitative data, which were linked to the trial data, contradicted the reporting of adverse events somewhat, suggesting that there may have been unreported adverse events in the quantitative analysis of outcomes. 118 Future trials therefore need to incorporate more robust data capture mechanisms with better triangulation of sources to record staff injuries. All future quantitative research should better track and report the spontaneous and planned workplace adaptations that occur during the study, and consider which adaptations can be made in advance as part of the intervention implementation to better facilitate staff acceptance and manage risks.
The qualitative evidence highlighted that senior care home managers were aware of the potential for additional costs associated with shock-absorbing flooring related to the workplace adaptations required to manage risks to staff. These included costs related to staffing levels, training and equipment upgrades. To date, researchers have not incorporated the potential of these additional costs (associated with the intervention) into economic evaluations, which should be considered in future. Based on the existing economic data (of sports flooring),119 we conclude that, if the very low-quality evidence were true (i.e. that shock-absorbing floors decrease injuries without increasing falls), then shock-absorbing flooring would be a dominant strategy (i.e. would be less costly and result in better health outcomes). These conclusions are subject to change, however, with better-quality evidence and a more comprehensive assessment of costs. If the higher-quality evidence (that shock-absorbing flooring makes little difference to injury and falls rates)50 were to be more widely confirmed with other settings and floors, then the costs of the intervention would be likely to outweigh the benefits. The intervention floor (a novel underlay) assessed in Mackey et al. 50 was compared with a plywood underlay to give the study floors comparable thicknesses and provide an element of masking to the study design (both study groups had vinyl overlays and concrete subfloors). It is feasible that an alternative control group (with no underlay and a concrete subfloor) may have produced a different result.
In terms of the overall completeness and applicability of the evidence, there are gaps with regard to high-quality evidence in hospitals, and alternative brands/designs of novel floors, sports floors, carpets and wooden subfloors. Few of the studies measured our primary outcomes, and the way outcomes were defined and measured differed across studies, an issue which has also been highlighted elsewhere. 123–125 Future activities are required to establish a core outcome set for flooring interventions, and then to design studies that can measure these, as well as control for potential confounding.
Certainty of the evidence
We used the GRADE approach to summarising the certainty of the evidence. Following this approach, randomised studies without important limitations provide high-quality evidence, whereas observational studies without special strengths or important limitations provide low-quality evidence. We did not upgrade any of the evidence from observational studies on the grounds of any special strengths. Special strengths could include having a large magnitude of effect, a dose–response gradient, or when the effect of plausible residual confounding works is in the opposite direction to the observed effect; it is rare to upgrade the quality of evidence when important limitations are considered to be present,84 as was the case with the evidence in this review.
The quality of observational evidence tended to be downgraded further owing to risk of bias (with uncontrolled confounding being the predominant problem). Hospital-based RCT evidence was downgraded because of imprecision (i.e. wide CIs expressing uncertainty as to where the intervention effects may lie), as were fracture outcomes. A couple of issues related to inconsistency (i.e. heterogeneous study effects) were present in the care home data for falls rates and hip fractures, and, occasionally, we downgraded the evidence because of concerns around publication bias.
In Gustavsson et al. ,52 the measurement of our primary outcome (injurious falls rate) was considered plausible, but was not analysed or reported. In Donald et al. ,105 the data were not reported fully, precluding inclusion in the meta-analysis (relating to falls resulting in injuries); however, owing to the size of the study, this was unlikely to have a substantive bearing on the findings. For Mackey et al. ,50 the adverse events data had not been published in full, although they were summarised for the purposes of inclusion in this review. We were unable to summarise any of the adverse events data as rates or risks, because of unknown denominators; for this reason, we downgraded this outcome for indirectness. The adverse events data in Mackey et al. 50 were also considered indirect evidence as they did not fully fit our inclusion criteria. Although the adverse events data in this study were collected as part of a randomised trial, it was the residents’ rooms that were individually randomised, rather than the staff, making the observation of staff outcomes more of a before-and-after design nested within the trial. We still included these data because of the importance of the outcome and the known difficulties of obtaining data on adverse events. 126
Owing to all of these limitations, the evidence in favour of shock-absorbing flooring was graded as being of very low quality, whereas some high- and moderate-quality evidence exists based on Mackey et al. ,50 which found one specific shock-absorbing floor (SmartCells underlay) no more beneficial than a plywood underlay in a care home.
Potential biases in the review process
Some of our decision-making processes through the course of this review could be considered contestable. For example, we opted to include very low-quality evidence and incorporated data considered to be at high risk of bias into our analyses. We included unpublished data and derived data, which may have been less trustworthy. We have attempted to guard against these decisions by providing cautionary conclusions, emphasising the findings from more robust evidence when available and undertaking sensitivity analyses to check the influence of these decisions on the findings. We estimated the design effect of the included cluster randomised trial for our secondary outcomes, which were not analysed in the trial report, despite us having access to the original patient data. 77 This approach was taken as re-analysing the original data was considered outside the scope of this review owing to time and resource issues. As a pilot study, it was very small for a cluster randomised trial, contributing minimal data to the analyses, and sensitivity analyses around the choice of ICC demonstrated that this approach was likely to have negligible impact on the review findings.
Our review primarily focused on older adults as the target population, and staff were included only in relation to adverse events for quantitative outcomes. Limited literature exists around other outcomes in staff, such as comfort, fatigue96 and pain,31 as well as laboratory-style experiments testing the influence of flooring on the forces required to push and pull various items of wheeled equipment relevant to care settings, which have not been included in this review. 25,127,128 The qualitative data highlighted these outcomes; however, we did not consider them priorities in the quantitative outcomes list. We attempted to obtain missing data to support the analysis of our prioritised outcomes and incorporated these when possible. However, some of our communication attempts and/or data requests to study authors were unsuccessful, either because of the time that had passed since the study was conducted76 or non-response. 102,105
Agreement and disagreements with other studies or reviews
Systematic reviews covering flooring materials are sparse. The Cochrane systematic review19 on falls prevention in hospitals and care homes excluded studies on shock-absorbing flooring, with the rationale that the intent of the intervention is to reduce fall injuries, rather than falls. A Cochrane review129 on hospital environments has been conducted; however, it is outdated (the last search was in 2006), and, with different inclusion criteria, subsequently included only two flooring studies. 105,130 A 2019 review131 of floor finishes with a facility management focus and no quality assessment included 71 articles (not all primary research) covering issues such as the influence of flooring finishes on indoor air quality, infection control, recyclability, maintenance, durability, cost, comfort, noise, aesthetics, healing, flame resistance, ease of movement, glare and safety. The section on safety advocates for shock-absorbing flooring (defined as linoleum sheets and carpet only) and is not comprehensive, mentioning two studies82,105 and other literature reviews. 132,133
The present review is based on an update of the clinical effectiveness and cost-effectiveness sections of a previous scoping review. 20 As a scoping review, it was descriptive in nature, in line with standard scoping review methodology,134 and did not contain any quality appraisal or meta-analyses. New studies and fuller reports have also been published since the original search of the scoping review, which have subsequently been included in this systematic review. 49–54,106 Therefore, to our knowledge, this is the first comprehensive systematic review on shock-absorbing flooring interventions for fall-related injury prevention.
The scoping review did, however, include a broader range of literature on shock-absorbing flooring, including laboratory-based and biomechanical studies exploring outcomes such as impact absorption, gait and balance. 32–41,43–48,67,130,135–149 The high-quality data relating to the ineffectiveness of novel flooring in care homes for reducing injury rates50 is counterintuitive to laboratory studies, which often indicate the superior shock absorbency in these floors and their comparability to hip protectors in terms of impact absorption. 26,37,136 Without an overlay, the novel underlay used in the care home trial (SmartCells) has been demonstrated to attenuate peak force by up to 33.7%, compared with 2 mm of rigid flooring, in a simulated fall to the hip,33 and by 80% in a simulated fall to the back of the head. 35 Explanatory factors for the negative findings in this review and their disconnect from the wider laboratory-based research may relate to:
-
the underlying assumptions of laboratory-based research associated with (1) the biofidelity of test systems, (2) the types of fall-related impacts simulated and (3) the type of impact required to sustain injury (and, conversely, the degree of impact attenuation required to prevent injury)
-
co-interventions (e.g. hip protectors) negating the power of the study to detect a change attributable to flooring
-
study populations having relatively low tissue tolerance values such that injuries occurred even for scenarios in which shock-absorbing floors reduced impact forces
-
setting characteristics, such as grab bars or staff vigilance, moderating the intervention effect
-
fall dynamics and environmental factors resulting in falls with impact sites and injury mechanisms not primarily associated with floors (e.g. walls, furniture, mobility aids).
These hypotheses would require further exploration to confirm or refute their basis. The laboratory research has indicated that shock-absorbing flooring can achieve greater impact reduction to head impacts35 and sensitivity analyses in our review (that included unpublished unadjusted data) identified a possible signal that head injuries may indeed be reduced in practice. This may imply that shock-absorbing floors need to achieve a higher force attenuation to successfully reduce injuries, making certain injuries (such as head injuries) more preventable than others (such as hip fractures). Alternatively, the higher force attenuation that can be achieved for head impacts and a higher baseline risk of head injuries (vs. hip fractures)115 may translate into a louder signal, which is easier to detect in the clinical research. Indeed, the fracture data in this review were generally too imprecise to detect a signal and further studies are likely to improve our understanding of potential effects.
Further biomechanical studies have been conducted on pushing tasks involving floor-based lift devices and wheelchairs. 25,127,150 One of these studies demonstrated increased pushing forces for a novel underlay (Sorbothane™, Sorbothane, Leyland, UK) that was not evaluated by any of the studies in the present review and is not in widespread use as a flooring material. 127 Both carpet and novel underlay (SmartCells) have been shown to increase the pushing forces required to initiate and sustain a manual wheelchair and floor-based lift; however, the addition of carpet has been shown to be more influential than a novel underlay to the measured hand forces. 25,150 Long-term care staff’s subjective ratings of pushing difficulty across different flooring conditions were all low for wheelchairs and motor-driven lifts (< 3 points on a 5-point scale),25,150 and higher for conventional lifts on carpet with or without shock-absorbing underlay. 25 It is considered significantly more difficult to wheel objects across carpet than across vinyl on concrete subfloors,25,150 and, although the introduction of a novel underlay did not significantly influence subjective difficulty ratings for wheelchairs and motor-driven lifts,25,150 it did for conventional lifts. 25 For conventional lifts,25 carpet with or without the novel shock-absorbing underlay exerted forces above recommended tolerance limits. 151 The type of lift used is highly influential, with motor-driven lifts negating the problems experienced with conventional lifts. 25 The qualitative research in the present review covered flooring brands different from the SmartCells underlay; in one study, a sports floor (Tarkett Omnisports Excel) was likened to carpet and staff expressed considerable concerns about pushing tasks. 118 In comparison to the SmartCells underlay, when Kradal, Omnisports Excel and carpet are laid, they are visibly different to a standard vinyl floor covering; we could speculate that this may also influence perceptions. The biomechanical literature complements the qualitative findings of the review by emphasising the important interactions between equipment types, flooring materials and pushing forces required, which indicate the potential for risk mitigation strategies to help alleviate the risks of adverse events and increased staff stress.
One of the concerns surrounding shock-absorbing flooring is whether or not it may inadvertently increase the risk of falling based on evidence that surfaces with extremely low levels of stiffness can influence balance control. 34 Our meta-analyses of falls rates per 1000 person-days and risk of being a faller were all non-significant, supporting the possibility that shock-absorbing flooring does not affect falls risk. Some of these analyses were imprecise, however, particularly in relation to evidence from RCTs in hospital settings, sports floors and carpets. We found very low-quality evidence in hospitals that the rate of falls did not increase with shock-absorbing flooring, and moderate- and high-quality evidence in care homes that falls rates and faller risk were not affected by SmartsCells flooring. These findings are in keeping with indirect evidence from the biomechanical-based literature, which suggests that, in general, individuals are able to maintain their balance on carpet36,138,139 and novel shock-absorbing floors. 33,34,36,38,152,153 Carpets and more compliant surfaces have been contraindicated, however, for their effects on balance in situations when sensory input is affected (e.g. with poor visual cues). 32,138,146 The majority of the biomechanical studies are conducted with healthy adults; however, some evidence exists based in clinical populations. Older inpatients have been observed to walk faster, with longer strides, on carpet than on vinyl,130 but these findings have been contradicted in a study of stroke patients who found carpet more challenging than parquetry. 39 One study has compared the abilities of inpatients (17 with stroke, 10 with Parkinson’s disease and 10 undergoing general geriatric rehabilitation) to perform the Timed Up and Go test on SmartCells, Tarkett Omnisports Excel and hospital-grade vinyl, and found no significant differences between flooring types (precision not reported). 153 This same study found no differences in patient-reported comfort and stability using visual analogue scales. 153 The current direct and indirect evidence, therefore, appears promising with regard to suggesting that falls are not increased on shock-absorbing floors; however, the evidence is imprecise in hospital settings, and biomechanical evidence of clinical populations is sparse.
Chapter 7 Conclusions
Implications for practice
The evidence suggests that one type of novel shock-absorbing floor may not be effective in care homes, compared with rigid flooring; however, gaps still exist in the knowledge. There is very low-quality evidence that shock-absorbing flooring may reduce injuries in hospitals and care homes, without increasing falls, and that wooden subfloors may result in fewer hip fractures than concrete subfloors. The economic evidence (based on sports flooring) suggests that, if injurious falls are reduced and the number of falls not increased, then shock-absorbing flooring is likely to be a dominant strategy (i.e. costs would be lower and QALYs increased). The evidence in favour of shock-absorbing flooring is, however, of very low quality, meaning that future research may change our understanding and there is much uncertainty. If future research indicates an increased risk of falling on shock-absorbing flooring, then the economic evidence suggests that this could result in an undesirable reduction in QALYs, even if injurious falls were reduced.
The review findings indicate that introducing shock-absorbing flooring to care settings has wider workplace implications, meaning that adaptations may be required in staffing, equipment and processes. Research confirms that wheeled equipment can be more challenging for staff to manoeuvre on shock-absorbing floors. However, evidence indicates both that adaptations can be made to accommodate this and that there is no overall increased risk of flooring-related staff injuries (very low-quality evidence). The evidence indicates that, if planning to install shock-absorbing flooring, it is important to consider the wider impacts (and related costs) on the workplace and how best to manage these; the current economic evidence has not evaluated these costs.
Implications for research
We have prioritised the following recommendations for research:
-
The current evidence base is diverse concerning how outcomes are defined, prioritised, measured, analysed and reported. In addition, there are complexities related to unit of analysis (i.e. individuals may experience multiple falls in different setting locations, and each fall may result in multiple injuries of different severities), which complicate analyses and future syntheses. Therefore, a fundamental step required in the field is the establishment of a clearly defined core outcome set, which includes recommendations for measurement, analysis and reporting. This piece of research should include a discussion around the relative merits and disadvantages of measuring injuries (and falls) as a product of the number of person-days, falls or even ‘active’ exposure time. This would require input from researchers, statisticians, clinicians, health and social care managers, policy-makers, and public and patient members, and should be designed to complement related core outcome sets (e.g. in community-based injurious falls prevention and hip protectors). 2,65
-
The majority of quantitative studies included in this review were observational, judged to be at serious risk of bias, and did not address our primary outcomes of injurious falls rate and falls rate. Certain questions (e.g. related to common flooring types, such as carpets and different subfloors) may lend themselves well to observational study designs; however, these should be designed to address the above core outcome set and to comprehensively deal with potential confounding. Other questions (particularly those addressing new flooring interventions) lend themselves more readily to pragmatic RCT designs (of which there is a paucity). Co-interventions, which are broadly implemented in care settings, will need to be carefully considered in the design of future studies.
-
There is a dearth of robust research on the effectiveness of shock-absorbing flooring in hospital settings. Hospitals differ from care homes, for example in terms of the population characteristics (e.g. with patients experiencing acute illness or episodes of reduced function), equipment in use, environmental characteristics and patient turnover. Future research should address this gap.
-
This review indicates that implementing shock-absorbing flooring leads to adaptations in the workplace. Future research therefore needs to plan for these adaptations as part of the study design. For example, implementation studies should be accompanied by process evaluations and risk management plans to better mitigate, measure, manage and evaluate the risks to staff. Investigators could define the ‘shock-absorbing flooring intervention’ more broadly when devising the study research question to involve the implementation of a package of measures for the protection of patients and staff (such as new equipment more suitable for use on softer surfaces, an additional staff member to support manual handling activities). As part of these considerations, further research and innovation is required to identify how best to adapt the workplace to accommodate shock-absorbing flooring.
-
There is currently limited high-quality economic evidence exploring the implementation of different flooring interventions. Future economic evaluations should –
-
provide improved specifications of the alternatives evaluated
-
distinguish falls by severity and type
-
specify the processes by which reductions in type of falls were expected to lead to improved health
-
use appropriate time frames, particularly when mortality is included
-
provide greater details (perhaps in an impact inventory) to enable different definitions of costs to be used in estimated ICERs; consideration should also be given to the costs of additional workplace adaptations.
-
-
With the present uncertainty surrounding current flooring solutions, research and innovation is required to establish the specifications for improved products to support fall-related injury prevention in care settings. A multidisciplinary approach will be required to validate a set of mechanical properties for floors (measuring shock absorbency and push and pull forces) and establish the minimally important differences required to make a meaningful difference in practice.
We are unaware of any ongoing studies in these areas.
Acknowledgements
This review was developed and delivered through the support and guidance of the Advisory Board members: Nadra Ahmed (National Care Association, Rochester, UK), Margaret Bell (public involvement member), Liz Burden (public involvement member), Alison Cracknell (Leeds Teaching Hospitals NHS Trust, Leeds, UK), Jonathan Stewart (Health Estates and Facilities Management Association, Liverpool, UK), Joleen Tobias (public involvement member), Julie Windsor (NHS England/Improvement, London, UK) and Anna Winfield (Leeds Teaching Hospitals NHS Trust).
The public involvement members (Margaret Bell, Liz Burden and Joleen Tobias) additionally supported the protocol development, communication of the risk-of-bias assessments and GRADE assessments, development of the Plain English summary, and dissemination activities.
We would like to thank Ngianga Li Kandala for his statistical support and advice, and Carl Hanger and Johanna Gustavsson for their co-operation, time and generous supply of unpublished data for incorporation in this review.
The Health and Safety Executive supported 10 days of Olanrewaju Okunribido’s time in kind on this project.
Contributions of authors
Amy Drahota (https://orcid.org/0000-0001-9772-0220) (Reader in Health and Social Care Evidence and Evaluation) contributed to the conception and design of the review; the acquisition, analysis and interpretation of the data; and drafting the final report.
Lambert M Felix (https://orcid.org/0000-0001-6517-9089) (Senior Research Associate, systematic reviews) contributed to the design of the review; the acquisition, analysis and interpretation of the data; and drafting the final report.
James Raftery (https://orcid.org/0000-0003-1094-8578) (Professor, Health Economics) contributed to the design of the review; the acquisition, analysis and interpretation of data; and drafting the final report.
Bethany E Keenan (https://orcid.org/0000-0001-7787-2892) (Research Fellow, Medical Engineering) contributed to the conception and design of the review, and the acquisition and interpretation of data.
Chantelle C Lachance (https://orcid.org/0000-0001-5755-5160) (Visiting Researcher, Knowledge Synthesis and Injury Prevention) contributed to the conception and design of the review, and the acquisition of data.
Dawn C Mackey (https://orcid.org/0000-0001-9854-1486) (Associate Professor, Ageing and Population Health) contributed to the conception and design of the review, and the acquisition and interpretation of data.
Chris Markham (https://orcid.org/0000-0001-8398-9333) (Head of School, Qualitative Research) contributed to the acquisition, analysis and interpretation of data.
Andrew C Laing (https://orcid.org/0000-0001-8128-011X) (Associate Professor, Injury Biomechanics and Ageing) contributed to the conception and design of the review.
Kirsten Farrell-Savage (https://orcid.org/0000-0002-2139-9095) (External Promotion and Liaison Lead, Communications and Public Involvement) contributed to the acquisition of data.
Olanrewaju Okunribido (https://orcid.org/0000-0003-4996-4890) (Ergonomics and Human Factors Specialist) contributed to data acquisition.
All authors critically revised the final report for important intellectual content and gave final approval, and agree to be accountable for all aspects of the work.
Publications
Lachance C, Felix L, Drahota A, Farrell-Savage K, Keenan B, Okunribido O, et al. The Shock-Absorbing Flooring Effectiveness SysTematic (SAFEST) review: a protocol. Poster presented at the Canadian Association on Gerontology, 24–26 October 2019, Moncton, NB, Canada.
Drahota AK, Keenan BE, Lachance C, Felix L, Raftery JP, Farrell-Savage KR, Mackey D. The SAFEST review: the Shock-Absorbing Flooring Effectiveness SysTematic review in care settings. Innov Aging 2019;3(Suppl. 1):S492–3. Poster presented at the Gerontological Society of America Annual Scientific Meeting, 13–17 November 2019, Austin, TX, USA.
Drahota A, Felix LM, Keenan BE, Lachance CC, Laing A, Mackey DC, et al. Protocol for the SAFEST review: the Shock-Absorbing Flooring Effectiveness SysTematic review including older adults and staff in hospitals and care homes. BMJ Open 2020;10:e032315.
Drahota A, Felix LM, Raftery J, Keenan BE, Lachance CC, Mackey D, et al. The SAFEST review: a mixed methods systematic review of shock-absorbing flooring for fall-related injury prevention. BMC Geriatrics 2022;22:32.
Data-sharing statement
Most technical data are included in the main report, appendices and supplementary materials. Project files are available on the Open Science Framework (https://osf.io/ev6xs/). Any additional data can be obtained from the corresponding author on request.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Drahota A, Felix LM, Raftery J, Keenan BE, Lachance CC, Mackey D, et al. The SAFEST review: a mixed methods systematic review of shock-absorbing flooring for fall-related injury prevention. BMC Geriatrics 2022;22. https://doi.org/10.1186/s12877-021-02670-4.
- Lamb SE, Jørstad-Stein EC, Hauer K, Becker C. Prevention of Falls Network Europe and Outcomes Consensus Group . Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc 2005;53:1618-22. https://doi.org/10.1111/j.1532-5415.2005.53455.x.
- James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev 2020;26:i3-i11. https://doi.org/10.1136/injuryprev-2019-043286.
- Dhargave P, Sendhilkumar R. Prevalence of risk factors for falls among elderly people living in long-term care homes. J Clin Gerontology Geriatr 2016;7:99-103. https://doi.org/10.1016/j.jcgg.2016.03.004.
- NHS Improvement . The Incidence and Costs of Inpatient Falls in Hospitals 2017.
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35:ii37-ii41. https://doi.org/10.1093/ageing/afl084.
- National Institute for Health and Care Excellence (NICE) . Falls in Older People: Assessing Risk and Prevention 2013.
- Zhao YL, Kim H. Older adult inpatient falls in acute care hospitals: intrinsic, extrinsic, and environmental factors. J Gerontol Nurs 2015;41:29-43. https://doi.org/10.3928/00989134-20150616-05.
- Kim J, Kim S, Park J, Lee E. Multilevel factors influencing falls of patients in hospital: the impact of nurse staffing. J Nurs Manag 2019;27:1011-19. https://doi.org/10.1111/jonm.12765.
- Severo IM, Almeida Mde A, Kuchenbecker R, Vieira DF, Weschenfelder ME, Pinto LR, et al. Risk factors for falls in hospitalized adult patients: an integrative review. Rev Esc Enferm USP 2014;48:540-54. https://doi.org/10.1590/S0080-623420140000300021.
- Ek S, Rizzuto D, Fratiglioni L, Johnell K, Xu W, Welmer AK. Risk profiles for injurious falls in people over 60: a population-based cohort study. J Gerontol A Biol Sci Med Sci 2018;73:233-9. https://doi.org/10.1093/gerona/glx115.
- Marks R, Allegrante JP, Ronald MacKenzie C, Lane JM. Hip fractures among the elderly: causes, consequences and control. Ageing Res Rev 2003;2:57-93. https://doi.org/10.1016/S1568-1637(02)00045-4.
- Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr 2013;56:407-15. https://doi.org/10.1016/j.archger.2012.12.006.
- Schoene D, Heller C, Aung YN, Sieber CC, Kemmler W, Freiberger E. A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls?. Clin Interv Aging 2019;14:701-19. https://doi.org/10.2147/CIA.S197857.
- Suzuki T, Sonoda S, Misawa K, Saitoh E, Shimizu Y, Kotake T. Incidence and consequence of falls in inpatient rehabilitation of stroke patients. Exp Aging Res 2005;31:457-69. https://doi.org/10.1080/03610730500206881.
- Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM. Factors related to functional prognosis in elderly patients after accidental hip fractures: a prospective cohort study. BMC Geriatr 2014;14. https://doi.org/10.1186/1471-2318-14-124.
- Royal College of Physicians . National Audit of Inpatient Falls (NAIF). Audit Report 2020 2020.
- Papadimitriou N, Tsilidis KK, Orfanos P, Benetou V, Ntzani EE, Soerjomataram I, et al. Burden of hip fracture using disability-adjusted life-years: a pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health 2017;2:e239-e246. https://doi.org/10.1016/S2468-2667(17)30046-4.
- Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018;9. https://doi.org/10.1002/14651858.CD005465.pub4.
- Lachance CC, Jurkowski MP, Dymarz AC, Robinovitch SN, Feldman F, Laing AC, et al. Compliant flooring to prevent fall-related injuries in older adults: a scoping review of biomechanical efficacy, clinical effectiveness, cost-effectiveness, and workplace safety. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0171652.
- Morello RT, Barker AL, Watts JJ, Haines T, Zavarsek SS, Hill KD, et al. The extra resource burden of in-hospital falls: a cost of falls study. Med J Aust 2015;203. https://doi.org/10.5694/mja15.00296.
- Baris VK, Intepeler SS, Yeginboy EY. The cost of serious patient fall-related injuries at hospitals in Turkey: a matched case–control study. Clin Nurs Res 2018;27:162-79. https://doi.org/10.1177/1054773816671521.
- Ruiz-Adame M, Correa M. A systematic review of the indirect and social costs studies in fragility fractures. Osteoporos Int 2020;31:1205-16. https://doi.org/10.1007/s00198-020-05319-x.
- Svedbom A, Hernlund E, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 2013;8. https://doi.org/10.1007/s11657-013-0137-0.
- Lachance CC, Korall AM, Russell CM, Feldman F, Robinovitch SN, Mackey DC. External hand forces exerted by long-term care staff to push floor-based lifts: effects of flooring system and resident weight. Hum Factors 2016;58:927-43. https://doi.org/10.1177/0018720816644083.
- Keenan BE, Hallas K, Drahota AK, Evans SL. A comparison of floor surfaces for injury prevention in care settings: impact forces and horizontal pulling force required to move wheeled equipment. Osteoporos Int 2020;31:2383-94. https://doi.org/10.1007/s00198-020-05520-y.
- Boyer J, Lin JH, Chang CC. Description and analysis of hand forces in medicine cart pushing tasks. Appl Ergon 2013;44:48-57. https://doi.org/10.1016/j.apergo.2012.04.008.
- Waters TR, Dick R, Lowe B, Werren D, Parsons K. Ergonomic assessment of floor-based and overhead lifts. Am J Safe Patient Handl Mov 2012;2:119-13.
- Mohammed S, Singh D, Johnson G, Xu P, McCluskey J, Harbison R. Evaluation of occupational risk factors for healthcare workers through analysis of the florida workers’ compensation claims database. Occup Dis Environ Med 2014;2:77-85. https://doi.org/10.4236/odem.2014.24009.
- Ngan K, Drebit S, Siow S, Yu S, Keen D, Alamgir H. Risks and causes of musculoskeletal injuries among health care workers. Occup Med 2010;60:389-94. https://doi.org/10.1093/occmed/kqq052.
- Wahlström J, Ostman C, Leijon O. The effect of flooring on musculoskeletal symptoms in the lower extremities and low back among female nursing assistants. Ergonomics 2012;55:248-55. https://doi.org/10.1080/00140139.2011.583360.
- Redfern MS, Moore PL, Yarsky CM. The influence of flooring on standing balance among older persons. Hum Factors 1997;39:445-55. https://doi.org/10.1518/001872097778827043.
- Laing AC, Robinovitch SN. Low stiffness floors can attenuate fall-related femoral impact forces by up to 50% without substantially impairing balance in older women. Accid Anal Prev 2009;41:642-50. https://doi.org/10.1016/j.aap.2009.03.001.
- Wright AD, Laing AC. The influence of novel compliant floors on balance control in elderly women – a biomechanical study. Accid Anal Prev 2011;43:1480-7. https://doi.org/10.1016/j.aap.2011.02.028.
- Wright AD, Laing AC. The influence of headform orientation and flooring systems on impact dynamics during simulated fall-related head impacts. Med Eng Phys 2012;34:1071-8. https://doi.org/10.1016/j.medengphy.2011.11.012.
- Wright AD, Heckman GA, McIlroy WE, Laing AC. Novel safety floors do not influence early compensatory balance reactions in older adults. Gait Posture 2014;40:160-5. https://doi.org/10.1016/j.gaitpost.2014.03.015.
- Glinka MN, Karakolis T, Callaghan JP, Laing AC. Characterization of the protective capacity of flooring systems using force-deflection profiling. Med Eng Phys 2013;35:108-15. https://doi.org/10.1016/j.medengphy.2012.04.006.
- Glinka MN, Cheema KP, Robinovitch SN, Laing AC. Quantification of the trade-off between force attenuation and balance impairment in the design of compliant safety floors. J Appl Biomech 2013;29:563-72. https://doi.org/10.1123/jab.29.5.563.
- Stephens JM, Goldie PA. Walking speed on parquetry and carpet after stroke: effect of surface and retest reliability. Clin Rehabil 1999;13:171-81. https://doi.org/10.1191/026921599668553798.
- Beach R, Bigelow K, Jackson K. Effect of Compliant Flooring on Postural Stability in an Older Adult Population n.d.
- Hanger H, Hurley K, White A. Low Impact Flooring – Does It Reduce Falls or Injury? n.d.
- Strang AJ, Haworth J, Hieronymus M, Walsh M, Smart LJ. Structural changes in postural sway lend insight into effects of balance training, vision, and support surface on postural control in a healthy population. Eur J Appl Physiol 2011;111:1485-95. https://doi.org/10.1007/s00421-010-1770-6.
- Weaver T, Laing A. The Influence of Safety Flooring on Reactive Stepping n.d.
- Nabhani F, Bamford JS. Impact properties of floor coverings and their role during simulated hip fractures. J Mater Process Technol 2004;153:139-44. https://doi.org/10.1016/j.jmatprotec.2004.04.211.
- Maki BE, Fernie GR. Impact attenuation of floor coverings in simulated falling accidents. Appl Ergon 1990;21:107-14. https://doi.org/10.1016/0003-6870(90)90132-H.
- Minns J, Nabhani F, Bamford JS. Can flooring and underlay materials reduce hip fractures in older people?. Nurs Older People 2004;16:16-20. https://doi.org/10.7748/nop2004.07.16.5.16.c2320.
- Casalena JA, Ovaert TC, Cavanagh PR, Streit DA. The Penn State Safety Floor: Part I – design parameters associated with walking deflections. J Biomech Eng 1998;120:518-26. https://doi.org/10.1115/1.2798022.
- Casalena JA, Badre-Alam A, Ovaert TC, Cavanagh PR, Streit DA. The Penn State Safety Floor: Part II – reduction of fall-related peak impact forces on the femur. J Biomech Eng 1998;120:527-32. https://doi.org/10.1115/1.2798023.
- Hanger HC. Low-impact flooring: does it reduce fall-related injuries?. J Am Med Dir Assoc 2017;18:588-91. https://doi.org/10.1016/j.jamda.2017.01.012.
- Mackey DC, Lachance CC, Wang PT, Feldman F, Laing AC, Leung PM, et al. The Flooring for Injury Prevention (FLIP) study of compliant flooring for the prevention of fall-related injuries in long-term care: a randomized trial. PLOS Med 2019;16. https://doi.org/10.1371/journal.pmed.1002843.
- Gustavsson J, Rahm G, Jernbro C, Nilson F. Effects of impact-absorbing flooring in residential care from the perspectives of enrolled nurses. J Hous Elderly 2017;31:367-81. https://doi.org/10.1080/02763893.2017.1335670.
- Gustavsson J, Bonander C, Nilson F. A quasi-experimental evaluation of compliant flooring in a residential care setting. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0201290.
- Gustavsson J, Jernbro C, Nilson F. There is more to life than risk avoidance – elderly people’s experiences of falls, fall-injuries and compliant flooring. Int J Qual Stud Health Well-Being 2018;13. https://doi.org/10.1080/17482631.2018.1479586.
- Lachance CC, Zaborska VO, Leung PM, Feldman F, Robinovitch SN, Mackey DC. Perceptions about compliant flooring from senior managers in long-term care. J Hous Elderly 2018;32:194-210. https://doi.org/10.1080/02763893.2018.1431584.
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019) n.d. www.training.cochrane.org/handbook (accessed 1 November 2020).
- Lockwood C, Porrit K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Joanna Briggs Institute Reviewer’s Manual. n.d.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. https://doi.org/10.1001/jama.283.15.2008.
- Higgins JPT, Lasserson T, Chandler J, Tovey D, Thomas J, Flemyng E, et al. Methodological Expectations of Cochrane Intervention Reviews. London: Cochrane; 2020.
- Lizarondo L, Stern C, Carrier J, Godfrey C, Rieger K, Salmond S, et al. JBI Manual for Evidence Synthesis. n.d.
- Higgins JP, Ramsay C, Reeves BC, Deeks JJ, Shea B, Valentine JC, et al. Issues relating to study design and risk of bias when including non-randomized studies in systematic reviews on the effects of interventions. Res Synth Methods 2013;4:12-25. https://doi.org/10.1002/jrsm.1056.
- Mitnitski A, Howlett SE, Rockwood K. Heterogeneity of human aging and its assessment. J Gerontol A Biol Sci Med Sci 2017;72:877-84. https://doi.org/10.1093/gerona/glw089.
- Kim S, Jazwinski SM. Quantitative measures of healthy aging and biological age. Healthy Aging Res 2015;4. https://doi.org/10.12715/har.2015.4.26.
- Ward D, Drahota A, Gal D, Severs M, Dean TP. Care home versus hospital and own home environments for rehabilitation of older people. Cochrane Database Syst Rev 2008;4. https://doi.org/10.1002/14651858.CD003164.pub2.
- Cameron ID, Robinovitch S, Birge S, Kannus P, Khan K, Lauritzen J, et al. Hip protectors: recommendations for conducting clinical trials – an international consensus statement (part II). Osteoporos Int 2010;21:1-10. https://doi.org/10.1007/s00198-009-1055-2.
- Lachance CC, Mackey DC. Feasibility of compliant flooring in long-term care: results from a stakeholder symposium. Can J Aging 2018;37:84-9. https://doi.org/10.1017/S0714980817000551.
- Drahota A, Felix LM, Keenan BE, Lachance CC, Laing A, Mackey DC, et al. Protocol for the SAFEST review: the Shock-Absorbing Flooring Effectiveness SysTematic review including older adults and staff in hospitals and care homes. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-032315.
- Rigby J, O’Connor M. Retaining older staff members in care homes and hospices in England and Australia: the impact of environment. Int J Palliat Nurs 2012;18:235-9. https://doi.org/10.12968/ijpn.2012.18.5.235.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275-83. https://doi.org/10.1136/bmj.313.7052.275.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013;346. https://doi.org/10.1136/bmj.f1049.
- Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment: a review and consolidation of quality assessment. PharmacoEconomics 2006;24:355-71. https://doi.org/10.2165/00019053-200624040-00006.
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366. https://doi.org/10.1136/bmj.l4898.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- Cannon J, Silvestri S, Munro M. Imaging choices in occult hip fracture. J Emerg Med 2009;37:144-52. https://doi.org/10.1016/j.jemermed.2007.12.039.
- Dominguez S, Liu P, Roberts C, Mandell M, Richman PB. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs – a study of emergency department patients. Acad Emerg Med 2005;12:366-9. https://doi.org/10.1111/j.1553-2712.2005.tb01959.x.
- Simpson A, Lamb S, Roberts PJ, Gardner TN, Evans JG. Does the type of flooring affect the risk of hip fracture?. Age Ageing 2004;33:242-6. https://doi.org/10.1093/ageing/afh071.
- Drahota AK, Ward D, Udell JE, Soilemezi D, Ogollah R, Higgins B, et al. Pilot cluster randomised controlled trial of flooring to reduce injuries from falls in wards for older people. Age Ageing 2013;42:633-40. https://doi.org/10.1093/ageing/aft067.
- Gulliford MC, Adams G, Ukoumunne OC, Latinovic R, Chinn S, Campbell MJ. Intraclass correlation coefficient and outcome prevalence are associated in clustered binary data. J Clin Epidemiol 2005;58:246-51. https://doi.org/10.1016/j.jclinepi.2004.08.012.
- Hill AM, McPhail SM, Waldron N, Etherton-Beer C, Ingram K, Flicker L, et al. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet 2015;385:2592-9. https://doi.org/10.1016/S0140-6736(14)61945-0.
- Barker AL, Morello RT, Wolfe R, Brand CA, Haines TP, Hill KD, et al. 6-PACK programme to decrease fall injuries in acute hospitals: cluster randomised controlled trial. BMJ 2016;352. https://doi.org/10.1136/bmj.h6781.
- Efthimiou O. Practical guide to the meta-analysis of rare events. Evid Based Ment Health 2018;21:72-6. https://doi.org/10.1136/eb-2018-102911.
- Lange B. The Impact of Absorbent Floor in Reducing Hip Fractures: A Cost–Utility Analysis Among Institutionalized Elderly 2012.
- HM Treasury . National Statistics. GDP Deflators at Market Prices, and Money GDP March 2020 (Quarterly National Accounts) n.d. www.gov.uk/government/statistics/gdp-deflators-at-market-prices-and-money-gdp-march-2020-quarterly-national-accounts (accessed 24 March 2021).
- Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. The GRADE Working Group; 2013.
- Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 2: how to make an overall CERQual assessment of confidence and create a Summary of Qualitative Findings table. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0689-2.
- Munthe-Kaas H, Bohren MA, Glenton C, Lewin S, Noyes J, Tuncalp O, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 3: how to assess methodological limitations. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0690-9.
- Noyes J, Booth A, Lewin S, Carlsen B, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 6: how to assess relevance of the data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0693-6.
- Colvin CJ, Garside R, Wainwright M, Munthe-Kaas H, Glenton C, Bohren MA, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 4: how to assess coherence. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0691-8.
- Glenton C, Carlsen B, Lewin S, Munthe-Kaas H, Colvin CJ, Tuncalp O, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 5: how to assess adequacy of data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0692-7.
- Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch 2006;13.
- Carvalho C, de Brito J, Flores-Colen I, Pereira C. Inspection, diagnosis, and rehabilitation system for vinyl and linoleum floorings in health infrastructures. J Perform Constr Facil 2018;32. https://doi.org/10.1061/(ASCE)CF.1943-5509.0001229.
- Anderson RL, Mackel DC, Stoler BS, Mallison GF. Carpeting in hospitals: an epidemiological evaluation. J Clin Microbiol 1982;15:408-15. https://doi.org/10.1128/JCM.15.3.408-415.1982.
- Ling C, Henderson S, Henderson R, Henderson M, Pedro T, Pang L. Cost benefit considerations of preventing elderly falls through environmental modifications to homes in Hana, Maui. Hawaii Med J 2008;67:65-8.
- Nabavi SH, Hatami ST, Norouzi F, Gerivani Z, Hatami SE, Ziarat HM, et al. Prevalence of fall and its related factors among older people in Bojnurd in 2015. Salmand Iran J Ageing 2016;11:466-73. https://doi.org/10.21859/sija-1103466.
- Vlodaver Z, Ortega HW, Arms J, Vander Velden H, Smith GA. Throw rug-related injuries treated in US EDs: are children the same as adults?. Am J Emerg Med 2014;32:1494-8. https://doi.org/10.1016/j.ajem.2014.09.024.
- Harris DD. The influence of flooring on environmental stressors: a study of three flooring materials in a hospital. HERD 2015;8:9-29. https://doi.org/10.1177/1937586715573730.
- Yarme J, Yarme H. Flooring and safety. Nurs Homes Long Term Care Manag 2001;50:82-3.
- Thorne C. Flooring for geriatric wards: report of an investigation at West Middlesex Hospital. The Builder 1963:557-9.
- Hignett S, Wolf L, Taylor E, Griffiths P. Firefighting to innovation: using human factors and ergonomics to tackle slip, trip, and fall risks in hospitals. Hum Factors 2015;57:1195-207. https://doi.org/10.1177/0018720815593642.
- Singh S. Floor Finish Selection in Hospital Design: A Survey of Facility Managers 2017.
- Warren CJ, Hanger HC. Fall and fracture rates following a change from carpet to vinyl floor coverings in a geriatric rehabilitation hospital. A longitudinal, observational study. Clin Rehabil 2013;27:258-63. https://doi.org/10.1177/0269215512455530.
- Knoefel F, Patrick L, Taylor J, Goubran R. Dual-stiffness flooring: can it reduce fracture rates associated with falls?. J Am Med Dir Assoc 2013;14:303-5. https://doi.org/10.1016/j.jamda.2012.12.077.
- Healey F. Does flooring type affect risk of injury in older in-patients?. Nurs Times 1994;90:40-1.
- Harris D. A material world: a comparative study of flooring material influence on patient safety, satisfaction, and quality of care. J Inter Des 2017;42:85-104. https://doi.org/10.1111/joid.12100.
- Donald IP, Pitt K, Armstrong E, Shuttleworth H. Preventing falls on an elderly care rehabilitation ward. Clin Rehabil 2000;14:178-85. https://doi.org/10.1191/026921500677888641.
- Hanger HC, Wilkinson TJ. Low-impact (compliant) flooring and staff injuries [published online ahead of print July 06 2020]. Disabil Rehabil 2020. https://doi.org/10.1080/09638288.2020.1786174.
- Drahota A, Gal D, Windsor J, Dixon S, Udell J, Ward D, et al. Pilot cluster randomised controlled trial of flooring to reduce injuries from falls in elderly care units: study protocol. Inj Prev 2011;17. https://doi.org/10.1136/injuryprev-2011-040154.
- Udell J. Fall and Injury Prevention Interventions: An Exploration Using Three Complementary Methodologies 2013.
- Lachance CC, Feldman F, Laing AC, Leung PM, Robinovitch SN, Mackey DC. Study protocol for the Flooring for Injury Prevention (FLIP) study: a randomised controlled trial in long-term care. Inj Prev 2016;22:453-60. https://doi.org/10.1136/injuryprev-2016-042008.
- Gustavsson J, Bonander C, Andersson R, Nilson F. Investigating the fall-injury reducing effect of impact absorbing flooring among female nursing home residents: initial results. Inj Prev 2015;21:320-4. https://doi.org/10.1136/injuryprev-2014-041468.
- Gustavsson J. Preventing fall injuries among elderly in residential care facilities with impact absorbing flooring. Inj Prev 2017;23. https://doi.org/10.1136/injuryprev-2017-042560.107.
- Gustavsson J. Evaluating compliant flooring as a fall injury reducing measure in a residential care setting. Inj Prev 2018;24:A225-A6. https://doi.org/10.1136/injuryprevention-2018-safety.623.
- Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 2007;18:805-35. https://doi.org/10.1097/EDE.0b013e3181577511.
- de Boer MR, Waterlander WE, Kuijper LD, Steenhuis IH, Twisk JW. Testing for baseline differences in randomized controlled trials: an unhealthy research behavior that is hard to eradicate. Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0162-z.
- Trinh LTT, Assareh H, Wood M, Addison-Wilson C, Sathiyaseelan Y. Falls in hospital causing injury. J Healthc Qual 2020;42:1-11. https://doi.org/10.1097/JHQ.0000000000000179.
- Eldridge S, Campbell M, Campbell M, Drahota A, Giraudeau B, Higgins J, et al. Revised Cochrane Risk of Bias Tool for Randomised Trials (RoB 2.0): Additional Considerations for Cluster-Randomised Trials n.d. https://sites.google.com/site/riskofbiastool/welcome/rob-2-0-tool/archive-rob-2-0-cluster-randomized-trials-2016 (accessed 1 October 2020).
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7454.1490.
- Drahota A, Ward D, Soilemezi D, Udell J, Latimer N, Hallas K, et al. The HIP-HOP Flooring Study: Helping Injury Prevention in Hospitalised Older People: Pilot Cluster Randomised Controlled Trial of Flooring to Reduce Injuries from Falls in Elderly Care Units: Final Report n.d. https://researchportal.port.ac.uk/portal/en/publications/the-hiphop-flooring-study-helping-injury-prevention-in-hospitalised-older-people(e426fc53-4e56-451d-a7d0-a54002f25e21).html (accessed 1 November 2020).
- Latimer N, Dixon S, Drahota AK, Severs M. Cost–utility analysis of a shock-absorbing floor intervention to prevent injuries from falls in hospital wards for older people. Age Ageing 2013;42:641-5. https://doi.org/10.1093/ageing/aft076.
- Zacker C, Shea D. An economic evaluation of energy-absorbing flooring to prevent hip fractures. Int J Technol Assess Health Care 1998;14:446-57. https://doi.org/10.1017/s0266462300011429.
- Ryen L, Svensson M. Modelling the cost-effectiveness of impact-absorbing flooring in Swedish residential care facilities. Eur J Public Health 2016;26:407-11. https://doi.org/10.1093/eurpub/ckv197.
- Njogu F, Brown P. Cost Effectiveness of Impact Absorbent Flooring in Reducing Fractures Among Institutionalized Elderly. Auckland: University of Auckland; 2008.
- Schwenk M, Lauenroth A, Stock C, Moreno RR, Oster P, McHugh G, et al. Definitions and methods of measuring and reporting on injurious falls in randomised controlled fall prevention trials: a systematic review. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-50.
- O’Malley N, Clifford AM, Comber L, Coote S. Fall definitions, faller classifications and outcomes used in falls research among people with multiple sclerosis: a systematic review [published online ahead of print July 06 2020]. Disabil Rehabil 2020. https://doi.org/10.1080/09638288.2020.1786173.
- Copsey B, Hopewell S, Becker C, Cameron ID, Lamb SE. Appraising the uptake and use of recommendations for a common outcome data set for clinical trials: a case study in fall injury prevention. Trials 2016;17. https://doi.org/10.1186/s13063-016-1259-7.
- Zorzela L, Loke YK, Ioannidis JP, Golder S, Santaguida P, Altman DG, et al. PRISMA harms checklist: improving harms reporting in systematic reviews. BMJ 2016;352. https://doi.org/10.1136/bmj.i157.
- Minns J, Tracey S. Wheelchair pushing forces over a vinyl and a new shock-absorbing flooring. Br J Occup Ther 2011;74:41-3. https://doi.org/10.4276/030802211X12947686093684.
- Al-Eisawi KW, Kerk CJ, Congleton JJ, Amendola AA, Jenkins OC, Gaines W. Factors affecting minimum push and pull forces of manual carts. Appl Ergon 1999;30:235-45. https://doi.org/10.1016/S0003-6870(98)00019-2.
- Drahota A, Ward D, Mackenzie H, Stores R, Higgins B, Gal D, et al. Sensory environment on health-related outcomes of hospital patients. Cochrane Database Syst Rev 2012;3. https://doi.org/10.1002/14651858.CD005315.pub2.
- Willmott M. The effect of a vinyl floor surface and a carpeted floor surface upon walking in elderly hospital inpatients. Age Ageing 1986;15:119-20. https://doi.org/10.1093/ageing/15.2.119.
- Dixit MK, Singh S, Lavy S, Yan W. Floor finish selection in health-care facilities: a systematic literature review. Facilities 2019;37:897-918. https://doi.org/10.1108/F-03-2018-0042.
- Drahota A, Gal D, Windsor J. Flooring as an intervention to reduce injuries from falls in healthcare settings: an overview. Qual Ageing Older Adults 2007;8:3-9. https://doi.org/10.1108/14717794200700002.
- Tse T. The environment and falls prevention: do environmental modifications make a difference?. Aust Occup Ther J 2005;54:271-81. https://doi.org/10.1111/j.1440-1630.2005.00525.x.
- Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141-6. https://doi.org/10.1097/XEB.0000000000000050.
- Bhan S, Levine I, Laing AC. The influence of body mass index and gender on the impact attenuation properties of flooring systems. J Appl Biomech 2013;29:731-9. https://doi.org/10.1123/jab.29.6.731.
- Bhan S, Levine IC, Laing AC. Energy absorption during impact on the proximal femur is affected by body mass index and flooring surface. J Biomech 2014;47:2391-7. https://doi.org/10.1016/j.jbiomech.2014.04.026.
- Chesney DA, Axelson PW. Preliminary test method for the determination of surface firmness wheelchair propulsion. IEEE Trans Rehabil Eng 1996;4:182-7. https://doi.org/10.1109/86.536773.
- Dickinson JI, Shroyer JL, Elias JW, Hutton JT, Gentry GM. The effect of selected residential carpet and pad on the balance of healthy older adults. Environ Behav 2001;33:279-95. https://doi.org/10.1177/00139160121972990.
- Dickinson JI, Shroyer JL, Elias JW. The influence of commercial-grade carpet on postural sway and balance strategy among older adults. Gerontologist 2002;42:552-9. https://doi.org/10.1093/geront/42.4.552.
- Finlay O, Beringer T. Effects of floor coverings on measurement of gait and plantar pressure. Physiotherapy 2007;93:144-50. https://doi.org/10.1016/j.physio.2006.11.014.
- Gardner TN, Simpson AH, Booth C, Sprukkelhorst P, Evans M, Kenwright J, et al. Measurement of impact force, simulation of fall and hip fracture. Med Eng Phys 1998;20:57-65. https://doi.org/10.1016/S1350-4533(97)00041-6.
- Glaser RM, Sawka MN, Wilde SW, Woodrow BK, Suryaprasad AG. Energy cost and cardiopulmonary responses for wheelchair locomotion and walking on tile and on carpet. Paraplegia 1981;19:220-6. https://doi.org/10.1038/sc.1981.45.
- Hales M, Johnson JD, Asbury G, Evans N. Influence of floor covering composition on force attenuation during falls, wheelchair mobility, and slip resistance. AATCC Rev 2015;15:44-53. https://doi.org/10.14504/ar.15.6.4.
- Koontz AM, Cooper RA, Boninger ML, Yang Y, Impink BG, van der Woude LH. A kinetic analysis of manual wheelchair propulsion during start-up on select indoor and outdoor surfaces. J Rehabil Res Dev 2005;42:447-58. https://doi.org/10.1682/jrrd.2004.08.0106.
- Li N, Tsushima E, Tsushima H. Comparison of impact force attenuation by various combinations of hip protector and flooring material using a simplified fall-impact simulation device. J Biomech 2013;46:1140-6. https://doi.org/10.1016/j.jbiomech.2013.01.007.
- Lord SR, Clark RD, Webster IW. Visual acuity and contrast sensitivity in relation to falls in an elderly population. Age Ageing 1991;20:175-81. https://doi.org/10.1093/ageing/20.3.175.
- McGill SM, Callaghan JP. Impact forces following the unexpected removal of a chair while sitting. Accid Anal Prev 1999;31:85-9. https://doi.org/10.1016/s0001-4575(98)00048-7.
- Nabhani F, Bamford J. Mechanical testing of hip protectors. J Mater Process Technol 2002;124:311-8. https://doi.org/10.1016/S0924-0136(02)00200-5.
- Soangra R, Jones B, Lockhart TE. Effects of anti-fatigue flooring on gait parameters. Proceedings of the Human Factors and Ergonomics Society 54th Annual Meeting 2010;54:2019-22. https://doi.org/10.1177/154193121005402324.
- Lachance CC, Korall AMB, Russell CM, Feldman F, Robinovitch SN, Mackey DC. Hand forces exerted by long-term care staff when pushing wheelchairs on compliant and non-compliant flooring. Appl Ergon 2018;71:95-101. https://doi.org/10.1016/j.apergo.2018.04.009.
- Snook SH, Ciriello VM. The design of manual handling tasks: revised tables of maximum acceptable weights and forces. Ergonomics 1991;34:1197-213. https://doi.org/10.1080/00140139108964855.
- Knoefel FD, Mousseau M, Berry M. Pilot study to assess mobility safety on a dual-stiffness floor. Can J Geriatr 2008;11:110-2.
- Losco EL, Hanger HC, Wilkinson TJ. Ease of walking on low-impact flooring in frail older people. J Am Med Dir Assoc 2019;20:385-6. https://doi.org/10.1016/j.jamda.2018.12.008.
Appendix 1 Search strategies
| Number | Search strategy |
|---|---|
| MEDLINE (date range searched: 1 May 2016–29 September 2019; date of last search: 29 September 2019) | |
| 1 | MH “Wounds and Injuries+” |
| 2 | MH “Accidental Falls/PC” |
| 3 | MH “Hip Fractures+/PC” |
| 4 | Fall# |
| 5 | Faller# |
| 6 | S1 OR S2 OR S3 OR S4 OR S5 |
| 7 | MH “Aged+” |
| 8 | MH “Middle Aged” |
| 9 | Older |
| 10 | Senior# |
| 11 | elderly |
| 12 | S7 OR S8 OR S9 OR S10 OR S11 |
| 13 | S6 AND S12 |
| 14 | MH “Residential Facilities+” |
| 15 | MH “Long-Term Care” |
| 16 | MH “Institutionalization” |
| 17 | MH “Hospitalization” |
| 18 | MH “Subacute Care” |
| 19 | MH “Hospitals+” |
| 20 | MH “Hospital Units” |
| 21 | MH “Rehabilitation Centers” |
| 22 | MH “Inpatients” |
| 23 | MH “Geriatric Assessment” |
| 24 | (“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “hospital”) N3 (care or ward# or hospital) |
| 25 | (rehabilitation or geriatric) N1 (ward# or hospital# or unit# or department#) |
| 26 | Hostel# or nursing home# |
| 27 | inpatient |
| 28 | resident# |
| 29 | institution# |
| 30 | S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 |
| 31 | S13 and S30 |
| 32 | floor* NOT (pelvic floor OR sinus OR mouth) |
| 33 | carpet* |
| 34 | ground surface# |
| 35 | smartcell* |
| 36 | tarkett |
| 37 | softile |
| 38 | sorbashock |
| 39 | forbo |
| 40 | kradal |
| 41 | noraplan |
| 42 | MH “Floors and Floorcoverings” |
| 43 | S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 |
| 44 | S31 AND S43 |
| 45 | MH “Animals+” |
| 46 | MH “Humans” |
| 47 | S45 NOT S46 |
| 48 | S44 NOT S47 |
| 49 |
S44 NOT S47 Limiters: date of publication – 1 May 2016 |
| CINAHL (date range searched: 1 May 2016–29 September 2019; date of last search: 29 September 2019) | |
| 1 | MH “Wounds and Injuries+” |
| 2 | (MH “Accidental Falls/PC/RF”) |
| 3 | (MH “Hip Fractures+/PC”) |
| 4 | Fall# |
| 5 | Faller# |
| 6 | S1 OR S2 OR S3 OR S4 OR S5 |
| 7 | (MH “Aged+”) |
| 8 | (MH “Middle Age”) |
| 9 | Older |
| 10 | Senior# |
| 11 | elderly |
| 12 | S7 OR S8 OR S9 OR S10 OR S11 |
| 13 | S6 AND S12 |
| 14 | (MH “Residential Facilities+”) |
| 15 | (MH “Long Term Care”) |
| 16 | (MH “Institutionalization+”) |
| 17 | MH “Hospitalization” |
| 18 | (MH “Subacute Care”) |
| 19 | (MH “Hospitals+”) |
| 20 | MH “Hospital Units” |
| 21 | (MH “Rehabilitation Centers”) |
| 22 | (MH “Inpatients”) |
| 23 | (MH “Geriatric Assessment”) |
| 24 | (“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “halfway” or “intermediate” or “hospital”) N3 (care or ward# or hospital) |
| 25 | (rehabilitation or geriatric) N1 (ward# or hospital# or unit# or department#) |
| 26 | hostel# or nursing home# |
| 27 | inpatient |
| 28 | resident# |
| 29 | institution# |
| 30 | S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 |
| 31 | S13 and S30 |
| 32 | floor* NOT (pelvic floor OR sinus OR mouth) |
| 33 | carpet* |
| 34 | ground surface# |
| 35 | smartcell* |
| 36 | tarkett |
| 37 | softile |
| 38 | sorbashock |
| 39 | forbo |
| 40 | kradal |
| 41 | noraplan |
| 42 | MH “Floors and Floorcoverings” |
| 43 | S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 |
| 44 | S31 AND S43 |
| 45 | MH “Animals+” |
| 46 | MH “Human” |
| 47 | S45 NOT S46 |
| 48 | S44 NOT S47 |
| 49 |
S44 NOT S47 Limiters: date of publication – 1 May 2016 |
| AgeLine (date range searched: 1 May 2016–23 November 2019; date of last search 23 November 2019) | |
| 1 | DE “Falls” |
| 2 | DE “Fractures” OR DE “Hip Injuries” |
| 3 | falls |
| 4 | faller# |
| 5 | DE “Accidents” OR DE “Falls” OR DE “Injuries” |
| 6 | S1 OR S2 OR S3 OR S4 OR S5 |
| 7 | DE “Board and Care Homes” OR DE “Homes for the Elderly” OR DE “Long Term Care” |
| 8 | DE “Acute Care” OR DE “Ambulatory Care” OR DE “Postoperative Care” OR DE “Subacute Care” OR DE “Hospitalization” OR DE “Inpatient Services” OR DE “Long Term Care” OR DE “For Profit Nursing Homes” OR DE “Homes for the Elderly” OR DE “Institutional Care” OR DE “Institutionalized Populations” OR DE “Intermediate Care” OR DE “Nonprofit Nursing Homes” OR DE “Nursing Homes” |
| 9 | DE “Institutionalization” OR DE “Nursing Home Placement” |
| 10 | DE “Hospitals” OR DE “Psychiatric Hospitals” OR DE “Teaching Hospitals” OR DE “Veterans Affairs Medical Centers” |
| 11 | DE “Inpatients” |
| 12 | DE “Geriatric Assessment” |
| 13 | (“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “halfway” or “intermediate” or “hospital”) N3 (care or ward# or hospital) |
| 14 | (rehabilitation or geriatric) N1 (ward# or hospital# or unit# or department#) |
| 15 | (hostel# or nursing home#) OR inpatient OR resident# |
| 16 | S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 |
| 17 | floor* NOT (pelvic floor OR sinus OR mouth) |
| 18 | carpet* |
| 19 | ground surface# |
| 20 | smartcell* |
| 21 | tarkett |
| 22 | softile |
| 23 | sorbashock |
| 24 | forbo |
| 25 | kradal |
| 26 | noraplan |
| 27 | S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 |
| 28 | S6 AND S16 AND S27 |
| 29 |
S6 AND S16 AND S27 Limiters: publication year – 2016–19 |
| Scopus (date range searched: 1 May 2016–29 September 2019; date of last search: 29 September 2019) | |
| 1 | Fall |
| 2 | faller |
| 3 | #1 OR #2 |
| 4 | Older |
| 5 | Senior |
| 6 | elderly |
| 7 | #4 OR #5 OR #6 |
| 8 | #3 AND #7 |
| 9 | (“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “halfway” or “intermediate” or “hospital”) W/3 (care or ward or hospital) |
| 10 | (“rehabilitation” or “geriatric”) W/1(ward or hospital or unit or department) |
| 11 | hostel or “nursing home” |
| 12 | inpatient |
| 13 | resident |
| 14 | institution |
| 15 | #9 OR #10 OR #12 OR #13 OR #14 |
| 16 | #8 AND #15 |
| 17 | floor* |
| 18 | (“pelvic floor” OR sinus OR mouth) |
| 19 | #17 AND NOT #18 |
| 20 | carpet* |
| 21 | “ground surface” |
| 22 | smartcell* |
| 23 | tarkett |
| 24 | softile |
| 25 | sorbashock |
| 26 | forbo |
| 27 | kradal |
| 28 | noraplan |
| 29 | #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 |
| 30 | #16 AND #29 |
| Web of Science (date range searched: 1 May 2016–29 September 2019; date of last search: 29 September 2019) | |
| 1 | fall$ |
| 2 | faller$ |
| 3 | #1 OR #2 |
| 4 | Older |
| 5 | Senior$ |
| 6 | elderly |
| 7 | #4 OR #5 OR #6 |
| 8 | #3 AND #7 |
| 9 | (“rehabilitation ward$” OR “rehabilitation hospital$” OR “rehabilitation unit$” OR “rehabilitation department$” OR “geriatric ward$” OR “geriatric hospital$” OR “geriatric unit$” OR “geriatric department$”) |
| 10 | ((“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “hospital”) AND (“care” or “ward$” or “hospital$”)) |
| 11 | hostel$ or nursing home$ |
| 12 | inpatient |
| 13 | resident$ |
| 14 | institution$ |
| 15 | #9 OR #10 OR #12 OR #13 OR #14 |
| 16 | #8 AND #15 |
| 17 | floor* NOT (pelvic floor OR sinus OR mouth) |
| 18 | carpet* |
| 19 | ground surface$ |
| 20 | smartcell* |
| 21 | tarkett |
| 22 | softile |
| 23 | sorbashock |
| 24 | forbo |
| 25 | kradal |
| 26 | noraplan |
| 27 | #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 |
| 28 | #16 AND #27 |
| 29 | #16 AND #27 Timespan=2016-2019 |
| ProQuest Dissertations & Theses (date range searched: 1 May 2016–3 October 2019; date of last search: 3 October 2019) | |
| 1 | MESH “Wounds and Injuries+” |
| 2 | MESH “Accidental Falls” |
| 3 | MESH “Hip Fractures “ |
| 4 | Fall? |
| 5 | Faller? |
| 6 | S1 OR S2 OR S3 OR S4 OR S5 |
| 7 | MESH “Aged” |
| 8 | MESH “Middle Aged” |
| 9 | Older |
| 10 | Senior? |
| 11 | elderly |
| 12 | S7 OR S8 OR S9 OR S10 OR S11 |
| 13 | S6 AND S12 |
| 14 | MESH “Residential Facilities” |
| 15 | MESH “Long-Term Care” |
| 16 | MESH “Institutionalization” |
| 17 | MESH “Hospitalization” |
| 18 | MESH “Subacute Care” |
| 19 | MESH “Hospitals” |
| 20 | MESH “Hospital Units” |
| 21 | MESH “Rehabilitation Centers” |
| 22 | MESH “Inpatients” |
| 23 | MESH “Geriatric Assessment” |
| 24 | (“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “hospital”) N/3 (care or ward? or hospital) |
| 25 | (rehabilitation or geriatric) N/1 (ward? or hospital? or unit? or department?) |
| 26 | Hostel? or nursing home? |
| 27 | inpatient |
| 28 | resident? |
| 29 | institution? |
| 30 | S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 |
| 31 | S13 and S30 |
| 32 | floor* NOT (pelvic floor OR sinus OR mouth) |
| 33 | carpet* |
| 34 | ground surface? |
| 35 | smartcell* |
| 36 | tarkett |
| 37 | softile |
| 38 | sorbashock |
| 39 | forbo |
| 40 | kradal |
| 41 | noraplan |
| 42 | MESH “Floors and Floorcoverings” |
| 43 | S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 |
| 44 | S31 AND S43 |
| 45 | MESH “Animals” |
| 46 | MESH “Humans” |
| 47 | S45 NOT S46 |
| 48 | S44 NOT S47 |
| 49 |
S44 NOT S47 Limiters: date of publication – 1 May 2016 |
| OpenGrey (date range searched: inception to 1 April 2020; date of last search: 1 April 2020) | |
| (“Floor coverings” OR “Flooring” OR “carpet” OR “ground surface” OR “SmartCell” OR “Tarkett” OR “Softile” OR “Sorbashock” OR “Kradal” OR “Forbo” OR “Noraplan”) AND (“aged” OR “older” OR “senior*” OR “elderly”) | |
| WHO International Clinical Trials Registry Platform (date range searched: 1 May 2016–3 October 2019; date of last search: 3 October 2019) | |
| Condition | fall* OR injur* OR older OR elder* OR aged OR senior* |
| AND intervention | Carpet* OR ground surface* OR Smartcell OR Tarkett OR Softile OR Sorbashock OR Kradal OR Forbo OR Noraplan OR floor* NOT sinus NOT pelvic floor NOT mouth |
| ClinicalTrials.gov (date range searched: 1 May 2016–1 April 2020; date of last search: 1 April 2020) | |
| Other terms | “residential” OR “Long-Term Care” OR “institutional” OR “Subacute” OR “hospitals” OR “hospital” OR “rehabilitation” OR “inpatients” OR “long stay” OR “long term” OR “acute” OR “sub-acute” OR “geriatric” |
| Condition or disease | falls OR fall OR injury OR injuries OR older OR elderly OR elders OR aged OR senior OR seniors |
| Intervention/treatment | “carpet” OR “SmartCell” OR “Tarkett” OR “Softile” OR “Sorbashock” OR “Kradal” OR “Forbo” OR “Noraplan” OR “floor” OR “floors” OR “flooring” NOT (“sinus” OR “pelvic floor” OR “mouth”) |
| First posted from | 1 May 2016 to 1 April 2020 |
| NHS EED and Health Technology Assessment database (date range searched: inception to 11 November 2019; date of last search: 11 November 2019) | |
| 1 | fall$ |
| 2 | faller$ |
| 3 | #1 OR #2 |
| 4 | Older |
| 5 | Senior$ |
| 6 | elderly |
| 7 | #4 OR #5 OR #6 |
| 8 | #3 AND #7 |
| 9 | (“rehabilitation ward$” OR “rehabilitation hospital$” OR “rehabilitation unit$” OR “rehabilitation department$” OR “geriatric ward$” OR “geriatric hospital$” OR “geriatric unit$” OR “geriatric department$”) |
| 10 | ((“long stay” or “long term” or “acute” or “sub-acute” or “subacute” or “residential” or “hospital”) AND (“care” or “ward$” or “hospital$”)) |
| 11 | hostel$ or nursing home$ |
| 12 | inpatient |
| 13 | resident$ |
| 14 | institution$ |
| 15 | #9 OR #10 OR #12 OR #13 OR #14 |
| 16 | #8 AND #15 |
| 17 | floor* NOT (pelvic floor OR sinus OR mouth) |
| 18 | carpet* |
| 19 | ground surface$ |
| 20 | smartcell* |
| 21 | tarkett |
| 22 | softile |
| 23 | sorbashock |
| 24 | forbo |
| 25 | kradal |
| 26 | noraplan |
| 27 | #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 |
| 28 | #16 AND #27 |
| 29 | #16 AND #27 Timespan=2016-2019 |
| Agency for Healthcare Research and Quality (date range searched: entire website; date of last search: 22 April 2020) | |
| flooring OR carpet OR ground surface OR SmartCell OR Tarkett OR Softile OR Sorbashock OR Kradal OR Forbo OR Noraplan | |
| The National Institute for Occupational Safety and Health (date range searched: 1 May 2016–22 April 2020; date of last search: 22 April 2020) | |
|
CARPET OR SMARTCELL OR TARKETT OR SOFTILE OR SORBASHOCK OR KRADAL OR FORBO OR NORAPLAN OR floor* - published from 05-2016 In Title (Advanced Search) |
|
| US Center for Health Design (date range searched: 2016–1 May 2019; date of last search: 1 May 2019) | |
|
Fall and Floor 54 items – manually went through to identify research studies from 2016 to current: 3 records |
|
| Parachute Canada (date range searched: entire website; date of last search: 22 April 2020) | |
|
Flooring Carpet Ground surface SmartCell Tarkett Softile Sorbashock Kradal Forbo Noraplan |
|
Appendix 2 Risk-of-bias tables (quantitative studies)
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias arising from the randomisation process | ||
| Was the allocation sequence random? | It is stated that patients were randomly assigned a floor type, but it is not fully explained how the randomisation sequence was generated:Using randomized envelopes for each risk group, patients were assigned a floor group (carpet or vinyl) and a physiotherapy group (conventional physiotherapy or additional exercise) | Probably yes |
| Was the allocation sequence concealed until participants were enrolled and assigned to interventions? | The study report does not provide information on the allocation process used to preserve concealment (i.e. whether or not the envelopes were serially numbered, sealed and opaque):Using randomized envelopes | No information |
| Did baseline differences between intervention groups suggest a problem with the randomisation process? | The baseline characteristics presented in table 1 of Donald et al.105 suggest that the two groups were relatively similar; however, more females were assigned to carpet (92.8%) than to vinyl (69.2%):The mean age and Barthel score for the groups on admission were similar in all groups, and baseline characteristics are shown in table 1 | Probably no |
| Risk-of-bias judgement |
Falls resulting in injuries, fractures, hip fractures, fallers: Allocation sequence was random, but there is no information about concealment of allocation sequence; any baseline differences observed between intervention groups appear to be compatible with chance |
Some concerns |
| 2. Risk of bias due to deviations from the intended interventions (effect of assignment to intervention) | ||
| Were participants aware of their assigned intervention during the trial? | It is not clear if an accompanying patient information sheet provided some details about the intervention. Nonetheless, participants would have been aware whether they were being nursed on carpet or vinyl:Written consent was obtained from patients and carers | Yes |
| Were carers and people delivering the interventions aware of participants’ assigned intervention during the trial? | Both of the interventions, carpet and vinyl flooring, were delivered in the same hospital, but in different bays. It is probable that nurses would have been aware of the study and assigned interventions | Probably yes |
| Were there deviations from the intended intervention that arose because of the experimental context? | It is stated that there was deviation from the intended intervention, but it is unlikely to be due to experimental context:Compliance with allocation was reasonable – two patients allocated to carpet were nursed on vinyl because they required side-rooms | Probably no |
| Was an appropriate analysis used to estimate the effect of assignment to intervention? | Although the authors state that an intention-to-treat analysis was used, the write-up of the results implies that an ‘as treated’ analysis may have been used, as it reports in terms of those who were ‘nursed in a carpeted room’ or ‘nursed on vinyl’ rather than in terms of those who were randomised to carpet or vinyl (although the deviations were few, it is not clear in which group the two deviating participants were analysed):Data on falls were available for every patient, and intention-to-treat analysis was used for the incidence of falls | Probably yes |
| Risk-of-bias judgement |
Falls resulting in injuries, fractures, hip fractures, fallers: Participants and people delivering the interventions were aware of interventions groups during the trial; deviations from intended intervention were unlikely to be due to experimental context. An appropriate analysis appears to have been used to estimate the effect of assignment to intervention |
Low |
| 3. Risk of bias as a result of missing data | ||
| Were data for this outcome available for all, or nearly all, participants randomised? |
Falls resulting in injuries: Reporting of injuries in each group is not clear (we do not know if the faller in the vinyl group sustained a minor injury, and it says ‘a third’ of falls resulted in minor injury, without a clear figure) |
No information |
| Fracture, hip fracture:No falls resulted in fracture | Yes | |
| Fallers:Data on falls were available for every patient, and intention-to-treat analysis was used for the incidence of falls | Yes | |
| Risk-of-bias judgement | Falls resulting in injuries | No information |
|
Fracture, hip fracture, fallers: Outcome data were available for all randomised participants |
Low | |
| 4. Risk of bias in measurement of the outcome | ||
| Was the method of measuring the outcome inappropriate? |
Falls resulting in injuries, fracture, hip fracture: Definition of injuries and data acquisition methods not described |
No information |
|
Fallers: A standardised method was used to measure the outcome – |
Probably no | |
| Could measurement or ascertainment of the outcome have differed between intervention groups? |
Falls resulting in injuries, fractures, hip fractures; fallers: The study was conducted in one ward, so it is likely that the processes were the same for all patients – |
Probably no |
| Were outcome assessors aware of the intervention received by study participants? |
Falls resulting in injuries, fractures, hip fractures, fallers: Both of the interventions, carpet and vinyl flooring, were delivered in the same hospital, but in different bays. Accident forms were completed by the nursing staff, so assessors were probably aware |
Probably yes |
| Could assessment of the outcome have been influenced by knowledge of intervention received? |
Falls resulting in injuries, fallers: Possibly for falls and injuries, as the outcome ascertainment relies on individuals completing an incident report form and classifying the event as a fall. These are observer-reported outcomes involving some judgment |
Probably yes |
|
Fracture, hip fracture: Less likely for fractures (as more objective); observer-reported outcomes not involving judgement |
Probably no | |
| Is it likely that assessment of the outcome was influenced by knowledge of intervention received? |
Falls resulting in injuries, fractures, hip fractures, fallers: There is a possibility that staff had more concerns about carpet, so it is possible that the assessment of the outcomes was influenced by knowledge of the intervention (more so for injuries and fallers). If health-care providers have concerns about carpet, they are more likely to be influenced by the knowledge of the intervention received – |
Probably no |
| Risk-of-bias judgement |
Falls resulting in injuries, fallers: Method of measuring the outcome was not inappropriate; measurement of the outcome did not differ between intervention groups; assessment of the outcome could have been influenced by knowledge of the intervention received; and it is unlikely that assessment of the outcome was influenced by knowledge of intervention received |
High |
|
Fracture, hip fracture: Method of measuring the outcome was not inappropriate; measurement or ascertainment of the outcome did not differ between intervention groups; and assessment of the outcome could not have been influenced by knowledge of the intervention received |
Some concerns | |
| 5. Risk of bias in selection of the reported result | ||
| Were the data that produced this result analysed in accordance with a prespecified analysis plan that was finalised before unblinded outcome data were available for analysis? |
Falls resulting in injuries, fractures, hip fractures, fallers: Protocol is unavailable to compare the planned measurement and analysis with the reported ones. Moreover, there is insufficient information in the methods section to make any judgement |
No information |
| Is the numerical result being assessed likely to have been selected, on the basis of the results, from multiple eligible outcome measurements (e.g. scales, definitions, time points) within the outcome domain? |
Falls resulting in injuries, fractures, hip fractures, fallers: It is unlikely, but cannot be certain as the protocol is not available |
Probably no |
| Is the numerical result being assessed likely to have been selected, on the basis of the results, from multiple eligible analyses of the data? |
Falls resulting in injuries: Not fully reported because of low counts, so unclear how many occurred in each group – |
Probably yes |
|
Fracture, hip fracture: It is stated that there were no fractures in either of the groups |
No | |
|
Fallers: Proportion of fallers is explicitly stated for each group |
No | |
| Risk-of-bias judgement | Falls resulting in injuries | High |
| Fractures, hip fractures, fallers | Some concerns | |
| Overall risk of bias | Falls resulting in injuries, fallers | High |
| Fractures, hip fractures | Some concerns | |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1a. Risk of bias arising from the randomisation process | ||
| Was the allocation sequence random? | Randomisation process for allocation sequence is explicitly stated:Sites were allocated to intervention or control groups by an independent statistician using a computer-generated random list, in blocks of four | Yes |
| Is it unlikely that the allocation sequence was subverted? | Allocation sequence was conducted by an independent statistician:The sequence and blocking was not revealed to the researchers until after the sites had been allocated. After sites received full governance approval, the researchers contacted the statistician to reveal the group allocation. The final three sites were randomised at the same time | Yes |
| Were there baseline imbalances that suggest a problem with the randomisation process? | Although there were some baseline differences between intervention groups, these are more likely to be due to chance:Participants were of similar age, fracture risk and functionality across groups, but there were more males, use of ambulatory aids and transfers between bays [. . .] in the intervention group [. . .]. More people were admitted with instability in the control group [. . . and] had more co-morbidities associated with fall risk [. . .] | Probably no |
| Risk-of-bias judgement |
All outcomes: Allocation sequence was random, allocation concealment was adequate, and baseline imbalances are unlikely to be due to problem with randomisation process |
Low |
| 1b. Risk of bias arising from the timing of identification and recruitment of participants in relation to timing of randomisation | ||
| Were all the individual participants identified before randomisation of clusters (and, if the trial specifically recruited patients, were they all recruited before randomisation of clusters)? |
Falls, fractures, injuries: Although the study area bay in each site was chosen prior to randomisation, recruitment of study participants took place post randomisation of clusters – |
No |
|
Adverse events: Staff were not recruited; staff were those working on the wards that were identified prior to randomisation |
Yes | |
| Is it likely that selection of individual participants was affected by knowledge of the intervention? |
Falls, fractures, injuries: All adults admitted to a bed in the study area were eligible to participate in the study. The study monitored any internal transfers within the ward to identify if staff were allocating high-risk patients to bays with intervention flooring because they thought it would help them –Drahota et al. 118 Reproduced with permission from Dunhill Medical Trust |
Probably no |
| Adverse events | Not applicable | |
| Were there baseline imbalances that suggest differential identification or recruitment of individual participants between arms? |
Falls, fractures, injuries: There was a tendency from the hospital staff to transfer patients between bays within a ward. Although the proportion of internal transfers was higher in the intervention group (13.3%) than in the control group (8.1%), the difference was not statistically significant. It is also possible that the transfers were made as a result of clinical needs, rather than the trial context:Drahota et al. 118 Reproduced with permission from Dunhill Medical Trust |
Probably no |
| Adverse events | Not applicable | |
| Risk-of-bias judgement |
All outcomes: Staff were not recruited and identified prior to randomisation. Patients were recruited after randomisation of the clusters; selection of individual participants is not affected by knowledge of the intervention, and baseline imbalances do not suggest differential recruitment of individual participants between trial arms |
Low |
| 2. Risk of bias due to deviations from the intended interventions (effect of assignment to intervention) | ||
| Were participants aware that they were in a trial? | Recruitment processes suggest that participants were aware of the trial:Patients who are to be admitted or transferred to the study area [. . .] will be informed about the study through a participant information sheet. [. . .] The patients or consultees will be able to contact the research team prior to participating in the trial should they have any questionsDrahota et al.107 | Yes |
| Were participants aware of their assigned intervention during the trial? | No masking was incorporated into the study | Yes |
| Were carers and trial personnel aware of participants’ assigned intervention during the trial? | No masking was incorporated into the study | Yes |
| Were there deviations from the intended intervention beyond what would be expected in usual practice? | Although there was a tendency for the staff to move high-risk fallers into the study areas at intervention sites, strategies were put in place to discourage changes in practice of internal transfers:The study site will notify the researchers [. . .] when a new patient is admitted (sending them the [. . .] reason for internal transfer if made). Internal transfers will be monitored to ensure that staff are not allocating high-risk patients to the new flooring because they think it may help themDrahota et al.107 | Probably no |
| Risk-of-bias judgement |
All outcomes: Both participants and study personnel were aware of the trial; participants and strategies were in place to ensure that there were no deviations from the intended intervention |
Low |
| 3. Risk of bias due to missing data | ||
| Were data for this outcome available for all, or nearly all, clusters randomised? |
All outcomes: All sites remained in the study and results were presented accordingly. The trial recruitment and participant flow are summarised in figure 1 of Drahota et al. :77 |
Yes |
| Were outcome data available for all, or nearly all, participants within clusters? | Falls, fractures, injuries:Four participants withdrew from the study; one from the intervention group for reasons unrelated to the flooring and three from the control group for unknown reasons | Yes |
|
Adverse events: We do not know how many staff are included in each cluster. The qualitative component of the study indicates that it is possible that there would have been more staff experiencing an adverse event than was actually documented using the adverse events form |
Probably no | |
| Are the proportions of missing outcome data and reasons for missing outcome data similar across intervention groups? | Falls, fractures, injuries | Not applicable |
|
Adverse events: There are no data on the number of staff at the outset |
No information | |
| Is there evidence that results were robust to the presence of missing outcome data? | Falls, fractures, injuries | Not applicable |
|
Adverse events: The result is narrative summary based on the documented adverse event forms. It is unlikely that there would be any big change to the narrative summary even if the missed data were included |
Probably yes | |
| Risk-of-bias judgement |
Falls, fractures, injuries: Outcome data available for all clusters, and participants within clusters |
Low |
|
Adverse events: There is evidence of missing outcome data for individuals within clusters; however, owing to the low counts, these data are unlikely to change the results |
Low | |
| 4. Risk of bias in measurement of the outcome | ||
| Were outcome assessors aware that a trial was taking place? | The study was not blinded:Sites were informed of their group allocation at the beginning of the baseline period to facilitate the flooring installation. No masking was incorporated into the study | Yes |
| Were outcome assessors aware of the intervention received by study participants? | The study was not blinded:As this study was not blinded it is potentially subject to detection bias, whereby staff at intervention sites may have been better at reporting the falls and possibly better at reporting those that resulted in no injury (which would have affected the injury rates as well as the falls rates)Drahota et al.118 Reproduced with permission from Dunhill Medical Trust | Probably yes |
| Was the assessment of the outcome likely to be influenced by knowledge of intervention received? | Appropriate data collection processes were followed to ensure that outcome assessment was not influenced by knowledge of intervention received:Prior to the onset of data collection, staff at each site were trained in the study protocol. Standardised forms were implemented across the sites to record baseline characteristics, falls, and injuries, for the purposes of the study. We conducted checks during ward audits, and by cross checking submitted forms through-out the study period, to ensure that data were being logged appropriately. Data monitoring was conducted through-out the study period and any anomalies or inconsistencies were followed up. All data was double-entered into encrypted datasets and verified for accuracyDrahota et al.118 Reproduced with permission from Dunhill Medical Trust | Probably no |
| Risk-of-bias judgement |
All outcomes: Outcome assessors were aware that participants were in a trial and of the intervention received by the participants; outcome assessment was unlikely to be influenced by knowledge of intervention received |
Low |
| 5. Risk of bias in selection of the reported result | ||
| Are the reported outcome data likely to have been selected, on the basis of the results, from multiple outcome measurements (e.g. scales, definitions, time points) within the outcome domain? | All reported outcomes are explicitly presented as proposed in the protocol | No |
| Are the reported outcome data likely to have been selected, on the basis of the results, from multiple analyses of the data? | All reported outcome data are as per the analysis plan | No |
| Risk-of-bias judgement |
All outcomes: No selective outcome reporting based on results from either multiple outcome measurements or multiple data analyses |
Low |
| Overall risk of bias | All outcomes | Low |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? |
All outcomes: Allocation of participants to rooms was non-random and monitored by staff – |
Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? |
All outcomes: Fall events were assigned to one of the flooring groups depending on the participants’ location of fall, irrespective of whether the participant resided in an apartment with either intervention or control flooring. The intervention flooring was not installed in bathrooms, which were considered control areas. This suggests that participants residing in an apartment with the intervention floor who sustained a fall in their bathroom were assigned to the control group – |
Yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? | All outcomes:During the study period, following initiatives from staff or relatives, four fall prone participants were moved from rooms with regular flooring to rooms with compliant flooring | Probably yes |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains and for time-varying confounding? |
Falls rate per 1000 person-days, number of falls resulting in injuries: Although multivariate analysis was conducted, important covariates such as history of falls/fractures and incontinence were not reported or considered in the analyses. Moreover, regression matching was undertaken to account for those who fell on both floors, but perhaps some additional attention should have been paid to those four participants who moved rooms (regular to compliant) – |
Probably no |
|
Number of fractures, number of hip fractures: Data were provided via personal communication and have not been adjusted for important confounding |
No | |
| Risk-of-bias judgement |
All outcomes: Some important confounding domains were not measured or reported |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? |
Falls rate per 1000 person-days: All residents living at the studied unit were invited to participate in the study and written consent was collected, with 94% of residents agreeing to participate |
Probably no |
|
Number of falls resulting in injuries, number of fractures, number of hip fractures: Fall events were selected into the analysis, rather than the individuals. Selection of events was based on whether or not an individual was considered to have received the intervention at the time of the fall. Seven falls were excluded as the injuries (unclear severities) were determined to be caused by something other than the floor (unclear from which groups); however, it is unlikely that these data would have had much influence on the findings – |
Probably no | |
| Do start of follow-up and start of intervention coincide for most participants? |
Falls rate per 1000 person-days: All falls were recorded on a falls registration form and one of the items collected was about type of flooring – |
Probably yes |
|
Number of falls resulting in injuries, number of fractures, number of hip fractures: Events were assigned to intervention based on the location of the fall; therefore, the start of the intervention is taken as when the participant made impact with the floor – |
Probably yes | |
| Risk-of-bias judgement |
All outcomes: All participants who would have been eligible for the target trial were invited to participate in the study; data that were excluded from the analyses were unlikely to influence the findings and may not have been associated with the intervention; and, for each participant, start of follow-up and start of intervention coincided |
Low |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? |
All outcomes: Intervention group comprised of compliant flooring, whereas control group included regular flooring of vinyl, linoleum or ceramic tiles – |
Yes |
| Was the information used to define intervention groups recorded at the start of the intervention? |
Falls rate per 1000 person-days: Participants were continuously recruited, based on when they moved in, during the study period. The allocation of the rooms was non-random and monitored by the staff |
Yes |
|
Number of falls resulting in injuries, number of fractures, number of hip fractures: The intervention groups were defined by the fall events, which were assigned to an intervention group based on the location of fall – |
Yes | |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? |
All outcomes: Intervention status was classified on an ongoing basis as part of the surveillance system – |
Probably no |
| Risk-of-bias judgement |
All outcomes: (1) Intervention status is well defined and (2) intervention definition is based solely on information collected at the time of intervention |
Low |
| 4. Risk of bias due to deviations from intended interventions | ||
| Were important co-interventions balanced across intervention groups? | Residents were wearing hip protectors in 13.4% of all falls. This is not beyond what might be expected in usual practice. There was no significant difference in the proportion of falls involving hip protectors between groups, although this added protection was slightly higher in the intervention group (intervention, 18%; control, 14%) | Probably yes |
| Was the intervention implemented successfully for most participants? | Falls were excluded if they occurred on non-floor surfaces (mattress or fall mat; n = 65), outside (n = 5) or if the injury outcome was caused by something other than the floor (n = 7; unclear from which groups). Of 851 falls, 9.1% were excluded | Probably yes |
| Did study participants adhere to the assigned intervention regimen? | Owing to the design of the study, the intervention was administered once at the time of each fall, as the unit of analysis was the fall event, rather than the participant. So, although participants did switch between groups, it was not possible for falls to switch between groups. Falls not adhering to the flooring intervention were excluded at the sample selection stage | Probably yes |
| Risk-of-bias judgement |
All outcomes: Important co-interventions (hip protectors) were balanced across intervention groups and there were no deviations from the intended interventions that were likely to affect the outcome |
Low |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? | Figure 2 in Gustavsson et al.52 summarises recruitment and participant flow. There is a discrepancy in the reported number of falls between figure 2 and table 2. We have confirmed the correct data following contact with the study author. Only those who had at least one fall were included in the analysis. Five falls were excluded from the analysis because data on key variables were missing –Sixty-five falls occurred on other surfaces than the two compared in this study (mattress and fall mat), five falls occurred outside and 7 falls were excluded as the injury outcome was caused by something other than flooring, leaving 774 fall events relevant to include in the analysis | Probably yes |
| Were participants excluded because of missing data on intervention status? | It is unclear what the ‘key variables’ were that resulted in the five exclusions due to missing data | No information |
| Were participants excluded because of missing data on other variables needed for the analysis? | Table 1 in Gustavsson et al.52 lists the variables with missing data, detailing missing information on visual impairment, cognitive impairment, sedatives and walking ability related to up to four fallers | Probably yes |
| Are the proportion of participants and reasons for missing data similar across interventions? | The information about the intervention assignment of the five excluded falls is not provided | No information |
| Is there evidence that results were robust to the presence of missing data? | As there were only five falls reported as excluded because of missing data, it is unlikely that these will have influenced the results | Probably no |
| Risk-of-bias judgement |
All outcomes: Data were reasonably complete |
Low |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? |
Falls rate per 1000 person-days, number of falls resulting in injuries: All falls were registered in accordance with the organisation’s existing injury surveillance system. The classification of injuries and severity may have been subject to influence – |
Probably yes |
|
Number of fractures, number of hip fractures: Fractures are unlikely to have been influenced by knowledge of the intervention |
Probably no | |
| Were outcome assessors aware of the intervention received by study participants? |
All outcomes: Although all falls were registered in accordance with the organisation’s existing injury surveillance system, it is possible that the outcome assessors were aware of the interventions: type of flooring was one of the items included in the audit forms and the study was not blinded |
Yes |
| Were the methods of outcome assessment comparable across intervention groups? |
Falls rate per 1000 person-days: All falls were registered in accordance with the organisation’s existing injury surveillance system. Outcomes are clearly defined – |
Probably yes |
| Number of falls resulting in injuries, number of fractures, number of hip fractures:‘minor’ (minor bruises or abrasions not requiring assistance from health professional; reduction in physical function [. . .] for at least three days), ‘moderate’ (wounds, bruises, sprains, cuts requiring a medical/health professional examination [. . .], X-ray, suture) or ‘severe’ (medically recorded fracture, head or internal injury requiring accident and emergency or inpatient treatment)© 2018 Gustavsson et al.52 This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited | Probably yes | |
| Were any systematic errors in measurement of the outcome related to intervention received? | It is unclear whether or not any validity checks were undertaken to identify systematic errors | No information |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of falls resulting in injuries: The methods of outcome assessment were comparable across intervention groups, the outcome measure is only minimally influenced by knowledge of the intervention received by study participants, and any error in measuring the outcome is likely to be only minimally related to intervention status |
Moderate |
|
Number of fractures, number of hip fractures: The methods of outcome assessment were comparable across intervention groups, the outcome measure is unlikely to be influenced by knowledge of the intervention received by study participants, and any error in measuring the outcome is likely to be only minimally related to intervention status |
Low | |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? |
Falls rate per 1000 person-days, number of falls resulting in injuries: Reported effect estimates are as specified in the methods; however, no protocol is available |
Probably no |
|
Number of fractures, number of hip fractures: Count data were received via personal communication |
Not applicable | |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention–outcome relationship? |
Falls rate per 1000 person-days, number of falls resulting in injuries: Reported effect estimates are as specified in the methods. The paper presents sensitivity analyses and demonstrates transparency in the different ways the data were explored |
Probably no |
|
Number of fractures, number of hip fractures: Unanalysed count data were received via personal communication; they have not been adjusted for confounding |
Not applicable | |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? |
Falls rate per 1000 person-days, number of falls resulting in injuries: Reported effect estimates are available for all eligible participants |
Probably no |
|
Number of fractures, number of hip fractures: Count data were received via personal communication |
Not applicable | |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of falls resulting in injuries: The outcome measurements and analyses are clearly defined and both internally and externally consistent; there is no indication of selection of the reported analysis from among multiple analyses, and there is no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results |
Moderate |
|
Number of fractures, number of hip fractures: Fractures were obtained through personal communication only and were not reported |
Serious | |
| Overall risk of bias | All outcomes | Serious |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? | The study was conducted in a natural environment, and participants were assigned to the intervention groups without any randomisation:Patients were allocated a bed space on the ward by nursing staff who were not involved in the running of this trial. Allocation was based on bed availability, as well as clinical need, such as proximity to nursing station | Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? | Analyses were based on where the falls occurred:Staff recorded where each fall occurred on the ward, using a map of ward layout attached to each QIER [Quality Incident Event Reporting] form | Probably yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? | The intervention areas consisting of rooms 1–3 were located closer to the nursing station, and it is possible that sicker patients were transferred from control rooms to intervention rooms for closer monitoring:Falls occurred throughout the ward, but with greater frequency in the single rooms. These single rooms were closer to the nursing station and therefore were used for patients who were sicker or needed closer observationAny bias might result in the sickest and/or more delirious patients to be placed closest to the nursing station (rooms 1 to 3, LIF [low-impact flooring]), thus negatively affecting fall rates for LIFs | Probably yes |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains and for time-varying confounding? | The analysis method does not take into account any of the confounding factors:Nonparametric (Wilcoxon rank-sum test) comparisons between cohorts were made. Categorical variables were compared using χ2 analyses | Probably no |
| Risk-of-bias judgement |
All outcomes: The study did not control for any of the important confounding domains |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? | All patients admitted to the ward during the study period were selected to participate in the study. However, only bedroom fallers were included in the analyses | Probably no |
| Do start of follow-up and start of intervention coincide for most participants? |
Injurious falls rate per 1000 person-days, falls rate per 1000 person-days: Standard procedures were followed for documenting falls. Exposure to the intervention would have coincided with admission to the ward, when follow-up would have started – |
Probably yes |
|
Number of falls resulting in injuries, number of fractures, number of hip fractures: The population of interest for the study were those who had sustained a bedroom fall during their hospitalisation; so, for these outcomes, the start of follow-up and exposure to the intervention (landing on the floor) would have coincided for patients once they fell |
Probably yes | |
| Risk-of-bias judgement |
All outcomes: (1) All participants who would have been eligible for the target trial were invited to participate in the study; data that were excluded from the analyses were unlikely to influence the findings and may not have been associated with the intervention; and (2) for each participant, start of follow-up and start of intervention coincided |
Low |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? | Intervention groups comprised three different low-impact floorings [(1) SmartCell, (2) Tarkett Excel Omnisport and (3) Kradal], whereas the control group consisted of standard vinyl flooring:12 bed spaces were covered by one of the LIFs, and 8 bed spaces were surrounded by standard vinyl flooring (3–4 mm thick) laid on subflooring of concrete. The corridor, dining room, and wet areas (bathrooms and toilets) did not have LIF installed | Yes |
| Was the information used to define intervention groups recorded at the start of the intervention? | Information about the intervention received was recorded at the time of the intervention and verified:Location of the patient’s bedroom (and fall) was cross checked with our computerized patient management system | Yes |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? | Outcome reporting in the QIER system was checked against the computerised patient management system to ensure that information about intervention status is captured accurately:Staff recorded where each fall occurred on the ward, using a map of ward layout attached to each QIER form. Location of the patient’s bedroom (and fall) was cross checked with our computerized patient management system | Probably no |
| Risk-of-bias judgement |
All outcomes: (1) Intervention status is well defined and (2) intervention definition is based solely on information collected at the time of intervention |
Low |
| 4. Risk of bias due to deviations from intended intervention | ||
| Were important co-interventions balanced across intervention groups? | Data on co-interventions are not described in the paper, so it is unknown if they were balanced across groups:This injury mitigation approach [LIF] is complementary to, and does not replace, existing fall prevention program | No information |
| Was the intervention implemented successfully for most participants? | Only ‘bedroom falls’ that occurred in the intervention and control areas were included in the study | Probably yes |
| Did study participants adhere to the assigned intervention regime? | ‘Bedroom falls’ formed part of the inclusion criteria and data were analysed at the level of falls. The intervention was administered once at the time of each fall. So, although it may have been possible for participants to switch between groups (if they were transferred to another area in the ward), it was not possible for falls to switch between groups | Probably yes |
| Risk-of-bias judgement |
All outcomes: No information is reported on important co-interventions to determine if there is a deviation from the intended intervention |
No information |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? | The population of interest for the study includes those who sustained a fall during their hospitalisation. As standard procedures were followed for documenting falls, it is likely that outcome data were available for all selected participants:Staff recorded where each fall occurred on the ward, using a map of ward layout attached to each QIER form. Location of the patient’s bedroom (and fall) was cross checked with our computerized patient management system | Probably yes |
| Were participants excluded due to missing data on intervention status? | As standard procedures were followed for documenting falls, it is likely that outcome data were available for all selected participants | Probably no |
| Were participants excluded due to missing data on other variables needed for the analysis? | The study did not undertake additional analysis to explore the effect of confounding | No |
| Risk-of-bias judgement |
All outcomes: Data appear reasonably complete |
Low |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? |
Falls rate per 1000 person-days, injurious falls rate per 1000 person-days: All falls and fall-related injuries were prospectively monitored using the established normal QIER system |
Probably no |
| Fall with injuries, fracture, hip fracture:To avoid investigator bias, the severity of injury assigned by the clinical and quality teams was used | Probably no | |
| Were outcome assessors aware of the intervention received by study participants? | The study was not blinded. Moreover, both the intervention and control floors were laid in the same ward | Yes |
| Were the methods of outcome assessment comparable across intervention groups? | Standardised procedures were followed for outcome assessment:[A]ll falls and fall-related injuries were prospectively monitored, using the established normal quality incident event reporting (QIER) system | Probably yes |
| Were any systematic errors in measurement of the outcome related to intervention received? | Standardised procedures were in place for measurement of outcome. Moreover, recording of outcome in the QIER form was cross checked with electronic records:Staff recorded where each fall occurred on the ward, using a map of ward layout attached to each QIER form. Location of the patient’s bedroom (and fall) was cross checked with our computerized patient management system | Probably no |
| Risk-of-bias judgement |
All outcomes: Methods of outcome assessment were comparable across intervention groups; outcome measure was unlikely to be influenced by knowledge of the intervention received by study participants; and any error in measuring the outcome is unrelated to intervention status |
Low |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? |
Injurious falls rate per 1000 person-days, falls rate per 1000 person-days: Data were received via personal communication to support the review analysis. Reported effect estimates are as specified in the methods; however, no protocol is available |
Probably no |
|
Number of falls resulting in injuries, number of fractures, number of hip fractures: Reported effect estimates are as specified in the methods; however, no protocol is available |
Probably no | |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention-outcome relationship? |
Injurious falls rate per 1000 person-days, falls rate per 1000 person-days: Reported effect estimates present only partial information, such as medians, ranges, and p-values for rates. Further data were provided by the study author that enabled calculation of the RaRs. The data for injurious falls rate were analysed using a non-parametric test in the published report, to show a ‘non-significant trend’; when these personally communicated data were entered into the meta-analysis (a parametric test) they became significant. We have highlighted this issue in the main body of the review (see Chapter 3, Injurious falls rate per 1000 person-days) |
Probably no |
|
Number of falls resulting in injuries, number of fractures, number of hip fractures: Descriptive data are presented in the report. There is no indication of selective reporting of effect estimates |
Probably no | |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? |
All outcomes: Reported effect estimates are based on all participants selected for the analyses. We have subgrouped the analyses by flooring type in the review (as planned in our review protocol), through personally communicated data. The study report presents all intervention groups together to improve power: |
Probably no |
| Risk-of-bias judgement |
All outcomes: The outcome measurements and analyses are clearly defined and both internally and externally consistent; there is no indication of selection of the reported analysis from among multiple analyses; and there is no indication of selection of the cohort or subgroups for analysis and reporting based on the results |
Moderate |
| Overall risk of bias | All outcomes | Serious |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? | Staff characteristics such as age, sex, roles and pre-existing conditions may have influenced the outcomes | Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? |
All injuries to staff that occurred in those wards were noted, irrespective of where the injured person normally worked The intervention ward moved to a different location with the same staffing and case mix, but this time with standard floors Judgement: participants could switch between intervention and control groups, both in the concurrent control condition, and in the before–after control condition |
Yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? |
During the concurrent control period, switches between groups were related to where staff were at the time of injury. It is possible that staff at risk of injury were scheduled to work on wards without the flooring to mitigate risk, but we have no way of knowing this For the before–after comparison, all staff were moved to the new ward, regardless of any predisposing factors |
Probably no |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains and for time-varying confounding? | The authors were limited by the data they had available to them, which meant that an analysis that controls for confounding was not feasible. The analysis they did undertake was probably OK for the data they had; however, it was not an analysis that controlled for confounding | No |
| Risk-of-bias judgement |
Adverse events: The study did not control for any of the important confounding domains |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? | Selection into the study was not based on particular staff characteristics. Any staff reporting an injury would have been assessed:All staff injuries reported on the Safety1st system from January 2013 to December 2018 were obtained | No |
| Do start of follow-up and start of intervention coincide for most participants? | The data collection period (January 2013–December 2018) coincides with the intervention period and the follow-up period. It is possible that there was a degree of staff turnover during the study; however, new staff entering the ward would have begun follow-up at the same time as their exposure started | Probably yes |
| Risk-of-bias judgement |
Adverse events: (1) All participants who would have been eligible for the target trial were invited to participate in the study; data that were excluded from the analyses were unlikely to influence the findings and may not have been associated with the intervention; and (2) for each participant, start of follow up and start of intervention coincided |
Low |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? | The intervention consisted of the LIF ward, whereas the control group consisted of the remaining three wards with standard flooring | Yes |
| Was the information used to define intervention groups recorded at the start of the intervention? | The LIF ward was compared to three controlled wards | Yes |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? | It is stated that ‘All injuries to staff that occurred in those wards were noted, irrespective of where the injured person normally worked’. As the injury was documented in an electronic system that was confirmed by a senior manager, it is unlikely that the knowledge of the outcome influenced the intervention status | Probably no |
| Risk-of-bias judgement |
Adverse events: The intervention status is well defined and intervention definition is based solely on information collected at the time of intervention |
Low |
| 4. Risk of bias due to deviations from intended intervention | ||
| Were there deviations from the intended intervention beyond what would be expected in usual practice? | We do not know how many of the injuries in the intervention ward occurred in the bays with the intervention flooring versus elsewhere in the same ward; however, it is likely that any deviations were part of usual practice. There is a possibility that staff changed their way of working to accommodate the increased risk of adverse events on the intervention floor; however, this has not been measured/reported in the study for us to know for sure | Probably no |
| Risk-of-bias judgement |
Adverse events: Any deviations from intended intervention reflected usual practice |
Low |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? |
Adverse events (staff injuries per month): All injuries meeting the inclusion criteria, documented in the quality reporting system, were included in the analysis |
Probably yes |
|
Adverse events (injury rates per 100 staff working days): The numbers of staff who are not injured are not recorded and therefore were not available to us, meaning a denominator population could not be determined. We were able to measure number of staff injured, but not the rate of injuries |
No | |
| Were participants excluded due to missing data on intervention status? |
Adverse events (staff injuries per month): Study participant data were directly obtained from the QIER system that included outcome as well as the intervention status |
Probably no |
|
Adverse events (injury rates per 100 staff working days): Outcome was not reported or analysed |
No information | |
| Were participants excluded due to missing data on other variables needed for the analysis? |
Adverse events (staff injuries per month): There is no indication of any participants being excluded |
Probably no |
| Adverse events (injury rates per 100 staff working days):The numbers of staff who are not injured were not recorded, which precluded calculations of time related hazard ratios. [. . .] the numbers of staff injured per month for each of the wards were compared [. . .] No adjustments for age, gender of staff or patient case mix [. . .] were made | Probably yes | |
| Risk-of-bias judgement |
Adverse events (staff injuries per month): Data are reasonably complete |
Low |
|
Adverse events (injury rates per 100 staff working days): Outcome not measured or reported |
No information | |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? | Outcomes are self-reported and assigned to the group based on the ward location at the time of injury, even if the staff worked in a different ward with the alternate flooring. Absence of blinding of the flooring surfaces can further increase the risk of bias | Probably yes |
| Were outcome assessors aware of the intervention received by study participants? |
There is no blinding of the flooring surfaces, so staff initially reporting their injuries would have been aware Assessors retrospectively rating the eligibility of the injuries reported for inclusion in the study also do not appear to be blinded |
Yes |
| Were the methods of outcome assessment comparable across intervention groups? |
Initial reporting of outcomes: outcomes are self-reported through the QIER system, which is then checked by the senior manager. This process is similar in both groups Classification of injuries for inclusion: categorisation system explained. The authors do acknowledge, however, that there were a large number of non-specified injury data, which made drawing conclusions about types of injuries sustained difficult. ‘Injuries not stated’ were included in the analysis of injuries per month |
Yes |
| Were any systematic errors in measurement of the outcome related to intervention received? | No information | |
| Risk-of-bias judgement |
Adverse events: The methods of outcome assessment were comparable across intervention groups; the outcome measure is only minimally influenced by knowledge of the intervention received, and any error in measuring the outcome is only minimally related to intervention status |
Moderate |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? | No protocol is available to determine whether or not the analyses followed a prespecified plan, although the data available to the researchers were somewhat limited | No |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention–outcome relationship? | Data for the analyses of injuries per month were dealt with at the ward level, based on retrospective acquisition of injuries in the institutional incident reporting system. The analyses were limited by the data available to the researchers. It is unlikely that the authors performed multiple analyses prior to selecting one for reporting | Probably no |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? | Data from three control wards were averaged together and not reported separately. As there is no prespecified plan, it is unclear if any exploration of subgroups was conducted prior to making this decision | Probably no |
| Risk-of-bias judgement |
Adverse events: The outcome measurements and analyses are clearly defined and internally consistent. There is no indication of selection of the reported analysis from among multiple analyses; there is no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results |
Moderate |
| Overall risk of bias | Adverse events | Serious |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? | The floors being compared were in different usage areas (the carpets were in sitting rooms and an acute admission ward; the vinyl was in bedrooms and a rehabilitation ward), and it is likely that patient risk factors differed between the carpet and vinyl groups:Since the carpeted areas included a joint assessment ward, there was a slightly higher likelihood that some patients falling on carpet suffered from dementia | Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? | Assignment to intervention was based on location of the fall, that is the type of flooring at the time of fall. However, it was possible for participants to switch groups (i.e. move from the vinyl bedroom to the carpeted dining area), which could have been influenced by time-varying confounding. The groups to which participants were analysed would inadvertently be based on their follow-up time spent on either carpet or vinyl:213 forms were separated into those involving falls on carpet, and those involving falls on vinyl, and the incidence of injury for each of these groups was obtained, and it was not possible to determine how long each patient spent in carpeted rather than vinyl-floored areas | Probably yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? | As carpet was in the dining areas, it is possible that the healthier/more active participants were more exposed to carpets, whereas those who are refined to bed were more likely to be limited to vinyl exposure. One ward had carpet in the bedded areas and this ward was more likely to have people with dementia. It is unclear if those more likely to go to the dining room were also more likely to injure themselves | Probably yes |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains and for time-varying confounding? | Healthier/more active patients may have received more exposure to carpet (those refined to bedrooms would have had more exposure to vinyl); however, exposure time could not have been measured in this study. As patients’ health improved, they may have switched groups, which implies the possible presence of time-varying confounding. There were no attempts to control for potential confounding:The age and sex of each patient who fell was also recorded, so that any difference in the composition of the two experimental groups could be seenResults were analysed using the chi-square test. Since the degree of freedom equalled one, Yates’ correction was incorporated | Probably no |
| Risk-of-bias judgement |
Number of falls resulting in injuries: The study did not control for any of the important confounding domains |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? | It is not clear how the random selection was carried out, but it is unlikely to be based on participant characteristics:This investigation retrospectively analysed a sample of 225 accident forms selected at random | Probably no |
| Do start of follow-up and start of intervention coincide for most participants? | Patients would have been admitted to the ward, followed up and exposed to the intervention simultaneously | Probably yes |
| Risk-of-bias judgement |
Number of falls resulting in injuries: (1) All participants who would have been eligible for the target trial were invited to participate in the study; and (2) for each participant, start of follow up and start of intervention coincided |
Low |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? | Intervention groups comprised carpet and vinyl flooring. Out of 225 incident report forms, ‘four accident forms had to be excluded as they did not contain enough information on where the fall occurred’, implying that the majority of cases were clearly defined | Yes |
| Was the information used to define intervention groups recorded at the start of the intervention? | Information to define intervention groups was recorded at the point of fall (when participants received the intervention: carpet or vinyl) | Yes |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? | It was a retrospective study. Staff would have had no reason to misclassify the intervention, as they would have had no knowledge that the study was due to take place at the time of completing the incident report forms | Probably no |
| Risk-of-bias judgement |
Number of falls resulting in injuries: Intervention status is well defined and the intervention definition is based solely on information collected at the time of intervention |
Low |
| 4. Risk of bias due to deviations from intended interventions | ||
| Were important co-interventions balanced across intervention groups? | Co-interventions (e.g. hip protectors, fall mats) were not mentioned in the study report | No information |
| Was the intervention implemented successfully for most participants? | The unit of analysis was falls and only falls that occurred on the comparison floors were included | Probably yes |
| Did study participants adhere to the assigned intervention regime? | The unit of analysis was the fall event, rather than the participant. The intervention was administered once at the time of each fall. So, although it may have been possible for participants to switch between groups, it was not possible for falls to switch between groups | Probably yes |
| Risk-of-bias judgement |
Number of falls resulting in injuries: No information is reported on important co-interventions to determine if there is a deviation from the intended intervention |
No information |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? | The ideal ‘target RCT’ would be to assign fallers to land on carpet or vinyl floors, and follow them up for injury status. In this study, a sample population of fallers was obtained from 225 randomly selected incident report forms (it is unclear how many incident reports there were in total) over 4 years, which could mimic the recruitment of participants to the ‘target randomised trial’. Of these, 12 (5.3%) were not included in the analysis of outcomes. So nearly all outcome data were available | Probably yes |
| Were participants excluded because of missing data on intervention status? | Four accident forms had to be excluded as they did not contain enough information on where the fall occurred. Another eight forms were excluded because they recorded injuries unrelated to the type of flooring (e.g. scalds) | Yes |
| Were participants excluded because of missing data on other variables needed for the analysis? | Very few variables were used in the analysis and there is no report of any additional analyses undertaken, so it is unlikely that participants were excluded on the basis of other missing data | No |
| Are the proportion of participants and reasons for missing data similar across interventions? | Information not provided. It would not be possible to determine which groups the participants were from who had missing intervention status | No information |
| Is there evidence that results were robust to the presence of missing data? | If the four excluded accident forms that had missing intervention status all presented injuries and all belonged to the carpet group, this would have had minimal impact on the findings | Probably yes |
| Risk-of-bias judgement |
Number of falls resulting in injuries: Data were reasonably complete |
Low |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? | Outcome data were collected retrospectively from a standard form used by the elderly unit. The study used a broad definition for ‘injury’, encompassing minor to severe injuries, suggesting that any mention of injury or pain would be classified as an injury. It is possible that some subjective judgement may have come into play (e.g. the eight forms that were excluded because of injuries deemed unrelated to flooring are not fully explained – just one example of scalds is given):For the purpose of this study injury was defined as any graze, bruise, laceration or fracture, and also any fall that resulted in the patient complaining of pain, even if there was no visible lesion | Probably yes |
| Were outcome assessors aware of the intervention received by study participants? | It is not reported whether or not there was any blinding; however, it appears likely that those collecting data from the incident reports were not blinded, as they were documenting the intervention status and the outcome status from the same incident report | Probably yes |
| Were the methods of outcome assessment comparable across intervention groups? | All outcomes were documented by the same elderly care unit. The authors suggest that it appears that very few falls had gone unrecorded; however, the data do not support this presumption. About 81% of the overall falls in the study had an injury outcome (91% on vinyl and 14.8% on carpet), so it is possible that staff in the carpeted areas were more likely to document non-injurious falls than those in the vinyl areas. It is difficult to know if the results could be due to this bias, random error, confounding or a real intervention effect, but the proportion of injurious falls on vinyl is very high:The interpretation of the results depended on nursing staff filling in the accident forms in a similar way across different flooring areas. The results supported the belief that very few falls had gone unrecorded, since they reflected previous research which suggests about half of falls in older people result in some injury | Probably yes |
| Were any systematic errors in measurement of the outcome related to intervention received? | It is possible that ‘complaint of pain’ was more likely to be documented in the vinyl group, if more patients in the carpet group had dementia, which may have made it harder to ascertain pain. This problem is likely to be already captured in the assessment of confounding | Probably yes |
| Risk-of-bias judgement |
Number of falls resulting in injuries: The outcome measure was subjective (i.e. vulnerable to influence by knowledge of the intervention received by study participants) and the outcome was assessed by assessors aware of the intervention received by study participants |
Serious |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? | There is no protocol or prespecified plan on which to base a judgement. Falls are classified as injurious or not; it is not clear if the classification of injury was specified in advance or not | No information |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention–outcome relationship? | One analysis was presented in this study, based on limited data. It is unlikely that different analyses were run and selectively reported, because of the limitations in the data | Probably no |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? | One analysis was presented in this study, based on limited data. There is no indication of any subgroups being explored | Probably no |
| Risk-of-bias judgement |
Number of falls resulting in injuries: The outcome measurements are clearly defined and internally consistent. There is no indication of selection of the reported analysis from among multiple analyses. There is no indication of selection of the cohort or subgroups for analysis and reporting on the basis of the results |
Moderate |
| Overall risk of bias | Number of falls resulting in injuries | Serious |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? | Allocation of participants to room was non-random, residents assessed with high risk of fall were selected to stay in rooms with DSF:Two resident bedrooms and bathrooms in the rehabilitation section have DSF flooring (SmartCells flooring) installed. Residents assessed with high risk of fall are selected to stay in these rooms | Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? | It was possible for participants to switch between groups depending on where they fell and analysis was based on where participants fell; therefore, participants’ follow-up was according to the intervention they received:Audit forms provide details regarding age, sex, osteoporosis, number of medications, previous falls, type of flooring (normal vs. DSF), time of day, type of injury, and resulting actions | Yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? | Residents were allocated to the intervention flooring if they were at high risk of falling and were in the rehabilitation section. Therefore, switches between groups were likely to be related to prognostic factors for the outcome | Probably yes |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains and for time-varying confounding? | Analysis plan is not fully reported, and the data provided for fractures and injurious falls do not appear to adjust for any confounding (despite mentioning ‘covariates’). The study did not measure/report on all of our specified ‘important’ confounders: comorbidities (osteoporosis only), mobility, visual impairment, cognitive status, continence problems and history of fractures were missing from the report:Patients allocated to DSF flooring rooms were comparable with their counterparts in the regular flooring rooms on the previously mentioned factors except that they were significantly younger and took significantly fewer medications; these factors were thus treated as covariates in the analyses | Probably no |
| Risk-of-bias judgement |
Number of falls resulting in injuries, number of fractures: Most of the prespecified confounding domains were not measured |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? | Selection into the study/analysis was based on whether or not a resident fell (start of intervention was impact with the floor). All falls in the intervention group were included, but only every third fall in the control group was included. Therefore, selection into the study for controls was based on characteristics (timing of fall) observed after the start of the intervention:Looking at the 2009 data, it was determined that there were approximately three times as many falls on regular flooring than on the DSF, so it was agreed to use data from every third fall on regular flooring (chronologically) | Yes |
| Were the post-intervention variables that influenced selection likely to be associated with intervention? | As there were approximately three times as many falls on regular flooring than on the intervention flooring, data were selected from every third fall for the regular flooring | Yes |
| Were the post-intervention variables that influenced selection likely to be influenced by the outcome or a cause of the outcome? | Selection may have been influenced by the outcome of interest. The rule-based system of selecting every third fall in the control group would not have been a cause of fractures or injurious falls. However, because no blinding appears to have been employed in the selection process, we cannot rule out that the researchers may have been influenced, for example on when to stop selecting control data (there were three more in the control group than intervention group), or from which number to start selecting data:Over the study period, there were 449 documented falls. There were 82 falls on the DSF, and these were compared with the first 85 identified by taking every third of the remaining 282 falls on regular flooring | Probably yes |
| Do start of follow-up and start of intervention coincide for most participants? | A standardised process was followed for tracking fall incidents, suggesting that participants are monitored from the time they received the intervention:[F]all incidents were tracked using a standard form that collects date/time and location of fall, consequences of the fall for the resident, contributing factors, and the care plan | Probably yes |
| Were adjustment techniques used that are likely to correct for the presence of selection biases? | The study did not undertake any adjustment techniques to address selection bias | No |
| Risk-of-bias judgement |
Number of falls resulting in injuries, number of fractures: Selection into the study was related (but not very strongly) to intervention and outcome, and was not adjusted for in analyses |
Serious |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? |
Intervention groups were defined by falls occurring in rooms with DSF or normal flooring Location of fall was documented on the incident report forms. Depending on the quality of reporting, it should have been relatively simple to classify the intervention status of each fall. The authors provide no indication that data on intervention status were missing |
Yes |
| Was the information used to define intervention groups recorded at the start of the intervention? | A standard form was used to track falls. The location of the fall was documented at the time of the fall (start of intervention) | Yes |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? | Half of the data were collected retrospectively from incident forms. The retrospective data were unlikely to have been influenced. Even the prospective data are unlikely to have been influenced by knowledge of the outcome, as it is relatively objective as to whether or not someone falls on a particular floor. Classification could have been ambiguous around a door threshold, but falls are more likely to occur by the bedside or bathroom than anywhere else | Probably no |
| Risk-of-bias judgement |
Number of falls resulting in injuries, number of fractures: Intervention status is well defined, and the intervention definition is based solely on information collected at the time of intervention |
Low |
| 4. Bias due to deviations from intended interventions | ||
| Were important co-interventions balanced across intervention groups? | Co-interventions (e.g. hip protectors, fall mats) were not mentioned in the study report | No information |
| Was the intervention implemented successfully for most participants? | The unit of analysis was falls and only falls that occurred on the comparison floors were included | Probably yes |
| Did study participants adhere to the assigned intervention regime? | The unit of analysis was the fall event, rather than the participant. The intervention was administered once at the time of each fall. So, although it may have been possible for participants to switch between groups, it was not possible for falls to switch between groups | Probably yes |
| Risk-of-bias judgement |
Number of falls resulting in injuries, number of fractures: No information is reported on important co-interventions to determine if there is a deviation from the intended intervention |
No information |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? | The study does not indicate that there were any missing data or how any missing data were dealt with | No information |
| Were participants excluded due to missing data on intervention status? | The study does not indicate that there were any missing data or how any missing data were dealt with | No information |
| Were participants excluded due to missing data on other variables needed for the analysis? | The study does not indicate that there were any missing data or how any missing data were dealt with | No information |
| Risk-of-bias judgement |
Number of falls resulting in injuries, number of fractures: No information is reported about missing data |
No information |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? |
Number of falls resulting in injuries: Although fall incidents were collected using a standard form, the outcomes require some judgement to record. The study does not provide a definition for ‘fall’, making it more likely that some non-injurious falls were missed; this would affect the overall risk of injury |
Probably yes |
|
Number of fractures: Objective outcome not requiring judgement; although there is a risk of basing the judgement on clinical features (the report does not confirm whether or not the fractures were radiologically confirmed), the risk is minimal |
Probably no | |
| Were outcome assessors aware of the intervention received by study participants? | The type of flooring was one of the items included in the audit forms. Approximately half of the data were collected retrospectively and half were collected prospectively, using the same data collection forms. The prospective data collection could have been more open to bias as outcome assessors may have been more aware of the study at this point. The data extraction from the incident report forms was also not blinded | Yes |
| Were the methods of outcome assessment comparable across intervention groups? | All outcomes came from the incident report forms. This appears similar across groups; however, the researchers have not provided a definition of falls:Like most nursing homes, Mountain View Manor tracks fall incidents using a standard form that collects date/time and location of fall, consequences of the fall for the resident, contributing factors, and the care plan | Probably yes |
| Were any systematic errors in measurement of the outcome related to intervention received? | There is a risk of this as a result of outcome assessors not being blinded. It is unlikely that the recording of fractures would be affected; however, the types of injuries and, particularly, the number of people with no injuries could have been influenced if those documenting the falls were more likely to log a non-injurious fall on the intervention floor. This would influence the risk scores for injuries and fractures | Probably yes |
| Risk-of-bias judgement |
Number of falls resulting in injuries: The outcome measure was subjective (i.e. vulnerable to influence by knowledge of the intervention received by study participants) and the outcome was assessed by assessors aware of the intervention received by study participants |
Serious |
|
Number of fractures: The methods of outcome assessment were comparable across groups; the outcome measure is only minimally influenced by knowledge of the intervention received by study participants and any error in measuring the outcome is only minimally related to intervention status |
Moderate | |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? |
Falls resulting in injuries: The authors provide a breakdown of the injury types; however, they present these as percentage score only and it is unclear how these add up. For example, the types of injuries add up to 31.6% in the intervention group (although it is unclear if the injury types are independent), but the number of falls resulting in injury is stated as 53%; the numbers do not match. So there is a query over how injuries have been classified and reported |
Probably yes |
|
Number of fractures: It is reported that there were no fractures in the intervention group but it is unclear if there were any hip fractures in the 2.4% of the participants in the control group who sustained a fracture |
Probably yes | |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention–outcome relationship? | The report does not present the results of the outcomes as per the statistical analysis plan. Only descriptive and narrative data are presented (percentage scores):Injury rate and type comparisons based on chi-square analyses, and prediction of room type allocation based on the number of injuries sustained using logistic regression, were conductedAlthough a number of trends were identified, there was insufficient power to attain statistical significance | Yes |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? | There does not appear to be any exploration of subgroups | Probably no |
| Risk-of-bias judgement |
Number of falls resulting in injuries, number of fractures: There is a high risk of selective reporting from among multiple analyses |
Serious |
| Overall risk of bias | Number of falls resulting in injuries, number of fractures | Serious |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias arising from the randomisation process | ||
| Was the allocation sequence random? | At the outset, the study rooms were randomised using a computerised random number generator. Subsequently, new participants were assigned to the study room based on room availability and this was not determined by the flooring type. As the trial had adequate allocation concealment and blinding, the strategies adopted by the care home were unlikely to cause any selection bias:Randomization was stratified by residential village (4 villages total) in blocks of 4 rooms with 1 : 1 allocation. Randomization was performed by the principal investigator using a computerized random-number generatorDuring follow-up, long term care staff assigned incoming residents to rooms on a first come, first served basis, which was mandatory practice; flooring was not considered when making room assignments | Yes |
| Was the allocation sequence concealed until participants were enrolled and assigned to interventions? | It is stated that the allocation sequence was ‘concealed from residents, residents’ families, LTC staff (outcome assessors), and FLIP Study research assistants involved in data collection and analysis’. Moreover, implementation of blinding strategies ensured adequate allocation concealment during the follow-up:The sequence was shared immediately after generation with the flooring installation team and an on-site project manager at the LTC site to enable room renovations; neither party was involved in data collection or analysis(i) the flooring installation team, LTC residents and their families, and LTC staff were unaware of the specific research questions throughout the trial; and (ii) LTC residents, their families, and LTC staff were also unaware of the types or numbers of floors under evaluation | Probably yes |
| Did baseline differences between intervention groups suggest a problem with the randomisation process? | Although there were some baseline differences between intervention groups, these are likely to have occurred because of chance. The analyses included a multivariate model that would have accounted for these differences:Baseline resident characteristics were well balanced between intervention and control groups across a range of demographic, medical history, mobility, and medication variables, with some exceptions | Probably no |
| Risk-of-bias judgement |
All outcomes: Allocation sequence was adequately concealed; any baseline differences observed between intervention groups appear to be compatible with chance; and the allocation sequence was random |
Low |
| 2. Risk of bias due to deviations from the intended interventions (effect of assignment to intervention) | ||
| Were participants aware of their assigned intervention during the trial? | Adequate measures were adopted to ensure blinding of the assigned intervention from the care home residents and their families:Intervention and control flooring were covered with the same hospital-grade vinyl, and thus, intervention and control rooms looked identical | No |
| Were carers and people delivering the interventions aware of participants’ assigned intervention during the trial? | Adequate measures were adopted to ensure blinding of the assigned intervention from the care home staff, who were unaware of the specific research questions or the types or numbers of floors under investigation:(i) the flooring installation team, LTC residents and their families, and LTC staff were unaware of the specific research questions throughout the trial; and (ii) LTC residents, their families, and LTC staff were also unaware of the types or numbers of floors under evaluation | No |
| Was an appropriate analysis used to estimate the effect of assignment to intervention? | The outcomes were analysed as prespecified:We conducted intent-to-treat analyses using a two-tailed significance level of 0.05 | Yes |
| Risk-of-bias judgement |
All outcomes: Participants, carers, and people delivering the interventions were unaware of intervention groups during the trial; and an appropriate analysis was used to estimate the effect of assignment to intervention |
Low |
| 3. Risk of bias due to missing data | ||
| Were data for this outcome available for all, or nearly all, participants randomised? | During the intervention period, there were 184 participants in the intervention group and 173 in the control group. The study relied on the data being completed by the care home staff in the event of a fall. Although the report does not describe the number of missing outcome data, owing to the attempted masking of outcome assessors, it is less likely that ‘missingness’ would differ substantially between groups. It can be derived from the tables presented in Mackey et al.50 that there were 20 falls missing (out of 1009) from the intervention group, and 23 falls missing (out of 898) from the control group in the analysis of outcomes (about 2% of the falls data were not included in the analysis); these missing data are unlikely to have influenced the findings | Probably yes |
| Risk-of-bias judgement |
All outcomes: Outcome data were available for all randomised participants |
Low |
| 4. Risk of bias in measurement of the outcome | ||
| Was the method of measuring the outcome inappropriate? |
All outcomes: Data were collected using standardised forms and from multiple sources It is stated in Mackey et al. 50 that all ‘data collection activities were retrospective and involved only secondary and deidentified data’:© 2019 Mackey et al. 50 This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited |
No |
| Could measurement or ascertainment of the outcome have differed between intervention groups? | It is stated that the care home followed its standard practice, which was to complete an incident form within 24 hours of participants’ sustaining a fall. Care home staff were not aware of the research question or of the different floor types. Data were collected using the same standardised systems for both study groups:Information from incident forms, resident charts, and hospital records were used to assess the nature and extent of fall-related injuries, including injury type, location, and severity | Probably no |
| Were outcome assessors aware of the intervention received by study participants? | The researchers made attempts to blind staff at the care home and the research assistants involved in data collection:Randomization was [. . .] concealed from [. . .] LTC staff (outcome assessors), and FLIP study research assistants involved in data collection | Probably no |
| Risk-of-bias judgement |
All outcomes: The method of measuring the outcomes was appropriate, measurement of the outcomes did not differ between intervention groups and the outcome assessors were unaware of the intervention received by study participants |
Low |
| 5. Risk of bias in selection of the reported result | ||
| Were the data that produced this result analysed in accordance with a prespecified analysis plan that was finalised before unblinded outcome data were available for analysis? |
Although there were changes made to the prespecified analysis plan, these are explicitly stated with a reasonable rationale and the decisions were made prior to the initiation of data analysis The statistical analysis plan for the primary outcome was changed from Poisson models (specified in the protocol) to negative binomial regression models, which provided a better fit for the data: |
Yes |
| Is the numerical result being assessed likely to have been selected, on the basis of the results, from multiple eligible outcome measurements (e.g. scales, definitions, time points) within the outcome domain? | Comparison with the protocol suggests that all reported results correspond to all intended outcome measurements | No |
| Is the numerical result being assessed likely to have been selected, on the basis of the results, from multiple eligible analyses of the data? | It is unlikely that there has been selective outcome reporting on the basis of the results. The only concern is related to adverse events (not assessed here),a which were specified in the protocol but not reported in the final report. Our data on adverse events are therefore based on a personal communication with the author, and we have been unable to undertake a full risk-of-bias assessment on this outcome (it would require an assessment with the ROBINS-I tool and a fuller report of the findings owing to the nested study design). Number of falls resulting in injuries was not a prespecified outcome for this study, but was calculated for the purposes of the systematic review; this outcome was significant, but the study reports on prespecified outcomes only, which were non-significant | No |
| Risk-of-bias judgement |
Injurious falls rate per 1000 person-days, falls rate per 1000 person-days, number of falls resulting in injuries, number of fractures, number of hip fractures, number of fallers: The data were analysed in accordance with a prespecified plan that was finalised before unblinded outcome data were available for analysis. The results being assessed are unlikely to have been selected, on the basis of the results, from multiple outcome measurements within the outcome domain, and reported outcome data are unlikely to have been selected, on the basis of the results, from multiple analyses of the data |
Low |
| Overall risk of bias | All outcomes | Low |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? | This was an observational study in which the groups were not assigned randomly and different room types had different floor coverings; hence, the potential for confounding cannot be ruled out | Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? | Analysis was based on which intervention (flooring type) participants received at the time of sustaining a fall | Yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? | Certain types of people may be more likely than others to move between the flooring types, and these types of people may also be more or less likely to experience the outcome of interest. Those people with bedside commodes, or who use incontinence products, may have been less exposed (unsupervised) to concrete/no carpet, so there may have been a relationship between level of continence and switches between interventions:The anomalous feature of table 4 is clearly the low risk of hip fractures being incurred from falls on uncarpeted concrete floors [. . .] These falls mostly occurred in bathrooms and toilets, 65% of which had this type of flooring compared with less than 6% of other rooms | Probably yes |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains and for time-varying confounding? | RRs were calculated without any adjustments made for potential confounding | No |
| Risk-of-bias judgement |
Number of hip fractures: Confounding domains were not measured or controlled for |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? | All residents who were recorded in the homes’ records as having sustained a fracture in a fall had been correctly identified:Thirty-four residential care homes [. . .] agreed to take part in the study [. . .] Data were collated with clinical records from the Accident and Emergency service [. . .] In order to validate reporting of hip fractures, the radiographs of the residents reported to have had a fracture were reviewed | No |
| Do start of follow-up and start of intervention coincide for most participants? | The population of interest for the study includes those who had sustained a fall. The start of the intervention is the point at which a person impacts with the floor and each new fall is considered an independent case. Any fracture that occurred shortly after receiving the intervention would have been picked up | Probably yes |
| Risk-of-bias judgement |
Number of hip fractures: (1) All participants who would have been eligible for the target trial were included in the study and (2) for each participant, start of follow up and start of intervention coincided |
Low |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? | The definition of intervention groups in this study is reliant on how clearly the populations were defined, as they did not appear to use a standard definition for falls. The report does not state how similar the classifications of falls were across sites. The discussion alludes to possible differences in the classification of residents in bathrooms and toilets (mostly uncarpeted concrete floors):The floor types were classified as: i. Wood subfloor with no carpet; ii. Wood subfloor with carpet; iii. Concrete subfloor with no carpet; iv. Concrete subfloor with carpetIt may be that falls in bathrooms and toilets were atypical in one way or another. Possibly staff were particularly vigilant during such falls and reported milder or less complete falls than were reported elsewhere in the homes | Probably no |
| Was the information used to define intervention groups recorded at the start of the intervention? | Information was collected at the time of intervention, along with the location of falls relating to the intervention group:Data on the number and location of falls were recorded prospectively for a minimum of 2 years from the falls register of each home | Yes |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? | The discussion alludes to possible differences in the classification of residents in bathrooms and toilets (mostly uncarpeted concrete floors). Although all fractures were likely to be detected across all intervention groups, it is possible that those without a fracture were differentially classified as receiving the intervention or not:Possibly staff were particularly vigilant during such falls and reported milder or less complete falls than were reported elsewhere in the homes | Probably yes |
| Risk-of-bias judgement |
Number of hip fractures: Intervention status is not well defined |
Serious |
| 4. Risk of bias due to deviations from intended interventions | ||
| Were important co-interventions balanced across intervention groups? | Important co-interventions (e.g. hip protectors, fall mats) were not mentioned as being measured in the report | No information |
| Was the intervention implemented successfully for most participants? | The unit of analysis was falls. A standard definition for falls (e.g. coming to rest on the ground or lower level) was not provided, so it is unclear whether or not all participants received the intervention as described:It may be that falls in bathrooms and toilets were atypical in one way or another. Possibly staff were particularly vigilant during such falls and reported milder or less complete falls than were reported elsewhere in the homes | Probably no |
| Did study participants adhere to the assigned intervention regimen? | The unit of analysis was the fall event, rather than the participant. The intervention was administered once at the time of each fall. So, although it may have been possible for participants to switch between groups, it was not possible for falls to switch between groups | Probably yes |
| Risk-of-bias judgement |
Number of hip fractures: No information is reported on important co-interventions to determine whether or not these indicated deviations from intended interventions; however, there were indications of deviations from the intended interventions in terms of implementation that were likely to affect the outcome, and the analyses were unable to accommodate this |
Serious |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? | Outcome data were available for all of those who were classified into the respective groups:This confirmed that all the residents that were recorded in the homes’ records as having sustained a fracture in a fall had been correctly identified | Probably yes |
| Were participants excluded because of missing data on intervention status? | The paper does not report any exclusions. It is unclear if people without fractures were excluded because of missing data on intervention status:Data on the number and location of falls were recorded prospectively for a minimum of 2 years from the falls register of each home. These data were collated with clinical records from the Accident and Emergency service [. . .] Comparability of the recording of falls in the different homes was assessed | Probably no |
| Were participants excluded because of missing data on other variables needed for the analysis? | The study does not report undertaking additional analyses to control for confounding factors | Probably no |
| Risk-of-bias judgement |
Number of hip fractures: Data were reasonably complete |
Low |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? | The identification of fractures is unlikely to have been influenced by knowledge of the intervention; however, the identification of those who fell without a fracture could have been related to the intervention, affecting the fracture risk. This issue has been captured under the risk-of-bias domain for classification of the intervention:The anomalous feature of table 4 is clearly the low risk of hip fractures being incurred from falls on uncarpeted concrete floors [. . .] Possibly staff were particularly vigilant during such falls and reported milder or less complete falls than were reported elsewhere in the homes | Probably no |
| Were outcome assessors aware of the intervention received by study participants? | Outcome assessors also record the location of fall | Probably yes |
| Were the methods of outcome assessment comparable across intervention groups? | Outcome of interest is an objective measure that was radiologically diagnosed by the same trust, meaning that they are likely to be comparable across intervention groups | Probably yes |
| Were any systematic errors in measurement of the outcome related to intervention received? | Outcome of interest is an objective measure that was radiologically diagnosed by the same trust | Probably no |
| Risk-of-bias judgement |
Number of hip fractures: Methods of outcome assessment were comparable across intervention groups, and the outcome measure was unlikely to be influenced by knowledge of the intervention received by study participants |
Low |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? | Throughout the report, the terms ‘hip fracture’ and ‘fracture’ are used interchangeably, but, based on the title, rationale/introduction and data collection description in the methods, it can be inferred that the focus was always on hip fracture | Probably no |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention–outcome relationship? | The statistical analysis plan is not well described to rule out bias. There is inconsistency in the reporting of the effect estimate: on page 244, it is reported as OR in the text but as relative risk in the tables | Probably yes |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? | Reported effect estimates are based on all participants selected for the analysis | Probably no |
| Risk-of-bias judgement |
Number of hip fractures: Probable risk of selective reporting from among multiple analyses |
Serious |
| Overall risk of bias | Number of hip fractures | Serious |
| Signalling questionsa | Supporting statement | Response |
|---|---|---|
| 1. Risk of bias due to confounding | ||
| Is there potential for confounding of the effect of intervention in this study? | The interventions occurred at different time periods and each ward acted as its own control; hence, the participants are likely to be different:The data on falls and any subsequent fractures for the 12 months preceding and 12 months following the change in flooring was retrieved for each ward. Thus each ward acted as its own control | Yes |
| Was the analysis based on splitting participants’ follow-up time according to intervention received? | The data on falls and any subsequent fractures for the 12 months preceding and 12 months following the change in flooring was retrieved from the Quality Improvement Event Reporting forms for each ward. As the interventions do not occur concurrently, there is a chance that an individual receives both of the interventions, depending on the timing of their hospitalisation | Yes |
| Were intervention discontinuations or switches likely to be related to factors that are prognostic for the outcome? | Interventions do not occur concurrently, so there is a chance that an individual receives both of the interventions, but this is more related to the timing of their hospitalisation than to prognostic factors | Probably no |
| Did the authors use an appropriate analysis method that controlled for all the important confounding domains? |
Falls rate per 1000 person-days, number of fractures: The analysis method used for rate calculation is not reported. Table 1 in Warren and Hanger101 suggests that the intervention groups differ by sex and mean length of stay. However, there is no report of an analysis method that would take into account of all the important confounding domains: |
Probably no |
| Did the authors control for any post-intervention variables that could have been affected by the intervention? | The report does not suggest that the analysis methods adjusted for any post-intervention variables | Probably no |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: Confounding domains were not measured or controlled for |
Serious |
| 2. Risk of bias due to selection of participants | ||
| Was selection of participants into the study (or into the analysis) based on participant characteristics observed after the start of intervention? | All patients admitted to the ward during the study period participated in the study:The data on falls and any subsequent fractures for the 12 months preceding and 12 months following the change in flooring was retrieved for each ward. The nursing staff were not aware of this study and no changes were made in the falls reporting process over the study period | No |
| Do start of follow-up and start of intervention coincide for most participants? |
Falls rate per 1000 person-days: Each individual would have been exposed to the intervention on admission to the ward, the same point at which follow-up for falls would have begun: |
Probably yes |
|
Number of fractures: Number of fractures is measured from the point of falling on the floor (number of fractures per 100 falls), with each new fall being considered an independent case. For this outcome, the start of intervention is implicitly defined as the point at which an individual falls on the floor, which is also the point from which they were followed up |
Probably yes | |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: All participants who would have been eligible for the target trial were included in the study; for each participant, start of follow-up and start of intervention coincided |
Low |
| 3. Risk of bias due to classification of intervention | ||
| Were intervention groups clearly defined? | Interventions comprised vinyl flooring and carpet | Yes |
| Was the information used to define intervention groups recorded at the start of the intervention? |
As the information about the intervention received is available from the audit form, the likelihood of misclassification is minimal |
Probably yes |
| Could classification of intervention status have been affected by knowledge of the outcome or risk of the outcome? | Standard procedures were followed for recording outcome, the nursing staff were not aware of this study, and no changes were made in the falls reporting process over the study period | Probably no |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: Intervention status is well defined, and the definition is based solely on information collected at the time of intervention |
Low |
| 4. Risk of bias due to deviations from intended intervention | ||
| Were important co-interventions balanced across intervention groups? | Co-interventions (e.g. hip protectors, fall mats) were not mentioned in the study report | No information |
| Was the intervention implemented successfully for most participants? | The study design was orientated around a system-wide implementation plan of the intervention flooring, covering all patient areas:In six of these wards over a two-year period, the carpet floor covering in all patient areas was replaced with a non-slip vinyl | Probably yes |
| Did study participants adhere to the assigned intervention regime? | Owing to the nature of the study design and situational context, it was unlikely that participants were able to switch between groups | Probably yes |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: No information is reported regarding important co-interventions to determine whether or not there is a deviation from the intended intervention |
No information |
| 5. Risk of bias due to missing data | ||
| Were outcome data available for all, or nearly all, participants? | The data on falls and any subsequent fractures for the 12 months preceding and 12 months following the change in flooring were retrieved for each ward, from the Quality Improvement Event Reporting forms | Probably yes |
| Were participants excluded because of missing data on intervention status? | The paper does not report on any exclusions. Owing to the time frames facilitating the clear depiction of intervention status, it seems unlikely that participants were excluded because of missing data on intervention status | Probably no |
| Were participants excluded because of missing data on other variables needed for the analysis? | The study does not report undertaking additional analyses to control for confounding factors | Not applicable |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: Data were reasonably complete |
Low |
| 6. Risk of bias in measurement of the outcome | ||
| Could the outcome measure have been influenced by knowledge of the intervention received? | The data on falls and any subsequent fractures for the 12 months preceding and 12 months following the change in flooring were retrieved for each ward, from the Quality Improvement Event Reporting forms. Moreover, the nursing staff who completed the form were not aware of this study and no changes were made in the falls reporting process over the study period | Probably no |
| Were outcome assessors aware of the intervention received by study participants? | Although the nursing staff are not aware of the study, they would have been aware of the flooring intervention | Probably yes |
| Were the methods of outcome assessment comparable across intervention groups? | [N]o changes were made in the falls reporting process over the study period | Probably yes |
| Were any systematic errors in measurement of the outcome related to intervention received? | This appears unlikely, as outcome assessors were unaware of the study and the methods of outcome ascertainment did not change over the course of the study | Probably no |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: The methods of outcome assessment were comparable across intervention groups, the outcome measure was unlikely to be influenced by knowledge of the intervention received by study participants (i.e. is objective), and any error in measuring the outcome is unrelated to intervention status |
Low |
| 7. Risk of bias in selection of the reported result | ||
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple outcome measurements within the outcome domain? |
Falls rate per 1000 person-days, number of fractures: Fall-related injuries would probably have been recorded, but only fractures were reported; there is no discussion of other injuries. There were 26 fractures, but it is not clear how many were hip fractures. There is no protocol available for this study, but the methods section appears congruent with what is reported in the results |
Probably no |
| Is the reported effect estimate likely to be selected, on the basis of the results, from multiple analyses of the intervention–outcome relationship? | There is no prespecified statistical analysis plan to rule out bias. Relatively straightforward analyses have been undertaken on the data and it appears unlikely that these would have been selectively reported (they are non-significant) | Probably no |
| Is the reported effect estimate likely to be selected, on the basis of the results, from different subgroups? | Subgroups are presented for falls rates, but alongside the data for all participants combined, so it is unlikely that effect estimates have been selected based on different subgroups | Probably no |
| Risk-of-bias judgement |
Falls rate per 1000 person-days, number of fractures: The outcome measurements and analyses are clearly defined and internally consistent and there is no indication of selection of the reported analysis from among multiple analyses, or selection of the cohort for analysis and reporting on the basis of the results |
Moderate |
| Overall risk of bias | Falls rate per 1000 person-days, number of fractures | Serious |
Appendix 3 Evidence profile table (hospitals)
| Outcome/study type | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Overall certainty of evidence | Comments |
|---|---|---|---|---|---|---|---|
| Injurious falls rate per 1000 person-days | |||||||
| RCTs | Not serious | Not serious | Not serious | Very serious | None |
⊕⊕◯◯ Low |
Wide CI that crosses the line of no effect, and small sample size |
| All studies | Serious | Not serious | Not serious | None | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of confounding |
| Falls rate per 1000 person-days | |||||||
| RCTs | Not serious | Not serious | Not serious | Very serious | None |
⊕⊕◯◯ Low |
Wide CI that crosses the line of no effect, and small sample size |
| All studies | Serious | Not serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of confounding |
| Number of falls resulting in injury | |||||||
| All studies | Very serious | Very serious | Not serious | Not serious | Publication bias strongly suspected |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of bias due to confounding and measurement of the outcome. Some concerns in selection of the reported result. Substantial heterogeneity (I2 = 73%; CIs of the studies do not overlap). Donald et al.105 is not included because of insufficient reporting |
| Number of fractures | |||||||
| RCTs | Not serious | Not serious | Not serious | Very serious | None |
⊕⊕◯◯ Low |
Few events and wide CI crossing the line of no effect |
| All studies | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of bias due to confounding. Wide CI that crosses the line of no effect, and small sample sizes |
| Number of hip fractures | |||||||
| RCTs | Not serious | Not serious | Not serious | Very serious | None |
⊕⊕◯◯ Low |
Few events and wide CI crossing the line of no effect |
| All studies | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of bias due to confounding. Few events and wide CI crossing the line of no effect |
| Number of fallers | |||||||
| RCTs | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Some concerns in the randomisation process, measurement of the outcome and selection of the reported result. Wide CI that crosses the line of no effect, and small sample sizes |
| Adverse events | |||||||
| RCTs | Not serious | Not serious | Serious | Very serious | None |
⊕◯◯◯ Very low |
Downgraded because there were very few data. Outcome not preferred reporting of rates per 100 working days (denominator not known), making objective comparison difficult |
| Observational studies | Serious | Not serious | Serious | Serious | None |
⊕◯◯◯ Very low |
Downgraded because of serious risk of confounding, and concerns about measurement of outcomes and selective reporting. Outcome not preferred reporting of rates per 100 working days (denominator not known), making objective comparison difficult. There were a limited number of events in each arm and no description of variance |
Appendix 4 Evidence profile table (care homes)
| Outcome/study type | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Overall certainty of evidence | Comments |
|---|---|---|---|---|---|---|---|
| Injurious falls rate per 1000 person-days | |||||||
| RCTs | Not serious | Not serious | Not serious | Not serious | None |
⊕⊕⊕⊕ High |
|
| All studies | Not serious | Not serious | Not serious | Not serious | Publication bias strongly suspected |
⊕◯◯◯ Very low |
The outcome could have reasonably been calculated from Gustavsson et al.52 using intention-to-treat principles (as was done for falls rates), but could not be derived from the available data, so is not included |
| Falls rate per 1000 person-days | |||||||
| RCTs | Not serious | Not serious | Not serious | Serious | None |
⊕⊕⊕◯ Moderate |
Wide CI that crosses the line of no effect |
| All studies | Very serious | Serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of confounding and some concerns about measurement of outcome and selective reporting. Substantial heterogeneity (I2 = 89%; CIs of the studies do not overlap and show opposite effects). Wide CI that crosses the line of no effect |
| Number of falls resulting in injury | |||||||
| All studies | Very serious | Not serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of bias due to confounding, selection of participants, measurement of outcome and selective reporting |
| Number of fractures | |||||||
| RCTs | Not serious | Not serious | Not serious | Very serious | None |
⊕⊕◯◯ Low |
Few events and wide CI that crosses the line of no effect |
| All studies | Very serious | Not serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Based on observational evidence. High risk of bias due to confounding, selection of participants, selective reporting and some concerns about measurement of outcome. Downgraded because of wide CI that crosses the line of no effect |
| Number of hip fractures | |||||||
| RCTs | Not serious | Not serious | Not serious | Very serious | None |
⊕⊕◯◯ Low |
Few events and wide CI that crosses the line of no effect |
| All studies | Very serious | Serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
High risk of bias due to confounding, classification of the intervention, deviation from intervention, and selective reporting; substantial heterogeneity (I2 = 73%), with CIs that do not overlap and show opposite effects |
| Number of fallers | |||||||
| RCTs | Not serious | Not serious | Not serious | Not serious | None |
⊕⊕⊕⊕ High |
|
| Adverse events | |||||||
| All studies | Not assessed | Not serious | Serious | Not assessed | Publication bias strongly suspected |
⊕◯◯◯ Very low |
Based on observational evidence. Nested study design (before-and-after study) within RCT: does not fit our inclusion criteria (indirect evidence). Information obtained via personal communication. Outcome presented in protocol, but not published (separate publication planned) |
Appendix 5 Evidence profile table (flooring types)
| Outcome/floor type | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Overall certainty of evidence | Comments |
|---|---|---|---|---|---|---|---|---|
| Injurious falls rate per 1000 person-days | ||||||||
| Novel | RCT and observational study | Serious | Not serious | Not serious | Not serious | Publication bias strongly suspected |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding. The outcome could have been calculated from Gustavsson et al.52 using intention-to-treat principles, but could not be derived from available data |
| Sports | RCT and observational study | Serious | Not serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding |
| Falls rate per 1000 person-days | ||||||||
| Novel | RCT and observational studies | Very serious | Serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding and concerns in measurement of outcome and selective reporting. Data are heterogeneous (I2 = 74%, CIs do not all overlap) |
| Sports | RCT and observational study | Serious | Not serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding. Wide CI including no effect |
| Number of falls resulting in injuries | ||||||||
| Novel | RCT and observational studies | Very serious | Not serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of bias in the following domains: confounding, selection of participants, measurement of outcomes, and selective reporting |
| Sports | RCT and observational study | Very serious | Not serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of bias related to confounding. Wide CI including no effect |
| Carpet | Observational study | Very serious | Not serious | Not serious | Not serious | Publication bias strongly suspected |
⊕◯◯◯ Very low |
Observational evidence with high risk of bias related to confounding, measurement of outcome, and concerns for selective reporting. Donald et al.105 not included because of insufficient reporting |
| Number of fractures | ||||||||
| Novel | RCT and observational study | Serious | Not serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding, and concerns for selective reporting. Wide CI including no effect |
| Sports | RCT and observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding, and concerns for selective reporting. Few events and wide CI including no effect |
| Carpet | RCT | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Observational evidence with concerns across risk-of-bias domains. Very small study with no events observed |
| Number of hip fractures | ||||||||
| Novel | RCT and observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding, and concerns for selection of the reported result. Wide CI including no effect |
| Sports | RCT and observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of confounding, and concerns for selective reporting. Few events; wide CI including no effect |
| Carpet | Observational study | Very serious | Serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of bias in the following domains: confounding, classification of interventions, deviations from the intervention, and selection of the reported results. Substantial heterogeneity (I2 = 86%, CIs do not overlap), with carpet on different subfloors showing opposite effects. Wide CI including no effect |
| Wood | Observational study | Very serious | Serious | Not serious | Not serious | None |
⊕◯◯◯ Very low |
Observational evidence with high risk of bias due to confounding, classification of interventions, deviations from the intervention, and selective reporting. Substantial heterogeneity (I2 = 86%, CIs do not overlap), with carpeted/uncarpeted wood showing opposite effects |
| Number of fallers | ||||||||
| Novel | RCT | Not serious | Not serious | Not serious | Not serious | None |
⊕⊕⊕⊕ High |
|
| Sports | RCT | Not serious | Not serious | Not serious | Serious | None |
⊕⊕⊕◯ Moderate |
Wide CI including no effect |
| Carpet | RCT | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
High risk of bias in outcome measurement and concerns with randomisation and selective reporting. Few events with wide CI |
| Adverse events | ||||||||
| Novel | Observational study | Not assessed | Not serious | Serious | Not assessed | Publication bias strongly suspected |
⊕◯◯◯ Very low |
Observational evidence. Nested before-and-after study within RCT: does not fit our inclusion criteria (indirect evidence). Information obtained via personal communication; outcome presented in protocol but not published (separate publication planned) |
| Sports | RCT | Not serious | Not serious | Serious | Very serious | None |
⊕◯◯◯ Very low |
Downgraded because there were very few data. Outcome not preferred reporting of rates per 100 working days (denominator not known), making objective comparison difficult |
Appendix 6 Subgroup analyses
| Outcomea | Subgroup effect estimates | Test for subgroup differencesb | |||
|---|---|---|---|---|---|
| Setting (RCTs) | Hospitals | Care homes | |||
| Injurious falls rate, RaR (95% CI) | 0.58 (0.18 to 1.91) | 0.91 (0.62 to 1.32) | – | – | χ2 = 0.50, df = 1 (p = 0.48), I2 = 0% |
| Falls rate, RaR (95% CI) | 1.07 (0.64 to 1.81) | 1.21 (0.87 to 1.68) | – | – | χ2 = 0.14, df = 1 (p = 0.71), I2 = 0% |
| Number of fractures (M–H; participants), OR (95% CI) | 0.33 (0.01 to 8.13) | 0.74 (0.29 to 1.92) | – | – | χ2 = 0.23, df = 1 (p = 0.63), I2 = 0% |
| Number of hip fractures (M–H; participants), OR (95% CI) | 0.33 (0.01 to 8.15) | 0.94 (0.13 to 6.74) | – | – | χ2 = 0.30, df = 1 (p = 0.59), I2 = 0% |
| Number of fallers, RR (95% CI) | 2.25 (0.56 to 9.04) | 1.03 (0.89 to 1.18) | – | – | χ2 = 1.20, df = 1 (p = 0.27), I2 = 16.4% |
| Fracture rate, RaR (95% CI) | 0.21 (0.01 to 5.25) | 0.83 (0.33 to 2.10) | – | – | χ2 = 0.66, df = 1 (p = 0.42), I2 = 0% |
| Setting (all studies) | Hospitals | Care homes | |||
| Injurious falls rate, RaR (95% CI) | 0.55 (0.36 to 0.84) | 0.91 (0.62 to 1.32) | – | – | χ2 = 3.05, df = 1 (p = 0.08), I2 = 67.2% |
| Falls rate, RaR (95% CI) | 0.88 (0.71 to 1.09) | 0.87 (0.47 to 1.62) | – | – | χ2 = 0.00, df = 1 (p = 0.98), I2 = 0% |
| Falls resulting in injuries, RR (95% CI) | 0.39 (0.15 to 1.02) | 0.80 (0.70 to 0.91) | – | – | χ2 = 2.08, df = 1 (p = 0.15), I2 = 51.9% |
| Number of fractures (M–H; participants), OR (95% CI) | 0.28 (0.04 to 1.77) | 0.74 (0.29 to 1.92) | – | – | χ2 = 0.86, df = 1 (p = 0.35), I2 = 0% |
| Number of fractures (M–H; falls), OR (95% CI) | 0.30 (0.05 to 1.92) | 0.61 (0.26 to 1.48) | – | – | χ2 = 0.48, df = 1 (p = 0.49), I2 = 0% |
| Number of hip fractures (M–H; participants), OR (95% CI) | 0.88 (0.12 to 6.47) | 0.94 (0.13 to 6.74) | – | – | χ2 = 0.00, df = 1 (p = 0.96), I2 = 0% |
| Number of hip fractures (M–H; falls), OR (95% CI) | 0.92 (0.13 to 6.65) | 1.17 (0.77 to 1.80) | – | – | χ2 = 0.06, df = 1 (p = 0.81), I2 = 0% |
| Number of fallers, RR (95% CI) | 2.25 (0.56 to 9.04) | 1.03 (0.89 to 1.18) | – | – | χ2 = 1.20, df = 1 (p = 0.27), I2 = 16.4% |
| Number of head injuries (participants), RR (95% CI) | 0.39 (0.10 to 1.51) | 0.60 (0.24 to 1.51) | – | – | χ2 = 0.26, df = 1 (p = 0.61), I2 = 0% |
| Number of head injuries (falls), RR (95% CI) | 0.45 (0.12 to 1.77) | 0.56 (0.22 to 1.45) | – | – | χ2 = 0.07, df = 1 (p = 0.80), I2 = 0% |
| Fracture rate, RaR (95% CI) | 0.24 (0.04 to 1.52) | 0.83 (0.33 to 2.10) | – | – | χ2 = 1.39, df = 1 (p = 0.24), I2 = 28.2% |
| Study design (all settings) | RCTs | Prospective cohort | Retrospective cohort | ||
| Injurious falls rate, RaR (95% CI) | 0.87 (0.61 to 1.25) | 0.54 (0.35 to 0.86) | – | – | χ2 = 2.56, df = 1 (p = 0.11), I2 = 61.0% |
| Falls rate, RaR (95% CI) | 1.17 (0.89 to 1.54) | 0.74 (0.57 to 0.97) | – | – | χ2 = 5.44, df = 1 (p = 0.02), I2 = 81.6% |
| Falls resulting in injuries, RR (95% CI) | 0.77 (0.67 to 0.88) | 0.68 (0.51 to 0.89) | 0.41 (0.07 to 2.35) | – | χ2 = 1.10, df = 2 (p = 0.58), I2 = 0% |
| Number of fractures (M–H; participants), OR (95% CI) | 0.69 (0.28 to 1.70) | 0.25 (0.03 to 2.48) | – | – | χ2 = 0.64, df = 1 (p = 0.43), I2 = 0% |
| Number of fractures (M–H; falls), OR (95% CI) | 0.66 (0.27 to 1.61) | 0.30 (0.03 to 2.89) | 0.20 (0.01 to 4.28) | – | χ2 = 0.85, df = 2 (p = 0.65), I2 = 0% |
| Number of hip fractures (M–H; participants), OR (95% CI) | 0.68 (0.13 to 3.49) | 2.37 (0.10 to 58.90) | – | – | χ2 = 0.46, df = 1 (p = 0.50), I2 = 0% |
| Number of hip fractures (M–H; falls), OR (95% CI) | 0.64 (0.13 to 3.29) | 1.21 (0.78 to 1.86) | – | – | χ2 = 0.30, df = 1 (p = 0.59), I2 = 0% |
| Number of head injuries (participants), RR (95% CI) | 0.60 (0.24 to 1.51) | 0.39 (0.10 to 1.51) | – | – | χ2 = 0.26, df = 1 (p = 0.61), I2 = 0% |
| Number of head injuries (falls), RR (95% CI) | 0.56 (0.22 to 1.45) | 0.45 (0.12 to 1.77) | – | – | χ2 = 0.07, df = 1 (p = 0.80), I2 = 0% |
| Fracture rate, RaR (95% CI) | 0.75 (0.31 to 1.82) | 0.26 (0.03 to 2.45) | – | – | χ2 = 0.75, df = 1 (p = 0.39), I2 = 0% |
| Study design (hospitals) | RCTs | Prospective cohort | Retrospective cohort | ||
| Injurious falls rate, RaR (95% CI) | 0.58 (0.18 to 1.91) | 0.54 (0.35 to 0.86) | – | – | χ2 = 0.01, df = 1 (p = 0.92), I2 = 0% |
| Falls rate, RaR (95% CI) | 1.07 (0.64 to 1.81) | 0.85 (0.67 to 1.07) | – | – | χ2 = 0.67, df = 1 (p = 0.41), I2 = 0% |
| Falls resulting in injuries, RR (95% CI) | 0.54 (0.12 to 2.40) | 0.64 (0.44 to 0.95) | 0.16 (0.06 to 0.40) | – | χ2 = 7.65, df = 2 (p = 0.02), I2 = 73.9% |
| Number of fractures (M–H; participants), OR (95% CI) | 0.33 (0.01 to 8.13) | 0.25 (0.03 to 2.48) | – | – | χ2 = 0.02, df = 1 (p = 0.90), I2 = 0% |
| Number of hip fractures (M–H; participants), OR (95% CI) | 0.33 (0.01 to 8.15) | 2.37 (0.10 to 58.90) | – | – | χ2 = 0.72, df = 1 (p = 0.40), I2 = 0% |
| Study design (care homes) | RCTs | Prospective cohort | Retrospective cohort | ||
| Falls rate, RaR (95% CI) | 1.21 (0.87 to 1.68) | 0.64 (0.51 to 0.82) | – | – | χ2 = 9.28, df = 1 (p = 0.002), I2 = 89.2% |
| Falls resulting in injuries, RR (95% CI) | 0.77 (0.67 to 0.89) | 0.71 (0.48 to 1.05) | 0.95 (0.72 to 1.25) | – | χ2 = 2.14, df = 2 (p = 0.34), I2 = 6.7% |
| Number of fractures (M–H; falls), OR (95% CI) | 0.71 (0.28 to 1.81) | – | 0.20 (0.01 to 4.28) | – | χ2 = 0.59, df = 1 (p = 0.44), I2 = 0% |
| Number of hip fractures (M–H; falls), OR (95% CI) | 0.89 (0.13 to 6.33) | 1.19 (0.77 to 1.84) | – | – | χ2 = 0.08, df = 1 (p = 0.78), I2 = 0% |
| Flooring type (RCTs) | Novel | Sports | Carpet | Wood | |
| Injurious falls rate, RaR (95% CI) | 0.91 (0.62 to 1.32) | 0.58 (0.18 to 1.91) | – | – | χ2 = 0.50, df = 1 (p = 0.48), I2 = 0% |
| Falls rate, RaR (95% CI) | 1.21 (0.87 to 1.68) | 1.07 (0.64 to 1.81) | – | – | χ2 = 0.14, df = 1 (p = 0.71), I2 = 0% |
| Number of fractures (M–H; participants), OR (95% CI) | 0.74 (0.29 to 1.92) | 0.33 (0.01 to 8.13) | – | – | χ2 = 0.23, df = 1 (p = 0.63), I2 = 0% |
| Number of hip fractures (M–H; participants), OR (95% CI) | 0.94 (0.13 to 6.74) | 0.33 (0.01 to 8.15) | – | – | χ2 = 0.30, df = 1 (p = 0.59), I2 = 0% |
| Number of fallers, RR (95% CI) | 1.03 (0.89 to 1.18) | 1.40 (0.63 to 3.10) | 6.50 (0.86 to 49.30) | – | χ2 = 3.68, df = 2 (p = 0.16), I2 = 45.7% |
| Flooring type (all studies) | Novel | Sports | Carpet | Wood | |
| Injurious falls rate, RaR (95% CI) | 0.80 (0.59 to 1.09) | 0.46 (0.23 to 0.92) | – | – | χ2 = 2.01, df = 1 (p = 0.16), I2 = 50.2% |
| Falls rate, RaR (95% CI) | 0.89 (0.65 to 1.24) | 0.85 (0.56 to 1.28) | – | – | χ2 = 0.04, df = 1 (p = 0.84), I2 = 0% |
| Falls resulting in injuries, RR (95% CI) | 0.79 (0.70 to 0.88) | 0.58 (0.30 to 1.12) | 0.16 (0.07 to 0.40) | – | All subgroups: χ2 = 12.09, df = 2 (p = 0.002), I2 = 83.5%; Excluding carpet: χ2 = 0.61, df = 1 (p = 0.44), I2 = 0% |
| Number of fractures (M–H; participants), OR (95% CI) | 0.67 (0.28 to 1.59) | 0.31 (0.03 to 3.07) | – | – | χ2 = 0.37, df = 1 (p = 0.54), I2 = 0% |
| Number of fractures (M–H; falls), OR (95% CI) | 0.59 (0.27 to 1.33) | 0.33 (0.03 to 3.25) | – | – | χ2 = 0.23, df = 1 (p = 0.63), I2 = 0% |
| Number of hip fractures (M–H; participants), OR (95% CI) | 1.25 (0.24 to 6.47) | 0.33 (0.01 to 8.15) | – | – | χ2 = 0.53, df = 1 (p = 0.47), I2 = 0% |
| Number of hip fractures (M–H; falls), OR (95% CI) | 1.29 (0.25 to 6.53) | 0.30 (0.01 to 7.70) | 1.19 (0.77 to 1.84) | 0.59 (0.45 to 0.78) | Excluding wood: χ2 = 0.69, df = 2 (p = 0.71), I2 = 0%; Excluding carpet: χ2 = 1.03, df = 2 (p = 0.60), I2 = 0% |
| Number of fallers, RR (95% CI) | 1.03 (0.89 to 1.18) | 1.40 (0.63 to 3.10) | 6.50 (0.86 to 49.30) | – | χ2 = 3.68, df = 2 (p = 0.16), I2 = 45.7% |
| Number of head injuries (participants), RR (95% CI) | 0.59 (0.27 to 1.28) | 0.19 (0.01 to 3.71) | – | – | χ2 = 0.53, df = 1 (p = 0.47), I2 = 0% |
| Number of head injuries (falls), RR (95% CI) | 0.59 (0.27 to 1.31) | 0.22 (0.01 to 4.44) | – | – | χ2 = 0.39, df = 1 (p = 0.53), I2 = 0% |
Appendix 7 Sensitivity analyses
| Outcome: sensitivity analysis | All settings | Hospitals | Care homes | Flooring types (all studies)a | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RCTs | All studies | RCTs | All studies | RCTs | All studies | Novel | Sports | Carpet | Wood | |
| Injurious falls rate, RaR (95% CI) | ||||||||||
| Main analysis | 0.87 (0.61 to 1.25) | 0.71 (0.48 to 1.04) | 0.58 (0.18 to 1.91) | 0.55 (0.36 to 0.84) | 0.91 (0.62 to 1.32) | – | 0.80 (0.59 to 1.09) | 0.46 (0.23 to 0.92) | – | – |
| Adjusted model (Mackey50) | 1.03 (0.72 to 1.47) | 0.75 (0.43 to 1.29) | – | – | 0.91 (0.75 to 1.59) | – | 0.84 (0.55 to 1.27) | – | – | – |
| Falls rate, RaR (95% CI) | ||||||||||
| Main analysis | 1.17 (0.89 to 1.54) | 0.89 (0.67 to 1.18) | 1.07 (0.64 to 1.81) | 0.88 (0.71 to 1.09) | 1.21 (0.87 to 1.68) | 0.87 (0.47 to 1.62) | 0.89 (0.65 to 1.24) | 0.85 (0.56 to 1.28) | – | – |
| Adjusted model (Mackey50) | 1.24 (0.93 to 1.64) | 0.91 (0.67 to 1.25) | – | – | 1.32 (0.94 to 1.84) | 0.91 (0.45 to 1.83) | 0.91 (0.64 to 1.31) | – | – | – |
| Unpublished data (Gustavsson52) | – | 0.87 (0.63 to 1.21) | – | – | – | 0.84 (0.42 to 1.68) | 0.88 (0.60 to 1.27) | – | – | – |
| Unpublished data (Hanger49) | – | 0.89 (0.67 to 1.19) | – | 0.89 (0.72 to 1.11) | – | – | 0.89 (0.65 to 1.24) | 0.85 (0.56 to 1.28) | – | – |
| Number of falls resulting in injuries, RR (95% CI) | ||||||||||
| Main analysis | – | 0.69 (0.52 to 0.90) | – | 0.39 (0.15 to 1.02) | – | 0.80 (0.70 to 0.91) | 0.75 (0.66 to 0.86) | 0.58 (0.30 to 1.12) | 0.16 (0.07 to 0.40) | – |
| ICC = 0.023 (Drahota77) | – | 0.68 (0.52 to 0.89) | – | 0.40 (0.16 to 0.97) | – | – | – | 0.57 (0.31 to 1.07) | – | – |
| ICC = 0.092 (Drahota77) | – | 0.69 (0.53 to 0.90) | – | 0.38 (0.13 to 1.08) | – | – | – | 0.58 (0.29 to 1.16) | – | – |
| Unpublished data (Hanger49) | – | 0.68 (0.52 to 0.89) | – | 0.39 (0.15 to 1.01) | – | – | – | – | – | – |
| Removing carpet (Healey103) | – | 0.78 (0.70 to 0.87) | – | 0.64 (0.44 to 0.93) | – | – | – | – | – | – |
| Number of fractures, OR (95% CI) | ||||||||||
| Main analysis (M–H; UoA: participants) | 0.69 (0.28 to 1.70) | 0.59 (0.26 to 1.35) | 0.33 (0.01 to 8.13) | 0.28 (0.04 to 1.77) | 0.74 (0.29 to 1.92) | – | 0.67 (0.28 to 1.59) | 0.31 (0.03 to 3.07) | – | – |
| M–H; UoA: falls | – | 0.53 (0.24 to 1.17) | – | – | – | 0.61 (0.26 to 1.48) | 0.59 (0.27 to 1.33) | 0.33 (0.03 to 3.25) | – | – |
| Peto; UoA: participants | 0.68 (0.27 to 1.70) | 0.58 (0.25 to 1.33) | 0.13 (0.00 to 6.76) | 0.24 (0.04 to 1.40) | 0.74 (0.29 to 1.91) | – | 0.67 (0.28 to 1.61) | 0.13 (0.01 to 2.08) | – | – |
| Peto; UoA: falls | – | 0.51 (0.23 to 1.13) | – | – | – | 0.70 (0.34 to 1.42) | 0.58 (0.25 to 1.32) | 0.14 (0.01 to 2.20) | – | – |
| Peto; UoA: participants; ICC = 0.0065 (Drahota77) | 0.68 (0.27 to 1.70) | 0.58 (0.25 to 1.33) | 0.13 (0.00 to 6.73) | 0.24 (0.04 to 1.40) | – | – | – | 0.13 (0.01 to 2.07) | – | – |
| Peto; UoA: falls; ICC = 0.0065 (Drahota77) | – | 0.51 (0.23 to 1.13) | – | – | – | – | – | 0.14 (0.01 to 2.22) | – | – |
| M–H; UoA: participants; ICC = 0.0065 (Drahota77) | 0.69 (0.28 to 1.70) | 0.59 (0.26 to 1.35) | 0.33 (0.01 to 8.09) | 0.28 (0.04 to 1.77) | – | – | – | 0.31 (0.03 to 3.06) | – | – |
| M–H; UoA: falls; ICC = 0.0065 (Drahota77) | – | 0.53 (0.24 to 1.17) | – | – | – | – | – | 0.33 (0.03 to 3.28) | – | – |
| Peto; UoA: participants; ICC = 0.026 (Drahota77) | 0.68 (0.27 to 1.70) | 0.58 (0.25 to 1.33) | 0.13 (0.00 to 6.74) | 0.24 (0.04 to 1.40) | – | – | – | 0.13 (0.01 to 2.07) | – | – |
| Peto; UoA: falls; ICC = 0.026 (Drahota77) | – | 0.51 (0.23 to 1.13) | – | – | – | – | – | 0.14 (0.01 to 2.27) | – | – |
| M–H; UoA: participants; ICC = 0.026 (Drahota77) | 0.69 (0.28 to 1.70) | 0.59 (0.26 to 1.35) | 0.33 (0.01 to 8.10) | 0.28 (0.04 to 1.77) | – | – | – | 0.31 (0.03 to 3.06) | – | – |
| M–H; UoA: falls; ICC = 0.026 (Drahota77) | – | 0.53 (0.24 to 1.17) | – | – | – | – | – | 0.33 (0.03 to 3.34) | – | – |
| Peto; UoA: participants; unpublished data (Hanger49) | – | 0.57 (0.25 to 1.32) | – | 0.23 (0.04 to 1.38) | – | – | – | – | – | – |
| Peto; UoA: falls; unpublished data (Hanger49) | – | 0.51 (0.23 to 1.13) | – | – | – | – | – | – | – | – |
| M–H; UoA: participants; unpublished data (Hanger49) | – | 0.59 (0.25 to 1.35) | – | 0.27 (0.04 to 1.75) | – | – | – | – | – | – |
| M–H; UoA: falls; unpublished data (Hanger49) | – | 0.53 (0.24 to 1.16) | – | – | – | – | – | – | – | – |
| M–H; UoA: participants; including Lange82 | – | 0.58 (0.26 to 1.30) | – | – | – | 0.71 (0.29 to 1.76) | 0.65 (0.29 to 1.49) | – | – | – |
| M–H; UoA: falls; including Lange82 | – | 0.56 (0.26 to 1.19) | – | – | – | 0.64 (0.28 to 1.50) | 0.62 (0.28 to 1.35) | – | – | – |
| M–H; UoA: falls; including Gustavsson52 | – | 0.62 (0.32 to 1.21) | – | – | – | 0.70 (0.34 to 1.45) | 0.67 (0.34 to 1.34) | – | – | – |
| Number of hip fractures, OR (95% CI) | ||||||||||
| Main analysis (M–H; UoA: participants) | 0.68 (0.13 to 3.49) | 0.91 (0.22 to 3.70) | 0.33 (0.01 to 8.15) | 0.88 (0.12 to 6.47) | 0.94 (0.13 to 6.74) | – | 1.25 (0.24 to 6.47) | 0.33 (0.01 to 8.15) | – | – |
| M–H; UoA: falls | – | 1.16 (0.77 to 1.76) | – | – | – | 1.17 (0.77 to 1.80) | 1.29 (0.25 to 6.53) | 0.30 (0.01 to 7.70) | 1.19 (0.77 to 1.84) | 0.59 (0.45 to 0.78) |
| Peto; UoA: participants | 0.64 (0.11 to 3.69) | 0.92 (0.18 to 4.59) | 0.13 (0.00 to 6.79) | 0.88 (0.05 to 14.23) | 0.94 (0.13 to 6.73) | – | 1.36 (0.23 to 7.91) | 0.13 (0.00 to 6.79) | – | – |
| Peto; UoA: falls | – | 1.16 (0.78 to 1.73) | – | – | – | 1.17 (0.78 to 1.75) | 1.35 (0.23 to 7.85) | 0.13 (0.00 to 6.38) | 1.18 (0.78 to 1.78) | 0.60 (0.46 to 0.78) |
| Peto; UoA: participants; ICC = 0.001 (Drahota77) | 0.63 (0.11 to 3.69) | 0.92 (0.18 to 4.58) | 0.13 (0.00 to 6.76) | 0.88 (0.05 to 14.20) | – | – | – | 0.13 (0.00 to 6.76) | – | – |
| Peto; UoA: falls; ICC = 0.001 (Drahota77) | – | 1.16 (0.78 to 1.73) | – | – | – | – | – | 0.13 (0.00 to 6.41) | – | – |
| M–H; UoA: participants; ICC = 0.001 (Drahota77) | 0.68 (0.13 to 3.48) | 0.91 (0.22 to 3.69) | 0.33 (0.01 to 8.11) | 0.88 (0.12 to 6.45) | – | – | – | 0.33 (0.01 to 8.11) | – | – |
| M–H; UoA: falls; ICC = 0.001 (Drahota77) | – | 1.16 (0.77 to 1.76) | – | – | – | – | – | 0.30 (0.01 to 7.73) | – | – |
| Peto; UoA: participants; ICC = 0.004 (Drahota77) | 0.63 (0.11 to 3.69) | 0.92 (0.18 to 4.58) | 0.13 (0.00 to 6.74) | 0.88 (0.05 to 14.18) | – | – | – | 0.13 (0.00 to 6.74) | – | – |
| Peto; UoA: falls; ICC = 0.004 (Drahota77) | – | 1.16 (0.78 to 1.73) | – | – | – | – | – | 0.13 (0.00 to 6.57) | – | – |
| M–H; UoA: participants; ICC = 0.004 (Drahota77) | 0.68 (0.13 to 3.48) | 0.91 (0.22 to 3.69) | 0.33 (0.01 to 8.10) | 0.88 (0.12 to 6.44) | – | – | – | 0.33 (0.01 to 8.10) | – | – |
| M–H; UoA: falls; ICC = 0.004 (Drahota77) | – | 1.16 (0.77 to 1.76) | – | – | – | – | – | 0.31 (0.01 to 7.94) | – | – |
| Peto; UoA: participants; unpublished data (Hanger49) | – | 0.92 (0.18 to 4.57) | – | 0.87 (0.05 to 14.10) | – | – | – | – | – | – |
| Peto; UoA: falls; unpublished data (Hanger49) | – | 1.16 (0.78 to 1.73) | – | – | – | – | – | – | – | – |
| M–H; UoA: participants; unpublished data (Hanger49) | – | 0.90 (0.22 to 3.68) | – | 0.87 (0.12 to 6.41) | – | – | – | – | – | – |
| M–H; UoA: falls; unpublished data (Hanger49) | – | 1.16 (0.77 to 1.76) | – | – | – | – | – | – | – | – |
| Peto; UoA: falls; Simpson76 regrouped | – | 1.10 (0.73 to 1.65) | – | – | – | 1.10 (0.73 to 1.66) | – | – | 1.11 (0.73 to 1.70) | 0.60 (0.46 to 0.79) |
| M–H; UoA: falls; Simpson76 regrouped | – | 1.10 (0.72 to 1.67) | – | – | – | 1.11 (0.72 to 1.70) | – | – | 1.12 (0.72 to 1.73) | 0.59 (0.45 to 0.79) |
| M–H; UoA: falls; including Gustavsson52 | – | 1.11 (0.74 to 1.65) | – | – | – | 1.12 (0.74 to 1.68) | 0.80 (0.24 to 2.67) | – | – | – |
| Number of fallers, RR (95% CI) | ||||||||||
| Main analysis | 1.28 (0.73 to 2.25) | – | 2.25 (0.56 to 9.04) | – | 1.03 (0.89 to 1.18) | – | 1.03 (0.89 to 1.18) | 1.40 (0.63 to 3.10) | 6.50 (0.86 to 49.3) | – |
| ICC = 0.01 (Drahota77) | 1.26 (0.75 to 2.11) | – | 2.21 (0.56 to 8.78) | – | – | – | – | 1.40 (0.71 to 2.73) | – | – |
| ICC = 0.04 (Drahota77) | 1.31 (0.69 to 2.50) | – | 2.32 (0.56 to 9.55) | – | – | – | – | 1.40 (0.51 to 3.80) | – | – |
| Low risk of bias (excluding Donald105) | 1.04 (0.90 to 1.19) | – | 1.40 (0.63 to 3.10) | – | – | – | – | – | – | – |
| Number of head injuries, RR (95% CI) | ||||||||||
| Main analysis (UoA: participants) | 0.60 (0.24 to 1.51) | 0.52 (0.24 to 1.12) | – | 0.39 (0.10 to 1.51) | 0.60 (0.24 to 1.51) | – | 0.59 (0.27 to 1.28) | 0.19 (0.01 to 3.71) | – | – |
| UoA: falls | 0.57 (0.22 to 1.45) | 0.53 (0.24 to 1.14) | – | 0.45 (0.12 to 1.77) | 0.57 (0.22 to 1.45) | – | 0.59 (0.27 to 1.31) | 0.22 (0.01 to 4.44) | – | – |
| UoA: participant; unpublished data (Hanger49) | – | 0.59 (0.27 to 1.29) | – | 0.57 (0.13 to 2.48) | – | – | – | – | – | – |
| UoA: falls; unpublished data (Hanger49) | – | 0.59 (0.27 to 1.31) | – | 0.67 (0.15 to 2.93) | – | – | – | – | – | – |
| UoA: falls; unpublished data (Gustavsson52) | – | 0.55 (0.31 to 0.97) | – | – | – | 0.57 (0.31 to 1.07) | 0.59 (0.33 to 1.04) | – | – | – |
| Rate of fractures, RaR (95% CI) | ||||||||||
| Main analysis | 0.75 (0.31 to 1.82) | 0.65 (0.28 to 1.48) | 0.21 (0.01 to 5.25) | 0.24 (0.04 to 1.52) | 0.83 (0.33 to 2.10) | – | – | – | – | – |
| ICC = 0.001 (Drahota77) | 0.74 (0.30 to 1.81) | 0.64 (0.28 to 1.47) | 0.21 (0.01 to 4.75) | 0.24 (0.04 to 1.49) | – | – | – | – | – | – |
| ICC = 0.004 (Drahota77) | 0.75 (0.31 to 1.85) | 0.65 (0.28 to 1.50) | 0.21 (0.01 to 6.38) | 0.24 (0.04 to 1.58) | – | – | – | – | – | – |
| Including Lange82 | – | 0.64 (0.29 to 1.42) | – | – | 0.80 (0.33 to 1.94) | – | – | – | – | – |
| Rate of hip fractures, RaR (95% CI) | ||||||||||
| Main analysis | 0.73 (0.13 to 4.01) | 0.94 (0.21 to 4.23) | 0.26 (0.01 to 7.78) | 0.82 (0.08 to 8.51) | 1.04 (0.15 to 7.36) | – | – | – | – | – |
| ICC = 0.001 (Drahota77) | 0.72 (0.13 to 3.89) | 0.93 (0.21 to 4.12) | 0.26 (0.01 to 7.00) | 0.79 (0.08 to 7.94) | – | – | – | – | – | – |
| ICC = 0.004 (Drahota77) | 0.75 (0.13 to 4.23) | 0.97 (0.21 to 4.42) | 0.26 (0.01 to 9.54) | 0.88 (0.08 to 9.64) | – | – | – | – | – | – |
Appendix 8 Evidence profile table (head-to-head comparisons)
| Outcome/comparison | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Overall certainty of evidence | Comments |
|---|---|---|---|---|---|---|---|---|
| Injurious falls rate per 1000 person-days | ||||||||
| Kradal vs. SmartCells | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Kradal vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| SmartCells vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Falls rate per 1000 person-days | ||||||||
| Kradal vs. SmartCells | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Kradal vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI close to the line of no effect, and high risk of bias due to confounding |
| SmartCells vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Number of falls resulting in injuries | ||||||||
| Kradal vs. SmartCells | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Kradal vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| SmartCells vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Number of fractures | ||||||||
| Kradal vs. SmartCells | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Kradal vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded as study was too small to measure this outcome |
| SmartCells vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Number of hip fractures | ||||||||
| Kradal vs. SmartCells | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Kradal vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded as study was too small to measure this outcome |
| SmartCells vs. Tarkett Omnisports Excel | Observational study | Serious | Not serious | Not serious | Very serious | None |
⊕◯◯◯ Very low |
Based on one observational study. Downgraded because of wide CI that crosses the line of no effect, and high risk of bias due to confounding |
| Number of fallers | ||||||||
| Kradal vs. SmartCells | No data available | |||||||
| Kradal vs. Tarkett Omnisports Excel | No data available | |||||||
| SmartCells vs. Tarkett Omnisports Excel | No data available | |||||||
| Adverse events | ||||||||
| Kradal vs. SmartCells | No data available | |||||||
| Kradal vs. Tarkett Omnisports Excel | No data available | |||||||
| SmartCells vs. Tarkett Omnisports Excel | No data available | |||||||
Appendix 9 Evidence profile table (qualitative findings)
| Review finding | Studies | Methodological limitations | Relevance | Coherence | Adequacy | Overall assessment of confidence | Explanation of judgement |
|---|---|---|---|---|---|---|---|
| Shock-absorbing flooring is viewed by many as a potential solution to help protect people from fall-related injuries, with a potential side effect of improving environmental comfort | Four studies51,53,54,118 | No or very minor concerns (three studies with minor methodological limitations and one study with some concerns) | No or very minor concerns (studies covered the perspectives of patients, visitors, residents and various staff groups) | Moderate concerns (some outliers within studies, but reasonably consistent across studies) | No or very minor concerns (four studies with mostly unequivocal findings owing to rich data, representing a range of views) |
⊕⊕⊕◯ Moderate confidence |
This finding should be read alongside the second synthesised finding. The finding has been rated down for coherence because, if read in isolation, it does not provide a complete picture of the review findings |
| Changing a floor has consequences for the wider system (e.g. affecting the ease of moving equipment), potentially leading to further adaptations and adjustments in behaviours, attitudes, equipment, processes and staffing | Four studies51,54,68,118 | Minor concerns (two studies with minor limitations; one study with some concerns contributed to the types of adjustments listed – concerns unlikely to have affected the findings; the study with the biggest limitations did not alter the findings) | No or very minor concerns (the studies covered care homes and hospitals, and the perspectives of patients, visitors and various staff groups) | Minor concerns (the finding does not attempt to explain how things may change, as there was variability in this even within studies) | Minor concerns (largely unequivocal findings from three studies; this finding aims to be more descriptive than explanatory and the data cover a broad scope of contexts) |
⊕⊕⊕⊕ High confidence |
|
| Installation may be an initial concern, but can be effectively managed; however, cost and funding considerations need to extend beyond the initial purchase and installation to consider potential adaptations in staffing/processes/equipment, and potential cost savings from fall-related injury prevention (should the floor be effective) | Two studies54,118 | Minor concerns (one study contributed more to the idea that the installation can be effectively managed, and lacked reporting of reflexivity, but researchers were independent of the flooring company and not employed by the NHS trusts that managed the installation process) | Minor concerns (partial relevance as the finding that installation can be effectively managed is specific to UK-based hospitals with a sports floor; the cost considerations relate more to senior care home managers in Canada; the finding is congruent with the second review finding, which draws on wider evidence) | Minor concerns (some evidence suggesting some senior care home managers did not think beyond the initial floor purchase and installation. The trial report associated with Drahota et al.118 reported a 20- to 30-cm slit along a weld in a new floor, which was probably a result of the installation process; this was repaired and resolved) | Moderate concerns (only two studies: one in UK hospitals describing the installation process, and one in Canadian care homes describing funding considerations. Although the finding is largely descriptive and makes intuitive sense, these topics have not been validated across different settings and contexts) |
⊕⊕⊕◯ Moderate confidence |
Two studies with data from two settings (hospitals in the UK and care homes in Canada). There were minor concerns for methodological limitations, relevance and coherence, and moderate concerns for the adequacy of data owing to the number of data contributing to the finding |
List of abbreviations
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- CHEERS
- Consolidated Health Economic Evaluation Reporting Standards
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- df
- degrees of freedom
- GBP
- Great British pounds
- GDP
- gross domestic product
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- JBI
- Joanna Briggs Institute
- NHS EED
- NHS Economic Evaluation Database
- OR
- odds ratio
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QALY
- quality-adjusted life-year
- RaR
- rate ratio
- RCT
- randomised controlled trial
- RoB 2.0
- Risk of Bias tool version 2.0
- ROBINS-I
- Risk Of Bias In Non-randomized Studies – of Interventions
- RR
- risk ratio
- WHO
- World Health Organization
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/ZOWL2323).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.